User login
Shift-work disorder
The burden of shift-work disorder (SWD) is multifactorial—affecting relationships, health, and work performance. Lack of support, research, and treatment for SWD has economic and safety consequences for society in general. In this supplement, sleep experts suggest practical steps to relieve the adverse effects of SWD.
The burden of shift-work disorder (SWD) is multifactorial—affecting relationships, health, and work performance. Lack of support, research, and treatment for SWD has economic and safety consequences for society in general. In this supplement, sleep experts suggest practical steps to relieve the adverse effects of SWD.
The burden of shift-work disorder (SWD) is multifactorial—affecting relationships, health, and work performance. Lack of support, research, and treatment for SWD has economic and safety consequences for society in general. In this supplement, sleep experts suggest practical steps to relieve the adverse effects of SWD.
Support
Support for the publication of this supplement was provided by Cephalon, Inc. Editorial assistance was provided by Anthemis Consulting Ltd and supported by Cephalon, Inc.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily represent those of Cephalon, Inc., or the publishers. Any procedures, medications, or other courses of diagnosis or treatment discussed or suggested by the authors should not be used by clinicians without evaluation of their patients’ conditions and possible contraindications or dangers in use, review of any applicable manufacturer’s product information, and comparisons with the recommendations of other authorities. Content may include product information that is inconsistent with or outside the approved labeling for these products in the United States. Before prescribing any medication, you must familiarize yourself with the manufacturer’s product information.
This material was submitted by Anthemis Consulting Ltd on behalf of the authors. It has been edited and peer reviewed by The Journal of Family Practice.
Managing Acid-Related Disorders Through the Ages of Mankind
A supplement to Internal Medicine News supported by a restricted grant from TAP Pharmaceutical Products, Inc.
Symposium Highlights of articles based on presentations given at a continuing medical education symposium held on October 22, 2002, in Seattle, Wash.

To view the supplement, click the image above.
A supplement to Internal Medicine News supported by a restricted grant from TAP Pharmaceutical Products, Inc.
Symposium Highlights of articles based on presentations given at a continuing medical education symposium held on October 22, 2002, in Seattle, Wash.

To view the supplement, click the image above.
A supplement to Internal Medicine News supported by a restricted grant from TAP Pharmaceutical Products, Inc.
Symposium Highlights of articles based on presentations given at a continuing medical education symposium held on October 22, 2002, in Seattle, Wash.

To view the supplement, click the image above.
The Role of Incretin-Based Therapies in Treating Patients with Type 2 Diabetes Mellitus
Supplement Editor:
Laurence Kennedy, MD
Contents
Incretin-based therapies for type 2 diabetes mellitus: New therapeutic mechanisms
Laurence Kennedy, MD
Current antihyperglycemic treatment strategies for patients with type 2 diabetes mellitus
Lawrence Blonde, MD
Role of the incretin pathway in the pathogenesis of type 2 diabetes mellitus
Jeffrey S. Freeman, DO
Patient and treatment perspectives: Revisiting the link between type 2 diabetes, weight gain, and cardiovascular risk
Anne L. Peters, MD, CDE
Advances in therapy for type 2 diabetes: GLP-1 receptor agonists and DPP-4 inhibitors
