User login
Children and COVID: Downward trend reverses with small increase in new cases
A small increase in new cases brought COVID-19’s latest losing streak to an end at 4 weeks, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
The 40,656 new cases reported bring the U.S. cumulative count of child COVID-19 cases to over 14.8 million since the pandemic began, which represents 18.4% of all cases, the AAP and CHA said in their weekly report based on state-level data.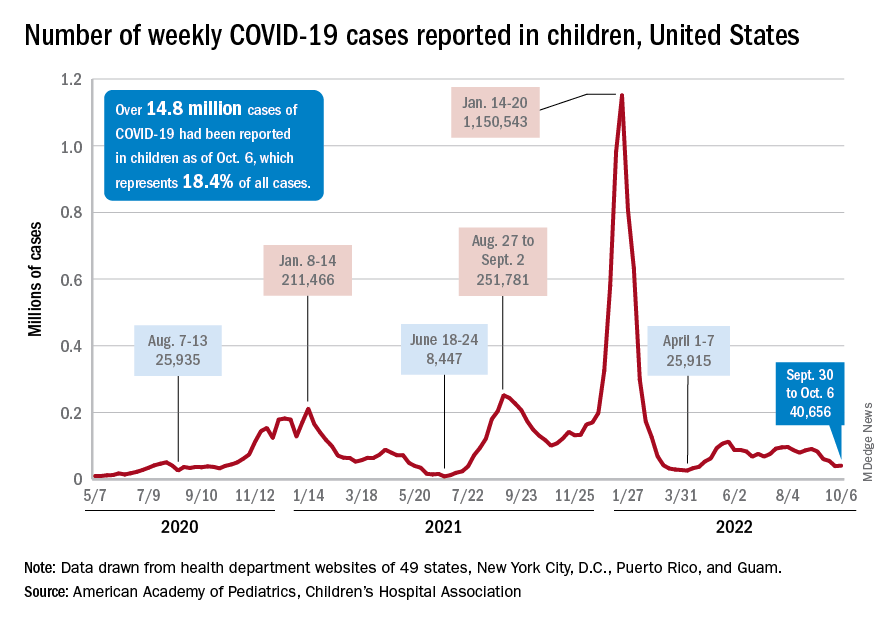
The increase in new cases was not reflected in emergency department visits or hospital admissions, which both continued sustained declines that started in August. In the week from Sept. 27 to Oct. 4, the 7-day averages for ED visits with diagnosed COVID were down by 21.5% (age 0-11), 27.3% (12-15), and 18.2% (16-17), the Centers for Disease Control and Prevention said, while the most recent 7-day average for new admissions – 127 per day for Oct. 2-8 – among children aged 0-17 years with confirmed COVID was down from 161 per day the previous week, a drop of over 21%.
The state-level data that are currently available (several states are no longer reporting) show Alaska (25.5%) and Vermont (25.4%) have the highest proportions of cumulative cases in children, and Florida (12.3%) and Utah (13.5%) have the lowest. Rhode Island has the highest rate of COVID-19 per 100,000 children at 40,427, while Missouri has the lowest at 14,252. The national average is 19,687 per 100,000, the AAP and CHA reported.
Taking a look at vaccination
Vaccinations were up slightly in children aged 12-17 years, as 20,000 initial doses were given during the week of Sept. 29 to Oct. 5, compared with 17,000 and 18,000 the previous 2 weeks. Initial vaccinations in younger children, however, continued declines dating back to August, the AAP said in its weekly vaccination trends report.
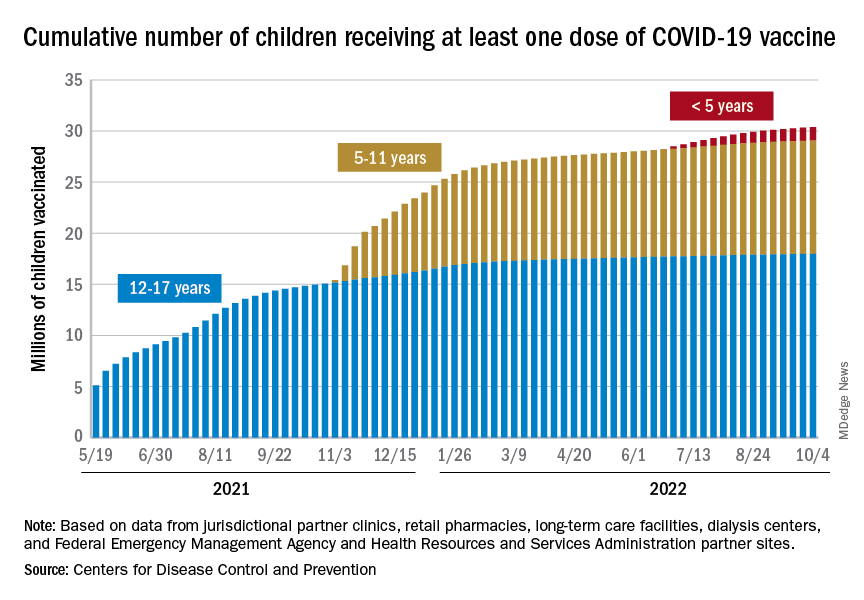
The District of Columbia and Massachusetts have the most highly vaccinated groups of 12- to 17-year-olds, as 100% and 95%, respectively, have received initial doses, while Wyoming (39%) and Idaho (42%) have the lowest. D.C. (73%) and Vermont (68%) have the highest proportions of vaccinated 5- to 11-year-olds, and Alabama (17%) and Mississippi (18%) have the lowest. For children under age 5 years, those in D.C. (33%) and Vermont (26%) are the most likely to have received an initial COVID vaccination, while Alabama, Louisiana, and Mississippi share national-low rates of 2%, the AAP said its report, which is based on CDC data.
When all states and territories are combined, 71% of children aged 12-17 have received at least one dose of vaccine, as have 38.6% of all children 5-11 years old and 6.7% of those under age 5. Almost 61% of the nation’s 16- to 17-year-olds have been fully vaccinated, along with 31.5% of those aged 5-11 and 2.4% of children younger than 5 years, the CDC said on its COVID Data Tracker.
About 42 million children – 58% of the population under the age of 18 years – have not received any vaccine yet, the AAP noted. Meanwhile, CDC data indicate that 36 children died of COVID in the last week, with pediatric deaths now totaling 1,781 over the course of the pandemic.
A small increase in new cases brought COVID-19’s latest losing streak to an end at 4 weeks, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
The 40,656 new cases reported bring the U.S. cumulative count of child COVID-19 cases to over 14.8 million since the pandemic began, which represents 18.4% of all cases, the AAP and CHA said in their weekly report based on state-level data.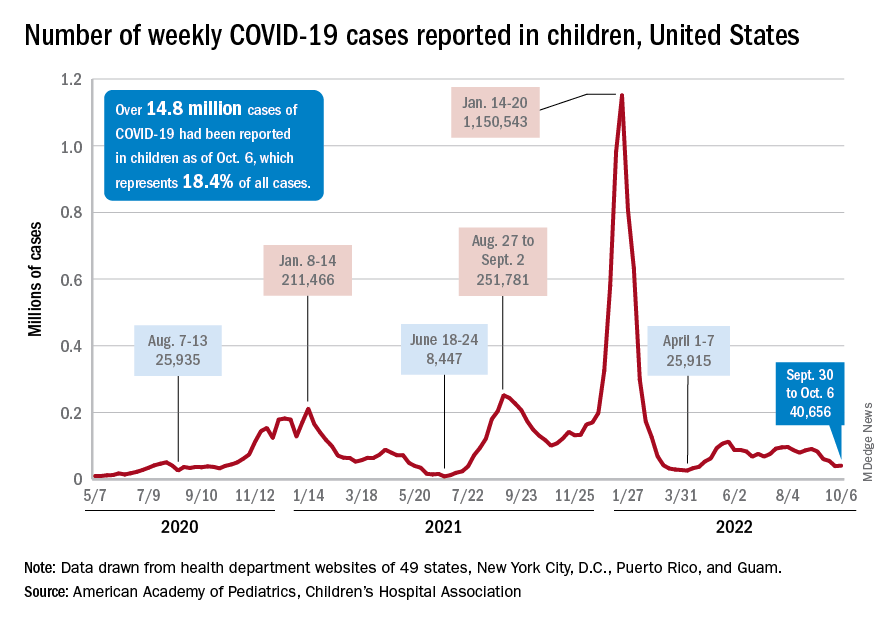
The increase in new cases was not reflected in emergency department visits or hospital admissions, which both continued sustained declines that started in August. In the week from Sept. 27 to Oct. 4, the 7-day averages for ED visits with diagnosed COVID were down by 21.5% (age 0-11), 27.3% (12-15), and 18.2% (16-17), the Centers for Disease Control and Prevention said, while the most recent 7-day average for new admissions – 127 per day for Oct. 2-8 – among children aged 0-17 years with confirmed COVID was down from 161 per day the previous week, a drop of over 21%.
The state-level data that are currently available (several states are no longer reporting) show Alaska (25.5%) and Vermont (25.4%) have the highest proportions of cumulative cases in children, and Florida (12.3%) and Utah (13.5%) have the lowest. Rhode Island has the highest rate of COVID-19 per 100,000 children at 40,427, while Missouri has the lowest at 14,252. The national average is 19,687 per 100,000, the AAP and CHA reported.
Taking a look at vaccination
Vaccinations were up slightly in children aged 12-17 years, as 20,000 initial doses were given during the week of Sept. 29 to Oct. 5, compared with 17,000 and 18,000 the previous 2 weeks. Initial vaccinations in younger children, however, continued declines dating back to August, the AAP said in its weekly vaccination trends report.
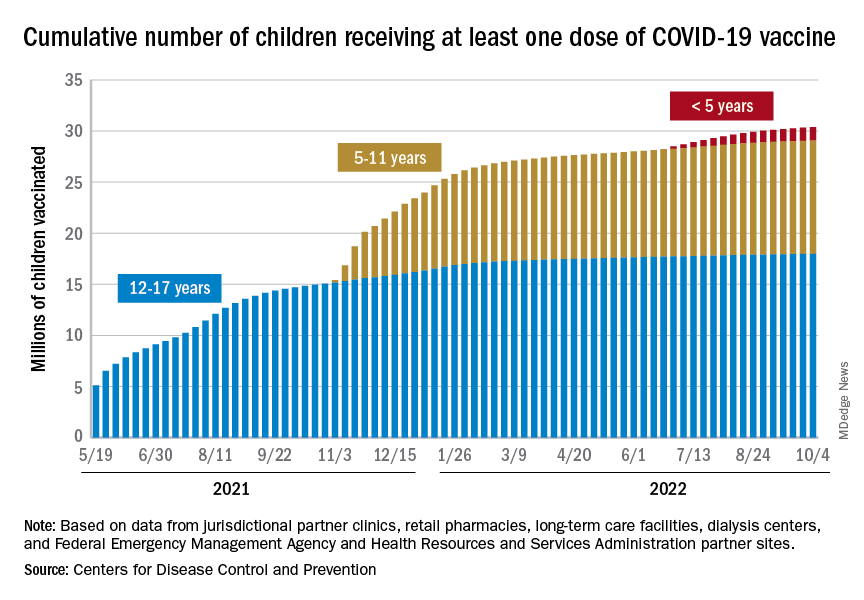
The District of Columbia and Massachusetts have the most highly vaccinated groups of 12- to 17-year-olds, as 100% and 95%, respectively, have received initial doses, while Wyoming (39%) and Idaho (42%) have the lowest. D.C. (73%) and Vermont (68%) have the highest proportions of vaccinated 5- to 11-year-olds, and Alabama (17%) and Mississippi (18%) have the lowest. For children under age 5 years, those in D.C. (33%) and Vermont (26%) are the most likely to have received an initial COVID vaccination, while Alabama, Louisiana, and Mississippi share national-low rates of 2%, the AAP said its report, which is based on CDC data.
When all states and territories are combined, 71% of children aged 12-17 have received at least one dose of vaccine, as have 38.6% of all children 5-11 years old and 6.7% of those under age 5. Almost 61% of the nation’s 16- to 17-year-olds have been fully vaccinated, along with 31.5% of those aged 5-11 and 2.4% of children younger than 5 years, the CDC said on its COVID Data Tracker.
About 42 million children – 58% of the population under the age of 18 years – have not received any vaccine yet, the AAP noted. Meanwhile, CDC data indicate that 36 children died of COVID in the last week, with pediatric deaths now totaling 1,781 over the course of the pandemic.
A small increase in new cases brought COVID-19’s latest losing streak to an end at 4 weeks, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
The 40,656 new cases reported bring the U.S. cumulative count of child COVID-19 cases to over 14.8 million since the pandemic began, which represents 18.4% of all cases, the AAP and CHA said in their weekly report based on state-level data.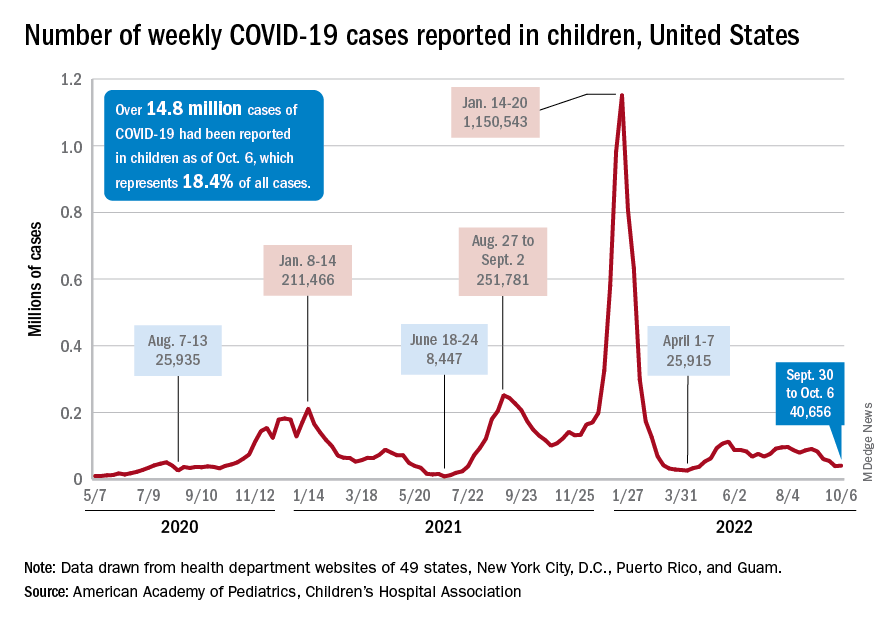
The increase in new cases was not reflected in emergency department visits or hospital admissions, which both continued sustained declines that started in August. In the week from Sept. 27 to Oct. 4, the 7-day averages for ED visits with diagnosed COVID were down by 21.5% (age 0-11), 27.3% (12-15), and 18.2% (16-17), the Centers for Disease Control and Prevention said, while the most recent 7-day average for new admissions – 127 per day for Oct. 2-8 – among children aged 0-17 years with confirmed COVID was down from 161 per day the previous week, a drop of over 21%.
The state-level data that are currently available (several states are no longer reporting) show Alaska (25.5%) and Vermont (25.4%) have the highest proportions of cumulative cases in children, and Florida (12.3%) and Utah (13.5%) have the lowest. Rhode Island has the highest rate of COVID-19 per 100,000 children at 40,427, while Missouri has the lowest at 14,252. The national average is 19,687 per 100,000, the AAP and CHA reported.
Taking a look at vaccination
Vaccinations were up slightly in children aged 12-17 years, as 20,000 initial doses were given during the week of Sept. 29 to Oct. 5, compared with 17,000 and 18,000 the previous 2 weeks. Initial vaccinations in younger children, however, continued declines dating back to August, the AAP said in its weekly vaccination trends report.
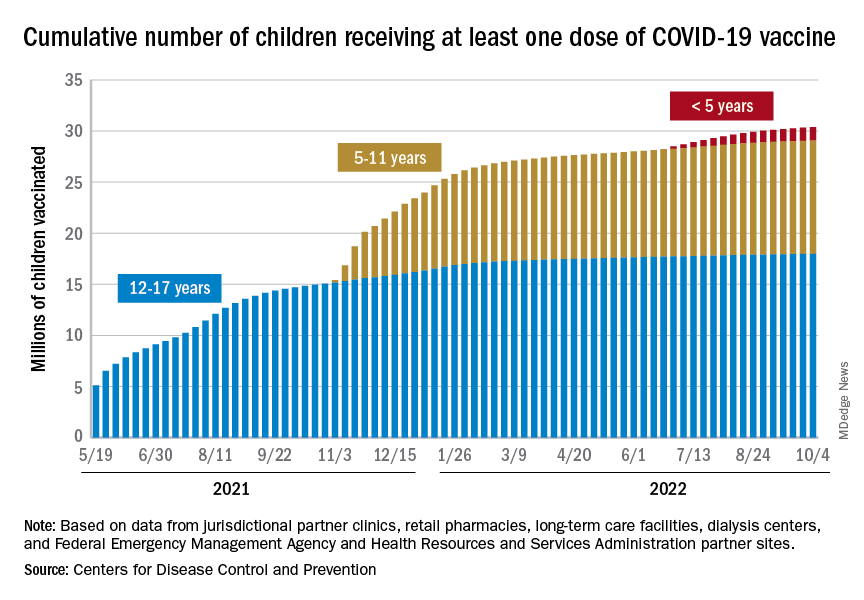
The District of Columbia and Massachusetts have the most highly vaccinated groups of 12- to 17-year-olds, as 100% and 95%, respectively, have received initial doses, while Wyoming (39%) and Idaho (42%) have the lowest. D.C. (73%) and Vermont (68%) have the highest proportions of vaccinated 5- to 11-year-olds, and Alabama (17%) and Mississippi (18%) have the lowest. For children under age 5 years, those in D.C. (33%) and Vermont (26%) are the most likely to have received an initial COVID vaccination, while Alabama, Louisiana, and Mississippi share national-low rates of 2%, the AAP said its report, which is based on CDC data.
When all states and territories are combined, 71% of children aged 12-17 have received at least one dose of vaccine, as have 38.6% of all children 5-11 years old and 6.7% of those under age 5. Almost 61% of the nation’s 16- to 17-year-olds have been fully vaccinated, along with 31.5% of those aged 5-11 and 2.4% of children younger than 5 years, the CDC said on its COVID Data Tracker.
About 42 million children – 58% of the population under the age of 18 years – have not received any vaccine yet, the AAP noted. Meanwhile, CDC data indicate that 36 children died of COVID in the last week, with pediatric deaths now totaling 1,781 over the course of the pandemic.
Mother-to-child transmission of SARS-CoV-2 may be underestimated
ANAHEIM, CALIF. – The rate of mother-to-child transmission of SARS-CoV-2 infection is likely higher than the current estimate of 2%-8%, suggests a recent study using cord blood serology to determine incidence. The study was presented at the American Academy of Pediatrics National Conference.
