User login
Current Approach to Acne Management: A Community-Based Analysis
Issues in Hepatitis B Virus Infection
Supplement Editor:
William D. Carey, MD
Contents
The prevalence and natural history of hepatitis B in the 21st century
William D. Carey, MD
Risk of hepatocellular carcinoma in hepatitis B and prevention through treatment
Morris Sherman, MD, PhD
Understanding cultural barriers in hepatitis B virus infection
Tram T. Tran, MD
Hepatitis B treatment: Current best practices, avoiding resistance
Robert G. Gish, MD
Monotherapy vs multiple-drug therapy: The experts debate
Robert G. Gish, MD, and Pierre M. Gholam,MD
Management of hepatitis B in pregnancy: Weighing the options
Tram T. Tran, MD
Strategies for managing coinfection with hepatitis B virus and HIV
Morris Sherman, MD, PhD
Supplement Editor:
William D. Carey, MD
Contents
The prevalence and natural history of hepatitis B in the 21st century
William D. Carey, MD
Risk of hepatocellular carcinoma in hepatitis B and prevention through treatment
Morris Sherman, MD, PhD
Understanding cultural barriers in hepatitis B virus infection
Tram T. Tran, MD
Hepatitis B treatment: Current best practices, avoiding resistance
Robert G. Gish, MD
Monotherapy vs multiple-drug therapy: The experts debate
Robert G. Gish, MD, and Pierre M. Gholam,MD
Management of hepatitis B in pregnancy: Weighing the options
Tram T. Tran, MD
Strategies for managing coinfection with hepatitis B virus and HIV
Morris Sherman, MD, PhD
Supplement Editor:
William D. Carey, MD
Contents
The prevalence and natural history of hepatitis B in the 21st century
William D. Carey, MD
Risk of hepatocellular carcinoma in hepatitis B and prevention through treatment
Morris Sherman, MD, PhD
Understanding cultural barriers in hepatitis B virus infection
Tram T. Tran, MD
Hepatitis B treatment: Current best practices, avoiding resistance
Robert G. Gish, MD
Monotherapy vs multiple-drug therapy: The experts debate
Robert G. Gish, MD, and Pierre M. Gholam,MD
Management of hepatitis B in pregnancy: Weighing the options
Tram T. Tran, MD
Strategies for managing coinfection with hepatitis B virus and HIV
Morris Sherman, MD, PhD
Proceedings of the 2008 Heart-Brain Summit
Supplement Editor:
Marc S. Penn, MD, PhD
Contents
Preface
Earl E. Bakken, MD, HonC, Hon DSc (3), Hon DHL (2)
Introduction: Heart-brain medicine: Update 2008
Marc S. Penn, MD, PhD, and Earl E. Bakken, MD, HonC, Hon DSc (3), Hon DHL (2)
Bakken Lecture: The brain, the heart, and therapeutic hypothermia
Patrick M. Kochanek, MD
Session 1: Pathways Involved in Neuromodulation of Risks in Coronary Artery Disease
Depression and heart rate variability in patients with coronary heart disease
Robert M. Carney, PhD, and Kenneth E. Freedland, PhD
Autonomic function and prognosis
Michael S. Lauer, MD
Vagal tone and the inflammatory reflex
Julian F. Thayer, PhD
Inflammation, atherosclerosis, and arterial thrombosis: Role of the scavenger receptors CD36
Roy L. Silverstein, MD
Pioneer Award Address: Ignorance isn't biased: Comments on receiving the Pioneer Award
David S. Goldstein, MD, PhD
Session II: Measures and Strategies for Modulation of Heart-Brain Interactions
Heart rate variability with deep breathing as a clinical test of cardiovagal function
Robert W. Shields, Jr, MD
Basic research models for the study of underlying mechanisms of electrical neuromodulation and ischemi heart-brain interactions
Mike J.L. DeJongste, MD, PhD, FESC; Gert J. TerHorst, PhD; and Robert D. Foreman, PhD
Session III: Annual Review of Key Papers in Heart-Brain Medicine
Key papers in the field published during the year prior to the Summit were discussed; two of those papers are reported here.
Cardiac sympathetic denervation preceding motor signs in Parkinson disease
David S. Goldstein, MD, PhD; Yehonatan Sharabi, MD; Barbara I. Karp, MD; Oladi Bentho; Ahmed Saleem, MD; Karel Pacak, MD, PhD; and Graeme Eisenhofer, PhD
Supine low-frequency power of heart rate variability reflects baroreflex function, not cardiac sympathetic innervation
Jeffrey P. Moak, MD; David S. Goldstein, MD, PhD; Basil A. Eldadah, MD, PhD; Ahmed Saleem, MD; Courtney Holmes, CMT; Sandra Pechnik, RN; and Yehonatan Sharabi, MD
Session IV: Code Lavender—Strategies for Implementing Heart-Brain Medicine
Is posttraumatic stress disorder related to development of heart disease? An update
Laura D. Kubzansky, PhD, and Karestan C. Koenen, PhD
Creating a healing environment: Rationale and research overview
Jone Geimer-Flanders, DO
Redesigning the neurocritical care unit to enhance family participation and improve outcomes
Owen Samuels, MD
Session V: Insights into Neuromodulation of Cardiovascular Function
Neuromodulation of cardiac pain and cerebral vasculature: Neural mechanisms
Robert D. Foreman, PhD, and Chao Qin, MD, PhD
Pinacidil induces vascular dilation and hyperemia in vivo and does not impact biophysical properties of neurons and astrocytes in vitro
Rosa Cao; Bryan T. Higashikubo; Jessica Cardin; Ulf Knoblich; Raddy Ramos, PhD; Mark T. Nelson, PhD; Christopher I. Moore, PhD; and Joshua C. Brumberg, PhD
The polyvagal theory: New insights into adaptive reactions of the autonomic nervous system
Stephen W. Porges, PhD
Poster Abstracts
Abstract 1: Insulin use does not protect against restenosis in diabetic patients presenting with acute coronary syndrome or symptomatic angina
Matthew C. Becker, MD; John M. Galla, MD; Saif Anwaruddin, MD; Samir Kapadia, MD; and Richard A. Krasuski, MD
Abstract 2: Postoperative statin use and lower LDL cholesterol concentration are associated with reduced incidence of stroke
Matthew C. Becker, John M. Galla, Ryan P. Daly, Femi Philip, Peter Zimbwa, Stephen O. Chen, Chen H. Chow, Tingfei Hu, Richard A. Krasuski, and Arman T. Askari
Abstract 3: Brain edema and blood-brain barrier leakage influence antiepileptic drug levels
Giulia Betto, Vincent Fazio, Damir Janigro, and Chaitali Ghosh
Abstract 4: CPAP treatment vs conservative treatment in mild obstructive sleep apnea: Implications on cardiovascular morbidity
Kumar Budur, MD, and Nattapong Jaimchariyatam, MD
Abstract 5: New bioinformatics program identifies behavioral medicine interventions for epidemic cardiovascular disease in the developing world: Analysis of multidisciplinary findings for launching a new global public health initiative in heart-brain medicine
William C. Bushell, PhD
Abstract 6: Do systemic inflammation and blood-brain barrier failure play a role in pediatric psychosis?
Erin Carlton, Tatiana Falcone, Ayush Batra, Vince Fazio, Kathleen Franco, and Damir Janigro
Abstract 7: Brain, heart, and education
Linda Bryant Caviness, PhD
Abstract 8: Tobacco smoke mediates a monocytic and endothelial proinflammatory activation that synergistically affects BBB integrity
L. Cucullo, T. Sathe, M. Hossain, and D. Janigro
Abstract 9: Dynamic changes in ECG predict poor outcome after aneurysmal subarachnoid hemorrhage (aSAH)
H.A. Elsharkawy, MD; S.M. El Hadi, MD, PhD; J.E. Tetzlaff, MD; and J.J. Provencio, MD, FCCM
Abstract 10: Mechanism studies of malformation of cortical development by prenatal exposure of combined methylazoxymethanol and thalidomide
Q. Fan, S. Ramakrishna, N. Marchi, V. Fazio, K. Hallene, and D. Janigro
Abstract 11: Proapolipoprotein A1 demonstrates improved potential as a serum marker for brain metastases without vascular disease interference
Vince Fazio, Peter Mazzone, Nicola Marchi, Thomas Masaryk, and Damir Janigro
Abstract 12: Biofeedback-assisted stress management training to reverse myocardial remodeling in patients with end-stage heart failure
Dana L. Frank, BS; Mary E. Klecka, BA; Jerry Kiffer, MA; Heather Henrickson, PhD; Michael G. McKee, PhD; and Christine S. Moravec, PhD
Abstract 13: Nitric oxide and arginine metabolism in depression: Effect of a serotonin-norepinephrine reuptake inhibitor
Angelos Halaris, John Piletz, Omer Iqbal, Debra Hoppensteadt, Jawed Fareed, He Zhu, James Sinacore, and C. Lindsay DeVane
Abstract 14: Association between excessive daytime sleepiness and oxygen desaturation in obstructive sleep apnea syndrome: Nadir oxygen saturation vs mean oxygen saturation vs time spent below 90% oxygen saturation—which is important?
Nattapong Jaimchariyatam, MD, and Kumar Budur, MD
Abstract 15: Endotoxin preconditioning of the CNS: Microglia activation and neuroprotection
Walid Jalabi, Ranjan Dutta, Yongming Jin, Gerson Criste, Xinghua Yin, Grahame J. Kidd, and Bruce D. Trapp
Abstract 16: Pilot of stress reduction strategies for patients after a coronary event
R. Lindquist, D. Windenburg, K. Savik, and U. Bronas
Abstract 17: Cerebrovascular substrates of seizures after cardiopulmonary bypass
Rebecca O’Dwyer, Tim Wehner, Dileep Nair, Giulia Betto, Nicola Marchi, and Damir Janigro
Abstract 18: Depression and whole blood serotonin in patients with coronary heart disease from the heart and soul study
Lawson Wulsin, Dominique Musselman, Christian Otte, Erica Bruce, Sadia Ali, and Mary Whooley
Abstract 19: Gender differences prominent in linking anxiety to long-term mortality among the elderly
Jianping Zhang, MD, PhD; Boaz Kahana, PhD; Eva Kahana, PhD; Bo Hu, PhD; and Leo Pozuelo, MD
Abstract 20: Temporal lobe and sinus node: A case report provides evidence for bidirectional effects
Rebecca O’Dwyer, MD; Andreas Alexopoulos, MD, MPH; Walid Saliba, MD; Imad Najm, MD; and Richard Burgess, MD, PhD
Supplement Editor:
Marc S. Penn, MD, PhD
Contents
Preface
Earl E. Bakken, MD, HonC, Hon DSc (3), Hon DHL (2)
Introduction: Heart-brain medicine: Update 2008
Marc S. Penn, MD, PhD, and Earl E. Bakken, MD, HonC, Hon DSc (3), Hon DHL (2)
Bakken Lecture: The brain, the heart, and therapeutic hypothermia
Patrick M. Kochanek, MD
Session 1: Pathways Involved in Neuromodulation of Risks in Coronary Artery Disease
Depression and heart rate variability in patients with coronary heart disease
Robert M. Carney, PhD, and Kenneth E. Freedland, PhD
Autonomic function and prognosis
Michael S. Lauer, MD
Vagal tone and the inflammatory reflex
Julian F. Thayer, PhD
Inflammation, atherosclerosis, and arterial thrombosis: Role of the scavenger receptors CD36
Roy L. Silverstein, MD
Pioneer Award Address: Ignorance isn't biased: Comments on receiving the Pioneer Award
David S. Goldstein, MD, PhD
Session II: Measures and Strategies for Modulation of Heart-Brain Interactions
Heart rate variability with deep breathing as a clinical test of cardiovagal function
Robert W. Shields, Jr, MD
Basic research models for the study of underlying mechanisms of electrical neuromodulation and ischemi heart-brain interactions
Mike J.L. DeJongste, MD, PhD, FESC; Gert J. TerHorst, PhD; and Robert D. Foreman, PhD
Session III: Annual Review of Key Papers in Heart-Brain Medicine
Key papers in the field published during the year prior to the Summit were discussed; two of those papers are reported here.
Cardiac sympathetic denervation preceding motor signs in Parkinson disease
David S. Goldstein, MD, PhD; Yehonatan Sharabi, MD; Barbara I. Karp, MD; Oladi Bentho; Ahmed Saleem, MD; Karel Pacak, MD, PhD; and Graeme Eisenhofer, PhD
Supine low-frequency power of heart rate variability reflects baroreflex function, not cardiac sympathetic innervation
Jeffrey P. Moak, MD; David S. Goldstein, MD, PhD; Basil A. Eldadah, MD, PhD; Ahmed Saleem, MD; Courtney Holmes, CMT; Sandra Pechnik, RN; and Yehonatan Sharabi, MD
Session IV: Code Lavender—Strategies for Implementing Heart-Brain Medicine
Is posttraumatic stress disorder related to development of heart disease? An update
Laura D. Kubzansky, PhD, and Karestan C. Koenen, PhD
Creating a healing environment: Rationale and research overview
Jone Geimer-Flanders, DO
Redesigning the neurocritical care unit to enhance family participation and improve outcomes
Owen Samuels, MD
Session V: Insights into Neuromodulation of Cardiovascular Function
Neuromodulation of cardiac pain and cerebral vasculature: Neural mechanisms
Robert D. Foreman, PhD, and Chao Qin, MD, PhD
Pinacidil induces vascular dilation and hyperemia in vivo and does not impact biophysical properties of neurons and astrocytes in vitro
Rosa Cao; Bryan T. Higashikubo; Jessica Cardin; Ulf Knoblich; Raddy Ramos, PhD; Mark T. Nelson, PhD; Christopher I. Moore, PhD; and Joshua C. Brumberg, PhD
The polyvagal theory: New insights into adaptive reactions of the autonomic nervous system
Stephen W. Porges, PhD
Poster Abstracts
Abstract 1: Insulin use does not protect against restenosis in diabetic patients presenting with acute coronary syndrome or symptomatic angina
Matthew C. Becker, MD; John M. Galla, MD; Saif Anwaruddin, MD; Samir Kapadia, MD; and Richard A. Krasuski, MD
Abstract 2: Postoperative statin use and lower LDL cholesterol concentration are associated with reduced incidence of stroke
Matthew C. Becker, John M. Galla, Ryan P. Daly, Femi Philip, Peter Zimbwa, Stephen O. Chen, Chen H. Chow, Tingfei Hu, Richard A. Krasuski, and Arman T. Askari
Abstract 3: Brain edema and blood-brain barrier leakage influence antiepileptic drug levels
Giulia Betto, Vincent Fazio, Damir Janigro, and Chaitali Ghosh
Abstract 4: CPAP treatment vs conservative treatment in mild obstructive sleep apnea: Implications on cardiovascular morbidity
Kumar Budur, MD, and Nattapong Jaimchariyatam, MD
Abstract 5: New bioinformatics program identifies behavioral medicine interventions for epidemic cardiovascular disease in the developing world: Analysis of multidisciplinary findings for launching a new global public health initiative in heart-brain medicine
William C. Bushell, PhD
Abstract 6: Do systemic inflammation and blood-brain barrier failure play a role in pediatric psychosis?
Erin Carlton, Tatiana Falcone, Ayush Batra, Vince Fazio, Kathleen Franco, and Damir Janigro
Abstract 7: Brain, heart, and education
Linda Bryant Caviness, PhD
Abstract 8: Tobacco smoke mediates a monocytic and endothelial proinflammatory activation that synergistically affects BBB integrity
L. Cucullo, T. Sathe, M. Hossain, and D. Janigro
Abstract 9: Dynamic changes in ECG predict poor outcome after aneurysmal subarachnoid hemorrhage (aSAH)
H.A. Elsharkawy, MD; S.M. El Hadi, MD, PhD; J.E. Tetzlaff, MD; and J.J. Provencio, MD, FCCM
Abstract 10: Mechanism studies of malformation of cortical development by prenatal exposure of combined methylazoxymethanol and thalidomide
Q. Fan, S. Ramakrishna, N. Marchi, V. Fazio, K. Hallene, and D. Janigro
Abstract 11: Proapolipoprotein A1 demonstrates improved potential as a serum marker for brain metastases without vascular disease interference
Vince Fazio, Peter Mazzone, Nicola Marchi, Thomas Masaryk, and Damir Janigro
Abstract 12: Biofeedback-assisted stress management training to reverse myocardial remodeling in patients with end-stage heart failure
Dana L. Frank, BS; Mary E. Klecka, BA; Jerry Kiffer, MA; Heather Henrickson, PhD; Michael G. McKee, PhD; and Christine S. Moravec, PhD
Abstract 13: Nitric oxide and arginine metabolism in depression: Effect of a serotonin-norepinephrine reuptake inhibitor
Angelos Halaris, John Piletz, Omer Iqbal, Debra Hoppensteadt, Jawed Fareed, He Zhu, James Sinacore, and C. Lindsay DeVane
Abstract 14: Association between excessive daytime sleepiness and oxygen desaturation in obstructive sleep apnea syndrome: Nadir oxygen saturation vs mean oxygen saturation vs time spent below 90% oxygen saturation—which is important?
