User login
Youth perfectionism: Too much of a good thing
SAN FRANCISCO – Maladaptive perfectionism contributes to and is a risk factor for many common psychiatric disorders in children and adolescents, panelists said at the annual conference of the Anxiety and Depression Association of America.
“Perfectionism isn’t a disorder, it’s a personality style. Some of the kids who come in don’t meet criteria for any psychiatric disorder, they just have this personality style that really warrants treatment, because it is getting in the way of their living happy and productive lives. But I would say most of the time we see overlap with DSM Axis I disorders,” said Deborah Ledley, PhD, a clinical psychologist at the Children’s and Adult Center for OCD and Anxiety in Plymouth Meeting, Pa.
“Basically, when people present with multiple disorders and underlying perfectionism, it might actually be more effective to target the perfectionism, rather than treating each disorder sequentially,” according to Dr. Ledley. “Do we really need to treat social anxiety and panic disorder, and a subclinical eating disorder, or can we say, ‘This person is a perfectionist – let us treat that and see if we can remit all those disorders.’”
That strategy often has proved successful for Dr. Ledley and her fellow panelist Lynne Siqueland, PhD, who also practices at the center. Both specialize in cognitive-behavioral therapy (CBT). They were quick to note that there are essentially no published studies on CBT for pediatric perfectionism. Nonetheless, they have found CBT to be quite effective in clinical practice, with the caveat that the standard, full-speed-ahead, 12-sessions-and-we’re done manualized approach to CBT as often applied to anxiety disorders, depression, and other CBT-amenable disorders will not work for perfectionistic youths.
Dr. Ledley agreed. “We are not rushing with these patients,” she said. “This is so different from the way we are with an OCD patient, for example. When I have an OCD patient, I have the initial session with the parents, then an assessment session with the kid, then in the next session, I do some psychoeducation, and in the session after that, I’m doing exposures, because I work fast. Working with perfectionist kids is different: I have to earn their trust. I tell them a lot of stories about patients I’ve worked with who are just like them.”
How to spot maladaptive perfectionism
When the therapists meet with the parents for the first time – generally without the kids present – what they hear over and over again is, “My child is wound like a spring.” These are generally children who excel at everything: school, sports, music lessons, and other activities. And they are stressed out.
“These are the kids who are working on their Beethoven at age 8, trying to master the Moonlight Sonata. But the parents say the child is too hard on himself, freaking out over a grade less than 100% on a small quiz,” Dr. Ledley observed.
Sometimes, though, perfectionism backfires even in grade school, and the parents’ concern is not that their child is super accomplished yet not enjoying it, but rather that their kid has great potential and never gets anything done because of procrastination or an inability to hand in work that is less than perfect.
Dr. Ledley said when she first meets a perfectionist child, she typically sees a kid who looks perfect, has impeccable manners, and is mature beyond their years.
“They’re invested in coming across as successful in every way. They definitely do not let their guard down when you first meet them. But with these kids who look so perfect, we feel that there’s this fragility and fear, and delicacy lurking just below the surface. It’s almost like they’re afraid they’re going to break because they’re so held together,” according to the psychologist.
Once trust has been established and the youth has drawn up a requested list of the pros and cons of their perfectionism, Dr. Siqueland said, she hears a familiar refrain: “No freedom, no fun, no choice, no time for friends, tired all the time, and no sleep. That’s the usual list of the kids.”
The notion that hard-driving parents typically are at fault for pushing their child into perfectionism is a misconception.
“In our practice, I would say it’s self-induced perfectionism in 75% of cases,” according to Dr. Siqueland.
Treatment tips
After spending considerable time establishing rapport with a perfectionist youth, Dr. Ledley and Dr. Siqueland emphasize three key messages:
1. While on the surface your perfectionist strategy makes sense, enabling you to bask in positive feedback from teachers, coaches, friends, and in some cases your parents, it simply can’t be kept up long term.
“To the ones who really want to go to college and med school, I just say, ‘It’s not going to work there. You’ll not survive college. Or maybe college, but certainly not med school. So are you going to fix it now or fix it later? If you want med school as a goal, let’s help you get there,’ ” Dr. Siqueland said.
2. Therapy is not about changing your values.
“They fear that, if they don’t push and sacrifice, they’re going to be average, or even a slacker – and slacker might be worse than average,” Dr. Siqueland continued.
“We tell them it’s OK to have a drive for excellence, to go after your dream, and to take pride in good work well done. These are your values, and that’s great. We are not in the business of turning you into a slacker,” Dr. Ledley added.
3. Perfectionism takes away choices.
Therapy is all about helping you to live your life rather than having anxiety order you around. You can learn to have freedom, fun, choice, and sleep while in most cases doing as well as or better than before on your grades.
For clinicians who are inexperienced in addressing perfectionism in youth, Dr. Ledley and Dr. Siqueland recommended as a useful primer “The Perfectionism Workbook for Teens” (Oakland, Calif.: New Harbinger Publications, 2016).
They reported having no financial conflicts of interest.
SAN FRANCISCO – Maladaptive perfectionism contributes to and is a risk factor for many common psychiatric disorders in children and adolescents, panelists said at the annual conference of the Anxiety and Depression Association of America.
“Perfectionism isn’t a disorder, it’s a personality style. Some of the kids who come in don’t meet criteria for any psychiatric disorder, they just have this personality style that really warrants treatment, because it is getting in the way of their living happy and productive lives. But I would say most of the time we see overlap with DSM Axis I disorders,” said Deborah Ledley, PhD, a clinical psychologist at the Children’s and Adult Center for OCD and Anxiety in Plymouth Meeting, Pa.
“Basically, when people present with multiple disorders and underlying perfectionism, it might actually be more effective to target the perfectionism, rather than treating each disorder sequentially,” according to Dr. Ledley. “Do we really need to treat social anxiety and panic disorder, and a subclinical eating disorder, or can we say, ‘This person is a perfectionist – let us treat that and see if we can remit all those disorders.’”
That strategy often has proved successful for Dr. Ledley and her fellow panelist Lynne Siqueland, PhD, who also practices at the center. Both specialize in cognitive-behavioral therapy (CBT). They were quick to note that there are essentially no published studies on CBT for pediatric perfectionism. Nonetheless, they have found CBT to be quite effective in clinical practice, with the caveat that the standard, full-speed-ahead, 12-sessions-and-we’re done manualized approach to CBT as often applied to anxiety disorders, depression, and other CBT-amenable disorders will not work for perfectionistic youths.
Dr. Ledley agreed. “We are not rushing with these patients,” she said. “This is so different from the way we are with an OCD patient, for example. When I have an OCD patient, I have the initial session with the parents, then an assessment session with the kid, then in the next session, I do some psychoeducation, and in the session after that, I’m doing exposures, because I work fast. Working with perfectionist kids is different: I have to earn their trust. I tell them a lot of stories about patients I’ve worked with who are just like them.”
How to spot maladaptive perfectionism
When the therapists meet with the parents for the first time – generally without the kids present – what they hear over and over again is, “My child is wound like a spring.” These are generally children who excel at everything: school, sports, music lessons, and other activities. And they are stressed out.
“These are the kids who are working on their Beethoven at age 8, trying to master the Moonlight Sonata. But the parents say the child is too hard on himself, freaking out over a grade less than 100% on a small quiz,” Dr. Ledley observed.
Sometimes, though, perfectionism backfires even in grade school, and the parents’ concern is not that their child is super accomplished yet not enjoying it, but rather that their kid has great potential and never gets anything done because of procrastination or an inability to hand in work that is less than perfect.
Dr. Ledley said when she first meets a perfectionist child, she typically sees a kid who looks perfect, has impeccable manners, and is mature beyond their years.
“They’re invested in coming across as successful in every way. They definitely do not let their guard down when you first meet them. But with these kids who look so perfect, we feel that there’s this fragility and fear, and delicacy lurking just below the surface. It’s almost like they’re afraid they’re going to break because they’re so held together,” according to the psychologist.
Once trust has been established and the youth has drawn up a requested list of the pros and cons of their perfectionism, Dr. Siqueland said, she hears a familiar refrain: “No freedom, no fun, no choice, no time for friends, tired all the time, and no sleep. That’s the usual list of the kids.”
The notion that hard-driving parents typically are at fault for pushing their child into perfectionism is a misconception.
“In our practice, I would say it’s self-induced perfectionism in 75% of cases,” according to Dr. Siqueland.
Treatment tips
After spending considerable time establishing rapport with a perfectionist youth, Dr. Ledley and Dr. Siqueland emphasize three key messages:
1. While on the surface your perfectionist strategy makes sense, enabling you to bask in positive feedback from teachers, coaches, friends, and in some cases your parents, it simply can’t be kept up long term.
“To the ones who really want to go to college and med school, I just say, ‘It’s not going to work there. You’ll not survive college. Or maybe college, but certainly not med school. So are you going to fix it now or fix it later? If you want med school as a goal, let’s help you get there,’ ” Dr. Siqueland said.
2. Therapy is not about changing your values.
“They fear that, if they don’t push and sacrifice, they’re going to be average, or even a slacker – and slacker might be worse than average,” Dr. Siqueland continued.
“We tell them it’s OK to have a drive for excellence, to go after your dream, and to take pride in good work well done. These are your values, and that’s great. We are not in the business of turning you into a slacker,” Dr. Ledley added.
3. Perfectionism takes away choices.
Therapy is all about helping you to live your life rather than having anxiety order you around. You can learn to have freedom, fun, choice, and sleep while in most cases doing as well as or better than before on your grades.
For clinicians who are inexperienced in addressing perfectionism in youth, Dr. Ledley and Dr. Siqueland recommended as a useful primer “The Perfectionism Workbook for Teens” (Oakland, Calif.: New Harbinger Publications, 2016).
They reported having no financial conflicts of interest.
SAN FRANCISCO – Maladaptive perfectionism contributes to and is a risk factor for many common psychiatric disorders in children and adolescents, panelists said at the annual conference of the Anxiety and Depression Association of America.
“Perfectionism isn’t a disorder, it’s a personality style. Some of the kids who come in don’t meet criteria for any psychiatric disorder, they just have this personality style that really warrants treatment, because it is getting in the way of their living happy and productive lives. But I would say most of the time we see overlap with DSM Axis I disorders,” said Deborah Ledley, PhD, a clinical psychologist at the Children’s and Adult Center for OCD and Anxiety in Plymouth Meeting, Pa.
“Basically, when people present with multiple disorders and underlying perfectionism, it might actually be more effective to target the perfectionism, rather than treating each disorder sequentially,” according to Dr. Ledley. “Do we really need to treat social anxiety and panic disorder, and a subclinical eating disorder, or can we say, ‘This person is a perfectionist – let us treat that and see if we can remit all those disorders.’”
That strategy often has proved successful for Dr. Ledley and her fellow panelist Lynne Siqueland, PhD, who also practices at the center. Both specialize in cognitive-behavioral therapy (CBT). They were quick to note that there are essentially no published studies on CBT for pediatric perfectionism. Nonetheless, they have found CBT to be quite effective in clinical practice, with the caveat that the standard, full-speed-ahead, 12-sessions-and-we’re done manualized approach to CBT as often applied to anxiety disorders, depression, and other CBT-amenable disorders will not work for perfectionistic youths.
Dr. Ledley agreed. “We are not rushing with these patients,” she said. “This is so different from the way we are with an OCD patient, for example. When I have an OCD patient, I have the initial session with the parents, then an assessment session with the kid, then in the next session, I do some psychoeducation, and in the session after that, I’m doing exposures, because I work fast. Working with perfectionist kids is different: I have to earn their trust. I tell them a lot of stories about patients I’ve worked with who are just like them.”
How to spot maladaptive perfectionism
When the therapists meet with the parents for the first time – generally without the kids present – what they hear over and over again is, “My child is wound like a spring.” These are generally children who excel at everything: school, sports, music lessons, and other activities. And they are stressed out.
“These are the kids who are working on their Beethoven at age 8, trying to master the Moonlight Sonata. But the parents say the child is too hard on himself, freaking out over a grade less than 100% on a small quiz,” Dr. Ledley observed.
Sometimes, though, perfectionism backfires even in grade school, and the parents’ concern is not that their child is super accomplished yet not enjoying it, but rather that their kid has great potential and never gets anything done because of procrastination or an inability to hand in work that is less than perfect.
Dr. Ledley said when she first meets a perfectionist child, she typically sees a kid who looks perfect, has impeccable manners, and is mature beyond their years.
“They’re invested in coming across as successful in every way. They definitely do not let their guard down when you first meet them. But with these kids who look so perfect, we feel that there’s this fragility and fear, and delicacy lurking just below the surface. It’s almost like they’re afraid they’re going to break because they’re so held together,” according to the psychologist.
Once trust has been established and the youth has drawn up a requested list of the pros and cons of their perfectionism, Dr. Siqueland said, she hears a familiar refrain: “No freedom, no fun, no choice, no time for friends, tired all the time, and no sleep. That’s the usual list of the kids.”
The notion that hard-driving parents typically are at fault for pushing their child into perfectionism is a misconception.
“In our practice, I would say it’s self-induced perfectionism in 75% of cases,” according to Dr. Siqueland.
Treatment tips
After spending considerable time establishing rapport with a perfectionist youth, Dr. Ledley and Dr. Siqueland emphasize three key messages:
1. While on the surface your perfectionist strategy makes sense, enabling you to bask in positive feedback from teachers, coaches, friends, and in some cases your parents, it simply can’t be kept up long term.
“To the ones who really want to go to college and med school, I just say, ‘It’s not going to work there. You’ll not survive college. Or maybe college, but certainly not med school. So are you going to fix it now or fix it later? If you want med school as a goal, let’s help you get there,’ ” Dr. Siqueland said.
2. Therapy is not about changing your values.
“They fear that, if they don’t push and sacrifice, they’re going to be average, or even a slacker – and slacker might be worse than average,” Dr. Siqueland continued.
“We tell them it’s OK to have a drive for excellence, to go after your dream, and to take pride in good work well done. These are your values, and that’s great. We are not in the business of turning you into a slacker,” Dr. Ledley added.
3. Perfectionism takes away choices.
Therapy is all about helping you to live your life rather than having anxiety order you around. You can learn to have freedom, fun, choice, and sleep while in most cases doing as well as or better than before on your grades.
For clinicians who are inexperienced in addressing perfectionism in youth, Dr. Ledley and Dr. Siqueland recommended as a useful primer “The Perfectionism Workbook for Teens” (Oakland, Calif.: New Harbinger Publications, 2016).
They reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM THE ANXIETY AND DEPRESSION CONFERENCE 2017
Little treatments show big promise for youth psychiatric problems
SAN FRANCISCO – Very brief, outside-the-box therapeutic interventions are racking up respectable efficacy scores in randomized, controlled trials addressing a variety of common psychiatric problems in youths, Jessica L. Schleider observed at the annual conference of the Anxiety and Depression Association of America.
The impetus for developing very brief interventions – or VBIs, as they are known in psychotherapy research parlance – is mounting recognition that conventional treatment approaches have by and large failed children and adolescents who have mental health problems, explained Ms. Schleider, a doctoral candidate in clinical psychology at Harvard University in Cambridge, Mass.
According to data from the Centers for Disease Control and Prevention and the Child Mind Institute, only 20% of American children and adolescents who have significant mental health problems access mental health services. And among those who do, only a minority complete their planned course of treatment.
Reimbursable treatment plans for youth mental health problems typically entail about 16 sessions. Yet national insurance reimbursement data indicate those youths who do access treatment attend on average fewer than four sessions.
“Given that the current model just doesn’t seem to be meeting the needs of kids and families across the country, novel approaches are going to be necessary to really reduce the burden of youth mental illness on a broad scale,” Ms. Schleider asserted.
She characterized VBIs as an example of what is often referred to in TED Talks as “disruptive innovation.” VBIs are intended to extend the reach of youth mental health services by offering interventions that are brief, affordable, accessible, and scalable. It’s a concept that has captured the imagination of officials at the National Institute of Mental Health, which is funding her VBI work and that of others under the institute’s experimental therapeutics initiative.
