User login
Tackling unhealthy substance use using USPSTF guidance and a 1-question tool
References
- US Preventive Services Task Force. Unhealthy drug use: screening [final recommendation statement]. Published June 9, 2020. https://uspreventiveservicestaskforce.org/uspstf/recommendation/drug-use-illicit-screening. Accessed July 28, 2020.
- US Preventive Services Task Force. Illicit drug use in children, adolescents, and young adults: primary care-based interventions [final recommendation statement]. Published May 26, 2020. https://uspreventiveservicestaskforce.org/uspstf/recommendation/drug-use-illicit-primary-care-interventions-for-children-and-adolescents. Accessed July 28, 2020.
- US Preventive Services Task Force. Prevention and cessation of tobacco use in children and adolescents: primary care interventions [final recommendation statement]. Published April 28, 2020. https://uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-and-nicotine-use-prevention-in-children-and-adolescents-primary-care-interventions. Accessed July 28, 2020.
- National Institute on Drug Abuse. NIDA Quick Screen v 1.0. www.drugabuse.gov/sites/default/files/pdf/nmassist.pdf. Accessed July 28, 2020.
- US Preventive Services Task Force. Tobacco smoking cessation in adults, including pregnant women: behavioral and pharmacotherapy interventions [update in progress]. Published September 21, 2015. https://uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions. Accessed July 28, 2020.
References
- US Preventive Services Task Force. Unhealthy drug use: screening [final recommendation statement]. Published June 9, 2020. https://uspreventiveservicestaskforce.org/uspstf/recommendation/drug-use-illicit-screening. Accessed July 28, 2020.
- US Preventive Services Task Force. Illicit drug use in children, adolescents, and young adults: primary care-based interventions [final recommendation statement]. Published May 26, 2020. https://uspreventiveservicestaskforce.org/uspstf/recommendation/drug-use-illicit-primary-care-interventions-for-children-and-adolescents. Accessed July 28, 2020.
- US Preventive Services Task Force. Prevention and cessation of tobacco use in children and adolescents: primary care interventions [final recommendation statement]. Published April 28, 2020. https://uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-and-nicotine-use-prevention-in-children-and-adolescents-primary-care-interventions. Accessed July 28, 2020.
- National Institute on Drug Abuse. NIDA Quick Screen v 1.0. www.drugabuse.gov/sites/default/files/pdf/nmassist.pdf. Accessed July 28, 2020.
- US Preventive Services Task Force. Tobacco smoking cessation in adults, including pregnant women: behavioral and pharmacotherapy interventions [update in progress]. Published September 21, 2015. https://uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions. Accessed July 28, 2020.
References
- US Preventive Services Task Force. Unhealthy drug use: screening [final recommendation statement]. Published June 9, 2020. https://uspreventiveservicestaskforce.org/uspstf/recommendation/drug-use-illicit-screening. Accessed July 28, 2020.
- US Preventive Services Task Force. Illicit drug use in children, adolescents, and young adults: primary care-based interventions [final recommendation statement]. Published May 26, 2020. https://uspreventiveservicestaskforce.org/uspstf/recommendation/drug-use-illicit-primary-care-interventions-for-children-and-adolescents. Accessed July 28, 2020.
- US Preventive Services Task Force. Prevention and cessation of tobacco use in children and adolescents: primary care interventions [final recommendation statement]. Published April 28, 2020. https://uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-and-nicotine-use-prevention-in-children-and-adolescents-primary-care-interventions. Accessed July 28, 2020.
- National Institute on Drug Abuse. NIDA Quick Screen v 1.0. www.drugabuse.gov/sites/default/files/pdf/nmassist.pdf. Accessed July 28, 2020.
- US Preventive Services Task Force. Tobacco smoking cessation in adults, including pregnant women: behavioral and pharmacotherapy interventions [update in progress]. Published September 21, 2015. https://uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions. Accessed July 28, 2020.
AMA urges change after dramatic increase in illicit opioid fatalities
In the past 5 years, there has been a significant drop in the use of prescription opioids and in deaths associated with such use; but at the same time there’s been a dramatic increase in fatalities involving illicit opioids and stimulants, a new report from the American Medical Association (AMA) Opioid Task Force shows.
Although the medical community has made some important progress against the opioid epidemic, with a 37% reduction in opioid prescribing since 2013, illicit drugs are now the dominant reason why drug overdoses kill more than 70,000 people each year, the report says.
In an effort to improve the situation, the AMA Opioid Task Force is urging the removal of barriers to evidence-based care for patients who have pain and for those who have substance use disorders (SUDs). The report notes that “red tape and misguided policies are grave dangers” to these patients.
“It is critically important as we see drug overdoses increasing that we work towards reducing barriers of care for substance use abusers,” Task Force Chair Patrice A. Harris, MD, said in an interview.
“At present, the status quo is killing far too many of our loved ones and wreaking havoc in our communities,” she said.
Dr. Harris noted that “a more coordinated/integrated approach” is needed to help individuals with SUDs.
“It is vitally important that these individuals can get access to treatment. Everyone deserves the opportunity for care,” she added.
Dramatic increases
The report cites figures from the Centers for Disease Control and Prevention that indicate the following regarding the period from the beginning of 2015 to the end of 2019:
- Deaths involving illicitly manufactured and fentanyl analogues increased from 5,766 to 36,509.
- Deaths involving stimulants such as increased from 4,402 to 16,279.
- Deaths involving cocaine increased from 5,496 to 15,974.
- Deaths involving heroin increased from 10,788 to 14,079.
- Deaths involving prescription opioids decreased from 12,269 to 11,904.
The report notes that deaths involving prescription opioids peaked in July 2017 at 15,003.
Some good news
In addition to the 37% reduction in opioid prescribing in recent years, the AMA lists other points of progress, such as a large increase in prescription drug monitoring program registrations. More than 1.8 million physicians and other healthcare professionals now participate in these programs.
Also, more physicians are now certified to treat opioid use disorder. More than 85,000 physicians, as well as a growing number of nurse practitioners and physician assistants, are now certified to treat patients in the office with buprenorphine. This represents an increase of more than 50,000 from 2017.
Access to naloxone is also increasing. More than 1 million naloxone prescriptions were dispensed in 2019 – nearly double the amount in 2018. This represents a 649% increase from 2017.
“We have made some good progress, but we can’t declare victory, and there are far too many barriers to getting treatment for substance use disorder,” Dr. Harris said.
“Policymakers, public health officials, and insurance companies need to come together to create a system where there are no barriers to care for people with substance use disorder and for those needing pain medications,” she added.
At present, prior authorization is often needed before these patients can receive medication. “This involves quite a bit of administration, filling in forms, making phone calls, and this is stopping people getting the care they need,” said Dr. Harris.
“This is a highly regulated environment. There are also regulations on the amount of methadone that can be prescribed and for the prescription of buprenorphine, which has to be initiated in person,” she said.
Will COVID-19 bring change?
Dr. Harris noted that some of these regulations have been relaxed during the COVID-19 crisis so that physicians could ensure that patients have continued access to medication, and she suggested that this may pave the way for the future.
“We need now to look at this carefully and have a conversation about whether these relaxations can be continued. But this would have to be evidence based. Perhaps we can use experience from the COVID-19 period to guide future policy on this,” she said.
The report highlights that despite medical society and patient advocacy, only 21 states and the District of Columbia have enacted laws that limit public and private insurers from imposing prior authorization requirements on SUD services or medications.
The Task Force urges removal of remaining prior authorizations, step therapy, and other inappropriate administrative burdens that delay or deny care for Food and Drug Administration–approved medications used as part of medication-assisted treatment for opioid use disorder.
The organization is also calling for better implementation of mental health and substance use disorder parity laws that require health insurers to provide the same level of benefits for mental health and SUD treatment and services that they do for medical/surgical care.
At present, only a few states have taken meaningful action to enact or enforce those laws, the report notes.
The Task Force also recommends the implementation of systems to track overdose and mortality trends to provide equitable public health interventions. These measures would include comprehensive, disaggregated racial and ethnic data collection related to testing, hospitalization, and mortality associated with opioids and other substances.
“We know that ending the drug overdose epidemic will not be easy, but if policymakers allow the status quo to continue, it will be impossible,” Dr. Harris said.
“ Physicians will continue to do our part. We urge policymakers to do theirs,” she added.
A version of this article originally appeared on Medscape.com.
In the past 5 years, there has been a significant drop in the use of prescription opioids and in deaths associated with such use; but at the same time there’s been a dramatic increase in fatalities involving illicit opioids and stimulants, a new report from the American Medical Association (AMA) Opioid Task Force shows.
Although the medical community has made some important progress against the opioid epidemic, with a 37% reduction in opioid prescribing since 2013, illicit drugs are now the dominant reason why drug overdoses kill more than 70,000 people each year, the report says.
In an effort to improve the situation, the AMA Opioid Task Force is urging the removal of barriers to evidence-based care for patients who have pain and for those who have substance use disorders (SUDs). The report notes that “red tape and misguided policies are grave dangers” to these patients.
“It is critically important as we see drug overdoses increasing that we work towards reducing barriers of care for substance use abusers,” Task Force Chair Patrice A. Harris, MD, said in an interview.
“At present, the status quo is killing far too many of our loved ones and wreaking havoc in our communities,” she said.
Dr. Harris noted that “a more coordinated/integrated approach” is needed to help individuals with SUDs.
“It is vitally important that these individuals can get access to treatment. Everyone deserves the opportunity for care,” she added.
Dramatic increases
The report cites figures from the Centers for Disease Control and Prevention that indicate the following regarding the period from the beginning of 2015 to the end of 2019:
- Deaths involving illicitly manufactured and fentanyl analogues increased from 5,766 to 36,509.
- Deaths involving stimulants such as increased from 4,402 to 16,279.
- Deaths involving cocaine increased from 5,496 to 15,974.
- Deaths involving heroin increased from 10,788 to 14,079.
- Deaths involving prescription opioids decreased from 12,269 to 11,904.
The report notes that deaths involving prescription opioids peaked in July 2017 at 15,003.
Some good news
In addition to the 37% reduction in opioid prescribing in recent years, the AMA lists other points of progress, such as a large increase in prescription drug monitoring program registrations. More than 1.8 million physicians and other healthcare professionals now participate in these programs.
Also, more physicians are now certified to treat opioid use disorder. More than 85,000 physicians, as well as a growing number of nurse practitioners and physician assistants, are now certified to treat patients in the office with buprenorphine. This represents an increase of more than 50,000 from 2017.
Access to naloxone is also increasing. More than 1 million naloxone prescriptions were dispensed in 2019 – nearly double the amount in 2018. This represents a 649% increase from 2017.
“We have made some good progress, but we can’t declare victory, and there are far too many barriers to getting treatment for substance use disorder,” Dr. Harris said.
“Policymakers, public health officials, and insurance companies need to come together to create a system where there are no barriers to care for people with substance use disorder and for those needing pain medications,” she added.
At present, prior authorization is often needed before these patients can receive medication. “This involves quite a bit of administration, filling in forms, making phone calls, and this is stopping people getting the care they need,” said Dr. Harris.
“This is a highly regulated environment. There are also regulations on the amount of methadone that can be prescribed and for the prescription of buprenorphine, which has to be initiated in person,” she said.
Will COVID-19 bring change?
Dr. Harris noted that some of these regulations have been relaxed during the COVID-19 crisis so that physicians could ensure that patients have continued access to medication, and she suggested that this may pave the way for the future.
“We need now to look at this carefully and have a conversation about whether these relaxations can be continued. But this would have to be evidence based. Perhaps we can use experience from the COVID-19 period to guide future policy on this,” she said.
The report highlights that despite medical society and patient advocacy, only 21 states and the District of Columbia have enacted laws that limit public and private insurers from imposing prior authorization requirements on SUD services or medications.
The Task Force urges removal of remaining prior authorizations, step therapy, and other inappropriate administrative burdens that delay or deny care for Food and Drug Administration–approved medications used as part of medication-assisted treatment for opioid use disorder.
The organization is also calling for better implementation of mental health and substance use disorder parity laws that require health insurers to provide the same level of benefits for mental health and SUD treatment and services that they do for medical/surgical care.
At present, only a few states have taken meaningful action to enact or enforce those laws, the report notes.
The Task Force also recommends the implementation of systems to track overdose and mortality trends to provide equitable public health interventions. These measures would include comprehensive, disaggregated racial and ethnic data collection related to testing, hospitalization, and mortality associated with opioids and other substances.
“We know that ending the drug overdose epidemic will not be easy, but if policymakers allow the status quo to continue, it will be impossible,” Dr. Harris said.
“ Physicians will continue to do our part. We urge policymakers to do theirs,” she added.
A version of this article originally appeared on Medscape.com.
In the past 5 years, there has been a significant drop in the use of prescription opioids and in deaths associated with such use; but at the same time there’s been a dramatic increase in fatalities involving illicit opioids and stimulants, a new report from the American Medical Association (AMA) Opioid Task Force shows.
Although the medical community has made some important progress against the opioid epidemic, with a 37% reduction in opioid prescribing since 2013, illicit drugs are now the dominant reason why drug overdoses kill more than 70,000 people each year, the report says.
In an effort to improve the situation, the AMA Opioid Task Force is urging the removal of barriers to evidence-based care for patients who have pain and for those who have substance use disorders (SUDs). The report notes that “red tape and misguided policies are grave dangers” to these patients.
“It is critically important as we see drug overdoses increasing that we work towards reducing barriers of care for substance use abusers,” Task Force Chair Patrice A. Harris, MD, said in an interview.
“At present, the status quo is killing far too many of our loved ones and wreaking havoc in our communities,” she said.
Dr. Harris noted that “a more coordinated/integrated approach” is needed to help individuals with SUDs.
“It is vitally important that these individuals can get access to treatment. Everyone deserves the opportunity for care,” she added.
Dramatic increases
The report cites figures from the Centers for Disease Control and Prevention that indicate the following regarding the period from the beginning of 2015 to the end of 2019:
- Deaths involving illicitly manufactured and fentanyl analogues increased from 5,766 to 36,509.
- Deaths involving stimulants such as increased from 4,402 to 16,279.
- Deaths involving cocaine increased from 5,496 to 15,974.
- Deaths involving heroin increased from 10,788 to 14,079.
- Deaths involving prescription opioids decreased from 12,269 to 11,904.
The report notes that deaths involving prescription opioids peaked in July 2017 at 15,003.
Some good news
In addition to the 37% reduction in opioid prescribing in recent years, the AMA lists other points of progress, such as a large increase in prescription drug monitoring program registrations. More than 1.8 million physicians and other healthcare professionals now participate in these programs.
Also, more physicians are now certified to treat opioid use disorder. More than 85,000 physicians, as well as a growing number of nurse practitioners and physician assistants, are now certified to treat patients in the office with buprenorphine. This represents an increase of more than 50,000 from 2017.
Access to naloxone is also increasing. More than 1 million naloxone prescriptions were dispensed in 2019 – nearly double the amount in 2018. This represents a 649% increase from 2017.
“We have made some good progress, but we can’t declare victory, and there are far too many barriers to getting treatment for substance use disorder,” Dr. Harris said.
“Policymakers, public health officials, and insurance companies need to come together to create a system where there are no barriers to care for people with substance use disorder and for those needing pain medications,” she added.
At present, prior authorization is often needed before these patients can receive medication. “This involves quite a bit of administration, filling in forms, making phone calls, and this is stopping people getting the care they need,” said Dr. Harris.
“This is a highly regulated environment. There are also regulations on the amount of methadone that can be prescribed and for the prescription of buprenorphine, which has to be initiated in person,” she said.
Will COVID-19 bring change?
Dr. Harris noted that some of these regulations have been relaxed during the COVID-19 crisis so that physicians could ensure that patients have continued access to medication, and she suggested that this may pave the way for the future.
“We need now to look at this carefully and have a conversation about whether these relaxations can be continued. But this would have to be evidence based. Perhaps we can use experience from the COVID-19 period to guide future policy on this,” she said.
The report highlights that despite medical society and patient advocacy, only 21 states and the District of Columbia have enacted laws that limit public and private insurers from imposing prior authorization requirements on SUD services or medications.
The Task Force urges removal of remaining prior authorizations, step therapy, and other inappropriate administrative burdens that delay or deny care for Food and Drug Administration–approved medications used as part of medication-assisted treatment for opioid use disorder.
The organization is also calling for better implementation of mental health and substance use disorder parity laws that require health insurers to provide the same level of benefits for mental health and SUD treatment and services that they do for medical/surgical care.
At present, only a few states have taken meaningful action to enact or enforce those laws, the report notes.
The Task Force also recommends the implementation of systems to track overdose and mortality trends to provide equitable public health interventions. These measures would include comprehensive, disaggregated racial and ethnic data collection related to testing, hospitalization, and mortality associated with opioids and other substances.
“We know that ending the drug overdose epidemic will not be easy, but if policymakers allow the status quo to continue, it will be impossible,” Dr. Harris said.
“ Physicians will continue to do our part. We urge policymakers to do theirs,” she added.
A version of this article originally appeared on Medscape.com.
Stress, COVID-19 contribute to mental health concerns in college students
Socioeconomic, technological, cultural, and historical conditions are contributing to a mental health crisis among college students in the United States, according to Anthony L. Rostain, MD, MA, in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
A recent National College Health Assessment published in fall of 2018 by the American College Health Association found that one in four college students had some kind of diagnosable mental illness, and 44% had symptoms of depression within the past year.
The assessment also found that college students felt overwhelmed (86%), felt sad (68%), felt very lonely (63%), had overwhelming anxiety (62%), experienced feelings of hopelessness (53%), or were depressed to the point where functioning was difficult (41%), all of which was higher than in previous years. Students also were more likely than in previous years to engage in interpersonal violence (17%), seriously consider suicide (11%), intentionally hurt themselves (7.4%), and attempt suicide (1.9%). According to the organization Active Minds, suicide is a leading cause of death in college students.
This shift in mental health for individuals in Generation Z, those born between the mid-1990s and early 2010s, can be attributed to historical events since the turn of the century, Dr. Rostain said at the meeting, presented by Global Academy for Medical Education. The Sept. 11, 2001, attacks, wars in Iraq and Afghanistan, the financial crisis of 2007-2008, school shootings, globalization leading to economic uncertainty, the 24-hour news cycle and continuous media exposure, and the influence of the Internet have all influenced Gen Z’s identity.
“Growing up immersed in the Internet certainly has its advantages, but also maybe created some vulnerabilities in our young people,” he said.
Concerns about climate change, the burden of higher education and student debt, and the COVID-19 pandemic also have contributed to anxiety in this group. In a spring survey of students published by Active Minds about COVID-19 and its impact on mental health, 91% of students reported having stress or anxiety, 81% were disappointed or sad, 80% said they felt lonely or isolated, 56% had relocated as a result of the pandemic, and 48% reported financial setbacks tied to COVID-19.
“Anxiety seems to have become a feature of modern life,” said Dr. Rostain, who is director of education at the department of psychiatry and professor of psychiatry at the Hospital of the University of Pennsylvania in Philadelphia.
“Our culture, which often has a prominent emotional tone of fear, tends to promote cognitive distortions in which everyone is perceiving danger at every turn.” in this group, he noted. While people should be washing their hands and staying safe through social distancing during the pandemic, “we don’t want people to stop functioning, planning the future, and really in college students’ case, studying and getting ready for their careers,” he said. Parents can hinder those goals through intensively parenting or “overparenting” their children, which can result in destructive perfectionism, anxiety and depression, abject fear of failure and risk avoidance, and a focus on the external aspects of life rather than internal feelings.
Heavier alcohol use and amphetamine use also is on the rise in college students, Dr. Rostain said. Increased stimulant use in young adults is attributed to greater access to prescription drugs prior to college, greater prevalence of attention-deficit/hyperactivity disorder (ADHD), peer pressure, and influence from marketing and media messaging, he said. Another important change is the rise of smartphones and the Internet, which might drive the need to be constantly connected and compete for attention.
“This is the first generation who had constant access to the Internet. Smartphones in particular are everywhere, and we think this is another important factor in considering what might be happening to young people,” Dr. Rostain said.
Developing problem-solving and conflict resolution skills, developing coping mechanisms, being able to regulate emotions, finding optimism toward the future, having access to mental health services, and having cultural or religious beliefs with a negative view of suicide are all protective factors that promote resiliency in young people, Dr. Rostain said. Other protective factors include the development of socio-emotional readiness skills, such as conscientiousness, self-management, interpersonal skills, self-control, task persistence, risk management, self-acceptance, and having an open mindset or seeking help when needed. However, he noted, family is one area that can be both a help or a risk to mental health.
“Family attachments and supportive relationships in the family are really critical in predicting good outcomes. By the same token, families that are conflicted, where there’s a lot of stress or there’s a lot of turmoil and/or where resources are not available, that may be a risk factor to coping in young adulthood,” he said.
Individual resilience can be developed through learning from mistakes and overcoming mindset barriers, such as feelings of not belonging, concerns about disappointing one’s parents, worries about not making it, or fears of being different.
On campus, best practices and emerging trends include wellness and resiliency programs, reducing stigma, engagement from students, training of faculty and staff, crisis management plans, telehealth counseling, substance abuse programs, postvention support after suicide, collaboration with mental health providers, and support for diverse populations.
“The best schools are the ones that promote communication and that invite families to be involved early on because parents and families can be and need to be educated about what to do to prevent adverse outcomes of young people who are really at risk,” Dr. Rostain said. “It takes a village to raise a child, and it takes the same village to bring someone from adolescence to young adulthood.”
Family-based intervention has also shown promise, he said, but clinicians should watch for signs that a family is not willing to undergo therapy, is scapegoating a college student, or there are signs of boundary violations, violence, or sexual abuse in the family – or attempts to undermine treatment.
Specific to COVID-19, campus mental health services should focus on routine, self-care, physical activity, and connections with other people while also space for grieving lost experiences, facing uncertainty, developing resilience, and finding meaning. In the family, challenges around COVID-19 can include issues of physical distancing and quarantine, anxiety about becoming infected with the virus, economic insecurity, managing conflicts, setting and enforcing boundaries in addition to providing mutual support, and finding new meaning during the pandemic.
“I think these are the challenges, but we think this whole process of people living together and handling life in a way they’ve never expected to may hold some silver linings,” Dr. Rostain said. “It may be a way of addressing many issues that were never addressed before the young person went off to college.”
Global Academy and this news organization are owned by the same parent company. Dr. Rostain reported receiving royalties from Routledge/Taylor Francis Group and St. Martin’s Press, scientific advisory board honoraria from Arbor and Shire/Takeda, consulting fees from the National Football League and Tris Pharmaceuticals, and has presented CME sessions for American Psychiatric Publishing, Global Medical Education, Shire/Takeda, and the U.S. Psychiatric Congress.
Socioeconomic, technological, cultural, and historical conditions are contributing to a mental health crisis among college students in the United States, according to Anthony L. Rostain, MD, MA, in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
A recent National College Health Assessment published in fall of 2018 by the American College Health Association found that one in four college students had some kind of diagnosable mental illness, and 44% had symptoms of depression within the past year.
The assessment also found that college students felt overwhelmed (86%), felt sad (68%), felt very lonely (63%), had overwhelming anxiety (62%), experienced feelings of hopelessness (53%), or were depressed to the point where functioning was difficult (41%), all of which was higher than in previous years. Students also were more likely than in previous years to engage in interpersonal violence (17%), seriously consider suicide (11%), intentionally hurt themselves (7.4%), and attempt suicide (1.9%). According to the organization Active Minds, suicide is a leading cause of death in college students.
This shift in mental health for individuals in Generation Z, those born between the mid-1990s and early 2010s, can be attributed to historical events since the turn of the century, Dr. Rostain said at the meeting, presented by Global Academy for Medical Education. The Sept. 11, 2001, attacks, wars in Iraq and Afghanistan, the financial crisis of 2007-2008, school shootings, globalization leading to economic uncertainty, the 24-hour news cycle and continuous media exposure, and the influence of the Internet have all influenced Gen Z’s identity.
“Growing up immersed in the Internet certainly has its advantages, but also maybe created some vulnerabilities in our young people,” he said.
Concerns about climate change, the burden of higher education and student debt, and the COVID-19 pandemic also have contributed to anxiety in this group. In a spring survey of students published by Active Minds about COVID-19 and its impact on mental health, 91% of students reported having stress or anxiety, 81% were disappointed or sad, 80% said they felt lonely or isolated, 56% had relocated as a result of the pandemic, and 48% reported financial setbacks tied to COVID-19.
“Anxiety seems to have become a feature of modern life,” said Dr. Rostain, who is director of education at the department of psychiatry and professor of psychiatry at the Hospital of the University of Pennsylvania in Philadelphia.
“Our culture, which often has a prominent emotional tone of fear, tends to promote cognitive distortions in which everyone is perceiving danger at every turn.” in this group, he noted. While people should be washing their hands and staying safe through social distancing during the pandemic, “we don’t want people to stop functioning, planning the future, and really in college students’ case, studying and getting ready for their careers,” he said. Parents can hinder those goals through intensively parenting or “overparenting” their children, which can result in destructive perfectionism, anxiety and depression, abject fear of failure and risk avoidance, and a focus on the external aspects of life rather than internal feelings.
Heavier alcohol use and amphetamine use also is on the rise in college students, Dr. Rostain said. Increased stimulant use in young adults is attributed to greater access to prescription drugs prior to college, greater prevalence of attention-deficit/hyperactivity disorder (ADHD), peer pressure, and influence from marketing and media messaging, he said. Another important change is the rise of smartphones and the Internet, which might drive the need to be constantly connected and compete for attention.
“This is the first generation who had constant access to the Internet. Smartphones in particular are everywhere, and we think this is another important factor in considering what might be happening to young people,” Dr. Rostain said.
Developing problem-solving and conflict resolution skills, developing coping mechanisms, being able to regulate emotions, finding optimism toward the future, having access to mental health services, and having cultural or religious beliefs with a negative view of suicide are all protective factors that promote resiliency in young people, Dr. Rostain said. Other protective factors include the development of socio-emotional readiness skills, such as conscientiousness, self-management, interpersonal skills, self-control, task persistence, risk management, self-acceptance, and having an open mindset or seeking help when needed. However, he noted, family is one area that can be both a help or a risk to mental health.
“Family attachments and supportive relationships in the family are really critical in predicting good outcomes. By the same token, families that are conflicted, where there’s a lot of stress or there’s a lot of turmoil and/or where resources are not available, that may be a risk factor to coping in young adulthood,” he said.
Individual resilience can be developed through learning from mistakes and overcoming mindset barriers, such as feelings of not belonging, concerns about disappointing one’s parents, worries about not making it, or fears of being different.
On campus, best practices and emerging trends include wellness and resiliency programs, reducing stigma, engagement from students, training of faculty and staff, crisis management plans, telehealth counseling, substance abuse programs, postvention support after suicide, collaboration with mental health providers, and support for diverse populations.
“The best schools are the ones that promote communication and that invite families to be involved early on because parents and families can be and need to be educated about what to do to prevent adverse outcomes of young people who are really at risk,” Dr. Rostain said. “It takes a village to raise a child, and it takes the same village to bring someone from adolescence to young adulthood.”
Family-based intervention has also shown promise, he said, but clinicians should watch for signs that a family is not willing to undergo therapy, is scapegoating a college student, or there are signs of boundary violations, violence, or sexual abuse in the family – or attempts to undermine treatment.
Specific to COVID-19, campus mental health services should focus on routine, self-care, physical activity, and connections with other people while also space for grieving lost experiences, facing uncertainty, developing resilience, and finding meaning. In the family, challenges around COVID-19 can include issues of physical distancing and quarantine, anxiety about becoming infected with the virus, economic insecurity, managing conflicts, setting and enforcing boundaries in addition to providing mutual support, and finding new meaning during the pandemic.
“I think these are the challenges, but we think this whole process of people living together and handling life in a way they’ve never expected to may hold some silver linings,” Dr. Rostain said. “It may be a way of addressing many issues that were never addressed before the young person went off to college.”
Global Academy and this news organization are owned by the same parent company. Dr. Rostain reported receiving royalties from Routledge/Taylor Francis Group and St. Martin’s Press, scientific advisory board honoraria from Arbor and Shire/Takeda, consulting fees from the National Football League and Tris Pharmaceuticals, and has presented CME sessions for American Psychiatric Publishing, Global Medical Education, Shire/Takeda, and the U.S. Psychiatric Congress.
Socioeconomic, technological, cultural, and historical conditions are contributing to a mental health crisis among college students in the United States, according to Anthony L. Rostain, MD, MA, in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
A recent National College Health Assessment published in fall of 2018 by the American College Health Association found that one in four college students had some kind of diagnosable mental illness, and 44% had symptoms of depression within the past year.
The assessment also found that college students felt overwhelmed (86%), felt sad (68%), felt very lonely (63%), had overwhelming anxiety (62%), experienced feelings of hopelessness (53%), or were depressed to the point where functioning was difficult (41%), all of which was higher than in previous years. Students also were more likely than in previous years to engage in interpersonal violence (17%), seriously consider suicide (11%), intentionally hurt themselves (7.4%), and attempt suicide (1.9%). According to the organization Active Minds, suicide is a leading cause of death in college students.
This shift in mental health for individuals in Generation Z, those born between the mid-1990s and early 2010s, can be attributed to historical events since the turn of the century, Dr. Rostain said at the meeting, presented by Global Academy for Medical Education. The Sept. 11, 2001, attacks, wars in Iraq and Afghanistan, the financial crisis of 2007-2008, school shootings, globalization leading to economic uncertainty, the 24-hour news cycle and continuous media exposure, and the influence of the Internet have all influenced Gen Z’s identity.
“Growing up immersed in the Internet certainly has its advantages, but also maybe created some vulnerabilities in our young people,” he said.
Concerns about climate change, the burden of higher education and student debt, and the COVID-19 pandemic also have contributed to anxiety in this group. In a spring survey of students published by Active Minds about COVID-19 and its impact on mental health, 91% of students reported having stress or anxiety, 81% were disappointed or sad, 80% said they felt lonely or isolated, 56% had relocated as a result of the pandemic, and 48% reported financial setbacks tied to COVID-19.
“Anxiety seems to have become a feature of modern life,” said Dr. Rostain, who is director of education at the department of psychiatry and professor of psychiatry at the Hospital of the University of Pennsylvania in Philadelphia.
“Our culture, which often has a prominent emotional tone of fear, tends to promote cognitive distortions in which everyone is perceiving danger at every turn.” in this group, he noted. While people should be washing their hands and staying safe through social distancing during the pandemic, “we don’t want people to stop functioning, planning the future, and really in college students’ case, studying and getting ready for their careers,” he said. Parents can hinder those goals through intensively parenting or “overparenting” their children, which can result in destructive perfectionism, anxiety and depression, abject fear of failure and risk avoidance, and a focus on the external aspects of life rather than internal feelings.
Heavier alcohol use and amphetamine use also is on the rise in college students, Dr. Rostain said. Increased stimulant use in young adults is attributed to greater access to prescription drugs prior to college, greater prevalence of attention-deficit/hyperactivity disorder (ADHD), peer pressure, and influence from marketing and media messaging, he said. Another important change is the rise of smartphones and the Internet, which might drive the need to be constantly connected and compete for attention.
“This is the first generation who had constant access to the Internet. Smartphones in particular are everywhere, and we think this is another important factor in considering what might be happening to young people,” Dr. Rostain said.
Developing problem-solving and conflict resolution skills, developing coping mechanisms, being able to regulate emotions, finding optimism toward the future, having access to mental health services, and having cultural or religious beliefs with a negative view of suicide are all protective factors that promote resiliency in young people, Dr. Rostain said. Other protective factors include the development of socio-emotional readiness skills, such as conscientiousness, self-management, interpersonal skills, self-control, task persistence, risk management, self-acceptance, and having an open mindset or seeking help when needed. However, he noted, family is one area that can be both a help or a risk to mental health.
“Family attachments and supportive relationships in the family are really critical in predicting good outcomes. By the same token, families that are conflicted, where there’s a lot of stress or there’s a lot of turmoil and/or where resources are not available, that may be a risk factor to coping in young adulthood,” he said.
Individual resilience can be developed through learning from mistakes and overcoming mindset barriers, such as feelings of not belonging, concerns about disappointing one’s parents, worries about not making it, or fears of being different.
On campus, best practices and emerging trends include wellness and resiliency programs, reducing stigma, engagement from students, training of faculty and staff, crisis management plans, telehealth counseling, substance abuse programs, postvention support after suicide, collaboration with mental health providers, and support for diverse populations.
“The best schools are the ones that promote communication and that invite families to be involved early on because parents and families can be and need to be educated about what to do to prevent adverse outcomes of young people who are really at risk,” Dr. Rostain said. “It takes a village to raise a child, and it takes the same village to bring someone from adolescence to young adulthood.”
Family-based intervention has also shown promise, he said, but clinicians should watch for signs that a family is not willing to undergo therapy, is scapegoating a college student, or there are signs of boundary violations, violence, or sexual abuse in the family – or attempts to undermine treatment.
Specific to COVID-19, campus mental health services should focus on routine, self-care, physical activity, and connections with other people while also space for grieving lost experiences, facing uncertainty, developing resilience, and finding meaning. In the family, challenges around COVID-19 can include issues of physical distancing and quarantine, anxiety about becoming infected with the virus, economic insecurity, managing conflicts, setting and enforcing boundaries in addition to providing mutual support, and finding new meaning during the pandemic.
“I think these are the challenges, but we think this whole process of people living together and handling life in a way they’ve never expected to may hold some silver linings,” Dr. Rostain said. “It may be a way of addressing many issues that were never addressed before the young person went off to college.”
Global Academy and this news organization are owned by the same parent company. Dr. Rostain reported receiving royalties from Routledge/Taylor Francis Group and St. Martin’s Press, scientific advisory board honoraria from Arbor and Shire/Takeda, consulting fees from the National Football League and Tris Pharmaceuticals, and has presented CME sessions for American Psychiatric Publishing, Global Medical Education, Shire/Takeda, and the U.S. Psychiatric Congress.
EXPERT ANALYSIS FROM CP/AACP 2020 PSYCHIATRY UPDATE
Some telepsychiatry ‘here to stay’ post COVID
The COVID-19 pandemic has changed life in numerous ways, including use of telehealth services for patients in all specialties. But telepsychiatry is an area not likely to go away even after the pandemic is over, according to Sanjay Gupta, MD.
The use of telepsychiatry has escalated significantly,” said Dr. Gupta, of the DENT Neurologic Institute, in Amherst, N.Y., in a bonus virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
About 90% of clinicians are performing telepsychiatry, Dr. Gupta noted, through methods such as phone consults, email, and video chat. As patients with psychiatric issues grapple with issues related to COVID-19 involving lockdowns, restrictions on travel, and consumption of news, they are presenting with addiction, depression, paranoia, mood lability, and other problems.
One issue immediately facing clinicians is whether to keep patients on long-acting injectables as a way to maintain psychological stability in patients with bipolar disorder, schizophrenia, and alcoholism – something Dr. Gupta and session moderator Henry A. Nasrallah, MD, advocated. “We should never stop the long-acting injectable to switch them to oral medication. Those patients are very likely to relapse,” Dr. Nasrallah said.
