User login
The Hospitalist only
Is a telehospitalist service right for you and your group?
Telemedicine “ripe for adoption” by hospitalists
For medical inpatients, the advent of virtual care began decades ago with telephones and the ability of physicians to give “verbal orders” while outside the hospital. It evolved into widespread adoption of pagers and is now ubiquitous through smart phones, texting, and HIPPA-compliant applications. In the past few years, inpatient telemedicine programs have been developed and studied including tele-ICU, telestroke, and now the telehospitalist.
Telemedicine is not new and has seen rapid adoption in the outpatient setting over the past decade,1 especially since the passing of telemedicine parity laws in 35 states to support equal reimbursement with face-to-face visits.2 In addition, 24 states have joined the Interstate Medical Licensure Compact (IMLC).3 This voluntary program provides an expedited pathway to licensure for qualified physicians who practice in multiple states. The goal is to increase access to care for patients in underserved and rural areas and to allow easier consultation through telemedicine. Combined, these two federal initiatives have lowered two major barriers to entry for telemedicine: reimbursement and credentialing.
Only a handful of papers have been published on the telehospitalist model with one of the first in 2007 in The Hospitalist reporting on the intersection between tele-ICU and telehospitalist care.4 More recent work describes the implementation of a telehospitalist program between a large university hospitalist program and a rural, critical access hospital.5 A key goal of this program, developed by Dr. Ethan Kuperman and colleagues at the University of Iowa, was to keep patients at the critical access hospital that previously would have been transferred. This has obvious benefits for patients, the critical access hospital, and the local community. It also benefited the tertiary care referral center, which was dealing with high occupancy rates. Keeping lower acuity patients at the critical access hospital helps maintain access for more complex patients at the referral center. This same principle has applied to the use of the tele-ICU where lower acuity ICU patients could remain in the small, rural ICU, and only those patients who the intensivist believes would benefit from a higher level of care in a tertiary center would be transferred.
As this study and others have shown, telemedicine is ripe for adoption by hospitalists. The bigger question is how should it fit into the current model of hospital medicine? There are several different applications we are familiar with and each has unique considerations. The first model, as applied in the Kuperman paper, is for a larger hospitalist program to provide a telehospitalist service to a smaller, unaffiliated hospital (for example, critical access hospitals) that employs nurse practitioners or physician assistants on site but can’t recruit or retain full-time hospitalist coverage. In this collaborative model of care, the local provider performs the physical exam but provides care under the guidance and supervision of a hospital medicine specialist. This is expected to improve outcomes and bring the benefits of hospital medicine, including improved outcomes and decreased hospital spending, to smaller communities.6 In this model, the critical access hospital pays a fee for the service and retains the billing to third party payers.
A variation on that model would provide telehospitalist services to other hospitals within an existing health care network (such as Kaiser Permanente, Intermountain Healthcare, government hospitals) that have different financial models with incentives to collaborate. The Veterans Health Administration is embarking on a pilot through the VA Office of Rural Health to provide a telehospitalist service to small rural VA hospitals using the consultative model during the day with a nurse practitioner at the local site and physician backup from the emergency department. Although existing night cross-coverage will be maintained by a physician on call, this telehospitalist service may also evolve into providing cross-coverage on nights and weekends.
A third would be like a locum tenens model in which telehospitalist services are contracted for short periods of time when coverage is needed for vacations or staff shortages. A fourth model of telehospitalist care would be to international areas in need of hospitalist expertise, like a medical mission model but without the expense or time required to travel. Other models will likely evolve based on the demand for services, supply of hospitalists, changes in regulations, and reimbursement.
Another important consideration is how this will evolve for the practicing hospitalist. Will we have dedicated virtual hospitalists, akin to the “nocturnist” who covers nights and weekends? Or will working on the telehospitalist service be in the rotation of duties like many programs have with teaching and “nonteaching” services, medical consultation, and even transition clinics and emergency department triage responsibilities? It could serve as a lower-intensity service that can be staffed during office-based time that would include scholarly work, quality improvement, and administrative duties. If financially viable, it could be mutually beneficial for both the provider and recipient sides of telehospitalist care.
For any of these models to work, technical aspects must be ironed-out. It is indispensable for the provider to have remote access to the electronic health record for data review, documentation, and placing orders if needed. Adequate broadband for effective video connection, accompanied by the appropriate HIPPA-compliant software and hardware must be in place. Although highly specialized hardware has been developed, including remote stethoscopes and otoscopes, the key component is a good camera and video screen on each end of the interaction. Based upon prior experience with telemedicine programs, establishment of trusting relationships with the receiving hospital staff, physicians, and nurse practitioners is also critical. Optimally, the telehospitalist would have an opportunity to travel to the remote site to meet with the local care team and learn about the local resources and community. Many other operational and logistical issues need to be considered and will be supported by the Society of Hospital Medicine through publications, online resources, and national and regional meeting educational content on telehospitalist programs.
As hospital medicine adopts the telehospitalist model, it brings with it important considerations. First, is how we embrace the concept of the medical virtualist, a term used to describe physicians who spend the majority or all of their time caring for patients using a virtual medium.7 We find it difficult to imagine spending all or the majority of our time as a virtual hospitalist, but years ago many could not imagine someone being a full-time hospitalist or nocturnist. Some individuals will see this as a career opportunity that allows them to work as a hospitalist regardless of where they live or where the hospital is located. That has obvious advantages for both career choice and the provision of hospital medicine expertise to low-resourced or low-volume settings, such as rural or international locations and nights and weekends.
Second, the telehospitalist model will require professional standards, training, reimbursement and coding adjustments, hardware and software development, and managing patient expectations for care.
Lastly, hospitals, health care systems, hospitalist groups, and even individual hospitalists will have to determine how best to take advantage of this innovative model of care to provide the highest possible quality, in a cost-efficient manner, that supports professional satisfaction and development.
Dr. Kaboli and Dr. Gutierrez are based at the Center for Access and Delivery Research and Evaluation (CADRE) at the Iowa City VA Healthcare System, the Veterans Rural Health Resource Center-Iowa City, VA Office of Rural Health, and the department of internal medicine, University of Iowa, both in Iowa City.
References
1. Barnett ML et al. Trends in telemedicine use in a large commercially insured population, 2005-2017. JAMA. 2018;320(20):2147-9.
2. American Telemedicine Association State Policy Resource Center. 2018; http://www.americantelemed.org/main/policy-page/state-policy-resource-center. Accessed 2018 Dec 14.
3. Interstate Medical Licensure Compact 2018; https://imlcc.org/. Accessed 2018 Dec 14.
4. Hengehold D. The telehospitalist. The Hospitalist. 2007;7(July). https://www.the-hospitalist.org/hospitalist/article/123381/telehospitalist. Accessed 2018 Dec 14.
5. Kuperman EF et al. The virtual hospitalist: A single-site implementation bringing hospitalist coverage to critical access hospitals. J Hosp Med. 2018;13(11):759-63.
6. Peterson MC. A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clinic proceedings. 2009;84(3):248-54.
7. Nochomovitz M, Sharma R. Is it time for a new medical specialty?: The medical virtualist. JAMA. 2018;319(5):437-8.
Telemedicine “ripe for adoption” by hospitalists
Telemedicine “ripe for adoption” by hospitalists
For medical inpatients, the advent of virtual care began decades ago with telephones and the ability of physicians to give “verbal orders” while outside the hospital. It evolved into widespread adoption of pagers and is now ubiquitous through smart phones, texting, and HIPPA-compliant applications. In the past few years, inpatient telemedicine programs have been developed and studied including tele-ICU, telestroke, and now the telehospitalist.
Telemedicine is not new and has seen rapid adoption in the outpatient setting over the past decade,1 especially since the passing of telemedicine parity laws in 35 states to support equal reimbursement with face-to-face visits.2 In addition, 24 states have joined the Interstate Medical Licensure Compact (IMLC).3 This voluntary program provides an expedited pathway to licensure for qualified physicians who practice in multiple states. The goal is to increase access to care for patients in underserved and rural areas and to allow easier consultation through telemedicine. Combined, these two federal initiatives have lowered two major barriers to entry for telemedicine: reimbursement and credentialing.
Only a handful of papers have been published on the telehospitalist model with one of the first in 2007 in The Hospitalist reporting on the intersection between tele-ICU and telehospitalist care.4 More recent work describes the implementation of a telehospitalist program between a large university hospitalist program and a rural, critical access hospital.5 A key goal of this program, developed by Dr. Ethan Kuperman and colleagues at the University of Iowa, was to keep patients at the critical access hospital that previously would have been transferred. This has obvious benefits for patients, the critical access hospital, and the local community. It also benefited the tertiary care referral center, which was dealing with high occupancy rates. Keeping lower acuity patients at the critical access hospital helps maintain access for more complex patients at the referral center. This same principle has applied to the use of the tele-ICU where lower acuity ICU patients could remain in the small, rural ICU, and only those patients who the intensivist believes would benefit from a higher level of care in a tertiary center would be transferred.
As this study and others have shown, telemedicine is ripe for adoption by hospitalists. The bigger question is how should it fit into the current model of hospital medicine? There are several different applications we are familiar with and each has unique considerations. The first model, as applied in the Kuperman paper, is for a larger hospitalist program to provide a telehospitalist service to a smaller, unaffiliated hospital (for example, critical access hospitals) that employs nurse practitioners or physician assistants on site but can’t recruit or retain full-time hospitalist coverage. In this collaborative model of care, the local provider performs the physical exam but provides care under the guidance and supervision of a hospital medicine specialist. This is expected to improve outcomes and bring the benefits of hospital medicine, including improved outcomes and decreased hospital spending, to smaller communities.6 In this model, the critical access hospital pays a fee for the service and retains the billing to third party payers.
A variation on that model would provide telehospitalist services to other hospitals within an existing health care network (such as Kaiser Permanente, Intermountain Healthcare, government hospitals) that have different financial models with incentives to collaborate. The Veterans Health Administration is embarking on a pilot through the VA Office of Rural Health to provide a telehospitalist service to small rural VA hospitals using the consultative model during the day with a nurse practitioner at the local site and physician backup from the emergency department. Although existing night cross-coverage will be maintained by a physician on call, this telehospitalist service may also evolve into providing cross-coverage on nights and weekends.
A third would be like a locum tenens model in which telehospitalist services are contracted for short periods of time when coverage is needed for vacations or staff shortages. A fourth model of telehospitalist care would be to international areas in need of hospitalist expertise, like a medical mission model but without the expense or time required to travel. Other models will likely evolve based on the demand for services, supply of hospitalists, changes in regulations, and reimbursement.
Another important consideration is how this will evolve for the practicing hospitalist. Will we have dedicated virtual hospitalists, akin to the “nocturnist” who covers nights and weekends? Or will working on the telehospitalist service be in the rotation of duties like many programs have with teaching and “nonteaching” services, medical consultation, and even transition clinics and emergency department triage responsibilities? It could serve as a lower-intensity service that can be staffed during office-based time that would include scholarly work, quality improvement, and administrative duties. If financially viable, it could be mutually beneficial for both the provider and recipient sides of telehospitalist care.
For any of these models to work, technical aspects must be ironed-out. It is indispensable for the provider to have remote access to the electronic health record for data review, documentation, and placing orders if needed. Adequate broadband for effective video connection, accompanied by the appropriate HIPPA-compliant software and hardware must be in place. Although highly specialized hardware has been developed, including remote stethoscopes and otoscopes, the key component is a good camera and video screen on each end of the interaction. Based upon prior experience with telemedicine programs, establishment of trusting relationships with the receiving hospital staff, physicians, and nurse practitioners is also critical. Optimally, the telehospitalist would have an opportunity to travel to the remote site to meet with the local care team and learn about the local resources and community. Many other operational and logistical issues need to be considered and will be supported by the Society of Hospital Medicine through publications, online resources, and national and regional meeting educational content on telehospitalist programs.
As hospital medicine adopts the telehospitalist model, it brings with it important considerations. First, is how we embrace the concept of the medical virtualist, a term used to describe physicians who spend the majority or all of their time caring for patients using a virtual medium.7 We find it difficult to imagine spending all or the majority of our time as a virtual hospitalist, but years ago many could not imagine someone being a full-time hospitalist or nocturnist. Some individuals will see this as a career opportunity that allows them to work as a hospitalist regardless of where they live or where the hospital is located. That has obvious advantages for both career choice and the provision of hospital medicine expertise to low-resourced or low-volume settings, such as rural or international locations and nights and weekends.
Second, the telehospitalist model will require professional standards, training, reimbursement and coding adjustments, hardware and software development, and managing patient expectations for care.
Lastly, hospitals, health care systems, hospitalist groups, and even individual hospitalists will have to determine how best to take advantage of this innovative model of care to provide the highest possible quality, in a cost-efficient manner, that supports professional satisfaction and development.
Dr. Kaboli and Dr. Gutierrez are based at the Center for Access and Delivery Research and Evaluation (CADRE) at the Iowa City VA Healthcare System, the Veterans Rural Health Resource Center-Iowa City, VA Office of Rural Health, and the department of internal medicine, University of Iowa, both in Iowa City.
References
1. Barnett ML et al. Trends in telemedicine use in a large commercially insured population, 2005-2017. JAMA. 2018;320(20):2147-9.
2. American Telemedicine Association State Policy Resource Center. 2018; http://www.americantelemed.org/main/policy-page/state-policy-resource-center. Accessed 2018 Dec 14.
3. Interstate Medical Licensure Compact 2018; https://imlcc.org/. Accessed 2018 Dec 14.
4. Hengehold D. The telehospitalist. The Hospitalist. 2007;7(July). https://www.the-hospitalist.org/hospitalist/article/123381/telehospitalist. Accessed 2018 Dec 14.
5. Kuperman EF et al. The virtual hospitalist: A single-site implementation bringing hospitalist coverage to critical access hospitals. J Hosp Med. 2018;13(11):759-63.
6. Peterson MC. A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clinic proceedings. 2009;84(3):248-54.
7. Nochomovitz M, Sharma R. Is it time for a new medical specialty?: The medical virtualist. JAMA. 2018;319(5):437-8.
For medical inpatients, the advent of virtual care began decades ago with telephones and the ability of physicians to give “verbal orders” while outside the hospital. It evolved into widespread adoption of pagers and is now ubiquitous through smart phones, texting, and HIPPA-compliant applications. In the past few years, inpatient telemedicine programs have been developed and studied including tele-ICU, telestroke, and now the telehospitalist.
Telemedicine is not new and has seen rapid adoption in the outpatient setting over the past decade,1 especially since the passing of telemedicine parity laws in 35 states to support equal reimbursement with face-to-face visits.2 In addition, 24 states have joined the Interstate Medical Licensure Compact (IMLC).3 This voluntary program provides an expedited pathway to licensure for qualified physicians who practice in multiple states. The goal is to increase access to care for patients in underserved and rural areas and to allow easier consultation through telemedicine. Combined, these two federal initiatives have lowered two major barriers to entry for telemedicine: reimbursement and credentialing.
Only a handful of papers have been published on the telehospitalist model with one of the first in 2007 in The Hospitalist reporting on the intersection between tele-ICU and telehospitalist care.4 More recent work describes the implementation of a telehospitalist program between a large university hospitalist program and a rural, critical access hospital.5 A key goal of this program, developed by Dr. Ethan Kuperman and colleagues at the University of Iowa, was to keep patients at the critical access hospital that previously would have been transferred. This has obvious benefits for patients, the critical access hospital, and the local community. It also benefited the tertiary care referral center, which was dealing with high occupancy rates. Keeping lower acuity patients at the critical access hospital helps maintain access for more complex patients at the referral center. This same principle has applied to the use of the tele-ICU where lower acuity ICU patients could remain in the small, rural ICU, and only those patients who the intensivist believes would benefit from a higher level of care in a tertiary center would be transferred.
As this study and others have shown, telemedicine is ripe for adoption by hospitalists. The bigger question is how should it fit into the current model of hospital medicine? There are several different applications we are familiar with and each has unique considerations. The first model, as applied in the Kuperman paper, is for a larger hospitalist program to provide a telehospitalist service to a smaller, unaffiliated hospital (for example, critical access hospitals) that employs nurse practitioners or physician assistants on site but can’t recruit or retain full-time hospitalist coverage. In this collaborative model of care, the local provider performs the physical exam but provides care under the guidance and supervision of a hospital medicine specialist. This is expected to improve outcomes and bring the benefits of hospital medicine, including improved outcomes and decreased hospital spending, to smaller communities.6 In this model, the critical access hospital pays a fee for the service and retains the billing to third party payers.
A variation on that model would provide telehospitalist services to other hospitals within an existing health care network (such as Kaiser Permanente, Intermountain Healthcare, government hospitals) that have different financial models with incentives to collaborate. The Veterans Health Administration is embarking on a pilot through the VA Office of Rural Health to provide a telehospitalist service to small rural VA hospitals using the consultative model during the day with a nurse practitioner at the local site and physician backup from the emergency department. Although existing night cross-coverage will be maintained by a physician on call, this telehospitalist service may also evolve into providing cross-coverage on nights and weekends.
A third would be like a locum tenens model in which telehospitalist services are contracted for short periods of time when coverage is needed for vacations or staff shortages. A fourth model of telehospitalist care would be to international areas in need of hospitalist expertise, like a medical mission model but without the expense or time required to travel. Other models will likely evolve based on the demand for services, supply of hospitalists, changes in regulations, and reimbursement.
