User login
Embedding diversity, equity, inclusion, and justice in hospital medicine
A road map for success
The language of equality in America’s founding was never truly embraced, resulting in a painful legacy of slavery, racial injustice, and gender inequality inherited by all generations. However, for as long as America has fallen short of this unfulfilled promise, individuals have dedicated their lives to the tireless work of correcting injustice. Although the process has been painstakingly slow, our nation has incrementally inched toward the promised vision of equality, and these efforts continue today. With increased attention to social justice movements such as #MeToo and Black Lives Matter, our collective social consciousness may be finally waking up to the systemic injustices embedded into our fundamental institutions.
Medicine is not immune to these injustices. Persistent underrepresentation of women and minorities remains in medical school faculty and the broader physician workforce, and the same inequities exist in hospital medicine.1-6 The report by the Association of American Medical Colleges (AAMC) on diversity in medicine highlights the impact widespread implicit and explicit bias has on creating exclusionary environments, exemplified by research demonstrating lower promotion rates in non-White faculty.7-8 The report calls us, as physicians, to a broader mission: “Focusing solely on increasing compositional diversity along the academic continuum is insufficient. To effectively enact institutional change at academic medical centers ... leaders must focus their efforts on developing inclusive, equity-minded environments.”7
We have a clear moral imperative to correct these shortcomings for our profession and our patients. It is incumbent on our institutions and hospital medicine groups (HMGs) to embark on the necessary process of systemic institutional change to address inequality and justice within our field.
A road map for DEI and justice in hospital medicine
The policies and biases allowing these inequities to persist have existed for decades, and superficial efforts will not bring sufficient change. Our institutions require new building blocks from which the foundation of a wholly inclusive and equal system of practice can be constructed. Encouragingly, some institutions and HMGs have taken steps to modernize their practices. We offer examples and suggestions of concrete practices to begin this journey, organizing these efforts into three broad categories:
1. Recruitment and retention
2. Scholarship, mentorship, and sponsorship
3. Community engagement and partnership.
Recruitment and retention
Improving equity and inclusion begins with recruitment. Search and hiring committees should be assembled intentionally, with gender balance, and ideally with diversity or equity experts invited to join. All members should receive unconscious bias training. For example, the University of Colorado utilizes a toolkit to ensure appropriate steps are followed in the recruitment process, including predetermined candidate selection criteria that are ranked in advance.
Job descriptions should be reviewed by a diversity expert, ensuring unbiased and ungendered language within written text. Advertisements should be wide-reaching, and the committee should consider asking applicants for a diversity statement. Interviews should include a variety of interviewers and interview types (e.g., 1:1, group, etc.). Letters of recommendation deserve special scrutiny; letters for women and minorities may be at risk of being shorter and less record focused, and may be subject to less professional respect, such as use of first names over honorifics or titles.
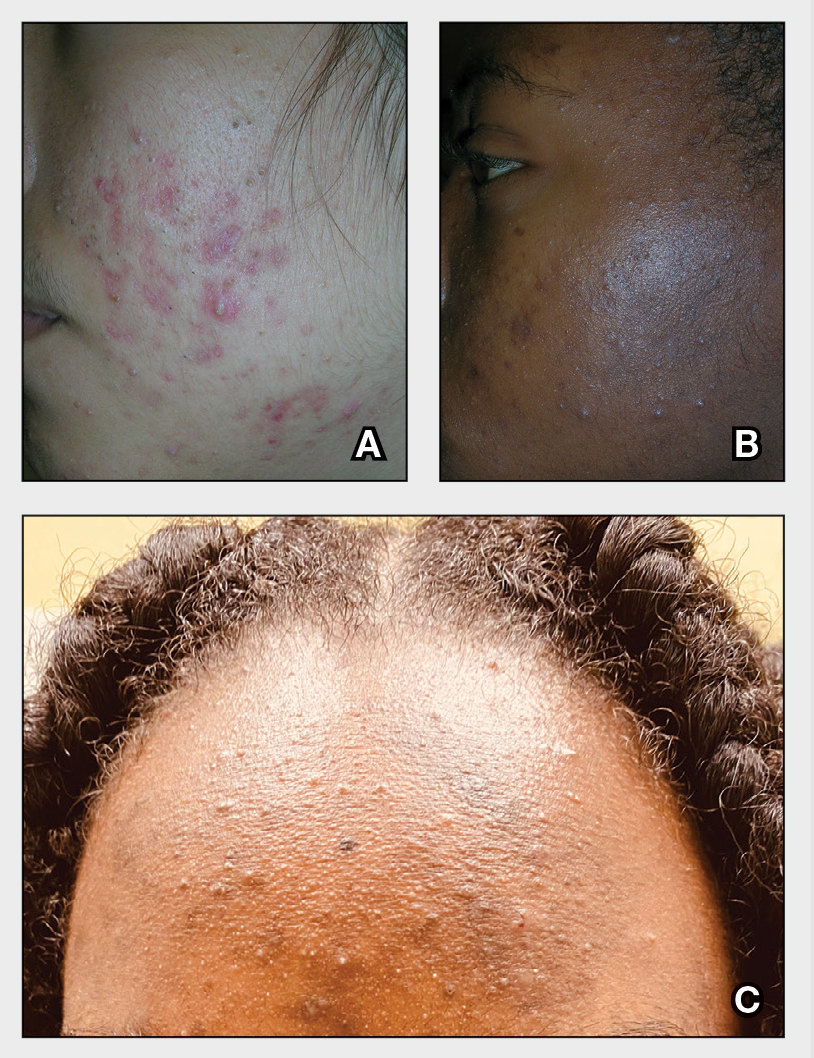
Once candidates are hired, institutions and HMGs should prioritize developing strategies to improve retention of a diverse workforce. This includes special attention to workplace culture, and thoughtfully striving for cultural intelligence within the group. Some examples may include developing affinity groups, such as underrepresented in medicine (UIM), women in medicine (WIM), or LGBTQ+ groups. Affinity groups provide a safe space for members and allies to support and uplift each other. Institutional and HMG leaders must educate themselves and their members on the importance of language (see table), and the more insidious forms of bias and discrimination that adversely affect workplace culture. Microinsults and microinvalidations, for example, can hurt and result in failure to recruit or turnover. 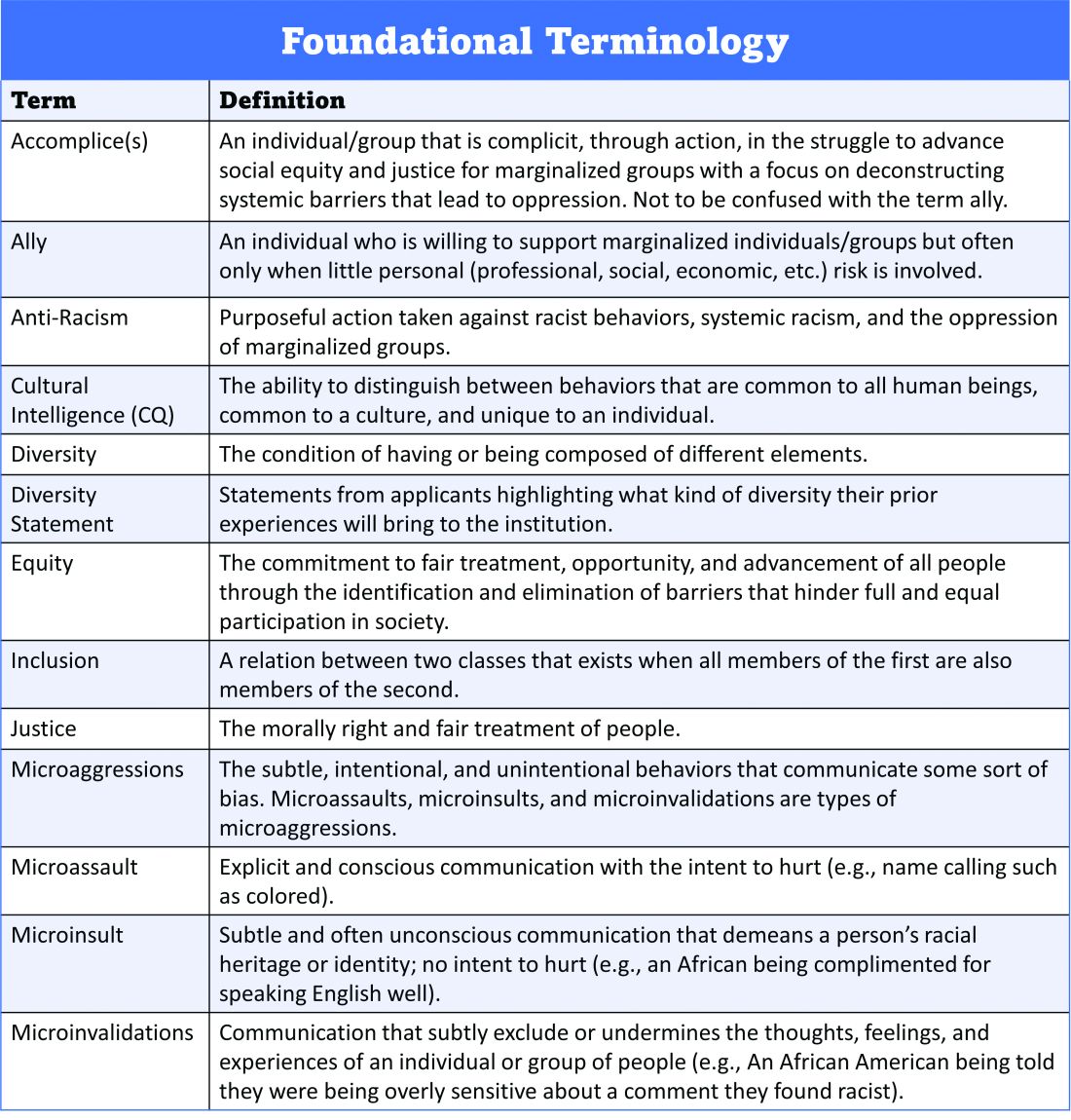
Conducting exit interviews when any hospitalist leaves is important to learn how to improve, but holding ‘stay’ interviews is mission critical. Stay interviews are an opportunity for HMG leaders to proactively understand why hospitalists stay, and what can be done to create more inclusive and equitable environments to retain them. This process creates psychological safety that brings challenges to the fore to be addressed, and spotlights best practices to be maintained and scaled.
Scholarship, mentorship, and sponsorship
Women and minorities are known to be over-mentored and under-sponsored. Sponsorship is defined by Ayyala et al. as “active support by someone appropriately placed in the organization who has significant influence on decision making processes or structures and who is advocating for the career advancement of an individual and recommends them for leadership roles, awards, or high-profile speaking opportunities.”9 While the goal of mentorship is professional development, sponsorship emphasizes professional advancement. Deliberate steps to both mentor and then sponsor diverse hospitalists and future hospitalists (including trainees) are important to ensure equity.
More inclusive HMGs can be bolstered by prioritizing peer education on the professional imperative that we have a diverse workforce and equitable, just workplaces. Academic institutions may use existing structures such as grand rounds to provide education on these crucial topics, and all HMGs can host journal clubs and professional development sessions on leadership competencies that foster inclusion and equity. Sessions coordinated by women and minorities are also a form of justice, by helping overcome barriers to career advancement. Diverse faculty presenting in educational venues will result in content that is relevant to more audience members and will exemplify that leaders and experts are of all races, ethnicities, genders, ages, and abilities.
Groups should prioritize mentoring trainees and early-career hospitalists on scholarly projects that examine equity in opportunities of care, which signals that this science is valued as much as basic research. When used to demonstrate areas needing improvement, these projects can drive meaningful change. Even projects as straightforward as studying diversity in conference presenters, disparities in adherence to guidelines, or QI projects on how race is portrayed in the medical record can be powerful tools in advancing equity.
A key part of mentoring is training hospitalists and future hospitalists in how to be an upstander, as in how to intervene when a peer or patient is affected by bias, harassment, or discrimination. Receiving such training can prepare hospitalists for these nearly inevitable experiences and receiving training during usual work hours communicates that this is a valuable and necessary professional competency.
Community engagement and partnership
Institutions and HMGs should deliberately work to promote community engagement and partnership within their groups. Beyond promoting health equity, community engagement also fosters inclusivity by allowing community members to share their ideas and give recommendations to the institutions that serve them.
There is a growing body of literature that demonstrates how disadvantages by individual and neighborhood-level socioeconomic status (SES) contribute to disparities in specific disease conditions.10-11 Strategies to narrow the gap in SES disadvantages may help reduce race-related health disparities. Institutions that engage the community and develop programs to promote health equity can do so through bidirectional exchange of knowledge and mutual benefit.
An institution-specific example is Medicine for the Greater Good at Johns Hopkins. The founders of this program wrote, “health is not synonymous with medicine. To truly care for our patients and their communities, health care professionals must understand how to deliver equitable health care that meets the needs of the diverse populations we care for. The mission of Medicine for the Greater Good is to promote health and wellness beyond the confines of the hospital through an interactive and engaging partnership with the community ...” Community engagement also provides an opportunity for growing the cultural intelligence of institutions and HMGs.
Tools for advancing comprehensive change – Repurposing PDSA cycles
Whether institutions and HMGs are at the beginning of their journey or further along in the work of reducing disparities, having a systematic approach for implementing and refining policies and procedures can cultivate more inclusive and equitable environments. Thankfully, hospitalists are already equipped with the fundamental tools needed to advance change across their institutions – QI processes in the form of Plan-Do-Study-Act (PDSA) cycles.
They allow a continuous cycle of successful incremental change based on direct evidence and experience. Any efforts to deconstruct systematic bias within our organizations must also be a continual process. Our female colleagues and colleagues of color need our institutions to engage unceasingly to bring about the equality they deserve. To that end, PDSA cycles are an apt tool to utilize in this work as they can naturally function in a never-ending process of improvement.
With PDSA as a model, we envision a cycle with steps that are intentionally purposed to fit the needs of equitable institutional change: Target-Engage-Assess-Modify. As highlighted (see graphic), these modifications ensure that stakeholders (i.e., those that unequal practices and policies affect the most) are engaged early and remain involved throughout the cycle. 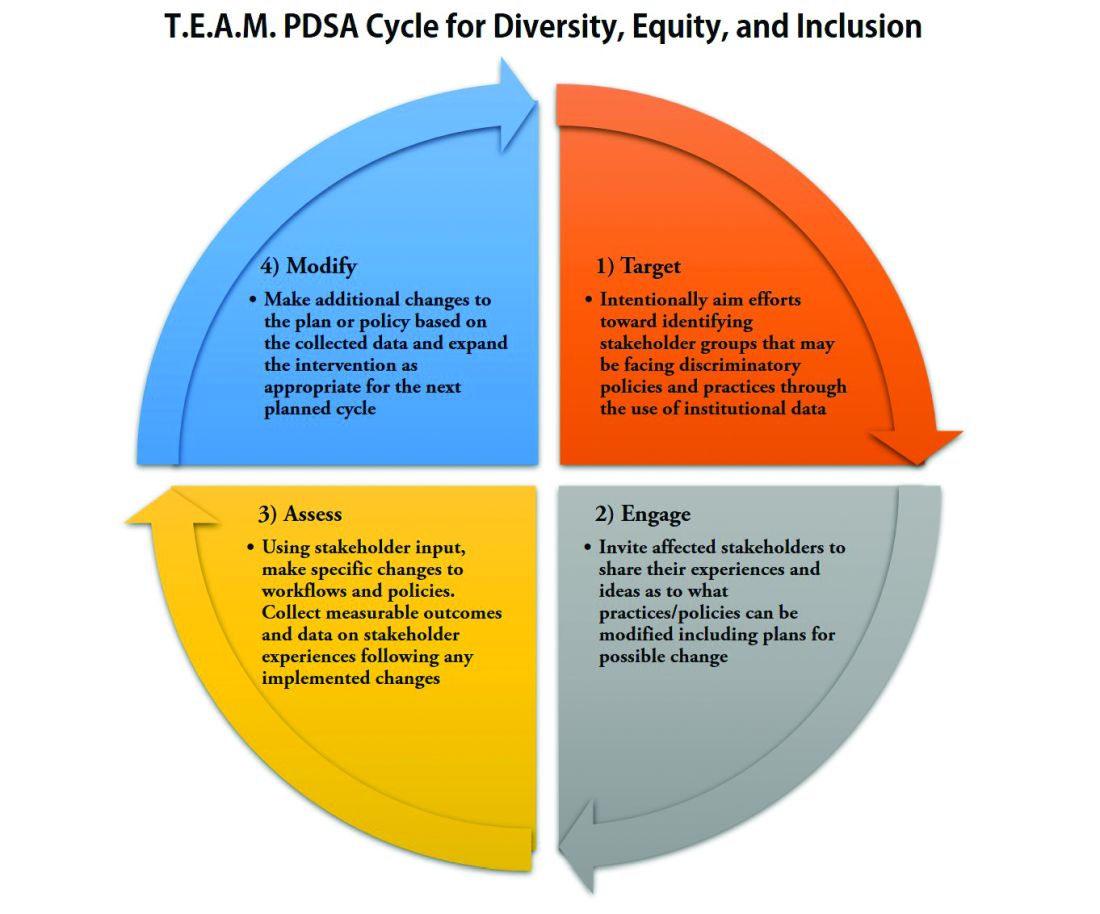
As hospitalists, we have significant work ahead to ensure that we develop and maintain a diverse, equitable and inclusive workforce. This work to bring change will not be easy and will require a considerable investment of time and resources. However, with the strategies and tools that we have outlined, our institutions and HMGs can start the change needed in our profession for our patients and the workforce. In doing so, we can all be accomplices in the fight to achieve racial and gender equity, and social justice.
Dr. Delapenha and Dr. Kisuule are based in the department of internal medicine, division of hospital medicine, at the Johns Hopkins University, Baltimore. Dr. Martin is based in the department of medicine, section of hospital medicine at the University of Chicago. Dr. Barrett is a hospitalist in the department of internal medicine, University of New Mexico, Albuquerque.
References
1. Diversity in Medicine: Facts and Figures 2019: Figure 19. Percentage of physicians by sex, 2018. AAMC website.
2. Diversity in Medicine: Facts and Figures 2019. Figure 16. Percentage of full-time U.S. medical school faculty by sex and race/ethnicity, 2018. AAMC website.
3. Diversity in Medicine: Facts and Figures 2019. Figure 15. Percentage of full-time U.S. medical school faculty by race/ethnicity, 2018. AAMC website.
4. Diversity in Medicine: Facts and Figures 2019. Figure 6. Percentage of acceptees to U.S. medical schools by race/ethnicity (alone), academic year 2018-2019. AAMC website.
5. Diversity in Medicine: Facts and Figures 2019 Figure 18. Percentage of all active physicians by race/ethnicity, 2018. AAMC website.
6. Herzke C et al. Gender issues in academic hospital medicine: A national survey of hospitalist leaders. J Gen Intern Med. 2020;35(6):1641-6.
7. Diversity in Medicine: Facts and Figures 2019. Fostering diversity and inclusion. AAMC website.
8. Diversity in Medicine: Facts and Figures 2019. Executive summary. AAMC website.
9. Ayyala MS et al. Mentorship is not enough: Exploring sponsorship and its role in career advancement in academic medicine. Acad Med. 2019;94(1):94-100.
10. Ejike OC et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. 2021 Apr 15;203(8):987-97.
11. Galiatsatos P et al. The effect of community socioeconomic status on sepsis-attributable mortality. J Crit Care. 2018 Aug;46:129-33.
A road map for success
A road map for success
The language of equality in America’s founding was never truly embraced, resulting in a painful legacy of slavery, racial injustice, and gender inequality inherited by all generations. However, for as long as America has fallen short of this unfulfilled promise, individuals have dedicated their lives to the tireless work of correcting injustice. Although the process has been painstakingly slow, our nation has incrementally inched toward the promised vision of equality, and these efforts continue today. With increased attention to social justice movements such as #MeToo and Black Lives Matter, our collective social consciousness may be finally waking up to the systemic injustices embedded into our fundamental institutions.
Medicine is not immune to these injustices. Persistent underrepresentation of women and minorities remains in medical school faculty and the broader physician workforce, and the same inequities exist in hospital medicine.1-6 The report by the Association of American Medical Colleges (AAMC) on diversity in medicine highlights the impact widespread implicit and explicit bias has on creating exclusionary environments, exemplified by research demonstrating lower promotion rates in non-White faculty.7-8 The report calls us, as physicians, to a broader mission: “Focusing solely on increasing compositional diversity along the academic continuum is insufficient. To effectively enact institutional change at academic medical centers ... leaders must focus their efforts on developing inclusive, equity-minded environments.”7
We have a clear moral imperative to correct these shortcomings for our profession and our patients. It is incumbent on our institutions and hospital medicine groups (HMGs) to embark on the necessary process of systemic institutional change to address inequality and justice within our field.
A road map for DEI and justice in hospital medicine
The policies and biases allowing these inequities to persist have existed for decades, and superficial efforts will not bring sufficient change. Our institutions require new building blocks from which the foundation of a wholly inclusive and equal system of practice can be constructed. Encouragingly, some institutions and HMGs have taken steps to modernize their practices. We offer examples and suggestions of concrete practices to begin this journey, organizing these efforts into three broad categories:
1. Recruitment and retention
2. Scholarship, mentorship, and sponsorship
3. Community engagement and partnership.
Recruitment and retention
Improving equity and inclusion begins with recruitment. Search and hiring committees should be assembled intentionally, with gender balance, and ideally with diversity or equity experts invited to join. All members should receive unconscious bias training. For example, the University of Colorado utilizes a toolkit to ensure appropriate steps are followed in the recruitment process, including predetermined candidate selection criteria that are ranked in advance.
Job descriptions should be reviewed by a diversity expert, ensuring unbiased and ungendered language within written text. Advertisements should be wide-reaching, and the committee should consider asking applicants for a diversity statement. Interviews should include a variety of interviewers and interview types (e.g., 1:1, group, etc.). Letters of recommendation deserve special scrutiny; letters for women and minorities may be at risk of being shorter and less record focused, and may be subject to less professional respect, such as use of first names over honorifics or titles.
Once candidates are hired, institutions and HMGs should prioritize developing strategies to improve retention of a diverse workforce. This includes special attention to workplace culture, and thoughtfully striving for cultural intelligence within the group. Some examples may include developing affinity groups, such as underrepresented in medicine (UIM), women in medicine (WIM), or LGBTQ+ groups. Affinity groups provide a safe space for members and allies to support and uplift each other. Institutional and HMG leaders must educate themselves and their members on the importance of language (see table), and the more insidious forms of bias and discrimination that adversely affect workplace culture. Microinsults and microinvalidations, for example, can hurt and result in failure to recruit or turnover. 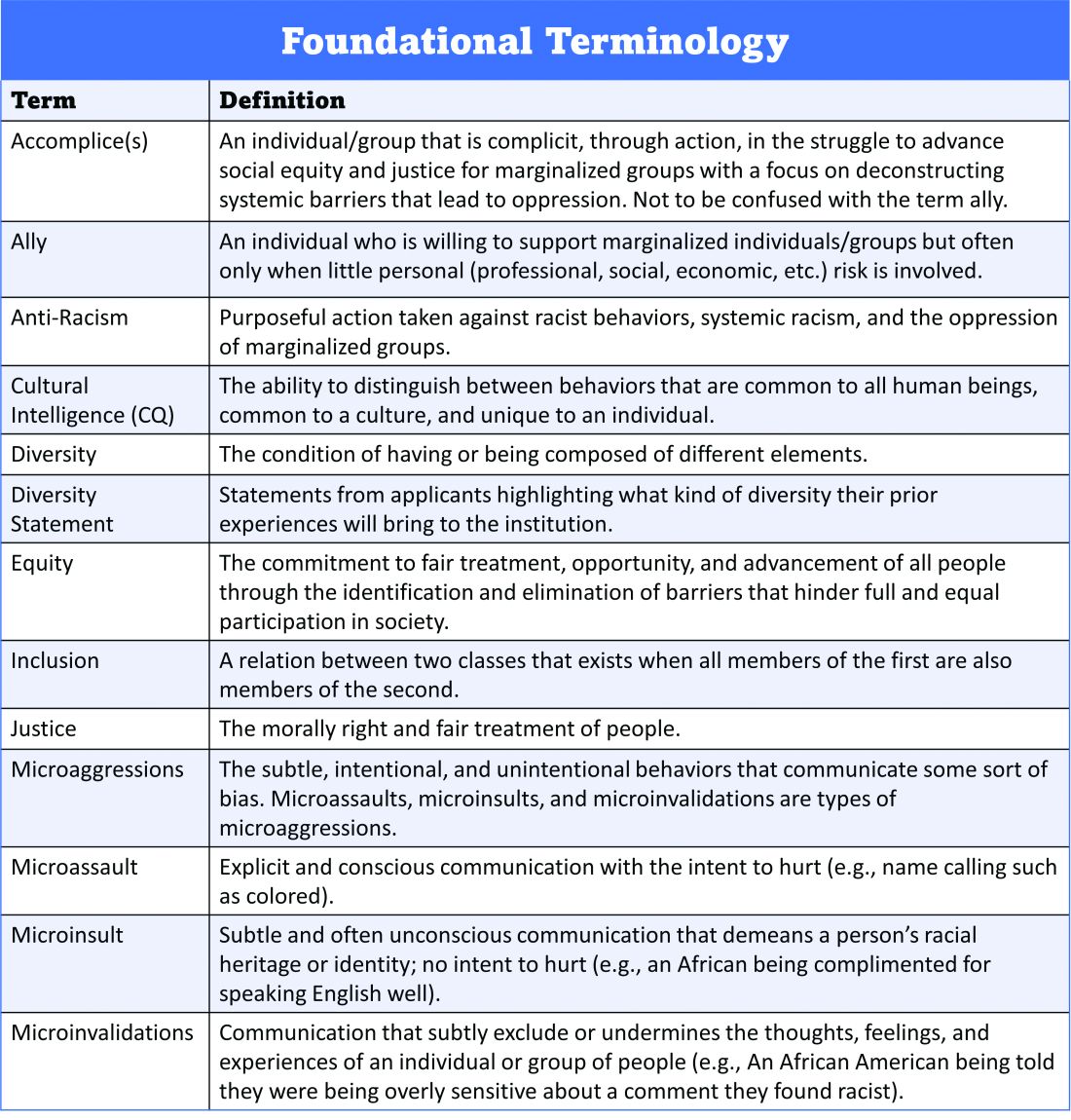
Conducting exit interviews when any hospitalist leaves is important to learn how to improve, but holding ‘stay’ interviews is mission critical. Stay interviews are an opportunity for HMG leaders to proactively understand why hospitalists stay, and what can be done to create more inclusive and equitable environments to retain them. This process creates psychological safety that brings challenges to the fore to be addressed, and spotlights best practices to be maintained and scaled.
Scholarship, mentorship, and sponsorship
Women and minorities are known to be over-mentored and under-sponsored. Sponsorship is defined by Ayyala et al. as “active support by someone appropriately placed in the organization who has significant influence on decision making processes or structures and who is advocating for the career advancement of an individual and recommends them for leadership roles, awards, or high-profile speaking opportunities.”9 While the goal of mentorship is professional development, sponsorship emphasizes professional advancement. Deliberate steps to both mentor and then sponsor diverse hospitalists and future hospitalists (including trainees) are important to ensure equity.
More inclusive HMGs can be bolstered by prioritizing peer education on the professional imperative that we have a diverse workforce and equitable, just workplaces. Academic institutions may use existing structures such as grand rounds to provide education on these crucial topics, and all HMGs can host journal clubs and professional development sessions on leadership competencies that foster inclusion and equity. Sessions coordinated by women and minorities are also a form of justice, by helping overcome barriers to career advancement. Diverse faculty presenting in educational venues will result in content that is relevant to more audience members and will exemplify that leaders and experts are of all races, ethnicities, genders, ages, and abilities.
Groups should prioritize mentoring trainees and early-career hospitalists on scholarly projects that examine equity in opportunities of care, which signals that this science is valued as much as basic research. When used to demonstrate areas needing improvement, these projects can drive meaningful change. Even projects as straightforward as studying diversity in conference presenters, disparities in adherence to guidelines, or QI projects on how race is portrayed in the medical record can be powerful tools in advancing equity.
A key part of mentoring is training hospitalists and future hospitalists in how to be an upstander, as in how to intervene when a peer or patient is affected by bias, harassment, or discrimination. Receiving such training can prepare hospitalists for these nearly inevitable experiences and receiving training during usual work hours communicates that this is a valuable and necessary professional competency.
Community engagement and partnership
Institutions and HMGs should deliberately work to promote community engagement and partnership within their groups. Beyond promoting health equity, community engagement also fosters inclusivity by allowing community members to share their ideas and give recommendations to the institutions that serve them.
There is a growing body of literature that demonstrates how disadvantages by individual and neighborhood-level socioeconomic status (SES) contribute to disparities in specific disease conditions.10-11 Strategies to narrow the gap in SES disadvantages may help reduce race-related health disparities. Institutions that engage the community and develop programs to promote health equity can do so through bidirectional exchange of knowledge and mutual benefit.
An institution-specific example is Medicine for the Greater Good at Johns Hopkins. The founders of this program wrote, “health is not synonymous with medicine. To truly care for our patients and their communities, health care professionals must understand how to deliver equitable health care that meets the needs of the diverse populations we care for. The mission of Medicine for the Greater Good is to promote health and wellness beyond the confines of the hospital through an interactive and engaging partnership with the community ...” Community engagement also provides an opportunity for growing the cultural intelligence of institutions and HMGs.
Tools for advancing comprehensive change – Repurposing PDSA cycles
Whether institutions and HMGs are at the beginning of their journey or further along in the work of reducing disparities, having a systematic approach for implementing and refining policies and procedures can cultivate more inclusive and equitable environments. Thankfully, hospitalists are already equipped with the fundamental tools needed to advance change across their institutions – QI processes in the form of Plan-Do-Study-Act (PDSA) cycles.
They allow a continuous cycle of successful incremental change based on direct evidence and experience. Any efforts to deconstruct systematic bias within our organizations must also be a continual process. Our female colleagues and colleagues of color need our institutions to engage unceasingly to bring about the equality they deserve. To that end, PDSA cycles are an apt tool to utilize in this work as they can naturally function in a never-ending process of improvement.
With PDSA as a model, we envision a cycle with steps that are intentionally purposed to fit the needs of equitable institutional change: Target-Engage-Assess-Modify. As highlighted (see graphic), these modifications ensure that stakeholders (i.e., those that unequal practices and policies affect the most) are engaged early and remain involved throughout the cycle. 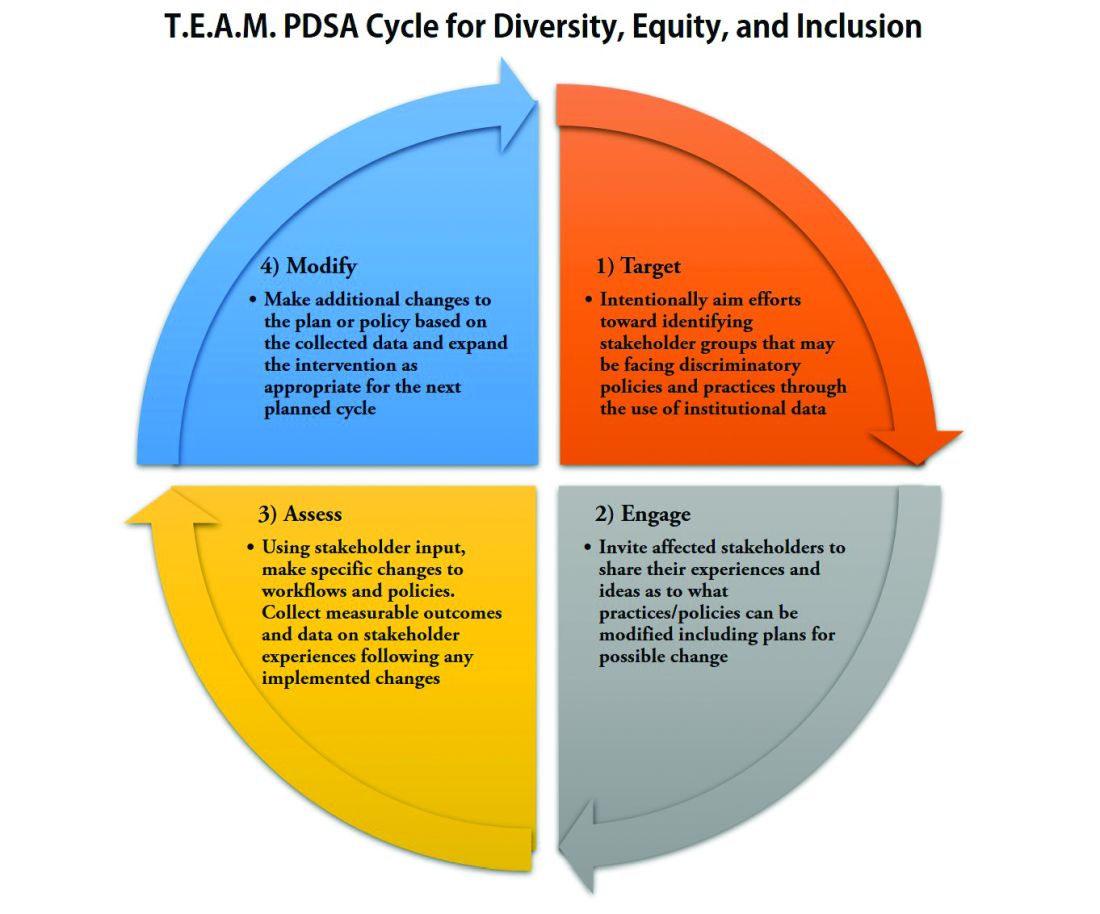
As hospitalists, we have significant work ahead to ensure that we develop and maintain a diverse, equitable and inclusive workforce. This work to bring change will not be easy and will require a considerable investment of time and resources. However, with the strategies and tools that we have outlined, our institutions and HMGs can start the change needed in our profession for our patients and the workforce. In doing so, we can all be accomplices in the fight to achieve racial and gender equity, and social justice.
