User login
Recognizing autophonia in patients with anorexia nervosa
Anorexia nervosa can affect a number of systems of the body, including the otolaryngologic presentation of autophonia1,2—a rare hyperperception of an abnormally intense hearing of one’s own voice and respiratory sounds.2 The most common cause of autophonia in patients with anorexia is a patulous (patent) eustachian tube, which can be caused by extreme weight loss.2,3
Significant reduction in the quantity of fat tissue at the location of the eustachian tube can cause patency.3 This creates an abnormal connection between the nasopharynx and tympanic membrane, in which sounds are transmitted directly from the oral cavity to the middle ear, causing autophonia, tinnitus, or sound distortion.4
What are the symptoms?Patients often report hearing their own voice more loudly in the affected ear. This can be distressing, and they might become preoccupied with the sound of their voice—thus affecting quality of life.2,4
The intensity of symptoms varies: from a mild sensation of a clogged ear to extremely bothersome discomfort much like a middle-ear infection.2,4 Autophonia, however, cannot be relieved by conventional therapies for those conditions.2,3
A patulous eustachian tube is difficult to detect and can be misdiagnosed as another condition. Pregnancy, stress, fatigue, radiation therapy, hormonal therapy, and dramatic weight loss also can cause a patulous eustachian tube.2
How is the diagnosis made?The diagnosis of autophonia is clinical and begins with a detailed history. Symptoms often appear within the time frame of rapid weight loss and without evidence of infection or other illness.2,3 The clinical examination is otherwise unremarkable.2,4
Is there treatment?To improve the patient’s comfort and quality of life, intervention is required, best provided by an integrated team of medical specialists. Weight gain, of course, is the treatment goal in anorexia, but this is a complex process often marked by relapse; a detailed discussion of treatment strategies is beyond the scope of this “Pearl.” Symptoms usually diminish as fatty tissue is restored upon successful treatment of anorexia, which closes the abnormal eustachian tube opening.2,3
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Olthoff A, Laskawi R, Kruse E. Successful treatment of autophonia with botulinum toxin: case report. Ann Otol Rhinol Laryngol. 2007;116(8):594-598.
2. Godbole M, Key A. Autophonia in anorexia nervosa. Int J Eat Disord. 2010;43(5):480-482.
3. Karwautz A, Hafferl A, Ungar D, et al. Patulous eustachian tube in a case of adolescent anorexia nervosa. Int J Eat Disord. 1999;25(3):353-355.
4. Dornhoffer JL, Leuwer R, Schwager K, et al. A practical guide to the eustachian tube. New York, NY: Springer; 2014:23-41.
Anorexia nervosa can affect a number of systems of the body, including the otolaryngologic presentation of autophonia1,2—a rare hyperperception of an abnormally intense hearing of one’s own voice and respiratory sounds.2 The most common cause of autophonia in patients with anorexia is a patulous (patent) eustachian tube, which can be caused by extreme weight loss.2,3
Significant reduction in the quantity of fat tissue at the location of the eustachian tube can cause patency.3 This creates an abnormal connection between the nasopharynx and tympanic membrane, in which sounds are transmitted directly from the oral cavity to the middle ear, causing autophonia, tinnitus, or sound distortion.4
What are the symptoms?Patients often report hearing their own voice more loudly in the affected ear. This can be distressing, and they might become preoccupied with the sound of their voice—thus affecting quality of life.2,4
The intensity of symptoms varies: from a mild sensation of a clogged ear to extremely bothersome discomfort much like a middle-ear infection.2,4 Autophonia, however, cannot be relieved by conventional therapies for those conditions.2,3
A patulous eustachian tube is difficult to detect and can be misdiagnosed as another condition. Pregnancy, stress, fatigue, radiation therapy, hormonal therapy, and dramatic weight loss also can cause a patulous eustachian tube.2
How is the diagnosis made?The diagnosis of autophonia is clinical and begins with a detailed history. Symptoms often appear within the time frame of rapid weight loss and without evidence of infection or other illness.2,3 The clinical examination is otherwise unremarkable.2,4
Is there treatment?To improve the patient’s comfort and quality of life, intervention is required, best provided by an integrated team of medical specialists. Weight gain, of course, is the treatment goal in anorexia, but this is a complex process often marked by relapse; a detailed discussion of treatment strategies is beyond the scope of this “Pearl.” Symptoms usually diminish as fatty tissue is restored upon successful treatment of anorexia, which closes the abnormal eustachian tube opening.2,3
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Anorexia nervosa can affect a number of systems of the body, including the otolaryngologic presentation of autophonia1,2—a rare hyperperception of an abnormally intense hearing of one’s own voice and respiratory sounds.2 The most common cause of autophonia in patients with anorexia is a patulous (patent) eustachian tube, which can be caused by extreme weight loss.2,3
Significant reduction in the quantity of fat tissue at the location of the eustachian tube can cause patency.3 This creates an abnormal connection between the nasopharynx and tympanic membrane, in which sounds are transmitted directly from the oral cavity to the middle ear, causing autophonia, tinnitus, or sound distortion.4
What are the symptoms?Patients often report hearing their own voice more loudly in the affected ear. This can be distressing, and they might become preoccupied with the sound of their voice—thus affecting quality of life.2,4
The intensity of symptoms varies: from a mild sensation of a clogged ear to extremely bothersome discomfort much like a middle-ear infection.2,4 Autophonia, however, cannot be relieved by conventional therapies for those conditions.2,3
A patulous eustachian tube is difficult to detect and can be misdiagnosed as another condition. Pregnancy, stress, fatigue, radiation therapy, hormonal therapy, and dramatic weight loss also can cause a patulous eustachian tube.2
How is the diagnosis made?The diagnosis of autophonia is clinical and begins with a detailed history. Symptoms often appear within the time frame of rapid weight loss and without evidence of infection or other illness.2,3 The clinical examination is otherwise unremarkable.2,4
Is there treatment?To improve the patient’s comfort and quality of life, intervention is required, best provided by an integrated team of medical specialists. Weight gain, of course, is the treatment goal in anorexia, but this is a complex process often marked by relapse; a detailed discussion of treatment strategies is beyond the scope of this “Pearl.” Symptoms usually diminish as fatty tissue is restored upon successful treatment of anorexia, which closes the abnormal eustachian tube opening.2,3
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Olthoff A, Laskawi R, Kruse E. Successful treatment of autophonia with botulinum toxin: case report. Ann Otol Rhinol Laryngol. 2007;116(8):594-598.
2. Godbole M, Key A. Autophonia in anorexia nervosa. Int J Eat Disord. 2010;43(5):480-482.
3. Karwautz A, Hafferl A, Ungar D, et al. Patulous eustachian tube in a case of adolescent anorexia nervosa. Int J Eat Disord. 1999;25(3):353-355.
4. Dornhoffer JL, Leuwer R, Schwager K, et al. A practical guide to the eustachian tube. New York, NY: Springer; 2014:23-41.
1. Olthoff A, Laskawi R, Kruse E. Successful treatment of autophonia with botulinum toxin: case report. Ann Otol Rhinol Laryngol. 2007;116(8):594-598.
2. Godbole M, Key A. Autophonia in anorexia nervosa. Int J Eat Disord. 2010;43(5):480-482.
3. Karwautz A, Hafferl A, Ungar D, et al. Patulous eustachian tube in a case of adolescent anorexia nervosa. Int J Eat Disord. 1999;25(3):353-355.
4. Dornhoffer JL, Leuwer R, Schwager K, et al. A practical guide to the eustachian tube. New York, NY: Springer; 2014:23-41.
Teaching trainees how to discern professional boundaries
Psychiatrists often serve as risk-management consultants for our medical colleagues. As part of this role, psychiatrists working with trainees— including resident physicians, medical students, and physician assistant students— have an opportunity to emphasize the importance of professional boundaries.1 Discussing appropriate professional boundaries and describing what might represent a violation of these boundaries is meaningful because a good understanding of these concepts promotes high-quality treatment and minimizes professional liability.2
Physical boundaries
Psychiatric patients might be agitated or display potentially dangerous behaviors; discussing the importance of body language and contact between physicians and their patients is, therefore, first and foremost, a matter of safety. Students who can recognize the signs and symptoms of agitation and maintain a safe distance between themselves and their patients are less likely to be injured.
Addressing romantic and sexual relationships between patients and their health care providers also is necessary. One study reported that 21% of medical students surveyed might not regard sexual contact with a patient as inappropriate.3 An adequate discussion of this topic is necessary to protect trainees and patients from a catastrophic misstep.
Emotional boundaries
Maintaining appropriate emotional boundaries is necessary in psychiatry. Given the prevalence of mental illness and substance abuse, many trainees have personal experience with psychiatric illness outside of their training. Discussing issues of transference and countertransference with students will prepare them for intense emotional reactions they will experience while working in psychiatry. Students who feel comfortable recognizing their own countertransference feelings and discussing them in supervision with their attending psychiatrist will be more successful in addressing the complex interpersonal challenges that their patients face.
Personal and informational boundaries
Discussing personal and informational boundaries can protect trainees from uncomfortable experiences in their non-clinical lives. Although, in previous decades, we needed to discourage students only from sharing their home address and telephone number with patients, the Internet and social media have made it easier for patients to discover personal information about their treatment team. Addressing issues related to social networks and instructing students on how to appropriately address and decline requests for personal information can prevent unwanted boundary crossings.
Psychiatrists are well suited to discuss these issues with trainees. In doing so, we can help them become knowledgeable health care providers—no matter which medical discipline they specialize in.
Disclosure
The author reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Duckworth KS, Kahn MW, Gutheil TG. Roles, quandaries, and remedies: teaching professional boundaries to medical students. Harv Rev Psychiatry. 1994;1(5):266-270.
2. Gutheil TG, Gabbard GO. The concept of boundaries in clinical practice: theoretical and risk-management dimensions. Am J Psychiatry. 1993;150(2):188-196.
3. White GE. Medical students’ learning needs about setting and maintaining social and sexual boundaries: a report. Med Educ. 2003;37(11):1017-1019.
Psychiatrists often serve as risk-management consultants for our medical colleagues. As part of this role, psychiatrists working with trainees— including resident physicians, medical students, and physician assistant students— have an opportunity to emphasize the importance of professional boundaries.1 Discussing appropriate professional boundaries and describing what might represent a violation of these boundaries is meaningful because a good understanding of these concepts promotes high-quality treatment and minimizes professional liability.2
Physical boundaries
Psychiatric patients might be agitated or display potentially dangerous behaviors; discussing the importance of body language and contact between physicians and their patients is, therefore, first and foremost, a matter of safety. Students who can recognize the signs and symptoms of agitation and maintain a safe distance between themselves and their patients are less likely to be injured.
Addressing romantic and sexual relationships between patients and their health care providers also is necessary. One study reported that 21% of medical students surveyed might not regard sexual contact with a patient as inappropriate.3 An adequate discussion of this topic is necessary to protect trainees and patients from a catastrophic misstep.
Emotional boundaries
Maintaining appropriate emotional boundaries is necessary in psychiatry. Given the prevalence of mental illness and substance abuse, many trainees have personal experience with psychiatric illness outside of their training. Discussing issues of transference and countertransference with students will prepare them for intense emotional reactions they will experience while working in psychiatry. Students who feel comfortable recognizing their own countertransference feelings and discussing them in supervision with their attending psychiatrist will be more successful in addressing the complex interpersonal challenges that their patients face.
Personal and informational boundaries
Discussing personal and informational boundaries can protect trainees from uncomfortable experiences in their non-clinical lives. Although, in previous decades, we needed to discourage students only from sharing their home address and telephone number with patients, the Internet and social media have made it easier for patients to discover personal information about their treatment team. Addressing issues related to social networks and instructing students on how to appropriately address and decline requests for personal information can prevent unwanted boundary crossings.
Psychiatrists are well suited to discuss these issues with trainees. In doing so, we can help them become knowledgeable health care providers—no matter which medical discipline they specialize in.
Disclosure
The author reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Psychiatrists often serve as risk-management consultants for our medical colleagues. As part of this role, psychiatrists working with trainees— including resident physicians, medical students, and physician assistant students— have an opportunity to emphasize the importance of professional boundaries.1 Discussing appropriate professional boundaries and describing what might represent a violation of these boundaries is meaningful because a good understanding of these concepts promotes high-quality treatment and minimizes professional liability.2
Physical boundaries
Psychiatric patients might be agitated or display potentially dangerous behaviors; discussing the importance of body language and contact between physicians and their patients is, therefore, first and foremost, a matter of safety. Students who can recognize the signs and symptoms of agitation and maintain a safe distance between themselves and their patients are less likely to be injured.
Addressing romantic and sexual relationships between patients and their health care providers also is necessary. One study reported that 21% of medical students surveyed might not regard sexual contact with a patient as inappropriate.3 An adequate discussion of this topic is necessary to protect trainees and patients from a catastrophic misstep.
Emotional boundaries
Maintaining appropriate emotional boundaries is necessary in psychiatry. Given the prevalence of mental illness and substance abuse, many trainees have personal experience with psychiatric illness outside of their training. Discussing issues of transference and countertransference with students will prepare them for intense emotional reactions they will experience while working in psychiatry. Students who feel comfortable recognizing their own countertransference feelings and discussing them in supervision with their attending psychiatrist will be more successful in addressing the complex interpersonal challenges that their patients face.
Personal and informational boundaries
Discussing personal and informational boundaries can protect trainees from uncomfortable experiences in their non-clinical lives. Although, in previous decades, we needed to discourage students only from sharing their home address and telephone number with patients, the Internet and social media have made it easier for patients to discover personal information about their treatment team. Addressing issues related to social networks and instructing students on how to appropriately address and decline requests for personal information can prevent unwanted boundary crossings.
Psychiatrists are well suited to discuss these issues with trainees. In doing so, we can help them become knowledgeable health care providers—no matter which medical discipline they specialize in.
Disclosure
The author reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Duckworth KS, Kahn MW, Gutheil TG. Roles, quandaries, and remedies: teaching professional boundaries to medical students. Harv Rev Psychiatry. 1994;1(5):266-270.
2. Gutheil TG, Gabbard GO. The concept of boundaries in clinical practice: theoretical and risk-management dimensions. Am J Psychiatry. 1993;150(2):188-196.
3. White GE. Medical students’ learning needs about setting and maintaining social and sexual boundaries: a report. Med Educ. 2003;37(11):1017-1019.
1. Duckworth KS, Kahn MW, Gutheil TG. Roles, quandaries, and remedies: teaching professional boundaries to medical students. Harv Rev Psychiatry. 1994;1(5):266-270.
2. Gutheil TG, Gabbard GO. The concept of boundaries in clinical practice: theoretical and risk-management dimensions. Am J Psychiatry. 1993;150(2):188-196.
3. White GE. Medical students’ learning needs about setting and maintaining social and sexual boundaries: a report. Med Educ. 2003;37(11):1017-1019.
What stalking victims need to restore their mental and somatic health
The obsessive pursuit of another has long been described in fiction and the scientific literature, but was conceptualized as “stalking” only relatively recently—first, under the guise of celebrity stalking and, later, as a public health issue recognized as affecting the general population. A useful working definition of stalking is “… the willful, malicious, and repeated following of and harassing of another person that threatens his/her safety.”1
Stalking victims report numerous, severe, life-changing effects from being stalked, including physical, social, and psychological harm. They typically experience mood, anxiety, and posttraumatic stress symptoms that require prompt evaluation and treatment.
Prevalence and other characteristics
Stalking and its subsequent victimization are common. Here are statistics:
• in the United States, approximately 1 million women and 370,000 men are stalked annually
• women are 3 times more likely to be stalked than raped2
• lifetime prevalence of stalking victimization is 20% (women, 23.5%; men, 10.5%)
• 75% of stalking victims are women
• 77% of stalking emerges from a prior acquaintance, including 49% that originated in a romantic relationship
• 33% of stalking encounters eventually lead to physical violence; slightly >10% of encounters lead to sexual violence
• stalking persists for an extended period; on average, almost 2 years.3
Penalties. Stalking can result in intervention by the criminal justice system. Legal sanctions levied on the perpetrator vary, depending on (among other variables) the severity of stalking; type of stalking; motive of the stalker; and the strength of incriminating evidence. Surprisingly, the outcome of the perpetrator’s prosecution (arrest, conviction, length of sentence) is unrelated to whether the victim reported continued stalking at follow-up.4,5
What are the symptoms and the damage? Given the intrusive nature of stalking behaviors and the extended period during which stalking persists, victims typically experience harmful psychological effects that range from subclinical symptoms to overt psychiatric disorders.
Stalking can have a profound impact on the victim and result in numerous psychological symptoms that become the focus of clinical attention. The typically chronic nature of stalking probably plays a significant role in its contributions to its victims’ psychological distress.6 Melton7 found that the most common adverse effect of stalking was related to the emotional impact of being stalked—with victims feeling scared, depressed, humiliated, embarrassed, distrustful of others, and angry or hateful.
Stalking victims report traumatic stress, hypervigilance, excessive fear, and anxiety coupled with disruptions in employment and social interactions.8 Many report having become highly distrustful or suspicious (44%); fearful (42%); nervous (31%); angry (27%); paranoid (36%); and depressed (21%). In general, victims have elevated scores on the Trauma Symptom Checklist.9
Stalking in the setting of intimate partner abuse is associated with harmful outcomes for the victim. These include repeat physical violence, psychological distress, and impaired physical or mental health, or both.3,7,10
Stalking victims who are female; had a prior relationship with the stalker; have experienced a greater variety of stalking behaviors; are divorced or separated; and have received government assistance were found to be more likely to experience multiple negative outcomes from stalking.11
Effects on mental health. Stalking victims have a higher incidence of mental disorders and comorbid illnesses compared with the general population,12 with the most robust associations identified between stalking victimization, major depressive disorder, and panic disorder. Stalking contributes to symptoms of posttraumatic stress disorder,13 and there is an association between posttraumatic stress and poor general health.14 Stalking victims report higher current use of psychotropic medications.12
Victims who blame themselves for being stalked report a significantly higher severity of depression, anxiety, and posttraumatic stress symptoms. Those who ruminate more about the stalking experience, or who explicitly emphasize the terror of stalking to a greater extent, also report a significantly higher severity of symptoms.15
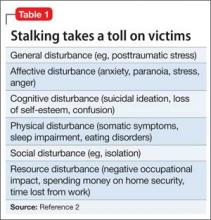
Spitzberg3 reported that stalking victimization has several possible effects on victims (Table 1).
Coping by movement. Victims might attempt to cope with stalking through several means,2 including:
• moving away—trying to avoid contact with the stalker
• moving with—negotiating a more acceptable form of relationship with the stalker
• moving against—attempting to harm, constrain, or punish the stalker
• moving inward—seeking self-control or self-actualization
• moving outward—seeking the assistance of others.
The degree of a victim’s symptoms correlates partially with the severity of stalking. However, other variables play a crucial role in explaining the level of distress among stalking victims15; these include the types of coping strategies adopted by victims. Self-blame, catastrophizing, and rumination are significantly associated with maladjustment; on the other hand, positive reappraisal—thoughts of attaching a positive meaning to the event, in terms of personal growth—is associated with greater psychological adjustment.
The more stalking a victim experiences (and, presumably, experiences greater distress), the greater the variety of coping strategies she (he) employs.16
How should stalking victims be treated?
Stalking victims are an underserved population. Practitioners often are unsure how to address stalking; furthermore, available treatments can be ineffective.
There is a great deal of variability in what professionals who work with stalking victims believe is appropriate practice. Services provided to victims vary widely,17 and the field has not yet come to a consensus on best practices.16
Proceed case by case. Practitioners must understand the nuances of each case to consider what might work at a particular point in time, and information from victims can help guide decision-making.16 Evidence suggests that stalking victims can feel frustrated in their attempt to seek help, particularly from the criminal justice system; it is possible that such bad experiences may dissuade them from seeking help later.5,8,18 It is worth noting that, as the frequency of stalking decreases for any given victim, her (his) perception of safety increases and distress diminishes.16
Few communities have attempted to address systemically the problem of stalking. Existing anti-stalking programs have focused on the criminal justice aspects of intervention,8 with less emphasis on treating victims.
Some stalking victims rely on friends and family for support and assistance, but research shows that most reach out to agencies for assistance and, generally, seek help from multiple sources.18 Typically, stalking victims are served by 2 types of victim service organizations:
• specialized, small, private and nonprofit agencies (eg, domestic violence shelters, rape crisis centers, victims’ rights advocacy organizations)
• small units housed in police departments and prosecutors’ offices.17
Note: When victims seek services at criminal justice agencies, they may be feeling particularly unsafe and distressed. This underscores the importance of co-locating victim service providers and criminal justice agencies.16
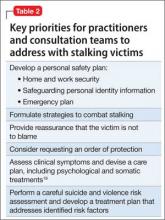
Stalking victims might benefit from multi-disciplinary team consultation, including input from psychiatric, psychotherapeutic, and law enforcement or security professionals. Key priorities for practitioners to address with stalking victims are given in Table 2.19
Stalking behavior does not significantly decrease when victims are in contact with victim services.16 Practitioners can integrate this prospect into their understanding of stalking when they work with victims: That is, it is likely that the problem will not go away quickly, even with intervention.
Victims’ needs remain great and broad-based. Spence-Diehl et al17 conducted a survey of service providers for stalking victims, evaluating the needs of those victims and the response of their communities. Some of their recommendations for better meeting victims’ needs are in Table 3.16
Keeping victims at the center
Several authors have written about the need to return to a victim-centered model of care. This approach (1) puts the victim’s understanding of her (his) situation at the center of victim assistance work and (2) views service providers as consultants in the decision-making process.20,21 The victim-centered approach to treatment, in which the client has a greater voice and degree of control over interventions, is associated with positive outcomes.22,23
At the heart of a client-centered model of victim assistance is the provider’s ability to listen to a victim’s story and respond in a nonjudgmental manner. This approach honors the victim’s circumstances and her personal understanding of risk.21
Bottom Line
Stalking victims are a distinctive population, experiencing numerous emotional, physical, and social effects of their stalking over an extended period. Services to treat this underserved population need to be further developed. A multifaceted approach to treating victims incorporates psychological, somatic, and practical interventions, and a victim-centered approach is associated with better outcomes.
Related Resources
• Harmon RB, O’Connor M. Forcier A, et al. The impact of anti-stalking training on front line service providers: using the anti-stalking training evaluation protocol (ASTEP). J Forensic Science. 2004;49(5):1050-1055.
• Spitzberg BH, Cupach WR. The state of the art of stalking: taking stock of the emerging literature. Aggression and Violence Behavior. 2007;12(1):64-86.
Disclosure
The author reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Meloy JR, Gothard S. Demographic and clinical comparison of obsessional followers and offenders with mental disorders. Am J Psychiatry. 1995;152(2):258-263.
2. Tjaden P, Thoennes N. Stalking in America: findings from the National Violence Against Women Survey. National Institute of Justice and Centers for Disease Control and Prevention. https://www.ncjrs.gov/pdffiles/169592.pdf. Published April 1998. Accessed March 25, 2015.
3. Spitzberg BH. The tactical topography of stalking victimization and management. Trauma, Violence, & Abuse. 2002;3(4):261-288.
4. McFarlane J, Willson P, Lemmey D, et al. Women filing assault charges on an intimate partner: criminal justice outcome and future violence experienced. Violence Against Women. 2000;6(4):396-408.
5. Melton HC. Stalking in the context of domestic violence: findings on the criminal justice system. Women & Criminal Justice. 2004;15:33-58.
6. Davies KE, Frieze IH. Research on stalking: what do we know and where do we go? Violence Vict. 2000;15(4):473-487.
7. Melton HC. Stalking in the context of intimate partner abuse: in the victims’ words. Feminist Criminology. 2007;2(4):346-363.
8. Spence-Diehl E. Intensive case management for victims of stalking: a pilot test evaluation. Brief Treatment Crisis Intervention. 2004;4(4):323-341.
9. Brewster MP. An exploration of the experiences and needs of former intimate stalking victims: final report submitted to the National Institute of Justice. West Chester, PA: West Chester University; 1997.
10. Logan TK, Shannon L, Cole J, et al. The impact of differential patterns of physical violence and stalking on mental health and help-seeking among women with protective orders. Violence Against Women. 2006;12(9):866-886.
11. Johnson MC, Kercher GA. Identifying predictors of negative psychological reactions to stalking victimization. J Interpers Violence. 2009;24(5):866-882.
12. Kuehner C, Gass P, Dressing H. Increased risk of mental disorders among lifetime victims of stalking—findings from a community study. Eur Psychiatry. 2007;22(3):142-145.
13. Basile KC, Arias I, Desai S, et al. The differential association of intimate partner physical, sexual, psychological, and stalking violence and post-traumatic stress symptoms in a nationally representative sample of women. J Traumatic Stress. 2004;17(5):413-421.
14. Kamphuis JH, Emmelkamp PM. Traumatic distress among support-seeking female victims of stalking. Am J Psychiatry. 2001;158(5):795-798.
15. Kraaij V, Arensman E, Garnefski N, et al. The role of cognitive coping in female victims of stalking. J Interpers Violence. 2007;22(12):1603-1612.
16. Bennett Cattaneo L, Cho S, Botuck S. Describing intimate partner stalking over time: an effort to inform victim-centered service provision. J Interpers Violence. 2011;26(17):3428-3454.
17. Spence-Diehl E, Potocky-Tripodi M. Victims of stalking: a study of service needs as perceived by victim services practitioners. J Interpers Violence. 2001;16(1):86-94.
18. Galeazzi GM, Buc˘ar-Ruc˘man A, DeFazio L, et al. Experiences of stalking victims and requests for help in three European countries. A survey. European Journal of Criminal Policy Research. 2009;15:243-260.
19. McEwan T, Purcell R. Assessing and surviving stalkers. Presented at: 45th Annual Meeting of American Academy of Psychiatry and the Law; October 2014; Chicago IL.
20. Cattaneo LB, Goodman LA. New directions in IPV risk assessment: an empowerment approach to risk management. In: Kendall-Tackett K, Giacomoni S, eds. Intimate partner violence. Kingston, NJ: Civic Research Institute; 2007:1-17.
21. Goodman LA, Epstein D. Listening to battered women: a survivor-centered approach to advocacy, mental health, and justice. Washington DC: American Psychological Association; 2008.
22. Cattaneo LB, Goodman LA. Through the lens of jurisprudence: the relationship between empowerment in the court system and well-being for intimate partner violence victims. J Interpers Violence. 2010;25(3):481-502.
23. Zweig JM, Burt MR. Predicting women’s perceptions of domestic violence and sexual assault agency helpfulness: what matters to program clients? Violence Against Women. 2007;13(11):1149-1178.
The obsessive pursuit of another has long been described in fiction and the scientific literature, but was conceptualized as “stalking” only relatively recently—first, under the guise of celebrity stalking and, later, as a public health issue recognized as affecting the general population. A useful working definition of stalking is “… the willful, malicious, and repeated following of and harassing of another person that threatens his/her safety.”1
Stalking victims report numerous, severe, life-changing effects from being stalked, including physical, social, and psychological harm. They typically experience mood, anxiety, and posttraumatic stress symptoms that require prompt evaluation and treatment.
Prevalence and other characteristics
Stalking and its subsequent victimization are common. Here are statistics:
• in the United States, approximately 1 million women and 370,000 men are stalked annually
• women are 3 times more likely to be stalked than raped2
• lifetime prevalence of stalking victimization is 20% (women, 23.5%; men, 10.5%)
• 75% of stalking victims are women
• 77% of stalking emerges from a prior acquaintance, including 49% that originated in a romantic relationship
• 33% of stalking encounters eventually lead to physical violence; slightly >10% of encounters lead to sexual violence
• stalking persists for an extended period; on average, almost 2 years.3
Penalties. Stalking can result in intervention by the criminal justice system. Legal sanctions levied on the perpetrator vary, depending on (among other variables) the severity of stalking; type of stalking; motive of the stalker; and the strength of incriminating evidence. Surprisingly, the outcome of the perpetrator’s prosecution (arrest, conviction, length of sentence) is unrelated to whether the victim reported continued stalking at follow-up.4,5
What are the symptoms and the damage? Given the intrusive nature of stalking behaviors and the extended period during which stalking persists, victims typically experience harmful psychological effects that range from subclinical symptoms to overt psychiatric disorders.
Stalking can have a profound impact on the victim and result in numerous psychological symptoms that become the focus of clinical attention. The typically chronic nature of stalking probably plays a significant role in its contributions to its victims’ psychological distress.6 Melton7 found that the most common adverse effect of stalking was related to the emotional impact of being stalked—with victims feeling scared, depressed, humiliated, embarrassed, distrustful of others, and angry or hateful.
Stalking victims report traumatic stress, hypervigilance, excessive fear, and anxiety coupled with disruptions in employment and social interactions.8 Many report having become highly distrustful or suspicious (44%); fearful (42%); nervous (31%); angry (27%); paranoid (36%); and depressed (21%). In general, victims have elevated scores on the Trauma Symptom Checklist.9
Stalking in the setting of intimate partner abuse is associated with harmful outcomes for the victim. These include repeat physical violence, psychological distress, and impaired physical or mental health, or both.3,7,10
Stalking victims who are female; had a prior relationship with the stalker; have experienced a greater variety of stalking behaviors; are divorced or separated; and have received government assistance were found to be more likely to experience multiple negative outcomes from stalking.11
Effects on mental health. Stalking victims have a higher incidence of mental disorders and comorbid illnesses compared with the general population,12 with the most robust associations identified between stalking victimization, major depressive disorder, and panic disorder. Stalking contributes to symptoms of posttraumatic stress disorder,13 and there is an association between posttraumatic stress and poor general health.14 Stalking victims report higher current use of psychotropic medications.12
Victims who blame themselves for being stalked report a significantly higher severity of depression, anxiety, and posttraumatic stress symptoms. Those who ruminate more about the stalking experience, or who explicitly emphasize the terror of stalking to a greater extent, also report a significantly higher severity of symptoms.15
Spitzberg3 reported that stalking victimization has several possible effects on victims (Table 1).
Coping by movement. Victims might attempt to cope with stalking through several means,2 including:
• moving away—trying to avoid contact with the stalker
• moving with—negotiating a more acceptable form of relationship with the stalker
• moving against—attempting to harm, constrain, or punish the stalker
• moving inward—seeking self-control or self-actualization
• moving outward—seeking the assistance of others.
The degree of a victim’s symptoms correlates partially with the severity of stalking. However, other variables play a crucial role in explaining the level of distress among stalking victims15; these include the types of coping strategies adopted by victims. Self-blame, catastrophizing, and rumination are significantly associated with maladjustment; on the other hand, positive reappraisal—thoughts of attaching a positive meaning to the event, in terms of personal growth—is associated with greater psychological adjustment.
The more stalking a victim experiences (and, presumably, experiences greater distress), the greater the variety of coping strategies she (he) employs.16
How should stalking victims be treated?
Stalking victims are an underserved population. Practitioners often are unsure how to address stalking; furthermore, available treatments can be ineffective.
There is a great deal of variability in what professionals who work with stalking victims believe is appropriate practice. Services provided to victims vary widely,17 and the field has not yet come to a consensus on best practices.16
Proceed case by case. Practitioners must understand the nuances of each case to consider what might work at a particular point in time, and information from victims can help guide decision-making.16 Evidence suggests that stalking victims can feel frustrated in their attempt to seek help, particularly from the criminal justice system; it is possible that such bad experiences may dissuade them from seeking help later.5,8,18 It is worth noting that, as the frequency of stalking decreases for any given victim, her (his) perception of safety increases and distress diminishes.16
Few communities have attempted to address systemically the problem of stalking. Existing anti-stalking programs have focused on the criminal justice aspects of intervention,8 with less emphasis on treating victims.
Some stalking victims rely on friends and family for support and assistance, but research shows that most reach out to agencies for assistance and, generally, seek help from multiple sources.18 Typically, stalking victims are served by 2 types of victim service organizations:
• specialized, small, private and nonprofit agencies (eg, domestic violence shelters, rape crisis centers, victims’ rights advocacy organizations)
• small units housed in police departments and prosecutors’ offices.17
Note: When victims seek services at criminal justice agencies, they may be feeling particularly unsafe and distressed. This underscores the importance of co-locating victim service providers and criminal justice agencies.16
Stalking victims might benefit from multi-disciplinary team consultation, including input from psychiatric, psychotherapeutic, and law enforcement or security professionals. Key priorities for practitioners to address with stalking victims are given in Table 2.19
Stalking behavior does not significantly decrease when victims are in contact with victim services.16 Practitioners can integrate this prospect into their understanding of stalking when they work with victims: That is, it is likely that the problem will not go away quickly, even with intervention.
Victims’ needs remain great and broad-based. Spence-Diehl et al17 conducted a survey of service providers for stalking victims, evaluating the needs of those victims and the response of their communities. Some of their recommendations for better meeting victims’ needs are in Table 3.16
Keeping victims at the center
Several authors have written about the need to return to a victim-centered model of care. This approach (1) puts the victim’s understanding of her (his) situation at the center of victim assistance work and (2) views service providers as consultants in the decision-making process.20,21 The victim-centered approach to treatment, in which the client has a greater voice and degree of control over interventions, is associated with positive outcomes.22,23
At the heart of a client-centered model of victim assistance is the provider’s ability to listen to a victim’s story and respond in a nonjudgmental manner. This approach honors the victim’s circumstances and her personal understanding of risk.21
Bottom Line
Stalking victims are a distinctive population, experiencing numerous emotional, physical, and social effects of their stalking over an extended period. Services to treat this underserved population need to be further developed. A multifaceted approach to treating victims incorporates psychological, somatic, and practical interventions, and a victim-centered approach is associated with better outcomes.
Related Resources
• Harmon RB, O’Connor M. Forcier A, et al. The impact of anti-stalking training on front line service providers: using the anti-stalking training evaluation protocol (ASTEP). J Forensic Science. 2004;49(5):1050-1055.
