User login
The Hospitalist only
Nontraditional specialty physicians supplement hospitalist staffing
More HMGs cover inpatient and ED settings
Our profession continues to experience steady growth, and demand for hospitalist physicians exceeds supply. In a recent article in The Hospitalist, Andrew White, MD, SFHM, highlighted the fact that most hospital medicine groups (HMGs) are constantly recruiting and open positions are not uncommon.
When we think about recruitment and staffing, I bet many of us think principally of physicians trained in the general medicine specialties of internal medicine, family medicine, and pediatrics. Yet, to help meet demand for hospital-based clinicians, HMGs sometimes turn to physicians certified in emergency medicine, critical care, geriatric medicine, palliative care, and other fields.
To gain a better understanding of the diversity within our profession, the Society of Hospital Medicine’s State of Hospital Medicine survey asked HMGs whether they employ at least one physician in these various specialties. Results published in the recently released 2018 State of Hospital Medicine (SoHM) Report show significant differences among groups, affected by location, group size, and type of employer.
At the core of our profession are physicians trained in internal medicine, present in 99.2% of adult medicine HMGs throughout the United States. No surprise given that our field was founded by internists and remains a popular career choice for IM residency graduates. Family physicians follow, with the highest percentage of groups employing at least one FP located in the southern United States at 70.3% and lowest in the west at 54.7%. Small-sized groups – fewer than 10 full-time equivalents (FTEs) – were also more likely to employ FPs.
This speaks to the challenge – often faced by smaller hospitals – of covering both adult and pediatric patient populations and limited workforce availability. Pediatrics- and internal medicine/pediatrics–trained physicians help meet this need and were prevalent within small-sized groups. Another distinction found in the report is that, while 92.1% of multistate hospitalist management companies employed family physicians, only 28.8% of academic university settings did so. Partly because of Accreditation Council for Graduate Medical Education requirements for IM-certified teaching attending for internal medicine residents, FP and other specialties are filling some non–teaching hospitalist positions within our academic programs.
What may be surprising is that emergency medicine and critical care had the largest increase in representation in hospital medicine. The two specialties showed similar growth trends, with a larger presence in the South and Midwest states and 56% of multistate hospitalist management companies employing them. Small- to medium-sized groups of up to 20 FTEs were also more likely to have physicians from these fields, with up to 44% of groups doing so. This is a significant change from 2016, when less than 3.4% of all HMGs overall had a physician certified in emergency or critical care medicine.
This finding seems to coincide with the growth in hospital medicine groups who are covering both ED and inpatient services. For small and rural hospitals, it has become necessary and beneficial to have physicians capable of covering both clinical settings.
Contrast this with geriatric medicine and palliative care. Here, we saw these two specialties to be present in our academic institutions at 26.8% and 22.5%, respectively. Large-sized HMGs were more likely to employ them, whereas their presence in multistate management groups or private multispecialty/primary care groups was quite low. Compared with our last survey in 2016, their overall prevalence in HMGs hasn’t changed significantly. Whether this will be different in the future with our aging population will be interesting to follow.
Published biannually, the SoHM report provides insight into these and other market-based dynamics that shape hospital medicine. The demand for hospital-based clinicians and the demands of acute inpatient care are leading to the broad and inclusive nature of hospital medicine. Our staffing will continue to be met not only by internal medicine and family medicine physicians but also through these other specialties joining our ranks and adding diversity to our profession.
Dr. Sites is the executive medical director of acute medicine at Providence St. Joseph Health, Oregon, and a member of SHM’s Practice Analysis Committee. She leads the hospital medicine programs and is involved in strategy development and alignment of acute inpatient medicine services at eight member hospitals. She has been a practicing hospitalist for 20 years and volunteers on medical mission trips to Guatemala annually.
More HMGs cover inpatient and ED settings
More HMGs cover inpatient and ED settings
Our profession continues to experience steady growth, and demand for hospitalist physicians exceeds supply. In a recent article in The Hospitalist, Andrew White, MD, SFHM, highlighted the fact that most hospital medicine groups (HMGs) are constantly recruiting and open positions are not uncommon.
When we think about recruitment and staffing, I bet many of us think principally of physicians trained in the general medicine specialties of internal medicine, family medicine, and pediatrics. Yet, to help meet demand for hospital-based clinicians, HMGs sometimes turn to physicians certified in emergency medicine, critical care, geriatric medicine, palliative care, and other fields.
To gain a better understanding of the diversity within our profession, the Society of Hospital Medicine’s State of Hospital Medicine survey asked HMGs whether they employ at least one physician in these various specialties. Results published in the recently released 2018 State of Hospital Medicine (SoHM) Report show significant differences among groups, affected by location, group size, and type of employer.
At the core of our profession are physicians trained in internal medicine, present in 99.2% of adult medicine HMGs throughout the United States. No surprise given that our field was founded by internists and remains a popular career choice for IM residency graduates. Family physicians follow, with the highest percentage of groups employing at least one FP located in the southern United States at 70.3% and lowest in the west at 54.7%. Small-sized groups – fewer than 10 full-time equivalents (FTEs) – were also more likely to employ FPs.
This speaks to the challenge – often faced by smaller hospitals – of covering both adult and pediatric patient populations and limited workforce availability. Pediatrics- and internal medicine/pediatrics–trained physicians help meet this need and were prevalent within small-sized groups. Another distinction found in the report is that, while 92.1% of multistate hospitalist management companies employed family physicians, only 28.8% of academic university settings did so. Partly because of Accreditation Council for Graduate Medical Education requirements for IM-certified teaching attending for internal medicine residents, FP and other specialties are filling some non–teaching hospitalist positions within our academic programs.
What may be surprising is that emergency medicine and critical care had the largest increase in representation in hospital medicine. The two specialties showed similar growth trends, with a larger presence in the South and Midwest states and 56% of multistate hospitalist management companies employing them. Small- to medium-sized groups of up to 20 FTEs were also more likely to have physicians from these fields, with up to 44% of groups doing so. This is a significant change from 2016, when less than 3.4% of all HMGs overall had a physician certified in emergency or critical care medicine.
This finding seems to coincide with the growth in hospital medicine groups who are covering both ED and inpatient services. For small and rural hospitals, it has become necessary and beneficial to have physicians capable of covering both clinical settings.
Contrast this with geriatric medicine and palliative care. Here, we saw these two specialties to be present in our academic institutions at 26.8% and 22.5%, respectively. Large-sized HMGs were more likely to employ them, whereas their presence in multistate management groups or private multispecialty/primary care groups was quite low. Compared with our last survey in 2016, their overall prevalence in HMGs hasn’t changed significantly. Whether this will be different in the future with our aging population will be interesting to follow.
Published biannually, the SoHM report provides insight into these and other market-based dynamics that shape hospital medicine. The demand for hospital-based clinicians and the demands of acute inpatient care are leading to the broad and inclusive nature of hospital medicine. Our staffing will continue to be met not only by internal medicine and family medicine physicians but also through these other specialties joining our ranks and adding diversity to our profession.
Dr. Sites is the executive medical director of acute medicine at Providence St. Joseph Health, Oregon, and a member of SHM’s Practice Analysis Committee. She leads the hospital medicine programs and is involved in strategy development and alignment of acute inpatient medicine services at eight member hospitals. She has been a practicing hospitalist for 20 years and volunteers on medical mission trips to Guatemala annually.
Our profession continues to experience steady growth, and demand for hospitalist physicians exceeds supply. In a recent article in The Hospitalist, Andrew White, MD, SFHM, highlighted the fact that most hospital medicine groups (HMGs) are constantly recruiting and open positions are not uncommon.
When we think about recruitment and staffing, I bet many of us think principally of physicians trained in the general medicine specialties of internal medicine, family medicine, and pediatrics. Yet, to help meet demand for hospital-based clinicians, HMGs sometimes turn to physicians certified in emergency medicine, critical care, geriatric medicine, palliative care, and other fields.
To gain a better understanding of the diversity within our profession, the Society of Hospital Medicine’s State of Hospital Medicine survey asked HMGs whether they employ at least one physician in these various specialties. Results published in the recently released 2018 State of Hospital Medicine (SoHM) Report show significant differences among groups, affected by location, group size, and type of employer.
At the core of our profession are physicians trained in internal medicine, present in 99.2% of adult medicine HMGs throughout the United States. No surprise given that our field was founded by internists and remains a popular career choice for IM residency graduates. Family physicians follow, with the highest percentage of groups employing at least one FP located in the southern United States at 70.3% and lowest in the west at 54.7%. Small-sized groups – fewer than 10 full-time equivalents (FTEs) – were also more likely to employ FPs.
This speaks to the challenge – often faced by smaller hospitals – of covering both adult and pediatric patient populations and limited workforce availability. Pediatrics- and internal medicine/pediatrics–trained physicians help meet this need and were prevalent within small-sized groups. Another distinction found in the report is that, while 92.1% of multistate hospitalist management companies employed family physicians, only 28.8% of academic university settings did so. Partly because of Accreditation Council for Graduate Medical Education requirements for IM-certified teaching attending for internal medicine residents, FP and other specialties are filling some non–teaching hospitalist positions within our academic programs.
What may be surprising is that emergency medicine and critical care had the largest increase in representation in hospital medicine. The two specialties showed similar growth trends, with a larger presence in the South and Midwest states and 56% of multistate hospitalist management companies employing them. Small- to medium-sized groups of up to 20 FTEs were also more likely to have physicians from these fields, with up to 44% of groups doing so. This is a significant change from 2016, when less than 3.4% of all HMGs overall had a physician certified in emergency or critical care medicine.
This finding seems to coincide with the growth in hospital medicine groups who are covering both ED and inpatient services. For small and rural hospitals, it has become necessary and beneficial to have physicians capable of covering both clinical settings.
Contrast this with geriatric medicine and palliative care. Here, we saw these two specialties to be present in our academic institutions at 26.8% and 22.5%, respectively. Large-sized HMGs were more likely to employ them, whereas their presence in multistate management groups or private multispecialty/primary care groups was quite low. Compared with our last survey in 2016, their overall prevalence in HMGs hasn’t changed significantly. Whether this will be different in the future with our aging population will be interesting to follow.
Published biannually, the SoHM report provides insight into these and other market-based dynamics that shape hospital medicine. The demand for hospital-based clinicians and the demands of acute inpatient care are leading to the broad and inclusive nature of hospital medicine. Our staffing will continue to be met not only by internal medicine and family medicine physicians but also through these other specialties joining our ranks and adding diversity to our profession.
Dr. Sites is the executive medical director of acute medicine at Providence St. Joseph Health, Oregon, and a member of SHM’s Practice Analysis Committee. She leads the hospital medicine programs and is involved in strategy development and alignment of acute inpatient medicine services at eight member hospitals. She has been a practicing hospitalist for 20 years and volunteers on medical mission trips to Guatemala annually.
In search of high-value care
Six steps that can help your team
U.S. spending on health care is growing rapidly and expected to reach 19.7% of gross domestic product by 2026.1 In response, the Centers for Medicare and Medicaid Services and national organizations such as the American Board of Internal Medicine (ABIM) and the American College of Physicians (ACP) have launched initiatives to ensure that the value being delivered to patients is on par with the escalating cost of care.
Over the past 10 years, I have led and advised hundreds of small- and large-scale projects that focused on improving patient care quality and cost. Below, I share what I, along with other leaders in high-value care, have observed that it takes to implement successful and lasting improvements – for the benefit of patients and hospitals.
A brief history of high-value care
When compared to other wealthy countries, the United States spends disproportionately more money on health care. In 2016, U.S. health care spending was $3.3 trillion1, or $10,348 per person.2 Hospital care alone was responsible for a third of health spending and amounted to $1.1 trillion in 20161. By 2026, national health spending is projected to reach $5.7 trillion1.
In response to escalating health care costs, CMS and other payers have shifted toward value-based reimbursements that tie payments to health care facilities and clinicians to their performance on selected quality, cost, and efficiency measures. For example, under the CMS Merit-based Incentive Payment System (MIPS), 5% of clinicians’ revenue in 2020 is tied to their 2018 performance in four categories: Quality, Cost, Improvement Activities, and Promoting Interoperability. The percentage of revenue at risk will increase to 9% in 2022, based on 2020 performance.