Dr. Delapenha and Dr. Kisuule are based in the department of internal medicine, division of hospital medicine, at the Johns Hopkins University, Baltimore. Dr. Martin is based in the department of medicine, section of hospital medicine at the University of Chicago. Dr. Barrett is a hospitalist in the department of internal medicine, University of New Mexico, Albuquerque.
References
1. Diversity in Medicine: Facts and Figures 2019: Figure 19. Percentage of physicians by sex, 2018. AAMC website.
2. Diversity in Medicine: Facts and Figures 2019. Figure 16. Percentage of full-time U.S. medical school faculty by sex and race/ethnicity, 2018. AAMC website.
3. Diversity in Medicine: Facts and Figures 2019. Figure 15. Percentage of full-time U.S. medical school faculty by race/ethnicity, 2018. AAMC website.
4. Diversity in Medicine: Facts and Figures 2019. Figure 6. Percentage of acceptees to U.S. medical schools by race/ethnicity (alone), academic year 2018-2019. AAMC website.
5. Diversity in Medicine: Facts and Figures 2019 Figure 18. Percentage of all active physicians by race/ethnicity, 2018. AAMC website.
6. Herzke C et al. Gender issues in academic hospital medicine: A national survey of hospitalist leaders. J Gen Intern Med. 2020;35(6):1641-6.
7. Diversity in Medicine: Facts and Figures 2019. Fostering diversity and inclusion. AAMC website.
8. Diversity in Medicine: Facts and Figures 2019. Executive summary. AAMC website.
9. Ayyala MS et al. Mentorship is not enough: Exploring sponsorship and its role in career advancement in academic medicine. Acad Med. 2019;94(1):94-100.
10. Ejike OC et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. 2021 Apr 15;203(8):987-97.
11. Galiatsatos P et al. The effect of community socioeconomic status on sepsis-attributable mortality. J Crit Care. 2018 Aug;46:129-33.
The language of equality in America’s founding was never truly embraced, resulting in a painful legacy of slavery, racial injustice, and gender inequality inherited by all generations. However, for as long as America has fallen short of this unfulfilled promise, individuals have dedicated their lives to the tireless work of correcting injustice. Although the process has been painstakingly slow, our nation has incrementally inched toward the promised vision of equality, and these efforts continue today. With increased attention to social justice movements such as #MeToo and Black Lives Matter, our collective social consciousness may be finally waking up to the systemic injustices embedded into our fundamental institutions.
Medicine is not immune to these injustices. Persistent underrepresentation of women and minorities remains in medical school faculty and the broader physician workforce, and the same inequities exist in hospital medicine.1-6 The report by the Association of American Medical Colleges (AAMC) on diversity in medicine highlights the impact widespread implicit and explicit bias has on creating exclusionary environments, exemplified by research demonstrating lower promotion rates in non-White faculty.7-8 The report calls us, as physicians, to a broader mission: “Focusing solely on increasing compositional diversity along the academic continuum is insufficient. To effectively enact institutional change at academic medical centers ... leaders must focus their efforts on developing inclusive, equity-minded environments.”7
We have a clear moral imperative to correct these shortcomings for our profession and our patients. It is incumbent on our institutions and hospital medicine groups (HMGs) to embark on the necessary process of systemic institutional change to address inequality and justice within our field.
A road map for DEI and justice in hospital medicine
The policies and biases allowing these inequities to persist have existed for decades, and superficial efforts will not bring sufficient change. Our institutions require new building blocks from which the foundation of a wholly inclusive and equal system of practice can be constructed. Encouragingly, some institutions and HMGs have taken steps to modernize their practices. We offer examples and suggestions of concrete practices to begin this journey, organizing these efforts into three broad categories:
1. Recruitment and retention
2. Scholarship, mentorship, and sponsorship
3. Community engagement and partnership.
Recruitment and retention
Improving equity and inclusion begins with recruitment. Search and hiring committees should be assembled intentionally, with gender balance, and ideally with diversity or equity experts invited to join. All members should receive unconscious bias training. For example, the University of Colorado utilizes a toolkit to ensure appropriate steps are followed in the recruitment process, including predetermined candidate selection criteria that are ranked in advance.
Job descriptions should be reviewed by a diversity expert, ensuring unbiased and ungendered language within written text. Advertisements should be wide-reaching, and the committee should consider asking applicants for a diversity statement. Interviews should include a variety of interviewers and interview types (e.g., 1:1, group, etc.). Letters of recommendation deserve special scrutiny; letters for women and minorities may be at risk of being shorter and less record focused, and may be subject to less professional respect, such as use of first names over honorifics or titles.
Once candidates are hired, institutions and HMGs should prioritize developing strategies to improve retention of a diverse workforce. This includes special attention to workplace culture, and thoughtfully striving for cultural intelligence within the group. Some examples may include developing affinity groups, such as underrepresented in medicine (UIM), women in medicine (WIM), or LGBTQ+ groups. Affinity groups provide a safe space for members and allies to support and uplift each other. Institutional and HMG leaders must educate themselves and their members on the importance of language (see table), and the more insidious forms of bias and discrimination that adversely affect workplace culture. Microinsults and microinvalidations, for example, can hurt and result in failure to recruit or turnover. 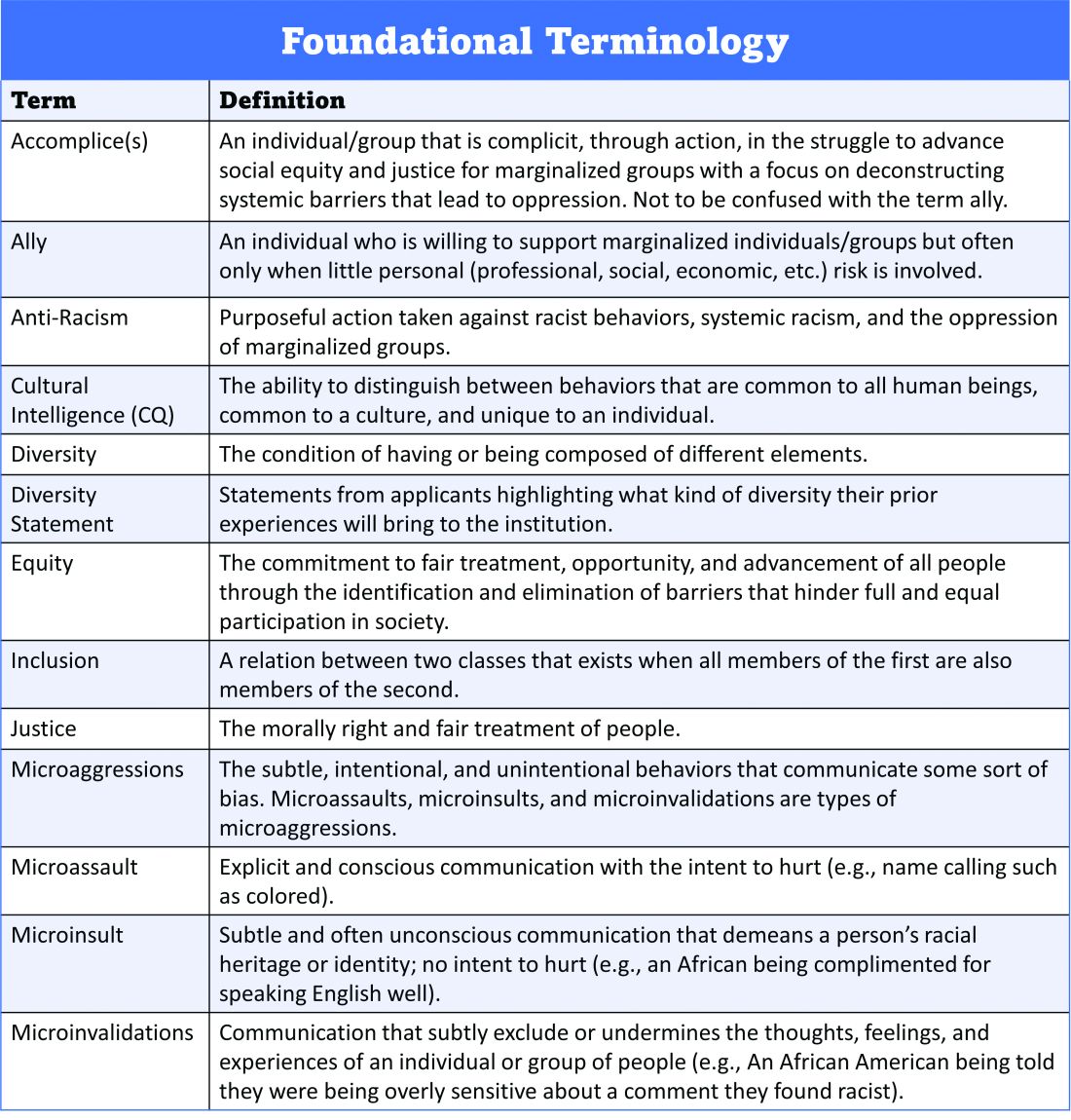
Conducting exit interviews when any hospitalist leaves is important to learn how to improve, but holding ‘stay’ interviews is mission critical. Stay interviews are an opportunity for HMG leaders to proactively understand why hospitalists stay, and what can be done to create more inclusive and equitable environments to retain them. This process creates psychological safety that brings challenges to the fore to be addressed, and spotlights best practices to be maintained and scaled.
Scholarship, mentorship, and sponsorship
Women and minorities are known to be over-mentored and under-sponsored. Sponsorship is defined by Ayyala et al. as “active support by someone appropriately placed in the organization who has significant influence on decision making processes or structures and who is advocating for the career advancement of an individual and recommends them for leadership roles, awards, or high-profile speaking opportunities.”9 While the goal of mentorship is professional development, sponsorship emphasizes professional advancement. Deliberate steps to both mentor and then sponsor diverse hospitalists and future hospitalists (including trainees) are important to ensure equity.
More inclusive HMGs can be bolstered by prioritizing peer education on the professional imperative that we have a diverse workforce and equitable, just workplaces. Academic institutions may use existing structures such as grand rounds to provide education on these crucial topics, and all HMGs can host journal clubs and professional development sessions on leadership competencies that foster inclusion and equity. Sessions coordinated by women and minorities are also a form of justice, by helping overcome barriers to career advancement. Diverse faculty presenting in educational venues will result in content that is relevant to more audience members and will exemplify that leaders and experts are of all races, ethnicities, genders, ages, and abilities.
Groups should prioritize mentoring trainees and early-career hospitalists on scholarly projects that examine equity in opportunities of care, which signals that this science is valued as much as basic research. When used to demonstrate areas needing improvement, these projects can drive meaningful change. Even projects as straightforward as studying diversity in conference presenters, disparities in adherence to guidelines, or QI projects on how race is portrayed in the medical record can be powerful tools in advancing equity.
A key part of mentoring is training hospitalists and future hospitalists in how to be an upstander, as in how to intervene when a peer or patient is affected by bias, harassment, or discrimination. Receiving such training can prepare hospitalists for these nearly inevitable experiences and receiving training during usual work hours communicates that this is a valuable and necessary professional competency.
Community engagement and partnership
Institutions and HMGs should deliberately work to promote community engagement and partnership within their groups. Beyond promoting health equity, community engagement also fosters inclusivity by allowing community members to share their ideas and give recommendations to the institutions that serve them.
There is a growing body of literature that demonstrates how disadvantages by individual and neighborhood-level socioeconomic status (SES) contribute to disparities in specific disease conditions.10-11 Strategies to narrow the gap in SES disadvantages may help reduce race-related health disparities. Institutions that engage the community and develop programs to promote health equity can do so through bidirectional exchange of knowledge and mutual benefit.
An institution-specific example is Medicine for the Greater Good at Johns Hopkins. The founders of this program wrote, “health is not synonymous with medicine. To truly care for our patients and their communities, health care professionals must understand how to deliver equitable health care that meets the needs of the diverse populations we care for. The mission of Medicine for the Greater Good is to promote health and wellness beyond the confines of the hospital through an interactive and engaging partnership with the community ...” Community engagement also provides an opportunity for growing the cultural intelligence of institutions and HMGs.
Tools for advancing comprehensive change – Repurposing PDSA cycles
Whether institutions and HMGs are at the beginning of their journey or further along in the work of reducing disparities, having a systematic approach for implementing and refining policies and procedures can cultivate more inclusive and equitable environments. Thankfully, hospitalists are already equipped with the fundamental tools needed to advance change across their institutions – QI processes in the form of Plan-Do-Study-Act (PDSA) cycles.
They allow a continuous cycle of successful incremental change based on direct evidence and experience. Any efforts to deconstruct systematic bias within our organizations must also be a continual process. Our female colleagues and colleagues of color need our institutions to engage unceasingly to bring about the equality they deserve. To that end, PDSA cycles are an apt tool to utilize in this work as they can naturally function in a never-ending process of improvement.
With PDSA as a model, we envision a cycle with steps that are intentionally purposed to fit the needs of equitable institutional change: Target-Engage-Assess-Modify. As highlighted (see graphic), these modifications ensure that stakeholders (i.e., those that unequal practices and policies affect the most) are engaged early and remain involved throughout the cycle. 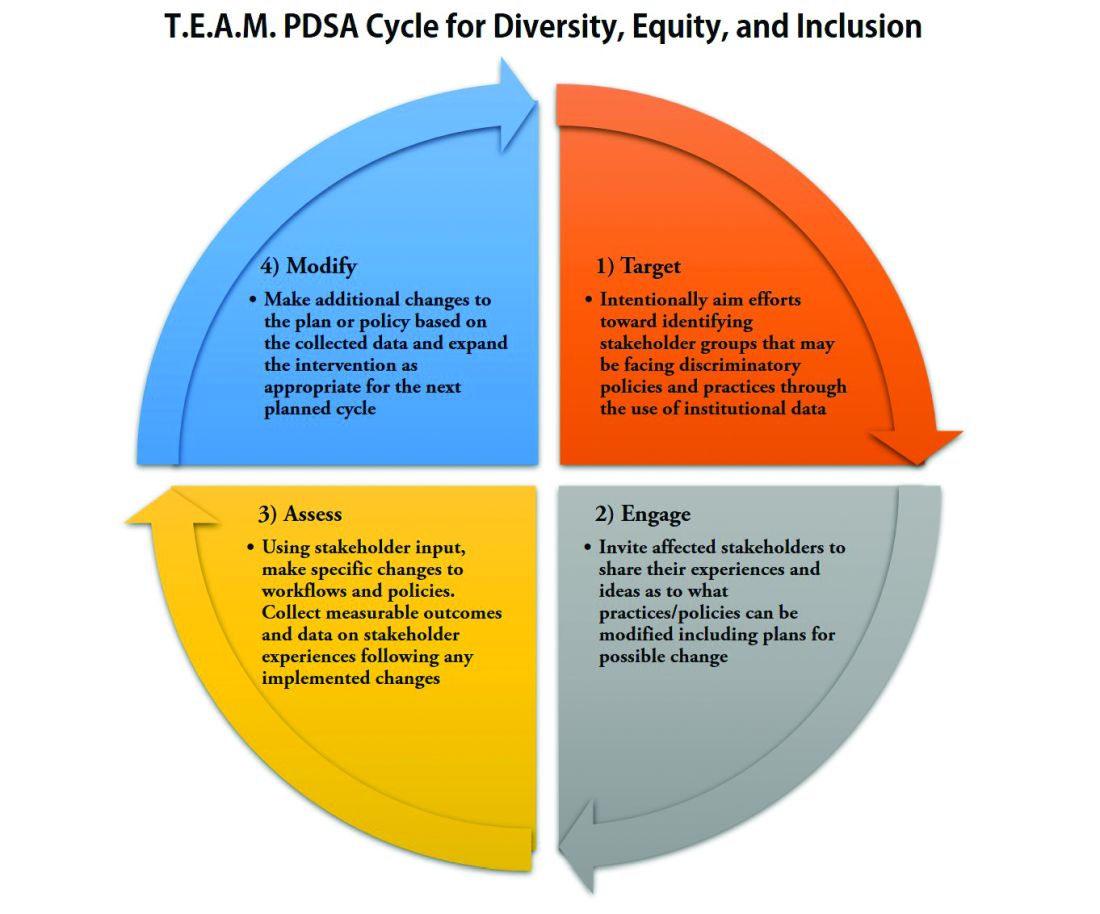
As hospitalists, we have significant work ahead to ensure that we develop and maintain a diverse, equitable and inclusive workforce. This work to bring change will not be easy and will require a considerable investment of time and resources. However, with the strategies and tools that we have outlined, our institutions and HMGs can start the change needed in our profession for our patients and the workforce. In doing so, we can all be accomplices in the fight to achieve racial and gender equity, and social justice.
Dr. Delapenha and Dr. Kisuule are based in the department of internal medicine, division of hospital medicine, at the Johns Hopkins University, Baltimore. Dr. Martin is based in the department of medicine, section of hospital medicine at the University of Chicago. Dr. Barrett is a hospitalist in the department of internal medicine, University of New Mexico, Albuquerque.
References
1. Diversity in Medicine: Facts and Figures 2019: Figure 19. Percentage of physicians by sex, 2018. AAMC website.
2. Diversity in Medicine: Facts and Figures 2019. Figure 16. Percentage of full-time U.S. medical school faculty by sex and race/ethnicity, 2018. AAMC website.
3. Diversity in Medicine: Facts and Figures 2019. Figure 15. Percentage of full-time U.S. medical school faculty by race/ethnicity, 2018. AAMC website.
4. Diversity in Medicine: Facts and Figures 2019. Figure 6. Percentage of acceptees to U.S. medical schools by race/ethnicity (alone), academic year 2018-2019. AAMC website.
5. Diversity in Medicine: Facts and Figures 2019 Figure 18. Percentage of all active physicians by race/ethnicity, 2018. AAMC website.
6. Herzke C et al. Gender issues in academic hospital medicine: A national survey of hospitalist leaders. J Gen Intern Med. 2020;35(6):1641-6.
7. Diversity in Medicine: Facts and Figures 2019. Fostering diversity and inclusion. AAMC website.
8. Diversity in Medicine: Facts and Figures 2019. Executive summary. AAMC website.
9. Ayyala MS et al. Mentorship is not enough: Exploring sponsorship and its role in career advancement in academic medicine. Acad Med. 2019;94(1):94-100.
10. Ejike OC et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. 2021 Apr 15;203(8):987-97.
11. Galiatsatos P et al. The effect of community socioeconomic status on sepsis-attributable mortality. J Crit Care. 2018 Aug;46:129-33.
Acne Vulgaris
THE COMPARISON
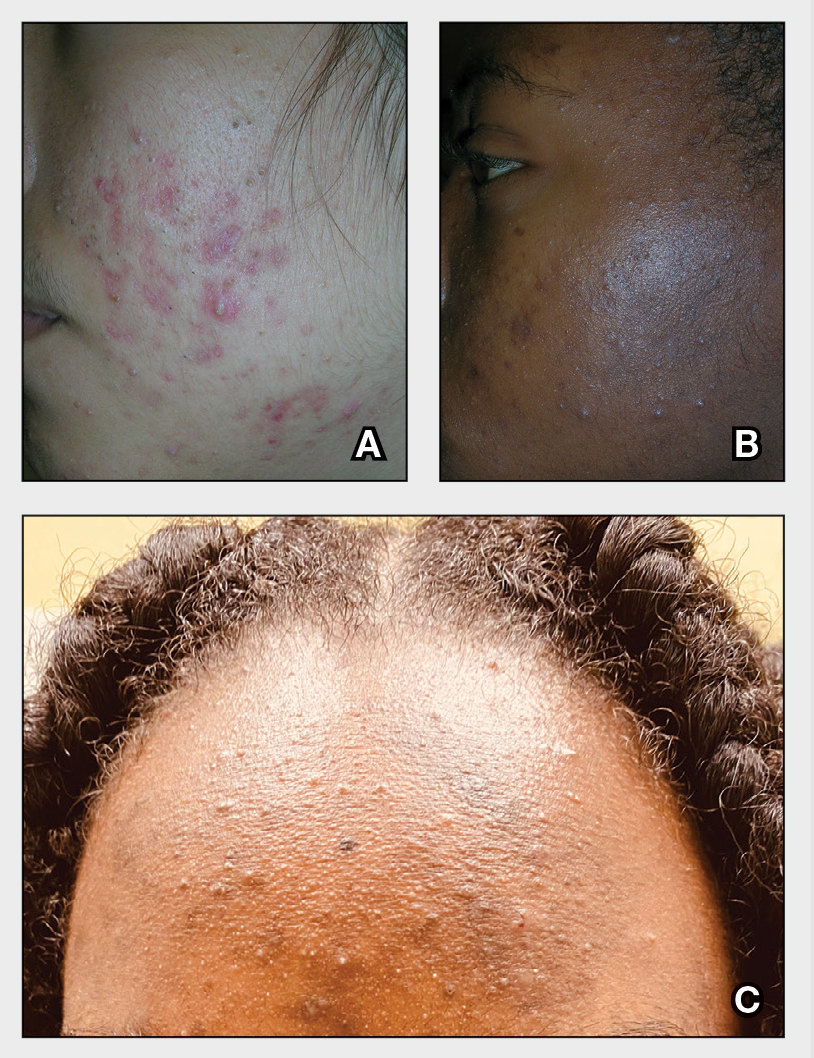
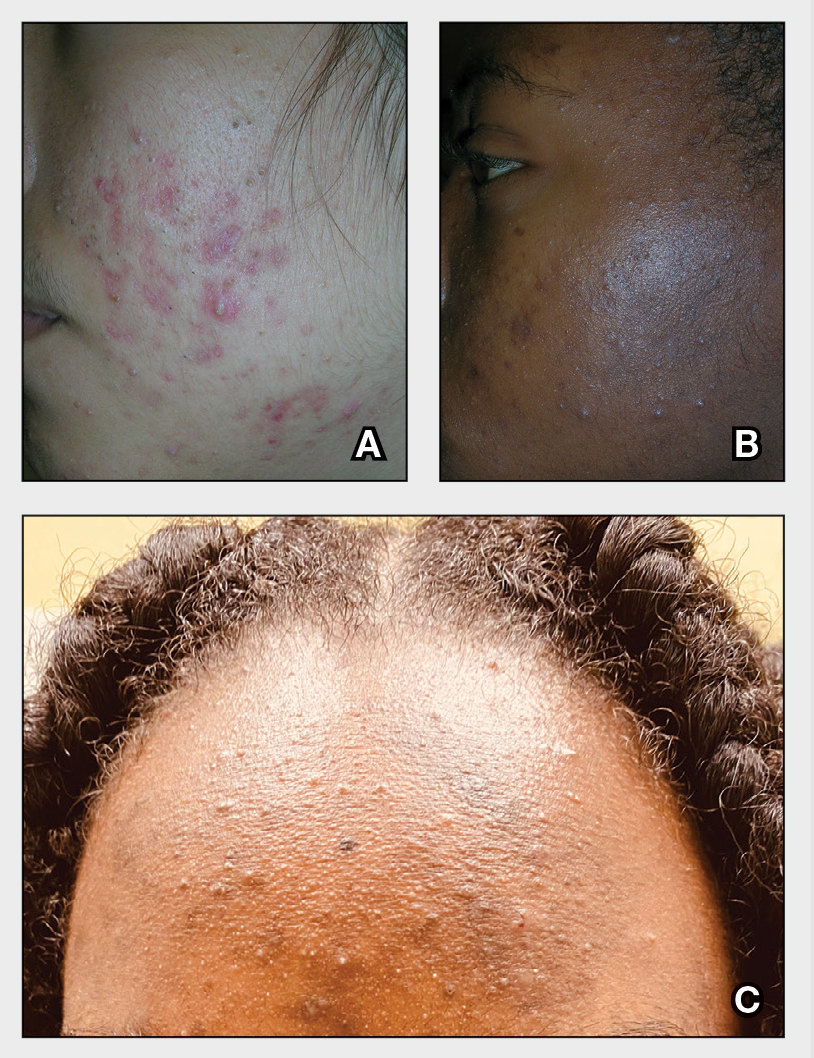
A A 27-year-old Hispanic woman with comedonal and inflammatory acne. Erythema is prominent around the inflammatory lesions. Note the pustule on the cheek surrounded by pink color.
B A teenaged Black boy with acne papules and pustules on the face. There are comedones, hyperpigmented macules, and pustules on the cheek.
C A teenaged Black girl with pomade acne. The patient used various hair care products, which obstructed the pilosebaceous units on the forehead.
Epidemiology
Acne is a leading dermatologic condition in individuals with skin of color in the United States.1
Key clinical features in people with darker skin tones include:
- erythematous or hyperpigmented papules or comedones
- hyperpigmented macules and postinflammatory hyperpigmentation (PIH)
- increased risk for keloidal scars.2
Worth noting
- Patients with darker skin tones may be more concerned with the dark marks (also referred to as scars or manchas in Spanish) than the acne itself. This PIH may be viewed by patients as the major problem.
- Acne medications such as azelaic acid and some retinoids (when applied appropriately) can treat both acne and PIH.3
- Irritation from topical acne medications, including retinoid dermatitis, may lead to more PIH. Using noncomedogenic moisturizers and applying medication appropriately (ie, a pea-sized amount of topical retinoid per application) may help limit irritation.4,5
- One type of acne seen more commonly, although not exclusively, in Black patients is pomade acne, which principally appears on the forehead and is associated with use of hair care and styling products (Figure, C).
Health disparity highlight
Disparities in access to health care exist for those with dermatologic concerns. According to one study, African American (28.5%) and Hispanic patients (23.9%) were less likely to be seen by a dermatologist solely for the diagnosis of a dermatologic condition compared to Asian and Pacific Islander patients (36.7%) or White patients (43.2%).1
Noting that isotretinoin is the most potent systemic therapy for severe cystic acne vulgaris, Bell et al6 reported that Black patients had lower odds of receiving isotretinoin compared to White patients. Hispanic patients had lower odds of receiving a topical retinoid, tretinoin, than non-Hispanic patients.6
- Davis SA, Narahari S, Feldman SR, et al. Top dermatologic conditions in patients of color: an analysis of nationally representative data. J Drugs Dermatol. 2012;11:466-473.
- Alexis AF, Woolery-Lloyd H, Williams K, et al. Racial/ethnic variations in acne: implications for treatment and skin care recommendations for acne patients with skin of color. J Drugs Dermatol. 2021;20:716-725.
- Woolery-Lloyd HC, Keri J, Doig S. Retinoids and azelaic acid to treat acne and hyperpigmentation in skin of color. J Drugs Dermatol. 2013;12:434-437.
- Grayson C, Heath C. Tips for addressing common conditions affecting pediatric and adolescent patients with skin of color [published online March 2, 2021]. Pediatr Dermatol. doi:10.1111/pde.14525
- Alexis AD, Harper JC, Stein Gold L, et al. Treating acne in patients with skin of color. Semin Cutan Med Surg. 2018;37(suppl 3):S71-S73.
- Bell MA, Whang KA, Thomas J, et al. Racial and ethnic disparities in access to emerging and frontline therapies in common dermatological conditions: a cross-sectional study. J Natl Med Assoc. 2020;112:650-653.
THE COMPARISON
A A 27-year-old Hispanic woman with comedonal and inflammatory acne. Erythema is prominent around the inflammatory lesions. Note the pustule on the cheek surrounded by pink color.
B A teenaged Black boy with acne papules and pustules on the face. There are comedones, hyperpigmented macules, and pustules on the cheek.
C A teenaged Black girl with pomade acne. The patient used various hair care products, which obstructed the pilosebaceous units on the forehead.
Epidemiology
Acne is a leading dermatologic condition in individuals with skin of color in the United States.1
Key clinical features in people with darker skin tones include:
- erythematous or hyperpigmented papules or comedones
- hyperpigmented macules and postinflammatory hyperpigmentation (PIH)
- increased risk for keloidal scars.2
Worth noting
- Patients with darker skin tones may be more concerned with the dark marks (also referred to as scars or manchas in Spanish) than the acne itself. This PIH may be viewed by patients as the major problem.
- Acne medications such as azelaic acid and some retinoids (when applied appropriately) can treat both acne and PIH.3
- Irritation from topical acne medications, including retinoid dermatitis, may lead to more PIH. Using noncomedogenic moisturizers and applying medication appropriately (ie, a pea-sized amount of topical retinoid per application) may help limit irritation.4,5
- One type of acne seen more commonly, although not exclusively, in Black patients is pomade acne, which principally appears on the forehead and is associated with use of hair care and styling products (Figure, C).
Health disparity highlight
Disparities in access to health care exist for those with dermatologic concerns. According to one study, African American (28.5%) and Hispanic patients (23.9%) were less likely to be seen by a dermatologist solely for the diagnosis of a dermatologic condition compared to Asian and Pacific Islander patients (36.7%) or White patients (43.2%).1
Noting that isotretinoin is the most potent systemic therapy for severe cystic acne vulgaris, Bell et al6 reported that Black patients had lower odds of receiving isotretinoin compared to White patients. Hispanic patients had lower odds of receiving a topical retinoid, tretinoin, than non-Hispanic patients.6
THE COMPARISON
A A 27-year-old Hispanic woman with comedonal and inflammatory acne. Erythema is prominent around the inflammatory lesions. Note the pustule on the cheek surrounded by pink color.
B A teenaged Black boy with acne papules and pustules on the face. There are comedones, hyperpigmented macules, and pustules on the cheek.
C A teenaged Black girl with pomade acne. The patient used various hair care products, which obstructed the pilosebaceous units on the forehead.
Epidemiology
Acne is a leading dermatologic condition in individuals with skin of color in the United States.1
Key clinical features in people with darker skin tones include:
- erythematous or hyperpigmented papules or comedones
- hyperpigmented macules and postinflammatory hyperpigmentation (PIH)
- increased risk for keloidal scars.2
Worth noting
- Patients with darker skin tones may be more concerned with the dark marks (also referred to as scars or manchas in Spanish) than the acne itself. This PIH may be viewed by patients as the major problem.
- Acne medications such as azelaic acid and some retinoids (when applied appropriately) can treat both acne and PIH.3
- Irritation from topical acne medications, including retinoid dermatitis, may lead to more PIH. Using noncomedogenic moisturizers and applying medication appropriately (ie, a pea-sized amount of topical retinoid per application) may help limit irritation.4,5
- One type of acne seen more commonly, although not exclusively, in Black patients is pomade acne, which principally appears on the forehead and is associated with use of hair care and styling products (Figure, C).