• Spitzberg BH, Cupach WR. The state of the art of stalking: taking stock of the emerging literature. Aggression and Violence Behavior. 2007;12(1):64-86.
Disclosure
The author reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
The obsessive pursuit of another has long been described in fiction and the scientific literature, but was conceptualized as “stalking” only relatively recently—first, under the guise of celebrity stalking and, later, as a public health issue recognized as affecting the general population. A useful working definition of stalking is “… the willful, malicious, and repeated following of and harassing of another person that threatens his/her safety.”1
Stalking victims report numerous, severe, life-changing effects from being stalked, including physical, social, and psychological harm. They typically experience mood, anxiety, and posttraumatic stress symptoms that require prompt evaluation and treatment.
Prevalence and other characteristics
Stalking and its subsequent victimization are common. Here are statistics:
• in the United States, approximately 1 million women and 370,000 men are stalked annually
• women are 3 times more likely to be stalked than raped2
• lifetime prevalence of stalking victimization is 20% (women, 23.5%; men, 10.5%)
• 75% of stalking victims are women
• 77% of stalking emerges from a prior acquaintance, including 49% that originated in a romantic relationship
• 33% of stalking encounters eventually lead to physical violence; slightly >10% of encounters lead to sexual violence
• stalking persists for an extended period; on average, almost 2 years.3
Penalties. Stalking can result in intervention by the criminal justice system. Legal sanctions levied on the perpetrator vary, depending on (among other variables) the severity of stalking; type of stalking; motive of the stalker; and the strength of incriminating evidence. Surprisingly, the outcome of the perpetrator’s prosecution (arrest, conviction, length of sentence) is unrelated to whether the victim reported continued stalking at follow-up.4,5
What are the symptoms and the damage? Given the intrusive nature of stalking behaviors and the extended period during which stalking persists, victims typically experience harmful psychological effects that range from subclinical symptoms to overt psychiatric disorders.
Stalking can have a profound impact on the victim and result in numerous psychological symptoms that become the focus of clinical attention. The typically chronic nature of stalking probably plays a significant role in its contributions to its victims’ psychological distress.6 Melton7 found that the most common adverse effect of stalking was related to the emotional impact of being stalked—with victims feeling scared, depressed, humiliated, embarrassed, distrustful of others, and angry or hateful.
Stalking victims report traumatic stress, hypervigilance, excessive fear, and anxiety coupled with disruptions in employment and social interactions.8 Many report having become highly distrustful or suspicious (44%); fearful (42%); nervous (31%); angry (27%); paranoid (36%); and depressed (21%). In general, victims have elevated scores on the Trauma Symptom Checklist.9
Stalking in the setting of intimate partner abuse is associated with harmful outcomes for the victim. These include repeat physical violence, psychological distress, and impaired physical or mental health, or both.3,7,10
Stalking victims who are female; had a prior relationship with the stalker; have experienced a greater variety of stalking behaviors; are divorced or separated; and have received government assistance were found to be more likely to experience multiple negative outcomes from stalking.11
Effects on mental health. Stalking victims have a higher incidence of mental disorders and comorbid illnesses compared with the general population,12 with the most robust associations identified between stalking victimization, major depressive disorder, and panic disorder. Stalking contributes to symptoms of posttraumatic stress disorder,13 and there is an association between posttraumatic stress and poor general health.14 Stalking victims report higher current use of psychotropic medications.12
Victims who blame themselves for being stalked report a significantly higher severity of depression, anxiety, and posttraumatic stress symptoms. Those who ruminate more about the stalking experience, or who explicitly emphasize the terror of stalking to a greater extent, also report a significantly higher severity of symptoms.15
Spitzberg3 reported that stalking victimization has several possible effects on victims (Table 1).
Coping by movement. Victims might attempt to cope with stalking through several means,2 including:
• moving away—trying to avoid contact with the stalker
• moving with—negotiating a more acceptable form of relationship with the stalker
• moving against—attempting to harm, constrain, or punish the stalker
• moving inward—seeking self-control or self-actualization
• moving outward—seeking the assistance of others.
The degree of a victim’s symptoms correlates partially with the severity of stalking. However, other variables play a crucial role in explaining the level of distress among stalking victims15; these include the types of coping strategies adopted by victims. Self-blame, catastrophizing, and rumination are significantly associated with maladjustment; on the other hand, positive reappraisal—thoughts of attaching a positive meaning to the event, in terms of personal growth—is associated with greater psychological adjustment.
The more stalking a victim experiences (and, presumably, experiences greater distress), the greater the variety of coping strategies she (he) employs.16
How should stalking victims be treated?
Stalking victims are an underserved population. Practitioners often are unsure how to address stalking; furthermore, available treatments can be ineffective.
There is a great deal of variability in what professionals who work with stalking victims believe is appropriate practice. Services provided to victims vary widely,17 and the field has not yet come to a consensus on best practices.16
Proceed case by case. Practitioners must understand the nuances of each case to consider what might work at a particular point in time, and information from victims can help guide decision-making.16 Evidence suggests that stalking victims can feel frustrated in their attempt to seek help, particularly from the criminal justice system; it is possible that such bad experiences may dissuade them from seeking help later.5,8,18 It is worth noting that, as the frequency of stalking decreases for any given victim, her (his) perception of safety increases and distress diminishes.16
Few communities have attempted to address systemically the problem of stalking. Existing anti-stalking programs have focused on the criminal justice aspects of intervention,8 with less emphasis on treating victims.
Some stalking victims rely on friends and family for support and assistance, but research shows that most reach out to agencies for assistance and, generally, seek help from multiple sources.18 Typically, stalking victims are served by 2 types of victim service organizations:
• specialized, small, private and nonprofit agencies (eg, domestic violence shelters, rape crisis centers, victims’ rights advocacy organizations)
• small units housed in police departments and prosecutors’ offices.17
Note: When victims seek services at criminal justice agencies, they may be feeling particularly unsafe and distressed. This underscores the importance of co-locating victim service providers and criminal justice agencies.16
Stalking victims might benefit from multi-disciplinary team consultation, including input from psychiatric, psychotherapeutic, and law enforcement or security professionals. Key priorities for practitioners to address with stalking victims are given in Table 2.19
Stalking behavior does not significantly decrease when victims are in contact with victim services.16 Practitioners can integrate this prospect into their understanding of stalking when they work with victims: That is, it is likely that the problem will not go away quickly, even with intervention.
Victims’ needs remain great and broad-based. Spence-Diehl et al17 conducted a survey of service providers for stalking victims, evaluating the needs of those victims and the response of their communities. Some of their recommendations for better meeting victims’ needs are in Table 3.16
Keeping victims at the center
Several authors have written about the need to return to a victim-centered model of care. This approach (1) puts the victim’s understanding of her (his) situation at the center of victim assistance work and (2) views service providers as consultants in the decision-making process.20,21 The victim-centered approach to treatment, in which the client has a greater voice and degree of control over interventions, is associated with positive outcomes.22,23
At the heart of a client-centered model of victim assistance is the provider’s ability to listen to a victim’s story and respond in a nonjudgmental manner. This approach honors the victim’s circumstances and her personal understanding of risk.21
Bottom Line
Stalking victims are a distinctive population, experiencing numerous emotional, physical, and social effects of their stalking over an extended period. Services to treat this underserved population need to be further developed. A multifaceted approach to treating victims incorporates psychological, somatic, and practical interventions, and a victim-centered approach is associated with better outcomes.
Related Resources
• Harmon RB, O’Connor M. Forcier A, et al. The impact of anti-stalking training on front line service providers: using the anti-stalking training evaluation protocol (ASTEP). J Forensic Science. 2004;49(5):1050-1055.
• Spitzberg BH, Cupach WR. The state of the art of stalking: taking stock of the emerging literature. Aggression and Violence Behavior. 2007;12(1):64-86.
Disclosure
The author reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Meloy JR, Gothard S. Demographic and clinical comparison of obsessional followers and offenders with mental disorders. Am J Psychiatry. 1995;152(2):258-263.
2. Tjaden P, Thoennes N. Stalking in America: findings from the National Violence Against Women Survey. National Institute of Justice and Centers for Disease Control and Prevention. https://www.ncjrs.gov/pdffiles/169592.pdf. Published April 1998. Accessed March 25, 2015.
3. Spitzberg BH. The tactical topography of stalking victimization and management. Trauma, Violence, & Abuse. 2002;3(4):261-288.
4. McFarlane J, Willson P, Lemmey D, et al. Women filing assault charges on an intimate partner: criminal justice outcome and future violence experienced. Violence Against Women. 2000;6(4):396-408.
5. Melton HC. Stalking in the context of domestic violence: findings on the criminal justice system. Women & Criminal Justice. 2004;15:33-58.
6. Davies KE, Frieze IH. Research on stalking: what do we know and where do we go? Violence Vict. 2000;15(4):473-487.
7. Melton HC. Stalking in the context of intimate partner abuse: in the victims’ words. Feminist Criminology. 2007;2(4):346-363.
8. Spence-Diehl E. Intensive case management for victims of stalking: a pilot test evaluation. Brief Treatment Crisis Intervention. 2004;4(4):323-341.
9. Brewster MP. An exploration of the experiences and needs of former intimate stalking victims: final report submitted to the National Institute of Justice. West Chester, PA: West Chester University; 1997.
10. Logan TK, Shannon L, Cole J, et al. The impact of differential patterns of physical violence and stalking on mental health and help-seeking among women with protective orders. Violence Against Women. 2006;12(9):866-886.
11. Johnson MC, Kercher GA. Identifying predictors of negative psychological reactions to stalking victimization. J Interpers Violence. 2009;24(5):866-882.
12. Kuehner C, Gass P, Dressing H. Increased risk of mental disorders among lifetime victims of stalking—findings from a community study. Eur Psychiatry. 2007;22(3):142-145.
13. Basile KC, Arias I, Desai S, et al. The differential association of intimate partner physical, sexual, psychological, and stalking violence and post-traumatic stress symptoms in a nationally representative sample of women. J Traumatic Stress. 2004;17(5):413-421.
14. Kamphuis JH, Emmelkamp PM. Traumatic distress among support-seeking female victims of stalking. Am J Psychiatry. 2001;158(5):795-798.
15. Kraaij V, Arensman E, Garnefski N, et al. The role of cognitive coping in female victims of stalking. J Interpers Violence. 2007;22(12):1603-1612.
16. Bennett Cattaneo L, Cho S, Botuck S. Describing intimate partner stalking over time: an effort to inform victim-centered service provision. J Interpers Violence. 2011;26(17):3428-3454.
17. Spence-Diehl E, Potocky-Tripodi M. Victims of stalking: a study of service needs as perceived by victim services practitioners. J Interpers Violence. 2001;16(1):86-94.
18. Galeazzi GM, Buc˘ar-Ruc˘man A, DeFazio L, et al. Experiences of stalking victims and requests for help in three European countries. A survey. European Journal of Criminal Policy Research. 2009;15:243-260.
19. McEwan T, Purcell R. Assessing and surviving stalkers. Presented at: 45th Annual Meeting of American Academy of Psychiatry and the Law; October 2014; Chicago IL.
20. Cattaneo LB, Goodman LA. New directions in IPV risk assessment: an empowerment approach to risk management. In: Kendall-Tackett K, Giacomoni S, eds. Intimate partner violence. Kingston, NJ: Civic Research Institute; 2007:1-17.
21. Goodman LA, Epstein D. Listening to battered women: a survivor-centered approach to advocacy, mental health, and justice. Washington DC: American Psychological Association; 2008.
22. Cattaneo LB, Goodman LA. Through the lens of jurisprudence: the relationship between empowerment in the court system and well-being for intimate partner violence victims. J Interpers Violence. 2010;25(3):481-502.
23. Zweig JM, Burt MR. Predicting women’s perceptions of domestic violence and sexual assault agency helpfulness: what matters to program clients? Violence Against Women. 2007;13(11):1149-1178.
1. Meloy JR, Gothard S. Demographic and clinical comparison of obsessional followers and offenders with mental disorders. Am J Psychiatry. 1995;152(2):258-263.
2. Tjaden P, Thoennes N. Stalking in America: findings from the National Violence Against Women Survey. National Institute of Justice and Centers for Disease Control and Prevention. https://www.ncjrs.gov/pdffiles/169592.pdf. Published April 1998. Accessed March 25, 2015.
3. Spitzberg BH. The tactical topography of stalking victimization and management. Trauma, Violence, & Abuse. 2002;3(4):261-288.
4. McFarlane J, Willson P, Lemmey D, et al. Women filing assault charges on an intimate partner: criminal justice outcome and future violence experienced. Violence Against Women. 2000;6(4):396-408.
5. Melton HC. Stalking in the context of domestic violence: findings on the criminal justice system. Women & Criminal Justice. 2004;15:33-58.
6. Davies KE, Frieze IH. Research on stalking: what do we know and where do we go? Violence Vict. 2000;15(4):473-487.
7. Melton HC. Stalking in the context of intimate partner abuse: in the victims’ words. Feminist Criminology. 2007;2(4):346-363.
8. Spence-Diehl E. Intensive case management for victims of stalking: a pilot test evaluation. Brief Treatment Crisis Intervention. 2004;4(4):323-341.
9. Brewster MP. An exploration of the experiences and needs of former intimate stalking victims: final report submitted to the National Institute of Justice. West Chester, PA: West Chester University; 1997.
10. Logan TK, Shannon L, Cole J, et al. The impact of differential patterns of physical violence and stalking on mental health and help-seeking among women with protective orders. Violence Against Women. 2006;12(9):866-886.
11. Johnson MC, Kercher GA. Identifying predictors of negative psychological reactions to stalking victimization. J Interpers Violence. 2009;24(5):866-882.
12. Kuehner C, Gass P, Dressing H. Increased risk of mental disorders among lifetime victims of stalking—findings from a community study. Eur Psychiatry. 2007;22(3):142-145.
13. Basile KC, Arias I, Desai S, et al. The differential association of intimate partner physical, sexual, psychological, and stalking violence and post-traumatic stress symptoms in a nationally representative sample of women. J Traumatic Stress. 2004;17(5):413-421.
14. Kamphuis JH, Emmelkamp PM. Traumatic distress among support-seeking female victims of stalking. Am J Psychiatry. 2001;158(5):795-798.
15. Kraaij V, Arensman E, Garnefski N, et al. The role of cognitive coping in female victims of stalking. J Interpers Violence. 2007;22(12):1603-1612.
16. Bennett Cattaneo L, Cho S, Botuck S. Describing intimate partner stalking over time: an effort to inform victim-centered service provision. J Interpers Violence. 2011;26(17):3428-3454.
17. Spence-Diehl E, Potocky-Tripodi M. Victims of stalking: a study of service needs as perceived by victim services practitioners. J Interpers Violence. 2001;16(1):86-94.
18. Galeazzi GM, Buc˘ar-Ruc˘man A, DeFazio L, et al. Experiences of stalking victims and requests for help in three European countries. A survey. European Journal of Criminal Policy Research. 2009;15:243-260.
19. McEwan T, Purcell R. Assessing and surviving stalkers. Presented at: 45th Annual Meeting of American Academy of Psychiatry and the Law; October 2014; Chicago IL.
20. Cattaneo LB, Goodman LA. New directions in IPV risk assessment: an empowerment approach to risk management. In: Kendall-Tackett K, Giacomoni S, eds. Intimate partner violence. Kingston, NJ: Civic Research Institute; 2007:1-17.
21. Goodman LA, Epstein D. Listening to battered women: a survivor-centered approach to advocacy, mental health, and justice. Washington DC: American Psychological Association; 2008.
22. Cattaneo LB, Goodman LA. Through the lens of jurisprudence: the relationship between empowerment in the court system and well-being for intimate partner violence victims. J Interpers Violence. 2010;25(3):481-502.
23. Zweig JM, Burt MR. Predicting women’s perceptions of domestic violence and sexual assault agency helpfulness: what matters to program clients? Violence Against Women. 2007;13(11):1149-1178.
Fatigue after depression responds to therapy. What are the next steps?
Fatigue and depression can be viewed as a “vicious cycle”: Fatigue can be a symptom of major depression, and fatigue can be a risk factor for depression.1 For example, fatigue associated with a general medical condition or traumatic brain injury can be a risk factor for developing major depressive disorder (MDD).1-3 It isn’t surprising that fatigue has been studied as a predictor of relapse after previous response to treatment in patients with MDD.
Despite the observed association between fatigue and depression, their underlying relationship often is unclear. The literature does not differentiate among fatigue associated with depression, fatigue as a treatment-emergent adverse effect, and fatigue as a residual symptom of depression that is partially responsive to treatment.4,5 To complicate the situation, many medications used to treat MDD can cause fatigue.
Patients often describe fatigue as (1) feeling tired, exhausted, or drained and (2) lacking energy and motivation. Fatigue can be related to impaired wakefulness but is believed to be a different entity than sleepiness.6 Residual fatigue can affect social, cognitive, emotional, and physical health.
We reviewed the literature about fatigue as a symptom of MDD by conducting a search of Medline, PubMed, and Google Scholar, using keywords depression, fatigue, residual symptoms, and treatment. We chose the papers cited in this article based on our consensus and because these publications represent expert opinion or the highest quality evidence available.
Residual fatigue has an effect on prognosis
Fatigue is a common symptom of MDD that persists in 20% to 30% of patients whose symptoms of depression otherwise remit.4,7-9 Several studies have linked residual fatigue with the overall prognosis of MDD.5 Data from a prospective study demonstrate that depressed patients have a higher risk of relapse when they continue to report symptoms of fatigue after their symptoms of depression have otherwise entered partial remission.10 Another study demonstrated that the severity of residual symptoms of depression is a strong predictor of another major depressive episode.11
In a large-scale study, the prevalence of residual fatigue after adequate treatment of MDD in both partial responders and remitters was 84.6%.12 The same study showed that one-third of patients who had been treated for MDD had persistent and clinically significant fatigue, which could suggest a relationship between fatigue and selective serotonin reuptake inhibitors (SSRIs) and other antidepressants.
Another study demonstrated that 64.6% of patients who responded to antidepressant treatment and who had baseline fatigue continued to exhibit symptoms of fatigue after an adequate trial of an antidepressant.13
Neurobiological considerations
Studies have shown that the neuronal circuits that malfunction in fatigue are different from those that malfunction in depression.14 Although the neurobiology of fatigue has not been determined, decreased neuronal activity in the prefrontal circuits has been associated with symptoms of fatigue.15
In addition, evidence from the literature shows a decrease in hormone secretion16 and cognitive abilities in patients exhibiting symptoms of fatigue.17 These findings have led some experts to hypothesize that symptoms of fatigue associated with depression could be the result of (1) immune dysregulation18 and (2) an inability of available antidepressants to target the underlying biology of the disorder.2
Despite the hypothesis that fatigue associated with depression might be biologically related to immune dysregulation, some authors continue to point to an imbalance in neurotransmitters—norepinephrine, histamine, dopamine, acetylcholine—as being associated with fatigue.14 For example, a study demonstrated that drugs targeting noradrenergic reuptake inhibition were more effective at preventing a relapse of fatigue compared with serotonergic drugs.19 Another study showed improvement in energy with an increase in the plasma level of desipramine, which affects noradrenergic neurotransmission.20
Inflammatory cytokines also have been explored in the search for an understanding of the etiology of fatigue and depression.21 Physical and mental stress promote the release of cytokines, which activate the immune system by inducing an inflammatory response; this response has been etiologically linked to depressive disorders.22 Furthermore, studies have demonstrated an elevated level of inflammatory cytokines in patients who have MDD— suggesting that MDD is associated with a chronic low level of inflammation that crosses the blood−brain barrier.23
Clinical considerations: A role for rating scales?
Despite the significance of residual fatigue on the quality of life of patients who have MDD, most common rating scales, such as the Hamilton Depression Rating Scale24 and the Montgomery-Åsberg Depression Rating Scale,25 have limited sensitivity for measuring fatigue.26 The Fatigue Associated with Depression (FAsD)27 questionnaire, designed according to FDA guidelines,28 is used to assess fatigue associated with depression. The final version of the FAsD includes 13 items: a 6-item experience subscale and a 7-item impact subscale.
Is the FAsD helpful? The experience subscale of the FAsD assesses how often the patient experiences different aspects of fatigue (tiredness, exhaustion, lack of energy, physical weakness, and a feeling that everything requires too much effort). The impact subscale of the FAsD assesses the effect of fatigue on daily life.
The overall FAsD score is calculated by taking the mean of each subscale; a change of 0.67 on the experience subscale and 0.57 on the impact subscale are considered clinically meaningful.27 The measurement properties of the questionnaire showed internal consistency, reliability, and validity in testing. Researchers note, however, that FAsD does not include items to assess the impact of fatigue on cognition. This means that the FAsD might not distinguish between physical and mental aspects of fatigue.
Treatment
It isn’t surprising that residual depression can increase health care utilization and economic burden, including such indirect costs as lost productivity and wages.29 Despite these impacts, there is a paucity of studies evaluating the relationship between residual symptoms, such as fatigue, and work productivity. It has been established that improving a depressed patient’s level of energy correlates with improved performance at work.
Treating fatigue as a residual symptom of MDD can be complicated because symptoms of fatigue might be:
• a discrete symptom of MDD
• a prodromal symptom of another disorder
• an adverse effect of an antidepressant.2,30
It is a major clinical problem, therefore, that antidepressants can alleviate and cause symptoms of fatigue.31 Treatment strategy should focus on identifying antidepressants that are less likely to cause fatigue (ie, noradrenergic or dopaminergic drugs, or both). Adjunctive treatments to target residual fatigue also can be used.32
There are limited published data on the effective treatment of residual fatigue in patients with MDD. Given the absence of sufficient evidence, agents that promote noradrenergic and dopaminergic neurotransmission have been the treatment of choice when targeting fatigue in depressed patients.2,14,21,33
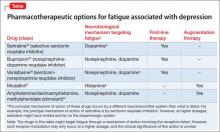
The Table34-37 lists potential treatment options often used to treat fatigue associated with depression.
SSRIs. Treatment with SSRIs has been associated with a low probability of achieving remission when targeting fatigue as a symptom of MDD.21
One study reported that, after 8 weeks of treatment with an SSRI, treatment-emergent adverse events, such as worsening fatigue and weakness, were observed—along with an overall lack of efficacy in targeting all symptoms of depression.38
Another study demonstrated positive effects when a noradrenergic agent was added to an SSRI in partial responders who continued to complain of residual fatigue.33
However, studies that compared the effects of SSRIs with those of antidepressants that have pronoradrenergic effects showed that the 2 mechanisms of action were not significantly different from each other in their ability to resolve residual symptoms of fatigue.21 A limiting factor might be that these studies were retrospective and did not analyze the efficacy of a noradrenergic agent as an adjunct for alleviating symptoms of fatigue.39
Bupropion. This commonly used medication for fatigue is believed to cause a significantly lower level of fatigue compared with SSRIs.40 The potential utility of bupropion in this area could be a reflection of its mechanism of action—ie, the drug targets both noradrenergic and dopaminergic neurotransmission.41
A study comparing bupropion with SSRIs in targeting somatic symptoms of depression reported a small but statistically significant difference in favor of the bupropion-treated group. However, this finding was confounded by the small effect size and difficulty quantifying somatic symptoms.40
Stimulants and modafinil. Psycho-stimulants have been shown to be efficacious for depression and fatigue, both as monotherapy and adjunctively.39,42
Modafinil has demonstrated efficacy in open-label trials for improving residual fatigue, but failed to separate from placebo in controlled trials.43 At least 1 other failed study has been published examining modafinil as a treatment for fatigue associated with depression.43
Adjunctive therapy with CNS stimulants, such as amphetamine/dextroamphetamine and methylphenidate, has been used to treat fatigue, with positive results.16 Modafinil and stimulants also could be tried as an augmentation strategy to other antidepressants; such use is off-label and should be attempted only after careful consideration.16
Exercise might be a nonpharmacotherapeutic modality that targets the underlying physiology associated with fatigue. Exercise releases endorphins, which can affect overall brain chemistry and which have been theorized to diminish symptoms of fatigue and depression.44 Consider exercise in addition to treatment with an antidepressant in selected patients.45
To sum up
In general, the literature does not recommend one medication as superior to any other for treating fatigue that is a residual symptom of depression. Such hesitation suggests that more empirical studies are needed to determine what is the best and proper management of treating fatigue associated with depression.
Bottom LinE
Fatigue can be a symptom of major depressive disorder (MDD) or a risk factor for depression. Fatigue has been studied as a predictor of relapse after previous response to treatment in patients with MDD. Residual fatigue can affect social, cognitive, emotional, and physical health and can result in increased utilization of health care services. A number of treatment options are available; none has been shown to be superior to the others.
Related Resources
• Leone SS. A disabling combination: fatigue and depression. Br J Psychiatry. 2010;197(2):86-87.
• Targum SD, Fava M. Fatigue as a residual symptom of depression. Innov Clin Neurosci. 2011;8(10):40-43.
• Illiades C. How to fight depression fatigue. Everyday Health. http://www.everydayhealth.com/health-report/major-depression-living-well/fight-depression-fatigue.aspx.
• Kerr M. Depression and fatigue: a vicious cycle. Healthline. http://www.healthline.com/health/depression/fatigue.
Drug Brand Names
Amphetamine/dextroamphetamine • Adderall
Bupropion • Wellbutrin
Desipramine • Norpramin
Methylphenidate • Ritalin
Modafinil • Provigil
Sertraline • Zoloft
Venlafaxine • Effexor
Disclosures
Dr. Sohail reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Macaluso has conducted clinical trials research as principal investigator for the following pharmaceutical manufacturers in the past 12 months: AbbVie, Inc.; Alkermes; AssureRx Health, Inc.; Eisai Co., Ltd.; FORUM Pharmaceuticals, Inc.; Janssen Pharmaceuticals, Inc.; and Naurex Inc. All clinical trial and study contracts were with, and payments were made to, University of Kansas Medical Center Research Institute, Kansas City, Kansas, a research institute affiliated with University of Kansas School of Medicine−Wichita.
1. Schönberger M, Herrberg M, Ponsford J. Fatigue as a cause, not a consequence of depression and daytime sleepiness: a cross-lagged analysis. J Head Trauma Rehabil. 2014;29(5):427-431.
2. Demyttenaere K, De Fruyt J, Stahl, SM. The many faces of fatigue in major depressive disorder. Int J Neuropsychopharmacol. 2005;8(1):93-105.
3. Skapinakis P, Lewis G, Mavreas V. Temporal relations between unexplained fatigue and depression: longitudinal data from an international study in primary care. Psychosom Med. 2004;66(3):330-335.
4. Nierenberg AA, Husain MM, Trivedi MH, et al. Residual symptoms after remission of major depressive disorder with citalopram and risk of relapse: a STAR*D report. Psychol Med. 2010;40(1):41-50.
5. Kennedy N, Paykel ES. Residual symptoms at remission from depression: impact on long-term outcome. J Affect Disord. 2004;80(2-3):135-144.
6. Shen J, Barbera J, Shapiro CM. Distinguishing sleepiness and fatigue: focus on definition and measurement. Sleep Med Rev. 2006;10:63-76.
7. Nierenberg AA, Keefe BR, Leslie VC, et al. Residual symptoms in depressed patients who respond acutely to fluoxetine. J Clin Psychiatry. 1999;60(4):221-225.
8. Tylee A, Gastpar M, Lépine JP, et al. DEPRES II (Depression Research in European Society II): a patient survey of the symptoms, disability and current management of depression in the community. DEPRES Steering Committee. Int Clin Psychopharmacol. 1999;14(3):139-151.
9. Marcus SM, Young EA, Kerber KB, et al. Gender differences in depression: findings from the STAR*D study. J Affect Disord. 2005;87(2-3):141-150.
10. Paykel ES, Ramana, R, Cooper Z, et al. Residual symptoms after partial remission: an important outcome in depression. Psychol Med. 1995;25(6):1171-1180.
11. Bockting CL, Spinhoven P, Koeter MW, et al; Depression Evaluation Longitudinal Therapy Assessment Study Group. Prediction of recurrence in recurrent depression and the influence of consecutive episodes on vulnerability for depression: a 2-year prospective study. J Clin Psychiatry. 2006;67(5):747-755.
12. Greco T, Eckert G, Kroenke K. The outcome of physical symptoms with treatment of depression. J Gen Intern Med. 2004;19(8):813-818.
13. McClintock SM, Husain MM, Wisniewski SR, et al. Residual symptoms in depressed outpatients who respond by 50% but do not remit to antidepressant medication. J Clin Psychopharmacol. 2011;31(2):180-186.
14. Stahl SM, Zhang L, Damatarca C, et al. Brain circuits determine destiny in depression: a novel approach to the psychopharmacology of wakefulness, fatigue, and executive dysfunction in major depressive disorder. J Clin Psychiatry. 2003;64(suppl 14):6-17.
15. MacHale SM, Law´rie SM, Cavanagh JT, et al. Cerebral perfusion in chronic fatigue syndrome and depression. Br J Psychiatry. 2000;176:550-556.
16. Paykel ES. Achieving gains beyond response. Acta Psychiatrica Scandinavica Suppl. 2002;(415):12-17.
17. van den Heuvel OA, Groenewegen HJ, Barkhof F, et al. Frontostriatal system in planning complexity: a parametric functional magnetic resonance version of Tower of London task. Neuroimage. 2003;18(2):367-374.
18. Jaremka LM, Fagundes CP, Glaser R, et al. Loneliness predicts pain, depression, and fatigue: understanding the role of immune dysregulation. Psychoneuroendocrinology. 2013;38(8):1310-1317.
19. Delgado PL, Charney DS, Price LH, et al. Serotonin function and the mechanism of antidepressant action. Reversal of antidepressant-induced remission by rapid depletion of plasma tryptophan. Arch Gen Psychiatry. 1990;47(5):411-418.
20. Nelson JC, Mazure C, Quinlan DM, et al. Drug-responsive symptoms in melancholia. Arch Gen Psychiatry. 1984;41(7):663-668.
21. Fava M, Ball S, Nelson, JC, et al. Clinical relevance of fatigue as a residual symptom in major depressive disorder. Depress Anxiety. 2014;31(3):250-257.
22. Anisman H, Merali Z, Poulter MO, et al. Cytokines as a precipitant of depressive illness: animal and human studies. Curr Pharm Des. 2005;11(8):963-972.
23. Simon NM, McNamara K, Chow CW, et al. A detailed examination of cytokine abnormalities in major depressive disorder. Eur Neuropsychopharmacol. 2008;18(3):230-233.
24. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56-62.
25. Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382-389.
26. Matza LS, Phillips GA, Revicki DA, et al. Development and validation of a patient-report measure of fatigue associated with depression. J Affect Disord. 2011;134(1-3):294-303.
27. Matza LS, Wyrwich KW, Phillips GA, et al. The Fatigue Associated with Depression Questionnaire (FAsD): responsiveness and responder definition. Qual Life Res. 2013;22(2):351-360.
28. Guidance for industry. Patient-reported outcome measures: use in medical product development to support labeling claims. Food and Drug Administration. http://www.fda. gov/downloads/Drugs/Guidances/UCM193282.pdf. Published December 2009. Accessed May 7, 2015.
29. Knoth RL, Bolge SC, Kim E, et al. Effect of inadequate response to treatment in patients with depression. Am J Manag Care. 2010;16(8):e188-e196.
30. Fava M. Symptoms of fatigue and cognitive/executive dysfunction in major depressive disorder before and after antidepressant treatment. J Clin Psychiatry. 2003;64(suppl 14):30-34.
31. Chang T, Fava M. The future of psychopharmacology of depression. J Clin Psychiatry. 2010;71(8):971-975.
32. Baldwin DS, Papakostas GI. Symptoms of fatigue and sleepiness in major depressive disorder. J Clin Psychiatry. 2006;67(suppl 6):9-15.
33. Ball SG, Dellva MA, D’Souza D, et al. A double-blind, placebo-controlled study of augmentation with LY2216684 for major depressive disorder patients who are partial responders to selective serotonin reuptake inhibitors [abstract P 05]. Int J Psych Clin Pract. 2010;14(suppl 1):19.
34. Stahl SM. Using secondary binding properties to select a not so elective serotonin reuptake inhibitor. J Clin Psychiatry. 1998;59(12):642-643.
35. Stahl SM. Essential psychopharmacology: neuroscientific basis and practical applications. 2nd ed. New York, NY: Cambridge University Press; 2000.
36. Bymaster FP, Katner JS, Nelson DL, et al. Atomoxetine increases extracellular levels of norepinephrine and dopamine in prefrontal cortex of rat: a potential mechanism for efficacy in attention deficit/hyperactivity disorder. Neuropsychopharmacology. 2002;27(5):699-711.
37. Scammell TE, Estabrooke IV, McCarthy MT, et al. Hypothalamic arousal regions are activated during modafinil-induced wakefulness. J Neurosci. 2000;20(22):8620-8628.
38. Daly EJ, Trivedi MH, Fava M, et al. The relationship between adverse events during selective serotonin reuptake inhibitor treatment for major depressive disorder and nonremission in the suicide assessment methodology study. J Clin Psychopharmacol. 2011;31(1):31-38.
39. Nelson JC. A review of the efficacy of serotonergic and noradrenergic reuptake inhibitors for treatment of major depression. Biol Psychiatry. 1999;46(9):1301-1308.
40. Papakostas GI, Nutt DJ, Hallett LA, et al. Resolution of sleepiness and fatigue in major depressive disorder: a comparison of bupropion and the selective serotonin reuptake inhibitors. Biol Psychiatry. 2006;60(12):1350-1355.
41. Fava M, Rush AJ, Thase ME, et al. 15 years of clinical experience with bupropion HCl: from bupropion to bupropion SR to bupropion XL. Prim Care Companion J Clin Psychiatry. 2005;7(3):106-113.
