User login
Cotempla XR-ODT approved for children, adolescents with ADHD
The Food and Drug Administration has approved the first methylphenidate extended-release orally disintegrating tablet for treating ADHD in patients aged 6-17 years old, Neos Therapeutics announced June 19.
The company said the approval came after a phase III trial showed that treatment in a laboratory classroom with the drug, called Cotempla XR-ODT, showed a significant improvement in attention-deficit/hyperactivity disorder symptom control when compared with a placebo across the classroom day (placebo-subtracted difference of –11). The onset of effect was shown at 1 hour post-dose and lasted through 12 hours. No serious adverse events were reported during the trial, and the adverse event profile was consistent with the established safety profile for other extended-release methylphenidate products.
Cotempla XR-ODT will be available commercially in a portable, child-resistant blister pack in the fall of 2017.
Find the full press release on Neos Therapeutics website.
The Food and Drug Administration has approved the first methylphenidate extended-release orally disintegrating tablet for treating ADHD in patients aged 6-17 years old, Neos Therapeutics announced June 19.
The company said the approval came after a phase III trial showed that treatment in a laboratory classroom with the drug, called Cotempla XR-ODT, showed a significant improvement in attention-deficit/hyperactivity disorder symptom control when compared with a placebo across the classroom day (placebo-subtracted difference of –11). The onset of effect was shown at 1 hour post-dose and lasted through 12 hours. No serious adverse events were reported during the trial, and the adverse event profile was consistent with the established safety profile for other extended-release methylphenidate products.
Cotempla XR-ODT will be available commercially in a portable, child-resistant blister pack in the fall of 2017.
Find the full press release on Neos Therapeutics website.
The Food and Drug Administration has approved the first methylphenidate extended-release orally disintegrating tablet for treating ADHD in patients aged 6-17 years old, Neos Therapeutics announced June 19.
The company said the approval came after a phase III trial showed that treatment in a laboratory classroom with the drug, called Cotempla XR-ODT, showed a significant improvement in attention-deficit/hyperactivity disorder symptom control when compared with a placebo across the classroom day (placebo-subtracted difference of –11). The onset of effect was shown at 1 hour post-dose and lasted through 12 hours. No serious adverse events were reported during the trial, and the adverse event profile was consistent with the established safety profile for other extended-release methylphenidate products.
Cotempla XR-ODT will be available commercially in a portable, child-resistant blister pack in the fall of 2017.
Find the full press release on Neos Therapeutics website.
Mydayis approved for teens, adults with ADHD
The Food and Drug Administration has approved a once-a-day treatment for patients aged 13 years and older with ADHD, Shire announced June 20 in a press release.
The approval of Mydayis was based on results from 16 clinical studies evaluating the medication in more than 1,600 adolescents (aged 13-17 years) and adults with attention-deficit/hyperactivity disorder. In the placebo-controlled clinical studies, Mydayis significantly improved symptoms of ADHD, as measured by the ADHD-RS-IV and the Permanent Product Measure of Performance (PERMP), in adults and adolescents. Improvement on the PERMP reached statistical significance beginning at 2 or 4 hours post dose and lasting up to 16 hours post dose.
The medication, an amphetamine product, consists of three different types of drug-releasing beads.
“With this approval, we hope to help patients who need a once-daily treatment option,” Flemming Ornskov, MD, MPH, said in a press release. Dr. Ornskov is CEO of Shire.
It is estimated that 4.4% of adults have ADHD in the United States, and 50%-66% of children with ADHD may continue to have symptoms of the disorder as adults.
Mydayis will be commercially available in the United States in the third quarter of 2017.
Read the full press release here.
The Food and Drug Administration has approved a once-a-day treatment for patients aged 13 years and older with ADHD, Shire announced June 20 in a press release.
The approval of Mydayis was based on results from 16 clinical studies evaluating the medication in more than 1,600 adolescents (aged 13-17 years) and adults with attention-deficit/hyperactivity disorder. In the placebo-controlled clinical studies, Mydayis significantly improved symptoms of ADHD, as measured by the ADHD-RS-IV and the Permanent Product Measure of Performance (PERMP), in adults and adolescents. Improvement on the PERMP reached statistical significance beginning at 2 or 4 hours post dose and lasting up to 16 hours post dose.
The medication, an amphetamine product, consists of three different types of drug-releasing beads.
“With this approval, we hope to help patients who need a once-daily treatment option,” Flemming Ornskov, MD, MPH, said in a press release. Dr. Ornskov is CEO of Shire.
It is estimated that 4.4% of adults have ADHD in the United States, and 50%-66% of children with ADHD may continue to have symptoms of the disorder as adults.
Mydayis will be commercially available in the United States in the third quarter of 2017.
Read the full press release here.
The Food and Drug Administration has approved a once-a-day treatment for patients aged 13 years and older with ADHD, Shire announced June 20 in a press release.
The approval of Mydayis was based on results from 16 clinical studies evaluating the medication in more than 1,600 adolescents (aged 13-17 years) and adults with attention-deficit/hyperactivity disorder. In the placebo-controlled clinical studies, Mydayis significantly improved symptoms of ADHD, as measured by the ADHD-RS-IV and the Permanent Product Measure of Performance (PERMP), in adults and adolescents. Improvement on the PERMP reached statistical significance beginning at 2 or 4 hours post dose and lasting up to 16 hours post dose.
The medication, an amphetamine product, consists of three different types of drug-releasing beads.
“With this approval, we hope to help patients who need a once-daily treatment option,” Flemming Ornskov, MD, MPH, said in a press release. Dr. Ornskov is CEO of Shire.
It is estimated that 4.4% of adults have ADHD in the United States, and 50%-66% of children with ADHD may continue to have symptoms of the disorder as adults.
Mydayis will be commercially available in the United States in the third quarter of 2017.
Read the full press release here.
Impairment persists despite treatment in adult ADHD
SAN DIEGO – Despite treatment with short- or long-acting medications, adults with attention-deficit/hyperactivity disorder report more impairment than do non-ADHD adults across several domains of daily life, and at certain times of day.
The findings, from a study presented at the annual meeting of the American Psychiatric Association, suggest that adults with ADHD have burdens that may persist despite medication.
The studies compared a cohort of 616 adults with a self-reported ADHD diagnosis and at least 6 months on medication, including short-acting stimulants, long-acting agents, or a combination of these. The researchers also recruited a comparison cohort of 200 non-ADHD adults.
“Interestingly, there was not only a difference between ADHD and non-ADHD groups, but there was also significant impairment reported among patients who are currently being treated for ADHD,” Alexandra Khachatryan, MPH, of Shire Pharmaceuticals, the study’s senior author, said in an interview. Ms. Khachatryan and her colleagues presented the findings at the APA.
For example, 44% of the ADHD respondents reported that the afternoon was the most challenging time of day, compared with 29% of non-ADHD participants (P less than .001). Mid-morning also was significantly more challenging for the ADHD group, with 26% reporting difficulties, compared with 17% of the non-ADHD cohort (P less than .01).
Other statistically significant between-group differences were seen related to managing affect and emotions, sustaining effort, working memory and recall, and interpersonal relationships.
“In addition to the burden patients report across the day, they also expressed significant challenges with psychosocial functioning and managing the demands of work, social, and family life despite treatment,” said Norman Atkins, PhD, of Shire, a coauthor of the study.
A separate poster by the same research group, using the same study data from the cohort of 616 currently treated adult ADHD patients (mean age 39, 70% female) looked at self-reported impairment across daily life domains by patients under different medication regimens.
Patients in the cohort were treated with short-acting stimulants (n = 166), long-acting stimulants (n = 201), or augmentation strategies (n = 249). The researchers found that afternoons and evenings were most difficult for patients regardless of treatment approach.
Ms. Khachatryan said the study was intended to help clinicians “understand what we’re offering patients and if we’re adequately meeting the needs of patients across the day. And we found that adults experience burden across the day despite being treated, and what they report as the most challenging times of day are the afternoon and evening hours,” when work, family, and household obligations are likely to be present.
Dr. Atkins added: “From an ADHD management perspective, the key takeaway is that these impairments occur across multiple settings and are most problematic at certain times of the day. It’s important for providers to have a meaningful conversation with their patients about their day-to-day challenges to fully appreciate how ADHD impacts their functioning so they can best optimize care.”
The researchers acknowledged as limitations of their study its high number of women participants, potentially reducing the generalizability of its findings; the reliance on self-reported outcomes; and between-group differences for the ADHD and non-ADHD groups that included differences in mean age (39 vs. 43, respectively) and full-time employment status (57% vs. 42%).
The study was sponsored by Shire Pharmaceuticals, with three of its five coauthors employed by the company.
SAN DIEGO – Despite treatment with short- or long-acting medications, adults with attention-deficit/hyperactivity disorder report more impairment than do non-ADHD adults across several domains of daily life, and at certain times of day.
The findings, from a study presented at the annual meeting of the American Psychiatric Association, suggest that adults with ADHD have burdens that may persist despite medication.
The studies compared a cohort of 616 adults with a self-reported ADHD diagnosis and at least 6 months on medication, including short-acting stimulants, long-acting agents, or a combination of these. The researchers also recruited a comparison cohort of 200 non-ADHD adults.
“Interestingly, there was not only a difference between ADHD and non-ADHD groups, but there was also significant impairment reported among patients who are currently being treated for ADHD,” Alexandra Khachatryan, MPH, of Shire Pharmaceuticals, the study’s senior author, said in an interview. Ms. Khachatryan and her colleagues presented the findings at the APA.
For example, 44% of the ADHD respondents reported that the afternoon was the most challenging time of day, compared with 29% of non-ADHD participants (P less than .001). Mid-morning also was significantly more challenging for the ADHD group, with 26% reporting difficulties, compared with 17% of the non-ADHD cohort (P less than .01).
Other statistically significant between-group differences were seen related to managing affect and emotions, sustaining effort, working memory and recall, and interpersonal relationships.
“In addition to the burden patients report across the day, they also expressed significant challenges with psychosocial functioning and managing the demands of work, social, and family life despite treatment,” said Norman Atkins, PhD, of Shire, a coauthor of the study.
A separate poster by the same research group, using the same study data from the cohort of 616 currently treated adult ADHD patients (mean age 39, 70% female) looked at self-reported impairment across daily life domains by patients under different medication regimens.
Patients in the cohort were treated with short-acting stimulants (n = 166), long-acting stimulants (n = 201), or augmentation strategies (n = 249). The researchers found that afternoons and evenings were most difficult for patients regardless of treatment approach.
Ms. Khachatryan said the study was intended to help clinicians “understand what we’re offering patients and if we’re adequately meeting the needs of patients across the day. And we found that adults experience burden across the day despite being treated, and what they report as the most challenging times of day are the afternoon and evening hours,” when work, family, and household obligations are likely to be present.
Dr. Atkins added: “From an ADHD management perspective, the key takeaway is that these impairments occur across multiple settings and are most problematic at certain times of the day. It’s important for providers to have a meaningful conversation with their patients about their day-to-day challenges to fully appreciate how ADHD impacts their functioning so they can best optimize care.”
The researchers acknowledged as limitations of their study its high number of women participants, potentially reducing the generalizability of its findings; the reliance on self-reported outcomes; and between-group differences for the ADHD and non-ADHD groups that included differences in mean age (39 vs. 43, respectively) and full-time employment status (57% vs. 42%).
The study was sponsored by Shire Pharmaceuticals, with three of its five coauthors employed by the company.
SAN DIEGO – Despite treatment with short- or long-acting medications, adults with attention-deficit/hyperactivity disorder report more impairment than do non-ADHD adults across several domains of daily life, and at certain times of day.
The findings, from a study presented at the annual meeting of the American Psychiatric Association, suggest that adults with ADHD have burdens that may persist despite medication.
The studies compared a cohort of 616 adults with a self-reported ADHD diagnosis and at least 6 months on medication, including short-acting stimulants, long-acting agents, or a combination of these. The researchers also recruited a comparison cohort of 200 non-ADHD adults.
“Interestingly, there was not only a difference between ADHD and non-ADHD groups, but there was also significant impairment reported among patients who are currently being treated for ADHD,” Alexandra Khachatryan, MPH, of Shire Pharmaceuticals, the study’s senior author, said in an interview. Ms. Khachatryan and her colleagues presented the findings at the APA.
For example, 44% of the ADHD respondents reported that the afternoon was the most challenging time of day, compared with 29% of non-ADHD participants (P less than .001). Mid-morning also was significantly more challenging for the ADHD group, with 26% reporting difficulties, compared with 17% of the non-ADHD cohort (P less than .01).
Other statistically significant between-group differences were seen related to managing affect and emotions, sustaining effort, working memory and recall, and interpersonal relationships.
“In addition to the burden patients report across the day, they also expressed significant challenges with psychosocial functioning and managing the demands of work, social, and family life despite treatment,” said Norman Atkins, PhD, of Shire, a coauthor of the study.
A separate poster by the same research group, using the same study data from the cohort of 616 currently treated adult ADHD patients (mean age 39, 70% female) looked at self-reported impairment across daily life domains by patients under different medication regimens.
Patients in the cohort were treated with short-acting stimulants (n = 166), long-acting stimulants (n = 201), or augmentation strategies (n = 249). The researchers found that afternoons and evenings were most difficult for patients regardless of treatment approach.
Ms. Khachatryan said the study was intended to help clinicians “understand what we’re offering patients and if we’re adequately meeting the needs of patients across the day. And we found that adults experience burden across the day despite being treated, and what they report as the most challenging times of day are the afternoon and evening hours,” when work, family, and household obligations are likely to be present.
Dr. Atkins added: “From an ADHD management perspective, the key takeaway is that these impairments occur across multiple settings and are most problematic at certain times of the day. It’s important for providers to have a meaningful conversation with their patients about their day-to-day challenges to fully appreciate how ADHD impacts their functioning so they can best optimize care.”
The researchers acknowledged as limitations of their study its high number of women participants, potentially reducing the generalizability of its findings; the reliance on self-reported outcomes; and between-group differences for the ADHD and non-ADHD groups that included differences in mean age (39 vs. 43, respectively) and full-time employment status (57% vs. 42%).
The study was sponsored by Shire Pharmaceuticals, with three of its five coauthors employed by the company.
AT APA
ADHD – not OCD – called the key comorbidity in pediatric hoarding
SAN FRANCISCO – Most of the pediatric hoarding literature focuses on hoarding accompanied by obsessive-compulsive disorder. But, “I want to highlight that [attention-deficit/hyperactivity disorder] is across the board something that seems to come up in child hoarding behaviors quite a bit, mirroring the adult literature, which is that hoarding behavior may be much more strongly associated with ADHD than it is with OCD,” Jennifer M. Park, PhD, said at the annual conference of the Anxiety and Depression Association of America.
Multiple studies have established that the prevalence of child hoarding is 2%-3.7%. Onset is typically at age 11-15 years. The course is chronic, and it’s a condition that typically exacerbates over time.
“A lot of the adult literature has shown that hoarding behavior actually starts in childhood. In many retrospective reports, adults say, ‘I’ve had these problems ever since I was a kid,’ ” according to Dr. Park, a psychologist affiliated with Stanford (Calif.) University.
Yet childhood hoarding is not widely perceived as problematic. Indeed, many parents and clinicians view it as developmentally appropriate. That’s to a great extent because the presentation of child hoarding behavior often is very different from and less disturbing than adult hoarding for the obvious reason that parents can limit the amount of clutter in the home.
“I have a bunch of kids who have quite significant hoarding behavior, but the parents are really on top of making sure all of that is left in the closet or within the child’s playroom, or maybe a certain section of the house,” Dr. Park said. “They’re able to keep it contained.”
Also, children and young adolescents lack the resources to accumulate massive clutter. They can’t drive, and have little or no money, so they can’t go on compulsive shopping sprees. “What I have seen in the kids that I work with is they make up for that by collecting things like paper and sticks, rocks, wrappers – anything that might be free, or knickknacks they can pick up along the way,” she said.
The cognitive-behavioral model of hoarding was first described 2 decades ago. It names three main factors as key to maintaining hoarding behaviors: emotional attachment and beliefs associated with one’s possessions, often including anthropomorphization; avoidance behaviors due to severe distress at the prospect of discarding stuff; and information-processing deficits.
“The idea here is that deficits in executive function – things like planning, organization, and inhibition – these are known in an extensive literature to be really strongly associated with ADHD, and executive function deficits link well with hoarding disorder as well,” Dr. Park continued.
Dr. Park was the first author of a recent multicenter study of 431 youths aged 6-17 diagnosed with OCD. They were participants in the OCD Collaborative Genetics Study and the OCD Collaborative Genetics Association Study, during which they completed the Behavior Rating Inventory of Executive Functioning (BRIEF) and the Hoarding Rating Scale–Interview. Clinically significant levels of hoarding compulsions were identified in 113 subjects. Compared with the group with OCD but not hoarding, the OCD/hoarding group had significantly lower scores – meaning problematic deficits – on nearly all of the executive function subscales on the BRIEF, including working memory, emotional control, and planning/organization.
The two groups did not differ significantly in the prevalence of full DSM-IV ADHD. But the hoarding group had significantly more inattention and hyperactivity symptoms, and in a multivariate analysis adjusted for age, sex, and ADHD symptoms, deficits in executive function as measured on the BRIEF instrument were the strongest predictor of hoarding severity in the study population (J Psychiatr Res. 2016 Nov;82:141-8).
In another study by Dr. Park and her coinvestigators involving 99 youth diagnosed with ADHD, the severity of inattention and hyperactivity/impulsivity predicted clinically significant hoarding, whereas nonhoarding OCD symptoms did not (J Atten Disord. 2016 Jul;20[7]:617-26).
In an earlier report by other investigators on 109 children seeking treatment for an anxiety disorder, 22% of the study population proved to have elevated levels of hoarding symptoms. They scored significantly higher than the nonhoarding group on measures of obsession-compulsion, anxiety, inattention, thought problems, rule breaking, aggression, social problems, major depression, and overall functional impairment. But of note, attention problems were a significantly stronger predictor of hoarding symptoms than were OCD or anxiety symptoms (J Anxiety Disord. 2015 Dec;36:9-14).
Discussant Eric Storch, PhD, said that it’s important for clinicians and parents to start taking child hoarding seriously as a legitimate treatment target.