Jaime A. Davidson, MD
Redefining treatment success in type 2 diabetes mellitus: Comprehensive targeting of core defects
William T. Cefalu, MD; Robert J. Richards, MD; and Lydia Y. Melendez-Ramirez, MD
Supplement Editor:
Laurence Kennedy, MD
Contents
Incretin-based therapies for type 2 diabetes mellitus: New therapeutic mechanisms
Laurence Kennedy, MD
Current antihyperglycemic treatment strategies for patients with type 2 diabetes mellitus
Lawrence Blonde, MD
Role of the incretin pathway in the pathogenesis of type 2 diabetes mellitus
Jeffrey S. Freeman, DO
Patient and treatment perspectives: Revisiting the link between type 2 diabetes, weight gain, and cardiovascular risk
Anne L. Peters, MD, CDE
Advances in therapy for type 2 diabetes: GLP-1 receptor agonists and DPP-4 inhibitors
Jaime A. Davidson, MD
Redefining treatment success in type 2 diabetes mellitus: Comprehensive targeting of core defects
William T. Cefalu, MD; Robert J. Richards, MD; and Lydia Y. Melendez-Ramirez, MD
Supplement Editor:
Laurence Kennedy, MD
Contents
Incretin-based therapies for type 2 diabetes mellitus: New therapeutic mechanisms
Laurence Kennedy, MD
Current antihyperglycemic treatment strategies for patients with type 2 diabetes mellitus
Lawrence Blonde, MD
Role of the incretin pathway in the pathogenesis of type 2 diabetes mellitus
Jeffrey S. Freeman, DO
Patient and treatment perspectives: Revisiting the link between type 2 diabetes, weight gain, and cardiovascular risk
Anne L. Peters, MD, CDE
Advances in therapy for type 2 diabetes: GLP-1 receptor agonists and DPP-4 inhibitors
Jaime A. Davidson, MD
Redefining treatment success in type 2 diabetes mellitus: Comprehensive targeting of core defects
William T. Cefalu, MD; Robert J. Richards, MD; and Lydia Y. Melendez-Ramirez, MD
Update: Options in Endometrial Ablation
Proceedings of the 4th Annual Perioperative Medicine Summit
Supplement Editor:
Amir K. Jaffer, MD, FHM
Associate Editors:
David L. Hepner, MD, and Franklin A. Michota, MD, FHM
Contents
Public reporting and pay-for-performance programs in perioperative medicine
Peter Lindenauer, MD MSc
Cardiac risk stratification for noncardiac surgery: Update from the American College of Cardiology/American Heart Association 2007 guidelines
Lee A. Fleisher, MD
Perioperative care of the elderly patient: An update
Robert M. Palmer, MD, MPH
The role of testing in the preoperative evaluation
David L. Hepner, MD
Perioperative fluid management: Progress despite lingering controversies
Mark A. Hamilton, MBBS, MRCP, FRCA
Giving anesthesiologists what they want: How to write a useful preoperative consult
David Lubarsky, MD, MBA, and Keith Candiotti, MD
Perioperative management of warfarin and antiplatelet therapy
Amir K. Jaffer, MD, FHM
Prevention of venous thromboembolism after surgery
Franklin A. Michota, MD, FHM
Perioperative management of diabetes: Translating evidence into practice
Luigi F. Meneghini, MD, MBA
Postoperative pulmonary complications: An update on risk assessment and reduction
Gerald W. Smetana, MD
Postoperative gastrointestinal tract dysfunction: An overview of causes and management strategies
Michael G. (Monty) Mythen, MD
Case studies in perioperative management: Challenges, controversies, and common ground
Steven L. Cohn, MD, and BobbieJean Sweitzer, MD
Statins and noncardiac surgery: Current evidence and practical considerations
Don Poldermans, MD, PhD
The experts debate: perioperative beta-blockade for noncardiac surgery patients—proven safe or not?
Don Poldermans, MD, PhD, and P.J. Devereaux, MD, PhD
Perioperative considerations for patients with liver disease
Paul Martin, MD
Perioperative management of obstructive sleep apnea: Ready for prime time?