Nattapong Jaimchariyatam, MD, and Kumar Budur, MD
Abstract 15: Endotoxin preconditioning of the CNS: Microglia activation and neuroprotection
Walid Jalabi, Ranjan Dutta, Yongming Jin, Gerson Criste, Xinghua Yin, Grahame J. Kidd, and Bruce D. Trapp
Abstract 16: Pilot of stress reduction strategies for patients after a coronary event
R. Lindquist, D. Windenburg, K. Savik, and U. Bronas
Abstract 17: Cerebrovascular substrates of seizures after cardiopulmonary bypass
Rebecca O’Dwyer, Tim Wehner, Dileep Nair, Giulia Betto, Nicola Marchi, and Damir Janigro
Abstract 18: Depression and whole blood serotonin in patients with coronary heart disease from the heart and soul study
Lawson Wulsin, Dominique Musselman, Christian Otte, Erica Bruce, Sadia Ali, and Mary Whooley
Abstract 19: Gender differences prominent in linking anxiety to long-term mortality among the elderly
Jianping Zhang, MD, PhD; Boaz Kahana, PhD; Eva Kahana, PhD; Bo Hu, PhD; and Leo Pozuelo, MD
Abstract 20: Temporal lobe and sinus node: A case report provides evidence for bidirectional effects
Rebecca O’Dwyer, MD; Andreas Alexopoulos, MD, MPH; Walid Saliba, MD; Imad Najm, MD; and Richard Burgess, MD, PhD
Supplement Editor:
Marc S. Penn, MD, PhD
Contents
Preface
Earl E. Bakken, MD, HonC, Hon DSc (3), Hon DHL (2)
Introduction: Heart-brain medicine: Update 2008
Marc S. Penn, MD, PhD, and Earl E. Bakken, MD, HonC, Hon DSc (3), Hon DHL (2)
Bakken Lecture: The brain, the heart, and therapeutic hypothermia
Patrick M. Kochanek, MD
Session 1: Pathways Involved in Neuromodulation of Risks in Coronary Artery Disease
Depression and heart rate variability in patients with coronary heart disease
Robert M. Carney, PhD, and Kenneth E. Freedland, PhD
Autonomic function and prognosis
Michael S. Lauer, MD
Vagal tone and the inflammatory reflex
Julian F. Thayer, PhD
Inflammation, atherosclerosis, and arterial thrombosis: Role of the scavenger receptors CD36
Roy L. Silverstein, MD
Pioneer Award Address: Ignorance isn't biased: Comments on receiving the Pioneer Award
David S. Goldstein, MD, PhD
Session II: Measures and Strategies for Modulation of Heart-Brain Interactions
Heart rate variability with deep breathing as a clinical test of cardiovagal function
Robert W. Shields, Jr, MD
Basic research models for the study of underlying mechanisms of electrical neuromodulation and ischemi heart-brain interactions
Mike J.L. DeJongste, MD, PhD, FESC; Gert J. TerHorst, PhD; and Robert D. Foreman, PhD
Session III: Annual Review of Key Papers in Heart-Brain Medicine
Key papers in the field published during the year prior to the Summit were discussed; two of those papers are reported here.
Cardiac sympathetic denervation preceding motor signs in Parkinson disease
David S. Goldstein, MD, PhD; Yehonatan Sharabi, MD; Barbara I. Karp, MD; Oladi Bentho; Ahmed Saleem, MD; Karel Pacak, MD, PhD; and Graeme Eisenhofer, PhD
Supine low-frequency power of heart rate variability reflects baroreflex function, not cardiac sympathetic innervation
Jeffrey P. Moak, MD; David S. Goldstein, MD, PhD; Basil A. Eldadah, MD, PhD; Ahmed Saleem, MD; Courtney Holmes, CMT; Sandra Pechnik, RN; and Yehonatan Sharabi, MD
Session IV: Code Lavender—Strategies for Implementing Heart-Brain Medicine
Is posttraumatic stress disorder related to development of heart disease? An update
Laura D. Kubzansky, PhD, and Karestan C. Koenen, PhD
Creating a healing environment: Rationale and research overview
Jone Geimer-Flanders, DO
Redesigning the neurocritical care unit to enhance family participation and improve outcomes
Owen Samuels, MD
Session V: Insights into Neuromodulation of Cardiovascular Function
Neuromodulation of cardiac pain and cerebral vasculature: Neural mechanisms
Robert D. Foreman, PhD, and Chao Qin, MD, PhD
Pinacidil induces vascular dilation and hyperemia in vivo and does not impact biophysical properties of neurons and astrocytes in vitro
Rosa Cao; Bryan T. Higashikubo; Jessica Cardin; Ulf Knoblich; Raddy Ramos, PhD; Mark T. Nelson, PhD; Christopher I. Moore, PhD; and Joshua C. Brumberg, PhD
The polyvagal theory: New insights into adaptive reactions of the autonomic nervous system
Stephen W. Porges, PhD
Poster Abstracts
Abstract 1: Insulin use does not protect against restenosis in diabetic patients presenting with acute coronary syndrome or symptomatic angina
Matthew C. Becker, MD; John M. Galla, MD; Saif Anwaruddin, MD; Samir Kapadia, MD; and Richard A. Krasuski, MD
Abstract 2: Postoperative statin use and lower LDL cholesterol concentration are associated with reduced incidence of stroke
Matthew C. Becker, John M. Galla, Ryan P. Daly, Femi Philip, Peter Zimbwa, Stephen O. Chen, Chen H. Chow, Tingfei Hu, Richard A. Krasuski, and Arman T. Askari
Abstract 3: Brain edema and blood-brain barrier leakage influence antiepileptic drug levels
Giulia Betto, Vincent Fazio, Damir Janigro, and Chaitali Ghosh
Abstract 4: CPAP treatment vs conservative treatment in mild obstructive sleep apnea: Implications on cardiovascular morbidity
Kumar Budur, MD, and Nattapong Jaimchariyatam, MD
Abstract 5: New bioinformatics program identifies behavioral medicine interventions for epidemic cardiovascular disease in the developing world: Analysis of multidisciplinary findings for launching a new global public health initiative in heart-brain medicine
William C. Bushell, PhD
Abstract 6: Do systemic inflammation and blood-brain barrier failure play a role in pediatric psychosis?
Erin Carlton, Tatiana Falcone, Ayush Batra, Vince Fazio, Kathleen Franco, and Damir Janigro
Abstract 7: Brain, heart, and education
Linda Bryant Caviness, PhD
Abstract 8: Tobacco smoke mediates a monocytic and endothelial proinflammatory activation that synergistically affects BBB integrity
L. Cucullo, T. Sathe, M. Hossain, and D. Janigro
Abstract 9: Dynamic changes in ECG predict poor outcome after aneurysmal subarachnoid hemorrhage (aSAH)
H.A. Elsharkawy, MD; S.M. El Hadi, MD, PhD; J.E. Tetzlaff, MD; and J.J. Provencio, MD, FCCM
Abstract 10: Mechanism studies of malformation of cortical development by prenatal exposure of combined methylazoxymethanol and thalidomide
Q. Fan, S. Ramakrishna, N. Marchi, V. Fazio, K. Hallene, and D. Janigro
Abstract 11: Proapolipoprotein A1 demonstrates improved potential as a serum marker for brain metastases without vascular disease interference
Vince Fazio, Peter Mazzone, Nicola Marchi, Thomas Masaryk, and Damir Janigro
Abstract 12: Biofeedback-assisted stress management training to reverse myocardial remodeling in patients with end-stage heart failure
Dana L. Frank, BS; Mary E. Klecka, BA; Jerry Kiffer, MA; Heather Henrickson, PhD; Michael G. McKee, PhD; and Christine S. Moravec, PhD
Abstract 13: Nitric oxide and arginine metabolism in depression: Effect of a serotonin-norepinephrine reuptake inhibitor
Angelos Halaris, John Piletz, Omer Iqbal, Debra Hoppensteadt, Jawed Fareed, He Zhu, James Sinacore, and C. Lindsay DeVane
Abstract 14: Association between excessive daytime sleepiness and oxygen desaturation in obstructive sleep apnea syndrome: Nadir oxygen saturation vs mean oxygen saturation vs time spent below 90% oxygen saturation—which is important?
Nattapong Jaimchariyatam, MD, and Kumar Budur, MD
Abstract 15: Endotoxin preconditioning of the CNS: Microglia activation and neuroprotection
Walid Jalabi, Ranjan Dutta, Yongming Jin, Gerson Criste, Xinghua Yin, Grahame J. Kidd, and Bruce D. Trapp
Abstract 16: Pilot of stress reduction strategies for patients after a coronary event
R. Lindquist, D. Windenburg, K. Savik, and U. Bronas
Abstract 17: Cerebrovascular substrates of seizures after cardiopulmonary bypass
Rebecca O’Dwyer, Tim Wehner, Dileep Nair, Giulia Betto, Nicola Marchi, and Damir Janigro
Abstract 18: Depression and whole blood serotonin in patients with coronary heart disease from the heart and soul study
Lawson Wulsin, Dominique Musselman, Christian Otte, Erica Bruce, Sadia Ali, and Mary Whooley
Abstract 19: Gender differences prominent in linking anxiety to long-term mortality among the elderly
Jianping Zhang, MD, PhD; Boaz Kahana, PhD; Eva Kahana, PhD; Bo Hu, PhD; and Leo Pozuelo, MD
Abstract 20: Temporal lobe and sinus node: A case report provides evidence for bidirectional effects
Rebecca O’Dwyer, MD; Andreas Alexopoulos, MD, MPH; Walid Saliba, MD; Imad Najm, MD; and Richard Burgess, MD, PhD
Platelet Response in Acute Coronary Syndromes
Supplement Editors:
Deepak L. Bhatt, MD, MPH, and W. Frank Peacock, MD
Contents
Importance of platelets and platelet response in acute coronary syndromes
Kandice Kottke-Marchant, MD, PhD
Novel antiplatelet strategies in acute coronary syndromes
Marc S. Sabatine, MD, MPH
The current state of antiplatelet therapy in acute coronary syndromes: The data and the real word
John H. Alexander, MD, MHSc
Platelet response in practice: Applying new insights and tools for testing and treatment
Deepak L. Bhatt, MD, MPH; Kandice Kottke-Marchant, MD, PhD; John H. Alexander, MD, MHSc; W. Frank Peacock, MD; and Marc S. Sabatine, MD, MPH
Supplement Editors:
Deepak L. Bhatt, MD, MPH, and W. Frank Peacock, MD
Contents
Importance of platelets and platelet response in acute coronary syndromes
Kandice Kottke-Marchant, MD, PhD
Novel antiplatelet strategies in acute coronary syndromes
Marc S. Sabatine, MD, MPH
The current state of antiplatelet therapy in acute coronary syndromes: The data and the real word
John H. Alexander, MD, MHSc
Platelet response in practice: Applying new insights and tools for testing and treatment
Deepak L. Bhatt, MD, MPH; Kandice Kottke-Marchant, MD, PhD; John H. Alexander, MD, MHSc; W. Frank Peacock, MD; and Marc S. Sabatine, MD, MPH
Supplement Editors:
Deepak L. Bhatt, MD, MPH, and W. Frank Peacock, MD
Contents
Importance of platelets and platelet response in acute coronary syndromes
Kandice Kottke-Marchant, MD, PhD
Novel antiplatelet strategies in acute coronary syndromes
Marc S. Sabatine, MD, MPH
The current state of antiplatelet therapy in acute coronary syndromes: The data and the real word
John H. Alexander, MD, MHSc
Platelet response in practice: Applying new insights and tools for testing and treatment
Deepak L. Bhatt, MD, MPH; Kandice Kottke-Marchant, MD, PhD; John H. Alexander, MD, MHSc; W. Frank Peacock, MD; and Marc S. Sabatine, MD, MPH
Perioperative Medicine Summit 2009
Summit Director:
Amir K. Jaffer, MD
Contents
Abstract 1: Pulmonary hypertension is an important predictor of perioperative outcomes in patients undergoing noncardiac surgery
Roop Kaw, MD; Esteban Walker, PhD; Vinay Pasupuleti, MD, PhD; Abhishek Deshpande, MD, PhD; Tarek Hamieh, MD; and Omar A. Minai, MD
Abstract 2: Analysis of administrative practices and residency training curricula in academic anesthesiology programs
David Hepner, A.R. Bader, D. Correll, L.C. Tsen, B.S. Segal, and A.M. Bader
Abstract 3: Is percent body fat a better predictor of surgical site infection risk than body mass index?
Emily Waisbren, BS; Angela M. Bader, MD, MPH; Heather Rosen, MD, MPH; Selwyn O. Rogers, Jr., MD, MPH; and Elof Eriksson, MD, PhD
Abstract 4: A nomogram for prediction of survival for patients undergoing elective major noncardiac surgery
Y. Olivia Xu-Cai, MD; and Michael W. Kattan, PhD
Abstract 5: Sustainability of an osteoporosis pathway
Catherine Gibb, MBBS, FRACP; Christopher Butcher, FRACS; Lesley Thomas, BNsg; and Jennifer Pink, BPharm
Abstract 6: Length of hospital stay is predicted by comorbidities
Catherine Gibb, MBBS, FRACP; and Professor Villis Marshall, FRACS
Abstract 7: Generalization of the POISE and Mangano studies on beta-blocker use in the perioperative period
Matthieu Touchette, MD; Odile Paquette, MD; Catherine St-Georges, MD; and Luc Lanthier, MD, MSc
Abstract 8: Impact of antihypertensive medication on perioperative period
Matthieu Touchette, MD; Odile Paquette, MD; Catherine St-Georges, MD; Danielle Pilon, MD, MSc; and Luc Lanthier, MD, MSc
Abstract 9: An analysis of preoperative testing protocols in academic anesthesiology programs
David Hepner, A.R. Bader, D. Correll, L.C. Tsen, B.S. Segal, and A.M. Bader
Abstract 10: Preoperative biomarkers of inflammation, ischemia, and heart failure and outcomes of vascular surgery
Matthew Griffee, MD; Ansgar Brambrink, MD, PhD; and Thomas Barrett, MD
Abstract 11: Alcohol-related predictors of postoperative delirium in major head and neck cancer surgery
Harrison Weed, MD; Summit Shah, BS; Xin He, PhD; Amit Agrawal, MD; Enver Ozer, MD; and David E. Schuller, MD
Abstract 12: Intraoperative coagulopathy: A low-volume treatment protocol that completely replaces fresh frozen plasma
Peter Kallas, MD; Mary Lou Green, MHS; and Anjali Desai, MD
Abstract 13: Is the Berlin Questionnaire an effective screening tool for obstructive sleep apnea in the preoperative total joint replacement population?
Peter Kallas, MD; Mark Schumacher; Mona Lazar, DO; and Anjali Desai, MD
Abstract 14: The impact of preoperative medical optimization on head and neck cancer surgery
Christopher Tan, MBBS; Catherine Gibb, MBBS, FRACP; and Suren Krishnan, MBBS, FRACS
Abstract 15: Reconceptualizing the preoperative process
Ross Kerridge, MBBS, FRCA, FANZCA
Abstract 16: Development of an electronic medical record smart set form to increase standardization, consistency, and compliance with ACC/AHA perioperative guidelines
Anitha Rajamanickam, MD; Ali Usmani, MD; Ajay Kumar, MD; and Brian Harte, MD
Abstract 17: Development of a perioperative electronic medical record research and quality improvement database
Anitha Rajamanickam, MD; Ali Usmani, MD; Feza Remzi, MD; Brian Harte, MD; and Ajay Kumar, MD
Abstract 18: An innovative perioperative/consultative curriculum for third-year internal medicine residents
Alex Rico, MD; Joshua Lenchus, DO; and Amir Jaffer, MD
Abstract 19: Preoperative medicine infobutton
Terrence J. Adam, MD, PhD
Abstract 20: Nurse practitioners: Bridging the gap in perioperative care
Sally Morgan, RN, MS, ANP-BC, ACNS-BC; and Angela Wright, RN, MSN, APRN, BC
Abstract 21: Intubation training of deploying far forward combat medical personnel with the video laryngoscope
Ben Boedeker, MD; Mary Barak-Bernhagen, BS; Kirsten Boedeker; and W. Bosseau Murray, MD
Abstract 22: The establishment of a perioperative skin integrity committee
Jeanne Lanchester, RN, MEd; Ann Leary, BSN, RNC; and Susan Vargas, AD, RN
Abstract 23: Development and implementation of a perianesthesia integrative care committee
Jeanne Lanchester, RN, MEd; Jeanette Cote, BWN, RN; Terri Jamros, RN; Charla Delillo, RN; Sherie Lavoie, BSN, RN; Jennifer Therminos, SN; Joan Compagnone, RN; and Nicole Engel, MSN, RN
Abstract 24: Development of a screening system to identify patients preoperatively who may benefit from a postoperative hospitalist consult
Elizabeth Marlow, MD, MA; and Chad Whelan, MD
Abstract 25: An algorithm for preoperative screening and management of sleep apnea: Have we created a monster?
