User login
Should lithium and ECT be used concurrently in geriatric patients?
Delirium has been described as a potential complication of concurrent lithium and electroconvulsive therapy (ECT) for depression, in association with a range of serum lithium levels. Although debate persists about the safety of continuing previously established lithium therapy during a course of ECT for mood symptoms, withholding lithium for 24 hours before administering ECT and measuring the serum lithium level before ECT were found to decrease the risk of post-ECT neurocognitive effects.1
We have found that the conventional practice of holding lithium for 24 hours before ECT might need to be re-evaluated in geriatric patients, as the following case demonstrates. Only 24 hours of holding lithium therapy might result in a lithium level sufficient to contribute to delirium after ECT.
CASE REPORT
An older woman with recurrent unipolar psychotic depression
Mrs. A, age 81, was admitted to the hospital with a 1-week history of depressed mood, anhedonia, insomnia, anergia, anorexia, and nihilistic somatic delusions that her organs were “rotting and shutting down.” Treatment included nortriptyline, 40 mg/d; lithium, 150 mg/d; and haloperidol, 0.5 mg/d. Her serum lithium level was 0.3 mEq/L (reference range, 0.6 to 1.2 mEq/L); the serum nortriptyline level was 68 ng/mL (reference range, 50 to 150 ng/mL). CT of the head and an electrocardiogram were unremarkable.
A twice-weekly course of ECT was initiated.
The day before Treatment 1 of ECT, the serum lithium level (drawn 12 hours after the last dose) was 0.4 mEq/L. Lithium was withheld 24 hours before ECT; nortriptyline and haloperidol were continued at prescribed dosages.
Right unilateral stimulation was used at 50%/mC energy (Thymatron DG, with methohexital anesthesia, and succinylcholine for muscle relaxation). Seizure duration, measured by EEG, was 57 seconds.
Mrs. A developed postictal delirium after the first 2 ECT sessions. The serum lithium level was unchanged. Subsequently, lithium treatment was discontinued and ECT was continued; once lithium was stopped, delirium resolved. ECT sessions 3 and 4 were uneventful, with no post-treatment delirium. Seizure duration for Treatment 4 was 58 seconds. She started breathing easily after all ECT sessions.
After Treatment 4, Mrs. A experienced full remission of depressive and psychotic symptoms. Repeat CT of head, after Treatment 4, was unchanged from baseline.
What is the role of lithium?
Mrs. A did not exhibit typical signs of lithium intoxication (diarrhea, vomiting, tremor). Notably, lithium has an intrinsic anticholinergic activity2; concurrent nortriptyline, a secondary amine tricyclic antidepressant with fewer anticholinergic side effects than other tricyclics,2 could precipitate delirium in a vulnerable patient secondary to excessive cumulative anticholinergic exposure.
No prolonged time-to-respiration or time-to-awakening occurred during treatments in which concurrent lithium and ECT were used; seizure duration with and without concurrent lithium was relatively similar.
There are potential complications of concurrent use of lithium and ECT:
• prolongation of the duration of muscle paralysis and apnea induced by commonly used neuromuscular-blocking agents (eg, succinylcholine)
• post-ECT cognitive disturbance.1,3,4
There is debate about the safety of continuing lithium during, or in close proximity to, ECT. In a case series of 12 patients who underwent combined lithium therapy and ECT, the authors concluded that this combination can be safe, regardless of age, as long as appropriate clinical monitoring is provided.4 In Mrs. A’s case, once post-ECT delirium was noted, lithium was discontinued for subsequent ECT sessions.
Because further ECT was uneventful without lithium, and no other clear acute cause of delirium could be identified, we concluded that lithium likely played a role in Mrs. A’s delirium. Notably, nortriptyline had been continued, suggesting that the degree of anticholinergic blockade provided by nortriptyline was insufficient to provoke delirium post-ECT in the absence of potentiation of this effect, as it had been when lithium also was used initially.
Guidelines for dosing and serum lithium concentrations in geriatric patients are not well-established; the current traditional range of 0.6 to 1.2 mEq/L, is too high for geriatric patients and can result in episodes of lithium toxicity, including delirium.5 Although our patient’s lithium level was below the reference range for all patients, a level of 0.3 mEq/L can be considered at the low end of the reference range for geriatric patients.5 Inasmuch as the lithium-assisted post-ECT delirium could represent a clinical sign of lithium toxicity, perhaps even a subtherapeutic level in a certain patient could be paradoxically “toxic.”
Although the serum lithium level in our patient remained below the toxic level for the general population (>1.5 mEq/L), delirium in a geriatric patient could result from:
• age-related changes in the pharmacokinetics of lithium, a water-soluble drug; these changes reduce renal clearance of the drug and extend plasma elimination half-life of a single dose to 36 hours, with the result that lithium remains in the body longer and necessitating a lower dosage (ie, a dosage that yields a serum level of approximately 0.5 mEq/L)
• the CNS tissue concentration of lithium, which can be high even though the serum level is not toxic
• an age-related increase in blood-brain barrier permeability, making the barrier more porous for drugs
• changes in blood-brain barrier permeability by post-ECT biochemical induction, with subsequent increased drug availability in the CNS.5,6
What we recommend
Possible interactions between lithium and ECT that lead to ECT-associated delirium need further elucidation, but discontinuing lithium during the course of ECT in a geriatric patient warrants your consideration. Following a safe interval after the last ECT session, lithium likely can be safely re-introduced 1) if there is clinical need and 2) as long as clinical surveillance for cognitive side effects is provided— especially if ECT will need to be reconsidered in the future.
Two additional considerations:
• Actively reassess lithium dosing in all geriatric psychiatric patients, especially those with renal insufficiency and other systemic metabolic considerations.
• Actively examine the use of all other anticholinergic agents in the course of evaluating a patient’s candidacy for ECT.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. American Psychiatric Association. The practice of electroconvulsive therapy: recommendations for treatment, training, and privileging. A task force report of the American Psychiatric Association. 2nd ed. Washington, DC: American Psychiatric Publishing; 2001.
2. Chew ML, Mulsant BH, Pollock BG, et al. Anticholinergic activity of 107 medications commonly used by older adults. J Am Geriatr Soc. 2008;56(7):1333-1341.
3. Hill GE, Wong KC, Hodges MR. Potentiation of succinylcholine neuromuscular blockade by lithium carbonate. Anesthesiology. 1976;44(5):439-442.
4. Dolenc TJ, Rasmussen KG. The safety of electroconvulsive therapy and lithium in combination: a case series and review of the literature. J ECT. 2005;21(3):165-170.
5. Shulman KI. Lithium for older adults with bipolar disorder: should it still be considered a first line agent? Drugs Aging. 2010;27(8):607-615.
6. Grandjean EM, Aubry JM. Lithium: updated human knowledge using an evidence-based approach. Part II: clinical pharmacology and therapeutic monitoring. CNS Drugs. 2009;23(4):331-349.
Delirium has been described as a potential complication of concurrent lithium and electroconvulsive therapy (ECT) for depression, in association with a range of serum lithium levels. Although debate persists about the safety of continuing previously established lithium therapy during a course of ECT for mood symptoms, withholding lithium for 24 hours before administering ECT and measuring the serum lithium level before ECT were found to decrease the risk of post-ECT neurocognitive effects.1
We have found that the conventional practice of holding lithium for 24 hours before ECT might need to be re-evaluated in geriatric patients, as the following case demonstrates. Only 24 hours of holding lithium therapy might result in a lithium level sufficient to contribute to delirium after ECT.
CASE REPORT
An older woman with recurrent unipolar psychotic depression
Mrs. A, age 81, was admitted to the hospital with a 1-week history of depressed mood, anhedonia, insomnia, anergia, anorexia, and nihilistic somatic delusions that her organs were “rotting and shutting down.” Treatment included nortriptyline, 40 mg/d; lithium, 150 mg/d; and haloperidol, 0.5 mg/d. Her serum lithium level was 0.3 mEq/L (reference range, 0.6 to 1.2 mEq/L); the serum nortriptyline level was 68 ng/mL (reference range, 50 to 150 ng/mL). CT of the head and an electrocardiogram were unremarkable.
A twice-weekly course of ECT was initiated.
The day before Treatment 1 of ECT, the serum lithium level (drawn 12 hours after the last dose) was 0.4 mEq/L. Lithium was withheld 24 hours before ECT; nortriptyline and haloperidol were continued at prescribed dosages.
Right unilateral stimulation was used at 50%/mC energy (Thymatron DG, with methohexital anesthesia, and succinylcholine for muscle relaxation). Seizure duration, measured by EEG, was 57 seconds.
Mrs. A developed postictal delirium after the first 2 ECT sessions. The serum lithium level was unchanged. Subsequently, lithium treatment was discontinued and ECT was continued; once lithium was stopped, delirium resolved. ECT sessions 3 and 4 were uneventful, with no post-treatment delirium. Seizure duration for Treatment 4 was 58 seconds. She started breathing easily after all ECT sessions.
After Treatment 4, Mrs. A experienced full remission of depressive and psychotic symptoms. Repeat CT of head, after Treatment 4, was unchanged from baseline.
What is the role of lithium?
Mrs. A did not exhibit typical signs of lithium intoxication (diarrhea, vomiting, tremor). Notably, lithium has an intrinsic anticholinergic activity2; concurrent nortriptyline, a secondary amine tricyclic antidepressant with fewer anticholinergic side effects than other tricyclics,2 could precipitate delirium in a vulnerable patient secondary to excessive cumulative anticholinergic exposure.
No prolonged time-to-respiration or time-to-awakening occurred during treatments in which concurrent lithium and ECT were used; seizure duration with and without concurrent lithium was relatively similar.
There are potential complications of concurrent use of lithium and ECT:
• prolongation of the duration of muscle paralysis and apnea induced by commonly used neuromuscular-blocking agents (eg, succinylcholine)
• post-ECT cognitive disturbance.1,3,4
There is debate about the safety of continuing lithium during, or in close proximity to, ECT. In a case series of 12 patients who underwent combined lithium therapy and ECT, the authors concluded that this combination can be safe, regardless of age, as long as appropriate clinical monitoring is provided.4 In Mrs. A’s case, once post-ECT delirium was noted, lithium was discontinued for subsequent ECT sessions.
Because further ECT was uneventful without lithium, and no other clear acute cause of delirium could be identified, we concluded that lithium likely played a role in Mrs. A’s delirium. Notably, nortriptyline had been continued, suggesting that the degree of anticholinergic blockade provided by nortriptyline was insufficient to provoke delirium post-ECT in the absence of potentiation of this effect, as it had been when lithium also was used initially.
Guidelines for dosing and serum lithium concentrations in geriatric patients are not well-established; the current traditional range of 0.6 to 1.2 mEq/L, is too high for geriatric patients and can result in episodes of lithium toxicity, including delirium.5 Although our patient’s lithium level was below the reference range for all patients, a level of 0.3 mEq/L can be considered at the low end of the reference range for geriatric patients.5 Inasmuch as the lithium-assisted post-ECT delirium could represent a clinical sign of lithium toxicity, perhaps even a subtherapeutic level in a certain patient could be paradoxically “toxic.”
Although the serum lithium level in our patient remained below the toxic level for the general population (>1.5 mEq/L), delirium in a geriatric patient could result from:
• age-related changes in the pharmacokinetics of lithium, a water-soluble drug; these changes reduce renal clearance of the drug and extend plasma elimination half-life of a single dose to 36 hours, with the result that lithium remains in the body longer and necessitating a lower dosage (ie, a dosage that yields a serum level of approximately 0.5 mEq/L)
• the CNS tissue concentration of lithium, which can be high even though the serum level is not toxic
• an age-related increase in blood-brain barrier permeability, making the barrier more porous for drugs
• changes in blood-brain barrier permeability by post-ECT biochemical induction, with subsequent increased drug availability in the CNS.5,6
What we recommend
Possible interactions between lithium and ECT that lead to ECT-associated delirium need further elucidation, but discontinuing lithium during the course of ECT in a geriatric patient warrants your consideration. Following a safe interval after the last ECT session, lithium likely can be safely re-introduced 1) if there is clinical need and 2) as long as clinical surveillance for cognitive side effects is provided— especially if ECT will need to be reconsidered in the future.
Two additional considerations:
• Actively reassess lithium dosing in all geriatric psychiatric patients, especially those with renal insufficiency and other systemic metabolic considerations.
• Actively examine the use of all other anticholinergic agents in the course of evaluating a patient’s candidacy for ECT.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Delirium has been described as a potential complication of concurrent lithium and electroconvulsive therapy (ECT) for depression, in association with a range of serum lithium levels. Although debate persists about the safety of continuing previously established lithium therapy during a course of ECT for mood symptoms, withholding lithium for 24 hours before administering ECT and measuring the serum lithium level before ECT were found to decrease the risk of post-ECT neurocognitive effects.1
We have found that the conventional practice of holding lithium for 24 hours before ECT might need to be re-evaluated in geriatric patients, as the following case demonstrates. Only 24 hours of holding lithium therapy might result in a lithium level sufficient to contribute to delirium after ECT.
CASE REPORT
An older woman with recurrent unipolar psychotic depression
Mrs. A, age 81, was admitted to the hospital with a 1-week history of depressed mood, anhedonia, insomnia, anergia, anorexia, and nihilistic somatic delusions that her organs were “rotting and shutting down.” Treatment included nortriptyline, 40 mg/d; lithium, 150 mg/d; and haloperidol, 0.5 mg/d. Her serum lithium level was 0.3 mEq/L (reference range, 0.6 to 1.2 mEq/L); the serum nortriptyline level was 68 ng/mL (reference range, 50 to 150 ng/mL). CT of the head and an electrocardiogram were unremarkable.
A twice-weekly course of ECT was initiated.
The day before Treatment 1 of ECT, the serum lithium level (drawn 12 hours after the last dose) was 0.4 mEq/L. Lithium was withheld 24 hours before ECT; nortriptyline and haloperidol were continued at prescribed dosages.
Right unilateral stimulation was used at 50%/mC energy (Thymatron DG, with methohexital anesthesia, and succinylcholine for muscle relaxation). Seizure duration, measured by EEG, was 57 seconds.
Mrs. A developed postictal delirium after the first 2 ECT sessions. The serum lithium level was unchanged. Subsequently, lithium treatment was discontinued and ECT was continued; once lithium was stopped, delirium resolved. ECT sessions 3 and 4 were uneventful, with no post-treatment delirium. Seizure duration for Treatment 4 was 58 seconds. She started breathing easily after all ECT sessions.
After Treatment 4, Mrs. A experienced full remission of depressive and psychotic symptoms. Repeat CT of head, after Treatment 4, was unchanged from baseline.
What is the role of lithium?
Mrs. A did not exhibit typical signs of lithium intoxication (diarrhea, vomiting, tremor). Notably, lithium has an intrinsic anticholinergic activity2; concurrent nortriptyline, a secondary amine tricyclic antidepressant with fewer anticholinergic side effects than other tricyclics,2 could precipitate delirium in a vulnerable patient secondary to excessive cumulative anticholinergic exposure.
No prolonged time-to-respiration or time-to-awakening occurred during treatments in which concurrent lithium and ECT were used; seizure duration with and without concurrent lithium was relatively similar.
There are potential complications of concurrent use of lithium and ECT:
• prolongation of the duration of muscle paralysis and apnea induced by commonly used neuromuscular-blocking agents (eg, succinylcholine)
• post-ECT cognitive disturbance.1,3,4
There is debate about the safety of continuing lithium during, or in close proximity to, ECT. In a case series of 12 patients who underwent combined lithium therapy and ECT, the authors concluded that this combination can be safe, regardless of age, as long as appropriate clinical monitoring is provided.4 In Mrs. A’s case, once post-ECT delirium was noted, lithium was discontinued for subsequent ECT sessions.
Because further ECT was uneventful without lithium, and no other clear acute cause of delirium could be identified, we concluded that lithium likely played a role in Mrs. A’s delirium. Notably, nortriptyline had been continued, suggesting that the degree of anticholinergic blockade provided by nortriptyline was insufficient to provoke delirium post-ECT in the absence of potentiation of this effect, as it had been when lithium also was used initially.
Guidelines for dosing and serum lithium concentrations in geriatric patients are not well-established; the current traditional range of 0.6 to 1.2 mEq/L, is too high for geriatric patients and can result in episodes of lithium toxicity, including delirium.5 Although our patient’s lithium level was below the reference range for all patients, a level of 0.3 mEq/L can be considered at the low end of the reference range for geriatric patients.5 Inasmuch as the lithium-assisted post-ECT delirium could represent a clinical sign of lithium toxicity, perhaps even a subtherapeutic level in a certain patient could be paradoxically “toxic.”
Although the serum lithium level in our patient remained below the toxic level for the general population (>1.5 mEq/L), delirium in a geriatric patient could result from:
• age-related changes in the pharmacokinetics of lithium, a water-soluble drug; these changes reduce renal clearance of the drug and extend plasma elimination half-life of a single dose to 36 hours, with the result that lithium remains in the body longer and necessitating a lower dosage (ie, a dosage that yields a serum level of approximately 0.5 mEq/L)
• the CNS tissue concentration of lithium, which can be high even though the serum level is not toxic
• an age-related increase in blood-brain barrier permeability, making the barrier more porous for drugs
• changes in blood-brain barrier permeability by post-ECT biochemical induction, with subsequent increased drug availability in the CNS.5,6
What we recommend
Possible interactions between lithium and ECT that lead to ECT-associated delirium need further elucidation, but discontinuing lithium during the course of ECT in a geriatric patient warrants your consideration. Following a safe interval after the last ECT session, lithium likely can be safely re-introduced 1) if there is clinical need and 2) as long as clinical surveillance for cognitive side effects is provided— especially if ECT will need to be reconsidered in the future.
Two additional considerations:
• Actively reassess lithium dosing in all geriatric psychiatric patients, especially those with renal insufficiency and other systemic metabolic considerations.
• Actively examine the use of all other anticholinergic agents in the course of evaluating a patient’s candidacy for ECT.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. American Psychiatric Association. The practice of electroconvulsive therapy: recommendations for treatment, training, and privileging. A task force report of the American Psychiatric Association. 2nd ed. Washington, DC: American Psychiatric Publishing; 2001.
2. Chew ML, Mulsant BH, Pollock BG, et al. Anticholinergic activity of 107 medications commonly used by older adults. J Am Geriatr Soc. 2008;56(7):1333-1341.
3. Hill GE, Wong KC, Hodges MR. Potentiation of succinylcholine neuromuscular blockade by lithium carbonate. Anesthesiology. 1976;44(5):439-442.
4. Dolenc TJ, Rasmussen KG. The safety of electroconvulsive therapy and lithium in combination: a case series and review of the literature. J ECT. 2005;21(3):165-170.
5. Shulman KI. Lithium for older adults with bipolar disorder: should it still be considered a first line agent? Drugs Aging. 2010;27(8):607-615.
6. Grandjean EM, Aubry JM. Lithium: updated human knowledge using an evidence-based approach. Part II: clinical pharmacology and therapeutic monitoring. CNS Drugs. 2009;23(4):331-349.
1. American Psychiatric Association. The practice of electroconvulsive therapy: recommendations for treatment, training, and privileging. A task force report of the American Psychiatric Association. 2nd ed. Washington, DC: American Psychiatric Publishing; 2001.
2. Chew ML, Mulsant BH, Pollock BG, et al. Anticholinergic activity of 107 medications commonly used by older adults. J Am Geriatr Soc. 2008;56(7):1333-1341.
3. Hill GE, Wong KC, Hodges MR. Potentiation of succinylcholine neuromuscular blockade by lithium carbonate. Anesthesiology. 1976;44(5):439-442.
4. Dolenc TJ, Rasmussen KG. The safety of electroconvulsive therapy and lithium in combination: a case series and review of the literature. J ECT. 2005;21(3):165-170.
5. Shulman KI. Lithium for older adults with bipolar disorder: should it still be considered a first line agent? Drugs Aging. 2010;27(8):607-615.
6. Grandjean EM, Aubry JM. Lithium: updated human knowledge using an evidence-based approach. Part II: clinical pharmacology and therapeutic monitoring. CNS Drugs. 2009;23(4):331-349.
Current and novel therapeutic approaches in myelodysplastic syndromes
Myelodysplastic syndromes (MDS) are a heterogeneous group of hematologic neoplasms with an annual incidence of 4.1 cases per 100,000 Americans. Patients with MDS suffer from chronic cytopenias that may lead to recurrent transfusions, infections, and increased risk for bleeding. They are also at risk for progression to acute myeloid leukemia. Allogeneic hematopoietic cell transplantation is the only potentially curative treatment for MDS, although 3 drugs have been approved by the US Food and Drug Administration for its treatment: lenalidomide, 5-azacitidine, and decitabine.
Click on the PDF icon at the top of this introduction to read the full article.
Myelodysplastic syndromes (MDS) are a heterogeneous group of hematologic neoplasms with an annual incidence of 4.1 cases per 100,000 Americans. Patients with MDS suffer from chronic cytopenias that may lead to recurrent transfusions, infections, and increased risk for bleeding. They are also at risk for progression to acute myeloid leukemia. Allogeneic hematopoietic cell transplantation is the only potentially curative treatment for MDS, although 3 drugs have been approved by the US Food and Drug Administration for its treatment: lenalidomide, 5-azacitidine, and decitabine.
Click on the PDF icon at the top of this introduction to read the full article.
Myelodysplastic syndromes (MDS) are a heterogeneous group of hematologic neoplasms with an annual incidence of 4.1 cases per 100,000 Americans. Patients with MDS suffer from chronic cytopenias that may lead to recurrent transfusions, infections, and increased risk for bleeding. They are also at risk for progression to acute myeloid leukemia. Allogeneic hematopoietic cell transplantation is the only potentially curative treatment for MDS, although 3 drugs have been approved by the US Food and Drug Administration for its treatment: lenalidomide, 5-azacitidine, and decitabine.
Click on the PDF icon at the top of this introduction to read the full article.
Delirium in the hospital: Emphasis on the management of geriatric patients
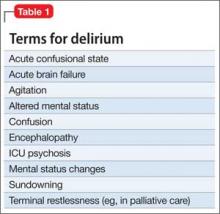
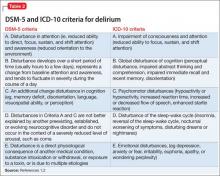
Although delirium has many descriptive terms (Table 1), a common unifying term is “acute global cognitive dysfunction,” now recognized as delirium; a consensus supported by DSM-51 and ICD-102 (Table 2). According to DSM-5, the essential feature is a disturbance of attention or awareness that is accompanied by a change in baseline cognition that cannot be explained by another preexisting, established, or evolving neurocognitive disorder (the newly named DSM-5 entity for dementia syndromes).1 Because delirium affects the cortex diffusely, psychiatric symptoms can include cognitive, mood, anxiety, or psychotic symptoms. Because many systemic illnesses can induce delirium, the differential diagnosis spans all organ systems.
Three subtypes
Delirium can be classified, based on symptoms,3,4 into 3 subtypes: hyperactive-hyperalert, hypoactive-hypoalert, and mixed delirium. Hyperactive patients present with restlessness and agitation. Hypoactive patients are lethargic, confused, slow to respond to questions, and often appear depressed. The differential prognostic significance of these subtypes has been examined in the literature, with conflicting results. Rabinowitz5 reported that hypoactive delirium has the worst prognosis, while Marcantonio et al6 indicated that the hyperactive subtype is associated with the highest mortality rate. Mixed delirium, with periods of both hyperactivity and hypoactivity, is the most common type of delirium.7
A prodromal phase, characterized by anxiety, frequent requests for nursing and medical assistance, decreased attention, restlessness, vivid dreams, disorientation immediately after awakening, and hallucinations, can occur before an episode of full-spectrum delirium; this prodromal state often is identified retrospectively —after the patient is in an episode of delirium.8,9
Evidence-based guidelines aim to improve recognition and clinical management.10-13 Disruptive behavior is the main reason for psychiatric referral in delirium.14,15 Delayed psychiatric consultation because of non-recognition of delirium is related to variables such as older age; history of a pre-existing, comorbid neurocognitive disorder; and the clinical appearance of hypoactive delirium.14
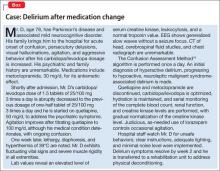
The case of Mr. D (Box),16 illustrates how the emergence of antipsychotic-associated neuroleptic malignant syndrome (NMS) can complicate antipsychotic treatment of delirium in a geriatric medical patient, although delirium also is a common presentation in NMS.17 Delirium developed after an increase in carbidopa/levodopa, which has central dopaminergic effects that can precipitate delirium, particularly in a geriatric patient with preexisting comorbid neurocognitive disorder. Further complicating Mr. D’s delirium presentation was the development of NMS, which had a multifactorial causation, such as the use of dopamine antagonists (ie, quetiapine, metoclopramide), and an abrupt decrease of a dopaminergic agent (ie, carbidopa/levodopa), all inducing a central dopamine relative hypoactivity.
Epidemiology
Delirium is more common in older patients,15 and is seen in 30% to 40% of hospitalized geriatric patients.18 Delirium in older patients, compared with other adults, is associated with more severe cognitive impairment.19 It is common among geriatric surgical patients (15% to 62%)20 with a peak 2 to 5 days postoperatively for hip fracture,21 and often is seen in ICU patients (70% to 87%).20 However, Spronk et al22 found that delirium is significantly under-recognized in the ICU. Nearly 90% of terminally ill patients become delirious before death.23 Terminal delirium often is unrecognized and can interfere with assessment of other clinical problems.24 A preexisting history of comorbid neurocognitive disorder was evident in as many as two-thirds of delirium cases.25
Pathophysiology and risk factors
The pathophysiology of delirium has been characterized as an imbalance of CNS metabolism, including decreased blood flow in various regions of the brain that may normalize once delirium resolves.26 Studies describe the simultaneous decrease of cholinergic transmission and dopaminergic excess.27,28 Predisposing and precipitating factors for delirium that are of particular importance in geriatric patients include:
• advanced age
• CNS disease
• infection
• cognitive impairment
• male sex
• poor nutrition
• dehydration and other metabolic abnormalities
• cardiovascular events
• substance use
• medication
• sensory deprivation (eg, impaired vision or hearing)
• sleep deprivation
• low level of physical activity.27,29,30
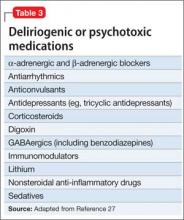
Table 3 lists the most common delirium-provocative medications.27
Evaluation and psychometric scales
The EEG can be useful in evaluating delirium, especially in clinically ambiguous cases. EEG findings may indicate generalized slowing or dropout of the posterior dominant rhythm, and generalized slow theta and delta waves, findings that are more common in delirium than in other neurocognitive disorders and other psychiatric illnesses. The EEG must be interpreted in the context of the delirium diagnostic workup, because abnormalities seen in other neurocognitive disorders can overlap with those of delirium.31
The EEG referral should specify the clinical suspicion of delirium to help interpret the results. Delirium cases in which the patient’s previous cognitive status is unknown may benefit from EEG evaluation, such as:
• in possible status epilepticus
• when delirium improvement has reached a plateau at a lower level of cognitive function than before onset of delirium
• when the patient is unable or unwilling to complete a psychiatric interview.27
Assessment instruments are available to diagnose and monitor delirium (Table 4). Typically, delirium assessment includes examining levels of arousal, psychomotor activity, cognition (ie, orientation, attention, and memory), and perceptual disturbances.
Psychometrically, a review of Table 4 suggests that validity appeared stable with adequate specificity (64% to 99%) but more variable sensitivity (36% to 100%). These reliability parameters also will be affected by the classification system (ie, DSM vs ICD) and the cut-off score employed.32 Most measures (eg, Confusion Assessment Method [CAM], CAM-ICU) provide an adequate sample of behavioral (ie, level of alertness), motor (ie, psychomotor activity), and cognitive (ie, orientation, attention, memory, and receptive language) function, with the exception of the Global Attentiveness Rating, which is a 2-minute open conversation protocol between physician and patient.
Some measures are stand-alone instruments, such as the Memorial Delirium Assessment Scale, whereas the CAM requires administration of separate cognitive screens, including the Mini-Mental State Examination (MMSE) and Digit Span.33 Instruments to detect delirium in critically ill patients are a more recent development. Wong et al34 reported that the most widely studied tool was the CAM. Obtaining collateral information from family, caregivers, and hospital staff is essential, particularly given the fluctuating nature of delirium.
Management
Prevention. Identify patients at high risk of delirium so that preventive strategies can be employed. Multi-component, nonpharmacotherapeutic interventions are used in clinical settings but few randomized trials have been conducted. The contributing effectiveness of individual components is not well-studied, but most include staff education to increase awareness of delirium. Of 3 multi-component intervention randomized trials, 2 reported a significantly lower incidence of delirium in the intervention group.35-37 Implementation of a multi-component protocol in medical/ surgical units was associated with a significant reduction in use of restraints.38
As in Mr. D’s case, complex drug regimens, particularly for CNS illness, can increase the risk of delirium. Considering the medication profile for patients with complex systemic illness—in particular, minimizing the use anticholinergics and dopamine agonists— may be crucial in preventing delirium.
Prophylactic administration of antipsychotics may reduce the risk of developing postoperative delirium.39 Studies of the use of these agents were characterized by small sample sizes and selected groups of patient populations. Of the 4 randomized studies evaluating prophylactic antipsychotics (vs placebo), 3 found a lower incidence of delirium in the intervention groups.39-41
A study of haloperidol in post-GI surgery patients showed a reduced occurrence of delirium,40 whereas its prophylactic use in patients undergoing hip surgery42 did not reduce the incidence of delirium compared with placebo, but did decrease severity when delirium occurred.42
Risperidone39 in post-cardiac surgery and olanzapine41 perioperatively in patients undergoing total knee or hip replacement have been shown to decrease delirium severity and duration. Targeted prophylaxis with risperidone43 in post-cardiac surgery patients who showed disturbed cognition but did not meet criteria for delirium reduced the number of patients requiring medication, compared with placebo.43
Dexmedetomidine, an α-2 adrenergic receptor agonist, compared with propofol or midazolam in post-cardiac valve surgery patients, resulted in a decreased incidence of delirium but no difference in delirium duration, hospital length of stay, or use of other medications.44 However, other studies have shown that dexmedetomidine reduces ICU length of stay and duration of mechanical ventilation.45
Treatment. Management of hospitalized medically ill geriatric patients with delirium is challenging and requires a comprehensive approach. The first step in delirium management is prompt identification and management of systemic medical disturbances associated with the delirium episode. First-line, nonpharmacotherapeutic strategies for patients with delirium include:
• reorientation
• behavioral interventions (eg, use of clear instructions and frequent eye contact with patients)
• environmental interventions (eg, minimal noise, adequate lighting, and limited room and staff changes)
• avoidance of physical restraints.46
Consider employing family members or hospital staff sitters to stay with the patient and to reassure, reorient, and watch for agitation and other unsafe behaviors (eg, attempted elopement). Psychoeducation for the patient and family on the phenomenology of delirium can be helpful.
The use of drug treatment strategies should be integrated into a comprehensive approach that includes the routine use of nondrug measures.46 Using medications for treating hypoactive delirium, formerly controversial, now has wider acceptance.47,48 A few high-quality randomized trials have been performed.25,49,50
Pharmacotherapy, especially in frail patients, should be initiated at the lowest starting dosage and titrated cautiously to clinical effect and for the shortest period of time necessary. Antipsychotics are preferred agents for treating all subtypes of delirium; haloperidol is widely used.46,51,52 However, antipsychotics, including haloperidol, can be associated with adverse neurologic effects such as extrapyramidal symptoms (EPS) and NMS.
Although reported less frequently than with haloperidol, other agents have been implicated in development of EPS and NMS, including atypical antipsychotics and antiemetic dopamine antagonists, particularly in parkinsonism-prone patients.53 Strategies that can minimize such risks in geriatric inpatients with delirium include oral, rather than parenteral, use of antipsychotics—preferential use of atypical over typical antipsychotics— and lowest effective dosages.54
In controlled trials, atypical antipsychotics for delirium showed efficacy compared with haloperidol.52,55 However, there is no research that demonstrates any advantage of one atypical over another.25
In Mr. D’s case, the most important intervention for managing delirium caused by NMS is to discontinue all dopamine antagonists and treat agitation with judicious doses of a benzodiazepine, with supportive care.17 In cases of sudden discontinuation or a dosage decrease of dopamine agonists, these medications should be resumed or optimized to minimize the risk of NMS-associated rhabdomyolysis and subsequent renal failure.17 Antipsychotics carry an increased risk of stroke and mortality in older patients with established or evolving neurocognitive disorders56,57 and can cause prolongation of the QTc interval.57
Other medications that could be used for delirium include cholinesterase inhibitors58,59 (although larger trials and a systematic review did not support this use60), and 5-HT receptor antagonists,61 such as trazodone. Benzodiazepines, such as lorazepam, are first-line treatment for delirium associated with seizures or withdrawal from alcohol, sedatives, hypnotics, and anxiolytics and for delirium caused by NMS. Be cautious about using benzodiazepines in geriatric patients because of a risk of respiratory depression, falls, sedation, and amnesia.
Geriatric patients with alcoholism and those with malnutrition are prone to thiamine and vitamin B12 deficiencies, which can induce delirium. Laboratory assessment and consideration of supplementation is recommended. Despite high occurrence of delirium in hospitalized older adults with preexisting comorbid neurocognitive disorders, there is no standard care for delirium comorbid with another neurocognitive disorder.62 Clinical practice guidelines for older patients receiving palliative care have been developed63; the goal is to minimize suffering and discomfort in patients in palliative care.64
Post-delirium prophylaxis. Medications for delirium usually can be tapered and discontinued once the episode has resolved and the patient is stable; it is common to discontinue medications when the patient has been symptom-free for 1 week.65 Some patients (eg, with end-stage liver disease, disseminated cancer) are prone to recurrent or to prolonged or chronic delirium. A period of post-recovery treatment with antipsychotics—even indefinite treatment in some cases—should be considered.
Post-delirium debriefing and aftercare. The psychological complications of delirium are distressing for the patient and his (her) caregivers. Psychiatric complications associated with delirium, including acute stress disorder—which might predict posttraumatic stress disorder—have been explored; early recognition and treatment may improve long-term outcomes.66 After recovery from acute delirium, cognitive assessment (eg, MMSE67 or Montreal Cognitive Assessment68) is recommended to validate current cognitive status because patients may have persistent decrement in cognitive function compared with pre-delirium condition, even after recovery from the acute episode.
Post-delirium debriefing may help patients who have recovered from a delirium episode. Patients may fear that their brief period of hallucinations might represent the onset of a chronic-relapsing psychotic disorder. Allow patients to communicate their distress about the delirium episode and give them the opportunity to talk through the experience. Brief them on the possibility that delirium will recur and advise them to seek emergency medical care in case of recurrence. Advise patients to monitor and maintain a normal sleep-wake cycle.
Family members can watch for syndromal recurrence of delirium. They should be encouraged to discuss their reaction to having seen their relative in a delirious state.
