User login
How an ‘ad hoc’ hospitalist model evolved during India’s COVID surge
Hospital administrators recognize the efficiencies
A year after the start of the COVID-19 pandemic, as the United States was getting a reprieve in new cases from its winter surge, the opposite was happening in the rest of the world. In India, a deadly second wave hit, crippling the health care system in the country for months.
Yugandhar Bhatt, MBBS, MD, a consultant pulmonologist with Yashoda Hospital–Malakpet in Hyderabad, India, told this news organization that someone looking at his hospital before the pandemic – a 400-bed multispecialty care unit – would see patients being treated for respiratory failure secondary to exacerbation of chronic obstructive pulmonary disease, bronchial asthma, community-acquired pneumonia, and heart failure. About 30-40 patients per day were treated on an outpatient basis, and more than 30 people were admitted as inpatients.
“After [the] COVID-19 surge, our hospital totally divided into COVID and non-COVID [wards], in which COVID patients occupied 70% of [the] total,” he said. About half of COVID-19 patients were in the ICU, with half of those patients requiring supplemental oxygen.
During the first wave in India, which lasted from May to December 2020, 50% of patients who were intubated were discharged. The percentage of extubated patients decreased to 20% in the second wave, Dr. Bhatt said.
The death toll during the second wave of COVID-19 cases was unlike anything India has seen previously. Between March 1 and June 29, 2021, an estimated 19.24 million individuals were newly infected with COVID-19 and 241,206 patients died, according to Our World in Data, a project of the Global Change Data Lab. When the second wave peaked on May 22, more than 4,000 people were dying each day.
“All hospitals [in India] were treating COVID-19 more than any other acute or chronic disease,” Ramesh Adhikari, MD, MS, SFHM, a hospitalist with Franciscan Health in Lafayette, Ind., said in an interview.
Challenges arose in treating COVID-19 in India that ran counter to how medicine was usually performed. Physicians were seeing more inpatient cases than usual – and more patients in general. The change, Dr. Adhikari said, forced health care providers to think outside the box.
An ‘on-the-fly’ hospitalist model
Patients in India access health care by visiting a hospital or primary health center and then are referred out to consultants – specialist doctors – if needed. While India has universal health coverage, it is a multi-payer system that includes approximately 37% of the population covered under the government plan, a large number of private health care facilities and no caps on cost-sharing for the patient. Initiatives like Rashtriya Swasthya Bima Yojana in 2008 and Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana in 2018 have attempted to close the gap and raise the number of lower-income individuals in India covered under the government plan and reduce out-of-pocket spending. Out-of-pocket payments still consist of about 70% of total health expenditures, according to the Commonwealth Fund.
“There is not much scope for a hospitalist because it’s so cash driven,” Shyam Odeti, MD, SFHM, section chief, hospital medicine, at the Carilion Clinic in Roanoke, Va., said in an interview. “For a hospitalist, there is no urgency in getting them out of the hospital. There was no need for much efficiency before.”
The first issue during the second wave was figuring out which consultants would care for COVID-19 patients. As there is no dedicated specialty for infectious disease in India, the responsibilities fell to internists and critical care medicine consultants who volunteered. Both are considered small specialties in India. They became “makeshift hospitalists” who learned as they went and became the experts in COVID-19 care, treating their own patients while making themselves available for consultations, Dr. Odeti said.
While no official hospital medicine model in India exists like in the United States, the second COVID-19 surge caused these consultants to begin thinking like hospitalists. Tenets of hospital medicine – like team-based treatment across specialties – arose out of necessity during the crisis. “They were trying to implement a hospitalist model because that’s the only way they could treat COVID-19,” said Dr. Adhikari, an editorial advisory board member for the Hospitalist.
“Even in the U.S. when we started the hospitalist model, it started out of necessity. It’s a combination of creating efficiencies and improving quality,” Dr. Odeti said. “It’s the same thing in India. It’s borne of necessity, but it was [done] at a rapid pace.”
Problems with patient flow
The next issue was triaging patients in the hospital based on COVID-19 severity. When the second wave began, hospitals in India ran out of beds and experienced staff shortages like in many countries. But this situation “was unusual for the health system,” according to Dr. Odeti, who is also an editorial board member for the Hospitalist.
“We never had that issue. There were so many patients wanting to come to the hospital, and so there was this rush.” There was no process to triage patients to determine who needed to stay. “Everybody got put into the hospital,” he said.
Once it was determined who would take care of patients with COVID-19, access to supplies became the primary problem, Dr. Adhikari explained. Lack of oxygen, ventilators, and critical medicines like the antiviral drug remdesivir were and continue to be in short supply. “I had friends who [said] they could not admit patients because they were worried if their oxygen supply [went] low in the middle of the night. They will treat the patients who were already admitted versus taking new patients. That had caused problems for the administrators,” Dr. Adhikari added.
It is also a source of additional stress for the physicians. Where patients flow through a hospital medicine model in the United States, a system that might include case managers, social workers, pharmacists, physician advocates, and other professionals to keep a patient’s care on track, the physician is the go-to person in India for patient care. While physicians provide access to medications and remain available to a patient’s family, those duties become much harder when caring for a greater number of patients during the pandemic. “That has led to some unrealistic expectations among the patients,” Dr. Adhikari said.
Dr. Bhatt said “more than half” of a physician’s time in India is spent counseling patients on concerns about COVID-19. “Awareness about the disease is limited from the patient and patient’s family perspective, as [there is] too much apprehension toward the nature of [the] disease,” he added. “Theoretical discussions collected from social media” obstruct the physician from executing his or her duties.
Physicians in India have had to contend with physical violence from patients and individuals on the street, Dr. Adhikari added. Workplace violence was already a concern – for years, the Indian Medical Association has cited a statistic that 75% of doctors in India have experienced violence at work (Indian J Psychiatry. 2019 Apr;61[Suppl 4]:S782-5). But the threat of violence against physicians has sharply increased during the COVID-19 pandemic. Disruptions to daily life through lockdowns “made people fearful, anxious, and sometimes they have found it difficult to access emergency treatment,” according to a letter published by Karthikeyan Iyengar and colleagues in the Postgraduate Medical Journal. In response to the restlessness, irritation, and despair resulting from hospitals closing their doors, “people have shown their frustration by verbally abusing and threatening to physically assault doctors and other health care workers,” the authors wrote.
A telemedicine boon in India
Back in the United States, hospitalists with family and friends in India were trying to figure out how to help. Some were working through the day, only to answer calls and WhatsApp messages from loved ones at night. “Everyone knows a physician or someone who’s your colleague, who owns a hospital or runs a hospital, or one of the family members is sick,” Dr. Adhikari said.
These U.S.-based hospitalists were burning the candle at both ends, helping with the pandemic in both countries. Physicians in India were posing questions to U.S. colleagues who they saw as having the most recent evidence for COVID-19 treatment. Out of the 180 physicians he trained with in India, Dr. Odeti said 110 of the physicians were in a large WhatsApp group chat that was constantly exchanging messages and serving as “kind of a friendly support group.”
In Dr. Odeti’s group chat, physicians helped one another find hospital beds for patients who reached out to them. “The first couple of weeks, there was no proper way for people to know where [patients] were based. There was no way to find if this hospital had a bed, so they reached out to any doctors they knew,” he said.
While he said it was emotionally draining, “at the same time, we felt a responsibility toward colleagues in India,” Dr. Odeti said, noting that as COVID-19 cases have decreased in India, the requests have been less frequent.
Because of concerns about traveling to India during the pandemic while on a J-1, H-1B, or other visa with the United States, directly helping friends and family in India seemed out of reach. But many hospitalists of Indian origin instead turned to telemedicine to help their colleagues. Telemedicine had already been steadily growing in India, but was accelerated by the pandemic. The current ratio of doctors to patients in India is 0.62 to 1,000 – lower than recommendations from the World Health Organization. That makes telemedicine a unique opportunity for one physician in India to reach many patients regardless of location.
Dr. Adhikari said he helped out his colleagues in India by performing consults for their patients. “They were just worried because they did not ‘know where to go, or what to get,” he said. “I was treating more patients in India than I was actually treating here.”
In March 2020, the Indian Ministry of Health and Family Welfare released telemedicine practice guidelines for the country, which relaxed regulations on privacy requirements and has been credited in part for giving telemedicine an additional boost during the pandemic. “That makes it easy for people to reach out but also has its own problems,” Dr. Adhikari said.
Monitoring of milder COVID-19 cases that don’t require hospitalization can be performed by a nurse who calls every few hours to check on a patient, make recommendations, and text treatment plans. “The telemedicine platforms are being adopted really fast,” Dr. Adhikari said. “The platforms were built in no time.”
According to NewZoo, a games market data analytics company, India has 345.9 million smartphone users as of 2019 – the second highest number of users in the world after China. Dr. Odeti said he believes telemedicine will be widely adopted.
“In India, they are very proactive in accepting these kinds of methods, so I’m sure they will,” he said. “Governments were trying to do it before the pandemic, because access to care is a problem in India. There are villages which are very, very remote.”
Reversion to old systems
After the peak in late May, new COVID-19 cases in India began to decrease, and the second wave waned on a national level. Hospitals began to get the supplies they needed, beds are available, and patients aren’t as sick as before, according to Dr. Adhikari. The federal government has begun issuing supplies to patients in each state, including COVID-19 vaccines. “The peak for the second wave is gone,” he said.
What remains is a group of physicians trained in how to triage patients and create efficiencies in a hospital setting. Could those skills be put to use elsewhere in India after the pandemic?
According to Dr. Bhatt, the patient care model is likely to revert to the system that existed before. “Whatever the changes, interims of bed occupancy, cost of ICU will be temporary [and] will change to normal,” he said. “But awareness about masks [and] sanitizing methods will be permanent.”
Dr. Adhikari believes that not utilizing the skills of newly minted hospitalists in India would be a missed opportunity. “This is a silver lining from COVID-19, that hospital medicine plays a vital role in the sickest patients, whether it is in India or the U.S. or anywhere,” he said. “I think the model of hospital medicine should be adopted. It’s not: ‘Should it really be adopted or not?’ It should be. There is a huge potential in doing inpatient coordinated [care], having people dedicated in the hospital.”
There are tangible benefits to creating efficiencies in India’s health system, Dr. Odeti said. Length of stay for sicker patients “was much longer” at 10-14 days during the second wave, compared with the United States, before lowering to around 5 days. “These hospitals right now are learning the efficient ways of doing it: when to send [patients] out, how to send them out, how to [perform] service-based practices, creating processes which were nonexistent before.”
While he doesn’t personally believe physicians will adopt a full-fledged hospitalist model unless the payer structure in India changes, “these people are at an advantage with this extra set of skills,” he said. “I think all the knowledge that these people have are going to come in handy.”
Opportunities for growth
Dr. Odeti sees the potential for the hospitalist model to grow in India – if not into its own specialty, then in how critical care consultants handle sicker patients and handoffs.
“The critical care clinician cannot keep the patient from the time they are admitted to the ICU until the discharge, so there will be a need for the transition,” Dr. Odeti said. “In the past, there were not many capabilities in Indian health systems to take care of these extremely sick patients, and now it is evolving. I think that is one more thing that will help.”
Dr. Adhikari said hospital systems in India are beginning to realize how having dedicated hospital physicians could benefit them. In India, “if you’re sick, you go to your doctor, you get treated and you disappear,” he said. The next time, you may see the same doctor or a completely different doctor. “There’s no system there, so it’s really hard for hospital medicine as such because patients, when they are very sick, they just come to the ER. They’re not followed by their primary care.”
Anecdotally, Dr. Odeti sees patients already adapting to having access to a physician for asking questions normally answered by primary care physicians. “I think primary care will come into play,” he said. “When I was doing a Zoom call for patients, they were asking me questions about sciatica. I think they are getting comfortable with this technology.”
A hospitalist model could even be applied to specific diseases with a large population of patients. Hospital administrators “have seen this for the first time, how efficient it could be if they had their own hospitalists and actually run it. So that’s the part that has crossed their minds,” Dr. Adhikari said. “How they will apply it going forward, other than during the COVID-19 pandemic, depends on the size of the hospital and the volume of the patients for a particular disease.”
“You can see in certain areas there is large growth for hospital medicine. But to rise to the level of the United States and how we do it, India needs bigger health systems to adopt the model,” Dr. Adhikari said.
Hospital administrators recognize the efficiencies
Hospital administrators recognize the efficiencies
A year after the start of the COVID-19 pandemic, as the United States was getting a reprieve in new cases from its winter surge, the opposite was happening in the rest of the world. In India, a deadly second wave hit, crippling the health care system in the country for months.
Yugandhar Bhatt, MBBS, MD, a consultant pulmonologist with Yashoda Hospital–Malakpet in Hyderabad, India, told this news organization that someone looking at his hospital before the pandemic – a 400-bed multispecialty care unit – would see patients being treated for respiratory failure secondary to exacerbation of chronic obstructive pulmonary disease, bronchial asthma, community-acquired pneumonia, and heart failure. About 30-40 patients per day were treated on an outpatient basis, and more than 30 people were admitted as inpatients.
“After [the] COVID-19 surge, our hospital totally divided into COVID and non-COVID [wards], in which COVID patients occupied 70% of [the] total,” he said. About half of COVID-19 patients were in the ICU, with half of those patients requiring supplemental oxygen.
During the first wave in India, which lasted from May to December 2020, 50% of patients who were intubated were discharged. The percentage of extubated patients decreased to 20% in the second wave, Dr. Bhatt said.
The death toll during the second wave of COVID-19 cases was unlike anything India has seen previously. Between March 1 and June 29, 2021, an estimated 19.24 million individuals were newly infected with COVID-19 and 241,206 patients died, according to Our World in Data, a project of the Global Change Data Lab. When the second wave peaked on May 22, more than 4,000 people were dying each day.
“All hospitals [in India] were treating COVID-19 more than any other acute or chronic disease,” Ramesh Adhikari, MD, MS, SFHM, a hospitalist with Franciscan Health in Lafayette, Ind., said in an interview.
Challenges arose in treating COVID-19 in India that ran counter to how medicine was usually performed. Physicians were seeing more inpatient cases than usual – and more patients in general. The change, Dr. Adhikari said, forced health care providers to think outside the box.
An ‘on-the-fly’ hospitalist model
Patients in India access health care by visiting a hospital or primary health center and then are referred out to consultants – specialist doctors – if needed. While India has universal health coverage, it is a multi-payer system that includes approximately 37% of the population covered under the government plan, a large number of private health care facilities and no caps on cost-sharing for the patient. Initiatives like Rashtriya Swasthya Bima Yojana in 2008 and Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana in 2018 have attempted to close the gap and raise the number of lower-income individuals in India covered under the government plan and reduce out-of-pocket spending. Out-of-pocket payments still consist of about 70% of total health expenditures, according to the Commonwealth Fund.
“There is not much scope for a hospitalist because it’s so cash driven,” Shyam Odeti, MD, SFHM, section chief, hospital medicine, at the Carilion Clinic in Roanoke, Va., said in an interview. “For a hospitalist, there is no urgency in getting them out of the hospital. There was no need for much efficiency before.”
The first issue during the second wave was figuring out which consultants would care for COVID-19 patients. As there is no dedicated specialty for infectious disease in India, the responsibilities fell to internists and critical care medicine consultants who volunteered. Both are considered small specialties in India. They became “makeshift hospitalists” who learned as they went and became the experts in COVID-19 care, treating their own patients while making themselves available for consultations, Dr. Odeti said.
While no official hospital medicine model in India exists like in the United States, the second COVID-19 surge caused these consultants to begin thinking like hospitalists. Tenets of hospital medicine – like team-based treatment across specialties – arose out of necessity during the crisis. “They were trying to implement a hospitalist model because that’s the only way they could treat COVID-19,” said Dr. Adhikari, an editorial advisory board member for the Hospitalist.
“Even in the U.S. when we started the hospitalist model, it started out of necessity. It’s a combination of creating efficiencies and improving quality,” Dr. Odeti said. “It’s the same thing in India. It’s borne of necessity, but it was [done] at a rapid pace.”
Problems with patient flow
The next issue was triaging patients in the hospital based on COVID-19 severity. When the second wave began, hospitals in India ran out of beds and experienced staff shortages like in many countries. But this situation “was unusual for the health system,” according to Dr. Odeti, who is also an editorial board member for the Hospitalist.
“We never had that issue. There were so many patients wanting to come to the hospital, and so there was this rush.” There was no process to triage patients to determine who needed to stay. “Everybody got put into the hospital,” he said.
Once it was determined who would take care of patients with COVID-19, access to supplies became the primary problem, Dr. Adhikari explained. Lack of oxygen, ventilators, and critical medicines like the antiviral drug remdesivir were and continue to be in short supply. “I had friends who [said] they could not admit patients because they were worried if their oxygen supply [went] low in the middle of the night. They will treat the patients who were already admitted versus taking new patients. That had caused problems for the administrators,” Dr. Adhikari added.