“Cord blood screening is a potential tool to identify SARS-CoV-2 infected and/or exposed neonates who should then be followed for long-term consequences of mother-to-child transmission,” Amy Yeh, MD, an assistant professor of clinical pediatrics at the University of Southern California, Los Angeles, told attendees at the meeting.
Dr. Yeh and her colleagues collected cord blood from more than 500 mothers at LAC+USC Medical Center from October 2021 to April 2022 and tested them for IgG antibodies against three SARS-CoV-2 antigens: nucleoprotein (N), receptor-binding domain (RBD), and spike protein (S1). Results with an IgG mean fluorescence intensity (MFI) above 700 were considered positive for IgG antibodies. A positive result for N as well as RBD or S1 indicated a natural infection while a positive result for only RBD or S1 indicated a vaccine response or past infection.
The researchers also tested a subset of the IgG positive samples for IgM and IgA antibodies against N, S1, and RBD, with an IgM MFI greater than 24 and an IgA MFI greater than 102 used as the thresholds for positive results.
Among 384 cord blood samples analyzed, 85.4% were positive for IgG against RBD, indicating that the mother had SARS-CoV-2 immunity from either a past infection or vaccination. Of these anti-RBD positive samples, 60.7% were anti-N IgG negative, suggesting that N had waned since vaccination or the past infection.
Since the other 39.3% that were anti-N IgG positive suggest a past maternal infection, the researchers assessed these 129 samples for IgM and IgA antibodies against RBD. They found that 16 of them had high levels of anti-RBD IgA and/or IgM antibodies, pointing to a rate of mother-to-child-transmission of up to 12.4%.
Sallie Permar, MD, PhD, a professor and the chair of pediatrics at Weill Cornell Medicine in New York, who was not involved in the research, said most studies of placental transmission have focused on virologic testing, such as PCR. “Serologic tests for congenital infections are inherently challenged by the transfer of maternal IgG across the placenta and therefore must rely on non-IgG isotype response detection, which have inherently been more susceptible to false-positive results than IgG-based tests,” Dr. Permar said.
Also, “it is unclear if virologic testing was performed in the infants, which, if positive in the same infants for which cord blood IgM/IgA responses were identified, could further validate positive serologic findings,” added Dr. Permar, who is also pediatrician-in-chief at New York-Presbyterian Komansky Children’s Hospital.
Given these limitations, Dr. Permar reiterated that diagnostics for congenital SARS-CoV-2 continue to evolve, even if congenital SARS-CoV-2 infection currently appears rare. Dr. Permar said she agreed with Dr. Yeh that following those who do develop this infection is important.
“There have been initial reports of neurodevelopmental and other outcomes from long-term follow-up cohorts of infants exposed to SARS-CoV-2 infection in utero with variable results and it should continue to be pursued using cohorts both enrolled early in the pandemic and those enrolled more recently after population-level immunity to SARS-CoV-2 was achieved,” said Dr. Permar.
Dr. Permar serves as a consultant to Moderna, Pfizer, Merck, Dynavax, and Hoopika on their CMV vaccine programs and has led sponsored research programs with Moderna and Merck. Information on study funding and on disclosures for Dr. Yeh was unavailable.
ANAHEIM, CALIF. – The rate of mother-to-child transmission of SARS-CoV-2 infection is likely higher than the current estimate of 2%-8%, suggests a recent study using cord blood serology to determine incidence. The study was presented at the American Academy of Pediatrics National Conference.
“Cord blood screening is a potential tool to identify SARS-CoV-2 infected and/or exposed neonates who should then be followed for long-term consequences of mother-to-child transmission,” Amy Yeh, MD, an assistant professor of clinical pediatrics at the University of Southern California, Los Angeles, told attendees at the meeting.
Dr. Yeh and her colleagues collected cord blood from more than 500 mothers at LAC+USC Medical Center from October 2021 to April 2022 and tested them for IgG antibodies against three SARS-CoV-2 antigens: nucleoprotein (N), receptor-binding domain (RBD), and spike protein (S1). Results with an IgG mean fluorescence intensity (MFI) above 700 were considered positive for IgG antibodies. A positive result for N as well as RBD or S1 indicated a natural infection while a positive result for only RBD or S1 indicated a vaccine response or past infection.
The researchers also tested a subset of the IgG positive samples for IgM and IgA antibodies against N, S1, and RBD, with an IgM MFI greater than 24 and an IgA MFI greater than 102 used as the thresholds for positive results.
Among 384 cord blood samples analyzed, 85.4% were positive for IgG against RBD, indicating that the mother had SARS-CoV-2 immunity from either a past infection or vaccination. Of these anti-RBD positive samples, 60.7% were anti-N IgG negative, suggesting that N had waned since vaccination or the past infection.
Since the other 39.3% that were anti-N IgG positive suggest a past maternal infection, the researchers assessed these 129 samples for IgM and IgA antibodies against RBD. They found that 16 of them had high levels of anti-RBD IgA and/or IgM antibodies, pointing to a rate of mother-to-child-transmission of up to 12.4%.
Sallie Permar, MD, PhD, a professor and the chair of pediatrics at Weill Cornell Medicine in New York, who was not involved in the research, said most studies of placental transmission have focused on virologic testing, such as PCR. “Serologic tests for congenital infections are inherently challenged by the transfer of maternal IgG across the placenta and therefore must rely on non-IgG isotype response detection, which have inherently been more susceptible to false-positive results than IgG-based tests,” Dr. Permar said.
Also, “it is unclear if virologic testing was performed in the infants, which, if positive in the same infants for which cord blood IgM/IgA responses were identified, could further validate positive serologic findings,” added Dr. Permar, who is also pediatrician-in-chief at New York-Presbyterian Komansky Children’s Hospital.
Given these limitations, Dr. Permar reiterated that diagnostics for congenital SARS-CoV-2 continue to evolve, even if congenital SARS-CoV-2 infection currently appears rare. Dr. Permar said she agreed with Dr. Yeh that following those who do develop this infection is important.
“There have been initial reports of neurodevelopmental and other outcomes from long-term follow-up cohorts of infants exposed to SARS-CoV-2 infection in utero with variable results and it should continue to be pursued using cohorts both enrolled early in the pandemic and those enrolled more recently after population-level immunity to SARS-CoV-2 was achieved,” said Dr. Permar.
Dr. Permar serves as a consultant to Moderna, Pfizer, Merck, Dynavax, and Hoopika on their CMV vaccine programs and has led sponsored research programs with Moderna and Merck. Information on study funding and on disclosures for Dr. Yeh was unavailable.
ANAHEIM, CALIF. – The rate of mother-to-child transmission of SARS-CoV-2 infection is likely higher than the current estimate of 2%-8%, suggests a recent study using cord blood serology to determine incidence. The study was presented at the American Academy of Pediatrics National Conference.
“Cord blood screening is a potential tool to identify SARS-CoV-2 infected and/or exposed neonates who should then be followed for long-term consequences of mother-to-child transmission,” Amy Yeh, MD, an assistant professor of clinical pediatrics at the University of Southern California, Los Angeles, told attendees at the meeting.
Dr. Yeh and her colleagues collected cord blood from more than 500 mothers at LAC+USC Medical Center from October 2021 to April 2022 and tested them for IgG antibodies against three SARS-CoV-2 antigens: nucleoprotein (N), receptor-binding domain (RBD), and spike protein (S1). Results with an IgG mean fluorescence intensity (MFI) above 700 were considered positive for IgG antibodies. A positive result for N as well as RBD or S1 indicated a natural infection while a positive result for only RBD or S1 indicated a vaccine response or past infection.
The researchers also tested a subset of the IgG positive samples for IgM and IgA antibodies against N, S1, and RBD, with an IgM MFI greater than 24 and an IgA MFI greater than 102 used as the thresholds for positive results.
Among 384 cord blood samples analyzed, 85.4% were positive for IgG against RBD, indicating that the mother had SARS-CoV-2 immunity from either a past infection or vaccination. Of these anti-RBD positive samples, 60.7% were anti-N IgG negative, suggesting that N had waned since vaccination or the past infection.
Since the other 39.3% that were anti-N IgG positive suggest a past maternal infection, the researchers assessed these 129 samples for IgM and IgA antibodies against RBD. They found that 16 of them had high levels of anti-RBD IgA and/or IgM antibodies, pointing to a rate of mother-to-child-transmission of up to 12.4%.
Sallie Permar, MD, PhD, a professor and the chair of pediatrics at Weill Cornell Medicine in New York, who was not involved in the research, said most studies of placental transmission have focused on virologic testing, such as PCR. “Serologic tests for congenital infections are inherently challenged by the transfer of maternal IgG across the placenta and therefore must rely on non-IgG isotype response detection, which have inherently been more susceptible to false-positive results than IgG-based tests,” Dr. Permar said.
Also, “it is unclear if virologic testing was performed in the infants, which, if positive in the same infants for which cord blood IgM/IgA responses were identified, could further validate positive serologic findings,” added Dr. Permar, who is also pediatrician-in-chief at New York-Presbyterian Komansky Children’s Hospital.
Given these limitations, Dr. Permar reiterated that diagnostics for congenital SARS-CoV-2 continue to evolve, even if congenital SARS-CoV-2 infection currently appears rare. Dr. Permar said she agreed with Dr. Yeh that following those who do develop this infection is important.
“There have been initial reports of neurodevelopmental and other outcomes from long-term follow-up cohorts of infants exposed to SARS-CoV-2 infection in utero with variable results and it should continue to be pursued using cohorts both enrolled early in the pandemic and those enrolled more recently after population-level immunity to SARS-CoV-2 was achieved,” said Dr. Permar.
Dr. Permar serves as a consultant to Moderna, Pfizer, Merck, Dynavax, and Hoopika on their CMV vaccine programs and has led sponsored research programs with Moderna and Merck. Information on study funding and on disclosures for Dr. Yeh was unavailable.
AT AAP 2022
Three COVID scenarios that could spell trouble for the fall
As the United States enters a third fall with COVID-19, the virus for many is seemingly gone – or at least out of mind. But for those keeping watch, it is far from forgotten as deaths and infections continue to mount at a lower but steady pace.
What does that mean for the upcoming months? Experts predict different scenarios, some more dire than others – with one more encouraging.
In the United States, more than 300 people still die every day from COVID and more than 44,000 new daily cases are reported, according to the Centers for Disease Control and Prevention.
But progress is undeniable. The stark daily death tolls of 2020 have plummeted. Vaccines and treatments have dramatically reduced severe illness, and mask requirements have mostly turned to personal preference.
among them more-resistant variants coupled with waning immunity, the potential for a “twindemic” with a flu/COVID onslaught, and underuse of lifesaving vaccines and treatments.
Variants loom/waning immunity
Omicron variant BA.5 still makes up about 80% of infections in the United States, followed by BA4.6, according to the CDC, but other subvariants are emerging and showing signs of resistance to current antiviral treatments.
Eric Topol, MD, founder and director of the Scripps Research Translational Institute in San Diego, said about COVID this fall: “There will be another wave, magnitude unknown.”
He said subvariants XBB and BQ.1.1 “have extreme levels of immune evasion and both could pose a challenge,” explaining that XBB is more likely to cause trouble than BQ.1.1 because it is even more resistant to natural or vaccine-induced immunity.
Dr. Topol pointed to new research on those variants in a preprint posted on bioRxiv. The authors’ conclusion: “These results suggest that current herd immunity and BA.5 vaccine boosters may not provide sufficiently broad protection against infection.”
Another variant to watch, some experts say, is Omicron subvariant BA.2.75.2, which has shown resistance to antiviral treatments. It is also growing at a rather alarming rate, says Michael Sweat, PhD, director of the Medical University of South Carolina Center for Global Health in Charleston. That subvariant currently makes up under 2% of U.S. cases but has spread to at least 55 countries and 43 U.S. states after first appearing at the end of last year globally and in mid-June in the United States.
A non–peer-reviewed preprint study from Sweden found that the variant in blood samples was neutralized on average “at titers approximately 6.5 times lower than BA.5, making BA.2.75.2 the most [neutralization-resistant] variant evaluated to date.”
Katelyn Jetelina, PhD, assistant professor in the department of epidemiology at University of Texas Health Science Center, Houston, said in an interview the U.S. waves often follow Europe’s, and Europe has seen a recent spike in cases and hospitalizations not related to Omicron subvariants, but to weather changes, waning immunity, and changes in behavior.
The World Health Organization reported on Oct. 5 that, while cases were down in every other region of the world, Europe’s numbers stand out, with an 8% increase in cases from the week before.
Dr. Jetelina cited events such as Oktoberfest in Germany, which ended in the first week of October after drawing nearly 6 million people over 2 weeks, as a potential contributor, and people heading indoors as weather patterns change in Europe.
Ali Mokdad, PhD, chief strategy officer for population health at the University of Washington, Seattle, said in an interview he is less worried about the documented variants we know about than he is about the potential for a new immune-escape variety yet to emerge.
“Right now we know the Chinese are gearing up to open up the country, and because they have low immunity and little infection, we expect in China there will be a lot of spread of Omicron,” he said. “It’s possible because of the number of infections we could see a new variant.”
Dr. Mokdad said waning immunity could also leave populations vulnerable to variants.
“Even if you get infected, after about 5 months, you’re susceptible again. Remember, most of the infections from Omicron happened in January or February 2022, and we had two waves after that,” he said.
The new bivalent vaccines tweaked to target some Omicron variants will help, Dr. Mokdad said, but he noted, “people are very reluctant to take it.”
Jennifer Nuzzo, DrPH, professor of epidemiology and director of the Pandemic Center at Brown University, Providence, R.I., worries that in the United States we have less ability this year to track variants as funding has receded for testing kits and testing sites. Most people are testing at home – which doesn’t show up in the numbers – and the United States is relying more on other countries’ data to spot trends.
“I think we’re just going to have less visibility into the circulation of this virus,” she said in an interview.
‘Twindemic’: COVID and flu
Dr. Jetelina noted Australia and New Zealand just wrapped up a flu season that saw flu numbers returning to normal after a sharp drop in the last 2 years, and North America typically follows suit.
“We do expect flu will be here in the United States and probably at levels that we saw prepandemic. We’re all holding our breath to see how our health systems hold up with COVID-19 and flu. We haven’t really experienced that yet,” she said.
There is some disagreement, however, about the possibility of a so-called “twindemic” of influenza and COVID.
Richard Webby, PhD, an infectious disease specialist at St. Jude Children’s Research Hospital in Memphis, said in an interview he thinks the possibility of both viruses spiking at the same time is unlikely.
“That’s not to say we won’t get flu and COVID activity in the same winter,” he explained, “but I think both roaring at the same time is unlikely.”
As an indicator, he said, at the beginning of the flu season last year in the Northern Hemisphere, flu activity started to pick up, but when the Omicron variant came along, “flu just wasn’t able to compete in that same environment and flu numbers dropped right off.” Previous literature suggests that when one virus is spiking it’s hard for another respiratory virus to take hold.
Vaccine, treatment underuse
Another threat is vaccines, boosters, and treatments sitting on shelves.
Dr. Sweat referred to frustration with vaccine uptake that seems to be “frozen in amber.”
As of Oct. 4, only 5.3% of people in the United States who were eligible had received the updated booster launched in early September.
Dr. Nuzzo said boosters for people at least 65 years old will be key to severity of COVID this season.
“I think that’s probably the biggest factor going into the fall and winter,” she said.
Only 38% of people at least 50 years old and 45% of those at least 65 years old had gotten a second booster as of early October.
“If we do nothing else, we have to increase booster uptake in that group,” Dr. Nuzzo said.
She said the treatment nirmatrelvir/ritonavir (Paxlovid, Pfizer) for treating mild to moderate COVID-19 in patients at high risk for severe disease is greatly underused, often because providers aren’t prescribing it because they don’t think it helps, are worried about drug interactions, or are worried about its “rebound” effect.
Dr. Nuzzo urged greater use of the drug and education on how to manage drug interactions.
“We have very strong data that it does help keep people out of hospital. Sure, there may be a rebound, but that pales in comparison to the risk of being hospitalized,” she said.
Calm COVID season?
Not all predictions are dire. There is another little-talked-about scenario, Dr. Sweat said – that we could be in for a calm COVID season, and those who seem to be only mildly concerned about COVID may find those thoughts justified in the numbers.
Omicron blew through with such strength, he noted, that it may have left wide immunity in its wake. Because variants seem to be staying in the Omicron family, that may signal optimism.
“If the next variant is a descendant of the Omicron lineage, I would suspect that all these people who just got infected will have some protection, not perfect, but quite a bit of protection,” Dr. Sweat said.
Dr. Topol, Dr. Nuzzo, Dr. Sweat, Dr. Webby, Dr. Mokdad, and Dr. Jetelina reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As the United States enters a third fall with COVID-19, the virus for many is seemingly gone – or at least out of mind. But for those keeping watch, it is far from forgotten as deaths and infections continue to mount at a lower but steady pace.
What does that mean for the upcoming months? Experts predict different scenarios, some more dire than others – with one more encouraging.
In the United States, more than 300 people still die every day from COVID and more than 44,000 new daily cases are reported, according to the Centers for Disease Control and Prevention.
But progress is undeniable. The stark daily death tolls of 2020 have plummeted. Vaccines and treatments have dramatically reduced severe illness, and mask requirements have mostly turned to personal preference.
among them more-resistant variants coupled with waning immunity, the potential for a “twindemic” with a flu/COVID onslaught, and underuse of lifesaving vaccines and treatments.
Variants loom/waning immunity
Omicron variant BA.5 still makes up about 80% of infections in the United States, followed by BA4.6, according to the CDC, but other subvariants are emerging and showing signs of resistance to current antiviral treatments.
Eric Topol, MD, founder and director of the Scripps Research Translational Institute in San Diego, said about COVID this fall: “There will be another wave, magnitude unknown.”
He said subvariants XBB and BQ.1.1 “have extreme levels of immune evasion and both could pose a challenge,” explaining that XBB is more likely to cause trouble than BQ.1.1 because it is even more resistant to natural or vaccine-induced immunity.
Dr. Topol pointed to new research on those variants in a preprint posted on bioRxiv. The authors’ conclusion: “These results suggest that current herd immunity and BA.5 vaccine boosters may not provide sufficiently broad protection against infection.”
Another variant to watch, some experts say, is Omicron subvariant BA.2.75.2, which has shown resistance to antiviral treatments. It is also growing at a rather alarming rate, says Michael Sweat, PhD, director of the Medical University of South Carolina Center for Global Health in Charleston. That subvariant currently makes up under 2% of U.S. cases but has spread to at least 55 countries and 43 U.S. states after first appearing at the end of last year globally and in mid-June in the United States.
A non–peer-reviewed preprint study from Sweden found that the variant in blood samples was neutralized on average “at titers approximately 6.5 times lower than BA.5, making BA.2.75.2 the most [neutralization-resistant] variant evaluated to date.”
Katelyn Jetelina, PhD, assistant professor in the department of epidemiology at University of Texas Health Science Center, Houston, said in an interview the U.S. waves often follow Europe’s, and Europe has seen a recent spike in cases and hospitalizations not related to Omicron subvariants, but to weather changes, waning immunity, and changes in behavior.
