User login
Try behavioral interventions for chronic insomnia
“The greatest medicine of all is teaching people how not to need it.” – Hippocrates
For many years, over-the-counter and prescription medications indicated for sleep problems/disorders have been available to patients. But the side effects associated with some of these medications are many. In light of the numerous nonpharmacologic interventions that are available to patients, they should be offered first when appropriate.
One of the top nonpharmacologic interventions is cognitive-behavioral therapy for insomnia, or CBT-I, which the American Academy of Sleep Medicine’s clinical guidelines say should be used as initial treatment if possible.1 Elements of CBT-I include cognitive therapy, which is aimed at reducing dysfunctional beliefs about sleep. Common distortions expressed by patients include: “I cannot sleep without medications” and “I must get 8 hours of sleep to feel refreshed and function well the next day.” It helps in dealing with anxiety and catastrophic thinking to establish realistic expectations and treatment related to insomnia.
CBT-I can be delivered in the form of monotherapy or in a combined manner. The individual components include psychoeducation, behavioral strategies, cognitive therapy, and relaxation training. CBT-I combines cognitive therapy with behavioral interventions. Behavioral elements include stimulus control therapy and sleep restriction therapy. Relaxation therapy might or might not be included. Sleep hygiene education usually is a part of it.2
Two other kinds of CBT that can be effective options are telephone-based CBT-I and Internet-based CBT-I.3,4 Meanwhile, among the disadvantages of CBT for insomnia are longer duration of therapy and lack of skilled clinicians.5
Many other kinds of behavioral interventions are available to patients with problems related to sleep, including stimulus control therapy, relaxation therapy, exercise therapy, and sleep restriction therapy.
Stimulus control therapy
This is a strategy aimed at strengthening the association of bed and bedroom to sleep, establishing a consistent sleep-wake rhythm, and reducing the activities that might interfere with sleep. This behavioral therapy is based on the idea that arousal occurs as a conditioned response to the stimulus of sleep environment, and it is among the most effective behavioral treatments.6,7 Strategies include the following:
1. Lie down with the intention of sleeping when sleepy.
2. Do not watch television, read, eat or worry while in bed. Use bed only for sleep and sex.
3. Get out of bed if unable to fall asleep within 10-15 minutes and go to another room. Return to bed only when sleepy. Do not watch the clock. Repeat this step as many times as necessary throughout the night.
4. Set an alarm clock to wake up at a fixed time each morning, including weekends, regardless of how much sleep you got during the night.
5. Do not take a nap during the day.
The goal of these strategies is to extinguish negative associations between bed and undesirable outcomes, such as wakefulness and frustration. One study showed that stimulus control participants, unlike control group participants, experienced significant improvement at follow-up for total sleep time, sleep efficiency, and sleep quality.8
Relaxation therapy
This encompasses different techniques that produce a relaxation response and reduce somatic arousal. It can be implemented before each sleep period. Progressive muscle relaxation, autogenic training, and biofeedback help reduce somatic arousal. Attention-focused procedures, such as imagery training and meditation, tend to lower presleep cognitive arousal (for example, intrusive thoughts, racing minds).9 Slow paced breathing prior to onset of sleep enhances vagal activity, which results in improved sleep parameters.10 One study showed improved quality of sleep and cognitive functions in the elderly by self-relaxation training.11
Exercise training
Participating in physical exercise can be useful in the treatment of insomnia.12 One randomized, controlled trial found that exercising regularly for at least 150 minutes per week was optimal.13 Another study found that, among overweight and obese men with insomnia, aerobic exercise over a 6-month period reduced difficulty in initiating and improving sleep.14
Sleep restriction therapy
The goal of this therapy is to increase the homeostatic drive to sleep. This is carried out by limiting the amount of time spent in bed to the same amount of time that the person reports sleeping. Naps are not allowed. Patients improve with increased drive to sleep in successive nights. In patients with bipolar disorder, however, sleep restriction should be used with caution as it can trigger manic episodes.15
Always ask about sleep
Clinicians should always ask patients about sleep during visits. Sleep duration and sleep quality should be assessed. Insomnia, which is an independent condition, may or may not coexist with other conditions. It is important to determine whether another sleep disorder, or a physical (such as pain, heart, or lung disease), neurological (such as Parkinson’s disease or cerebrovascular disease), or psychiatric disorder (such as depressive illness, anxiety disorder, or substance misuse) is the primary diagnosis. Treatment of insomnia can improve comorbidities.16
In addition, it is important to teach patients about basic sleep hygiene, which includes abiding by a consistent bedtime, and avoiding coffee, alcohol, and nicotine. Eliminating a bedroom clock, not exercising in the late afternoon/early evening, and consuming light bedtime snacks are other measures that can be taken. Avoiding the prolonged use of light-emitting screens before bedtime is another positive step.17
In conclusion, cognitive and behavioral methods are just as effective as prescription medications for short-term treatment of chronic insomnia and should be considered as first line before considering medications. The beneficial effects of CBT-I, in contrast to those produced by medication, might last well beyond the termination of active treatment.
References
1. J Clin Sleep Med. 2008 Oct 15;4(5):487-504.
2. J Clin Psychol. 2010;66(11):1148-60.
3. Sleep. 2013 Mar 1;36(3):353-62.
4. Sleep Med Rev. 2016 Dec;30:1-10.
5. BMC Family Prac. 2012;13:40.
6. Sleep. 2006 Nov;29(11):1398-414.
7. Behavioral Treatments for Sleep Disorders. 1991. doi: 10.1016/13978-0-12-381522-4.00002-X.
8. Behav Modif 1998 Jan;22(1):3-28.
9. Am Fam Physician. 1999 Jun;59(11):3029-38.
10. Psychophysiology. 2015 Mar;52(3):388-96.
11. J Clin Nursing. 2013 April 10. doi: 10.1111/jocn.12096.
12. J Physiother. 2012;58(3):157-63.
13. J Sleep Res. 2015 Oct;24(5):526-34.
14 Sleep Med. 2016 Sep;25:113-121.
15. Am J Psychiatry. 2013 Jul;170(7):716-20.
16. JAMA Intern Med. 2015 Sep;175(9):1461-72.
17. Proc Natl Acad Sci USA. 2015;112(4):1232-7.
Dr. Lamba is a psychiatrist and medical director at Bayridge Hospital in Lynn, Mass. Dr. Rana is assistant professor of pediatrics at Boston University.
“The greatest medicine of all is teaching people how not to need it.” – Hippocrates
For many years, over-the-counter and prescription medications indicated for sleep problems/disorders have been available to patients. But the side effects associated with some of these medications are many. In light of the numerous nonpharmacologic interventions that are available to patients, they should be offered first when appropriate.
One of the top nonpharmacologic interventions is cognitive-behavioral therapy for insomnia, or CBT-I, which the American Academy of Sleep Medicine’s clinical guidelines say should be used as initial treatment if possible.1 Elements of CBT-I include cognitive therapy, which is aimed at reducing dysfunctional beliefs about sleep. Common distortions expressed by patients include: “I cannot sleep without medications” and “I must get 8 hours of sleep to feel refreshed and function well the next day.” It helps in dealing with anxiety and catastrophic thinking to establish realistic expectations and treatment related to insomnia.
CBT-I can be delivered in the form of monotherapy or in a combined manner. The individual components include psychoeducation, behavioral strategies, cognitive therapy, and relaxation training. CBT-I combines cognitive therapy with behavioral interventions. Behavioral elements include stimulus control therapy and sleep restriction therapy. Relaxation therapy might or might not be included. Sleep hygiene education usually is a part of it.2
Two other kinds of CBT that can be effective options are telephone-based CBT-I and Internet-based CBT-I.3,4 Meanwhile, among the disadvantages of CBT for insomnia are longer duration of therapy and lack of skilled clinicians.5
Many other kinds of behavioral interventions are available to patients with problems related to sleep, including stimulus control therapy, relaxation therapy, exercise therapy, and sleep restriction therapy.
Stimulus control therapy
This is a strategy aimed at strengthening the association of bed and bedroom to sleep, establishing a consistent sleep-wake rhythm, and reducing the activities that might interfere with sleep. This behavioral therapy is based on the idea that arousal occurs as a conditioned response to the stimulus of sleep environment, and it is among the most effective behavioral treatments.6,7 Strategies include the following:
1. Lie down with the intention of sleeping when sleepy.
2. Do not watch television, read, eat or worry while in bed. Use bed only for sleep and sex.
3. Get out of bed if unable to fall asleep within 10-15 minutes and go to another room. Return to bed only when sleepy. Do not watch the clock. Repeat this step as many times as necessary throughout the night.
4. Set an alarm clock to wake up at a fixed time each morning, including weekends, regardless of how much sleep you got during the night.
5. Do not take a nap during the day.
The goal of these strategies is to extinguish negative associations between bed and undesirable outcomes, such as wakefulness and frustration. One study showed that stimulus control participants, unlike control group participants, experienced significant improvement at follow-up for total sleep time, sleep efficiency, and sleep quality.8
Relaxation therapy
This encompasses different techniques that produce a relaxation response and reduce somatic arousal. It can be implemented before each sleep period. Progressive muscle relaxation, autogenic training, and biofeedback help reduce somatic arousal. Attention-focused procedures, such as imagery training and meditation, tend to lower presleep cognitive arousal (for example, intrusive thoughts, racing minds).9 Slow paced breathing prior to onset of sleep enhances vagal activity, which results in improved sleep parameters.10 One study showed improved quality of sleep and cognitive functions in the elderly by self-relaxation training.11
Exercise training
Participating in physical exercise can be useful in the treatment of insomnia.12 One randomized, controlled trial found that exercising regularly for at least 150 minutes per week was optimal.13 Another study found that, among overweight and obese men with insomnia, aerobic exercise over a 6-month period reduced difficulty in initiating and improving sleep.14
Sleep restriction therapy
The goal of this therapy is to increase the homeostatic drive to sleep. This is carried out by limiting the amount of time spent in bed to the same amount of time that the person reports sleeping. Naps are not allowed. Patients improve with increased drive to sleep in successive nights. In patients with bipolar disorder, however, sleep restriction should be used with caution as it can trigger manic episodes.15
Always ask about sleep
Clinicians should always ask patients about sleep during visits. Sleep duration and sleep quality should be assessed. Insomnia, which is an independent condition, may or may not coexist with other conditions. It is important to determine whether another sleep disorder, or a physical (such as pain, heart, or lung disease), neurological (such as Parkinson’s disease or cerebrovascular disease), or psychiatric disorder (such as depressive illness, anxiety disorder, or substance misuse) is the primary diagnosis. Treatment of insomnia can improve comorbidities.16
In addition, it is important to teach patients about basic sleep hygiene, which includes abiding by a consistent bedtime, and avoiding coffee, alcohol, and nicotine. Eliminating a bedroom clock, not exercising in the late afternoon/early evening, and consuming light bedtime snacks are other measures that can be taken. Avoiding the prolonged use of light-emitting screens before bedtime is another positive step.17
In conclusion, cognitive and behavioral methods are just as effective as prescription medications for short-term treatment of chronic insomnia and should be considered as first line before considering medications. The beneficial effects of CBT-I, in contrast to those produced by medication, might last well beyond the termination of active treatment.
References
1. J Clin Sleep Med. 2008 Oct 15;4(5):487-504.
2. J Clin Psychol. 2010;66(11):1148-60.
3. Sleep. 2013 Mar 1;36(3):353-62.
4. Sleep Med Rev. 2016 Dec;30:1-10.
5. BMC Family Prac. 2012;13:40.
6. Sleep. 2006 Nov;29(11):1398-414.
7. Behavioral Treatments for Sleep Disorders. 1991. doi: 10.1016/13978-0-12-381522-4.00002-X.
8. Behav Modif 1998 Jan;22(1):3-28.
9. Am Fam Physician. 1999 Jun;59(11):3029-38.
10. Psychophysiology. 2015 Mar;52(3):388-96.
11. J Clin Nursing. 2013 April 10. doi: 10.1111/jocn.12096.
12. J Physiother. 2012;58(3):157-63.
13. J Sleep Res. 2015 Oct;24(5):526-34.
14 Sleep Med. 2016 Sep;25:113-121.
15. Am J Psychiatry. 2013 Jul;170(7):716-20.
16. JAMA Intern Med. 2015 Sep;175(9):1461-72.
17. Proc Natl Acad Sci USA. 2015;112(4):1232-7.
Dr. Lamba is a psychiatrist and medical director at Bayridge Hospital in Lynn, Mass. Dr. Rana is assistant professor of pediatrics at Boston University.
“The greatest medicine of all is teaching people how not to need it.” – Hippocrates
For many years, over-the-counter and prescription medications indicated for sleep problems/disorders have been available to patients. But the side effects associated with some of these medications are many. In light of the numerous nonpharmacologic interventions that are available to patients, they should be offered first when appropriate.
One of the top nonpharmacologic interventions is cognitive-behavioral therapy for insomnia, or CBT-I, which the American Academy of Sleep Medicine’s clinical guidelines say should be used as initial treatment if possible.1 Elements of CBT-I include cognitive therapy, which is aimed at reducing dysfunctional beliefs about sleep. Common distortions expressed by patients include: “I cannot sleep without medications” and “I must get 8 hours of sleep to feel refreshed and function well the next day.” It helps in dealing with anxiety and catastrophic thinking to establish realistic expectations and treatment related to insomnia.
CBT-I can be delivered in the form of monotherapy or in a combined manner. The individual components include psychoeducation, behavioral strategies, cognitive therapy, and relaxation training. CBT-I combines cognitive therapy with behavioral interventions. Behavioral elements include stimulus control therapy and sleep restriction therapy. Relaxation therapy might or might not be included. Sleep hygiene education usually is a part of it.2
Two other kinds of CBT that can be effective options are telephone-based CBT-I and Internet-based CBT-I.3,4 Meanwhile, among the disadvantages of CBT for insomnia are longer duration of therapy and lack of skilled clinicians.5
Many other kinds of behavioral interventions are available to patients with problems related to sleep, including stimulus control therapy, relaxation therapy, exercise therapy, and sleep restriction therapy.
Stimulus control therapy
This is a strategy aimed at strengthening the association of bed and bedroom to sleep, establishing a consistent sleep-wake rhythm, and reducing the activities that might interfere with sleep. This behavioral therapy is based on the idea that arousal occurs as a conditioned response to the stimulus of sleep environment, and it is among the most effective behavioral treatments.6,7 Strategies include the following:
1. Lie down with the intention of sleeping when sleepy.
2. Do not watch television, read, eat or worry while in bed. Use bed only for sleep and sex.
3. Get out of bed if unable to fall asleep within 10-15 minutes and go to another room. Return to bed only when sleepy. Do not watch the clock. Repeat this step as many times as necessary throughout the night.
4. Set an alarm clock to wake up at a fixed time each morning, including weekends, regardless of how much sleep you got during the night.
5. Do not take a nap during the day.
The goal of these strategies is to extinguish negative associations between bed and undesirable outcomes, such as wakefulness and frustration. One study showed that stimulus control participants, unlike control group participants, experienced significant improvement at follow-up for total sleep time, sleep efficiency, and sleep quality.8
Relaxation therapy
This encompasses different techniques that produce a relaxation response and reduce somatic arousal. It can be implemented before each sleep period. Progressive muscle relaxation, autogenic training, and biofeedback help reduce somatic arousal. Attention-focused procedures, such as imagery training and meditation, tend to lower presleep cognitive arousal (for example, intrusive thoughts, racing minds).9 Slow paced breathing prior to onset of sleep enhances vagal activity, which results in improved sleep parameters.10 One study showed improved quality of sleep and cognitive functions in the elderly by self-relaxation training.11
Exercise training
Participating in physical exercise can be useful in the treatment of insomnia.12 One randomized, controlled trial found that exercising regularly for at least 150 minutes per week was optimal.13 Another study found that, among overweight and obese men with insomnia, aerobic exercise over a 6-month period reduced difficulty in initiating and improving sleep.14
Sleep restriction therapy
The goal of this therapy is to increase the homeostatic drive to sleep. This is carried out by limiting the amount of time spent in bed to the same amount of time that the person reports sleeping. Naps are not allowed. Patients improve with increased drive to sleep in successive nights. In patients with bipolar disorder, however, sleep restriction should be used with caution as it can trigger manic episodes.15
Always ask about sleep
Clinicians should always ask patients about sleep during visits. Sleep duration and sleep quality should be assessed. Insomnia, which is an independent condition, may or may not coexist with other conditions. It is important to determine whether another sleep disorder, or a physical (such as pain, heart, or lung disease), neurological (such as Parkinson’s disease or cerebrovascular disease), or psychiatric disorder (such as depressive illness, anxiety disorder, or substance misuse) is the primary diagnosis. Treatment of insomnia can improve comorbidities.16
In addition, it is important to teach patients about basic sleep hygiene, which includes abiding by a consistent bedtime, and avoiding coffee, alcohol, and nicotine. Eliminating a bedroom clock, not exercising in the late afternoon/early evening, and consuming light bedtime snacks are other measures that can be taken. Avoiding the prolonged use of light-emitting screens before bedtime is another positive step.17
In conclusion, cognitive and behavioral methods are just as effective as prescription medications for short-term treatment of chronic insomnia and should be considered as first line before considering medications. The beneficial effects of CBT-I, in contrast to those produced by medication, might last well beyond the termination of active treatment.
References
1. J Clin Sleep Med. 2008 Oct 15;4(5):487-504.
2. J Clin Psychol. 2010;66(11):1148-60.
3. Sleep. 2013 Mar 1;36(3):353-62.
4. Sleep Med Rev. 2016 Dec;30:1-10.
5. BMC Family Prac. 2012;13:40.
6. Sleep. 2006 Nov;29(11):1398-414.
7. Behavioral Treatments for Sleep Disorders. 1991. doi: 10.1016/13978-0-12-381522-4.00002-X.
8. Behav Modif 1998 Jan;22(1):3-28.
9. Am Fam Physician. 1999 Jun;59(11):3029-38.
10. Psychophysiology. 2015 Mar;52(3):388-96.
11. J Clin Nursing. 2013 April 10. doi: 10.1111/jocn.12096.
12. J Physiother. 2012;58(3):157-63.
13. J Sleep Res. 2015 Oct;24(5):526-34.
14 Sleep Med. 2016 Sep;25:113-121.
15. Am J Psychiatry. 2013 Jul;170(7):716-20.
16. JAMA Intern Med. 2015 Sep;175(9):1461-72.
17. Proc Natl Acad Sci USA. 2015;112(4):1232-7.
Dr. Lamba is a psychiatrist and medical director at Bayridge Hospital in Lynn, Mass. Dr. Rana is assistant professor of pediatrics at Boston University.
Who is in charge here?
My first patient of the afternoon was a simple hypertension follow-up, or so I thought as I was walking into the room. She was a healthy 50-year-old woman with no medical problems other than her blood pressure, which was measured at 130/76 in the office. Her heart and lungs were normal, she had no chest pain or shortness of breath, and she was taking her medications without any problem. All simple enough. I complimented her on how she was doing, told her to continue her medications, and return in 6 months.
She put up her hand and said, “Wait a minute.”
Then she pulled out her smartphone. She tapped open an app, and handed it to me so I could look at a graph of her home blood pressures. The graph had all of her readings from the last 4 months, taken 2-3 times a day. It had automatically labeled each blood pressure in green, yellow, or red to indicate whether they were normal, higher than normal, or elevated, respectively.
Of course, the app creators had determined that a ‘green’ (normal) systolic pressure was less than 120 mm Hg. Values above that were yellow (higher than normal), until a systolic pressure of 130, at which point they became red (elevated). This is consistent with the most recent American Heart Association guidelines, but these guidelines have been the subject of a lot of controversy. There are many, including myself, who believe that the correct systolic pressure to define hypertension should be 140 for many patients, rather than 130. The app disagrees, and patients using the app see the app’s definition of hypertension every time they enter a blood pressure. In the case of my patient, since normal was indicated only by a systolic of less than 120 (which is a relatively rare event), I had to explain the difference between normal blood pressure and her blood pressure goal, and why the two were not the same.
Later that afternoon I was seeing a 60-year-old male who had electrical cardioversion of his atrial fibrillation 2 weeks prior to the visit. He had been sent home, as is usually the case, on an antiarrhythmic and an oral anticoagulant. He was feeling fine and had not noticed any palpitations, chest discomfort, or shortness of breath. I listened to his heart and lungs, which sounded normal, and I told him it sounded like he was doing well. Then he said, “I have an Apple watch.” I had a feeling I knew what was coming next.
He handed me his iPhone and asked me if I could review his rhythm strips. For those unacquainted with the new Apple watch, all he had to do to obtain those strips was open an EKG app and touch the crown of his watch with a finger from his other hand. This essentially made an electrical connection from his left to right arm, allowing the watch to generate a one-lead EKG tracing. The device then provides a computer-generated rhythm strip and sends that image and an interpretation of it to an iPhone, which is connected to the watch via Bluetooth. These results can then be shared or printed out as a pdf document.