It is also a source of additional stress for the physicians. Where patients flow through a hospital medicine model in the United States, a system that might include case managers, social workers, pharmacists, physician advocates, and other professionals to keep a patient’s care on track, the physician is the go-to person in India for patient care. While physicians provide access to medications and remain available to a patient’s family, those duties become much harder when caring for a greater number of patients during the pandemic. “That has led to some unrealistic expectations among the patients,” Dr. Adhikari said.
Dr. Bhatt said “more than half” of a physician’s time in India is spent counseling patients on concerns about COVID-19. “Awareness about the disease is limited from the patient and patient’s family perspective, as [there is] too much apprehension toward the nature of [the] disease,” he added. “Theoretical discussions collected from social media” obstruct the physician from executing his or her duties.
Physicians in India have had to contend with physical violence from patients and individuals on the street, Dr. Adhikari added. Workplace violence was already a concern – for years, the Indian Medical Association has cited a statistic that 75% of doctors in India have experienced violence at work (Indian J Psychiatry. 2019 Apr;61[Suppl 4]:S782-5). But the threat of violence against physicians has sharply increased during the COVID-19 pandemic. Disruptions to daily life through lockdowns “made people fearful, anxious, and sometimes they have found it difficult to access emergency treatment,” according to a letter published by Karthikeyan Iyengar and colleagues in the Postgraduate Medical Journal. In response to the restlessness, irritation, and despair resulting from hospitals closing their doors, “people have shown their frustration by verbally abusing and threatening to physically assault doctors and other health care workers,” the authors wrote.
A telemedicine boon in India
Back in the United States, hospitalists with family and friends in India were trying to figure out how to help. Some were working through the day, only to answer calls and WhatsApp messages from loved ones at night. “Everyone knows a physician or someone who’s your colleague, who owns a hospital or runs a hospital, or one of the family members is sick,” Dr. Adhikari said.
These U.S.-based hospitalists were burning the candle at both ends, helping with the pandemic in both countries. Physicians in India were posing questions to U.S. colleagues who they saw as having the most recent evidence for COVID-19 treatment. Out of the 180 physicians he trained with in India, Dr. Odeti said 110 of the physicians were in a large WhatsApp group chat that was constantly exchanging messages and serving as “kind of a friendly support group.”
In Dr. Odeti’s group chat, physicians helped one another find hospital beds for patients who reached out to them. “The first couple of weeks, there was no proper way for people to know where [patients] were based. There was no way to find if this hospital had a bed, so they reached out to any doctors they knew,” he said.
While he said it was emotionally draining, “at the same time, we felt a responsibility toward colleagues in India,” Dr. Odeti said, noting that as COVID-19 cases have decreased in India, the requests have been less frequent.
Because of concerns about traveling to India during the pandemic while on a J-1, H-1B, or other visa with the United States, directly helping friends and family in India seemed out of reach. But many hospitalists of Indian origin instead turned to telemedicine to help their colleagues. Telemedicine had already been steadily growing in India, but was accelerated by the pandemic. The current ratio of doctors to patients in India is 0.62 to 1,000 – lower than recommendations from the World Health Organization. That makes telemedicine a unique opportunity for one physician in India to reach many patients regardless of location.
Dr. Adhikari said he helped out his colleagues in India by performing consults for their patients. “They were just worried because they did not ‘know where to go, or what to get,” he said. “I was treating more patients in India than I was actually treating here.”
In March 2020, the Indian Ministry of Health and Family Welfare released telemedicine practice guidelines for the country, which relaxed regulations on privacy requirements and has been credited in part for giving telemedicine an additional boost during the pandemic. “That makes it easy for people to reach out but also has its own problems,” Dr. Adhikari said.
Monitoring of milder COVID-19 cases that don’t require hospitalization can be performed by a nurse who calls every few hours to check on a patient, make recommendations, and text treatment plans. “The telemedicine platforms are being adopted really fast,” Dr. Adhikari said. “The platforms were built in no time.”
According to NewZoo, a games market data analytics company, India has 345.9 million smartphone users as of 2019 – the second highest number of users in the world after China. Dr. Odeti said he believes telemedicine will be widely adopted.
“In India, they are very proactive in accepting these kinds of methods, so I’m sure they will,” he said. “Governments were trying to do it before the pandemic, because access to care is a problem in India. There are villages which are very, very remote.”
Reversion to old systems
After the peak in late May, new COVID-19 cases in India began to decrease, and the second wave waned on a national level. Hospitals began to get the supplies they needed, beds are available, and patients aren’t as sick as before, according to Dr. Adhikari. The federal government has begun issuing supplies to patients in each state, including COVID-19 vaccines. “The peak for the second wave is gone,” he said.
What remains is a group of physicians trained in how to triage patients and create efficiencies in a hospital setting. Could those skills be put to use elsewhere in India after the pandemic?
According to Dr. Bhatt, the patient care model is likely to revert to the system that existed before. “Whatever the changes, interims of bed occupancy, cost of ICU will be temporary [and] will change to normal,” he said. “But awareness about masks [and] sanitizing methods will be permanent.”
Dr. Adhikari believes that not utilizing the skills of newly minted hospitalists in India would be a missed opportunity. “This is a silver lining from COVID-19, that hospital medicine plays a vital role in the sickest patients, whether it is in India or the U.S. or anywhere,” he said. “I think the model of hospital medicine should be adopted. It’s not: ‘Should it really be adopted or not?’ It should be. There is a huge potential in doing inpatient coordinated [care], having people dedicated in the hospital.”
There are tangible benefits to creating efficiencies in India’s health system, Dr. Odeti said. Length of stay for sicker patients “was much longer” at 10-14 days during the second wave, compared with the United States, before lowering to around 5 days. “These hospitals right now are learning the efficient ways of doing it: when to send [patients] out, how to send them out, how to [perform] service-based practices, creating processes which were nonexistent before.”
While he doesn’t personally believe physicians will adopt a full-fledged hospitalist model unless the payer structure in India changes, “these people are at an advantage with this extra set of skills,” he said. “I think all the knowledge that these people have are going to come in handy.”
Opportunities for growth
Dr. Odeti sees the potential for the hospitalist model to grow in India – if not into its own specialty, then in how critical care consultants handle sicker patients and handoffs.
“The critical care clinician cannot keep the patient from the time they are admitted to the ICU until the discharge, so there will be a need for the transition,” Dr. Odeti said. “In the past, there were not many capabilities in Indian health systems to take care of these extremely sick patients, and now it is evolving. I think that is one more thing that will help.”
Dr. Adhikari said hospital systems in India are beginning to realize how having dedicated hospital physicians could benefit them. In India, “if you’re sick, you go to your doctor, you get treated and you disappear,” he said. The next time, you may see the same doctor or a completely different doctor. “There’s no system there, so it’s really hard for hospital medicine as such because patients, when they are very sick, they just come to the ER. They’re not followed by their primary care.”
Anecdotally, Dr. Odeti sees patients already adapting to having access to a physician for asking questions normally answered by primary care physicians. “I think primary care will come into play,” he said. “When I was doing a Zoom call for patients, they were asking me questions about sciatica. I think they are getting comfortable with this technology.”
A hospitalist model could even be applied to specific diseases with a large population of patients. Hospital administrators “have seen this for the first time, how efficient it could be if they had their own hospitalists and actually run it. So that’s the part that has crossed their minds,” Dr. Adhikari said. “How they will apply it going forward, other than during the COVID-19 pandemic, depends on the size of the hospital and the volume of the patients for a particular disease.”
“You can see in certain areas there is large growth for hospital medicine. But to rise to the level of the United States and how we do it, India needs bigger health systems to adopt the model,” Dr. Adhikari said.
A year after the start of the COVID-19 pandemic, as the United States was getting a reprieve in new cases from its winter surge, the opposite was happening in the rest of the world. In India, a deadly second wave hit, crippling the health care system in the country for months.
Yugandhar Bhatt, MBBS, MD, a consultant pulmonologist with Yashoda Hospital–Malakpet in Hyderabad, India, told this news organization that someone looking at his hospital before the pandemic – a 400-bed multispecialty care unit – would see patients being treated for respiratory failure secondary to exacerbation of chronic obstructive pulmonary disease, bronchial asthma, community-acquired pneumonia, and heart failure. About 30-40 patients per day were treated on an outpatient basis, and more than 30 people were admitted as inpatients.
“After [the] COVID-19 surge, our hospital totally divided into COVID and non-COVID [wards], in which COVID patients occupied 70% of [the] total,” he said. About half of COVID-19 patients were in the ICU, with half of those patients requiring supplemental oxygen.
During the first wave in India, which lasted from May to December 2020, 50% of patients who were intubated were discharged. The percentage of extubated patients decreased to 20% in the second wave, Dr. Bhatt said.
The death toll during the second wave of COVID-19 cases was unlike anything India has seen previously. Between March 1 and June 29, 2021, an estimated 19.24 million individuals were newly infected with COVID-19 and 241,206 patients died, according to Our World in Data, a project of the Global Change Data Lab. When the second wave peaked on May 22, more than 4,000 people were dying each day.
“All hospitals [in India] were treating COVID-19 more than any other acute or chronic disease,” Ramesh Adhikari, MD, MS, SFHM, a hospitalist with Franciscan Health in Lafayette, Ind., said in an interview.
Challenges arose in treating COVID-19 in India that ran counter to how medicine was usually performed. Physicians were seeing more inpatient cases than usual – and more patients in general. The change, Dr. Adhikari said, forced health care providers to think outside the box.
An ‘on-the-fly’ hospitalist model
Patients in India access health care by visiting a hospital or primary health center and then are referred out to consultants – specialist doctors – if needed. While India has universal health coverage, it is a multi-payer system that includes approximately 37% of the population covered under the government plan, a large number of private health care facilities and no caps on cost-sharing for the patient. Initiatives like Rashtriya Swasthya Bima Yojana in 2008 and Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana in 2018 have attempted to close the gap and raise the number of lower-income individuals in India covered under the government plan and reduce out-of-pocket spending. Out-of-pocket payments still consist of about 70% of total health expenditures, according to the Commonwealth Fund.
“There is not much scope for a hospitalist because it’s so cash driven,” Shyam Odeti, MD, SFHM, section chief, hospital medicine, at the Carilion Clinic in Roanoke, Va., said in an interview. “For a hospitalist, there is no urgency in getting them out of the hospital. There was no need for much efficiency before.”
The first issue during the second wave was figuring out which consultants would care for COVID-19 patients. As there is no dedicated specialty for infectious disease in India, the responsibilities fell to internists and critical care medicine consultants who volunteered. Both are considered small specialties in India. They became “makeshift hospitalists” who learned as they went and became the experts in COVID-19 care, treating their own patients while making themselves available for consultations, Dr. Odeti said.
While no official hospital medicine model in India exists like in the United States, the second COVID-19 surge caused these consultants to begin thinking like hospitalists. Tenets of hospital medicine – like team-based treatment across specialties – arose out of necessity during the crisis. “They were trying to implement a hospitalist model because that’s the only way they could treat COVID-19,” said Dr. Adhikari, an editorial advisory board member for the Hospitalist.
“Even in the U.S. when we started the hospitalist model, it started out of necessity. It’s a combination of creating efficiencies and improving quality,” Dr. Odeti said. “It’s the same thing in India. It’s borne of necessity, but it was [done] at a rapid pace.”
Problems with patient flow
The next issue was triaging patients in the hospital based on COVID-19 severity. When the second wave began, hospitals in India ran out of beds and experienced staff shortages like in many countries. But this situation “was unusual for the health system,” according to Dr. Odeti, who is also an editorial board member for the Hospitalist.
“We never had that issue. There were so many patients wanting to come to the hospital, and so there was this rush.” There was no process to triage patients to determine who needed to stay. “Everybody got put into the hospital,” he said.
Once it was determined who would take care of patients with COVID-19, access to supplies became the primary problem, Dr. Adhikari explained. Lack of oxygen, ventilators, and critical medicines like the antiviral drug remdesivir were and continue to be in short supply. “I had friends who [said] they could not admit patients because they were worried if their oxygen supply [went] low in the middle of the night. They will treat the patients who were already admitted versus taking new patients. That had caused problems for the administrators,” Dr. Adhikari added.
It is also a source of additional stress for the physicians. Where patients flow through a hospital medicine model in the United States, a system that might include case managers, social workers, pharmacists, physician advocates, and other professionals to keep a patient’s care on track, the physician is the go-to person in India for patient care. While physicians provide access to medications and remain available to a patient’s family, those duties become much harder when caring for a greater number of patients during the pandemic. “That has led to some unrealistic expectations among the patients,” Dr. Adhikari said.
Dr. Bhatt said “more than half” of a physician’s time in India is spent counseling patients on concerns about COVID-19. “Awareness about the disease is limited from the patient and patient’s family perspective, as [there is] too much apprehension toward the nature of [the] disease,” he added. “Theoretical discussions collected from social media” obstruct the physician from executing his or her duties.
Physicians in India have had to contend with physical violence from patients and individuals on the street, Dr. Adhikari added. Workplace violence was already a concern – for years, the Indian Medical Association has cited a statistic that 75% of doctors in India have experienced violence at work (Indian J Psychiatry. 2019 Apr;61[Suppl 4]:S782-5). But the threat of violence against physicians has sharply increased during the COVID-19 pandemic. Disruptions to daily life through lockdowns “made people fearful, anxious, and sometimes they have found it difficult to access emergency treatment,” according to a letter published by Karthikeyan Iyengar and colleagues in the Postgraduate Medical Journal. In response to the restlessness, irritation, and despair resulting from hospitals closing their doors, “people have shown their frustration by verbally abusing and threatening to physically assault doctors and other health care workers,” the authors wrote.
A telemedicine boon in India
Back in the United States, hospitalists with family and friends in India were trying to figure out how to help. Some were working through the day, only to answer calls and WhatsApp messages from loved ones at night. “Everyone knows a physician or someone who’s your colleague, who owns a hospital or runs a hospital, or one of the family members is sick,” Dr. Adhikari said.
These U.S.-based hospitalists were burning the candle at both ends, helping with the pandemic in both countries. Physicians in India were posing questions to U.S. colleagues who they saw as having the most recent evidence for COVID-19 treatment. Out of the 180 physicians he trained with in India, Dr. Odeti said 110 of the physicians were in a large WhatsApp group chat that was constantly exchanging messages and serving as “kind of a friendly support group.”
In Dr. Odeti’s group chat, physicians helped one another find hospital beds for patients who reached out to them. “The first couple of weeks, there was no proper way for people to know where [patients] were based. There was no way to find if this hospital had a bed, so they reached out to any doctors they knew,” he said.
While he said it was emotionally draining, “at the same time, we felt a responsibility toward colleagues in India,” Dr. Odeti said, noting that as COVID-19 cases have decreased in India, the requests have been less frequent.
Because of concerns about traveling to India during the pandemic while on a J-1, H-1B, or other visa with the United States, directly helping friends and family in India seemed out of reach. But many hospitalists of Indian origin instead turned to telemedicine to help their colleagues. Telemedicine had already been steadily growing in India, but was accelerated by the pandemic. The current ratio of doctors to patients in India is 0.62 to 1,000 – lower than recommendations from the World Health Organization. That makes telemedicine a unique opportunity for one physician in India to reach many patients regardless of location.
Dr. Adhikari said he helped out his colleagues in India by performing consults for their patients. “They were just worried because they did not ‘know where to go, or what to get,” he said. “I was treating more patients in India than I was actually treating here.”
In March 2020, the Indian Ministry of Health and Family Welfare released telemedicine practice guidelines for the country, which relaxed regulations on privacy requirements and has been credited in part for giving telemedicine an additional boost during the pandemic. “That makes it easy for people to reach out but also has its own problems,” Dr. Adhikari said.
Monitoring of milder COVID-19 cases that don’t require hospitalization can be performed by a nurse who calls every few hours to check on a patient, make recommendations, and text treatment plans. “The telemedicine platforms are being adopted really fast,” Dr. Adhikari said. “The platforms were built in no time.”
According to NewZoo, a games market data analytics company, India has 345.9 million smartphone users as of 2019 – the second highest number of users in the world after China. Dr. Odeti said he believes telemedicine will be widely adopted.
“In India, they are very proactive in accepting these kinds of methods, so I’m sure they will,” he said. “Governments were trying to do it before the pandemic, because access to care is a problem in India. There are villages which are very, very remote.”
Reversion to old systems
After the peak in late May, new COVID-19 cases in India began to decrease, and the second wave waned on a national level. Hospitals began to get the supplies they needed, beds are available, and patients aren’t as sick as before, according to Dr. Adhikari. The federal government has begun issuing supplies to patients in each state, including COVID-19 vaccines. “The peak for the second wave is gone,” he said.
What remains is a group of physicians trained in how to triage patients and create efficiencies in a hospital setting. Could those skills be put to use elsewhere in India after the pandemic?
According to Dr. Bhatt, the patient care model is likely to revert to the system that existed before. “Whatever the changes, interims of bed occupancy, cost of ICU will be temporary [and] will change to normal,” he said. “But awareness about masks [and] sanitizing methods will be permanent.”