Health disparity highlight
Disparities in access to health care exist for those with dermatologic concerns. According to one study, African American (28.5%) and Hispanic patients (23.9%) were less likely to be seen by a dermatologist solely for the diagnosis of a dermatologic condition compared to Asian and Pacific Islander patients (36.7%) or White patients (43.2%).1
Noting that isotretinoin is the most potent systemic therapy for severe cystic acne vulgaris, Bell et al6 reported that Black patients had lower odds of receiving isotretinoin compared to White patients. Hispanic patients had lower odds of receiving a topical retinoid, tretinoin, than non-Hispanic patients.6
- Davis SA, Narahari S, Feldman SR, et al. Top dermatologic conditions in patients of color: an analysis of nationally representative data. J Drugs Dermatol. 2012;11:466-473.
- Alexis AF, Woolery-Lloyd H, Williams K, et al. Racial/ethnic variations in acne: implications for treatment and skin care recommendations for acne patients with skin of color. J Drugs Dermatol. 2021;20:716-725.
- Woolery-Lloyd HC, Keri J, Doig S. Retinoids and azelaic acid to treat acne and hyperpigmentation in skin of color. J Drugs Dermatol. 2013;12:434-437.
- Grayson C, Heath C. Tips for addressing common conditions affecting pediatric and adolescent patients with skin of color [published online March 2, 2021]. Pediatr Dermatol. doi:10.1111/pde.14525
- Alexis AD, Harper JC, Stein Gold L, et al. Treating acne in patients with skin of color. Semin Cutan Med Surg. 2018;37(suppl 3):S71-S73.
- Bell MA, Whang KA, Thomas J, et al. Racial and ethnic disparities in access to emerging and frontline therapies in common dermatological conditions: a cross-sectional study. J Natl Med Assoc. 2020;112:650-653.
- Davis SA, Narahari S, Feldman SR, et al. Top dermatologic conditions in patients of color: an analysis of nationally representative data. J Drugs Dermatol. 2012;11:466-473.
- Alexis AF, Woolery-Lloyd H, Williams K, et al. Racial/ethnic variations in acne: implications for treatment and skin care recommendations for acne patients with skin of color. J Drugs Dermatol. 2021;20:716-725.
- Woolery-Lloyd HC, Keri J, Doig S. Retinoids and azelaic acid to treat acne and hyperpigmentation in skin of color. J Drugs Dermatol. 2013;12:434-437.
- Grayson C, Heath C. Tips for addressing common conditions affecting pediatric and adolescent patients with skin of color [published online March 2, 2021]. Pediatr Dermatol. doi:10.1111/pde.14525
- Alexis AD, Harper JC, Stein Gold L, et al. Treating acne in patients with skin of color. Semin Cutan Med Surg. 2018;37(suppl 3):S71-S73.
- Bell MA, Whang KA, Thomas J, et al. Racial and ethnic disparities in access to emerging and frontline therapies in common dermatological conditions: a cross-sectional study. J Natl Med Assoc. 2020;112:650-653.
Eurocentric standards of beauty are no longer dominant, experts agree
Addressing current standards of beauty at the Skin of Color Update 2021, dermatologists speaking about attitudes within four ethnic groups recounted a similar story: .
This change is relevant to dermatologists consulting with patients for cosmetic procedures. Four dermatologists who recounted the types of procedures their patients are requesting each reported that more patients are seeking cosmetic enhancements that accentuate rather than modify ethnic features.
Lips in Black, Asian, and Arab ethnic groups are just one example.
“Where several years ago, the conversation was really about lip reductions – how we can deemphasize the lip – I am now seeing lots of women of color coming in to ask about lip augmentation, looking to highlight their lips as a point of beauty,” reported Michelle Henry, MD, a dermatologist who practices in New York City.
She is not alone. Others participating on the same panel spoke of a growing interest among their patients to maintain or even emphasize the same ethnic features – including but not limited to lip shape and size that they were once anxious to modify.
In Asian patients, “the goal is not to Westernize,” agreed Annie Chiu, MD, a dermatologist who practices in North Redondo Beach, Calif. For lips, she spoke of the “50-50 ratio” of upper and lower lip symmetry that is consistent with a traditional Asian characteristic.
Like Dr. Henry, Dr. Chiu said that many requests for cosmetic work now involve accentuating Asian features, such as the oval shape of the face, rather than steps to modify this shape. This is a relatively recent change.
“I am finding that more of my patients want to improve the esthetic balance to optimize the appearance within their own ethnicity,” she said.
In the United Arab Emirates (UAE), Hassan Galadari, MD, an American-trained physician who is assistant professor of dermatology at the UAE University in Dubai, recently conducted a poll of his patients. In order of importance, full lips came after wide eyes, a straight nose, and a sharp jaw line. Full cheeks and a round face completed a list that diverges from the California-blond prototype.
Although Angelina Jolie was selected over several Lebanese actresses as a first choice for an icon of beauty in this same poll, Dr. Galadari pointed out that this actress has many of the features, including wide eyes, a straight nose, and full lips, that are consistent with traditional features of Arab beauty.
Perceptions of beauty are not just changing within ethnic groups but reflected in mass culture. Dr. Henry pointed to a published comparison of the “World’s Most Beautiful” list from People magazine in 2017 relative to 1990. Of the 50 celebrities on the list in 1990, 88% were Fitzpatrick skin types I-III. Only 12% were types IV-VI, which increased to almost 30% of the 135 celebrities on the list in 2017 (P = .01). In 1990, just one celebrity (2%) was of mixed race, which increased to 10.4% in 2017.
Among Hispanic women, the changes in attitude are perhaps best captured among younger relative to older patients requesting cosmetic work, according to Maritza I. Perez, MD, professor of dermatology, University of Connecticut, Farmington. She said that her younger patients are less likely to seek rhinoplasty and blepharoplasty relative to her older patients, a reflection perhaps of comfort with their natural looks.
However, “the celebration of Latinas as beautiful, seductive, and sexual is hardly new,” she said, indicating that younger Hispanic patients are probably not driven to modify their ethnic features because they are already widely admired. “Six of the 10 women crowned Miss Universe in the last decade were from Latin American countries,” she noted.
The general willingness of patients within ethnic groups and society as a whole to see ethnic features as admirable and attractive was generally regarded by all the panelists as a positive development.
Dr. Henry, who said she was “encouraged” by such trends as “the natural hair movement” and diminishing interest among her darker patients in lightening skin pigment, said, “I definitely see a change among my patients in regard to their goals.”
For clinicians offering consults to patients seeking cosmetic work, Dr. Henry recommended being aware and sensitive to this evolution in order to offer appropriate care.
Dr. Chiu, emphasizing the pride that many of her patients take in their Asian features, made the same recommendation. She credited globalization and social media for attitudes that have allowed an embrace of what are now far more inclusive standards of beauty.
Dr. Henry reports financial relationships with Allergan and Merz. Dr. Chiu has financial relationships with AbbVie, Cynosure, Merz, Revance, and Solta. Dr. Galadari reports financial relationships with nine pharmaceutical companies, including Allergan, Merz, Revance, and Fillmed Laboratories. Dr. Perez reports no relevant conflicts of interest.
Addressing current standards of beauty at the Skin of Color Update 2021, dermatologists speaking about attitudes within four ethnic groups recounted a similar story: .
This change is relevant to dermatologists consulting with patients for cosmetic procedures. Four dermatologists who recounted the types of procedures their patients are requesting each reported that more patients are seeking cosmetic enhancements that accentuate rather than modify ethnic features.
Lips in Black, Asian, and Arab ethnic groups are just one example.
“Where several years ago, the conversation was really about lip reductions – how we can deemphasize the lip – I am now seeing lots of women of color coming in to ask about lip augmentation, looking to highlight their lips as a point of beauty,” reported Michelle Henry, MD, a dermatologist who practices in New York City.
She is not alone. Others participating on the same panel spoke of a growing interest among their patients to maintain or even emphasize the same ethnic features – including but not limited to lip shape and size that they were once anxious to modify.
In Asian patients, “the goal is not to Westernize,” agreed Annie Chiu, MD, a dermatologist who practices in North Redondo Beach, Calif. For lips, she spoke of the “50-50 ratio” of upper and lower lip symmetry that is consistent with a traditional Asian characteristic.
Like Dr. Henry, Dr. Chiu said that many requests for cosmetic work now involve accentuating Asian features, such as the oval shape of the face, rather than steps to modify this shape. This is a relatively recent change.
“I am finding that more of my patients want to improve the esthetic balance to optimize the appearance within their own ethnicity,” she said.
In the United Arab Emirates (UAE), Hassan Galadari, MD, an American-trained physician who is assistant professor of dermatology at the UAE University in Dubai, recently conducted a poll of his patients. In order of importance, full lips came after wide eyes, a straight nose, and a sharp jaw line. Full cheeks and a round face completed a list that diverges from the California-blond prototype.
Although Angelina Jolie was selected over several Lebanese actresses as a first choice for an icon of beauty in this same poll, Dr. Galadari pointed out that this actress has many of the features, including wide eyes, a straight nose, and full lips, that are consistent with traditional features of Arab beauty.
Perceptions of beauty are not just changing within ethnic groups but reflected in mass culture. Dr. Henry pointed to a published comparison of the “World’s Most Beautiful” list from People magazine in 2017 relative to 1990. Of the 50 celebrities on the list in 1990, 88% were Fitzpatrick skin types I-III. Only 12% were types IV-VI, which increased to almost 30% of the 135 celebrities on the list in 2017 (P = .01). In 1990, just one celebrity (2%) was of mixed race, which increased to 10.4% in 2017.
Among Hispanic women, the changes in attitude are perhaps best captured among younger relative to older patients requesting cosmetic work, according to Maritza I. Perez, MD, professor of dermatology, University of Connecticut, Farmington. She said that her younger patients are less likely to seek rhinoplasty and blepharoplasty relative to her older patients, a reflection perhaps of comfort with their natural looks.
However, “the celebration of Latinas as beautiful, seductive, and sexual is hardly new,” she said, indicating that younger Hispanic patients are probably not driven to modify their ethnic features because they are already widely admired. “Six of the 10 women crowned Miss Universe in the last decade were from Latin American countries,” she noted.
The general willingness of patients within ethnic groups and society as a whole to see ethnic features as admirable and attractive was generally regarded by all the panelists as a positive development.
Dr. Henry, who said she was “encouraged” by such trends as “the natural hair movement” and diminishing interest among her darker patients in lightening skin pigment, said, “I definitely see a change among my patients in regard to their goals.”
For clinicians offering consults to patients seeking cosmetic work, Dr. Henry recommended being aware and sensitive to this evolution in order to offer appropriate care.
Dr. Chiu, emphasizing the pride that many of her patients take in their Asian features, made the same recommendation. She credited globalization and social media for attitudes that have allowed an embrace of what are now far more inclusive standards of beauty.
Dr. Henry reports financial relationships with Allergan and Merz. Dr. Chiu has financial relationships with AbbVie, Cynosure, Merz, Revance, and Solta. Dr. Galadari reports financial relationships with nine pharmaceutical companies, including Allergan, Merz, Revance, and Fillmed Laboratories. Dr. Perez reports no relevant conflicts of interest.
Addressing current standards of beauty at the Skin of Color Update 2021, dermatologists speaking about attitudes within four ethnic groups recounted a similar story: .
This change is relevant to dermatologists consulting with patients for cosmetic procedures. Four dermatologists who recounted the types of procedures their patients are requesting each reported that more patients are seeking cosmetic enhancements that accentuate rather than modify ethnic features.
Lips in Black, Asian, and Arab ethnic groups are just one example.
“Where several years ago, the conversation was really about lip reductions – how we can deemphasize the lip – I am now seeing lots of women of color coming in to ask about lip augmentation, looking to highlight their lips as a point of beauty,” reported Michelle Henry, MD, a dermatologist who practices in New York City.
She is not alone. Others participating on the same panel spoke of a growing interest among their patients to maintain or even emphasize the same ethnic features – including but not limited to lip shape and size that they were once anxious to modify.
In Asian patients, “the goal is not to Westernize,” agreed Annie Chiu, MD, a dermatologist who practices in North Redondo Beach, Calif. For lips, she spoke of the “50-50 ratio” of upper and lower lip symmetry that is consistent with a traditional Asian characteristic.
Like Dr. Henry, Dr. Chiu said that many requests for cosmetic work now involve accentuating Asian features, such as the oval shape of the face, rather than steps to modify this shape. This is a relatively recent change.
“I am finding that more of my patients want to improve the esthetic balance to optimize the appearance within their own ethnicity,” she said.
In the United Arab Emirates (UAE), Hassan Galadari, MD, an American-trained physician who is assistant professor of dermatology at the UAE University in Dubai, recently conducted a poll of his patients. In order of importance, full lips came after wide eyes, a straight nose, and a sharp jaw line. Full cheeks and a round face completed a list that diverges from the California-blond prototype.
Although Angelina Jolie was selected over several Lebanese actresses as a first choice for an icon of beauty in this same poll, Dr. Galadari pointed out that this actress has many of the features, including wide eyes, a straight nose, and full lips, that are consistent with traditional features of Arab beauty.
Perceptions of beauty are not just changing within ethnic groups but reflected in mass culture. Dr. Henry pointed to a published comparison of the “World’s Most Beautiful” list from People magazine in 2017 relative to 1990. Of the 50 celebrities on the list in 1990, 88% were Fitzpatrick skin types I-III. Only 12% were types IV-VI, which increased to almost 30% of the 135 celebrities on the list in 2017 (P = .01). In 1990, just one celebrity (2%) was of mixed race, which increased to 10.4% in 2017.
Among Hispanic women, the changes in attitude are perhaps best captured among younger relative to older patients requesting cosmetic work, according to Maritza I. Perez, MD, professor of dermatology, University of Connecticut, Farmington. She said that her younger patients are less likely to seek rhinoplasty and blepharoplasty relative to her older patients, a reflection perhaps of comfort with their natural looks.
However, “the celebration of Latinas as beautiful, seductive, and sexual is hardly new,” she said, indicating that younger Hispanic patients are probably not driven to modify their ethnic features because they are already widely admired. “Six of the 10 women crowned Miss Universe in the last decade were from Latin American countries,” she noted.
The general willingness of patients within ethnic groups and society as a whole to see ethnic features as admirable and attractive was generally regarded by all the panelists as a positive development.
Dr. Henry, who said she was “encouraged” by such trends as “the natural hair movement” and diminishing interest among her darker patients in lightening skin pigment, said, “I definitely see a change among my patients in regard to their goals.”
For clinicians offering consults to patients seeking cosmetic work, Dr. Henry recommended being aware and sensitive to this evolution in order to offer appropriate care.
Dr. Chiu, emphasizing the pride that many of her patients take in their Asian features, made the same recommendation. She credited globalization and social media for attitudes that have allowed an embrace of what are now far more inclusive standards of beauty.
Dr. Henry reports financial relationships with Allergan and Merz. Dr. Chiu has financial relationships with AbbVie, Cynosure, Merz, Revance, and Solta. Dr. Galadari reports financial relationships with nine pharmaceutical companies, including Allergan, Merz, Revance, and Fillmed Laboratories. Dr. Perez reports no relevant conflicts of interest.
FROM SOC 2021
Workplace mistreatment common among emergency medicine residents
published online Aug. 19 in JAMA Network Open.
The survey of more than 6,000 residents found that almost 1 in 2 respondents had been exposed to some form of workplace mistreatment in the previous year, including gender and racial discrimination, physical abuse, or sexual harassment.
“The last study on mistreatment in EM residency training in the United States occurred more than 25 years ago,” said Michelle D. Lall, MD, associate professor of medicine at Emory University, Atlanta. “These findings provide a current look. Mistreatment occurs frequently in EM residency training nationally, and it occurs more frequently in women, racial/ethnic minorities, and those who identify as LGBTQ+,” Dr. Lall added. “Additionally, we found an association between experiencing mistreatment at least a few times per month and having suicidal thoughts.”
Negative sequelae from workplace mistreatment
Dr. Lall explained that workplace mistreatment and institutional responses to such behaviors have been linked to hostile work environments for physicians. In previous research, workplace mistreatment has been found to negatively affect individuals’ sense of self, a phenomenon that not only hindered professional productivity but also increased a variety of other negative factors, such as stress, job dissatisfaction, negative workplace behaviors, and turnover. Perhaps not surprisingly, workplace discrimination has also been shown to have negative effects on physical and mental health.
Despite such findings, little is known about the current state of workplace mistreatment among EM residents. This led the investigators to examine the prevalence, types, and sources of such perceived treatment during their training. In addition, the researchers assessed the association between mistreatment and suicidal ideation. Insights into these problems, they say, may spur leaders in the field to develop and implement strategies to help new physicians maintain their well-being throughout their careers.
“A 2019 study by Yue-Yung Hu and associates looked at discrimination, abuse, harassment, and burnout in surgical residents, and they found that mistreatment occurs frequently among general surgery residents, especially women,” Dr. Lall said. “Our study group felt it was important to look at the rates of mistreatment among EM residents nationally in order to obtain baseline data and to use this data to identify and promote educational interventions to reduce workplace mistreatment.”
Emergency residents surveyed
To achieve these ends, Dr. Lall and colleagues sent a survey to all individuals enrolled in EM residencies accredited by the Accreditation Council for Graduate Medical Education who had participated in the 2020 American Board of Emergency Medicine in-training examination. The 35-item multiple-choice survey asked residents to self-report the frequency, sources, and types of mistreatment they had experienced during their training. Suicidal thoughts were assessed by asking residents whether they had considered taking their own life.
Respondents categorized the frequency of mistreatment as never having occurred, having occurred a few times a year, a few times a month, a few times a week, or every day. The investigators created a composite indicator for the study’s primary comparisons that represented the maximum reported frequency of any single exposure. Responses were categorized according to the frequency of mistreatment exposure as either no exposure, exposures a few times per year, or exposures a few times or more per month (including a few times per week or every day).
Almost half report mistreatment
The survey was sent to 8,162 eligible residents in EM. Of those, 6,503 (79.7%) completed the entire survey. Respondents were primarily male (62.1%) and non-Hispanic White (64.0%); 2,620 residents (34.1%) were from other racial/ethnic groups. Of the respondents, 483 residents (6.6%) identified as lesbian, gay, bisexual, transgender, queer, or other (LGBTQ+); 5,951 residents (77.5%) were married or in a relationship.
It was found that 3,463 (45.1%) of participants reported having been exposed to some sort of workplace mistreatment during the most recent academic year. A common source of mistreatment was patients and/or their families. These caused a total of 1,234 events.
Gender discrimination was reported by 2,104 residents (29.5%), 1,635 of whom were women. The most common source of such discrimination was patients or patients’ family members (1,027 women; 184 men). Other sources included nurses or staff (331 women; 59 men).
Racial discrimination was common. It was reported by 1,284 residents; 907 residents were from racial/ethnic groups other than White. Among non-White racial/ethnic groups, 248 residents reported being exposed to racial discrimination at least a few times per month. The most common source of racial discrimination was patients or their family members.
Discrimination based on sexual orientation or gender identity was reported by 220 residents. Once again, the majority of LGBTQ+ residents indicated that patients or their families were the primary source. More than 1,000 residents (n = 1047) reported sexual harassment; among these residents, 721 were women. Patients and/or patients’ family members were the most common source of such discrimination, followed by nurses and staff.
A total of 2,069 residents reported verbal or emotional abuse, including 806 women and 1,212 men. Patients/patients’ family members were the most common source, followed by attending physicians. Physical abuse was reported by 331 respondents. Physical abuse was primarily attributed to patients/patients’ families.
Suicidal thoughts were reported by 178 residents; the prevalence was comparable with respect to gender (2.4% men; 2.4% women) and race/ethnicity (2.4% non-Hispanic White; 2.7% other racial/ethnic groups). Adjusted models revealed that the prevalence for suicidal thoughts was greater among residents who identified as LGBTQ+ (odds ratio [OR], 2.04; 99% confidence interval, 1.04-3.99). An association was found between suicidal thoughts and having experienced mistreatment at least a few times each month (OR, 5.83; 99% CI, 3.70-9.20).
Identifying sources key to stemming mistreatment
These findings, the researchers say, demonstrate the alarming frequency with which workplace mistreatment occurs for EM residents. The survey also found that such mistreatment was more common among residents from racial/ethnic minority populations, women, and residents who identify as LGBTQ+. Perhaps most disturbingly, the occurrence of workplace mistreatment was found to be associated with suicidal thoughts.
The researchers say that although it is likely that residents in many medical specialties experience similar mistreatment to some degree, such treatment should never be considered acceptable. Indeed, Dr. Lall said that identifying sources of mistreatment may help both institutions and individuals determine interventions necessary for improving the well-being of EM residents.
“The first step is recognizing, based on our data, that mistreatment is experienced frequently in EM training in the United States,” she said. “Future qualitative studies of residents and program leaders may help identify which systems, programs, or cultural factors were associated with lower rates of mistreatment in some institutions and higher rates in others.
“Identifying these factors and developing and promoting best practices to minimize workplace mistreatment during residency may help optimize the professional career experience and improve the personal and professional well-being of physicians throughout their lives,” Dr. Lall added.
Commenting on the findings for this article, Karl Y. Bilimoria, MD, of Northwestern University, Chicago, noted that these surveys clearly lay out actionable opportunities to improve trainee mistreatment. “Given that much of the mistreatment of EM residents comes from patients and families, the solutions must be appropriately tailored to address those sources,” Dr. Bilimoria noted.
“Programs need to actively work even more to protect their trainees and faculty from this mistreatment, as it has severe effects and often leads to, or worsens, burnout,” he added.
Funding for statistical analysis was provided by the American Board of Emergency Medicine. Dr. Lall and Dr. Bilimoria reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
published online Aug. 19 in JAMA Network Open.
The survey of more than 6,000 residents found that almost 1 in 2 respondents had been exposed to some form of workplace mistreatment in the previous year, including gender and racial discrimination, physical abuse, or sexual harassment.
“The last study on mistreatment in EM residency training in the United States occurred more than 25 years ago,” said Michelle D. Lall, MD, associate professor of medicine at Emory University, Atlanta. “These findings provide a current look. Mistreatment occurs frequently in EM residency training nationally, and it occurs more frequently in women, racial/ethnic minorities, and those who identify as LGBTQ+,” Dr. Lall added. “Additionally, we found an association between experiencing mistreatment at least a few times per month and having suicidal thoughts.”
Negative sequelae from workplace mistreatment
Dr. Lall explained that workplace mistreatment and institutional responses to such behaviors have been linked to hostile work environments for physicians. In previous research, workplace mistreatment has been found to negatively affect individuals’ sense of self, a phenomenon that not only hindered professional productivity but also increased a variety of other negative factors, such as stress, job dissatisfaction, negative workplace behaviors, and turnover. Perhaps not surprisingly, workplace discrimination has also been shown to have negative effects on physical and mental health.
Despite such findings, little is known about the current state of workplace mistreatment among EM residents. This led the investigators to examine the prevalence, types, and sources of such perceived treatment during their training. In addition, the researchers assessed the association between mistreatment and suicidal ideation. Insights into these problems, they say, may spur leaders in the field to develop and implement strategies to help new physicians maintain their well-being throughout their careers.
“A 2019 study by Yue-Yung Hu and associates looked at discrimination, abuse, harassment, and burnout in surgical residents, and they found that mistreatment occurs frequently among general surgery residents, especially women,” Dr. Lall said. “Our study group felt it was important to look at the rates of mistreatment among EM residents nationally in order to obtain baseline data and to use this data to identify and promote educational interventions to reduce workplace mistreatment.”
Emergency residents surveyed
To achieve these ends, Dr. Lall and colleagues sent a survey to all individuals enrolled in EM residencies accredited by the Accreditation Council for Graduate Medical Education who had participated in the 2020 American Board of Emergency Medicine in-training examination. The 35-item multiple-choice survey asked residents to self-report the frequency, sources, and types of mistreatment they had experienced during their training. Suicidal thoughts were assessed by asking residents whether they had considered taking their own life.
Respondents categorized the frequency of mistreatment as never having occurred, having occurred a few times a year, a few times a month, a few times a week, or every day. The investigators created a composite indicator for the study’s primary comparisons that represented the maximum reported frequency of any single exposure. Responses were categorized according to the frequency of mistreatment exposure as either no exposure, exposures a few times per year, or exposures a few times or more per month (including a few times per week or every day).
Almost half report mistreatment
The survey was sent to 8,162 eligible residents in EM. Of those, 6,503 (79.7%) completed the entire survey. Respondents were primarily male (62.1%) and non-Hispanic White (64.0%); 2,620 residents (34.1%) were from other racial/ethnic groups. Of the respondents, 483 residents (6.6%) identified as lesbian, gay, bisexual, transgender, queer, or other (LGBTQ+); 5,951 residents (77.5%) were married or in a relationship.
It was found that 3,463 (45.1%) of participants reported having been exposed to some sort of workplace mistreatment during the most recent academic year. A common source of mistreatment was patients and/or their families. These caused a total of 1,234 events.
Gender discrimination was reported by 2,104 residents (29.5%), 1,635 of whom were women. The most common source of such discrimination was patients or patients’ family members (1,027 women; 184 men). Other sources included nurses or staff (331 women; 59 men).
Racial discrimination was common. It was reported by 1,284 residents; 907 residents were from racial/ethnic groups other than White. Among non-White racial/ethnic groups, 248 residents reported being exposed to racial discrimination at least a few times per month. The most common source of racial discrimination was patients or their family members.
Discrimination based on sexual orientation or gender identity was reported by 220 residents. Once again, the majority of LGBTQ+ residents indicated that patients or their families were the primary source. More than 1,000 residents (n = 1047) reported sexual harassment; among these residents, 721 were women. Patients and/or patients’ family members were the most common source of such discrimination, followed by nurses and staff.
A total of 2,069 residents reported verbal or emotional abuse, including 806 women and 1,212 men. Patients/patients’ family members were the most common source, followed by attending physicians. Physical abuse was reported by 331 respondents. Physical abuse was primarily attributed to patients/patients’ families.
Suicidal thoughts were reported by 178 residents; the prevalence was comparable with respect to gender (2.4% men; 2.4% women) and race/ethnicity (2.4% non-Hispanic White; 2.7% other racial/ethnic groups). Adjusted models revealed that the prevalence for suicidal thoughts was greater among residents who identified as LGBTQ+ (odds ratio [OR], 2.04; 99% confidence interval, 1.04-3.99). An association was found between suicidal thoughts and having experienced mistreatment at least a few times each month (OR, 5.83; 99% CI, 3.70-9.20).
Identifying sources key to stemming mistreatment
These findings, the researchers say, demonstrate the alarming frequency with which workplace mistreatment occurs for EM residents. The survey also found that such mistreatment was more common among residents from racial/ethnic minority populations, women, and residents who identify as LGBTQ+. Perhaps most disturbingly, the occurrence of workplace mistreatment was found to be associated with suicidal thoughts.
The researchers say that although it is likely that residents in many medical specialties experience similar mistreatment to some degree, such treatment should never be considered acceptable. Indeed, Dr. Lall said that identifying sources of mistreatment may help both institutions and individuals determine interventions necessary for improving the well-being of EM residents.
“The first step is recognizing, based on our data, that mistreatment is experienced frequently in EM training in the United States,” she said. “Future qualitative studies of residents and program leaders may help identify which systems, programs, or cultural factors were associated with lower rates of mistreatment in some institutions and higher rates in others.
“Identifying these factors and developing and promoting best practices to minimize workplace mistreatment during residency may help optimize the professional career experience and improve the personal and professional well-being of physicians throughout their lives,” Dr. Lall added.
Commenting on the findings for this article, Karl Y. Bilimoria, MD, of Northwestern University, Chicago, noted that these surveys clearly lay out actionable opportunities to improve trainee mistreatment. “Given that much of the mistreatment of EM residents comes from patients and families, the solutions must be appropriately tailored to address those sources,” Dr. Bilimoria noted.
“Programs need to actively work even more to protect their trainees and faculty from this mistreatment, as it has severe effects and often leads to, or worsens, burnout,” he added.
Funding for statistical analysis was provided by the American Board of Emergency Medicine. Dr. Lall and Dr. Bilimoria reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
published online Aug. 19 in JAMA Network Open.
The survey of more than 6,000 residents found that almost 1 in 2 respondents had been exposed to some form of workplace mistreatment in the previous year, including gender and racial discrimination, physical abuse, or sexual harassment.
“The last study on mistreatment in EM residency training in the United States occurred more than 25 years ago,” said Michelle D. Lall, MD, associate professor of medicine at Emory University, Atlanta. “These findings provide a current look. Mistreatment occurs frequently in EM residency training nationally, and it occurs more frequently in women, racial/ethnic minorities, and those who identify as LGBTQ+,” Dr. Lall added. “Additionally, we found an association between experiencing mistreatment at least a few times per month and having suicidal thoughts.”
Negative sequelae from workplace mistreatment
Dr. Lall explained that workplace mistreatment and institutional responses to such behaviors have been linked to hostile work environments for physicians. In previous research, workplace mistreatment has been found to negatively affect individuals’ sense of self, a phenomenon that not only hindered professional productivity but also increased a variety of other negative factors, such as stress, job dissatisfaction, negative workplace behaviors, and turnover. Perhaps not surprisingly, workplace discrimination has also been shown to have negative effects on physical and mental health.
Despite such findings, little is known about the current state of workplace mistreatment among EM residents. This led the investigators to examine the prevalence, types, and sources of such perceived treatment during their training. In addition, the researchers assessed the association between mistreatment and suicidal ideation. Insights into these problems, they say, may spur leaders in the field to develop and implement strategies to help new physicians maintain their well-being throughout their careers.
“A 2019 study by Yue-Yung Hu and associates looked at discrimination, abuse, harassment, and burnout in surgical residents, and they found that mistreatment occurs frequently among general surgery residents, especially women,” Dr. Lall said. “Our study group felt it was important to look at the rates of mistreatment among EM residents nationally in order to obtain baseline data and to use this data to identify and promote educational interventions to reduce workplace mistreatment.”
Emergency residents surveyed
To achieve these ends, Dr. Lall and colleagues sent a survey to all individuals enrolled in EM residencies accredited by the Accreditation Council for Graduate Medical Education who had participated in the 2020 American Board of Emergency Medicine in-training examination. The 35-item multiple-choice survey asked residents to self-report the frequency, sources, and types of mistreatment they had experienced during their training. Suicidal thoughts were assessed by asking residents whether they had considered taking their own life.
Respondents categorized the frequency of mistreatment as never having occurred, having occurred a few times a year, a few times a month, a few times a week, or every day. The investigators created a composite indicator for the study’s primary comparisons that represented the maximum reported frequency of any single exposure. Responses were categorized according to the frequency of mistreatment exposure as either no exposure, exposures a few times per year, or exposures a few times or more per month (including a few times per week or every day).
Almost half report mistreatment
The survey was sent to 8,162 eligible residents in EM. Of those, 6,503 (79.7%) completed the entire survey. Respondents were primarily male (62.1%) and non-Hispanic White (64.0%); 2,620 residents (34.1%) were from other racial/ethnic groups. Of the respondents, 483 residents (6.6%) identified as lesbian, gay, bisexual, transgender, queer, or other (LGBTQ+); 5,951 residents (77.5%) were married or in a relationship.
It was found that 3,463 (45.1%) of participants reported having been exposed to some sort of workplace mistreatment during the most recent academic year. A common source of mistreatment was patients and/or their families. These caused a total of 1,234 events.
Gender discrimination was reported by 2,104 residents (29.5%), 1,635 of whom were women. The most common source of such discrimination was patients or patients’ family members (1,027 women; 184 men). Other sources included nurses or staff (331 women; 59 men).
Racial discrimination was common. It was reported by 1,284 residents; 907 residents were from racial/ethnic groups other than White. Among non-White racial/ethnic groups, 248 residents reported being exposed to racial discrimination at least a few times per month. The most common source of racial discrimination was patients or their family members.
Discrimination based on sexual orientation or gender identity was reported by 220 residents. Once again, the majority of LGBTQ+ residents indicated that patients or their families were the primary source. More than 1,000 residents (n = 1047) reported sexual harassment; among these residents, 721 were women. Patients and/or patients’ family members were the most common source of such discrimination, followed by nurses and staff.