The patient wanted to know if the smartphone’s interpretation of those rhythm strips was correct, and if he was really having frequent asymptomatic recurrence of his atrial fibrillation. Unsurprising to me or anyone who has used one of these (or other) phone-based EKG devices, the watch-generated rhythm strips looked clean and clear and the interpretation was spot on. It correctly identified his frequent asymptomatic episodes of atrial fibrillation. This was important information, which markedly affected his medical care.
These two very different examples are early indications that the way that we will be collecting information will rapidly and radically change over the next few years. It has always been clear that making long-term decisions about the treatment of hypertension based on a single reading in the office setting is not optimal. It has been equally clear that a single office EKG provides a limited snapshot into the frequency of intermittent atrial fibrillation. Deciding how to treat patients has never been easy and many decisions are plagued with ambiguity. Having limited information is a blessing and a curse; it’s quick and easy to review a small amount of data, but there is a nagging recognition that those data are only a distant representation of a patient’s real health outside of the office.
As we move forward we will increasingly have the ability to see a patient’s physiologic parameters where and when those values are most important: during the countless hours when they are not in our offices. The new American Heart Association hypertension guideline, issued in late 2017, has placed increased emphasis on ambulatory blood pressure monitoring. Determining how to use all this new information will be a challenge. It will take time to become comfortable with interpreting and making sense of an incredible number of data points. For example, if a patient checks his blood pressure twice a day for 3 months, his efforts will generate 180 separate blood pressure readings! You can bet there is going to be a good deal of inconsistency in those readings, making interpretation challenging. There will also probably be a few high readings, such as the occasional 190/110, which are likely to cause concern and anxiety in patients. There is little question that the availability of such detailed information holds the potential to allow us to make better decisions. The challenge will be in deciding how to use it to actually improve – not just complicate – patient care.
What are your thoughts on this? Feel free to email us at [email protected].
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on twitter (@doctornotte).
My first patient of the afternoon was a simple hypertension follow-up, or so I thought as I was walking into the room. She was a healthy 50-year-old woman with no medical problems other than her blood pressure, which was measured at 130/76 in the office. Her heart and lungs were normal, she had no chest pain or shortness of breath, and she was taking her medications without any problem. All simple enough. I complimented her on how she was doing, told her to continue her medications, and return in 6 months.
She put up her hand and said, “Wait a minute.”
Then she pulled out her smartphone. She tapped open an app, and handed it to me so I could look at a graph of her home blood pressures. The graph had all of her readings from the last 4 months, taken 2-3 times a day. It had automatically labeled each blood pressure in green, yellow, or red to indicate whether they were normal, higher than normal, or elevated, respectively.
Of course, the app creators had determined that a ‘green’ (normal) systolic pressure was less than 120 mm Hg. Values above that were yellow (higher than normal), until a systolic pressure of 130, at which point they became red (elevated). This is consistent with the most recent American Heart Association guidelines, but these guidelines have been the subject of a lot of controversy. There are many, including myself, who believe that the correct systolic pressure to define hypertension should be 140 for many patients, rather than 130. The app disagrees, and patients using the app see the app’s definition of hypertension every time they enter a blood pressure. In the case of my patient, since normal was indicated only by a systolic of less than 120 (which is a relatively rare event), I had to explain the difference between normal blood pressure and her blood pressure goal, and why the two were not the same.
Later that afternoon I was seeing a 60-year-old male who had electrical cardioversion of his atrial fibrillation 2 weeks prior to the visit. He had been sent home, as is usually the case, on an antiarrhythmic and an oral anticoagulant. He was feeling fine and had not noticed any palpitations, chest discomfort, or shortness of breath. I listened to his heart and lungs, which sounded normal, and I told him it sounded like he was doing well. Then he said, “I have an Apple watch.” I had a feeling I knew what was coming next.
He handed me his iPhone and asked me if I could review his rhythm strips. For those unacquainted with the new Apple watch, all he had to do to obtain those strips was open an EKG app and touch the crown of his watch with a finger from his other hand. This essentially made an electrical connection from his left to right arm, allowing the watch to generate a one-lead EKG tracing. The device then provides a computer-generated rhythm strip and sends that image and an interpretation of it to an iPhone, which is connected to the watch via Bluetooth. These results can then be shared or printed out as a pdf document.
The patient wanted to know if the smartphone’s interpretation of those rhythm strips was correct, and if he was really having frequent asymptomatic recurrence of his atrial fibrillation. Unsurprising to me or anyone who has used one of these (or other) phone-based EKG devices, the watch-generated rhythm strips looked clean and clear and the interpretation was spot on. It correctly identified his frequent asymptomatic episodes of atrial fibrillation. This was important information, which markedly affected his medical care.
These two very different examples are early indications that the way that we will be collecting information will rapidly and radically change over the next few years. It has always been clear that making long-term decisions about the treatment of hypertension based on a single reading in the office setting is not optimal. It has been equally clear that a single office EKG provides a limited snapshot into the frequency of intermittent atrial fibrillation. Deciding how to treat patients has never been easy and many decisions are plagued with ambiguity. Having limited information is a blessing and a curse; it’s quick and easy to review a small amount of data, but there is a nagging recognition that those data are only a distant representation of a patient’s real health outside of the office.
As we move forward we will increasingly have the ability to see a patient’s physiologic parameters where and when those values are most important: during the countless hours when they are not in our offices. The new American Heart Association hypertension guideline, issued in late 2017, has placed increased emphasis on ambulatory blood pressure monitoring. Determining how to use all this new information will be a challenge. It will take time to become comfortable with interpreting and making sense of an incredible number of data points. For example, if a patient checks his blood pressure twice a day for 3 months, his efforts will generate 180 separate blood pressure readings! You can bet there is going to be a good deal of inconsistency in those readings, making interpretation challenging. There will also probably be a few high readings, such as the occasional 190/110, which are likely to cause concern and anxiety in patients. There is little question that the availability of such detailed information holds the potential to allow us to make better decisions. The challenge will be in deciding how to use it to actually improve – not just complicate – patient care.
What are your thoughts on this? Feel free to email us at [email protected].
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on twitter (@doctornotte).
My first patient of the afternoon was a simple hypertension follow-up, or so I thought as I was walking into the room. She was a healthy 50-year-old woman with no medical problems other than her blood pressure, which was measured at 130/76 in the office. Her heart and lungs were normal, she had no chest pain or shortness of breath, and she was taking her medications without any problem. All simple enough. I complimented her on how she was doing, told her to continue her medications, and return in 6 months.
She put up her hand and said, “Wait a minute.”
Then she pulled out her smartphone. She tapped open an app, and handed it to me so I could look at a graph of her home blood pressures. The graph had all of her readings from the last 4 months, taken 2-3 times a day. It had automatically labeled each blood pressure in green, yellow, or red to indicate whether they were normal, higher than normal, or elevated, respectively.
Of course, the app creators had determined that a ‘green’ (normal) systolic pressure was less than 120 mm Hg. Values above that were yellow (higher than normal), until a systolic pressure of 130, at which point they became red (elevated). This is consistent with the most recent American Heart Association guidelines, but these guidelines have been the subject of a lot of controversy. There are many, including myself, who believe that the correct systolic pressure to define hypertension should be 140 for many patients, rather than 130. The app disagrees, and patients using the app see the app’s definition of hypertension every time they enter a blood pressure. In the case of my patient, since normal was indicated only by a systolic of less than 120 (which is a relatively rare event), I had to explain the difference between normal blood pressure and her blood pressure goal, and why the two were not the same.
Later that afternoon I was seeing a 60-year-old male who had electrical cardioversion of his atrial fibrillation 2 weeks prior to the visit. He had been sent home, as is usually the case, on an antiarrhythmic and an oral anticoagulant. He was feeling fine and had not noticed any palpitations, chest discomfort, or shortness of breath. I listened to his heart and lungs, which sounded normal, and I told him it sounded like he was doing well. Then he said, “I have an Apple watch.” I had a feeling I knew what was coming next.
He handed me his iPhone and asked me if I could review his rhythm strips. For those unacquainted with the new Apple watch, all he had to do to obtain those strips was open an EKG app and touch the crown of his watch with a finger from his other hand. This essentially made an electrical connection from his left to right arm, allowing the watch to generate a one-lead EKG tracing. The device then provides a computer-generated rhythm strip and sends that image and an interpretation of it to an iPhone, which is connected to the watch via Bluetooth. These results can then be shared or printed out as a pdf document.
The patient wanted to know if the smartphone’s interpretation of those rhythm strips was correct, and if he was really having frequent asymptomatic recurrence of his atrial fibrillation. Unsurprising to me or anyone who has used one of these (or other) phone-based EKG devices, the watch-generated rhythm strips looked clean and clear and the interpretation was spot on. It correctly identified his frequent asymptomatic episodes of atrial fibrillation. This was important information, which markedly affected his medical care.
These two very different examples are early indications that the way that we will be collecting information will rapidly and radically change over the next few years. It has always been clear that making long-term decisions about the treatment of hypertension based on a single reading in the office setting is not optimal. It has been equally clear that a single office EKG provides a limited snapshot into the frequency of intermittent atrial fibrillation. Deciding how to treat patients has never been easy and many decisions are plagued with ambiguity. Having limited information is a blessing and a curse; it’s quick and easy to review a small amount of data, but there is a nagging recognition that those data are only a distant representation of a patient’s real health outside of the office.
As we move forward we will increasingly have the ability to see a patient’s physiologic parameters where and when those values are most important: during the countless hours when they are not in our offices. The new American Heart Association hypertension guideline, issued in late 2017, has placed increased emphasis on ambulatory blood pressure monitoring. Determining how to use all this new information will be a challenge. It will take time to become comfortable with interpreting and making sense of an incredible number of data points. For example, if a patient checks his blood pressure twice a day for 3 months, his efforts will generate 180 separate blood pressure readings! You can bet there is going to be a good deal of inconsistency in those readings, making interpretation challenging. There will also probably be a few high readings, such as the occasional 190/110, which are likely to cause concern and anxiety in patients. There is little question that the availability of such detailed information holds the potential to allow us to make better decisions. The challenge will be in deciding how to use it to actually improve – not just complicate – patient care.
What are your thoughts on this? Feel free to email us at [email protected].
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on twitter (@doctornotte).
Motherhood and the working psychiatrist
Raising a child is difficult. For working professional women, including doctors, that difficulty extends beyond bottles, bath time, and burping; it impacts day-to-day physiological function, time management, and emotional well-being.
The 1950s upheld a family model with traditional gender roles. By 1960, the family portrait of a breadwinner father and a stay-at-home mother with one or more children comprised 62% of American households.1 Precipitous changes occurred over the next decades as the housing market soared, education costs increased, and divorce rates rose. The 1980s ushered the arrival of women’s power suits and the notion of women “having it all.”1
Fast-forward to modern times. Medicine is changing, too. Women are slowly but surely starting to rise in this once male-led field. In 2017, for the first time more women than men enrolled in medical schools in the United States.2 In a 2015 report, the Association of American Medical Colleges found that 57% of residents who were pursuing psychiatry were women.3 And the median age of women applying to medical school who enrolled in 2017 or 2018 was 23 years.4
Choosing to parent as a physician poses challenges for women and men alike. As the rates of women in medicine and psychiatry are increasing, this article focuses on unique obstacles faced by mothers and aims to:
- explore the dueling duties of mothers who practice medicine
- consider the dilemma women face when returning to the workforce during the postpartum period
- discuss options for enhanced recognition and care of maternal and child well-being.
Duty: Being both parent and physician
The working psychiatrist mother has a duty to her patients and profession—not to mention a duty to her child. The demands are endless on both sides. No matter what stage of her professional career (medical school, residency, fellowship, or beyond) she chooses to begin motherhood, the responsibilities and expectations can be overwhelming. Doctor appointments, nausea and vomiting, fatigue, discomfort, and stress do not fit well within a schedule of intensive studying, working 24-hour shifts, navigating complex schedules, treating patients, and sorting out the financial heft of loan repayment, home ownership, contract negotiation, or relocation.5
Psychiatry carries a notable dichotomy of lecturing at length on the importance of maternal-infant attachment. John Bowlby argued that a child’s attachment to the mother is instinctual and primary, noting that early loss creates true mourning due to the primal ties of child to mother.6 Bowlby also asserted that personality development and psychopathology are rooted in the concept of attachment and the emotional security built through early childhood experiences.6
Continue to: Dr. Donald Winnnicott introduced the concept of...
Dr. Donald Winnicott introduced the concept of a “good-enough” mother in 1953.7 Today, although Winnicott’s teachings are explored in psychiatry training programs and practice, his concept does not resonate with many working mothers. Most physicians strive for perfection while struggling to balance their personal and professional lives.7
It’s no wonder that tales abound of female physicians being praised for their ability to take on grueling shifts up to their due date, forego lunch to pump breast milk, or cover shifts beyond child daycare closing times. This raises an interesting dilemma: Is the primary goal the efficiency of promoting commerce, patient numbers, and the workings of the health care system? Or is it the wellness of expecting mothers and the development and attachment of an infant to the parent? Is the goal to slowly and carefully craft our next generation of young humans? Or is there a way to “have it all”?
Dilemma: Misperceptions after returning to work
As they regain control of their bodies, sleep, and overall health, women who return to work during the postpartum period battle a myriad of misperceptions along with the logistical hurdles of breast-feeding. In a study of surgical residencies, 61% of program directors reported that female trainees’ work was negatively affected by becoming parents.8 But other evidence suggests there is a disparity between perception and reality.
As a result, misperceptions can negatively affect maternity leave or lactation time. Women often rightfully fear they may be viewed as taking leisure time or making convenient excuses to shirk responsibility, rather than focusing on the necessities for recovery, care, and bonding. Such pressures can lead to burnout and resentment. The struggle with breast-feeding is pervasive across all medical specialties. In a 2018 survey of 347 women who had children during surgical residency, 39% of respondents strongly considered leaving their training, 95.6% indicated that breast-feeding was important to them, and 58.1% stopped breast-feeding earlier than desired due to challenges faced in the workplace, such as poor access to lactation facilities and difficulty leaving the operating room to express milk.11
The American Academy of Pediatrics (AAP) recommends exclusive breast-feeding through 6 months of the postpartum period, and continued breast-feeding until the infant is at least 12 months old. Breast-feeding confers benefits to both the infant and mother, including positive impacts on the child’s cognitive development and health into adulthood, as well as higher productivity and lower absenteeism for breast-feeding mothers.12 By 2009, only 23 states had adopted laws to encourage breast-feeding in the workplace. In 2010, the United States government enacted the “reasonable break time” provision in Section 4207 of the Patient Protection and Affordable Care Act (ACA), which requires all employers to provide a period of time and private space other than a bathroom in which female employees can express milk for a child up to age 1.12
Continue to: In 2016...
In 2016, a follow-up national survey of employed women explored workplace changes after the ACA, and noted that only 40% of women had access to both break time and a private space for lactation.13 If the goal is to give working women a true choice of whether to continue breast-feeding after returning to work, these mothers need to be provided with the proper social and structural supports in order to allow for that personal decision.14
Discussion: Barriers to change
Breast-feeding, it has been argued, is the most enduring investment in women’s physical, cognitive, and social capacities, and provides protection for children against death, disease, and poverty.15 Research has shown that breast-feeding every child until age 1 would yield medical benefits, including fewer infections, increased intelligence in children, protection against breast cancer in mothers, and economic savings of $300 billion for the United States.15
We are no longer in the 1950s, but modern times still present challenges for mothers who are working as physicians. Although the AAP recommends that new parents receive 12 weeks leave from work, policies for faculty at the 12 top medical schools in the United States offer new mothers only approximately 2 months of paid leave.16 There also are problems of inconsistency among approaches to parenthood in graduate medical education (GME) training, different specialty clinical requirements, and different residency training programs. These factors all contribute to negative attitudes towards parenthood.17
We know the barriers for women.18 With more women entering the medical profession, we need to continue finding creative and workable solutions as these problems become more pressing.19 In a 2018 Time article, Lily Rothman wrote, “you can’t talk about breastfeeding in the United States without pointing out that every other wealthy country has found a way to accommodate breastfeeding mothers, and usually in the form of lengthy paid maternity leave.”20 However, maternity leave in the United States today dictates that mothers return to work while their children would still benefit from nursing.21
When it comes to GME and medical institutions, programs could look at barriers such as lack of accommodations for trainees who are pregnant or have young children. Addressing these barriers could include making private lactation rooms available and instituting flexible scheduling. It would be best if scheduling accommodations and policies were established by an institution’s administration, rather than leaving coverage up to the students or residents. Going further, institutions could consider offering flexible maternity leave and work schedules, allowing breaks for those who are breast-feeding, and creating lactation facilities.22 This could take the form of a breast-feeding support program that fits available budget resources.23
Continue to: Psychiatrists frequently discuss...
Psychiatrists frequently discuss Winnicott’s “good-enough mother” concept, with the mother transitioning from focusing on her baby’s needs to her own sense of personhood that is unable to respond to her baby’s every wish.6 This concept was established well before the shifting demographics of the nuclear family, the short maternity leaves and early returns to work, early separation of one’s infants to childcare settings, and experiences with pumped lactation milk that working mothers experience today. Is it any wonder childbearing female psychiatrists face a special kind of working-mother guilt?
1. Collins G. When everything changed: the amazing journey of American women from 1960 to the present. New York, NY: Little, Brown and Company; 2009;271, 301.
2. AAMCNews. More women than men enrolled in U.S. medical schools in 2017. Association of American Medical Colleges. https://news.aamc.org/press-releases/article/applicant-enrollment-2017/. Published December 18, 2017. Accessed November 21, 2018.
3. Vassar L. How medical specialties vary by gender. American Medical Association. https://wire.ama-assn.org/education/how-medical-specialties-vary-gender. Published February 18, 2015. Accessed November 21, 2018.
4. Association of American Medical Colleges. Table A-6: age of applicants to U.S. medical schools at anticipated matriculation by sex and race/ethnicity, 2014-2015 through 2017-2018. https://www.aamc.org/download/321468/data/factstablea6.pdf. Published November 30, 2017. Accessed February 7, 2019.
5. Jones V. Best time to have a baby as a physician? It depends. Doximity. https://opmed.doximity.com/articles/the-best-time-to-have-a-baby-as-a-physician-it-depends-c8064a92156c. Published September 11, 2017. Accessed November 21, 2018.
6. Mitchell SA, Black MJ. The British object relations school: W.R.D. Fairbairn and D.W. Winnicott. In: Freud and beyond: a history of modern psychoanalytic thought. New York, NY: Basic Books; 1995:125-126, 137.
7. Ratnapalan S, Batty H. To be good enough. Can Fam Physician. 2009;55(3):239-242.
8. Sandler BJ, Tackett JJ, Longo WE, et al. Pregnancy and parenthood among surgery residents: results of the first nationwide survey of general surgery residency program Directors. J Am Coll Surg. 2016;222(6):1090-1096.
9. Kmec JA. Are motherhood penalties and fatherhood bonuses warranted? Comparing pro-work behaviors and conditions of mothers, fathers, and non-parents. Social Science Research. 2011;40(2):444-459.
10. Hampton R. Working moms don’t deserve the blame for unfair work expectations. Slate. https://slate.com/human-interest/2018/05/working-moms-dont-deserve-blame-for-unfair-work-expectations.html. Published May 18, 2018. Accessed November 25, 2018.
11. Rangel EL, Smink DS, Castillo-Angeles M, et al. Pregnancy and motherhood during surgical training. JAMA Surgery. 2018;153(7):644-652.
12. Murtagh L, Moulton AD. Working mothers, breastfeeding, and the law. Am J Public Health. 2011;101(2):217-223.
13. Kozhimannil KB, Jou J, Gjerdingen DK, et al. Access to workplace accommodations to support breastfeeding after passage of the Affordable Care Act. Womens Health Issues. 2016;26(1):6-13.
14. Dinour LM, Bai YK. Breastfeeding: the illusion of choice. Womens Health Issues. 2016;26(5):479-482.
15. Hansen K. Breastfeeding: a smart investment in people and in economies. Lancet. 2016;387(10017):416.
16. Greenfield R. Even America’s top doctors aren’t getting the parental leave doctors recommend. Bloomberg. https://www.bloomberg.com/news/articles/2018-02-13/even-america-s-top-doctors-aren-t-getting-the-parental-leave-doctors-recommend. Published February 13, 2018. Accessed November 21, 2018.
17. Humphries LS, Lyon S, Garza R, et al. Parental leave policies in graduate medical education: a systematic review. American J Surg. 2017;214(4):634-639.