Rising health care costs put a burden not just on the federal and state budgets, but on individual and family budgets as well. Out-of-pocket spending grew 3.9% in 2016 to $352.5 billion1 and is expected to increase in the future. High health care costs rightfully bring into question the value individual consumers of health care services are getting in return. If value is defined as the level of benefit achieved for a given cost, what is high-value care? The 2013 Institute of Medicine report3 defined high-value care as “the best care for the patient, with the optimal result for the circumstances, delivered at the right price.” It goes beyond a set of quality and cost measures used by payers to affect provider reimbursement and is driven by day-to-day individual providers’ decisions that affect individual patients’ outcomes and their cost of care.
High-value care has been embraced by national organizations. In 2012, the ABIM Foundation launched the Choosing Wisely initiative to support and promote conversations between clinicians and patients in choosing care that is truly necessary, supported by evidence, and free from harm. The result was an evidence-based list of recommendations from 540 specialty societies, including the Society of Hospital Medicine. The SHM – Adult Hospital Medicine list4 features the following “Five things physicians and patients should question”:
- Don’t place, or leave in place, urinary catheters for incontinence or convenience or monitoring of output for non–critically ill patients.
- Don’t prescribe medications for stress ulcer prophylaxis to medical inpatients unless at high risk for GI complications.
- Avoid transfusions of red blood cells for arbitrary hemoglobin or hematocrit thresholds and in the absence of symptoms of active coronary disease, heart failure, or stroke.
- Don’t order continuous telemetry monitoring outside of the ICU without using a protocol that governs continuation.
- Don’t perform repetitive CBC and chemistry testing in the face of clinical and lab stability.
The ACP launched a high-value care initiative that offers learning resources for clinicians and medical educators, clinical guidelines, and best practice advice. In 2012, a workgroup of internists convened by ACP developed a list of 37 clinical situations in which medical tests are commonly used but do not provide high value.5 Seven of those situations are applicable to adult hospital medicine.
High-value care today: What the experts say
More than 5 years later, what progress have hospitalists made in adopting high-value care practices? To answer this and other questions, I reached out to three national experts in high-value care in hospital medicine: Amit Pahwa, MD, assistant professor of medicine and pediatrics at Johns Hopkins University, Baltimore, and a course director of “Topics in interdisciplinary medicine: High-value health care”; Christopher Petrilli, MD, clinical assistant professor in the department of medicine at New York University Langone Health and clinical lead, Manhattan campus, value-based management; and Charlie Wray, DO, MS, assistant professor of medicine at the University of California in San Francisco and a coauthor of an article on high-value care in hospital medicine published recently in the Journal of General Internal Medicine6.
The experts agree that awareness of high-value care among practicing physicians and medical trainees has increased in the last few years. Major professional publications have highlighted the topic, including The Journal of Hospital Medicine’s “Things We Do For No Reason” series, JAMA’s “Teachable Moments,” and the American Journal of Medicine’s recurring column dedicated to high-value care practice. Leading teaching institutions have built high-value care curricula as a part of their medical student and resident training. However, widespread adoption has been slow and sometimes difficult.
The barriers to adoption of high-value practices among hospitalists are numerous and deep rooted in historical practices and culture. As Dr. Petrilli said, the “culture of overordering [diagnostic tests] is hard to break.” Hospitalists may not have well-developed relationships with patients, or time to explain why some tests or treatments are unnecessary. There is a lack of cost transparency, including the cost of the tests themselves and the downstream costs of additional tests and follow-ups. The best intended interventions fail to produce durable change unless they are seamlessly integrated into a hospitalist’s daily workflow.
Six steps to implementing a successful high-value care initiative
What can hospitalists do to improve the value of care they provide to their patients and hospital partners?
1. Identify high-value care opportunities at your hospital.
Dr. Wray pointed out that “all high-value care is local.” Start by looking at the national guidelines and talking to your senior clinical leaders and colleagues. Review your hospital data to identify opportunities and understand the root causes, including variability among providers.
If you choose to analyze and present provider-specific data, first be transparent on why you are doing that. Your goal is not to tell physicians how to practice or to score them, but instead, to promote adoption of evidence-based high-value care by identifying and discussing provider practice variations, and to generate possible solutions. Second, make sure that the data you present is credible and trustworthy by clearly outlining the data source, time frame, sample size per provider, any inclusion and exclusion criteria, attribution logic, and severity adjustment methodology. Third, expect initial pushback as transparency and change can be scary. But most doctors are inherently competitive and will want to be the best at caring for their patients.
2. Assemble the team.
Identify an executive sponsor – a senior clinical executive (for example, the chief medical officer or vice president of medical affairs) whose role is to help engage stakeholders, secure resources, and remove barriers. When assembling the rest of the team, include a representative from each major stakeholder group, but keep the team small enough to be effective. For example, if your project focuses on improving telemetry utilization, seek representation from hospitalists, cardiologists, nurses, utilization managers, and possibly IT. Look for people with the relevant knowledge and experience who are respected by their peers and can influence opinion.
3. Design a sustainable solution.
To be sustainable, a solution must be evidence based, well integrated in provider workflow, and have acceptable impact on daily workload (e.g., additional time per patient). If an estimated impact is significant, you need to discuss adding resources or negotiating trade-offs.
A great example of a sustainable solution, aimed to control overutilization of telemetry and urinary catheters, is the one implemented by Dr. Wray and his team.7 They designed an EHR-based “silent” indicator that clearly signaled an active telemetry or urinary catheter order for each patient. Clicking on the indicator directed a provider to a “manage order” screen where she could cancel the order, if necessary.
4. Engage providers.
You may design the best solution, but it will not succeed unless it is embraced by others. To engage providers, you must clearly communicate why the change is urgently needed for the benefit of their patients, hospital, or community, and appeal to their minds, hearts, and competitive nature.
For example, if you are focusing on overutilization of urinary catheters, you may share your hospital’s urinary catheter device utilization ratio (# of indwelling catheter days/# patient days) against national benchmarks, or the impact on hospital catheter–associated urinary tract infections (CAUTI) rates to appeal to the physicians’ minds. Often, data alone are not enough to move people to action. You must appeal to their hearts by sharing stories of real patients whose lives were affected by preventable CAUTI. Leverage physicians’ competitive nature by using provider-specific data to compare against their peers to spark a discussion.
5. Evaluate impact.
Even before you implement a solution, select metrics to measure impact and set SMART (specific, measurable, achievable, relevant, and time-bound) goals. As your implementation moves forward, do not let up or give up – continue to evaluate impact, remove barriers, refine your solution to get back on track if needed, and constantly communicate to share ongoing project results and lessons learned.
6. Sustain improvements.
Sustainable improvements require well-designed solutions integrated into provider workflow, but that is just the first step. Once you demonstrate the impact, consider including the metric (e.g., telemetry or urinary catheter utilization) in your team and/or individual provider performance dashboard, regularly reviewing and discussing performance during your team meetings to maintain engagement, and if needed, making improvements to get back on track.
Successful adoption of high-value care practices requires a disciplined approach to design and implement solutions that are patient-centric, evidence-based, data-driven and integrated in provider workflow.
Dr. Farah is a hospitalist, Physician Advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. From the Centers for Medicare & Medicaid Services: National Health Expenditure Projections 2018-2027.
2. Peterson-Kaiser Health System Tracker: How does health spending in the U.S. compare to other countries?
3. Creating a new culture of care, in “Best care at lower cost: The path to continuously learning health care in America.” (Washington: National Academies Press, 2013, pp. 255-80).
4. Choosing Wisely: SHM – Adult Hospital Medicine; Five things physicians and patients should question.
5. Qaseem A et al. Appropriate use of screening and diagnostic tests to foster high-value, cost-conscious care. Ann Intern Med. 2012 Jan 17;156(2):147-9.
6. Cho HJ et al. Right care in hospital medicine: Co-creation of ten opportunities in overuse and underuse for improving value in hospital medicine. J Gen Intern Med. 2018 Jun;33(6):804-6.
7. Wray CM et al. Improving value by reducing unnecessary telemetry and urinary catheter utilization in hospitalized patients. Am J Med. 2017 Sep;130(9):1037-41.
Six steps that can help your team
Six steps that can help your team
U.S. spending on health care is growing rapidly and expected to reach 19.7% of gross domestic product by 2026.1 In response, the Centers for Medicare and Medicaid Services and national organizations such as the American Board of Internal Medicine (ABIM) and the American College of Physicians (ACP) have launched initiatives to ensure that the value being delivered to patients is on par with the escalating cost of care.
Over the past 10 years, I have led and advised hundreds of small- and large-scale projects that focused on improving patient care quality and cost. Below, I share what I, along with other leaders in high-value care, have observed that it takes to implement successful and lasting improvements – for the benefit of patients and hospitals.
A brief history of high-value care
When compared to other wealthy countries, the United States spends disproportionately more money on health care. In 2016, U.S. health care spending was $3.3 trillion1, or $10,348 per person.2 Hospital care alone was responsible for a third of health spending and amounted to $1.1 trillion in 20161. By 2026, national health spending is projected to reach $5.7 trillion1.
In response to escalating health care costs, CMS and other payers have shifted toward value-based reimbursements that tie payments to health care facilities and clinicians to their performance on selected quality, cost, and efficiency measures. For example, under the CMS Merit-based Incentive Payment System (MIPS), 5% of clinicians’ revenue in 2020 is tied to their 2018 performance in four categories: Quality, Cost, Improvement Activities, and Promoting Interoperability. The percentage of revenue at risk will increase to 9% in 2022, based on 2020 performance.
Rising health care costs put a burden not just on the federal and state budgets, but on individual and family budgets as well. Out-of-pocket spending grew 3.9% in 2016 to $352.5 billion1 and is expected to increase in the future. High health care costs rightfully bring into question the value individual consumers of health care services are getting in return. If value is defined as the level of benefit achieved for a given cost, what is high-value care? The 2013 Institute of Medicine report3 defined high-value care as “the best care for the patient, with the optimal result for the circumstances, delivered at the right price.” It goes beyond a set of quality and cost measures used by payers to affect provider reimbursement and is driven by day-to-day individual providers’ decisions that affect individual patients’ outcomes and their cost of care.
High-value care has been embraced by national organizations. In 2012, the ABIM Foundation launched the Choosing Wisely initiative to support and promote conversations between clinicians and patients in choosing care that is truly necessary, supported by evidence, and free from harm. The result was an evidence-based list of recommendations from 540 specialty societies, including the Society of Hospital Medicine. The SHM – Adult Hospital Medicine list4 features the following “Five things physicians and patients should question”:
- Don’t place, or leave in place, urinary catheters for incontinence or convenience or monitoring of output for non–critically ill patients.
- Don’t prescribe medications for stress ulcer prophylaxis to medical inpatients unless at high risk for GI complications.
- Avoid transfusions of red blood cells for arbitrary hemoglobin or hematocrit thresholds and in the absence of symptoms of active coronary disease, heart failure, or stroke.
- Don’t order continuous telemetry monitoring outside of the ICU without using a protocol that governs continuation.
- Don’t perform repetitive CBC and chemistry testing in the face of clinical and lab stability.
The ACP launched a high-value care initiative that offers learning resources for clinicians and medical educators, clinical guidelines, and best practice advice. In 2012, a workgroup of internists convened by ACP developed a list of 37 clinical situations in which medical tests are commonly used but do not provide high value.5 Seven of those situations are applicable to adult hospital medicine.
High-value care today: What the experts say
More than 5 years later, what progress have hospitalists made in adopting high-value care practices? To answer this and other questions, I reached out to three national experts in high-value care in hospital medicine: Amit Pahwa, MD, assistant professor of medicine and pediatrics at Johns Hopkins University, Baltimore, and a course director of “Topics in interdisciplinary medicine: High-value health care”; Christopher Petrilli, MD, clinical assistant professor in the department of medicine at New York University Langone Health and clinical lead, Manhattan campus, value-based management; and Charlie Wray, DO, MS, assistant professor of medicine at the University of California in San Francisco and a coauthor of an article on high-value care in hospital medicine published recently in the Journal of General Internal Medicine6.
The experts agree that awareness of high-value care among practicing physicians and medical trainees has increased in the last few years. Major professional publications have highlighted the topic, including The Journal of Hospital Medicine’s “Things We Do For No Reason” series, JAMA’s “Teachable Moments,” and the American Journal of Medicine’s recurring column dedicated to high-value care practice. Leading teaching institutions have built high-value care curricula as a part of their medical student and resident training. However, widespread adoption has been slow and sometimes difficult.