Another important consideration is how this will evolve for the practicing hospitalist. Will we have dedicated virtual hospitalists, akin to the “nocturnist” who covers nights and weekends? Or will working on the telehospitalist service be in the rotation of duties like many programs have with teaching and “nonteaching” services, medical consultation, and even transition clinics and emergency department triage responsibilities? It could serve as a lower-intensity service that can be staffed during office-based time that would include scholarly work, quality improvement, and administrative duties. If financially viable, it could be mutually beneficial for both the provider and recipient sides of telehospitalist care.
For any of these models to work, technical aspects must be ironed-out. It is indispensable for the provider to have remote access to the electronic health record for data review, documentation, and placing orders if needed. Adequate broadband for effective video connection, accompanied by the appropriate HIPPA-compliant software and hardware must be in place. Although highly specialized hardware has been developed, including remote stethoscopes and otoscopes, the key component is a good camera and video screen on each end of the interaction. Based upon prior experience with telemedicine programs, establishment of trusting relationships with the receiving hospital staff, physicians, and nurse practitioners is also critical. Optimally, the telehospitalist would have an opportunity to travel to the remote site to meet with the local care team and learn about the local resources and community. Many other operational and logistical issues need to be considered and will be supported by the Society of Hospital Medicine through publications, online resources, and national and regional meeting educational content on telehospitalist programs.
As hospital medicine adopts the telehospitalist model, it brings with it important considerations. First, is how we embrace the concept of the medical virtualist, a term used to describe physicians who spend the majority or all of their time caring for patients using a virtual medium.7 We find it difficult to imagine spending all or the majority of our time as a virtual hospitalist, but years ago many could not imagine someone being a full-time hospitalist or nocturnist. Some individuals will see this as a career opportunity that allows them to work as a hospitalist regardless of where they live or where the hospital is located. That has obvious advantages for both career choice and the provision of hospital medicine expertise to low-resourced or low-volume settings, such as rural or international locations and nights and weekends.
Second, the telehospitalist model will require professional standards, training, reimbursement and coding adjustments, hardware and software development, and managing patient expectations for care.
Lastly, hospitals, health care systems, hospitalist groups, and even individual hospitalists will have to determine how best to take advantage of this innovative model of care to provide the highest possible quality, in a cost-efficient manner, that supports professional satisfaction and development.
Dr. Kaboli and Dr. Gutierrez are based at the Center for Access and Delivery Research and Evaluation (CADRE) at the Iowa City VA Healthcare System, the Veterans Rural Health Resource Center-Iowa City, VA Office of Rural Health, and the department of internal medicine, University of Iowa, both in Iowa City.
References
1. Barnett ML et al. Trends in telemedicine use in a large commercially insured population, 2005-2017. JAMA. 2018;320(20):2147-9.
2. American Telemedicine Association State Policy Resource Center. 2018; http://www.americantelemed.org/main/policy-page/state-policy-resource-center. Accessed 2018 Dec 14.
3. Interstate Medical Licensure Compact 2018; https://imlcc.org/. Accessed 2018 Dec 14.
4. Hengehold D. The telehospitalist. The Hospitalist. 2007;7(July). https://www.the-hospitalist.org/hospitalist/article/123381/telehospitalist. Accessed 2018 Dec 14.
5. Kuperman EF et al. The virtual hospitalist: A single-site implementation bringing hospitalist coverage to critical access hospitals. J Hosp Med. 2018;13(11):759-63.
6. Peterson MC. A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clinic proceedings. 2009;84(3):248-54.
7. Nochomovitz M, Sharma R. Is it time for a new medical specialty?: The medical virtualist. JAMA. 2018;319(5):437-8.
Advance care planning codes not being used
Starting in 2016, the Centers for Medicare & Medicaid Services began paying physicians for advance care planning discussions with the approval of two new codes: 99497 and 99498. The codes pay about $86 for the first 30 minutes of a face-to-face conversation with a patient, family member, and/or surrogate and about $75 for additional sessions. Services can be furnished in both inpatient and ambulatory settings, and payment is not limited to particular physician specialties.
In 2016, health care professionals in New England (Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont) billed Medicare 26,522 times for the advance care planning (ACP) codes for a total of 24,536 patients, which represented less than 1% of Medicare beneficiaries in New England at the time, according to Kimberly Pelland, MPH, of Healthcentric Advisors, Providence, R.I., and her colleagues. Most claims were billed in the office, followed by in nursing homes, and in hospitals; 40% of conversations occurred during an annual wellness visit (JAMA Intern Med. 2019 March 11. doi:10.1001/jamainternmed.2018.8107).
Internists billed Medicare the most for ACP claims (65%), followed by family physicians (22%) gerontologists (5%), and oncologist/hematologists (0.3%), according to the analysis based on 2016 Medicare claims data and Census Bureau data. A greater proportion of patients with ACP claims were female, aged 85 years or older, enrolled in hospice, and died in the study year. Patients had higher odds of having an ACP claim if they were older and had lower income, and if they had cancer, heart failure, stroke, chronic kidney disease, or dementia. Male patients who were Asian, black, and Hispanic had lower chances of having an ACP claim.
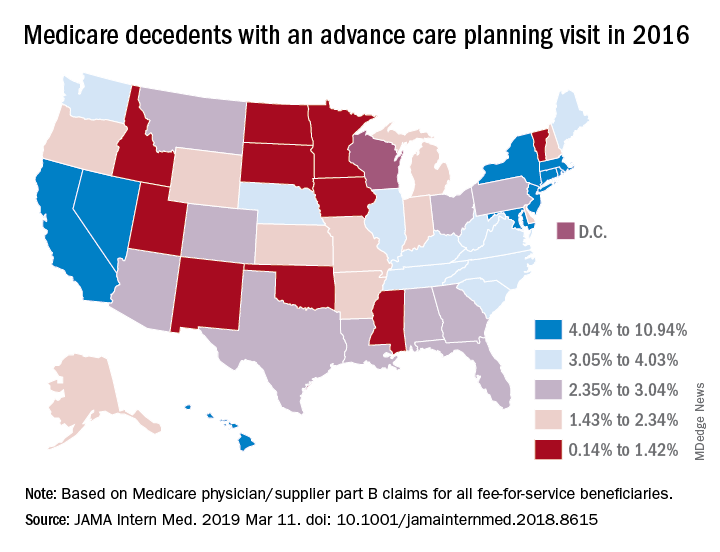
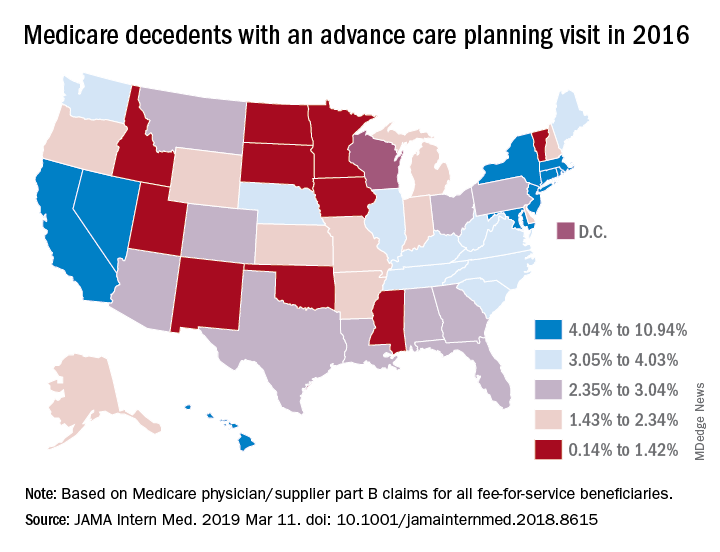
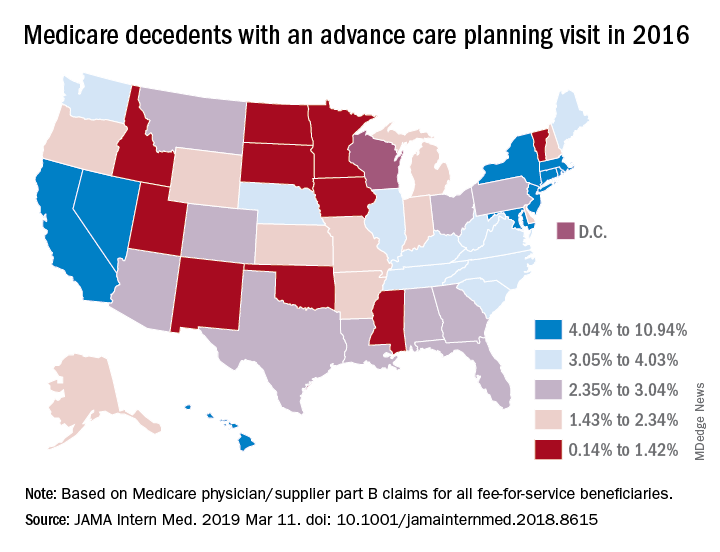
In a related study, Emmanuelle Belanger, PhD, of Brown University, Providence, R.I., and her colleagues examined national Medicare data from 2016 to the third quarter of 2017. Across the United States, 2% of Medicare patients aged 65 years and older received advance care planning services that were billed under the ACP codes (JAMA Intern Med. 2019 March 11. doi: 10.1001/jamainternmed.2018.8615). Visits billed under the ACP codes increased from 538,275 to 633,214 during the same time period. Claim rates were higher among patients who died within the study period, reaching 3% in 2016 and 6% in 2017. The percentage of decedents with an ACP billed visit varied strongly across states, with states such as North Dakota, South Dakota, and Wyoming having the fewest ACP visits billed and states such as California and Nevada having the most. ACP billed visits increased in all settings in 2017, but primarily in hospitals and nursing homes. Nationally, internists billed the codes most (48%), followed by family physicians (28%).
While the two studies indicate low usage of the ACP codes, many physicians are discussing advance care planning with their patients, said Mary M. Newman, MD, an internist based in Lutherville, Md., and former American College of Physicians adviser to the American Medical Association Relative Scale Value Update Committee (RUC).
“What cannot be captured by tracking under Medicare claims data are those shorter conversations that we have frequently,” Dr. Newman said in an interview. “If we have a short conversation about advance care planning, it gets folded into our evaluation and management visit. It’s not going to be separately billed.”
At the same time, some patients are not ready to discuss end-of-life options and decline the discussions when asked, Dr. Newman said. Particularly for healthier patients, end of life care is not a primary focus, she noted.
“Not everybody’s ready to have an advance care planning [discussion] that lasts 16-45 minutes,” she said. “Many people over age 65 are not ready to deal with advance care planning in their day-to-day lives, and it may not be what they wish to discuss. I offer the option to patients and some say, ‘Yes, I’d love to,’ and others decline or postpone.”
Low usage of the ACP codes may be associated with lack of awareness, uncertainty about appropriate code use, or associated billing that is not part of the standard workflow, Ankita Mehta, MD, of Mount Sinai in New York wrote an editorial accompanying the studies (JAMA Intern Med. 2019 March 11. doi:10.1001/jamainternmed.2018.8105).
“Regardless, the low rates of utilization of ACP codes is alarming and highlights the need to create strategies to integrate ACP discussions into standard practice and build ACP documentation and billing in clinical workflow,” Dr. Mehta said.
Dr. Newman agreed that more education among physicians is needed.
“The amount of education clinicians have received varies tremendously across the geography of the country,” she said. “I think the codes are going to be slowly adopted. The challenge to us is to make sure we’re all better educated on palliative care as people age and get sick and that we are sensitive to our patients explicit and implicit needs for these discussions.”
Starting in 2016, the Centers for Medicare & Medicaid Services began paying physicians for advance care planning discussions with the approval of two new codes: 99497 and 99498. The codes pay about $86 for the first 30 minutes of a face-to-face conversation with a patient, family member, and/or surrogate and about $75 for additional sessions. Services can be furnished in both inpatient and ambulatory settings, and payment is not limited to particular physician specialties.
In 2016, health care professionals in New England (Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont) billed Medicare 26,522 times for the advance care planning (ACP) codes for a total of 24,536 patients, which represented less than 1% of Medicare beneficiaries in New England at the time, according to Kimberly Pelland, MPH, of Healthcentric Advisors, Providence, R.I., and her colleagues. Most claims were billed in the office, followed by in nursing homes, and in hospitals; 40% of conversations occurred during an annual wellness visit (JAMA Intern Med. 2019 March 11. doi:10.1001/jamainternmed.2018.8107).
Internists billed Medicare the most for ACP claims (65%), followed by family physicians (22%) gerontologists (5%), and oncologist/hematologists (0.3%), according to the analysis based on 2016 Medicare claims data and Census Bureau data. A greater proportion of patients with ACP claims were female, aged 85 years or older, enrolled in hospice, and died in the study year. Patients had higher odds of having an ACP claim if they were older and had lower income, and if they had cancer, heart failure, stroke, chronic kidney disease, or dementia. Male patients who were Asian, black, and Hispanic had lower chances of having an ACP claim.
In a related study, Emmanuelle Belanger, PhD, of Brown University, Providence, R.I., and her colleagues examined national Medicare data from 2016 to the third quarter of 2017. Across the United States, 2% of Medicare patients aged 65 years and older received advance care planning services that were billed under the ACP codes (JAMA Intern Med. 2019 March 11. doi: 10.1001/jamainternmed.2018.8615). Visits billed under the ACP codes increased from 538,275 to 633,214 during the same time period. Claim rates were higher among patients who died within the study period, reaching 3% in 2016 and 6% in 2017. The percentage of decedents with an ACP billed visit varied strongly across states, with states such as North Dakota, South Dakota, and Wyoming having the fewest ACP visits billed and states such as California and Nevada having the most. ACP billed visits increased in all settings in 2017, but primarily in hospitals and nursing homes. Nationally, internists billed the codes most (48%), followed by family physicians (28%).
While the two studies indicate low usage of the ACP codes, many physicians are discussing advance care planning with their patients, said Mary M. Newman, MD, an internist based in Lutherville, Md., and former American College of Physicians adviser to the American Medical Association Relative Scale Value Update Committee (RUC).
“What cannot be captured by tracking under Medicare claims data are those shorter conversations that we have frequently,” Dr. Newman said in an interview. “If we have a short conversation about advance care planning, it gets folded into our evaluation and management visit. It’s not going to be separately billed.”
At the same time, some patients are not ready to discuss end-of-life options and decline the discussions when asked, Dr. Newman said. Particularly for healthier patients, end of life care is not a primary focus, she noted.
“Not everybody’s ready to have an advance care planning [discussion] that lasts 16-45 minutes,” she said. “Many people over age 65 are not ready to deal with advance care planning in their day-to-day lives, and it may not be what they wish to discuss. I offer the option to patients and some say, ‘Yes, I’d love to,’ and others decline or postpone.”
Low usage of the ACP codes may be associated with lack of awareness, uncertainty about appropriate code use, or associated billing that is not part of the standard workflow, Ankita Mehta, MD, of Mount Sinai in New York wrote an editorial accompanying the studies (JAMA Intern Med. 2019 March 11. doi:10.1001/jamainternmed.2018.8105).
“Regardless, the low rates of utilization of ACP codes is alarming and highlights the need to create strategies to integrate ACP discussions into standard practice and build ACP documentation and billing in clinical workflow,” Dr. Mehta said.
Dr. Newman agreed that more education among physicians is needed.
“The amount of education clinicians have received varies tremendously across the geography of the country,” she said. “I think the codes are going to be slowly adopted. The challenge to us is to make sure we’re all better educated on palliative care as people age and get sick and that we are sensitive to our patients explicit and implicit needs for these discussions.”
Starting in 2016, the Centers for Medicare & Medicaid Services began paying physicians for advance care planning discussions with the approval of two new codes: 99497 and 99498. The codes pay about $86 for the first 30 minutes of a face-to-face conversation with a patient, family member, and/or surrogate and about $75 for additional sessions. Services can be furnished in both inpatient and ambulatory settings, and payment is not limited to particular physician specialties.
In 2016, health care professionals in New England (Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont) billed Medicare 26,522 times for the advance care planning (ACP) codes for a total of 24,536 patients, which represented less than 1% of Medicare beneficiaries in New England at the time, according to Kimberly Pelland, MPH, of Healthcentric Advisors, Providence, R.I., and her colleagues. Most claims were billed in the office, followed by in nursing homes, and in hospitals; 40% of conversations occurred during an annual wellness visit (JAMA Intern Med. 2019 March 11. doi:10.1001/jamainternmed.2018.8107).
Internists billed Medicare the most for ACP claims (65%), followed by family physicians (22%) gerontologists (5%), and oncologist/hematologists (0.3%), according to the analysis based on 2016 Medicare claims data and Census Bureau data. A greater proportion of patients with ACP claims were female, aged 85 years or older, enrolled in hospice, and died in the study year. Patients had higher odds of having an ACP claim if they were older and had lower income, and if they had cancer, heart failure, stroke, chronic kidney disease, or dementia. Male patients who were Asian, black, and Hispanic had lower chances of having an ACP claim.
In a related study, Emmanuelle Belanger, PhD, of Brown University, Providence, R.I., and her colleagues examined national Medicare data from 2016 to the third quarter of 2017. Across the United States, 2% of Medicare patients aged 65 years and older received advance care planning services that were billed under the ACP codes (JAMA Intern Med. 2019 March 11. doi: 10.1001/jamainternmed.2018.8615). Visits billed under the ACP codes increased from 538,275 to 633,214 during the same time period. Claim rates were higher among patients who died within the study period, reaching 3% in 2016 and 6% in 2017. The percentage of decedents with an ACP billed visit varied strongly across states, with states such as North Dakota, South Dakota, and Wyoming having the fewest ACP visits billed and states such as California and Nevada having the most. ACP billed visits increased in all settings in 2017, but primarily in hospitals and nursing homes. Nationally, internists billed the codes most (48%), followed by family physicians (28%).