Health care systems with integrated electronic medical records should list “delirium, resolved” on the patient’s illness profile or problem list and alert the patient’s primary care provider to the delirium history to avoid future exposure to delirium-provocative medications, and to prompt the provider to assume an active role in post-delirium care, including delirium recurrence surveillance, medication adjustment, risk factor management, and post-recovery cognitive assessment.
Bottom Line
Evaluation of delirium in geriatric patients includes clinical vigilance and screening, differentiating delirium from other neurocognitive disorders, and identifying and treating underlying causes. Perioperative use of antipsychotics may reduce the incidence of delirium, although hospital length of stay generally has not been reduced with prophylaxis. Management interventions include staff education, systematic screening, use of multicomponent interventions, and pharmacologic interventions.
Related Resources
• Downing LJ, Caprio TV, Lyness JM. Geriatric psychiatry review: differential diagnosis and treatment of the 3 D’s - delirium, dementia, and depression. Curr Psychiatry Rep. 2013;15(6):365.
• Brooks PB. Postoperative delirium in elderly patients. Am J Nurs. 2012;112(9):38-49.
Drug Brand Names
Carbidopa/levodopa • Sinemet Midazolam • Versed
Dexmedetomidine • Precedex Olanzapine • Zyprexa
Haloperidol • Haldol Propofol • Diprivan
Lithium • Eskalith, Lithobid Quetiapine • Seroquel
Lorazepam • Ativan Risperidone • Risperdal
Metoclopramide • Reglan Trazodone • Desyrel
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders, fifth edition. Washington, DC: American Psychiatric Association; 2013.
2. World Health Organization. The ICD-10 classification of mental and behavioural disorders. Diagnostic criteria for research. Geneva, Switzerland: WHO; 1993.
3. Lipowski ZJ. Delirium in the elderly patient. N Engl J Med. 1989;320(9):578-582.
4. Meagher DJ, Trzepacz PT. Motoric subtypes of delirium. Semin Clin Neuropsychiatry. 2000;5(2):75-85.
5. Rabinowitz T. Delirium: an important (but often unrecognized) clinical syndrome. Curr Psychiatry Rep. 2002;4(3):202-208.
6. Marcantonio ER, Ta T, Duthie E, et al. Delirium severity and psychomotor types: their relationship with outcomes after hip fracture repair. Am J Geriatr Soc. 2002;50(5):850-857.
7. Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. 2001;286(21):2703-2710.
8. Duppils GS, Wikblad K. Delirium: behavioural changes before and during the prodromal phase. J Clin Nurs. 2004;13(5):609-616.
9. de Jonghe JF, Kalisvaart KJ, Dijkstra M, et al. Early symptoms in the prodromal phase of delirium: a prospective cohort study in elderly patients undergoing hip surgery. Am J Geriatr Psychiatry. 2007;15(2):112-121.
10. Cook IA. Guideline watch: practice guideline for the treatment of patients with delirium. Arlington, VA: American Psychiatric Publishing; 2004.
11. Hogan D, Gage L, Bruto V, et al. National guidelines for seniors’ mental health: the assessment and treatment of delirium. Canadian Journal of Geriatrics. 2006;9(suppl 2):S42-51.
12. Leentjens AF, Diefenbacher A. A survey of delirium guidelines in Europe. J Psychosom Res. 2006;61(1):123-128.
13. Tropea J, Slee JA, Brand CA, et al. Clinical practice guidelines for the management of delirium in older people in Australia. Australas J Ageing. 2008;27(3):150-156.
14. Mittal D, Majithia D, Kennedy R, et al. Differences in characteristics and outcome of delirium as based on referral patterns. Psychosomatics. 2006;47(5):367-375.
15. Grover S, Subodh BN, Avasthi A, et al. Prevalence and clinical profile of delirium: a study from a tertiary-care hospital in north India. Gen Hosp Psychiatry. 2009;31(1): 25-29.
16. Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12): 941-948.
17. Strawn JR, Keck PE Jr, Caroff SN. Neuroleptic malignant syndrome. Am J Psychiatry. 2007;164(6):870-876.
18. Dobmejer K. Delirium in elderly medical patients. Clinical Geriatrics. 1996;4:43-68.
19. Leentjens AF, Maclullich AM, Meagher DJ. Delirium, Cinderella no more...? J Psychosom Res. 2008;65(3):205.
20. Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol. 2009;5(4):210-220.
21. Streubel PN, Ricci WM, Gardner MJ. Fragility fractures: preoperative, perioperative, and postoperative management. Current Orthopaedic Practice. 2009;20(5):482-489.
22. Spronk PE, Riekerk B, Hofhuis J, et al. Occurrence of delirium is severely underestimated in the ICU during daily care. Intensive Care Med. 2009;35(7):1276-1280.
23. Lawlor PG, Gagnon B, Mancini IL, et al. Occurrence, causes, and outcome of delirium in patients with advanced cancer: a prospective study. Arch Intern Med. 2000;160(6):786-794.
24. Ganzini L. Care of patients with delirium at the end of life. Annals of Long-Term Care. 2007;15(3):35-40.
25. Bourne RS, Tahir TA, Borthwick M, et al. Drug treatment of delirium: past, present and future. J Psychosom Res. 2008;65(3):273-282.
26. Yokota H, Ogawa S, Kurokawa A, et al. Regional cerebral blood flow in delirium patients. Psychiatry Clin Neurosci. 2003;57(3):337-339.
27. Maldonado JR. Pathoetiological model of delirium: a comprehensive understanding of the neurobiology of delirium and an evidence-based approach to prevention and treatment. Crit Care Clin. 2008;24(4):789-856, ix.
28. Trzepacz PT. Is there a final common neural pathway in delirium? Focus on acetylcholine and dopamine. Semin Clin Neuropsychiatry. 2000;5(2):132-148.
29. Inouye SK. The dilemma of delirium: clinical and research controversies regarding diagnosis and evaluation of delirium in hospitalized elderly medical patients. Am J Med. 1994;97(3):278-288.
30. Laurila JV, Laakkonen ML, Tilvis RS, et al. Predisposing and precipitating factors for delirium in a frail geriatric population. J Psychosom Res. 2008;65(3):249-254.
31. Morandi A, McCurley J, Vasilevskis EE, et al. Tools to detect delirium superimposed on dementia: a systematic review. J Am Geriatr Soc. 2012;60(11):2005-2013.
32. Kazmierski J, Kowman M, Banach M, et al. The use of DSM-IV and ICD-10 criteria and diagnostic scales for delirium among cardiac surgery patients: results from the IPDACS study. J Neuropsychiatry Clin Neurosci. 2010; 22(4):426-432.
33. Breitbart W, Rosenfeld B, Roth A, et al. The Memorial Delirium Rating Scale. J Pain Symptom Manage. 1997;13(3):128-137.
34. Wong CL, Holroyd-Leduc J, Simel DL, et al. Does this patient have delirium?: value of bedside instruments. JAMA. 2010;304(7):779-786.
35. Marcantonio ER, Flacker JM, Wright RJ, et al. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2011;49(5):516-522.
36. Lundström M, Edlund A, Karlsson S, et al. A multifactorial intervention program reduces the duration of delirium, length of hospitalization, and mortality in delirious patients. J Am Geriatr Soc. 2005;53(4):622-628.
37. Lundström M, Olofsson B, Stenvall M, et al. Postoperative delirium in old patients with femoral neck fracture: a randomized intervention study. Aging Clin Exp Res. 2007; 19(3):178-186.
38. Kratz A. Use of the acute confusion protocol: a research utilization project. J Nurs Care Qual. 2008;23(4):331-337.
39. Prakanrattana U, Prapaitrakool S. Efficacy of risperidone for prevention of postoperative delirium in cardiac surgery. Anaesth Intensive Care. 2007;35(5):714-719.
40. Kaneko T, Cai J, Ishikura T, et al. Prophylactic consecutive administration of haloperidol can reduce the occurrence of postoperative delirium in gastrointestinal surgery. Yonago Acta Medica. 1999;42:179-184.
41. Larsen KA, Kelly SE, Stern TA, et al. Administration of olanzapine to prevent postoperative delirium in elderly joint-replacement patients: a randomized, controlled trial. Psychosomatics. 2010;51(5):409-418.
42. Kalisvaart KJ, de Jonghe JF, Bogaards MJ, et al. Haloperidol prophylaxis for elderly hip-surgery patients at risk for delirium: a randomized placebo-controlled study. J Am Geriatr Soc. 2005;53(10):1658-1666.
43. Hakim SM, Othman AI, Naoum DO. Early treatment with risperidone for subsyndromal delirium after on-pump cardiac surgery in the elderly: a randomized trial. Anesthesiology. 2012;116(5):987-997.
44. Maldonado JR, Wysong A, van der Starre PJ, et al. Dexmedetomidine and the reduction of postoperative delirium after cardiac surgery. Psychosomatics. 2009;50(3): 206-217.
45. Short J. Use of dexmedetomidine for primary sedation in a general intensive care unit. Crit Care Nurse. 2010;30(1): 29-38; quiz 39.
46. Practice guideline for the treatment of patients with delirium. American Psychiatric Association [Comment in: Treatment of patients with delirium. Am J Psychiatry. 2000.]. Am J Psychiatry. 1999;156(suppl 5):1-20.
47. Maldonado JR. Delirium in the acute care setting: characteristics, diagnosis, and treatment. Crit Care Clin. 2008;24(4):657-722, vii.
48. Platt MM, Breitbart W, Smith M, et al. Efficacy of neuroleptics for hypoactive delirium. J Neuropsychiatry Clin Neurosci. 1994;6(1):66-67.
49. Lonergan E, Britton AM, Luxenberg J, et al. Antipsychotics for delirium. Cochrane Database Syst Rev. 2007;(2):CD005594.
50. Seitz DP, Gill SS, van Zyl LT. Antipsychotics in the treatment of delirium: a systematic review. J Clin Psychiatry. 2007;68(1):11-21.
51. Breitbart W, Marotta R, Platt MM, et al. A double-blind trial of haloperidol, chlorpromazine, and lorazepam in the treatment of delirium in hospitalized AIDS patients. Am J Psychiatry. 1996;153(2):231-237.
52. Hu H, Deng W, Yang H, et al. Olanzapine and haloperidol for senile delirium: a randomized controlled observation. Chinese Journal of Clinical Rehabilitation. 2006;10(42): 188-190.
53. Friedman JH, Fernandez HH. Atypical antipsychotics in Parkinson-sensitive populations. J Geriatr Psychiatry Neurol. 2002;15(3):156-170.
54. Seitz DP, Gill SS. Neuroleptic malignant syndrome complicating antipsychotic treatment of delirium or agitation in medical and surgical patients: case reports and a review of the literature. Psychosomatics. 2009; 50(1):8-15.
55. Han CS, Kim YK. A double-blind trial of risperidone and haloperidol for the treatment of delirium. Psychosomatics. 2004;45(4):297-301.
56. Sink KM, Holden KF, Yaffe K. Pharmacological treatment of neuropsychiatric symptoms of dementia: a review of the evidence. JAMA. 2005;293(5):596-608.
57. Hermann N, Lanctôt KL. Atypical antipsychotics for neuropsychiatric symptoms of dementia: malignant or maligned? Drug Saf. 2006;29(10):833-843.
58. Noyan MA, Elbi H, Aksu H. Donepezil for anticholinergic drug intoxication: a case report. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27(5):885-887.
59. Gleason OC. Donepezil for postoperative delirium. Psychosomatics. 2003;44(5):437-438.
60. Overshott R, Karim S, Burns A. Cholinesterase inhibitors for delirium. Cochrane Database Syst Rev. 2008;(1): CD005317.
61. Davis MP. Does trazodone have a role in palliating symptoms? Support Care Cancer. 2007;15(2):221-224.
62. Fick DM, Agostini JV, Inouye SK. Delirium superimposed on dementia: a systematic review. J Am Geriatr Soc. 2002; 50(10):1723-1732.
63. Brajtman S, Wright D, Hogan D, et al. Developing guidelines for the assessment and treatment of delirium in older adults at the end of life. Can Geriatr J. 2011;14(2):40-50.
64. Caraceni A, Simonetti F. Palliating delirium in patients with cancer. Lancet Oncol. 2009;10(2):164-172.
65. Alexopoulos GS, Streim J, Carpenter D, et al; Expert Consensus Panel for using Antipsychotic Drugs in Older Patients. Using antipsychotic agents in older patients. J Clin Psychiatry. 2004;65(suppl 2):5-99; discussion 100-102; quiz 103-104.
66. Granja C, Gomes E, Amaro A, et al. Understanding posttraumatic stress disorder-related symptoms after critical care: the early illness amnesia hypothesis. Crit Care Med. 2008;36(10):2801-2809.
67. Ringdal GI, Ringdal K, Juliebø V, et al. Using the Mini- Mental State Examination to screen for delirium in elderly patients with hip fracture. Dement Geriatr Cogn Disord. 2011;32(6):394-400.
68. Olson RA, Chhanabhai T, McKenzie M. Feasibility study of the Montreal Cognitive Assessment (MoCA) in patients with brain metastases. Support Care Cancer. 2008;16(11):1273-1278.
Although delirium has many descriptive terms (Table 1), a common unifying term is “acute global cognitive dysfunction,” now recognized as delirium; a consensus supported by DSM-51 and ICD-102 (Table 2). According to DSM-5, the essential feature is a disturbance of attention or awareness that is accompanied by a change in baseline cognition that cannot be explained by another preexisting, established, or evolving neurocognitive disorder (the newly named DSM-5 entity for dementia syndromes).1 Because delirium affects the cortex diffusely, psychiatric symptoms can include cognitive, mood, anxiety, or psychotic symptoms. Because many systemic illnesses can induce delirium, the differential diagnosis spans all organ systems.
Three subtypes
Delirium can be classified, based on symptoms,3,4 into 3 subtypes: hyperactive-hyperalert, hypoactive-hypoalert, and mixed delirium. Hyperactive patients present with restlessness and agitation. Hypoactive patients are lethargic, confused, slow to respond to questions, and often appear depressed. The differential prognostic significance of these subtypes has been examined in the literature, with conflicting results. Rabinowitz5 reported that hypoactive delirium has the worst prognosis, while Marcantonio et al6 indicated that the hyperactive subtype is associated with the highest mortality rate. Mixed delirium, with periods of both hyperactivity and hypoactivity, is the most common type of delirium.7
A prodromal phase, characterized by anxiety, frequent requests for nursing and medical assistance, decreased attention, restlessness, vivid dreams, disorientation immediately after awakening, and hallucinations, can occur before an episode of full-spectrum delirium; this prodromal state often is identified retrospectively —after the patient is in an episode of delirium.8,9
Evidence-based guidelines aim to improve recognition and clinical management.10-13 Disruptive behavior is the main reason for psychiatric referral in delirium.14,15 Delayed psychiatric consultation because of non-recognition of delirium is related to variables such as older age; history of a pre-existing, comorbid neurocognitive disorder; and the clinical appearance of hypoactive delirium.14
The case of Mr. D (Box),16 illustrates how the emergence of antipsychotic-associated neuroleptic malignant syndrome (NMS) can complicate antipsychotic treatment of delirium in a geriatric medical patient, although delirium also is a common presentation in NMS.17 Delirium developed after an increase in carbidopa/levodopa, which has central dopaminergic effects that can precipitate delirium, particularly in a geriatric patient with preexisting comorbid neurocognitive disorder. Further complicating Mr. D’s delirium presentation was the development of NMS, which had a multifactorial causation, such as the use of dopamine antagonists (ie, quetiapine, metoclopramide), and an abrupt decrease of a dopaminergic agent (ie, carbidopa/levodopa), all inducing a central dopamine relative hypoactivity.
Epidemiology
Delirium is more common in older patients,15 and is seen in 30% to 40% of hospitalized geriatric patients.18 Delirium in older patients, compared with other adults, is associated with more severe cognitive impairment.19 It is common among geriatric surgical patients (15% to 62%)20 with a peak 2 to 5 days postoperatively for hip fracture,21 and often is seen in ICU patients (70% to 87%).20 However, Spronk et al22 found that delirium is significantly under-recognized in the ICU. Nearly 90% of terminally ill patients become delirious before death.23 Terminal delirium often is unrecognized and can interfere with assessment of other clinical problems.24 A preexisting history of comorbid neurocognitive disorder was evident in as many as two-thirds of delirium cases.25
Pathophysiology and risk factors
The pathophysiology of delirium has been characterized as an imbalance of CNS metabolism, including decreased blood flow in various regions of the brain that may normalize once delirium resolves.26 Studies describe the simultaneous decrease of cholinergic transmission and dopaminergic excess.27,28 Predisposing and precipitating factors for delirium that are of particular importance in geriatric patients include:
• advanced age
• CNS disease
• infection
• cognitive impairment
• male sex
• poor nutrition
• dehydration and other metabolic abnormalities
• cardiovascular events
• substance use
• medication
• sensory deprivation (eg, impaired vision or hearing)
• sleep deprivation
• low level of physical activity.27,29,30
Table 3 lists the most common delirium-provocative medications.27
Evaluation and psychometric scales
The EEG can be useful in evaluating delirium, especially in clinically ambiguous cases. EEG findings may indicate generalized slowing or dropout of the posterior dominant rhythm, and generalized slow theta and delta waves, findings that are more common in delirium than in other neurocognitive disorders and other psychiatric illnesses. The EEG must be interpreted in the context of the delirium diagnostic workup, because abnormalities seen in other neurocognitive disorders can overlap with those of delirium.31
The EEG referral should specify the clinical suspicion of delirium to help interpret the results. Delirium cases in which the patient’s previous cognitive status is unknown may benefit from EEG evaluation, such as:
• in possible status epilepticus
• when delirium improvement has reached a plateau at a lower level of cognitive function than before onset of delirium
• when the patient is unable or unwilling to complete a psychiatric interview.27
Assessment instruments are available to diagnose and monitor delirium (Table 4). Typically, delirium assessment includes examining levels of arousal, psychomotor activity, cognition (ie, orientation, attention, and memory), and perceptual disturbances.
Psychometrically, a review of Table 4 suggests that validity appeared stable with adequate specificity (64% to 99%) but more variable sensitivity (36% to 100%). These reliability parameters also will be affected by the classification system (ie, DSM vs ICD) and the cut-off score employed.32 Most measures (eg, Confusion Assessment Method [CAM], CAM-ICU) provide an adequate sample of behavioral (ie, level of alertness), motor (ie, psychomotor activity), and cognitive (ie, orientation, attention, memory, and receptive language) function, with the exception of the Global Attentiveness Rating, which is a 2-minute open conversation protocol between physician and patient.
Some measures are stand-alone instruments, such as the Memorial Delirium Assessment Scale, whereas the CAM requires administration of separate cognitive screens, including the Mini-Mental State Examination (MMSE) and Digit Span.33 Instruments to detect delirium in critically ill patients are a more recent development. Wong et al34 reported that the most widely studied tool was the CAM. Obtaining collateral information from family, caregivers, and hospital staff is essential, particularly given the fluctuating nature of delirium.
Management
Prevention. Identify patients at high risk of delirium so that preventive strategies can be employed. Multi-component, nonpharmacotherapeutic interventions are used in clinical settings but few randomized trials have been conducted. The contributing effectiveness of individual components is not well-studied, but most include staff education to increase awareness of delirium. Of 3 multi-component intervention randomized trials, 2 reported a significantly lower incidence of delirium in the intervention group.35-37 Implementation of a multi-component protocol in medical/ surgical units was associated with a significant reduction in use of restraints.38
As in Mr. D’s case, complex drug regimens, particularly for CNS illness, can increase the risk of delirium. Considering the medication profile for patients with complex systemic illness—in particular, minimizing the use anticholinergics and dopamine agonists— may be crucial in preventing delirium.
Prophylactic administration of antipsychotics may reduce the risk of developing postoperative delirium.39 Studies of the use of these agents were characterized by small sample sizes and selected groups of patient populations. Of the 4 randomized studies evaluating prophylactic antipsychotics (vs placebo), 3 found a lower incidence of delirium in the intervention groups.39-41
A study of haloperidol in post-GI surgery patients showed a reduced occurrence of delirium,40 whereas its prophylactic use in patients undergoing hip surgery42 did not reduce the incidence of delirium compared with placebo, but did decrease severity when delirium occurred.42
Risperidone39 in post-cardiac surgery and olanzapine41 perioperatively in patients undergoing total knee or hip replacement have been shown to decrease delirium severity and duration. Targeted prophylaxis with risperidone43 in post-cardiac surgery patients who showed disturbed cognition but did not meet criteria for delirium reduced the number of patients requiring medication, compared with placebo.43
Dexmedetomidine, an α-2 adrenergic receptor agonist, compared with propofol or midazolam in post-cardiac valve surgery patients, resulted in a decreased incidence of delirium but no difference in delirium duration, hospital length of stay, or use of other medications.44 However, other studies have shown that dexmedetomidine reduces ICU length of stay and duration of mechanical ventilation.45
Treatment. Management of hospitalized medically ill geriatric patients with delirium is challenging and requires a comprehensive approach. The first step in delirium management is prompt identification and management of systemic medical disturbances associated with the delirium episode. First-line, nonpharmacotherapeutic strategies for patients with delirium include:
• reorientation
• behavioral interventions (eg, use of clear instructions and frequent eye contact with patients)
• environmental interventions (eg, minimal noise, adequate lighting, and limited room and staff changes)
• avoidance of physical restraints.46
Consider employing family members or hospital staff sitters to stay with the patient and to reassure, reorient, and watch for agitation and other unsafe behaviors (eg, attempted elopement). Psychoeducation for the patient and family on the phenomenology of delirium can be helpful.
The use of drug treatment strategies should be integrated into a comprehensive approach that includes the routine use of nondrug measures.46 Using medications for treating hypoactive delirium, formerly controversial, now has wider acceptance.47,48 A few high-quality randomized trials have been performed.25,49,50
Pharmacotherapy, especially in frail patients, should be initiated at the lowest starting dosage and titrated cautiously to clinical effect and for the shortest period of time necessary. Antipsychotics are preferred agents for treating all subtypes of delirium; haloperidol is widely used.46,51,52 However, antipsychotics, including haloperidol, can be associated with adverse neurologic effects such as extrapyramidal symptoms (EPS) and NMS.
Although reported less frequently than with haloperidol, other agents have been implicated in development of EPS and NMS, including atypical antipsychotics and antiemetic dopamine antagonists, particularly in parkinsonism-prone patients.53 Strategies that can minimize such risks in geriatric inpatients with delirium include oral, rather than parenteral, use of antipsychotics—preferential use of atypical over typical antipsychotics— and lowest effective dosages.54
In controlled trials, atypical antipsychotics for delirium showed efficacy compared with haloperidol.52,55 However, there is no research that demonstrates any advantage of one atypical over another.25
In Mr. D’s case, the most important intervention for managing delirium caused by NMS is to discontinue all dopamine antagonists and treat agitation with judicious doses of a benzodiazepine, with supportive care.17 In cases of sudden discontinuation or a dosage decrease of dopamine agonists, these medications should be resumed or optimized to minimize the risk of NMS-associated rhabdomyolysis and subsequent renal failure.17 Antipsychotics carry an increased risk of stroke and mortality in older patients with established or evolving neurocognitive disorders56,57 and can cause prolongation of the QTc interval.57
Other medications that could be used for delirium include cholinesterase inhibitors58,59 (although larger trials and a systematic review did not support this use60), and 5-HT receptor antagonists,61 such as trazodone. Benzodiazepines, such as lorazepam, are first-line treatment for delirium associated with seizures or withdrawal from alcohol, sedatives, hypnotics, and anxiolytics and for delirium caused by NMS. Be cautious about using benzodiazepines in geriatric patients because of a risk of respiratory depression, falls, sedation, and amnesia.
Geriatric patients with alcoholism and those with malnutrition are prone to thiamine and vitamin B12 deficiencies, which can induce delirium. Laboratory assessment and consideration of supplementation is recommended. Despite high occurrence of delirium in hospitalized older adults with preexisting comorbid neurocognitive disorders, there is no standard care for delirium comorbid with another neurocognitive disorder.62 Clinical practice guidelines for older patients receiving palliative care have been developed63; the goal is to minimize suffering and discomfort in patients in palliative care.64
Post-delirium prophylaxis. Medications for delirium usually can be tapered and discontinued once the episode has resolved and the patient is stable; it is common to discontinue medications when the patient has been symptom-free for 1 week.65 Some patients (eg, with end-stage liver disease, disseminated cancer) are prone to recurrent or to prolonged or chronic delirium. A period of post-recovery treatment with antipsychotics—even indefinite treatment in some cases—should be considered.
Post-delirium debriefing and aftercare. The psychological complications of delirium are distressing for the patient and his (her) caregivers. Psychiatric complications associated with delirium, including acute stress disorder—which might predict posttraumatic stress disorder—have been explored; early recognition and treatment may improve long-term outcomes.66 After recovery from acute delirium, cognitive assessment (eg, MMSE67 or Montreal Cognitive Assessment68) is recommended to validate current cognitive status because patients may have persistent decrement in cognitive function compared with pre-delirium condition, even after recovery from the acute episode.
Post-delirium debriefing may help patients who have recovered from a delirium episode. Patients may fear that their brief period of hallucinations might represent the onset of a chronic-relapsing psychotic disorder. Allow patients to communicate their distress about the delirium episode and give them the opportunity to talk through the experience. Brief them on the possibility that delirium will recur and advise them to seek emergency medical care in case of recurrence. Advise patients to monitor and maintain a normal sleep-wake cycle.
Family members can watch for syndromal recurrence of delirium. They should be encouraged to discuss their reaction to having seen their relative in a delirious state.
Health care systems with integrated electronic medical records should list “delirium, resolved” on the patient’s illness profile or problem list and alert the patient’s primary care provider to the delirium history to avoid future exposure to delirium-provocative medications, and to prompt the provider to assume an active role in post-delirium care, including delirium recurrence surveillance, medication adjustment, risk factor management, and post-recovery cognitive assessment.
Bottom Line
Evaluation of delirium in geriatric patients includes clinical vigilance and screening, differentiating delirium from other neurocognitive disorders, and identifying and treating underlying causes. Perioperative use of antipsychotics may reduce the incidence of delirium, although hospital length of stay generally has not been reduced with prophylaxis. Management interventions include staff education, systematic screening, use of multicomponent interventions, and pharmacologic interventions.
Related Resources
• Downing LJ, Caprio TV, Lyness JM. Geriatric psychiatry review: differential diagnosis and treatment of the 3 D’s - delirium, dementia, and depression. Curr Psychiatry Rep. 2013;15(6):365.
• Brooks PB. Postoperative delirium in elderly patients. Am J Nurs. 2012;112(9):38-49.
Drug Brand Names
Carbidopa/levodopa • Sinemet Midazolam • Versed
Dexmedetomidine • Precedex Olanzapine • Zyprexa
Haloperidol • Haldol Propofol • Diprivan
Lithium • Eskalith, Lithobid Quetiapine • Seroquel
Lorazepam • Ativan Risperidone • Risperdal
Metoclopramide • Reglan Trazodone • Desyrel
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Although delirium has many descriptive terms (Table 1), a common unifying term is “acute global cognitive dysfunction,” now recognized as delirium; a consensus supported by DSM-51 and ICD-102 (Table 2). According to DSM-5, the essential feature is a disturbance of attention or awareness that is accompanied by a change in baseline cognition that cannot be explained by another preexisting, established, or evolving neurocognitive disorder (the newly named DSM-5 entity for dementia syndromes).1 Because delirium affects the cortex diffusely, psychiatric symptoms can include cognitive, mood, anxiety, or psychotic symptoms. Because many systemic illnesses can induce delirium, the differential diagnosis spans all organ systems.
Three subtypes
Delirium can be classified, based on symptoms,3,4 into 3 subtypes: hyperactive-hyperalert, hypoactive-hypoalert, and mixed delirium. Hyperactive patients present with restlessness and agitation. Hypoactive patients are lethargic, confused, slow to respond to questions, and often appear depressed. The differential prognostic significance of these subtypes has been examined in the literature, with conflicting results. Rabinowitz5 reported that hypoactive delirium has the worst prognosis, while Marcantonio et al6 indicated that the hyperactive subtype is associated with the highest mortality rate. Mixed delirium, with periods of both hyperactivity and hypoactivity, is the most common type of delirium.7
A prodromal phase, characterized by anxiety, frequent requests for nursing and medical assistance, decreased attention, restlessness, vivid dreams, disorientation immediately after awakening, and hallucinations, can occur before an episode of full-spectrum delirium; this prodromal state often is identified retrospectively —after the patient is in an episode of delirium.8,9
Evidence-based guidelines aim to improve recognition and clinical management.10-13 Disruptive behavior is the main reason for psychiatric referral in delirium.14,15 Delayed psychiatric consultation because of non-recognition of delirium is related to variables such as older age; history of a pre-existing, comorbid neurocognitive disorder; and the clinical appearance of hypoactive delirium.14
The case of Mr. D (Box),16 illustrates how the emergence of antipsychotic-associated neuroleptic malignant syndrome (NMS) can complicate antipsychotic treatment of delirium in a geriatric medical patient, although delirium also is a common presentation in NMS.17 Delirium developed after an increase in carbidopa/levodopa, which has central dopaminergic effects that can precipitate delirium, particularly in a geriatric patient with preexisting comorbid neurocognitive disorder. Further complicating Mr. D’s delirium presentation was the development of NMS, which had a multifactorial causation, such as the use of dopamine antagonists (ie, quetiapine, metoclopramide), and an abrupt decrease of a dopaminergic agent (ie, carbidopa/levodopa), all inducing a central dopamine relative hypoactivity.
Epidemiology
Delirium is more common in older patients,15 and is seen in 30% to 40% of hospitalized geriatric patients.18 Delirium in older patients, compared with other adults, is associated with more severe cognitive impairment.19 It is common among geriatric surgical patients (15% to 62%)20 with a peak 2 to 5 days postoperatively for hip fracture,21 and often is seen in ICU patients (70% to 87%).20 However, Spronk et al22 found that delirium is significantly under-recognized in the ICU. Nearly 90% of terminally ill patients become delirious before death.23 Terminal delirium often is unrecognized and can interfere with assessment of other clinical problems.24 A preexisting history of comorbid neurocognitive disorder was evident in as many as two-thirds of delirium cases.25
Pathophysiology and risk factors
The pathophysiology of delirium has been characterized as an imbalance of CNS metabolism, including decreased blood flow in various regions of the brain that may normalize once delirium resolves.26 Studies describe the simultaneous decrease of cholinergic transmission and dopaminergic excess.27,28 Predisposing and precipitating factors for delirium that are of particular importance in geriatric patients include:
• advanced age
• CNS disease
• infection
• cognitive impairment
• male sex
• poor nutrition
• dehydration and other metabolic abnormalities
• cardiovascular events
• substance use
• medication
• sensory deprivation (eg, impaired vision or hearing)
• sleep deprivation
• low level of physical activity.27,29,30
Table 3 lists the most common delirium-provocative medications.27
Evaluation and psychometric scales
The EEG can be useful in evaluating delirium, especially in clinically ambiguous cases. EEG findings may indicate generalized slowing or dropout of the posterior dominant rhythm, and generalized slow theta and delta waves, findings that are more common in delirium than in other neurocognitive disorders and other psychiatric illnesses. The EEG must be interpreted in the context of the delirium diagnostic workup, because abnormalities seen in other neurocognitive disorders can overlap with those of delirium.31
The EEG referral should specify the clinical suspicion of delirium to help interpret the results. Delirium cases in which the patient’s previous cognitive status is unknown may benefit from EEG evaluation, such as:
• in possible status epilepticus
• when delirium improvement has reached a plateau at a lower level of cognitive function than before onset of delirium
• when the patient is unable or unwilling to complete a psychiatric interview.27
Assessment instruments are available to diagnose and monitor delirium (Table 4). Typically, delirium assessment includes examining levels of arousal, psychomotor activity, cognition (ie, orientation, attention, and memory), and perceptual disturbances.
Psychometrically, a review of Table 4 suggests that validity appeared stable with adequate specificity (64% to 99%) but more variable sensitivity (36% to 100%). These reliability parameters also will be affected by the classification system (ie, DSM vs ICD) and the cut-off score employed.32 Most measures (eg, Confusion Assessment Method [CAM], CAM-ICU) provide an adequate sample of behavioral (ie, level of alertness), motor (ie, psychomotor activity), and cognitive (ie, orientation, attention, memory, and receptive language) function, with the exception of the Global Attentiveness Rating, which is a 2-minute open conversation protocol between physician and patient.
Some measures are stand-alone instruments, such as the Memorial Delirium Assessment Scale, whereas the CAM requires administration of separate cognitive screens, including the Mini-Mental State Examination (MMSE) and Digit Span.33 Instruments to detect delirium in critically ill patients are a more recent development. Wong et al34 reported that the most widely studied tool was the CAM. Obtaining collateral information from family, caregivers, and hospital staff is essential, particularly given the fluctuating nature of delirium.
Management
Prevention. Identify patients at high risk of delirium so that preventive strategies can be employed. Multi-component, nonpharmacotherapeutic interventions are used in clinical settings but few randomized trials have been conducted. The contributing effectiveness of individual components is not well-studied, but most include staff education to increase awareness of delirium. Of 3 multi-component intervention randomized trials, 2 reported a significantly lower incidence of delirium in the intervention group.35-37 Implementation of a multi-component protocol in medical/ surgical units was associated with a significant reduction in use of restraints.38
As in Mr. D’s case, complex drug regimens, particularly for CNS illness, can increase the risk of delirium. Considering the medication profile for patients with complex systemic illness—in particular, minimizing the use anticholinergics and dopamine agonists— may be crucial in preventing delirium.
Prophylactic administration of antipsychotics may reduce the risk of developing postoperative delirium.39 Studies of the use of these agents were characterized by small sample sizes and selected groups of patient populations. Of the 4 randomized studies evaluating prophylactic antipsychotics (vs placebo), 3 found a lower incidence of delirium in the intervention groups.39-41
A study of haloperidol in post-GI surgery patients showed a reduced occurrence of delirium,40 whereas its prophylactic use in patients undergoing hip surgery42 did not reduce the incidence of delirium compared with placebo, but did decrease severity when delirium occurred.42
Risperidone39 in post-cardiac surgery and olanzapine41 perioperatively in patients undergoing total knee or hip replacement have been shown to decrease delirium severity and duration. Targeted prophylaxis with risperidone43 in post-cardiac surgery patients who showed disturbed cognition but did not meet criteria for delirium reduced the number of patients requiring medication, compared with placebo.43
Dexmedetomidine, an α-2 adrenergic receptor agonist, compared with propofol or midazolam in post-cardiac valve surgery patients, resulted in a decreased incidence of delirium but no difference in delirium duration, hospital length of stay, or use of other medications.44 However, other studies have shown that dexmedetomidine reduces ICU length of stay and duration of mechanical ventilation.45
Treatment. Management of hospitalized medically ill geriatric patients with delirium is challenging and requires a comprehensive approach. The first step in delirium management is prompt identification and management of systemic medical disturbances associated with the delirium episode. First-line, nonpharmacotherapeutic strategies for patients with delirium include:
• reorientation
• behavioral interventions (eg, use of clear instructions and frequent eye contact with patients)
• environmental interventions (eg, minimal noise, adequate lighting, and limited room and staff changes)
• avoidance of physical restraints.46
Consider employing family members or hospital staff sitters to stay with the patient and to reassure, reorient, and watch for agitation and other unsafe behaviors (eg, attempted elopement). Psychoeducation for the patient and family on the phenomenology of delirium can be helpful.