During the pandemic, clinicians need to find “safe and novel ways of providing the injection,” and several methods have been pioneered. For example, if a patient with schizophrenia is on lockdown, a nurse can visit monthly or bimonthly to administer an injection, check on the patient’s mental status, and assess whether that patient needs an adjustment to their medication. Other clinics are offering “drive-by” injections to patients who arrive by car, and a nurse wearing a mask and a face shield administers the injection from the car window. Monthly naltrexone also can be administered using one of these methods, and telepsychiatry can be used to monitor patients, Dr. Gupta noted at the meeting, presented by Global Academy for Medical Education.
“In my clinic, what happens is the injection room is set up just next to the door, so they don’t have to walk deep into the clinic,” Dr. Gupta said. “They walk in, go to the left, [and] there’s the injection room. They sit, get an injection, they’re out. It’s kept smooth.”
Choosing the right telehealth option
Clinicians should be aware of important regulatory changes that occurred that made widespread telehealth more appealing during the COVID-19 pandemic. Payment parity with in-office visits makes telehealth a viable consideration, while some states have begun offering telehealth licenses to practice across state lines. There is wide variation with regard to which states provide licensure and prescribing privileges for out-of-state clinicians without seeing those patients in person. “The most important thing: The psychiatry service is provided in the state where the patient is located,” Dr. Gupta said. Clinicians should check with that state’s board to figure out specific requirements. “Preferably if you get it in writing, it’s good for you,” he said.
Deciding who the clinician is seeing – consulting with patients or other physicians/clinicians – and what type of visits a clinician will conduct is an important step in transitioning to telepsychiatry. Visits from evaluation through ongoing care are possible through telepsychiatry, or a clinician can opt to see just second opinion visits, Dr. Gupta said. It is also important to consider the technical ability of the patient to do video conferencing.
As HIPAA requirements for privacy have relaxed, clinicians now have an array of teleconferencing options to choose from; platforms such as FaceTime, Doximity, Vidyo, Doxy.me, Zoom, and video chat through EMR are popular options. However, when regular HIPAA requirements are reinstated after the pandemic, clinicians will need to find a compliant platform and sign a business associate agreement to stay within the law.
“Right now, my preferred use is FaceTime,” Dr. Gupta said. “Quick, simple, easy to use. A lot of people have an iPhone, and they know how to do it. I usually have the patient call me and I don’t use my personal iPhone; my clinic has an iPhone.”
How a clinician looks during a telepsychiatry visit is also important. Lighting, position of the camera, and clothing should all be considered. Keep the camera at eye level, test the lighting in the room where the call will take place, and use artificial lighting sources behind a computer, Dr. Gupta said. Other tips for telepsychiatry visits include silencing devices and microphones before a session begins, wearing solid-colored clothes, and having an identification badge visible to the patient. Sessions should be free of background distractions, such as a dog barking or a child interrupting, with the goal of creating an environment where the patient feels free to answer questions.
Contingency planning is a must for video visits, Dr. Gupta said. “I think the simplest thing is to see the patient. But all the stuff that’s the wraparound is really hard, because issues can arise suddenly, and we need to plan.” If a patient has a medical issue or becomes actively suicidal during a session, it is important to know contact information for the local police and crisis services. Clinicians also must plan for technology failure and provide alternative options for continuing the sessions, such as by phone.
Selecting patients for telepsychiatry
Not all patients will make the transition to telepsychiatry. “You can’t do telepsychiatry with everyone. It is a risk, so pick and choose,” Dr. Gupta said.
“Safety is a big consideration for conducting a telepsychiatry visit, especially when other health care providers are present. For example, when performing telehealth visits in a clinic, nursing home, or correctional facility, “I feel a lot more comfortable if there’s another health care clinician there,” Dr. Gupta said.
Clinicians may want to avoid a telepsychiatry visit for a patient in their own home for reasons of safety, reliability, and privacy. A longitudinal history with collateral information from friends or relatives can be helpful, but some subtle signs and body language may get missed over video, compared with an in-person visit. Sometimes you may not see if the patient is using substances. You have to really reconsider if [there] is violence and self-injurious behavior,” he said.
Discussing the pros and cons of telepsychiatry is important to obtaining patient consent. While consent requirements have relaxed under the COVID-19 pandemic, consent should ideally be obtained in writing, but can also be obtained verbally during a crisis. A plan should be developed for what will happen in the case of technology failure. “The patient should also know you’re maintaining privacy, you’re maintaining confidentiality, but there is a risk of hacking,” Dr. Gupta said. “Those things can happen, [and] there are no guarantees.”
If a patient is uncomfortable after beginning telepsychiatry, moving to in-person visits is also an option. “Many times, I do that if I’m not getting a good handle on things,” Dr. Gupta said. Situations where patients insist on in-patient visits over telepsychiatry are rare in his experience, Dr. Gupta noted, and are usually the result of the patient being unfamiliar with the technology. In cases where a patient cannot be talked through a technology barrier, visits can be done in the clinic while taking proper precautions.
“If it is a first-time visit, then I do it in the clinic,” Dr. Gupta said. “They come in, they have a face mask, and we use our group therapy room. The patients sit in a social-distanced fashion. But then, you document why you did this in-person visit like that.”
Documentation during COVID-19 also includes identifying the patient at the first visit, the nature of the visit (teleconference or other), parties present, referencing the pandemic, writing the location of the patient and the clinician, noting the patient’s satisfaction, evaluating the patient’s mental status, and recording what technology was used and any technical issues that were encountered.
Some populations of patients are better suited to telepsychiatry than others. It is more convenient for chronically psychiatrically ill patients in group homes and their staff to communicate through telepsychiatry, Dr. Gupta said. Consultation liaison in hospitals and emergency departments through telepsychiatry can limit the spread of infection, while increased access and convenience occurs as telepsychiatry is implemented in correctional facilities and nursing homes.
“What we are doing now, some of it is here to stay,” Dr. Gupta said.
In situations where a patient needs to switch providers, clinicians should continue to follow that patient until his first patient visit with that new provider. It is also important to set boundaries and apply some level of formality to the telepsychiatry visit, which means seeing the patient in a secure location where he can speak freely and privately.
“The best practices are [to] maintain faith [and] fidelity of the psychiatric assessment,” Dr. Gupta said. “Keep the trust and do your best to maintain patient privacy, because the privacy is not the same as it may be in a face-to-face session when you use televideo.”
Global Academy and this news organization are owned by the same parent company.
Dr. Gupta reported no relevant financial disclosures. Dr. Nasrallah disclosed serving as a consultant for and on the speakers bureaus of several pharmaceutical companies, including Alkermes, Janssen, and Lundbeck. He also disclosed serving on the speakers bureau of Otsuka.
The COVID-19 pandemic has changed life in numerous ways, including use of telehealth services for patients in all specialties. But telepsychiatry is an area not likely to go away even after the pandemic is over, according to Sanjay Gupta, MD.
The use of telepsychiatry has escalated significantly,” said Dr. Gupta, of the DENT Neurologic Institute, in Amherst, N.Y., in a bonus virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
About 90% of clinicians are performing telepsychiatry, Dr. Gupta noted, through methods such as phone consults, email, and video chat. As patients with psychiatric issues grapple with issues related to COVID-19 involving lockdowns, restrictions on travel, and consumption of news, they are presenting with addiction, depression, paranoia, mood lability, and other problems.
One issue immediately facing clinicians is whether to keep patients on long-acting injectables as a way to maintain psychological stability in patients with bipolar disorder, schizophrenia, and alcoholism – something Dr. Gupta and session moderator Henry A. Nasrallah, MD, advocated. “We should never stop the long-acting injectable to switch them to oral medication. Those patients are very likely to relapse,” Dr. Nasrallah said.
During the pandemic, clinicians need to find “safe and novel ways of providing the injection,” and several methods have been pioneered. For example, if a patient with schizophrenia is on lockdown, a nurse can visit monthly or bimonthly to administer an injection, check on the patient’s mental status, and assess whether that patient needs an adjustment to their medication. Other clinics are offering “drive-by” injections to patients who arrive by car, and a nurse wearing a mask and a face shield administers the injection from the car window. Monthly naltrexone also can be administered using one of these methods, and telepsychiatry can be used to monitor patients, Dr. Gupta noted at the meeting, presented by Global Academy for Medical Education.
“In my clinic, what happens is the injection room is set up just next to the door, so they don’t have to walk deep into the clinic,” Dr. Gupta said. “They walk in, go to the left, [and] there’s the injection room. They sit, get an injection, they’re out. It’s kept smooth.”
Choosing the right telehealth option
Clinicians should be aware of important regulatory changes that occurred that made widespread telehealth more appealing during the COVID-19 pandemic. Payment parity with in-office visits makes telehealth a viable consideration, while some states have begun offering telehealth licenses to practice across state lines. There is wide variation with regard to which states provide licensure and prescribing privileges for out-of-state clinicians without seeing those patients in person. “The most important thing: The psychiatry service is provided in the state where the patient is located,” Dr. Gupta said. Clinicians should check with that state’s board to figure out specific requirements. “Preferably if you get it in writing, it’s good for you,” he said.
Deciding who the clinician is seeing – consulting with patients or other physicians/clinicians – and what type of visits a clinician will conduct is an important step in transitioning to telepsychiatry. Visits from evaluation through ongoing care are possible through telepsychiatry, or a clinician can opt to see just second opinion visits, Dr. Gupta said. It is also important to consider the technical ability of the patient to do video conferencing.
As HIPAA requirements for privacy have relaxed, clinicians now have an array of teleconferencing options to choose from; platforms such as FaceTime, Doximity, Vidyo, Doxy.me, Zoom, and video chat through EMR are popular options. However, when regular HIPAA requirements are reinstated after the pandemic, clinicians will need to find a compliant platform and sign a business associate agreement to stay within the law.
“Right now, my preferred use is FaceTime,” Dr. Gupta said. “Quick, simple, easy to use. A lot of people have an iPhone, and they know how to do it. I usually have the patient call me and I don’t use my personal iPhone; my clinic has an iPhone.”
How a clinician looks during a telepsychiatry visit is also important. Lighting, position of the camera, and clothing should all be considered. Keep the camera at eye level, test the lighting in the room where the call will take place, and use artificial lighting sources behind a computer, Dr. Gupta said. Other tips for telepsychiatry visits include silencing devices and microphones before a session begins, wearing solid-colored clothes, and having an identification badge visible to the patient. Sessions should be free of background distractions, such as a dog barking or a child interrupting, with the goal of creating an environment where the patient feels free to answer questions.
Contingency planning is a must for video visits, Dr. Gupta said. “I think the simplest thing is to see the patient. But all the stuff that’s the wraparound is really hard, because issues can arise suddenly, and we need to plan.” If a patient has a medical issue or becomes actively suicidal during a session, it is important to know contact information for the local police and crisis services. Clinicians also must plan for technology failure and provide alternative options for continuing the sessions, such as by phone.
Selecting patients for telepsychiatry
Not all patients will make the transition to telepsychiatry. “You can’t do telepsychiatry with everyone. It is a risk, so pick and choose,” Dr. Gupta said.
“Safety is a big consideration for conducting a telepsychiatry visit, especially when other health care providers are present. For example, when performing telehealth visits in a clinic, nursing home, or correctional facility, “I feel a lot more comfortable if there’s another health care clinician there,” Dr. Gupta said.
Clinicians may want to avoid a telepsychiatry visit for a patient in their own home for reasons of safety, reliability, and privacy. A longitudinal history with collateral information from friends or relatives can be helpful, but some subtle signs and body language may get missed over video, compared with an in-person visit. Sometimes you may not see if the patient is using substances. You have to really reconsider if [there] is violence and self-injurious behavior,” he said.
Discussing the pros and cons of telepsychiatry is important to obtaining patient consent. While consent requirements have relaxed under the COVID-19 pandemic, consent should ideally be obtained in writing, but can also be obtained verbally during a crisis. A plan should be developed for what will happen in the case of technology failure. “The patient should also know you’re maintaining privacy, you’re maintaining confidentiality, but there is a risk of hacking,” Dr. Gupta said. “Those things can happen, [and] there are no guarantees.”
If a patient is uncomfortable after beginning telepsychiatry, moving to in-person visits is also an option. “Many times, I do that if I’m not getting a good handle on things,” Dr. Gupta said. Situations where patients insist on in-patient visits over telepsychiatry are rare in his experience, Dr. Gupta noted, and are usually the result of the patient being unfamiliar with the technology. In cases where a patient cannot be talked through a technology barrier, visits can be done in the clinic while taking proper precautions.
“If it is a first-time visit, then I do it in the clinic,” Dr. Gupta said. “They come in, they have a face mask, and we use our group therapy room. The patients sit in a social-distanced fashion. But then, you document why you did this in-person visit like that.”
Documentation during COVID-19 also includes identifying the patient at the first visit, the nature of the visit (teleconference or other), parties present, referencing the pandemic, writing the location of the patient and the clinician, noting the patient’s satisfaction, evaluating the patient’s mental status, and recording what technology was used and any technical issues that were encountered.
Some populations of patients are better suited to telepsychiatry than others. It is more convenient for chronically psychiatrically ill patients in group homes and their staff to communicate through telepsychiatry, Dr. Gupta said. Consultation liaison in hospitals and emergency departments through telepsychiatry can limit the spread of infection, while increased access and convenience occurs as telepsychiatry is implemented in correctional facilities and nursing homes.
“What we are doing now, some of it is here to stay,” Dr. Gupta said.
In situations where a patient needs to switch providers, clinicians should continue to follow that patient until his first patient visit with that new provider. It is also important to set boundaries and apply some level of formality to the telepsychiatry visit, which means seeing the patient in a secure location where he can speak freely and privately.
“The best practices are [to] maintain faith [and] fidelity of the psychiatric assessment,” Dr. Gupta said. “Keep the trust and do your best to maintain patient privacy, because the privacy is not the same as it may be in a face-to-face session when you use televideo.”
Global Academy and this news organization are owned by the same parent company.
Dr. Gupta reported no relevant financial disclosures. Dr. Nasrallah disclosed serving as a consultant for and on the speakers bureaus of several pharmaceutical companies, including Alkermes, Janssen, and Lundbeck. He also disclosed serving on the speakers bureau of Otsuka.
The COVID-19 pandemic has changed life in numerous ways, including use of telehealth services for patients in all specialties. But telepsychiatry is an area not likely to go away even after the pandemic is over, according to Sanjay Gupta, MD.
The use of telepsychiatry has escalated significantly,” said Dr. Gupta, of the DENT Neurologic Institute, in Amherst, N.Y., in a bonus virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
About 90% of clinicians are performing telepsychiatry, Dr. Gupta noted, through methods such as phone consults, email, and video chat. As patients with psychiatric issues grapple with issues related to COVID-19 involving lockdowns, restrictions on travel, and consumption of news, they are presenting with addiction, depression, paranoia, mood lability, and other problems.
One issue immediately facing clinicians is whether to keep patients on long-acting injectables as a way to maintain psychological stability in patients with bipolar disorder, schizophrenia, and alcoholism – something Dr. Gupta and session moderator Henry A. Nasrallah, MD, advocated. “We should never stop the long-acting injectable to switch them to oral medication. Those patients are very likely to relapse,” Dr. Nasrallah said.
During the pandemic, clinicians need to find “safe and novel ways of providing the injection,” and several methods have been pioneered. For example, if a patient with schizophrenia is on lockdown, a nurse can visit monthly or bimonthly to administer an injection, check on the patient’s mental status, and assess whether that patient needs an adjustment to their medication. Other clinics are offering “drive-by” injections to patients who arrive by car, and a nurse wearing a mask and a face shield administers the injection from the car window. Monthly naltrexone also can be administered using one of these methods, and telepsychiatry can be used to monitor patients, Dr. Gupta noted at the meeting, presented by Global Academy for Medical Education.
“In my clinic, what happens is the injection room is set up just next to the door, so they don’t have to walk deep into the clinic,” Dr. Gupta said. “They walk in, go to the left, [and] there’s the injection room. They sit, get an injection, they’re out. It’s kept smooth.”
Choosing the right telehealth option
Clinicians should be aware of important regulatory changes that occurred that made widespread telehealth more appealing during the COVID-19 pandemic. Payment parity with in-office visits makes telehealth a viable consideration, while some states have begun offering telehealth licenses to practice across state lines. There is wide variation with regard to which states provide licensure and prescribing privileges for out-of-state clinicians without seeing those patients in person. “The most important thing: The psychiatry service is provided in the state where the patient is located,” Dr. Gupta said. Clinicians should check with that state’s board to figure out specific requirements. “Preferably if you get it in writing, it’s good for you,” he said.
Deciding who the clinician is seeing – consulting with patients or other physicians/clinicians – and what type of visits a clinician will conduct is an important step in transitioning to telepsychiatry. Visits from evaluation through ongoing care are possible through telepsychiatry, or a clinician can opt to see just second opinion visits, Dr. Gupta said. It is also important to consider the technical ability of the patient to do video conferencing.
As HIPAA requirements for privacy have relaxed, clinicians now have an array of teleconferencing options to choose from; platforms such as FaceTime, Doximity, Vidyo, Doxy.me, Zoom, and video chat through EMR are popular options. However, when regular HIPAA requirements are reinstated after the pandemic, clinicians will need to find a compliant platform and sign a business associate agreement to stay within the law.
“Right now, my preferred use is FaceTime,” Dr. Gupta said. “Quick, simple, easy to use. A lot of people have an iPhone, and they know how to do it. I usually have the patient call me and I don’t use my personal iPhone; my clinic has an iPhone.”
How a clinician looks during a telepsychiatry visit is also important. Lighting, position of the camera, and clothing should all be considered. Keep the camera at eye level, test the lighting in the room where the call will take place, and use artificial lighting sources behind a computer, Dr. Gupta said. Other tips for telepsychiatry visits include silencing devices and microphones before a session begins, wearing solid-colored clothes, and having an identification badge visible to the patient. Sessions should be free of background distractions, such as a dog barking or a child interrupting, with the goal of creating an environment where the patient feels free to answer questions.
Contingency planning is a must for video visits, Dr. Gupta said. “I think the simplest thing is to see the patient. But all the stuff that’s the wraparound is really hard, because issues can arise suddenly, and we need to plan.” If a patient has a medical issue or becomes actively suicidal during a session, it is important to know contact information for the local police and crisis services. Clinicians also must plan for technology failure and provide alternative options for continuing the sessions, such as by phone.
Selecting patients for telepsychiatry
Not all patients will make the transition to telepsychiatry. “You can’t do telepsychiatry with everyone. It is a risk, so pick and choose,” Dr. Gupta said.
“Safety is a big consideration for conducting a telepsychiatry visit, especially when other health care providers are present. For example, when performing telehealth visits in a clinic, nursing home, or correctional facility, “I feel a lot more comfortable if there’s another health care clinician there,” Dr. Gupta said.
Clinicians may want to avoid a telepsychiatry visit for a patient in their own home for reasons of safety, reliability, and privacy. A longitudinal history with collateral information from friends or relatives can be helpful, but some subtle signs and body language may get missed over video, compared with an in-person visit. Sometimes you may not see if the patient is using substances. You have to really reconsider if [there] is violence and self-injurious behavior,” he said.
Discussing the pros and cons of telepsychiatry is important to obtaining patient consent. While consent requirements have relaxed under the COVID-19 pandemic, consent should ideally be obtained in writing, but can also be obtained verbally during a crisis. A plan should be developed for what will happen in the case of technology failure. “The patient should also know you’re maintaining privacy, you’re maintaining confidentiality, but there is a risk of hacking,” Dr. Gupta said. “Those things can happen, [and] there are no guarantees.”
If a patient is uncomfortable after beginning telepsychiatry, moving to in-person visits is also an option. “Many times, I do that if I’m not getting a good handle on things,” Dr. Gupta said. Situations where patients insist on in-patient visits over telepsychiatry are rare in his experience, Dr. Gupta noted, and are usually the result of the patient being unfamiliar with the technology. In cases where a patient cannot be talked through a technology barrier, visits can be done in the clinic while taking proper precautions.
“If it is a first-time visit, then I do it in the clinic,” Dr. Gupta said. “They come in, they have a face mask, and we use our group therapy room. The patients sit in a social-distanced fashion. But then, you document why you did this in-person visit like that.”
Documentation during COVID-19 also includes identifying the patient at the first visit, the nature of the visit (teleconference or other), parties present, referencing the pandemic, writing the location of the patient and the clinician, noting the patient’s satisfaction, evaluating the patient’s mental status, and recording what technology was used and any technical issues that were encountered.
Some populations of patients are better suited to telepsychiatry than others. It is more convenient for chronically psychiatrically ill patients in group homes and their staff to communicate through telepsychiatry, Dr. Gupta said. Consultation liaison in hospitals and emergency departments through telepsychiatry can limit the spread of infection, while increased access and convenience occurs as telepsychiatry is implemented in correctional facilities and nursing homes.
“What we are doing now, some of it is here to stay,” Dr. Gupta said.
In situations where a patient needs to switch providers, clinicians should continue to follow that patient until his first patient visit with that new provider. It is also important to set boundaries and apply some level of formality to the telepsychiatry visit, which means seeing the patient in a secure location where he can speak freely and privately.
“The best practices are [to] maintain faith [and] fidelity of the psychiatric assessment,” Dr. Gupta said. “Keep the trust and do your best to maintain patient privacy, because the privacy is not the same as it may be in a face-to-face session when you use televideo.”
Global Academy and this news organization are owned by the same parent company.
Dr. Gupta reported no relevant financial disclosures. Dr. Nasrallah disclosed serving as a consultant for and on the speakers bureaus of several pharmaceutical companies, including Alkermes, Janssen, and Lundbeck. He also disclosed serving on the speakers bureau of Otsuka.
EXPERT ANALYSIS FROM CP/AACP 2020 PSYCHIATRY UPDATE
Managing amidst COVID-19 (and everything else that ails us)
This year, medical media has been dominated by reporting on the devastating COVID-19 pandemic. Many studies and analyses have shown that staying at home, social distancing, quarantining of close contacts, and wearing face masks and face shields are effective ways of preventing spread.
Although initially there were no known effective treatments for severe COVID-19 infection (other than oxygen and ventilator support), we now know that dexamethasone,1 remdesivir,2 and convalescent plasma3 are effective in lessening the severity of illness and perhaps preventing death. That said, we will continue to struggle with COVID-19 for the foreseeable future.
But other medical illnesses actually predominate in terms of morbidity and mortality, even during this pandemic. For example, although there has been an average of roughly 5600 COVID-19-related deaths per week for the past 4 months,4 there are, on average, more than 54,000 deaths per week in the United States from other causes.5 This means that we must continue to tend to the other health care needs of our patients even as we deal with COVID-19.
In that light, JFP continues to publish practical, evidence-based clinical reviews designed to keep family physicians and other primary health care clinicians up to date on a variety of topics. For instance, in this issue of JFP, we have articles on:
- Opioid prescribing. Although opioids have risks, they remain potent medications for relief from acute pain, as well as cancer-related pain and chronic pain not sufficiently treated with other medications. Mahvan et al provide expert advice on maximizing benefit and minimizing the risks of opioid prescribing.
- Secondary ischemic stroke prevention. For patients who have suffered a transient ischemic attack or minor stroke, a mainstay of prevention is antiplatelet therapy. Aspirin alone used to be the treatment of choice, but research has demonstrated the value of adding another antiplatelet agent. Helmer et al’s thorough review reminds us that the antiplatelet drug of choice, in addition to aspirin, is clopidogrel, which should be used only for the first 30 days after the event because of an increased bleeding risk.
- Combatting Clostridioides difficile infection. CDI has been a difficult condition to treat, especially in high-risk patients. Zukauckas et al provide a comprehensive review of diagnosis and management. Vancomycin is now the drug of choice, and fecal transplant is highly effective in preventing recurrent CDI.
This diverse range of timely, practical, evidence-based guidance—in addition to coverage of COVID-19 and other rapidly emerging medical news stories—can all be found on our Web site at www.mdedge.com/familymedicine. We remain committed to supplying you with all of the information you need to provide your patients with the very best care—no matter what brings them in to see you.
1. Low-cost dexamethasone reduces death by up to one third in hospitalized patients with severe respiratory complications of COVID-19. Recovery: Randomised Evaluation of COVID-19 Therapy Web site. June 16, 2020. www.recoverytrial.net/news/low-cost-dexamethasone-reduces-death-by-up-to-one-third-in-hospitalised-patients-with-severe-respiratory-complications-of-covid-19. Accessed July 1, 2020.
2. Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of Covid-19—preliminary report [published online ahead of print]. N Engl J Med. doi: 10.1056/NEJMoa2007764.
3. Li L, Zhang W, Hu Y, et. al. Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and life-threatening COVID-19: a randomized clinical trial [published online ahead of print]. JAMA. doi:10.1001/jama.2020.10044.
4. Stokes EK, Zambrano LD, Anderson KN, et al. Coronavirus disease 2019 case surveillance—United States, January 22–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:759-765.
5. Xu J, Murphy SL, Kochanek KD, et al. Mortality in the United States, 2018. NCHS Data Brief. 2020;1-8.
This year, medical media has been dominated by reporting on the devastating COVID-19 pandemic. Many studies and analyses have shown that staying at home, social distancing, quarantining of close contacts, and wearing face masks and face shields are effective ways of preventing spread.
Although initially there were no known effective treatments for severe COVID-19 infection (other than oxygen and ventilator support), we now know that dexamethasone,1 remdesivir,2 and convalescent plasma3 are effective in lessening the severity of illness and perhaps preventing death. That said, we will continue to struggle with COVID-19 for the foreseeable future.
But other medical illnesses actually predominate in terms of morbidity and mortality, even during this pandemic. For example, although there has been an average of roughly 5600 COVID-19-related deaths per week for the past 4 months,4 there are, on average, more than 54,000 deaths per week in the United States from other causes.5 This means that we must continue to tend to the other health care needs of our patients even as we deal with COVID-19.
In that light, JFP continues to publish practical, evidence-based clinical reviews designed to keep family physicians and other primary health care clinicians up to date on a variety of topics. For instance, in this issue of JFP, we have articles on:
- Opioid prescribing. Although opioids have risks, they remain potent medications for relief from acute pain, as well as cancer-related pain and chronic pain not sufficiently treated with other medications. Mahvan et al provide expert advice on maximizing benefit and minimizing the risks of opioid prescribing.
- Secondary ischemic stroke prevention. For patients who have suffered a transient ischemic attack or minor stroke, a mainstay of prevention is antiplatelet therapy. Aspirin alone used to be the treatment of choice, but research has demonstrated the value of adding another antiplatelet agent. Helmer et al’s thorough review reminds us that the antiplatelet drug of choice, in addition to aspirin, is clopidogrel, which should be used only for the first 30 days after the event because of an increased bleeding risk.
- Combatting Clostridioides difficile infection. CDI has been a difficult condition to treat, especially in high-risk patients. Zukauckas et al provide a comprehensive review of diagnosis and management. Vancomycin is now the drug of choice, and fecal transplant is highly effective in preventing recurrent CDI.
This diverse range of timely, practical, evidence-based guidance—in addition to coverage of COVID-19 and other rapidly emerging medical news stories—can all be found on our Web site at www.mdedge.com/familymedicine. We remain committed to supplying you with all of the information you need to provide your patients with the very best care—no matter what brings them in to see you.
This year, medical media has been dominated by reporting on the devastating COVID-19 pandemic. Many studies and analyses have shown that staying at home, social distancing, quarantining of close contacts, and wearing face masks and face shields are effective ways of preventing spread.
Although initially there were no known effective treatments for severe COVID-19 infection (other than oxygen and ventilator support), we now know that dexamethasone,1 remdesivir,2 and convalescent plasma3 are effective in lessening the severity of illness and perhaps preventing death. That said, we will continue to struggle with COVID-19 for the foreseeable future.
But other medical illnesses actually predominate in terms of morbidity and mortality, even during this pandemic. For example, although there has been an average of roughly 5600 COVID-19-related deaths per week for the past 4 months,4 there are, on average, more than 54,000 deaths per week in the United States from other causes.5 This means that we must continue to tend to the other health care needs of our patients even as we deal with COVID-19.
In that light, JFP continues to publish practical, evidence-based clinical reviews designed to keep family physicians and other primary health care clinicians up to date on a variety of topics. For instance, in this issue of JFP, we have articles on:
- Opioid prescribing. Although opioids have risks, they remain potent medications for relief from acute pain, as well as cancer-related pain and chronic pain not sufficiently treated with other medications. Mahvan et al provide expert advice on maximizing benefit and minimizing the risks of opioid prescribing.
- Secondary ischemic stroke prevention. For patients who have suffered a transient ischemic attack or minor stroke, a mainstay of prevention is antiplatelet therapy. Aspirin alone used to be the treatment of choice, but research has demonstrated the value of adding another antiplatelet agent. Helmer et al’s thorough review reminds us that the antiplatelet drug of choice, in addition to aspirin, is clopidogrel, which should be used only for the first 30 days after the event because of an increased bleeding risk.
- Combatting Clostridioides difficile infection. CDI has been a difficult condition to treat, especially in high-risk patients. Zukauckas et al provide a comprehensive review of diagnosis and management. Vancomycin is now the drug of choice, and fecal transplant is highly effective in preventing recurrent CDI.
This diverse range of timely, practical, evidence-based guidance—in addition to coverage of COVID-19 and other rapidly emerging medical news stories—can all be found on our Web site at www.mdedge.com/familymedicine. We remain committed to supplying you with all of the information you need to provide your patients with the very best care—no matter what brings them in to see you.
1. Low-cost dexamethasone reduces death by up to one third in hospitalized patients with severe respiratory complications of COVID-19. Recovery: Randomised Evaluation of COVID-19 Therapy Web site. June 16, 2020. www.recoverytrial.net/news/low-cost-dexamethasone-reduces-death-by-up-to-one-third-in-hospitalised-patients-with-severe-respiratory-complications-of-covid-19. Accessed July 1, 2020.
2. Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of Covid-19—preliminary report [published online ahead of print]. N Engl J Med. doi: 10.1056/NEJMoa2007764.
3. Li L, Zhang W, Hu Y, et. al. Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and life-threatening COVID-19: a randomized clinical trial [published online ahead of print]. JAMA. doi:10.1001/jama.2020.10044.
4. Stokes EK, Zambrano LD, Anderson KN, et al. Coronavirus disease 2019 case surveillance—United States, January 22–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:759-765.
5. Xu J, Murphy SL, Kochanek KD, et al. Mortality in the United States, 2018. NCHS Data Brief. 2020;1-8.
1. Low-cost dexamethasone reduces death by up to one third in hospitalized patients with severe respiratory complications of COVID-19. Recovery: Randomised Evaluation of COVID-19 Therapy Web site. June 16, 2020. www.recoverytrial.net/news/low-cost-dexamethasone-reduces-death-by-up-to-one-third-in-hospitalised-patients-with-severe-respiratory-complications-of-covid-19. Accessed July 1, 2020.
2. Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of Covid-19—preliminary report [published online ahead of print]. N Engl J Med. doi: 10.1056/NEJMoa2007764.
3. Li L, Zhang W, Hu Y, et. al. Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and life-threatening COVID-19: a randomized clinical trial [published online ahead of print]. JAMA. doi:10.1001/jama.2020.10044.
4. Stokes EK, Zambrano LD, Anderson KN, et al. Coronavirus disease 2019 case surveillance—United States, January 22–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:759-765.
5. Xu J, Murphy SL, Kochanek KD, et al. Mortality in the United States, 2018. NCHS Data Brief. 2020;1-8.
Travel times to opioid addiction programs drive a lack of access to treatment
If US pharmacies were permitted to dispense methadone for opioid use disorder (OUD) it would improve national access to treatment and save costs, new research suggests.
Under current federal regulations, only opioid treatment programs (OTPs) are permitted to dispense methadone maintenance treatment. This stands in sharp contrast to how methadone is dispensed in Canada, Australia, and the United Kingdom, where patients can obtain daily doses of methadone maintenance from community pharmacies.
“It’s challenging for patients in many parts of the US to access methadone treatment,” Robert Kleinman, MD, of Stanford University School of Medicine, Stanford, California, said in a JAMA Psychiatry podcast.
“It’s important for policymakers to consider strategies that enhance access to methadone maintenance treatment, in that it’s associated with large reductions in mortality from opioid use disorder. One possibility is to use pharmacies as dispensing sites,” said Kleinman.
The study was published online July 15 in JAMA Psychiatry.
An Hour vs 10 Minutes
Kleinman examined how pharmacy-based dispensing would affect drive times to the nearest OTP for the general US population. The analysis included all 1682 OTP locations, 69,475 unique pharmacy locations, and 72,443 census tracts.
The average drive time to OTPs in the US is 20.4 minutes vs a drive time of 4.5 minutes to pharmacies.
Driving times to OTPs are particularly long in nonmetropolitan counties while pharmacies remain “relatively easily accessible” in nonmetropolitan counties, he said.
In “micropolitan” counties, for example, the drive time to OTPs was 48.4 minutes vs 7 minutes to pharmacies. In the most rural counties, the drive time to OTPs is 60.9 minutes vs 9.1 minutes to pharmacies.
“This suggests that pharmacy-based dispensing has the potential to reduce urban or rural inequities, and access to methadone treatment,” Kleinman said.
In a mileage cost analysis, Kleinman determined that the average cost of one-way trip to an OTP in the US is $3.12 compared with 45 cents to a pharmacy. In the most rural counties, the average cost one-way is $11.10 vs $1.27 to a pharmacy.
Kleinman says decreasing drive times, distance, and costs for patients seeking methadone treatment by allowing pharmacies to dispense the medication may help achieve several public health goals.
“Patients dissuaded from obtaining treatment because of extended travel, particularly patients with disabilities, unreliable access to transportation, or from rural regions, would have reduced barriers to care. Quality of life may be increased for the more than 380,000 individuals currently receiving methadone treatment if less time is spent commuting,” he writes.
Time for Change
The authors of an accompanying editorial, say the “regulatory burden” on methadone provision in the US “effectively prohibits the integration of methadone prescribing into primary care, even in rural communities where there may exist no specialty substance use treatment options.”
However, federal and state agencies are starting to take action to expand geographic access to methadone treatment, note Paul Joudrey, MD, MPH, and coauthors from Yale School of Medicine, New Haven, Connecticut.
, and Ohio and Kentucky have passed laws to allow greater use of federally qualified health centers and other facilities for methadone dispensing.
“While these policies are welcomed, the results here by Kleinman and others suggest they fall short of needed expansion if patients’ rights to evidence-based care for OUD are to be ensured. Importantly, even with broad adoption of mobile or pharmacy-based dispensing, patients would still face a long drive time to a central OTP before starting methadone,” Joudrey and colleagues write.
In their view, the only way to address this barrier is to modify federal law, and this “should be urgently pursued in the context of the ongoing overdose epidemic. It is time for policies that truly support methadone treatment for OUD as opposed to focusing on diversion.”
This article first appeared on Medscape.com.
If US pharmacies were permitted to dispense methadone for opioid use disorder (OUD) it would improve national access to treatment and save costs, new research suggests.
Under current federal regulations, only opioid treatment programs (OTPs) are permitted to dispense methadone maintenance treatment. This stands in sharp contrast to how methadone is dispensed in Canada, Australia, and the United Kingdom, where patients can obtain daily doses of methadone maintenance from community pharmacies.
“It’s challenging for patients in many parts of the US to access methadone treatment,” Robert Kleinman, MD, of Stanford University School of Medicine, Stanford, California, said in a JAMA Psychiatry podcast.
“It’s important for policymakers to consider strategies that enhance access to methadone maintenance treatment, in that it’s associated with large reductions in mortality from opioid use disorder. One possibility is to use pharmacies as dispensing sites,” said Kleinman.