18. Raju TNK. Continued barriers for breast-feeding in public and the workplace. J Pediatr. 2006;148(5):677-679.
19. Stewart DE, Robinson GE. Combining motherhood with psychiatric training and practice. Can J Psychiatry. 1985;30(1):28-34.
20. Rothman L. D esperate women, desperate doctors and the surprising history behind the breastfeeding debate. Time. http://time.com/5353068/breastfeeding-debate-history/. Published July 31, 2018. Accessed November 21, 2018.
21. Livingston G. Among 41 nations, U.S. is the outlier when it comes to paid parental leave. Pew Research Center. http://www.pewresearch.org/fact-tank/2016/09/26/u-s-lacks-mandated-paid-parental-leave/. Published September 26, 2016. Accessed November 21, 2018.
22. McCluskey PD. Long hours, short leaves force moms to reconsider jobs as surgeons. Boston Globe. https://www.bostonglobe.com/metro/2018/03/21/new-survey-says-female-surgical-residents-struggle-balance-training-motherhood/2ENQU1aPZmIJYy20iaRlLL/story.html. Published March 21, 2018. Accessed November 21, 2018.
23. Dinour LM, Szaro JM. Employer-based programs to support breastfeeding among working mothers: a systematic review. Breastfeeding Med. 2017;12:131-141.
Raising a child is difficult. For working professional women, including doctors, that difficulty extends beyond bottles, bath time, and burping; it impacts day-to-day physiological function, time management, and emotional well-being.
The 1950s upheld a family model with traditional gender roles. By 1960, the family portrait of a breadwinner father and a stay-at-home mother with one or more children comprised 62% of American households.1 Precipitous changes occurred over the next decades as the housing market soared, education costs increased, and divorce rates rose. The 1980s ushered the arrival of women’s power suits and the notion of women “having it all.”1
Fast-forward to modern times. Medicine is changing, too. Women are slowly but surely starting to rise in this once male-led field. In 2017, for the first time more women than men enrolled in medical schools in the United States.2 In a 2015 report, the Association of American Medical Colleges found that 57% of residents who were pursuing psychiatry were women.3 And the median age of women applying to medical school who enrolled in 2017 or 2018 was 23 years.4
Choosing to parent as a physician poses challenges for women and men alike. As the rates of women in medicine and psychiatry are increasing, this article focuses on unique obstacles faced by mothers and aims to:
- explore the dueling duties of mothers who practice medicine
- consider the dilemma women face when returning to the workforce during the postpartum period
- discuss options for enhanced recognition and care of maternal and child well-being.
Duty: Being both parent and physician
The working psychiatrist mother has a duty to her patients and profession—not to mention a duty to her child. The demands are endless on both sides. No matter what stage of her professional career (medical school, residency, fellowship, or beyond) she chooses to begin motherhood, the responsibilities and expectations can be overwhelming. Doctor appointments, nausea and vomiting, fatigue, discomfort, and stress do not fit well within a schedule of intensive studying, working 24-hour shifts, navigating complex schedules, treating patients, and sorting out the financial heft of loan repayment, home ownership, contract negotiation, or relocation.5
Psychiatry carries a notable dichotomy of lecturing at length on the importance of maternal-infant attachment. John Bowlby argued that a child’s attachment to the mother is instinctual and primary, noting that early loss creates true mourning due to the primal ties of child to mother.6 Bowlby also asserted that personality development and psychopathology are rooted in the concept of attachment and the emotional security built through early childhood experiences.6
Continue to: Dr. Donald Winnnicott introduced the concept of...
Dr. Donald Winnicott introduced the concept of a “good-enough” mother in 1953.7 Today, although Winnicott’s teachings are explored in psychiatry training programs and practice, his concept does not resonate with many working mothers. Most physicians strive for perfection while struggling to balance their personal and professional lives.7
It’s no wonder that tales abound of female physicians being praised for their ability to take on grueling shifts up to their due date, forego lunch to pump breast milk, or cover shifts beyond child daycare closing times. This raises an interesting dilemma: Is the primary goal the efficiency of promoting commerce, patient numbers, and the workings of the health care system? Or is it the wellness of expecting mothers and the development and attachment of an infant to the parent? Is the goal to slowly and carefully craft our next generation of young humans? Or is there a way to “have it all”?
Dilemma: Misperceptions after returning to work
As they regain control of their bodies, sleep, and overall health, women who return to work during the postpartum period battle a myriad of misperceptions along with the logistical hurdles of breast-feeding. In a study of surgical residencies, 61% of program directors reported that female trainees’ work was negatively affected by becoming parents.8 But other evidence suggests there is a disparity between perception and reality.
As a result, misperceptions can negatively affect maternity leave or lactation time. Women often rightfully fear they may be viewed as taking leisure time or making convenient excuses to shirk responsibility, rather than focusing on the necessities for recovery, care, and bonding. Such pressures can lead to burnout and resentment. The struggle with breast-feeding is pervasive across all medical specialties. In a 2018 survey of 347 women who had children during surgical residency, 39% of respondents strongly considered leaving their training, 95.6% indicated that breast-feeding was important to them, and 58.1% stopped breast-feeding earlier than desired due to challenges faced in the workplace, such as poor access to lactation facilities and difficulty leaving the operating room to express milk.11
The American Academy of Pediatrics (AAP) recommends exclusive breast-feeding through 6 months of the postpartum period, and continued breast-feeding until the infant is at least 12 months old. Breast-feeding confers benefits to both the infant and mother, including positive impacts on the child’s cognitive development and health into adulthood, as well as higher productivity and lower absenteeism for breast-feeding mothers.12 By 2009, only 23 states had adopted laws to encourage breast-feeding in the workplace. In 2010, the United States government enacted the “reasonable break time” provision in Section 4207 of the Patient Protection and Affordable Care Act (ACA), which requires all employers to provide a period of time and private space other than a bathroom in which female employees can express milk for a child up to age 1.12
Continue to: In 2016...
In 2016, a follow-up national survey of employed women explored workplace changes after the ACA, and noted that only 40% of women had access to both break time and a private space for lactation.13 If the goal is to give working women a true choice of whether to continue breast-feeding after returning to work, these mothers need to be provided with the proper social and structural supports in order to allow for that personal decision.14
Discussion: Barriers to change
Breast-feeding, it has been argued, is the most enduring investment in women’s physical, cognitive, and social capacities, and provides protection for children against death, disease, and poverty.15 Research has shown that breast-feeding every child until age 1 would yield medical benefits, including fewer infections, increased intelligence in children, protection against breast cancer in mothers, and economic savings of $300 billion for the United States.15
We are no longer in the 1950s, but modern times still present challenges for mothers who are working as physicians. Although the AAP recommends that new parents receive 12 weeks leave from work, policies for faculty at the 12 top medical schools in the United States offer new mothers only approximately 2 months of paid leave.16 There also are problems of inconsistency among approaches to parenthood in graduate medical education (GME) training, different specialty clinical requirements, and different residency training programs. These factors all contribute to negative attitudes towards parenthood.17
We know the barriers for women.18 With more women entering the medical profession, we need to continue finding creative and workable solutions as these problems become more pressing.19 In a 2018 Time article, Lily Rothman wrote, “you can’t talk about breastfeeding in the United States without pointing out that every other wealthy country has found a way to accommodate breastfeeding mothers, and usually in the form of lengthy paid maternity leave.”20 However, maternity leave in the United States today dictates that mothers return to work while their children would still benefit from nursing.21
When it comes to GME and medical institutions, programs could look at barriers such as lack of accommodations for trainees who are pregnant or have young children. Addressing these barriers could include making private lactation rooms available and instituting flexible scheduling. It would be best if scheduling accommodations and policies were established by an institution’s administration, rather than leaving coverage up to the students or residents. Going further, institutions could consider offering flexible maternity leave and work schedules, allowing breaks for those who are breast-feeding, and creating lactation facilities.22 This could take the form of a breast-feeding support program that fits available budget resources.23
Continue to: Psychiatrists frequently discuss...
Psychiatrists frequently discuss Winnicott’s “good-enough mother” concept, with the mother transitioning from focusing on her baby’s needs to her own sense of personhood that is unable to respond to her baby’s every wish.6 This concept was established well before the shifting demographics of the nuclear family, the short maternity leaves and early returns to work, early separation of one’s infants to childcare settings, and experiences with pumped lactation milk that working mothers experience today. Is it any wonder childbearing female psychiatrists face a special kind of working-mother guilt?
Raising a child is difficult. For working professional women, including doctors, that difficulty extends beyond bottles, bath time, and burping; it impacts day-to-day physiological function, time management, and emotional well-being.
The 1950s upheld a family model with traditional gender roles. By 1960, the family portrait of a breadwinner father and a stay-at-home mother with one or more children comprised 62% of American households.1 Precipitous changes occurred over the next decades as the housing market soared, education costs increased, and divorce rates rose. The 1980s ushered the arrival of women’s power suits and the notion of women “having it all.”1
Fast-forward to modern times. Medicine is changing, too. Women are slowly but surely starting to rise in this once male-led field. In 2017, for the first time more women than men enrolled in medical schools in the United States.2 In a 2015 report, the Association of American Medical Colleges found that 57% of residents who were pursuing psychiatry were women.3 And the median age of women applying to medical school who enrolled in 2017 or 2018 was 23 years.4
Choosing to parent as a physician poses challenges for women and men alike. As the rates of women in medicine and psychiatry are increasing, this article focuses on unique obstacles faced by mothers and aims to:
- explore the dueling duties of mothers who practice medicine
- consider the dilemma women face when returning to the workforce during the postpartum period
- discuss options for enhanced recognition and care of maternal and child well-being.
Duty: Being both parent and physician
The working psychiatrist mother has a duty to her patients and profession—not to mention a duty to her child. The demands are endless on both sides. No matter what stage of her professional career (medical school, residency, fellowship, or beyond) she chooses to begin motherhood, the responsibilities and expectations can be overwhelming. Doctor appointments, nausea and vomiting, fatigue, discomfort, and stress do not fit well within a schedule of intensive studying, working 24-hour shifts, navigating complex schedules, treating patients, and sorting out the financial heft of loan repayment, home ownership, contract negotiation, or relocation.5
Psychiatry carries a notable dichotomy of lecturing at length on the importance of maternal-infant attachment. John Bowlby argued that a child’s attachment to the mother is instinctual and primary, noting that early loss creates true mourning due to the primal ties of child to mother.6 Bowlby also asserted that personality development and psychopathology are rooted in the concept of attachment and the emotional security built through early childhood experiences.6
Continue to: Dr. Donald Winnnicott introduced the concept of...
Dr. Donald Winnicott introduced the concept of a “good-enough” mother in 1953.7 Today, although Winnicott’s teachings are explored in psychiatry training programs and practice, his concept does not resonate with many working mothers. Most physicians strive for perfection while struggling to balance their personal and professional lives.7
It’s no wonder that tales abound of female physicians being praised for their ability to take on grueling shifts up to their due date, forego lunch to pump breast milk, or cover shifts beyond child daycare closing times. This raises an interesting dilemma: Is the primary goal the efficiency of promoting commerce, patient numbers, and the workings of the health care system? Or is it the wellness of expecting mothers and the development and attachment of an infant to the parent? Is the goal to slowly and carefully craft our next generation of young humans? Or is there a way to “have it all”?
Dilemma: Misperceptions after returning to work
As they regain control of their bodies, sleep, and overall health, women who return to work during the postpartum period battle a myriad of misperceptions along with the logistical hurdles of breast-feeding. In a study of surgical residencies, 61% of program directors reported that female trainees’ work was negatively affected by becoming parents.8 But other evidence suggests there is a disparity between perception and reality.
As a result, misperceptions can negatively affect maternity leave or lactation time. Women often rightfully fear they may be viewed as taking leisure time or making convenient excuses to shirk responsibility, rather than focusing on the necessities for recovery, care, and bonding. Such pressures can lead to burnout and resentment. The struggle with breast-feeding is pervasive across all medical specialties. In a 2018 survey of 347 women who had children during surgical residency, 39% of respondents strongly considered leaving their training, 95.6% indicated that breast-feeding was important to them, and 58.1% stopped breast-feeding earlier than desired due to challenges faced in the workplace, such as poor access to lactation facilities and difficulty leaving the operating room to express milk.11
The American Academy of Pediatrics (AAP) recommends exclusive breast-feeding through 6 months of the postpartum period, and continued breast-feeding until the infant is at least 12 months old. Breast-feeding confers benefits to both the infant and mother, including positive impacts on the child’s cognitive development and health into adulthood, as well as higher productivity and lower absenteeism for breast-feeding mothers.12 By 2009, only 23 states had adopted laws to encourage breast-feeding in the workplace. In 2010, the United States government enacted the “reasonable break time” provision in Section 4207 of the Patient Protection and Affordable Care Act (ACA), which requires all employers to provide a period of time and private space other than a bathroom in which female employees can express milk for a child up to age 1.12
Continue to: In 2016...
In 2016, a follow-up national survey of employed women explored workplace changes after the ACA, and noted that only 40% of women had access to both break time and a private space for lactation.13 If the goal is to give working women a true choice of whether to continue breast-feeding after returning to work, these mothers need to be provided with the proper social and structural supports in order to allow for that personal decision.14
Discussion: Barriers to change
Breast-feeding, it has been argued, is the most enduring investment in women’s physical, cognitive, and social capacities, and provides protection for children against death, disease, and poverty.15 Research has shown that breast-feeding every child until age 1 would yield medical benefits, including fewer infections, increased intelligence in children, protection against breast cancer in mothers, and economic savings of $300 billion for the United States.15
We are no longer in the 1950s, but modern times still present challenges for mothers who are working as physicians. Although the AAP recommends that new parents receive 12 weeks leave from work, policies for faculty at the 12 top medical schools in the United States offer new mothers only approximately 2 months of paid leave.16 There also are problems of inconsistency among approaches to parenthood in graduate medical education (GME) training, different specialty clinical requirements, and different residency training programs. These factors all contribute to negative attitudes towards parenthood.17
We know the barriers for women.18 With more women entering the medical profession, we need to continue finding creative and workable solutions as these problems become more pressing.19 In a 2018 Time article, Lily Rothman wrote, “you can’t talk about breastfeeding in the United States without pointing out that every other wealthy country has found a way to accommodate breastfeeding mothers, and usually in the form of lengthy paid maternity leave.”20 However, maternity leave in the United States today dictates that mothers return to work while their children would still benefit from nursing.21
When it comes to GME and medical institutions, programs could look at barriers such as lack of accommodations for trainees who are pregnant or have young children. Addressing these barriers could include making private lactation rooms available and instituting flexible scheduling. It would be best if scheduling accommodations and policies were established by an institution’s administration, rather than leaving coverage up to the students or residents. Going further, institutions could consider offering flexible maternity leave and work schedules, allowing breaks for those who are breast-feeding, and creating lactation facilities.22 This could take the form of a breast-feeding support program that fits available budget resources.23
Continue to: Psychiatrists frequently discuss...
Psychiatrists frequently discuss Winnicott’s “good-enough mother” concept, with the mother transitioning from focusing on her baby’s needs to her own sense of personhood that is unable to respond to her baby’s every wish.6 This concept was established well before the shifting demographics of the nuclear family, the short maternity leaves and early returns to work, early separation of one’s infants to childcare settings, and experiences with pumped lactation milk that working mothers experience today. Is it any wonder childbearing female psychiatrists face a special kind of working-mother guilt?
1. Collins G. When everything changed: the amazing journey of American women from 1960 to the present. New York, NY: Little, Brown and Company; 2009;271, 301.
2. AAMCNews. More women than men enrolled in U.S. medical schools in 2017. Association of American Medical Colleges. https://news.aamc.org/press-releases/article/applicant-enrollment-2017/. Published December 18, 2017. Accessed November 21, 2018.
3. Vassar L. How medical specialties vary by gender. American Medical Association. https://wire.ama-assn.org/education/how-medical-specialties-vary-gender. Published February 18, 2015. Accessed November 21, 2018.
4. Association of American Medical Colleges. Table A-6: age of applicants to U.S. medical schools at anticipated matriculation by sex and race/ethnicity, 2014-2015 through 2017-2018. https://www.aamc.org/download/321468/data/factstablea6.pdf. Published November 30, 2017. Accessed February 7, 2019.
5. Jones V. Best time to have a baby as a physician? It depends. Doximity. https://opmed.doximity.com/articles/the-best-time-to-have-a-baby-as-a-physician-it-depends-c8064a92156c. Published September 11, 2017. Accessed November 21, 2018.
6. Mitchell SA, Black MJ. The British object relations school: W.R.D. Fairbairn and D.W. Winnicott. In: Freud and beyond: a history of modern psychoanalytic thought. New York, NY: Basic Books; 1995:125-126, 137.
7. Ratnapalan S, Batty H. To be good enough. Can Fam Physician. 2009;55(3):239-242.
8. Sandler BJ, Tackett JJ, Longo WE, et al. Pregnancy and parenthood among surgery residents: results of the first nationwide survey of general surgery residency program Directors. J Am Coll Surg. 2016;222(6):1090-1096.
9. Kmec JA. Are motherhood penalties and fatherhood bonuses warranted? Comparing pro-work behaviors and conditions of mothers, fathers, and non-parents. Social Science Research. 2011;40(2):444-459.
10. Hampton R. Working moms don’t deserve the blame for unfair work expectations. Slate. https://slate.com/human-interest/2018/05/working-moms-dont-deserve-blame-for-unfair-work-expectations.html. Published May 18, 2018. Accessed November 25, 2018.
11. Rangel EL, Smink DS, Castillo-Angeles M, et al. Pregnancy and motherhood during surgical training. JAMA Surgery. 2018;153(7):644-652.
12. Murtagh L, Moulton AD. Working mothers, breastfeeding, and the law. Am J Public Health. 2011;101(2):217-223.
13. Kozhimannil KB, Jou J, Gjerdingen DK, et al. Access to workplace accommodations to support breastfeeding after passage of the Affordable Care Act. Womens Health Issues. 2016;26(1):6-13.
14. Dinour LM, Bai YK. Breastfeeding: the illusion of choice. Womens Health Issues. 2016;26(5):479-482.
15. Hansen K. Breastfeeding: a smart investment in people and in economies. Lancet. 2016;387(10017):416.
16. Greenfield R. Even America’s top doctors aren’t getting the parental leave doctors recommend. Bloomberg. https://www.bloomberg.com/news/articles/2018-02-13/even-america-s-top-doctors-aren-t-getting-the-parental-leave-doctors-recommend. Published February 13, 2018. Accessed November 21, 2018.
17. Humphries LS, Lyon S, Garza R, et al. Parental leave policies in graduate medical education: a systematic review. American J Surg. 2017;214(4):634-639.
18. Raju TNK. Continued barriers for breast-feeding in public and the workplace. J Pediatr. 2006;148(5):677-679.
19. Stewart DE, Robinson GE. Combining motherhood with psychiatric training and practice. Can J Psychiatry. 1985;30(1):28-34.
20. Rothman L. D esperate women, desperate doctors and the surprising history behind the breastfeeding debate. Time. http://time.com/5353068/breastfeeding-debate-history/. Published July 31, 2018. Accessed November 21, 2018.
21. Livingston G. Among 41 nations, U.S. is the outlier when it comes to paid parental leave. Pew Research Center. http://www.pewresearch.org/fact-tank/2016/09/26/u-s-lacks-mandated-paid-parental-leave/. Published September 26, 2016. Accessed November 21, 2018.
22. McCluskey PD. Long hours, short leaves force moms to reconsider jobs as surgeons. Boston Globe. https://www.bostonglobe.com/metro/2018/03/21/new-survey-says-female-surgical-residents-struggle-balance-training-motherhood/2ENQU1aPZmIJYy20iaRlLL/story.html. Published March 21, 2018. Accessed November 21, 2018.
23. Dinour LM, Szaro JM. Employer-based programs to support breastfeeding among working mothers: a systematic review. Breastfeeding Med. 2017;12:131-141.
1. Collins G. When everything changed: the amazing journey of American women from 1960 to the present. New York, NY: Little, Brown and Company; 2009;271, 301.
2. AAMCNews. More women than men enrolled in U.S. medical schools in 2017. Association of American Medical Colleges. https://news.aamc.org/press-releases/article/applicant-enrollment-2017/. Published December 18, 2017. Accessed November 21, 2018.
3. Vassar L. How medical specialties vary by gender. American Medical Association. https://wire.ama-assn.org/education/how-medical-specialties-vary-gender. Published February 18, 2015. Accessed November 21, 2018.
4. Association of American Medical Colleges. Table A-6: age of applicants to U.S. medical schools at anticipated matriculation by sex and race/ethnicity, 2014-2015 through 2017-2018. https://www.aamc.org/download/321468/data/factstablea6.pdf. Published November 30, 2017. Accessed February 7, 2019.