A total of 2,069 residents reported verbal or emotional abuse, including 806 women and 1,212 men. Patients/patients’ family members were the most common source, followed by attending physicians. Physical abuse was reported by 331 respondents. Physical abuse was primarily attributed to patients/patients’ families.
Suicidal thoughts were reported by 178 residents; the prevalence was comparable with respect to gender (2.4% men; 2.4% women) and race/ethnicity (2.4% non-Hispanic White; 2.7% other racial/ethnic groups). Adjusted models revealed that the prevalence for suicidal thoughts was greater among residents who identified as LGBTQ+ (odds ratio [OR], 2.04; 99% confidence interval, 1.04-3.99). An association was found between suicidal thoughts and having experienced mistreatment at least a few times each month (OR, 5.83; 99% CI, 3.70-9.20).
Identifying sources key to stemming mistreatment
These findings, the researchers say, demonstrate the alarming frequency with which workplace mistreatment occurs for EM residents. The survey also found that such mistreatment was more common among residents from racial/ethnic minority populations, women, and residents who identify as LGBTQ+. Perhaps most disturbingly, the occurrence of workplace mistreatment was found to be associated with suicidal thoughts.
The researchers say that although it is likely that residents in many medical specialties experience similar mistreatment to some degree, such treatment should never be considered acceptable. Indeed, Dr. Lall said that identifying sources of mistreatment may help both institutions and individuals determine interventions necessary for improving the well-being of EM residents.
“The first step is recognizing, based on our data, that mistreatment is experienced frequently in EM training in the United States,” she said. “Future qualitative studies of residents and program leaders may help identify which systems, programs, or cultural factors were associated with lower rates of mistreatment in some institutions and higher rates in others.
“Identifying these factors and developing and promoting best practices to minimize workplace mistreatment during residency may help optimize the professional career experience and improve the personal and professional well-being of physicians throughout their lives,” Dr. Lall added.
Commenting on the findings for this article, Karl Y. Bilimoria, MD, of Northwestern University, Chicago, noted that these surveys clearly lay out actionable opportunities to improve trainee mistreatment. “Given that much of the mistreatment of EM residents comes from patients and families, the solutions must be appropriately tailored to address those sources,” Dr. Bilimoria noted.
“Programs need to actively work even more to protect their trainees and faculty from this mistreatment, as it has severe effects and often leads to, or worsens, burnout,” he added.
Funding for statistical analysis was provided by the American Board of Emergency Medicine. Dr. Lall and Dr. Bilimoria reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
PHM 2021: Achieving gender equity in medicine
PHM 2021 session
Accelerating Patient Care and Healthcare Workforce Diversity and Inclusion
Presenter
Julie Silver, MD
Session summary
Gender inequity in medicine has been well documented and further highlighted by the tremendous impact of the COVID-19 pandemic on women in medicine. While more women than men are entering medical schools across the U.S., women still struggle to reach the highest levels of academic rank, achieve leadership positions of power and influence, receive fair equitable pay, attain leadership roles in national societies, and receive funding from national agencies. They also continue to face discrimination and implicit and explicit biases. Women of color or from other minority backgrounds face even greater barriers and biases. Despite being a specialty in which women represent almost 70% of the workforce, pediatrics is not immune to these disparities.
In her PHM21 plenary on Aug. 3, 2021, Dr. Julie Silver, a national expert in gender equity disparities, detailed the landscape for women in medicine and proposed some solutions to accelerate systemic change for gender equity. In order to understand and mitigate gender inequity, Dr. Silver encouraged the PHM community to identify influential “gatekeepers” of promotion, advancement, and salary compensation. In academic medicine medical schools, funding agencies, professional societies, and journals are the gatekeepers to advancement and compensation for women. Women are traditionally underrepresented as members and influential leaders of these gatekeeping organizations and in their recognition structures, therefore their advancement, compensation, and wellbeing are hindered.
Key takeaways
- Critical mass theory will not help alleviate gender inequity in medicine, as women make up a critical mass in pediatrics and are still experiencing stark inequities. Critical actor leaders are needed to highlight disparities and drive change even once a critical mass is reached.
- Our current diversity, equity, and inclusion (DEI) efforts are ineffective and are creating an “illusion of fairness that causes majority group members to become less sensitive to recognizing discrimination against minorities.” Many of the activities that are considered citizenship, including committees focused on DEI efforts, should be counted as scholarship, and appropriately compensated to ensure promotion of our women and minority colleagues.
- Male allies are critical to documenting, disseminating, and addressing gender inequality. Without the support of men in the field, we will see little progress.
- While there are numerous advocacy angles we can take when advocating for gender equity, the most effective will be the financial angle. Gender pay gaps at the start of a career can lead to roughly 2 million dollars of salary loss for a woman over the course of her career. In order to alleviate those salary pay gaps our institutions must not expect women to negotiate for fair pay, make salary benchmarks transparent, continue to monitor and conduct research on compensation disparities, and attempt to alleviate the weight of educational debt.
- COVID-19 is causing immense stress on women in medicine, and the impact could be disastrous. We must recognize and reward the “4th shift” women are working for COVID-19–related activities at home and at work, and put measures in place to #GiveHerAReasonToStay in health care.
- Men and other women leaders have a responsibility to sponsor the many and well-qualified women in medicine for awards, committees, and speaking engagements. These opportunities are key markers of success in academic medicine and are critical to advancement and salary compensation.
Dr. Casillas is the internal medicine-pediatric chief resident for the University of Cincinnati/Cincinnati Children’s Internal Medicine-Pediatric program. His career goal is to serve as a hospitalist for children and adults, and he is interested in health equity and Latinx health. Dr. O’Toole is a pediatric and adult hospitalist at Cincinnati Children’s Hospital Medical Center and University of Cincinnati Medical Center, and a professor of pediatrics and internal medicine at the University of Cincinnati College of Medicine. She serves as program director of Cincinnati’s Combined Internal Medicine and Pediatrics Residency Program.
PHM 2021 session
Accelerating Patient Care and Healthcare Workforce Diversity and Inclusion
Presenter
Julie Silver, MD
Session summary
Gender inequity in medicine has been well documented and further highlighted by the tremendous impact of the COVID-19 pandemic on women in medicine. While more women than men are entering medical schools across the U.S., women still struggle to reach the highest levels of academic rank, achieve leadership positions of power and influence, receive fair equitable pay, attain leadership roles in national societies, and receive funding from national agencies. They also continue to face discrimination and implicit and explicit biases. Women of color or from other minority backgrounds face even greater barriers and biases. Despite being a specialty in which women represent almost 70% of the workforce, pediatrics is not immune to these disparities.
In her PHM21 plenary on Aug. 3, 2021, Dr. Julie Silver, a national expert in gender equity disparities, detailed the landscape for women in medicine and proposed some solutions to accelerate systemic change for gender equity. In order to understand and mitigate gender inequity, Dr. Silver encouraged the PHM community to identify influential “gatekeepers” of promotion, advancement, and salary compensation. In academic medicine medical schools, funding agencies, professional societies, and journals are the gatekeepers to advancement and compensation for women. Women are traditionally underrepresented as members and influential leaders of these gatekeeping organizations and in their recognition structures, therefore their advancement, compensation, and wellbeing are hindered.
Key takeaways
- Critical mass theory will not help alleviate gender inequity in medicine, as women make up a critical mass in pediatrics and are still experiencing stark inequities. Critical actor leaders are needed to highlight disparities and drive change even once a critical mass is reached.
- Our current diversity, equity, and inclusion (DEI) efforts are ineffective and are creating an “illusion of fairness that causes majority group members to become less sensitive to recognizing discrimination against minorities.” Many of the activities that are considered citizenship, including committees focused on DEI efforts, should be counted as scholarship, and appropriately compensated to ensure promotion of our women and minority colleagues.
- Male allies are critical to documenting, disseminating, and addressing gender inequality. Without the support of men in the field, we will see little progress.
- While there are numerous advocacy angles we can take when advocating for gender equity, the most effective will be the financial angle. Gender pay gaps at the start of a career can lead to roughly 2 million dollars of salary loss for a woman over the course of her career. In order to alleviate those salary pay gaps our institutions must not expect women to negotiate for fair pay, make salary benchmarks transparent, continue to monitor and conduct research on compensation disparities, and attempt to alleviate the weight of educational debt.
- COVID-19 is causing immense stress on women in medicine, and the impact could be disastrous. We must recognize and reward the “4th shift” women are working for COVID-19–related activities at home and at work, and put measures in place to #GiveHerAReasonToStay in health care.
- Men and other women leaders have a responsibility to sponsor the many and well-qualified women in medicine for awards, committees, and speaking engagements. These opportunities are key markers of success in academic medicine and are critical to advancement and salary compensation.
Dr. Casillas is the internal medicine-pediatric chief resident for the University of Cincinnati/Cincinnati Children’s Internal Medicine-Pediatric program. His career goal is to serve as a hospitalist for children and adults, and he is interested in health equity and Latinx health. Dr. O’Toole is a pediatric and adult hospitalist at Cincinnati Children’s Hospital Medical Center and University of Cincinnati Medical Center, and a professor of pediatrics and internal medicine at the University of Cincinnati College of Medicine. She serves as program director of Cincinnati’s Combined Internal Medicine and Pediatrics Residency Program.
PHM 2021 session
Accelerating Patient Care and Healthcare Workforce Diversity and Inclusion
Presenter
Julie Silver, MD
Session summary
Gender inequity in medicine has been well documented and further highlighted by the tremendous impact of the COVID-19 pandemic on women in medicine. While more women than men are entering medical schools across the U.S., women still struggle to reach the highest levels of academic rank, achieve leadership positions of power and influence, receive fair equitable pay, attain leadership roles in national societies, and receive funding from national agencies. They also continue to face discrimination and implicit and explicit biases. Women of color or from other minority backgrounds face even greater barriers and biases. Despite being a specialty in which women represent almost 70% of the workforce, pediatrics is not immune to these disparities.
In her PHM21 plenary on Aug. 3, 2021, Dr. Julie Silver, a national expert in gender equity disparities, detailed the landscape for women in medicine and proposed some solutions to accelerate systemic change for gender equity. In order to understand and mitigate gender inequity, Dr. Silver encouraged the PHM community to identify influential “gatekeepers” of promotion, advancement, and salary compensation. In academic medicine medical schools, funding agencies, professional societies, and journals are the gatekeepers to advancement and compensation for women. Women are traditionally underrepresented as members and influential leaders of these gatekeeping organizations and in their recognition structures, therefore their advancement, compensation, and wellbeing are hindered.
Key takeaways
- Critical mass theory will not help alleviate gender inequity in medicine, as women make up a critical mass in pediatrics and are still experiencing stark inequities. Critical actor leaders are needed to highlight disparities and drive change even once a critical mass is reached.
- Our current diversity, equity, and inclusion (DEI) efforts are ineffective and are creating an “illusion of fairness that causes majority group members to become less sensitive to recognizing discrimination against minorities.” Many of the activities that are considered citizenship, including committees focused on DEI efforts, should be counted as scholarship, and appropriately compensated to ensure promotion of our women and minority colleagues.
- Male allies are critical to documenting, disseminating, and addressing gender inequality. Without the support of men in the field, we will see little progress.
- While there are numerous advocacy angles we can take when advocating for gender equity, the most effective will be the financial angle. Gender pay gaps at the start of a career can lead to roughly 2 million dollars of salary loss for a woman over the course of her career. In order to alleviate those salary pay gaps our institutions must not expect women to negotiate for fair pay, make salary benchmarks transparent, continue to monitor and conduct research on compensation disparities, and attempt to alleviate the weight of educational debt.
- COVID-19 is causing immense stress on women in medicine, and the impact could be disastrous. We must recognize and reward the “4th shift” women are working for COVID-19–related activities at home and at work, and put measures in place to #GiveHerAReasonToStay in health care.
- Men and other women leaders have a responsibility to sponsor the many and well-qualified women in medicine for awards, committees, and speaking engagements. These opportunities are key markers of success in academic medicine and are critical to advancement and salary compensation.
Dr. Casillas is the internal medicine-pediatric chief resident for the University of Cincinnati/Cincinnati Children’s Internal Medicine-Pediatric program. His career goal is to serve as a hospitalist for children and adults, and he is interested in health equity and Latinx health. Dr. O’Toole is a pediatric and adult hospitalist at Cincinnati Children’s Hospital Medical Center and University of Cincinnati Medical Center, and a professor of pediatrics and internal medicine at the University of Cincinnati College of Medicine. She serves as program director of Cincinnati’s Combined Internal Medicine and Pediatrics Residency Program.
Cavernous gender gap in Medicare payments to cardiologists
Women cardiologists receive dramatically smaller payments from the U.S. Centers for Medicare & Medicaid Services (CMS) than their male counterparts, new research suggests.
An analysis of 2016 claims data revealed male cardiologists received on average 45% more reimbursement than women in the inpatient setting, with the median payment 39% higher ($62,897 vs. $45,288).
In the outpatient setting, men received on average 62% more annual CMS payments, with the median payment 75% higher ($91,053 vs. $51,975; P < .001 for both).
The difference remained significant after the exclusion of the top and bottom 2.5% of earning physicians and cardiology subspecialties, like electrophysiology and interventional cardiology, with high procedural volumes and greater gender imbalances.
“This is one study among others which demonstrates a wage gap between men and women in medicine in cardiology,” lead author Inbar Raber, MD, Beth Israel Deaconess Medical Center, Boston, said in an interview. “I hope by increasing awareness [and] understanding of possible etiologies, it will enable some sustainable solutions, and those include access to additional support staff and equitable models surrounding parental leave and childcare support.”
The study, published online September 8 in JAMA Cardiology, comes on the heels of a recent cross-sectional analysis that put cardiology at the bottom of 13 internal medicine subspecialties with just 21% female faculty representation and one of only three specialties in which women’s median salaries did not reach 90% of men’s.
The new findings build on a 2017 report that showed Medicare payments to women physicians in 2013 were 55% of those to male physicians across all specialties.
“It can be disheartening, especially as an early career woman cardiologist, seeing these differences, but I think the responsibility on all of us is to take these observations and really try to understand more deeply why they exist,” Nosheen Reza, MD, from the University of Pennsylvania, Philadelphia, and coauthor of the cross-sectional analysis, told this news organization.
Several factors could be contributing to the disparity, but “it’s not gender discrimination from Medicare,” Dr. Raber said. “The gap in reimbursement is really driven by the types and the volume of charges submitted.”
Indeed, a direct comparison of the three most common inpatient and outpatient billing codes showed no difference in payments between the sexes.
Men, however, submitted 24% more median inpatient charges to CMS than women (1,190 vs. 959), and 94% more outpatient charges (1,685 vs. 870).
Men also submitted slightly more unique billing codes (median inpatient, 10 vs. 9; median outpatient, 11 vs. 8).
Notably, women made up just 13% of the 17,524 cardiologists who received CMS payments in the inpatient setting in 2016 and 13% of the 16,929 cardiologists who did so in the outpatient setting.
Louisiana had the dubious distinction of having the largest gender gap in mean CMS payments, with male cardiologists earning $145,323 (235%) more than women, whereas women cardiologists in Vermont out-earned men by $31,483 (38%).
Overall, male cardiologists had more years in practice than women cardiologists and cared for slightly older Medicare beneficiaries.
Differences in CMS payments persisted, however, after adjustment for years since graduation, physician subspecialty, number of charges, number of unique billing codes, and patient complexity. The resulting β coefficient was -0.06, which translates into women receiving an average of 94% of the CMS payments received by men.
“The first takeaway, if you were really crass and focused on the bottom line, might be: ‘Hey, let me get a few more male cardiologists because they’re going to bring more into the organization.’ But we shouldn’t do that because, unless you link these data with quality outcomes, they’re an interesting observation and hypothesis-generating,” said Sharonne Hayes, MD, coauthor of the 2017 report and professor of cardiovascular medicine at Mayo Clinic in Rochester, Minn., where she has served as director of diversity and inclusion for a decade.
She noted that there are multiple examples that the style of medicine women practice, on average, may be more effective, may be more outcomes based, and may save lives, as suggested by a recent analysis of hospitalized Medicare beneficiaries.
“The gap was not much different, like within 1% or so, but when you take that over the literally millions of Medicare patients cared for each year by hospitalists, that’s a substantial number of people,” Dr. Hayes said. “So, I think we need to take a step back, and we have to include these observations on studies like this and better understand the compensation gaps.”
She pointed out that the present study lacks data on full-time-equivalent status but that female physicians are more likely to work part-time, thus reducing the volume of claims.
Women might also care for different patient populations. “I practice in a women’s heart clinic and take care of [spontaneous coronary artery dissection] SCAD patients where the average age of SCAD is 42. So, the vast majority of patients I see on a day-to-day basis aren’t going to be Medicare age,” observed Dr. Hayes.
The differences in charges might also reflect the increased obligations in nonreimbursed work that women can have, Dr. Raber said. These can be things like mentoring, teaching roles, and serving on committees, which is a hypothesis supported by a 2021 study that showed women physicians spend more time on these “citizenship tasks” than men.
Finally, there could be organizational barriers that affect women’s clinical volumes, including less access to support from health care personnel. Added support is especially important, though, amid a 100-year pandemic, the women agreed.
“Within the first year of the pandemic, we saw women leaving the workforce in droves across all sectors, including medicine, including academic medicine. And, as the pandemic goes on without any signs of abatement, those threats continue to exist and continue to be amplified,” Dr. Reza said.
The groundswell of support surrounding the importance of diversity, equity, and inclusion initiatives across the board has helped bring attention to the issue, she said. Some institutions, including the National Institutes of Health, are making efforts to extend relief to women with young families, caregivers, or those in academic medicine who, for example, need extensions on grants or bridge funding.
“There’s certainly a lot left to do, but I do think within the last year, there’s been an acceleration of literature that has come out, not only pointing out the disparities, but pointing out that perhaps women physicians do have better outcomes and are better liked by their patients and that losing women in the workforce would be a huge detriment to the field overall,” Dr. Reza said.
Dr. Raber, Dr. Reza, and Dr. Hayes reports no relevant financial relationships. Coauthor conflict of interest disclosures are listed in the paper.
A version of this article first appeared on Medscape.com.
Women cardiologists receive dramatically smaller payments from the U.S. Centers for Medicare & Medicaid Services (CMS) than their male counterparts, new research suggests.
An analysis of 2016 claims data revealed male cardiologists received on average 45% more reimbursement than women in the inpatient setting, with the median payment 39% higher ($62,897 vs. $45,288).
In the outpatient setting, men received on average 62% more annual CMS payments, with the median payment 75% higher ($91,053 vs. $51,975; P < .001 for both).
The difference remained significant after the exclusion of the top and bottom 2.5% of earning physicians and cardiology subspecialties, like electrophysiology and interventional cardiology, with high procedural volumes and greater gender imbalances.
“This is one study among others which demonstrates a wage gap between men and women in medicine in cardiology,” lead author Inbar Raber, MD, Beth Israel Deaconess Medical Center, Boston, said in an interview. “I hope by increasing awareness [and] understanding of possible etiologies, it will enable some sustainable solutions, and those include access to additional support staff and equitable models surrounding parental leave and childcare support.”
The study, published online September 8 in JAMA Cardiology, comes on the heels of a recent cross-sectional analysis that put cardiology at the bottom of 13 internal medicine subspecialties with just 21% female faculty representation and one of only three specialties in which women’s median salaries did not reach 90% of men’s.
The new findings build on a 2017 report that showed Medicare payments to women physicians in 2013 were 55% of those to male physicians across all specialties.
“It can be disheartening, especially as an early career woman cardiologist, seeing these differences, but I think the responsibility on all of us is to take these observations and really try to understand more deeply why they exist,” Nosheen Reza, MD, from the University of Pennsylvania, Philadelphia, and coauthor of the cross-sectional analysis, told this news organization.
Several factors could be contributing to the disparity, but “it’s not gender discrimination from Medicare,” Dr. Raber said. “The gap in reimbursement is really driven by the types and the volume of charges submitted.”
Indeed, a direct comparison of the three most common inpatient and outpatient billing codes showed no difference in payments between the sexes.
Men, however, submitted 24% more median inpatient charges to CMS than women (1,190 vs. 959), and 94% more outpatient charges (1,685 vs. 870).
Men also submitted slightly more unique billing codes (median inpatient, 10 vs. 9; median outpatient, 11 vs. 8).
Notably, women made up just 13% of the 17,524 cardiologists who received CMS payments in the inpatient setting in 2016 and 13% of the 16,929 cardiologists who did so in the outpatient setting.
Louisiana had the dubious distinction of having the largest gender gap in mean CMS payments, with male cardiologists earning $145,323 (235%) more than women, whereas women cardiologists in Vermont out-earned men by $31,483 (38%).
Overall, male cardiologists had more years in practice than women cardiologists and cared for slightly older Medicare beneficiaries.
Differences in CMS payments persisted, however, after adjustment for years since graduation, physician subspecialty, number of charges, number of unique billing codes, and patient complexity. The resulting β coefficient was -0.06, which translates into women receiving an average of 94% of the CMS payments received by men.
“The first takeaway, if you were really crass and focused on the bottom line, might be: ‘Hey, let me get a few more male cardiologists because they’re going to bring more into the organization.’ But we shouldn’t do that because, unless you link these data with quality outcomes, they’re an interesting observation and hypothesis-generating,” said Sharonne Hayes, MD, coauthor of the 2017 report and professor of cardiovascular medicine at Mayo Clinic in Rochester, Minn., where she has served as director of diversity and inclusion for a decade.
She noted that there are multiple examples that the style of medicine women practice, on average, may be more effective, may be more outcomes based, and may save lives, as suggested by a recent analysis of hospitalized Medicare beneficiaries.
“The gap was not much different, like within 1% or so, but when you take that over the literally millions of Medicare patients cared for each year by hospitalists, that’s a substantial number of people,” Dr. Hayes said. “So, I think we need to take a step back, and we have to include these observations on studies like this and better understand the compensation gaps.”
She pointed out that the present study lacks data on full-time-equivalent status but that female physicians are more likely to work part-time, thus reducing the volume of claims.
Women might also care for different patient populations. “I practice in a women’s heart clinic and take care of [spontaneous coronary artery dissection] SCAD patients where the average age of SCAD is 42. So, the vast majority of patients I see on a day-to-day basis aren’t going to be Medicare age,” observed Dr. Hayes.
The differences in charges might also reflect the increased obligations in nonreimbursed work that women can have, Dr. Raber said. These can be things like mentoring, teaching roles, and serving on committees, which is a hypothesis supported by a 2021 study that showed women physicians spend more time on these “citizenship tasks” than men.
Finally, there could be organizational barriers that affect women’s clinical volumes, including less access to support from health care personnel. Added support is especially important, though, amid a 100-year pandemic, the women agreed.
“Within the first year of the pandemic, we saw women leaving the workforce in droves across all sectors, including medicine, including academic medicine. And, as the pandemic goes on without any signs of abatement, those threats continue to exist and continue to be amplified,” Dr. Reza said.
The groundswell of support surrounding the importance of diversity, equity, and inclusion initiatives across the board has helped bring attention to the issue, she said. Some institutions, including the National Institutes of Health, are making efforts to extend relief to women with young families, caregivers, or those in academic medicine who, for example, need extensions on grants or bridge funding.
“There’s certainly a lot left to do, but I do think within the last year, there’s been an acceleration of literature that has come out, not only pointing out the disparities, but pointing out that perhaps women physicians do have better outcomes and are better liked by their patients and that losing women in the workforce would be a huge detriment to the field overall,” Dr. Reza said.
Dr. Raber, Dr. Reza, and Dr. Hayes reports no relevant financial relationships. Coauthor conflict of interest disclosures are listed in the paper.
A version of this article first appeared on Medscape.com.
Women cardiologists receive dramatically smaller payments from the U.S. Centers for Medicare & Medicaid Services (CMS) than their male counterparts, new research suggests.
An analysis of 2016 claims data revealed male cardiologists received on average 45% more reimbursement than women in the inpatient setting, with the median payment 39% higher ($62,897 vs. $45,288).
In the outpatient setting, men received on average 62% more annual CMS payments, with the median payment 75% higher ($91,053 vs. $51,975; P < .001 for both).
The difference remained significant after the exclusion of the top and bottom 2.5% of earning physicians and cardiology subspecialties, like electrophysiology and interventional cardiology, with high procedural volumes and greater gender imbalances.
“This is one study among others which demonstrates a wage gap between men and women in medicine in cardiology,” lead author Inbar Raber, MD, Beth Israel Deaconess Medical Center, Boston, said in an interview. “I hope by increasing awareness [and] understanding of possible etiologies, it will enable some sustainable solutions, and those include access to additional support staff and equitable models surrounding parental leave and childcare support.”
The study, published online September 8 in JAMA Cardiology, comes on the heels of a recent cross-sectional analysis that put cardiology at the bottom of 13 internal medicine subspecialties with just 21% female faculty representation and one of only three specialties in which women’s median salaries did not reach 90% of men’s.
The new findings build on a 2017 report that showed Medicare payments to women physicians in 2013 were 55% of those to male physicians across all specialties.
“It can be disheartening, especially as an early career woman cardiologist, seeing these differences, but I think the responsibility on all of us is to take these observations and really try to understand more deeply why they exist,” Nosheen Reza, MD, from the University of Pennsylvania, Philadelphia, and coauthor of the cross-sectional analysis, told this news organization.
Several factors could be contributing to the disparity, but “it’s not gender discrimination from Medicare,” Dr. Raber said. “The gap in reimbursement is really driven by the types and the volume of charges submitted.”
Indeed, a direct comparison of the three most common inpatient and outpatient billing codes showed no difference in payments between the sexes.
Men, however, submitted 24% more median inpatient charges to CMS than women (1,190 vs. 959), and 94% more outpatient charges (1,685 vs. 870).
Men also submitted slightly more unique billing codes (median inpatient, 10 vs. 9; median outpatient, 11 vs. 8).
Notably, women made up just 13% of the 17,524 cardiologists who received CMS payments in the inpatient setting in 2016 and 13% of the 16,929 cardiologists who did so in the outpatient setting.
Louisiana had the dubious distinction of having the largest gender gap in mean CMS payments, with male cardiologists earning $145,323 (235%) more than women, whereas women cardiologists in Vermont out-earned men by $31,483 (38%).
Overall, male cardiologists had more years in practice than women cardiologists and cared for slightly older Medicare beneficiaries.
Differences in CMS payments persisted, however, after adjustment for years since graduation, physician subspecialty, number of charges, number of unique billing codes, and patient complexity. The resulting β coefficient was -0.06, which translates into women receiving an average of 94% of the CMS payments received by men.
“The first takeaway, if you were really crass and focused on the bottom line, might be: ‘Hey, let me get a few more male cardiologists because they’re going to bring more into the organization.’ But we shouldn’t do that because, unless you link these data with quality outcomes, they’re an interesting observation and hypothesis-generating,” said Sharonne Hayes, MD, coauthor of the 2017 report and professor of cardiovascular medicine at Mayo Clinic in Rochester, Minn., where she has served as director of diversity and inclusion for a decade.
She noted that there are multiple examples that the style of medicine women practice, on average, may be more effective, may be more outcomes based, and may save lives, as suggested by a recent analysis of hospitalized Medicare beneficiaries.
“The gap was not much different, like within 1% or so, but when you take that over the literally millions of Medicare patients cared for each year by hospitalists, that’s a substantial number of people,” Dr. Hayes said. “So, I think we need to take a step back, and we have to include these observations on studies like this and better understand the compensation gaps.”
She pointed out that the present study lacks data on full-time-equivalent status but that female physicians are more likely to work part-time, thus reducing the volume of claims.
Women might also care for different patient populations. “I practice in a women’s heart clinic and take care of [spontaneous coronary artery dissection] SCAD patients where the average age of SCAD is 42. So, the vast majority of patients I see on a day-to-day basis aren’t going to be Medicare age,” observed Dr. Hayes.
The differences in charges might also reflect the increased obligations in nonreimbursed work that women can have, Dr. Raber said. These can be things like mentoring, teaching roles, and serving on committees, which is a hypothesis supported by a 2021 study that showed women physicians spend more time on these “citizenship tasks” than men.
Finally, there could be organizational barriers that affect women’s clinical volumes, including less access to support from health care personnel. Added support is especially important, though, amid a 100-year pandemic, the women agreed.
“Within the first year of the pandemic, we saw women leaving the workforce in droves across all sectors, including medicine, including academic medicine. And, as the pandemic goes on without any signs of abatement, those threats continue to exist and continue to be amplified,” Dr. Reza said.
The groundswell of support surrounding the importance of diversity, equity, and inclusion initiatives across the board has helped bring attention to the issue, she said. Some institutions, including the National Institutes of Health, are making efforts to extend relief to women with young families, caregivers, or those in academic medicine who, for example, need extensions on grants or bridge funding.
“There’s certainly a lot left to do, but I do think within the last year, there’s been an acceleration of literature that has come out, not only pointing out the disparities, but pointing out that perhaps women physicians do have better outcomes and are better liked by their patients and that losing women in the workforce would be a huge detriment to the field overall,” Dr. Reza said.
Dr. Raber, Dr. Reza, and Dr. Hayes reports no relevant financial relationships. Coauthor conflict of interest disclosures are listed in the paper.
A version of this article first appeared on Medscape.com.
Unequal resource distribution underlies lung cancer disparities
Lung cancer disparities are reversible, but it will take changes at the social policy and organizational levels to do it, according to Ray Osarogiagbon, MBBS, a medical oncologist in the thoracic oncology program at Baptist Cancer Center, Memphis.
Much of the issue comes down to unequal distribution of services across the country, with less high-end care available in areas hardest hit by lung cancer, which are often areas with higher percentages of Black people, Dr. Osarogiagbon said. He addressed the issues – which he conceptualizes as “avoidable differences” – in a plenary presentation at the virtual 2021 World Conference on Lung Cancer.
He said that much of disparity research has focused on patient-level issues, but it has the least potential to effect change and also has “the unpleasant side effect of stigmatizing the victims of disparate health care delivery.”
Better to look at the big picture. “We have to focus on the areas where we are most likely to be successful, the social policy level, next the organizational level, and then providers,” he said.
Kentucky, followed by Mississippi, Arkansas, Tennessee, West Virginia, and Alabama, has the highest lung cancer burden in the United States. While lung cancer has been on the decline for decades nationwide, some counties in those states in particular continue to struggle with rising lung cancer mortality.
Dr. Osarogiagbon’s own health care system, which serves western Tennessee as well as eastern Arkansas and northern Mississippi, sees about 1,300 lung cancer cases annually, more than many states in the United States.
Regional disparities in lung cancer care span the entirety of available services, from unequal access to tobacco cessation and other preventive measures straight through to access to leading-edge systemic therapies. Disparities are particularly acute with more recent advances such as immunotherapy and low-dose CT screening.
One recent study, for instance, found that several southern states with high lung cancer burdens had screening rates below 4%, while several New England states had rates ranging to over 15%.
“There is a mismatch between the places were lung cancer kills and the places where we have invested in low-dose CT scan facilities,” Dr. Osarogiagbon said. As a side effect, White patients have better access,
It’s not, he said, that Black people are more likely to refuse such services, as least as far as clinical trials go.
Black patients are significantly underrepresented in pharmaceutical industry trials. Part of the issues is that areas hardest hit by lung cancer are often also ones less likely to have the infrastructure to support trials.
But on an equal playing field, Black patients are at least as eager as White patients to sign up for a trial. Dr. Osarogiagbon and colleagues found that, if offered the chance, almost 60% of Black patients said they would participate in a trial versus 53.4% of White patients. If access were equal, there would be “no race-based disparities” in trial participation, he said.
It’s also emerging that Black patients might benefit more from innovations such as immune checkpoint inhibitors treatment and low-dose CT screening, which means that, if they were included in more trials, companies would likely have stronger study results.
It’s something they should pay attention to, if for no other reason than it would help their bottom line, Dr. Osarogiagbon said.
Curative surgery for early-stage lung tumors is another issue. At the county level in the United States, he and his team found that it’s offered to anywhere from 13% to 92% of patients who qualify.
“Counties in the lowest quartile for receipt of surgery were those with a high proportion of non-Hispanic Black subjects, high poverty and uninsured rates, low surgeon-to-population ratio, and nonmetropolitan status,” they found.
Dr. Osarogiagbon is a consultant for and/or has stock in a number of companies, including AstraZeneca, Eli Lilly, and Genentech.
