User login
Hospital managers identify barriers to antimicrobial stewardship
Antimicrobial stewardship programs are being introduced in hospitals internationally amidst the problem of escalating antimicrobial resistance. But sustained behavioral change in the area of antibiotic prescribing has been difficult to achieve.
While we have an understanding of doctors’ roles in antibiotic optimization within hospital contexts, the role of hospital management in successes or failures of antimicrobial stewardship programs (and optimization of antibiotics more broadly) has not been explored. Our new study published in the Journal of Hospital Infection examines this very question – the role of the manager as an enabler, or indeed a barrier, to antibiotic optimization.
Researchers in the study performed semistructured interviews with 23 hospital managers at three hospitals in two different states in Australia to specifically examine their opinions on antibiotic resistance, antibiotic governance, and their roles as senior management. The results illustrate how hospital managers prioritize financial pressures and immediate clinical demands over longer-term issues such as antibiotic prescribing and resistance. Here is an example of those pressures, described by one manager:
“I think the problem is [antimicrobial stewardship] in a competitive market. Are the waiting lists more newsworthy than antibiotic prescribing? Absolutely. You get more adverse events happening because of the waiting lists. … So, of course it’s not going to be the [antibiotic] prescribing that comes up to the top of that.” –Departmental Director
The study results also showed how managers find it challenging to comprehend, or act on the basis of, antibiotic-prescribing audits and had little faith in the value of data on antibiotic use and appropriateness. Other clinical areas with more clearly defined targets (and consequences for failing to meet targets) were prioritized over antibiotic prescribing in medical management decision making. Managers also found it difficult to influence the behavior of doctors and thought that it was a clinical responsibility to improve practice. In the words of one:
“I am a believer in delegated accountability and people on the shop floor knowing what they’re doing and being held accountable for it.” – Divisional Director
Managers perceived that there was limited accountability among doctors for antibiotic use and limited education and feedback to doctors:
“Those figures [on suboptimal prescribing] you give me, I haven’t heard them before. So, that in itself is a problem, and I would suggest you’d probably find a large number of medical staff haven’t been exposed to that.”
– Divisional Director
This study was performed in three hospitals with active antimicrobial stewardship programs. In Australia, as is becoming the pattern in countries within the Organisation for Economic Co-operation and Development (OECD), there is a legislative requirement for hospitals to have an effective antimicrobial stewardship program. And yet, meaningful sustained change in antibiotic prescribing is elusive, as evidenced by national antibiotic-prescribing data. The study results raise the important question of who is perceived as responsible for antibiotic-prescribing improvement and the actual and potential role of hospital managers in enacting change. It seems likely that both “top-down” influence (by managers and executive) and “bottom-up” influence (clinician-driven processes) will be required for effective and sustained practice change.
It is also clear from the results of this study that hospital managers do not perceive clear or immediate consequences for failing to improve antibiotic prescribing, and the perceived “distant” threat of antimicrobial resistance is not prioritized among other competing pressures. In addition, the widespread nature of antibiotic use makes it difficult to audit and even more difficult to communicate the extent of the problem.
These data would suggest that to move forward we need to look at an incentive structure for antibiotic-prescribing improvements or consequences in the short term for failing to optimize antibiotic use, and clearly defined goals for antibiotic optimization in hospitals.
Jennifer Broom, MBChB, PhD, is an infectious diseases physician at the Sunshine Coast Hospital and Health Service and an associate professor of medicine at the University of Queensland, Brisbane, Australia. Alex Broom, PhD, is professor of sociology in the School of Social Sciences at the University of New South Wales, Sydney.
Antimicrobial stewardship programs are being introduced in hospitals internationally amidst the problem of escalating antimicrobial resistance. But sustained behavioral change in the area of antibiotic prescribing has been difficult to achieve.
While we have an understanding of doctors’ roles in antibiotic optimization within hospital contexts, the role of hospital management in successes or failures of antimicrobial stewardship programs (and optimization of antibiotics more broadly) has not been explored. Our new study published in the Journal of Hospital Infection examines this very question – the role of the manager as an enabler, or indeed a barrier, to antibiotic optimization.
Researchers in the study performed semistructured interviews with 23 hospital managers at three hospitals in two different states in Australia to specifically examine their opinions on antibiotic resistance, antibiotic governance, and their roles as senior management. The results illustrate how hospital managers prioritize financial pressures and immediate clinical demands over longer-term issues such as antibiotic prescribing and resistance. Here is an example of those pressures, described by one manager:
“I think the problem is [antimicrobial stewardship] in a competitive market. Are the waiting lists more newsworthy than antibiotic prescribing? Absolutely. You get more adverse events happening because of the waiting lists. … So, of course it’s not going to be the [antibiotic] prescribing that comes up to the top of that.” –Departmental Director
The study results also showed how managers find it challenging to comprehend, or act on the basis of, antibiotic-prescribing audits and had little faith in the value of data on antibiotic use and appropriateness. Other clinical areas with more clearly defined targets (and consequences for failing to meet targets) were prioritized over antibiotic prescribing in medical management decision making. Managers also found it difficult to influence the behavior of doctors and thought that it was a clinical responsibility to improve practice. In the words of one:
“I am a believer in delegated accountability and people on the shop floor knowing what they’re doing and being held accountable for it.” – Divisional Director
Managers perceived that there was limited accountability among doctors for antibiotic use and limited education and feedback to doctors:
“Those figures [on suboptimal prescribing] you give me, I haven’t heard them before. So, that in itself is a problem, and I would suggest you’d probably find a large number of medical staff haven’t been exposed to that.”
– Divisional Director
This study was performed in three hospitals with active antimicrobial stewardship programs. In Australia, as is becoming the pattern in countries within the Organisation for Economic Co-operation and Development (OECD), there is a legislative requirement for hospitals to have an effective antimicrobial stewardship program. And yet, meaningful sustained change in antibiotic prescribing is elusive, as evidenced by national antibiotic-prescribing data. The study results raise the important question of who is perceived as responsible for antibiotic-prescribing improvement and the actual and potential role of hospital managers in enacting change. It seems likely that both “top-down” influence (by managers and executive) and “bottom-up” influence (clinician-driven processes) will be required for effective and sustained practice change.
It is also clear from the results of this study that hospital managers do not perceive clear or immediate consequences for failing to improve antibiotic prescribing, and the perceived “distant” threat of antimicrobial resistance is not prioritized among other competing pressures. In addition, the widespread nature of antibiotic use makes it difficult to audit and even more difficult to communicate the extent of the problem.
These data would suggest that to move forward we need to look at an incentive structure for antibiotic-prescribing improvements or consequences in the short term for failing to optimize antibiotic use, and clearly defined goals for antibiotic optimization in hospitals.
Jennifer Broom, MBChB, PhD, is an infectious diseases physician at the Sunshine Coast Hospital and Health Service and an associate professor of medicine at the University of Queensland, Brisbane, Australia. Alex Broom, PhD, is professor of sociology in the School of Social Sciences at the University of New South Wales, Sydney.
Antimicrobial stewardship programs are being introduced in hospitals internationally amidst the problem of escalating antimicrobial resistance. But sustained behavioral change in the area of antibiotic prescribing has been difficult to achieve.
While we have an understanding of doctors’ roles in antibiotic optimization within hospital contexts, the role of hospital management in successes or failures of antimicrobial stewardship programs (and optimization of antibiotics more broadly) has not been explored. Our new study published in the Journal of Hospital Infection examines this very question – the role of the manager as an enabler, or indeed a barrier, to antibiotic optimization.
Researchers in the study performed semistructured interviews with 23 hospital managers at three hospitals in two different states in Australia to specifically examine their opinions on antibiotic resistance, antibiotic governance, and their roles as senior management. The results illustrate how hospital managers prioritize financial pressures and immediate clinical demands over longer-term issues such as antibiotic prescribing and resistance. Here is an example of those pressures, described by one manager:
“I think the problem is [antimicrobial stewardship] in a competitive market. Are the waiting lists more newsworthy than antibiotic prescribing? Absolutely. You get more adverse events happening because of the waiting lists. … So, of course it’s not going to be the [antibiotic] prescribing that comes up to the top of that.” –Departmental Director
The study results also showed how managers find it challenging to comprehend, or act on the basis of, antibiotic-prescribing audits and had little faith in the value of data on antibiotic use and appropriateness. Other clinical areas with more clearly defined targets (and consequences for failing to meet targets) were prioritized over antibiotic prescribing in medical management decision making. Managers also found it difficult to influence the behavior of doctors and thought that it was a clinical responsibility to improve practice. In the words of one:
“I am a believer in delegated accountability and people on the shop floor knowing what they’re doing and being held accountable for it.” – Divisional Director
Managers perceived that there was limited accountability among doctors for antibiotic use and limited education and feedback to doctors:
“Those figures [on suboptimal prescribing] you give me, I haven’t heard them before. So, that in itself is a problem, and I would suggest you’d probably find a large number of medical staff haven’t been exposed to that.”
– Divisional Director
This study was performed in three hospitals with active antimicrobial stewardship programs. In Australia, as is becoming the pattern in countries within the Organisation for Economic Co-operation and Development (OECD), there is a legislative requirement for hospitals to have an effective antimicrobial stewardship program. And yet, meaningful sustained change in antibiotic prescribing is elusive, as evidenced by national antibiotic-prescribing data. The study results raise the important question of who is perceived as responsible for antibiotic-prescribing improvement and the actual and potential role of hospital managers in enacting change. It seems likely that both “top-down” influence (by managers and executive) and “bottom-up” influence (clinician-driven processes) will be required for effective and sustained practice change.
It is also clear from the results of this study that hospital managers do not perceive clear or immediate consequences for failing to improve antibiotic prescribing, and the perceived “distant” threat of antimicrobial resistance is not prioritized among other competing pressures. In addition, the widespread nature of antibiotic use makes it difficult to audit and even more difficult to communicate the extent of the problem.
These data would suggest that to move forward we need to look at an incentive structure for antibiotic-prescribing improvements or consequences in the short term for failing to optimize antibiotic use, and clearly defined goals for antibiotic optimization in hospitals.
Jennifer Broom, MBChB, PhD, is an infectious diseases physician at the Sunshine Coast Hospital and Health Service and an associate professor of medicine at the University of Queensland, Brisbane, Australia. Alex Broom, PhD, is professor of sociology in the School of Social Sciences at the University of New South Wales, Sydney.
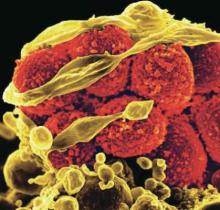
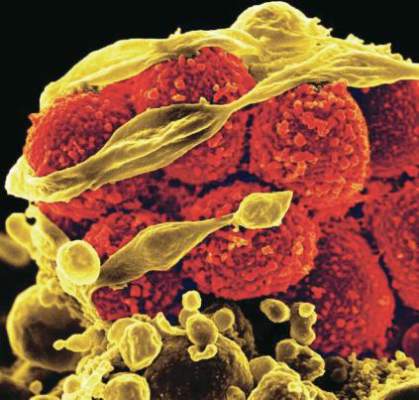
MRSA patients report signs of stigma tied to illness
About half of individuals infected with methicillin-resistant Staphylococcus aureus report feeling stigmatized in interactions with hospital staff, data from a survey of 61 adult patients show.