The World Health Organization reported on Oct. 5 that, while cases were down in every other region of the world, Europe’s numbers stand out, with an 8% increase in cases from the week before.
Dr. Jetelina cited events such as Oktoberfest in Germany, which ended in the first week of October after drawing nearly 6 million people over 2 weeks, as a potential contributor, and people heading indoors as weather patterns change in Europe.
Ali Mokdad, PhD, chief strategy officer for population health at the University of Washington, Seattle, said in an interview he is less worried about the documented variants we know about than he is about the potential for a new immune-escape variety yet to emerge.
“Right now we know the Chinese are gearing up to open up the country, and because they have low immunity and little infection, we expect in China there will be a lot of spread of Omicron,” he said. “It’s possible because of the number of infections we could see a new variant.”
Dr. Mokdad said waning immunity could also leave populations vulnerable to variants.
“Even if you get infected, after about 5 months, you’re susceptible again. Remember, most of the infections from Omicron happened in January or February 2022, and we had two waves after that,” he said.
The new bivalent vaccines tweaked to target some Omicron variants will help, Dr. Mokdad said, but he noted, “people are very reluctant to take it.”
Jennifer Nuzzo, DrPH, professor of epidemiology and director of the Pandemic Center at Brown University, Providence, R.I., worries that in the United States we have less ability this year to track variants as funding has receded for testing kits and testing sites. Most people are testing at home – which doesn’t show up in the numbers – and the United States is relying more on other countries’ data to spot trends.
“I think we’re just going to have less visibility into the circulation of this virus,” she said in an interview.
‘Twindemic’: COVID and flu
Dr. Jetelina noted Australia and New Zealand just wrapped up a flu season that saw flu numbers returning to normal after a sharp drop in the last 2 years, and North America typically follows suit.
“We do expect flu will be here in the United States and probably at levels that we saw prepandemic. We’re all holding our breath to see how our health systems hold up with COVID-19 and flu. We haven’t really experienced that yet,” she said.
There is some disagreement, however, about the possibility of a so-called “twindemic” of influenza and COVID.
Richard Webby, PhD, an infectious disease specialist at St. Jude Children’s Research Hospital in Memphis, said in an interview he thinks the possibility of both viruses spiking at the same time is unlikely.
“That’s not to say we won’t get flu and COVID activity in the same winter,” he explained, “but I think both roaring at the same time is unlikely.”
As an indicator, he said, at the beginning of the flu season last year in the Northern Hemisphere, flu activity started to pick up, but when the Omicron variant came along, “flu just wasn’t able to compete in that same environment and flu numbers dropped right off.” Previous literature suggests that when one virus is spiking it’s hard for another respiratory virus to take hold.
Vaccine, treatment underuse
Another threat is vaccines, boosters, and treatments sitting on shelves.
Dr. Sweat referred to frustration with vaccine uptake that seems to be “frozen in amber.”
As of Oct. 4, only 5.3% of people in the United States who were eligible had received the updated booster launched in early September.
Dr. Nuzzo said boosters for people at least 65 years old will be key to severity of COVID this season.
“I think that’s probably the biggest factor going into the fall and winter,” she said.
Only 38% of people at least 50 years old and 45% of those at least 65 years old had gotten a second booster as of early October.
“If we do nothing else, we have to increase booster uptake in that group,” Dr. Nuzzo said.
She said the treatment nirmatrelvir/ritonavir (Paxlovid, Pfizer) for treating mild to moderate COVID-19 in patients at high risk for severe disease is greatly underused, often because providers aren’t prescribing it because they don’t think it helps, are worried about drug interactions, or are worried about its “rebound” effect.
Dr. Nuzzo urged greater use of the drug and education on how to manage drug interactions.
“We have very strong data that it does help keep people out of hospital. Sure, there may be a rebound, but that pales in comparison to the risk of being hospitalized,” she said.
Calm COVID season?
Not all predictions are dire. There is another little-talked-about scenario, Dr. Sweat said – that we could be in for a calm COVID season, and those who seem to be only mildly concerned about COVID may find those thoughts justified in the numbers.
Omicron blew through with such strength, he noted, that it may have left wide immunity in its wake. Because variants seem to be staying in the Omicron family, that may signal optimism.
“If the next variant is a descendant of the Omicron lineage, I would suspect that all these people who just got infected will have some protection, not perfect, but quite a bit of protection,” Dr. Sweat said.
Dr. Topol, Dr. Nuzzo, Dr. Sweat, Dr. Webby, Dr. Mokdad, and Dr. Jetelina reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As the United States enters a third fall with COVID-19, the virus for many is seemingly gone – or at least out of mind. But for those keeping watch, it is far from forgotten as deaths and infections continue to mount at a lower but steady pace.
What does that mean for the upcoming months? Experts predict different scenarios, some more dire than others – with one more encouraging.
In the United States, more than 300 people still die every day from COVID and more than 44,000 new daily cases are reported, according to the Centers for Disease Control and Prevention.
But progress is undeniable. The stark daily death tolls of 2020 have plummeted. Vaccines and treatments have dramatically reduced severe illness, and mask requirements have mostly turned to personal preference.
among them more-resistant variants coupled with waning immunity, the potential for a “twindemic” with a flu/COVID onslaught, and underuse of lifesaving vaccines and treatments.
Variants loom/waning immunity
Omicron variant BA.5 still makes up about 80% of infections in the United States, followed by BA4.6, according to the CDC, but other subvariants are emerging and showing signs of resistance to current antiviral treatments.
Eric Topol, MD, founder and director of the Scripps Research Translational Institute in San Diego, said about COVID this fall: “There will be another wave, magnitude unknown.”
He said subvariants XBB and BQ.1.1 “have extreme levels of immune evasion and both could pose a challenge,” explaining that XBB is more likely to cause trouble than BQ.1.1 because it is even more resistant to natural or vaccine-induced immunity.
Dr. Topol pointed to new research on those variants in a preprint posted on bioRxiv. The authors’ conclusion: “These results suggest that current herd immunity and BA.5 vaccine boosters may not provide sufficiently broad protection against infection.”
Another variant to watch, some experts say, is Omicron subvariant BA.2.75.2, which has shown resistance to antiviral treatments. It is also growing at a rather alarming rate, says Michael Sweat, PhD, director of the Medical University of South Carolina Center for Global Health in Charleston. That subvariant currently makes up under 2% of U.S. cases but has spread to at least 55 countries and 43 U.S. states after first appearing at the end of last year globally and in mid-June in the United States.
A non–peer-reviewed preprint study from Sweden found that the variant in blood samples was neutralized on average “at titers approximately 6.5 times lower than BA.5, making BA.2.75.2 the most [neutralization-resistant] variant evaluated to date.”
Katelyn Jetelina, PhD, assistant professor in the department of epidemiology at University of Texas Health Science Center, Houston, said in an interview the U.S. waves often follow Europe’s, and Europe has seen a recent spike in cases and hospitalizations not related to Omicron subvariants, but to weather changes, waning immunity, and changes in behavior.
The World Health Organization reported on Oct. 5 that, while cases were down in every other region of the world, Europe’s numbers stand out, with an 8% increase in cases from the week before.
Dr. Jetelina cited events such as Oktoberfest in Germany, which ended in the first week of October after drawing nearly 6 million people over 2 weeks, as a potential contributor, and people heading indoors as weather patterns change in Europe.
Ali Mokdad, PhD, chief strategy officer for population health at the University of Washington, Seattle, said in an interview he is less worried about the documented variants we know about than he is about the potential for a new immune-escape variety yet to emerge.
“Right now we know the Chinese are gearing up to open up the country, and because they have low immunity and little infection, we expect in China there will be a lot of spread of Omicron,” he said. “It’s possible because of the number of infections we could see a new variant.”
Dr. Mokdad said waning immunity could also leave populations vulnerable to variants.
“Even if you get infected, after about 5 months, you’re susceptible again. Remember, most of the infections from Omicron happened in January or February 2022, and we had two waves after that,” he said.
The new bivalent vaccines tweaked to target some Omicron variants will help, Dr. Mokdad said, but he noted, “people are very reluctant to take it.”
Jennifer Nuzzo, DrPH, professor of epidemiology and director of the Pandemic Center at Brown University, Providence, R.I., worries that in the United States we have less ability this year to track variants as funding has receded for testing kits and testing sites. Most people are testing at home – which doesn’t show up in the numbers – and the United States is relying more on other countries’ data to spot trends.
“I think we’re just going to have less visibility into the circulation of this virus,” she said in an interview.
‘Twindemic’: COVID and flu
Dr. Jetelina noted Australia and New Zealand just wrapped up a flu season that saw flu numbers returning to normal after a sharp drop in the last 2 years, and North America typically follows suit.
“We do expect flu will be here in the United States and probably at levels that we saw prepandemic. We’re all holding our breath to see how our health systems hold up with COVID-19 and flu. We haven’t really experienced that yet,” she said.
There is some disagreement, however, about the possibility of a so-called “twindemic” of influenza and COVID.
Richard Webby, PhD, an infectious disease specialist at St. Jude Children’s Research Hospital in Memphis, said in an interview he thinks the possibility of both viruses spiking at the same time is unlikely.
“That’s not to say we won’t get flu and COVID activity in the same winter,” he explained, “but I think both roaring at the same time is unlikely.”
As an indicator, he said, at the beginning of the flu season last year in the Northern Hemisphere, flu activity started to pick up, but when the Omicron variant came along, “flu just wasn’t able to compete in that same environment and flu numbers dropped right off.” Previous literature suggests that when one virus is spiking it’s hard for another respiratory virus to take hold.
Vaccine, treatment underuse
Another threat is vaccines, boosters, and treatments sitting on shelves.
Dr. Sweat referred to frustration with vaccine uptake that seems to be “frozen in amber.”
As of Oct. 4, only 5.3% of people in the United States who were eligible had received the updated booster launched in early September.
Dr. Nuzzo said boosters for people at least 65 years old will be key to severity of COVID this season.
“I think that’s probably the biggest factor going into the fall and winter,” she said.
Only 38% of people at least 50 years old and 45% of those at least 65 years old had gotten a second booster as of early October.
“If we do nothing else, we have to increase booster uptake in that group,” Dr. Nuzzo said.
She said the treatment nirmatrelvir/ritonavir (Paxlovid, Pfizer) for treating mild to moderate COVID-19 in patients at high risk for severe disease is greatly underused, often because providers aren’t prescribing it because they don’t think it helps, are worried about drug interactions, or are worried about its “rebound” effect.
Dr. Nuzzo urged greater use of the drug and education on how to manage drug interactions.
“We have very strong data that it does help keep people out of hospital. Sure, there may be a rebound, but that pales in comparison to the risk of being hospitalized,” she said.
Calm COVID season?
Not all predictions are dire. There is another little-talked-about scenario, Dr. Sweat said – that we could be in for a calm COVID season, and those who seem to be only mildly concerned about COVID may find those thoughts justified in the numbers.
Omicron blew through with such strength, he noted, that it may have left wide immunity in its wake. Because variants seem to be staying in the Omicron family, that may signal optimism.
“If the next variant is a descendant of the Omicron lineage, I would suspect that all these people who just got infected will have some protection, not perfect, but quite a bit of protection,” Dr. Sweat said.
Dr. Topol, Dr. Nuzzo, Dr. Sweat, Dr. Webby, Dr. Mokdad, and Dr. Jetelina reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MD and APP-only care benefit patients in the ED
A provider-only patient care protocol was safe and efficient for delivery of emergency department care in response to pandemic-related staff shortages, based on data from nearly 3,000 patients.
The COVID-19 pandemic sparked a shortage of health care personnel, according to Tanveer Gaibi, MD, of INOVA Fairfax Hospital, Falls Church, Va., and colleagues. To help manage these challenges, the INOVA emergency department developed a Provider-Only Patients (POP) protocol for patients who required minimal nursing care.
In a study presented at the American College of Emergency Physicians 2022 Scientific Assembly, the researchers reported the outcomes of a cohort of patients with suspected COVID-19 who were treated in the emergency department using the POP protocol between Dec. 1, 2021, and Jan. 15, 2022. The patients ranged in age from 21 to 64, and all presented with COVID-19-related complaints, with an Emergency Severity Index (ESI) of 4 or 5, with 1 being the most urgent and 5 being the least urgent.
Patients were triaged by a physician or nurse to determine POP status. The researchers reviewed data from a total of 640 patients treated via the POP protocol and 2,386 patients who were not POP with ESI of 4 or 5.
Overall, the mean time from when a patient was initially seen by a provider to the discharge disposition was 48 minutes shorter for POP, and the mean time from discharge disposition placement to leaving the ED was 66 minutes shorter. None of the POP-protocol patients were readmitted within 72 hours of discharge. The researchers estimated that the 640 patients in the POP protocol saved approximately 1892.27 hours of nursing and 705.1 provider hours during the study period, and no additional physician hours or advanced-practice provider hours were needed.
The study findings suggest that POP holds up as a safe, efficient, and effective process that can reduce discharge length of stay and provider to disposition times. Although more research is needed, the POP model also may be considered to address staffing challenges unrelated to the pandemic, the researchers concluded.
“This study was conducted at [a] time when our emergency department was experiencing a sudden and disproportionate increase in volume related to the Omicron variant of COVID-19,” Dr. Gaibi told this news organization. “This novel process was developed by brainstorming untested ways of managing this increased demand. The research study was a natural outcome once the process was implemented,” he said.
“Once barriers to implementing this process were overcome, we were not surprised by the results,” Dr. Gaibi said. “Subtracting at the time for nursing process was anticipated to shorten cycle times.”
The clinical implications of POP relate to generalizability outside of the pandemic setting, Dr. Gaibi noted. “We anticipate that POP could be used for patients with minor complaints to greatly shorten their time in the emergency department,” he said.
“Potential barriers to the generalized use of POP relate, in part, to local administrative barriers related to nursing assessments,” Dr. Gaibi explained. “Further, POP patients should be simple and require little or no testing. Keeping to this strict definition of the provider-only patient may be a pitfall in terms of its hard wiring,” he added.
Looking ahead, more research is needed to study POP in ED patients with minor complaints not necessarily related to COVID-19, Dr. Gaibi said.
The study received no outside funding. The researchers disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A provider-only patient care protocol was safe and efficient for delivery of emergency department care in response to pandemic-related staff shortages, based on data from nearly 3,000 patients.
The COVID-19 pandemic sparked a shortage of health care personnel, according to Tanveer Gaibi, MD, of INOVA Fairfax Hospital, Falls Church, Va., and colleagues. To help manage these challenges, the INOVA emergency department developed a Provider-Only Patients (POP) protocol for patients who required minimal nursing care.
In a study presented at the American College of Emergency Physicians 2022 Scientific Assembly, the researchers reported the outcomes of a cohort of patients with suspected COVID-19 who were treated in the emergency department using the POP protocol between Dec. 1, 2021, and Jan. 15, 2022. The patients ranged in age from 21 to 64, and all presented with COVID-19-related complaints, with an Emergency Severity Index (ESI) of 4 or 5, with 1 being the most urgent and 5 being the least urgent.
Patients were triaged by a physician or nurse to determine POP status. The researchers reviewed data from a total of 640 patients treated via the POP protocol and 2,386 patients who were not POP with ESI of 4 or 5.
Overall, the mean time from when a patient was initially seen by a provider to the discharge disposition was 48 minutes shorter for POP, and the mean time from discharge disposition placement to leaving the ED was 66 minutes shorter. None of the POP-protocol patients were readmitted within 72 hours of discharge. The researchers estimated that the 640 patients in the POP protocol saved approximately 1892.27 hours of nursing and 705.1 provider hours during the study period, and no additional physician hours or advanced-practice provider hours were needed.
The study findings suggest that POP holds up as a safe, efficient, and effective process that can reduce discharge length of stay and provider to disposition times. Although more research is needed, the POP model also may be considered to address staffing challenges unrelated to the pandemic, the researchers concluded.
“This study was conducted at [a] time when our emergency department was experiencing a sudden and disproportionate increase in volume related to the Omicron variant of COVID-19,” Dr. Gaibi told this news organization. “This novel process was developed by brainstorming untested ways of managing this increased demand. The research study was a natural outcome once the process was implemented,” he said.
“Once barriers to implementing this process were overcome, we were not surprised by the results,” Dr. Gaibi said. “Subtracting at the time for nursing process was anticipated to shorten cycle times.”
The clinical implications of POP relate to generalizability outside of the pandemic setting, Dr. Gaibi noted. “We anticipate that POP could be used for patients with minor complaints to greatly shorten their time in the emergency department,” he said.
“Potential barriers to the generalized use of POP relate, in part, to local administrative barriers related to nursing assessments,” Dr. Gaibi explained. “Further, POP patients should be simple and require little or no testing. Keeping to this strict definition of the provider-only patient may be a pitfall in terms of its hard wiring,” he added.
Looking ahead, more research is needed to study POP in ED patients with minor complaints not necessarily related to COVID-19, Dr. Gaibi said.
The study received no outside funding. The researchers disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A provider-only patient care protocol was safe and efficient for delivery of emergency department care in response to pandemic-related staff shortages, based on data from nearly 3,000 patients.
The COVID-19 pandemic sparked a shortage of health care personnel, according to Tanveer Gaibi, MD, of INOVA Fairfax Hospital, Falls Church, Va., and colleagues. To help manage these challenges, the INOVA emergency department developed a Provider-Only Patients (POP) protocol for patients who required minimal nursing care.
In a study presented at the American College of Emergency Physicians 2022 Scientific Assembly, the researchers reported the outcomes of a cohort of patients with suspected COVID-19 who were treated in the emergency department using the POP protocol between Dec. 1, 2021, and Jan. 15, 2022. The patients ranged in age from 21 to 64, and all presented with COVID-19-related complaints, with an Emergency Severity Index (ESI) of 4 or 5, with 1 being the most urgent and 5 being the least urgent.
Patients were triaged by a physician or nurse to determine POP status. The researchers reviewed data from a total of 640 patients treated via the POP protocol and 2,386 patients who were not POP with ESI of 4 or 5.
Overall, the mean time from when a patient was initially seen by a provider to the discharge disposition was 48 minutes shorter for POP, and the mean time from discharge disposition placement to leaving the ED was 66 minutes shorter. None of the POP-protocol patients were readmitted within 72 hours of discharge. The researchers estimated that the 640 patients in the POP protocol saved approximately 1892.27 hours of nursing and 705.1 provider hours during the study period, and no additional physician hours or advanced-practice provider hours were needed.
The study findings suggest that POP holds up as a safe, efficient, and effective process that can reduce discharge length of stay and provider to disposition times. Although more research is needed, the POP model also may be considered to address staffing challenges unrelated to the pandemic, the researchers concluded.
“This study was conducted at [a] time when our emergency department was experiencing a sudden and disproportionate increase in volume related to the Omicron variant of COVID-19,” Dr. Gaibi told this news organization. “This novel process was developed by brainstorming untested ways of managing this increased demand. The research study was a natural outcome once the process was implemented,” he said.