The barriers to adoption of high-value practices among hospitalists are numerous and deep rooted in historical practices and culture. As Dr. Petrilli said, the “culture of overordering [diagnostic tests] is hard to break.” Hospitalists may not have well-developed relationships with patients, or time to explain why some tests or treatments are unnecessary. There is a lack of cost transparency, including the cost of the tests themselves and the downstream costs of additional tests and follow-ups. The best intended interventions fail to produce durable change unless they are seamlessly integrated into a hospitalist’s daily workflow.
Six steps to implementing a successful high-value care initiative
What can hospitalists do to improve the value of care they provide to their patients and hospital partners?
1. Identify high-value care opportunities at your hospital.
Dr. Wray pointed out that “all high-value care is local.” Start by looking at the national guidelines and talking to your senior clinical leaders and colleagues. Review your hospital data to identify opportunities and understand the root causes, including variability among providers.
If you choose to analyze and present provider-specific data, first be transparent on why you are doing that. Your goal is not to tell physicians how to practice or to score them, but instead, to promote adoption of evidence-based high-value care by identifying and discussing provider practice variations, and to generate possible solutions. Second, make sure that the data you present is credible and trustworthy by clearly outlining the data source, time frame, sample size per provider, any inclusion and exclusion criteria, attribution logic, and severity adjustment methodology. Third, expect initial pushback as transparency and change can be scary. But most doctors are inherently competitive and will want to be the best at caring for their patients.
2. Assemble the team.
Identify an executive sponsor – a senior clinical executive (for example, the chief medical officer or vice president of medical affairs) whose role is to help engage stakeholders, secure resources, and remove barriers. When assembling the rest of the team, include a representative from each major stakeholder group, but keep the team small enough to be effective. For example, if your project focuses on improving telemetry utilization, seek representation from hospitalists, cardiologists, nurses, utilization managers, and possibly IT. Look for people with the relevant knowledge and experience who are respected by their peers and can influence opinion.
3. Design a sustainable solution.
To be sustainable, a solution must be evidence based, well integrated in provider workflow, and have acceptable impact on daily workload (e.g., additional time per patient). If an estimated impact is significant, you need to discuss adding resources or negotiating trade-offs.
A great example of a sustainable solution, aimed to control overutilization of telemetry and urinary catheters, is the one implemented by Dr. Wray and his team.7 They designed an EHR-based “silent” indicator that clearly signaled an active telemetry or urinary catheter order for each patient. Clicking on the indicator directed a provider to a “manage order” screen where she could cancel the order, if necessary.
4. Engage providers.
You may design the best solution, but it will not succeed unless it is embraced by others. To engage providers, you must clearly communicate why the change is urgently needed for the benefit of their patients, hospital, or community, and appeal to their minds, hearts, and competitive nature.
For example, if you are focusing on overutilization of urinary catheters, you may share your hospital’s urinary catheter device utilization ratio (# of indwelling catheter days/# patient days) against national benchmarks, or the impact on hospital catheter–associated urinary tract infections (CAUTI) rates to appeal to the physicians’ minds. Often, data alone are not enough to move people to action. You must appeal to their hearts by sharing stories of real patients whose lives were affected by preventable CAUTI. Leverage physicians’ competitive nature by using provider-specific data to compare against their peers to spark a discussion.
5. Evaluate impact.
Even before you implement a solution, select metrics to measure impact and set SMART (specific, measurable, achievable, relevant, and time-bound) goals. As your implementation moves forward, do not let up or give up – continue to evaluate impact, remove barriers, refine your solution to get back on track if needed, and constantly communicate to share ongoing project results and lessons learned.
6. Sustain improvements.
Sustainable improvements require well-designed solutions integrated into provider workflow, but that is just the first step. Once you demonstrate the impact, consider including the metric (e.g., telemetry or urinary catheter utilization) in your team and/or individual provider performance dashboard, regularly reviewing and discussing performance during your team meetings to maintain engagement, and if needed, making improvements to get back on track.
Successful adoption of high-value care practices requires a disciplined approach to design and implement solutions that are patient-centric, evidence-based, data-driven and integrated in provider workflow.
Dr. Farah is a hospitalist, Physician Advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. From the Centers for Medicare & Medicaid Services: National Health Expenditure Projections 2018-2027.
2. Peterson-Kaiser Health System Tracker: How does health spending in the U.S. compare to other countries?
3. Creating a new culture of care, in “Best care at lower cost: The path to continuously learning health care in America.” (Washington: National Academies Press, 2013, pp. 255-80).
4. Choosing Wisely: SHM – Adult Hospital Medicine; Five things physicians and patients should question.
5. Qaseem A et al. Appropriate use of screening and diagnostic tests to foster high-value, cost-conscious care. Ann Intern Med. 2012 Jan 17;156(2):147-9.
6. Cho HJ et al. Right care in hospital medicine: Co-creation of ten opportunities in overuse and underuse for improving value in hospital medicine. J Gen Intern Med. 2018 Jun;33(6):804-6.
7. Wray CM et al. Improving value by reducing unnecessary telemetry and urinary catheter utilization in hospitalized patients. Am J Med. 2017 Sep;130(9):1037-41.
U.S. spending on health care is growing rapidly and expected to reach 19.7% of gross domestic product by 2026.1 In response, the Centers for Medicare and Medicaid Services and national organizations such as the American Board of Internal Medicine (ABIM) and the American College of Physicians (ACP) have launched initiatives to ensure that the value being delivered to patients is on par with the escalating cost of care.
Over the past 10 years, I have led and advised hundreds of small- and large-scale projects that focused on improving patient care quality and cost. Below, I share what I, along with other leaders in high-value care, have observed that it takes to implement successful and lasting improvements – for the benefit of patients and hospitals.
A brief history of high-value care
When compared to other wealthy countries, the United States spends disproportionately more money on health care. In 2016, U.S. health care spending was $3.3 trillion1, or $10,348 per person.2 Hospital care alone was responsible for a third of health spending and amounted to $1.1 trillion in 20161. By 2026, national health spending is projected to reach $5.7 trillion1.
In response to escalating health care costs, CMS and other payers have shifted toward value-based reimbursements that tie payments to health care facilities and clinicians to their performance on selected quality, cost, and efficiency measures. For example, under the CMS Merit-based Incentive Payment System (MIPS), 5% of clinicians’ revenue in 2020 is tied to their 2018 performance in four categories: Quality, Cost, Improvement Activities, and Promoting Interoperability. The percentage of revenue at risk will increase to 9% in 2022, based on 2020 performance.
Rising health care costs put a burden not just on the federal and state budgets, but on individual and family budgets as well. Out-of-pocket spending grew 3.9% in 2016 to $352.5 billion1 and is expected to increase in the future. High health care costs rightfully bring into question the value individual consumers of health care services are getting in return. If value is defined as the level of benefit achieved for a given cost, what is high-value care? The 2013 Institute of Medicine report3 defined high-value care as “the best care for the patient, with the optimal result for the circumstances, delivered at the right price.” It goes beyond a set of quality and cost measures used by payers to affect provider reimbursement and is driven by day-to-day individual providers’ decisions that affect individual patients’ outcomes and their cost of care.
High-value care has been embraced by national organizations. In 2012, the ABIM Foundation launched the Choosing Wisely initiative to support and promote conversations between clinicians and patients in choosing care that is truly necessary, supported by evidence, and free from harm. The result was an evidence-based list of recommendations from 540 specialty societies, including the Society of Hospital Medicine. The SHM – Adult Hospital Medicine list4 features the following “Five things physicians and patients should question”:
- Don’t place, or leave in place, urinary catheters for incontinence or convenience or monitoring of output for non–critically ill patients.
- Don’t prescribe medications for stress ulcer prophylaxis to medical inpatients unless at high risk for GI complications.
- Avoid transfusions of red blood cells for arbitrary hemoglobin or hematocrit thresholds and in the absence of symptoms of active coronary disease, heart failure, or stroke.
- Don’t order continuous telemetry monitoring outside of the ICU without using a protocol that governs continuation.
- Don’t perform repetitive CBC and chemistry testing in the face of clinical and lab stability.
The ACP launched a high-value care initiative that offers learning resources for clinicians and medical educators, clinical guidelines, and best practice advice. In 2012, a workgroup of internists convened by ACP developed a list of 37 clinical situations in which medical tests are commonly used but do not provide high value.5 Seven of those situations are applicable to adult hospital medicine.
High-value care today: What the experts say
More than 5 years later, what progress have hospitalists made in adopting high-value care practices? To answer this and other questions, I reached out to three national experts in high-value care in hospital medicine: Amit Pahwa, MD, assistant professor of medicine and pediatrics at Johns Hopkins University, Baltimore, and a course director of “Topics in interdisciplinary medicine: High-value health care”; Christopher Petrilli, MD, clinical assistant professor in the department of medicine at New York University Langone Health and clinical lead, Manhattan campus, value-based management; and Charlie Wray, DO, MS, assistant professor of medicine at the University of California in San Francisco and a coauthor of an article on high-value care in hospital medicine published recently in the Journal of General Internal Medicine6.
The experts agree that awareness of high-value care among practicing physicians and medical trainees has increased in the last few years. Major professional publications have highlighted the topic, including The Journal of Hospital Medicine’s “Things We Do For No Reason” series, JAMA’s “Teachable Moments,” and the American Journal of Medicine’s recurring column dedicated to high-value care practice. Leading teaching institutions have built high-value care curricula as a part of their medical student and resident training. However, widespread adoption has been slow and sometimes difficult.
The barriers to adoption of high-value practices among hospitalists are numerous and deep rooted in historical practices and culture. As Dr. Petrilli said, the “culture of overordering [diagnostic tests] is hard to break.” Hospitalists may not have well-developed relationships with patients, or time to explain why some tests or treatments are unnecessary. There is a lack of cost transparency, including the cost of the tests themselves and the downstream costs of additional tests and follow-ups. The best intended interventions fail to produce durable change unless they are seamlessly integrated into a hospitalist’s daily workflow.
Six steps to implementing a successful high-value care initiative
What can hospitalists do to improve the value of care they provide to their patients and hospital partners?
1. Identify high-value care opportunities at your hospital.
Dr. Wray pointed out that “all high-value care is local.” Start by looking at the national guidelines and talking to your senior clinical leaders and colleagues. Review your hospital data to identify opportunities and understand the root causes, including variability among providers.
If you choose to analyze and present provider-specific data, first be transparent on why you are doing that. Your goal is not to tell physicians how to practice or to score them, but instead, to promote adoption of evidence-based high-value care by identifying and discussing provider practice variations, and to generate possible solutions. Second, make sure that the data you present is credible and trustworthy by clearly outlining the data source, time frame, sample size per provider, any inclusion and exclusion criteria, attribution logic, and severity adjustment methodology. Third, expect initial pushback as transparency and change can be scary. But most doctors are inherently competitive and will want to be the best at caring for their patients.
2. Assemble the team.
Identify an executive sponsor – a senior clinical executive (for example, the chief medical officer or vice president of medical affairs) whose role is to help engage stakeholders, secure resources, and remove barriers. When assembling the rest of the team, include a representative from each major stakeholder group, but keep the team small enough to be effective. For example, if your project focuses on improving telemetry utilization, seek representation from hospitalists, cardiologists, nurses, utilization managers, and possibly IT. Look for people with the relevant knowledge and experience who are respected by their peers and can influence opinion.
3. Design a sustainable solution.
To be sustainable, a solution must be evidence based, well integrated in provider workflow, and have acceptable impact on daily workload (e.g., additional time per patient). If an estimated impact is significant, you need to discuss adding resources or negotiating trade-offs.
A great example of a sustainable solution, aimed to control overutilization of telemetry and urinary catheters, is the one implemented by Dr. Wray and his team.7 They designed an EHR-based “silent” indicator that clearly signaled an active telemetry or urinary catheter order for each patient. Clicking on the indicator directed a provider to a “manage order” screen where she could cancel the order, if necessary.
4. Engage providers.
You may design the best solution, but it will not succeed unless it is embraced by others. To engage providers, you must clearly communicate why the change is urgently needed for the benefit of their patients, hospital, or community, and appeal to their minds, hearts, and competitive nature.
For example, if you are focusing on overutilization of urinary catheters, you may share your hospital’s urinary catheter device utilization ratio (# of indwelling catheter days/# patient days) against national benchmarks, or the impact on hospital catheter–associated urinary tract infections (CAUTI) rates to appeal to the physicians’ minds. Often, data alone are not enough to move people to action. You must appeal to their hearts by sharing stories of real patients whose lives were affected by preventable CAUTI. Leverage physicians’ competitive nature by using provider-specific data to compare against their peers to spark a discussion.