“Hospital care for people who carry MRSA calls for a dedicated and patient-centered approach in both the way the care is delivered ... as well as the way the care is organized at the institutional level,” wrote Babette Rump, MD, of the Regional Health Service Utrecht region, Zeist, the Netherlands, and her coauthors (J Hosp Infect. 2016. doi: 10.1016/j.jhin.2016.09.010). “Prevention of unnecessary intrusive measures, while as the same time applying appropriate precautionary measures, is key to successful and respectful MRSA management.”
Dr. Rump and her associates set out to identify and quantify stigma tied to MRSA and “explore its association with mental health within a country with a MRSA ‘search and destroy’ policy.” In the Netherlands and Scandinavian countries, this policy includes isolating MRSA carriers, wearing personal protective equipment, and disinfecting the room after patients are discharged (Antimicrob Resist Infect Control. 2014 Jan 15;3[1]3). The U.S. Centers for Disease Control and Prevention, in its 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings, recommends similar methods, including application of infection control precautions during patient care and environmental measures, such as cleaning and disinfection of the patient care environment and dedicated single-patient use of noncritical equipment.
In the current study, 60-item questionnaires were provided to all adult patients at two hospitals and two regional health services who had acquired MRSA between Oct. 1, 2013, and April 1, 2014. Stigma was assessed using the 40-item Berger HIV Stigma Scale, reported Dr. Rump.
Overall, 56% of survey respondents reported stigma, including 14% who reported clear stigma and 42% who reported suggestive stigma. The remaining 44% reported no stigma. A total of 80% of the patients received MRSA eradication treatment, which was strongly associated with higher stigma, the researchers noted.
Written comments provided by 40 patients (68%) along with the questionnaires “offer valuable insights to set the focus for improvement,” the researchers said.
The most frequent comments involved patients’ perceived organizational problems with the hospital (8 patients), lack of staff knowledge (4 patients), as well as little attention paid to patient perspectives (4 patients) and unnecessarily intrusive treatments (3 patients). Also of note, 5 patients blamed and 2 “shamed” the hospital as their source of MRSA.
The results were limited by several factors, including the small study size, the researchers wrote. However, the findings suggest that “a substantial proportion of people that carry MRSA experience signs of stigma and that anticipation on MRSA-associated stigma is warranted,” they said.
The researchers had no financial conflicts to disclose.
About half of individuals infected with methicillin-resistant Staphylococcus aureus report feeling stigmatized in interactions with hospital staff, data from a survey of 61 adult patients show.
“Hospital care for people who carry MRSA calls for a dedicated and patient-centered approach in both the way the care is delivered ... as well as the way the care is organized at the institutional level,” wrote Babette Rump, MD, of the Regional Health Service Utrecht region, Zeist, the Netherlands, and her coauthors (J Hosp Infect. 2016. doi: 10.1016/j.jhin.2016.09.010). “Prevention of unnecessary intrusive measures, while as the same time applying appropriate precautionary measures, is key to successful and respectful MRSA management.”
Dr. Rump and her associates set out to identify and quantify stigma tied to MRSA and “explore its association with mental health within a country with a MRSA ‘search and destroy’ policy.” In the Netherlands and Scandinavian countries, this policy includes isolating MRSA carriers, wearing personal protective equipment, and disinfecting the room after patients are discharged (Antimicrob Resist Infect Control. 2014 Jan 15;3[1]3). The U.S. Centers for Disease Control and Prevention, in its 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings, recommends similar methods, including application of infection control precautions during patient care and environmental measures, such as cleaning and disinfection of the patient care environment and dedicated single-patient use of noncritical equipment.
In the current study, 60-item questionnaires were provided to all adult patients at two hospitals and two regional health services who had acquired MRSA between Oct. 1, 2013, and April 1, 2014. Stigma was assessed using the 40-item Berger HIV Stigma Scale, reported Dr. Rump.
Overall, 56% of survey respondents reported stigma, including 14% who reported clear stigma and 42% who reported suggestive stigma. The remaining 44% reported no stigma. A total of 80% of the patients received MRSA eradication treatment, which was strongly associated with higher stigma, the researchers noted.
Written comments provided by 40 patients (68%) along with the questionnaires “offer valuable insights to set the focus for improvement,” the researchers said.
The most frequent comments involved patients’ perceived organizational problems with the hospital (8 patients), lack of staff knowledge (4 patients), as well as little attention paid to patient perspectives (4 patients) and unnecessarily intrusive treatments (3 patients). Also of note, 5 patients blamed and 2 “shamed” the hospital as their source of MRSA.
The results were limited by several factors, including the small study size, the researchers wrote. However, the findings suggest that “a substantial proportion of people that carry MRSA experience signs of stigma and that anticipation on MRSA-associated stigma is warranted,” they said.
The researchers had no financial conflicts to disclose.
About half of individuals infected with methicillin-resistant Staphylococcus aureus report feeling stigmatized in interactions with hospital staff, data from a survey of 61 adult patients show.
“Hospital care for people who carry MRSA calls for a dedicated and patient-centered approach in both the way the care is delivered ... as well as the way the care is organized at the institutional level,” wrote Babette Rump, MD, of the Regional Health Service Utrecht region, Zeist, the Netherlands, and her coauthors (J Hosp Infect. 2016. doi: 10.1016/j.jhin.2016.09.010). “Prevention of unnecessary intrusive measures, while as the same time applying appropriate precautionary measures, is key to successful and respectful MRSA management.”
Dr. Rump and her associates set out to identify and quantify stigma tied to MRSA and “explore its association with mental health within a country with a MRSA ‘search and destroy’ policy.” In the Netherlands and Scandinavian countries, this policy includes isolating MRSA carriers, wearing personal protective equipment, and disinfecting the room after patients are discharged (Antimicrob Resist Infect Control. 2014 Jan 15;3[1]3). The U.S. Centers for Disease Control and Prevention, in its 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings, recommends similar methods, including application of infection control precautions during patient care and environmental measures, such as cleaning and disinfection of the patient care environment and dedicated single-patient use of noncritical equipment.
In the current study, 60-item questionnaires were provided to all adult patients at two hospitals and two regional health services who had acquired MRSA between Oct. 1, 2013, and April 1, 2014. Stigma was assessed using the 40-item Berger HIV Stigma Scale, reported Dr. Rump.
Overall, 56% of survey respondents reported stigma, including 14% who reported clear stigma and 42% who reported suggestive stigma. The remaining 44% reported no stigma. A total of 80% of the patients received MRSA eradication treatment, which was strongly associated with higher stigma, the researchers noted.
Written comments provided by 40 patients (68%) along with the questionnaires “offer valuable insights to set the focus for improvement,” the researchers said.
The most frequent comments involved patients’ perceived organizational problems with the hospital (8 patients), lack of staff knowledge (4 patients), as well as little attention paid to patient perspectives (4 patients) and unnecessarily intrusive treatments (3 patients). Also of note, 5 patients blamed and 2 “shamed” the hospital as their source of MRSA.
The results were limited by several factors, including the small study size, the researchers wrote. However, the findings suggest that “a substantial proportion of people that carry MRSA experience signs of stigma and that anticipation on MRSA-associated stigma is warranted,” they said.
The researchers had no financial conflicts to disclose.
FROM THE JOURNAL OF HOSPITAL INFECTION
Key clinical point: Adults with methicillin-resistant Staphylococcus aureus (MRSA) are susceptible to stigma.
Major finding: Approximately half (56%) of adults being treated for MRSA reported stigma associated with their illness.
Data source: A cross-sectional study including 61 adults with MRSA.
Disclosures: The researchers had no financial conflicts to disclose.
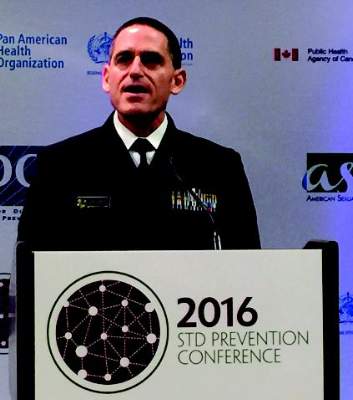
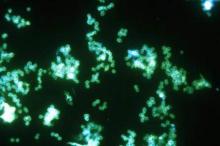
Gonorrhea cluster shows increased antibiotic resistance
ATLANTA – A cluster of gonorrhea cases from the state of Hawaii has been identified as the first in the United States to show decreased susceptibility to ceftriaxone and azithromycin, the two most commonly prescribed drugs used to treat the infection.
“We’re seeing new, troubling signs that our current gonorrhea treatment is losing its effectiveness [but] we’ve not seen a treatment failure in the U.S.,” explained Jonathan Mermin, MD, director of the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, during a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
Isolates were collected from seven individuals in Hawaii during April and May of this year, all of which showed “dramatically higher levels” of resistance to azithromycin in laboratory testing than has normally been seen in the U.S. While large-scale resistance to azithromycin is something the CDC has watched for several months, four of these seven isolates also demonstrated less vulnerability to ceftriaxone, the first time that has occurred. Since 2010, the recommended treatment for gonorrhea has consisted of a single ceftriaxone shot and an oral dose of azithromycin; having a cluster with increased resistance to both is problematic on several levels, infectious disease experts say.
According to Alan Katz, MD, of the University of Hawaii in Honolulu, “the state of Hawaii has been a seminal site for monitoring Neisseria gonorrhoeae resistance, and the Hawaii state Department of Health has been one of the original CDC gonococcal isolate surveillance program surveillance sites since its inception in 1986.” Hawaii typically sees more gonorrhea cases than the rest of the country, partially due its location between the U.S. and Asia, the latter of which Dr. Katz explained is “where we believe many [drug]-resistant strains originate.”
Currently, trials are underway to identify a new treatment that can replace the current regimen, with promising early results. The drug in question, known as ETX0914, is a single-dose oral therapy that would substitute for ceftriaxone in the currently recommended treatment protocol. Stephanie N. Taylor, MD, of Louisiana State University in New Orleans, shared results of a randomized controlled trial, in which 179 subjects – 167 males and 12 females – received either 2g or 3g doses of only ETX0914, or only ceftriaxone.
A total of 47 subjects received the 3g ETX0914 dose, while 49 subjects received the 2g dose, and the rest received ceftriaxone. All patients (47/47) receiving the 3g dose were cured, and 98% (48/49) in the 2g dose were cured, with only 21 subjects (12%) in the entire study population reporting mild side effects.
“We are very pleased with these results and look forward to seeing ETX0914 advance through additional clinical trials,” Dr. Taylor said in a statement.
