User login
The Hospitalist only
Medicare’s two-midnight rule
What hospitalists must know
Most hospitalists’ training likely included caring for patients in the ambulatory clinic, urgent care, and ED settings. One of the most important aspects of medical training is deciding which of the patients seen in these settings need to “be admitted” to a hospital because of risk, severity of illness, and/or need for certain medical services. In this context, “admit” is a synonym for “hospitalize.”
However, in today’s health care system, in which hospitalization costs are usually borne by a third-party payer, “admit” can have a very different meaning. For most payers, “admit” means “hospitalize as inpatient.” This is distinct from “hospitalize as an outpatient.” (“Observation” or “obs” is the most common example of a hospitalization as an outpatient.) In the medical payer world, inpatient and outpatient are often referred to as “statuses.” The distinction between inpatient versus outpatient status can affect payment and is based on rules that a hospital and payer have agreed upon. (Inpatient hospital care is generally paid at a higher rate than outpatient hospital care.) It is important for hospitalists to have a basic understanding of these rules because it can affect hospital billing, the hospitalist’s professional fees, beneficiary liability, and payer denials of inpatient care.
For years, Medicare’s definition of an inpatient hospitalization was primarily based on an expectation of a hospitalization of at least 24 hours and a physician’s judgment of the beneficiary’s need for inpatient hospital services. This judgment was to be based on the physician’s assessment of the patient’s severity of illness, the risk of an adverse outcome, and the hospital services required. (The exact definition by Centers for Medicare & Medicaid Services is much longer and can be found in the Medicare Benefits Policy Manual.1) Under Medicare, defining a hospitalization as inpatient versus outpatient is especially important because they are billed to different Medicare programs (Part A for inpatient, Part B for outpatient), and both hospital reimbursement and the patient liability can vary significantly.
Not surprisingly, CMS found that how physicians were making status decisions for medically similar hospitalized patients varied greatly. CMS noted two major concerns: an overuse of inpatient for patients hospitalized overnight leading to increased charges to CMS and multiday observation hospitalizations for lower-acuity patients leading to excessive liability for Medicare beneficiaries. (Observation stays are billed under Part B, under which the beneficiary generally has a 20% copay.)
To address these concerns, in October 2013, CMS adjusted the definition of inpatient to include “the two-midnight rule.” Basically, CMS said that, in order to qualify for inpatient, the admitting physician should expect the beneficiary to require hospital care spanning at least two midnights, rather than the previous 24-hour benchmark, regardless of the severity of illness or risk of adverse outcome. (There are exceptions and exemptions to the two-midnight rule, which are discussed later in this article.)
The idea of the two-midnight rule was to address the two concerns noted above. Under this rule, most expected overnight hospitalizations should be outpatients, even if they are more than 24 hours in length, and any medically necessary outpatient hospitalization should be “converted” to inpatient if and when it is clear that a second midnight of hospitalization is medically necessary.
In January 2016, CMS amended the two-midnight rule to recognize, as it had done prior to October 2013, that some hospitalizations, based on physician judgment, would be appropriate for inpatient without an expectation of a hospitalization that spans at least two midnights. Unfortunately, CMS has not been forthcoming with guidance of examples of which hospitalizations would fall into this new category, other than to say they expect the use of this new provision would generally not be appropriate for a hospital stay of less than 24 hours.
As of today, physicians should order inpatient services under the following three situations:
- The physician expects the beneficiary to require hospital care spanning at least two midnights.
- The physician provides a service on Medicare’s inpatient-only list.
- The physician expects the beneficiary to require hospital care for less than two midnights but feels that inpatient services are nevertheless appropriate.
This most recently updated version of the two-midnight rule can be found in Section 42 CFR §412.3 of the Code of Federal Regulations.2 Each of these three situations warrants additional discussion.
Care expected to span two midnights
The first situation is the one most applicable to hospitalists. In this circumstance there are three key points to remember.
The first point is that the two-midnight rule is based on a reasonable expectation of a need for hospitalization for at least two nights, not the actual length of hospitalization. Auditors, based on long-standing guidance from the CMS, should consider only the information known (or that should have been known) to the provider at the time the inpatient decision is made.
For example, if the expectation of the need for hospitalization of at least 2 midnights is well documented in the admission note, but the beneficiary improves more rapidly than expected and can be discharged before the second midnight, billing Medicare under Part A for inpatient admission remains appropriate. Auditors may look for provider documentation describing the unexpected improvement, and while such documentation is not an absolute requirement, its presence can be helpful in defending inpatient billing.
Other situations in which there can be an expectation of hospitalization of at least two midnights, but the actual length of stay does not meet this benchmark, are death, patients leaving against medical advice, or transfer to another hospital. For example, if a patient is hospitalized as an inpatient for bacterial endocarditis, and the documented plan of care includes at least 2 days of IV antibiotics and monitoring of cultures, inpatient remains appropriate even if the patient signs out against medical advice the following day.
The second key point to understand is that a night must be “medically necessary” to count toward the two-midnight benchmark. Hospital time spent receiving custodial care, because of excessive delays, or incurred because of the convenience of the beneficiary or provider does not count toward the two-midnight benchmark. For example, imagine a patient hospitalized with chest pain on Saturday evening and the attending physician determines that the patient requires serial cardiac isoenzymes and ECGs followed, most likely, by a noninvasive stress test. The attending physician, knowing that the hospital does not offer stress testing on Sunday, expects the patient to remain hospitalized at least until Monday, thus two midnights. However, in this situation, the second midnight (Sunday night) was not medically necessary and does not count toward the two midnight expectation.
The third key point to know is that the clock for calculating the two-midnight rule begins when the beneficiary starts receiving hospital care, not when the inpatient order is placed. Further, care that starts in the ED or at another hospital counts, too. In contrast, care at an outpatient clinic, an urgent care facility, or waiting-room time in an ED does not count.
When CMS implemented the two-midnight rule in 2013, they said that they would be open to exceptions. The first and only exception to date to the two-midnight rule is newly initiated and unanticipated mechanical ventilation. (This excludes anticipated intubations related to other care, such as procedures.) For example, inpatient is appropriate for a patient who requires hospitalization for an anaphylactic reaction or a drug overdose and needs intubation and mechanical ventilation, even if discharge is expected before a second midnight of hospital care.
CMS’s inpatient-only list
Each year, CMS publishes a list of procedures that CMS will pay only under Part A (that is, as inpatient). This list is updated quarterly (Addendum E) and can be found on the CMS website.3 Hospitalizations associated with the procedures on this list should always be inpatient, regardless of the expected length of stay.
It is important to note that the inpatient-only list is dynamic; it is revised annually, and procedures can come on or off the list. Notably, in January 2018, elective total knee replacements and laparoscopic radical prostatectomies came off the inpatient-only list. Most surgeons and proceduralists know whether the procedure they are performing is on this list, and they should advise hospitalists accordingly if the hospitalist is to be the attending of record and will be writing the admission order.
Inpatient services are nevertheless appropriate
The third situation, in which an inpatient admission is appropriate even when the admitting provider does not expect a two-midnight stay, was added to the two-midnight rule in January 2016. CMS states that the factors used in making this determination can be based on physician judgment and documented in the medical record.
At first reading, one might think that CMS is, in effect, returning to the definition of an inpatient prior to the two-midnight rule’s implementation in 2013. However, CMS has not offered clear guidance for its use, and they did not remove any of the previous two-midnight rule guidance. In the absence of clear guidance, hospitalists may be best served by not using this latest change to the two-midnight rule in determining which Medicare beneficiary hospitalizations are appropriate for inpatient designation.
A final, and critical, point about the two-midnight rule is that it only applies to traditional Medicare, and it does not apply to other payers, including commercial insurance and Medicaid. Medicare Advantage plans may or may not follow the two-midnight rule, depending on their contract with the hospital. Which patients are appropriate for inpatient designations are usually determined by the individual contract that the hospital has signed with that payer.
A better understanding of the two-midnight rule including to whom it applies, when it applies, and how to apply it will help you accurately determine which hospitalizations are appropriate for inpatient payment. With this understanding you will quickly become the hero of your hospital’s case managers and billing department.
Dr. Locke is senior physician advisor at the Johns Hopkins Hospital in Baltimore and president-elect of the American College of Physician Advisors. Dr. Hu is executive director of physician advisor services at the University of North Carolina Health Care System, Chapel Hill, and president of the American College of Physician Advisors.
References
1. Medicare Benefit Policy Manual. Chapter 1 - Inpatient Hospital Services Covered Under Part A. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/bp102c01.pdf.
2. Code of Federal Regulations. https://www.ecfr.gov/cgi-bin/text-idx?SID=958ee67a826285698204a34e1e5d6406&node=42:2.0.1.2.12.1.47.3&rgn=div8.
3. Current Procedural Terminology, Fourth Edition. https://www.cms.gov/apps/ama/license.asp?file=/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Downloads/CMS-1695-FC-2019-OPPS-FR-Addenda.zip.
What hospitalists must know
What hospitalists must know
Most hospitalists’ training likely included caring for patients in the ambulatory clinic, urgent care, and ED settings. One of the most important aspects of medical training is deciding which of the patients seen in these settings need to “be admitted” to a hospital because of risk, severity of illness, and/or need for certain medical services. In this context, “admit” is a synonym for “hospitalize.”
However, in today’s health care system, in which hospitalization costs are usually borne by a third-party payer, “admit” can have a very different meaning. For most payers, “admit” means “hospitalize as inpatient.” This is distinct from “hospitalize as an outpatient.” (“Observation” or “obs” is the most common example of a hospitalization as an outpatient.) In the medical payer world, inpatient and outpatient are often referred to as “statuses.” The distinction between inpatient versus outpatient status can affect payment and is based on rules that a hospital and payer have agreed upon. (Inpatient hospital care is generally paid at a higher rate than outpatient hospital care.) It is important for hospitalists to have a basic understanding of these rules because it can affect hospital billing, the hospitalist’s professional fees, beneficiary liability, and payer denials of inpatient care.
For years, Medicare’s definition of an inpatient hospitalization was primarily based on an expectation of a hospitalization of at least 24 hours and a physician’s judgment of the beneficiary’s need for inpatient hospital services. This judgment was to be based on the physician’s assessment of the patient’s severity of illness, the risk of an adverse outcome, and the hospital services required. (The exact definition by Centers for Medicare & Medicaid Services is much longer and can be found in the Medicare Benefits Policy Manual.1) Under Medicare, defining a hospitalization as inpatient versus outpatient is especially important because they are billed to different Medicare programs (Part A for inpatient, Part B for outpatient), and both hospital reimbursement and the patient liability can vary significantly.
Not surprisingly, CMS found that how physicians were making status decisions for medically similar hospitalized patients varied greatly. CMS noted two major concerns: an overuse of inpatient for patients hospitalized overnight leading to increased charges to CMS and multiday observation hospitalizations for lower-acuity patients leading to excessive liability for Medicare beneficiaries. (Observation stays are billed under Part B, under which the beneficiary generally has a 20% copay.)
To address these concerns, in October 2013, CMS adjusted the definition of inpatient to include “the two-midnight rule.” Basically, CMS said that, in order to qualify for inpatient, the admitting physician should expect the beneficiary to require hospital care spanning at least two midnights, rather than the previous 24-hour benchmark, regardless of the severity of illness or risk of adverse outcome. (There are exceptions and exemptions to the two-midnight rule, which are discussed later in this article.)
The idea of the two-midnight rule was to address the two concerns noted above. Under this rule, most expected overnight hospitalizations should be outpatients, even if they are more than 24 hours in length, and any medically necessary outpatient hospitalization should be “converted” to inpatient if and when it is clear that a second midnight of hospitalization is medically necessary.
In January 2016, CMS amended the two-midnight rule to recognize, as it had done prior to October 2013, that some hospitalizations, based on physician judgment, would be appropriate for inpatient without an expectation of a hospitalization that spans at least two midnights. Unfortunately, CMS has not been forthcoming with guidance of examples of which hospitalizations would fall into this new category, other than to say they expect the use of this new provision would generally not be appropriate for a hospital stay of less than 24 hours.
As of today, physicians should order inpatient services under the following three situations:
- The physician expects the beneficiary to require hospital care spanning at least two midnights.
- The physician provides a service on Medicare’s inpatient-only list.
- The physician expects the beneficiary to require hospital care for less than two midnights but feels that inpatient services are nevertheless appropriate.
This most recently updated version of the two-midnight rule can be found in Section 42 CFR §412.3 of the Code of Federal Regulations.2 Each of these three situations warrants additional discussion.
Care expected to span two midnights
The first situation is the one most applicable to hospitalists. In this circumstance there are three key points to remember.
The first point is that the two-midnight rule is based on a reasonable expectation of a need for hospitalization for at least two nights, not the actual length of hospitalization. Auditors, based on long-standing guidance from the CMS, should consider only the information known (or that should have been known) to the provider at the time the inpatient decision is made.
For example, if the expectation of the need for hospitalization of at least 2 midnights is well documented in the admission note, but the beneficiary improves more rapidly than expected and can be discharged before the second midnight, billing Medicare under Part A for inpatient admission remains appropriate. Auditors may look for provider documentation describing the unexpected improvement, and while such documentation is not an absolute requirement, its presence can be helpful in defending inpatient billing.
Other situations in which there can be an expectation of hospitalization of at least two midnights, but the actual length of stay does not meet this benchmark, are death, patients leaving against medical advice, or transfer to another hospital. For example, if a patient is hospitalized as an inpatient for bacterial endocarditis, and the documented plan of care includes at least 2 days of IV antibiotics and monitoring of cultures, inpatient remains appropriate even if the patient signs out against medical advice the following day.
The second key point to understand is that a night must be “medically necessary” to count toward the two-midnight benchmark. Hospital time spent receiving custodial care, because of excessive delays, or incurred because of the convenience of the beneficiary or provider does not count toward the two-midnight benchmark. For example, imagine a patient hospitalized with chest pain on Saturday evening and the attending physician determines that the patient requires serial cardiac isoenzymes and ECGs followed, most likely, by a noninvasive stress test. The attending physician, knowing that the hospital does not offer stress testing on Sunday, expects the patient to remain hospitalized at least until Monday, thus two midnights. However, in this situation, the second midnight (Sunday night) was not medically necessary and does not count toward the two midnight expectation.
The third key point to know is that the clock for calculating the two-midnight rule begins when the beneficiary starts receiving hospital care, not when the inpatient order is placed. Further, care that starts in the ED or at another hospital counts, too. In contrast, care at an outpatient clinic, an urgent care facility, or waiting-room time in an ED does not count.
When CMS implemented the two-midnight rule in 2013, they said that they would be open to exceptions. The first and only exception to date to the two-midnight rule is newly initiated and unanticipated mechanical ventilation. (This excludes anticipated intubations related to other care, such as procedures.) For example, inpatient is appropriate for a patient who requires hospitalization for an anaphylactic reaction or a drug overdose and needs intubation and mechanical ventilation, even if discharge is expected before a second midnight of hospital care.
CMS’s inpatient-only list
Each year, CMS publishes a list of procedures that CMS will pay only under Part A (that is, as inpatient). This list is updated quarterly (Addendum E) and can be found on the CMS website.3 Hospitalizations associated with the procedures on this list should always be inpatient, regardless of the expected length of stay.
It is important to note that the inpatient-only list is dynamic; it is revised annually, and procedures can come on or off the list. Notably, in January 2018, elective total knee replacements and laparoscopic radical prostatectomies came off the inpatient-only list. Most surgeons and proceduralists know whether the procedure they are performing is on this list, and they should advise hospitalists accordingly if the hospitalist is to be the attending of record and will be writing the admission order.
Inpatient services are nevertheless appropriate
The third situation, in which an inpatient admission is appropriate even when the admitting provider does not expect a two-midnight stay, was added to the two-midnight rule in January 2016. CMS states that the factors used in making this determination can be based on physician judgment and documented in the medical record.
At first reading, one might think that CMS is, in effect, returning to the definition of an inpatient prior to the two-midnight rule’s implementation in 2013. However, CMS has not offered clear guidance for its use, and they did not remove any of the previous two-midnight rule guidance. In the absence of clear guidance, hospitalists may be best served by not using this latest change to the two-midnight rule in determining which Medicare beneficiary hospitalizations are appropriate for inpatient designation.
A final, and critical, point about the two-midnight rule is that it only applies to traditional Medicare, and it does not apply to other payers, including commercial insurance and Medicaid. Medicare Advantage plans may or may not follow the two-midnight rule, depending on their contract with the hospital. Which patients are appropriate for inpatient designations are usually determined by the individual contract that the hospital has signed with that payer.
A better understanding of the two-midnight rule including to whom it applies, when it applies, and how to apply it will help you accurately determine which hospitalizations are appropriate for inpatient payment. With this understanding you will quickly become the hero of your hospital’s case managers and billing department.
Dr. Locke is senior physician advisor at the Johns Hopkins Hospital in Baltimore and president-elect of the American College of Physician Advisors. Dr. Hu is executive director of physician advisor services at the University of North Carolina Health Care System, Chapel Hill, and president of the American College of Physician Advisors.
References
1. Medicare Benefit Policy Manual. Chapter 1 - Inpatient Hospital Services Covered Under Part A. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/bp102c01.pdf.
2. Code of Federal Regulations. https://www.ecfr.gov/cgi-bin/text-idx?SID=958ee67a826285698204a34e1e5d6406&node=42:2.0.1.2.12.1.47.3&rgn=div8.
3. Current Procedural Terminology, Fourth Edition. https://www.cms.gov/apps/ama/license.asp?file=/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Downloads/CMS-1695-FC-2019-OPPS-FR-Addenda.zip.
Most hospitalists’ training likely included caring for patients in the ambulatory clinic, urgent care, and ED settings. One of the most important aspects of medical training is deciding which of the patients seen in these settings need to “be admitted” to a hospital because of risk, severity of illness, and/or need for certain medical services. In this context, “admit” is a synonym for “hospitalize.”
However, in today’s health care system, in which hospitalization costs are usually borne by a third-party payer, “admit” can have a very different meaning. For most payers, “admit” means “hospitalize as inpatient.” This is distinct from “hospitalize as an outpatient.” (“Observation” or “obs” is the most common example of a hospitalization as an outpatient.) In the medical payer world, inpatient and outpatient are often referred to as “statuses.” The distinction between inpatient versus outpatient status can affect payment and is based on rules that a hospital and payer have agreed upon. (Inpatient hospital care is generally paid at a higher rate than outpatient hospital care.) It is important for hospitalists to have a basic understanding of these rules because it can affect hospital billing, the hospitalist’s professional fees, beneficiary liability, and payer denials of inpatient care.
For years, Medicare’s definition of an inpatient hospitalization was primarily based on an expectation of a hospitalization of at least 24 hours and a physician’s judgment of the beneficiary’s need for inpatient hospital services. This judgment was to be based on the physician’s assessment of the patient’s severity of illness, the risk of an adverse outcome, and the hospital services required. (The exact definition by Centers for Medicare & Medicaid Services is much longer and can be found in the Medicare Benefits Policy Manual.1) Under Medicare, defining a hospitalization as inpatient versus outpatient is especially important because they are billed to different Medicare programs (Part A for inpatient, Part B for outpatient), and both hospital reimbursement and the patient liability can vary significantly.
Not surprisingly, CMS found that how physicians were making status decisions for medically similar hospitalized patients varied greatly. CMS noted two major concerns: an overuse of inpatient for patients hospitalized overnight leading to increased charges to CMS and multiday observation hospitalizations for lower-acuity patients leading to excessive liability for Medicare beneficiaries. (Observation stays are billed under Part B, under which the beneficiary generally has a 20% copay.)
To address these concerns, in October 2013, CMS adjusted the definition of inpatient to include “the two-midnight rule.” Basically, CMS said that, in order to qualify for inpatient, the admitting physician should expect the beneficiary to require hospital care spanning at least two midnights, rather than the previous 24-hour benchmark, regardless of the severity of illness or risk of adverse outcome. (There are exceptions and exemptions to the two-midnight rule, which are discussed later in this article.)
The idea of the two-midnight rule was to address the two concerns noted above. Under this rule, most expected overnight hospitalizations should be outpatients, even if they are more than 24 hours in length, and any medically necessary outpatient hospitalization should be “converted” to inpatient if and when it is clear that a second midnight of hospitalization is medically necessary.
In January 2016, CMS amended the two-midnight rule to recognize, as it had done prior to October 2013, that some hospitalizations, based on physician judgment, would be appropriate for inpatient without an expectation of a hospitalization that spans at least two midnights. Unfortunately, CMS has not been forthcoming with guidance of examples of which hospitalizations would fall into this new category, other than to say they expect the use of this new provision would generally not be appropriate for a hospital stay of less than 24 hours.
As of today, physicians should order inpatient services under the following three situations:
- The physician expects the beneficiary to require hospital care spanning at least two midnights.
- The physician provides a service on Medicare’s inpatient-only list.
- The physician expects the beneficiary to require hospital care for less than two midnights but feels that inpatient services are nevertheless appropriate.
This most recently updated version of the two-midnight rule can be found in Section 42 CFR §412.3 of the Code of Federal Regulations.2 Each of these three situations warrants additional discussion.
Care expected to span two midnights
The first situation is the one most applicable to hospitalists. In this circumstance there are three key points to remember.
The first point is that the two-midnight rule is based on a reasonable expectation of a need for hospitalization for at least two nights, not the actual length of hospitalization. Auditors, based on long-standing guidance from the CMS, should consider only the information known (or that should have been known) to the provider at the time the inpatient decision is made.
For example, if the expectation of the need for hospitalization of at least 2 midnights is well documented in the admission note, but the beneficiary improves more rapidly than expected and can be discharged before the second midnight, billing Medicare under Part A for inpatient admission remains appropriate. Auditors may look for provider documentation describing the unexpected improvement, and while such documentation is not an absolute requirement, its presence can be helpful in defending inpatient billing.