While the two studies indicate low usage of the ACP codes, many physicians are discussing advance care planning with their patients, said Mary M. Newman, MD, an internist based in Lutherville, Md., and former American College of Physicians adviser to the American Medical Association Relative Scale Value Update Committee (RUC).
“What cannot be captured by tracking under Medicare claims data are those shorter conversations that we have frequently,” Dr. Newman said in an interview. “If we have a short conversation about advance care planning, it gets folded into our evaluation and management visit. It’s not going to be separately billed.”
At the same time, some patients are not ready to discuss end-of-life options and decline the discussions when asked, Dr. Newman said. Particularly for healthier patients, end of life care is not a primary focus, she noted.
“Not everybody’s ready to have an advance care planning [discussion] that lasts 16-45 minutes,” she said. “Many people over age 65 are not ready to deal with advance care planning in their day-to-day lives, and it may not be what they wish to discuss. I offer the option to patients and some say, ‘Yes, I’d love to,’ and others decline or postpone.”
Low usage of the ACP codes may be associated with lack of awareness, uncertainty about appropriate code use, or associated billing that is not part of the standard workflow, Ankita Mehta, MD, of Mount Sinai in New York wrote an editorial accompanying the studies (JAMA Intern Med. 2019 March 11. doi:10.1001/jamainternmed.2018.8105).
“Regardless, the low rates of utilization of ACP codes is alarming and highlights the need to create strategies to integrate ACP discussions into standard practice and build ACP documentation and billing in clinical workflow,” Dr. Mehta said.
Dr. Newman agreed that more education among physicians is needed.
“The amount of education clinicians have received varies tremendously across the geography of the country,” she said. “I think the codes are going to be slowly adopted. The challenge to us is to make sure we’re all better educated on palliative care as people age and get sick and that we are sensitive to our patients explicit and implicit needs for these discussions.”
Prior authorization an increasing burden
The use of prior authorization for prescriptions and medical services has continued to increase in recent years, despite the consequences to continuity of care, according to a survey by the American Medical Association.

and 41% said that PA for medical services has done the same. The corresponding numbers for 5-year decreases in PAs were 2% and 1%, the AMA reported March 12.
Results of the survey, conducted in December 2018, also show that 85% of physicians believe that prior authorization sometimes, often, or always has a negative effect on the continuity of patients’ care. Almost 70% of respondents said that it is somewhat or extremely difficult to determine when PA is required for a prescription or medical service, and only 8% reported contracting with a health plan that offers programs to exempt physicians from the PA process, the AMA said.
“Physicians follow insurance protocols for prior authorization that require faxing recurring paperwork, multiple phone calls, and hours spent on hold. At the same time, patients’ lives can hang in the balance until health plans decide if needed care will qualify for insurance coverage,” AMA President Barbara L. McAneny, MD, said in a statement.
In January 2018, two organizations representing insurers – America’s Health Insurance Plans and the Blue Cross Blue Shield Association – signed onto a joint consensus statement with the AMA and other health care groups that provided five areas for improvement of the PA process. The current survey results show that “most health plans are not making meaningful progress on reforming the cumbersome prior authorization process,” the AMA said.
The use of prior authorization for prescriptions and medical services has continued to increase in recent years, despite the consequences to continuity of care, according to a survey by the American Medical Association.

and 41% said that PA for medical services has done the same. The corresponding numbers for 5-year decreases in PAs were 2% and 1%, the AMA reported March 12.
Results of the survey, conducted in December 2018, also show that 85% of physicians believe that prior authorization sometimes, often, or always has a negative effect on the continuity of patients’ care. Almost 70% of respondents said that it is somewhat or extremely difficult to determine when PA is required for a prescription or medical service, and only 8% reported contracting with a health plan that offers programs to exempt physicians from the PA process, the AMA said.
“Physicians follow insurance protocols for prior authorization that require faxing recurring paperwork, multiple phone calls, and hours spent on hold. At the same time, patients’ lives can hang in the balance until health plans decide if needed care will qualify for insurance coverage,” AMA President Barbara L. McAneny, MD, said in a statement.
In January 2018, two organizations representing insurers – America’s Health Insurance Plans and the Blue Cross Blue Shield Association – signed onto a joint consensus statement with the AMA and other health care groups that provided five areas for improvement of the PA process. The current survey results show that “most health plans are not making meaningful progress on reforming the cumbersome prior authorization process,” the AMA said.
The use of prior authorization for prescriptions and medical services has continued to increase in recent years, despite the consequences to continuity of care, according to a survey by the American Medical Association.

and 41% said that PA for medical services has done the same. The corresponding numbers for 5-year decreases in PAs were 2% and 1%, the AMA reported March 12.
Results of the survey, conducted in December 2018, also show that 85% of physicians believe that prior authorization sometimes, often, or always has a negative effect on the continuity of patients’ care. Almost 70% of respondents said that it is somewhat or extremely difficult to determine when PA is required for a prescription or medical service, and only 8% reported contracting with a health plan that offers programs to exempt physicians from the PA process, the AMA said.
“Physicians follow insurance protocols for prior authorization that require faxing recurring paperwork, multiple phone calls, and hours spent on hold. At the same time, patients’ lives can hang in the balance until health plans decide if needed care will qualify for insurance coverage,” AMA President Barbara L. McAneny, MD, said in a statement.
In January 2018, two organizations representing insurers – America’s Health Insurance Plans and the Blue Cross Blue Shield Association – signed onto a joint consensus statement with the AMA and other health care groups that provided five areas for improvement of the PA process. The current survey results show that “most health plans are not making meaningful progress on reforming the cumbersome prior authorization process,” the AMA said.
Hospitalist scheduling: A search for balance
Survey says ...
Scheduling. Has there ever been such a simple word that is so complex? A simple Internet search of hospitalist scheduling returns thousands of possible discussions, leaving readers to conclude that the possibilities are endless and the challenges great. The answer certainly is not a one-size-fits-all approach.
Hospitalist scheduling is one of the key sections in the 2018 State of Hospital Medicine (SoHM) report; the 2018 report delves deeper into hospitalist scheduling than ever before.
For those of you who have been regular users of prior SoHM reports, you should be pleasantly surprised to find new comparative values: There are nearly 50% more pages dedicated just to scheduling!
For those readers who have never subscribed to the SoHM Report, this is your chance to study how other groups approach hospitalist schedules.
Why is hospitalist scheduling such a hot topic? For one, flexible and sustainable scheduling is an important contributor to job satisfaction. It is important for hospitalists to have a high degree of input into managing and effecting change for personal work-life balance.
As John Nelson, MD, MHM, a cofounder of the Society of Hospital Medicine, wrote recently in The Hospitalist, “an optimal schedule alone isn’t the key to preventing it [burnout], but maybe a good schedule can reduce your risk you’ll suffer from it.”
Secondly, ensuring that the hospitalist team is right sized – that is, scheduling hospitalists in the right place at the right time – is an art. Using resources, such as the 2018 SoHM report, to identify quantifiable comparisons enables hospitalist groups to continuously ensure the hospitalist schedule meets the clinical demands while optimizing the hospitalist group’s schedule.
Unfilled positions
The 2018 SoHM report features a new section on unfilled positions that may provide insight and better understanding about how your group compares to others, as it relates to properly evaluating your recruitment pipeline.
For hospital medicine groups (HMGs) serving adults only, two out of three groups have unfilled positions, and about half of pediatric-only hospitalist groups have unfilled positions. Andrew White, MD, SFHM, associate professor of medicine at the University of Washington, Seattle, provided us with a deep-dive discussion of this topic in a recent article in The Hospitalist.
If your group has historically had more unfilled positions than the respondents, it might mean your group should consider different strategies to close the gap. It may also lead to conversations about how to rethink the schedule to better meet the demands of clinical care with limited resources.
So, with all these unfilled positions, how are hospitalist groups filling the gap? Not all groups are using locum tenens to fill those unfilled positions. About a third of hospitalist groups reported leaving those gaps uncovered.
The most commonly reported tactic to fill in the gaps was voluntary extra shifts by existing hospitalists (physicians and/or nurse practioners/physician assistants). This approach is used by 70% of hospitalist groups. The second most-used tactic was “moonlighters” or PRN physicians (57.4%). Thirdly, was use of locum tenens physicians.
With these baselines, we will be able to better track and trend the industry going forward.
Scheduling methodologies
For pediatric practices, the fixed rotating block scheduling has decreased over the two survey periods (16.7% versus 6.7%).
Even though the 7-on/7-off schedule remains quite popular among adult-only HMGs, many seasoned hospitalists wonder whether this is sustainable through all seasons of life. Some hospitalists have said a 7-on/7-off schedule is like turning on and off your personal life and that it takes a day or 2 to recover from 7 consecutive 12-hour days.
On the other hand, a fixed schedule is the easiest to explain, and many new hospitalists are requesting a fixed schedule. Even so, a fixed schedule may not allow for enough flexibility to adapt the schedule to the demands of patient care.
Nonetheless, a fixed schedule remains a very popular scheduling pattern. Does this scheduling model lead to burnout? Does this scheduling model increase or decrease elasticity? The debate of flexible versus fixed schedules continues!
Results by shift type
Very simply, the length of individual shifts has not changed much in prior years. For adult-only practices, most all day and night shifts are 12 hours in length. For pediatric-only HMGs, most day shifts are about 10 hours, and most night shifts are about 13 hours.
Most evening or swing shifts for adult-only practices are about 10 hours, which is a slight decrease from 2016. Pediatric-only practices’ evening shifts are about 8 hours in length.
A new question this year is about daytime admitters. For adult hospitalist groups, over half of groups have daytime admitters. For pediatric groups, nearly three out of four groups have daytime dedicated admitters. Also, the larger the group size, the more likely it is to have a dedicated daytime admitter.
Nocturnists remain in demand! Over 80% of adult hospitalist groups have on-site hospitalists at night. About a quarter of pediatric-only practices have nocturnists.
Scheduled workload distribution
One way of scheduling patient assignments is the phenomenon of unit-based assignments, or geographic rounding. As this has become more prevalent, the SHM Practice Analysis Committee recommended adding a question about unit-based assignments to the 2018 SoHM report.
The adoption of unit-based assignments is higher in academic groups (54.3%), as well as among hospitalists employed at a “hospital, health system or integrated delivery system” (47.4%), than in other group practice models.
Just as with the presence of daytime admitters, the larger the group the more likely it has some form of unit-based assignments. Further study would be needed to determine whether there is a link between the presence of daytime admitters and successful unit-based assignments for daytime rounders.
What’s the verdict?
Hospitalist scheduling will continue to evolve. It’s a never-ending balance of what’s best for patients and what’s best for hospitalists (and likely many other key stakeholders).
Scheduling is personal. Scheduling is an art form. The biggest question in this topic area is: Has anyone figured out the ‘secret sauce’ to hospitalist scheduling? Go online to SHM’s HMX to start the discussion!
Ms. Trask is national vice president of the Hospital Medicine Service Line at Catholic Health Initiatives in Englewood, Colo. She is also a member of The Hospitalist’s editorial advisory board.
Survey says ...
Survey says ...
Scheduling. Has there ever been such a simple word that is so complex? A simple Internet search of hospitalist scheduling returns thousands of possible discussions, leaving readers to conclude that the possibilities are endless and the challenges great. The answer certainly is not a one-size-fits-all approach.
Hospitalist scheduling is one of the key sections in the 2018 State of Hospital Medicine (SoHM) report; the 2018 report delves deeper into hospitalist scheduling than ever before.
For those of you who have been regular users of prior SoHM reports, you should be pleasantly surprised to find new comparative values: There are nearly 50% more pages dedicated just to scheduling!
For those readers who have never subscribed to the SoHM Report, this is your chance to study how other groups approach hospitalist schedules.
Why is hospitalist scheduling such a hot topic? For one, flexible and sustainable scheduling is an important contributor to job satisfaction. It is important for hospitalists to have a high degree of input into managing and effecting change for personal work-life balance.
As John Nelson, MD, MHM, a cofounder of the Society of Hospital Medicine, wrote recently in The Hospitalist, “an optimal schedule alone isn’t the key to preventing it [burnout], but maybe a good schedule can reduce your risk you’ll suffer from it.”
Secondly, ensuring that the hospitalist team is right sized – that is, scheduling hospitalists in the right place at the right time – is an art. Using resources, such as the 2018 SoHM report, to identify quantifiable comparisons enables hospitalist groups to continuously ensure the hospitalist schedule meets the clinical demands while optimizing the hospitalist group’s schedule.
Unfilled positions
The 2018 SoHM report features a new section on unfilled positions that may provide insight and better understanding about how your group compares to others, as it relates to properly evaluating your recruitment pipeline.
For hospital medicine groups (HMGs) serving adults only, two out of three groups have unfilled positions, and about half of pediatric-only hospitalist groups have unfilled positions. Andrew White, MD, SFHM, associate professor of medicine at the University of Washington, Seattle, provided us with a deep-dive discussion of this topic in a recent article in The Hospitalist.
If your group has historically had more unfilled positions than the respondents, it might mean your group should consider different strategies to close the gap. It may also lead to conversations about how to rethink the schedule to better meet the demands of clinical care with limited resources.
So, with all these unfilled positions, how are hospitalist groups filling the gap? Not all groups are using locum tenens to fill those unfilled positions. About a third of hospitalist groups reported leaving those gaps uncovered.
The most commonly reported tactic to fill in the gaps was voluntary extra shifts by existing hospitalists (physicians and/or nurse practioners/physician assistants). This approach is used by 70% of hospitalist groups. The second most-used tactic was “moonlighters” or PRN physicians (57.4%). Thirdly, was use of locum tenens physicians.
With these baselines, we will be able to better track and trend the industry going forward.
Scheduling methodologies
For pediatric practices, the fixed rotating block scheduling has decreased over the two survey periods (16.7% versus 6.7%).
Even though the 7-on/7-off schedule remains quite popular among adult-only HMGs, many seasoned hospitalists wonder whether this is sustainable through all seasons of life. Some hospitalists have said a 7-on/7-off schedule is like turning on and off your personal life and that it takes a day or 2 to recover from 7 consecutive 12-hour days.
On the other hand, a fixed schedule is the easiest to explain, and many new hospitalists are requesting a fixed schedule. Even so, a fixed schedule may not allow for enough flexibility to adapt the schedule to the demands of patient care.
Nonetheless, a fixed schedule remains a very popular scheduling pattern. Does this scheduling model lead to burnout? Does this scheduling model increase or decrease elasticity? The debate of flexible versus fixed schedules continues!
Results by shift type
Very simply, the length of individual shifts has not changed much in prior years. For adult-only practices, most all day and night shifts are 12 hours in length. For pediatric-only HMGs, most day shifts are about 10 hours, and most night shifts are about 13 hours.
Most evening or swing shifts for adult-only practices are about 10 hours, which is a slight decrease from 2016. Pediatric-only practices’ evening shifts are about 8 hours in length.
A new question this year is about daytime admitters. For adult hospitalist groups, over half of groups have daytime admitters. For pediatric groups, nearly three out of four groups have daytime dedicated admitters. Also, the larger the group size, the more likely it is to have a dedicated daytime admitter.
Nocturnists remain in demand! Over 80% of adult hospitalist groups have on-site hospitalists at night. About a quarter of pediatric-only practices have nocturnists.
Scheduled workload distribution
One way of scheduling patient assignments is the phenomenon of unit-based assignments, or geographic rounding. As this has become more prevalent, the SHM Practice Analysis Committee recommended adding a question about unit-based assignments to the 2018 SoHM report.
The adoption of unit-based assignments is higher in academic groups (54.3%), as well as among hospitalists employed at a “hospital, health system or integrated delivery system” (47.4%), than in other group practice models.
Just as with the presence of daytime admitters, the larger the group the more likely it has some form of unit-based assignments. Further study would be needed to determine whether there is a link between the presence of daytime admitters and successful unit-based assignments for daytime rounders.
What’s the verdict?
Hospitalist scheduling will continue to evolve. It’s a never-ending balance of what’s best for patients and what’s best for hospitalists (and likely many other key stakeholders).
Scheduling is personal. Scheduling is an art form. The biggest question in this topic area is: Has anyone figured out the ‘secret sauce’ to hospitalist scheduling? Go online to SHM’s HMX to start the discussion!
Ms. Trask is national vice president of the Hospital Medicine Service Line at Catholic Health Initiatives in Englewood, Colo. She is also a member of The Hospitalist’s editorial advisory board.
Scheduling. Has there ever been such a simple word that is so complex? A simple Internet search of hospitalist scheduling returns thousands of possible discussions, leaving readers to conclude that the possibilities are endless and the challenges great. The answer certainly is not a one-size-fits-all approach.
Hospitalist scheduling is one of the key sections in the 2018 State of Hospital Medicine (SoHM) report; the 2018 report delves deeper into hospitalist scheduling than ever before.
For those of you who have been regular users of prior SoHM reports, you should be pleasantly surprised to find new comparative values: There are nearly 50% more pages dedicated just to scheduling!
For those readers who have never subscribed to the SoHM Report, this is your chance to study how other groups approach hospitalist schedules.