For now, health care providers are encouraged to continue with the currently recommended drug therapy, which is still effective. In a statement, Gail Bolan, MD, director of the Division of STD Prevention at the CDC, reminded providers that infections should be treated immediately in order for the drugs to have their full impact.
“All health care providers should also promptly report any suspected treatment failure to local health officials and CDC to ensure rapid response to cases or clusters of concern,” she added.
ATLANTA – A cluster of gonorrhea cases from the state of Hawaii has been identified as the first in the United States to show decreased susceptibility to ceftriaxone and azithromycin, the two most commonly prescribed drugs used to treat the infection.
“We’re seeing new, troubling signs that our current gonorrhea treatment is losing its effectiveness [but] we’ve not seen a treatment failure in the U.S.,” explained Jonathan Mermin, MD, director of the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, during a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
Isolates were collected from seven individuals in Hawaii during April and May of this year, all of which showed “dramatically higher levels” of resistance to azithromycin in laboratory testing than has normally been seen in the U.S. While large-scale resistance to azithromycin is something the CDC has watched for several months, four of these seven isolates also demonstrated less vulnerability to ceftriaxone, the first time that has occurred. Since 2010, the recommended treatment for gonorrhea has consisted of a single ceftriaxone shot and an oral dose of azithromycin; having a cluster with increased resistance to both is problematic on several levels, infectious disease experts say.
According to Alan Katz, MD, of the University of Hawaii in Honolulu, “the state of Hawaii has been a seminal site for monitoring Neisseria gonorrhoeae resistance, and the Hawaii state Department of Health has been one of the original CDC gonococcal isolate surveillance program surveillance sites since its inception in 1986.” Hawaii typically sees more gonorrhea cases than the rest of the country, partially due its location between the U.S. and Asia, the latter of which Dr. Katz explained is “where we believe many [drug]-resistant strains originate.”
Currently, trials are underway to identify a new treatment that can replace the current regimen, with promising early results. The drug in question, known as ETX0914, is a single-dose oral therapy that would substitute for ceftriaxone in the currently recommended treatment protocol. Stephanie N. Taylor, MD, of Louisiana State University in New Orleans, shared results of a randomized controlled trial, in which 179 subjects – 167 males and 12 females – received either 2g or 3g doses of only ETX0914, or only ceftriaxone.
A total of 47 subjects received the 3g ETX0914 dose, while 49 subjects received the 2g dose, and the rest received ceftriaxone. All patients (47/47) receiving the 3g dose were cured, and 98% (48/49) in the 2g dose were cured, with only 21 subjects (12%) in the entire study population reporting mild side effects.
“We are very pleased with these results and look forward to seeing ETX0914 advance through additional clinical trials,” Dr. Taylor said in a statement.
For now, health care providers are encouraged to continue with the currently recommended drug therapy, which is still effective. In a statement, Gail Bolan, MD, director of the Division of STD Prevention at the CDC, reminded providers that infections should be treated immediately in order for the drugs to have their full impact.
“All health care providers should also promptly report any suspected treatment failure to local health officials and CDC to ensure rapid response to cases or clusters of concern,” she added.
ATLANTA – A cluster of gonorrhea cases from the state of Hawaii has been identified as the first in the United States to show decreased susceptibility to ceftriaxone and azithromycin, the two most commonly prescribed drugs used to treat the infection.
“We’re seeing new, troubling signs that our current gonorrhea treatment is losing its effectiveness [but] we’ve not seen a treatment failure in the U.S.,” explained Jonathan Mermin, MD, director of the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, during a conference on STD prevention sponsored by the Centers for Disease Control and Prevention.
Isolates were collected from seven individuals in Hawaii during April and May of this year, all of which showed “dramatically higher levels” of resistance to azithromycin in laboratory testing than has normally been seen in the U.S. While large-scale resistance to azithromycin is something the CDC has watched for several months, four of these seven isolates also demonstrated less vulnerability to ceftriaxone, the first time that has occurred. Since 2010, the recommended treatment for gonorrhea has consisted of a single ceftriaxone shot and an oral dose of azithromycin; having a cluster with increased resistance to both is problematic on several levels, infectious disease experts say.
According to Alan Katz, MD, of the University of Hawaii in Honolulu, “the state of Hawaii has been a seminal site for monitoring Neisseria gonorrhoeae resistance, and the Hawaii state Department of Health has been one of the original CDC gonococcal isolate surveillance program surveillance sites since its inception in 1986.” Hawaii typically sees more gonorrhea cases than the rest of the country, partially due its location between the U.S. and Asia, the latter of which Dr. Katz explained is “where we believe many [drug]-resistant strains originate.”
Currently, trials are underway to identify a new treatment that can replace the current regimen, with promising early results. The drug in question, known as ETX0914, is a single-dose oral therapy that would substitute for ceftriaxone in the currently recommended treatment protocol. Stephanie N. Taylor, MD, of Louisiana State University in New Orleans, shared results of a randomized controlled trial, in which 179 subjects – 167 males and 12 females – received either 2g or 3g doses of only ETX0914, or only ceftriaxone.
A total of 47 subjects received the 3g ETX0914 dose, while 49 subjects received the 2g dose, and the rest received ceftriaxone. All patients (47/47) receiving the 3g dose were cured, and 98% (48/49) in the 2g dose were cured, with only 21 subjects (12%) in the entire study population reporting mild side effects.
“We are very pleased with these results and look forward to seeing ETX0914 advance through additional clinical trials,” Dr. Taylor said in a statement.
For now, health care providers are encouraged to continue with the currently recommended drug therapy, which is still effective. In a statement, Gail Bolan, MD, director of the Division of STD Prevention at the CDC, reminded providers that infections should be treated immediately in order for the drugs to have their full impact.
“All health care providers should also promptly report any suspected treatment failure to local health officials and CDC to ensure rapid response to cases or clusters of concern,” she added.
AT THE 2016 STD PREVENTION CONFERENCE
Update on the third international consensus definitions for sepsis and septic shock
Sepsis is the primary cause of death from infection. Early identification and treatment of sepsis is important in improving patient outcomes. The consensus conference sought to differentiate sepsis, which is defined as “life-threatening organ dysfunction caused by a dysregulated host response to infection” from uncomplicated infection.
Sepsis was last classified in a 2001 guideline that based its definition on the presence of two or more systemic inflammatory response syndrome (SIRS) criteria, which included an elevated temperature, heart rate higher than 90 bpm, respiratory rate higher than 20 breaths per minute, and a white blood cell count greater than greater than 12,000 mcL or less than 4,000 mcL or greater than 10% immature bands.
The problem with the SIRS definition of sepsis is that while it reflects a response to infection, it does not sufficiently distinguish between individuals with infections and those with a dysregulated response that leads to a poor prognosis, which is the definition of sepsis. The current consensus conference redefines sepsis with a more direct emphasis on organ dysfunction, as this is the aspect of sepsis that is most clearly linked to patient outcomes.
In the consensus conference document, sepsis is defined as a “life-threatening organ dysfunction caused by a dysregulated host response to infection.” The guidelines recommend using the quick version of the sequential (sepsis-related) organ failure assessment score (qSOFA) to identify patients with sepsis. In its long form, the SOFA used seven clinical and laboratory data points for completion, and is best suited to use in an intensive care setting where detailed data are available. The qSOFA score has only three criteria and by being easier to use can aid in rapid identification of sepsis and the patients most likely to deteriorate from sepsis.
The qSOFA criteria predict poor outcome in patients with infection who have two or more of the following: respiratory rate greater than or equal to 22 breaths/min, new or worsened altered mentation, or systolic blood pressure less than or equal to 100 mm Hg. Unlike the full SOFA score, the qSOFA does not require any laboratory testing and so can be performed in the office or bedside on a hospital floor. The qSOFA does not necessarily define sepsis, rather it identifies patients at a higher risk of hospital death or prolonged ICU stay. The consensus conference suggests that “qSOFA criteria be used to prompt clinicians to further investigate for organ dysfunction, initiate or escalate therapy as appropriate, and consider referral to critical care or increase the frequency of monitoring, if such actions have not already been undertaken.” The task force suggested that the qSOFA score may be a helpful adjunct to best clinical judgment for identifying patients who might benefit from a higher level of care.
Septic shock is defined as a subset of sepsis in which profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk for death than sepsis alone. Septic shock can be identified when, after adequate fluid resuscitation, the patient requires vasopressor therapy to maintain mean arterial pressure of at least 65 mm Hg and has a serum lactate level greater than 2 mmol/L.
Once sepsis is suspected, prompt therapy needs to be started as per the Surviving Sepsis Campaign Guidelines. The qSOFA criteria can be used to identify patients at high risk for morbidity and mortality. Within 3 hours, a lactate level should be obtained as well as blood cultures from two separate sites drawn prior to administration of antibiotics (but do not delay antibiotic administration). Empiric broad-spectrum antibiotics should be given within 45 minutes of the identification of sepsis. Antibiotic choice will vary per clinician/institution preference, but should likely include coverage for Pseudomonas and MRSA (piperacillin/tazobactam and vancomycin, for example). Antibiotics should be reassessed daily for de-escalation. Administer 30 mL/kg crystalloid for hypotension or lactate greater than or equal to 4 mmol/L. Within 6 hours, vasopressors should be given for hypotension that does not respond to initial fluid resuscitation to maintain a mean arterial pressure (MAP) of at least 65mm Hg. In the event of persistent hypotension after initial fluid administration (MAP under 65 mm Hg) or if initial lactate was greater than or equal to 4 mmol/L, volume status and tissue perfusion should be reassessed and lactate should be rechecked if it was initially elevated.
The bottom line
A 2016 international task force recommended that the definition of sepsis should be changed to emphasize organ dysfunction rather than a systemic inflammatory response. Use of the qSOFA score, which relies only on clinically observable data rather than laboratory evaluation, is recommended to identify patients at high risk for morbidity and mortality. Early recognition of sepsis and evaluation with qSOFT should facilitate early treatment and improve survival.
References
Singer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) FRCP; JAMA. 2016;315[8]:801-10. doi: 10.1001/jama.2016.0287.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003 Apr;31(4):1250-6.
Singer M, Deutschman CS, Seymour C, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016 Feb 23;315(8):801-10.
Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004 Mar;32(3):858-73.
Dr. Mills is assistant residency program director and assistant professor in the department of family and community medicine and department of physiology at Sidney Kimmel Medical College at Thomas Jefferson University. Dr. Botti is a second-year resident in the family medicine residency program department of family and community medicine at Sidney Kimmel Medical College at Thomas Jefferson University. Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia.
Sepsis is the primary cause of death from infection. Early identification and treatment of sepsis is important in improving patient outcomes. The consensus conference sought to differentiate sepsis, which is defined as “life-threatening organ dysfunction caused by a dysregulated host response to infection” from uncomplicated infection.
Sepsis was last classified in a 2001 guideline that based its definition on the presence of two or more systemic inflammatory response syndrome (SIRS) criteria, which included an elevated temperature, heart rate higher than 90 bpm, respiratory rate higher than 20 breaths per minute, and a white blood cell count greater than greater than 12,000 mcL or less than 4,000 mcL or greater than 10% immature bands.