42. Candy M, Jones CB, Williams R, et al. Psychostimulants for depression. Cochrane Database Syst Rev. 2008;(2):CD006722. doi: 10.1002/14651858.CD006722.pub2.
43. Lam JY, Freeman MK, Cates ME. Modafinil augmentation for residual symptoms of fatigue in patients with a partial response to antidepressants. Ann Pharmacother. 2007;41(6):1005-1012.
44. Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clinical Psychol Rev. 2001;21(1):33-61.
45. Trivedi MH, Greer TL, Grannemann BD, et al. Exercise as an augmentation strategy for treatment of major depression. J Psychiatr Pract. 2006;12(4):205-213.
Fatigue and depression can be viewed as a “vicious cycle”: Fatigue can be a symptom of major depression, and fatigue can be a risk factor for depression.1 For example, fatigue associated with a general medical condition or traumatic brain injury can be a risk factor for developing major depressive disorder (MDD).1-3 It isn’t surprising that fatigue has been studied as a predictor of relapse after previous response to treatment in patients with MDD.
Despite the observed association between fatigue and depression, their underlying relationship often is unclear. The literature does not differentiate among fatigue associated with depression, fatigue as a treatment-emergent adverse effect, and fatigue as a residual symptom of depression that is partially responsive to treatment.4,5 To complicate the situation, many medications used to treat MDD can cause fatigue.
Patients often describe fatigue as (1) feeling tired, exhausted, or drained and (2) lacking energy and motivation. Fatigue can be related to impaired wakefulness but is believed to be a different entity than sleepiness.6 Residual fatigue can affect social, cognitive, emotional, and physical health.
We reviewed the literature about fatigue as a symptom of MDD by conducting a search of Medline, PubMed, and Google Scholar, using keywords depression, fatigue, residual symptoms, and treatment. We chose the papers cited in this article based on our consensus and because these publications represent expert opinion or the highest quality evidence available.
Residual fatigue has an effect on prognosis
Fatigue is a common symptom of MDD that persists in 20% to 30% of patients whose symptoms of depression otherwise remit.4,7-9 Several studies have linked residual fatigue with the overall prognosis of MDD.5 Data from a prospective study demonstrate that depressed patients have a higher risk of relapse when they continue to report symptoms of fatigue after their symptoms of depression have otherwise entered partial remission.10 Another study demonstrated that the severity of residual symptoms of depression is a strong predictor of another major depressive episode.11
In a large-scale study, the prevalence of residual fatigue after adequate treatment of MDD in both partial responders and remitters was 84.6%.12 The same study showed that one-third of patients who had been treated for MDD had persistent and clinically significant fatigue, which could suggest a relationship between fatigue and selective serotonin reuptake inhibitors (SSRIs) and other antidepressants.
Another study demonstrated that 64.6% of patients who responded to antidepressant treatment and who had baseline fatigue continued to exhibit symptoms of fatigue after an adequate trial of an antidepressant.13
Neurobiological considerations
Studies have shown that the neuronal circuits that malfunction in fatigue are different from those that malfunction in depression.14 Although the neurobiology of fatigue has not been determined, decreased neuronal activity in the prefrontal circuits has been associated with symptoms of fatigue.15
In addition, evidence from the literature shows a decrease in hormone secretion16 and cognitive abilities in patients exhibiting symptoms of fatigue.17 These findings have led some experts to hypothesize that symptoms of fatigue associated with depression could be the result of (1) immune dysregulation18 and (2) an inability of available antidepressants to target the underlying biology of the disorder.2
Despite the hypothesis that fatigue associated with depression might be biologically related to immune dysregulation, some authors continue to point to an imbalance in neurotransmitters—norepinephrine, histamine, dopamine, acetylcholine—as being associated with fatigue.14 For example, a study demonstrated that drugs targeting noradrenergic reuptake inhibition were more effective at preventing a relapse of fatigue compared with serotonergic drugs.19 Another study showed improvement in energy with an increase in the plasma level of desipramine, which affects noradrenergic neurotransmission.20
Inflammatory cytokines also have been explored in the search for an understanding of the etiology of fatigue and depression.21 Physical and mental stress promote the release of cytokines, which activate the immune system by inducing an inflammatory response; this response has been etiologically linked to depressive disorders.22 Furthermore, studies have demonstrated an elevated level of inflammatory cytokines in patients who have MDD— suggesting that MDD is associated with a chronic low level of inflammation that crosses the blood−brain barrier.23
Clinical considerations: A role for rating scales?
Despite the significance of residual fatigue on the quality of life of patients who have MDD, most common rating scales, such as the Hamilton Depression Rating Scale24 and the Montgomery-Åsberg Depression Rating Scale,25 have limited sensitivity for measuring fatigue.26 The Fatigue Associated with Depression (FAsD)27 questionnaire, designed according to FDA guidelines,28 is used to assess fatigue associated with depression. The final version of the FAsD includes 13 items: a 6-item experience subscale and a 7-item impact subscale.
Is the FAsD helpful? The experience subscale of the FAsD assesses how often the patient experiences different aspects of fatigue (tiredness, exhaustion, lack of energy, physical weakness, and a feeling that everything requires too much effort). The impact subscale of the FAsD assesses the effect of fatigue on daily life.
The overall FAsD score is calculated by taking the mean of each subscale; a change of 0.67 on the experience subscale and 0.57 on the impact subscale are considered clinically meaningful.27 The measurement properties of the questionnaire showed internal consistency, reliability, and validity in testing. Researchers note, however, that FAsD does not include items to assess the impact of fatigue on cognition. This means that the FAsD might not distinguish between physical and mental aspects of fatigue.
Treatment
It isn’t surprising that residual depression can increase health care utilization and economic burden, including such indirect costs as lost productivity and wages.29 Despite these impacts, there is a paucity of studies evaluating the relationship between residual symptoms, such as fatigue, and work productivity. It has been established that improving a depressed patient’s level of energy correlates with improved performance at work.
Treating fatigue as a residual symptom of MDD can be complicated because symptoms of fatigue might be:
• a discrete symptom of MDD
• a prodromal symptom of another disorder
• an adverse effect of an antidepressant.2,30
It is a major clinical problem, therefore, that antidepressants can alleviate and cause symptoms of fatigue.31 Treatment strategy should focus on identifying antidepressants that are less likely to cause fatigue (ie, noradrenergic or dopaminergic drugs, or both). Adjunctive treatments to target residual fatigue also can be used.32
There are limited published data on the effective treatment of residual fatigue in patients with MDD. Given the absence of sufficient evidence, agents that promote noradrenergic and dopaminergic neurotransmission have been the treatment of choice when targeting fatigue in depressed patients.2,14,21,33
The Table34-37 lists potential treatment options often used to treat fatigue associated with depression.
SSRIs. Treatment with SSRIs has been associated with a low probability of achieving remission when targeting fatigue as a symptom of MDD.21
One study reported that, after 8 weeks of treatment with an SSRI, treatment-emergent adverse events, such as worsening fatigue and weakness, were observed—along with an overall lack of efficacy in targeting all symptoms of depression.38
Another study demonstrated positive effects when a noradrenergic agent was added to an SSRI in partial responders who continued to complain of residual fatigue.33
However, studies that compared the effects of SSRIs with those of antidepressants that have pronoradrenergic effects showed that the 2 mechanisms of action were not significantly different from each other in their ability to resolve residual symptoms of fatigue.21 A limiting factor might be that these studies were retrospective and did not analyze the efficacy of a noradrenergic agent as an adjunct for alleviating symptoms of fatigue.39
Bupropion. This commonly used medication for fatigue is believed to cause a significantly lower level of fatigue compared with SSRIs.40 The potential utility of bupropion in this area could be a reflection of its mechanism of action—ie, the drug targets both noradrenergic and dopaminergic neurotransmission.41
A study comparing bupropion with SSRIs in targeting somatic symptoms of depression reported a small but statistically significant difference in favor of the bupropion-treated group. However, this finding was confounded by the small effect size and difficulty quantifying somatic symptoms.40
Stimulants and modafinil. Psycho-stimulants have been shown to be efficacious for depression and fatigue, both as monotherapy and adjunctively.39,42
Modafinil has demonstrated efficacy in open-label trials for improving residual fatigue, but failed to separate from placebo in controlled trials.43 At least 1 other failed study has been published examining modafinil as a treatment for fatigue associated with depression.43
Adjunctive therapy with CNS stimulants, such as amphetamine/dextroamphetamine and methylphenidate, has been used to treat fatigue, with positive results.16 Modafinil and stimulants also could be tried as an augmentation strategy to other antidepressants; such use is off-label and should be attempted only after careful consideration.16
Exercise might be a nonpharmacotherapeutic modality that targets the underlying physiology associated with fatigue. Exercise releases endorphins, which can affect overall brain chemistry and which have been theorized to diminish symptoms of fatigue and depression.44 Consider exercise in addition to treatment with an antidepressant in selected patients.45
To sum up
In general, the literature does not recommend one medication as superior to any other for treating fatigue that is a residual symptom of depression. Such hesitation suggests that more empirical studies are needed to determine what is the best and proper management of treating fatigue associated with depression.
Bottom LinE
Fatigue can be a symptom of major depressive disorder (MDD) or a risk factor for depression. Fatigue has been studied as a predictor of relapse after previous response to treatment in patients with MDD. Residual fatigue can affect social, cognitive, emotional, and physical health and can result in increased utilization of health care services. A number of treatment options are available; none has been shown to be superior to the others.
Related Resources
• Leone SS. A disabling combination: fatigue and depression. Br J Psychiatry. 2010;197(2):86-87.
• Targum SD, Fava M. Fatigue as a residual symptom of depression. Innov Clin Neurosci. 2011;8(10):40-43.
• Illiades C. How to fight depression fatigue. Everyday Health. http://www.everydayhealth.com/health-report/major-depression-living-well/fight-depression-fatigue.aspx.
• Kerr M. Depression and fatigue: a vicious cycle. Healthline. http://www.healthline.com/health/depression/fatigue.
Drug Brand Names
Amphetamine/dextroamphetamine • Adderall
Bupropion • Wellbutrin
Desipramine • Norpramin
Methylphenidate • Ritalin
Modafinil • Provigil
Sertraline • Zoloft
Venlafaxine • Effexor
Disclosures
Dr. Sohail reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Macaluso has conducted clinical trials research as principal investigator for the following pharmaceutical manufacturers in the past 12 months: AbbVie, Inc.; Alkermes; AssureRx Health, Inc.; Eisai Co., Ltd.; FORUM Pharmaceuticals, Inc.; Janssen Pharmaceuticals, Inc.; and Naurex Inc. All clinical trial and study contracts were with, and payments were made to, University of Kansas Medical Center Research Institute, Kansas City, Kansas, a research institute affiliated with University of Kansas School of Medicine−Wichita.
Fatigue and depression can be viewed as a “vicious cycle”: Fatigue can be a symptom of major depression, and fatigue can be a risk factor for depression.1 For example, fatigue associated with a general medical condition or traumatic brain injury can be a risk factor for developing major depressive disorder (MDD).1-3 It isn’t surprising that fatigue has been studied as a predictor of relapse after previous response to treatment in patients with MDD.
Despite the observed association between fatigue and depression, their underlying relationship often is unclear. The literature does not differentiate among fatigue associated with depression, fatigue as a treatment-emergent adverse effect, and fatigue as a residual symptom of depression that is partially responsive to treatment.4,5 To complicate the situation, many medications used to treat MDD can cause fatigue.
Patients often describe fatigue as (1) feeling tired, exhausted, or drained and (2) lacking energy and motivation. Fatigue can be related to impaired wakefulness but is believed to be a different entity than sleepiness.6 Residual fatigue can affect social, cognitive, emotional, and physical health.
We reviewed the literature about fatigue as a symptom of MDD by conducting a search of Medline, PubMed, and Google Scholar, using keywords depression, fatigue, residual symptoms, and treatment. We chose the papers cited in this article based on our consensus and because these publications represent expert opinion or the highest quality evidence available.
Residual fatigue has an effect on prognosis
Fatigue is a common symptom of MDD that persists in 20% to 30% of patients whose symptoms of depression otherwise remit.4,7-9 Several studies have linked residual fatigue with the overall prognosis of MDD.5 Data from a prospective study demonstrate that depressed patients have a higher risk of relapse when they continue to report symptoms of fatigue after their symptoms of depression have otherwise entered partial remission.10 Another study demonstrated that the severity of residual symptoms of depression is a strong predictor of another major depressive episode.11
In a large-scale study, the prevalence of residual fatigue after adequate treatment of MDD in both partial responders and remitters was 84.6%.12 The same study showed that one-third of patients who had been treated for MDD had persistent and clinically significant fatigue, which could suggest a relationship between fatigue and selective serotonin reuptake inhibitors (SSRIs) and other antidepressants.
Another study demonstrated that 64.6% of patients who responded to antidepressant treatment and who had baseline fatigue continued to exhibit symptoms of fatigue after an adequate trial of an antidepressant.13
Neurobiological considerations
Studies have shown that the neuronal circuits that malfunction in fatigue are different from those that malfunction in depression.14 Although the neurobiology of fatigue has not been determined, decreased neuronal activity in the prefrontal circuits has been associated with symptoms of fatigue.15
In addition, evidence from the literature shows a decrease in hormone secretion16 and cognitive abilities in patients exhibiting symptoms of fatigue.17 These findings have led some experts to hypothesize that symptoms of fatigue associated with depression could be the result of (1) immune dysregulation18 and (2) an inability of available antidepressants to target the underlying biology of the disorder.2
Despite the hypothesis that fatigue associated with depression might be biologically related to immune dysregulation, some authors continue to point to an imbalance in neurotransmitters—norepinephrine, histamine, dopamine, acetylcholine—as being associated with fatigue.14 For example, a study demonstrated that drugs targeting noradrenergic reuptake inhibition were more effective at preventing a relapse of fatigue compared with serotonergic drugs.19 Another study showed improvement in energy with an increase in the plasma level of desipramine, which affects noradrenergic neurotransmission.20
Inflammatory cytokines also have been explored in the search for an understanding of the etiology of fatigue and depression.21 Physical and mental stress promote the release of cytokines, which activate the immune system by inducing an inflammatory response; this response has been etiologically linked to depressive disorders.22 Furthermore, studies have demonstrated an elevated level of inflammatory cytokines in patients who have MDD— suggesting that MDD is associated with a chronic low level of inflammation that crosses the blood−brain barrier.23
Clinical considerations: A role for rating scales?
Despite the significance of residual fatigue on the quality of life of patients who have MDD, most common rating scales, such as the Hamilton Depression Rating Scale24 and the Montgomery-Åsberg Depression Rating Scale,25 have limited sensitivity for measuring fatigue.26 The Fatigue Associated with Depression (FAsD)27 questionnaire, designed according to FDA guidelines,28 is used to assess fatigue associated with depression. The final version of the FAsD includes 13 items: a 6-item experience subscale and a 7-item impact subscale.
Is the FAsD helpful? The experience subscale of the FAsD assesses how often the patient experiences different aspects of fatigue (tiredness, exhaustion, lack of energy, physical weakness, and a feeling that everything requires too much effort). The impact subscale of the FAsD assesses the effect of fatigue on daily life.
The overall FAsD score is calculated by taking the mean of each subscale; a change of 0.67 on the experience subscale and 0.57 on the impact subscale are considered clinically meaningful.27 The measurement properties of the questionnaire showed internal consistency, reliability, and validity in testing. Researchers note, however, that FAsD does not include items to assess the impact of fatigue on cognition. This means that the FAsD might not distinguish between physical and mental aspects of fatigue.
Treatment
It isn’t surprising that residual depression can increase health care utilization and economic burden, including such indirect costs as lost productivity and wages.29 Despite these impacts, there is a paucity of studies evaluating the relationship between residual symptoms, such as fatigue, and work productivity. It has been established that improving a depressed patient’s level of energy correlates with improved performance at work.
Treating fatigue as a residual symptom of MDD can be complicated because symptoms of fatigue might be:
• a discrete symptom of MDD
• a prodromal symptom of another disorder
• an adverse effect of an antidepressant.2,30
It is a major clinical problem, therefore, that antidepressants can alleviate and cause symptoms of fatigue.31 Treatment strategy should focus on identifying antidepressants that are less likely to cause fatigue (ie, noradrenergic or dopaminergic drugs, or both). Adjunctive treatments to target residual fatigue also can be used.32
There are limited published data on the effective treatment of residual fatigue in patients with MDD. Given the absence of sufficient evidence, agents that promote noradrenergic and dopaminergic neurotransmission have been the treatment of choice when targeting fatigue in depressed patients.2,14,21,33
The Table34-37 lists potential treatment options often used to treat fatigue associated with depression.
SSRIs. Treatment with SSRIs has been associated with a low probability of achieving remission when targeting fatigue as a symptom of MDD.21
One study reported that, after 8 weeks of treatment with an SSRI, treatment-emergent adverse events, such as worsening fatigue and weakness, were observed—along with an overall lack of efficacy in targeting all symptoms of depression.38
Another study demonstrated positive effects when a noradrenergic agent was added to an SSRI in partial responders who continued to complain of residual fatigue.33
However, studies that compared the effects of SSRIs with those of antidepressants that have pronoradrenergic effects showed that the 2 mechanisms of action were not significantly different from each other in their ability to resolve residual symptoms of fatigue.21 A limiting factor might be that these studies were retrospective and did not analyze the efficacy of a noradrenergic agent as an adjunct for alleviating symptoms of fatigue.39
Bupropion. This commonly used medication for fatigue is believed to cause a significantly lower level of fatigue compared with SSRIs.40 The potential utility of bupropion in this area could be a reflection of its mechanism of action—ie, the drug targets both noradrenergic and dopaminergic neurotransmission.41
A study comparing bupropion with SSRIs in targeting somatic symptoms of depression reported a small but statistically significant difference in favor of the bupropion-treated group. However, this finding was confounded by the small effect size and difficulty quantifying somatic symptoms.40
Stimulants and modafinil. Psycho-stimulants have been shown to be efficacious for depression and fatigue, both as monotherapy and adjunctively.39,42
Modafinil has demonstrated efficacy in open-label trials for improving residual fatigue, but failed to separate from placebo in controlled trials.43 At least 1 other failed study has been published examining modafinil as a treatment for fatigue associated with depression.43
Adjunctive therapy with CNS stimulants, such as amphetamine/dextroamphetamine and methylphenidate, has been used to treat fatigue, with positive results.16 Modafinil and stimulants also could be tried as an augmentation strategy to other antidepressants; such use is off-label and should be attempted only after careful consideration.16
Exercise might be a nonpharmacotherapeutic modality that targets the underlying physiology associated with fatigue. Exercise releases endorphins, which can affect overall brain chemistry and which have been theorized to diminish symptoms of fatigue and depression.44 Consider exercise in addition to treatment with an antidepressant in selected patients.45
To sum up
In general, the literature does not recommend one medication as superior to any other for treating fatigue that is a residual symptom of depression. Such hesitation suggests that more empirical studies are needed to determine what is the best and proper management of treating fatigue associated with depression.
Bottom LinE
Fatigue can be a symptom of major depressive disorder (MDD) or a risk factor for depression. Fatigue has been studied as a predictor of relapse after previous response to treatment in patients with MDD. Residual fatigue can affect social, cognitive, emotional, and physical health and can result in increased utilization of health care services. A number of treatment options are available; none has been shown to be superior to the others.
Related Resources
• Leone SS. A disabling combination: fatigue and depression. Br J Psychiatry. 2010;197(2):86-87.
• Targum SD, Fava M. Fatigue as a residual symptom of depression. Innov Clin Neurosci. 2011;8(10):40-43.
• Illiades C. How to fight depression fatigue. Everyday Health. http://www.everydayhealth.com/health-report/major-depression-living-well/fight-depression-fatigue.aspx.
• Kerr M. Depression and fatigue: a vicious cycle. Healthline. http://www.healthline.com/health/depression/fatigue.
Drug Brand Names
Amphetamine/dextroamphetamine • Adderall
Bupropion • Wellbutrin
Desipramine • Norpramin
Methylphenidate • Ritalin
Modafinil • Provigil
Sertraline • Zoloft
Venlafaxine • Effexor
Disclosures
Dr. Sohail reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Macaluso has conducted clinical trials research as principal investigator for the following pharmaceutical manufacturers in the past 12 months: AbbVie, Inc.; Alkermes; AssureRx Health, Inc.; Eisai Co., Ltd.; FORUM Pharmaceuticals, Inc.; Janssen Pharmaceuticals, Inc.; and Naurex Inc. All clinical trial and study contracts were with, and payments were made to, University of Kansas Medical Center Research Institute, Kansas City, Kansas, a research institute affiliated with University of Kansas School of Medicine−Wichita.
1. Schönberger M, Herrberg M, Ponsford J. Fatigue as a cause, not a consequence of depression and daytime sleepiness: a cross-lagged analysis. J Head Trauma Rehabil. 2014;29(5):427-431.
2. Demyttenaere K, De Fruyt J, Stahl, SM. The many faces of fatigue in major depressive disorder. Int J Neuropsychopharmacol. 2005;8(1):93-105.
3. Skapinakis P, Lewis G, Mavreas V. Temporal relations between unexplained fatigue and depression: longitudinal data from an international study in primary care. Psychosom Med. 2004;66(3):330-335.
4. Nierenberg AA, Husain MM, Trivedi MH, et al. Residual symptoms after remission of major depressive disorder with citalopram and risk of relapse: a STAR*D report. Psychol Med. 2010;40(1):41-50.
5. Kennedy N, Paykel ES. Residual symptoms at remission from depression: impact on long-term outcome. J Affect Disord. 2004;80(2-3):135-144.
6. Shen J, Barbera J, Shapiro CM. Distinguishing sleepiness and fatigue: focus on definition and measurement. Sleep Med Rev. 2006;10:63-76.
7. Nierenberg AA, Keefe BR, Leslie VC, et al. Residual symptoms in depressed patients who respond acutely to fluoxetine. J Clin Psychiatry. 1999;60(4):221-225.
8. Tylee A, Gastpar M, Lépine JP, et al. DEPRES II (Depression Research in European Society II): a patient survey of the symptoms, disability and current management of depression in the community. DEPRES Steering Committee. Int Clin Psychopharmacol. 1999;14(3):139-151.
9. Marcus SM, Young EA, Kerber KB, et al. Gender differences in depression: findings from the STAR*D study. J Affect Disord. 2005;87(2-3):141-150.
10. Paykel ES, Ramana, R, Cooper Z, et al. Residual symptoms after partial remission: an important outcome in depression. Psychol Med. 1995;25(6):1171-1180.
11. Bockting CL, Spinhoven P, Koeter MW, et al; Depression Evaluation Longitudinal Therapy Assessment Study Group. Prediction of recurrence in recurrent depression and the influence of consecutive episodes on vulnerability for depression: a 2-year prospective study. J Clin Psychiatry. 2006;67(5):747-755.
12. Greco T, Eckert G, Kroenke K. The outcome of physical symptoms with treatment of depression. J Gen Intern Med. 2004;19(8):813-818.
13. McClintock SM, Husain MM, Wisniewski SR, et al. Residual symptoms in depressed outpatients who respond by 50% but do not remit to antidepressant medication. J Clin Psychopharmacol. 2011;31(2):180-186.
14. Stahl SM, Zhang L, Damatarca C, et al. Brain circuits determine destiny in depression: a novel approach to the psychopharmacology of wakefulness, fatigue, and executive dysfunction in major depressive disorder. J Clin Psychiatry. 2003;64(suppl 14):6-17.
15. MacHale SM, Law´rie SM, Cavanagh JT, et al. Cerebral perfusion in chronic fatigue syndrome and depression. Br J Psychiatry. 2000;176:550-556.
16. Paykel ES. Achieving gains beyond response. Acta Psychiatrica Scandinavica Suppl. 2002;(415):12-17.
17. van den Heuvel OA, Groenewegen HJ, Barkhof F, et al. Frontostriatal system in planning complexity: a parametric functional magnetic resonance version of Tower of London task. Neuroimage. 2003;18(2):367-374.
18. Jaremka LM, Fagundes CP, Glaser R, et al. Loneliness predicts pain, depression, and fatigue: understanding the role of immune dysregulation. Psychoneuroendocrinology. 2013;38(8):1310-1317.
19. Delgado PL, Charney DS, Price LH, et al. Serotonin function and the mechanism of antidepressant action. Reversal of antidepressant-induced remission by rapid depletion of plasma tryptophan. Arch Gen Psychiatry. 1990;47(5):411-418.
20. Nelson JC, Mazure C, Quinlan DM, et al. Drug-responsive symptoms in melancholia. Arch Gen Psychiatry. 1984;41(7):663-668.
21. Fava M, Ball S, Nelson, JC, et al. Clinical relevance of fatigue as a residual symptom in major depressive disorder. Depress Anxiety. 2014;31(3):250-257.
22. Anisman H, Merali Z, Poulter MO, et al. Cytokines as a precipitant of depressive illness: animal and human studies. Curr Pharm Des. 2005;11(8):963-972.
23. Simon NM, McNamara K, Chow CW, et al. A detailed examination of cytokine abnormalities in major depressive disorder. Eur Neuropsychopharmacol. 2008;18(3):230-233.
24. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56-62.
25. Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382-389.
26. Matza LS, Phillips GA, Revicki DA, et al. Development and validation of a patient-report measure of fatigue associated with depression. J Affect Disord. 2011;134(1-3):294-303.
27. Matza LS, Wyrwich KW, Phillips GA, et al. The Fatigue Associated with Depression Questionnaire (FAsD): responsiveness and responder definition. Qual Life Res. 2013;22(2):351-360.
28. Guidance for industry. Patient-reported outcome measures: use in medical product development to support labeling claims. Food and Drug Administration. http://www.fda. gov/downloads/Drugs/Guidances/UCM193282.pdf. Published December 2009. Accessed May 7, 2015.
29. Knoth RL, Bolge SC, Kim E, et al. Effect of inadequate response to treatment in patients with depression. Am J Manag Care. 2010;16(8):e188-e196.
30. Fava M. Symptoms of fatigue and cognitive/executive dysfunction in major depressive disorder before and after antidepressant treatment. J Clin Psychiatry. 2003;64(suppl 14):30-34.
31. Chang T, Fava M. The future of psychopharmacology of depression. J Clin Psychiatry. 2010;71(8):971-975.
32. Baldwin DS, Papakostas GI. Symptoms of fatigue and sleepiness in major depressive disorder. J Clin Psychiatry. 2006;67(suppl 6):9-15.
33. Ball SG, Dellva MA, D’Souza D, et al. A double-blind, placebo-controlled study of augmentation with LY2216684 for major depressive disorder patients who are partial responders to selective serotonin reuptake inhibitors [abstract P 05]. Int J Psych Clin Pract. 2010;14(suppl 1):19.
34. Stahl SM. Using secondary binding properties to select a not so elective serotonin reuptake inhibitor. J Clin Psychiatry. 1998;59(12):642-643.
35. Stahl SM. Essential psychopharmacology: neuroscientific basis and practical applications. 2nd ed. New York, NY: Cambridge University Press; 2000.
36. Bymaster FP, Katner JS, Nelson DL, et al. Atomoxetine increases extracellular levels of norepinephrine and dopamine in prefrontal cortex of rat: a potential mechanism for efficacy in attention deficit/hyperactivity disorder. Neuropsychopharmacology. 2002;27(5):699-711.
37. Scammell TE, Estabrooke IV, McCarthy MT, et al. Hypothalamic arousal regions are activated during modafinil-induced wakefulness. J Neurosci. 2000;20(22):8620-8628.
38. Daly EJ, Trivedi MH, Fava M, et al. The relationship between adverse events during selective serotonin reuptake inhibitor treatment for major depressive disorder and nonremission in the suicide assessment methodology study. J Clin Psychopharmacol. 2011;31(1):31-38.
39. Nelson JC. A review of the efficacy of serotonergic and noradrenergic reuptake inhibitors for treatment of major depression. Biol Psychiatry. 1999;46(9):1301-1308.
40. Papakostas GI, Nutt DJ, Hallett LA, et al. Resolution of sleepiness and fatigue in major depressive disorder: a comparison of bupropion and the selective serotonin reuptake inhibitors. Biol Psychiatry. 2006;60(12):1350-1355.
41. Fava M, Rush AJ, Thase ME, et al. 15 years of clinical experience with bupropion HCl: from bupropion to bupropion SR to bupropion XL. Prim Care Companion J Clin Psychiatry. 2005;7(3):106-113.
42. Candy M, Jones CB, Williams R, et al. Psychostimulants for depression. Cochrane Database Syst Rev. 2008;(2):CD006722. doi: 10.1002/14651858.CD006722.pub2.
43. Lam JY, Freeman MK, Cates ME. Modafinil augmentation for residual symptoms of fatigue in patients with a partial response to antidepressants. Ann Pharmacother. 2007;41(6):1005-1012.
44. Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clinical Psychol Rev. 2001;21(1):33-61.
45. Trivedi MH, Greer TL, Grannemann BD, et al. Exercise as an augmentation strategy for treatment of major depression. J Psychiatr Pract. 2006;12(4):205-213.
1. Schönberger M, Herrberg M, Ponsford J. Fatigue as a cause, not a consequence of depression and daytime sleepiness: a cross-lagged analysis. J Head Trauma Rehabil. 2014;29(5):427-431.
2. Demyttenaere K, De Fruyt J, Stahl, SM. The many faces of fatigue in major depressive disorder. Int J Neuropsychopharmacol. 2005;8(1):93-105.
3. Skapinakis P, Lewis G, Mavreas V. Temporal relations between unexplained fatigue and depression: longitudinal data from an international study in primary care. Psychosom Med. 2004;66(3):330-335.
4. Nierenberg AA, Husain MM, Trivedi MH, et al. Residual symptoms after remission of major depressive disorder with citalopram and risk of relapse: a STAR*D report. Psychol Med. 2010;40(1):41-50.
5. Kennedy N, Paykel ES. Residual symptoms at remission from depression: impact on long-term outcome. J Affect Disord. 2004;80(2-3):135-144.
6. Shen J, Barbera J, Shapiro CM. Distinguishing sleepiness and fatigue: focus on definition and measurement. Sleep Med Rev. 2006;10:63-76.
7. Nierenberg AA, Keefe BR, Leslie VC, et al. Residual symptoms in depressed patients who respond acutely to fluoxetine. J Clin Psychiatry. 1999;60(4):221-225.
8. Tylee A, Gastpar M, Lépine JP, et al. DEPRES II (Depression Research in European Society II): a patient survey of the symptoms, disability and current management of depression in the community. DEPRES Steering Committee. Int Clin Psychopharmacol. 1999;14(3):139-151.
9. Marcus SM, Young EA, Kerber KB, et al. Gender differences in depression: findings from the STAR*D study. J Affect Disord. 2005;87(2-3):141-150.
10. Paykel ES, Ramana, R, Cooper Z, et al. Residual symptoms after partial remission: an important outcome in depression. Psychol Med. 1995;25(6):1171-1180.
11. Bockting CL, Spinhoven P, Koeter MW, et al; Depression Evaluation Longitudinal Therapy Assessment Study Group. Prediction of recurrence in recurrent depression and the influence of consecutive episodes on vulnerability for depression: a 2-year prospective study. J Clin Psychiatry. 2006;67(5):747-755.
12. Greco T, Eckert G, Kroenke K. The outcome of physical symptoms with treatment of depression. J Gen Intern Med. 2004;19(8):813-818.
13. McClintock SM, Husain MM, Wisniewski SR, et al. Residual symptoms in depressed outpatients who respond by 50% but do not remit to antidepressant medication. J Clin Psychopharmacol. 2011;31(2):180-186.
14. Stahl SM, Zhang L, Damatarca C, et al. Brain circuits determine destiny in depression: a novel approach to the psychopharmacology of wakefulness, fatigue, and executive dysfunction in major depressive disorder. J Clin Psychiatry. 2003;64(suppl 14):6-17.
15. MacHale SM, Law´rie SM, Cavanagh JT, et al. Cerebral perfusion in chronic fatigue syndrome and depression. Br J Psychiatry. 2000;176:550-556.
16. Paykel ES. Achieving gains beyond response. Acta Psychiatrica Scandinavica Suppl. 2002;(415):12-17.
17. van den Heuvel OA, Groenewegen HJ, Barkhof F, et al. Frontostriatal system in planning complexity: a parametric functional magnetic resonance version of Tower of London task. Neuroimage. 2003;18(2):367-374.
18. Jaremka LM, Fagundes CP, Glaser R, et al. Loneliness predicts pain, depression, and fatigue: understanding the role of immune dysregulation. Psychoneuroendocrinology. 2013;38(8):1310-1317.
19. Delgado PL, Charney DS, Price LH, et al. Serotonin function and the mechanism of antidepressant action. Reversal of antidepressant-induced remission by rapid depletion of plasma tryptophan. Arch Gen Psychiatry. 1990;47(5):411-418.
20. Nelson JC, Mazure C, Quinlan DM, et al. Drug-responsive symptoms in melancholia. Arch Gen Psychiatry. 1984;41(7):663-668.
21. Fava M, Ball S, Nelson, JC, et al. Clinical relevance of fatigue as a residual symptom in major depressive disorder. Depress Anxiety. 2014;31(3):250-257.
22. Anisman H, Merali Z, Poulter MO, et al. Cytokines as a precipitant of depressive illness: animal and human studies. Curr Pharm Des. 2005;11(8):963-972.
23. Simon NM, McNamara K, Chow CW, et al. A detailed examination of cytokine abnormalities in major depressive disorder. Eur Neuropsychopharmacol. 2008;18(3):230-233.
24. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56-62.
25. Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382-389.
26. Matza LS, Phillips GA, Revicki DA, et al. Development and validation of a patient-report measure of fatigue associated with depression. J Affect Disord. 2011;134(1-3):294-303.
27. Matza LS, Wyrwich KW, Phillips GA, et al. The Fatigue Associated with Depression Questionnaire (FAsD): responsiveness and responder definition. Qual Life Res. 2013;22(2):351-360.