Dr. Adhikari believes that not utilizing the skills of newly minted hospitalists in India would be a missed opportunity. “This is a silver lining from COVID-19, that hospital medicine plays a vital role in the sickest patients, whether it is in India or the U.S. or anywhere,” he said. “I think the model of hospital medicine should be adopted. It’s not: ‘Should it really be adopted or not?’ It should be. There is a huge potential in doing inpatient coordinated [care], having people dedicated in the hospital.”
There are tangible benefits to creating efficiencies in India’s health system, Dr. Odeti said. Length of stay for sicker patients “was much longer” at 10-14 days during the second wave, compared with the United States, before lowering to around 5 days. “These hospitals right now are learning the efficient ways of doing it: when to send [patients] out, how to send them out, how to [perform] service-based practices, creating processes which were nonexistent before.”
While he doesn’t personally believe physicians will adopt a full-fledged hospitalist model unless the payer structure in India changes, “these people are at an advantage with this extra set of skills,” he said. “I think all the knowledge that these people have are going to come in handy.”
Opportunities for growth
Dr. Odeti sees the potential for the hospitalist model to grow in India – if not into its own specialty, then in how critical care consultants handle sicker patients and handoffs.
“The critical care clinician cannot keep the patient from the time they are admitted to the ICU until the discharge, so there will be a need for the transition,” Dr. Odeti said. “In the past, there were not many capabilities in Indian health systems to take care of these extremely sick patients, and now it is evolving. I think that is one more thing that will help.”
Dr. Adhikari said hospital systems in India are beginning to realize how having dedicated hospital physicians could benefit them. In India, “if you’re sick, you go to your doctor, you get treated and you disappear,” he said. The next time, you may see the same doctor or a completely different doctor. “There’s no system there, so it’s really hard for hospital medicine as such because patients, when they are very sick, they just come to the ER. They’re not followed by their primary care.”
Anecdotally, Dr. Odeti sees patients already adapting to having access to a physician for asking questions normally answered by primary care physicians. “I think primary care will come into play,” he said. “When I was doing a Zoom call for patients, they were asking me questions about sciatica. I think they are getting comfortable with this technology.”
A hospitalist model could even be applied to specific diseases with a large population of patients. Hospital administrators “have seen this for the first time, how efficient it could be if they had their own hospitalists and actually run it. So that’s the part that has crossed their minds,” Dr. Adhikari said. “How they will apply it going forward, other than during the COVID-19 pandemic, depends on the size of the hospital and the volume of the patients for a particular disease.”
“You can see in certain areas there is large growth for hospital medicine. But to rise to the level of the United States and how we do it, India needs bigger health systems to adopt the model,” Dr. Adhikari said.
ITP after COVID-19 Vaccination at the Salisbury VA Healthcare System: Case Studies
Background
An association between vaccines and the rare development of immune thrombocytopenic purpura (ITP) has been reported in the literature. More recently, there have been a few case reports published describing patients developing ITP shortly after COVID- 19 vaccination, but this has not been reported specifically in the Veteran population. The SVAHCS has three cases of Veterans diagnosed with new or relapsed ITP within two months of receiving the second COVID-19 vaccine (all Pfizer brand). The treatment(s) and current outcome for each patient is summarized below.
Case Reports
Case 1 is a 78-year-old male Veteran who received his second COVID-19 vaccine on 2/10/21. Patient was diagnosed with ITP 4/27/21, hospitalized multiple times and treated with pulse dexamethasone, prednisone taper, rituximab IV weekly and romiplostim injections. Currently, patient has a thrombocytosis and romiplostim injections are on hold. Case 2 is a 90-yearold male Veteran who received his second COVID-19 vaccine on 3/16/21. Patient was diagnosed on 5/3/21 and treated with pulse dexamethasone, prednisone taper and rituximab IV weekly. Platelet count is currently normal. Case 3 is a 75-year-old male Veteran who received his second COVID-19 vaccine on 2/1/21. He has a history of ITP diagnosed 12/12/14 that has been well controlled with weekly romiplostim injections until 4/9/21. Patient was hospitalized and treated with pulse dexamethasone and prednisone taper. Upon discharge, therapy was changed from romiplostim to fostamatinib. Currently, platelet count recovered and is stable.
Conclusions
The two Veterans with de novo ITP exhibited resistant disease and had prolonged treatment courses, taking approximately a month to recover their platelet counts. In contrast, the Veteran with relapsed ITP exhibited a faster recovery period of approximately two weeks. In the safety trials conducted for the Pfizer COVID-19 vaccine, participants received vaccination or placebo and had a follow-up for an average of two months which may explain why ITP was not reported as a possible association until after marketing. After treating the above cases, the SVAHCS plans to use thrombopoietin receptor agonists (TPO-RAs) earlier in the treatment of ITP that may be associated with the COVID-19 vaccine as this has recently been recommended in case reports from the general population.
Background
An association between vaccines and the rare development of immune thrombocytopenic purpura (ITP) has been reported in the literature. More recently, there have been a few case reports published describing patients developing ITP shortly after COVID- 19 vaccination, but this has not been reported specifically in the Veteran population. The SVAHCS has three cases of Veterans diagnosed with new or relapsed ITP within two months of receiving the second COVID-19 vaccine (all Pfizer brand). The treatment(s) and current outcome for each patient is summarized below.
Case Reports
Case 1 is a 78-year-old male Veteran who received his second COVID-19 vaccine on 2/10/21. Patient was diagnosed with ITP 4/27/21, hospitalized multiple times and treated with pulse dexamethasone, prednisone taper, rituximab IV weekly and romiplostim injections. Currently, patient has a thrombocytosis and romiplostim injections are on hold. Case 2 is a 90-yearold male Veteran who received his second COVID-19 vaccine on 3/16/21. Patient was diagnosed on 5/3/21 and treated with pulse dexamethasone, prednisone taper and rituximab IV weekly. Platelet count is currently normal. Case 3 is a 75-year-old male Veteran who received his second COVID-19 vaccine on 2/1/21. He has a history of ITP diagnosed 12/12/14 that has been well controlled with weekly romiplostim injections until 4/9/21. Patient was hospitalized and treated with pulse dexamethasone and prednisone taper. Upon discharge, therapy was changed from romiplostim to fostamatinib. Currently, platelet count recovered and is stable.
Conclusions
The two Veterans with de novo ITP exhibited resistant disease and had prolonged treatment courses, taking approximately a month to recover their platelet counts. In contrast, the Veteran with relapsed ITP exhibited a faster recovery period of approximately two weeks. In the safety trials conducted for the Pfizer COVID-19 vaccine, participants received vaccination or placebo and had a follow-up for an average of two months which may explain why ITP was not reported as a possible association until after marketing. After treating the above cases, the SVAHCS plans to use thrombopoietin receptor agonists (TPO-RAs) earlier in the treatment of ITP that may be associated with the COVID-19 vaccine as this has recently been recommended in case reports from the general population.
Background
An association between vaccines and the rare development of immune thrombocytopenic purpura (ITP) has been reported in the literature. More recently, there have been a few case reports published describing patients developing ITP shortly after COVID- 19 vaccination, but this has not been reported specifically in the Veteran population. The SVAHCS has three cases of Veterans diagnosed with new or relapsed ITP within two months of receiving the second COVID-19 vaccine (all Pfizer brand). The treatment(s) and current outcome for each patient is summarized below.
Case Reports
Case 1 is a 78-year-old male Veteran who received his second COVID-19 vaccine on 2/10/21. Patient was diagnosed with ITP 4/27/21, hospitalized multiple times and treated with pulse dexamethasone, prednisone taper, rituximab IV weekly and romiplostim injections. Currently, patient has a thrombocytosis and romiplostim injections are on hold. Case 2 is a 90-yearold male Veteran who received his second COVID-19 vaccine on 3/16/21. Patient was diagnosed on 5/3/21 and treated with pulse dexamethasone, prednisone taper and rituximab IV weekly. Platelet count is currently normal. Case 3 is a 75-year-old male Veteran who received his second COVID-19 vaccine on 2/1/21. He has a history of ITP diagnosed 12/12/14 that has been well controlled with weekly romiplostim injections until 4/9/21. Patient was hospitalized and treated with pulse dexamethasone and prednisone taper. Upon discharge, therapy was changed from romiplostim to fostamatinib. Currently, platelet count recovered and is stable.
Conclusions
The two Veterans with de novo ITP exhibited resistant disease and had prolonged treatment courses, taking approximately a month to recover their platelet counts. In contrast, the Veteran with relapsed ITP exhibited a faster recovery period of approximately two weeks. In the safety trials conducted for the Pfizer COVID-19 vaccine, participants received vaccination or placebo and had a follow-up for an average of two months which may explain why ITP was not reported as a possible association until after marketing. After treating the above cases, the SVAHCS plans to use thrombopoietin receptor agonists (TPO-RAs) earlier in the treatment of ITP that may be associated with the COVID-19 vaccine as this has recently been recommended in case reports from the general population.
COVID-19 spares lung function in young adults
Here’s some encouraging news for once regarding SARS-CoV-2 infections: A study of young adults for whom prepandemic spirometry data were available showed that COVID-19 did not have a significant impact on lung function, even among patients with asthma.
Among 853 Swedish men and women (mean age, 22 years) who were part of a birth cohort study, there were no significant differences in either forced expiratory volume in 1 second (FEV1) or in the ratio of FEV1 to forced vital capacity, reported Ida Mogensen, MD, PhD, a postdoctoral fellow at the Karolinska Institute in Stockholm.
“We found no effect of COVID-19 on spirometric lung function in generally healthy adults,” she said in an oral abstract presented at the European Respiratory Society 2021 International Congress.
The findings echo those of a small study that involved 73 children and adolescents with COVID-19 and 45 uninfected control persons. The investigators in that study, which was also presented at ERS 2021, found that there were no significant differences in the frequency of abnormal pulmonary function measures between case patients and control patients (abstract OA1303).
“The findings from these two studies provide important reassurance about the impact of COVID infection on lung function in children and young adults,” commented Anita Simonds, MD, an honorary consultant in respiratory and sleep medicine at the Royal Brompton Hospital, London.
“We know already that this group is less likely to suffer severe illness if they contract the virus, and these studies, which importantly include comparator groups without COVID-19, show that they are also less likely to suffer long-term consequences with respect to lung function,” she said. Dr. Simonds was not involved in either study.
Young adult study
Dr. Mogenson and colleagues assessed data on 853 participants in the BAMSE Project, a prospective birth cohort study that included 4,089 children born in Stockholm from 1994 to 1996. Of the participants, 147 had asthma. They have been regularly followed with questionnaires on respiratory symptoms and medications. In addition, at 8 and 16 years’ follow-up, spirometry measures and fractional exhaled nitric oxide (FeNO) levels were assessed, allergic sensitization tests were administered, and blood eosinophil levels were measured.
In 2020 and 2021, during the pandemic, the participants underwent spirometry testing and were assessed for antibodies against SARS-CoV-2, and they self-reported use of inhaled corticosteroids.
The investigators defined asthma as any physician diagnosis and asthma symptoms and/or asthma medication use within the previous year. Participants were determined to be COVID-19 seropositive if they had IgG antibodies to the SARS-CoV-2 spike greater than 25.09 AU/mL, IgM antibodies greater than 14.42 AU/mL, or IgA antibodies greater than 2.61 AU/mL, as measured with enzyme-linked immunosorbent assay.
Participants who had been vaccinated against COVID-19 were excluded.
No significant decreases
A total of 243 participants, including 38 with asthma, were seropositive for SARS-CoV-2 antibodies. The mean change in lung function from before the pandemic to the study end date during the pandemic were not significantly different between seropositive participants and seronegative participants or IgM-positive participants and seronegative participants.
Similarly, there were no significant differences in lung function between seropositive and seronegative participants in an analysis that was adjusted for sex, body mass index, smoking status, or prepandemic lung function.
Although there was a trend toward slightly lower function among seropositive participants with asthma in comparison with seronegative patients with asthma, it was not statistically significant, Dr. Mogenson said.
There were also no significant decreases in lung function from the prepandemic measure to the present in any of the inflammatory parameters, including blood eosinophil levels, FeNO, allergic sensitization, or inhaled corticosteroid use.
Potential misclassification
In the question-and-answer period that followed the presentation, session comoderator Sam Bayat, MD, PhD, from the University of Grenoble (France), who was not involved in the study, noted that “some subjects can have positive serology without any symptoms, while others can have symptomatic disease and a couple of months later they have negative serology.”
He asked Dr. Mogenson whether they had included in their study participants with symptomatic COVID-19 and whether that would change the findings.
“We did not have access to RNA testing, so we only had serology, and of course some participants could be wrongly classified to have disease – probably around 15%,” she acknowledged.
She noted that there were no significant changes in lung function among patients who reported having respiratory symptoms.
The study was funded by the Swedish Research Council, the Swedish Heart-Lung Foundation, the Swedish Research Council for Health, Working Life and Welfare, the Karolinska Institutet, Formas, the European Research Council, and Region Stockholm. Dr. Mogenson, Dr. Simonds, and Dr. Bayat disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Here’s some encouraging news for once regarding SARS-CoV-2 infections: A study of young adults for whom prepandemic spirometry data were available showed that COVID-19 did not have a significant impact on lung function, even among patients with asthma.
Among 853 Swedish men and women (mean age, 22 years) who were part of a birth cohort study, there were no significant differences in either forced expiratory volume in 1 second (FEV1) or in the ratio of FEV1 to forced vital capacity, reported Ida Mogensen, MD, PhD, a postdoctoral fellow at the Karolinska Institute in Stockholm.
“We found no effect of COVID-19 on spirometric lung function in generally healthy adults,” she said in an oral abstract presented at the European Respiratory Society 2021 International Congress.
The findings echo those of a small study that involved 73 children and adolescents with COVID-19 and 45 uninfected control persons. The investigators in that study, which was also presented at ERS 2021, found that there were no significant differences in the frequency of abnormal pulmonary function measures between case patients and control patients (abstract OA1303).
“The findings from these two studies provide important reassurance about the impact of COVID infection on lung function in children and young adults,” commented Anita Simonds, MD, an honorary consultant in respiratory and sleep medicine at the Royal Brompton Hospital, London.
“We know already that this group is less likely to suffer severe illness if they contract the virus, and these studies, which importantly include comparator groups without COVID-19, show that they are also less likely to suffer long-term consequences with respect to lung function,” she said. Dr. Simonds was not involved in either study.
Young adult study
Dr. Mogenson and colleagues assessed data on 853 participants in the BAMSE Project, a prospective birth cohort study that included 4,089 children born in Stockholm from 1994 to 1996. Of the participants, 147 had asthma. They have been regularly followed with questionnaires on respiratory symptoms and medications. In addition, at 8 and 16 years’ follow-up, spirometry measures and fractional exhaled nitric oxide (FeNO) levels were assessed, allergic sensitization tests were administered, and blood eosinophil levels were measured.
In 2020 and 2021, during the pandemic, the participants underwent spirometry testing and were assessed for antibodies against SARS-CoV-2, and they self-reported use of inhaled corticosteroids.
The investigators defined asthma as any physician diagnosis and asthma symptoms and/or asthma medication use within the previous year. Participants were determined to be COVID-19 seropositive if they had IgG antibodies to the SARS-CoV-2 spike greater than 25.09 AU/mL, IgM antibodies greater than 14.42 AU/mL, or IgA antibodies greater than 2.61 AU/mL, as measured with enzyme-linked immunosorbent assay.
Participants who had been vaccinated against COVID-19 were excluded.
No significant decreases
A total of 243 participants, including 38 with asthma, were seropositive for SARS-CoV-2 antibodies. The mean change in lung function from before the pandemic to the study end date during the pandemic were not significantly different between seropositive participants and seronegative participants or IgM-positive participants and seronegative participants.
Similarly, there were no significant differences in lung function between seropositive and seronegative participants in an analysis that was adjusted for sex, body mass index, smoking status, or prepandemic lung function.
Although there was a trend toward slightly lower function among seropositive participants with asthma in comparison with seronegative patients with asthma, it was not statistically significant, Dr. Mogenson said.
There were also no significant decreases in lung function from the prepandemic measure to the present in any of the inflammatory parameters, including blood eosinophil levels, FeNO, allergic sensitization, or inhaled corticosteroid use.
Potential misclassification
In the question-and-answer period that followed the presentation, session comoderator Sam Bayat, MD, PhD, from the University of Grenoble (France), who was not involved in the study, noted that “some subjects can have positive serology without any symptoms, while others can have symptomatic disease and a couple of months later they have negative serology.”
He asked Dr. Mogenson whether they had included in their study participants with symptomatic COVID-19 and whether that would change the findings.
“We did not have access to RNA testing, so we only had serology, and of course some participants could be wrongly classified to have disease – probably around 15%,” she acknowledged.
She noted that there were no significant changes in lung function among patients who reported having respiratory symptoms.