5. Jones V. Best time to have a baby as a physician? It depends. Doximity. https://opmed.doximity.com/articles/the-best-time-to-have-a-baby-as-a-physician-it-depends-c8064a92156c. Published September 11, 2017. Accessed November 21, 2018.
6. Mitchell SA, Black MJ. The British object relations school: W.R.D. Fairbairn and D.W. Winnicott. In: Freud and beyond: a history of modern psychoanalytic thought. New York, NY: Basic Books; 1995:125-126, 137.
7. Ratnapalan S, Batty H. To be good enough. Can Fam Physician. 2009;55(3):239-242.
8. Sandler BJ, Tackett JJ, Longo WE, et al. Pregnancy and parenthood among surgery residents: results of the first nationwide survey of general surgery residency program Directors. J Am Coll Surg. 2016;222(6):1090-1096.
9. Kmec JA. Are motherhood penalties and fatherhood bonuses warranted? Comparing pro-work behaviors and conditions of mothers, fathers, and non-parents. Social Science Research. 2011;40(2):444-459.
10. Hampton R. Working moms don’t deserve the blame for unfair work expectations. Slate. https://slate.com/human-interest/2018/05/working-moms-dont-deserve-blame-for-unfair-work-expectations.html. Published May 18, 2018. Accessed November 25, 2018.
11. Rangel EL, Smink DS, Castillo-Angeles M, et al. Pregnancy and motherhood during surgical training. JAMA Surgery. 2018;153(7):644-652.
12. Murtagh L, Moulton AD. Working mothers, breastfeeding, and the law. Am J Public Health. 2011;101(2):217-223.
13. Kozhimannil KB, Jou J, Gjerdingen DK, et al. Access to workplace accommodations to support breastfeeding after passage of the Affordable Care Act. Womens Health Issues. 2016;26(1):6-13.
14. Dinour LM, Bai YK. Breastfeeding: the illusion of choice. Womens Health Issues. 2016;26(5):479-482.
15. Hansen K. Breastfeeding: a smart investment in people and in economies. Lancet. 2016;387(10017):416.
16. Greenfield R. Even America’s top doctors aren’t getting the parental leave doctors recommend. Bloomberg. https://www.bloomberg.com/news/articles/2018-02-13/even-america-s-top-doctors-aren-t-getting-the-parental-leave-doctors-recommend. Published February 13, 2018. Accessed November 21, 2018.
17. Humphries LS, Lyon S, Garza R, et al. Parental leave policies in graduate medical education: a systematic review. American J Surg. 2017;214(4):634-639.
18. Raju TNK. Continued barriers for breast-feeding in public and the workplace. J Pediatr. 2006;148(5):677-679.
19. Stewart DE, Robinson GE. Combining motherhood with psychiatric training and practice. Can J Psychiatry. 1985;30(1):28-34.
20. Rothman L. D esperate women, desperate doctors and the surprising history behind the breastfeeding debate. Time. http://time.com/5353068/breastfeeding-debate-history/. Published July 31, 2018. Accessed November 21, 2018.
21. Livingston G. Among 41 nations, U.S. is the outlier when it comes to paid parental leave. Pew Research Center. http://www.pewresearch.org/fact-tank/2016/09/26/u-s-lacks-mandated-paid-parental-leave/. Published September 26, 2016. Accessed November 21, 2018.
22. McCluskey PD. Long hours, short leaves force moms to reconsider jobs as surgeons. Boston Globe. https://www.bostonglobe.com/metro/2018/03/21/new-survey-says-female-surgical-residents-struggle-balance-training-motherhood/2ENQU1aPZmIJYy20iaRlLL/story.html. Published March 21, 2018. Accessed November 21, 2018.
23. Dinour LM, Szaro JM. Employer-based programs to support breastfeeding among working mothers: a systematic review. Breastfeeding Med. 2017;12:131-141.
Career Choices: Addiction psychiatry
Editor’s note: Career Choices features a psychiatry resident/fellow interviewing a psychiatrist about why he or she has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths.
In this Career Choices, Saeed Ahmed, MD, talked with Cornel Stanciu, MD. Dr. Stanciu is an addiction psychiatrist at Dartmouth’s Geisel School of Medicine, where he is an Assistant Professor, and serves as the Director of Addiction Services at New Hampshire Hospital. He provides support to clinicians managing patients with addictive disorders in a multitude of settings, and also assists with policy making and delivery of addiction care at the state level. He is also the author of Deciphering the Addicted Brain, a guide to help families and the general public better understand addictive disorders.
Dr. Ahmed: What attracted you to pursue subspecialty training in addictive disorders?
Dr. Stanciu: In the early stages of my training, I frequently encountered individuals with medical and mental health disorders whose treatment was impacted by underlying substance use. I soon came to realize any attempts at (for example) managing hypertension in someone with cocaine use disorder, or managing schizophrenia in someone with ongoing cannabis use, were futile. Almost all of my patients receiving treatment for mental health disorders were dependent on tobacco or other substances, and most were interested in cessation. Through mentorship from addiction-trained residency faculty members, I was able to get a taste of the neurobiologic complexities of the disease, something that left me with a desire to develop a deeper understanding of the disease process. Witnessing strikingly positive outcomes with implementation of evidence-based treatment modalities further solidified my path to subspecialty training. Even during that early phase, because I expressed interest in managing these conditions, I was immediately put in a position to share and disseminate any newly acquired knowledge to other specialties as well as the public.
Dr. Ahmed: Could one manage addictive disorders with just general psychiatry training, and what are the differences between the different paths to certification that a resident could undertake?
Dr. Stanciu: Addictive disorders fall under the general umbrella of psychiatric care. Most individuals with these disorders exhibit some degree of mental illness. Medical school curriculum offers on average 2 hours of addiction-related didactics during 4 years. General psychiatry training programs vary significantly in the type of exposure to addiction—some residencies have an affiliated addiction fellowship, others have addiction-trained psychiatrists on staff, but most have none. Ultimately, there is great variability in the degree of comfort in working with individuals with addictive disorders post-residency. Being able to prescribe medications for the treatment of addictive disorders is very different from being familiar with the latest evidence-based recommendations and guidelines; the latter is
Addiction medicine is a fairly new route initially intended to allow non-psychiatric specialties access to addictive disorders training and certification. This is offered through the American Board of Preventive Medicine. There are currently 2 routes to sitting for the exam: through completion of a 1-year addiction medicine fellowship, or through the “practice pathway” still available until 2020. To be eligible for the latter, individuals must provide documentation of clinical experience post-residency, which is quantified as number of hours spent treating patients with addictions, plus any additional courses or training, and must be endorsed by a certified addictionologist.
Continue to: What was your fellowship experience link...
Dr. Ahmed: What was your fellowship experience like, and what should one consider when choosing a program?
Dr. Stanciu: I completed my fellowship training through Dartmouth’s Geisel School of Medicine, and the experience was tremendously valuable. In evaluating programs, one of the starting points is whether you have interest in a formal research track, because several programs include an optional year for that. Most programs tend to provide exposure to the Veterans Affairs system. The 1 year should provide you with broad exposure to all possible settings, all addictive disorders and patient populations, and all treatment modalities, in addition to rigorous didactic sessions. The ideal program should include rotations through methadone treatment centers, intensive outpatient programs, pain and interdisciplinary clinics, detoxification units, and centers for treatment of adolescent and young adults, as well as general medical settings and infectious disease clinics. There should also be close collaboration with psychologists who can provide training in evidence-based therapeutic modalities. During this year, it is vital to expand your knowledge of the ethical and legal regulations of treatment programs, state and federal requirements, insurance complexities, and requirements for privacy and protection of health information. The size of these programs can vary significantly, which may limit the one-on-one time devoted to your training, which is something I personally valued. My faculty was very supportive of academic endeavors, providing guidance, funding, and encouragement for attending and presenting at conferences, publishing papers, and other academic pursuits. Additionally, faculty should be current with emerging literature and willing to develop or implement new protocols and evaluate new pharmacologic therapies.
Dr. Ahmed: What are some of the career options and work settings for addiction psychiatrists?
Dr. Stanciu: Addiction psychiatrists work in numerous settings and various capacities. They can provide subspecialty care directly by seeing patients in outpatient clinics or inpatient addiction treatment centers for detoxification or rehabilitation, or they can work with dual-diagnosis populations in inpatient units. The expansion of telemedicine also holds promise for a role through virtual services. Indirectly, they can serve as a resource for expertise in the field through consultations in medical and psychiatric settings, or through policy making by working with the legislature and public health departments. Additionally, they can help create and integrate new knowledge into practice and educate future generations of physicians and the public.
Dr. Ahmed: What are some of the prevalent disorders and reasons for consultation that you encounter in your daily practice?
Continue to: Dr. Stanciu's response...
Dr. Stanciu: This can vary significantly depending on the setting, geographical region, and demographics of the population. My main non-administrative responsibilities are primarily consultative assisting clinicians at a 200-bed psychiatric hospital to address co-occurring addictive disorders. In short-term units, I am primarily asked to provide input on issues related to various toxidromes and withdrawals and the use of relapse prevention medications for alcohol use disorders as well as the use of buprenorphine or other forms of medication-assisted treatment. I work closely with licensed drug and alcohol counselors in implementing brief interventions as well as facilitating outpatient treatment referrals. Clinicians in longer term units may consult on issues related to pain management in individuals who have addictive disorders, the use of evidence-based pharmacologic agents to address cravings, or the use of relapse prevention medications for someone close to discharge. In terms of specific drugs of abuse, although opioids have recently received a tremendous amount of attention due to the visible costs through overdose deaths, the magnitude of individuals who are losing years of quality life through the use of alcohol and tobacco is significant, and hence this is a large portion of the conditions I encounter. I have also seen an abundance of marijuana use due to decreased perception of harm and increased access.
Dr. Ahmed: What are some of the challenges in working in this field?
Dr. Stanciu: Historically, funding for services has been an issue for clinicians working primarily with addictive disorders from the standpoint of reimbursement, patient access to evidence-based pharmacotherapy, and ability to collaborate with existing levels of care. In recent years, federal funding and policies have changed this, and after numerous studies have found increased cost savings, commercial insurances are providing coverage. A significant challenge also has been public stigma and dealing with a condition that is relapsing-remitting, poorly understood by other specialties and the general public, and sometimes labeled as a defect of character. Several efforts in education have lessened this; however, the impact still takes a toll on patients, who may feel ashamed of their disorder and sometimes are hesitant to take medications because they may believe that they are not “clean” if they depend on a medication for remission. Lastly, recent changes in marijuana policies make conversations about this drug quite difficult because patients often view it as harmless, and the laws governing legality and indications for therapeutic use are slightly ahead of the evidence.
Dr. Ahmed: In what direction do you believe the subspecialty is headed?
Dr. Stanciu: Currently, there are approximately 1,000 certified addiction psychiatrists for the 45 million Americans who have addictive disorders. Smoking and other forms of tobacco use pose significant threats to the 2020 Healthy People Tobacco Use objectives. There is a significant demand for addictionologists in both public and private sectors. As with mental health, demand exceeds supply, and efforts are underway to expand downstream education and increase access to specialists. Several federal laws have been put in place to remove barriers and expand access to care and have paved the way to a brighter future. One is the Affordable Care Act, which requires all insurances including Medicaid to cover the cost of treatment. Second is the Mental Health Parity and Addiction Equity Act, which ensures that the duration and dollar amount of coverage for substance use disorders is comparable to that of medical and surgical care.
Continue to: Another exciting possibility...
Another exciting possibility comes from the world of pharmaceuticals. Some medications have modest efficacy for addressing addictive disorders; however, historically these have been poorly utilized. Enhanced understanding of the neurobiology combined with increased insurance reimbursement should prompt research and new drug development. Some promising agents are already in the pipeline. Research into molecular and gene therapy as a way to better individualize care is also underway.
Going forward, I think we will also encounter a different landscape of drugs. Synthetic agents are emerging and increasing in popularity. Alarmingly, public perception of harm is decreasing. When it comes to cannabis use, I see a rise in pathologic use and the ramifications of this will have a drastic impact, particularly on patients with mental health conditions. We will need to undertake better efforts in monitoring, staying updated, and providing public education campaigns.
Dr. Ahmed: What advice do you have for trainees contemplating subspecialty training in addiction psychiatry?
Dr. Stanciu: I cannot emphasize enough the importance of mentorship. The American Academy of Addiction Psychiatry has a robust system for connecting mentees with mentors at all stages in their careers. This can be extremely helpful, especially in situations where the residency program does not have addiction-trained faculty or rotations through treatment centers. Joining such an organization also grants you access to resources that can help further your enthusiasm. Those interested should also familiarize themselves with currently available pharmacotherapeutic treatments that have evidence supporting efficacy for various addictive disorders, and begin to incorporate these medications into general mental health practice, along with attempts at motivational interviewing. For example, begin discussing naltrexone with patients who have comorbid alcohol use disorders and are interested in reducing their drinking; and varenicline with patients who smoke and are interested in quitting. The outcomes should automatically elicit an interest in pursuing further training in the field!
Editor’s note: Career Choices features a psychiatry resident/fellow interviewing a psychiatrist about why he or she has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths.
In this Career Choices, Saeed Ahmed, MD, talked with Cornel Stanciu, MD. Dr. Stanciu is an addiction psychiatrist at Dartmouth’s Geisel School of Medicine, where he is an Assistant Professor, and serves as the Director of Addiction Services at New Hampshire Hospital. He provides support to clinicians managing patients with addictive disorders in a multitude of settings, and also assists with policy making and delivery of addiction care at the state level. He is also the author of Deciphering the Addicted Brain, a guide to help families and the general public better understand addictive disorders.
Dr. Ahmed: What attracted you to pursue subspecialty training in addictive disorders?
Dr. Stanciu: In the early stages of my training, I frequently encountered individuals with medical and mental health disorders whose treatment was impacted by underlying substance use. I soon came to realize any attempts at (for example) managing hypertension in someone with cocaine use disorder, or managing schizophrenia in someone with ongoing cannabis use, were futile. Almost all of my patients receiving treatment for mental health disorders were dependent on tobacco or other substances, and most were interested in cessation. Through mentorship from addiction-trained residency faculty members, I was able to get a taste of the neurobiologic complexities of the disease, something that left me with a desire to develop a deeper understanding of the disease process. Witnessing strikingly positive outcomes with implementation of evidence-based treatment modalities further solidified my path to subspecialty training. Even during that early phase, because I expressed interest in managing these conditions, I was immediately put in a position to share and disseminate any newly acquired knowledge to other specialties as well as the public.
Dr. Ahmed: Could one manage addictive disorders with just general psychiatry training, and what are the differences between the different paths to certification that a resident could undertake?
Dr. Stanciu: Addictive disorders fall under the general umbrella of psychiatric care. Most individuals with these disorders exhibit some degree of mental illness. Medical school curriculum offers on average 2 hours of addiction-related didactics during 4 years. General psychiatry training programs vary significantly in the type of exposure to addiction—some residencies have an affiliated addiction fellowship, others have addiction-trained psychiatrists on staff, but most have none. Ultimately, there is great variability in the degree of comfort in working with individuals with addictive disorders post-residency. Being able to prescribe medications for the treatment of addictive disorders is very different from being familiar with the latest evidence-based recommendations and guidelines; the latter is
Addiction medicine is a fairly new route initially intended to allow non-psychiatric specialties access to addictive disorders training and certification. This is offered through the American Board of Preventive Medicine. There are currently 2 routes to sitting for the exam: through completion of a 1-year addiction medicine fellowship, or through the “practice pathway” still available until 2020. To be eligible for the latter, individuals must provide documentation of clinical experience post-residency, which is quantified as number of hours spent treating patients with addictions, plus any additional courses or training, and must be endorsed by a certified addictionologist.
Continue to: What was your fellowship experience link...
Dr. Ahmed: What was your fellowship experience like, and what should one consider when choosing a program?
Dr. Stanciu: I completed my fellowship training through Dartmouth’s Geisel School of Medicine, and the experience was tremendously valuable. In evaluating programs, one of the starting points is whether you have interest in a formal research track, because several programs include an optional year for that. Most programs tend to provide exposure to the Veterans Affairs system. The 1 year should provide you with broad exposure to all possible settings, all addictive disorders and patient populations, and all treatment modalities, in addition to rigorous didactic sessions. The ideal program should include rotations through methadone treatment centers, intensive outpatient programs, pain and interdisciplinary clinics, detoxification units, and centers for treatment of adolescent and young adults, as well as general medical settings and infectious disease clinics. There should also be close collaboration with psychologists who can provide training in evidence-based therapeutic modalities. During this year, it is vital to expand your knowledge of the ethical and legal regulations of treatment programs, state and federal requirements, insurance complexities, and requirements for privacy and protection of health information. The size of these programs can vary significantly, which may limit the one-on-one time devoted to your training, which is something I personally valued. My faculty was very supportive of academic endeavors, providing guidance, funding, and encouragement for attending and presenting at conferences, publishing papers, and other academic pursuits. Additionally, faculty should be current with emerging literature and willing to develop or implement new protocols and evaluate new pharmacologic therapies.
Dr. Ahmed: What are some of the career options and work settings for addiction psychiatrists?
Dr. Stanciu: Addiction psychiatrists work in numerous settings and various capacities. They can provide subspecialty care directly by seeing patients in outpatient clinics or inpatient addiction treatment centers for detoxification or rehabilitation, or they can work with dual-diagnosis populations in inpatient units. The expansion of telemedicine also holds promise for a role through virtual services. Indirectly, they can serve as a resource for expertise in the field through consultations in medical and psychiatric settings, or through policy making by working with the legislature and public health departments. Additionally, they can help create and integrate new knowledge into practice and educate future generations of physicians and the public.
Dr. Ahmed: What are some of the prevalent disorders and reasons for consultation that you encounter in your daily practice?
Continue to: Dr. Stanciu's response...
Dr. Stanciu: This can vary significantly depending on the setting, geographical region, and demographics of the population. My main non-administrative responsibilities are primarily consultative assisting clinicians at a 200-bed psychiatric hospital to address co-occurring addictive disorders. In short-term units, I am primarily asked to provide input on issues related to various toxidromes and withdrawals and the use of relapse prevention medications for alcohol use disorders as well as the use of buprenorphine or other forms of medication-assisted treatment. I work closely with licensed drug and alcohol counselors in implementing brief interventions as well as facilitating outpatient treatment referrals. Clinicians in longer term units may consult on issues related to pain management in individuals who have addictive disorders, the use of evidence-based pharmacologic agents to address cravings, or the use of relapse prevention medications for someone close to discharge. In terms of specific drugs of abuse, although opioids have recently received a tremendous amount of attention due to the visible costs through overdose deaths, the magnitude of individuals who are losing years of quality life through the use of alcohol and tobacco is significant, and hence this is a large portion of the conditions I encounter. I have also seen an abundance of marijuana use due to decreased perception of harm and increased access.
Dr. Ahmed: What are some of the challenges in working in this field?
Dr. Stanciu: Historically, funding for services has been an issue for clinicians working primarily with addictive disorders from the standpoint of reimbursement, patient access to evidence-based pharmacotherapy, and ability to collaborate with existing levels of care. In recent years, federal funding and policies have changed this, and after numerous studies have found increased cost savings, commercial insurances are providing coverage. A significant challenge also has been public stigma and dealing with a condition that is relapsing-remitting, poorly understood by other specialties and the general public, and sometimes labeled as a defect of character. Several efforts in education have lessened this; however, the impact still takes a toll on patients, who may feel ashamed of their disorder and sometimes are hesitant to take medications because they may believe that they are not “clean” if they depend on a medication for remission. Lastly, recent changes in marijuana policies make conversations about this drug quite difficult because patients often view it as harmless, and the laws governing legality and indications for therapeutic use are slightly ahead of the evidence.
Dr. Ahmed: In what direction do you believe the subspecialty is headed?
Dr. Stanciu: Currently, there are approximately 1,000 certified addiction psychiatrists for the 45 million Americans who have addictive disorders. Smoking and other forms of tobacco use pose significant threats to the 2020 Healthy People Tobacco Use objectives. There is a significant demand for addictionologists in both public and private sectors. As with mental health, demand exceeds supply, and efforts are underway to expand downstream education and increase access to specialists. Several federal laws have been put in place to remove barriers and expand access to care and have paved the way to a brighter future. One is the Affordable Care Act, which requires all insurances including Medicaid to cover the cost of treatment. Second is the Mental Health Parity and Addiction Equity Act, which ensures that the duration and dollar amount of coverage for substance use disorders is comparable to that of medical and surgical care.
Continue to: Another exciting possibility...