28. Guidance for industry. Patient-reported outcome measures: use in medical product development to support labeling claims. Food and Drug Administration. http://www.fda. gov/downloads/Drugs/Guidances/UCM193282.pdf. Published December 2009. Accessed May 7, 2015.
29. Knoth RL, Bolge SC, Kim E, et al. Effect of inadequate response to treatment in patients with depression. Am J Manag Care. 2010;16(8):e188-e196.
30. Fava M. Symptoms of fatigue and cognitive/executive dysfunction in major depressive disorder before and after antidepressant treatment. J Clin Psychiatry. 2003;64(suppl 14):30-34.
31. Chang T, Fava M. The future of psychopharmacology of depression. J Clin Psychiatry. 2010;71(8):971-975.
32. Baldwin DS, Papakostas GI. Symptoms of fatigue and sleepiness in major depressive disorder. J Clin Psychiatry. 2006;67(suppl 6):9-15.
33. Ball SG, Dellva MA, D’Souza D, et al. A double-blind, placebo-controlled study of augmentation with LY2216684 for major depressive disorder patients who are partial responders to selective serotonin reuptake inhibitors [abstract P 05]. Int J Psych Clin Pract. 2010;14(suppl 1):19.
34. Stahl SM. Using secondary binding properties to select a not so elective serotonin reuptake inhibitor. J Clin Psychiatry. 1998;59(12):642-643.
35. Stahl SM. Essential psychopharmacology: neuroscientific basis and practical applications. 2nd ed. New York, NY: Cambridge University Press; 2000.
36. Bymaster FP, Katner JS, Nelson DL, et al. Atomoxetine increases extracellular levels of norepinephrine and dopamine in prefrontal cortex of rat: a potential mechanism for efficacy in attention deficit/hyperactivity disorder. Neuropsychopharmacology. 2002;27(5):699-711.
37. Scammell TE, Estabrooke IV, McCarthy MT, et al. Hypothalamic arousal regions are activated during modafinil-induced wakefulness. J Neurosci. 2000;20(22):8620-8628.
38. Daly EJ, Trivedi MH, Fava M, et al. The relationship between adverse events during selective serotonin reuptake inhibitor treatment for major depressive disorder and nonremission in the suicide assessment methodology study. J Clin Psychopharmacol. 2011;31(1):31-38.
39. Nelson JC. A review of the efficacy of serotonergic and noradrenergic reuptake inhibitors for treatment of major depression. Biol Psychiatry. 1999;46(9):1301-1308.
40. Papakostas GI, Nutt DJ, Hallett LA, et al. Resolution of sleepiness and fatigue in major depressive disorder: a comparison of bupropion and the selective serotonin reuptake inhibitors. Biol Psychiatry. 2006;60(12):1350-1355.
41. Fava M, Rush AJ, Thase ME, et al. 15 years of clinical experience with bupropion HCl: from bupropion to bupropion SR to bupropion XL. Prim Care Companion J Clin Psychiatry. 2005;7(3):106-113.
42. Candy M, Jones CB, Williams R, et al. Psychostimulants for depression. Cochrane Database Syst Rev. 2008;(2):CD006722. doi: 10.1002/14651858.CD006722.pub2.
43. Lam JY, Freeman MK, Cates ME. Modafinil augmentation for residual symptoms of fatigue in patients with a partial response to antidepressants. Ann Pharmacother. 2007;41(6):1005-1012.
44. Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clinical Psychol Rev. 2001;21(1):33-61.
45. Trivedi MH, Greer TL, Grannemann BD, et al. Exercise as an augmentation strategy for treatment of major depression. J Psychiatr Pract. 2006;12(4):205-213.
Epithelial Ovarian Cancer: Management of Advanced Disease
Edited by: Arthur T. Skarin, MD, FACP, FCCP
Epithelial ovarian cancer is the fifth leading cause of cancer death among women in the United States. Most women with ovarian cancer present at an advanced stage (International Federation of Gynecology and Obstetrics stage III), for which the standard treatment remains cytoreductive surgery followed by platinum- and taxane-based combination chemotherapy. Although this treatment frequently is curative for patients with early-stage disease, more than 60% of women with advanced disease will develop recurrent disease with progressively shorter disease-free intervals. However, there are many clinical trials in progress that are aimed at refining current therapy and evaluating different approaches to postoperative therapy, with the goal of improving prognosis and quality of life.
To read the full article in PDF:
Edited by: Arthur T. Skarin, MD, FACP, FCCP
Epithelial ovarian cancer is the fifth leading cause of cancer death among women in the United States. Most women with ovarian cancer present at an advanced stage (International Federation of Gynecology and Obstetrics stage III), for which the standard treatment remains cytoreductive surgery followed by platinum- and taxane-based combination chemotherapy. Although this treatment frequently is curative for patients with early-stage disease, more than 60% of women with advanced disease will develop recurrent disease with progressively shorter disease-free intervals. However, there are many clinical trials in progress that are aimed at refining current therapy and evaluating different approaches to postoperative therapy, with the goal of improving prognosis and quality of life.
To read the full article in PDF:
Edited by: Arthur T. Skarin, MD, FACP, FCCP
Epithelial ovarian cancer is the fifth leading cause of cancer death among women in the United States. Most women with ovarian cancer present at an advanced stage (International Federation of Gynecology and Obstetrics stage III), for which the standard treatment remains cytoreductive surgery followed by platinum- and taxane-based combination chemotherapy. Although this treatment frequently is curative for patients with early-stage disease, more than 60% of women with advanced disease will develop recurrent disease with progressively shorter disease-free intervals. However, there are many clinical trials in progress that are aimed at refining current therapy and evaluating different approaches to postoperative therapy, with the goal of improving prognosis and quality of life.
To read the full article in PDF:
Stand by me! Reducing the risk of injurious falls in older adults
Falls and fall-related injuries are common in older adults Every year, 30% of those who are 65 and older fall,1 and the consequences are potentially serious. Falls are the primary cause of hip fracture, which requires an extensive period of rehabilitation. However, rehabilitation does not always restore the older adult to his or her preinjury functional state. In fact, at 6 to 12 months after a hip fracture, 22% to 75% of elderly patients have not recovered their prefracture ambulatory or functional status.2
Falls are also the most common cause of traumatic brain injury in older adults,3 often resulting in long-term cognitive and emotional problems and pain that compromise quality of life. Falls can be fatal and in fact are the leading cause of death from injury in older adults.4
Practitioners can reduce fall-related injury5 and potentially improve quality of life by screening older adults yearly, performing a focused history and examination when necessary, and implementing evidence-based interventions.
RISK FACTORS
A single identifiable factor may account for only a small portion of the fall risk. Falls in older adults are, in general, multifactorial and can be caused by medical conditions (eg, sarcopenia, particularly of the lower limbs, vision loss, urinary incontinence, neuropathies), cognitive impairment, medications such as psychotropic drugs, and home hazards such as area rugs, extension cords, and dimly lit stairways.
The strongest predictors of falls are a recent fall and the presence of a gait or balance disorder.6
SCREENING TESTS
Joint guidelines from the American Geriatrics Society and British Geriatrics Society,7 published in 2011, recommend that practitioners screen older adults yearly for fall risk by asking two questions: “Have you fallen in the past year?” and “Are you having difficulty with gait or balance?” A negative response to both questions suggests a low risk of falling in the near future. Patients with two or more falls, a balance or gait problem (subjective or objective), or history of a fall requiring medical attention should undergo a focused history and physical examination plus a multifactorial risk assessment.
A report of one fall without injury should prompt a simple office-based test of balance. Examples of tests include the Get Up and Go, the Timed Up and Go, and the One-Legged Stance (the Unipedal Stance).
In the Get Up and Go test, patients sit comfortably in a chair with a straight back. They rise from the chair, stand still, walk a short distance (about 3 meters), turn around, walk back to the chair, and sit down.8 The clinician notes any deviation from a confident, smooth performance.
In the Timed Up and Go test, the clinician records the time it takes for the patient to rise from a hardback chair, walk 10 feet (3 meters), turn, return to the chair, and sit down.9 Most older adults complete this test in less than 10 seconds. Taking longer than 14 seconds is associated with a high risk of falls.10
For the One-Legged Stance test, the clinician asks the patient to stand on one leg. A patient without significant balance issues is able to stand for at least 5 seconds.11
Figure 1 summarizes the approach for a community-dwelling patient who presents to the outpatient setting. A complete multifactorial risk assessment may require a dedicated appointment or referral to a specialist such as a geriatrician, physiatrist, or neurologist.
WHAT INFORMATION DOES A FOCUSED HISTORY INCLUDE?
The fall-focused history includes:
A detailed description of the circumstances of the fall or falls, symptoms (such as dizziness), and injuries or other consequences of the fall.7
A medication review. Table 1 includes commonly prescribed drug classes associated with increased fall risk.12 Be especially vigilant for eyedrops used to treat glaucoma (some can potentiate bradycardia) and for psychotropic drugs.
Drug regimens with a high psychotropic burden can be identified with the Drug Burden Index13 or the Anticholinergic Risk Scale,14 but these scales are cumbersome and are usually used only as part of a research study. The updated Beers criteria15 and use of a structured medication review such as the START and STOPP algorithms16 can help prune unnecessary, inappropriate, and high-risk medications such as:
- Selective serotonin reuptake inhibitors in the absence of current major depression. These drugs increase the risk of falls and decrease bone density.17
- Proton pump inhibitors in the absence of a true indication for this drug class to treat reflux. Drugs in this class reduce bone density and increase the risk of hip fracture after 1 year of continuous use18
- Cholinesterase inhibitors in the absence of demonstrated benefit to dementia symptoms for the particular patient. Drugs in this class are associated with falls, hip fracture, bradycardia, and possible need for pacemaker placement.19
Review of activities of daily living (ADLs). A functional assessment of the patient’s ability to complete ADLs helps identify targets for therapy. Assess whether the patient is afraid of falling and, if so, what impact this fear has on ADLs. This can help determine whether the fear protects the patient from performing risky tasks, or harms the patient by contributing to deconditioning.
Medical conditions. Consider chronic conditions that can impair mobility and increase fall risk. These include urinary incontinence, cognitive impairment (eg, dementia), neuropathy, degenerative neurologic conditions such as Parkinson disease, and degenerative arthritis. Osteoporosis increases the risk of fracture in a fall. Vitamin D deficiency increases both fall and fracture risk.20
PHYSICAL EXAMINATION FINDINGS
Assess the patient’s vision, proprioception, reflexes, and cortical, extrapyramidal, and cerebellar function.7
Perform a detailed assessment of the patient’s gait, balance, and mobility. Assess the lower extremities for joint and nerve function, muscle strength, and range of motion.7 The use of brain imaging, if appropriate, is guided by gait abnormalities. Unexpected findings such as neuropathy may require referrals for further evaluation.
Examine the patient’s feet and footwear for signs of poor fit and for styles that may be inappropriate for someone at risk of falling, such as high heels.
Conduct a cardiovascular examination. In addition to assessing heart rate and rhythm and checking for heart murmurs, evaluate the patient for postural changes in heart rate and blood pressure. Wait at least 2 minutes before asking the patient to change position from supine to seated and from seated to standing. A longer interval (3 to 5 minutes) can be used depending on the patient’s history. For example, an older adult reporting a syncopal episode standing by the kitchen sink may need a longer standing interval prior to blood pressure measurement than an older adult who falls right after standing up from a chair.
If there is a strong suspicion that an orthostatic condition contributed to a fall but it is not possible to elicit orthostasis in the office, it may be necessary to refer the patient for tilt-table testing. If the circumstances suggest that pressure along the neck, or turning the neck, contributed to a fall, referral for carotid sinus stimulation may be appropriate. If there is a concern that a brady- or tachyarrhythmia contributed to the fall, a referral for 24- or 48-hour Holter monitoring or a 30-day loop monitor may be indicated.
Assess the patient’s mental status. Cognitive impairment itself is an independent predictor of falls7 because it can reduce processing speed and impair executive function.21 Executive dysfunction may contribute to falls by causing problems with multitasking, drug compliance, and judgment. The presence and severity of cognitive impairment may affect recommendation options (see below), so the assessment should include a screening test. Consider using the Mini-Cog, which requires the patient to recall three words and draw an analog clock (Figure 2).22
Some cognitive screening tests validated for use in the general older population include the General Practitioner Assessment of Cognition and the Memory Impairment Screen.23 More involved cognitive testing such as the Folstein Mini-Mental State Examination, Montreal Cognitive Assessment, and the Saint Louis University Mental Status Examination are routinely performed in a geriatric or neurologic setting. The Folstein is a proprietary test; the other two are not.
Conditions such as circulatory disease, chronic obstructive pulmonary disease, depression, and arthritis are associated with a higher risk of falling, even with adjustment for drug use and other potential confounding factors.24
A brief mood assessment is part of the multifactorial assessment because mood disorders in older adults can lead to deconditioning, drug noncompliance, and other conditions that lead to falls and fall-related injuries. Options for screening include the Geriatric Depression Scale (15 or 30 questions) and the Patient Health Questionnaire (the PHQ-2 or the PHQ-9).7
WHAT ARE THE EVIDENCE-BASED INTERVENTIONS?
In general, interventions are chosen according to the risks identified by the assessment; multiple interventions are usually necessary. It is ineffective to identify risk factors without providing intervention.25
Specific interventions with recommendation levels A and B are listed in Table 2.7 Level A interventions are specifically supported by strong evidence and should be recommended. Of note, although vitamin D3 may not be bioequivalent to vitamin D2, studies in older adults have not consistently found a clinically different outcome, and either may be supplemented in the community-dwelling elderly. Except for vitamin D, these interventions target community-dwelling older adults who are cognitively intact.
Home assessments are effective in high-risk patients, such as those with poor vision and those who were recently hospitalized. The goal is to improve safety, particularly during patient transfers, with education and training provided by an occupational or physical therapist or other geriatric specialist. The benefit of home assessment and environmental modification is greater when combined with other strategies and in general should not be implemented alone.
Exercise is an important intervention. The number needed to treat (NNT) to prevent one fall in older people over the course of at least 12 weeks is 16.26 This compares favorably with interventions that are commonly used in the general population, such as aspirin therapy as secondary prevention for cardiovascular disease (NNT for 1 year = 50)27 and statin therapy to prevent one death from a cardiovascular event over 5 years in people with known heart disease (NNT = 83).28
Exercise recommendations should be customized to the patient. The amount and type of exercise depends on the patient’s baseline physical activity, medication use including antiplatelet and anticoagulant therapy, home environment, cardiac and pulmonary reserve, vision and hearing deficits, and comorbidities including neuropathy and arthritis.
The well-known risks associated with exercise include myocardial infarction and cardiac arrest, as well as falls and fractures. However, the benefits extend beyond fall risk and include improvements in physical function, glycemic control, cardiopulmonary reserve, bone density, arthritic pain, mood, and cognition. Exercise can also help manage weight, reduce sarcopenia, and increase opportunities for socialization. In most positive trials, the exercise interventions lasted longer than 12 weeks, had variable intensity, and occurred 1 to 3 times per week.
The American College of Sports Medicine recommends that older adults perform aerobic exercise 3 to 5 times per week, 20 to 60 minutes per session (the lower ranges are for frail elderly patients).29 It also recommends resistance training 2 to 4 days per week, 20 to 45 minutes per session, depending on the patient’s level of frailty and conditioning.30 Most older adults do not exercise enough.
Interventions listed at the bottom of Table 2 do not, in general, have enough evidence to support or discourage their use; these are level C recommendations. However, these interventions may be considered for certain individuals. For example, older adults with diabetic neuropathy are often unaware of their foot position when they walk. Additionally, those with diabetic neuropathy may have slower generation of ankle and knee strength compared with age-matched controls. These patients may benefit from targeted physical therapy to strengthen ankle and knee extensors and to retrain stride and speed to improve both gait and safety awareness.
Patients who wear shoes that fit poorly, have high heels, or are not laced or buckled have a higher risk of falls.31 Consider recommending footwear that has a firm, low, rubber heel and a sole with a large surface contact area, which may help reduce the risk of falling.32 Advise patients to wear shoes when they are at home and to avoid using slippers and going barefoot.33
Cataract surgery, another level C intervention, is associated with fewer fall-related injuries, particularly hip fracture.34 Noncataract vision interventions (such as exchanging progressive or bifocal lenses for single-lens glasses) may be effective in select patients if distorted vision in the lower fields of view increases the risk of falling, particularly outdoors.35
INTERVENTIONS FOR SPECIAL POPULATIONS
Falls occur more frequently in mobile residents of long-term care facilities than in community-dwelling adults.7 Institutional residents are older and more frail, have more cognitive impairment, and are prescribed more medications. Half of long-term care residents fall at least once a year.7
The data support giving combined calcium and vitamin D supplementation to older adults in long-term care facilities to reduce fracture rates.36 The NNT to prevent one hip fracture is about 111.37 Hip protectors in this setting may reduce the risk of a hip fracture but also may increase the risk of a pelvic fracture. They do not alter the risk of falling.38
Collaborative interventions can help reduce the fall risk in older adults in the nursing home.39 Input from medical, psychosocial, nursing, podiatric, dietary, and therapy services can be solicited and incorporated into an individualized fall prevention program. The program can also include modifications in the environment to improve safety and reduce fall risk.
The benefits of exercise in reducing injurious falls in long-term care is less clear than in the community, likely because of the heterogeneity of both the long-term care population and the studied interventions. Exercise has other benefits, however. It maintains a person’s ability to complete ADLs, improves mood, reduces hyperglycemia, and improves quality of life. Some studies have found a greater risk of falling with exercise therapy as independence increased.40 However, a meta-analysis in 2013 found that exercise interventions, ranging from 3 to 24 months and consisting mainly of balance and resistance training, reduced the risk of falls by 23%.41 Mixing several types of exercises was helpful. Studies of a longer duration with exercise sessions at least 2 to 3 times per week demonstrated the most benefit.41 There was no statistically significant reduction in fracture risk in this meta-analysis,41 although, possibly, more participants would have been needed for a longer period to demonstrate a benefit. Additionally, no study combined osteoporosis treatment with exercise interventions.
WHAT EVIDENCE EXISTS FOR PATIENTS WITH COGNITIVE IMPAIRMENT?
Currently, there are no specific evidence-based recommendations for fall prevention in community-dwelling older adults with cognitive impairment and dementia.7 Cognitively impaired adults are typically excluded from community studies of fall prevention. The one study that specifically investigated community-dwelling adults with cognitive impairment was not able to demonstrate a fall reduction with multifactorial intervention.42
PREVENTING FALLS IN ELDERLY PATIENTS WHO RECENTLY HAD A STROKE
Falls are common in patients who have had a cerebrovascular event. Up to 7% of patients fall in the first week after a stroke. In the year after a stroke, 55% to 75% of patients experience a fall.43 Falls account for the most common medical complication after a stroke.44
Several small studies found that vitamin D supplementation after a stroke reduced both the rate of falls and the number of people who fall.45 Additional interventions such as exercise, medication, and visual aids have been studied, but there is little evidence to support their use. Mobile patients who have lower-extremity hemiparesis after a stroke may develop osteoporosis in the affected limb, so evaluation and appropriate pharmacologic therapy may be considered.
- Tromp AM, Pluijm SM, Smit JH, Deeg DJ, Bouter LM, Lips P. Fall-risk screening test: a prospective study on predictors for falls in community-dwelling elderly. J Clin Epidemiol 2001; 54:837–844.
- Binder EF, Brown M, Sinacore DR, Steger-May K, Yarasheski KE, Schechtman KB. Effects of extended outpatient rehabilitation after hip fracture: a randomized controlled trial. JAMA 2004; 292:837–846.
- Sterling DA, O’Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma 2001; 50:116–119.
- Centers for Disease Control and Prevention (CDC). Web-based Injury Statistics Query and Reporting System (WISQARSTM). www.cdc.gov/injury/wisqars. Accessed April 8, 2015.
- Tinetti ME, Baker DI, King M, et al. Effect of dissemination of evidence in reducing injuries from falls. N Engl J Med 2008; 359:252–261.
- Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall? JAMA 2007; 297:77–86.
- Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 2011; 59:148–157.
- Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the “get-up and go” test. Arch Phys Med Rehabil 1986; 67:387–389.
- Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991; 39:142–148.
- Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther 2000; 80:896–903.
- Springer BA, Marin R, Cyhan T, Roberts H, Gill NW. Normative values for the unipedal stance test with eyes open and closed. J Geriatr Phys Ther 2007; 30:8–15.
- Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc 1999; 47:30–39.
- Hilmer SN, Mager DE, Simonsick EM, et al. A drug burden index to define the functional burden of medications in older people. Arch Intern Med 2007; 167:781–787.
- Rudolph JL, Salow MJ, Angelini MC, McGlinchey RE. The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch Intern Med 2008; 168:508–513.
- American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2012; 60:616–631.
- Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther 2008; 46:72–83.
- Sterke CS, Ziere G, van Beeck EF, Looman CW, van der Cammen TJ. Dose-response relationship between selective serotonin re-uptake inhibitors and injurious falls: a study in nursing home residents with dementia. Br J Clin Pharmacol 2012; 73:812–820.
- Khalili H, Huang ES, Jacobson BC, Camargo CA Jr, Feskanich D, Chan AT. Use of proton pump inhibitors and risk of hip fracture in relation to dietary and lifestyle factors: a prospective cohort study. BMJ 2012; 344:e372.
- Gill SS, Anderson GM, Fischer HD, et al. Syncope and its consequences in patients with dementia receiving cholinesterase inhibitors: a population-based cohort study. Arch Intern Med 2009; 169:867–873.
- Janssen HC, Samson MM, Verhaar HJ. Vitamin D deficiency, muscle function, and falls in elderly people. Am J Clin Nutr 2002; 75:611–615.
- Muir SW, Gopaul K, Montero Odasso MM. The role of cognitive impairment in fall risk among older adults: a systematic review and meta-analysis. Age Ageing 2012; 41:299–308.
- Borson S, Scanlan J, Brush M, Vitaliano P, Dokmak A. The Mini-Cog: a cognitive ‘vital signs’ measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry 2000; 15:1021–1027.
- Cordell CB, Borson S, Boustani M, et al; Medicare Detection of Cognitive Impairment Workgroup. Alzheimer’s Association recommendations for operationalizing the detection of cognitive impairment during the Medicare Annual Wellness Visit in a primary care setting. Alzheimers Dement 2013; 9:141–150.
- Lawlor DA, Patel R, Ebrahim S. Association between falls in elderly women and chronic diseases and drug use: cross sectional study. BMJ 2003; 327:712–717.
- Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ 2002; 325:128.
- Chang JT, Morton SC, Rubenstein LZ, et al. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials. BMJ 2004; 328:680.
- Antithrombotic Trialists’ (ATT) Collaboration; Baigent C, Blackwell L, Collins R, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 2009; 373:1849–1860.
- Baigent C, Keech A, Kearney PM, et al; Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005; 366:1267–1278.
- Mazzeo RS; American College of Sports Medicine (ACSM). Exercise and the older adult. ACSM Current Comment. www.acsm.org/docs/current-comments/exerciseandtheolderadult.pdf. Accessed April 8, 2015.
- Willoughby DS; American College of Sports Medicine (ACSM). Resistance training and the older adult. ACSM Current Comment. www.acsm.org/docs/current-comments/resistancetrainingandtheoa.pdf. Accessed April 8, 2015.
- Tencer AF, Koepsell TD, Wolf ME, et al. Biomechanical properties of shoes and risk of falls in older adults. J Am Geriatr Soc 2004; 52:1840–1846.
- Lord SR, Bashford GM. Shoe characteristics and balance in older women. J Am Geriatr Soc 1996; 44:429–433.
- Kelsey JL, Procter-Gray E, Nguyen US, Li W, Kiel DP, Hannan MT. Footwear and falls in the home among older individuals in the MOBILIZE Boston Study. Footwear Sci 2010; 2:123–129.
- Tseng VL, Yu F, Lum F, Coleman AL. Risk of fractures following cataract surgery in Medicare beneficiaries. JAMA 2012; 308:493–501.
- Cumming RG, Ivers R, Clemson L, et al. Improving vision to prevent falls in frail older people: a randomized trial. J Am Geriatr Soc 2007; 55:175–181.
- Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, et al. Effect of vitamin D on falls: a meta-analysis. JAMA 2004; 291:1999–2006.
- Avenell A, Mak JCS, O’Connell D. Vitamin D and vitamin D analogues for preventing fractures in postmenopausal women and older men. Cochrane Database Syst Rev 2014; 4:CD000227.
- Santesso N, Carrasco-Labra A, Brignardello-Petersen R. Hip protectors for preventing hip fractures in older people. Cochrane Database Syst Rev 2014; 3:CD001255.
- Messinger-Rapport B, Dumas LG. Falls in the nursing home: a collaborative approach. Nurs Clin North Am 2009; 44:187–195.
- Faber MJ, Bosscher RJ, Chin A, Paw MJ, van Wieringen PC. Effects of exercise programs on falls and mobility in frail and pre-frail older adults: a multicenter randomized controlled trial. Arch Phys Med Rehabil 2006; 87:885–896.
- Silva RB, Eslick GD, Duque G. Exercise for falls and fracture prevention in long term care facilities: a systematic review and meta-analysis. J Am Med Dir Assoc 2013; 14:685–689.e2.
- Shaw FE, Bond J, Richardson DA, et al. Multifactorial intervention after a fall in older people with cognitive impairment and dementia presenting to the accident and emergency department: randomised controlled trial. BMJ 2003; 326:73.
- Ashburn A, Hyndman D, Pickering R, Yardley L, Harris S. Predicting people with stroke at risk of falls. Age Ageing 2008; 37:270–276.
- Davenport RJ, Dennis MS, Wellwood I, Warlow CP. Complications after acute stroke. Stroke 1996; 27:415–420.
- Verheyden GS, Weerdesteyn V, Pickering RM, et al. Interventions for preventing falls in people after stroke. Cochrane Database Syst Rev 2013; 5:CD008728.
Falls and fall-related injuries are common in older adults Every year, 30% of those who are 65 and older fall,1 and the consequences are potentially serious. Falls are the primary cause of hip fracture, which requires an extensive period of rehabilitation. However, rehabilitation does not always restore the older adult to his or her preinjury functional state. In fact, at 6 to 12 months after a hip fracture, 22% to 75% of elderly patients have not recovered their prefracture ambulatory or functional status.2
Falls are also the most common cause of traumatic brain injury in older adults,3 often resulting in long-term cognitive and emotional problems and pain that compromise quality of life. Falls can be fatal and in fact are the leading cause of death from injury in older adults.4
Practitioners can reduce fall-related injury5 and potentially improve quality of life by screening older adults yearly, performing a focused history and examination when necessary, and implementing evidence-based interventions.
RISK FACTORS
A single identifiable factor may account for only a small portion of the fall risk. Falls in older adults are, in general, multifactorial and can be caused by medical conditions (eg, sarcopenia, particularly of the lower limbs, vision loss, urinary incontinence, neuropathies), cognitive impairment, medications such as psychotropic drugs, and home hazards such as area rugs, extension cords, and dimly lit stairways.
The strongest predictors of falls are a recent fall and the presence of a gait or balance disorder.6
SCREENING TESTS
Joint guidelines from the American Geriatrics Society and British Geriatrics Society,7 published in 2011, recommend that practitioners screen older adults yearly for fall risk by asking two questions: “Have you fallen in the past year?” and “Are you having difficulty with gait or balance?” A negative response to both questions suggests a low risk of falling in the near future. Patients with two or more falls, a balance or gait problem (subjective or objective), or history of a fall requiring medical attention should undergo a focused history and physical examination plus a multifactorial risk assessment.
A report of one fall without injury should prompt a simple office-based test of balance. Examples of tests include the Get Up and Go, the Timed Up and Go, and the One-Legged Stance (the Unipedal Stance).
In the Get Up and Go test, patients sit comfortably in a chair with a straight back. They rise from the chair, stand still, walk a short distance (about 3 meters), turn around, walk back to the chair, and sit down.8 The clinician notes any deviation from a confident, smooth performance.
In the Timed Up and Go test, the clinician records the time it takes for the patient to rise from a hardback chair, walk 10 feet (3 meters), turn, return to the chair, and sit down.9 Most older adults complete this test in less than 10 seconds. Taking longer than 14 seconds is associated with a high risk of falls.10
For the One-Legged Stance test, the clinician asks the patient to stand on one leg. A patient without significant balance issues is able to stand for at least 5 seconds.11
Figure 1 summarizes the approach for a community-dwelling patient who presents to the outpatient setting. A complete multifactorial risk assessment may require a dedicated appointment or referral to a specialist such as a geriatrician, physiatrist, or neurologist.
WHAT INFORMATION DOES A FOCUSED HISTORY INCLUDE?
The fall-focused history includes:
A detailed description of the circumstances of the fall or falls, symptoms (such as dizziness), and injuries or other consequences of the fall.7
A medication review. Table 1 includes commonly prescribed drug classes associated with increased fall risk.12 Be especially vigilant for eyedrops used to treat glaucoma (some can potentiate bradycardia) and for psychotropic drugs.
Drug regimens with a high psychotropic burden can be identified with the Drug Burden Index13 or the Anticholinergic Risk Scale,14 but these scales are cumbersome and are usually used only as part of a research study. The updated Beers criteria15 and use of a structured medication review such as the START and STOPP algorithms16 can help prune unnecessary, inappropriate, and high-risk medications such as:
- Selective serotonin reuptake inhibitors in the absence of current major depression. These drugs increase the risk of falls and decrease bone density.17
- Proton pump inhibitors in the absence of a true indication for this drug class to treat reflux. Drugs in this class reduce bone density and increase the risk of hip fracture after 1 year of continuous use18
- Cholinesterase inhibitors in the absence of demonstrated benefit to dementia symptoms for the particular patient. Drugs in this class are associated with falls, hip fracture, bradycardia, and possible need for pacemaker placement.19
Review of activities of daily living (ADLs). A functional assessment of the patient’s ability to complete ADLs helps identify targets for therapy. Assess whether the patient is afraid of falling and, if so, what impact this fear has on ADLs. This can help determine whether the fear protects the patient from performing risky tasks, or harms the patient by contributing to deconditioning.
Medical conditions. Consider chronic conditions that can impair mobility and increase fall risk. These include urinary incontinence, cognitive impairment (eg, dementia), neuropathy, degenerative neurologic conditions such as Parkinson disease, and degenerative arthritis. Osteoporosis increases the risk of fracture in a fall. Vitamin D deficiency increases both fall and fracture risk.20
PHYSICAL EXAMINATION FINDINGS
Assess the patient’s vision, proprioception, reflexes, and cortical, extrapyramidal, and cerebellar function.7
Perform a detailed assessment of the patient’s gait, balance, and mobility. Assess the lower extremities for joint and nerve function, muscle strength, and range of motion.7 The use of brain imaging, if appropriate, is guided by gait abnormalities. Unexpected findings such as neuropathy may require referrals for further evaluation.
Examine the patient’s feet and footwear for signs of poor fit and for styles that may be inappropriate for someone at risk of falling, such as high heels.
Conduct a cardiovascular examination. In addition to assessing heart rate and rhythm and checking for heart murmurs, evaluate the patient for postural changes in heart rate and blood pressure. Wait at least 2 minutes before asking the patient to change position from supine to seated and from seated to standing. A longer interval (3 to 5 minutes) can be used depending on the patient’s history. For example, an older adult reporting a syncopal episode standing by the kitchen sink may need a longer standing interval prior to blood pressure measurement than an older adult who falls right after standing up from a chair.
If there is a strong suspicion that an orthostatic condition contributed to a fall but it is not possible to elicit orthostasis in the office, it may be necessary to refer the patient for tilt-table testing. If the circumstances suggest that pressure along the neck, or turning the neck, contributed to a fall, referral for carotid sinus stimulation may be appropriate. If there is a concern that a brady- or tachyarrhythmia contributed to the fall, a referral for 24- or 48-hour Holter monitoring or a 30-day loop monitor may be indicated.
Assess the patient’s mental status. Cognitive impairment itself is an independent predictor of falls7 because it can reduce processing speed and impair executive function.21 Executive dysfunction may contribute to falls by causing problems with multitasking, drug compliance, and judgment. The presence and severity of cognitive impairment may affect recommendation options (see below), so the assessment should include a screening test. Consider using the Mini-Cog, which requires the patient to recall three words and draw an analog clock (Figure 2).22
Some cognitive screening tests validated for use in the general older population include the General Practitioner Assessment of Cognition and the Memory Impairment Screen.23 More involved cognitive testing such as the Folstein Mini-Mental State Examination, Montreal Cognitive Assessment, and the Saint Louis University Mental Status Examination are routinely performed in a geriatric or neurologic setting. The Folstein is a proprietary test; the other two are not.
Conditions such as circulatory disease, chronic obstructive pulmonary disease, depression, and arthritis are associated with a higher risk of falling, even with adjustment for drug use and other potential confounding factors.24
A brief mood assessment is part of the multifactorial assessment because mood disorders in older adults can lead to deconditioning, drug noncompliance, and other conditions that lead to falls and fall-related injuries. Options for screening include the Geriatric Depression Scale (15 or 30 questions) and the Patient Health Questionnaire (the PHQ-2 or the PHQ-9).7
WHAT ARE THE EVIDENCE-BASED INTERVENTIONS?
In general, interventions are chosen according to the risks identified by the assessment; multiple interventions are usually necessary. It is ineffective to identify risk factors without providing intervention.25
Specific interventions with recommendation levels A and B are listed in Table 2.7 Level A interventions are specifically supported by strong evidence and should be recommended. Of note, although vitamin D3 may not be bioequivalent to vitamin D2, studies in older adults have not consistently found a clinically different outcome, and either may be supplemented in the community-dwelling elderly. Except for vitamin D, these interventions target community-dwelling older adults who are cognitively intact.