The use of drug treatment strategies should be integrated into a comprehensive approach that includes the routine use of nondrug measures.46 Using medications for treating hypoactive delirium, formerly controversial, now has wider acceptance.47,48 A few high-quality randomized trials have been performed.25,49,50
Pharmacotherapy, especially in frail patients, should be initiated at the lowest starting dosage and titrated cautiously to clinical effect and for the shortest period of time necessary. Antipsychotics are preferred agents for treating all subtypes of delirium; haloperidol is widely used.46,51,52 However, antipsychotics, including haloperidol, can be associated with adverse neurologic effects such as extrapyramidal symptoms (EPS) and NMS.
Although reported less frequently than with haloperidol, other agents have been implicated in development of EPS and NMS, including atypical antipsychotics and antiemetic dopamine antagonists, particularly in parkinsonism-prone patients.53 Strategies that can minimize such risks in geriatric inpatients with delirium include oral, rather than parenteral, use of antipsychotics—preferential use of atypical over typical antipsychotics— and lowest effective dosages.54
In controlled trials, atypical antipsychotics for delirium showed efficacy compared with haloperidol.52,55 However, there is no research that demonstrates any advantage of one atypical over another.25
In Mr. D’s case, the most important intervention for managing delirium caused by NMS is to discontinue all dopamine antagonists and treat agitation with judicious doses of a benzodiazepine, with supportive care.17 In cases of sudden discontinuation or a dosage decrease of dopamine agonists, these medications should be resumed or optimized to minimize the risk of NMS-associated rhabdomyolysis and subsequent renal failure.17 Antipsychotics carry an increased risk of stroke and mortality in older patients with established or evolving neurocognitive disorders56,57 and can cause prolongation of the QTc interval.57
Other medications that could be used for delirium include cholinesterase inhibitors58,59 (although larger trials and a systematic review did not support this use60), and 5-HT receptor antagonists,61 such as trazodone. Benzodiazepines, such as lorazepam, are first-line treatment for delirium associated with seizures or withdrawal from alcohol, sedatives, hypnotics, and anxiolytics and for delirium caused by NMS. Be cautious about using benzodiazepines in geriatric patients because of a risk of respiratory depression, falls, sedation, and amnesia.
Geriatric patients with alcoholism and those with malnutrition are prone to thiamine and vitamin B12 deficiencies, which can induce delirium. Laboratory assessment and consideration of supplementation is recommended. Despite high occurrence of delirium in hospitalized older adults with preexisting comorbid neurocognitive disorders, there is no standard care for delirium comorbid with another neurocognitive disorder.62 Clinical practice guidelines for older patients receiving palliative care have been developed63; the goal is to minimize suffering and discomfort in patients in palliative care.64
Post-delirium prophylaxis. Medications for delirium usually can be tapered and discontinued once the episode has resolved and the patient is stable; it is common to discontinue medications when the patient has been symptom-free for 1 week.65 Some patients (eg, with end-stage liver disease, disseminated cancer) are prone to recurrent or to prolonged or chronic delirium. A period of post-recovery treatment with antipsychotics—even indefinite treatment in some cases—should be considered.
Post-delirium debriefing and aftercare. The psychological complications of delirium are distressing for the patient and his (her) caregivers. Psychiatric complications associated with delirium, including acute stress disorder—which might predict posttraumatic stress disorder—have been explored; early recognition and treatment may improve long-term outcomes.66 After recovery from acute delirium, cognitive assessment (eg, MMSE67 or Montreal Cognitive Assessment68) is recommended to validate current cognitive status because patients may have persistent decrement in cognitive function compared with pre-delirium condition, even after recovery from the acute episode.
Post-delirium debriefing may help patients who have recovered from a delirium episode. Patients may fear that their brief period of hallucinations might represent the onset of a chronic-relapsing psychotic disorder. Allow patients to communicate their distress about the delirium episode and give them the opportunity to talk through the experience. Brief them on the possibility that delirium will recur and advise them to seek emergency medical care in case of recurrence. Advise patients to monitor and maintain a normal sleep-wake cycle.
Family members can watch for syndromal recurrence of delirium. They should be encouraged to discuss their reaction to having seen their relative in a delirious state.
Health care systems with integrated electronic medical records should list “delirium, resolved” on the patient’s illness profile or problem list and alert the patient’s primary care provider to the delirium history to avoid future exposure to delirium-provocative medications, and to prompt the provider to assume an active role in post-delirium care, including delirium recurrence surveillance, medication adjustment, risk factor management, and post-recovery cognitive assessment.
Bottom Line
Evaluation of delirium in geriatric patients includes clinical vigilance and screening, differentiating delirium from other neurocognitive disorders, and identifying and treating underlying causes. Perioperative use of antipsychotics may reduce the incidence of delirium, although hospital length of stay generally has not been reduced with prophylaxis. Management interventions include staff education, systematic screening, use of multicomponent interventions, and pharmacologic interventions.
Related Resources
• Downing LJ, Caprio TV, Lyness JM. Geriatric psychiatry review: differential diagnosis and treatment of the 3 D’s - delirium, dementia, and depression. Curr Psychiatry Rep. 2013;15(6):365.
• Brooks PB. Postoperative delirium in elderly patients. Am J Nurs. 2012;112(9):38-49.
Drug Brand Names
Carbidopa/levodopa • Sinemet Midazolam • Versed
Dexmedetomidine • Precedex Olanzapine • Zyprexa
Haloperidol • Haldol Propofol • Diprivan
Lithium • Eskalith, Lithobid Quetiapine • Seroquel
Lorazepam • Ativan Risperidone • Risperdal
Metoclopramide • Reglan Trazodone • Desyrel
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders, fifth edition. Washington, DC: American Psychiatric Association; 2013.
2. World Health Organization. The ICD-10 classification of mental and behavioural disorders. Diagnostic criteria for research. Geneva, Switzerland: WHO; 1993.
3. Lipowski ZJ. Delirium in the elderly patient. N Engl J Med. 1989;320(9):578-582.
4. Meagher DJ, Trzepacz PT. Motoric subtypes of delirium. Semin Clin Neuropsychiatry. 2000;5(2):75-85.
5. Rabinowitz T. Delirium: an important (but often unrecognized) clinical syndrome. Curr Psychiatry Rep. 2002;4(3):202-208.
6. Marcantonio ER, Ta T, Duthie E, et al. Delirium severity and psychomotor types: their relationship with outcomes after hip fracture repair. Am J Geriatr Soc. 2002;50(5):850-857.
7. Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. 2001;286(21):2703-2710.
8. Duppils GS, Wikblad K. Delirium: behavioural changes before and during the prodromal phase. J Clin Nurs. 2004;13(5):609-616.
9. de Jonghe JF, Kalisvaart KJ, Dijkstra M, et al. Early symptoms in the prodromal phase of delirium: a prospective cohort study in elderly patients undergoing hip surgery. Am J Geriatr Psychiatry. 2007;15(2):112-121.
10. Cook IA. Guideline watch: practice guideline for the treatment of patients with delirium. Arlington, VA: American Psychiatric Publishing; 2004.
11. Hogan D, Gage L, Bruto V, et al. National guidelines for seniors’ mental health: the assessment and treatment of delirium. Canadian Journal of Geriatrics. 2006;9(suppl 2):S42-51.
12. Leentjens AF, Diefenbacher A. A survey of delirium guidelines in Europe. J Psychosom Res. 2006;61(1):123-128.
13. Tropea J, Slee JA, Brand CA, et al. Clinical practice guidelines for the management of delirium in older people in Australia. Australas J Ageing. 2008;27(3):150-156.
14. Mittal D, Majithia D, Kennedy R, et al. Differences in characteristics and outcome of delirium as based on referral patterns. Psychosomatics. 2006;47(5):367-375.
15. Grover S, Subodh BN, Avasthi A, et al. Prevalence and clinical profile of delirium: a study from a tertiary-care hospital in north India. Gen Hosp Psychiatry. 2009;31(1): 25-29.
16. Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12): 941-948.
17. Strawn JR, Keck PE Jr, Caroff SN. Neuroleptic malignant syndrome. Am J Psychiatry. 2007;164(6):870-876.
18. Dobmejer K. Delirium in elderly medical patients. Clinical Geriatrics. 1996;4:43-68.
19. Leentjens AF, Maclullich AM, Meagher DJ. Delirium, Cinderella no more...? J Psychosom Res. 2008;65(3):205.
20. Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol. 2009;5(4):210-220.
21. Streubel PN, Ricci WM, Gardner MJ. Fragility fractures: preoperative, perioperative, and postoperative management. Current Orthopaedic Practice. 2009;20(5):482-489.
22. Spronk PE, Riekerk B, Hofhuis J, et al. Occurrence of delirium is severely underestimated in the ICU during daily care. Intensive Care Med. 2009;35(7):1276-1280.
23. Lawlor PG, Gagnon B, Mancini IL, et al. Occurrence, causes, and outcome of delirium in patients with advanced cancer: a prospective study. Arch Intern Med. 2000;160(6):786-794.
24. Ganzini L. Care of patients with delirium at the end of life. Annals of Long-Term Care. 2007;15(3):35-40.
25. Bourne RS, Tahir TA, Borthwick M, et al. Drug treatment of delirium: past, present and future. J Psychosom Res. 2008;65(3):273-282.
26. Yokota H, Ogawa S, Kurokawa A, et al. Regional cerebral blood flow in delirium patients. Psychiatry Clin Neurosci. 2003;57(3):337-339.
27. Maldonado JR. Pathoetiological model of delirium: a comprehensive understanding of the neurobiology of delirium and an evidence-based approach to prevention and treatment. Crit Care Clin. 2008;24(4):789-856, ix.
28. Trzepacz PT. Is there a final common neural pathway in delirium? Focus on acetylcholine and dopamine. Semin Clin Neuropsychiatry. 2000;5(2):132-148.
29. Inouye SK. The dilemma of delirium: clinical and research controversies regarding diagnosis and evaluation of delirium in hospitalized elderly medical patients. Am J Med. 1994;97(3):278-288.
30. Laurila JV, Laakkonen ML, Tilvis RS, et al. Predisposing and precipitating factors for delirium in a frail geriatric population. J Psychosom Res. 2008;65(3):249-254.
31. Morandi A, McCurley J, Vasilevskis EE, et al. Tools to detect delirium superimposed on dementia: a systematic review. J Am Geriatr Soc. 2012;60(11):2005-2013.
32. Kazmierski J, Kowman M, Banach M, et al. The use of DSM-IV and ICD-10 criteria and diagnostic scales for delirium among cardiac surgery patients: results from the IPDACS study. J Neuropsychiatry Clin Neurosci. 2010; 22(4):426-432.
33. Breitbart W, Rosenfeld B, Roth A, et al. The Memorial Delirium Rating Scale. J Pain Symptom Manage. 1997;13(3):128-137.
34. Wong CL, Holroyd-Leduc J, Simel DL, et al. Does this patient have delirium?: value of bedside instruments. JAMA. 2010;304(7):779-786.
35. Marcantonio ER, Flacker JM, Wright RJ, et al. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2011;49(5):516-522.
36. Lundström M, Edlund A, Karlsson S, et al. A multifactorial intervention program reduces the duration of delirium, length of hospitalization, and mortality in delirious patients. J Am Geriatr Soc. 2005;53(4):622-628.
37. Lundström M, Olofsson B, Stenvall M, et al. Postoperative delirium in old patients with femoral neck fracture: a randomized intervention study. Aging Clin Exp Res. 2007; 19(3):178-186.
38. Kratz A. Use of the acute confusion protocol: a research utilization project. J Nurs Care Qual. 2008;23(4):331-337.
39. Prakanrattana U, Prapaitrakool S. Efficacy of risperidone for prevention of postoperative delirium in cardiac surgery. Anaesth Intensive Care. 2007;35(5):714-719.
40. Kaneko T, Cai J, Ishikura T, et al. Prophylactic consecutive administration of haloperidol can reduce the occurrence of postoperative delirium in gastrointestinal surgery. Yonago Acta Medica. 1999;42:179-184.
41. Larsen KA, Kelly SE, Stern TA, et al. Administration of olanzapine to prevent postoperative delirium in elderly joint-replacement patients: a randomized, controlled trial. Psychosomatics. 2010;51(5):409-418.
42. Kalisvaart KJ, de Jonghe JF, Bogaards MJ, et al. Haloperidol prophylaxis for elderly hip-surgery patients at risk for delirium: a randomized placebo-controlled study. J Am Geriatr Soc. 2005;53(10):1658-1666.
43. Hakim SM, Othman AI, Naoum DO. Early treatment with risperidone for subsyndromal delirium after on-pump cardiac surgery in the elderly: a randomized trial. Anesthesiology. 2012;116(5):987-997.
44. Maldonado JR, Wysong A, van der Starre PJ, et al. Dexmedetomidine and the reduction of postoperative delirium after cardiac surgery. Psychosomatics. 2009;50(3): 206-217.
45. Short J. Use of dexmedetomidine for primary sedation in a general intensive care unit. Crit Care Nurse. 2010;30(1): 29-38; quiz 39.
46. Practice guideline for the treatment of patients with delirium. American Psychiatric Association [Comment in: Treatment of patients with delirium. Am J Psychiatry. 2000.]. Am J Psychiatry. 1999;156(suppl 5):1-20.
47. Maldonado JR. Delirium in the acute care setting: characteristics, diagnosis, and treatment. Crit Care Clin. 2008;24(4):657-722, vii.
48. Platt MM, Breitbart W, Smith M, et al. Efficacy of neuroleptics for hypoactive delirium. J Neuropsychiatry Clin Neurosci. 1994;6(1):66-67.
49. Lonergan E, Britton AM, Luxenberg J, et al. Antipsychotics for delirium. Cochrane Database Syst Rev. 2007;(2):CD005594.
50. Seitz DP, Gill SS, van Zyl LT. Antipsychotics in the treatment of delirium: a systematic review. J Clin Psychiatry. 2007;68(1):11-21.
51. Breitbart W, Marotta R, Platt MM, et al. A double-blind trial of haloperidol, chlorpromazine, and lorazepam in the treatment of delirium in hospitalized AIDS patients. Am J Psychiatry. 1996;153(2):231-237.
52. Hu H, Deng W, Yang H, et al. Olanzapine and haloperidol for senile delirium: a randomized controlled observation. Chinese Journal of Clinical Rehabilitation. 2006;10(42): 188-190.
53. Friedman JH, Fernandez HH. Atypical antipsychotics in Parkinson-sensitive populations. J Geriatr Psychiatry Neurol. 2002;15(3):156-170.
54. Seitz DP, Gill SS. Neuroleptic malignant syndrome complicating antipsychotic treatment of delirium or agitation in medical and surgical patients: case reports and a review of the literature. Psychosomatics. 2009; 50(1):8-15.
55. Han CS, Kim YK. A double-blind trial of risperidone and haloperidol for the treatment of delirium. Psychosomatics. 2004;45(4):297-301.
56. Sink KM, Holden KF, Yaffe K. Pharmacological treatment of neuropsychiatric symptoms of dementia: a review of the evidence. JAMA. 2005;293(5):596-608.
57. Hermann N, Lanctôt KL. Atypical antipsychotics for neuropsychiatric symptoms of dementia: malignant or maligned? Drug Saf. 2006;29(10):833-843.
58. Noyan MA, Elbi H, Aksu H. Donepezil for anticholinergic drug intoxication: a case report. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27(5):885-887.
59. Gleason OC. Donepezil for postoperative delirium. Psychosomatics. 2003;44(5):437-438.
60. Overshott R, Karim S, Burns A. Cholinesterase inhibitors for delirium. Cochrane Database Syst Rev. 2008;(1): CD005317.
61. Davis MP. Does trazodone have a role in palliating symptoms? Support Care Cancer. 2007;15(2):221-224.
62. Fick DM, Agostini JV, Inouye SK. Delirium superimposed on dementia: a systematic review. J Am Geriatr Soc. 2002; 50(10):1723-1732.
63. Brajtman S, Wright D, Hogan D, et al. Developing guidelines for the assessment and treatment of delirium in older adults at the end of life. Can Geriatr J. 2011;14(2):40-50.
64. Caraceni A, Simonetti F. Palliating delirium in patients with cancer. Lancet Oncol. 2009;10(2):164-172.
65. Alexopoulos GS, Streim J, Carpenter D, et al; Expert Consensus Panel for using Antipsychotic Drugs in Older Patients. Using antipsychotic agents in older patients. J Clin Psychiatry. 2004;65(suppl 2):5-99; discussion 100-102; quiz 103-104.
66. Granja C, Gomes E, Amaro A, et al. Understanding posttraumatic stress disorder-related symptoms after critical care: the early illness amnesia hypothesis. Crit Care Med. 2008;36(10):2801-2809.
67. Ringdal GI, Ringdal K, Juliebø V, et al. Using the Mini- Mental State Examination to screen for delirium in elderly patients with hip fracture. Dement Geriatr Cogn Disord. 2011;32(6):394-400.
68. Olson RA, Chhanabhai T, McKenzie M. Feasibility study of the Montreal Cognitive Assessment (MoCA) in patients with brain metastases. Support Care Cancer. 2008;16(11):1273-1278.
1. Diagnostic and statistical manual of mental disorders, fifth edition. Washington, DC: American Psychiatric Association; 2013.
2. World Health Organization. The ICD-10 classification of mental and behavioural disorders. Diagnostic criteria for research. Geneva, Switzerland: WHO; 1993.
3. Lipowski ZJ. Delirium in the elderly patient. N Engl J Med. 1989;320(9):578-582.
4. Meagher DJ, Trzepacz PT. Motoric subtypes of delirium. Semin Clin Neuropsychiatry. 2000;5(2):75-85.
5. Rabinowitz T. Delirium: an important (but often unrecognized) clinical syndrome. Curr Psychiatry Rep. 2002;4(3):202-208.
6. Marcantonio ER, Ta T, Duthie E, et al. Delirium severity and psychomotor types: their relationship with outcomes after hip fracture repair. Am J Geriatr Soc. 2002;50(5):850-857.
7. Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. 2001;286(21):2703-2710.
8. Duppils GS, Wikblad K. Delirium: behavioural changes before and during the prodromal phase. J Clin Nurs. 2004;13(5):609-616.
9. de Jonghe JF, Kalisvaart KJ, Dijkstra M, et al. Early symptoms in the prodromal phase of delirium: a prospective cohort study in elderly patients undergoing hip surgery. Am J Geriatr Psychiatry. 2007;15(2):112-121.
10. Cook IA. Guideline watch: practice guideline for the treatment of patients with delirium. Arlington, VA: American Psychiatric Publishing; 2004.
11. Hogan D, Gage L, Bruto V, et al. National guidelines for seniors’ mental health: the assessment and treatment of delirium. Canadian Journal of Geriatrics. 2006;9(suppl 2):S42-51.
12. Leentjens AF, Diefenbacher A. A survey of delirium guidelines in Europe. J Psychosom Res. 2006;61(1):123-128.
13. Tropea J, Slee JA, Brand CA, et al. Clinical practice guidelines for the management of delirium in older people in Australia. Australas J Ageing. 2008;27(3):150-156.
14. Mittal D, Majithia D, Kennedy R, et al. Differences in characteristics and outcome of delirium as based on referral patterns. Psychosomatics. 2006;47(5):367-375.
15. Grover S, Subodh BN, Avasthi A, et al. Prevalence and clinical profile of delirium: a study from a tertiary-care hospital in north India. Gen Hosp Psychiatry. 2009;31(1): 25-29.
16. Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12): 941-948.
17. Strawn JR, Keck PE Jr, Caroff SN. Neuroleptic malignant syndrome. Am J Psychiatry. 2007;164(6):870-876.
18. Dobmejer K. Delirium in elderly medical patients. Clinical Geriatrics. 1996;4:43-68.
19. Leentjens AF, Maclullich AM, Meagher DJ. Delirium, Cinderella no more...? J Psychosom Res. 2008;65(3):205.
20. Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol. 2009;5(4):210-220.
21. Streubel PN, Ricci WM, Gardner MJ. Fragility fractures: preoperative, perioperative, and postoperative management. Current Orthopaedic Practice. 2009;20(5):482-489.
22. Spronk PE, Riekerk B, Hofhuis J, et al. Occurrence of delirium is severely underestimated in the ICU during daily care. Intensive Care Med. 2009;35(7):1276-1280.
23. Lawlor PG, Gagnon B, Mancini IL, et al. Occurrence, causes, and outcome of delirium in patients with advanced cancer: a prospective study. Arch Intern Med. 2000;160(6):786-794.
24. Ganzini L. Care of patients with delirium at the end of life. Annals of Long-Term Care. 2007;15(3):35-40.
25. Bourne RS, Tahir TA, Borthwick M, et al. Drug treatment of delirium: past, present and future. J Psychosom Res. 2008;65(3):273-282.
26. Yokota H, Ogawa S, Kurokawa A, et al. Regional cerebral blood flow in delirium patients. Psychiatry Clin Neurosci. 2003;57(3):337-339.
27. Maldonado JR. Pathoetiological model of delirium: a comprehensive understanding of the neurobiology of delirium and an evidence-based approach to prevention and treatment. Crit Care Clin. 2008;24(4):789-856, ix.
28. Trzepacz PT. Is there a final common neural pathway in delirium? Focus on acetylcholine and dopamine. Semin Clin Neuropsychiatry. 2000;5(2):132-148.
29. Inouye SK. The dilemma of delirium: clinical and research controversies regarding diagnosis and evaluation of delirium in hospitalized elderly medical patients. Am J Med. 1994;97(3):278-288.
30. Laurila JV, Laakkonen ML, Tilvis RS, et al. Predisposing and precipitating factors for delirium in a frail geriatric population. J Psychosom Res. 2008;65(3):249-254.
31. Morandi A, McCurley J, Vasilevskis EE, et al. Tools to detect delirium superimposed on dementia: a systematic review. J Am Geriatr Soc. 2012;60(11):2005-2013.
32. Kazmierski J, Kowman M, Banach M, et al. The use of DSM-IV and ICD-10 criteria and diagnostic scales for delirium among cardiac surgery patients: results from the IPDACS study. J Neuropsychiatry Clin Neurosci. 2010; 22(4):426-432.
33. Breitbart W, Rosenfeld B, Roth A, et al. The Memorial Delirium Rating Scale. J Pain Symptom Manage. 1997;13(3):128-137.
34. Wong CL, Holroyd-Leduc J, Simel DL, et al. Does this patient have delirium?: value of bedside instruments. JAMA. 2010;304(7):779-786.
35. Marcantonio ER, Flacker JM, Wright RJ, et al. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2011;49(5):516-522.
36. Lundström M, Edlund A, Karlsson S, et al. A multifactorial intervention program reduces the duration of delirium, length of hospitalization, and mortality in delirious patients. J Am Geriatr Soc. 2005;53(4):622-628.
37. Lundström M, Olofsson B, Stenvall M, et al. Postoperative delirium in old patients with femoral neck fracture: a randomized intervention study. Aging Clin Exp Res. 2007; 19(3):178-186.
38. Kratz A. Use of the acute confusion protocol: a research utilization project. J Nurs Care Qual. 2008;23(4):331-337.
39. Prakanrattana U, Prapaitrakool S. Efficacy of risperidone for prevention of postoperative delirium in cardiac surgery. Anaesth Intensive Care. 2007;35(5):714-719.
40. Kaneko T, Cai J, Ishikura T, et al. Prophylactic consecutive administration of haloperidol can reduce the occurrence of postoperative delirium in gastrointestinal surgery. Yonago Acta Medica. 1999;42:179-184.
41. Larsen KA, Kelly SE, Stern TA, et al. Administration of olanzapine to prevent postoperative delirium in elderly joint-replacement patients: a randomized, controlled trial. Psychosomatics. 2010;51(5):409-418.
42. Kalisvaart KJ, de Jonghe JF, Bogaards MJ, et al. Haloperidol prophylaxis for elderly hip-surgery patients at risk for delirium: a randomized placebo-controlled study. J Am Geriatr Soc. 2005;53(10):1658-1666.
43. Hakim SM, Othman AI, Naoum DO. Early treatment with risperidone for subsyndromal delirium after on-pump cardiac surgery in the elderly: a randomized trial. Anesthesiology. 2012;116(5):987-997.
44. Maldonado JR, Wysong A, van der Starre PJ, et al. Dexmedetomidine and the reduction of postoperative delirium after cardiac surgery. Psychosomatics. 2009;50(3): 206-217.
45. Short J. Use of dexmedetomidine for primary sedation in a general intensive care unit. Crit Care Nurse. 2010;30(1): 29-38; quiz 39.
46. Practice guideline for the treatment of patients with delirium. American Psychiatric Association [Comment in: Treatment of patients with delirium. Am J Psychiatry. 2000.]. Am J Psychiatry. 1999;156(suppl 5):1-20.
47. Maldonado JR. Delirium in the acute care setting: characteristics, diagnosis, and treatment. Crit Care Clin. 2008;24(4):657-722, vii.
48. Platt MM, Breitbart W, Smith M, et al. Efficacy of neuroleptics for hypoactive delirium. J Neuropsychiatry Clin Neurosci. 1994;6(1):66-67.
49. Lonergan E, Britton AM, Luxenberg J, et al. Antipsychotics for delirium. Cochrane Database Syst Rev. 2007;(2):CD005594.
50. Seitz DP, Gill SS, van Zyl LT. Antipsychotics in the treatment of delirium: a systematic review. J Clin Psychiatry. 2007;68(1):11-21.
51. Breitbart W, Marotta R, Platt MM, et al. A double-blind trial of haloperidol, chlorpromazine, and lorazepam in the treatment of delirium in hospitalized AIDS patients. Am J Psychiatry. 1996;153(2):231-237.
52. Hu H, Deng W, Yang H, et al. Olanzapine and haloperidol for senile delirium: a randomized controlled observation. Chinese Journal of Clinical Rehabilitation. 2006;10(42): 188-190.
53. Friedman JH, Fernandez HH. Atypical antipsychotics in Parkinson-sensitive populations. J Geriatr Psychiatry Neurol. 2002;15(3):156-170.
54. Seitz DP, Gill SS. Neuroleptic malignant syndrome complicating antipsychotic treatment of delirium or agitation in medical and surgical patients: case reports and a review of the literature. Psychosomatics. 2009; 50(1):8-15.
55. Han CS, Kim YK. A double-blind trial of risperidone and haloperidol for the treatment of delirium. Psychosomatics. 2004;45(4):297-301.
56. Sink KM, Holden KF, Yaffe K. Pharmacological treatment of neuropsychiatric symptoms of dementia: a review of the evidence. JAMA. 2005;293(5):596-608.
57. Hermann N, Lanctôt KL. Atypical antipsychotics for neuropsychiatric symptoms of dementia: malignant or maligned? Drug Saf. 2006;29(10):833-843.
58. Noyan MA, Elbi H, Aksu H. Donepezil for anticholinergic drug intoxication: a case report. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27(5):885-887.
59. Gleason OC. Donepezil for postoperative delirium. Psychosomatics. 2003;44(5):437-438.
60. Overshott R, Karim S, Burns A. Cholinesterase inhibitors for delirium. Cochrane Database Syst Rev. 2008;(1): CD005317.
61. Davis MP. Does trazodone have a role in palliating symptoms? Support Care Cancer. 2007;15(2):221-224.
62. Fick DM, Agostini JV, Inouye SK. Delirium superimposed on dementia: a systematic review. J Am Geriatr Soc. 2002; 50(10):1723-1732.
63. Brajtman S, Wright D, Hogan D, et al. Developing guidelines for the assessment and treatment of delirium in older adults at the end of life. Can Geriatr J. 2011;14(2):40-50.
64. Caraceni A, Simonetti F. Palliating delirium in patients with cancer. Lancet Oncol. 2009;10(2):164-172.
65. Alexopoulos GS, Streim J, Carpenter D, et al; Expert Consensus Panel for using Antipsychotic Drugs in Older Patients. Using antipsychotic agents in older patients. J Clin Psychiatry. 2004;65(suppl 2):5-99; discussion 100-102; quiz 103-104.
66. Granja C, Gomes E, Amaro A, et al. Understanding posttraumatic stress disorder-related symptoms after critical care: the early illness amnesia hypothesis. Crit Care Med. 2008;36(10):2801-2809.
67. Ringdal GI, Ringdal K, Juliebø V, et al. Using the Mini- Mental State Examination to screen for delirium in elderly patients with hip fracture. Dement Geriatr Cogn Disord. 2011;32(6):394-400.
68. Olson RA, Chhanabhai T, McKenzie M. Feasibility study of the Montreal Cognitive Assessment (MoCA) in patients with brain metastases. Support Care Cancer. 2008;16(11):1273-1278.
A cognitive-behavioral strategy for preventing suicide
Many mental health practitioners have had training in cognitive-behavioral therapy (CBT)—short-term, evidence-based psychotherapy for treating a variety of psychiatric conditions (eg, posttraumatic stress disorder) and medical comorbidities (eg, insomnia)—but only some are knowledgeable about how to best use CBT with a suicidal patient. This article provides a clinician-friendly summary of a 10-session evidence-based outpatient1-3 and an adapted 6 to 8 session inpatient4,5 cognitive-behavioral protocol (known as Post-Admission Cognitive Therapy [PACT]) that is designed to help patients who have suicide-related thoughts and/or behaviors.
3 phases of CBT for suicide prevention
An average of 9 hours of individual CBT for the prevention of suicide has been reported to reduce the likelihood of repeat suicide attempts in approximately 50% of patients.1 Here, we introduce you to 3 phases of CBT for preventing suicide—phases that are the same for outpatients or inpatients. Our aim is to help you become familiar with CBT strategies that can be adapted for your treatment setting and used to intervene with vulnerable patients who are at risk for suicidal self-directed violence. A thorough assessment of the patient’s psychiatric diagnosis and history, presenting problems, and risk and protective factors for suicide must be completed before treatment begins.
Phase I. The patient is asked to tell a story associated with his (her) most recent episode of suicidal thoughts or behavior, or both. This narrative serves as 1) a foundation for planning treatment and 2) a model for understanding how best to deactivate the wish to die through the process of psychotherapy.
Phase II. The patient is assisted with modifying underdeveloped or overdeveloped skills that are most closely associated with the risk of triggering a suicidal crisis. For example, a patient with underdeveloped skills in regulating anger and hatred toward himself is taught to modulate these problematic emotions more effectively. In addition, effective problem-solving strategies are reviewed and practiced.
Phase III. The patient is guided through a relapse prevention task. The purpose of this exercise is to 1) highlight skills learned during therapy and 2) allow the patient to practice effective problem-solving strategies that are aimed at minimizing the recurrence of suicidal self-directed violence.
Theorectical basis for preventing suicide with CBT
Aaron Beck, in 1979,6 proposed that a person’s biopsychosocial vulnerabilities can interact with suicidal thoughts and behaviors to produce a state that Beck labeled the “suicide mode.” Once produced, a suicide mode can become activated by cognitive, affective, motivational, and behavioral systems.
The frequency and severity of suicide mode activation can increase over time, especially for persons who do not have protective factors and those who have a history of self-directed violence—in particular, attempted suicide. Moreover, some persons might experience a chronic state of suicide mode activation and, therefore, remain at elevated risk of suicide. Once a suicide-specific mode is activated, the person considers suicide the only option for solving his life problems. Suicide might be considered a rational decision at this point.6
The hypothesized mechanism of action associated with CBT for preventing suicide can be described as:
• deactivation of the suicide mode
• modification of the structure and content of the suicide mode
• construction and practice of more adaptive structural modes to promote a desire to live.
The underlying philosophy of this intervention is that the suicide mode occurs independently of psychiatric diagnoses and must be targeted directly; treatment therefore is transdiagnostic.7 In other words, instead of addressing a symptom of a psychiatric disorder, treatment directly targets suicide-related ideation and behaviors (Table 1).
Using that framework, psychiatric diagnoses are conceptualized in terms of how the associated symptoms contribute to the activation, maintenance, and exacerbation of the suicide mode.
Protocol for preventing suicide
The outpatient protocol1-3 comprises 10, 45- to 50-minute weekly individual psychotherapy sessions, with an allowance for booster sessions (as needed), until the patient is able to complete the relapse prevention task in Phase III. The inpatient protocol4,5 comprises 6, 90-minute individual psychotherapy sessions, with an allowance for 2 booster sessions (as needed) during the inpatient stay and as many as 4 telephone booster sessions after discharge.
Phase I: Tell the suicide story
Engage the patient in treatment. To increase adherence to treatment and minimize the risk of drop-out, practitioners are encouraged to establish a strong, early therapeutic alliance with the patient. Showing genuine empathy and providing a safe, supportive, and nonjudgmental environment are instrumental for engaging patients in treatment. The practitioner listens carefully to the patient’s narrative, provides periodic summaries to check on accurate understanding, and keeps interruptions to a minimum.
Collaboratively generate a safety plan. A crisis response plan or safety plan—an individualized, hierarchically arranged, written list of coping strategies to be implemented during a suicide crisis—is developed as soon as possible. Guidance on how to develop a structured safety plan has been provided by Stanley and Brown.8,9
Practitioners must ensure that the safety plan contains contact information that the patient can use to reach the practitioner, the clinic, the on-call provider (if available), the local 24-hour emergency department, and the 24/7 National Suicide Prevention Lifeline (800-273-TALK [8255]). Discussion of how to limit access to lethal means also is important.
Because safety planning is a collaborative process, it is imperative that practitioners check on the patient’s willingness to follow the safety plan and help him overcome perceived obstacles in implementation. Copies of the plan can be kept at different locations and shared with family members, friends, or both with the patient’s permission.
Develop a cognitive-behavioral conceptualization. The cognitive-behavioral conceptualization is an individualized map of a patient’s automatic thoughts (eg, “I am going to get fired today”), conditional assumptions (“If I get fired, then my life is over”), and core beliefs (“I am an utter failure”) that are activated before, during, and after suicidal self-directed violence. To develop that conceptualization, the patient is asked to tell a story about his (her) most recent suicidal crisis (the Box, offers a sample script) and to describe reactions to having survived a suicide attempt. (Note: Patients who report regret after an attempt are at greatest risk for dying by suicide.10)
This activity gives the patient an opportunity to disclose details surrounding his suicidal thoughts and actions, and might allow for a cathartic experience through storytelling. As practitioners listen to the suicide narrative, they collect data on the patient’s early childhood experiences (typically, suicide-activating events), associated automatic thoughts and images, emotional responses, and subsequent behaviors.
Based on this information, a cognitive-behavioral case conceptualization diagram (Figure 1, and Table 2) is generated collaboratively with the patienta and used to personalize treatment planning.
a Judith Beck offers sample case conceptualization diagrams in Cognitive behavior therapy: Basics and beyond, 2nd ed. New York, New York: Guilford Press; 2011.
Phase II: Build skills
Build skills to prevent episodes of suicidal self-directed violence. Information obtained from the conceptualization is used to generate an individualized cognitive-behavioral plan of intervention. The overall goal is to determine skill-based problem areas that are associated with the most recent episode of suicidal self-directed violence.