“We know that if you start treatment early, you’re more likely to be successful versus when you start at age 57 and the clutter is 9 or 10 on a scale of 10,” said Dr. Storch, professor of pediatrics and director of clinical research for developmental pediatrics at the University of South Florida, Tampa.
Dr. Park reported having no financial conflicts of interest regarding her presentation.
SAN FRANCISCO – Most of the pediatric hoarding literature focuses on hoarding accompanied by obsessive-compulsive disorder. But, “I want to highlight that [attention-deficit/hyperactivity disorder] is across the board something that seems to come up in child hoarding behaviors quite a bit, mirroring the adult literature, which is that hoarding behavior may be much more strongly associated with ADHD than it is with OCD,” Jennifer M. Park, PhD, said at the annual conference of the Anxiety and Depression Association of America.
Multiple studies have established that the prevalence of child hoarding is 2%-3.7%. Onset is typically at age 11-15 years. The course is chronic, and it’s a condition that typically exacerbates over time.
“A lot of the adult literature has shown that hoarding behavior actually starts in childhood. In many retrospective reports, adults say, ‘I’ve had these problems ever since I was a kid,’ ” according to Dr. Park, a psychologist affiliated with Stanford (Calif.) University.
Yet childhood hoarding is not widely perceived as problematic. Indeed, many parents and clinicians view it as developmentally appropriate. That’s to a great extent because the presentation of child hoarding behavior often is very different from and less disturbing than adult hoarding for the obvious reason that parents can limit the amount of clutter in the home.
“I have a bunch of kids who have quite significant hoarding behavior, but the parents are really on top of making sure all of that is left in the closet or within the child’s playroom, or maybe a certain section of the house,” Dr. Park said. “They’re able to keep it contained.”
Also, children and young adolescents lack the resources to accumulate massive clutter. They can’t drive, and have little or no money, so they can’t go on compulsive shopping sprees. “What I have seen in the kids that I work with is they make up for that by collecting things like paper and sticks, rocks, wrappers – anything that might be free, or knickknacks they can pick up along the way,” she said.
The cognitive-behavioral model of hoarding was first described 2 decades ago. It names three main factors as key to maintaining hoarding behaviors: emotional attachment and beliefs associated with one’s possessions, often including anthropomorphization; avoidance behaviors due to severe distress at the prospect of discarding stuff; and information-processing deficits.
“The idea here is that deficits in executive function – things like planning, organization, and inhibition – these are known in an extensive literature to be really strongly associated with ADHD, and executive function deficits link well with hoarding disorder as well,” Dr. Park continued.
Dr. Park was the first author of a recent multicenter study of 431 youths aged 6-17 diagnosed with OCD. They were participants in the OCD Collaborative Genetics Study and the OCD Collaborative Genetics Association Study, during which they completed the Behavior Rating Inventory of Executive Functioning (BRIEF) and the Hoarding Rating Scale–Interview. Clinically significant levels of hoarding compulsions were identified in 113 subjects. Compared with the group with OCD but not hoarding, the OCD/hoarding group had significantly lower scores – meaning problematic deficits – on nearly all of the executive function subscales on the BRIEF, including working memory, emotional control, and planning/organization.
The two groups did not differ significantly in the prevalence of full DSM-IV ADHD. But the hoarding group had significantly more inattention and hyperactivity symptoms, and in a multivariate analysis adjusted for age, sex, and ADHD symptoms, deficits in executive function as measured on the BRIEF instrument were the strongest predictor of hoarding severity in the study population (J Psychiatr Res. 2016 Nov;82:141-8).
In another study by Dr. Park and her coinvestigators involving 99 youth diagnosed with ADHD, the severity of inattention and hyperactivity/impulsivity predicted clinically significant hoarding, whereas nonhoarding OCD symptoms did not (J Atten Disord. 2016 Jul;20[7]:617-26).
In an earlier report by other investigators on 109 children seeking treatment for an anxiety disorder, 22% of the study population proved to have elevated levels of hoarding symptoms. They scored significantly higher than the nonhoarding group on measures of obsession-compulsion, anxiety, inattention, thought problems, rule breaking, aggression, social problems, major depression, and overall functional impairment. But of note, attention problems were a significantly stronger predictor of hoarding symptoms than were OCD or anxiety symptoms (J Anxiety Disord. 2015 Dec;36:9-14).
Discussant Eric Storch, PhD, said that it’s important for clinicians and parents to start taking child hoarding seriously as a legitimate treatment target.
“We know that if you start treatment early, you’re more likely to be successful versus when you start at age 57 and the clutter is 9 or 10 on a scale of 10,” said Dr. Storch, professor of pediatrics and director of clinical research for developmental pediatrics at the University of South Florida, Tampa.
Dr. Park reported having no financial conflicts of interest regarding her presentation.
SAN FRANCISCO – Most of the pediatric hoarding literature focuses on hoarding accompanied by obsessive-compulsive disorder. But, “I want to highlight that [attention-deficit/hyperactivity disorder] is across the board something that seems to come up in child hoarding behaviors quite a bit, mirroring the adult literature, which is that hoarding behavior may be much more strongly associated with ADHD than it is with OCD,” Jennifer M. Park, PhD, said at the annual conference of the Anxiety and Depression Association of America.
Multiple studies have established that the prevalence of child hoarding is 2%-3.7%. Onset is typically at age 11-15 years. The course is chronic, and it’s a condition that typically exacerbates over time.
“A lot of the adult literature has shown that hoarding behavior actually starts in childhood. In many retrospective reports, adults say, ‘I’ve had these problems ever since I was a kid,’ ” according to Dr. Park, a psychologist affiliated with Stanford (Calif.) University.
Yet childhood hoarding is not widely perceived as problematic. Indeed, many parents and clinicians view it as developmentally appropriate. That’s to a great extent because the presentation of child hoarding behavior often is very different from and less disturbing than adult hoarding for the obvious reason that parents can limit the amount of clutter in the home.
“I have a bunch of kids who have quite significant hoarding behavior, but the parents are really on top of making sure all of that is left in the closet or within the child’s playroom, or maybe a certain section of the house,” Dr. Park said. “They’re able to keep it contained.”
Also, children and young adolescents lack the resources to accumulate massive clutter. They can’t drive, and have little or no money, so they can’t go on compulsive shopping sprees. “What I have seen in the kids that I work with is they make up for that by collecting things like paper and sticks, rocks, wrappers – anything that might be free, or knickknacks they can pick up along the way,” she said.
The cognitive-behavioral model of hoarding was first described 2 decades ago. It names three main factors as key to maintaining hoarding behaviors: emotional attachment and beliefs associated with one’s possessions, often including anthropomorphization; avoidance behaviors due to severe distress at the prospect of discarding stuff; and information-processing deficits.
“The idea here is that deficits in executive function – things like planning, organization, and inhibition – these are known in an extensive literature to be really strongly associated with ADHD, and executive function deficits link well with hoarding disorder as well,” Dr. Park continued.
Dr. Park was the first author of a recent multicenter study of 431 youths aged 6-17 diagnosed with OCD. They were participants in the OCD Collaborative Genetics Study and the OCD Collaborative Genetics Association Study, during which they completed the Behavior Rating Inventory of Executive Functioning (BRIEF) and the Hoarding Rating Scale–Interview. Clinically significant levels of hoarding compulsions were identified in 113 subjects. Compared with the group with OCD but not hoarding, the OCD/hoarding group had significantly lower scores – meaning problematic deficits – on nearly all of the executive function subscales on the BRIEF, including working memory, emotional control, and planning/organization.
The two groups did not differ significantly in the prevalence of full DSM-IV ADHD. But the hoarding group had significantly more inattention and hyperactivity symptoms, and in a multivariate analysis adjusted for age, sex, and ADHD symptoms, deficits in executive function as measured on the BRIEF instrument were the strongest predictor of hoarding severity in the study population (J Psychiatr Res. 2016 Nov;82:141-8).
In another study by Dr. Park and her coinvestigators involving 99 youth diagnosed with ADHD, the severity of inattention and hyperactivity/impulsivity predicted clinically significant hoarding, whereas nonhoarding OCD symptoms did not (J Atten Disord. 2016 Jul;20[7]:617-26).
In an earlier report by other investigators on 109 children seeking treatment for an anxiety disorder, 22% of the study population proved to have elevated levels of hoarding symptoms. They scored significantly higher than the nonhoarding group on measures of obsession-compulsion, anxiety, inattention, thought problems, rule breaking, aggression, social problems, major depression, and overall functional impairment. But of note, attention problems were a significantly stronger predictor of hoarding symptoms than were OCD or anxiety symptoms (J Anxiety Disord. 2015 Dec;36:9-14).
Discussant Eric Storch, PhD, said that it’s important for clinicians and parents to start taking child hoarding seriously as a legitimate treatment target.
“We know that if you start treatment early, you’re more likely to be successful versus when you start at age 57 and the clutter is 9 or 10 on a scale of 10,” said Dr. Storch, professor of pediatrics and director of clinical research for developmental pediatrics at the University of South Florida, Tampa.
Dr. Park reported having no financial conflicts of interest regarding her presentation.
EXPERT ANALYSIS FROM ANXIETY AND DEPRESSION CONFERENCE 2017
What role does asthma medication have in ADHD or depression?
Asthma medications comprise several drug classes, including leukotriene antagonists and steroid-based inhalers. These drugs have been implicated in behavioral changes, such as increased hyperactivity, similar to symptoms of attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD)1; this scenario is more of a concern in children than adults. This raises the question of whether these medications are physiologically linked to behavioral symptoms because of a suggested association with serotonin.2,3 If this is the case, it is necessary to identify and evaluate possible psychiatric effects of these asthma agents.
How asthma medications work
Some asthma agents, such as montelukast, act as either leukotriene-related enzyme inhibitors (arachidonate 5-lipoxygenase) or leukotriene receptor antagonists. These drugs block production of inflammatory leukotrienes, which cause bronchoconstriction. Leukotrienes also can trigger cytokine synthesis, which can modulate leukotriene receptor function. Therefore, leukotriene antagonists could interfere with cytokine function.3,4
Corticosteroid inhalers suppress inflammatory genes by reversing histone acetylation of inflammatory genes involved in asthma. These inhalers have been shown to reduce cytokine levels in patients with chronic lung disease and those with moderate to
Possible link between asthma and serotonin
Serotonin plays an integral role in observable, dysfunctional behaviors seen in disorders such as ADHD and ODD. In previous studies, serotonin modulated the cytokine network, and patients with asthma had elevated levels of plasma serotonin.2,3 These findings imply that asthma medications could be involved in altering levels of both cytokines and serotonin. Pretorius2 emphasized the importance of monitoring serotonin levels in children who exhibit behavioral dysfunction based on these observations:
- Persons with asthma presenting with medical symptoms have elevated serotonin levels.
- Decreased serotonin levels have been associated with ADHD and ODD; medications for ADHD have been shown to increase serotonin levels.
- Asthma medications have been shown to decrease serotonin levels.2,3
Asthma medications might be partially responsible for behavioral disturbances, and therapeutic management should integrate the role of serotonin with asthma therapy.2,3
Clinical considerations
Therapeutic management of asthma should consider psychiatric conditions and treatments. Future research should investigate the overall predisposition for behavioral dysfunction in persons with respiratory syncytial virus, a precursor for asthma. Once an asthma patient’s risk of a psychiatric disorder has been identified, the clinician can determine the most effective medications for treating the condition. If potential medications or genetic or environmental factors are identified, we might expect a move toward personalized care in the not too distant future.
1. Saricoban HE, Ozen A, Harmanci K, et al. Common behavioral problems among children with asthma: is there a role of asthma treatment? Ann Allergy Asthma Immunol. 2011;106(3):200-204.
2. Pretorius E. Asthma medication may influence the psychological functioning of children. Med Hypotheses. 2004;63(3):409-413.
3. Ménard G, Turmei V, Bissonnette EY. Serotonin modulates the cytokine network in the lung: involvement of prostaglandin E2. Clin Exp Immunol. 2007;150(2):340-348.
4. Rola-Pleszczynski M, Stankova J. Cytokine-leukotriene receptor interactions. Scientific World Journal. 2007;7:1348-1358.
5. Kaur M, Reynolds S, Smyth LJ, et al. The effects of corticosteroids on cytokine production from asthma lung lymphocytes. Int Immunopharmacol. 2014;23(2):581-584.
6. Honda R, Ichiyama T, Sunagawa S, et al. Inhaled corticosteroid therapy reduces cytokine levels in sputum from very preterm infants with chronic lung disease. Acta Paediatr. 2009;98(1):118-122.
7. Pretorius E. Corticosteroids, depression and the role of serotonin. Rev Neurosci. 2004;15(2):109-116.
Asthma medications comprise several drug classes, including leukotriene antagonists and steroid-based inhalers. These drugs have been implicated in behavioral changes, such as increased hyperactivity, similar to symptoms of attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD)1; this scenario is more of a concern in children than adults. This raises the question of whether these medications are physiologically linked to behavioral symptoms because of a suggested association with serotonin.2,3 If this is the case, it is necessary to identify and evaluate possible psychiatric effects of these asthma agents.
How asthma medications work
Some asthma agents, such as montelukast, act as either leukotriene-related enzyme inhibitors (arachidonate 5-lipoxygenase) or leukotriene receptor antagonists. These drugs block production of inflammatory leukotrienes, which cause bronchoconstriction. Leukotrienes also can trigger cytokine synthesis, which can modulate leukotriene receptor function. Therefore, leukotriene antagonists could interfere with cytokine function.3,4
Corticosteroid inhalers suppress inflammatory genes by reversing histone acetylation of inflammatory genes involved in asthma. These inhalers have been shown to reduce cytokine levels in patients with chronic lung disease and those with moderate to
Possible link between asthma and serotonin
Serotonin plays an integral role in observable, dysfunctional behaviors seen in disorders such as ADHD and ODD. In previous studies, serotonin modulated the cytokine network, and patients with asthma had elevated levels of plasma serotonin.2,3 These findings imply that asthma medications could be involved in altering levels of both cytokines and serotonin. Pretorius2 emphasized the importance of monitoring serotonin levels in children who exhibit behavioral dysfunction based on these observations:
- Persons with asthma presenting with medical symptoms have elevated serotonin levels.
- Decreased serotonin levels have been associated with ADHD and ODD; medications for ADHD have been shown to increase serotonin levels.
- Asthma medications have been shown to decrease serotonin levels.2,3
Asthma medications might be partially responsible for behavioral disturbances, and therapeutic management should integrate the role of serotonin with asthma therapy.2,3
Clinical considerations
Therapeutic management of asthma should consider psychiatric conditions and treatments. Future research should investigate the overall predisposition for behavioral dysfunction in persons with respiratory syncytial virus, a precursor for asthma. Once an asthma patient’s risk of a psychiatric disorder has been identified, the clinician can determine the most effective medications for treating the condition. If potential medications or genetic or environmental factors are identified, we might expect a move toward personalized care in the not too distant future.
Asthma medications comprise several drug classes, including leukotriene antagonists and steroid-based inhalers. These drugs have been implicated in behavioral changes, such as increased hyperactivity, similar to symptoms of attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD)1; this scenario is more of a concern in children than adults. This raises the question of whether these medications are physiologically linked to behavioral symptoms because of a suggested association with serotonin.2,3 If this is the case, it is necessary to identify and evaluate possible psychiatric effects of these asthma agents.
How asthma medications work
Some asthma agents, such as montelukast, act as either leukotriene-related enzyme inhibitors (arachidonate 5-lipoxygenase) or leukotriene receptor antagonists. These drugs block production of inflammatory leukotrienes, which cause bronchoconstriction. Leukotrienes also can trigger cytokine synthesis, which can modulate leukotriene receptor function. Therefore, leukotriene antagonists could interfere with cytokine function.3,4
Corticosteroid inhalers suppress inflammatory genes by reversing histone acetylation of inflammatory genes involved in asthma. These inhalers have been shown to reduce cytokine levels in patients with chronic lung disease and those with moderate to
Possible link between asthma and serotonin
Serotonin plays an integral role in observable, dysfunctional behaviors seen in disorders such as ADHD and ODD. In previous studies, serotonin modulated the cytokine network, and patients with asthma had elevated levels of plasma serotonin.2,3 These findings imply that asthma medications could be involved in altering levels of both cytokines and serotonin. Pretorius2 emphasized the importance of monitoring serotonin levels in children who exhibit behavioral dysfunction based on these observations:
- Persons with asthma presenting with medical symptoms have elevated serotonin levels.
- Decreased serotonin levels have been associated with ADHD and ODD; medications for ADHD have been shown to increase serotonin levels.
- Asthma medications have been shown to decrease serotonin levels.2,3
Asthma medications might be partially responsible for behavioral disturbances, and therapeutic management should integrate the role of serotonin with asthma therapy.2,3
Clinical considerations
Therapeutic management of asthma should consider psychiatric conditions and treatments. Future research should investigate the overall predisposition for behavioral dysfunction in persons with respiratory syncytial virus, a precursor for asthma. Once an asthma patient’s risk of a psychiatric disorder has been identified, the clinician can determine the most effective medications for treating the condition. If potential medications or genetic or environmental factors are identified, we might expect a move toward personalized care in the not too distant future.
1. Saricoban HE, Ozen A, Harmanci K, et al. Common behavioral problems among children with asthma: is there a role of asthma treatment? Ann Allergy Asthma Immunol. 2011;106(3):200-204.
2. Pretorius E. Asthma medication may influence the psychological functioning of children. Med Hypotheses. 2004;63(3):409-413.
3. Ménard G, Turmei V, Bissonnette EY. Serotonin modulates the cytokine network in the lung: involvement of prostaglandin E2. Clin Exp Immunol. 2007;150(2):340-348.
4. Rola-Pleszczynski M, Stankova J. Cytokine-leukotriene receptor interactions. Scientific World Journal. 2007;7:1348-1358.
5. Kaur M, Reynolds S, Smyth LJ, et al. The effects of corticosteroids on cytokine production from asthma lung lymphocytes. Int Immunopharmacol. 2014;23(2):581-584.
6. Honda R, Ichiyama T, Sunagawa S, et al. Inhaled corticosteroid therapy reduces cytokine levels in sputum from very preterm infants with chronic lung disease. Acta Paediatr. 2009;98(1):118-122.