The study was funded by the Swedish Research Council, the Swedish Heart-Lung Foundation, the Swedish Research Council for Health, Working Life and Welfare, the Karolinska Institutet, Formas, the European Research Council, and Region Stockholm. Dr. Mogenson, Dr. Simonds, and Dr. Bayat disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Here’s some encouraging news for once regarding SARS-CoV-2 infections: A study of young adults for whom prepandemic spirometry data were available showed that COVID-19 did not have a significant impact on lung function, even among patients with asthma.
Among 853 Swedish men and women (mean age, 22 years) who were part of a birth cohort study, there were no significant differences in either forced expiratory volume in 1 second (FEV1) or in the ratio of FEV1 to forced vital capacity, reported Ida Mogensen, MD, PhD, a postdoctoral fellow at the Karolinska Institute in Stockholm.
“We found no effect of COVID-19 on spirometric lung function in generally healthy adults,” she said in an oral abstract presented at the European Respiratory Society 2021 International Congress.
The findings echo those of a small study that involved 73 children and adolescents with COVID-19 and 45 uninfected control persons. The investigators in that study, which was also presented at ERS 2021, found that there were no significant differences in the frequency of abnormal pulmonary function measures between case patients and control patients (abstract OA1303).
“The findings from these two studies provide important reassurance about the impact of COVID infection on lung function in children and young adults,” commented Anita Simonds, MD, an honorary consultant in respiratory and sleep medicine at the Royal Brompton Hospital, London.
“We know already that this group is less likely to suffer severe illness if they contract the virus, and these studies, which importantly include comparator groups without COVID-19, show that they are also less likely to suffer long-term consequences with respect to lung function,” she said. Dr. Simonds was not involved in either study.
Young adult study
Dr. Mogenson and colleagues assessed data on 853 participants in the BAMSE Project, a prospective birth cohort study that included 4,089 children born in Stockholm from 1994 to 1996. Of the participants, 147 had asthma. They have been regularly followed with questionnaires on respiratory symptoms and medications. In addition, at 8 and 16 years’ follow-up, spirometry measures and fractional exhaled nitric oxide (FeNO) levels were assessed, allergic sensitization tests were administered, and blood eosinophil levels were measured.
In 2020 and 2021, during the pandemic, the participants underwent spirometry testing and were assessed for antibodies against SARS-CoV-2, and they self-reported use of inhaled corticosteroids.
The investigators defined asthma as any physician diagnosis and asthma symptoms and/or asthma medication use within the previous year. Participants were determined to be COVID-19 seropositive if they had IgG antibodies to the SARS-CoV-2 spike greater than 25.09 AU/mL, IgM antibodies greater than 14.42 AU/mL, or IgA antibodies greater than 2.61 AU/mL, as measured with enzyme-linked immunosorbent assay.
Participants who had been vaccinated against COVID-19 were excluded.
No significant decreases
A total of 243 participants, including 38 with asthma, were seropositive for SARS-CoV-2 antibodies. The mean change in lung function from before the pandemic to the study end date during the pandemic were not significantly different between seropositive participants and seronegative participants or IgM-positive participants and seronegative participants.
Similarly, there were no significant differences in lung function between seropositive and seronegative participants in an analysis that was adjusted for sex, body mass index, smoking status, or prepandemic lung function.
Although there was a trend toward slightly lower function among seropositive participants with asthma in comparison with seronegative patients with asthma, it was not statistically significant, Dr. Mogenson said.
There were also no significant decreases in lung function from the prepandemic measure to the present in any of the inflammatory parameters, including blood eosinophil levels, FeNO, allergic sensitization, or inhaled corticosteroid use.
Potential misclassification
In the question-and-answer period that followed the presentation, session comoderator Sam Bayat, MD, PhD, from the University of Grenoble (France), who was not involved in the study, noted that “some subjects can have positive serology without any symptoms, while others can have symptomatic disease and a couple of months later they have negative serology.”
He asked Dr. Mogenson whether they had included in their study participants with symptomatic COVID-19 and whether that would change the findings.
“We did not have access to RNA testing, so we only had serology, and of course some participants could be wrongly classified to have disease – probably around 15%,” she acknowledged.
She noted that there were no significant changes in lung function among patients who reported having respiratory symptoms.
The study was funded by the Swedish Research Council, the Swedish Heart-Lung Foundation, the Swedish Research Council for Health, Working Life and Welfare, the Karolinska Institutet, Formas, the European Research Council, and Region Stockholm. Dr. Mogenson, Dr. Simonds, and Dr. Bayat disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sweeping new vaccine mandates will impact most U.S. workers
, including sweeping vaccine mandates that will affect 100 million American workers, nearly two-thirds of the country’s workforce.
“As your president, I’m announcing tonight a new plan to get more Americans vaccinated to combat those blocking public health,” he said Sept. 9.
As part of a six-part plan unveiled in a speech from the State Dining Room of the White House, President Biden said he would require vaccinations for nearly 4 million federal workers and the employees of companies that contract with the federal government.
He has also directed the Occupational Safety and Health Administration to develop a rule that will require large employers -- those with at least 100 employees -- to ensure their workers are vaccinated or tested weekly.
Nearly 17 million health care workers will face new vaccine mandates as part of the conditions of participation in the Medicare and Medicaid programs.
President Biden said the federal government will require staff at federally funded Head Start programs and schools to be vaccinated. He’s also calling on all states to mandate vaccines for teachers.
“A distinct minority of Americans, supported by a distinct minority of elected officials, are keeping us from turning the corner,” PresidentBiden said. “These pandemic politics, as I refer to them, are making people sick, causing unvaccinated people to die.”
One public health official said he was glad to see the president’s bold action.
“What I saw today was the federal government trying to use its powers to create greater safety in the American population,” said Ashish K. Jha, MD, dean of the school of public health at Brown University, Providence, R.I., in a call with reporters after the speech.
National Nurses United, the largest union of registered nurses in the United States, issued a statement in support of President Biden’s new vaccination requirements, but pushed back on his language.
“…as advocates for public health, registered nurses want to be extremely clear: There is no such thing as a pandemic of only the unvaccinated. The science of epidemiology tells us there is just one deadly, global pandemic that has not yet ended, and we are all in it together. To get out of it, we must act together. All of us,” the statement says.
A host of other professional groups, including the American Medical Association and the Association of State and Territorial Health Officials, also issued statements of support for President Biden’s plan.
But the plan was not well received by all.
“I will pursue every legal option available to the state of Georgia to stop this blatantly unlawful overreach by the Biden Administration,” said Georgia Governor Brian Kemp, a Republican, in a Tweet.
The National Council for Occupational Safety and Health called the plan “a missed opportunity” because it failed to include workplace protections for essential workers such as grocery, postal, and transit workers.
“Social distancing, improved ventilation, shift rotation, and protective equipment to reduce exposure are important components of an overall plan to reduce risk and stop the virus. These tools are missing from the new steps President Biden announced today,” said Jessica Martinez, co-executive director of the group.
In addition to the new vaccination requirements, President Biden said extra doses would be on the way for people who have already been fully vaccinated in order to protect against waning immunity, starting on Sept. 20. But he noted that those plans would be contingent on the Food and Drug Administration’s approval for third doses and the Centers for Disease Control and Prevention’s recommendation of the shots.
President Biden pledged to use the Defense Production Act to ramp up production of at-home tests, which have been selling out across the nation as the Delta variant spreads.
He also announced plans to expand access to COVID-19 testing, including offering testing for free at thousands of pharmacies nationwide and getting major retailers to sell at-home COVID-19 tests at cost.
The BinaxNow test kit, which currently retails for $23.99, will now cost about $15 for two tests at Kroger, Amazon, and Walmart, according to the White House. Food banks and community health centers will get free tests, too.
He called on states to set up COVID-19 testing programs at all schools.
Jha said that in his view, the big, game-changing news out of the president’s speech was the expansion of testing.
“Our country has failed to deploy tests in a way that can really bring this pandemic under control,” Jha said. “There are plenty of reasons, data, experience to indicate that if these were widely available, it would make a dramatic difference in reducing infection numbers across our country.”.
Dr. Jha said the private market had not worked effectively to make testing more widely available, so it was “absolutely a requirement of the federal government to step in and make testing more widely available,” he said.
President Biden also announced new economic stimulus programs, saying he’s expanding loan programs to small businesses and streamlining the loan forgiveness process.
President Biden said he’s boosting help for overburdened hospitals, doubling the number of federal surge response teams sent to hard-hit areas to reduce the strain on local health care workers. He said he would increase the pace of antibody treatments to states by 50%.
“We made so much progress during the past 7 months of this pandemic. Even so, we remain at a critical moment, a critical time,” he said. “We have the tools. Now, we just have to finish the job with truth, with science, with confidence and together as one nation.”
A version of this article first appeared on WebMD.com.
, including sweeping vaccine mandates that will affect 100 million American workers, nearly two-thirds of the country’s workforce.
“As your president, I’m announcing tonight a new plan to get more Americans vaccinated to combat those blocking public health,” he said Sept. 9.
As part of a six-part plan unveiled in a speech from the State Dining Room of the White House, President Biden said he would require vaccinations for nearly 4 million federal workers and the employees of companies that contract with the federal government.
He has also directed the Occupational Safety and Health Administration to develop a rule that will require large employers -- those with at least 100 employees -- to ensure their workers are vaccinated or tested weekly.
Nearly 17 million health care workers will face new vaccine mandates as part of the conditions of participation in the Medicare and Medicaid programs.
President Biden said the federal government will require staff at federally funded Head Start programs and schools to be vaccinated. He’s also calling on all states to mandate vaccines for teachers.
“A distinct minority of Americans, supported by a distinct minority of elected officials, are keeping us from turning the corner,” PresidentBiden said. “These pandemic politics, as I refer to them, are making people sick, causing unvaccinated people to die.”
One public health official said he was glad to see the president’s bold action.
“What I saw today was the federal government trying to use its powers to create greater safety in the American population,” said Ashish K. Jha, MD, dean of the school of public health at Brown University, Providence, R.I., in a call with reporters after the speech.
National Nurses United, the largest union of registered nurses in the United States, issued a statement in support of President Biden’s new vaccination requirements, but pushed back on his language.
“…as advocates for public health, registered nurses want to be extremely clear: There is no such thing as a pandemic of only the unvaccinated. The science of epidemiology tells us there is just one deadly, global pandemic that has not yet ended, and we are all in it together. To get out of it, we must act together. All of us,” the statement says.
A host of other professional groups, including the American Medical Association and the Association of State and Territorial Health Officials, also issued statements of support for President Biden’s plan.
But the plan was not well received by all.
“I will pursue every legal option available to the state of Georgia to stop this blatantly unlawful overreach by the Biden Administration,” said Georgia Governor Brian Kemp, a Republican, in a Tweet.
The National Council for Occupational Safety and Health called the plan “a missed opportunity” because it failed to include workplace protections for essential workers such as grocery, postal, and transit workers.
“Social distancing, improved ventilation, shift rotation, and protective equipment to reduce exposure are important components of an overall plan to reduce risk and stop the virus. These tools are missing from the new steps President Biden announced today,” said Jessica Martinez, co-executive director of the group.
In addition to the new vaccination requirements, President Biden said extra doses would be on the way for people who have already been fully vaccinated in order to protect against waning immunity, starting on Sept. 20. But he noted that those plans would be contingent on the Food and Drug Administration’s approval for third doses and the Centers for Disease Control and Prevention’s recommendation of the shots.
President Biden pledged to use the Defense Production Act to ramp up production of at-home tests, which have been selling out across the nation as the Delta variant spreads.
He also announced plans to expand access to COVID-19 testing, including offering testing for free at thousands of pharmacies nationwide and getting major retailers to sell at-home COVID-19 tests at cost.
The BinaxNow test kit, which currently retails for $23.99, will now cost about $15 for two tests at Kroger, Amazon, and Walmart, according to the White House. Food banks and community health centers will get free tests, too.
He called on states to set up COVID-19 testing programs at all schools.
Jha said that in his view, the big, game-changing news out of the president’s speech was the expansion of testing.
“Our country has failed to deploy tests in a way that can really bring this pandemic under control,” Jha said. “There are plenty of reasons, data, experience to indicate that if these were widely available, it would make a dramatic difference in reducing infection numbers across our country.”.
Dr. Jha said the private market had not worked effectively to make testing more widely available, so it was “absolutely a requirement of the federal government to step in and make testing more widely available,” he said.
President Biden also announced new economic stimulus programs, saying he’s expanding loan programs to small businesses and streamlining the loan forgiveness process.
President Biden said he’s boosting help for overburdened hospitals, doubling the number of federal surge response teams sent to hard-hit areas to reduce the strain on local health care workers. He said he would increase the pace of antibody treatments to states by 50%.
“We made so much progress during the past 7 months of this pandemic. Even so, we remain at a critical moment, a critical time,” he said. “We have the tools. Now, we just have to finish the job with truth, with science, with confidence and together as one nation.”
A version of this article first appeared on WebMD.com.
, including sweeping vaccine mandates that will affect 100 million American workers, nearly two-thirds of the country’s workforce.
“As your president, I’m announcing tonight a new plan to get more Americans vaccinated to combat those blocking public health,” he said Sept. 9.
As part of a six-part plan unveiled in a speech from the State Dining Room of the White House, President Biden said he would require vaccinations for nearly 4 million federal workers and the employees of companies that contract with the federal government.
He has also directed the Occupational Safety and Health Administration to develop a rule that will require large employers -- those with at least 100 employees -- to ensure their workers are vaccinated or tested weekly.
Nearly 17 million health care workers will face new vaccine mandates as part of the conditions of participation in the Medicare and Medicaid programs.
President Biden said the federal government will require staff at federally funded Head Start programs and schools to be vaccinated. He’s also calling on all states to mandate vaccines for teachers.
“A distinct minority of Americans, supported by a distinct minority of elected officials, are keeping us from turning the corner,” PresidentBiden said. “These pandemic politics, as I refer to them, are making people sick, causing unvaccinated people to die.”
One public health official said he was glad to see the president’s bold action.
“What I saw today was the federal government trying to use its powers to create greater safety in the American population,” said Ashish K. Jha, MD, dean of the school of public health at Brown University, Providence, R.I., in a call with reporters after the speech.
National Nurses United, the largest union of registered nurses in the United States, issued a statement in support of President Biden’s new vaccination requirements, but pushed back on his language.
“…as advocates for public health, registered nurses want to be extremely clear: There is no such thing as a pandemic of only the unvaccinated. The science of epidemiology tells us there is just one deadly, global pandemic that has not yet ended, and we are all in it together. To get out of it, we must act together. All of us,” the statement says.
A host of other professional groups, including the American Medical Association and the Association of State and Territorial Health Officials, also issued statements of support for President Biden’s plan.
But the plan was not well received by all.
“I will pursue every legal option available to the state of Georgia to stop this blatantly unlawful overreach by the Biden Administration,” said Georgia Governor Brian Kemp, a Republican, in a Tweet.
The National Council for Occupational Safety and Health called the plan “a missed opportunity” because it failed to include workplace protections for essential workers such as grocery, postal, and transit workers.
“Social distancing, improved ventilation, shift rotation, and protective equipment to reduce exposure are important components of an overall plan to reduce risk and stop the virus. These tools are missing from the new steps President Biden announced today,” said Jessica Martinez, co-executive director of the group.
In addition to the new vaccination requirements, President Biden said extra doses would be on the way for people who have already been fully vaccinated in order to protect against waning immunity, starting on Sept. 20. But he noted that those plans would be contingent on the Food and Drug Administration’s approval for third doses and the Centers for Disease Control and Prevention’s recommendation of the shots.
President Biden pledged to use the Defense Production Act to ramp up production of at-home tests, which have been selling out across the nation as the Delta variant spreads.
He also announced plans to expand access to COVID-19 testing, including offering testing for free at thousands of pharmacies nationwide and getting major retailers to sell at-home COVID-19 tests at cost.
The BinaxNow test kit, which currently retails for $23.99, will now cost about $15 for two tests at Kroger, Amazon, and Walmart, according to the White House. Food banks and community health centers will get free tests, too.
He called on states to set up COVID-19 testing programs at all schools.
Jha said that in his view, the big, game-changing news out of the president’s speech was the expansion of testing.
“Our country has failed to deploy tests in a way that can really bring this pandemic under control,” Jha said. “There are plenty of reasons, data, experience to indicate that if these were widely available, it would make a dramatic difference in reducing infection numbers across our country.”.
Dr. Jha said the private market had not worked effectively to make testing more widely available, so it was “absolutely a requirement of the federal government to step in and make testing more widely available,” he said.
President Biden also announced new economic stimulus programs, saying he’s expanding loan programs to small businesses and streamlining the loan forgiveness process.
President Biden said he’s boosting help for overburdened hospitals, doubling the number of federal surge response teams sent to hard-hit areas to reduce the strain on local health care workers. He said he would increase the pace of antibody treatments to states by 50%.
“We made so much progress during the past 7 months of this pandemic. Even so, we remain at a critical moment, a critical time,” he said. “We have the tools. Now, we just have to finish the job with truth, with science, with confidence and together as one nation.”
A version of this article first appeared on WebMD.com.