“Once barriers to implementing this process were overcome, we were not surprised by the results,” Dr. Gaibi said. “Subtracting at the time for nursing process was anticipated to shorten cycle times.”
The clinical implications of POP relate to generalizability outside of the pandemic setting, Dr. Gaibi noted. “We anticipate that POP could be used for patients with minor complaints to greatly shorten their time in the emergency department,” he said.
“Potential barriers to the generalized use of POP relate, in part, to local administrative barriers related to nursing assessments,” Dr. Gaibi explained. “Further, POP patients should be simple and require little or no testing. Keeping to this strict definition of the provider-only patient may be a pitfall in terms of its hard wiring,” he added.
Looking ahead, more research is needed to study POP in ED patients with minor complaints not necessarily related to COVID-19, Dr. Gaibi said.
The study received no outside funding. The researchers disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACEP 2022
Evusheld PrEP may protect immunocompromised patients from severe COVID-19
Tixagevimab copackaged with cilgavimab (Evusheld) is a safe and effective preexposure prophylaxis (PrEP) in patients undergoing B-cell-depleting therapies who have poor immune response to COVID-19 vaccination and are at high risk for serious COVID-19 illness, a small, single-site study suggests.
Evusheld, the only COVID-19 PrEP option available, has Emergency Use Authorization (EUA) from the Food and Drug Administration for treatment of immunocompromised patients who may not respond sufficiently to COVID-19 vaccination and patients who’ve had a severe adverse reaction to COVID-19 vaccination.
“We report the largest real-world experience of Evusheld in this population, and our findings are encouraging,” lead study author Cassandra Calabrese, DO, rheumatologist and infectious disease specialist at Cleveland Clinic, said in an interview.
“Of 412 patients who received Evusheld, 12 [2.9%] developed breakthrough COVID-19, with 11 having mild courses and 1 who required hospitalization but recovered,” she added.
“Our data suggest that Evusheld PrEP, in combination with aggressive outpatient treatment of COVID-19, is likely effective in lowering risk of severe COVID in this vulnerable group.
“Practitioners who care for patients with immune-mediated inflammatory diseases should triage high-risk patients for Evusheld as well as rapid diagnosis and aggressive outpatient therapy if infected,” Dr. Calabrese advised.
For the study, Dr. Calabrese and colleagues at Cleveland Clinic searched the health care system pharmacy records for patients with immune‐mediated inflammatory diseases (IMIDs) or inborn errors of humoral immunity (IEI) who met the criteria to receive Evusheld. The researchers included patients on B-cell-depleting therapies or with humoral IEI who had received at least one dose of Evusheld and were later diagnosed with COVID-19, and they excluded those treated with B-cell-depleting therapies for cancer.
EVUSHELD was well tolerated
After extracting data on COVID-19 infection, vaccination status, and outcomes, they found that, between Jan. 18 and May 28, 2022, 412 patients with IMIDs or humoral IEI received Evusheld. No deaths occurred among these patients and, overall, they tolerated the medication well.
All 12 patients who experienced breakthrough COVID-19 infection were treated with B-cell-depleting therapies. Among the 12 patients:
- Six patients developed infection 13-84 (median 19) days after receiving 150 mg/150 mg tixagevimab/cilgavimab.
- Six patients developed infection 19-72 (median of 38.5) days after either a single dose of 300 mg/300 mg or a second dose of 150 mg/150 mg.
- Eleven patients had mild illness and recovered at home; one patient was hospitalized and treated with high-flow oxygen. All cases had been vaccinated against COVID-19 (five received two vaccinations, six received three, and one received four).
- One possible serious adverse event involved a patient with COVID-19 and immune-mediated thrombocytopenia (ITP) who was hospitalized soon after receiving Evusheld with ITP flare that resolved with intravenous immunoglobulin.
Dr. Calabrese acknowledged limitations to the study, including few patients, lack of a comparator group, and the study period falling during the Omicron wave.
“Also, nine of the breakthrough cases received additional COVID-19 therapy (oral antiviral or monoclonal antibody), which falls within standard of care for this high-risk group but prevents ascribing effectiveness to individual components of the regimen,” she added.
“Evusheld is authorized for PrEP against COVID-19 in patients at high risk for severe COVID due to suboptimal vaccine responses. This includes patients receiving B-cell-depleting drugs like rituximab, and patients with inborn errors of humoral immunity,” Dr. Calabrese explained.
“It is well known that this group of patients is at very high risk for severe COVID and death, even when fully vaccinated, and it has become clear that more strategies are needed to protect this vulnerable group, including use of Evusheld as well as aggressive treatment if infected,” she added.
Evusheld not always easy to obtain
Although the medication has been available in the United States since January 2022, Dr. Calabrese said, patients may not receive it because of barriers including lack of both awareness and access.
Davey Smith, MD, professor of medicine and head of infectious diseases and global public health at the University of California San Diego, in La Jolla, said in an interview that he was not surprised by the results, but added that the study was conducted in too few patients to draw any strong conclusions or affect patient care.
“This small study that showed that breakthrough infections occurred but were generally mild, provides a small glimpse of real-world use of tixagevimab/cilgavimab as PrEP for immunocompromised persons,” said Dr. Smith, who was not involved in the study.
“In the setting of Omicron and vaccination, I would expect the same outcomes reported even without the treatment,” he added.
Dr. Smith recommends larger related randomized, controlled trials to provide clinicians with sufficient data to guide them in their patient care.
Graham Snyder, MD, associate professor in the division of infectious diseases at the University of Pittsburgh and medical director of infection prevention and hospital epidemiology at the University of Pittsburgh Medical Center, noted that the study “adds to a quickly growing literature on the real-world benefits of tixagevimab/cilgavimab to protect vulnerable individuals with weakened immune systems from the complications of COVID-19.
“This study provides a modest addition to our understanding of the role and benefit of Evusheld,” Dr. Snyder said in an interview. “By characterizing only patients who have received Evusheld without an untreated comparison group, we can’t draw any inference about the extent of benefit the agent provided to these patients.
“Substantial data already show that this agent is effective in preventing complications of COVID-19 infection in immunocompromised individuals,” added Dr. Snyder, who was not involved in the study.
“ ‘Immunocompromised’ represents a very diverse set of clinical conditions,” he said. “The research agenda should therefore focus on a more refined description of the effect in specific populations and a continued understanding of the effect of Evusheld in the context of updated vaccination strategies and changing virus ecology.”
Dr. Calabrese and her colleagues wrote that larger, controlled trials are underway.
FDA: Evusheld may not neutralize certain SARS-CoV-2 variants
“The biggest unanswered question is how Evusheld will hold up against new variants,” Dr. Calabrese said.
In an Oct. 3, 2022, update, the Food and Drug Administration released a statement about the risk of developing COVID-19 from SARS-CoV-2 variants that are not neutralized by Evusheld. The statement mentions an updated fact sheet that describes reduced protection from Evusheld against the Omicron subvariant BA.4.6, which accounted for nearly 13% of all new COVID-19 cases in the United States in the week ending Oct. 1.
There was no outside funding for the study. Dr. Smith reported no relevant financial conflicts of interest. Dr. Snyder said he is an unpaid adviser to an AstraZeneca observational study that’s assessing the real-world effectiveness of Evusheld.
Tixagevimab copackaged with cilgavimab (Evusheld) is a safe and effective preexposure prophylaxis (PrEP) in patients undergoing B-cell-depleting therapies who have poor immune response to COVID-19 vaccination and are at high risk for serious COVID-19 illness, a small, single-site study suggests.
Evusheld, the only COVID-19 PrEP option available, has Emergency Use Authorization (EUA) from the Food and Drug Administration for treatment of immunocompromised patients who may not respond sufficiently to COVID-19 vaccination and patients who’ve had a severe adverse reaction to COVID-19 vaccination.
“We report the largest real-world experience of Evusheld in this population, and our findings are encouraging,” lead study author Cassandra Calabrese, DO, rheumatologist and infectious disease specialist at Cleveland Clinic, said in an interview.
“Of 412 patients who received Evusheld, 12 [2.9%] developed breakthrough COVID-19, with 11 having mild courses and 1 who required hospitalization but recovered,” she added.
“Our data suggest that Evusheld PrEP, in combination with aggressive outpatient treatment of COVID-19, is likely effective in lowering risk of severe COVID in this vulnerable group.
“Practitioners who care for patients with immune-mediated inflammatory diseases should triage high-risk patients for Evusheld as well as rapid diagnosis and aggressive outpatient therapy if infected,” Dr. Calabrese advised.
For the study, Dr. Calabrese and colleagues at Cleveland Clinic searched the health care system pharmacy records for patients with immune‐mediated inflammatory diseases (IMIDs) or inborn errors of humoral immunity (IEI) who met the criteria to receive Evusheld. The researchers included patients on B-cell-depleting therapies or with humoral IEI who had received at least one dose of Evusheld and were later diagnosed with COVID-19, and they excluded those treated with B-cell-depleting therapies for cancer.
EVUSHELD was well tolerated
After extracting data on COVID-19 infection, vaccination status, and outcomes, they found that, between Jan. 18 and May 28, 2022, 412 patients with IMIDs or humoral IEI received Evusheld. No deaths occurred among these patients and, overall, they tolerated the medication well.
All 12 patients who experienced breakthrough COVID-19 infection were treated with B-cell-depleting therapies. Among the 12 patients:
- Six patients developed infection 13-84 (median 19) days after receiving 150 mg/150 mg tixagevimab/cilgavimab.
- Six patients developed infection 19-72 (median of 38.5) days after either a single dose of 300 mg/300 mg or a second dose of 150 mg/150 mg.
- Eleven patients had mild illness and recovered at home; one patient was hospitalized and treated with high-flow oxygen. All cases had been vaccinated against COVID-19 (five received two vaccinations, six received three, and one received four).
- One possible serious adverse event involved a patient with COVID-19 and immune-mediated thrombocytopenia (ITP) who was hospitalized soon after receiving Evusheld with ITP flare that resolved with intravenous immunoglobulin.
Dr. Calabrese acknowledged limitations to the study, including few patients, lack of a comparator group, and the study period falling during the Omicron wave.
“Also, nine of the breakthrough cases received additional COVID-19 therapy (oral antiviral or monoclonal antibody), which falls within standard of care for this high-risk group but prevents ascribing effectiveness to individual components of the regimen,” she added.
“Evusheld is authorized for PrEP against COVID-19 in patients at high risk for severe COVID due to suboptimal vaccine responses. This includes patients receiving B-cell-depleting drugs like rituximab, and patients with inborn errors of humoral immunity,” Dr. Calabrese explained.
“It is well known that this group of patients is at very high risk for severe COVID and death, even when fully vaccinated, and it has become clear that more strategies are needed to protect this vulnerable group, including use of Evusheld as well as aggressive treatment if infected,” she added.
Evusheld not always easy to obtain
Although the medication has been available in the United States since January 2022, Dr. Calabrese said, patients may not receive it because of barriers including lack of both awareness and access.
Davey Smith, MD, professor of medicine and head of infectious diseases and global public health at the University of California San Diego, in La Jolla, said in an interview that he was not surprised by the results, but added that the study was conducted in too few patients to draw any strong conclusions or affect patient care.
“This small study that showed that breakthrough infections occurred but were generally mild, provides a small glimpse of real-world use of tixagevimab/cilgavimab as PrEP for immunocompromised persons,” said Dr. Smith, who was not involved in the study.
“In the setting of Omicron and vaccination, I would expect the same outcomes reported even without the treatment,” he added.
Dr. Smith recommends larger related randomized, controlled trials to provide clinicians with sufficient data to guide them in their patient care.
Graham Snyder, MD, associate professor in the division of infectious diseases at the University of Pittsburgh and medical director of infection prevention and hospital epidemiology at the University of Pittsburgh Medical Center, noted that the study “adds to a quickly growing literature on the real-world benefits of tixagevimab/cilgavimab to protect vulnerable individuals with weakened immune systems from the complications of COVID-19.
“This study provides a modest addition to our understanding of the role and benefit of Evusheld,” Dr. Snyder said in an interview. “By characterizing only patients who have received Evusheld without an untreated comparison group, we can’t draw any inference about the extent of benefit the agent provided to these patients.
“Substantial data already show that this agent is effective in preventing complications of COVID-19 infection in immunocompromised individuals,” added Dr. Snyder, who was not involved in the study.
“ ‘Immunocompromised’ represents a very diverse set of clinical conditions,” he said. “The research agenda should therefore focus on a more refined description of the effect in specific populations and a continued understanding of the effect of Evusheld in the context of updated vaccination strategies and changing virus ecology.”
Dr. Calabrese and her colleagues wrote that larger, controlled trials are underway.
FDA: Evusheld may not neutralize certain SARS-CoV-2 variants
“The biggest unanswered question is how Evusheld will hold up against new variants,” Dr. Calabrese said.
In an Oct. 3, 2022, update, the Food and Drug Administration released a statement about the risk of developing COVID-19 from SARS-CoV-2 variants that are not neutralized by Evusheld. The statement mentions an updated fact sheet that describes reduced protection from Evusheld against the Omicron subvariant BA.4.6, which accounted for nearly 13% of all new COVID-19 cases in the United States in the week ending Oct. 1.
There was no outside funding for the study. Dr. Smith reported no relevant financial conflicts of interest. Dr. Snyder said he is an unpaid adviser to an AstraZeneca observational study that’s assessing the real-world effectiveness of Evusheld.
Tixagevimab copackaged with cilgavimab (Evusheld) is a safe and effective preexposure prophylaxis (PrEP) in patients undergoing B-cell-depleting therapies who have poor immune response to COVID-19 vaccination and are at high risk for serious COVID-19 illness, a small, single-site study suggests.
Evusheld, the only COVID-19 PrEP option available, has Emergency Use Authorization (EUA) from the Food and Drug Administration for treatment of immunocompromised patients who may not respond sufficiently to COVID-19 vaccination and patients who’ve had a severe adverse reaction to COVID-19 vaccination.
“We report the largest real-world experience of Evusheld in this population, and our findings are encouraging,” lead study author Cassandra Calabrese, DO, rheumatologist and infectious disease specialist at Cleveland Clinic, said in an interview.
“Of 412 patients who received Evusheld, 12 [2.9%] developed breakthrough COVID-19, with 11 having mild courses and 1 who required hospitalization but recovered,” she added.
“Our data suggest that Evusheld PrEP, in combination with aggressive outpatient treatment of COVID-19, is likely effective in lowering risk of severe COVID in this vulnerable group.
“Practitioners who care for patients with immune-mediated inflammatory diseases should triage high-risk patients for Evusheld as well as rapid diagnosis and aggressive outpatient therapy if infected,” Dr. Calabrese advised.
For the study, Dr. Calabrese and colleagues at Cleveland Clinic searched the health care system pharmacy records for patients with immune‐mediated inflammatory diseases (IMIDs) or inborn errors of humoral immunity (IEI) who met the criteria to receive Evusheld. The researchers included patients on B-cell-depleting therapies or with humoral IEI who had received at least one dose of Evusheld and were later diagnosed with COVID-19, and they excluded those treated with B-cell-depleting therapies for cancer.
EVUSHELD was well tolerated
After extracting data on COVID-19 infection, vaccination status, and outcomes, they found that, between Jan. 18 and May 28, 2022, 412 patients with IMIDs or humoral IEI received Evusheld. No deaths occurred among these patients and, overall, they tolerated the medication well.
All 12 patients who experienced breakthrough COVID-19 infection were treated with B-cell-depleting therapies. Among the 12 patients:
- Six patients developed infection 13-84 (median 19) days after receiving 150 mg/150 mg tixagevimab/cilgavimab.
- Six patients developed infection 19-72 (median of 38.5) days after either a single dose of 300 mg/300 mg or a second dose of 150 mg/150 mg.
- Eleven patients had mild illness and recovered at home; one patient was hospitalized and treated with high-flow oxygen. All cases had been vaccinated against COVID-19 (five received two vaccinations, six received three, and one received four).
- One possible serious adverse event involved a patient with COVID-19 and immune-mediated thrombocytopenia (ITP) who was hospitalized soon after receiving Evusheld with ITP flare that resolved with intravenous immunoglobulin.
Dr. Calabrese acknowledged limitations to the study, including few patients, lack of a comparator group, and the study period falling during the Omicron wave.
“Also, nine of the breakthrough cases received additional COVID-19 therapy (oral antiviral or monoclonal antibody), which falls within standard of care for this high-risk group but prevents ascribing effectiveness to individual components of the regimen,” she added.
“Evusheld is authorized for PrEP against COVID-19 in patients at high risk for severe COVID due to suboptimal vaccine responses. This includes patients receiving B-cell-depleting drugs like rituximab, and patients with inborn errors of humoral immunity,” Dr. Calabrese explained.
“It is well known that this group of patients is at very high risk for severe COVID and death, even when fully vaccinated, and it has become clear that more strategies are needed to protect this vulnerable group, including use of Evusheld as well as aggressive treatment if infected,” she added.
Evusheld not always easy to obtain
Although the medication has been available in the United States since January 2022, Dr. Calabrese said, patients may not receive it because of barriers including lack of both awareness and access.
Davey Smith, MD, professor of medicine and head of infectious diseases and global public health at the University of California San Diego, in La Jolla, said in an interview that he was not surprised by the results, but added that the study was conducted in too few patients to draw any strong conclusions or affect patient care.
“This small study that showed that breakthrough infections occurred but were generally mild, provides a small glimpse of real-world use of tixagevimab/cilgavimab as PrEP for immunocompromised persons,” said Dr. Smith, who was not involved in the study.
“In the setting of Omicron and vaccination, I would expect the same outcomes reported even without the treatment,” he added.
Dr. Smith recommends larger related randomized, controlled trials to provide clinicians with sufficient data to guide them in their patient care.
Graham Snyder, MD, associate professor in the division of infectious diseases at the University of Pittsburgh and medical director of infection prevention and hospital epidemiology at the University of Pittsburgh Medical Center, noted that the study “adds to a quickly growing literature on the real-world benefits of tixagevimab/cilgavimab to protect vulnerable individuals with weakened immune systems from the complications of COVID-19.
“This study provides a modest addition to our understanding of the role and benefit of Evusheld,” Dr. Snyder said in an interview. “By characterizing only patients who have received Evusheld without an untreated comparison group, we can’t draw any inference about the extent of benefit the agent provided to these patients.
“Substantial data already show that this agent is effective in preventing complications of COVID-19 infection in immunocompromised individuals,” added Dr. Snyder, who was not involved in the study.
“ ‘Immunocompromised’ represents a very diverse set of clinical conditions,” he said. “The research agenda should therefore focus on a more refined description of the effect in specific populations and a continued understanding of the effect of Evusheld in the context of updated vaccination strategies and changing virus ecology.”
Dr. Calabrese and her colleagues wrote that larger, controlled trials are underway.
FDA: Evusheld may not neutralize certain SARS-CoV-2 variants
“The biggest unanswered question is how Evusheld will hold up against new variants,” Dr. Calabrese said.