Home assessments are effective in high-risk patients, such as those with poor vision and those who were recently hospitalized. The goal is to improve safety, particularly during patient transfers, with education and training provided by an occupational or physical therapist or other geriatric specialist. The benefit of home assessment and environmental modification is greater when combined with other strategies and in general should not be implemented alone.
Exercise is an important intervention. The number needed to treat (NNT) to prevent one fall in older people over the course of at least 12 weeks is 16.26 This compares favorably with interventions that are commonly used in the general population, such as aspirin therapy as secondary prevention for cardiovascular disease (NNT for 1 year = 50)27 and statin therapy to prevent one death from a cardiovascular event over 5 years in people with known heart disease (NNT = 83).28
Exercise recommendations should be customized to the patient. The amount and type of exercise depends on the patient’s baseline physical activity, medication use including antiplatelet and anticoagulant therapy, home environment, cardiac and pulmonary reserve, vision and hearing deficits, and comorbidities including neuropathy and arthritis.
The well-known risks associated with exercise include myocardial infarction and cardiac arrest, as well as falls and fractures. However, the benefits extend beyond fall risk and include improvements in physical function, glycemic control, cardiopulmonary reserve, bone density, arthritic pain, mood, and cognition. Exercise can also help manage weight, reduce sarcopenia, and increase opportunities for socialization. In most positive trials, the exercise interventions lasted longer than 12 weeks, had variable intensity, and occurred 1 to 3 times per week.
The American College of Sports Medicine recommends that older adults perform aerobic exercise 3 to 5 times per week, 20 to 60 minutes per session (the lower ranges are for frail elderly patients).29 It also recommends resistance training 2 to 4 days per week, 20 to 45 minutes per session, depending on the patient’s level of frailty and conditioning.30 Most older adults do not exercise enough.
Interventions listed at the bottom of Table 2 do not, in general, have enough evidence to support or discourage their use; these are level C recommendations. However, these interventions may be considered for certain individuals. For example, older adults with diabetic neuropathy are often unaware of their foot position when they walk. Additionally, those with diabetic neuropathy may have slower generation of ankle and knee strength compared with age-matched controls. These patients may benefit from targeted physical therapy to strengthen ankle and knee extensors and to retrain stride and speed to improve both gait and safety awareness.
Patients who wear shoes that fit poorly, have high heels, or are not laced or buckled have a higher risk of falls.31 Consider recommending footwear that has a firm, low, rubber heel and a sole with a large surface contact area, which may help reduce the risk of falling.32 Advise patients to wear shoes when they are at home and to avoid using slippers and going barefoot.33
Cataract surgery, another level C intervention, is associated with fewer fall-related injuries, particularly hip fracture.34 Noncataract vision interventions (such as exchanging progressive or bifocal lenses for single-lens glasses) may be effective in select patients if distorted vision in the lower fields of view increases the risk of falling, particularly outdoors.35
INTERVENTIONS FOR SPECIAL POPULATIONS
Falls occur more frequently in mobile residents of long-term care facilities than in community-dwelling adults.7 Institutional residents are older and more frail, have more cognitive impairment, and are prescribed more medications. Half of long-term care residents fall at least once a year.7
The data support giving combined calcium and vitamin D supplementation to older adults in long-term care facilities to reduce fracture rates.36 The NNT to prevent one hip fracture is about 111.37 Hip protectors in this setting may reduce the risk of a hip fracture but also may increase the risk of a pelvic fracture. They do not alter the risk of falling.38
Collaborative interventions can help reduce the fall risk in older adults in the nursing home.39 Input from medical, psychosocial, nursing, podiatric, dietary, and therapy services can be solicited and incorporated into an individualized fall prevention program. The program can also include modifications in the environment to improve safety and reduce fall risk.
The benefits of exercise in reducing injurious falls in long-term care is less clear than in the community, likely because of the heterogeneity of both the long-term care population and the studied interventions. Exercise has other benefits, however. It maintains a person’s ability to complete ADLs, improves mood, reduces hyperglycemia, and improves quality of life. Some studies have found a greater risk of falling with exercise therapy as independence increased.40 However, a meta-analysis in 2013 found that exercise interventions, ranging from 3 to 24 months and consisting mainly of balance and resistance training, reduced the risk of falls by 23%.41 Mixing several types of exercises was helpful. Studies of a longer duration with exercise sessions at least 2 to 3 times per week demonstrated the most benefit.41 There was no statistically significant reduction in fracture risk in this meta-analysis,41 although, possibly, more participants would have been needed for a longer period to demonstrate a benefit. Additionally, no study combined osteoporosis treatment with exercise interventions.
WHAT EVIDENCE EXISTS FOR PATIENTS WITH COGNITIVE IMPAIRMENT?
Currently, there are no specific evidence-based recommendations for fall prevention in community-dwelling older adults with cognitive impairment and dementia.7 Cognitively impaired adults are typically excluded from community studies of fall prevention. The one study that specifically investigated community-dwelling adults with cognitive impairment was not able to demonstrate a fall reduction with multifactorial intervention.42
PREVENTING FALLS IN ELDERLY PATIENTS WHO RECENTLY HAD A STROKE
Falls are common in patients who have had a cerebrovascular event. Up to 7% of patients fall in the first week after a stroke. In the year after a stroke, 55% to 75% of patients experience a fall.43 Falls account for the most common medical complication after a stroke.44
Several small studies found that vitamin D supplementation after a stroke reduced both the rate of falls and the number of people who fall.45 Additional interventions such as exercise, medication, and visual aids have been studied, but there is little evidence to support their use. Mobile patients who have lower-extremity hemiparesis after a stroke may develop osteoporosis in the affected limb, so evaluation and appropriate pharmacologic therapy may be considered.
Falls and fall-related injuries are common in older adults Every year, 30% of those who are 65 and older fall,1 and the consequences are potentially serious. Falls are the primary cause of hip fracture, which requires an extensive period of rehabilitation. However, rehabilitation does not always restore the older adult to his or her preinjury functional state. In fact, at 6 to 12 months after a hip fracture, 22% to 75% of elderly patients have not recovered their prefracture ambulatory or functional status.2
Falls are also the most common cause of traumatic brain injury in older adults,3 often resulting in long-term cognitive and emotional problems and pain that compromise quality of life. Falls can be fatal and in fact are the leading cause of death from injury in older adults.4
Practitioners can reduce fall-related injury5 and potentially improve quality of life by screening older adults yearly, performing a focused history and examination when necessary, and implementing evidence-based interventions.
RISK FACTORS
A single identifiable factor may account for only a small portion of the fall risk. Falls in older adults are, in general, multifactorial and can be caused by medical conditions (eg, sarcopenia, particularly of the lower limbs, vision loss, urinary incontinence, neuropathies), cognitive impairment, medications such as psychotropic drugs, and home hazards such as area rugs, extension cords, and dimly lit stairways.
The strongest predictors of falls are a recent fall and the presence of a gait or balance disorder.6
SCREENING TESTS
Joint guidelines from the American Geriatrics Society and British Geriatrics Society,7 published in 2011, recommend that practitioners screen older adults yearly for fall risk by asking two questions: “Have you fallen in the past year?” and “Are you having difficulty with gait or balance?” A negative response to both questions suggests a low risk of falling in the near future. Patients with two or more falls, a balance or gait problem (subjective or objective), or history of a fall requiring medical attention should undergo a focused history and physical examination plus a multifactorial risk assessment.
A report of one fall without injury should prompt a simple office-based test of balance. Examples of tests include the Get Up and Go, the Timed Up and Go, and the One-Legged Stance (the Unipedal Stance).
In the Get Up and Go test, patients sit comfortably in a chair with a straight back. They rise from the chair, stand still, walk a short distance (about 3 meters), turn around, walk back to the chair, and sit down.8 The clinician notes any deviation from a confident, smooth performance.
In the Timed Up and Go test, the clinician records the time it takes for the patient to rise from a hardback chair, walk 10 feet (3 meters), turn, return to the chair, and sit down.9 Most older adults complete this test in less than 10 seconds. Taking longer than 14 seconds is associated with a high risk of falls.10
For the One-Legged Stance test, the clinician asks the patient to stand on one leg. A patient without significant balance issues is able to stand for at least 5 seconds.11
Figure 1 summarizes the approach for a community-dwelling patient who presents to the outpatient setting. A complete multifactorial risk assessment may require a dedicated appointment or referral to a specialist such as a geriatrician, physiatrist, or neurologist.
WHAT INFORMATION DOES A FOCUSED HISTORY INCLUDE?
The fall-focused history includes:
A detailed description of the circumstances of the fall or falls, symptoms (such as dizziness), and injuries or other consequences of the fall.7
A medication review. Table 1 includes commonly prescribed drug classes associated with increased fall risk.12 Be especially vigilant for eyedrops used to treat glaucoma (some can potentiate bradycardia) and for psychotropic drugs.
Drug regimens with a high psychotropic burden can be identified with the Drug Burden Index13 or the Anticholinergic Risk Scale,14 but these scales are cumbersome and are usually used only as part of a research study. The updated Beers criteria15 and use of a structured medication review such as the START and STOPP algorithms16 can help prune unnecessary, inappropriate, and high-risk medications such as:
- Selective serotonin reuptake inhibitors in the absence of current major depression. These drugs increase the risk of falls and decrease bone density.17
- Proton pump inhibitors in the absence of a true indication for this drug class to treat reflux. Drugs in this class reduce bone density and increase the risk of hip fracture after 1 year of continuous use18
- Cholinesterase inhibitors in the absence of demonstrated benefit to dementia symptoms for the particular patient. Drugs in this class are associated with falls, hip fracture, bradycardia, and possible need for pacemaker placement.19
Review of activities of daily living (ADLs). A functional assessment of the patient’s ability to complete ADLs helps identify targets for therapy. Assess whether the patient is afraid of falling and, if so, what impact this fear has on ADLs. This can help determine whether the fear protects the patient from performing risky tasks, or harms the patient by contributing to deconditioning.
Medical conditions. Consider chronic conditions that can impair mobility and increase fall risk. These include urinary incontinence, cognitive impairment (eg, dementia), neuropathy, degenerative neurologic conditions such as Parkinson disease, and degenerative arthritis. Osteoporosis increases the risk of fracture in a fall. Vitamin D deficiency increases both fall and fracture risk.20
PHYSICAL EXAMINATION FINDINGS
Assess the patient’s vision, proprioception, reflexes, and cortical, extrapyramidal, and cerebellar function.7
Perform a detailed assessment of the patient’s gait, balance, and mobility. Assess the lower extremities for joint and nerve function, muscle strength, and range of motion.7 The use of brain imaging, if appropriate, is guided by gait abnormalities. Unexpected findings such as neuropathy may require referrals for further evaluation.
Examine the patient’s feet and footwear for signs of poor fit and for styles that may be inappropriate for someone at risk of falling, such as high heels.
Conduct a cardiovascular examination. In addition to assessing heart rate and rhythm and checking for heart murmurs, evaluate the patient for postural changes in heart rate and blood pressure. Wait at least 2 minutes before asking the patient to change position from supine to seated and from seated to standing. A longer interval (3 to 5 minutes) can be used depending on the patient’s history. For example, an older adult reporting a syncopal episode standing by the kitchen sink may need a longer standing interval prior to blood pressure measurement than an older adult who falls right after standing up from a chair.
If there is a strong suspicion that an orthostatic condition contributed to a fall but it is not possible to elicit orthostasis in the office, it may be necessary to refer the patient for tilt-table testing. If the circumstances suggest that pressure along the neck, or turning the neck, contributed to a fall, referral for carotid sinus stimulation may be appropriate. If there is a concern that a brady- or tachyarrhythmia contributed to the fall, a referral for 24- or 48-hour Holter monitoring or a 30-day loop monitor may be indicated.
Assess the patient’s mental status. Cognitive impairment itself is an independent predictor of falls7 because it can reduce processing speed and impair executive function.21 Executive dysfunction may contribute to falls by causing problems with multitasking, drug compliance, and judgment. The presence and severity of cognitive impairment may affect recommendation options (see below), so the assessment should include a screening test. Consider using the Mini-Cog, which requires the patient to recall three words and draw an analog clock (Figure 2).22
Some cognitive screening tests validated for use in the general older population include the General Practitioner Assessment of Cognition and the Memory Impairment Screen.23 More involved cognitive testing such as the Folstein Mini-Mental State Examination, Montreal Cognitive Assessment, and the Saint Louis University Mental Status Examination are routinely performed in a geriatric or neurologic setting. The Folstein is a proprietary test; the other two are not.
Conditions such as circulatory disease, chronic obstructive pulmonary disease, depression, and arthritis are associated with a higher risk of falling, even with adjustment for drug use and other potential confounding factors.24
A brief mood assessment is part of the multifactorial assessment because mood disorders in older adults can lead to deconditioning, drug noncompliance, and other conditions that lead to falls and fall-related injuries. Options for screening include the Geriatric Depression Scale (15 or 30 questions) and the Patient Health Questionnaire (the PHQ-2 or the PHQ-9).7
WHAT ARE THE EVIDENCE-BASED INTERVENTIONS?
In general, interventions are chosen according to the risks identified by the assessment; multiple interventions are usually necessary. It is ineffective to identify risk factors without providing intervention.25
Specific interventions with recommendation levels A and B are listed in Table 2.7 Level A interventions are specifically supported by strong evidence and should be recommended. Of note, although vitamin D3 may not be bioequivalent to vitamin D2, studies in older adults have not consistently found a clinically different outcome, and either may be supplemented in the community-dwelling elderly. Except for vitamin D, these interventions target community-dwelling older adults who are cognitively intact.
Home assessments are effective in high-risk patients, such as those with poor vision and those who were recently hospitalized. The goal is to improve safety, particularly during patient transfers, with education and training provided by an occupational or physical therapist or other geriatric specialist. The benefit of home assessment and environmental modification is greater when combined with other strategies and in general should not be implemented alone.
Exercise is an important intervention. The number needed to treat (NNT) to prevent one fall in older people over the course of at least 12 weeks is 16.26 This compares favorably with interventions that are commonly used in the general population, such as aspirin therapy as secondary prevention for cardiovascular disease (NNT for 1 year = 50)27 and statin therapy to prevent one death from a cardiovascular event over 5 years in people with known heart disease (NNT = 83).28
Exercise recommendations should be customized to the patient. The amount and type of exercise depends on the patient’s baseline physical activity, medication use including antiplatelet and anticoagulant therapy, home environment, cardiac and pulmonary reserve, vision and hearing deficits, and comorbidities including neuropathy and arthritis.
The well-known risks associated with exercise include myocardial infarction and cardiac arrest, as well as falls and fractures. However, the benefits extend beyond fall risk and include improvements in physical function, glycemic control, cardiopulmonary reserve, bone density, arthritic pain, mood, and cognition. Exercise can also help manage weight, reduce sarcopenia, and increase opportunities for socialization. In most positive trials, the exercise interventions lasted longer than 12 weeks, had variable intensity, and occurred 1 to 3 times per week.
The American College of Sports Medicine recommends that older adults perform aerobic exercise 3 to 5 times per week, 20 to 60 minutes per session (the lower ranges are for frail elderly patients).29 It also recommends resistance training 2 to 4 days per week, 20 to 45 minutes per session, depending on the patient’s level of frailty and conditioning.30 Most older adults do not exercise enough.
Interventions listed at the bottom of Table 2 do not, in general, have enough evidence to support or discourage their use; these are level C recommendations. However, these interventions may be considered for certain individuals. For example, older adults with diabetic neuropathy are often unaware of their foot position when they walk. Additionally, those with diabetic neuropathy may have slower generation of ankle and knee strength compared with age-matched controls. These patients may benefit from targeted physical therapy to strengthen ankle and knee extensors and to retrain stride and speed to improve both gait and safety awareness.
Patients who wear shoes that fit poorly, have high heels, or are not laced or buckled have a higher risk of falls.31 Consider recommending footwear that has a firm, low, rubber heel and a sole with a large surface contact area, which may help reduce the risk of falling.32 Advise patients to wear shoes when they are at home and to avoid using slippers and going barefoot.33
Cataract surgery, another level C intervention, is associated with fewer fall-related injuries, particularly hip fracture.34 Noncataract vision interventions (such as exchanging progressive or bifocal lenses for single-lens glasses) may be effective in select patients if distorted vision in the lower fields of view increases the risk of falling, particularly outdoors.35
INTERVENTIONS FOR SPECIAL POPULATIONS
Falls occur more frequently in mobile residents of long-term care facilities than in community-dwelling adults.7 Institutional residents are older and more frail, have more cognitive impairment, and are prescribed more medications. Half of long-term care residents fall at least once a year.7
The data support giving combined calcium and vitamin D supplementation to older adults in long-term care facilities to reduce fracture rates.36 The NNT to prevent one hip fracture is about 111.37 Hip protectors in this setting may reduce the risk of a hip fracture but also may increase the risk of a pelvic fracture. They do not alter the risk of falling.38
Collaborative interventions can help reduce the fall risk in older adults in the nursing home.39 Input from medical, psychosocial, nursing, podiatric, dietary, and therapy services can be solicited and incorporated into an individualized fall prevention program. The program can also include modifications in the environment to improve safety and reduce fall risk.
The benefits of exercise in reducing injurious falls in long-term care is less clear than in the community, likely because of the heterogeneity of both the long-term care population and the studied interventions. Exercise has other benefits, however. It maintains a person’s ability to complete ADLs, improves mood, reduces hyperglycemia, and improves quality of life. Some studies have found a greater risk of falling with exercise therapy as independence increased.40 However, a meta-analysis in 2013 found that exercise interventions, ranging from 3 to 24 months and consisting mainly of balance and resistance training, reduced the risk of falls by 23%.41 Mixing several types of exercises was helpful. Studies of a longer duration with exercise sessions at least 2 to 3 times per week demonstrated the most benefit.41 There was no statistically significant reduction in fracture risk in this meta-analysis,41 although, possibly, more participants would have been needed for a longer period to demonstrate a benefit. Additionally, no study combined osteoporosis treatment with exercise interventions.
WHAT EVIDENCE EXISTS FOR PATIENTS WITH COGNITIVE IMPAIRMENT?
Currently, there are no specific evidence-based recommendations for fall prevention in community-dwelling older adults with cognitive impairment and dementia.7 Cognitively impaired adults are typically excluded from community studies of fall prevention. The one study that specifically investigated community-dwelling adults with cognitive impairment was not able to demonstrate a fall reduction with multifactorial intervention.42
PREVENTING FALLS IN ELDERLY PATIENTS WHO RECENTLY HAD A STROKE
Falls are common in patients who have had a cerebrovascular event. Up to 7% of patients fall in the first week after a stroke. In the year after a stroke, 55% to 75% of patients experience a fall.43 Falls account for the most common medical complication after a stroke.44
Several small studies found that vitamin D supplementation after a stroke reduced both the rate of falls and the number of people who fall.45 Additional interventions such as exercise, medication, and visual aids have been studied, but there is little evidence to support their use. Mobile patients who have lower-extremity hemiparesis after a stroke may develop osteoporosis in the affected limb, so evaluation and appropriate pharmacologic therapy may be considered.
- Tromp AM, Pluijm SM, Smit JH, Deeg DJ, Bouter LM, Lips P. Fall-risk screening test: a prospective study on predictors for falls in community-dwelling elderly. J Clin Epidemiol 2001; 54:837–844.
- Binder EF, Brown M, Sinacore DR, Steger-May K, Yarasheski KE, Schechtman KB. Effects of extended outpatient rehabilitation after hip fracture: a randomized controlled trial. JAMA 2004; 292:837–846.
- Sterling DA, O’Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma 2001; 50:116–119.
- Centers for Disease Control and Prevention (CDC). Web-based Injury Statistics Query and Reporting System (WISQARSTM). www.cdc.gov/injury/wisqars. Accessed April 8, 2015.
- Tinetti ME, Baker DI, King M, et al. Effect of dissemination of evidence in reducing injuries from falls. N Engl J Med 2008; 359:252–261.
- Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall? JAMA 2007; 297:77–86.
- Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 2011; 59:148–157.
- Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the “get-up and go” test. Arch Phys Med Rehabil 1986; 67:387–389.
- Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991; 39:142–148.
- Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther 2000; 80:896–903.
- Springer BA, Marin R, Cyhan T, Roberts H, Gill NW. Normative values for the unipedal stance test with eyes open and closed. J Geriatr Phys Ther 2007; 30:8–15.
- Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc 1999; 47:30–39.
- Hilmer SN, Mager DE, Simonsick EM, et al. A drug burden index to define the functional burden of medications in older people. Arch Intern Med 2007; 167:781–787.
- Rudolph JL, Salow MJ, Angelini MC, McGlinchey RE. The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch Intern Med 2008; 168:508–513.
- American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2012; 60:616–631.
- Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther 2008; 46:72–83.
- Sterke CS, Ziere G, van Beeck EF, Looman CW, van der Cammen TJ. Dose-response relationship between selective serotonin re-uptake inhibitors and injurious falls: a study in nursing home residents with dementia. Br J Clin Pharmacol 2012; 73:812–820.
- Khalili H, Huang ES, Jacobson BC, Camargo CA Jr, Feskanich D, Chan AT. Use of proton pump inhibitors and risk of hip fracture in relation to dietary and lifestyle factors: a prospective cohort study. BMJ 2012; 344:e372.
- Gill SS, Anderson GM, Fischer HD, et al. Syncope and its consequences in patients with dementia receiving cholinesterase inhibitors: a population-based cohort study. Arch Intern Med 2009; 169:867–873.
- Janssen HC, Samson MM, Verhaar HJ. Vitamin D deficiency, muscle function, and falls in elderly people. Am J Clin Nutr 2002; 75:611–615.
- Muir SW, Gopaul K, Montero Odasso MM. The role of cognitive impairment in fall risk among older adults: a systematic review and meta-analysis. Age Ageing 2012; 41:299–308.
- Borson S, Scanlan J, Brush M, Vitaliano P, Dokmak A. The Mini-Cog: a cognitive ‘vital signs’ measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry 2000; 15:1021–1027.
- Cordell CB, Borson S, Boustani M, et al; Medicare Detection of Cognitive Impairment Workgroup. Alzheimer’s Association recommendations for operationalizing the detection of cognitive impairment during the Medicare Annual Wellness Visit in a primary care setting. Alzheimers Dement 2013; 9:141–150.
- Lawlor DA, Patel R, Ebrahim S. Association between falls in elderly women and chronic diseases and drug use: cross sectional study. BMJ 2003; 327:712–717.
- Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ 2002; 325:128.
- Chang JT, Morton SC, Rubenstein LZ, et al. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials. BMJ 2004; 328:680.
- Antithrombotic Trialists’ (ATT) Collaboration; Baigent C, Blackwell L, Collins R, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 2009; 373:1849–1860.
- Baigent C, Keech A, Kearney PM, et al; Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005; 366:1267–1278.
- Mazzeo RS; American College of Sports Medicine (ACSM). Exercise and the older adult. ACSM Current Comment. www.acsm.org/docs/current-comments/exerciseandtheolderadult.pdf. Accessed April 8, 2015.
- Willoughby DS; American College of Sports Medicine (ACSM). Resistance training and the older adult. ACSM Current Comment. www.acsm.org/docs/current-comments/resistancetrainingandtheoa.pdf. Accessed April 8, 2015.
- Tencer AF, Koepsell TD, Wolf ME, et al. Biomechanical properties of shoes and risk of falls in older adults. J Am Geriatr Soc 2004; 52:1840–1846.
- Lord SR, Bashford GM. Shoe characteristics and balance in older women. J Am Geriatr Soc 1996; 44:429–433.
- Kelsey JL, Procter-Gray E, Nguyen US, Li W, Kiel DP, Hannan MT. Footwear and falls in the home among older individuals in the MOBILIZE Boston Study. Footwear Sci 2010; 2:123–129.
- Tseng VL, Yu F, Lum F, Coleman AL. Risk of fractures following cataract surgery in Medicare beneficiaries. JAMA 2012; 308:493–501.
- Cumming RG, Ivers R, Clemson L, et al. Improving vision to prevent falls in frail older people: a randomized trial. J Am Geriatr Soc 2007; 55:175–181.
- Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, et al. Effect of vitamin D on falls: a meta-analysis. JAMA 2004; 291:1999–2006.
- Avenell A, Mak JCS, O’Connell D. Vitamin D and vitamin D analogues for preventing fractures in postmenopausal women and older men. Cochrane Database Syst Rev 2014; 4:CD000227.
- Santesso N, Carrasco-Labra A, Brignardello-Petersen R. Hip protectors for preventing hip fractures in older people. Cochrane Database Syst Rev 2014; 3:CD001255.
- Messinger-Rapport B, Dumas LG. Falls in the nursing home: a collaborative approach. Nurs Clin North Am 2009; 44:187–195.
- Faber MJ, Bosscher RJ, Chin A, Paw MJ, van Wieringen PC. Effects of exercise programs on falls and mobility in frail and pre-frail older adults: a multicenter randomized controlled trial. Arch Phys Med Rehabil 2006; 87:885–896.
- Silva RB, Eslick GD, Duque G. Exercise for falls and fracture prevention in long term care facilities: a systematic review and meta-analysis. J Am Med Dir Assoc 2013; 14:685–689.e2.
- Shaw FE, Bond J, Richardson DA, et al. Multifactorial intervention after a fall in older people with cognitive impairment and dementia presenting to the accident and emergency department: randomised controlled trial. BMJ 2003; 326:73.
- Ashburn A, Hyndman D, Pickering R, Yardley L, Harris S. Predicting people with stroke at risk of falls. Age Ageing 2008; 37:270–276.
- Davenport RJ, Dennis MS, Wellwood I, Warlow CP. Complications after acute stroke. Stroke 1996; 27:415–420.
- Verheyden GS, Weerdesteyn V, Pickering RM, et al. Interventions for preventing falls in people after stroke. Cochrane Database Syst Rev 2013; 5:CD008728.
- Tromp AM, Pluijm SM, Smit JH, Deeg DJ, Bouter LM, Lips P. Fall-risk screening test: a prospective study on predictors for falls in community-dwelling elderly. J Clin Epidemiol 2001; 54:837–844.
- Binder EF, Brown M, Sinacore DR, Steger-May K, Yarasheski KE, Schechtman KB. Effects of extended outpatient rehabilitation after hip fracture: a randomized controlled trial. JAMA 2004; 292:837–846.
- Sterling DA, O’Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma 2001; 50:116–119.
- Centers for Disease Control and Prevention (CDC). Web-based Injury Statistics Query and Reporting System (WISQARSTM). www.cdc.gov/injury/wisqars. Accessed April 8, 2015.
- Tinetti ME, Baker DI, King M, et al. Effect of dissemination of evidence in reducing injuries from falls. N Engl J Med 2008; 359:252–261.
- Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall? JAMA 2007; 297:77–86.
- Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 2011; 59:148–157.
- Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the “get-up and go” test. Arch Phys Med Rehabil 1986; 67:387–389.
- Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991; 39:142–148.
- Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther 2000; 80:896–903.
- Springer BA, Marin R, Cyhan T, Roberts H, Gill NW. Normative values for the unipedal stance test with eyes open and closed. J Geriatr Phys Ther 2007; 30:8–15.
- Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc 1999; 47:30–39.
- Hilmer SN, Mager DE, Simonsick EM, et al. A drug burden index to define the functional burden of medications in older people. Arch Intern Med 2007; 167:781–787.
- Rudolph JL, Salow MJ, Angelini MC, McGlinchey RE. The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch Intern Med 2008; 168:508–513.
- American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2012; 60:616–631.
- Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther 2008; 46:72–83.
- Sterke CS, Ziere G, van Beeck EF, Looman CW, van der Cammen TJ. Dose-response relationship between selective serotonin re-uptake inhibitors and injurious falls: a study in nursing home residents with dementia. Br J Clin Pharmacol 2012; 73:812–820.
- Khalili H, Huang ES, Jacobson BC, Camargo CA Jr, Feskanich D, Chan AT. Use of proton pump inhibitors and risk of hip fracture in relation to dietary and lifestyle factors: a prospective cohort study. BMJ 2012; 344:e372.
- Gill SS, Anderson GM, Fischer HD, et al. Syncope and its consequences in patients with dementia receiving cholinesterase inhibitors: a population-based cohort study. Arch Intern Med 2009; 169:867–873.
- Janssen HC, Samson MM, Verhaar HJ. Vitamin D deficiency, muscle function, and falls in elderly people. Am J Clin Nutr 2002; 75:611–615.
- Muir SW, Gopaul K, Montero Odasso MM. The role of cognitive impairment in fall risk among older adults: a systematic review and meta-analysis. Age Ageing 2012; 41:299–308.
- Borson S, Scanlan J, Brush M, Vitaliano P, Dokmak A. The Mini-Cog: a cognitive ‘vital signs’ measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry 2000; 15:1021–1027.
- Cordell CB, Borson S, Boustani M, et al; Medicare Detection of Cognitive Impairment Workgroup. Alzheimer’s Association recommendations for operationalizing the detection of cognitive impairment during the Medicare Annual Wellness Visit in a primary care setting. Alzheimers Dement 2013; 9:141–150.
- Lawlor DA, Patel R, Ebrahim S. Association between falls in elderly women and chronic diseases and drug use: cross sectional study. BMJ 2003; 327:712–717.
- Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ 2002; 325:128.
- Chang JT, Morton SC, Rubenstein LZ, et al. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials. BMJ 2004; 328:680.
- Antithrombotic Trialists’ (ATT) Collaboration; Baigent C, Blackwell L, Collins R, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 2009; 373:1849–1860.
- Baigent C, Keech A, Kearney PM, et al; Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005; 366:1267–1278.
- Mazzeo RS; American College of Sports Medicine (ACSM). Exercise and the older adult. ACSM Current Comment. www.acsm.org/docs/current-comments/exerciseandtheolderadult.pdf. Accessed April 8, 2015.
- Willoughby DS; American College of Sports Medicine (ACSM). Resistance training and the older adult. ACSM Current Comment. www.acsm.org/docs/current-comments/resistancetrainingandtheoa.pdf. Accessed April 8, 2015.
- Tencer AF, Koepsell TD, Wolf ME, et al. Biomechanical properties of shoes and risk of falls in older adults. J Am Geriatr Soc 2004; 52:1840–1846.
- Lord SR, Bashford GM. Shoe characteristics and balance in older women. J Am Geriatr Soc 1996; 44:429–433.
- Kelsey JL, Procter-Gray E, Nguyen US, Li W, Kiel DP, Hannan MT. Footwear and falls in the home among older individuals in the MOBILIZE Boston Study. Footwear Sci 2010; 2:123–129.
- Tseng VL, Yu F, Lum F, Coleman AL. Risk of fractures following cataract surgery in Medicare beneficiaries. JAMA 2012; 308:493–501.
- Cumming RG, Ivers R, Clemson L, et al. Improving vision to prevent falls in frail older people: a randomized trial. J Am Geriatr Soc 2007; 55:175–181.
- Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, et al. Effect of vitamin D on falls: a meta-analysis. JAMA 2004; 291:1999–2006.
- Avenell A, Mak JCS, O’Connell D. Vitamin D and vitamin D analogues for preventing fractures in postmenopausal women and older men. Cochrane Database Syst Rev 2014; 4:CD000227.
- Santesso N, Carrasco-Labra A, Brignardello-Petersen R. Hip protectors for preventing hip fractures in older people. Cochrane Database Syst Rev 2014; 3:CD001255.
- Messinger-Rapport B, Dumas LG. Falls in the nursing home: a collaborative approach. Nurs Clin North Am 2009; 44:187–195.
- Faber MJ, Bosscher RJ, Chin A, Paw MJ, van Wieringen PC. Effects of exercise programs on falls and mobility in frail and pre-frail older adults: a multicenter randomized controlled trial. Arch Phys Med Rehabil 2006; 87:885–896.
- Silva RB, Eslick GD, Duque G. Exercise for falls and fracture prevention in long term care facilities: a systematic review and meta-analysis. J Am Med Dir Assoc 2013; 14:685–689.e2.
- Shaw FE, Bond J, Richardson DA, et al. Multifactorial intervention after a fall in older people with cognitive impairment and dementia presenting to the accident and emergency department: randomised controlled trial. BMJ 2003; 326:73.
- Ashburn A, Hyndman D, Pickering R, Yardley L, Harris S. Predicting people with stroke at risk of falls. Age Ageing 2008; 37:270–276.
- Davenport RJ, Dennis MS, Wellwood I, Warlow CP. Complications after acute stroke. Stroke 1996; 27:415–420.
- Verheyden GS, Weerdesteyn V, Pickering RM, et al. Interventions for preventing falls in people after stroke. Cochrane Database Syst Rev 2013; 5:CD008728.
KEY POINTS
- Practitioners can reduce fall-related injury by screening older adults yearly with questions about problems with balance and gait, performing a focused history and examination when necessary, and implementing evidence-based interventions.
- Cognitive impairment itself is an independent predictor of falls because it can reduce processing speed and impair executive function.
- An exercise program with resistance, balance, and gait training is usually prescribed to patients at high risk, along with a home assessment and withdrawal or minimization of psychoactive and antipsychotic medications.
- Combined calcium and vitamin D supplements should be given to most older adults in long-term care facilities to reduce fracture rates.
- There are no specific evidence-based recommendations for fall prevention in community-living older adults with cognitive impairment or dementia.
Penicillin allergy: A practical guide for clinicians
Most patients who report that they are allergic to penicillin can ultimately receive penicillin or a penicillin-type antibiotic again after an appropriate evaluation and, possibly, treatment. This course of action decreases the need for broad-spectrum antibiotics,1–4 reduces health care costs, and prevents the development of multidrug-resistant pathogens.5
About 10% of the general population say that they are allergic to penicillin.1,6,7 Although the prevalence of life-threatening anaphylactic reactions to penicillin has been estimated to be between 0.02% and 0.04%,6 the most common reaction is a cutaneous eruption. Since anaphylactic reactions are mediated by immunoglobulin E (IgE), evaluation of patients with a history of penicillin allergy by penicillin skin testing is recommended to rule out IgE-mediated reactions.