Pandemic-related school closures tied to mental health inequities
Back-to-school jitters are heightened this year, as children head back to the risk of COVID transmission in class, but one upside to the return of in-person school may be better mental health for students.
New research shows that virtual schooling, which dominated in many districts last year, was associated with worse mental health outcomes for students – especially older ones – and youth from Black, Hispanic, or lower-income families were hit hardest because they experienced the most closures.
“Schools with lower funding may have had more difficulty meeting guidelines for safe reopening, including updates to ventilation systems and finding the physical space to create safe distancing between children,” explained lead author Matt Hawrilenko, PhD, of the department of psychiatry and behavioral sciences at the University of Washington, Seattle, in an interview.
“In the context of complex school reopening decisions that balance competing risks and benefits, these findings suggest that allocating funding to support safe in-person instruction may reduce mental health inequities associated with race/ethnicity and income,” he and his coauthors noted in the study, published in JAMA Network Open. “Ensuring that all students have access to additional educational and mental health resources must be an important public health priority, met with appropriate funding and work force augmentation, during and beyond the COVID-19 pandemic.”
The study used a cross-sectional population-based survey of 2,324 parents of school-age children in the United States. It was administered in English and Spanish via web and telephone between Dec. 2 and Dec. 21, 2020, and used the parent-report version of the Strengths and Difficulties Questionnaire (SDQ) to assess mental health difficulties of one child per family in four domains: emotional problems, peer problems, conduct, and hyperactivity. Parents were also asked about what kind of schooling their child had received in the last year (remote, in-person, or hybrid) and about demographic information such as child age, gender, household income, parent race and ethnicity, and parent education.
The results showed that, during the 2020 school year, 58.0% of children attended school remotely, 24% attended fully in person, and 18.0% attended in a hybrid format. “Fully remote schooling was strongly patterned along lines of parent race and ethnicity as well as income,” the authors noted. “Parents of 336 children attending school in person (65.8%) but of 597 children attending school fully remotely (44.5%) were White, whereas all other racial/ethnic groups had larger proportions of children attending school fully remotely (P < .001).”
In terms of mental health, the findings showed that older children who attended school remotely had more difficulties, compared with those who attended in-person – but among younger children, remote learning was comparable or slightly better for mental health.
Specifically, “a child aged 17 years attending school remotely would be expected to have a total difficulty score 2.4 points higher than a child of the same age attending school in person, corresponding to a small effect size in favor of in-person schooling,” the authors wrote. “Conversely, a child aged 4 years attending school remotely would be expected to have a total difficulty score 0.5 points lower than a child of the same age attending school in person, corresponding to a very small effect size in favor of remote schooling.”
Age of child proves critical
“Our best estimate is that remote schooling was associated with no difference in mental health difficulties at age 6, and with slightly more difficulties with each year of age after that, with differences most clearly apparent for high school–aged kids,” explained Dr. Hawrilenko, adding the finding suggests that school reopenings should prioritize older children.
However, “what kids are doing at home matters,” he added. “In the youngest age group, the biggest work kids are doing in school and childcare settings is social and emotional development. … Finding opportunities for regular, safe social interactions with peers – perhaps during outdoor playdates – can help them build those skills.”
He emphasized with the anticipated starts and stutters of the new school year there is an important role that doctors can play.
“First, they can help families assess their own risk profile, and whether it makes sense for their children to attend school in person or remotely [to the extent that is an option]. Second, they can help families think through how school closures might impact their child specifically. For those kids who wind up with long chunks of remote schooling, scheduling in regular interactions with other kids in safe ways could make a big difference. Another driver of child anxiety might be learning loss, and this is a good place to reinforce that not every mental health problem needs a mental health solution.
“A lot of kids might be rightfully anxious about having fallen behind over the pandemic. These kids are preparing to transition to college or to the workforce and may be feeling increasingly behind while approaching these moments of transition. Pointing families toward the resources to help them navigate these issues could go a long way to helping quell child anxiety.”
Research helps fill vacuum
Elizabeth A. Stuart, PhD, who was not involved in the study, said in an interview that this research is particularly valuable because there have been very few data on this topic, especially on a large-scale national sample.
“Sadly, many of the results are not surprising,” said Dr. Stuart, a statistician and professor of mental health at Johns Hopkins University, Baltimore. “Data have shown significant mental health challenges for adults during the pandemic, and it is not surprising that children and youth would experience that as well, especially for those whose daily routines and structures changed dramatically and who were not able to be interacting in-person with teachers, staff, and classmates. This is an important reminder that schools provide not just academic instruction for students, but that the social interactions and other services (such as behavioral health supports, meals, and connections with other social services) students might receive in school are crucial.
“It has been heartening to see a stronger commitment to getting students safely back into school this fall across the country, and that the Centers for Disease Control and Prevention highlighted the benefits of in-person schooling in their COVID-19–related guidance for schools.”
Dr. Stuart added that, as students return to classes, it will be important for schools to tackle ongoing mental health challenges.
“Some students may be struggling in obvious ways; for others it may be harder to identify. It will also be important to continue to monitor children’s and youth mental health … as returning to in-person school may bring its own challenges. ”
Dr. Hawrilenko agreed.
“From a policy perspective, I am quite frankly terrified about how these inequities – in particular, learning loss – might play out long after school closures are a distant memory,” he said. “It is critical to provide schools the resources not just to minimize risk when reopening, but additional funding for workforce augmentation – both for mental health staffing and for additional educational support – to help students navigate the months and years over which they transition back into the classroom.”
Dr. Hawrilenko and Dr. Stuart had no disclosures.
Back-to-school jitters are heightened this year, as children head back to the risk of COVID transmission in class, but one upside to the return of in-person school may be better mental health for students.
New research shows that virtual schooling, which dominated in many districts last year, was associated with worse mental health outcomes for students – especially older ones – and youth from Black, Hispanic, or lower-income families were hit hardest because they experienced the most closures.
“Schools with lower funding may have had more difficulty meeting guidelines for safe reopening, including updates to ventilation systems and finding the physical space to create safe distancing between children,” explained lead author Matt Hawrilenko, PhD, of the department of psychiatry and behavioral sciences at the University of Washington, Seattle, in an interview.
“In the context of complex school reopening decisions that balance competing risks and benefits, these findings suggest that allocating funding to support safe in-person instruction may reduce mental health inequities associated with race/ethnicity and income,” he and his coauthors noted in the study, published in JAMA Network Open. “Ensuring that all students have access to additional educational and mental health resources must be an important public health priority, met with appropriate funding and work force augmentation, during and beyond the COVID-19 pandemic.”
The study used a cross-sectional population-based survey of 2,324 parents of school-age children in the United States. It was administered in English and Spanish via web and telephone between Dec. 2 and Dec. 21, 2020, and used the parent-report version of the Strengths and Difficulties Questionnaire (SDQ) to assess mental health difficulties of one child per family in four domains: emotional problems, peer problems, conduct, and hyperactivity. Parents were also asked about what kind of schooling their child had received in the last year (remote, in-person, or hybrid) and about demographic information such as child age, gender, household income, parent race and ethnicity, and parent education.
The results showed that, during the 2020 school year, 58.0% of children attended school remotely, 24% attended fully in person, and 18.0% attended in a hybrid format. “Fully remote schooling was strongly patterned along lines of parent race and ethnicity as well as income,” the authors noted. “Parents of 336 children attending school in person (65.8%) but of 597 children attending school fully remotely (44.5%) were White, whereas all other racial/ethnic groups had larger proportions of children attending school fully remotely (P < .001).”
In terms of mental health, the findings showed that older children who attended school remotely had more difficulties, compared with those who attended in-person – but among younger children, remote learning was comparable or slightly better for mental health.
Specifically, “a child aged 17 years attending school remotely would be expected to have a total difficulty score 2.4 points higher than a child of the same age attending school in person, corresponding to a small effect size in favor of in-person schooling,” the authors wrote. “Conversely, a child aged 4 years attending school remotely would be expected to have a total difficulty score 0.5 points lower than a child of the same age attending school in person, corresponding to a very small effect size in favor of remote schooling.”
Age of child proves critical
“Our best estimate is that remote schooling was associated with no difference in mental health difficulties at age 6, and with slightly more difficulties with each year of age after that, with differences most clearly apparent for high school–aged kids,” explained Dr. Hawrilenko, adding the finding suggests that school reopenings should prioritize older children.
However, “what kids are doing at home matters,” he added. “In the youngest age group, the biggest work kids are doing in school and childcare settings is social and emotional development. … Finding opportunities for regular, safe social interactions with peers – perhaps during outdoor playdates – can help them build those skills.”
He emphasized with the anticipated starts and stutters of the new school year there is an important role that doctors can play.
“First, they can help families assess their own risk profile, and whether it makes sense for their children to attend school in person or remotely [to the extent that is an option]. Second, they can help families think through how school closures might impact their child specifically. For those kids who wind up with long chunks of remote schooling, scheduling in regular interactions with other kids in safe ways could make a big difference. Another driver of child anxiety might be learning loss, and this is a good place to reinforce that not every mental health problem needs a mental health solution.
“A lot of kids might be rightfully anxious about having fallen behind over the pandemic. These kids are preparing to transition to college or to the workforce and may be feeling increasingly behind while approaching these moments of transition. Pointing families toward the resources to help them navigate these issues could go a long way to helping quell child anxiety.”
Research helps fill vacuum
Elizabeth A. Stuart, PhD, who was not involved in the study, said in an interview that this research is particularly valuable because there have been very few data on this topic, especially on a large-scale national sample.
“Sadly, many of the results are not surprising,” said Dr. Stuart, a statistician and professor of mental health at Johns Hopkins University, Baltimore. “Data have shown significant mental health challenges for adults during the pandemic, and it is not surprising that children and youth would experience that as well, especially for those whose daily routines and structures changed dramatically and who were not able to be interacting in-person with teachers, staff, and classmates. This is an important reminder that schools provide not just academic instruction for students, but that the social interactions and other services (such as behavioral health supports, meals, and connections with other social services) students might receive in school are crucial.
“It has been heartening to see a stronger commitment to getting students safely back into school this fall across the country, and that the Centers for Disease Control and Prevention highlighted the benefits of in-person schooling in their COVID-19–related guidance for schools.”
Dr. Stuart added that, as students return to classes, it will be important for schools to tackle ongoing mental health challenges.
“Some students may be struggling in obvious ways; for others it may be harder to identify. It will also be important to continue to monitor children’s and youth mental health … as returning to in-person school may bring its own challenges. ”
Dr. Hawrilenko agreed.
“From a policy perspective, I am quite frankly terrified about how these inequities – in particular, learning loss – might play out long after school closures are a distant memory,” he said. “It is critical to provide schools the resources not just to minimize risk when reopening, but additional funding for workforce augmentation – both for mental health staffing and for additional educational support – to help students navigate the months and years over which they transition back into the classroom.”
Dr. Hawrilenko and Dr. Stuart had no disclosures.
Back-to-school jitters are heightened this year, as children head back to the risk of COVID transmission in class, but one upside to the return of in-person school may be better mental health for students.
New research shows that virtual schooling, which dominated in many districts last year, was associated with worse mental health outcomes for students – especially older ones – and youth from Black, Hispanic, or lower-income families were hit hardest because they experienced the most closures.
“Schools with lower funding may have had more difficulty meeting guidelines for safe reopening, including updates to ventilation systems and finding the physical space to create safe distancing between children,” explained lead author Matt Hawrilenko, PhD, of the department of psychiatry and behavioral sciences at the University of Washington, Seattle, in an interview.
“In the context of complex school reopening decisions that balance competing risks and benefits, these findings suggest that allocating funding to support safe in-person instruction may reduce mental health inequities associated with race/ethnicity and income,” he and his coauthors noted in the study, published in JAMA Network Open. “Ensuring that all students have access to additional educational and mental health resources must be an important public health priority, met with appropriate funding and work force augmentation, during and beyond the COVID-19 pandemic.”
The study used a cross-sectional population-based survey of 2,324 parents of school-age children in the United States. It was administered in English and Spanish via web and telephone between Dec. 2 and Dec. 21, 2020, and used the parent-report version of the Strengths and Difficulties Questionnaire (SDQ) to assess mental health difficulties of one child per family in four domains: emotional problems, peer problems, conduct, and hyperactivity. Parents were also asked about what kind of schooling their child had received in the last year (remote, in-person, or hybrid) and about demographic information such as child age, gender, household income, parent race and ethnicity, and parent education.
The results showed that, during the 2020 school year, 58.0% of children attended school remotely, 24% attended fully in person, and 18.0% attended in a hybrid format. “Fully remote schooling was strongly patterned along lines of parent race and ethnicity as well as income,” the authors noted. “Parents of 336 children attending school in person (65.8%) but of 597 children attending school fully remotely (44.5%) were White, whereas all other racial/ethnic groups had larger proportions of children attending school fully remotely (P < .001).”
In terms of mental health, the findings showed that older children who attended school remotely had more difficulties, compared with those who attended in-person – but among younger children, remote learning was comparable or slightly better for mental health.
Specifically, “a child aged 17 years attending school remotely would be expected to have a total difficulty score 2.4 points higher than a child of the same age attending school in person, corresponding to a small effect size in favor of in-person schooling,” the authors wrote. “Conversely, a child aged 4 years attending school remotely would be expected to have a total difficulty score 0.5 points lower than a child of the same age attending school in person, corresponding to a very small effect size in favor of remote schooling.”
Age of child proves critical
“Our best estimate is that remote schooling was associated with no difference in mental health difficulties at age 6, and with slightly more difficulties with each year of age after that, with differences most clearly apparent for high school–aged kids,” explained Dr. Hawrilenko, adding the finding suggests that school reopenings should prioritize older children.
However, “what kids are doing at home matters,” he added. “In the youngest age group, the biggest work kids are doing in school and childcare settings is social and emotional development. … Finding opportunities for regular, safe social interactions with peers – perhaps during outdoor playdates – can help them build those skills.”
He emphasized with the anticipated starts and stutters of the new school year there is an important role that doctors can play.
“First, they can help families assess their own risk profile, and whether it makes sense for their children to attend school in person or remotely [to the extent that is an option]. Second, they can help families think through how school closures might impact their child specifically. For those kids who wind up with long chunks of remote schooling, scheduling in regular interactions with other kids in safe ways could make a big difference. Another driver of child anxiety might be learning loss, and this is a good place to reinforce that not every mental health problem needs a mental health solution.
“A lot of kids might be rightfully anxious about having fallen behind over the pandemic. These kids are preparing to transition to college or to the workforce and may be feeling increasingly behind while approaching these moments of transition. Pointing families toward the resources to help them navigate these issues could go a long way to helping quell child anxiety.”
Research helps fill vacuum
Elizabeth A. Stuart, PhD, who was not involved in the study, said in an interview that this research is particularly valuable because there have been very few data on this topic, especially on a large-scale national sample.
“Sadly, many of the results are not surprising,” said Dr. Stuart, a statistician and professor of mental health at Johns Hopkins University, Baltimore. “Data have shown significant mental health challenges for adults during the pandemic, and it is not surprising that children and youth would experience that as well, especially for those whose daily routines and structures changed dramatically and who were not able to be interacting in-person with teachers, staff, and classmates. This is an important reminder that schools provide not just academic instruction for students, but that the social interactions and other services (such as behavioral health supports, meals, and connections with other social services) students might receive in school are crucial.
“It has been heartening to see a stronger commitment to getting students safely back into school this fall across the country, and that the Centers for Disease Control and Prevention highlighted the benefits of in-person schooling in their COVID-19–related guidance for schools.”
Dr. Stuart added that, as students return to classes, it will be important for schools to tackle ongoing mental health challenges.
“Some students may be struggling in obvious ways; for others it may be harder to identify. It will also be important to continue to monitor children’s and youth mental health … as returning to in-person school may bring its own challenges. ”
Dr. Hawrilenko agreed.
“From a policy perspective, I am quite frankly terrified about how these inequities – in particular, learning loss – might play out long after school closures are a distant memory,” he said. “It is critical to provide schools the resources not just to minimize risk when reopening, but additional funding for workforce augmentation – both for mental health staffing and for additional educational support – to help students navigate the months and years over which they transition back into the classroom.”
Dr. Hawrilenko and Dr. Stuart had no disclosures.
FROM JAMA NETWORK OPEN
COVID-19 linked to rise in suicide-related ED visits among youth
After a steep decline in the first months of the COVID-19 pandemic, youth with suicidal thoughts and behaviors visiting an emergency department (ED) resurged with an overrepresentation among girls and children without a prior psychiatric history, according to a cross-sectional study conducted at Kaiser Permanente Northern California.
The latest findings, published in JAMA Psychiatry, are highly consistent with Centers for Disease Control and Prevention data published a few months earlier in the Morbidity and Mortality Weekly Report that looked at these trends among young people aged 12-25 before and during the pandemic. In addition, the new data suggest that prevention efforts might be particularly helpful for these young people and their families.