In an Oct. 3, 2022, update, the Food and Drug Administration released a statement about the risk of developing COVID-19 from SARS-CoV-2 variants that are not neutralized by Evusheld. The statement mentions an updated fact sheet that describes reduced protection from Evusheld against the Omicron subvariant BA.4.6, which accounted for nearly 13% of all new COVID-19 cases in the United States in the week ending Oct. 1.
There was no outside funding for the study. Dr. Smith reported no relevant financial conflicts of interest. Dr. Snyder said he is an unpaid adviser to an AstraZeneca observational study that’s assessing the real-world effectiveness of Evusheld.
FROM RMD OPEN
Is another COVID-19 booster really needed?
Many countries around the globe are starting to roll out another booster of the COVID-19 vaccine but, with public interest waning and a sense of normalcy firmly installed in our minds, this may prove an ill-fated effort, unless authorities can provide a coherent answer to the question “Is another jab really needed?” (The short answer is a firm “yes,” of course.)
In what we could call the “chronic” phase of the pandemic, most countries have now settled for a certain number of daily cases and a (relatively low) number of complications and deaths. It’s the vaccines that have afforded us this peace of mind, lest we forget. But they are different to other vaccines that we are more familiar with, such as the MMR that we get as kids and then forget about for the rest of our lives. As good as the different COVID-19 vaccines are, they never came with the promise of generating lifelong antibodies. We knew early on that the immunity they provide slowly wanes with time. That doesn’t mean that those who have their vaccination records up to date (which included a booster probably earlier in 2022) are suddenly exposed. Data suggest that although people several months past their last booster would now be more prone to getting reinfected, the protection against severe disease still hangs around 85%. In other words, their chances of ending up in the hospital are low.
Why worry, then, about further boosting the immune system? The same studies show that an additional jab would increase this percentage up to 99%. Is this roughly 10% improvement really worth another worldwide vaccination campaign? Well, this is a numbers game, after all. The current form of the virus is extremely infectious, and the Northern Hemisphere is heading toward the cold months of the year, which we have seen in past years increases COVID-19 contagions, as you would expect from any airborne virus. Thus, it’s easy to expect a new peak in the number of cases, especially considering that we are not going to apply any of the usual restrictions to prevent this. In these conditions, extending the safety net to a further 10% of the population would substantially reduce the total number of victims. It seems like a good investment of resources.
We can be more surgical about it and direct this new vaccination campaign to the population most likely to end up in the hospital. People with concomitant pathologies are at the top of the list, but it’s also an age issue. On the basis of different studies of the most common ages of admission, the cutoff point for the booster varies from country to country, with the lowest being 50 and in other cases hovering around 65 years of age. Given the safety of these vaccines, if we can afford it, the wider we cast the net, the better, but at least we should make every effort to fully vaccinate the higher age brackets.
The final question is which vaccine to give. There are confounding studies about the importance of switching to Omicron-specific jabs, which are finally available. Although this seems like a good idea, since Omicron infections elicit a more effective range of antibodies and new variants seem to better escape our defenses, recent studies suggest that there actually may not be so much difference with the old formula.
The conclusion? This regimen of yearly boosters for some may be the scenario for the upcoming years, similar to what we already do for the flu, so we should get used to it.
Dr. Macip is associate professor, department of molecular and cellular biology, University of Leicester (England). He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Many countries around the globe are starting to roll out another booster of the COVID-19 vaccine but, with public interest waning and a sense of normalcy firmly installed in our minds, this may prove an ill-fated effort, unless authorities can provide a coherent answer to the question “Is another jab really needed?” (The short answer is a firm “yes,” of course.)
In what we could call the “chronic” phase of the pandemic, most countries have now settled for a certain number of daily cases and a (relatively low) number of complications and deaths. It’s the vaccines that have afforded us this peace of mind, lest we forget. But they are different to other vaccines that we are more familiar with, such as the MMR that we get as kids and then forget about for the rest of our lives. As good as the different COVID-19 vaccines are, they never came with the promise of generating lifelong antibodies. We knew early on that the immunity they provide slowly wanes with time. That doesn’t mean that those who have their vaccination records up to date (which included a booster probably earlier in 2022) are suddenly exposed. Data suggest that although people several months past their last booster would now be more prone to getting reinfected, the protection against severe disease still hangs around 85%. In other words, their chances of ending up in the hospital are low.
Why worry, then, about further boosting the immune system? The same studies show that an additional jab would increase this percentage up to 99%. Is this roughly 10% improvement really worth another worldwide vaccination campaign? Well, this is a numbers game, after all. The current form of the virus is extremely infectious, and the Northern Hemisphere is heading toward the cold months of the year, which we have seen in past years increases COVID-19 contagions, as you would expect from any airborne virus. Thus, it’s easy to expect a new peak in the number of cases, especially considering that we are not going to apply any of the usual restrictions to prevent this. In these conditions, extending the safety net to a further 10% of the population would substantially reduce the total number of victims. It seems like a good investment of resources.
We can be more surgical about it and direct this new vaccination campaign to the population most likely to end up in the hospital. People with concomitant pathologies are at the top of the list, but it’s also an age issue. On the basis of different studies of the most common ages of admission, the cutoff point for the booster varies from country to country, with the lowest being 50 and in other cases hovering around 65 years of age. Given the safety of these vaccines, if we can afford it, the wider we cast the net, the better, but at least we should make every effort to fully vaccinate the higher age brackets.
The final question is which vaccine to give. There are confounding studies about the importance of switching to Omicron-specific jabs, which are finally available. Although this seems like a good idea, since Omicron infections elicit a more effective range of antibodies and new variants seem to better escape our defenses, recent studies suggest that there actually may not be so much difference with the old formula.
The conclusion? This regimen of yearly boosters for some may be the scenario for the upcoming years, similar to what we already do for the flu, so we should get used to it.
Dr. Macip is associate professor, department of molecular and cellular biology, University of Leicester (England). He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Many countries around the globe are starting to roll out another booster of the COVID-19 vaccine but, with public interest waning and a sense of normalcy firmly installed in our minds, this may prove an ill-fated effort, unless authorities can provide a coherent answer to the question “Is another jab really needed?” (The short answer is a firm “yes,” of course.)
In what we could call the “chronic” phase of the pandemic, most countries have now settled for a certain number of daily cases and a (relatively low) number of complications and deaths. It’s the vaccines that have afforded us this peace of mind, lest we forget. But they are different to other vaccines that we are more familiar with, such as the MMR that we get as kids and then forget about for the rest of our lives. As good as the different COVID-19 vaccines are, they never came with the promise of generating lifelong antibodies. We knew early on that the immunity they provide slowly wanes with time. That doesn’t mean that those who have their vaccination records up to date (which included a booster probably earlier in 2022) are suddenly exposed. Data suggest that although people several months past their last booster would now be more prone to getting reinfected, the protection against severe disease still hangs around 85%. In other words, their chances of ending up in the hospital are low.
Why worry, then, about further boosting the immune system? The same studies show that an additional jab would increase this percentage up to 99%. Is this roughly 10% improvement really worth another worldwide vaccination campaign? Well, this is a numbers game, after all. The current form of the virus is extremely infectious, and the Northern Hemisphere is heading toward the cold months of the year, which we have seen in past years increases COVID-19 contagions, as you would expect from any airborne virus. Thus, it’s easy to expect a new peak in the number of cases, especially considering that we are not going to apply any of the usual restrictions to prevent this. In these conditions, extending the safety net to a further 10% of the population would substantially reduce the total number of victims. It seems like a good investment of resources.
We can be more surgical about it and direct this new vaccination campaign to the population most likely to end up in the hospital. People with concomitant pathologies are at the top of the list, but it’s also an age issue. On the basis of different studies of the most common ages of admission, the cutoff point for the booster varies from country to country, with the lowest being 50 and in other cases hovering around 65 years of age. Given the safety of these vaccines, if we can afford it, the wider we cast the net, the better, but at least we should make every effort to fully vaccinate the higher age brackets.
The final question is which vaccine to give. There are confounding studies about the importance of switching to Omicron-specific jabs, which are finally available. Although this seems like a good idea, since Omicron infections elicit a more effective range of antibodies and new variants seem to better escape our defenses, recent studies suggest that there actually may not be so much difference with the old formula.
The conclusion? This regimen of yearly boosters for some may be the scenario for the upcoming years, similar to what we already do for the flu, so we should get used to it.
Dr. Macip is associate professor, department of molecular and cellular biology, University of Leicester (England). He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Children and COVID: Weekly cases dropped by 57% in September
The last full week of September brought a 4th straight week of declines in the number of new COVID-19 cases reported among children, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, with the month of September bringing a decline of about 57% in reported cases for the 45 states and territories that are still releasing pediatric COVID data on their health department websites, the AAP and CHA said in their joint weekly report.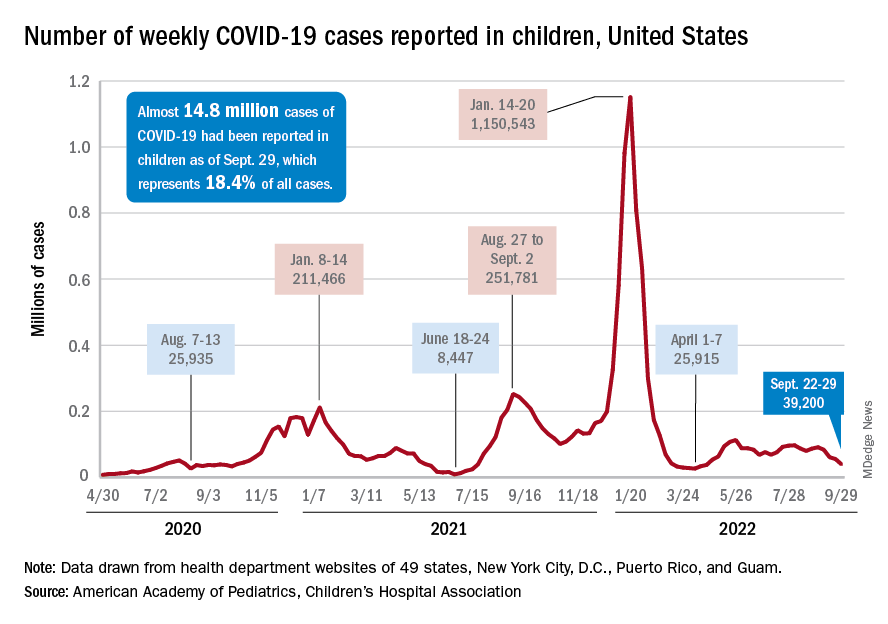
New cases dropped in all four regions after the Northeast and West had seen increases the previous week, and the distribution of cases for the latest week was fairly even, with the Midwest and Northeast right around 10,000, the South slightly over 10,000, and the West under 10,000 by about the same amount. At the state level, the largest increases – around 1.5% – over the last 2 weeks occurred in Kentucky and Nevada, the AAP/CHA data show.
The cumulative number of COVID-19 cases in children was almost 14.8 million as of Sept. 29, with children representing 18.4% of all cases since the pandemic began, the AAP and CHA said. The Centers for Disease Control and Prevention, which is able to use a uniform age range of 0-17 years, puts total cases at 15.2 million and the proportion of child cases at 17.4%. Total deaths in children from COVID as of Oct. 3 were 1,745, the CDC reported.
New vaccinations, in the meantime, are being added in numbers only slightly higher than new cases. Initial COVID vaccinations for the week of Sept. 22-28 were about 44,000 for children under 5 years of age (down from 51,000 the week before), 24,000 for children aged 5-11 years (down from 28,000), and 17,000 for those aged 12-17 (down from 18,000), the AAP said in its weekly vaccination report.
To look at it another way, the total proportion of children under 5 years of age who had received at least one dose of COVID vaccine as of Sept. 28 was 6.5%, compared with 6.4% on Sept. 21, while the corresponding rates for children aged 5-11 and 12-17 were unchanged at 38.5% and 70.9%. The 12- to 17-year-olds, in fact, have been stuck at 70.9% since Sept. 13, according to data from the CDC.
In a recent study published in Vaccine, investigators attributed the discrepancies between age groups at least partly to the acceptance of misinformation about vaccine safety in general and the COVID-19 vaccines in particular.
“All of the misconceptions we studied focused in one way or another on the safety of vaccination, and that explains why people’s misbeliefs about vaccinating kids are so highly related to their concerns about vaccines in general. Unfortunately, those concerns weigh even more heavily when adults consider vaccinating children,” lead author Dan Romer, PhD, of the University of Pennsylvania, Philadelphia, said in a written statement.
The last full week of September brought a 4th straight week of declines in the number of new COVID-19 cases reported among children, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, with the month of September bringing a decline of about 57% in reported cases for the 45 states and territories that are still releasing pediatric COVID data on their health department websites, the AAP and CHA said in their joint weekly report.
New cases dropped in all four regions after the Northeast and West had seen increases the previous week, and the distribution of cases for the latest week was fairly even, with the Midwest and Northeast right around 10,000, the South slightly over 10,000, and the West under 10,000 by about the same amount. At the state level, the largest increases – around 1.5% – over the last 2 weeks occurred in Kentucky and Nevada, the AAP/CHA data show.
The cumulative number of COVID-19 cases in children was almost 14.8 million as of Sept. 29, with children representing 18.4% of all cases since the pandemic began, the AAP and CHA said. The Centers for Disease Control and Prevention, which is able to use a uniform age range of 0-17 years, puts total cases at 15.2 million and the proportion of child cases at 17.4%. Total deaths in children from COVID as of Oct. 3 were 1,745, the CDC reported.
New vaccinations, in the meantime, are being added in numbers only slightly higher than new cases. Initial COVID vaccinations for the week of Sept. 22-28 were about 44,000 for children under 5 years of age (down from 51,000 the week before), 24,000 for children aged 5-11 years (down from 28,000), and 17,000 for those aged 12-17 (down from 18,000), the AAP said in its weekly vaccination report.
To look at it another way, the total proportion of children under 5 years of age who had received at least one dose of COVID vaccine as of Sept. 28 was 6.5%, compared with 6.4% on Sept. 21, while the corresponding rates for children aged 5-11 and 12-17 were unchanged at 38.5% and 70.9%. The 12- to 17-year-olds, in fact, have been stuck at 70.9% since Sept. 13, according to data from the CDC.
In a recent study published in Vaccine, investigators attributed the discrepancies between age groups at least partly to the acceptance of misinformation about vaccine safety in general and the COVID-19 vaccines in particular.
“All of the misconceptions we studied focused in one way or another on the safety of vaccination, and that explains why people’s misbeliefs about vaccinating kids are so highly related to their concerns about vaccines in general. Unfortunately, those concerns weigh even more heavily when adults consider vaccinating children,” lead author Dan Romer, PhD, of the University of Pennsylvania, Philadelphia, said in a written statement.
The last full week of September brought a 4th straight week of declines in the number of new COVID-19 cases reported among children, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, with the month of September bringing a decline of about 57% in reported cases for the 45 states and territories that are still releasing pediatric COVID data on their health department websites, the AAP and CHA said in their joint weekly report.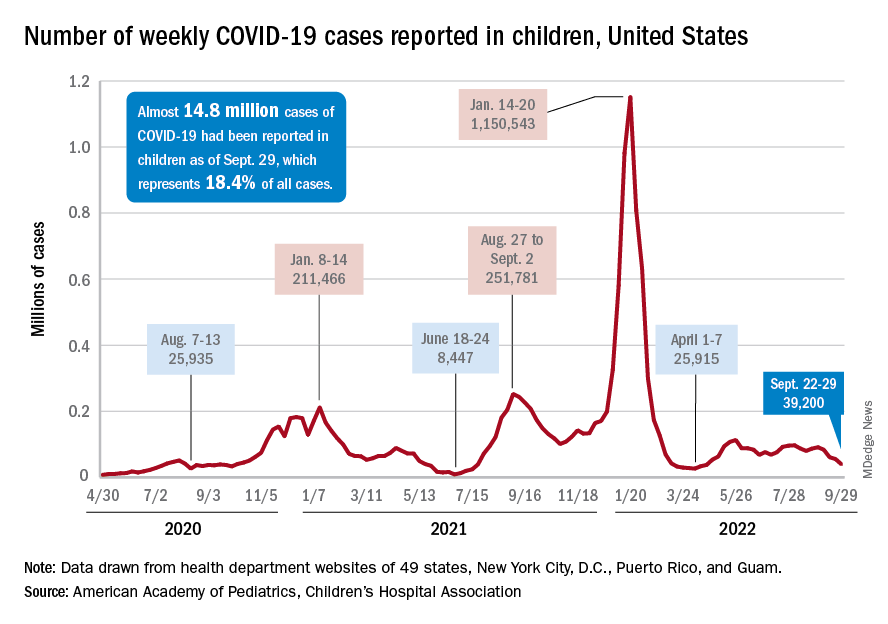
New cases dropped in all four regions after the Northeast and West had seen increases the previous week, and the distribution of cases for the latest week was fairly even, with the Midwest and Northeast right around 10,000, the South slightly over 10,000, and the West under 10,000 by about the same amount. At the state level, the largest increases – around 1.5% – over the last 2 weeks occurred in Kentucky and Nevada, the AAP/CHA data show.
The cumulative number of COVID-19 cases in children was almost 14.8 million as of Sept. 29, with children representing 18.4% of all cases since the pandemic began, the AAP and CHA said. The Centers for Disease Control and Prevention, which is able to use a uniform age range of 0-17 years, puts total cases at 15.2 million and the proportion of child cases at 17.4%. Total deaths in children from COVID as of Oct. 3 were 1,745, the CDC reported.
New vaccinations, in the meantime, are being added in numbers only slightly higher than new cases. Initial COVID vaccinations for the week of Sept. 22-28 were about 44,000 for children under 5 years of age (down from 51,000 the week before), 24,000 for children aged 5-11 years (down from 28,000), and 17,000 for those aged 12-17 (down from 18,000), the AAP said in its weekly vaccination report.
To look at it another way, the total proportion of children under 5 years of age who had received at least one dose of COVID vaccine as of Sept. 28 was 6.5%, compared with 6.4% on Sept. 21, while the corresponding rates for children aged 5-11 and 12-17 were unchanged at 38.5% and 70.9%. The 12- to 17-year-olds, in fact, have been stuck at 70.9% since Sept. 13, according to data from the CDC.
In a recent study published in Vaccine, investigators attributed the discrepancies between age groups at least partly to the acceptance of misinformation about vaccine safety in general and the COVID-19 vaccines in particular.
“All of the misconceptions we studied focused in one way or another on the safety of vaccination, and that explains why people’s misbeliefs about vaccinating kids are so highly related to their concerns about vaccines in general. Unfortunately, those concerns weigh even more heavily when adults consider vaccinating children,” lead author Dan Romer, PhD, of the University of Pennsylvania, Philadelphia, said in a written statement.
Shortage of family physicians in Canada intensified during pandemic
A higher percentage of family physicians quit during the early months of the pandemic than the average yearly percentage that did in the prior decade, according to data from Canada.