7. Pretorius E. Corticosteroids, depression and the role of serotonin. Rev Neurosci. 2004;15(2):109-116.
1. Saricoban HE, Ozen A, Harmanci K, et al. Common behavioral problems among children with asthma: is there a role of asthma treatment? Ann Allergy Asthma Immunol. 2011;106(3):200-204.
2. Pretorius E. Asthma medication may influence the psychological functioning of children. Med Hypotheses. 2004;63(3):409-413.
3. Ménard G, Turmei V, Bissonnette EY. Serotonin modulates the cytokine network in the lung: involvement of prostaglandin E2. Clin Exp Immunol. 2007;150(2):340-348.
4. Rola-Pleszczynski M, Stankova J. Cytokine-leukotriene receptor interactions. Scientific World Journal. 2007;7:1348-1358.
5. Kaur M, Reynolds S, Smyth LJ, et al. The effects of corticosteroids on cytokine production from asthma lung lymphocytes. Int Immunopharmacol. 2014;23(2):581-584.
6. Honda R, Ichiyama T, Sunagawa S, et al. Inhaled corticosteroid therapy reduces cytokine levels in sputum from very preterm infants with chronic lung disease. Acta Paediatr. 2009;98(1):118-122.
7. Pretorius E. Corticosteroids, depression and the role of serotonin. Rev Neurosci. 2004;15(2):109-116.
FDA approves generic Strattera for pediatric, adult ADHD patients
The Food and Drug Administration has approved the first generic versions of Strattera (atomoxetine) for the treatment of attention-deficit/hyperactivity disorder, the agency announced May 30.
Apotex, Teva Pharmaceuticals USA, Aurobindo Pharma, and Glenmark Pharmaceuticals all gained approval to market generic atomoxetine at various strengths. All versions must be sold with a patient medication guide describing the uses and risks of atomoxetine and must also include a boxed warning detailing the potential for increased risk of suicidal ideation in children and adolescents.
“Today’s approvals mark an important step forward in bringing consumers additional treatments that have met the FDA’s rigorous standards. Quickly bringing generics to market so patients have more options to treat their conditions is a top priority for the FDA,” Kathleen Uhl, MD, director of the Office of Generic Drugs in the FDA’s Center for Drug Evaluation and Research, said in a press release.
Find the full press release on the FDA website.
The Food and Drug Administration has approved the first generic versions of Strattera (atomoxetine) for the treatment of attention-deficit/hyperactivity disorder, the agency announced May 30.
Apotex, Teva Pharmaceuticals USA, Aurobindo Pharma, and Glenmark Pharmaceuticals all gained approval to market generic atomoxetine at various strengths. All versions must be sold with a patient medication guide describing the uses and risks of atomoxetine and must also include a boxed warning detailing the potential for increased risk of suicidal ideation in children and adolescents.
“Today’s approvals mark an important step forward in bringing consumers additional treatments that have met the FDA’s rigorous standards. Quickly bringing generics to market so patients have more options to treat their conditions is a top priority for the FDA,” Kathleen Uhl, MD, director of the Office of Generic Drugs in the FDA’s Center for Drug Evaluation and Research, said in a press release.
Find the full press release on the FDA website.
The Food and Drug Administration has approved the first generic versions of Strattera (atomoxetine) for the treatment of attention-deficit/hyperactivity disorder, the agency announced May 30.
Apotex, Teva Pharmaceuticals USA, Aurobindo Pharma, and Glenmark Pharmaceuticals all gained approval to market generic atomoxetine at various strengths. All versions must be sold with a patient medication guide describing the uses and risks of atomoxetine and must also include a boxed warning detailing the potential for increased risk of suicidal ideation in children and adolescents.
“Today’s approvals mark an important step forward in bringing consumers additional treatments that have met the FDA’s rigorous standards. Quickly bringing generics to market so patients have more options to treat their conditions is a top priority for the FDA,” Kathleen Uhl, MD, director of the Office of Generic Drugs in the FDA’s Center for Drug Evaluation and Research, said in a press release.
Find the full press release on the FDA website.
ADHD medication may lower risk of motor vehicle crashes
Men with ADHD had a 38% lower risk of motor vehicle crashes (MVCs) when receiving ADHD medication, compared with months off medication. Women had a 42% lower risk, according to the results of a U.S. study.
Estimates suggested that up to 22% of MVCs in patients with ADHD could have been avoided if they had received medication during the whole length of the study, reported Zheng Chang, PhD, of the Karolinska Institutet, Sweden, and his colleagues (JAMA Psychiatry. 2017 May 10. doi: 10.1001/jamapsychiatry.2017.0659)
“This study is the first, to date, to demonstrate a long-term association between receiving ADHD medication and decreased MVCs,” said Dr. Chang and his associates. If this result demonstrates a protective effect, it is possible that continuous ADHD medication use might lead to lower risk of other problems, such as substance abuse disorder, or provide long-term improvements in life functioning for people with ADHD.
This study was supported by grants from the Swedish Research Council and the National Institute of Mental Health, as well as grants to two of the researchers from the Swedish Research Council for Health, Working Life and Welfare, and the National Institute on Drug Abuse. Dr. Chang and the other researchers had no relevant financial disclosures, except for Henrik Larsson, PhD, who received some speaker’s fees and research grants from pharmaceutical companies outside this work.
Prescribing medication to ADHD patients does not guarantee they will take it. Therefore, there is a chance that some of the motor vehicle crashes that occurred during a month when a patient reportedly was on medication may have occurred on a day when the patient had not actually taken medication. Also, using ED visits to measure the number of MVCs has a major drawback: vehicular accidents do not necessarily result in ED visits. Therefore, the study by Chang et al. may not accurately report the benefits of ADHD medication on safe driving.
Management of ADHD is not limited to school or the workplace but extends to other aspects of life, such as driving, which clinicians must consider when prescribing. It also is important to keep in mind, while prescribing, that the progression of ADHD often involves a decrease in hyperactivity during adulthood, while inattention and impulsivity may continue, and that the latter two traits can lead to distracted driving. Another important variable is that MVCs involving individuals with ADHD often happen later in the evening, when their medications may have worn off.
Customizing and improving ADHD pharmacotherapy, while being mindful of effects, is the most sensible way forward.
Vishal Madaan, MD, and Daniel J. Cox, PhD, are at the University of Virginia Health System in Charlottesville. Dr. Madaan reported receiving research support from Forest, Purdue, Aevi Genomic Medicine (formerly Medgenics), Sunovion, and Pfizer, as well as receiving royalties from Taylor & Francis. Dr. Cox reported receiving research support from the National Institutes of Health, Purdue, Johnson & Johnson, and Dexcom. They made these remarks in a commentary accompanying the study by Dr. Chang et al. (JAMA Psychiatry. 2017 May 10. doi: 10.1001/jamapsychiatry.2017.0659).
Prescribing medication to ADHD patients does not guarantee they will take it. Therefore, there is a chance that some of the motor vehicle crashes that occurred during a month when a patient reportedly was on medication may have occurred on a day when the patient had not actually taken medication. Also, using ED visits to measure the number of MVCs has a major drawback: vehicular accidents do not necessarily result in ED visits. Therefore, the study by Chang et al. may not accurately report the benefits of ADHD medication on safe driving.
Management of ADHD is not limited to school or the workplace but extends to other aspects of life, such as driving, which clinicians must consider when prescribing. It also is important to keep in mind, while prescribing, that the progression of ADHD often involves a decrease in hyperactivity during adulthood, while inattention and impulsivity may continue, and that the latter two traits can lead to distracted driving. Another important variable is that MVCs involving individuals with ADHD often happen later in the evening, when their medications may have worn off.
Customizing and improving ADHD pharmacotherapy, while being mindful of effects, is the most sensible way forward.
Vishal Madaan, MD, and Daniel J. Cox, PhD, are at the University of Virginia Health System in Charlottesville. Dr. Madaan reported receiving research support from Forest, Purdue, Aevi Genomic Medicine (formerly Medgenics), Sunovion, and Pfizer, as well as receiving royalties from Taylor & Francis. Dr. Cox reported receiving research support from the National Institutes of Health, Purdue, Johnson & Johnson, and Dexcom. They made these remarks in a commentary accompanying the study by Dr. Chang et al. (JAMA Psychiatry. 2017 May 10. doi: 10.1001/jamapsychiatry.2017.0659).
Prescribing medication to ADHD patients does not guarantee they will take it. Therefore, there is a chance that some of the motor vehicle crashes that occurred during a month when a patient reportedly was on medication may have occurred on a day when the patient had not actually taken medication. Also, using ED visits to measure the number of MVCs has a major drawback: vehicular accidents do not necessarily result in ED visits. Therefore, the study by Chang et al. may not accurately report the benefits of ADHD medication on safe driving.
Management of ADHD is not limited to school or the workplace but extends to other aspects of life, such as driving, which clinicians must consider when prescribing. It also is important to keep in mind, while prescribing, that the progression of ADHD often involves a decrease in hyperactivity during adulthood, while inattention and impulsivity may continue, and that the latter two traits can lead to distracted driving. Another important variable is that MVCs involving individuals with ADHD often happen later in the evening, when their medications may have worn off.
Customizing and improving ADHD pharmacotherapy, while being mindful of effects, is the most sensible way forward.
Vishal Madaan, MD, and Daniel J. Cox, PhD, are at the University of Virginia Health System in Charlottesville. Dr. Madaan reported receiving research support from Forest, Purdue, Aevi Genomic Medicine (formerly Medgenics), Sunovion, and Pfizer, as well as receiving royalties from Taylor & Francis. Dr. Cox reported receiving research support from the National Institutes of Health, Purdue, Johnson & Johnson, and Dexcom. They made these remarks in a commentary accompanying the study by Dr. Chang et al. (JAMA Psychiatry. 2017 May 10. doi: 10.1001/jamapsychiatry.2017.0659).
Men with ADHD had a 38% lower risk of motor vehicle crashes (MVCs) when receiving ADHD medication, compared with months off medication. Women had a 42% lower risk, according to the results of a U.S. study.
Estimates suggested that up to 22% of MVCs in patients with ADHD could have been avoided if they had received medication during the whole length of the study, reported Zheng Chang, PhD, of the Karolinska Institutet, Sweden, and his colleagues (JAMA Psychiatry. 2017 May 10. doi: 10.1001/jamapsychiatry.2017.0659)
“This study is the first, to date, to demonstrate a long-term association between receiving ADHD medication and decreased MVCs,” said Dr. Chang and his associates. If this result demonstrates a protective effect, it is possible that continuous ADHD medication use might lead to lower risk of other problems, such as substance abuse disorder, or provide long-term improvements in life functioning for people with ADHD.
This study was supported by grants from the Swedish Research Council and the National Institute of Mental Health, as well as grants to two of the researchers from the Swedish Research Council for Health, Working Life and Welfare, and the National Institute on Drug Abuse. Dr. Chang and the other researchers had no relevant financial disclosures, except for Henrik Larsson, PhD, who received some speaker’s fees and research grants from pharmaceutical companies outside this work.
Men with ADHD had a 38% lower risk of motor vehicle crashes (MVCs) when receiving ADHD medication, compared with months off medication. Women had a 42% lower risk, according to the results of a U.S. study.
Estimates suggested that up to 22% of MVCs in patients with ADHD could have been avoided if they had received medication during the whole length of the study, reported Zheng Chang, PhD, of the Karolinska Institutet, Sweden, and his colleagues (JAMA Psychiatry. 2017 May 10. doi: 10.1001/jamapsychiatry.2017.0659)
“This study is the first, to date, to demonstrate a long-term association between receiving ADHD medication and decreased MVCs,” said Dr. Chang and his associates. If this result demonstrates a protective effect, it is possible that continuous ADHD medication use might lead to lower risk of other problems, such as substance abuse disorder, or provide long-term improvements in life functioning for people with ADHD.
This study was supported by grants from the Swedish Research Council and the National Institute of Mental Health, as well as grants to two of the researchers from the Swedish Research Council for Health, Working Life and Welfare, and the National Institute on Drug Abuse. Dr. Chang and the other researchers had no relevant financial disclosures, except for Henrik Larsson, PhD, who received some speaker’s fees and research grants from pharmaceutical companies outside this work.
FROM JAMA PSYCHIATRY
Key clinical point:
Major finding: Patients with ADHD have 22% less risk for motor vehicle crashes when they are on medication.
Data source: Data were gathered from commercial insurance claims of a national cohort of 2,319,450 patients with ADHD and ED visits for motor vehicle crashes.
Disclosures: This study was supported by grants from the Swedish Research Council and the National Institute of Mental Health, as well grants to two of the researchers from the Swedish Research Council for Health, Working Life and Welfare, and the National Institute on Drug Abuse. Dr. Chang and the other researchers had no relevant financial disclosures, except for Dr. Larsson who received some speaker’s fees and research grants from pharmaceutical companies outside this work.
Racial, ethnic differences exist ADHD treatment of Medicaid-enrolled youth
, reported Janet R. Cummings, PhD, and her associates at the Rollins School of Public Health at Emory University, Atlanta.
Overall, quality of care for Medicaid-enrolled children receiving ADHD treatment is poor. Of those who initiated medications, 59% visited a provider within 30 days, 64% received at least two other doctor visits, and 38% received combined treatment with any psychotherapy visit. Sixty percent did not fill the ADHD prescription for enough days, 70% had no psychotherapy visit, and 42% stopped treatment.
The percentage that had any follow-up visit in the initiation phase was lower among African American children than among white children (56% vs. 61%, P less than .001), while Hispanic children were more likely than were white children to receive adequate follow-up in the initiation phase (63% vs. 61%; P less than .001) as well as in the C&M phase (71% vs. 63%; P less than .001). In children who continued medication, African American and Hispanic children were more likely than were white children to receive any psychotherapy (42% and 49% vs. 35%; P less than .001).
“The adjusted rate of discontinuing medication was 22.4% points higher (P less than .001) among African American versus white youth and 16.7% points higher (P less than .001) among Hispanic versus white youth,” Dr. Cummings and her associates said. “These findings are in line with research indicating that racial/ethnic minority parents may prefer psychosocial treatments over medication for ADHD.”
In terms of stopping treatment, the percentages were significantly higher among African American (51%) and Hispanic (45%) children than among white children at 36% (P less than .001).
“Higher rates of medication discontinuation among minority youth could be due to differences in cultural health beliefs and/or concerns about ADHD medication treatment. African American parents are less likely than white parents to conceptualize ADHD as a medical condition requiring treatment and may be less willing to administer psychotropic medication to a child due to beliefs about medication efficacy and side effects. ADHD medication is associated with an increased risk of adverse effects ... and a substantial proportion of treatment discontinuation is due to these adverse effects,” the researchers said.
Read more in Pediatrics (2017 May 16. doi: 10.1542/ peds. 2016-2444).
, reported Janet R. Cummings, PhD, and her associates at the Rollins School of Public Health at Emory University, Atlanta.
Overall, quality of care for Medicaid-enrolled children receiving ADHD treatment is poor. Of those who initiated medications, 59% visited a provider within 30 days, 64% received at least two other doctor visits, and 38% received combined treatment with any psychotherapy visit. Sixty percent did not fill the ADHD prescription for enough days, 70% had no psychotherapy visit, and 42% stopped treatment.
The percentage that had any follow-up visit in the initiation phase was lower among African American children than among white children (56% vs. 61%, P less than .001), while Hispanic children were more likely than were white children to receive adequate follow-up in the initiation phase (63% vs. 61%; P less than .001) as well as in the C&M phase (71% vs. 63%; P less than .001). In children who continued medication, African American and Hispanic children were more likely than were white children to receive any psychotherapy (42% and 49% vs. 35%; P less than .001).
“The adjusted rate of discontinuing medication was 22.4% points higher (P less than .001) among African American versus white youth and 16.7% points higher (P less than .001) among Hispanic versus white youth,” Dr. Cummings and her associates said. “These findings are in line with research indicating that racial/ethnic minority parents may prefer psychosocial treatments over medication for ADHD.”
In terms of stopping treatment, the percentages were significantly higher among African American (51%) and Hispanic (45%) children than among white children at 36% (P less than .001).
“Higher rates of medication discontinuation among minority youth could be due to differences in cultural health beliefs and/or concerns about ADHD medication treatment. African American parents are less likely than white parents to conceptualize ADHD as a medical condition requiring treatment and may be less willing to administer psychotropic medication to a child due to beliefs about medication efficacy and side effects. ADHD medication is associated with an increased risk of adverse effects ... and a substantial proportion of treatment discontinuation is due to these adverse effects,” the researchers said.
Read more in Pediatrics (2017 May 16. doi: 10.1542/ peds. 2016-2444).
, reported Janet R. Cummings, PhD, and her associates at the Rollins School of Public Health at Emory University, Atlanta.
Overall, quality of care for Medicaid-enrolled children receiving ADHD treatment is poor. Of those who initiated medications, 59% visited a provider within 30 days, 64% received at least two other doctor visits, and 38% received combined treatment with any psychotherapy visit. Sixty percent did not fill the ADHD prescription for enough days, 70% had no psychotherapy visit, and 42% stopped treatment.
The percentage that had any follow-up visit in the initiation phase was lower among African American children than among white children (56% vs. 61%, P less than .001), while Hispanic children were more likely than were white children to receive adequate follow-up in the initiation phase (63% vs. 61%; P less than .001) as well as in the C&M phase (71% vs. 63%; P less than .001). In children who continued medication, African American and Hispanic children were more likely than were white children to receive any psychotherapy (42% and 49% vs. 35%; P less than .001).
“The adjusted rate of discontinuing medication was 22.4% points higher (P less than .001) among African American versus white youth and 16.7% points higher (P less than .001) among Hispanic versus white youth,” Dr. Cummings and her associates said. “These findings are in line with research indicating that racial/ethnic minority parents may prefer psychosocial treatments over medication for ADHD.”
In terms of stopping treatment, the percentages were significantly higher among African American (51%) and Hispanic (45%) children than among white children at 36% (P less than .001).
“Higher rates of medication discontinuation among minority youth could be due to differences in cultural health beliefs and/or concerns about ADHD medication treatment. African American parents are less likely than white parents to conceptualize ADHD as a medical condition requiring treatment and may be less willing to administer psychotropic medication to a child due to beliefs about medication efficacy and side effects. ADHD medication is associated with an increased risk of adverse effects ... and a substantial proportion of treatment discontinuation is due to these adverse effects,” the researchers said.