Ms. Schleider coauthored a recent meta-analysis of 50 randomized, controlled trials of single-session interventions (SSIs) for mental health problems in a collective 10,508 youths. The investigators found that the treatment effect size varied by the target problem. The largest effect size documented – 1.05, which is a strong benefit – was for SSIs targeting eating disorders. The weakest was for the 18 randomized trials addressing substance abuse, with an effect size of a mere 0.08 (J Am Acad Child Adolesc Psychiatry. 2017 Feb;56[2]:107-15).
“The mean effect size across all categories is 0.32, which is decent. It’s in the small-to-medium range,” she noted. “But if you zoom in on the most common types of youth mental health problems – anxiety, conduct, and depression – we see that the overall effect of those single-session programs compares surprisingly well to the full-length treatments that we have, further supporting a possible value as an element of our mental health system.”
For SSIs addressing anxiety, for example, the mean posttreatment effect size was 0.56, compared with 0.61 for conventional multisession programs. For conduct problems, SSIs produced a mean effect size of 0.54, versus 0.46 for full-length treatment programs. And while the effect size of SSIs for depression was small, at 0.18, the same might be said for the 0.28 mean effect size for standard depression therapy programs.
Mean SSI treatment effect sizes were larger for children than for adolescents, at 0.42, compared with 0.19.
Ms. Schleider also presented highlights of a published randomized, double-blind trial of a self-administered computer-guided SSI she and her coauthor have developed. That SSI is designed to briefly teach troubled adolescents a growth personality mindset: that is, the belief that personal traits such as shyness, sadness, and intelligence are malleable through effort and hard work, rather than static and unchangeable.
“Kids with fixed mindsets tend to fare worse than those with growth mindsets,” she said. “They give up prematurely in response to social and academic stress, and they engage in a lot more negative self talk.
The intervention borrows from the achievement motivation theory developed by Carol S. Dweck, Ph.D., professor of psychology at Stanford (Calif.) University and author of the book, “Mindset: the New Psychology of Success.”
The trial randomized 96 subjects aged 12-15 years to a half hour spent on a computer with the growth mindset intervention or a shared feelings control. These were teens with elevated levels of internalizing problems. Eighty-four percent of them met criteria for anxiety by the SCARED CHILD (Screen for Child Anxiety Related Disorders – Child Version) or for depression via the CDI (Children’s Depression Inventory). Subjects were followed up immediately post treatment and again at 3, 6, and 9 months, with 74% of the original group participating in the final follow-up.
The guided growth mindset group showed significant reductions from baseline in CDI and SCARED scores at every follow-up point, while the control group remained unchanged.
“What I see as the bottom line are the 9-month follow-up effects: All effect sizes for youth- and parent-reported outcomes of anxiety and depression are in the small-to-medium range,” Ms. Schleider said. “But this is quite promising, I think, for a 30-minute intervention that kids can complete on their own.”
Also, the mindset intervention strengthened postintervention measures of the adolescents’ perceived control. On a postintervention, laboratory-based, standardized social stress test, the mindset intervention group achieved physiologic recovery more than three times faster than did the controls, as assessed via electrodermal activity.
Ms. Schleider called the study results “promising and exciting.” She is now working with therapists at McLean Hospital, Belmont, Mass., to see whether administering the growth mindset intervention at the start of youth intensive cognitive-behavioral therapy for anxiety results in improved treatment outcomes.
“By teaching kids that change is possible, it might improve their engagement in CBT or reduce their dropout rates,” she noted.
Ms. Schleider is also pilot studying a parent-directed growth mindset intervention to learn whether it improves parents’ attitude toward psychotherapy and seeking services for a troubled child.
Her randomized trial was supported by the National Institute of Mental Health, the American Psychological Association, and the Harvard Center on the Developing Child. She reported having no financial conflicts.
SAN FRANCISCO – Very brief, outside-the-box therapeutic interventions are racking up respectable efficacy scores in randomized, controlled trials addressing a variety of common psychiatric problems in youths, Jessica L. Schleider observed at the annual conference of the Anxiety and Depression Association of America.
The impetus for developing very brief interventions – or VBIs, as they are known in psychotherapy research parlance – is mounting recognition that conventional treatment approaches have by and large failed children and adolescents who have mental health problems, explained Ms. Schleider, a doctoral candidate in clinical psychology at Harvard University in Cambridge, Mass.
According to data from the Centers for Disease Control and Prevention and the Child Mind Institute, only 20% of American children and adolescents who have significant mental health problems access mental health services. And among those who do, only a minority complete their planned course of treatment.
Reimbursable treatment plans for youth mental health problems typically entail about 16 sessions. Yet national insurance reimbursement data indicate those youths who do access treatment attend on average fewer than four sessions.
“Given that the current model just doesn’t seem to be meeting the needs of kids and families across the country, novel approaches are going to be necessary to really reduce the burden of youth mental illness on a broad scale,” Ms. Schleider asserted.
She characterized VBIs as an example of what is often referred to in TED Talks as “disruptive innovation.” VBIs are intended to extend the reach of youth mental health services by offering interventions that are brief, affordable, accessible, and scalable. It’s a concept that has captured the imagination of officials at the National Institute of Mental Health, which is funding her VBI work and that of others under the institute’s experimental therapeutics initiative.
Ms. Schleider coauthored a recent meta-analysis of 50 randomized, controlled trials of single-session interventions (SSIs) for mental health problems in a collective 10,508 youths. The investigators found that the treatment effect size varied by the target problem. The largest effect size documented – 1.05, which is a strong benefit – was for SSIs targeting eating disorders. The weakest was for the 18 randomized trials addressing substance abuse, with an effect size of a mere 0.08 (J Am Acad Child Adolesc Psychiatry. 2017 Feb;56[2]:107-15).
“The mean effect size across all categories is 0.32, which is decent. It’s in the small-to-medium range,” she noted. “But if you zoom in on the most common types of youth mental health problems – anxiety, conduct, and depression – we see that the overall effect of those single-session programs compares surprisingly well to the full-length treatments that we have, further supporting a possible value as an element of our mental health system.”
For SSIs addressing anxiety, for example, the mean posttreatment effect size was 0.56, compared with 0.61 for conventional multisession programs. For conduct problems, SSIs produced a mean effect size of 0.54, versus 0.46 for full-length treatment programs. And while the effect size of SSIs for depression was small, at 0.18, the same might be said for the 0.28 mean effect size for standard depression therapy programs.
Mean SSI treatment effect sizes were larger for children than for adolescents, at 0.42, compared with 0.19.
Ms. Schleider also presented highlights of a published randomized, double-blind trial of a self-administered computer-guided SSI she and her coauthor have developed. That SSI is designed to briefly teach troubled adolescents a growth personality mindset: that is, the belief that personal traits such as shyness, sadness, and intelligence are malleable through effort and hard work, rather than static and unchangeable.
“Kids with fixed mindsets tend to fare worse than those with growth mindsets,” she said. “They give up prematurely in response to social and academic stress, and they engage in a lot more negative self talk.
The intervention borrows from the achievement motivation theory developed by Carol S. Dweck, Ph.D., professor of psychology at Stanford (Calif.) University and author of the book, “Mindset: the New Psychology of Success.”
The trial randomized 96 subjects aged 12-15 years to a half hour spent on a computer with the growth mindset intervention or a shared feelings control. These were teens with elevated levels of internalizing problems. Eighty-four percent of them met criteria for anxiety by the SCARED CHILD (Screen for Child Anxiety Related Disorders – Child Version) or for depression via the CDI (Children’s Depression Inventory). Subjects were followed up immediately post treatment and again at 3, 6, and 9 months, with 74% of the original group participating in the final follow-up.
The guided growth mindset group showed significant reductions from baseline in CDI and SCARED scores at every follow-up point, while the control group remained unchanged.
“What I see as the bottom line are the 9-month follow-up effects: All effect sizes for youth- and parent-reported outcomes of anxiety and depression are in the small-to-medium range,” Ms. Schleider said. “But this is quite promising, I think, for a 30-minute intervention that kids can complete on their own.”
Also, the mindset intervention strengthened postintervention measures of the adolescents’ perceived control. On a postintervention, laboratory-based, standardized social stress test, the mindset intervention group achieved physiologic recovery more than three times faster than did the controls, as assessed via electrodermal activity.
Ms. Schleider called the study results “promising and exciting.” She is now working with therapists at McLean Hospital, Belmont, Mass., to see whether administering the growth mindset intervention at the start of youth intensive cognitive-behavioral therapy for anxiety results in improved treatment outcomes.
“By teaching kids that change is possible, it might improve their engagement in CBT or reduce their dropout rates,” she noted.
Ms. Schleider is also pilot studying a parent-directed growth mindset intervention to learn whether it improves parents’ attitude toward psychotherapy and seeking services for a troubled child.
Her randomized trial was supported by the National Institute of Mental Health, the American Psychological Association, and the Harvard Center on the Developing Child. She reported having no financial conflicts.
SAN FRANCISCO – Very brief, outside-the-box therapeutic interventions are racking up respectable efficacy scores in randomized, controlled trials addressing a variety of common psychiatric problems in youths, Jessica L. Schleider observed at the annual conference of the Anxiety and Depression Association of America.
The impetus for developing very brief interventions – or VBIs, as they are known in psychotherapy research parlance – is mounting recognition that conventional treatment approaches have by and large failed children and adolescents who have mental health problems, explained Ms. Schleider, a doctoral candidate in clinical psychology at Harvard University in Cambridge, Mass.
According to data from the Centers for Disease Control and Prevention and the Child Mind Institute, only 20% of American children and adolescents who have significant mental health problems access mental health services. And among those who do, only a minority complete their planned course of treatment.
Reimbursable treatment plans for youth mental health problems typically entail about 16 sessions. Yet national insurance reimbursement data indicate those youths who do access treatment attend on average fewer than four sessions.
“Given that the current model just doesn’t seem to be meeting the needs of kids and families across the country, novel approaches are going to be necessary to really reduce the burden of youth mental illness on a broad scale,” Ms. Schleider asserted.
She characterized VBIs as an example of what is often referred to in TED Talks as “disruptive innovation.” VBIs are intended to extend the reach of youth mental health services by offering interventions that are brief, affordable, accessible, and scalable. It’s a concept that has captured the imagination of officials at the National Institute of Mental Health, which is funding her VBI work and that of others under the institute’s experimental therapeutics initiative.
Ms. Schleider coauthored a recent meta-analysis of 50 randomized, controlled trials of single-session interventions (SSIs) for mental health problems in a collective 10,508 youths. The investigators found that the treatment effect size varied by the target problem. The largest effect size documented – 1.05, which is a strong benefit – was for SSIs targeting eating disorders. The weakest was for the 18 randomized trials addressing substance abuse, with an effect size of a mere 0.08 (J Am Acad Child Adolesc Psychiatry. 2017 Feb;56[2]:107-15).
“The mean effect size across all categories is 0.32, which is decent. It’s in the small-to-medium range,” she noted. “But if you zoom in on the most common types of youth mental health problems – anxiety, conduct, and depression – we see that the overall effect of those single-session programs compares surprisingly well to the full-length treatments that we have, further supporting a possible value as an element of our mental health system.”
For SSIs addressing anxiety, for example, the mean posttreatment effect size was 0.56, compared with 0.61 for conventional multisession programs. For conduct problems, SSIs produced a mean effect size of 0.54, versus 0.46 for full-length treatment programs. And while the effect size of SSIs for depression was small, at 0.18, the same might be said for the 0.28 mean effect size for standard depression therapy programs.
Mean SSI treatment effect sizes were larger for children than for adolescents, at 0.42, compared with 0.19.
Ms. Schleider also presented highlights of a published randomized, double-blind trial of a self-administered computer-guided SSI she and her coauthor have developed. That SSI is designed to briefly teach troubled adolescents a growth personality mindset: that is, the belief that personal traits such as shyness, sadness, and intelligence are malleable through effort and hard work, rather than static and unchangeable.
“Kids with fixed mindsets tend to fare worse than those with growth mindsets,” she said. “They give up prematurely in response to social and academic stress, and they engage in a lot more negative self talk.
The intervention borrows from the achievement motivation theory developed by Carol S. Dweck, Ph.D., professor of psychology at Stanford (Calif.) University and author of the book, “Mindset: the New Psychology of Success.”
The trial randomized 96 subjects aged 12-15 years to a half hour spent on a computer with the growth mindset intervention or a shared feelings control. These were teens with elevated levels of internalizing problems. Eighty-four percent of them met criteria for anxiety by the SCARED CHILD (Screen for Child Anxiety Related Disorders – Child Version) or for depression via the CDI (Children’s Depression Inventory). Subjects were followed up immediately post treatment and again at 3, 6, and 9 months, with 74% of the original group participating in the final follow-up.
The guided growth mindset group showed significant reductions from baseline in CDI and SCARED scores at every follow-up point, while the control group remained unchanged.
“What I see as the bottom line are the 9-month follow-up effects: All effect sizes for youth- and parent-reported outcomes of anxiety and depression are in the small-to-medium range,” Ms. Schleider said. “But this is quite promising, I think, for a 30-minute intervention that kids can complete on their own.”
Also, the mindset intervention strengthened postintervention measures of the adolescents’ perceived control. On a postintervention, laboratory-based, standardized social stress test, the mindset intervention group achieved physiologic recovery more than three times faster than did the controls, as assessed via electrodermal activity.
Ms. Schleider called the study results “promising and exciting.” She is now working with therapists at McLean Hospital, Belmont, Mass., to see whether administering the growth mindset intervention at the start of youth intensive cognitive-behavioral therapy for anxiety results in improved treatment outcomes.
“By teaching kids that change is possible, it might improve their engagement in CBT or reduce their dropout rates,” she noted.
Ms. Schleider is also pilot studying a parent-directed growth mindset intervention to learn whether it improves parents’ attitude toward psychotherapy and seeking services for a troubled child.
Her randomized trial was supported by the National Institute of Mental Health, the American Psychological Association, and the Harvard Center on the Developing Child. She reported having no financial conflicts.
EXPERT ANALYSIS FROM THE ANXIETY AND DEPRESSION CONFERENCE 2017
Transcranial magnetic stimulation shows promise in autism spectrum disorder
SAN FRANCISCO – , Eric Hollander, MD, said at the annual conference of the Anxiety and Depression Association of America.
“It’s a promising tool. There’s a lot of hope. There have been a range of scattered studies. But there is still a lot more work that needs to be done in terms of defining the optimal target structures in the brain, the dose and frequency of treatment, and which symptoms respond best,” said Dr. Hollander, director of the autism and obsessive-compulsive spectrum program as well as the anxiety and depression program at Albert Einstein College of Medicine in New York.
The authors characterized transcranial magnetic stimulation (TMS) for autism spectrum disorder (ASD) as “a novel, possibly transformative approach” but added a strong cautionary note.
“The available literature on the TMS use in ASD is preliminary, composed of studies with methodological limitations. Thus, off-label clinical rTMS [repetitive TMS] use for therapeutic interventions in ASD without an investigational device exemption and outside of an IRB [institutional review board]-approved research trial is premature pending further, adequately powered and controlled trials,” according to the white paper by the TMS in ASD Consensus Group (Autism Res. 2016 Feb;9[2]:184-203).
ASD support groups are eager to see TMS developed as a treatment, Dr. Hollander said. This is largely a result of the 2016 publication of a nonfiction book entitled, “Switched On: A Memoir of Brain Change and Emotional Awakening” (New York: Spiegel & Grau, 2016). Author John Elder Robison is a high-functioning individual with ASD who describes his dramatic improvement in response to TMS therapy in an early clinical trial conducted at Boston’s Beth Israel Deaconess Medical Center.
Dr. Hollander has been extensively involved in pioneering studies of TMS for the treatment of depression – currently its only Food and Drug Administration–approved indication – as well as for obsessive-compulsive disorder. His recent work on TMS for the treatment of ASD has focused on the noninvasive therapy’s ability to favorably affect the excitatory/inhibitory imbalance that characterizes ASD. This imbalance is tied chiefly to abnormal glutamatergic and gamma-aminobutyric acid–ergic neurotransmission in the neocortex, cerebellum, hippocampus, and amygdala. The imbalance is thought to be responsible for the cognitive, sensory, learning, memory, and motor deficits, as well as increased propensity for seizures, associated with ASD.