The study was published online July 15 in JAMA Psychiatry.
An Hour vs 10 Minutes
Kleinman examined how pharmacy-based dispensing would affect drive times to the nearest OTP for the general US population. The analysis included all 1682 OTP locations, 69,475 unique pharmacy locations, and 72,443 census tracts.
The average drive time to OTPs in the US is 20.4 minutes vs a drive time of 4.5 minutes to pharmacies.
Driving times to OTPs are particularly long in nonmetropolitan counties while pharmacies remain “relatively easily accessible” in nonmetropolitan counties, he said.
In “micropolitan” counties, for example, the drive time to OTPs was 48.4 minutes vs 7 minutes to pharmacies. In the most rural counties, the drive time to OTPs is 60.9 minutes vs 9.1 minutes to pharmacies.
“This suggests that pharmacy-based dispensing has the potential to reduce urban or rural inequities, and access to methadone treatment,” Kleinman said.
In a mileage cost analysis, Kleinman determined that the average cost of one-way trip to an OTP in the US is $3.12 compared with 45 cents to a pharmacy. In the most rural counties, the average cost one-way is $11.10 vs $1.27 to a pharmacy.
Kleinman says decreasing drive times, distance, and costs for patients seeking methadone treatment by allowing pharmacies to dispense the medication may help achieve several public health goals.
“Patients dissuaded from obtaining treatment because of extended travel, particularly patients with disabilities, unreliable access to transportation, or from rural regions, would have reduced barriers to care. Quality of life may be increased for the more than 380,000 individuals currently receiving methadone treatment if less time is spent commuting,” he writes.
Time for Change
The authors of an accompanying editorial, say the “regulatory burden” on methadone provision in the US “effectively prohibits the integration of methadone prescribing into primary care, even in rural communities where there may exist no specialty substance use treatment options.”
However, federal and state agencies are starting to take action to expand geographic access to methadone treatment, note Paul Joudrey, MD, MPH, and coauthors from Yale School of Medicine, New Haven, Connecticut.
, and Ohio and Kentucky have passed laws to allow greater use of federally qualified health centers and other facilities for methadone dispensing.
“While these policies are welcomed, the results here by Kleinman and others suggest they fall short of needed expansion if patients’ rights to evidence-based care for OUD are to be ensured. Importantly, even with broad adoption of mobile or pharmacy-based dispensing, patients would still face a long drive time to a central OTP before starting methadone,” Joudrey and colleagues write.
In their view, the only way to address this barrier is to modify federal law, and this “should be urgently pursued in the context of the ongoing overdose epidemic. It is time for policies that truly support methadone treatment for OUD as opposed to focusing on diversion.”
This article first appeared on Medscape.com.
If US pharmacies were permitted to dispense methadone for opioid use disorder (OUD) it would improve national access to treatment and save costs, new research suggests.
Under current federal regulations, only opioid treatment programs (OTPs) are permitted to dispense methadone maintenance treatment. This stands in sharp contrast to how methadone is dispensed in Canada, Australia, and the United Kingdom, where patients can obtain daily doses of methadone maintenance from community pharmacies.
“It’s challenging for patients in many parts of the US to access methadone treatment,” Robert Kleinman, MD, of Stanford University School of Medicine, Stanford, California, said in a JAMA Psychiatry podcast.
“It’s important for policymakers to consider strategies that enhance access to methadone maintenance treatment, in that it’s associated with large reductions in mortality from opioid use disorder. One possibility is to use pharmacies as dispensing sites,” said Kleinman.
The study was published online July 15 in JAMA Psychiatry.
An Hour vs 10 Minutes
Kleinman examined how pharmacy-based dispensing would affect drive times to the nearest OTP for the general US population. The analysis included all 1682 OTP locations, 69,475 unique pharmacy locations, and 72,443 census tracts.
The average drive time to OTPs in the US is 20.4 minutes vs a drive time of 4.5 minutes to pharmacies.
Driving times to OTPs are particularly long in nonmetropolitan counties while pharmacies remain “relatively easily accessible” in nonmetropolitan counties, he said.
In “micropolitan” counties, for example, the drive time to OTPs was 48.4 minutes vs 7 minutes to pharmacies. In the most rural counties, the drive time to OTPs is 60.9 minutes vs 9.1 minutes to pharmacies.
“This suggests that pharmacy-based dispensing has the potential to reduce urban or rural inequities, and access to methadone treatment,” Kleinman said.
In a mileage cost analysis, Kleinman determined that the average cost of one-way trip to an OTP in the US is $3.12 compared with 45 cents to a pharmacy. In the most rural counties, the average cost one-way is $11.10 vs $1.27 to a pharmacy.
Kleinman says decreasing drive times, distance, and costs for patients seeking methadone treatment by allowing pharmacies to dispense the medication may help achieve several public health goals.
“Patients dissuaded from obtaining treatment because of extended travel, particularly patients with disabilities, unreliable access to transportation, or from rural regions, would have reduced barriers to care. Quality of life may be increased for the more than 380,000 individuals currently receiving methadone treatment if less time is spent commuting,” he writes.
Time for Change
The authors of an accompanying editorial, say the “regulatory burden” on methadone provision in the US “effectively prohibits the integration of methadone prescribing into primary care, even in rural communities where there may exist no specialty substance use treatment options.”
However, federal and state agencies are starting to take action to expand geographic access to methadone treatment, note Paul Joudrey, MD, MPH, and coauthors from Yale School of Medicine, New Haven, Connecticut.
, and Ohio and Kentucky have passed laws to allow greater use of federally qualified health centers and other facilities for methadone dispensing.
“While these policies are welcomed, the results here by Kleinman and others suggest they fall short of needed expansion if patients’ rights to evidence-based care for OUD are to be ensured. Importantly, even with broad adoption of mobile or pharmacy-based dispensing, patients would still face a long drive time to a central OTP before starting methadone,” Joudrey and colleagues write.
In their view, the only way to address this barrier is to modify federal law, and this “should be urgently pursued in the context of the ongoing overdose epidemic. It is time for policies that truly support methadone treatment for OUD as opposed to focusing on diversion.”
This article first appeared on Medscape.com.
Tips and tools for safe opioid prescribing
CASE
Marcelo G* is a 46-year-old man who presented to our family medicine clinic with a complex medical history including end-stage renal disease (ESRD) and hemodialysis, chronic anemia, peripheral vascular disease, venous thromboembolism and anticoagulation, major depressive disorder, osteoarthritis, and lumbosacral radiculopathy. His current medications included vitamin B complex, cholecalciferol, atorvastatin, warfarin, acetaminophen, diclofenac gel, and capsaicin cream. Mr. G reported bothersome bilateral knee and back pain despite physical therapy and consistent use of his current medications in addition to occasional intra-articular glucocorticoid injections. He mentioned that he had benefited in the past from intermittent opioid use.
How would you manage this patient’s care?
*The patient’s name has been changed to protect his identity.
In 2013, an estimated 191 million prescriptions for opioids were written by health care providers, which is the equivalent of all adults living in the United States having their own opioid prescription.1 This large expansion in opioid prescribing and use has also led to a rise in opioid overdose deaths, whether from prescribed or illicit use.1 The Centers for Disease Control and Prevention (CDC) points out that each day, approximately 128 Americans die from an opioid overdose.1 Deaths that occur from opioid overdose often involve the prescribed opioids methadone, oxycodone, and hydrocodone, the illicit opioid heroin, and, of particular concern, prescription and illicit fentanyl.1
The extent of this problem has sparked the development of health safety initiatives and research efforts. Through production quotas, the US Drug Enforcement Administration (DEA) reduced the number of opioids produced across all schedule I and schedule II lists in 2017 by as much as 25%.2 The DEA again reduced the amounts produced in 2018.3 For 2020, the DEA has determined that the production quotas and assessment of annual needs are sufficient.4
The CDC has also promoted access to naloxone and prevention initiatives; pharmacies in some states have standing orders for naloxone, and medical personnel and law enforcement now carry it.1,5 Finally, new research has identified risk factors that influence one’s potential for addiction, such as mental illness, history of substance and alcohol abuse, and a low income.6 Interestingly, while numerous initiatives and strategies have been implemented across health systems, there is little evidence that demonstrates how implementation of safe prescribing strategies has affected overall patient safety and avoidance of opioid-related harms.
Nevertheless, concerns related to opioids are especially important for primary care providers, who manage many patients with acute and chronic diseases and disorders that require pain control.7 Family physicians write more opioid prescriptions than any other specialty,8 and they are therefore uniquely positioned to protect patients, improve the quality of their care, and ultimately produce a meaningful public health impact. This article provides a guide to safe opioid prescribing.
Continue to: Use the patient interview to ensure that Tx aligns with patient goals
Use the patient interview to ensure that Tx aligns with patient goals
For patients presenting with chronic pain, conduct a complete general history and physical examination that includes a review of available records; a medical, surgical, social, family, medication, and allergy history; a review of systems; and documentation of any psychiatric comorbidities (ie, depression, anxiety, psychiatric disorders, personality traits). Inquiries about social history and current medications should explore the possibility of previous and current substance use and misuse.
While causes of pain can be assessed through physical examination and diagnostic tests, the patient interview is an invaluable source of information. No single means of assessment has consistently demonstrated superiority over another in measuring pain, and numerous standard assessment tools are available (TABLE 19-13).14 Unidimensional tools are often easy and quick ways to assess pain intensity. Multidimensional tools, although more time intensive, are designed to gather more subjective information about the patient’s pain. Finally, use an instrument such as the 9-item Patient Health Questionnaire (PHQ-9) to screen patients for psychological distress.15,16
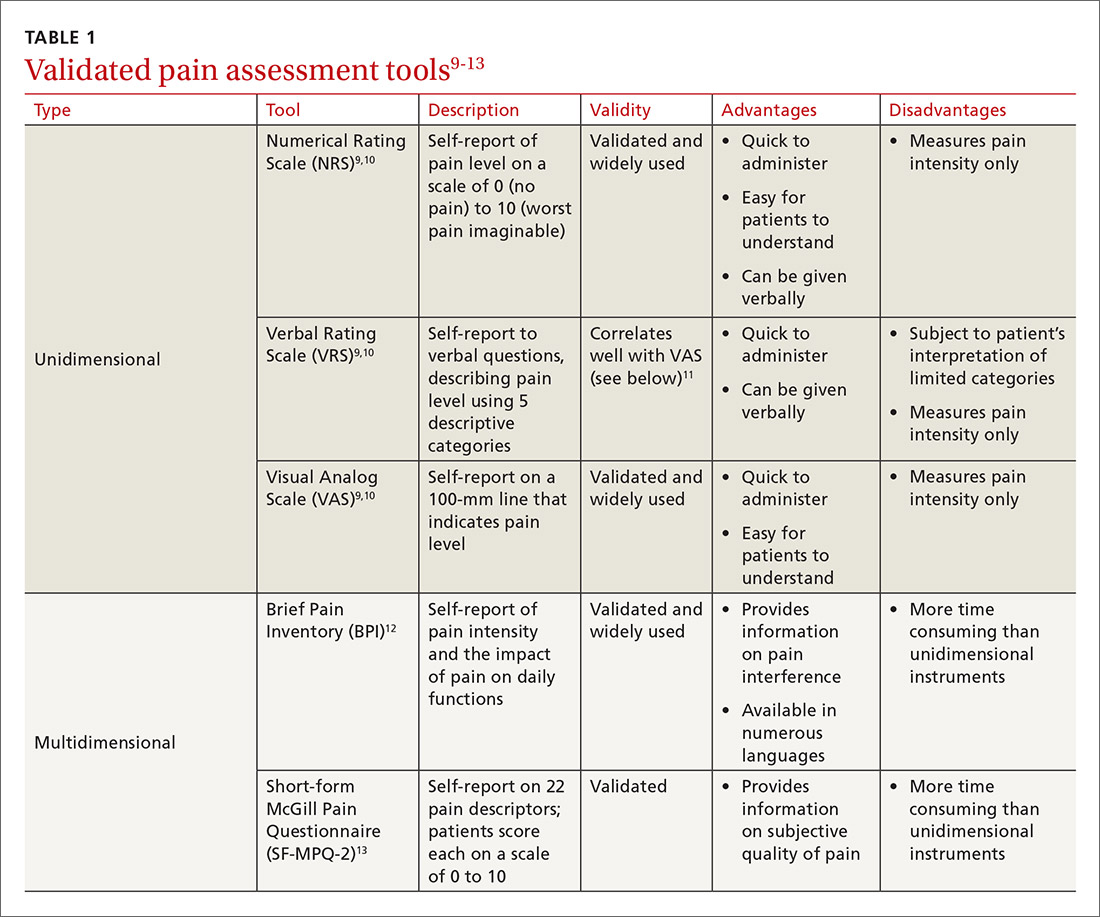
Provide an environment for patients to openly discuss their experiences, expectations, preferences, fears, and coping efforts, as well as the impact that pain has had on their lives.17,18 Without this foundational understanding, medical treatment may work against the patient’s goals. An empathic approach allows for effective communication, shared decision making, and ultimately, an avenue for individualized therapy.
Balancing treatment with risk mitigation
The challenge of managing chronic pain is to balance treating the patient with the basic principle of nonmaleficence (primum non nocere: “first, do no harm”). The literature has shown that risk factors such as a family history of substance abuse or sexual abuse, younger age, and psychological disease may be linked to greater risk for opioid misuse.19,20 However, despite the many risk-screening tools available, no single instrument has reliably and accurately predicted those at higher propensity for prescription addiction. In fact, risk-screening tools as a whole remain unregulated by the US Food and Drug Administration (FDA) and other authorities.21 Still, screening tools provide useful information as one component of the risk-mitigation process.
Screening tools. The tools most commonly used clinically to stratify risk prior to prescribing opioids are the 5-item Opioid Risk Tool (ORT),22 the revised 24-item Screener and Opioid Assessment for Patients with Pain (SOAPP-R),23 which are patient self-administered assessments, and the 7-item clinician-administered DIRE (Diagnosis, Intractability, Risk, Efficacy).24 Given the subtle differences in criteria and the time required for each of these risk assessments, we recommend choosing one based on site-specific resources and overall clinician comfort.25 Risk stratification helps to determine the optimal frequency and intensity of monitoring, not necessarily to deny care to “high-risk” patients.
Continue to: In fact, just as the "universal precautions"...
In fact, just as the “universal precautions” approach has been applied to infection control, many have suggested using a similar approach to pain management. Risk screening should never be misunderstood as an attempt to diminish or undermine the patient’s burden of pain. By routinely conducting thorough and respectful inquiries of risk factors for all patients, clinicians can reduce stigma, improve care, and contain overall risk.26,27
Monitoring programs and patient agreements. In addition to risk-screening tools, the CDC recommends using state prescription drug monitoring programs (PDMP) and urine drug testing (UDT) data to confirm the use of prescribed and illicit substances.28 All 50 states have implemented PDMPs.29 Consider incorporating these components into controlled-substance agreements, which ultimately aim to promote safety and trust between patients and providers. Of course, such agreements do not eliminate all risks associated with opioid prescribing, nor do they guarantee the absence of adverse outcomes. However, when used correctly, they can provide safeguards to reduce misuse and abuse. They also have the potential to preserve the patient-provider relationship, as opposed to providers cursorily refusing to prescribe opioids altogether. The term “controlled-substance agreement” is preferable to “pain contract” or “narcotic contract” as the latter 2 terms may feel stigmatizing and threatening.30
Risk evaluation and mitigation strategy (REMS). In an effort to ensure that benefits of opioid analgesics continue to outweigh the risks, the FDA approved the extended-release (ER)/long-acting (LA) opioid analgesics shared system REMS. Under this REMS, a consortium of ER/LA opioid manufacturers is mandated to provide prescriber education in the form of accredited continuing education and patient educational materials, available at https://opioidanalgesicrems.com/RpcUI/home.u.
CASE
After reviewing Mr. G’s chart and conducting a history, we learned that his bilateral knee osteoarthritis was atraumatic and likely due to overuse—although possibly affected by major trauma in a motor vehicle accident 5 years earlier. Imaging also revealed multilevel disc degeneration contributing to his radicular back pain, which seemed to be worse on days after working as a caterer. Poor lifting form at work may have contributed to his pain. Nevertheless, he had been consistent with medical follow-up and denied current or past use of illicit substances. Per the numeric rating scale (NRS), he reported 8 out of 10 pain in his knees and 6 out of 10 in his back. In addition to obtaining a PHQ-9 score of 4, we conducted a DIRE assessment and obtained a score of 19 out of a possible 21, indicating that he may be a good candidate for long-term opioid analgesia.
Criteria for prescribing opioids and for guiding treatment goals
Prescribing an opioid requires establishing a medical necessity based on 3 criteria:31
- pain of moderate-to-severe degree
- a physical diagnosis or suspected organic problem
- documented treatment failure of a noncontrolled substance, adjuvant agents, physician-ordered physical therapy, structured exercise program, and interventional techniques.
Continue to: Treatment goals should be established...
Treatment goals should be established and understood by the prescriber and patient prior to initiation of opioids.28 Overarching treatment goals for all opioids prescribed are pain relief (but not necessarily a focus on pain scores), improvement in functional activity, and minimization of adverse effects, with the latter 2 goals taking precedence.31 To assess outcomes, formally measure progress toward goals from baseline evaluations. This can be achieved through repeated use of validated tools such as those mentioned earlier, or may be more broadly considered as progress toward employment status or increasing participation in activities.31 All pain management plans involving opioids should include continued efforts with nonpharmacologic therapy (eg, exercise therapy, weight loss, behavioral training) and nonopioid pharmacologic therapy (eg, nonsteroidal anti-inflammatory drugs, tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors, anticonvulsants).28
Have an “exit strategy.” As part of goal setting, also consider how therapy will be discontinued if benefits do not outweigh the risks of harm.28 Weigh functional status gains against adverse opioid consequences using the PEG scale (pain, enjoyment of life, and general activity) (TABLE 232).33 Improvements of 30% from baseline have been deemed clinically meaningful by some,32 but not all benefits will be easy to quantify. At the start of treatment dialogue, use the term “therapeutic trial” instead of ”treatment plan” to more effectively convey that opioids will be continued only if safe and effective, and will be prescribed at the lowest effective dose as one component of the multimodal approach to pain.30
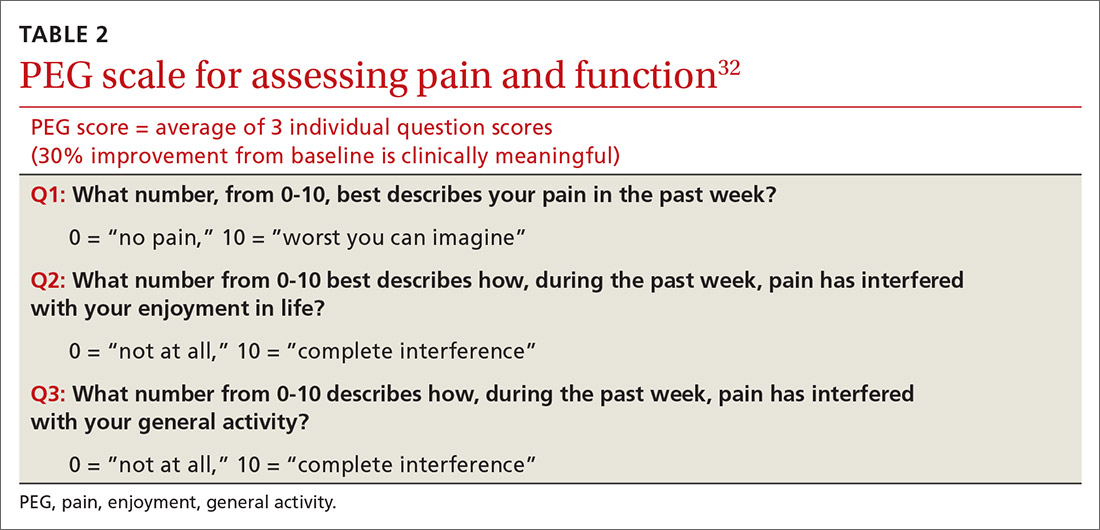
Initiation of treatment: Opioid selection and dosing
When initiating opioid therapy, prescribe an immediate-release, short-acting agent instead of an ER/LA formulation.28
For moderate pain, first consider tramadol, codeine, tapentadol, or hydrocodone.31 Second-line agents for moderate pain are hydrocodone or oxycodone.31
For severe pain, first-line agents include hydrocodone, oxycodone, hydromorphone, or morphine.31 Second-line agents for severe pain are fentanyl and, with careful supervision or referral to a pain specialist, methadone or buprenorphine.31
Continue to: Of special note...
Of special note,

At the start, prescribe the lowest effective dosage (referring to the product labeling for guidance) and calculate total daily dose in terms of morphine milligram equivalents (MME) (TABLE 335-37).28 Exercise caution when considering opioids for patients with respiratory sleep disorders and for patients ≥ 65 years due to altered pharmacokinetics in the elderly population.38 Also make dose adjustments for renal and hepatic insufficiency (TABLE 435).
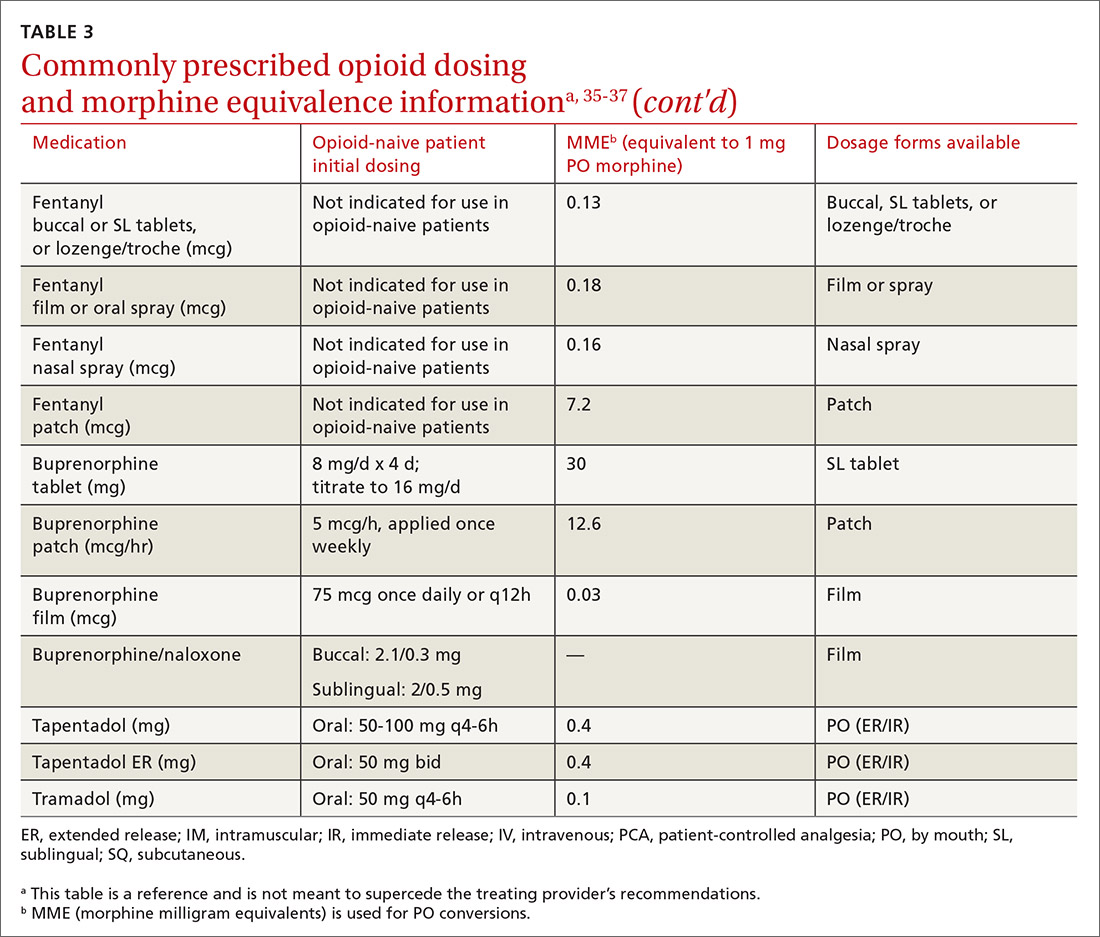
Doses between 20 to 50 MME/d are considered relatively low dosages.28 Be cautious when prescribing an opioid at any dosage, and reassess evidence of individual benefits and risks before increasing the dosage to ≥ 50 MME/d.28 Regard a dosage of 90 MME/d as maximal.28 While there is no analgesic ceiling, doses greater than 90 MME/d are associated with risk for overdose and should prompt referral to a pain specialist.31 Veterans Administration guidelines cite strong evidence that risk for overdose and death significantly increases at a range of 20 to 50 MME/d.33 Daily doses exceeding 90 MME/d should be documented with rational justification.28
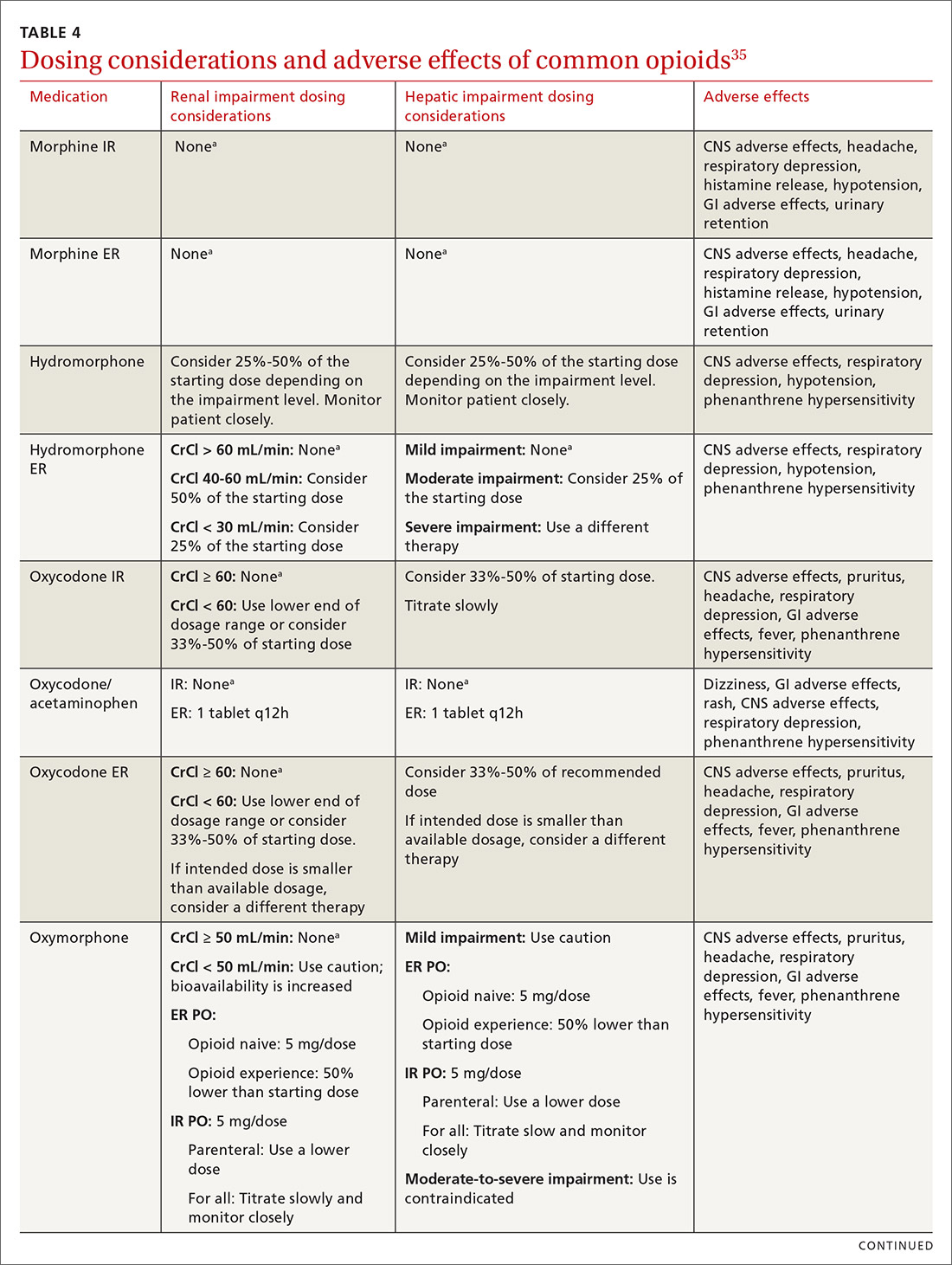
CASE
Noncontrolled medications are preferred in the treatment of chronic pain. However, the utility of adjuvant options such as NSAIDs, duloxetine, or gabapentin were limited in Mr. G’s case due to his ESRD. Calcium channel α2-δ ligands may have been effective in reducing symptoms of neuropathic pain but would have had limited efficacy against osteoarthritis. Based on his low risk for opioid misuse, we decided to start Mr. G on oxycodone 2.5 mg PO, every 6 hours as needed for moderate-to-severe pain, and to follow up in 1 month. We also explained proper lifting form to him and encouraged him to continue with physical therapy.
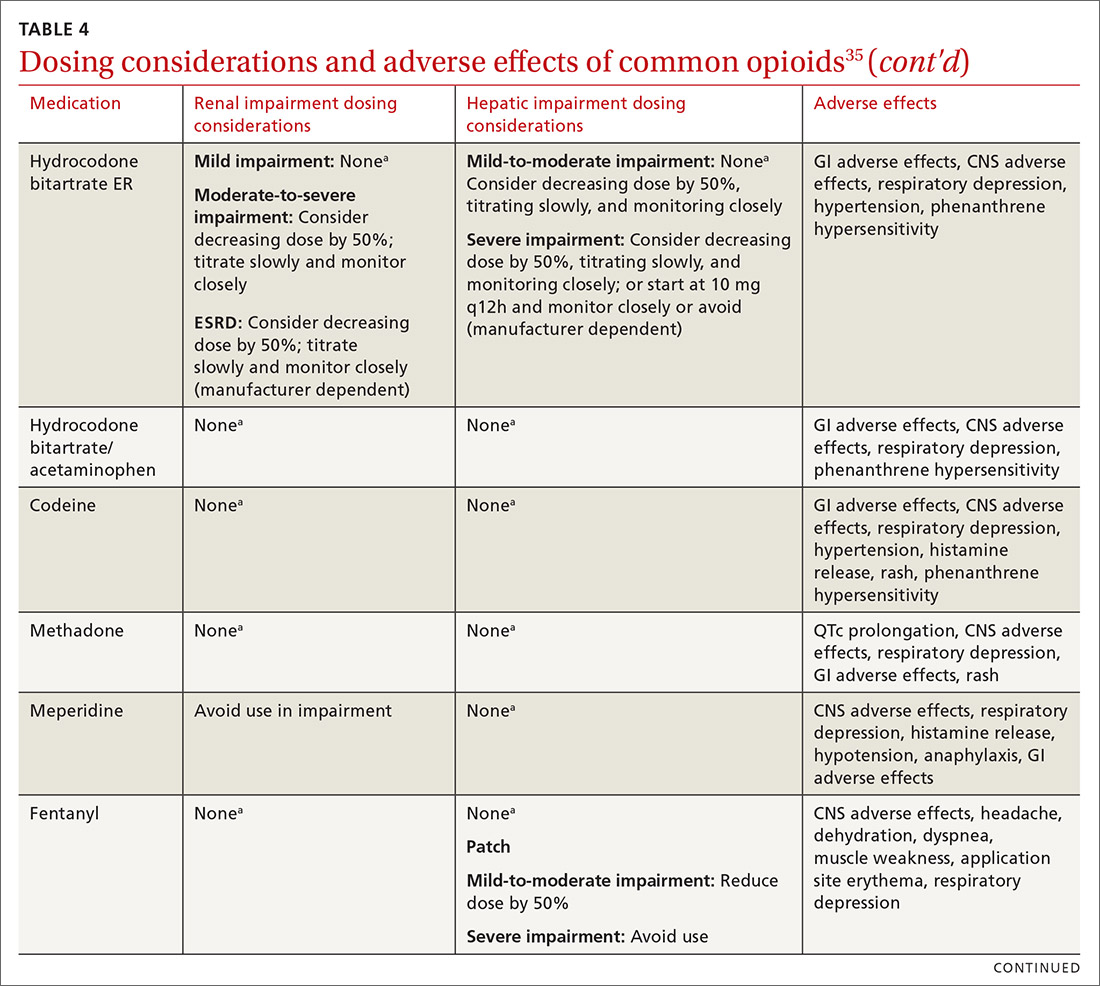
Deciding to continue therapy with opioids
There is a lack of convincing evidence that opioid use beyond 6 months improves quality of life; patients do not report a significant reduction in pain beyond this time.28 Thus, a repeat evaluation of continued medical necessity is essential before deciding in favor of ongoing, long-term treatment with opioids. Continue prescribing opioids only if there is meaningful pain relief and improved function that outweighs the harms that may be expected for a given patient.31 With all patients, consider prescribing naloxone to accompany dispensed opioid prescriptions.28 This is particularly important for those at risk for misuse (history of overdose, history of substance use disorder, dosages ≥ 50 MME/d, or concurrent benzodiazepine use). Resources for prescribing naloxone in primary care settings can be found through Prescribe to Prevent at http://prescribetoprevent.org. Due to the established risk of overdose, avoid, if possible, concomitant prescriptions of benzodiazepines and opioids.31
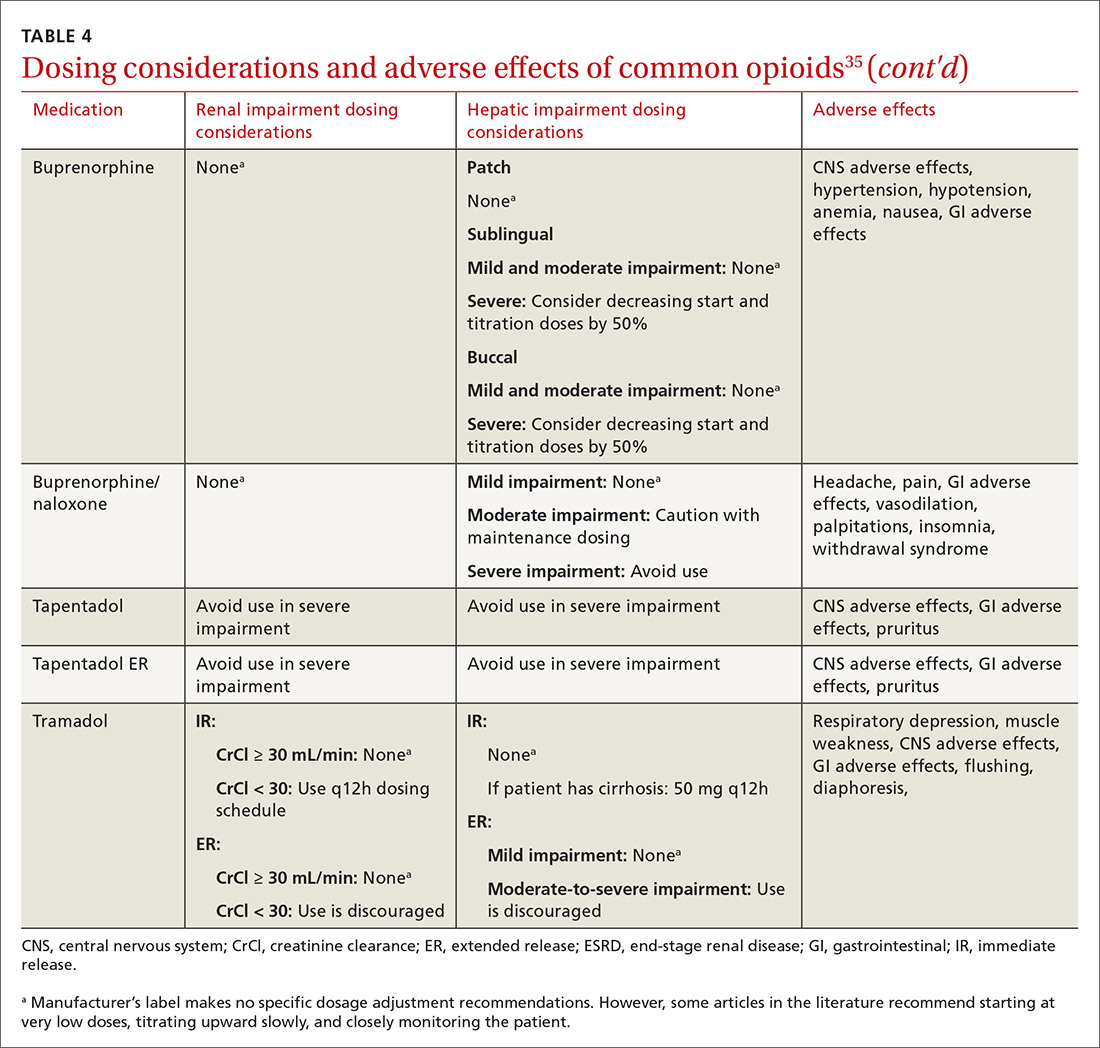
Continue to: Follow-up and monitoring
Follow-up and monitoring
Responsiveness to opioids varies greatly among individuals.38,39 An opioid that leads to a therapeutic analgesic effect in one patient may cause adverse events or toxicity in another. Periodically reassess the appropriateness of chronic opioid therapy and modify treatment based on its ability to meet therapeutic goals. While practice behaviors and clinic policies vary across institutions, risk stratification can provide guidance on the frequency and intensity of follow-up and monitoring. Kaye et al21 describe a triage system in which low-risk patients may be managed by a primary care provider with routine follow-up and reassessment every 3 months.21 Moderate-risk patients may warrant additional management by specialists and a monthly follow-up. High-risk patients may need referrals to interdisciplinary pain centers or addiction specialists.21
Along these lines, the CDC recommends conducting a PDMP review and UDT before initiating therapy, followed by a periodic PDMP (every 1-3 months) and a UDT at least annually. Keep in mind, providers should follow their state-specific regulations, as monitoring requirements may vary. In addition, clinicians should always be alert to adverse reactions (TABLE 435) and sudden behavior changes such as respiratory depression, nausea, constipation, pruritus, cognitive impairment, falls, motor vehicle accidents, and aberrant behaviors. Under these circumstances, consider a dose reduction and, in certain cases, discontinuation.