Read more in Pediatrics (2017 May 16. doi: 10.1542/ peds. 2016-2444).
FROM PEDIATRICS
Adult ADHD: Pharmacologic treatment in the DSM-5 era
Attention-deficit/hyperactivity disorder (ADHD) is common; it affects 5% to 7% of children1,2 and 4% to 5% of all adults.3,4 Pediatric ADHD often persists into adulthood, as 65% of individuals diagnosed as children retain impairing symptoms by age 25.4
The prevalence of ADHD in childhood is 2 to 3 times greater among boys than girls, but more comparable between the sexes in adulthood.2 Symptoms could be more easily overlooked in women because of the greater prominence of hyperactivity and impulsivity-type symptoms in men.5
Untreated ADHD is associated with significant costs. Adults with ADHD have increased unemployment rates, poor work performance, and comparatively lower educational performance.6,7 Compared with non-ADHD adults, those with ADHD have:
- more traffic violations and accidents and a higher rate of criminal convictions and incarcerations8,9
- a mortality rate almost 2 times higher, with the greatest differences seen in deaths by suicide and accidents.10,11
Adults with ADHD also are more likely to have a comorbid psychiatric disorder—in particular, substance use11—and often are in treatment for other mental or substance use disorders. Among adults who meet diagnostic criteria for ADHD, approximately only 10% are receiving treatment for ADHD symptoms.3,12
Changes in DSM-5
Revisions within DSM-5 simplify ADHD’s diagnosis—and make it more difficult to ignore in
DSM-5 also provides examples of behaviors more commonly found in adults, such as “feelings of restlessness,” compared with DSM-IV’s “often runs about or climbs excessively in situations in which it is inappropriate.” Finally, ADHD now may be diagnosed in a person with an autism spectrum disorder who meets diagnostic criteria for both disorders.13,14
Identifying ADHD in adults
ADHD diagnosis in adults is made through careful clinical interviewing. For example, ask about what factors motivated an individual to seek evaluation for ADHD. Often, patients present after a change in responsibility at work or at home, such as a promotion or birth/adoption of a new child.
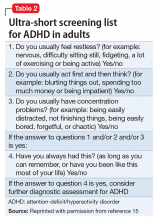
Consider incorporating a brief screen for adult ADHD in all new outpatient evaluations (Table 2).15 Screen for other psychiatric disorders as well; comorbidity with ADHD is high, and hyperactivity and inattention symptoms may result from anxiety, depression, or substance use.
Screen for learning disorders, which can present with ADHD symptoms (such as poor concentration) when the individual attempts difficult tasks. Evaluate for risk factors associated with ADHD medications, such as a history of cardiac problems, hypertension, or tachycardia. A family history of ADHD is found in approximately 80% of cases.16,17 Determine the presence of ADHD symptoms in childhood. A careful review of the educational history often reveals long-term underachievement and struggles in school. Patients may report a chronic history of poor attention or feelings of restlessness in school. Sometimes problems do not become apparent until high school or college; some individuals, especially those with high intelligence, compensate for deficits and show fewer overt symptoms of impairment until later in their education.18Occupational history also may be revealing:
- How are they performing at work?
- Have they changed jobs multiple times in a short period?
- Do they have difficulty organizing tasks?
Subtle ADHD signs include time of arrival to appointments (eg, late or extremely early), missing data on intake paperwork, and a history of losing keys or phones.
Neuropsychological testing. Some clinicians routinely include neuropsychological testing in an adult ADHD evaluation, but these studies have shown inconsistent cognitive deficits in people with ADHD.19,20 No distinct psychometric cognitive test or profile is diagnostic of ADHD or its subtypes.21
Treatment and follow-up care
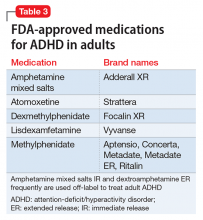
Four general categories of medications are used to treat ADHD in children and adults:
After starting a patient on medication, at each follow-up appointment ask about new cardiac symptoms or diagnoses, new family history of cardiac problems, or new medications. Measure pulse and blood pressure every 1 to 3 months. Measure vital signs more frequently during titration and weaning periods.23
Stimulant medications
Amphetamines have dual action: they block the reuptake of dopamine and noradrenaline by competitive inhibition of the transporters and promote the release of dopamine and noradrenaline by competitive inhibition of the intraneuronal vesicular monoamine transporter.24
For most amphetamine products, including dextroamphetamine and amphetamine mixed salts, the target dosage is approximately 0.5 mg/kg. Start at a lower dosage, however, and rapidly titrate weekly so patients can adjust to the medication while not becoming frustrated with a lack of efficacy. Some patients may require short-acting forms with dosing 3 times per day, and twice daily dosing is not uncommon with extended-release (ER) formulations.
Metabolism of most amphetamine products—with the exception of lisdexamfetamine—involves the cytochrome P450 (CYP) enzyme CYP2D6, leading to the formation of the metabolite 4-hydroxyamphetamine.25 The pharmacokinetics of lisdexamfetamine in slow or ultra-rapid CYP2D6 metabolizers has not been evaluated (Shire US Inc., written communication, July 2014).
Agents that alter urinary pH can affect blood levels of amphetamine. Acidifying agents decrease amphetamine blood levels, while alkalinizing agents increase amphetamine blood levels.26
Lisdexamfetamine contains L-lysine, an essential amino acid, covalently bound to d-amphetamine via an amide linking group.27 After absorption, lisdexamfetamine is metabolized by rate-limited, enzymatic hydrolysis to yield d-amphetamine and L-lysine.24,28,29 A starting dose of 40 mg is advised; twice-daily dosing rarely is required.
A meta-analysis of 5 randomized, controlled trials in the treatment of adult ADHD showed a response rate of 70% for lisdexamfetamine compared with 37% for placebo. Trial duration ranged from 4 to 14 weeks, with dosages of 30 to 70 mg/d.30 Another analysis of data from lisdexamfetamine trials predicted an effect size of 1.07 for European adults, which is larger than the 0.8 threshold for large effect sizes.31
Methylphenidate products. Methylphenidate’s main action is through enhancement of dopamine signaling by blockade of the dopamine transporter, leading to increases in extracellular dopamine as well as norepinephrine.22,32 Optimized dosing is generally 1 mg/kg per day, and dosing up to 80 to 120 mg/d is not unusual.33
Dexmethylphenidate is the more pharmacologically active enantiomer of racemic methylphenidate and is twice as potent.34-36 Target dosing of dexmethylphenidate should be one-half as much (ie, 0.5 mg/kg per day) as other methylphenidate products.37
Managing stimulants’ side effects
Amphetamines’ side effects may include insomnia, dry mouth, decreased appetite, weight loss, headaches, and anxiety. To help minimize sleep problems, advise patients to take a second immediate-release dose at noon, rather than later in the afternoon. The longer-acting formulation taken once per day in the morning may be offered as an alternative. Some patients may experience improved sleep because of diminished bedtime ruminations.
Oral rinses, such as Biotène, could help reduce discomfort associated with dry mouth. Pilocarpine, which stimulates saliva production, is another option if rinses are not effective. To address decreased appetite, advise patients to take their medication after they eat. Switching from an immediate-release amphetamine to a longer-acting formulation also may lessen symptoms. Lisdexamfetamine might be a good choice for adults with ADHD who have undergone bariatric surgeries because it is absorbed in the small bowel.38
Methylphenidate has no interactions with CYP enzymes, making it an attractive option for patients taking CYP inhibiting or stimulating medications.39 The most common side effects of methylphenidate products include appetite loss, insomnia, irritability, and tachycardia. Some side effects will abate after 1 to 2 weeks of treatment, but persistence of insomnia and appetite loss may require a decrease in dosage. In rare cases, methylphenidate may produce tics, exacerbate an existing tic disorder, or produce mania or psychosis.40,41 Methylphenidate inhibits the metabolism of tricyclic antidepressants; use methylphenidate with caution in patients taking monoamine oxidase inhibitors.42,43Cardiovascular risks. Possible cardiovascular risks associated with stimulant use have gained widespread attention, although research has not demonstrated an increased risk of serious cardiovascular events in young and middle-aged adults receiving stimulant medications for ADHD.44 Nonetheless, obtain a thorough medical history in adult patients, including cardiac history, family history of cardiac disease, history of any cardiac symptoms, and a medication history. Baseline ECG is not required.45
Screen for a family history of sudden death in a young person, sudden death during exercise, cardiac arrhythmia, cardiomyopathies (including hypertrophic cardiomyopathy, dilated cardiomyopathy, and right ventricular cardiomyopathy), prolonged QT interval, short QT syndrome, Brugada syndrome, Wolff-Parkinson-White syndrome, Marfan syndrome, and an event requiring resuscitation in a family member younger than 35, including syncope requiring rescuscitation.23 If fainting spells, palpitations, chest pain, or other symptoms suggest preexisting cardiovascular disease, refer the patient promptly to a cardiologist.
Peripheral vasculopathy, including Raynaud’s phenomenon, is a lesser known side effect associated with stimulants.46 Symptoms are usually mild, but in rare instances stimulants are associated with digital ulceration or soft tissue breakdown.47 Advise patients to tell you if they experience any new symptoms of numbness, pain, skin color changes, or sensitivity to temperature in fingers and toes. Signs and symptoms generally improve after dosage reduction or discontinuation of the stimulant medication.46 Referral to a rheumatologist might be appropriate if symptoms persist.
A noradrenergic medication
Atomoxetine is a potent, selective inhibitor of the presynaptic noradrenaline transporter that increases the availability of extracellular noradrenaline in the prefrontal cortex.48,49 Atomoxetine may be a good alternative for adult patients with ADHD and comorbid anxiety.50
For adults, the optimal starting dosage is 40 mg in the morning for 1 week, followed by an increase to 80 mg. Insufficient dosing is common with atomoxetine, and the dosage could be increased to 100 mg/d.51 Dosing twice per day may be associated with higher rates of insomnia.
Atomoxetine’s efficacy for managing ADHD in adults has been consistently demonstrated by 6 placebo-controlled trials of 10 to 16 weeks, 3 placebo-controlled 6-month trials, and a 1-year maintenance-of-response trial.52 Atomoxetine was found to have an effect size of 0.45 (medium) (number needed to treat [NNT] = 5).53-55The most common adverse effects include nausea, dry mouth, insomnia, and erectile dysfunction. Small increases in heart rate and blood pressure have been reported, so use this medication with caution in patients for whom this might be problematic. Atomoxetine is metabolized by CYP2D6; 7% of white individuals have a genotype corresponding to a nonfunctional CYP2D6 enzyme.56-58
Alpha-2 adrenergic agonists
Clonidine and guanfacine are antihypertensive drugs that induce peripheral sympathoinhibition via the stimulation of receptors. Clonidine binds equally to adrenergic receptor subtypes α-2A, α-2B, and α-2C (as well as to α-1 and β subtypes, histamine receptors, and possibly dopamine receptors).59,60 Guanfacine binds preferentially to postsynaptic α-2A adrenoceptors in the prefrontal cortex, which have been implicated in attentional and organizational functions.61,62
ER guanfacine and ER clonidine are FDA-approved as monotherapy for ADHD in children and adolescents.
Efficacy in adults. A small (N = 17), double-blind, placebo-controlled, crossover study comparing immediate-release guanfacine and dextroamphetamine found that both medications significantly reduced adult ADHD symptoms, as measured with the DSM-IV Adult Behavior Checklist for Adults.63
No trials have been published regarding the efficacy of ER clonidine in adults with ADHD; adverse effects including sedation, bradycardia, and hypotension may limit its use. One study compared the supplemental use of ER guanfacine (1 to 6 mg/d) or a matching placebo in 26 adults with ADHD who had suboptimal response to stimulant-only treatment. After 10 weeks, both the guanfacine ER and placebo groups showed statistically significant improvements in ADHD symptoms and general functioning. The treatments did not differ in efficacy, safety, or tolerability.64
Adverse events. Compared with clonidine, guanfacine has less CNS depressant and hypotensive activity.58 A phase I trial of ER guanfacine in healthy adults found its single-dose pharmacokinetic properties in 1-, 2-, and 4-mg tablets appeared to be statistically linear. Somnolence—the most common treatment-emergent adverse effect—occurred in 33 of 52 participants (63.5%). All mean vital-sign measurements and ECG parameters remained within normal limits after dosing, and no marked changes from baseline measurements were noted.65
Antidepressants
Antidepressants used in ADHD treatment include bupropion and tricyclic antidepressants.
Bupropion is a noradrenaline and dopamine reuptake inhibitor and is considered to be a mild psychostimulant because of its amphetamine-derived chemical structure.66,67 It generally is considered a third-line medication when stimulants have not improved ADHD symptoms or are not tolerated.
A 2011 meta-analysis examined 5 randomized, controlled trials including 175 adults treated with bupropion for ADHD. Bupropion was found to be more effective than placebo (NNT = 5), although bupropion’s therapeutic benefits were not observed until weeks 5 and 6. Its effects were less pronounced than those of methylphenidate. Mean daily dosages were 362 mg for the bupropion SR trials and 393 mg for the bupropion XL trial.68
Tricyclics. Desipramine and nortriptyline have been found to be efficacious in childhood ADHD,69,70 although cardiovascular risk and toxicity in overdose limit their use.71
1. Polanczyk G, de Lima MS, Horta BL, et al. The worldwide prevalence of ADHD: a systemic review and metaregression analysis. Am J Psychiatry. 2007;164(6):942-948.
2. Simon V, Czobor P, Bálint S, et al. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br J Psychiatry. 2009;194(3):204-211.
3. Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163(4):716-723.
4. Faraone S, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36(2):159-165.
5. Gershon J. A meta-analytic review of gender differences in ADHD. J Atten Disord. 2002;5(3):143-154.
6. Halmøy A, Fasmer OB, Gillberg C, et al. Occupational outcome in adult ADHD: impact of symptom profile, comorbid psychiatric problems, and treatment: a cross-sectional study of 414 clinically diagnosed adult ADHD patients. J Atten Disord. 2009;13(2):175-187.
7. Kuriyan AB, Pelham WE Jr, Molina BS, et al. Young adult educational and vocational outcomes of children diagnosed with ADHD. J Abnorm Child Psychol. 2013;41(1):27-41.
8. Murphy K, Barkley RA. Attention deficit hyperactivity disorder in adults: comorbidities and adaptive impairment. Compr Psychiatry. 1996;37(6):393-401.
9. Mannuzza S, Klein RG, Mouton JL 3rd. Lifetime criminality among boys with attention deficit hyperactivity disorder: a prospective follow-up study into adulthood using official arrest records. Psychiatry Res. 2008;160(3):237-246.
10. Dalsgaard S, Østergaard SD, Leckman JF, et al. Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: a nationwide cohort study. Lancet. 2015;385(9983):2190-2196.
11. Barbaresi WJ, Colligan RC, Weaver AL, et al. Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: a prospective study. Pediatrics. 2013;131(4):637-644.
12. Babcock T, Ornstein CS. Comorbidity and its impact in adult patients with attention-deficit/hyperactivity disorder: a primary care perspective. Postgrad Med. 2009;121(3):73-82.
13. Attention-deficit/hyperactivity disorder. In: Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:59-66.
14. Attention-deficit/hyperactivity disorder. In: Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000:78-85.
15. Kooij JJS. Adult ADHD: diagnostic assessment and treatment. 3rd ed. Amsterdam, Netherlands: Springer; 2013:34.
16. Faraone SV, Khan SA. Candidate gene studies of attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2006;67(suppl 8):13-20.
17. Neale BM, Medland SE, Ripke S, et al; Psychiatric GWAS Consortium: ADHD Subgroup. Meta-analysis of genome-wide association studies of attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2010;49(9):884-897.
18. Milioni AL, Chaim TM, Cavallet M, et al. High IQ may “mask” the diagnosis of ADHD by compensating for deficits in executive functions in treatment-naïve adults with ADHD [published online October 30, 2014]. J Atten Disord. pii: 1087054714554933.
19. Rapport MD, Chung KM, Shore G, et al. Upgrading the science and technology of assessment and diagnosis: laboratory and clinic-based assessment of children with ADHD. J Clin Child Psychol. 2000;29(4):555-568.
20. Woods SP, Lovejoy DW, Ball JD. Neuropsychological characteristics of adults with ADHD: a comprehensive review of initial studies. Clin Neuropsychol. 2002;16(1):12-34.
21. Lange KW, Hauser J, Lange KM, et al. Utility of cognitive neuropsychological assessment in attention-deficit/hyperactivity disorder. Atten Defic Hyperact Disord. 2014;6(4):241-248.
22. Arnold LE. Methylphenidate vs. amphetamine: comparative review. J Atten Disord. 2000;3(4):200-211.
23. Vetter VL Elia J, Erickson, C, et al; American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee; American Heart Association Council on Cardiovascular Nursing. Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder [corrected]: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing [Erratum in: Circulation. 2009;120(7):e55-e59]. Circulation. 2008;117(18):2407-2423.
24. Seiden LS, Sabol KE, Ricaurte GA. Amphetamine: effects on catecholamine systems and behavior. Annu Rev Pharmacol Toxicol. 1993;33:639-677.
25. Wu D, Otton SV, Inaba T, et al. Interactions of amphetamine analogs with human liver CYP2D6. Biochem Pharmacol. 1997;53(11):1605-1612.
26. Vyvanse [package insert]. Lexington, MA: Shire Pharmaceuticals; 2015.
27. Pennick M. Absorption of lisdexamfetamine dimesylate and its enzymatic conversion to d-amphetamine. Neuropsychiatr Dis Treat. 2010;6:317-327.
28. Heal DJ, Smith SL, Gosden J, et al. Amphetamine, past and present—a pharmacological and clinical perspective. J Psychopharmacol. 2013;27(6):479-496.
29. Krishnan SM, Pennick M, Stark JG. Metabolism, distribution and elimination of lisdexamfetamine dimesylate: open-label, single-centre, phase I study in healthy adult volunteers. Clin Drug Invest. 2008;28(12):745-755.