Lung cancer disparities are reversible, but it will take changes at the social policy and organizational levels to do it, according to Ray Osarogiagbon, MBBS, a medical oncologist in the thoracic oncology program at Baptist Cancer Center, Memphis.
Much of the issue comes down to unequal distribution of services across the country, with less high-end care available in areas hardest hit by lung cancer, which are often areas with higher percentages of Black people, Dr. Osarogiagbon said. He addressed the issues – which he conceptualizes as “avoidable differences” – in a plenary presentation at the virtual 2021 World Conference on Lung Cancer.
He said that much of disparity research has focused on patient-level issues, but it has the least potential to effect change and also has “the unpleasant side effect of stigmatizing the victims of disparate health care delivery.”
Better to look at the big picture. “We have to focus on the areas where we are most likely to be successful, the social policy level, next the organizational level, and then providers,” he said.
Kentucky, followed by Mississippi, Arkansas, Tennessee, West Virginia, and Alabama, has the highest lung cancer burden in the United States. While lung cancer has been on the decline for decades nationwide, some counties in those states in particular continue to struggle with rising lung cancer mortality.
Dr. Osarogiagbon’s own health care system, which serves western Tennessee as well as eastern Arkansas and northern Mississippi, sees about 1,300 lung cancer cases annually, more than many states in the United States.
Regional disparities in lung cancer care span the entirety of available services, from unequal access to tobacco cessation and other preventive measures straight through to access to leading-edge systemic therapies. Disparities are particularly acute with more recent advances such as immunotherapy and low-dose CT screening.
One recent study, for instance, found that several southern states with high lung cancer burdens had screening rates below 4%, while several New England states had rates ranging to over 15%.
“There is a mismatch between the places were lung cancer kills and the places where we have invested in low-dose CT scan facilities,” Dr. Osarogiagbon said. As a side effect, White patients have better access,
It’s not, he said, that Black people are more likely to refuse such services, as least as far as clinical trials go.
Black patients are significantly underrepresented in pharmaceutical industry trials. Part of the issues is that areas hardest hit by lung cancer are often also ones less likely to have the infrastructure to support trials.
But on an equal playing field, Black patients are at least as eager as White patients to sign up for a trial. Dr. Osarogiagbon and colleagues found that, if offered the chance, almost 60% of Black patients said they would participate in a trial versus 53.4% of White patients. If access were equal, there would be “no race-based disparities” in trial participation, he said.
It’s also emerging that Black patients might benefit more from innovations such as immune checkpoint inhibitors treatment and low-dose CT screening, which means that, if they were included in more trials, companies would likely have stronger study results.
It’s something they should pay attention to, if for no other reason than it would help their bottom line, Dr. Osarogiagbon said.
Curative surgery for early-stage lung tumors is another issue. At the county level in the United States, he and his team found that it’s offered to anywhere from 13% to 92% of patients who qualify.
“Counties in the lowest quartile for receipt of surgery were those with a high proportion of non-Hispanic Black subjects, high poverty and uninsured rates, low surgeon-to-population ratio, and nonmetropolitan status,” they found.
Dr. Osarogiagbon is a consultant for and/or has stock in a number of companies, including AstraZeneca, Eli Lilly, and Genentech.
Lung cancer disparities are reversible, but it will take changes at the social policy and organizational levels to do it, according to Ray Osarogiagbon, MBBS, a medical oncologist in the thoracic oncology program at Baptist Cancer Center, Memphis.
Much of the issue comes down to unequal distribution of services across the country, with less high-end care available in areas hardest hit by lung cancer, which are often areas with higher percentages of Black people, Dr. Osarogiagbon said. He addressed the issues – which he conceptualizes as “avoidable differences” – in a plenary presentation at the virtual 2021 World Conference on Lung Cancer.
He said that much of disparity research has focused on patient-level issues, but it has the least potential to effect change and also has “the unpleasant side effect of stigmatizing the victims of disparate health care delivery.”
Better to look at the big picture. “We have to focus on the areas where we are most likely to be successful, the social policy level, next the organizational level, and then providers,” he said.
Kentucky, followed by Mississippi, Arkansas, Tennessee, West Virginia, and Alabama, has the highest lung cancer burden in the United States. While lung cancer has been on the decline for decades nationwide, some counties in those states in particular continue to struggle with rising lung cancer mortality.
Dr. Osarogiagbon’s own health care system, which serves western Tennessee as well as eastern Arkansas and northern Mississippi, sees about 1,300 lung cancer cases annually, more than many states in the United States.
Regional disparities in lung cancer care span the entirety of available services, from unequal access to tobacco cessation and other preventive measures straight through to access to leading-edge systemic therapies. Disparities are particularly acute with more recent advances such as immunotherapy and low-dose CT screening.
One recent study, for instance, found that several southern states with high lung cancer burdens had screening rates below 4%, while several New England states had rates ranging to over 15%.
“There is a mismatch between the places were lung cancer kills and the places where we have invested in low-dose CT scan facilities,” Dr. Osarogiagbon said. As a side effect, White patients have better access,
It’s not, he said, that Black people are more likely to refuse such services, as least as far as clinical trials go.
Black patients are significantly underrepresented in pharmaceutical industry trials. Part of the issues is that areas hardest hit by lung cancer are often also ones less likely to have the infrastructure to support trials.
But on an equal playing field, Black patients are at least as eager as White patients to sign up for a trial. Dr. Osarogiagbon and colleagues found that, if offered the chance, almost 60% of Black patients said they would participate in a trial versus 53.4% of White patients. If access were equal, there would be “no race-based disparities” in trial participation, he said.
It’s also emerging that Black patients might benefit more from innovations such as immune checkpoint inhibitors treatment and low-dose CT screening, which means that, if they were included in more trials, companies would likely have stronger study results.
It’s something they should pay attention to, if for no other reason than it would help their bottom line, Dr. Osarogiagbon said.
Curative surgery for early-stage lung tumors is another issue. At the county level in the United States, he and his team found that it’s offered to anywhere from 13% to 92% of patients who qualify.
“Counties in the lowest quartile for receipt of surgery were those with a high proportion of non-Hispanic Black subjects, high poverty and uninsured rates, low surgeon-to-population ratio, and nonmetropolitan status,” they found.
Dr. Osarogiagbon is a consultant for and/or has stock in a number of companies, including AstraZeneca, Eli Lilly, and Genentech.
FROM WCLC 2021
Gender equity and gynecologic surgery: Ensuring a culture of diversity and inclusion
A workplace environment conducive to success includes equal access to resources and opportunities, work-life integration, freedom from gender discrimination and sexual harassment, and supportive leadership. With focused leadership that is accountable for actionable interventions through measurable outcomes, it is possible to create an equitable, safe, and dignified workplace for all ObGyns.
Recently, obstetrics and gynecology has become the only surgical specialty in which a majority of practitioners are women. Since the 1990s, women in ObGyn have composed the majority of trainees, and 2012 marked the first year that more than half of the American College of Obstetricians and Gynecologists (ACOG) Fellows in practice were women.1
Despite the large proportion of women within the specialty, ongoing gender-based inequities continue. Many of these inequities are rooted in our pervasive societal views of behavioral norms based on biologic or perceived sex, otherwise known as “gender,” roles.2 The cultural gender role for men embodies characteristics that are bold, competitive, decisive, analytical; qualities for women include modesty, nurturing, and accommodating in interactions with others. Such male-typed traits and behaviors are termed “agentic” because they involve human agency, whereas female-typed traits and behaviors are termed “communal.”3
Gender biases remain widespread, even among health care providers.4 When gender roles are applied to medical specialties, there is an assumption that women tend toward “communal” specialties, such as pediatrics or family practice, whereas men are better suited for technical or procedural specialties.5 ObGyn is an outlier in this schema because its procedural and surgical aspects would characterize the specialty as “agentic,” yet the majority of ObGyn trainees and physicians are women.
Biases related to gender impact many aspects of practice for the ObGyn, including:
- surgical education and training
- the gender wage gap
- interpersonal interactions and sexual harassment
- advancement and promotion.
Surgical education and training
The message that desirable characteristics for leadership and autonomy are aligned with masculinity is enforced early in medical culture, and it supports the ubiquity of deep-seated stereotypes about gender roles in medicine. For example, the language used for letters of recommendation for women applying to residency and fellowship highlight communal language (nurturing, warm), whereas those for men more typically use agentic terms (decisive, strong, future leader).6 During ObGyn surgical training, women residents receive more negative evaluations than men from nurses throughout training, and they report spending more effort to nurture these relationships, including changing communication in order to engage assistance from nurses.7
Similarly, women trainees receive harsher and more contradictory feedback from attending physicians.8 For example, a woman resident may be criticized for failing to develop independence and execute complete plans for patient care; later, she might be labeled as “rogue” and told that she should engage with and seek input from supervising faculty when independently executing a treatment plan.
Even when attempting to apply feedback in the operating room, women trainees are afforded less surgical autonomy than men trainees.9 These factors contribute to lower surgical confidence in women trainees despite their having the same technical skills as men, as measured by the Fundamentals of Laparoscopic Surgery skills exam.10
Continue to: The gender wage gap...
The gender wage gap
The mean salary for women ObGyns remains lower than that for men at every academic rank, with the differences ranging from $54,700 at the assistant professor rank to $183,200 for the department chair position.11 Notably, the pay discrepancy persists after adjustments are made for common salary-influencing metrics, such as experience, practice construct, and academic productivity.12 The gender salary gap is further identified for women subspecialists, as women reproductive endocrinology and infertility specialists and gynecologic oncologists earn $67,000 and $120,000 less, respectively, than men colleagues.13,14
While the gender wage gap often is attributed to women’s desire to work part time, similar rates of graduating women and men medical students in 2018 ranked schedule flexibility as important, suggesting that work-life balance is related to an individual’s generation rather than gender.11
Parenting status specifically adversely affects women physicians, with an ascribed “motherhood penalty” and “fatherhood bonus” phenomenon: women physicians who became parents lost an additional 6% salary, whereas men physicians saw a salary increase of 4% with parenthood.15
Most worrisome for the specialty is evidence of declining wages for ObGyns relative to other fields. “Occupational segregation”16 refers to the pronounced negative effect on earnings as more women enter a given field, which has been described in other professions.17 Overall, ObGyn salaries are the lowest among surgical specialties18 and show evidence of decline corresponding to the increasing numbers of women in the field.16
Interpersonal interactions and sexual harassment
In the workplace, women in ObGyn face more interpersonal relationship friction than men. Practicing women ObGyns report differing treatment by nurses as compared to men,19 noting that additional time and effort are required to nurture professional relationships. Additionally, nurses and trainees20 evaluate practicing women ObGyns more harshly than they evaluate men. Further, women gynecologic surgeons experience gender bias from patients, as patients endorse a preference to have a woman gynecologist but prefer a man gynecologic surgeon.21
In addition to gender bias, the experience of gender harassment, including sexual harassment, is common, as two-thirds of women gynecologists report workplace harassment, 90% of which is attributed to gender.22 This rate is 3 times higher than that for men, with a senior colleague in a position of power within the same organization reported to be the harasser to women in 91% of occurrences.
Advancement and promotion
Within academia, women faculty face specific career-limiting barriers related to gender. Rates of academic promotion and leadership opportunities remain lower for women than for men faculty. Although there has been more women representation in ObGyn over the past 20 years, the number of women serving as department chairs, cancer center directors, editors-in-chief, or on a board of directors remains lower than what would be expected by representation ratios.23 (Representation ratios were calculated as the proportion of ObGyn department-based leadership roles held by women in 2019 divided by the proportion of women ObGyn residents in 1990; representation ratios <1.0 indicate underrepresentation of women). This lag in attainment of leadership roles is compounded by the difficulties women faculty experience in finding mentorship and sponsorship,24 which are known benefits to career advancement.
Having fewer women hold leadership roles also negatively influences those in training. For example, a survey of emergency medicine and ObGyn residents identified an implicit gender bias that men and women residents favored men for leadership roles.25 This difference, however, was not significant when division chiefs and department chairs were women, which suggests that visibility of women leaders positively influences the stereotype perception of men and women trainees.4
Continue to: Blueprint for change...
Blueprint for change
While the issues surrounding gender bias are widespread, solutions exist to create gender equity within ObGyn. Efforts to change individual behavior and organizational culture should start with an understanding of the current environment.
Multiple studies have promoted the concept of “culture change,”26,27 which parallels a standard change process. A critical aspect of change is that individuals and organizations maintain the status quo until something prompts a desire to achieve a different way of being. As data regarding the breadth and impact of gender bias emerge and awareness is raised, there is recognition that the status quo is not achieving the goals of the department or institution. This may occur through the result of loss of physician talent, reduced access for vulnerable patient populations, or lower financial productivity.
Once change is considered, it must deliberately be pursued through a specific process. The first actionable step is to assess the existing state and then identify prior barriers to and current opportunities for success. A validated instrument that has been applied for this purpose is the Diversity Engagement Survey, a 22-item questionnaire that assesses 8 domains of organizational inclusion on a 5-point Likert scale (see TABLE).28 This tool not only provides a measure of institutional culture but also obtains characteristics of the respondents so that it additionally assesses how engaged specific groups are within the organization. Once baseline data are obtained, an action plan can be formulated and enacted. This cycle of assessment, system influences, plan, and act should be continued until the desired changes are achieved.
It is critically important to identify objective, measurable outcomes to assure that the interventions are moving the culture toward enhanced gender equity. As the ideal state is achieved, development of practices and enforceable policies help to ensure the longevity of cultural changes. Furthermore, periodic re-evaluation of the existing organizational culture will confirm the maintenance of gender equity objectives.
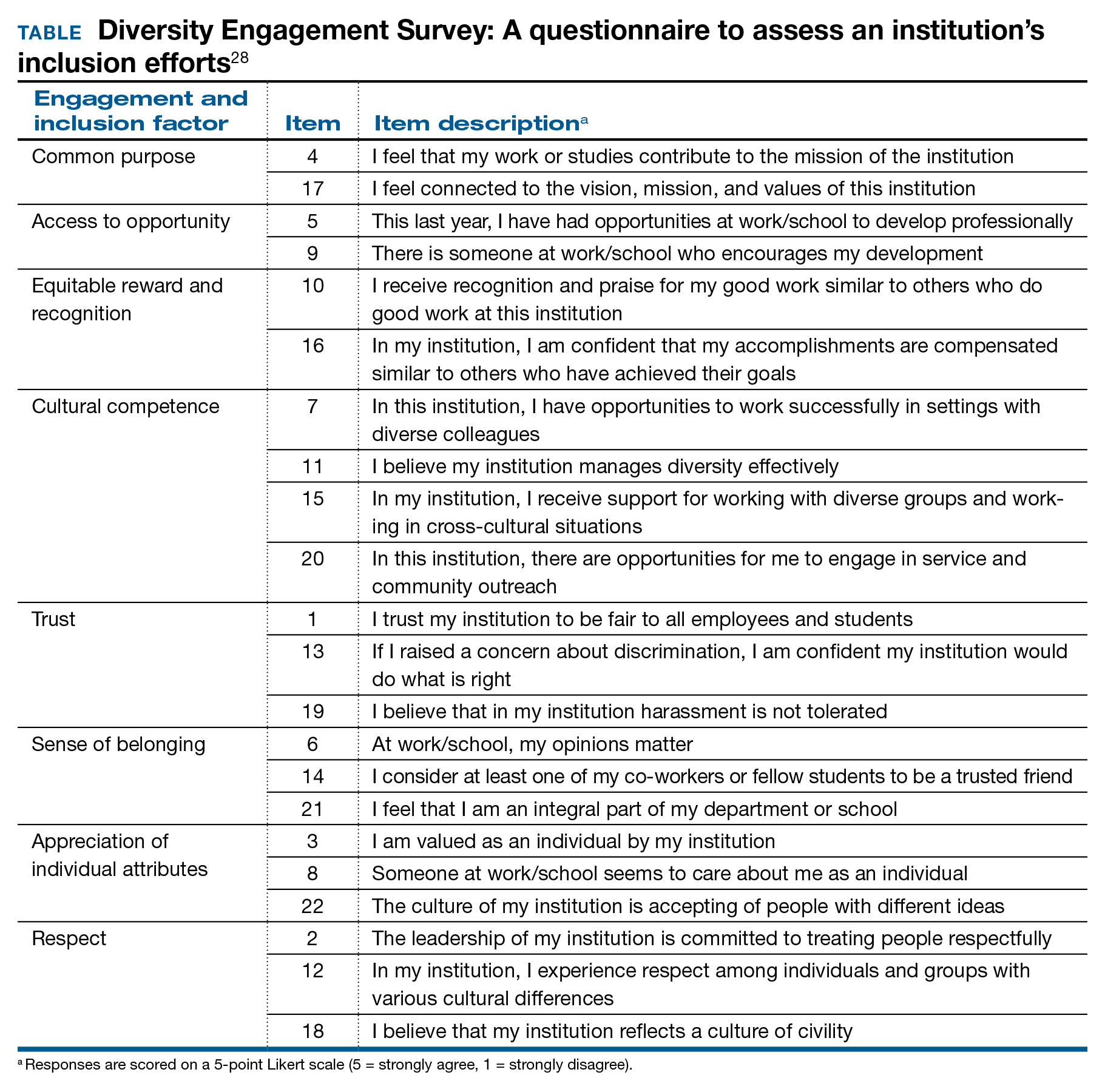
Solutions toward gender equity
Gender inequity may arise from societal gender roles, but it is incumbent on health care organizations to create an environment free from gender bias and gender harassment. An imperative first step is to identify the occurrence of gender discrimination.
The HITS (Hurt, Insulted, Threatened with harm, or Screamed at) screening tool has been used effectively with surgical residents to identify the prevalence of and most common types of abuse.29 This instrument could be adapted and administered to ObGyns in practice or in training. These data should inform the need for system-level antisexist training as well as enforcement of zero-tolerance policies.
Organizations have the ability to create a salary-only compensation model for physicians within the same specialty regardless of academic rank or academic productivity, which has been demonstrated to eliminate gender pay disparity.30 Additional measures to achieve gender equity involve antisexist hiring processes31 and transparency in metrics for job performance, salary, and promotion.32
While health care organizations are obliged to construct a gender-equitable culture, efforts can be made on the individual level. Implicit bias is ascribed to the unconscious attitudes and stereotypes people conclude about groups. The Implicit Association Test (IAT) is a validated instrument that provides the respondent with information about one’s own implicit biases. By uncovering gender bias “blind spots,” an individual can work to consciously overcome these stereotypes. Extending from the mental reframing required for overturning implicit biases, individuals can learn to identify and intervene in real-world situations. This concept of “being an upstander” denotes stepping in and standing up when an inappropriate situation arises33 (see “Case example: Being an upstander”). The targeted individual may not have the ability or safety to navigate through a confrontation, but an upstander might be able to assist the target with empowerment, verbalization of needs, and support.
Lastly, mentorship and sponsorship are critical factors for professional development and career advancement. Bidirectional mentorship identifies benefit for the mentee and the mentor whereby the junior faculty obtain career development and support and the senior faculty may learn new teaching or communication skills.34
A final word
As recognized advocates for women’s health, we must intentionally move toward a workplace that is equitable, safe, and dignified for all ObGyns. Ensuring gender equity within obstetrics and gynecology is everyone’s responsibility. ●
Dr. Bethany Wain is attending a departmental conference and is talking with another member of her division when Dr. Joselle, her division director, approaches. He is accompanied by the Visiting Professor, an internationally reputable and dynamic man, a content expert in the field of work in which Dr. Wain is interested and has published. Dr. Joselle introduces the Visiting Professor formally, using his title of “doctor.” He then introduces Dr. Wain by her abridged first name, Beth.
As an upstander, the Visiting Professor quickly addresses Dr. Wain by her title and uses the situation as a platform to highlight the need to maintain professional address in the professional environment. He then adds that women, who are usually junior in academic rank, confer more benefit to being addressed formally and receiving visibility and respect for their work in a public forum. In this way, the Visiting Professor amplifies Dr. Wain’s work and status and demonstrates the standard of using professional address for women and men.
- Rayburn WF. The Obstetrician-Gynecologist Workforce in the United States: Facts, Figures, and Implications, 2017. Washington, DC: American Congress of Obstetricians and Gynecologists; 2017.
- Carnes M. Commentary: deconstructing gender differences. Acad Med. 2010;85:575-577.
- Eagly AH. The his and hers of prosocial behavior: an examination of the social psychology of gender. Am Psychol. 2009;64:644-658.
- Salles A, Awad M, Goldin L, et al. Estimating implicit and explicit gender bias among health care professionals and surgeons. JAMA Netw Open. 2019;2:e196545.
- Carnes M, Bartels CM, Kaatz A, et al. Why is John more likely to become department chair than Jennifer? Trans Am Clin Climatol Assoc. 2015;126:197-214.
- Hoffman A, Grant, W, McCormick, et al. Gendered differences in letters of recommendation for transplant surgery fellowship applicants. J Surg Edu. 2019;76:427-432.
- Galvin SL, Parlier AB, Martino E, et al. Gender bias in nurse evaluations of residents in obstetrics and gynecology. Obstet Gynecol. 2015;126(suppl 4):7S-12S.
- Gerull KM, Loe M, Seiler K, et al. Assessing gender bias in qualitative evaluations of surgical residents. Am J Surg. 2019;217:306-313.
- Meyerson SL, Sternbach JM, Zwischenberger JB, et al. The effect of gender on resident autonomy in the operating room. J Surg Educ. 2017;74:e111-e118.
- Flyckt RL, White EE, Goodman LR, et al. The use of laparoscopy simulation to explore gender differences in resident surgical confidence. Obstet Gynecol Int. 2017;2017:1945801.
- Heisler CA, Mark K, Ton J, et al. Has a critical mass of women resulted in gender equity in gynecologic surgery? Am J Obstet Gynecol. 2020;223:665-673.
- Warner AS, Lehmann LS. Gender wage disparities in medicine: time to close the gap. J Gen Intern Med. 2019;34:1334-1336.
- Gilbert SB, Allshouse A, Skaznik-Wikiel ME. Gender inequality in salaries among reproductive endocrinology and infertility specialists in the United States. Fertil Steril. 2019;111:1194-1200.
- Croft KM, Rauh LA, Orr JW, et al. Compensation differences by gender in gynecologic oncology. Society of Gynecologic Oncology Annual Meeting on Women’s Cancer. 2020. https://sgo.confex.com /sgo/2020/meetingapp.cgi/Paper/15762. 2020. Accessed April 1, 2020.
- Wang SS, Ackerman S. The motherhood penalty: is it alive and well in 2020? J Am Coll Radiol. 2020;17:688-689.
- Pelley E, Carnes M. When a specialty becomes “women’s work”: trends in and implications of specialty gender segregation in medicine. Acad Med. 2020;95:1499-1506.
- Hegewisch A, Hartmann H. Occupational segregation and the gender wage gap: a job half done. Institute for Women’s Policy Research. 2014. https://iwpr.org/iwpr-issues/employment-and-earnings /occupational-segregation-and-the-gender-wage-gap-a-job-half -done/. Accessed August 26, 2021.
- Greenberg CC. Association for Academic Surgery presidential address: sticky floors and glass ceilings. J Surg Res. 2017;219:ix-xviii.
- Dossett LA, Vitous CA, Lindquist K, et al. Women surgeons’ experiences of interprofessional workplace conflict. JAMA Netw Open. 2020;3:e2019843.
- Morgan HK, Purkis JA, Porter AC, et al. Student evaluation of faculty physicians: gender differences in teaching evaluations. J Womens Health (Larchmt). 2016;25:453-456.
- Childs AJ, Friedman WH, Schwartz MP, et al. Female patients’ sex preferences in selection of gynecologists and surgeons. South Med J. 2005;98:405-408.
- Brown J, Drury L, Raub K, et al. Workplace harassment and discrimination in gynecology: results of the AAGL Member Survey. J Minim Invasive Gynecol. 2019;26:838-846.
- Temkin AM, Rubinsak L, Benoit MF, et al. Take me to your leader: reporting structures and equity in academic gynecologic oncology. Gynecol Oncol. 2020;157:759-764.
- Shakil S, Redberg RF. Gender disparities in sponsorship—how they perpetuate the glass ceiling. JAMA Intern Med. 2017;177:582.
- Hansen M, Schoonover A, Skarica B, et al. Implicit gender bias among US resident physicians. BMC Med Ed. 2019;19:396.
- Estrada M, Burnett M, Campbell AG, et al. Improving underrepresented minority student persistence in STEM. CBE Life Sci Educ. 2016;15:es5.
- Carnes M, Handelsman J, Sheridan J. Diversity in academic medicine: the stages of change model. J Womens Health (Larchmt). 2005;14:471-475.
- Person SD, Jordan CG, Allison JJ, et al. Measuring diversity and inclusion in academic medicine. The Diversity Engagement Survey. Acad Med. 2015;90:1675-1683.
- Fitzgerald CA, Smith RN, Luo-Owen X, et al. Screening for harassment, abuse, and discrimination among surgery residents: an EAST multicenter trial. Am Surg. 2019;85:456-461.
- Hayes SN, Noseworthy JH, Farrugia G. A structured compensation plan results in equitable physician compensation: a single-center analysis. Mayo Clin Proc. 2020;95:35-43.
- Devine PG, Forscher PS, Cox WT, et al. A gender bias habit-breaking intervention led to increased hiring of female faculty in STEMM departments. J Exp Soc Psychol. 2017;73:211-215.
- Morgan AU, Chaiyachati KH, Weissman GE, et al. Eliminating genderbased bias in academic medicine: more than naming the “elephant in the room.” J Gen Intern Med. 2018;33:966-968.
- Mello MM, Jagsi R. Standing up against gender bias and harassment— a matter of professional ethics. N Engl J Med. 2020;382:1385-1387.
- Burgess A, van Diggele C, Mellis C. Mentorship in the health profession: a review. Clin Teach. 2018;15:197-202.
A workplace environment conducive to success includes equal access to resources and opportunities, work-life integration, freedom from gender discrimination and sexual harassment, and supportive leadership. With focused leadership that is accountable for actionable interventions through measurable outcomes, it is possible to create an equitable, safe, and dignified workplace for all ObGyns.
Recently, obstetrics and gynecology has become the only surgical specialty in which a majority of practitioners are women. Since the 1990s, women in ObGyn have composed the majority of trainees, and 2012 marked the first year that more than half of the American College of Obstetricians and Gynecologists (ACOG) Fellows in practice were women.1
Despite the large proportion of women within the specialty, ongoing gender-based inequities continue. Many of these inequities are rooted in our pervasive societal views of behavioral norms based on biologic or perceived sex, otherwise known as “gender,” roles.2 The cultural gender role for men embodies characteristics that are bold, competitive, decisive, analytical; qualities for women include modesty, nurturing, and accommodating in interactions with others. Such male-typed traits and behaviors are termed “agentic” because they involve human agency, whereas female-typed traits and behaviors are termed “communal.”3
Gender biases remain widespread, even among health care providers.4 When gender roles are applied to medical specialties, there is an assumption that women tend toward “communal” specialties, such as pediatrics or family practice, whereas men are better suited for technical or procedural specialties.5 ObGyn is an outlier in this schema because its procedural and surgical aspects would characterize the specialty as “agentic,” yet the majority of ObGyn trainees and physicians are women.
Biases related to gender impact many aspects of practice for the ObGyn, including:
- surgical education and training
- the gender wage gap
- interpersonal interactions and sexual harassment
- advancement and promotion.
Surgical education and training
The message that desirable characteristics for leadership and autonomy are aligned with masculinity is enforced early in medical culture, and it supports the ubiquity of deep-seated stereotypes about gender roles in medicine. For example, the language used for letters of recommendation for women applying to residency and fellowship highlight communal language (nurturing, warm), whereas those for men more typically use agentic terms (decisive, strong, future leader).6 During ObGyn surgical training, women residents receive more negative evaluations than men from nurses throughout training, and they report spending more effort to nurture these relationships, including changing communication in order to engage assistance from nurses.7
Similarly, women trainees receive harsher and more contradictory feedback from attending physicians.8 For example, a woman resident may be criticized for failing to develop independence and execute complete plans for patient care; later, she might be labeled as “rogue” and told that she should engage with and seek input from supervising faculty when independently executing a treatment plan.
Even when attempting to apply feedback in the operating room, women trainees are afforded less surgical autonomy than men trainees.9 These factors contribute to lower surgical confidence in women trainees despite their having the same technical skills as men, as measured by the Fundamentals of Laparoscopic Surgery skills exam.10
Continue to: The gender wage gap...
The gender wage gap
The mean salary for women ObGyns remains lower than that for men at every academic rank, with the differences ranging from $54,700 at the assistant professor rank to $183,200 for the department chair position.11 Notably, the pay discrepancy persists after adjustments are made for common salary-influencing metrics, such as experience, practice construct, and academic productivity.12 The gender salary gap is further identified for women subspecialists, as women reproductive endocrinology and infertility specialists and gynecologic oncologists earn $67,000 and $120,000 less, respectively, than men colleagues.13,14
While the gender wage gap often is attributed to women’s desire to work part time, similar rates of graduating women and men medical students in 2018 ranked schedule flexibility as important, suggesting that work-life balance is related to an individual’s generation rather than gender.11
Parenting status specifically adversely affects women physicians, with an ascribed “motherhood penalty” and “fatherhood bonus” phenomenon: women physicians who became parents lost an additional 6% salary, whereas men physicians saw a salary increase of 4% with parenthood.15
Most worrisome for the specialty is evidence of declining wages for ObGyns relative to other fields. “Occupational segregation”16 refers to the pronounced negative effect on earnings as more women enter a given field, which has been described in other professions.17 Overall, ObGyn salaries are the lowest among surgical specialties18 and show evidence of decline corresponding to the increasing numbers of women in the field.16
Interpersonal interactions and sexual harassment
In the workplace, women in ObGyn face more interpersonal relationship friction than men. Practicing women ObGyns report differing treatment by nurses as compared to men,19 noting that additional time and effort are required to nurture professional relationships. Additionally, nurses and trainees20 evaluate practicing women ObGyns more harshly than they evaluate men. Further, women gynecologic surgeons experience gender bias from patients, as patients endorse a preference to have a woman gynecologist but prefer a man gynecologic surgeon.21
In addition to gender bias, the experience of gender harassment, including sexual harassment, is common, as two-thirds of women gynecologists report workplace harassment, 90% of which is attributed to gender.22 This rate is 3 times higher than that for men, with a senior colleague in a position of power within the same organization reported to be the harasser to women in 91% of occurrences.
Advancement and promotion
Within academia, women faculty face specific career-limiting barriers related to gender. Rates of academic promotion and leadership opportunities remain lower for women than for men faculty. Although there has been more women representation in ObGyn over the past 20 years, the number of women serving as department chairs, cancer center directors, editors-in-chief, or on a board of directors remains lower than what would be expected by representation ratios.23 (Representation ratios were calculated as the proportion of ObGyn department-based leadership roles held by women in 2019 divided by the proportion of women ObGyn residents in 1990; representation ratios <1.0 indicate underrepresentation of women). This lag in attainment of leadership roles is compounded by the difficulties women faculty experience in finding mentorship and sponsorship,24 which are known benefits to career advancement.
Having fewer women hold leadership roles also negatively influences those in training. For example, a survey of emergency medicine and ObGyn residents identified an implicit gender bias that men and women residents favored men for leadership roles.25 This difference, however, was not significant when division chiefs and department chairs were women, which suggests that visibility of women leaders positively influences the stereotype perception of men and women trainees.4
Continue to: Blueprint for change...
Blueprint for change
While the issues surrounding gender bias are widespread, solutions exist to create gender equity within ObGyn. Efforts to change individual behavior and organizational culture should start with an understanding of the current environment.
Multiple studies have promoted the concept of “culture change,”26,27 which parallels a standard change process. A critical aspect of change is that individuals and organizations maintain the status quo until something prompts a desire to achieve a different way of being. As data regarding the breadth and impact of gender bias emerge and awareness is raised, there is recognition that the status quo is not achieving the goals of the department or institution. This may occur through the result of loss of physician talent, reduced access for vulnerable patient populations, or lower financial productivity.