Shirin Shafazand, MD, MS
Nuts and bolts of preoperative clinics: The view from three institutions
Angela M. Bader, MD, MPH; BobbieJean Sweitzer, MD; and Ajay Kumar, MD
Perioperative management of anemia: Limits of blood transfusion and alternatives to it
Ajay Kumar, MD
Medicolegal issues in perioperative medicine: Lessons from real cases
Franklin A. Michota, MD, FHM, and Matthew J. Donnelly, Esq
Perioperative medication management: General principles and practical applications
Christopher Whinney, MD
Supplement Editor:
Amir K. Jaffer, MD, FHM
Associate Editors:
David L. Hepner, MD, and Franklin A. Michota, MD, FHM
Contents
Public reporting and pay-for-performance programs in perioperative medicine
Peter Lindenauer, MD MSc
Cardiac risk stratification for noncardiac surgery: Update from the American College of Cardiology/American Heart Association 2007 guidelines
Lee A. Fleisher, MD
Perioperative care of the elderly patient: An update
Robert M. Palmer, MD, MPH
The role of testing in the preoperative evaluation
David L. Hepner, MD
Perioperative fluid management: Progress despite lingering controversies
Mark A. Hamilton, MBBS, MRCP, FRCA
Giving anesthesiologists what they want: How to write a useful preoperative consult
David Lubarsky, MD, MBA, and Keith Candiotti, MD
Perioperative management of warfarin and antiplatelet therapy
Amir K. Jaffer, MD, FHM
Prevention of venous thromboembolism after surgery
Franklin A. Michota, MD, FHM
Perioperative management of diabetes: Translating evidence into practice
Luigi F. Meneghini, MD, MBA
Postoperative pulmonary complications: An update on risk assessment and reduction
Gerald W. Smetana, MD
Postoperative gastrointestinal tract dysfunction: An overview of causes and management strategies
Michael G. (Monty) Mythen, MD
Case studies in perioperative management: Challenges, controversies, and common ground
Steven L. Cohn, MD, and BobbieJean Sweitzer, MD
Statins and noncardiac surgery: Current evidence and practical considerations
Don Poldermans, MD, PhD
The experts debate: perioperative beta-blockade for noncardiac surgery patients—proven safe or not?
Don Poldermans, MD, PhD, and P.J. Devereaux, MD, PhD
Perioperative considerations for patients with liver disease
Paul Martin, MD
Perioperative management of obstructive sleep apnea: Ready for prime time?
Shirin Shafazand, MD, MS
Nuts and bolts of preoperative clinics: The view from three institutions
Angela M. Bader, MD, MPH; BobbieJean Sweitzer, MD; and Ajay Kumar, MD
Perioperative management of anemia: Limits of blood transfusion and alternatives to it
Ajay Kumar, MD
Medicolegal issues in perioperative medicine: Lessons from real cases
Franklin A. Michota, MD, FHM, and Matthew J. Donnelly, Esq
Perioperative medication management: General principles and practical applications
Christopher Whinney, MD
Supplement Editor:
Amir K. Jaffer, MD, FHM
Associate Editors:
David L. Hepner, MD, and Franklin A. Michota, MD, FHM
Contents
Public reporting and pay-for-performance programs in perioperative medicine
Peter Lindenauer, MD MSc
Cardiac risk stratification for noncardiac surgery: Update from the American College of Cardiology/American Heart Association 2007 guidelines
Lee A. Fleisher, MD
Perioperative care of the elderly patient: An update
Robert M. Palmer, MD, MPH
The role of testing in the preoperative evaluation
David L. Hepner, MD
Perioperative fluid management: Progress despite lingering controversies
Mark A. Hamilton, MBBS, MRCP, FRCA
Giving anesthesiologists what they want: How to write a useful preoperative consult
David Lubarsky, MD, MBA, and Keith Candiotti, MD
Perioperative management of warfarin and antiplatelet therapy
Amir K. Jaffer, MD, FHM
Prevention of venous thromboembolism after surgery
Franklin A. Michota, MD, FHM
Perioperative management of diabetes: Translating evidence into practice
Luigi F. Meneghini, MD, MBA
Postoperative pulmonary complications: An update on risk assessment and reduction
Gerald W. Smetana, MD
Postoperative gastrointestinal tract dysfunction: An overview of causes and management strategies
Michael G. (Monty) Mythen, MD
Case studies in perioperative management: Challenges, controversies, and common ground
Steven L. Cohn, MD, and BobbieJean Sweitzer, MD
Statins and noncardiac surgery: Current evidence and practical considerations
Don Poldermans, MD, PhD
The experts debate: perioperative beta-blockade for noncardiac surgery patients—proven safe or not?
Don Poldermans, MD, PhD, and P.J. Devereaux, MD, PhD
Perioperative considerations for patients with liver disease
Paul Martin, MD
Perioperative management of obstructive sleep apnea: Ready for prime time?