30. Maneeton N, Maneeton B, Suttajit S, et al. Exploratory meta-analysis on lisdexamfetamine versus placebo in adult ADHD. Drug Des Devel Ther. 2014;8:1685-1693.
31. Fridman M, Hodgkins P, Kahle JS, et al. Predicted effect size of lisdexamfetamine treatment of attention deficit/hyperactivity disorder (ADHD) in European adults: estimates based on indirect analysis using a systematic review and meta-regression analysis. Eur Psychiatry. 2015;30(4):521-527.
32. Markowitz JS, DeVane CL, Pestreich L, et al. Session 1-87-differentiation of d-, L- and dl-methylphenidate through in vitro pharmacological screening. In: Abstracts: Oral and Poster Presentations of the NCDEU 45th Annual Meeting; June 6-9, 2005; Boca Raton, FL:186.
33. Spencer T, Biederman J, Wilens T, et al. A large, double-blind, randomized clinical trial of methylphenidate in the treatment of adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2005;57(5):456-463.
34. Teo SK, Stirling DI, Thomas SD, et al. Neurobehavioral effects of racemic threo-methylphenidate and its D and L enantiomers in rats. Pharmacol Biochem Behav. 2003;74(3):747-754.
35. Ding YS, Fowler JS, Volkow ND, et al. Chiral drugs: comparison of the pharmacokinetics of [11C]d-threo and L-threo-methylphenidate in the human and baboon brain. Psychopharmacol (Berl). 1997;131(1):71-78.
36. Davids E, Zhang K, Tarazi FI, et al. Stereoselective effects of methylphenidate on motor hyperactivity in juvenile rats induced by neonatal 6-hydroxydopamine lesioning. Psychopharmacol (Berl). 2002;160(1):92-98.
37. Srinivas NR, Hubbard JW, Quinn D, et al. Enantioselective pharmacokinetics and pharmacodynamics of dl-threo-methylphenidate in children with attention deficit hyperactivity disorder. Clin Pharmacol Ther. 1992;52(5):561-568.
38. Ermer JC, Haffey MB, Doll WJ, et al. Pharmacokinetics of lisdexamfetamine dimesylate after targeted gastrointestinal release or oral administration in healthy adults. Drug Metab Dispos. 2012;40(2):290-297.
39. DeVane CL, Markowitz JS, Carson SW, et al. Single-dose pharmacokinetics of methylphenidate in CYP2D6 extensive and poor metabolizers. J Clin Psychopharmacol. 2000;20(3):347-349.
40. Graham J, Coghill D. Adverse effects of pharmacotherapies for attention-deficit hyperactivity disorder: epidemiology, prevention and management. CNS Drugs. 2008;22(3):213-237.
41. Ross RG. Psychotic and manic-like symptoms during stimulant treatment of attention deficit hyperactivity disorder. Am J Psychiatry. 2006;163(7):1149-1152.
42. Shelton Clauson A, Elliott ES, Watson BD, et al. Coadministration of phenelzine and methylphenidate for treatment-resistant depression. Ann Pharmacother. 2004;38(3):508.
43. Markowitz JS, Patrick KS. Pharmacokinetic and pharmacodynamic drug interactions in the treatment of attention-deficit hyperactivity disorder. Clin Pharmacokinet. 2001;40(10):753-772.
44. Habel LA, Cooper WO, Sox CM, et al. ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. JAMA. 2011;306(24):2673-2683.
45. Graham J, Banaschewski T, Buitelaar J, et al; European Guidelines Group. European guidelines on managing adverse effects of medication for ADHD. Eur Child Adolesc Psychiatry. 2011;20(1):17-37.
46. Goldman W, Seltzer R, Reuman P. Association between treatment with central nervous system stimulants and Raynaud’s syndrome in children: a retrospective case-control study of rheumatology patients. Arthritis Rheum. 2008;58(2):563-566.
47. Syed RH, Moore TL. Methylphenidate and dextroamphetamine-induced peripheral vasculopathy. J Clin Rheum. 2008;14(1):30-33.
48. Wilens TE. Mechanism of action of agents in attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2006;67(suppl 8):32-38.
49. Bymaster FP, Katner JS, Nelson DL, et al. Atomoxetine increases extracellular levels of norepinephrine and dopamine in prefrontal cortex of rat: a potential mechanism for efficacy in attention deficit/hyperactivity disorder. Neuropsychopharmacology. 2002;27(5):699-711.
50. Adler LA, Liebowitz M, Kronenberger W, et al. Atomoxetine treatment in adults with attention-deficit/hyperactivity disorder and comorbid social anxiety disorder. Depress Anxiety. 2009;26(3):212-221.
51. Clemow DB. Suboptimal dosing of Strattera (atomoxetine) for ADHD patients. Postgrad Med. 2014;126(5):196-198.
52. Camporeale A, Porsdal V, De Bruyckere K, et al. Safety and tolerability of atomoxetine in treatment of attention deficit hyperactivity disorder in adult patients: an integrated analysis of 15 clinical trials. J Psychopharmacol. 2015;29(1):3-14.
53. Young JL, Sarkis E, Qiao M, et al. Once-daily treatment with atomoxetine in adults with attention-deficit/hyperactivity disorder: a 24-week, randomized, double-blind, placebo-controlled trial. Clin Neuropharmacol. 2011;34(2):51-60.
54. Bitter I, Angyalosi A, Czobor P. Pharmacological treatment of adult ADHD. Curr Opin Psychiatry. 2012;25(6):529-534.
55. Faraone SV, Glatt SJ. A comparison of the efficacy of medications for adult attention-deficit/hyperactivity disorder using meta-analysis of effect sizes. J Clin Psychiatry. 2010;71(6):754-763.
56. Ring BJ, Gillespie JS, Eckstein JA, et al. Identification of the human cytochromes P450 responsible for atomoxetine metabolism. Drug Metab Dispos. 2002;30(3):319-323.
57. Farid NA, Bergstrom RF, Ziege EA, et al. Single-dose and steady state pharmacokinetics of tomoxetine in normal subjects. J Clin Pharmacol. 1985;25(4):296-301.
58. Mizutani T. PM frequencies of major CYPs in Asians and Caucasians. Drug Metab Rev. 2003;35(2-3):99-106.
59. Jasper JR, Lesnick JD, Chang LK, et al. Ligand efficacy and potency at recombinant alpha2 adrenergic receptors: agonist-mediated [35S]GTPgammaS binding. Biochem Pharmacol. 1998;55(7):1035-1043.
60. Ruggiero S, Clavenna A, Reale L, et al. Guanfacine for attention deficit and hyperactivity disorder in pediatrics: a systematic review and meta-analysis. Eur Neuropsychopharmacol. 2014;24(10):1578-1590.
61. Arnsten AF, Pliszka SR. Catecholamine influences on prefrontal cortical function: relevance to treatment of attention deficit/hyperactivity disorder and related disorders. Pharmacol Biochem Behav. 2011;99(2):211-216.
62. Uhlén S, Wikberg JE. Delineation of rat kidney alpha 2A- and alpha 2B-adrenoceptors with [3H]RX821002 radioligand binding: computer modelling reveals that guanfacine is an alpha 2A-selective compound. Eur J Pharmacol. 1991;202(2):235-243.
63. Taylor FB, Russo J. Comparing guanfacine and dextroamphetamine for the treatment of adult attention deficit/hyperactivity disorder. J Clin Psychopharmacol. 2001;21(2):223-228.
64. Butterfield ME, Saal J, Young B, et al. Supplementary guanfacine hydrochloride as a treatment of attention deficit hyperactivity disorder in adults: a double blind, placebo-controlled study. Psychiatry Res. 2016;236:136-141.
65. Swearingen D, Pennick M, Shojaei A, et al. A phase I, randomized, open-label, crossover study of the single-dose pharmacokinetic properties of guanfacine extended-release 1-, 2-, and 4-mg tablets in healthy adults. Clin Ther. 2007;29(4):617-625.
66. Cooper BR, Wang CM, Cox RF. Evidence that the acute behavioral and electrophysiological effects of bupropion (Wellbutrin) are mediated by a noradrenergic mechanism. Neuropsychopharmacology. 1994;11(2):133-141.
67. Reimherr FW, Hedges DW, Strong RE, et al. Bupropion SR in adults with ADHD: a short-term, placebo-controlled trial. Neuropsychiatr Dis Treat. 2005;1(3):245-251.
68. Maneeton N, Maneeton B, Srisurapanont M, et al. Bupropion for adults with attention-deficit hyperactivity disorder: meta-analysis of randomized, placebo-controlled trials. Psychiatry Clin Neurosci. 2011;65(7):611-617.
69. Biederman J, Baldessarini RJ, Wright V, et al. A double-blind placebo controlled study of desipramine in the treatment of ADD: I. Efficacy. J Am Acad Child Adolesc Psychiatry. 1989;28(5):777-784.
70. Spencer T, Biederman J, Wilens T, et al. Nortriptyline treatment of children with attention-deficit hyperactivity disorder and tic disorder or Tourette’s syndrome. J Am Acad Child Adolesc Psychiatry. 1993;32(1):205-210.
71. Bond DJ, Hadjipavlou G, Lam RW, et al. The Canadian Network for Mood and Anxiety Treatments (CANMAT) task force recommendations for the management of patients with mood disorders and comorbid attention-deficit/hyperactivity disorder. Ann Clin Psychiatry. 2012;24(1):23-37.
Attention-deficit/hyperactivity disorder (ADHD) is common; it affects 5% to 7% of children1,2 and 4% to 5% of all adults.3,4 Pediatric ADHD often persists into adulthood, as 65% of individuals diagnosed as children retain impairing symptoms by age 25.4
The prevalence of ADHD in childhood is 2 to 3 times greater among boys than girls, but more comparable between the sexes in adulthood.2 Symptoms could be more easily overlooked in women because of the greater prominence of hyperactivity and impulsivity-type symptoms in men.5
Untreated ADHD is associated with significant costs. Adults with ADHD have increased unemployment rates, poor work performance, and comparatively lower educational performance.6,7 Compared with non-ADHD adults, those with ADHD have:
- more traffic violations and accidents and a higher rate of criminal convictions and incarcerations8,9
- a mortality rate almost 2 times higher, with the greatest differences seen in deaths by suicide and accidents.10,11
Adults with ADHD also are more likely to have a comorbid psychiatric disorder—in particular, substance use11—and often are in treatment for other mental or substance use disorders. Among adults who meet diagnostic criteria for ADHD, approximately only 10% are receiving treatment for ADHD symptoms.3,12
Changes in DSM-5
Revisions within DSM-5 simplify ADHD’s diagnosis—and make it more difficult to ignore in
DSM-5 also provides examples of behaviors more commonly found in adults, such as “feelings of restlessness,” compared with DSM-IV’s “often runs about or climbs excessively in situations in which it is inappropriate.” Finally, ADHD now may be diagnosed in a person with an autism spectrum disorder who meets diagnostic criteria for both disorders.13,14
Identifying ADHD in adults
ADHD diagnosis in adults is made through careful clinical interviewing. For example, ask about what factors motivated an individual to seek evaluation for ADHD. Often, patients present after a change in responsibility at work or at home, such as a promotion or birth/adoption of a new child.
Consider incorporating a brief screen for adult ADHD in all new outpatient evaluations (Table 2).15 Screen for other psychiatric disorders as well; comorbidity with ADHD is high, and hyperactivity and inattention symptoms may result from anxiety, depression, or substance use.
Screen for learning disorders, which can present with ADHD symptoms (such as poor concentration) when the individual attempts difficult tasks. Evaluate for risk factors associated with ADHD medications, such as a history of cardiac problems, hypertension, or tachycardia. A family history of ADHD is found in approximately 80% of cases.16,17 Determine the presence of ADHD symptoms in childhood. A careful review of the educational history often reveals long-term underachievement and struggles in school. Patients may report a chronic history of poor attention or feelings of restlessness in school. Sometimes problems do not become apparent until high school or college; some individuals, especially those with high intelligence, compensate for deficits and show fewer overt symptoms of impairment until later in their education.18Occupational history also may be revealing:
- How are they performing at work?
- Have they changed jobs multiple times in a short period?
- Do they have difficulty organizing tasks?
Subtle ADHD signs include time of arrival to appointments (eg, late or extremely early), missing data on intake paperwork, and a history of losing keys or phones.
Neuropsychological testing. Some clinicians routinely include neuropsychological testing in an adult ADHD evaluation, but these studies have shown inconsistent cognitive deficits in people with ADHD.19,20 No distinct psychometric cognitive test or profile is diagnostic of ADHD or its subtypes.21
Treatment and follow-up care
Four general categories of medications are used to treat ADHD in children and adults:
After starting a patient on medication, at each follow-up appointment ask about new cardiac symptoms or diagnoses, new family history of cardiac problems, or new medications. Measure pulse and blood pressure every 1 to 3 months. Measure vital signs more frequently during titration and weaning periods.23
Stimulant medications
Amphetamines have dual action: they block the reuptake of dopamine and noradrenaline by competitive inhibition of the transporters and promote the release of dopamine and noradrenaline by competitive inhibition of the intraneuronal vesicular monoamine transporter.24
For most amphetamine products, including dextroamphetamine and amphetamine mixed salts, the target dosage is approximately 0.5 mg/kg. Start at a lower dosage, however, and rapidly titrate weekly so patients can adjust to the medication while not becoming frustrated with a lack of efficacy. Some patients may require short-acting forms with dosing 3 times per day, and twice daily dosing is not uncommon with extended-release (ER) formulations.
Metabolism of most amphetamine products—with the exception of lisdexamfetamine—involves the cytochrome P450 (CYP) enzyme CYP2D6, leading to the formation of the metabolite 4-hydroxyamphetamine.25 The pharmacokinetics of lisdexamfetamine in slow or ultra-rapid CYP2D6 metabolizers has not been evaluated (Shire US Inc., written communication, July 2014).
Agents that alter urinary pH can affect blood levels of amphetamine. Acidifying agents decrease amphetamine blood levels, while alkalinizing agents increase amphetamine blood levels.26
Lisdexamfetamine contains L-lysine, an essential amino acid, covalently bound to d-amphetamine via an amide linking group.27 After absorption, lisdexamfetamine is metabolized by rate-limited, enzymatic hydrolysis to yield d-amphetamine and L-lysine.24,28,29 A starting dose of 40 mg is advised; twice-daily dosing rarely is required.
A meta-analysis of 5 randomized, controlled trials in the treatment of adult ADHD showed a response rate of 70% for lisdexamfetamine compared with 37% for placebo. Trial duration ranged from 4 to 14 weeks, with dosages of 30 to 70 mg/d.30 Another analysis of data from lisdexamfetamine trials predicted an effect size of 1.07 for European adults, which is larger than the 0.8 threshold for large effect sizes.31
Methylphenidate products. Methylphenidate’s main action is through enhancement of dopamine signaling by blockade of the dopamine transporter, leading to increases in extracellular dopamine as well as norepinephrine.22,32 Optimized dosing is generally 1 mg/kg per day, and dosing up to 80 to 120 mg/d is not unusual.33
Dexmethylphenidate is the more pharmacologically active enantiomer of racemic methylphenidate and is twice as potent.34-36 Target dosing of dexmethylphenidate should be one-half as much (ie, 0.5 mg/kg per day) as other methylphenidate products.37
Managing stimulants’ side effects
Amphetamines’ side effects may include insomnia, dry mouth, decreased appetite, weight loss, headaches, and anxiety. To help minimize sleep problems, advise patients to take a second immediate-release dose at noon, rather than later in the afternoon. The longer-acting formulation taken once per day in the morning may be offered as an alternative. Some patients may experience improved sleep because of diminished bedtime ruminations.
Oral rinses, such as Biotène, could help reduce discomfort associated with dry mouth. Pilocarpine, which stimulates saliva production, is another option if rinses are not effective. To address decreased appetite, advise patients to take their medication after they eat. Switching from an immediate-release amphetamine to a longer-acting formulation also may lessen symptoms. Lisdexamfetamine might be a good choice for adults with ADHD who have undergone bariatric surgeries because it is absorbed in the small bowel.38
Methylphenidate has no interactions with CYP enzymes, making it an attractive option for patients taking CYP inhibiting or stimulating medications.39 The most common side effects of methylphenidate products include appetite loss, insomnia, irritability, and tachycardia. Some side effects will abate after 1 to 2 weeks of treatment, but persistence of insomnia and appetite loss may require a decrease in dosage. In rare cases, methylphenidate may produce tics, exacerbate an existing tic disorder, or produce mania or psychosis.40,41 Methylphenidate inhibits the metabolism of tricyclic antidepressants; use methylphenidate with caution in patients taking monoamine oxidase inhibitors.42,43Cardiovascular risks. Possible cardiovascular risks associated with stimulant use have gained widespread attention, although research has not demonstrated an increased risk of serious cardiovascular events in young and middle-aged adults receiving stimulant medications for ADHD.44 Nonetheless, obtain a thorough medical history in adult patients, including cardiac history, family history of cardiac disease, history of any cardiac symptoms, and a medication history. Baseline ECG is not required.45
Screen for a family history of sudden death in a young person, sudden death during exercise, cardiac arrhythmia, cardiomyopathies (including hypertrophic cardiomyopathy, dilated cardiomyopathy, and right ventricular cardiomyopathy), prolonged QT interval, short QT syndrome, Brugada syndrome, Wolff-Parkinson-White syndrome, Marfan syndrome, and an event requiring resuscitation in a family member younger than 35, including syncope requiring rescuscitation.23 If fainting spells, palpitations, chest pain, or other symptoms suggest preexisting cardiovascular disease, refer the patient promptly to a cardiologist.
Peripheral vasculopathy, including Raynaud’s phenomenon, is a lesser known side effect associated with stimulants.46 Symptoms are usually mild, but in rare instances stimulants are associated with digital ulceration or soft tissue breakdown.47 Advise patients to tell you if they experience any new symptoms of numbness, pain, skin color changes, or sensitivity to temperature in fingers and toes. Signs and symptoms generally improve after dosage reduction or discontinuation of the stimulant medication.46 Referral to a rheumatologist might be appropriate if symptoms persist.