Another exciting possibility comes from the world of pharmaceuticals. Some medications have modest efficacy for addressing addictive disorders; however, historically these have been poorly utilized. Enhanced understanding of the neurobiology combined with increased insurance reimbursement should prompt research and new drug development. Some promising agents are already in the pipeline. Research into molecular and gene therapy as a way to better individualize care is also underway.
Going forward, I think we will also encounter a different landscape of drugs. Synthetic agents are emerging and increasing in popularity. Alarmingly, public perception of harm is decreasing. When it comes to cannabis use, I see a rise in pathologic use and the ramifications of this will have a drastic impact, particularly on patients with mental health conditions. We will need to undertake better efforts in monitoring, staying updated, and providing public education campaigns.
Dr. Ahmed: What advice do you have for trainees contemplating subspecialty training in addiction psychiatry?
Dr. Stanciu: I cannot emphasize enough the importance of mentorship. The American Academy of Addiction Psychiatry has a robust system for connecting mentees with mentors at all stages in their careers. This can be extremely helpful, especially in situations where the residency program does not have addiction-trained faculty or rotations through treatment centers. Joining such an organization also grants you access to resources that can help further your enthusiasm. Those interested should also familiarize themselves with currently available pharmacotherapeutic treatments that have evidence supporting efficacy for various addictive disorders, and begin to incorporate these medications into general mental health practice, along with attempts at motivational interviewing. For example, begin discussing naltrexone with patients who have comorbid alcohol use disorders and are interested in reducing their drinking; and varenicline with patients who smoke and are interested in quitting. The outcomes should automatically elicit an interest in pursuing further training in the field!
Editor’s note: Career Choices features a psychiatry resident/fellow interviewing a psychiatrist about why he or she has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths.
In this Career Choices, Saeed Ahmed, MD, talked with Cornel Stanciu, MD. Dr. Stanciu is an addiction psychiatrist at Dartmouth’s Geisel School of Medicine, where he is an Assistant Professor, and serves as the Director of Addiction Services at New Hampshire Hospital. He provides support to clinicians managing patients with addictive disorders in a multitude of settings, and also assists with policy making and delivery of addiction care at the state level. He is also the author of Deciphering the Addicted Brain, a guide to help families and the general public better understand addictive disorders.
Dr. Ahmed: What attracted you to pursue subspecialty training in addictive disorders?
Dr. Stanciu: In the early stages of my training, I frequently encountered individuals with medical and mental health disorders whose treatment was impacted by underlying substance use. I soon came to realize any attempts at (for example) managing hypertension in someone with cocaine use disorder, or managing schizophrenia in someone with ongoing cannabis use, were futile. Almost all of my patients receiving treatment for mental health disorders were dependent on tobacco or other substances, and most were interested in cessation. Through mentorship from addiction-trained residency faculty members, I was able to get a taste of the neurobiologic complexities of the disease, something that left me with a desire to develop a deeper understanding of the disease process. Witnessing strikingly positive outcomes with implementation of evidence-based treatment modalities further solidified my path to subspecialty training. Even during that early phase, because I expressed interest in managing these conditions, I was immediately put in a position to share and disseminate any newly acquired knowledge to other specialties as well as the public.
Dr. Ahmed: Could one manage addictive disorders with just general psychiatry training, and what are the differences between the different paths to certification that a resident could undertake?
Dr. Stanciu: Addictive disorders fall under the general umbrella of psychiatric care. Most individuals with these disorders exhibit some degree of mental illness. Medical school curriculum offers on average 2 hours of addiction-related didactics during 4 years. General psychiatry training programs vary significantly in the type of exposure to addiction—some residencies have an affiliated addiction fellowship, others have addiction-trained psychiatrists on staff, but most have none. Ultimately, there is great variability in the degree of comfort in working with individuals with addictive disorders post-residency. Being able to prescribe medications for the treatment of addictive disorders is very different from being familiar with the latest evidence-based recommendations and guidelines; the latter is
Addiction medicine is a fairly new route initially intended to allow non-psychiatric specialties access to addictive disorders training and certification. This is offered through the American Board of Preventive Medicine. There are currently 2 routes to sitting for the exam: through completion of a 1-year addiction medicine fellowship, or through the “practice pathway” still available until 2020. To be eligible for the latter, individuals must provide documentation of clinical experience post-residency, which is quantified as number of hours spent treating patients with addictions, plus any additional courses or training, and must be endorsed by a certified addictionologist.
Continue to: What was your fellowship experience link...
Dr. Ahmed: What was your fellowship experience like, and what should one consider when choosing a program?
Dr. Stanciu: I completed my fellowship training through Dartmouth’s Geisel School of Medicine, and the experience was tremendously valuable. In evaluating programs, one of the starting points is whether you have interest in a formal research track, because several programs include an optional year for that. Most programs tend to provide exposure to the Veterans Affairs system. The 1 year should provide you with broad exposure to all possible settings, all addictive disorders and patient populations, and all treatment modalities, in addition to rigorous didactic sessions. The ideal program should include rotations through methadone treatment centers, intensive outpatient programs, pain and interdisciplinary clinics, detoxification units, and centers for treatment of adolescent and young adults, as well as general medical settings and infectious disease clinics. There should also be close collaboration with psychologists who can provide training in evidence-based therapeutic modalities. During this year, it is vital to expand your knowledge of the ethical and legal regulations of treatment programs, state and federal requirements, insurance complexities, and requirements for privacy and protection of health information. The size of these programs can vary significantly, which may limit the one-on-one time devoted to your training, which is something I personally valued. My faculty was very supportive of academic endeavors, providing guidance, funding, and encouragement for attending and presenting at conferences, publishing papers, and other academic pursuits. Additionally, faculty should be current with emerging literature and willing to develop or implement new protocols and evaluate new pharmacologic therapies.
Dr. Ahmed: What are some of the career options and work settings for addiction psychiatrists?
Dr. Stanciu: Addiction psychiatrists work in numerous settings and various capacities. They can provide subspecialty care directly by seeing patients in outpatient clinics or inpatient addiction treatment centers for detoxification or rehabilitation, or they can work with dual-diagnosis populations in inpatient units. The expansion of telemedicine also holds promise for a role through virtual services. Indirectly, they can serve as a resource for expertise in the field through consultations in medical and psychiatric settings, or through policy making by working with the legislature and public health departments. Additionally, they can help create and integrate new knowledge into practice and educate future generations of physicians and the public.
Dr. Ahmed: What are some of the prevalent disorders and reasons for consultation that you encounter in your daily practice?
Continue to: Dr. Stanciu's response...
Dr. Stanciu: This can vary significantly depending on the setting, geographical region, and demographics of the population. My main non-administrative responsibilities are primarily consultative assisting clinicians at a 200-bed psychiatric hospital to address co-occurring addictive disorders. In short-term units, I am primarily asked to provide input on issues related to various toxidromes and withdrawals and the use of relapse prevention medications for alcohol use disorders as well as the use of buprenorphine or other forms of medication-assisted treatment. I work closely with licensed drug and alcohol counselors in implementing brief interventions as well as facilitating outpatient treatment referrals. Clinicians in longer term units may consult on issues related to pain management in individuals who have addictive disorders, the use of evidence-based pharmacologic agents to address cravings, or the use of relapse prevention medications for someone close to discharge. In terms of specific drugs of abuse, although opioids have recently received a tremendous amount of attention due to the visible costs through overdose deaths, the magnitude of individuals who are losing years of quality life through the use of alcohol and tobacco is significant, and hence this is a large portion of the conditions I encounter. I have also seen an abundance of marijuana use due to decreased perception of harm and increased access.
Dr. Ahmed: What are some of the challenges in working in this field?
Dr. Stanciu: Historically, funding for services has been an issue for clinicians working primarily with addictive disorders from the standpoint of reimbursement, patient access to evidence-based pharmacotherapy, and ability to collaborate with existing levels of care. In recent years, federal funding and policies have changed this, and after numerous studies have found increased cost savings, commercial insurances are providing coverage. A significant challenge also has been public stigma and dealing with a condition that is relapsing-remitting, poorly understood by other specialties and the general public, and sometimes labeled as a defect of character. Several efforts in education have lessened this; however, the impact still takes a toll on patients, who may feel ashamed of their disorder and sometimes are hesitant to take medications because they may believe that they are not “clean” if they depend on a medication for remission. Lastly, recent changes in marijuana policies make conversations about this drug quite difficult because patients often view it as harmless, and the laws governing legality and indications for therapeutic use are slightly ahead of the evidence.
Dr. Ahmed: In what direction do you believe the subspecialty is headed?
Dr. Stanciu: Currently, there are approximately 1,000 certified addiction psychiatrists for the 45 million Americans who have addictive disorders. Smoking and other forms of tobacco use pose significant threats to the 2020 Healthy People Tobacco Use objectives. There is a significant demand for addictionologists in both public and private sectors. As with mental health, demand exceeds supply, and efforts are underway to expand downstream education and increase access to specialists. Several federal laws have been put in place to remove barriers and expand access to care and have paved the way to a brighter future. One is the Affordable Care Act, which requires all insurances including Medicaid to cover the cost of treatment. Second is the Mental Health Parity and Addiction Equity Act, which ensures that the duration and dollar amount of coverage for substance use disorders is comparable to that of medical and surgical care.
Continue to: Another exciting possibility...
Another exciting possibility comes from the world of pharmaceuticals. Some medications have modest efficacy for addressing addictive disorders; however, historically these have been poorly utilized. Enhanced understanding of the neurobiology combined with increased insurance reimbursement should prompt research and new drug development. Some promising agents are already in the pipeline. Research into molecular and gene therapy as a way to better individualize care is also underway.
Going forward, I think we will also encounter a different landscape of drugs. Synthetic agents are emerging and increasing in popularity. Alarmingly, public perception of harm is decreasing. When it comes to cannabis use, I see a rise in pathologic use and the ramifications of this will have a drastic impact, particularly on patients with mental health conditions. We will need to undertake better efforts in monitoring, staying updated, and providing public education campaigns.
Dr. Ahmed: What advice do you have for trainees contemplating subspecialty training in addiction psychiatry?
Dr. Stanciu: I cannot emphasize enough the importance of mentorship. The American Academy of Addiction Psychiatry has a robust system for connecting mentees with mentors at all stages in their careers. This can be extremely helpful, especially in situations where the residency program does not have addiction-trained faculty or rotations through treatment centers. Joining such an organization also grants you access to resources that can help further your enthusiasm. Those interested should also familiarize themselves with currently available pharmacotherapeutic treatments that have evidence supporting efficacy for various addictive disorders, and begin to incorporate these medications into general mental health practice, along with attempts at motivational interviewing. For example, begin discussing naltrexone with patients who have comorbid alcohol use disorders and are interested in reducing their drinking; and varenicline with patients who smoke and are interested in quitting. The outcomes should automatically elicit an interest in pursuing further training in the field!
Shining a spotlight on physician well-being, more
Shining a spotlight on physician well-being
In “Physician impairment”1 (C
Dr. Farrell’s article does not acknowledge the rule of law. I do not understand why anyone wanting to help physicians would not want them to be aware of their employment rights under the ADA or advise that their ADA rights protect them from unwarranted medical inquiries and referrals to physician health programs (PHPs) or other entities for evaluation.
Dr. Farrell also claims that burnout, poor well-being, and mental disorders cause medical errors and low quality of patient care, but there are many reasons to doubt that this is the case.3,4 Readers should be wary of medical journal articles that cover topics related to physician well-being. Articles related to PHPs, in particular, typically paint an overly rosy picture of the effectiveness of these programs and fail to note important problematic aspects.5,6
Nicholas D. Lawson, MD
Georgetown University Law Center
Washington, DC
References
1. Lawson ND. Physician impairment. Current Psychiatry. 2017;16(10):8.
2. Farrell H. Physician impairment: a need for prevention. Current Psychiatry. 2018;17(9):41-44.
3. Lawson ND. Burnout is not associated with increased medical errors. Mayo Clin Proc. 2018;93(11):1683.
4. Tyssen R. What is the level of burnout that impairs functioning? J Intern Med. 2018;283(6):594-596.
5. Lawson ND, Boyd JW. Flaws in the methods and reporting of physician health program outcome studies. Gen Hosp Psychiatry. 2018;54:65-66.
6. Lawson ND, Boyd JW. Physician health program outcome data should be viewed with caution. Judges J. 2018;57(4):36.
The author responds
I thank Dr. Lawson for his interest in my article. In this extremely challenging work that we do as psychiatrists, which can sometimes be quite isolating, there is a long continuum of experience, reward, and challenge. Dr. Lawson’s research and publication on the topic of physician’s health issues are very much respected and appreciated. In fact, I see no conflict between Dr. Lawson’s letter and my 2018 column on the prevention of impairment.
Given the extensive continuum of our work, my article on physician’s health issues sought to shine a bright spotlight solely on the topic of prevention. As colleagues, there is significant value in supporting rather than reporting one another. Awareness of and sensitivity to physician vulnerability, early detection, and prevention will hopefully continue to gain traction in the future.
By putting the focus on proactively helping colleagues, my hope is that my article will spark an ongoing conversation about how we can work collaboratively to make well-being a priority.
Dr. Lawson’s thoughtful letter is much appreciated because it continues the discussion by shining a spotlight further down the continuum. He focuses on the aftermath of impairment and aptly points out the complications in reporting, confusion about duty, and the protections provided by the ADA. Also, I support Dr. Lawson’s cautions regarding PHPs—all the more reason to join together in shifting the dialogue from management of a crisis to prevention of it.
Helen M. Farrell, MD
Lecturer
Harvard Medical School
Psychiatrist
Beth Israel Deaconess Medical Center
Boston, Massachusetts
Continue to: Neuropolitics
Neuropolitics: Psychiatrists’ responsibility
Regarding Dr. Nasrallah’s editorial “Neuropolitics in the age of extremism: Brain regions involved in hatred” (C
I agree with Dr. Nasrallah that “even the most skillful psychiatrists” cannot “repair a nation caught up in poisonous emotional turmoil”—at least not by employing clinical skills alone. But that doesn’t mean we shouldn’t try, and the American Psychiatric Association (APA) ethics code (Sections 1.2, 3, and 7) compels us to speak out when our patients or the public are being harmed by public policy.1 We are much more likely to have an impact when we speak with one voice, as is the case with professional medical organizations such as the APA. In December 2018, APA President Dr. Altha J. Stewart issued a call to action addressing “the current climate of hateful and divisive rhetoric that leads to senseless violence and tragic loss of life,” stating “… we members must speak out, use our specialized training and expertise for the public’s benefit, and apply it to not only healing, but also preventing psychological trauma and senseless tragedies.”2
James L. Fleming, MD
Psychiatric Medical Care
Lee’s Summit, Missouri
References
1. American Psychiatric Association. The principles of medical ethics with annotations especially applicable to psychiatry, 2013 edition. https://www.psychiatry.org/psychiatrists/practice/ethics. Published 2013. Accessed February 5, 2019.
2. Stewart A, Pozios, V. Forget about staying in our lane: let’s connect the dots. American Psychiatric Association Publishing. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2018.12a20. Published December 3, 2018. Accessed February 3, 2019.
Shining a spotlight on physician well-being
In “Physician impairment”1 (C
Dr. Farrell’s article does not acknowledge the rule of law. I do not understand why anyone wanting to help physicians would not want them to be aware of their employment rights under the ADA or advise that their ADA rights protect them from unwarranted medical inquiries and referrals to physician health programs (PHPs) or other entities for evaluation.
Dr. Farrell also claims that burnout, poor well-being, and mental disorders cause medical errors and low quality of patient care, but there are many reasons to doubt that this is the case.3,4 Readers should be wary of medical journal articles that cover topics related to physician well-being. Articles related to PHPs, in particular, typically paint an overly rosy picture of the effectiveness of these programs and fail to note important problematic aspects.5,6
Nicholas D. Lawson, MD
Georgetown University Law Center
Washington, DC
References
1. Lawson ND. Physician impairment. Current Psychiatry. 2017;16(10):8.
2. Farrell H. Physician impairment: a need for prevention. Current Psychiatry. 2018;17(9):41-44.
3. Lawson ND. Burnout is not associated with increased medical errors. Mayo Clin Proc. 2018;93(11):1683.
4. Tyssen R. What is the level of burnout that impairs functioning? J Intern Med. 2018;283(6):594-596.
5. Lawson ND, Boyd JW. Flaws in the methods and reporting of physician health program outcome studies. Gen Hosp Psychiatry. 2018;54:65-66.
6. Lawson ND, Boyd JW. Physician health program outcome data should be viewed with caution. Judges J. 2018;57(4):36.
The author responds
I thank Dr. Lawson for his interest in my article. In this extremely challenging work that we do as psychiatrists, which can sometimes be quite isolating, there is a long continuum of experience, reward, and challenge. Dr. Lawson’s research and publication on the topic of physician’s health issues are very much respected and appreciated. In fact, I see no conflict between Dr. Lawson’s letter and my 2018 column on the prevention of impairment.
Given the extensive continuum of our work, my article on physician’s health issues sought to shine a bright spotlight solely on the topic of prevention. As colleagues, there is significant value in supporting rather than reporting one another. Awareness of and sensitivity to physician vulnerability, early detection, and prevention will hopefully continue to gain traction in the future.
By putting the focus on proactively helping colleagues, my hope is that my article will spark an ongoing conversation about how we can work collaboratively to make well-being a priority.
Dr. Lawson’s thoughtful letter is much appreciated because it continues the discussion by shining a spotlight further down the continuum. He focuses on the aftermath of impairment and aptly points out the complications in reporting, confusion about duty, and the protections provided by the ADA. Also, I support Dr. Lawson’s cautions regarding PHPs—all the more reason to join together in shifting the dialogue from management of a crisis to prevention of it.
Helen M. Farrell, MD
Lecturer
Harvard Medical School
Psychiatrist
Beth Israel Deaconess Medical Center
Boston, Massachusetts
Continue to: Neuropolitics
Neuropolitics: Psychiatrists’ responsibility
Regarding Dr. Nasrallah’s editorial “Neuropolitics in the age of extremism: Brain regions involved in hatred” (C
I agree with Dr. Nasrallah that “even the most skillful psychiatrists” cannot “repair a nation caught up in poisonous emotional turmoil”—at least not by employing clinical skills alone. But that doesn’t mean we shouldn’t try, and the American Psychiatric Association (APA) ethics code (Sections 1.2, 3, and 7) compels us to speak out when our patients or the public are being harmed by public policy.1 We are much more likely to have an impact when we speak with one voice, as is the case with professional medical organizations such as the APA. In December 2018, APA President Dr. Altha J. Stewart issued a call to action addressing “the current climate of hateful and divisive rhetoric that leads to senseless violence and tragic loss of life,” stating “… we members must speak out, use our specialized training and expertise for the public’s benefit, and apply it to not only healing, but also preventing psychological trauma and senseless tragedies.”2
James L. Fleming, MD
Psychiatric Medical Care
Lee’s Summit, Missouri
References
1. American Psychiatric Association. The principles of medical ethics with annotations especially applicable to psychiatry, 2013 edition. https://www.psychiatry.org/psychiatrists/practice/ethics. Published 2013. Accessed February 5, 2019.
2. Stewart A, Pozios, V. Forget about staying in our lane: let’s connect the dots. American Psychiatric Association Publishing. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2018.12a20. Published December 3, 2018. Accessed February 3, 2019.
Shining a spotlight on physician well-being
In “Physician impairment”1 (C
Dr. Farrell’s article does not acknowledge the rule of law. I do not understand why anyone wanting to help physicians would not want them to be aware of their employment rights under the ADA or advise that their ADA rights protect them from unwarranted medical inquiries and referrals to physician health programs (PHPs) or other entities for evaluation.
Dr. Farrell also claims that burnout, poor well-being, and mental disorders cause medical errors and low quality of patient care, but there are many reasons to doubt that this is the case.3,4 Readers should be wary of medical journal articles that cover topics related to physician well-being. Articles related to PHPs, in particular, typically paint an overly rosy picture of the effectiveness of these programs and fail to note important problematic aspects.5,6
Nicholas D. Lawson, MD
Georgetown University Law Center
Washington, DC
References
1. Lawson ND. Physician impairment. Current Psychiatry. 2017;16(10):8.
2. Farrell H. Physician impairment: a need for prevention. Current Psychiatry. 2018;17(9):41-44.
3. Lawson ND. Burnout is not associated with increased medical errors. Mayo Clin Proc. 2018;93(11):1683.
4. Tyssen R. What is the level of burnout that impairs functioning? J Intern Med. 2018;283(6):594-596.
5. Lawson ND, Boyd JW. Flaws in the methods and reporting of physician health program outcome studies. Gen Hosp Psychiatry. 2018;54:65-66.