The problem with the SIRS definition of sepsis is that while it reflects a response to infection, it does not sufficiently distinguish between individuals with infections and those with a dysregulated response that leads to a poor prognosis, which is the definition of sepsis. The current consensus conference redefines sepsis with a more direct emphasis on organ dysfunction, as this is the aspect of sepsis that is most clearly linked to patient outcomes.
In the consensus conference document, sepsis is defined as a “life-threatening organ dysfunction caused by a dysregulated host response to infection.” The guidelines recommend using the quick version of the sequential (sepsis-related) organ failure assessment score (qSOFA) to identify patients with sepsis. In its long form, the SOFA used seven clinical and laboratory data points for completion, and is best suited to use in an intensive care setting where detailed data are available. The qSOFA score has only three criteria and by being easier to use can aid in rapid identification of sepsis and the patients most likely to deteriorate from sepsis.
The qSOFA criteria predict poor outcome in patients with infection who have two or more of the following: respiratory rate greater than or equal to 22 breaths/min, new or worsened altered mentation, or systolic blood pressure less than or equal to 100 mm Hg. Unlike the full SOFA score, the qSOFA does not require any laboratory testing and so can be performed in the office or bedside on a hospital floor. The qSOFA does not necessarily define sepsis, rather it identifies patients at a higher risk of hospital death or prolonged ICU stay. The consensus conference suggests that “qSOFA criteria be used to prompt clinicians to further investigate for organ dysfunction, initiate or escalate therapy as appropriate, and consider referral to critical care or increase the frequency of monitoring, if such actions have not already been undertaken.” The task force suggested that the qSOFA score may be a helpful adjunct to best clinical judgment for identifying patients who might benefit from a higher level of care.
Septic shock is defined as a subset of sepsis in which profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk for death than sepsis alone. Septic shock can be identified when, after adequate fluid resuscitation, the patient requires vasopressor therapy to maintain mean arterial pressure of at least 65 mm Hg and has a serum lactate level greater than 2 mmol/L.
Once sepsis is suspected, prompt therapy needs to be started as per the Surviving Sepsis Campaign Guidelines. The qSOFA criteria can be used to identify patients at high risk for morbidity and mortality. Within 3 hours, a lactate level should be obtained as well as blood cultures from two separate sites drawn prior to administration of antibiotics (but do not delay antibiotic administration). Empiric broad-spectrum antibiotics should be given within 45 minutes of the identification of sepsis. Antibiotic choice will vary per clinician/institution preference, but should likely include coverage for Pseudomonas and MRSA (piperacillin/tazobactam and vancomycin, for example). Antibiotics should be reassessed daily for de-escalation. Administer 30 mL/kg crystalloid for hypotension or lactate greater than or equal to 4 mmol/L. Within 6 hours, vasopressors should be given for hypotension that does not respond to initial fluid resuscitation to maintain a mean arterial pressure (MAP) of at least 65mm Hg. In the event of persistent hypotension after initial fluid administration (MAP under 65 mm Hg) or if initial lactate was greater than or equal to 4 mmol/L, volume status and tissue perfusion should be reassessed and lactate should be rechecked if it was initially elevated.
The bottom line
A 2016 international task force recommended that the definition of sepsis should be changed to emphasize organ dysfunction rather than a systemic inflammatory response. Use of the qSOFA score, which relies only on clinically observable data rather than laboratory evaluation, is recommended to identify patients at high risk for morbidity and mortality. Early recognition of sepsis and evaluation with qSOFT should facilitate early treatment and improve survival.
References
Singer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) FRCP; JAMA. 2016;315[8]:801-10. doi: 10.1001/jama.2016.0287.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003 Apr;31(4):1250-6.
Singer M, Deutschman CS, Seymour C, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016 Feb 23;315(8):801-10.
Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004 Mar;32(3):858-73.
Dr. Mills is assistant residency program director and assistant professor in the department of family and community medicine and department of physiology at Sidney Kimmel Medical College at Thomas Jefferson University. Dr. Botti is a second-year resident in the family medicine residency program department of family and community medicine at Sidney Kimmel Medical College at Thomas Jefferson University. Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia.
Sepsis is the primary cause of death from infection. Early identification and treatment of sepsis is important in improving patient outcomes. The consensus conference sought to differentiate sepsis, which is defined as “life-threatening organ dysfunction caused by a dysregulated host response to infection” from uncomplicated infection.
Sepsis was last classified in a 2001 guideline that based its definition on the presence of two or more systemic inflammatory response syndrome (SIRS) criteria, which included an elevated temperature, heart rate higher than 90 bpm, respiratory rate higher than 20 breaths per minute, and a white blood cell count greater than greater than 12,000 mcL or less than 4,000 mcL or greater than 10% immature bands.
The problem with the SIRS definition of sepsis is that while it reflects a response to infection, it does not sufficiently distinguish between individuals with infections and those with a dysregulated response that leads to a poor prognosis, which is the definition of sepsis. The current consensus conference redefines sepsis with a more direct emphasis on organ dysfunction, as this is the aspect of sepsis that is most clearly linked to patient outcomes.
In the consensus conference document, sepsis is defined as a “life-threatening organ dysfunction caused by a dysregulated host response to infection.” The guidelines recommend using the quick version of the sequential (sepsis-related) organ failure assessment score (qSOFA) to identify patients with sepsis. In its long form, the SOFA used seven clinical and laboratory data points for completion, and is best suited to use in an intensive care setting where detailed data are available. The qSOFA score has only three criteria and by being easier to use can aid in rapid identification of sepsis and the patients most likely to deteriorate from sepsis.
The qSOFA criteria predict poor outcome in patients with infection who have two or more of the following: respiratory rate greater than or equal to 22 breaths/min, new or worsened altered mentation, or systolic blood pressure less than or equal to 100 mm Hg. Unlike the full SOFA score, the qSOFA does not require any laboratory testing and so can be performed in the office or bedside on a hospital floor. The qSOFA does not necessarily define sepsis, rather it identifies patients at a higher risk of hospital death or prolonged ICU stay. The consensus conference suggests that “qSOFA criteria be used to prompt clinicians to further investigate for organ dysfunction, initiate or escalate therapy as appropriate, and consider referral to critical care or increase the frequency of monitoring, if such actions have not already been undertaken.” The task force suggested that the qSOFA score may be a helpful adjunct to best clinical judgment for identifying patients who might benefit from a higher level of care.
Septic shock is defined as a subset of sepsis in which profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk for death than sepsis alone. Septic shock can be identified when, after adequate fluid resuscitation, the patient requires vasopressor therapy to maintain mean arterial pressure of at least 65 mm Hg and has a serum lactate level greater than 2 mmol/L.
Once sepsis is suspected, prompt therapy needs to be started as per the Surviving Sepsis Campaign Guidelines. The qSOFA criteria can be used to identify patients at high risk for morbidity and mortality. Within 3 hours, a lactate level should be obtained as well as blood cultures from two separate sites drawn prior to administration of antibiotics (but do not delay antibiotic administration). Empiric broad-spectrum antibiotics should be given within 45 minutes of the identification of sepsis. Antibiotic choice will vary per clinician/institution preference, but should likely include coverage for Pseudomonas and MRSA (piperacillin/tazobactam and vancomycin, for example). Antibiotics should be reassessed daily for de-escalation. Administer 30 mL/kg crystalloid for hypotension or lactate greater than or equal to 4 mmol/L. Within 6 hours, vasopressors should be given for hypotension that does not respond to initial fluid resuscitation to maintain a mean arterial pressure (MAP) of at least 65mm Hg. In the event of persistent hypotension after initial fluid administration (MAP under 65 mm Hg) or if initial lactate was greater than or equal to 4 mmol/L, volume status and tissue perfusion should be reassessed and lactate should be rechecked if it was initially elevated.
The bottom line
A 2016 international task force recommended that the definition of sepsis should be changed to emphasize organ dysfunction rather than a systemic inflammatory response. Use of the qSOFA score, which relies only on clinically observable data rather than laboratory evaluation, is recommended to identify patients at high risk for morbidity and mortality. Early recognition of sepsis and evaluation with qSOFT should facilitate early treatment and improve survival.
References
Singer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) FRCP; JAMA. 2016;315[8]:801-10. doi: 10.1001/jama.2016.0287.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003 Apr;31(4):1250-6.
Singer M, Deutschman CS, Seymour C, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016 Feb 23;315(8):801-10.
Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004 Mar;32(3):858-73.
Dr. Mills is assistant residency program director and assistant professor in the department of family and community medicine and department of physiology at Sidney Kimmel Medical College at Thomas Jefferson University. Dr. Botti is a second-year resident in the family medicine residency program department of family and community medicine at Sidney Kimmel Medical College at Thomas Jefferson University. Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia.
Checklist may prompt cuts in unneeded antibiotic prescriptions
Primary care practitioners’ use of a seven-item checklist may reduce the number of pediatric patients with respiratory tract infections who are prescribed unnecessary antibiotics, a prognostic cohort study suggests.
The study revealed short illness (a duration of illness of 3 days or less), temperature (a body temperature of 37.8°C or greater at presentation), age (being under 2 years), intercostal or subcostal recession, wheeze on auscultation, asthma, and vomiting (moderate or severe in the previous 24 hours) were each independently associated with hospital admission (P less than .01 for all associations).
The checklist includes these seven characteristics or risk variables (short illness, temperature, age, recession, wheeze, asthma, and vomiting [mnemonic STARWAVe]). To use the checklist, a primary care practitioner would assign one point for the presence of each item in a patient then add up all of the points to determine that patient’s risk level for future hospital admission for respiratory tract infection. A score of 1 point or less, observed in 5,593 (67%) cases would be considered indicative of a very low rate of risk for hospitalization (0.3%, 0.2%-0.4%). A score of 2 or 3 points, found for 2,520 (30%) children, would be considered as a normal level of risk (1.5%, 1.0%-1.9%), and a score of 4 or more points, seen in 204 (3%) children, would signify a high risk level (11.8%, 7.3%-16.2%).
Of the 8,394 children assessed, 78 (0.9%; 95% confidence interval, 0.7%-1.2%) were admitted to a hospital. Most were admitted on days 2-7 (33, 42%) and on days 8-30 (30, 39%) following recruitment. Only 15 (19%) were admitted on the day of recruitment (day 1).
“Many clinicians report that they prescribe antibiotics just in case, to mitigate perceived risk of future hospital admission and complications, and that failing to provide a prescription for a child who subsequently becomes seriously unwell is professionally unacceptable. If primary care clinicians could identify children at low (or very low) risk of such future complications, the reduced clinical uncertainty could lead to a reduced use of antibiotics in these groups of patients,” wrote first author Alastair Hay, MD, from the Centre for Academic Primary Care in the School of Social and Community Medicine at the University of Bristol (England), and his colleagues.