Other situations in which there can be an expectation of hospitalization of at least two midnights, but the actual length of stay does not meet this benchmark, are death, patients leaving against medical advice, or transfer to another hospital. For example, if a patient is hospitalized as an inpatient for bacterial endocarditis, and the documented plan of care includes at least 2 days of IV antibiotics and monitoring of cultures, inpatient remains appropriate even if the patient signs out against medical advice the following day.
The second key point to understand is that a night must be “medically necessary” to count toward the two-midnight benchmark. Hospital time spent receiving custodial care, because of excessive delays, or incurred because of the convenience of the beneficiary or provider does not count toward the two-midnight benchmark. For example, imagine a patient hospitalized with chest pain on Saturday evening and the attending physician determines that the patient requires serial cardiac isoenzymes and ECGs followed, most likely, by a noninvasive stress test. The attending physician, knowing that the hospital does not offer stress testing on Sunday, expects the patient to remain hospitalized at least until Monday, thus two midnights. However, in this situation, the second midnight (Sunday night) was not medically necessary and does not count toward the two midnight expectation.
The third key point to know is that the clock for calculating the two-midnight rule begins when the beneficiary starts receiving hospital care, not when the inpatient order is placed. Further, care that starts in the ED or at another hospital counts, too. In contrast, care at an outpatient clinic, an urgent care facility, or waiting-room time in an ED does not count.
When CMS implemented the two-midnight rule in 2013, they said that they would be open to exceptions. The first and only exception to date to the two-midnight rule is newly initiated and unanticipated mechanical ventilation. (This excludes anticipated intubations related to other care, such as procedures.) For example, inpatient is appropriate for a patient who requires hospitalization for an anaphylactic reaction or a drug overdose and needs intubation and mechanical ventilation, even if discharge is expected before a second midnight of hospital care.
CMS’s inpatient-only list
Each year, CMS publishes a list of procedures that CMS will pay only under Part A (that is, as inpatient). This list is updated quarterly (Addendum E) and can be found on the CMS website.3 Hospitalizations associated with the procedures on this list should always be inpatient, regardless of the expected length of stay.
It is important to note that the inpatient-only list is dynamic; it is revised annually, and procedures can come on or off the list. Notably, in January 2018, elective total knee replacements and laparoscopic radical prostatectomies came off the inpatient-only list. Most surgeons and proceduralists know whether the procedure they are performing is on this list, and they should advise hospitalists accordingly if the hospitalist is to be the attending of record and will be writing the admission order.
Inpatient services are nevertheless appropriate
The third situation, in which an inpatient admission is appropriate even when the admitting provider does not expect a two-midnight stay, was added to the two-midnight rule in January 2016. CMS states that the factors used in making this determination can be based on physician judgment and documented in the medical record.
At first reading, one might think that CMS is, in effect, returning to the definition of an inpatient prior to the two-midnight rule’s implementation in 2013. However, CMS has not offered clear guidance for its use, and they did not remove any of the previous two-midnight rule guidance. In the absence of clear guidance, hospitalists may be best served by not using this latest change to the two-midnight rule in determining which Medicare beneficiary hospitalizations are appropriate for inpatient designation.
A final, and critical, point about the two-midnight rule is that it only applies to traditional Medicare, and it does not apply to other payers, including commercial insurance and Medicaid. Medicare Advantage plans may or may not follow the two-midnight rule, depending on their contract with the hospital. Which patients are appropriate for inpatient designations are usually determined by the individual contract that the hospital has signed with that payer.
A better understanding of the two-midnight rule including to whom it applies, when it applies, and how to apply it will help you accurately determine which hospitalizations are appropriate for inpatient payment. With this understanding you will quickly become the hero of your hospital’s case managers and billing department.
Dr. Locke is senior physician advisor at the Johns Hopkins Hospital in Baltimore and president-elect of the American College of Physician Advisors. Dr. Hu is executive director of physician advisor services at the University of North Carolina Health Care System, Chapel Hill, and president of the American College of Physician Advisors.
References
1. Medicare Benefit Policy Manual. Chapter 1 - Inpatient Hospital Services Covered Under Part A. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/bp102c01.pdf.
2. Code of Federal Regulations. https://www.ecfr.gov/cgi-bin/text-idx?SID=958ee67a826285698204a34e1e5d6406&node=42:2.0.1.2.12.1.47.3&rgn=div8.
3. Current Procedural Terminology, Fourth Edition. https://www.cms.gov/apps/ama/license.asp?file=/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Downloads/CMS-1695-FC-2019-OPPS-FR-Addenda.zip.
Disruptive behavior on the job linked to depression, burnout
SAN DIEGO – Hospitals pay a price for bad behavior by staff in the workplace, results of a large multicenter study suggest.
A work culture in which disruptive behavior is tolerated can have consequences. Research on this topic has linked disruptive behavior by staff in the health care setting to increased frequency of medical errors and lower quality of care (Am J Med Qual. 2011 Sep-Oct;26(5):372-9; J Caring Sci. 2016 Sep 1;5(3):241-9). This new study, based on a workplace culture survey of 7,923 health care workers and 325 work settings at 16 hospitals in a large West Coast health care system, found , researchers found. The paper was presented by study lead Allison Hadley, MD, of Duke Children’s Hospital, Durham, N.C., at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
The investigators developed a novel survey scale for evaluating disruptive behaviors in the health care setting. The objective was to look at the associations between disruptive behavior, teamwork, safety culture, burnout, and depression. Disruptive behaviors included turning backs or hanging up the phone before a conversation is over, bullying or trying to publicly humiliate other staff, making inappropriate comments (with sexual, racial, religious, or ethnic slurs), and physical aggression (such as throwing, hitting, and pushing).
San Francisco internist Alan H. Rosenstein, MD, who studies disruptive behavior in medicine, said in an interview that the findings confirm anecdotal experience of medical staff. “One of the downsides of disruptive behavior is very unsatisfied and unhappy people,” he said
The investigators used a t-test analysis to study the strength of the association between disruptive behavior and work culture in health care work settings. They found a statistically significant association between less disruptive behavior and lower levels of burnout and depression among staff (t = 6.4 and t = 4.1, respectively, P less than .001) and higher levels of teamwork, safety culture, and work-life balance (t = 10.2, t = 9.5 and t = 5.8, respectively, P less than .001). Settings in which disruptive behaviors were more common were more likely to have poor teamwork culture (P less than .001) and safety climate (P less than .001), and higher rates of depression (P less than .001). Settings in which disruptive behaviors were more common were more likely to have poor teamwork culture (P less than .001) and safety climate (P less than .001), and higher rates of depression (P less than .001).
Bullying was reported at about 40% of workplaces with low teamwork levels, compared with nearly 20% in those with high teamwork levels.
Physical aggression was reported in nearly 20% of those workplaces with low teamwork levels, compared with 5% in workplaces with high teamwork levels (P less than .001).
Researchers also found that disruptive behaviors were least common during day shifts and more common among health care workers who care for both adults and children than among those who care for only adults. “Teamwork, safety culture, and work-life balance were highest in those [hospital] units with the least disruptive behaviors,” said Dr. Hadley.
Overall, the highest positive correlation was found between higher levels of teamwork and lower levels of disruptive behavior, Dr. Hadley said. If a hospital department is trying to address one issue to improve disruptive behavior, she’d suggest it “focus on teamwork first. I hope that would have the greatest impact.”
Dr. Rosenstein, who has conducted several studies on disruptive behavior, said the key to improving the workplace is to “build a culture based on the mission of providing patient care. It’s not to save a dollar, to make a dollar. The mission is patient care.”
What’s next? Dr. Hadley said her team is continuing to work on developing a scale to measure disruptive behavior in the workplace.
No study funding was reported. Dr. Hadley and Dr. Rosenstein reported no relevant disclosures.
SOURCE: Hadley A et al. CCC48, Abstract 114.
SAN DIEGO – Hospitals pay a price for bad behavior by staff in the workplace, results of a large multicenter study suggest.
A work culture in which disruptive behavior is tolerated can have consequences. Research on this topic has linked disruptive behavior by staff in the health care setting to increased frequency of medical errors and lower quality of care (Am J Med Qual. 2011 Sep-Oct;26(5):372-9; J Caring Sci. 2016 Sep 1;5(3):241-9). This new study, based on a workplace culture survey of 7,923 health care workers and 325 work settings at 16 hospitals in a large West Coast health care system, found , researchers found. The paper was presented by study lead Allison Hadley, MD, of Duke Children’s Hospital, Durham, N.C., at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
The investigators developed a novel survey scale for evaluating disruptive behaviors in the health care setting. The objective was to look at the associations between disruptive behavior, teamwork, safety culture, burnout, and depression. Disruptive behaviors included turning backs or hanging up the phone before a conversation is over, bullying or trying to publicly humiliate other staff, making inappropriate comments (with sexual, racial, religious, or ethnic slurs), and physical aggression (such as throwing, hitting, and pushing).
San Francisco internist Alan H. Rosenstein, MD, who studies disruptive behavior in medicine, said in an interview that the findings confirm anecdotal experience of medical staff. “One of the downsides of disruptive behavior is very unsatisfied and unhappy people,” he said
The investigators used a t-test analysis to study the strength of the association between disruptive behavior and work culture in health care work settings. They found a statistically significant association between less disruptive behavior and lower levels of burnout and depression among staff (t = 6.4 and t = 4.1, respectively, P less than .001) and higher levels of teamwork, safety culture, and work-life balance (t = 10.2, t = 9.5 and t = 5.8, respectively, P less than .001). Settings in which disruptive behaviors were more common were more likely to have poor teamwork culture (P less than .001) and safety climate (P less than .001), and higher rates of depression (P less than .001). Settings in which disruptive behaviors were more common were more likely to have poor teamwork culture (P less than .001) and safety climate (P less than .001), and higher rates of depression (P less than .001).
Bullying was reported at about 40% of workplaces with low teamwork levels, compared with nearly 20% in those with high teamwork levels.
Physical aggression was reported in nearly 20% of those workplaces with low teamwork levels, compared with 5% in workplaces with high teamwork levels (P less than .001).
Researchers also found that disruptive behaviors were least common during day shifts and more common among health care workers who care for both adults and children than among those who care for only adults. “Teamwork, safety culture, and work-life balance were highest in those [hospital] units with the least disruptive behaviors,” said Dr. Hadley.
Overall, the highest positive correlation was found between higher levels of teamwork and lower levels of disruptive behavior, Dr. Hadley said. If a hospital department is trying to address one issue to improve disruptive behavior, she’d suggest it “focus on teamwork first. I hope that would have the greatest impact.”
Dr. Rosenstein, who has conducted several studies on disruptive behavior, said the key to improving the workplace is to “build a culture based on the mission of providing patient care. It’s not to save a dollar, to make a dollar. The mission is patient care.”
What’s next? Dr. Hadley said her team is continuing to work on developing a scale to measure disruptive behavior in the workplace.
No study funding was reported. Dr. Hadley and Dr. Rosenstein reported no relevant disclosures.
SOURCE: Hadley A et al. CCC48, Abstract 114.
SAN DIEGO – Hospitals pay a price for bad behavior by staff in the workplace, results of a large multicenter study suggest.
A work culture in which disruptive behavior is tolerated can have consequences. Research on this topic has linked disruptive behavior by staff in the health care setting to increased frequency of medical errors and lower quality of care (Am J Med Qual. 2011 Sep-Oct;26(5):372-9; J Caring Sci. 2016 Sep 1;5(3):241-9). This new study, based on a workplace culture survey of 7,923 health care workers and 325 work settings at 16 hospitals in a large West Coast health care system, found , researchers found. The paper was presented by study lead Allison Hadley, MD, of Duke Children’s Hospital, Durham, N.C., at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
The investigators developed a novel survey scale for evaluating disruptive behaviors in the health care setting. The objective was to look at the associations between disruptive behavior, teamwork, safety culture, burnout, and depression. Disruptive behaviors included turning backs or hanging up the phone before a conversation is over, bullying or trying to publicly humiliate other staff, making inappropriate comments (with sexual, racial, religious, or ethnic slurs), and physical aggression (such as throwing, hitting, and pushing).
San Francisco internist Alan H. Rosenstein, MD, who studies disruptive behavior in medicine, said in an interview that the findings confirm anecdotal experience of medical staff. “One of the downsides of disruptive behavior is very unsatisfied and unhappy people,” he said
The investigators used a t-test analysis to study the strength of the association between disruptive behavior and work culture in health care work settings. They found a statistically significant association between less disruptive behavior and lower levels of burnout and depression among staff (t = 6.4 and t = 4.1, respectively, P less than .001) and higher levels of teamwork, safety culture, and work-life balance (t = 10.2, t = 9.5 and t = 5.8, respectively, P less than .001). Settings in which disruptive behaviors were more common were more likely to have poor teamwork culture (P less than .001) and safety climate (P less than .001), and higher rates of depression (P less than .001). Settings in which disruptive behaviors were more common were more likely to have poor teamwork culture (P less than .001) and safety climate (P less than .001), and higher rates of depression (P less than .001).
Bullying was reported at about 40% of workplaces with low teamwork levels, compared with nearly 20% in those with high teamwork levels.
Physical aggression was reported in nearly 20% of those workplaces with low teamwork levels, compared with 5% in workplaces with high teamwork levels (P less than .001).
Researchers also found that disruptive behaviors were least common during day shifts and more common among health care workers who care for both adults and children than among those who care for only adults. “Teamwork, safety culture, and work-life balance were highest in those [hospital] units with the least disruptive behaviors,” said Dr. Hadley.
Overall, the highest positive correlation was found between higher levels of teamwork and lower levels of disruptive behavior, Dr. Hadley said. If a hospital department is trying to address one issue to improve disruptive behavior, she’d suggest it “focus on teamwork first. I hope that would have the greatest impact.”
Dr. Rosenstein, who has conducted several studies on disruptive behavior, said the key to improving the workplace is to “build a culture based on the mission of providing patient care. It’s not to save a dollar, to make a dollar. The mission is patient care.”
What’s next? Dr. Hadley said her team is continuing to work on developing a scale to measure disruptive behavior in the workplace.
No study funding was reported. Dr. Hadley and Dr. Rosenstein reported no relevant disclosures.
SOURCE: Hadley A et al. CCC48, Abstract 114.
REPORTING FROM CCC48
Culture change needed to improve gender inequalities in medicine
LONDON –
“Gender equality is everyone’s business,” Sarah Hawkes, MBBS, PhD, a professor of global public health at University College London (England), said at the event.
“We’re not talking about women taking over the shop, but women being given an equal opportunity to run the shop. It doesn’t matter where we place ourselves on the gender spectrum as far as advancing equality in science is concerned. What matters is that we all, irrespective of gender, call ourselves feminists.”
For years, women have been “underrepresented in positions of power and leadership, undervalued, and experience discrimination and gender-based violence in scientific and health disciplines across the world,” according to an editorial in the British-based journal (Lancet. 2019;393:493). Such inequalities are compounded and hard to separate from other inequalities, including ethnicity, disability, class, geography, and sexuality.
Despite efforts to readdress the predominantly male culture of medicine, the problem of gender inequality remains “stubbornly persistent,” the editorial said.
“We have spent years being told that the problem lies with us as individuals and that we just need to be better, stronger, more vocal, as women,” Dr. Hawkes observed. “But what really needs to happen is for change to happen in places that hold power.” She further argued: “We don’t need any more individual change; we need organizational and institutional norm change.”
Gender inequality has a long history, and not just in medicine, said British journalist Caroline Criado-Perez OBE, who gave a keynote speech. Ms. Criado-Perez, who is a well-respected feminist campaigner, noted that the world was largely “modeled to fit men.” From architecture to transport, and even crash-test dummies, everything was largely modeled on, or to accommodate, the male rather than the female body.
“I don’t need to tell you that women are 50% more likely to be misdiagnosed following a heart attack” than men. There is no more urgent need to challenge gender inequality than in medicine, Women are dying because of the gender data gap in medicine,” she asserted. “In medical research, in medical education, in medical practice, it needs to be closed as a matter of urgency.”
Original data published in the Advancing Women in Science, Medicine and Global Health special edition of The Lancet found that only 31% of biomedical research papers published in 2016 reported outcomes for both men and women (Lancet. 2019;393:550-9). Reporting of sex differences was somewhat better in clinical or public health-related research papers, at 67% and 69%, respectively. Sex-differences were more likely to be reported if a woman was one of the key authors, Cassidy R. Sugimoto, PhD, associate professor of informatics at Indiana University in Bloomington, and associates, observed in their paper.
That said, women often have to fight to be included as an author on a paper, even when they have done the majority of the work, the event participants highlighted. Women were still less likely than men to be named as the first or last author on a paper, as well as be less likely to receive research funding to enable them to do the work in the first place (Lancet. 2018;393:531-40).
“Was it really you?” was a question sometimes asked of a woman named as a lead or first author, noted Sonia Gandhi, MD, PhD, group leader of the Neurodegeneration Biology Laboratory at the Francis Crick Institute in Cambridge (England). Women network differently to men, Dr. Gandhi observed, and not necessarily in networks that forward careers. Women were also often questioned about their productivity, and regardless of any training on unconscious bias, women were still at a disadvantage if they took a career break to have children.
Women’s credentials and capabilities were often felt to be less respected by male colleagues, and there was talk of being met with microaggressions in the workplace, as in one example given by Nana Odom, MSc, a clinical engineer at the Royal United Hospital Bath (England). She was told “you’re not an engineer, because I have not got a set of screwdrivers and sit at a computer and program.” Such comments can deeply affect a person, Dr. Odom said. “Sometimes I feel that if I don’t go into the workshop and open up a bit of kit that I am not an engineer, but it’s so unconscious, it carries on with you.” These types of stories need to be told so then they can be properly addressed when they do happen, she said.
Female representation is so important, said F. Gigi Osler, MD, head of otolaryngology-head and neck surgery at St. Boniface Hospital in Winnipeg. Dr. Osler is the 2018-2019 president of the Canadian Medical Association, the eighth woman to hold this prestigious position in the organization’s 151 years of operation. She also happens to be the first female surgeon and the first woman of color in the role. “When I stepped into the presidency last August, I thought very long and very hard about how I was going to use my voice and this platform,” Dr. Osler said. “It became very clear to me after I started how important representation was. I can’t tell you how many women, young women, and women of color...have come up to me to say, ‘I’m so excited to have you in this position. I’ve never seen someone who looks like me in that type of leadership position,’ ” she observed.
“As leaders, I think we can advocate for structures and processes,” Dr. Osler added, “I think we set the culture.” Leaders have the responsibility for creating and nurturing and fostering a professional, respectful, and inclusive environment, she said.
“We need more strong leaders, we need more diversity in leadership.” Dr. Osler was keen to point out that greater diversity does not mean only women, but other groups as well. “Look around the room. Who is not here? How can I make it easier for them to get here?”
Another strong female role model at the event was Dame Sally Davies, the Chief Medical Officer for England, a hematologist by training. Not only is she the first female in that role, she will also become the first female Master of Trinity College Cambridge starting in October 2019, a role dominated by men for more than 500 years.
All people, women and men, need to be given fair opportunity, Dame Sally said. Addressing structural issues can help, she said. “We need role models, mentors, and champions,” she said, noting that there were differences between the three. “Mentors give you advice, they get to know you, and they help you think through your issue. Champions may not have time for that, but they know you are good,” and they are putting you forward for opportunities.
“If the system isn’t right, or we are treated badly, we need to call it out,” Dame Sally said. “I do think that we often let things pass that we shouldn’t.” A classic situation is where a woman may suggest something at a meeting and it is ignored, but when a man says the same thing it is taken on board. That kind of behavior needs to stop and be addressed when it happens, by everyone at the table, she said.
Dr. Hawkes observed in her summing up of the day: “Throughout the history of health, change comes about not just through action at the top, but also from action from the bottom up.” She added: “The question is how do we make that change happen?” That’s where the next phase of research needs to take place, she suggested, “we need to actually see, in a very evidence-informed way, what actually works to make and sustain change.”
No financial disclosures were reported by any of the speakers quoted.
SOURCE: Lancet. 2019;393:493–610, e6-e28
LONDON –
“Gender equality is everyone’s business,” Sarah Hawkes, MBBS, PhD, a professor of global public health at University College London (England), said at the event.
“We’re not talking about women taking over the shop, but women being given an equal opportunity to run the shop. It doesn’t matter where we place ourselves on the gender spectrum as far as advancing equality in science is concerned. What matters is that we all, irrespective of gender, call ourselves feminists.”
For years, women have been “underrepresented in positions of power and leadership, undervalued, and experience discrimination and gender-based violence in scientific and health disciplines across the world,” according to an editorial in the British-based journal (Lancet. 2019;393:493). Such inequalities are compounded and hard to separate from other inequalities, including ethnicity, disability, class, geography, and sexuality.
Despite efforts to readdress the predominantly male culture of medicine, the problem of gender inequality remains “stubbornly persistent,” the editorial said.
“We have spent years being told that the problem lies with us as individuals and that we just need to be better, stronger, more vocal, as women,” Dr. Hawkes observed. “But what really needs to happen is for change to happen in places that hold power.” She further argued: “We don’t need any more individual change; we need organizational and institutional norm change.”
Gender inequality has a long history, and not just in medicine, said British journalist Caroline Criado-Perez OBE, who gave a keynote speech. Ms. Criado-Perez, who is a well-respected feminist campaigner, noted that the world was largely “modeled to fit men.” From architecture to transport, and even crash-test dummies, everything was largely modeled on, or to accommodate, the male rather than the female body.
“I don’t need to tell you that women are 50% more likely to be misdiagnosed following a heart attack” than men. There is no more urgent need to challenge gender inequality than in medicine, Women are dying because of the gender data gap in medicine,” she asserted. “In medical research, in medical education, in medical practice, it needs to be closed as a matter of urgency.”
Original data published in the Advancing Women in Science, Medicine and Global Health special edition of The Lancet found that only 31% of biomedical research papers published in 2016 reported outcomes for both men and women (Lancet. 2019;393:550-9). Reporting of sex differences was somewhat better in clinical or public health-related research papers, at 67% and 69%, respectively. Sex-differences were more likely to be reported if a woman was one of the key authors, Cassidy R. Sugimoto, PhD, associate professor of informatics at Indiana University in Bloomington, and associates, observed in their paper.