Deborah C. Richman, MBChB, FFA(SA); Jorge M. Mallea, MD; Paul S. Richman, MD; and Pater S.A. Glass, MBChB
Abstract 26: Constructing a collaborative neuroscience hospitalist program
Rachel Thompson, MD; Christy Gilmore, MD; Kamal Ajam, MD; and Jennifer Thompson, MD
Abstract 27: The development of algorithms for preoperative management of antiplatelet and anticoagulation therapy in patients undergoing surgical or invasive procedures
Catherine McGowan, MSN, and Patricia Kidik, MSN
Abstract 28: Surgeon-initiated preoperative screening: A new approach
Christina Johnson, RN, PA-C; and Edward J. denBraven, CRNA
Abstract 29: A new process for ensuring the safety of patients having anesthesia outside of the operating room
Ellen Leary, MSN; Catherine McGowan, MSN; Kathleen McGrath, MSN; Sheila McCabe Hassan, MSN; and Theresa Kennedy, MSN
Abstract 30: Establishing a virtual preoperative evaluation clinic
Corey Zetterman, MD; Bobbie J. Sweitzer, MD; and Ben H. Boedeker, MD
Abstract 31: Perioperative hypoxemia and rhabdomyolysis in a medically complicated patient
Sarah Bodin, MD
Abstract 32: How soon is too soon? General anesthesia after coronary intervention with bare metal stents
Meghan Tadel, MD
Abstract 33: Can patients with critical aortic stenosis undergo noncardiac surgery without intervening aortic valve replacement?
M. Chadi Alraies, MD; Abdul Alraiyes, MD; Anitha Rajamanickam, MD; and Frank Michota, MD
Abstract 34: Is it safe to operate on cocaine-positive patients?
M. Chadi Alraies, MD; Abdul Hamid Alraiyes, MD; and Brian Harte, MD
Abstract 35: To intensive care or not?
Mona Lazar, DO; and Peter Kallas, MD
Abstract 36: Predicting surgical complications from liver disease
Mona Lazar, DO, and Peter Kallas, MD
Abstract 37: Preoperative coronary angiography: Friend or foe?
Ross Kerridge, MBBS, FRCA, FANZCA
Abstract 38: Heparin-induced thrombocytopenia with low molecular weight heparin after total knee replacement
Steven Cohn, MD
Abstract 39: Patient with Parkinson’s disease treated with implanted deep brain stimulators for laparotomy
Deborah C. Richman, MBChB, FFA(SA); Daryn H. Moller, MD; and Khoa N. Nguyen, MD
Abstract 40: Ethical dilemma in the preoperative assessment clinic: Can a patient refuse an indicated cardiac workup? Can we refuse to anesthetize?
Deborah C. Richman, MBChB, FFA(SA)
Abstract 41: Coronary artery bypass grafting as a precipitatin factor in diabetic ketoacidosis in type 2 diabetes
Vishal Sehgral, MD, and Abbas Kitabchi, MD
Summit Director:
Amir K. Jaffer, MD
Contents
Abstract 1: Pulmonary hypertension is an important predictor of perioperative outcomes in patients undergoing noncardiac surgery
Roop Kaw, MD; Esteban Walker, PhD; Vinay Pasupuleti, MD, PhD; Abhishek Deshpande, MD, PhD; Tarek Hamieh, MD; and Omar A. Minai, MD
Abstract 2: Analysis of administrative practices and residency training curricula in academic anesthesiology programs
David Hepner, A.R. Bader, D. Correll, L.C. Tsen, B.S. Segal, and A.M. Bader
Abstract 3: Is percent body fat a better predictor of surgical site infection risk than body mass index?
Emily Waisbren, BS; Angela M. Bader, MD, MPH; Heather Rosen, MD, MPH; Selwyn O. Rogers, Jr., MD, MPH; and Elof Eriksson, MD, PhD
Abstract 4: A nomogram for prediction of survival for patients undergoing elective major noncardiac surgery
Y. Olivia Xu-Cai, MD; and Michael W. Kattan, PhD
Abstract 5: Sustainability of an osteoporosis pathway
Catherine Gibb, MBBS, FRACP; Christopher Butcher, FRACS; Lesley Thomas, BNsg; and Jennifer Pink, BPharm
Abstract 6: Length of hospital stay is predicted by comorbidities
Catherine Gibb, MBBS, FRACP; and Professor Villis Marshall, FRACS
Abstract 7: Generalization of the POISE and Mangano studies on beta-blocker use in the perioperative period
Matthieu Touchette, MD; Odile Paquette, MD; Catherine St-Georges, MD; and Luc Lanthier, MD, MSc
Abstract 8: Impact of antihypertensive medication on perioperative period
Matthieu Touchette, MD; Odile Paquette, MD; Catherine St-Georges, MD; Danielle Pilon, MD, MSc; and Luc Lanthier, MD, MSc
Abstract 9: An analysis of preoperative testing protocols in academic anesthesiology programs
David Hepner, A.R. Bader, D. Correll, L.C. Tsen, B.S. Segal, and A.M. Bader
Abstract 10: Preoperative biomarkers of inflammation, ischemia, and heart failure and outcomes of vascular surgery
Matthew Griffee, MD; Ansgar Brambrink, MD, PhD; and Thomas Barrett, MD
Abstract 11: Alcohol-related predictors of postoperative delirium in major head and neck cancer surgery
Harrison Weed, MD; Summit Shah, BS; Xin He, PhD; Amit Agrawal, MD; Enver Ozer, MD; and David E. Schuller, MD
Abstract 12: Intraoperative coagulopathy: A low-volume treatment protocol that completely replaces fresh frozen plasma
Peter Kallas, MD; Mary Lou Green, MHS; and Anjali Desai, MD
Abstract 13: Is the Berlin Questionnaire an effective screening tool for obstructive sleep apnea in the preoperative total joint replacement population?
Peter Kallas, MD; Mark Schumacher; Mona Lazar, DO; and Anjali Desai, MD
Abstract 14: The impact of preoperative medical optimization on head and neck cancer surgery
Christopher Tan, MBBS; Catherine Gibb, MBBS, FRACP; and Suren Krishnan, MBBS, FRACS
Abstract 15: Reconceptualizing the preoperative process
Ross Kerridge, MBBS, FRCA, FANZCA
Abstract 16: Development of an electronic medical record smart set form to increase standardization, consistency, and compliance with ACC/AHA perioperative guidelines
Anitha Rajamanickam, MD; Ali Usmani, MD; Ajay Kumar, MD; and Brian Harte, MD
Abstract 17: Development of a perioperative electronic medical record research and quality improvement database
Anitha Rajamanickam, MD; Ali Usmani, MD; Feza Remzi, MD; Brian Harte, MD; and Ajay Kumar, MD
Abstract 18: An innovative perioperative/consultative curriculum for third-year internal medicine residents
Alex Rico, MD; Joshua Lenchus, DO; and Amir Jaffer, MD
Abstract 19: Preoperative medicine infobutton
Terrence J. Adam, MD, PhD
Abstract 20: Nurse practitioners: Bridging the gap in perioperative care
Sally Morgan, RN, MS, ANP-BC, ACNS-BC; and Angela Wright, RN, MSN, APRN, BC
Abstract 21: Intubation training of deploying far forward combat medical personnel with the video laryngoscope
Ben Boedeker, MD; Mary Barak-Bernhagen, BS; Kirsten Boedeker; and W. Bosseau Murray, MD
Abstract 22: The establishment of a perioperative skin integrity committee
Jeanne Lanchester, RN, MEd; Ann Leary, BSN, RNC; and Susan Vargas, AD, RN
Abstract 23: Development and implementation of a perianesthesia integrative care committee
Jeanne Lanchester, RN, MEd; Jeanette Cote, BWN, RN; Terri Jamros, RN; Charla Delillo, RN; Sherie Lavoie, BSN, RN; Jennifer Therminos, SN; Joan Compagnone, RN; and Nicole Engel, MSN, RN
Abstract 24: Development of a screening system to identify patients preoperatively who may benefit from a postoperative hospitalist consult
Elizabeth Marlow, MD, MA; and Chad Whelan, MD
Abstract 25: An algorithm for preoperative screening and management of sleep apnea: Have we created a monster?
Deborah C. Richman, MBChB, FFA(SA); Jorge M. Mallea, MD; Paul S. Richman, MD; and Pater S.A. Glass, MBChB
Abstract 26: Constructing a collaborative neuroscience hospitalist program
Rachel Thompson, MD; Christy Gilmore, MD; Kamal Ajam, MD; and Jennifer Thompson, MD
Abstract 27: The development of algorithms for preoperative management of antiplatelet and anticoagulation therapy in patients undergoing surgical or invasive procedures
Catherine McGowan, MSN, and Patricia Kidik, MSN
Abstract 28: Surgeon-initiated preoperative screening: A new approach
Christina Johnson, RN, PA-C; and Edward J. denBraven, CRNA
Abstract 29: A new process for ensuring the safety of patients having anesthesia outside of the operating room
Ellen Leary, MSN; Catherine McGowan, MSN; Kathleen McGrath, MSN; Sheila McCabe Hassan, MSN; and Theresa Kennedy, MSN
Abstract 30: Establishing a virtual preoperative evaluation clinic
Corey Zetterman, MD; Bobbie J. Sweitzer, MD; and Ben H. Boedeker, MD
Abstract 31: Perioperative hypoxemia and rhabdomyolysis in a medically complicated patient
Sarah Bodin, MD
Abstract 32: How soon is too soon? General anesthesia after coronary intervention with bare metal stents
Meghan Tadel, MD
Abstract 33: Can patients with critical aortic stenosis undergo noncardiac surgery without intervening aortic valve replacement?
M. Chadi Alraies, MD; Abdul Alraiyes, MD; Anitha Rajamanickam, MD; and Frank Michota, MD
Abstract 34: Is it safe to operate on cocaine-positive patients?
M. Chadi Alraies, MD; Abdul Hamid Alraiyes, MD; and Brian Harte, MD
Abstract 35: To intensive care or not?
Mona Lazar, DO; and Peter Kallas, MD
Abstract 36: Predicting surgical complications from liver disease
Mona Lazar, DO, and Peter Kallas, MD
Abstract 37: Preoperative coronary angiography: Friend or foe?
Ross Kerridge, MBBS, FRCA, FANZCA
Abstract 38: Heparin-induced thrombocytopenia with low molecular weight heparin after total knee replacement
Steven Cohn, MD
Abstract 39: Patient with Parkinson’s disease treated with implanted deep brain stimulators for laparotomy
Deborah C. Richman, MBChB, FFA(SA); Daryn H. Moller, MD; and Khoa N. Nguyen, MD
Abstract 40: Ethical dilemma in the preoperative assessment clinic: Can a patient refuse an indicated cardiac workup? Can we refuse to anesthetize?
Deborah C. Richman, MBChB, FFA(SA)
Abstract 41: Coronary artery bypass grafting as a precipitatin factor in diabetic ketoacidosis in type 2 diabetes
Vishal Sehgral, MD, and Abbas Kitabchi, MD
Summit Director:
Amir K. Jaffer, MD
Contents
Abstract 1: Pulmonary hypertension is an important predictor of perioperative outcomes in patients undergoing noncardiac surgery
Roop Kaw, MD; Esteban Walker, PhD; Vinay Pasupuleti, MD, PhD; Abhishek Deshpande, MD, PhD; Tarek Hamieh, MD; and Omar A. Minai, MD
Abstract 2: Analysis of administrative practices and residency training curricula in academic anesthesiology programs
David Hepner, A.R. Bader, D. Correll, L.C. Tsen, B.S. Segal, and A.M. Bader
Abstract 3: Is percent body fat a better predictor of surgical site infection risk than body mass index?
Emily Waisbren, BS; Angela M. Bader, MD, MPH; Heather Rosen, MD, MPH; Selwyn O. Rogers, Jr., MD, MPH; and Elof Eriksson, MD, PhD
Abstract 4: A nomogram for prediction of survival for patients undergoing elective major noncardiac surgery
Y. Olivia Xu-Cai, MD; and Michael W. Kattan, PhD
Abstract 5: Sustainability of an osteoporosis pathway
Catherine Gibb, MBBS, FRACP; Christopher Butcher, FRACS; Lesley Thomas, BNsg; and Jennifer Pink, BPharm
Abstract 6: Length of hospital stay is predicted by comorbidities
Catherine Gibb, MBBS, FRACP; and Professor Villis Marshall, FRACS
Abstract 7: Generalization of the POISE and Mangano studies on beta-blocker use in the perioperative period
Matthieu Touchette, MD; Odile Paquette, MD; Catherine St-Georges, MD; and Luc Lanthier, MD, MSc
Abstract 8: Impact of antihypertensive medication on perioperative period
Matthieu Touchette, MD; Odile Paquette, MD; Catherine St-Georges, MD; Danielle Pilon, MD, MSc; and Luc Lanthier, MD, MSc
Abstract 9: An analysis of preoperative testing protocols in academic anesthesiology programs
David Hepner, A.R. Bader, D. Correll, L.C. Tsen, B.S. Segal, and A.M. Bader
Abstract 10: Preoperative biomarkers of inflammation, ischemia, and heart failure and outcomes of vascular surgery
Matthew Griffee, MD; Ansgar Brambrink, MD, PhD; and Thomas Barrett, MD
Abstract 11: Alcohol-related predictors of postoperative delirium in major head and neck cancer surgery
Harrison Weed, MD; Summit Shah, BS; Xin He, PhD; Amit Agrawal, MD; Enver Ozer, MD; and David E. Schuller, MD
Abstract 12: Intraoperative coagulopathy: A low-volume treatment protocol that completely replaces fresh frozen plasma
Peter Kallas, MD; Mary Lou Green, MHS; and Anjali Desai, MD
Abstract 13: Is the Berlin Questionnaire an effective screening tool for obstructive sleep apnea in the preoperative total joint replacement population?
Peter Kallas, MD; Mark Schumacher; Mona Lazar, DO; and Anjali Desai, MD
Abstract 14: The impact of preoperative medical optimization on head and neck cancer surgery
Christopher Tan, MBBS; Catherine Gibb, MBBS, FRACP; and Suren Krishnan, MBBS, FRACS
Abstract 15: Reconceptualizing the preoperative process
Ross Kerridge, MBBS, FRCA, FANZCA
Abstract 16: Development of an electronic medical record smart set form to increase standardization, consistency, and compliance with ACC/AHA perioperative guidelines
Anitha Rajamanickam, MD; Ali Usmani, MD; Ajay Kumar, MD; and Brian Harte, MD
Abstract 17: Development of a perioperative electronic medical record research and quality improvement database
Anitha Rajamanickam, MD; Ali Usmani, MD; Feza Remzi, MD; Brian Harte, MD; and Ajay Kumar, MD
Abstract 18: An innovative perioperative/consultative curriculum for third-year internal medicine residents
Alex Rico, MD; Joshua Lenchus, DO; and Amir Jaffer, MD
Abstract 19: Preoperative medicine infobutton
Terrence J. Adam, MD, PhD
Abstract 20: Nurse practitioners: Bridging the gap in perioperative care
Sally Morgan, RN, MS, ANP-BC, ACNS-BC; and Angela Wright, RN, MSN, APRN, BC
Abstract 21: Intubation training of deploying far forward combat medical personnel with the video laryngoscope
Ben Boedeker, MD; Mary Barak-Bernhagen, BS; Kirsten Boedeker; and W. Bosseau Murray, MD
Abstract 22: The establishment of a perioperative skin integrity committee
Jeanne Lanchester, RN, MEd; Ann Leary, BSN, RNC; and Susan Vargas, AD, RN
Abstract 23: Development and implementation of a perianesthesia integrative care committee
Jeanne Lanchester, RN, MEd; Jeanette Cote, BWN, RN; Terri Jamros, RN; Charla Delillo, RN; Sherie Lavoie, BSN, RN; Jennifer Therminos, SN; Joan Compagnone, RN; and Nicole Engel, MSN, RN
Abstract 24: Development of a screening system to identify patients preoperatively who may benefit from a postoperative hospitalist consult
Elizabeth Marlow, MD, MA; and Chad Whelan, MD
Abstract 25: An algorithm for preoperative screening and management of sleep apnea: Have we created a monster?