These researchers conducted the study based on a structured, blinded review of the medical records from children aged between 3 months and 16 years presenting with acute cough (less than or equal to 28 days) and respiratory tract infection treated by 519 general practitioners in 247 practices in England between July 2011 and June 2013. The primary study outcome was hospital admission for respiratory tract infection within 30 days.
Additionally, a multivariable model was employed to detect factors associated with increased risk of hospital admission. As measured by receiver operating characteristic curve analysis, the accuracy of the STARWAVe score checklist in predicting risk groups and associated risk of hospitalization was found to be high (0.81; 95% CI, 0.77-0.86). The suggested probability of hospital admission for children who did not have any of the seven characteristics included in the checklist was found to be exceptionally low (0.14%).
Significantly associated parent-reported variables included both moderate or severe vomiting and severe fever, each in the previous 24 hours. Significant clinician-reported variables included intercostal or subcostal recession and wheeze on auscultation.
“The main value of our results is to reduce clinical uncertainty and antibiotic use in children least likely to benefit from them, namely those at very low risk of future hospital admission,” Dr. Hay and his associates noted in The Lancet Respiratory Medicine (Lancet Respir Med. 2016 Sep 1. doi: 10.1016/S2213-2600(16)30223-5).
Funding for this study was provided by the National Institute for Health Research and sponsored by the University of Bristol. Only one of the study’s authors, Dr. Peter Muir, reported ties to industry sources.
There are few efficacious interventions for respiratory tract infection available to primary care clinicians beyond offering reassurance and self-management advice, so the modest benefit offered by antibiotics can persuade general practitioners to prescribe them.
To derive (and validate) a clinical prediction rule to improve targeted antibiotic prescribing in children with respiratory tract infections, Hay et al determined the seven characteristics independently associated (P less than .01 for all associations) with hospital admission for children presenting to primary care physicians with cough and respiratory tract infection (STARWAVe). Using this seven-item checklist to help structure point-of-care assessment for this patient population should predict the risk of hospital admission with remarkable accuracy (area under the received operating characteristic curve, 0.81; 95% CI, 0.76-0.85).
STARWAVe offers primary care clinicians an evidence-based practical tool to help guide antibiotic prescription decisions and, through shared decision-making, has the potential to reduce antibiotic prescription based on prognostic uncertainty or on nonmedical grounds.
If STARWAVe leads to an increase in antibiotic prescription (to 90%) in high-risk children and a parallel halving of prescription to those at low risk of hospital admission, it could achieve a 10% overall reduction in primary care antibiotic prescriptions for respiratory tract infections.
These comments are excerpted from a commentary by Dr. Christopher C. Winchester from Oxford PharmaGenesis and Durham University (England), Alison Chisholm, MSc, from the Respiratory Effectiveness Group in Cambridge (England), and Dr. David Price from the University of Aberdeen (Scotland) and the Observational and Pragmatic Research Institute in Singapore. Dr. Winchester and Dr. Price disclosed financial relationships with numerous industry sources; Ms. Chisholm indicated no financial relationships relevant to this article. Funded information was not provided. (Lancet Respir Med. 2016 Sep 1. doi: 10.1016/S2213-2600(16)30272-7).
There are few efficacious interventions for respiratory tract infection available to primary care clinicians beyond offering reassurance and self-management advice, so the modest benefit offered by antibiotics can persuade general practitioners to prescribe them.
To derive (and validate) a clinical prediction rule to improve targeted antibiotic prescribing in children with respiratory tract infections, Hay et al determined the seven characteristics independently associated (P less than .01 for all associations) with hospital admission for children presenting to primary care physicians with cough and respiratory tract infection (STARWAVe). Using this seven-item checklist to help structure point-of-care assessment for this patient population should predict the risk of hospital admission with remarkable accuracy (area under the received operating characteristic curve, 0.81; 95% CI, 0.76-0.85).
STARWAVe offers primary care clinicians an evidence-based practical tool to help guide antibiotic prescription decisions and, through shared decision-making, has the potential to reduce antibiotic prescription based on prognostic uncertainty or on nonmedical grounds.
If STARWAVe leads to an increase in antibiotic prescription (to 90%) in high-risk children and a parallel halving of prescription to those at low risk of hospital admission, it could achieve a 10% overall reduction in primary care antibiotic prescriptions for respiratory tract infections.
These comments are excerpted from a commentary by Dr. Christopher C. Winchester from Oxford PharmaGenesis and Durham University (England), Alison Chisholm, MSc, from the Respiratory Effectiveness Group in Cambridge (England), and Dr. David Price from the University of Aberdeen (Scotland) and the Observational and Pragmatic Research Institute in Singapore. Dr. Winchester and Dr. Price disclosed financial relationships with numerous industry sources; Ms. Chisholm indicated no financial relationships relevant to this article. Funded information was not provided. (Lancet Respir Med. 2016 Sep 1. doi: 10.1016/S2213-2600(16)30272-7).
There are few efficacious interventions for respiratory tract infection available to primary care clinicians beyond offering reassurance and self-management advice, so the modest benefit offered by antibiotics can persuade general practitioners to prescribe them.
To derive (and validate) a clinical prediction rule to improve targeted antibiotic prescribing in children with respiratory tract infections, Hay et al determined the seven characteristics independently associated (P less than .01 for all associations) with hospital admission for children presenting to primary care physicians with cough and respiratory tract infection (STARWAVe). Using this seven-item checklist to help structure point-of-care assessment for this patient population should predict the risk of hospital admission with remarkable accuracy (area under the received operating characteristic curve, 0.81; 95% CI, 0.76-0.85).
STARWAVe offers primary care clinicians an evidence-based practical tool to help guide antibiotic prescription decisions and, through shared decision-making, has the potential to reduce antibiotic prescription based on prognostic uncertainty or on nonmedical grounds.
If STARWAVe leads to an increase in antibiotic prescription (to 90%) in high-risk children and a parallel halving of prescription to those at low risk of hospital admission, it could achieve a 10% overall reduction in primary care antibiotic prescriptions for respiratory tract infections.
These comments are excerpted from a commentary by Dr. Christopher C. Winchester from Oxford PharmaGenesis and Durham University (England), Alison Chisholm, MSc, from the Respiratory Effectiveness Group in Cambridge (England), and Dr. David Price from the University of Aberdeen (Scotland) and the Observational and Pragmatic Research Institute in Singapore. Dr. Winchester and Dr. Price disclosed financial relationships with numerous industry sources; Ms. Chisholm indicated no financial relationships relevant to this article. Funded information was not provided. (Lancet Respir Med. 2016 Sep 1. doi: 10.1016/S2213-2600(16)30272-7).
Primary care practitioners’ use of a seven-item checklist may reduce the number of pediatric patients with respiratory tract infections who are prescribed unnecessary antibiotics, a prognostic cohort study suggests.
The study revealed short illness (a duration of illness of 3 days or less), temperature (a body temperature of 37.8°C or greater at presentation), age (being under 2 years), intercostal or subcostal recession, wheeze on auscultation, asthma, and vomiting (moderate or severe in the previous 24 hours) were each independently associated with hospital admission (P less than .01 for all associations).
The checklist includes these seven characteristics or risk variables (short illness, temperature, age, recession, wheeze, asthma, and vomiting [mnemonic STARWAVe]). To use the checklist, a primary care practitioner would assign one point for the presence of each item in a patient then add up all of the points to determine that patient’s risk level for future hospital admission for respiratory tract infection. A score of 1 point or less, observed in 5,593 (67%) cases would be considered indicative of a very low rate of risk for hospitalization (0.3%, 0.2%-0.4%). A score of 2 or 3 points, found for 2,520 (30%) children, would be considered as a normal level of risk (1.5%, 1.0%-1.9%), and a score of 4 or more points, seen in 204 (3%) children, would signify a high risk level (11.8%, 7.3%-16.2%).
Of the 8,394 children assessed, 78 (0.9%; 95% confidence interval, 0.7%-1.2%) were admitted to a hospital. Most were admitted on days 2-7 (33, 42%) and on days 8-30 (30, 39%) following recruitment. Only 15 (19%) were admitted on the day of recruitment (day 1).
“Many clinicians report that they prescribe antibiotics just in case, to mitigate perceived risk of future hospital admission and complications, and that failing to provide a prescription for a child who subsequently becomes seriously unwell is professionally unacceptable. If primary care clinicians could identify children at low (or very low) risk of such future complications, the reduced clinical uncertainty could lead to a reduced use of antibiotics in these groups of patients,” wrote first author Alastair Hay, MD, from the Centre for Academic Primary Care in the School of Social and Community Medicine at the University of Bristol (England), and his colleagues.
These researchers conducted the study based on a structured, blinded review of the medical records from children aged between 3 months and 16 years presenting with acute cough (less than or equal to 28 days) and respiratory tract infection treated by 519 general practitioners in 247 practices in England between July 2011 and June 2013. The primary study outcome was hospital admission for respiratory tract infection within 30 days.
Additionally, a multivariable model was employed to detect factors associated with increased risk of hospital admission. As measured by receiver operating characteristic curve analysis, the accuracy of the STARWAVe score checklist in predicting risk groups and associated risk of hospitalization was found to be high (0.81; 95% CI, 0.77-0.86). The suggested probability of hospital admission for children who did not have any of the seven characteristics included in the checklist was found to be exceptionally low (0.14%).
Significantly associated parent-reported variables included both moderate or severe vomiting and severe fever, each in the previous 24 hours. Significant clinician-reported variables included intercostal or subcostal recession and wheeze on auscultation.
“The main value of our results is to reduce clinical uncertainty and antibiotic use in children least likely to benefit from them, namely those at very low risk of future hospital admission,” Dr. Hay and his associates noted in The Lancet Respiratory Medicine (Lancet Respir Med. 2016 Sep 1. doi: 10.1016/S2213-2600(16)30223-5).
Funding for this study was provided by the National Institute for Health Research and sponsored by the University of Bristol. Only one of the study’s authors, Dr. Peter Muir, reported ties to industry sources.
Primary care practitioners’ use of a seven-item checklist may reduce the number of pediatric patients with respiratory tract infections who are prescribed unnecessary antibiotics, a prognostic cohort study suggests.
The study revealed short illness (a duration of illness of 3 days or less), temperature (a body temperature of 37.8°C or greater at presentation), age (being under 2 years), intercostal or subcostal recession, wheeze on auscultation, asthma, and vomiting (moderate or severe in the previous 24 hours) were each independently associated with hospital admission (P less than .01 for all associations).
The checklist includes these seven characteristics or risk variables (short illness, temperature, age, recession, wheeze, asthma, and vomiting [mnemonic STARWAVe]). To use the checklist, a primary care practitioner would assign one point for the presence of each item in a patient then add up all of the points to determine that patient’s risk level for future hospital admission for respiratory tract infection. A score of 1 point or less, observed in 5,593 (67%) cases would be considered indicative of a very low rate of risk for hospitalization (0.3%, 0.2%-0.4%). A score of 2 or 3 points, found for 2,520 (30%) children, would be considered as a normal level of risk (1.5%, 1.0%-1.9%), and a score of 4 or more points, seen in 204 (3%) children, would signify a high risk level (11.8%, 7.3%-16.2%).