The researchers conducted two analyses of billing claims data for family physicians practicing in Ontario. They examined data for a period from 2010 to 2019 – before the onset of the pandemic – and from 2019 through 2020. The findings were published in Annals of Family Medicine.
Overall, the proportion of family physicians who stopped working rose from an average of 1.6% each year for the period between 2010 and 2019 to 3% in the period from 2019 to 2020. The pandemic data set included 12,247 physicians in Ontario. Of these, 385 (3.1%) reported no billings in the first 6 months of the pandemic.
Compared with family physicians billing for work during the pandemic, those reporting no billings were significantly more likely to be 75 years or older (13.0% vs. 3.4%), to have patient panels of less than 500 patients (40.0% vs. 25.8%), and to be eligible for fee-for-service reimbursement (37.7% vs. 24.9%; P less than .001 for all). The family physicians who reported no billing early in the pandemic also had fewer billing days in the previous year (mean of 73 days vs. 101 days, P less than .001).
In a regression analysis, the absolute increase in the percentage of family physicians who stopped working was 0.3% per year from 2010 to 2019, but rose to 1.2% between 2019 and 2020.
Challenges to family physicians in Ontario in the early months of the COVID-19 pandemic included reduced revenue, inability to keep offices fully staffed, and problems obtaining enough personal protective equipment. Such challenges may have prompted some family physicians to stop working prematurely, but more research is needed in other settings, wrote study author Tara Kiran, MD, of the University of Toronto, and colleagues.
“There were a lot of stories and suggestions that more family physicians were choosing to retire due to COVID,” Michael Green, MD, a coauthor of the paper, said in an interview. “Given the preexisting shortages we thought it would be important to see if this was true, and how big of an issue it was,” he said.
Although the absolute number of primary care physicians who stopped working is small, the implications are large given the ongoing shortage of family physicians in Canada, the researchers wrote.
The characteristics of physicians stopping work, such as older age and smaller practice size, were consistent with that of physicians preparing for retirement, the researchers noted. In addition, 56% of the family physicians who stopped working during the pandemic practiced in a patient enrollment model, in which patients are enrolled and between 15% and 70% of payment is based on age and sex. In this study, approximately 80% of physicians worked in this model. The remaining 20% operated in independent, fee-for-service practices.
“Although we cannot directly attribute causation, we hypothesize that some family physicians accelerated their retirement plans because of the pandemic,” the researchers noted. They proposed that possible reasons include health concerns, increased costs of infection prevention and control, reduced revenue from office visits, and burnout. The current study did not examine these issues.
Additional studies are needed to understand the impact on population health, the researchers concluded, but they estimated that the number of family physicians who stopped work during the pandemic would have provided care for approximately 170,000 patients.
The study findings reflect a genuine turnover by family physicians, vs. a departure from family practice to a fellowship and practice in another specialty, Dr. Green said. “We looked at physician billings to determine who stopped practicing, so we report only on those who stopped billing the Ontario Health Insurance Program altogether,” he explained.
The ongoing pandemic accelerated the issue of an upcoming wave of physician retirements and added to an already large number of people without a family physician, Dr. Green noted.
“We know there will be significant shortages of family physicians if we don’t modernize our ways of delivering primary care,” said Dr. Green. More research is needed on how to support family doctors with teams and administrative supports to allow them to provide high quality care to more patients, he said. Better models to estimate health workforce needs in primary care are needed as well, he added.
In the United States, a physician shortage has been growing since before the pandemic, according to a report published in 2021 by the Association of American Medical Colleges. In this report, “The Complexities of Physician Supply and Demand: Projections from 2019 to 2034,” the authors specifically projected a primary care physician shortage of 17,800 to 48,000 by 2034. This projection is in part based on an increase in the percentage of the U.S. population aged 65 years and older, which will increase the demand for care, according to the authors. The report also confirmed that many U.S. physicians are approaching retirement age and that more than two of five active physicians will be 65 years or older within the next 10 years.
However, the authors of this U.S. report acknowledged that the impact of the pandemic on existing primary care shortages remains unclear.
“There are still many unknowns about the direct short-term and long-term impacts of COVID-19 on the physician workforce, and it may be several years before those impacts are clearly understood,” they said in the executive summary of their report.
Alison N. Huffstetler, MD, a coauthor of a recent report that tried to identify the active primary care workforce in Virginia, said, “We know from other research that there are not enough primary care doctors, right now, to do the work that needs to be done – some citations have noted it would take a primary care doc over 20 hours a day just to provide preventive care.
“As our population continues to age, live longer, and need more complex care management, we must ensure we have an accountable, accessible, and knowledgeable primary care network to care for our communities,” she said.
Current state of primary care in Virginia
The study by Dr. Huffstetler, of Virginia Commonwealth University, Richmond, and colleagues was published in Annals of Family Medicine. It used a novel strategy involving the analysis of state all-payer claims data to determine how many physicians were practicing primary care in Virginia.
The researchers used the National Plan and Provider Enumeration System (NPPES) and the Virginia All-Payer Claims Database (VA-APCD) and identified all Virginia physicians and their specialties through the NPPES between 2015 and 2019. Active physicians were defined as those with at least one claim in the VA-APCD during the study period. They identified 20,976 active physicians in Virginia, 28.1% of whom were classified as primary care. Of these, 52% were family medicine physicians, 18.5% were internal medicine physicians, 16.8% were pediatricians, 11.8% were ob.gyns., and 0.5% were other specialists.
Clinician specialties were identified via specialty codes from the NPPES. Physicians were identified as primary care providers in two ways. The first way was by identifying those who had a National Uniform Claim Committee (NUCC) taxonomy of family medicine. The NUCC identifies a provider’s specialty using several levels of classification based on board certification and subspecialty certification data. The second identifier was having been a physician who had billed for at least 10 wellness visit codes from Jan. 1, 2019, through Dec. 31, 2019.
Over the 5-year study period (2015-2019), the counts and percentages of primary care physicians in the workforce remained stable, and the overall number of physicians in the state increased by 3.5%, the researchers noted. A total of 60.45% of all physicians and 60.87% of primary care physicians remained active, and 11.66% of all physicians had a claim in only 1 of the 5 years.
How distribution and access impact patients
In an interview, Dr. Huffstetler said the study she and colleagues authored “offers a transparent and reproducible process for identifying primary care physicians in a state, where they practice, and what changes in staffing occur over time.”
“In Virginia, this is particularly important, as we recently expanded Medicaid, making primary care more affordable for over 500,000 people,” she said. “We also saw the importance of distribution and accessibility to primary care over the past 3 years of COVID. In order to adequately prepare for community needs in the coming years, we must know who is providing primary care, and where they are.”
However, the model used in this study has its limitations, Dr. Huffstetler said, including the lack of a definitive definition of primary care using claims data.
“We used a data-informed wellness visit threshold, but it is likely that primary care is delivered in some locations without claims that are reflected by a wellness visit, and we hope to look at scope in the future to help refine these results,” she said.
Canadian study shows pandemic’s impact on patient care
“The pandemic’s impact on primary care remains palpable, and Dr. Kiran’s team has done an excellent analysis on the practice trends during the past several years,” Dr. Huffstetler said.
“The Canadian analysis uses claims in a similar manner to our study; however, it appears that they already knew who the FPs were in Ontario,” Dr. Huffstetler noted. “Their claims threshold of 50 for active practice was higher than ours, at only 1. Should those FPs have moved to a different specialty, the physicians would still have claims for the patients seen in other subspecialties. As such, I don’t suspect that their analysis miscalculated those that transitioned, rather than stopped practice,” she explained.
The Ontario study was supported by the Initial Credential Evaluation Service, which is funded by the Ontario Ministry of Health and the Ministry of Long-Term Care, as well as by the Canadian Institutes of Health Research. Additional support came from the INSPIRE Primary Health Care Research Program, which is also funded by the Ontario Ministry of Health and Long-Term Care. The researchers had no financial conflicts to disclose.
The Virginia study was supported by the Department of Medical Assistance Services and the National Center for Advancing Translational Sciences. The researchers had no financial conflicts to disclose.
The supply and demand report was conducted for the AAMC by IHS Markit, a global information company.
A higher percentage of family physicians quit during the early months of the pandemic than the average yearly percentage that did in the prior decade, according to data from Canada.
The researchers conducted two analyses of billing claims data for family physicians practicing in Ontario. They examined data for a period from 2010 to 2019 – before the onset of the pandemic – and from 2019 through 2020. The findings were published in Annals of Family Medicine.
Overall, the proportion of family physicians who stopped working rose from an average of 1.6% each year for the period between 2010 and 2019 to 3% in the period from 2019 to 2020. The pandemic data set included 12,247 physicians in Ontario. Of these, 385 (3.1%) reported no billings in the first 6 months of the pandemic.
Compared with family physicians billing for work during the pandemic, those reporting no billings were significantly more likely to be 75 years or older (13.0% vs. 3.4%), to have patient panels of less than 500 patients (40.0% vs. 25.8%), and to be eligible for fee-for-service reimbursement (37.7% vs. 24.9%; P less than .001 for all). The family physicians who reported no billing early in the pandemic also had fewer billing days in the previous year (mean of 73 days vs. 101 days, P less than .001).
In a regression analysis, the absolute increase in the percentage of family physicians who stopped working was 0.3% per year from 2010 to 2019, but rose to 1.2% between 2019 and 2020.
Challenges to family physicians in Ontario in the early months of the COVID-19 pandemic included reduced revenue, inability to keep offices fully staffed, and problems obtaining enough personal protective equipment. Such challenges may have prompted some family physicians to stop working prematurely, but more research is needed in other settings, wrote study author Tara Kiran, MD, of the University of Toronto, and colleagues.
“There were a lot of stories and suggestions that more family physicians were choosing to retire due to COVID,” Michael Green, MD, a coauthor of the paper, said in an interview. “Given the preexisting shortages we thought it would be important to see if this was true, and how big of an issue it was,” he said.
Although the absolute number of primary care physicians who stopped working is small, the implications are large given the ongoing shortage of family physicians in Canada, the researchers wrote.
The characteristics of physicians stopping work, such as older age and smaller practice size, were consistent with that of physicians preparing for retirement, the researchers noted. In addition, 56% of the family physicians who stopped working during the pandemic practiced in a patient enrollment model, in which patients are enrolled and between 15% and 70% of payment is based on age and sex. In this study, approximately 80% of physicians worked in this model. The remaining 20% operated in independent, fee-for-service practices.
“Although we cannot directly attribute causation, we hypothesize that some family physicians accelerated their retirement plans because of the pandemic,” the researchers noted. They proposed that possible reasons include health concerns, increased costs of infection prevention and control, reduced revenue from office visits, and burnout. The current study did not examine these issues.
Additional studies are needed to understand the impact on population health, the researchers concluded, but they estimated that the number of family physicians who stopped work during the pandemic would have provided care for approximately 170,000 patients.
The study findings reflect a genuine turnover by family physicians, vs. a departure from family practice to a fellowship and practice in another specialty, Dr. Green said. “We looked at physician billings to determine who stopped practicing, so we report only on those who stopped billing the Ontario Health Insurance Program altogether,” he explained.
The ongoing pandemic accelerated the issue of an upcoming wave of physician retirements and added to an already large number of people without a family physician, Dr. Green noted.
“We know there will be significant shortages of family physicians if we don’t modernize our ways of delivering primary care,” said Dr. Green. More research is needed on how to support family doctors with teams and administrative supports to allow them to provide high quality care to more patients, he said. Better models to estimate health workforce needs in primary care are needed as well, he added.
In the United States, a physician shortage has been growing since before the pandemic, according to a report published in 2021 by the Association of American Medical Colleges. In this report, “The Complexities of Physician Supply and Demand: Projections from 2019 to 2034,” the authors specifically projected a primary care physician shortage of 17,800 to 48,000 by 2034. This projection is in part based on an increase in the percentage of the U.S. population aged 65 years and older, which will increase the demand for care, according to the authors. The report also confirmed that many U.S. physicians are approaching retirement age and that more than two of five active physicians will be 65 years or older within the next 10 years.
However, the authors of this U.S. report acknowledged that the impact of the pandemic on existing primary care shortages remains unclear.
“There are still many unknowns about the direct short-term and long-term impacts of COVID-19 on the physician workforce, and it may be several years before those impacts are clearly understood,” they said in the executive summary of their report.
Alison N. Huffstetler, MD, a coauthor of a recent report that tried to identify the active primary care workforce in Virginia, said, “We know from other research that there are not enough primary care doctors, right now, to do the work that needs to be done – some citations have noted it would take a primary care doc over 20 hours a day just to provide preventive care.
“As our population continues to age, live longer, and need more complex care management, we must ensure we have an accountable, accessible, and knowledgeable primary care network to care for our communities,” she said.
Current state of primary care in Virginia
The study by Dr. Huffstetler, of Virginia Commonwealth University, Richmond, and colleagues was published in Annals of Family Medicine. It used a novel strategy involving the analysis of state all-payer claims data to determine how many physicians were practicing primary care in Virginia.
The researchers used the National Plan and Provider Enumeration System (NPPES) and the Virginia All-Payer Claims Database (VA-APCD) and identified all Virginia physicians and their specialties through the NPPES between 2015 and 2019. Active physicians were defined as those with at least one claim in the VA-APCD during the study period. They identified 20,976 active physicians in Virginia, 28.1% of whom were classified as primary care. Of these, 52% were family medicine physicians, 18.5% were internal medicine physicians, 16.8% were pediatricians, 11.8% were ob.gyns., and 0.5% were other specialists.
Clinician specialties were identified via specialty codes from the NPPES. Physicians were identified as primary care providers in two ways. The first way was by identifying those who had a National Uniform Claim Committee (NUCC) taxonomy of family medicine. The NUCC identifies a provider’s specialty using several levels of classification based on board certification and subspecialty certification data. The second identifier was having been a physician who had billed for at least 10 wellness visit codes from Jan. 1, 2019, through Dec. 31, 2019.
Over the 5-year study period (2015-2019), the counts and percentages of primary care physicians in the workforce remained stable, and the overall number of physicians in the state increased by 3.5%, the researchers noted. A total of 60.45% of all physicians and 60.87% of primary care physicians remained active, and 11.66% of all physicians had a claim in only 1 of the 5 years.
How distribution and access impact patients
In an interview, Dr. Huffstetler said the study she and colleagues authored “offers a transparent and reproducible process for identifying primary care physicians in a state, where they practice, and what changes in staffing occur over time.”
“In Virginia, this is particularly important, as we recently expanded Medicaid, making primary care more affordable for over 500,000 people,” she said. “We also saw the importance of distribution and accessibility to primary care over the past 3 years of COVID. In order to adequately prepare for community needs in the coming years, we must know who is providing primary care, and where they are.”
However, the model used in this study has its limitations, Dr. Huffstetler said, including the lack of a definitive definition of primary care using claims data.
“We used a data-informed wellness visit threshold, but it is likely that primary care is delivered in some locations without claims that are reflected by a wellness visit, and we hope to look at scope in the future to help refine these results,” she said.
Canadian study shows pandemic’s impact on patient care
“The pandemic’s impact on primary care remains palpable, and Dr. Kiran’s team has done an excellent analysis on the practice trends during the past several years,” Dr. Huffstetler said.
“The Canadian analysis uses claims in a similar manner to our study; however, it appears that they already knew who the FPs were in Ontario,” Dr. Huffstetler noted. “Their claims threshold of 50 for active practice was higher than ours, at only 1. Should those FPs have moved to a different specialty, the physicians would still have claims for the patients seen in other subspecialties. As such, I don’t suspect that their analysis miscalculated those that transitioned, rather than stopped practice,” she explained.
The Ontario study was supported by the Initial Credential Evaluation Service, which is funded by the Ontario Ministry of Health and the Ministry of Long-Term Care, as well as by the Canadian Institutes of Health Research. Additional support came from the INSPIRE Primary Health Care Research Program, which is also funded by the Ontario Ministry of Health and Long-Term Care. The researchers had no financial conflicts to disclose.
The Virginia study was supported by the Department of Medical Assistance Services and the National Center for Advancing Translational Sciences. The researchers had no financial conflicts to disclose.
The supply and demand report was conducted for the AAMC by IHS Markit, a global information company.
A higher percentage of family physicians quit during the early months of the pandemic than the average yearly percentage that did in the prior decade, according to data from Canada.
The researchers conducted two analyses of billing claims data for family physicians practicing in Ontario. They examined data for a period from 2010 to 2019 – before the onset of the pandemic – and from 2019 through 2020. The findings were published in Annals of Family Medicine.
Overall, the proportion of family physicians who stopped working rose from an average of 1.6% each year for the period between 2010 and 2019 to 3% in the period from 2019 to 2020. The pandemic data set included 12,247 physicians in Ontario. Of these, 385 (3.1%) reported no billings in the first 6 months of the pandemic.
Compared with family physicians billing for work during the pandemic, those reporting no billings were significantly more likely to be 75 years or older (13.0% vs. 3.4%), to have patient panels of less than 500 patients (40.0% vs. 25.8%), and to be eligible for fee-for-service reimbursement (37.7% vs. 24.9%; P less than .001 for all). The family physicians who reported no billing early in the pandemic also had fewer billing days in the previous year (mean of 73 days vs. 101 days, P less than .001).
In a regression analysis, the absolute increase in the percentage of family physicians who stopped working was 0.3% per year from 2010 to 2019, but rose to 1.2% between 2019 and 2020.
Challenges to family physicians in Ontario in the early months of the COVID-19 pandemic included reduced revenue, inability to keep offices fully staffed, and problems obtaining enough personal protective equipment. Such challenges may have prompted some family physicians to stop working prematurely, but more research is needed in other settings, wrote study author Tara Kiran, MD, of the University of Toronto, and colleagues.
“There were a lot of stories and suggestions that more family physicians were choosing to retire due to COVID,” Michael Green, MD, a coauthor of the paper, said in an interview. “Given the preexisting shortages we thought it would be important to see if this was true, and how big of an issue it was,” he said.
Although the absolute number of primary care physicians who stopped working is small, the implications are large given the ongoing shortage of family physicians in Canada, the researchers wrote.
The characteristics of physicians stopping work, such as older age and smaller practice size, were consistent with that of physicians preparing for retirement, the researchers noted. In addition, 56% of the family physicians who stopped working during the pandemic practiced in a patient enrollment model, in which patients are enrolled and between 15% and 70% of payment is based on age and sex. In this study, approximately 80% of physicians worked in this model. The remaining 20% operated in independent, fee-for-service practices.
“Although we cannot directly attribute causation, we hypothesize that some family physicians accelerated their retirement plans because of the pandemic,” the researchers noted. They proposed that possible reasons include health concerns, increased costs of infection prevention and control, reduced revenue from office visits, and burnout. The current study did not examine these issues.
Additional studies are needed to understand the impact on population health, the researchers concluded, but they estimated that the number of family physicians who stopped work during the pandemic would have provided care for approximately 170,000 patients.
