User login
Metabolites implicated in CHD development in African Americans
Selected metabolic biomarkers may influence disease risk and progression in African American and White persons in different ways, a cohort study of the landmark Jackson Heart Study has found.
The investigators identified 22 specific metabolites that seem to influence incident CHD risk in African American patients – 13 metabolites that were also replicated in a multiethnic population and 9 novel metabolites that include N-acylamides and leucine, a branched-chain amino acid.
“To our knowledge, this is the first time that an N-acylamide as a class of molecule has been shown to be associated with incident coronary heart disease,” lead study author Daniel E. Cruz, MD, an instructor at Harvard Medical School in the division of cardiovascular medicine at Beth Israel Deaconess Medical Center in Boston, said in an interview.
The researchers analyzed targeted plasma metabolomic profiles of 2,346 participants in the Jackson Heart Study, a prospective population-based cohort study in the Mississippi city that included 5,306 African American patients evaluated over 15 years. They then performed a replication analysis of CHD-associated metabolites among 1,588 multiethnic participants in the Women’s Health Initiative, another population-based cohort study that included 161,808 postmenopausal women, also over 15 years. In all, the study, published in JAMA Cardiology, identified 46 metabolites that were associated with incident CHD up to 16 years before the incident event
Dr. Cruz said the “most interesting” findings were the roles of the N-acylamide linoleoyl ethanolamide and leucine. The former is of interest “because it is a lipid-signaling molecule that has been shown to have anti-inflammatory effects on macrophages; the influence and effects on macrophages are of particular interest because of macrophages’ central role in atherosclerosis and coronary heart disease,” he said.
Leucine draws interest because, in this study population, it was linked to a reduced risk of incident CHD. The researchers cited four previous studies in predominantly non-Hispanic White populations that found no association between branched-chain amino acids and incident CHD in Circulation, Stroke Circulation: Genomic and Precision Medicine, and Atherosclerosis. Other branched-amino acids included in the analysis trended toward a decreased risk of CHD, but those didn’t achieve the same statistical significance as that of leucine, Dr. Cruz said.
“In some of the analyses we did, there was a subset of metabolites that the associations with CHD appeared to be different between self-identified African Americans in the Jackson cohort vs. self-identified non-Hispanic Whites, and leucine was one of them,” Dr. Cruz said.
He emphasized that this study “is not a genetic analysis” because the participants self-identified their race. “So our next step is to figure out why this difference appears between these self-identified groups,” Dr. Cruz said. “We suspect environmental factors play a role – psychological stress, diet, income level, to name a few – but we are also interested to see if there are genetic causes.”
The results “are not clinically applicable,” Dr. Cruz said, but they do point to a need for more ethnically and racially diverse study populations. “The big picture is that, before we go implementing novel biomarkers into clinical practice, we need to make sure that they are accurate across different populations of people,” he said. “The only way to do this is to study different groups with the same rigor and vigor and thoughtfulness as any other group.”
These findings fall in line with other studies that found other nonmetabolomic biomarkers have countervailing effects on CHD risk in African Americans and non-Hispanic Whites, said Christie M. Ballantyne, MD, chief of cardiology at Baylor College of Medicine in Houston. For example, African Americans have been found to have lower triglyceride and HDL cholesterol levels than those of Whites.
The study “points out that there may be important biological differences in the metabolic pathways and abnormalities in the development of CHD between races,” Dr. Ballantyne said. “This further emphasizes both the importance and challenge of testing therapies in multiple racial/ethnic groups and with more even representation between men and women.”
Combining metabolomic profiling along with other biomarkers and possibly genetics may be helpful to “personalize” therapies in the future, he added.
Dr. Cruz and Dr. Ballantyne have no relevant relationships to disclose.
Selected metabolic biomarkers may influence disease risk and progression in African American and White persons in different ways, a cohort study of the landmark Jackson Heart Study has found.
The investigators identified 22 specific metabolites that seem to influence incident CHD risk in African American patients – 13 metabolites that were also replicated in a multiethnic population and 9 novel metabolites that include N-acylamides and leucine, a branched-chain amino acid.
“To our knowledge, this is the first time that an N-acylamide as a class of molecule has been shown to be associated with incident coronary heart disease,” lead study author Daniel E. Cruz, MD, an instructor at Harvard Medical School in the division of cardiovascular medicine at Beth Israel Deaconess Medical Center in Boston, said in an interview.
The researchers analyzed targeted plasma metabolomic profiles of 2,346 participants in the Jackson Heart Study, a prospective population-based cohort study in the Mississippi city that included 5,306 African American patients evaluated over 15 years. They then performed a replication analysis of CHD-associated metabolites among 1,588 multiethnic participants in the Women’s Health Initiative, another population-based cohort study that included 161,808 postmenopausal women, also over 15 years. In all, the study, published in JAMA Cardiology, identified 46 metabolites that were associated with incident CHD up to 16 years before the incident event
Dr. Cruz said the “most interesting” findings were the roles of the N-acylamide linoleoyl ethanolamide and leucine. The former is of interest “because it is a lipid-signaling molecule that has been shown to have anti-inflammatory effects on macrophages; the influence and effects on macrophages are of particular interest because of macrophages’ central role in atherosclerosis and coronary heart disease,” he said.
Leucine draws interest because, in this study population, it was linked to a reduced risk of incident CHD. The researchers cited four previous studies in predominantly non-Hispanic White populations that found no association between branched-chain amino acids and incident CHD in Circulation, Stroke Circulation: Genomic and Precision Medicine, and Atherosclerosis. Other branched-amino acids included in the analysis trended toward a decreased risk of CHD, but those didn’t achieve the same statistical significance as that of leucine, Dr. Cruz said.
“In some of the analyses we did, there was a subset of metabolites that the associations with CHD appeared to be different between self-identified African Americans in the Jackson cohort vs. self-identified non-Hispanic Whites, and leucine was one of them,” Dr. Cruz said.
He emphasized that this study “is not a genetic analysis” because the participants self-identified their race. “So our next step is to figure out why this difference appears between these self-identified groups,” Dr. Cruz said. “We suspect environmental factors play a role – psychological stress, diet, income level, to name a few – but we are also interested to see if there are genetic causes.”
The results “are not clinically applicable,” Dr. Cruz said, but they do point to a need for more ethnically and racially diverse study populations. “The big picture is that, before we go implementing novel biomarkers into clinical practice, we need to make sure that they are accurate across different populations of people,” he said. “The only way to do this is to study different groups with the same rigor and vigor and thoughtfulness as any other group.”
These findings fall in line with other studies that found other nonmetabolomic biomarkers have countervailing effects on CHD risk in African Americans and non-Hispanic Whites, said Christie M. Ballantyne, MD, chief of cardiology at Baylor College of Medicine in Houston. For example, African Americans have been found to have lower triglyceride and HDL cholesterol levels than those of Whites.
The study “points out that there may be important biological differences in the metabolic pathways and abnormalities in the development of CHD between races,” Dr. Ballantyne said. “This further emphasizes both the importance and challenge of testing therapies in multiple racial/ethnic groups and with more even representation between men and women.”
Combining metabolomic profiling along with other biomarkers and possibly genetics may be helpful to “personalize” therapies in the future, he added.
Dr. Cruz and Dr. Ballantyne have no relevant relationships to disclose.
Selected metabolic biomarkers may influence disease risk and progression in African American and White persons in different ways, a cohort study of the landmark Jackson Heart Study has found.
The investigators identified 22 specific metabolites that seem to influence incident CHD risk in African American patients – 13 metabolites that were also replicated in a multiethnic population and 9 novel metabolites that include N-acylamides and leucine, a branched-chain amino acid.
“To our knowledge, this is the first time that an N-acylamide as a class of molecule has been shown to be associated with incident coronary heart disease,” lead study author Daniel E. Cruz, MD, an instructor at Harvard Medical School in the division of cardiovascular medicine at Beth Israel Deaconess Medical Center in Boston, said in an interview.
The researchers analyzed targeted plasma metabolomic profiles of 2,346 participants in the Jackson Heart Study, a prospective population-based cohort study in the Mississippi city that included 5,306 African American patients evaluated over 15 years. They then performed a replication analysis of CHD-associated metabolites among 1,588 multiethnic participants in the Women’s Health Initiative, another population-based cohort study that included 161,808 postmenopausal women, also over 15 years. In all, the study, published in JAMA Cardiology, identified 46 metabolites that were associated with incident CHD up to 16 years before the incident event
Dr. Cruz said the “most interesting” findings were the roles of the N-acylamide linoleoyl ethanolamide and leucine. The former is of interest “because it is a lipid-signaling molecule that has been shown to have anti-inflammatory effects on macrophages; the influence and effects on macrophages are of particular interest because of macrophages’ central role in atherosclerosis and coronary heart disease,” he said.
Leucine draws interest because, in this study population, it was linked to a reduced risk of incident CHD. The researchers cited four previous studies in predominantly non-Hispanic White populations that found no association between branched-chain amino acids and incident CHD in Circulation, Stroke Circulation: Genomic and Precision Medicine, and Atherosclerosis. Other branched-amino acids included in the analysis trended toward a decreased risk of CHD, but those didn’t achieve the same statistical significance as that of leucine, Dr. Cruz said.
“In some of the analyses we did, there was a subset of metabolites that the associations with CHD appeared to be different between self-identified African Americans in the Jackson cohort vs. self-identified non-Hispanic Whites, and leucine was one of them,” Dr. Cruz said.
He emphasized that this study “is not a genetic analysis” because the participants self-identified their race. “So our next step is to figure out why this difference appears between these self-identified groups,” Dr. Cruz said. “We suspect environmental factors play a role – psychological stress, diet, income level, to name a few – but we are also interested to see if there are genetic causes.”
The results “are not clinically applicable,” Dr. Cruz said, but they do point to a need for more ethnically and racially diverse study populations. “The big picture is that, before we go implementing novel biomarkers into clinical practice, we need to make sure that they are accurate across different populations of people,” he said. “The only way to do this is to study different groups with the same rigor and vigor and thoughtfulness as any other group.”
These findings fall in line with other studies that found other nonmetabolomic biomarkers have countervailing effects on CHD risk in African Americans and non-Hispanic Whites, said Christie M. Ballantyne, MD, chief of cardiology at Baylor College of Medicine in Houston. For example, African Americans have been found to have lower triglyceride and HDL cholesterol levels than those of Whites.
The study “points out that there may be important biological differences in the metabolic pathways and abnormalities in the development of CHD between races,” Dr. Ballantyne said. “This further emphasizes both the importance and challenge of testing therapies in multiple racial/ethnic groups and with more even representation between men and women.”
Combining metabolomic profiling along with other biomarkers and possibly genetics may be helpful to “personalize” therapies in the future, he added.
Dr. Cruz and Dr. Ballantyne have no relevant relationships to disclose.
FROM JAMA CARDIOLOGY
Gender Disparities in Income Among Board-Certified Dermatologists
Although the number of female graduates from US medical schools has steadily increased,1 several studies since the 1970s indicate that a disparity exists in salary, academic rank, and promotion among female and male physicians across multiple specialties.2-8 Proposed explanations include women working fewer hours, having lower productivity rates, undernegotiating compensation, and underbilling for the same services. However, when controlling for variables such as time, experience, specialty, rank, and research activities, this gap unequivocally persists. There are limited data on this topic in dermatology, a field in which women comprise more than half of the working population.6,7 Most analyses of gender disparities in dermatology are based on data primarily from academic dermatologists, which may not be representative of the larger population of dermatologists.8,9 The purpose of this study is to determine if an income disparity exists between male and female physicians in dermatology, including those in private practice and those who are specialty trained.
Methods
Population—We performed a cross-sectional self-reported survey to examine compensation of male and female board-certified dermatologists (MDs/DOs). Several populations of dermatologists were surveyed in August and September 2018. Approximately 20% of the members of the American Academy of Dermatology were randomly selected and sent a link to the survey. Additionally, a survey link was emailed to members of the Association of Professors of Dermatology, American College of Mohs Surgery, and American Society for Dermatologic Surgery. A link to the survey also was published on “The Board Certified Dermatologists” Facebook group.
Statistical Analysis—Descriptive statistics were used to summarize the distribution of variables overall and within gender (male or female). Not all respondents completed every section, and duplicates and incomplete responses were removed. Variables were compared between genders using t tests (continuous), the Pearson χ2 test (nominal), or the Cochran-Mantel-Haenszel test (ordinal). For categorical variables with small cell counts, an exact χ2 test for small samples was used. For continuous variables, t test P values were calculated using either pooled or Satterthwaithe approximation.
To analyze the effect of different variables on total income using multivariate and univariate linear regression, the income variable was transformed into a continuous variable by using midpoints of the categories. Univariate linear regression was used to assess the effect and significance of each variable on total annual income. Variables that were found to have a P value of less than .05 (α=.05) were deemed as significant predictors of total annual income. These variables were added to a multivariate linear regression model to determine their effect on income when adjusting for other significant (and approaching significance) factors. In addition, variables that were found to have a P value of less than .2 (α=.05) were added to the multivariate linear regression model to assess significance of these specific variables when adjusting for other factors. In this way, we tested and accounted for a multitude of variables as potential sources of confounding.
Results
Demographics—Our survey was emailed to 3079 members of the American Academy of Dermatology, and 277 responses were received. Approximately 144 additional responses were obtained collectively from links sent to the directories of the Association of Professors of Dermatology, American College of Mohs Surgery, and American Society for Dermatologic Surgery and from social media. Of these respondents, 53.65% (213/397) were female and 46.35% (184/397) were male. When stratifying by race/ethnicity, 77.33% identified as White; 13.85% identified as Asian; 6.3% identified as Black or African American, Hispanic/Latino, and Native American; and 2.52% chose not to respond. Although most male and female respondents were White, a significantly higher proportion of female respondents identified as Asian or Black/African American/Hispanic/Latino/Native American (P=.0006). We found that race/ethnicity did not significantly impact income (P=.2736). All US Census regions were represented in this study, and geographic distribution as well as population density of practice location (ie, rural, suburban, urban setting) did not differ significantly between males and females (P=.5982 and P=.1007, respectively) and did not significantly impact income (P=.3225 and P=.10663, respectively).

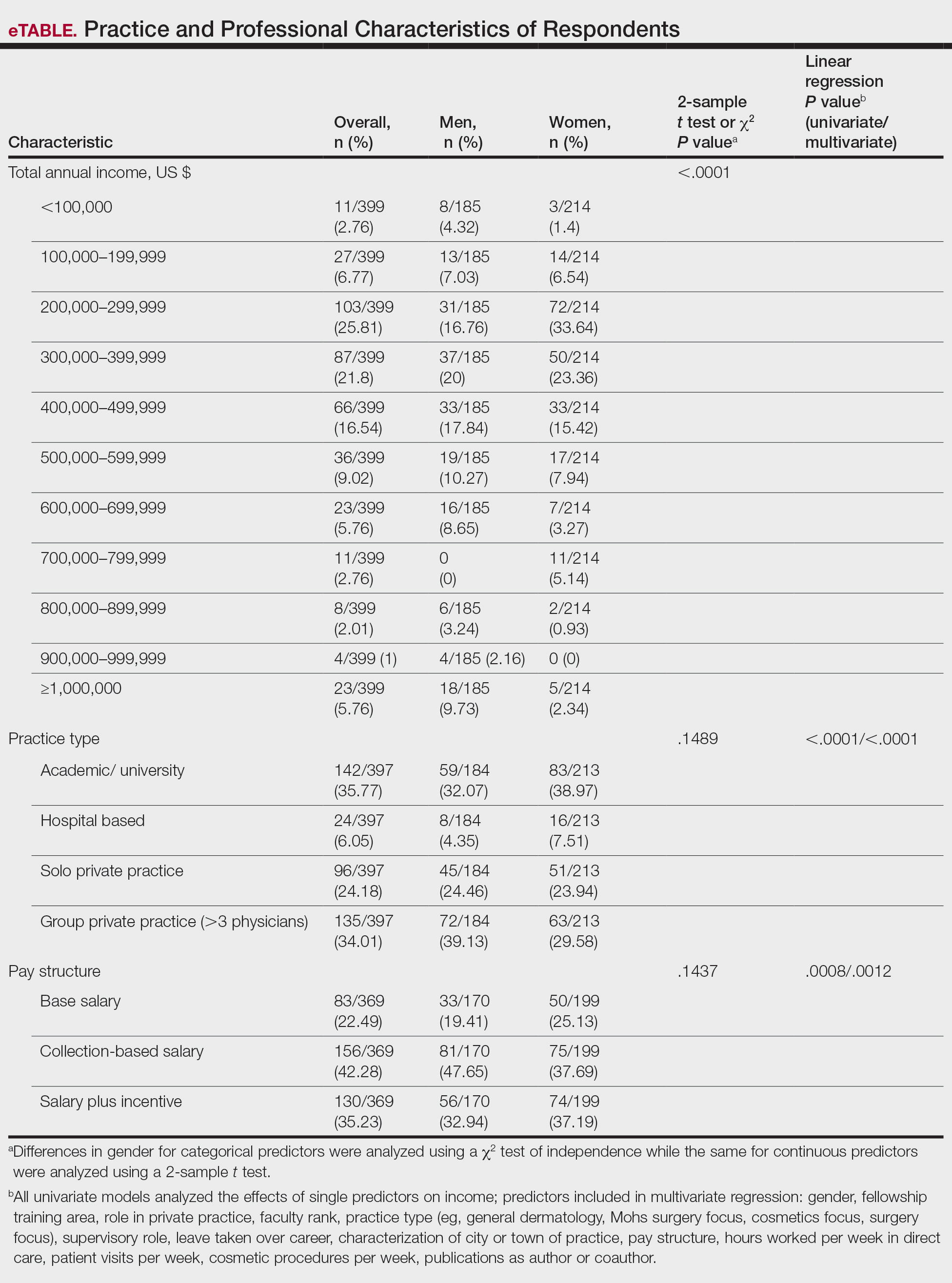
Income—Total annual income was defined as the aggregate sum of all types of financial compensation received in 1 calendar year (eg, salary, bonuses, benefits) and was elicited as an ordinal variable in income brackets of US $100,000. Overall, χ2 analysis showed a statistically significant difference in annual total income between male and female dermatologists (P<.0001), with a higher proportion of males in the highest pay bracket (Figure). Gender remained a statistically significant predictor of income on both univariate and multivariate linear regression analyses (P=.0002 and P<.0001, respectively), indicating that gender has a significant impact on compensation, even after controlling for other variables (eTable). Of note, males in this sample were on average older and in practice longer than females (approximately 6 years, P<.0001). However, when univariate linear regression was performed, both age (P=.8281) and number of years since residency or fellowship completion (P=.8743) were not significant predictors of income.
Practice Type—There were no statistically significant differences between men and women in practice type (P=.1489), including academic/university, hospital based, and solo and group private practice; pay structure (P=.1437), including base salary, collection-based salary, or salary plus incentive; holding a supervisory role (P=.0846); or having ownership of a practice (P=.3565)(eTable). Most respondents were in solo or group private practice (58.2%) and had a component of productivity-based compensation (77.5%). In addition, 62% of private practice dermatologists (133/212) had an ownership interest in their practice. As expected, univariate and multivariate regression analyses showed that practice type, pay structure, supervisory roles, and employee vs ownership roles were significant predictors of income (P<.05)(eTable).
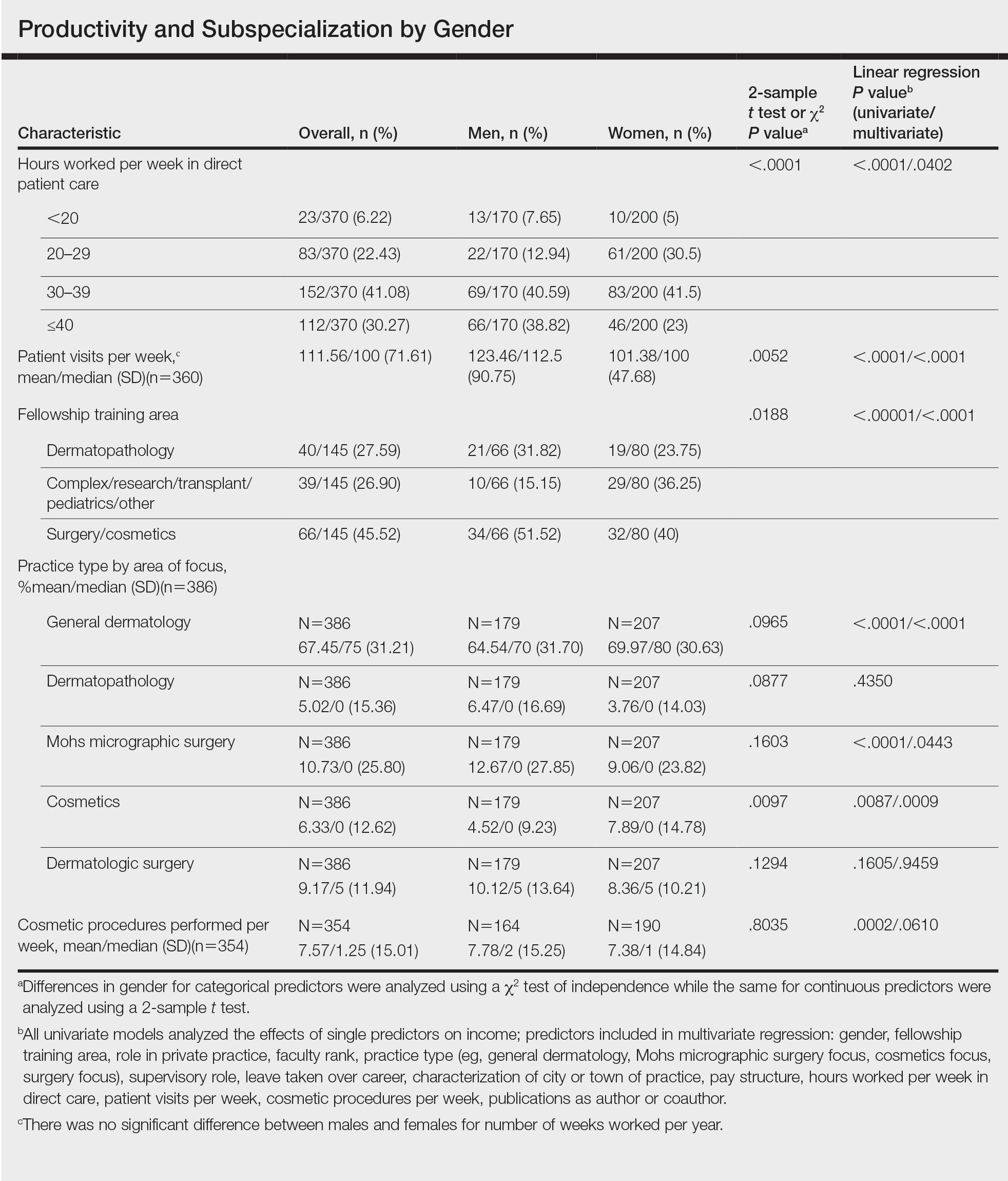
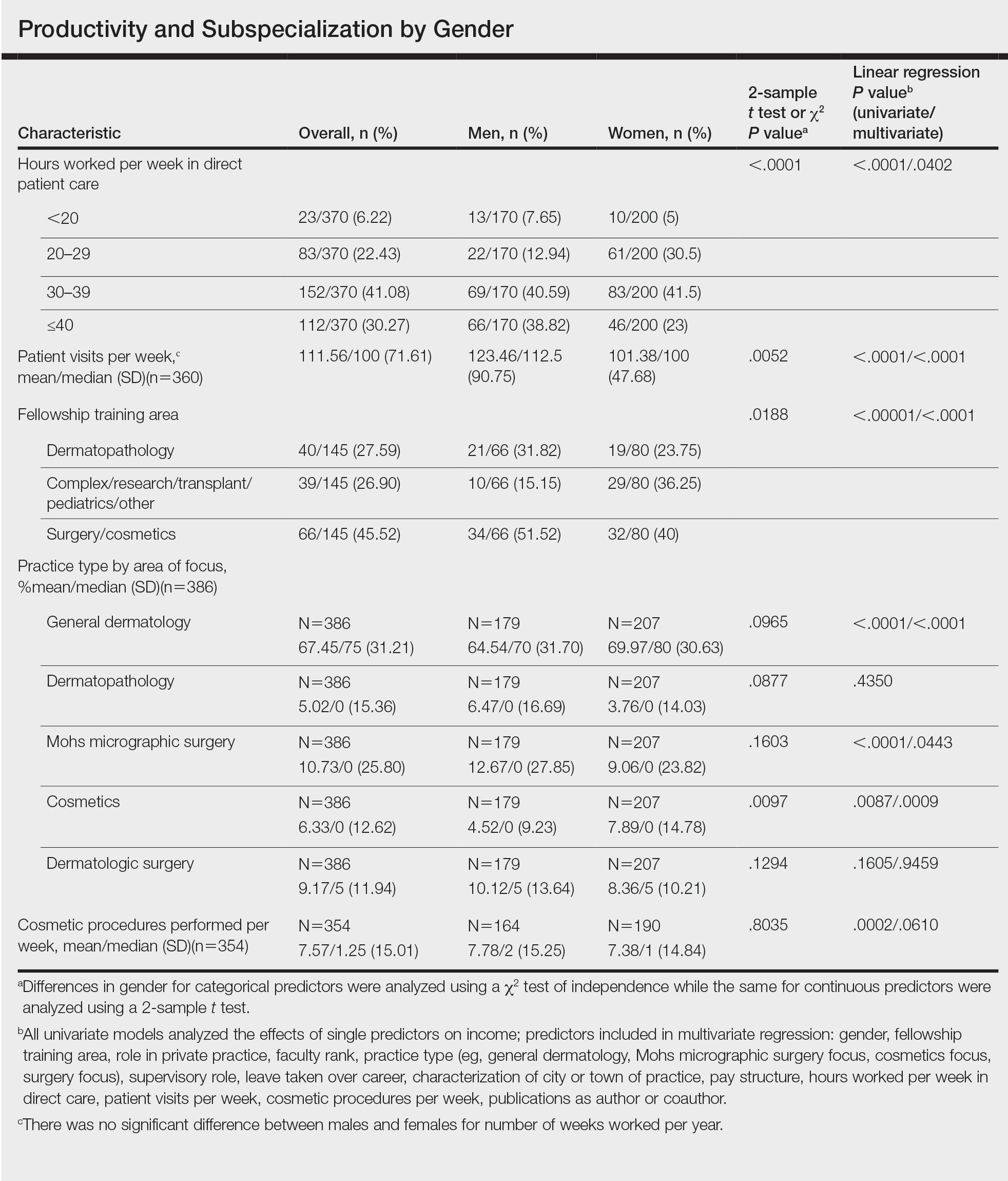
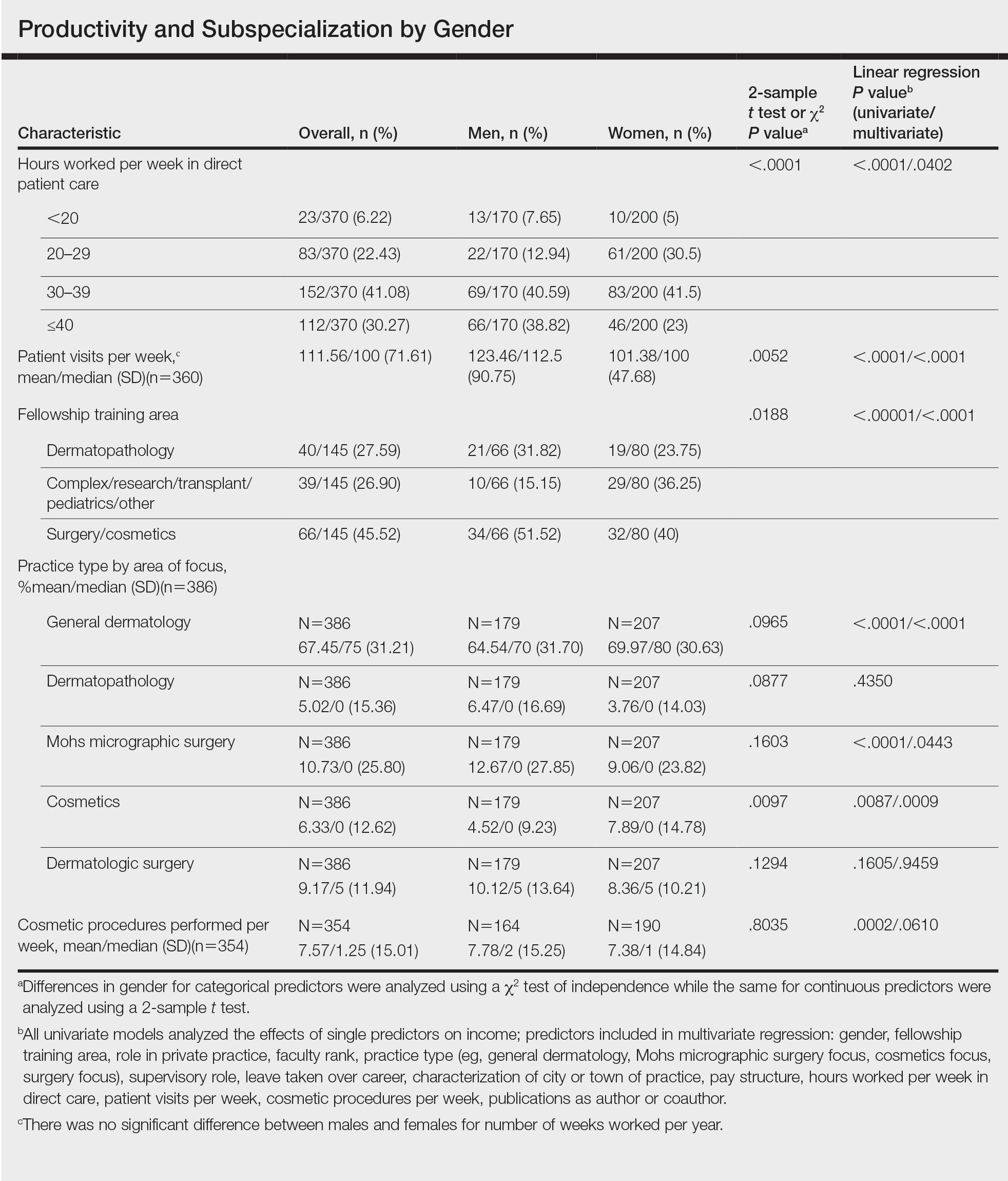
Work Productivity—Statistically significant differences were found between men and women in hours worked per week in direct patient care (P<.0001) and in patient visits per week (P=.0052), with a higher percentage of men working more than 40 hours per week and men seeing an average of approximately 22 more patients per week than women. In the subgroup of all dermatologists working more than 40 hours per week, a statistically significant difference in income persisted between males and females (P=.0001). Hours worked per week and patient visits per week were statistically significant predictors of income on both univariate and multivariate regression analyses (P<.05)(Table).