Additionally, in cases of pain unresponsive to escalating opioid doses, include opioid-induced hyperalgesia (OIH) in the differential. Dose reductions, opioid rotations, and office-based detoxifications are all options for the treatment of OIH.40 Assessment of pain and function can be accomplished using the PEG scale (TABLE 2).32
CASE
Two weeks into Mr. G’s initial regimen, he called to report no change in pain or functional status. We increased his dose to 5 mg PO every 6 hours as needed. At his 1-month follow-up appointment, he reported his pain as 6/10 and no adverse effects. We again increased his dose to 10 mg PO every 6 hours as needed, with follow-up in another month.
Discontinuation and tapering of opioids
Indications for discontinuing opioids are patient request, resolution of pain, doses ≥ 90 MME/d (in which case a pain specialist should be consulted), inadequate response, untoward adverse effects, and abuse and misuse.1,31,41 However, providers may also face the challenge of working with patients for whom the benefit of opioid therapy is uncertain but who do not have an absolute contraindication. Guidance on this matter may be found in a 2017 systematic review of studies on reducing or discontinuing long-term opioid therapy.42 Although evidence on the whole was low quality, it showed that tapering or discontinuing opioids may actually reduce pain and improve function and quality of life.
Continue to: When working with a patient to taper treatment
When working with a patient to taper treatment, consider using a multidisciplinary approach. Also, assess the patient’s pain level and perception of needs for opioids, make clear the substantial effort that will be asked of the patient, and agree on coping strategies the patient can use to manage the taper.31,43 While the evidence does not appear to support one tapering regimen over another, we can offer some recommendations on ways to individualize a tapering regimen (TABLE 5).1,31,41,43,44
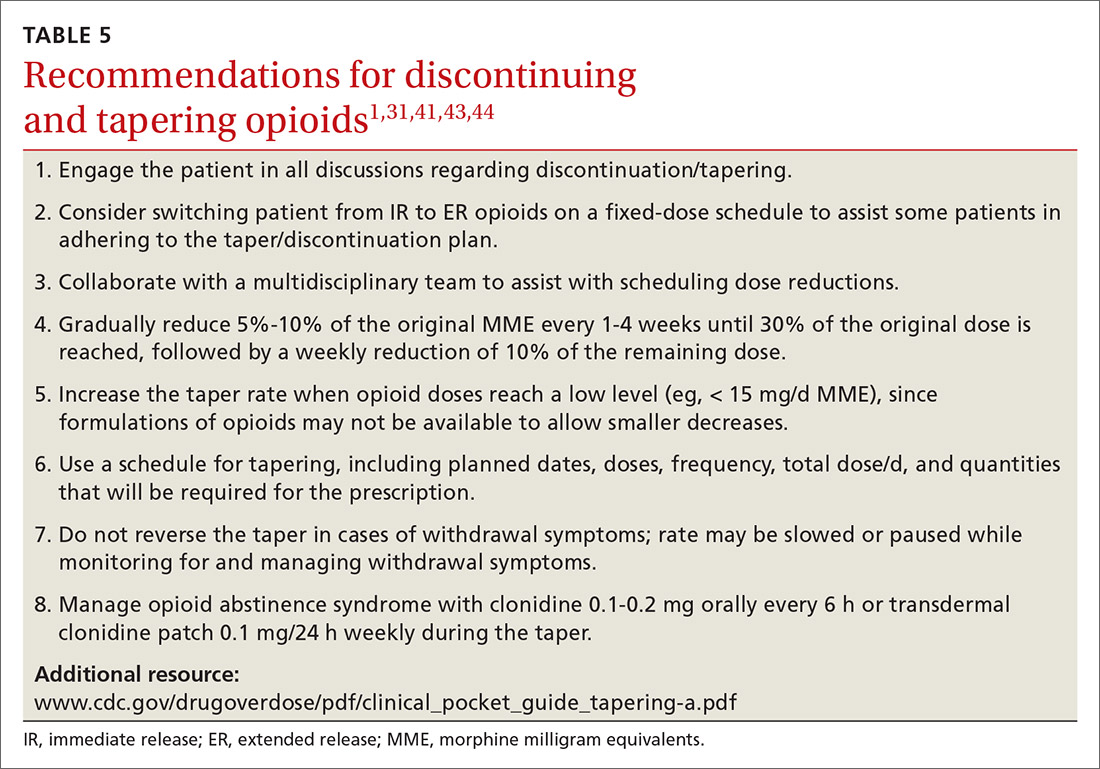
General recommendations. Gradually reduce the original MME dose by 5% to 10% every week to every 4 weeks, with frequent follow-up and adjustments as needed based on the individual’s response.1,31,41,43 In the event that the patient does not tolerate this dose-reduction schedule, tapering can be slowed further.31 Avoid abrupt discontinuation.33 Opioid abstinence syndrome, a myriad of symptoms caused by deprivation of opioids in physiologically dependent individuals, although rare, can occur during tapering and can be managed with clonidine 0.1 to 0.2 mg orally every 6 hours or transdermal clonidine patch 0.1 mg/24 hours weekly during the taper.31
Tapering of long-term opioid treatment is not without risk. Immediate risks include withdrawal syndrome, hyperalgesia, and dropout, while ongoing issues are potential relapse, problems in increasing and maintaining function, and medicolegal implications.43 Withdrawal symptoms begin 2 to 3 half-lives after the last dose of opioid, and resolution varies depending on the duration of use, the most recent dose, and speed of tapering.43 In general, a patient needs 20% to 25% of the previous day’s dose to prevent withdrawal symptoms.31 Increased pain appears to be a brief, time-limited occurance.43 Dropout and relapse tend to be attributed to patient factors such as depressive symptoms and higher pain scores at initiation of the taper.43 Low pain at the end of tapering has been shown to predict long-term abstinence from opioids.43
CASE
Two months into his oxycodone regimen, Mr. G reported improved functional status at his catering job and overall improved quality of life. He had improved his lifting form and was attending biweekly physical therapy sessions. His pain score was 3/10. He expressed a desire to “not get hooked on opioids,” and mentioned he had “tried stopping the medicine last week” but experienced withdrawal symptoms. We discussed and prescribed the following 5-week taper plan: 2.5 mg reduction of oxycodone per dose, every 2 weeks x 2. Then 2.5 mg PO every 6 hours as needed x 1 week before stopping.
Organizing your approach
To optimize the chance for success in opioid treatment and to heighten vigilance and minimize harm to patients, we believe an organized approach is key (TABLE 614,22-24,28,30-32), particularly since this class of medication lacks strong evidence to support its long-term use.
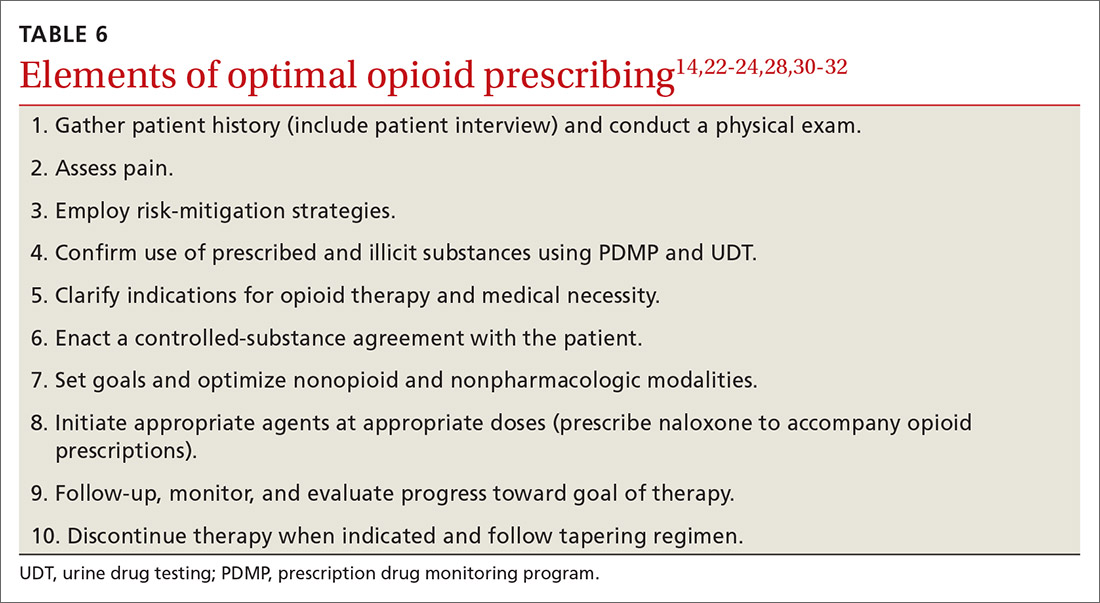
CORRESPONDENCE
Tracy Mahvan, PharmD, BCGP, University of Wyoming, School of Pharmacy, 1000 East University Avenue, Laramie, WY 82071; [email protected].
1. CDC. Opioid overdose. www.cdc.gov/drugoverdose/opioids/prescribed.html. Accessed June 26, 2020.
2. DEA, Department of Justice. Established aggregate production quotas for schedule I and II controlled substances and assessment of annual needs for the list I chemicals ephedrine, pseudoephedrine, and phenylpropanolamine for 2017. www.deadiversion.usdoj.gov/fed_regs/quotas/2016/fr1005.htm. Accessed June 26, 2020.
3. DEA, Department of Justice. Established aggregate production quotas for schedule I and II controlled substances and assessment of annual needs for the list I chemicals ephedrine, pseudoephedrine, and phenylpropanolamine for 2018. www.deadiversion.usdoj.gov/fed_regs/quotas/2017/fr1108.htm. Accessed June 26, 2020.
4. DEA, Department of Justice. Established aggregate production quotas for schedule I and II controlled substances and assessment of annual needs for the list I chemicals ephedrine, pseudoephedrine, and phenylpropanolamine for 2020. www.deadiversion.usdoj.gov/fed_regs/quotas/2019/fr1202.htm. Accessed June 26, 2020.
5. US Department of Veterans Affairs. Pharmacy benefits management services: academic detailing service—opioid overdose education & naloxone distribution (OEND). www.pbm.va.gov/AcademicDetailingService/Opioid_Overdose_Education_and_Naloxone_Distribution.asp. Accessed June 26, 2020.
6. McCarberg BH. Pain management in primary care: strategies to mitigate opioid misuse, abuse, and diversion. Postgrad Med. 2011;123:119-130.
7. Dean L. Tramadol therapy and CYP2D6 genotype. In: Pratt V, McLeod H, Rubinstein W, et al (eds). Medical Genetics Summaries [Internet]. Bethesda, Md: National Center for Biotechnology Information (US); 2015. www.ncbi.nlm.nih.gov/books/NBK315950/. Accessed June 26, 2020.
8. Chen JH, Humphreys K, Shah NH, et al. Distribution of opioids by different types of Medicare prescribers. JAMA Intern Med. 2016;176:259-261.
9. Jensen MP, Karoly P. Self-report scales and procedures for assessing pain in adults. In: Turk DC, Melzack R, eds. Handbook of Pain Assessment. 3rd ed. New York, NY: Guilford Press; 2011;19-41.
10. Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005; 14:798-804.
11. Ohnhaus EE, Adler R. Methodological problems in the measurement of pain: a comparison between the verbal rating scale and the visual analogue scale. Pain. 1975;1:379-384.
12. Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23:129-138.
13. Dworkin RH, Turk DC, Revicki DA, et al. Development and initial validation of an expanded and revised version of the short-form McGill Pain Questionnaire (SF-MPQ-2). Pain. 2009;144:35-42.
14. Dansie EJ, Turk DC. Assessment of patients with chronic pain. Br J Anaesth. 2013;111:19-25.
15. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-613.
16. Choi Y, Mayer TG, Williams MJ, Gatchel RJ. What is the best screening test for depression in chronic spinal pain patients? Spine J. 2014;14:1175-1182.
17. Practice guidelines for chronic pain management: an updated report by the American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine. Anesthesiology. 2010;122:810-833.
18. Gallagher RM. Empathy: a timeless skill for the pain medicine toolbox. Pain Med. 2006;7:213-214.
19. Koyyalagunta D, Bruera E, Aigner C, et al. Risk stratification of opioid misuse among patients with cancer pain using the SOAPP-SF. Pain Med. 2013;14:667-675.
20. Trescot AM, Helm S, Hansen H, et al. Opioids in the management of chronic non-cancer pain: an update of American Society of the Interventional Pain Physicians’ (ASIPP) guidelines. Pain Physician. 2008;11:S5-S62.
21. Kaye AD, Jones MR, Kaye AM, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse (part 2). Pain Physician. 2017;20:S111-S133.
22. Webster LR, Webster RM. Predicting aberrant behaviors in opioid‐treated patients: preliminary validation of the Opioid Risk Tool. Pain Med. 2005;6:432-442.
23. Butler SF, Fernandez K, Benoit C, et al. Validation of the revised screener and opioid assessment for patients with pain (SOAPP-R). J Pain. 2008;9:360-372.
24. Belgrade MJ, Schamber CD, Lindgren BR. The DIRE score: predicting outcomes of opioid prescribing for chronic pain. J Pain. 2006;7:671-681.
25. Fine PG, Finnegan T, Portenoy RK. Protect your patients, protect your practice: practical risk assessment in the structuring of opioid therapy in chronic pain. J Fam Pract. 2010;59(9 suppl 2):S1-16.
26. Gourlay DL, Heit HA, Almahrezi A. Universal precautions in pain medicine: a rational approach to the treatment of chronic pain. Pain Med. 2005;6:107-112.
27. Manubay JM, Muchow C, Sullivan MA. Prescription drug abuse: epidemiology, regulatory issues, chronic pain management with narcotic analgesics. Prim Care. 2011;38:71-90.
28. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm Rep. 2016;65:1-49.
29. Prescription Drug Monitoring Program Training and Technical Assistance Center. State PDMP profiles and contacts. www.pdmpassist.org/State. Accessed June 26, 2020.
30. Tobin DG, Andrews R, Becker WC. Prescribing opioids in primary care: Safely starting, monitoring, and stopping. Cleve Clin J Med. 2016;83:207-215.
31. Manchikanti L, Kaye AM, Knezevis NN, et al. Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of Interventional Pain Physicians (ASIPP) guidelines. Pain Physician. 2017;20:S3-S92.
32. HHS. Checklist for prescribing opioids for chronic pain. www.cdc.gov/drugoverdose/pdf/PDO_Checklist-a.pdf. Accessed June 26, 2020.
33. VA/DoD. VA/DoD clinical practice guideline for opioid therapy for chronic pain. www.healthquality.va.gov/guidelines/Pain/cot/VADoDOTCPG022717.pdf. Accessed June 26, 2020.
34. Nuckols TK, Anderson L, Popescu I, et al. Opioid prescribing: a systematic review and critical appraisal of guidelines for chronic pain. Ann Intern Med. 2014;160:38-47.
35. Lexi-Comp Online. Hudson (OH): Wolters Kluwer Clinical Drug Information, Inc; 2018. https://online.lexi.com/lco/action/login. Accessed July 9, 2020.
36. CMS. Opioid oral morphine milligram equivalent (MME) conversion factors. www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/Opioid-Morphine-EQ-Conversion-Factors-Aug-2017.pdf. Accessed June 26, 2020.
37. Cupp M. Equianalgesic dosing of opioids for pain management. Pharmacist’s Letter/Prescriber’s Letter. 2018:340406. Stockton (CA): Therapeutic Research Center, LLC; 2018. www.nhms.org/sites/default/files/Pdfs/Opioid-Comparison-Chart-Prescriber-Letter-2012.pdf. Accessed June 26, 2020.
38. Smith HS. Variations in opioid responsiveness. Pain Physician. 2008;11:237-248.
39. Bronstein K, Passik S, Munitz L, et al. Can clinicians accurately predict which patients are misusing their medications? J Pain. 2011;12(suppl):P3.
40. Silverman SM. Opioid induced hyperalgesia: clinical implications for the pain practitioner. Pain Physician. 2009;12:679-684.
41. Busse JW, Craigie S, Juurlink DN, et al. Guideline for opioid therapy and chronic non-cancer pain. CMAJ. 2017;189:E659-E666.
42. Frank JW, Lovejoy TI, Becker WC, et al. Patient outcomes in dose reduction or discontinuation of long-term opioid therapy: a systematic review. Ann Intern Med. 2017;167:181-191.
43. Berna C, Kulich RJ, Rathmell JP. Tapering long-term opioid therapy in chronic non-cancer pain: evidence and recommendations for everyday practice. Mayo Clin Proc. 2015;90:828-842.
44. Washington State Agency Medical Director’s Group. Interagency guideline on prescribing opioids for pain. June 2015. www.agencymeddirectors.wa.gov/Files/2015AMDGOpioidGuideline.pdf. Accessed June 26, 2020.
CASE
Marcelo G* is a 46-year-old man who presented to our family medicine clinic with a complex medical history including end-stage renal disease (ESRD) and hemodialysis, chronic anemia, peripheral vascular disease, venous thromboembolism and anticoagulation, major depressive disorder, osteoarthritis, and lumbosacral radiculopathy. His current medications included vitamin B complex, cholecalciferol, atorvastatin, warfarin, acetaminophen, diclofenac gel, and capsaicin cream. Mr. G reported bothersome bilateral knee and back pain despite physical therapy and consistent use of his current medications in addition to occasional intra-articular glucocorticoid injections. He mentioned that he had benefited in the past from intermittent opioid use.
How would you manage this patient’s care?
*The patient’s name has been changed to protect his identity.
In 2013, an estimated 191 million prescriptions for opioids were written by health care providers, which is the equivalent of all adults living in the United States having their own opioid prescription.1 This large expansion in opioid prescribing and use has also led to a rise in opioid overdose deaths, whether from prescribed or illicit use.1 The Centers for Disease Control and Prevention (CDC) points out that each day, approximately 128 Americans die from an opioid overdose.1 Deaths that occur from opioid overdose often involve the prescribed opioids methadone, oxycodone, and hydrocodone, the illicit opioid heroin, and, of particular concern, prescription and illicit fentanyl.1
The extent of this problem has sparked the development of health safety initiatives and research efforts. Through production quotas, the US Drug Enforcement Administration (DEA) reduced the number of opioids produced across all schedule I and schedule II lists in 2017 by as much as 25%.2 The DEA again reduced the amounts produced in 2018.3 For 2020, the DEA has determined that the production quotas and assessment of annual needs are sufficient.4
The CDC has also promoted access to naloxone and prevention initiatives; pharmacies in some states have standing orders for naloxone, and medical personnel and law enforcement now carry it.1,5 Finally, new research has identified risk factors that influence one’s potential for addiction, such as mental illness, history of substance and alcohol abuse, and a low income.6 Interestingly, while numerous initiatives and strategies have been implemented across health systems, there is little evidence that demonstrates how implementation of safe prescribing strategies has affected overall patient safety and avoidance of opioid-related harms.
Nevertheless, concerns related to opioids are especially important for primary care providers, who manage many patients with acute and chronic diseases and disorders that require pain control.7 Family physicians write more opioid prescriptions than any other specialty,8 and they are therefore uniquely positioned to protect patients, improve the quality of their care, and ultimately produce a meaningful public health impact. This article provides a guide to safe opioid prescribing.
Continue to: Use the patient interview to ensure that Tx aligns with patient goals
Use the patient interview to ensure that Tx aligns with patient goals
For patients presenting with chronic pain, conduct a complete general history and physical examination that includes a review of available records; a medical, surgical, social, family, medication, and allergy history; a review of systems; and documentation of any psychiatric comorbidities (ie, depression, anxiety, psychiatric disorders, personality traits). Inquiries about social history and current medications should explore the possibility of previous and current substance use and misuse.
While causes of pain can be assessed through physical examination and diagnostic tests, the patient interview is an invaluable source of information. No single means of assessment has consistently demonstrated superiority over another in measuring pain, and numerous standard assessment tools are available (TABLE 19-13).14 Unidimensional tools are often easy and quick ways to assess pain intensity. Multidimensional tools, although more time intensive, are designed to gather more subjective information about the patient’s pain. Finally, use an instrument such as the 9-item Patient Health Questionnaire (PHQ-9) to screen patients for psychological distress.15,16
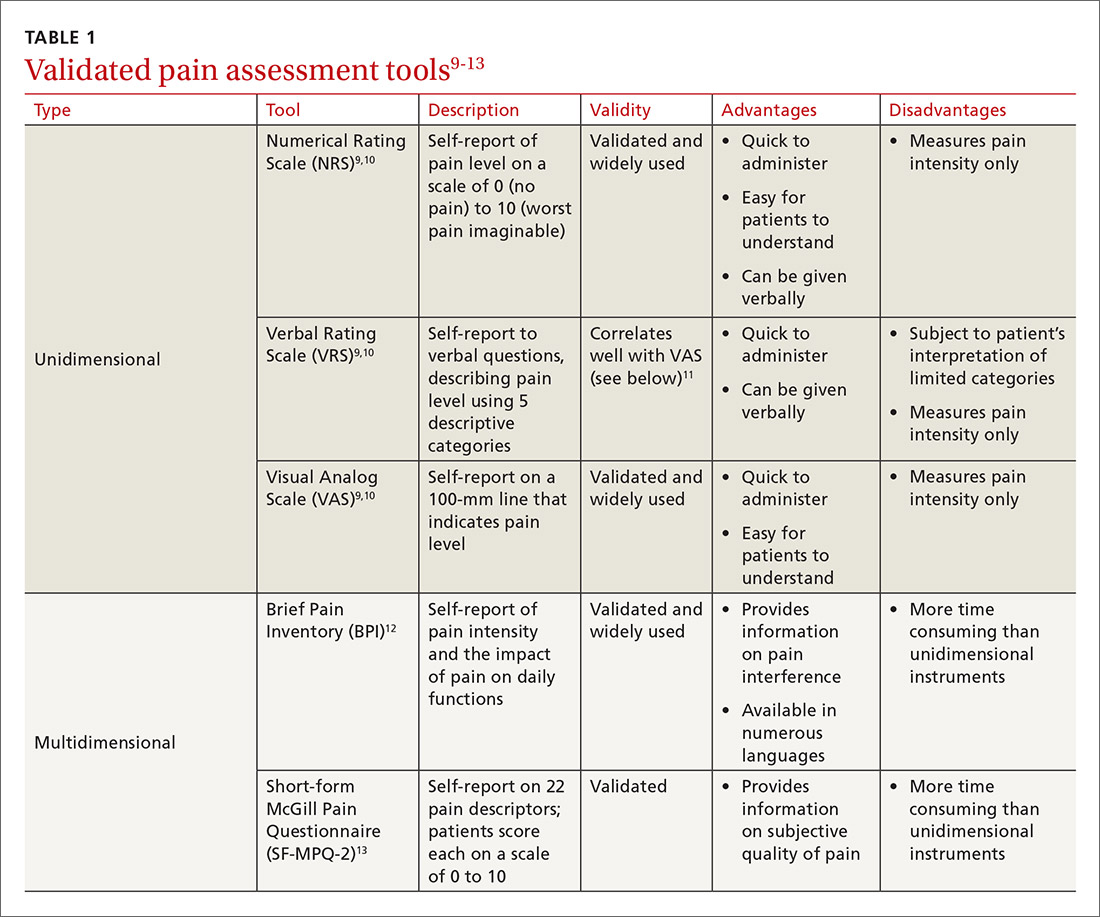
Provide an environment for patients to openly discuss their experiences, expectations, preferences, fears, and coping efforts, as well as the impact that pain has had on their lives.17,18 Without this foundational understanding, medical treatment may work against the patient’s goals. An empathic approach allows for effective communication, shared decision making, and ultimately, an avenue for individualized therapy.
Balancing treatment with risk mitigation
The challenge of managing chronic pain is to balance treating the patient with the basic principle of nonmaleficence (primum non nocere: “first, do no harm”). The literature has shown that risk factors such as a family history of substance abuse or sexual abuse, younger age, and psychological disease may be linked to greater risk for opioid misuse.19,20 However, despite the many risk-screening tools available, no single instrument has reliably and accurately predicted those at higher propensity for prescription addiction. In fact, risk-screening tools as a whole remain unregulated by the US Food and Drug Administration (FDA) and other authorities.21 Still, screening tools provide useful information as one component of the risk-mitigation process.
Screening tools. The tools most commonly used clinically to stratify risk prior to prescribing opioids are the 5-item Opioid Risk Tool (ORT),22 the revised 24-item Screener and Opioid Assessment for Patients with Pain (SOAPP-R),23 which are patient self-administered assessments, and the 7-item clinician-administered DIRE (Diagnosis, Intractability, Risk, Efficacy).24 Given the subtle differences in criteria and the time required for each of these risk assessments, we recommend choosing one based on site-specific resources and overall clinician comfort.25 Risk stratification helps to determine the optimal frequency and intensity of monitoring, not necessarily to deny care to “high-risk” patients.
Continue to: In fact, just as the "universal precautions"...
In fact, just as the “universal precautions” approach has been applied to infection control, many have suggested using a similar approach to pain management. Risk screening should never be misunderstood as an attempt to diminish or undermine the patient’s burden of pain. By routinely conducting thorough and respectful inquiries of risk factors for all patients, clinicians can reduce stigma, improve care, and contain overall risk.26,27
Monitoring programs and patient agreements. In addition to risk-screening tools, the CDC recommends using state prescription drug monitoring programs (PDMP) and urine drug testing (UDT) data to confirm the use of prescribed and illicit substances.28 All 50 states have implemented PDMPs.29 Consider incorporating these components into controlled-substance agreements, which ultimately aim to promote safety and trust between patients and providers. Of course, such agreements do not eliminate all risks associated with opioid prescribing, nor do they guarantee the absence of adverse outcomes. However, when used correctly, they can provide safeguards to reduce misuse and abuse. They also have the potential to preserve the patient-provider relationship, as opposed to providers cursorily refusing to prescribe opioids altogether. The term “controlled-substance agreement” is preferable to “pain contract” or “narcotic contract” as the latter 2 terms may feel stigmatizing and threatening.30
Risk evaluation and mitigation strategy (REMS). In an effort to ensure that benefits of opioid analgesics continue to outweigh the risks, the FDA approved the extended-release (ER)/long-acting (LA) opioid analgesics shared system REMS. Under this REMS, a consortium of ER/LA opioid manufacturers is mandated to provide prescriber education in the form of accredited continuing education and patient educational materials, available at https://opioidanalgesicrems.com/RpcUI/home.u.
CASE
After reviewing Mr. G’s chart and conducting a history, we learned that his bilateral knee osteoarthritis was atraumatic and likely due to overuse—although possibly affected by major trauma in a motor vehicle accident 5 years earlier. Imaging also revealed multilevel disc degeneration contributing to his radicular back pain, which seemed to be worse on days after working as a caterer. Poor lifting form at work may have contributed to his pain. Nevertheless, he had been consistent with medical follow-up and denied current or past use of illicit substances. Per the numeric rating scale (NRS), he reported 8 out of 10 pain in his knees and 6 out of 10 in his back. In addition to obtaining a PHQ-9 score of 4, we conducted a DIRE assessment and obtained a score of 19 out of a possible 21, indicating that he may be a good candidate for long-term opioid analgesia.
Criteria for prescribing opioids and for guiding treatment goals
Prescribing an opioid requires establishing a medical necessity based on 3 criteria:31
- pain of moderate-to-severe degree
- a physical diagnosis or suspected organic problem
- documented treatment failure of a noncontrolled substance, adjuvant agents, physician-ordered physical therapy, structured exercise program, and interventional techniques.
Continue to: Treatment goals should be established...
Treatment goals should be established and understood by the prescriber and patient prior to initiation of opioids.28 Overarching treatment goals for all opioids prescribed are pain relief (but not necessarily a focus on pain scores), improvement in functional activity, and minimization of adverse effects, with the latter 2 goals taking precedence.31 To assess outcomes, formally measure progress toward goals from baseline evaluations. This can be achieved through repeated use of validated tools such as those mentioned earlier, or may be more broadly considered as progress toward employment status or increasing participation in activities.31 All pain management plans involving opioids should include continued efforts with nonpharmacologic therapy (eg, exercise therapy, weight loss, behavioral training) and nonopioid pharmacologic therapy (eg, nonsteroidal anti-inflammatory drugs, tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors, anticonvulsants).28
Have an “exit strategy.” As part of goal setting, also consider how therapy will be discontinued if benefits do not outweigh the risks of harm.28 Weigh functional status gains against adverse opioid consequences using the PEG scale (pain, enjoyment of life, and general activity) (TABLE 232).33 Improvements of 30% from baseline have been deemed clinically meaningful by some,32 but not all benefits will be easy to quantify. At the start of treatment dialogue, use the term “therapeutic trial” instead of ”treatment plan” to more effectively convey that opioids will be continued only if safe and effective, and will be prescribed at the lowest effective dose as one component of the multimodal approach to pain.30
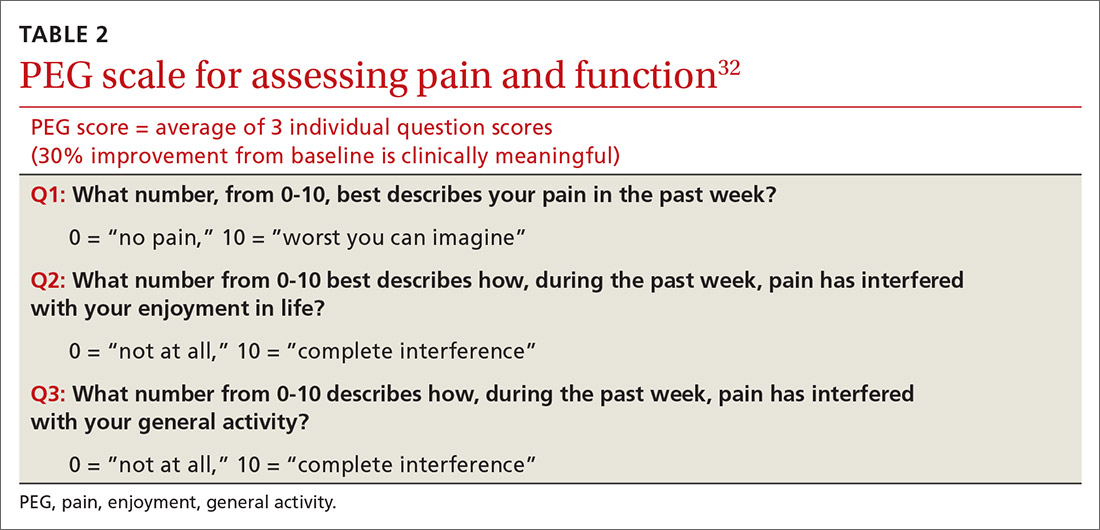
Initiation of treatment: Opioid selection and dosing
When initiating opioid therapy, prescribe an immediate-release, short-acting agent instead of an ER/LA formulation.28
For moderate pain, first consider tramadol, codeine, tapentadol, or hydrocodone.31 Second-line agents for moderate pain are hydrocodone or oxycodone.31
For severe pain, first-line agents include hydrocodone, oxycodone, hydromorphone, or morphine.31 Second-line agents for severe pain are fentanyl and, with careful supervision or referral to a pain specialist, methadone or buprenorphine.31
Continue to: Of special note...
Of special note,

At the start, prescribe the lowest effective dosage (referring to the product labeling for guidance) and calculate total daily dose in terms of morphine milligram equivalents (MME) (TABLE 335-37).28 Exercise caution when considering opioids for patients with respiratory sleep disorders and for patients ≥ 65 years due to altered pharmacokinetics in the elderly population.38 Also make dose adjustments for renal and hepatic insufficiency (TABLE 435).