Practitioner and patient collaboratively identify skills that are underdeveloped and ones that are overdeveloped so that they can be addressed systematically. In general, based on our clinical experience with suicidal patients, we recommend focusing on skills captured within ≥1 of the deficit domains in Table 3. Explanation of the various cognitive-behavioral strategies used in this phase of treatment is beyond the scope of this article, but 2 activities that highlight the clinical work conducted in this phase are described in the following sections. We selected those activities because they are easy to implement and, we have found, receive overall patient acceptability.
For a detailed understanding of strategies used in Phase II of CBT for preventing suicide, see Related Resources. In addition, the book Choosing to live: How to defeat suicide through cognitive therapy11 can serve as a self-help guide for patients to follow through with CBT skill-building strategies.
Sample activity #1: Construct a ‘hope box.’ One activity that you can use to help a patient cope with suicide-activating core beliefs (eg, “My life is worthless”) involves construction of a so-called hope box. The box helps the patient directly challenge his extreme distress, by being reminded of previous successes, positive experiences, and reasons for living. The process of constructing a hope box allows the patient to work on modifying his problematic core beliefs (eg, worthlessness, helplessness, incapable of being loved).
It can be helpful to have the patient construct his hope box during a session, to ensure that everything that is put in the box is truly helpful and personalized. Items included vary from patient to patient, and might consist of pictures of loved ones, a favorite poem, a prayer, coping cards (see next section), or all of these. For example, one of our patients chose to include a picture of herself in her early 20s as a reminder of a positive, fulfilling time in her life; this gave her hope that it is possible to experience those feelings again.
Bush et alb at the National Center for Telehealth and Technology have developed a Virtual Hope Box, a free mobile application for tablets and smartphones (compatible with Android and iOS operating systems) that patients can use under the guidance of their practitioner.
bwww.t2.health.mil/apps/virtual-hope-box
Sample activity #2: Generate coping cards. Effective problem-solving skills can be promoted by having the patient construct coping cards —wallet-size cards generated collaboratively in session. Coping cards are note cards that a patient keeps nearby to cope better during a difficult situation. They provide an easily accessible way to jump-start adaptive thinking during a suicidal crisis. The patient is encouraged to use coping cards to practice adaptive thinking even when not in a crisis.
There are 3 kinds of coping cards:
• place a suicide-relevant automatic thought or core belief on one side of the card; on the other side, place an alternative, more adaptive response
• write a list of coping strategies
• write instructions to motivate or “activate” the patient toward completing a specific goal (Figure 2).
Phase III: Prevent relapse
Complete relapse prevention task. Relapse prevention is a common CBT strategy that aims to strengthen self-management to minimize likelihood of returning to a previously stopped behavior. For patients who present only with suicidal thoughts, relapse prevention is directed at identifying triggers and minimizing the occurrence and/ or intensity of such thoughts in the future. For patients who present with suicidal self-directed violence, relapse prevention is directed at identifying triggers for suicidal actions and reducing the likelihood of acting on suicidal urges. The brief guidance provided below will familiarize you with each of the relapse prevention steps, which may be completed in multiple sessions.
Step 1: Provide psychoeducation
Explain the difference between a lapse and a relapse. In general, you want the patient to understand that, although suicidal thoughts might persist and recur over time, suicidal self-directed violence must be prevented. Describe the purpose of the relapse prevention task (ie, to minimize the chance that suicidal thinking and actions will recur); address questions and concerns; and obtain permission to begin the procedure. Assure the patient that this is a collaborative activity and you will be in the room to ensure comfort and safety.
STEP 2: Retell the suicide story
Ask the patient to imagine the chain of events, thoughts, and feelings that led to the most recent episode of suicide ideation or suicidal self-directed violence. Tell the patient that you want him to construct a movie script to describe the chain of events that resulted in the suicide crisis —but to do so slowly, taking enough time to describe the details of each scene of the movie.
Step 3: Apply CBT skills
Ask the patient again to take you through the sequence of events leading to the most recent episode of suicide ideation or suicidal self-directed violence. This time, however, direct him to use the skills learned in therapy to appropriately respond cognitively, affectively, and behaviorally to move further away from the suicide outcome.
If the patient is moving too fast or neglecting important points, stop and ask about alternative ways of thinking, feeling, and behaving. Use as much time as needed until the patient is able to demonstrate solid learning of at least several learned CBT strategies to prevent suicidal self-directed violence.
Step 4: Generalize learning to prepare for future suicidal crises
In this stage —given your knowledge of the patient’s psychosocial history, cognitive- behavioral conceptualization, and suicide mode triggers —you collaboratively create a future scenario that is likely to activate suicidal self-directed violence. Question the patient about possible coping strategies, provide helpful feedback, guide him through each link in the chain of events, and propose additional alternative strategies if he is clearly neglecting important points of the intervention.
Step 5: Debrief and summarize lessons learned
Debrief the patient by providing a summary of the skills he has learned in therapy, congratulate him for completing this final therapeutic task, and assess overall emotional reaction to this activity. Remind him that mood fluctuations and future setbacks, in the form of lapses, are expected. Give him the option to request booster sessions and make plans for next steps in accomplishing general goals of therapy.
Treatment can be terminated when the patient is able to complete the relapse prevention task. If he is not ready or able to complete this exercise successfully, you can extend treatment. The duration of the extension is left to the practitioner’s judgment, based on the overall treatment plan. Brown and colleagues2 have reported a maximum number of 24 outpatient sessions (for patients who need additional booster sessions); based on clinical experience, it is reasonable to assume that it would be highly unlikely for a patient not to meet treatment objectives after a methodical course of outpatient CBT.
In cases in which goals of treatment have not been met, consultation with colleagues, review of adherence problems, and consideration of obstacles for treatment efficacy would be recommended.
A checklist can be used to determine whether a patient is ready to end treatment. Variables that can be considered in assessing readiness for termination include:
• reduced scores on self-report measures for a number of weeks
• evidence of enhanced problem-solving
• engagement in adjunctive health care services
• development of a social support system.
Post-Admission Cognitive Therapy (PACT)
An inpatient cognitive-behavioral protocol for the prevention of suicide, adapted from the efficacious outpatient model, is being evaluated at the Walter Reed National Military Medical Center, Bethesda, Maryland, and Fort Belvoir Community Hospital, Fort Belvoir, Virginia. The inpatient intervention is called PACT; components are summarized in Table 4.
Bottom Line
Cognitive-behavioral therapy for preventing suicide is an efficacious protocol for reducing the recurrence of suicidal self-directed violence. Post-Admission Cognitive Therapy is the adapted inpatient treatment package. You are encouraged to gain additional training and supervision on the delivery of these interventions to your high-risk suicidal patients.
Related Resources
• Academy of Cognitive Therapy. www.academyofct.org.
• National Suicide Prevention Lifeline. www.suicide preventionlifeline.org.
• Wenzel A, Brown GK, Beck AT. Cognitive therapy for suicidal patients: scientific and clinical applications. Washington, DC: American Psychological Association; 2009.
Disclosures
Support for research on inpatient cognitive-behavioral therapy for the prevention of suicide provided to Principal Investigator, Dr. Ghahramanlou-Holloway by the Department of Defense, Congressionally Directed Medical Research Program (W81XWH-08-2-0172), Military Operational Medicine Research Program (W81XWH-11-2-0106), and the National Alliance for Research on Schizophrenia and Depression (15219).
1. Brown GK, Ten Have T, Henriques GR, et al. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. JAMA. 2005;294(5):563-570.
2. Brown GK, Henriques GR, Ratto C, et al. Cognitive therapy treatment manual for suicide attempters. Philadelphia, PA: University of Pennsylvania; 2002 (unpublished).
3. Berk MS, Henriques GR, Warman DM, et al. A cognitive therapy intervention for suicide attempters: an overview of the treatment and case examples. Cogn Behav Pract. 2004;11(3):265-277.
4. Ghahramanlou-Holloway M, Cox D, Greene F. Post-admission cognitive therapy: a brief intervention for psychiatric inpatients admitted after a suicide attempt. Cogn Behav Pract. 2012;19(2):233-244.
5. Neely L, Irwin K, Carreno Ponce JT, et al. Post Admission Cognitive Therapy (PACT) for the prevention of suicide in military personnel with histories of trauma: treatment development and case example. Clinical Case Studies. 2013;12(6):457-473.
6. Beck AT. Cognitive therapy and the emotional disorders. New York, NY: Penguin Group; 1979.
7. Ghahramanlou-Holloway M, Brown GK, Beck AT. Suicide. In: Whisman M, ed. Adapting cognitive therapy for depression: managing complexity and comorbidity. New York, NY: Guilford Press; 2008:159-184.
8. Stanley B, Brown GK. Safety planning intervention: a brief intervention to mitigate suicide risk. Cogn Behav Pract. 2012;19(2):256-264.
9. Stanley B, Brown GK. Safety plan treatment manual to reduce suicide risk: veteran version. http://www. mentalhealth.va.gov/docs/va_safety_planning_manual. pdf. Published August 20, 2008. Accessed July 2, 2014.
10. Henriques G, Wenzel A, Brown GK, et al. Suicide attempters’ reaction to survival as a risk factor for eventual suicide. Am J Psychiatry. 2005;162(11):2180-2182.
11. Ellis TE, Newman CF. Choosing to live: How to defeat suicide through cognitive therapy. Oakland, CA: New Harbinger Publications, Inc; 1996.
Many mental health practitioners have had training in cognitive-behavioral therapy (CBT)—short-term, evidence-based psychotherapy for treating a variety of psychiatric conditions (eg, posttraumatic stress disorder) and medical comorbidities (eg, insomnia)—but only some are knowledgeable about how to best use CBT with a suicidal patient. This article provides a clinician-friendly summary of a 10-session evidence-based outpatient1-3 and an adapted 6 to 8 session inpatient4,5 cognitive-behavioral protocol (known as Post-Admission Cognitive Therapy [PACT]) that is designed to help patients who have suicide-related thoughts and/or behaviors.
3 phases of CBT for suicide prevention
An average of 9 hours of individual CBT for the prevention of suicide has been reported to reduce the likelihood of repeat suicide attempts in approximately 50% of patients.1 Here, we introduce you to 3 phases of CBT for preventing suicide—phases that are the same for outpatients or inpatients. Our aim is to help you become familiar with CBT strategies that can be adapted for your treatment setting and used to intervene with vulnerable patients who are at risk for suicidal self-directed violence. A thorough assessment of the patient’s psychiatric diagnosis and history, presenting problems, and risk and protective factors for suicide must be completed before treatment begins.
Phase I. The patient is asked to tell a story associated with his (her) most recent episode of suicidal thoughts or behavior, or both. This narrative serves as 1) a foundation for planning treatment and 2) a model for understanding how best to deactivate the wish to die through the process of psychotherapy.
Phase II. The patient is assisted with modifying underdeveloped or overdeveloped skills that are most closely associated with the risk of triggering a suicidal crisis. For example, a patient with underdeveloped skills in regulating anger and hatred toward himself is taught to modulate these problematic emotions more effectively. In addition, effective problem-solving strategies are reviewed and practiced.
Phase III. The patient is guided through a relapse prevention task. The purpose of this exercise is to 1) highlight skills learned during therapy and 2) allow the patient to practice effective problem-solving strategies that are aimed at minimizing the recurrence of suicidal self-directed violence.
Theorectical basis for preventing suicide with CBT
Aaron Beck, in 1979,6 proposed that a person’s biopsychosocial vulnerabilities can interact with suicidal thoughts and behaviors to produce a state that Beck labeled the “suicide mode.” Once produced, a suicide mode can become activated by cognitive, affective, motivational, and behavioral systems.
The frequency and severity of suicide mode activation can increase over time, especially for persons who do not have protective factors and those who have a history of self-directed violence—in particular, attempted suicide. Moreover, some persons might experience a chronic state of suicide mode activation and, therefore, remain at elevated risk of suicide. Once a suicide-specific mode is activated, the person considers suicide the only option for solving his life problems. Suicide might be considered a rational decision at this point.6
The hypothesized mechanism of action associated with CBT for preventing suicide can be described as:
• deactivation of the suicide mode
• modification of the structure and content of the suicide mode
• construction and practice of more adaptive structural modes to promote a desire to live.
The underlying philosophy of this intervention is that the suicide mode occurs independently of psychiatric diagnoses and must be targeted directly; treatment therefore is transdiagnostic.7 In other words, instead of addressing a symptom of a psychiatric disorder, treatment directly targets suicide-related ideation and behaviors (Table 1).
Using that framework, psychiatric diagnoses are conceptualized in terms of how the associated symptoms contribute to the activation, maintenance, and exacerbation of the suicide mode.
Protocol for preventing suicide
The outpatient protocol1-3 comprises 10, 45- to 50-minute weekly individual psychotherapy sessions, with an allowance for booster sessions (as needed), until the patient is able to complete the relapse prevention task in Phase III. The inpatient protocol4,5 comprises 6, 90-minute individual psychotherapy sessions, with an allowance for 2 booster sessions (as needed) during the inpatient stay and as many as 4 telephone booster sessions after discharge.
Phase I: Tell the suicide story
Engage the patient in treatment. To increase adherence to treatment and minimize the risk of drop-out, practitioners are encouraged to establish a strong, early therapeutic alliance with the patient. Showing genuine empathy and providing a safe, supportive, and nonjudgmental environment are instrumental for engaging patients in treatment. The practitioner listens carefully to the patient’s narrative, provides periodic summaries to check on accurate understanding, and keeps interruptions to a minimum.
Collaboratively generate a safety plan. A crisis response plan or safety plan—an individualized, hierarchically arranged, written list of coping strategies to be implemented during a suicide crisis—is developed as soon as possible. Guidance on how to develop a structured safety plan has been provided by Stanley and Brown.8,9
Practitioners must ensure that the safety plan contains contact information that the patient can use to reach the practitioner, the clinic, the on-call provider (if available), the local 24-hour emergency department, and the 24/7 National Suicide Prevention Lifeline (800-273-TALK [8255]). Discussion of how to limit access to lethal means also is important.
Because safety planning is a collaborative process, it is imperative that practitioners check on the patient’s willingness to follow the safety plan and help him overcome perceived obstacles in implementation. Copies of the plan can be kept at different locations and shared with family members, friends, or both with the patient’s permission.
Develop a cognitive-behavioral conceptualization. The cognitive-behavioral conceptualization is an individualized map of a patient’s automatic thoughts (eg, “I am going to get fired today”), conditional assumptions (“If I get fired, then my life is over”), and core beliefs (“I am an utter failure”) that are activated before, during, and after suicidal self-directed violence. To develop that conceptualization, the patient is asked to tell a story about his (her) most recent suicidal crisis (the Box, offers a sample script) and to describe reactions to having survived a suicide attempt. (Note: Patients who report regret after an attempt are at greatest risk for dying by suicide.10)
This activity gives the patient an opportunity to disclose details surrounding his suicidal thoughts and actions, and might allow for a cathartic experience through storytelling. As practitioners listen to the suicide narrative, they collect data on the patient’s early childhood experiences (typically, suicide-activating events), associated automatic thoughts and images, emotional responses, and subsequent behaviors.
Based on this information, a cognitive-behavioral case conceptualization diagram (Figure 1, and Table 2) is generated collaboratively with the patienta and used to personalize treatment planning.
a Judith Beck offers sample case conceptualization diagrams in Cognitive behavior therapy: Basics and beyond, 2nd ed. New York, New York: Guilford Press; 2011.
Phase II: Build skills
Build skills to prevent episodes of suicidal self-directed violence. Information obtained from the conceptualization is used to generate an individualized cognitive-behavioral plan of intervention. The overall goal is to determine skill-based problem areas that are associated with the most recent episode of suicidal self-directed violence.
Practitioner and patient collaboratively identify skills that are underdeveloped and ones that are overdeveloped so that they can be addressed systematically. In general, based on our clinical experience with suicidal patients, we recommend focusing on skills captured within ≥1 of the deficit domains in Table 3. Explanation of the various cognitive-behavioral strategies used in this phase of treatment is beyond the scope of this article, but 2 activities that highlight the clinical work conducted in this phase are described in the following sections. We selected those activities because they are easy to implement and, we have found, receive overall patient acceptability.
For a detailed understanding of strategies used in Phase II of CBT for preventing suicide, see Related Resources. In addition, the book Choosing to live: How to defeat suicide through cognitive therapy11 can serve as a self-help guide for patients to follow through with CBT skill-building strategies.
Sample activity #1: Construct a ‘hope box.’ One activity that you can use to help a patient cope with suicide-activating core beliefs (eg, “My life is worthless”) involves construction of a so-called hope box. The box helps the patient directly challenge his extreme distress, by being reminded of previous successes, positive experiences, and reasons for living. The process of constructing a hope box allows the patient to work on modifying his problematic core beliefs (eg, worthlessness, helplessness, incapable of being loved).
It can be helpful to have the patient construct his hope box during a session, to ensure that everything that is put in the box is truly helpful and personalized. Items included vary from patient to patient, and might consist of pictures of loved ones, a favorite poem, a prayer, coping cards (see next section), or all of these. For example, one of our patients chose to include a picture of herself in her early 20s as a reminder of a positive, fulfilling time in her life; this gave her hope that it is possible to experience those feelings again.
Bush et alb at the National Center for Telehealth and Technology have developed a Virtual Hope Box, a free mobile application for tablets and smartphones (compatible with Android and iOS operating systems) that patients can use under the guidance of their practitioner.
bwww.t2.health.mil/apps/virtual-hope-box
Sample activity #2: Generate coping cards. Effective problem-solving skills can be promoted by having the patient construct coping cards —wallet-size cards generated collaboratively in session. Coping cards are note cards that a patient keeps nearby to cope better during a difficult situation. They provide an easily accessible way to jump-start adaptive thinking during a suicidal crisis. The patient is encouraged to use coping cards to practice adaptive thinking even when not in a crisis.
There are 3 kinds of coping cards:
• place a suicide-relevant automatic thought or core belief on one side of the card; on the other side, place an alternative, more adaptive response
• write a list of coping strategies
• write instructions to motivate or “activate” the patient toward completing a specific goal (Figure 2).
Phase III: Prevent relapse
Complete relapse prevention task. Relapse prevention is a common CBT strategy that aims to strengthen self-management to minimize likelihood of returning to a previously stopped behavior. For patients who present only with suicidal thoughts, relapse prevention is directed at identifying triggers and minimizing the occurrence and/ or intensity of such thoughts in the future. For patients who present with suicidal self-directed violence, relapse prevention is directed at identifying triggers for suicidal actions and reducing the likelihood of acting on suicidal urges. The brief guidance provided below will familiarize you with each of the relapse prevention steps, which may be completed in multiple sessions.
Step 1: Provide psychoeducation
Explain the difference between a lapse and a relapse. In general, you want the patient to understand that, although suicidal thoughts might persist and recur over time, suicidal self-directed violence must be prevented. Describe the purpose of the relapse prevention task (ie, to minimize the chance that suicidal thinking and actions will recur); address questions and concerns; and obtain permission to begin the procedure. Assure the patient that this is a collaborative activity and you will be in the room to ensure comfort and safety.
STEP 2: Retell the suicide story
Ask the patient to imagine the chain of events, thoughts, and feelings that led to the most recent episode of suicide ideation or suicidal self-directed violence. Tell the patient that you want him to construct a movie script to describe the chain of events that resulted in the suicide crisis —but to do so slowly, taking enough time to describe the details of each scene of the movie.
Step 3: Apply CBT skills
Ask the patient again to take you through the sequence of events leading to the most recent episode of suicide ideation or suicidal self-directed violence. This time, however, direct him to use the skills learned in therapy to appropriately respond cognitively, affectively, and behaviorally to move further away from the suicide outcome.
If the patient is moving too fast or neglecting important points, stop and ask about alternative ways of thinking, feeling, and behaving. Use as much time as needed until the patient is able to demonstrate solid learning of at least several learned CBT strategies to prevent suicidal self-directed violence.
Step 4: Generalize learning to prepare for future suicidal crises
In this stage —given your knowledge of the patient’s psychosocial history, cognitive- behavioral conceptualization, and suicide mode triggers —you collaboratively create a future scenario that is likely to activate suicidal self-directed violence. Question the patient about possible coping strategies, provide helpful feedback, guide him through each link in the chain of events, and propose additional alternative strategies if he is clearly neglecting important points of the intervention.
Step 5: Debrief and summarize lessons learned
Debrief the patient by providing a summary of the skills he has learned in therapy, congratulate him for completing this final therapeutic task, and assess overall emotional reaction to this activity. Remind him that mood fluctuations and future setbacks, in the form of lapses, are expected. Give him the option to request booster sessions and make plans for next steps in accomplishing general goals of therapy.
Treatment can be terminated when the patient is able to complete the relapse prevention task. If he is not ready or able to complete this exercise successfully, you can extend treatment. The duration of the extension is left to the practitioner’s judgment, based on the overall treatment plan. Brown and colleagues2 have reported a maximum number of 24 outpatient sessions (for patients who need additional booster sessions); based on clinical experience, it is reasonable to assume that it would be highly unlikely for a patient not to meet treatment objectives after a methodical course of outpatient CBT.
In cases in which goals of treatment have not been met, consultation with colleagues, review of adherence problems, and consideration of obstacles for treatment efficacy would be recommended.
A checklist can be used to determine whether a patient is ready to end treatment. Variables that can be considered in assessing readiness for termination include:
• reduced scores on self-report measures for a number of weeks
• evidence of enhanced problem-solving
• engagement in adjunctive health care services
• development of a social support system.
Post-Admission Cognitive Therapy (PACT)
An inpatient cognitive-behavioral protocol for the prevention of suicide, adapted from the efficacious outpatient model, is being evaluated at the Walter Reed National Military Medical Center, Bethesda, Maryland, and Fort Belvoir Community Hospital, Fort Belvoir, Virginia. The inpatient intervention is called PACT; components are summarized in Table 4.
Bottom Line
Cognitive-behavioral therapy for preventing suicide is an efficacious protocol for reducing the recurrence of suicidal self-directed violence. Post-Admission Cognitive Therapy is the adapted inpatient treatment package. You are encouraged to gain additional training and supervision on the delivery of these interventions to your high-risk suicidal patients.
Related Resources
• Academy of Cognitive Therapy. www.academyofct.org.
• National Suicide Prevention Lifeline. www.suicide preventionlifeline.org.
• Wenzel A, Brown GK, Beck AT. Cognitive therapy for suicidal patients: scientific and clinical applications. Washington, DC: American Psychological Association; 2009.
Disclosures
Support for research on inpatient cognitive-behavioral therapy for the prevention of suicide provided to Principal Investigator, Dr. Ghahramanlou-Holloway by the Department of Defense, Congressionally Directed Medical Research Program (W81XWH-08-2-0172), Military Operational Medicine Research Program (W81XWH-11-2-0106), and the National Alliance for Research on Schizophrenia and Depression (15219).
Many mental health practitioners have had training in cognitive-behavioral therapy (CBT)—short-term, evidence-based psychotherapy for treating a variety of psychiatric conditions (eg, posttraumatic stress disorder) and medical comorbidities (eg, insomnia)—but only some are knowledgeable about how to best use CBT with a suicidal patient. This article provides a clinician-friendly summary of a 10-session evidence-based outpatient1-3 and an adapted 6 to 8 session inpatient4,5 cognitive-behavioral protocol (known as Post-Admission Cognitive Therapy [PACT]) that is designed to help patients who have suicide-related thoughts and/or behaviors.
3 phases of CBT for suicide prevention
An average of 9 hours of individual CBT for the prevention of suicide has been reported to reduce the likelihood of repeat suicide attempts in approximately 50% of patients.1 Here, we introduce you to 3 phases of CBT for preventing suicide—phases that are the same for outpatients or inpatients. Our aim is to help you become familiar with CBT strategies that can be adapted for your treatment setting and used to intervene with vulnerable patients who are at risk for suicidal self-directed violence. A thorough assessment of the patient’s psychiatric diagnosis and history, presenting problems, and risk and protective factors for suicide must be completed before treatment begins.
Phase I. The patient is asked to tell a story associated with his (her) most recent episode of suicidal thoughts or behavior, or both. This narrative serves as 1) a foundation for planning treatment and 2) a model for understanding how best to deactivate the wish to die through the process of psychotherapy.
Phase II. The patient is assisted with modifying underdeveloped or overdeveloped skills that are most closely associated with the risk of triggering a suicidal crisis. For example, a patient with underdeveloped skills in regulating anger and hatred toward himself is taught to modulate these problematic emotions more effectively. In addition, effective problem-solving strategies are reviewed and practiced.
Phase III. The patient is guided through a relapse prevention task. The purpose of this exercise is to 1) highlight skills learned during therapy and 2) allow the patient to practice effective problem-solving strategies that are aimed at minimizing the recurrence of suicidal self-directed violence.
Theorectical basis for preventing suicide with CBT
Aaron Beck, in 1979,6 proposed that a person’s biopsychosocial vulnerabilities can interact with suicidal thoughts and behaviors to produce a state that Beck labeled the “suicide mode.” Once produced, a suicide mode can become activated by cognitive, affective, motivational, and behavioral systems.
The frequency and severity of suicide mode activation can increase over time, especially for persons who do not have protective factors and those who have a history of self-directed violence—in particular, attempted suicide. Moreover, some persons might experience a chronic state of suicide mode activation and, therefore, remain at elevated risk of suicide. Once a suicide-specific mode is activated, the person considers suicide the only option for solving his life problems. Suicide might be considered a rational decision at this point.6
The hypothesized mechanism of action associated with CBT for preventing suicide can be described as:
• deactivation of the suicide mode
• modification of the structure and content of the suicide mode
• construction and practice of more adaptive structural modes to promote a desire to live.
The underlying philosophy of this intervention is that the suicide mode occurs independently of psychiatric diagnoses and must be targeted directly; treatment therefore is transdiagnostic.7 In other words, instead of addressing a symptom of a psychiatric disorder, treatment directly targets suicide-related ideation and behaviors (Table 1).
Using that framework, psychiatric diagnoses are conceptualized in terms of how the associated symptoms contribute to the activation, maintenance, and exacerbation of the suicide mode.
Protocol for preventing suicide
The outpatient protocol1-3 comprises 10, 45- to 50-minute weekly individual psychotherapy sessions, with an allowance for booster sessions (as needed), until the patient is able to complete the relapse prevention task in Phase III. The inpatient protocol4,5 comprises 6, 90-minute individual psychotherapy sessions, with an allowance for 2 booster sessions (as needed) during the inpatient stay and as many as 4 telephone booster sessions after discharge.
Phase I: Tell the suicide story
Engage the patient in treatment. To increase adherence to treatment and minimize the risk of drop-out, practitioners are encouraged to establish a strong, early therapeutic alliance with the patient. Showing genuine empathy and providing a safe, supportive, and nonjudgmental environment are instrumental for engaging patients in treatment. The practitioner listens carefully to the patient’s narrative, provides periodic summaries to check on accurate understanding, and keeps interruptions to a minimum.
Collaboratively generate a safety plan. A crisis response plan or safety plan—an individualized, hierarchically arranged, written list of coping strategies to be implemented during a suicide crisis—is developed as soon as possible. Guidance on how to develop a structured safety plan has been provided by Stanley and Brown.8,9
Practitioners must ensure that the safety plan contains contact information that the patient can use to reach the practitioner, the clinic, the on-call provider (if available), the local 24-hour emergency department, and the 24/7 National Suicide Prevention Lifeline (800-273-TALK [8255]). Discussion of how to limit access to lethal means also is important.
Because safety planning is a collaborative process, it is imperative that practitioners check on the patient’s willingness to follow the safety plan and help him overcome perceived obstacles in implementation. Copies of the plan can be kept at different locations and shared with family members, friends, or both with the patient’s permission.
Develop a cognitive-behavioral conceptualization. The cognitive-behavioral conceptualization is an individualized map of a patient’s automatic thoughts (eg, “I am going to get fired today”), conditional assumptions (“If I get fired, then my life is over”), and core beliefs (“I am an utter failure”) that are activated before, during, and after suicidal self-directed violence. To develop that conceptualization, the patient is asked to tell a story about his (her) most recent suicidal crisis (the Box, offers a sample script) and to describe reactions to having survived a suicide attempt. (Note: Patients who report regret after an attempt are at greatest risk for dying by suicide.10)
This activity gives the patient an opportunity to disclose details surrounding his suicidal thoughts and actions, and might allow for a cathartic experience through storytelling. As practitioners listen to the suicide narrative, they collect data on the patient’s early childhood experiences (typically, suicide-activating events), associated automatic thoughts and images, emotional responses, and subsequent behaviors.
Based on this information, a cognitive-behavioral case conceptualization diagram (Figure 1, and Table 2) is generated collaboratively with the patienta and used to personalize treatment planning.
a Judith Beck offers sample case conceptualization diagrams in Cognitive behavior therapy: Basics and beyond, 2nd ed. New York, New York: Guilford Press; 2011.
Phase II: Build skills
Build skills to prevent episodes of suicidal self-directed violence. Information obtained from the conceptualization is used to generate an individualized cognitive-behavioral plan of intervention. The overall goal is to determine skill-based problem areas that are associated with the most recent episode of suicidal self-directed violence.
Practitioner and patient collaboratively identify skills that are underdeveloped and ones that are overdeveloped so that they can be addressed systematically. In general, based on our clinical experience with suicidal patients, we recommend focusing on skills captured within ≥1 of the deficit domains in Table 3. Explanation of the various cognitive-behavioral strategies used in this phase of treatment is beyond the scope of this article, but 2 activities that highlight the clinical work conducted in this phase are described in the following sections. We selected those activities because they are easy to implement and, we have found, receive overall patient acceptability.
For a detailed understanding of strategies used in Phase II of CBT for preventing suicide, see Related Resources. In addition, the book Choosing to live: How to defeat suicide through cognitive therapy11 can serve as a self-help guide for patients to follow through with CBT skill-building strategies.
Sample activity #1: Construct a ‘hope box.’ One activity that you can use to help a patient cope with suicide-activating core beliefs (eg, “My life is worthless”) involves construction of a so-called hope box. The box helps the patient directly challenge his extreme distress, by being reminded of previous successes, positive experiences, and reasons for living. The process of constructing a hope box allows the patient to work on modifying his problematic core beliefs (eg, worthlessness, helplessness, incapable of being loved).
It can be helpful to have the patient construct his hope box during a session, to ensure that everything that is put in the box is truly helpful and personalized. Items included vary from patient to patient, and might consist of pictures of loved ones, a favorite poem, a prayer, coping cards (see next section), or all of these. For example, one of our patients chose to include a picture of herself in her early 20s as a reminder of a positive, fulfilling time in her life; this gave her hope that it is possible to experience those feelings again.
Bush et alb at the National Center for Telehealth and Technology have developed a Virtual Hope Box, a free mobile application for tablets and smartphones (compatible with Android and iOS operating systems) that patients can use under the guidance of their practitioner.
bwww.t2.health.mil/apps/virtual-hope-box
Sample activity #2: Generate coping cards. Effective problem-solving skills can be promoted by having the patient construct coping cards —wallet-size cards generated collaboratively in session. Coping cards are note cards that a patient keeps nearby to cope better during a difficult situation. They provide an easily accessible way to jump-start adaptive thinking during a suicidal crisis. The patient is encouraged to use coping cards to practice adaptive thinking even when not in a crisis.
There are 3 kinds of coping cards:
• place a suicide-relevant automatic thought or core belief on one side of the card; on the other side, place an alternative, more adaptive response
• write a list of coping strategies
• write instructions to motivate or “activate” the patient toward completing a specific goal (Figure 2).
Phase III: Prevent relapse
Complete relapse prevention task. Relapse prevention is a common CBT strategy that aims to strengthen self-management to minimize likelihood of returning to a previously stopped behavior. For patients who present only with suicidal thoughts, relapse prevention is directed at identifying triggers and minimizing the occurrence and/ or intensity of such thoughts in the future. For patients who present with suicidal self-directed violence, relapse prevention is directed at identifying triggers for suicidal actions and reducing the likelihood of acting on suicidal urges. The brief guidance provided below will familiarize you with each of the relapse prevention steps, which may be completed in multiple sessions.
Step 1: Provide psychoeducation
Explain the difference between a lapse and a relapse. In general, you want the patient to understand that, although suicidal thoughts might persist and recur over time, suicidal self-directed violence must be prevented. Describe the purpose of the relapse prevention task (ie, to minimize the chance that suicidal thinking and actions will recur); address questions and concerns; and obtain permission to begin the procedure. Assure the patient that this is a collaborative activity and you will be in the room to ensure comfort and safety.
STEP 2: Retell the suicide story
Ask the patient to imagine the chain of events, thoughts, and feelings that led to the most recent episode of suicide ideation or suicidal self-directed violence. Tell the patient that you want him to construct a movie script to describe the chain of events that resulted in the suicide crisis —but to do so slowly, taking enough time to describe the details of each scene of the movie.
Step 3: Apply CBT skills
Ask the patient again to take you through the sequence of events leading to the most recent episode of suicide ideation or suicidal self-directed violence. This time, however, direct him to use the skills learned in therapy to appropriately respond cognitively, affectively, and behaviorally to move further away from the suicide outcome.
If the patient is moving too fast or neglecting important points, stop and ask about alternative ways of thinking, feeling, and behaving. Use as much time as needed until the patient is able to demonstrate solid learning of at least several learned CBT strategies to prevent suicidal self-directed violence.
Step 4: Generalize learning to prepare for future suicidal crises
In this stage —given your knowledge of the patient’s psychosocial history, cognitive- behavioral conceptualization, and suicide mode triggers —you collaboratively create a future scenario that is likely to activate suicidal self-directed violence. Question the patient about possible coping strategies, provide helpful feedback, guide him through each link in the chain of events, and propose additional alternative strategies if he is clearly neglecting important points of the intervention.
Step 5: Debrief and summarize lessons learned
Debrief the patient by providing a summary of the skills he has learned in therapy, congratulate him for completing this final therapeutic task, and assess overall emotional reaction to this activity. Remind him that mood fluctuations and future setbacks, in the form of lapses, are expected. Give him the option to request booster sessions and make plans for next steps in accomplishing general goals of therapy.
Treatment can be terminated when the patient is able to complete the relapse prevention task. If he is not ready or able to complete this exercise successfully, you can extend treatment. The duration of the extension is left to the practitioner’s judgment, based on the overall treatment plan. Brown and colleagues2 have reported a maximum number of 24 outpatient sessions (for patients who need additional booster sessions); based on clinical experience, it is reasonable to assume that it would be highly unlikely for a patient not to meet treatment objectives after a methodical course of outpatient CBT.
In cases in which goals of treatment have not been met, consultation with colleagues, review of adherence problems, and consideration of obstacles for treatment efficacy would be recommended.
A checklist can be used to determine whether a patient is ready to end treatment. Variables that can be considered in assessing readiness for termination include:
• reduced scores on self-report measures for a number of weeks
• evidence of enhanced problem-solving
• engagement in adjunctive health care services
• development of a social support system.
Post-Admission Cognitive Therapy (PACT)
An inpatient cognitive-behavioral protocol for the prevention of suicide, adapted from the efficacious outpatient model, is being evaluated at the Walter Reed National Military Medical Center, Bethesda, Maryland, and Fort Belvoir Community Hospital, Fort Belvoir, Virginia. The inpatient intervention is called PACT; components are summarized in Table 4.