This excitatory/inhibitory imbalance is marked by increased cortical excitability and decreased inhibition within the densely packed cortical minicolumns of neurons, which are organized into pathways and circuits.
“You can use TMS as a treatment, or you can use it as a research probe to look at these mechanisms by turning on or off pathways,” the psychiatrist explained. “These densely packed minicolumns are like wires with poor insulation, which results in impairment in the ability to distinguish a stimulus from background noise. In the pathologic condition, you’re getting a rapid firing which doesn’t really differentiate what’s a true signal from what’s background noise.”
Therapeutically, TMS can be employed to improve that signal-to-noise ratio, either by reducing excitation or increasing inhibition. Potential TMS targets in autism include the anterior cingulate cortex, the supplementary or presupplementary motor area, the dorsal medial prefrontal cortex, the dorsal lateral prefrontal cortex, and the cerebellum. More than a dozen published TMS studies – albeit open-label, uncontrolled, and featuring only handfuls of patients – have demonstrated long-lasting improvements in the two core symptom domains of ASD: reduced repetitive behaviors and improved social relatedness and interpersonal functioning, Dr. Hollander said.
A wide range of associated noncore symptoms, including disruptive behaviors such as self-injury or aggression, impulse control, social anxiety, and depression, also might be targeted.
“In our clinical practice, we tend to treat adults with ASD who have a lot of OCD [obsessive-compulsive disorder] and repetitive behavior symptoms but also mood or anxiety symptoms or PTSD [posttraumatic stress disorder] symptoms as a result of earlier bullying. You can adapt your treatment to the target symptoms, so if there’s a lot of OCD-type symptoms, you might use low-frequency TMS at 1 Hz to target the supplementary motor area. If people are coming in with depressive symptoms, you can use the dorsolateral prefrontal cortex depression target. If they have a lot of anxiety, you can target the right frontal anxiety loop with low-frequency TMS. Or with a lot of PTSD symptoms, you can use high-frequency stimulation of the dorsolateral prefrontal cortex at 20 Hz,” Dr. Hollander said.
An important caveat, however, is that ASD is associated with an increased risk of seizures and other EEG abnormalities, so low-frequency TMS generally is preferable because of its greater safety.
Another challenge is administering TMS in children.
“Kids move around a lot, so you’re probably going to be using briefer stimulation parameters like theta burst stimulation rather than longer treatment parameters,” Dr. Hollander said.
That being said, there are more than two dozen published studies of TMS for treatment of children and adolescents, and surveys indicate that these patients generally find it quite tolerable. Dr. Hollander noted that in one study, children and adolescents ranked it somewhere between watching television and a long car ride. This placed TMS on the midrange of a tolerability scale: not as good as having a birthday party or playing a game, but better than going to the dentist, throwing up, or, in last place, getting a shot. Of the 39 youngsters, 34 indicated that they would recommend TMS to a friend.
Dr. Hollander reported receiving research funding from the National Institute of Mental Health, the National Institute on Drug Abuse, and the National Institute of Neurological Disorders and Stroke. He serves as a consultant to roughly half a dozen pharmaceutical companies.
SAN FRANCISCO – , Eric Hollander, MD, said at the annual conference of the Anxiety and Depression Association of America.
“It’s a promising tool. There’s a lot of hope. There have been a range of scattered studies. But there is still a lot more work that needs to be done in terms of defining the optimal target structures in the brain, the dose and frequency of treatment, and which symptoms respond best,” said Dr. Hollander, director of the autism and obsessive-compulsive spectrum program as well as the anxiety and depression program at Albert Einstein College of Medicine in New York.
The authors characterized transcranial magnetic stimulation (TMS) for autism spectrum disorder (ASD) as “a novel, possibly transformative approach” but added a strong cautionary note.
“The available literature on the TMS use in ASD is preliminary, composed of studies with methodological limitations. Thus, off-label clinical rTMS [repetitive TMS] use for therapeutic interventions in ASD without an investigational device exemption and outside of an IRB [institutional review board]-approved research trial is premature pending further, adequately powered and controlled trials,” according to the white paper by the TMS in ASD Consensus Group (Autism Res. 2016 Feb;9[2]:184-203).
ASD support groups are eager to see TMS developed as a treatment, Dr. Hollander said. This is largely a result of the 2016 publication of a nonfiction book entitled, “Switched On: A Memoir of Brain Change and Emotional Awakening” (New York: Spiegel & Grau, 2016). Author John Elder Robison is a high-functioning individual with ASD who describes his dramatic improvement in response to TMS therapy in an early clinical trial conducted at Boston’s Beth Israel Deaconess Medical Center.
Dr. Hollander has been extensively involved in pioneering studies of TMS for the treatment of depression – currently its only Food and Drug Administration–approved indication – as well as for obsessive-compulsive disorder. His recent work on TMS for the treatment of ASD has focused on the noninvasive therapy’s ability to favorably affect the excitatory/inhibitory imbalance that characterizes ASD. This imbalance is tied chiefly to abnormal glutamatergic and gamma-aminobutyric acid–ergic neurotransmission in the neocortex, cerebellum, hippocampus, and amygdala. The imbalance is thought to be responsible for the cognitive, sensory, learning, memory, and motor deficits, as well as increased propensity for seizures, associated with ASD.
This excitatory/inhibitory imbalance is marked by increased cortical excitability and decreased inhibition within the densely packed cortical minicolumns of neurons, which are organized into pathways and circuits.
“You can use TMS as a treatment, or you can use it as a research probe to look at these mechanisms by turning on or off pathways,” the psychiatrist explained. “These densely packed minicolumns are like wires with poor insulation, which results in impairment in the ability to distinguish a stimulus from background noise. In the pathologic condition, you’re getting a rapid firing which doesn’t really differentiate what’s a true signal from what’s background noise.”
Therapeutically, TMS can be employed to improve that signal-to-noise ratio, either by reducing excitation or increasing inhibition. Potential TMS targets in autism include the anterior cingulate cortex, the supplementary or presupplementary motor area, the dorsal medial prefrontal cortex, the dorsal lateral prefrontal cortex, and the cerebellum. More than a dozen published TMS studies – albeit open-label, uncontrolled, and featuring only handfuls of patients – have demonstrated long-lasting improvements in the two core symptom domains of ASD: reduced repetitive behaviors and improved social relatedness and interpersonal functioning, Dr. Hollander said.
A wide range of associated noncore symptoms, including disruptive behaviors such as self-injury or aggression, impulse control, social anxiety, and depression, also might be targeted.
“In our clinical practice, we tend to treat adults with ASD who have a lot of OCD [obsessive-compulsive disorder] and repetitive behavior symptoms but also mood or anxiety symptoms or PTSD [posttraumatic stress disorder] symptoms as a result of earlier bullying. You can adapt your treatment to the target symptoms, so if there’s a lot of OCD-type symptoms, you might use low-frequency TMS at 1 Hz to target the supplementary motor area. If people are coming in with depressive symptoms, you can use the dorsolateral prefrontal cortex depression target. If they have a lot of anxiety, you can target the right frontal anxiety loop with low-frequency TMS. Or with a lot of PTSD symptoms, you can use high-frequency stimulation of the dorsolateral prefrontal cortex at 20 Hz,” Dr. Hollander said.
An important caveat, however, is that ASD is associated with an increased risk of seizures and other EEG abnormalities, so low-frequency TMS generally is preferable because of its greater safety.
Another challenge is administering TMS in children.
“Kids move around a lot, so you’re probably going to be using briefer stimulation parameters like theta burst stimulation rather than longer treatment parameters,” Dr. Hollander said.
That being said, there are more than two dozen published studies of TMS for treatment of children and adolescents, and surveys indicate that these patients generally find it quite tolerable. Dr. Hollander noted that in one study, children and adolescents ranked it somewhere between watching television and a long car ride. This placed TMS on the midrange of a tolerability scale: not as good as having a birthday party or playing a game, but better than going to the dentist, throwing up, or, in last place, getting a shot. Of the 39 youngsters, 34 indicated that they would recommend TMS to a friend.
Dr. Hollander reported receiving research funding from the National Institute of Mental Health, the National Institute on Drug Abuse, and the National Institute of Neurological Disorders and Stroke. He serves as a consultant to roughly half a dozen pharmaceutical companies.
SAN FRANCISCO – , Eric Hollander, MD, said at the annual conference of the Anxiety and Depression Association of America.
“It’s a promising tool. There’s a lot of hope. There have been a range of scattered studies. But there is still a lot more work that needs to be done in terms of defining the optimal target structures in the brain, the dose and frequency of treatment, and which symptoms respond best,” said Dr. Hollander, director of the autism and obsessive-compulsive spectrum program as well as the anxiety and depression program at Albert Einstein College of Medicine in New York.
The authors characterized transcranial magnetic stimulation (TMS) for autism spectrum disorder (ASD) as “a novel, possibly transformative approach” but added a strong cautionary note.
“The available literature on the TMS use in ASD is preliminary, composed of studies with methodological limitations. Thus, off-label clinical rTMS [repetitive TMS] use for therapeutic interventions in ASD without an investigational device exemption and outside of an IRB [institutional review board]-approved research trial is premature pending further, adequately powered and controlled trials,” according to the white paper by the TMS in ASD Consensus Group (Autism Res. 2016 Feb;9[2]:184-203).
ASD support groups are eager to see TMS developed as a treatment, Dr. Hollander said. This is largely a result of the 2016 publication of a nonfiction book entitled, “Switched On: A Memoir of Brain Change and Emotional Awakening” (New York: Spiegel & Grau, 2016). Author John Elder Robison is a high-functioning individual with ASD who describes his dramatic improvement in response to TMS therapy in an early clinical trial conducted at Boston’s Beth Israel Deaconess Medical Center.
Dr. Hollander has been extensively involved in pioneering studies of TMS for the treatment of depression – currently its only Food and Drug Administration–approved indication – as well as for obsessive-compulsive disorder. His recent work on TMS for the treatment of ASD has focused on the noninvasive therapy’s ability to favorably affect the excitatory/inhibitory imbalance that characterizes ASD. This imbalance is tied chiefly to abnormal glutamatergic and gamma-aminobutyric acid–ergic neurotransmission in the neocortex, cerebellum, hippocampus, and amygdala. The imbalance is thought to be responsible for the cognitive, sensory, learning, memory, and motor deficits, as well as increased propensity for seizures, associated with ASD.
This excitatory/inhibitory imbalance is marked by increased cortical excitability and decreased inhibition within the densely packed cortical minicolumns of neurons, which are organized into pathways and circuits.
“You can use TMS as a treatment, or you can use it as a research probe to look at these mechanisms by turning on or off pathways,” the psychiatrist explained. “These densely packed minicolumns are like wires with poor insulation, which results in impairment in the ability to distinguish a stimulus from background noise. In the pathologic condition, you’re getting a rapid firing which doesn’t really differentiate what’s a true signal from what’s background noise.”
Therapeutically, TMS can be employed to improve that signal-to-noise ratio, either by reducing excitation or increasing inhibition. Potential TMS targets in autism include the anterior cingulate cortex, the supplementary or presupplementary motor area, the dorsal medial prefrontal cortex, the dorsal lateral prefrontal cortex, and the cerebellum. More than a dozen published TMS studies – albeit open-label, uncontrolled, and featuring only handfuls of patients – have demonstrated long-lasting improvements in the two core symptom domains of ASD: reduced repetitive behaviors and improved social relatedness and interpersonal functioning, Dr. Hollander said.
A wide range of associated noncore symptoms, including disruptive behaviors such as self-injury or aggression, impulse control, social anxiety, and depression, also might be targeted.
“In our clinical practice, we tend to treat adults with ASD who have a lot of OCD [obsessive-compulsive disorder] and repetitive behavior symptoms but also mood or anxiety symptoms or PTSD [posttraumatic stress disorder] symptoms as a result of earlier bullying. You can adapt your treatment to the target symptoms, so if there’s a lot of OCD-type symptoms, you might use low-frequency TMS at 1 Hz to target the supplementary motor area. If people are coming in with depressive symptoms, you can use the dorsolateral prefrontal cortex depression target. If they have a lot of anxiety, you can target the right frontal anxiety loop with low-frequency TMS. Or with a lot of PTSD symptoms, you can use high-frequency stimulation of the dorsolateral prefrontal cortex at 20 Hz,” Dr. Hollander said.
An important caveat, however, is that ASD is associated with an increased risk of seizures and other EEG abnormalities, so low-frequency TMS generally is preferable because of its greater safety.
Another challenge is administering TMS in children.
“Kids move around a lot, so you’re probably going to be using briefer stimulation parameters like theta burst stimulation rather than longer treatment parameters,” Dr. Hollander said.
That being said, there are more than two dozen published studies of TMS for treatment of children and adolescents, and surveys indicate that these patients generally find it quite tolerable. Dr. Hollander noted that in one study, children and adolescents ranked it somewhere between watching television and a long car ride. This placed TMS on the midrange of a tolerability scale: not as good as having a birthday party or playing a game, but better than going to the dentist, throwing up, or, in last place, getting a shot. Of the 39 youngsters, 34 indicated that they would recommend TMS to a friend.
Dr. Hollander reported receiving research funding from the National Institute of Mental Health, the National Institute on Drug Abuse, and the National Institute of Neurological Disorders and Stroke. He serves as a consultant to roughly half a dozen pharmaceutical companies.
EXPERT ANALYSIS FROM THE ANXIETY AND DEPRESSION CONFERENCE 2017
Tweaking CBT to boost outcomes in GAD
SAN FRANCISCO – The search is on for ways to refine cognitive-behavioral therapy for generalized anxiety disorder in order to improve upon current relatively modest success rates.
Cognitive-behavioral therapy (CBT) is less effective for generalized anxiety disorder (GAD) than for the other anxiety disorders. Only about one-half of patients are improved post-treatment, and less than one-third reach recovery, noted Richard E. Zinbarg, PhD, at the annual conference of the Anxiety and Depression Association of America.
At a session on advances in treatment of GAD, investigators presented randomized clinical trials assessing a variety of specific strategies aimed at enhancing the effectiveness of CBT in evidence-based fashion. The trials included a study of the impact of having patients keep a worry outcome journal, an exploration of the potential deleterious effects of a phenomenon known as relaxation-induced anxiety, and a study of the effectiveness of emotion regulation therapy, a relatively recent form of psychotherapy that’s part of the so-called “third wave” of CBT.
Worry outcome journal
Lucas LaFreniere observed that while CBT has been broadly shown to be effective for GAD, the various forms of CBT are packages of components that often include psychoeducation, stimulus control, behavioral experiments, exposure, cognitive reframing, relaxation training, and other elements in various combinations and sequences. Almost none of these specific components has been evaluated formally to learn whether they are pulling their weight therapeutically and making a positive contribution to outcomes.
Mr. LaFreniere, a doctoral student in clinical psychology at Pennsylvania State University in Hershey, presented a randomized trial of one such component, worry outcome monitoring, which currently is incorporated in some but not all CBT programs for GAD. Mr. LaFreniere and his coinvestigators developed a version of worry outcome monitoring they dubbed the worry outcome journal, or WOJ, which he characterized as “a brief ecological momentary intervention for worry.”
The WOJ works like this: At four random times per day, WOJ users receive a phone message to drop what they’re doing and record on a chart what they’re currently worrying about. They briefly note the date and time, the content of their worry, the distress it’s causing on a 1-7 scale, how much time they’re spending thinking about it, and their prediction as to the likelihood that this negative event actually will come to pass, which by the nature of their illness generally is unrealistically sky high early on in treatment. Later, they return to record whether the worrisome outcome occurred. The WOJ data are often reviewed in session.
The hypothesis was that the WOJ would reduce worry by aiding GAD patients in attending to their worries more thoroughly and objectively, recognizing in the moment the high cost of their worrying in terms of distress and cognitive interference, forming more realistic predictions about the future, and changing their conviction that excessive worrying is a worthwhile use of their time.
“One thing that particularly motivates me as a treatment researcher is the idea that those with GAD could be making themselves chronically miserable in an effort to protect themselves from future catastrophes that likely are not even going to happen. That’s a lot of human suffering that isn’t necessary. What we can do to help with that, we should do,” Mr. LaFreniere said.