A noradrenergic medication
Atomoxetine is a potent, selective inhibitor of the presynaptic noradrenaline transporter that increases the availability of extracellular noradrenaline in the prefrontal cortex.48,49 Atomoxetine may be a good alternative for adult patients with ADHD and comorbid anxiety.50
For adults, the optimal starting dosage is 40 mg in the morning for 1 week, followed by an increase to 80 mg. Insufficient dosing is common with atomoxetine, and the dosage could be increased to 100 mg/d.51 Dosing twice per day may be associated with higher rates of insomnia.
Atomoxetine’s efficacy for managing ADHD in adults has been consistently demonstrated by 6 placebo-controlled trials of 10 to 16 weeks, 3 placebo-controlled 6-month trials, and a 1-year maintenance-of-response trial.52 Atomoxetine was found to have an effect size of 0.45 (medium) (number needed to treat [NNT] = 5).53-55The most common adverse effects include nausea, dry mouth, insomnia, and erectile dysfunction. Small increases in heart rate and blood pressure have been reported, so use this medication with caution in patients for whom this might be problematic. Atomoxetine is metabolized by CYP2D6; 7% of white individuals have a genotype corresponding to a nonfunctional CYP2D6 enzyme.56-58
Alpha-2 adrenergic agonists
Clonidine and guanfacine are antihypertensive drugs that induce peripheral sympathoinhibition via the stimulation of receptors. Clonidine binds equally to adrenergic receptor subtypes α-2A, α-2B, and α-2C (as well as to α-1 and β subtypes, histamine receptors, and possibly dopamine receptors).59,60 Guanfacine binds preferentially to postsynaptic α-2A adrenoceptors in the prefrontal cortex, which have been implicated in attentional and organizational functions.61,62
ER guanfacine and ER clonidine are FDA-approved as monotherapy for ADHD in children and adolescents.
Efficacy in adults. A small (N = 17), double-blind, placebo-controlled, crossover study comparing immediate-release guanfacine and dextroamphetamine found that both medications significantly reduced adult ADHD symptoms, as measured with the DSM-IV Adult Behavior Checklist for Adults.63
No trials have been published regarding the efficacy of ER clonidine in adults with ADHD; adverse effects including sedation, bradycardia, and hypotension may limit its use. One study compared the supplemental use of ER guanfacine (1 to 6 mg/d) or a matching placebo in 26 adults with ADHD who had suboptimal response to stimulant-only treatment. After 10 weeks, both the guanfacine ER and placebo groups showed statistically significant improvements in ADHD symptoms and general functioning. The treatments did not differ in efficacy, safety, or tolerability.64
Adverse events. Compared with clonidine, guanfacine has less CNS depressant and hypotensive activity.58 A phase I trial of ER guanfacine in healthy adults found its single-dose pharmacokinetic properties in 1-, 2-, and 4-mg tablets appeared to be statistically linear. Somnolence—the most common treatment-emergent adverse effect—occurred in 33 of 52 participants (63.5%). All mean vital-sign measurements and ECG parameters remained within normal limits after dosing, and no marked changes from baseline measurements were noted.65
Antidepressants
Antidepressants used in ADHD treatment include bupropion and tricyclic antidepressants.
Bupropion is a noradrenaline and dopamine reuptake inhibitor and is considered to be a mild psychostimulant because of its amphetamine-derived chemical structure.66,67 It generally is considered a third-line medication when stimulants have not improved ADHD symptoms or are not tolerated.
A 2011 meta-analysis examined 5 randomized, controlled trials including 175 adults treated with bupropion for ADHD. Bupropion was found to be more effective than placebo (NNT = 5), although bupropion’s therapeutic benefits were not observed until weeks 5 and 6. Its effects were less pronounced than those of methylphenidate. Mean daily dosages were 362 mg for the bupropion SR trials and 393 mg for the bupropion XL trial.68
Tricyclics. Desipramine and nortriptyline have been found to be efficacious in childhood ADHD,69,70 although cardiovascular risk and toxicity in overdose limit their use.71
Attention-deficit/hyperactivity disorder (ADHD) is common; it affects 5% to 7% of children1,2 and 4% to 5% of all adults.3,4 Pediatric ADHD often persists into adulthood, as 65% of individuals diagnosed as children retain impairing symptoms by age 25.4
The prevalence of ADHD in childhood is 2 to 3 times greater among boys than girls, but more comparable between the sexes in adulthood.2 Symptoms could be more easily overlooked in women because of the greater prominence of hyperactivity and impulsivity-type symptoms in men.5
Untreated ADHD is associated with significant costs. Adults with ADHD have increased unemployment rates, poor work performance, and comparatively lower educational performance.6,7 Compared with non-ADHD adults, those with ADHD have:
- more traffic violations and accidents and a higher rate of criminal convictions and incarcerations8,9
- a mortality rate almost 2 times higher, with the greatest differences seen in deaths by suicide and accidents.10,11
Adults with ADHD also are more likely to have a comorbid psychiatric disorder—in particular, substance use11—and often are in treatment for other mental or substance use disorders. Among adults who meet diagnostic criteria for ADHD, approximately only 10% are receiving treatment for ADHD symptoms.3,12
Changes in DSM-5
Revisions within DSM-5 simplify ADHD’s diagnosis—and make it more difficult to ignore in
DSM-5 also provides examples of behaviors more commonly found in adults, such as “feelings of restlessness,” compared with DSM-IV’s “often runs about or climbs excessively in situations in which it is inappropriate.” Finally, ADHD now may be diagnosed in a person with an autism spectrum disorder who meets diagnostic criteria for both disorders.13,14
Identifying ADHD in adults
ADHD diagnosis in adults is made through careful clinical interviewing. For example, ask about what factors motivated an individual to seek evaluation for ADHD. Often, patients present after a change in responsibility at work or at home, such as a promotion or birth/adoption of a new child.
Consider incorporating a brief screen for adult ADHD in all new outpatient evaluations (Table 2).15 Screen for other psychiatric disorders as well; comorbidity with ADHD is high, and hyperactivity and inattention symptoms may result from anxiety, depression, or substance use.
Screen for learning disorders, which can present with ADHD symptoms (such as poor concentration) when the individual attempts difficult tasks. Evaluate for risk factors associated with ADHD medications, such as a history of cardiac problems, hypertension, or tachycardia. A family history of ADHD is found in approximately 80% of cases.16,17 Determine the presence of ADHD symptoms in childhood. A careful review of the educational history often reveals long-term underachievement and struggles in school. Patients may report a chronic history of poor attention or feelings of restlessness in school. Sometimes problems do not become apparent until high school or college; some individuals, especially those with high intelligence, compensate for deficits and show fewer overt symptoms of impairment until later in their education.18Occupational history also may be revealing:
- How are they performing at work?
- Have they changed jobs multiple times in a short period?
- Do they have difficulty organizing tasks?
Subtle ADHD signs include time of arrival to appointments (eg, late or extremely early), missing data on intake paperwork, and a history of losing keys or phones.
Neuropsychological testing. Some clinicians routinely include neuropsychological testing in an adult ADHD evaluation, but these studies have shown inconsistent cognitive deficits in people with ADHD.19,20 No distinct psychometric cognitive test or profile is diagnostic of ADHD or its subtypes.21
Treatment and follow-up care
Four general categories of medications are used to treat ADHD in children and adults:
After starting a patient on medication, at each follow-up appointment ask about new cardiac symptoms or diagnoses, new family history of cardiac problems, or new medications. Measure pulse and blood pressure every 1 to 3 months. Measure vital signs more frequently during titration and weaning periods.23
Stimulant medications
Amphetamines have dual action: they block the reuptake of dopamine and noradrenaline by competitive inhibition of the transporters and promote the release of dopamine and noradrenaline by competitive inhibition of the intraneuronal vesicular monoamine transporter.24
For most amphetamine products, including dextroamphetamine and amphetamine mixed salts, the target dosage is approximately 0.5 mg/kg. Start at a lower dosage, however, and rapidly titrate weekly so patients can adjust to the medication while not becoming frustrated with a lack of efficacy. Some patients may require short-acting forms with dosing 3 times per day, and twice daily dosing is not uncommon with extended-release (ER) formulations.
Metabolism of most amphetamine products—with the exception of lisdexamfetamine—involves the cytochrome P450 (CYP) enzyme CYP2D6, leading to the formation of the metabolite 4-hydroxyamphetamine.25 The pharmacokinetics of lisdexamfetamine in slow or ultra-rapid CYP2D6 metabolizers has not been evaluated (Shire US Inc., written communication, July 2014).
Agents that alter urinary pH can affect blood levels of amphetamine. Acidifying agents decrease amphetamine blood levels, while alkalinizing agents increase amphetamine blood levels.26
Lisdexamfetamine contains L-lysine, an essential amino acid, covalently bound to d-amphetamine via an amide linking group.27 After absorption, lisdexamfetamine is metabolized by rate-limited, enzymatic hydrolysis to yield d-amphetamine and L-lysine.24,28,29 A starting dose of 40 mg is advised; twice-daily dosing rarely is required.
A meta-analysis of 5 randomized, controlled trials in the treatment of adult ADHD showed a response rate of 70% for lisdexamfetamine compared with 37% for placebo. Trial duration ranged from 4 to 14 weeks, with dosages of 30 to 70 mg/d.30 Another analysis of data from lisdexamfetamine trials predicted an effect size of 1.07 for European adults, which is larger than the 0.8 threshold for large effect sizes.31
Methylphenidate products. Methylphenidate’s main action is through enhancement of dopamine signaling by blockade of the dopamine transporter, leading to increases in extracellular dopamine as well as norepinephrine.22,32 Optimized dosing is generally 1 mg/kg per day, and dosing up to 80 to 120 mg/d is not unusual.33
Dexmethylphenidate is the more pharmacologically active enantiomer of racemic methylphenidate and is twice as potent.34-36 Target dosing of dexmethylphenidate should be one-half as much (ie, 0.5 mg/kg per day) as other methylphenidate products.37
Managing stimulants’ side effects
Amphetamines’ side effects may include insomnia, dry mouth, decreased appetite, weight loss, headaches, and anxiety. To help minimize sleep problems, advise patients to take a second immediate-release dose at noon, rather than later in the afternoon. The longer-acting formulation taken once per day in the morning may be offered as an alternative. Some patients may experience improved sleep because of diminished bedtime ruminations.
Oral rinses, such as Biotène, could help reduce discomfort associated with dry mouth. Pilocarpine, which stimulates saliva production, is another option if rinses are not effective. To address decreased appetite, advise patients to take their medication after they eat. Switching from an immediate-release amphetamine to a longer-acting formulation also may lessen symptoms. Lisdexamfetamine might be a good choice for adults with ADHD who have undergone bariatric surgeries because it is absorbed in the small bowel.38
Methylphenidate has no interactions with CYP enzymes, making it an attractive option for patients taking CYP inhibiting or stimulating medications.39 The most common side effects of methylphenidate products include appetite loss, insomnia, irritability, and tachycardia. Some side effects will abate after 1 to 2 weeks of treatment, but persistence of insomnia and appetite loss may require a decrease in dosage. In rare cases, methylphenidate may produce tics, exacerbate an existing tic disorder, or produce mania or psychosis.40,41 Methylphenidate inhibits the metabolism of tricyclic antidepressants; use methylphenidate with caution in patients taking monoamine oxidase inhibitors.42,43Cardiovascular risks. Possible cardiovascular risks associated with stimulant use have gained widespread attention, although research has not demonstrated an increased risk of serious cardiovascular events in young and middle-aged adults receiving stimulant medications for ADHD.44 Nonetheless, obtain a thorough medical history in adult patients, including cardiac history, family history of cardiac disease, history of any cardiac symptoms, and a medication history. Baseline ECG is not required.45
Screen for a family history of sudden death in a young person, sudden death during exercise, cardiac arrhythmia, cardiomyopathies (including hypertrophic cardiomyopathy, dilated cardiomyopathy, and right ventricular cardiomyopathy), prolonged QT interval, short QT syndrome, Brugada syndrome, Wolff-Parkinson-White syndrome, Marfan syndrome, and an event requiring resuscitation in a family member younger than 35, including syncope requiring rescuscitation.23 If fainting spells, palpitations, chest pain, or other symptoms suggest preexisting cardiovascular disease, refer the patient promptly to a cardiologist.
Peripheral vasculopathy, including Raynaud’s phenomenon, is a lesser known side effect associated with stimulants.46 Symptoms are usually mild, but in rare instances stimulants are associated with digital ulceration or soft tissue breakdown.47 Advise patients to tell you if they experience any new symptoms of numbness, pain, skin color changes, or sensitivity to temperature in fingers and toes. Signs and symptoms generally improve after dosage reduction or discontinuation of the stimulant medication.46 Referral to a rheumatologist might be appropriate if symptoms persist.
A noradrenergic medication
Atomoxetine is a potent, selective inhibitor of the presynaptic noradrenaline transporter that increases the availability of extracellular noradrenaline in the prefrontal cortex.48,49 Atomoxetine may be a good alternative for adult patients with ADHD and comorbid anxiety.50
For adults, the optimal starting dosage is 40 mg in the morning for 1 week, followed by an increase to 80 mg. Insufficient dosing is common with atomoxetine, and the dosage could be increased to 100 mg/d.51 Dosing twice per day may be associated with higher rates of insomnia.
Atomoxetine’s efficacy for managing ADHD in adults has been consistently demonstrated by 6 placebo-controlled trials of 10 to 16 weeks, 3 placebo-controlled 6-month trials, and a 1-year maintenance-of-response trial.52 Atomoxetine was found to have an effect size of 0.45 (medium) (number needed to treat [NNT] = 5).53-55The most common adverse effects include nausea, dry mouth, insomnia, and erectile dysfunction. Small increases in heart rate and blood pressure have been reported, so use this medication with caution in patients for whom this might be problematic. Atomoxetine is metabolized by CYP2D6; 7% of white individuals have a genotype corresponding to a nonfunctional CYP2D6 enzyme.56-58
Alpha-2 adrenergic agonists
Clonidine and guanfacine are antihypertensive drugs that induce peripheral sympathoinhibition via the stimulation of receptors. Clonidine binds equally to adrenergic receptor subtypes α-2A, α-2B, and α-2C (as well as to α-1 and β subtypes, histamine receptors, and possibly dopamine receptors).59,60 Guanfacine binds preferentially to postsynaptic α-2A adrenoceptors in the prefrontal cortex, which have been implicated in attentional and organizational functions.61,62
ER guanfacine and ER clonidine are FDA-approved as monotherapy for ADHD in children and adolescents.
Efficacy in adults. A small (N = 17), double-blind, placebo-controlled, crossover study comparing immediate-release guanfacine and dextroamphetamine found that both medications significantly reduced adult ADHD symptoms, as measured with the DSM-IV Adult Behavior Checklist for Adults.63
No trials have been published regarding the efficacy of ER clonidine in adults with ADHD; adverse effects including sedation, bradycardia, and hypotension may limit its use. One study compared the supplemental use of ER guanfacine (1 to 6 mg/d) or a matching placebo in 26 adults with ADHD who had suboptimal response to stimulant-only treatment. After 10 weeks, both the guanfacine ER and placebo groups showed statistically significant improvements in ADHD symptoms and general functioning. The treatments did not differ in efficacy, safety, or tolerability.64
Adverse events. Compared with clonidine, guanfacine has less CNS depressant and hypotensive activity.58 A phase I trial of ER guanfacine in healthy adults found its single-dose pharmacokinetic properties in 1-, 2-, and 4-mg tablets appeared to be statistically linear. Somnolence—the most common treatment-emergent adverse effect—occurred in 33 of 52 participants (63.5%). All mean vital-sign measurements and ECG parameters remained within normal limits after dosing, and no marked changes from baseline measurements were noted.65
Antidepressants
Antidepressants used in ADHD treatment include bupropion and tricyclic antidepressants.
Bupropion is a noradrenaline and dopamine reuptake inhibitor and is considered to be a mild psychostimulant because of its amphetamine-derived chemical structure.66,67 It generally is considered a third-line medication when stimulants have not improved ADHD symptoms or are not tolerated.
A 2011 meta-analysis examined 5 randomized, controlled trials including 175 adults treated with bupropion for ADHD. Bupropion was found to be more effective than placebo (NNT = 5), although bupropion’s therapeutic benefits were not observed until weeks 5 and 6. Its effects were less pronounced than those of methylphenidate. Mean daily dosages were 362 mg for the bupropion SR trials and 393 mg for the bupropion XL trial.68
Tricyclics. Desipramine and nortriptyline have been found to be efficacious in childhood ADHD,69,70 although cardiovascular risk and toxicity in overdose limit their use.71
1. Polanczyk G, de Lima MS, Horta BL, et al. The worldwide prevalence of ADHD: a systemic review and metaregression analysis. Am J Psychiatry. 2007;164(6):942-948.
2. Simon V, Czobor P, Bálint S, et al. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br J Psychiatry. 2009;194(3):204-211.
3. Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163(4):716-723.
4. Faraone S, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36(2):159-165.
5. Gershon J. A meta-analytic review of gender differences in ADHD. J Atten Disord. 2002;5(3):143-154.
6. Halmøy A, Fasmer OB, Gillberg C, et al. Occupational outcome in adult ADHD: impact of symptom profile, comorbid psychiatric problems, and treatment: a cross-sectional study of 414 clinically diagnosed adult ADHD patients. J Atten Disord. 2009;13(2):175-187.
7. Kuriyan AB, Pelham WE Jr, Molina BS, et al. Young adult educational and vocational outcomes of children diagnosed with ADHD. J Abnorm Child Psychol. 2013;41(1):27-41.
8. Murphy K, Barkley RA. Attention deficit hyperactivity disorder in adults: comorbidities and adaptive impairment. Compr Psychiatry. 1996;37(6):393-401.
9. Mannuzza S, Klein RG, Mouton JL 3rd. Lifetime criminality among boys with attention deficit hyperactivity disorder: a prospective follow-up study into adulthood using official arrest records. Psychiatry Res. 2008;160(3):237-246.
10. Dalsgaard S, Østergaard SD, Leckman JF, et al. Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: a nationwide cohort study. Lancet. 2015;385(9983):2190-2196.
11. Barbaresi WJ, Colligan RC, Weaver AL, et al. Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: a prospective study. Pediatrics. 2013;131(4):637-644.
12. Babcock T, Ornstein CS. Comorbidity and its impact in adult patients with attention-deficit/hyperactivity disorder: a primary care perspective. Postgrad Med. 2009;121(3):73-82.