The study findings reflect a genuine turnover by family physicians, vs. a departure from family practice to a fellowship and practice in another specialty, Dr. Green said. “We looked at physician billings to determine who stopped practicing, so we report only on those who stopped billing the Ontario Health Insurance Program altogether,” he explained.
The ongoing pandemic accelerated the issue of an upcoming wave of physician retirements and added to an already large number of people without a family physician, Dr. Green noted.
“We know there will be significant shortages of family physicians if we don’t modernize our ways of delivering primary care,” said Dr. Green. More research is needed on how to support family doctors with teams and administrative supports to allow them to provide high quality care to more patients, he said. Better models to estimate health workforce needs in primary care are needed as well, he added.
In the United States, a physician shortage has been growing since before the pandemic, according to a report published in 2021 by the Association of American Medical Colleges. In this report, “The Complexities of Physician Supply and Demand: Projections from 2019 to 2034,” the authors specifically projected a primary care physician shortage of 17,800 to 48,000 by 2034. This projection is in part based on an increase in the percentage of the U.S. population aged 65 years and older, which will increase the demand for care, according to the authors. The report also confirmed that many U.S. physicians are approaching retirement age and that more than two of five active physicians will be 65 years or older within the next 10 years.
However, the authors of this U.S. report acknowledged that the impact of the pandemic on existing primary care shortages remains unclear.
“There are still many unknowns about the direct short-term and long-term impacts of COVID-19 on the physician workforce, and it may be several years before those impacts are clearly understood,” they said in the executive summary of their report.
Alison N. Huffstetler, MD, a coauthor of a recent report that tried to identify the active primary care workforce in Virginia, said, “We know from other research that there are not enough primary care doctors, right now, to do the work that needs to be done – some citations have noted it would take a primary care doc over 20 hours a day just to provide preventive care.
“As our population continues to age, live longer, and need more complex care management, we must ensure we have an accountable, accessible, and knowledgeable primary care network to care for our communities,” she said.
Current state of primary care in Virginia
The study by Dr. Huffstetler, of Virginia Commonwealth University, Richmond, and colleagues was published in Annals of Family Medicine. It used a novel strategy involving the analysis of state all-payer claims data to determine how many physicians were practicing primary care in Virginia.
The researchers used the National Plan and Provider Enumeration System (NPPES) and the Virginia All-Payer Claims Database (VA-APCD) and identified all Virginia physicians and their specialties through the NPPES between 2015 and 2019. Active physicians were defined as those with at least one claim in the VA-APCD during the study period. They identified 20,976 active physicians in Virginia, 28.1% of whom were classified as primary care. Of these, 52% were family medicine physicians, 18.5% were internal medicine physicians, 16.8% were pediatricians, 11.8% were ob.gyns., and 0.5% were other specialists.
Clinician specialties were identified via specialty codes from the NPPES. Physicians were identified as primary care providers in two ways. The first way was by identifying those who had a National Uniform Claim Committee (NUCC) taxonomy of family medicine. The NUCC identifies a provider’s specialty using several levels of classification based on board certification and subspecialty certification data. The second identifier was having been a physician who had billed for at least 10 wellness visit codes from Jan. 1, 2019, through Dec. 31, 2019.
Over the 5-year study period (2015-2019), the counts and percentages of primary care physicians in the workforce remained stable, and the overall number of physicians in the state increased by 3.5%, the researchers noted. A total of 60.45% of all physicians and 60.87% of primary care physicians remained active, and 11.66% of all physicians had a claim in only 1 of the 5 years.
How distribution and access impact patients
In an interview, Dr. Huffstetler said the study she and colleagues authored “offers a transparent and reproducible process for identifying primary care physicians in a state, where they practice, and what changes in staffing occur over time.”
“In Virginia, this is particularly important, as we recently expanded Medicaid, making primary care more affordable for over 500,000 people,” she said. “We also saw the importance of distribution and accessibility to primary care over the past 3 years of COVID. In order to adequately prepare for community needs in the coming years, we must know who is providing primary care, and where they are.”
However, the model used in this study has its limitations, Dr. Huffstetler said, including the lack of a definitive definition of primary care using claims data.
“We used a data-informed wellness visit threshold, but it is likely that primary care is delivered in some locations without claims that are reflected by a wellness visit, and we hope to look at scope in the future to help refine these results,” she said.
Canadian study shows pandemic’s impact on patient care
“The pandemic’s impact on primary care remains palpable, and Dr. Kiran’s team has done an excellent analysis on the practice trends during the past several years,” Dr. Huffstetler said.
“The Canadian analysis uses claims in a similar manner to our study; however, it appears that they already knew who the FPs were in Ontario,” Dr. Huffstetler noted. “Their claims threshold of 50 for active practice was higher than ours, at only 1. Should those FPs have moved to a different specialty, the physicians would still have claims for the patients seen in other subspecialties. As such, I don’t suspect that their analysis miscalculated those that transitioned, rather than stopped practice,” she explained.
The Ontario study was supported by the Initial Credential Evaluation Service, which is funded by the Ontario Ministry of Health and the Ministry of Long-Term Care, as well as by the Canadian Institutes of Health Research. Additional support came from the INSPIRE Primary Health Care Research Program, which is also funded by the Ontario Ministry of Health and Long-Term Care. The researchers had no financial conflicts to disclose.
The Virginia study was supported by the Department of Medical Assistance Services and the National Center for Advancing Translational Sciences. The researchers had no financial conflicts to disclose.
The supply and demand report was conducted for the AAMC by IHS Markit, a global information company.
FROM ANNALS OF FAMILY MEDICINE
Sore throat becoming dominant COVID symptom: Reports
according to recent reports in the United Kingdom.
The shift could be a cause of concern for the fall. As the main symptoms of the coronavirus change, people could spread the virus without realizing it.
“Many people are still using the government guidelines about symptoms, which are wrong,” Tim Spector, a professor of genetic epidemiology at King’s College London, told the Independent.
Prof. Spector cofounded the COVID ZOE app, which is part of the world’s largest COVID-19 study. Throughout the pandemic, researchers have used data from the app to track changes in symptoms.
“At the moment, COVID starts in two-thirds of people with a sore throat,” he said. “Fever and loss of smell are really rare now, so many old people may not think they’ve got COVID. They’d say it’s a cold and not be tested.”
COVID-19 infections in the United Kingdom increased 14% at the end of September, according to data from the U.K.’s Office for National Statistics. More than 1.1 million people tested positive during the week ending Sept. 20, up from 927,000 cases the week before. The numbers continue to increase in England and Wales, with an uncertain trend in Northern Ireland and Scotland.
The fall wave of infections has likely arrived in the United Kingdom, Prof. Spector told the Independent. Omicron variants continue to evolve and are escaping immunity from previous infection and vaccination, which he expects to continue into the winter.
But with reduced testing and surveillance of new variants, public health experts have voiced concerns about tracking the latest variants and COVID-19 trends.
“We can only detect variants or know what’s coming by doing sequencing from PCR testing, and that’s not going on anywhere near the extent it was a year ago,” Lawrence Young, a professor of virology at the University of Warwick, Coventry, England, told the Independent.
“People are going to get various infections over the winter but won’t know what they are because free tests aren’t available,” he said. “It’s going to be a problem.”
COVID-19 cases are also increasing across Europe, which could mark the first regional spike since the BA.5 wave, according to the latest data from the European CDC. (In the past, increases in Europe have signaled a trend to come in other regions.)
People aged 65 and older have been hit the hardest, the data shows, with cases rising 9% from the previous week. Hospitalizations remain stable for now, although 14 of 27 countries in the European region have noted an upward trend.
“Changes in population mixing following the summer break are likely to be the main driver of these increases, with no indication of changes in the distribution of circulating variants,” the European CDC said.
For now, most COVID-19 numbers are still falling in the United States, according to a weekly CDC update published Sept. 30. About 47,000 cases are being reported each day, marking a 13% decrease from the week before. Hospitalizations dropped 7%, and deaths dropped 6%.
At the same time, test positivity rose slightly last week, from 9.6% to 9.8%. Wastewater surveillance indicates that 53% of sites in the United States reported a decrease in virus levels, while 41% reported an increase last week.
The CDC encouraged people to get the updated Omicron-targeted booster shot for the fall. About 7.5 million Americans have received the updated vaccine. Half of the eligible population in the United States hasn’t received any booster dose yet.
“Bivalent boosters help restore protection that might have gone down since your last dose – and they also give extra protection for you and those around you against all lineages of the Omicron variant,” the CDC wrote. “The more people who stay up to date on vaccinations, the better chance we have of avoiding a possible surge in COVID-19 illness later this fall and winter.”
A version of this article first appeared on WebMD.com.
according to recent reports in the United Kingdom.
The shift could be a cause of concern for the fall. As the main symptoms of the coronavirus change, people could spread the virus without realizing it.
“Many people are still using the government guidelines about symptoms, which are wrong,” Tim Spector, a professor of genetic epidemiology at King’s College London, told the Independent.
Prof. Spector cofounded the COVID ZOE app, which is part of the world’s largest COVID-19 study. Throughout the pandemic, researchers have used data from the app to track changes in symptoms.
“At the moment, COVID starts in two-thirds of people with a sore throat,” he said. “Fever and loss of smell are really rare now, so many old people may not think they’ve got COVID. They’d say it’s a cold and not be tested.”
COVID-19 infections in the United Kingdom increased 14% at the end of September, according to data from the U.K.’s Office for National Statistics. More than 1.1 million people tested positive during the week ending Sept. 20, up from 927,000 cases the week before. The numbers continue to increase in England and Wales, with an uncertain trend in Northern Ireland and Scotland.
The fall wave of infections has likely arrived in the United Kingdom, Prof. Spector told the Independent. Omicron variants continue to evolve and are escaping immunity from previous infection and vaccination, which he expects to continue into the winter.
But with reduced testing and surveillance of new variants, public health experts have voiced concerns about tracking the latest variants and COVID-19 trends.
“We can only detect variants or know what’s coming by doing sequencing from PCR testing, and that’s not going on anywhere near the extent it was a year ago,” Lawrence Young, a professor of virology at the University of Warwick, Coventry, England, told the Independent.
“People are going to get various infections over the winter but won’t know what they are because free tests aren’t available,” he said. “It’s going to be a problem.”
COVID-19 cases are also increasing across Europe, which could mark the first regional spike since the BA.5 wave, according to the latest data from the European CDC. (In the past, increases in Europe have signaled a trend to come in other regions.)
People aged 65 and older have been hit the hardest, the data shows, with cases rising 9% from the previous week. Hospitalizations remain stable for now, although 14 of 27 countries in the European region have noted an upward trend.
“Changes in population mixing following the summer break are likely to be the main driver of these increases, with no indication of changes in the distribution of circulating variants,” the European CDC said.
For now, most COVID-19 numbers are still falling in the United States, according to a weekly CDC update published Sept. 30. About 47,000 cases are being reported each day, marking a 13% decrease from the week before. Hospitalizations dropped 7%, and deaths dropped 6%.
At the same time, test positivity rose slightly last week, from 9.6% to 9.8%. Wastewater surveillance indicates that 53% of sites in the United States reported a decrease in virus levels, while 41% reported an increase last week.
The CDC encouraged people to get the updated Omicron-targeted booster shot for the fall. About 7.5 million Americans have received the updated vaccine. Half of the eligible population in the United States hasn’t received any booster dose yet.
“Bivalent boosters help restore protection that might have gone down since your last dose – and they also give extra protection for you and those around you against all lineages of the Omicron variant,” the CDC wrote. “The more people who stay up to date on vaccinations, the better chance we have of avoiding a possible surge in COVID-19 illness later this fall and winter.”
A version of this article first appeared on WebMD.com.
according to recent reports in the United Kingdom.
The shift could be a cause of concern for the fall. As the main symptoms of the coronavirus change, people could spread the virus without realizing it.
“Many people are still using the government guidelines about symptoms, which are wrong,” Tim Spector, a professor of genetic epidemiology at King’s College London, told the Independent.
Prof. Spector cofounded the COVID ZOE app, which is part of the world’s largest COVID-19 study. Throughout the pandemic, researchers have used data from the app to track changes in symptoms.
“At the moment, COVID starts in two-thirds of people with a sore throat,” he said. “Fever and loss of smell are really rare now, so many old people may not think they’ve got COVID. They’d say it’s a cold and not be tested.”
COVID-19 infections in the United Kingdom increased 14% at the end of September, according to data from the U.K.’s Office for National Statistics. More than 1.1 million people tested positive during the week ending Sept. 20, up from 927,000 cases the week before. The numbers continue to increase in England and Wales, with an uncertain trend in Northern Ireland and Scotland.
The fall wave of infections has likely arrived in the United Kingdom, Prof. Spector told the Independent. Omicron variants continue to evolve and are escaping immunity from previous infection and vaccination, which he expects to continue into the winter.
But with reduced testing and surveillance of new variants, public health experts have voiced concerns about tracking the latest variants and COVID-19 trends.
“We can only detect variants or know what’s coming by doing sequencing from PCR testing, and that’s not going on anywhere near the extent it was a year ago,” Lawrence Young, a professor of virology at the University of Warwick, Coventry, England, told the Independent.
“People are going to get various infections over the winter but won’t know what they are because free tests aren’t available,” he said. “It’s going to be a problem.”
COVID-19 cases are also increasing across Europe, which could mark the first regional spike since the BA.5 wave, according to the latest data from the European CDC. (In the past, increases in Europe have signaled a trend to come in other regions.)
People aged 65 and older have been hit the hardest, the data shows, with cases rising 9% from the previous week. Hospitalizations remain stable for now, although 14 of 27 countries in the European region have noted an upward trend.
“Changes in population mixing following the summer break are likely to be the main driver of these increases, with no indication of changes in the distribution of circulating variants,” the European CDC said.
For now, most COVID-19 numbers are still falling in the United States, according to a weekly CDC update published Sept. 30. About 47,000 cases are being reported each day, marking a 13% decrease from the week before. Hospitalizations dropped 7%, and deaths dropped 6%.
At the same time, test positivity rose slightly last week, from 9.6% to 9.8%. Wastewater surveillance indicates that 53% of sites in the United States reported a decrease in virus levels, while 41% reported an increase last week.
The CDC encouraged people to get the updated Omicron-targeted booster shot for the fall. About 7.5 million Americans have received the updated vaccine. Half of the eligible population in the United States hasn’t received any booster dose yet.
“Bivalent boosters help restore protection that might have gone down since your last dose – and they also give extra protection for you and those around you against all lineages of the Omicron variant,” the CDC wrote. “The more people who stay up to date on vaccinations, the better chance we have of avoiding a possible surge in COVID-19 illness later this fall and winter.”
A version of this article first appeared on WebMD.com.
Breakthrough COVID studies lend support to use of new boosters in immunosuppressed patients
People with immune-mediated inflammatory diseases who are taking immunosuppressants don’t mount as strong of an immune defense against the Omicron variant as they did against the original SARS-CoV-2 wild-type virus, according to two studies published in Annals of the Rheumatic Diseases. One of the studies further showed that vaccinated individuals taking immunosuppressants have poorer cross-neutralizing responses to Omicron than do healthy vaccinated individuals, even after three doses of the COVID-19 mRNA vaccines.
“We carefully suggest that if Omicron-specific vaccination can be administered, it may be an effective way to reduce the risk of breakthrough infections in patients with autoimmune rheumatic disease,” Sang Tae Choi, MD, PhD, of the University College of Medicine, Seoul, Korea, and one of the authors of the study on cross-neutralizing protection, told this news organization. “However, further research is needed on Omicron-specific vaccine effectiveness in patients with immune dysfunctions. We believe that these study results can be of great benefit in determining the strategy of vaccination in the future.”
The earlier study, published in July, examined the ability of COVID-19 vaccines to induce cross-reactive antibody responses against Omicron infections in patients with autoimmune rheumatic diseases (ARDs). The observational study involved 149 patients with ARDs and 94 health care workers as controls, all of whom provided blood samples a median 15 weeks after their second COVID vaccine dose or a median 8 weeks after their third dose. A little more than two-thirds of the patients (68.5%) had received a third mRNA vaccine dose. None of the participants previously had COVID-19.
The researchers compared the rate of breakthrough infections with the Omicron variant to the neutralizing responses in patients’ blood, specifically the cross-neutralizing antibody responses because the original mRNA vaccines targeted a different variant than Omicron. Breakthrough infections were assessed by survey questions.
“Our findings suggested that neither primary series vaccinations nor booster doses are sufficient to induce Omicron-neutralizing responses above the threshold in patients with ARDs, although responses were noticeably increased following the third dose of an mRNA vaccine,” write Woo-Joong Kim, of the Chung-Ang University College of Medicine, Seoul, Korea, and his colleagues. “This impairment of cross-neutralization responses across most of our patients contrasts starkly with a potent elicitation of the Omicron-neutralizing responses after the third vaccination in healthy recipients.”
The average neutralizing responses against the original SARS-CoV-2 strain were similar in both groups: 76% in patients with ARDs and 72% in health care workers after the second dose. The mean response after a third dose was 97% in health care workers and 88% in patients.
The average cross-neutralizing response against the Omicron variant was far lower, particularly in those with rheumatic disease: only 11.5%, which rose to 27% after the third dose. Only 39% of the patient sera showed neutralization of Omicron, even after the third dose. Meanwhile, the mean cross-neutralizing response in health care workers was 18% after the second dose and 50% after the third.
When the researchers compared seropositivity rates against the original virus to neutralizing responses against Omicron, the association between these was stronger in health care workers than in those with ARDs. In fact, among patients with ARDs who seroconverted, only 41% showed any response against Omicron. Among all the patients, most of those who didn’t respond to Omicron (93.5%) had initially seroconverted.
The researchers also looked at the ability to neutralize Omicron on the basis of disease in those who received three doses of the vaccine. About half of those with lupus (52%) showed any neutralization against Omicron, compared with 25% of those with rheumatoid arthritis, 37.5% of those with ankylosing spondylitis, 33% of those with Behçet snydrome, and all of those with adult-onset Still’s disease.
The rate of breakthrough infections was lower in patients (19%) than in health care workers (33%). A similar pattern was seen in the more recent study published Sept. 5. Researchers used data from a prospective cohort study in the Netherlands to examine incidence and severity of Omicron breakthrough infections in patients with immune-mediated inflammatory diseases. The researchers compared infection rates and severity among 1,593 vaccinated patients with inflammatory disease who were taking immunosuppressants and 579 vaccinated controls (418 patients with inflammatory disease not on immunosuppressants and 161 healthy controls).
One in five patients with inflammatory disease (21%) were taking immunosuppressants that substantially impair antibodies, such as anti-CD20 therapy, S1P modulators, or mycophenolate mofetil combination therapy, and 48% of these patients seroconverted after primary vaccination, compared with 96% of patients taking other immunosuppressants and 98% of controls.
Breakthrough infection rates were similar between the control group (31%) and those taking immunosuppressants (30%). Only three participants had severe disease requiring hospitalization: one control and two patients taking immunosuppressants.