On the other hand, this was a matter that cried out for a controlled trial because of the possibility that attempts to reduce worry might have unintended harmful consequences.
“Those with GAD have positive beliefs about worry. They believe it’s useful: it motivates, buffers emotional shifts, facilitates problem solving, and marks you as caring and conscientious – good personality traits,” he explained.
His study included 51 GAD patients randomized to 10 days using the WOJ or to a thought log control condition in which prompted by their cell phone four times daily, they recorded whatever everyday thought was on their mind at the moment. An example drawn from personal experience, Mr. LaFreniere said, might be “I love enchiladas!”
Outcome measures evaluated at baseline, again at 10 days upon conclusion of the intervention, and finally at 30 days of follow-up were the Penn State Worry Questionnaire, the GAD Questionnaire for DSM-IV, and the Meta-Cognitions Questionnaire subscales for positive beliefs about worry, uncontrollability of one’s thoughts, and negative beliefs about worry.
“The big reveal was that 91% of their worries did not come true,” he reported.
The primary outcome was reduction in worries as measured by the Penn State Questionnaire. The WOJ group showed a significant reduction, compared with controls, immediately post-treatment – which remained significant, albeit attenuated to a moderate effect size, at 30 days.
At day 10, 18 of 29 WOJ users no longer met diagnostic criteria for GAD, compared with 6 of 22 controls. By day 30, however, there was no significant between-group difference on this secondary endpoint.
The WOJ group showed a significantly greater reduction than controls on the secondary endpoint of uncontrollability of beliefs at both days 10 and 30.
“The WOJ may be a viable ecological momentary intervention for reducing worry in GAD. Therapist-free use of WOJ led to decreased worrying after only 10 days. It’s quite possible that longer practice may yield even stronger results. After all, for a normal CBT protocol, we’re looking at 8-20 weeks of treatment,” Mr. LaFreniere observed.
“I’d like to underscore that there was no harm done: The WOJ didn’t increase detrimental beliefs about worry,” he added. “We had a worry ourselves as researchers – disconfirmed by the trial – that patients may take the non-occurrence of their worries as some kind of proof that worry prevented those bad things from happening.”
Mr. LaFreniere is interested in studying the WOJ for worry reduction in non-GAD populations.
“Worry can be very high in other anxiety disorders, major depressive disorder, bipolar disorders, and in insomnia. The WOJ is highly cost-effective and easy to disseminate. It could very easily be made into a smartphone app,” he said.
Relaxation-induced anxiety
Relaxation training often is incorporated in treatment packages for GAD. Yet, it’s possible that one reason CBT is only modestly effective for GAD is because of relaxation-induced anxiety (RIA), an understudied phenomenon defined as a paradoxical increase in the physiological, behavioral, and cognitive aspects of anxiety when a person tries to relax.
“It has been theorized that individuals who are especially concerned with maintaining control over physical and psychological processes find relaxation vulnerable, unpleasant, and activating. Thus, discomfort with perceived lack of control during relaxed moments – an inability to let go – may result in unsought increase in anxiety during therapeutic attempts at relaxation,” according to Michelle G. Newman, PhD, professor of psychology at Penn State.
She presented a secondary analysis of a published randomized clinical trial she coauthored (J Consult Clin Psychol. 2002 Apr;70[2]:288-98) in which 41 participants with GAD were assigned to CBT with relaxation therapy using standard progressive muscle relaxation techniques or to self-control desensitization. Relaxation therapy and relaxation-induced anxiety ratings were recorded at each session. Outcomes were assessed post-treatment and at 6, 12, and 24 months of follow-up using the Penn State Worry Questionnaire, the State-Trait Anxiety Inventory, the Hamilton Anxiety Rating Scale, and the Clinician Severity Rating for GAD symptoms. In addition, immediately after each in-session relaxation practice, patients were asked to rate on a 9-point scale how much they noticed an increase in anxiety during the relaxation session.
All subjects improved significantly, but those with a lower peak RIA – defined as the highest level of RIA experienced in any of the 14 treatment sessions – had significantly fewer GAD symptoms at the end of therapy as well as at 2-year follow-up. Peak RIA was unrelated to baseline GAD symptom severity or change over time in anxiety symptoms. However, patients whose peak RIA occurred during the last several treatment sessions showed less improvement in GAD symptoms at the conclusion of treatment than those whose peak came earlier.
The clinical implications of these findings are that therapists who use progressive muscle relaxation in the treatment of GAD should assess RIA at the conclusion of every session, and if a patient reports moderate or higher RIA, the duration of the relaxation training portion of therapy should not be shortened until after several consecutive sessions of lower RIA have been reported, according to Dr. Newman.
Emotion regulation therapy
Megan E. Renna brought attendees up to speed on emotion regulation therapy (ERT), a third wave variant of CBT that incorporates principles from more traditional CBT, such as skills training and exposure, supplemented by teaching emotion regulation skills. Those skills include the development of present moment awareness and cultivation of compassion. Both are grounded in research on motivational and regulatory learning mechanisms related to threat vs. safety and reward versus loss.
As detailed in a recent review article for which she was first author (Front Psychol. 2017 Feb 6;8:98), ERT is a manualized, mechanism-targeted treatment for what she termed “distress disorders”; namely, GAD and major depressive disorder, which are highly comorbid, share key underlying temperamental features, and for whom adequate therapeutic success is all too often elusive. ERT appears to be particularly useful during the emerging adulthood years and across a broad range of ethnic and racial patients, according to Ms. Renna, a PhD student in clinical psychology at Hunter College in New York.
The efficacy of the original 20-session, individual therapy version of ERT was established in a study of 20 GAD patients, half of whom also had major depression (Depress Anxiety. 2015 Aug;32[8]:614-23). But Ms. Renna said ERT’s developers – Douglas S. Mennin, PhD, of Hunter College, and David M. Fresco, PhD, of Kent State (Ohio) University, are interested in determining the minimum effective therapeutic dose of ERT. They have conducted an open randomized trial of a 16-session version of ERT in which the results proved similar to those seen with 20 sessions. Now they’re carrying out a study of 8 vs. 16 sessions. The study is ongoing, but at first look, the results with 8 sessions of ERT appear similar to 16, Ms. Renna said.
None of the speakers reported having any financial conflicts of interest.
SAN FRANCISCO – The search is on for ways to refine cognitive-behavioral therapy for generalized anxiety disorder in order to improve upon current relatively modest success rates.
Cognitive-behavioral therapy (CBT) is less effective for generalized anxiety disorder (GAD) than for the other anxiety disorders. Only about one-half of patients are improved post-treatment, and less than one-third reach recovery, noted Richard E. Zinbarg, PhD, at the annual conference of the Anxiety and Depression Association of America.
At a session on advances in treatment of GAD, investigators presented randomized clinical trials assessing a variety of specific strategies aimed at enhancing the effectiveness of CBT in evidence-based fashion. The trials included a study of the impact of having patients keep a worry outcome journal, an exploration of the potential deleterious effects of a phenomenon known as relaxation-induced anxiety, and a study of the effectiveness of emotion regulation therapy, a relatively recent form of psychotherapy that’s part of the so-called “third wave” of CBT.
Worry outcome journal
Lucas LaFreniere observed that while CBT has been broadly shown to be effective for GAD, the various forms of CBT are packages of components that often include psychoeducation, stimulus control, behavioral experiments, exposure, cognitive reframing, relaxation training, and other elements in various combinations and sequences. Almost none of these specific components has been evaluated formally to learn whether they are pulling their weight therapeutically and making a positive contribution to outcomes.
Mr. LaFreniere, a doctoral student in clinical psychology at Pennsylvania State University in Hershey, presented a randomized trial of one such component, worry outcome monitoring, which currently is incorporated in some but not all CBT programs for GAD. Mr. LaFreniere and his coinvestigators developed a version of worry outcome monitoring they dubbed the worry outcome journal, or WOJ, which he characterized as “a brief ecological momentary intervention for worry.”
The WOJ works like this: At four random times per day, WOJ users receive a phone message to drop what they’re doing and record on a chart what they’re currently worrying about. They briefly note the date and time, the content of their worry, the distress it’s causing on a 1-7 scale, how much time they’re spending thinking about it, and their prediction as to the likelihood that this negative event actually will come to pass, which by the nature of their illness generally is unrealistically sky high early on in treatment. Later, they return to record whether the worrisome outcome occurred. The WOJ data are often reviewed in session.
The hypothesis was that the WOJ would reduce worry by aiding GAD patients in attending to their worries more thoroughly and objectively, recognizing in the moment the high cost of their worrying in terms of distress and cognitive interference, forming more realistic predictions about the future, and changing their conviction that excessive worrying is a worthwhile use of their time.
“One thing that particularly motivates me as a treatment researcher is the idea that those with GAD could be making themselves chronically miserable in an effort to protect themselves from future catastrophes that likely are not even going to happen. That’s a lot of human suffering that isn’t necessary. What we can do to help with that, we should do,” Mr. LaFreniere said.
On the other hand, this was a matter that cried out for a controlled trial because of the possibility that attempts to reduce worry might have unintended harmful consequences.
“Those with GAD have positive beliefs about worry. They believe it’s useful: it motivates, buffers emotional shifts, facilitates problem solving, and marks you as caring and conscientious – good personality traits,” he explained.
His study included 51 GAD patients randomized to 10 days using the WOJ or to a thought log control condition in which prompted by their cell phone four times daily, they recorded whatever everyday thought was on their mind at the moment. An example drawn from personal experience, Mr. LaFreniere said, might be “I love enchiladas!”
Outcome measures evaluated at baseline, again at 10 days upon conclusion of the intervention, and finally at 30 days of follow-up were the Penn State Worry Questionnaire, the GAD Questionnaire for DSM-IV, and the Meta-Cognitions Questionnaire subscales for positive beliefs about worry, uncontrollability of one’s thoughts, and negative beliefs about worry.
“The big reveal was that 91% of their worries did not come true,” he reported.
The primary outcome was reduction in worries as measured by the Penn State Questionnaire. The WOJ group showed a significant reduction, compared with controls, immediately post-treatment – which remained significant, albeit attenuated to a moderate effect size, at 30 days.
At day 10, 18 of 29 WOJ users no longer met diagnostic criteria for GAD, compared with 6 of 22 controls. By day 30, however, there was no significant between-group difference on this secondary endpoint.
The WOJ group showed a significantly greater reduction than controls on the secondary endpoint of uncontrollability of beliefs at both days 10 and 30.
“The WOJ may be a viable ecological momentary intervention for reducing worry in GAD. Therapist-free use of WOJ led to decreased worrying after only 10 days. It’s quite possible that longer practice may yield even stronger results. After all, for a normal CBT protocol, we’re looking at 8-20 weeks of treatment,” Mr. LaFreniere observed.
“I’d like to underscore that there was no harm done: The WOJ didn’t increase detrimental beliefs about worry,” he added. “We had a worry ourselves as researchers – disconfirmed by the trial – that patients may take the non-occurrence of their worries as some kind of proof that worry prevented those bad things from happening.”
Mr. LaFreniere is interested in studying the WOJ for worry reduction in non-GAD populations.
“Worry can be very high in other anxiety disorders, major depressive disorder, bipolar disorders, and in insomnia. The WOJ is highly cost-effective and easy to disseminate. It could very easily be made into a smartphone app,” he said.
Relaxation-induced anxiety
Relaxation training often is incorporated in treatment packages for GAD. Yet, it’s possible that one reason CBT is only modestly effective for GAD is because of relaxation-induced anxiety (RIA), an understudied phenomenon defined as a paradoxical increase in the physiological, behavioral, and cognitive aspects of anxiety when a person tries to relax.
“It has been theorized that individuals who are especially concerned with maintaining control over physical and psychological processes find relaxation vulnerable, unpleasant, and activating. Thus, discomfort with perceived lack of control during relaxed moments – an inability to let go – may result in unsought increase in anxiety during therapeutic attempts at relaxation,” according to Michelle G. Newman, PhD, professor of psychology at Penn State.
She presented a secondary analysis of a published randomized clinical trial she coauthored (J Consult Clin Psychol. 2002 Apr;70[2]:288-98) in which 41 participants with GAD were assigned to CBT with relaxation therapy using standard progressive muscle relaxation techniques or to self-control desensitization. Relaxation therapy and relaxation-induced anxiety ratings were recorded at each session. Outcomes were assessed post-treatment and at 6, 12, and 24 months of follow-up using the Penn State Worry Questionnaire, the State-Trait Anxiety Inventory, the Hamilton Anxiety Rating Scale, and the Clinician Severity Rating for GAD symptoms. In addition, immediately after each in-session relaxation practice, patients were asked to rate on a 9-point scale how much they noticed an increase in anxiety during the relaxation session.
All subjects improved significantly, but those with a lower peak RIA – defined as the highest level of RIA experienced in any of the 14 treatment sessions – had significantly fewer GAD symptoms at the end of therapy as well as at 2-year follow-up. Peak RIA was unrelated to baseline GAD symptom severity or change over time in anxiety symptoms. However, patients whose peak RIA occurred during the last several treatment sessions showed less improvement in GAD symptoms at the conclusion of treatment than those whose peak came earlier.
The clinical implications of these findings are that therapists who use progressive muscle relaxation in the treatment of GAD should assess RIA at the conclusion of every session, and if a patient reports moderate or higher RIA, the duration of the relaxation training portion of therapy should not be shortened until after several consecutive sessions of lower RIA have been reported, according to Dr. Newman.
Emotion regulation therapy
Megan E. Renna brought attendees up to speed on emotion regulation therapy (ERT), a third wave variant of CBT that incorporates principles from more traditional CBT, such as skills training and exposure, supplemented by teaching emotion regulation skills. Those skills include the development of present moment awareness and cultivation of compassion. Both are grounded in research on motivational and regulatory learning mechanisms related to threat vs. safety and reward versus loss.
As detailed in a recent review article for which she was first author (Front Psychol. 2017 Feb 6;8:98), ERT is a manualized, mechanism-targeted treatment for what she termed “distress disorders”; namely, GAD and major depressive disorder, which are highly comorbid, share key underlying temperamental features, and for whom adequate therapeutic success is all too often elusive. ERT appears to be particularly useful during the emerging adulthood years and across a broad range of ethnic and racial patients, according to Ms. Renna, a PhD student in clinical psychology at Hunter College in New York.
The efficacy of the original 20-session, individual therapy version of ERT was established in a study of 20 GAD patients, half of whom also had major depression (Depress Anxiety. 2015 Aug;32[8]:614-23). But Ms. Renna said ERT’s developers – Douglas S. Mennin, PhD, of Hunter College, and David M. Fresco, PhD, of Kent State (Ohio) University, are interested in determining the minimum effective therapeutic dose of ERT. They have conducted an open randomized trial of a 16-session version of ERT in which the results proved similar to those seen with 20 sessions. Now they’re carrying out a study of 8 vs. 16 sessions. The study is ongoing, but at first look, the results with 8 sessions of ERT appear similar to 16, Ms. Renna said.
None of the speakers reported having any financial conflicts of interest.
SAN FRANCISCO – The search is on for ways to refine cognitive-behavioral therapy for generalized anxiety disorder in order to improve upon current relatively modest success rates.
Cognitive-behavioral therapy (CBT) is less effective for generalized anxiety disorder (GAD) than for the other anxiety disorders. Only about one-half of patients are improved post-treatment, and less than one-third reach recovery, noted Richard E. Zinbarg, PhD, at the annual conference of the Anxiety and Depression Association of America.
At a session on advances in treatment of GAD, investigators presented randomized clinical trials assessing a variety of specific strategies aimed at enhancing the effectiveness of CBT in evidence-based fashion. The trials included a study of the impact of having patients keep a worry outcome journal, an exploration of the potential deleterious effects of a phenomenon known as relaxation-induced anxiety, and a study of the effectiveness of emotion regulation therapy, a relatively recent form of psychotherapy that’s part of the so-called “third wave” of CBT.
Worry outcome journal
Lucas LaFreniere observed that while CBT has been broadly shown to be effective for GAD, the various forms of CBT are packages of components that often include psychoeducation, stimulus control, behavioral experiments, exposure, cognitive reframing, relaxation training, and other elements in various combinations and sequences. Almost none of these specific components has been evaluated formally to learn whether they are pulling their weight therapeutically and making a positive contribution to outcomes.