Bottom Line
Cognitive-behavioral therapy for preventing suicide is an efficacious protocol for reducing the recurrence of suicidal self-directed violence. Post-Admission Cognitive Therapy is the adapted inpatient treatment package. You are encouraged to gain additional training and supervision on the delivery of these interventions to your high-risk suicidal patients.
Related Resources
• Academy of Cognitive Therapy. www.academyofct.org.
• National Suicide Prevention Lifeline. www.suicide preventionlifeline.org.
• Wenzel A, Brown GK, Beck AT. Cognitive therapy for suicidal patients: scientific and clinical applications. Washington, DC: American Psychological Association; 2009.
Disclosures
Support for research on inpatient cognitive-behavioral therapy for the prevention of suicide provided to Principal Investigator, Dr. Ghahramanlou-Holloway by the Department of Defense, Congressionally Directed Medical Research Program (W81XWH-08-2-0172), Military Operational Medicine Research Program (W81XWH-11-2-0106), and the National Alliance for Research on Schizophrenia and Depression (15219).
1. Brown GK, Ten Have T, Henriques GR, et al. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. JAMA. 2005;294(5):563-570.
2. Brown GK, Henriques GR, Ratto C, et al. Cognitive therapy treatment manual for suicide attempters. Philadelphia, PA: University of Pennsylvania; 2002 (unpublished).
3. Berk MS, Henriques GR, Warman DM, et al. A cognitive therapy intervention for suicide attempters: an overview of the treatment and case examples. Cogn Behav Pract. 2004;11(3):265-277.
4. Ghahramanlou-Holloway M, Cox D, Greene F. Post-admission cognitive therapy: a brief intervention for psychiatric inpatients admitted after a suicide attempt. Cogn Behav Pract. 2012;19(2):233-244.
5. Neely L, Irwin K, Carreno Ponce JT, et al. Post Admission Cognitive Therapy (PACT) for the prevention of suicide in military personnel with histories of trauma: treatment development and case example. Clinical Case Studies. 2013;12(6):457-473.
6. Beck AT. Cognitive therapy and the emotional disorders. New York, NY: Penguin Group; 1979.
7. Ghahramanlou-Holloway M, Brown GK, Beck AT. Suicide. In: Whisman M, ed. Adapting cognitive therapy for depression: managing complexity and comorbidity. New York, NY: Guilford Press; 2008:159-184.
8. Stanley B, Brown GK. Safety planning intervention: a brief intervention to mitigate suicide risk. Cogn Behav Pract. 2012;19(2):256-264.
9. Stanley B, Brown GK. Safety plan treatment manual to reduce suicide risk: veteran version. http://www. mentalhealth.va.gov/docs/va_safety_planning_manual. pdf. Published August 20, 2008. Accessed July 2, 2014.
10. Henriques G, Wenzel A, Brown GK, et al. Suicide attempters’ reaction to survival as a risk factor for eventual suicide. Am J Psychiatry. 2005;162(11):2180-2182.
11. Ellis TE, Newman CF. Choosing to live: How to defeat suicide through cognitive therapy. Oakland, CA: New Harbinger Publications, Inc; 1996.
1. Brown GK, Ten Have T, Henriques GR, et al. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. JAMA. 2005;294(5):563-570.
2. Brown GK, Henriques GR, Ratto C, et al. Cognitive therapy treatment manual for suicide attempters. Philadelphia, PA: University of Pennsylvania; 2002 (unpublished).
3. Berk MS, Henriques GR, Warman DM, et al. A cognitive therapy intervention for suicide attempters: an overview of the treatment and case examples. Cogn Behav Pract. 2004;11(3):265-277.
4. Ghahramanlou-Holloway M, Cox D, Greene F. Post-admission cognitive therapy: a brief intervention for psychiatric inpatients admitted after a suicide attempt. Cogn Behav Pract. 2012;19(2):233-244.
5. Neely L, Irwin K, Carreno Ponce JT, et al. Post Admission Cognitive Therapy (PACT) for the prevention of suicide in military personnel with histories of trauma: treatment development and case example. Clinical Case Studies. 2013;12(6):457-473.
6. Beck AT. Cognitive therapy and the emotional disorders. New York, NY: Penguin Group; 1979.
7. Ghahramanlou-Holloway M, Brown GK, Beck AT. Suicide. In: Whisman M, ed. Adapting cognitive therapy for depression: managing complexity and comorbidity. New York, NY: Guilford Press; 2008:159-184.
8. Stanley B, Brown GK. Safety planning intervention: a brief intervention to mitigate suicide risk. Cogn Behav Pract. 2012;19(2):256-264.
9. Stanley B, Brown GK. Safety plan treatment manual to reduce suicide risk: veteran version. http://www. mentalhealth.va.gov/docs/va_safety_planning_manual. pdf. Published August 20, 2008. Accessed July 2, 2014.
10. Henriques G, Wenzel A, Brown GK, et al. Suicide attempters’ reaction to survival as a risk factor for eventual suicide. Am J Psychiatry. 2005;162(11):2180-2182.
11. Ellis TE, Newman CF. Choosing to live: How to defeat suicide through cognitive therapy. Oakland, CA: New Harbinger Publications, Inc; 1996.
How to talk to patients and their family after a diagnosis of mild cognitive impairment
Mild cognitive impairment (MCI) is a transitional clinical stage between normal aging and dementia. Together with aging, it is considered the most significant risk factor for developing dementia, often the Alzheimer’s type.1
MCI is a challenging neuropsychiatric diagnosis to discuss with patients and their family because it is characterized by overlapping features of normal aging and because of its heterogeneity of etiology, clinical presentation, and outcome.2,3 The evolution to dementia and the lack of effective treatments for preventing or forestalling this outcome can be difficult to address—particularly when the patient is in good health and has been leading a productive life.
Successful communication is key
You can take steps to communicate in a helpful way, build a strong treatment alliance, and reduce the potential for the iatrogenic effects of disclosing this diagnosis and its prognostic implications.
Clarify that your findings are consistent with the patient’s or family’s report of sustained and concerning change in cognition and, depending on the patient, concurrent alterations in affect, behavior, or both. Emphasize that these changes are disproportionately severe relative to expectations for the patient’s age and are not caused by psychiatric or clear-cut medical factors.
Highlight contexts in which the patient’s symptoms are likely to become more disruptive and impaired, and situations in which the patient can be expected to function more effectively.
Provide evidence-based support for the rate of progression of symptoms and functional impairment.3
Emphasize that major lifestyle adjustments usually are unnecessary in the absence of progression, especially for patients who are retired or not involved in endeavors that involve significant cognitive and executive functioning demands.
Discuss the role that cognition-enhancing medications might play in managing symptoms.4
Address indications for additional services, including formal psychiatric care for patients who have concomitant affective or behavioral symptoms and who are highly distressed by the diagnosis. Pair these services with longitudinal monitoring for possible exacerbation of symptoms.
Identify psychiatric, medical, and lifestyle factors that can increase the risk of dementia. Depending on the patient’s history, this might include diabetes, hypertension, elevated lipid levels, obesity, smoking, head trauma, depression, physical inactivity, and lack of intellectual stimulation.
Review compensatory strategies. In MCI predominantly amnestic type, for example, having the patient make systematic lists for shopping and other activities of daily living, as well as establishing routines for organizaton, can bolster successful coping.
If psychometric testing was not utilized to establish the diagnosis, discussion can include the value of performing such an assessment for a more finely tuned profile of preserved and impaired neurobehavioral functions. Such a profile can include test patterns that 1) have prognostic value with regard to the likelihood of progression to dementia and 2) establish a baseline against which you can assess stability or progression over time.5
Disclosure
Dr. Pollak reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging- Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):270-279.
2. Ellison JM, Harper DG, Berlow Y, et al. Beyond the “C” in MCI: noncognitive symptoms in amnestic and non-amnestic mild cognitive impairment. CNS Spectr. 2008;13(1):66-72.
3. Goveas JS, Dixon-Holbrook M, Kerwin D, et al. Mild cognitive impairment: how can you be sure? Current Psychiatry. 2008;7(4):36-40, 46-50.
4. Doody RS, Ferris SH, Salloway S, et al. Donepezil treatment of patients with MCI: a 48-week randomized, placebo-controlled trial. Neurology. 2009;72(18):1555-1561.
5. Summers MJ, Saunders NL. Neuropsychological measures predict decline to Alzheimer’s dementia from mild cognitive impairment. Neuropsychology. 2012;26(4):498-508.
Mild cognitive impairment (MCI) is a transitional clinical stage between normal aging and dementia. Together with aging, it is considered the most significant risk factor for developing dementia, often the Alzheimer’s type.1
MCI is a challenging neuropsychiatric diagnosis to discuss with patients and their family because it is characterized by overlapping features of normal aging and because of its heterogeneity of etiology, clinical presentation, and outcome.2,3 The evolution to dementia and the lack of effective treatments for preventing or forestalling this outcome can be difficult to address—particularly when the patient is in good health and has been leading a productive life.
Successful communication is key
You can take steps to communicate in a helpful way, build a strong treatment alliance, and reduce the potential for the iatrogenic effects of disclosing this diagnosis and its prognostic implications.
Clarify that your findings are consistent with the patient’s or family’s report of sustained and concerning change in cognition and, depending on the patient, concurrent alterations in affect, behavior, or both. Emphasize that these changes are disproportionately severe relative to expectations for the patient’s age and are not caused by psychiatric or clear-cut medical factors.
Highlight contexts in which the patient’s symptoms are likely to become more disruptive and impaired, and situations in which the patient can be expected to function more effectively.
Provide evidence-based support for the rate of progression of symptoms and functional impairment.3
Emphasize that major lifestyle adjustments usually are unnecessary in the absence of progression, especially for patients who are retired or not involved in endeavors that involve significant cognitive and executive functioning demands.
Discuss the role that cognition-enhancing medications might play in managing symptoms.4
Address indications for additional services, including formal psychiatric care for patients who have concomitant affective or behavioral symptoms and who are highly distressed by the diagnosis. Pair these services with longitudinal monitoring for possible exacerbation of symptoms.
Identify psychiatric, medical, and lifestyle factors that can increase the risk of dementia. Depending on the patient’s history, this might include diabetes, hypertension, elevated lipid levels, obesity, smoking, head trauma, depression, physical inactivity, and lack of intellectual stimulation.
Review compensatory strategies. In MCI predominantly amnestic type, for example, having the patient make systematic lists for shopping and other activities of daily living, as well as establishing routines for organizaton, can bolster successful coping.
If psychometric testing was not utilized to establish the diagnosis, discussion can include the value of performing such an assessment for a more finely tuned profile of preserved and impaired neurobehavioral functions. Such a profile can include test patterns that 1) have prognostic value with regard to the likelihood of progression to dementia and 2) establish a baseline against which you can assess stability or progression over time.5
Disclosure
Dr. Pollak reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Mild cognitive impairment (MCI) is a transitional clinical stage between normal aging and dementia. Together with aging, it is considered the most significant risk factor for developing dementia, often the Alzheimer’s type.1
MCI is a challenging neuropsychiatric diagnosis to discuss with patients and their family because it is characterized by overlapping features of normal aging and because of its heterogeneity of etiology, clinical presentation, and outcome.2,3 The evolution to dementia and the lack of effective treatments for preventing or forestalling this outcome can be difficult to address—particularly when the patient is in good health and has been leading a productive life.
Successful communication is key
You can take steps to communicate in a helpful way, build a strong treatment alliance, and reduce the potential for the iatrogenic effects of disclosing this diagnosis and its prognostic implications.
Clarify that your findings are consistent with the patient’s or family’s report of sustained and concerning change in cognition and, depending on the patient, concurrent alterations in affect, behavior, or both. Emphasize that these changes are disproportionately severe relative to expectations for the patient’s age and are not caused by psychiatric or clear-cut medical factors.
Highlight contexts in which the patient’s symptoms are likely to become more disruptive and impaired, and situations in which the patient can be expected to function more effectively.
Provide evidence-based support for the rate of progression of symptoms and functional impairment.3
Emphasize that major lifestyle adjustments usually are unnecessary in the absence of progression, especially for patients who are retired or not involved in endeavors that involve significant cognitive and executive functioning demands.
Discuss the role that cognition-enhancing medications might play in managing symptoms.4
Address indications for additional services, including formal psychiatric care for patients who have concomitant affective or behavioral symptoms and who are highly distressed by the diagnosis. Pair these services with longitudinal monitoring for possible exacerbation of symptoms.
Identify psychiatric, medical, and lifestyle factors that can increase the risk of dementia. Depending on the patient’s history, this might include diabetes, hypertension, elevated lipid levels, obesity, smoking, head trauma, depression, physical inactivity, and lack of intellectual stimulation.
Review compensatory strategies. In MCI predominantly amnestic type, for example, having the patient make systematic lists for shopping and other activities of daily living, as well as establishing routines for organizaton, can bolster successful coping.
If psychometric testing was not utilized to establish the diagnosis, discussion can include the value of performing such an assessment for a more finely tuned profile of preserved and impaired neurobehavioral functions. Such a profile can include test patterns that 1) have prognostic value with regard to the likelihood of progression to dementia and 2) establish a baseline against which you can assess stability or progression over time.5
Disclosure
Dr. Pollak reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging- Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):270-279.
2. Ellison JM, Harper DG, Berlow Y, et al. Beyond the “C” in MCI: noncognitive symptoms in amnestic and non-amnestic mild cognitive impairment. CNS Spectr. 2008;13(1):66-72.
3. Goveas JS, Dixon-Holbrook M, Kerwin D, et al. Mild cognitive impairment: how can you be sure? Current Psychiatry. 2008;7(4):36-40, 46-50.
4. Doody RS, Ferris SH, Salloway S, et al. Donepezil treatment of patients with MCI: a 48-week randomized, placebo-controlled trial. Neurology. 2009;72(18):1555-1561.
5. Summers MJ, Saunders NL. Neuropsychological measures predict decline to Alzheimer’s dementia from mild cognitive impairment. Neuropsychology. 2012;26(4):498-508.
1. Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging- Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):270-279.
2. Ellison JM, Harper DG, Berlow Y, et al. Beyond the “C” in MCI: noncognitive symptoms in amnestic and non-amnestic mild cognitive impairment. CNS Spectr. 2008;13(1):66-72.
3. Goveas JS, Dixon-Holbrook M, Kerwin D, et al. Mild cognitive impairment: how can you be sure? Current Psychiatry. 2008;7(4):36-40, 46-50.
4. Doody RS, Ferris SH, Salloway S, et al. Donepezil treatment of patients with MCI: a 48-week randomized, placebo-controlled trial. Neurology. 2009;72(18):1555-1561.
5. Summers MJ, Saunders NL. Neuropsychological measures predict decline to Alzheimer’s dementia from mild cognitive impairment. Neuropsychology. 2012;26(4):498-508.
Avoid hospitalization for severe and enduring anorexia nervosa by personalizing your care
Severe and enduring anorexia nervosa (SE-AN) is persistent anorexia nervosa (AN) lasting for ≥7 years with or without a history of treatment. Evidence points to the effectiveness of a patient-tailored plan for treating SE-AN over any universal fix. Proper medication, therapeutic alliance, and strategic discharge planning are the ingredients for treating SE-AN that avoids re-hospitalization (Table).
Nutritional support and pharmacotherapy required
Comprehensive metabolic analysis and initiating nutrition should be the first priority for the medical team. Starved-state patients can have electrolyte and metabolic derangements that place them at risk of fatal arrhythmias or multi-system organ failure. Do not hesitate to initiate nasogastric tube feeding under the observation of a certified nutritionist when necessary for survival. A double-blind, randomized controlled trial demonstrated the benefit of olanzapine compared with placebo to increase body mass index (BMI) of hospitalized AN patients. Olanzapine was titrated from 2.5 to 10 mg/d over a 13-week period, and was associated with higher patient achievement of a BMI > 18.5 kg/m2.1
Although the patient is receiving nutritional support in conjunction with psychotropic medication, the road to BMI recovery can be long. Don’t forget that SE-AN can be incapacitating. In SE-AN, the fear of gaining weight is so severe that the idea of starvation-induced death initially might seem more palatable. Although counterintuitive, as the patient recovers metabolically, self-image deteriorates. Statements praising any new weight gain can derail any therapeutic relationship.
Therapeutic alliance is key
Establishing high-quality therapeutic alliance, as measured by the Helping Relationships Questionnaire, has been shown to have a positive outcome on eating disorder symptoms and comorbid depressed mood in later phases of SE-AN treatment.2,3 Although therapeutic alliance is individualized, maintaining open communication and reiterating how it is the patient’s decision to consume whole food at a level at which the feeding tube can be discontinued are good places to start treatment.
Proper discharge timing and transition to outpatient care for SE-AN patients is paramount. In multicenter studies, treatment ends too early in 57.8% of patients; discharge at sub-ideal BMI is linked to rehospitalization.3 Slower weight gain and delayed establishment of therapeutic alliance are predictors of patients who exit treatment programs too early.3 Clinicians who remain vigilant for the above metrics are less likely to feed into the unacceptably high rate of treatment failure for SE-AN.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Bissada H, Tasca GA, Barber AM, et al. Olanzapine in the treatment of low body weight and obsessive thinking in women with anorexia nervosa: a randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2008;165(10):1281-1288.
2. Stiles-Shields C, Touyz S, Hay P, et al. Therapeutic alliance in two treatments for adults with severe and enduring anorexia nervosa. Int J Eat Disord. 2013;46(8):783-789.
3. Sly R, Morgan JF, Mountford VA, et al. Predicting premature termination of hospitalised treatment for anorexia nervosa: the roles of therapeutic alliance, motivation, and behaviour change. Eat Behav. 2013;14(2):119-123.
Severe and enduring anorexia nervosa (SE-AN) is persistent anorexia nervosa (AN) lasting for ≥7 years with or without a history of treatment. Evidence points to the effectiveness of a patient-tailored plan for treating SE-AN over any universal fix. Proper medication, therapeutic alliance, and strategic discharge planning are the ingredients for treating SE-AN that avoids re-hospitalization (Table).
Nutritional support and pharmacotherapy required
Comprehensive metabolic analysis and initiating nutrition should be the first priority for the medical team. Starved-state patients can have electrolyte and metabolic derangements that place them at risk of fatal arrhythmias or multi-system organ failure. Do not hesitate to initiate nasogastric tube feeding under the observation of a certified nutritionist when necessary for survival. A double-blind, randomized controlled trial demonstrated the benefit of olanzapine compared with placebo to increase body mass index (BMI) of hospitalized AN patients. Olanzapine was titrated from 2.5 to 10 mg/d over a 13-week period, and was associated with higher patient achievement of a BMI > 18.5 kg/m2.1
Although the patient is receiving nutritional support in conjunction with psychotropic medication, the road to BMI recovery can be long. Don’t forget that SE-AN can be incapacitating. In SE-AN, the fear of gaining weight is so severe that the idea of starvation-induced death initially might seem more palatable. Although counterintuitive, as the patient recovers metabolically, self-image deteriorates. Statements praising any new weight gain can derail any therapeutic relationship.
Therapeutic alliance is key
Establishing high-quality therapeutic alliance, as measured by the Helping Relationships Questionnaire, has been shown to have a positive outcome on eating disorder symptoms and comorbid depressed mood in later phases of SE-AN treatment.2,3 Although therapeutic alliance is individualized, maintaining open communication and reiterating how it is the patient’s decision to consume whole food at a level at which the feeding tube can be discontinued are good places to start treatment.
Proper discharge timing and transition to outpatient care for SE-AN patients is paramount. In multicenter studies, treatment ends too early in 57.8% of patients; discharge at sub-ideal BMI is linked to rehospitalization.3 Slower weight gain and delayed establishment of therapeutic alliance are predictors of patients who exit treatment programs too early.3 Clinicians who remain vigilant for the above metrics are less likely to feed into the unacceptably high rate of treatment failure for SE-AN.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Severe and enduring anorexia nervosa (SE-AN) is persistent anorexia nervosa (AN) lasting for ≥7 years with or without a history of treatment. Evidence points to the effectiveness of a patient-tailored plan for treating SE-AN over any universal fix. Proper medication, therapeutic alliance, and strategic discharge planning are the ingredients for treating SE-AN that avoids re-hospitalization (Table).
Nutritional support and pharmacotherapy required
Comprehensive metabolic analysis and initiating nutrition should be the first priority for the medical team. Starved-state patients can have electrolyte and metabolic derangements that place them at risk of fatal arrhythmias or multi-system organ failure. Do not hesitate to initiate nasogastric tube feeding under the observation of a certified nutritionist when necessary for survival. A double-blind, randomized controlled trial demonstrated the benefit of olanzapine compared with placebo to increase body mass index (BMI) of hospitalized AN patients. Olanzapine was titrated from 2.5 to 10 mg/d over a 13-week period, and was associated with higher patient achievement of a BMI > 18.5 kg/m2.1
Although the patient is receiving nutritional support in conjunction with psychotropic medication, the road to BMI recovery can be long. Don’t forget that SE-AN can be incapacitating. In SE-AN, the fear of gaining weight is so severe that the idea of starvation-induced death initially might seem more palatable. Although counterintuitive, as the patient recovers metabolically, self-image deteriorates. Statements praising any new weight gain can derail any therapeutic relationship.
Therapeutic alliance is key
Establishing high-quality therapeutic alliance, as measured by the Helping Relationships Questionnaire, has been shown to have a positive outcome on eating disorder symptoms and comorbid depressed mood in later phases of SE-AN treatment.2,3 Although therapeutic alliance is individualized, maintaining open communication and reiterating how it is the patient’s decision to consume whole food at a level at which the feeding tube can be discontinued are good places to start treatment.
Proper discharge timing and transition to outpatient care for SE-AN patients is paramount. In multicenter studies, treatment ends too early in 57.8% of patients; discharge at sub-ideal BMI is linked to rehospitalization.3 Slower weight gain and delayed establishment of therapeutic alliance are predictors of patients who exit treatment programs too early.3 Clinicians who remain vigilant for the above metrics are less likely to feed into the unacceptably high rate of treatment failure for SE-AN.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Bissada H, Tasca GA, Barber AM, et al. Olanzapine in the treatment of low body weight and obsessive thinking in women with anorexia nervosa: a randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2008;165(10):1281-1288.
2. Stiles-Shields C, Touyz S, Hay P, et al. Therapeutic alliance in two treatments for adults with severe and enduring anorexia nervosa. Int J Eat Disord. 2013;46(8):783-789.
3. Sly R, Morgan JF, Mountford VA, et al. Predicting premature termination of hospitalised treatment for anorexia nervosa: the roles of therapeutic alliance, motivation, and behaviour change. Eat Behav. 2013;14(2):119-123.
1. Bissada H, Tasca GA, Barber AM, et al. Olanzapine in the treatment of low body weight and obsessive thinking in women with anorexia nervosa: a randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2008;165(10):1281-1288.
2. Stiles-Shields C, Touyz S, Hay P, et al. Therapeutic alliance in two treatments for adults with severe and enduring anorexia nervosa. Int J Eat Disord. 2013;46(8):783-789.
3. Sly R, Morgan JF, Mountford VA, et al. Predicting premature termination of hospitalised treatment for anorexia nervosa: the roles of therapeutic alliance, motivation, and behaviour change. Eat Behav. 2013;14(2):119-123.
Take caution: Look for DISTURBED behaviors when you assess violence risk
A common misconception is that persons who are mentally ill are inherently dangerous. However, there is, at most, a weak overall relationship between mental illness and violence. Increased violence is more likely to occur during periods of acute psychiatric symptoms.1 Because few patients evaluated in most clinical settings will commit a violent act, it is important to assess for specific risk factors for violence to guide clinical decision making.
The acronym DISTURBED can be a reminder about important patient-specific features that correlate with violence. There are several variables to consider when identifying persons who are more likely to commit acts of violence.2
Demographics. Young age, male sex, cognitive deficits, less formal education, unemployment, financial hardship, and homelessness are associated with an increased risk of violence. A person’s living environment and ongoing social circumstances are important considerations when assessing violence risk.
Impulsivity. Persons who display impulsive behaviors generally are more likely to behave violently. This is particularly true in persons who have been given a diagnosis of antisocial personality disorder or borderline personality disorder. Impulsivity often can be treated with medication, behavioral therapy, and other psychotherapeutic modalities.
Substance use is associated with an increased risk of violence in people with and without other mental health issues. Alcohol can increase the likelihood of violence through intoxication, withdrawal, or brain changes related to chronic drinking. Some illicit drugs are associated with violence, including phencyclidine, cocaine, methamphetamine, inhalants, anabolic steroids, and so-called bath salts. Be cautious when treating a patient who is intoxicated with one or more of these substances.
Threats. Persons who express a threat are more likely to behave violently3; those who voice threats against an identified target should be taken seriously. The more specific the threat, the more consideration it should be given. In a clinical setting, the potential target should be informed as soon as possible about the threat. If a patient is voicing a threat against a person outside the clinical setting, you may have a duty to protect by reporting that threat to law enforcement.
Untreated psychosis. Be of patients who have untreated or undertreated symptoms, including psychosis and substance intoxication. Patients in a triage setting or who are newly admitted to an inpatient unit often present the greatest risk because their symptoms have not been treated. People with paranoid delusions are at a higher risk of assaulting their perceived persecutors. Those who are highly disorganized also are more prone to lash out and commit a violent act.4,5
Repeat violence. The best predictor of violence is a history of violence. The severity of the violent acts is an important consideration. Even a person who has only a single (known) past violent act can pose a high risk if the act was murder, rape, or another highly violent assault. Learning details about past assaults, through reviewing available records or gathering collateral information, is important when assessing violence risk.
Behaviors. There are physical warning signs that often are observed immediately before a person commits a violent act. Potential warning signs include: punching a wall or breaking objects; tightening of facial muscles; clenching of fists; and pacing. These behaviors suggest a risk of imminent violence and should be closely monitored when assessing a patient who might be prone to violence. If a patient does not respond to redirection, he (she) may require staff intervention.
Eagerness. Much like when assessing the risk of suicide, intent is an important consideration in assessing the risk of violence. A person who is eager to commit an act of violence presents significant risk. Basic inquiries about homicidal ideation are insufficient; instead, explore potential responses to situations that might have a direct impact on the individual patient. For example, if the patient has had frequent disagreements with a family member, inquiring about hypothetical violent scenarios involving that family member would be valuable.
Distress. Persons who are concerned about safety often are inclined to lash out in perceived self-defense. For example, fear often is reported by psychiatric inpatients immediately before they commit an act of violence. In inpatient psychiatric units, providing a quiet room, or a similar amenity, can help prevent an assault by a patient who feels cornered or afraid. The staff can ease patients’ concerns by taking a calm and caring approach to addressing their needs.
Valuable tool for maintaining a safe environment
We recommend that clinicians—especially those who have little clinical experience (medical students, residents)—refer to this mnemonic before starting work in emergency and inpatient psychiatric settings— 2 settings in which assessment of violence risk is common. The mnemonic will help when gathering information to assess important risk factors for violence.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Steadman HJ, Mulvey EP, Monahan J, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55(5):393-401.
2. Tardiff K. Clinical risk assessment of violence. In: Simon RI, Tardiff K, eds. Textbook of violence assessment and management. Arlington, VA: American Psychiatric Publishing, Inc; 2008:3-16.
3. Maier GJ. Managing threatening behavior. The role of talk down and talk up. J Psychosoc Nurs Ment Health Serv. 1996;34(6):25-30.
4. McNiel DE, Binder RL. The relationship between acute psychiatric symptoms, diagnosis, and short-term risk of violence. Hosp Community Psychiatry. 1994;45(2): 133-137.
5. Krakowski M, Czobor P, Chou JC. Course of violence in patients with schizophrenia: relationship to clinical symptoms. Schizophr Bull. 1999;25(3):505-517.
A common misconception is that persons who are mentally ill are inherently dangerous. However, there is, at most, a weak overall relationship between mental illness and violence. Increased violence is more likely to occur during periods of acute psychiatric symptoms.1 Because few patients evaluated in most clinical settings will commit a violent act, it is important to assess for specific risk factors for violence to guide clinical decision making.
The acronym DISTURBED can be a reminder about important patient-specific features that correlate with violence. There are several variables to consider when identifying persons who are more likely to commit acts of violence.2
Demographics. Young age, male sex, cognitive deficits, less formal education, unemployment, financial hardship, and homelessness are associated with an increased risk of violence. A person’s living environment and ongoing social circumstances are important considerations when assessing violence risk.
Impulsivity. Persons who display impulsive behaviors generally are more likely to behave violently. This is particularly true in persons who have been given a diagnosis of antisocial personality disorder or borderline personality disorder. Impulsivity often can be treated with medication, behavioral therapy, and other psychotherapeutic modalities.
Substance use is associated with an increased risk of violence in people with and without other mental health issues. Alcohol can increase the likelihood of violence through intoxication, withdrawal, or brain changes related to chronic drinking. Some illicit drugs are associated with violence, including phencyclidine, cocaine, methamphetamine, inhalants, anabolic steroids, and so-called bath salts. Be cautious when treating a patient who is intoxicated with one or more of these substances.
Threats. Persons who express a threat are more likely to behave violently3; those who voice threats against an identified target should be taken seriously. The more specific the threat, the more consideration it should be given. In a clinical setting, the potential target should be informed as soon as possible about the threat. If a patient is voicing a threat against a person outside the clinical setting, you may have a duty to protect by reporting that threat to law enforcement.
Untreated psychosis. Be of patients who have untreated or undertreated symptoms, including psychosis and substance intoxication. Patients in a triage setting or who are newly admitted to an inpatient unit often present the greatest risk because their symptoms have not been treated. People with paranoid delusions are at a higher risk of assaulting their perceived persecutors. Those who are highly disorganized also are more prone to lash out and commit a violent act.4,5
Repeat violence. The best predictor of violence is a history of violence. The severity of the violent acts is an important consideration. Even a person who has only a single (known) past violent act can pose a high risk if the act was murder, rape, or another highly violent assault. Learning details about past assaults, through reviewing available records or gathering collateral information, is important when assessing violence risk.
Behaviors. There are physical warning signs that often are observed immediately before a person commits a violent act. Potential warning signs include: punching a wall or breaking objects; tightening of facial muscles; clenching of fists; and pacing. These behaviors suggest a risk of imminent violence and should be closely monitored when assessing a patient who might be prone to violence. If a patient does not respond to redirection, he (she) may require staff intervention.
Eagerness. Much like when assessing the risk of suicide, intent is an important consideration in assessing the risk of violence. A person who is eager to commit an act of violence presents significant risk. Basic inquiries about homicidal ideation are insufficient; instead, explore potential responses to situations that might have a direct impact on the individual patient. For example, if the patient has had frequent disagreements with a family member, inquiring about hypothetical violent scenarios involving that family member would be valuable.
Distress. Persons who are concerned about safety often are inclined to lash out in perceived self-defense. For example, fear often is reported by psychiatric inpatients immediately before they commit an act of violence. In inpatient psychiatric units, providing a quiet room, or a similar amenity, can help prevent an assault by a patient who feels cornered or afraid. The staff can ease patients’ concerns by taking a calm and caring approach to addressing their needs.
Valuable tool for maintaining a safe environment
We recommend that clinicians—especially those who have little clinical experience (medical students, residents)—refer to this mnemonic before starting work in emergency and inpatient psychiatric settings— 2 settings in which assessment of violence risk is common. The mnemonic will help when gathering information to assess important risk factors for violence.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
A common misconception is that persons who are mentally ill are inherently dangerous. However, there is, at most, a weak overall relationship between mental illness and violence. Increased violence is more likely to occur during periods of acute psychiatric symptoms.1 Because few patients evaluated in most clinical settings will commit a violent act, it is important to assess for specific risk factors for violence to guide clinical decision making.
The acronym DISTURBED can be a reminder about important patient-specific features that correlate with violence. There are several variables to consider when identifying persons who are more likely to commit acts of violence.2
Demographics. Young age, male sex, cognitive deficits, less formal education, unemployment, financial hardship, and homelessness are associated with an increased risk of violence. A person’s living environment and ongoing social circumstances are important considerations when assessing violence risk.
Impulsivity. Persons who display impulsive behaviors generally are more likely to behave violently. This is particularly true in persons who have been given a diagnosis of antisocial personality disorder or borderline personality disorder. Impulsivity often can be treated with medication, behavioral therapy, and other psychotherapeutic modalities.
Substance use is associated with an increased risk of violence in people with and without other mental health issues. Alcohol can increase the likelihood of violence through intoxication, withdrawal, or brain changes related to chronic drinking. Some illicit drugs are associated with violence, including phencyclidine, cocaine, methamphetamine, inhalants, anabolic steroids, and so-called bath salts. Be cautious when treating a patient who is intoxicated with one or more of these substances.
Threats. Persons who express a threat are more likely to behave violently3; those who voice threats against an identified target should be taken seriously. The more specific the threat, the more consideration it should be given. In a clinical setting, the potential target should be informed as soon as possible about the threat. If a patient is voicing a threat against a person outside the clinical setting, you may have a duty to protect by reporting that threat to law enforcement.
Untreated psychosis. Be of patients who have untreated or undertreated symptoms, including psychosis and substance intoxication. Patients in a triage setting or who are newly admitted to an inpatient unit often present the greatest risk because their symptoms have not been treated. People with paranoid delusions are at a higher risk of assaulting their perceived persecutors. Those who are highly disorganized also are more prone to lash out and commit a violent act.4,5
Repeat violence. The best predictor of violence is a history of violence. The severity of the violent acts is an important consideration. Even a person who has only a single (known) past violent act can pose a high risk if the act was murder, rape, or another highly violent assault. Learning details about past assaults, through reviewing available records or gathering collateral information, is important when assessing violence risk.
Behaviors. There are physical warning signs that often are observed immediately before a person commits a violent act. Potential warning signs include: punching a wall or breaking objects; tightening of facial muscles; clenching of fists; and pacing. These behaviors suggest a risk of imminent violence and should be closely monitored when assessing a patient who might be prone to violence. If a patient does not respond to redirection, he (she) may require staff intervention.
Eagerness. Much like when assessing the risk of suicide, intent is an important consideration in assessing the risk of violence. A person who is eager to commit an act of violence presents significant risk. Basic inquiries about homicidal ideation are insufficient; instead, explore potential responses to situations that might have a direct impact on the individual patient. For example, if the patient has had frequent disagreements with a family member, inquiring about hypothetical violent scenarios involving that family member would be valuable.
Distress. Persons who are concerned about safety often are inclined to lash out in perceived self-defense. For example, fear often is reported by psychiatric inpatients immediately before they commit an act of violence. In inpatient psychiatric units, providing a quiet room, or a similar amenity, can help prevent an assault by a patient who feels cornered or afraid. The staff can ease patients’ concerns by taking a calm and caring approach to addressing their needs.
Valuable tool for maintaining a safe environment
We recommend that clinicians—especially those who have little clinical experience (medical students, residents)—refer to this mnemonic before starting work in emergency and inpatient psychiatric settings— 2 settings in which assessment of violence risk is common. The mnemonic will help when gathering information to assess important risk factors for violence.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Steadman HJ, Mulvey EP, Monahan J, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55(5):393-401.