Why is hospitalist scheduling such a hot topic? For one, flexible and sustainable scheduling is an important contributor to job satisfaction. It is important for hospitalists to have a high degree of input into managing and effecting change for personal work-life balance.
As John Nelson, MD, MHM, a cofounder of the Society of Hospital Medicine, wrote recently in The Hospitalist, “an optimal schedule alone isn’t the key to preventing it [burnout], but maybe a good schedule can reduce your risk you’ll suffer from it.”
Secondly, ensuring that the hospitalist team is right sized – that is, scheduling hospitalists in the right place at the right time – is an art. Using resources, such as the 2018 SoHM report, to identify quantifiable comparisons enables hospitalist groups to continuously ensure the hospitalist schedule meets the clinical demands while optimizing the hospitalist group’s schedule.
Unfilled positions
The 2018 SoHM report features a new section on unfilled positions that may provide insight and better understanding about how your group compares to others, as it relates to properly evaluating your recruitment pipeline.
For hospital medicine groups (HMGs) serving adults only, two out of three groups have unfilled positions, and about half of pediatric-only hospitalist groups have unfilled positions. Andrew White, MD, SFHM, associate professor of medicine at the University of Washington, Seattle, provided us with a deep-dive discussion of this topic in a recent article in The Hospitalist.
If your group has historically had more unfilled positions than the respondents, it might mean your group should consider different strategies to close the gap. It may also lead to conversations about how to rethink the schedule to better meet the demands of clinical care with limited resources.
So, with all these unfilled positions, how are hospitalist groups filling the gap? Not all groups are using locum tenens to fill those unfilled positions. About a third of hospitalist groups reported leaving those gaps uncovered.
The most commonly reported tactic to fill in the gaps was voluntary extra shifts by existing hospitalists (physicians and/or nurse practioners/physician assistants). This approach is used by 70% of hospitalist groups. The second most-used tactic was “moonlighters” or PRN physicians (57.4%). Thirdly, was use of locum tenens physicians.
With these baselines, we will be able to better track and trend the industry going forward.
Scheduling methodologies
For pediatric practices, the fixed rotating block scheduling has decreased over the two survey periods (16.7% versus 6.7%).
Even though the 7-on/7-off schedule remains quite popular among adult-only HMGs, many seasoned hospitalists wonder whether this is sustainable through all seasons of life. Some hospitalists have said a 7-on/7-off schedule is like turning on and off your personal life and that it takes a day or 2 to recover from 7 consecutive 12-hour days.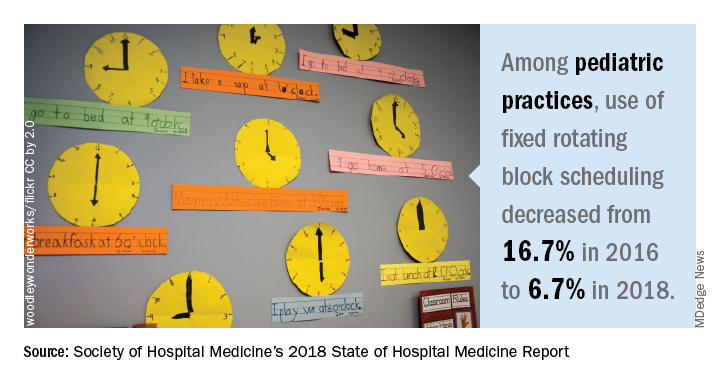
On the other hand, a fixed schedule is the easiest to explain, and many new hospitalists are requesting a fixed schedule. Even so, a fixed schedule may not allow for enough flexibility to adapt the schedule to the demands of patient care.
Nonetheless, a fixed schedule remains a very popular scheduling pattern. Does this scheduling model lead to burnout? Does this scheduling model increase or decrease elasticity? The debate of flexible versus fixed schedules continues!
Results by shift type
Very simply, the length of individual shifts has not changed much in prior years. For adult-only practices, most all day and night shifts are 12 hours in length. For pediatric-only HMGs, most day shifts are about 10 hours, and most night shifts are about 13 hours.
Most evening or swing shifts for adult-only practices are about 10 hours, which is a slight decrease from 2016. Pediatric-only practices’ evening shifts are about 8 hours in length.
A new question this year is about daytime admitters. For adult hospitalist groups, over half of groups have daytime admitters. For pediatric groups, nearly three out of four groups have daytime dedicated admitters. Also, the larger the group size, the more likely it is to have a dedicated daytime admitter.
Nocturnists remain in demand! Over 80% of adult hospitalist groups have on-site hospitalists at night. About a quarter of pediatric-only practices have nocturnists.
Scheduled workload distribution
One way of scheduling patient assignments is the phenomenon of unit-based assignments, or geographic rounding. As this has become more prevalent, the SHM Practice Analysis Committee recommended adding a question about unit-based assignments to the 2018 SoHM report.
The adoption of unit-based assignments is higher in academic groups (54.3%), as well as among hospitalists employed at a “hospital, health system or integrated delivery system” (47.4%), than in other group practice models.
Just as with the presence of daytime admitters, the larger the group the more likely it has some form of unit-based assignments. Further study would be needed to determine whether there is a link between the presence of daytime admitters and successful unit-based assignments for daytime rounders.
What’s the verdict?
Hospitalist scheduling will continue to evolve. It’s a never-ending balance of what’s best for patients and what’s best for hospitalists (and likely many other key stakeholders).
Scheduling is personal. Scheduling is an art form. The biggest question in this topic area is: Has anyone figured out the ‘secret sauce’ to hospitalist scheduling? Go online to SHM’s HMX to start the discussion!
Ms. Trask is national vice president of the Hospital Medicine Service Line at Catholic Health Initiatives in Englewood, Colo. She is also a member of The Hospitalist’s editorial advisory board.
Groups of physicians produce more accurate diagnoses than individuals
Groups of physicians and trainees diagnose clinical cases with more accuracy than individuals, according to a study of solo and aggregate diagnoses collected through an online medical teaching platform.
“These findings suggest that using the concept of collective intelligence to pool many physicians’ diagnoses could be a scalable approach to improve diagnostic accuracy,” wrote lead author Michael L. Barnett, MD, of Harvard University in Boston and his coauthors, adding that “groups of all sizes outperformed individual subspecialists on cases in their own subspecialty.” The study was published online in JAMA Network Open.
This cross-sectional study examined 1,572 cases solved within the Human Diagnosis Project (Human Dx) system, an online platform for authoring and diagnosing teaching cases. The system presents real-life cases from clinical practices and asks respondents to generate ranked differential diagnoses. Cases are tagged for specialties based on both intended diagnoses and the top diagnoses chosen by respondents. All cases used in this study were authored between May 7, 2014, and October 5, 2016, and had 10 or more respondents.
Of the 2,069 attending physicians and fellows, residents, and medical students (users) who solved cases within the Human Dx system, 1,452 (70.2%) were trained in internal medicine, 1,228 (59.4%) were residents or fellows, 431 (20.8%) were attending physicians, and 410 (19.8%) were medical students. To create a collective differential, Dr. Barnett and his colleagues aggregated the responses of up to nine participants via a weighted combination of each clinician’s top three diagnoses, which they dubbed “collective intelligence.”
The diagnostic accuracy for groups of nine was 85.6% (95% confidence interval, 83.9%-87.4%), compared with individual users at 62.5% (95% CI, 60.1%-64.9%), a difference of 23% (95% CI, 14.9%-31.2%; P less than .001). Groups of five saw a 17.8% difference in accuracy versus an individual (95% CI, 14.0%-21.6%; P less than .001), compared with 12.5% for groups of two (95% CI, 9.3%-15.8%; P less than .001). Taken together, these seem to underline an association between larger groups and increased accuracy.
Individual specialists solved cases in their particular areas with a diagnostic accuracy of 66.3% (95% CI, 59.1%-73.5%), compared with nonmatched specialty accuracy of 63.9% (95% CI, 56.6%-71.2%). Groups, however, outperformed specialists across the board: 77.7% accuracy for a group of 2 (95% CI, 70.1%-84.6%; P less than .001) and 85.5% accuracy for a group of 9 (95% CI, 75.1%-95.9%; P less than .001).
The coauthors shared the limitations of their study, including the possibility that the users who contributed these cases to Human Dx may not be representative of the medical community as a whole. They also noted that, while their 431 attending physicians constituted the “largest number ... to date in a study of collective intelligence,” trainees still made up almost 80% of users. In addition, they acknowledged that Human Dx was not designed to generate collective diagnoses nor assess collective intelligence; another platform created with that ability in mind may have returned different results. Finally, they were unable to assess how exactly greater accuracy would have been linked to changes in treatment, calling it “an important question for future work.”
The authors disclosed several conflicts of interest. One doctor reported receiving personal fees from Greylock McKinnon Associates; another reported receiving personal fees from the Human Diagnosis Project and serving as their nonprofit director during the study. A third doctor reported consulting for a company that makes patient-safety monitoring systems and receiving compensation from a not-for-profit incubator, along with having equity in three medical data and software companies.
SOURCE: Barnett ML et al. JAMA Netw Open. 2019 Mar 1. doi: 10.1001/jamanetworkopen.2019.0096.
Although this study from Barnett et al. is not the silver bullet for misdiagnosis, better understanding why physicians make mistakes is a necessary and valuable undertaking, according to Stephan D. Fihn, MD, of the University of Washington, Seattle.
In the past, the “correct” diagnostic approach included making a list of potential diagnoses and systematically ruling them out one by one, a process conveyed via clinicopathologic conferences in teaching hospitals. These, Dr. Fihn recalled, lasted until medical educators recognized them as “more ... theatrical events than meaningful teaching exercises” and understood that master clinicians did not actually think in the manner this approach modeled. Since then, the maturation of cognitive psychology and “a growing literature” have made diagnostic error seem like a common, sometimes unavoidable element of being human.
What can be done? Computers have always been a possibility, but “none have achieved the breadth of content and accuracy necessary to be adopted to any great extent,” Dr. Fihn wrote. Another option is crowdsourcing, as described in this study from Barnett and colleagues. Their approach has its pitfalls: A 62.5% level of diagnostic accuracy from individuals is not very high, which suggests either difficult cases or a preponderance of inexperienced clinicians who may benefit from collective intelligence even more. Regardless, he stated, “clinicians need to be cognizant of their own inherent limitations and acknowledge fallibility”; being humble and willing to seek advice “remain important, albeit imperfect, antidotes to misdiagnosis.”
These comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Mar 1. doi: 10.1001/jamanetworkopen.2019.1071 ). No conflicts of interest were reported.
Although this study from Barnett et al. is not the silver bullet for misdiagnosis, better understanding why physicians make mistakes is a necessary and valuable undertaking, according to Stephan D. Fihn, MD, of the University of Washington, Seattle.
In the past, the “correct” diagnostic approach included making a list of potential diagnoses and systematically ruling them out one by one, a process conveyed via clinicopathologic conferences in teaching hospitals. These, Dr. Fihn recalled, lasted until medical educators recognized them as “more ... theatrical events than meaningful teaching exercises” and understood that master clinicians did not actually think in the manner this approach modeled. Since then, the maturation of cognitive psychology and “a growing literature” have made diagnostic error seem like a common, sometimes unavoidable element of being human.
What can be done? Computers have always been a possibility, but “none have achieved the breadth of content and accuracy necessary to be adopted to any great extent,” Dr. Fihn wrote. Another option is crowdsourcing, as described in this study from Barnett and colleagues. Their approach has its pitfalls: A 62.5% level of diagnostic accuracy from individuals is not very high, which suggests either difficult cases or a preponderance of inexperienced clinicians who may benefit from collective intelligence even more. Regardless, he stated, “clinicians need to be cognizant of their own inherent limitations and acknowledge fallibility”; being humble and willing to seek advice “remain important, albeit imperfect, antidotes to misdiagnosis.”
These comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Mar 1. doi: 10.1001/jamanetworkopen.2019.1071 ). No conflicts of interest were reported.
Although this study from Barnett et al. is not the silver bullet for misdiagnosis, better understanding why physicians make mistakes is a necessary and valuable undertaking, according to Stephan D. Fihn, MD, of the University of Washington, Seattle.
In the past, the “correct” diagnostic approach included making a list of potential diagnoses and systematically ruling them out one by one, a process conveyed via clinicopathologic conferences in teaching hospitals. These, Dr. Fihn recalled, lasted until medical educators recognized them as “more ... theatrical events than meaningful teaching exercises” and understood that master clinicians did not actually think in the manner this approach modeled. Since then, the maturation of cognitive psychology and “a growing literature” have made diagnostic error seem like a common, sometimes unavoidable element of being human.
What can be done? Computers have always been a possibility, but “none have achieved the breadth of content and accuracy necessary to be adopted to any great extent,” Dr. Fihn wrote. Another option is crowdsourcing, as described in this study from Barnett and colleagues. Their approach has its pitfalls: A 62.5% level of diagnostic accuracy from individuals is not very high, which suggests either difficult cases or a preponderance of inexperienced clinicians who may benefit from collective intelligence even more. Regardless, he stated, “clinicians need to be cognizant of their own inherent limitations and acknowledge fallibility”; being humble and willing to seek advice “remain important, albeit imperfect, antidotes to misdiagnosis.”
These comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Mar 1. doi: 10.1001/jamanetworkopen.2019.1071 ). No conflicts of interest were reported.
Groups of physicians and trainees diagnose clinical cases with more accuracy than individuals, according to a study of solo and aggregate diagnoses collected through an online medical teaching platform.
“These findings suggest that using the concept of collective intelligence to pool many physicians’ diagnoses could be a scalable approach to improve diagnostic accuracy,” wrote lead author Michael L. Barnett, MD, of Harvard University in Boston and his coauthors, adding that “groups of all sizes outperformed individual subspecialists on cases in their own subspecialty.” The study was published online in JAMA Network Open.
This cross-sectional study examined 1,572 cases solved within the Human Diagnosis Project (Human Dx) system, an online platform for authoring and diagnosing teaching cases. The system presents real-life cases from clinical practices and asks respondents to generate ranked differential diagnoses. Cases are tagged for specialties based on both intended diagnoses and the top diagnoses chosen by respondents. All cases used in this study were authored between May 7, 2014, and October 5, 2016, and had 10 or more respondents.
Of the 2,069 attending physicians and fellows, residents, and medical students (users) who solved cases within the Human Dx system, 1,452 (70.2%) were trained in internal medicine, 1,228 (59.4%) were residents or fellows, 431 (20.8%) were attending physicians, and 410 (19.8%) were medical students. To create a collective differential, Dr. Barnett and his colleagues aggregated the responses of up to nine participants via a weighted combination of each clinician’s top three diagnoses, which they dubbed “collective intelligence.”
The diagnostic accuracy for groups of nine was 85.6% (95% confidence interval, 83.9%-87.4%), compared with individual users at 62.5% (95% CI, 60.1%-64.9%), a difference of 23% (95% CI, 14.9%-31.2%; P less than .001). Groups of five saw a 17.8% difference in accuracy versus an individual (95% CI, 14.0%-21.6%; P less than .001), compared with 12.5% for groups of two (95% CI, 9.3%-15.8%; P less than .001). Taken together, these seem to underline an association between larger groups and increased accuracy.
Individual specialists solved cases in their particular areas with a diagnostic accuracy of 66.3% (95% CI, 59.1%-73.5%), compared with nonmatched specialty accuracy of 63.9% (95% CI, 56.6%-71.2%). Groups, however, outperformed specialists across the board: 77.7% accuracy for a group of 2 (95% CI, 70.1%-84.6%; P less than .001) and 85.5% accuracy for a group of 9 (95% CI, 75.1%-95.9%; P less than .001).
The coauthors shared the limitations of their study, including the possibility that the users who contributed these cases to Human Dx may not be representative of the medical community as a whole. They also noted that, while their 431 attending physicians constituted the “largest number ... to date in a study of collective intelligence,” trainees still made up almost 80% of users. In addition, they acknowledged that Human Dx was not designed to generate collective diagnoses nor assess collective intelligence; another platform created with that ability in mind may have returned different results. Finally, they were unable to assess how exactly greater accuracy would have been linked to changes in treatment, calling it “an important question for future work.”
The authors disclosed several conflicts of interest. One doctor reported receiving personal fees from Greylock McKinnon Associates; another reported receiving personal fees from the Human Diagnosis Project and serving as their nonprofit director during the study. A third doctor reported consulting for a company that makes patient-safety monitoring systems and receiving compensation from a not-for-profit incubator, along with having equity in three medical data and software companies.
SOURCE: Barnett ML et al. JAMA Netw Open. 2019 Mar 1. doi: 10.1001/jamanetworkopen.2019.0096.
Groups of physicians and trainees diagnose clinical cases with more accuracy than individuals, according to a study of solo and aggregate diagnoses collected through an online medical teaching platform.
“These findings suggest that using the concept of collective intelligence to pool many physicians’ diagnoses could be a scalable approach to improve diagnostic accuracy,” wrote lead author Michael L. Barnett, MD, of Harvard University in Boston and his coauthors, adding that “groups of all sizes outperformed individual subspecialists on cases in their own subspecialty.” The study was published online in JAMA Network Open.
This cross-sectional study examined 1,572 cases solved within the Human Diagnosis Project (Human Dx) system, an online platform for authoring and diagnosing teaching cases. The system presents real-life cases from clinical practices and asks respondents to generate ranked differential diagnoses. Cases are tagged for specialties based on both intended diagnoses and the top diagnoses chosen by respondents. All cases used in this study were authored between May 7, 2014, and October 5, 2016, and had 10 or more respondents.