5. Evaluate impact.
Even before you implement a solution, select metrics to measure impact and set SMART (specific, measurable, achievable, relevant, and time-bound) goals. As your implementation moves forward, do not let up or give up – continue to evaluate impact, remove barriers, refine your solution to get back on track if needed, and constantly communicate to share ongoing project results and lessons learned.
6. Sustain improvements.
Sustainable improvements require well-designed solutions integrated into provider workflow, but that is just the first step. Once you demonstrate the impact, consider including the metric (e.g., telemetry or urinary catheter utilization) in your team and/or individual provider performance dashboard, regularly reviewing and discussing performance during your team meetings to maintain engagement, and if needed, making improvements to get back on track.
Successful adoption of high-value care practices requires a disciplined approach to design and implement solutions that are patient-centric, evidence-based, data-driven and integrated in provider workflow.
Dr. Farah is a hospitalist, Physician Advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. From the Centers for Medicare & Medicaid Services: National Health Expenditure Projections 2018-2027.
2. Peterson-Kaiser Health System Tracker: How does health spending in the U.S. compare to other countries?
3. Creating a new culture of care, in “Best care at lower cost: The path to continuously learning health care in America.” (Washington: National Academies Press, 2013, pp. 255-80).
4. Choosing Wisely: SHM – Adult Hospital Medicine; Five things physicians and patients should question.
5. Qaseem A et al. Appropriate use of screening and diagnostic tests to foster high-value, cost-conscious care. Ann Intern Med. 2012 Jan 17;156(2):147-9.
6. Cho HJ et al. Right care in hospital medicine: Co-creation of ten opportunities in overuse and underuse for improving value in hospital medicine. J Gen Intern Med. 2018 Jun;33(6):804-6.
7. Wray CM et al. Improving value by reducing unnecessary telemetry and urinary catheter utilization in hospitalized patients. Am J Med. 2017 Sep;130(9):1037-41.
Hospitalist Career Goals Should Flow from Passion and Purpose
By Surinder Yadav, MD
For many new or job-changing hospitalists, finding your next position may be your main focus. It’s easy to imagine that once you land a job, the rest of your career will fall easily into place.
But hospital medicine is demanding stuff, and you can get so busy meeting the needs of others that you lose sight of your own. Eventually survival mode kicks in, and your drive and passion begin to fade.
In order to maintain a sense of forward momentum and job satisfaction, it helps to set annual goals. What could you accomplish this year that would really get you excited about your career? What skills could take your practice to the next level? Are your current actions in sync with your values and life purpose?
Here are some tips I've learned through the years:
Base goals on your passion
To get the most satisfaction from your career, start by identifying your passion. Why did you select medicine as a career, and how does it relate to your life purpose? Once you are clear on what motivates you to get up in the morning, you can set your goals to help drive and sustain that passion.
Set goals that are measurable
If you don’t have goals you can measure, it’s too easy to let them slide when you get busy with other obligations. Examples of some measurable goals I’ve set for my own career include taking leadership courses in project management and people management.
Once you’ve established your goals and determined how you will measure your progress and success, create a timeline for achieving each milestone. Also, consider finding an accountability partner who will check in with you now and then to make sure you're on track.
Be realistic
Goals that are admirable but not attainable are a waste of the paper they are written on. Make sure you have the resources you need to achieve your specific goals so that you have no roadblocks to success.
A final thought: One of the benefits of working for a physician partnership like Vituity is flexibility. You'll have more leeway to create a work schedule that allows you time for yourself. Work-life balance is great for your career longevity, and we believe it’s also good for your patients. When you feel rested and fulfilled, you have more energy and compassion to give to others.
Surinder Yadav, MD, is Vituity’s Vice President of Hospital Medicine Operations.
To learn more about satisfying medical careers at Vituity, please visit http://www.vituity.com/careers.
By Surinder Yadav, MD
For many new or job-changing hospitalists, finding your next position may be your main focus. It’s easy to imagine that once you land a job, the rest of your career will fall easily into place.
But hospital medicine is demanding stuff, and you can get so busy meeting the needs of others that you lose sight of your own. Eventually survival mode kicks in, and your drive and passion begin to fade.
In order to maintain a sense of forward momentum and job satisfaction, it helps to set annual goals. What could you accomplish this year that would really get you excited about your career? What skills could take your practice to the next level? Are your current actions in sync with your values and life purpose?
Here are some tips I've learned through the years:
Base goals on your passion
To get the most satisfaction from your career, start by identifying your passion. Why did you select medicine as a career, and how does it relate to your life purpose? Once you are clear on what motivates you to get up in the morning, you can set your goals to help drive and sustain that passion.
Set goals that are measurable
If you don’t have goals you can measure, it’s too easy to let them slide when you get busy with other obligations. Examples of some measurable goals I’ve set for my own career include taking leadership courses in project management and people management.
Once you’ve established your goals and determined how you will measure your progress and success, create a timeline for achieving each milestone. Also, consider finding an accountability partner who will check in with you now and then to make sure you're on track.
Be realistic
Goals that are admirable but not attainable are a waste of the paper they are written on. Make sure you have the resources you need to achieve your specific goals so that you have no roadblocks to success.
A final thought: One of the benefits of working for a physician partnership like Vituity is flexibility. You'll have more leeway to create a work schedule that allows you time for yourself. Work-life balance is great for your career longevity, and we believe it’s also good for your patients. When you feel rested and fulfilled, you have more energy and compassion to give to others.
Surinder Yadav, MD, is Vituity’s Vice President of Hospital Medicine Operations.
To learn more about satisfying medical careers at Vituity, please visit http://www.vituity.com/careers.
By Surinder Yadav, MD
For many new or job-changing hospitalists, finding your next position may be your main focus. It’s easy to imagine that once you land a job, the rest of your career will fall easily into place.
But hospital medicine is demanding stuff, and you can get so busy meeting the needs of others that you lose sight of your own. Eventually survival mode kicks in, and your drive and passion begin to fade.
In order to maintain a sense of forward momentum and job satisfaction, it helps to set annual goals. What could you accomplish this year that would really get you excited about your career? What skills could take your practice to the next level? Are your current actions in sync with your values and life purpose?
Here are some tips I've learned through the years:
Base goals on your passion
To get the most satisfaction from your career, start by identifying your passion. Why did you select medicine as a career, and how does it relate to your life purpose? Once you are clear on what motivates you to get up in the morning, you can set your goals to help drive and sustain that passion.
Set goals that are measurable
If you don’t have goals you can measure, it’s too easy to let them slide when you get busy with other obligations. Examples of some measurable goals I’ve set for my own career include taking leadership courses in project management and people management.
Once you’ve established your goals and determined how you will measure your progress and success, create a timeline for achieving each milestone. Also, consider finding an accountability partner who will check in with you now and then to make sure you're on track.
Be realistic
Goals that are admirable but not attainable are a waste of the paper they are written on. Make sure you have the resources you need to achieve your specific goals so that you have no roadblocks to success.
A final thought: One of the benefits of working for a physician partnership like Vituity is flexibility. You'll have more leeway to create a work schedule that allows you time for yourself. Work-life balance is great for your career longevity, and we believe it’s also good for your patients. When you feel rested and fulfilled, you have more energy and compassion to give to others.
Surinder Yadav, MD, is Vituity’s Vice President of Hospital Medicine Operations.
To learn more about satisfying medical careers at Vituity, please visit http://www.vituity.com/careers.
ONC’s Dr. Rucker: Era of provider-controlled data is over
“The era of the provider controlling all of this, I think this is over,” Donald Rucker, MD, head of the Office of the National Coordinator (ONC) for Health Information Technology within the Department of Health and Human Services, said at an annual conference on health data and innovation. We need a “formal path to put patients back in control of their medical data.”
That path can be found in a pair of proposed rules issued earlier this year, one from the Centers for Medicare & Medicaid Services and the other from ONC, that are designed to give patients that control.
With smartphone apps under development that will allow patient access to health care data from a single point of entry, “technology now allows us to move from having to go portal to portal to portal to really having us in control,” Dr. Rucker said. “I think it is going to transform [health care] in the same way that the smartphone app has transformed other sectors. We are very excited about that.”
Access to data and information should further the transition to value-based care as patients become the center of the decision tree, Dr. Rucker said, making decisions based on benefits in a way that is not possible now.
“In particular, we think patients are going to start being able to shop for care,” he said, adding that if “they don’t like the price of the care they are getting, they are going to be able to move their business elsewhere.”
To that end, he said that much of the talk about interoperability “is really a conversation about affordability and the vast expenses in health care and how you get some control over that.”
“The era of the provider controlling all of this, I think this is over,” Donald Rucker, MD, head of the Office of the National Coordinator (ONC) for Health Information Technology within the Department of Health and Human Services, said at an annual conference on health data and innovation. We need a “formal path to put patients back in control of their medical data.”
That path can be found in a pair of proposed rules issued earlier this year, one from the Centers for Medicare & Medicaid Services and the other from ONC, that are designed to give patients that control.
With smartphone apps under development that will allow patient access to health care data from a single point of entry, “technology now allows us to move from having to go portal to portal to portal to really having us in control,” Dr. Rucker said. “I think it is going to transform [health care] in the same way that the smartphone app has transformed other sectors. We are very excited about that.”
Access to data and information should further the transition to value-based care as patients become the center of the decision tree, Dr. Rucker said, making decisions based on benefits in a way that is not possible now.
“In particular, we think patients are going to start being able to shop for care,” he said, adding that if “they don’t like the price of the care they are getting, they are going to be able to move their business elsewhere.”
To that end, he said that much of the talk about interoperability “is really a conversation about affordability and the vast expenses in health care and how you get some control over that.”
“The era of the provider controlling all of this, I think this is over,” Donald Rucker, MD, head of the Office of the National Coordinator (ONC) for Health Information Technology within the Department of Health and Human Services, said at an annual conference on health data and innovation. We need a “formal path to put patients back in control of their medical data.”
That path can be found in a pair of proposed rules issued earlier this year, one from the Centers for Medicare & Medicaid Services and the other from ONC, that are designed to give patients that control.
With smartphone apps under development that will allow patient access to health care data from a single point of entry, “technology now allows us to move from having to go portal to portal to portal to really having us in control,” Dr. Rucker said. “I think it is going to transform [health care] in the same way that the smartphone app has transformed other sectors. We are very excited about that.”
Access to data and information should further the transition to value-based care as patients become the center of the decision tree, Dr. Rucker said, making decisions based on benefits in a way that is not possible now.
“In particular, we think patients are going to start being able to shop for care,” he said, adding that if “they don’t like the price of the care they are getting, they are going to be able to move their business elsewhere.”
To that end, he said that much of the talk about interoperability “is really a conversation about affordability and the vast expenses in health care and how you get some control over that.”
REPORTING FROM HEALTH DATAPALOOZA 2019
Malpractice: More lawsuits does not equal more relocations
David M. Studdert of Stanford (Calif.) University and his colleagues analyzed data from Medicare and the National Practitioner Data Bank (NPDB) to assess associations between the number of paid malpractice claims that doctors accrued and exits from medical practice, changes in clinical volume, geographic relocation, and change in practice-group size. The study population included 480,894 physicians who had 68,956 paid claims from 2003 to 2015. Of the study group, 89% had no claims, 9% had one claim, and the remaining 2% had two or more claims that accounted for 40% of all claims. Nearly three-quarters of the doctors studied were men, and the majority of specialties were internal medicine (17%), general practice/family medicine (15%), emergency medicine (7%), radiology (6%), and anesthesiology (6%).
Physicians with a higher number of claims against them did not relocate at a greater rate than physicians who had fewer or no claims, the investigators wrote in the New England Journal of Medicine.
More claims against a doctor were associated with a higher likelihood of leaving medicine and more shifts into smaller practice settings. For instance, physicians with one claim had 9% higher odds of leaving the practice than doctors with no claims, and physicians with five or more claims had a 45% higher chance of leaving medicine than doctors with no claims, the researchers found.
In addition, investigators found that doctors with two to four claims had 50%-60% higher odds of entering solo practice than physicians with no claims, and physicians with five or more claims had nearly 150% higher odds of moving to solo practice than doctors who had never been sued. Physicians with three or more claims were more likely to be male, work in surgical specialties, and be at least age 50 years.
The study addresses concerns that physicians with troubling legal records were moving across state lines for a fresh start, Mr. Studdert said in an interview. “We were surprised to find that physicians who accumulated multiple malpractice claims were no more likely to relocate their practices than physicians without claims. The National Practitioner Data Bank probably has something to do with that.”