Education and Fellowship Training—No significant difference existed between males and females in type of undergraduate school attended, namely public or private institutions (P=.1090), but a significant difference existed within type of medical school education, with a higher percentage of females attending private medical schools (53.03%) compared to males (38.24%)(P=.0045). However, type of undergraduate or medical school attended had no impact on income (P=.9103). A higher percentage of males (27.32%) completed additional advanced degrees, such as a master of business administration or a master of public health, compared to females (16.9%)(P=.0122). However, the completion of additional advanced degrees had no significant impact on income (P=.2379). No statistical significance existed between males and females in number of residencies completed (P=.3236), and residencies completed had no significant impact on income (P=.4584).
Of 397 respondents, approximately one-third of respondents completed fellowship training (36.5%). Fellowships included dermatopathology, surgery/cosmetics, and other (encompassing complex medical, research, transplant, and pediatric dermatology). Although similar percentages of men and women completed fellowship training, men and women differed significantly by type of fellowship completed (P=.0188). There were similar rates of dermatopathology and surgical fellowship completion between genders but almost 3 times the number of females who completed other fellowships. Type of fellowship training was a statistically significant predictor of income on both univariate and multivariate regression analyses (P<.00001 and P<.0001, respectively).
Work Activity—Respondents were asked to estimate the amount of time devoted to general dermatology, dermatopathology, Mohs micrographic surgery, cosmetics, and dermatologic surgery in their practices (Table). Women devoted a significantly higher average percentage of time to cosmetics (7.89%) compared to men (4.52%)(P=.0097). The number of cosmetic procedures performed per week was not statistically significantly different between men and women (P=.8035) but was a significant factor for income on univariate regression analysis (P=.0002). Time spent performing dermatologic surgery, general dermatology, or Mohs micrographic surgery did not significantly differ between men and women but was found to significantly influence income.
Academic Dermatology—Among the respondents working in academic settings, χ2 analysis identified a significant difference in the faculty rank between males and females, with a tendency for lower academic rank in females (P=.0508). Assistant professorship was comprised of 35% of men vs 51% of women, whereas full professorship consisted of 26% of men but only 13% of women. Academic rank was found to be a significant predictor of income, with higher rank associated with higher income (P<.0001 on univariate regression analysis). However, when adjusting for other factors, academic rank was no longer a significant predictor of income (P=.0840 on multivariate regression analysis). No significant difference existed between men and women in funding received from the National Institutes of Health, conduction of clinical trials, or authorship of scientific publications, and these factors were not found to have a significant impact on income.
Work Leave—Male and female dermatologists showed a statistically significant difference in maternity or Family and Medical Leave Act (FMLA) leave taken over their careers, with 56.03% of females reporting leave taken compared to 6.78% of males (P<.0001). Women reported a significantly higher average number of weeks of maternity or FMLA leave taken over their careers (12.92 weeks) compared to men (2.42 weeks) (P<.0001). However, upon univariate regression analysis, whether or not maternity or FMLA leave was taken over their careers (P=.2005), the number of times that maternity or FMLA leave was taken (P=.4350), and weeks of maternity or FMLA leave taken (P=.4057) were all not significant predictors of income.
Comment
This study sought to investigate the relationship between income and gender in dermatology, and our results demonstrated that statistically significant differences in total annual income exist between male and female dermatologists, with male dermatologists earning a significantly higher income, approximately an additional $80,000. Our results are consistent with other studies of US physician income, which have found a gender gap ranging from $13,399 to $82,000 that persists even when controlling for factors such as specialty choice, practice setting, rank and role in practice, work hours, vacation/leave taken, and others.2-7,10-15
There was a significant difference in rank of male and female academic dermatologists, with fewer females at higher academic ranks. These results are consistent with numerous studies in academic dermatology that show underrepresentation of women at higher academic ranks and leadership positions.8,9,16-18 Poor negotiation may contribute to differences in both rank and income.19,20 There are conflicting data on research productivity of academic dermatologists and length of career, first and senior authorship, and quality and academic impact, all of which add complexity to this topic.8,9,12,16-18,20-23Male and female dermatologists reported significant differences in productivity, with male dermatologists working more hours and seeing more patients per week than female dermatologists. These results are consistent with other studies of dermatologists4,24 and other physicians.12 Regardless, gender was still found to have a significant impact on income even when controlling for differences in productivity and FMLA leave taken. These results are consistent with numerous studies of US physicians that found a gender gap in income even when controlling for hours worked.12,23 Although fellowship training as a whole was found to significantly impact income, our results do not characterize whether the impact on income was positive or negative for each type of fellowship. Fellowship training in specialties such as internal medicine or general surgery likewise has variable effects on income.24,25
A comprehensive survey design and significant data elicited from dermatologists working in private practice for the first time served as the main strengths of this study. Limitations included self-reported design, categorical ranges, and limited sample size in subgroups. Future directions include deeper analysis of subgroups, including fellowship-trained dermatologists, dermatologists working more than 40 hours per week, and female dermatologists by race/ethnicity.
Conclusion
We have demonstrated that self-reported discrepancies in salary between male and female dermatologists exist, with male dermatologists earning a significantly higher annual salary than their female counterparts. This study identified and stratified several career factors that comprise the broad field and practice of dermatology. Even when controlling for these variations, we have demonstrated that gender alone remains a significant predictor of income, indicating that an unexplained income gap between the 2 genders exists in dermatology.
- Association of American Medical Colleges. Table B-2.2: Total Graduates by U.S. Medical School and Sex, 2015-2016 through 2019-2020. December 3, 2020. Accessed October 12, 2021. https://www.aamc.org/download/321532/data/factstableb2-2.pdf
- Willett LL, Halvorsen AJ, McDonald FS, et al. Gender differences in salary of internal medicine residency directors: a national survey. Am J Med. 2015;128:659-665.
- Weeks WB, Wallace AE, Mackenzie TA. Gender differences in anesthesiologists’ annual incomes. Anesthesiology. 2007;106:806-811.
- Weeks WB, Wallace AE. Gender differences in ophthalmologists’ annual incomes. Ophthalmology. 2007;114:1696-1701.
- Singh A, Burke CA, Larive B, et al. Do gender disparities persist in gastroenterology after 10 years of practice? Am J Gastroenterol. 2008;103:1589-1595.
- Desai T, Ali S, Fang X, et al. Equal work for unequal pay: the gender reimbursement gap for healthcare providers in the United States. Postgrad Med J. 2016;92:571-575.
- Jena AB, Olenski AR, Blumenthal DM. Sex differences in physician salary in US public medical schools. JAMA Intern Med. 2016;176:1294-1304.
- John AM, Gupta AB, John ES, et al. A gender-based comparison of promotion and research productivity in academic dermatology. Dermatol Online J. 2016;22:13030/qt1hx610pf.
- Sadeghpour M, Bernstein I, Ko C, et al. Role of sex in academic dermatology: results from a national survey. Arch Dermatol. 2012;148:809-814.
- Gilbert SB, Allshouse A, Skaznik-Wikiel ME. Gender inequality in salaries among reproductive endocrinology and infertility subspecialists in the United States. Fertil Steril. 2019;111:1194-1200.
- Jagsi R, Griffith KA, Stewart A, et al. Gender differences in the salaries of physician researchers. JAMA. 2012;307:2410-2417. doi:10.1001/jama.2012.6183
- Apaydin EA, Chen PGC, Friedberg MW, et al. Differences in physician income by gender in a multiregion survey. J Gen Intern Med. 2018;33:1574-1581.
- Read S, Butkus R, Weissman A, et al. Compensation disparities by gender in internal medicine. Ann Intern Med. 2018;169:658-661.
- Guss ZD, Chen Q, Hu C, et al. Differences in physician compensation between men and women at United States public academic radiation oncology departments. Int J Radiat Oncol Biol Phys. 2019;103:314-319.
- Lo Sasso AT, Richards MR, Chou CF, et al. The $16,819 pay gap for newly trained physicians: the unexplained trend of men earning more than women. Health Aff (Millwood). 2011;30:193-201.
- Shah A, Jalal S, Khosa F. Influences for gender disparity in dermatology in North America. Int J Dermatol. 2018;57:171-176.
- Shi CR, Olbricht S, Vleugels RA, et al. Sex and leadership in academic dermatology: a nationwide survey. J Am Acad Dermatol. 2017;77:782-784.
- Shih AF, Sun W, Yick C, et al. Trends in scholarly productivity of dermatology faculty by academic status and gender. J Am Acad Dermatol. 2019;80:1774-1776.
- Sarfaty S, Kolb D, Barnett R, et al. Negotiation in academic medicine: a necessary career skill. J Womens Health (Larchmt). 2007;16:235-244.
- Jacobson CC, Nguyen JC, Kimball AB. Gender and parenting significantly affect work hours of recent dermatology program graduates. Arch Dermatol. 2004;140:191-196.
- Feramisco JD, Leitenberger JJ, Redfern SI, et al. A gender gap in the dermatology literature? Cross-sectional analysis of manuscript authorship trends in dermatology journals during 3 decades. J Am Acad Dermatol. 2009;60:63-69.
- Bendels MHK, Dietz MC, Brüggmann D, et al. Gender disparities in high-quality dermatology research: a descriptive bibliometric study on scientific authorships. BMJ Open. 2018;8:e020089.
- Seabury SA, Chandra A, Jena AB. Trends in the earnings of male and female health care professionals in the United States, 1987 to 2010. JAMA Intern Med. 2013;173:1748-1750.
- Baimas-George M, Fleischer B, Slakey D, et al. Is it all about the money? Not all surgical subspecialization leads to higher lifetime revenue when compared to general surgery. J Surg Educ. 2017;74:E62-E66.
- Leigh JP, Tancredi D, Jerant A, et al. Lifetime earnings for physicians across specialties. Med Care. 2012;50:1093-1101.
Although the number of female graduates from US medical schools has steadily increased,1 several studies since the 1970s indicate that a disparity exists in salary, academic rank, and promotion among female and male physicians across multiple specialties.2-8 Proposed explanations include women working fewer hours, having lower productivity rates, undernegotiating compensation, and underbilling for the same services. However, when controlling for variables such as time, experience, specialty, rank, and research activities, this gap unequivocally persists. There are limited data on this topic in dermatology, a field in which women comprise more than half of the working population.6,7 Most analyses of gender disparities in dermatology are based on data primarily from academic dermatologists, which may not be representative of the larger population of dermatologists.8,9 The purpose of this study is to determine if an income disparity exists between male and female physicians in dermatology, including those in private practice and those who are specialty trained.
Methods
Population—We performed a cross-sectional self-reported survey to examine compensation of male and female board-certified dermatologists (MDs/DOs). Several populations of dermatologists were surveyed in August and September 2018. Approximately 20% of the members of the American Academy of Dermatology were randomly selected and sent a link to the survey. Additionally, a survey link was emailed to members of the Association of Professors of Dermatology, American College of Mohs Surgery, and American Society for Dermatologic Surgery. A link to the survey also was published on “The Board Certified Dermatologists” Facebook group.
Statistical Analysis—Descriptive statistics were used to summarize the distribution of variables overall and within gender (male or female). Not all respondents completed every section, and duplicates and incomplete responses were removed. Variables were compared between genders using t tests (continuous), the Pearson χ2 test (nominal), or the Cochran-Mantel-Haenszel test (ordinal). For categorical variables with small cell counts, an exact χ2 test for small samples was used. For continuous variables, t test P values were calculated using either pooled or Satterthwaithe approximation.
To analyze the effect of different variables on total income using multivariate and univariate linear regression, the income variable was transformed into a continuous variable by using midpoints of the categories. Univariate linear regression was used to assess the effect and significance of each variable on total annual income. Variables that were found to have a P value of less than .05 (α=.05) were deemed as significant predictors of total annual income. These variables were added to a multivariate linear regression model to determine their effect on income when adjusting for other significant (and approaching significance) factors. In addition, variables that were found to have a P value of less than .2 (α=.05) were added to the multivariate linear regression model to assess significance of these specific variables when adjusting for other factors. In this way, we tested and accounted for a multitude of variables as potential sources of confounding.
Results
Demographics—Our survey was emailed to 3079 members of the American Academy of Dermatology, and 277 responses were received. Approximately 144 additional responses were obtained collectively from links sent to the directories of the Association of Professors of Dermatology, American College of Mohs Surgery, and American Society for Dermatologic Surgery and from social media. Of these respondents, 53.65% (213/397) were female and 46.35% (184/397) were male. When stratifying by race/ethnicity, 77.33% identified as White; 13.85% identified as Asian; 6.3% identified as Black or African American, Hispanic/Latino, and Native American; and 2.52% chose not to respond. Although most male and female respondents were White, a significantly higher proportion of female respondents identified as Asian or Black/African American/Hispanic/Latino/Native American (P=.0006). We found that race/ethnicity did not significantly impact income (P=.2736). All US Census regions were represented in this study, and geographic distribution as well as population density of practice location (ie, rural, suburban, urban setting) did not differ significantly between males and females (P=.5982 and P=.1007, respectively) and did not significantly impact income (P=.3225 and P=.10663, respectively).

Income—Total annual income was defined as the aggregate sum of all types of financial compensation received in 1 calendar year (eg, salary, bonuses, benefits) and was elicited as an ordinal variable in income brackets of US $100,000. Overall, χ2 analysis showed a statistically significant difference in annual total income between male and female dermatologists (P<.0001), with a higher proportion of males in the highest pay bracket (Figure). Gender remained a statistically significant predictor of income on both univariate and multivariate linear regression analyses (P=.0002 and P<.0001, respectively), indicating that gender has a significant impact on compensation, even after controlling for other variables (eTable). Of note, males in this sample were on average older and in practice longer than females (approximately 6 years, P<.0001). However, when univariate linear regression was performed, both age (P=.8281) and number of years since residency or fellowship completion (P=.8743) were not significant predictors of income.
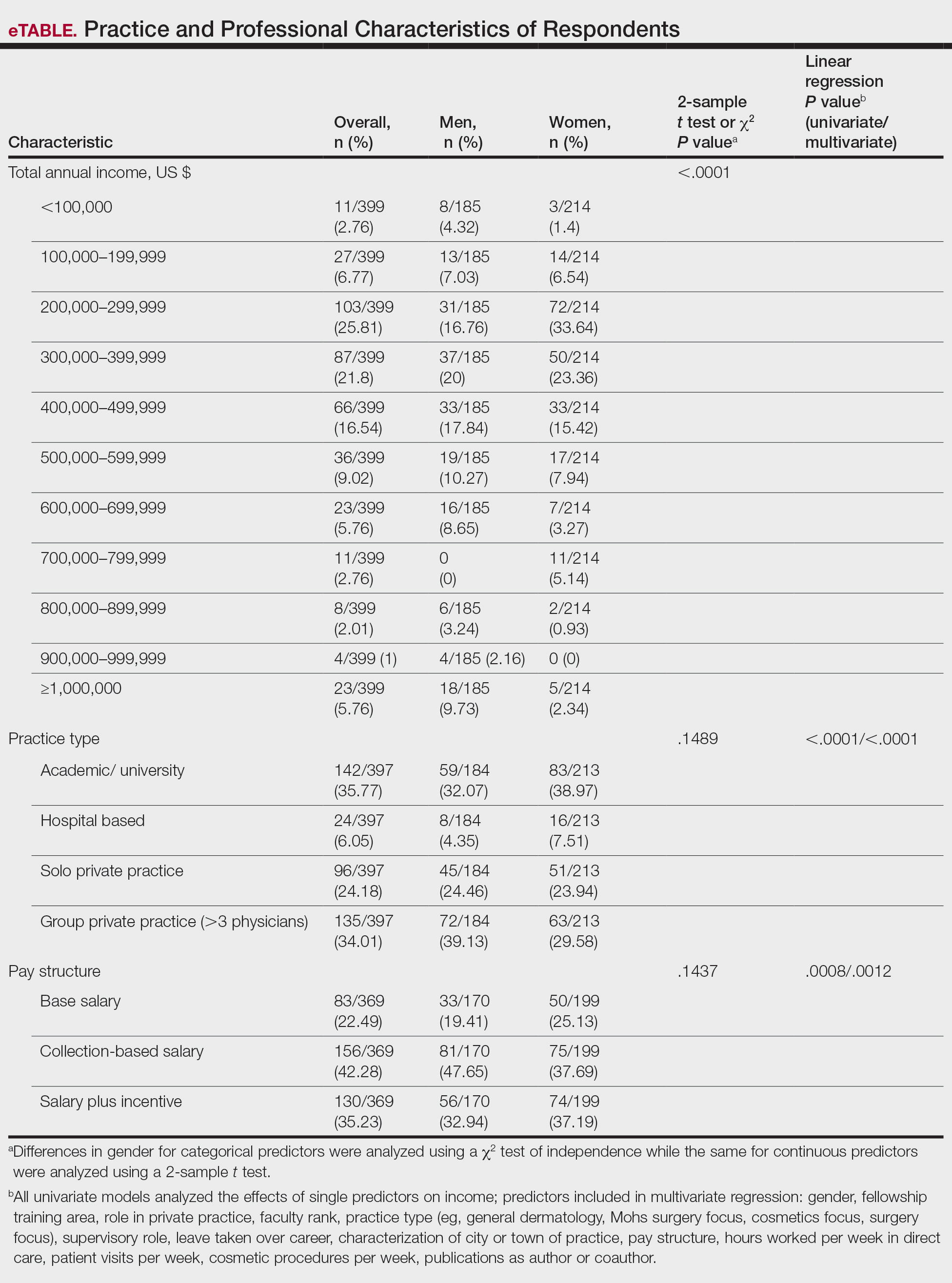
Practice Type—There were no statistically significant differences between men and women in practice type (P=.1489), including academic/university, hospital based, and solo and group private practice; pay structure (P=.1437), including base salary, collection-based salary, or salary plus incentive; holding a supervisory role (P=.0846); or having ownership of a practice (P=.3565)(eTable). Most respondents were in solo or group private practice (58.2%) and had a component of productivity-based compensation (77.5%). In addition, 62% of private practice dermatologists (133/212) had an ownership interest in their practice. As expected, univariate and multivariate regression analyses showed that practice type, pay structure, supervisory roles, and employee vs ownership roles were significant predictors of income (P<.05)(eTable).
Work Productivity—Statistically significant differences were found between men and women in hours worked per week in direct patient care (P<.0001) and in patient visits per week (P=.0052), with a higher percentage of men working more than 40 hours per week and men seeing an average of approximately 22 more patients per week than women. In the subgroup of all dermatologists working more than 40 hours per week, a statistically significant difference in income persisted between males and females (P=.0001). Hours worked per week and patient visits per week were statistically significant predictors of income on both univariate and multivariate regression analyses (P<.05)(Table).
Education and Fellowship Training—No significant difference existed between males and females in type of undergraduate school attended, namely public or private institutions (P=.1090), but a significant difference existed within type of medical school education, with a higher percentage of females attending private medical schools (53.03%) compared to males (38.24%)(P=.0045). However, type of undergraduate or medical school attended had no impact on income (P=.9103). A higher percentage of males (27.32%) completed additional advanced degrees, such as a master of business administration or a master of public health, compared to females (16.9%)(P=.0122). However, the completion of additional advanced degrees had no significant impact on income (P=.2379). No statistical significance existed between males and females in number of residencies completed (P=.3236), and residencies completed had no significant impact on income (P=.4584).
Of 397 respondents, approximately one-third of respondents completed fellowship training (36.5%). Fellowships included dermatopathology, surgery/cosmetics, and other (encompassing complex medical, research, transplant, and pediatric dermatology). Although similar percentages of men and women completed fellowship training, men and women differed significantly by type of fellowship completed (P=.0188). There were similar rates of dermatopathology and surgical fellowship completion between genders but almost 3 times the number of females who completed other fellowships. Type of fellowship training was a statistically significant predictor of income on both univariate and multivariate regression analyses (P<.00001 and P<.0001, respectively).
Work Activity—Respondents were asked to estimate the amount of time devoted to general dermatology, dermatopathology, Mohs micrographic surgery, cosmetics, and dermatologic surgery in their practices (Table). Women devoted a significantly higher average percentage of time to cosmetics (7.89%) compared to men (4.52%)(P=.0097). The number of cosmetic procedures performed per week was not statistically significantly different between men and women (P=.8035) but was a significant factor for income on univariate regression analysis (P=.0002). Time spent performing dermatologic surgery, general dermatology, or Mohs micrographic surgery did not significantly differ between men and women but was found to significantly influence income.