Once change is considered, it must deliberately be pursued through a specific process. The first actionable step is to assess the existing state and then identify prior barriers to and current opportunities for success. A validated instrument that has been applied for this purpose is the Diversity Engagement Survey, a 22-item questionnaire that assesses 8 domains of organizational inclusion on a 5-point Likert scale (see TABLE).28 This tool not only provides a measure of institutional culture but also obtains characteristics of the respondents so that it additionally assesses how engaged specific groups are within the organization. Once baseline data are obtained, an action plan can be formulated and enacted. This cycle of assessment, system influences, plan, and act should be continued until the desired changes are achieved.
It is critically important to identify objective, measurable outcomes to assure that the interventions are moving the culture toward enhanced gender equity. As the ideal state is achieved, development of practices and enforceable policies help to ensure the longevity of cultural changes. Furthermore, periodic re-evaluation of the existing organizational culture will confirm the maintenance of gender equity objectives.
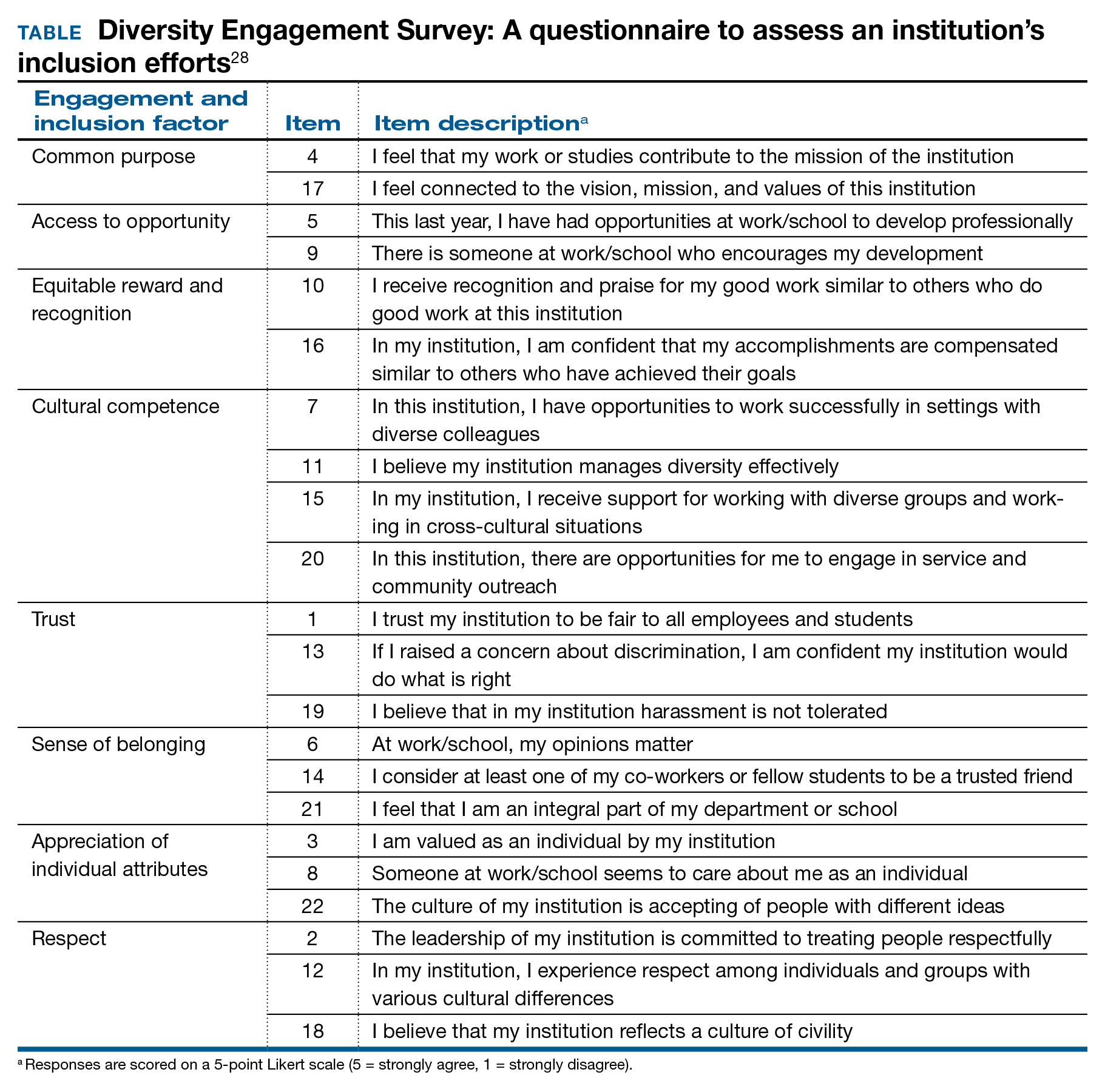
Solutions toward gender equity
Gender inequity may arise from societal gender roles, but it is incumbent on health care organizations to create an environment free from gender bias and gender harassment. An imperative first step is to identify the occurrence of gender discrimination.
The HITS (Hurt, Insulted, Threatened with harm, or Screamed at) screening tool has been used effectively with surgical residents to identify the prevalence of and most common types of abuse.29 This instrument could be adapted and administered to ObGyns in practice or in training. These data should inform the need for system-level antisexist training as well as enforcement of zero-tolerance policies.
Organizations have the ability to create a salary-only compensation model for physicians within the same specialty regardless of academic rank or academic productivity, which has been demonstrated to eliminate gender pay disparity.30 Additional measures to achieve gender equity involve antisexist hiring processes31 and transparency in metrics for job performance, salary, and promotion.32
While health care organizations are obliged to construct a gender-equitable culture, efforts can be made on the individual level. Implicit bias is ascribed to the unconscious attitudes and stereotypes people conclude about groups. The Implicit Association Test (IAT) is a validated instrument that provides the respondent with information about one’s own implicit biases. By uncovering gender bias “blind spots,” an individual can work to consciously overcome these stereotypes. Extending from the mental reframing required for overturning implicit biases, individuals can learn to identify and intervene in real-world situations. This concept of “being an upstander” denotes stepping in and standing up when an inappropriate situation arises33 (see “Case example: Being an upstander”). The targeted individual may not have the ability or safety to navigate through a confrontation, but an upstander might be able to assist the target with empowerment, verbalization of needs, and support.
Lastly, mentorship and sponsorship are critical factors for professional development and career advancement. Bidirectional mentorship identifies benefit for the mentee and the mentor whereby the junior faculty obtain career development and support and the senior faculty may learn new teaching or communication skills.34
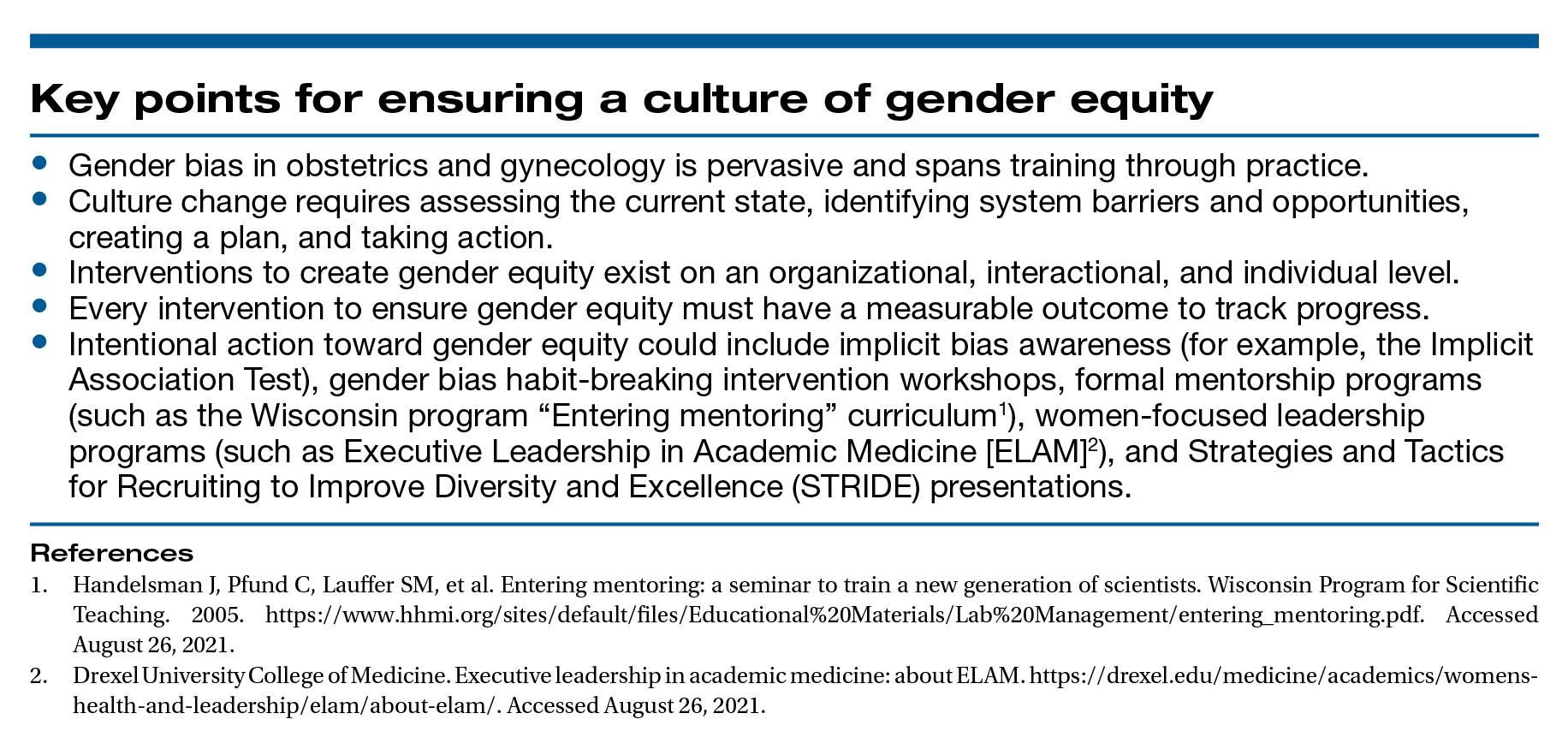
A final word
As recognized advocates for women’s health, we must intentionally move toward a workplace that is equitable, safe, and dignified for all ObGyns. Ensuring gender equity within obstetrics and gynecology is everyone’s responsibility. ●
Dr. Bethany Wain is attending a departmental conference and is talking with another member of her division when Dr. Joselle, her division director, approaches. He is accompanied by the Visiting Professor, an internationally reputable and dynamic man, a content expert in the field of work in which Dr. Wain is interested and has published. Dr. Joselle introduces the Visiting Professor formally, using his title of “doctor.” He then introduces Dr. Wain by her abridged first name, Beth.
As an upstander, the Visiting Professor quickly addresses Dr. Wain by her title and uses the situation as a platform to highlight the need to maintain professional address in the professional environment. He then adds that women, who are usually junior in academic rank, confer more benefit to being addressed formally and receiving visibility and respect for their work in a public forum. In this way, the Visiting Professor amplifies Dr. Wain’s work and status and demonstrates the standard of using professional address for women and men.
A workplace environment conducive to success includes equal access to resources and opportunities, work-life integration, freedom from gender discrimination and sexual harassment, and supportive leadership. With focused leadership that is accountable for actionable interventions through measurable outcomes, it is possible to create an equitable, safe, and dignified workplace for all ObGyns.
Recently, obstetrics and gynecology has become the only surgical specialty in which a majority of practitioners are women. Since the 1990s, women in ObGyn have composed the majority of trainees, and 2012 marked the first year that more than half of the American College of Obstetricians and Gynecologists (ACOG) Fellows in practice were women.1
Despite the large proportion of women within the specialty, ongoing gender-based inequities continue. Many of these inequities are rooted in our pervasive societal views of behavioral norms based on biologic or perceived sex, otherwise known as “gender,” roles.2 The cultural gender role for men embodies characteristics that are bold, competitive, decisive, analytical; qualities for women include modesty, nurturing, and accommodating in interactions with others. Such male-typed traits and behaviors are termed “agentic” because they involve human agency, whereas female-typed traits and behaviors are termed “communal.”3
Gender biases remain widespread, even among health care providers.4 When gender roles are applied to medical specialties, there is an assumption that women tend toward “communal” specialties, such as pediatrics or family practice, whereas men are better suited for technical or procedural specialties.5 ObGyn is an outlier in this schema because its procedural and surgical aspects would characterize the specialty as “agentic,” yet the majority of ObGyn trainees and physicians are women.
Biases related to gender impact many aspects of practice for the ObGyn, including:
- surgical education and training
- the gender wage gap
- interpersonal interactions and sexual harassment
- advancement and promotion.
Surgical education and training
The message that desirable characteristics for leadership and autonomy are aligned with masculinity is enforced early in medical culture, and it supports the ubiquity of deep-seated stereotypes about gender roles in medicine. For example, the language used for letters of recommendation for women applying to residency and fellowship highlight communal language (nurturing, warm), whereas those for men more typically use agentic terms (decisive, strong, future leader).6 During ObGyn surgical training, women residents receive more negative evaluations than men from nurses throughout training, and they report spending more effort to nurture these relationships, including changing communication in order to engage assistance from nurses.7
Similarly, women trainees receive harsher and more contradictory feedback from attending physicians.8 For example, a woman resident may be criticized for failing to develop independence and execute complete plans for patient care; later, she might be labeled as “rogue” and told that she should engage with and seek input from supervising faculty when independently executing a treatment plan.
Even when attempting to apply feedback in the operating room, women trainees are afforded less surgical autonomy than men trainees.9 These factors contribute to lower surgical confidence in women trainees despite their having the same technical skills as men, as measured by the Fundamentals of Laparoscopic Surgery skills exam.10
Continue to: The gender wage gap...
The gender wage gap
The mean salary for women ObGyns remains lower than that for men at every academic rank, with the differences ranging from $54,700 at the assistant professor rank to $183,200 for the department chair position.11 Notably, the pay discrepancy persists after adjustments are made for common salary-influencing metrics, such as experience, practice construct, and academic productivity.12 The gender salary gap is further identified for women subspecialists, as women reproductive endocrinology and infertility specialists and gynecologic oncologists earn $67,000 and $120,000 less, respectively, than men colleagues.13,14
While the gender wage gap often is attributed to women’s desire to work part time, similar rates of graduating women and men medical students in 2018 ranked schedule flexibility as important, suggesting that work-life balance is related to an individual’s generation rather than gender.11
Parenting status specifically adversely affects women physicians, with an ascribed “motherhood penalty” and “fatherhood bonus” phenomenon: women physicians who became parents lost an additional 6% salary, whereas men physicians saw a salary increase of 4% with parenthood.15
Most worrisome for the specialty is evidence of declining wages for ObGyns relative to other fields. “Occupational segregation”16 refers to the pronounced negative effect on earnings as more women enter a given field, which has been described in other professions.17 Overall, ObGyn salaries are the lowest among surgical specialties18 and show evidence of decline corresponding to the increasing numbers of women in the field.16
Interpersonal interactions and sexual harassment
In the workplace, women in ObGyn face more interpersonal relationship friction than men. Practicing women ObGyns report differing treatment by nurses as compared to men,19 noting that additional time and effort are required to nurture professional relationships. Additionally, nurses and trainees20 evaluate practicing women ObGyns more harshly than they evaluate men. Further, women gynecologic surgeons experience gender bias from patients, as patients endorse a preference to have a woman gynecologist but prefer a man gynecologic surgeon.21
In addition to gender bias, the experience of gender harassment, including sexual harassment, is common, as two-thirds of women gynecologists report workplace harassment, 90% of which is attributed to gender.22 This rate is 3 times higher than that for men, with a senior colleague in a position of power within the same organization reported to be the harasser to women in 91% of occurrences.
Advancement and promotion
Within academia, women faculty face specific career-limiting barriers related to gender. Rates of academic promotion and leadership opportunities remain lower for women than for men faculty. Although there has been more women representation in ObGyn over the past 20 years, the number of women serving as department chairs, cancer center directors, editors-in-chief, or on a board of directors remains lower than what would be expected by representation ratios.23 (Representation ratios were calculated as the proportion of ObGyn department-based leadership roles held by women in 2019 divided by the proportion of women ObGyn residents in 1990; representation ratios <1.0 indicate underrepresentation of women). This lag in attainment of leadership roles is compounded by the difficulties women faculty experience in finding mentorship and sponsorship,24 which are known benefits to career advancement.
Having fewer women hold leadership roles also negatively influences those in training. For example, a survey of emergency medicine and ObGyn residents identified an implicit gender bias that men and women residents favored men for leadership roles.25 This difference, however, was not significant when division chiefs and department chairs were women, which suggests that visibility of women leaders positively influences the stereotype perception of men and women trainees.4
Continue to: Blueprint for change...
Blueprint for change
While the issues surrounding gender bias are widespread, solutions exist to create gender equity within ObGyn. Efforts to change individual behavior and organizational culture should start with an understanding of the current environment.
Multiple studies have promoted the concept of “culture change,”26,27 which parallels a standard change process. A critical aspect of change is that individuals and organizations maintain the status quo until something prompts a desire to achieve a different way of being. As data regarding the breadth and impact of gender bias emerge and awareness is raised, there is recognition that the status quo is not achieving the goals of the department or institution. This may occur through the result of loss of physician talent, reduced access for vulnerable patient populations, or lower financial productivity.
Once change is considered, it must deliberately be pursued through a specific process. The first actionable step is to assess the existing state and then identify prior barriers to and current opportunities for success. A validated instrument that has been applied for this purpose is the Diversity Engagement Survey, a 22-item questionnaire that assesses 8 domains of organizational inclusion on a 5-point Likert scale (see TABLE).28 This tool not only provides a measure of institutional culture but also obtains characteristics of the respondents so that it additionally assesses how engaged specific groups are within the organization. Once baseline data are obtained, an action plan can be formulated and enacted. This cycle of assessment, system influences, plan, and act should be continued until the desired changes are achieved.
It is critically important to identify objective, measurable outcomes to assure that the interventions are moving the culture toward enhanced gender equity. As the ideal state is achieved, development of practices and enforceable policies help to ensure the longevity of cultural changes. Furthermore, periodic re-evaluation of the existing organizational culture will confirm the maintenance of gender equity objectives.
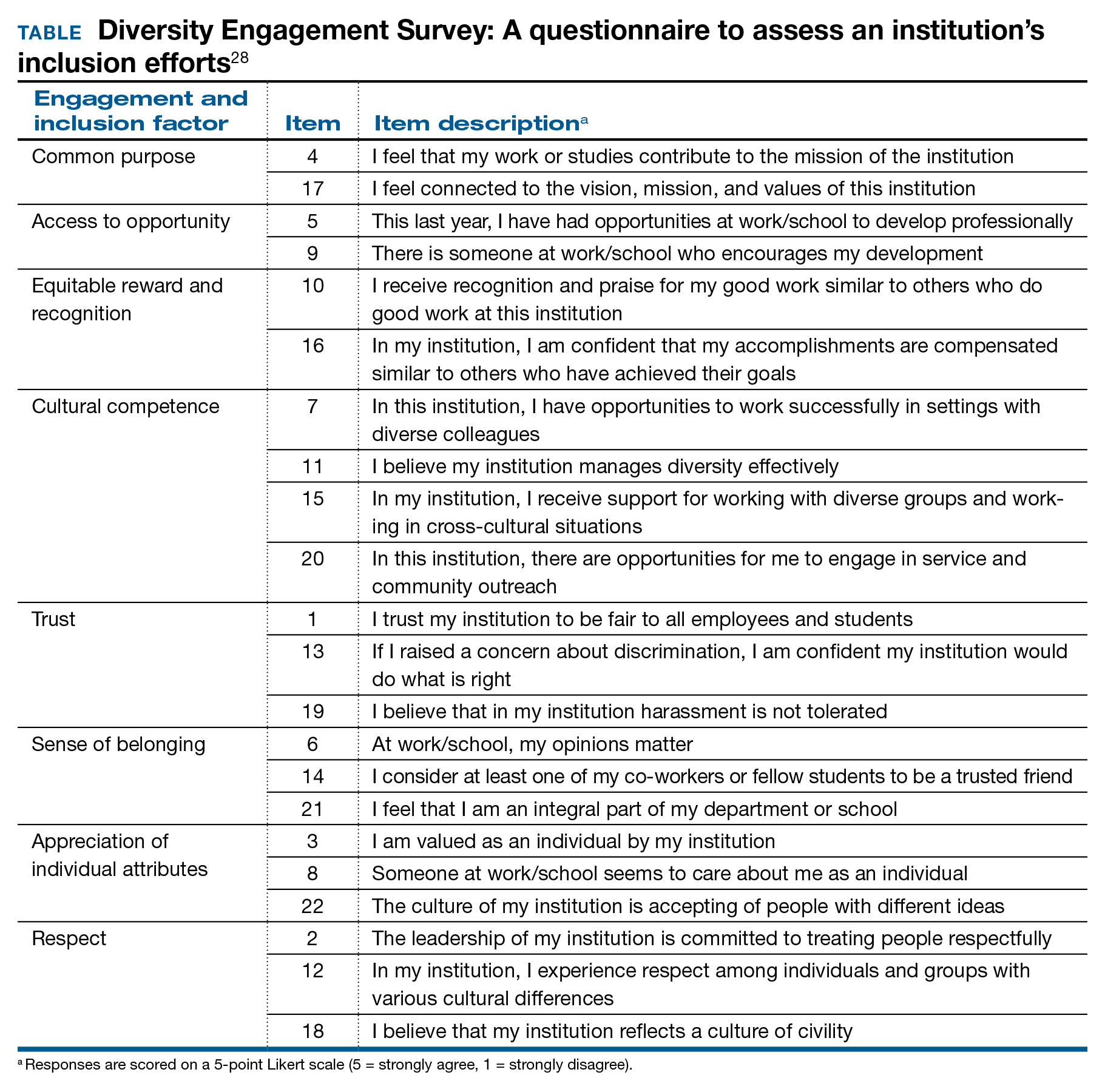
Solutions toward gender equity
Gender inequity may arise from societal gender roles, but it is incumbent on health care organizations to create an environment free from gender bias and gender harassment. An imperative first step is to identify the occurrence of gender discrimination.
The HITS (Hurt, Insulted, Threatened with harm, or Screamed at) screening tool has been used effectively with surgical residents to identify the prevalence of and most common types of abuse.29 This instrument could be adapted and administered to ObGyns in practice or in training. These data should inform the need for system-level antisexist training as well as enforcement of zero-tolerance policies.
Organizations have the ability to create a salary-only compensation model for physicians within the same specialty regardless of academic rank or academic productivity, which has been demonstrated to eliminate gender pay disparity.30 Additional measures to achieve gender equity involve antisexist hiring processes31 and transparency in metrics for job performance, salary, and promotion.32
While health care organizations are obliged to construct a gender-equitable culture, efforts can be made on the individual level. Implicit bias is ascribed to the unconscious attitudes and stereotypes people conclude about groups. The Implicit Association Test (IAT) is a validated instrument that provides the respondent with information about one’s own implicit biases. By uncovering gender bias “blind spots,” an individual can work to consciously overcome these stereotypes. Extending from the mental reframing required for overturning implicit biases, individuals can learn to identify and intervene in real-world situations. This concept of “being an upstander” denotes stepping in and standing up when an inappropriate situation arises33 (see “Case example: Being an upstander”). The targeted individual may not have the ability or safety to navigate through a confrontation, but an upstander might be able to assist the target with empowerment, verbalization of needs, and support.
Lastly, mentorship and sponsorship are critical factors for professional development and career advancement. Bidirectional mentorship identifies benefit for the mentee and the mentor whereby the junior faculty obtain career development and support and the senior faculty may learn new teaching or communication skills.34
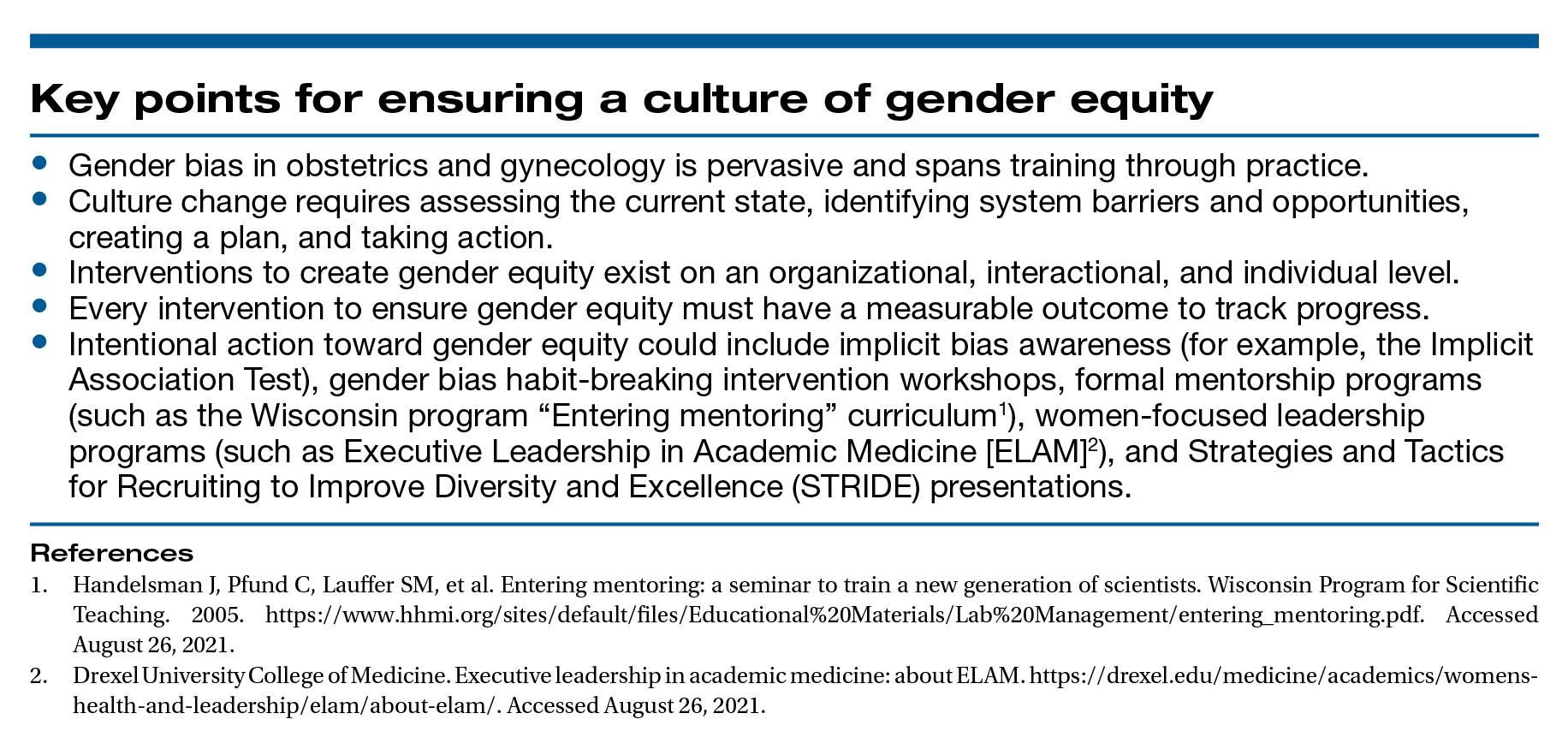
A final word
As recognized advocates for women’s health, we must intentionally move toward a workplace that is equitable, safe, and dignified for all ObGyns. Ensuring gender equity within obstetrics and gynecology is everyone’s responsibility. ●
Dr. Bethany Wain is attending a departmental conference and is talking with another member of her division when Dr. Joselle, her division director, approaches. He is accompanied by the Visiting Professor, an internationally reputable and dynamic man, a content expert in the field of work in which Dr. Wain is interested and has published. Dr. Joselle introduces the Visiting Professor formally, using his title of “doctor.” He then introduces Dr. Wain by her abridged first name, Beth.
As an upstander, the Visiting Professor quickly addresses Dr. Wain by her title and uses the situation as a platform to highlight the need to maintain professional address in the professional environment. He then adds that women, who are usually junior in academic rank, confer more benefit to being addressed formally and receiving visibility and respect for their work in a public forum. In this way, the Visiting Professor amplifies Dr. Wain’s work and status and demonstrates the standard of using professional address for women and men.
- Rayburn WF. The Obstetrician-Gynecologist Workforce in the United States: Facts, Figures, and Implications, 2017. Washington, DC: American Congress of Obstetricians and Gynecologists; 2017.
- Carnes M. Commentary: deconstructing gender differences. Acad Med. 2010;85:575-577.
- Eagly AH. The his and hers of prosocial behavior: an examination of the social psychology of gender. Am Psychol. 2009;64:644-658.
- Salles A, Awad M, Goldin L, et al. Estimating implicit and explicit gender bias among health care professionals and surgeons. JAMA Netw Open. 2019;2:e196545.
- Carnes M, Bartels CM, Kaatz A, et al. Why is John more likely to become department chair than Jennifer? Trans Am Clin Climatol Assoc. 2015;126:197-214.
- Hoffman A, Grant, W, McCormick, et al. Gendered differences in letters of recommendation for transplant surgery fellowship applicants. J Surg Edu. 2019;76:427-432.
- Galvin SL, Parlier AB, Martino E, et al. Gender bias in nurse evaluations of residents in obstetrics and gynecology. Obstet Gynecol. 2015;126(suppl 4):7S-12S.
- Gerull KM, Loe M, Seiler K, et al. Assessing gender bias in qualitative evaluations of surgical residents. Am J Surg. 2019;217:306-313.
- Meyerson SL, Sternbach JM, Zwischenberger JB, et al. The effect of gender on resident autonomy in the operating room. J Surg Educ. 2017;74:e111-e118.
- Flyckt RL, White EE, Goodman LR, et al. The use of laparoscopy simulation to explore gender differences in resident surgical confidence. Obstet Gynecol Int. 2017;2017:1945801.
- Heisler CA, Mark K, Ton J, et al. Has a critical mass of women resulted in gender equity in gynecologic surgery? Am J Obstet Gynecol. 2020;223:665-673.
- Warner AS, Lehmann LS. Gender wage disparities in medicine: time to close the gap. J Gen Intern Med. 2019;34:1334-1336.
- Gilbert SB, Allshouse A, Skaznik-Wikiel ME. Gender inequality in salaries among reproductive endocrinology and infertility specialists in the United States. Fertil Steril. 2019;111:1194-1200.
- Croft KM, Rauh LA, Orr JW, et al. Compensation differences by gender in gynecologic oncology. Society of Gynecologic Oncology Annual Meeting on Women’s Cancer. 2020. https://sgo.confex.com /sgo/2020/meetingapp.cgi/Paper/15762. 2020. Accessed April 1, 2020.
- Wang SS, Ackerman S. The motherhood penalty: is it alive and well in 2020? J Am Coll Radiol. 2020;17:688-689.
- Pelley E, Carnes M. When a specialty becomes “women’s work”: trends in and implications of specialty gender segregation in medicine. Acad Med. 2020;95:1499-1506.
- Hegewisch A, Hartmann H. Occupational segregation and the gender wage gap: a job half done. Institute for Women’s Policy Research. 2014. https://iwpr.org/iwpr-issues/employment-and-earnings /occupational-segregation-and-the-gender-wage-gap-a-job-half -done/. Accessed August 26, 2021.
- Greenberg CC. Association for Academic Surgery presidential address: sticky floors and glass ceilings. J Surg Res. 2017;219:ix-xviii.
- Dossett LA, Vitous CA, Lindquist K, et al. Women surgeons’ experiences of interprofessional workplace conflict. JAMA Netw Open. 2020;3:e2019843.
- Morgan HK, Purkis JA, Porter AC, et al. Student evaluation of faculty physicians: gender differences in teaching evaluations. J Womens Health (Larchmt). 2016;25:453-456.
- Childs AJ, Friedman WH, Schwartz MP, et al. Female patients’ sex preferences in selection of gynecologists and surgeons. South Med J. 2005;98:405-408.
- Brown J, Drury L, Raub K, et al. Workplace harassment and discrimination in gynecology: results of the AAGL Member Survey. J Minim Invasive Gynecol. 2019;26:838-846.
- Temkin AM, Rubinsak L, Benoit MF, et al. Take me to your leader: reporting structures and equity in academic gynecologic oncology. Gynecol Oncol. 2020;157:759-764.
