User login
Negligent management of labor is the top cause of lawsuits against ob.gyns, a study of legal claims shows.
Researchers with national medical liability insurer, Coverys, analyzed 472 ob.gyn.–related claims from their database that closed between 2013 and 2017. Of the claims, 37% stemmed from alleged negligence during labor management, while 14% resulted from inappropriate management of pregnancy, and 12% were associated with negligent patient monitoring. And 11% resulted from an alleged delay in performing cesarean section, according to the report.
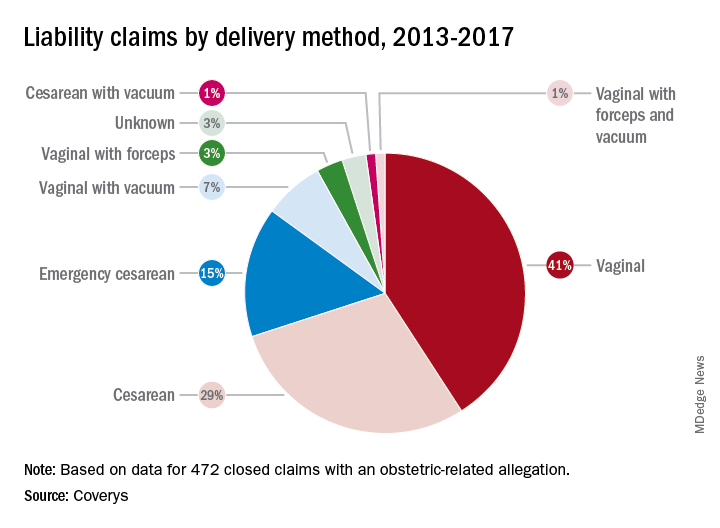
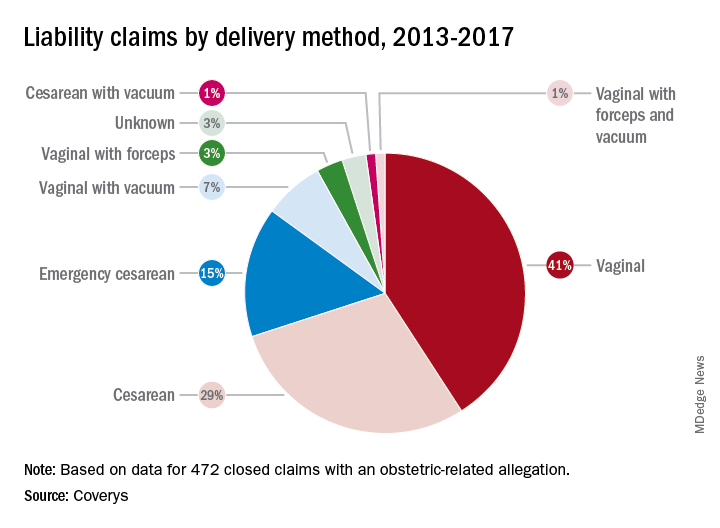
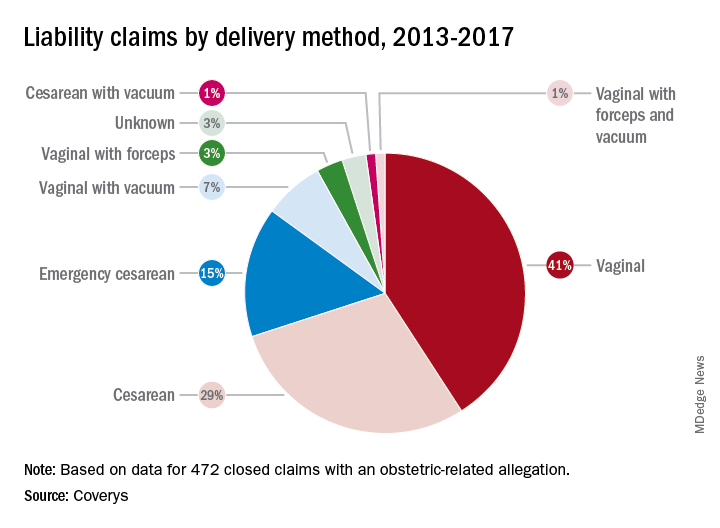
More than half of the obstetric-related claims involved patients with at least one known comorbidity (58%), most commonly diabetes and obesity. Hypertension was the third most frequent risk factor associated with patient claims, followed by post-40 week gestation and macrosomia. Vaginal births were responsible for more claims than cesarean sections (52% vs. 45%); vaginal births also resulted in more than three times as many claims as did emergency cesareans.
Nearly all obstetrics claims resulted in injuries or death to babies (90%), with 41% of claims associated with neurologic injuries, 37% related to shoulder dystocia/brachial plexus injuries, and 34% ending in fetal demise, including stillbirth. Other claims included congenital injuries, chorioamnionitis, and lacerations/contusions.
Of 60 claims that included communication breakdowns as a key factor, 28% were associated with communication failures between physicians, while 28% were associated with communication breakdowns between doctors and nurses. Of the communication mishap cases, 17% were associated with communication failures among physicians and mid-level providers and 10% were associated with breakdowns in communication between physicians and patients.
The Coverys report includes guidance for ob.gyns. on reducing their legal risk when caring for patients in labor. Some primary tips include:
- Require fetal heart rate (FHR) interpretation training. All obstetric providers and staff should undergo training on the interpretation of FHR patterns before treating obstetric patients.