Deborah C. Richman, MBChB, FFA(SA); Jorge M. Mallea, MD; Paul S. Richman, MD; and Pater S.A. Glass, MBChB
Abstract 26: Constructing a collaborative neuroscience hospitalist program
Rachel Thompson, MD; Christy Gilmore, MD; Kamal Ajam, MD; and Jennifer Thompson, MD
Abstract 27: The development of algorithms for preoperative management of antiplatelet and anticoagulation therapy in patients undergoing surgical or invasive procedures
Catherine McGowan, MSN, and Patricia Kidik, MSN
Abstract 28: Surgeon-initiated preoperative screening: A new approach
Christina Johnson, RN, PA-C; and Edward J. denBraven, CRNA
Abstract 29: A new process for ensuring the safety of patients having anesthesia outside of the operating room
Ellen Leary, MSN; Catherine McGowan, MSN; Kathleen McGrath, MSN; Sheila McCabe Hassan, MSN; and Theresa Kennedy, MSN
Abstract 30: Establishing a virtual preoperative evaluation clinic
Corey Zetterman, MD; Bobbie J. Sweitzer, MD; and Ben H. Boedeker, MD
Abstract 31: Perioperative hypoxemia and rhabdomyolysis in a medically complicated patient
Sarah Bodin, MD
Abstract 32: How soon is too soon? General anesthesia after coronary intervention with bare metal stents
Meghan Tadel, MD
Abstract 33: Can patients with critical aortic stenosis undergo noncardiac surgery without intervening aortic valve replacement?
M. Chadi Alraies, MD; Abdul Alraiyes, MD; Anitha Rajamanickam, MD; and Frank Michota, MD
Abstract 34: Is it safe to operate on cocaine-positive patients?
M. Chadi Alraies, MD; Abdul Hamid Alraiyes, MD; and Brian Harte, MD
Abstract 35: To intensive care or not?
Mona Lazar, DO; and Peter Kallas, MD
Abstract 36: Predicting surgical complications from liver disease
Mona Lazar, DO, and Peter Kallas, MD
Abstract 37: Preoperative coronary angiography: Friend or foe?
Ross Kerridge, MBBS, FRCA, FANZCA
Abstract 38: Heparin-induced thrombocytopenia with low molecular weight heparin after total knee replacement
Steven Cohn, MD
Abstract 39: Patient with Parkinson’s disease treated with implanted deep brain stimulators for laparotomy
Deborah C. Richman, MBChB, FFA(SA); Daryn H. Moller, MD; and Khoa N. Nguyen, MD
Abstract 40: Ethical dilemma in the preoperative assessment clinic: Can a patient refuse an indicated cardiac workup? Can we refuse to anesthetize?
Deborah C. Richman, MBChB, FFA(SA)
Abstract 41: Coronary artery bypass grafting as a precipitatin factor in diabetic ketoacidosis in type 2 diabetes
Vishal Sehgral, MD, and Abbas Kitabchi, MD
Changing the Face of Acne Therapy
Multidisciplinary Management of ADHF
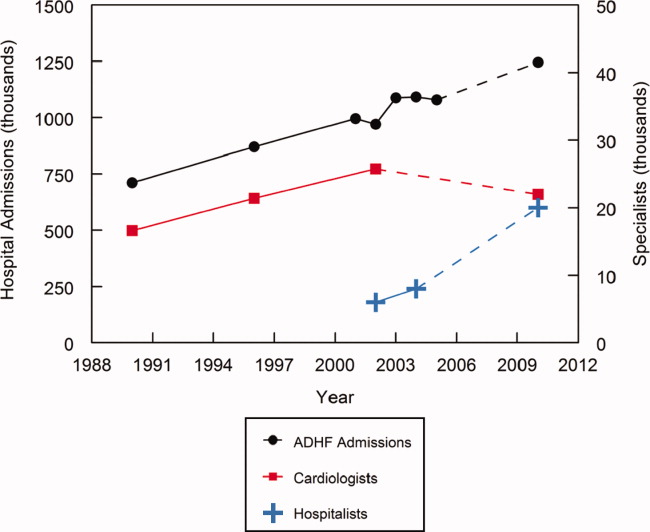
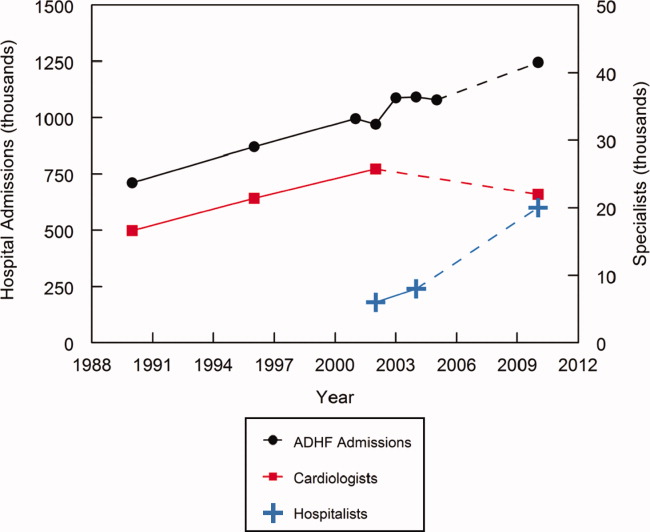
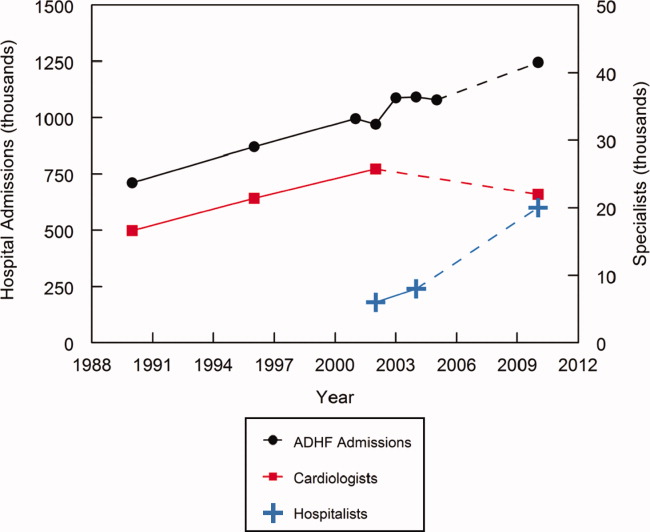
Acute decompensated heart failure (ADHF) is a common disorder that is frequently managed by hospitalists. This management is expected to expand over the next several years because of a continuing increase in the number of ADHF admissions coupled with a plateau or possible decline in the number of practicing cardiologists (Figure 1).114 In addition, 12% of fellowship training positions in cardiology were eliminated between 1995 and 2001, and the fact that the current number of training positions is inadequate to meet future demands is not recognized.15, 16 Given the severity of this disorder, the limited data from randomized, controlled clinical trials,17 and the limitations of current treatment, this management can be both challenging and rewarding. The goal of this special supplement of the Journal of Hospital Medicine is to assist hospitalists in this endeavor by summarizing the currently available data and treatment options and presenting a rational evidence‐based algorithm for the management of ADHF.
A multidisciplinary approach to heart failure has been shown to reduce cost, decrease length of stay, curtail readmissions, and improve compliance.1820 By leading and coordinating teams of physicians, pharmacists, nurses, nutritionists, physical therapists, and case managers and by developing and implementing indications for cardiology consultation, hospitalists can facilitate this multidisciplinary approach.21, 22 However, it is important to remember that hospitalists do not replace cardiologists, who remain a valuable and key component of this multidisciplinary team. Their input is vital in developing care pathways and criteria for consultation, and they, along with primary care physicians, will be the primary source of patient care following hospital discharge. Good communication between hospitalists and cardiologists is essential to optimize the care of patients with ADHF.
Maximizing the efficacy of ADHF care requires a thorough understanding of (1) the causes and potential treatments for the patient's acute decompensation, (2) the management of the patient's chronic heart failure, and (3) potential future therapies. Strategies to improve the continuum of heart failure care have been employed to help improve patient outcomes.23 For example, hospital‐based disease management programs have consistently been shown to optimize care and reduce rehospitalization rates in patients with heart failure.24 These programs involve a multidisciplinary, multifaceted approach to care in order to provide a continuum of care extending from hospitalization and into a patient's home environment.
Because of their practice location and experience, hospitalists are uniquely suited to influence acute inpatient care.25 They see patients in a variety of hospital settings and consequently tend to think of the entire system and not just an isolated component or patient.14 In addition, they have a vested interest in hospital quality improvement measures and are frequently involved in evaluating policies and procedures and developing and implementing clinical pathways, guidelines, and decision‐support tools.26 Data demonstrate that compliance is greater with evidence‐based guidelines and core performance measures when inpatient care is directed by a hospitalist.2730 Improved compliance with selected quality measures in patients with acute myocardial infarction and congestive heart failure has been observed when hospitals implement standardized admission and discharge orders.31, 32
Numerous transitions, such as outpatient to inpatient, intensive care unit to ward, and ward to home, occur during hospitalization, and these transitions are frequently associated with changes in the patient's medication regimen. During an acute illness, chronic medications may be held or discontinued, long‐acting medications may be changed to short‐acting ones to better titrate dose and achieve tighter control, and closed formularies may necessitate substituting 1 medication for another.33 A breakdown in communication during hospitalization‐associated transitions commonly affects medication regimens and can adversely impact patient care.3436 In a prospective evaluation, 53.6% [95% confidence interval (CI): 45.7%61.6%] of patients admitted to the hospital had at least 1 unintended discrepancy between their admission medication orders and their chronic outpatient regimen; 38.6% of these discrepancies were considered a potential threat to the patient.34 Likewise, 49% of patients being discharged from the hospital in another evaluation had an unexplained discrepancy between their preadmission and discharge medications.36 As a result, the Joint Commission on Accreditation of Healthcare Organizations now requires accredited facilities to perform medication reconciliation whenever a patient changes service, setting, provider, or level of care and new medication orders are written.37 This reconciliation is especially important in patients with heart failure, for whom polypharmacy is common and noncompliance with appropriate treatment regimens substantially increases readmission rates.3842
During these transition periods, hospitalists can play an important role in bridging the communication gap and providing this medication reconciliation.33 For example, actively involving hospitalists in all aspects of the reconciliation process at 1 institution resulted in a 4‐fold increase in consistency with preadmission medications.43 Similarly, because of the number of discharge summaries that they write, hospitalists are well suited to lead implementation of new policies and procedures to ensure compliance with recent changes in the Joint Commission on Accreditation of Healthcare Organizations requirements regarding these summaries.
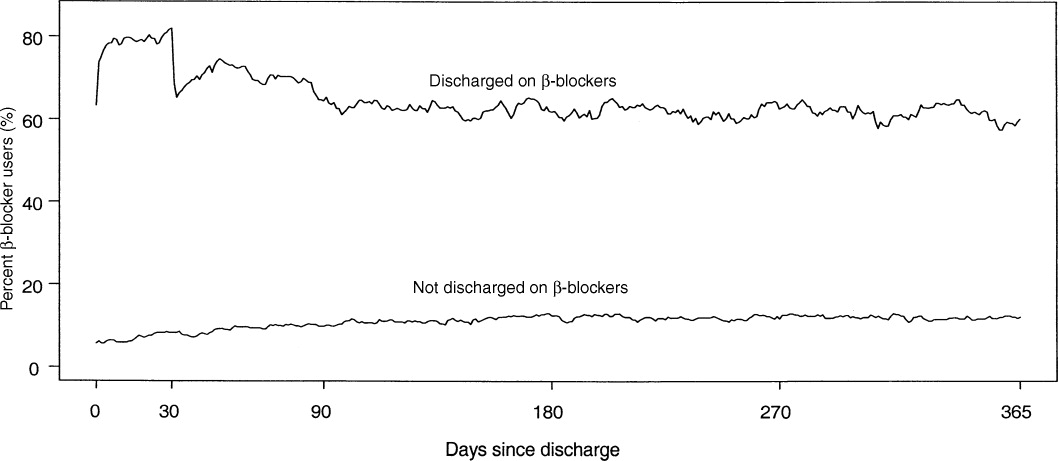
In addition to playing an active role in acute patient management, hospitalists can substantially influence long‐term care and outcomes. Consequently, hospitalists must be well versed in the management of chronic heart failure. Patients are intensely focused on their illness during the hospitalization period, and this focus enhances opportunities for meaningful education and behavior modification. Numerous studies have demonstrated that adherence to long‐term therapy is improved when this therapy is initiated before or at hospital discharge.4446 In an evaluation of data from the Organized Program To Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure Registry (OPTIMIZE‐HF), the prescription of a ‐blocker at discharge was associated with a significant reduction in 60‐ to 90‐day mortality [hazard ratio (HR): 0.48; 95% CI: 0.30‐0.79], and prescription of an angiotensin‐converting enzyme inhibitor or angiotensin receptor blocker at discharge was associated with a significant reduction in 60‐ to 90‐day mortality and/or rehospitalization (HR: 0.51; 95% CI: 0.34‐0.78).47 In the Cardiac Hospitalization Atherosclerosis Management Program (CHAMP), emphasizing initiation of chronic therapy prior to hospital discharge was associated with 3.0‐fold greater angiotensin‐converting enzyme inhibitor use and 3.2‐fold greater ‐blocker use at 1 year (both P 0.01).46 Similarly, in patients surviving acute myocardial infarction, the strongest predictor of ‐blocker use at 30 days following discharge was receipt of a ‐blocker prescription at the time of discharge (HR: 15.8; 95% CI: 10.8‐23.3), and this beneficial effect was sustained for up to a year (Figure 2).44 Likewise, in patients with ADHF, the prevalence of ‐blocker therapy at 60 days was significantly increased when this therapy was initiated before discharge (91%) versus after discharge (73%; P 0.001).45 This predischarge initiation of chronic therapy has been shown to reduce morbidity and mortality.
An awareness of new therapies for ADHF that are in late stages of clinical development can improve understanding of the complex pathophysiology of ADHF and enhance appropriate adaptation of these therapies once they become clinically available. These new therapies represent an attempt to improve on existing therapies, and consequently, they fall into the same 3 general categories as current therapies: diuretics, vasodilators, and inotropic agents.48, 49 Vasopressin receptor antagonists and adenosine receptor antagonists represent an attempt to stimulate aquaresis without inducing hyponatremia, hypokalemia, diminished glomerular filtration, or adverse neurohormonal activation;4854 endothelin receptor antagonists and newer natriuretic peptides represent an attempt to stimulate vasodilation and improve cardiac output without diminishing renal function;49, 55 and myosin activators and sodium‐potassium adenosine triphosphatase inhibitors represent an attempt to enhance contractility without inducing arrhythmogenicity or increasing mortality risk4859 (Table 1).
| Class/MOA | Agent(s) | Advantages/Disadvantages | References |
|---|---|---|---|
| |||
| Vasopressin receptor antagonists | Tolvaptan | Induce aquaresis without natriuresis | deGoma et al.48 |
| Conivaptan | Potentially avoid hyponatremia and hypokalemia | Tang and Hobbs49 | |
| Lixivaptan | Konstam et al.50 | ||
| SR‐121463b | Schrier et al.51 | ||
| Schweiger and Zdanowicz52 | |||
| Adenosine A1 receptor antagonists | Rolofylline | Increase renal blood flow | Tang and Hobbs49 |
| BG‐9719 | Increase intraglomerular hydraulic pressure | deGoma et al.48 | |
| BG‐9928 | May produce diuresis without adversely affecting glomerular filtration and renal function | Givertz et al.53 Greenberg et al.54 | |
| Endothelin receptor antagonists | Tezosentan | Potent vasodilator | Tang and Hobbs49 |
| Improves cardiac output | McMurray et al.55 | ||
| Hemodynamic effects have not translated into an improvement in heart failure symptoms or risk of death. | |||
| Natriuretic peptides | Ularitide | Resists inactivation by neutral endopeptidase | deGoma et al.48 |
| Improves filling pressures and dyspnea scores | Mitrovic et al.59 | ||
| No apparent deleterious effect on short‐term renal function | |||
| Myosin activators | CK‐1827452 | Tries to dissociate inotropy from arrhythmogenicity | deGoma et al.48 |
| Enhances contractility by targeting myocardial myosin, the force generating cardiac enzymes | Cytokinetics56 | ||
| Still very early in clinical development (just entered phase 2) | |||
| Sodium‐potassium ATPase inhibitors | Istaroxime | Tries to dissociate inotropy from arrhythmogenicity | deGoma et al.48 |
| Enhances contractility by stimulating calcium entry into the sarcolemmal Na/Ca exchanger | Blair et al.57 | ||
| Lusitropic | Cleland et al.58 | ||
| Still very early in clinical development (just completed first phase 2 trial) | |||
Finally, although major advancements in the medical therapy of heart failure patients have substantially improved outcomes,60 technological advances in mechanical devices,61 including automatic implantable cardioverter defibrillators, cardiac resynchronization therapy, and ventricular assist devices, as well as advances in the surgical treatment of heart failure,62 have also been used to support the failing heart. Heart failure patients being treated with mechanical devices, as well as those following cardiac transplant, require unique care. As more mechanical and surgical innovations emerge, nonpharmacologic therapy will continue to evolve as a cornerstone of the management strategy in heart failure patients. Hospitalists will need to rely on care pathways, criteria for consultation, and good communication with cardiologists to optimize the care of these patients. Hospitalists should work with their cardiology colleagues in their local institution to develop appropriate criteria for cardiology consultation, and everyone should be educated on these criteria.