Shirin Shafazand, MD, MS
Nuts and bolts of preoperative clinics: The view from three institutions
Angela M. Bader, MD, MPH; BobbieJean Sweitzer, MD; and Ajay Kumar, MD
Perioperative management of anemia: Limits of blood transfusion and alternatives to it
Ajay Kumar, MD
Medicolegal issues in perioperative medicine: Lessons from real cases
Franklin A. Michota, MD, FHM, and Matthew J. Donnelly, Esq
Perioperative medication management: General principles and practical applications
Christopher Whinney, MD
Fixed-Combination Monotherapy With Clindamycin 1%-Benzoyl Peroxide 5% Gel: Focus on Acne Patient Benefits and Clinical Use
Advanced energy systems for laparoscopic gynecology procedures
Dr Brill: Probably no surgical instrument defines the gynecologist more than the Kleppinger forceps, the first bipolar device used for tubal ligation. It remains an important part of our armamentarium despite thermal spread, smoke, char, tissue sticking, and inconsistent hemostasis,1-5 shortcomings that have led to the development of newer bipolar electrosurgical devices—the LigaSure™ Vessel Sealing System, PlasmaKinetic (PK) platform, and ENSEAL®. These energy-based surgical devices offer added functionality—coagulation and cutting in a single instrument—as well as increased efficiency. These instruments offer specific features that appeal to gynecologic surgeons who have different needs and preferences. Ultrasonic energy technology has also advanced significantly, with instruments such as the Harmonic ACE®, which both cuts and coagulates at the point of impact for use in soft-tissue incisions and transections.
Dr Brill: Probably no surgical instrument defines the gynecologist more than the Kleppinger forceps, the first bipolar device used for tubal ligation. It remains an important part of our armamentarium despite thermal spread, smoke, char, tissue sticking, and inconsistent hemostasis,1-5 shortcomings that have led to the development of newer bipolar electrosurgical devices—the LigaSure™ Vessel Sealing System, PlasmaKinetic (PK) platform, and ENSEAL®. These energy-based surgical devices offer added functionality—coagulation and cutting in a single instrument—as well as increased efficiency. These instruments offer specific features that appeal to gynecologic surgeons who have different needs and preferences. Ultrasonic energy technology has also advanced significantly, with instruments such as the Harmonic ACE®, which both cuts and coagulates at the point of impact for use in soft-tissue incisions and transections.
Dr Brill: Probably no surgical instrument defines the gynecologist more than the Kleppinger forceps, the first bipolar device used for tubal ligation. It remains an important part of our armamentarium despite thermal spread, smoke, char, tissue sticking, and inconsistent hemostasis,1-5 shortcomings that have led to the development of newer bipolar electrosurgical devices—the LigaSure™ Vessel Sealing System, PlasmaKinetic (PK) platform, and ENSEAL®. These energy-based surgical devices offer added functionality—coagulation and cutting in a single instrument—as well as increased efficiency. These instruments offer specific features that appeal to gynecologic surgeons who have different needs and preferences. Ultrasonic energy technology has also advanced significantly, with instruments such as the Harmonic ACE®, which both cuts and coagulates at the point of impact for use in soft-tissue incisions and transections.