Established by Congress in 1986, the NPDB was started, in part, to restrict the ability of incompetent physicians to move across states to hide their track records. By requiring hospitals to query doctors records before granting them clinical privileges and encouraging physician groups, health plans, and professional societies to do the same, the NPDB has “almost certainly increased the difficulty of relocation for physicians with legal problems,” the authors noted in the study.
A primary takeaway from the analysis is that, while a single malpractice claim is a relatively weak signal that a quality problem exists, multiple paid claims over a relatively short period of time are a strong signal that a physician may have a quality deficiency, Mr. Studdert said in the interview.
“Regulators and malpractice insurers should be paying closer attention to this signal,” he added. “To the extent that physicians are aware of a colleague’s checkered malpractice history, they may have a role to play too. Vigilance about signs of further problems, for one, but also careful thought about the wisdom of referring patients to such physicians.”
Michelle M. Mello, JD, PhD, and Mr. Studdert both reported receiving grants from SUMIT Insurance during the conduct of the study.
Source: Studdert DM et al. N Engl J Med. 2019 Mar 28. doi: 10.1056/NEJMsa1809981.
David M. Studdert of Stanford (Calif.) University and his colleagues analyzed data from Medicare and the National Practitioner Data Bank (NPDB) to assess associations between the number of paid malpractice claims that doctors accrued and exits from medical practice, changes in clinical volume, geographic relocation, and change in practice-group size. The study population included 480,894 physicians who had 68,956 paid claims from 2003 to 2015. Of the study group, 89% had no claims, 9% had one claim, and the remaining 2% had two or more claims that accounted for 40% of all claims. Nearly three-quarters of the doctors studied were men, and the majority of specialties were internal medicine (17%), general practice/family medicine (15%), emergency medicine (7%), radiology (6%), and anesthesiology (6%).
Physicians with a higher number of claims against them did not relocate at a greater rate than physicians who had fewer or no claims, the investigators wrote in the New England Journal of Medicine.
More claims against a doctor were associated with a higher likelihood of leaving medicine and more shifts into smaller practice settings. For instance, physicians with one claim had 9% higher odds of leaving the practice than doctors with no claims, and physicians with five or more claims had a 45% higher chance of leaving medicine than doctors with no claims, the researchers found.
In addition, investigators found that doctors with two to four claims had 50%-60% higher odds of entering solo practice than physicians with no claims, and physicians with five or more claims had nearly 150% higher odds of moving to solo practice than doctors who had never been sued. Physicians with three or more claims were more likely to be male, work in surgical specialties, and be at least age 50 years.
The study addresses concerns that physicians with troubling legal records were moving across state lines for a fresh start, Mr. Studdert said in an interview. “We were surprised to find that physicians who accumulated multiple malpractice claims were no more likely to relocate their practices than physicians without claims. The National Practitioner Data Bank probably has something to do with that.”
Established by Congress in 1986, the NPDB was started, in part, to restrict the ability of incompetent physicians to move across states to hide their track records. By requiring hospitals to query doctors records before granting them clinical privileges and encouraging physician groups, health plans, and professional societies to do the same, the NPDB has “almost certainly increased the difficulty of relocation for physicians with legal problems,” the authors noted in the study.
A primary takeaway from the analysis is that, while a single malpractice claim is a relatively weak signal that a quality problem exists, multiple paid claims over a relatively short period of time are a strong signal that a physician may have a quality deficiency, Mr. Studdert said in the interview.
“Regulators and malpractice insurers should be paying closer attention to this signal,” he added. “To the extent that physicians are aware of a colleague’s checkered malpractice history, they may have a role to play too. Vigilance about signs of further problems, for one, but also careful thought about the wisdom of referring patients to such physicians.”
Michelle M. Mello, JD, PhD, and Mr. Studdert both reported receiving grants from SUMIT Insurance during the conduct of the study.
Source: Studdert DM et al. N Engl J Med. 2019 Mar 28. doi: 10.1056/NEJMsa1809981.
David M. Studdert of Stanford (Calif.) University and his colleagues analyzed data from Medicare and the National Practitioner Data Bank (NPDB) to assess associations between the number of paid malpractice claims that doctors accrued and exits from medical practice, changes in clinical volume, geographic relocation, and change in practice-group size. The study population included 480,894 physicians who had 68,956 paid claims from 2003 to 2015. Of the study group, 89% had no claims, 9% had one claim, and the remaining 2% had two or more claims that accounted for 40% of all claims. Nearly three-quarters of the doctors studied were men, and the majority of specialties were internal medicine (17%), general practice/family medicine (15%), emergency medicine (7%), radiology (6%), and anesthesiology (6%).
Physicians with a higher number of claims against them did not relocate at a greater rate than physicians who had fewer or no claims, the investigators wrote in the New England Journal of Medicine.
More claims against a doctor were associated with a higher likelihood of leaving medicine and more shifts into smaller practice settings. For instance, physicians with one claim had 9% higher odds of leaving the practice than doctors with no claims, and physicians with five or more claims had a 45% higher chance of leaving medicine than doctors with no claims, the researchers found.
In addition, investigators found that doctors with two to four claims had 50%-60% higher odds of entering solo practice than physicians with no claims, and physicians with five or more claims had nearly 150% higher odds of moving to solo practice than doctors who had never been sued. Physicians with three or more claims were more likely to be male, work in surgical specialties, and be at least age 50 years.
The study addresses concerns that physicians with troubling legal records were moving across state lines for a fresh start, Mr. Studdert said in an interview. “We were surprised to find that physicians who accumulated multiple malpractice claims were no more likely to relocate their practices than physicians without claims. The National Practitioner Data Bank probably has something to do with that.”
Established by Congress in 1986, the NPDB was started, in part, to restrict the ability of incompetent physicians to move across states to hide their track records. By requiring hospitals to query doctors records before granting them clinical privileges and encouraging physician groups, health plans, and professional societies to do the same, the NPDB has “almost certainly increased the difficulty of relocation for physicians with legal problems,” the authors noted in the study.
A primary takeaway from the analysis is that, while a single malpractice claim is a relatively weak signal that a quality problem exists, multiple paid claims over a relatively short period of time are a strong signal that a physician may have a quality deficiency, Mr. Studdert said in the interview.
“Regulators and malpractice insurers should be paying closer attention to this signal,” he added. “To the extent that physicians are aware of a colleague’s checkered malpractice history, they may have a role to play too. Vigilance about signs of further problems, for one, but also careful thought about the wisdom of referring patients to such physicians.”
Michelle M. Mello, JD, PhD, and Mr. Studdert both reported receiving grants from SUMIT Insurance during the conduct of the study.
Source: Studdert DM et al. N Engl J Med. 2019 Mar 28. doi: 10.1056/NEJMsa1809981.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Gender wage gap varies by specialty
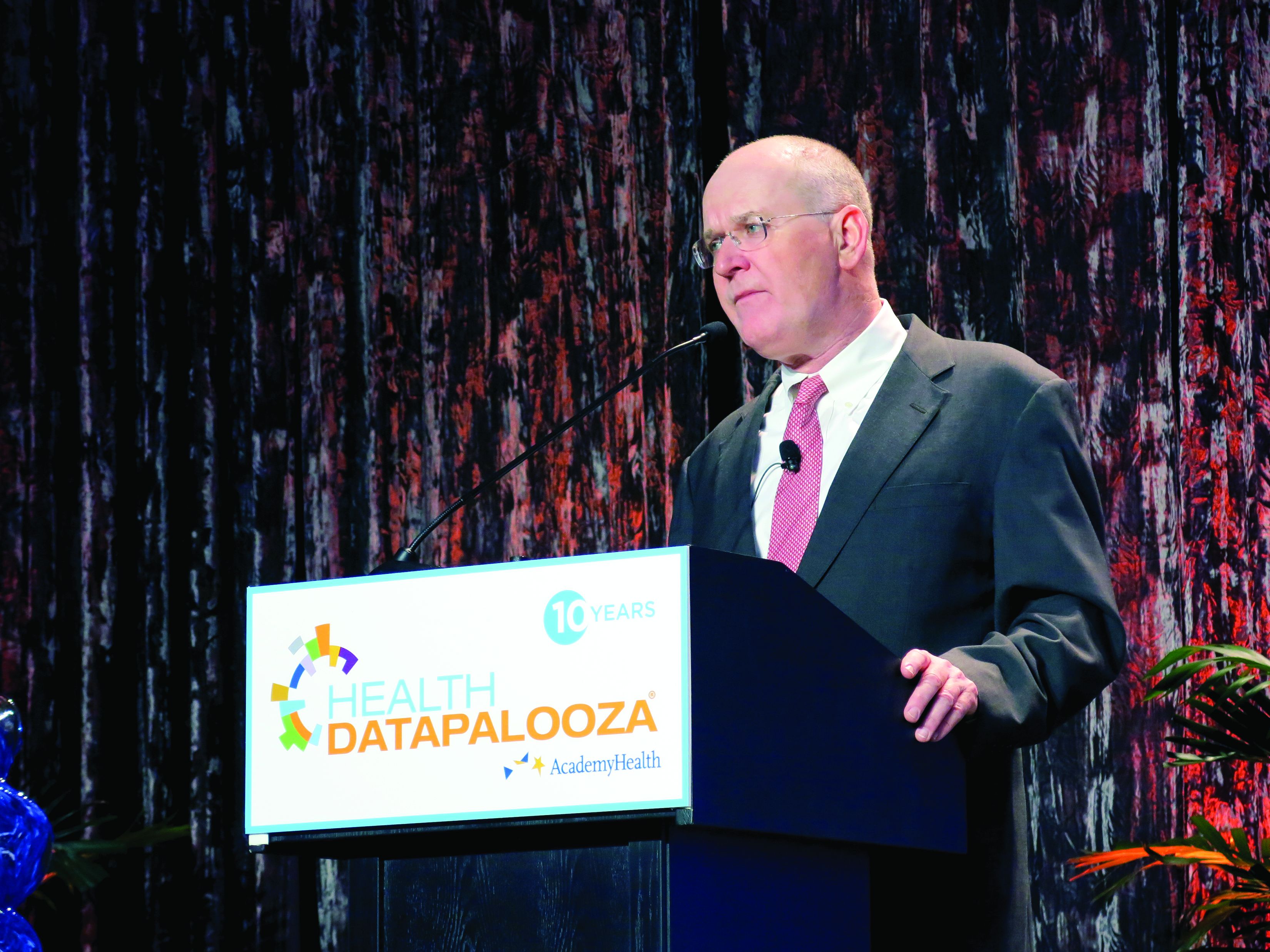
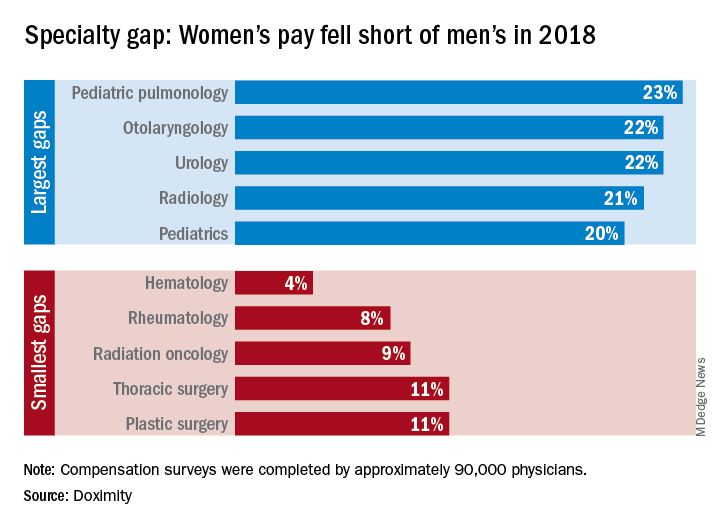
There is no specialty in which women physicians make as much as men, but hematology came the closest in 2018, according to a new survey by the medical social network Doximity.