That said, women often have to fight to be included as an author on a paper, even when they have done the majority of the work, the event participants highlighted. Women were still less likely than men to be named as the first or last author on a paper, as well as be less likely to receive research funding to enable them to do the work in the first place (Lancet. 2018;393:531-40).
“Was it really you?” was a question sometimes asked of a woman named as a lead or first author, noted Sonia Gandhi, MD, PhD, group leader of the Neurodegeneration Biology Laboratory at the Francis Crick Institute in Cambridge (England). Women network differently to men, Dr. Gandhi observed, and not necessarily in networks that forward careers. Women were also often questioned about their productivity, and regardless of any training on unconscious bias, women were still at a disadvantage if they took a career break to have children.
Women’s credentials and capabilities were often felt to be less respected by male colleagues, and there was talk of being met with microaggressions in the workplace, as in one example given by Nana Odom, MSc, a clinical engineer at the Royal United Hospital Bath (England). She was told “you’re not an engineer, because I have not got a set of screwdrivers and sit at a computer and program.” Such comments can deeply affect a person, Dr. Odom said. “Sometimes I feel that if I don’t go into the workshop and open up a bit of kit that I am not an engineer, but it’s so unconscious, it carries on with you.” These types of stories need to be told so then they can be properly addressed when they do happen, she said.
Female representation is so important, said F. Gigi Osler, MD, head of otolaryngology-head and neck surgery at St. Boniface Hospital in Winnipeg. Dr. Osler is the 2018-2019 president of the Canadian Medical Association, the eighth woman to hold this prestigious position in the organization’s 151 years of operation. She also happens to be the first female surgeon and the first woman of color in the role. “When I stepped into the presidency last August, I thought very long and very hard about how I was going to use my voice and this platform,” Dr. Osler said. “It became very clear to me after I started how important representation was. I can’t tell you how many women, young women, and women of color...have come up to me to say, ‘I’m so excited to have you in this position. I’ve never seen someone who looks like me in that type of leadership position,’ ” she observed.
“As leaders, I think we can advocate for structures and processes,” Dr. Osler added, “I think we set the culture.” Leaders have the responsibility for creating and nurturing and fostering a professional, respectful, and inclusive environment, she said.
“We need more strong leaders, we need more diversity in leadership.” Dr. Osler was keen to point out that greater diversity does not mean only women, but other groups as well. “Look around the room. Who is not here? How can I make it easier for them to get here?”
Another strong female role model at the event was Dame Sally Davies, the Chief Medical Officer for England, a hematologist by training. Not only is she the first female in that role, she will also become the first female Master of Trinity College Cambridge starting in October 2019, a role dominated by men for more than 500 years.
All people, women and men, need to be given fair opportunity, Dame Sally said. Addressing structural issues can help, she said. “We need role models, mentors, and champions,” she said, noting that there were differences between the three. “Mentors give you advice, they get to know you, and they help you think through your issue. Champions may not have time for that, but they know you are good,” and they are putting you forward for opportunities.
“If the system isn’t right, or we are treated badly, we need to call it out,” Dame Sally said. “I do think that we often let things pass that we shouldn’t.” A classic situation is where a woman may suggest something at a meeting and it is ignored, but when a man says the same thing it is taken on board. That kind of behavior needs to stop and be addressed when it happens, by everyone at the table, she said.
Dr. Hawkes observed in her summing up of the day: “Throughout the history of health, change comes about not just through action at the top, but also from action from the bottom up.” She added: “The question is how do we make that change happen?” That’s where the next phase of research needs to take place, she suggested, “we need to actually see, in a very evidence-informed way, what actually works to make and sustain change.”
No financial disclosures were reported by any of the speakers quoted.
SOURCE: Lancet. 2019;393:493–610, e6-e28
LONDON –
“Gender equality is everyone’s business,” Sarah Hawkes, MBBS, PhD, a professor of global public health at University College London (England), said at the event.
“We’re not talking about women taking over the shop, but women being given an equal opportunity to run the shop. It doesn’t matter where we place ourselves on the gender spectrum as far as advancing equality in science is concerned. What matters is that we all, irrespective of gender, call ourselves feminists.”
For years, women have been “underrepresented in positions of power and leadership, undervalued, and experience discrimination and gender-based violence in scientific and health disciplines across the world,” according to an editorial in the British-based journal (Lancet. 2019;393:493). Such inequalities are compounded and hard to separate from other inequalities, including ethnicity, disability, class, geography, and sexuality.
Despite efforts to readdress the predominantly male culture of medicine, the problem of gender inequality remains “stubbornly persistent,” the editorial said.
“We have spent years being told that the problem lies with us as individuals and that we just need to be better, stronger, more vocal, as women,” Dr. Hawkes observed. “But what really needs to happen is for change to happen in places that hold power.” She further argued: “We don’t need any more individual change; we need organizational and institutional norm change.”
Gender inequality has a long history, and not just in medicine, said British journalist Caroline Criado-Perez OBE, who gave a keynote speech. Ms. Criado-Perez, who is a well-respected feminist campaigner, noted that the world was largely “modeled to fit men.” From architecture to transport, and even crash-test dummies, everything was largely modeled on, or to accommodate, the male rather than the female body.
“I don’t need to tell you that women are 50% more likely to be misdiagnosed following a heart attack” than men. There is no more urgent need to challenge gender inequality than in medicine, Women are dying because of the gender data gap in medicine,” she asserted. “In medical research, in medical education, in medical practice, it needs to be closed as a matter of urgency.”
Original data published in the Advancing Women in Science, Medicine and Global Health special edition of The Lancet found that only 31% of biomedical research papers published in 2016 reported outcomes for both men and women (Lancet. 2019;393:550-9). Reporting of sex differences was somewhat better in clinical or public health-related research papers, at 67% and 69%, respectively. Sex-differences were more likely to be reported if a woman was one of the key authors, Cassidy R. Sugimoto, PhD, associate professor of informatics at Indiana University in Bloomington, and associates, observed in their paper.
That said, women often have to fight to be included as an author on a paper, even when they have done the majority of the work, the event participants highlighted. Women were still less likely than men to be named as the first or last author on a paper, as well as be less likely to receive research funding to enable them to do the work in the first place (Lancet. 2018;393:531-40).
“Was it really you?” was a question sometimes asked of a woman named as a lead or first author, noted Sonia Gandhi, MD, PhD, group leader of the Neurodegeneration Biology Laboratory at the Francis Crick Institute in Cambridge (England). Women network differently to men, Dr. Gandhi observed, and not necessarily in networks that forward careers. Women were also often questioned about their productivity, and regardless of any training on unconscious bias, women were still at a disadvantage if they took a career break to have children.
Women’s credentials and capabilities were often felt to be less respected by male colleagues, and there was talk of being met with microaggressions in the workplace, as in one example given by Nana Odom, MSc, a clinical engineer at the Royal United Hospital Bath (England). She was told “you’re not an engineer, because I have not got a set of screwdrivers and sit at a computer and program.” Such comments can deeply affect a person, Dr. Odom said. “Sometimes I feel that if I don’t go into the workshop and open up a bit of kit that I am not an engineer, but it’s so unconscious, it carries on with you.” These types of stories need to be told so then they can be properly addressed when they do happen, she said.
Female representation is so important, said F. Gigi Osler, MD, head of otolaryngology-head and neck surgery at St. Boniface Hospital in Winnipeg. Dr. Osler is the 2018-2019 president of the Canadian Medical Association, the eighth woman to hold this prestigious position in the organization’s 151 years of operation. She also happens to be the first female surgeon and the first woman of color in the role. “When I stepped into the presidency last August, I thought very long and very hard about how I was going to use my voice and this platform,” Dr. Osler said. “It became very clear to me after I started how important representation was. I can’t tell you how many women, young women, and women of color...have come up to me to say, ‘I’m so excited to have you in this position. I’ve never seen someone who looks like me in that type of leadership position,’ ” she observed.
“As leaders, I think we can advocate for structures and processes,” Dr. Osler added, “I think we set the culture.” Leaders have the responsibility for creating and nurturing and fostering a professional, respectful, and inclusive environment, she said.
“We need more strong leaders, we need more diversity in leadership.” Dr. Osler was keen to point out that greater diversity does not mean only women, but other groups as well. “Look around the room. Who is not here? How can I make it easier for them to get here?”
Another strong female role model at the event was Dame Sally Davies, the Chief Medical Officer for England, a hematologist by training. Not only is she the first female in that role, she will also become the first female Master of Trinity College Cambridge starting in October 2019, a role dominated by men for more than 500 years.
All people, women and men, need to be given fair opportunity, Dame Sally said. Addressing structural issues can help, she said. “We need role models, mentors, and champions,” she said, noting that there were differences between the three. “Mentors give you advice, they get to know you, and they help you think through your issue. Champions may not have time for that, but they know you are good,” and they are putting you forward for opportunities.
“If the system isn’t right, or we are treated badly, we need to call it out,” Dame Sally said. “I do think that we often let things pass that we shouldn’t.” A classic situation is where a woman may suggest something at a meeting and it is ignored, but when a man says the same thing it is taken on board. That kind of behavior needs to stop and be addressed when it happens, by everyone at the table, she said.
Dr. Hawkes observed in her summing up of the day: “Throughout the history of health, change comes about not just through action at the top, but also from action from the bottom up.” She added: “The question is how do we make that change happen?” That’s where the next phase of research needs to take place, she suggested, “we need to actually see, in a very evidence-informed way, what actually works to make and sustain change.”
No financial disclosures were reported by any of the speakers quoted.
SOURCE: Lancet. 2019;393:493–610, e6-e28
FROM A LAUNCH EVENT HELD BY THE LANCET
ONC aims to help docs, patients with information sharing in proposed rule
The Office of the National Coordinator of Health Information Technology is looking to adopt standardized application programming interfaces (APIs) in an effort to boost interoperability of health data.
The Department of Health & Human Services office posted a proposed rule Feb. 11, 2019, that would, according to an agency press release, “help allow individuals to securely and easily access structured and unstructured EHI [electronic health information] formats using smartphones and other mobile devices.”
“We think our rule is going to help reduce burden and improve care,” Michael Lipinski, director of the Regulatory Affairs Division in the ONC Office of Policy, said in an interview. “It is going to do that through technology. With the APIs, you should be able to get to your information easier and have it readily available. Whether that is from another health care provider or using other health care products through the API to improve care, you will have that ability between the certified API and the information blocking policies to use third party developers and their products.”
The proposed rule also included a requirement that EHRs certified by ONC be able to easily export information contained within the EHR and make the format used to extract and export the data contained within the EHR publicly available.
“Another third party developer can build to that and offer competing services to pull that information out,” Mr. Lipinski said. “That would obviously help if you were choosing to switch [EHRs] if you didn’t like the features you were getting from your EHR. ... That functionality should help if you want to do that.”
The standardizing of APIs to help the delivery of data will go hand in hand with information blocking aspects of the proposed rule, which defines the few exceptions where an activity would not be considered information blocking, such as when engaging in practices will prevent patient harm; engaging in consistent, nondiscriminatory practices to protect patient privacy; and implementing practices to promote the security of health information.
Mr. Lipinski said these changes will help prevent providers from hiding behind HIPAA rules as the excuse to not share patient information, which will help with care coordination. “From a provider’s perspective, this should help them get more access to information, more access in a structured way and then easily get and share that information.”
Ultimately, Mr. Lipinski said, the goal is “to increase competition and lower cost while still improving the quality of care for patients.”
The Office of the National Coordinator of Health Information Technology is looking to adopt standardized application programming interfaces (APIs) in an effort to boost interoperability of health data.
The Department of Health & Human Services office posted a proposed rule Feb. 11, 2019, that would, according to an agency press release, “help allow individuals to securely and easily access structured and unstructured EHI [electronic health information] formats using smartphones and other mobile devices.”
“We think our rule is going to help reduce burden and improve care,” Michael Lipinski, director of the Regulatory Affairs Division in the ONC Office of Policy, said in an interview. “It is going to do that through technology. With the APIs, you should be able to get to your information easier and have it readily available. Whether that is from another health care provider or using other health care products through the API to improve care, you will have that ability between the certified API and the information blocking policies to use third party developers and their products.”
The proposed rule also included a requirement that EHRs certified by ONC be able to easily export information contained within the EHR and make the format used to extract and export the data contained within the EHR publicly available.
“Another third party developer can build to that and offer competing services to pull that information out,” Mr. Lipinski said. “That would obviously help if you were choosing to switch [EHRs] if you didn’t like the features you were getting from your EHR. ... That functionality should help if you want to do that.”
The standardizing of APIs to help the delivery of data will go hand in hand with information blocking aspects of the proposed rule, which defines the few exceptions where an activity would not be considered information blocking, such as when engaging in practices will prevent patient harm; engaging in consistent, nondiscriminatory practices to protect patient privacy; and implementing practices to promote the security of health information.
Mr. Lipinski said these changes will help prevent providers from hiding behind HIPAA rules as the excuse to not share patient information, which will help with care coordination. “From a provider’s perspective, this should help them get more access to information, more access in a structured way and then easily get and share that information.”
Ultimately, Mr. Lipinski said, the goal is “to increase competition and lower cost while still improving the quality of care for patients.”
The Office of the National Coordinator of Health Information Technology is looking to adopt standardized application programming interfaces (APIs) in an effort to boost interoperability of health data.
The Department of Health & Human Services office posted a proposed rule Feb. 11, 2019, that would, according to an agency press release, “help allow individuals to securely and easily access structured and unstructured EHI [electronic health information] formats using smartphones and other mobile devices.”
“We think our rule is going to help reduce burden and improve care,” Michael Lipinski, director of the Regulatory Affairs Division in the ONC Office of Policy, said in an interview. “It is going to do that through technology. With the APIs, you should be able to get to your information easier and have it readily available. Whether that is from another health care provider or using other health care products through the API to improve care, you will have that ability between the certified API and the information blocking policies to use third party developers and their products.”
The proposed rule also included a requirement that EHRs certified by ONC be able to easily export information contained within the EHR and make the format used to extract and export the data contained within the EHR publicly available.
“Another third party developer can build to that and offer competing services to pull that information out,” Mr. Lipinski said. “That would obviously help if you were choosing to switch [EHRs] if you didn’t like the features you were getting from your EHR. ... That functionality should help if you want to do that.”
The standardizing of APIs to help the delivery of data will go hand in hand with information blocking aspects of the proposed rule, which defines the few exceptions where an activity would not be considered information blocking, such as when engaging in practices will prevent patient harm; engaging in consistent, nondiscriminatory practices to protect patient privacy; and implementing practices to promote the security of health information.
Mr. Lipinski said these changes will help prevent providers from hiding behind HIPAA rules as the excuse to not share patient information, which will help with care coordination. “From a provider’s perspective, this should help them get more access to information, more access in a structured way and then easily get and share that information.”
Ultimately, Mr. Lipinski said, the goal is “to increase competition and lower cost while still improving the quality of care for patients.”
Benefiting from an egalitarian hospital culture
Cultural change linked to improved outcomes
Health care experts have long known of a link between patient outcomes and a hospital’s organizational culture, according to an article in the New York Times by Pauline W. Chen, MD.
“Heart attack patients who are treated at hospitals where nurses feel powerless and senior management is only sporadically involved in patient care tend to fare more poorly than patients hospitalized at institutions where nurses are asked regularly for their input and chief executives hold regular meetings with clinicians to review patient results,” she wrote.
But there is hope for change, Dr. Chen noted, and it’s demonstrable, citing a group of researchers that has written about strategies targeting hospital organizational culture called “Leadership Saves Lives.” The researchers showed hospitals could create significant cultural changes, which could impact patient outcomes, in just 2 years.
“Leadership Saves Lives requires that each hospital create a ‘Guiding Coalition,’ a group of staff members from across the entire institution. The coalition members participate in regular workshops, discussions, and national forums on ways hospitals might improve, then help their respective hospital translate newfound ideas and information into clinical practice,” she wrote.
The researchers monitored heart attack patients to assess the effect of Leadership Saves Lives in 10 hospitals that had below average patient outcomes. Over 2 years, all 10 hospitals changed significantly, but 6 hospitals experienced particularly profound cultural transformations.
“The staff of these hospitals spoke of an institutional shift from ‘because I said so’ to ‘focusing on the why’s,’ ” Dr. Chen wrote. “Instead of accepting that every heart attack patient had to undergo certain testing or take specific drugs because the chief of the department or administrator had previously established such clinical protocols, for example, it became more important to provide the data that proved such rituals were actually helpful. Staff members in these hospitals also said they received, and appreciated, increased support from senior management and a newfound freedom to voice opinions in ‘more of an equal role, no matter what position you are.’ ”
The degree of an institution’s cultural change was directly linked to patient outcomes, the researchers found. Indeed, hospitals that made more substantial changes in their work culture realized larger and more sustained drops in heart attack mortality rates.
References
1. Chen PW. A More Egalitarian Hospital Culture Is Better for Everyone. New York Times. https://www.nytimes.com/2018/05/31/well/live/doctors-patients-hospital-culture-better-health.html. Published May 31, 2018. Accessed June 1, 2018.
2. Curry LA et al. Organizational culture change in U.S. hospitals: A mixed methods longitudinal intervention study. Implementation Science. 2015 Mar 7. doi: 10.1186/s13012-015-0218-0. Accessed June 18, 2018.
Cultural change linked to improved outcomes
Cultural change linked to improved outcomes
Health care experts have long known of a link between patient outcomes and a hospital’s organizational culture, according to an article in the New York Times by Pauline W. Chen, MD.
“Heart attack patients who are treated at hospitals where nurses feel powerless and senior management is only sporadically involved in patient care tend to fare more poorly than patients hospitalized at institutions where nurses are asked regularly for their input and chief executives hold regular meetings with clinicians to review patient results,” she wrote.
But there is hope for change, Dr. Chen noted, and it’s demonstrable, citing a group of researchers that has written about strategies targeting hospital organizational culture called “Leadership Saves Lives.” The researchers showed hospitals could create significant cultural changes, which could impact patient outcomes, in just 2 years.
“Leadership Saves Lives requires that each hospital create a ‘Guiding Coalition,’ a group of staff members from across the entire institution. The coalition members participate in regular workshops, discussions, and national forums on ways hospitals might improve, then help their respective hospital translate newfound ideas and information into clinical practice,” she wrote.
The researchers monitored heart attack patients to assess the effect of Leadership Saves Lives in 10 hospitals that had below average patient outcomes. Over 2 years, all 10 hospitals changed significantly, but 6 hospitals experienced particularly profound cultural transformations.
“The staff of these hospitals spoke of an institutional shift from ‘because I said so’ to ‘focusing on the why’s,’ ” Dr. Chen wrote. “Instead of accepting that every heart attack patient had to undergo certain testing or take specific drugs because the chief of the department or administrator had previously established such clinical protocols, for example, it became more important to provide the data that proved such rituals were actually helpful. Staff members in these hospitals also said they received, and appreciated, increased support from senior management and a newfound freedom to voice opinions in ‘more of an equal role, no matter what position you are.’ ”
The degree of an institution’s cultural change was directly linked to patient outcomes, the researchers found. Indeed, hospitals that made more substantial changes in their work culture realized larger and more sustained drops in heart attack mortality rates.
References
1. Chen PW. A More Egalitarian Hospital Culture Is Better for Everyone. New York Times. https://www.nytimes.com/2018/05/31/well/live/doctors-patients-hospital-culture-better-health.html. Published May 31, 2018. Accessed June 1, 2018.
2. Curry LA et al. Organizational culture change in U.S. hospitals: A mixed methods longitudinal intervention study. Implementation Science. 2015 Mar 7. doi: 10.1186/s13012-015-0218-0. Accessed June 18, 2018.
Health care experts have long known of a link between patient outcomes and a hospital’s organizational culture, according to an article in the New York Times by Pauline W. Chen, MD.
“Heart attack patients who are treated at hospitals where nurses feel powerless and senior management is only sporadically involved in patient care tend to fare more poorly than patients hospitalized at institutions where nurses are asked regularly for their input and chief executives hold regular meetings with clinicians to review patient results,” she wrote.
But there is hope for change, Dr. Chen noted, and it’s demonstrable, citing a group of researchers that has written about strategies targeting hospital organizational culture called “Leadership Saves Lives.” The researchers showed hospitals could create significant cultural changes, which could impact patient outcomes, in just 2 years.
“Leadership Saves Lives requires that each hospital create a ‘Guiding Coalition,’ a group of staff members from across the entire institution. The coalition members participate in regular workshops, discussions, and national forums on ways hospitals might improve, then help their respective hospital translate newfound ideas and information into clinical practice,” she wrote.
The researchers monitored heart attack patients to assess the effect of Leadership Saves Lives in 10 hospitals that had below average patient outcomes. Over 2 years, all 10 hospitals changed significantly, but 6 hospitals experienced particularly profound cultural transformations.
“The staff of these hospitals spoke of an institutional shift from ‘because I said so’ to ‘focusing on the why’s,’ ” Dr. Chen wrote. “Instead of accepting that every heart attack patient had to undergo certain testing or take specific drugs because the chief of the department or administrator had previously established such clinical protocols, for example, it became more important to provide the data that proved such rituals were actually helpful. Staff members in these hospitals also said they received, and appreciated, increased support from senior management and a newfound freedom to voice opinions in ‘more of an equal role, no matter what position you are.’ ”
The degree of an institution’s cultural change was directly linked to patient outcomes, the researchers found. Indeed, hospitals that made more substantial changes in their work culture realized larger and more sustained drops in heart attack mortality rates.
References
1. Chen PW. A More Egalitarian Hospital Culture Is Better for Everyone. New York Times. https://www.nytimes.com/2018/05/31/well/live/doctors-patients-hospital-culture-better-health.html. Published May 31, 2018. Accessed June 1, 2018.
2. Curry LA et al. Organizational culture change in U.S. hospitals: A mixed methods longitudinal intervention study. Implementation Science. 2015 Mar 7. doi: 10.1186/s13012-015-0218-0. Accessed June 18, 2018.