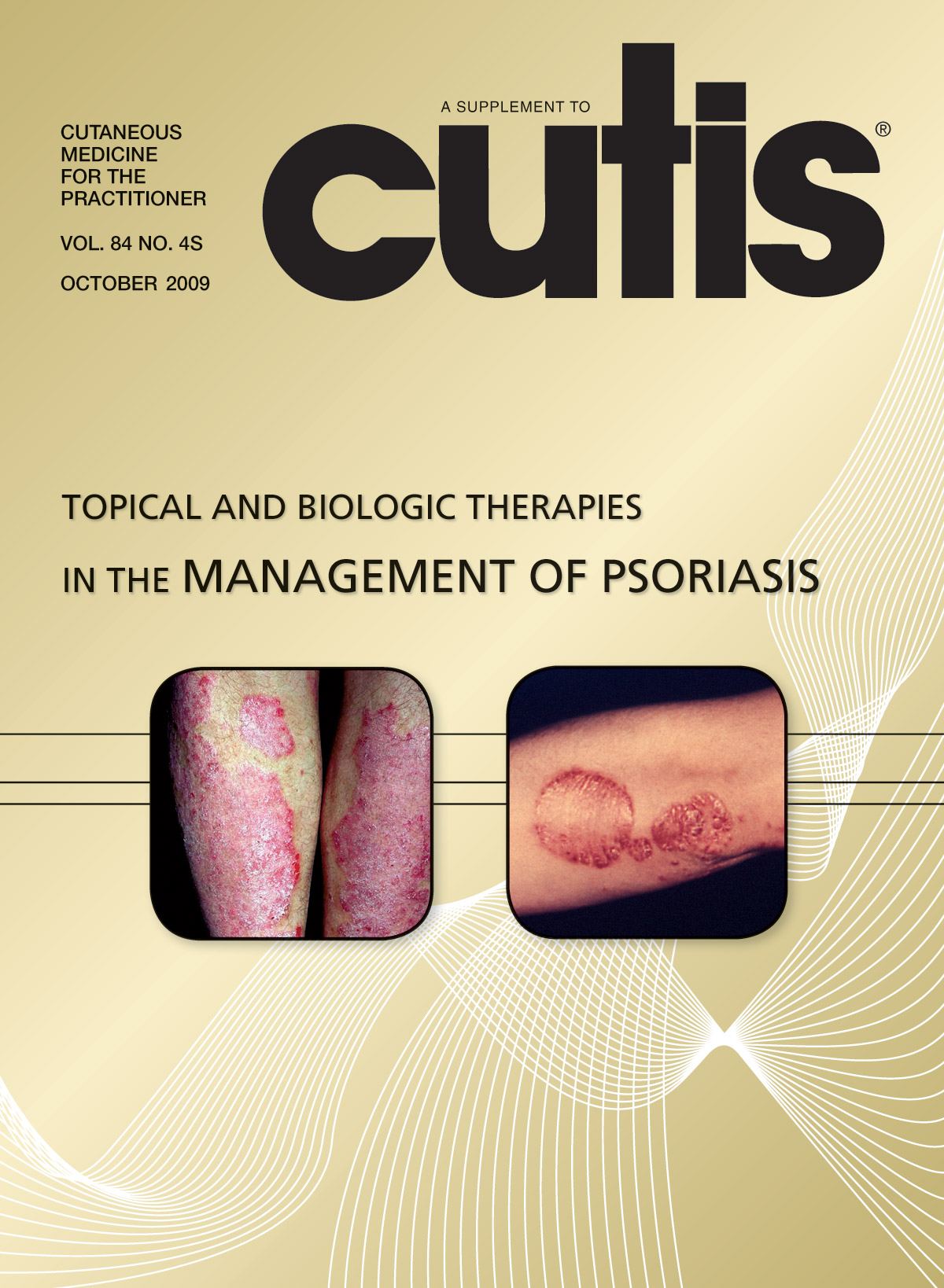
Topical and Biologic Therapies in the Management of Psoriasis
Postmenopausal Osteoporosis: Fracture Risk and Prevention
This monograph reviews advances in our understanding of the pathophysiology of postmenopausal osteoporosis and new recommendations for best practices in diagnosis and treatment. In Part 1, bone expert Michael R. McClung, MD, comments on new findings concerning bone metabolism. In Part 2, health care providers discuss how to identify and manage postmenopausal osteoporosis patients at risk for fracture.
This monograph reviews advances in our understanding of the pathophysiology of postmenopausal osteoporosis and new recommendations for best practices in diagnosis and treatment. In Part 1, bone expert Michael R. McClung, MD, comments on new findings concerning bone metabolism. In Part 2, health care providers discuss how to identify and manage postmenopausal osteoporosis patients at risk for fracture.
This monograph reviews advances in our understanding of the pathophysiology of postmenopausal osteoporosis and new recommendations for best practices in diagnosis and treatment. In Part 1, bone expert Michael R. McClung, MD, comments on new findings concerning bone metabolism. In Part 2, health care providers discuss how to identify and manage postmenopausal osteoporosis patients at risk for fracture.