The subsequent discussions in this supplement expand on these topics. First, I review the presentation and early recognition, risk stratification, and treatment of patients with ADHF and the role of the hospitalist in this assessment and treatment process. Next, Dr. Khan and Dr. Heywood review the role of diuretics, vasodilators, and ultrafiltration in the management of patients with volume overload and high filling pressures and conclude with a discussion of potential future pharmacologic treatment options, such as tolvaptan and rolofylline, and nonpharmacologic modalities, such as wireless hemodynamic monitoring through implanted devices. Finally, Dr. Michota and I discuss bridging the gap between evidence and practice in the management of patients with ADHF. We review the evidence‐based guidelines that are currently available; discuss the appropriate location for treatment based on the patient's initial history and physical, radiographic, and laboratory findings; provide a practical algorithm for this treatment; and discuss means to transition care from the inpatient setting to the outpatient setting in a manner that enhances compliance with long‐term therapy and reduces recidivism. Given the anticipated growth in ADHF and the need for hospitalists to manage this disease together with cardiologists and others, we believe that the provided information will be helpful in the management of ADHF.
- ,.National Hospital Discharge Survey: annual summary, 1996.Vital Health Stat.1999;13(140):1–46.
- ,,,.Hospitalization of patients with heart failure: National Hospital Discharge Survey, 1985 to 1995.Am Heart J.1999;137(2):352–360.
- ,,.National Hospital Discharge Survey: 2001 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2004;13(156):1–198.
- ,,.National Hospital Discharge Survey: 2002 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2005;13(158):1–199.
- ,,.National Hospital Discharge Survey: 2005 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2007;13(165):1–209.
- ,,.National Hospital Discharge Survey: 2004 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2006;13(162):1–209.
- ,,.National Hospital Discharge Survey: 2003 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2006;13(160):1–206.
- Division for Heart Disease and Stroke Prevention. Heart failure fact sheet. Available at: http://www.cdc.gov/dhdsp/library/fs_heart_failure_longdesc.htm. Accessed September2008.
- US Census Bureau. Projected population of the United States, by age and sex: 2000 to 2050. Available at: http://www.census.gov/population/www/projections/usinterimproj/natprojtab02a.pdf. Accessed September2008.
- ,,,.Demographics and cardiology, 1950–2050.J Am Coll Cardiol.2000;35(4):1067–1081.
- 35th Bethesda Conference.Cardiology's workforce crisis: a pragmatic approach. Bethesda, Maryland, 17–18 October 2003.J Am Coll Cardiol.2004;44(2):216–275.
- ,.The evolution of the hospitalist movement in the USA.Clin Med.2002;2(4):327–330.
- .Hospitalists in the United States—mission accomplished or work in progress?N Engl J Med.2004;350(19):1935–1936.
- .Identifying strategies to improve outcomes and reduce costs—a role for the hospitalist.Curr Opin Pulm Med.2004;10(suppl):S19–S22.
- ,.Cardiovascular manpower: the looming crisis.Circulation.2004;109(7):817–820.
- ,.The United States cardiovascular care deficit.Circulation.2004;109(7):821–823.
- Heart Failure Society of America.Evaluation and management of patients with acute decompensated heart failure.J Card Fail.2006;12(1):e86–e103.
- ,,,.Reduction in heart failure events by the addition of a clinical pharmacist to the heart failure management team. Results of the Pharmacist in Heart Failure Assessment Recommendation and Monitoring (PHARM) study.Arch Intern Med.1999;159(16):1939–1945.
- ,,,,.Impact of care at a multidisciplinary congestive heart failure clinic: a randomized trial.CMAJ.2005;173(1):40–45.
- ,.Implementing a congestive heart failure disease management program to decrease length of stay and cost.J Cardiovasc Nurs.1999;14(1):55–74.
- ,,,,.The core competencies in hospital medicine: a framework for curriculum development by the Society of Hospital Medicine.J Hosp Med.2006;1(suppl 1):2–95.
- ,,, et al.ASHP‐SHM joint statement on hospitalist‐pharmacist collaboration.J Hosp Med.2008;3(suppl 3). doi://10.1002/jhm.315. Available at: http://www3.interscience.wiley.com.
- ,,,,,.Heart failure: improving the continuum of care.Care Manag J.2006;7(2):58–63.
- ,,.Strategies to reduce hospitalization in the management of heart failure.Lippincotts Case Manag.2005;10(6 suppl):S1–S15.
- .Improving the management of patients after myocardial infarction, from admission to discharge.Clin Ther.2006;28(10):1509–1539.
- .The role of hospitalists in the management of acute decompensated heart failure.Am Heart Hosp J.2005;3(2):111–117.
- ,,,,.Quality of care for patients hospitalized with heart failure: assessing the impact of hospitalists.Arch Intern Med.2002;162(11):1251–1256.
- ,.Productive interdisciplinary team relationships: the hospitalist and the case manager.Lippincotts Case Manag.2006;11(3):160–164.
- .Use of pay for performance in a community hospital private hospitalist group: a preliminary report.Trans Am Clin Climatol Assoc.2007;118:263–272.
- ,,.Comparison of practice patterns of hospitalists and community physicians in the care of patients with congestive heart failure.J Hosp Med.2008;3(1):35–41.
- ,,,,,.Integrating “best of care” protocols into clinicians' workflow via care provider order entry: impact on quality‐of‐care indicators for acute myocardial infarction.J Am Med Inform Assoc.2006;13(2):188–196.
- ,,, et al.Improved compliance with quality measures at hospital discharge with a computerized physician order entry system.Am Heart J.2006;151(3):643–653.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,,, et al.Unintended medication discrepancies at the time of hospital admission.Arch Intern Med.2005;165(4):424–429.
- ,,,,,.Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients.Am J Health Syst Pharm.2004;61(16):1689–1695.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166(5):565–571.
- Joint Commission on Accreditation of Healthcare Organizations. Using medication reconciliation to prevent errors. Sentinel Event Alert #35. Available at: http://www.jointcommission.org/sentinelevents/sentineleventalert/sea_35.htm. Accessed September2008.
- ,,,.Precipitating factors leading to decompensation of heart failure: traits among urban blacks.Arch Intern Med.1988;148(9):2013–2016.
- ,,,,.Early readmission of elderly patients with congestive heart failure.J Am Geriatr Soc.1990;38(12):1290–1295.
- ,.Observation unit management of heart failure.Emerg Med Clin North Am.2001;19(1):209–232.
- ,,, et al.Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Failure National Registry (ADHERE).Am Heart J.2005;149(2):209–216.
- ,,, et al.Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure.JAMA.2006;296(18):2217–2226.
- . Eliminating drug errors: hospitals adopt medication reconciliation to improve patient safety. Available at: http://www.acponline.org/clinical_information/journals_publications/acp_hospitalist/may07/drug_errors.htm. Accessed September2008.
- ,,, et al.Outpatient adherence to beta‐blocker therapy after acute myocardial infarction.JAm Coll Cardiol.2002;40(9):1589–1595.
- ,.Predischarge initiation of carvedilol in patients hospitalized for decompensated heart failure.Am J Cardiol.2004;93(9A):74B–76B.
- ,,,.Improved treatment of coronary heart disease by implementation of a Cardiac Hospitalization Atherosclerosis Management Program (CHAMP).Am J Cardiol.2001;87(7):819–822.
- ,,, et al.Association between performance measures and clinical outcomes for patients hospitalized with heart failure.JAMA.2007;297(1):61–70.
- ,,,.Emerging therapies for the management of decompensated heart failure: from bench to bedside.J Am Coll Cardiol.2006;48(12):2397–2409.
- ,.Novel strategies for the management of acute decompensated heart failure.Curr Cardiol Rev.2005;1(1):1–5.
- ,,, et al.Effects of oral tolvaptan in patients hospitalized for worsening heart failure: the EVEREST outcome trial.JAMA.2007;297(12):1319–1331.
- ,,, et al.Tolvaptan, a selective oral vasopressin V2‐receptor antagonist, for hyponatremia.N Engl J Med.2006;355(20):2099–2112.
- ,.Vasopressin‐receptor antagonists in heart failure.Am J Health Syst Pharm.2008;65(9):807–817.
- ,,,,.The effects of KW‐3902, an adenosine A1‐receptor antagonist, on diuresis and renal function in patients with acute decompensated heart failure and renal impairment or diuretic resistance.J Am Coll Cardiol.2007;50(16):1551–1560.
- ,,, et al.Effects of multiple oral doses of an A1 adenosine antagonist, BG9928, in patients with heart failure: results of a placebo‐controlled, dose‐escalation study.J Am Coll Cardiol.2007;50(7):600–606.
- ,,, et al.Effects of tezosentan on symptoms and clinical outcomes in patients with acute heart failure: the VERITAS randomized controlled trials.JAMA.2007;298(17):2009–2019.
- CK‐1827452. Cytokinetics Web site. Available at: http://www.cytokinetics.com/ck_1827452. Accessed September2008.
- ,,, et al.Rationale and design of the hemodynamic, echocardiographic and neurohormonal effects of istaroxime, a novel intravenous inotropic and lusitropic agent: a randomized controlled trial in patients hospitalized with heart failure (HORIZON‐HF) trial.Am J Ther.2008;15(3):231–240.
- ,,, et al.Clinical trials update from the American College of Cardiology 2008: CARISMA, TRENDS, meta‐analysis of Cox‐2 studies, HAT, ON‐TARGET, HYVET, ACCOMPLISH, MOMENTUM, PROTECT, HORIZON‐HF and REVERSE.Eur J Heart Fail.2008;10(6):614–620.
- ,,, et al.Haemodynamic and clinical effects of ularitide in decompensated heart failure.Eur Heart J.2006;27(23):2823–2832.
- ,,.Mechanical support in acute and chronic heart failure.Curr Cardiol Rep.2008;10(3):168–175.
- ,.Devices in acute heart failure.Crit Care Med.2008;36(1 suppl):S121–S128.
- ,.Advances in the surgical treatment of heart failure.Curr Opin Cardiol.2008;23(3):249–253.
Acute decompensated heart failure (ADHF) is a common disorder that is frequently managed by hospitalists. This management is expected to expand over the next several years because of a continuing increase in the number of ADHF admissions coupled with a plateau or possible decline in the number of practicing cardiologists (Figure 1).114 In addition, 12% of fellowship training positions in cardiology were eliminated between 1995 and 2001, and the fact that the current number of training positions is inadequate to meet future demands is not recognized.15, 16 Given the severity of this disorder, the limited data from randomized, controlled clinical trials,17 and the limitations of current treatment, this management can be both challenging and rewarding. The goal of this special supplement of the Journal of Hospital Medicine is to assist hospitalists in this endeavor by summarizing the currently available data and treatment options and presenting a rational evidence‐based algorithm for the management of ADHF.
A multidisciplinary approach to heart failure has been shown to reduce cost, decrease length of stay, curtail readmissions, and improve compliance.1820 By leading and coordinating teams of physicians, pharmacists, nurses, nutritionists, physical therapists, and case managers and by developing and implementing indications for cardiology consultation, hospitalists can facilitate this multidisciplinary approach.21, 22 However, it is important to remember that hospitalists do not replace cardiologists, who remain a valuable and key component of this multidisciplinary team. Their input is vital in developing care pathways and criteria for consultation, and they, along with primary care physicians, will be the primary source of patient care following hospital discharge. Good communication between hospitalists and cardiologists is essential to optimize the care of patients with ADHF.
Maximizing the efficacy of ADHF care requires a thorough understanding of (1) the causes and potential treatments for the patient's acute decompensation, (2) the management of the patient's chronic heart failure, and (3) potential future therapies. Strategies to improve the continuum of heart failure care have been employed to help improve patient outcomes.23 For example, hospital‐based disease management programs have consistently been shown to optimize care and reduce rehospitalization rates in patients with heart failure.24 These programs involve a multidisciplinary, multifaceted approach to care in order to provide a continuum of care extending from hospitalization and into a patient's home environment.
Because of their practice location and experience, hospitalists are uniquely suited to influence acute inpatient care.25 They see patients in a variety of hospital settings and consequently tend to think of the entire system and not just an isolated component or patient.14 In addition, they have a vested interest in hospital quality improvement measures and are frequently involved in evaluating policies and procedures and developing and implementing clinical pathways, guidelines, and decision‐support tools.26 Data demonstrate that compliance is greater with evidence‐based guidelines and core performance measures when inpatient care is directed by a hospitalist.2730 Improved compliance with selected quality measures in patients with acute myocardial infarction and congestive heart failure has been observed when hospitals implement standardized admission and discharge orders.31, 32
Numerous transitions, such as outpatient to inpatient, intensive care unit to ward, and ward to home, occur during hospitalization, and these transitions are frequently associated with changes in the patient's medication regimen. During an acute illness, chronic medications may be held or discontinued, long‐acting medications may be changed to short‐acting ones to better titrate dose and achieve tighter control, and closed formularies may necessitate substituting 1 medication for another.33 A breakdown in communication during hospitalization‐associated transitions commonly affects medication regimens and can adversely impact patient care.3436 In a prospective evaluation, 53.6% [95% confidence interval (CI): 45.7%61.6%] of patients admitted to the hospital had at least 1 unintended discrepancy between their admission medication orders and their chronic outpatient regimen; 38.6% of these discrepancies were considered a potential threat to the patient.34 Likewise, 49% of patients being discharged from the hospital in another evaluation had an unexplained discrepancy between their preadmission and discharge medications.36 As a result, the Joint Commission on Accreditation of Healthcare Organizations now requires accredited facilities to perform medication reconciliation whenever a patient changes service, setting, provider, or level of care and new medication orders are written.37 This reconciliation is especially important in patients with heart failure, for whom polypharmacy is common and noncompliance with appropriate treatment regimens substantially increases readmission rates.3842
During these transition periods, hospitalists can play an important role in bridging the communication gap and providing this medication reconciliation.33 For example, actively involving hospitalists in all aspects of the reconciliation process at 1 institution resulted in a 4‐fold increase in consistency with preadmission medications.43 Similarly, because of the number of discharge summaries that they write, hospitalists are well suited to lead implementation of new policies and procedures to ensure compliance with recent changes in the Joint Commission on Accreditation of Healthcare Organizations requirements regarding these summaries.
In addition to playing an active role in acute patient management, hospitalists can substantially influence long‐term care and outcomes. Consequently, hospitalists must be well versed in the management of chronic heart failure. Patients are intensely focused on their illness during the hospitalization period, and this focus enhances opportunities for meaningful education and behavior modification. Numerous studies have demonstrated that adherence to long‐term therapy is improved when this therapy is initiated before or at hospital discharge.4446 In an evaluation of data from the Organized Program To Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure Registry (OPTIMIZE‐HF), the prescription of a ‐blocker at discharge was associated with a significant reduction in 60‐ to 90‐day mortality [hazard ratio (HR): 0.48; 95% CI: 0.30‐0.79], and prescription of an angiotensin‐converting enzyme inhibitor or angiotensin receptor blocker at discharge was associated with a significant reduction in 60‐ to 90‐day mortality and/or rehospitalization (HR: 0.51; 95% CI: 0.34‐0.78).47 In the Cardiac Hospitalization Atherosclerosis Management Program (CHAMP), emphasizing initiation of chronic therapy prior to hospital discharge was associated with 3.0‐fold greater angiotensin‐converting enzyme inhibitor use and 3.2‐fold greater ‐blocker use at 1 year (both P 0.01).46 Similarly, in patients surviving acute myocardial infarction, the strongest predictor of ‐blocker use at 30 days following discharge was receipt of a ‐blocker prescription at the time of discharge (HR: 15.8; 95% CI: 10.8‐23.3), and this beneficial effect was sustained for up to a year (Figure 2).44 Likewise, in patients with ADHF, the prevalence of ‐blocker therapy at 60 days was significantly increased when this therapy was initiated before discharge (91%) versus after discharge (73%; P 0.001).45 This predischarge initiation of chronic therapy has been shown to reduce morbidity and mortality.