Public insurance income limits and hospitalizations for low-income children
Vulnerable populations at greater risk
Background: Medicaid and the Children’s Health Insurance Program (CHIP) provide health care to over 30 million children in the United States.1,2 As a result, low-income children have had increased access to health care, of all forms, which has increased the utilization of primary care and decreased unnecessary ED visits and hospitalizations. However, this comes at a high cost, both at the state and national level. Medicaid currently subsidizes more than 50% of every state’s public insurance program, spending about $100 billion/year in health care payments for children.3 Given this hefty price tag, there have been myriad strategies proposed to help decrease these costs. One such strategy, includes decreasing enrollment in public insurance through decreasing income eligibility thresholds. As a result, many children from low-income families would lose their public insurance and be eligible for commercial insurance only. Consequently, this would place an undue financial burden on these families and the health care systems that care for them. Furthermore, it is anticipated that poor health care outcomes would increase in these vulnerable populations.
Study design: Retrospective cohort study using 2014 State Inpatient Databases.
Setting: Pediatric hospitalizations (aged less than 18 years) from 14 states during 2014 with public insurance listed as the primary payer. This encompassed about 30% of family households in the United States in 2014.
Synopsis: Simulations were done at three different thresholds of the federal poverty level (FPL), including less than 100%, less than 200% and less than 300%. Of the families included, 43% lived below 300%, 27% below 200% and 11% below 100% of the FPL. Of note, public insurance FPL eligibility limits tended to be lower in states with a greater percentage of the population being below 300% of the FPL. The results, of these reductions, were as follows:
- If reduced to less than 300% of the FPL, about 155,000 hospitalizations became ineligible for reimbursement. The median per-hospitalization estimated costs ranged from approximately $6,000 to approximately $10,000, accumulating $1.2 billion in estimated costs.
- If reduced to less than 200% of the FPL, about 440,000 hospitalizations became ineligible for reimbursement. The median per-hospitalization estimated costs ranged from approximately $2,000 to approximately $10,000, accumulating $3.1 billion in estimated costs.
- If reduced to less than 100% of the FPL, about 650,000 hospitalizations became ineligible for reimbursement. The median per-hospitalization estimated costs ranged from approximately $2,000 to approximately $10,000, accumulating $4.4 billion in estimated costs.
If these reductions occurred, healthy newborns would be disproportionately affected by them, which is important to note because newborn hospitalization is one of the fastest-rising costs in pediatric care. In fact, it can range from approximately $700 to approximately $2,000 per hospitalization, which may represent a huge financial strain for families that are unable to secure commercial insurance. Furthermore, with the average hospitalization of non-newborns ranging from $3,000 to $10,000, it is likely that this cost would constitute a fairly large percentage of a low income family’s annual income, which may represent an untenable financial burden.
Thus, if these families are unable to obtain commercial insurance and/or pay these debts, the financial burden will shift to the institutions that care for these vulnerable populations.
Bottom line: If public insurance eligibility thresholds were decreased, a large number of pediatric hospitalizations would become ineligible for coverage, which would shift the costs to families and institutions that are already financially strained and likely result in poor health care outcomes for some of our most vulnerable pediatric patients.
Citation: Bettenhausen JL et al. The effect of lowering public insurance income limits on hospitalizations for low-income children. Pediatrics. 2018 Aug. doi: 10.1542/peds.2017-3486.
Dr. Darden is a pediatric hospitalist at Phoenix Children’s Hospital and clinical assistant professor, University of Arizona, Phoenix.
References
1. The Henry J. Kaiser Family Foundation. Total Medicaid Spending. 2016. Available at: http://kff.org/medicaid/state-indicator/total-medicaid-spending/.
2. Medicaid and CHIP Payment and Access Commission. Trends in Medicaid Spending. 2016. Available at https://www.macpac.gov/wp-content/uploads/2016/06/Trends-in-Medicaid-Spending.pdf.
3. Medicaid and CHIP Payment and Access Commission. Medicaid’s share of state budgets. 2017. Available at: https://www.macpac.gov/subtopic/medicaids-share-of-state-budgets/.
Vulnerable populations at greater risk
Vulnerable populations at greater risk
Background: Medicaid and the Children’s Health Insurance Program (CHIP) provide health care to over 30 million children in the United States.1,2 As a result, low-income children have had increased access to health care, of all forms, which has increased the utilization of primary care and decreased unnecessary ED visits and hospitalizations. However, this comes at a high cost, both at the state and national level. Medicaid currently subsidizes more than 50% of every state’s public insurance program, spending about $100 billion/year in health care payments for children.3 Given this hefty price tag, there have been myriad strategies proposed to help decrease these costs. One such strategy, includes decreasing enrollment in public insurance through decreasing income eligibility thresholds. As a result, many children from low-income families would lose their public insurance and be eligible for commercial insurance only. Consequently, this would place an undue financial burden on these families and the health care systems that care for them. Furthermore, it is anticipated that poor health care outcomes would increase in these vulnerable populations.
Study design: Retrospective cohort study using 2014 State Inpatient Databases.
Setting: Pediatric hospitalizations (aged less than 18 years) from 14 states during 2014 with public insurance listed as the primary payer. This encompassed about 30% of family households in the United States in 2014.
Synopsis: Simulations were done at three different thresholds of the federal poverty level (FPL), including less than 100%, less than 200% and less than 300%. Of the families included, 43% lived below 300%, 27% below 200% and 11% below 100% of the FPL. Of note, public insurance FPL eligibility limits tended to be lower in states with a greater percentage of the population being below 300% of the FPL. The results, of these reductions, were as follows:
- If reduced to less than 300% of the FPL, about 155,000 hospitalizations became ineligible for reimbursement. The median per-hospitalization estimated costs ranged from approximately $6,000 to approximately $10,000, accumulating $1.2 billion in estimated costs.
- If reduced to less than 200% of the FPL, about 440,000 hospitalizations became ineligible for reimbursement. The median per-hospitalization estimated costs ranged from approximately $2,000 to approximately $10,000, accumulating $3.1 billion in estimated costs.
- If reduced to less than 100% of the FPL, about 650,000 hospitalizations became ineligible for reimbursement. The median per-hospitalization estimated costs ranged from approximately $2,000 to approximately $10,000, accumulating $4.4 billion in estimated costs.
If these reductions occurred, healthy newborns would be disproportionately affected by them, which is important to note because newborn hospitalization is one of the fastest-rising costs in pediatric care. In fact, it can range from approximately $700 to approximately $2,000 per hospitalization, which may represent a huge financial strain for families that are unable to secure commercial insurance. Furthermore, with the average hospitalization of non-newborns ranging from $3,000 to $10,000, it is likely that this cost would constitute a fairly large percentage of a low income family’s annual income, which may represent an untenable financial burden.
Thus, if these families are unable to obtain commercial insurance and/or pay these debts, the financial burden will shift to the institutions that care for these vulnerable populations.
Bottom line: If public insurance eligibility thresholds were decreased, a large number of pediatric hospitalizations would become ineligible for coverage, which would shift the costs to families and institutions that are already financially strained and likely result in poor health care outcomes for some of our most vulnerable pediatric patients.
Citation: Bettenhausen JL et al. The effect of lowering public insurance income limits on hospitalizations for low-income children. Pediatrics. 2018 Aug. doi: 10.1542/peds.2017-3486.
Dr. Darden is a pediatric hospitalist at Phoenix Children’s Hospital and clinical assistant professor, University of Arizona, Phoenix.
References
1. The Henry J. Kaiser Family Foundation. Total Medicaid Spending. 2016. Available at: http://kff.org/medicaid/state-indicator/total-medicaid-spending/.
2. Medicaid and CHIP Payment and Access Commission. Trends in Medicaid Spending. 2016. Available at https://www.macpac.gov/wp-content/uploads/2016/06/Trends-in-Medicaid-Spending.pdf.
3. Medicaid and CHIP Payment and Access Commission. Medicaid’s share of state budgets. 2017. Available at: https://www.macpac.gov/subtopic/medicaids-share-of-state-budgets/.
Background: Medicaid and the Children’s Health Insurance Program (CHIP) provide health care to over 30 million children in the United States.1,2 As a result, low-income children have had increased access to health care, of all forms, which has increased the utilization of primary care and decreased unnecessary ED visits and hospitalizations. However, this comes at a high cost, both at the state and national level. Medicaid currently subsidizes more than 50% of every state’s public insurance program, spending about $100 billion/year in health care payments for children.3 Given this hefty price tag, there have been myriad strategies proposed to help decrease these costs. One such strategy, includes decreasing enrollment in public insurance through decreasing income eligibility thresholds. As a result, many children from low-income families would lose their public insurance and be eligible for commercial insurance only. Consequently, this would place an undue financial burden on these families and the health care systems that care for them. Furthermore, it is anticipated that poor health care outcomes would increase in these vulnerable populations.
Study design: Retrospective cohort study using 2014 State Inpatient Databases.
Setting: Pediatric hospitalizations (aged less than 18 years) from 14 states during 2014 with public insurance listed as the primary payer. This encompassed about 30% of family households in the United States in 2014.
Synopsis: Simulations were done at three different thresholds of the federal poverty level (FPL), including less than 100%, less than 200% and less than 300%. Of the families included, 43% lived below 300%, 27% below 200% and 11% below 100% of the FPL. Of note, public insurance FPL eligibility limits tended to be lower in states with a greater percentage of the population being below 300% of the FPL. The results, of these reductions, were as follows:
- If reduced to less than 300% of the FPL, about 155,000 hospitalizations became ineligible for reimbursement. The median per-hospitalization estimated costs ranged from approximately $6,000 to approximately $10,000, accumulating $1.2 billion in estimated costs.
- If reduced to less than 200% of the FPL, about 440,000 hospitalizations became ineligible for reimbursement. The median per-hospitalization estimated costs ranged from approximately $2,000 to approximately $10,000, accumulating $3.1 billion in estimated costs.
- If reduced to less than 100% of the FPL, about 650,000 hospitalizations became ineligible for reimbursement. The median per-hospitalization estimated costs ranged from approximately $2,000 to approximately $10,000, accumulating $4.4 billion in estimated costs.
If these reductions occurred, healthy newborns would be disproportionately affected by them, which is important to note because newborn hospitalization is one of the fastest-rising costs in pediatric care. In fact, it can range from approximately $700 to approximately $2,000 per hospitalization, which may represent a huge financial strain for families that are unable to secure commercial insurance. Furthermore, with the average hospitalization of non-newborns ranging from $3,000 to $10,000, it is likely that this cost would constitute a fairly large percentage of a low income family’s annual income, which may represent an untenable financial burden.
Thus, if these families are unable to obtain commercial insurance and/or pay these debts, the financial burden will shift to the institutions that care for these vulnerable populations.
Bottom line: If public insurance eligibility thresholds were decreased, a large number of pediatric hospitalizations would become ineligible for coverage, which would shift the costs to families and institutions that are already financially strained and likely result in poor health care outcomes for some of our most vulnerable pediatric patients.
Citation: Bettenhausen JL et al. The effect of lowering public insurance income limits on hospitalizations for low-income children. Pediatrics. 2018 Aug. doi: 10.1542/peds.2017-3486.
Dr. Darden is a pediatric hospitalist at Phoenix Children’s Hospital and clinical assistant professor, University of Arizona, Phoenix.
References
1. The Henry J. Kaiser Family Foundation. Total Medicaid Spending. 2016. Available at: http://kff.org/medicaid/state-indicator/total-medicaid-spending/.
2. Medicaid and CHIP Payment and Access Commission. Trends in Medicaid Spending. 2016. Available at https://www.macpac.gov/wp-content/uploads/2016/06/Trends-in-Medicaid-Spending.pdf.
3. Medicaid and CHIP Payment and Access Commission. Medicaid’s share of state budgets. 2017. Available at: https://www.macpac.gov/subtopic/medicaids-share-of-state-budgets/.
Anxiety, depression, burnout higher in physician mothers caring for others at home
Physicians who are also mothers have a higher risk of burnout and mood and anxiety disorders if they are also caring for someone with a serious illness or disability outside of work, according to a cross-sectional survey reported in a letter in JAMA Internal Medicine.
“Our findings highlight the additional caregiving responsibilities of some women physicians and the potential consequences of these additional responsibilities for their behavioral health and careers,” wrote Veronica Yank, MD, of the department of medicine at the University of California, San Francisco, and her colleagues.
“To reduce burnout and improve workforce retention, health care systems should develop new approaches to identify and address the needs of these physician mothers,” they wrote.
The researchers used data from a June-July 2016 online survey of respondents from the Physicians Moms Group online community. Approximately 16,059 members saw the posting for the survey, and 5,613 United States–based mothers participated.
Among the questions was one on non–work related caregiving responsibilities that asked whether the respondent provided “regular care or assistance to a friend or family member with a serious health problem, long-term illness or disability” during the last year. Other questions assessed alcohol and drug use, history of a mood or anxiety disorder, career satisfaction and burnout.
Among the 16.4% of respondents who had additional caregiving responsibilities outside of work for someone chronically or seriously ill or disabled, nearly half (48.3%) said they cared for ill parents, 16.9% for children or infants, 7.7% for a partner, and 28.6% for another relative. In addition, 16.7% of respondents had such caregiving responsibilities for more than one person.
The women with these extra caregiving responsibilities were 21% more likely to have a mood or anxiety disorder (adjusted relative risk, 1.21; P = .02) and 25% more likely to report burnout (aRR, 1.25; P = .007), compared with those who did not have such extra responsibilities.
There were no significant differences, however, on rates of career satisfaction, risky drinking behaviors, or substance abuse between physician mothers who did have additional caregiving responsibilities and those who did not.
Among the study’s limitations were its cross-sectional nature, use of a convenience sample that may not be generalizable or representative, and lack of data on fathers or non-parent physicians for comparison.
SOURCE: Yank V et al. JAMA Intern Med. 2019 Jan 28. doi: 10.1001/jamainternmed.2018.6411.
Physicians who are also mothers have a higher risk of burnout and mood and anxiety disorders if they are also caring for someone with a serious illness or disability outside of work, according to a cross-sectional survey reported in a letter in JAMA Internal Medicine.
“Our findings highlight the additional caregiving responsibilities of some women physicians and the potential consequences of these additional responsibilities for their behavioral health and careers,” wrote Veronica Yank, MD, of the department of medicine at the University of California, San Francisco, and her colleagues.
“To reduce burnout and improve workforce retention, health care systems should develop new approaches to identify and address the needs of these physician mothers,” they wrote.
The researchers used data from a June-July 2016 online survey of respondents from the Physicians Moms Group online community. Approximately 16,059 members saw the posting for the survey, and 5,613 United States–based mothers participated.
Among the questions was one on non–work related caregiving responsibilities that asked whether the respondent provided “regular care or assistance to a friend or family member with a serious health problem, long-term illness or disability” during the last year. Other questions assessed alcohol and drug use, history of a mood or anxiety disorder, career satisfaction and burnout.
Among the 16.4% of respondents who had additional caregiving responsibilities outside of work for someone chronically or seriously ill or disabled, nearly half (48.3%) said they cared for ill parents, 16.9% for children or infants, 7.7% for a partner, and 28.6% for another relative. In addition, 16.7% of respondents had such caregiving responsibilities for more than one person.
The women with these extra caregiving responsibilities were 21% more likely to have a mood or anxiety disorder (adjusted relative risk, 1.21; P = .02) and 25% more likely to report burnout (aRR, 1.25; P = .007), compared with those who did not have such extra responsibilities.
There were no significant differences, however, on rates of career satisfaction, risky drinking behaviors, or substance abuse between physician mothers who did have additional caregiving responsibilities and those who did not.
Among the study’s limitations were its cross-sectional nature, use of a convenience sample that may not be generalizable or representative, and lack of data on fathers or non-parent physicians for comparison.
SOURCE: Yank V et al. JAMA Intern Med. 2019 Jan 28. doi: 10.1001/jamainternmed.2018.6411.
Physicians who are also mothers have a higher risk of burnout and mood and anxiety disorders if they are also caring for someone with a serious illness or disability outside of work, according to a cross-sectional survey reported in a letter in JAMA Internal Medicine.
“Our findings highlight the additional caregiving responsibilities of some women physicians and the potential consequences of these additional responsibilities for their behavioral health and careers,” wrote Veronica Yank, MD, of the department of medicine at the University of California, San Francisco, and her colleagues.
“To reduce burnout and improve workforce retention, health care systems should develop new approaches to identify and address the needs of these physician mothers,” they wrote.
The researchers used data from a June-July 2016 online survey of respondents from the Physicians Moms Group online community. Approximately 16,059 members saw the posting for the survey, and 5,613 United States–based mothers participated.
Among the questions was one on non–work related caregiving responsibilities that asked whether the respondent provided “regular care or assistance to a friend or family member with a serious health problem, long-term illness or disability” during the last year. Other questions assessed alcohol and drug use, history of a mood or anxiety disorder, career satisfaction and burnout.
Among the 16.4% of respondents who had additional caregiving responsibilities outside of work for someone chronically or seriously ill or disabled, nearly half (48.3%) said they cared for ill parents, 16.9% for children or infants, 7.7% for a partner, and 28.6% for another relative. In addition, 16.7% of respondents had such caregiving responsibilities for more than one person.
The women with these extra caregiving responsibilities were 21% more likely to have a mood or anxiety disorder (adjusted relative risk, 1.21; P = .02) and 25% more likely to report burnout (aRR, 1.25; P = .007), compared with those who did not have such extra responsibilities.
There were no significant differences, however, on rates of career satisfaction, risky drinking behaviors, or substance abuse between physician mothers who did have additional caregiving responsibilities and those who did not.
Among the study’s limitations were its cross-sectional nature, use of a convenience sample that may not be generalizable or representative, and lack of data on fathers or non-parent physicians for comparison.
SOURCE: Yank V et al. JAMA Intern Med. 2019 Jan 28. doi: 10.1001/jamainternmed.2018.6411.
FROM JAMA INTERNAL MEDICINE
Key clinical point:
Major finding: Risk of anxiety and mood disorders is 21% higher and burnout is 25% higher among physician mothers with extra caregiving at home.
Study details: The findings are based on an online cross-sectional survey of 5,613 United States–based physician mothers conducted from June to July 2016.
Disclosures: No single entity directly funded the study, but the authors were supported by a variety of grants from foundations and the National Institutes of Health at the time it was completed. One coauthor is founder of Equity Quotient, a company that provides gender equity culture analytics for institutions, and another has consulted for Amgen and Vizient and receives stock options as an Equity Quotient advisory board member.
Source: Yank V et al. JAMA Internal Medicine. 2018 Jan 28. doi: 10.1001/jamainternmed.2018.6411.
New or existing drugs? Both fuel price inflation
Inflation in existing drugs’ prices and the debut of new drugs are both contributing to the overall rising costs of pharmaceuticals.
.
For oral and injectable specialty drugs, costs increased 20.6% and 12.5%, respectively, with 71.1% and 52.4% attributable to new drugs. Costs of oral and injectable generic drugs grew by 4.4% and 7.3%, also driven by entrants into the market.
Researchers looked at monthly wholesale acquisition costs of 24,877 National Drug Codes for oral drugs and 3,049 injectable drugs from 2005 to 2016. They compared them with pharmacy claims from the UPMC Health Plan, which offers insurance products to more than 3.2 million members across the spectrum of private and public arenas.
“Our analyses yielded three main findings,” explained Inmaculada Hernandez, PharmD, PhD, University of Pittsburgh, and her colleagues in a report published in the January 2019 issue of Health Affairs.
“First, costs increased considerably faster than inflation across all drug classes, and increases were highest for oral specialty drugs and lowest for oral generics,” Dr. Hernandez and her colleagues wrote.
“Second, rising costs of brand-name drugs were driven by inflation in the prices of widely used existing drugs,” they added. A combination of new products and price inflation in existing drugs drove the rising costs of specialty drugs, with new drugs accounting for a larger share of the price increases.
Third, “existing generics tended to decrease the average cost of generic drugs,” Dr. Hernandez noted. However, new generic products cost more than those already on the market, which fueled the annual increases in average costs.
The authors noted that their estimates demonstrate the role of inflation on pharmaceutical cost increases and support policy efforts to control that inflation.
“In the current value-based landscape, increasing drug costs attributable to new products can sometimes be justified on the basis of improved outcomes,” Dr. Hernandez and colleagues stated. “However, rising costs due to inflation do not reflect improved value for patients.”
The researchers noted that the data are limited by the lack of rebate information, which is generally proprietary. Thus, “the contribution of existing drugs may have been lower than we estimated,” they noted. In addition, “because the magnitude of rebates has increased in the past decade, our findings likely overestimated cost increases for brand-name drugs.” The researchers also didn’t examine the effect of drugs transitioning from brand to generic offerings.
The authors provided no disclosures.
SOURCE: Hernandez I et al. Health Aff (Millwood). 2019 Jan 2019. doi: 10.1377/hlthaff.2018.05147.
Inflation in existing drugs’ prices and the debut of new drugs are both contributing to the overall rising costs of pharmaceuticals.
.
For oral and injectable specialty drugs, costs increased 20.6% and 12.5%, respectively, with 71.1% and 52.4% attributable to new drugs. Costs of oral and injectable generic drugs grew by 4.4% and 7.3%, also driven by entrants into the market.
Researchers looked at monthly wholesale acquisition costs of 24,877 National Drug Codes for oral drugs and 3,049 injectable drugs from 2005 to 2016. They compared them with pharmacy claims from the UPMC Health Plan, which offers insurance products to more than 3.2 million members across the spectrum of private and public arenas.
“Our analyses yielded three main findings,” explained Inmaculada Hernandez, PharmD, PhD, University of Pittsburgh, and her colleagues in a report published in the January 2019 issue of Health Affairs.
“First, costs increased considerably faster than inflation across all drug classes, and increases were highest for oral specialty drugs and lowest for oral generics,” Dr. Hernandez and her colleagues wrote.