- Strengthen communication. Health professionals should use the same language when describing electronic fetal-monitoring patterns. Such terminology should be used consistently through all medical record entries and communications regarding patient cases.
- Craft and maintain fetal-monitoring policies. Develop evidence-based policies and procedures around fetal monitoring during labor that outline when each type of monitoring should be used based on each patient case and circumstance.
- Keep doctors informed. Develop protocols that ensure physicians remain in the loop regarding the condition of the patient and which includes communication strategies for contacting doctors when the patient’s condition changes or requires oversight.
Negligent management of labor is the top cause of lawsuits against ob.gyns, a study of legal claims shows.
Researchers with national medical liability insurer, Coverys, analyzed 472 ob.gyn.–related claims from their database that closed between 2013 and 2017. Of the claims, 37% stemmed from alleged negligence during labor management, while 14% resulted from inappropriate management of pregnancy, and 12% were associated with negligent patient monitoring. And 11% resulted from an alleged delay in performing cesarean section, according to the report.
More than half of the obstetric-related claims involved patients with at least one known comorbidity (58%), most commonly diabetes and obesity. Hypertension was the third most frequent risk factor associated with patient claims, followed by post-40 week gestation and macrosomia. Vaginal births were responsible for more claims than cesarean sections (52% vs. 45%); vaginal births also resulted in more than three times as many claims as did emergency cesareans.
Nearly all obstetrics claims resulted in injuries or death to babies (90%), with 41% of claims associated with neurologic injuries, 37% related to shoulder dystocia/brachial plexus injuries, and 34% ending in fetal demise, including stillbirth. Other claims included congenital injuries, chorioamnionitis, and lacerations/contusions.
Of 60 claims that included communication breakdowns as a key factor, 28% were associated with communication failures between physicians, while 28% were associated with communication breakdowns between doctors and nurses. Of the communication mishap cases, 17% were associated with communication failures among physicians and mid-level providers and 10% were associated with breakdowns in communication between physicians and patients.
The Coverys report includes guidance for ob.gyns. on reducing their legal risk when caring for patients in labor. Some primary tips include:
- Require fetal heart rate (FHR) interpretation training. All obstetric providers and staff should undergo training on the interpretation of FHR patterns before treating obstetric patients.
- Strengthen communication. Health professionals should use the same language when describing electronic fetal-monitoring patterns. Such terminology should be used consistently through all medical record entries and communications regarding patient cases.
- Craft and maintain fetal-monitoring policies. Develop evidence-based policies and procedures around fetal monitoring during labor that outline when each type of monitoring should be used based on each patient case and circumstance.
- Keep doctors informed. Develop protocols that ensure physicians remain in the loop regarding the condition of the patient and which includes communication strategies for contacting doctors when the patient’s condition changes or requires oversight.
Negligent management of labor is the top cause of lawsuits against ob.gyns, a study of legal claims shows.
Researchers with national medical liability insurer, Coverys, analyzed 472 ob.gyn.–related claims from their database that closed between 2013 and 2017. Of the claims, 37% stemmed from alleged negligence during labor management, while 14% resulted from inappropriate management of pregnancy, and 12% were associated with negligent patient monitoring. And 11% resulted from an alleged delay in performing cesarean section, according to the report.
More than half of the obstetric-related claims involved patients with at least one known comorbidity (58%), most commonly diabetes and obesity. Hypertension was the third most frequent risk factor associated with patient claims, followed by post-40 week gestation and macrosomia. Vaginal births were responsible for more claims than cesarean sections (52% vs. 45%); vaginal births also resulted in more than three times as many claims as did emergency cesareans.
Nearly all obstetrics claims resulted in injuries or death to babies (90%), with 41% of claims associated with neurologic injuries, 37% related to shoulder dystocia/brachial plexus injuries, and 34% ending in fetal demise, including stillbirth. Other claims included congenital injuries, chorioamnionitis, and lacerations/contusions.
Of 60 claims that included communication breakdowns as a key factor, 28% were associated with communication failures between physicians, while 28% were associated with communication breakdowns between doctors and nurses. Of the communication mishap cases, 17% were associated with communication failures among physicians and mid-level providers and 10% were associated with breakdowns in communication between physicians and patients.
The Coverys report includes guidance for ob.gyns. on reducing their legal risk when caring for patients in labor. Some primary tips include:
- Require fetal heart rate (FHR) interpretation training. All obstetric providers and staff should undergo training on the interpretation of FHR patterns before treating obstetric patients.
- Strengthen communication. Health professionals should use the same language when describing electronic fetal-monitoring patterns. Such terminology should be used consistently through all medical record entries and communications regarding patient cases.
- Craft and maintain fetal-monitoring policies. Develop evidence-based policies and procedures around fetal monitoring during labor that outline when each type of monitoring should be used based on each patient case and circumstance.
- Keep doctors informed. Develop protocols that ensure physicians remain in the loop regarding the condition of the patient and which includes communication strategies for contacting doctors when the patient’s condition changes or requires oversight.
Key clinical point: Consistent use of fetal-monitoring protocols is recommended to reduce potential legal risks.
Major finding Of 472 claims, 37% stemmed from alleged negligence during labor management.
Study details: Analysis of 472 ob.gyn.–related claims closed between 2013 and 2017.
Disclosures: Coverys is a national medical professional liability insurer.