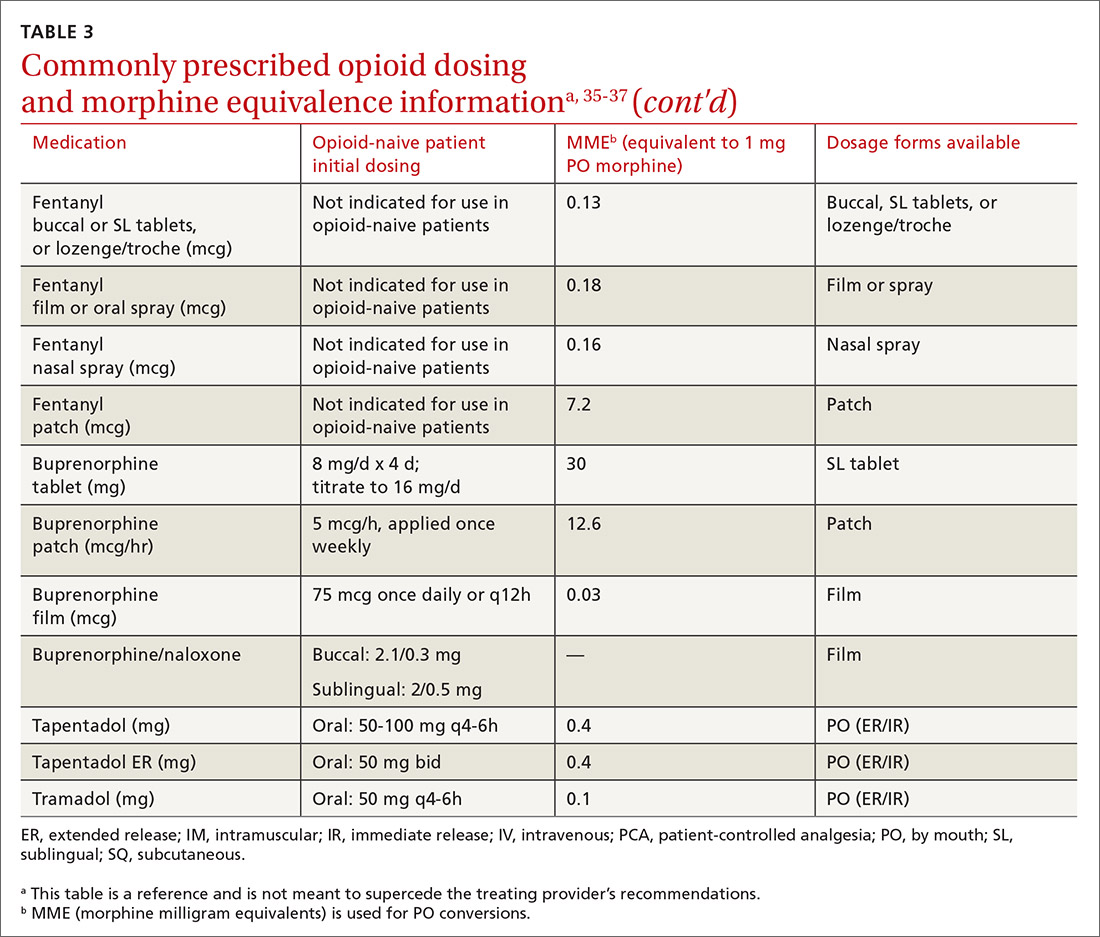
Doses between 20 to 50 MME/d are considered relatively low dosages.28 Be cautious when prescribing an opioid at any dosage, and reassess evidence of individual benefits and risks before increasing the dosage to ≥ 50 MME/d.28 Regard a dosage of 90 MME/d as maximal.28 While there is no analgesic ceiling, doses greater than 90 MME/d are associated with risk for overdose and should prompt referral to a pain specialist.31 Veterans Administration guidelines cite strong evidence that risk for overdose and death significantly increases at a range of 20 to 50 MME/d.33 Daily doses exceeding 90 MME/d should be documented with rational justification.28
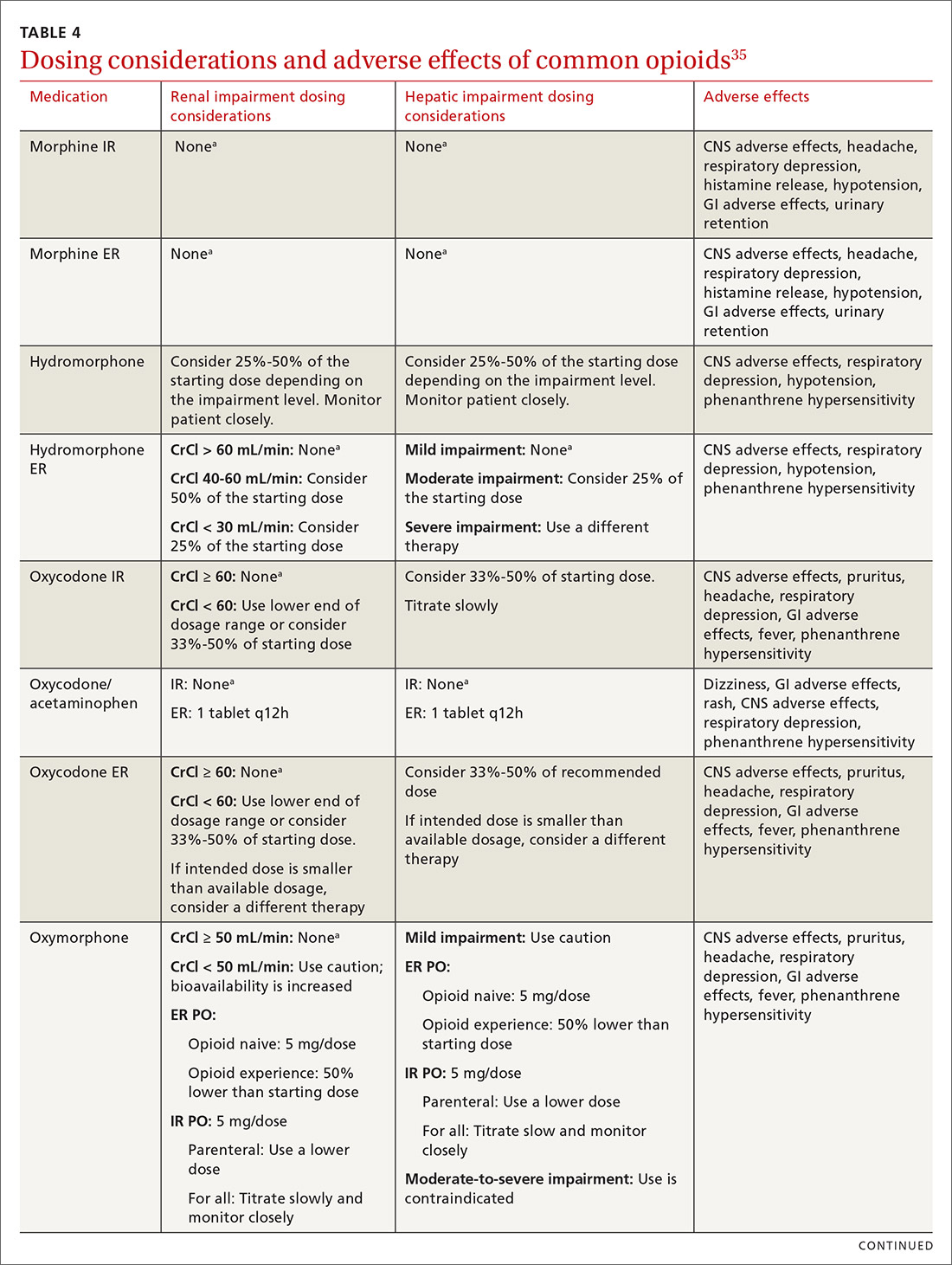
CASE
Noncontrolled medications are preferred in the treatment of chronic pain. However, the utility of adjuvant options such as NSAIDs, duloxetine, or gabapentin were limited in Mr. G’s case due to his ESRD. Calcium channel α2-δ ligands may have been effective in reducing symptoms of neuropathic pain but would have had limited efficacy against osteoarthritis. Based on his low risk for opioid misuse, we decided to start Mr. G on oxycodone 2.5 mg PO, every 6 hours as needed for moderate-to-severe pain, and to follow up in 1 month. We also explained proper lifting form to him and encouraged him to continue with physical therapy.
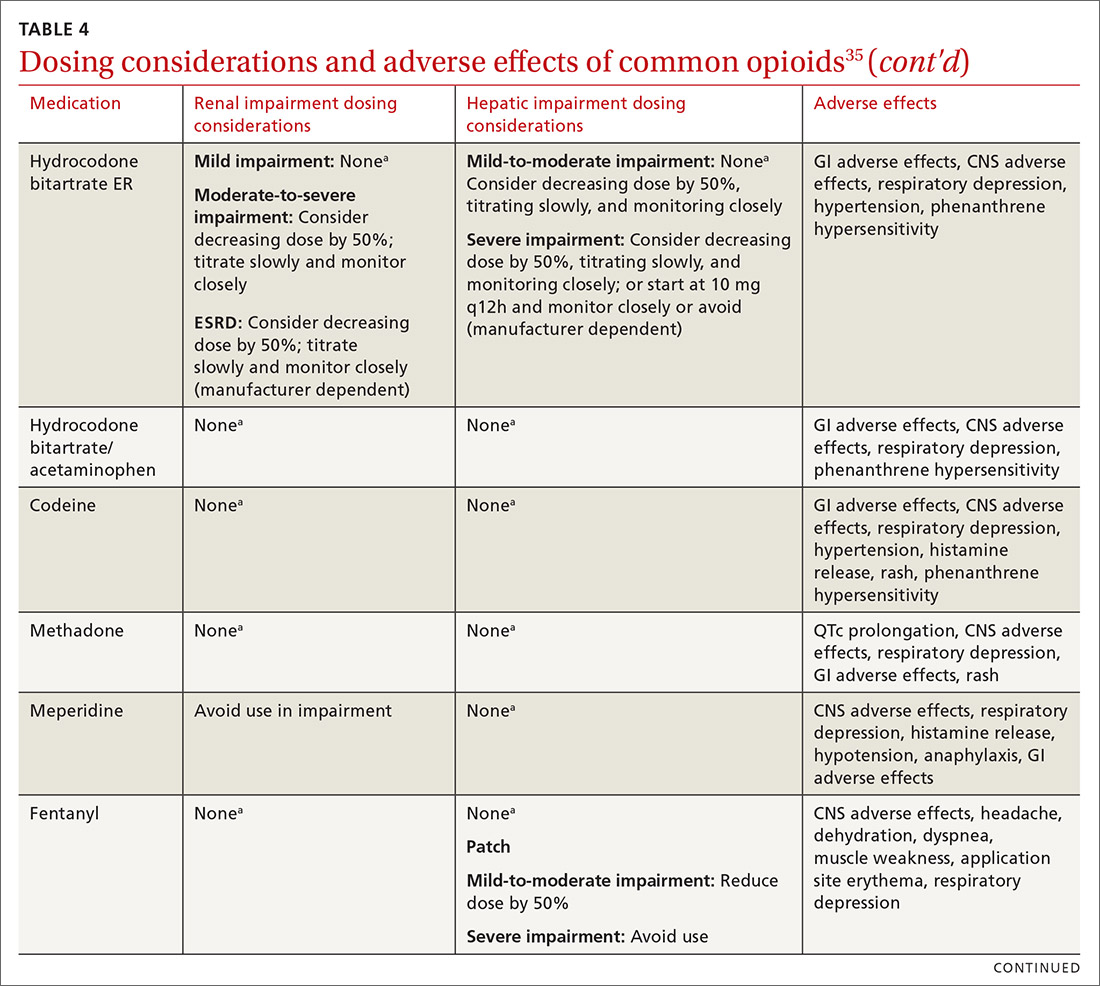
Deciding to continue therapy with opioids
There is a lack of convincing evidence that opioid use beyond 6 months improves quality of life; patients do not report a significant reduction in pain beyond this time.28 Thus, a repeat evaluation of continued medical necessity is essential before deciding in favor of ongoing, long-term treatment with opioids. Continue prescribing opioids only if there is meaningful pain relief and improved function that outweighs the harms that may be expected for a given patient.31 With all patients, consider prescribing naloxone to accompany dispensed opioid prescriptions.28 This is particularly important for those at risk for misuse (history of overdose, history of substance use disorder, dosages ≥ 50 MME/d, or concurrent benzodiazepine use). Resources for prescribing naloxone in primary care settings can be found through Prescribe to Prevent at http://prescribetoprevent.org. Due to the established risk of overdose, avoid, if possible, concomitant prescriptions of benzodiazepines and opioids.31
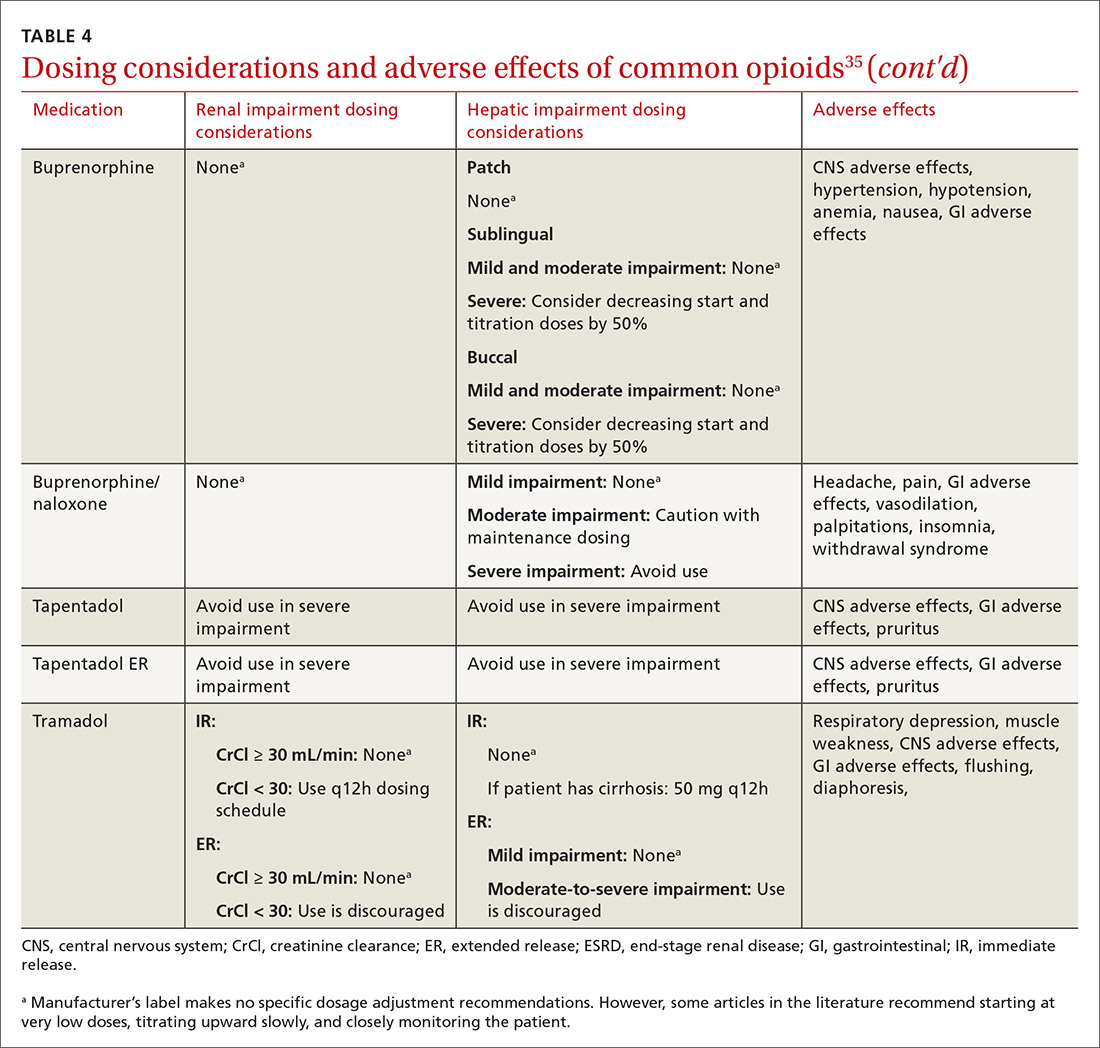
Continue to: Follow-up and monitoring
Follow-up and monitoring
Responsiveness to opioids varies greatly among individuals.38,39 An opioid that leads to a therapeutic analgesic effect in one patient may cause adverse events or toxicity in another. Periodically reassess the appropriateness of chronic opioid therapy and modify treatment based on its ability to meet therapeutic goals. While practice behaviors and clinic policies vary across institutions, risk stratification can provide guidance on the frequency and intensity of follow-up and monitoring. Kaye et al21 describe a triage system in which low-risk patients may be managed by a primary care provider with routine follow-up and reassessment every 3 months.21 Moderate-risk patients may warrant additional management by specialists and a monthly follow-up. High-risk patients may need referrals to interdisciplinary pain centers or addiction specialists.21
Along these lines, the CDC recommends conducting a PDMP review and UDT before initiating therapy, followed by a periodic PDMP (every 1-3 months) and a UDT at least annually. Keep in mind, providers should follow their state-specific regulations, as monitoring requirements may vary. In addition, clinicians should always be alert to adverse reactions (TABLE 435) and sudden behavior changes such as respiratory depression, nausea, constipation, pruritus, cognitive impairment, falls, motor vehicle accidents, and aberrant behaviors. Under these circumstances, consider a dose reduction and, in certain cases, discontinuation.
Additionally, in cases of pain unresponsive to escalating opioid doses, include opioid-induced hyperalgesia (OIH) in the differential. Dose reductions, opioid rotations, and office-based detoxifications are all options for the treatment of OIH.40 Assessment of pain and function can be accomplished using the PEG scale (TABLE 2).32
CASE
Two weeks into Mr. G’s initial regimen, he called to report no change in pain or functional status. We increased his dose to 5 mg PO every 6 hours as needed. At his 1-month follow-up appointment, he reported his pain as 6/10 and no adverse effects. We again increased his dose to 10 mg PO every 6 hours as needed, with follow-up in another month.
Discontinuation and tapering of opioids
Indications for discontinuing opioids are patient request, resolution of pain, doses ≥ 90 MME/d (in which case a pain specialist should be consulted), inadequate response, untoward adverse effects, and abuse and misuse.1,31,41 However, providers may also face the challenge of working with patients for whom the benefit of opioid therapy is uncertain but who do not have an absolute contraindication. Guidance on this matter may be found in a 2017 systematic review of studies on reducing or discontinuing long-term opioid therapy.42 Although evidence on the whole was low quality, it showed that tapering or discontinuing opioids may actually reduce pain and improve function and quality of life.
Continue to: When working with a patient to taper treatment
When working with a patient to taper treatment, consider using a multidisciplinary approach. Also, assess the patient’s pain level and perception of needs for opioids, make clear the substantial effort that will be asked of the patient, and agree on coping strategies the patient can use to manage the taper.31,43 While the evidence does not appear to support one tapering regimen over another, we can offer some recommendations on ways to individualize a tapering regimen (TABLE 5).1,31,41,43,44
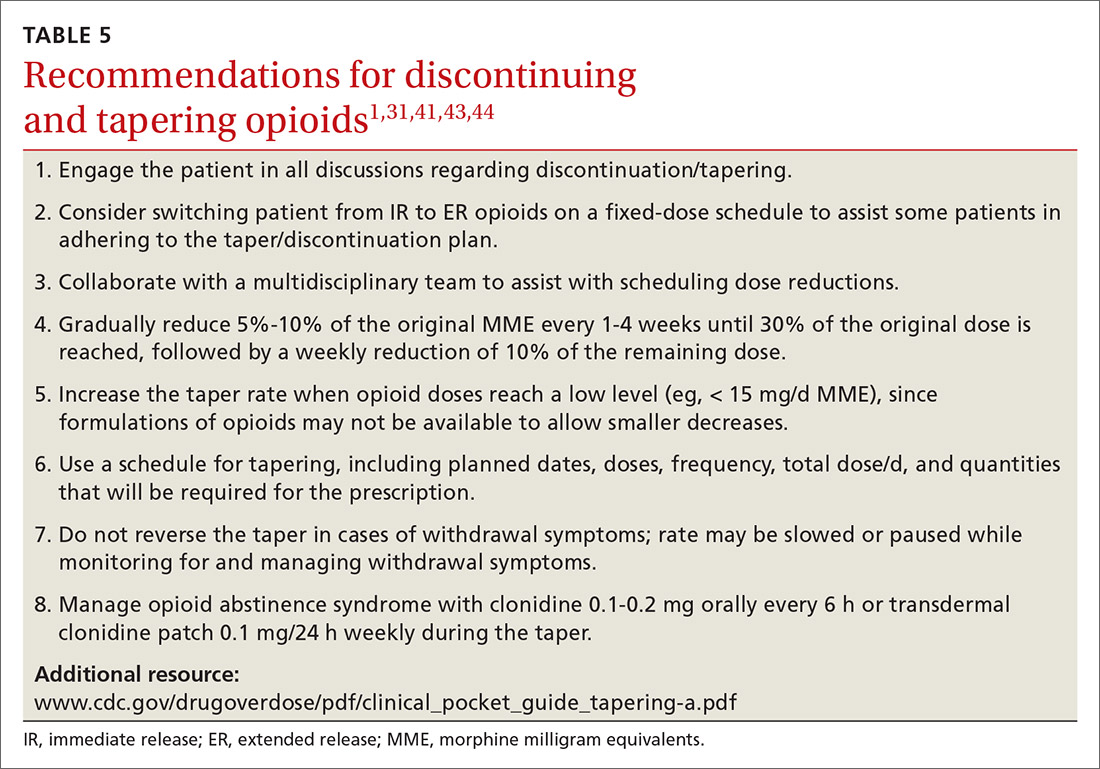
General recommendations. Gradually reduce the original MME dose by 5% to 10% every week to every 4 weeks, with frequent follow-up and adjustments as needed based on the individual’s response.1,31,41,43 In the event that the patient does not tolerate this dose-reduction schedule, tapering can be slowed further.31 Avoid abrupt discontinuation.33 Opioid abstinence syndrome, a myriad of symptoms caused by deprivation of opioids in physiologically dependent individuals, although rare, can occur during tapering and can be managed with clonidine 0.1 to 0.2 mg orally every 6 hours or transdermal clonidine patch 0.1 mg/24 hours weekly during the taper.31
Tapering of long-term opioid treatment is not without risk. Immediate risks include withdrawal syndrome, hyperalgesia, and dropout, while ongoing issues are potential relapse, problems in increasing and maintaining function, and medicolegal implications.43 Withdrawal symptoms begin 2 to 3 half-lives after the last dose of opioid, and resolution varies depending on the duration of use, the most recent dose, and speed of tapering.43 In general, a patient needs 20% to 25% of the previous day’s dose to prevent withdrawal symptoms.31 Increased pain appears to be a brief, time-limited occurance.43 Dropout and relapse tend to be attributed to patient factors such as depressive symptoms and higher pain scores at initiation of the taper.43 Low pain at the end of tapering has been shown to predict long-term abstinence from opioids.43
CASE
Two months into his oxycodone regimen, Mr. G reported improved functional status at his catering job and overall improved quality of life. He had improved his lifting form and was attending biweekly physical therapy sessions. His pain score was 3/10. He expressed a desire to “not get hooked on opioids,” and mentioned he had “tried stopping the medicine last week” but experienced withdrawal symptoms. We discussed and prescribed the following 5-week taper plan: 2.5 mg reduction of oxycodone per dose, every 2 weeks x 2. Then 2.5 mg PO every 6 hours as needed x 1 week before stopping.
Organizing your approach
To optimize the chance for success in opioid treatment and to heighten vigilance and minimize harm to patients, we believe an organized approach is key (TABLE 614,22-24,28,30-32), particularly since this class of medication lacks strong evidence to support its long-term use.
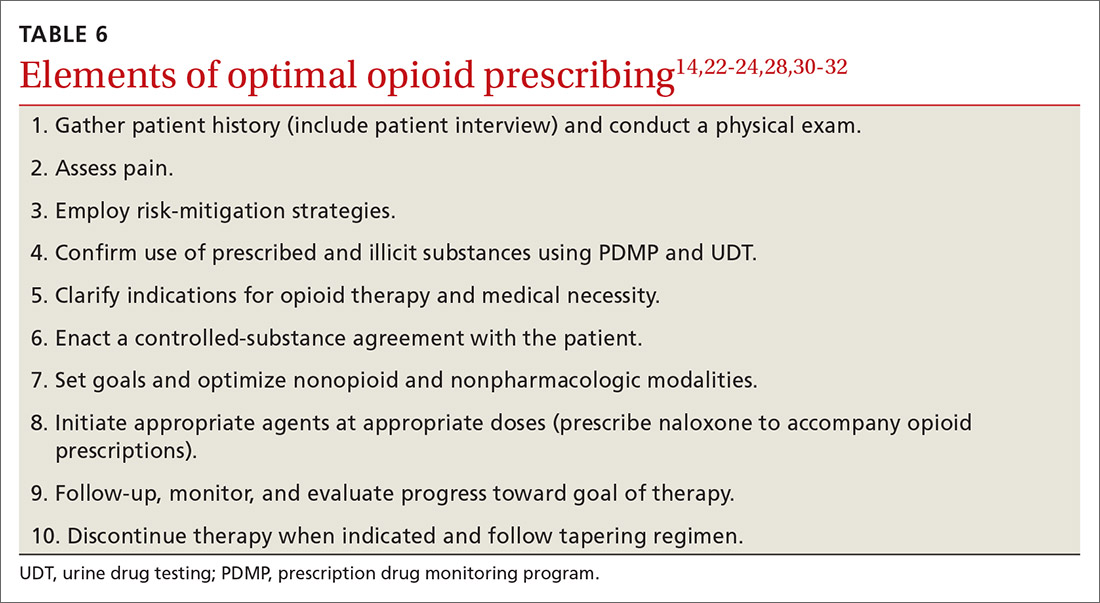
CORRESPONDENCE
Tracy Mahvan, PharmD, BCGP, University of Wyoming, School of Pharmacy, 1000 East University Avenue, Laramie, WY 82071; [email protected].
CASE
Marcelo G* is a 46-year-old man who presented to our family medicine clinic with a complex medical history including end-stage renal disease (ESRD) and hemodialysis, chronic anemia, peripheral vascular disease, venous thromboembolism and anticoagulation, major depressive disorder, osteoarthritis, and lumbosacral radiculopathy. His current medications included vitamin B complex, cholecalciferol, atorvastatin, warfarin, acetaminophen, diclofenac gel, and capsaicin cream. Mr. G reported bothersome bilateral knee and back pain despite physical therapy and consistent use of his current medications in addition to occasional intra-articular glucocorticoid injections. He mentioned that he had benefited in the past from intermittent opioid use.
How would you manage this patient’s care?
*The patient’s name has been changed to protect his identity.
In 2013, an estimated 191 million prescriptions for opioids were written by health care providers, which is the equivalent of all adults living in the United States having their own opioid prescription.1 This large expansion in opioid prescribing and use has also led to a rise in opioid overdose deaths, whether from prescribed or illicit use.1 The Centers for Disease Control and Prevention (CDC) points out that each day, approximately 128 Americans die from an opioid overdose.1 Deaths that occur from opioid overdose often involve the prescribed opioids methadone, oxycodone, and hydrocodone, the illicit opioid heroin, and, of particular concern, prescription and illicit fentanyl.1
The extent of this problem has sparked the development of health safety initiatives and research efforts. Through production quotas, the US Drug Enforcement Administration (DEA) reduced the number of opioids produced across all schedule I and schedule II lists in 2017 by as much as 25%.2 The DEA again reduced the amounts produced in 2018.3 For 2020, the DEA has determined that the production quotas and assessment of annual needs are sufficient.4
The CDC has also promoted access to naloxone and prevention initiatives; pharmacies in some states have standing orders for naloxone, and medical personnel and law enforcement now carry it.1,5 Finally, new research has identified risk factors that influence one’s potential for addiction, such as mental illness, history of substance and alcohol abuse, and a low income.6 Interestingly, while numerous initiatives and strategies have been implemented across health systems, there is little evidence that demonstrates how implementation of safe prescribing strategies has affected overall patient safety and avoidance of opioid-related harms.
Nevertheless, concerns related to opioids are especially important for primary care providers, who manage many patients with acute and chronic diseases and disorders that require pain control.7 Family physicians write more opioid prescriptions than any other specialty,8 and they are therefore uniquely positioned to protect patients, improve the quality of their care, and ultimately produce a meaningful public health impact. This article provides a guide to safe opioid prescribing.
Continue to: Use the patient interview to ensure that Tx aligns with patient goals
Use the patient interview to ensure that Tx aligns with patient goals
For patients presenting with chronic pain, conduct a complete general history and physical examination that includes a review of available records; a medical, surgical, social, family, medication, and allergy history; a review of systems; and documentation of any psychiatric comorbidities (ie, depression, anxiety, psychiatric disorders, personality traits). Inquiries about social history and current medications should explore the possibility of previous and current substance use and misuse.
While causes of pain can be assessed through physical examination and diagnostic tests, the patient interview is an invaluable source of information. No single means of assessment has consistently demonstrated superiority over another in measuring pain, and numerous standard assessment tools are available (TABLE 19-13).14 Unidimensional tools are often easy and quick ways to assess pain intensity. Multidimensional tools, although more time intensive, are designed to gather more subjective information about the patient’s pain. Finally, use an instrument such as the 9-item Patient Health Questionnaire (PHQ-9) to screen patients for psychological distress.15,16
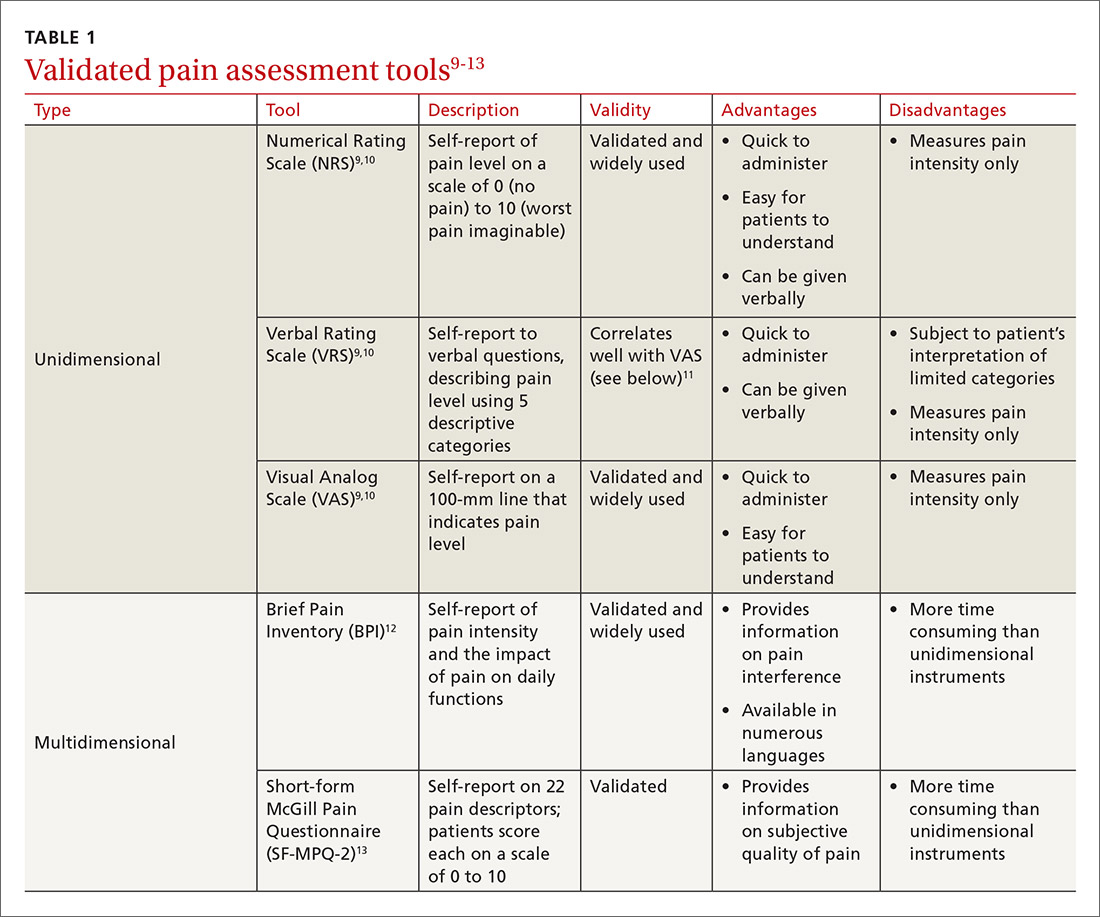
Provide an environment for patients to openly discuss their experiences, expectations, preferences, fears, and coping efforts, as well as the impact that pain has had on their lives.17,18 Without this foundational understanding, medical treatment may work against the patient’s goals. An empathic approach allows for effective communication, shared decision making, and ultimately, an avenue for individualized therapy.
Balancing treatment with risk mitigation
The challenge of managing chronic pain is to balance treating the patient with the basic principle of nonmaleficence (primum non nocere: “first, do no harm”). The literature has shown that risk factors such as a family history of substance abuse or sexual abuse, younger age, and psychological disease may be linked to greater risk for opioid misuse.19,20 However, despite the many risk-screening tools available, no single instrument has reliably and accurately predicted those at higher propensity for prescription addiction. In fact, risk-screening tools as a whole remain unregulated by the US Food and Drug Administration (FDA) and other authorities.21 Still, screening tools provide useful information as one component of the risk-mitigation process.
Screening tools. The tools most commonly used clinically to stratify risk prior to prescribing opioids are the 5-item Opioid Risk Tool (ORT),22 the revised 24-item Screener and Opioid Assessment for Patients with Pain (SOAPP-R),23 which are patient self-administered assessments, and the 7-item clinician-administered DIRE (Diagnosis, Intractability, Risk, Efficacy).24 Given the subtle differences in criteria and the time required for each of these risk assessments, we recommend choosing one based on site-specific resources and overall clinician comfort.25 Risk stratification helps to determine the optimal frequency and intensity of monitoring, not necessarily to deny care to “high-risk” patients.
Continue to: In fact, just as the "universal precautions"...
In fact, just as the “universal precautions” approach has been applied to infection control, many have suggested using a similar approach to pain management. Risk screening should never be misunderstood as an attempt to diminish or undermine the patient’s burden of pain. By routinely conducting thorough and respectful inquiries of risk factors for all patients, clinicians can reduce stigma, improve care, and contain overall risk.26,27
Monitoring programs and patient agreements. In addition to risk-screening tools, the CDC recommends using state prescription drug monitoring programs (PDMP) and urine drug testing (UDT) data to confirm the use of prescribed and illicit substances.28 All 50 states have implemented PDMPs.29 Consider incorporating these components into controlled-substance agreements, which ultimately aim to promote safety and trust between patients and providers. Of course, such agreements do not eliminate all risks associated with opioid prescribing, nor do they guarantee the absence of adverse outcomes. However, when used correctly, they can provide safeguards to reduce misuse and abuse. They also have the potential to preserve the patient-provider relationship, as opposed to providers cursorily refusing to prescribe opioids altogether. The term “controlled-substance agreement” is preferable to “pain contract” or “narcotic contract” as the latter 2 terms may feel stigmatizing and threatening.30
Risk evaluation and mitigation strategy (REMS). In an effort to ensure that benefits of opioid analgesics continue to outweigh the risks, the FDA approved the extended-release (ER)/long-acting (LA) opioid analgesics shared system REMS. Under this REMS, a consortium of ER/LA opioid manufacturers is mandated to provide prescriber education in the form of accredited continuing education and patient educational materials, available at https://opioidanalgesicrems.com/RpcUI/home.u.