“As suicide-related encounters have made up more ED volume during the pandemic, increasing ED-based interventions, staff trained in addressing emergency mental health needs, and aftercare resources may also be valuable in addressing the needs of this population,” wrote Kathryn K. Erickson-Ridout, MD, PhD, first author of the more recent study and an adjunct investigator with the Kaiser Permanente Division of Research, Oakland, Calif.
“While these results suggest many of our youth are coping well through the pandemic, we need to be vigilant as health care workers,” she said in an interview.
Dr. Ridout and associates evaluated suicide-related ED visits among children aged 5-17 years presenting to EDs in the Kaiser Permanente Northern California system. Four periods in 2020 were compared with the same four periods in 2019.
In the first period, March through May 2020, the incidence rate ratio (IRR) of suicide-related ED visits among children and adolescents fell more than 40% (IRR, 0.53; P < .001) relative to the same months in 2019. This is consistent with a broader decline in other types of ED visits during the beginning of the COVID-19 pandemic.
In the periods of June through August and September to Dec. 15, suicide-related ED visits increased, reaching prepandemic levels overall but with differences between genders. In girls, an increase in the first period reached significance (IRR, 1.19; P = .04) and then climbed even higher in the second (hazard ratio, 1.22; P < .001).
Youth present with no prior psychiatric history
Among boys, the increase relative to 2019 in the first period was modest and nonsignificant (IRR, 1.05; P = .26) In the second period, suicide-related ED visits fell and the difference relative to the same period in 2019 reached statistical significance (IRR, 0.81; P = .02).
Other characteristics of suicide-related ED visits during the pandemic were also different from those observed in 2019. One was an increase in visits from youth with no prior history of mental health or suicide-related outpatient visits.
“This finding may suggest that a youth’s first presentation to the ED for suicidal thoughts and behaviors differed during the pandemic, compared to prior to the pandemic,” Dr. Erickson-Ridout explained. “Mental health comorbidities first diagnosed at the ED encounter may suggest an increased complexity at first presentation.”
These data are remarkably similar to ED visits for suicide attempts that were reported by the CDC several months earlier. The CDC data were drawn from the National Syndromic Surveillance Program, which captures data from 71% of the EDs in the United States.
Measured from March 29 to April 25, 2020, ED visits for a suicide attempt declined by more than 25% in both girls and boys, but by early May, those visits were already starting to return to prepandemic levels, particularly among girls, according to the CDC report. When evaluated from July 26 through Aug. 22, 2020, the mean weekly ED visits for suspected suicide attempts had increased 26.2% among girls but only 10.8% among boys, compared with the same period in 2019.
‘More severe distress’ found among girls
In the most recent period evaluated, starting Feb. 21, 2021, and extending to March 20, , compared with the same period in 2019. For boys, the increase was 3.7%.
Higher rates of suicide attempts among girls have been reported by others independent of the COVID-19 pandemic, but the CDC investigators led by Ellen Yard, PhD, a researcher in the CDC’s National Center for Environmental Health, Chamblee, Ga., reported that others have also found greater suicide ideation and attempts by girls during the pandemic.
Neither study was designed to isolate the reason or reasons for an increase in suicide-related ED visits overall or among girls specifically, but Dr. Yard and her coinvestigators speculated that social distancing and isolation during the COVID-19 pandemic might be affecting girls more.
The faster increase in suicide attempts among girls compared with boys “speaks to the importance of upstream prevention to prevent this group from becoming suicidal in the first place as well as improving suicide care both during and after ED visits,” said Dr. Yard, who was interviewed about this research.
For clinicians, she recommended “scaling up adoption of evidence-based best practice.” She cited two such resources from the National Action Alliance for Suicide Prevention (NAASP). One resource is the Best Practices in Care Transitions for Individuals with Suicide Risk: Inpatient Care to Outpatient Care; the other is called Recommended Standard Care. Both are available online for free from the NAASP.
Dr. Erickson-Ridout and Dr. Yard reported no potential conflicts of interest.
After a steep decline in the first months of the COVID-19 pandemic, youth with suicidal thoughts and behaviors visiting an emergency department (ED) resurged with an overrepresentation among girls and children without a prior psychiatric history, according to a cross-sectional study conducted at Kaiser Permanente Northern California.
The latest findings, published in JAMA Psychiatry, are highly consistent with Centers for Disease Control and Prevention data published a few months earlier in the Morbidity and Mortality Weekly Report that looked at these trends among young people aged 12-25 before and during the pandemic. In addition, the new data suggest that prevention efforts might be particularly helpful for these young people and their families.
“As suicide-related encounters have made up more ED volume during the pandemic, increasing ED-based interventions, staff trained in addressing emergency mental health needs, and aftercare resources may also be valuable in addressing the needs of this population,” wrote Kathryn K. Erickson-Ridout, MD, PhD, first author of the more recent study and an adjunct investigator with the Kaiser Permanente Division of Research, Oakland, Calif.
“While these results suggest many of our youth are coping well through the pandemic, we need to be vigilant as health care workers,” she said in an interview.
Dr. Ridout and associates evaluated suicide-related ED visits among children aged 5-17 years presenting to EDs in the Kaiser Permanente Northern California system. Four periods in 2020 were compared with the same four periods in 2019.
In the first period, March through May 2020, the incidence rate ratio (IRR) of suicide-related ED visits among children and adolescents fell more than 40% (IRR, 0.53; P < .001) relative to the same months in 2019. This is consistent with a broader decline in other types of ED visits during the beginning of the COVID-19 pandemic.
In the periods of June through August and September to Dec. 15, suicide-related ED visits increased, reaching prepandemic levels overall but with differences between genders. In girls, an increase in the first period reached significance (IRR, 1.19; P = .04) and then climbed even higher in the second (hazard ratio, 1.22; P < .001).
Youth present with no prior psychiatric history
Among boys, the increase relative to 2019 in the first period was modest and nonsignificant (IRR, 1.05; P = .26) In the second period, suicide-related ED visits fell and the difference relative to the same period in 2019 reached statistical significance (IRR, 0.81; P = .02).
Other characteristics of suicide-related ED visits during the pandemic were also different from those observed in 2019. One was an increase in visits from youth with no prior history of mental health or suicide-related outpatient visits.
“This finding may suggest that a youth’s first presentation to the ED for suicidal thoughts and behaviors differed during the pandemic, compared to prior to the pandemic,” Dr. Erickson-Ridout explained. “Mental health comorbidities first diagnosed at the ED encounter may suggest an increased complexity at first presentation.”
These data are remarkably similar to ED visits for suicide attempts that were reported by the CDC several months earlier. The CDC data were drawn from the National Syndromic Surveillance Program, which captures data from 71% of the EDs in the United States.
Measured from March 29 to April 25, 2020, ED visits for a suicide attempt declined by more than 25% in both girls and boys, but by early May, those visits were already starting to return to prepandemic levels, particularly among girls, according to the CDC report. When evaluated from July 26 through Aug. 22, 2020, the mean weekly ED visits for suspected suicide attempts had increased 26.2% among girls but only 10.8% among boys, compared with the same period in 2019.
‘More severe distress’ found among girls
In the most recent period evaluated, starting Feb. 21, 2021, and extending to March 20, , compared with the same period in 2019. For boys, the increase was 3.7%.
Higher rates of suicide attempts among girls have been reported by others independent of the COVID-19 pandemic, but the CDC investigators led by Ellen Yard, PhD, a researcher in the CDC’s National Center for Environmental Health, Chamblee, Ga., reported that others have also found greater suicide ideation and attempts by girls during the pandemic.
Neither study was designed to isolate the reason or reasons for an increase in suicide-related ED visits overall or among girls specifically, but Dr. Yard and her coinvestigators speculated that social distancing and isolation during the COVID-19 pandemic might be affecting girls more.
The faster increase in suicide attempts among girls compared with boys “speaks to the importance of upstream prevention to prevent this group from becoming suicidal in the first place as well as improving suicide care both during and after ED visits,” said Dr. Yard, who was interviewed about this research.
For clinicians, she recommended “scaling up adoption of evidence-based best practice.” She cited two such resources from the National Action Alliance for Suicide Prevention (NAASP). One resource is the Best Practices in Care Transitions for Individuals with Suicide Risk: Inpatient Care to Outpatient Care; the other is called Recommended Standard Care. Both are available online for free from the NAASP.
Dr. Erickson-Ridout and Dr. Yard reported no potential conflicts of interest.
After a steep decline in the first months of the COVID-19 pandemic, youth with suicidal thoughts and behaviors visiting an emergency department (ED) resurged with an overrepresentation among girls and children without a prior psychiatric history, according to a cross-sectional study conducted at Kaiser Permanente Northern California.
The latest findings, published in JAMA Psychiatry, are highly consistent with Centers for Disease Control and Prevention data published a few months earlier in the Morbidity and Mortality Weekly Report that looked at these trends among young people aged 12-25 before and during the pandemic. In addition, the new data suggest that prevention efforts might be particularly helpful for these young people and their families.
“As suicide-related encounters have made up more ED volume during the pandemic, increasing ED-based interventions, staff trained in addressing emergency mental health needs, and aftercare resources may also be valuable in addressing the needs of this population,” wrote Kathryn K. Erickson-Ridout, MD, PhD, first author of the more recent study and an adjunct investigator with the Kaiser Permanente Division of Research, Oakland, Calif.
“While these results suggest many of our youth are coping well through the pandemic, we need to be vigilant as health care workers,” she said in an interview.
Dr. Ridout and associates evaluated suicide-related ED visits among children aged 5-17 years presenting to EDs in the Kaiser Permanente Northern California system. Four periods in 2020 were compared with the same four periods in 2019.
In the first period, March through May 2020, the incidence rate ratio (IRR) of suicide-related ED visits among children and adolescents fell more than 40% (IRR, 0.53; P < .001) relative to the same months in 2019. This is consistent with a broader decline in other types of ED visits during the beginning of the COVID-19 pandemic.
In the periods of June through August and September to Dec. 15, suicide-related ED visits increased, reaching prepandemic levels overall but with differences between genders. In girls, an increase in the first period reached significance (IRR, 1.19; P = .04) and then climbed even higher in the second (hazard ratio, 1.22; P < .001).
Youth present with no prior psychiatric history
Among boys, the increase relative to 2019 in the first period was modest and nonsignificant (IRR, 1.05; P = .26) In the second period, suicide-related ED visits fell and the difference relative to the same period in 2019 reached statistical significance (IRR, 0.81; P = .02).
Other characteristics of suicide-related ED visits during the pandemic were also different from those observed in 2019. One was an increase in visits from youth with no prior history of mental health or suicide-related outpatient visits.
“This finding may suggest that a youth’s first presentation to the ED for suicidal thoughts and behaviors differed during the pandemic, compared to prior to the pandemic,” Dr. Erickson-Ridout explained. “Mental health comorbidities first diagnosed at the ED encounter may suggest an increased complexity at first presentation.”
These data are remarkably similar to ED visits for suicide attempts that were reported by the CDC several months earlier. The CDC data were drawn from the National Syndromic Surveillance Program, which captures data from 71% of the EDs in the United States.
Measured from March 29 to April 25, 2020, ED visits for a suicide attempt declined by more than 25% in both girls and boys, but by early May, those visits were already starting to return to prepandemic levels, particularly among girls, according to the CDC report. When evaluated from July 26 through Aug. 22, 2020, the mean weekly ED visits for suspected suicide attempts had increased 26.2% among girls but only 10.8% among boys, compared with the same period in 2019.
‘More severe distress’ found among girls
In the most recent period evaluated, starting Feb. 21, 2021, and extending to March 20, , compared with the same period in 2019. For boys, the increase was 3.7%.
Higher rates of suicide attempts among girls have been reported by others independent of the COVID-19 pandemic, but the CDC investigators led by Ellen Yard, PhD, a researcher in the CDC’s National Center for Environmental Health, Chamblee, Ga., reported that others have also found greater suicide ideation and attempts by girls during the pandemic.
Neither study was designed to isolate the reason or reasons for an increase in suicide-related ED visits overall or among girls specifically, but Dr. Yard and her coinvestigators speculated that social distancing and isolation during the COVID-19 pandemic might be affecting girls more.
The faster increase in suicide attempts among girls compared with boys “speaks to the importance of upstream prevention to prevent this group from becoming suicidal in the first place as well as improving suicide care both during and after ED visits,” said Dr. Yard, who was interviewed about this research.
For clinicians, she recommended “scaling up adoption of evidence-based best practice.” She cited two such resources from the National Action Alliance for Suicide Prevention (NAASP). One resource is the Best Practices in Care Transitions for Individuals with Suicide Risk: Inpatient Care to Outpatient Care; the other is called Recommended Standard Care. Both are available online for free from the NAASP.
Dr. Erickson-Ridout and Dr. Yard reported no potential conflicts of interest.
FROM JAMA PSYCHIATRY
COVID vaccine response in patients with solid tumors
Among cancer patients with solid tumors, the response to the COVID-19 vaccine 6 months after receiving a second dose was as good as that of the general population, according to new findings from a case-control study.
The BNT162b2, or Pfizer-BioNTech, vaccine (Comirnaty) was previously shown to have good short-term efficacy, immunogenicity, and safety in cancer patients with solid tumors, but little is known about longer-term efficacy in this population, say the investigators.
They assessed responses 6 months after a second dose of the vaccine.
Serologic tests showed that 122 of 154 patients with solid tumors who were actively undergoing cancer treatment (79%) and 114 of 135 age-matched health care workers who served as control persons (84%) were seropositive at 6 months (P = .32).
Most (81%) of the patients with cancer who were seronegative were receiving chemotherapy, the researchers report.
One case of severe COVID-19 that required hospitalization occurred among the solid-tumor group; none occurred among the control persons, they also note.
The findings were published online on Sept. 2 in Cancer Discovery.
“In our study we saw that in all outcomes, including immunogenicity, infectivity rate throughout the 6-month period, and safety, patients with solid tumors depicted a similar trend as the general population,” commented lead author Irit Ben-Aharon, MD, PhD, director of the division of oncology at Rambam Health Care Campus, Haifa, Israel, in an American Association for Cancer Research press statement.
However, she and her coauthors stressed the importance of continuing to follow guidance, such as social distancing and mask wearing, for reducing COVID-19 transmission. “Due to uncertainty of the extended efficacy of the vaccine in the general population and recent reports on rising infection rates among vaccinated individuals, adherence to health care risk reduction recommendations is cardinal,” they write.
The mean age of the control persons in the study was 63 years, and the mean age of the case patients was 66 years. The most common cancers were gastrointestinal (36%), lung (23%), breast (17%), and genitourinary (11%). Treatment protocols included chemotherapy (62%), biological agents (36%), and immunotherapy (30%). Some patients received more than one type of treatment.
All of the reported adverse effects associated with vaccination had resolved at the time of follow-up.
These data can “help inform recommendations surrounding the prioritization of different groups for booster vaccines,” Dr. Ben-Aharon adds.
In fact, recently updated guidelines from the National Comprehensive Cancer Network state that cancer patients with solid tumors who are receiving treatment within 1 year of their initial vaccine dose should be prioritized for a booster vaccine.
The study was partially supported by the Israel Cancer Research Fund. Serologic testing of the control cohort was supported by the Ministry of Health, Israel. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Among cancer patients with solid tumors, the response to the COVID-19 vaccine 6 months after receiving a second dose was as good as that of the general population, according to new findings from a case-control study.
The BNT162b2, or Pfizer-BioNTech, vaccine (Comirnaty) was previously shown to have good short-term efficacy, immunogenicity, and safety in cancer patients with solid tumors, but little is known about longer-term efficacy in this population, say the investigators.
They assessed responses 6 months after a second dose of the vaccine.
Serologic tests showed that 122 of 154 patients with solid tumors who were actively undergoing cancer treatment (79%) and 114 of 135 age-matched health care workers who served as control persons (84%) were seropositive at 6 months (P = .32).
Most (81%) of the patients with cancer who were seronegative were receiving chemotherapy, the researchers report.
One case of severe COVID-19 that required hospitalization occurred among the solid-tumor group; none occurred among the control persons, they also note.
The findings were published online on Sept. 2 in Cancer Discovery.
“In our study we saw that in all outcomes, including immunogenicity, infectivity rate throughout the 6-month period, and safety, patients with solid tumors depicted a similar trend as the general population,” commented lead author Irit Ben-Aharon, MD, PhD, director of the division of oncology at Rambam Health Care Campus, Haifa, Israel, in an American Association for Cancer Research press statement.
However, she and her coauthors stressed the importance of continuing to follow guidance, such as social distancing and mask wearing, for reducing COVID-19 transmission. “Due to uncertainty of the extended efficacy of the vaccine in the general population and recent reports on rising infection rates among vaccinated individuals, adherence to health care risk reduction recommendations is cardinal,” they write.
The mean age of the control persons in the study was 63 years, and the mean age of the case patients was 66 years. The most common cancers were gastrointestinal (36%), lung (23%), breast (17%), and genitourinary (11%). Treatment protocols included chemotherapy (62%), biological agents (36%), and immunotherapy (30%). Some patients received more than one type of treatment.