6. Lawson ND, Boyd JW. Physician health program outcome data should be viewed with caution. Judges J. 2018;57(4):36.
The author responds
I thank Dr. Lawson for his interest in my article. In this extremely challenging work that we do as psychiatrists, which can sometimes be quite isolating, there is a long continuum of experience, reward, and challenge. Dr. Lawson’s research and publication on the topic of physician’s health issues are very much respected and appreciated. In fact, I see no conflict between Dr. Lawson’s letter and my 2018 column on the prevention of impairment.
Given the extensive continuum of our work, my article on physician’s health issues sought to shine a bright spotlight solely on the topic of prevention. As colleagues, there is significant value in supporting rather than reporting one another. Awareness of and sensitivity to physician vulnerability, early detection, and prevention will hopefully continue to gain traction in the future.
By putting the focus on proactively helping colleagues, my hope is that my article will spark an ongoing conversation about how we can work collaboratively to make well-being a priority.
Dr. Lawson’s thoughtful letter is much appreciated because it continues the discussion by shining a spotlight further down the continuum. He focuses on the aftermath of impairment and aptly points out the complications in reporting, confusion about duty, and the protections provided by the ADA. Also, I support Dr. Lawson’s cautions regarding PHPs—all the more reason to join together in shifting the dialogue from management of a crisis to prevention of it.
Helen M. Farrell, MD
Lecturer
Harvard Medical School
Psychiatrist
Beth Israel Deaconess Medical Center
Boston, Massachusetts
Continue to: Neuropolitics
Neuropolitics: Psychiatrists’ responsibility
Regarding Dr. Nasrallah’s editorial “Neuropolitics in the age of extremism: Brain regions involved in hatred” (C
I agree with Dr. Nasrallah that “even the most skillful psychiatrists” cannot “repair a nation caught up in poisonous emotional turmoil”—at least not by employing clinical skills alone. But that doesn’t mean we shouldn’t try, and the American Psychiatric Association (APA) ethics code (Sections 1.2, 3, and 7) compels us to speak out when our patients or the public are being harmed by public policy.1 We are much more likely to have an impact when we speak with one voice, as is the case with professional medical organizations such as the APA. In December 2018, APA President Dr. Altha J. Stewart issued a call to action addressing “the current climate of hateful and divisive rhetoric that leads to senseless violence and tragic loss of life,” stating “… we members must speak out, use our specialized training and expertise for the public’s benefit, and apply it to not only healing, but also preventing psychological trauma and senseless tragedies.”2
James L. Fleming, MD
Psychiatric Medical Care
Lee’s Summit, Missouri
References
1. American Psychiatric Association. The principles of medical ethics with annotations especially applicable to psychiatry, 2013 edition. https://www.psychiatry.org/psychiatrists/practice/ethics. Published 2013. Accessed February 5, 2019.
2. Stewart A, Pozios, V. Forget about staying in our lane: let’s connect the dots. American Psychiatric Association Publishing. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2018.12a20. Published December 3, 2018. Accessed February 3, 2019.
Psychiatry and neurology: Sister neuroscience specialties with different approaches to the brain
Neurologists and psychiatrists diagnose and treat disorders of the brain’s hardware and software, respectively. The brain is a physically tangible structure, while its mind is virtual and intangible.
Not surprisingly, neurology and psychiatry have very different approaches to the assessment and treatment of brain and mind disorders. It reminds me of ophthalmology, where some of the faculty focus on the hardware of the eye (cornea, lens, and retina) while others focus on the major function of the eye—vision. Similarly, the mind is the major function of the brain.
Clinical neuroscience represents the shared foundational underpinnings of neurologists and psychiatrists, but their management of brain and mind disorders is understandably quite different, albeit with the same final goal: to repair and restore the structure and function of this divinely complex organ, the command and control center of the human soul and behavior.
In Table 1, I compare and contrast the clinical approaches of these 2 sister clinical neuroscience specialties, beyond the shared standard medical templates of history of present illness, medical history, social history, family history, review of systems, and physical examination.
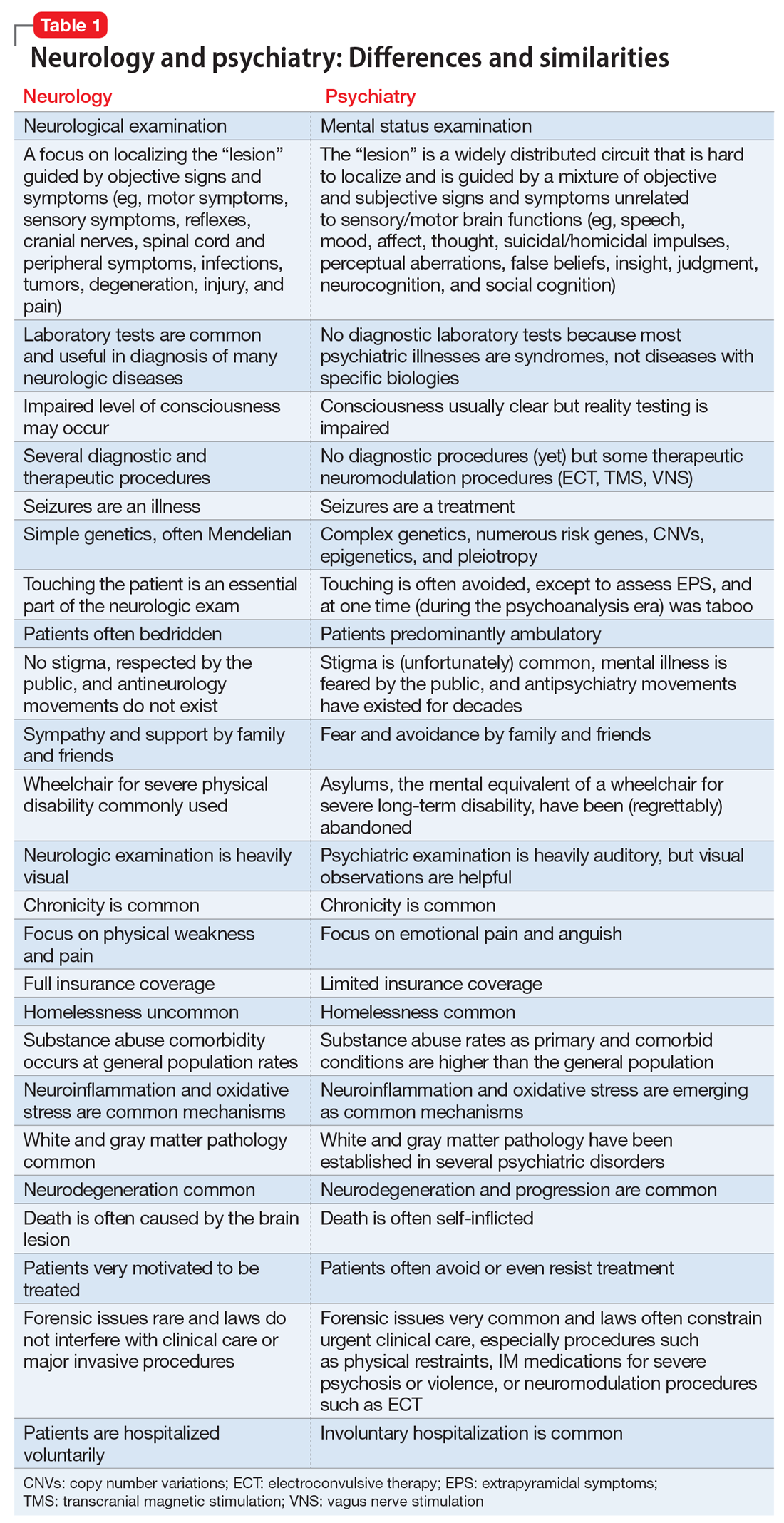
Despite those many differences in assessing and treating neurologic vs psychiatric disorders of the brain, there is an indisputable fact: Every neurologic disorder is associated with psychiatric manifestations, and every psychiatric illness is associated with neurologic symptoms. The brain is the most complex structure in the universe; its development requires the expression of 50% of the human genome, and its major task is to generate a mind that enables every human being to navigate the biopsychosocial imperatives of life. Any brain lesion, regardless of size and location, will disrupt the integrity of the mind in one way or another, such as speaking, thinking, fantasizing, arguing, understanding, feeling, remembering, plotting, enjoying, socializing, or courting. The bottom line is that every patient with a brain/mind disorder should ideally receive both neurologic and psychiatric evaluation, and the requisite dual interventions as necessary.1 If the focus is exclusively on either the brain or the mind, clinical and functional outcomes for the patient will be suboptimal.
Neuropsychiatrists and behavioral neurologists represent excellent bridges across these 2 sister specialties. There are twice as many psychiatrists as neurologists, but very few neuropsychiatrists or behavioral neurologists. The American Board of Psychiatry and Neurology (ABPN) has approved several board certifications for both specialties, and several subspecialties as well (Table 2). When will the ABPN approve neuropsychiatry and behavioral neurology as subspecialties, to facilitate the integration of the brain and the mind,2 and to bridge the chasm between disorders of the brain and mind?
To comment on this editorial or other topics of interest: [email protected].
1. Nasrallah HA. Toward the era of transformational neuropsychiatry. Asian J Psychiatr. 2015;17:140-141.
2. Nasrallah HA. Reintegrating psychiatry and neurology is long overdue: Part 1. April 30, 2014. https://www.cmeinstitute.com/pages/lets-talk.aspx?bid=72. Accessed February 11, 2019.
Neurologists and psychiatrists diagnose and treat disorders of the brain’s hardware and software, respectively. The brain is a physically tangible structure, while its mind is virtual and intangible.
Not surprisingly, neurology and psychiatry have very different approaches to the assessment and treatment of brain and mind disorders. It reminds me of ophthalmology, where some of the faculty focus on the hardware of the eye (cornea, lens, and retina) while others focus on the major function of the eye—vision. Similarly, the mind is the major function of the brain.
Clinical neuroscience represents the shared foundational underpinnings of neurologists and psychiatrists, but their management of brain and mind disorders is understandably quite different, albeit with the same final goal: to repair and restore the structure and function of this divinely complex organ, the command and control center of the human soul and behavior.
In Table 1, I compare and contrast the clinical approaches of these 2 sister clinical neuroscience specialties, beyond the shared standard medical templates of history of present illness, medical history, social history, family history, review of systems, and physical examination.
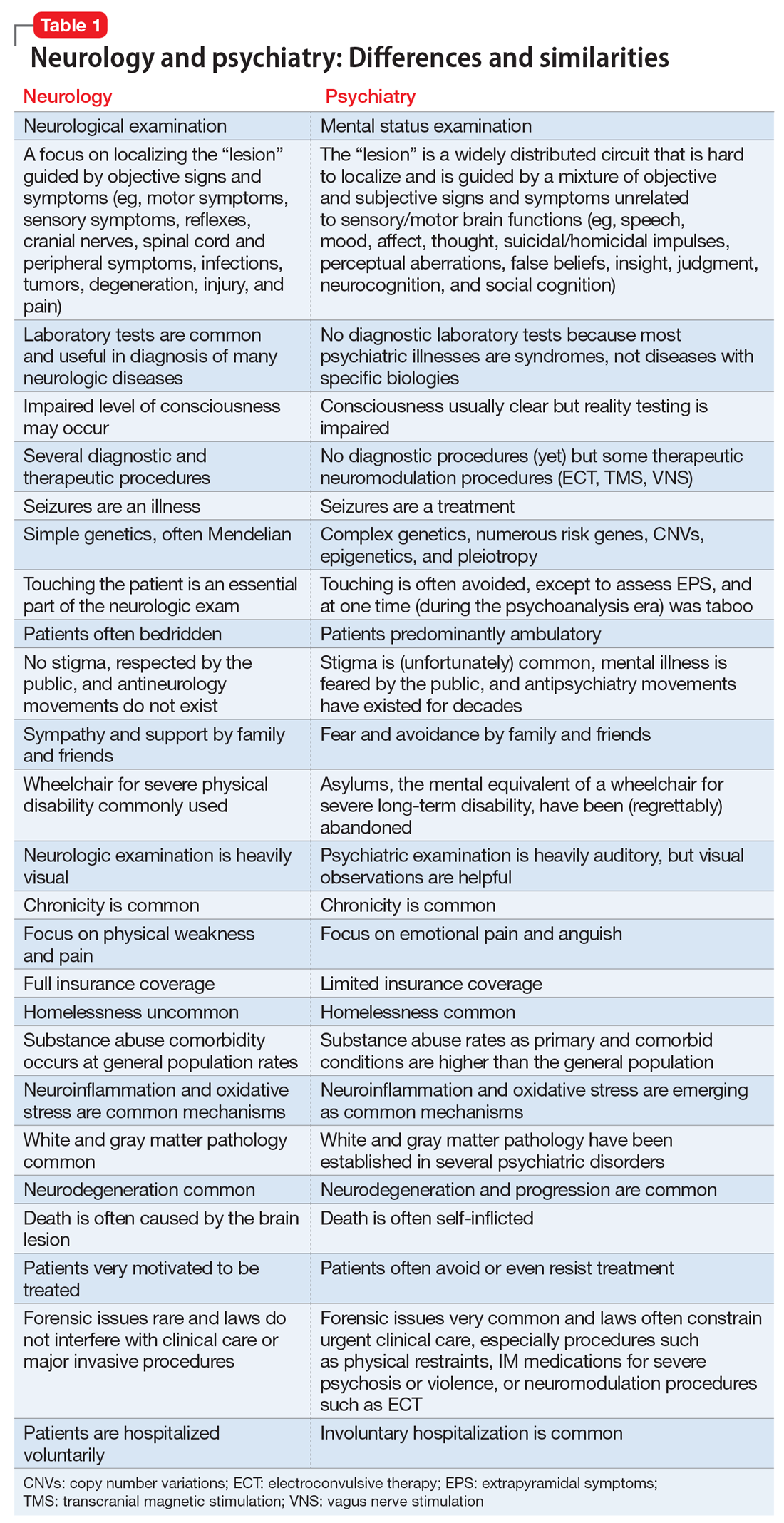
Despite those many differences in assessing and treating neurologic vs psychiatric disorders of the brain, there is an indisputable fact: Every neurologic disorder is associated with psychiatric manifestations, and every psychiatric illness is associated with neurologic symptoms. The brain is the most complex structure in the universe; its development requires the expression of 50% of the human genome, and its major task is to generate a mind that enables every human being to navigate the biopsychosocial imperatives of life. Any brain lesion, regardless of size and location, will disrupt the integrity of the mind in one way or another, such as speaking, thinking, fantasizing, arguing, understanding, feeling, remembering, plotting, enjoying, socializing, or courting. The bottom line is that every patient with a brain/mind disorder should ideally receive both neurologic and psychiatric evaluation, and the requisite dual interventions as necessary.1 If the focus is exclusively on either the brain or the mind, clinical and functional outcomes for the patient will be suboptimal.
Neuropsychiatrists and behavioral neurologists represent excellent bridges across these 2 sister specialties. There are twice as many psychiatrists as neurologists, but very few neuropsychiatrists or behavioral neurologists. The American Board of Psychiatry and Neurology (ABPN) has approved several board certifications for both specialties, and several subspecialties as well (Table 2). When will the ABPN approve neuropsychiatry and behavioral neurology as subspecialties, to facilitate the integration of the brain and the mind,2 and to bridge the chasm between disorders of the brain and mind?
To comment on this editorial or other topics of interest: [email protected].
Neurologists and psychiatrists diagnose and treat disorders of the brain’s hardware and software, respectively. The brain is a physically tangible structure, while its mind is virtual and intangible.
Not surprisingly, neurology and psychiatry have very different approaches to the assessment and treatment of brain and mind disorders. It reminds me of ophthalmology, where some of the faculty focus on the hardware of the eye (cornea, lens, and retina) while others focus on the major function of the eye—vision. Similarly, the mind is the major function of the brain.
Clinical neuroscience represents the shared foundational underpinnings of neurologists and psychiatrists, but their management of brain and mind disorders is understandably quite different, albeit with the same final goal: to repair and restore the structure and function of this divinely complex organ, the command and control center of the human soul and behavior.
In Table 1, I compare and contrast the clinical approaches of these 2 sister clinical neuroscience specialties, beyond the shared standard medical templates of history of present illness, medical history, social history, family history, review of systems, and physical examination.
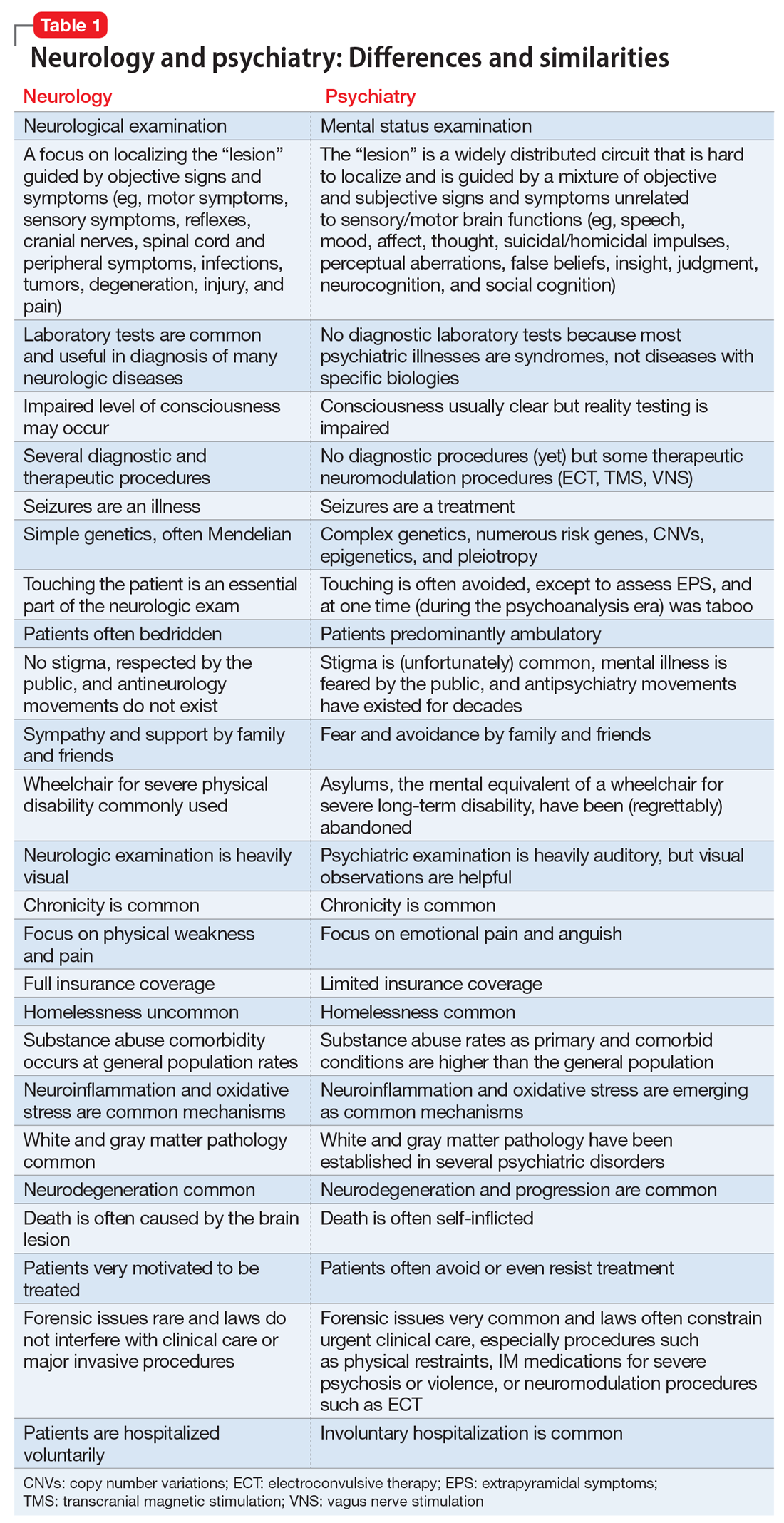
Despite those many differences in assessing and treating neurologic vs psychiatric disorders of the brain, there is an indisputable fact: Every neurologic disorder is associated with psychiatric manifestations, and every psychiatric illness is associated with neurologic symptoms. The brain is the most complex structure in the universe; its development requires the expression of 50% of the human genome, and its major task is to generate a mind that enables every human being to navigate the biopsychosocial imperatives of life. Any brain lesion, regardless of size and location, will disrupt the integrity of the mind in one way or another, such as speaking, thinking, fantasizing, arguing, understanding, feeling, remembering, plotting, enjoying, socializing, or courting. The bottom line is that every patient with a brain/mind disorder should ideally receive both neurologic and psychiatric evaluation, and the requisite dual interventions as necessary.1 If the focus is exclusively on either the brain or the mind, clinical and functional outcomes for the patient will be suboptimal.