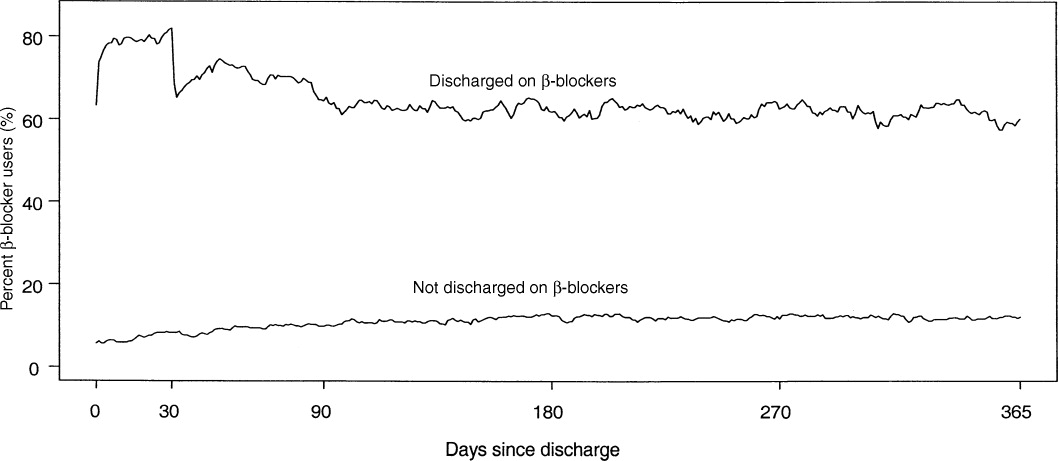
An awareness of new therapies for ADHF that are in late stages of clinical development can improve understanding of the complex pathophysiology of ADHF and enhance appropriate adaptation of these therapies once they become clinically available. These new therapies represent an attempt to improve on existing therapies, and consequently, they fall into the same 3 general categories as current therapies: diuretics, vasodilators, and inotropic agents.48, 49 Vasopressin receptor antagonists and adenosine receptor antagonists represent an attempt to stimulate aquaresis without inducing hyponatremia, hypokalemia, diminished glomerular filtration, or adverse neurohormonal activation;4854 endothelin receptor antagonists and newer natriuretic peptides represent an attempt to stimulate vasodilation and improve cardiac output without diminishing renal function;49, 55 and myosin activators and sodium‐potassium adenosine triphosphatase inhibitors represent an attempt to enhance contractility without inducing arrhythmogenicity or increasing mortality risk4859 (Table 1).
| Class/MOA | Agent(s) | Advantages/Disadvantages | References |
|---|---|---|---|
| |||
| Vasopressin receptor antagonists | Tolvaptan | Induce aquaresis without natriuresis | deGoma et al.48 |
| Conivaptan | Potentially avoid hyponatremia and hypokalemia | Tang and Hobbs49 | |
| Lixivaptan | Konstam et al.50 | ||
| SR‐121463b | Schrier et al.51 | ||
| Schweiger and Zdanowicz52 | |||
| Adenosine A1 receptor antagonists | Rolofylline | Increase renal blood flow | Tang and Hobbs49 |
| BG‐9719 | Increase intraglomerular hydraulic pressure | deGoma et al.48 | |
| BG‐9928 | May produce diuresis without adversely affecting glomerular filtration and renal function | Givertz et al.53 Greenberg et al.54 | |
| Endothelin receptor antagonists | Tezosentan | Potent vasodilator | Tang and Hobbs49 |
| Improves cardiac output | McMurray et al.55 | ||
| Hemodynamic effects have not translated into an improvement in heart failure symptoms or risk of death. | |||
| Natriuretic peptides | Ularitide | Resists inactivation by neutral endopeptidase | deGoma et al.48 |
| Improves filling pressures and dyspnea scores | Mitrovic et al.59 | ||
| No apparent deleterious effect on short‐term renal function | |||
| Myosin activators | CK‐1827452 | Tries to dissociate inotropy from arrhythmogenicity | deGoma et al.48 |
| Enhances contractility by targeting myocardial myosin, the force generating cardiac enzymes | Cytokinetics56 | ||
| Still very early in clinical development (just entered phase 2) | |||
| Sodium‐potassium ATPase inhibitors | Istaroxime | Tries to dissociate inotropy from arrhythmogenicity | deGoma et al.48 |
| Enhances contractility by stimulating calcium entry into the sarcolemmal Na/Ca exchanger | Blair et al.57 | ||
| Lusitropic | Cleland et al.58 | ||
| Still very early in clinical development (just completed first phase 2 trial) | |||
Finally, although major advancements in the medical therapy of heart failure patients have substantially improved outcomes,60 technological advances in mechanical devices,61 including automatic implantable cardioverter defibrillators, cardiac resynchronization therapy, and ventricular assist devices, as well as advances in the surgical treatment of heart failure,62 have also been used to support the failing heart. Heart failure patients being treated with mechanical devices, as well as those following cardiac transplant, require unique care. As more mechanical and surgical innovations emerge, nonpharmacologic therapy will continue to evolve as a cornerstone of the management strategy in heart failure patients. Hospitalists will need to rely on care pathways, criteria for consultation, and good communication with cardiologists to optimize the care of these patients. Hospitalists should work with their cardiology colleagues in their local institution to develop appropriate criteria for cardiology consultation, and everyone should be educated on these criteria.
The subsequent discussions in this supplement expand on these topics. First, I review the presentation and early recognition, risk stratification, and treatment of patients with ADHF and the role of the hospitalist in this assessment and treatment process. Next, Dr. Khan and Dr. Heywood review the role of diuretics, vasodilators, and ultrafiltration in the management of patients with volume overload and high filling pressures and conclude with a discussion of potential future pharmacologic treatment options, such as tolvaptan and rolofylline, and nonpharmacologic modalities, such as wireless hemodynamic monitoring through implanted devices. Finally, Dr. Michota and I discuss bridging the gap between evidence and practice in the management of patients with ADHF. We review the evidence‐based guidelines that are currently available; discuss the appropriate location for treatment based on the patient's initial history and physical, radiographic, and laboratory findings; provide a practical algorithm for this treatment; and discuss means to transition care from the inpatient setting to the outpatient setting in a manner that enhances compliance with long‐term therapy and reduces recidivism. Given the anticipated growth in ADHF and the need for hospitalists to manage this disease together with cardiologists and others, we believe that the provided information will be helpful in the management of ADHF.
Acute decompensated heart failure (ADHF) is a common disorder that is frequently managed by hospitalists. This management is expected to expand over the next several years because of a continuing increase in the number of ADHF admissions coupled with a plateau or possible decline in the number of practicing cardiologists (Figure 1).114 In addition, 12% of fellowship training positions in cardiology were eliminated between 1995 and 2001, and the fact that the current number of training positions is inadequate to meet future demands is not recognized.15, 16 Given the severity of this disorder, the limited data from randomized, controlled clinical trials,17 and the limitations of current treatment, this management can be both challenging and rewarding. The goal of this special supplement of the Journal of Hospital Medicine is to assist hospitalists in this endeavor by summarizing the currently available data and treatment options and presenting a rational evidence‐based algorithm for the management of ADHF.
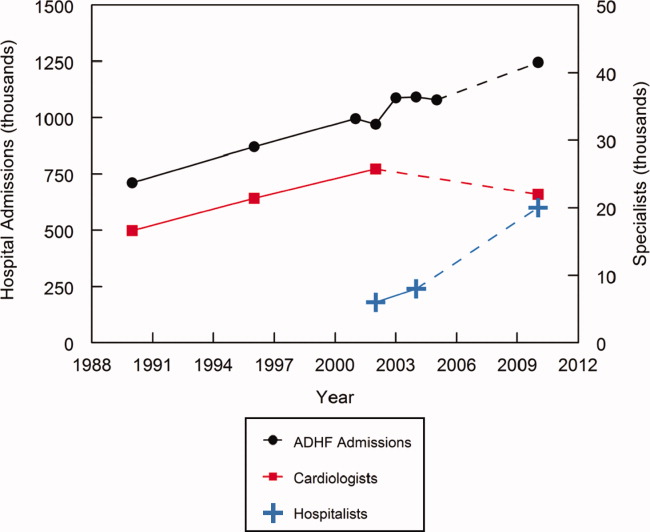
A multidisciplinary approach to heart failure has been shown to reduce cost, decrease length of stay, curtail readmissions, and improve compliance.1820 By leading and coordinating teams of physicians, pharmacists, nurses, nutritionists, physical therapists, and case managers and by developing and implementing indications for cardiology consultation, hospitalists can facilitate this multidisciplinary approach.21, 22 However, it is important to remember that hospitalists do not replace cardiologists, who remain a valuable and key component of this multidisciplinary team. Their input is vital in developing care pathways and criteria for consultation, and they, along with primary care physicians, will be the primary source of patient care following hospital discharge. Good communication between hospitalists and cardiologists is essential to optimize the care of patients with ADHF.
Maximizing the efficacy of ADHF care requires a thorough understanding of (1) the causes and potential treatments for the patient's acute decompensation, (2) the management of the patient's chronic heart failure, and (3) potential future therapies. Strategies to improve the continuum of heart failure care have been employed to help improve patient outcomes.23 For example, hospital‐based disease management programs have consistently been shown to optimize care and reduce rehospitalization rates in patients with heart failure.24 These programs involve a multidisciplinary, multifaceted approach to care in order to provide a continuum of care extending from hospitalization and into a patient's home environment.
Because of their practice location and experience, hospitalists are uniquely suited to influence acute inpatient care.25 They see patients in a variety of hospital settings and consequently tend to think of the entire system and not just an isolated component or patient.14 In addition, they have a vested interest in hospital quality improvement measures and are frequently involved in evaluating policies and procedures and developing and implementing clinical pathways, guidelines, and decision‐support tools.26 Data demonstrate that compliance is greater with evidence‐based guidelines and core performance measures when inpatient care is directed by a hospitalist.2730 Improved compliance with selected quality measures in patients with acute myocardial infarction and congestive heart failure has been observed when hospitals implement standardized admission and discharge orders.31, 32
Numerous transitions, such as outpatient to inpatient, intensive care unit to ward, and ward to home, occur during hospitalization, and these transitions are frequently associated with changes in the patient's medication regimen. During an acute illness, chronic medications may be held or discontinued, long‐acting medications may be changed to short‐acting ones to better titrate dose and achieve tighter control, and closed formularies may necessitate substituting 1 medication for another.33 A breakdown in communication during hospitalization‐associated transitions commonly affects medication regimens and can adversely impact patient care.3436 In a prospective evaluation, 53.6% [95% confidence interval (CI): 45.7%61.6%] of patients admitted to the hospital had at least 1 unintended discrepancy between their admission medication orders and their chronic outpatient regimen; 38.6% of these discrepancies were considered a potential threat to the patient.34 Likewise, 49% of patients being discharged from the hospital in another evaluation had an unexplained discrepancy between their preadmission and discharge medications.36 As a result, the Joint Commission on Accreditation of Healthcare Organizations now requires accredited facilities to perform medication reconciliation whenever a patient changes service, setting, provider, or level of care and new medication orders are written.37 This reconciliation is especially important in patients with heart failure, for whom polypharmacy is common and noncompliance with appropriate treatment regimens substantially increases readmission rates.3842
During these transition periods, hospitalists can play an important role in bridging the communication gap and providing this medication reconciliation.33 For example, actively involving hospitalists in all aspects of the reconciliation process at 1 institution resulted in a 4‐fold increase in consistency with preadmission medications.43 Similarly, because of the number of discharge summaries that they write, hospitalists are well suited to lead implementation of new policies and procedures to ensure compliance with recent changes in the Joint Commission on Accreditation of Healthcare Organizations requirements regarding these summaries.
In addition to playing an active role in acute patient management, hospitalists can substantially influence long‐term care and outcomes. Consequently, hospitalists must be well versed in the management of chronic heart failure. Patients are intensely focused on their illness during the hospitalization period, and this focus enhances opportunities for meaningful education and behavior modification. Numerous studies have demonstrated that adherence to long‐term therapy is improved when this therapy is initiated before or at hospital discharge.4446 In an evaluation of data from the Organized Program To Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure Registry (OPTIMIZE‐HF), the prescription of a ‐blocker at discharge was associated with a significant reduction in 60‐ to 90‐day mortality [hazard ratio (HR): 0.48; 95% CI: 0.30‐0.79], and prescription of an angiotensin‐converting enzyme inhibitor or angiotensin receptor blocker at discharge was associated with a significant reduction in 60‐ to 90‐day mortality and/or rehospitalization (HR: 0.51; 95% CI: 0.34‐0.78).47 In the Cardiac Hospitalization Atherosclerosis Management Program (CHAMP), emphasizing initiation of chronic therapy prior to hospital discharge was associated with 3.0‐fold greater angiotensin‐converting enzyme inhibitor use and 3.2‐fold greater ‐blocker use at 1 year (both P 0.01).46 Similarly, in patients surviving acute myocardial infarction, the strongest predictor of ‐blocker use at 30 days following discharge was receipt of a ‐blocker prescription at the time of discharge (HR: 15.8; 95% CI: 10.8‐23.3), and this beneficial effect was sustained for up to a year (Figure 2).44 Likewise, in patients with ADHF, the prevalence of ‐blocker therapy at 60 days was significantly increased when this therapy was initiated before discharge (91%) versus after discharge (73%; P 0.001).45 This predischarge initiation of chronic therapy has been shown to reduce morbidity and mortality.
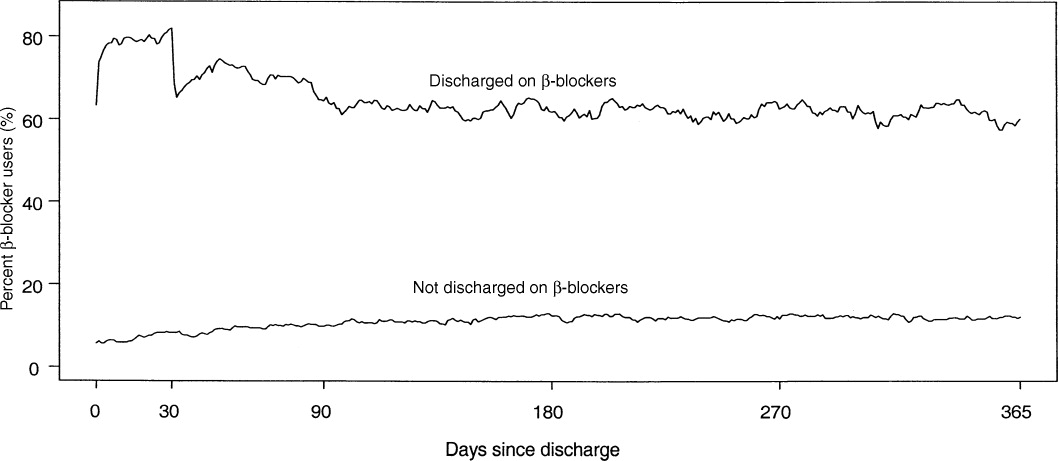
An awareness of new therapies for ADHF that are in late stages of clinical development can improve understanding of the complex pathophysiology of ADHF and enhance appropriate adaptation of these therapies once they become clinically available. These new therapies represent an attempt to improve on existing therapies, and consequently, they fall into the same 3 general categories as current therapies: diuretics, vasodilators, and inotropic agents.48, 49 Vasopressin receptor antagonists and adenosine receptor antagonists represent an attempt to stimulate aquaresis without inducing hyponatremia, hypokalemia, diminished glomerular filtration, or adverse neurohormonal activation;4854 endothelin receptor antagonists and newer natriuretic peptides represent an attempt to stimulate vasodilation and improve cardiac output without diminishing renal function;49, 55 and myosin activators and sodium‐potassium adenosine triphosphatase inhibitors represent an attempt to enhance contractility without inducing arrhythmogenicity or increasing mortality risk4859 (Table 1).
| Class/MOA | Agent(s) | Advantages/Disadvantages | References |
|---|---|---|---|
| |||
| Vasopressin receptor antagonists | Tolvaptan | Induce aquaresis without natriuresis | deGoma et al.48 |
| Conivaptan | Potentially avoid hyponatremia and hypokalemia | Tang and Hobbs49 | |
| Lixivaptan | Konstam et al.50 | ||
| SR‐121463b | Schrier et al.51 | ||
| Schweiger and Zdanowicz52 | |||
| Adenosine A1 receptor antagonists | Rolofylline | Increase renal blood flow | Tang and Hobbs49 |
| BG‐9719 | Increase intraglomerular hydraulic pressure | deGoma et al.48 | |
| BG‐9928 | May produce diuresis without adversely affecting glomerular filtration and renal function | Givertz et al.53 Greenberg et al.54 | |
| Endothelin receptor antagonists | Tezosentan | Potent vasodilator | Tang and Hobbs49 |
| Improves cardiac output | McMurray et al.55 | ||
| Hemodynamic effects have not translated into an improvement in heart failure symptoms or risk of death. | |||
| Natriuretic peptides | Ularitide | Resists inactivation by neutral endopeptidase | deGoma et al.48 |
| Improves filling pressures and dyspnea scores | Mitrovic et al.59 | ||
| No apparent deleterious effect on short‐term renal function | |||
| Myosin activators | CK‐1827452 | Tries to dissociate inotropy from arrhythmogenicity | deGoma et al.48 |
| Enhances contractility by targeting myocardial myosin, the force generating cardiac enzymes | Cytokinetics56 | ||
| Still very early in clinical development (just entered phase 2) | |||
| Sodium‐potassium ATPase inhibitors | Istaroxime | Tries to dissociate inotropy from arrhythmogenicity | deGoma et al.48 |
| Enhances contractility by stimulating calcium entry into the sarcolemmal Na/Ca exchanger | Blair et al.57 | ||
| Lusitropic | Cleland et al.58 | ||
| Still very early in clinical development (just completed first phase 2 trial) | |||
Finally, although major advancements in the medical therapy of heart failure patients have substantially improved outcomes,60 technological advances in mechanical devices,61 including automatic implantable cardioverter defibrillators, cardiac resynchronization therapy, and ventricular assist devices, as well as advances in the surgical treatment of heart failure,62 have also been used to support the failing heart. Heart failure patients being treated with mechanical devices, as well as those following cardiac transplant, require unique care. As more mechanical and surgical innovations emerge, nonpharmacologic therapy will continue to evolve as a cornerstone of the management strategy in heart failure patients. Hospitalists will need to rely on care pathways, criteria for consultation, and good communication with cardiologists to optimize the care of these patients. Hospitalists should work with their cardiology colleagues in their local institution to develop appropriate criteria for cardiology consultation, and everyone should be educated on these criteria.