Academic Dermatology—Among the respondents working in academic settings, χ2 analysis identified a significant difference in the faculty rank between males and females, with a tendency for lower academic rank in females (P=.0508). Assistant professorship was comprised of 35% of men vs 51% of women, whereas full professorship consisted of 26% of men but only 13% of women. Academic rank was found to be a significant predictor of income, with higher rank associated with higher income (P<.0001 on univariate regression analysis). However, when adjusting for other factors, academic rank was no longer a significant predictor of income (P=.0840 on multivariate regression analysis). No significant difference existed between men and women in funding received from the National Institutes of Health, conduction of clinical trials, or authorship of scientific publications, and these factors were not found to have a significant impact on income.
Work Leave—Male and female dermatologists showed a statistically significant difference in maternity or Family and Medical Leave Act (FMLA) leave taken over their careers, with 56.03% of females reporting leave taken compared to 6.78% of males (P<.0001). Women reported a significantly higher average number of weeks of maternity or FMLA leave taken over their careers (12.92 weeks) compared to men (2.42 weeks) (P<.0001). However, upon univariate regression analysis, whether or not maternity or FMLA leave was taken over their careers (P=.2005), the number of times that maternity or FMLA leave was taken (P=.4350), and weeks of maternity or FMLA leave taken (P=.4057) were all not significant predictors of income.
Comment
This study sought to investigate the relationship between income and gender in dermatology, and our results demonstrated that statistically significant differences in total annual income exist between male and female dermatologists, with male dermatologists earning a significantly higher income, approximately an additional $80,000. Our results are consistent with other studies of US physician income, which have found a gender gap ranging from $13,399 to $82,000 that persists even when controlling for factors such as specialty choice, practice setting, rank and role in practice, work hours, vacation/leave taken, and others.2-7,10-15
There was a significant difference in rank of male and female academic dermatologists, with fewer females at higher academic ranks. These results are consistent with numerous studies in academic dermatology that show underrepresentation of women at higher academic ranks and leadership positions.8,9,16-18 Poor negotiation may contribute to differences in both rank and income.19,20 There are conflicting data on research productivity of academic dermatologists and length of career, first and senior authorship, and quality and academic impact, all of which add complexity to this topic.8,9,12,16-18,20-23Male and female dermatologists reported significant differences in productivity, with male dermatologists working more hours and seeing more patients per week than female dermatologists. These results are consistent with other studies of dermatologists4,24 and other physicians.12 Regardless, gender was still found to have a significant impact on income even when controlling for differences in productivity and FMLA leave taken. These results are consistent with numerous studies of US physicians that found a gender gap in income even when controlling for hours worked.12,23 Although fellowship training as a whole was found to significantly impact income, our results do not characterize whether the impact on income was positive or negative for each type of fellowship. Fellowship training in specialties such as internal medicine or general surgery likewise has variable effects on income.24,25
A comprehensive survey design and significant data elicited from dermatologists working in private practice for the first time served as the main strengths of this study. Limitations included self-reported design, categorical ranges, and limited sample size in subgroups. Future directions include deeper analysis of subgroups, including fellowship-trained dermatologists, dermatologists working more than 40 hours per week, and female dermatologists by race/ethnicity.
Conclusion
We have demonstrated that self-reported discrepancies in salary between male and female dermatologists exist, with male dermatologists earning a significantly higher annual salary than their female counterparts. This study identified and stratified several career factors that comprise the broad field and practice of dermatology. Even when controlling for these variations, we have demonstrated that gender alone remains a significant predictor of income, indicating that an unexplained income gap between the 2 genders exists in dermatology.
Although the number of female graduates from US medical schools has steadily increased,1 several studies since the 1970s indicate that a disparity exists in salary, academic rank, and promotion among female and male physicians across multiple specialties.2-8 Proposed explanations include women working fewer hours, having lower productivity rates, undernegotiating compensation, and underbilling for the same services. However, when controlling for variables such as time, experience, specialty, rank, and research activities, this gap unequivocally persists. There are limited data on this topic in dermatology, a field in which women comprise more than half of the working population.6,7 Most analyses of gender disparities in dermatology are based on data primarily from academic dermatologists, which may not be representative of the larger population of dermatologists.8,9 The purpose of this study is to determine if an income disparity exists between male and female physicians in dermatology, including those in private practice and those who are specialty trained.
Methods
Population—We performed a cross-sectional self-reported survey to examine compensation of male and female board-certified dermatologists (MDs/DOs). Several populations of dermatologists were surveyed in August and September 2018. Approximately 20% of the members of the American Academy of Dermatology were randomly selected and sent a link to the survey. Additionally, a survey link was emailed to members of the Association of Professors of Dermatology, American College of Mohs Surgery, and American Society for Dermatologic Surgery. A link to the survey also was published on “The Board Certified Dermatologists” Facebook group.
Statistical Analysis—Descriptive statistics were used to summarize the distribution of variables overall and within gender (male or female). Not all respondents completed every section, and duplicates and incomplete responses were removed. Variables were compared between genders using t tests (continuous), the Pearson χ2 test (nominal), or the Cochran-Mantel-Haenszel test (ordinal). For categorical variables with small cell counts, an exact χ2 test for small samples was used. For continuous variables, t test P values were calculated using either pooled or Satterthwaithe approximation.
To analyze the effect of different variables on total income using multivariate and univariate linear regression, the income variable was transformed into a continuous variable by using midpoints of the categories. Univariate linear regression was used to assess the effect and significance of each variable on total annual income. Variables that were found to have a P value of less than .05 (α=.05) were deemed as significant predictors of total annual income. These variables were added to a multivariate linear regression model to determine their effect on income when adjusting for other significant (and approaching significance) factors. In addition, variables that were found to have a P value of less than .2 (α=.05) were added to the multivariate linear regression model to assess significance of these specific variables when adjusting for other factors. In this way, we tested and accounted for a multitude of variables as potential sources of confounding.
Results
Demographics—Our survey was emailed to 3079 members of the American Academy of Dermatology, and 277 responses were received. Approximately 144 additional responses were obtained collectively from links sent to the directories of the Association of Professors of Dermatology, American College of Mohs Surgery, and American Society for Dermatologic Surgery and from social media. Of these respondents, 53.65% (213/397) were female and 46.35% (184/397) were male. When stratifying by race/ethnicity, 77.33% identified as White; 13.85% identified as Asian; 6.3% identified as Black or African American, Hispanic/Latino, and Native American; and 2.52% chose not to respond. Although most male and female respondents were White, a significantly higher proportion of female respondents identified as Asian or Black/African American/Hispanic/Latino/Native American (P=.0006). We found that race/ethnicity did not significantly impact income (P=.2736). All US Census regions were represented in this study, and geographic distribution as well as population density of practice location (ie, rural, suburban, urban setting) did not differ significantly between males and females (P=.5982 and P=.1007, respectively) and did not significantly impact income (P=.3225 and P=.10663, respectively).

Income—Total annual income was defined as the aggregate sum of all types of financial compensation received in 1 calendar year (eg, salary, bonuses, benefits) and was elicited as an ordinal variable in income brackets of US $100,000. Overall, χ2 analysis showed a statistically significant difference in annual total income between male and female dermatologists (P<.0001), with a higher proportion of males in the highest pay bracket (Figure). Gender remained a statistically significant predictor of income on both univariate and multivariate linear regression analyses (P=.0002 and P<.0001, respectively), indicating that gender has a significant impact on compensation, even after controlling for other variables (eTable). Of note, males in this sample were on average older and in practice longer than females (approximately 6 years, P<.0001). However, when univariate linear regression was performed, both age (P=.8281) and number of years since residency or fellowship completion (P=.8743) were not significant predictors of income.
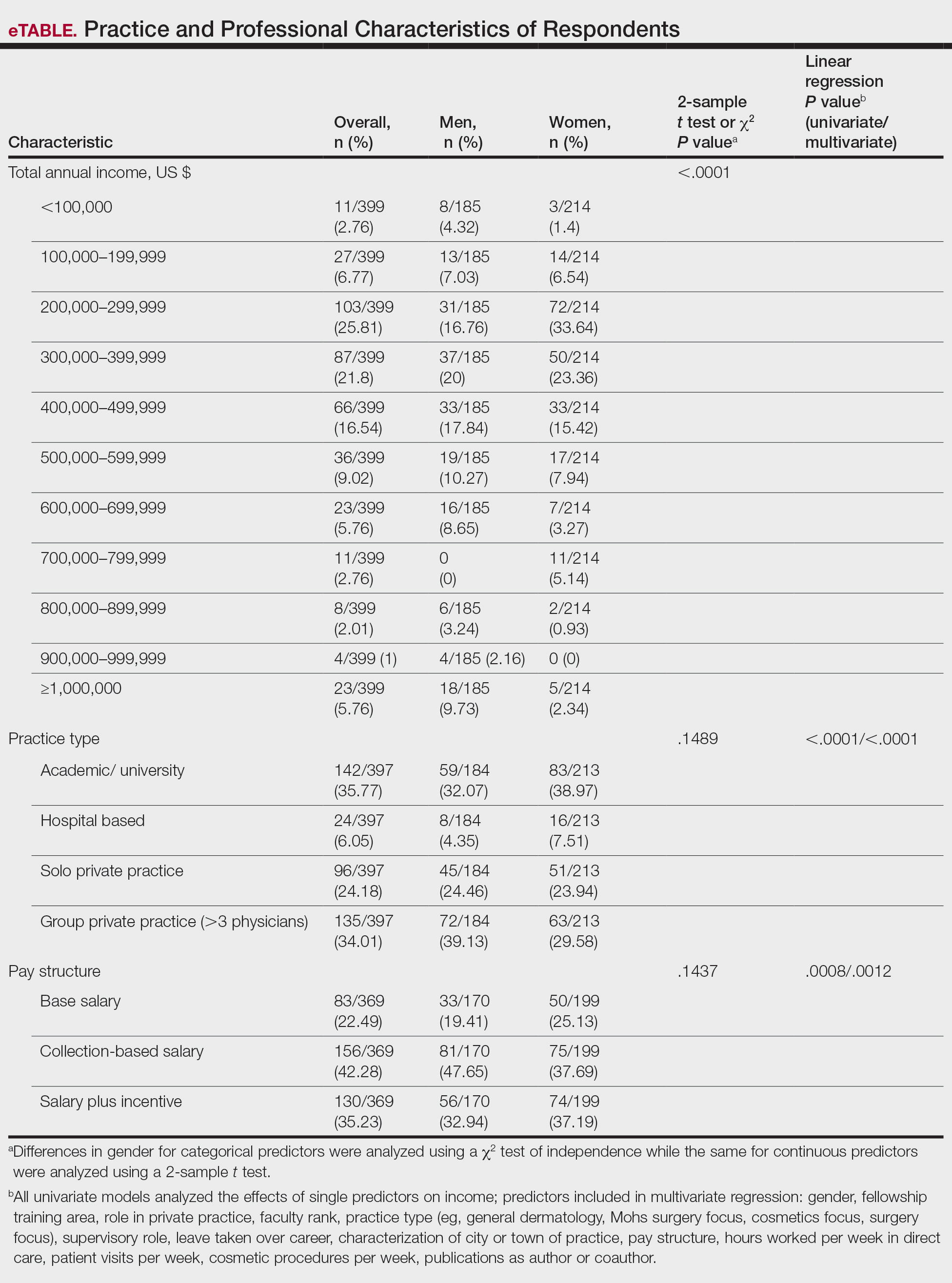
Practice Type—There were no statistically significant differences between men and women in practice type (P=.1489), including academic/university, hospital based, and solo and group private practice; pay structure (P=.1437), including base salary, collection-based salary, or salary plus incentive; holding a supervisory role (P=.0846); or having ownership of a practice (P=.3565)(eTable). Most respondents were in solo or group private practice (58.2%) and had a component of productivity-based compensation (77.5%). In addition, 62% of private practice dermatologists (133/212) had an ownership interest in their practice. As expected, univariate and multivariate regression analyses showed that practice type, pay structure, supervisory roles, and employee vs ownership roles were significant predictors of income (P<.05)(eTable).
Work Productivity—Statistically significant differences were found between men and women in hours worked per week in direct patient care (P<.0001) and in patient visits per week (P=.0052), with a higher percentage of men working more than 40 hours per week and men seeing an average of approximately 22 more patients per week than women. In the subgroup of all dermatologists working more than 40 hours per week, a statistically significant difference in income persisted between males and females (P=.0001). Hours worked per week and patient visits per week were statistically significant predictors of income on both univariate and multivariate regression analyses (P<.05)(Table).
Education and Fellowship Training—No significant difference existed between males and females in type of undergraduate school attended, namely public or private institutions (P=.1090), but a significant difference existed within type of medical school education, with a higher percentage of females attending private medical schools (53.03%) compared to males (38.24%)(P=.0045). However, type of undergraduate or medical school attended had no impact on income (P=.9103). A higher percentage of males (27.32%) completed additional advanced degrees, such as a master of business administration or a master of public health, compared to females (16.9%)(P=.0122). However, the completion of additional advanced degrees had no significant impact on income (P=.2379). No statistical significance existed between males and females in number of residencies completed (P=.3236), and residencies completed had no significant impact on income (P=.4584).
Of 397 respondents, approximately one-third of respondents completed fellowship training (36.5%). Fellowships included dermatopathology, surgery/cosmetics, and other (encompassing complex medical, research, transplant, and pediatric dermatology). Although similar percentages of men and women completed fellowship training, men and women differed significantly by type of fellowship completed (P=.0188). There were similar rates of dermatopathology and surgical fellowship completion between genders but almost 3 times the number of females who completed other fellowships. Type of fellowship training was a statistically significant predictor of income on both univariate and multivariate regression analyses (P<.00001 and P<.0001, respectively).
Work Activity—Respondents were asked to estimate the amount of time devoted to general dermatology, dermatopathology, Mohs micrographic surgery, cosmetics, and dermatologic surgery in their practices (Table). Women devoted a significantly higher average percentage of time to cosmetics (7.89%) compared to men (4.52%)(P=.0097). The number of cosmetic procedures performed per week was not statistically significantly different between men and women (P=.8035) but was a significant factor for income on univariate regression analysis (P=.0002). Time spent performing dermatologic surgery, general dermatology, or Mohs micrographic surgery did not significantly differ between men and women but was found to significantly influence income.
Academic Dermatology—Among the respondents working in academic settings, χ2 analysis identified a significant difference in the faculty rank between males and females, with a tendency for lower academic rank in females (P=.0508). Assistant professorship was comprised of 35% of men vs 51% of women, whereas full professorship consisted of 26% of men but only 13% of women. Academic rank was found to be a significant predictor of income, with higher rank associated with higher income (P<.0001 on univariate regression analysis). However, when adjusting for other factors, academic rank was no longer a significant predictor of income (P=.0840 on multivariate regression analysis). No significant difference existed between men and women in funding received from the National Institutes of Health, conduction of clinical trials, or authorship of scientific publications, and these factors were not found to have a significant impact on income.
Work Leave—Male and female dermatologists showed a statistically significant difference in maternity or Family and Medical Leave Act (FMLA) leave taken over their careers, with 56.03% of females reporting leave taken compared to 6.78% of males (P<.0001). Women reported a significantly higher average number of weeks of maternity or FMLA leave taken over their careers (12.92 weeks) compared to men (2.42 weeks) (P<.0001). However, upon univariate regression analysis, whether or not maternity or FMLA leave was taken over their careers (P=.2005), the number of times that maternity or FMLA leave was taken (P=.4350), and weeks of maternity or FMLA leave taken (P=.4057) were all not significant predictors of income.
Comment
This study sought to investigate the relationship between income and gender in dermatology, and our results demonstrated that statistically significant differences in total annual income exist between male and female dermatologists, with male dermatologists earning a significantly higher income, approximately an additional $80,000. Our results are consistent with other studies of US physician income, which have found a gender gap ranging from $13,399 to $82,000 that persists even when controlling for factors such as specialty choice, practice setting, rank and role in practice, work hours, vacation/leave taken, and others.2-7,10-15
There was a significant difference in rank of male and female academic dermatologists, with fewer females at higher academic ranks. These results are consistent with numerous studies in academic dermatology that show underrepresentation of women at higher academic ranks and leadership positions.8,9,16-18 Poor negotiation may contribute to differences in both rank and income.19,20 There are conflicting data on research productivity of academic dermatologists and length of career, first and senior authorship, and quality and academic impact, all of which add complexity to this topic.8,9,12,16-18,20-23Male and female dermatologists reported significant differences in productivity, with male dermatologists working more hours and seeing more patients per week than female dermatologists. These results are consistent with other studies of dermatologists4,24 and other physicians.12 Regardless, gender was still found to have a significant impact on income even when controlling for differences in productivity and FMLA leave taken. These results are consistent with numerous studies of US physicians that found a gender gap in income even when controlling for hours worked.12,23 Although fellowship training as a whole was found to significantly impact income, our results do not characterize whether the impact on income was positive or negative for each type of fellowship. Fellowship training in specialties such as internal medicine or general surgery likewise has variable effects on income.24,25
A comprehensive survey design and significant data elicited from dermatologists working in private practice for the first time served as the main strengths of this study. Limitations included self-reported design, categorical ranges, and limited sample size in subgroups. Future directions include deeper analysis of subgroups, including fellowship-trained dermatologists, dermatologists working more than 40 hours per week, and female dermatologists by race/ethnicity.
Conclusion
We have demonstrated that self-reported discrepancies in salary between male and female dermatologists exist, with male dermatologists earning a significantly higher annual salary than their female counterparts. This study identified and stratified several career factors that comprise the broad field and practice of dermatology. Even when controlling for these variations, we have demonstrated that gender alone remains a significant predictor of income, indicating that an unexplained income gap between the 2 genders exists in dermatology.
- Association of American Medical Colleges. Table B-2.2: Total Graduates by U.S. Medical School and Sex, 2015-2016 through 2019-2020. December 3, 2020. Accessed October 12, 2021. https://www.aamc.org/download/321532/data/factstableb2-2.pdf
- Willett LL, Halvorsen AJ, McDonald FS, et al. Gender differences in salary of internal medicine residency directors: a national survey. Am J Med. 2015;128:659-665.
- Weeks WB, Wallace AE, Mackenzie TA. Gender differences in anesthesiologists’ annual incomes. Anesthesiology. 2007;106:806-811.
- Weeks WB, Wallace AE. Gender differences in ophthalmologists’ annual incomes. Ophthalmology. 2007;114:1696-1701.
- Singh A, Burke CA, Larive B, et al. Do gender disparities persist in gastroenterology after 10 years of practice? Am J Gastroenterol. 2008;103:1589-1595.
- Desai T, Ali S, Fang X, et al. Equal work for unequal pay: the gender reimbursement gap for healthcare providers in the United States. Postgrad Med J. 2016;92:571-575.
- Jena AB, Olenski AR, Blumenthal DM. Sex differences in physician salary in US public medical schools. JAMA Intern Med. 2016;176:1294-1304.
- John AM, Gupta AB, John ES, et al. A gender-based comparison of promotion and research productivity in academic dermatology. Dermatol Online J. 2016;22:13030/qt1hx610pf.
- Sadeghpour M, Bernstein I, Ko C, et al. Role of sex in academic dermatology: results from a national survey. Arch Dermatol. 2012;148:809-814.
- Gilbert SB, Allshouse A, Skaznik-Wikiel ME. Gender inequality in salaries among reproductive endocrinology and infertility subspecialists in the United States. Fertil Steril. 2019;111:1194-1200.
- Jagsi R, Griffith KA, Stewart A, et al. Gender differences in the salaries of physician researchers. JAMA. 2012;307:2410-2417. doi:10.1001/jama.2012.6183
- Apaydin EA, Chen PGC, Friedberg MW, et al. Differences in physician income by gender in a multiregion survey. J Gen Intern Med. 2018;33:1574-1581.
- Read S, Butkus R, Weissman A, et al. Compensation disparities by gender in internal medicine. Ann Intern Med. 2018;169:658-661.
- Guss ZD, Chen Q, Hu C, et al. Differences in physician compensation between men and women at United States public academic radiation oncology departments. Int J Radiat Oncol Biol Phys. 2019;103:314-319.
- Lo Sasso AT, Richards MR, Chou CF, et al. The $16,819 pay gap for newly trained physicians: the unexplained trend of men earning more than women. Health Aff (Millwood). 2011;30:193-201.
- Shah A, Jalal S, Khosa F. Influences for gender disparity in dermatology in North America. Int J Dermatol. 2018;57:171-176.
- Shi CR, Olbricht S, Vleugels RA, et al. Sex and leadership in academic dermatology: a nationwide survey. J Am Acad Dermatol. 2017;77:782-784.
- Shih AF, Sun W, Yick C, et al. Trends in scholarly productivity of dermatology faculty by academic status and gender. J Am Acad Dermatol. 2019;80:1774-1776.
- Sarfaty S, Kolb D, Barnett R, et al. Negotiation in academic medicine: a necessary career skill. J Womens Health (Larchmt). 2007;16:235-244.
- Jacobson CC, Nguyen JC, Kimball AB. Gender and parenting significantly affect work hours of recent dermatology program graduates. Arch Dermatol. 2004;140:191-196.
- Feramisco JD, Leitenberger JJ, Redfern SI, et al. A gender gap in the dermatology literature? Cross-sectional analysis of manuscript authorship trends in dermatology journals during 3 decades. J Am Acad Dermatol. 2009;60:63-69.
- Bendels MHK, Dietz MC, Brüggmann D, et al. Gender disparities in high-quality dermatology research: a descriptive bibliometric study on scientific authorships. BMJ Open. 2018;8:e020089.
- Seabury SA, Chandra A, Jena AB. Trends in the earnings of male and female health care professionals in the United States, 1987 to 2010. JAMA Intern Med. 2013;173:1748-1750.
- Baimas-George M, Fleischer B, Slakey D, et al. Is it all about the money? Not all surgical subspecialization leads to higher lifetime revenue when compared to general surgery. J Surg Educ. 2017;74:E62-E66.
- Leigh JP, Tancredi D, Jerant A, et al. Lifetime earnings for physicians across specialties. Med Care. 2012;50:1093-1101.
- Association of American Medical Colleges. Table B-2.2: Total Graduates by U.S. Medical School and Sex, 2015-2016 through 2019-2020. December 3, 2020. Accessed October 12, 2021. https://www.aamc.org/download/321532/data/factstableb2-2.pdf
- Willett LL, Halvorsen AJ, McDonald FS, et al. Gender differences in salary of internal medicine residency directors: a national survey. Am J Med. 2015;128:659-665.
- Weeks WB, Wallace AE, Mackenzie TA. Gender differences in anesthesiologists’ annual incomes. Anesthesiology. 2007;106:806-811.
- Weeks WB, Wallace AE. Gender differences in ophthalmologists’ annual incomes. Ophthalmology. 2007;114:1696-1701.
- Singh A, Burke CA, Larive B, et al. Do gender disparities persist in gastroenterology after 10 years of practice? Am J Gastroenterol. 2008;103:1589-1595.
- Desai T, Ali S, Fang X, et al. Equal work for unequal pay: the gender reimbursement gap for healthcare providers in the United States. Postgrad Med J. 2016;92:571-575.
- Jena AB, Olenski AR, Blumenthal DM. Sex differences in physician salary in US public medical schools. JAMA Intern Med. 2016;176:1294-1304.
- John AM, Gupta AB, John ES, et al. A gender-based comparison of promotion and research productivity in academic dermatology. Dermatol Online J. 2016;22:13030/qt1hx610pf.
- Sadeghpour M, Bernstein I, Ko C, et al. Role of sex in academic dermatology: results from a national survey. Arch Dermatol. 2012;148:809-814.
- Gilbert SB, Allshouse A, Skaznik-Wikiel ME. Gender inequality in salaries among reproductive endocrinology and infertility subspecialists in the United States. Fertil Steril. 2019;111:1194-1200.
- Jagsi R, Griffith KA, Stewart A, et al. Gender differences in the salaries of physician researchers. JAMA. 2012;307:2410-2417. doi:10.1001/jama.2012.6183
- Apaydin EA, Chen PGC, Friedberg MW, et al. Differences in physician income by gender in a multiregion survey. J Gen Intern Med. 2018;33:1574-1581.
- Read S, Butkus R, Weissman A, et al. Compensation disparities by gender in internal medicine. Ann Intern Med. 2018;169:658-661.
- Guss ZD, Chen Q, Hu C, et al. Differences in physician compensation between men and women at United States public academic radiation oncology departments. Int J Radiat Oncol Biol Phys. 2019;103:314-319.
- Lo Sasso AT, Richards MR, Chou CF, et al. The $16,819 pay gap for newly trained physicians: the unexplained trend of men earning more than women. Health Aff (Millwood). 2011;30:193-201.
- Shah A, Jalal S, Khosa F. Influences for gender disparity in dermatology in North America. Int J Dermatol. 2018;57:171-176.
- Shi CR, Olbricht S, Vleugels RA, et al. Sex and leadership in academic dermatology: a nationwide survey. J Am Acad Dermatol. 2017;77:782-784.
- Shih AF, Sun W, Yick C, et al. Trends in scholarly productivity of dermatology faculty by academic status and gender. J Am Acad Dermatol. 2019;80:1774-1776.
- Sarfaty S, Kolb D, Barnett R, et al. Negotiation in academic medicine: a necessary career skill. J Womens Health (Larchmt). 2007;16:235-244.