“Second, rising costs of brand-name drugs were driven by inflation in the prices of widely used existing drugs,” they added. A combination of new products and price inflation in existing drugs drove the rising costs of specialty drugs, with new drugs accounting for a larger share of the price increases.
Third, “existing generics tended to decrease the average cost of generic drugs,” Dr. Hernandez noted. However, new generic products cost more than those already on the market, which fueled the annual increases in average costs.
The authors noted that their estimates demonstrate the role of inflation on pharmaceutical cost increases and support policy efforts to control that inflation.
“In the current value-based landscape, increasing drug costs attributable to new products can sometimes be justified on the basis of improved outcomes,” Dr. Hernandez and colleagues stated. “However, rising costs due to inflation do not reflect improved value for patients.”
The researchers noted that the data are limited by the lack of rebate information, which is generally proprietary. Thus, “the contribution of existing drugs may have been lower than we estimated,” they noted. In addition, “because the magnitude of rebates has increased in the past decade, our findings likely overestimated cost increases for brand-name drugs.” The researchers also didn’t examine the effect of drugs transitioning from brand to generic offerings.
The authors provided no disclosures.
SOURCE: Hernandez I et al. Health Aff (Millwood). 2019 Jan 2019. doi: 10.1377/hlthaff.2018.05147.
Inflation in existing drugs’ prices and the debut of new drugs are both contributing to the overall rising costs of pharmaceuticals.
.
For oral and injectable specialty drugs, costs increased 20.6% and 12.5%, respectively, with 71.1% and 52.4% attributable to new drugs. Costs of oral and injectable generic drugs grew by 4.4% and 7.3%, also driven by entrants into the market.
Researchers looked at monthly wholesale acquisition costs of 24,877 National Drug Codes for oral drugs and 3,049 injectable drugs from 2005 to 2016. They compared them with pharmacy claims from the UPMC Health Plan, which offers insurance products to more than 3.2 million members across the spectrum of private and public arenas.
“Our analyses yielded three main findings,” explained Inmaculada Hernandez, PharmD, PhD, University of Pittsburgh, and her colleagues in a report published in the January 2019 issue of Health Affairs.
“First, costs increased considerably faster than inflation across all drug classes, and increases were highest for oral specialty drugs and lowest for oral generics,” Dr. Hernandez and her colleagues wrote.
“Second, rising costs of brand-name drugs were driven by inflation in the prices of widely used existing drugs,” they added. A combination of new products and price inflation in existing drugs drove the rising costs of specialty drugs, with new drugs accounting for a larger share of the price increases.
Third, “existing generics tended to decrease the average cost of generic drugs,” Dr. Hernandez noted. However, new generic products cost more than those already on the market, which fueled the annual increases in average costs.
The authors noted that their estimates demonstrate the role of inflation on pharmaceutical cost increases and support policy efforts to control that inflation.
“In the current value-based landscape, increasing drug costs attributable to new products can sometimes be justified on the basis of improved outcomes,” Dr. Hernandez and colleagues stated. “However, rising costs due to inflation do not reflect improved value for patients.”
The researchers noted that the data are limited by the lack of rebate information, which is generally proprietary. Thus, “the contribution of existing drugs may have been lower than we estimated,” they noted. In addition, “because the magnitude of rebates has increased in the past decade, our findings likely overestimated cost increases for brand-name drugs.” The researchers also didn’t examine the effect of drugs transitioning from brand to generic offerings.
The authors provided no disclosures.
SOURCE: Hernandez I et al. Health Aff (Millwood). 2019 Jan 2019. doi: 10.1377/hlthaff.2018.05147.
FROM HEALTH AFFAIRS
Key clinical point: Price inflation in existing drugs and new product introductions are driving increases in pharmaceutical costs.
Major finding: 71% of oral specialty drug price increases during 2005-2019 are attributable to new products.
Study details: Researchers analyzed the wholesale acquisition prices of 24,877 oral drugs and 3,049 injectable drugs and compared them with pharmacy claims across all public and private insurance products offered by the UPMC Health Plan.
Disclosures: The authors provided no disclosures.
Source: Hernandez I et al. Health Aff (Millwood). 2019 Jan. doi: 10.1377/hlthaff.2018.05147.
The state of hospital medicine in 2018
Productivity, pay, and roles remain center stage
In a national health care environment undergoing unprecedented transformation, the specialty of hospital medicine appears to be an island of relative stability, a conclusion that is supported by the principal findings from SHM’s 2018 State of Hospital Medicine (SoHM) report.
The report of hospitalist group practice characteristics, as well as other key data defining the field’s current status, that the Society of Hospital Medicine puts out every 2 years reveals that overall salaries for hospitalist physicians are up by 3.8% since 2016. Although productivity, as measured by work relative value units (RVUs), remained largely flat over the same period, financial support per full-time equivalent (FTE) physician position to hospitalist groups from their hospitals and health systems is up significantly.
Total support per FTE averaged $176,657 in 2018, 12% higher than in 2016, noted Leslie Flores, MHA, SFHM, of Nelson Flores Hospital Medicine Consultants, and a member of SHM’s Practice Analysis Committee, which oversees the biennial survey. Compensation and productivity data were collected by the Medical Group Management Association and licensed by SHM for inclusion in its report.
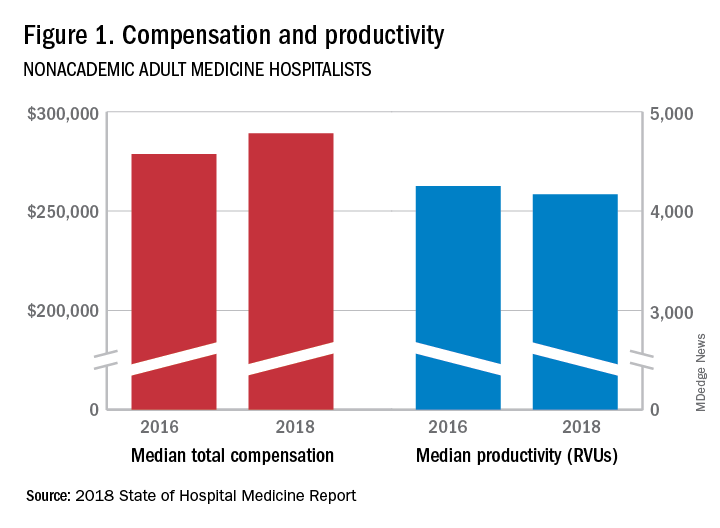
These findings – particularly the flat productivity – raise questions about long-term sustainability, Ms. Flores said. “What is going on? Do hospital administrators still recognize the value hospitalists bring to the operations and the quality of their hospitals? Or is paying the subsidy just a cost of doing business – a necessity for most hospitals in a setting where demand for hospitalist positions remains high?”
Andrew White, MD, FACP, SFHM, chair of SHM’s Practice Analysis Committee and director of the hospital medicine service at the University of Washington Medical Center, Seattle, said basic market forces dictate that it is “pretty much inconceivable” to run a modern hospital of any size without hospitalists.
“Clearly, demand outstrips supply, which drives up salaries and support, whether CEOs feel that the hospitalist group is earning that support or not,” Dr. White said. “The unfilled hospitalist positions we identified speak to ongoing projected greater demand than supply. That said, hospitalists and group leaders can’t be complacent and must collaborate effectively with hospitals to provide highly valuable services.” Turnover of hospitalist positions was up slightly, he noted, at 7.4% in 2018, from 6.9% in 2016, reversing a trend of previous years.
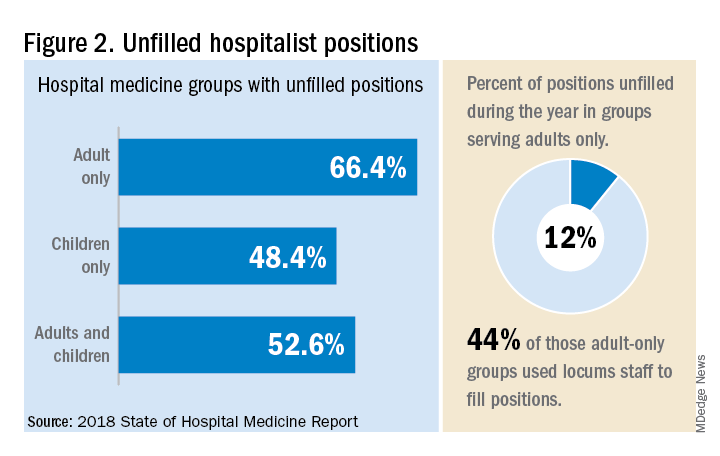
But will these trends continue at a time when hospitals face continued pressure to cut costs, as the hospital medicine subsidy may represent one of their largest cost centers? Because the size of hospitalist groups continues to grow, hospitals’ total subsidy for hospital medicine is going up faster than the percentage increase in support per FTE.
How do hospitalists use the SoHM report?
Dr. White called the 2018 SoHM report the “most representative and balanced sample to date” of hospitalist group practices, with some of the highest quality data, thanks to more robust participation in the survey by pediatric groups and improved distribution among hospitalist management companies and academic programs.
“Not that past reports had major flaws, but this version is more authoritative, reflecting an intentional effort by our Practice Analysis Committee to bring in more participants from key groups,” he said.
The biennial report has been around long enough to achieve brand recognition in the field as the most authoritative source of information regarding hospitalist practice, he added. “We worked hard this year to balance the participants, with more of our responses than in the past coming from multi-hospital groups, whether 4 to 5 sites, or 20 to 30.”
Surveys were conducted online in January and February of 2018 in response to invitations mailed and emailed to targeted hospital medicine group leaders. A total of 569 groups completed the survey, representing 8,889 hospitalist FTEs, approximately 16% of the total hospitalist workforce. Responses were presented in several categories, including by size of program, region and employment model. Groups that care for adults only represented 87.9% of the surveys, while groups that care for children only were 6.7% and groups that care for both adults and children were 5.4%.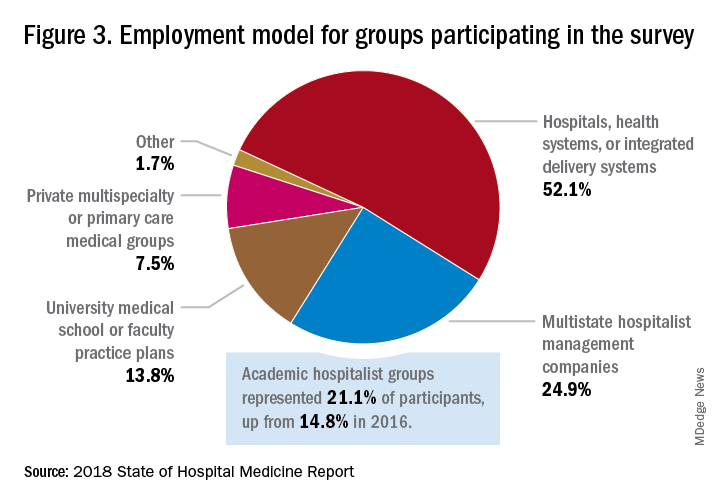
“This survey doesn’t tell us what should be best practice in hospital medicine,” Dr. White said, only what is actual current practice. He uses it in his own health system to not only contextualize and justify his group’s performance metrics for hospital administrators – relative to national and categorical averages – but also to see if the direction his group is following is consistent with what’s going on in the larger field.
“These data offer a very powerful resource regarding the trends in hospital medicine,” said Romil Chadha, MD, MPH, FACP, SFHM, associate division chief for operations in the division of hospital medicine at the University of Kentucky and UK Healthcare, Lexington. “It is my repository of data to go before my administrators for decisions that need to be made or to pilot new programs.”
Dr. Chadha also uses the data to help answer compensation, scheduling, and support questions from his group’s members.
Thomas McIlraith, MD, immediate past chairman of the hospital medicine department at Mercy Medical Group, Sacramento, Calif., said the report’s value is that it allows comparisons of salaries in different settings, and to see, for example, how night staffing is structured. “A lot of leaders I spoke to at SHM’s 2018 Leadership Academy in Vancouver were saying they didn’t feel up to parity with the national standards. You can use the report to look at the state of hospital medicine nationally and make comparisons,” he said.
Calls for more productivity
Roberta Himebaugh, MBA, SFHM, senior vice president of acute care services for the national hospitalist management company TeamHealth, and cochair of the SHM Practice Administrators Special Interest Group, said her company’s clients have traditionally asked for greater productivity from their hospitalist contracts as a way to decrease overall costs. Some markets are starting to see a change in that approach, she noted.
“Recently there’s been an increased focus on paying hospitalists to focus on quality rather than just productivity. Some of our clients are willing to pay for that, and we are trying to assign value to this non-billable time or adjust our productivity standards appropriately. I think hospitals definitely understand the value of non-billable services from hospitalists, but still will push us on the productivity targets,” Ms. Himebaugh said.
“I don’t believe hospital medicine can be sustainable long term on flat productivity or flat RVUs,” she added. “Yet the costs of burnout associated with pushing higher productivity are not sustainable, either.” So what are the answers? She said many inefficiencies are involved in responding to inquiries on the floor that could have been addressed another way, or waiting for the turnaround of diagnostic tests.
“Maybe we don’t need physicians to be in the hospital 24/7 if we have access to telehealth, or a partnership with the emergency department, or greater use of advanced care practice providers,” Ms. Himebaugh said. “Our hospitals are examining those options, and we have to look at how we can become more efficient and less costly. At TeamHealth, we are trying to staff for value – looking at patient flow patterns and adjusting our schedules accordingly. Is there a bolus of admissions tied to emergency department shift changes, or to certain days of the week? How can we move from the 12-hour shift that begins at 7 a.m. and ends at 7 p.m., and instead provide coverage for when the patients are there?”
Mark Williams, MD, MHM, chief of the division of hospital medicine at the University of Kentucky, Lexington, said he appreciates the volume of data in the report but wishes for even more survey participants, which could make the breakouts for subgroups such as academic hospitalists more robust. Other current sources of hospitalist salary data include the Association of American Medical Colleges (AAMC), which produces compensation reports to help medical schools and teaching hospitals with benchmarking, and the Faculty Practice Solution Center developed jointly by AAMC and Vizient to provide faculty practice plans with analytic tools. The Medical Group Management Association (MGMA) is another valuable source of information, some of which was licensed for inclusion in the SoHM report.
“There is no source of absolute truth that hospitalists can point to,” Dr. Williams said. “I will present my data and my administrators will reply: ‘We have our own data.’ Our institution has consistently ranked first or second nationwide for the sickest patients. We take more Medicaid and dually eligible patients, who have a lot of social issues. They take a lot of time to manage medically and the RVUs don’t reflect that. And yet I’m still judged by my RVUs generated per hospitalist. Hospital administrators understandably want to get the most productivity, and they are looking for their own data for average productivity numbers.”
Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., said that hospital medicine’s flat productivity trends would be difficult to sustain in the business world. But there aren’t easy or obvious ways to increase hospitalists’ productivity. The SoHM report also shows that as productivity increases, total compensation increases but at a lower rate, resulting in a gradual decrease in compensation per RVU.
Pressures to increase productivity can be a double-edged sword, Dr. Williams added. Demanding that doctors make more billable visits faster to generate more RVUs can be a recipe for burnout and turnover, with huge costs associated with recruiting replacements.
“If there was recent turnover of hospitalists at the hospital, with the need to find replacements, there may be institutional memory about that,” he said. “But where are hospitals spending their money? Bottom line, we still need to learn to cut our costs.”
How is hospitalist practice evolving?
In addition to payment and productivity data, the SoHM report provides a current picture of the evolving state of hospitalist group practices. A key thread is how the work hospitalists are doing, and the way they do it, is changing, with new information about comanagement roles, dedicated admitters, night coverage, geographic rounding, and the like.
Making greater use of nurse practitioners and physician assistants (NPs/PAs), may be one way to change the flat productivity trends, Dr. Brown said. With a cost per RVU that’s roughly half that of a doctor’s, NPs/PAs could contribute to the bottom line. But he sees surprisingly large variation in how hospitalist groups are using them. Typically, they are deployed at a ratio of four doctors to one NP/PA, but that ratio could be two to one or even one to one, he said.
Use of NPs/PAs by academic hospitalist groups is up, from 52.1% in 2016 to 75.7% in 2018. For adult-only groups, 76.8% had NPs/PAs, with higher rates in hospitals and health systems and lower rates in the West region. But a lot of groups are using these practitioners for nonproductive work, and some are failing to generate any billing income, Dr. Brown said.
“The rate at which NPs/PAs performed billable services was higher in physician-owned practices, resulting in a lower cost per RVU, suggesting that many practices may be underutilizing their NPs/PAs or not sharing the work.” Not every NP or PA wants to or is able to care for very complex patients, Dr. Brown said, “but you want a system where the NP and PA can work at the highest level permitted by state law.”
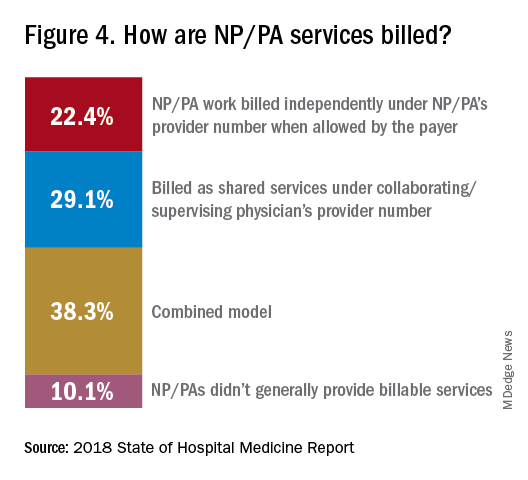
The predominant scheduling model of hospital medicine, 7 days on duty followed by 7 days off, has diminished somewhat in recent years. There appears to be some fluctuation and a gradual move away from 7 on/7 off toward some kind of variable approach, since the former may not be physically sustainable for the doctor over the long haul, Dr. Brown said. Some groups are experimenting with a combined approach.
“I think balancing workload with manpower has always been a challenge for our field. Maybe we should be working shorter shifts or fewer days and making sure our hospitalists aren’t ever sitting around idle,” he said. “And could we come in on nonclinical days to do administrative tasks? I think the solution is out there, but we haven’t created the algorithms to define that yet. If you could somehow use the data for volume, number of beds, nurse staffing, etc., by year and seasonally, you might be able to reliably predict census. This is about applying data hospitals already have in their electronic health records, but utilizing the data in ways that are more helpful.”
Dr. McIlraith added that a big driver of the future of hospital medicine will be the evolution of the EHR and the digitalization of health care, as hospitals learn how to leverage more of what’s in their EHRs. “The impact will grow for hospitalists through the creation and maturation of big data systems – and the learning that can be extracted from what’s contained in the electronic health record.”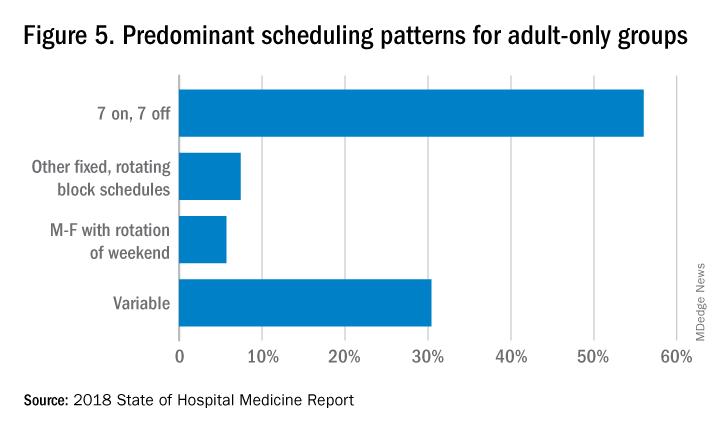
Another important question for hospitalist groups is their model of backup scheduling, to make sure there is a replacement available if a scheduled doctor calls in sick or if demand is unexpectedly high.
“In today’s world, this is how we have traditionally managed unpredictability,” Dr. Brown said. “You don’t know when you will need it, but if you need it, you want it immediately. So how do you pay for it – only when the doctor comes in, or also an amount just for being on call?” Some groups pay for both, he said, others for neither.
“We are a group of 70 hospitalists, and if someone is sick you can’t just shut down the service,” said Dr. Chadha. “We are one of the few to use incentives for both, which could include a 1-week decrease in clinical shifts in exchange for 2 weeks of backup. We have times with 25% usage of backup number 1, and 10% usage of backup number 2,” he noted. “But the goal is for our hospitalists to have assurances that there is a backup system and that it works.”
The presence of nocturnists in hospitals continues to rise, with 76.1% of adults-only groups having nocturnists, 27.6% of children-only groups, and 68.2% of adults and children groups. Geographic or unit-based hospital assignments have grown to 36.4% of adult-only groups.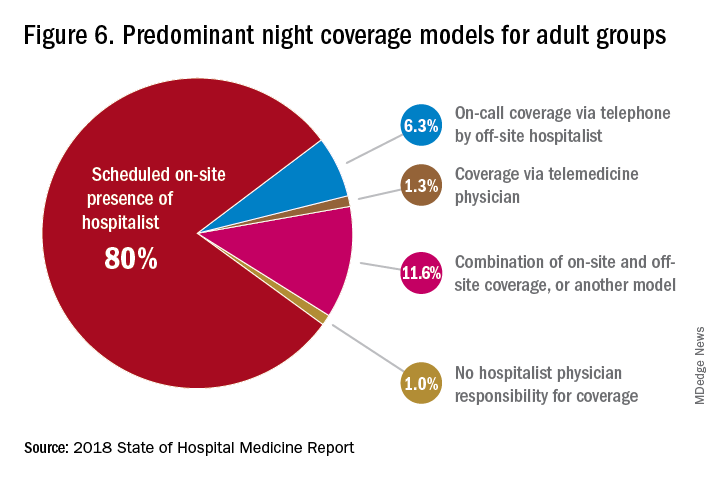
What are hospitalists’ other new roles?