Neuropsychiatrists and behavioral neurologists represent excellent bridges across these 2 sister specialties. There are twice as many psychiatrists as neurologists, but very few neuropsychiatrists or behavioral neurologists. The American Board of Psychiatry and Neurology (ABPN) has approved several board certifications for both specialties, and several subspecialties as well (Table 2). When will the ABPN approve neuropsychiatry and behavioral neurology as subspecialties, to facilitate the integration of the brain and the mind,2 and to bridge the chasm between disorders of the brain and mind?
To comment on this editorial or other topics of interest: [email protected].
1. Nasrallah HA. Toward the era of transformational neuropsychiatry. Asian J Psychiatr. 2015;17:140-141.
2. Nasrallah HA. Reintegrating psychiatry and neurology is long overdue: Part 1. April 30, 2014. https://www.cmeinstitute.com/pages/lets-talk.aspx?bid=72. Accessed February 11, 2019.
1. Nasrallah HA. Toward the era of transformational neuropsychiatry. Asian J Psychiatr. 2015;17:140-141.
2. Nasrallah HA. Reintegrating psychiatry and neurology is long overdue: Part 1. April 30, 2014. https://www.cmeinstitute.com/pages/lets-talk.aspx?bid=72. Accessed February 11, 2019.
Aerospace medicine and psychiatry
As part of my psychiatry residency training, I had the privilege to work with and learn from an aerospace psychiatrist. Aerospace medicine is a branch of preventive and occupational medicine in which aviators (pilots, aircrew, or astronauts) are subject to evaluation/treatment. The goal is to assess physical and mental health factors to mitigate risks, protect public safety, and ensure the aviators’ well-being.1,2 Aerospace psychiatry is a highly specialized area in which practitioners are trained to perform specific evaluations. In this article, I review those evaluations for those looking to gain insight into the field.
Aviation medical examination
Under Title 14 of the Code of Federal Regulations, the Federal Aviation Administration (FAA) requires aviators to be evaluated for medical certification by undergoing an aviation medical exam.2 In order to be deemed “fit for duty,” aviators must meet strict physical and mental health standards set by the FAA. The extent of these standards varies by the class of licensure (Table 13). Aviation medical exams are performed by any physician who has been designated by the FAA and completed the appropriate FAA aviation medical examiner (AME) training. Aviators who meet the medical standards for their licensure class are recommended for medical certification. If the AME brings up further questions due to the limits of the examination and/or a lack of medical records, the certification will likely be deferred pending further evaluation by an FAA-approved medical specialist and/or the receipt of additional medical records. Questions about a possible psychiatric diagnosis/history or substance use disorder will lead to referral to a psychiatrist familiar with aviation standards for further evaluation.
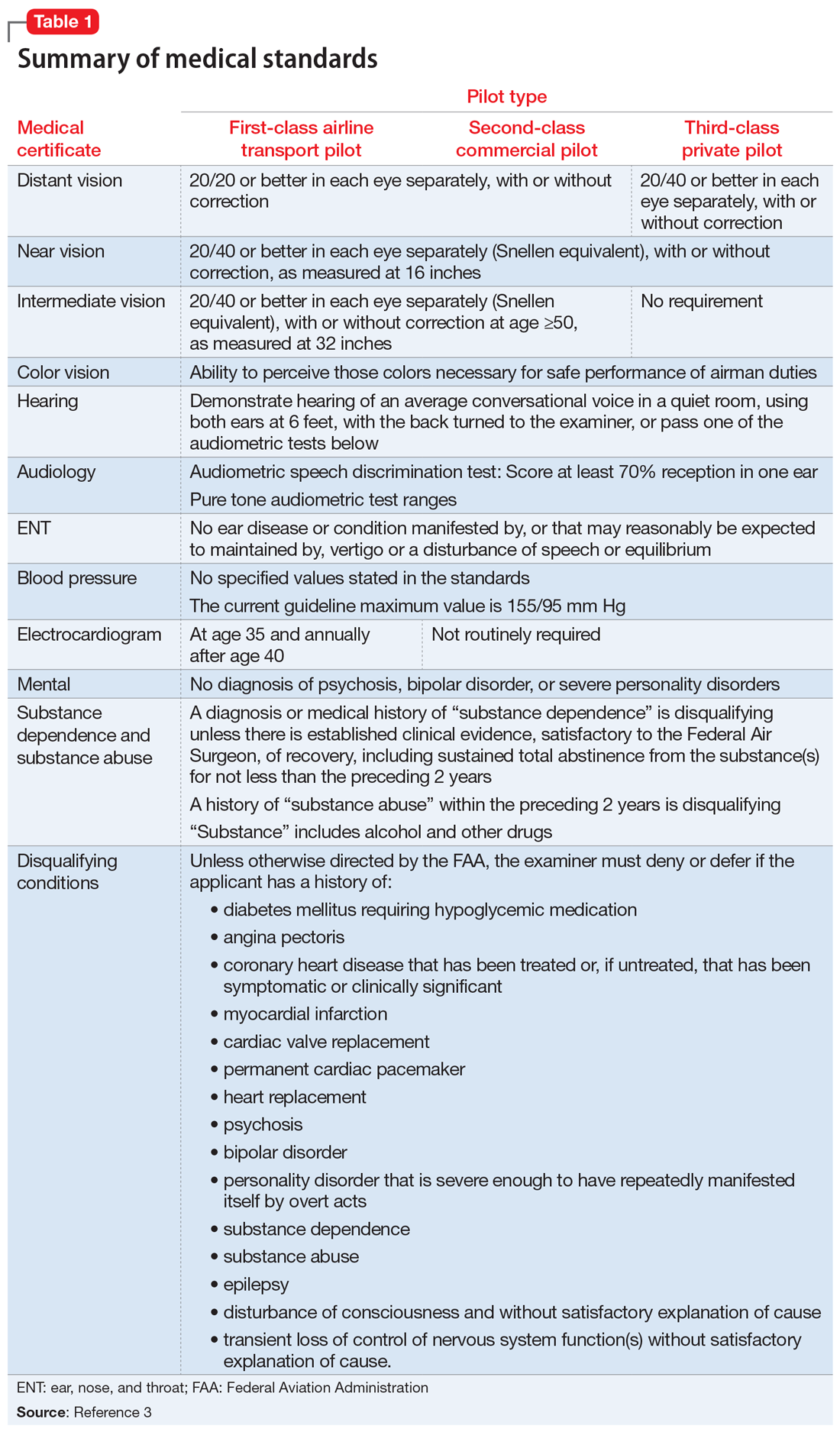
_
Special issuances and Conditions AMEs Can Issue
There are 15 disqualifying conditions for medical certification (Table 13). However, a special issuance of a medical certification may be granted if the aviator shows to the satisfaction of the aviation medical examiner that the duties of the licensure class can be performed without endangering the public safety and that the condition is deemed stable. This may be shown through additional medical evaluations/tests and/or records.
There are certain medical conditions for which an AME can issue a medical certificate without further review from other specialists; thus, an AME can review and follow the Conditions AMEs Can Issue (CACI) worksheet to recommend medical certification (Table 24). The CACI guidelines and worksheets are updated by the FAA regularly to ensure aviators’ health and minimize public risk.
Psychiatric & Psychological Evaluation
Aviators may be referred for Psychiatric and Psychological Evaluation (P&P) if an AME discovers additional concerns about psychiatric and neurocognitive disorders. These cases are not clear-cut. An example would be an aviator who was receiving a psychotropic medication in the past and reported past heavy alcohol use. The P&P includes a thorough psychiatric evaluation by an aerospace psychiatrist and extensive psychological testing by an aerospace psychologist. These clinicians also review collateral information and past medical/AME records. Aviators may be recommended for medical certification with special issuance or may be denied medical certification as a result of these examinations.
Human Intervention Motivation Study program
The Human Intervention Motivation Study (HIMS) program was established to provide an avenue whereby commercial pilots with active substance use disorders can be identified, treated, and successfully returned to active flight status.5 The goal of the HIMS program is to save lives and careers while enhancing flight safety. Physicians trained in HIMS evaluations follow the multifactorial addiction disease model. This evaluation is used to identify active substance use and initiate treatment, and to maintain sobriety and monitor aftercare adherence.
1. Bor R, Hubbard T. Aviation mental health: psychological implications for air transportation. Hampshire, England: Ashgate Publishing Limited; 2006.
2. US Department of Transportation Federal Aviation Administration. Medical certification. https://www.faa.gov/licenses_certificates/medical_certification/. Updated February 1, 2019. Accessed February 19, 2019.
3. US Department of Transportation Federal Aviation Administration. Summary of medical standards. https://www.faa.gov/about/office_org/headquarters_offices/avs/offices/aam/ame/guide/media/synopsis.pdf. Revised April 3, 2006. Accessed October 7, 2018.
4. US Department of Transportation Federal Aviation Administration. Guide for aviation medical examiners: CACI conditions. Revised April 3, 2006. https://www.faa.gov/about/office_org/headquarters_offices/avs/offices/aam/ame/guide/certification_ws/. Accessed October 8, 2018.
5. HIMS. About HIMS. http://www.himsprogram.com/Home/About. Accessed February 6, 2019.
As part of my psychiatry residency training, I had the privilege to work with and learn from an aerospace psychiatrist. Aerospace medicine is a branch of preventive and occupational medicine in which aviators (pilots, aircrew, or astronauts) are subject to evaluation/treatment. The goal is to assess physical and mental health factors to mitigate risks, protect public safety, and ensure the aviators’ well-being.1,2 Aerospace psychiatry is a highly specialized area in which practitioners are trained to perform specific evaluations. In this article, I review those evaluations for those looking to gain insight into the field.
Aviation medical examination
Under Title 14 of the Code of Federal Regulations, the Federal Aviation Administration (FAA) requires aviators to be evaluated for medical certification by undergoing an aviation medical exam.2 In order to be deemed “fit for duty,” aviators must meet strict physical and mental health standards set by the FAA. The extent of these standards varies by the class of licensure (Table 13). Aviation medical exams are performed by any physician who has been designated by the FAA and completed the appropriate FAA aviation medical examiner (AME) training. Aviators who meet the medical standards for their licensure class are recommended for medical certification. If the AME brings up further questions due to the limits of the examination and/or a lack of medical records, the certification will likely be deferred pending further evaluation by an FAA-approved medical specialist and/or the receipt of additional medical records. Questions about a possible psychiatric diagnosis/history or substance use disorder will lead to referral to a psychiatrist familiar with aviation standards for further evaluation.
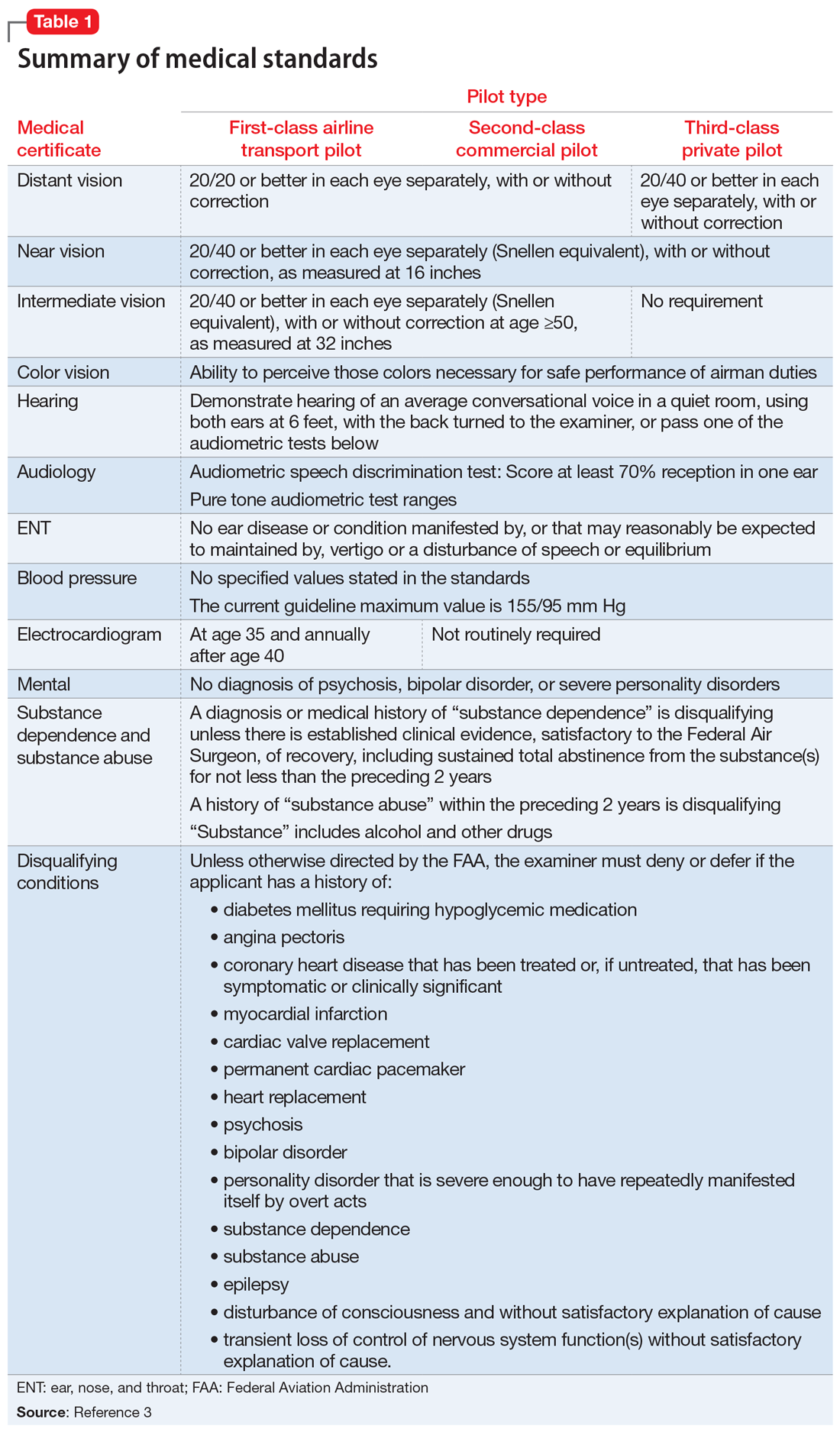
_
Special issuances and Conditions AMEs Can Issue
There are 15 disqualifying conditions for medical certification (Table 13). However, a special issuance of a medical certification may be granted if the aviator shows to the satisfaction of the aviation medical examiner that the duties of the licensure class can be performed without endangering the public safety and that the condition is deemed stable. This may be shown through additional medical evaluations/tests and/or records.
There are certain medical conditions for which an AME can issue a medical certificate without further review from other specialists; thus, an AME can review and follow the Conditions AMEs Can Issue (CACI) worksheet to recommend medical certification (Table 24). The CACI guidelines and worksheets are updated by the FAA regularly to ensure aviators’ health and minimize public risk.
Psychiatric & Psychological Evaluation
Aviators may be referred for Psychiatric and Psychological Evaluation (P&P) if an AME discovers additional concerns about psychiatric and neurocognitive disorders. These cases are not clear-cut. An example would be an aviator who was receiving a psychotropic medication in the past and reported past heavy alcohol use. The P&P includes a thorough psychiatric evaluation by an aerospace psychiatrist and extensive psychological testing by an aerospace psychologist. These clinicians also review collateral information and past medical/AME records. Aviators may be recommended for medical certification with special issuance or may be denied medical certification as a result of these examinations.
Human Intervention Motivation Study program
The Human Intervention Motivation Study (HIMS) program was established to provide an avenue whereby commercial pilots with active substance use disorders can be identified, treated, and successfully returned to active flight status.5 The goal of the HIMS program is to save lives and careers while enhancing flight safety. Physicians trained in HIMS evaluations follow the multifactorial addiction disease model. This evaluation is used to identify active substance use and initiate treatment, and to maintain sobriety and monitor aftercare adherence.
As part of my psychiatry residency training, I had the privilege to work with and learn from an aerospace psychiatrist. Aerospace medicine is a branch of preventive and occupational medicine in which aviators (pilots, aircrew, or astronauts) are subject to evaluation/treatment. The goal is to assess physical and mental health factors to mitigate risks, protect public safety, and ensure the aviators’ well-being.1,2 Aerospace psychiatry is a highly specialized area in which practitioners are trained to perform specific evaluations. In this article, I review those evaluations for those looking to gain insight into the field.
Aviation medical examination
Under Title 14 of the Code of Federal Regulations, the Federal Aviation Administration (FAA) requires aviators to be evaluated for medical certification by undergoing an aviation medical exam.2 In order to be deemed “fit for duty,” aviators must meet strict physical and mental health standards set by the FAA. The extent of these standards varies by the class of licensure (Table 13). Aviation medical exams are performed by any physician who has been designated by the FAA and completed the appropriate FAA aviation medical examiner (AME) training. Aviators who meet the medical standards for their licensure class are recommended for medical certification. If the AME brings up further questions due to the limits of the examination and/or a lack of medical records, the certification will likely be deferred pending further evaluation by an FAA-approved medical specialist and/or the receipt of additional medical records. Questions about a possible psychiatric diagnosis/history or substance use disorder will lead to referral to a psychiatrist familiar with aviation standards for further evaluation.
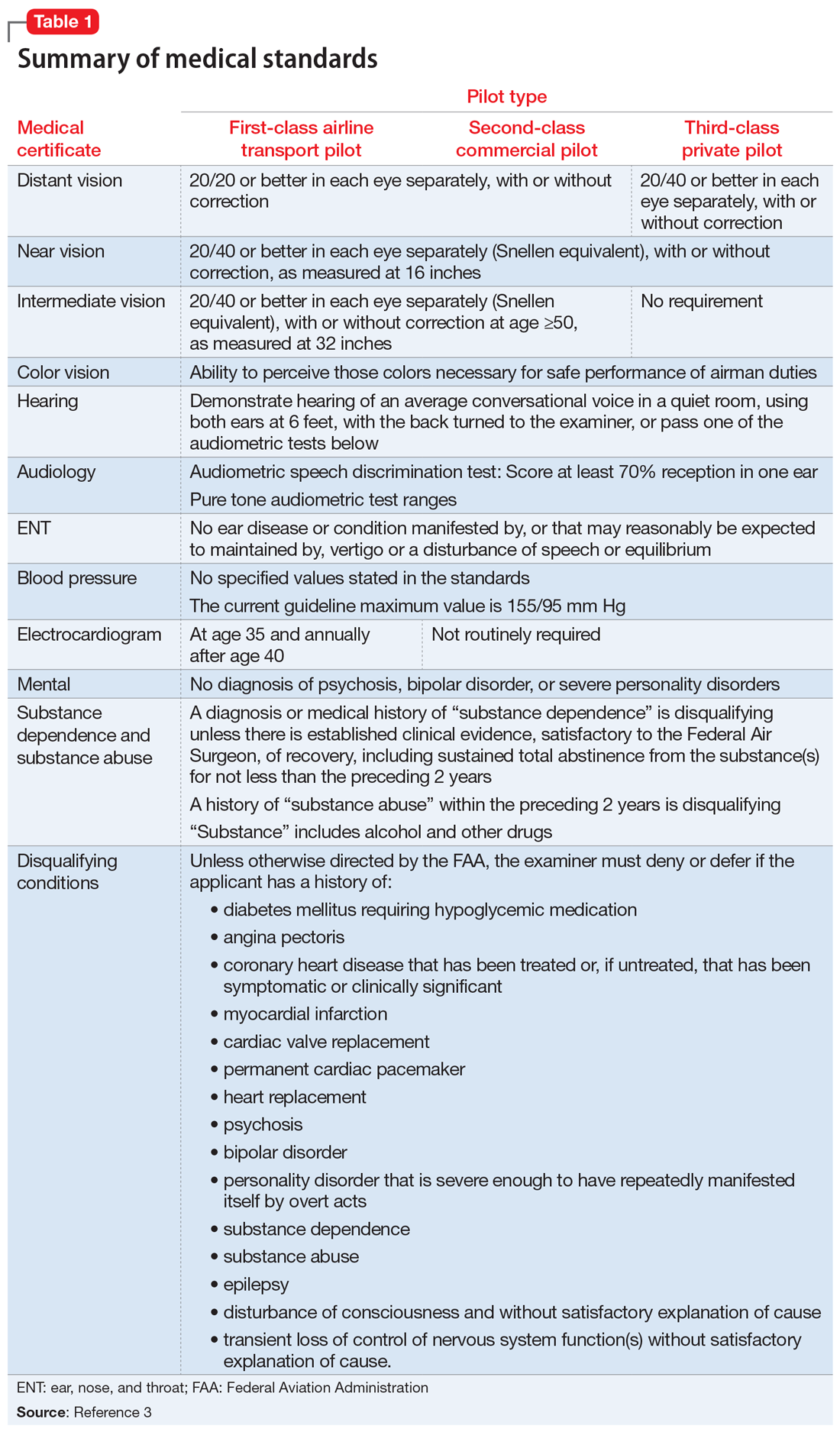
_
Special issuances and Conditions AMEs Can Issue
There are 15 disqualifying conditions for medical certification (Table 13). However, a special issuance of a medical certification may be granted if the aviator shows to the satisfaction of the aviation medical examiner that the duties of the licensure class can be performed without endangering the public safety and that the condition is deemed stable. This may be shown through additional medical evaluations/tests and/or records.