The subsequent discussions in this supplement expand on these topics. First, I review the presentation and early recognition, risk stratification, and treatment of patients with ADHF and the role of the hospitalist in this assessment and treatment process. Next, Dr. Khan and Dr. Heywood review the role of diuretics, vasodilators, and ultrafiltration in the management of patients with volume overload and high filling pressures and conclude with a discussion of potential future pharmacologic treatment options, such as tolvaptan and rolofylline, and nonpharmacologic modalities, such as wireless hemodynamic monitoring through implanted devices. Finally, Dr. Michota and I discuss bridging the gap between evidence and practice in the management of patients with ADHF. We review the evidence‐based guidelines that are currently available; discuss the appropriate location for treatment based on the patient's initial history and physical, radiographic, and laboratory findings; provide a practical algorithm for this treatment; and discuss means to transition care from the inpatient setting to the outpatient setting in a manner that enhances compliance with long‐term therapy and reduces recidivism. Given the anticipated growth in ADHF and the need for hospitalists to manage this disease together with cardiologists and others, we believe that the provided information will be helpful in the management of ADHF.
- ,.National Hospital Discharge Survey: annual summary, 1996.Vital Health Stat.1999;13(140):1–46.
- ,,,.Hospitalization of patients with heart failure: National Hospital Discharge Survey, 1985 to 1995.Am Heart J.1999;137(2):352–360.
- ,,.National Hospital Discharge Survey: 2001 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2004;13(156):1–198.
- ,,.National Hospital Discharge Survey: 2002 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2005;13(158):1–199.
- ,,.National Hospital Discharge Survey: 2005 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2007;13(165):1–209.
- ,,.National Hospital Discharge Survey: 2004 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2006;13(162):1–209.
- ,,.National Hospital Discharge Survey: 2003 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2006;13(160):1–206.
- Division for Heart Disease and Stroke Prevention. Heart failure fact sheet. Available at: http://www.cdc.gov/dhdsp/library/fs_heart_failure_longdesc.htm. Accessed September2008.
- US Census Bureau. Projected population of the United States, by age and sex: 2000 to 2050. Available at: http://www.census.gov/population/www/projections/usinterimproj/natprojtab02a.pdf. Accessed September2008.
- ,,,.Demographics and cardiology, 1950–2050.J Am Coll Cardiol.2000;35(4):1067–1081.
- 35th Bethesda Conference.Cardiology's workforce crisis: a pragmatic approach. Bethesda, Maryland, 17–18 October 2003.J Am Coll Cardiol.2004;44(2):216–275.
- ,.The evolution of the hospitalist movement in the USA.Clin Med.2002;2(4):327–330.
- .Hospitalists in the United States—mission accomplished or work in progress?N Engl J Med.2004;350(19):1935–1936.
- .Identifying strategies to improve outcomes and reduce costs—a role for the hospitalist.Curr Opin Pulm Med.2004;10(suppl):S19–S22.
- ,.Cardiovascular manpower: the looming crisis.Circulation.2004;109(7):817–820.
- ,.The United States cardiovascular care deficit.Circulation.2004;109(7):821–823.
- Heart Failure Society of America.Evaluation and management of patients with acute decompensated heart failure.J Card Fail.2006;12(1):e86–e103.
- ,,,.Reduction in heart failure events by the addition of a clinical pharmacist to the heart failure management team. Results of the Pharmacist in Heart Failure Assessment Recommendation and Monitoring (PHARM) study.Arch Intern Med.1999;159(16):1939–1945.
- ,,,,.Impact of care at a multidisciplinary congestive heart failure clinic: a randomized trial.CMAJ.2005;173(1):40–45.
- ,.Implementing a congestive heart failure disease management program to decrease length of stay and cost.J Cardiovasc Nurs.1999;14(1):55–74.
- ,,,,.The core competencies in hospital medicine: a framework for curriculum development by the Society of Hospital Medicine.J Hosp Med.2006;1(suppl 1):2–95.
- ,,, et al.ASHP‐SHM joint statement on hospitalist‐pharmacist collaboration.J Hosp Med.2008;3(suppl 3). doi://10.1002/jhm.315. Available at: http://www3.interscience.wiley.com.
- ,,,,,.Heart failure: improving the continuum of care.Care Manag J.2006;7(2):58–63.
- ,,.Strategies to reduce hospitalization in the management of heart failure.Lippincotts Case Manag.2005;10(6 suppl):S1–S15.
- .Improving the management of patients after myocardial infarction, from admission to discharge.Clin Ther.2006;28(10):1509–1539.
- .The role of hospitalists in the management of acute decompensated heart failure.Am Heart Hosp J.2005;3(2):111–117.
- ,,,,.Quality of care for patients hospitalized with heart failure: assessing the impact of hospitalists.Arch Intern Med.2002;162(11):1251–1256.
- ,.Productive interdisciplinary team relationships: the hospitalist and the case manager.Lippincotts Case Manag.2006;11(3):160–164.
- .Use of pay for performance in a community hospital private hospitalist group: a preliminary report.Trans Am Clin Climatol Assoc.2007;118:263–272.
- ,,.Comparison of practice patterns of hospitalists and community physicians in the care of patients with congestive heart failure.J Hosp Med.2008;3(1):35–41.
- ,,,,,.Integrating “best of care” protocols into clinicians' workflow via care provider order entry: impact on quality‐of‐care indicators for acute myocardial infarction.J Am Med Inform Assoc.2006;13(2):188–196.
- ,,, et al.Improved compliance with quality measures at hospital discharge with a computerized physician order entry system.Am Heart J.2006;151(3):643–653.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,,, et al.Unintended medication discrepancies at the time of hospital admission.Arch Intern Med.2005;165(4):424–429.
- ,,,,,.Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients.Am J Health Syst Pharm.2004;61(16):1689–1695.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166(5):565–571.
- Joint Commission on Accreditation of Healthcare Organizations. Using medication reconciliation to prevent errors. Sentinel Event Alert #35. Available at: http://www.jointcommission.org/sentinelevents/sentineleventalert/sea_35.htm. Accessed September2008.
- ,,,.Precipitating factors leading to decompensation of heart failure: traits among urban blacks.Arch Intern Med.1988;148(9):2013–2016.
- ,,,,.Early readmission of elderly patients with congestive heart failure.J Am Geriatr Soc.1990;38(12):1290–1295.
- ,.Observation unit management of heart failure.Emerg Med Clin North Am.2001;19(1):209–232.
- ,,, et al.Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Failure National Registry (ADHERE).Am Heart J.2005;149(2):209–216.
- ,,, et al.Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure.JAMA.2006;296(18):2217–2226.
- . Eliminating drug errors: hospitals adopt medication reconciliation to improve patient safety. Available at: http://www.acponline.org/clinical_information/journals_publications/acp_hospitalist/may07/drug_errors.htm. Accessed September2008.
- ,,, et al.Outpatient adherence to beta‐blocker therapy after acute myocardial infarction.JAm Coll Cardiol.2002;40(9):1589–1595.
- ,.Predischarge initiation of carvedilol in patients hospitalized for decompensated heart failure.Am J Cardiol.2004;93(9A):74B–76B.
- ,,,.Improved treatment of coronary heart disease by implementation of a Cardiac Hospitalization Atherosclerosis Management Program (CHAMP).Am J Cardiol.2001;87(7):819–822.
- ,,, et al.Association between performance measures and clinical outcomes for patients hospitalized with heart failure.JAMA.2007;297(1):61–70.
- ,,,.Emerging therapies for the management of decompensated heart failure: from bench to bedside.J Am Coll Cardiol.2006;48(12):2397–2409.
- ,.Novel strategies for the management of acute decompensated heart failure.Curr Cardiol Rev.2005;1(1):1–5.
- ,,, et al.Effects of oral tolvaptan in patients hospitalized for worsening heart failure: the EVEREST outcome trial.JAMA.2007;297(12):1319–1331.
- ,,, et al.Tolvaptan, a selective oral vasopressin V2‐receptor antagonist, for hyponatremia.N Engl J Med.2006;355(20):2099–2112.
- ,.Vasopressin‐receptor antagonists in heart failure.Am J Health Syst Pharm.2008;65(9):807–817.
- ,,,,.The effects of KW‐3902, an adenosine A1‐receptor antagonist, on diuresis and renal function in patients with acute decompensated heart failure and renal impairment or diuretic resistance.J Am Coll Cardiol.2007;50(16):1551–1560.
- ,,, et al.Effects of multiple oral doses of an A1 adenosine antagonist, BG9928, in patients with heart failure: results of a placebo‐controlled, dose‐escalation study.J Am Coll Cardiol.2007;50(7):600–606.
- ,,, et al.Effects of tezosentan on symptoms and clinical outcomes in patients with acute heart failure: the VERITAS randomized controlled trials.JAMA.2007;298(17):2009–2019.
- CK‐1827452. Cytokinetics Web site. Available at: http://www.cytokinetics.com/ck_1827452. Accessed September2008.
- ,,, et al.Rationale and design of the hemodynamic, echocardiographic and neurohormonal effects of istaroxime, a novel intravenous inotropic and lusitropic agent: a randomized controlled trial in patients hospitalized with heart failure (HORIZON‐HF) trial.Am J Ther.2008;15(3):231–240.
- ,,, et al.Clinical trials update from the American College of Cardiology 2008: CARISMA, TRENDS, meta‐analysis of Cox‐2 studies, HAT, ON‐TARGET, HYVET, ACCOMPLISH, MOMENTUM, PROTECT, HORIZON‐HF and REVERSE.Eur J Heart Fail.2008;10(6):614–620.
- ,,, et al.Haemodynamic and clinical effects of ularitide in decompensated heart failure.Eur Heart J.2006;27(23):2823–2832.
- ,,.Mechanical support in acute and chronic heart failure.Curr Cardiol Rep.2008;10(3):168–175.
- ,.Devices in acute heart failure.Crit Care Med.2008;36(1 suppl):S121–S128.
- ,.Advances in the surgical treatment of heart failure.Curr Opin Cardiol.2008;23(3):249–253.
- ,.National Hospital Discharge Survey: annual summary, 1996.Vital Health Stat.1999;13(140):1–46.
- ,,,.Hospitalization of patients with heart failure: National Hospital Discharge Survey, 1985 to 1995.Am Heart J.1999;137(2):352–360.
- ,,.National Hospital Discharge Survey: 2001 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2004;13(156):1–198.
- ,,.National Hospital Discharge Survey: 2002 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2005;13(158):1–199.
- ,,.National Hospital Discharge Survey: 2005 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2007;13(165):1–209.
- ,,.National Hospital Discharge Survey: 2004 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2006;13(162):1–209.
- ,,.National Hospital Discharge Survey: 2003 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2006;13(160):1–206.
- Division for Heart Disease and Stroke Prevention. Heart failure fact sheet. Available at: http://www.cdc.gov/dhdsp/library/fs_heart_failure_longdesc.htm. Accessed September2008.
- US Census Bureau. Projected population of the United States, by age and sex: 2000 to 2050. Available at: http://www.census.gov/population/www/projections/usinterimproj/natprojtab02a.pdf. Accessed September2008.
- ,,,.Demographics and cardiology, 1950–2050.J Am Coll Cardiol.2000;35(4):1067–1081.
- 35th Bethesda Conference.Cardiology's workforce crisis: a pragmatic approach. Bethesda, Maryland, 17–18 October 2003.J Am Coll Cardiol.2004;44(2):216–275.
- ,.The evolution of the hospitalist movement in the USA.Clin Med.2002;2(4):327–330.
- .Hospitalists in the United States—mission accomplished or work in progress?N Engl J Med.2004;350(19):1935–1936.
- .Identifying strategies to improve outcomes and reduce costs—a role for the hospitalist.Curr Opin Pulm Med.2004;10(suppl):S19–S22.
- ,.Cardiovascular manpower: the looming crisis.Circulation.2004;109(7):817–820.
- ,.The United States cardiovascular care deficit.Circulation.2004;109(7):821–823.
- Heart Failure Society of America.Evaluation and management of patients with acute decompensated heart failure.J Card Fail.2006;12(1):e86–e103.
- ,,,.Reduction in heart failure events by the addition of a clinical pharmacist to the heart failure management team. Results of the Pharmacist in Heart Failure Assessment Recommendation and Monitoring (PHARM) study.Arch Intern Med.1999;159(16):1939–1945.
- ,,,,.Impact of care at a multidisciplinary congestive heart failure clinic: a randomized trial.CMAJ.2005;173(1):40–45.
- ,.Implementing a congestive heart failure disease management program to decrease length of stay and cost.J Cardiovasc Nurs.1999;14(1):55–74.
- ,,,,.The core competencies in hospital medicine: a framework for curriculum development by the Society of Hospital Medicine.J Hosp Med.2006;1(suppl 1):2–95.
- ,,, et al.ASHP‐SHM joint statement on hospitalist‐pharmacist collaboration.J Hosp Med.2008;3(suppl 3). doi://10.1002/jhm.315. Available at: http://www3.interscience.wiley.com.
- ,,,,,.Heart failure: improving the continuum of care.Care Manag J.2006;7(2):58–63.
- ,,.Strategies to reduce hospitalization in the management of heart failure.Lippincotts Case Manag.2005;10(6 suppl):S1–S15.
- .Improving the management of patients after myocardial infarction, from admission to discharge.Clin Ther.2006;28(10):1509–1539.
- .The role of hospitalists in the management of acute decompensated heart failure.Am Heart Hosp J.2005;3(2):111–117.
- ,,,,.Quality of care for patients hospitalized with heart failure: assessing the impact of hospitalists.Arch Intern Med.2002;162(11):1251–1256.
- ,.Productive interdisciplinary team relationships: the hospitalist and the case manager.Lippincotts Case Manag.2006;11(3):160–164.
- .Use of pay for performance in a community hospital private hospitalist group: a preliminary report.Trans Am Clin Climatol Assoc.2007;118:263–272.
- ,,.Comparison of practice patterns of hospitalists and community physicians in the care of patients with congestive heart failure.J Hosp Med.2008;3(1):35–41.
- ,,,,,.Integrating “best of care” protocols into clinicians' workflow via care provider order entry: impact on quality‐of‐care indicators for acute myocardial infarction.J Am Med Inform Assoc.2006;13(2):188–196.
- ,,, et al.Improved compliance with quality measures at hospital discharge with a computerized physician order entry system.Am Heart J.2006;151(3):643–653.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,,, et al.Unintended medication discrepancies at the time of hospital admission.Arch Intern Med.2005;165(4):424–429.
- ,,,,,.Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients.Am J Health Syst Pharm.2004;61(16):1689–1695.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166(5):565–571.
- Joint Commission on Accreditation of Healthcare Organizations. Using medication reconciliation to prevent errors. Sentinel Event Alert #35. Available at: http://www.jointcommission.org/sentinelevents/sentineleventalert/sea_35.htm. Accessed September2008.
- ,,,.Precipitating factors leading to decompensation of heart failure: traits among urban blacks.Arch Intern Med.1988;148(9):2013–2016.
- ,,,,.Early readmission of elderly patients with congestive heart failure.J Am Geriatr Soc.1990;38(12):1290–1295.
- ,.Observation unit management of heart failure.Emerg Med Clin North Am.2001;19(1):209–232.