2. Tardiff K. Clinical risk assessment of violence. In: Simon RI, Tardiff K, eds. Textbook of violence assessment and management. Arlington, VA: American Psychiatric Publishing, Inc; 2008:3-16.
3. Maier GJ. Managing threatening behavior. The role of talk down and talk up. J Psychosoc Nurs Ment Health Serv. 1996;34(6):25-30.
4. McNiel DE, Binder RL. The relationship between acute psychiatric symptoms, diagnosis, and short-term risk of violence. Hosp Community Psychiatry. 1994;45(2): 133-137.
5. Krakowski M, Czobor P, Chou JC. Course of violence in patients with schizophrenia: relationship to clinical symptoms. Schizophr Bull. 1999;25(3):505-517.
1. Steadman HJ, Mulvey EP, Monahan J, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55(5):393-401.
2. Tardiff K. Clinical risk assessment of violence. In: Simon RI, Tardiff K, eds. Textbook of violence assessment and management. Arlington, VA: American Psychiatric Publishing, Inc; 2008:3-16.
3. Maier GJ. Managing threatening behavior. The role of talk down and talk up. J Psychosoc Nurs Ment Health Serv. 1996;34(6):25-30.
4. McNiel DE, Binder RL. The relationship between acute psychiatric symptoms, diagnosis, and short-term risk of violence. Hosp Community Psychiatry. 1994;45(2): 133-137.
5. Krakowski M, Czobor P, Chou JC. Course of violence in patients with schizophrenia: relationship to clinical symptoms. Schizophr Bull. 1999;25(3):505-517.
Take caution: Look for DISTURBED behaviors when you assess violence risk
A common misconception is that persons who are mentally ill are inherently dangerous. However, there is, at most, a weak overall relationship between mental illness and violence. Increased violence is more likely to occur during periods of acute psychiatric symptoms.1 Because few patients evaluated in most clinical settings will commit a violent act, it is important to assess for specific risk factors for violence to guide clinical decision making.
The acronym DISTURBED can be a reminder about important patient-specific features that correlate with violence. There are several variables to consider when identifying persons who are more likely to commit acts of violence.2
Demographics. Young age, male sex, cognitive deficits, less formal education, unemployment, financial hardship, and homelessness are associated with an increased risk of violence. A person’s living environment and ongoing social circumstances are important considerations when assessing violence risk.
Impulsivity. Persons who display impulsive behaviors generally are more likely to behave violently. This is particularly true in persons who have been given a diagnosis of antisocial personality disorder or borderline personality disorder. Impulsivity often can be treated with medication, behavioral therapy, and other psychotherapeutic modalities.
Substance use is associated with an increased risk of violence in people with and without other mental health issues. Alcohol can increase the likelihood of violence through intoxication, withdrawal, or brain changes related to chronic drinking. Some illicit drugs are associated with violence, including phencyclidine, cocaine, methamphetamine, inhalants, anabolic steroids, and so-called bath salts. Be cautious when treating a patient who is intoxicated with one or more of these substances.
Threats. Persons who express a threat are more likely to behave violently3; those who voice threats against an identified target should be taken seriously. The more specific the threat, the more consideration it should be given. In a clinical setting, the potential target should be informed as soon as possible about the threat. If a patient is voicing a threat against a person outside the clinical setting, you may have a duty to protect by reporting that threat to law enforcement.
Untreated psychosis. Be of patients who have untreated or undertreated symptoms, including psychosis and substance intoxication. Patients in a triage setting or who are newly admitted to an inpatient unit often present the greatest risk because their symptoms have not been treated. People with paranoid delusions are at a higher risk of assaulting their perceived persecutors. Those who are highly disorganized also are more prone to lash out and commit a violent act.4,5
Repeat violence. The best predictor of violence is a history of violence. The severity of the violent acts is an important consideration. Even a person who has only a single (known) past violent act can pose a high risk if the act was murder, rape, or another highly violent assault. Learning details about past assaults, through reviewing available records or gathering collateral information, is important when assessing violence risk.
Behaviors. There are physical warning signs that often are observed immediately before a person commits a violent act. Potential warning signs include: punching a wall or breaking objects; tightening of facial muscles; clenching of fists; and pacing. These behaviors suggest a risk of imminent violence and should be closely monitored when assessing a patient who might be prone to violence. If a patient does not respond to redirection, he (she) may require staff intervention.
Eagerness. Much like when assessing the risk of suicide, intent is an important consideration in assessing the risk of violence. A person who is eager to commit an act of violence presents significant risk. Basic inquiries about homicidal ideation are insufficient; instead, explore potential responses to situations that might have a direct impact on the individual patient. For example, if the patient has had frequent disagreements with a family member, inquiring about hypothetical violent scenarios involving that family member would be valuable.
Distress. Persons who are concerned about safety often are inclined to lash out in perceived self-defense. For example, fear often is reported by psychiatric inpatients immediately before they commit an act of violence. In inpatient psychiatric units, providing a quiet room, or a similar amenity, can help prevent an assault by a patient who feels cornered or afraid. The staff can ease patients’ concerns by taking a calm and caring approach to addressing their needs.
Valuable tool for maintaining a safe environment
We recommend that clinicians—especially those who have little clinical experience (medical students, residents)—refer to this mnemonic before starting work in emergency and inpatient psychiatric settings— 2 settings in which assessment of violence risk is common. The mnemonic will help when gathering information to assess important risk factors for violence.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Steadman HJ, Mulvey EP, Monahan J, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55(5):393-401.
2. Tardiff K. Clinical risk assessment of violence. In: Simon RI, Tardiff K, eds. Textbook of violence assessment and management. Arlington, VA: American Psychiatric Publishing, Inc; 2008:3-16.
3. Maier GJ. Managing threatening behavior. The role of talk down and talk up. J Psychosoc Nurs Ment Health Serv. 1996;34(6):25-30.
4. McNiel DE, Binder RL. The relationship between acute psychiatric symptoms, diagnosis, and short-term risk of violence. Hosp Community Psychiatry. 1994;45(2): 133-137.
5. Krakowski M, Czobor P, Chou JC. Course of violence in patients with schizophrenia: relationship to clinical symptoms. Schizophr Bull. 1999;25(3):505-517.
A common misconception is that persons who are mentally ill are inherently dangerous. However, there is, at most, a weak overall relationship between mental illness and violence. Increased violence is more likely to occur during periods of acute psychiatric symptoms.1 Because few patients evaluated in most clinical settings will commit a violent act, it is important to assess for specific risk factors for violence to guide clinical decision making.
The acronym DISTURBED can be a reminder about important patient-specific features that correlate with violence. There are several variables to consider when identifying persons who are more likely to commit acts of violence.2
Demographics. Young age, male sex, cognitive deficits, less formal education, unemployment, financial hardship, and homelessness are associated with an increased risk of violence. A person’s living environment and ongoing social circumstances are important considerations when assessing violence risk.
Impulsivity. Persons who display impulsive behaviors generally are more likely to behave violently. This is particularly true in persons who have been given a diagnosis of antisocial personality disorder or borderline personality disorder. Impulsivity often can be treated with medication, behavioral therapy, and other psychotherapeutic modalities.
Substance use is associated with an increased risk of violence in people with and without other mental health issues. Alcohol can increase the likelihood of violence through intoxication, withdrawal, or brain changes related to chronic drinking. Some illicit drugs are associated with violence, including phencyclidine, cocaine, methamphetamine, inhalants, anabolic steroids, and so-called bath salts. Be cautious when treating a patient who is intoxicated with one or more of these substances.
Threats. Persons who express a threat are more likely to behave violently3; those who voice threats against an identified target should be taken seriously. The more specific the threat, the more consideration it should be given. In a clinical setting, the potential target should be informed as soon as possible about the threat. If a patient is voicing a threat against a person outside the clinical setting, you may have a duty to protect by reporting that threat to law enforcement.
Untreated psychosis. Be of patients who have untreated or undertreated symptoms, including psychosis and substance intoxication. Patients in a triage setting or who are newly admitted to an inpatient unit often present the greatest risk because their symptoms have not been treated. People with paranoid delusions are at a higher risk of assaulting their perceived persecutors. Those who are highly disorganized also are more prone to lash out and commit a violent act.4,5
Repeat violence. The best predictor of violence is a history of violence. The severity of the violent acts is an important consideration. Even a person who has only a single (known) past violent act can pose a high risk if the act was murder, rape, or another highly violent assault. Learning details about past assaults, through reviewing available records or gathering collateral information, is important when assessing violence risk.
Behaviors. There are physical warning signs that often are observed immediately before a person commits a violent act. Potential warning signs include: punching a wall or breaking objects; tightening of facial muscles; clenching of fists; and pacing. These behaviors suggest a risk of imminent violence and should be closely monitored when assessing a patient who might be prone to violence. If a patient does not respond to redirection, he (she) may require staff intervention.
Eagerness. Much like when assessing the risk of suicide, intent is an important consideration in assessing the risk of violence. A person who is eager to commit an act of violence presents significant risk. Basic inquiries about homicidal ideation are insufficient; instead, explore potential responses to situations that might have a direct impact on the individual patient. For example, if the patient has had frequent disagreements with a family member, inquiring about hypothetical violent scenarios involving that family member would be valuable.
Distress. Persons who are concerned about safety often are inclined to lash out in perceived self-defense. For example, fear often is reported by psychiatric inpatients immediately before they commit an act of violence. In inpatient psychiatric units, providing a quiet room, or a similar amenity, can help prevent an assault by a patient who feels cornered or afraid. The staff can ease patients’ concerns by taking a calm and caring approach to addressing their needs.
Valuable tool for maintaining a safe environment
We recommend that clinicians—especially those who have little clinical experience (medical students, residents)—refer to this mnemonic before starting work in emergency and inpatient psychiatric settings— 2 settings in which assessment of violence risk is common. The mnemonic will help when gathering information to assess important risk factors for violence.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
A common misconception is that persons who are mentally ill are inherently dangerous. However, there is, at most, a weak overall relationship between mental illness and violence. Increased violence is more likely to occur during periods of acute psychiatric symptoms.1 Because few patients evaluated in most clinical settings will commit a violent act, it is important to assess for specific risk factors for violence to guide clinical decision making.
The acronym DISTURBED can be a reminder about important patient-specific features that correlate with violence. There are several variables to consider when identifying persons who are more likely to commit acts of violence.2
Demographics. Young age, male sex, cognitive deficits, less formal education, unemployment, financial hardship, and homelessness are associated with an increased risk of violence. A person’s living environment and ongoing social circumstances are important considerations when assessing violence risk.
Impulsivity. Persons who display impulsive behaviors generally are more likely to behave violently. This is particularly true in persons who have been given a diagnosis of antisocial personality disorder or borderline personality disorder. Impulsivity often can be treated with medication, behavioral therapy, and other psychotherapeutic modalities.
Substance use is associated with an increased risk of violence in people with and without other mental health issues. Alcohol can increase the likelihood of violence through intoxication, withdrawal, or brain changes related to chronic drinking. Some illicit drugs are associated with violence, including phencyclidine, cocaine, methamphetamine, inhalants, anabolic steroids, and so-called bath salts. Be cautious when treating a patient who is intoxicated with one or more of these substances.
Threats. Persons who express a threat are more likely to behave violently3; those who voice threats against an identified target should be taken seriously. The more specific the threat, the more consideration it should be given. In a clinical setting, the potential target should be informed as soon as possible about the threat. If a patient is voicing a threat against a person outside the clinical setting, you may have a duty to protect by reporting that threat to law enforcement.
Untreated psychosis. Be of patients who have untreated or undertreated symptoms, including psychosis and substance intoxication. Patients in a triage setting or who are newly admitted to an inpatient unit often present the greatest risk because their symptoms have not been treated. People with paranoid delusions are at a higher risk of assaulting their perceived persecutors. Those who are highly disorganized also are more prone to lash out and commit a violent act.4,5
Repeat violence. The best predictor of violence is a history of violence. The severity of the violent acts is an important consideration. Even a person who has only a single (known) past violent act can pose a high risk if the act was murder, rape, or another highly violent assault. Learning details about past assaults, through reviewing available records or gathering collateral information, is important when assessing violence risk.
Behaviors. There are physical warning signs that often are observed immediately before a person commits a violent act. Potential warning signs include: punching a wall or breaking objects; tightening of facial muscles; clenching of fists; and pacing. These behaviors suggest a risk of imminent violence and should be closely monitored when assessing a patient who might be prone to violence. If a patient does not respond to redirection, he (she) may require staff intervention.
Eagerness. Much like when assessing the risk of suicide, intent is an important consideration in assessing the risk of violence. A person who is eager to commit an act of violence presents significant risk. Basic inquiries about homicidal ideation are insufficient; instead, explore potential responses to situations that might have a direct impact on the individual patient. For example, if the patient has had frequent disagreements with a family member, inquiring about hypothetical violent scenarios involving that family member would be valuable.
Distress. Persons who are concerned about safety often are inclined to lash out in perceived self-defense. For example, fear often is reported by psychiatric inpatients immediately before they commit an act of violence. In inpatient psychiatric units, providing a quiet room, or a similar amenity, can help prevent an assault by a patient who feels cornered or afraid. The staff can ease patients’ concerns by taking a calm and caring approach to addressing their needs.
Valuable tool for maintaining a safe environment
We recommend that clinicians—especially those who have little clinical experience (medical students, residents)—refer to this mnemonic before starting work in emergency and inpatient psychiatric settings— 2 settings in which assessment of violence risk is common. The mnemonic will help when gathering information to assess important risk factors for violence.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Steadman HJ, Mulvey EP, Monahan J, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55(5):393-401.
2. Tardiff K. Clinical risk assessment of violence. In: Simon RI, Tardiff K, eds. Textbook of violence assessment and management. Arlington, VA: American Psychiatric Publishing, Inc; 2008:3-16.
3. Maier GJ. Managing threatening behavior. The role of talk down and talk up. J Psychosoc Nurs Ment Health Serv. 1996;34(6):25-30.
4. McNiel DE, Binder RL. The relationship between acute psychiatric symptoms, diagnosis, and short-term risk of violence. Hosp Community Psychiatry. 1994;45(2): 133-137.
5. Krakowski M, Czobor P, Chou JC. Course of violence in patients with schizophrenia: relationship to clinical symptoms. Schizophr Bull. 1999;25(3):505-517.
1. Steadman HJ, Mulvey EP, Monahan J, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55(5):393-401.
2. Tardiff K. Clinical risk assessment of violence. In: Simon RI, Tardiff K, eds. Textbook of violence assessment and management. Arlington, VA: American Psychiatric Publishing, Inc; 2008:3-16.
3. Maier GJ. Managing threatening behavior. The role of talk down and talk up. J Psychosoc Nurs Ment Health Serv. 1996;34(6):25-30.
4. McNiel DE, Binder RL. The relationship between acute psychiatric symptoms, diagnosis, and short-term risk of violence. Hosp Community Psychiatry. 1994;45(2): 133-137.
5. Krakowski M, Czobor P, Chou JC. Course of violence in patients with schizophrenia: relationship to clinical symptoms. Schizophr Bull. 1999;25(3):505-517.
IV Antibiotic Duration in Children
Rationally defining the appropriate duration of intravenous (IV) antibiotics for children with bacterial infections is challenging. For example, how long should a 2‐week‐old infant with a urinary tract infection (UTI) caused by Escherichia coli (E coli) be treated intravenously if the infant has responded to treatment and is back to baseline within 1 to 2 days? What if the blood culture was also positive for E coli? What are the risks and benefits of continuing IV antibiotics?
Such questions are common for pediatric hospitalists. Bacterial infections remain a relatively frequent cause of pediatric hospitalization, especially in neonates where 5 of the top 10 causes of hospitalizations are related to bacterial infections.[1] For some conditions, children remain hospitalized after clinical improvement simply for ongoing provision of IV antibiotics. Alternatively, some children are discharged home with a peripherally inserted central catheter (PICC) to complete an IV course.
The decision regarding the duration of IV antibiotics varies according to the condition for which the antibiotic is prescribed and often by practitioner or hospital. Many recommendations are numerically based (eg, 10 days for group B Streptococcus [GBS] bacteremia, 21 days for E coli meningitis), without taking into account patient‐level factors such as initial severity or response to therapy. These concrete recommendations may in fact be preferred by some practitioners, as suggested by a former chairman of the Committee on Infectious Disease for the American Academy of Pediatrics (AAP): The Red Book is designed for people who make decisions. It cannot waffle on an issue. It has to make a positive recommendation even if the data are incomplete.[2] A potential downside of this mentality, however, is that some practitioners may then feel obligated to follow these recommendations despite the lack of supportive evidence.
EXTENDING IV ANTIBIOTICS BEYOND CLINICAL RECOVERY
What is the rationale for continuing IV antibiotics in infants whose symptoms have completely resolved? Several factors likely drive these decisions: prevention of recurrences, concerns about bioavailability of enteral antibiotics and patient compliance, adherence to expert recommendations/guidelines, and perhaps a general sense that more is betterthat serious infections and/or their sequelae require more aggressive treatments.
Recurrence of a potentially life‐threatening infection is an understandable concern. Even when symptoms have resolved and there is documented clearance of the infection, such clearance does not necessarily signify that the body has rid itself of the pathogen completely. Some infections are deep seated and may warrant continuing treatment despite apparent recovery. To some, the risks of prolonging IV therapy may seem inconsequential when juxtaposed to a potentially devastating recurrence. However, in many conditions, recurrences may be related to host issues or ongoing exposures rather than inadequate treatment of the original infection. Recurrent UTIs, for example, are more likely in infants with urologic abnormalities,[3] and recurrent GBS bacteremia has been associated with GBS colonization of maternal breast milk and/or maternal mastitis.[4, 5, 6, 7] Although it is tempting to extend IV courses to prevent recurrences, it is not clear that the benefits of such an approach outweigh the risks.
Concerns over enteral absorption and bioavailability are also understandable, especially in young infants. The superior efficacy of IV over oral antibiotics in general is well accepted for many pediatric conditions, and in some cases (eg, septic shock) it would be unethical to perform a head‐to‐head trial. However, the lack of any published trials (to our knowledge) in pediatrics confirming the superiority of IV antibiotics suggests that oral antibiotic absorption is sufficient for many infections. Even in neonates, several studies have demonstrated that therapeutic serum levels are easily reached with oral dosing of amoxicillin in term and preterm neonates.[8, 9]
For the remainder of this review, the published recommendations and available evidence behind the duration of IV therapy are summarized for 4 bacterial infections in children in which IV antibiotic therapy often continues after clinical recovery: meningitis, bacteremia, UTI, and acute osteomyelitis. We conclude by proposing additional considerations for IV antibiotic durations, especially in situations where guidelines and/or evidence are either nonexistent, dated, conflicting, or contrary to evidence from published studies.
BACTERIAL MENINGITIS
The Infectious Disease Society of America and the British National Institute for Clinical Evidence have both published guidelines with pediatric recommendations for duration of therapy in bacterial meningitis,[10, 11] though the recommendations differ somewhat for 3 of the 4 most common pathogens, and are not always concordant with evidence from randomized controlled trials (Table 1).[12, 13, 14]
| Pathogen | IDSA | NICE | Minimum Range Achieving Equivalent Outcomes in Recent Randomized Trials |
|---|---|---|---|
| |||
| Group B Streptococcus | 1421 days | 14 days | None available |
| Neisseria meningititis | 7 days | 7 days | 15 days[12, 13, 14] |
| Haemophilus influenzae type b | 7 days | 10 days | 45 days[12, 13] |
| Streptococcus pneumoniae | 1014 days | 14 days | 45 days[12, 13] |
A recent meta‐analysis on duration of therapy in meningitis included 5 open‐label trials of ceftriaxone for bacterial meningitis in children.[12] These trials included the 3 most common pathogens and were categorized as short‐course (47 days, n=196 patients) and long‐course (714 days, n=187 patients) therapy. There was no significant difference in clinical success or long‐term neurological complications between groups. Subsequently, a multicountry trial enrolled over 1000 children 2 months to 12 years of age with meningitis caused by Haemophilus influenzae type b, Streptococcus pneumonia, or Neisseria meningititis who were stable after 5 days of IV ceftriaxone therapy and randomized them to receive placebo or an additional 5 days of ceftriaxone.[13] Patients with persistence of seizures, bacteremia, abscess or distant infections, or who were judged to be deteriorating or still severely ill at the 5‐day point were excluded (4.7% of the children who were recruited on day 0). There were no significant differences in bacteriologic failures, clinical failures, or clinical sequelae in survivors. The authors concluded that ceftriaxone can be discontinued in children with bacterial meningitis who are clinically stable after 5 days of IV therapy. Further trials in developed countries are needed.
BACTEREMIA
Because of routine vaccination against H influenzae type b and S pneumoniae, bacteremia beyond the first few months of life in otherwise healthy children is now rare.[15] Even in infants too young to benefit directly from vaccination, the epidemiology of bacteremia has changed considerably over the last few decades, with E coli and GBS constituting the majority (65%77%) of cases.[16, 17] We will limit this review on bacteremia to these 2 organisms in young infants.
Most cases of E coli bacteremia are associated with UTI (91%98%),[16, 17] and most bacteremic UTIs (88%92%) are caused by E coli.[18, 19, 20, 21] There are no official recommendations for the duration of treatment of bacteremic UTI, and only a limited amount of evidence can be gleaned from existing studies. In a trial of oral cefixime for infants aged 1 to 24 months with UTI, all 13 infants with bacteremia fared well whether they received oral cefixime only or IV cefotaxime for 3 days followed by oral cefixime.[18] In a study on length of IV antibiotic therapy in over 12,000 infants 6 months old with UTI, the presence of bacteremia predicted longer IV treatment length (bacteremia was present in 0.5% of the short IV group vs 0.8% of the long IV group, P=0.02) but did not predict treatment failure, defined as readmission within 30 days.[3] In a multicenter investigation of 229 infants 3 months old with bacteremic UTI, the duration of parenteral antibiotics was extremely variable (range, 117 days) and was not associated with treatment failure, defined as recurrent UTI caused by the same organism within 30 days (mean duration 7.8 days in the treatment‐failure group vs 7.7 days in the no‐failure group, P=0.99).[21] In summary, there is no evidence to support a prolonged course (ie, >35 days) of IV antibiotics for bacteremic UTI.
For bacteremia caused by GBS, although the Red Book Committee on Infectious Disease recommends 10 days of IV antibiotics,[22] to our knowledge there are no experimental or observational investigations to support this recommendation. Although available studies suggest that IV courses of at least 10 days are generally provided,[7, 23] no studies have compared outcomes of infants treated with short versus long courses. However, in a study that included 29 full‐term neonates with GBS bacteremia, all 29 had responded initially to 48 hours of intravenous antibiotics (defined as being asymptomatic and fed enterally), and were then treated successfully with high‐dose oral amoxicillin for the remainder of the course, with no recurrences.[8] Although recurrences are estimated to occur in 0.5% to 3% of babies treated for GBS infections, many recurrences are associated with exposure factors such as GBS colonization of the breast milk.[4, 5, 6, 7] In summary, although 10 or more days of IV antibiotic therapy remains a common published recommendation, there is no supportive evidence. More research is needed to assess whether shorter IV courses are safe.
UTI
Most UTIs can be treated with oral antibiotics.[24] In its practice parameter on febrile UTIs in infants 2 months to 2 years of age, the AAP recommends oral antibiotics for well‐appearing children.[25] This recommendation is supported by a recent Cochrane review on the topic,[26] and at least 3 additional trials that have demonstrated that long IV courses do not yield better outcomes than shorter IV courses or oral only courses.[27, 28, 29]
However, all of these trials exclude infants 1 month old, and there are no published recommendations for the 2‐month‐old age group. The study by Brady et al. on >12,000 infants 6 months old with UTI demonstrated no significant differences in UTI readmission rates between infants who were given 4 days of IV antibiotics versus those who were given 4 days.[3] There were 3,383 infants 30 days old in this study, and about one‐third of these babies received a short IV course. Failure rates were nearly identical in each group (2.3% in short course vs 2.4% in long course) even after risk adjustment (personal communication with Patrick Brady, MD, on February 7, 2014). Magin et al. describe 172 neonates (median age 19 days) with UTI who were treated intravenously for a median duration of 4 days (interquartile range, 36 days) and did not experience treatment failures or relapses.[30]
In summary, most cases of UTI can be managed with oral antibiotics. Uncertainty remains over the optimal approach for infants 1 to 2 months old, an age range not considered in current published guidelines. Current evidence suggests that IV treatment for 3 to 4 days followed by oral therapy may be sufficient treatment in this age group.
ACUTE OSTEOMYELITIS
Given the excellent blood supply to rapidly growing tissues in children, shorter durations of IV therapy have been studied with increasing frequency. A 2002 systematic review included 12 prospective cohort studies with at least 6 months of follow‐up.[31] Studies were stratified into 7 days or >7 days IV therapy, and there were no differences in cure rates. Subsequently, a large Finnish trial reported on 131 children who received an initial short IV course (24 days) followed by 20 versus 30 total days of therapy with very low treatment failure rates.[32]
The largest study from the United States to date analyzed nearly 2000 cases of osteomyelitis from 29 hospitals.[33] This study defined a prolonged IV course by placement of a central venous catheter. The rates of prolonged IV therapy varied significantly across hospitals, ranging from 10% to 95% of patients, without detectable differences in outcomes. Furthermore, the readmission rate for catheter related complications (3%) was nearly as high as the overall treatment failure rate (4%5%). Recently, Arnold et al. reported 8 years' experience with a management algorithm to guide the transition to oral antibiotics in pediatric osteoarticular infections in a patient specific manner.[34] This study included 194 patients (154 uncomplicated and 40 complicated cases), all with culture‐proven disease. Transition to oral antibiotics occurred based on resolution of fever and pain, improved function of the affected region, and a C‐reactive protein level of 3 mg/dL, and occurred at an average of 10 days into the treatment course. These authors also provided extensive information about complications to demonstrate that the proposed strategy can be used with a wide range of patients and pathogens. There was a single microbiologic treatment failure after oral step‐down therapy in a complicated osteoarticular infection, with a retained bony fragment. This study represents a successful example of a patient‐centered approach to IV antibiotic duration.
A PATIENT‐CENTERED APPROACH
Returning to the example above of the 2‐week‐old with UTI (with or without bacteremia), there are no published guidelines and only limited available evidence to help guide the duration of IV antibiotics in this case. When standards of care (eg, from published guidelines, review articles, textbooks, or local expert guidance) are nonexistent, conflicting, dated, or contrary to existing evidence, patient‐level factors can be incorporated into the decision‐making process (Table 2). In these cases, tailoring the IV antibiotic course to the individual's response (referred to in 1 review as the ultimate bioassay of the therapy[2]), while also weighing risks and benefits of ongoing therapy, is a logical approach.
| Consideration | Description |
|---|---|
| |
| Severity of initial infection | If concern of recurrence is the justification for a longer IV course, then a more prolonged course might be considered for a more severe initial presentation (eg, septic shock, multisystem organ failure, intensive care unit admission). |
| Response to therapy | Continued IV antibiotics might be warranted in patients who are still symptomatic (eg, fever, vomiting). Inflammatory markers have been used to guide therapy in osteomyelitis.[34] |
| Patient compliance | If a child does not tolerate oral antibiotics or there are concerns about family adherence, a longer IV course may be considered. |
| Family preferences | Shared decision making can be employed, especially when there is no clear evidence supporting a specific duration. |
| Assessment of harms of ongoing hospitalization and/or prolonged IV therapy | See Table 3 |
SEVERITY OF INITIAL INFECTION AND RESPONSE TO THERAPY
The severity of the initial infection, whether in terms of presentation or clinical recovery, can factor into the duration of therapy. Provision of a longer IV course to prevent (albeit theoretically) a recurrence makes more logical sense in an infant with GBS bacteremia who was ill enough to warrant intensive care unit admission than in an infant whose only symptom was a fever. Similarly, most practitioners would be reluctant to stop IV antibiotics and discharge a patient with a bacterial infection who is persistently febrile or vomiting. Although the use of inflammatory markers and other clinical symptoms to guide therapy has been limited to osteomyelitis, this approach might be useful and should be studied in other conditions.
SHARED DECISION MAKING
Shared decision making can also be employed. Parents of sick, hospitalized children generally prefer to be involved in the decision‐making process.[35] For a parent who has concerns about their child's well‐being in the hospital, or has multiple other children at home, competing career obligations, and/or limited family support, the burden of ongoing hospitalization can be significant, and should be factored into decision making. Involving parents in medical decisions may lead to a reduction in utilization for some conditions.[36]
ASSESSMENT OF RISKS/COSTS
The risks and costs of pediatric hospitalization and prolonged IV antibiotics are well described in the literature and are summarized in Table 3. Although the benefits of prolonging IV antibiotics in a child who has recovered from an acute bacterial infection are largely theoretical, many of the risks are concrete and quantifiable. For example, a young infant being treated for a bacteremic UTI may run out of potential IV sites and need a PICC line to continue IV therapy, which according to a recent review of 2574 PICC lines has a 21% complication rate. This rate is even higher in children for whom the PICC line indication was provision of antibiotics (27%) and for infants 1 year of age (44%).[37] Moreover, this procedure often requires sedation or anesthesia for placement, which has both known and unknown risks, including concerns about subsequent adverse effects on development in young children.[38] Nosocomial exposure to seasonal viruses poses an additional risk to hospitalized children.[39]
| Harm of Intravenous Antibiotic Therapy | Description or Example |
|---|---|
| |
| Complications from peripheral IV catheter | Leading source of pain and distress for hospitalized children.[44] |
| Serious complications can occur following IV infiltrates.[45] | |
| Complications from PICC line | Approximately 20% overall complication rate (44% in infants 1 year old).[37] |
| Complications led to rehospitalization of 3% of children being treated with prolonged antibiotics for osteomyelitis.[33] | |
| When thrombosis occurs (up to 9% risk in neonates[46]), 3 months of anticoagulation is recommended.[47] | |
| Complications may arise from sedation/anesthesia necessary to place catheter. Anesthesia has been associated with adverse behavioral or developmental outcomes in children 4 years of age.[38] | |
| Risk of nosocomial infection while hospitalized | An estimated 6% of hospital RSV infections are nosocomial, which are associated with a more prolonged LOS than hospitalizations for community‐acquired RSV.[39] |
| Medication error | In 1 investigation, serious medication errors occurred in 22 per 1,000 patient‐days in a large children's hospital.[48] |
| Emotional and financial burdens | Hospitalization can pose a significant strain on the child, parents, and siblings. |
| Financial costs to healthcare system | In 2003, infection‐related hospitalizations in infants had an average cost of $4,000 (average LOS 3.5 days).[1] |
| Harms associated with prolonged courses of antibiotics in general (IV or PO) | Antibiotic resistance, diarrhea (including Clostridium difficile), allergic reactions, increased costs.[49] |
These additional considerations for the duration of IV antibiotics are not evidence based and should not be used to justify an IV duration that differs dramatically from an accepted standard of care. These are merely considerations that incorporate clinical judgment and a comprehensive analysis of risks and benefits in situations where the available evidence is suboptimal. This approach can be adopted both as a framework for future research and directly in clinical practice.
CONCLUSION
In an era of increasing focus on overtreatment/waste,[40] patient safety,[41] and patient‐centered care,[42] the duration of IV antibiotics for common bacterial infections is a prime target for improving pediatric healthcare value. As emphasized by Michael Porter recently in The New England Journal of Medicine, value should always be defined around the customer.[43] A high‐value approach to IV antibiotic duration incorporates a rigorous assessment of risks and benefits that focuses on best evidence and patient‐level factors.
In discussing published guidelines in a review on bacterial meningitis therapy, Michael Radetsky noted that [R]ecommended criteria, even if provisional, may inadvertently become invested with an independent power to force submission and prohibit deviation. The danger is that sensitivity to individual responsiveness and variability will be lost.[2] Guidelines are useful tools in pediatrics and should continue to be used to direct IV antibiotic durations for bacterial infections in children. However, the emphasis on fixed durations of IV antibiotics might not always serve the best interest of the patient. When guidelines are lacking or contradictory, patient factors should also be considered.
Acknowledgements
The authors thank Ellen R. Wald, MD, and Kenneth B. Roberts, MD, for their thoughtful and valuable additions to this review.
Disclosure: Nothing to report.
- , , , , . Infectious disease hospitalizations among infants in the United States. Pediatrics. 2008;121(2):244–252.
- . Duration of treatment in bacterial meningitis: a historical inquiry. Pediatr Infect Dis J. 1990;9(1):2–9.
- , , . Length of intravenous antibiotic therapy and treatment failure in infants with urinary tract infections. Pediatrics. 2010;126(2):196–203.
- , , , et al. Group B streptococci in milk and late neonatal infections: an analysis of cases in the literature. Arch Dis Child Fetal Neonatal Ed. 2014;99(1):F41–F47.
- , , . Recurrent late‐onset group B Streptococcus sepsis in a preterm infant acquired by expressed breastmilk transmission: a case report. Breastfeed Med. 2013;8(1):134–136.
- , , , , , . Late‐onset and recurrent neonatal Group B streptococcal disease associated with breast‐milk transmission. Pediatr Dev Pathol. 2003;6(3):251–256.
- , , , , . A 5‐year review of recurrent group B streptococcal disease: lessons from twin infants. Clin Infect Dis. 2000;30(2):282–287.
- , , , et al. Therapeutic amoxicillin levels achieved with oral administration in term neonates. Eur J Clin Pharmacol. 2007;63(7):657–662.
- , , , , , . Population pharmacokinetics and dosing of amoxicillin in (pre)term neonates. Ther Drug Monit. 2006;28(2):226–231.
- , , , et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004;39(9):1267–1284.
- , , , , , . Management of bacterial meningitis and meningococcal septicaemia in children and young people: summary of NICE guidance. BMJ. 2010;340:c3209.
- , , , , . Short versus long duration of antibiotic therapy for bacterial meningitis: a meta‐analysis of randomised controlled trials in children. Arch Dis Child. 2009;94(8):607–614.
- , , , et al. 5 versus 10 days of treatment with ceftriaxone for bacterial meningitis in children: a double‐blind randomised equivalence study. Lancet. 2011;377(9780):1837–1845.
- , , , et al. Ceftriaxone as effective as long‐acting chloramphenicol in short‐course treatment of meningococcal meningitis during epidemics: a randomised non‐inferiority study. Lancet. 2005;366(9482):308–313.
- , , , et al. Changing epidemiology of outpatient bacteremia in 3‐ to 36‐month‐old children after the introduction of the heptavalent‐conjugated pneumococcal vaccine. Pediatr Infect Dis J. 2006;25(4):293–300.
- , , , et al. Epidemiology of bacteremia in febrile infants in the United States. Pediatrics. 2013;132(6):990–996.
- , , . Changing epidemiology of bacteremia in infants aged 1 week to 3 months. Pediatrics. 2012;129(3):e590–e596.
- , , , et al. Oral versus initial intravenous therapy for urinary tract infections in young febrile children. Pediatrics. 1999;104(1 pt 1):79–86.
- , , , , . Bacteremic urinary tract infection in children. Pediatr Infect Dis J. 2000;19(7):630–634.