Mr. LaFreniere, a doctoral student in clinical psychology at Pennsylvania State University in Hershey, presented a randomized trial of one such component, worry outcome monitoring, which currently is incorporated in some but not all CBT programs for GAD. Mr. LaFreniere and his coinvestigators developed a version of worry outcome monitoring they dubbed the worry outcome journal, or WOJ, which he characterized as “a brief ecological momentary intervention for worry.”
The WOJ works like this: At four random times per day, WOJ users receive a phone message to drop what they’re doing and record on a chart what they’re currently worrying about. They briefly note the date and time, the content of their worry, the distress it’s causing on a 1-7 scale, how much time they’re spending thinking about it, and their prediction as to the likelihood that this negative event actually will come to pass, which by the nature of their illness generally is unrealistically sky high early on in treatment. Later, they return to record whether the worrisome outcome occurred. The WOJ data are often reviewed in session.
The hypothesis was that the WOJ would reduce worry by aiding GAD patients in attending to their worries more thoroughly and objectively, recognizing in the moment the high cost of their worrying in terms of distress and cognitive interference, forming more realistic predictions about the future, and changing their conviction that excessive worrying is a worthwhile use of their time.
“One thing that particularly motivates me as a treatment researcher is the idea that those with GAD could be making themselves chronically miserable in an effort to protect themselves from future catastrophes that likely are not even going to happen. That’s a lot of human suffering that isn’t necessary. What we can do to help with that, we should do,” Mr. LaFreniere said.
On the other hand, this was a matter that cried out for a controlled trial because of the possibility that attempts to reduce worry might have unintended harmful consequences.
“Those with GAD have positive beliefs about worry. They believe it’s useful: it motivates, buffers emotional shifts, facilitates problem solving, and marks you as caring and conscientious – good personality traits,” he explained.
His study included 51 GAD patients randomized to 10 days using the WOJ or to a thought log control condition in which prompted by their cell phone four times daily, they recorded whatever everyday thought was on their mind at the moment. An example drawn from personal experience, Mr. LaFreniere said, might be “I love enchiladas!”
Outcome measures evaluated at baseline, again at 10 days upon conclusion of the intervention, and finally at 30 days of follow-up were the Penn State Worry Questionnaire, the GAD Questionnaire for DSM-IV, and the Meta-Cognitions Questionnaire subscales for positive beliefs about worry, uncontrollability of one’s thoughts, and negative beliefs about worry.
“The big reveal was that 91% of their worries did not come true,” he reported.
The primary outcome was reduction in worries as measured by the Penn State Questionnaire. The WOJ group showed a significant reduction, compared with controls, immediately post-treatment – which remained significant, albeit attenuated to a moderate effect size, at 30 days.
At day 10, 18 of 29 WOJ users no longer met diagnostic criteria for GAD, compared with 6 of 22 controls. By day 30, however, there was no significant between-group difference on this secondary endpoint.
The WOJ group showed a significantly greater reduction than controls on the secondary endpoint of uncontrollability of beliefs at both days 10 and 30.
“The WOJ may be a viable ecological momentary intervention for reducing worry in GAD. Therapist-free use of WOJ led to decreased worrying after only 10 days. It’s quite possible that longer practice may yield even stronger results. After all, for a normal CBT protocol, we’re looking at 8-20 weeks of treatment,” Mr. LaFreniere observed.
“I’d like to underscore that there was no harm done: The WOJ didn’t increase detrimental beliefs about worry,” he added. “We had a worry ourselves as researchers – disconfirmed by the trial – that patients may take the non-occurrence of their worries as some kind of proof that worry prevented those bad things from happening.”
Mr. LaFreniere is interested in studying the WOJ for worry reduction in non-GAD populations.
“Worry can be very high in other anxiety disorders, major depressive disorder, bipolar disorders, and in insomnia. The WOJ is highly cost-effective and easy to disseminate. It could very easily be made into a smartphone app,” he said.
Relaxation-induced anxiety
Relaxation training often is incorporated in treatment packages for GAD. Yet, it’s possible that one reason CBT is only modestly effective for GAD is because of relaxation-induced anxiety (RIA), an understudied phenomenon defined as a paradoxical increase in the physiological, behavioral, and cognitive aspects of anxiety when a person tries to relax.
“It has been theorized that individuals who are especially concerned with maintaining control over physical and psychological processes find relaxation vulnerable, unpleasant, and activating. Thus, discomfort with perceived lack of control during relaxed moments – an inability to let go – may result in unsought increase in anxiety during therapeutic attempts at relaxation,” according to Michelle G. Newman, PhD, professor of psychology at Penn State.
She presented a secondary analysis of a published randomized clinical trial she coauthored (J Consult Clin Psychol. 2002 Apr;70[2]:288-98) in which 41 participants with GAD were assigned to CBT with relaxation therapy using standard progressive muscle relaxation techniques or to self-control desensitization. Relaxation therapy and relaxation-induced anxiety ratings were recorded at each session. Outcomes were assessed post-treatment and at 6, 12, and 24 months of follow-up using the Penn State Worry Questionnaire, the State-Trait Anxiety Inventory, the Hamilton Anxiety Rating Scale, and the Clinician Severity Rating for GAD symptoms. In addition, immediately after each in-session relaxation practice, patients were asked to rate on a 9-point scale how much they noticed an increase in anxiety during the relaxation session.
All subjects improved significantly, but those with a lower peak RIA – defined as the highest level of RIA experienced in any of the 14 treatment sessions – had significantly fewer GAD symptoms at the end of therapy as well as at 2-year follow-up. Peak RIA was unrelated to baseline GAD symptom severity or change over time in anxiety symptoms. However, patients whose peak RIA occurred during the last several treatment sessions showed less improvement in GAD symptoms at the conclusion of treatment than those whose peak came earlier.
The clinical implications of these findings are that therapists who use progressive muscle relaxation in the treatment of GAD should assess RIA at the conclusion of every session, and if a patient reports moderate or higher RIA, the duration of the relaxation training portion of therapy should not be shortened until after several consecutive sessions of lower RIA have been reported, according to Dr. Newman.
Emotion regulation therapy
Megan E. Renna brought attendees up to speed on emotion regulation therapy (ERT), a third wave variant of CBT that incorporates principles from more traditional CBT, such as skills training and exposure, supplemented by teaching emotion regulation skills. Those skills include the development of present moment awareness and cultivation of compassion. Both are grounded in research on motivational and regulatory learning mechanisms related to threat vs. safety and reward versus loss.
As detailed in a recent review article for which she was first author (Front Psychol. 2017 Feb 6;8:98), ERT is a manualized, mechanism-targeted treatment for what she termed “distress disorders”; namely, GAD and major depressive disorder, which are highly comorbid, share key underlying temperamental features, and for whom adequate therapeutic success is all too often elusive. ERT appears to be particularly useful during the emerging adulthood years and across a broad range of ethnic and racial patients, according to Ms. Renna, a PhD student in clinical psychology at Hunter College in New York.
The efficacy of the original 20-session, individual therapy version of ERT was established in a study of 20 GAD patients, half of whom also had major depression (Depress Anxiety. 2015 Aug;32[8]:614-23). But Ms. Renna said ERT’s developers – Douglas S. Mennin, PhD, of Hunter College, and David M. Fresco, PhD, of Kent State (Ohio) University, are interested in determining the minimum effective therapeutic dose of ERT. They have conducted an open randomized trial of a 16-session version of ERT in which the results proved similar to those seen with 20 sessions. Now they’re carrying out a study of 8 vs. 16 sessions. The study is ongoing, but at first look, the results with 8 sessions of ERT appear similar to 16, Ms. Renna said.
None of the speakers reported having any financial conflicts of interest.
EXPERT ANALYSIS FROM THE ANXIETY AND DEPRESSION CONFERENCE 2017
Transcranial magnetic stimulation shows more promise in refractory OCD
SAN FRANCISCO – Mounting evidence suggests that transcranial magnetic stimulation is an effective noninvasive therapy for obsessive-compulsive disorder refractory to first-line medications, Eric Hollander, MD, said at the annual conference of the Anxiety and Depression Association of America.
A novel treatment for obsessive-compulsive disorder (OCD) would be most welcome. This is a disorder that’s common – affecting 2%-3% of the population – debilitating, and notoriously tough to treat. Roughly half of patients with OCD don’t respond to first-line therapy, which is selective serotonin reuptake inhibitors, cognitive-behavioral therapy, or both, according to Dr. Hollander, director of the autism and obsessive-compulsive spectrum program as well as the anxiety and depression program at Albert Einstein College of Medicine in New York.
Four companies now have FDA-cleared TMS devices indicated for treatment of major depression: Brainsway, which markets a dTMS device, and Neuronetics, MagVenture, and Magstim, which sell repetitive TMS (rTMS) devices that do not penetrate as deeply beneath the skull as dTMS and therefore target different brain structures.
TMS for OCD is, at present, off-label therapy. Yet, there is now sufficient experience derived from formal clinical trials and off-label use in clinical practice to be able to state that the standard target area for rTMS is the supplementary motor area (SMA), according to Dr. Hollander.
He was senior author of a randomized open-label pilot study involving 50 consecutive OCD patients refractory to SSRIs. Half were assigned to a popular second-line strategy: augmentation with antipsychotic agents. The other half received five 20-minute-long rTMS sessions per week for 3 weeks using low-frequency 1 Hz bilateral stimulation of the SMA.
At 3 weeks, the treatment response rate as defined by at least a 25% reduction from baseline on the Yale-Brown Obsessive-Compulsive Scale (YBOCS) was 68% in the rTMS group, compared with 24% in the control arm. Thus, rTMS was better than treatment as usual (J Psychopharmacol. 2016 Jun;30[6]:568-78).
“That’s considerable improvement after only 3 weeks of stimulation, which is a very short time, compared to other OCD treatments,” the psychiatrist noted.
In another study, Dr. Hollander and his coinvestigators used the same rTMS regimen targeting the SMA in 22 SSRI-refractory OCD patients. After 3 weeks of rTMS, 12 of the 22 were treatment responders and 3 patients were in remission.
Moreover, these effects were long-lasting. At 6 months, 13 patients were responders and 4 were in remission, and, at 12 months – nearly a year after their relatively brief course of rTMS – there were 12 responders and 3 remitters.
Participants also showed significant reductions on both the Hamilton Depression Rating Scale (HAM-D) and the Hamilton Anxiety Rating Scale (HAM-A), effects that were sustained during follow-up, although the improvement in OCD symptoms was more impressive, he said.
Other investigators also have reported positive results using rTMS for OCD, with the first publication coming from Italian investigators more than a decade ago (Int J Neuropsychopharmacol. 2006 Feb;9[1]:95-100).
Studies of dTMS for OCD are a more recent development. In 2016, investigators reported on 40 OCD patients treated double-blind with either high-stimulation dTMS at 20 Hz, low-stimulation at 1 Hz, or a sham magnetic coil daily for 5 weeks. The target areas were the medial prefrontal and anterior cingulate cortices, areas too deep to be reached using rTMS. At the 5-week mark, the patients who received high-stimulation dTMS showed a mean 26% improvement in YBOCS scores, compared with a 6% reduction in the low-stimulation and sham-treatment arms.
In this study, electroencephalogram evoked potential responses over the anterior cingulate cortex correlated with clinical response, thus providing a welcome biomarker of treatment efficacy.
How TMS works in OCD
TMS involves placing a coil on the scalp to create a magnetic pulse that passes through the skull and achieves predictable changes in neuronal activity in brain tissue, either exciting or deactivating target regions depending upon whether high- or low-frequency TMS is applied.
Brain imaging studies show that OCD is characterized by hyperactivation of the medial frontal cortex and the SMA. The dysfunctional circuitry of OCD has been worked out. It’s striatally based, involving frontal-striatal-thalamic circuits. The SMA sits right above the anterior cingulate cortex and provides access to these key pathways. Basically, increased neuronal activity in the frontal lobes of OCD patients results in miscommunication with the striatal and thalamic regions, with resultant thalamic hyperactivity. This failure of cortical inhibition leads to persistent intrusive thoughts and behaviors, Dr. Hollander explained.
The neural circuitry of OCD is distinct from that of other anxiety disorders, and it appears that TMS is not as effective in those disorders as in OCD, he added.
The anterior cingulate is one step closer than the SMA to the frontal-striatal-thalamic circuits, which are of particular therapeutic interest in OCD, and it’s accessible by dTMS. Anterior cingulate activity is decreased in OCD. When high-frequency dTMS revs up that activity, the result is symptomatic improvement. Of note, the anterior cingulate also is the target for cingulotomy, an established surgical treatment for OCD.
Dr. Hollander reported receiving research funding from the National Institute of Mental Health, the National Institute on Drug Abuse, and the National Institute of Neurological Disorders and Stroke. He serves as a consultant to a number of pharmaceutical companies.
SAN FRANCISCO – Mounting evidence suggests that transcranial magnetic stimulation is an effective noninvasive therapy for obsessive-compulsive disorder refractory to first-line medications, Eric Hollander, MD, said at the annual conference of the Anxiety and Depression Association of America.
A novel treatment for obsessive-compulsive disorder (OCD) would be most welcome. This is a disorder that’s common – affecting 2%-3% of the population – debilitating, and notoriously tough to treat. Roughly half of patients with OCD don’t respond to first-line therapy, which is selective serotonin reuptake inhibitors, cognitive-behavioral therapy, or both, according to Dr. Hollander, director of the autism and obsessive-compulsive spectrum program as well as the anxiety and depression program at Albert Einstein College of Medicine in New York.
Four companies now have FDA-cleared TMS devices indicated for treatment of major depression: Brainsway, which markets a dTMS device, and Neuronetics, MagVenture, and Magstim, which sell repetitive TMS (rTMS) devices that do not penetrate as deeply beneath the skull as dTMS and therefore target different brain structures.
TMS for OCD is, at present, off-label therapy. Yet, there is now sufficient experience derived from formal clinical trials and off-label use in clinical practice to be able to state that the standard target area for rTMS is the supplementary motor area (SMA), according to Dr. Hollander.
He was senior author of a randomized open-label pilot study involving 50 consecutive OCD patients refractory to SSRIs. Half were assigned to a popular second-line strategy: augmentation with antipsychotic agents. The other half received five 20-minute-long rTMS sessions per week for 3 weeks using low-frequency 1 Hz bilateral stimulation of the SMA.
At 3 weeks, the treatment response rate as defined by at least a 25% reduction from baseline on the Yale-Brown Obsessive-Compulsive Scale (YBOCS) was 68% in the rTMS group, compared with 24% in the control arm. Thus, rTMS was better than treatment as usual (J Psychopharmacol. 2016 Jun;30[6]:568-78).
“That’s considerable improvement after only 3 weeks of stimulation, which is a very short time, compared to other OCD treatments,” the psychiatrist noted.
In another study, Dr. Hollander and his coinvestigators used the same rTMS regimen targeting the SMA in 22 SSRI-refractory OCD patients. After 3 weeks of rTMS, 12 of the 22 were treatment responders and 3 patients were in remission.
Moreover, these effects were long-lasting. At 6 months, 13 patients were responders and 4 were in remission, and, at 12 months – nearly a year after their relatively brief course of rTMS – there were 12 responders and 3 remitters.
Participants also showed significant reductions on both the Hamilton Depression Rating Scale (HAM-D) and the Hamilton Anxiety Rating Scale (HAM-A), effects that were sustained during follow-up, although the improvement in OCD symptoms was more impressive, he said.
Other investigators also have reported positive results using rTMS for OCD, with the first publication coming from Italian investigators more than a decade ago (Int J Neuropsychopharmacol. 2006 Feb;9[1]:95-100).
Studies of dTMS for OCD are a more recent development. In 2016, investigators reported on 40 OCD patients treated double-blind with either high-stimulation dTMS at 20 Hz, low-stimulation at 1 Hz, or a sham magnetic coil daily for 5 weeks. The target areas were the medial prefrontal and anterior cingulate cortices, areas too deep to be reached using rTMS. At the 5-week mark, the patients who received high-stimulation dTMS showed a mean 26% improvement in YBOCS scores, compared with a 6% reduction in the low-stimulation and sham-treatment arms.