This review outlines a practical approach to evaluating a suspected IgE-mediated reaction to penicillin, with key points in the history and diagnostic testing. We also review subsequent management and cross-reactivity with other beta-lactam-containing antibiotics.
EVALUATING ALLERGIC PATIENTS
Evaluation of patients with a history of penicillin allergy can be improved with an understanding of the classification of drug reactions, risk factors for allergy, and the pathophysiology of penicillin allergy.
Classification of drug reactions
Adverse drug reactions include all unintended pharmacologic effects of a drug and can be classified as predictable (type A) or unpredictable (type B). Predictable reactions are dose-dependent, are related to the known pharmacologic actions of the medication, and occur in otherwise healthy individuals. Unpredictable reactions are further classified into drug intolerance, drug idiosyncrasy, drug allergy, and pseudoallergic reactions.8,9
Penicillin allergy can manifest as any hypersensitivity reaction of the Gell and Coombs classification (Table 1).9 Type I (immediate) and type IV (delayed) reactions are the most common types of reactions that occur with antibiotics and should be classified based on the onset of symptoms as immediate (within 1 hour) or delayed (days or weeks).8
Risk factors for IgE-mediated reaction
Risk factors for a hypersensitivity reaction include frequent or repetitive courses of penicillin10 and high-dose parenteral (rather than oral) administration.
Age and atopy are not risk factors for penicillin allergy.7 However, atopy increases the risk of a more severe anaphylactic reaction to penicillin, and anaphylactic reactions are most commonly reported between the ages of 20 and 49.6
Pathophysiology of penicillin allergy
All penicillins share a common core ring structure (beta-lactam and thiazolidine rings) but differ in their side chains (R group) (Figure 1).
Under physiologic conditions, the core ring structure is metabolized into major (penicilloyl) and minor (penicillin itself, penicilloate and penilloate) antigenic determinants that may trigger an immediate IgE-dependent response.9 In the United States, commercial forms of antigenic determinates for skin testing exist in the form of penicillin G (minor determinant) and penicilloyl-polylysine, better known as Prepen (major determinant).
Immediate-type reactions to similar antibiotics such as aminopenicillins and cephalosporins may be caused by IgE antibodies against the R-group side chain rather than the core penicillin major and minor determinants.11
Questions to ask patients who have a history of penicillin allergy
Patients should be questioned closely about previous and current reactions to penicillin and should undergo skin-prick and intradermal testing, followed by graded-dose challenge or drug tolerance desensitization (Figure 2).
Questions to ask patients who have a history of penicillin allergy (Table 2)9,12 include the following:
Do you remember the details of the reaction? These include the route of administration, the time between the dose of penicillin and the appearance of symptoms, and how the reaction was managed.
Immediate reactions (ie, IgE-mediated, or Gell and Coombs type I) usually occur within the first hour after the first dose of the antibiotic, although they occasionally take up to 2 hours to occur, especially if the medication is taken orally and is taken with food. Symptoms consistent with IgE-mediated reactions include urticaria (most common), pruritus, angioedema, laryngeal edema, wheezing, shortness of breath, presyncope or syncope, hypotension, and cardiorespiratory collapse.
In contrast, symptoms of a non–IgE-mediated reaction are delayed in onset, occurring after days of treatment. They include nonpruritic maculopapular eruptions, hemolytic anemia, serum sickness, Stevens-Johnson syndrome, drug rash with eosinophilia and systemic symptoms, acute interstitial nephritis, and toxic epidermal necrolysis.9
If the patient has had severe non–IgE-mediated reactions to penicillin (eg, Stevens-Johnson syndrome, toxic epidermal necrolysis, acute interstitial nephritis, hemolytic anemia, or serum sickness) in the past, skin testing, graded-dose challenge, and desensitization are contraindicated.
How many years ago did the reaction occur? Most patients lose their sensitivity to penicillin over time.7,13–15 Nearly 50% of patients with IgE-mediated penicillin allergy lose their sensitivity within 5 years of the reaction,15 increasing to 80% or more by 10 years.13
How was the reaction managed? What was the outcome? Use of and positive response to epinephrine and histamine 1 receptor antagonists (antihistamines) with resolution or significant improvement of symptoms within a few hours may indicate an IgE-mediated reaction.
What was the indication for penicillin? Many cutaneous reactions are a result of an underlying viral or bacterial infection. For example, up to 90% of patients with Epstein-Barr virus infection develop a maculopapular rash when given penicillin.16
Have you tolerated other forms of penicillin since the reaction? Sometimes the patient has already tolerated other beta-lactams such as aminopenicillins, cephalosporins, and semisynthetic penicillins (piperacillin-tazobactam). Patients who tolerate other beta-lactams without adverse reactions are not allergic to beta-lactams.
Diagnostic tests
Skin testing. The only validated test for diagnosing IgE-mediated reactions caused by penicillin is the immediate hypersensitivity skin test,9 which should be performed by a board-certified allergist. The test consists of skin-prick and intradermal testing with the major determinant (penicilloyl-polylysine), the minor determinant (penicillin G), a negative control (normal saline), and a positive control (histamine). Minor-determinant mix is not commercially available in the United States.
Results of skin-prick testing are read 15 minutes after application. A positive response is a wheal at least 3 mm larger in diameter (with equivalent erythema) than the negative control done simultaneously. Intradermal testing is only done after a negative skin-prick test. If the allergic reaction was severe (ie, anaphylaxis), skin testing should be done at least 4 to 6 weeks after the reaction.
A history of severe non–IgE-mediated reaction to penicillin is a contraindication to skin-prick testing for penicillin allergy. The positive predictive value of penicillin skin testing is 50%, and the negative predictive value is 97%.3,7,9,13
Commercial in vitro testing (serum-specific IgE assays) for IgE-mediated hypersensitivity to penicillin is inferior to skin testing in terms of the negative predictive value and is not a suitable substitute for penicillin skin testing.
MANAGING PENICILLIN ALLERGY
If skin testing is positive, use another antibiotic, or refer for desensitization
If penicillin skin testing is positive (Figure 2), use another antibiotic that is equally efficacious. Patients who absolutely need a beta-lactam may undergo drug desensitization, performed by a board-certified allergist.
During desensitization, patients receive progressively higher doses of the drug every 15 to 20 minutes subcutaneously or intravenously, or every 20 to 30 minutes orally, until a full therapeutic dose is tolerated. Most protocols begin with a dose ranging from 1/10,000 to 1/1,000 of the final dose, depending on the severity of the allergic reaction.9,17
Using modern protocols, the success rate for tolerance induction is extremely high (75% to 100% in patients with cystic fibrosis, a group with a high rate of drug allergy18–20).
Drug desensitization is contraindicated in patients with non–IgE-mediated reactions.
If skin testing is negative, refer for graded-dose challenge
If skin testing is negative (Figure 2), graded-dose challenge is recommended. This procedure must be done by a board-certified allergist. If the original reaction was life-threatening, graded-dose challenge may entail giving 1/100 of the therapeutic dose. Then, if no reaction occurs during a brief observation period (usually 30 minutes), a full dose is given. However, many patients can start with 1/10 or even a full dose of the drug, especially if the original reaction was limited to the skin and the penicillin skin test is negative.
Graded-dose challenge is contraindicated if the original reaction was a severe non–IgE-mediated reaction.
UNDERSTANDING CROSS-REACTIVITY OF PENICILLIN
Penicillin is the only antibiotic for which skin testing is reliable and validated. If a drug that cross-reacts with penicillin is needed, it is important to know the rate of cross-reactivity (Table 3). The rate of cross-reactivity between penicillin and aminopenicillins (amoxicillin and ampicillin) is less than 1.3% in the United States.10,21 However, the cross-reactivity rate among aminopenicillins and cephalosporins is between 10% to 40%. For that reason, patients with prior reactions to aminopenicillins should avoid cephalosporins that share identical R-chain side groups with aminopenicillins.9,22
The rate of cross-reactivity between penicillin and cephalosporins was reported as 10% 40 years ago.23,24 But this was with early, first-generation cephalosporins that may have been contaminated with penicillin. The cross-reactivity rate with cephalosporins today is 3%.25 In general, first- and second-generation cephalosporins cause more allergic reactions than third- and fourth-generation cephalosporins.26
Patients with a history of penicillin allergy who require a cephalosporin should still undergo penicillin skin testing. Skin testing with cephalosporins has not been validated. However, skin testing with nonirritating concentrations of cephalosporins9 may be done to elucidate IgE reactions.
In a study by Romano et al,27 110 patients who had positive results on penicillin skin testing completed graded-dose challenge with the carbapenem antibiotic imipenem. The rate of cross-reactivity between penicillin and imipenem was less than 1%.
Monobactam antibiotics do not cross-react with other beta-lactams, except ceftazidime with aztreonam. This is probably because of similarities in their chemical structure.
- Park M, Markus P, Matesic D, Li JT. Safety and effectiveness of a preoperative allergy clinic in decreasing vancomycin use in patients with a history of penicillin allergy. Ann Allergy Asthma Immunol 2006; 97:681–687.
- Arroliga ME, Radojicic C, Gordon SM, et al. A prospective observational study of the effect of penicillin skin testing on antibiotic use in the intensive care unit. Infect Control Hosp Epidemiol 2003; 24:347–350.
- del Real GA, Rose ME, Ramirez-Atamoros MT, et al. Penicillin skin testing in patients with a history of beta-lactam allergy. Ann Allergy Asthma Immunol 2007; 98:355–359.
- Nadarajah K, Green GR, Naglak M. Clinical outcomes of penicillin skin testing. Ann Allergy Asthma Immunol 2005; 95:541–545.
- Harris AD, Sauberman L, Kabbash L, Greineder DK, Samore MH. Penicillin skin testing: a way to optimize antibiotic utilization. Am J Med 1999; 107:166–168.
- Idsoe O, Guthe T, Willcox RR, de Weck AL. Nature and extent of penicillin side-reactions, with particular reference to fatalities from anaphylactic shock. Bull World Health Organ 1968; 38:159–188.
- Gadde J, Spence M, Wheeler B, Adkinson NF Jr. Clinical experience with penicillin skin testing in a large inner-city STD clinic. JAMA 1993; 270:2456–2463.
- Johansson SG, Bieber T, Dahl R, et al. Revised nomenclature for allergy for global use: report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol 2004; 113:832–836.
- Joint Task Force on Practice Parameters; American Academy of Allergy, Asthma and Immunology; American College of Allergy, Asthma and Immunology; Joint Council of Allergy, Asthma and Immunology. Drug allergy: an updated practice parameter. Ann Allergy Asthma Immunol 2010; 105:259–273.
- Park MA, Matesic D, Markus PJ, Li JT. Female sex as a risk factor for penicillin allergy. Ann Allergy Asthma Immunol 2007; 99:54–58.
- Moreno E, Macias E, Davila I, Laffond E, Ruiz A, Lorente F. Hypersensitivity reactions to cephalosporins. Expert Opin Drug Saf 2008; 7:295–304.
- Salkind AR, Cuddy PG, Foxworth JW. The rational clinical examination. Is this patient allergic to penicillin? An evidence-based analysis of the likelihood of penicillin allergy. JAMA 2001; 285:2498–2505.
- Sullivan TJ, Wedner HJ, Shatz GS, Yecies LD, Parker CW. Skin testing to detect penicillin allergy. J Allergy Clin Immunol 1981; 68:171–180.
- Macy E, Schatz M, Lin C, Poon KY. The falling rate of positive penicillin skin tests from 1995 to 2007. Perm J 2009; 13:12–18.
- Blanca M, Torres MJ, Garcia JJ, et al. Natural evolution of skin test sensitivity in patients allergic to beta-lactam antibiotics. J Allergy Clin Immunol 1999; 103:918–924.
- Patel BM. Skin rash with infectious mononucleosis and ampicillin. Pediatrics 1967; 40:910–911.
- Liu A, Fanning L, Chong H, et al. Desensitization regimens for drug allergy: state of the art in the 21st century. Clin Exp Allergy 2011; 41:1679–1688.
- Burrows JA, Toon M, Bell SC. Antibiotic desensitization in adults with cystic fibrosis. Respirology 2003; 8:359–364.
- Turvey SE, Cronin B, Arnold AD, Dioun AF. Antibiotic desensitization for the allergic patient: 5 years of experience and practice. Ann Allergy Asthma Immunol 2004; 92:426–432.
- Legere HJ 3rd, Palis RI, Rodriguez Bouza T, Uluer AZ, Castells MC. A safe protocol for rapid desensitization in patients with cystic fibrosis and antibiotic hypersensitivity. J Cyst Fibros 2009; 8:418–424.
- Lin E, Saxon A, Riedl M. Penicillin allergy: value of including amoxicillin as a determinant in penicillin skin testing. Int Arch Allergy Immunol 2010; 152:313–318.
- Dickson SD, Salazar KC. Diagnosis and management of immediate hypersensitivity reactions to cephalosporins. Clin Rev Allergy Immunol 2013; 45:131–142.
- Dash CH. Penicillin allergy and the cephalosporins. J Antimicrob Chemother 1975; 1(suppl 3):107–118.
- Petz LD. Immunologic cross-reactivity between penicillins and cephalosporins: a review. J Infect Dis 1978; 137(suppl):S74–S79.
- American Academy of Allergy Asthma & Immunology. Cephalosporin administration to patients with a history of penicillin allergy. www.aaaai.org/Aaaai/media/MediaLibrary/PDF%20Documents/Practice%20and%20Parameters/Cephalosporin-administration-2009.pdf. Accessed April 2, 2015.
- Fonacier L, Hirschberg R, Gerson S. Adverse drug reactions to cephalosporins in hospitalized patients with a history of penicillin allergy. Allergy Asthma Proc 2005; 26:135–141.
- Romano A, Viola M, Gueant-Rodriguez RM, Gaeta F, Pettinato R, Gueant JL. Imipenem in patients with immediate hypersensitivity to penicillins. N Engl J Med 2006; 354:2835–2837.
Most patients who report that they are allergic to penicillin can ultimately receive penicillin or a penicillin-type antibiotic again after an appropriate evaluation and, possibly, treatment. This course of action decreases the need for broad-spectrum antibiotics,1–4 reduces health care costs, and prevents the development of multidrug-resistant pathogens.5
About 10% of the general population say that they are allergic to penicillin.1,6,7 Although the prevalence of life-threatening anaphylactic reactions to penicillin has been estimated to be between 0.02% and 0.04%,6 the most common reaction is a cutaneous eruption. Since anaphylactic reactions are mediated by immunoglobulin E (IgE), evaluation of patients with a history of penicillin allergy by penicillin skin testing is recommended to rule out IgE-mediated reactions.
This review outlines a practical approach to evaluating a suspected IgE-mediated reaction to penicillin, with key points in the history and diagnostic testing. We also review subsequent management and cross-reactivity with other beta-lactam-containing antibiotics.
EVALUATING ALLERGIC PATIENTS
Evaluation of patients with a history of penicillin allergy can be improved with an understanding of the classification of drug reactions, risk factors for allergy, and the pathophysiology of penicillin allergy.
Classification of drug reactions
Adverse drug reactions include all unintended pharmacologic effects of a drug and can be classified as predictable (type A) or unpredictable (type B). Predictable reactions are dose-dependent, are related to the known pharmacologic actions of the medication, and occur in otherwise healthy individuals. Unpredictable reactions are further classified into drug intolerance, drug idiosyncrasy, drug allergy, and pseudoallergic reactions.8,9
Penicillin allergy can manifest as any hypersensitivity reaction of the Gell and Coombs classification (Table 1).9 Type I (immediate) and type IV (delayed) reactions are the most common types of reactions that occur with antibiotics and should be classified based on the onset of symptoms as immediate (within 1 hour) or delayed (days or weeks).8
Risk factors for IgE-mediated reaction
Risk factors for a hypersensitivity reaction include frequent or repetitive courses of penicillin10 and high-dose parenteral (rather than oral) administration.
Age and atopy are not risk factors for penicillin allergy.7 However, atopy increases the risk of a more severe anaphylactic reaction to penicillin, and anaphylactic reactions are most commonly reported between the ages of 20 and 49.6
Pathophysiology of penicillin allergy
All penicillins share a common core ring structure (beta-lactam and thiazolidine rings) but differ in their side chains (R group) (Figure 1).
Under physiologic conditions, the core ring structure is metabolized into major (penicilloyl) and minor (penicillin itself, penicilloate and penilloate) antigenic determinants that may trigger an immediate IgE-dependent response.9 In the United States, commercial forms of antigenic determinates for skin testing exist in the form of penicillin G (minor determinant) and penicilloyl-polylysine, better known as Prepen (major determinant).
Immediate-type reactions to similar antibiotics such as aminopenicillins and cephalosporins may be caused by IgE antibodies against the R-group side chain rather than the core penicillin major and minor determinants.11
Questions to ask patients who have a history of penicillin allergy
Patients should be questioned closely about previous and current reactions to penicillin and should undergo skin-prick and intradermal testing, followed by graded-dose challenge or drug tolerance desensitization (Figure 2).
Questions to ask patients who have a history of penicillin allergy (Table 2)9,12 include the following:
Do you remember the details of the reaction? These include the route of administration, the time between the dose of penicillin and the appearance of symptoms, and how the reaction was managed.
Immediate reactions (ie, IgE-mediated, or Gell and Coombs type I) usually occur within the first hour after the first dose of the antibiotic, although they occasionally take up to 2 hours to occur, especially if the medication is taken orally and is taken with food. Symptoms consistent with IgE-mediated reactions include urticaria (most common), pruritus, angioedema, laryngeal edema, wheezing, shortness of breath, presyncope or syncope, hypotension, and cardiorespiratory collapse.
In contrast, symptoms of a non–IgE-mediated reaction are delayed in onset, occurring after days of treatment. They include nonpruritic maculopapular eruptions, hemolytic anemia, serum sickness, Stevens-Johnson syndrome, drug rash with eosinophilia and systemic symptoms, acute interstitial nephritis, and toxic epidermal necrolysis.9
If the patient has had severe non–IgE-mediated reactions to penicillin (eg, Stevens-Johnson syndrome, toxic epidermal necrolysis, acute interstitial nephritis, hemolytic anemia, or serum sickness) in the past, skin testing, graded-dose challenge, and desensitization are contraindicated.
How many years ago did the reaction occur? Most patients lose their sensitivity to penicillin over time.7,13–15 Nearly 50% of patients with IgE-mediated penicillin allergy lose their sensitivity within 5 years of the reaction,15 increasing to 80% or more by 10 years.13
How was the reaction managed? What was the outcome? Use of and positive response to epinephrine and histamine 1 receptor antagonists (antihistamines) with resolution or significant improvement of symptoms within a few hours may indicate an IgE-mediated reaction.
What was the indication for penicillin? Many cutaneous reactions are a result of an underlying viral or bacterial infection. For example, up to 90% of patients with Epstein-Barr virus infection develop a maculopapular rash when given penicillin.16
Have you tolerated other forms of penicillin since the reaction? Sometimes the patient has already tolerated other beta-lactams such as aminopenicillins, cephalosporins, and semisynthetic penicillins (piperacillin-tazobactam). Patients who tolerate other beta-lactams without adverse reactions are not allergic to beta-lactams.
Diagnostic tests
Skin testing. The only validated test for diagnosing IgE-mediated reactions caused by penicillin is the immediate hypersensitivity skin test,9 which should be performed by a board-certified allergist. The test consists of skin-prick and intradermal testing with the major determinant (penicilloyl-polylysine), the minor determinant (penicillin G), a negative control (normal saline), and a positive control (histamine). Minor-determinant mix is not commercially available in the United States.
Results of skin-prick testing are read 15 minutes after application. A positive response is a wheal at least 3 mm larger in diameter (with equivalent erythema) than the negative control done simultaneously. Intradermal testing is only done after a negative skin-prick test. If the allergic reaction was severe (ie, anaphylaxis), skin testing should be done at least 4 to 6 weeks after the reaction.
A history of severe non–IgE-mediated reaction to penicillin is a contraindication to skin-prick testing for penicillin allergy. The positive predictive value of penicillin skin testing is 50%, and the negative predictive value is 97%.3,7,9,13
Commercial in vitro testing (serum-specific IgE assays) for IgE-mediated hypersensitivity to penicillin is inferior to skin testing in terms of the negative predictive value and is not a suitable substitute for penicillin skin testing.
MANAGING PENICILLIN ALLERGY
If skin testing is positive, use another antibiotic, or refer for desensitization
If penicillin skin testing is positive (Figure 2), use another antibiotic that is equally efficacious. Patients who absolutely need a beta-lactam may undergo drug desensitization, performed by a board-certified allergist.
During desensitization, patients receive progressively higher doses of the drug every 15 to 20 minutes subcutaneously or intravenously, or every 20 to 30 minutes orally, until a full therapeutic dose is tolerated. Most protocols begin with a dose ranging from 1/10,000 to 1/1,000 of the final dose, depending on the severity of the allergic reaction.9,17
Using modern protocols, the success rate for tolerance induction is extremely high (75% to 100% in patients with cystic fibrosis, a group with a high rate of drug allergy18–20).
Drug desensitization is contraindicated in patients with non–IgE-mediated reactions.
If skin testing is negative, refer for graded-dose challenge
If skin testing is negative (Figure 2), graded-dose challenge is recommended. This procedure must be done by a board-certified allergist. If the original reaction was life-threatening, graded-dose challenge may entail giving 1/100 of the therapeutic dose. Then, if no reaction occurs during a brief observation period (usually 30 minutes), a full dose is given. However, many patients can start with 1/10 or even a full dose of the drug, especially if the original reaction was limited to the skin and the penicillin skin test is negative.
Graded-dose challenge is contraindicated if the original reaction was a severe non–IgE-mediated reaction.
UNDERSTANDING CROSS-REACTIVITY OF PENICILLIN
Penicillin is the only antibiotic for which skin testing is reliable and validated. If a drug that cross-reacts with penicillin is needed, it is important to know the rate of cross-reactivity (Table 3). The rate of cross-reactivity between penicillin and aminopenicillins (amoxicillin and ampicillin) is less than 1.3% in the United States.10,21 However, the cross-reactivity rate among aminopenicillins and cephalosporins is between 10% to 40%. For that reason, patients with prior reactions to aminopenicillins should avoid cephalosporins that share identical R-chain side groups with aminopenicillins.9,22
The rate of cross-reactivity between penicillin and cephalosporins was reported as 10% 40 years ago.23,24 But this was with early, first-generation cephalosporins that may have been contaminated with penicillin. The cross-reactivity rate with cephalosporins today is 3%.25 In general, first- and second-generation cephalosporins cause more allergic reactions than third- and fourth-generation cephalosporins.26
Patients with a history of penicillin allergy who require a cephalosporin should still undergo penicillin skin testing. Skin testing with cephalosporins has not been validated. However, skin testing with nonirritating concentrations of cephalosporins9 may be done to elucidate IgE reactions.
In a study by Romano et al,27 110 patients who had positive results on penicillin skin testing completed graded-dose challenge with the carbapenem antibiotic imipenem. The rate of cross-reactivity between penicillin and imipenem was less than 1%.
Monobactam antibiotics do not cross-react with other beta-lactams, except ceftazidime with aztreonam. This is probably because of similarities in their chemical structure.
Most patients who report that they are allergic to penicillin can ultimately receive penicillin or a penicillin-type antibiotic again after an appropriate evaluation and, possibly, treatment. This course of action decreases the need for broad-spectrum antibiotics,1–4 reduces health care costs, and prevents the development of multidrug-resistant pathogens.5
About 10% of the general population say that they are allergic to penicillin.1,6,7 Although the prevalence of life-threatening anaphylactic reactions to penicillin has been estimated to be between 0.02% and 0.04%,6 the most common reaction is a cutaneous eruption. Since anaphylactic reactions are mediated by immunoglobulin E (IgE), evaluation of patients with a history of penicillin allergy by penicillin skin testing is recommended to rule out IgE-mediated reactions.
This review outlines a practical approach to evaluating a suspected IgE-mediated reaction to penicillin, with key points in the history and diagnostic testing. We also review subsequent management and cross-reactivity with other beta-lactam-containing antibiotics.
EVALUATING ALLERGIC PATIENTS
Evaluation of patients with a history of penicillin allergy can be improved with an understanding of the classification of drug reactions, risk factors for allergy, and the pathophysiology of penicillin allergy.
Classification of drug reactions
Adverse drug reactions include all unintended pharmacologic effects of a drug and can be classified as predictable (type A) or unpredictable (type B). Predictable reactions are dose-dependent, are related to the known pharmacologic actions of the medication, and occur in otherwise healthy individuals. Unpredictable reactions are further classified into drug intolerance, drug idiosyncrasy, drug allergy, and pseudoallergic reactions.8,9
Penicillin allergy can manifest as any hypersensitivity reaction of the Gell and Coombs classification (Table 1).9 Type I (immediate) and type IV (delayed) reactions are the most common types of reactions that occur with antibiotics and should be classified based on the onset of symptoms as immediate (within 1 hour) or delayed (days or weeks).8
Risk factors for IgE-mediated reaction
Risk factors for a hypersensitivity reaction include frequent or repetitive courses of penicillin10 and high-dose parenteral (rather than oral) administration.
Age and atopy are not risk factors for penicillin allergy.7 However, atopy increases the risk of a more severe anaphylactic reaction to penicillin, and anaphylactic reactions are most commonly reported between the ages of 20 and 49.6
Pathophysiology of penicillin allergy
All penicillins share a common core ring structure (beta-lactam and thiazolidine rings) but differ in their side chains (R group) (Figure 1).
Under physiologic conditions, the core ring structure is metabolized into major (penicilloyl) and minor (penicillin itself, penicilloate and penilloate) antigenic determinants that may trigger an immediate IgE-dependent response.9 In the United States, commercial forms of antigenic determinates for skin testing exist in the form of penicillin G (minor determinant) and penicilloyl-polylysine, better known as Prepen (major determinant).
Immediate-type reactions to similar antibiotics such as aminopenicillins and cephalosporins may be caused by IgE antibodies against the R-group side chain rather than the core penicillin major and minor determinants.11
Questions to ask patients who have a history of penicillin allergy
Patients should be questioned closely about previous and current reactions to penicillin and should undergo skin-prick and intradermal testing, followed by graded-dose challenge or drug tolerance desensitization (Figure 2).
Questions to ask patients who have a history of penicillin allergy (Table 2)9,12 include the following:
Do you remember the details of the reaction? These include the route of administration, the time between the dose of penicillin and the appearance of symptoms, and how the reaction was managed.
Immediate reactions (ie, IgE-mediated, or Gell and Coombs type I) usually occur within the first hour after the first dose of the antibiotic, although they occasionally take up to 2 hours to occur, especially if the medication is taken orally and is taken with food. Symptoms consistent with IgE-mediated reactions include urticaria (most common), pruritus, angioedema, laryngeal edema, wheezing, shortness of breath, presyncope or syncope, hypotension, and cardiorespiratory collapse.
In contrast, symptoms of a non–IgE-mediated reaction are delayed in onset, occurring after days of treatment. They include nonpruritic maculopapular eruptions, hemolytic anemia, serum sickness, Stevens-Johnson syndrome, drug rash with eosinophilia and systemic symptoms, acute interstitial nephritis, and toxic epidermal necrolysis.9
If the patient has had severe non–IgE-mediated reactions to penicillin (eg, Stevens-Johnson syndrome, toxic epidermal necrolysis, acute interstitial nephritis, hemolytic anemia, or serum sickness) in the past, skin testing, graded-dose challenge, and desensitization are contraindicated.
How many years ago did the reaction occur? Most patients lose their sensitivity to penicillin over time.7,13–15 Nearly 50% of patients with IgE-mediated penicillin allergy lose their sensitivity within 5 years of the reaction,15 increasing to 80% or more by 10 years.13
How was the reaction managed? What was the outcome? Use of and positive response to epinephrine and histamine 1 receptor antagonists (antihistamines) with resolution or significant improvement of symptoms within a few hours may indicate an IgE-mediated reaction.
What was the indication for penicillin? Many cutaneous reactions are a result of an underlying viral or bacterial infection. For example, up to 90% of patients with Epstein-Barr virus infection develop a maculopapular rash when given penicillin.16
Have you tolerated other forms of penicillin since the reaction? Sometimes the patient has already tolerated other beta-lactams such as aminopenicillins, cephalosporins, and semisynthetic penicillins (piperacillin-tazobactam). Patients who tolerate other beta-lactams without adverse reactions are not allergic to beta-lactams.
Diagnostic tests
Skin testing. The only validated test for diagnosing IgE-mediated reactions caused by penicillin is the immediate hypersensitivity skin test,9 which should be performed by a board-certified allergist. The test consists of skin-prick and intradermal testing with the major determinant (penicilloyl-polylysine), the minor determinant (penicillin G), a negative control (normal saline), and a positive control (histamine). Minor-determinant mix is not commercially available in the United States.
Results of skin-prick testing are read 15 minutes after application. A positive response is a wheal at least 3 mm larger in diameter (with equivalent erythema) than the negative control done simultaneously. Intradermal testing is only done after a negative skin-prick test. If the allergic reaction was severe (ie, anaphylaxis), skin testing should be done at least 4 to 6 weeks after the reaction.
A history of severe non–IgE-mediated reaction to penicillin is a contraindication to skin-prick testing for penicillin allergy. The positive predictive value of penicillin skin testing is 50%, and the negative predictive value is 97%.3,7,9,13
Commercial in vitro testing (serum-specific IgE assays) for IgE-mediated hypersensitivity to penicillin is inferior to skin testing in terms of the negative predictive value and is not a suitable substitute for penicillin skin testing.
MANAGING PENICILLIN ALLERGY
If skin testing is positive, use another antibiotic, or refer for desensitization
If penicillin skin testing is positive (Figure 2), use another antibiotic that is equally efficacious. Patients who absolutely need a beta-lactam may undergo drug desensitization, performed by a board-certified allergist.
During desensitization, patients receive progressively higher doses of the drug every 15 to 20 minutes subcutaneously or intravenously, or every 20 to 30 minutes orally, until a full therapeutic dose is tolerated. Most protocols begin with a dose ranging from 1/10,000 to 1/1,000 of the final dose, depending on the severity of the allergic reaction.9,17
Using modern protocols, the success rate for tolerance induction is extremely high (75% to 100% in patients with cystic fibrosis, a group with a high rate of drug allergy18–20).
Drug desensitization is contraindicated in patients with non–IgE-mediated reactions.
If skin testing is negative, refer for graded-dose challenge
If skin testing is negative (Figure 2), graded-dose challenge is recommended. This procedure must be done by a board-certified allergist. If the original reaction was life-threatening, graded-dose challenge may entail giving 1/100 of the therapeutic dose. Then, if no reaction occurs during a brief observation period (usually 30 minutes), a full dose is given. However, many patients can start with 1/10 or even a full dose of the drug, especially if the original reaction was limited to the skin and the penicillin skin test is negative.
Graded-dose challenge is contraindicated if the original reaction was a severe non–IgE-mediated reaction.
UNDERSTANDING CROSS-REACTIVITY OF PENICILLIN
Penicillin is the only antibiotic for which skin testing is reliable and validated. If a drug that cross-reacts with penicillin is needed, it is important to know the rate of cross-reactivity (Table 3). The rate of cross-reactivity between penicillin and aminopenicillins (amoxicillin and ampicillin) is less than 1.3% in the United States.10,21 However, the cross-reactivity rate among aminopenicillins and cephalosporins is between 10% to 40%. For that reason, patients with prior reactions to aminopenicillins should avoid cephalosporins that share identical R-chain side groups with aminopenicillins.9,22
The rate of cross-reactivity between penicillin and cephalosporins was reported as 10% 40 years ago.23,24 But this was with early, first-generation cephalosporins that may have been contaminated with penicillin. The cross-reactivity rate with cephalosporins today is 3%.25 In general, first- and second-generation cephalosporins cause more allergic reactions than third- and fourth-generation cephalosporins.26
Patients with a history of penicillin allergy who require a cephalosporin should still undergo penicillin skin testing. Skin testing with cephalosporins has not been validated. However, skin testing with nonirritating concentrations of cephalosporins9 may be done to elucidate IgE reactions.
In a study by Romano et al,27 110 patients who had positive results on penicillin skin testing completed graded-dose challenge with the carbapenem antibiotic imipenem. The rate of cross-reactivity between penicillin and imipenem was less than 1%.
Monobactam antibiotics do not cross-react with other beta-lactams, except ceftazidime with aztreonam. This is probably because of similarities in their chemical structure.
- Park M, Markus P, Matesic D, Li JT. Safety and effectiveness of a preoperative allergy clinic in decreasing vancomycin use in patients with a history of penicillin allergy. Ann Allergy Asthma Immunol 2006; 97:681–687.
- Arroliga ME, Radojicic C, Gordon SM, et al. A prospective observational study of the effect of penicillin skin testing on antibiotic use in the intensive care unit. Infect Control Hosp Epidemiol 2003; 24:347–350.
- del Real GA, Rose ME, Ramirez-Atamoros MT, et al. Penicillin skin testing in patients with a history of beta-lactam allergy. Ann Allergy Asthma Immunol 2007; 98:355–359.
- Nadarajah K, Green GR, Naglak M. Clinical outcomes of penicillin skin testing. Ann Allergy Asthma Immunol 2005; 95:541–545.
- Harris AD, Sauberman L, Kabbash L, Greineder DK, Samore MH. Penicillin skin testing: a way to optimize antibiotic utilization. Am J Med 1999; 107:166–168.
- Idsoe O, Guthe T, Willcox RR, de Weck AL. Nature and extent of penicillin side-reactions, with particular reference to fatalities from anaphylactic shock. Bull World Health Organ 1968; 38:159–188.