- , , , , , . Urine testing and urinary tract infections in febrile infants seen in office settings: the Pediatric Research in Office Settings' Febrile Infant Study. Arch Pediatr Adolesc Med. 2002;156(1):44–54.
- , , , , , . Management of bacteremic urinary tract infections in infants less than 3 months of age. Abstract presented at: Pediatric Academic Societies Annual Meeting; May 5, 2014; Vancouver BC, Canada.
- , , , . Red Book: 2009 Report of the Committee on Infectious Diseases. 28th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2012.
- , . Recurrent group B streptococcal bacteremia. Clin Pediatr (Phila). 2012;51(9):884–887.
- , , , . Antibiotics for treating lower urinary tract infection in children. Cochrane Database Syst Rev. 2012;8:CD006857.
- . Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011;128(3):595–610.
- , , . Antibiotics for acute pyelonephritis in children. Cochrane Database Syst Rev. 2007(4):CD003772.
- , , , et al. Randomized trial of oral versus sequential IV/oral antibiotic for acute pyelonephritis in children. Pediatrics. 2012;129(2):e269–e275.
- , , , et al. Prospective, randomized trial comparing short and long intravenous antibiotic treatment of acute pyelonephritis in children: dimercaptosuccinic acid scintigraphic evaluation at 9 months. Pediatrics. 2008;121(3):e553–e560.
- , , , et al. Randomised trial of oral versus sequential intravenous/oral cephalosporins in children with pyelonephritis. Eur J Pediatr. 2008;167(9):1037–1047.
- , , , , . Efficacy of short‐term intravenous antibiotic in neonates with urinary tract infection. Pediatr Emerg Care. 2007;23(2):83–86.
- , , , , , . Shorter courses of parenteral antibiotic therapy do not appear to influence response rates for children with acute hematogenous osteomyelitis: a systematic review. BMC Infect Dis. 2002;2:16.
- , , , . Short‐ versus long‐term antimicrobial treatment for acute hematogenous osteomyelitis of childhood: prospective, randomized trial on 131 culture‐positive cases. Pediatr Infect Dis J. 2010;29(12):1123–1128.
- , , , , , . Prolonged intravenous therapy versus early transition to oral antimicrobial therapy for acute osteomyelitis in children. Pediatrics. 2009;123(2):636–642.
- , , , et al. Acute bacterial osteoarticular infections: eight‐year analysis of C‐reactive protein for oral step‐down therapy. Pediatrics. 2012;130(4):e821–e828.
- , , , , , . Parental decision‐making preferences in the pediatric intensive care unit. Crit Care Med. 2012;40(10):2876–2882.
- , , , , . An assessment of the shared‐decision model in parents of children with acute otitis media. Pediatrics. 2005;116(6):1267–1275.
- , , , , . Risk factors for peripherally inserted central venous catheter complications in children. JAMA Pediatr. 2013;167(5):429–435.
- , , . Current clinical evidence on the effect of general anesthesia on neurodevelopment in children: an updated systematic review with meta‐regression. PLoS One. 2014;9(1):e85760.
- , , , et al. Nosocomial respiratory syncytial virus infection in Canadian pediatric hospitals: a Pediatric Investigators Collaborative Network on Infections in Canada Study. Pediatrics. 1997;100(6):943–946.
- , . Eliminating waste in US health care. JAMA. 2012;307(14):1513–1516.
- , , . Safely doing less: a missing component of the patient safety dialogue. Pediatrics. 2011;128(6):e1596–e1597.
- Committee On Hospital Care and Institute For Patient‐ and Family‐Centered Care. Patient‐ and family‐centered care and the pediatrician's role. Pediatrics. 2012;129(2):394–404.
- . What is value in health care? N Engl J Med. 2010;363(26):2477–2481.
- , , , , . Prevalence and source of pain in pediatric inpatients. Pain. 1996;68(1):25–31.
- , , , . Acute compartment syndrome of the upper extremity in children: diagnosis, management, and outcomes. J Child Orthop. 2013;7(3):225–233.
- , , , , . Neonatal central venous catheter thrombosis: diagnosis, management and outcome. Blood Coagul Fibrinolysis. 2014;25(2):97–106.
- , , , et al. Antithrombotic therapy in neonates and children: antithrombotic therapy and prevention of thrombosis, 9th ed: American C ollege of Chest Physicians Evidence‐Based Clinical Practice Guidelines. Chest. 2012;141(2 suppl):e737S–801S.
- , , , et al. Effect of computer order entry on prevention of serious medication errors in hospitalized children. Pediatrics. 2008;121(3):e421–e427.
- Duration and cessation of antimicrobial treatment. J Hosp Med. 2012;7(suppl 1):S22–S33.
Rationally defining the appropriate duration of intravenous (IV) antibiotics for children with bacterial infections is challenging. For example, how long should a 2‐week‐old infant with a urinary tract infection (UTI) caused by Escherichia coli (E coli) be treated intravenously if the infant has responded to treatment and is back to baseline within 1 to 2 days? What if the blood culture was also positive for E coli? What are the risks and benefits of continuing IV antibiotics?
Such questions are common for pediatric hospitalists. Bacterial infections remain a relatively frequent cause of pediatric hospitalization, especially in neonates where 5 of the top 10 causes of hospitalizations are related to bacterial infections.[1] For some conditions, children remain hospitalized after clinical improvement simply for ongoing provision of IV antibiotics. Alternatively, some children are discharged home with a peripherally inserted central catheter (PICC) to complete an IV course.
The decision regarding the duration of IV antibiotics varies according to the condition for which the antibiotic is prescribed and often by practitioner or hospital. Many recommendations are numerically based (eg, 10 days for group B Streptococcus [GBS] bacteremia, 21 days for E coli meningitis), without taking into account patient‐level factors such as initial severity or response to therapy. These concrete recommendations may in fact be preferred by some practitioners, as suggested by a former chairman of the Committee on Infectious Disease for the American Academy of Pediatrics (AAP): The Red Book is designed for people who make decisions. It cannot waffle on an issue. It has to make a positive recommendation even if the data are incomplete.[2] A potential downside of this mentality, however, is that some practitioners may then feel obligated to follow these recommendations despite the lack of supportive evidence.
EXTENDING IV ANTIBIOTICS BEYOND CLINICAL RECOVERY
What is the rationale for continuing IV antibiotics in infants whose symptoms have completely resolved? Several factors likely drive these decisions: prevention of recurrences, concerns about bioavailability of enteral antibiotics and patient compliance, adherence to expert recommendations/guidelines, and perhaps a general sense that more is betterthat serious infections and/or their sequelae require more aggressive treatments.
Recurrence of a potentially life‐threatening infection is an understandable concern. Even when symptoms have resolved and there is documented clearance of the infection, such clearance does not necessarily signify that the body has rid itself of the pathogen completely. Some infections are deep seated and may warrant continuing treatment despite apparent recovery. To some, the risks of prolonging IV therapy may seem inconsequential when juxtaposed to a potentially devastating recurrence. However, in many conditions, recurrences may be related to host issues or ongoing exposures rather than inadequate treatment of the original infection. Recurrent UTIs, for example, are more likely in infants with urologic abnormalities,[3] and recurrent GBS bacteremia has been associated with GBS colonization of maternal breast milk and/or maternal mastitis.[4, 5, 6, 7] Although it is tempting to extend IV courses to prevent recurrences, it is not clear that the benefits of such an approach outweigh the risks.
Concerns over enteral absorption and bioavailability are also understandable, especially in young infants. The superior efficacy of IV over oral antibiotics in general is well accepted for many pediatric conditions, and in some cases (eg, septic shock) it would be unethical to perform a head‐to‐head trial. However, the lack of any published trials (to our knowledge) in pediatrics confirming the superiority of IV antibiotics suggests that oral antibiotic absorption is sufficient for many infections. Even in neonates, several studies have demonstrated that therapeutic serum levels are easily reached with oral dosing of amoxicillin in term and preterm neonates.[8, 9]
For the remainder of this review, the published recommendations and available evidence behind the duration of IV therapy are summarized for 4 bacterial infections in children in which IV antibiotic therapy often continues after clinical recovery: meningitis, bacteremia, UTI, and acute osteomyelitis. We conclude by proposing additional considerations for IV antibiotic durations, especially in situations where guidelines and/or evidence are either nonexistent, dated, conflicting, or contrary to evidence from published studies.
BACTERIAL MENINGITIS
The Infectious Disease Society of America and the British National Institute for Clinical Evidence have both published guidelines with pediatric recommendations for duration of therapy in bacterial meningitis,[10, 11] though the recommendations differ somewhat for 3 of the 4 most common pathogens, and are not always concordant with evidence from randomized controlled trials (Table 1).[12, 13, 14]
| Pathogen | IDSA | NICE | Minimum Range Achieving Equivalent Outcomes in Recent Randomized Trials |
|---|---|---|---|
| |||
| Group B Streptococcus | 1421 days | 14 days | None available |
| Neisseria meningititis | 7 days | 7 days | 15 days[12, 13, 14] |
| Haemophilus influenzae type b | 7 days | 10 days | 45 days[12, 13] |
| Streptococcus pneumoniae | 1014 days | 14 days | 45 days[12, 13] |
A recent meta‐analysis on duration of therapy in meningitis included 5 open‐label trials of ceftriaxone for bacterial meningitis in children.[12] These trials included the 3 most common pathogens and were categorized as short‐course (47 days, n=196 patients) and long‐course (714 days, n=187 patients) therapy. There was no significant difference in clinical success or long‐term neurological complications between groups. Subsequently, a multicountry trial enrolled over 1000 children 2 months to 12 years of age with meningitis caused by Haemophilus influenzae type b, Streptococcus pneumonia, or Neisseria meningititis who were stable after 5 days of IV ceftriaxone therapy and randomized them to receive placebo or an additional 5 days of ceftriaxone.[13] Patients with persistence of seizures, bacteremia, abscess or distant infections, or who were judged to be deteriorating or still severely ill at the 5‐day point were excluded (4.7% of the children who were recruited on day 0). There were no significant differences in bacteriologic failures, clinical failures, or clinical sequelae in survivors. The authors concluded that ceftriaxone can be discontinued in children with bacterial meningitis who are clinically stable after 5 days of IV therapy. Further trials in developed countries are needed.
BACTEREMIA
Because of routine vaccination against H influenzae type b and S pneumoniae, bacteremia beyond the first few months of life in otherwise healthy children is now rare.[15] Even in infants too young to benefit directly from vaccination, the epidemiology of bacteremia has changed considerably over the last few decades, with E coli and GBS constituting the majority (65%77%) of cases.[16, 17] We will limit this review on bacteremia to these 2 organisms in young infants.
Most cases of E coli bacteremia are associated with UTI (91%98%),[16, 17] and most bacteremic UTIs (88%92%) are caused by E coli.[18, 19, 20, 21] There are no official recommendations for the duration of treatment of bacteremic UTI, and only a limited amount of evidence can be gleaned from existing studies. In a trial of oral cefixime for infants aged 1 to 24 months with UTI, all 13 infants with bacteremia fared well whether they received oral cefixime only or IV cefotaxime for 3 days followed by oral cefixime.[18] In a study on length of IV antibiotic therapy in over 12,000 infants 6 months old with UTI, the presence of bacteremia predicted longer IV treatment length (bacteremia was present in 0.5% of the short IV group vs 0.8% of the long IV group, P=0.02) but did not predict treatment failure, defined as readmission within 30 days.[3] In a multicenter investigation of 229 infants 3 months old with bacteremic UTI, the duration of parenteral antibiotics was extremely variable (range, 117 days) and was not associated with treatment failure, defined as recurrent UTI caused by the same organism within 30 days (mean duration 7.8 days in the treatment‐failure group vs 7.7 days in the no‐failure group, P=0.99).[21] In summary, there is no evidence to support a prolonged course (ie, >35 days) of IV antibiotics for bacteremic UTI.
For bacteremia caused by GBS, although the Red Book Committee on Infectious Disease recommends 10 days of IV antibiotics,[22] to our knowledge there are no experimental or observational investigations to support this recommendation. Although available studies suggest that IV courses of at least 10 days are generally provided,[7, 23] no studies have compared outcomes of infants treated with short versus long courses. However, in a study that included 29 full‐term neonates with GBS bacteremia, all 29 had responded initially to 48 hours of intravenous antibiotics (defined as being asymptomatic and fed enterally), and were then treated successfully with high‐dose oral amoxicillin for the remainder of the course, with no recurrences.[8] Although recurrences are estimated to occur in 0.5% to 3% of babies treated for GBS infections, many recurrences are associated with exposure factors such as GBS colonization of the breast milk.[4, 5, 6, 7] In summary, although 10 or more days of IV antibiotic therapy remains a common published recommendation, there is no supportive evidence. More research is needed to assess whether shorter IV courses are safe.
UTI
Most UTIs can be treated with oral antibiotics.[24] In its practice parameter on febrile UTIs in infants 2 months to 2 years of age, the AAP recommends oral antibiotics for well‐appearing children.[25] This recommendation is supported by a recent Cochrane review on the topic,[26] and at least 3 additional trials that have demonstrated that long IV courses do not yield better outcomes than shorter IV courses or oral only courses.[27, 28, 29]
However, all of these trials exclude infants 1 month old, and there are no published recommendations for the 2‐month‐old age group. The study by Brady et al. on >12,000 infants 6 months old with UTI demonstrated no significant differences in UTI readmission rates between infants who were given 4 days of IV antibiotics versus those who were given 4 days.[3] There were 3,383 infants 30 days old in this study, and about one‐third of these babies received a short IV course. Failure rates were nearly identical in each group (2.3% in short course vs 2.4% in long course) even after risk adjustment (personal communication with Patrick Brady, MD, on February 7, 2014). Magin et al. describe 172 neonates (median age 19 days) with UTI who were treated intravenously for a median duration of 4 days (interquartile range, 36 days) and did not experience treatment failures or relapses.[30]
In summary, most cases of UTI can be managed with oral antibiotics. Uncertainty remains over the optimal approach for infants 1 to 2 months old, an age range not considered in current published guidelines. Current evidence suggests that IV treatment for 3 to 4 days followed by oral therapy may be sufficient treatment in this age group.
ACUTE OSTEOMYELITIS
Given the excellent blood supply to rapidly growing tissues in children, shorter durations of IV therapy have been studied with increasing frequency. A 2002 systematic review included 12 prospective cohort studies with at least 6 months of follow‐up.[31] Studies were stratified into 7 days or >7 days IV therapy, and there were no differences in cure rates. Subsequently, a large Finnish trial reported on 131 children who received an initial short IV course (24 days) followed by 20 versus 30 total days of therapy with very low treatment failure rates.[32]
The largest study from the United States to date analyzed nearly 2000 cases of osteomyelitis from 29 hospitals.[33] This study defined a prolonged IV course by placement of a central venous catheter. The rates of prolonged IV therapy varied significantly across hospitals, ranging from 10% to 95% of patients, without detectable differences in outcomes. Furthermore, the readmission rate for catheter related complications (3%) was nearly as high as the overall treatment failure rate (4%5%). Recently, Arnold et al. reported 8 years' experience with a management algorithm to guide the transition to oral antibiotics in pediatric osteoarticular infections in a patient specific manner.[34] This study included 194 patients (154 uncomplicated and 40 complicated cases), all with culture‐proven disease. Transition to oral antibiotics occurred based on resolution of fever and pain, improved function of the affected region, and a C‐reactive protein level of 3 mg/dL, and occurred at an average of 10 days into the treatment course. These authors also provided extensive information about complications to demonstrate that the proposed strategy can be used with a wide range of patients and pathogens. There was a single microbiologic treatment failure after oral step‐down therapy in a complicated osteoarticular infection, with a retained bony fragment. This study represents a successful example of a patient‐centered approach to IV antibiotic duration.
A PATIENT‐CENTERED APPROACH
Returning to the example above of the 2‐week‐old with UTI (with or without bacteremia), there are no published guidelines and only limited available evidence to help guide the duration of IV antibiotics in this case. When standards of care (eg, from published guidelines, review articles, textbooks, or local expert guidance) are nonexistent, conflicting, dated, or contrary to existing evidence, patient‐level factors can be incorporated into the decision‐making process (Table 2). In these cases, tailoring the IV antibiotic course to the individual's response (referred to in 1 review as the ultimate bioassay of the therapy[2]), while also weighing risks and benefits of ongoing therapy, is a logical approach.
| Consideration | Description |
|---|---|
| |
| Severity of initial infection | If concern of recurrence is the justification for a longer IV course, then a more prolonged course might be considered for a more severe initial presentation (eg, septic shock, multisystem organ failure, intensive care unit admission). |
| Response to therapy | Continued IV antibiotics might be warranted in patients who are still symptomatic (eg, fever, vomiting). Inflammatory markers have been used to guide therapy in osteomyelitis.[34] |
| Patient compliance | If a child does not tolerate oral antibiotics or there are concerns about family adherence, a longer IV course may be considered. |
| Family preferences | Shared decision making can be employed, especially when there is no clear evidence supporting a specific duration. |
| Assessment of harms of ongoing hospitalization and/or prolonged IV therapy | See Table 3 |
SEVERITY OF INITIAL INFECTION AND RESPONSE TO THERAPY
The severity of the initial infection, whether in terms of presentation or clinical recovery, can factor into the duration of therapy. Provision of a longer IV course to prevent (albeit theoretically) a recurrence makes more logical sense in an infant with GBS bacteremia who was ill enough to warrant intensive care unit admission than in an infant whose only symptom was a fever. Similarly, most practitioners would be reluctant to stop IV antibiotics and discharge a patient with a bacterial infection who is persistently febrile or vomiting. Although the use of inflammatory markers and other clinical symptoms to guide therapy has been limited to osteomyelitis, this approach might be useful and should be studied in other conditions.
SHARED DECISION MAKING
Shared decision making can also be employed. Parents of sick, hospitalized children generally prefer to be involved in the decision‐making process.[35] For a parent who has concerns about their child's well‐being in the hospital, or has multiple other children at home, competing career obligations, and/or limited family support, the burden of ongoing hospitalization can be significant, and should be factored into decision making. Involving parents in medical decisions may lead to a reduction in utilization for some conditions.[36]
ASSESSMENT OF RISKS/COSTS
The risks and costs of pediatric hospitalization and prolonged IV antibiotics are well described in the literature and are summarized in Table 3. Although the benefits of prolonging IV antibiotics in a child who has recovered from an acute bacterial infection are largely theoretical, many of the risks are concrete and quantifiable. For example, a young infant being treated for a bacteremic UTI may run out of potential IV sites and need a PICC line to continue IV therapy, which according to a recent review of 2574 PICC lines has a 21% complication rate. This rate is even higher in children for whom the PICC line indication was provision of antibiotics (27%) and for infants 1 year of age (44%).[37] Moreover, this procedure often requires sedation or anesthesia for placement, which has both known and unknown risks, including concerns about subsequent adverse effects on development in young children.[38] Nosocomial exposure to seasonal viruses poses an additional risk to hospitalized children.[39]
| Harm of Intravenous Antibiotic Therapy | Description or Example |
|---|---|
| |
| Complications from peripheral IV catheter | Leading source of pain and distress for hospitalized children.[44] |
| Serious complications can occur following IV infiltrates.[45] | |
| Complications from PICC line | Approximately 20% overall complication rate (44% in infants 1 year old).[37] |
| Complications led to rehospitalization of 3% of children being treated with prolonged antibiotics for osteomyelitis.[33] | |
| When thrombosis occurs (up to 9% risk in neonates[46]), 3 months of anticoagulation is recommended.[47] | |
| Complications may arise from sedation/anesthesia necessary to place catheter. Anesthesia has been associated with adverse behavioral or developmental outcomes in children 4 years of age.[38] | |
| Risk of nosocomial infection while hospitalized | An estimated 6% of hospital RSV infections are nosocomial, which are associated with a more prolonged LOS than hospitalizations for community‐acquired RSV.[39] |
| Medication error | In 1 investigation, serious medication errors occurred in 22 per 1,000 patient‐days in a large children's hospital.[48] |
| Emotional and financial burdens | Hospitalization can pose a significant strain on the child, parents, and siblings. |
| Financial costs to healthcare system | In 2003, infection‐related hospitalizations in infants had an average cost of $4,000 (average LOS 3.5 days).[1] |
| Harms associated with prolonged courses of antibiotics in general (IV or PO) | Antibiotic resistance, diarrhea (including Clostridium difficile), allergic reactions, increased costs.[49] |
These additional considerations for the duration of IV antibiotics are not evidence based and should not be used to justify an IV duration that differs dramatically from an accepted standard of care. These are merely considerations that incorporate clinical judgment and a comprehensive analysis of risks and benefits in situations where the available evidence is suboptimal. This approach can be adopted both as a framework for future research and directly in clinical practice.
CONCLUSION
In an era of increasing focus on overtreatment/waste,[40] patient safety,[41] and patient‐centered care,[42] the duration of IV antibiotics for common bacterial infections is a prime target for improving pediatric healthcare value. As emphasized by Michael Porter recently in The New England Journal of Medicine, value should always be defined around the customer.[43] A high‐value approach to IV antibiotic duration incorporates a rigorous assessment of risks and benefits that focuses on best evidence and patient‐level factors.
In discussing published guidelines in a review on bacterial meningitis therapy, Michael Radetsky noted that [R]ecommended criteria, even if provisional, may inadvertently become invested with an independent power to force submission and prohibit deviation. The danger is that sensitivity to individual responsiveness and variability will be lost.[2] Guidelines are useful tools in pediatrics and should continue to be used to direct IV antibiotic durations for bacterial infections in children. However, the emphasis on fixed durations of IV antibiotics might not always serve the best interest of the patient. When guidelines are lacking or contradictory, patient factors should also be considered.
Acknowledgements
The authors thank Ellen R. Wald, MD, and Kenneth B. Roberts, MD, for their thoughtful and valuable additions to this review.
Disclosure: Nothing to report.
Rationally defining the appropriate duration of intravenous (IV) antibiotics for children with bacterial infections is challenging. For example, how long should a 2‐week‐old infant with a urinary tract infection (UTI) caused by Escherichia coli (E coli) be treated intravenously if the infant has responded to treatment and is back to baseline within 1 to 2 days? What if the blood culture was also positive for E coli? What are the risks and benefits of continuing IV antibiotics?
Such questions are common for pediatric hospitalists. Bacterial infections remain a relatively frequent cause of pediatric hospitalization, especially in neonates where 5 of the top 10 causes of hospitalizations are related to bacterial infections.[1] For some conditions, children remain hospitalized after clinical improvement simply for ongoing provision of IV antibiotics. Alternatively, some children are discharged home with a peripherally inserted central catheter (PICC) to complete an IV course.
The decision regarding the duration of IV antibiotics varies according to the condition for which the antibiotic is prescribed and often by practitioner or hospital. Many recommendations are numerically based (eg, 10 days for group B Streptococcus [GBS] bacteremia, 21 days for E coli meningitis), without taking into account patient‐level factors such as initial severity or response to therapy. These concrete recommendations may in fact be preferred by some practitioners, as suggested by a former chairman of the Committee on Infectious Disease for the American Academy of Pediatrics (AAP): The Red Book is designed for people who make decisions. It cannot waffle on an issue. It has to make a positive recommendation even if the data are incomplete.[2] A potential downside of this mentality, however, is that some practitioners may then feel obligated to follow these recommendations despite the lack of supportive evidence.
EXTENDING IV ANTIBIOTICS BEYOND CLINICAL RECOVERY
What is the rationale for continuing IV antibiotics in infants whose symptoms have completely resolved? Several factors likely drive these decisions: prevention of recurrences, concerns about bioavailability of enteral antibiotics and patient compliance, adherence to expert recommendations/guidelines, and perhaps a general sense that more is betterthat serious infections and/or their sequelae require more aggressive treatments.
Recurrence of a potentially life‐threatening infection is an understandable concern. Even when symptoms have resolved and there is documented clearance of the infection, such clearance does not necessarily signify that the body has rid itself of the pathogen completely. Some infections are deep seated and may warrant continuing treatment despite apparent recovery. To some, the risks of prolonging IV therapy may seem inconsequential when juxtaposed to a potentially devastating recurrence. However, in many conditions, recurrences may be related to host issues or ongoing exposures rather than inadequate treatment of the original infection. Recurrent UTIs, for example, are more likely in infants with urologic abnormalities,[3] and recurrent GBS bacteremia has been associated with GBS colonization of maternal breast milk and/or maternal mastitis.[4, 5, 6, 7] Although it is tempting to extend IV courses to prevent recurrences, it is not clear that the benefits of such an approach outweigh the risks.
Concerns over enteral absorption and bioavailability are also understandable, especially in young infants. The superior efficacy of IV over oral antibiotics in general is well accepted for many pediatric conditions, and in some cases (eg, septic shock) it would be unethical to perform a head‐to‐head trial. However, the lack of any published trials (to our knowledge) in pediatrics confirming the superiority of IV antibiotics suggests that oral antibiotic absorption is sufficient for many infections. Even in neonates, several studies have demonstrated that therapeutic serum levels are easily reached with oral dosing of amoxicillin in term and preterm neonates.[8, 9]
For the remainder of this review, the published recommendations and available evidence behind the duration of IV therapy are summarized for 4 bacterial infections in children in which IV antibiotic therapy often continues after clinical recovery: meningitis, bacteremia, UTI, and acute osteomyelitis. We conclude by proposing additional considerations for IV antibiotic durations, especially in situations where guidelines and/or evidence are either nonexistent, dated, conflicting, or contrary to evidence from published studies.
BACTERIAL MENINGITIS
The Infectious Disease Society of America and the British National Institute for Clinical Evidence have both published guidelines with pediatric recommendations for duration of therapy in bacterial meningitis,[10, 11] though the recommendations differ somewhat for 3 of the 4 most common pathogens, and are not always concordant with evidence from randomized controlled trials (Table 1).[12, 13, 14]
| Pathogen | IDSA | NICE | Minimum Range Achieving Equivalent Outcomes in Recent Randomized Trials |
|---|---|---|---|
| |||
| Group B Streptococcus | 1421 days | 14 days | None available |
| Neisseria meningititis | 7 days | 7 days | 15 days[12, 13, 14] |
| Haemophilus influenzae type b | 7 days | 10 days | 45 days[12, 13] |
| Streptococcus pneumoniae | 1014 days | 14 days | 45 days[12, 13] |
A recent meta‐analysis on duration of therapy in meningitis included 5 open‐label trials of ceftriaxone for bacterial meningitis in children.[12] These trials included the 3 most common pathogens and were categorized as short‐course (47 days, n=196 patients) and long‐course (714 days, n=187 patients) therapy. There was no significant difference in clinical success or long‐term neurological complications between groups. Subsequently, a multicountry trial enrolled over 1000 children 2 months to 12 years of age with meningitis caused by Haemophilus influenzae type b, Streptococcus pneumonia, or Neisseria meningititis who were stable after 5 days of IV ceftriaxone therapy and randomized them to receive placebo or an additional 5 days of ceftriaxone.[13] Patients with persistence of seizures, bacteremia, abscess or distant infections, or who were judged to be deteriorating or still severely ill at the 5‐day point were excluded (4.7% of the children who were recruited on day 0). There were no significant differences in bacteriologic failures, clinical failures, or clinical sequelae in survivors. The authors concluded that ceftriaxone can be discontinued in children with bacterial meningitis who are clinically stable after 5 days of IV therapy. Further trials in developed countries are needed.
BACTEREMIA
Because of routine vaccination against H influenzae type b and S pneumoniae, bacteremia beyond the first few months of life in otherwise healthy children is now rare.[15] Even in infants too young to benefit directly from vaccination, the epidemiology of bacteremia has changed considerably over the last few decades, with E coli and GBS constituting the majority (65%77%) of cases.[16, 17] We will limit this review on bacteremia to these 2 organisms in young infants.
Most cases of E coli bacteremia are associated with UTI (91%98%),[16, 17] and most bacteremic UTIs (88%92%) are caused by E coli.[18, 19, 20, 21] There are no official recommendations for the duration of treatment of bacteremic UTI, and only a limited amount of evidence can be gleaned from existing studies. In a trial of oral cefixime for infants aged 1 to 24 months with UTI, all 13 infants with bacteremia fared well whether they received oral cefixime only or IV cefotaxime for 3 days followed by oral cefixime.[18] In a study on length of IV antibiotic therapy in over 12,000 infants 6 months old with UTI, the presence of bacteremia predicted longer IV treatment length (bacteremia was present in 0.5% of the short IV group vs 0.8% of the long IV group, P=0.02) but did not predict treatment failure, defined as readmission within 30 days.[3] In a multicenter investigation of 229 infants 3 months old with bacteremic UTI, the duration of parenteral antibiotics was extremely variable (range, 117 days) and was not associated with treatment failure, defined as recurrent UTI caused by the same organism within 30 days (mean duration 7.8 days in the treatment‐failure group vs 7.7 days in the no‐failure group, P=0.99).[21] In summary, there is no evidence to support a prolonged course (ie, >35 days) of IV antibiotics for bacteremic UTI.
For bacteremia caused by GBS, although the Red Book Committee on Infectious Disease recommends 10 days of IV antibiotics,[22] to our knowledge there are no experimental or observational investigations to support this recommendation. Although available studies suggest that IV courses of at least 10 days are generally provided,[7, 23] no studies have compared outcomes of infants treated with short versus long courses. However, in a study that included 29 full‐term neonates with GBS bacteremia, all 29 had responded initially to 48 hours of intravenous antibiotics (defined as being asymptomatic and fed enterally), and were then treated successfully with high‐dose oral amoxicillin for the remainder of the course, with no recurrences.[8] Although recurrences are estimated to occur in 0.5% to 3% of babies treated for GBS infections, many recurrences are associated with exposure factors such as GBS colonization of the breast milk.[4, 5, 6, 7] In summary, although 10 or more days of IV antibiotic therapy remains a common published recommendation, there is no supportive evidence. More research is needed to assess whether shorter IV courses are safe.
UTI
Most UTIs can be treated with oral antibiotics.[24] In its practice parameter on febrile UTIs in infants 2 months to 2 years of age, the AAP recommends oral antibiotics for well‐appearing children.[25] This recommendation is supported by a recent Cochrane review on the topic,[26] and at least 3 additional trials that have demonstrated that long IV courses do not yield better outcomes than shorter IV courses or oral only courses.[27, 28, 29]
However, all of these trials exclude infants 1 month old, and there are no published recommendations for the 2‐month‐old age group. The study by Brady et al. on >12,000 infants 6 months old with UTI demonstrated no significant differences in UTI readmission rates between infants who were given 4 days of IV antibiotics versus those who were given 4 days.[3] There were 3,383 infants 30 days old in this study, and about one‐third of these babies received a short IV course. Failure rates were nearly identical in each group (2.3% in short course vs 2.4% in long course) even after risk adjustment (personal communication with Patrick Brady, MD, on February 7, 2014). Magin et al. describe 172 neonates (median age 19 days) with UTI who were treated intravenously for a median duration of 4 days (interquartile range, 36 days) and did not experience treatment failures or relapses.[30]
In summary, most cases of UTI can be managed with oral antibiotics. Uncertainty remains over the optimal approach for infants 1 to 2 months old, an age range not considered in current published guidelines. Current evidence suggests that IV treatment for 3 to 4 days followed by oral therapy may be sufficient treatment in this age group.
ACUTE OSTEOMYELITIS
Given the excellent blood supply to rapidly growing tissues in children, shorter durations of IV therapy have been studied with increasing frequency. A 2002 systematic review included 12 prospective cohort studies with at least 6 months of follow‐up.[31] Studies were stratified into 7 days or >7 days IV therapy, and there were no differences in cure rates. Subsequently, a large Finnish trial reported on 131 children who received an initial short IV course (24 days) followed by 20 versus 30 total days of therapy with very low treatment failure rates.[32]
The largest study from the United States to date analyzed nearly 2000 cases of osteomyelitis from 29 hospitals.[33] This study defined a prolonged IV course by placement of a central venous catheter. The rates of prolonged IV therapy varied significantly across hospitals, ranging from 10% to 95% of patients, without detectable differences in outcomes. Furthermore, the readmission rate for catheter related complications (3%) was nearly as high as the overall treatment failure rate (4%5%). Recently, Arnold et al. reported 8 years' experience with a management algorithm to guide the transition to oral antibiotics in pediatric osteoarticular infections in a patient specific manner.[34] This study included 194 patients (154 uncomplicated and 40 complicated cases), all with culture‐proven disease. Transition to oral antibiotics occurred based on resolution of fever and pain, improved function of the affected region, and a C‐reactive protein level of 3 mg/dL, and occurred at an average of 10 days into the treatment course. These authors also provided extensive information about complications to demonstrate that the proposed strategy can be used with a wide range of patients and pathogens. There was a single microbiologic treatment failure after oral step‐down therapy in a complicated osteoarticular infection, with a retained bony fragment. This study represents a successful example of a patient‐centered approach to IV antibiotic duration.
A PATIENT‐CENTERED APPROACH
Returning to the example above of the 2‐week‐old with UTI (with or without bacteremia), there are no published guidelines and only limited available evidence to help guide the duration of IV antibiotics in this case. When standards of care (eg, from published guidelines, review articles, textbooks, or local expert guidance) are nonexistent, conflicting, dated, or contrary to existing evidence, patient‐level factors can be incorporated into the decision‐making process (Table 2). In these cases, tailoring the IV antibiotic course to the individual's response (referred to in 1 review as the ultimate bioassay of the therapy[2]), while also weighing risks and benefits of ongoing therapy, is a logical approach.
| Consideration | Description |
|---|---|
| |
| Severity of initial infection | If concern of recurrence is the justification for a longer IV course, then a more prolonged course might be considered for a more severe initial presentation (eg, septic shock, multisystem organ failure, intensive care unit admission). |
| Response to therapy | Continued IV antibiotics might be warranted in patients who are still symptomatic (eg, fever, vomiting). Inflammatory markers have been used to guide therapy in osteomyelitis.[34] |
| Patient compliance | If a child does not tolerate oral antibiotics or there are concerns about family adherence, a longer IV course may be considered. |
| Family preferences | Shared decision making can be employed, especially when there is no clear evidence supporting a specific duration. |
| Assessment of harms of ongoing hospitalization and/or prolonged IV therapy | See Table 3 |
SEVERITY OF INITIAL INFECTION AND RESPONSE TO THERAPY
The severity of the initial infection, whether in terms of presentation or clinical recovery, can factor into the duration of therapy. Provision of a longer IV course to prevent (albeit theoretically) a recurrence makes more logical sense in an infant with GBS bacteremia who was ill enough to warrant intensive care unit admission than in an infant whose only symptom was a fever. Similarly, most practitioners would be reluctant to stop IV antibiotics and discharge a patient with a bacterial infection who is persistently febrile or vomiting. Although the use of inflammatory markers and other clinical symptoms to guide therapy has been limited to osteomyelitis, this approach might be useful and should be studied in other conditions.