“In both studies, the controls had similar or higher rates of breakthrough infections, compared with the immunosuppressed,” noted Alfred Kim, MD, an assistant professor of medicine at Washington University, St Louis, but he added, “one has to consider differences in mitigation strategies, such as masking, that may explain these findings.” That is, patients taking immunosuppressants may be taking fewer risks in the community or have fewer potential exposures, especially in the Korean study, wherein the controls were health care workers.
A greater disparity in infections occurred when considering seroconversion rates. Breakthrough incidence was 38% among those taking immunosuppressants who did not seroconvert, compared with 29% among those who did. A similar trend was seen in breakthrough incidence between those taking strongly antibody-impairing immunosuppressants (36% breakthrough rate) and those taking other immunosuppressants (28%).
Among those taking immunosuppressants who seroconverted, a primary series of vaccination reduced the risk of a breakthrough infection by 29%. Protection became more robust with a booster or prior infection, both of which reduced breakthrough infection risk by 39% in those taking immunosuppressants who seroconverted.
“We demonstrate in patients with immune-mediated inflammatory diseases on immunosuppressants that additional vaccinations are associated with decreased risk of SARS-CoV-2 Omicron breakthrough infections,” wrote Eileen W. Stalman, MD, PhD, of Amsterdam UMC in the Netherlands, and her colleagues.
Though neither study broke down immune response or breakthrough infection based on individual medications, Kim said that previous research allows one to extrapolate “that prior culprits of poor vaccine responses [such as B-cell depleting drugs, mycophenolate, and TNF [tumor necrosis factor] inhibitors will continue to bear the greatest burden in breakthrough infection, including Omicron.”
Overall, he found the data from both studies relatively consistent with one another.
“Those on immunosuppression, particularly mechanisms that have been established as risk factors for poor vaccine responses, are at risk of breakthrough infection during the era of Omicron,” Dr. Kim said.
The earlier study from Korea also found that “the median time between the third-dose vaccination and the date of confirmed breakthrough infection in patients with ARDs was significantly shorter, compared with that in health care workers” at just 93 days in patients versus 122 days in health care workers. They postulated that this population’s limited neutralization of Omicron explained this short-lived protection.
Most of the patients with breakthrough infections (74%) in that study showed no neutralization against Omicron, including the only two hospitalized patients, both of whom had strong responses against the original SARS-CoV-2 strain. The significant decline over time of neutralization against Omicron suggested “the potential for a substantial loss of the protection from breakthrough infection,” the authors write.
“The third dose of an mRNA vaccine could improve the cross-neutralization of the SARS-CoV-2 Omicron variant in patients with autoimmune rheumatic disease [although] more than half of the patients failed to generate Omicron-neutralizing antibodies,” Tae Choi said in an interview. “Our study sheds light on the relative deficiency of the Omicron-specific neutralizing responses in patients with autoimmune rheumatic disease and their anticipated vulnerability to breakthrough infection.”
The message for clinicians, Dr. Kim said, is to “continue to urge our patients to maintain additional and boosting doses per guidance, use pre-exposure prophylaxis such as Evusheld, and continue other mitigation strategies as they have done.”
The Dutch study was funded by The Netherlands Organization for Health Research and Development; the Korean study used no external funding.
The authors of the Korean study had no disclosures. The Dutch study’s authors reported a wide range of disclosures involving more than a dozen pharmaceutical companies but not including Pfizer or Moderna. Dr. Kim’s industry disclosures include Alexion, ANI, AstraZeneca, Aurinia, Exagen, Foghorn Therapeutics, GlaxoSmithKline, Kypha, and Pfizer.
A version of this article first appeared on Medscape.com.
People with immune-mediated inflammatory diseases who are taking immunosuppressants don’t mount as strong of an immune defense against the Omicron variant as they did against the original SARS-CoV-2 wild-type virus, according to two studies published in Annals of the Rheumatic Diseases. One of the studies further showed that vaccinated individuals taking immunosuppressants have poorer cross-neutralizing responses to Omicron than do healthy vaccinated individuals, even after three doses of the COVID-19 mRNA vaccines.
“We carefully suggest that if Omicron-specific vaccination can be administered, it may be an effective way to reduce the risk of breakthrough infections in patients with autoimmune rheumatic disease,” Sang Tae Choi, MD, PhD, of the University College of Medicine, Seoul, Korea, and one of the authors of the study on cross-neutralizing protection, told this news organization. “However, further research is needed on Omicron-specific vaccine effectiveness in patients with immune dysfunctions. We believe that these study results can be of great benefit in determining the strategy of vaccination in the future.”
The earlier study, published in July, examined the ability of COVID-19 vaccines to induce cross-reactive antibody responses against Omicron infections in patients with autoimmune rheumatic diseases (ARDs). The observational study involved 149 patients with ARDs and 94 health care workers as controls, all of whom provided blood samples a median 15 weeks after their second COVID vaccine dose or a median 8 weeks after their third dose. A little more than two-thirds of the patients (68.5%) had received a third mRNA vaccine dose. None of the participants previously had COVID-19.
The researchers compared the rate of breakthrough infections with the Omicron variant to the neutralizing responses in patients’ blood, specifically the cross-neutralizing antibody responses because the original mRNA vaccines targeted a different variant than Omicron. Breakthrough infections were assessed by survey questions.
“Our findings suggested that neither primary series vaccinations nor booster doses are sufficient to induce Omicron-neutralizing responses above the threshold in patients with ARDs, although responses were noticeably increased following the third dose of an mRNA vaccine,” write Woo-Joong Kim, of the Chung-Ang University College of Medicine, Seoul, Korea, and his colleagues. “This impairment of cross-neutralization responses across most of our patients contrasts starkly with a potent elicitation of the Omicron-neutralizing responses after the third vaccination in healthy recipients.”
The average neutralizing responses against the original SARS-CoV-2 strain were similar in both groups: 76% in patients with ARDs and 72% in health care workers after the second dose. The mean response after a third dose was 97% in health care workers and 88% in patients.
The average cross-neutralizing response against the Omicron variant was far lower, particularly in those with rheumatic disease: only 11.5%, which rose to 27% after the third dose. Only 39% of the patient sera showed neutralization of Omicron, even after the third dose. Meanwhile, the mean cross-neutralizing response in health care workers was 18% after the second dose and 50% after the third.
When the researchers compared seropositivity rates against the original virus to neutralizing responses against Omicron, the association between these was stronger in health care workers than in those with ARDs. In fact, among patients with ARDs who seroconverted, only 41% showed any response against Omicron. Among all the patients, most of those who didn’t respond to Omicron (93.5%) had initially seroconverted.
The researchers also looked at the ability to neutralize Omicron on the basis of disease in those who received three doses of the vaccine. About half of those with lupus (52%) showed any neutralization against Omicron, compared with 25% of those with rheumatoid arthritis, 37.5% of those with ankylosing spondylitis, 33% of those with Behçet snydrome, and all of those with adult-onset Still’s disease.
The rate of breakthrough infections was lower in patients (19%) than in health care workers (33%). A similar pattern was seen in the more recent study published Sept. 5. Researchers used data from a prospective cohort study in the Netherlands to examine incidence and severity of Omicron breakthrough infections in patients with immune-mediated inflammatory diseases. The researchers compared infection rates and severity among 1,593 vaccinated patients with inflammatory disease who were taking immunosuppressants and 579 vaccinated controls (418 patients with inflammatory disease not on immunosuppressants and 161 healthy controls).
One in five patients with inflammatory disease (21%) were taking immunosuppressants that substantially impair antibodies, such as anti-CD20 therapy, S1P modulators, or mycophenolate mofetil combination therapy, and 48% of these patients seroconverted after primary vaccination, compared with 96% of patients taking other immunosuppressants and 98% of controls.
Breakthrough infection rates were similar between the control group (31%) and those taking immunosuppressants (30%). Only three participants had severe disease requiring hospitalization: one control and two patients taking immunosuppressants.
“In both studies, the controls had similar or higher rates of breakthrough infections, compared with the immunosuppressed,” noted Alfred Kim, MD, an assistant professor of medicine at Washington University, St Louis, but he added, “one has to consider differences in mitigation strategies, such as masking, that may explain these findings.” That is, patients taking immunosuppressants may be taking fewer risks in the community or have fewer potential exposures, especially in the Korean study, wherein the controls were health care workers.
A greater disparity in infections occurred when considering seroconversion rates. Breakthrough incidence was 38% among those taking immunosuppressants who did not seroconvert, compared with 29% among those who did. A similar trend was seen in breakthrough incidence between those taking strongly antibody-impairing immunosuppressants (36% breakthrough rate) and those taking other immunosuppressants (28%).
Among those taking immunosuppressants who seroconverted, a primary series of vaccination reduced the risk of a breakthrough infection by 29%. Protection became more robust with a booster or prior infection, both of which reduced breakthrough infection risk by 39% in those taking immunosuppressants who seroconverted.
“We demonstrate in patients with immune-mediated inflammatory diseases on immunosuppressants that additional vaccinations are associated with decreased risk of SARS-CoV-2 Omicron breakthrough infections,” wrote Eileen W. Stalman, MD, PhD, of Amsterdam UMC in the Netherlands, and her colleagues.
Though neither study broke down immune response or breakthrough infection based on individual medications, Kim said that previous research allows one to extrapolate “that prior culprits of poor vaccine responses [such as B-cell depleting drugs, mycophenolate, and TNF [tumor necrosis factor] inhibitors will continue to bear the greatest burden in breakthrough infection, including Omicron.”
Overall, he found the data from both studies relatively consistent with one another.
“Those on immunosuppression, particularly mechanisms that have been established as risk factors for poor vaccine responses, are at risk of breakthrough infection during the era of Omicron,” Dr. Kim said.
The earlier study from Korea also found that “the median time between the third-dose vaccination and the date of confirmed breakthrough infection in patients with ARDs was significantly shorter, compared with that in health care workers” at just 93 days in patients versus 122 days in health care workers. They postulated that this population’s limited neutralization of Omicron explained this short-lived protection.
Most of the patients with breakthrough infections (74%) in that study showed no neutralization against Omicron, including the only two hospitalized patients, both of whom had strong responses against the original SARS-CoV-2 strain. The significant decline over time of neutralization against Omicron suggested “the potential for a substantial loss of the protection from breakthrough infection,” the authors write.
“The third dose of an mRNA vaccine could improve the cross-neutralization of the SARS-CoV-2 Omicron variant in patients with autoimmune rheumatic disease [although] more than half of the patients failed to generate Omicron-neutralizing antibodies,” Tae Choi said in an interview. “Our study sheds light on the relative deficiency of the Omicron-specific neutralizing responses in patients with autoimmune rheumatic disease and their anticipated vulnerability to breakthrough infection.”
The message for clinicians, Dr. Kim said, is to “continue to urge our patients to maintain additional and boosting doses per guidance, use pre-exposure prophylaxis such as Evusheld, and continue other mitigation strategies as they have done.”
The Dutch study was funded by The Netherlands Organization for Health Research and Development; the Korean study used no external funding.
The authors of the Korean study had no disclosures. The Dutch study’s authors reported a wide range of disclosures involving more than a dozen pharmaceutical companies but not including Pfizer or Moderna. Dr. Kim’s industry disclosures include Alexion, ANI, AstraZeneca, Aurinia, Exagen, Foghorn Therapeutics, GlaxoSmithKline, Kypha, and Pfizer.
A version of this article first appeared on Medscape.com.
People with immune-mediated inflammatory diseases who are taking immunosuppressants don’t mount as strong of an immune defense against the Omicron variant as they did against the original SARS-CoV-2 wild-type virus, according to two studies published in Annals of the Rheumatic Diseases. One of the studies further showed that vaccinated individuals taking immunosuppressants have poorer cross-neutralizing responses to Omicron than do healthy vaccinated individuals, even after three doses of the COVID-19 mRNA vaccines.
“We carefully suggest that if Omicron-specific vaccination can be administered, it may be an effective way to reduce the risk of breakthrough infections in patients with autoimmune rheumatic disease,” Sang Tae Choi, MD, PhD, of the University College of Medicine, Seoul, Korea, and one of the authors of the study on cross-neutralizing protection, told this news organization. “However, further research is needed on Omicron-specific vaccine effectiveness in patients with immune dysfunctions. We believe that these study results can be of great benefit in determining the strategy of vaccination in the future.”
The earlier study, published in July, examined the ability of COVID-19 vaccines to induce cross-reactive antibody responses against Omicron infections in patients with autoimmune rheumatic diseases (ARDs). The observational study involved 149 patients with ARDs and 94 health care workers as controls, all of whom provided blood samples a median 15 weeks after their second COVID vaccine dose or a median 8 weeks after their third dose. A little more than two-thirds of the patients (68.5%) had received a third mRNA vaccine dose. None of the participants previously had COVID-19.
The researchers compared the rate of breakthrough infections with the Omicron variant to the neutralizing responses in patients’ blood, specifically the cross-neutralizing antibody responses because the original mRNA vaccines targeted a different variant than Omicron. Breakthrough infections were assessed by survey questions.
“Our findings suggested that neither primary series vaccinations nor booster doses are sufficient to induce Omicron-neutralizing responses above the threshold in patients with ARDs, although responses were noticeably increased following the third dose of an mRNA vaccine,” write Woo-Joong Kim, of the Chung-Ang University College of Medicine, Seoul, Korea, and his colleagues. “This impairment of cross-neutralization responses across most of our patients contrasts starkly with a potent elicitation of the Omicron-neutralizing responses after the third vaccination in healthy recipients.”
The average neutralizing responses against the original SARS-CoV-2 strain were similar in both groups: 76% in patients with ARDs and 72% in health care workers after the second dose. The mean response after a third dose was 97% in health care workers and 88% in patients.
The average cross-neutralizing response against the Omicron variant was far lower, particularly in those with rheumatic disease: only 11.5%, which rose to 27% after the third dose. Only 39% of the patient sera showed neutralization of Omicron, even after the third dose. Meanwhile, the mean cross-neutralizing response in health care workers was 18% after the second dose and 50% after the third.
When the researchers compared seropositivity rates against the original virus to neutralizing responses against Omicron, the association between these was stronger in health care workers than in those with ARDs. In fact, among patients with ARDs who seroconverted, only 41% showed any response against Omicron. Among all the patients, most of those who didn’t respond to Omicron (93.5%) had initially seroconverted.
The researchers also looked at the ability to neutralize Omicron on the basis of disease in those who received three doses of the vaccine. About half of those with lupus (52%) showed any neutralization against Omicron, compared with 25% of those with rheumatoid arthritis, 37.5% of those with ankylosing spondylitis, 33% of those with Behçet snydrome, and all of those with adult-onset Still’s disease.
The rate of breakthrough infections was lower in patients (19%) than in health care workers (33%). A similar pattern was seen in the more recent study published Sept. 5. Researchers used data from a prospective cohort study in the Netherlands to examine incidence and severity of Omicron breakthrough infections in patients with immune-mediated inflammatory diseases. The researchers compared infection rates and severity among 1,593 vaccinated patients with inflammatory disease who were taking immunosuppressants and 579 vaccinated controls (418 patients with inflammatory disease not on immunosuppressants and 161 healthy controls).
One in five patients with inflammatory disease (21%) were taking immunosuppressants that substantially impair antibodies, such as anti-CD20 therapy, S1P modulators, or mycophenolate mofetil combination therapy, and 48% of these patients seroconverted after primary vaccination, compared with 96% of patients taking other immunosuppressants and 98% of controls.
Breakthrough infection rates were similar between the control group (31%) and those taking immunosuppressants (30%). Only three participants had severe disease requiring hospitalization: one control and two patients taking immunosuppressants.
“In both studies, the controls had similar or higher rates of breakthrough infections, compared with the immunosuppressed,” noted Alfred Kim, MD, an assistant professor of medicine at Washington University, St Louis, but he added, “one has to consider differences in mitigation strategies, such as masking, that may explain these findings.” That is, patients taking immunosuppressants may be taking fewer risks in the community or have fewer potential exposures, especially in the Korean study, wherein the controls were health care workers.
A greater disparity in infections occurred when considering seroconversion rates. Breakthrough incidence was 38% among those taking immunosuppressants who did not seroconvert, compared with 29% among those who did. A similar trend was seen in breakthrough incidence between those taking strongly antibody-impairing immunosuppressants (36% breakthrough rate) and those taking other immunosuppressants (28%).
Among those taking immunosuppressants who seroconverted, a primary series of vaccination reduced the risk of a breakthrough infection by 29%. Protection became more robust with a booster or prior infection, both of which reduced breakthrough infection risk by 39% in those taking immunosuppressants who seroconverted.
“We demonstrate in patients with immune-mediated inflammatory diseases on immunosuppressants that additional vaccinations are associated with decreased risk of SARS-CoV-2 Omicron breakthrough infections,” wrote Eileen W. Stalman, MD, PhD, of Amsterdam UMC in the Netherlands, and her colleagues.
Though neither study broke down immune response or breakthrough infection based on individual medications, Kim said that previous research allows one to extrapolate “that prior culprits of poor vaccine responses [such as B-cell depleting drugs, mycophenolate, and TNF [tumor necrosis factor] inhibitors will continue to bear the greatest burden in breakthrough infection, including Omicron.”
Overall, he found the data from both studies relatively consistent with one another.
“Those on immunosuppression, particularly mechanisms that have been established as risk factors for poor vaccine responses, are at risk of breakthrough infection during the era of Omicron,” Dr. Kim said.
The earlier study from Korea also found that “the median time between the third-dose vaccination and the date of confirmed breakthrough infection in patients with ARDs was significantly shorter, compared with that in health care workers” at just 93 days in patients versus 122 days in health care workers. They postulated that this population’s limited neutralization of Omicron explained this short-lived protection.
Most of the patients with breakthrough infections (74%) in that study showed no neutralization against Omicron, including the only two hospitalized patients, both of whom had strong responses against the original SARS-CoV-2 strain. The significant decline over time of neutralization against Omicron suggested “the potential for a substantial loss of the protection from breakthrough infection,” the authors write.
“The third dose of an mRNA vaccine could improve the cross-neutralization of the SARS-CoV-2 Omicron variant in patients with autoimmune rheumatic disease [although] more than half of the patients failed to generate Omicron-neutralizing antibodies,” Tae Choi said in an interview. “Our study sheds light on the relative deficiency of the Omicron-specific neutralizing responses in patients with autoimmune rheumatic disease and their anticipated vulnerability to breakthrough infection.”
The message for clinicians, Dr. Kim said, is to “continue to urge our patients to maintain additional and boosting doses per guidance, use pre-exposure prophylaxis such as Evusheld, and continue other mitigation strategies as they have done.”
The Dutch study was funded by The Netherlands Organization for Health Research and Development; the Korean study used no external funding.
The authors of the Korean study had no disclosures. The Dutch study’s authors reported a wide range of disclosures involving more than a dozen pharmaceutical companies but not including Pfizer or Moderna. Dr. Kim’s industry disclosures include Alexion, ANI, AstraZeneca, Aurinia, Exagen, Foghorn Therapeutics, GlaxoSmithKline, Kypha, and Pfizer.
A version of this article first appeared on Medscape.com.