In this study, electroencephalogram evoked potential responses over the anterior cingulate cortex correlated with clinical response, thus providing a welcome biomarker of treatment efficacy.
How TMS works in OCD
TMS involves placing a coil on the scalp to create a magnetic pulse that passes through the skull and achieves predictable changes in neuronal activity in brain tissue, either exciting or deactivating target regions depending upon whether high- or low-frequency TMS is applied.
Brain imaging studies show that OCD is characterized by hyperactivation of the medial frontal cortex and the SMA. The dysfunctional circuitry of OCD has been worked out. It’s striatally based, involving frontal-striatal-thalamic circuits. The SMA sits right above the anterior cingulate cortex and provides access to these key pathways. Basically, increased neuronal activity in the frontal lobes of OCD patients results in miscommunication with the striatal and thalamic regions, with resultant thalamic hyperactivity. This failure of cortical inhibition leads to persistent intrusive thoughts and behaviors, Dr. Hollander explained.
The neural circuitry of OCD is distinct from that of other anxiety disorders, and it appears that TMS is not as effective in those disorders as in OCD, he added.
The anterior cingulate is one step closer than the SMA to the frontal-striatal-thalamic circuits, which are of particular therapeutic interest in OCD, and it’s accessible by dTMS. Anterior cingulate activity is decreased in OCD. When high-frequency dTMS revs up that activity, the result is symptomatic improvement. Of note, the anterior cingulate also is the target for cingulotomy, an established surgical treatment for OCD.
Dr. Hollander reported receiving research funding from the National Institute of Mental Health, the National Institute on Drug Abuse, and the National Institute of Neurological Disorders and Stroke. He serves as a consultant to a number of pharmaceutical companies.
SAN FRANCISCO – Mounting evidence suggests that transcranial magnetic stimulation is an effective noninvasive therapy for obsessive-compulsive disorder refractory to first-line medications, Eric Hollander, MD, said at the annual conference of the Anxiety and Depression Association of America.
A novel treatment for obsessive-compulsive disorder (OCD) would be most welcome. This is a disorder that’s common – affecting 2%-3% of the population – debilitating, and notoriously tough to treat. Roughly half of patients with OCD don’t respond to first-line therapy, which is selective serotonin reuptake inhibitors, cognitive-behavioral therapy, or both, according to Dr. Hollander, director of the autism and obsessive-compulsive spectrum program as well as the anxiety and depression program at Albert Einstein College of Medicine in New York.
Four companies now have FDA-cleared TMS devices indicated for treatment of major depression: Brainsway, which markets a dTMS device, and Neuronetics, MagVenture, and Magstim, which sell repetitive TMS (rTMS) devices that do not penetrate as deeply beneath the skull as dTMS and therefore target different brain structures.
TMS for OCD is, at present, off-label therapy. Yet, there is now sufficient experience derived from formal clinical trials and off-label use in clinical practice to be able to state that the standard target area for rTMS is the supplementary motor area (SMA), according to Dr. Hollander.
He was senior author of a randomized open-label pilot study involving 50 consecutive OCD patients refractory to SSRIs. Half were assigned to a popular second-line strategy: augmentation with antipsychotic agents. The other half received five 20-minute-long rTMS sessions per week for 3 weeks using low-frequency 1 Hz bilateral stimulation of the SMA.
At 3 weeks, the treatment response rate as defined by at least a 25% reduction from baseline on the Yale-Brown Obsessive-Compulsive Scale (YBOCS) was 68% in the rTMS group, compared with 24% in the control arm. Thus, rTMS was better than treatment as usual (J Psychopharmacol. 2016 Jun;30[6]:568-78).
“That’s considerable improvement after only 3 weeks of stimulation, which is a very short time, compared to other OCD treatments,” the psychiatrist noted.
In another study, Dr. Hollander and his coinvestigators used the same rTMS regimen targeting the SMA in 22 SSRI-refractory OCD patients. After 3 weeks of rTMS, 12 of the 22 were treatment responders and 3 patients were in remission.
Moreover, these effects were long-lasting. At 6 months, 13 patients were responders and 4 were in remission, and, at 12 months – nearly a year after their relatively brief course of rTMS – there were 12 responders and 3 remitters.
Participants also showed significant reductions on both the Hamilton Depression Rating Scale (HAM-D) and the Hamilton Anxiety Rating Scale (HAM-A), effects that were sustained during follow-up, although the improvement in OCD symptoms was more impressive, he said.
Other investigators also have reported positive results using rTMS for OCD, with the first publication coming from Italian investigators more than a decade ago (Int J Neuropsychopharmacol. 2006 Feb;9[1]:95-100).
Studies of dTMS for OCD are a more recent development. In 2016, investigators reported on 40 OCD patients treated double-blind with either high-stimulation dTMS at 20 Hz, low-stimulation at 1 Hz, or a sham magnetic coil daily for 5 weeks. The target areas were the medial prefrontal and anterior cingulate cortices, areas too deep to be reached using rTMS. At the 5-week mark, the patients who received high-stimulation dTMS showed a mean 26% improvement in YBOCS scores, compared with a 6% reduction in the low-stimulation and sham-treatment arms.
In this study, electroencephalogram evoked potential responses over the anterior cingulate cortex correlated with clinical response, thus providing a welcome biomarker of treatment efficacy.
How TMS works in OCD
TMS involves placing a coil on the scalp to create a magnetic pulse that passes through the skull and achieves predictable changes in neuronal activity in brain tissue, either exciting or deactivating target regions depending upon whether high- or low-frequency TMS is applied.
Brain imaging studies show that OCD is characterized by hyperactivation of the medial frontal cortex and the SMA. The dysfunctional circuitry of OCD has been worked out. It’s striatally based, involving frontal-striatal-thalamic circuits. The SMA sits right above the anterior cingulate cortex and provides access to these key pathways. Basically, increased neuronal activity in the frontal lobes of OCD patients results in miscommunication with the striatal and thalamic regions, with resultant thalamic hyperactivity. This failure of cortical inhibition leads to persistent intrusive thoughts and behaviors, Dr. Hollander explained.
The neural circuitry of OCD is distinct from that of other anxiety disorders, and it appears that TMS is not as effective in those disorders as in OCD, he added.
The anterior cingulate is one step closer than the SMA to the frontal-striatal-thalamic circuits, which are of particular therapeutic interest in OCD, and it’s accessible by dTMS. Anterior cingulate activity is decreased in OCD. When high-frequency dTMS revs up that activity, the result is symptomatic improvement. Of note, the anterior cingulate also is the target for cingulotomy, an established surgical treatment for OCD.
Dr. Hollander reported receiving research funding from the National Institute of Mental Health, the National Institute on Drug Abuse, and the National Institute of Neurological Disorders and Stroke. He serves as a consultant to a number of pharmaceutical companies.
EXPERT ANALYSIS FROM THE ANXIETY AND DEPRESSION CONFERENCE 2017
Who’s best suited for Internet-based CBT?
SAN FRANCISCO – Nearly 6% of patients deteriorated during Internet-based cognitive-behavioral therapy (iCBT) in an individual patient data meta-analysis totaling 2,866 participants in 29 published clinical trials, Alexander Rozental, PhD, reported at the annual conference of the Anxiety and Depression Association of America.
On the other hand, the meta-analysis also highlighted the hazards of doing nothing for patients experiencing mental distress: 17.4% of patients deteriorated while in wait-list control groups in the 29 trials, a rate of harm triple the 5.8% deterioration rate in patients during iCBT, added Dr. Rozental, a clinical psychologist at Stockholm University.
This meta-analysis is one of the very few studies to look at the negative effects of a psychologic treatment. Psychotherapy research has focused almost entirely on the positive effects. That’s at odds with the way pharmacologic research is conducted, in which reporting of adverse events is mandatory, he noted.
Of patients in the meta-analysis, 61% sought treatment for anxiety disorders, 20% for depression, and the rest for erectile dysfunction, pathological gambling, or relationship problems.
iCBT is particularly popular in Sweden, where it was developed two decades ago as a means of disseminating evidence-based, manualized therapy to a broad population in a highly cost-effective manner. This form of psychotherapy typically entails 8 to 12 weekly treatment modules, with weekly assignments, predetermined deadlines, texts and exercises, and regular, albeit relatively brief, contact with a therapist via secure email.
Dr. Rozental and his coinvestigators reviewed individual patient data in search of predictors of treatment success or deterioration. A profile emerged of the patients least likely to deteriorate while on iCBT: older age, university-educated, in a stable relationship, and with a higher level of symptoms pretreatment.
“You might interpret the findings as an indicator for matching the right type of treatment to the right patient. Perhaps those [who] are younger, have less than a university degree, and are not in a relationship might be better off in a face to face treatment, at least in terms of preventing deterioration,” he observed in an interview. “This makes sense if you think about the amount of work you have to do on your own in Internet-based psychological treatments, which include limited access to a therapist and require reading a lot of text material.”
Patients participating in iCBT who fit that profile might need extra support from a therapist in order to improve, Dr. Rozental added.
He reported having no financial conflicts regarding his study, which was funded by the Swedish Research Council for Health, Working Life, and Welfare.
SAN FRANCISCO – Nearly 6% of patients deteriorated during Internet-based cognitive-behavioral therapy (iCBT) in an individual patient data meta-analysis totaling 2,866 participants in 29 published clinical trials, Alexander Rozental, PhD, reported at the annual conference of the Anxiety and Depression Association of America.
On the other hand, the meta-analysis also highlighted the hazards of doing nothing for patients experiencing mental distress: 17.4% of patients deteriorated while in wait-list control groups in the 29 trials, a rate of harm triple the 5.8% deterioration rate in patients during iCBT, added Dr. Rozental, a clinical psychologist at Stockholm University.
This meta-analysis is one of the very few studies to look at the negative effects of a psychologic treatment. Psychotherapy research has focused almost entirely on the positive effects. That’s at odds with the way pharmacologic research is conducted, in which reporting of adverse events is mandatory, he noted.
Of patients in the meta-analysis, 61% sought treatment for anxiety disorders, 20% for depression, and the rest for erectile dysfunction, pathological gambling, or relationship problems.
iCBT is particularly popular in Sweden, where it was developed two decades ago as a means of disseminating evidence-based, manualized therapy to a broad population in a highly cost-effective manner. This form of psychotherapy typically entails 8 to 12 weekly treatment modules, with weekly assignments, predetermined deadlines, texts and exercises, and regular, albeit relatively brief, contact with a therapist via secure email.
Dr. Rozental and his coinvestigators reviewed individual patient data in search of predictors of treatment success or deterioration. A profile emerged of the patients least likely to deteriorate while on iCBT: older age, university-educated, in a stable relationship, and with a higher level of symptoms pretreatment.
“You might interpret the findings as an indicator for matching the right type of treatment to the right patient. Perhaps those [who] are younger, have less than a university degree, and are not in a relationship might be better off in a face to face treatment, at least in terms of preventing deterioration,” he observed in an interview. “This makes sense if you think about the amount of work you have to do on your own in Internet-based psychological treatments, which include limited access to a therapist and require reading a lot of text material.”
Patients participating in iCBT who fit that profile might need extra support from a therapist in order to improve, Dr. Rozental added.
He reported having no financial conflicts regarding his study, which was funded by the Swedish Research Council for Health, Working Life, and Welfare.
SAN FRANCISCO – Nearly 6% of patients deteriorated during Internet-based cognitive-behavioral therapy (iCBT) in an individual patient data meta-analysis totaling 2,866 participants in 29 published clinical trials, Alexander Rozental, PhD, reported at the annual conference of the Anxiety and Depression Association of America.
On the other hand, the meta-analysis also highlighted the hazards of doing nothing for patients experiencing mental distress: 17.4% of patients deteriorated while in wait-list control groups in the 29 trials, a rate of harm triple the 5.8% deterioration rate in patients during iCBT, added Dr. Rozental, a clinical psychologist at Stockholm University.
This meta-analysis is one of the very few studies to look at the negative effects of a psychologic treatment. Psychotherapy research has focused almost entirely on the positive effects. That’s at odds with the way pharmacologic research is conducted, in which reporting of adverse events is mandatory, he noted.
Of patients in the meta-analysis, 61% sought treatment for anxiety disorders, 20% for depression, and the rest for erectile dysfunction, pathological gambling, or relationship problems.
iCBT is particularly popular in Sweden, where it was developed two decades ago as a means of disseminating evidence-based, manualized therapy to a broad population in a highly cost-effective manner. This form of psychotherapy typically entails 8 to 12 weekly treatment modules, with weekly assignments, predetermined deadlines, texts and exercises, and regular, albeit relatively brief, contact with a therapist via secure email.
Dr. Rozental and his coinvestigators reviewed individual patient data in search of predictors of treatment success or deterioration. A profile emerged of the patients least likely to deteriorate while on iCBT: older age, university-educated, in a stable relationship, and with a higher level of symptoms pretreatment.
“You might interpret the findings as an indicator for matching the right type of treatment to the right patient. Perhaps those [who] are younger, have less than a university degree, and are not in a relationship might be better off in a face to face treatment, at least in terms of preventing deterioration,” he observed in an interview. “This makes sense if you think about the amount of work you have to do on your own in Internet-based psychological treatments, which include limited access to a therapist and require reading a lot of text material.”
Patients participating in iCBT who fit that profile might need extra support from a therapist in order to improve, Dr. Rozental added.
He reported having no financial conflicts regarding his study, which was funded by the Swedish Research Council for Health, Working Life, and Welfare.
AT THE ANXIETY AND DEPRESSION CONFERENCE 2017
Key clinical point:
Major finding: Slightly less than 6% of patients deteriorated while participating in Internet-based cognitive-behavioral therapy, mostly for anxiety disorders or depression.
Data source: This individual patient data meta-analysis involved 2,866 participants in 29 published clinical trials of internet-based cognitive-behavioral therapy.
Disclosures: The study was funded by the Swedish Research Council for Health, Working Life, and Welfare. The presenter reported having no financial conflicts.
Almost one-third of Syrian refugees in U.S. met PTSD criteria
SAN FRANCISCO – Nearly one-third of adult Syrian civil war refugees who have resettled in the Detroit area meet diagnostic criteria for posttraumatic stress disorder, according to preliminary results of an ongoing study presented by Arash Javanbakht, MD, at the annual conference of the Anxiety and Depression Association of America.
That’s comparable to PTSD rates documented in Vietnam War combat veterans.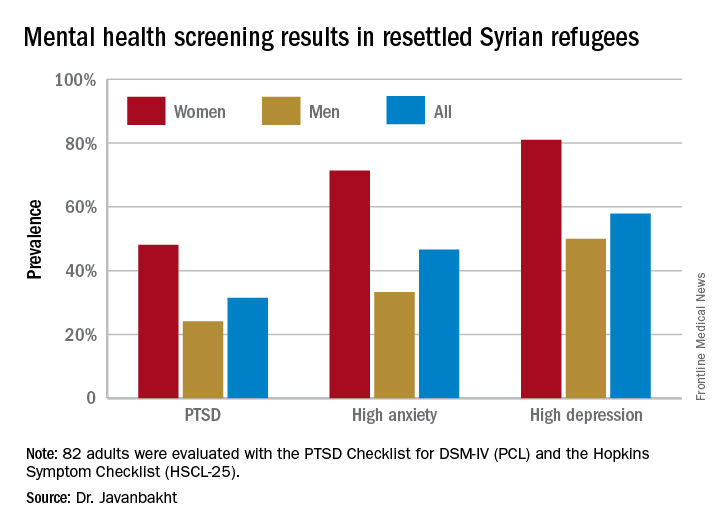
“Based on these data, mental health care for Syrian refugees resettling in the U.S. is highly needed,” he observed.
Michigan has a large population of Syrian war refugees. All who settle in southeastern Michigan undergo an initial health examination at Arab American and Chaldean Council primary care clinics staffed by bilingual teams. More than 90% of eligible adult refugees who have been invited to join Dr. Javanbakht’s mental health screening study have opted to participate. This extraordinarily high recruitment rate suggests that the findings are generalizable to the broader Syrian refugee community throughout the United States in his view.