“We have a large group of 50 doctors, with about 40 FTEs, and we are evolving from the traditional generalist role toward more subspecialty comanagement,” said Bryan Huang, MD, physician adviser and associate clinical professor in the division of hospital medicine at the University of California–San Diego. “Our hospitalists are asking what it means to be an academic hospitalist as our teaching roles have shrunk.”
Dr. Huang recently took on a new role as physician adviser for his hospital in such areas as utilization review, patient flow, and length of stay. “I’m spearheading a work group to address quality issues – all of which involve collaboration with other professionals. We also developed an admitting role here for a hospitalist whose sole role for the day is to admit patients.” Nationally up to 51.2% of hospitalist groups utilize a dedicated daytime admitter.
The report found that hospital services for which hospitalists are more likely to be attendings than consultants include GI/liver, 78.4%; palliative care, 77.3%; neurology/stroke, 73.6%; oncology, 67.8%; cardiology, 56.9%; and critical care, 50.7%. Conditions where hospitalists are more likely to consult rather than admit and attend include neurosurgery, orthopedics, general surgery, cardiovascular surgery, and other surgical subspecialties.
Other hospital services routinely provided by adult-only hospitalists include care of patients in an ICU setting (62.7%); primary responsibility for observation units (54.6%); primary clinical responsibility for rapid response teams (48.8%); primary responsibility for code blue or cardiac arrest teams (43.8%); nighttime admissions or tuck-in services (33.9%); and medical procedures (31.5%). For pediatric hospital medicine groups, care of healthy newborns and medical procedures were among the most common services provided, while for hospitalists serving adults and children, rapid response teams, ICUs, and specialty units were most common.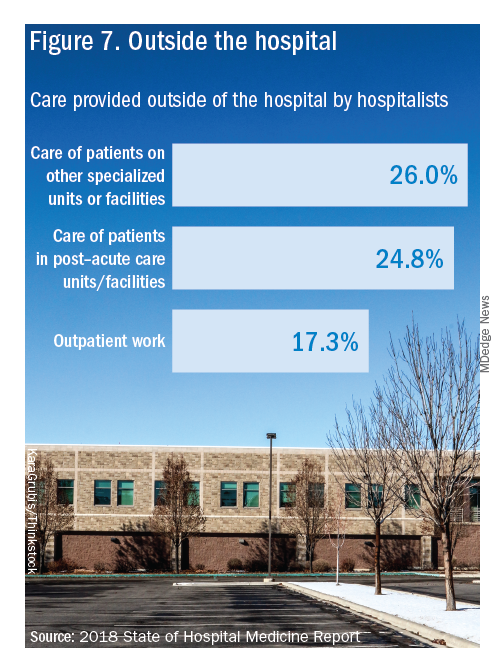
New models of payment for health care
As the larger health care system is being transformed by new payment models and benefit structures, including accountable care organizations (ACOs), value-based purchasing, bundled payments, and other forms of population-based coverage – which is described as a volume-to-value shift in health care – how are these new models affecting hospitalists?
Observers say penetration of these new models varies widely by locality but they haven’t had much direct impact on hospitalists’ practices – at least not yet. However, as hospitals and health systems find themselves needing to learn new ways to invest their resources differently in response to these trends, what matters to the hospital should be of great importance to the hospitalist group.
“I haven’t seen a lot of dramatic changes in how hospitalists engage with value-based purchasing,” Dr. White said. “If we know that someone is part of an ACO, the instinctual – and right – response is to treat them like any other patient. But we still need to be committed to not waste resources.”
Hospitalists are the best people to understand the intricacies of how the health care system works under value-based approaches, Dr. Huang said. “That’s why so many hospitalists have taken leadership positions in their hospitals. I think all of this translates to the practical, day-to-day work of hospitalists, reflected in our focus on readmissions and length of stay.”
Dr. Williams said the health care system still hasn’t turned the corner from fee-for-service to value-based purchasing. “It still represents a tiny fraction of the income of hospitalists. Hospitals still have to focus on the bottom line, as fee-for-service reimbursement for hospitalized patients continues to get squeezed, and ACOs aren’t exactly paying premium rates either. Ask almost any hospital CEO what drives their bottom line today and the answer is volume – along with optimizing productivity. Pretty much every place I look, the future does not look terribly rosy for hospitals.”
Ms. Himebaugh said she is bullish on hospital medicine, in the sense that it’s unlikely to go away anytime soon. “Hospitalists are needed and provide value. But I don’t think we have devised the right model yet. I’m not sure our current model is sustainable. We need to find new models we can afford that don’t require squeezing our providers.”
For more information about the 2018 State of Hospital Medicine Report, contact SHM’s Practice Management Department at: [email protected] or call 800-843-3360. See also: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/.
Productivity, pay, and roles remain center stage
Productivity, pay, and roles remain center stage
In a national health care environment undergoing unprecedented transformation, the specialty of hospital medicine appears to be an island of relative stability, a conclusion that is supported by the principal findings from SHM’s 2018 State of Hospital Medicine (SoHM) report.
The report of hospitalist group practice characteristics, as well as other key data defining the field’s current status, that the Society of Hospital Medicine puts out every 2 years reveals that overall salaries for hospitalist physicians are up by 3.8% since 2016. Although productivity, as measured by work relative value units (RVUs), remained largely flat over the same period, financial support per full-time equivalent (FTE) physician position to hospitalist groups from their hospitals and health systems is up significantly.
Total support per FTE averaged $176,657 in 2018, 12% higher than in 2016, noted Leslie Flores, MHA, SFHM, of Nelson Flores Hospital Medicine Consultants, and a member of SHM’s Practice Analysis Committee, which oversees the biennial survey. Compensation and productivity data were collected by the Medical Group Management Association and licensed by SHM for inclusion in its report.
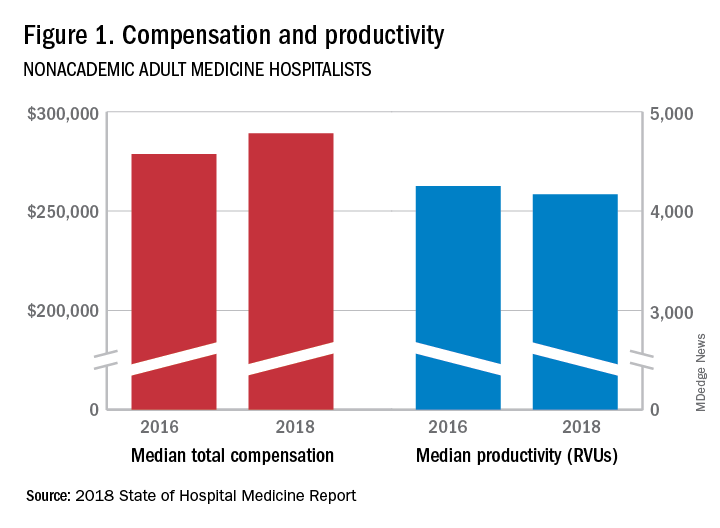
These findings – particularly the flat productivity – raise questions about long-term sustainability, Ms. Flores said. “What is going on? Do hospital administrators still recognize the value hospitalists bring to the operations and the quality of their hospitals? Or is paying the subsidy just a cost of doing business – a necessity for most hospitals in a setting where demand for hospitalist positions remains high?”
Andrew White, MD, FACP, SFHM, chair of SHM’s Practice Analysis Committee and director of the hospital medicine service at the University of Washington Medical Center, Seattle, said basic market forces dictate that it is “pretty much inconceivable” to run a modern hospital of any size without hospitalists.
“Clearly, demand outstrips supply, which drives up salaries and support, whether CEOs feel that the hospitalist group is earning that support or not,” Dr. White said. “The unfilled hospitalist positions we identified speak to ongoing projected greater demand than supply. That said, hospitalists and group leaders can’t be complacent and must collaborate effectively with hospitals to provide highly valuable services.” Turnover of hospitalist positions was up slightly, he noted, at 7.4% in 2018, from 6.9% in 2016, reversing a trend of previous years.
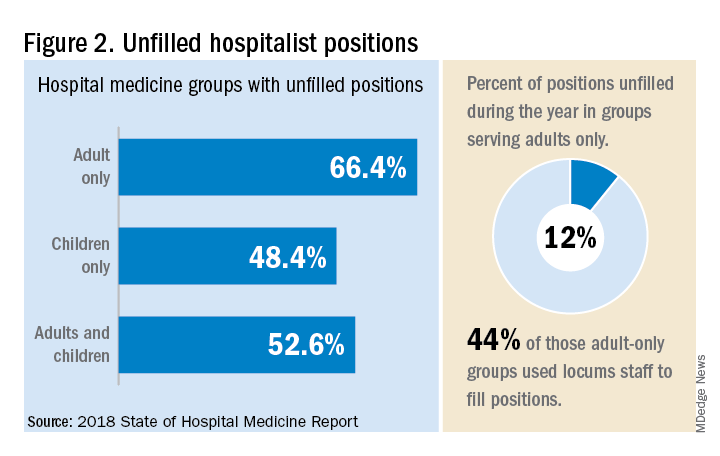
But will these trends continue at a time when hospitals face continued pressure to cut costs, as the hospital medicine subsidy may represent one of their largest cost centers? Because the size of hospitalist groups continues to grow, hospitals’ total subsidy for hospital medicine is going up faster than the percentage increase in support per FTE.
How do hospitalists use the SoHM report?
Dr. White called the 2018 SoHM report the “most representative and balanced sample to date” of hospitalist group practices, with some of the highest quality data, thanks to more robust participation in the survey by pediatric groups and improved distribution among hospitalist management companies and academic programs.
“Not that past reports had major flaws, but this version is more authoritative, reflecting an intentional effort by our Practice Analysis Committee to bring in more participants from key groups,” he said.
The biennial report has been around long enough to achieve brand recognition in the field as the most authoritative source of information regarding hospitalist practice, he added. “We worked hard this year to balance the participants, with more of our responses than in the past coming from multi-hospital groups, whether 4 to 5 sites, or 20 to 30.”
Surveys were conducted online in January and February of 2018 in response to invitations mailed and emailed to targeted hospital medicine group leaders. A total of 569 groups completed the survey, representing 8,889 hospitalist FTEs, approximately 16% of the total hospitalist workforce. Responses were presented in several categories, including by size of program, region and employment model. Groups that care for adults only represented 87.9% of the surveys, while groups that care for children only were 6.7% and groups that care for both adults and children were 5.4%.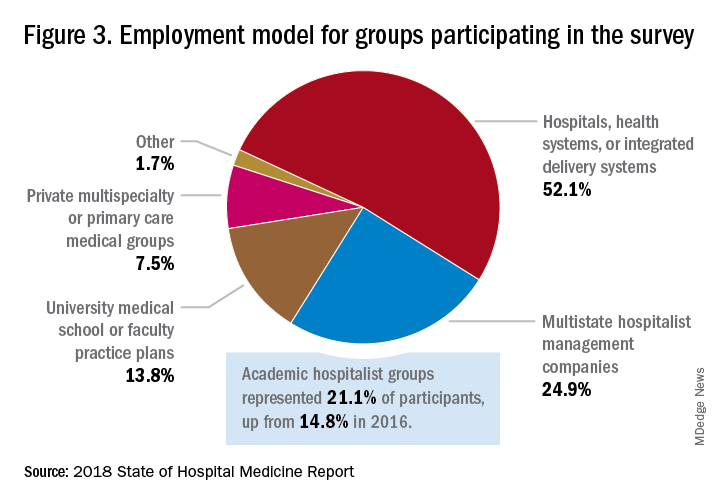
“This survey doesn’t tell us what should be best practice in hospital medicine,” Dr. White said, only what is actual current practice. He uses it in his own health system to not only contextualize and justify his group’s performance metrics for hospital administrators – relative to national and categorical averages – but also to see if the direction his group is following is consistent with what’s going on in the larger field.
“These data offer a very powerful resource regarding the trends in hospital medicine,” said Romil Chadha, MD, MPH, FACP, SFHM, associate division chief for operations in the division of hospital medicine at the University of Kentucky and UK Healthcare, Lexington. “It is my repository of data to go before my administrators for decisions that need to be made or to pilot new programs.”
Dr. Chadha also uses the data to help answer compensation, scheduling, and support questions from his group’s members.
Thomas McIlraith, MD, immediate past chairman of the hospital medicine department at Mercy Medical Group, Sacramento, Calif., said the report’s value is that it allows comparisons of salaries in different settings, and to see, for example, how night staffing is structured. “A lot of leaders I spoke to at SHM’s 2018 Leadership Academy in Vancouver were saying they didn’t feel up to parity with the national standards. You can use the report to look at the state of hospital medicine nationally and make comparisons,” he said.
Calls for more productivity
Roberta Himebaugh, MBA, SFHM, senior vice president of acute care services for the national hospitalist management company TeamHealth, and cochair of the SHM Practice Administrators Special Interest Group, said her company’s clients have traditionally asked for greater productivity from their hospitalist contracts as a way to decrease overall costs. Some markets are starting to see a change in that approach, she noted.
“Recently there’s been an increased focus on paying hospitalists to focus on quality rather than just productivity. Some of our clients are willing to pay for that, and we are trying to assign value to this non-billable time or adjust our productivity standards appropriately. I think hospitals definitely understand the value of non-billable services from hospitalists, but still will push us on the productivity targets,” Ms. Himebaugh said.
“I don’t believe hospital medicine can be sustainable long term on flat productivity or flat RVUs,” she added. “Yet the costs of burnout associated with pushing higher productivity are not sustainable, either.” So what are the answers? She said many inefficiencies are involved in responding to inquiries on the floor that could have been addressed another way, or waiting for the turnaround of diagnostic tests.
“Maybe we don’t need physicians to be in the hospital 24/7 if we have access to telehealth, or a partnership with the emergency department, or greater use of advanced care practice providers,” Ms. Himebaugh said. “Our hospitals are examining those options, and we have to look at how we can become more efficient and less costly. At TeamHealth, we are trying to staff for value – looking at patient flow patterns and adjusting our schedules accordingly. Is there a bolus of admissions tied to emergency department shift changes, or to certain days of the week? How can we move from the 12-hour shift that begins at 7 a.m. and ends at 7 p.m., and instead provide coverage for when the patients are there?”
Mark Williams, MD, MHM, chief of the division of hospital medicine at the University of Kentucky, Lexington, said he appreciates the volume of data in the report but wishes for even more survey participants, which could make the breakouts for subgroups such as academic hospitalists more robust. Other current sources of hospitalist salary data include the Association of American Medical Colleges (AAMC), which produces compensation reports to help medical schools and teaching hospitals with benchmarking, and the Faculty Practice Solution Center developed jointly by AAMC and Vizient to provide faculty practice plans with analytic tools. The Medical Group Management Association (MGMA) is another valuable source of information, some of which was licensed for inclusion in the SoHM report.
“There is no source of absolute truth that hospitalists can point to,” Dr. Williams said. “I will present my data and my administrators will reply: ‘We have our own data.’ Our institution has consistently ranked first or second nationwide for the sickest patients. We take more Medicaid and dually eligible patients, who have a lot of social issues. They take a lot of time to manage medically and the RVUs don’t reflect that. And yet I’m still judged by my RVUs generated per hospitalist. Hospital administrators understandably want to get the most productivity, and they are looking for their own data for average productivity numbers.”
Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., said that hospital medicine’s flat productivity trends would be difficult to sustain in the business world. But there aren’t easy or obvious ways to increase hospitalists’ productivity. The SoHM report also shows that as productivity increases, total compensation increases but at a lower rate, resulting in a gradual decrease in compensation per RVU.
Pressures to increase productivity can be a double-edged sword, Dr. Williams added. Demanding that doctors make more billable visits faster to generate more RVUs can be a recipe for burnout and turnover, with huge costs associated with recruiting replacements.
“If there was recent turnover of hospitalists at the hospital, with the need to find replacements, there may be institutional memory about that,” he said. “But where are hospitals spending their money? Bottom line, we still need to learn to cut our costs.”
How is hospitalist practice evolving?
In addition to payment and productivity data, the SoHM report provides a current picture of the evolving state of hospitalist group practices. A key thread is how the work hospitalists are doing, and the way they do it, is changing, with new information about comanagement roles, dedicated admitters, night coverage, geographic rounding, and the like.
Making greater use of nurse practitioners and physician assistants (NPs/PAs), may be one way to change the flat productivity trends, Dr. Brown said. With a cost per RVU that’s roughly half that of a doctor’s, NPs/PAs could contribute to the bottom line. But he sees surprisingly large variation in how hospitalist groups are using them. Typically, they are deployed at a ratio of four doctors to one NP/PA, but that ratio could be two to one or even one to one, he said.
Use of NPs/PAs by academic hospitalist groups is up, from 52.1% in 2016 to 75.7% in 2018. For adult-only groups, 76.8% had NPs/PAs, with higher rates in hospitals and health systems and lower rates in the West region. But a lot of groups are using these practitioners for nonproductive work, and some are failing to generate any billing income, Dr. Brown said.
“The rate at which NPs/PAs performed billable services was higher in physician-owned practices, resulting in a lower cost per RVU, suggesting that many practices may be underutilizing their NPs/PAs or not sharing the work.” Not every NP or PA wants to or is able to care for very complex patients, Dr. Brown said, “but you want a system where the NP and PA can work at the highest level permitted by state law.”
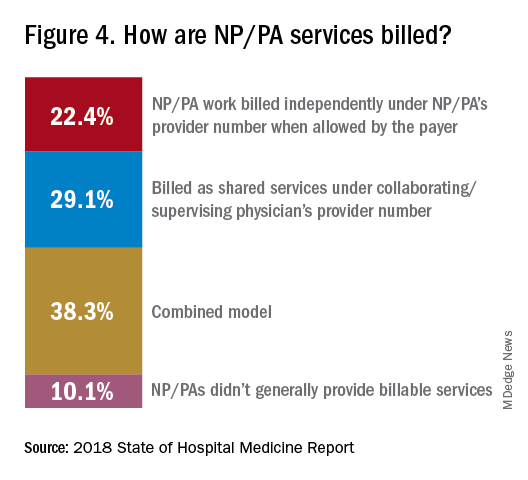
The predominant scheduling model of hospital medicine, 7 days on duty followed by 7 days off, has diminished somewhat in recent years. There appears to be some fluctuation and a gradual move away from 7 on/7 off toward some kind of variable approach, since the former may not be physically sustainable for the doctor over the long haul, Dr. Brown said. Some groups are experimenting with a combined approach.
“I think balancing workload with manpower has always been a challenge for our field. Maybe we should be working shorter shifts or fewer days and making sure our hospitalists aren’t ever sitting around idle,” he said. “And could we come in on nonclinical days to do administrative tasks? I think the solution is out there, but we haven’t created the algorithms to define that yet. If you could somehow use the data for volume, number of beds, nurse staffing, etc., by year and seasonally, you might be able to reliably predict census. This is about applying data hospitals already have in their electronic health records, but utilizing the data in ways that are more helpful.”
Dr. McIlraith added that a big driver of the future of hospital medicine will be the evolution of the EHR and the digitalization of health care, as hospitals learn how to leverage more of what’s in their EHRs. “The impact will grow for hospitalists through the creation and maturation of big data systems – and the learning that can be extracted from what’s contained in the electronic health record.”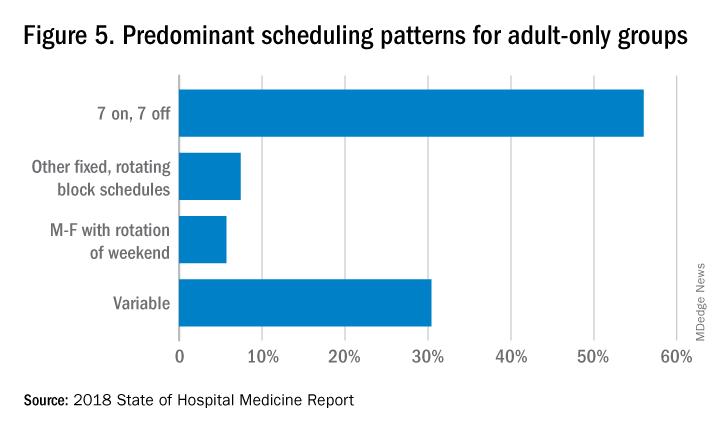
Another important question for hospitalist groups is their model of backup scheduling, to make sure there is a replacement available if a scheduled doctor calls in sick or if demand is unexpectedly high.
“In today’s world, this is how we have traditionally managed unpredictability,” Dr. Brown said. “You don’t know when you will need it, but if you need it, you want it immediately. So how do you pay for it – only when the doctor comes in, or also an amount just for being on call?” Some groups pay for both, he said, others for neither.
“We are a group of 70 hospitalists, and if someone is sick you can’t just shut down the service,” said Dr. Chadha. “We are one of the few to use incentives for both, which could include a 1-week decrease in clinical shifts in exchange for 2 weeks of backup. We have times with 25% usage of backup number 1, and 10% usage of backup number 2,” he noted. “But the goal is for our hospitalists to have assurances that there is a backup system and that it works.”
The presence of nocturnists in hospitals continues to rise, with 76.1% of adults-only groups having nocturnists, 27.6% of children-only groups, and 68.2% of adults and children groups. Geographic or unit-based hospital assignments have grown to 36.4% of adult-only groups.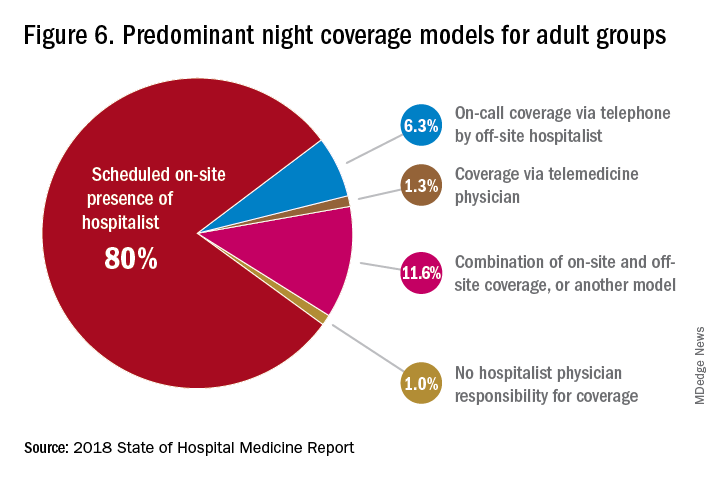
What are hospitalists’ other new roles?