SHARED DECISION MAKING
Shared decision making can also be employed. Parents of sick, hospitalized children generally prefer to be involved in the decision‐making process.[35] For a parent who has concerns about their child's well‐being in the hospital, or has multiple other children at home, competing career obligations, and/or limited family support, the burden of ongoing hospitalization can be significant, and should be factored into decision making. Involving parents in medical decisions may lead to a reduction in utilization for some conditions.[36]
ASSESSMENT OF RISKS/COSTS
The risks and costs of pediatric hospitalization and prolonged IV antibiotics are well described in the literature and are summarized in Table 3. Although the benefits of prolonging IV antibiotics in a child who has recovered from an acute bacterial infection are largely theoretical, many of the risks are concrete and quantifiable. For example, a young infant being treated for a bacteremic UTI may run out of potential IV sites and need a PICC line to continue IV therapy, which according to a recent review of 2574 PICC lines has a 21% complication rate. This rate is even higher in children for whom the PICC line indication was provision of antibiotics (27%) and for infants 1 year of age (44%).[37] Moreover, this procedure often requires sedation or anesthesia for placement, which has both known and unknown risks, including concerns about subsequent adverse effects on development in young children.[38] Nosocomial exposure to seasonal viruses poses an additional risk to hospitalized children.[39]
| Harm of Intravenous Antibiotic Therapy | Description or Example |
|---|---|
| |
| Complications from peripheral IV catheter | Leading source of pain and distress for hospitalized children.[44] |
| Serious complications can occur following IV infiltrates.[45] | |
| Complications from PICC line | Approximately 20% overall complication rate (44% in infants 1 year old).[37] |
| Complications led to rehospitalization of 3% of children being treated with prolonged antibiotics for osteomyelitis.[33] | |
| When thrombosis occurs (up to 9% risk in neonates[46]), 3 months of anticoagulation is recommended.[47] | |
| Complications may arise from sedation/anesthesia necessary to place catheter. Anesthesia has been associated with adverse behavioral or developmental outcomes in children 4 years of age.[38] | |
| Risk of nosocomial infection while hospitalized | An estimated 6% of hospital RSV infections are nosocomial, which are associated with a more prolonged LOS than hospitalizations for community‐acquired RSV.[39] |
| Medication error | In 1 investigation, serious medication errors occurred in 22 per 1,000 patient‐days in a large children's hospital.[48] |
| Emotional and financial burdens | Hospitalization can pose a significant strain on the child, parents, and siblings. |
| Financial costs to healthcare system | In 2003, infection‐related hospitalizations in infants had an average cost of $4,000 (average LOS 3.5 days).[1] |
| Harms associated with prolonged courses of antibiotics in general (IV or PO) | Antibiotic resistance, diarrhea (including Clostridium difficile), allergic reactions, increased costs.[49] |
These additional considerations for the duration of IV antibiotics are not evidence based and should not be used to justify an IV duration that differs dramatically from an accepted standard of care. These are merely considerations that incorporate clinical judgment and a comprehensive analysis of risks and benefits in situations where the available evidence is suboptimal. This approach can be adopted both as a framework for future research and directly in clinical practice.
CONCLUSION
In an era of increasing focus on overtreatment/waste,[40] patient safety,[41] and patient‐centered care,[42] the duration of IV antibiotics for common bacterial infections is a prime target for improving pediatric healthcare value. As emphasized by Michael Porter recently in The New England Journal of Medicine, value should always be defined around the customer.[43] A high‐value approach to IV antibiotic duration incorporates a rigorous assessment of risks and benefits that focuses on best evidence and patient‐level factors.
In discussing published guidelines in a review on bacterial meningitis therapy, Michael Radetsky noted that [R]ecommended criteria, even if provisional, may inadvertently become invested with an independent power to force submission and prohibit deviation. The danger is that sensitivity to individual responsiveness and variability will be lost.[2] Guidelines are useful tools in pediatrics and should continue to be used to direct IV antibiotic durations for bacterial infections in children. However, the emphasis on fixed durations of IV antibiotics might not always serve the best interest of the patient. When guidelines are lacking or contradictory, patient factors should also be considered.
Acknowledgements
The authors thank Ellen R. Wald, MD, and Kenneth B. Roberts, MD, for their thoughtful and valuable additions to this review.
Disclosure: Nothing to report.
- , , , , . Infectious disease hospitalizations among infants in the United States. Pediatrics. 2008;121(2):244–252.
- . Duration of treatment in bacterial meningitis: a historical inquiry. Pediatr Infect Dis J. 1990;9(1):2–9.
- , , . Length of intravenous antibiotic therapy and treatment failure in infants with urinary tract infections. Pediatrics. 2010;126(2):196–203.
- , , , et al. Group B streptococci in milk and late neonatal infections: an analysis of cases in the literature. Arch Dis Child Fetal Neonatal Ed. 2014;99(1):F41–F47.
- , , . Recurrent late‐onset group B Streptococcus sepsis in a preterm infant acquired by expressed breastmilk transmission: a case report. Breastfeed Med. 2013;8(1):134–136.
- , , , , , . Late‐onset and recurrent neonatal Group B streptococcal disease associated with breast‐milk transmission. Pediatr Dev Pathol. 2003;6(3):251–256.
- , , , , . A 5‐year review of recurrent group B streptococcal disease: lessons from twin infants. Clin Infect Dis. 2000;30(2):282–287.
- , , , et al. Therapeutic amoxicillin levels achieved with oral administration in term neonates. Eur J Clin Pharmacol. 2007;63(7):657–662.
- , , , , , . Population pharmacokinetics and dosing of amoxicillin in (pre)term neonates. Ther Drug Monit. 2006;28(2):226–231.
- , , , et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004;39(9):1267–1284.
- , , , , , . Management of bacterial meningitis and meningococcal septicaemia in children and young people: summary of NICE guidance. BMJ. 2010;340:c3209.
- , , , , . Short versus long duration of antibiotic therapy for bacterial meningitis: a meta‐analysis of randomised controlled trials in children. Arch Dis Child. 2009;94(8):607–614.
- , , , et al. 5 versus 10 days of treatment with ceftriaxone for bacterial meningitis in children: a double‐blind randomised equivalence study. Lancet. 2011;377(9780):1837–1845.
- , , , et al. Ceftriaxone as effective as long‐acting chloramphenicol in short‐course treatment of meningococcal meningitis during epidemics: a randomised non‐inferiority study. Lancet. 2005;366(9482):308–313.
- , , , et al. Changing epidemiology of outpatient bacteremia in 3‐ to 36‐month‐old children after the introduction of the heptavalent‐conjugated pneumococcal vaccine. Pediatr Infect Dis J. 2006;25(4):293–300.
- , , , et al. Epidemiology of bacteremia in febrile infants in the United States. Pediatrics. 2013;132(6):990–996.
- , , . Changing epidemiology of bacteremia in infants aged 1 week to 3 months. Pediatrics. 2012;129(3):e590–e596.
- , , , et al. Oral versus initial intravenous therapy for urinary tract infections in young febrile children. Pediatrics. 1999;104(1 pt 1):79–86.
- , , , , . Bacteremic urinary tract infection in children. Pediatr Infect Dis J. 2000;19(7):630–634.
- , , , , , . Urine testing and urinary tract infections in febrile infants seen in office settings: the Pediatric Research in Office Settings' Febrile Infant Study. Arch Pediatr Adolesc Med. 2002;156(1):44–54.
- , , , , , . Management of bacteremic urinary tract infections in infants less than 3 months of age. Abstract presented at: Pediatric Academic Societies Annual Meeting; May 5, 2014; Vancouver BC, Canada.
- , , , . Red Book: 2009 Report of the Committee on Infectious Diseases. 28th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2012.
- , . Recurrent group B streptococcal bacteremia. Clin Pediatr (Phila). 2012;51(9):884–887.
- , , , . Antibiotics for treating lower urinary tract infection in children. Cochrane Database Syst Rev. 2012;8:CD006857.
- . Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011;128(3):595–610.
- , , . Antibiotics for acute pyelonephritis in children. Cochrane Database Syst Rev. 2007(4):CD003772.
- , , , et al. Randomized trial of oral versus sequential IV/oral antibiotic for acute pyelonephritis in children. Pediatrics. 2012;129(2):e269–e275.
- , , , et al. Prospective, randomized trial comparing short and long intravenous antibiotic treatment of acute pyelonephritis in children: dimercaptosuccinic acid scintigraphic evaluation at 9 months. Pediatrics. 2008;121(3):e553–e560.
- , , , et al. Randomised trial of oral versus sequential intravenous/oral cephalosporins in children with pyelonephritis. Eur J Pediatr. 2008;167(9):1037–1047.
- , , , , . Efficacy of short‐term intravenous antibiotic in neonates with urinary tract infection. Pediatr Emerg Care. 2007;23(2):83–86.
- , , , , , . Shorter courses of parenteral antibiotic therapy do not appear to influence response rates for children with acute hematogenous osteomyelitis: a systematic review. BMC Infect Dis. 2002;2:16.
- , , , . Short‐ versus long‐term antimicrobial treatment for acute hematogenous osteomyelitis of childhood: prospective, randomized trial on 131 culture‐positive cases. Pediatr Infect Dis J. 2010;29(12):1123–1128.
- , , , , , . Prolonged intravenous therapy versus early transition to oral antimicrobial therapy for acute osteomyelitis in children. Pediatrics. 2009;123(2):636–642.
- , , , et al. Acute bacterial osteoarticular infections: eight‐year analysis of C‐reactive protein for oral step‐down therapy. Pediatrics. 2012;130(4):e821–e828.
- , , , , , . Parental decision‐making preferences in the pediatric intensive care unit. Crit Care Med. 2012;40(10):2876–2882.
- , , , , . An assessment of the shared‐decision model in parents of children with acute otitis media. Pediatrics. 2005;116(6):1267–1275.
- , , , , . Risk factors for peripherally inserted central venous catheter complications in children. JAMA Pediatr. 2013;167(5):429–435.
- , , . Current clinical evidence on the effect of general anesthesia on neurodevelopment in children: an updated systematic review with meta‐regression. PLoS One. 2014;9(1):e85760.
- , , , et al. Nosocomial respiratory syncytial virus infection in Canadian pediatric hospitals: a Pediatric Investigators Collaborative Network on Infections in Canada Study. Pediatrics. 1997;100(6):943–946.
- , . Eliminating waste in US health care. JAMA. 2012;307(14):1513–1516.
- , , . Safely doing less: a missing component of the patient safety dialogue. Pediatrics. 2011;128(6):e1596–e1597.
- Committee On Hospital Care and Institute For Patient‐ and Family‐Centered Care. Patient‐ and family‐centered care and the pediatrician's role. Pediatrics. 2012;129(2):394–404.
- . What is value in health care? N Engl J Med. 2010;363(26):2477–2481.
- , , , , . Prevalence and source of pain in pediatric inpatients. Pain. 1996;68(1):25–31.
- , , , . Acute compartment syndrome of the upper extremity in children: diagnosis, management, and outcomes. J Child Orthop. 2013;7(3):225–233.
- , , , , . Neonatal central venous catheter thrombosis: diagnosis, management and outcome. Blood Coagul Fibrinolysis. 2014;25(2):97–106.
- , , , et al. Antithrombotic therapy in neonates and children: antithrombotic therapy and prevention of thrombosis, 9th ed: American C ollege of Chest Physicians Evidence‐Based Clinical Practice Guidelines. Chest. 2012;141(2 suppl):e737S–801S.
- , , , et al. Effect of computer order entry on prevention of serious medication errors in hospitalized children. Pediatrics. 2008;121(3):e421–e427.
- Duration and cessation of antimicrobial treatment. J Hosp Med. 2012;7(suppl 1):S22–S33.
- , , , , . Infectious disease hospitalizations among infants in the United States. Pediatrics. 2008;121(2):244–252.
- . Duration of treatment in bacterial meningitis: a historical inquiry. Pediatr Infect Dis J. 1990;9(1):2–9.
- , , . Length of intravenous antibiotic therapy and treatment failure in infants with urinary tract infections. Pediatrics. 2010;126(2):196–203.
- , , , et al. Group B streptococci in milk and late neonatal infections: an analysis of cases in the literature. Arch Dis Child Fetal Neonatal Ed. 2014;99(1):F41–F47.
- , , . Recurrent late‐onset group B Streptococcus sepsis in a preterm infant acquired by expressed breastmilk transmission: a case report. Breastfeed Med. 2013;8(1):134–136.
- , , , , , . Late‐onset and recurrent neonatal Group B streptococcal disease associated with breast‐milk transmission. Pediatr Dev Pathol. 2003;6(3):251–256.
- , , , , . A 5‐year review of recurrent group B streptococcal disease: lessons from twin infants. Clin Infect Dis. 2000;30(2):282–287.
- , , , et al. Therapeutic amoxicillin levels achieved with oral administration in term neonates. Eur J Clin Pharmacol. 2007;63(7):657–662.
- , , , , , . Population pharmacokinetics and dosing of amoxicillin in (pre)term neonates. Ther Drug Monit. 2006;28(2):226–231.
- , , , et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004;39(9):1267–1284.
- , , , , , . Management of bacterial meningitis and meningococcal septicaemia in children and young people: summary of NICE guidance. BMJ. 2010;340:c3209.
- , , , , . Short versus long duration of antibiotic therapy for bacterial meningitis: a meta‐analysis of randomised controlled trials in children. Arch Dis Child. 2009;94(8):607–614.
- , , , et al. 5 versus 10 days of treatment with ceftriaxone for bacterial meningitis in children: a double‐blind randomised equivalence study. Lancet. 2011;377(9780):1837–1845.
- , , , et al. Ceftriaxone as effective as long‐acting chloramphenicol in short‐course treatment of meningococcal meningitis during epidemics: a randomised non‐inferiority study. Lancet. 2005;366(9482):308–313.
- , , , et al. Changing epidemiology of outpatient bacteremia in 3‐ to 36‐month‐old children after the introduction of the heptavalent‐conjugated pneumococcal vaccine. Pediatr Infect Dis J. 2006;25(4):293–300.
- , , , et al. Epidemiology of bacteremia in febrile infants in the United States. Pediatrics. 2013;132(6):990–996.
- , , . Changing epidemiology of bacteremia in infants aged 1 week to 3 months. Pediatrics. 2012;129(3):e590–e596.
- , , , et al. Oral versus initial intravenous therapy for urinary tract infections in young febrile children. Pediatrics. 1999;104(1 pt 1):79–86.
- , , , , . Bacteremic urinary tract infection in children. Pediatr Infect Dis J. 2000;19(7):630–634.
- , , , , , . Urine testing and urinary tract infections in febrile infants seen in office settings: the Pediatric Research in Office Settings' Febrile Infant Study. Arch Pediatr Adolesc Med. 2002;156(1):44–54.
- , , , , , . Management of bacteremic urinary tract infections in infants less than 3 months of age. Abstract presented at: Pediatric Academic Societies Annual Meeting; May 5, 2014; Vancouver BC, Canada.
- , , , . Red Book: 2009 Report of the Committee on Infectious Diseases. 28th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2012.
- , . Recurrent group B streptococcal bacteremia. Clin Pediatr (Phila). 2012;51(9):884–887.
- , , , . Antibiotics for treating lower urinary tract infection in children. Cochrane Database Syst Rev. 2012;8:CD006857.
- . Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011;128(3):595–610.
- , , . Antibiotics for acute pyelonephritis in children. Cochrane Database Syst Rev. 2007(4):CD003772.
- , , , et al. Randomized trial of oral versus sequential IV/oral antibiotic for acute pyelonephritis in children. Pediatrics. 2012;129(2):e269–e275.
- , , , et al. Prospective, randomized trial comparing short and long intravenous antibiotic treatment of acute pyelonephritis in children: dimercaptosuccinic acid scintigraphic evaluation at 9 months. Pediatrics. 2008;121(3):e553–e560.
- , , , et al. Randomised trial of oral versus sequential intravenous/oral cephalosporins in children with pyelonephritis. Eur J Pediatr. 2008;167(9):1037–1047.
- , , , , . Efficacy of short‐term intravenous antibiotic in neonates with urinary tract infection. Pediatr Emerg Care. 2007;23(2):83–86.
- , , , , , . Shorter courses of parenteral antibiotic therapy do not appear to influence response rates for children with acute hematogenous osteomyelitis: a systematic review. BMC Infect Dis. 2002;2:16.
- , , , . Short‐ versus long‐term antimicrobial treatment for acute hematogenous osteomyelitis of childhood: prospective, randomized trial on 131 culture‐positive cases. Pediatr Infect Dis J. 2010;29(12):1123–1128.
- , , , , , . Prolonged intravenous therapy versus early transition to oral antimicrobial therapy for acute osteomyelitis in children. Pediatrics. 2009;123(2):636–642.
- , , , et al. Acute bacterial osteoarticular infections: eight‐year analysis of C‐reactive protein for oral step‐down therapy. Pediatrics. 2012;130(4):e821–e828.
- , , , , , . Parental decision‐making preferences in the pediatric intensive care unit. Crit Care Med. 2012;40(10):2876–2882.
- , , , , . An assessment of the shared‐decision model in parents of children with acute otitis media. Pediatrics. 2005;116(6):1267–1275.
- , , , , . Risk factors for peripherally inserted central venous catheter complications in children. JAMA Pediatr. 2013;167(5):429–435.
- , , . Current clinical evidence on the effect of general anesthesia on neurodevelopment in children: an updated systematic review with meta‐regression. PLoS One. 2014;9(1):e85760.
- , , , et al. Nosocomial respiratory syncytial virus infection in Canadian pediatric hospitals: a Pediatric Investigators Collaborative Network on Infections in Canada Study. Pediatrics. 1997;100(6):943–946.
- , . Eliminating waste in US health care. JAMA. 2012;307(14):1513–1516.
- , , . Safely doing less: a missing component of the patient safety dialogue. Pediatrics. 2011;128(6):e1596–e1597.
- Committee On Hospital Care and Institute For Patient‐ and Family‐Centered Care. Patient‐ and family‐centered care and the pediatrician's role. Pediatrics. 2012;129(2):394–404.
- . What is value in health care? N Engl J Med. 2010;363(26):2477–2481.
- , , , , . Prevalence and source of pain in pediatric inpatients. Pain. 1996;68(1):25–31.
- , , , . Acute compartment syndrome of the upper extremity in children: diagnosis, management, and outcomes. J Child Orthop. 2013;7(3):225–233.
- , , , , . Neonatal central venous catheter thrombosis: diagnosis, management and outcome. Blood Coagul Fibrinolysis. 2014;25(2):97–106.
- , , , et al. Antithrombotic therapy in neonates and children: antithrombotic therapy and prevention of thrombosis, 9th ed: American C ollege of Chest Physicians Evidence‐Based Clinical Practice Guidelines. Chest. 2012;141(2 suppl):e737S–801S.
- , , , et al. Effect of computer order entry on prevention of serious medication errors in hospitalized children. Pediatrics. 2008;121(3):e421–e427.
- Duration and cessation of antimicrobial treatment. J Hosp Med. 2012;7(suppl 1):S22–S33.
Survey: ObGyns’ salaries rose slightly in 2013
The 2014 Medscape Compensation Report surveyed more than 24,000 physicians in 25 specialties. Five percent of respondents were ObGyns, whose mean income rose slightly to $243,000 in 2013 from $242,000 in 2012, up from $220,000 in 2011.1–3 The highest ObGyn earners lived in the Great Lakes and North Central regions.1
Survey findings
Men make more than women. In 2013, male ObGyns reported earning $256,000; female ObGyns reported $229,000 in mean income. However, women felt more satisfied with their salary (47% of women vs 38% of men). Regardless of gender, ObGyns were slightly less happy with their income than all physicians (50% satisfied).1
Among all female physicians, more were employed than self-employed; the opposite was true for male physicians.4 Half of all graduating physicians are now female, and demographics show that 62% of all female physicians are younger than age 45.1
Practice settings are key to income. Sixty percent of ObGyns indicated they would choose medicine again as a career; 43% would choose their own specialty. However, only 25% of ObGyns would make the same decision about practice setting.1
In 2013, employed and self-employed ObGyns reported nearly the same mean income: $243,000 versus $246,000, respectively. However, when broken down by specific practice setting, the highest earners were ObGyns who worked for health-care organizations, at $273,000. Additional 2013 mean earnings ranked by work setting were1:
- multispecialty office-based group practices, $271,000
- single-specialty office-based group practices, $255,000
- hospitals, $228,000
- solo office-based practices, $212,000
- outpatient clinics, $207,000.
In 2013, 49% of employed physicians worked in hospitals or in groups owned by a hospital, while 21% were employed by private groups. Other employment situations included community health centers, corporate laboratories, correction institutions, military bases, and nursing homes.4
ACO participation grows. In 2013, 37% of ObGyns either participated in an Accountable Care Organization (ACO) or planned on joining an ACO within the next year.1 This was an increase from 25% in 2012.2,3
In the most recent report, 2% chose concierge practices (also known as direct primary care) and 5% opted for cash-only practices.1 In 2012, only 1% of ObGyns opted for concierge practices, and 3% for cash-only practices.2,3
Related article: Is private ObGyn practice on its way out? Lucia DiVenere, MA (October 2011)
Employment over private practice? In 2013, physicians were enticed to seek employment by the financial challenges of private practice (38%); not having to be concerned about administrative issues (29%); and working shorter and more regular hours (19%). Other reported benefits of employment were academic opportunities, better life−work balance, more vacation time, and no loss of income during vacation. More than half (53%) of employed physicians who were previously self-employed felt that patient care was superior now that they were employed, and 37% thought it was about the same.4
Related article: Mean income for ObGyns increased in 2012. Deborah Reale (News for your Practice; August 2013)
Career satisfaction
ObGyns were close to the bottom among all physicians (48%) when it came to overall career satisfaction, tied with nephrologists, surgeons, and pulmonologists. The most satisfied physicians were dermatologists (65%); the least satisfied were plastic surgeons (45%).1
What drives you? In 2013, more ObGyns (41%) than all physicians (33%) reported that the most rewarding part of their job was their relationships with patients. Thirty percent of ObGyns chose being good at their jobs; 8% chose making good money; and 2% found nothing rewarding about the job.1
How much patient time do you spend? The majority (58%) of ObGyns reported spending more than 40 hours per week with patients and 16 minutes or less (66%) per patient.1 In 2012, 60% of ObGyn respondents reported spending 16 minutes or less per patient.2,3
Anticipating the effects of the Affordable Care Act
Under the Affordable Care Act (ACA), an organization’s revenue will still be determined largely by the volume generated by physicians. The percentage of ObGyns who saw 50 to 124 patients per week increased from 57% in 2012 to 69% in 2013 (TABLE).1,2
In 2013, 53% of ObGyns still were undecided about health-insurance exchange participation—the same percentage as all survey respondents. Among ObGyns, 30% would participate, and 17% would not participate.1
Related article: As the Affordable Care Act comes of age, a look behind the headlines. Lucia DiVenere, MA (Practice Management; January 2014)
Almost half (49%) of ObGyns expect their income under the ACA to decrease. About 45% of ObGyns did not foresee any change, and 5% believed their incomes would increase (1% didn’t know) under the ACA. ObGyns also anticipated a higher workload, a decline in quality of patient care and access, and reduced ability to make decisions.1
Almost one-third of ObGyns dropped poorly paying insurers. In 2013, 29% of ObGyns said they regularly drop insurers who pay poorly, but 46% said they keep their insurers year after year. In 2012, 26% of ObGyns said they drop insurers who pay the least or create the most trouble; 29% said they keep all insurers.2,3 Private insurance paid for 63% of patient visits to ObGyns in 2013.1
Fewer ObGyns indicated they would see Medicare and Medicaid patients. In 2013, 20% of self-employed and 5% of employed ObGyns said that they plan to stop taking new Medicare or Medicaid patients. More employed (72%) than self-employed (46%) ObGyns reported that they would continue seeing new and current Medicare and Medicaid patients.1
Related article: Medicare and Medicaid are on the brink of insolvency, and you’re not just a bystander. Robert L. Barbieri, MD (Editorial; October 2011)
In 2012, 15% of ObGyn respondents planned to stop taking new Medicare or Medicaid patients, but 53% of ObGyn respondents said they would continue to see current patients and would take on new Medicare or Medicaid patients.2,3
TELL US WHAT YOU THINK! Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
- Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
- Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
- Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
- Kane L. Employed vs self-employed: Who is better off? Medscape Web site. http://www.medscape.com/features/slideshow/public/employed-doctors. Published March 11, 2014. Accessed June 2, 2014.
The 2014 Medscape Compensation Report surveyed more than 24,000 physicians in 25 specialties. Five percent of respondents were ObGyns, whose mean income rose slightly to $243,000 in 2013 from $242,000 in 2012, up from $220,000 in 2011.1–3 The highest ObGyn earners lived in the Great Lakes and North Central regions.1
Survey findings
Men make more than women. In 2013, male ObGyns reported earning $256,000; female ObGyns reported $229,000 in mean income. However, women felt more satisfied with their salary (47% of women vs 38% of men). Regardless of gender, ObGyns were slightly less happy with their income than all physicians (50% satisfied).1
Among all female physicians, more were employed than self-employed; the opposite was true for male physicians.4 Half of all graduating physicians are now female, and demographics show that 62% of all female physicians are younger than age 45.1
Practice settings are key to income. Sixty percent of ObGyns indicated they would choose medicine again as a career; 43% would choose their own specialty. However, only 25% of ObGyns would make the same decision about practice setting.1
In 2013, employed and self-employed ObGyns reported nearly the same mean income: $243,000 versus $246,000, respectively. However, when broken down by specific practice setting, the highest earners were ObGyns who worked for health-care organizations, at $273,000. Additional 2013 mean earnings ranked by work setting were1:
- multispecialty office-based group practices, $271,000
- single-specialty office-based group practices, $255,000
- hospitals, $228,000
- solo office-based practices, $212,000
- outpatient clinics, $207,000.
In 2013, 49% of employed physicians worked in hospitals or in groups owned by a hospital, while 21% were employed by private groups. Other employment situations included community health centers, corporate laboratories, correction institutions, military bases, and nursing homes.4
ACO participation grows. In 2013, 37% of ObGyns either participated in an Accountable Care Organization (ACO) or planned on joining an ACO within the next year.1 This was an increase from 25% in 2012.2,3
In the most recent report, 2% chose concierge practices (also known as direct primary care) and 5% opted for cash-only practices.1 In 2012, only 1% of ObGyns opted for concierge practices, and 3% for cash-only practices.2,3
Related article: Is private ObGyn practice on its way out? Lucia DiVenere, MA (October 2011)
Employment over private practice? In 2013, physicians were enticed to seek employment by the financial challenges of private practice (38%); not having to be concerned about administrative issues (29%); and working shorter and more regular hours (19%). Other reported benefits of employment were academic opportunities, better life−work balance, more vacation time, and no loss of income during vacation. More than half (53%) of employed physicians who were previously self-employed felt that patient care was superior now that they were employed, and 37% thought it was about the same.4
Related article: Mean income for ObGyns increased in 2012. Deborah Reale (News for your Practice; August 2013)
Career satisfaction
ObGyns were close to the bottom among all physicians (48%) when it came to overall career satisfaction, tied with nephrologists, surgeons, and pulmonologists. The most satisfied physicians were dermatologists (65%); the least satisfied were plastic surgeons (45%).1
What drives you? In 2013, more ObGyns (41%) than all physicians (33%) reported that the most rewarding part of their job was their relationships with patients. Thirty percent of ObGyns chose being good at their jobs; 8% chose making good money; and 2% found nothing rewarding about the job.1
How much patient time do you spend? The majority (58%) of ObGyns reported spending more than 40 hours per week with patients and 16 minutes or less (66%) per patient.1 In 2012, 60% of ObGyn respondents reported spending 16 minutes or less per patient.2,3
Anticipating the effects of the Affordable Care Act
Under the Affordable Care Act (ACA), an organization’s revenue will still be determined largely by the volume generated by physicians. The percentage of ObGyns who saw 50 to 124 patients per week increased from 57% in 2012 to 69% in 2013 (TABLE).1,2
In 2013, 53% of ObGyns still were undecided about health-insurance exchange participation—the same percentage as all survey respondents. Among ObGyns, 30% would participate, and 17% would not participate.1
Related article: As the Affordable Care Act comes of age, a look behind the headlines. Lucia DiVenere, MA (Practice Management; January 2014)
Almost half (49%) of ObGyns expect their income under the ACA to decrease. About 45% of ObGyns did not foresee any change, and 5% believed their incomes would increase (1% didn’t know) under the ACA. ObGyns also anticipated a higher workload, a decline in quality of patient care and access, and reduced ability to make decisions.1
Almost one-third of ObGyns dropped poorly paying insurers. In 2013, 29% of ObGyns said they regularly drop insurers who pay poorly, but 46% said they keep their insurers year after year. In 2012, 26% of ObGyns said they drop insurers who pay the least or create the most trouble; 29% said they keep all insurers.2,3 Private insurance paid for 63% of patient visits to ObGyns in 2013.1
Fewer ObGyns indicated they would see Medicare and Medicaid patients. In 2013, 20% of self-employed and 5% of employed ObGyns said that they plan to stop taking new Medicare or Medicaid patients. More employed (72%) than self-employed (46%) ObGyns reported that they would continue seeing new and current Medicare and Medicaid patients.1
Related article: Medicare and Medicaid are on the brink of insolvency, and you’re not just a bystander. Robert L. Barbieri, MD (Editorial; October 2011)
In 2012, 15% of ObGyn respondents planned to stop taking new Medicare or Medicaid patients, but 53% of ObGyn respondents said they would continue to see current patients and would take on new Medicare or Medicaid patients.2,3
TELL US WHAT YOU THINK! Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
The 2014 Medscape Compensation Report surveyed more than 24,000 physicians in 25 specialties. Five percent of respondents were ObGyns, whose mean income rose slightly to $243,000 in 2013 from $242,000 in 2012, up from $220,000 in 2011.1–3 The highest ObGyn earners lived in the Great Lakes and North Central regions.1
Survey findings
Men make more than women. In 2013, male ObGyns reported earning $256,000; female ObGyns reported $229,000 in mean income. However, women felt more satisfied with their salary (47% of women vs 38% of men). Regardless of gender, ObGyns were slightly less happy with their income than all physicians (50% satisfied).1
Among all female physicians, more were employed than self-employed; the opposite was true for male physicians.4 Half of all graduating physicians are now female, and demographics show that 62% of all female physicians are younger than age 45.1
Practice settings are key to income. Sixty percent of ObGyns indicated they would choose medicine again as a career; 43% would choose their own specialty. However, only 25% of ObGyns would make the same decision about practice setting.1
In 2013, employed and self-employed ObGyns reported nearly the same mean income: $243,000 versus $246,000, respectively. However, when broken down by specific practice setting, the highest earners were ObGyns who worked for health-care organizations, at $273,000. Additional 2013 mean earnings ranked by work setting were1:
- multispecialty office-based group practices, $271,000
- single-specialty office-based group practices, $255,000
- hospitals, $228,000
- solo office-based practices, $212,000
- outpatient clinics, $207,000.
In 2013, 49% of employed physicians worked in hospitals or in groups owned by a hospital, while 21% were employed by private groups. Other employment situations included community health centers, corporate laboratories, correction institutions, military bases, and nursing homes.4
ACO participation grows. In 2013, 37% of ObGyns either participated in an Accountable Care Organization (ACO) or planned on joining an ACO within the next year.1 This was an increase from 25% in 2012.2,3
In the most recent report, 2% chose concierge practices (also known as direct primary care) and 5% opted for cash-only practices.1 In 2012, only 1% of ObGyns opted for concierge practices, and 3% for cash-only practices.2,3
Related article: Is private ObGyn practice on its way out? Lucia DiVenere, MA (October 2011)
Employment over private practice? In 2013, physicians were enticed to seek employment by the financial challenges of private practice (38%); not having to be concerned about administrative issues (29%); and working shorter and more regular hours (19%). Other reported benefits of employment were academic opportunities, better life−work balance, more vacation time, and no loss of income during vacation. More than half (53%) of employed physicians who were previously self-employed felt that patient care was superior now that they were employed, and 37% thought it was about the same.4
Related article: Mean income for ObGyns increased in 2012. Deborah Reale (News for your Practice; August 2013)
Career satisfaction
ObGyns were close to the bottom among all physicians (48%) when it came to overall career satisfaction, tied with nephrologists, surgeons, and pulmonologists. The most satisfied physicians were dermatologists (65%); the least satisfied were plastic surgeons (45%).1
What drives you? In 2013, more ObGyns (41%) than all physicians (33%) reported that the most rewarding part of their job was their relationships with patients. Thirty percent of ObGyns chose being good at their jobs; 8% chose making good money; and 2% found nothing rewarding about the job.1
How much patient time do you spend? The majority (58%) of ObGyns reported spending more than 40 hours per week with patients and 16 minutes or less (66%) per patient.1 In 2012, 60% of ObGyn respondents reported spending 16 minutes or less per patient.2,3
Anticipating the effects of the Affordable Care Act
Under the Affordable Care Act (ACA), an organization’s revenue will still be determined largely by the volume generated by physicians. The percentage of ObGyns who saw 50 to 124 patients per week increased from 57% in 2012 to 69% in 2013 (TABLE).1,2
In 2013, 53% of ObGyns still were undecided about health-insurance exchange participation—the same percentage as all survey respondents. Among ObGyns, 30% would participate, and 17% would not participate.1
Related article: As the Affordable Care Act comes of age, a look behind the headlines. Lucia DiVenere, MA (Practice Management; January 2014)
Almost half (49%) of ObGyns expect their income under the ACA to decrease. About 45% of ObGyns did not foresee any change, and 5% believed their incomes would increase (1% didn’t know) under the ACA. ObGyns also anticipated a higher workload, a decline in quality of patient care and access, and reduced ability to make decisions.1
Almost one-third of ObGyns dropped poorly paying insurers. In 2013, 29% of ObGyns said they regularly drop insurers who pay poorly, but 46% said they keep their insurers year after year. In 2012, 26% of ObGyns said they drop insurers who pay the least or create the most trouble; 29% said they keep all insurers.2,3 Private insurance paid for 63% of patient visits to ObGyns in 2013.1
Fewer ObGyns indicated they would see Medicare and Medicaid patients. In 2013, 20% of self-employed and 5% of employed ObGyns said that they plan to stop taking new Medicare or Medicaid patients. More employed (72%) than self-employed (46%) ObGyns reported that they would continue seeing new and current Medicare and Medicaid patients.1
Related article: Medicare and Medicaid are on the brink of insolvency, and you’re not just a bystander. Robert L. Barbieri, MD (Editorial; October 2011)
In 2012, 15% of ObGyn respondents planned to stop taking new Medicare or Medicaid patients, but 53% of ObGyn respondents said they would continue to see current patients and would take on new Medicare or Medicaid patients.2,3
TELL US WHAT YOU THINK! Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
- Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
- Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
- Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
- Kane L. Employed vs self-employed: Who is better off? Medscape Web site. http://www.medscape.com/features/slideshow/public/employed-doctors. Published March 11, 2014. Accessed June 2, 2014.
- Peckham C. Medscape OB/GYN Compensation Report 2014. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 15, 2014. Accessed June 2, 2014.
- Medscape News. Ob/Gyn Compensation Report 2013. Medscape Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
- Reale D. Mean income for ObGyns increased in 2012. OBG Manag. 2013;25(8):34–36.
- Kane L. Employed vs self-employed: Who is better off? Medscape Web site. http://www.medscape.com/features/slideshow/public/employed-doctors. Published March 11, 2014. Accessed June 2, 2014.