The screening tools employed in the study are the PTSD Checklist, DSM-IV version (PCL), and the Hopkins Symptom Checklist (HSCL-25), which contains 10 anxiety questions and 15 depression questions.
Of the first 82 adult Syrian refugees evaluated, 26 (31.5%) were diagnosed as having PTSD on the basis of a PCL total score of 40 or more plus fulfillment of the DSM-IV diagnostic criteria for the disorder. In fact, this subgroup had a mean PCL score of 62.3. The prevalence of PTSD was twice as great in women, compared with men (see graphic).
Clinically impactful anxiety symptoms as defined by an HSCL-25 anxiety score greater than 1.79 was present in 38 refugees (47%), and clinically meaningful depressive symptoms were present in 47 (58%).
Anxiety, depression, and PTSD all were tightly correlated, complicating the clinical challenges, the psychiatrist noted.
Enrollment in the study is ongoing, but a first pass examination of a participant population that’s now twice the size of that in his presentation at the conference continues to show similar results, according to Dr. Javanbakht.
Dr. Javanbakht reported having no financial conflicts of interest regarding the study, which was funded by the state of Michigan and the Detroit Wayne Mental Health Authority.
SAN FRANCISCO – Nearly one-third of adult Syrian civil war refugees who have resettled in the Detroit area meet diagnostic criteria for posttraumatic stress disorder, according to preliminary results of an ongoing study presented by Arash Javanbakht, MD, at the annual conference of the Anxiety and Depression Association of America.
That’s comparable to PTSD rates documented in Vietnam War combat veterans.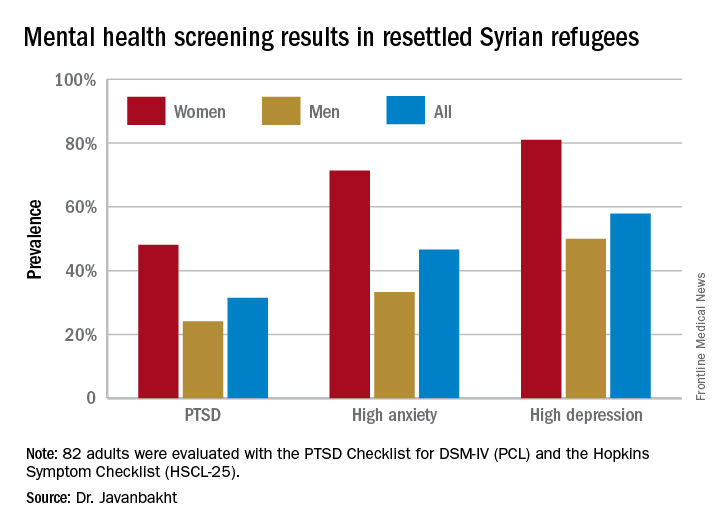
“Based on these data, mental health care for Syrian refugees resettling in the U.S. is highly needed,” he observed.
Michigan has a large population of Syrian war refugees. All who settle in southeastern Michigan undergo an initial health examination at Arab American and Chaldean Council primary care clinics staffed by bilingual teams. More than 90% of eligible adult refugees who have been invited to join Dr. Javanbakht’s mental health screening study have opted to participate. This extraordinarily high recruitment rate suggests that the findings are generalizable to the broader Syrian refugee community throughout the United States in his view.
The screening tools employed in the study are the PTSD Checklist, DSM-IV version (PCL), and the Hopkins Symptom Checklist (HSCL-25), which contains 10 anxiety questions and 15 depression questions.
Of the first 82 adult Syrian refugees evaluated, 26 (31.5%) were diagnosed as having PTSD on the basis of a PCL total score of 40 or more plus fulfillment of the DSM-IV diagnostic criteria for the disorder. In fact, this subgroup had a mean PCL score of 62.3. The prevalence of PTSD was twice as great in women, compared with men (see graphic).
Clinically impactful anxiety symptoms as defined by an HSCL-25 anxiety score greater than 1.79 was present in 38 refugees (47%), and clinically meaningful depressive symptoms were present in 47 (58%).
Anxiety, depression, and PTSD all were tightly correlated, complicating the clinical challenges, the psychiatrist noted.
Enrollment in the study is ongoing, but a first pass examination of a participant population that’s now twice the size of that in his presentation at the conference continues to show similar results, according to Dr. Javanbakht.
Dr. Javanbakht reported having no financial conflicts of interest regarding the study, which was funded by the state of Michigan and the Detroit Wayne Mental Health Authority.
SAN FRANCISCO – Nearly one-third of adult Syrian civil war refugees who have resettled in the Detroit area meet diagnostic criteria for posttraumatic stress disorder, according to preliminary results of an ongoing study presented by Arash Javanbakht, MD, at the annual conference of the Anxiety and Depression Association of America.
That’s comparable to PTSD rates documented in Vietnam War combat veterans.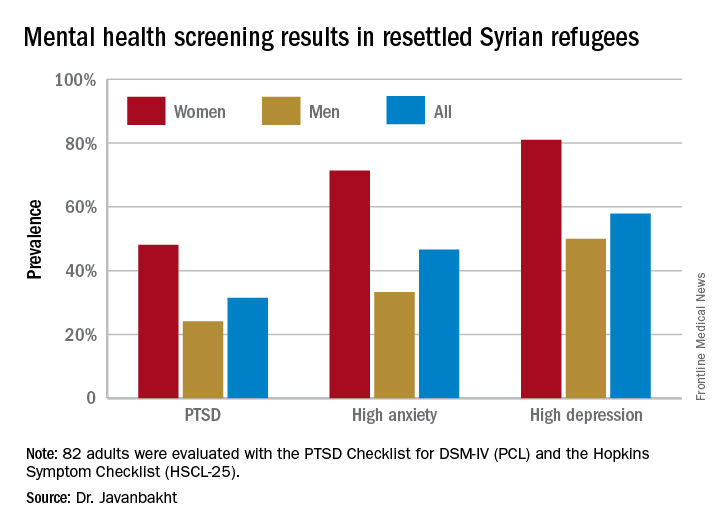
“Based on these data, mental health care for Syrian refugees resettling in the U.S. is highly needed,” he observed.
Michigan has a large population of Syrian war refugees. All who settle in southeastern Michigan undergo an initial health examination at Arab American and Chaldean Council primary care clinics staffed by bilingual teams. More than 90% of eligible adult refugees who have been invited to join Dr. Javanbakht’s mental health screening study have opted to participate. This extraordinarily high recruitment rate suggests that the findings are generalizable to the broader Syrian refugee community throughout the United States in his view.
The screening tools employed in the study are the PTSD Checklist, DSM-IV version (PCL), and the Hopkins Symptom Checklist (HSCL-25), which contains 10 anxiety questions and 15 depression questions.
Of the first 82 adult Syrian refugees evaluated, 26 (31.5%) were diagnosed as having PTSD on the basis of a PCL total score of 40 or more plus fulfillment of the DSM-IV diagnostic criteria for the disorder. In fact, this subgroup had a mean PCL score of 62.3. The prevalence of PTSD was twice as great in women, compared with men (see graphic).
Clinically impactful anxiety symptoms as defined by an HSCL-25 anxiety score greater than 1.79 was present in 38 refugees (47%), and clinically meaningful depressive symptoms were present in 47 (58%).
Anxiety, depression, and PTSD all were tightly correlated, complicating the clinical challenges, the psychiatrist noted.
Enrollment in the study is ongoing, but a first pass examination of a participant population that’s now twice the size of that in his presentation at the conference continues to show similar results, according to Dr. Javanbakht.
Dr. Javanbakht reported having no financial conflicts of interest regarding the study, which was funded by the state of Michigan and the Detroit Wayne Mental Health Authority.
AT THE ANXIETY AND DEPRESSION CONFERENCE 2017
Key clinical point:
Major finding: One-third of adult Syrian war refugees who have resettled in Michigan have posttraumatic stress disorder.
Data source: This ongoing cross-sectional study initially screened 82 adult Syrian civil war refugees for PTSD, anxiety, and depression.
Disclosures: This ongoing study is funded by the state of Michigan and the Detroit Wayne Mental Health Authority. The presenter reported having no financial conflicts of interest.
Anhedonia emerges as a major transdiagnostic treatment target
SAN FRANCISCO – Anhedonia is the symptom dimension that cuts most strongly across the diagnostic boundaries of anxiety and depression and contributes most to the characteristically poor quality of life in both, Emily C. Livermore reported at the annual conference of the Anxiety and Depression Association of America.
“Our results suggest that anhedonia may have a disproportionate impact on disability from depression and anxiety and may be an important target for tailoring treatment and assessing treatment outcomes,” declared Ms. Livermore, a doctoral student in clinical psychology at Stanford (Calif.) University.
She presented a study of 121 adults with anxiety or depressive symptoms. The study was conducted under the auspices of the National Institute of Mental Health’s Research Domain Criteria (RDoC) initiative. The RDoC program is intended to promote a new way of studying mental disorders based on dimensional psychological constructs independent of traditional psychiatric diagnoses, which in some circles are now dismissed as “silos.” In keeping with the RDoC goals, Ms. Livermore and her coinvestigators examined diagnosis-independent dimensions of symptoms and how they affected quality of life.
The investigators obtained a comprehensive picture of the participants’ symptoms and quality of life by having them complete the Penn State Worry Questionnaire, the Mood and Anxiety Symptoms Questionnaire, the Depression Anxiety Stress Scale, and the World Health Organization Quality of Life – Brief Version.
The investigators then mapped the symptoms and their interconnections in order to identify what they called transdiagnostic symptom factor dimensions. They found four of them, which they termed anhedonia, worry, tension, and anxious arousal, a dimension encompassing physical symptoms including shortness of breath and heart palpitations.
Next, using regression analyses, they examined the relationship between levels of those four symptom factor dimensions and the four quality of life domains captured in the WHO instrument, namely, physical, psychologic, environmental, and social quality of life. Study participants averaged unhealthily low quality of life scores on two of these domains – the psychological and social – as defined by scores more than one standard deviation below normative.
Of the four symptom dimensions, anhedonia stood out as having moderate to-strong negative associations with all four quality of life domains. The other three symptom dimensions showed no or only weak associations with the four quality of life domains, with the exception of anxious arousal, which displayed a moderate relationship with physical quality of life.
Ms. Livermore reported having no financial conflicts regarding the study, which was funded by the National Institute of Mental Health.
SAN FRANCISCO – Anhedonia is the symptom dimension that cuts most strongly across the diagnostic boundaries of anxiety and depression and contributes most to the characteristically poor quality of life in both, Emily C. Livermore reported at the annual conference of the Anxiety and Depression Association of America.
“Our results suggest that anhedonia may have a disproportionate impact on disability from depression and anxiety and may be an important target for tailoring treatment and assessing treatment outcomes,” declared Ms. Livermore, a doctoral student in clinical psychology at Stanford (Calif.) University.
She presented a study of 121 adults with anxiety or depressive symptoms. The study was conducted under the auspices of the National Institute of Mental Health’s Research Domain Criteria (RDoC) initiative. The RDoC program is intended to promote a new way of studying mental disorders based on dimensional psychological constructs independent of traditional psychiatric diagnoses, which in some circles are now dismissed as “silos.” In keeping with the RDoC goals, Ms. Livermore and her coinvestigators examined diagnosis-independent dimensions of symptoms and how they affected quality of life.
The investigators obtained a comprehensive picture of the participants’ symptoms and quality of life by having them complete the Penn State Worry Questionnaire, the Mood and Anxiety Symptoms Questionnaire, the Depression Anxiety Stress Scale, and the World Health Organization Quality of Life – Brief Version.
The investigators then mapped the symptoms and their interconnections in order to identify what they called transdiagnostic symptom factor dimensions. They found four of them, which they termed anhedonia, worry, tension, and anxious arousal, a dimension encompassing physical symptoms including shortness of breath and heart palpitations.
Next, using regression analyses, they examined the relationship between levels of those four symptom factor dimensions and the four quality of life domains captured in the WHO instrument, namely, physical, psychologic, environmental, and social quality of life. Study participants averaged unhealthily low quality of life scores on two of these domains – the psychological and social – as defined by scores more than one standard deviation below normative.
Of the four symptom dimensions, anhedonia stood out as having moderate to-strong negative associations with all four quality of life domains. The other three symptom dimensions showed no or only weak associations with the four quality of life domains, with the exception of anxious arousal, which displayed a moderate relationship with physical quality of life.
Ms. Livermore reported having no financial conflicts regarding the study, which was funded by the National Institute of Mental Health.
SAN FRANCISCO – Anhedonia is the symptom dimension that cuts most strongly across the diagnostic boundaries of anxiety and depression and contributes most to the characteristically poor quality of life in both, Emily C. Livermore reported at the annual conference of the Anxiety and Depression Association of America.
“Our results suggest that anhedonia may have a disproportionate impact on disability from depression and anxiety and may be an important target for tailoring treatment and assessing treatment outcomes,” declared Ms. Livermore, a doctoral student in clinical psychology at Stanford (Calif.) University.
She presented a study of 121 adults with anxiety or depressive symptoms. The study was conducted under the auspices of the National Institute of Mental Health’s Research Domain Criteria (RDoC) initiative. The RDoC program is intended to promote a new way of studying mental disorders based on dimensional psychological constructs independent of traditional psychiatric diagnoses, which in some circles are now dismissed as “silos.” In keeping with the RDoC goals, Ms. Livermore and her coinvestigators examined diagnosis-independent dimensions of symptoms and how they affected quality of life.
The investigators obtained a comprehensive picture of the participants’ symptoms and quality of life by having them complete the Penn State Worry Questionnaire, the Mood and Anxiety Symptoms Questionnaire, the Depression Anxiety Stress Scale, and the World Health Organization Quality of Life – Brief Version.
The investigators then mapped the symptoms and their interconnections in order to identify what they called transdiagnostic symptom factor dimensions. They found four of them, which they termed anhedonia, worry, tension, and anxious arousal, a dimension encompassing physical symptoms including shortness of breath and heart palpitations.
Next, using regression analyses, they examined the relationship between levels of those four symptom factor dimensions and the four quality of life domains captured in the WHO instrument, namely, physical, psychologic, environmental, and social quality of life. Study participants averaged unhealthily low quality of life scores on two of these domains – the psychological and social – as defined by scores more than one standard deviation below normative.
Of the four symptom dimensions, anhedonia stood out as having moderate to-strong negative associations with all four quality of life domains. The other three symptom dimensions showed no or only weak associations with the four quality of life domains, with the exception of anxious arousal, which displayed a moderate relationship with physical quality of life.
Ms. Livermore reported having no financial conflicts regarding the study, which was funded by the National Institute of Mental Health.
AT THE ANXIETY AND DEPRESSION CONFERENCE 2017
Key clinical point:
Major finding: Anhedonia has a disproportionate negative impact on all of the major quality of life domains in both anxiety and depression.
Data source: A cross-sectional study of 121 adults with clinically significant anxiety or depression symptoms.
Disclosures: The presenter reported having no financial conflicts regarding the study, which was funded by the National Institute of Mental Health.
ADHD – not OCD – called the key comorbidity in pediatric hoarding
SAN FRANCISCO – Most of the pediatric hoarding literature focuses on hoarding accompanied by obsessive-compulsive disorder. But, “I want to highlight that [attention-deficit/hyperactivity disorder] is across the board something that seems to come up in child hoarding behaviors quite a bit, mirroring the adult literature, which is that hoarding behavior may be much more strongly associated with ADHD than it is with OCD,” Jennifer M. Park, PhD, said at the annual conference of the Anxiety and Depression Association of America.
Multiple studies have established that the prevalence of child hoarding is 2%-3.7%. Onset is typically at age 11-15 years. The course is chronic, and it’s a condition that typically exacerbates over time.
“A lot of the adult literature has shown that hoarding behavior actually starts in childhood. In many retrospective reports, adults say, ‘I’ve had these problems ever since I was a kid,’ ” according to Dr. Park, a psychologist affiliated with Stanford (Calif.) University.
Yet childhood hoarding is not widely perceived as problematic. Indeed, many parents and clinicians view it as developmentally appropriate. That’s to a great extent because the presentation of child hoarding behavior often is very different from and less disturbing than adult hoarding for the obvious reason that parents can limit the amount of clutter in the home.