CASE
After reviewing Mr. G’s chart and conducting a history, we learned that his bilateral knee osteoarthritis was atraumatic and likely due to overuse—although possibly affected by major trauma in a motor vehicle accident 5 years earlier. Imaging also revealed multilevel disc degeneration contributing to his radicular back pain, which seemed to be worse on days after working as a caterer. Poor lifting form at work may have contributed to his pain. Nevertheless, he had been consistent with medical follow-up and denied current or past use of illicit substances. Per the numeric rating scale (NRS), he reported 8 out of 10 pain in his knees and 6 out of 10 in his back. In addition to obtaining a PHQ-9 score of 4, we conducted a DIRE assessment and obtained a score of 19 out of a possible 21, indicating that he may be a good candidate for long-term opioid analgesia.
Criteria for prescribing opioids and for guiding treatment goals
Prescribing an opioid requires establishing a medical necessity based on 3 criteria:31
- pain of moderate-to-severe degree
- a physical diagnosis or suspected organic problem
- documented treatment failure of a noncontrolled substance, adjuvant agents, physician-ordered physical therapy, structured exercise program, and interventional techniques.
Continue to: Treatment goals should be established...
Treatment goals should be established and understood by the prescriber and patient prior to initiation of opioids.28 Overarching treatment goals for all opioids prescribed are pain relief (but not necessarily a focus on pain scores), improvement in functional activity, and minimization of adverse effects, with the latter 2 goals taking precedence.31 To assess outcomes, formally measure progress toward goals from baseline evaluations. This can be achieved through repeated use of validated tools such as those mentioned earlier, or may be more broadly considered as progress toward employment status or increasing participation in activities.31 All pain management plans involving opioids should include continued efforts with nonpharmacologic therapy (eg, exercise therapy, weight loss, behavioral training) and nonopioid pharmacologic therapy (eg, nonsteroidal anti-inflammatory drugs, tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors, anticonvulsants).28
Have an “exit strategy.” As part of goal setting, also consider how therapy will be discontinued if benefits do not outweigh the risks of harm.28 Weigh functional status gains against adverse opioid consequences using the PEG scale (pain, enjoyment of life, and general activity) (TABLE 232).33 Improvements of 30% from baseline have been deemed clinically meaningful by some,32 but not all benefits will be easy to quantify. At the start of treatment dialogue, use the term “therapeutic trial” instead of ”treatment plan” to more effectively convey that opioids will be continued only if safe and effective, and will be prescribed at the lowest effective dose as one component of the multimodal approach to pain.30
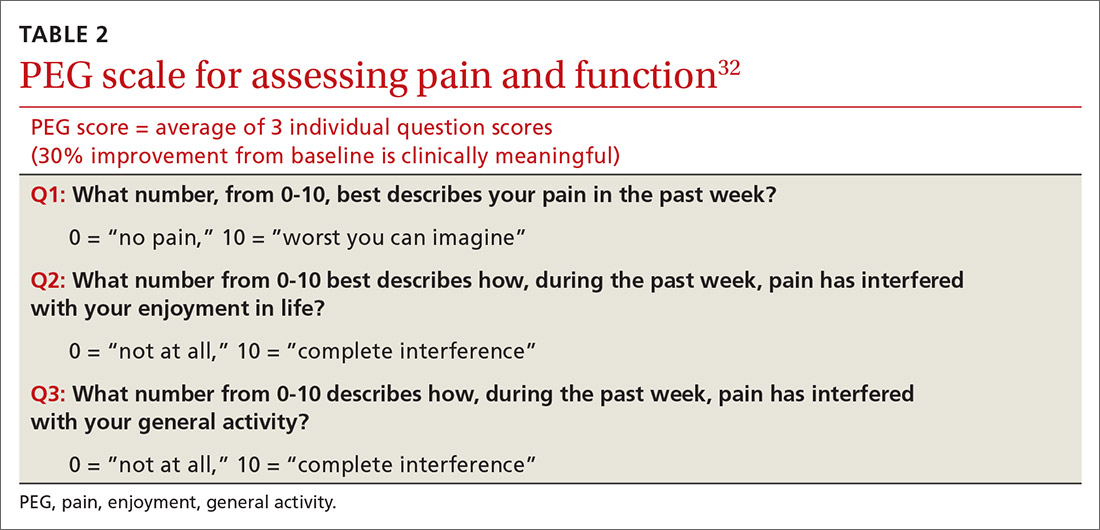
Initiation of treatment: Opioid selection and dosing
When initiating opioid therapy, prescribe an immediate-release, short-acting agent instead of an ER/LA formulation.28
For moderate pain, first consider tramadol, codeine, tapentadol, or hydrocodone.31 Second-line agents for moderate pain are hydrocodone or oxycodone.31
For severe pain, first-line agents include hydrocodone, oxycodone, hydromorphone, or morphine.31 Second-line agents for severe pain are fentanyl and, with careful supervision or referral to a pain specialist, methadone or buprenorphine.31
Continue to: Of special note...
Of special note,

At the start, prescribe the lowest effective dosage (referring to the product labeling for guidance) and calculate total daily dose in terms of morphine milligram equivalents (MME) (TABLE 335-37).28 Exercise caution when considering opioids for patients with respiratory sleep disorders and for patients ≥ 65 years due to altered pharmacokinetics in the elderly population.38 Also make dose adjustments for renal and hepatic insufficiency (TABLE 435).
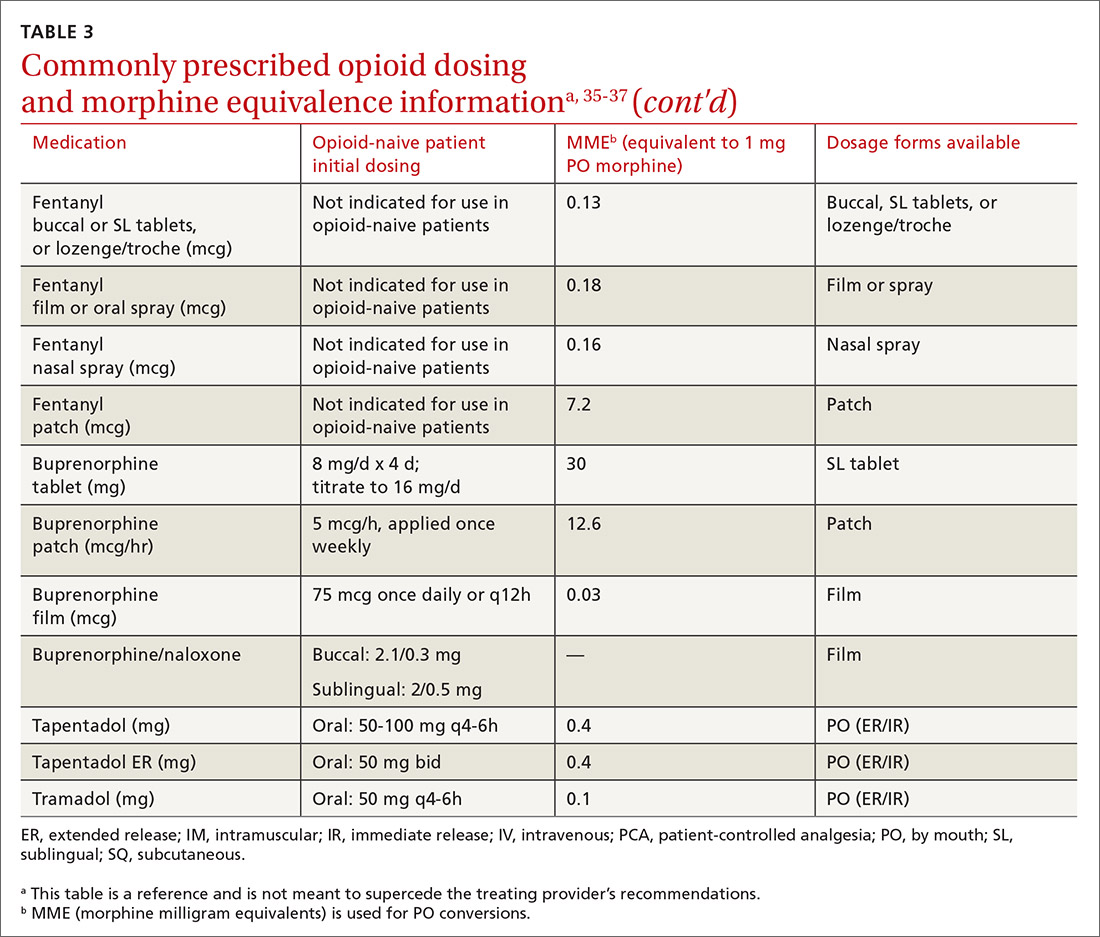
Doses between 20 to 50 MME/d are considered relatively low dosages.28 Be cautious when prescribing an opioid at any dosage, and reassess evidence of individual benefits and risks before increasing the dosage to ≥ 50 MME/d.28 Regard a dosage of 90 MME/d as maximal.28 While there is no analgesic ceiling, doses greater than 90 MME/d are associated with risk for overdose and should prompt referral to a pain specialist.31 Veterans Administration guidelines cite strong evidence that risk for overdose and death significantly increases at a range of 20 to 50 MME/d.33 Daily doses exceeding 90 MME/d should be documented with rational justification.28
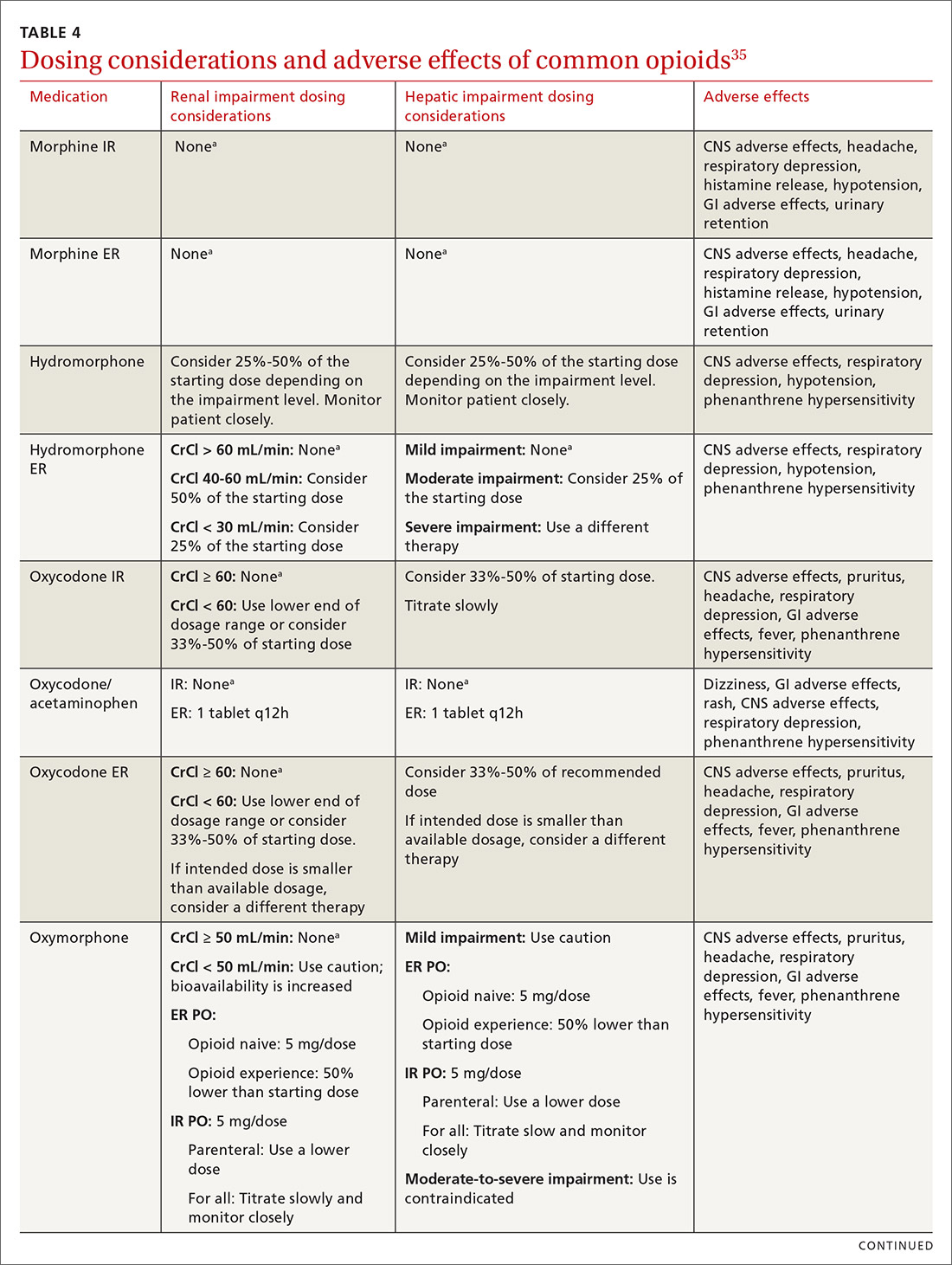
CASE
Noncontrolled medications are preferred in the treatment of chronic pain. However, the utility of adjuvant options such as NSAIDs, duloxetine, or gabapentin were limited in Mr. G’s case due to his ESRD. Calcium channel α2-δ ligands may have been effective in reducing symptoms of neuropathic pain but would have had limited efficacy against osteoarthritis. Based on his low risk for opioid misuse, we decided to start Mr. G on oxycodone 2.5 mg PO, every 6 hours as needed for moderate-to-severe pain, and to follow up in 1 month. We also explained proper lifting form to him and encouraged him to continue with physical therapy.
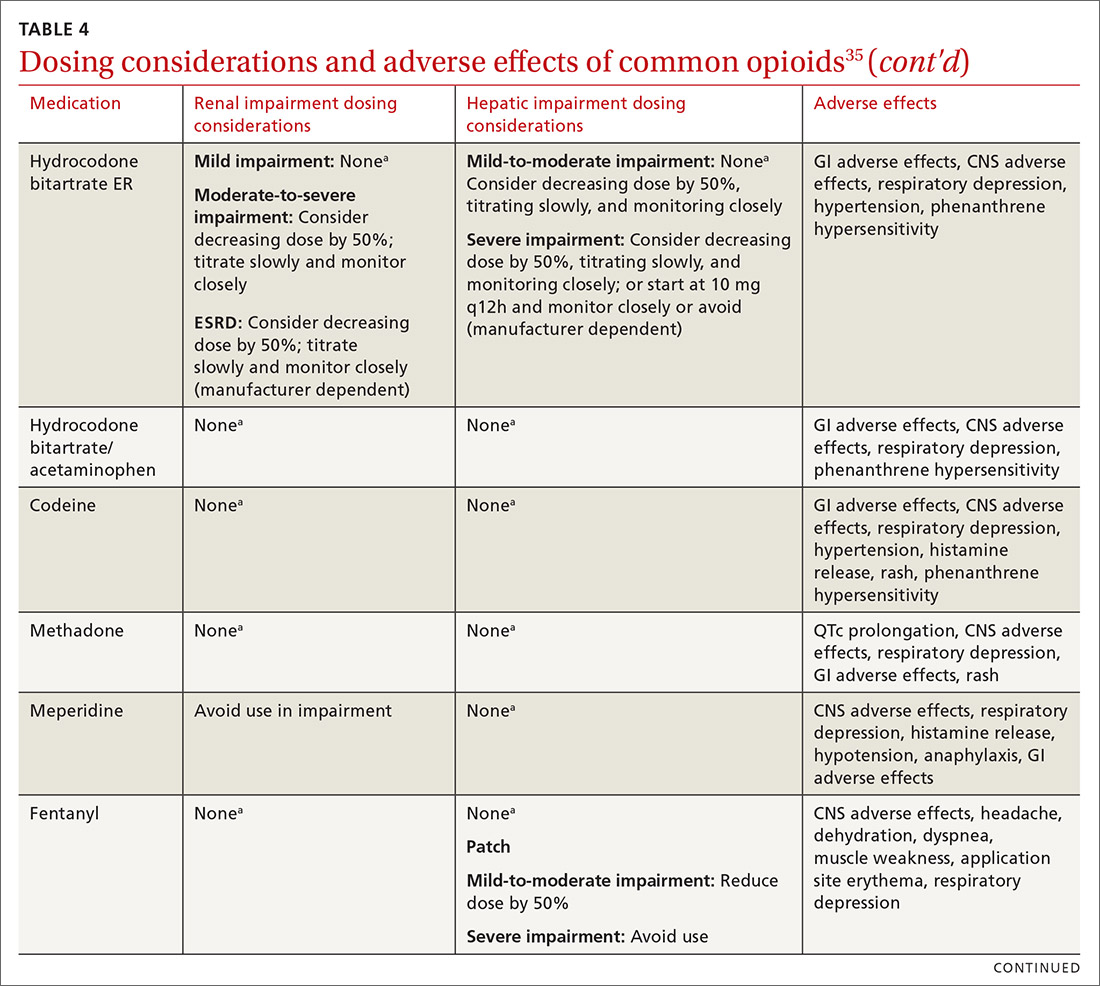
Deciding to continue therapy with opioids
There is a lack of convincing evidence that opioid use beyond 6 months improves quality of life; patients do not report a significant reduction in pain beyond this time.28 Thus, a repeat evaluation of continued medical necessity is essential before deciding in favor of ongoing, long-term treatment with opioids. Continue prescribing opioids only if there is meaningful pain relief and improved function that outweighs the harms that may be expected for a given patient.31 With all patients, consider prescribing naloxone to accompany dispensed opioid prescriptions.28 This is particularly important for those at risk for misuse (history of overdose, history of substance use disorder, dosages ≥ 50 MME/d, or concurrent benzodiazepine use). Resources for prescribing naloxone in primary care settings can be found through Prescribe to Prevent at http://prescribetoprevent.org. Due to the established risk of overdose, avoid, if possible, concomitant prescriptions of benzodiazepines and opioids.31
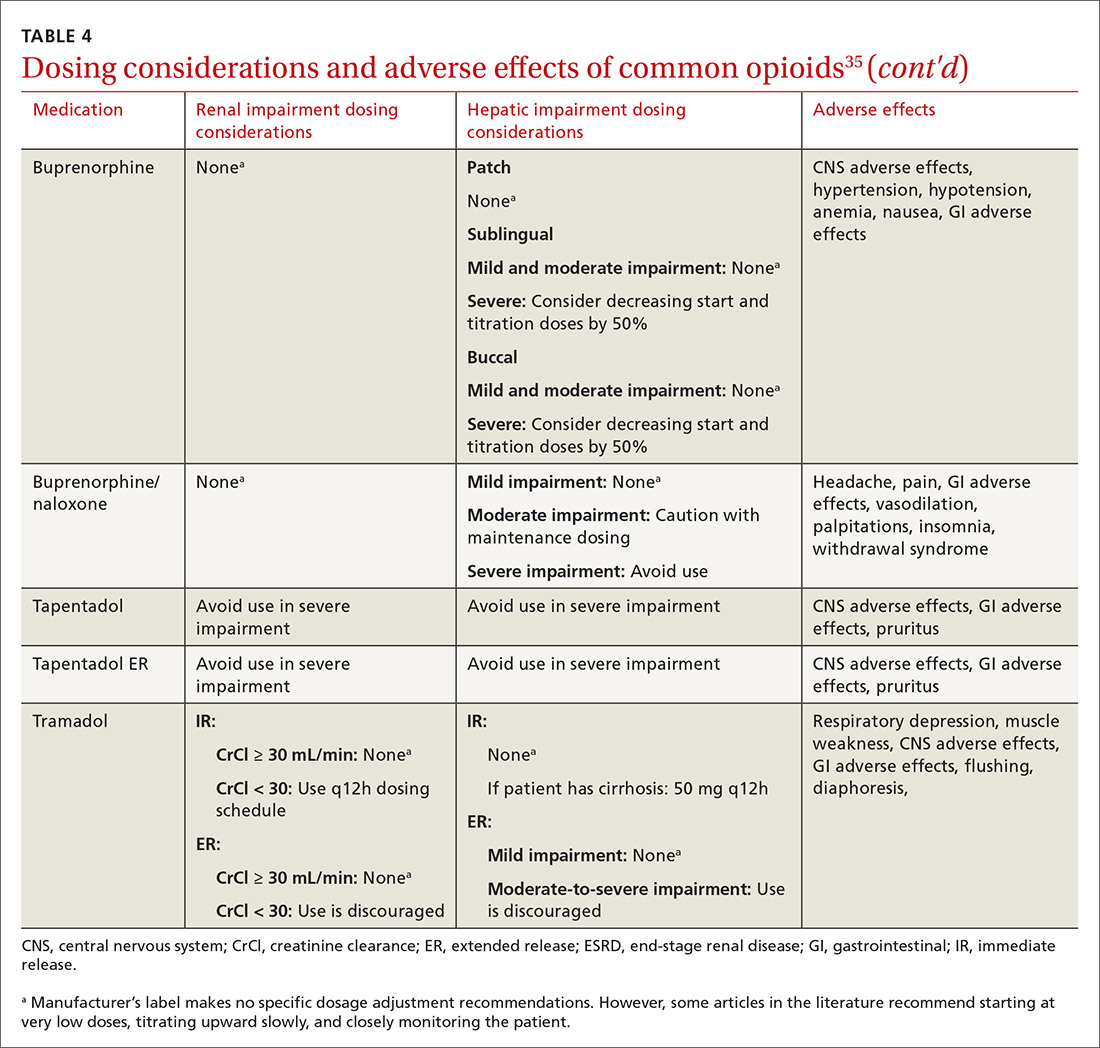
Continue to: Follow-up and monitoring
Follow-up and monitoring
Responsiveness to opioids varies greatly among individuals.38,39 An opioid that leads to a therapeutic analgesic effect in one patient may cause adverse events or toxicity in another. Periodically reassess the appropriateness of chronic opioid therapy and modify treatment based on its ability to meet therapeutic goals. While practice behaviors and clinic policies vary across institutions, risk stratification can provide guidance on the frequency and intensity of follow-up and monitoring. Kaye et al21 describe a triage system in which low-risk patients may be managed by a primary care provider with routine follow-up and reassessment every 3 months.21 Moderate-risk patients may warrant additional management by specialists and a monthly follow-up. High-risk patients may need referrals to interdisciplinary pain centers or addiction specialists.21
Along these lines, the CDC recommends conducting a PDMP review and UDT before initiating therapy, followed by a periodic PDMP (every 1-3 months) and a UDT at least annually. Keep in mind, providers should follow their state-specific regulations, as monitoring requirements may vary. In addition, clinicians should always be alert to adverse reactions (TABLE 435) and sudden behavior changes such as respiratory depression, nausea, constipation, pruritus, cognitive impairment, falls, motor vehicle accidents, and aberrant behaviors. Under these circumstances, consider a dose reduction and, in certain cases, discontinuation.
Additionally, in cases of pain unresponsive to escalating opioid doses, include opioid-induced hyperalgesia (OIH) in the differential. Dose reductions, opioid rotations, and office-based detoxifications are all options for the treatment of OIH.40 Assessment of pain and function can be accomplished using the PEG scale (TABLE 2).32
CASE
Two weeks into Mr. G’s initial regimen, he called to report no change in pain or functional status. We increased his dose to 5 mg PO every 6 hours as needed. At his 1-month follow-up appointment, he reported his pain as 6/10 and no adverse effects. We again increased his dose to 10 mg PO every 6 hours as needed, with follow-up in another month.
Discontinuation and tapering of opioids
Indications for discontinuing opioids are patient request, resolution of pain, doses ≥ 90 MME/d (in which case a pain specialist should be consulted), inadequate response, untoward adverse effects, and abuse and misuse.1,31,41 However, providers may also face the challenge of working with patients for whom the benefit of opioid therapy is uncertain but who do not have an absolute contraindication. Guidance on this matter may be found in a 2017 systematic review of studies on reducing or discontinuing long-term opioid therapy.42 Although evidence on the whole was low quality, it showed that tapering or discontinuing opioids may actually reduce pain and improve function and quality of life.
Continue to: When working with a patient to taper treatment
When working with a patient to taper treatment, consider using a multidisciplinary approach. Also, assess the patient’s pain level and perception of needs for opioids, make clear the substantial effort that will be asked of the patient, and agree on coping strategies the patient can use to manage the taper.31,43 While the evidence does not appear to support one tapering regimen over another, we can offer some recommendations on ways to individualize a tapering regimen (TABLE 5).1,31,41,43,44
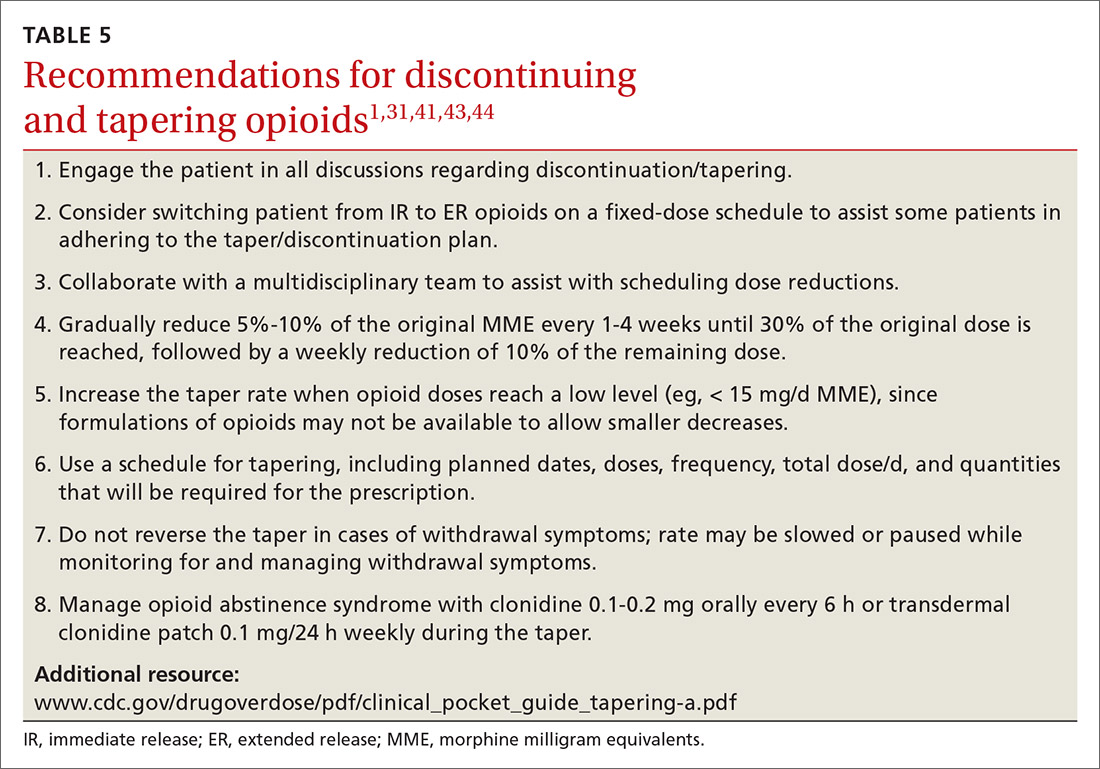
General recommendations. Gradually reduce the original MME dose by 5% to 10% every week to every 4 weeks, with frequent follow-up and adjustments as needed based on the individual’s response.1,31,41,43 In the event that the patient does not tolerate this dose-reduction schedule, tapering can be slowed further.31 Avoid abrupt discontinuation.33 Opioid abstinence syndrome, a myriad of symptoms caused by deprivation of opioids in physiologically dependent individuals, although rare, can occur during tapering and can be managed with clonidine 0.1 to 0.2 mg orally every 6 hours or transdermal clonidine patch 0.1 mg/24 hours weekly during the taper.31
Tapering of long-term opioid treatment is not without risk. Immediate risks include withdrawal syndrome, hyperalgesia, and dropout, while ongoing issues are potential relapse, problems in increasing and maintaining function, and medicolegal implications.43 Withdrawal symptoms begin 2 to 3 half-lives after the last dose of opioid, and resolution varies depending on the duration of use, the most recent dose, and speed of tapering.43 In general, a patient needs 20% to 25% of the previous day’s dose to prevent withdrawal symptoms.31 Increased pain appears to be a brief, time-limited occurance.43 Dropout and relapse tend to be attributed to patient factors such as depressive symptoms and higher pain scores at initiation of the taper.43 Low pain at the end of tapering has been shown to predict long-term abstinence from opioids.43
CASE
Two months into his oxycodone regimen, Mr. G reported improved functional status at his catering job and overall improved quality of life. He had improved his lifting form and was attending biweekly physical therapy sessions. His pain score was 3/10. He expressed a desire to “not get hooked on opioids,” and mentioned he had “tried stopping the medicine last week” but experienced withdrawal symptoms. We discussed and prescribed the following 5-week taper plan: 2.5 mg reduction of oxycodone per dose, every 2 weeks x 2. Then 2.5 mg PO every 6 hours as needed x 1 week before stopping.
Organizing your approach
To optimize the chance for success in opioid treatment and to heighten vigilance and minimize harm to patients, we believe an organized approach is key (TABLE 614,22-24,28,30-32), particularly since this class of medication lacks strong evidence to support its long-term use.
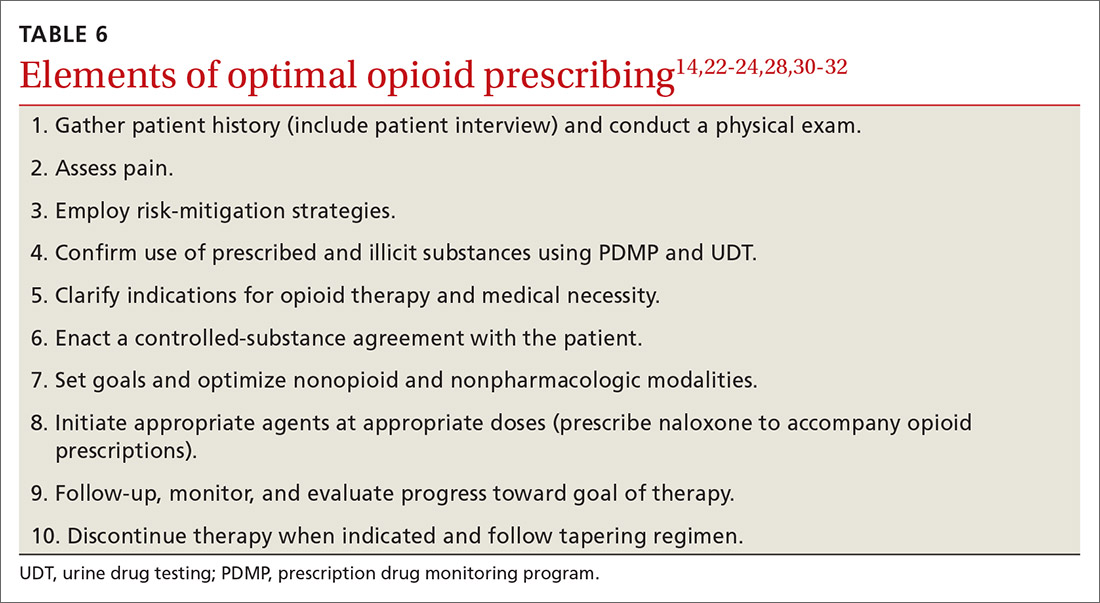
CORRESPONDENCE
Tracy Mahvan, PharmD, BCGP, University of Wyoming, School of Pharmacy, 1000 East University Avenue, Laramie, WY 82071; [email protected].
1. CDC. Opioid overdose. www.cdc.gov/drugoverdose/opioids/prescribed.html. Accessed June 26, 2020.
2. DEA, Department of Justice. Established aggregate production quotas for schedule I and II controlled substances and assessment of annual needs for the list I chemicals ephedrine, pseudoephedrine, and phenylpropanolamine for 2017. www.deadiversion.usdoj.gov/fed_regs/quotas/2016/fr1005.htm. Accessed June 26, 2020.
3. DEA, Department of Justice. Established aggregate production quotas for schedule I and II controlled substances and assessment of annual needs for the list I chemicals ephedrine, pseudoephedrine, and phenylpropanolamine for 2018. www.deadiversion.usdoj.gov/fed_regs/quotas/2017/fr1108.htm. Accessed June 26, 2020.
4. DEA, Department of Justice. Established aggregate production quotas for schedule I and II controlled substances and assessment of annual needs for the list I chemicals ephedrine, pseudoephedrine, and phenylpropanolamine for 2020. www.deadiversion.usdoj.gov/fed_regs/quotas/2019/fr1202.htm. Accessed June 26, 2020.
5. US Department of Veterans Affairs. Pharmacy benefits management services: academic detailing service—opioid overdose education & naloxone distribution (OEND). www.pbm.va.gov/AcademicDetailingService/Opioid_Overdose_Education_and_Naloxone_Distribution.asp. Accessed June 26, 2020.
6. McCarberg BH. Pain management in primary care: strategies to mitigate opioid misuse, abuse, and diversion. Postgrad Med. 2011;123:119-130.
7. Dean L. Tramadol therapy and CYP2D6 genotype. In: Pratt V, McLeod H, Rubinstein W, et al (eds). Medical Genetics Summaries [Internet]. Bethesda, Md: National Center for Biotechnology Information (US); 2015. www.ncbi.nlm.nih.gov/books/NBK315950/. Accessed June 26, 2020.
8. Chen JH, Humphreys K, Shah NH, et al. Distribution of opioids by different types of Medicare prescribers. JAMA Intern Med. 2016;176:259-261.
9. Jensen MP, Karoly P. Self-report scales and procedures for assessing pain in adults. In: Turk DC, Melzack R, eds. Handbook of Pain Assessment. 3rd ed. New York, NY: Guilford Press; 2011;19-41.
10. Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005; 14:798-804.
11. Ohnhaus EE, Adler R. Methodological problems in the measurement of pain: a comparison between the verbal rating scale and the visual analogue scale. Pain. 1975;1:379-384.
12. Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23:129-138.
13. Dworkin RH, Turk DC, Revicki DA, et al. Development and initial validation of an expanded and revised version of the short-form McGill Pain Questionnaire (SF-MPQ-2). Pain. 2009;144:35-42.
14. Dansie EJ, Turk DC. Assessment of patients with chronic pain. Br J Anaesth. 2013;111:19-25.
15. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-613.
16. Choi Y, Mayer TG, Williams MJ, Gatchel RJ. What is the best screening test for depression in chronic spinal pain patients? Spine J. 2014;14:1175-1182.
17. Practice guidelines for chronic pain management: an updated report by the American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine. Anesthesiology. 2010;122:810-833.
18. Gallagher RM. Empathy: a timeless skill for the pain medicine toolbox. Pain Med. 2006;7:213-214.
19. Koyyalagunta D, Bruera E, Aigner C, et al. Risk stratification of opioid misuse among patients with cancer pain using the SOAPP-SF. Pain Med. 2013;14:667-675.
20. Trescot AM, Helm S, Hansen H, et al. Opioids in the management of chronic non-cancer pain: an update of American Society of the Interventional Pain Physicians’ (ASIPP) guidelines. Pain Physician. 2008;11:S5-S62.
21. Kaye AD, Jones MR, Kaye AM, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse (part 2). Pain Physician. 2017;20:S111-S133.
22. Webster LR, Webster RM. Predicting aberrant behaviors in opioid‐treated patients: preliminary validation of the Opioid Risk Tool. Pain Med. 2005;6:432-442.
23. Butler SF, Fernandez K, Benoit C, et al. Validation of the revised screener and opioid assessment for patients with pain (SOAPP-R). J Pain. 2008;9:360-372.
24. Belgrade MJ, Schamber CD, Lindgren BR. The DIRE score: predicting outcomes of opioid prescribing for chronic pain. J Pain. 2006;7:671-681.