- Gadde J, Spence M, Wheeler B, Adkinson NF Jr. Clinical experience with penicillin skin testing in a large inner-city STD clinic. JAMA 1993; 270:2456–2463.
- Johansson SG, Bieber T, Dahl R, et al. Revised nomenclature for allergy for global use: report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol 2004; 113:832–836.
- Joint Task Force on Practice Parameters; American Academy of Allergy, Asthma and Immunology; American College of Allergy, Asthma and Immunology; Joint Council of Allergy, Asthma and Immunology. Drug allergy: an updated practice parameter. Ann Allergy Asthma Immunol 2010; 105:259–273.
- Park MA, Matesic D, Markus PJ, Li JT. Female sex as a risk factor for penicillin allergy. Ann Allergy Asthma Immunol 2007; 99:54–58.
- Moreno E, Macias E, Davila I, Laffond E, Ruiz A, Lorente F. Hypersensitivity reactions to cephalosporins. Expert Opin Drug Saf 2008; 7:295–304.
- Salkind AR, Cuddy PG, Foxworth JW. The rational clinical examination. Is this patient allergic to penicillin? An evidence-based analysis of the likelihood of penicillin allergy. JAMA 2001; 285:2498–2505.
- Sullivan TJ, Wedner HJ, Shatz GS, Yecies LD, Parker CW. Skin testing to detect penicillin allergy. J Allergy Clin Immunol 1981; 68:171–180.
- Macy E, Schatz M, Lin C, Poon KY. The falling rate of positive penicillin skin tests from 1995 to 2007. Perm J 2009; 13:12–18.
- Blanca M, Torres MJ, Garcia JJ, et al. Natural evolution of skin test sensitivity in patients allergic to beta-lactam antibiotics. J Allergy Clin Immunol 1999; 103:918–924.
- Patel BM. Skin rash with infectious mononucleosis and ampicillin. Pediatrics 1967; 40:910–911.
- Liu A, Fanning L, Chong H, et al. Desensitization regimens for drug allergy: state of the art in the 21st century. Clin Exp Allergy 2011; 41:1679–1688.
- Burrows JA, Toon M, Bell SC. Antibiotic desensitization in adults with cystic fibrosis. Respirology 2003; 8:359–364.
- Turvey SE, Cronin B, Arnold AD, Dioun AF. Antibiotic desensitization for the allergic patient: 5 years of experience and practice. Ann Allergy Asthma Immunol 2004; 92:426–432.
- Legere HJ 3rd, Palis RI, Rodriguez Bouza T, Uluer AZ, Castells MC. A safe protocol for rapid desensitization in patients with cystic fibrosis and antibiotic hypersensitivity. J Cyst Fibros 2009; 8:418–424.
- Lin E, Saxon A, Riedl M. Penicillin allergy: value of including amoxicillin as a determinant in penicillin skin testing. Int Arch Allergy Immunol 2010; 152:313–318.
- Dickson SD, Salazar KC. Diagnosis and management of immediate hypersensitivity reactions to cephalosporins. Clin Rev Allergy Immunol 2013; 45:131–142.
- Dash CH. Penicillin allergy and the cephalosporins. J Antimicrob Chemother 1975; 1(suppl 3):107–118.
- Petz LD. Immunologic cross-reactivity between penicillins and cephalosporins: a review. J Infect Dis 1978; 137(suppl):S74–S79.
- American Academy of Allergy Asthma & Immunology. Cephalosporin administration to patients with a history of penicillin allergy. www.aaaai.org/Aaaai/media/MediaLibrary/PDF%20Documents/Practice%20and%20Parameters/Cephalosporin-administration-2009.pdf. Accessed April 2, 2015.
- Fonacier L, Hirschberg R, Gerson S. Adverse drug reactions to cephalosporins in hospitalized patients with a history of penicillin allergy. Allergy Asthma Proc 2005; 26:135–141.
- Romano A, Viola M, Gueant-Rodriguez RM, Gaeta F, Pettinato R, Gueant JL. Imipenem in patients with immediate hypersensitivity to penicillins. N Engl J Med 2006; 354:2835–2837.
- Park M, Markus P, Matesic D, Li JT. Safety and effectiveness of a preoperative allergy clinic in decreasing vancomycin use in patients with a history of penicillin allergy. Ann Allergy Asthma Immunol 2006; 97:681–687.
- Arroliga ME, Radojicic C, Gordon SM, et al. A prospective observational study of the effect of penicillin skin testing on antibiotic use in the intensive care unit. Infect Control Hosp Epidemiol 2003; 24:347–350.
- del Real GA, Rose ME, Ramirez-Atamoros MT, et al. Penicillin skin testing in patients with a history of beta-lactam allergy. Ann Allergy Asthma Immunol 2007; 98:355–359.
- Nadarajah K, Green GR, Naglak M. Clinical outcomes of penicillin skin testing. Ann Allergy Asthma Immunol 2005; 95:541–545.
- Harris AD, Sauberman L, Kabbash L, Greineder DK, Samore MH. Penicillin skin testing: a way to optimize antibiotic utilization. Am J Med 1999; 107:166–168.
- Idsoe O, Guthe T, Willcox RR, de Weck AL. Nature and extent of penicillin side-reactions, with particular reference to fatalities from anaphylactic shock. Bull World Health Organ 1968; 38:159–188.
- Gadde J, Spence M, Wheeler B, Adkinson NF Jr. Clinical experience with penicillin skin testing in a large inner-city STD clinic. JAMA 1993; 270:2456–2463.
- Johansson SG, Bieber T, Dahl R, et al. Revised nomenclature for allergy for global use: report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol 2004; 113:832–836.
- Joint Task Force on Practice Parameters; American Academy of Allergy, Asthma and Immunology; American College of Allergy, Asthma and Immunology; Joint Council of Allergy, Asthma and Immunology. Drug allergy: an updated practice parameter. Ann Allergy Asthma Immunol 2010; 105:259–273.
- Park MA, Matesic D, Markus PJ, Li JT. Female sex as a risk factor for penicillin allergy. Ann Allergy Asthma Immunol 2007; 99:54–58.
- Moreno E, Macias E, Davila I, Laffond E, Ruiz A, Lorente F. Hypersensitivity reactions to cephalosporins. Expert Opin Drug Saf 2008; 7:295–304.
- Salkind AR, Cuddy PG, Foxworth JW. The rational clinical examination. Is this patient allergic to penicillin? An evidence-based analysis of the likelihood of penicillin allergy. JAMA 2001; 285:2498–2505.
- Sullivan TJ, Wedner HJ, Shatz GS, Yecies LD, Parker CW. Skin testing to detect penicillin allergy. J Allergy Clin Immunol 1981; 68:171–180.
- Macy E, Schatz M, Lin C, Poon KY. The falling rate of positive penicillin skin tests from 1995 to 2007. Perm J 2009; 13:12–18.
- Blanca M, Torres MJ, Garcia JJ, et al. Natural evolution of skin test sensitivity in patients allergic to beta-lactam antibiotics. J Allergy Clin Immunol 1999; 103:918–924.
- Patel BM. Skin rash with infectious mononucleosis and ampicillin. Pediatrics 1967; 40:910–911.
- Liu A, Fanning L, Chong H, et al. Desensitization regimens for drug allergy: state of the art in the 21st century. Clin Exp Allergy 2011; 41:1679–1688.
- Burrows JA, Toon M, Bell SC. Antibiotic desensitization in adults with cystic fibrosis. Respirology 2003; 8:359–364.
- Turvey SE, Cronin B, Arnold AD, Dioun AF. Antibiotic desensitization for the allergic patient: 5 years of experience and practice. Ann Allergy Asthma Immunol 2004; 92:426–432.
- Legere HJ 3rd, Palis RI, Rodriguez Bouza T, Uluer AZ, Castells MC. A safe protocol for rapid desensitization in patients with cystic fibrosis and antibiotic hypersensitivity. J Cyst Fibros 2009; 8:418–424.
- Lin E, Saxon A, Riedl M. Penicillin allergy: value of including amoxicillin as a determinant in penicillin skin testing. Int Arch Allergy Immunol 2010; 152:313–318.
- Dickson SD, Salazar KC. Diagnosis and management of immediate hypersensitivity reactions to cephalosporins. Clin Rev Allergy Immunol 2013; 45:131–142.
- Dash CH. Penicillin allergy and the cephalosporins. J Antimicrob Chemother 1975; 1(suppl 3):107–118.
- Petz LD. Immunologic cross-reactivity between penicillins and cephalosporins: a review. J Infect Dis 1978; 137(suppl):S74–S79.
- American Academy of Allergy Asthma & Immunology. Cephalosporin administration to patients with a history of penicillin allergy. www.aaaai.org/Aaaai/media/MediaLibrary/PDF%20Documents/Practice%20and%20Parameters/Cephalosporin-administration-2009.pdf. Accessed April 2, 2015.
- Fonacier L, Hirschberg R, Gerson S. Adverse drug reactions to cephalosporins in hospitalized patients with a history of penicillin allergy. Allergy Asthma Proc 2005; 26:135–141.
- Romano A, Viola M, Gueant-Rodriguez RM, Gaeta F, Pettinato R, Gueant JL. Imipenem in patients with immediate hypersensitivity to penicillins. N Engl J Med 2006; 354:2835–2837.
KEY POINTS
- The prevalence of reported penicillin allergy is 10% in the general population. However, more than 90% of these patients are found not to be allergic to penicillin after skin testing.
- In patients found to have penicillin allergy, the frequency of positive results on skin testing decreases by 10% per year of avoidance. Therefore, 80% to 100% of patients are expected to test negative for penicillin allergy by 10 years after their reaction.
- Skin testing for penicillin allergy is only useful for type 1 IgE-mediated reactions. However, in properly selected patients, the negative predictive value of penicillin skin testing is nearly 97%.
- The rate of cross-reactivity between penicillin and cephalosporins is approximately 3%.
Why CMS’ plan to unbundle global surgery periods should be scrapped
Sometimes it’s difficult to figure out which way is forward. For the past few years, private insurers and the federal government (through the Medicare program) have been experimenting with and putting in place different ways of paying physicians for the care they provide. Many alternatives are designed to increase value for our nation’s health care dollars and improve quality of care, often through care coordination. Most involve different ways of “bundling” care—paying a single sum for a patient’s episode of care rather than separate payments each time a physician encounters a patient.
For more than 20 years, Medicare has bundled most surgeries, paying 1 sum to the physician and requiring only 1 copayment from the beneficiary patient. In this way, when a patient needs surgery, Medicare pays the surgeon 1 payment for preparation the day before surgery, for the surgery itself, and for either 10 or 90 days of follow-up care, depending on the specific procedure involved (TABLE 1). Similarly the patient has had 1 copay for the entire episode of care. This bundling is called global surgical codes, and it applies to coding, billing, and reimbursement.
Table 1: CMS description of 10- and 90-day global codes Minor procedures: 10-day postoperative period
Major procedures: 90-day postoperative period
|
This approach may change soon—and not for the better. In this article, I describe how the federal Centers for Medicare and Medicaid Services (CMS) plan to eliminate global surgery bundling, as well as the efforts under way by the American Congress of Obstetricians and Gynecologists (ACOG) and other organizations to stop the proposed change.
The CMS plan to eliminate surgical bundling
In a significant twist from the trend toward bundling and care coordination, CMS finalized its proposed policy in its 2015 Medicare Physician Fee Schedule final rule to transition all 10- and 90-day global surgical codes to 0-day global surgical codes by 2017 and 2018, respectively. Beginning in 2017 for 10-day global codes and 2018 for 90-day codes, physicians will be paid separately for the day of surgery and for evaluation and management (E&M) provided on the day before and any days after. Patients will have copays for each physician intervention.
CMS has decided to move forward with this change despite overwhelming concern and opposition on the part of both patients and physicians. This change would affect more than 4,200 services on the Medicare Physician Fee Schedule—well over one-third of the 9,900 current procedural terminology (CPT) codes.
The new codes and increased paperwork and billing are daunting, and would result in an estimated 63 million additional claims per year to account for postsurgical E&M services. The cost to CMS alone for this huge new mountain of claims may be as high as $95 million per year. Moreover, under the new system, patients may not return for the full range of follow-up care needed if they get billed for every visit, possibly resulting in poorer outcomes.
CMS’ justification for unbundling
CMS argues that this change is needed because many surgeons are failing to provide as much care (as many E&M follow-up visits) as they’re paid to deliver under the 10- and 90-day codes. As evidence, CMS points to 3 reports published by the Department of Health and Human Services Office of Inspector General:
- An April 2009 report from the field of ocular surgery found that physicians provided fewer E&M services than were included in 201 of 300 examined global surgery fees. The cost of these undelivered services was approximately $97.6 million.1
- A May 2012 report from the field of cardiac surgery found that physicians provided fewer E&M services than were included in 132 global surgery fees of the 300 surgeries examined. The cost: $14.6 million.2
- Another May 2012 report, this one from the field of musculoskeletal surgery, found that physicians provided fewer E&M services than were included in 165 global surgery fees of the 300 surgeries examined. The cost for these undelivered services: $49 million.3
Based largely on these reports, CMS has determined that it cannot verify the number of visits, level of service, and relative costs of the services included in a global package, in large part because the current valuation methodology relies on survey data estimating the resources used in a typical case, instead of on actual data.
In each of these reports, the Inspector General also found smaller numbers of cases where surgeons provided more E&M care than was covered under the global payment. In each report, the Inspector General suggests that CMS should do more to identify and correctly value misvalued codes. ACOG Vice President for Health Policy Barbara Levy, MD, who is also chair of the Relative Value Scale Update Committee, or RUC, makes a compelling case that the RUC has identified and corrected many global surgical codes since these reports were issued and is in the process of revising more codes. She also argues that the RUC is the appropriate place to address these issues.
Policy analysis finds that total RVUs would decline
CMS has indicated that it intends to use a formula for converting the 10- and 90-day global services into 0-day services by simply reducing the work relative value units (RVUs) for the service by the number of work RVUs in the postoperative visits. The American College of Surgeons asked Health Policy Alternatives (HPA), a consulting firm, to analyze the CMS decision. HPA found that “systematically convert[ing] all global surgical codes to 0-day global codes by backing out of the bundled E&M services reduces the total RVUs and each component (work, practice expense, and malpractice) for surgical codes. Specifically, for surgical specialties, the impact of this transition on all Medicare reimbursed codes results in the following reductions:
- overall payment decrease of 1.8%
- payment decrease of 0.8% for work
- payment decrease of 2% for practice expense
- payment decrease of 9.2% for malpractice.
This modeling resulted in a total overall payment increase of 0.1% for generalists and a payment increase of 0.3% for medical specialists.”4
HPA’s findings related to the malpractice component are especially interesting for the ObGyn specialty. “Model results demonstrate that this policy results in significant redistribution of malpractice away from the main specialty provider of the surgical procedure into the entire group of providers (surgical and nonsurgical),” notes the HPA report.4 “Most impacted will be specialties with higher malpractice expenses, such as neurosurgeons and cardiac surgeons.”4 We could add ObGyns to that list.
ACOG cites numerous objections
ACOG is deeply involved in opposing this new CMS policy and preventing it from ever going into effect, working on our own, in coalition with our medical organization colleagues and patient organizations, and working closely with the US Congress.
ACOG and 28 other medical organizations, including the American Medical Association (AMA), summarized our opposition in a letter to US House and Senate Democratic and Republican leaders in December 2014, saying that this new policy:
Detracts from quality of care, impedes patient access, and complicates patient copays
- Patients will be responsible for copays on each service, including follow-up visits. This could considerably increase the administrative burden on patients. Worse, it could discourage them from returning for needed follow-up care.
- In the hospital critical care setting, the global payment structure allows the surgeon to oversee and coordinate care related to the patient’s recovery. Without the global structure, care will be fragmented and providers may compete to see patients and bill for the care they provide.
Undermines Medicare reform initiatives
- CMS initiatives for payment are all moving toward larger bundled payments. Deconstruction of the current payment structure for physicians is counterintuitive to the end goal of providing more comprehensive and coordinated care for the patient.
- Current bipartisan, bicameral legislation to repeal and replace the flawed sustainable growth rate formula calls for “a period of stability” in physician pay to allow physicians to transition to alternative payment models. The proposal to unbundle global surgical periods will add new complexities to an already flawed system and stymie progress.
Increases administrative burden
- The administrative burden on surgical practices and CMS (and its contractors) will be significant. Eliminating the global package will result in 63 million additional claims per year, adding unnecessary costs to our health care system.
Obstructs clinical registry data collection and quality improvement
- Surgeons will have less ability to collect information on patient outcomes in clinical registries, undermining many of the most meaningful quality improvement initiatives.5
Additional ACOG concerns
ACOG added these concerns to our opposition to the CMS plan:
- The change will not accurately account for physician work, practice expense, and malpractice risk for services performed.
- Thousands of new codes and/or values will need to be created for postoperative care because the supplies and equipment needed for postoperative care are not included in the E&M codes that will be used to report in-hospital and outpatient postoperative services (TABLE 2).
- Liability costs of a specific service should be derived from those of the performing specialties. Under the CMS plan, the liability costs associated with postoperative work would be removed from the primary service and artificially diluted by the wide mix of specialties performing all types of E&M services. Without global periods, a one-size-fits-all approach to professional liability insurance will be unsustainable and result in great disparities between the actual and realized malpractice costs for many physician specialties.
Table 2: Other postoperative care services currently bundled into global surgical packages
|
We have important allies
The American Association of Retired Persons (AARP) joined us in September 2014, when it formally asked CMS to abandon this new policy. In a letter to CMS Administrator Marilyn Tavenner, AARP noted that, “from a beneficiary perspective, we are concerned that this unbundling could produce considerable confusion and cause beneficiaries to receive multiple explanations of Medicare benefits (and incur separate cost-sharing obligations) related to a single surgical procedure….[G]iven the obvious methodological uncertainty and complexity involved in determining appropriate values for a very large number of ‘new’ 0-day global services, and the likely confusion surrounding the resulting increase in Medicare claims, AARP has serious doubts regarding the benefit of this unbundling proposal. We suggest [that] CMS consider other available alternatives, including the re-valuation of global services whose current values are believed to be incorrect.”6
Also in September, 27 Republican and Democratic members of Congress wrote a strong letter to CMS echoing the medical community’s concerns. The letter and many months of congressional leadership have been spearheaded by Representatives Larry Bucshon, MD, and Ami Bera, MD—demonstrating the value of having physicians in elective office. Other physician members of Congress who have provided outstanding leadership include ACOG Fellows and Representatives Michael Burgess, MD, and Phil Roe, MD, as well as Representatives Tom Price, MD; Andy Harris, MD; Joe Heck, DO; Charles Boustany, MD; Raul Ruiz, MD; and Dan Benishek, MD.
This important group of physician leaders, ACOG, AARP, and the surgical community are hard at work to derail or significantly delay what most physicians and policy analysts see as a very bad idea.
Congress takes action
In April 2015, Congress passed HR2, the Medicare Access and CHIP Reauthorization Bill, which most notably repealed the Medicare Sustainable Growth Rate formula. Included in this law is an important provision to halt implementation of CMS’ plan to unbundle all 10- and 90-day global codes.
Section 523 of that law requires CMS to periodically collect information on the services that surgeons furnish during these global periods, beginning no later than 2017, and use that information to ensure that the bundled payment amounts for surgical services are accurate. The Secretary of Health and Human Services is given the authority to withhold a portion of payment for services with a 10- or 90-day global period to incentivize the reporting of information. The Secretary can stop collecting this information from surgeons once the needed data can be obtained through other mechanisms, such as clinical data registries and electronic medical records.
Congressmen Bucshon and Bera championed this provision, along with nearly all physician members of the US House of Representatives. This change ensures a thorough, data-driven approach to appropriately valuing surgical services, including those provided by ObGyn subspecialists, such as urogynecologists and gynecologic oncologists.
Acknowledgment
The author thanks Barbara Levy, MD, ACOG Vice President for Health Policy, for her helpful comments.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Department of Health and Human Services, Office of Inspector General. Nationwide Review of Evaluation and Management Services Included in Eye and Ocular Adnexa Global Surgery Fees for Calendar Year 2005. A-05-07-00077. Washington, DC: Department of Health and Human Services; April 2009.
2. Department of Health and Human Services, Office of Inspector General. Cardiovascular Global Surgery Fees Often Did Not Reflect the Number of Evaluation and Management Services Provided. A-05-09-00054. Washington, DC: Department of Health and Human Services; May 2012.
3. Department of Health and Human Services, Office of Inspector General. Musculoskeletal Global Surgery Fees Often Did Not Reflect the Number of Evaluation and Management Services Provided. A-05-09-00053. Washington, DC: Department of Health and Human Services; May 2012.
4. Summary of Initial Modeling Results of the CMS Policy to Transition 10- and 90-Day Global Surgery Codes to 0-Day Global Surgery Codes. Washington, DC: Health Policy Alternatives; January 9, 2015.
5. American Congress of Obstetricians and Gynecologists joint letter to Congress; December 2, 2014.
6. American Association of Retired Persons letter to Marilyn Tavenner, Administrator, Centers for Medicare and Medicaid Services; September 2, 2014.
Sometimes it’s difficult to figure out which way is forward. For the past few years, private insurers and the federal government (through the Medicare program) have been experimenting with and putting in place different ways of paying physicians for the care they provide. Many alternatives are designed to increase value for our nation’s health care dollars and improve quality of care, often through care coordination. Most involve different ways of “bundling” care—paying a single sum for a patient’s episode of care rather than separate payments each time a physician encounters a patient.
For more than 20 years, Medicare has bundled most surgeries, paying 1 sum to the physician and requiring only 1 copayment from the beneficiary patient. In this way, when a patient needs surgery, Medicare pays the surgeon 1 payment for preparation the day before surgery, for the surgery itself, and for either 10 or 90 days of follow-up care, depending on the specific procedure involved (TABLE 1). Similarly the patient has had 1 copay for the entire episode of care. This bundling is called global surgical codes, and it applies to coding, billing, and reimbursement.
Table 1: CMS description of 10- and 90-day global codes Minor procedures: 10-day postoperative period
Major procedures: 90-day postoperative period
|
This approach may change soon—and not for the better. In this article, I describe how the federal Centers for Medicare and Medicaid Services (CMS) plan to eliminate global surgery bundling, as well as the efforts under way by the American Congress of Obstetricians and Gynecologists (ACOG) and other organizations to stop the proposed change.
The CMS plan to eliminate surgical bundling
In a significant twist from the trend toward bundling and care coordination, CMS finalized its proposed policy in its 2015 Medicare Physician Fee Schedule final rule to transition all 10- and 90-day global surgical codes to 0-day global surgical codes by 2017 and 2018, respectively. Beginning in 2017 for 10-day global codes and 2018 for 90-day codes, physicians will be paid separately for the day of surgery and for evaluation and management (E&M) provided on the day before and any days after. Patients will have copays for each physician intervention.
CMS has decided to move forward with this change despite overwhelming concern and opposition on the part of both patients and physicians. This change would affect more than 4,200 services on the Medicare Physician Fee Schedule—well over one-third of the 9,900 current procedural terminology (CPT) codes.
The new codes and increased paperwork and billing are daunting, and would result in an estimated 63 million additional claims per year to account for postsurgical E&M services. The cost to CMS alone for this huge new mountain of claims may be as high as $95 million per year. Moreover, under the new system, patients may not return for the full range of follow-up care needed if they get billed for every visit, possibly resulting in poorer outcomes.
CMS’ justification for unbundling
CMS argues that this change is needed because many surgeons are failing to provide as much care (as many E&M follow-up visits) as they’re paid to deliver under the 10- and 90-day codes. As evidence, CMS points to 3 reports published by the Department of Health and Human Services Office of Inspector General:
- An April 2009 report from the field of ocular surgery found that physicians provided fewer E&M services than were included in 201 of 300 examined global surgery fees. The cost of these undelivered services was approximately $97.6 million.1
- A May 2012 report from the field of cardiac surgery found that physicians provided fewer E&M services than were included in 132 global surgery fees of the 300 surgeries examined. The cost: $14.6 million.2
- Another May 2012 report, this one from the field of musculoskeletal surgery, found that physicians provided fewer E&M services than were included in 165 global surgery fees of the 300 surgeries examined. The cost for these undelivered services: $49 million.3
Based largely on these reports, CMS has determined that it cannot verify the number of visits, level of service, and relative costs of the services included in a global package, in large part because the current valuation methodology relies on survey data estimating the resources used in a typical case, instead of on actual data.
In each of these reports, the Inspector General also found smaller numbers of cases where surgeons provided more E&M care than was covered under the global payment. In each report, the Inspector General suggests that CMS should do more to identify and correctly value misvalued codes. ACOG Vice President for Health Policy Barbara Levy, MD, who is also chair of the Relative Value Scale Update Committee, or RUC, makes a compelling case that the RUC has identified and corrected many global surgical codes since these reports were issued and is in the process of revising more codes. She also argues that the RUC is the appropriate place to address these issues.
Policy analysis finds that total RVUs would decline
CMS has indicated that it intends to use a formula for converting the 10- and 90-day global services into 0-day services by simply reducing the work relative value units (RVUs) for the service by the number of work RVUs in the postoperative visits. The American College of Surgeons asked Health Policy Alternatives (HPA), a consulting firm, to analyze the CMS decision. HPA found that “systematically convert[ing] all global surgical codes to 0-day global codes by backing out of the bundled E&M services reduces the total RVUs and each component (work, practice expense, and malpractice) for surgical codes. Specifically, for surgical specialties, the impact of this transition on all Medicare reimbursed codes results in the following reductions:
- overall payment decrease of 1.8%
- payment decrease of 0.8% for work
- payment decrease of 2% for practice expense
- payment decrease of 9.2% for malpractice.
This modeling resulted in a total overall payment increase of 0.1% for generalists and a payment increase of 0.3% for medical specialists.”4
HPA’s findings related to the malpractice component are especially interesting for the ObGyn specialty. “Model results demonstrate that this policy results in significant redistribution of malpractice away from the main specialty provider of the surgical procedure into the entire group of providers (surgical and nonsurgical),” notes the HPA report.4 “Most impacted will be specialties with higher malpractice expenses, such as neurosurgeons and cardiac surgeons.”4 We could add ObGyns to that list.
ACOG cites numerous objections
ACOG is deeply involved in opposing this new CMS policy and preventing it from ever going into effect, working on our own, in coalition with our medical organization colleagues and patient organizations, and working closely with the US Congress.
ACOG and 28 other medical organizations, including the American Medical Association (AMA), summarized our opposition in a letter to US House and Senate Democratic and Republican leaders in December 2014, saying that this new policy:
Detracts from quality of care, impedes patient access, and complicates patient copays
- Patients will be responsible for copays on each service, including follow-up visits. This could considerably increase the administrative burden on patients. Worse, it could discourage them from returning for needed follow-up care.
- In the hospital critical care setting, the global payment structure allows the surgeon to oversee and coordinate care related to the patient’s recovery. Without the global structure, care will be fragmented and providers may compete to see patients and bill for the care they provide.
Undermines Medicare reform initiatives
- CMS initiatives for payment are all moving toward larger bundled payments. Deconstruction of the current payment structure for physicians is counterintuitive to the end goal of providing more comprehensive and coordinated care for the patient.
- Current bipartisan, bicameral legislation to repeal and replace the flawed sustainable growth rate formula calls for “a period of stability” in physician pay to allow physicians to transition to alternative payment models. The proposal to unbundle global surgical periods will add new complexities to an already flawed system and stymie progress.
Increases administrative burden
- The administrative burden on surgical practices and CMS (and its contractors) will be significant. Eliminating the global package will result in 63 million additional claims per year, adding unnecessary costs to our health care system.
Obstructs clinical registry data collection and quality improvement
- Surgeons will have less ability to collect information on patient outcomes in clinical registries, undermining many of the most meaningful quality improvement initiatives.5
Additional ACOG concerns
ACOG added these concerns to our opposition to the CMS plan:
- The change will not accurately account for physician work, practice expense, and malpractice risk for services performed.
- Thousands of new codes and/or values will need to be created for postoperative care because the supplies and equipment needed for postoperative care are not included in the E&M codes that will be used to report in-hospital and outpatient postoperative services (TABLE 2).
- Liability costs of a specific service should be derived from those of the performing specialties. Under the CMS plan, the liability costs associated with postoperative work would be removed from the primary service and artificially diluted by the wide mix of specialties performing all types of E&M services. Without global periods, a one-size-fits-all approach to professional liability insurance will be unsustainable and result in great disparities between the actual and realized malpractice costs for many physician specialties.
Table 2: Other postoperative care services currently bundled into global surgical packages
|
We have important allies
The American Association of Retired Persons (AARP) joined us in September 2014, when it formally asked CMS to abandon this new policy. In a letter to CMS Administrator Marilyn Tavenner, AARP noted that, “from a beneficiary perspective, we are concerned that this unbundling could produce considerable confusion and cause beneficiaries to receive multiple explanations of Medicare benefits (and incur separate cost-sharing obligations) related to a single surgical procedure….[G]iven the obvious methodological uncertainty and complexity involved in determining appropriate values for a very large number of ‘new’ 0-day global services, and the likely confusion surrounding the resulting increase in Medicare claims, AARP has serious doubts regarding the benefit of this unbundling proposal. We suggest [that] CMS consider other available alternatives, including the re-valuation of global services whose current values are believed to be incorrect.”6
Also in September, 27 Republican and Democratic members of Congress wrote a strong letter to CMS echoing the medical community’s concerns. The letter and many months of congressional leadership have been spearheaded by Representatives Larry Bucshon, MD, and Ami Bera, MD—demonstrating the value of having physicians in elective office. Other physician members of Congress who have provided outstanding leadership include ACOG Fellows and Representatives Michael Burgess, MD, and Phil Roe, MD, as well as Representatives Tom Price, MD; Andy Harris, MD; Joe Heck, DO; Charles Boustany, MD; Raul Ruiz, MD; and Dan Benishek, MD.
This important group of physician leaders, ACOG, AARP, and the surgical community are hard at work to derail or significantly delay what most physicians and policy analysts see as a very bad idea.
Congress takes action
In April 2015, Congress passed HR2, the Medicare Access and CHIP Reauthorization Bill, which most notably repealed the Medicare Sustainable Growth Rate formula. Included in this law is an important provision to halt implementation of CMS’ plan to unbundle all 10- and 90-day global codes.
Section 523 of that law requires CMS to periodically collect information on the services that surgeons furnish during these global periods, beginning no later than 2017, and use that information to ensure that the bundled payment amounts for surgical services are accurate. The Secretary of Health and Human Services is given the authority to withhold a portion of payment for services with a 10- or 90-day global period to incentivize the reporting of information. The Secretary can stop collecting this information from surgeons once the needed data can be obtained through other mechanisms, such as clinical data registries and electronic medical records.
Congressmen Bucshon and Bera championed this provision, along with nearly all physician members of the US House of Representatives. This change ensures a thorough, data-driven approach to appropriately valuing surgical services, including those provided by ObGyn subspecialists, such as urogynecologists and gynecologic oncologists.
Acknowledgment
The author thanks Barbara Levy, MD, ACOG Vice President for Health Policy, for her helpful comments.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Sometimes it’s difficult to figure out which way is forward. For the past few years, private insurers and the federal government (through the Medicare program) have been experimenting with and putting in place different ways of paying physicians for the care they provide. Many alternatives are designed to increase value for our nation’s health care dollars and improve quality of care, often through care coordination. Most involve different ways of “bundling” care—paying a single sum for a patient’s episode of care rather than separate payments each time a physician encounters a patient.
For more than 20 years, Medicare has bundled most surgeries, paying 1 sum to the physician and requiring only 1 copayment from the beneficiary patient. In this way, when a patient needs surgery, Medicare pays the surgeon 1 payment for preparation the day before surgery, for the surgery itself, and for either 10 or 90 days of follow-up care, depending on the specific procedure involved (TABLE 1). Similarly the patient has had 1 copay for the entire episode of care. This bundling is called global surgical codes, and it applies to coding, billing, and reimbursement.
Table 1: CMS description of 10- and 90-day global codes Minor procedures: 10-day postoperative period
Major procedures: 90-day postoperative period
|
This approach may change soon—and not for the better. In this article, I describe how the federal Centers for Medicare and Medicaid Services (CMS) plan to eliminate global surgery bundling, as well as the efforts under way by the American Congress of Obstetricians and Gynecologists (ACOG) and other organizations to stop the proposed change.
The CMS plan to eliminate surgical bundling
In a significant twist from the trend toward bundling and care coordination, CMS finalized its proposed policy in its 2015 Medicare Physician Fee Schedule final rule to transition all 10- and 90-day global surgical codes to 0-day global surgical codes by 2017 and 2018, respectively. Beginning in 2017 for 10-day global codes and 2018 for 90-day codes, physicians will be paid separately for the day of surgery and for evaluation and management (E&M) provided on the day before and any days after. Patients will have copays for each physician intervention.
CMS has decided to move forward with this change despite overwhelming concern and opposition on the part of both patients and physicians. This change would affect more than 4,200 services on the Medicare Physician Fee Schedule—well over one-third of the 9,900 current procedural terminology (CPT) codes.
The new codes and increased paperwork and billing are daunting, and would result in an estimated 63 million additional claims per year to account for postsurgical E&M services. The cost to CMS alone for this huge new mountain of claims may be as high as $95 million per year. Moreover, under the new system, patients may not return for the full range of follow-up care needed if they get billed for every visit, possibly resulting in poorer outcomes.