- Shakil S, Redberg RF. Gender disparities in sponsorship—how they perpetuate the glass ceiling. JAMA Intern Med. 2017;177:582.
- Hansen M, Schoonover A, Skarica B, et al. Implicit gender bias among US resident physicians. BMC Med Ed. 2019;19:396.
- Estrada M, Burnett M, Campbell AG, et al. Improving underrepresented minority student persistence in STEM. CBE Life Sci Educ. 2016;15:es5.
- Carnes M, Handelsman J, Sheridan J. Diversity in academic medicine: the stages of change model. J Womens Health (Larchmt). 2005;14:471-475.
- Person SD, Jordan CG, Allison JJ, et al. Measuring diversity and inclusion in academic medicine. The Diversity Engagement Survey. Acad Med. 2015;90:1675-1683.
- Fitzgerald CA, Smith RN, Luo-Owen X, et al. Screening for harassment, abuse, and discrimination among surgery residents: an EAST multicenter trial. Am Surg. 2019;85:456-461.
- Hayes SN, Noseworthy JH, Farrugia G. A structured compensation plan results in equitable physician compensation: a single-center analysis. Mayo Clin Proc. 2020;95:35-43.
- Devine PG, Forscher PS, Cox WT, et al. A gender bias habit-breaking intervention led to increased hiring of female faculty in STEMM departments. J Exp Soc Psychol. 2017;73:211-215.
- Morgan AU, Chaiyachati KH, Weissman GE, et al. Eliminating genderbased bias in academic medicine: more than naming the “elephant in the room.” J Gen Intern Med. 2018;33:966-968.
- Mello MM, Jagsi R. Standing up against gender bias and harassment— a matter of professional ethics. N Engl J Med. 2020;382:1385-1387.
- Burgess A, van Diggele C, Mellis C. Mentorship in the health profession: a review. Clin Teach. 2018;15:197-202.
- Rayburn WF. The Obstetrician-Gynecologist Workforce in the United States: Facts, Figures, and Implications, 2017. Washington, DC: American Congress of Obstetricians and Gynecologists; 2017.
- Carnes M. Commentary: deconstructing gender differences. Acad Med. 2010;85:575-577.
- Eagly AH. The his and hers of prosocial behavior: an examination of the social psychology of gender. Am Psychol. 2009;64:644-658.
- Salles A, Awad M, Goldin L, et al. Estimating implicit and explicit gender bias among health care professionals and surgeons. JAMA Netw Open. 2019;2:e196545.
- Carnes M, Bartels CM, Kaatz A, et al. Why is John more likely to become department chair than Jennifer? Trans Am Clin Climatol Assoc. 2015;126:197-214.
- Hoffman A, Grant, W, McCormick, et al. Gendered differences in letters of recommendation for transplant surgery fellowship applicants. J Surg Edu. 2019;76:427-432.
- Galvin SL, Parlier AB, Martino E, et al. Gender bias in nurse evaluations of residents in obstetrics and gynecology. Obstet Gynecol. 2015;126(suppl 4):7S-12S.
- Gerull KM, Loe M, Seiler K, et al. Assessing gender bias in qualitative evaluations of surgical residents. Am J Surg. 2019;217:306-313.
- Meyerson SL, Sternbach JM, Zwischenberger JB, et al. The effect of gender on resident autonomy in the operating room. J Surg Educ. 2017;74:e111-e118.
- Flyckt RL, White EE, Goodman LR, et al. The use of laparoscopy simulation to explore gender differences in resident surgical confidence. Obstet Gynecol Int. 2017;2017:1945801.
- Heisler CA, Mark K, Ton J, et al. Has a critical mass of women resulted in gender equity in gynecologic surgery? Am J Obstet Gynecol. 2020;223:665-673.
- Warner AS, Lehmann LS. Gender wage disparities in medicine: time to close the gap. J Gen Intern Med. 2019;34:1334-1336.
- Gilbert SB, Allshouse A, Skaznik-Wikiel ME. Gender inequality in salaries among reproductive endocrinology and infertility specialists in the United States. Fertil Steril. 2019;111:1194-1200.
- Croft KM, Rauh LA, Orr JW, et al. Compensation differences by gender in gynecologic oncology. Society of Gynecologic Oncology Annual Meeting on Women’s Cancer. 2020. https://sgo.confex.com /sgo/2020/meetingapp.cgi/Paper/15762. 2020. Accessed April 1, 2020.
- Wang SS, Ackerman S. The motherhood penalty: is it alive and well in 2020? J Am Coll Radiol. 2020;17:688-689.
- Pelley E, Carnes M. When a specialty becomes “women’s work”: trends in and implications of specialty gender segregation in medicine. Acad Med. 2020;95:1499-1506.
- Hegewisch A, Hartmann H. Occupational segregation and the gender wage gap: a job half done. Institute for Women’s Policy Research. 2014. https://iwpr.org/iwpr-issues/employment-and-earnings /occupational-segregation-and-the-gender-wage-gap-a-job-half -done/. Accessed August 26, 2021.
- Greenberg CC. Association for Academic Surgery presidential address: sticky floors and glass ceilings. J Surg Res. 2017;219:ix-xviii.
- Dossett LA, Vitous CA, Lindquist K, et al. Women surgeons’ experiences of interprofessional workplace conflict. JAMA Netw Open. 2020;3:e2019843.
- Morgan HK, Purkis JA, Porter AC, et al. Student evaluation of faculty physicians: gender differences in teaching evaluations. J Womens Health (Larchmt). 2016;25:453-456.
- Childs AJ, Friedman WH, Schwartz MP, et al. Female patients’ sex preferences in selection of gynecologists and surgeons. South Med J. 2005;98:405-408.
- Brown J, Drury L, Raub K, et al. Workplace harassment and discrimination in gynecology: results of the AAGL Member Survey. J Minim Invasive Gynecol. 2019;26:838-846.
- Temkin AM, Rubinsak L, Benoit MF, et al. Take me to your leader: reporting structures and equity in academic gynecologic oncology. Gynecol Oncol. 2020;157:759-764.
- Shakil S, Redberg RF. Gender disparities in sponsorship—how they perpetuate the glass ceiling. JAMA Intern Med. 2017;177:582.
- Hansen M, Schoonover A, Skarica B, et al. Implicit gender bias among US resident physicians. BMC Med Ed. 2019;19:396.
- Estrada M, Burnett M, Campbell AG, et al. Improving underrepresented minority student persistence in STEM. CBE Life Sci Educ. 2016;15:es5.
- Carnes M, Handelsman J, Sheridan J. Diversity in academic medicine: the stages of change model. J Womens Health (Larchmt). 2005;14:471-475.
- Person SD, Jordan CG, Allison JJ, et al. Measuring diversity and inclusion in academic medicine. The Diversity Engagement Survey. Acad Med. 2015;90:1675-1683.
- Fitzgerald CA, Smith RN, Luo-Owen X, et al. Screening for harassment, abuse, and discrimination among surgery residents: an EAST multicenter trial. Am Surg. 2019;85:456-461.
- Hayes SN, Noseworthy JH, Farrugia G. A structured compensation plan results in equitable physician compensation: a single-center analysis. Mayo Clin Proc. 2020;95:35-43.
- Devine PG, Forscher PS, Cox WT, et al. A gender bias habit-breaking intervention led to increased hiring of female faculty in STEMM departments. J Exp Soc Psychol. 2017;73:211-215.
- Morgan AU, Chaiyachati KH, Weissman GE, et al. Eliminating genderbased bias in academic medicine: more than naming the “elephant in the room.” J Gen Intern Med. 2018;33:966-968.
- Mello MM, Jagsi R. Standing up against gender bias and harassment— a matter of professional ethics. N Engl J Med. 2020;382:1385-1387.
- Burgess A, van Diggele C, Mellis C. Mentorship in the health profession: a review. Clin Teach. 2018;15:197-202.
Increasing Skin of Color Publications in the Dermatology Literature: A Call to Action
The US population is becoming more diverse. By 2044, it is predicted that there will be a majority minority population in the United States.1 Therefore, it is imperative to continue to develop educational mechanisms for all dermatologists to increase and maintain competency in skin of color dermatology, which will contribute to the achievement of health equity for patients with all skin tones and hair types.
Not only is clinical skin of color education necessary, but diversity, equity, and inclusion (DEI) education for dermatologists also is critical. Clinical examination,2 diagnosis, and treatment of skin and hair disorders across the skin of color spectrum with cultural humility is essential to achieve health equity. If trainees, dermatologists, other specialists, and primary care clinicians are not frequently exposed to patients with darker skin tones and coily hair, the nuances in diagnosing and treating these patients must be learned in alternate ways.
To ready the nation’s physicians and clinicians to care for the growing diverse population, exposure to more images of dermatologic diseases in those with darker skin tones in journal articles, textbooks, conference lectures, and online dermatology image libraries is necessary to help close the skin of color training and practice gap.3,4 The following initiatives demonstrate how Cutis has sought to address these educational gaps and remains committed to improving DEI education in dermatology.
Collaboration With the Skin of Color Society
The Skin of Color Society (SOCS), which was founded in 2004 by Dr. Susan C. Taylor, is a dermatologic organization with more than 800 members representing 32 countries. Its mission includes promoting awareness and excellence within skin of color dermatology through research, education, and mentorship. The SOCS has utilized strategic partnerships with national and international dermatologists, as well as professional medical organizations and community, industry, and corporate groups, to ultimately ensure that patients with skin of color receive the expert care they deserve.5 In 2017, Cutis published the inaugural article in its collaboration with the SOCS,6 and more articles, which undergo regular peer review, continue to be published quarterly (https://www.mdedge.com/dermatology/skin-color).
Increase Number of Journal Articles on Skin of Color Topics
Increasing the number of journal articles on skin of color–related topics needs to be intentional, as it is a tool that has been identified as a necessary part of enhancing awareness and subsequently improving patient care. Wilson et al7 used stringent criteria to review all articles published from January 2018 to October 2020 in 52 dermatology journals for inclusion of topics on skin of color, hair in patients with skin of color, diversity and inclusion, and socioeconomic and health care disparities in the skin of color population. The journals they reviewed included publications based on continents with majority skin of color populations, such as Asia, as well as those with minority skin of color populations, such as Europe. During the study period, the percentage of articles covering skin of color ranged from 2.04% to 61.8%, with an average of 16.8%.7
The total number of Cutis articles published during the study period was 709, with 132 (18.62%) meeting the investigators’ criteria for articles on skin of color; these included case reports in which at least 1 patient with skin of color was featured.7 Overall, Cutis ranked 16th of the 52 journals for inclusion of skin of color content. Cutis was one of only a few journals based in North America, a non–skin-of-color–predominant continent, to make the top 16 in this study.7
Some of the 132 skin of color articles published in Cutis were the result of the journal’s collaboration with the SOCS. Through this collaboration, articles were published on a variety of skin of color topics, including DEI (6), alopecia and hair care (5), dermoscopy/optical coherence tomography imaging (1), atopic dermatitis (1), cosmetics (1), hidradenitis suppurativa (1), pigmentation (1), rosacea (1), and skin cancer (2). These articles also resulted in a number of podcast discussions (https://www.mdedge.com/podcasts/dermatology-weekly), including one on dealing with DEI, one on pigmentation, and one on dermoscopy/optical coherence tomography imaging. The latter featured the SOCS Scientific Symposium poster winners in 2020.
The number of articles published specifically through Cutis’s collaboration with the SOCS accounted for only a small part of the journal’s 132 skin of color articles identified in the study by Wilson et al.7 We speculate that Cutis’s display of intentional commitment to supporting the inclusion of skin of color articles in the journal may in turn encourage its broader readership to submit more skin of color–focused articles for peer review.
Wilson et al7 specifically remarked that “Cutis’s [Skin of Color] section in each issue is a promising idea.” They also highlighted Clinics in Dermatology for committing an entire issue to skin of color; however, despite this initiative, Clinics in Dermatology still ranked 35th of 52 journals with regard to the overall percentage of skin of color articles published.7 This suggests that a journal publishing one special issue on skin of color annually is a helpful addition to the literature, but increasing the number of articles related to skin of color in each journal issue, similar to Cutis, will ultimately result in a higher overall number of skin of color articles in the dermatology literature.
Both Amuzie et al4 and Wilson et al7 concluded that the higher a journal’s impact factor, the lower the number of skin of color articles published.However, skin of color articles published in high-impact journals received a higher number of citations than those in other lower-impact journals.4 High-impact journals may use Cutis as a model for increasing the number of skin of color articles they publish, which will have a notable impact on increasing skin of color knowledge and educating dermatologists.
Coverage of Diversity, Equity, and Inclusion
In another study, Bray et al8 conducted a PubMed search of articles indexed for MEDLINE from January 2008 to July 2019 to quantify the number of articles specifically focused on DEI in a variety of medical specialties. The field of dermatology had the highest number of articles published on DEI (25) compared to the other specialties, including family medicine (23), orthopedic surgery (12), internal medicine (9), general surgery (7), radiology (6), ophthalmology (2), and anesthesiology (2).8 However, Wilson et al7 found that, out of all the categories of skin of color articles published in dermatology journals during their study period, those focused on DEI made up less than 1% of the total number of articles. Dermatology is off to a great start compared to other specialties, but there is still more work to do in dermatology for DEI. Cutis’s collaboration with the SOCS has resulted in 6 DEI articles published since 2017.
Think Beyond Dermatology Education
The collaboration between Cutis and the SOCS was established to create a series of articles dedicated to increasing the skin of color dermatology knowledge base of the Cutis readership and beyond; however, increased readership and more citations are needed to amplify the reach of the articles published by these skin of color experts. Cutis’s collaboration with SOCS is one mechanism to increase the skin of color literature, but skin of color and DEI articles outside of this collaboration should continue to be published in each issue of Cutis.
The collaboration between SOCS and Cutis was and continues to be a forward-thinking step toward improving skin of color dermatology education, but there is still work to be done across the medical literature with regard to increasing intentional publication of skin of color articles. Nondermatologist clinicians in the Cutis readership benefit from knowledge of skin of color, as all specialties and primary care will see increased patient diversity in their examination rooms.
To further ensure that primary care is not left behind, Cutis has partnered with The Journal of Family Practice to produce a new column called Dx Across the Skin of Color Spectrum (https://www.mdedge.com/dermatology/dx-across-skin-color-spectrum), which is co-published in both journals.9,10 These one-page fact sheets highlight images of dermatologic conditions in skin of color as well as images of the same condition in lighter skin, a concept suggested by Cutis Associate Editor, Dr. Candrice R. Heath. The goal of this new column is to increase the accurate diagnosis of dermatologic conditions in skin of color and to highlight health disparities related to a particular condition in an easy-to-understand format. Uniquely, Dr. Heath co-authors this content with family physician Dr. Richard P. Usatine.
Final Thoughts
The entire community of medical journals should continue to develop creative ways to educate their readership. Medical professionals stay up-to-date on best practices through journal articles, textbooks, conferences, and even podcasts. Therefore, it is best to incorporate skin of color knowledge throughout all educational programming, particularly through enduring materials such as journal articles. Wilson et al7 suggested that a minimum of 16.8% of a dermatology journal’s articles in each issue should focus on skin of color in addition to special focus issues, as this will work toward more equitable dermatologic care.
Knowledge is only part of the equation; compassionate care with cultural humility is the other part. Publishing scientific facts about biology and structure, diagnosis, and treatment selection in skin of color, as well as committing to lifelong learning about the differences in our patients despite the absence of shared life or cultural experiences, may be the key to truly impacting health equity.11 We believe that together we will get there one journal article and one citation at a time.
- Colby SL, Ortman JM. Projections of the size and composition of the U.S. population: 2014 to 2060. United States Census Bureau website. Published March 2015. Accessed August 11, 2021. https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf
- Grayson C, Heath C. An approach to examining tightly coiled hair among patients with hair loss in race-discordant patient-physician interactions. JAMA Dermatol. 2021;157:505-506. doi:10.1001/jamadermatol.2021.0338
- Alvarado SM, Feng H. Representation of dark skin images of common dermatologic conditions in educational resources: a cross-sectional analysis. J Am Acad Dermatol. 2021;84:1427-1431. doi:10.1016/j.jaad.2020.06.041
- Amuzie AU, Jia JL, Taylor SC, et al. Skin-of-color article representation in dermatology literature 2009-2019: higher citation counts and opportunities for inclusion [published online March 24, 2021]. J Am Acad Dermatol. doi:10.1016/j.jaad.2021.03.063
- Learn more about SOCS. Skin of Color Society website. Accessed August 11, 2021. https://skinofcolorsociety.org/about-socs/
- Subash J, Tull R, McMichael A. Diversity in dermatology: a society devoted to skin of color. Cutis. 2017;99:322-324.
- Wilson BN, Sun M, Ashbaugh AG, et al. Assessment of skin of colorand diversity and inclusion content of dermatologic published literature: an analysis and call to action [published online April 20, 2021]. Int J Womens Dermatol. https://doi.org/10.1016/j.ijwd.2021.04.001
- Bray JK, McMichael AJ, Huang WW, et al. Publication rates on the topic of racial and ethnic diversity in dermatology versus other specialties. Dermatol Online J. 2020;26:13030/qt094243gp.
- Heath CR, Usatine R. Atopic dermatitis. Cutis. 2021;107:332. doi:10.12788/cutis.0274
- Heath CR, Usatine R. Psoriasis. Cutis. 2021;108:56. doi:10.12788/cutis.0298
- Jones N, Heath CR. Hair at the intersection of dermatology and anthropology: a conversation on race and relationships [published online August 3, 2021]. Pediatr Dermatol. doi:10.1111/pde.14721
The US population is becoming more diverse. By 2044, it is predicted that there will be a majority minority population in the United States.1 Therefore, it is imperative to continue to develop educational mechanisms for all dermatologists to increase and maintain competency in skin of color dermatology, which will contribute to the achievement of health equity for patients with all skin tones and hair types.
Not only is clinical skin of color education necessary, but diversity, equity, and inclusion (DEI) education for dermatologists also is critical. Clinical examination,2 diagnosis, and treatment of skin and hair disorders across the skin of color spectrum with cultural humility is essential to achieve health equity. If trainees, dermatologists, other specialists, and primary care clinicians are not frequently exposed to patients with darker skin tones and coily hair, the nuances in diagnosing and treating these patients must be learned in alternate ways.
To ready the nation’s physicians and clinicians to care for the growing diverse population, exposure to more images of dermatologic diseases in those with darker skin tones in journal articles, textbooks, conference lectures, and online dermatology image libraries is necessary to help close the skin of color training and practice gap.3,4 The following initiatives demonstrate how Cutis has sought to address these educational gaps and remains committed to improving DEI education in dermatology.
Collaboration With the Skin of Color Society
The Skin of Color Society (SOCS), which was founded in 2004 by Dr. Susan C. Taylor, is a dermatologic organization with more than 800 members representing 32 countries. Its mission includes promoting awareness and excellence within skin of color dermatology through research, education, and mentorship. The SOCS has utilized strategic partnerships with national and international dermatologists, as well as professional medical organizations and community, industry, and corporate groups, to ultimately ensure that patients with skin of color receive the expert care they deserve.5 In 2017, Cutis published the inaugural article in its collaboration with the SOCS,6 and more articles, which undergo regular peer review, continue to be published quarterly (https://www.mdedge.com/dermatology/skin-color).
Increase Number of Journal Articles on Skin of Color Topics
Increasing the number of journal articles on skin of color–related topics needs to be intentional, as it is a tool that has been identified as a necessary part of enhancing awareness and subsequently improving patient care. Wilson et al7 used stringent criteria to review all articles published from January 2018 to October 2020 in 52 dermatology journals for inclusion of topics on skin of color, hair in patients with skin of color, diversity and inclusion, and socioeconomic and health care disparities in the skin of color population. The journals they reviewed included publications based on continents with majority skin of color populations, such as Asia, as well as those with minority skin of color populations, such as Europe. During the study period, the percentage of articles covering skin of color ranged from 2.04% to 61.8%, with an average of 16.8%.7
The total number of Cutis articles published during the study period was 709, with 132 (18.62%) meeting the investigators’ criteria for articles on skin of color; these included case reports in which at least 1 patient with skin of color was featured.7 Overall, Cutis ranked 16th of the 52 journals for inclusion of skin of color content. Cutis was one of only a few journals based in North America, a non–skin-of-color–predominant continent, to make the top 16 in this study.7
Some of the 132 skin of color articles published in Cutis were the result of the journal’s collaboration with the SOCS. Through this collaboration, articles were published on a variety of skin of color topics, including DEI (6), alopecia and hair care (5), dermoscopy/optical coherence tomography imaging (1), atopic dermatitis (1), cosmetics (1), hidradenitis suppurativa (1), pigmentation (1), rosacea (1), and skin cancer (2). These articles also resulted in a number of podcast discussions (https://www.mdedge.com/podcasts/dermatology-weekly), including one on dealing with DEI, one on pigmentation, and one on dermoscopy/optical coherence tomography imaging. The latter featured the SOCS Scientific Symposium poster winners in 2020.
The number of articles published specifically through Cutis’s collaboration with the SOCS accounted for only a small part of the journal’s 132 skin of color articles identified in the study by Wilson et al.7 We speculate that Cutis’s display of intentional commitment to supporting the inclusion of skin of color articles in the journal may in turn encourage its broader readership to submit more skin of color–focused articles for peer review.
Wilson et al7 specifically remarked that “Cutis’s [Skin of Color] section in each issue is a promising idea.” They also highlighted Clinics in Dermatology for committing an entire issue to skin of color; however, despite this initiative, Clinics in Dermatology still ranked 35th of 52 journals with regard to the overall percentage of skin of color articles published.7 This suggests that a journal publishing one special issue on skin of color annually is a helpful addition to the literature, but increasing the number of articles related to skin of color in each journal issue, similar to Cutis, will ultimately result in a higher overall number of skin of color articles in the dermatology literature.
Both Amuzie et al4 and Wilson et al7 concluded that the higher a journal’s impact factor, the lower the number of skin of color articles published.However, skin of color articles published in high-impact journals received a higher number of citations than those in other lower-impact journals.4 High-impact journals may use Cutis as a model for increasing the number of skin of color articles they publish, which will have a notable impact on increasing skin of color knowledge and educating dermatologists.
Coverage of Diversity, Equity, and Inclusion
In another study, Bray et al8 conducted a PubMed search of articles indexed for MEDLINE from January 2008 to July 2019 to quantify the number of articles specifically focused on DEI in a variety of medical specialties. The field of dermatology had the highest number of articles published on DEI (25) compared to the other specialties, including family medicine (23), orthopedic surgery (12), internal medicine (9), general surgery (7), radiology (6), ophthalmology (2), and anesthesiology (2).8 However, Wilson et al7 found that, out of all the categories of skin of color articles published in dermatology journals during their study period, those focused on DEI made up less than 1% of the total number of articles. Dermatology is off to a great start compared to other specialties, but there is still more work to do in dermatology for DEI. Cutis’s collaboration with the SOCS has resulted in 6 DEI articles published since 2017.
Think Beyond Dermatology Education
The collaboration between Cutis and the SOCS was established to create a series of articles dedicated to increasing the skin of color dermatology knowledge base of the Cutis readership and beyond; however, increased readership and more citations are needed to amplify the reach of the articles published by these skin of color experts. Cutis’s collaboration with SOCS is one mechanism to increase the skin of color literature, but skin of color and DEI articles outside of this collaboration should continue to be published in each issue of Cutis.
The collaboration between SOCS and Cutis was and continues to be a forward-thinking step toward improving skin of color dermatology education, but there is still work to be done across the medical literature with regard to increasing intentional publication of skin of color articles. Nondermatologist clinicians in the Cutis readership benefit from knowledge of skin of color, as all specialties and primary care will see increased patient diversity in their examination rooms.
To further ensure that primary care is not left behind, Cutis has partnered with The Journal of Family Practice to produce a new column called Dx Across the Skin of Color Spectrum (https://www.mdedge.com/dermatology/dx-across-skin-color-spectrum), which is co-published in both journals.9,10 These one-page fact sheets highlight images of dermatologic conditions in skin of color as well as images of the same condition in lighter skin, a concept suggested by Cutis Associate Editor, Dr. Candrice R. Heath. The goal of this new column is to increase the accurate diagnosis of dermatologic conditions in skin of color and to highlight health disparities related to a particular condition in an easy-to-understand format. Uniquely, Dr. Heath co-authors this content with family physician Dr. Richard P. Usatine.
Final Thoughts
The entire community of medical journals should continue to develop creative ways to educate their readership. Medical professionals stay up-to-date on best practices through journal articles, textbooks, conferences, and even podcasts. Therefore, it is best to incorporate skin of color knowledge throughout all educational programming, particularly through enduring materials such as journal articles. Wilson et al7 suggested that a minimum of 16.8% of a dermatology journal’s articles in each issue should focus on skin of color in addition to special focus issues, as this will work toward more equitable dermatologic care.
Knowledge is only part of the equation; compassionate care with cultural humility is the other part. Publishing scientific facts about biology and structure, diagnosis, and treatment selection in skin of color, as well as committing to lifelong learning about the differences in our patients despite the absence of shared life or cultural experiences, may be the key to truly impacting health equity.11 We believe that together we will get there one journal article and one citation at a time.
The US population is becoming more diverse. By 2044, it is predicted that there will be a majority minority population in the United States.1 Therefore, it is imperative to continue to develop educational mechanisms for all dermatologists to increase and maintain competency in skin of color dermatology, which will contribute to the achievement of health equity for patients with all skin tones and hair types.
Not only is clinical skin of color education necessary, but diversity, equity, and inclusion (DEI) education for dermatologists also is critical. Clinical examination,2 diagnosis, and treatment of skin and hair disorders across the skin of color spectrum with cultural humility is essential to achieve health equity. If trainees, dermatologists, other specialists, and primary care clinicians are not frequently exposed to patients with darker skin tones and coily hair, the nuances in diagnosing and treating these patients must be learned in alternate ways.
To ready the nation’s physicians and clinicians to care for the growing diverse population, exposure to more images of dermatologic diseases in those with darker skin tones in journal articles, textbooks, conference lectures, and online dermatology image libraries is necessary to help close the skin of color training and practice gap.3,4 The following initiatives demonstrate how Cutis has sought to address these educational gaps and remains committed to improving DEI education in dermatology.
Collaboration With the Skin of Color Society
The Skin of Color Society (SOCS), which was founded in 2004 by Dr. Susan C. Taylor, is a dermatologic organization with more than 800 members representing 32 countries. Its mission includes promoting awareness and excellence within skin of color dermatology through research, education, and mentorship. The SOCS has utilized strategic partnerships with national and international dermatologists, as well as professional medical organizations and community, industry, and corporate groups, to ultimately ensure that patients with skin of color receive the expert care they deserve.5 In 2017, Cutis published the inaugural article in its collaboration with the SOCS,6 and more articles, which undergo regular peer review, continue to be published quarterly (https://www.mdedge.com/dermatology/skin-color).
Increase Number of Journal Articles on Skin of Color Topics
Increasing the number of journal articles on skin of color–related topics needs to be intentional, as it is a tool that has been identified as a necessary part of enhancing awareness and subsequently improving patient care. Wilson et al7 used stringent criteria to review all articles published from January 2018 to October 2020 in 52 dermatology journals for inclusion of topics on skin of color, hair in patients with skin of color, diversity and inclusion, and socioeconomic and health care disparities in the skin of color population. The journals they reviewed included publications based on continents with majority skin of color populations, such as Asia, as well as those with minority skin of color populations, such as Europe. During the study period, the percentage of articles covering skin of color ranged from 2.04% to 61.8%, with an average of 16.8%.7
The total number of Cutis articles published during the study period was 709, with 132 (18.62%) meeting the investigators’ criteria for articles on skin of color; these included case reports in which at least 1 patient with skin of color was featured.7 Overall, Cutis ranked 16th of the 52 journals for inclusion of skin of color content. Cutis was one of only a few journals based in North America, a non–skin-of-color–predominant continent, to make the top 16 in this study.7
Some of the 132 skin of color articles published in Cutis were the result of the journal’s collaboration with the SOCS. Through this collaboration, articles were published on a variety of skin of color topics, including DEI (6), alopecia and hair care (5), dermoscopy/optical coherence tomography imaging (1), atopic dermatitis (1), cosmetics (1), hidradenitis suppurativa (1), pigmentation (1), rosacea (1), and skin cancer (2). These articles also resulted in a number of podcast discussions (https://www.mdedge.com/podcasts/dermatology-weekly), including one on dealing with DEI, one on pigmentation, and one on dermoscopy/optical coherence tomography imaging. The latter featured the SOCS Scientific Symposium poster winners in 2020.
The number of articles published specifically through Cutis’s collaboration with the SOCS accounted for only a small part of the journal’s 132 skin of color articles identified in the study by Wilson et al.7 We speculate that Cutis’s display of intentional commitment to supporting the inclusion of skin of color articles in the journal may in turn encourage its broader readership to submit more skin of color–focused articles for peer review.
Wilson et al7 specifically remarked that “Cutis’s [Skin of Color] section in each issue is a promising idea.” They also highlighted Clinics in Dermatology for committing an entire issue to skin of color; however, despite this initiative, Clinics in Dermatology still ranked 35th of 52 journals with regard to the overall percentage of skin of color articles published.7 This suggests that a journal publishing one special issue on skin of color annually is a helpful addition to the literature, but increasing the number of articles related to skin of color in each journal issue, similar to Cutis, will ultimately result in a higher overall number of skin of color articles in the dermatology literature.
Both Amuzie et al4 and Wilson et al7 concluded that the higher a journal’s impact factor, the lower the number of skin of color articles published.However, skin of color articles published in high-impact journals received a higher number of citations than those in other lower-impact journals.4 High-impact journals may use Cutis as a model for increasing the number of skin of color articles they publish, which will have a notable impact on increasing skin of color knowledge and educating dermatologists.
Coverage of Diversity, Equity, and Inclusion
In another study, Bray et al8 conducted a PubMed search of articles indexed for MEDLINE from January 2008 to July 2019 to quantify the number of articles specifically focused on DEI in a variety of medical specialties. The field of dermatology had the highest number of articles published on DEI (25) compared to the other specialties, including family medicine (23), orthopedic surgery (12), internal medicine (9), general surgery (7), radiology (6), ophthalmology (2), and anesthesiology (2).8 However, Wilson et al7 found that, out of all the categories of skin of color articles published in dermatology journals during their study period, those focused on DEI made up less than 1% of the total number of articles. Dermatology is off to a great start compared to other specialties, but there is still more work to do in dermatology for DEI. Cutis’s collaboration with the SOCS has resulted in 6 DEI articles published since 2017.
Think Beyond Dermatology Education
The collaboration between Cutis and the SOCS was established to create a series of articles dedicated to increasing the skin of color dermatology knowledge base of the Cutis readership and beyond; however, increased readership and more citations are needed to amplify the reach of the articles published by these skin of color experts. Cutis’s collaboration with SOCS is one mechanism to increase the skin of color literature, but skin of color and DEI articles outside of this collaboration should continue to be published in each issue of Cutis.
The collaboration between SOCS and Cutis was and continues to be a forward-thinking step toward improving skin of color dermatology education, but there is still work to be done across the medical literature with regard to increasing intentional publication of skin of color articles. Nondermatologist clinicians in the Cutis readership benefit from knowledge of skin of color, as all specialties and primary care will see increased patient diversity in their examination rooms.
To further ensure that primary care is not left behind, Cutis has partnered with The Journal of Family Practice to produce a new column called Dx Across the Skin of Color Spectrum (https://www.mdedge.com/dermatology/dx-across-skin-color-spectrum), which is co-published in both journals.9,10 These one-page fact sheets highlight images of dermatologic conditions in skin of color as well as images of the same condition in lighter skin, a concept suggested by Cutis Associate Editor, Dr. Candrice R. Heath. The goal of this new column is to increase the accurate diagnosis of dermatologic conditions in skin of color and to highlight health disparities related to a particular condition in an easy-to-understand format. Uniquely, Dr. Heath co-authors this content with family physician Dr. Richard P. Usatine.
Final Thoughts
The entire community of medical journals should continue to develop creative ways to educate their readership. Medical professionals stay up-to-date on best practices through journal articles, textbooks, conferences, and even podcasts. Therefore, it is best to incorporate skin of color knowledge throughout all educational programming, particularly through enduring materials such as journal articles. Wilson et al7 suggested that a minimum of 16.8% of a dermatology journal’s articles in each issue should focus on skin of color in addition to special focus issues, as this will work toward more equitable dermatologic care.