25. Fine PG, Finnegan T, Portenoy RK. Protect your patients, protect your practice: practical risk assessment in the structuring of opioid therapy in chronic pain. J Fam Pract. 2010;59(9 suppl 2):S1-16.
26. Gourlay DL, Heit HA, Almahrezi A. Universal precautions in pain medicine: a rational approach to the treatment of chronic pain. Pain Med. 2005;6:107-112.
27. Manubay JM, Muchow C, Sullivan MA. Prescription drug abuse: epidemiology, regulatory issues, chronic pain management with narcotic analgesics. Prim Care. 2011;38:71-90.
28. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm Rep. 2016;65:1-49.
29. Prescription Drug Monitoring Program Training and Technical Assistance Center. State PDMP profiles and contacts. www.pdmpassist.org/State. Accessed June 26, 2020.
30. Tobin DG, Andrews R, Becker WC. Prescribing opioids in primary care: Safely starting, monitoring, and stopping. Cleve Clin J Med. 2016;83:207-215.
31. Manchikanti L, Kaye AM, Knezevis NN, et al. Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of Interventional Pain Physicians (ASIPP) guidelines. Pain Physician. 2017;20:S3-S92.
32. HHS. Checklist for prescribing opioids for chronic pain. www.cdc.gov/drugoverdose/pdf/PDO_Checklist-a.pdf. Accessed June 26, 2020.
33. VA/DoD. VA/DoD clinical practice guideline for opioid therapy for chronic pain. www.healthquality.va.gov/guidelines/Pain/cot/VADoDOTCPG022717.pdf. Accessed June 26, 2020.
34. Nuckols TK, Anderson L, Popescu I, et al. Opioid prescribing: a systematic review and critical appraisal of guidelines for chronic pain. Ann Intern Med. 2014;160:38-47.
35. Lexi-Comp Online. Hudson (OH): Wolters Kluwer Clinical Drug Information, Inc; 2018. https://online.lexi.com/lco/action/login. Accessed July 9, 2020.
36. CMS. Opioid oral morphine milligram equivalent (MME) conversion factors. www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/Opioid-Morphine-EQ-Conversion-Factors-Aug-2017.pdf. Accessed June 26, 2020.
37. Cupp M. Equianalgesic dosing of opioids for pain management. Pharmacist’s Letter/Prescriber’s Letter. 2018:340406. Stockton (CA): Therapeutic Research Center, LLC; 2018. www.nhms.org/sites/default/files/Pdfs/Opioid-Comparison-Chart-Prescriber-Letter-2012.pdf. Accessed June 26, 2020.
38. Smith HS. Variations in opioid responsiveness. Pain Physician. 2008;11:237-248.
39. Bronstein K, Passik S, Munitz L, et al. Can clinicians accurately predict which patients are misusing their medications? J Pain. 2011;12(suppl):P3.
40. Silverman SM. Opioid induced hyperalgesia: clinical implications for the pain practitioner. Pain Physician. 2009;12:679-684.
41. Busse JW, Craigie S, Juurlink DN, et al. Guideline for opioid therapy and chronic non-cancer pain. CMAJ. 2017;189:E659-E666.
42. Frank JW, Lovejoy TI, Becker WC, et al. Patient outcomes in dose reduction or discontinuation of long-term opioid therapy: a systematic review. Ann Intern Med. 2017;167:181-191.
43. Berna C, Kulich RJ, Rathmell JP. Tapering long-term opioid therapy in chronic non-cancer pain: evidence and recommendations for everyday practice. Mayo Clin Proc. 2015;90:828-842.
44. Washington State Agency Medical Director’s Group. Interagency guideline on prescribing opioids for pain. June 2015. www.agencymeddirectors.wa.gov/Files/2015AMDGOpioidGuideline.pdf. Accessed June 26, 2020.
1. CDC. Opioid overdose. www.cdc.gov/drugoverdose/opioids/prescribed.html. Accessed June 26, 2020.
2. DEA, Department of Justice. Established aggregate production quotas for schedule I and II controlled substances and assessment of annual needs for the list I chemicals ephedrine, pseudoephedrine, and phenylpropanolamine for 2017. www.deadiversion.usdoj.gov/fed_regs/quotas/2016/fr1005.htm. Accessed June 26, 2020.
3. DEA, Department of Justice. Established aggregate production quotas for schedule I and II controlled substances and assessment of annual needs for the list I chemicals ephedrine, pseudoephedrine, and phenylpropanolamine for 2018. www.deadiversion.usdoj.gov/fed_regs/quotas/2017/fr1108.htm. Accessed June 26, 2020.
4. DEA, Department of Justice. Established aggregate production quotas for schedule I and II controlled substances and assessment of annual needs for the list I chemicals ephedrine, pseudoephedrine, and phenylpropanolamine for 2020. www.deadiversion.usdoj.gov/fed_regs/quotas/2019/fr1202.htm. Accessed June 26, 2020.
5. US Department of Veterans Affairs. Pharmacy benefits management services: academic detailing service—opioid overdose education & naloxone distribution (OEND). www.pbm.va.gov/AcademicDetailingService/Opioid_Overdose_Education_and_Naloxone_Distribution.asp. Accessed June 26, 2020.
6. McCarberg BH. Pain management in primary care: strategies to mitigate opioid misuse, abuse, and diversion. Postgrad Med. 2011;123:119-130.
7. Dean L. Tramadol therapy and CYP2D6 genotype. In: Pratt V, McLeod H, Rubinstein W, et al (eds). Medical Genetics Summaries [Internet]. Bethesda, Md: National Center for Biotechnology Information (US); 2015. www.ncbi.nlm.nih.gov/books/NBK315950/. Accessed June 26, 2020.
8. Chen JH, Humphreys K, Shah NH, et al. Distribution of opioids by different types of Medicare prescribers. JAMA Intern Med. 2016;176:259-261.
9. Jensen MP, Karoly P. Self-report scales and procedures for assessing pain in adults. In: Turk DC, Melzack R, eds. Handbook of Pain Assessment. 3rd ed. New York, NY: Guilford Press; 2011;19-41.
10. Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005; 14:798-804.
11. Ohnhaus EE, Adler R. Methodological problems in the measurement of pain: a comparison between the verbal rating scale and the visual analogue scale. Pain. 1975;1:379-384.
12. Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23:129-138.
13. Dworkin RH, Turk DC, Revicki DA, et al. Development and initial validation of an expanded and revised version of the short-form McGill Pain Questionnaire (SF-MPQ-2). Pain. 2009;144:35-42.
14. Dansie EJ, Turk DC. Assessment of patients with chronic pain. Br J Anaesth. 2013;111:19-25.
15. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-613.
16. Choi Y, Mayer TG, Williams MJ, Gatchel RJ. What is the best screening test for depression in chronic spinal pain patients? Spine J. 2014;14:1175-1182.
17. Practice guidelines for chronic pain management: an updated report by the American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine. Anesthesiology. 2010;122:810-833.
18. Gallagher RM. Empathy: a timeless skill for the pain medicine toolbox. Pain Med. 2006;7:213-214.
19. Koyyalagunta D, Bruera E, Aigner C, et al. Risk stratification of opioid misuse among patients with cancer pain using the SOAPP-SF. Pain Med. 2013;14:667-675.
20. Trescot AM, Helm S, Hansen H, et al. Opioids in the management of chronic non-cancer pain: an update of American Society of the Interventional Pain Physicians’ (ASIPP) guidelines. Pain Physician. 2008;11:S5-S62.
21. Kaye AD, Jones MR, Kaye AM, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse (part 2). Pain Physician. 2017;20:S111-S133.
22. Webster LR, Webster RM. Predicting aberrant behaviors in opioid‐treated patients: preliminary validation of the Opioid Risk Tool. Pain Med. 2005;6:432-442.
23. Butler SF, Fernandez K, Benoit C, et al. Validation of the revised screener and opioid assessment for patients with pain (SOAPP-R). J Pain. 2008;9:360-372.
24. Belgrade MJ, Schamber CD, Lindgren BR. The DIRE score: predicting outcomes of opioid prescribing for chronic pain. J Pain. 2006;7:671-681.
25. Fine PG, Finnegan T, Portenoy RK. Protect your patients, protect your practice: practical risk assessment in the structuring of opioid therapy in chronic pain. J Fam Pract. 2010;59(9 suppl 2):S1-16.
26. Gourlay DL, Heit HA, Almahrezi A. Universal precautions in pain medicine: a rational approach to the treatment of chronic pain. Pain Med. 2005;6:107-112.
27. Manubay JM, Muchow C, Sullivan MA. Prescription drug abuse: epidemiology, regulatory issues, chronic pain management with narcotic analgesics. Prim Care. 2011;38:71-90.
28. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm Rep. 2016;65:1-49.
29. Prescription Drug Monitoring Program Training and Technical Assistance Center. State PDMP profiles and contacts. www.pdmpassist.org/State. Accessed June 26, 2020.
30. Tobin DG, Andrews R, Becker WC. Prescribing opioids in primary care: Safely starting, monitoring, and stopping. Cleve Clin J Med. 2016;83:207-215.
31. Manchikanti L, Kaye AM, Knezevis NN, et al. Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of Interventional Pain Physicians (ASIPP) guidelines. Pain Physician. 2017;20:S3-S92.
32. HHS. Checklist for prescribing opioids for chronic pain. www.cdc.gov/drugoverdose/pdf/PDO_Checklist-a.pdf. Accessed June 26, 2020.
33. VA/DoD. VA/DoD clinical practice guideline for opioid therapy for chronic pain. www.healthquality.va.gov/guidelines/Pain/cot/VADoDOTCPG022717.pdf. Accessed June 26, 2020.
34. Nuckols TK, Anderson L, Popescu I, et al. Opioid prescribing: a systematic review and critical appraisal of guidelines for chronic pain. Ann Intern Med. 2014;160:38-47.
35. Lexi-Comp Online. Hudson (OH): Wolters Kluwer Clinical Drug Information, Inc; 2018. https://online.lexi.com/lco/action/login. Accessed July 9, 2020.
36. CMS. Opioid oral morphine milligram equivalent (MME) conversion factors. www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/Opioid-Morphine-EQ-Conversion-Factors-Aug-2017.pdf. Accessed June 26, 2020.
37. Cupp M. Equianalgesic dosing of opioids for pain management. Pharmacist’s Letter/Prescriber’s Letter. 2018:340406. Stockton (CA): Therapeutic Research Center, LLC; 2018. www.nhms.org/sites/default/files/Pdfs/Opioid-Comparison-Chart-Prescriber-Letter-2012.pdf. Accessed June 26, 2020.
38. Smith HS. Variations in opioid responsiveness. Pain Physician. 2008;11:237-248.
39. Bronstein K, Passik S, Munitz L, et al. Can clinicians accurately predict which patients are misusing their medications? J Pain. 2011;12(suppl):P3.
40. Silverman SM. Opioid induced hyperalgesia: clinical implications for the pain practitioner. Pain Physician. 2009;12:679-684.
41. Busse JW, Craigie S, Juurlink DN, et al. Guideline for opioid therapy and chronic non-cancer pain. CMAJ. 2017;189:E659-E666.
42. Frank JW, Lovejoy TI, Becker WC, et al. Patient outcomes in dose reduction or discontinuation of long-term opioid therapy: a systematic review. Ann Intern Med. 2017;167:181-191.
43. Berna C, Kulich RJ, Rathmell JP. Tapering long-term opioid therapy in chronic non-cancer pain: evidence and recommendations for everyday practice. Mayo Clin Proc. 2015;90:828-842.
44. Washington State Agency Medical Director’s Group. Interagency guideline on prescribing opioids for pain. June 2015. www.agencymeddirectors.wa.gov/Files/2015AMDGOpioidGuideline.pdf. Accessed June 26, 2020.
PRACTICE RECOMMENDATIONS
› Use a screening instrument such as the Opioid Risk Tool or the DIRE assessment to gauge a patient’s risk of opioid misuse and determine the frequency of monitoring. C
› Give as much priority to improving functional activity and minimizing adverse opioid effects as you do to relieving pain. C
› Prescribe an immediate-release, short-acting agent at first instead of a long-acting formulation; start with the lowest effective dosage and calculate total daily dose in terms of morphine milligram equivalents (MME). C
› Reduce the original MME dose by 5% to 10% every week when discontinuing an opioid. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Revisiting Xanax amid the coronavirus crisis
One of the more alarming trends that has emerged during the coronavirus crisis is the concomitant rise in the use of benzodiazepines, such as Xanax. It has been reported that at-risk individuals began seeking prescription anxiolytics as early as mid-February with a consequent peak of 34% the following month, coinciding with the World Health Organization’s declaration of a global pandemic.1
Consistent with the available literature indicating that women are twice as likely to be affected by anxiety disorders, the prescription spikes were almost double when compared with those of their male counterparts.2 The pandemic has instilled a sense of fear in people, leading to social repercussions, such as estrangement, insomnia, and paranoia for at-risk populations.3,4
“Benzos” are commonly prescribed to help people sleep or to assist them in overcoming a host of anxiety disorders. The rapid onset of effects make Xanax a desirable and efficacious benzodiazepine.5 The use of these medications might not be an immediate cause for concern because patients might be taking it as intended. Nevertheless, clinicians are shying away from medical management in favor of counseling or therapy.
Dangerous trends
Numerous factors might contribute to this grim scenario, including patient dependence on benzodiazepines, paranoia about engaging with health care professionals because of fear tied to potential COVID-19 exposure, and/or increased access to illicit counterfeit pills from drug dealers or the dark web markets.
Lessons can be gleaned from the most extensive dark web drug busts in Britain’s history, in which a deluge of “pharmaceutical grade” Xanax pills made it to the hands of drug dealers and consumers between 2015 and 2017.6 A similar phenomenon emerged stateside.7 Virtually indistinguishable from recognized 2-mg Xanax pills, these fake pills posed a serious challenge to forensic scientists.8 The threat of overdose is very real for users targeted by the counterfeit Xanax trade, especially since those at risk often bypass professional health care guidelines.
In broad daylight, the drug dealers ran their operations revolving around two fake Xanax products: a primary knockoff and a limited edition – and vastly more potent “Red Devil” variant that was intentionally dyed for branding purposes. Because the “Red Devil” formulations contained 2.5 times the dose of the 2-mg pill, it had even more pronounced tolerance, dependence, and withdrawal effects (for example, panic attacks, anxiety, and/or hallucinations) – fatal consequences for users involved in consuming other drugs, such as alcohol or opioids. Preexisting drug users tend to gravitate toward benzodiazepines, such as alprazolam (Xanax), perhaps in part, because of its relatively rapid onset of action. Xanax also is known for inducing proeuphoric states at higher doses, hence the appeal of the “Red Devil” pills.
Benzodiazepines, as a class of drugs, facilitate the neurotransmitter gamma-aminobutryric acid’s (GABA) effect on the brain, producing anxiolytic, hypnotic, and/or anticonvulsant states within the user.9 Unbeknownst to numerous users is the fact that drugs such as alcohol and opioids, like Xanax, also serve as respiratory depressants, overriding the brain’s governance of the breathing mechanism. This, in turn, leads to unintended overdose deaths, even among seasoned drug seekers.
Overdose deaths have been steadily climbing over the years because it is common for some users to consume alcohol while being on Xanax therapy – without realizing that both substances are depressants and that taking them together can lead to side effects such as respiratory depression.
Forensic cases also have revealed that preexisting opioid consumers were drawn to Xanax; the drug’s potent mechanism of action would likely appeal to habituated users. A typical behavioral pattern has emerged among users and must be addressed. According to Australian Professor Shane Darke: “So they take their Xanax, they take their painkiller, then they get drunk, that could be enough to kill them.”
Fatalities are more likely when benzodiazepines are combined with other drug classes or if the existing supply is contaminated or laced (for example, with fentanyl).8
As far as deaths by accidental benzodiazepine overdose are concerned, a similar epidemic has been recorded in the United States. In 2013, almost one-third of all prescription overdose deaths can be attributed to the use of benzodiazepines (for example, Xanax, Valium, and Ativan). However, media attention has been considerably muted, especially when compared with that of narcotic abuse. This is even more puzzling when taking into account that three-quarters of benzodiazepine mortalities co-occur within the context of narcotic consumption. Substance Abuse and Mental Health Services Administration data confirm the ubiquitous nature of benzodiazepine (such as alprazolam) coprescriptions, accounting for roughly half of the 176,000 emergency department cases for 2011. The Centers for Disease Control and Prevention noted that there was a 67% increase in benzodiazepine prescriptions between 1996 and 2013, which warranted more stringent regulations for this particular class of drugs.
In 2016, the CDC issued new guidelines for opioid use acknowledging the danger of benzodiazepine coprescriptions. Food and Drug Administration “black box” warnings now grace the prescriptions of both of these drug classes.10 This trend remains on an upward trajectory, even more so during the pandemic, as there are 9.7 million prescriptions of anxiolytics/hypnotics such as Xanax, Ativan, and Klonopin in the United States as of March 2020, which represents a 10% increase over the previous year. , as well as the implementation of urine drug screening monitoring for drug adherence/compliance and diversion in those with suspected benzodiazepine addiction or a history of polysubstance abuse.11,12
Clinical correlates
For patients who present acutely with Xanax toxicity in the emergency room setting, we will need to initially stabilize the vital signs and address the ongoing symptoms. It is advisable to arrange health care accommodations for patients with physical dependence to monitor and treat their withdrawal symptoms. The patient should be enrolled in a comprehensive addiction facility after undergoing formal detoxification; a tapered treatment protocol will need to be implemented because quitting “cold turkey” can lead to convulsions and, in some cases, death. Patient education, talk therapy, and alternatives to benzodiazepines should be discussed with the clinician.13,145
However, to truly address the elephant in the room, we will need to consider institutional reforms to prevent a similar situation from arising in the future. Primary care physician shortages are compounded by changes in insurance policies. Nurses and physician assistants will need to be trained to manage benzodiazepine prescriptions. If there are community shortages in physicians, patients might turn to illegal means to secure their benzodiazepine supply, and it is imperative that we have the necessary fellowship and education programs to educate nonphysician health care clinicians with benzodiazepine management. Because physicians were prescribing benzodiazepines liberally, the Prescription Drug Monitoring Programs (PDMP) was enacted to monitor physician practices. Unfortunately, this ultimately intimidated physicians and effectively curbed reasonable physician prescribing patterns. It might be necessary to revisit existing prescription monitoring programs, encourage drug evaluations and guidelines based on evidence-based medicine and embrace telemedicine in order to facilitate patient-physician communication.
As of now, it is too early to prescribe Xanax routinely for ongoing anxiety experienced during the coronavirus crisis, and several physicians are cautious about prescribing antianxiety medications for more than a few months.17 Surprisingly, researchers in Barcelona have even explored the role of Xanax as potentially inhibiting Mpro, the primary protease of coronavirus, thereby forestalling the virus’s ability to replicate.16 However, it is worth noting that, given the preliminary nature of the results, any attempts at conclusively integrating Xanax within the context of coronavirus therapy would be premature.
References
1. Luhby T. Anti-anxiety medication prescriptions up 34% since coronavirus. CNN. 2020 Apr 16.
2. Women and Anxiety. Anxiety and Depression Association of America.
3. Shigemura J et al. Psychiatry Clin Neurosci. 2012 Apr 7;74(4):281-2.
4. Petersen A. More people are taking drugs for anxiety and insomnia, and doctors are worried. The Wall Street Journal. 2020 May 25.
5. Downey M. Xanax overdose and related deaths. National Drug & Alcohol Research Centre. UNSW Sydney.
6. Bryant B. Fake Xanax: The UK’s biggest ever dark net drugs bust. BBC. 2018 Mar 10.
7. Reinberg S. Fatal overdoses rising from sedatives like Valium, Xanax. HealthDay. 2016 Feb.
8. Is counterfeit Xanax dangerous? American Addiction Centers. Updated 2018 Nov 14.
9. McLaren E. Xanax history and statistics. Drugabuse.com.
10. Benzodiazepines and opioids. National Institute on Drug Abuse. 2018 Mar 15.
11. Choudhry Z et al. J Psychiatry. 2015;18(5). doi: 10.4172/2378-5756.1000319.
12. Islam FA et al. Current Psychiatry. 2018 Dec 17(12):43-4.
13. Adams M. Xanax death rate on the rise. White Sands Treatment. 2017 Sept.NEED LINK
14. Storrs C. Benzodiazepine overdose deaths soared in recent years, study finds. CNN. 2016 Feb. 18.
15. Hanscom DA. Plan A – Thrive and survive COVID-19. Back in Control. 2020.
16. Smith C. Xanax, a common anxiety medication, might actually block coronavirus. BGR. 2020 May 29.
Dr. Islam is a medical adviser for the International Maternal and Child Health Foundation (IMCHF), Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Islam disclosed no relevant financial relationships.
Mr. Choudhry is a research assistant at the IMCHF. He has no disclosures.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF and is Mr. Choudhry’s father. He has no disclosures.
One of the more alarming trends that has emerged during the coronavirus crisis is the concomitant rise in the use of benzodiazepines, such as Xanax. It has been reported that at-risk individuals began seeking prescription anxiolytics as early as mid-February with a consequent peak of 34% the following month, coinciding with the World Health Organization’s declaration of a global pandemic.1
Consistent with the available literature indicating that women are twice as likely to be affected by anxiety disorders, the prescription spikes were almost double when compared with those of their male counterparts.2 The pandemic has instilled a sense of fear in people, leading to social repercussions, such as estrangement, insomnia, and paranoia for at-risk populations.3,4
“Benzos” are commonly prescribed to help people sleep or to assist them in overcoming a host of anxiety disorders. The rapid onset of effects make Xanax a desirable and efficacious benzodiazepine.5 The use of these medications might not be an immediate cause for concern because patients might be taking it as intended. Nevertheless, clinicians are shying away from medical management in favor of counseling or therapy.
Dangerous trends
Numerous factors might contribute to this grim scenario, including patient dependence on benzodiazepines, paranoia about engaging with health care professionals because of fear tied to potential COVID-19 exposure, and/or increased access to illicit counterfeit pills from drug dealers or the dark web markets.
Lessons can be gleaned from the most extensive dark web drug busts in Britain’s history, in which a deluge of “pharmaceutical grade” Xanax pills made it to the hands of drug dealers and consumers between 2015 and 2017.6 A similar phenomenon emerged stateside.7 Virtually indistinguishable from recognized 2-mg Xanax pills, these fake pills posed a serious challenge to forensic scientists.8 The threat of overdose is very real for users targeted by the counterfeit Xanax trade, especially since those at risk often bypass professional health care guidelines.
In broad daylight, the drug dealers ran their operations revolving around two fake Xanax products: a primary knockoff and a limited edition – and vastly more potent “Red Devil” variant that was intentionally dyed for branding purposes. Because the “Red Devil” formulations contained 2.5 times the dose of the 2-mg pill, it had even more pronounced tolerance, dependence, and withdrawal effects (for example, panic attacks, anxiety, and/or hallucinations) – fatal consequences for users involved in consuming other drugs, such as alcohol or opioids. Preexisting drug users tend to gravitate toward benzodiazepines, such as alprazolam (Xanax), perhaps in part, because of its relatively rapid onset of action. Xanax also is known for inducing proeuphoric states at higher doses, hence the appeal of the “Red Devil” pills.
Benzodiazepines, as a class of drugs, facilitate the neurotransmitter gamma-aminobutryric acid’s (GABA) effect on the brain, producing anxiolytic, hypnotic, and/or anticonvulsant states within the user.9 Unbeknownst to numerous users is the fact that drugs such as alcohol and opioids, like Xanax, also serve as respiratory depressants, overriding the brain’s governance of the breathing mechanism. This, in turn, leads to unintended overdose deaths, even among seasoned drug seekers.
Overdose deaths have been steadily climbing over the years because it is common for some users to consume alcohol while being on Xanax therapy – without realizing that both substances are depressants and that taking them together can lead to side effects such as respiratory depression.
Forensic cases also have revealed that preexisting opioid consumers were drawn to Xanax; the drug’s potent mechanism of action would likely appeal to habituated users. A typical behavioral pattern has emerged among users and must be addressed. According to Australian Professor Shane Darke: “So they take their Xanax, they take their painkiller, then they get drunk, that could be enough to kill them.”
Fatalities are more likely when benzodiazepines are combined with other drug classes or if the existing supply is contaminated or laced (for example, with fentanyl).8
As far as deaths by accidental benzodiazepine overdose are concerned, a similar epidemic has been recorded in the United States. In 2013, almost one-third of all prescription overdose deaths can be attributed to the use of benzodiazepines (for example, Xanax, Valium, and Ativan). However, media attention has been considerably muted, especially when compared with that of narcotic abuse. This is even more puzzling when taking into account that three-quarters of benzodiazepine mortalities co-occur within the context of narcotic consumption. Substance Abuse and Mental Health Services Administration data confirm the ubiquitous nature of benzodiazepine (such as alprazolam) coprescriptions, accounting for roughly half of the 176,000 emergency department cases for 2011. The Centers for Disease Control and Prevention noted that there was a 67% increase in benzodiazepine prescriptions between 1996 and 2013, which warranted more stringent regulations for this particular class of drugs.
In 2016, the CDC issued new guidelines for opioid use acknowledging the danger of benzodiazepine coprescriptions. Food and Drug Administration “black box” warnings now grace the prescriptions of both of these drug classes.10 This trend remains on an upward trajectory, even more so during the pandemic, as there are 9.7 million prescriptions of anxiolytics/hypnotics such as Xanax, Ativan, and Klonopin in the United States as of March 2020, which represents a 10% increase over the previous year. , as well as the implementation of urine drug screening monitoring for drug adherence/compliance and diversion in those with suspected benzodiazepine addiction or a history of polysubstance abuse.11,12
Clinical correlates
For patients who present acutely with Xanax toxicity in the emergency room setting, we will need to initially stabilize the vital signs and address the ongoing symptoms. It is advisable to arrange health care accommodations for patients with physical dependence to monitor and treat their withdrawal symptoms. The patient should be enrolled in a comprehensive addiction facility after undergoing formal detoxification; a tapered treatment protocol will need to be implemented because quitting “cold turkey” can lead to convulsions and, in some cases, death. Patient education, talk therapy, and alternatives to benzodiazepines should be discussed with the clinician.13,145
However, to truly address the elephant in the room, we will need to consider institutional reforms to prevent a similar situation from arising in the future. Primary care physician shortages are compounded by changes in insurance policies. Nurses and physician assistants will need to be trained to manage benzodiazepine prescriptions. If there are community shortages in physicians, patients might turn to illegal means to secure their benzodiazepine supply, and it is imperative that we have the necessary fellowship and education programs to educate nonphysician health care clinicians with benzodiazepine management. Because physicians were prescribing benzodiazepines liberally, the Prescription Drug Monitoring Programs (PDMP) was enacted to monitor physician practices. Unfortunately, this ultimately intimidated physicians and effectively curbed reasonable physician prescribing patterns. It might be necessary to revisit existing prescription monitoring programs, encourage drug evaluations and guidelines based on evidence-based medicine and embrace telemedicine in order to facilitate patient-physician communication.
As of now, it is too early to prescribe Xanax routinely for ongoing anxiety experienced during the coronavirus crisis, and several physicians are cautious about prescribing antianxiety medications for more than a few months.17 Surprisingly, researchers in Barcelona have even explored the role of Xanax as potentially inhibiting Mpro, the primary protease of coronavirus, thereby forestalling the virus’s ability to replicate.16 However, it is worth noting that, given the preliminary nature of the results, any attempts at conclusively integrating Xanax within the context of coronavirus therapy would be premature.
References
1. Luhby T. Anti-anxiety medication prescriptions up 34% since coronavirus. CNN. 2020 Apr 16.
2. Women and Anxiety. Anxiety and Depression Association of America.
3. Shigemura J et al. Psychiatry Clin Neurosci. 2012 Apr 7;74(4):281-2.
4. Petersen A. More people are taking drugs for anxiety and insomnia, and doctors are worried. The Wall Street Journal. 2020 May 25.
5. Downey M. Xanax overdose and related deaths. National Drug & Alcohol Research Centre. UNSW Sydney.
6. Bryant B. Fake Xanax: The UK’s biggest ever dark net drugs bust. BBC. 2018 Mar 10.
7. Reinberg S. Fatal overdoses rising from sedatives like Valium, Xanax. HealthDay. 2016 Feb.
8. Is counterfeit Xanax dangerous? American Addiction Centers. Updated 2018 Nov 14.
9. McLaren E. Xanax history and statistics. Drugabuse.com.
10. Benzodiazepines and opioids. National Institute on Drug Abuse. 2018 Mar 15.
11. Choudhry Z et al. J Psychiatry. 2015;18(5). doi: 10.4172/2378-5756.1000319.
12. Islam FA et al. Current Psychiatry. 2018 Dec 17(12):43-4.
13. Adams M. Xanax death rate on the rise. White Sands Treatment. 2017 Sept.NEED LINK
14. Storrs C. Benzodiazepine overdose deaths soared in recent years, study finds. CNN. 2016 Feb. 18.
15. Hanscom DA. Plan A – Thrive and survive COVID-19. Back in Control. 2020.
16. Smith C. Xanax, a common anxiety medication, might actually block coronavirus. BGR. 2020 May 29.
Dr. Islam is a medical adviser for the International Maternal and Child Health Foundation (IMCHF), Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Islam disclosed no relevant financial relationships.
Mr. Choudhry is a research assistant at the IMCHF. He has no disclosures.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF and is Mr. Choudhry’s father. He has no disclosures.
One of the more alarming trends that has emerged during the coronavirus crisis is the concomitant rise in the use of benzodiazepines, such as Xanax. It has been reported that at-risk individuals began seeking prescription anxiolytics as early as mid-February with a consequent peak of 34% the following month, coinciding with the World Health Organization’s declaration of a global pandemic.1
Consistent with the available literature indicating that women are twice as likely to be affected by anxiety disorders, the prescription spikes were almost double when compared with those of their male counterparts.2 The pandemic has instilled a sense of fear in people, leading to social repercussions, such as estrangement, insomnia, and paranoia for at-risk populations.3,4
“Benzos” are commonly prescribed to help people sleep or to assist them in overcoming a host of anxiety disorders. The rapid onset of effects make Xanax a desirable and efficacious benzodiazepine.5 The use of these medications might not be an immediate cause for concern because patients might be taking it as intended. Nevertheless, clinicians are shying away from medical management in favor of counseling or therapy.
Dangerous trends
Numerous factors might contribute to this grim scenario, including patient dependence on benzodiazepines, paranoia about engaging with health care professionals because of fear tied to potential COVID-19 exposure, and/or increased access to illicit counterfeit pills from drug dealers or the dark web markets.
Lessons can be gleaned from the most extensive dark web drug busts in Britain’s history, in which a deluge of “pharmaceutical grade” Xanax pills made it to the hands of drug dealers and consumers between 2015 and 2017.6 A similar phenomenon emerged stateside.7 Virtually indistinguishable from recognized 2-mg Xanax pills, these fake pills posed a serious challenge to forensic scientists.8 The threat of overdose is very real for users targeted by the counterfeit Xanax trade, especially since those at risk often bypass professional health care guidelines.
In broad daylight, the drug dealers ran their operations revolving around two fake Xanax products: a primary knockoff and a limited edition – and vastly more potent “Red Devil” variant that was intentionally dyed for branding purposes. Because the “Red Devil” formulations contained 2.5 times the dose of the 2-mg pill, it had even more pronounced tolerance, dependence, and withdrawal effects (for example, panic attacks, anxiety, and/or hallucinations) – fatal consequences for users involved in consuming other drugs, such as alcohol or opioids. Preexisting drug users tend to gravitate toward benzodiazepines, such as alprazolam (Xanax), perhaps in part, because of its relatively rapid onset of action. Xanax also is known for inducing proeuphoric states at higher doses, hence the appeal of the “Red Devil” pills.
Benzodiazepines, as a class of drugs, facilitate the neurotransmitter gamma-aminobutryric acid’s (GABA) effect on the brain, producing anxiolytic, hypnotic, and/or anticonvulsant states within the user.9 Unbeknownst to numerous users is the fact that drugs such as alcohol and opioids, like Xanax, also serve as respiratory depressants, overriding the brain’s governance of the breathing mechanism. This, in turn, leads to unintended overdose deaths, even among seasoned drug seekers.
Overdose deaths have been steadily climbing over the years because it is common for some users to consume alcohol while being on Xanax therapy – without realizing that both substances are depressants and that taking them together can lead to side effects such as respiratory depression.
Forensic cases also have revealed that preexisting opioid consumers were drawn to Xanax; the drug’s potent mechanism of action would likely appeal to habituated users. A typical behavioral pattern has emerged among users and must be addressed. According to Australian Professor Shane Darke: “So they take their Xanax, they take their painkiller, then they get drunk, that could be enough to kill them.”
Fatalities are more likely when benzodiazepines are combined with other drug classes or if the existing supply is contaminated or laced (for example, with fentanyl).8
As far as deaths by accidental benzodiazepine overdose are concerned, a similar epidemic has been recorded in the United States. In 2013, almost one-third of all prescription overdose deaths can be attributed to the use of benzodiazepines (for example, Xanax, Valium, and Ativan). However, media attention has been considerably muted, especially when compared with that of narcotic abuse. This is even more puzzling when taking into account that three-quarters of benzodiazepine mortalities co-occur within the context of narcotic consumption. Substance Abuse and Mental Health Services Administration data confirm the ubiquitous nature of benzodiazepine (such as alprazolam) coprescriptions, accounting for roughly half of the 176,000 emergency department cases for 2011. The Centers for Disease Control and Prevention noted that there was a 67% increase in benzodiazepine prescriptions between 1996 and 2013, which warranted more stringent regulations for this particular class of drugs.
In 2016, the CDC issued new guidelines for opioid use acknowledging the danger of benzodiazepine coprescriptions. Food and Drug Administration “black box” warnings now grace the prescriptions of both of these drug classes.10 This trend remains on an upward trajectory, even more so during the pandemic, as there are 9.7 million prescriptions of anxiolytics/hypnotics such as Xanax, Ativan, and Klonopin in the United States as of March 2020, which represents a 10% increase over the previous year. , as well as the implementation of urine drug screening monitoring for drug adherence/compliance and diversion in those with suspected benzodiazepine addiction or a history of polysubstance abuse.11,12
Clinical correlates
For patients who present acutely with Xanax toxicity in the emergency room setting, we will need to initially stabilize the vital signs and address the ongoing symptoms. It is advisable to arrange health care accommodations for patients with physical dependence to monitor and treat their withdrawal symptoms. The patient should be enrolled in a comprehensive addiction facility after undergoing formal detoxification; a tapered treatment protocol will need to be implemented because quitting “cold turkey” can lead to convulsions and, in some cases, death. Patient education, talk therapy, and alternatives to benzodiazepines should be discussed with the clinician.13,145
However, to truly address the elephant in the room, we will need to consider institutional reforms to prevent a similar situation from arising in the future. Primary care physician shortages are compounded by changes in insurance policies. Nurses and physician assistants will need to be trained to manage benzodiazepine prescriptions. If there are community shortages in physicians, patients might turn to illegal means to secure their benzodiazepine supply, and it is imperative that we have the necessary fellowship and education programs to educate nonphysician health care clinicians with benzodiazepine management. Because physicians were prescribing benzodiazepines liberally, the Prescription Drug Monitoring Programs (PDMP) was enacted to monitor physician practices. Unfortunately, this ultimately intimidated physicians and effectively curbed reasonable physician prescribing patterns. It might be necessary to revisit existing prescription monitoring programs, encourage drug evaluations and guidelines based on evidence-based medicine and embrace telemedicine in order to facilitate patient-physician communication.