- Jacobson CC, Nguyen JC, Kimball AB. Gender and parenting significantly affect work hours of recent dermatology program graduates. Arch Dermatol. 2004;140:191-196.
- Feramisco JD, Leitenberger JJ, Redfern SI, et al. A gender gap in the dermatology literature? Cross-sectional analysis of manuscript authorship trends in dermatology journals during 3 decades. J Am Acad Dermatol. 2009;60:63-69.
- Bendels MHK, Dietz MC, Brüggmann D, et al. Gender disparities in high-quality dermatology research: a descriptive bibliometric study on scientific authorships. BMJ Open. 2018;8:e020089.
- Seabury SA, Chandra A, Jena AB. Trends in the earnings of male and female health care professionals in the United States, 1987 to 2010. JAMA Intern Med. 2013;173:1748-1750.
- Baimas-George M, Fleischer B, Slakey D, et al. Is it all about the money? Not all surgical subspecialization leads to higher lifetime revenue when compared to general surgery. J Surg Educ. 2017;74:E62-E66.
- Leigh JP, Tancredi D, Jerant A, et al. Lifetime earnings for physicians across specialties. Med Care. 2012;50:1093-1101.
Practice Points
- In this survey-based cross-sectional study, a statistically significant income disparity between male and female dermatologists was found.
- Although several differences were identified between male and female dermatologists that contribute to income, gender remained a statistically significant predictor of income, and this disparity could not be explained by other factors.
Sickle cell raises risk for stillbirth
Both sickle cell trait and sickle cell disease were significantly associated with an increased risk of stillbirth, based on data from more than 50,000 women.
Pregnant women with sickle cell disease (SCD) are at increased risk of complications, including stillbirth, but many women with the disease in the United States lack access to specialty care, Silvia P. Canelón, PhD, of the University of Pennsylvania, Philadelphia, and colleagues wrote. Sickle cell trait (SCT), defined as one abnormal allele of the hemoglobin gene, is not considered a disease state because many carriers are asymptomatic, and therefore even less likely to be assessed for potential complications. “However, it is possible for people with SCT to experience sickling of red blood cells under severe hypoxia, dehydration, and hyperthermia. This condition can lead to severe medical complications for sickle cell carriers, including fetal loss, splenic infarction, exercise-related sudden death, and others,” they noted.
In a study published in JAMA Network Open, the researchers reviewed data from 63,334 deliveries in 50,560 women between Jan. 1, 2010, and Aug. 15, 2017, at four quaternary academic medical centers in Pennsylvania. Of these, 1,904 had SCT but not SCD, and 164 had SCD. The mean age of the women was 29.5 years, and approximately 56% were single at the time of delivery. A majority (87%) of the study population was Rhesus-factor positive, 47.0% were Black or African American, 33.7% were White, and 45.2% had ABO blood type O.
Risk factors for stillbirth used in the analysis included SCD, numbers of pain crises and blood transfusions before delivery, delivery episode (to represent parity), history of cesarean delivery, multiple gestation, age, marital status, race and ethnicity, ABO blood type, Rhesus factor, and year of delivery.
Overall, the prevalence of stillbirth in women with SCT was 1.1%, compared with 0.8% in the general study population, and was significantly associated with increased risk of stillbirth after controlling for multiple risk factors. The adjusted odds ratio was 8.94 for stillbirth risk in women with SCT, compared with women without SCT (P = .045), although the risk was greater among women with SCD, compared with those without SCD (aOR, 26.40).
“In addition, the stratified analysis found Black or African American patients with SCD to be at higher risk of stillbirth, compared with Black or African American patients without SCD (aOR, 3.59),” but no significant association was noted between stillbirth and SCT, the researchers wrote. Stillbirth rates were 1.1% in Black or African American women overall, 2.7% in those with SCD, and 1.0% in those with SCT. Overall, multiple gestation was associated with an increased risk of stillbirth (aOR, 4.68), while a history of cesarean delivery and being married at the time of delivery were associated with decreased risk (aOR, 0.44 and 0.72, respectively).
The lack of association between stillbirth and SCT in Black or African American patients supports some previous research, but contradicts other studies, the researchers wrote. “Ultimately, it may be impossible to disentangle the risks due to the disease and those due to disparities associated with the disease that have resulted from longstanding inequity and stigma,” they said. The findings also suggest that biological mechanisms of SCT may contribute to severe clinical complications, and therefore “invite a more critical examination of the assumption that SCT is not a disease state.”
The study findings were limited by several factors including the lack of assessment of SCT independent of other comorbidities, such as hypertension, preeclampsia, diabetes, and obesity, and by the use of billing codes that could misclassify patients, the researchers noted.
However, the results support some findings from previous studies of the potential health complications for pregnant SCT patients. The large study population highlights the need to identify women’s SCT status during obstetric care, and to provide both pregnancy guidance for SCT patients and systemic support of comprehensive care for SCD and SCT patients, they concluded.
Disparities may drive stillbirth in sickle cell trait women
“There is a paucity of research evaluating sickle cell trait and the risk of adverse pregnancy outcomes such as stillbirth,” Iris Krishna, MD, of Emory University, Atlanta, said in an interview. “Prior studies evaluating the risk of stillbirth have yielded mixed results, and an increased risk of stillbirth in women with sickle cell trait has not been established. This study is unique in that it attempts to address how racial inequities and health disparities may contribute to risk of stillbirth in women with sickle cell trait.”
Although the study findings suggest an increased risk of stillbirth in women with sickle cell trait, an analysis stratified for Black or African American patients showed no association, Dr. Krishna said. “The prevalence of stillbirth was noted to be 1% among Black or African American patients with sickle cell trait compared to the prevalence of stillbirth of 1.1% among Black or African American women with no sickle cell trait or disease. Although, sickle cell trait or sickle cell disease can be found in any racial or ethnic group, it disproportionately affects Black or African Americans, with a sickle cell trait carrier rate of approximately 1 in 10. The mixed findings in this study amongst racial/ethnic groups further suggest that there is more research needed before an association between stillbirth and sickle cell trait can be supported.”
As for clinical implications, “it is well established that for women with sickle cell trait there is an increased risk of urinary tract infections in pregnancy,” said Dr. Krishna. “Women with sickle cell trait should have a urine culture performed at their first prenatal visit and each trimester. At this time, studies evaluating risk of stillbirth in women with sickle cell trait have yielded conflicting results, and current consensus is that women with sickle cell trait are not at increased risk. In comparison, women with sickle cell disease are at increased risk for stillbirth and adverse pregnancy outcomes. Women with sickle cell disease should be followed closely during pregnancy and fetal surveillance implemented at 32 weeks, if not sooner, to reduce risk of stillbirth.
“Prior studies evaluating risk of stillbirth in women with sickle cell trait consist of retrospective cohorts with small study populations,” Dr. Krishna added. Notably, the current study was limited by the inability to adjust for comorbidities including diabetes, hypertension, and obesity, that are not only associated with an increased risk for stillbirth, but also disproportionately common among Black women.
“More studies are needed evaluating the relationship between these comorbidities as well as studies specifically evaluating how race affects care and pregnancy outcomes,” Dr. Krisha emphasized.
The study was funded by the University of Pennsylvania department of biostatistics, epidemiology, and informatics. Lead author Dr. Canelón disclosed grants from the Centers for Disease Control and Prevention, Clinical and Translational Science Awards, and grants from the National Institutes of Health outside the submitted work. Dr. Krishna had no financial conflicts to disclose, but serves on the editorial advisory board of Ob.Gyn News.
Both sickle cell trait and sickle cell disease were significantly associated with an increased risk of stillbirth, based on data from more than 50,000 women.
Pregnant women with sickle cell disease (SCD) are at increased risk of complications, including stillbirth, but many women with the disease in the United States lack access to specialty care, Silvia P. Canelón, PhD, of the University of Pennsylvania, Philadelphia, and colleagues wrote. Sickle cell trait (SCT), defined as one abnormal allele of the hemoglobin gene, is not considered a disease state because many carriers are asymptomatic, and therefore even less likely to be assessed for potential complications. “However, it is possible for people with SCT to experience sickling of red blood cells under severe hypoxia, dehydration, and hyperthermia. This condition can lead to severe medical complications for sickle cell carriers, including fetal loss, splenic infarction, exercise-related sudden death, and others,” they noted.
In a study published in JAMA Network Open, the researchers reviewed data from 63,334 deliveries in 50,560 women between Jan. 1, 2010, and Aug. 15, 2017, at four quaternary academic medical centers in Pennsylvania. Of these, 1,904 had SCT but not SCD, and 164 had SCD. The mean age of the women was 29.5 years, and approximately 56% were single at the time of delivery. A majority (87%) of the study population was Rhesus-factor positive, 47.0% were Black or African American, 33.7% were White, and 45.2% had ABO blood type O.
Risk factors for stillbirth used in the analysis included SCD, numbers of pain crises and blood transfusions before delivery, delivery episode (to represent parity), history of cesarean delivery, multiple gestation, age, marital status, race and ethnicity, ABO blood type, Rhesus factor, and year of delivery.
Overall, the prevalence of stillbirth in women with SCT was 1.1%, compared with 0.8% in the general study population, and was significantly associated with increased risk of stillbirth after controlling for multiple risk factors. The adjusted odds ratio was 8.94 for stillbirth risk in women with SCT, compared with women without SCT (P = .045), although the risk was greater among women with SCD, compared with those without SCD (aOR, 26.40).
“In addition, the stratified analysis found Black or African American patients with SCD to be at higher risk of stillbirth, compared with Black or African American patients without SCD (aOR, 3.59),” but no significant association was noted between stillbirth and SCT, the researchers wrote. Stillbirth rates were 1.1% in Black or African American women overall, 2.7% in those with SCD, and 1.0% in those with SCT. Overall, multiple gestation was associated with an increased risk of stillbirth (aOR, 4.68), while a history of cesarean delivery and being married at the time of delivery were associated with decreased risk (aOR, 0.44 and 0.72, respectively).
The lack of association between stillbirth and SCT in Black or African American patients supports some previous research, but contradicts other studies, the researchers wrote. “Ultimately, it may be impossible to disentangle the risks due to the disease and those due to disparities associated with the disease that have resulted from longstanding inequity and stigma,” they said. The findings also suggest that biological mechanisms of SCT may contribute to severe clinical complications, and therefore “invite a more critical examination of the assumption that SCT is not a disease state.”
The study findings were limited by several factors including the lack of assessment of SCT independent of other comorbidities, such as hypertension, preeclampsia, diabetes, and obesity, and by the use of billing codes that could misclassify patients, the researchers noted.
However, the results support some findings from previous studies of the potential health complications for pregnant SCT patients. The large study population highlights the need to identify women’s SCT status during obstetric care, and to provide both pregnancy guidance for SCT patients and systemic support of comprehensive care for SCD and SCT patients, they concluded.
Disparities may drive stillbirth in sickle cell trait women
“There is a paucity of research evaluating sickle cell trait and the risk of adverse pregnancy outcomes such as stillbirth,” Iris Krishna, MD, of Emory University, Atlanta, said in an interview. “Prior studies evaluating the risk of stillbirth have yielded mixed results, and an increased risk of stillbirth in women with sickle cell trait has not been established. This study is unique in that it attempts to address how racial inequities and health disparities may contribute to risk of stillbirth in women with sickle cell trait.”
Although the study findings suggest an increased risk of stillbirth in women with sickle cell trait, an analysis stratified for Black or African American patients showed no association, Dr. Krishna said. “The prevalence of stillbirth was noted to be 1% among Black or African American patients with sickle cell trait compared to the prevalence of stillbirth of 1.1% among Black or African American women with no sickle cell trait or disease. Although, sickle cell trait or sickle cell disease can be found in any racial or ethnic group, it disproportionately affects Black or African Americans, with a sickle cell trait carrier rate of approximately 1 in 10. The mixed findings in this study amongst racial/ethnic groups further suggest that there is more research needed before an association between stillbirth and sickle cell trait can be supported.”
As for clinical implications, “it is well established that for women with sickle cell trait there is an increased risk of urinary tract infections in pregnancy,” said Dr. Krishna. “Women with sickle cell trait should have a urine culture performed at their first prenatal visit and each trimester. At this time, studies evaluating risk of stillbirth in women with sickle cell trait have yielded conflicting results, and current consensus is that women with sickle cell trait are not at increased risk. In comparison, women with sickle cell disease are at increased risk for stillbirth and adverse pregnancy outcomes. Women with sickle cell disease should be followed closely during pregnancy and fetal surveillance implemented at 32 weeks, if not sooner, to reduce risk of stillbirth.
“Prior studies evaluating risk of stillbirth in women with sickle cell trait consist of retrospective cohorts with small study populations,” Dr. Krishna added. Notably, the current study was limited by the inability to adjust for comorbidities including diabetes, hypertension, and obesity, that are not only associated with an increased risk for stillbirth, but also disproportionately common among Black women.
“More studies are needed evaluating the relationship between these comorbidities as well as studies specifically evaluating how race affects care and pregnancy outcomes,” Dr. Krisha emphasized.
The study was funded by the University of Pennsylvania department of biostatistics, epidemiology, and informatics. Lead author Dr. Canelón disclosed grants from the Centers for Disease Control and Prevention, Clinical and Translational Science Awards, and grants from the National Institutes of Health outside the submitted work. Dr. Krishna had no financial conflicts to disclose, but serves on the editorial advisory board of Ob.Gyn News.
Both sickle cell trait and sickle cell disease were significantly associated with an increased risk of stillbirth, based on data from more than 50,000 women.
Pregnant women with sickle cell disease (SCD) are at increased risk of complications, including stillbirth, but many women with the disease in the United States lack access to specialty care, Silvia P. Canelón, PhD, of the University of Pennsylvania, Philadelphia, and colleagues wrote. Sickle cell trait (SCT), defined as one abnormal allele of the hemoglobin gene, is not considered a disease state because many carriers are asymptomatic, and therefore even less likely to be assessed for potential complications. “However, it is possible for people with SCT to experience sickling of red blood cells under severe hypoxia, dehydration, and hyperthermia. This condition can lead to severe medical complications for sickle cell carriers, including fetal loss, splenic infarction, exercise-related sudden death, and others,” they noted.
In a study published in JAMA Network Open, the researchers reviewed data from 63,334 deliveries in 50,560 women between Jan. 1, 2010, and Aug. 15, 2017, at four quaternary academic medical centers in Pennsylvania. Of these, 1,904 had SCT but not SCD, and 164 had SCD. The mean age of the women was 29.5 years, and approximately 56% were single at the time of delivery. A majority (87%) of the study population was Rhesus-factor positive, 47.0% were Black or African American, 33.7% were White, and 45.2% had ABO blood type O.
Risk factors for stillbirth used in the analysis included SCD, numbers of pain crises and blood transfusions before delivery, delivery episode (to represent parity), history of cesarean delivery, multiple gestation, age, marital status, race and ethnicity, ABO blood type, Rhesus factor, and year of delivery.
Overall, the prevalence of stillbirth in women with SCT was 1.1%, compared with 0.8% in the general study population, and was significantly associated with increased risk of stillbirth after controlling for multiple risk factors. The adjusted odds ratio was 8.94 for stillbirth risk in women with SCT, compared with women without SCT (P = .045), although the risk was greater among women with SCD, compared with those without SCD (aOR, 26.40).
“In addition, the stratified analysis found Black or African American patients with SCD to be at higher risk of stillbirth, compared with Black or African American patients without SCD (aOR, 3.59),” but no significant association was noted between stillbirth and SCT, the researchers wrote. Stillbirth rates were 1.1% in Black or African American women overall, 2.7% in those with SCD, and 1.0% in those with SCT. Overall, multiple gestation was associated with an increased risk of stillbirth (aOR, 4.68), while a history of cesarean delivery and being married at the time of delivery were associated with decreased risk (aOR, 0.44 and 0.72, respectively).
The lack of association between stillbirth and SCT in Black or African American patients supports some previous research, but contradicts other studies, the researchers wrote. “Ultimately, it may be impossible to disentangle the risks due to the disease and those due to disparities associated with the disease that have resulted from longstanding inequity and stigma,” they said. The findings also suggest that biological mechanisms of SCT may contribute to severe clinical complications, and therefore “invite a more critical examination of the assumption that SCT is not a disease state.”
The study findings were limited by several factors including the lack of assessment of SCT independent of other comorbidities, such as hypertension, preeclampsia, diabetes, and obesity, and by the use of billing codes that could misclassify patients, the researchers noted.
However, the results support some findings from previous studies of the potential health complications for pregnant SCT patients. The large study population highlights the need to identify women’s SCT status during obstetric care, and to provide both pregnancy guidance for SCT patients and systemic support of comprehensive care for SCD and SCT patients, they concluded.
Disparities may drive stillbirth in sickle cell trait women
“There is a paucity of research evaluating sickle cell trait and the risk of adverse pregnancy outcomes such as stillbirth,” Iris Krishna, MD, of Emory University, Atlanta, said in an interview. “Prior studies evaluating the risk of stillbirth have yielded mixed results, and an increased risk of stillbirth in women with sickle cell trait has not been established. This study is unique in that it attempts to address how racial inequities and health disparities may contribute to risk of stillbirth in women with sickle cell trait.”
Although the study findings suggest an increased risk of stillbirth in women with sickle cell trait, an analysis stratified for Black or African American patients showed no association, Dr. Krishna said. “The prevalence of stillbirth was noted to be 1% among Black or African American patients with sickle cell trait compared to the prevalence of stillbirth of 1.1% among Black or African American women with no sickle cell trait or disease. Although, sickle cell trait or sickle cell disease can be found in any racial or ethnic group, it disproportionately affects Black or African Americans, with a sickle cell trait carrier rate of approximately 1 in 10. The mixed findings in this study amongst racial/ethnic groups further suggest that there is more research needed before an association between stillbirth and sickle cell trait can be supported.”
As for clinical implications, “it is well established that for women with sickle cell trait there is an increased risk of urinary tract infections in pregnancy,” said Dr. Krishna. “Women with sickle cell trait should have a urine culture performed at their first prenatal visit and each trimester. At this time, studies evaluating risk of stillbirth in women with sickle cell trait have yielded conflicting results, and current consensus is that women with sickle cell trait are not at increased risk. In comparison, women with sickle cell disease are at increased risk for stillbirth and adverse pregnancy outcomes. Women with sickle cell disease should be followed closely during pregnancy and fetal surveillance implemented at 32 weeks, if not sooner, to reduce risk of stillbirth.
“Prior studies evaluating risk of stillbirth in women with sickle cell trait consist of retrospective cohorts with small study populations,” Dr. Krishna added. Notably, the current study was limited by the inability to adjust for comorbidities including diabetes, hypertension, and obesity, that are not only associated with an increased risk for stillbirth, but also disproportionately common among Black women.
“More studies are needed evaluating the relationship between these comorbidities as well as studies specifically evaluating how race affects care and pregnancy outcomes,” Dr. Krisha emphasized.
The study was funded by the University of Pennsylvania department of biostatistics, epidemiology, and informatics. Lead author Dr. Canelón disclosed grants from the Centers for Disease Control and Prevention, Clinical and Translational Science Awards, and grants from the National Institutes of Health outside the submitted work. Dr. Krishna had no financial conflicts to disclose, but serves on the editorial advisory board of Ob.Gyn News.
FROM JAMA NETWORK OPEN
Congress OKs Veterans Affairs Expansive New Maternal Care Program
It’s called the Momnibus—the Black Maternal Health Momnibus Act of 2021 (HR 959) with 12 bills addressing “every dimension of the maternal health crisis in America.” The first bill in the Momnibus to pass Congress is the Protecting Moms Who Served act, which sets up a $15 million maternal care program within the US Department of Veterans Affairs (VA). “There has never been a comprehensive evaluation of how our nation’s growing maternal mortality crisis is impacting our women veterans, even though they may be at higher risk due to their service,” said Sen. Tammy Duckworth (D-IL), a co-sponsor of the Momnibus. The bill has passed Congress and awaits President Biden’s signature.
Rep. Lauren Underwood (D-IL) along with Rep. Alma Adams (D- NC-12), Sen. Cory Booker D-NJ), and members of the Black Maternal Health Caucus reintroduced the bill (first introduced last year). According to Rep. Underwood, the act would codify and strengthen the VA maternity care coordination programs. It also will require the US Government Accountability Office to report the deaths of pregnant and postpartum veterans and to focus on any racial or ethnic disparities. The bill passed overwhelmingly, 414 to 9 and awaits President Biden’s signature.
The Momnibus’s cute name represents a very serious purpose. “Maternal mortality has historically been used as a key indicator of the health of a population,” say researchers from National Vital Statistics Reports. But American mothers are dying at the highest rate in the developed world, and the numbers have been rising dramatically. Between 1987, when the Centers for Disease Control and Prevention (CDC) launched the Pregnancy Mortality Surveillance System in 2017, the latest year for available data, the number of reported pregnancy-related deaths in the United States rose steadily from 7.2 deaths per 100,000 live births to 17.3 per 100,000.
The maternal morbidity crisis is particularly stark among certain groups of women. Black women are acutely at risk, dying at 3 to 4 times the rate of White women (41.7 deaths per 100,000 live births), and one-third higher than the next highest risk group, Native American women (28.3 deaths per 100,000 live births).
But just how accurate have the data been? The study published in National Vital Statistics Report found that using a checkbox for “cause of death” specifying maternal death identified more than triple the number of maternal deaths. Without the checkbox item, maternal mortality rates in 2015 and 2016 would have been reported as 8.7 deaths per 100,000 live births, compared with 8.9 in 2002. With the checkbox, the rate would be reported as 20.9 per 100,000 live births in 2015 and 21.8/100,000 in 2016.
The CDC states that the reasons for the rising numbers are unclear; advances in identification have improved over time, for one. But by and large, the women are dying of preventable causes, such as hypertension, diabetes mellitus, and chronic heart disease. Nearly 60% of maternal deaths are deemed preventable.
Black and other minority women, though, may be dying of biases. Researchers from Beth Israel and Harvard cite studies that have found racial and ethnic disparities in obstetric care delivery. Non-Hispanic Blacks women, Hispanic women, and Asian women, for instance, have lower odds of labor induction when compared with that of White women. The odds of receiving an episiotomy are lower in non-Hispanic Black and Hispanic women. The Listening to Mothers survey III found that 24% of participants perceived discrimination during birth hospitalization, predominantly among Black or Hispanic women and uninsured women.
A maternal health equity advocacy group, 4Kira4Moms, was founded by the husband of Kira Johnson who died of hemorrhage following a routine scheduled cesarean section. In the recovery room, her catheter began turning pink with blood. For 10 hours, her husband said, he and her family begged the medical staff for help but were told his wife was not a priority. Thus, the Momnibus also contains the Kira Johnson Act, which will establish funding for community-based groups to provide Black pregnant women with more support.
Among other changes, the Momnibus will:
- Make critical investments in social determinants of health that influence maternal health outcomes, such as housing, transportation, and nutrition;
- Provide funding to community-based organizations that are working to improve maternal health outcomes and promote equity;
- Comprehensively study the unique maternal health risks facing pregnant and postpartum veterans and support VA maternity care coordination programs;
- Support mothers with mental health conditions and substance use disorders; and
- Promote innovative payment models to incentivize high-quality maternity care and nonclinical perinatal support
A variety of recent bills in Congress address maternal health. The Mothers and Offspring Mortality and Morbidity Awareness (MOMMA) Act, for instance, also would specifically address maternal health disparities by improving data collection and reporting, improving maternal care, and advancing respectful, equitable care. It also would extend Medicaid and the Children’s Health Insurance Program coverage. Katie Shea Barrett, MPH, executive director of March for Moms, a coalition of families, health care practitioners, policy makers, and partners advocating for mothers’ and families’ health, notes in an essay for thehill.com that Medicaid coverage ends about 60 days postpartum, although half of the maternal deaths happen between 42 days and 1 year postpartum.
She writes: “[W]e have to directly address the disproportionate impact of maternal mortality on women of color by training providers in offering care that is culturally competent and free of implicit bias. Health systems must be aware and respectful of cultural norms when providing care and be mindful of buying into stereotypes based on race, ethnicity, and even underlying medical conditions like diabetes, which often lead to perceived discrimination and perpetuate systems of injustice.”
In April, Vice President Kamala Harris called for sweeping action to curb racial inequities in pregnancy and childbirth. In an email Q&A with STAT, she said, “With every day that goes by and every woman who dies, the need for action grows more urgent.”
It’s called the Momnibus—the Black Maternal Health Momnibus Act of 2021 (HR 959) with 12 bills addressing “every dimension of the maternal health crisis in America.” The first bill in the Momnibus to pass Congress is the Protecting Moms Who Served act, which sets up a $15 million maternal care program within the US Department of Veterans Affairs (VA). “There has never been a comprehensive evaluation of how our nation’s growing maternal mortality crisis is impacting our women veterans, even though they may be at higher risk due to their service,” said Sen. Tammy Duckworth (D-IL), a co-sponsor of the Momnibus. The bill has passed Congress and awaits President Biden’s signature.
Rep. Lauren Underwood (D-IL) along with Rep. Alma Adams (D- NC-12), Sen. Cory Booker D-NJ), and members of the Black Maternal Health Caucus reintroduced the bill (first introduced last year). According to Rep. Underwood, the act would codify and strengthen the VA maternity care coordination programs. It also will require the US Government Accountability Office to report the deaths of pregnant and postpartum veterans and to focus on any racial or ethnic disparities. The bill passed overwhelmingly, 414 to 9 and awaits President Biden’s signature.