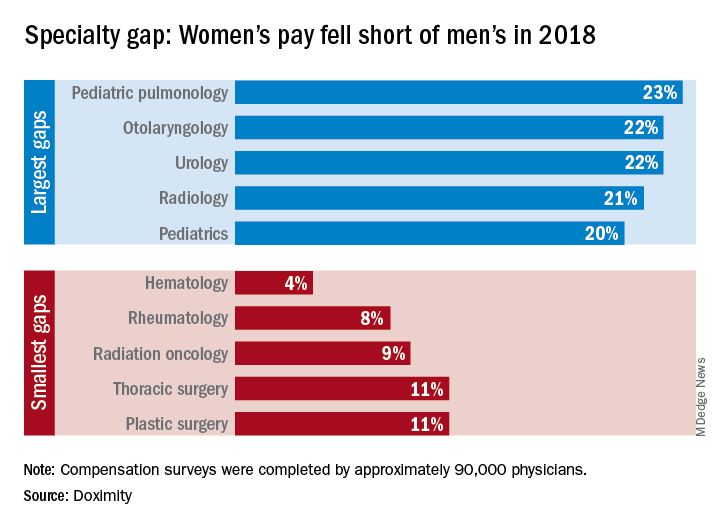
Female hematologists averaged $309,000 in earnings in 2018, just 4% less than their male counterparts, who brought in an average of $323,000. Rheumatology had the next-smallest gap, 8%, between women and men, followed by radiation oncology at 9% and thoracic surgery and plastic surgery at 11% each, Doximity reported March 26. All of the 90,000 physicians involved in the survey worked at least 40 hours per week.
At the other end of the scale is pediatric pulmonology, home of the largest gender wage gap. Average compensation for women in the specialty was $195,000, or 23% less than the $253,000 that men received. Women in otolaryngology and urology were next, earning 22% less than men in those specialties, while women in radiology and pediatrics averaged 21% and 20% less, respectively, than men, Doximity said in its report.
The gender wage gap has been persistent, but the latest data show that it is starting to close as the earnings curve for male physicians flattened in 2018 while pay increased for female physicians.
“Compensation transparency is a powerful force. As more data becomes available to us, exposing the pay gap between men and women, we see more movements to rectify this issue,” said Christopher Whaley, PhD, of the University of California, Berkeley, School of Public Health, who was lead author of the study.
To account for differences in specialty, geography, and physician-specific factors, the Doximity researchers used “a multivariate regression with fixed effects for provider specialty and [metropolitan statistical area].” They also controlled for how long each physician has been in practice and their self-reported average hours worked.
There is no specialty in which women physicians make as much as men, but hematology came the closest in 2018, according to a new survey by the medical social network Doximity.
Female hematologists averaged $309,000 in earnings in 2018, just 4% less than their male counterparts, who brought in an average of $323,000. Rheumatology had the next-smallest gap, 8%, between women and men, followed by radiation oncology at 9% and thoracic surgery and plastic surgery at 11% each, Doximity reported March 26. All of the 90,000 physicians involved in the survey worked at least 40 hours per week.
At the other end of the scale is pediatric pulmonology, home of the largest gender wage gap. Average compensation for women in the specialty was $195,000, or 23% less than the $253,000 that men received. Women in otolaryngology and urology were next, earning 22% less than men in those specialties, while women in radiology and pediatrics averaged 21% and 20% less, respectively, than men, Doximity said in its report.
The gender wage gap has been persistent, but the latest data show that it is starting to close as the earnings curve for male physicians flattened in 2018 while pay increased for female physicians.
“Compensation transparency is a powerful force. As more data becomes available to us, exposing the pay gap between men and women, we see more movements to rectify this issue,” said Christopher Whaley, PhD, of the University of California, Berkeley, School of Public Health, who was lead author of the study.
To account for differences in specialty, geography, and physician-specific factors, the Doximity researchers used “a multivariate regression with fixed effects for provider specialty and [metropolitan statistical area].” They also controlled for how long each physician has been in practice and their self-reported average hours worked.
There is no specialty in which women physicians make as much as men, but hematology came the closest in 2018, according to a new survey by the medical social network Doximity.
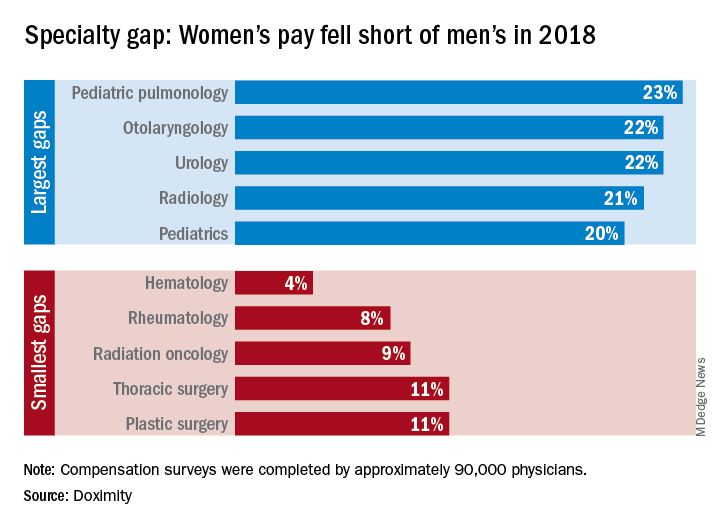
Female hematologists averaged $309,000 in earnings in 2018, just 4% less than their male counterparts, who brought in an average of $323,000. Rheumatology had the next-smallest gap, 8%, between women and men, followed by radiation oncology at 9% and thoracic surgery and plastic surgery at 11% each, Doximity reported March 26. All of the 90,000 physicians involved in the survey worked at least 40 hours per week.
At the other end of the scale is pediatric pulmonology, home of the largest gender wage gap. Average compensation for women in the specialty was $195,000, or 23% less than the $253,000 that men received. Women in otolaryngology and urology were next, earning 22% less than men in those specialties, while women in radiology and pediatrics averaged 21% and 20% less, respectively, than men, Doximity said in its report.
The gender wage gap has been persistent, but the latest data show that it is starting to close as the earnings curve for male physicians flattened in 2018 while pay increased for female physicians.
“Compensation transparency is a powerful force. As more data becomes available to us, exposing the pay gap between men and women, we see more movements to rectify this issue,” said Christopher Whaley, PhD, of the University of California, Berkeley, School of Public Health, who was lead author of the study.
To account for differences in specialty, geography, and physician-specific factors, the Doximity researchers used “a multivariate regression with fixed effects for provider specialty and [metropolitan statistical area].” They also controlled for how long each physician has been in practice and their self-reported average hours worked.
Hospital medicine grows globally
Hospital medicine is growing in popularity in some foreign countries, speakers said during Monday afternoon’s session, “International Hospital Medicine in the United Arab Emirates, Brazil and Holland.” The presenters discussed some of the history of hospital medicine in each of those countries as well as some current challenges.
Hospital medicine in the Netherlands started in about 2012, said Marjolein de Boom, MD, a hospitalist at Haaglanden Medical Centre. The country has its own 3-year training program for hospitalists, who first started to work in hospitals in the country in 2015. “It’s a relatively new and young specialty,” said Dr. de Boom, with 39 hospitalists in the country working in 8 of the 80 Dutch hospitals. Another 25 or so hospitalists are in training, “so it’s a growing profession,” she said. A Dutch chapter of SHM has been in place since 2017.
Hospitals in the Netherlands permit physicians to serve as hospitalists in different specialties depending on their needs. For example, Dr. de Boom works in the oncology department, as well as the surgical and trauma surgery units. One challenge has been to get more physicians interested in the hospitalist program because it’s newer and not as well-known, she said.
Hospital medicine in the United Arab Emirates also is a newer concept. The American model of hospital medicine was first introduced to the region in 2014 by the Cleveland Clinic in Abu Dhabi, said Mahmoud Al-Hawamdeh, MD, MBA, SFHM, FACP, chair of hospital medicine at the medical center. “Before that, inpatient hospital care was done by traditional family and internal medicine physicians, general practitioners, and residents,” he said.
There are 43 hospitalists at Cleveland Clinic, Abu Dhabi, said Dr. Al-Hawamdeh. They cover about 50%-60% of inpatient services, as well as handle admissions for vascular surgery, ophthalmology, and some general services; they also comanage postcardiac surgery care, he said. “It has been a tremendous success to implement hospital medicine in the care for the inpatient with improved quality metrics, reduced length of stay, and improved patient satisfaction.”
However, there are some challenges, such as educating patients and families about the role of hospitalists, cultural barriers, and the lack of a postdischarge follow-up network and institutions such as skilled nursing facilities. Dr. Al-Hawamdeh worked with physicians from Johns Hopkins Aramco Healthcare and Hamad Medical Corporation to establish an SHM Middle East chapter in 2016.
In Brazil, hospital medicine started to take hold in 2004, said Guilherme Barcellos, MD, SFHM. At that time, just a few doctors were true hospitalists. Dr. Barcellos helped create two hospitalist societies in the country. Hospitalists balancing multiple jobs is still very common, but decreasing, he said, while hospital employment and medical group participation is increasing.
“It was a high-pressure environment, crying out for efficiency, that drove forward Brazilian hospital medicine,” Dr. Barcellos said, “together with new reimbursement models, surgical redesigns, primary care recognition and structure.”
Some challenges remain in Brazil as well, he said. Fancy private hospitals announce they have hospitalists when they may not. In addition, the role of generalists and subspecialists, and the role of certifications, is not always clear. But hospitalists are gaining a foothold, participating in a Choosing Wisely initiative in the country and organizing several conferences.
Hospital medicine is growing in popularity in some foreign countries, speakers said during Monday afternoon’s session, “International Hospital Medicine in the United Arab Emirates, Brazil and Holland.” The presenters discussed some of the history of hospital medicine in each of those countries as well as some current challenges.
Hospital medicine in the Netherlands started in about 2012, said Marjolein de Boom, MD, a hospitalist at Haaglanden Medical Centre. The country has its own 3-year training program for hospitalists, who first started to work in hospitals in the country in 2015. “It’s a relatively new and young specialty,” said Dr. de Boom, with 39 hospitalists in the country working in 8 of the 80 Dutch hospitals. Another 25 or so hospitalists are in training, “so it’s a growing profession,” she said. A Dutch chapter of SHM has been in place since 2017.
Hospitals in the Netherlands permit physicians to serve as hospitalists in different specialties depending on their needs. For example, Dr. de Boom works in the oncology department, as well as the surgical and trauma surgery units. One challenge has been to get more physicians interested in the hospitalist program because it’s newer and not as well-known, she said.
Hospital medicine in the United Arab Emirates also is a newer concept. The American model of hospital medicine was first introduced to the region in 2014 by the Cleveland Clinic in Abu Dhabi, said Mahmoud Al-Hawamdeh, MD, MBA, SFHM, FACP, chair of hospital medicine at the medical center. “Before that, inpatient hospital care was done by traditional family and internal medicine physicians, general practitioners, and residents,” he said.
There are 43 hospitalists at Cleveland Clinic, Abu Dhabi, said Dr. Al-Hawamdeh. They cover about 50%-60% of inpatient services, as well as handle admissions for vascular surgery, ophthalmology, and some general services; they also comanage postcardiac surgery care, he said. “It has been a tremendous success to implement hospital medicine in the care for the inpatient with improved quality metrics, reduced length of stay, and improved patient satisfaction.”
However, there are some challenges, such as educating patients and families about the role of hospitalists, cultural barriers, and the lack of a postdischarge follow-up network and institutions such as skilled nursing facilities. Dr. Al-Hawamdeh worked with physicians from Johns Hopkins Aramco Healthcare and Hamad Medical Corporation to establish an SHM Middle East chapter in 2016.
In Brazil, hospital medicine started to take hold in 2004, said Guilherme Barcellos, MD, SFHM. At that time, just a few doctors were true hospitalists. Dr. Barcellos helped create two hospitalist societies in the country. Hospitalists balancing multiple jobs is still very common, but decreasing, he said, while hospital employment and medical group participation is increasing.
“It was a high-pressure environment, crying out for efficiency, that drove forward Brazilian hospital medicine,” Dr. Barcellos said, “together with new reimbursement models, surgical redesigns, primary care recognition and structure.”
Some challenges remain in Brazil as well, he said. Fancy private hospitals announce they have hospitalists when they may not. In addition, the role of generalists and subspecialists, and the role of certifications, is not always clear. But hospitalists are gaining a foothold, participating in a Choosing Wisely initiative in the country and organizing several conferences.
Hospital medicine is growing in popularity in some foreign countries, speakers said during Monday afternoon’s session, “International Hospital Medicine in the United Arab Emirates, Brazil and Holland.” The presenters discussed some of the history of hospital medicine in each of those countries as well as some current challenges.