13. Attention-deficit/hyperactivity disorder. In: Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:59-66.
14. Attention-deficit/hyperactivity disorder. In: Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000:78-85.
15. Kooij JJS. Adult ADHD: diagnostic assessment and treatment. 3rd ed. Amsterdam, Netherlands: Springer; 2013:34.
16. Faraone SV, Khan SA. Candidate gene studies of attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2006;67(suppl 8):13-20.
17. Neale BM, Medland SE, Ripke S, et al; Psychiatric GWAS Consortium: ADHD Subgroup. Meta-analysis of genome-wide association studies of attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2010;49(9):884-897.
18. Milioni AL, Chaim TM, Cavallet M, et al. High IQ may “mask” the diagnosis of ADHD by compensating for deficits in executive functions in treatment-naïve adults with ADHD [published online October 30, 2014]. J Atten Disord. pii: 1087054714554933.
19. Rapport MD, Chung KM, Shore G, et al. Upgrading the science and technology of assessment and diagnosis: laboratory and clinic-based assessment of children with ADHD. J Clin Child Psychol. 2000;29(4):555-568.
20. Woods SP, Lovejoy DW, Ball JD. Neuropsychological characteristics of adults with ADHD: a comprehensive review of initial studies. Clin Neuropsychol. 2002;16(1):12-34.
21. Lange KW, Hauser J, Lange KM, et al. Utility of cognitive neuropsychological assessment in attention-deficit/hyperactivity disorder. Atten Defic Hyperact Disord. 2014;6(4):241-248.
22. Arnold LE. Methylphenidate vs. amphetamine: comparative review. J Atten Disord. 2000;3(4):200-211.
23. Vetter VL Elia J, Erickson, C, et al; American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee; American Heart Association Council on Cardiovascular Nursing. Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder [corrected]: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing [Erratum in: Circulation. 2009;120(7):e55-e59]. Circulation. 2008;117(18):2407-2423.
24. Seiden LS, Sabol KE, Ricaurte GA. Amphetamine: effects on catecholamine systems and behavior. Annu Rev Pharmacol Toxicol. 1993;33:639-677.
25. Wu D, Otton SV, Inaba T, et al. Interactions of amphetamine analogs with human liver CYP2D6. Biochem Pharmacol. 1997;53(11):1605-1612.
26. Vyvanse [package insert]. Lexington, MA: Shire Pharmaceuticals; 2015.
27. Pennick M. Absorption of lisdexamfetamine dimesylate and its enzymatic conversion to d-amphetamine. Neuropsychiatr Dis Treat. 2010;6:317-327.
28. Heal DJ, Smith SL, Gosden J, et al. Amphetamine, past and present—a pharmacological and clinical perspective. J Psychopharmacol. 2013;27(6):479-496.
29. Krishnan SM, Pennick M, Stark JG. Metabolism, distribution and elimination of lisdexamfetamine dimesylate: open-label, single-centre, phase I study in healthy adult volunteers. Clin Drug Invest. 2008;28(12):745-755.
30. Maneeton N, Maneeton B, Suttajit S, et al. Exploratory meta-analysis on lisdexamfetamine versus placebo in adult ADHD. Drug Des Devel Ther. 2014;8:1685-1693.
31. Fridman M, Hodgkins P, Kahle JS, et al. Predicted effect size of lisdexamfetamine treatment of attention deficit/hyperactivity disorder (ADHD) in European adults: estimates based on indirect analysis using a systematic review and meta-regression analysis. Eur Psychiatry. 2015;30(4):521-527.
32. Markowitz JS, DeVane CL, Pestreich L, et al. Session 1-87-differentiation of d-, L- and dl-methylphenidate through in vitro pharmacological screening. In: Abstracts: Oral and Poster Presentations of the NCDEU 45th Annual Meeting; June 6-9, 2005; Boca Raton, FL:186.
33. Spencer T, Biederman J, Wilens T, et al. A large, double-blind, randomized clinical trial of methylphenidate in the treatment of adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2005;57(5):456-463.
34. Teo SK, Stirling DI, Thomas SD, et al. Neurobehavioral effects of racemic threo-methylphenidate and its D and L enantiomers in rats. Pharmacol Biochem Behav. 2003;74(3):747-754.
35. Ding YS, Fowler JS, Volkow ND, et al. Chiral drugs: comparison of the pharmacokinetics of [11C]d-threo and L-threo-methylphenidate in the human and baboon brain. Psychopharmacol (Berl). 1997;131(1):71-78.
36. Davids E, Zhang K, Tarazi FI, et al. Stereoselective effects of methylphenidate on motor hyperactivity in juvenile rats induced by neonatal 6-hydroxydopamine lesioning. Psychopharmacol (Berl). 2002;160(1):92-98.
37. Srinivas NR, Hubbard JW, Quinn D, et al. Enantioselective pharmacokinetics and pharmacodynamics of dl-threo-methylphenidate in children with attention deficit hyperactivity disorder. Clin Pharmacol Ther. 1992;52(5):561-568.
38. Ermer JC, Haffey MB, Doll WJ, et al. Pharmacokinetics of lisdexamfetamine dimesylate after targeted gastrointestinal release or oral administration in healthy adults. Drug Metab Dispos. 2012;40(2):290-297.
39. DeVane CL, Markowitz JS, Carson SW, et al. Single-dose pharmacokinetics of methylphenidate in CYP2D6 extensive and poor metabolizers. J Clin Psychopharmacol. 2000;20(3):347-349.
40. Graham J, Coghill D. Adverse effects of pharmacotherapies for attention-deficit hyperactivity disorder: epidemiology, prevention and management. CNS Drugs. 2008;22(3):213-237.
41. Ross RG. Psychotic and manic-like symptoms during stimulant treatment of attention deficit hyperactivity disorder. Am J Psychiatry. 2006;163(7):1149-1152.
42. Shelton Clauson A, Elliott ES, Watson BD, et al. Coadministration of phenelzine and methylphenidate for treatment-resistant depression. Ann Pharmacother. 2004;38(3):508.
43. Markowitz JS, Patrick KS. Pharmacokinetic and pharmacodynamic drug interactions in the treatment of attention-deficit hyperactivity disorder. Clin Pharmacokinet. 2001;40(10):753-772.
44. Habel LA, Cooper WO, Sox CM, et al. ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. JAMA. 2011;306(24):2673-2683.
45. Graham J, Banaschewski T, Buitelaar J, et al; European Guidelines Group. European guidelines on managing adverse effects of medication for ADHD. Eur Child Adolesc Psychiatry. 2011;20(1):17-37.
46. Goldman W, Seltzer R, Reuman P. Association between treatment with central nervous system stimulants and Raynaud’s syndrome in children: a retrospective case-control study of rheumatology patients. Arthritis Rheum. 2008;58(2):563-566.
47. Syed RH, Moore TL. Methylphenidate and dextroamphetamine-induced peripheral vasculopathy. J Clin Rheum. 2008;14(1):30-33.
48. Wilens TE. Mechanism of action of agents in attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2006;67(suppl 8):32-38.
49. Bymaster FP, Katner JS, Nelson DL, et al. Atomoxetine increases extracellular levels of norepinephrine and dopamine in prefrontal cortex of rat: a potential mechanism for efficacy in attention deficit/hyperactivity disorder. Neuropsychopharmacology. 2002;27(5):699-711.
50. Adler LA, Liebowitz M, Kronenberger W, et al. Atomoxetine treatment in adults with attention-deficit/hyperactivity disorder and comorbid social anxiety disorder. Depress Anxiety. 2009;26(3):212-221.
51. Clemow DB. Suboptimal dosing of Strattera (atomoxetine) for ADHD patients. Postgrad Med. 2014;126(5):196-198.
52. Camporeale A, Porsdal V, De Bruyckere K, et al. Safety and tolerability of atomoxetine in treatment of attention deficit hyperactivity disorder in adult patients: an integrated analysis of 15 clinical trials. J Psychopharmacol. 2015;29(1):3-14.
53. Young JL, Sarkis E, Qiao M, et al. Once-daily treatment with atomoxetine in adults with attention-deficit/hyperactivity disorder: a 24-week, randomized, double-blind, placebo-controlled trial. Clin Neuropharmacol. 2011;34(2):51-60.
54. Bitter I, Angyalosi A, Czobor P. Pharmacological treatment of adult ADHD. Curr Opin Psychiatry. 2012;25(6):529-534.
55. Faraone SV, Glatt SJ. A comparison of the efficacy of medications for adult attention-deficit/hyperactivity disorder using meta-analysis of effect sizes. J Clin Psychiatry. 2010;71(6):754-763.
56. Ring BJ, Gillespie JS, Eckstein JA, et al. Identification of the human cytochromes P450 responsible for atomoxetine metabolism. Drug Metab Dispos. 2002;30(3):319-323.
57. Farid NA, Bergstrom RF, Ziege EA, et al. Single-dose and steady state pharmacokinetics of tomoxetine in normal subjects. J Clin Pharmacol. 1985;25(4):296-301.
58. Mizutani T. PM frequencies of major CYPs in Asians and Caucasians. Drug Metab Rev. 2003;35(2-3):99-106.
59. Jasper JR, Lesnick JD, Chang LK, et al. Ligand efficacy and potency at recombinant alpha2 adrenergic receptors: agonist-mediated [35S]GTPgammaS binding. Biochem Pharmacol. 1998;55(7):1035-1043.
60. Ruggiero S, Clavenna A, Reale L, et al. Guanfacine for attention deficit and hyperactivity disorder in pediatrics: a systematic review and meta-analysis. Eur Neuropsychopharmacol. 2014;24(10):1578-1590.
61. Arnsten AF, Pliszka SR. Catecholamine influences on prefrontal cortical function: relevance to treatment of attention deficit/hyperactivity disorder and related disorders. Pharmacol Biochem Behav. 2011;99(2):211-216.
62. Uhlén S, Wikberg JE. Delineation of rat kidney alpha 2A- and alpha 2B-adrenoceptors with [3H]RX821002 radioligand binding: computer modelling reveals that guanfacine is an alpha 2A-selective compound. Eur J Pharmacol. 1991;202(2):235-243.
63. Taylor FB, Russo J. Comparing guanfacine and dextroamphetamine for the treatment of adult attention deficit/hyperactivity disorder. J Clin Psychopharmacol. 2001;21(2):223-228.
64. Butterfield ME, Saal J, Young B, et al. Supplementary guanfacine hydrochloride as a treatment of attention deficit hyperactivity disorder in adults: a double blind, placebo-controlled study. Psychiatry Res. 2016;236:136-141.
65. Swearingen D, Pennick M, Shojaei A, et al. A phase I, randomized, open-label, crossover study of the single-dose pharmacokinetic properties of guanfacine extended-release 1-, 2-, and 4-mg tablets in healthy adults. Clin Ther. 2007;29(4):617-625.
66. Cooper BR, Wang CM, Cox RF. Evidence that the acute behavioral and electrophysiological effects of bupropion (Wellbutrin) are mediated by a noradrenergic mechanism. Neuropsychopharmacology. 1994;11(2):133-141.
67. Reimherr FW, Hedges DW, Strong RE, et al. Bupropion SR in adults with ADHD: a short-term, placebo-controlled trial. Neuropsychiatr Dis Treat. 2005;1(3):245-251.
68. Maneeton N, Maneeton B, Srisurapanont M, et al. Bupropion for adults with attention-deficit hyperactivity disorder: meta-analysis of randomized, placebo-controlled trials. Psychiatry Clin Neurosci. 2011;65(7):611-617.
69. Biederman J, Baldessarini RJ, Wright V, et al. A double-blind placebo controlled study of desipramine in the treatment of ADD: I. Efficacy. J Am Acad Child Adolesc Psychiatry. 1989;28(5):777-784.
70. Spencer T, Biederman J, Wilens T, et al. Nortriptyline treatment of children with attention-deficit hyperactivity disorder and tic disorder or Tourette’s syndrome. J Am Acad Child Adolesc Psychiatry. 1993;32(1):205-210.
71. Bond DJ, Hadjipavlou G, Lam RW, et al. The Canadian Network for Mood and Anxiety Treatments (CANMAT) task force recommendations for the management of patients with mood disorders and comorbid attention-deficit/hyperactivity disorder. Ann Clin Psychiatry. 2012;24(1):23-37.
1. Polanczyk G, de Lima MS, Horta BL, et al. The worldwide prevalence of ADHD: a systemic review and metaregression analysis. Am J Psychiatry. 2007;164(6):942-948.
2. Simon V, Czobor P, Bálint S, et al. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br J Psychiatry. 2009;194(3):204-211.
3. Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163(4):716-723.
4. Faraone S, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36(2):159-165.
5. Gershon J. A meta-analytic review of gender differences in ADHD. J Atten Disord. 2002;5(3):143-154.
6. Halmøy A, Fasmer OB, Gillberg C, et al. Occupational outcome in adult ADHD: impact of symptom profile, comorbid psychiatric problems, and treatment: a cross-sectional study of 414 clinically diagnosed adult ADHD patients. J Atten Disord. 2009;13(2):175-187.
7. Kuriyan AB, Pelham WE Jr, Molina BS, et al. Young adult educational and vocational outcomes of children diagnosed with ADHD. J Abnorm Child Psychol. 2013;41(1):27-41.
8. Murphy K, Barkley RA. Attention deficit hyperactivity disorder in adults: comorbidities and adaptive impairment. Compr Psychiatry. 1996;37(6):393-401.
9. Mannuzza S, Klein RG, Mouton JL 3rd. Lifetime criminality among boys with attention deficit hyperactivity disorder: a prospective follow-up study into adulthood using official arrest records. Psychiatry Res. 2008;160(3):237-246.
10. Dalsgaard S, Østergaard SD, Leckman JF, et al. Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: a nationwide cohort study. Lancet. 2015;385(9983):2190-2196.
11. Barbaresi WJ, Colligan RC, Weaver AL, et al. Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: a prospective study. Pediatrics. 2013;131(4):637-644.
12. Babcock T, Ornstein CS. Comorbidity and its impact in adult patients with attention-deficit/hyperactivity disorder: a primary care perspective. Postgrad Med. 2009;121(3):73-82.
13. Attention-deficit/hyperactivity disorder. In: Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:59-66.
14. Attention-deficit/hyperactivity disorder. In: Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000:78-85.
15. Kooij JJS. Adult ADHD: diagnostic assessment and treatment. 3rd ed. Amsterdam, Netherlands: Springer; 2013:34.
16. Faraone SV, Khan SA. Candidate gene studies of attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2006;67(suppl 8):13-20.
17. Neale BM, Medland SE, Ripke S, et al; Psychiatric GWAS Consortium: ADHD Subgroup. Meta-analysis of genome-wide association studies of attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2010;49(9):884-897.
18. Milioni AL, Chaim TM, Cavallet M, et al. High IQ may “mask” the diagnosis of ADHD by compensating for deficits in executive functions in treatment-naïve adults with ADHD [published online October 30, 2014]. J Atten Disord. pii: 1087054714554933.
19. Rapport MD, Chung KM, Shore G, et al. Upgrading the science and technology of assessment and diagnosis: laboratory and clinic-based assessment of children with ADHD. J Clin Child Psychol. 2000;29(4):555-568.
20. Woods SP, Lovejoy DW, Ball JD. Neuropsychological characteristics of adults with ADHD: a comprehensive review of initial studies. Clin Neuropsychol. 2002;16(1):12-34.
21. Lange KW, Hauser J, Lange KM, et al. Utility of cognitive neuropsychological assessment in attention-deficit/hyperactivity disorder. Atten Defic Hyperact Disord. 2014;6(4):241-248.
22. Arnold LE. Methylphenidate vs. amphetamine: comparative review. J Atten Disord. 2000;3(4):200-211.
23. Vetter VL Elia J, Erickson, C, et al; American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee; American Heart Association Council on Cardiovascular Nursing. Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder [corrected]: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing [Erratum in: Circulation. 2009;120(7):e55-e59]. Circulation. 2008;117(18):2407-2423.
24. Seiden LS, Sabol KE, Ricaurte GA. Amphetamine: effects on catecholamine systems and behavior. Annu Rev Pharmacol Toxicol. 1993;33:639-677.
25. Wu D, Otton SV, Inaba T, et al. Interactions of amphetamine analogs with human liver CYP2D6. Biochem Pharmacol. 1997;53(11):1605-1612.
26. Vyvanse [package insert]. Lexington, MA: Shire Pharmaceuticals; 2015.
27. Pennick M. Absorption of lisdexamfetamine dimesylate and its enzymatic conversion to d-amphetamine. Neuropsychiatr Dis Treat. 2010;6:317-327.
28. Heal DJ, Smith SL, Gosden J, et al. Amphetamine, past and present—a pharmacological and clinical perspective. J Psychopharmacol. 2013;27(6):479-496.
29. Krishnan SM, Pennick M, Stark JG. Metabolism, distribution and elimination of lisdexamfetamine dimesylate: open-label, single-centre, phase I study in healthy adult volunteers. Clin Drug Invest. 2008;28(12):745-755.
30. Maneeton N, Maneeton B, Suttajit S, et al. Exploratory meta-analysis on lisdexamfetamine versus placebo in adult ADHD. Drug Des Devel Ther. 2014;8:1685-1693.
31. Fridman M, Hodgkins P, Kahle JS, et al. Predicted effect size of lisdexamfetamine treatment of attention deficit/hyperactivity disorder (ADHD) in European adults: estimates based on indirect analysis using a systematic review and meta-regression analysis. Eur Psychiatry. 2015;30(4):521-527.
32. Markowitz JS, DeVane CL, Pestreich L, et al. Session 1-87-differentiation of d-, L- and dl-methylphenidate through in vitro pharmacological screening. In: Abstracts: Oral and Poster Presentations of the NCDEU 45th Annual Meeting; June 6-9, 2005; Boca Raton, FL:186.
33. Spencer T, Biederman J, Wilens T, et al. A large, double-blind, randomized clinical trial of methylphenidate in the treatment of adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2005;57(5):456-463.
34. Teo SK, Stirling DI, Thomas SD, et al. Neurobehavioral effects of racemic threo-methylphenidate and its D and L enantiomers in rats. Pharmacol Biochem Behav. 2003;74(3):747-754.