The Momnibus’s cute name represents a very serious purpose. “Maternal mortality has historically been used as a key indicator of the health of a population,” say researchers from National Vital Statistics Reports. But American mothers are dying at the highest rate in the developed world, and the numbers have been rising dramatically. Between 1987, when the Centers for Disease Control and Prevention (CDC) launched the Pregnancy Mortality Surveillance System in 2017, the latest year for available data, the number of reported pregnancy-related deaths in the United States rose steadily from 7.2 deaths per 100,000 live births to 17.3 per 100,000.
The maternal morbidity crisis is particularly stark among certain groups of women. Black women are acutely at risk, dying at 3 to 4 times the rate of White women (41.7 deaths per 100,000 live births), and one-third higher than the next highest risk group, Native American women (28.3 deaths per 100,000 live births).
But just how accurate have the data been? The study published in National Vital Statistics Report found that using a checkbox for “cause of death” specifying maternal death identified more than triple the number of maternal deaths. Without the checkbox item, maternal mortality rates in 2015 and 2016 would have been reported as 8.7 deaths per 100,000 live births, compared with 8.9 in 2002. With the checkbox, the rate would be reported as 20.9 per 100,000 live births in 2015 and 21.8/100,000 in 2016.
The CDC states that the reasons for the rising numbers are unclear; advances in identification have improved over time, for one. But by and large, the women are dying of preventable causes, such as hypertension, diabetes mellitus, and chronic heart disease. Nearly 60% of maternal deaths are deemed preventable.
Black and other minority women, though, may be dying of biases. Researchers from Beth Israel and Harvard cite studies that have found racial and ethnic disparities in obstetric care delivery. Non-Hispanic Blacks women, Hispanic women, and Asian women, for instance, have lower odds of labor induction when compared with that of White women. The odds of receiving an episiotomy are lower in non-Hispanic Black and Hispanic women. The Listening to Mothers survey III found that 24% of participants perceived discrimination during birth hospitalization, predominantly among Black or Hispanic women and uninsured women.
A maternal health equity advocacy group, 4Kira4Moms, was founded by the husband of Kira Johnson who died of hemorrhage following a routine scheduled cesarean section. In the recovery room, her catheter began turning pink with blood. For 10 hours, her husband said, he and her family begged the medical staff for help but were told his wife was not a priority. Thus, the Momnibus also contains the Kira Johnson Act, which will establish funding for community-based groups to provide Black pregnant women with more support.
Among other changes, the Momnibus will:
- Make critical investments in social determinants of health that influence maternal health outcomes, such as housing, transportation, and nutrition;
- Provide funding to community-based organizations that are working to improve maternal health outcomes and promote equity;
- Comprehensively study the unique maternal health risks facing pregnant and postpartum veterans and support VA maternity care coordination programs;
- Support mothers with mental health conditions and substance use disorders; and
- Promote innovative payment models to incentivize high-quality maternity care and nonclinical perinatal support
A variety of recent bills in Congress address maternal health. The Mothers and Offspring Mortality and Morbidity Awareness (MOMMA) Act, for instance, also would specifically address maternal health disparities by improving data collection and reporting, improving maternal care, and advancing respectful, equitable care. It also would extend Medicaid and the Children’s Health Insurance Program coverage. Katie Shea Barrett, MPH, executive director of March for Moms, a coalition of families, health care practitioners, policy makers, and partners advocating for mothers’ and families’ health, notes in an essay for thehill.com that Medicaid coverage ends about 60 days postpartum, although half of the maternal deaths happen between 42 days and 1 year postpartum.
She writes: “[W]e have to directly address the disproportionate impact of maternal mortality on women of color by training providers in offering care that is culturally competent and free of implicit bias. Health systems must be aware and respectful of cultural norms when providing care and be mindful of buying into stereotypes based on race, ethnicity, and even underlying medical conditions like diabetes, which often lead to perceived discrimination and perpetuate systems of injustice.”
In April, Vice President Kamala Harris called for sweeping action to curb racial inequities in pregnancy and childbirth. In an email Q&A with STAT, she said, “With every day that goes by and every woman who dies, the need for action grows more urgent.”
It’s called the Momnibus—the Black Maternal Health Momnibus Act of 2021 (HR 959) with 12 bills addressing “every dimension of the maternal health crisis in America.” The first bill in the Momnibus to pass Congress is the Protecting Moms Who Served act, which sets up a $15 million maternal care program within the US Department of Veterans Affairs (VA). “There has never been a comprehensive evaluation of how our nation’s growing maternal mortality crisis is impacting our women veterans, even though they may be at higher risk due to their service,” said Sen. Tammy Duckworth (D-IL), a co-sponsor of the Momnibus. The bill has passed Congress and awaits President Biden’s signature.
Rep. Lauren Underwood (D-IL) along with Rep. Alma Adams (D- NC-12), Sen. Cory Booker D-NJ), and members of the Black Maternal Health Caucus reintroduced the bill (first introduced last year). According to Rep. Underwood, the act would codify and strengthen the VA maternity care coordination programs. It also will require the US Government Accountability Office to report the deaths of pregnant and postpartum veterans and to focus on any racial or ethnic disparities. The bill passed overwhelmingly, 414 to 9 and awaits President Biden’s signature.
The Momnibus’s cute name represents a very serious purpose. “Maternal mortality has historically been used as a key indicator of the health of a population,” say researchers from National Vital Statistics Reports. But American mothers are dying at the highest rate in the developed world, and the numbers have been rising dramatically. Between 1987, when the Centers for Disease Control and Prevention (CDC) launched the Pregnancy Mortality Surveillance System in 2017, the latest year for available data, the number of reported pregnancy-related deaths in the United States rose steadily from 7.2 deaths per 100,000 live births to 17.3 per 100,000.
The maternal morbidity crisis is particularly stark among certain groups of women. Black women are acutely at risk, dying at 3 to 4 times the rate of White women (41.7 deaths per 100,000 live births), and one-third higher than the next highest risk group, Native American women (28.3 deaths per 100,000 live births).
But just how accurate have the data been? The study published in National Vital Statistics Report found that using a checkbox for “cause of death” specifying maternal death identified more than triple the number of maternal deaths. Without the checkbox item, maternal mortality rates in 2015 and 2016 would have been reported as 8.7 deaths per 100,000 live births, compared with 8.9 in 2002. With the checkbox, the rate would be reported as 20.9 per 100,000 live births in 2015 and 21.8/100,000 in 2016.
The CDC states that the reasons for the rising numbers are unclear; advances in identification have improved over time, for one. But by and large, the women are dying of preventable causes, such as hypertension, diabetes mellitus, and chronic heart disease. Nearly 60% of maternal deaths are deemed preventable.
Black and other minority women, though, may be dying of biases. Researchers from Beth Israel and Harvard cite studies that have found racial and ethnic disparities in obstetric care delivery. Non-Hispanic Blacks women, Hispanic women, and Asian women, for instance, have lower odds of labor induction when compared with that of White women. The odds of receiving an episiotomy are lower in non-Hispanic Black and Hispanic women. The Listening to Mothers survey III found that 24% of participants perceived discrimination during birth hospitalization, predominantly among Black or Hispanic women and uninsured women.
A maternal health equity advocacy group, 4Kira4Moms, was founded by the husband of Kira Johnson who died of hemorrhage following a routine scheduled cesarean section. In the recovery room, her catheter began turning pink with blood. For 10 hours, her husband said, he and her family begged the medical staff for help but were told his wife was not a priority. Thus, the Momnibus also contains the Kira Johnson Act, which will establish funding for community-based groups to provide Black pregnant women with more support.
Among other changes, the Momnibus will:
- Make critical investments in social determinants of health that influence maternal health outcomes, such as housing, transportation, and nutrition;
- Provide funding to community-based organizations that are working to improve maternal health outcomes and promote equity;
- Comprehensively study the unique maternal health risks facing pregnant and postpartum veterans and support VA maternity care coordination programs;
- Support mothers with mental health conditions and substance use disorders; and
- Promote innovative payment models to incentivize high-quality maternity care and nonclinical perinatal support
A variety of recent bills in Congress address maternal health. The Mothers and Offspring Mortality and Morbidity Awareness (MOMMA) Act, for instance, also would specifically address maternal health disparities by improving data collection and reporting, improving maternal care, and advancing respectful, equitable care. It also would extend Medicaid and the Children’s Health Insurance Program coverage. Katie Shea Barrett, MPH, executive director of March for Moms, a coalition of families, health care practitioners, policy makers, and partners advocating for mothers’ and families’ health, notes in an essay for thehill.com that Medicaid coverage ends about 60 days postpartum, although half of the maternal deaths happen between 42 days and 1 year postpartum.
She writes: “[W]e have to directly address the disproportionate impact of maternal mortality on women of color by training providers in offering care that is culturally competent and free of implicit bias. Health systems must be aware and respectful of cultural norms when providing care and be mindful of buying into stereotypes based on race, ethnicity, and even underlying medical conditions like diabetes, which often lead to perceived discrimination and perpetuate systems of injustice.”
In April, Vice President Kamala Harris called for sweeping action to curb racial inequities in pregnancy and childbirth. In an email Q&A with STAT, she said, “With every day that goes by and every woman who dies, the need for action grows more urgent.”
Non–health care municipal services cut severe maternal morbidity rates
Municipal budget allocations can affect severe maternal morbidity (SMM) rates, a cross-sectional study published in JAMA Network Open reported.
Led by Felix M. Muchomba, PhD, an assistant professor at Rutgers University School of Social Work in New Brunswick, N.J., the study found that local expenditures on fire and ambulance, transportation, health, housing, and libraries were negatively associated with SMM. Specifically, annual per-capita expenditures of $1,000 and higher in these categories were associated with a 35.4%-67.3% lower risk of SMM: odds ratios, 0.33 (95% confidence interval, 0.15-0.72) to 0.65 (95% CI, 0.46-0.91).
In contrast, expenditures on police were positively associated with SMM: OR, 1.15 (95% CI, 1.04-1.28).
In the first study of environmental services spending and SMM done at the municipal level – others have focused on state and county funding – Dr. Muchomba’s group analyzed 2008-2018 birth files linked to maternal hospital discharge records and U.S. Census municipal expenditures data.
The study’s cohort comprised 1,001,410 mothers giving birth in New Jersey hospitals with a mean age of 29.8 years. Of these,10.9 % were Asian, 14.8% were Black, 28.0% were Hispanic, and 44.7% were White.
Per-capita municipal expenditures were reviewed for a broad range of city services: education, public health, fire and ambulance, parks, recreation, natural resources, housing, community development, public welfare; police; transportation, and libraries. “Each year municipalities spend about $600 billion nationwide on local services, investing far more than counties do,” Dr. Muchomba said.
Among developed nations, the United States has a rate of high maternal morbidity, a determinant of maternal mortality, and New Jersey has one of the highest rates in the country, although, paradoxically, it has one of the lowest state poverty rates and one of the highest state income levels, he added, said explaining the impetus for the study.
Previous research has found that state and local investment in non–health specific services can reduce infant mortality rates (IMR). Last year, for example, a national study of 2000-2016 data led by Neal D. Goldstein, PhD, MRI, an assistant professor of epidemiology and biostatistics at Drexel University in Philadelphia, reported that a $0.30 per-person increase in environmental spending was associated with a decrease of 0.03 deaths per 1,000 live births, and a $0.73 per-person increase in social services spending was associated with a decrease of 0.02 deaths per 1,000 live births. “IMR is reflective of, and amenable to broad social, economic, and health care delivery contexts within a society. State and local governments, via increased social and environmental expenditures, have the potential to reduce, albeit not eliminate, IMR disparities,” Dr. Goldstein’s group wrote in Pediatrics.
According to Aimee J. Palumbo, PhD, MPH, an assistant professor in the department of epidemiology & biostatistics in the College of Public Health at Temple University in Philadelphia, who was not involved in the study, the current study’s results are broadly consistent with those of the Goldstein study, of which she is a coauthor, in that it shows spending on public welfare is associated with better outcomes following birth.
“This analysis, however, is done at the municipality level, which allows it to evaluate variations in spending that occur at more local levels, rather than the state level like ours,” she said in an interview. “The researchers are also able to control for individual-level factors,” which is good as it is really suggestive of the impact that spending has on outcomes after controlling for some individual characteristics.”
Both studies speak to the importance of exploring funding for social services and specific programs that affect health, Dr. Palumbo added.
Services that affect nonmedical determinants of health broadly affect how people live their daily lives, Dr. Muchomba said – where they live, how they get to work and to medical appointments, where they shop, how they engage in recreation.
“Housing is very important for mothers since it provides a safe space to shelter during pregnancy and during recovery from childbirth. It’s a safe place to store medications and to prepare healthy food,” he continued. “But much of the housing in New Jersey is very expensive, and some mothers may have to decide between paying the rent and buying healthy food.”
In other benefits, local services spending provides transportation to jobs and health care, bus shelters, effective waste management, viable sidewalks, safe crosswalks, and public exercise venues that help to reduce obesity.
The category that Dr. Muchomba is most often asked about is libraries. “Why libraries? Our hypothesis is that libraries provide some low-income people with their only access to computers and the Internet. They’re a major resource for information and a proxy for the delivery of other services,” he said. In addition, many libraries offer English as a second language classes, which may increase health literacy among immigrants.
A major objective of the 2020 Maternal Health Action Plan of the U.S. Department of Health & Human Services is to better target resources by identifying problem spots for maternal morbidity and mortality. “Our findings strongly suggest that surveillance at the municipal level, a level rarely considered in studies of health outcomes, would be important for success in such efforts,” the authors wrote.
Dr. Muchomba believes doctors can have a role to play in targeting of spending for local services that can reduce maternal morbidity and mortality. “Many physicians are engaged in community health outreach efforts. As respected people in the community, they need to be aware of these other determinants of health that may be driving maternal morbidity rates in their communities.”
This research was supported by the Robert Wood Johnson Foundation, the National Center for Advancing Translational Sciences, the U.S. Department of Health & Human Services Health Resources and Service Administration and the Child Health Institute of New Jersey. Dr. Muchomba reported a grant from Eunice Kennedy Shriver National Institute of Child Health and Human Development outside of the submitted work. Dr. Palumbo had no potential competing interests to disclose.
Municipal budget allocations can affect severe maternal morbidity (SMM) rates, a cross-sectional study published in JAMA Network Open reported.
Led by Felix M. Muchomba, PhD, an assistant professor at Rutgers University School of Social Work in New Brunswick, N.J., the study found that local expenditures on fire and ambulance, transportation, health, housing, and libraries were negatively associated with SMM. Specifically, annual per-capita expenditures of $1,000 and higher in these categories were associated with a 35.4%-67.3% lower risk of SMM: odds ratios, 0.33 (95% confidence interval, 0.15-0.72) to 0.65 (95% CI, 0.46-0.91).
In contrast, expenditures on police were positively associated with SMM: OR, 1.15 (95% CI, 1.04-1.28).
In the first study of environmental services spending and SMM done at the municipal level – others have focused on state and county funding – Dr. Muchomba’s group analyzed 2008-2018 birth files linked to maternal hospital discharge records and U.S. Census municipal expenditures data.
The study’s cohort comprised 1,001,410 mothers giving birth in New Jersey hospitals with a mean age of 29.8 years. Of these,10.9 % were Asian, 14.8% were Black, 28.0% were Hispanic, and 44.7% were White.
Per-capita municipal expenditures were reviewed for a broad range of city services: education, public health, fire and ambulance, parks, recreation, natural resources, housing, community development, public welfare; police; transportation, and libraries. “Each year municipalities spend about $600 billion nationwide on local services, investing far more than counties do,” Dr. Muchomba said.
Among developed nations, the United States has a rate of high maternal morbidity, a determinant of maternal mortality, and New Jersey has one of the highest rates in the country, although, paradoxically, it has one of the lowest state poverty rates and one of the highest state income levels, he added, said explaining the impetus for the study.
Previous research has found that state and local investment in non–health specific services can reduce infant mortality rates (IMR). Last year, for example, a national study of 2000-2016 data led by Neal D. Goldstein, PhD, MRI, an assistant professor of epidemiology and biostatistics at Drexel University in Philadelphia, reported that a $0.30 per-person increase in environmental spending was associated with a decrease of 0.03 deaths per 1,000 live births, and a $0.73 per-person increase in social services spending was associated with a decrease of 0.02 deaths per 1,000 live births. “IMR is reflective of, and amenable to broad social, economic, and health care delivery contexts within a society. State and local governments, via increased social and environmental expenditures, have the potential to reduce, albeit not eliminate, IMR disparities,” Dr. Goldstein’s group wrote in Pediatrics.
According to Aimee J. Palumbo, PhD, MPH, an assistant professor in the department of epidemiology & biostatistics in the College of Public Health at Temple University in Philadelphia, who was not involved in the study, the current study’s results are broadly consistent with those of the Goldstein study, of which she is a coauthor, in that it shows spending on public welfare is associated with better outcomes following birth.
“This analysis, however, is done at the municipality level, which allows it to evaluate variations in spending that occur at more local levels, rather than the state level like ours,” she said in an interview. “The researchers are also able to control for individual-level factors,” which is good as it is really suggestive of the impact that spending has on outcomes after controlling for some individual characteristics.”
Both studies speak to the importance of exploring funding for social services and specific programs that affect health, Dr. Palumbo added.
Services that affect nonmedical determinants of health broadly affect how people live their daily lives, Dr. Muchomba said – where they live, how they get to work and to medical appointments, where they shop, how they engage in recreation.
“Housing is very important for mothers since it provides a safe space to shelter during pregnancy and during recovery from childbirth. It’s a safe place to store medications and to prepare healthy food,” he continued. “But much of the housing in New Jersey is very expensive, and some mothers may have to decide between paying the rent and buying healthy food.”
In other benefits, local services spending provides transportation to jobs and health care, bus shelters, effective waste management, viable sidewalks, safe crosswalks, and public exercise venues that help to reduce obesity.
The category that Dr. Muchomba is most often asked about is libraries. “Why libraries? Our hypothesis is that libraries provide some low-income people with their only access to computers and the Internet. They’re a major resource for information and a proxy for the delivery of other services,” he said. In addition, many libraries offer English as a second language classes, which may increase health literacy among immigrants.
A major objective of the 2020 Maternal Health Action Plan of the U.S. Department of Health & Human Services is to better target resources by identifying problem spots for maternal morbidity and mortality. “Our findings strongly suggest that surveillance at the municipal level, a level rarely considered in studies of health outcomes, would be important for success in such efforts,” the authors wrote.
Dr. Muchomba believes doctors can have a role to play in targeting of spending for local services that can reduce maternal morbidity and mortality. “Many physicians are engaged in community health outreach efforts. As respected people in the community, they need to be aware of these other determinants of health that may be driving maternal morbidity rates in their communities.”
This research was supported by the Robert Wood Johnson Foundation, the National Center for Advancing Translational Sciences, the U.S. Department of Health & Human Services Health Resources and Service Administration and the Child Health Institute of New Jersey. Dr. Muchomba reported a grant from Eunice Kennedy Shriver National Institute of Child Health and Human Development outside of the submitted work. Dr. Palumbo had no potential competing interests to disclose.
Municipal budget allocations can affect severe maternal morbidity (SMM) rates, a cross-sectional study published in JAMA Network Open reported.
Led by Felix M. Muchomba, PhD, an assistant professor at Rutgers University School of Social Work in New Brunswick, N.J., the study found that local expenditures on fire and ambulance, transportation, health, housing, and libraries were negatively associated with SMM. Specifically, annual per-capita expenditures of $1,000 and higher in these categories were associated with a 35.4%-67.3% lower risk of SMM: odds ratios, 0.33 (95% confidence interval, 0.15-0.72) to 0.65 (95% CI, 0.46-0.91).
In contrast, expenditures on police were positively associated with SMM: OR, 1.15 (95% CI, 1.04-1.28).
In the first study of environmental services spending and SMM done at the municipal level – others have focused on state and county funding – Dr. Muchomba’s group analyzed 2008-2018 birth files linked to maternal hospital discharge records and U.S. Census municipal expenditures data.
The study’s cohort comprised 1,001,410 mothers giving birth in New Jersey hospitals with a mean age of 29.8 years. Of these,10.9 % were Asian, 14.8% were Black, 28.0% were Hispanic, and 44.7% were White.
Per-capita municipal expenditures were reviewed for a broad range of city services: education, public health, fire and ambulance, parks, recreation, natural resources, housing, community development, public welfare; police; transportation, and libraries. “Each year municipalities spend about $600 billion nationwide on local services, investing far more than counties do,” Dr. Muchomba said.
Among developed nations, the United States has a rate of high maternal morbidity, a determinant of maternal mortality, and New Jersey has one of the highest rates in the country, although, paradoxically, it has one of the lowest state poverty rates and one of the highest state income levels, he added, said explaining the impetus for the study.
Previous research has found that state and local investment in non–health specific services can reduce infant mortality rates (IMR). Last year, for example, a national study of 2000-2016 data led by Neal D. Goldstein, PhD, MRI, an assistant professor of epidemiology and biostatistics at Drexel University in Philadelphia, reported that a $0.30 per-person increase in environmental spending was associated with a decrease of 0.03 deaths per 1,000 live births, and a $0.73 per-person increase in social services spending was associated with a decrease of 0.02 deaths per 1,000 live births. “IMR is reflective of, and amenable to broad social, economic, and health care delivery contexts within a society. State and local governments, via increased social and environmental expenditures, have the potential to reduce, albeit not eliminate, IMR disparities,” Dr. Goldstein’s group wrote in Pediatrics.
According to Aimee J. Palumbo, PhD, MPH, an assistant professor in the department of epidemiology & biostatistics in the College of Public Health at Temple University in Philadelphia, who was not involved in the study, the current study’s results are broadly consistent with those of the Goldstein study, of which she is a coauthor, in that it shows spending on public welfare is associated with better outcomes following birth.
“This analysis, however, is done at the municipality level, which allows it to evaluate variations in spending that occur at more local levels, rather than the state level like ours,” she said in an interview. “The researchers are also able to control for individual-level factors,” which is good as it is really suggestive of the impact that spending has on outcomes after controlling for some individual characteristics.”
Both studies speak to the importance of exploring funding for social services and specific programs that affect health, Dr. Palumbo added.
Services that affect nonmedical determinants of health broadly affect how people live their daily lives, Dr. Muchomba said – where they live, how they get to work and to medical appointments, where they shop, how they engage in recreation.
“Housing is very important for mothers since it provides a safe space to shelter during pregnancy and during recovery from childbirth. It’s a safe place to store medications and to prepare healthy food,” he continued. “But much of the housing in New Jersey is very expensive, and some mothers may have to decide between paying the rent and buying healthy food.”
In other benefits, local services spending provides transportation to jobs and health care, bus shelters, effective waste management, viable sidewalks, safe crosswalks, and public exercise venues that help to reduce obesity.
The category that Dr. Muchomba is most often asked about is libraries. “Why libraries? Our hypothesis is that libraries provide some low-income people with their only access to computers and the Internet. They’re a major resource for information and a proxy for the delivery of other services,” he said. In addition, many libraries offer English as a second language classes, which may increase health literacy among immigrants.
A major objective of the 2020 Maternal Health Action Plan of the U.S. Department of Health & Human Services is to better target resources by identifying problem spots for maternal morbidity and mortality. “Our findings strongly suggest that surveillance at the municipal level, a level rarely considered in studies of health outcomes, would be important for success in such efforts,” the authors wrote.
Dr. Muchomba believes doctors can have a role to play in targeting of spending for local services that can reduce maternal morbidity and mortality. “Many physicians are engaged in community health outreach efforts. As respected people in the community, they need to be aware of these other determinants of health that may be driving maternal morbidity rates in their communities.”
This research was supported by the Robert Wood Johnson Foundation, the National Center for Advancing Translational Sciences, the U.S. Department of Health & Human Services Health Resources and Service Administration and the Child Health Institute of New Jersey. Dr. Muchomba reported a grant from Eunice Kennedy Shriver National Institute of Child Health and Human Development outside of the submitted work. Dr. Palumbo had no potential competing interests to disclose.
JAMA NETWORK OPEN
High-poverty areas host more firearm-related youth deaths
Higher poverty concentration at the county level significantly increased the risk of firearm-related deaths in children and youth aged 5-24 years in the United States, based on a review of approximately 67,000 fatalities.
Firearms are the second-leading cause of death in children and young adults in the United States, according to data from the Centers for Disease Control and Prevention, wrote Jefferson T. Barrett, MD, of The Children’s Hospital at Montefiore, New York, and colleagues. County-level poverty has been associated with increased injury mortality in children, but the association between county-level poverty and firearm-related mortality in particular has not been well studied.
In a cross-sectional study published in JAMA Pediatrics, 67,905 firearm-related deaths in children and youth aged 5-24 years that occurred between Jan. 1, 2007, and Dec. 31, 2016 were analyzed. The deaths included 42,512 homicides (62.6%), 23,034 suicides (33.9%), and 1,627 unintentional deaths (2.4%).
County poverty data were acquired from the U.S. Census Bureau. County-level poverty was divided into five categories based on percentage of the population living below the federal poverty level: 0%-4.9%, 5%-9.9%, 10%-14.9%, 15%-19.9%, and 20% or more.
Overall, 88.6% of the total deaths were in males. Notably, 44.8% of total firearm-related deaths and 63.9% of homicides occurred in non-Hispanic Blacks, who make up only 14% of the youth population in the United States, the researchers wrote.
The total number of firearm-related deaths was 248 in the lowest quintile of poverty concentration, followed by 6,841, 18,551, 27,305, and 14,960 in the remaining quintiles.