“We have a large group of 50 doctors, with about 40 FTEs, and we are evolving from the traditional generalist role toward more subspecialty comanagement,” said Bryan Huang, MD, physician adviser and associate clinical professor in the division of hospital medicine at the University of California–San Diego. “Our hospitalists are asking what it means to be an academic hospitalist as our teaching roles have shrunk.”
Dr. Huang recently took on a new role as physician adviser for his hospital in such areas as utilization review, patient flow, and length of stay. “I’m spearheading a work group to address quality issues – all of which involve collaboration with other professionals. We also developed an admitting role here for a hospitalist whose sole role for the day is to admit patients.” Nationally up to 51.2% of hospitalist groups utilize a dedicated daytime admitter.
The report found that hospital services for which hospitalists are more likely to be attendings than consultants include GI/liver, 78.4%; palliative care, 77.3%; neurology/stroke, 73.6%; oncology, 67.8%; cardiology, 56.9%; and critical care, 50.7%. Conditions where hospitalists are more likely to consult rather than admit and attend include neurosurgery, orthopedics, general surgery, cardiovascular surgery, and other surgical subspecialties.
Other hospital services routinely provided by adult-only hospitalists include care of patients in an ICU setting (62.7%); primary responsibility for observation units (54.6%); primary clinical responsibility for rapid response teams (48.8%); primary responsibility for code blue or cardiac arrest teams (43.8%); nighttime admissions or tuck-in services (33.9%); and medical procedures (31.5%). For pediatric hospital medicine groups, care of healthy newborns and medical procedures were among the most common services provided, while for hospitalists serving adults and children, rapid response teams, ICUs, and specialty units were most common.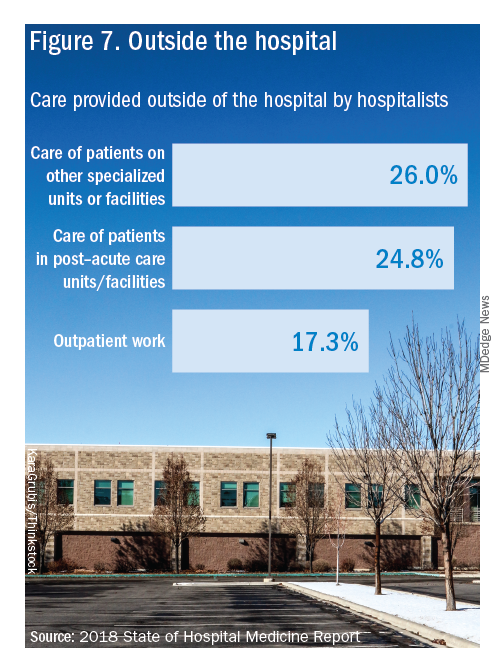
New models of payment for health care
As the larger health care system is being transformed by new payment models and benefit structures, including accountable care organizations (ACOs), value-based purchasing, bundled payments, and other forms of population-based coverage – which is described as a volume-to-value shift in health care – how are these new models affecting hospitalists?
Observers say penetration of these new models varies widely by locality but they haven’t had much direct impact on hospitalists’ practices – at least not yet. However, as hospitals and health systems find themselves needing to learn new ways to invest their resources differently in response to these trends, what matters to the hospital should be of great importance to the hospitalist group.
“I haven’t seen a lot of dramatic changes in how hospitalists engage with value-based purchasing,” Dr. White said. “If we know that someone is part of an ACO, the instinctual – and right – response is to treat them like any other patient. But we still need to be committed to not waste resources.”
Hospitalists are the best people to understand the intricacies of how the health care system works under value-based approaches, Dr. Huang said. “That’s why so many hospitalists have taken leadership positions in their hospitals. I think all of this translates to the practical, day-to-day work of hospitalists, reflected in our focus on readmissions and length of stay.”
Dr. Williams said the health care system still hasn’t turned the corner from fee-for-service to value-based purchasing. “It still represents a tiny fraction of the income of hospitalists. Hospitals still have to focus on the bottom line, as fee-for-service reimbursement for hospitalized patients continues to get squeezed, and ACOs aren’t exactly paying premium rates either. Ask almost any hospital CEO what drives their bottom line today and the answer is volume – along with optimizing productivity. Pretty much every place I look, the future does not look terribly rosy for hospitals.”
Ms. Himebaugh said she is bullish on hospital medicine, in the sense that it’s unlikely to go away anytime soon. “Hospitalists are needed and provide value. But I don’t think we have devised the right model yet. I’m not sure our current model is sustainable. We need to find new models we can afford that don’t require squeezing our providers.”
For more information about the 2018 State of Hospital Medicine Report, contact SHM’s Practice Management Department at: [email protected] or call 800-843-3360. See also: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/.
In a national health care environment undergoing unprecedented transformation, the specialty of hospital medicine appears to be an island of relative stability, a conclusion that is supported by the principal findings from SHM’s 2018 State of Hospital Medicine (SoHM) report.
The report of hospitalist group practice characteristics, as well as other key data defining the field’s current status, that the Society of Hospital Medicine puts out every 2 years reveals that overall salaries for hospitalist physicians are up by 3.8% since 2016. Although productivity, as measured by work relative value units (RVUs), remained largely flat over the same period, financial support per full-time equivalent (FTE) physician position to hospitalist groups from their hospitals and health systems is up significantly.
Total support per FTE averaged $176,657 in 2018, 12% higher than in 2016, noted Leslie Flores, MHA, SFHM, of Nelson Flores Hospital Medicine Consultants, and a member of SHM’s Practice Analysis Committee, which oversees the biennial survey. Compensation and productivity data were collected by the Medical Group Management Association and licensed by SHM for inclusion in its report.
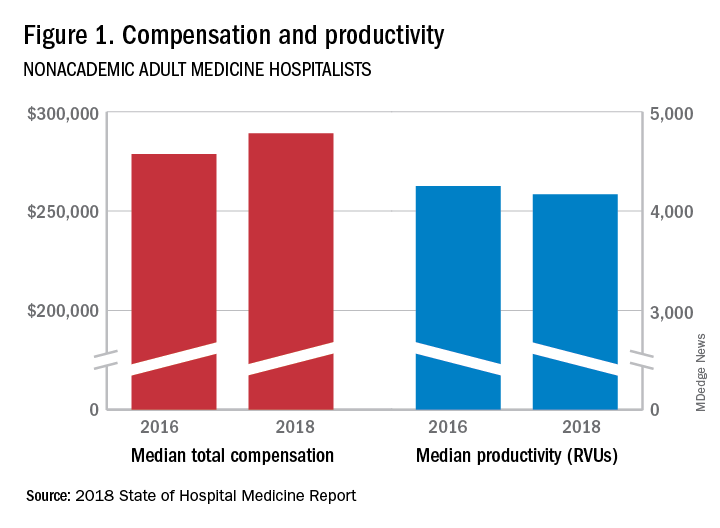
These findings – particularly the flat productivity – raise questions about long-term sustainability, Ms. Flores said. “What is going on? Do hospital administrators still recognize the value hospitalists bring to the operations and the quality of their hospitals? Or is paying the subsidy just a cost of doing business – a necessity for most hospitals in a setting where demand for hospitalist positions remains high?”
Andrew White, MD, FACP, SFHM, chair of SHM’s Practice Analysis Committee and director of the hospital medicine service at the University of Washington Medical Center, Seattle, said basic market forces dictate that it is “pretty much inconceivable” to run a modern hospital of any size without hospitalists.
“Clearly, demand outstrips supply, which drives up salaries and support, whether CEOs feel that the hospitalist group is earning that support or not,” Dr. White said. “The unfilled hospitalist positions we identified speak to ongoing projected greater demand than supply. That said, hospitalists and group leaders can’t be complacent and must collaborate effectively with hospitals to provide highly valuable services.” Turnover of hospitalist positions was up slightly, he noted, at 7.4% in 2018, from 6.9% in 2016, reversing a trend of previous years.
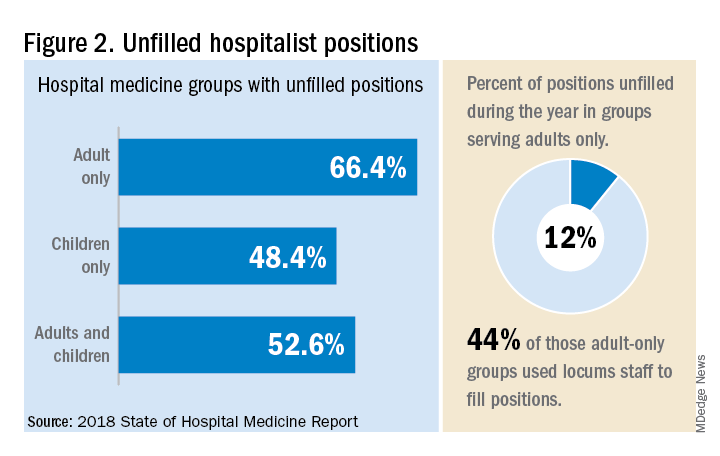
But will these trends continue at a time when hospitals face continued pressure to cut costs, as the hospital medicine subsidy may represent one of their largest cost centers? Because the size of hospitalist groups continues to grow, hospitals’ total subsidy for hospital medicine is going up faster than the percentage increase in support per FTE.
How do hospitalists use the SoHM report?
Dr. White called the 2018 SoHM report the “most representative and balanced sample to date” of hospitalist group practices, with some of the highest quality data, thanks to more robust participation in the survey by pediatric groups and improved distribution among hospitalist management companies and academic programs.
“Not that past reports had major flaws, but this version is more authoritative, reflecting an intentional effort by our Practice Analysis Committee to bring in more participants from key groups,” he said.
The biennial report has been around long enough to achieve brand recognition in the field as the most authoritative source of information regarding hospitalist practice, he added. “We worked hard this year to balance the participants, with more of our responses than in the past coming from multi-hospital groups, whether 4 to 5 sites, or 20 to 30.”
Surveys were conducted online in January and February of 2018 in response to invitations mailed and emailed to targeted hospital medicine group leaders. A total of 569 groups completed the survey, representing 8,889 hospitalist FTEs, approximately 16% of the total hospitalist workforce. Responses were presented in several categories, including by size of program, region and employment model. Groups that care for adults only represented 87.9% of the surveys, while groups that care for children only were 6.7% and groups that care for both adults and children were 5.4%.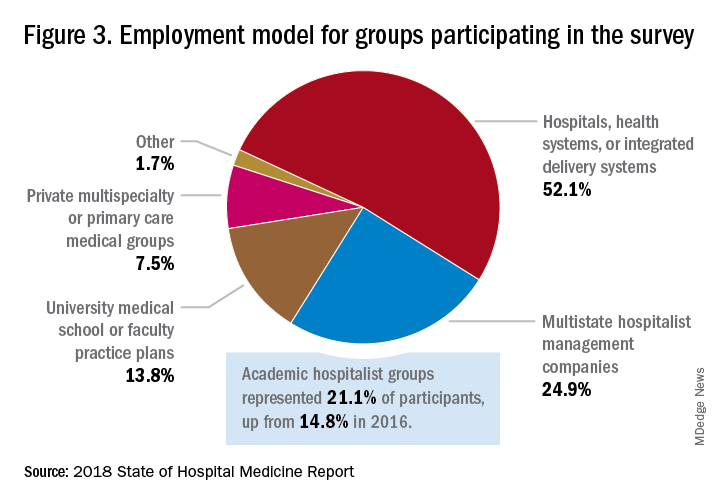
“This survey doesn’t tell us what should be best practice in hospital medicine,” Dr. White said, only what is actual current practice. He uses it in his own health system to not only contextualize and justify his group’s performance metrics for hospital administrators – relative to national and categorical averages – but also to see if the direction his group is following is consistent with what’s going on in the larger field.
“These data offer a very powerful resource regarding the trends in hospital medicine,” said Romil Chadha, MD, MPH, FACP, SFHM, associate division chief for operations in the division of hospital medicine at the University of Kentucky and UK Healthcare, Lexington. “It is my repository of data to go before my administrators for decisions that need to be made or to pilot new programs.”
Dr. Chadha also uses the data to help answer compensation, scheduling, and support questions from his group’s members.
Thomas McIlraith, MD, immediate past chairman of the hospital medicine department at Mercy Medical Group, Sacramento, Calif., said the report’s value is that it allows comparisons of salaries in different settings, and to see, for example, how night staffing is structured. “A lot of leaders I spoke to at SHM’s 2018 Leadership Academy in Vancouver were saying they didn’t feel up to parity with the national standards. You can use the report to look at the state of hospital medicine nationally and make comparisons,” he said.
Calls for more productivity
Roberta Himebaugh, MBA, SFHM, senior vice president of acute care services for the national hospitalist management company TeamHealth, and cochair of the SHM Practice Administrators Special Interest Group, said her company’s clients have traditionally asked for greater productivity from their hospitalist contracts as a way to decrease overall costs. Some markets are starting to see a change in that approach, she noted.
“Recently there’s been an increased focus on paying hospitalists to focus on quality rather than just productivity. Some of our clients are willing to pay for that, and we are trying to assign value to this non-billable time or adjust our productivity standards appropriately. I think hospitals definitely understand the value of non-billable services from hospitalists, but still will push us on the productivity targets,” Ms. Himebaugh said.
“I don’t believe hospital medicine can be sustainable long term on flat productivity or flat RVUs,” she added. “Yet the costs of burnout associated with pushing higher productivity are not sustainable, either.” So what are the answers? She said many inefficiencies are involved in responding to inquiries on the floor that could have been addressed another way, or waiting for the turnaround of diagnostic tests.
“Maybe we don’t need physicians to be in the hospital 24/7 if we have access to telehealth, or a partnership with the emergency department, or greater use of advanced care practice providers,” Ms. Himebaugh said. “Our hospitals are examining those options, and we have to look at how we can become more efficient and less costly. At TeamHealth, we are trying to staff for value – looking at patient flow patterns and adjusting our schedules accordingly. Is there a bolus of admissions tied to emergency department shift changes, or to certain days of the week? How can we move from the 12-hour shift that begins at 7 a.m. and ends at 7 p.m., and instead provide coverage for when the patients are there?”
Mark Williams, MD, MHM, chief of the division of hospital medicine at the University of Kentucky, Lexington, said he appreciates the volume of data in the report but wishes for even more survey participants, which could make the breakouts for subgroups such as academic hospitalists more robust. Other current sources of hospitalist salary data include the Association of American Medical Colleges (AAMC), which produces compensation reports to help medical schools and teaching hospitals with benchmarking, and the Faculty Practice Solution Center developed jointly by AAMC and Vizient to provide faculty practice plans with analytic tools. The Medical Group Management Association (MGMA) is another valuable source of information, some of which was licensed for inclusion in the SoHM report.
“There is no source of absolute truth that hospitalists can point to,” Dr. Williams said. “I will present my data and my administrators will reply: ‘We have our own data.’ Our institution has consistently ranked first or second nationwide for the sickest patients. We take more Medicaid and dually eligible patients, who have a lot of social issues. They take a lot of time to manage medically and the RVUs don’t reflect that. And yet I’m still judged by my RVUs generated per hospitalist. Hospital administrators understandably want to get the most productivity, and they are looking for their own data for average productivity numbers.”
Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., said that hospital medicine’s flat productivity trends would be difficult to sustain in the business world. But there aren’t easy or obvious ways to increase hospitalists’ productivity. The SoHM report also shows that as productivity increases, total compensation increases but at a lower rate, resulting in a gradual decrease in compensation per RVU.
Pressures to increase productivity can be a double-edged sword, Dr. Williams added. Demanding that doctors make more billable visits faster to generate more RVUs can be a recipe for burnout and turnover, with huge costs associated with recruiting replacements.
“If there was recent turnover of hospitalists at the hospital, with the need to find replacements, there may be institutional memory about that,” he said. “But where are hospitals spending their money? Bottom line, we still need to learn to cut our costs.”
How is hospitalist practice evolving?
In addition to payment and productivity data, the SoHM report provides a current picture of the evolving state of hospitalist group practices. A key thread is how the work hospitalists are doing, and the way they do it, is changing, with new information about comanagement roles, dedicated admitters, night coverage, geographic rounding, and the like.
Making greater use of nurse practitioners and physician assistants (NPs/PAs), may be one way to change the flat productivity trends, Dr. Brown said. With a cost per RVU that’s roughly half that of a doctor’s, NPs/PAs could contribute to the bottom line. But he sees surprisingly large variation in how hospitalist groups are using them. Typically, they are deployed at a ratio of four doctors to one NP/PA, but that ratio could be two to one or even one to one, he said.
Use of NPs/PAs by academic hospitalist groups is up, from 52.1% in 2016 to 75.7% in 2018. For adult-only groups, 76.8% had NPs/PAs, with higher rates in hospitals and health systems and lower rates in the West region. But a lot of groups are using these practitioners for nonproductive work, and some are failing to generate any billing income, Dr. Brown said.
“The rate at which NPs/PAs performed billable services was higher in physician-owned practices, resulting in a lower cost per RVU, suggesting that many practices may be underutilizing their NPs/PAs or not sharing the work.” Not every NP or PA wants to or is able to care for very complex patients, Dr. Brown said, “but you want a system where the NP and PA can work at the highest level permitted by state law.”
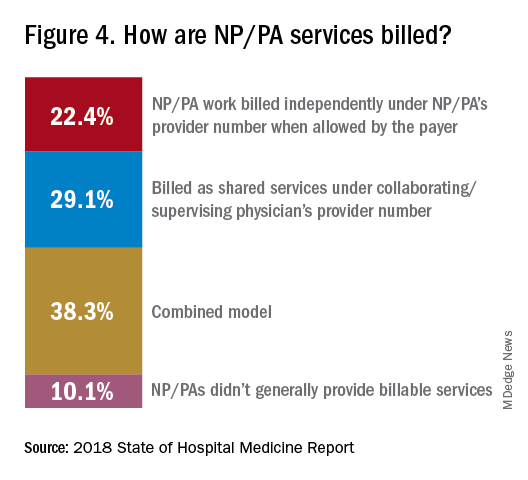
The predominant scheduling model of hospital medicine, 7 days on duty followed by 7 days off, has diminished somewhat in recent years. There appears to be some fluctuation and a gradual move away from 7 on/7 off toward some kind of variable approach, since the former may not be physically sustainable for the doctor over the long haul, Dr. Brown said. Some groups are experimenting with a combined approach.
“I think balancing workload with manpower has always been a challenge for our field. Maybe we should be working shorter shifts or fewer days and making sure our hospitalists aren’t ever sitting around idle,” he said. “And could we come in on nonclinical days to do administrative tasks? I think the solution is out there, but we haven’t created the algorithms to define that yet. If you could somehow use the data for volume, number of beds, nurse staffing, etc., by year and seasonally, you might be able to reliably predict census. This is about applying data hospitals already have in their electronic health records, but utilizing the data in ways that are more helpful.”
Dr. McIlraith added that a big driver of the future of hospital medicine will be the evolution of the EHR and the digitalization of health care, as hospitals learn how to leverage more of what’s in their EHRs. “The impact will grow for hospitalists through the creation and maturation of big data systems – and the learning that can be extracted from what’s contained in the electronic health record.”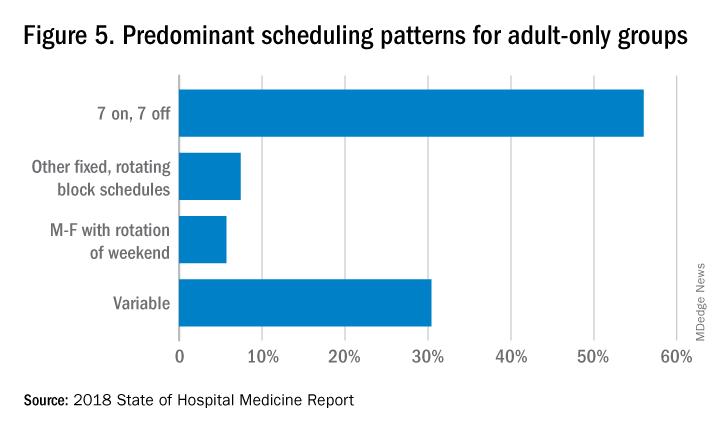
Another important question for hospitalist groups is their model of backup scheduling, to make sure there is a replacement available if a scheduled doctor calls in sick or if demand is unexpectedly high.
“In today’s world, this is how we have traditionally managed unpredictability,” Dr. Brown said. “You don’t know when you will need it, but if you need it, you want it immediately. So how do you pay for it – only when the doctor comes in, or also an amount just for being on call?” Some groups pay for both, he said, others for neither.
“We are a group of 70 hospitalists, and if someone is sick you can’t just shut down the service,” said Dr. Chadha. “We are one of the few to use incentives for both, which could include a 1-week decrease in clinical shifts in exchange for 2 weeks of backup. We have times with 25% usage of backup number 1, and 10% usage of backup number 2,” he noted. “But the goal is for our hospitalists to have assurances that there is a backup system and that it works.”
The presence of nocturnists in hospitals continues to rise, with 76.1% of adults-only groups having nocturnists, 27.6% of children-only groups, and 68.2% of adults and children groups. Geographic or unit-based hospital assignments have grown to 36.4% of adult-only groups.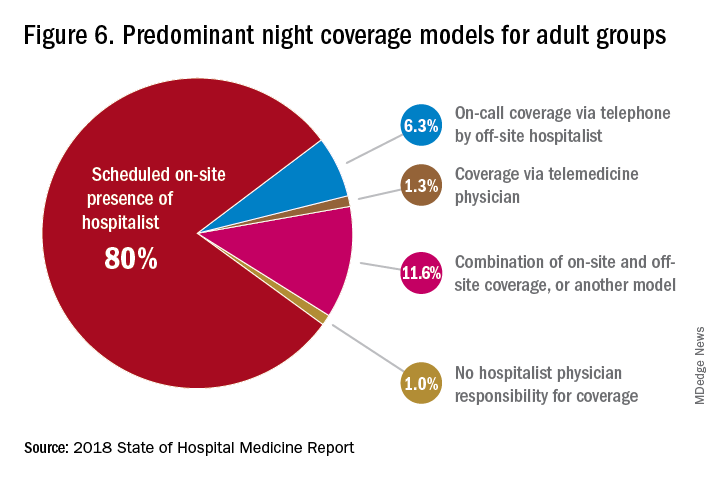
What are hospitalists’ other new roles?