Of the 2,069 attending physicians and fellows, residents, and medical students (users) who solved cases within the Human Dx system, 1,452 (70.2%) were trained in internal medicine, 1,228 (59.4%) were residents or fellows, 431 (20.8%) were attending physicians, and 410 (19.8%) were medical students. To create a collective differential, Dr. Barnett and his colleagues aggregated the responses of up to nine participants via a weighted combination of each clinician’s top three diagnoses, which they dubbed “collective intelligence.”
The diagnostic accuracy for groups of nine was 85.6% (95% confidence interval, 83.9%-87.4%), compared with individual users at 62.5% (95% CI, 60.1%-64.9%), a difference of 23% (95% CI, 14.9%-31.2%; P less than .001). Groups of five saw a 17.8% difference in accuracy versus an individual (95% CI, 14.0%-21.6%; P less than .001), compared with 12.5% for groups of two (95% CI, 9.3%-15.8%; P less than .001). Taken together, these seem to underline an association between larger groups and increased accuracy.
Individual specialists solved cases in their particular areas with a diagnostic accuracy of 66.3% (95% CI, 59.1%-73.5%), compared with nonmatched specialty accuracy of 63.9% (95% CI, 56.6%-71.2%). Groups, however, outperformed specialists across the board: 77.7% accuracy for a group of 2 (95% CI, 70.1%-84.6%; P less than .001) and 85.5% accuracy for a group of 9 (95% CI, 75.1%-95.9%; P less than .001).
The coauthors shared the limitations of their study, including the possibility that the users who contributed these cases to Human Dx may not be representative of the medical community as a whole. They also noted that, while their 431 attending physicians constituted the “largest number ... to date in a study of collective intelligence,” trainees still made up almost 80% of users. In addition, they acknowledged that Human Dx was not designed to generate collective diagnoses nor assess collective intelligence; another platform created with that ability in mind may have returned different results. Finally, they were unable to assess how exactly greater accuracy would have been linked to changes in treatment, calling it “an important question for future work.”
The authors disclosed several conflicts of interest. One doctor reported receiving personal fees from Greylock McKinnon Associates; another reported receiving personal fees from the Human Diagnosis Project and serving as their nonprofit director during the study. A third doctor reported consulting for a company that makes patient-safety monitoring systems and receiving compensation from a not-for-profit incubator, along with having equity in three medical data and software companies.
SOURCE: Barnett ML et al. JAMA Netw Open. 2019 Mar 1. doi: 10.1001/jamanetworkopen.2019.0096.
FROM JAMA NETWORK OPEN
AAP: Treating patients during disasters raises liability risks
In a 2019 technical report, the AAP outlines common claims that can arise when treating children during disasters and how certain circumstances can force you to deviate from routine medical practices. In an accompanying policy statement by the AAP committee on medical liability and risk management, recommendations are offered for how to prepare for and prevent such legal risks.
During disasters, liability dangers can increase when circumstances “devolve into an environment of limited choices for both patients and providers,” and you have fewer treatment options available to you, according to the guidance authored by New York pediatrician Dr. Robin L. Altman and her associates.
Common claims that stem from treating patients during disasters are negligence, abandonment, and lack of informed consent. The AAP technical report offers examples about how these accusations can occur, including:
- When during a disaster, you are forced to alter treatment because of scarce medical supplies or equipment, you may later be accused of negligence if the patient’s outcome is negatively affected by the modified treatment.
- When a disaster progresses to overwhelming conditions, and you must practice in an altered health care environment that demands atypical actions, such actions may later be questioned and be accused of providing suboptimal care. Documentation of medical decision making for instance, a primary defense for one’s actions, may be compromised because of an inoperable electronic medical record. Similarly, past medical history may be unavailable, which may impact the appropriateness of care provision.
- In chaotic conditions, you may have to stop treating some patients to focus their time and resources elsewhere, which may lead to an abandonment claim, defined as unilateral termination of a physician-patient relationship – without proper patient notice – when treatment is still required. An abandonment claim also may arise when you have to make decisions in extreme conditions about which patients to transfer or evacuate first and whom to leave behind.
- When providing medical care to children during disasters, a lack of informed consent claim can arise if adequate parental permission is unattainable. This may result from families that are separated or displaced children in need of medical care.
Other claims that can arise from providing care during disasters include HIPAA breaches, licensing violations, discrimination claims, and Emergency Medical Treatment and Labor Act (EMTALA) violations, among others.
To reduce liability risks, you should strive to understand liability risks and limitations during disasters and take steps to mitigate them by crafting a disaster readiness plan, according to the AAP policy statement. The plan should include provider and staff education on improving medical care during disasters and how best to document medical decisions made in disaster-affected health care environments. Proactively identifying obstacles to care during disasters also is key. You can use the AAP division of state government affairs as a resource; it can provide current information on disaster liability in the different states.
You also should understand potential limits to your medical malpractice insurance coverage during disasters and take steps to add coverage for identified gaps, according to the AAP guidelines.
AAP recommends that you advocate for your health center to have active disaster plans that cover children’s needs and for your hospital to conduct regular drills that test pediatric capabilities. Throughout the guidelines, the AAP calls on the U.S. Department of Health and Human Services to review current state and federal liability laws, and for the agency to recommend new laws that address disaster-response liability protections for doctors. HHS also should assess the liability coverage needs of physicians during crisis times and take action to reduce inconsistencies in state malpractice protections for volunteer physicians and nonvolunteer physicians, according to AAP.
The AAP policy statement is timely because of the number of recent disasters in the United States, said Dr. Altman, lead author of the two papers.
Citing the Federal Emergency Management Agency, Dr. Altman said there were 59 major disaster declarations and 16 emergency declarations in 2017, along with more than 300 mass shooting incidents and more than 110 other man-made disasters such as fires and industrial accidents.
“Disaster conditions can result in pediatric health care providers being faced with the need to address medical conditions outside of their scope of training and experience, without access to the usual fund of patient history and background information, without the usual input or consent from parents or guardians, without the usual assistance of data such as laboratory values or physiologic monitoring, and without knowledge of how long dire conditions will last,” Dr. Altman said in an AAP News statement. “In addition, this can occur within the backdrop of one’s own physical exhaustion, concerns for the safety of one’s own family members, and the risk of loss of valuable and expensive professional property and supplies.”
The AAP guidance can help pediatricians understand the unique professional liability risks that may occur when caring for pediatric patients and families during a disaster, she said.
“It is the hope that this will raise awareness, improve preparedness, and reduce potential deficiencies in professional liability protections for health care providers trying to do their best to care for patients during these infrequent, yet debilitating, events,” Dr. Altman said in the statement.
There was no external funding, and the authors indicated they had no relevant financial disclosures.
SOURCES: Pediatrics. 2019. doi: 10.1542/peds.2018-3892; Pediatrics. 2019. doi: 10.1542/peds.2018-3893.
In a 2019 technical report, the AAP outlines common claims that can arise when treating children during disasters and how certain circumstances can force you to deviate from routine medical practices. In an accompanying policy statement by the AAP committee on medical liability and risk management, recommendations are offered for how to prepare for and prevent such legal risks.
During disasters, liability dangers can increase when circumstances “devolve into an environment of limited choices for both patients and providers,” and you have fewer treatment options available to you, according to the guidance authored by New York pediatrician Dr. Robin L. Altman and her associates.
Common claims that stem from treating patients during disasters are negligence, abandonment, and lack of informed consent. The AAP technical report offers examples about how these accusations can occur, including:
- When during a disaster, you are forced to alter treatment because of scarce medical supplies or equipment, you may later be accused of negligence if the patient’s outcome is negatively affected by the modified treatment.
- When a disaster progresses to overwhelming conditions, and you must practice in an altered health care environment that demands atypical actions, such actions may later be questioned and be accused of providing suboptimal care. Documentation of medical decision making for instance, a primary defense for one’s actions, may be compromised because of an inoperable electronic medical record. Similarly, past medical history may be unavailable, which may impact the appropriateness of care provision.
- In chaotic conditions, you may have to stop treating some patients to focus their time and resources elsewhere, which may lead to an abandonment claim, defined as unilateral termination of a physician-patient relationship – without proper patient notice – when treatment is still required. An abandonment claim also may arise when you have to make decisions in extreme conditions about which patients to transfer or evacuate first and whom to leave behind.
- When providing medical care to children during disasters, a lack of informed consent claim can arise if adequate parental permission is unattainable. This may result from families that are separated or displaced children in need of medical care.
Other claims that can arise from providing care during disasters include HIPAA breaches, licensing violations, discrimination claims, and Emergency Medical Treatment and Labor Act (EMTALA) violations, among others.
To reduce liability risks, you should strive to understand liability risks and limitations during disasters and take steps to mitigate them by crafting a disaster readiness plan, according to the AAP policy statement. The plan should include provider and staff education on improving medical care during disasters and how best to document medical decisions made in disaster-affected health care environments. Proactively identifying obstacles to care during disasters also is key. You can use the AAP division of state government affairs as a resource; it can provide current information on disaster liability in the different states.
You also should understand potential limits to your medical malpractice insurance coverage during disasters and take steps to add coverage for identified gaps, according to the AAP guidelines.
AAP recommends that you advocate for your health center to have active disaster plans that cover children’s needs and for your hospital to conduct regular drills that test pediatric capabilities. Throughout the guidelines, the AAP calls on the U.S. Department of Health and Human Services to review current state and federal liability laws, and for the agency to recommend new laws that address disaster-response liability protections for doctors. HHS also should assess the liability coverage needs of physicians during crisis times and take action to reduce inconsistencies in state malpractice protections for volunteer physicians and nonvolunteer physicians, according to AAP.
The AAP policy statement is timely because of the number of recent disasters in the United States, said Dr. Altman, lead author of the two papers.
Citing the Federal Emergency Management Agency, Dr. Altman said there were 59 major disaster declarations and 16 emergency declarations in 2017, along with more than 300 mass shooting incidents and more than 110 other man-made disasters such as fires and industrial accidents.
“Disaster conditions can result in pediatric health care providers being faced with the need to address medical conditions outside of their scope of training and experience, without access to the usual fund of patient history and background information, without the usual input or consent from parents or guardians, without the usual assistance of data such as laboratory values or physiologic monitoring, and without knowledge of how long dire conditions will last,” Dr. Altman said in an AAP News statement. “In addition, this can occur within the backdrop of one’s own physical exhaustion, concerns for the safety of one’s own family members, and the risk of loss of valuable and expensive professional property and supplies.”
The AAP guidance can help pediatricians understand the unique professional liability risks that may occur when caring for pediatric patients and families during a disaster, she said.
“It is the hope that this will raise awareness, improve preparedness, and reduce potential deficiencies in professional liability protections for health care providers trying to do their best to care for patients during these infrequent, yet debilitating, events,” Dr. Altman said in the statement.
There was no external funding, and the authors indicated they had no relevant financial disclosures.
SOURCES: Pediatrics. 2019. doi: 10.1542/peds.2018-3892; Pediatrics. 2019. doi: 10.1542/peds.2018-3893.
In a 2019 technical report, the AAP outlines common claims that can arise when treating children during disasters and how certain circumstances can force you to deviate from routine medical practices. In an accompanying policy statement by the AAP committee on medical liability and risk management, recommendations are offered for how to prepare for and prevent such legal risks.
During disasters, liability dangers can increase when circumstances “devolve into an environment of limited choices for both patients and providers,” and you have fewer treatment options available to you, according to the guidance authored by New York pediatrician Dr. Robin L. Altman and her associates.
Common claims that stem from treating patients during disasters are negligence, abandonment, and lack of informed consent. The AAP technical report offers examples about how these accusations can occur, including:
- When during a disaster, you are forced to alter treatment because of scarce medical supplies or equipment, you may later be accused of negligence if the patient’s outcome is negatively affected by the modified treatment.
- When a disaster progresses to overwhelming conditions, and you must practice in an altered health care environment that demands atypical actions, such actions may later be questioned and be accused of providing suboptimal care. Documentation of medical decision making for instance, a primary defense for one’s actions, may be compromised because of an inoperable electronic medical record. Similarly, past medical history may be unavailable, which may impact the appropriateness of care provision.
- In chaotic conditions, you may have to stop treating some patients to focus their time and resources elsewhere, which may lead to an abandonment claim, defined as unilateral termination of a physician-patient relationship – without proper patient notice – when treatment is still required. An abandonment claim also may arise when you have to make decisions in extreme conditions about which patients to transfer or evacuate first and whom to leave behind.
- When providing medical care to children during disasters, a lack of informed consent claim can arise if adequate parental permission is unattainable. This may result from families that are separated or displaced children in need of medical care.
Other claims that can arise from providing care during disasters include HIPAA breaches, licensing violations, discrimination claims, and Emergency Medical Treatment and Labor Act (EMTALA) violations, among others.
To reduce liability risks, you should strive to understand liability risks and limitations during disasters and take steps to mitigate them by crafting a disaster readiness plan, according to the AAP policy statement. The plan should include provider and staff education on improving medical care during disasters and how best to document medical decisions made in disaster-affected health care environments. Proactively identifying obstacles to care during disasters also is key. You can use the AAP division of state government affairs as a resource; it can provide current information on disaster liability in the different states.
You also should understand potential limits to your medical malpractice insurance coverage during disasters and take steps to add coverage for identified gaps, according to the AAP guidelines.
AAP recommends that you advocate for your health center to have active disaster plans that cover children’s needs and for your hospital to conduct regular drills that test pediatric capabilities. Throughout the guidelines, the AAP calls on the U.S. Department of Health and Human Services to review current state and federal liability laws, and for the agency to recommend new laws that address disaster-response liability protections for doctors. HHS also should assess the liability coverage needs of physicians during crisis times and take action to reduce inconsistencies in state malpractice protections for volunteer physicians and nonvolunteer physicians, according to AAP.
The AAP policy statement is timely because of the number of recent disasters in the United States, said Dr. Altman, lead author of the two papers.
Citing the Federal Emergency Management Agency, Dr. Altman said there were 59 major disaster declarations and 16 emergency declarations in 2017, along with more than 300 mass shooting incidents and more than 110 other man-made disasters such as fires and industrial accidents.
“Disaster conditions can result in pediatric health care providers being faced with the need to address medical conditions outside of their scope of training and experience, without access to the usual fund of patient history and background information, without the usual input or consent from parents or guardians, without the usual assistance of data such as laboratory values or physiologic monitoring, and without knowledge of how long dire conditions will last,” Dr. Altman said in an AAP News statement. “In addition, this can occur within the backdrop of one’s own physical exhaustion, concerns for the safety of one’s own family members, and the risk of loss of valuable and expensive professional property and supplies.”
The AAP guidance can help pediatricians understand the unique professional liability risks that may occur when caring for pediatric patients and families during a disaster, she said.
“It is the hope that this will raise awareness, improve preparedness, and reduce potential deficiencies in professional liability protections for health care providers trying to do their best to care for patients during these infrequent, yet debilitating, events,” Dr. Altman said in the statement.
There was no external funding, and the authors indicated they had no relevant financial disclosures.
SOURCES: Pediatrics. 2019. doi: 10.1542/peds.2018-3892; Pediatrics. 2019. doi: 10.1542/peds.2018-3893.
Malpractice suits are less frequent – but more costly
Lawsuits against physicians declined across virtually all specialties by more than a quarter over a 10-year span, but the cost to manage legal challenges went up, a recent analysis finds.
From 2007 to 2016, the rate of claims dropped by 27% per 100 doctors from 5.1 to 3.7, according to a review of 124,000 cases by CRICO Strategies, a division of CRICO, the medical liability insurance provider for the Harvard medical community. CRICO’s database of claims contains about 30% of legal cases filed against health providers across the U.S.
For internists, the rate of lawsuits decreased by 35% between 2007 and 2016, according to CRICO data provided to MDedge News. Ob.gyns. saw a 44% drop in claims over the 10-year period, and surgeons experienced a 23% rate decrease. The analysis did not break down the rate of claims by other single subspecialists. Claims decreased by a combined 29% for cardiologists, dermatologists, endocrinologists, family physicians, gastroenterologists, hematologists/oncologists, hospitalists, infectious disease specialists, internists, nephrologists, neurologists, pulmonologists, and rheumatologists/immunologists, according to the report published in February 2019 on CRICO’s website.
The findings are consistent with prior research on claim trends, said Seth Seabury, PhD, a medical liability researcher and director of the Keck-Schaeffer Initiative for Population Health Policy at the University of Southern California, Los Angeles.
“Malpractice claim frequency has been falling pretty steadily for a while now, reflecting a number of factors including the widespread adoption of tort reform and other measures to shield physicians from malpractice risk,” Dr. Seabury said in an interview. “Interestingly, the decline seems greatest in the claims with lower potential stakes, as you see average indemnity holding flat or rising. Some of this likely reflects the unwillingness of attorneys to take cases with lower potential payouts, because of the high cost of litigating a malpractice case.”
While frequency went down, the cost to manage a legal claim went up, according to CRICO data. The price of defending a malpractice lawsuit rose an average of 3.5% annually over the 10-year period from $36,000 to $46,000. For cases that ended with no payment (indemnity) to plaintiffs, the cost to manage a case rose an average of 5% annually.