Of the 8,394 children assessed, 78 (0.9%; 95% confidence interval, 0.7%-1.2%) were admitted to a hospital. Most were admitted on days 2-7 (33, 42%) and on days 8-30 (30, 39%) following recruitment. Only 15 (19%) were admitted on the day of recruitment (day 1).
“Many clinicians report that they prescribe antibiotics just in case, to mitigate perceived risk of future hospital admission and complications, and that failing to provide a prescription for a child who subsequently becomes seriously unwell is professionally unacceptable. If primary care clinicians could identify children at low (or very low) risk of such future complications, the reduced clinical uncertainty could lead to a reduced use of antibiotics in these groups of patients,” wrote first author Alastair Hay, MD, from the Centre for Academic Primary Care in the School of Social and Community Medicine at the University of Bristol (England), and his colleagues.
These researchers conducted the study based on a structured, blinded review of the medical records from children aged between 3 months and 16 years presenting with acute cough (less than or equal to 28 days) and respiratory tract infection treated by 519 general practitioners in 247 practices in England between July 2011 and June 2013. The primary study outcome was hospital admission for respiratory tract infection within 30 days.
Additionally, a multivariable model was employed to detect factors associated with increased risk of hospital admission. As measured by receiver operating characteristic curve analysis, the accuracy of the STARWAVe score checklist in predicting risk groups and associated risk of hospitalization was found to be high (0.81; 95% CI, 0.77-0.86). The suggested probability of hospital admission for children who did not have any of the seven characteristics included in the checklist was found to be exceptionally low (0.14%).
Significantly associated parent-reported variables included both moderate or severe vomiting and severe fever, each in the previous 24 hours. Significant clinician-reported variables included intercostal or subcostal recession and wheeze on auscultation.
“The main value of our results is to reduce clinical uncertainty and antibiotic use in children least likely to benefit from them, namely those at very low risk of future hospital admission,” Dr. Hay and his associates noted in The Lancet Respiratory Medicine (Lancet Respir Med. 2016 Sep 1. doi: 10.1016/S2213-2600(16)30223-5).
Funding for this study was provided by the National Institute for Health Research and sponsored by the University of Bristol. Only one of the study’s authors, Dr. Peter Muir, reported ties to industry sources.
FROM THE LANCET RESPIRATORY MEDICINE
Key clinical point: Use of a checklist of seven characteristics independently associated with hospital admission for children presenting to primary care physicians with cough and respiratory tract infection may lead to more appropriate prescribing of antibiotics in this patient population.
Major finding: Only 0.9% of 8,394 pediatric patients presenting to primary care with acute cough and respiratory tract infections were admitted to hospitals. A checklist based on seven characteristics observed in study participants (short illness, temperature, age, recession, wheeze, asthma, and vomiting [mnemonic STARWAVe]) that were independently associated with hospital admission (P less than .01 for all associations) was developed to define three risk categories for future hospital admission for respiratory tract infection.
Data sources: A prognostic cohort study of children aged between 3 months and 16 years presenting with acute cough (28 days or fewer) and respiratory tract infection treated by 519 general practitioners in 247 practices in England between July 2011 and June 2013.
Disclosures: Funding for this study was provided by the National Institute for Health Research and sponsored by the University of Bristol. Only Dr. Peter Muir reported ties to industry sources.
New drugs poised to stem tide of antibacterial resistance in gonorrhea
ANNAPOLIS, MD. – Three novel treatments for gonorrhea, currently in late stages of development, could give clinicians an edge in the fight against antibacterial resistance, according to a federal health official.
The pathogen Neisseria gonorrhoeae is already showing signs of besting first-line therapy ceftriaxone in Japan and parts of Europe, said Carolyn Deal, PhD, chief of the sexually transmitted diseases branch at the National Institute of Allergy and Infectious Diseases (NIAID). And the Centers for Disease Control and Prevention lists N. gonorrhoeae among its “urgent” antibiotic resistance threats.
“I think we have a new superbug,” Dr. Deal said at the annual scientific meeting of the Infectious Diseases Society for Obstetrics and Gynecology. “In my opinion, it’s just a matter of time in this country.”
But three agents in late-stage clinical trials for uncomplicated urogenital gonorrhea offer promise in fighting the gram-negative bacteria, according to Dr. Deal. The first is solithromycin, manufactured by Cempra. The company has a phase III study underway to compare a single dose of oral solithromycin with intramuscular ceftriaxone plus oral azithromycin for urogenital gonorrhea.
The other two drugs are first-in-class antibacterial agents. In partnership with the NIAID, the company Entasis recently completed a phase II study of zoliflodacin, an oral agent in a novel class of topoisomerase inhibitors. A phase III trial is expected to begin in 2017, also in partnership with the NIAID, according to an Entasis document. The third agent is gepotidacin, a novel triazaacenaphthylene antibacterial agent currently being investigated by GlaxoSmithKline in a phase II study.
Because N. gonorrhoeae poses such an urgent threat, waiting to develop a vaccine is less feasible than working with companies to develop additional antibacterial agents, Dr. Deal said. But taking a compound out of the basic research lab and having enough data to get into the investigational new drug phase is a significant investment, she said, so pharmaceutical manufacturers look for as many indications for a drug as possible.
For instance, solithromycin was initially investigated for community-acquired pneumonia. Gepotidacin initially was developed in partnership with the NIAID and the Biomedical Advanced Research and Development Authority in case of an anthrax attack, Dr. Deal said. “The Entasis product is the only one specifically developed for Neisseria gonorrhoeae,” she said.
One reason that two of the drugs in the pipeline include N. gonorrhoeae as an indication is that the Food and Drug Administration has issued guidance on developing drugs in the area of uncomplicated gonorrhea. That guidance is lacking for nasopharyngeal and rectal gonorrhea, leaving a “vacuum” in the pipeline, Dr. Deal said. “Many of us have come to the conclusion that developing vaccines is the only real long-term solution.”
On Twitter @whitneymcknight
ANNAPOLIS, MD. – Three novel treatments for gonorrhea, currently in late stages of development, could give clinicians an edge in the fight against antibacterial resistance, according to a federal health official.
The pathogen Neisseria gonorrhoeae is already showing signs of besting first-line therapy ceftriaxone in Japan and parts of Europe, said Carolyn Deal, PhD, chief of the sexually transmitted diseases branch at the National Institute of Allergy and Infectious Diseases (NIAID). And the Centers for Disease Control and Prevention lists N. gonorrhoeae among its “urgent” antibiotic resistance threats.
“I think we have a new superbug,” Dr. Deal said at the annual scientific meeting of the Infectious Diseases Society for Obstetrics and Gynecology. “In my opinion, it’s just a matter of time in this country.”
But three agents in late-stage clinical trials for uncomplicated urogenital gonorrhea offer promise in fighting the gram-negative bacteria, according to Dr. Deal. The first is solithromycin, manufactured by Cempra. The company has a phase III study underway to compare a single dose of oral solithromycin with intramuscular ceftriaxone plus oral azithromycin for urogenital gonorrhea.
The other two drugs are first-in-class antibacterial agents. In partnership with the NIAID, the company Entasis recently completed a phase II study of zoliflodacin, an oral agent in a novel class of topoisomerase inhibitors. A phase III trial is expected to begin in 2017, also in partnership with the NIAID, according to an Entasis document. The third agent is gepotidacin, a novel triazaacenaphthylene antibacterial agent currently being investigated by GlaxoSmithKline in a phase II study.
Because N. gonorrhoeae poses such an urgent threat, waiting to develop a vaccine is less feasible than working with companies to develop additional antibacterial agents, Dr. Deal said. But taking a compound out of the basic research lab and having enough data to get into the investigational new drug phase is a significant investment, she said, so pharmaceutical manufacturers look for as many indications for a drug as possible.
For instance, solithromycin was initially investigated for community-acquired pneumonia. Gepotidacin initially was developed in partnership with the NIAID and the Biomedical Advanced Research and Development Authority in case of an anthrax attack, Dr. Deal said. “The Entasis product is the only one specifically developed for Neisseria gonorrhoeae,” she said.
One reason that two of the drugs in the pipeline include N. gonorrhoeae as an indication is that the Food and Drug Administration has issued guidance on developing drugs in the area of uncomplicated gonorrhea. That guidance is lacking for nasopharyngeal and rectal gonorrhea, leaving a “vacuum” in the pipeline, Dr. Deal said. “Many of us have come to the conclusion that developing vaccines is the only real long-term solution.”
On Twitter @whitneymcknight
ANNAPOLIS, MD. – Three novel treatments for gonorrhea, currently in late stages of development, could give clinicians an edge in the fight against antibacterial resistance, according to a federal health official.
The pathogen Neisseria gonorrhoeae is already showing signs of besting first-line therapy ceftriaxone in Japan and parts of Europe, said Carolyn Deal, PhD, chief of the sexually transmitted diseases branch at the National Institute of Allergy and Infectious Diseases (NIAID). And the Centers for Disease Control and Prevention lists N. gonorrhoeae among its “urgent” antibiotic resistance threats.
“I think we have a new superbug,” Dr. Deal said at the annual scientific meeting of the Infectious Diseases Society for Obstetrics and Gynecology. “In my opinion, it’s just a matter of time in this country.”
But three agents in late-stage clinical trials for uncomplicated urogenital gonorrhea offer promise in fighting the gram-negative bacteria, according to Dr. Deal. The first is solithromycin, manufactured by Cempra. The company has a phase III study underway to compare a single dose of oral solithromycin with intramuscular ceftriaxone plus oral azithromycin for urogenital gonorrhea.
The other two drugs are first-in-class antibacterial agents. In partnership with the NIAID, the company Entasis recently completed a phase II study of zoliflodacin, an oral agent in a novel class of topoisomerase inhibitors. A phase III trial is expected to begin in 2017, also in partnership with the NIAID, according to an Entasis document. The third agent is gepotidacin, a novel triazaacenaphthylene antibacterial agent currently being investigated by GlaxoSmithKline in a phase II study.
Because N. gonorrhoeae poses such an urgent threat, waiting to develop a vaccine is less feasible than working with companies to develop additional antibacterial agents, Dr. Deal said. But taking a compound out of the basic research lab and having enough data to get into the investigational new drug phase is a significant investment, she said, so pharmaceutical manufacturers look for as many indications for a drug as possible.
For instance, solithromycin was initially investigated for community-acquired pneumonia. Gepotidacin initially was developed in partnership with the NIAID and the Biomedical Advanced Research and Development Authority in case of an anthrax attack, Dr. Deal said. “The Entasis product is the only one specifically developed for Neisseria gonorrhoeae,” she said.