“I have a bunch of kids who have quite significant hoarding behavior, but the parents are really on top of making sure all of that is left in the closet or within the child’s playroom, or maybe a certain section of the house,” Dr. Park said. “They’re able to keep it contained.”
Also, children and young adolescents lack the resources to accumulate massive clutter. They can’t drive, and have little or no money, so they can’t go on compulsive shopping sprees. “What I have seen in the kids that I work with is they make up for that by collecting things like paper and sticks, rocks, wrappers – anything that might be free, or knickknacks they can pick up along the way,” she said.
The cognitive-behavioral model of hoarding was first described 2 decades ago. It names three main factors as key to maintaining hoarding behaviors: emotional attachment and beliefs associated with one’s possessions, often including anthropomorphization; avoidance behaviors due to severe distress at the prospect of discarding stuff; and information-processing deficits.
“The idea here is that deficits in executive function – things like planning, organization, and inhibition – these are known in an extensive literature to be really strongly associated with ADHD, and executive function deficits link well with hoarding disorder as well,” Dr. Park continued.
Dr. Park was the first author of a recent multicenter study of 431 youths aged 6-17 diagnosed with OCD. They were participants in the OCD Collaborative Genetics Study and the OCD Collaborative Genetics Association Study, during which they completed the Behavior Rating Inventory of Executive Functioning (BRIEF) and the Hoarding Rating Scale–Interview. Clinically significant levels of hoarding compulsions were identified in 113 subjects. Compared with the group with OCD but not hoarding, the OCD/hoarding group had significantly lower scores – meaning problematic deficits – on nearly all of the executive function subscales on the BRIEF, including working memory, emotional control, and planning/organization.
The two groups did not differ significantly in the prevalence of full DSM-IV ADHD. But the hoarding group had significantly more inattention and hyperactivity symptoms, and in a multivariate analysis adjusted for age, sex, and ADHD symptoms, deficits in executive function as measured on the BRIEF instrument were the strongest predictor of hoarding severity in the study population (J Psychiatr Res. 2016 Nov;82:141-8).
In another study by Dr. Park and her coinvestigators involving 99 youth diagnosed with ADHD, the severity of inattention and hyperactivity/impulsivity predicted clinically significant hoarding, whereas nonhoarding OCD symptoms did not (J Atten Disord. 2016 Jul;20[7]:617-26).
In an earlier report by other investigators on 109 children seeking treatment for an anxiety disorder, 22% of the study population proved to have elevated levels of hoarding symptoms. They scored significantly higher than the nonhoarding group on measures of obsession-compulsion, anxiety, inattention, thought problems, rule breaking, aggression, social problems, major depression, and overall functional impairment. But of note, attention problems were a significantly stronger predictor of hoarding symptoms than were OCD or anxiety symptoms (J Anxiety Disord. 2015 Dec;36:9-14).
Discussant Eric Storch, PhD, said that it’s important for clinicians and parents to start taking child hoarding seriously as a legitimate treatment target.
“We know that if you start treatment early, you’re more likely to be successful versus when you start at age 57 and the clutter is 9 or 10 on a scale of 10,” said Dr. Storch, professor of pediatrics and director of clinical research for developmental pediatrics at the University of South Florida, Tampa.
Dr. Park reported having no financial conflicts of interest regarding her presentation.
SAN FRANCISCO – Most of the pediatric hoarding literature focuses on hoarding accompanied by obsessive-compulsive disorder. But, “I want to highlight that [attention-deficit/hyperactivity disorder] is across the board something that seems to come up in child hoarding behaviors quite a bit, mirroring the adult literature, which is that hoarding behavior may be much more strongly associated with ADHD than it is with OCD,” Jennifer M. Park, PhD, said at the annual conference of the Anxiety and Depression Association of America.
Multiple studies have established that the prevalence of child hoarding is 2%-3.7%. Onset is typically at age 11-15 years. The course is chronic, and it’s a condition that typically exacerbates over time.
“A lot of the adult literature has shown that hoarding behavior actually starts in childhood. In many retrospective reports, adults say, ‘I’ve had these problems ever since I was a kid,’ ” according to Dr. Park, a psychologist affiliated with Stanford (Calif.) University.
Yet childhood hoarding is not widely perceived as problematic. Indeed, many parents and clinicians view it as developmentally appropriate. That’s to a great extent because the presentation of child hoarding behavior often is very different from and less disturbing than adult hoarding for the obvious reason that parents can limit the amount of clutter in the home.
“I have a bunch of kids who have quite significant hoarding behavior, but the parents are really on top of making sure all of that is left in the closet or within the child’s playroom, or maybe a certain section of the house,” Dr. Park said. “They’re able to keep it contained.”
Also, children and young adolescents lack the resources to accumulate massive clutter. They can’t drive, and have little or no money, so they can’t go on compulsive shopping sprees. “What I have seen in the kids that I work with is they make up for that by collecting things like paper and sticks, rocks, wrappers – anything that might be free, or knickknacks they can pick up along the way,” she said.
The cognitive-behavioral model of hoarding was first described 2 decades ago. It names three main factors as key to maintaining hoarding behaviors: emotional attachment and beliefs associated with one’s possessions, often including anthropomorphization; avoidance behaviors due to severe distress at the prospect of discarding stuff; and information-processing deficits.
“The idea here is that deficits in executive function – things like planning, organization, and inhibition – these are known in an extensive literature to be really strongly associated with ADHD, and executive function deficits link well with hoarding disorder as well,” Dr. Park continued.
Dr. Park was the first author of a recent multicenter study of 431 youths aged 6-17 diagnosed with OCD. They were participants in the OCD Collaborative Genetics Study and the OCD Collaborative Genetics Association Study, during which they completed the Behavior Rating Inventory of Executive Functioning (BRIEF) and the Hoarding Rating Scale–Interview. Clinically significant levels of hoarding compulsions were identified in 113 subjects. Compared with the group with OCD but not hoarding, the OCD/hoarding group had significantly lower scores – meaning problematic deficits – on nearly all of the executive function subscales on the BRIEF, including working memory, emotional control, and planning/organization.
The two groups did not differ significantly in the prevalence of full DSM-IV ADHD. But the hoarding group had significantly more inattention and hyperactivity symptoms, and in a multivariate analysis adjusted for age, sex, and ADHD symptoms, deficits in executive function as measured on the BRIEF instrument were the strongest predictor of hoarding severity in the study population (J Psychiatr Res. 2016 Nov;82:141-8).
In another study by Dr. Park and her coinvestigators involving 99 youth diagnosed with ADHD, the severity of inattention and hyperactivity/impulsivity predicted clinically significant hoarding, whereas nonhoarding OCD symptoms did not (J Atten Disord. 2016 Jul;20[7]:617-26).
In an earlier report by other investigators on 109 children seeking treatment for an anxiety disorder, 22% of the study population proved to have elevated levels of hoarding symptoms. They scored significantly higher than the nonhoarding group on measures of obsession-compulsion, anxiety, inattention, thought problems, rule breaking, aggression, social problems, major depression, and overall functional impairment. But of note, attention problems were a significantly stronger predictor of hoarding symptoms than were OCD or anxiety symptoms (J Anxiety Disord. 2015 Dec;36:9-14).
Discussant Eric Storch, PhD, said that it’s important for clinicians and parents to start taking child hoarding seriously as a legitimate treatment target.
“We know that if you start treatment early, you’re more likely to be successful versus when you start at age 57 and the clutter is 9 or 10 on a scale of 10,” said Dr. Storch, professor of pediatrics and director of clinical research for developmental pediatrics at the University of South Florida, Tampa.
Dr. Park reported having no financial conflicts of interest regarding her presentation.
SAN FRANCISCO – Most of the pediatric hoarding literature focuses on hoarding accompanied by obsessive-compulsive disorder. But, “I want to highlight that [attention-deficit/hyperactivity disorder] is across the board something that seems to come up in child hoarding behaviors quite a bit, mirroring the adult literature, which is that hoarding behavior may be much more strongly associated with ADHD than it is with OCD,” Jennifer M. Park, PhD, said at the annual conference of the Anxiety and Depression Association of America.
Multiple studies have established that the prevalence of child hoarding is 2%-3.7%. Onset is typically at age 11-15 years. The course is chronic, and it’s a condition that typically exacerbates over time.
“A lot of the adult literature has shown that hoarding behavior actually starts in childhood. In many retrospective reports, adults say, ‘I’ve had these problems ever since I was a kid,’ ” according to Dr. Park, a psychologist affiliated with Stanford (Calif.) University.
Yet childhood hoarding is not widely perceived as problematic. Indeed, many parents and clinicians view it as developmentally appropriate. That’s to a great extent because the presentation of child hoarding behavior often is very different from and less disturbing than adult hoarding for the obvious reason that parents can limit the amount of clutter in the home.
“I have a bunch of kids who have quite significant hoarding behavior, but the parents are really on top of making sure all of that is left in the closet or within the child’s playroom, or maybe a certain section of the house,” Dr. Park said. “They’re able to keep it contained.”
Also, children and young adolescents lack the resources to accumulate massive clutter. They can’t drive, and have little or no money, so they can’t go on compulsive shopping sprees. “What I have seen in the kids that I work with is they make up for that by collecting things like paper and sticks, rocks, wrappers – anything that might be free, or knickknacks they can pick up along the way,” she said.
The cognitive-behavioral model of hoarding was first described 2 decades ago. It names three main factors as key to maintaining hoarding behaviors: emotional attachment and beliefs associated with one’s possessions, often including anthropomorphization; avoidance behaviors due to severe distress at the prospect of discarding stuff; and information-processing deficits.
“The idea here is that deficits in executive function – things like planning, organization, and inhibition – these are known in an extensive literature to be really strongly associated with ADHD, and executive function deficits link well with hoarding disorder as well,” Dr. Park continued.
Dr. Park was the first author of a recent multicenter study of 431 youths aged 6-17 diagnosed with OCD. They were participants in the OCD Collaborative Genetics Study and the OCD Collaborative Genetics Association Study, during which they completed the Behavior Rating Inventory of Executive Functioning (BRIEF) and the Hoarding Rating Scale–Interview. Clinically significant levels of hoarding compulsions were identified in 113 subjects. Compared with the group with OCD but not hoarding, the OCD/hoarding group had significantly lower scores – meaning problematic deficits – on nearly all of the executive function subscales on the BRIEF, including working memory, emotional control, and planning/organization.
The two groups did not differ significantly in the prevalence of full DSM-IV ADHD. But the hoarding group had significantly more inattention and hyperactivity symptoms, and in a multivariate analysis adjusted for age, sex, and ADHD symptoms, deficits in executive function as measured on the BRIEF instrument were the strongest predictor of hoarding severity in the study population (J Psychiatr Res. 2016 Nov;82:141-8).
In another study by Dr. Park and her coinvestigators involving 99 youth diagnosed with ADHD, the severity of inattention and hyperactivity/impulsivity predicted clinically significant hoarding, whereas nonhoarding OCD symptoms did not (J Atten Disord. 2016 Jul;20[7]:617-26).
In an earlier report by other investigators on 109 children seeking treatment for an anxiety disorder, 22% of the study population proved to have elevated levels of hoarding symptoms. They scored significantly higher than the nonhoarding group on measures of obsession-compulsion, anxiety, inattention, thought problems, rule breaking, aggression, social problems, major depression, and overall functional impairment. But of note, attention problems were a significantly stronger predictor of hoarding symptoms than were OCD or anxiety symptoms (J Anxiety Disord. 2015 Dec;36:9-14).
Discussant Eric Storch, PhD, said that it’s important for clinicians and parents to start taking child hoarding seriously as a legitimate treatment target.
“We know that if you start treatment early, you’re more likely to be successful versus when you start at age 57 and the clutter is 9 or 10 on a scale of 10,” said Dr. Storch, professor of pediatrics and director of clinical research for developmental pediatrics at the University of South Florida, Tampa.
Dr. Park reported having no financial conflicts of interest regarding her presentation.
EXPERT ANALYSIS FROM ANXIETY AND DEPRESSION CONFERENCE 2017
Female predisposition to anxiety disorders may have prenatal origin
SAN FRANCISCO – Why are anxiety disorders twice as prevalent in women as in men? As in Hawaiian hula dancing, the expressive hands may tell the tale.
The ratio of the length of the index finger to ring finger – known as the 2D:4D ratio – is a physical trait that remains stable across the lifetimes of males and females. It’s also a reliable indicator of prenatal exposure to androgens. In female college students, the higher the 2D:4D ratio, the greater their level of ruminative thinking, which is known to be both a risk factor and maintenance factor for anxiety, Ellie Shuo Jin reported at the annual conference of the Anxiety and Depression Association of America.
The findings shed new light on the relationship between testosterone and anxiety disorders, according to Ms. Jin, a doctoral student at the University of Texas, Austin. The hormone previously has been linked to reduced levels of anxiety, an observation consistent with the lower prevalence of anxiety disorders in men. However, it has been unclear whether prenatal exposure to testosterone, which encourages organizational effects, or the activational effects of postnatal exposure to the hormone is most protective against anxiety disorders.
Ms. Jin found that prenatal testosterone exposure as reflected in a low 2D:4D ratio was associated with a lower level of repetitive negative thinking as measured using the Perseverative Thinking Questionnaire but only in the female students.
She reported having no financial conflicts of interest regarding her study.
SAN FRANCISCO – Why are anxiety disorders twice as prevalent in women as in men? As in Hawaiian hula dancing, the expressive hands may tell the tale.
The ratio of the length of the index finger to ring finger – known as the 2D:4D ratio – is a physical trait that remains stable across the lifetimes of males and females. It’s also a reliable indicator of prenatal exposure to androgens. In female college students, the higher the 2D:4D ratio, the greater their level of ruminative thinking, which is known to be both a risk factor and maintenance factor for anxiety, Ellie Shuo Jin reported at the annual conference of the Anxiety and Depression Association of America.
The findings shed new light on the relationship between testosterone and anxiety disorders, according to Ms. Jin, a doctoral student at the University of Texas, Austin. The hormone previously has been linked to reduced levels of anxiety, an observation consistent with the lower prevalence of anxiety disorders in men. However, it has been unclear whether prenatal exposure to testosterone, which encourages organizational effects, or the activational effects of postnatal exposure to the hormone is most protective against anxiety disorders.
Ms. Jin found that prenatal testosterone exposure as reflected in a low 2D:4D ratio was associated with a lower level of repetitive negative thinking as measured using the Perseverative Thinking Questionnaire but only in the female students.
She reported having no financial conflicts of interest regarding her study.
SAN FRANCISCO – Why are anxiety disorders twice as prevalent in women as in men? As in Hawaiian hula dancing, the expressive hands may tell the tale.
The ratio of the length of the index finger to ring finger – known as the 2D:4D ratio – is a physical trait that remains stable across the lifetimes of males and females. It’s also a reliable indicator of prenatal exposure to androgens. In female college students, the higher the 2D:4D ratio, the greater their level of ruminative thinking, which is known to be both a risk factor and maintenance factor for anxiety, Ellie Shuo Jin reported at the annual conference of the Anxiety and Depression Association of America.
The findings shed new light on the relationship between testosterone and anxiety disorders, according to Ms. Jin, a doctoral student at the University of Texas, Austin. The hormone previously has been linked to reduced levels of anxiety, an observation consistent with the lower prevalence of anxiety disorders in men. However, it has been unclear whether prenatal exposure to testosterone, which encourages organizational effects, or the activational effects of postnatal exposure to the hormone is most protective against anxiety disorders.
Ms. Jin found that prenatal testosterone exposure as reflected in a low 2D:4D ratio was associated with a lower level of repetitive negative thinking as measured using the Perseverative Thinking Questionnaire but only in the female students.
She reported having no financial conflicts of interest regarding her study.
AT THE ANXIETY AND DEPRESSION CONFERENCE 2017
Key clinical point:
Major finding: The higher the ratio of the length of the index finger to the ring finger on the left hand, the greater the predisposition to repetitive negative thinking in women but not in men.
Data source: This cross-sectional study correlated the 2D:4D digit ratio to levels of repetitive negative thinking in 103 college students.
Disclosures: The presenter reported having no financial conflicts regarding her study.