Knowledge is only part of the equation; compassionate care with cultural humility is the other part. Publishing scientific facts about biology and structure, diagnosis, and treatment selection in skin of color, as well as committing to lifelong learning about the differences in our patients despite the absence of shared life or cultural experiences, may be the key to truly impacting health equity.11 We believe that together we will get there one journal article and one citation at a time.
- Colby SL, Ortman JM. Projections of the size and composition of the U.S. population: 2014 to 2060. United States Census Bureau website. Published March 2015. Accessed August 11, 2021. https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf
- Grayson C, Heath C. An approach to examining tightly coiled hair among patients with hair loss in race-discordant patient-physician interactions. JAMA Dermatol. 2021;157:505-506. doi:10.1001/jamadermatol.2021.0338
- Alvarado SM, Feng H. Representation of dark skin images of common dermatologic conditions in educational resources: a cross-sectional analysis. J Am Acad Dermatol. 2021;84:1427-1431. doi:10.1016/j.jaad.2020.06.041
- Amuzie AU, Jia JL, Taylor SC, et al. Skin-of-color article representation in dermatology literature 2009-2019: higher citation counts and opportunities for inclusion [published online March 24, 2021]. J Am Acad Dermatol. doi:10.1016/j.jaad.2021.03.063
- Learn more about SOCS. Skin of Color Society website. Accessed August 11, 2021. https://skinofcolorsociety.org/about-socs/
- Subash J, Tull R, McMichael A. Diversity in dermatology: a society devoted to skin of color. Cutis. 2017;99:322-324.
- Wilson BN, Sun M, Ashbaugh AG, et al. Assessment of skin of colorand diversity and inclusion content of dermatologic published literature: an analysis and call to action [published online April 20, 2021]. Int J Womens Dermatol. https://doi.org/10.1016/j.ijwd.2021.04.001
- Bray JK, McMichael AJ, Huang WW, et al. Publication rates on the topic of racial and ethnic diversity in dermatology versus other specialties. Dermatol Online J. 2020;26:13030/qt094243gp.
- Heath CR, Usatine R. Atopic dermatitis. Cutis. 2021;107:332. doi:10.12788/cutis.0274
- Heath CR, Usatine R. Psoriasis. Cutis. 2021;108:56. doi:10.12788/cutis.0298
- Jones N, Heath CR. Hair at the intersection of dermatology and anthropology: a conversation on race and relationships [published online August 3, 2021]. Pediatr Dermatol. doi:10.1111/pde.14721
- Colby SL, Ortman JM. Projections of the size and composition of the U.S. population: 2014 to 2060. United States Census Bureau website. Published March 2015. Accessed August 11, 2021. https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf
- Grayson C, Heath C. An approach to examining tightly coiled hair among patients with hair loss in race-discordant patient-physician interactions. JAMA Dermatol. 2021;157:505-506. doi:10.1001/jamadermatol.2021.0338
- Alvarado SM, Feng H. Representation of dark skin images of common dermatologic conditions in educational resources: a cross-sectional analysis. J Am Acad Dermatol. 2021;84:1427-1431. doi:10.1016/j.jaad.2020.06.041
- Amuzie AU, Jia JL, Taylor SC, et al. Skin-of-color article representation in dermatology literature 2009-2019: higher citation counts and opportunities for inclusion [published online March 24, 2021]. J Am Acad Dermatol. doi:10.1016/j.jaad.2021.03.063
- Learn more about SOCS. Skin of Color Society website. Accessed August 11, 2021. https://skinofcolorsociety.org/about-socs/
- Subash J, Tull R, McMichael A. Diversity in dermatology: a society devoted to skin of color. Cutis. 2017;99:322-324.
- Wilson BN, Sun M, Ashbaugh AG, et al. Assessment of skin of colorand diversity and inclusion content of dermatologic published literature: an analysis and call to action [published online April 20, 2021]. Int J Womens Dermatol. https://doi.org/10.1016/j.ijwd.2021.04.001
- Bray JK, McMichael AJ, Huang WW, et al. Publication rates on the topic of racial and ethnic diversity in dermatology versus other specialties. Dermatol Online J. 2020;26:13030/qt094243gp.
- Heath CR, Usatine R. Atopic dermatitis. Cutis. 2021;107:332. doi:10.12788/cutis.0274
- Heath CR, Usatine R. Psoriasis. Cutis. 2021;108:56. doi:10.12788/cutis.0298
- Jones N, Heath CR. Hair at the intersection of dermatology and anthropology: a conversation on race and relationships [published online August 3, 2021]. Pediatr Dermatol. doi:10.1111/pde.14721
Practice Points
- Submitting more articles related to skin of color for peer review and publication will increase educational opportunities.
- Journals that publish skin of color articles play a critical role in reducing educational gaps and ultimately help improve patient care for those with skin of color.
Verrucous Scalp Plaque and Widespread Eruption
The Diagnosis: Pemphigus Foliaceous
Laboratory workup including a complete blood cell count with differential, comprehensive metabolic panel, antinuclear antibodies, Sjögren syndrome A and B antibodies, hepatitis profile, rapid plasma reagin, HIV screen, aldolase, anti–Jo-1, T-Spot TB test (Quest Diagnostics), and tissue cultures was unremarkable. Two 4-mm punch biopsies were obtained from the left cheek and upper back, both of which demonstrated intragranular acantholysis suggestive of pemphigus foliaceous (Figure 1A). A subsequent punch biopsy from the right lower abdomen sent for direct immunofluorescence demonstrated netlike positivity of IgG and C3 in the upper epidermis (Figure 1B), and serum sent for indirect immunofluorescence demonstrated intercellular IgG antibodies to desmoglein (Dsg) 1 on monkey esophagus and positive Dsg-1 antibodies on enzyme-linked immunosorbent assay, confirming the diagnosis.
The patient was started on a 60-mg prednisone taper as well as dapsone 50 mg daily; the dapsone was titrated up to 100 mg daily. After tapering down to 10 mg daily of prednisone over 2 months and continuing dapsone with minimal improvement, he was given 2 infusions of rituximab 1000 mg 2 weeks apart. The scalp plaque was dramatically improved at 3-month follow-up (Figure 2), with partial improvement of the cheek plaques (Figure 3). Dapsone was increased to 150 mg daily, and he was encouraged to use triamcinolone acetonide ointment 0.1% twice daily, which led to further improvement.


Pemphigus foliaceus is an autoimmune blistering disease that most commonly occurs in middle-aged adults. It generally is less common than pemphigus vulgaris, except in Finland, Tunisia, and Brazil, where there is an endemic condition with an identical clinical and histological presentation known as fogo selvagem.1
The pathogenesis of pemphigus foliaceous is characterized by IgG autoantibodies against Dsg-1, a transmembrane glycoprotein involved in the cellular adhesion of keratinocytes, which is preferentially expressed in the superficial epidermis.2-7 Dysfunction of Dsg-1 results in the separation of superficial epidermal cells, resulting in intraepidermal blisters.2,7 In contrast to pemphigus vulgaris, there typically is a lack of oral mucosal involvement due to compensation by Dsg-3 in the mucosa.4 Potential triggers for pemphigus foliaceous include exposure to UV radiation; radiotherapy; pregnancy; physiologic stress; and drugs, most commonly captopril, penicillamine, and thiols.8
Pemphigus foliaceous lesions clinically appear as eroded and crusted lesions on an erythematous base, commonly in a seborrheic distribution on the face, scalp, and trunk with sparing of the oral mucosa,2,6 but lesions can progress to a widespread and more severe exfoliative dermatitis.7 Lesions also can appear as psoriasiform plaques and often are initially misdiagnosed as psoriasis, particularly in patients with skin of color.9,10
Diagnosis of pemphigus foliaceous typically is made using a combination of histology as well as both direct and indirect immunofluorescence. Histologically, pemphigus foliaceus presents with subcorneal acantholysis, which is most prominent in the granular layer and occasionally the presence of neutrophils and eosinophils in the blister cavity.7 Direct immunofluorescence demonstrates netlike intercellular IgG and C3 in the upper portion of the epidermis.11 Indirect immunofluorescence can help detect circulating IgG antibodies to Dsg-1, with guinea pig esophagus being the ideal substrate.11,12
First-line treatment of pemphigus foliaceus consists of systemic glucocorticoid therapy, often administered with azathioprine, methotrexate, or mycophenolate mofetil.2,6,13 Although first-line treatment is effective in 60% to 80% of patients,2 relapsing cases can be treated with cyclophosphamide, intravenous immunoglobulin, immunoadsorption, plasmapheresis, or rituximab.2
Rituximab is a chimeric monoclonal antibody targeting CD20+ B cells, leading to decreased antibody production, which has been shown to be effective in treating severe and refractory cases of pemphigus foliaceus.6,13Rituximab with short-course prednisone has been found to be more effective in achieving complete remission at 24 months than prednisone alone.14 In patients with contraindications to systemic glucocorticoid therapy, rituximab has been shown as an effective first-line therapy.15 One-quarter of patients treated with rituximab relapsed within 2 years of treatment6 (average time to relapse, 6–26 months).16 High-dose rituximab regimens, along with a higher number of rituximab treatment cycles, have been shown to prolong time to relapse.6 Further, higher baseline levels of Dsg-1 antibody have been correlated to earlier relapse and can be used following rituximab therapy to monitor disease progression.6,16
The differential diagnosis for pemphigus foliaceous includes disseminated blastomycosis, hypertrophic lupus erythematosus, sebopsoriasis, and secondary syphilis. Disseminated blastomycosis presents with cutaneous manifestations such as nodules, papules, or pustules evolving over weeks to months into ulcers with subsequent scarring.17 Hypertrophic lupus erythematosus presents with papules and nodules with associated keratotic scaling on the face, palms, and extensor surfaces of the limbs.18 Sebopsoriasis is characterized by well-defined lesions with an overlying scale distributed on the scalp, face, and chest.19 Secondary syphilis presents as early hyperpigmented macules transitioning to acral papulosquamous lesions involving the palms and soles.20
- Hans-Filho G, Aoki V, Hans Bittner NR, et al. Fogo selvagem: endemic pemphigus foliaceus. An Bras Dermatol. 2018;93:638-650.
- Jenson KK, Burr DM, Edwards BC. Case report: reatment of refractory pemphigus foliaceus with rituximab. Practical Dermatology. February 2016:33-36. Accessed August 27, 2021. https://practicaldermatology.com/articles/2016-feb/case-report -treatment-of-refractory-pemphigus-foliaceus-with-rituximab -financial-matters-aad-asds-resources
- Amagai M, Hashimoto T, Green KJ, et al. Antigen-specific immunoadsorption of pathogenic autoantibodies in pemphigus foliaceus. J Invest Dermatol. 1995;104:895-901.
- Mahoney MG, Wang Z, Rothenberger K, et al. Explanations for the clinical and microscopic localization of lesions in pemphigus foliaceus and vulgaris. J Clin Invest. 1999;103:461-468.
- Oktarina DAM, Sokol E, Kramer D, et al. Endocytosis of IgG, desmoglein 1, and plakoglobin in pemphigus foliaceus patient skin. Front Immunol. 2019;10:1-12.
- Kraft M, Worm M. Pemphigus foliaceus-repeated treatment with rituximab 7 years after initial response: a case report. Front Med. 2018;5:315.
- Hale EK. Pemphigus foliaceous. Dermatol Online J. 2002;8:9.
- Tavakolpour S. Pemphigus trigger factors: special focus on pemphigus vulgaris and pemphigus foliaceus. Arch Dermatol Res. 2018;310:95-106.
- A boobaker J, Morar N, Ramdial PK, et al. Pemphigus in South Africa. Int J Dermatol. 2001;40:115-119.
- Austin E, Millsop JW, Ely H, et al. Psoriasiform pemphigus foliaceus in an African American female: an important clinical manifestation. J Drugs Dermatol. 2018;17:471.
- Arbache ST, Nogueira TG, Delgado L, et al. Immunofluorescence testing in the diagnosis of autoimmune blistering diseases: overview of 10-year experience. An Bras Dermatol. 2014;89:885-889.
- Sabolinski ML, Beutner EH, Krasny S, et al. Substrate specificity of antiepithelial antibodies of pemphigus vulgaris and pemphigus foliaceus sera in immunofluorescence tests on monkey and guinea pig esophagus sections. J Invest Dermatol. 1987;88:545-549.
- Palacios-Álvarez I, Riquelme-McLoughlin C, Curto-Barredo L, et al. Rituximab treatment of pemphigus foliaceus: a retrospective study of 12 patients. J Am Acad Dermatol. 2021;85:484-486.
- Murrell DF, Sprecher E. Rituximab and short-course prednisone as the new gold standard for new-onset pemphigus vulgaris and pemphigus foliaceus. Br J Dermatol. 2017;177:1143-1144.
- Gregoriou S, Efthymiou O, Stefanaki C, et al. Management of pemphigus vulgaris: challenges and solutions. Clin Cosmet Investig Dermatol. 2015;8:521-527.
- Saleh MA. A prospective study comparing patients with early and late relapsing pemphigus treated with rituximab. J Am Acad Dermatol. 2018;79:97-103.
- Castillo CG, Kauffman CA, Miceli MH. Blastomycosis. Infect Dis Clin North Am. 2016;30:247-264.
- Herzum A, Gasparini G, Emanuele C, et al. Atypical and rare forms of cutaneous lupus erythematosus: the importance of the diagnosis for the best management of patients. Dermatology. 2013;1-10.
- Tull TJ, Noy M, Bunker CB, et al. Sebopsoriasis in patients with HIV: a case series of 20 patients. Br J Dermatol. 2016; 173:813-815.
- Balagula Y, Mattei P, Wisco OJ, et al. The great imitator revised: the spectrum of atypical cutaneous manifestations of secondary syphilis. Int J Dermatol. 2014;53:1434-1441.
The Diagnosis: Pemphigus Foliaceous
Laboratory workup including a complete blood cell count with differential, comprehensive metabolic panel, antinuclear antibodies, Sjögren syndrome A and B antibodies, hepatitis profile, rapid plasma reagin, HIV screen, aldolase, anti–Jo-1, T-Spot TB test (Quest Diagnostics), and tissue cultures was unremarkable. Two 4-mm punch biopsies were obtained from the left cheek and upper back, both of which demonstrated intragranular acantholysis suggestive of pemphigus foliaceous (Figure 1A). A subsequent punch biopsy from the right lower abdomen sent for direct immunofluorescence demonstrated netlike positivity of IgG and C3 in the upper epidermis (Figure 1B), and serum sent for indirect immunofluorescence demonstrated intercellular IgG antibodies to desmoglein (Dsg) 1 on monkey esophagus and positive Dsg-1 antibodies on enzyme-linked immunosorbent assay, confirming the diagnosis.
The patient was started on a 60-mg prednisone taper as well as dapsone 50 mg daily; the dapsone was titrated up to 100 mg daily. After tapering down to 10 mg daily of prednisone over 2 months and continuing dapsone with minimal improvement, he was given 2 infusions of rituximab 1000 mg 2 weeks apart. The scalp plaque was dramatically improved at 3-month follow-up (Figure 2), with partial improvement of the cheek plaques (Figure 3). Dapsone was increased to 150 mg daily, and he was encouraged to use triamcinolone acetonide ointment 0.1% twice daily, which led to further improvement.


Pemphigus foliaceus is an autoimmune blistering disease that most commonly occurs in middle-aged adults. It generally is less common than pemphigus vulgaris, except in Finland, Tunisia, and Brazil, where there is an endemic condition with an identical clinical and histological presentation known as fogo selvagem.1
The pathogenesis of pemphigus foliaceous is characterized by IgG autoantibodies against Dsg-1, a transmembrane glycoprotein involved in the cellular adhesion of keratinocytes, which is preferentially expressed in the superficial epidermis.2-7 Dysfunction of Dsg-1 results in the separation of superficial epidermal cells, resulting in intraepidermal blisters.2,7 In contrast to pemphigus vulgaris, there typically is a lack of oral mucosal involvement due to compensation by Dsg-3 in the mucosa.4 Potential triggers for pemphigus foliaceous include exposure to UV radiation; radiotherapy; pregnancy; physiologic stress; and drugs, most commonly captopril, penicillamine, and thiols.8
Pemphigus foliaceous lesions clinically appear as eroded and crusted lesions on an erythematous base, commonly in a seborrheic distribution on the face, scalp, and trunk with sparing of the oral mucosa,2,6 but lesions can progress to a widespread and more severe exfoliative dermatitis.7 Lesions also can appear as psoriasiform plaques and often are initially misdiagnosed as psoriasis, particularly in patients with skin of color.9,10
Diagnosis of pemphigus foliaceous typically is made using a combination of histology as well as both direct and indirect immunofluorescence. Histologically, pemphigus foliaceus presents with subcorneal acantholysis, which is most prominent in the granular layer and occasionally the presence of neutrophils and eosinophils in the blister cavity.7 Direct immunofluorescence demonstrates netlike intercellular IgG and C3 in the upper portion of the epidermis.11 Indirect immunofluorescence can help detect circulating IgG antibodies to Dsg-1, with guinea pig esophagus being the ideal substrate.11,12
First-line treatment of pemphigus foliaceus consists of systemic glucocorticoid therapy, often administered with azathioprine, methotrexate, or mycophenolate mofetil.2,6,13 Although first-line treatment is effective in 60% to 80% of patients,2 relapsing cases can be treated with cyclophosphamide, intravenous immunoglobulin, immunoadsorption, plasmapheresis, or rituximab.2
Rituximab is a chimeric monoclonal antibody targeting CD20+ B cells, leading to decreased antibody production, which has been shown to be effective in treating severe and refractory cases of pemphigus foliaceus.6,13Rituximab with short-course prednisone has been found to be more effective in achieving complete remission at 24 months than prednisone alone.14 In patients with contraindications to systemic glucocorticoid therapy, rituximab has been shown as an effective first-line therapy.15 One-quarter of patients treated with rituximab relapsed within 2 years of treatment6 (average time to relapse, 6–26 months).16 High-dose rituximab regimens, along with a higher number of rituximab treatment cycles, have been shown to prolong time to relapse.6 Further, higher baseline levels of Dsg-1 antibody have been correlated to earlier relapse and can be used following rituximab therapy to monitor disease progression.6,16
The differential diagnosis for pemphigus foliaceous includes disseminated blastomycosis, hypertrophic lupus erythematosus, sebopsoriasis, and secondary syphilis. Disseminated blastomycosis presents with cutaneous manifestations such as nodules, papules, or pustules evolving over weeks to months into ulcers with subsequent scarring.17 Hypertrophic lupus erythematosus presents with papules and nodules with associated keratotic scaling on the face, palms, and extensor surfaces of the limbs.18 Sebopsoriasis is characterized by well-defined lesions with an overlying scale distributed on the scalp, face, and chest.19 Secondary syphilis presents as early hyperpigmented macules transitioning to acral papulosquamous lesions involving the palms and soles.20
The Diagnosis: Pemphigus Foliaceous
Laboratory workup including a complete blood cell count with differential, comprehensive metabolic panel, antinuclear antibodies, Sjögren syndrome A and B antibodies, hepatitis profile, rapid plasma reagin, HIV screen, aldolase, anti–Jo-1, T-Spot TB test (Quest Diagnostics), and tissue cultures was unremarkable. Two 4-mm punch biopsies were obtained from the left cheek and upper back, both of which demonstrated intragranular acantholysis suggestive of pemphigus foliaceous (Figure 1A). A subsequent punch biopsy from the right lower abdomen sent for direct immunofluorescence demonstrated netlike positivity of IgG and C3 in the upper epidermis (Figure 1B), and serum sent for indirect immunofluorescence demonstrated intercellular IgG antibodies to desmoglein (Dsg) 1 on monkey esophagus and positive Dsg-1 antibodies on enzyme-linked immunosorbent assay, confirming the diagnosis.
The patient was started on a 60-mg prednisone taper as well as dapsone 50 mg daily; the dapsone was titrated up to 100 mg daily. After tapering down to 10 mg daily of prednisone over 2 months and continuing dapsone with minimal improvement, he was given 2 infusions of rituximab 1000 mg 2 weeks apart. The scalp plaque was dramatically improved at 3-month follow-up (Figure 2), with partial improvement of the cheek plaques (Figure 3). Dapsone was increased to 150 mg daily, and he was encouraged to use triamcinolone acetonide ointment 0.1% twice daily, which led to further improvement.


Pemphigus foliaceus is an autoimmune blistering disease that most commonly occurs in middle-aged adults. It generally is less common than pemphigus vulgaris, except in Finland, Tunisia, and Brazil, where there is an endemic condition with an identical clinical and histological presentation known as fogo selvagem.1
The pathogenesis of pemphigus foliaceous is characterized by IgG autoantibodies against Dsg-1, a transmembrane glycoprotein involved in the cellular adhesion of keratinocytes, which is preferentially expressed in the superficial epidermis.2-7 Dysfunction of Dsg-1 results in the separation of superficial epidermal cells, resulting in intraepidermal blisters.2,7 In contrast to pemphigus vulgaris, there typically is a lack of oral mucosal involvement due to compensation by Dsg-3 in the mucosa.4 Potential triggers for pemphigus foliaceous include exposure to UV radiation; radiotherapy; pregnancy; physiologic stress; and drugs, most commonly captopril, penicillamine, and thiols.8
Pemphigus foliaceous lesions clinically appear as eroded and crusted lesions on an erythematous base, commonly in a seborrheic distribution on the face, scalp, and trunk with sparing of the oral mucosa,2,6 but lesions can progress to a widespread and more severe exfoliative dermatitis.7 Lesions also can appear as psoriasiform plaques and often are initially misdiagnosed as psoriasis, particularly in patients with skin of color.9,10
Diagnosis of pemphigus foliaceous typically is made using a combination of histology as well as both direct and indirect immunofluorescence. Histologically, pemphigus foliaceus presents with subcorneal acantholysis, which is most prominent in the granular layer and occasionally the presence of neutrophils and eosinophils in the blister cavity.7 Direct immunofluorescence demonstrates netlike intercellular IgG and C3 in the upper portion of the epidermis.11 Indirect immunofluorescence can help detect circulating IgG antibodies to Dsg-1, with guinea pig esophagus being the ideal substrate.11,12
First-line treatment of pemphigus foliaceus consists of systemic glucocorticoid therapy, often administered with azathioprine, methotrexate, or mycophenolate mofetil.2,6,13 Although first-line treatment is effective in 60% to 80% of patients,2 relapsing cases can be treated with cyclophosphamide, intravenous immunoglobulin, immunoadsorption, plasmapheresis, or rituximab.2
Rituximab is a chimeric monoclonal antibody targeting CD20+ B cells, leading to decreased antibody production, which has been shown to be effective in treating severe and refractory cases of pemphigus foliaceus.6,13Rituximab with short-course prednisone has been found to be more effective in achieving complete remission at 24 months than prednisone alone.14 In patients with contraindications to systemic glucocorticoid therapy, rituximab has been shown as an effective first-line therapy.15 One-quarter of patients treated with rituximab relapsed within 2 years of treatment6 (average time to relapse, 6–26 months).16 High-dose rituximab regimens, along with a higher number of rituximab treatment cycles, have been shown to prolong time to relapse.6 Further, higher baseline levels of Dsg-1 antibody have been correlated to earlier relapse and can be used following rituximab therapy to monitor disease progression.6,16
The differential diagnosis for pemphigus foliaceous includes disseminated blastomycosis, hypertrophic lupus erythematosus, sebopsoriasis, and secondary syphilis. Disseminated blastomycosis presents with cutaneous manifestations such as nodules, papules, or pustules evolving over weeks to months into ulcers with subsequent scarring.17 Hypertrophic lupus erythematosus presents with papules and nodules with associated keratotic scaling on the face, palms, and extensor surfaces of the limbs.18 Sebopsoriasis is characterized by well-defined lesions with an overlying scale distributed on the scalp, face, and chest.19 Secondary syphilis presents as early hyperpigmented macules transitioning to acral papulosquamous lesions involving the palms and soles.20
- Hans-Filho G, Aoki V, Hans Bittner NR, et al. Fogo selvagem: endemic pemphigus foliaceus. An Bras Dermatol. 2018;93:638-650.
- Jenson KK, Burr DM, Edwards BC. Case report: reatment of refractory pemphigus foliaceus with rituximab. Practical Dermatology. February 2016:33-36. Accessed August 27, 2021. https://practicaldermatology.com/articles/2016-feb/case-report -treatment-of-refractory-pemphigus-foliaceus-with-rituximab -financial-matters-aad-asds-resources
- Amagai M, Hashimoto T, Green KJ, et al. Antigen-specific immunoadsorption of pathogenic autoantibodies in pemphigus foliaceus. J Invest Dermatol. 1995;104:895-901.
- Mahoney MG, Wang Z, Rothenberger K, et al. Explanations for the clinical and microscopic localization of lesions in pemphigus foliaceus and vulgaris. J Clin Invest. 1999;103:461-468.
- Oktarina DAM, Sokol E, Kramer D, et al. Endocytosis of IgG, desmoglein 1, and plakoglobin in pemphigus foliaceus patient skin. Front Immunol. 2019;10:1-12.
- Kraft M, Worm M. Pemphigus foliaceus-repeated treatment with rituximab 7 years after initial response: a case report. Front Med. 2018;5:315.
- Hale EK. Pemphigus foliaceous. Dermatol Online J. 2002;8:9.
- Tavakolpour S. Pemphigus trigger factors: special focus on pemphigus vulgaris and pemphigus foliaceus. Arch Dermatol Res. 2018;310:95-106.
- A boobaker J, Morar N, Ramdial PK, et al. Pemphigus in South Africa. Int J Dermatol. 2001;40:115-119.
- Austin E, Millsop JW, Ely H, et al. Psoriasiform pemphigus foliaceus in an African American female: an important clinical manifestation. J Drugs Dermatol. 2018;17:471.
- Arbache ST, Nogueira TG, Delgado L, et al. Immunofluorescence testing in the diagnosis of autoimmune blistering diseases: overview of 10-year experience. An Bras Dermatol. 2014;89:885-889.
- Sabolinski ML, Beutner EH, Krasny S, et al. Substrate specificity of antiepithelial antibodies of pemphigus vulgaris and pemphigus foliaceus sera in immunofluorescence tests on monkey and guinea pig esophagus sections. J Invest Dermatol. 1987;88:545-549.
- Palacios-Álvarez I, Riquelme-McLoughlin C, Curto-Barredo L, et al. Rituximab treatment of pemphigus foliaceus: a retrospective study of 12 patients. J Am Acad Dermatol. 2021;85:484-486.
- Murrell DF, Sprecher E. Rituximab and short-course prednisone as the new gold standard for new-onset pemphigus vulgaris and pemphigus foliaceus. Br J Dermatol. 2017;177:1143-1144.
- Gregoriou S, Efthymiou O, Stefanaki C, et al. Management of pemphigus vulgaris: challenges and solutions. Clin Cosmet Investig Dermatol. 2015;8:521-527.
- Saleh MA. A prospective study comparing patients with early and late relapsing pemphigus treated with rituximab. J Am Acad Dermatol. 2018;79:97-103.
- Castillo CG, Kauffman CA, Miceli MH. Blastomycosis. Infect Dis Clin North Am. 2016;30:247-264.
- Herzum A, Gasparini G, Emanuele C, et al. Atypical and rare forms of cutaneous lupus erythematosus: the importance of the diagnosis for the best management of patients. Dermatology. 2013;1-10.
- Tull TJ, Noy M, Bunker CB, et al. Sebopsoriasis in patients with HIV: a case series of 20 patients. Br J Dermatol. 2016; 173:813-815.
- Balagula Y, Mattei P, Wisco OJ, et al. The great imitator revised: the spectrum of atypical cutaneous manifestations of secondary syphilis. Int J Dermatol. 2014;53:1434-1441.
- Hans-Filho G, Aoki V, Hans Bittner NR, et al. Fogo selvagem: endemic pemphigus foliaceus. An Bras Dermatol. 2018;93:638-650.
- Jenson KK, Burr DM, Edwards BC. Case report: reatment of refractory pemphigus foliaceus with rituximab. Practical Dermatology. February 2016:33-36. Accessed August 27, 2021. https://practicaldermatology.com/articles/2016-feb/case-report -treatment-of-refractory-pemphigus-foliaceus-with-rituximab -financial-matters-aad-asds-resources
- Amagai M, Hashimoto T, Green KJ, et al. Antigen-specific immunoadsorption of pathogenic autoantibodies in pemphigus foliaceus. J Invest Dermatol. 1995;104:895-901.
- Mahoney MG, Wang Z, Rothenberger K, et al. Explanations for the clinical and microscopic localization of lesions in pemphigus foliaceus and vulgaris. J Clin Invest. 1999;103:461-468.
- Oktarina DAM, Sokol E, Kramer D, et al. Endocytosis of IgG, desmoglein 1, and plakoglobin in pemphigus foliaceus patient skin. Front Immunol. 2019;10:1-12.
- Kraft M, Worm M. Pemphigus foliaceus-repeated treatment with rituximab 7 years after initial response: a case report. Front Med. 2018;5:315.
- Hale EK. Pemphigus foliaceous. Dermatol Online J. 2002;8:9.
- Tavakolpour S. Pemphigus trigger factors: special focus on pemphigus vulgaris and pemphigus foliaceus. Arch Dermatol Res. 2018;310:95-106.
- A boobaker J, Morar N, Ramdial PK, et al. Pemphigus in South Africa. Int J Dermatol. 2001;40:115-119.
- Austin E, Millsop JW, Ely H, et al. Psoriasiform pemphigus foliaceus in an African American female: an important clinical manifestation. J Drugs Dermatol. 2018;17:471.
- Arbache ST, Nogueira TG, Delgado L, et al. Immunofluorescence testing in the diagnosis of autoimmune blistering diseases: overview of 10-year experience. An Bras Dermatol. 2014;89:885-889.
- Sabolinski ML, Beutner EH, Krasny S, et al. Substrate specificity of antiepithelial antibodies of pemphigus vulgaris and pemphigus foliaceus sera in immunofluorescence tests on monkey and guinea pig esophagus sections. J Invest Dermatol. 1987;88:545-549.
- Palacios-Álvarez I, Riquelme-McLoughlin C, Curto-Barredo L, et al. Rituximab treatment of pemphigus foliaceus: a retrospective study of 12 patients. J Am Acad Dermatol. 2021;85:484-486.
- Murrell DF, Sprecher E. Rituximab and short-course prednisone as the new gold standard for new-onset pemphigus vulgaris and pemphigus foliaceus. Br J Dermatol. 2017;177:1143-1144.
- Gregoriou S, Efthymiou O, Stefanaki C, et al. Management of pemphigus vulgaris: challenges and solutions. Clin Cosmet Investig Dermatol. 2015;8:521-527.
- Saleh MA. A prospective study comparing patients with early and late relapsing pemphigus treated with rituximab. J Am Acad Dermatol. 2018;79:97-103.
- Castillo CG, Kauffman CA, Miceli MH. Blastomycosis. Infect Dis Clin North Am. 2016;30:247-264.
- Herzum A, Gasparini G, Emanuele C, et al. Atypical and rare forms of cutaneous lupus erythematosus: the importance of the diagnosis for the best management of patients. Dermatology. 2013;1-10.
- Tull TJ, Noy M, Bunker CB, et al. Sebopsoriasis in patients with HIV: a case series of 20 patients. Br J Dermatol. 2016; 173:813-815.
- Balagula Y, Mattei P, Wisco OJ, et al. The great imitator revised: the spectrum of atypical cutaneous manifestations of secondary syphilis. Int J Dermatol. 2014;53:1434-1441.

A 40-year-old Black man presented for evaluation of a thick plaque throughout the scalp (top), scaly plaques on the cheeks (bottom), and a spreading rash on the trunk that had progressed over the last few months. He had no relevant medical history, took no medications, and was in a monogamous relationship with a female partner. He previously saw an outside dermatologist who gave him triamcinolone cream, which was mildly helpful. Physical examination revealed a thick verrucous plaque throughout the scalp extending onto the forehead; thick plaques on the cheeks; and numerous, thinly eroded lesions on the trunk. Biopsies and a laboratory workup were performed.