The upward trends in case management expenses are striking, particularly since the time to resolve cases has decreased, said Michelle Mello, PhD, a health research and policy professor at Stanford (Calif.) University. From 2007 to 2016, the average time to resolve a case dropped from 29 to 27 months, the CRICO report found.
“CRICO nods to disclosure and apology approaches as perhaps underlying the more encouraging trend in time to resolution, but it was surprising to me that such approaches have not translated into lower defense costs,” Dr. Mello said in an interview. “In particular, a lot is still being spent to manage cases that never result in a payment to the patient. My hope was that, as hospitals got better at communicating with patients about adverse events, including the fact that about three-quarters of them are not due to substandard care, there would be fewer claims involving such events and also less money spent dealing with such claims when they do arise.”
For cases that do end in payment, high payouts are on the rise. Cases that ended in payments of $1 million or more increased 4% over the 10-year time frame, while payments of $3 million to $11 million increased 7% annually, according to the CRICO report. Cases that ended in payment lower than $1 million dropped over the 10-year span.
The reasons behind increasing plaintiff payouts is uncertain, Dr. Seabury said.
“It’s hard to say exactly why high payouts are on the rise, as payout levels reflect a number of factors – [such as] economic damages, clinical severity, pain and suffering – that can be difficult to disentangle,” he said. “But it is probably concerning for doctors in the sense that, while claims are becoming less likely, when they do happen, it could be more catastrophic in the sense of having large damages that exceed the policy limit.”
Lawsuits against physicians declined across virtually all specialties by more than a quarter over a 10-year span, but the cost to manage legal challenges went up, a recent analysis finds.
From 2007 to 2016, the rate of claims dropped by 27% per 100 doctors from 5.1 to 3.7, according to a review of 124,000 cases by CRICO Strategies, a division of CRICO, the medical liability insurance provider for the Harvard medical community. CRICO’s database of claims contains about 30% of legal cases filed against health providers across the U.S.
For internists, the rate of lawsuits decreased by 35% between 2007 and 2016, according to CRICO data provided to MDedge News. Ob.gyns. saw a 44% drop in claims over the 10-year period, and surgeons experienced a 23% rate decrease. The analysis did not break down the rate of claims by other single subspecialists. Claims decreased by a combined 29% for cardiologists, dermatologists, endocrinologists, family physicians, gastroenterologists, hematologists/oncologists, hospitalists, infectious disease specialists, internists, nephrologists, neurologists, pulmonologists, and rheumatologists/immunologists, according to the report published in February 2019 on CRICO’s website.
The findings are consistent with prior research on claim trends, said Seth Seabury, PhD, a medical liability researcher and director of the Keck-Schaeffer Initiative for Population Health Policy at the University of Southern California, Los Angeles.
“Malpractice claim frequency has been falling pretty steadily for a while now, reflecting a number of factors including the widespread adoption of tort reform and other measures to shield physicians from malpractice risk,” Dr. Seabury said in an interview. “Interestingly, the decline seems greatest in the claims with lower potential stakes, as you see average indemnity holding flat or rising. Some of this likely reflects the unwillingness of attorneys to take cases with lower potential payouts, because of the high cost of litigating a malpractice case.”
While frequency went down, the cost to manage a legal claim went up, according to CRICO data. The price of defending a malpractice lawsuit rose an average of 3.5% annually over the 10-year period from $36,000 to $46,000. For cases that ended with no payment (indemnity) to plaintiffs, the cost to manage a case rose an average of 5% annually.
The upward trends in case management expenses are striking, particularly since the time to resolve cases has decreased, said Michelle Mello, PhD, a health research and policy professor at Stanford (Calif.) University. From 2007 to 2016, the average time to resolve a case dropped from 29 to 27 months, the CRICO report found.
“CRICO nods to disclosure and apology approaches as perhaps underlying the more encouraging trend in time to resolution, but it was surprising to me that such approaches have not translated into lower defense costs,” Dr. Mello said in an interview. “In particular, a lot is still being spent to manage cases that never result in a payment to the patient. My hope was that, as hospitals got better at communicating with patients about adverse events, including the fact that about three-quarters of them are not due to substandard care, there would be fewer claims involving such events and also less money spent dealing with such claims when they do arise.”
For cases that do end in payment, high payouts are on the rise. Cases that ended in payments of $1 million or more increased 4% over the 10-year time frame, while payments of $3 million to $11 million increased 7% annually, according to the CRICO report. Cases that ended in payment lower than $1 million dropped over the 10-year span.
The reasons behind increasing plaintiff payouts is uncertain, Dr. Seabury said.
“It’s hard to say exactly why high payouts are on the rise, as payout levels reflect a number of factors – [such as] economic damages, clinical severity, pain and suffering – that can be difficult to disentangle,” he said. “But it is probably concerning for doctors in the sense that, while claims are becoming less likely, when they do happen, it could be more catastrophic in the sense of having large damages that exceed the policy limit.”
Lawsuits against physicians declined across virtually all specialties by more than a quarter over a 10-year span, but the cost to manage legal challenges went up, a recent analysis finds.
From 2007 to 2016, the rate of claims dropped by 27% per 100 doctors from 5.1 to 3.7, according to a review of 124,000 cases by CRICO Strategies, a division of CRICO, the medical liability insurance provider for the Harvard medical community. CRICO’s database of claims contains about 30% of legal cases filed against health providers across the U.S.
For internists, the rate of lawsuits decreased by 35% between 2007 and 2016, according to CRICO data provided to MDedge News. Ob.gyns. saw a 44% drop in claims over the 10-year period, and surgeons experienced a 23% rate decrease. The analysis did not break down the rate of claims by other single subspecialists. Claims decreased by a combined 29% for cardiologists, dermatologists, endocrinologists, family physicians, gastroenterologists, hematologists/oncologists, hospitalists, infectious disease specialists, internists, nephrologists, neurologists, pulmonologists, and rheumatologists/immunologists, according to the report published in February 2019 on CRICO’s website.
The findings are consistent with prior research on claim trends, said Seth Seabury, PhD, a medical liability researcher and director of the Keck-Schaeffer Initiative for Population Health Policy at the University of Southern California, Los Angeles.
“Malpractice claim frequency has been falling pretty steadily for a while now, reflecting a number of factors including the widespread adoption of tort reform and other measures to shield physicians from malpractice risk,” Dr. Seabury said in an interview. “Interestingly, the decline seems greatest in the claims with lower potential stakes, as you see average indemnity holding flat or rising. Some of this likely reflects the unwillingness of attorneys to take cases with lower potential payouts, because of the high cost of litigating a malpractice case.”
While frequency went down, the cost to manage a legal claim went up, according to CRICO data. The price of defending a malpractice lawsuit rose an average of 3.5% annually over the 10-year period from $36,000 to $46,000. For cases that ended with no payment (indemnity) to plaintiffs, the cost to manage a case rose an average of 5% annually.
The upward trends in case management expenses are striking, particularly since the time to resolve cases has decreased, said Michelle Mello, PhD, a health research and policy professor at Stanford (Calif.) University. From 2007 to 2016, the average time to resolve a case dropped from 29 to 27 months, the CRICO report found.
“CRICO nods to disclosure and apology approaches as perhaps underlying the more encouraging trend in time to resolution, but it was surprising to me that such approaches have not translated into lower defense costs,” Dr. Mello said in an interview. “In particular, a lot is still being spent to manage cases that never result in a payment to the patient. My hope was that, as hospitals got better at communicating with patients about adverse events, including the fact that about three-quarters of them are not due to substandard care, there would be fewer claims involving such events and also less money spent dealing with such claims when they do arise.”
For cases that do end in payment, high payouts are on the rise. Cases that ended in payments of $1 million or more increased 4% over the 10-year time frame, while payments of $3 million to $11 million increased 7% annually, according to the CRICO report. Cases that ended in payment lower than $1 million dropped over the 10-year span.
The reasons behind increasing plaintiff payouts is uncertain, Dr. Seabury said.
“It’s hard to say exactly why high payouts are on the rise, as payout levels reflect a number of factors – [such as] economic damages, clinical severity, pain and suffering – that can be difficult to disentangle,” he said. “But it is probably concerning for doctors in the sense that, while claims are becoming less likely, when they do happen, it could be more catastrophic in the sense of having large damages that exceed the policy limit.”
Advancing coherence: Your “meta-leadership” objective
Learn to balance organizational priorities
For the many people who expect you to lead, your role – among others – is to create coherence. That coherence characterizes the logic and consistency of what you do in your organization. It assembles the individual work of many different people into a whole that functions well. Coherence in your workplace helps people make sense of what they are doing and why it matters.
Our very rational brain craves coherence. We assemble facts, emotions, ambitions and our life stories into narratives that define who we are, what we are doing, and why it is important. An effective organizational “metaleader” encourages that process for followers. It helps people make sense of the work side of their life.
When coherence is absent, the workplace is riddled with contradictions, unpredictability, and dissonance. People are expected to accomplish tasks for which the time, tools, and talent are missing. There is a perplexed swirl of high activity and low productivity. Expectations for high quality of care and patient satisfaction are contradicted by an overbearing workload, reams of paper work, and the low morale that leaves the work force lethargic. “What we are doing here and how we are doing it doesn’t make sense,” exemplifies the exasperation of working amid incoherence. The department does not drive together toward success-oriented performance. Instead, different people, priorities, and opportunities will be positioned in conflict with one another. For people in your group and those surrounding it, morale and motivation suffer. There is the risk that people will descend into malaise.
Creating coherence is a complex metaleadership process. A large health care center is a cacophony of priorities, of which advancing quality of care is but one. There are other objectives, some contradictory, that also absorb time and attention: achievement of financial benchmarks, promotion of professional careers, and the individual hopes and desires of patients. Systematically aligning those many priorities and objectives is a process of both design and leadership.
The metaleadership model is a strategy for building coherence amid the complexity of health care operations. For those unfamiliar with metaleadership: The prefix “meta-” refers to a wider perspective on what is happening, the people involved, and the overall combination of objectives. The three dimensions of practice are: 1) the Person of the metaleader – your own priorities, values and emotional intelligence; 2) the Situation – what is happening and what ought to be done about it; and 3) Connectivity of Effort, which leads down to subordinates, up to bosses, across to other internal departments, and beyond to external organizations and professionals.
In building connectivity of effort, the metaleader links the many sides of the work being accomplished. The intent is to balance – purposefully – different organizational objectives into a combined whole that gets the jobs done. Furthermore, that coherence links and adapts what people are doing to the situation at hand. And in essence, the person of the leader cannot lead broader coherence if not coherent in her or his own thinking, attitudes, and behaviors, so achievement of personal and professional clarity of purpose is important.
The question for you: How do you as a hospitalist leader create coherence in what you are leading given the changing priorities, actions, and turbulence of current health policy and the market?
The answers lie in the communication you foster and clarify. That communication demands clarity and diplomacy. It is multidirectional such that messages and information in your leading down, up, across, and beyond complement and inform one another.
An illustration of one pathway: You learn from senior management about cuts in the budget. You reflect with them on the choices implicit in those cuts. Perhaps there are better ways to reduce expenditures and increase revenues that offer an alternative pathway to a balanced budget? When communicating with your subordinates, you open conversation on ways to enhance efficiencies and assure quality. You explore avenues to partner with other departments within your institution on how you can link and leverage services and capabilities. And you consider your marketplace and the actions you can take to reinforce your department and assure the volume necessary to achieve budget and quality objectives. And through it all, you monitor the situation. What are the effects of the budget adjustments, and what can be done to sustain the coherence of the work and output of the department? It is a leadership process of constant situational awareness, personal commitment, and connectivity of effort.
An illustration of another pathway: Resist the change and argue forcefully for holding onto the current budget and workforce. Though you do not possess the authority to control larger budgetary decisions, you employ influence well beyond your authority. You recruit allies to your cause, advocates who believe in the purpose you are promoting. You build an alternative coherence, mindful of fostering friendship and minimizing alienation. You are recognized for the passion of your professional commitment and your capacity to uphold quality care and organizational balance.
Two very different pathways to crafting coherence. Leaders of each perceive their actions to advance priority coherence objectives. Apply this question to your own complex problem solving.
Metaleaders forge coherence through the narratives they build and the consistency with those themes and priorities. When everyone on your staff, from physicians to housekeeping personnel, can say “I am here to help save lives,” you know that your followers are on board with a shared mission. They recognize that their efforts contribute to that overall mission. Each person has a role to play, and her or his work fits with the efforts of others, and the bottom line accomplishments of the department.
The coherence you forge assists your followers to make sense of what they are doing and how it fits what others are doing. Work is fulfilling. Beyond that, in a turbulent health care system, you anticipate both problems and opportunities with strategies to meet them. You stay ahead of the game to ensure that people within and outside the department are aligned to maximize opportunities for success.
This is particularly important for the hospitalist. Your job is to fashion coherence on many levels. First, coherent patient care for the patient. Second, coherent interactions among professionals. Finally, organizational coherence, so one piece of the puzzle fits with others. And, when there is a need to recalculate, you adapt and develop solutions that fit the people and situation at hand.
Dr. Marcus is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is Director of the Program for Health Care Negotiation and Conflict Resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
Learn to balance organizational priorities
Learn to balance organizational priorities
For the many people who expect you to lead, your role – among others – is to create coherence. That coherence characterizes the logic and consistency of what you do in your organization. It assembles the individual work of many different people into a whole that functions well. Coherence in your workplace helps people make sense of what they are doing and why it matters.
Our very rational brain craves coherence. We assemble facts, emotions, ambitions and our life stories into narratives that define who we are, what we are doing, and why it is important. An effective organizational “metaleader” encourages that process for followers. It helps people make sense of the work side of their life.
When coherence is absent, the workplace is riddled with contradictions, unpredictability, and dissonance. People are expected to accomplish tasks for which the time, tools, and talent are missing. There is a perplexed swirl of high activity and low productivity. Expectations for high quality of care and patient satisfaction are contradicted by an overbearing workload, reams of paper work, and the low morale that leaves the work force lethargic. “What we are doing here and how we are doing it doesn’t make sense,” exemplifies the exasperation of working amid incoherence. The department does not drive together toward success-oriented performance. Instead, different people, priorities, and opportunities will be positioned in conflict with one another. For people in your group and those surrounding it, morale and motivation suffer. There is the risk that people will descend into malaise.
Creating coherence is a complex metaleadership process. A large health care center is a cacophony of priorities, of which advancing quality of care is but one. There are other objectives, some contradictory, that also absorb time and attention: achievement of financial benchmarks, promotion of professional careers, and the individual hopes and desires of patients. Systematically aligning those many priorities and objectives is a process of both design and leadership.
The metaleadership model is a strategy for building coherence amid the complexity of health care operations. For those unfamiliar with metaleadership: The prefix “meta-” refers to a wider perspective on what is happening, the people involved, and the overall combination of objectives. The three dimensions of practice are: 1) the Person of the metaleader – your own priorities, values and emotional intelligence; 2) the Situation – what is happening and what ought to be done about it; and 3) Connectivity of Effort, which leads down to subordinates, up to bosses, across to other internal departments, and beyond to external organizations and professionals.
In building connectivity of effort, the metaleader links the many sides of the work being accomplished. The intent is to balance – purposefully – different organizational objectives into a combined whole that gets the jobs done. Furthermore, that coherence links and adapts what people are doing to the situation at hand. And in essence, the person of the leader cannot lead broader coherence if not coherent in her or his own thinking, attitudes, and behaviors, so achievement of personal and professional clarity of purpose is important.
The question for you: How do you as a hospitalist leader create coherence in what you are leading given the changing priorities, actions, and turbulence of current health policy and the market?
The answers lie in the communication you foster and clarify. That communication demands clarity and diplomacy. It is multidirectional such that messages and information in your leading down, up, across, and beyond complement and inform one another.
An illustration of one pathway: You learn from senior management about cuts in the budget. You reflect with them on the choices implicit in those cuts. Perhaps there are better ways to reduce expenditures and increase revenues that offer an alternative pathway to a balanced budget? When communicating with your subordinates, you open conversation on ways to enhance efficiencies and assure quality. You explore avenues to partner with other departments within your institution on how you can link and leverage services and capabilities. And you consider your marketplace and the actions you can take to reinforce your department and assure the volume necessary to achieve budget and quality objectives. And through it all, you monitor the situation. What are the effects of the budget adjustments, and what can be done to sustain the coherence of the work and output of the department? It is a leadership process of constant situational awareness, personal commitment, and connectivity of effort.
An illustration of another pathway: Resist the change and argue forcefully for holding onto the current budget and workforce. Though you do not possess the authority to control larger budgetary decisions, you employ influence well beyond your authority. You recruit allies to your cause, advocates who believe in the purpose you are promoting. You build an alternative coherence, mindful of fostering friendship and minimizing alienation. You are recognized for the passion of your professional commitment and your capacity to uphold quality care and organizational balance.
Two very different pathways to crafting coherence. Leaders of each perceive their actions to advance priority coherence objectives. Apply this question to your own complex problem solving.
Metaleaders forge coherence through the narratives they build and the consistency with those themes and priorities. When everyone on your staff, from physicians to housekeeping personnel, can say “I am here to help save lives,” you know that your followers are on board with a shared mission. They recognize that their efforts contribute to that overall mission. Each person has a role to play, and her or his work fits with the efforts of others, and the bottom line accomplishments of the department.
The coherence you forge assists your followers to make sense of what they are doing and how it fits what others are doing. Work is fulfilling. Beyond that, in a turbulent health care system, you anticipate both problems and opportunities with strategies to meet them. You stay ahead of the game to ensure that people within and outside the department are aligned to maximize opportunities for success.