CMS’ justification for unbundling
CMS argues that this change is needed because many surgeons are failing to provide as much care (as many E&M follow-up visits) as they’re paid to deliver under the 10- and 90-day codes. As evidence, CMS points to 3 reports published by the Department of Health and Human Services Office of Inspector General:
- An April 2009 report from the field of ocular surgery found that physicians provided fewer E&M services than were included in 201 of 300 examined global surgery fees. The cost of these undelivered services was approximately $97.6 million.1
- A May 2012 report from the field of cardiac surgery found that physicians provided fewer E&M services than were included in 132 global surgery fees of the 300 surgeries examined. The cost: $14.6 million.2
- Another May 2012 report, this one from the field of musculoskeletal surgery, found that physicians provided fewer E&M services than were included in 165 global surgery fees of the 300 surgeries examined. The cost for these undelivered services: $49 million.3
Based largely on these reports, CMS has determined that it cannot verify the number of visits, level of service, and relative costs of the services included in a global package, in large part because the current valuation methodology relies on survey data estimating the resources used in a typical case, instead of on actual data.
In each of these reports, the Inspector General also found smaller numbers of cases where surgeons provided more E&M care than was covered under the global payment. In each report, the Inspector General suggests that CMS should do more to identify and correctly value misvalued codes. ACOG Vice President for Health Policy Barbara Levy, MD, who is also chair of the Relative Value Scale Update Committee, or RUC, makes a compelling case that the RUC has identified and corrected many global surgical codes since these reports were issued and is in the process of revising more codes. She also argues that the RUC is the appropriate place to address these issues.
Policy analysis finds that total RVUs would decline
CMS has indicated that it intends to use a formula for converting the 10- and 90-day global services into 0-day services by simply reducing the work relative value units (RVUs) for the service by the number of work RVUs in the postoperative visits. The American College of Surgeons asked Health Policy Alternatives (HPA), a consulting firm, to analyze the CMS decision. HPA found that “systematically convert[ing] all global surgical codes to 0-day global codes by backing out of the bundled E&M services reduces the total RVUs and each component (work, practice expense, and malpractice) for surgical codes. Specifically, for surgical specialties, the impact of this transition on all Medicare reimbursed codes results in the following reductions:
- overall payment decrease of 1.8%
- payment decrease of 0.8% for work
- payment decrease of 2% for practice expense
- payment decrease of 9.2% for malpractice.
This modeling resulted in a total overall payment increase of 0.1% for generalists and a payment increase of 0.3% for medical specialists.”4
HPA’s findings related to the malpractice component are especially interesting for the ObGyn specialty. “Model results demonstrate that this policy results in significant redistribution of malpractice away from the main specialty provider of the surgical procedure into the entire group of providers (surgical and nonsurgical),” notes the HPA report.4 “Most impacted will be specialties with higher malpractice expenses, such as neurosurgeons and cardiac surgeons.”4 We could add ObGyns to that list.
ACOG cites numerous objections
ACOG is deeply involved in opposing this new CMS policy and preventing it from ever going into effect, working on our own, in coalition with our medical organization colleagues and patient organizations, and working closely with the US Congress.
ACOG and 28 other medical organizations, including the American Medical Association (AMA), summarized our opposition in a letter to US House and Senate Democratic and Republican leaders in December 2014, saying that this new policy:
Detracts from quality of care, impedes patient access, and complicates patient copays
- Patients will be responsible for copays on each service, including follow-up visits. This could considerably increase the administrative burden on patients. Worse, it could discourage them from returning for needed follow-up care.
- In the hospital critical care setting, the global payment structure allows the surgeon to oversee and coordinate care related to the patient’s recovery. Without the global structure, care will be fragmented and providers may compete to see patients and bill for the care they provide.
Undermines Medicare reform initiatives
- CMS initiatives for payment are all moving toward larger bundled payments. Deconstruction of the current payment structure for physicians is counterintuitive to the end goal of providing more comprehensive and coordinated care for the patient.
- Current bipartisan, bicameral legislation to repeal and replace the flawed sustainable growth rate formula calls for “a period of stability” in physician pay to allow physicians to transition to alternative payment models. The proposal to unbundle global surgical periods will add new complexities to an already flawed system and stymie progress.
Increases administrative burden
- The administrative burden on surgical practices and CMS (and its contractors) will be significant. Eliminating the global package will result in 63 million additional claims per year, adding unnecessary costs to our health care system.
Obstructs clinical registry data collection and quality improvement
- Surgeons will have less ability to collect information on patient outcomes in clinical registries, undermining many of the most meaningful quality improvement initiatives.5
Additional ACOG concerns
ACOG added these concerns to our opposition to the CMS plan:
- The change will not accurately account for physician work, practice expense, and malpractice risk for services performed.
- Thousands of new codes and/or values will need to be created for postoperative care because the supplies and equipment needed for postoperative care are not included in the E&M codes that will be used to report in-hospital and outpatient postoperative services (TABLE 2).
- Liability costs of a specific service should be derived from those of the performing specialties. Under the CMS plan, the liability costs associated with postoperative work would be removed from the primary service and artificially diluted by the wide mix of specialties performing all types of E&M services. Without global periods, a one-size-fits-all approach to professional liability insurance will be unsustainable and result in great disparities between the actual and realized malpractice costs for many physician specialties.
Table 2: Other postoperative care services currently bundled into global surgical packages
|
We have important allies
The American Association of Retired Persons (AARP) joined us in September 2014, when it formally asked CMS to abandon this new policy. In a letter to CMS Administrator Marilyn Tavenner, AARP noted that, “from a beneficiary perspective, we are concerned that this unbundling could produce considerable confusion and cause beneficiaries to receive multiple explanations of Medicare benefits (and incur separate cost-sharing obligations) related to a single surgical procedure….[G]iven the obvious methodological uncertainty and complexity involved in determining appropriate values for a very large number of ‘new’ 0-day global services, and the likely confusion surrounding the resulting increase in Medicare claims, AARP has serious doubts regarding the benefit of this unbundling proposal. We suggest [that] CMS consider other available alternatives, including the re-valuation of global services whose current values are believed to be incorrect.”6
Also in September, 27 Republican and Democratic members of Congress wrote a strong letter to CMS echoing the medical community’s concerns. The letter and many months of congressional leadership have been spearheaded by Representatives Larry Bucshon, MD, and Ami Bera, MD—demonstrating the value of having physicians in elective office. Other physician members of Congress who have provided outstanding leadership include ACOG Fellows and Representatives Michael Burgess, MD, and Phil Roe, MD, as well as Representatives Tom Price, MD; Andy Harris, MD; Joe Heck, DO; Charles Boustany, MD; Raul Ruiz, MD; and Dan Benishek, MD.
This important group of physician leaders, ACOG, AARP, and the surgical community are hard at work to derail or significantly delay what most physicians and policy analysts see as a very bad idea.
Congress takes action
In April 2015, Congress passed HR2, the Medicare Access and CHIP Reauthorization Bill, which most notably repealed the Medicare Sustainable Growth Rate formula. Included in this law is an important provision to halt implementation of CMS’ plan to unbundle all 10- and 90-day global codes.
Section 523 of that law requires CMS to periodically collect information on the services that surgeons furnish during these global periods, beginning no later than 2017, and use that information to ensure that the bundled payment amounts for surgical services are accurate. The Secretary of Health and Human Services is given the authority to withhold a portion of payment for services with a 10- or 90-day global period to incentivize the reporting of information. The Secretary can stop collecting this information from surgeons once the needed data can be obtained through other mechanisms, such as clinical data registries and electronic medical records.
Congressmen Bucshon and Bera championed this provision, along with nearly all physician members of the US House of Representatives. This change ensures a thorough, data-driven approach to appropriately valuing surgical services, including those provided by ObGyn subspecialists, such as urogynecologists and gynecologic oncologists.
Acknowledgment
The author thanks Barbara Levy, MD, ACOG Vice President for Health Policy, for her helpful comments.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Department of Health and Human Services, Office of Inspector General. Nationwide Review of Evaluation and Management Services Included in Eye and Ocular Adnexa Global Surgery Fees for Calendar Year 2005. A-05-07-00077. Washington, DC: Department of Health and Human Services; April 2009.
2. Department of Health and Human Services, Office of Inspector General. Cardiovascular Global Surgery Fees Often Did Not Reflect the Number of Evaluation and Management Services Provided. A-05-09-00054. Washington, DC: Department of Health and Human Services; May 2012.
3. Department of Health and Human Services, Office of Inspector General. Musculoskeletal Global Surgery Fees Often Did Not Reflect the Number of Evaluation and Management Services Provided. A-05-09-00053. Washington, DC: Department of Health and Human Services; May 2012.
4. Summary of Initial Modeling Results of the CMS Policy to Transition 10- and 90-Day Global Surgery Codes to 0-Day Global Surgery Codes. Washington, DC: Health Policy Alternatives; January 9, 2015.
5. American Congress of Obstetricians and Gynecologists joint letter to Congress; December 2, 2014.
6. American Association of Retired Persons letter to Marilyn Tavenner, Administrator, Centers for Medicare and Medicaid Services; September 2, 2014.
1. Department of Health and Human Services, Office of Inspector General. Nationwide Review of Evaluation and Management Services Included in Eye and Ocular Adnexa Global Surgery Fees for Calendar Year 2005. A-05-07-00077. Washington, DC: Department of Health and Human Services; April 2009.
2. Department of Health and Human Services, Office of Inspector General. Cardiovascular Global Surgery Fees Often Did Not Reflect the Number of Evaluation and Management Services Provided. A-05-09-00054. Washington, DC: Department of Health and Human Services; May 2012.
3. Department of Health and Human Services, Office of Inspector General. Musculoskeletal Global Surgery Fees Often Did Not Reflect the Number of Evaluation and Management Services Provided. A-05-09-00053. Washington, DC: Department of Health and Human Services; May 2012.
4. Summary of Initial Modeling Results of the CMS Policy to Transition 10- and 90-Day Global Surgery Codes to 0-Day Global Surgery Codes. Washington, DC: Health Policy Alternatives; January 9, 2015.
5. American Congress of Obstetricians and Gynecologists joint letter to Congress; December 2, 2014.
6. American Association of Retired Persons letter to Marilyn Tavenner, Administrator, Centers for Medicare and Medicaid Services; September 2, 2014.
How to assess and treat birth-related depression in new fathers
Only recently has paternal postpartum depression (PPD) received much attention. Research has shown that maternal PPD is associated with negative outcomes in the child’s cognitive development and social and marital problems for the parents. Likewise, depressed fathers are less likely to play outside with their child and more likely to put the child to bed awake.1
Recent studies reported that 10.4% of men experienced depression within 12 month of delivery.1 Edmondson et al2 estimate the prevalence of paternal PPD to be 8% between birth and 3 months, 26% from 3 to 6 months, and 9% from 6 to 12 months.
Risk factors
Risk factors for paternal PPD have not been studied extensively. Some studies have shown that immaturity, lack of social support, first or unplanned pregnancies, marital relationship problems, and unemployment were the most common risk factors for depression in men postnatally.3 A history of depression and other psychiatric disorders also increases risk.4 Psychosocial factors, such as quality of the spousal relationship, parenting distress, and perceived parenting efficacy, contribute to paternal depression.
Similarly, depressed postpartum fathers experience higher levels of parenting distress and a lower sense of parenting efficacy.5 Interestingly, negative life events were associated with increased risk for depression in mothers, but not fathers.3
Clinical presentation
Paternal PPD symptoms appear within 12 months after the birth of the child and last for at least 2 weeks. Signs and symptoms of depression in men might not resemble those seen in postpartum women. Men tend to show aggression, increased or easy irritability, and agitation, and might not seek help for emotional issues as readily as women do. Typical symptoms of depression often are present, such as sleep disturbance or changes in sleep patterns, difficulty concentrating, memory problems, and feelings of worthlessness, hopelessness, inadequacy, and excess guilt with suicidal ideation.6
Making the diagnosis
Maternal PPD commonly is evaluated using the Edinburgh Postnatal Depression Scale- Partner (EDPS-P) or Postpartum Depression Screening Scale. However, studies are lacking to determine which diagnostic modality is most accurate for diagnosing paternal PPD.
A paternal PPD screening tool could include the EDPS-P administered to mothers. Edmonson et al2 determined an EDPS-P score of >10 was the optimal cut-off point for screening for paternal depression, with a sensitivity of 89.5% and a specificity of 78.2%, compared with a structured clinical interview. Fisher et al4 determined that the EDPS-P report was a reliable method for detecting paternal PPD compared with validated depression scales completed by fathers. Madsen et al5 determined the Gotland Male Depression Scale, which detects typical male depressive symptoms, also was effective in recognizing paternal PPD at 6 weeks postpartum.7
Treatment of paternal PPD
Specific treatment for paternal PPD has not been studied extensively. Psychotherapy targeted at interpersonal family relationships and parenting is indicated for mild depression, whereas a combination of psychotherapy and pharmacotherapy is recommended for moderate or severe depression.
Depending on specific patient factors, pharmacotherapy options include selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors, tricyclic antidepressants, and atypical antipsychotics.8 SSRIs often are used because of their efficacy and relative lack of serious side effects, as demonstrated in numerous trials.2 Recovery is more likely with combination therapy than monotherapy.9 Fathers with psychosis or suicidal ideation should be referred for inpatient treatment.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Paulson JF, Dauber S, Leiferman JA. Individual and combined effects of postpartum depression in mothers and fathers on parenting behavior. Pediatrics. 2006;118(2):659-668.
2. Edmondson OJ, Psychogiou L, Vlachos H, et al. Depression in fathers in the postnatal period: assessment of the Edinburgh Postnatal Depression Scale as a screening measure. J Affect Disord. 2010;125(1-3):365-368.
3. Schumacher M, Zubaran C, White G. Bringing birth-related paternal depression to the fore. Women Birth. 2008;21(2):65-70.
4. Fisher SD, Kopelman R, O’Hara MW. Partner report of paternal depression using the Edinburgh Postnatal Depression Scale-Partner. Arch Womens Ment Health. 2012;15(4):283-288.
5. Madsen SA, Juhl T. Paternal depression in the postnatal period assessed with traditional and male depression scales. Journal of Men’s Health and Gender. 2007;4(1):26-31.
6. Escribà-Agüir V, Artazcoz L. Gender differences in postpartum depression: a longitudinal cohort study. J Epidemiol Community Health. 2011;65(4):320-326.
7. Cuijpers P, van Straten A, Warmerdam L, et al. Psychotherapy versus the combination of psychotherapy and pharmacotherapy in the treatment of depression: a meta-analysis. Depress Anxiety. 2009;26(3):279-288.
8. Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation anti-depressants: a multiple-treatments meta-analysis. Lancet. 2009;373(9665):746-758.
9. Demontigny F, Girard ME, Lacharité C, et al. Psychosocial factors associated with paternal postnatal depression. J Affect Disord. 2013;15(150):44-49.
Only recently has paternal postpartum depression (PPD) received much attention. Research has shown that maternal PPD is associated with negative outcomes in the child’s cognitive development and social and marital problems for the parents. Likewise, depressed fathers are less likely to play outside with their child and more likely to put the child to bed awake.1
Recent studies reported that 10.4% of men experienced depression within 12 month of delivery.1 Edmondson et al2 estimate the prevalence of paternal PPD to be 8% between birth and 3 months, 26% from 3 to 6 months, and 9% from 6 to 12 months.
Risk factors
Risk factors for paternal PPD have not been studied extensively. Some studies have shown that immaturity, lack of social support, first or unplanned pregnancies, marital relationship problems, and unemployment were the most common risk factors for depression in men postnatally.3 A history of depression and other psychiatric disorders also increases risk.4 Psychosocial factors, such as quality of the spousal relationship, parenting distress, and perceived parenting efficacy, contribute to paternal depression.
Similarly, depressed postpartum fathers experience higher levels of parenting distress and a lower sense of parenting efficacy.5 Interestingly, negative life events were associated with increased risk for depression in mothers, but not fathers.3
Clinical presentation
Paternal PPD symptoms appear within 12 months after the birth of the child and last for at least 2 weeks. Signs and symptoms of depression in men might not resemble those seen in postpartum women. Men tend to show aggression, increased or easy irritability, and agitation, and might not seek help for emotional issues as readily as women do. Typical symptoms of depression often are present, such as sleep disturbance or changes in sleep patterns, difficulty concentrating, memory problems, and feelings of worthlessness, hopelessness, inadequacy, and excess guilt with suicidal ideation.6
Making the diagnosis
Maternal PPD commonly is evaluated using the Edinburgh Postnatal Depression Scale- Partner (EDPS-P) or Postpartum Depression Screening Scale. However, studies are lacking to determine which diagnostic modality is most accurate for diagnosing paternal PPD.
A paternal PPD screening tool could include the EDPS-P administered to mothers. Edmonson et al2 determined an EDPS-P score of >10 was the optimal cut-off point for screening for paternal depression, with a sensitivity of 89.5% and a specificity of 78.2%, compared with a structured clinical interview. Fisher et al4 determined that the EDPS-P report was a reliable method for detecting paternal PPD compared with validated depression scales completed by fathers. Madsen et al5 determined the Gotland Male Depression Scale, which detects typical male depressive symptoms, also was effective in recognizing paternal PPD at 6 weeks postpartum.7
Treatment of paternal PPD
Specific treatment for paternal PPD has not been studied extensively. Psychotherapy targeted at interpersonal family relationships and parenting is indicated for mild depression, whereas a combination of psychotherapy and pharmacotherapy is recommended for moderate or severe depression.
Depending on specific patient factors, pharmacotherapy options include selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors, tricyclic antidepressants, and atypical antipsychotics.8 SSRIs often are used because of their efficacy and relative lack of serious side effects, as demonstrated in numerous trials.2 Recovery is more likely with combination therapy than monotherapy.9 Fathers with psychosis or suicidal ideation should be referred for inpatient treatment.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Only recently has paternal postpartum depression (PPD) received much attention. Research has shown that maternal PPD is associated with negative outcomes in the child’s cognitive development and social and marital problems for the parents. Likewise, depressed fathers are less likely to play outside with their child and more likely to put the child to bed awake.1
Recent studies reported that 10.4% of men experienced depression within 12 month of delivery.1 Edmondson et al2 estimate the prevalence of paternal PPD to be 8% between birth and 3 months, 26% from 3 to 6 months, and 9% from 6 to 12 months.
Risk factors
Risk factors for paternal PPD have not been studied extensively. Some studies have shown that immaturity, lack of social support, first or unplanned pregnancies, marital relationship problems, and unemployment were the most common risk factors for depression in men postnatally.3 A history of depression and other psychiatric disorders also increases risk.4 Psychosocial factors, such as quality of the spousal relationship, parenting distress, and perceived parenting efficacy, contribute to paternal depression.
Similarly, depressed postpartum fathers experience higher levels of parenting distress and a lower sense of parenting efficacy.5 Interestingly, negative life events were associated with increased risk for depression in mothers, but not fathers.3
Clinical presentation
Paternal PPD symptoms appear within 12 months after the birth of the child and last for at least 2 weeks. Signs and symptoms of depression in men might not resemble those seen in postpartum women. Men tend to show aggression, increased or easy irritability, and agitation, and might not seek help for emotional issues as readily as women do. Typical symptoms of depression often are present, such as sleep disturbance or changes in sleep patterns, difficulty concentrating, memory problems, and feelings of worthlessness, hopelessness, inadequacy, and excess guilt with suicidal ideation.6
Making the diagnosis
Maternal PPD commonly is evaluated using the Edinburgh Postnatal Depression Scale- Partner (EDPS-P) or Postpartum Depression Screening Scale. However, studies are lacking to determine which diagnostic modality is most accurate for diagnosing paternal PPD.
A paternal PPD screening tool could include the EDPS-P administered to mothers. Edmonson et al2 determined an EDPS-P score of >10 was the optimal cut-off point for screening for paternal depression, with a sensitivity of 89.5% and a specificity of 78.2%, compared with a structured clinical interview. Fisher et al4 determined that the EDPS-P report was a reliable method for detecting paternal PPD compared with validated depression scales completed by fathers. Madsen et al5 determined the Gotland Male Depression Scale, which detects typical male depressive symptoms, also was effective in recognizing paternal PPD at 6 weeks postpartum.7
Treatment of paternal PPD
Specific treatment for paternal PPD has not been studied extensively. Psychotherapy targeted at interpersonal family relationships and parenting is indicated for mild depression, whereas a combination of psychotherapy and pharmacotherapy is recommended for moderate or severe depression.
Depending on specific patient factors, pharmacotherapy options include selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors, tricyclic antidepressants, and atypical antipsychotics.8 SSRIs often are used because of their efficacy and relative lack of serious side effects, as demonstrated in numerous trials.2 Recovery is more likely with combination therapy than monotherapy.9 Fathers with psychosis or suicidal ideation should be referred for inpatient treatment.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Paulson JF, Dauber S, Leiferman JA. Individual and combined effects of postpartum depression in mothers and fathers on parenting behavior. Pediatrics. 2006;118(2):659-668.
2. Edmondson OJ, Psychogiou L, Vlachos H, et al. Depression in fathers in the postnatal period: assessment of the Edinburgh Postnatal Depression Scale as a screening measure. J Affect Disord. 2010;125(1-3):365-368.
3. Schumacher M, Zubaran C, White G. Bringing birth-related paternal depression to the fore. Women Birth. 2008;21(2):65-70.
4. Fisher SD, Kopelman R, O’Hara MW. Partner report of paternal depression using the Edinburgh Postnatal Depression Scale-Partner. Arch Womens Ment Health. 2012;15(4):283-288.
5. Madsen SA, Juhl T. Paternal depression in the postnatal period assessed with traditional and male depression scales. Journal of Men’s Health and Gender. 2007;4(1):26-31.
6. Escribà-Agüir V, Artazcoz L. Gender differences in postpartum depression: a longitudinal cohort study. J Epidemiol Community Health. 2011;65(4):320-326.
7. Cuijpers P, van Straten A, Warmerdam L, et al. Psychotherapy versus the combination of psychotherapy and pharmacotherapy in the treatment of depression: a meta-analysis. Depress Anxiety. 2009;26(3):279-288.
8. Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation anti-depressants: a multiple-treatments meta-analysis. Lancet. 2009;373(9665):746-758.
9. Demontigny F, Girard ME, Lacharité C, et al. Psychosocial factors associated with paternal postnatal depression. J Affect Disord. 2013;15(150):44-49.
1. Paulson JF, Dauber S, Leiferman JA. Individual and combined effects of postpartum depression in mothers and fathers on parenting behavior. Pediatrics. 2006;118(2):659-668.
2. Edmondson OJ, Psychogiou L, Vlachos H, et al. Depression in fathers in the postnatal period: assessment of the Edinburgh Postnatal Depression Scale as a screening measure. J Affect Disord. 2010;125(1-3):365-368.
3. Schumacher M, Zubaran C, White G. Bringing birth-related paternal depression to the fore. Women Birth. 2008;21(2):65-70.
4. Fisher SD, Kopelman R, O’Hara MW. Partner report of paternal depression using the Edinburgh Postnatal Depression Scale-Partner. Arch Womens Ment Health. 2012;15(4):283-288.
5. Madsen SA, Juhl T. Paternal depression in the postnatal period assessed with traditional and male depression scales. Journal of Men’s Health and Gender. 2007;4(1):26-31.
6. Escribà-Agüir V, Artazcoz L. Gender differences in postpartum depression: a longitudinal cohort study. J Epidemiol Community Health. 2011;65(4):320-326.
7. Cuijpers P, van Straten A, Warmerdam L, et al. Psychotherapy versus the combination of psychotherapy and pharmacotherapy in the treatment of depression: a meta-analysis. Depress Anxiety. 2009;26(3):279-288.
8. Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation anti-depressants: a multiple-treatments meta-analysis. Lancet. 2009;373(9665):746-758.
9. Demontigny F, Girard ME, Lacharité C, et al. Psychosocial factors associated with paternal postnatal depression. J Affect Disord. 2013;15(150):44-49.
Some essentials to consider when opening a private psychiatric practice
Ah! the dream of opening private practice! Whether you’re a resident making less than minimum wage or a clinic employee seeing ever more patients, the allure is powerful. But, just because you’re whip-smart in matters of the mind, doesn’t mean you know how to run a business. To prevent your dream from succumbing to the siren’s allure, you’ll need to create a blueprint that gets you moving today, as well as prepare systems that will endure over the years.
Establish a business model
Before signing a lease or scheduling patients, think through these fundamental questions, not just from a clinical perspective but a business one as well:
• What kind of care would you like to provide? If you want to practice psychotherapy and medication, you’ll have fewer time slots to have to fill, but it may be more challenging to find patients who want and can afford psychotherapy from you as well.
• Where do you want to practice? Time spent commuting rarely produces income, so how close do you want your office to be to where you live? Being able to walk to work is wonderful, but is where you live the best location for your patients?
For example, downtown areas in big cities are good for providing a critical mass of patients, especially if you only want to manage patients’ medications. But if you want to see children and families, you should consider a location that is friendlier for them—usually more residential areas. Having a coffee shop nearby for waiting parents doesn’t hurt. If you work in a rural area, how easily can patients get to your office?
• Which hours do you want to work? Many patients will want to see you at “prime time”—before or after their work day or during the weekend. This might, not coincidentally, be when you don’t want to work. Consider whether there is room for compromise: Can you work 1 or 2 early or late days? Can you do 1 weekend day once in a while? If you want to see children, can you regularly be available after school?
• Will you accept insurance? Pros: The insurance companies will do the marketing for you; your practice will fill quickly; their checks don’t bounce; and, 98% of the time, the claims and payment process works just fine.
Cons: You will make less money per patient, in return for the higher volume of patients that are sent your way; the insurance companies won’t want to pay you more than they pay non-psychiatrists for psychotherapy; and the small amount of time that there are administrative problems can consume a disproportionate share of your sanity.
Run the numbers carefully
Next, think about the financial aspect. How much do you need to make, after you’ve paid business expenses and taxes, to be content? You might be tempted to work as many hours as possible, thinking that every hour off is an hour that you could have billed. Shifting your viewpoint from “hours lost” to “hours free” is a necessary approach to reduce burnout.
Once you have figured out your financial goal, do the math: multiply hours/ week × hourly rate × how many weeks/ year you’ll work to determine your annual income. Play around with the numbers to test your priorities, such as optimizing daily hours vs vacation time vs charging more or less.
Build your brand
This is your professional identity—the picture of your practice that your colleagues and future patients will see and that will start to get those hours filled. How will you convey your strengths and personality? The answer: Get out of the office.
• Take clinicians who will refer patients to you out to lunch (and pick up the tab).
• Give free talks to psychotherapists or primary care providers. Grand rounds, group practice meetings, or local clinical associations are potential venues. Give the organizer a menu of topic options that connect your clinical interests and theirs, and then create a dynamic presentation based on their feedback. Tip: Do not PowerPoint them to tears.
• Start blogging. If you enjoy writing, use a blog to showcase your talent and expertise. It is free advertising and makes you seem like a trusted authority. However, don’t start a blog unless you can commit to posting regularly.
Proceed thoughtfully; seek advice
As you think through the matrix of issues presented above, each set of answers may lead to a deeper set of questions. Consultation with a colleague or mentor can save you valuable time. Although you don’t have to have all the answers before you open your practice, spending time thinking through these and other issues beforehand will optimize the chance that your dream becomes a reality.
Disclosure
Dr. Braslow is the founder of Luminello.com.
Ah! the dream of opening private practice! Whether you’re a resident making less than minimum wage or a clinic employee seeing ever more patients, the allure is powerful. But, just because you’re whip-smart in matters of the mind, doesn’t mean you know how to run a business. To prevent your dream from succumbing to the siren’s allure, you’ll need to create a blueprint that gets you moving today, as well as prepare systems that will endure over the years.
Establish a business model
Before signing a lease or scheduling patients, think through these fundamental questions, not just from a clinical perspective but a business one as well:
• What kind of care would you like to provide? If you want to practice psychotherapy and medication, you’ll have fewer time slots to have to fill, but it may be more challenging to find patients who want and can afford psychotherapy from you as well.
• Where do you want to practice? Time spent commuting rarely produces income, so how close do you want your office to be to where you live? Being able to walk to work is wonderful, but is where you live the best location for your patients?
For example, downtown areas in big cities are good for providing a critical mass of patients, especially if you only want to manage patients’ medications. But if you want to see children and families, you should consider a location that is friendlier for them—usually more residential areas. Having a coffee shop nearby for waiting parents doesn’t hurt. If you work in a rural area, how easily can patients get to your office?
• Which hours do you want to work? Many patients will want to see you at “prime time”—before or after their work day or during the weekend. This might, not coincidentally, be when you don’t want to work. Consider whether there is room for compromise: Can you work 1 or 2 early or late days? Can you do 1 weekend day once in a while? If you want to see children, can you regularly be available after school?
• Will you accept insurance? Pros: The insurance companies will do the marketing for you; your practice will fill quickly; their checks don’t bounce; and, 98% of the time, the claims and payment process works just fine.
Cons: You will make less money per patient, in return for the higher volume of patients that are sent your way; the insurance companies won’t want to pay you more than they pay non-psychiatrists for psychotherapy; and the small amount of time that there are administrative problems can consume a disproportionate share of your sanity.
Run the numbers carefully
Next, think about the financial aspect. How much do you need to make, after you’ve paid business expenses and taxes, to be content? You might be tempted to work as many hours as possible, thinking that every hour off is an hour that you could have billed. Shifting your viewpoint from “hours lost” to “hours free” is a necessary approach to reduce burnout.
Once you have figured out your financial goal, do the math: multiply hours/ week × hourly rate × how many weeks/ year you’ll work to determine your annual income. Play around with the numbers to test your priorities, such as optimizing daily hours vs vacation time vs charging more or less.
Build your brand
This is your professional identity—the picture of your practice that your colleagues and future patients will see and that will start to get those hours filled. How will you convey your strengths and personality? The answer: Get out of the office.
• Take clinicians who will refer patients to you out to lunch (and pick up the tab).
• Give free talks to psychotherapists or primary care providers. Grand rounds, group practice meetings, or local clinical associations are potential venues. Give the organizer a menu of topic options that connect your clinical interests and theirs, and then create a dynamic presentation based on their feedback. Tip: Do not PowerPoint them to tears.
• Start blogging. If you enjoy writing, use a blog to showcase your talent and expertise. It is free advertising and makes you seem like a trusted authority. However, don’t start a blog unless you can commit to posting regularly.
Proceed thoughtfully; seek advice
As you think through the matrix of issues presented above, each set of answers may lead to a deeper set of questions. Consultation with a colleague or mentor can save you valuable time. Although you don’t have to have all the answers before you open your practice, spending time thinking through these and other issues beforehand will optimize the chance that your dream becomes a reality.
Disclosure
Dr. Braslow is the founder of Luminello.com.
Ah! the dream of opening private practice! Whether you’re a resident making less than minimum wage or a clinic employee seeing ever more patients, the allure is powerful. But, just because you’re whip-smart in matters of the mind, doesn’t mean you know how to run a business. To prevent your dream from succumbing to the siren’s allure, you’ll need to create a blueprint that gets you moving today, as well as prepare systems that will endure over the years.
Establish a business model
Before signing a lease or scheduling patients, think through these fundamental questions, not just from a clinical perspective but a business one as well:
• What kind of care would you like to provide? If you want to practice psychotherapy and medication, you’ll have fewer time slots to have to fill, but it may be more challenging to find patients who want and can afford psychotherapy from you as well.
• Where do you want to practice? Time spent commuting rarely produces income, so how close do you want your office to be to where you live? Being able to walk to work is wonderful, but is where you live the best location for your patients?
For example, downtown areas in big cities are good for providing a critical mass of patients, especially if you only want to manage patients’ medications. But if you want to see children and families, you should consider a location that is friendlier for them—usually more residential areas. Having a coffee shop nearby for waiting parents doesn’t hurt. If you work in a rural area, how easily can patients get to your office?
• Which hours do you want to work? Many patients will want to see you at “prime time”—before or after their work day or during the weekend. This might, not coincidentally, be when you don’t want to work. Consider whether there is room for compromise: Can you work 1 or 2 early or late days? Can you do 1 weekend day once in a while? If you want to see children, can you regularly be available after school?
• Will you accept insurance? Pros: The insurance companies will do the marketing for you; your practice will fill quickly; their checks don’t bounce; and, 98% of the time, the claims and payment process works just fine.
Cons: You will make less money per patient, in return for the higher volume of patients that are sent your way; the insurance companies won’t want to pay you more than they pay non-psychiatrists for psychotherapy; and the small amount of time that there are administrative problems can consume a disproportionate share of your sanity.
Run the numbers carefully
Next, think about the financial aspect. How much do you need to make, after you’ve paid business expenses and taxes, to be content? You might be tempted to work as many hours as possible, thinking that every hour off is an hour that you could have billed. Shifting your viewpoint from “hours lost” to “hours free” is a necessary approach to reduce burnout.
Once you have figured out your financial goal, do the math: multiply hours/ week × hourly rate × how many weeks/ year you’ll work to determine your annual income. Play around with the numbers to test your priorities, such as optimizing daily hours vs vacation time vs charging more or less.
Build your brand
This is your professional identity—the picture of your practice that your colleagues and future patients will see and that will start to get those hours filled. How will you convey your strengths and personality? The answer: Get out of the office.
• Take clinicians who will refer patients to you out to lunch (and pick up the tab).
• Give free talks to psychotherapists or primary care providers. Grand rounds, group practice meetings, or local clinical associations are potential venues. Give the organizer a menu of topic options that connect your clinical interests and theirs, and then create a dynamic presentation based on their feedback. Tip: Do not PowerPoint them to tears.
• Start blogging. If you enjoy writing, use a blog to showcase your talent and expertise. It is free advertising and makes you seem like a trusted authority. However, don’t start a blog unless you can commit to posting regularly.
Proceed thoughtfully; seek advice
As you think through the matrix of issues presented above, each set of answers may lead to a deeper set of questions. Consultation with a colleague or mentor can save you valuable time. Although you don’t have to have all the answers before you open your practice, spending time thinking through these and other issues beforehand will optimize the chance that your dream becomes a reality.
Disclosure
Dr. Braslow is the founder of Luminello.com.