One reason that two of the drugs in the pipeline include N. gonorrhoeae as an indication is that the Food and Drug Administration has issued guidance on developing drugs in the area of uncomplicated gonorrhea. That guidance is lacking for nasopharyngeal and rectal gonorrhea, leaving a “vacuum” in the pipeline, Dr. Deal said. “Many of us have come to the conclusion that developing vaccines is the only real long-term solution.”
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM IDSOG
Many patients with diabetic foot infections get unnecessary MRSA treatment
Many patients with diabetic foot infections receive methicillin-resistant Staphylococcus aureus antibiotics unnecessarily, according to Kelly Reveles, PharmD, and her associates.
Among the 318 patients with diabetic foot infections (DFIs) in the study, S. aureus was the most common pathogen, accounting for 146 cases. MRSA accounted for 47 of S. aureus cases, and 15% of overall cases. Although MRSA accounted for a relatively small number of cases, MRSA antibiotics were administered to 86% of all patients, resulting in 71% of all patients receiving the treatment unnecessarily.
Independent risk factors for MRSA DFI were male sex and bone involvement. Other risk factors included previous MRSA infection, more severe infection, and a higher white cell count. The most common comorbidities of DFI were hypertension, dyslipidemia, and obesity.
“The improper use of antibiotics unnecessarily exposes the patient to potential complications of the therapy. Furthermore, the overuse of antibiotics drives antimicrobial resistance and is likely to increase the health care burden,” the investigators wrote.
Find the full study in PLoS One (doi: 10.1371/journal.pone.0161658).
Many patients with diabetic foot infections receive methicillin-resistant Staphylococcus aureus antibiotics unnecessarily, according to Kelly Reveles, PharmD, and her associates.
Among the 318 patients with diabetic foot infections (DFIs) in the study, S. aureus was the most common pathogen, accounting for 146 cases. MRSA accounted for 47 of S. aureus cases, and 15% of overall cases. Although MRSA accounted for a relatively small number of cases, MRSA antibiotics were administered to 86% of all patients, resulting in 71% of all patients receiving the treatment unnecessarily.
Independent risk factors for MRSA DFI were male sex and bone involvement. Other risk factors included previous MRSA infection, more severe infection, and a higher white cell count. The most common comorbidities of DFI were hypertension, dyslipidemia, and obesity.
“The improper use of antibiotics unnecessarily exposes the patient to potential complications of the therapy. Furthermore, the overuse of antibiotics drives antimicrobial resistance and is likely to increase the health care burden,” the investigators wrote.
Find the full study in PLoS One (doi: 10.1371/journal.pone.0161658).
Many patients with diabetic foot infections receive methicillin-resistant Staphylococcus aureus antibiotics unnecessarily, according to Kelly Reveles, PharmD, and her associates.
Among the 318 patients with diabetic foot infections (DFIs) in the study, S. aureus was the most common pathogen, accounting for 146 cases. MRSA accounted for 47 of S. aureus cases, and 15% of overall cases. Although MRSA accounted for a relatively small number of cases, MRSA antibiotics were administered to 86% of all patients, resulting in 71% of all patients receiving the treatment unnecessarily.
Independent risk factors for MRSA DFI were male sex and bone involvement. Other risk factors included previous MRSA infection, more severe infection, and a higher white cell count. The most common comorbidities of DFI were hypertension, dyslipidemia, and obesity.
“The improper use of antibiotics unnecessarily exposes the patient to potential complications of the therapy. Furthermore, the overuse of antibiotics drives antimicrobial resistance and is likely to increase the health care burden,” the investigators wrote.
Find the full study in PLoS One (doi: 10.1371/journal.pone.0161658).
FROM PLOS ONE
WHO updates ranking of critically important antimicrobials
In light of increasing antibiotic resistance among pathogens, the World Health Organization has revised its global rankings of critically important antimicrobials used in human medicine, designating quinolones, third- and fourth-generation cephalosporins, macrolides and ketolides, and glycopeptides as among the highest-priority drugs in the world.
Peter C. Collignon, MBBS, of Canberra (Australia) Hospital and his colleagues on the WHO Advisory Group on Integrated Surveillance of Antimicrobial Resistance, created the rankings for use in developing risk management strategies related to antimicrobial use in food production animals. According to Dr. Collignon and his coauthors, the rankings are intended to help regulators and other stakeholders know which types of antimicrobials used in animals present potentially higher risks to human populations and help inform how this use might be better managed (e.g. restriction to single-animal therapy or prohibition of mass treatment and extra-label use) to minimize the risk of transmission of resistance to the human population.
WHO studies previously suggested that antimicrobials which currently have no veterinary equivalent (for example, carbapenems) “as well as any new class of antimicrobial developed for human therapy should not be used in animals.” Dr. Collignon’s WHO Advisory Group followed two essential criteria to designate antimicrobials of utmost importance to human health in the new study: 1. antimicrobials that are the sole, or one of limited available therapies, to treat serious bacterial infections in people and 2. antimicrobials used to treat infections in people caused by either (a) bacteria that may be transmitted to humans from nonhuman sources or (b) bacteria that may acquire resistance genes from nonhuman sources.
The highest-priority and most critically important antimicrobials are those which meet the criteria listed above and that are used in greatest volume or highest frequency by humans. Another criteria for prioritization involves antimicrobial classes where evidence suggests that the “transmission of resistant bacteria or resistance genes from nonhuman sources is already occurring, or has occurred previously.” Quinolones, third- and fourth-generation cephalosporins, macrolides and ketolides, and glycopeptides were the only antimicrobials that met all criteria for prioritization.
“Antimicrobial resistance remains a threat to human health and drivers of resistance act in all sectors; human, animal, and the environment,” the WHO Advisory Group concluded. “Prioritizing the antimicrobials that are critically important for humans is a valuable and strategic risk-management tool and will be improved with the evidence-based approach which is currently underway.”
Read the full study in Clinical Infectious Diseases (doi: 10.1093/cid/ciw475).
In light of increasing antibiotic resistance among pathogens, the World Health Organization has revised its global rankings of critically important antimicrobials used in human medicine, designating quinolones, third- and fourth-generation cephalosporins, macrolides and ketolides, and glycopeptides as among the highest-priority drugs in the world.
Peter C. Collignon, MBBS, of Canberra (Australia) Hospital and his colleagues on the WHO Advisory Group on Integrated Surveillance of Antimicrobial Resistance, created the rankings for use in developing risk management strategies related to antimicrobial use in food production animals. According to Dr. Collignon and his coauthors, the rankings are intended to help regulators and other stakeholders know which types of antimicrobials used in animals present potentially higher risks to human populations and help inform how this use might be better managed (e.g. restriction to single-animal therapy or prohibition of mass treatment and extra-label use) to minimize the risk of transmission of resistance to the human population.
WHO studies previously suggested that antimicrobials which currently have no veterinary equivalent (for example, carbapenems) “as well as any new class of antimicrobial developed for human therapy should not be used in animals.” Dr. Collignon’s WHO Advisory Group followed two essential criteria to designate antimicrobials of utmost importance to human health in the new study: 1. antimicrobials that are the sole, or one of limited available therapies, to treat serious bacterial infections in people and 2. antimicrobials used to treat infections in people caused by either (a) bacteria that may be transmitted to humans from nonhuman sources or (b) bacteria that may acquire resistance genes from nonhuman sources.
The highest-priority and most critically important antimicrobials are those which meet the criteria listed above and that are used in greatest volume or highest frequency by humans. Another criteria for prioritization involves antimicrobial classes where evidence suggests that the “transmission of resistant bacteria or resistance genes from nonhuman sources is already occurring, or has occurred previously.” Quinolones, third- and fourth-generation cephalosporins, macrolides and ketolides, and glycopeptides were the only antimicrobials that met all criteria for prioritization.
“Antimicrobial resistance remains a threat to human health and drivers of resistance act in all sectors; human, animal, and the environment,” the WHO Advisory Group concluded. “Prioritizing the antimicrobials that are critically important for humans is a valuable and strategic risk-management tool and will be improved with the evidence-based approach which is currently underway.”
Read the full study in Clinical Infectious Diseases (doi: 10.1093/cid/ciw475).
In light of increasing antibiotic resistance among pathogens, the World Health Organization has revised its global rankings of critically important antimicrobials used in human medicine, designating quinolones, third- and fourth-generation cephalosporins, macrolides and ketolides, and glycopeptides as among the highest-priority drugs in the world.
Peter C. Collignon, MBBS, of Canberra (Australia) Hospital and his colleagues on the WHO Advisory Group on Integrated Surveillance of Antimicrobial Resistance, created the rankings for use in developing risk management strategies related to antimicrobial use in food production animals. According to Dr. Collignon and his coauthors, the rankings are intended to help regulators and other stakeholders know which types of antimicrobials used in animals present potentially higher risks to human populations and help inform how this use might be better managed (e.g. restriction to single-animal therapy or prohibition of mass treatment and extra-label use) to minimize the risk of transmission of resistance to the human population.
WHO studies previously suggested that antimicrobials which currently have no veterinary equivalent (for example, carbapenems) “as well as any new class of antimicrobial developed for human therapy should not be used in animals.” Dr. Collignon’s WHO Advisory Group followed two essential criteria to designate antimicrobials of utmost importance to human health in the new study: 1. antimicrobials that are the sole, or one of limited available therapies, to treat serious bacterial infections in people and 2. antimicrobials used to treat infections in people caused by either (a) bacteria that may be transmitted to humans from nonhuman sources or (b) bacteria that may acquire resistance genes from nonhuman sources.
The highest-priority and most critically important antimicrobials are those which meet the criteria listed above and that are used in greatest volume or highest frequency by humans. Another criteria for prioritization involves antimicrobial classes where evidence suggests that the “transmission of resistant bacteria or resistance genes from nonhuman sources is already occurring, or has occurred previously.” Quinolones, third- and fourth-generation cephalosporins, macrolides and ketolides, and glycopeptides were the only antimicrobials that met all criteria for prioritization.
“Antimicrobial resistance remains a threat to human health and drivers of resistance act in all sectors; human, animal, and the environment,” the WHO Advisory Group concluded. “Prioritizing the antimicrobials that are critically important for humans is a valuable and strategic risk-management tool and will be improved with the evidence-based approach which is currently underway.”
Read the full study in Clinical Infectious Diseases (doi: 10.1093/cid/ciw475).
FROM CLINICAL INFECTIOUS DISEASES
Fourth U.S. case of mcr-1–resistance gene reported
A fourth case of bacterial infection harboring the mcr-1 gene has been reported in a child recently returned from a visit to the Caribbean, according to a case report published Sept. 9 in Morbidity and Mortality Weekly Report.
The mcr-1 gene, which confers resistance to the last-resort antibiotic colistin, was first reported in China and is the first plasmid-mediated colistin-resistance mechanism to be identified. Since its discovery in 2015, cases have been reported in Africa, Asia, Europe, South America, and North America.
In this case report, a young patient developed fever and bloody diarrhea 2 days before returning to the United States from a 2-week visit to the Caribbean. The child were treated with the paromomycin and a stool specimen was collected on June 16, with follow-up cultures on June 18 and June 23.