In a multivariate regression model that included demographics, urban versus rural, and statewide firearm prevalence, youth in counties with the highest quintile of poverty concentration had an increased rate of total firearm-related deaths (adjusted incidence rate ratio, 2.29), as well as increased rates of homicides, suicides, and unintentional deaths (aIRR, 3.55, 1.45, and 9.32, respectively), compared with those living in the lowest quintile of poverty concentration. Individuals in the highest poverty quintile accounted for 22.0% of total firearm-related deaths, 25.5% of homicides, 15.3% of suicides, and 25.1% of unintentional deaths.
The researchers also calculated the population-attributable fraction (PAF) and years of potential life lost. “The PAF represents the proportion of deaths associated with a particular exposure, which was concentrated county poverty in this study,” they explained. The PAF for all firearm-related deaths was 0.51, PAFs for homicides, suicides, and unintentional deaths were 0.66, 0.30, and 0.86, respectively. The PAF calculation translated to 34,292 firearm-related deaths that may not have occurred if youth in all counties had the same risk as those in counties with the lowest poverty concentration.
“Over the 10-year study period, we observed 3,833,105 years of potential life lost in youth aged 5-24 years from firearm-related deaths,” the researchers wrote.
The study findings were limited by several factors including the potential bias of a cross-section design, and inability to account for all the ways that county-level poverty might increase the risk of firearm-related death in children and teens, the researchers noted. Other potential limitations include possible misclassification of death, lack of data on individual family incomes, shifts in counties in the poverty categories over time, and the use of statewide, rather than countywide, estimates of firearm ownership.
However, the results are consistent with those of previous studies, and add that “mortality rates were consistent even after controlling for demographic variables, county urbanicity, and statewide firearm prevalence,” the researchers concluded.
Address structural racism to reduce disparities
“Firearm-related homicides among youth aged 5-24 years are among the causes of death with the greatest disparities,” based on CDC fatal injury reports, wrote Alice M. Ellyson, PhD, Frederick P. Rivara, MD, and Ali Rowhani-Rahbar, MD, all of the University of Washington, Seattle, in an accompanying editorial.
The current study builds on previous research, including studies showing an association between income inequality and firearm-related homicide, they said. More research is needed to determine how to intervene in the pathways between poverty and firearm-related death. For example, if access to high-quality health care is a factor, programs to increase access to health insurance, such as the Affordable Care Act and Children’s Health Insurance Program, or to increase access to high-quality trauma care may help reduce firearm-related death in youth.
“The study of where, how, and why racism operates as a factor in both poverty and firearm-related death must continue, especially considering the disparities consistently documented in Alaska Native or American Indian, Black, and Hispanic communities,” the editorialists wrote.
“Key potential mechanisms for reducing the consequences of poverty for firearm-related death are often denied to racial and ethnic minority groups through a variety of structures, policies, and systems in health care, employment, housing, transportation, and education,” they emphasized, and the impact of racism, not only on the pathways to poverty, but also on mediators between poverty and firearm-related death, must be explored.
Findings spotlight need to for poverty programs
The study was an interesting look at the specific relationship between poverty and firearm-related deaths in people aged younger than 25 years in the United States, Tim Joos, MD, of Seattle said in an interview.
“Although America is not a poor country, the combination of poverty within America and its unique gun culture seems to prove deadly for its youth,” Dr. Joos said. “The strongest relationship is between firearm-related homicide and poverty, but unintentional firearm deaths and poverty also are clearly linked, whereas the link between firearm-related suicide and poverty appears to be present, but small.”.
In the current study, “the authors note that firearm deaths are the second-leading cause of death among all people ages 15-24 years,” said Dr. Joos. “Many of us have followed children from infancy just to have them meet this untimely end as adolescents, wishing we had a vaccine or other remedy in our toolbelt for this particular scourge.
“As our country currently debates the size of the social safety net, this study is one of many that suggests government programs aimed at poverty alleviation would substantially contribute to the health of American youth,” Dr. Joos added.
The study received no outside funding. Lead author Dr. Barrett had no financial conflicts to disclose. Dr. Ellyson disclosed funds from the CDC, the state of Washington, and the Grandmothers Against Gun Violence Foundation for research outside the submitted work. Dr. Rivara disclosed funds from the National Institutes of Health, the State of Washington, and the National Collaborative on Gun Violence Research for research outside the submitted work. Dr. Rowhani-Rahbar disclosed funds from the CDC, National Institutes of Health, National Collaborative on Gun Violence Research, Fund for a Safer Future, and state of Washington for research outside the submitted work. Dr. Joos had no financial conflicts to disclose, but serves on the editorial advisory board of Pediatric News.
Higher poverty concentration at the county level significantly increased the risk of firearm-related deaths in children and youth aged 5-24 years in the United States, based on a review of approximately 67,000 fatalities.
Firearms are the second-leading cause of death in children and young adults in the United States, according to data from the Centers for Disease Control and Prevention, wrote Jefferson T. Barrett, MD, of The Children’s Hospital at Montefiore, New York, and colleagues. County-level poverty has been associated with increased injury mortality in children, but the association between county-level poverty and firearm-related mortality in particular has not been well studied.
In a cross-sectional study published in JAMA Pediatrics, 67,905 firearm-related deaths in children and youth aged 5-24 years that occurred between Jan. 1, 2007, and Dec. 31, 2016 were analyzed. The deaths included 42,512 homicides (62.6%), 23,034 suicides (33.9%), and 1,627 unintentional deaths (2.4%).
County poverty data were acquired from the U.S. Census Bureau. County-level poverty was divided into five categories based on percentage of the population living below the federal poverty level: 0%-4.9%, 5%-9.9%, 10%-14.9%, 15%-19.9%, and 20% or more.
Overall, 88.6% of the total deaths were in males. Notably, 44.8% of total firearm-related deaths and 63.9% of homicides occurred in non-Hispanic Blacks, who make up only 14% of the youth population in the United States, the researchers wrote.
The total number of firearm-related deaths was 248 in the lowest quintile of poverty concentration, followed by 6,841, 18,551, 27,305, and 14,960 in the remaining quintiles.
In a multivariate regression model that included demographics, urban versus rural, and statewide firearm prevalence, youth in counties with the highest quintile of poverty concentration had an increased rate of total firearm-related deaths (adjusted incidence rate ratio, 2.29), as well as increased rates of homicides, suicides, and unintentional deaths (aIRR, 3.55, 1.45, and 9.32, respectively), compared with those living in the lowest quintile of poverty concentration. Individuals in the highest poverty quintile accounted for 22.0% of total firearm-related deaths, 25.5% of homicides, 15.3% of suicides, and 25.1% of unintentional deaths.
The researchers also calculated the population-attributable fraction (PAF) and years of potential life lost. “The PAF represents the proportion of deaths associated with a particular exposure, which was concentrated county poverty in this study,” they explained. The PAF for all firearm-related deaths was 0.51, PAFs for homicides, suicides, and unintentional deaths were 0.66, 0.30, and 0.86, respectively. The PAF calculation translated to 34,292 firearm-related deaths that may not have occurred if youth in all counties had the same risk as those in counties with the lowest poverty concentration.
“Over the 10-year study period, we observed 3,833,105 years of potential life lost in youth aged 5-24 years from firearm-related deaths,” the researchers wrote.
The study findings were limited by several factors including the potential bias of a cross-section design, and inability to account for all the ways that county-level poverty might increase the risk of firearm-related death in children and teens, the researchers noted. Other potential limitations include possible misclassification of death, lack of data on individual family incomes, shifts in counties in the poverty categories over time, and the use of statewide, rather than countywide, estimates of firearm ownership.
However, the results are consistent with those of previous studies, and add that “mortality rates were consistent even after controlling for demographic variables, county urbanicity, and statewide firearm prevalence,” the researchers concluded.
Address structural racism to reduce disparities
“Firearm-related homicides among youth aged 5-24 years are among the causes of death with the greatest disparities,” based on CDC fatal injury reports, wrote Alice M. Ellyson, PhD, Frederick P. Rivara, MD, and Ali Rowhani-Rahbar, MD, all of the University of Washington, Seattle, in an accompanying editorial.
The current study builds on previous research, including studies showing an association between income inequality and firearm-related homicide, they said. More research is needed to determine how to intervene in the pathways between poverty and firearm-related death. For example, if access to high-quality health care is a factor, programs to increase access to health insurance, such as the Affordable Care Act and Children’s Health Insurance Program, or to increase access to high-quality trauma care may help reduce firearm-related death in youth.
“The study of where, how, and why racism operates as a factor in both poverty and firearm-related death must continue, especially considering the disparities consistently documented in Alaska Native or American Indian, Black, and Hispanic communities,” the editorialists wrote.
“Key potential mechanisms for reducing the consequences of poverty for firearm-related death are often denied to racial and ethnic minority groups through a variety of structures, policies, and systems in health care, employment, housing, transportation, and education,” they emphasized, and the impact of racism, not only on the pathways to poverty, but also on mediators between poverty and firearm-related death, must be explored.
Findings spotlight need to for poverty programs
The study was an interesting look at the specific relationship between poverty and firearm-related deaths in people aged younger than 25 years in the United States, Tim Joos, MD, of Seattle said in an interview.
“Although America is not a poor country, the combination of poverty within America and its unique gun culture seems to prove deadly for its youth,” Dr. Joos said. “The strongest relationship is between firearm-related homicide and poverty, but unintentional firearm deaths and poverty also are clearly linked, whereas the link between firearm-related suicide and poverty appears to be present, but small.”.
In the current study, “the authors note that firearm deaths are the second-leading cause of death among all people ages 15-24 years,” said Dr. Joos. “Many of us have followed children from infancy just to have them meet this untimely end as adolescents, wishing we had a vaccine or other remedy in our toolbelt for this particular scourge.
“As our country currently debates the size of the social safety net, this study is one of many that suggests government programs aimed at poverty alleviation would substantially contribute to the health of American youth,” Dr. Joos added.
The study received no outside funding. Lead author Dr. Barrett had no financial conflicts to disclose. Dr. Ellyson disclosed funds from the CDC, the state of Washington, and the Grandmothers Against Gun Violence Foundation for research outside the submitted work. Dr. Rivara disclosed funds from the National Institutes of Health, the State of Washington, and the National Collaborative on Gun Violence Research for research outside the submitted work. Dr. Rowhani-Rahbar disclosed funds from the CDC, National Institutes of Health, National Collaborative on Gun Violence Research, Fund for a Safer Future, and state of Washington for research outside the submitted work. Dr. Joos had no financial conflicts to disclose, but serves on the editorial advisory board of Pediatric News.
Higher poverty concentration at the county level significantly increased the risk of firearm-related deaths in children and youth aged 5-24 years in the United States, based on a review of approximately 67,000 fatalities.
Firearms are the second-leading cause of death in children and young adults in the United States, according to data from the Centers for Disease Control and Prevention, wrote Jefferson T. Barrett, MD, of The Children’s Hospital at Montefiore, New York, and colleagues. County-level poverty has been associated with increased injury mortality in children, but the association between county-level poverty and firearm-related mortality in particular has not been well studied.
In a cross-sectional study published in JAMA Pediatrics, 67,905 firearm-related deaths in children and youth aged 5-24 years that occurred between Jan. 1, 2007, and Dec. 31, 2016 were analyzed. The deaths included 42,512 homicides (62.6%), 23,034 suicides (33.9%), and 1,627 unintentional deaths (2.4%).
County poverty data were acquired from the U.S. Census Bureau. County-level poverty was divided into five categories based on percentage of the population living below the federal poverty level: 0%-4.9%, 5%-9.9%, 10%-14.9%, 15%-19.9%, and 20% or more.
Overall, 88.6% of the total deaths were in males. Notably, 44.8% of total firearm-related deaths and 63.9% of homicides occurred in non-Hispanic Blacks, who make up only 14% of the youth population in the United States, the researchers wrote.
The total number of firearm-related deaths was 248 in the lowest quintile of poverty concentration, followed by 6,841, 18,551, 27,305, and 14,960 in the remaining quintiles.
In a multivariate regression model that included demographics, urban versus rural, and statewide firearm prevalence, youth in counties with the highest quintile of poverty concentration had an increased rate of total firearm-related deaths (adjusted incidence rate ratio, 2.29), as well as increased rates of homicides, suicides, and unintentional deaths (aIRR, 3.55, 1.45, and 9.32, respectively), compared with those living in the lowest quintile of poverty concentration. Individuals in the highest poverty quintile accounted for 22.0% of total firearm-related deaths, 25.5% of homicides, 15.3% of suicides, and 25.1% of unintentional deaths.
The researchers also calculated the population-attributable fraction (PAF) and years of potential life lost. “The PAF represents the proportion of deaths associated with a particular exposure, which was concentrated county poverty in this study,” they explained. The PAF for all firearm-related deaths was 0.51, PAFs for homicides, suicides, and unintentional deaths were 0.66, 0.30, and 0.86, respectively. The PAF calculation translated to 34,292 firearm-related deaths that may not have occurred if youth in all counties had the same risk as those in counties with the lowest poverty concentration.
“Over the 10-year study period, we observed 3,833,105 years of potential life lost in youth aged 5-24 years from firearm-related deaths,” the researchers wrote.
The study findings were limited by several factors including the potential bias of a cross-section design, and inability to account for all the ways that county-level poverty might increase the risk of firearm-related death in children and teens, the researchers noted. Other potential limitations include possible misclassification of death, lack of data on individual family incomes, shifts in counties in the poverty categories over time, and the use of statewide, rather than countywide, estimates of firearm ownership.
However, the results are consistent with those of previous studies, and add that “mortality rates were consistent even after controlling for demographic variables, county urbanicity, and statewide firearm prevalence,” the researchers concluded.
Address structural racism to reduce disparities
“Firearm-related homicides among youth aged 5-24 years are among the causes of death with the greatest disparities,” based on CDC fatal injury reports, wrote Alice M. Ellyson, PhD, Frederick P. Rivara, MD, and Ali Rowhani-Rahbar, MD, all of the University of Washington, Seattle, in an accompanying editorial.
The current study builds on previous research, including studies showing an association between income inequality and firearm-related homicide, they said. More research is needed to determine how to intervene in the pathways between poverty and firearm-related death. For example, if access to high-quality health care is a factor, programs to increase access to health insurance, such as the Affordable Care Act and Children’s Health Insurance Program, or to increase access to high-quality trauma care may help reduce firearm-related death in youth.
“The study of where, how, and why racism operates as a factor in both poverty and firearm-related death must continue, especially considering the disparities consistently documented in Alaska Native or American Indian, Black, and Hispanic communities,” the editorialists wrote.
“Key potential mechanisms for reducing the consequences of poverty for firearm-related death are often denied to racial and ethnic minority groups through a variety of structures, policies, and systems in health care, employment, housing, transportation, and education,” they emphasized, and the impact of racism, not only on the pathways to poverty, but also on mediators between poverty and firearm-related death, must be explored.
Findings spotlight need to for poverty programs
The study was an interesting look at the specific relationship between poverty and firearm-related deaths in people aged younger than 25 years in the United States, Tim Joos, MD, of Seattle said in an interview.
“Although America is not a poor country, the combination of poverty within America and its unique gun culture seems to prove deadly for its youth,” Dr. Joos said. “The strongest relationship is between firearm-related homicide and poverty, but unintentional firearm deaths and poverty also are clearly linked, whereas the link between firearm-related suicide and poverty appears to be present, but small.”.
In the current study, “the authors note that firearm deaths are the second-leading cause of death among all people ages 15-24 years,” said Dr. Joos. “Many of us have followed children from infancy just to have them meet this untimely end as adolescents, wishing we had a vaccine or other remedy in our toolbelt for this particular scourge.
“As our country currently debates the size of the social safety net, this study is one of many that suggests government programs aimed at poverty alleviation would substantially contribute to the health of American youth,” Dr. Joos added.
The study received no outside funding. Lead author Dr. Barrett had no financial conflicts to disclose. Dr. Ellyson disclosed funds from the CDC, the state of Washington, and the Grandmothers Against Gun Violence Foundation for research outside the submitted work. Dr. Rivara disclosed funds from the National Institutes of Health, the State of Washington, and the National Collaborative on Gun Violence Research for research outside the submitted work. Dr. Rowhani-Rahbar disclosed funds from the CDC, National Institutes of Health, National Collaborative on Gun Violence Research, Fund for a Safer Future, and state of Washington for research outside the submitted work. Dr. Joos had no financial conflicts to disclose, but serves on the editorial advisory board of Pediatric News.
FROM JAMA PEDIATRICS
Sociocultural stigmas provide barriers to sexual health in gay and bisexual Hispanic men
Religion and masculine ideology remain significant social cultural barriers to sexual health in Hispanic gay or bisexual men, according to new qualitative research presented at the 2021 Association of Nurses in AIDS Care conference. The pilot study also found that these men learned more sexual health information from friends and social networks than from their health care professionals.
“There’s still so much we do not know about cultural factors and the different levels of influence that shape sexual health promotion beliefs among Latinos, but moreover in Latino same-gender–loving men,” lead author Lisvel Matos, MSN, FNP-C, WHNP-BC, a PhD candidate at Duke University’s School of Nursing, Durham, N.C., said in an interview. Ms. Matos prefers the term same-gender–loving men (SGLM) over men who have sex with men, as the latter term is more clinical and can be stigmatizing.
In Ms. Matos’ 10 years of working in nursing, she noticed that this lack of understanding about sexual health in Hispanic SGLM impeded culturally relevant interventions in this population. “When we don’t have the evidence to show what’s effective for these populations,” she said, “then we’re kind of working blind.”
To get a better sense of social cultural barriers that influence sexual health, Ms. Matos and colleagues conducted 60- to 75-minute interviews with Hispanic SGLM through the secure web conferencing app WebEx from October 2020 to October 2021. The study used the World Health Organization’s definition of sexual health: “a state of physical, emotional, mental and social well-being in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity.” The pilot study included 15 individuals, 8 of whom were born outside of the United States. The mean age of participants was 31.4 years, and 47% reported being single and sexually active. 93% of participants said they were aware of pre-exposure prophylaxis (PrEP), and 47% reported using PrEP.
Ms. Matos identified three common themes in barriers to sexual health in these men: sexual silence, religion, and machismo, a term meaning aggressive masculine pride and patriarchal ideas of manhood. “Because of social constructs, because of what it meant to be a man, [sexual health] was a very difficult subject in adolescence,” said one participant in a quote included on the poster. “I definitely believe in Christianity, and I think that has affected my sexual preference,” said another quoted individual. “It came into that Catholic guilt where you always feel bad.”
More than half of the study participants reported not having access to health care at one time in their life, because of lack of insurance or other factors such as feeling uncomfortable or even dehumanized by health care professionals. Most men said they learned about sexual health, including PrEP, from dating apps like Grindr or friend-based social media platforms rather than in care settings. Ms. Matos, who presented the study at the conference, received the Student Poster Research Award for her work.
The findings are “a good reminder for providers” that these barriers, which have been identified for decades, are still major impediments to sexual health in Hispanic SGLM, both individually and at the clinic level, Dalmacio Dennis Flores, PhD, ACRN, an assistant professor at the University of Pennsylvania School of Nursing, Philadelphia, said in an interview. He was not involved with the work. “We need to be in a space to normalize their attractions, behaviors, and identities and then help them to be more confident about it,” he noted.
Self-confidence as well as trust in sexual partners and health providers were factors that helped these men overcome this negative messaging and sociocultural stigmas, Ms. Matos found.
“The fact that [the researchers] have individual level data about the experiences of this group of men can inform how we develop clinic-level structures that can, for example, promote trust with the provider,” added Kamila Alexander, PhD, MPH, RN, an assistant professor and associate director of PhD and postdoctoral programs at Johns Hopkins University’s School of Nursing, Baltimore.
Dr. Alexander, who was not involved with the research, added that the small study is a good starting point to better inform culturally relevant care for populations marginalized by society, like Hispanic SGLM, and to challenge ingrained stereotypes around religion, masculinity, and sexuality. The researchers “highlighted these intersectional stigmas that have a lot to do with structural factors,” she said, “and those things are really ripe for intervention.”
Ms. Matos, Dr. Flores, and Dr. Alexander disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Religion and masculine ideology remain significant social cultural barriers to sexual health in Hispanic gay or bisexual men, according to new qualitative research presented at the 2021 Association of Nurses in AIDS Care conference. The pilot study also found that these men learned more sexual health information from friends and social networks than from their health care professionals.
“There’s still so much we do not know about cultural factors and the different levels of influence that shape sexual health promotion beliefs among Latinos, but moreover in Latino same-gender–loving men,” lead author Lisvel Matos, MSN, FNP-C, WHNP-BC, a PhD candidate at Duke University’s School of Nursing, Durham, N.C., said in an interview. Ms. Matos prefers the term same-gender–loving men (SGLM) over men who have sex with men, as the latter term is more clinical and can be stigmatizing.
In Ms. Matos’ 10 years of working in nursing, she noticed that this lack of understanding about sexual health in Hispanic SGLM impeded culturally relevant interventions in this population. “When we don’t have the evidence to show what’s effective for these populations,” she said, “then we’re kind of working blind.”
To get a better sense of social cultural barriers that influence sexual health, Ms. Matos and colleagues conducted 60- to 75-minute interviews with Hispanic SGLM through the secure web conferencing app WebEx from October 2020 to October 2021. The study used the World Health Organization’s definition of sexual health: “a state of physical, emotional, mental and social well-being in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity.” The pilot study included 15 individuals, 8 of whom were born outside of the United States. The mean age of participants was 31.4 years, and 47% reported being single and sexually active. 93% of participants said they were aware of pre-exposure prophylaxis (PrEP), and 47% reported using PrEP.
Ms. Matos identified three common themes in barriers to sexual health in these men: sexual silence, religion, and machismo, a term meaning aggressive masculine pride and patriarchal ideas of manhood. “Because of social constructs, because of what it meant to be a man, [sexual health] was a very difficult subject in adolescence,” said one participant in a quote included on the poster. “I definitely believe in Christianity, and I think that has affected my sexual preference,” said another quoted individual. “It came into that Catholic guilt where you always feel bad.”
More than half of the study participants reported not having access to health care at one time in their life, because of lack of insurance or other factors such as feeling uncomfortable or even dehumanized by health care professionals. Most men said they learned about sexual health, including PrEP, from dating apps like Grindr or friend-based social media platforms rather than in care settings. Ms. Matos, who presented the study at the conference, received the Student Poster Research Award for her work.
The findings are “a good reminder for providers” that these barriers, which have been identified for decades, are still major impediments to sexual health in Hispanic SGLM, both individually and at the clinic level, Dalmacio Dennis Flores, PhD, ACRN, an assistant professor at the University of Pennsylvania School of Nursing, Philadelphia, said in an interview. He was not involved with the work. “We need to be in a space to normalize their attractions, behaviors, and identities and then help them to be more confident about it,” he noted.
Self-confidence as well as trust in sexual partners and health providers were factors that helped these men overcome this negative messaging and sociocultural stigmas, Ms. Matos found.
“The fact that [the researchers] have individual level data about the experiences of this group of men can inform how we develop clinic-level structures that can, for example, promote trust with the provider,” added Kamila Alexander, PhD, MPH, RN, an assistant professor and associate director of PhD and postdoctoral programs at Johns Hopkins University’s School of Nursing, Baltimore.
Dr. Alexander, who was not involved with the research, added that the small study is a good starting point to better inform culturally relevant care for populations marginalized by society, like Hispanic SGLM, and to challenge ingrained stereotypes around religion, masculinity, and sexuality. The researchers “highlighted these intersectional stigmas that have a lot to do with structural factors,” she said, “and those things are really ripe for intervention.”
Ms. Matos, Dr. Flores, and Dr. Alexander disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Religion and masculine ideology remain significant social cultural barriers to sexual health in Hispanic gay or bisexual men, according to new qualitative research presented at the 2021 Association of Nurses in AIDS Care conference. The pilot study also found that these men learned more sexual health information from friends and social networks than from their health care professionals.
“There’s still so much we do not know about cultural factors and the different levels of influence that shape sexual health promotion beliefs among Latinos, but moreover in Latino same-gender–loving men,” lead author Lisvel Matos, MSN, FNP-C, WHNP-BC, a PhD candidate at Duke University’s School of Nursing, Durham, N.C., said in an interview. Ms. Matos prefers the term same-gender–loving men (SGLM) over men who have sex with men, as the latter term is more clinical and can be stigmatizing.
In Ms. Matos’ 10 years of working in nursing, she noticed that this lack of understanding about sexual health in Hispanic SGLM impeded culturally relevant interventions in this population. “When we don’t have the evidence to show what’s effective for these populations,” she said, “then we’re kind of working blind.”
To get a better sense of social cultural barriers that influence sexual health, Ms. Matos and colleagues conducted 60- to 75-minute interviews with Hispanic SGLM through the secure web conferencing app WebEx from October 2020 to October 2021. The study used the World Health Organization’s definition of sexual health: “a state of physical, emotional, mental and social well-being in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity.” The pilot study included 15 individuals, 8 of whom were born outside of the United States. The mean age of participants was 31.4 years, and 47% reported being single and sexually active. 93% of participants said they were aware of pre-exposure prophylaxis (PrEP), and 47% reported using PrEP.
Ms. Matos identified three common themes in barriers to sexual health in these men: sexual silence, religion, and machismo, a term meaning aggressive masculine pride and patriarchal ideas of manhood. “Because of social constructs, because of what it meant to be a man, [sexual health] was a very difficult subject in adolescence,” said one participant in a quote included on the poster. “I definitely believe in Christianity, and I think that has affected my sexual preference,” said another quoted individual. “It came into that Catholic guilt where you always feel bad.”