Hospital medicine in the Netherlands started in about 2012, said Marjolein de Boom, MD, a hospitalist at Haaglanden Medical Centre. The country has its own 3-year training program for hospitalists, who first started to work in hospitals in the country in 2015. “It’s a relatively new and young specialty,” said Dr. de Boom, with 39 hospitalists in the country working in 8 of the 80 Dutch hospitals. Another 25 or so hospitalists are in training, “so it’s a growing profession,” she said. A Dutch chapter of SHM has been in place since 2017.
Hospitals in the Netherlands permit physicians to serve as hospitalists in different specialties depending on their needs. For example, Dr. de Boom works in the oncology department, as well as the surgical and trauma surgery units. One challenge has been to get more physicians interested in the hospitalist program because it’s newer and not as well-known, she said.
Hospital medicine in the United Arab Emirates also is a newer concept. The American model of hospital medicine was first introduced to the region in 2014 by the Cleveland Clinic in Abu Dhabi, said Mahmoud Al-Hawamdeh, MD, MBA, SFHM, FACP, chair of hospital medicine at the medical center. “Before that, inpatient hospital care was done by traditional family and internal medicine physicians, general practitioners, and residents,” he said.
There are 43 hospitalists at Cleveland Clinic, Abu Dhabi, said Dr. Al-Hawamdeh. They cover about 50%-60% of inpatient services, as well as handle admissions for vascular surgery, ophthalmology, and some general services; they also comanage postcardiac surgery care, he said. “It has been a tremendous success to implement hospital medicine in the care for the inpatient with improved quality metrics, reduced length of stay, and improved patient satisfaction.”
However, there are some challenges, such as educating patients and families about the role of hospitalists, cultural barriers, and the lack of a postdischarge follow-up network and institutions such as skilled nursing facilities. Dr. Al-Hawamdeh worked with physicians from Johns Hopkins Aramco Healthcare and Hamad Medical Corporation to establish an SHM Middle East chapter in 2016.
In Brazil, hospital medicine started to take hold in 2004, said Guilherme Barcellos, MD, SFHM. At that time, just a few doctors were true hospitalists. Dr. Barcellos helped create two hospitalist societies in the country. Hospitalists balancing multiple jobs is still very common, but decreasing, he said, while hospital employment and medical group participation is increasing.
“It was a high-pressure environment, crying out for efficiency, that drove forward Brazilian hospital medicine,” Dr. Barcellos said, “together with new reimbursement models, surgical redesigns, primary care recognition and structure.”
Some challenges remain in Brazil as well, he said. Fancy private hospitals announce they have hospitalists when they may not. In addition, the role of generalists and subspecialists, and the role of certifications, is not always clear. But hospitalists are gaining a foothold, participating in a Choosing Wisely initiative in the country and organizing several conferences.
ABIM contests class-action lawsuit, asks judge to dismiss
Attorneys for the American Board of Internal Medicine have asked Judge Robert Kelly of the United States District Court for the Eastern District of Pennsylvania to dismiss a class-action lawsuit against the board’s maintenance of certification (MOC) program.
The legal challenge, filed Dec. 6, 2018, claims that ABIM charges inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification as a condition of employment.
The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their certification. On Jan. 23 of this year, the suit was amended to include racketeering and unjust enrichment claims.
In a motion filed March 18, attorneys for ABIM asserted that the plaintiffs fail to prove that board certification – initial certification and continuing certification – are two separate products that ABIM is unlawfully tying, and for that reason, their antitrust claims are invalid, according to the motion.
“Plaintiffs may disagree with ABIM and members of the medical community on whether ABIM certification provides them value, but their claims have no basis in the law,” Richard J. Baron, MD, ABIM president and CEO said in a statement. “With advances in medical science and technology occurring constantly, periodic assessments are critical to ensure internists are staying current and continuing to meet high performance standards in their field.”
Two other lawsuits challenging MOC, one against the American Board of Psychiatry and Neurology and another against the American Board of Radiology, are ongoing.
More than $200,000 has been raised by doctors and their supporters nationwide through a GoFundMe campaign launched by Practicing Physicians of America to pay for the plaintiffs’ legal costs.
Attorneys for the American Board of Internal Medicine have asked Judge Robert Kelly of the United States District Court for the Eastern District of Pennsylvania to dismiss a class-action lawsuit against the board’s maintenance of certification (MOC) program.
The legal challenge, filed Dec. 6, 2018, claims that ABIM charges inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification as a condition of employment.
The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their certification. On Jan. 23 of this year, the suit was amended to include racketeering and unjust enrichment claims.
In a motion filed March 18, attorneys for ABIM asserted that the plaintiffs fail to prove that board certification – initial certification and continuing certification – are two separate products that ABIM is unlawfully tying, and for that reason, their antitrust claims are invalid, according to the motion.
“Plaintiffs may disagree with ABIM and members of the medical community on whether ABIM certification provides them value, but their claims have no basis in the law,” Richard J. Baron, MD, ABIM president and CEO said in a statement. “With advances in medical science and technology occurring constantly, periodic assessments are critical to ensure internists are staying current and continuing to meet high performance standards in their field.”
Two other lawsuits challenging MOC, one against the American Board of Psychiatry and Neurology and another against the American Board of Radiology, are ongoing.
More than $200,000 has been raised by doctors and their supporters nationwide through a GoFundMe campaign launched by Practicing Physicians of America to pay for the plaintiffs’ legal costs.
Attorneys for the American Board of Internal Medicine have asked Judge Robert Kelly of the United States District Court for the Eastern District of Pennsylvania to dismiss a class-action lawsuit against the board’s maintenance of certification (MOC) program.
The legal challenge, filed Dec. 6, 2018, claims that ABIM charges inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification as a condition of employment.
The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their certification. On Jan. 23 of this year, the suit was amended to include racketeering and unjust enrichment claims.
In a motion filed March 18, attorneys for ABIM asserted that the plaintiffs fail to prove that board certification – initial certification and continuing certification – are two separate products that ABIM is unlawfully tying, and for that reason, their antitrust claims are invalid, according to the motion.
“Plaintiffs may disagree with ABIM and members of the medical community on whether ABIM certification provides them value, but their claims have no basis in the law,” Richard J. Baron, MD, ABIM president and CEO said in a statement. “With advances in medical science and technology occurring constantly, periodic assessments are critical to ensure internists are staying current and continuing to meet high performance standards in their field.”
Two other lawsuits challenging MOC, one against the American Board of Psychiatry and Neurology and another against the American Board of Radiology, are ongoing.
More than $200,000 has been raised by doctors and their supporters nationwide through a GoFundMe campaign launched by Practicing Physicians of America to pay for the plaintiffs’ legal costs.
Planning for change in hospitalist practice management
At Sunday’s HM19 pre-course “Oh, the Places We’ll Go! Practice Management Tools for Navigating the Changing Role of Your Hospital Medicine Group,” the theme was how to anticipate and embrace changing roles as hospital medicine groups are being asked to take on more responsibility.
“The scope of hospitalist practice is evolving rapidly, both clinically and in terms of all of the other things that hospitalists are being asked to do,” said Leslie Flores, MHA, SFHM, a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif., and course co-director, in an interview before the pre-course. “Our goals with this program are to help leaders position their hospitalist groups for success with this changing environment that they’re living in and the changing roles of hospitalists.”
In an audience poll at the beginning of the pre-course, attendees – a majority of whom were practicing hospitalists and managers of hospitalist groups – said their biggest challenge areas were related to compensation or workflows that have not evolved to match their changing role, and disagreements over who should admit patients.
One of the goals of the session was to give hospitalist leaders ideas to address these issues, which included information on how to implement better team-based care and interdisciplinary care models within their groups, as well as how to adjust their compensation, scheduling, and staffing models to prepare for this “new world of hospitalist medicine,” said Ms. Flores.
“One of the biggest sources of contention and stress that we see in hospitalist groups is that there’s just so much change, and it’s happening so rapidly, and people are having a hard time really figuring out how to deal with all of that,” she said.
The day began with John Nelson, MD, MHM, outlining the “Trends in Scope of Practice Evolution.” Dr. Nelson, a partner at Nelson Flores Hospital Medicine Consultants, medical director of Overlake Medical Center in Bellevue, Wash., and course co-director, said hospitalists are increasingly working more in outpatient care, post-acute care, and other specialty facilities. In addition, as group size increases, the likelihood a hospitalist group will be responsible for an observation or short stay unit increases, while a larger group is less likely to have a clinical responsibility for a code blue, cardiac arrest, or rapid response team.
Other topics in the pre-course focused on how to change the culture in a group to an environment where team members are empowered to ask questions or voice concerns, improve patient flow by removing reasons for delays in discharge, recruit the right team members to a group, handle transitions of care, and anticipate change in a group. In addition, the speakers participated in discussions where they shared their biggest successes and failures in practice as leaders and participated in a lightning round where they provided “off-the-cuff” responses to questions from Ms. Flores.
Although hospitalists did not create the current environment that is expanding their role in the health care system, they can position themselves to decide what the scope of their role is, said Dr. Nelson.
“What we should do is navigate our group through these changes in the way that’s going to be most effective for ourselves, the providers in our group, and our organization,” he said. “Those groups that try to dig their heels in or resist all change, they fail. . . and they frustrate themselves. So instead, if you engage in planning for changes in the scope of your practice, you have a chance to make it go the way you’d like it to go, and you’re going to be more satisfied.”
At Sunday’s HM19 pre-course “Oh, the Places We’ll Go! Practice Management Tools for Navigating the Changing Role of Your Hospital Medicine Group,” the theme was how to anticipate and embrace changing roles as hospital medicine groups are being asked to take on more responsibility.
“The scope of hospitalist practice is evolving rapidly, both clinically and in terms of all of the other things that hospitalists are being asked to do,” said Leslie Flores, MHA, SFHM, a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif., and course co-director, in an interview before the pre-course. “Our goals with this program are to help leaders position their hospitalist groups for success with this changing environment that they’re living in and the changing roles of hospitalists.”
In an audience poll at the beginning of the pre-course, attendees – a majority of whom were practicing hospitalists and managers of hospitalist groups – said their biggest challenge areas were related to compensation or workflows that have not evolved to match their changing role, and disagreements over who should admit patients.
One of the goals of the session was to give hospitalist leaders ideas to address these issues, which included information on how to implement better team-based care and interdisciplinary care models within their groups, as well as how to adjust their compensation, scheduling, and staffing models to prepare for this “new world of hospitalist medicine,” said Ms. Flores.
“One of the biggest sources of contention and stress that we see in hospitalist groups is that there’s just so much change, and it’s happening so rapidly, and people are having a hard time really figuring out how to deal with all of that,” she said.
The day began with John Nelson, MD, MHM, outlining the “Trends in Scope of Practice Evolution.” Dr. Nelson, a partner at Nelson Flores Hospital Medicine Consultants, medical director of Overlake Medical Center in Bellevue, Wash., and course co-director, said hospitalists are increasingly working more in outpatient care, post-acute care, and other specialty facilities. In addition, as group size increases, the likelihood a hospitalist group will be responsible for an observation or short stay unit increases, while a larger group is less likely to have a clinical responsibility for a code blue, cardiac arrest, or rapid response team.
Other topics in the pre-course focused on how to change the culture in a group to an environment where team members are empowered to ask questions or voice concerns, improve patient flow by removing reasons for delays in discharge, recruit the right team members to a group, handle transitions of care, and anticipate change in a group. In addition, the speakers participated in discussions where they shared their biggest successes and failures in practice as leaders and participated in a lightning round where they provided “off-the-cuff” responses to questions from Ms. Flores.
Although hospitalists did not create the current environment that is expanding their role in the health care system, they can position themselves to decide what the scope of their role is, said Dr. Nelson.
“What we should do is navigate our group through these changes in the way that’s going to be most effective for ourselves, the providers in our group, and our organization,” he said. “Those groups that try to dig their heels in or resist all change, they fail. . . and they frustrate themselves. So instead, if you engage in planning for changes in the scope of your practice, you have a chance to make it go the way you’d like it to go, and you’re going to be more satisfied.”
At Sunday’s HM19 pre-course “Oh, the Places We’ll Go! Practice Management Tools for Navigating the Changing Role of Your Hospital Medicine Group,” the theme was how to anticipate and embrace changing roles as hospital medicine groups are being asked to take on more responsibility.
“The scope of hospitalist practice is evolving rapidly, both clinically and in terms of all of the other things that hospitalists are being asked to do,” said Leslie Flores, MHA, SFHM, a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif., and course co-director, in an interview before the pre-course. “Our goals with this program are to help leaders position their hospitalist groups for success with this changing environment that they’re living in and the changing roles of hospitalists.”