This is particularly important for the hospitalist. Your job is to fashion coherence on many levels. First, coherent patient care for the patient. Second, coherent interactions among professionals. Finally, organizational coherence, so one piece of the puzzle fits with others. And, when there is a need to recalculate, you adapt and develop solutions that fit the people and situation at hand.
Dr. Marcus is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is Director of the Program for Health Care Negotiation and Conflict Resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
For the many people who expect you to lead, your role – among others – is to create coherence. That coherence characterizes the logic and consistency of what you do in your organization. It assembles the individual work of many different people into a whole that functions well. Coherence in your workplace helps people make sense of what they are doing and why it matters.
Our very rational brain craves coherence. We assemble facts, emotions, ambitions and our life stories into narratives that define who we are, what we are doing, and why it is important. An effective organizational “metaleader” encourages that process for followers. It helps people make sense of the work side of their life.
When coherence is absent, the workplace is riddled with contradictions, unpredictability, and dissonance. People are expected to accomplish tasks for which the time, tools, and talent are missing. There is a perplexed swirl of high activity and low productivity. Expectations for high quality of care and patient satisfaction are contradicted by an overbearing workload, reams of paper work, and the low morale that leaves the work force lethargic. “What we are doing here and how we are doing it doesn’t make sense,” exemplifies the exasperation of working amid incoherence. The department does not drive together toward success-oriented performance. Instead, different people, priorities, and opportunities will be positioned in conflict with one another. For people in your group and those surrounding it, morale and motivation suffer. There is the risk that people will descend into malaise.
Creating coherence is a complex metaleadership process. A large health care center is a cacophony of priorities, of which advancing quality of care is but one. There are other objectives, some contradictory, that also absorb time and attention: achievement of financial benchmarks, promotion of professional careers, and the individual hopes and desires of patients. Systematically aligning those many priorities and objectives is a process of both design and leadership.
The metaleadership model is a strategy for building coherence amid the complexity of health care operations. For those unfamiliar with metaleadership: The prefix “meta-” refers to a wider perspective on what is happening, the people involved, and the overall combination of objectives. The three dimensions of practice are: 1) the Person of the metaleader – your own priorities, values and emotional intelligence; 2) the Situation – what is happening and what ought to be done about it; and 3) Connectivity of Effort, which leads down to subordinates, up to bosses, across to other internal departments, and beyond to external organizations and professionals.
In building connectivity of effort, the metaleader links the many sides of the work being accomplished. The intent is to balance – purposefully – different organizational objectives into a combined whole that gets the jobs done. Furthermore, that coherence links and adapts what people are doing to the situation at hand. And in essence, the person of the leader cannot lead broader coherence if not coherent in her or his own thinking, attitudes, and behaviors, so achievement of personal and professional clarity of purpose is important.
The question for you: How do you as a hospitalist leader create coherence in what you are leading given the changing priorities, actions, and turbulence of current health policy and the market?
The answers lie in the communication you foster and clarify. That communication demands clarity and diplomacy. It is multidirectional such that messages and information in your leading down, up, across, and beyond complement and inform one another.
An illustration of one pathway: You learn from senior management about cuts in the budget. You reflect with them on the choices implicit in those cuts. Perhaps there are better ways to reduce expenditures and increase revenues that offer an alternative pathway to a balanced budget? When communicating with your subordinates, you open conversation on ways to enhance efficiencies and assure quality. You explore avenues to partner with other departments within your institution on how you can link and leverage services and capabilities. And you consider your marketplace and the actions you can take to reinforce your department and assure the volume necessary to achieve budget and quality objectives. And through it all, you monitor the situation. What are the effects of the budget adjustments, and what can be done to sustain the coherence of the work and output of the department? It is a leadership process of constant situational awareness, personal commitment, and connectivity of effort.
An illustration of another pathway: Resist the change and argue forcefully for holding onto the current budget and workforce. Though you do not possess the authority to control larger budgetary decisions, you employ influence well beyond your authority. You recruit allies to your cause, advocates who believe in the purpose you are promoting. You build an alternative coherence, mindful of fostering friendship and minimizing alienation. You are recognized for the passion of your professional commitment and your capacity to uphold quality care and organizational balance.
Two very different pathways to crafting coherence. Leaders of each perceive their actions to advance priority coherence objectives. Apply this question to your own complex problem solving.
Metaleaders forge coherence through the narratives they build and the consistency with those themes and priorities. When everyone on your staff, from physicians to housekeeping personnel, can say “I am here to help save lives,” you know that your followers are on board with a shared mission. They recognize that their efforts contribute to that overall mission. Each person has a role to play, and her or his work fits with the efforts of others, and the bottom line accomplishments of the department.
The coherence you forge assists your followers to make sense of what they are doing and how it fits what others are doing. Work is fulfilling. Beyond that, in a turbulent health care system, you anticipate both problems and opportunities with strategies to meet them. You stay ahead of the game to ensure that people within and outside the department are aligned to maximize opportunities for success.
This is particularly important for the hospitalist. Your job is to fashion coherence on many levels. First, coherent patient care for the patient. Second, coherent interactions among professionals. Finally, organizational coherence, so one piece of the puzzle fits with others. And, when there is a need to recalculate, you adapt and develop solutions that fit the people and situation at hand.
Dr. Marcus is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is Director of the Program for Health Care Negotiation and Conflict Resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
The ever-evolving scope of hospitalists’ clinical services
More care ‘beyond the walls’ of the hospital
The 2018 State of Hospital Medicine (SoHM) Report provides indispensable data about the scope of clinical services routinely provided by adult and pediatric hospitalists. This year’s SoHM report reveals that a growing number of Hospital Medicine Groups (HMGs) serving adults are involved in roles beyond the inpatient medical wards, including various surgical comanagement programs, outpatient care, and post-acute care services.
The survey also compares services provided by academic and nonacademic HMGs, which remain markedly different in some areas. As the landscape of health care continues to evolve, hospitalists transform their scope of services to meet the needs of the institutions and communities they serve.
In the previous three SoHM reports, it was well established that more than 87% of adult hospital medicine groups play some role in comanaging surgical patients. In this year’s SoHM report, that role was further stratified to capture the various subspecialties represented, and to identify whether the hospitalists generally served as admitting/attending physician or consultant.
Hospitalists’ roles in comanagement are most prominent for care of orthopedic and general surgery patients, but more than 50% of surveyed HMGs reported being involved in comanagement in some capacity with neurosurgery, obstetrics, and cardiovascular surgery. Additionally, almost 95% of surveyed adult HMGs reported that they provided comanagement services for at least one other surgical specialty that was not listed in the survey.
The report also displays comanagement services provided to various medical subspecialties, including neurology, GI/liver, oncology, and more. Of the medical subspecialties represented, adult HMGs comanaged GI/liver (98.2%) and oncology (97.7%) services more often than others.
Interestingly, more HMGs are providing care for patients beyond the walls of the hospital. In the 2018 SoHM report, over 17% of surveyed HMG respondents reported providing care in an outpatient setting, representing an increase of 6.5 percentage points over 2016. Most strikingly, from 2016 to 2018, there was a 12 percentage point increase in adult HMGs reporting services provided to post-acute care facilities (from 13.1% to 24.8%).
These trends were most notable in the Midwest region where nearly 28% of HMGs provide patient care in an outpatient setting and up to 34% in post-acute care facilities. In part, this trend may result from the increased emphasis on improving transitions of care, by providing prehospital preoperative services, postdischarge follow-up encounters, or offering posthospitalization extensivist care.
Within the hospital itself, there remain striking differences in certain services provided by academic and nonacademic HMGs serving adults. Nonacademic HMGs are far more likely to cover patients in an ICU than their academic counterparts (72.0% vs. 34.3%). In contrast, academic hospitalist groups were significantly more inclined to perform procedures. However, the report also showed that there was an overall downtrend of percentage of HMGs that cover patients in an ICU or perform procedures.
As the scope of hospitalist services continues to change over time, should there be concern for scope creep? It depends on how one might view the change. As health care becomes ever more complex, high-functioning HMGs are needed to navigate it, both within and beyond the hospital. Some might consider scope evolution to be a reflection of hospitalists being recognized for their ability to provide high-quality, efficient, and comprehensive care. Hospital medicine groups will likely continue to evolve to meet the needs of an ever-changing health care environment.
Dr. Kurian is chief of the academic division of hospital medicine at Northwell Health in New York. She is a member of the SHM Practice Analysis Committee.
More care ‘beyond the walls’ of the hospital
More care ‘beyond the walls’ of the hospital
The 2018 State of Hospital Medicine (SoHM) Report provides indispensable data about the scope of clinical services routinely provided by adult and pediatric hospitalists. This year’s SoHM report reveals that a growing number of Hospital Medicine Groups (HMGs) serving adults are involved in roles beyond the inpatient medical wards, including various surgical comanagement programs, outpatient care, and post-acute care services.
The survey also compares services provided by academic and nonacademic HMGs, which remain markedly different in some areas. As the landscape of health care continues to evolve, hospitalists transform their scope of services to meet the needs of the institutions and communities they serve.
In the previous three SoHM reports, it was well established that more than 87% of adult hospital medicine groups play some role in comanaging surgical patients. In this year’s SoHM report, that role was further stratified to capture the various subspecialties represented, and to identify whether the hospitalists generally served as admitting/attending physician or consultant.
Hospitalists’ roles in comanagement are most prominent for care of orthopedic and general surgery patients, but more than 50% of surveyed HMGs reported being involved in comanagement in some capacity with neurosurgery, obstetrics, and cardiovascular surgery. Additionally, almost 95% of surveyed adult HMGs reported that they provided comanagement services for at least one other surgical specialty that was not listed in the survey.
The report also displays comanagement services provided to various medical subspecialties, including neurology, GI/liver, oncology, and more. Of the medical subspecialties represented, adult HMGs comanaged GI/liver (98.2%) and oncology (97.7%) services more often than others.
Interestingly, more HMGs are providing care for patients beyond the walls of the hospital. In the 2018 SoHM report, over 17% of surveyed HMG respondents reported providing care in an outpatient setting, representing an increase of 6.5 percentage points over 2016. Most strikingly, from 2016 to 2018, there was a 12 percentage point increase in adult HMGs reporting services provided to post-acute care facilities (from 13.1% to 24.8%).
These trends were most notable in the Midwest region where nearly 28% of HMGs provide patient care in an outpatient setting and up to 34% in post-acute care facilities. In part, this trend may result from the increased emphasis on improving transitions of care, by providing prehospital preoperative services, postdischarge follow-up encounters, or offering posthospitalization extensivist care.
Within the hospital itself, there remain striking differences in certain services provided by academic and nonacademic HMGs serving adults. Nonacademic HMGs are far more likely to cover patients in an ICU than their academic counterparts (72.0% vs. 34.3%). In contrast, academic hospitalist groups were significantly more inclined to perform procedures. However, the report also showed that there was an overall downtrend of percentage of HMGs that cover patients in an ICU or perform procedures.
As the scope of hospitalist services continues to change over time, should there be concern for scope creep? It depends on how one might view the change. As health care becomes ever more complex, high-functioning HMGs are needed to navigate it, both within and beyond the hospital. Some might consider scope evolution to be a reflection of hospitalists being recognized for their ability to provide high-quality, efficient, and comprehensive care. Hospital medicine groups will likely continue to evolve to meet the needs of an ever-changing health care environment.
Dr. Kurian is chief of the academic division of hospital medicine at Northwell Health in New York. She is a member of the SHM Practice Analysis Committee.
The 2018 State of Hospital Medicine (SoHM) Report provides indispensable data about the scope of clinical services routinely provided by adult and pediatric hospitalists. This year’s SoHM report reveals that a growing number of Hospital Medicine Groups (HMGs) serving adults are involved in roles beyond the inpatient medical wards, including various surgical comanagement programs, outpatient care, and post-acute care services.
The survey also compares services provided by academic and nonacademic HMGs, which remain markedly different in some areas. As the landscape of health care continues to evolve, hospitalists transform their scope of services to meet the needs of the institutions and communities they serve.
In the previous three SoHM reports, it was well established that more than 87% of adult hospital medicine groups play some role in comanaging surgical patients. In this year’s SoHM report, that role was further stratified to capture the various subspecialties represented, and to identify whether the hospitalists generally served as admitting/attending physician or consultant.
Hospitalists’ roles in comanagement are most prominent for care of orthopedic and general surgery patients, but more than 50% of surveyed HMGs reported being involved in comanagement in some capacity with neurosurgery, obstetrics, and cardiovascular surgery. Additionally, almost 95% of surveyed adult HMGs reported that they provided comanagement services for at least one other surgical specialty that was not listed in the survey.
The report also displays comanagement services provided to various medical subspecialties, including neurology, GI/liver, oncology, and more. Of the medical subspecialties represented, adult HMGs comanaged GI/liver (98.2%) and oncology (97.7%) services more often than others.
Interestingly, more HMGs are providing care for patients beyond the walls of the hospital. In the 2018 SoHM report, over 17% of surveyed HMG respondents reported providing care in an outpatient setting, representing an increase of 6.5 percentage points over 2016. Most strikingly, from 2016 to 2018, there was a 12 percentage point increase in adult HMGs reporting services provided to post-acute care facilities (from 13.1% to 24.8%).
These trends were most notable in the Midwest region where nearly 28% of HMGs provide patient care in an outpatient setting and up to 34% in post-acute care facilities. In part, this trend may result from the increased emphasis on improving transitions of care, by providing prehospital preoperative services, postdischarge follow-up encounters, or offering posthospitalization extensivist care.
Within the hospital itself, there remain striking differences in certain services provided by academic and nonacademic HMGs serving adults. Nonacademic HMGs are far more likely to cover patients in an ICU than their academic counterparts (72.0% vs. 34.3%). In contrast, academic hospitalist groups were significantly more inclined to perform procedures. However, the report also showed that there was an overall downtrend of percentage of HMGs that cover patients in an ICU or perform procedures.
As the scope of hospitalist services continues to change over time, should there be concern for scope creep? It depends on how one might view the change. As health care becomes ever more complex, high-functioning HMGs are needed to navigate it, both within and beyond the hospital. Some might consider scope evolution to be a reflection of hospitalists being recognized for their ability to provide high-quality, efficient, and comprehensive care. Hospital medicine groups will likely continue to evolve to meet the needs of an ever-changing health care environment.
Dr. Kurian is chief of the academic division of hospital medicine at Northwell Health in New York. She is a member of the SHM Practice Analysis Committee.
Final ‘Vision’ report addresses MOC woes
Whatever you do, change the name.
That was key among the final recommendations the Vision Initiative Commission submitted to the American Board of Medical Specialties on how to improve the maintenance of certification process.
“A new term that communicates the concept, intent, and expectations of continuing certification programs should be adopted by the ABMS in order to reengage disaffected diplomates and assure the public and other stakeholders that the certificate has enduring meaning and value,” according to the final report. A new term was not suggested.
The commission recommended a continuing certification system with four aims:
- Become a meaningful, contemporary, and relevant professional development activity for diplomates that ensures they remain up-to-date in their specialty.
- Demonstrate a commitment to professional self-regulation to both diplomates and the public.
- Align with international and national standards for certification programs.
- Provide a specialty-based credential that would be of value to diplomates and to multiple stakeholders, including patients, families, the public, and health care institutions.
Testing methods and situations must be simplified and updated, according to the report, which was submitted to ABMS on Feb. 12. Continuing certification “must change to incorporate longitudinal and other innovative formative assessment strategies that support learning, identify knowledge and skills gaps, and help diplomates stay current. The ABMS Boards must offer an alternative to burdensome highly secure, point-in-time examinations of knowledge.” In addition, the boards “must no longer use a single point-in-time examination or a series of single point-in-time assessments as the sole method to determine certification status.”
Instead, the commission recommends that ABMS “move quickly to formative assessment formats that are not characterized by high-stakes summative outcomes (pass/fail), specified time frames for high-stakes assessment, or require burdensome testing formats (such as testing centers or remote proctoring) that are inconsistent with the desired goals for continuing certification – support learning; identify knowledge and skills gaps; and help diplomates stay current.”
The commission also defined how the certification process should be used by other stakeholders.
“ABMS must demonstrate and communicate that continuing certification has value, meaning, and purpose in the health care environment,” the report states. “Hospitals, health systems, payers, and other health care organizations can independently decide what factors are used in credentialing and privileging decisions. ABMS must inform these organizations that continuing certification should not be the only criterion used in these decisions, and these organizations should use a wide portfolio of criteria in these decisions. ABMS must encourage hospitals, health systems, payers, and other health care organizations to not deny credentialing or privileging to a physician solely on the basis of certification status.”
Additionally, the commission report states that “ABMS and the ABMS Boards should collaborate with specialty societies, the [continuing medical education/continuing professional development] community, and other expert stakeholders to develop the infrastructure to support learning activities that produce data-driven advances in clinical practice. The ABMS Boards must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage.”
The report adds that the boards “should readily accept existing activities that diplomates are doing to advance their clinical practice and to provide credit for performing low-resource, high-impact activities as part of their daily practice routine.”
The commission’s final report incorporates a number of changes that physicians offered based on a draft version of the report.
The American College of Physicians commented that it “objects to the use of data regarding quality measures for individual diplomate certification status, because physician-level measures of quality are flawed, and because physician-level data inevitably leads to physician-level documentation burden. Flawed performance measures also often inadequately adjust for patient comorbidities and socioeconomic status, which leads to assessments that do not reflect the actual quality of care.”