More than half of the study participants reported not having access to health care at one time in their life, because of lack of insurance or other factors such as feeling uncomfortable or even dehumanized by health care professionals. Most men said they learned about sexual health, including PrEP, from dating apps like Grindr or friend-based social media platforms rather than in care settings. Ms. Matos, who presented the study at the conference, received the Student Poster Research Award for her work.
The findings are “a good reminder for providers” that these barriers, which have been identified for decades, are still major impediments to sexual health in Hispanic SGLM, both individually and at the clinic level, Dalmacio Dennis Flores, PhD, ACRN, an assistant professor at the University of Pennsylvania School of Nursing, Philadelphia, said in an interview. He was not involved with the work. “We need to be in a space to normalize their attractions, behaviors, and identities and then help them to be more confident about it,” he noted.
Self-confidence as well as trust in sexual partners and health providers were factors that helped these men overcome this negative messaging and sociocultural stigmas, Ms. Matos found.
“The fact that [the researchers] have individual level data about the experiences of this group of men can inform how we develop clinic-level structures that can, for example, promote trust with the provider,” added Kamila Alexander, PhD, MPH, RN, an assistant professor and associate director of PhD and postdoctoral programs at Johns Hopkins University’s School of Nursing, Baltimore.
Dr. Alexander, who was not involved with the research, added that the small study is a good starting point to better inform culturally relevant care for populations marginalized by society, like Hispanic SGLM, and to challenge ingrained stereotypes around religion, masculinity, and sexuality. The researchers “highlighted these intersectional stigmas that have a lot to do with structural factors,” she said, “and those things are really ripe for intervention.”
Ms. Matos, Dr. Flores, and Dr. Alexander disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ANAC 2021
Black young adults: Remember this when facing discrimination
Joel Bervell recalls leaving his hometown of Seattle for the East Coast after being accepted into Yale University.
Still getting accustomed to the big move, Mr. Bervell, who had breezed through high school with straight As, went to see his chemistry professor for advice after getting a low grade on a test.
“He took one look at me and said, ‘Oh, if you’re on the football team, you don’t need to worry about it. So many people from the football team come into the class and end up dropping out, so if you need to drop this class, you can,’ ” Mr. Bervell says.
Mr. Bervell, who is Black, was not on the football team, nor did he receive a sports scholarship of any kind.
“For that professor to make an assumption of me, which to me felt like it was based on my race, made me less likely to want to go into a science field, where I felt like I was being judged before I even had a chance to prove myself,” Mr. Bervell says.
.
Researchers studied health data on 1,834 Americans ages 18-28 over a 10-year span. Findings show that the more instances of discrimination they experienced – including ageism, sexism, and racism – the more likely they were to face mental and behavioral struggles, like mental illness, drug use, severe psychological distress, and poor overall health.
Mr. Bervell, now 26, says he feels lucky that growing up, he was taught healthy ways to process his feelings and emotions.
“Instead of taking that and internalizing it, I said, ‘how can I use this to prove him wrong?’” he says. “Does that mean I need to work harder or does that mean I need to find a different mentor? Surround myself with different people?”
Mr. Bervell is currently a 3rd-year medical student at Washington State University.
When he’s not at the hospital seeing patients, you can find him educating his nearly 340,000 TikTok followers on topics like racial bias in medicine.
Acknowledge the impact
Most Black people don’t tie psychological distress to acts of racism, according to Rheeda Walker, PhD, psychology professor at the University of Houston and author of “The Unapologetic Guide to Black Mental Health” (Oakland, Calif.: New Harbinger Publications, 2020).
Many Black people even normalize it.
“Individuals deal with it [racism] as just another thing, like paying bills, going to work, and studying for class and not as the overwhelming psychological burden that it is,” says Dr. Walker.
And despite what some may say, racial discrimination is not merely “a thing of the past,” Dr. Walker says.
“Instead, discrimination has shifted form from more overt forms of discrimination to less obvious microaggression,” she says.
It’s also critical that young adults are taught how to deal with racism to avoid the risk of “internalizing that they deserve to be mistreated, and/or that they have to work twice as hard to overcome racism,” says Dr. Walker.
“Both scenarios can escalate hopelessness and worry, psychological features of depression and anxiety, respectively,” Dr. Walker says.
Embrace your emotions
Known around the office as “a big teddy bear,” Frederick Herman, a mortgage loan originator based in Charlotte, Va., was coaching a newer employee on how to make sales calls, a common practice in his line of work.
He says a day or 2 days later, his manager let him know that he had made an employee “very uncomfortable” by intimidating them while they were on the phone. Mr. Herman, 29, was told to watch his “aggressive” behavior.
“I’m a bigger Black man. I’m like 6’2, 300 lbs., somewhat muscular. So, if me talking or trying to coach her came off as intimidating, then there’s nothing that I could do or say differently than I was already doing to make her not feel intimidated,” Mr. Herman says.
“If a big teddy bear is now intimidating to you, that just tells me everything I need to know.”
This wasn’t the first time Mr. Herman had been reprimanded for being “too aggressive” or “showing off” when trying to help colleagues at work.
“I’ve had other experiences at work where I may not share my ideas, or I may get super anxious,” says Mr. Herman, a Black man of Haitian descent.
It’s important to allow yourself to feel your emotions after facing acts of discrimination, says Ebony Butler, PhD, a licensed psychologist and creator of My Therapy Cards, a card deck tailored for men, women, and teens of color, with self-care and reflection prompts.
This is a practice called “self-validation” and can reduce the tendency to blame oneself for the mistreatment, says Dr. Butler.
Mr. Herman, 29, says that he recently signed up for therapy to work through his struggles with anxiety.
Relaxation techniques, like grounding and mindfulness, can also be helpful, says Dr. Butler.
“Some example ways to practice grounding are immersing oneself in nature, walking bare feet on the ground, lying on the floor, practicing slow, deep breathing, or engaging the senses,” she says.
“When we are grounded and present, we can better manage our responses and plan our action steps.”
Utilize unique
If you find yourself in a racially charged school or workplace setting, don’t be intimidated, says Wendy Osefo, PhD, education professor at Johns Hopkins University, Baltimore, political commentator, and television personality.
Dr. Osefo made history in 2016 as the first Black woman to earn a PhD in public affairs/community development from Rutgers University.
“Your attitude should be that, no matter how different you might be, you belong, and you earned the right to occupy this space. You’re not less qualified than others who surround you,” she says.
Dr. Ofeso is also CEO of The 1954 Equity Project, an organization that gives minority students tools to succeed in higher education – like mentorships, peer support groups, and other resources and services – all while remaining their authentic selves.
No matter how uncomfortable it might be, staying true to who you are vs. conforming to the masses pays off, says Dr. Osefo.
“Being different is unique and allows you to bring a new and fresh perspective into an environment,” she says.
“Leaning into this uniqueness builds a level of confidence that will aid in your ability to be successful.”
A version of this article first appeared on WebMD.com.
Joel Bervell recalls leaving his hometown of Seattle for the East Coast after being accepted into Yale University.
Still getting accustomed to the big move, Mr. Bervell, who had breezed through high school with straight As, went to see his chemistry professor for advice after getting a low grade on a test.
“He took one look at me and said, ‘Oh, if you’re on the football team, you don’t need to worry about it. So many people from the football team come into the class and end up dropping out, so if you need to drop this class, you can,’ ” Mr. Bervell says.
Mr. Bervell, who is Black, was not on the football team, nor did he receive a sports scholarship of any kind.
“For that professor to make an assumption of me, which to me felt like it was based on my race, made me less likely to want to go into a science field, where I felt like I was being judged before I even had a chance to prove myself,” Mr. Bervell says.
.
Researchers studied health data on 1,834 Americans ages 18-28 over a 10-year span. Findings show that the more instances of discrimination they experienced – including ageism, sexism, and racism – the more likely they were to face mental and behavioral struggles, like mental illness, drug use, severe psychological distress, and poor overall health.
Mr. Bervell, now 26, says he feels lucky that growing up, he was taught healthy ways to process his feelings and emotions.
“Instead of taking that and internalizing it, I said, ‘how can I use this to prove him wrong?’” he says. “Does that mean I need to work harder or does that mean I need to find a different mentor? Surround myself with different people?”
Mr. Bervell is currently a 3rd-year medical student at Washington State University.
When he’s not at the hospital seeing patients, you can find him educating his nearly 340,000 TikTok followers on topics like racial bias in medicine.
Acknowledge the impact
Most Black people don’t tie psychological distress to acts of racism, according to Rheeda Walker, PhD, psychology professor at the University of Houston and author of “The Unapologetic Guide to Black Mental Health” (Oakland, Calif.: New Harbinger Publications, 2020).
Many Black people even normalize it.
“Individuals deal with it [racism] as just another thing, like paying bills, going to work, and studying for class and not as the overwhelming psychological burden that it is,” says Dr. Walker.
And despite what some may say, racial discrimination is not merely “a thing of the past,” Dr. Walker says.
“Instead, discrimination has shifted form from more overt forms of discrimination to less obvious microaggression,” she says.
It’s also critical that young adults are taught how to deal with racism to avoid the risk of “internalizing that they deserve to be mistreated, and/or that they have to work twice as hard to overcome racism,” says Dr. Walker.
“Both scenarios can escalate hopelessness and worry, psychological features of depression and anxiety, respectively,” Dr. Walker says.
Embrace your emotions
Known around the office as “a big teddy bear,” Frederick Herman, a mortgage loan originator based in Charlotte, Va., was coaching a newer employee on how to make sales calls, a common practice in his line of work.
He says a day or 2 days later, his manager let him know that he had made an employee “very uncomfortable” by intimidating them while they were on the phone. Mr. Herman, 29, was told to watch his “aggressive” behavior.
“I’m a bigger Black man. I’m like 6’2, 300 lbs., somewhat muscular. So, if me talking or trying to coach her came off as intimidating, then there’s nothing that I could do or say differently than I was already doing to make her not feel intimidated,” Mr. Herman says.
“If a big teddy bear is now intimidating to you, that just tells me everything I need to know.”
This wasn’t the first time Mr. Herman had been reprimanded for being “too aggressive” or “showing off” when trying to help colleagues at work.
“I’ve had other experiences at work where I may not share my ideas, or I may get super anxious,” says Mr. Herman, a Black man of Haitian descent.
It’s important to allow yourself to feel your emotions after facing acts of discrimination, says Ebony Butler, PhD, a licensed psychologist and creator of My Therapy Cards, a card deck tailored for men, women, and teens of color, with self-care and reflection prompts.
This is a practice called “self-validation” and can reduce the tendency to blame oneself for the mistreatment, says Dr. Butler.
Mr. Herman, 29, says that he recently signed up for therapy to work through his struggles with anxiety.
Relaxation techniques, like grounding and mindfulness, can also be helpful, says Dr. Butler.
“Some example ways to practice grounding are immersing oneself in nature, walking bare feet on the ground, lying on the floor, practicing slow, deep breathing, or engaging the senses,” she says.
“When we are grounded and present, we can better manage our responses and plan our action steps.”
Utilize unique
If you find yourself in a racially charged school or workplace setting, don’t be intimidated, says Wendy Osefo, PhD, education professor at Johns Hopkins University, Baltimore, political commentator, and television personality.
Dr. Osefo made history in 2016 as the first Black woman to earn a PhD in public affairs/community development from Rutgers University.
“Your attitude should be that, no matter how different you might be, you belong, and you earned the right to occupy this space. You’re not less qualified than others who surround you,” she says.
Dr. Ofeso is also CEO of The 1954 Equity Project, an organization that gives minority students tools to succeed in higher education – like mentorships, peer support groups, and other resources and services – all while remaining their authentic selves.
No matter how uncomfortable it might be, staying true to who you are vs. conforming to the masses pays off, says Dr. Osefo.
“Being different is unique and allows you to bring a new and fresh perspective into an environment,” she says.
“Leaning into this uniqueness builds a level of confidence that will aid in your ability to be successful.”
A version of this article first appeared on WebMD.com.
Joel Bervell recalls leaving his hometown of Seattle for the East Coast after being accepted into Yale University.
Still getting accustomed to the big move, Mr. Bervell, who had breezed through high school with straight As, went to see his chemistry professor for advice after getting a low grade on a test.
“He took one look at me and said, ‘Oh, if you’re on the football team, you don’t need to worry about it. So many people from the football team come into the class and end up dropping out, so if you need to drop this class, you can,’ ” Mr. Bervell says.
Mr. Bervell, who is Black, was not on the football team, nor did he receive a sports scholarship of any kind.
“For that professor to make an assumption of me, which to me felt like it was based on my race, made me less likely to want to go into a science field, where I felt like I was being judged before I even had a chance to prove myself,” Mr. Bervell says.
.
Researchers studied health data on 1,834 Americans ages 18-28 over a 10-year span. Findings show that the more instances of discrimination they experienced – including ageism, sexism, and racism – the more likely they were to face mental and behavioral struggles, like mental illness, drug use, severe psychological distress, and poor overall health.
Mr. Bervell, now 26, says he feels lucky that growing up, he was taught healthy ways to process his feelings and emotions.
“Instead of taking that and internalizing it, I said, ‘how can I use this to prove him wrong?’” he says. “Does that mean I need to work harder or does that mean I need to find a different mentor? Surround myself with different people?”
Mr. Bervell is currently a 3rd-year medical student at Washington State University.
When he’s not at the hospital seeing patients, you can find him educating his nearly 340,000 TikTok followers on topics like racial bias in medicine.
Acknowledge the impact
Most Black people don’t tie psychological distress to acts of racism, according to Rheeda Walker, PhD, psychology professor at the University of Houston and author of “The Unapologetic Guide to Black Mental Health” (Oakland, Calif.: New Harbinger Publications, 2020).
Many Black people even normalize it.
“Individuals deal with it [racism] as just another thing, like paying bills, going to work, and studying for class and not as the overwhelming psychological burden that it is,” says Dr. Walker.
And despite what some may say, racial discrimination is not merely “a thing of the past,” Dr. Walker says.
“Instead, discrimination has shifted form from more overt forms of discrimination to less obvious microaggression,” she says.
It’s also critical that young adults are taught how to deal with racism to avoid the risk of “internalizing that they deserve to be mistreated, and/or that they have to work twice as hard to overcome racism,” says Dr. Walker.
“Both scenarios can escalate hopelessness and worry, psychological features of depression and anxiety, respectively,” Dr. Walker says.
Embrace your emotions
Known around the office as “a big teddy bear,” Frederick Herman, a mortgage loan originator based in Charlotte, Va., was coaching a newer employee on how to make sales calls, a common practice in his line of work.
He says a day or 2 days later, his manager let him know that he had made an employee “very uncomfortable” by intimidating them while they were on the phone. Mr. Herman, 29, was told to watch his “aggressive” behavior.
“I’m a bigger Black man. I’m like 6’2, 300 lbs., somewhat muscular. So, if me talking or trying to coach her came off as intimidating, then there’s nothing that I could do or say differently than I was already doing to make her not feel intimidated,” Mr. Herman says.
“If a big teddy bear is now intimidating to you, that just tells me everything I need to know.”
This wasn’t the first time Mr. Herman had been reprimanded for being “too aggressive” or “showing off” when trying to help colleagues at work.
“I’ve had other experiences at work where I may not share my ideas, or I may get super anxious,” says Mr. Herman, a Black man of Haitian descent.
It’s important to allow yourself to feel your emotions after facing acts of discrimination, says Ebony Butler, PhD, a licensed psychologist and creator of My Therapy Cards, a card deck tailored for men, women, and teens of color, with self-care and reflection prompts.
This is a practice called “self-validation” and can reduce the tendency to blame oneself for the mistreatment, says Dr. Butler.
Mr. Herman, 29, says that he recently signed up for therapy to work through his struggles with anxiety.
Relaxation techniques, like grounding and mindfulness, can also be helpful, says Dr. Butler.
“Some example ways to practice grounding are immersing oneself in nature, walking bare feet on the ground, lying on the floor, practicing slow, deep breathing, or engaging the senses,” she says.
“When we are grounded and present, we can better manage our responses and plan our action steps.”
Utilize unique
If you find yourself in a racially charged school or workplace setting, don’t be intimidated, says Wendy Osefo, PhD, education professor at Johns Hopkins University, Baltimore, political commentator, and television personality.
Dr. Osefo made history in 2016 as the first Black woman to earn a PhD in public affairs/community development from Rutgers University.
“Your attitude should be that, no matter how different you might be, you belong, and you earned the right to occupy this space. You’re not less qualified than others who surround you,” she says.
Dr. Ofeso is also CEO of The 1954 Equity Project, an organization that gives minority students tools to succeed in higher education – like mentorships, peer support groups, and other resources and services – all while remaining their authentic selves.
No matter how uncomfortable it might be, staying true to who you are vs. conforming to the masses pays off, says Dr. Osefo.
“Being different is unique and allows you to bring a new and fresh perspective into an environment,” she says.
“Leaning into this uniqueness builds a level of confidence that will aid in your ability to be successful.”
A version of this article first appeared on WebMD.com.
Early-in-career family physician shares hopes for future of specialty
I became interested in becoming a physician during my very last semester of college. I volunteered in a hospital psychiatric department in the unit that provided electroconvulsive therapy to patients with severe mental health diagnoses. Although this was about 15 years ago, I still vividly remember the curiosity I had walking around the hospital looking around at all the doctors and nurses and wanting to understand what their day-to-day life was like helping people to optimize their health.
Up until that time, thankfully my family and I had been relatively healthy, and, outside of routine checkups, my time spent in a hospital or clinic was limited. Therefore, those months of volunteering at the hospital were the longest periods of time I’d spent around physicians and other health care professionals really witnessing firsthand the science and the art of medicine.
During my time volunteering I saw one patient over the course of several weeks who was catatonic when I first met her, but by the end of several electroconvulsive therapy treatments she had a subtle smile on her face and we were able to have a conversation. She was a younger Black woman like myself and at that moment I knew that I wanted to become a physician and be involved in people’s lives in such a unique manner.
I worked for several years before applying to medical school. During that time two of my jobs involved doing home visits with children, young adults, and their families. I once again experienced the connection that one can make with someone and their family over a short period of time when you actively listen, understand what is important to them, and work together.
After several years of this work I got accepted into medical school and excitedly started the path to becoming a physician. While the learning curve was difficult, I genuinely enjoyed every block of medical school, including learning the anatomy, pathophysiology, and pharmacology. I could not wait to be in front of patients to use this newfound knowledge to help solve their health problems.
‘There is no such thing as a single issue-struggle’
As I started the third year of medical school and clinical rotations, I found joy in being in hospitals and clinics. I also came to recognize that understanding the pharmacology of why metformin helps improve the hemoglobin A1c in people with diabetes is not necessarily one of the keys to helping people optimize their health. I started to talk with patients and all sorts of questions would come to mind. Where did they grow up? What did they identify as their culture? What did they do in their day to day? Did they have a home and support at that home? Are they someone’s caretaker? What are their hopes for the future? And the list goes on.
I ultimately chose family medicine as a specialty because, as Audre Lorde said, “there is no such thing as a single-issue struggle because we do not live single-issue lives,” and family medicine allows one to look at the intersections of people’s lives and how they affect their health and well-being.
I currently practice as a family medicine physician in a setting in which I provide a lot of sexual and reproductive health care. I welcome patients of all ages and genders, and this care includes preconception counseling, contraceptive counseling, prenatal and postpartum care, STI testing and treatment, abortion care, and routine preventive care – just to name a few.
I decided to specialize in sexual and reproductive health care within family medicine because of the historic discrimination and inequitable treatment that is often experienced by young Black persons when they seek care for their sexual health and/or reproductive choices. In addition, there is often stigma within communities when it comes to talking about sex, bodies, and pleasure.
Recently, after a few minutes with a patient, she shared with me that she just completed nursing school and was studying for her exams. We talked about what type of jobs she was looking to apply for and where she wanted to work. I expressed to her that I was proud of the hard work she put in to complete nursing school and commiserated with her about the challenges in schooling and studying that it takes to start in the health care field. The conversation eventually found its way to talking about her sexual and reproductive health care. She shared with me that she was interested in having a child; however, at this time she put those plans on hold because she was scared about the racism within health care and the unacceptable high rates of maternal mortality among Black women in this country.
I listened and shared that as someone who also identifies as a Black woman, I have similar fears and anxieties surrounding my own reproductive health future. During the visit with this patient, I used my training in family medicine to better understand her physical and mental health needs and reassured her that I was going to partner with her through her health care journey.
Hope for the future of family medicine
As I work on a day-to-day basis I often think about my hopes for patients, as well as my hopes for medicine and the field of family medicine. My hope for the future of family medicine is that we can continue to make meaningful connections with patients to help them optimize their health and well-being.
I imagine a system in which we have the time and support to do this for all of our patients regardless of their immigration status, socioeconomic status, or any other historically excluded status. My hope for the future of family medicine is that I can write a prescription for a medication or physical therapy, and the patient is able to fill the prescription without having to worry about the financial implications of paying for it. My hope for the future of family medicine is that patients can seek out care without the fear of discrimination or racism through an increasingly diverse work force. My hope for the future of family medicine is that these improvements become a reality and that as physicians we can appreciate the connections we make with patients and the impact this has on their overall health and well-being.
Dr. Lockley is a family medicine physician currently living in Harlem, N.Y., and a member of the editorial advisory board of Family Practice News. She currently works for Public Health Solutions’ Sexual and Reproductive Health Centers in Brooklyn, providing primary care and reproductive health care services there, and as an abortion provider throughout the New York region. She completed both medical school and residency in Philadelphia and then did a fellowship in reproductive health care and advocacy through the Family Health Center of Harlem and the Reproductive Health Access Project. She can be reached at [email protected].
I became interested in becoming a physician during my very last semester of college. I volunteered in a hospital psychiatric department in the unit that provided electroconvulsive therapy to patients with severe mental health diagnoses. Although this was about 15 years ago, I still vividly remember the curiosity I had walking around the hospital looking around at all the doctors and nurses and wanting to understand what their day-to-day life was like helping people to optimize their health.
Up until that time, thankfully my family and I had been relatively healthy, and, outside of routine checkups, my time spent in a hospital or clinic was limited. Therefore, those months of volunteering at the hospital were the longest periods of time I’d spent around physicians and other health care professionals really witnessing firsthand the science and the art of medicine.
During my time volunteering I saw one patient over the course of several weeks who was catatonic when I first met her, but by the end of several electroconvulsive therapy treatments she had a subtle smile on her face and we were able to have a conversation. She was a younger Black woman like myself and at that moment I knew that I wanted to become a physician and be involved in people’s lives in such a unique manner.
I worked for several years before applying to medical school. During that time two of my jobs involved doing home visits with children, young adults, and their families. I once again experienced the connection that one can make with someone and their family over a short period of time when you actively listen, understand what is important to them, and work together.
After several years of this work I got accepted into medical school and excitedly started the path to becoming a physician. While the learning curve was difficult, I genuinely enjoyed every block of medical school, including learning the anatomy, pathophysiology, and pharmacology. I could not wait to be in front of patients to use this newfound knowledge to help solve their health problems.
‘There is no such thing as a single issue-struggle’
As I started the third year of medical school and clinical rotations, I found joy in being in hospitals and clinics. I also came to recognize that understanding the pharmacology of why metformin helps improve the hemoglobin A1c in people with diabetes is not necessarily one of the keys to helping people optimize their health. I started to talk with patients and all sorts of questions would come to mind. Where did they grow up? What did they identify as their culture? What did they do in their day to day? Did they have a home and support at that home? Are they someone’s caretaker? What are their hopes for the future? And the list goes on.
I ultimately chose family medicine as a specialty because, as Audre Lorde said, “there is no such thing as a single-issue struggle because we do not live single-issue lives,” and family medicine allows one to look at the intersections of people’s lives and how they affect their health and well-being.
I currently practice as a family medicine physician in a setting in which I provide a lot of sexual and reproductive health care. I welcome patients of all ages and genders, and this care includes preconception counseling, contraceptive counseling, prenatal and postpartum care, STI testing and treatment, abortion care, and routine preventive care – just to name a few.
I decided to specialize in sexual and reproductive health care within family medicine because of the historic discrimination and inequitable treatment that is often experienced by young Black persons when they seek care for their sexual health and/or reproductive choices. In addition, there is often stigma within communities when it comes to talking about sex, bodies, and pleasure.
Recently, after a few minutes with a patient, she shared with me that she just completed nursing school and was studying for her exams. We talked about what type of jobs she was looking to apply for and where she wanted to work. I expressed to her that I was proud of the hard work she put in to complete nursing school and commiserated with her about the challenges in schooling and studying that it takes to start in the health care field. The conversation eventually found its way to talking about her sexual and reproductive health care. She shared with me that she was interested in having a child; however, at this time she put those plans on hold because she was scared about the racism within health care and the unacceptable high rates of maternal mortality among Black women in this country.
I listened and shared that as someone who also identifies as a Black woman, I have similar fears and anxieties surrounding my own reproductive health future. During the visit with this patient, I used my training in family medicine to better understand her physical and mental health needs and reassured her that I was going to partner with her through her health care journey.
Hope for the future of family medicine
As I work on a day-to-day basis I often think about my hopes for patients, as well as my hopes for medicine and the field of family medicine. My hope for the future of family medicine is that we can continue to make meaningful connections with patients to help them optimize their health and well-being.
I imagine a system in which we have the time and support to do this for all of our patients regardless of their immigration status, socioeconomic status, or any other historically excluded status. My hope for the future of family medicine is that I can write a prescription for a medication or physical therapy, and the patient is able to fill the prescription without having to worry about the financial implications of paying for it. My hope for the future of family medicine is that patients can seek out care without the fear of discrimination or racism through an increasingly diverse work force. My hope for the future of family medicine is that these improvements become a reality and that as physicians we can appreciate the connections we make with patients and the impact this has on their overall health and well-being.