All of the reported adverse effects associated with vaccination had resolved at the time of follow-up.
These data can “help inform recommendations surrounding the prioritization of different groups for booster vaccines,” Dr. Ben-Aharon adds.
In fact, recently updated guidelines from the National Comprehensive Cancer Network state that cancer patients with solid tumors who are receiving treatment within 1 year of their initial vaccine dose should be prioritized for a booster vaccine.
The study was partially supported by the Israel Cancer Research Fund. Serologic testing of the control cohort was supported by the Ministry of Health, Israel. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Among cancer patients with solid tumors, the response to the COVID-19 vaccine 6 months after receiving a second dose was as good as that of the general population, according to new findings from a case-control study.
The BNT162b2, or Pfizer-BioNTech, vaccine (Comirnaty) was previously shown to have good short-term efficacy, immunogenicity, and safety in cancer patients with solid tumors, but little is known about longer-term efficacy in this population, say the investigators.
They assessed responses 6 months after a second dose of the vaccine.
Serologic tests showed that 122 of 154 patients with solid tumors who were actively undergoing cancer treatment (79%) and 114 of 135 age-matched health care workers who served as control persons (84%) were seropositive at 6 months (P = .32).
Most (81%) of the patients with cancer who were seronegative were receiving chemotherapy, the researchers report.
One case of severe COVID-19 that required hospitalization occurred among the solid-tumor group; none occurred among the control persons, they also note.
The findings were published online on Sept. 2 in Cancer Discovery.
“In our study we saw that in all outcomes, including immunogenicity, infectivity rate throughout the 6-month period, and safety, patients with solid tumors depicted a similar trend as the general population,” commented lead author Irit Ben-Aharon, MD, PhD, director of the division of oncology at Rambam Health Care Campus, Haifa, Israel, in an American Association for Cancer Research press statement.
However, she and her coauthors stressed the importance of continuing to follow guidance, such as social distancing and mask wearing, for reducing COVID-19 transmission. “Due to uncertainty of the extended efficacy of the vaccine in the general population and recent reports on rising infection rates among vaccinated individuals, adherence to health care risk reduction recommendations is cardinal,” they write.
The mean age of the control persons in the study was 63 years, and the mean age of the case patients was 66 years. The most common cancers were gastrointestinal (36%), lung (23%), breast (17%), and genitourinary (11%). Treatment protocols included chemotherapy (62%), biological agents (36%), and immunotherapy (30%). Some patients received more than one type of treatment.
All of the reported adverse effects associated with vaccination had resolved at the time of follow-up.
These data can “help inform recommendations surrounding the prioritization of different groups for booster vaccines,” Dr. Ben-Aharon adds.
In fact, recently updated guidelines from the National Comprehensive Cancer Network state that cancer patients with solid tumors who are receiving treatment within 1 year of their initial vaccine dose should be prioritized for a booster vaccine.
The study was partially supported by the Israel Cancer Research Fund. Serologic testing of the control cohort was supported by the Ministry of Health, Israel. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Long COVID could spell kidney troubles down the line
Physicians caring for COVID-19 survivors should routinely check kidney function, which is often damaged by the SARS-CoV-2 virus months after both severe and milder cases, new research indicates.
The largest study to date with the longest follow-up of COVID-19-related kidney outcomes also found that every type of kidney problem, including end-stage kidney disease (ESKD), was far more common in COVID-19 survivors who were admitted to the ICU or experienced acute kidney injury (AKI) while hospitalized.
Researchers analyzed U.S. Veterans Health Administration data from more than 1.7 million patients, including more than 89,000 who tested positive for COVID-19, for the study, which was published online Sept. 1, 2021, in the Journal of the American Society of Nephrology.
The risk of kidney problems “is more robust or pronounced in people who have had severe infection, but present in even asymptomatic and mild disease, which shouldn’t be discounted. Those people represent the majority of those with COVID-19,” said senior author Ziyad Al-Aly, MD, of the Veteran Affairs St. Louis Health Care System.
“That’s why the results are important, because even in people with mild disease to start with, the risk of kidney problems is not trivial,” he told this news organization. “It’s smaller than in people who were in the ICU, but it’s not ... zero.”
Experts aren’t yet certain how COVID-19 can damage the kidneys, hypothesizing that several factors may be at play. The virus may directly infect kidney cells rich in ACE2 receptors, which are key to infection, said nephrologist F. Perry Wilson, MD, of Yale University, New Haven, Conn., and a member of Medscape’s advisory board.
Kidneys might also be particularly vulnerable to the inflammatory cascade or blood clotting often seen in COVID-19, Dr. Al-Aly and Wilson both suggested.
COVID-19 survivors more likely to have kidney damage than controls
“A lot of health systems either have or are establishing post-COVID care clinics, which we think should definitely incorporate a kidney component,” Dr. Al-Aly advised. “They should check patients’ blood and urine for kidney problems.”
This is particularly important because “kidney problems, for the most part, are painless and silent,” he added.
“Realizing 2 years down the road that someone has ESKD, where they need dialysis or a kidney transplant, is what we don’t want. We don’t want this to be unrecognized, uncared for, unattended to,” he said.
Dr. Al-Aly and colleagues evaluated VA health system records, including data from 89,216 patients who tested positive for COVID-19 between March 2020 and March 2021, as well as 1.7 million controls who did not have COVID-19. Over a median follow-up of about 5.5 months, participants’ estimated glomerular filtration rate and serum creatinine levels were tracked to assess kidney health and outcomes according to infection severity.
Results were striking, with COVID-19 survivors about one-third more likely than controls to have kidney damage or significant declines in kidney function between 1 and 6 months after infection. More than 4,700 COVID-19 survivors had lost at least 30% of their kidney function within a year, and these patients were 25% more likely to reach that level of decline than controls.
Additionally, COVID-19 survivors were nearly twice as likely to experience AKI and almost three times as likely to be diagnosed with ESKD as controls.
If your patient had COVID-19, ‘it’s reasonable to check kidney function’
“This information tells us that if your patient was sick with COVID-19 and comes for follow-up visits, it’s reasonable to check their kidney function,” Dr. Wilson, who was not involved with the research, told this news organization.
“Even for patients who were not hospitalized, if they were laid low or dehydrated ... it should be part of the post-COVID care package,” he said.
If just a fraction of the millions of COVID-19 survivors in the United States develop long-term kidney problems, the ripple effect on American health care could be substantial, Dr. Wilson and Dr. Al-Aly agreed.
“We’re still living in a pandemic, so it’s hard to tell the total impact,” Dr. Al-Aly said. “But this ultimately will contribute to a rise in burden of kidney disease. This and other long COVID manifestations are going to alter the landscape of clinical care and health care in the United States for a decade or more.”
Because renal problems can limit a patient’s treatment options for other major diseases, including diabetes and cancer, COVID-related kidney damage can ultimately impact survivability.
“There are a lot of medications you can’t use in people with advanced kidney problems,” Dr. Al-Aly said.
The main study limitation was that patients were mostly older White men (median age, 68 years), although more than 9,000 women were included in the VA data, Dr. Al-Aly noted. Additionally, controls were more likely to be younger, Black, living in long-term care, and have higher rates of chronic health conditions and medication use.
The experts agreed that ongoing research tracking kidney outcomes is crucial for years to come.
“We also need to be following a cohort of these patients as part of a research protocol where they come in every 6 months for a standard set of lab tests to really understand what’s going on with their kidneys,” Dr. Wilson said.
“Lastly – and a much tougher sell – is we need biopsies. It’s very hard to infer what’s going on in complex disease with the kidneys without biopsy tissue,” he added.
The study was funded by the American Society of Nephrology and the Department of Veterans Affairs. Dr. Al-Aly and Dr. Wilson reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Physicians caring for COVID-19 survivors should routinely check kidney function, which is often damaged by the SARS-CoV-2 virus months after both severe and milder cases, new research indicates.
The largest study to date with the longest follow-up of COVID-19-related kidney outcomes also found that every type of kidney problem, including end-stage kidney disease (ESKD), was far more common in COVID-19 survivors who were admitted to the ICU or experienced acute kidney injury (AKI) while hospitalized.
Researchers analyzed U.S. Veterans Health Administration data from more than 1.7 million patients, including more than 89,000 who tested positive for COVID-19, for the study, which was published online Sept. 1, 2021, in the Journal of the American Society of Nephrology.
The risk of kidney problems “is more robust or pronounced in people who have had severe infection, but present in even asymptomatic and mild disease, which shouldn’t be discounted. Those people represent the majority of those with COVID-19,” said senior author Ziyad Al-Aly, MD, of the Veteran Affairs St. Louis Health Care System.
“That’s why the results are important, because even in people with mild disease to start with, the risk of kidney problems is not trivial,” he told this news organization. “It’s smaller than in people who were in the ICU, but it’s not ... zero.”
Experts aren’t yet certain how COVID-19 can damage the kidneys, hypothesizing that several factors may be at play. The virus may directly infect kidney cells rich in ACE2 receptors, which are key to infection, said nephrologist F. Perry Wilson, MD, of Yale University, New Haven, Conn., and a member of Medscape’s advisory board.
Kidneys might also be particularly vulnerable to the inflammatory cascade or blood clotting often seen in COVID-19, Dr. Al-Aly and Wilson both suggested.
COVID-19 survivors more likely to have kidney damage than controls
“A lot of health systems either have or are establishing post-COVID care clinics, which we think should definitely incorporate a kidney component,” Dr. Al-Aly advised. “They should check patients’ blood and urine for kidney problems.”
This is particularly important because “kidney problems, for the most part, are painless and silent,” he added.
“Realizing 2 years down the road that someone has ESKD, where they need dialysis or a kidney transplant, is what we don’t want. We don’t want this to be unrecognized, uncared for, unattended to,” he said.
Dr. Al-Aly and colleagues evaluated VA health system records, including data from 89,216 patients who tested positive for COVID-19 between March 2020 and March 2021, as well as 1.7 million controls who did not have COVID-19. Over a median follow-up of about 5.5 months, participants’ estimated glomerular filtration rate and serum creatinine levels were tracked to assess kidney health and outcomes according to infection severity.
Results were striking, with COVID-19 survivors about one-third more likely than controls to have kidney damage or significant declines in kidney function between 1 and 6 months after infection. More than 4,700 COVID-19 survivors had lost at least 30% of their kidney function within a year, and these patients were 25% more likely to reach that level of decline than controls.
Additionally, COVID-19 survivors were nearly twice as likely to experience AKI and almost three times as likely to be diagnosed with ESKD as controls.
If your patient had COVID-19, ‘it’s reasonable to check kidney function’
“This information tells us that if your patient was sick with COVID-19 and comes for follow-up visits, it’s reasonable to check their kidney function,” Dr. Wilson, who was not involved with the research, told this news organization.
“Even for patients who were not hospitalized, if they were laid low or dehydrated ... it should be part of the post-COVID care package,” he said.
If just a fraction of the millions of COVID-19 survivors in the United States develop long-term kidney problems, the ripple effect on American health care could be substantial, Dr. Wilson and Dr. Al-Aly agreed.
“We’re still living in a pandemic, so it’s hard to tell the total impact,” Dr. Al-Aly said. “But this ultimately will contribute to a rise in burden of kidney disease. This and other long COVID manifestations are going to alter the landscape of clinical care and health care in the United States for a decade or more.”
Because renal problems can limit a patient’s treatment options for other major diseases, including diabetes and cancer, COVID-related kidney damage can ultimately impact survivability.
“There are a lot of medications you can’t use in people with advanced kidney problems,” Dr. Al-Aly said.
The main study limitation was that patients were mostly older White men (median age, 68 years), although more than 9,000 women were included in the VA data, Dr. Al-Aly noted. Additionally, controls were more likely to be younger, Black, living in long-term care, and have higher rates of chronic health conditions and medication use.
The experts agreed that ongoing research tracking kidney outcomes is crucial for years to come.
“We also need to be following a cohort of these patients as part of a research protocol where they come in every 6 months for a standard set of lab tests to really understand what’s going on with their kidneys,” Dr. Wilson said.
“Lastly – and a much tougher sell – is we need biopsies. It’s very hard to infer what’s going on in complex disease with the kidneys without biopsy tissue,” he added.
The study was funded by the American Society of Nephrology and the Department of Veterans Affairs. Dr. Al-Aly and Dr. Wilson reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Physicians caring for COVID-19 survivors should routinely check kidney function, which is often damaged by the SARS-CoV-2 virus months after both severe and milder cases, new research indicates.
The largest study to date with the longest follow-up of COVID-19-related kidney outcomes also found that every type of kidney problem, including end-stage kidney disease (ESKD), was far more common in COVID-19 survivors who were admitted to the ICU or experienced acute kidney injury (AKI) while hospitalized.
Researchers analyzed U.S. Veterans Health Administration data from more than 1.7 million patients, including more than 89,000 who tested positive for COVID-19, for the study, which was published online Sept. 1, 2021, in the Journal of the American Society of Nephrology.
The risk of kidney problems “is more robust or pronounced in people who have had severe infection, but present in even asymptomatic and mild disease, which shouldn’t be discounted. Those people represent the majority of those with COVID-19,” said senior author Ziyad Al-Aly, MD, of the Veteran Affairs St. Louis Health Care System.
“That’s why the results are important, because even in people with mild disease to start with, the risk of kidney problems is not trivial,” he told this news organization. “It’s smaller than in people who were in the ICU, but it’s not ... zero.”
Experts aren’t yet certain how COVID-19 can damage the kidneys, hypothesizing that several factors may be at play. The virus may directly infect kidney cells rich in ACE2 receptors, which are key to infection, said nephrologist F. Perry Wilson, MD, of Yale University, New Haven, Conn., and a member of Medscape’s advisory board.
Kidneys might also be particularly vulnerable to the inflammatory cascade or blood clotting often seen in COVID-19, Dr. Al-Aly and Wilson both suggested.
COVID-19 survivors more likely to have kidney damage than controls
“A lot of health systems either have or are establishing post-COVID care clinics, which we think should definitely incorporate a kidney component,” Dr. Al-Aly advised. “They should check patients’ blood and urine for kidney problems.”
This is particularly important because “kidney problems, for the most part, are painless and silent,” he added.
“Realizing 2 years down the road that someone has ESKD, where they need dialysis or a kidney transplant, is what we don’t want. We don’t want this to be unrecognized, uncared for, unattended to,” he said.
Dr. Al-Aly and colleagues evaluated VA health system records, including data from 89,216 patients who tested positive for COVID-19 between March 2020 and March 2021, as well as 1.7 million controls who did not have COVID-19. Over a median follow-up of about 5.5 months, participants’ estimated glomerular filtration rate and serum creatinine levels were tracked to assess kidney health and outcomes according to infection severity.
Results were striking, with COVID-19 survivors about one-third more likely than controls to have kidney damage or significant declines in kidney function between 1 and 6 months after infection. More than 4,700 COVID-19 survivors had lost at least 30% of their kidney function within a year, and these patients were 25% more likely to reach that level of decline than controls.
Additionally, COVID-19 survivors were nearly twice as likely to experience AKI and almost three times as likely to be diagnosed with ESKD as controls.
If your patient had COVID-19, ‘it’s reasonable to check kidney function’
“This information tells us that if your patient was sick with COVID-19 and comes for follow-up visits, it’s reasonable to check their kidney function,” Dr. Wilson, who was not involved with the research, told this news organization.
“Even for patients who were not hospitalized, if they were laid low or dehydrated ... it should be part of the post-COVID care package,” he said.
If just a fraction of the millions of COVID-19 survivors in the United States develop long-term kidney problems, the ripple effect on American health care could be substantial, Dr. Wilson and Dr. Al-Aly agreed.
“We’re still living in a pandemic, so it’s hard to tell the total impact,” Dr. Al-Aly said. “But this ultimately will contribute to a rise in burden of kidney disease. This and other long COVID manifestations are going to alter the landscape of clinical care and health care in the United States for a decade or more.”
Because renal problems can limit a patient’s treatment options for other major diseases, including diabetes and cancer, COVID-related kidney damage can ultimately impact survivability.
“There are a lot of medications you can’t use in people with advanced kidney problems,” Dr. Al-Aly said.
The main study limitation was that patients were mostly older White men (median age, 68 years), although more than 9,000 women were included in the VA data, Dr. Al-Aly noted. Additionally, controls were more likely to be younger, Black, living in long-term care, and have higher rates of chronic health conditions and medication use.
The experts agreed that ongoing research tracking kidney outcomes is crucial for years to come.
“We also need to be following a cohort of these patients as part of a research protocol where they come in every 6 months for a standard set of lab tests to really understand what’s going on with their kidneys,” Dr. Wilson said.
“Lastly – and a much tougher sell – is we need biopsies. It’s very hard to infer what’s going on in complex disease with the kidneys without biopsy tissue,” he added.
The study was funded by the American Society of Nephrology and the Department of Veterans Affairs. Dr. Al-Aly and Dr. Wilson reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Florida doctor won’t treat unvaccinated patients in person
Linda Marraccini, MD, sent a letter to patients that said those who aren’t vaccinated won’t be allowed to book in-person appointments at her practice now that the Food and Drug Administration has fully approved the Pfizer vaccine for general use, according to NBC Miami.