“We have a large group of 50 doctors, with about 40 FTEs, and we are evolving from the traditional generalist role toward more subspecialty comanagement,” said Bryan Huang, MD, physician adviser and associate clinical professor in the division of hospital medicine at the University of California–San Diego. “Our hospitalists are asking what it means to be an academic hospitalist as our teaching roles have shrunk.”
Dr. Huang recently took on a new role as physician adviser for his hospital in such areas as utilization review, patient flow, and length of stay. “I’m spearheading a work group to address quality issues – all of which involve collaboration with other professionals. We also developed an admitting role here for a hospitalist whose sole role for the day is to admit patients.” Nationally up to 51.2% of hospitalist groups utilize a dedicated daytime admitter.
The report found that hospital services for which hospitalists are more likely to be attendings than consultants include GI/liver, 78.4%; palliative care, 77.3%; neurology/stroke, 73.6%; oncology, 67.8%; cardiology, 56.9%; and critical care, 50.7%. Conditions where hospitalists are more likely to consult rather than admit and attend include neurosurgery, orthopedics, general surgery, cardiovascular surgery, and other surgical subspecialties.
Other hospital services routinely provided by adult-only hospitalists include care of patients in an ICU setting (62.7%); primary responsibility for observation units (54.6%); primary clinical responsibility for rapid response teams (48.8%); primary responsibility for code blue or cardiac arrest teams (43.8%); nighttime admissions or tuck-in services (33.9%); and medical procedures (31.5%). For pediatric hospital medicine groups, care of healthy newborns and medical procedures were among the most common services provided, while for hospitalists serving adults and children, rapid response teams, ICUs, and specialty units were most common.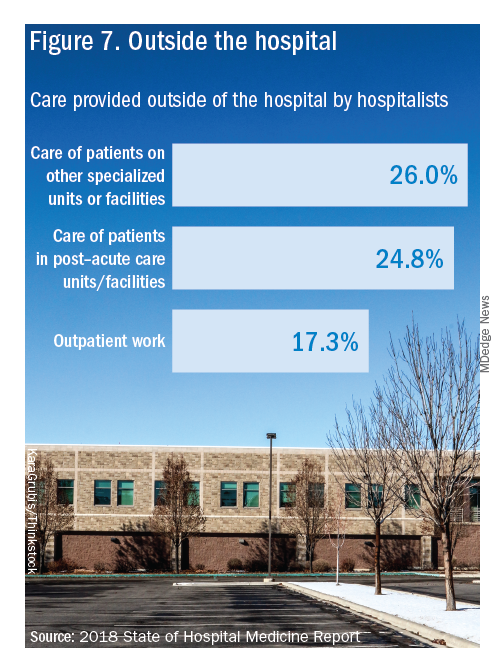
New models of payment for health care
As the larger health care system is being transformed by new payment models and benefit structures, including accountable care organizations (ACOs), value-based purchasing, bundled payments, and other forms of population-based coverage – which is described as a volume-to-value shift in health care – how are these new models affecting hospitalists?
Observers say penetration of these new models varies widely by locality but they haven’t had much direct impact on hospitalists’ practices – at least not yet. However, as hospitals and health systems find themselves needing to learn new ways to invest their resources differently in response to these trends, what matters to the hospital should be of great importance to the hospitalist group.
“I haven’t seen a lot of dramatic changes in how hospitalists engage with value-based purchasing,” Dr. White said. “If we know that someone is part of an ACO, the instinctual – and right – response is to treat them like any other patient. But we still need to be committed to not waste resources.”
Hospitalists are the best people to understand the intricacies of how the health care system works under value-based approaches, Dr. Huang said. “That’s why so many hospitalists have taken leadership positions in their hospitals. I think all of this translates to the practical, day-to-day work of hospitalists, reflected in our focus on readmissions and length of stay.”
Dr. Williams said the health care system still hasn’t turned the corner from fee-for-service to value-based purchasing. “It still represents a tiny fraction of the income of hospitalists. Hospitals still have to focus on the bottom line, as fee-for-service reimbursement for hospitalized patients continues to get squeezed, and ACOs aren’t exactly paying premium rates either. Ask almost any hospital CEO what drives their bottom line today and the answer is volume – along with optimizing productivity. Pretty much every place I look, the future does not look terribly rosy for hospitals.”
Ms. Himebaugh said she is bullish on hospital medicine, in the sense that it’s unlikely to go away anytime soon. “Hospitalists are needed and provide value. But I don’t think we have devised the right model yet. I’m not sure our current model is sustainable. We need to find new models we can afford that don’t require squeezing our providers.”
For more information about the 2018 State of Hospital Medicine Report, contact SHM’s Practice Management Department at: [email protected] or call 800-843-3360. See also: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/.
HIPAA compliance: Three cases to learn from
Data security experts say three HIPAA violations that resulted in significant fines by the Office for Civil Rights (OCR) in 2018 hold important lessons for health professionals about safeguarding records and training staff in HIPAA compliance.
Read on to learn how the cases unfolded and what knowledge practices can gain from the common HIPAA mistakes.
Who? Allergy Associates of Hartford, Conn.
What happened? A patient contacted a local television station to complain about a dispute between herself and a physician at Allergy Associates in Hartford, Conn. The disagreement stemmed from the office turning away the patient because she allegedly brought her service animal, according to a Nov. 26 announcement by the Department of Health & Human Services. The reporter contacted the doctor in question for a news story and, in responding, the physician disclosed protected patient information to the reporter.
What else? An OCR investigation determined that a privacy officer with Allergy Associates had instructed the physician not to respond to the media about the complaint or to respond with “no comment”; that advice was disregarded. The practice then failed to discipline the physician or take any corrective action following the disclosure, according to the OCR.
How much? The OCR imposed a $125,000 fine on the practice and a corrective action plan that includes 2 years of OCR monitoring.
Lessons learned: Had the practice disciplined the physician or taken corrective action after the disclosure, the OCR may not have penalized the group so severely, according to Jennifer Mitchell, a Cincinnati-based health law attorney and vice chair of the American Bar Association eHealth, Privacy, & Security Interest Group.
“In my opinion, the government levied these penalties because the provider did not sanction the doctor,” Ms. Mitchell said in an interview. “Health care entities need to take proper steps to remediate and, at a minimum, hold their workforce responsible for their behavior and ensure that it won’t happen again.”
The case emphasizes the need to train team members on media protocols and to ensure that protected health information is not mistakenly released. In addition to implementing policies and procedures, practices must also be willing to discipline health professionals when violations occur.
“A health care provider’s natural inclination is to defend themselves if they are being accused by a patient,” she said. “However, under the HIPAA rules, health care providers have to understand that they are prohibited from making such public statements about any patient.”
Who? Advanced Care Hospitalists of Lakeland, Fla.
What happened? Advanced Care Hospitalists (ACH) received billing services from an individual who represented himself to be affiliated with a Florida-based company named Doctor’s First Choice Billing. A local hospital later notified ACH that patient information, including names and Social Security numbers, were viewable on the First Choice website. ACH identified at least 400 patients affected by the breach and reported the breach to the OCR. However, ACH later determined that an additional 8,855 patients may have been affected and revised its OCR notification.
What else? During its investigation, the OCR found that the hospitalist group had never entered into a business associate agreement for billing services with First Choice, as required by HIPAA, and that the practice also failed to adopt any policies regarding business associate agreements until 2014, according to a Dec. 4 announcement from HHS.
How much? The OCR fined the practice $500,000 and also imposed a robust corrective action plan that includes an enterprise-wide risk analysis and the adoption of business associate agreements. Roger Severino, OCR director, called the case especially troubling because “the practice allowed the names and Social Security numbers of thousands of patients to be exposed on the Internet after it failed to follow basic security requirements under HIPAA.”
Lessons learned: The case illustrates the importance of having a business associate agreement in place for all third parties that may have access to protected health information, said Clinton Mikel, a Farmington Hills, Mich., health law attorney specializing in HIPAA compliance.
Under HIPAA, a business associate is defined as a person or entity, other than a member of the workforce of a covered entity, who “performs functions or activities on behalf of, or provides certain services to, a covered entity that involve access by the business associate to protected health information.”
HIPAA requires that covered entities enter into contracts with business associates to ensure appropriate safeguarding of protected health information.
“If your business associate has a breach, your practice must report the breach to OCR and your patients,” Mr. Mikel said in an interview. “The OCR will then investigate your practice and your relationship with the business associate. Just because the breach and fault clearly happened elsewhere, you will still be investigated, and could face a penalty if HIPAA requirements weren’t met.”
Who? Filefax of Northbrook, Ill.
What happened? The OCR opened an investigation after receiving an anonymous complaint that medical records obtained from Filefax, a company that provided storage, maintenance, and delivery of medical records for health professionals, were left unmonitored at a shredding and recycling facility. OCR’s investigation revealed that a person left the records of 2,150 patients at the recycling plant and that the records contained protected health information, according to an HHS announcement. It is unclear if the person worked for Filefax.
What else? The OCR discovered that, in a related incident, an individual who obtained medical records from Filefax left them unattended in an unlocked truck in the Filefax parking lot.
How much? The OCR imposed a $100,000 fine on Filefax. The company is no longer in business; however, a court-appointed liquidator has agreed to properly store and dispose of the remaining records.
Lessons learned: Although the case did not involve a health provider, the circumstances are applicable to physicians, particularly when practices move or close, Mr. Mikel said. In some cases, a former patient may contact a shuttered practice only to learn their record cannot be located, or worse, that a breach has occurred.
“[Such a case is] ripe for a patient to complain to OCR,” he said. “OCR doesn’t care if you’re closed or retired, they’re going to look.”
HIPAA requires thatcovered entities apply appropriate administrative, technical, and physical safeguards to protect the privacy of protected health information in any form when moving or closing. The safeguards must prevent prohibited uses and disclosures of protected health information in connection with the disposal of such information, according to the rule. The HHS provides guidance for the disposing of medical records; further, the American Academy of Family Physicians has created a checklist on closing a practice that addresses the transferring of medical records.
Without taking the correct measures, doctors may end up drawing scrutiny from OCR and face a potential fine if violations are found, experts said.
“Covered entities and business associates need to be aware that OCR is committed to enforcing HIPAA regardless of whether a covered entity is opening its doors or closing them,” Mr. Severino of the OCR said in a statement. “HIPAA still applies.”
Data security experts say three HIPAA violations that resulted in significant fines by the Office for Civil Rights (OCR) in 2018 hold important lessons for health professionals about safeguarding records and training staff in HIPAA compliance.
Read on to learn how the cases unfolded and what knowledge practices can gain from the common HIPAA mistakes.
Who? Allergy Associates of Hartford, Conn.
What happened? A patient contacted a local television station to complain about a dispute between herself and a physician at Allergy Associates in Hartford, Conn. The disagreement stemmed from the office turning away the patient because she allegedly brought her service animal, according to a Nov. 26 announcement by the Department of Health & Human Services. The reporter contacted the doctor in question for a news story and, in responding, the physician disclosed protected patient information to the reporter.
What else? An OCR investigation determined that a privacy officer with Allergy Associates had instructed the physician not to respond to the media about the complaint or to respond with “no comment”; that advice was disregarded. The practice then failed to discipline the physician or take any corrective action following the disclosure, according to the OCR.
How much? The OCR imposed a $125,000 fine on the practice and a corrective action plan that includes 2 years of OCR monitoring.
Lessons learned: Had the practice disciplined the physician or taken corrective action after the disclosure, the OCR may not have penalized the group so severely, according to Jennifer Mitchell, a Cincinnati-based health law attorney and vice chair of the American Bar Association eHealth, Privacy, & Security Interest Group.
“In my opinion, the government levied these penalties because the provider did not sanction the doctor,” Ms. Mitchell said in an interview. “Health care entities need to take proper steps to remediate and, at a minimum, hold their workforce responsible for their behavior and ensure that it won’t happen again.”
The case emphasizes the need to train team members on media protocols and to ensure that protected health information is not mistakenly released. In addition to implementing policies and procedures, practices must also be willing to discipline health professionals when violations occur.
“A health care provider’s natural inclination is to defend themselves if they are being accused by a patient,” she said. “However, under the HIPAA rules, health care providers have to understand that they are prohibited from making such public statements about any patient.”
Who? Advanced Care Hospitalists of Lakeland, Fla.
What happened? Advanced Care Hospitalists (ACH) received billing services from an individual who represented himself to be affiliated with a Florida-based company named Doctor’s First Choice Billing. A local hospital later notified ACH that patient information, including names and Social Security numbers, were viewable on the First Choice website. ACH identified at least 400 patients affected by the breach and reported the breach to the OCR. However, ACH later determined that an additional 8,855 patients may have been affected and revised its OCR notification.
What else? During its investigation, the OCR found that the hospitalist group had never entered into a business associate agreement for billing services with First Choice, as required by HIPAA, and that the practice also failed to adopt any policies regarding business associate agreements until 2014, according to a Dec. 4 announcement from HHS.
How much? The OCR fined the practice $500,000 and also imposed a robust corrective action plan that includes an enterprise-wide risk analysis and the adoption of business associate agreements. Roger Severino, OCR director, called the case especially troubling because “the practice allowed the names and Social Security numbers of thousands of patients to be exposed on the Internet after it failed to follow basic security requirements under HIPAA.”
Lessons learned: The case illustrates the importance of having a business associate agreement in place for all third parties that may have access to protected health information, said Clinton Mikel, a Farmington Hills, Mich., health law attorney specializing in HIPAA compliance.
Under HIPAA, a business associate is defined as a person or entity, other than a member of the workforce of a covered entity, who “performs functions or activities on behalf of, or provides certain services to, a covered entity that involve access by the business associate to protected health information.”
HIPAA requires that covered entities enter into contracts with business associates to ensure appropriate safeguarding of protected health information.
“If your business associate has a breach, your practice must report the breach to OCR and your patients,” Mr. Mikel said in an interview. “The OCR will then investigate your practice and your relationship with the business associate. Just because the breach and fault clearly happened elsewhere, you will still be investigated, and could face a penalty if HIPAA requirements weren’t met.”
Who? Filefax of Northbrook, Ill.
What happened? The OCR opened an investigation after receiving an anonymous complaint that medical records obtained from Filefax, a company that provided storage, maintenance, and delivery of medical records for health professionals, were left unmonitored at a shredding and recycling facility. OCR’s investigation revealed that a person left the records of 2,150 patients at the recycling plant and that the records contained protected health information, according to an HHS announcement. It is unclear if the person worked for Filefax.
What else? The OCR discovered that, in a related incident, an individual who obtained medical records from Filefax left them unattended in an unlocked truck in the Filefax parking lot.
How much? The OCR imposed a $100,000 fine on Filefax. The company is no longer in business; however, a court-appointed liquidator has agreed to properly store and dispose of the remaining records.
Lessons learned: Although the case did not involve a health provider, the circumstances are applicable to physicians, particularly when practices move or close, Mr. Mikel said. In some cases, a former patient may contact a shuttered practice only to learn their record cannot be located, or worse, that a breach has occurred.
“[Such a case is] ripe for a patient to complain to OCR,” he said. “OCR doesn’t care if you’re closed or retired, they’re going to look.”
HIPAA requires thatcovered entities apply appropriate administrative, technical, and physical safeguards to protect the privacy of protected health information in any form when moving or closing. The safeguards must prevent prohibited uses and disclosures of protected health information in connection with the disposal of such information, according to the rule. The HHS provides guidance for the disposing of medical records; further, the American Academy of Family Physicians has created a checklist on closing a practice that addresses the transferring of medical records.
Without taking the correct measures, doctors may end up drawing scrutiny from OCR and face a potential fine if violations are found, experts said.
“Covered entities and business associates need to be aware that OCR is committed to enforcing HIPAA regardless of whether a covered entity is opening its doors or closing them,” Mr. Severino of the OCR said in a statement. “HIPAA still applies.”
Data security experts say three HIPAA violations that resulted in significant fines by the Office for Civil Rights (OCR) in 2018 hold important lessons for health professionals about safeguarding records and training staff in HIPAA compliance.
Read on to learn how the cases unfolded and what knowledge practices can gain from the common HIPAA mistakes.
Who? Allergy Associates of Hartford, Conn.
What happened? A patient contacted a local television station to complain about a dispute between herself and a physician at Allergy Associates in Hartford, Conn. The disagreement stemmed from the office turning away the patient because she allegedly brought her service animal, according to a Nov. 26 announcement by the Department of Health & Human Services. The reporter contacted the doctor in question for a news story and, in responding, the physician disclosed protected patient information to the reporter.
What else? An OCR investigation determined that a privacy officer with Allergy Associates had instructed the physician not to respond to the media about the complaint or to respond with “no comment”; that advice was disregarded. The practice then failed to discipline the physician or take any corrective action following the disclosure, according to the OCR.
How much? The OCR imposed a $125,000 fine on the practice and a corrective action plan that includes 2 years of OCR monitoring.
Lessons learned: Had the practice disciplined the physician or taken corrective action after the disclosure, the OCR may not have penalized the group so severely, according to Jennifer Mitchell, a Cincinnati-based health law attorney and vice chair of the American Bar Association eHealth, Privacy, & Security Interest Group.
“In my opinion, the government levied these penalties because the provider did not sanction the doctor,” Ms. Mitchell said in an interview. “Health care entities need to take proper steps to remediate and, at a minimum, hold their workforce responsible for their behavior and ensure that it won’t happen again.”
The case emphasizes the need to train team members on media protocols and to ensure that protected health information is not mistakenly released. In addition to implementing policies and procedures, practices must also be willing to discipline health professionals when violations occur.
“A health care provider’s natural inclination is to defend themselves if they are being accused by a patient,” she said. “However, under the HIPAA rules, health care providers have to understand that they are prohibited from making such public statements about any patient.”
Who? Advanced Care Hospitalists of Lakeland, Fla.
What happened? Advanced Care Hospitalists (ACH) received billing services from an individual who represented himself to be affiliated with a Florida-based company named Doctor’s First Choice Billing. A local hospital later notified ACH that patient information, including names and Social Security numbers, were viewable on the First Choice website. ACH identified at least 400 patients affected by the breach and reported the breach to the OCR. However, ACH later determined that an additional 8,855 patients may have been affected and revised its OCR notification.
What else? During its investigation, the OCR found that the hospitalist group had never entered into a business associate agreement for billing services with First Choice, as required by HIPAA, and that the practice also failed to adopt any policies regarding business associate agreements until 2014, according to a Dec. 4 announcement from HHS.
How much? The OCR fined the practice $500,000 and also imposed a robust corrective action plan that includes an enterprise-wide risk analysis and the adoption of business associate agreements. Roger Severino, OCR director, called the case especially troubling because “the practice allowed the names and Social Security numbers of thousands of patients to be exposed on the Internet after it failed to follow basic security requirements under HIPAA.”
Lessons learned: The case illustrates the importance of having a business associate agreement in place for all third parties that may have access to protected health information, said Clinton Mikel, a Farmington Hills, Mich., health law attorney specializing in HIPAA compliance.
Under HIPAA, a business associate is defined as a person or entity, other than a member of the workforce of a covered entity, who “performs functions or activities on behalf of, or provides certain services to, a covered entity that involve access by the business associate to protected health information.”
HIPAA requires that covered entities enter into contracts with business associates to ensure appropriate safeguarding of protected health information.
“If your business associate has a breach, your practice must report the breach to OCR and your patients,” Mr. Mikel said in an interview. “The OCR will then investigate your practice and your relationship with the business associate. Just because the breach and fault clearly happened elsewhere, you will still be investigated, and could face a penalty if HIPAA requirements weren’t met.”
Who? Filefax of Northbrook, Ill.
What happened? The OCR opened an investigation after receiving an anonymous complaint that medical records obtained from Filefax, a company that provided storage, maintenance, and delivery of medical records for health professionals, were left unmonitored at a shredding and recycling facility. OCR’s investigation revealed that a person left the records of 2,150 patients at the recycling plant and that the records contained protected health information, according to an HHS announcement. It is unclear if the person worked for Filefax.
What else? The OCR discovered that, in a related incident, an individual who obtained medical records from Filefax left them unattended in an unlocked truck in the Filefax parking lot.
How much? The OCR imposed a $100,000 fine on Filefax. The company is no longer in business; however, a court-appointed liquidator has agreed to properly store and dispose of the remaining records.
Lessons learned: Although the case did not involve a health provider, the circumstances are applicable to physicians, particularly when practices move or close, Mr. Mikel said. In some cases, a former patient may contact a shuttered practice only to learn their record cannot be located, or worse, that a breach has occurred.
“[Such a case is] ripe for a patient to complain to OCR,” he said. “OCR doesn’t care if you’re closed or retired, they’re going to look.”
HIPAA requires thatcovered entities apply appropriate administrative, technical, and physical safeguards to protect the privacy of protected health information in any form when moving or closing. The safeguards must prevent prohibited uses and disclosures of protected health information in connection with the disposal of such information, according to the rule. The HHS provides guidance for the disposing of medical records; further, the American Academy of Family Physicians has created a checklist on closing a practice that addresses the transferring of medical records.
Without taking the correct measures, doctors may end up drawing scrutiny from OCR and face a potential fine if violations are found, experts said.
“Covered entities and business associates need to be aware that OCR is committed to enforcing HIPAA regardless of whether a covered entity is opening its doors or closing them,” Mr. Severino of the OCR said in a statement. “HIPAA still applies.”