35. Ding YS, Fowler JS, Volkow ND, et al. Chiral drugs: comparison of the pharmacokinetics of [11C]d-threo and L-threo-methylphenidate in the human and baboon brain. Psychopharmacol (Berl). 1997;131(1):71-78.
36. Davids E, Zhang K, Tarazi FI, et al. Stereoselective effects of methylphenidate on motor hyperactivity in juvenile rats induced by neonatal 6-hydroxydopamine lesioning. Psychopharmacol (Berl). 2002;160(1):92-98.
37. Srinivas NR, Hubbard JW, Quinn D, et al. Enantioselective pharmacokinetics and pharmacodynamics of dl-threo-methylphenidate in children with attention deficit hyperactivity disorder. Clin Pharmacol Ther. 1992;52(5):561-568.
38. Ermer JC, Haffey MB, Doll WJ, et al. Pharmacokinetics of lisdexamfetamine dimesylate after targeted gastrointestinal release or oral administration in healthy adults. Drug Metab Dispos. 2012;40(2):290-297.
39. DeVane CL, Markowitz JS, Carson SW, et al. Single-dose pharmacokinetics of methylphenidate in CYP2D6 extensive and poor metabolizers. J Clin Psychopharmacol. 2000;20(3):347-349.
40. Graham J, Coghill D. Adverse effects of pharmacotherapies for attention-deficit hyperactivity disorder: epidemiology, prevention and management. CNS Drugs. 2008;22(3):213-237.
41. Ross RG. Psychotic and manic-like symptoms during stimulant treatment of attention deficit hyperactivity disorder. Am J Psychiatry. 2006;163(7):1149-1152.
42. Shelton Clauson A, Elliott ES, Watson BD, et al. Coadministration of phenelzine and methylphenidate for treatment-resistant depression. Ann Pharmacother. 2004;38(3):508.
43. Markowitz JS, Patrick KS. Pharmacokinetic and pharmacodynamic drug interactions in the treatment of attention-deficit hyperactivity disorder. Clin Pharmacokinet. 2001;40(10):753-772.
44. Habel LA, Cooper WO, Sox CM, et al. ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. JAMA. 2011;306(24):2673-2683.
45. Graham J, Banaschewski T, Buitelaar J, et al; European Guidelines Group. European guidelines on managing adverse effects of medication for ADHD. Eur Child Adolesc Psychiatry. 2011;20(1):17-37.
46. Goldman W, Seltzer R, Reuman P. Association between treatment with central nervous system stimulants and Raynaud’s syndrome in children: a retrospective case-control study of rheumatology patients. Arthritis Rheum. 2008;58(2):563-566.
47. Syed RH, Moore TL. Methylphenidate and dextroamphetamine-induced peripheral vasculopathy. J Clin Rheum. 2008;14(1):30-33.
48. Wilens TE. Mechanism of action of agents in attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2006;67(suppl 8):32-38.
49. Bymaster FP, Katner JS, Nelson DL, et al. Atomoxetine increases extracellular levels of norepinephrine and dopamine in prefrontal cortex of rat: a potential mechanism for efficacy in attention deficit/hyperactivity disorder. Neuropsychopharmacology. 2002;27(5):699-711.
50. Adler LA, Liebowitz M, Kronenberger W, et al. Atomoxetine treatment in adults with attention-deficit/hyperactivity disorder and comorbid social anxiety disorder. Depress Anxiety. 2009;26(3):212-221.
51. Clemow DB. Suboptimal dosing of Strattera (atomoxetine) for ADHD patients. Postgrad Med. 2014;126(5):196-198.
52. Camporeale A, Porsdal V, De Bruyckere K, et al. Safety and tolerability of atomoxetine in treatment of attention deficit hyperactivity disorder in adult patients: an integrated analysis of 15 clinical trials. J Psychopharmacol. 2015;29(1):3-14.
53. Young JL, Sarkis E, Qiao M, et al. Once-daily treatment with atomoxetine in adults with attention-deficit/hyperactivity disorder: a 24-week, randomized, double-blind, placebo-controlled trial. Clin Neuropharmacol. 2011;34(2):51-60.
54. Bitter I, Angyalosi A, Czobor P. Pharmacological treatment of adult ADHD. Curr Opin Psychiatry. 2012;25(6):529-534.
55. Faraone SV, Glatt SJ. A comparison of the efficacy of medications for adult attention-deficit/hyperactivity disorder using meta-analysis of effect sizes. J Clin Psychiatry. 2010;71(6):754-763.
56. Ring BJ, Gillespie JS, Eckstein JA, et al. Identification of the human cytochromes P450 responsible for atomoxetine metabolism. Drug Metab Dispos. 2002;30(3):319-323.
57. Farid NA, Bergstrom RF, Ziege EA, et al. Single-dose and steady state pharmacokinetics of tomoxetine in normal subjects. J Clin Pharmacol. 1985;25(4):296-301.
58. Mizutani T. PM frequencies of major CYPs in Asians and Caucasians. Drug Metab Rev. 2003;35(2-3):99-106.
59. Jasper JR, Lesnick JD, Chang LK, et al. Ligand efficacy and potency at recombinant alpha2 adrenergic receptors: agonist-mediated [35S]GTPgammaS binding. Biochem Pharmacol. 1998;55(7):1035-1043.
60. Ruggiero S, Clavenna A, Reale L, et al. Guanfacine for attention deficit and hyperactivity disorder in pediatrics: a systematic review and meta-analysis. Eur Neuropsychopharmacol. 2014;24(10):1578-1590.
61. Arnsten AF, Pliszka SR. Catecholamine influences on prefrontal cortical function: relevance to treatment of attention deficit/hyperactivity disorder and related disorders. Pharmacol Biochem Behav. 2011;99(2):211-216.
62. Uhlén S, Wikberg JE. Delineation of rat kidney alpha 2A- and alpha 2B-adrenoceptors with [3H]RX821002 radioligand binding: computer modelling reveals that guanfacine is an alpha 2A-selective compound. Eur J Pharmacol. 1991;202(2):235-243.
63. Taylor FB, Russo J. Comparing guanfacine and dextroamphetamine for the treatment of adult attention deficit/hyperactivity disorder. J Clin Psychopharmacol. 2001;21(2):223-228.
64. Butterfield ME, Saal J, Young B, et al. Supplementary guanfacine hydrochloride as a treatment of attention deficit hyperactivity disorder in adults: a double blind, placebo-controlled study. Psychiatry Res. 2016;236:136-141.
65. Swearingen D, Pennick M, Shojaei A, et al. A phase I, randomized, open-label, crossover study of the single-dose pharmacokinetic properties of guanfacine extended-release 1-, 2-, and 4-mg tablets in healthy adults. Clin Ther. 2007;29(4):617-625.
66. Cooper BR, Wang CM, Cox RF. Evidence that the acute behavioral and electrophysiological effects of bupropion (Wellbutrin) are mediated by a noradrenergic mechanism. Neuropsychopharmacology. 1994;11(2):133-141.
67. Reimherr FW, Hedges DW, Strong RE, et al. Bupropion SR in adults with ADHD: a short-term, placebo-controlled trial. Neuropsychiatr Dis Treat. 2005;1(3):245-251.
68. Maneeton N, Maneeton B, Srisurapanont M, et al. Bupropion for adults with attention-deficit hyperactivity disorder: meta-analysis of randomized, placebo-controlled trials. Psychiatry Clin Neurosci. 2011;65(7):611-617.
69. Biederman J, Baldessarini RJ, Wright V, et al. A double-blind placebo controlled study of desipramine in the treatment of ADD: I. Efficacy. J Am Acad Child Adolesc Psychiatry. 1989;28(5):777-784.
70. Spencer T, Biederman J, Wilens T, et al. Nortriptyline treatment of children with attention-deficit hyperactivity disorder and tic disorder or Tourette’s syndrome. J Am Acad Child Adolesc Psychiatry. 1993;32(1):205-210.
71. Bond DJ, Hadjipavlou G, Lam RW, et al. The Canadian Network for Mood and Anxiety Treatments (CANMAT) task force recommendations for the management of patients with mood disorders and comorbid attention-deficit/hyperactivity disorder. Ann Clin Psychiatry. 2012;24(1):23-37.
Recreational marijuana use should not rule out ADHD stimulant treatment
SAN FRANCISCO – “If one is going to say ‘you need 6 months of abstinence from cannabis before I am going to treat your ADHD,’ that’s absurd. If [kids] are stoned all the time, no, but if it’s intermittent, it’s really not a factor,” according to James J. McGough, MD, director of the Attention Deficit Disorder Clinic at the University of California, Los Angeles.
There’s no evidence that ongoing stimulant treatment increases the risk of substance abuse, and “we must admit to ourselves that substance use among adolescents and young adults is normative. It happens,” even among well-adapted kids. “Think of your own past histories,” he said to an audience of psychiatrists and other medical professionals at a psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
“You have” to deal with substance abuse that’s ruining lives, but otherwise, “I’m comfortable giving a prescription under some circumstances even if I know [patients] are using drugs. It’s the extent and type of [drug use] that informs if we should prescribe or not,” said Dr. McGough, also a professor of clinical psychiatry at the university, but be careful to “really document what you’re doing.”
Misuse and diversion is mostly related to performance enhancement, especially at competitive universities, or when grades head south. Children and young adults in those situations, as well as smokers, drinkers, and those with conduct disorders, “are the ones you worry about.” If a Stanford medical school student at age 27 suddenly develops a horrible problem focusing, with no past ADHD history, “I’m a little suspicious,” he said, noting that people who malinger “tend to go off the scale in terms of endorsing symptoms.”
If misuse and abuse are a concern, extended-release stimulants, as well as nonstimulants, are better options than immediate-release formulations.
Audience members also were curious about alternative approaches for ADHD, but the news wasn’t very good.
For now, there’s no brain scan, test, or lab measurement that reliably detects ADHD. Even with neuropsychiatric testing, only half of children and adolescents will have executive-functioning deficits. The problem with computerized tests, meanwhile, is that a lot of children and adolescents with ADHD have no problem focusing on computer games, so they aren’t helpful for diagnosis.
“The gold standard for ADHD assessment remains a good interview,” and documenting DSM-5 criteria, he said.
As for alternative treatments, “what studies have shown is that if you are highly invested in the treatment and not blinded” to it, “you tend to think you do better. In good studies where they look at teachers who don’t know what’s going on, it doesn’t pan out,” he said. Metanalysis of neurofeedback hasn’t shown effect, nor have computer games to train focus; kids will get better at them with practice, but they haven’t been shown to improve ADHD.
The only exception is omega-3, but the effect size is barely measurable. “If you can get the kid so swallow those fish oil things, go for it, or they can eat salmon,” Dr. McGough said.
In short, medications remain the best option for treating the core symptoms of ADHD, first with stimulants then, as needed, nonstimulants.
But “you are not meeting your patients’ needs if you are only prescribing medications,” he said. Psychosocial education, family behavioral therapy, and school interventions – even things as simple as sitting toward the front of the class and having a little more time on tests – are critical for overall improvement.
It’s also important to let patients and families know that “they don’t have to be ashamed of this,” and the patients need to know why they are taking their medication, he said.
Too often, children are started on a low dose of medication and told to come back in a month. “That’s a waste of time, because it’s a whole month when the person is probably inadequately treated,” Dr. McGough said.
Instead, he has patients titrate up at first, with advice to cut back or stop and call if there are problems. The patient returns after 3 weeks, and the most effective, best-tolerated dose is selected for treatment.
Dr. McGough disclosed relationships with Purdue, Shire, Tris, Sunovion, NeuroSigma, and Neurovance.
SAN FRANCISCO – “If one is going to say ‘you need 6 months of abstinence from cannabis before I am going to treat your ADHD,’ that’s absurd. If [kids] are stoned all the time, no, but if it’s intermittent, it’s really not a factor,” according to James J. McGough, MD, director of the Attention Deficit Disorder Clinic at the University of California, Los Angeles.
There’s no evidence that ongoing stimulant treatment increases the risk of substance abuse, and “we must admit to ourselves that substance use among adolescents and young adults is normative. It happens,” even among well-adapted kids. “Think of your own past histories,” he said to an audience of psychiatrists and other medical professionals at a psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
“You have” to deal with substance abuse that’s ruining lives, but otherwise, “I’m comfortable giving a prescription under some circumstances even if I know [patients] are using drugs. It’s the extent and type of [drug use] that informs if we should prescribe or not,” said Dr. McGough, also a professor of clinical psychiatry at the university, but be careful to “really document what you’re doing.”
Misuse and diversion is mostly related to performance enhancement, especially at competitive universities, or when grades head south. Children and young adults in those situations, as well as smokers, drinkers, and those with conduct disorders, “are the ones you worry about.” If a Stanford medical school student at age 27 suddenly develops a horrible problem focusing, with no past ADHD history, “I’m a little suspicious,” he said, noting that people who malinger “tend to go off the scale in terms of endorsing symptoms.”
If misuse and abuse are a concern, extended-release stimulants, as well as nonstimulants, are better options than immediate-release formulations.
Audience members also were curious about alternative approaches for ADHD, but the news wasn’t very good.
For now, there’s no brain scan, test, or lab measurement that reliably detects ADHD. Even with neuropsychiatric testing, only half of children and adolescents will have executive-functioning deficits. The problem with computerized tests, meanwhile, is that a lot of children and adolescents with ADHD have no problem focusing on computer games, so they aren’t helpful for diagnosis.
“The gold standard for ADHD assessment remains a good interview,” and documenting DSM-5 criteria, he said.
As for alternative treatments, “what studies have shown is that if you are highly invested in the treatment and not blinded” to it, “you tend to think you do better. In good studies where they look at teachers who don’t know what’s going on, it doesn’t pan out,” he said. Metanalysis of neurofeedback hasn’t shown effect, nor have computer games to train focus; kids will get better at them with practice, but they haven’t been shown to improve ADHD.
The only exception is omega-3, but the effect size is barely measurable. “If you can get the kid so swallow those fish oil things, go for it, or they can eat salmon,” Dr. McGough said.
In short, medications remain the best option for treating the core symptoms of ADHD, first with stimulants then, as needed, nonstimulants.
But “you are not meeting your patients’ needs if you are only prescribing medications,” he said. Psychosocial education, family behavioral therapy, and school interventions – even things as simple as sitting toward the front of the class and having a little more time on tests – are critical for overall improvement.
It’s also important to let patients and families know that “they don’t have to be ashamed of this,” and the patients need to know why they are taking their medication, he said.
Too often, children are started on a low dose of medication and told to come back in a month. “That’s a waste of time, because it’s a whole month when the person is probably inadequately treated,” Dr. McGough said.
Instead, he has patients titrate up at first, with advice to cut back or stop and call if there are problems. The patient returns after 3 weeks, and the most effective, best-tolerated dose is selected for treatment.
Dr. McGough disclosed relationships with Purdue, Shire, Tris, Sunovion, NeuroSigma, and Neurovance.
SAN FRANCISCO – “If one is going to say ‘you need 6 months of abstinence from cannabis before I am going to treat your ADHD,’ that’s absurd. If [kids] are stoned all the time, no, but if it’s intermittent, it’s really not a factor,” according to James J. McGough, MD, director of the Attention Deficit Disorder Clinic at the University of California, Los Angeles.
There’s no evidence that ongoing stimulant treatment increases the risk of substance abuse, and “we must admit to ourselves that substance use among adolescents and young adults is normative. It happens,” even among well-adapted kids. “Think of your own past histories,” he said to an audience of psychiatrists and other medical professionals at a psychopharmacology update held by the American Academy of Child and Adolescent Psychiatry.
“You have” to deal with substance abuse that’s ruining lives, but otherwise, “I’m comfortable giving a prescription under some circumstances even if I know [patients] are using drugs. It’s the extent and type of [drug use] that informs if we should prescribe or not,” said Dr. McGough, also a professor of clinical psychiatry at the university, but be careful to “really document what you’re doing.”
Misuse and diversion is mostly related to performance enhancement, especially at competitive universities, or when grades head south. Children and young adults in those situations, as well as smokers, drinkers, and those with conduct disorders, “are the ones you worry about.” If a Stanford medical school student at age 27 suddenly develops a horrible problem focusing, with no past ADHD history, “I’m a little suspicious,” he said, noting that people who malinger “tend to go off the scale in terms of endorsing symptoms.”
If misuse and abuse are a concern, extended-release stimulants, as well as nonstimulants, are better options than immediate-release formulations.
Audience members also were curious about alternative approaches for ADHD, but the news wasn’t very good.
For now, there’s no brain scan, test, or lab measurement that reliably detects ADHD. Even with neuropsychiatric testing, only half of children and adolescents will have executive-functioning deficits. The problem with computerized tests, meanwhile, is that a lot of children and adolescents with ADHD have no problem focusing on computer games, so they aren’t helpful for diagnosis.
“The gold standard for ADHD assessment remains a good interview,” and documenting DSM-5 criteria, he said.
As for alternative treatments, “what studies have shown is that if you are highly invested in the treatment and not blinded” to it, “you tend to think you do better. In good studies where they look at teachers who don’t know what’s going on, it doesn’t pan out,” he said. Metanalysis of neurofeedback hasn’t shown effect, nor have computer games to train focus; kids will get better at them with practice, but they haven’t been shown to improve ADHD.
The only exception is omega-3, but the effect size is barely measurable. “If you can get the kid so swallow those fish oil things, go for it, or they can eat salmon,” Dr. McGough said.
In short, medications remain the best option for treating the core symptoms of ADHD, first with stimulants then, as needed, nonstimulants.
But “you are not meeting your patients’ needs if you are only prescribing medications,” he said. Psychosocial education, family behavioral therapy, and school interventions – even things as simple as sitting toward the front of the class and having a little more time on tests – are critical for overall improvement.
It’s also important to let patients and families know that “they don’t have to be ashamed of this,” and the patients need to know why they are taking their medication, he said.
Too often, children are started on a low dose of medication and told to come back in a month. “That’s a waste of time, because it’s a whole month when the person is probably inadequately treated,” Dr. McGough said.
Instead, he has patients titrate up at first, with advice to cut back or stop and call if there are problems. The patient returns after 3 weeks, and the most effective, best-tolerated dose is selected for treatment.
Dr. McGough disclosed relationships with Purdue, Shire, Tris, Sunovion, NeuroSigma, and Neurovance.