- ,,, et al.Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Failure National Registry (ADHERE).Am Heart J.2005;149(2):209–216.
- ,,, et al.Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure.JAMA.2006;296(18):2217–2226.
- . Eliminating drug errors: hospitals adopt medication reconciliation to improve patient safety. Available at: http://www.acponline.org/clinical_information/journals_publications/acp_hospitalist/may07/drug_errors.htm. Accessed September2008.
- ,,, et al.Outpatient adherence to beta‐blocker therapy after acute myocardial infarction.JAm Coll Cardiol.2002;40(9):1589–1595.
- ,.Predischarge initiation of carvedilol in patients hospitalized for decompensated heart failure.Am J Cardiol.2004;93(9A):74B–76B.
- ,,,.Improved treatment of coronary heart disease by implementation of a Cardiac Hospitalization Atherosclerosis Management Program (CHAMP).Am J Cardiol.2001;87(7):819–822.
- ,,, et al.Association between performance measures and clinical outcomes for patients hospitalized with heart failure.JAMA.2007;297(1):61–70.
- ,,,.Emerging therapies for the management of decompensated heart failure: from bench to bedside.J Am Coll Cardiol.2006;48(12):2397–2409.
- ,.Novel strategies for the management of acute decompensated heart failure.Curr Cardiol Rev.2005;1(1):1–5.
- ,,, et al.Effects of oral tolvaptan in patients hospitalized for worsening heart failure: the EVEREST outcome trial.JAMA.2007;297(12):1319–1331.
- ,,, et al.Tolvaptan, a selective oral vasopressin V2‐receptor antagonist, for hyponatremia.N Engl J Med.2006;355(20):2099–2112.
- ,.Vasopressin‐receptor antagonists in heart failure.Am J Health Syst Pharm.2008;65(9):807–817.
- ,,,,.The effects of KW‐3902, an adenosine A1‐receptor antagonist, on diuresis and renal function in patients with acute decompensated heart failure and renal impairment or diuretic resistance.J Am Coll Cardiol.2007;50(16):1551–1560.
- ,,, et al.Effects of multiple oral doses of an A1 adenosine antagonist, BG9928, in patients with heart failure: results of a placebo‐controlled, dose‐escalation study.J Am Coll Cardiol.2007;50(7):600–606.
- ,,, et al.Effects of tezosentan on symptoms and clinical outcomes in patients with acute heart failure: the VERITAS randomized controlled trials.JAMA.2007;298(17):2009–2019.
- CK‐1827452. Cytokinetics Web site. Available at: http://www.cytokinetics.com/ck_1827452. Accessed September2008.
- ,,, et al.Rationale and design of the hemodynamic, echocardiographic and neurohormonal effects of istaroxime, a novel intravenous inotropic and lusitropic agent: a randomized controlled trial in patients hospitalized with heart failure (HORIZON‐HF) trial.Am J Ther.2008;15(3):231–240.
- ,,, et al.Clinical trials update from the American College of Cardiology 2008: CARISMA, TRENDS, meta‐analysis of Cox‐2 studies, HAT, ON‐TARGET, HYVET, ACCOMPLISH, MOMENTUM, PROTECT, HORIZON‐HF and REVERSE.Eur J Heart Fail.2008;10(6):614–620.
- ,,, et al.Haemodynamic and clinical effects of ularitide in decompensated heart failure.Eur Heart J.2006;27(23):2823–2832.
- ,,.Mechanical support in acute and chronic heart failure.Curr Cardiol Rep.2008;10(3):168–175.
- ,.Devices in acute heart failure.Crit Care Med.2008;36(1 suppl):S121–S128.
- ,.Advances in the surgical treatment of heart failure.Curr Opin Cardiol.2008;23(3):249–253.
Innovations in Natural Antioxidants & Their Role in Dermatology
Proceedings of the Ethical Challenges in Surgical Innovation Summit
Supplement Editors:
Allen Bashour, MD, and Eric Kodish, MD
Contents
Most of the articles in this supplement were developed from audio transcripts of the summit’s presentations and panel discussions. The transcripts were edited by the Cleveland Clinic Journal of Medicine staff for clarity and conciseness, and were then review and revised/approved by the respective speaker or panelists. Exceptions are the articles followed by an asterisk (*) below, which were submitted as manuscripts by their authors.
From the summit directors*
Eric Kodish, MD, and Allen Bashour, MD
Editors and contributors
Welcome—Ethics in surgical innovation: Vigorous discussion will foster future progress
Delos M. Cosgrove, MD
Panel 1: Surgical Innovation and Ethical Dilemmas
Surgical innovation and ethical dilemmas: Precautions and proximity*
Joseph J. Fins, MD
Surgical innovation and ethical dilemmas: A panel discussion
Isador Lieberman, MD; James Herndon, MD; Joseph Hahn, MD; Joseph J. Fins, MD; and Ali Rezai, MD
Panel 2: Transplant Innovation and Ethical Challenges
Pushing the envelope in transplantation: Three lives at stake*
Pauline W. Chen, MD
Transplant innovation and ethical challenges: What have we learned? A collection of perspectives and panel discussion
Denton A. Cooley, MD; John J. Fung, MD, PhD; James B. Young, MD; Thomas E. Starzl, MD, PhD; Mark Siegler, MD; and Pauline W. Chen, MD
We have come far, but selecting organ recipients remains an ethical minefield—Denton A. Cooley, MD
Despite the odds, the transplant field has progressed rapidly—John J. Fung, MD, PhD
A continued need for evidence-based guidance—James B. Young, MD
What does—and does not—spur innovation?—Thomas E. Starzl, MD, PhD
Panel discussion—Moderated by Mark Siegler, MD
Keynote Address
Medical professionalism in a commercialized health care market*
Arnold S. Relman, MD
Panel 3: Inside the Operating Room
Inside the operating room—balancing the risks and benefi ts of new surgical procedures: A collection of perspectives and panel discussion
Joel D. Cooper, MD; Ralph V. Clayman, MD; Thomas M. Krummel, MD; Philip R. Schauer, MD; Christopher Thompson, MD, MHES; and Jonathan D. Moreno, PhD
How should we introduce and evaluate new procedures?—Joel D. Cooper, MD
Idea to implementation: A personal perspective on the development of laparoscopic nephrectomy—Ralph V. Clayman, MD
Special perspectives in infants and children—Thomas M. Krummel, MD
Bariatric surgery: What role for ethics as established procedures approach new frontiers?—Philip R. Schauer, MD
Natural orifice transluminal endoscopic surgery: Too much too soon?—Christopher Thompson, MD, MHES
Panel discussion—Moderated by Jonathan D. Moreno, PhD
Keynote Address
Will the United States maintain its position as a world leader in medical technology?
Thomas J. Fogarty, MD
Panel 4: Outside the Operating Room
Outside the operating room—economic, regulatory, and legal challenges: A collection of perspectives and panel discussion
Lawrence K. Altman, MD; Michael A. Mussallem; Rebecca Dresser, JD; Paul A. Lombardo, PhD, JD; Peter A. Ubel, MD; and Christopher L. White, Esq
Preface—Lawrence K. Altman, MD (Moderator)
A device company perspective: Serving patients is the key to sustainable success—Michael A. Mussallem
A regulatory and legal perspective: Issues in off-label device use—Rebecca Dresser, JD
A historical perspective: The more things change, the more they remain the same—Paul A. Lombardo, PhD, JD
An economic value perspective: Setting limits on health care can be ethical—Peter A. Ubel, MD
An industry perspective: Proactive self-regulation through an industry code of ethics—Christopher L. White, Esq
Panel discussion—Moderated by Lawrence K. Altman, MD
Panel 5: New Surgical Devices and Ethical Challenges
New surgical devices and ethical challenges: A collection of perspectives and panel discussion
Daniel Schultz, MD; Mary H. McGrath, MD, MPH; Thomas H. Murray, PhD; Roy K. Greenberg, MD; and Thomas J. Fogarty, MD
An FDA perspective on device regulation—Daniel Schultz, MD
Responsibilities of the media, FDA, and professional societies—Mary H. McGrath, MD, MPH
Promoting swift, safe, and smart innovation—Thomas H. Murray, PhD
Panel discussion—Moderated by Roy K. Greenberg, MD
Supplement Editors:
Allen Bashour, MD, and Eric Kodish, MD
Contents
Most of the articles in this supplement were developed from audio transcripts of the summit’s presentations and panel discussions. The transcripts were edited by the Cleveland Clinic Journal of Medicine staff for clarity and conciseness, and were then review and revised/approved by the respective speaker or panelists. Exceptions are the articles followed by an asterisk (*) below, which were submitted as manuscripts by their authors.
From the summit directors*
Eric Kodish, MD, and Allen Bashour, MD
Editors and contributors
Welcome—Ethics in surgical innovation: Vigorous discussion will foster future progress
Delos M. Cosgrove, MD
Panel 1: Surgical Innovation and Ethical Dilemmas
Surgical innovation and ethical dilemmas: Precautions and proximity*
Joseph J. Fins, MD
Surgical innovation and ethical dilemmas: A panel discussion
Isador Lieberman, MD; James Herndon, MD; Joseph Hahn, MD; Joseph J. Fins, MD; and Ali Rezai, MD
Panel 2: Transplant Innovation and Ethical Challenges
Pushing the envelope in transplantation: Three lives at stake*
Pauline W. Chen, MD
Transplant innovation and ethical challenges: What have we learned? A collection of perspectives and panel discussion
Denton A. Cooley, MD; John J. Fung, MD, PhD; James B. Young, MD; Thomas E. Starzl, MD, PhD; Mark Siegler, MD; and Pauline W. Chen, MD
We have come far, but selecting organ recipients remains an ethical minefield—Denton A. Cooley, MD
Despite the odds, the transplant field has progressed rapidly—John J. Fung, MD, PhD
A continued need for evidence-based guidance—James B. Young, MD
What does—and does not—spur innovation?—Thomas E. Starzl, MD, PhD
Panel discussion—Moderated by Mark Siegler, MD
Keynote Address
Medical professionalism in a commercialized health care market*
Arnold S. Relman, MD
Panel 3: Inside the Operating Room
Inside the operating room—balancing the risks and benefi ts of new surgical procedures: A collection of perspectives and panel discussion
Joel D. Cooper, MD; Ralph V. Clayman, MD; Thomas M. Krummel, MD; Philip R. Schauer, MD; Christopher Thompson, MD, MHES; and Jonathan D. Moreno, PhD
How should we introduce and evaluate new procedures?—Joel D. Cooper, MD
Idea to implementation: A personal perspective on the development of laparoscopic nephrectomy—Ralph V. Clayman, MD
Special perspectives in infants and children—Thomas M. Krummel, MD
Bariatric surgery: What role for ethics as established procedures approach new frontiers?—Philip R. Schauer, MD
Natural orifice transluminal endoscopic surgery: Too much too soon?—Christopher Thompson, MD, MHES
Panel discussion—Moderated by Jonathan D. Moreno, PhD
Keynote Address
Will the United States maintain its position as a world leader in medical technology?
Thomas J. Fogarty, MD
Panel 4: Outside the Operating Room
Outside the operating room—economic, regulatory, and legal challenges: A collection of perspectives and panel discussion
Lawrence K. Altman, MD; Michael A. Mussallem; Rebecca Dresser, JD; Paul A. Lombardo, PhD, JD; Peter A. Ubel, MD; and Christopher L. White, Esq
Preface—Lawrence K. Altman, MD (Moderator)
A device company perspective: Serving patients is the key to sustainable success—Michael A. Mussallem
A regulatory and legal perspective: Issues in off-label device use—Rebecca Dresser, JD
A historical perspective: The more things change, the more they remain the same—Paul A. Lombardo, PhD, JD
An economic value perspective: Setting limits on health care can be ethical—Peter A. Ubel, MD
An industry perspective: Proactive self-regulation through an industry code of ethics—Christopher L. White, Esq
Panel discussion—Moderated by Lawrence K. Altman, MD
Panel 5: New Surgical Devices and Ethical Challenges
New surgical devices and ethical challenges: A collection of perspectives and panel discussion
Daniel Schultz, MD; Mary H. McGrath, MD, MPH; Thomas H. Murray, PhD; Roy K. Greenberg, MD; and Thomas J. Fogarty, MD
An FDA perspective on device regulation—Daniel Schultz, MD
Responsibilities of the media, FDA, and professional societies—Mary H. McGrath, MD, MPH
Promoting swift, safe, and smart innovation—Thomas H. Murray, PhD
Panel discussion—Moderated by Roy K. Greenberg, MD
Supplement Editors:
Allen Bashour, MD, and Eric Kodish, MD
Contents
Most of the articles in this supplement were developed from audio transcripts of the summit’s presentations and panel discussions. The transcripts were edited by the Cleveland Clinic Journal of Medicine staff for clarity and conciseness, and were then review and revised/approved by the respective speaker or panelists. Exceptions are the articles followed by an asterisk (*) below, which were submitted as manuscripts by their authors.
From the summit directors*
Eric Kodish, MD, and Allen Bashour, MD
Editors and contributors
Welcome—Ethics in surgical innovation: Vigorous discussion will foster future progress
Delos M. Cosgrove, MD
Panel 1: Surgical Innovation and Ethical Dilemmas
Surgical innovation and ethical dilemmas: Precautions and proximity*
Joseph J. Fins, MD
Surgical innovation and ethical dilemmas: A panel discussion
Isador Lieberman, MD; James Herndon, MD; Joseph Hahn, MD; Joseph J. Fins, MD; and Ali Rezai, MD
Panel 2: Transplant Innovation and Ethical Challenges
Pushing the envelope in transplantation: Three lives at stake*
Pauline W. Chen, MD
Transplant innovation and ethical challenges: What have we learned? A collection of perspectives and panel discussion
Denton A. Cooley, MD; John J. Fung, MD, PhD; James B. Young, MD; Thomas E. Starzl, MD, PhD; Mark Siegler, MD; and Pauline W. Chen, MD
We have come far, but selecting organ recipients remains an ethical minefield—Denton A. Cooley, MD
Despite the odds, the transplant field has progressed rapidly—John J. Fung, MD, PhD
A continued need for evidence-based guidance—James B. Young, MD
What does—and does not—spur innovation?—Thomas E. Starzl, MD, PhD
Panel discussion—Moderated by Mark Siegler, MD
Keynote Address
Medical professionalism in a commercialized health care market*
Arnold S. Relman, MD
Panel 3: Inside the Operating Room
Inside the operating room—balancing the risks and benefi ts of new surgical procedures: A collection of perspectives and panel discussion
Joel D. Cooper, MD; Ralph V. Clayman, MD; Thomas M. Krummel, MD; Philip R. Schauer, MD; Christopher Thompson, MD, MHES; and Jonathan D. Moreno, PhD
How should we introduce and evaluate new procedures?—Joel D. Cooper, MD
Idea to implementation: A personal perspective on the development of laparoscopic nephrectomy—Ralph V. Clayman, MD
Special perspectives in infants and children—Thomas M. Krummel, MD
Bariatric surgery: What role for ethics as established procedures approach new frontiers?—Philip R. Schauer, MD
Natural orifice transluminal endoscopic surgery: Too much too soon?—Christopher Thompson, MD, MHES
Panel discussion—Moderated by Jonathan D. Moreno, PhD
Keynote Address
Will the United States maintain its position as a world leader in medical technology?
Thomas J. Fogarty, MD
Panel 4: Outside the Operating Room
Outside the operating room—economic, regulatory, and legal challenges: A collection of perspectives and panel discussion
Lawrence K. Altman, MD; Michael A. Mussallem; Rebecca Dresser, JD; Paul A. Lombardo, PhD, JD; Peter A. Ubel, MD; and Christopher L. White, Esq
Preface—Lawrence K. Altman, MD (Moderator)
A device company perspective: Serving patients is the key to sustainable success—Michael A. Mussallem
A regulatory and legal perspective: Issues in off-label device use—Rebecca Dresser, JD
A historical perspective: The more things change, the more they remain the same—Paul A. Lombardo, PhD, JD
An economic value perspective: Setting limits on health care can be ethical—Peter A. Ubel, MD
An industry perspective: Proactive self-regulation through an industry code of ethics—Christopher L. White, Esq
Panel discussion—Moderated by Lawrence K. Altman, MD
Panel 5: New Surgical Devices and Ethical Challenges
New surgical devices and ethical challenges: A collection of perspectives and panel discussion
Daniel Schultz, MD; Mary H. McGrath, MD, MPH; Thomas H. Murray, PhD; Roy K. Greenberg, MD; and Thomas J. Fogarty, MD
An FDA perspective on device regulation—Daniel Schultz, MD
Responsibilities of the media, FDA, and professional societies—Mary H. McGrath, MD, MPH
Promoting swift, safe, and smart innovation—Thomas H. Murray, PhD
Panel discussion—Moderated by Roy K. Greenberg, MD