As of now, it is too early to prescribe Xanax routinely for ongoing anxiety experienced during the coronavirus crisis, and several physicians are cautious about prescribing antianxiety medications for more than a few months.17 Surprisingly, researchers in Barcelona have even explored the role of Xanax as potentially inhibiting Mpro, the primary protease of coronavirus, thereby forestalling the virus’s ability to replicate.16 However, it is worth noting that, given the preliminary nature of the results, any attempts at conclusively integrating Xanax within the context of coronavirus therapy would be premature.
References
1. Luhby T. Anti-anxiety medication prescriptions up 34% since coronavirus. CNN. 2020 Apr 16.
2. Women and Anxiety. Anxiety and Depression Association of America.
3. Shigemura J et al. Psychiatry Clin Neurosci. 2012 Apr 7;74(4):281-2.
4. Petersen A. More people are taking drugs for anxiety and insomnia, and doctors are worried. The Wall Street Journal. 2020 May 25.
5. Downey M. Xanax overdose and related deaths. National Drug & Alcohol Research Centre. UNSW Sydney.
6. Bryant B. Fake Xanax: The UK’s biggest ever dark net drugs bust. BBC. 2018 Mar 10.
7. Reinberg S. Fatal overdoses rising from sedatives like Valium, Xanax. HealthDay. 2016 Feb.
8. Is counterfeit Xanax dangerous? American Addiction Centers. Updated 2018 Nov 14.
9. McLaren E. Xanax history and statistics. Drugabuse.com.
10. Benzodiazepines and opioids. National Institute on Drug Abuse. 2018 Mar 15.
11. Choudhry Z et al. J Psychiatry. 2015;18(5). doi: 10.4172/2378-5756.1000319.
12. Islam FA et al. Current Psychiatry. 2018 Dec 17(12):43-4.
13. Adams M. Xanax death rate on the rise. White Sands Treatment. 2017 Sept.NEED LINK
14. Storrs C. Benzodiazepine overdose deaths soared in recent years, study finds. CNN. 2016 Feb. 18.
15. Hanscom DA. Plan A – Thrive and survive COVID-19. Back in Control. 2020.
16. Smith C. Xanax, a common anxiety medication, might actually block coronavirus. BGR. 2020 May 29.
Dr. Islam is a medical adviser for the International Maternal and Child Health Foundation (IMCHF), Montreal, and is based in New York. He also is a postdoctoral fellow, psychopharmacologist, and a board-certified medical affairs specialist. Dr. Islam disclosed no relevant financial relationships.
Mr. Choudhry is a research assistant at the IMCHF. He has no disclosures.
Dr. Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF and is Mr. Choudhry’s father. He has no disclosures.
As a black psychiatrist, she is ‘exhausted’ and ‘furious’
I didn’t have any doctors in my family. The only doctor I knew was my pediatrician. At 6 years old – and this gives you a glimpse into my personality – I told my parents I did not think he was a good doctor. I said, “When I grow up to be a doctor, I’m going to be a better doctor than him.” Fast forward to 7th grade, when I saw an orthopedic surgeon for my scoliosis. He was phenomenal. He listened. He explained to me all of the science and medicine and his rationale for decisions. I thought, “That is the kind of doctor I want to be.”
I went to medical school at Penn and didn’t think psychiatry was a medical specialty. I thought it was just Freud and laying on couches. I thought, “Where’s the science, where’s the physiology, where’s the genetics?” I was headed toward surgery.
Then, I rotated with an incredible psychiatrist. I saw behavior was biological, chemical, electrical, and physiological. I realize, looking back, that I had an interest because there is mental illness in my family. And there is so much stigma against psychiatric illnesses and addiction. It’s shocking how badly our patients get treated in the general medicine construct. So, I thought, “This field has science, the human body, activism, and marginalized patients? This is for me!”
I went to Howard University, which was the most freeing time of my life. There was no code-switching, no working hard to be a “presentable” Black person. When I started interviewing for medical schools, I was told by someone I interviewed with at one school that I should straighten my hair if I wanted to get accepted. I marked that school off my list. I decided right then that I would rather not go to medical school than straighten my hair to get into medical school. I went to Penn; they accepted me without my hair straight.
Penn Med was majorly White. There were six of us who were Black in a class of about 150 people. There was this feeling like “we let you in” even though every single one of us who was there was clearly at the top of the game to have been able to get there. I loved Penn Med. My class was amazing. I became the first Black president of medical student government there and I won a lot of awards.
When I was finishing up, my dean at the time, who was a White woman, said, “I’m so proud of you. You came in a piece of coal and look how we shined you up. “What do you say? I have a smart mouth, so I said, “I was already shiny when I got here.” She said, “See, that’s part of your problem, you don’t know how to take a compliment.” That was 2002, and I still remember every word of that conversation.
I was on the psychiatry unit rounding as a medical student and introduced myself to a patient. He said, “What’s your name?” And I thought, here it comes. I said, “Nzinga Ajabu,” my name at the time. He said “Nzinga? You probably have a spear in your closet.” When I tell these stories to White people, they’re always shocked. When I tell these stories to Black people, they say, “Yeah, that sounds about right.”
You can talk to Black medical students, Black interns, Black residents. When patients say something racist to you, nobody speaks up for you, nobody. It should be the attending that professionally approaches the patient and says something, anything. But they just laugh uncomfortably, they let it pass, they pretend they didn’t hear it. Meanwhile, you are fuming, and injured, and have to maintain your professionalism. It happens all the time. When people say, “Oh, you don’t look like a doctor,” I know what that means, but someone else may not even notice it’s an insult. When they do notice an insult, they don’t have the language or the courage to address it. And it’s not always a patient leveling racial insults. It very often is the attending, the fellow, the resident, or another medical student.
These things happen to me less now because I’m in a position of power. I’d say most insults that come my way now are overwhelmingly unintentional. I call people out on it 95% of the time. The other 5% of the time, I’m either exhausted, or I’m in some power structure where I decide it’s too risky. And those are the days – when I decide it’s too risky for me to speak up – when I come home exhausted. Because there will always be a power dynamic, as long as I’m alive, where you can’t speak up because you’re a Black woman, and that just wears me out.
Ultimately, I opted out of academic medicine because I thought it was too constraining, that I wouldn’t be able to raise my voice and do the activism I needed to do. – I’m able to advocate for people who are marginalized by medicine and, in treating addiction, advocate for people who are marginalized by psychiatry, which is marginalized by medicine.
A bias people have is that when you talk about Black people, they think you are talking about poor people. When we talk about police brutality, or being pulled over by the police, or dying in childbirth, our colleagues don’t think that’s happening to us. They think that’s happening to “those” Black people. Regardless of my socioeconomic status, I still have a higher chance of dying in childbirth or dying from COVID.
COVID had already turned my work up to 100 – we had staff losing loved ones and coming down with fevers themselves. And I had just launched my podcast. Then they killed Breonna Taylor, Ahmaud Arbery, Amy Cooper called the cops on Christian Cooper, and they killed George Floyd. This is how it happens. Bam. Bam. Bam.
The series of killings turned up my work at Physicians for Criminal Justice Reform, but it also turned up my work as a mother. My boys are 13 and 14. I personally can’t watch some of the videos because I see my own sons. I was already tired. Now I’m exhausted, I’m furious and I’m desperate to protect my kids. They have this on their backs already. Both of them have already had to deal with overt racism – they’ve had this burden since they were 5 years old, if not younger. I have to teach them to fight this war. Should that be how it is?
Nzinga Harrison, MD, 43, is a psychiatrist and the cofounder and chief medical officer of Eleanor Health, a network of physician clinics that treats people affected by addiction in North Carolina and New Jersey. She is also a cofounder of Physicians for Criminal Justice Reform. and host of the new podcast In Recovery. Harrison was raised in Indianapolis, went to college at Howard University and received her MD from the Perelman School of Medicine at the University of Pennsylvania in 2002. Her mother was an elementary school teacher. Her father, an electrical engineer, was commander of the local Black Panther Militia. Both supported her love of math and science and brought her with them to picket lines and marches.
This article first appeared on Medscape.com.
I didn’t have any doctors in my family. The only doctor I knew was my pediatrician. At 6 years old – and this gives you a glimpse into my personality – I told my parents I did not think he was a good doctor. I said, “When I grow up to be a doctor, I’m going to be a better doctor than him.” Fast forward to 7th grade, when I saw an orthopedic surgeon for my scoliosis. He was phenomenal. He listened. He explained to me all of the science and medicine and his rationale for decisions. I thought, “That is the kind of doctor I want to be.”
I went to medical school at Penn and didn’t think psychiatry was a medical specialty. I thought it was just Freud and laying on couches. I thought, “Where’s the science, where’s the physiology, where’s the genetics?” I was headed toward surgery.
Then, I rotated with an incredible psychiatrist. I saw behavior was biological, chemical, electrical, and physiological. I realize, looking back, that I had an interest because there is mental illness in my family. And there is so much stigma against psychiatric illnesses and addiction. It’s shocking how badly our patients get treated in the general medicine construct. So, I thought, “This field has science, the human body, activism, and marginalized patients? This is for me!”
I went to Howard University, which was the most freeing time of my life. There was no code-switching, no working hard to be a “presentable” Black person. When I started interviewing for medical schools, I was told by someone I interviewed with at one school that I should straighten my hair if I wanted to get accepted. I marked that school off my list. I decided right then that I would rather not go to medical school than straighten my hair to get into medical school. I went to Penn; they accepted me without my hair straight.
Penn Med was majorly White. There were six of us who were Black in a class of about 150 people. There was this feeling like “we let you in” even though every single one of us who was there was clearly at the top of the game to have been able to get there. I loved Penn Med. My class was amazing. I became the first Black president of medical student government there and I won a lot of awards.
When I was finishing up, my dean at the time, who was a White woman, said, “I’m so proud of you. You came in a piece of coal and look how we shined you up. “What do you say? I have a smart mouth, so I said, “I was already shiny when I got here.” She said, “See, that’s part of your problem, you don’t know how to take a compliment.” That was 2002, and I still remember every word of that conversation.
I was on the psychiatry unit rounding as a medical student and introduced myself to a patient. He said, “What’s your name?” And I thought, here it comes. I said, “Nzinga Ajabu,” my name at the time. He said “Nzinga? You probably have a spear in your closet.” When I tell these stories to White people, they’re always shocked. When I tell these stories to Black people, they say, “Yeah, that sounds about right.”
You can talk to Black medical students, Black interns, Black residents. When patients say something racist to you, nobody speaks up for you, nobody. It should be the attending that professionally approaches the patient and says something, anything. But they just laugh uncomfortably, they let it pass, they pretend they didn’t hear it. Meanwhile, you are fuming, and injured, and have to maintain your professionalism. It happens all the time. When people say, “Oh, you don’t look like a doctor,” I know what that means, but someone else may not even notice it’s an insult. When they do notice an insult, they don’t have the language or the courage to address it. And it’s not always a patient leveling racial insults. It very often is the attending, the fellow, the resident, or another medical student.
These things happen to me less now because I’m in a position of power. I’d say most insults that come my way now are overwhelmingly unintentional. I call people out on it 95% of the time. The other 5% of the time, I’m either exhausted, or I’m in some power structure where I decide it’s too risky. And those are the days – when I decide it’s too risky for me to speak up – when I come home exhausted. Because there will always be a power dynamic, as long as I’m alive, where you can’t speak up because you’re a Black woman, and that just wears me out.
Ultimately, I opted out of academic medicine because I thought it was too constraining, that I wouldn’t be able to raise my voice and do the activism I needed to do. – I’m able to advocate for people who are marginalized by medicine and, in treating addiction, advocate for people who are marginalized by psychiatry, which is marginalized by medicine.
A bias people have is that when you talk about Black people, they think you are talking about poor people. When we talk about police brutality, or being pulled over by the police, or dying in childbirth, our colleagues don’t think that’s happening to us. They think that’s happening to “those” Black people. Regardless of my socioeconomic status, I still have a higher chance of dying in childbirth or dying from COVID.
COVID had already turned my work up to 100 – we had staff losing loved ones and coming down with fevers themselves. And I had just launched my podcast. Then they killed Breonna Taylor, Ahmaud Arbery, Amy Cooper called the cops on Christian Cooper, and they killed George Floyd. This is how it happens. Bam. Bam. Bam.
The series of killings turned up my work at Physicians for Criminal Justice Reform, but it also turned up my work as a mother. My boys are 13 and 14. I personally can’t watch some of the videos because I see my own sons. I was already tired. Now I’m exhausted, I’m furious and I’m desperate to protect my kids. They have this on their backs already. Both of them have already had to deal with overt racism – they’ve had this burden since they were 5 years old, if not younger. I have to teach them to fight this war. Should that be how it is?
Nzinga Harrison, MD, 43, is a psychiatrist and the cofounder and chief medical officer of Eleanor Health, a network of physician clinics that treats people affected by addiction in North Carolina and New Jersey. She is also a cofounder of Physicians for Criminal Justice Reform. and host of the new podcast In Recovery. Harrison was raised in Indianapolis, went to college at Howard University and received her MD from the Perelman School of Medicine at the University of Pennsylvania in 2002. Her mother was an elementary school teacher. Her father, an electrical engineer, was commander of the local Black Panther Militia. Both supported her love of math and science and brought her with them to picket lines and marches.
This article first appeared on Medscape.com.
I didn’t have any doctors in my family. The only doctor I knew was my pediatrician. At 6 years old – and this gives you a glimpse into my personality – I told my parents I did not think he was a good doctor. I said, “When I grow up to be a doctor, I’m going to be a better doctor than him.” Fast forward to 7th grade, when I saw an orthopedic surgeon for my scoliosis. He was phenomenal. He listened. He explained to me all of the science and medicine and his rationale for decisions. I thought, “That is the kind of doctor I want to be.”
I went to medical school at Penn and didn’t think psychiatry was a medical specialty. I thought it was just Freud and laying on couches. I thought, “Where’s the science, where’s the physiology, where’s the genetics?” I was headed toward surgery.
Then, I rotated with an incredible psychiatrist. I saw behavior was biological, chemical, electrical, and physiological. I realize, looking back, that I had an interest because there is mental illness in my family. And there is so much stigma against psychiatric illnesses and addiction. It’s shocking how badly our patients get treated in the general medicine construct. So, I thought, “This field has science, the human body, activism, and marginalized patients? This is for me!”
I went to Howard University, which was the most freeing time of my life. There was no code-switching, no working hard to be a “presentable” Black person. When I started interviewing for medical schools, I was told by someone I interviewed with at one school that I should straighten my hair if I wanted to get accepted. I marked that school off my list. I decided right then that I would rather not go to medical school than straighten my hair to get into medical school. I went to Penn; they accepted me without my hair straight.
Penn Med was majorly White. There were six of us who were Black in a class of about 150 people. There was this feeling like “we let you in” even though every single one of us who was there was clearly at the top of the game to have been able to get there. I loved Penn Med. My class was amazing. I became the first Black president of medical student government there and I won a lot of awards.
When I was finishing up, my dean at the time, who was a White woman, said, “I’m so proud of you. You came in a piece of coal and look how we shined you up. “What do you say? I have a smart mouth, so I said, “I was already shiny when I got here.” She said, “See, that’s part of your problem, you don’t know how to take a compliment.” That was 2002, and I still remember every word of that conversation.
I was on the psychiatry unit rounding as a medical student and introduced myself to a patient. He said, “What’s your name?” And I thought, here it comes. I said, “Nzinga Ajabu,” my name at the time. He said “Nzinga? You probably have a spear in your closet.” When I tell these stories to White people, they’re always shocked. When I tell these stories to Black people, they say, “Yeah, that sounds about right.”
You can talk to Black medical students, Black interns, Black residents. When patients say something racist to you, nobody speaks up for you, nobody. It should be the attending that professionally approaches the patient and says something, anything. But they just laugh uncomfortably, they let it pass, they pretend they didn’t hear it. Meanwhile, you are fuming, and injured, and have to maintain your professionalism. It happens all the time. When people say, “Oh, you don’t look like a doctor,” I know what that means, but someone else may not even notice it’s an insult. When they do notice an insult, they don’t have the language or the courage to address it. And it’s not always a patient leveling racial insults. It very often is the attending, the fellow, the resident, or another medical student.
These things happen to me less now because I’m in a position of power. I’d say most insults that come my way now are overwhelmingly unintentional. I call people out on it 95% of the time. The other 5% of the time, I’m either exhausted, or I’m in some power structure where I decide it’s too risky. And those are the days – when I decide it’s too risky for me to speak up – when I come home exhausted. Because there will always be a power dynamic, as long as I’m alive, where you can’t speak up because you’re a Black woman, and that just wears me out.
Ultimately, I opted out of academic medicine because I thought it was too constraining, that I wouldn’t be able to raise my voice and do the activism I needed to do. – I’m able to advocate for people who are marginalized by medicine and, in treating addiction, advocate for people who are marginalized by psychiatry, which is marginalized by medicine.
A bias people have is that when you talk about Black people, they think you are talking about poor people. When we talk about police brutality, or being pulled over by the police, or dying in childbirth, our colleagues don’t think that’s happening to us. They think that’s happening to “those” Black people. Regardless of my socioeconomic status, I still have a higher chance of dying in childbirth or dying from COVID.
COVID had already turned my work up to 100 – we had staff losing loved ones and coming down with fevers themselves. And I had just launched my podcast. Then they killed Breonna Taylor, Ahmaud Arbery, Amy Cooper called the cops on Christian Cooper, and they killed George Floyd. This is how it happens. Bam. Bam. Bam.
The series of killings turned up my work at Physicians for Criminal Justice Reform, but it also turned up my work as a mother. My boys are 13 and 14. I personally can’t watch some of the videos because I see my own sons. I was already tired. Now I’m exhausted, I’m furious and I’m desperate to protect my kids. They have this on their backs already. Both of them have already had to deal with overt racism – they’ve had this burden since they were 5 years old, if not younger. I have to teach them to fight this war. Should that be how it is?
Nzinga Harrison, MD, 43, is a psychiatrist and the cofounder and chief medical officer of Eleanor Health, a network of physician clinics that treats people affected by addiction in North Carolina and New Jersey. She is also a cofounder of Physicians for Criminal Justice Reform. and host of the new podcast In Recovery. Harrison was raised in Indianapolis, went to college at Howard University and received her MD from the Perelman School of Medicine at the University of Pennsylvania in 2002. Her mother was an elementary school teacher. Her father, an electrical engineer, was commander of the local Black Panther Militia. Both supported her love of math and science and brought her with them to picket lines and marches.
This article first appeared on Medscape.com.
Medication-assisted treatment in corrections: A life-saving intervention
Opioid overdose deaths in the United States have more than tripled in recent years, from 6.1 deaths per 100,000 individuals in 1999 to 20.7 per 100,000 individuals in 2018.1 Although the availability of medication-assisted treatment (MAT) has expanded over the past decade, this lifesaving treatment remains largely inaccessible to some of the most vulnerable members of our communities: opioid users facing reentry after incarceration.
Just as abstinence in the community brings a loss of tolerance to opioids, individuals who are incarcerated lose tolerance as well. Clinicians who treat patients with opioid use disorders (OUD) are accustomed to warning patients about the risk of returning to prior levels of use too quickly. Harm reduction strategies include using slowly, using with friends, and having naloxone on hand to prevent unintended overdose.
The risks of opioid use are magnified for those facing reentry; incarceration contributes to a loss of employment, social supports, and connection to care. Those changes can create an exceptionally stressful reentry period – one that places individuals at an acutely high risk of relapse and overdose. Within the first 2 years of release, an individual with a history of incarceration has a risk of death 3.5 times higher than that of someone in the general population. Within the first 2 weeks, those recently incarcerated are 129 times more likely to overdose on opioids and 12.7 times more likely to die than members of the general population.2
Treatment with MAT dramatically reduces deaths during this crucial period. In England, large national studies have shown a similar 75% decrease in all-cause mortality within the first 4 weeks of release among individuals with OUD.4 In California, the counties with the highest overdose death rates are consistently those with fewer opioid treatment programs, which suggests that access to treatment is necessary to prolong the lives of those suffering from OUD.5 In-custody overdose deaths are quite rare, and access to MAT during incarceration has decreased in-custody deaths by 74%.6
Decreased opioid overdose deaths is not the only outcome of MAT. Pharmacotherapy for OUD also has been shown to increase treatment retention,7 reduce reincarceration,8 prevent communicable infections,9 and decrease use of other illicit substances.10 The provision of MAT also has been shown to be cost effective.11
Despite those benefits, as of 2017, only 30 out of 5,100 jails and prisons in the United States provided treatment with methadone or buprenorphine.12 When individuals on maintenance therapy are incarcerated, most correctional facilities force them to taper and discontinue those medications. This practice can cause distressing withdrawal symptoms and actively increase the risk of death for these individuals.
Concerns related to the provision of MAT, and specifically buprenorphine, in the correctional health setting often are related to diversion. Although safe administration of opioid full and partial agonists is a priority, recent literature has suggested that buprenorphine is not a medication frequently used for euphoric properties. In fact, the literature suggests that individuals using illicit buprenorphine primarily do so to treat withdrawal symptoms and that illicit use diminishes with access to formal treatment.13,14
Another concern is that pharmacotherapy for OUD should not be used without adjunctive psychotherapies and social supports. While dual pharmacotherapy and psychotherapy is ideal, the American Society for Addiction Medicine 2020 National Practice Guidelines for the treatment of OUD state: “a patient’s decision to decline psychosocial treatment or the absence of available psychosocial treatment should not preclude or delay pharmacotherapy, with appropriate medication management.”15 Just as some patients wish to engage in mutual help or psychotherapeutic modalities only, some patients wish to engage only in psychopharmacologic interventions. Declaring one modality of treatment better, or worse, or more worthwhile is not borne out by the literature and often places clinicians’ preferences over the preferences of patients.
Individuals who suffer from substance use disorders are at high risk of incarceration, relapse, and overdose death. These patients also suffer from stigmatization from peers and health care workers alike, making the process of engaging in care incredibly burdensome. Because of the disease of addiction, many of our patients cannot envision a healthy future: a future with the potential for intimate relationships, meaningful community engagement, and a rich inner life. The provision of MAT is lifesaving and improves the chances of a successful reentry – an intuitive first step in a long, but worthwhile, journey.
References
1. Hedegaard H et al; National Center for Health Statistics. Drug overdose deaths in the United States, 1999–2018. NCHS Data Brief, 2020 Jan, No. 356.
2. Binswanger IA et al. N Engl J Med. 2007;356:157-65.
3. Green TC et al. JAMA Psychiatry. 2018;75(4):405-7.
4. Marsden J et al. Addiction. 2017;112(8):1408-18.
5. Joshi V and Urada D. State Targeted Response to the Opioid Crisis: California Strategic Plan. 2017 Aug 30.
6. Larney S et al. BMJ Open. 2014. doi: 10.1136/bmjopen-2013-004666.
7. Rich JD et al. Lancet. 2015;386(9991):350-9.
8. Deck D et al. J Addict Dis. 2009. 28(2):89-102.
9. MacArthur GJ et al. BMJ. 2012. doi: 10.1136/bmj.e5945.
10. Tsui J et al. J Subst Abuse Treat. 2019. 109:80-5.
11. Gisev N et al. Addiction. 2015 Dec;110(12):1975-84.
12. National Mental Health and Substance Use Policy Laboratory. “Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings.” HHS Publication No. PEP19-MATUSECJS. Rockville, Md.: Substance Abuse and Mental Health Services Administration, 2019.
13. Bazazi AR et al. J Addict Med. 2011;5(3):175-80.
14. Schuman-Olivier Z. et al. J Subst Abuse Treat. 2010 Jul;39(1):41-50.
15. Crotty K et al. J Addict Med. 2020;14(2)99-112.
Dr. Barnes is chief resident at San Mateo County Behavioral Health and Recovery Services in California. He disclosed no relevant financial relationships. Dr. Lenane is resident* at San Mateo County Behavioral Health and Recovery Services. He disclosed no relevant financial relationships. The opinions shared in this article represent the viewpoints of the authors and are not necessarily representative of the viewpoints or policies of their academic program or employer.
*This article was updated 7/9/2020.
Opioid overdose deaths in the United States have more than tripled in recent years, from 6.1 deaths per 100,000 individuals in 1999 to 20.7 per 100,000 individuals in 2018.1 Although the availability of medication-assisted treatment (MAT) has expanded over the past decade, this lifesaving treatment remains largely inaccessible to some of the most vulnerable members of our communities: opioid users facing reentry after incarceration.
Just as abstinence in the community brings a loss of tolerance to opioids, individuals who are incarcerated lose tolerance as well. Clinicians who treat patients with opioid use disorders (OUD) are accustomed to warning patients about the risk of returning to prior levels of use too quickly. Harm reduction strategies include using slowly, using with friends, and having naloxone on hand to prevent unintended overdose.
The risks of opioid use are magnified for those facing reentry; incarceration contributes to a loss of employment, social supports, and connection to care. Those changes can create an exceptionally stressful reentry period – one that places individuals at an acutely high risk of relapse and overdose. Within the first 2 years of release, an individual with a history of incarceration has a risk of death 3.5 times higher than that of someone in the general population. Within the first 2 weeks, those recently incarcerated are 129 times more likely to overdose on opioids and 12.7 times more likely to die than members of the general population.2
Treatment with MAT dramatically reduces deaths during this crucial period. In England, large national studies have shown a similar 75% decrease in all-cause mortality within the first 4 weeks of release among individuals with OUD.4 In California, the counties with the highest overdose death rates are consistently those with fewer opioid treatment programs, which suggests that access to treatment is necessary to prolong the lives of those suffering from OUD.5 In-custody overdose deaths are quite rare, and access to MAT during incarceration has decreased in-custody deaths by 74%.6
Decreased opioid overdose deaths is not the only outcome of MAT. Pharmacotherapy for OUD also has been shown to increase treatment retention,7 reduce reincarceration,8 prevent communicable infections,9 and decrease use of other illicit substances.10 The provision of MAT also has been shown to be cost effective.11
Despite those benefits, as of 2017, only 30 out of 5,100 jails and prisons in the United States provided treatment with methadone or buprenorphine.12 When individuals on maintenance therapy are incarcerated, most correctional facilities force them to taper and discontinue those medications. This practice can cause distressing withdrawal symptoms and actively increase the risk of death for these individuals.
Concerns related to the provision of MAT, and specifically buprenorphine, in the correctional health setting often are related to diversion. Although safe administration of opioid full and partial agonists is a priority, recent literature has suggested that buprenorphine is not a medication frequently used for euphoric properties. In fact, the literature suggests that individuals using illicit buprenorphine primarily do so to treat withdrawal symptoms and that illicit use diminishes with access to formal treatment.13,14
Another concern is that pharmacotherapy for OUD should not be used without adjunctive psychotherapies and social supports. While dual pharmacotherapy and psychotherapy is ideal, the American Society for Addiction Medicine 2020 National Practice Guidelines for the treatment of OUD state: “a patient’s decision to decline psychosocial treatment or the absence of available psychosocial treatment should not preclude or delay pharmacotherapy, with appropriate medication management.”15 Just as some patients wish to engage in mutual help or psychotherapeutic modalities only, some patients wish to engage only in psychopharmacologic interventions. Declaring one modality of treatment better, or worse, or more worthwhile is not borne out by the literature and often places clinicians’ preferences over the preferences of patients.
Individuals who suffer from substance use disorders are at high risk of incarceration, relapse, and overdose death. These patients also suffer from stigmatization from peers and health care workers alike, making the process of engaging in care incredibly burdensome. Because of the disease of addiction, many of our patients cannot envision a healthy future: a future with the potential for intimate relationships, meaningful community engagement, and a rich inner life. The provision of MAT is lifesaving and improves the chances of a successful reentry – an intuitive first step in a long, but worthwhile, journey.
References
1. Hedegaard H et al; National Center for Health Statistics. Drug overdose deaths in the United States, 1999–2018. NCHS Data Brief, 2020 Jan, No. 356.
2. Binswanger IA et al. N Engl J Med. 2007;356:157-65.
3. Green TC et al. JAMA Psychiatry. 2018;75(4):405-7.
4. Marsden J et al. Addiction. 2017;112(8):1408-18.
5. Joshi V and Urada D. State Targeted Response to the Opioid Crisis: California Strategic Plan. 2017 Aug 30.
6. Larney S et al. BMJ Open. 2014. doi: 10.1136/bmjopen-2013-004666.
7. Rich JD et al. Lancet. 2015;386(9991):350-9.
8. Deck D et al. J Addict Dis. 2009. 28(2):89-102.
9. MacArthur GJ et al. BMJ. 2012. doi: 10.1136/bmj.e5945.
10. Tsui J et al. J Subst Abuse Treat. 2019. 109:80-5.
11. Gisev N et al. Addiction. 2015 Dec;110(12):1975-84.
12. National Mental Health and Substance Use Policy Laboratory. “Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings.” HHS Publication No. PEP19-MATUSECJS. Rockville, Md.: Substance Abuse and Mental Health Services Administration, 2019.
13. Bazazi AR et al. J Addict Med. 2011;5(3):175-80.
14. Schuman-Olivier Z. et al. J Subst Abuse Treat. 2010 Jul;39(1):41-50.
15. Crotty K et al. J Addict Med. 2020;14(2)99-112.
Dr. Barnes is chief resident at San Mateo County Behavioral Health and Recovery Services in California. He disclosed no relevant financial relationships. Dr. Lenane is resident* at San Mateo County Behavioral Health and Recovery Services. He disclosed no relevant financial relationships. The opinions shared in this article represent the viewpoints of the authors and are not necessarily representative of the viewpoints or policies of their academic program or employer.
*This article was updated 7/9/2020.
Opioid overdose deaths in the United States have more than tripled in recent years, from 6.1 deaths per 100,000 individuals in 1999 to 20.7 per 100,000 individuals in 2018.1 Although the availability of medication-assisted treatment (MAT) has expanded over the past decade, this lifesaving treatment remains largely inaccessible to some of the most vulnerable members of our communities: opioid users facing reentry after incarceration.
Just as abstinence in the community brings a loss of tolerance to opioids, individuals who are incarcerated lose tolerance as well. Clinicians who treat patients with opioid use disorders (OUD) are accustomed to warning patients about the risk of returning to prior levels of use too quickly. Harm reduction strategies include using slowly, using with friends, and having naloxone on hand to prevent unintended overdose.
The risks of opioid use are magnified for those facing reentry; incarceration contributes to a loss of employment, social supports, and connection to care. Those changes can create an exceptionally stressful reentry period – one that places individuals at an acutely high risk of relapse and overdose. Within the first 2 years of release, an individual with a history of incarceration has a risk of death 3.5 times higher than that of someone in the general population. Within the first 2 weeks, those recently incarcerated are 129 times more likely to overdose on opioids and 12.7 times more likely to die than members of the general population.2
Treatment with MAT dramatically reduces deaths during this crucial period. In England, large national studies have shown a similar 75% decrease in all-cause mortality within the first 4 weeks of release among individuals with OUD.4 In California, the counties with the highest overdose death rates are consistently those with fewer opioid treatment programs, which suggests that access to treatment is necessary to prolong the lives of those suffering from OUD.5 In-custody overdose deaths are quite rare, and access to MAT during incarceration has decreased in-custody deaths by 74%.6
Decreased opioid overdose deaths is not the only outcome of MAT. Pharmacotherapy for OUD also has been shown to increase treatment retention,7 reduce reincarceration,8 prevent communicable infections,9 and decrease use of other illicit substances.10 The provision of MAT also has been shown to be cost effective.11
Despite those benefits, as of 2017, only 30 out of 5,100 jails and prisons in the United States provided treatment with methadone or buprenorphine.12 When individuals on maintenance therapy are incarcerated, most correctional facilities force them to taper and discontinue those medications. This practice can cause distressing withdrawal symptoms and actively increase the risk of death for these individuals.
Concerns related to the provision of MAT, and specifically buprenorphine, in the correctional health setting often are related to diversion. Although safe administration of opioid full and partial agonists is a priority, recent literature has suggested that buprenorphine is not a medication frequently used for euphoric properties. In fact, the literature suggests that individuals using illicit buprenorphine primarily do so to treat withdrawal symptoms and that illicit use diminishes with access to formal treatment.13,14
Another concern is that pharmacotherapy for OUD should not be used without adjunctive psychotherapies and social supports. While dual pharmacotherapy and psychotherapy is ideal, the American Society for Addiction Medicine 2020 National Practice Guidelines for the treatment of OUD state: “a patient’s decision to decline psychosocial treatment or the absence of available psychosocial treatment should not preclude or delay pharmacotherapy, with appropriate medication management.”15 Just as some patients wish to engage in mutual help or psychotherapeutic modalities only, some patients wish to engage only in psychopharmacologic interventions. Declaring one modality of treatment better, or worse, or more worthwhile is not borne out by the literature and often places clinicians’ preferences over the preferences of patients.
Individuals who suffer from substance use disorders are at high risk of incarceration, relapse, and overdose death. These patients also suffer from stigmatization from peers and health care workers alike, making the process of engaging in care incredibly burdensome. Because of the disease of addiction, many of our patients cannot envision a healthy future: a future with the potential for intimate relationships, meaningful community engagement, and a rich inner life. The provision of MAT is lifesaving and improves the chances of a successful reentry – an intuitive first step in a long, but worthwhile, journey.
References
1. Hedegaard H et al; National Center for Health Statistics. Drug overdose deaths in the United States, 1999–2018. NCHS Data Brief, 2020 Jan, No. 356.
2. Binswanger IA et al. N Engl J Med. 2007;356:157-65.
3. Green TC et al. JAMA Psychiatry. 2018;75(4):405-7.
4. Marsden J et al. Addiction. 2017;112(8):1408-18.
5. Joshi V and Urada D. State Targeted Response to the Opioid Crisis: California Strategic Plan. 2017 Aug 30.
6. Larney S et al. BMJ Open. 2014. doi: 10.1136/bmjopen-2013-004666.
7. Rich JD et al. Lancet. 2015;386(9991):350-9.
8. Deck D et al. J Addict Dis. 2009. 28(2):89-102.
9. MacArthur GJ et al. BMJ. 2012. doi: 10.1136/bmj.e5945.
10. Tsui J et al. J Subst Abuse Treat. 2019. 109:80-5.
11. Gisev N et al. Addiction. 2015 Dec;110(12):1975-84.
12. National Mental Health and Substance Use Policy Laboratory. “Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings.” HHS Publication No. PEP19-MATUSECJS. Rockville, Md.: Substance Abuse and Mental Health Services Administration, 2019.
13. Bazazi AR et al. J Addict Med. 2011;5(3):175-80.
14. Schuman-Olivier Z. et al. J Subst Abuse Treat. 2010 Jul;39(1):41-50.
15. Crotty K et al. J Addict Med. 2020;14(2)99-112.
Dr. Barnes is chief resident at San Mateo County Behavioral Health and Recovery Services in California. He disclosed no relevant financial relationships. Dr. Lenane is resident* at San Mateo County Behavioral Health and Recovery Services. He disclosed no relevant financial relationships. The opinions shared in this article represent the viewpoints of the authors and are not necessarily representative of the viewpoints or policies of their academic program or employer.
*This article was updated 7/9/2020.


