“This is a public health emergency – the health of the public takes priority over the rights of any given individual in this situation,” she wrote in the letter, which was obtained by NBC Miami.
“It appears that there is a lack of selflessness and concern for the burden on the health and well-being of our society from our encounters,” she wrote.
Dr. Marraccini said the policy is in the best interest of her other patients and doesn’t violate the Hippocratic oath. Patients who are having chemotherapy or who have weak immune systems face higher risks of being infected with the coronavirus.
“It’s not fair for people who are unvaccinated to harm other people,” she told Newsweek Sept. 4.
“The Hippocratic oath is very science based,” she said. “I am following the science. I’m applying this to the benefit of the sick.”
Dr. Marraccini said her new policy goes into effect on Sept. 15, and she will continue to see unvaccinated patients virtually during the next month until they find another health care provider.
She said that the response to her decision has been “99.9% favorable” and that she will make exceptions if patients can’t receive a shot because of hardships. Her office also provides the Johnson & Johnson vaccine.
“We’re not going to leave them out there in the cold,” she told Newsweek.
During the past month, COVID-19 cases have surged in Florida, reaching record-level highs of more than 20,000 cases per day. Cases began rising in the summer because of the more contagious Delta variant.
In late August, a group of doctors in southern Florida urged people to get vaccinated, citing their exhaustion and frustration with unvaccinated patients who make up the large majority of COVID-19 hospitalizations, according to Newsweek.
Other doctors have declined to treat unvaccinated patients in recent weeks. Jason Valentine, MD, a doctor in Mobile, Ala., said he would no longer see unvaccinated patients as of Oct. 1, according to AL.com.
Dr. Marraccini urged people to become informed about COVID-19 vaccines, as well as their role in reducing the surge of cases in the state. The pandemic “did not have to go on this long,” she said.
“Responsibility has to do with each individual,” she told Newsweek. “This is a global health issue, and everyone owns part of that responsibility.”
A version of this article first appeared on WebMD.com.
Linda Marraccini, MD, sent a letter to patients that said those who aren’t vaccinated won’t be allowed to book in-person appointments at her practice now that the Food and Drug Administration has fully approved the Pfizer vaccine for general use, according to NBC Miami.
“This is a public health emergency – the health of the public takes priority over the rights of any given individual in this situation,” she wrote in the letter, which was obtained by NBC Miami.
“It appears that there is a lack of selflessness and concern for the burden on the health and well-being of our society from our encounters,” she wrote.
Dr. Marraccini said the policy is in the best interest of her other patients and doesn’t violate the Hippocratic oath. Patients who are having chemotherapy or who have weak immune systems face higher risks of being infected with the coronavirus.
“It’s not fair for people who are unvaccinated to harm other people,” she told Newsweek Sept. 4.
“The Hippocratic oath is very science based,” she said. “I am following the science. I’m applying this to the benefit of the sick.”
Dr. Marraccini said her new policy goes into effect on Sept. 15, and she will continue to see unvaccinated patients virtually during the next month until they find another health care provider.
She said that the response to her decision has been “99.9% favorable” and that she will make exceptions if patients can’t receive a shot because of hardships. Her office also provides the Johnson & Johnson vaccine.
“We’re not going to leave them out there in the cold,” she told Newsweek.
During the past month, COVID-19 cases have surged in Florida, reaching record-level highs of more than 20,000 cases per day. Cases began rising in the summer because of the more contagious Delta variant.
In late August, a group of doctors in southern Florida urged people to get vaccinated, citing their exhaustion and frustration with unvaccinated patients who make up the large majority of COVID-19 hospitalizations, according to Newsweek.
Other doctors have declined to treat unvaccinated patients in recent weeks. Jason Valentine, MD, a doctor in Mobile, Ala., said he would no longer see unvaccinated patients as of Oct. 1, according to AL.com.
Dr. Marraccini urged people to become informed about COVID-19 vaccines, as well as their role in reducing the surge of cases in the state. The pandemic “did not have to go on this long,” she said.
“Responsibility has to do with each individual,” she told Newsweek. “This is a global health issue, and everyone owns part of that responsibility.”
A version of this article first appeared on WebMD.com.
Linda Marraccini, MD, sent a letter to patients that said those who aren’t vaccinated won’t be allowed to book in-person appointments at her practice now that the Food and Drug Administration has fully approved the Pfizer vaccine for general use, according to NBC Miami.
“This is a public health emergency – the health of the public takes priority over the rights of any given individual in this situation,” she wrote in the letter, which was obtained by NBC Miami.
“It appears that there is a lack of selflessness and concern for the burden on the health and well-being of our society from our encounters,” she wrote.
Dr. Marraccini said the policy is in the best interest of her other patients and doesn’t violate the Hippocratic oath. Patients who are having chemotherapy or who have weak immune systems face higher risks of being infected with the coronavirus.
“It’s not fair for people who are unvaccinated to harm other people,” she told Newsweek Sept. 4.
“The Hippocratic oath is very science based,” she said. “I am following the science. I’m applying this to the benefit of the sick.”
Dr. Marraccini said her new policy goes into effect on Sept. 15, and she will continue to see unvaccinated patients virtually during the next month until they find another health care provider.
She said that the response to her decision has been “99.9% favorable” and that she will make exceptions if patients can’t receive a shot because of hardships. Her office also provides the Johnson & Johnson vaccine.
“We’re not going to leave them out there in the cold,” she told Newsweek.
During the past month, COVID-19 cases have surged in Florida, reaching record-level highs of more than 20,000 cases per day. Cases began rising in the summer because of the more contagious Delta variant.
In late August, a group of doctors in southern Florida urged people to get vaccinated, citing their exhaustion and frustration with unvaccinated patients who make up the large majority of COVID-19 hospitalizations, according to Newsweek.
Other doctors have declined to treat unvaccinated patients in recent weeks. Jason Valentine, MD, a doctor in Mobile, Ala., said he would no longer see unvaccinated patients as of Oct. 1, according to AL.com.
Dr. Marraccini urged people to become informed about COVID-19 vaccines, as well as their role in reducing the surge of cases in the state. The pandemic “did not have to go on this long,” she said.
“Responsibility has to do with each individual,” she told Newsweek. “This is a global health issue, and everyone owns part of that responsibility.”
A version of this article first appeared on WebMD.com.
United States reaches 5 million cases of child COVID
Cases of child COVID-19 set a new 1-week record and the total number of children infected during the pandemic passed 5 million, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
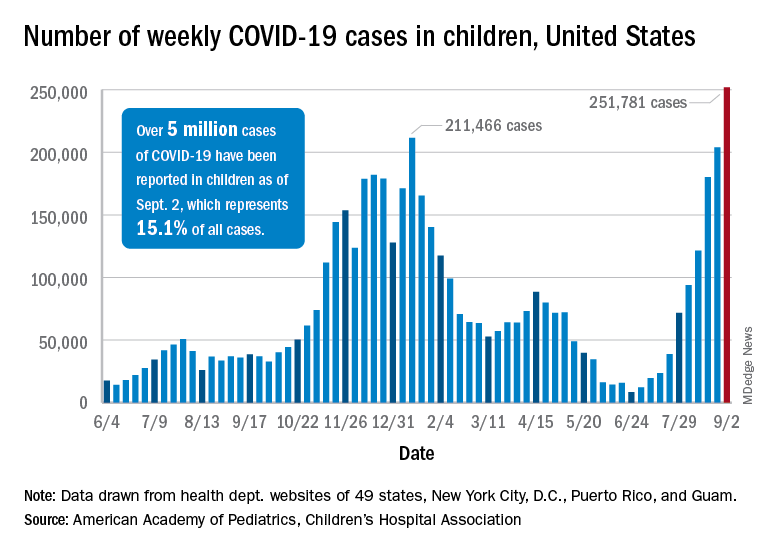
The nearly 282,000 new cases reported in the United States during the week ending Sept. 2 broke the record of 211,000 set in mid-January and brought the cumulative count to 5,049,465 children with COVID-19 since the pandemic began, the AAP and the CHA said in their weekly COVID report.
Hospitalizations in children aged 0-17 years have also reached record levels in recent days. The highest daily admission rate since the pandemic began, 0.51 per 100,000 population, was recorded on Sept. 2, less than 2 months after the nation saw its lowest child COVID admission rate for 1 day: 0.07 per 100,000 on July 4. That’s an increase of 629%, according to data from the Centers for Disease Control and Prevention.
Vaccinations in children, however, did not follow suit. New vaccinations in children aged 12-17 years dropped by 4.5% for the week ending Sept. 6, compared with the week before. Initiations were actually up almost 12% for children aged 16-17, but that was not enough to overcome the continued decline among 12- to 15-year-olds, the CDC said on its COVID Data Tracker.
Despite the decline in new vaccinations, those younger children passed a noteworthy group milestone: 50.9% of all 12- to 15-year-olds now have received at least one dose, with 38.6% having completed the regimen. The 16- to 17-year-olds got an earlier start and have reached 58.9% coverage for one dose and 47.6% for two, the CDC said.
A total of 12.2 million children aged 12-17 years had received at least one dose of COVID vaccine as of Sept. 6, of whom almost 9.5 million are fully vaccinated, based on the CDC data.
At the state level, Vermont has the highest rates for vaccine initiation (75%) and full vaccination (65%), with Massachusetts (75%/62%) and Connecticut (73%/59%) just behind. The other end of the scale is occupied by Wyoming (28% initiation/19% full vaccination), Alabama (32%/19%), and North Dakota (32%/23%), the AAP said in a separate report.
In a recent letter to the Food and Drug Administration, AAP President Lee Savio Beers, MD, said that the “Delta variant is surging at extremely alarming rates in every region of America. This surge is seriously impacting all populations, including children.” Dr. Beers urged the FDA to work “aggressively toward authorizing safe and effective COVID-19 vaccines for children under age 12 as soon as possible.”
Cases of child COVID-19 set a new 1-week record and the total number of children infected during the pandemic passed 5 million, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
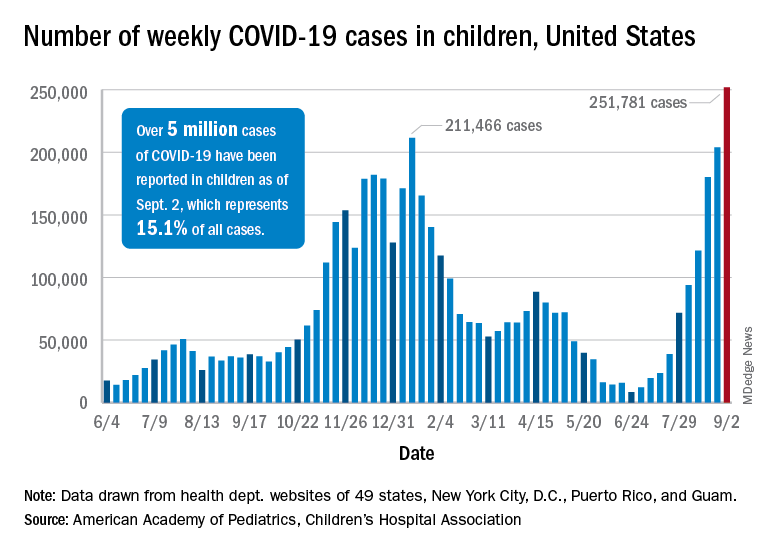
The nearly 282,000 new cases reported in the United States during the week ending Sept. 2 broke the record of 211,000 set in mid-January and brought the cumulative count to 5,049,465 children with COVID-19 since the pandemic began, the AAP and the CHA said in their weekly COVID report.
Hospitalizations in children aged 0-17 years have also reached record levels in recent days. The highest daily admission rate since the pandemic began, 0.51 per 100,000 population, was recorded on Sept. 2, less than 2 months after the nation saw its lowest child COVID admission rate for 1 day: 0.07 per 100,000 on July 4. That’s an increase of 629%, according to data from the Centers for Disease Control and Prevention.
Vaccinations in children, however, did not follow suit. New vaccinations in children aged 12-17 years dropped by 4.5% for the week ending Sept. 6, compared with the week before. Initiations were actually up almost 12% for children aged 16-17, but that was not enough to overcome the continued decline among 12- to 15-year-olds, the CDC said on its COVID Data Tracker.
Despite the decline in new vaccinations, those younger children passed a noteworthy group milestone: 50.9% of all 12- to 15-year-olds now have received at least one dose, with 38.6% having completed the regimen. The 16- to 17-year-olds got an earlier start and have reached 58.9% coverage for one dose and 47.6% for two, the CDC said.
A total of 12.2 million children aged 12-17 years had received at least one dose of COVID vaccine as of Sept. 6, of whom almost 9.5 million are fully vaccinated, based on the CDC data.
At the state level, Vermont has the highest rates for vaccine initiation (75%) and full vaccination (65%), with Massachusetts (75%/62%) and Connecticut (73%/59%) just behind. The other end of the scale is occupied by Wyoming (28% initiation/19% full vaccination), Alabama (32%/19%), and North Dakota (32%/23%), the AAP said in a separate report.
In a recent letter to the Food and Drug Administration, AAP President Lee Savio Beers, MD, said that the “Delta variant is surging at extremely alarming rates in every region of America. This surge is seriously impacting all populations, including children.” Dr. Beers urged the FDA to work “aggressively toward authorizing safe and effective COVID-19 vaccines for children under age 12 as soon as possible.”
Cases of child COVID-19 set a new 1-week record and the total number of children infected during the pandemic passed 5 million, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
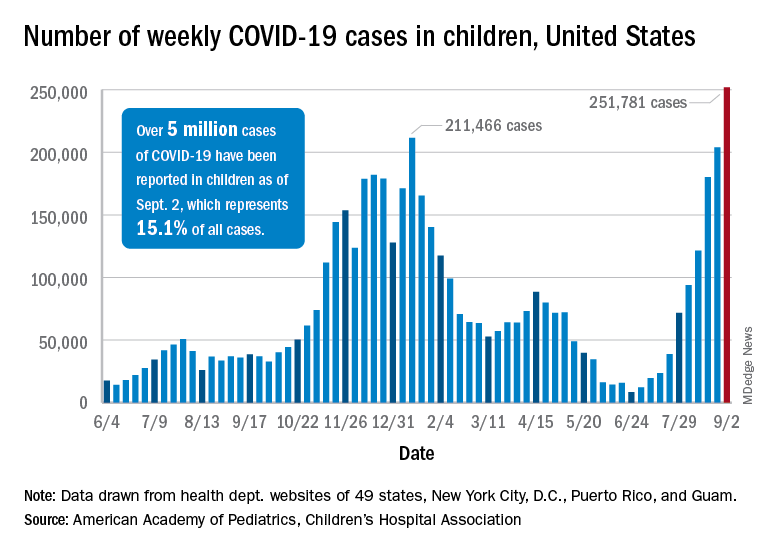
The nearly 282,000 new cases reported in the United States during the week ending Sept. 2 broke the record of 211,000 set in mid-January and brought the cumulative count to 5,049,465 children with COVID-19 since the pandemic began, the AAP and the CHA said in their weekly COVID report.
Hospitalizations in children aged 0-17 years have also reached record levels in recent days. The highest daily admission rate since the pandemic began, 0.51 per 100,000 population, was recorded on Sept. 2, less than 2 months after the nation saw its lowest child COVID admission rate for 1 day: 0.07 per 100,000 on July 4. That’s an increase of 629%, according to data from the Centers for Disease Control and Prevention.
Vaccinations in children, however, did not follow suit. New vaccinations in children aged 12-17 years dropped by 4.5% for the week ending Sept. 6, compared with the week before. Initiations were actually up almost 12% for children aged 16-17, but that was not enough to overcome the continued decline among 12- to 15-year-olds, the CDC said on its COVID Data Tracker.
Despite the decline in new vaccinations, those younger children passed a noteworthy group milestone: 50.9% of all 12- to 15-year-olds now have received at least one dose, with 38.6% having completed the regimen. The 16- to 17-year-olds got an earlier start and have reached 58.9% coverage for one dose and 47.6% for two, the CDC said.
A total of 12.2 million children aged 12-17 years had received at least one dose of COVID vaccine as of Sept. 6, of whom almost 9.5 million are fully vaccinated, based on the CDC data.
At the state level, Vermont has the highest rates for vaccine initiation (75%) and full vaccination (65%), with Massachusetts (75%/62%) and Connecticut (73%/59%) just behind. The other end of the scale is occupied by Wyoming (28% initiation/19% full vaccination), Alabama (32%/19%), and North Dakota (32%/23%), the AAP said in a separate report.
In a recent letter to the Food and Drug Administration, AAP President Lee Savio Beers, MD, said that the “Delta variant is surging at extremely alarming rates in every region of America. This surge is seriously impacting all populations, including children.” Dr. Beers urged the FDA to work “aggressively toward authorizing safe and effective COVID-19 vaccines for children under age 12 as soon as possible.”