All revealed Escherichia coli O157 harboring mcr-1. The isolates also carried a plasmid blaCMY-2 gene, which confers resistance to third-generation cephalosporins. Stool cultures taken on June 24 and July 1 were negative for E. coli O157 (MMWR. 2016 Sep 9. http://dx.doi.org/10.15585/mmwr.mm6536e3).
Family members in close contact with the patient also were tested; all were found to be negative. Similarly, 16 environmental samples collected from the kitchen and diaper-changing area of the patient’s home were negative for mcr-1.
Researchers reported that the patient was “typically healthy,” and the child’s diet included fruit, dairy products, and meat. While on vacation in the Caribbean, the child ate meat purchased at a live animal market but did not visit the market personally. The child also had contact with a pet dog and cat.
“At this time, CDC recommends that Enterobacteriaceae isolates with a colistin or polymyxin B MIC plus or minus 4 mcg/mL be tested for the presence of mcr-1; testing is available through CDC,” wrote Dr. Amber M. Vasquez and her colleagues from the Centers for Disease Control and Prevention. “Prompt reporting of mcr-1–carrying isolates to public health officials allows for a rapid response to identify transmission and limit further spread.”
A fourth case of bacterial infection harboring the mcr-1 gene has been reported in a child recently returned from a visit to the Caribbean, according to a case report published Sept. 9 in Morbidity and Mortality Weekly Report.
The mcr-1 gene, which confers resistance to the last-resort antibiotic colistin, was first reported in China and is the first plasmid-mediated colistin-resistance mechanism to be identified. Since its discovery in 2015, cases have been reported in Africa, Asia, Europe, South America, and North America.
In this case report, a young patient developed fever and bloody diarrhea 2 days before returning to the United States from a 2-week visit to the Caribbean. The child were treated with the paromomycin and a stool specimen was collected on June 16, with follow-up cultures on June 18 and June 23.
All revealed Escherichia coli O157 harboring mcr-1. The isolates also carried a plasmid blaCMY-2 gene, which confers resistance to third-generation cephalosporins. Stool cultures taken on June 24 and July 1 were negative for E. coli O157 (MMWR. 2016 Sep 9. http://dx.doi.org/10.15585/mmwr.mm6536e3).
Family members in close contact with the patient also were tested; all were found to be negative. Similarly, 16 environmental samples collected from the kitchen and diaper-changing area of the patient’s home were negative for mcr-1.
Researchers reported that the patient was “typically healthy,” and the child’s diet included fruit, dairy products, and meat. While on vacation in the Caribbean, the child ate meat purchased at a live animal market but did not visit the market personally. The child also had contact with a pet dog and cat.
“At this time, CDC recommends that Enterobacteriaceae isolates with a colistin or polymyxin B MIC plus or minus 4 mcg/mL be tested for the presence of mcr-1; testing is available through CDC,” wrote Dr. Amber M. Vasquez and her colleagues from the Centers for Disease Control and Prevention. “Prompt reporting of mcr-1–carrying isolates to public health officials allows for a rapid response to identify transmission and limit further spread.”
A fourth case of bacterial infection harboring the mcr-1 gene has been reported in a child recently returned from a visit to the Caribbean, according to a case report published Sept. 9 in Morbidity and Mortality Weekly Report.
The mcr-1 gene, which confers resistance to the last-resort antibiotic colistin, was first reported in China and is the first plasmid-mediated colistin-resistance mechanism to be identified. Since its discovery in 2015, cases have been reported in Africa, Asia, Europe, South America, and North America.
In this case report, a young patient developed fever and bloody diarrhea 2 days before returning to the United States from a 2-week visit to the Caribbean. The child were treated with the paromomycin and a stool specimen was collected on June 16, with follow-up cultures on June 18 and June 23.
All revealed Escherichia coli O157 harboring mcr-1. The isolates also carried a plasmid blaCMY-2 gene, which confers resistance to third-generation cephalosporins. Stool cultures taken on June 24 and July 1 were negative for E. coli O157 (MMWR. 2016 Sep 9. http://dx.doi.org/10.15585/mmwr.mm6536e3).
Family members in close contact with the patient also were tested; all were found to be negative. Similarly, 16 environmental samples collected from the kitchen and diaper-changing area of the patient’s home were negative for mcr-1.
Researchers reported that the patient was “typically healthy,” and the child’s diet included fruit, dairy products, and meat. While on vacation in the Caribbean, the child ate meat purchased at a live animal market but did not visit the market personally. The child also had contact with a pet dog and cat.
“At this time, CDC recommends that Enterobacteriaceae isolates with a colistin or polymyxin B MIC plus or minus 4 mcg/mL be tested for the presence of mcr-1; testing is available through CDC,” wrote Dr. Amber M. Vasquez and her colleagues from the Centers for Disease Control and Prevention. “Prompt reporting of mcr-1–carrying isolates to public health officials allows for a rapid response to identify transmission and limit further spread.”
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
Antibiotic susceptibility differs in transplant recipients
Antibiotic susceptibility in bacteria cultured from transplant recipients at a single hospital differed markedly from that in hospital-wide antibiograms, according to a report published in Diagnostic Microbiology and Infectious Disease.
Understanding the differences in antibiotic susceptibility among these highly immunocompromised patients can help guide treatment when they develop infection, and reduce the delay before they begin receiving appropriate antibiotics, said Rossana Rosa, MD, of Jackson Memorial Hospital, Miami, and her associates.
The investigators examined the antibiotic susceptibility of 1,889 isolates from blood and urine specimens taken from patients who had received solid-organ transplants at a single tertiary-care teaching hospital and then developed bacterial infections during a 2-year period. These patients included both children and adults who had received kidney, pancreas, liver, heart, lung, or intestinal transplants and were treated in numerous, “geographically distributed” units throughout the hospital. Their culture results were compared with those from 10,439 other patients with bacterial infections, which comprised the hospital-wide antibiograms developed every 6 months during the study period.
The Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa isolates from the transplant recipients showed markedly less susceptibility to first-line antibiotics than would have been predicted by the hospital-antibiograms. In particular, in the transplant recipients E. coli infections were resistant to trimethoprim-sulfamethoxazole, levofloxacin, and ceftriaxone; K. pneumoniae infections were resistant to every antibiotic except amikacin; and P. aeruginosa infections were resistant to levofloxacin, cefepime, and amikacin (Diag Microbiol Infect Dis. 2016 Aug 25. doi: 10.1016/j.diagmicrobio.2016.08.018).
“We advocate for the development of antibiograms specific to solid-organ transplant recipients. This may allow intrahospital comparisons and intertransplant-center monitoring of trends in antimicrobial resistance over time,” Dr. Rosa and her associates said.
Antibiotic susceptibility in bacteria cultured from transplant recipients at a single hospital differed markedly from that in hospital-wide antibiograms, according to a report published in Diagnostic Microbiology and Infectious Disease.
Understanding the differences in antibiotic susceptibility among these highly immunocompromised patients can help guide treatment when they develop infection, and reduce the delay before they begin receiving appropriate antibiotics, said Rossana Rosa, MD, of Jackson Memorial Hospital, Miami, and her associates.
The investigators examined the antibiotic susceptibility of 1,889 isolates from blood and urine specimens taken from patients who had received solid-organ transplants at a single tertiary-care teaching hospital and then developed bacterial infections during a 2-year period. These patients included both children and adults who had received kidney, pancreas, liver, heart, lung, or intestinal transplants and were treated in numerous, “geographically distributed” units throughout the hospital. Their culture results were compared with those from 10,439 other patients with bacterial infections, which comprised the hospital-wide antibiograms developed every 6 months during the study period.
The Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa isolates from the transplant recipients showed markedly less susceptibility to first-line antibiotics than would have been predicted by the hospital-antibiograms. In particular, in the transplant recipients E. coli infections were resistant to trimethoprim-sulfamethoxazole, levofloxacin, and ceftriaxone; K. pneumoniae infections were resistant to every antibiotic except amikacin; and P. aeruginosa infections were resistant to levofloxacin, cefepime, and amikacin (Diag Microbiol Infect Dis. 2016 Aug 25. doi: 10.1016/j.diagmicrobio.2016.08.018).
“We advocate for the development of antibiograms specific to solid-organ transplant recipients. This may allow intrahospital comparisons and intertransplant-center monitoring of trends in antimicrobial resistance over time,” Dr. Rosa and her associates said.
Antibiotic susceptibility in bacteria cultured from transplant recipients at a single hospital differed markedly from that in hospital-wide antibiograms, according to a report published in Diagnostic Microbiology and Infectious Disease.
Understanding the differences in antibiotic susceptibility among these highly immunocompromised patients can help guide treatment when they develop infection, and reduce the delay before they begin receiving appropriate antibiotics, said Rossana Rosa, MD, of Jackson Memorial Hospital, Miami, and her associates.
The investigators examined the antibiotic susceptibility of 1,889 isolates from blood and urine specimens taken from patients who had received solid-organ transplants at a single tertiary-care teaching hospital and then developed bacterial infections during a 2-year period. These patients included both children and adults who had received kidney, pancreas, liver, heart, lung, or intestinal transplants and were treated in numerous, “geographically distributed” units throughout the hospital. Their culture results were compared with those from 10,439 other patients with bacterial infections, which comprised the hospital-wide antibiograms developed every 6 months during the study period.
The Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa isolates from the transplant recipients showed markedly less susceptibility to first-line antibiotics than would have been predicted by the hospital-antibiograms. In particular, in the transplant recipients E. coli infections were resistant to trimethoprim-sulfamethoxazole, levofloxacin, and ceftriaxone; K. pneumoniae infections were resistant to every antibiotic except amikacin; and P. aeruginosa infections were resistant to levofloxacin, cefepime, and amikacin (Diag Microbiol Infect Dis. 2016 Aug 25. doi: 10.1016/j.diagmicrobio.2016.08.018).
“We advocate for the development of antibiograms specific to solid-organ transplant recipients. This may allow intrahospital comparisons and intertransplant-center monitoring of trends in antimicrobial resistance over time,” Dr. Rosa and her associates said.
FROM DIAGNOSTIC MICROBIOLOGY AND INFECTIOUS DISEASE
Key clinical point: Antibiotic susceptibility in bacteria cultured from transplant recipients differs markedly from that in hospital-wide antibiograms.
Major finding: In the transplant recipients, E. coli infections were resistant to trimethoprim-sulfamethoxazole, levofloxacin, and ceftriaxone; K. pneumoniae infections were resistant to every antibiotic except amikacin; and P. aeruginosa infections were resistant to levofloxacin, cefepime, and amikacin.
Data source: A single-center study comparing the antibiotic susceptibility of 1,889 bacterial isolates from transplant recipients with 10,439 isolates from other patients.
Disclosures: This study was not supported by funding from any public, commercial, or not-for-profit entities. Dr. Rosa and her associates reported having no relevant financial disclosures.