In an audience poll at the beginning of the pre-course, attendees – a majority of whom were practicing hospitalists and managers of hospitalist groups – said their biggest challenge areas were related to compensation or workflows that have not evolved to match their changing role, and disagreements over who should admit patients.
One of the goals of the session was to give hospitalist leaders ideas to address these issues, which included information on how to implement better team-based care and interdisciplinary care models within their groups, as well as how to adjust their compensation, scheduling, and staffing models to prepare for this “new world of hospitalist medicine,” said Ms. Flores.
“One of the biggest sources of contention and stress that we see in hospitalist groups is that there’s just so much change, and it’s happening so rapidly, and people are having a hard time really figuring out how to deal with all of that,” she said.
The day began with John Nelson, MD, MHM, outlining the “Trends in Scope of Practice Evolution.” Dr. Nelson, a partner at Nelson Flores Hospital Medicine Consultants, medical director of Overlake Medical Center in Bellevue, Wash., and course co-director, said hospitalists are increasingly working more in outpatient care, post-acute care, and other specialty facilities. In addition, as group size increases, the likelihood a hospitalist group will be responsible for an observation or short stay unit increases, while a larger group is less likely to have a clinical responsibility for a code blue, cardiac arrest, or rapid response team.
Other topics in the pre-course focused on how to change the culture in a group to an environment where team members are empowered to ask questions or voice concerns, improve patient flow by removing reasons for delays in discharge, recruit the right team members to a group, handle transitions of care, and anticipate change in a group. In addition, the speakers participated in discussions where they shared their biggest successes and failures in practice as leaders and participated in a lightning round where they provided “off-the-cuff” responses to questions from Ms. Flores.
Although hospitalists did not create the current environment that is expanding their role in the health care system, they can position themselves to decide what the scope of their role is, said Dr. Nelson.
“What we should do is navigate our group through these changes in the way that’s going to be most effective for ourselves, the providers in our group, and our organization,” he said. “Those groups that try to dig their heels in or resist all change, they fail. . . and they frustrate themselves. So instead, if you engage in planning for changes in the scope of your practice, you have a chance to make it go the way you’d like it to go, and you’re going to be more satisfied.”
FDA chief calls for stricter scrutiny of electronic health records
“What we really need is a much more tailored approach, so that we have appropriate oversight of EHRs when they’re doing things that could create risk for patients,” Dr. Gottlieb said in an interview with Kaiser Health News.
Dr. Gottlieb was responding to “Botched Operation,” a report published March 18 by KHN and Fortune magazine. The investigation found that the federal government has spent more than $36 billion over the past 10 years to switch doctors and hospitals from paper to digital records systems. In that time, thousands of reports of deaths, injuries, and near misses linked to EHRs have piled up in databases – including at least one run by the FDA.
Dr. Gottlieb said Congress would need to enact legislation to define when an EHR would require government oversight. He said that the digital records systems, which store a patient’s medical history, don’t fit neatly under the agency’s existing mandate to regulate items such as drugs and medical devices.
Dr. Gottlieb said the best approach might be to say that an EHR that has a certain capability becomes a medical device. He called EHRs a “unique tool,” noting that the risks posed by their use aren’t the same as for a traditional medical device implanted in a patient. “You need a much different regulatory scheme,” he said.
The 21st Century Cures Act of 2016 excludes the FDA from having oversight over EHRs as a medical device.
Dr. Gottlieb said that health IT companies could add new functions that would improve EHRs, but they have been reluctant to do so because they didn’t want their products to fall under FDA jurisdiction. He added that he was “not calling” for FDA to take over such a duty, however, and suggested that any new approach could be years away. Proponents have long argued that widespread use of EHRs can make medicine safer by alerting doctors to potential medical errors, though critics counter that software glitches and user errors may cause new varieties of medical mistakes.
How closely the FDA should watch over the digital medical record revolution has been controversial for years. The agency’s interest in the issue perked up after Congress decided in February 2009 to spend billions of dollars on digital medical records as part of an economic stimulus program.
At the time, many industry groups argued that FDA regulation would “stifle innovation” and stall the national drive to bring medicine into the modern era. Federal officials responsible for doling out billions in subsidies to doctors and hospitals generally sympathized with that view and were skeptical of allowing the FDA to play a role.
The debate became public in February 2010, when Jeffrey Shuren, MD, an FDA official, testified at a public hearing that the agency had tied 6 deaths and more than 200 injuries to health information technology. In all, the FDA said, it had logged 260 reports in the previous 2 years of “malfunctions with the potential for patient harm.”
The agency said the findings were based largely on reports voluntarily submitted to the FDA and suggested “significant clinical implications and public safety issues.” In one case cited, lab tests done in a hospital emergency department were sent to the wrong patient’s file. Since then, several government and private repositories have associated thousands of injuries, near misses, and deaths to EHR technology.
Dr. Shuren said in 2010 that the agency recognized that health information technology had great potential to improve patient care, but also needed oversight to “assure patient safety.”
While some safety proponents agree that EHRs offer tremendous benefits, they also see a greater opportunities to improve their safety.
Dean Sittig, PhD, a professor of bioinformatics and bioengineering at the University of Texas, Houston, said EHRs have improved safety within the health care system, but they have not eliminated errors to the extent that he would have expected. Federal officials were initially pushing for rapid adoption and ‘there wasn’t a lot of interest in talking about things that could go wrong,’ ” Dr. Sittig told KHN and Fortune.
Earlier in March, Gottlieb announced his resignation from the FDA. His last day is scheduled to be April 5.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente. KHN correspondents Sarah Jane Tribble, Sydney Lupkin, and Julie Rovner contributed to this report.
“What we really need is a much more tailored approach, so that we have appropriate oversight of EHRs when they’re doing things that could create risk for patients,” Dr. Gottlieb said in an interview with Kaiser Health News.
Dr. Gottlieb was responding to “Botched Operation,” a report published March 18 by KHN and Fortune magazine. The investigation found that the federal government has spent more than $36 billion over the past 10 years to switch doctors and hospitals from paper to digital records systems. In that time, thousands of reports of deaths, injuries, and near misses linked to EHRs have piled up in databases – including at least one run by the FDA.
Dr. Gottlieb said Congress would need to enact legislation to define when an EHR would require government oversight. He said that the digital records systems, which store a patient’s medical history, don’t fit neatly under the agency’s existing mandate to regulate items such as drugs and medical devices.
Dr. Gottlieb said the best approach might be to say that an EHR that has a certain capability becomes a medical device. He called EHRs a “unique tool,” noting that the risks posed by their use aren’t the same as for a traditional medical device implanted in a patient. “You need a much different regulatory scheme,” he said.
The 21st Century Cures Act of 2016 excludes the FDA from having oversight over EHRs as a medical device.
Dr. Gottlieb said that health IT companies could add new functions that would improve EHRs, but they have been reluctant to do so because they didn’t want their products to fall under FDA jurisdiction. He added that he was “not calling” for FDA to take over such a duty, however, and suggested that any new approach could be years away. Proponents have long argued that widespread use of EHRs can make medicine safer by alerting doctors to potential medical errors, though critics counter that software glitches and user errors may cause new varieties of medical mistakes.
How closely the FDA should watch over the digital medical record revolution has been controversial for years. The agency’s interest in the issue perked up after Congress decided in February 2009 to spend billions of dollars on digital medical records as part of an economic stimulus program.
At the time, many industry groups argued that FDA regulation would “stifle innovation” and stall the national drive to bring medicine into the modern era. Federal officials responsible for doling out billions in subsidies to doctors and hospitals generally sympathized with that view and were skeptical of allowing the FDA to play a role.
The debate became public in February 2010, when Jeffrey Shuren, MD, an FDA official, testified at a public hearing that the agency had tied 6 deaths and more than 200 injuries to health information technology. In all, the FDA said, it had logged 260 reports in the previous 2 years of “malfunctions with the potential for patient harm.”
The agency said the findings were based largely on reports voluntarily submitted to the FDA and suggested “significant clinical implications and public safety issues.” In one case cited, lab tests done in a hospital emergency department were sent to the wrong patient’s file. Since then, several government and private repositories have associated thousands of injuries, near misses, and deaths to EHR technology.
Dr. Shuren said in 2010 that the agency recognized that health information technology had great potential to improve patient care, but also needed oversight to “assure patient safety.”
While some safety proponents agree that EHRs offer tremendous benefits, they also see a greater opportunities to improve their safety.
Dean Sittig, PhD, a professor of bioinformatics and bioengineering at the University of Texas, Houston, said EHRs have improved safety within the health care system, but they have not eliminated errors to the extent that he would have expected. Federal officials were initially pushing for rapid adoption and ‘there wasn’t a lot of interest in talking about things that could go wrong,’ ” Dr. Sittig told KHN and Fortune.
Earlier in March, Gottlieb announced his resignation from the FDA. His last day is scheduled to be April 5.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente. KHN correspondents Sarah Jane Tribble, Sydney Lupkin, and Julie Rovner contributed to this report.
“What we really need is a much more tailored approach, so that we have appropriate oversight of EHRs when they’re doing things that could create risk for patients,” Dr. Gottlieb said in an interview with Kaiser Health News.
Dr. Gottlieb was responding to “Botched Operation,” a report published March 18 by KHN and Fortune magazine. The investigation found that the federal government has spent more than $36 billion over the past 10 years to switch doctors and hospitals from paper to digital records systems. In that time, thousands of reports of deaths, injuries, and near misses linked to EHRs have piled up in databases – including at least one run by the FDA.
Dr. Gottlieb said Congress would need to enact legislation to define when an EHR would require government oversight. He said that the digital records systems, which store a patient’s medical history, don’t fit neatly under the agency’s existing mandate to regulate items such as drugs and medical devices.
Dr. Gottlieb said the best approach might be to say that an EHR that has a certain capability becomes a medical device. He called EHRs a “unique tool,” noting that the risks posed by their use aren’t the same as for a traditional medical device implanted in a patient. “You need a much different regulatory scheme,” he said.
The 21st Century Cures Act of 2016 excludes the FDA from having oversight over EHRs as a medical device.
Dr. Gottlieb said that health IT companies could add new functions that would improve EHRs, but they have been reluctant to do so because they didn’t want their products to fall under FDA jurisdiction. He added that he was “not calling” for FDA to take over such a duty, however, and suggested that any new approach could be years away. Proponents have long argued that widespread use of EHRs can make medicine safer by alerting doctors to potential medical errors, though critics counter that software glitches and user errors may cause new varieties of medical mistakes.
How closely the FDA should watch over the digital medical record revolution has been controversial for years. The agency’s interest in the issue perked up after Congress decided in February 2009 to spend billions of dollars on digital medical records as part of an economic stimulus program.
At the time, many industry groups argued that FDA regulation would “stifle innovation” and stall the national drive to bring medicine into the modern era. Federal officials responsible for doling out billions in subsidies to doctors and hospitals generally sympathized with that view and were skeptical of allowing the FDA to play a role.
The debate became public in February 2010, when Jeffrey Shuren, MD, an FDA official, testified at a public hearing that the agency had tied 6 deaths and more than 200 injuries to health information technology. In all, the FDA said, it had logged 260 reports in the previous 2 years of “malfunctions with the potential for patient harm.”
The agency said the findings were based largely on reports voluntarily submitted to the FDA and suggested “significant clinical implications and public safety issues.” In one case cited, lab tests done in a hospital emergency department were sent to the wrong patient’s file. Since then, several government and private repositories have associated thousands of injuries, near misses, and deaths to EHR technology.
Dr. Shuren said in 2010 that the agency recognized that health information technology had great potential to improve patient care, but also needed oversight to “assure patient safety.”
While some safety proponents agree that EHRs offer tremendous benefits, they also see a greater opportunities to improve their safety.
Dean Sittig, PhD, a professor of bioinformatics and bioengineering at the University of Texas, Houston, said EHRs have improved safety within the health care system, but they have not eliminated errors to the extent that he would have expected. Federal officials were initially pushing for rapid adoption and ‘there wasn’t a lot of interest in talking about things that could go wrong,’ ” Dr. Sittig told KHN and Fortune.
Earlier in March, Gottlieb announced his resignation from the FDA. His last day is scheduled to be April 5.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente. KHN correspondents Sarah Jane Tribble, Sydney Lupkin, and Julie Rovner contributed to this report.