Similarly, the American Society of Hematology noted in a statement that it “disagrees with the commission’s recommendation to retain the reporting of practice improvement activities as part of continuous certification due to direct and indirect costs needed to fulfill this requirement on top of requirements for engagement in quality improvement mandated by insurers, institutions, and health systems.”
While the draft report recommended that specialty boards provide aggregated feedback to medical societies, a more individualized dissemination on the gaps in knowledge would be more helpful, according to Doug Henley, MD, CEO of the American Academy of Family Physicians, who said that a more individualized approach would help his organization better provide CME to its members to help fill in the knowledge gaps.
“If we can identify these and use other processes and then target at the individual level to seek improvement, I think that will be a better outcome rather than just x learners don’t do well in diabetic care,” he said in an interview. “That doesn’t really help me in terms of who needs the real education in diabetic care versus who needs it for heart failure.”
The final recommendation notes that ABMS member boards “must collaborate with professional and/or CME/CPD organizations to share data and information to guide and support diplomate engagement in continuing certification.”
The document further clarifies that the boards should examine “the aggregated results from assessments to identify knowledge, skills, and other competency gaps,” and the aggregated data should be shared with specialty societies, CME/CPD providers, quality improvement professionals, and other health care organizations.
One weakness in the draft noted by Dr. Henley was the lack of a more forceful tone within the recommendations. Even though AMBS is not bound by its recommendations, he said that he would like to see stronger language throughout the document.
“We would certainly hope that the ABMS and the member boards will follow the direction of the Vision Commission very directly and succinctly,” he said. “That is why we suggested that some of the recommendations from the Vision Commission should use words like ‘should’ and ‘must’ and not just ‘encourage’ and words like that.”
That recommendation was taken and implemented in the final document.
Societies differed in how often participation in the certification process should occur.
The American College of Rheumatology in its comments challenged a recommendation that certification should be structured to expect participation on an annual basis.
“The ACR supports the importance of ongoing learning,” it stated. “However, no discussion is provided as to how and why the recommendation for annual participation by diplomates was conceived. For some ABMS Boards, an annual requirement will increase physician burden unless continuing certification is modified to a formative pathway. If this recommendation is to be retained, the commission would be encouraged to emphasize that inclusion of annual participation should be part of an overall program structure plan that supports a formative approach to assessment. In addition, the ACR requests that ABMS Boards allow exceptions without penalty to be made to this annual requirement to all for live events.”
The American College of Cardiology took a different point of view with regard to this recommendation.
In its comments, ACC stated that it “concurs with this recommendation. Annual participation is a feature of the ACC’s proposed maintenance of certification solution. The ACC believes that ABMS boards should recognize, and make allowances for, physicians who may, for valid reasons (illness, sabbatical, medical or family issue) may not participate in MOC for a period of a year.” ACC generally concurred with the recommendations in the draft.
The final document presented the commission’s view that the ABMS member boards “need to engage with diplomates on an ongoing basis instead of every 2, 5, or 10 years. The ABMS Boards should develop a diplomate engagement strategy and support the idea that diplomates are committed to learning and continually improving their practice, skills, and competencies. The ABMS Boards should expect that diplomates would engage in some learning, assessment, or advancing practice work annually.”
The American Gastroenterological Association, in its comment letter on the draft, said it was “greatly concerned” about the inclusion of practice improvement data, noting it is “debatable whether it is even within the appropriate domain of the boards to assume responsibility for clinical practice performance and quality assurance.”
The final report states that ABMS “must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage,” and added that “when appropriate, taking advantage of other organizations’ quality improvement and reporting activities should be maximized to avoid additional burdens on diplomates.”
ABMS and its board are not bound to follow any of the recommendations contained within the report, but the commission states that it “expects that the ABMS and the ABMS Boards, in collaboration with professional organizations and other stakeholders, will prioritize these recommendations and develop the necessary strategies and infrastructure to implement them.”
Whatever you do, change the name.
That was key among the final recommendations the Vision Initiative Commission submitted to the American Board of Medical Specialties on how to improve the maintenance of certification process.
“A new term that communicates the concept, intent, and expectations of continuing certification programs should be adopted by the ABMS in order to reengage disaffected diplomates and assure the public and other stakeholders that the certificate has enduring meaning and value,” according to the final report. A new term was not suggested.
The commission recommended a continuing certification system with four aims:
- Become a meaningful, contemporary, and relevant professional development activity for diplomates that ensures they remain up-to-date in their specialty.
- Demonstrate a commitment to professional self-regulation to both diplomates and the public.
- Align with international and national standards for certification programs.
- Provide a specialty-based credential that would be of value to diplomates and to multiple stakeholders, including patients, families, the public, and health care institutions.
Testing methods and situations must be simplified and updated, according to the report, which was submitted to ABMS on Feb. 12. Continuing certification “must change to incorporate longitudinal and other innovative formative assessment strategies that support learning, identify knowledge and skills gaps, and help diplomates stay current. The ABMS Boards must offer an alternative to burdensome highly secure, point-in-time examinations of knowledge.” In addition, the boards “must no longer use a single point-in-time examination or a series of single point-in-time assessments as the sole method to determine certification status.”
Instead, the commission recommends that ABMS “move quickly to formative assessment formats that are not characterized by high-stakes summative outcomes (pass/fail), specified time frames for high-stakes assessment, or require burdensome testing formats (such as testing centers or remote proctoring) that are inconsistent with the desired goals for continuing certification – support learning; identify knowledge and skills gaps; and help diplomates stay current.”
The commission also defined how the certification process should be used by other stakeholders.
“ABMS must demonstrate and communicate that continuing certification has value, meaning, and purpose in the health care environment,” the report states. “Hospitals, health systems, payers, and other health care organizations can independently decide what factors are used in credentialing and privileging decisions. ABMS must inform these organizations that continuing certification should not be the only criterion used in these decisions, and these organizations should use a wide portfolio of criteria in these decisions. ABMS must encourage hospitals, health systems, payers, and other health care organizations to not deny credentialing or privileging to a physician solely on the basis of certification status.”
Additionally, the commission report states that “ABMS and the ABMS Boards should collaborate with specialty societies, the [continuing medical education/continuing professional development] community, and other expert stakeholders to develop the infrastructure to support learning activities that produce data-driven advances in clinical practice. The ABMS Boards must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage.”
The report adds that the boards “should readily accept existing activities that diplomates are doing to advance their clinical practice and to provide credit for performing low-resource, high-impact activities as part of their daily practice routine.”
The commission’s final report incorporates a number of changes that physicians offered based on a draft version of the report.
The American College of Physicians commented that it “objects to the use of data regarding quality measures for individual diplomate certification status, because physician-level measures of quality are flawed, and because physician-level data inevitably leads to physician-level documentation burden. Flawed performance measures also often inadequately adjust for patient comorbidities and socioeconomic status, which leads to assessments that do not reflect the actual quality of care.”
Similarly, the American Society of Hematology noted in a statement that it “disagrees with the commission’s recommendation to retain the reporting of practice improvement activities as part of continuous certification due to direct and indirect costs needed to fulfill this requirement on top of requirements for engagement in quality improvement mandated by insurers, institutions, and health systems.”
While the draft report recommended that specialty boards provide aggregated feedback to medical societies, a more individualized dissemination on the gaps in knowledge would be more helpful, according to Doug Henley, MD, CEO of the American Academy of Family Physicians, who said that a more individualized approach would help his organization better provide CME to its members to help fill in the knowledge gaps.
“If we can identify these and use other processes and then target at the individual level to seek improvement, I think that will be a better outcome rather than just x learners don’t do well in diabetic care,” he said in an interview. “That doesn’t really help me in terms of who needs the real education in diabetic care versus who needs it for heart failure.”
The final recommendation notes that ABMS member boards “must collaborate with professional and/or CME/CPD organizations to share data and information to guide and support diplomate engagement in continuing certification.”
The document further clarifies that the boards should examine “the aggregated results from assessments to identify knowledge, skills, and other competency gaps,” and the aggregated data should be shared with specialty societies, CME/CPD providers, quality improvement professionals, and other health care organizations.
One weakness in the draft noted by Dr. Henley was the lack of a more forceful tone within the recommendations. Even though AMBS is not bound by its recommendations, he said that he would like to see stronger language throughout the document.
“We would certainly hope that the ABMS and the member boards will follow the direction of the Vision Commission very directly and succinctly,” he said. “That is why we suggested that some of the recommendations from the Vision Commission should use words like ‘should’ and ‘must’ and not just ‘encourage’ and words like that.”
That recommendation was taken and implemented in the final document.
Societies differed in how often participation in the certification process should occur.
The American College of Rheumatology in its comments challenged a recommendation that certification should be structured to expect participation on an annual basis.
“The ACR supports the importance of ongoing learning,” it stated. “However, no discussion is provided as to how and why the recommendation for annual participation by diplomates was conceived. For some ABMS Boards, an annual requirement will increase physician burden unless continuing certification is modified to a formative pathway. If this recommendation is to be retained, the commission would be encouraged to emphasize that inclusion of annual participation should be part of an overall program structure plan that supports a formative approach to assessment. In addition, the ACR requests that ABMS Boards allow exceptions without penalty to be made to this annual requirement to all for live events.”
The American College of Cardiology took a different point of view with regard to this recommendation.
In its comments, ACC stated that it “concurs with this recommendation. Annual participation is a feature of the ACC’s proposed maintenance of certification solution. The ACC believes that ABMS boards should recognize, and make allowances for, physicians who may, for valid reasons (illness, sabbatical, medical or family issue) may not participate in MOC for a period of a year.” ACC generally concurred with the recommendations in the draft.
The final document presented the commission’s view that the ABMS member boards “need to engage with diplomates on an ongoing basis instead of every 2, 5, or 10 years. The ABMS Boards should develop a diplomate engagement strategy and support the idea that diplomates are committed to learning and continually improving their practice, skills, and competencies. The ABMS Boards should expect that diplomates would engage in some learning, assessment, or advancing practice work annually.”
The American Gastroenterological Association, in its comment letter on the draft, said it was “greatly concerned” about the inclusion of practice improvement data, noting it is “debatable whether it is even within the appropriate domain of the boards to assume responsibility for clinical practice performance and quality assurance.”
The final report states that ABMS “must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage,” and added that “when appropriate, taking advantage of other organizations’ quality improvement and reporting activities should be maximized to avoid additional burdens on diplomates.”
ABMS and its board are not bound to follow any of the recommendations contained within the report, but the commission states that it “expects that the ABMS and the ABMS Boards, in collaboration with professional organizations and other stakeholders, will prioritize these recommendations and develop the necessary strategies and infrastructure to implement them.”
Whatever you do, change the name.
That was key among the final recommendations the Vision Initiative Commission submitted to the American Board of Medical Specialties on how to improve the maintenance of certification process.
“A new term that communicates the concept, intent, and expectations of continuing certification programs should be adopted by the ABMS in order to reengage disaffected diplomates and assure the public and other stakeholders that the certificate has enduring meaning and value,” according to the final report. A new term was not suggested.
The commission recommended a continuing certification system with four aims:
- Become a meaningful, contemporary, and relevant professional development activity for diplomates that ensures they remain up-to-date in their specialty.
- Demonstrate a commitment to professional self-regulation to both diplomates and the public.
- Align with international and national standards for certification programs.
- Provide a specialty-based credential that would be of value to diplomates and to multiple stakeholders, including patients, families, the public, and health care institutions.
Testing methods and situations must be simplified and updated, according to the report, which was submitted to ABMS on Feb. 12. Continuing certification “must change to incorporate longitudinal and other innovative formative assessment strategies that support learning, identify knowledge and skills gaps, and help diplomates stay current. The ABMS Boards must offer an alternative to burdensome highly secure, point-in-time examinations of knowledge.” In addition, the boards “must no longer use a single point-in-time examination or a series of single point-in-time assessments as the sole method to determine certification status.”
Instead, the commission recommends that ABMS “move quickly to formative assessment formats that are not characterized by high-stakes summative outcomes (pass/fail), specified time frames for high-stakes assessment, or require burdensome testing formats (such as testing centers or remote proctoring) that are inconsistent with the desired goals for continuing certification – support learning; identify knowledge and skills gaps; and help diplomates stay current.”
The commission also defined how the certification process should be used by other stakeholders.
“ABMS must demonstrate and communicate that continuing certification has value, meaning, and purpose in the health care environment,” the report states. “Hospitals, health systems, payers, and other health care organizations can independently decide what factors are used in credentialing and privileging decisions. ABMS must inform these organizations that continuing certification should not be the only criterion used in these decisions, and these organizations should use a wide portfolio of criteria in these decisions. ABMS must encourage hospitals, health systems, payers, and other health care organizations to not deny credentialing or privileging to a physician solely on the basis of certification status.”
Additionally, the commission report states that “ABMS and the ABMS Boards should collaborate with specialty societies, the [continuing medical education/continuing professional development] community, and other expert stakeholders to develop the infrastructure to support learning activities that produce data-driven advances in clinical practice. The ABMS Boards must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage.”
The report adds that the boards “should readily accept existing activities that diplomates are doing to advance their clinical practice and to provide credit for performing low-resource, high-impact activities as part of their daily practice routine.”
The commission’s final report incorporates a number of changes that physicians offered based on a draft version of the report.
The American College of Physicians commented that it “objects to the use of data regarding quality measures for individual diplomate certification status, because physician-level measures of quality are flawed, and because physician-level data inevitably leads to physician-level documentation burden. Flawed performance measures also often inadequately adjust for patient comorbidities and socioeconomic status, which leads to assessments that do not reflect the actual quality of care.”
Similarly, the American Society of Hematology noted in a statement that it “disagrees with the commission’s recommendation to retain the reporting of practice improvement activities as part of continuous certification due to direct and indirect costs needed to fulfill this requirement on top of requirements for engagement in quality improvement mandated by insurers, institutions, and health systems.”
While the draft report recommended that specialty boards provide aggregated feedback to medical societies, a more individualized dissemination on the gaps in knowledge would be more helpful, according to Doug Henley, MD, CEO of the American Academy of Family Physicians, who said that a more individualized approach would help his organization better provide CME to its members to help fill in the knowledge gaps.
“If we can identify these and use other processes and then target at the individual level to seek improvement, I think that will be a better outcome rather than just x learners don’t do well in diabetic care,” he said in an interview. “That doesn’t really help me in terms of who needs the real education in diabetic care versus who needs it for heart failure.”
The final recommendation notes that ABMS member boards “must collaborate with professional and/or CME/CPD organizations to share data and information to guide and support diplomate engagement in continuing certification.”
The document further clarifies that the boards should examine “the aggregated results from assessments to identify knowledge, skills, and other competency gaps,” and the aggregated data should be shared with specialty societies, CME/CPD providers, quality improvement professionals, and other health care organizations.
One weakness in the draft noted by Dr. Henley was the lack of a more forceful tone within the recommendations. Even though AMBS is not bound by its recommendations, he said that he would like to see stronger language throughout the document.
“We would certainly hope that the ABMS and the member boards will follow the direction of the Vision Commission very directly and succinctly,” he said. “That is why we suggested that some of the recommendations from the Vision Commission should use words like ‘should’ and ‘must’ and not just ‘encourage’ and words like that.”
That recommendation was taken and implemented in the final document.
Societies differed in how often participation in the certification process should occur.
The American College of Rheumatology in its comments challenged a recommendation that certification should be structured to expect participation on an annual basis.
“The ACR supports the importance of ongoing learning,” it stated. “However, no discussion is provided as to how and why the recommendation for annual participation by diplomates was conceived. For some ABMS Boards, an annual requirement will increase physician burden unless continuing certification is modified to a formative pathway. If this recommendation is to be retained, the commission would be encouraged to emphasize that inclusion of annual participation should be part of an overall program structure plan that supports a formative approach to assessment. In addition, the ACR requests that ABMS Boards allow exceptions without penalty to be made to this annual requirement to all for live events.”
The American College of Cardiology took a different point of view with regard to this recommendation.
In its comments, ACC stated that it “concurs with this recommendation. Annual participation is a feature of the ACC’s proposed maintenance of certification solution. The ACC believes that ABMS boards should recognize, and make allowances for, physicians who may, for valid reasons (illness, sabbatical, medical or family issue) may not participate in MOC for a period of a year.” ACC generally concurred with the recommendations in the draft.
The final document presented the commission’s view that the ABMS member boards “need to engage with diplomates on an ongoing basis instead of every 2, 5, or 10 years. The ABMS Boards should develop a diplomate engagement strategy and support the idea that diplomates are committed to learning and continually improving their practice, skills, and competencies. The ABMS Boards should expect that diplomates would engage in some learning, assessment, or advancing practice work annually.”
The American Gastroenterological Association, in its comment letter on the draft, said it was “greatly concerned” about the inclusion of practice improvement data, noting it is “debatable whether it is even within the appropriate domain of the boards to assume responsibility for clinical practice performance and quality assurance.”
The final report states that ABMS “must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage,” and added that “when appropriate, taking advantage of other organizations’ quality improvement and reporting activities should be maximized to avoid additional burdens on diplomates.”
ABMS and its board are not bound to follow any of the recommendations contained within the report, but the commission states that it “expects that the ABMS and the ABMS Boards, in collaboration with professional organizations and other stakeholders, will prioritize these recommendations and develop the necessary strategies and infrastructure to implement them.”