Dr. Lockley is a family medicine physician currently living in Harlem, N.Y., and a member of the editorial advisory board of Family Practice News. She currently works for Public Health Solutions’ Sexual and Reproductive Health Centers in Brooklyn, providing primary care and reproductive health care services there, and as an abortion provider throughout the New York region. She completed both medical school and residency in Philadelphia and then did a fellowship in reproductive health care and advocacy through the Family Health Center of Harlem and the Reproductive Health Access Project. She can be reached at [email protected].
I became interested in becoming a physician during my very last semester of college. I volunteered in a hospital psychiatric department in the unit that provided electroconvulsive therapy to patients with severe mental health diagnoses. Although this was about 15 years ago, I still vividly remember the curiosity I had walking around the hospital looking around at all the doctors and nurses and wanting to understand what their day-to-day life was like helping people to optimize their health.
Up until that time, thankfully my family and I had been relatively healthy, and, outside of routine checkups, my time spent in a hospital or clinic was limited. Therefore, those months of volunteering at the hospital were the longest periods of time I’d spent around physicians and other health care professionals really witnessing firsthand the science and the art of medicine.
During my time volunteering I saw one patient over the course of several weeks who was catatonic when I first met her, but by the end of several electroconvulsive therapy treatments she had a subtle smile on her face and we were able to have a conversation. She was a younger Black woman like myself and at that moment I knew that I wanted to become a physician and be involved in people’s lives in such a unique manner.
I worked for several years before applying to medical school. During that time two of my jobs involved doing home visits with children, young adults, and their families. I once again experienced the connection that one can make with someone and their family over a short period of time when you actively listen, understand what is important to them, and work together.
After several years of this work I got accepted into medical school and excitedly started the path to becoming a physician. While the learning curve was difficult, I genuinely enjoyed every block of medical school, including learning the anatomy, pathophysiology, and pharmacology. I could not wait to be in front of patients to use this newfound knowledge to help solve their health problems.
‘There is no such thing as a single issue-struggle’
As I started the third year of medical school and clinical rotations, I found joy in being in hospitals and clinics. I also came to recognize that understanding the pharmacology of why metformin helps improve the hemoglobin A1c in people with diabetes is not necessarily one of the keys to helping people optimize their health. I started to talk with patients and all sorts of questions would come to mind. Where did they grow up? What did they identify as their culture? What did they do in their day to day? Did they have a home and support at that home? Are they someone’s caretaker? What are their hopes for the future? And the list goes on.
I ultimately chose family medicine as a specialty because, as Audre Lorde said, “there is no such thing as a single-issue struggle because we do not live single-issue lives,” and family medicine allows one to look at the intersections of people’s lives and how they affect their health and well-being.
I currently practice as a family medicine physician in a setting in which I provide a lot of sexual and reproductive health care. I welcome patients of all ages and genders, and this care includes preconception counseling, contraceptive counseling, prenatal and postpartum care, STI testing and treatment, abortion care, and routine preventive care – just to name a few.
I decided to specialize in sexual and reproductive health care within family medicine because of the historic discrimination and inequitable treatment that is often experienced by young Black persons when they seek care for their sexual health and/or reproductive choices. In addition, there is often stigma within communities when it comes to talking about sex, bodies, and pleasure.
Recently, after a few minutes with a patient, she shared with me that she just completed nursing school and was studying for her exams. We talked about what type of jobs she was looking to apply for and where she wanted to work. I expressed to her that I was proud of the hard work she put in to complete nursing school and commiserated with her about the challenges in schooling and studying that it takes to start in the health care field. The conversation eventually found its way to talking about her sexual and reproductive health care. She shared with me that she was interested in having a child; however, at this time she put those plans on hold because she was scared about the racism within health care and the unacceptable high rates of maternal mortality among Black women in this country.
I listened and shared that as someone who also identifies as a Black woman, I have similar fears and anxieties surrounding my own reproductive health future. During the visit with this patient, I used my training in family medicine to better understand her physical and mental health needs and reassured her that I was going to partner with her through her health care journey.
Hope for the future of family medicine
As I work on a day-to-day basis I often think about my hopes for patients, as well as my hopes for medicine and the field of family medicine. My hope for the future of family medicine is that we can continue to make meaningful connections with patients to help them optimize their health and well-being.
I imagine a system in which we have the time and support to do this for all of our patients regardless of their immigration status, socioeconomic status, or any other historically excluded status. My hope for the future of family medicine is that I can write a prescription for a medication or physical therapy, and the patient is able to fill the prescription without having to worry about the financial implications of paying for it. My hope for the future of family medicine is that patients can seek out care without the fear of discrimination or racism through an increasingly diverse work force. My hope for the future of family medicine is that these improvements become a reality and that as physicians we can appreciate the connections we make with patients and the impact this has on their overall health and well-being.
Dr. Lockley is a family medicine physician currently living in Harlem, N.Y., and a member of the editorial advisory board of Family Practice News. She currently works for Public Health Solutions’ Sexual and Reproductive Health Centers in Brooklyn, providing primary care and reproductive health care services there, and as an abortion provider throughout the New York region. She completed both medical school and residency in Philadelphia and then did a fellowship in reproductive health care and advocacy through the Family Health Center of Harlem and the Reproductive Health Access Project. She can be reached at [email protected].
Seborrheic dermatitis
THE COMPARISON
A Seborrheic dermatitis in a woman with brown-gray greasy scale, as well as petaloid papules and plaques that are especially prominent in the nasolabial folds.
B Seborrheic dermatitis in a man with erythema, scale, and mild postinflammatory hypopigmentation that are especially prominent in the nasolabial folds.
C Seborrheic dermatitis in a man with erythema, faint scale, and postinflammatory hypopigmentation that are especially prominent in the nasolabial folds.
D Seborrheic dermatitis in a man with erythema and scale of the eyebrows and glabellar region.
Seborrheic dermatitis (SD) is an inflammatory condition that is thought to be part of a response to Malassezia yeast. The scalp and face are most commonly affected, particularly the nasolabial folds, eyebrows, ears, postauricular areas, and beard area. Men also may have SD on the mid upper chest in association with chest hair. In infants, the scalp and body skin folds often are affected.
Epidemiology
SD affects patients of all ages: infants, adolescents, and adults. It is among the most common dermatologic diagnoses reported in Black patients in the United States.1
Key clinical features in darker skin tones
- In those with darker skin tones, arcuate, polycyclic, or petaloid (flower petallike) plaques may be present (FIGURE A). Also, hypopigmented patches and plaques may be prominent (FIGURES B AND C). The classic description includes thin pink patches and plaques with white greasy scale on the face (FIGURE D).
- The scalp may have diffuse scale or isolated scaly plaques.
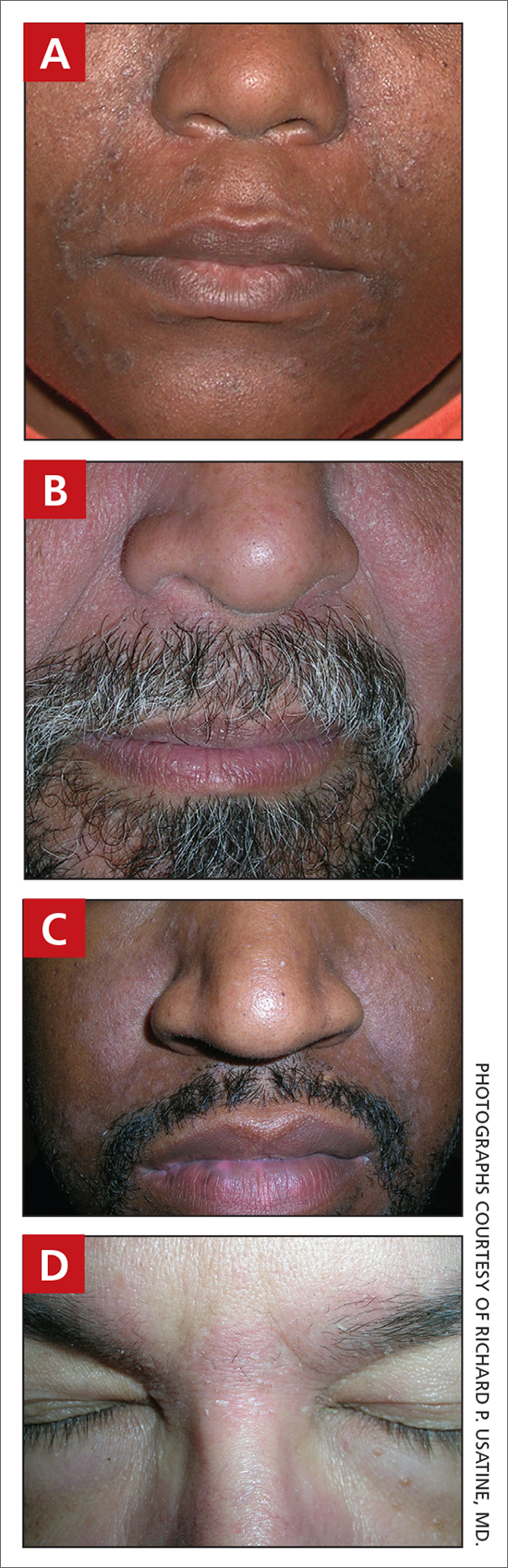
Worth noting
- In those with tightly coiled hair, there is a predisposition for dry hair and increased risk for breakage.
- Treatment plans for patients with SD often include frequent hair washing. However, in those with tightly coiled hair, the treatment plan may need to be modified due to hair texture, tendency for dryness, and washing frequency preferences. Washing the scalp at least every 1 to 2 weeks may be a preferred approach for those with tightly coiled hair at increased risk for dryness/breakage vs washing daily.2 In a sample of 201 caregivers of Black girls, Rucker Wright et al3 found that washing the hair more than once per week was not correlated with a lower prevalence of SD.
- If tightly coiled hair is temporarily straightened with heat (eg, blow-dryer, flat iron), adding a liquid-based treatment such as clobetasol solution or fluocinonide solution will cause the hair to revert to its normal curl pattern.
- It is appropriate to ask patients for their vehicle preference for medications.2 For example, if clobetasol is the treatment selected for the patient, the vehicle can reflect patient preference for a liquid, foam, cream, or ointment.
- Some antifungal/antiyeast shampoos may cause further hair dryness and breakage.
- Treatment may be delayed because patients often use various topical pomades and ointments to cover up the scale and help with pruritus.
- Diffuse scale of tinea capitis in school- aged children can be mistaken for SD, which leads to delayed diagnosis and treatment.
- Clinicians should become comfortable with scalp examinations in patients with tightly coiled hair. Patients with chief concerns related to their hair and scalp expect their clinicians to touch these areas. Avoid leaning in to examine the patient without touching the patient’s hair and scalp.2,4
Health disparity highlight
SD is among the most common cutaneous disorders diagnosed in patients with skin of color.1,5 Delay in recognition of SD in those with darker skin tones leads to delayed treatment. SD of the face can cause notable postinflammatory pigmentation alteration. Pigmentation changes in the skin further impact quality of life.
1. Alexis AF, Sergay AB, Taylor SC. Common dermatologic disorders in skin of color: a comparative practice survey. Cutis. 2007;80:387-394.
2. Grayson C, Heath C. Tips for addressing common conditions affecting pediatric and adolescent patients with skin of color [published online March 2, 2021]. Pediatr Dermatol. 2021;10.1111/ pde.14525
3. Rucker Wright D, Gathers R, Kapke A, et al. Hair care practices and their association with scalp and hair disorders in African American girls. J Am Acad Dermatol. 2011;64: 253-262. doi:10.1016/j.jaad.2010.05.037
4. Grayson C, Heath C. An approach to examining tightly coiled hair among patients with hair loss in race-discordant patientphysician interactions. JAMA Dermatol. 2021;157:505-506. doi:10.1001/jamadermatol.2021.0338
5. Gaulding JV, Gutierrez D, Bhatia BK, et al. Epidemiology of skin diseases in a diverse patient population. J Drugs Dermatol. 2018;17:1032-1036.
THE COMPARISON
A Seborrheic dermatitis in a woman with brown-gray greasy scale, as well as petaloid papules and plaques that are especially prominent in the nasolabial folds.
B Seborrheic dermatitis in a man with erythema, scale, and mild postinflammatory hypopigmentation that are especially prominent in the nasolabial folds.
C Seborrheic dermatitis in a man with erythema, faint scale, and postinflammatory hypopigmentation that are especially prominent in the nasolabial folds.
D Seborrheic dermatitis in a man with erythema and scale of the eyebrows and glabellar region.
Seborrheic dermatitis (SD) is an inflammatory condition that is thought to be part of a response to Malassezia yeast. The scalp and face are most commonly affected, particularly the nasolabial folds, eyebrows, ears, postauricular areas, and beard area. Men also may have SD on the mid upper chest in association with chest hair. In infants, the scalp and body skin folds often are affected.
Epidemiology
SD affects patients of all ages: infants, adolescents, and adults. It is among the most common dermatologic diagnoses reported in Black patients in the United States.1
Key clinical features in darker skin tones
- In those with darker skin tones, arcuate, polycyclic, or petaloid (flower petallike) plaques may be present (FIGURE A). Also, hypopigmented patches and plaques may be prominent (FIGURES B AND C). The classic description includes thin pink patches and plaques with white greasy scale on the face (FIGURE D).
- The scalp may have diffuse scale or isolated scaly plaques.
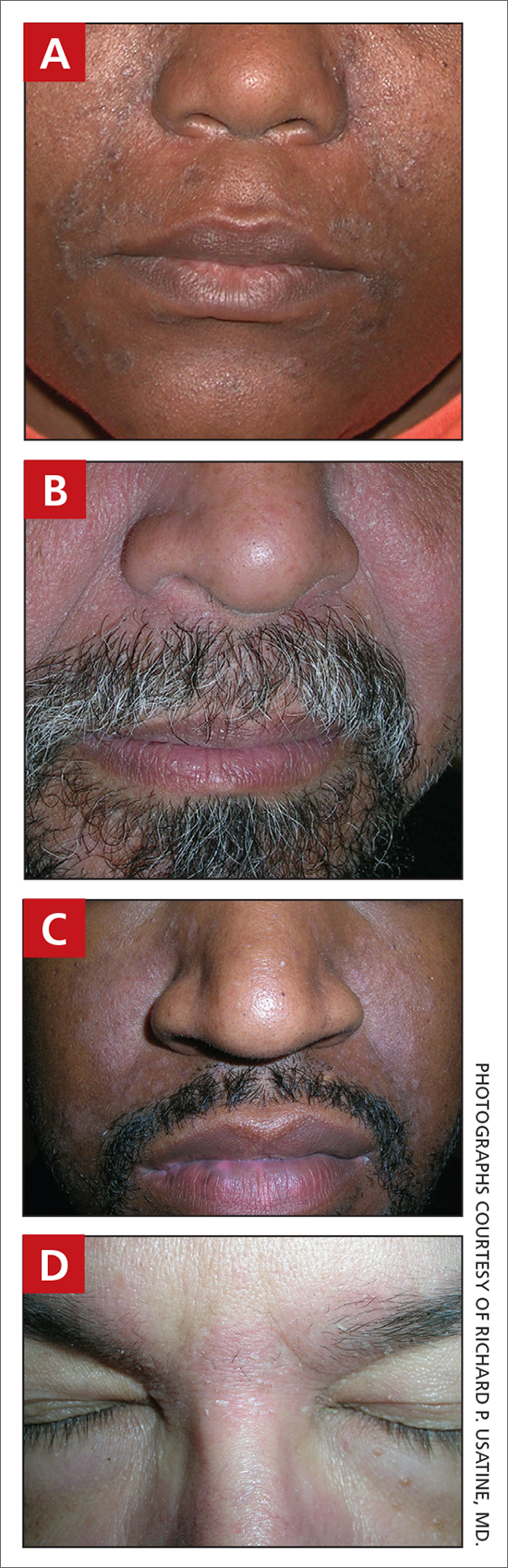
Worth noting
- In those with tightly coiled hair, there is a predisposition for dry hair and increased risk for breakage.
- Treatment plans for patients with SD often include frequent hair washing. However, in those with tightly coiled hair, the treatment plan may need to be modified due to hair texture, tendency for dryness, and washing frequency preferences. Washing the scalp at least every 1 to 2 weeks may be a preferred approach for those with tightly coiled hair at increased risk for dryness/breakage vs washing daily.2 In a sample of 201 caregivers of Black girls, Rucker Wright et al3 found that washing the hair more than once per week was not correlated with a lower prevalence of SD.
- If tightly coiled hair is temporarily straightened with heat (eg, blow-dryer, flat iron), adding a liquid-based treatment such as clobetasol solution or fluocinonide solution will cause the hair to revert to its normal curl pattern.
- It is appropriate to ask patients for their vehicle preference for medications.2 For example, if clobetasol is the treatment selected for the patient, the vehicle can reflect patient preference for a liquid, foam, cream, or ointment.
- Some antifungal/antiyeast shampoos may cause further hair dryness and breakage.
- Treatment may be delayed because patients often use various topical pomades and ointments to cover up the scale and help with pruritus.
- Diffuse scale of tinea capitis in school- aged children can be mistaken for SD, which leads to delayed diagnosis and treatment.
- Clinicians should become comfortable with scalp examinations in patients with tightly coiled hair. Patients with chief concerns related to their hair and scalp expect their clinicians to touch these areas. Avoid leaning in to examine the patient without touching the patient’s hair and scalp.2,4
Health disparity highlight
SD is among the most common cutaneous disorders diagnosed in patients with skin of color.1,5 Delay in recognition of SD in those with darker skin tones leads to delayed treatment. SD of the face can cause notable postinflammatory pigmentation alteration. Pigmentation changes in the skin further impact quality of life.
THE COMPARISON
A Seborrheic dermatitis in a woman with brown-gray greasy scale, as well as petaloid papules and plaques that are especially prominent in the nasolabial folds.
B Seborrheic dermatitis in a man with erythema, scale, and mild postinflammatory hypopigmentation that are especially prominent in the nasolabial folds.
C Seborrheic dermatitis in a man with erythema, faint scale, and postinflammatory hypopigmentation that are especially prominent in the nasolabial folds.
D Seborrheic dermatitis in a man with erythema and scale of the eyebrows and glabellar region.
Seborrheic dermatitis (SD) is an inflammatory condition that is thought to be part of a response to Malassezia yeast. The scalp and face are most commonly affected, particularly the nasolabial folds, eyebrows, ears, postauricular areas, and beard area. Men also may have SD on the mid upper chest in association with chest hair. In infants, the scalp and body skin folds often are affected.
Epidemiology
SD affects patients of all ages: infants, adolescents, and adults. It is among the most common dermatologic diagnoses reported in Black patients in the United States.1
Key clinical features in darker skin tones
- In those with darker skin tones, arcuate, polycyclic, or petaloid (flower petallike) plaques may be present (FIGURE A). Also, hypopigmented patches and plaques may be prominent (FIGURES B AND C). The classic description includes thin pink patches and plaques with white greasy scale on the face (FIGURE D).
- The scalp may have diffuse scale or isolated scaly plaques.
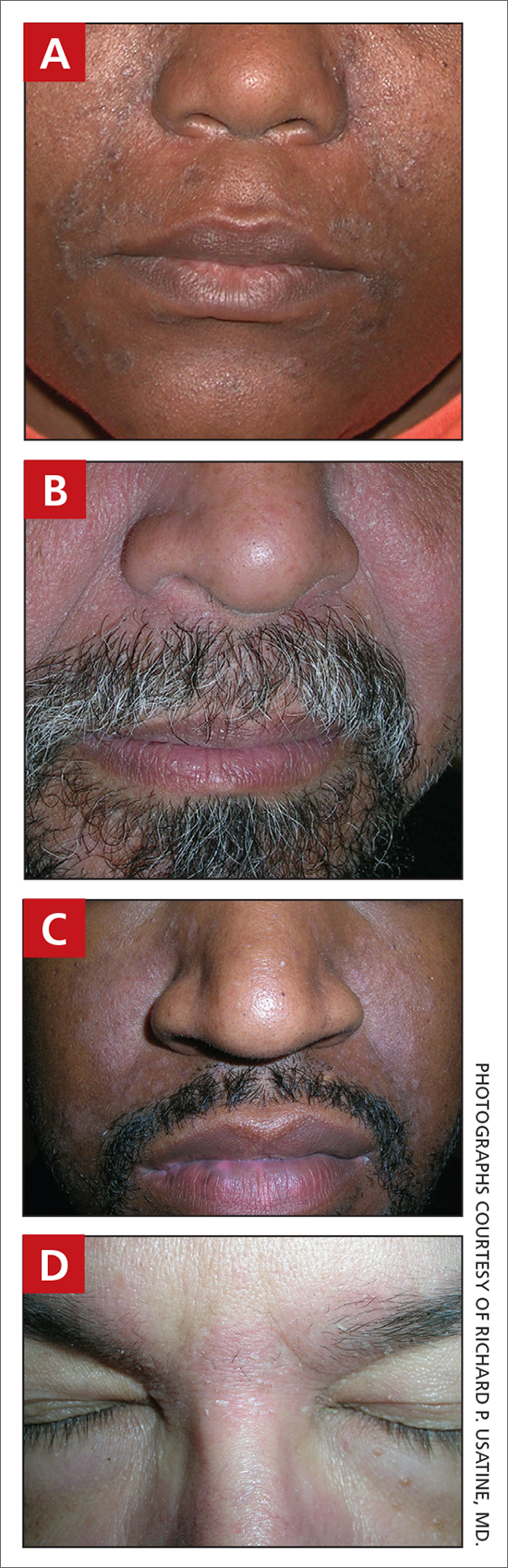
Worth noting
- In those with tightly coiled hair, there is a predisposition for dry hair and increased risk for breakage.
- Treatment plans for patients with SD often include frequent hair washing. However, in those with tightly coiled hair, the treatment plan may need to be modified due to hair texture, tendency for dryness, and washing frequency preferences. Washing the scalp at least every 1 to 2 weeks may be a preferred approach for those with tightly coiled hair at increased risk for dryness/breakage vs washing daily.2 In a sample of 201 caregivers of Black girls, Rucker Wright et al3 found that washing the hair more than once per week was not correlated with a lower prevalence of SD.
- If tightly coiled hair is temporarily straightened with heat (eg, blow-dryer, flat iron), adding a liquid-based treatment such as clobetasol solution or fluocinonide solution will cause the hair to revert to its normal curl pattern.
- It is appropriate to ask patients for their vehicle preference for medications.2 For example, if clobetasol is the treatment selected for the patient, the vehicle can reflect patient preference for a liquid, foam, cream, or ointment.
- Some antifungal/antiyeast shampoos may cause further hair dryness and breakage.
- Treatment may be delayed because patients often use various topical pomades and ointments to cover up the scale and help with pruritus.
- Diffuse scale of tinea capitis in school- aged children can be mistaken for SD, which leads to delayed diagnosis and treatment.
- Clinicians should become comfortable with scalp examinations in patients with tightly coiled hair. Patients with chief concerns related to their hair and scalp expect their clinicians to touch these areas. Avoid leaning in to examine the patient without touching the patient’s hair and scalp.2,4
Health disparity highlight
SD is among the most common cutaneous disorders diagnosed in patients with skin of color.1,5 Delay in recognition of SD in those with darker skin tones leads to delayed treatment. SD of the face can cause notable postinflammatory pigmentation alteration. Pigmentation changes in the skin further impact quality of life.
1. Alexis AF, Sergay AB, Taylor SC. Common dermatologic disorders in skin of color: a comparative practice survey. Cutis. 2007;80:387-394.
2. Grayson C, Heath C. Tips for addressing common conditions affecting pediatric and adolescent patients with skin of color [published online March 2, 2021]. Pediatr Dermatol. 2021;10.1111/ pde.14525
3. Rucker Wright D, Gathers R, Kapke A, et al. Hair care practices and their association with scalp and hair disorders in African American girls. J Am Acad Dermatol. 2011;64: 253-262. doi:10.1016/j.jaad.2010.05.037
4. Grayson C, Heath C. An approach to examining tightly coiled hair among patients with hair loss in race-discordant patientphysician interactions. JAMA Dermatol. 2021;157:505-506. doi:10.1001/jamadermatol.2021.0338
5. Gaulding JV, Gutierrez D, Bhatia BK, et al. Epidemiology of skin diseases in a diverse patient population. J Drugs Dermatol. 2018;17:1032-1036.
1. Alexis AF, Sergay AB, Taylor SC. Common dermatologic disorders in skin of color: a comparative practice survey. Cutis. 2007;80:387-394.
2. Grayson C, Heath C. Tips for addressing common conditions affecting pediatric and adolescent patients with skin of color [published online March 2, 2021]. Pediatr Dermatol. 2021;10.1111/ pde.14525
3. Rucker Wright D, Gathers R, Kapke A, et al. Hair care practices and their association with scalp and hair disorders in African American girls. J Am Acad Dermatol. 2011;64: 253-262. doi:10.1016/j.jaad.2010.05.037
4. Grayson C, Heath C. An approach to examining tightly coiled hair among patients with hair loss in race-discordant patientphysician interactions. JAMA Dermatol. 2021;157:505-506. doi:10.1001/jamadermatol.2021.0338
5. Gaulding JV, Gutierrez D, Bhatia BK, et al. Epidemiology of skin diseases in a diverse patient population. J Drugs Dermatol. 2018;17:1032-1036.