There are certain medical conditions for which an AME can issue a medical certificate without further review from other specialists; thus, an AME can review and follow the Conditions AMEs Can Issue (CACI) worksheet to recommend medical certification (Table 24). The CACI guidelines and worksheets are updated by the FAA regularly to ensure aviators’ health and minimize public risk.
Psychiatric & Psychological Evaluation
Aviators may be referred for Psychiatric and Psychological Evaluation (P&P) if an AME discovers additional concerns about psychiatric and neurocognitive disorders. These cases are not clear-cut. An example would be an aviator who was receiving a psychotropic medication in the past and reported past heavy alcohol use. The P&P includes a thorough psychiatric evaluation by an aerospace psychiatrist and extensive psychological testing by an aerospace psychologist. These clinicians also review collateral information and past medical/AME records. Aviators may be recommended for medical certification with special issuance or may be denied medical certification as a result of these examinations.
Human Intervention Motivation Study program
The Human Intervention Motivation Study (HIMS) program was established to provide an avenue whereby commercial pilots with active substance use disorders can be identified, treated, and successfully returned to active flight status.5 The goal of the HIMS program is to save lives and careers while enhancing flight safety. Physicians trained in HIMS evaluations follow the multifactorial addiction disease model. This evaluation is used to identify active substance use and initiate treatment, and to maintain sobriety and monitor aftercare adherence.
1. Bor R, Hubbard T. Aviation mental health: psychological implications for air transportation. Hampshire, England: Ashgate Publishing Limited; 2006.
2. US Department of Transportation Federal Aviation Administration. Medical certification. https://www.faa.gov/licenses_certificates/medical_certification/. Updated February 1, 2019. Accessed February 19, 2019.
3. US Department of Transportation Federal Aviation Administration. Summary of medical standards. https://www.faa.gov/about/office_org/headquarters_offices/avs/offices/aam/ame/guide/media/synopsis.pdf. Revised April 3, 2006. Accessed October 7, 2018.
4. US Department of Transportation Federal Aviation Administration. Guide for aviation medical examiners: CACI conditions. Revised April 3, 2006. https://www.faa.gov/about/office_org/headquarters_offices/avs/offices/aam/ame/guide/certification_ws/. Accessed October 8, 2018.
5. HIMS. About HIMS. http://www.himsprogram.com/Home/About. Accessed February 6, 2019.
1. Bor R, Hubbard T. Aviation mental health: psychological implications for air transportation. Hampshire, England: Ashgate Publishing Limited; 2006.
2. US Department of Transportation Federal Aviation Administration. Medical certification. https://www.faa.gov/licenses_certificates/medical_certification/. Updated February 1, 2019. Accessed February 19, 2019.
3. US Department of Transportation Federal Aviation Administration. Summary of medical standards. https://www.faa.gov/about/office_org/headquarters_offices/avs/offices/aam/ame/guide/media/synopsis.pdf. Revised April 3, 2006. Accessed October 7, 2018.
4. US Department of Transportation Federal Aviation Administration. Guide for aviation medical examiners: CACI conditions. Revised April 3, 2006. https://www.faa.gov/about/office_org/headquarters_offices/avs/offices/aam/ame/guide/certification_ws/. Accessed October 8, 2018.
5. HIMS. About HIMS. http://www.himsprogram.com/Home/About. Accessed February 6, 2019.
A.I. and U
There is a good chance that your car is equipped with a backup camera. It also may have sensors that alert you when there is another vehicle in one of your blind spots. These wonders of modern technology simply are vision enhancers much like an x-ray or an ultrasound. The sensors merely collect visual data, but the decision of what should be done with this additional information is up to you, just as you decide how to respond to your patient’s lab work and imaging studies.
If you have more disposable income than I do, you may have a vehicle that not only gathers information but also makes decisions based on what it senses by slowing down, applying the brakes, or adjusting the steering. My friends who own these semi-autonomous cars generally have given these control systems positive grades once they have experienced a few events in which the vehicle took over in what it considered a dangerous situation. However, even my friends who are fans of their semi-autonomous cars are uncomfortable about the widespread introduction of fully autonomous vehicles.
The practice of medicine is riding the crest of this same wave of artificial intelligence that promises, or some might say threatens, to remove humans from the driver’s seat (“A.I. Shows Promise Assisting Physicians,” by Cade Metz, The New York Times, Feb. 11, 2019). As reported in the New York Times, a team of physicians has created a system capable of making diagnoses based on a “neural network” that uses complex computer algorithms to learn by analyzing extremely large amounts of data. Once this system had been “taught” to identify certain medical conditions in EMRs, the team tasked the system with analyzing the records of nearly 600,000 patients at a women and children’s hospital in southern China. The investigators claim that the system was able to diagnose asthma with more than 90% accuracy, while physicians can diagnose with an accuracy of 80%-94%, and the system diagnosed gastrointestinal disease with 87% accuracy, well within the physicians’ accuracy range of 82%-90%.
Does this apparent success for A.I. mean that not only will you be vacating your place behind the wheel of your car, but also taking down your shingle and hanging up your stethoscope? Before you rush out and sign up for a federally-funded retraining program, you should remember that this study was done in China, where the privacy laws are somewhat skimpy and the data more voluminous by several scales of magnitude than here. Replicating their results and However, this report should serve as wake-up call to those of you who believe that making diagnoses is at the core of what makes you a physician. If sorting through pages of data to arrive at an explanation for your patients’ complaints is the intellectual challenge that keeps the practice of medicine fresh and exciting, you may want to start looking for other sources of mental stimulation.
A.I. isn’t going to replace the primary care physician. There still will need to be someone available at the initial point of contact who can do a physical exam, take, or at least review, the patient’s history, and then order the lab work and imaging studies that the A.I. system will use to make the diagnosis. In other words, the physician will be primarily responsible for data collection. You may feel that you are almost there already.
Will there be new roles for primary care physicians once A.I. systems are making the diagnoses? It is hard to imagine a fully autonomous health care system in which physicians completely disappear. But, now is the time to think seriously about how we are going to reinvent ourselves to adapt to the inevitable changes and continue as an (or could be "the") essential human element in an increasingly automated system.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
There is a good chance that your car is equipped with a backup camera. It also may have sensors that alert you when there is another vehicle in one of your blind spots. These wonders of modern technology simply are vision enhancers much like an x-ray or an ultrasound. The sensors merely collect visual data, but the decision of what should be done with this additional information is up to you, just as you decide how to respond to your patient’s lab work and imaging studies.
If you have more disposable income than I do, you may have a vehicle that not only gathers information but also makes decisions based on what it senses by slowing down, applying the brakes, or adjusting the steering. My friends who own these semi-autonomous cars generally have given these control systems positive grades once they have experienced a few events in which the vehicle took over in what it considered a dangerous situation. However, even my friends who are fans of their semi-autonomous cars are uncomfortable about the widespread introduction of fully autonomous vehicles.
The practice of medicine is riding the crest of this same wave of artificial intelligence that promises, or some might say threatens, to remove humans from the driver’s seat (“A.I. Shows Promise Assisting Physicians,” by Cade Metz, The New York Times, Feb. 11, 2019). As reported in the New York Times, a team of physicians has created a system capable of making diagnoses based on a “neural network” that uses complex computer algorithms to learn by analyzing extremely large amounts of data. Once this system had been “taught” to identify certain medical conditions in EMRs, the team tasked the system with analyzing the records of nearly 600,000 patients at a women and children’s hospital in southern China. The investigators claim that the system was able to diagnose asthma with more than 90% accuracy, while physicians can diagnose with an accuracy of 80%-94%, and the system diagnosed gastrointestinal disease with 87% accuracy, well within the physicians’ accuracy range of 82%-90%.
Does this apparent success for A.I. mean that not only will you be vacating your place behind the wheel of your car, but also taking down your shingle and hanging up your stethoscope? Before you rush out and sign up for a federally-funded retraining program, you should remember that this study was done in China, where the privacy laws are somewhat skimpy and the data more voluminous by several scales of magnitude than here. Replicating their results and However, this report should serve as wake-up call to those of you who believe that making diagnoses is at the core of what makes you a physician. If sorting through pages of data to arrive at an explanation for your patients’ complaints is the intellectual challenge that keeps the practice of medicine fresh and exciting, you may want to start looking for other sources of mental stimulation.
A.I. isn’t going to replace the primary care physician. There still will need to be someone available at the initial point of contact who can do a physical exam, take, or at least review, the patient’s history, and then order the lab work and imaging studies that the A.I. system will use to make the diagnosis. In other words, the physician will be primarily responsible for data collection. You may feel that you are almost there already.
Will there be new roles for primary care physicians once A.I. systems are making the diagnoses? It is hard to imagine a fully autonomous health care system in which physicians completely disappear. But, now is the time to think seriously about how we are going to reinvent ourselves to adapt to the inevitable changes and continue as an (or could be "the") essential human element in an increasingly automated system.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
There is a good chance that your car is equipped with a backup camera. It also may have sensors that alert you when there is another vehicle in one of your blind spots. These wonders of modern technology simply are vision enhancers much like an x-ray or an ultrasound. The sensors merely collect visual data, but the decision of what should be done with this additional information is up to you, just as you decide how to respond to your patient’s lab work and imaging studies.
If you have more disposable income than I do, you may have a vehicle that not only gathers information but also makes decisions based on what it senses by slowing down, applying the brakes, or adjusting the steering. My friends who own these semi-autonomous cars generally have given these control systems positive grades once they have experienced a few events in which the vehicle took over in what it considered a dangerous situation. However, even my friends who are fans of their semi-autonomous cars are uncomfortable about the widespread introduction of fully autonomous vehicles.
The practice of medicine is riding the crest of this same wave of artificial intelligence that promises, or some might say threatens, to remove humans from the driver’s seat (“A.I. Shows Promise Assisting Physicians,” by Cade Metz, The New York Times, Feb. 11, 2019). As reported in the New York Times, a team of physicians has created a system capable of making diagnoses based on a “neural network” that uses complex computer algorithms to learn by analyzing extremely large amounts of data. Once this system had been “taught” to identify certain medical conditions in EMRs, the team tasked the system with analyzing the records of nearly 600,000 patients at a women and children’s hospital in southern China. The investigators claim that the system was able to diagnose asthma with more than 90% accuracy, while physicians can diagnose with an accuracy of 80%-94%, and the system diagnosed gastrointestinal disease with 87% accuracy, well within the physicians’ accuracy range of 82%-90%.
Does this apparent success for A.I. mean that not only will you be vacating your place behind the wheel of your car, but also taking down your shingle and hanging up your stethoscope? Before you rush out and sign up for a federally-funded retraining program, you should remember that this study was done in China, where the privacy laws are somewhat skimpy and the data more voluminous by several scales of magnitude than here. Replicating their results and However, this report should serve as wake-up call to those of you who believe that making diagnoses is at the core of what makes you a physician. If sorting through pages of data to arrive at an explanation for your patients’ complaints is the intellectual challenge that keeps the practice of medicine fresh and exciting, you may want to start looking for other sources of mental stimulation.
A.I. isn’t going to replace the primary care physician. There still will need to be someone available at the initial point of contact who can do a physical exam, take, or at least review, the patient’s history, and then order the lab work and imaging studies that the A.I. system will use to make the diagnosis. In other words, the physician will be primarily responsible for data collection. You may feel that you are almost there already.
Will there be new roles for primary care physicians once A.I. systems are making the diagnoses? It is hard to imagine a fully autonomous health care system in which physicians completely disappear. But, now is the time to think seriously about how we are going to reinvent ourselves to adapt to the inevitable changes and continue as an (or could be "the") essential human element in an increasingly automated system.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
How are you at coping with transparency?
As reported in the Wall Street Journal, the current administration has proposed a suite of initiatives that could improve patients’ access to their health data, including doctors’ and hospitals’ electronic records as well as insurance claim information (“Rules to Ease Patient Access to Health Data Are Proposed,” by Anna Wilde Mathews, Feb. 11, 2019). One of the draft rules would mandate new technology standards that allow health information data to flow seamlessly between providers and hospitals using different electronic systems, a step that should have been taken well before the federal government began cajoling physicians into adopting not-ready-for-prime-time EMR systems and rewarding their “meaningful use.” Other rules are aimed at discouraging the patient-unfriendly practice of delaying and charging for the transfer of medical records.
Apple already has begun research and development on systems and tools that would allow patients to receive and store their health information on their smart phones and tablets. Arriving at the ED or a consulting physician, the patient would need only unlock his or her device to share his or her medical record.
These proposals are long overdue and in the long run should save providers and patients time and expense. As long as they also include rules mandating true transparency in hospital billing, these initiatives appear to be heading us in the right direction.
Do you create your office notes with the assumption that your patient will be reading them? Seventy-five years ago, physicians, many of whom were in solo practice, scrawled their notes as simple mnemonics. They could barely decipher their own scribbles. If they needed to share information with a consultant, it was with a phone call or dictated letter. You probably are more aware of creating a readable note because you rely on covering physicians ... and you know that the folks who pay you will be auditing your charts.
Depending on your patient mix, most of the notes you generate probably don’t contain many observations that you are hesitant to share with the patient. If you haven’t already discussed his body mass index with the patient you have described as “obese,” you aren’t doing your job. However, occasionally there are topics that have arisen in the family and social history that may not be pertinent to the patient’s current problem, but provide a more nuanced picture of her and serve as a mnemonic at a later visit. Will the patient mind if you include these tidbits in an electronic record that may be shared by a wide audience outside the confines of your exam room?
How do you deal with situations like this when the threat of transparency could interfere with our relationship with our patients? You could ask the patient, “ Do you mind if I include that event you just told me, in your EMR?” You could create a “shadow record” that includes information the patient prefers not to be shared and your own observations that you don’t feel comfortable sharing with the patient. Is this “shadow record” something electronic that could be redacted by simply toggling a clickable box? Or is it an old-fashioned paper note you keep in a separate file in a locked drawer in a file cabinet (if you even have a file cabinet)? I fear the lawyers would have something to say about both those options. The best solution may simply be to rely on your memory. If you have so many patients that you can’t remember those occasional sensitive issues that have been shared with you, then maybe you have too many patients.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater.” Email him at [email protected].
As reported in the Wall Street Journal, the current administration has proposed a suite of initiatives that could improve patients’ access to their health data, including doctors’ and hospitals’ electronic records as well as insurance claim information (“Rules to Ease Patient Access to Health Data Are Proposed,” by Anna Wilde Mathews, Feb. 11, 2019). One of the draft rules would mandate new technology standards that allow health information data to flow seamlessly between providers and hospitals using different electronic systems, a step that should have been taken well before the federal government began cajoling physicians into adopting not-ready-for-prime-time EMR systems and rewarding their “meaningful use.” Other rules are aimed at discouraging the patient-unfriendly practice of delaying and charging for the transfer of medical records.
Apple already has begun research and development on systems and tools that would allow patients to receive and store their health information on their smart phones and tablets. Arriving at the ED or a consulting physician, the patient would need only unlock his or her device to share his or her medical record.
These proposals are long overdue and in the long run should save providers and patients time and expense. As long as they also include rules mandating true transparency in hospital billing, these initiatives appear to be heading us in the right direction.
Do you create your office notes with the assumption that your patient will be reading them? Seventy-five years ago, physicians, many of whom were in solo practice, scrawled their notes as simple mnemonics. They could barely decipher their own scribbles. If they needed to share information with a consultant, it was with a phone call or dictated letter. You probably are more aware of creating a readable note because you rely on covering physicians ... and you know that the folks who pay you will be auditing your charts.
Depending on your patient mix, most of the notes you generate probably don’t contain many observations that you are hesitant to share with the patient. If you haven’t already discussed his body mass index with the patient you have described as “obese,” you aren’t doing your job. However, occasionally there are topics that have arisen in the family and social history that may not be pertinent to the patient’s current problem, but provide a more nuanced picture of her and serve as a mnemonic at a later visit. Will the patient mind if you include these tidbits in an electronic record that may be shared by a wide audience outside the confines of your exam room?
How do you deal with situations like this when the threat of transparency could interfere with our relationship with our patients? You could ask the patient, “ Do you mind if I include that event you just told me, in your EMR?” You could create a “shadow record” that includes information the patient prefers not to be shared and your own observations that you don’t feel comfortable sharing with the patient. Is this “shadow record” something electronic that could be redacted by simply toggling a clickable box? Or is it an old-fashioned paper note you keep in a separate file in a locked drawer in a file cabinet (if you even have a file cabinet)? I fear the lawyers would have something to say about both those options. The best solution may simply be to rely on your memory. If you have so many patients that you can’t remember those occasional sensitive issues that have been shared with you, then maybe you have too many patients.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater.” Email him at [email protected].
As reported in the Wall Street Journal, the current administration has proposed a suite of initiatives that could improve patients’ access to their health data, including doctors’ and hospitals’ electronic records as well as insurance claim information (“Rules to Ease Patient Access to Health Data Are Proposed,” by Anna Wilde Mathews, Feb. 11, 2019). One of the draft rules would mandate new technology standards that allow health information data to flow seamlessly between providers and hospitals using different electronic systems, a step that should have been taken well before the federal government began cajoling physicians into adopting not-ready-for-prime-time EMR systems and rewarding their “meaningful use.” Other rules are aimed at discouraging the patient-unfriendly practice of delaying and charging for the transfer of medical records.
Apple already has begun research and development on systems and tools that would allow patients to receive and store their health information on their smart phones and tablets. Arriving at the ED or a consulting physician, the patient would need only unlock his or her device to share his or her medical record.
These proposals are long overdue and in the long run should save providers and patients time and expense. As long as they also include rules mandating true transparency in hospital billing, these initiatives appear to be heading us in the right direction.
Do you create your office notes with the assumption that your patient will be reading them? Seventy-five years ago, physicians, many of whom were in solo practice, scrawled their notes as simple mnemonics. They could barely decipher their own scribbles. If they needed to share information with a consultant, it was with a phone call or dictated letter. You probably are more aware of creating a readable note because you rely on covering physicians ... and you know that the folks who pay you will be auditing your charts.
Depending on your patient mix, most of the notes you generate probably don’t contain many observations that you are hesitant to share with the patient. If you haven’t already discussed his body mass index with the patient you have described as “obese,” you aren’t doing your job. However, occasionally there are topics that have arisen in the family and social history that may not be pertinent to the patient’s current problem, but provide a more nuanced picture of her and serve as a mnemonic at a later visit. Will the patient mind if you include these tidbits in an electronic record that may be shared by a wide audience outside the confines of your exam room?
How do you deal with situations like this when the threat of transparency could interfere with our relationship with our patients? You could ask the patient, “ Do you mind if I include that event you just told me, in your EMR?” You could create a “shadow record” that includes information the patient prefers not to be shared and your own observations that you don’t feel comfortable sharing with the patient. Is this “shadow record” something electronic that could be redacted by simply toggling a clickable box? Or is it an old-fashioned paper note you keep in a separate file in a locked drawer in a file cabinet (if you even have a file cabinet)? I fear the lawyers would have something to say about both those options. The best solution may simply be to rely on your memory. If you have so many patients that you can’t remember those occasional sensitive issues that have been shared with you, then maybe you have too many patients.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater.” Email him at [email protected].
Adenovirus: More than just another viral illness
The mother of three looked tired and little worried. She wasn’t one to bring her kids to the pediatrician’s office with every minor illness, but her youngest had 3 days of fever, runny nose, cough, and little of her normal energy.
The pediatrician entered the room and smiled sympathetically.
“We ran tests for flu and RSV [respiratory syncytial virus] and it’s neither of those so. ...”
“So it’s just a virus that we don’t routinely test for and it’s going to need to run its course,” the mother finished his sentence. She knew the drill.
Before the doctor could leave the room though, the mother had one more question. “You don’t think it could be adenovirus do you?”
Most years, influenza and RSV command center stage, and adenovirus is relegated to the wings. It is not so much lack of disease or morbidity, but rather lack of recognition. Yes, we all learned in medical school that it is a cause of epidemic keratoconjunctivitis, but many adenoviral infections are clinically indistinguishable from infections caused by other viruses. Common symptoms – fever, cough, sore throat, and malaise – overlap with those caused by influenza. Like rhinovirus, adenovirus can cause common cold symptoms. Like RSV, it can cause bronchiolitis. Just like parainfluenza, it can cause croup. It can cause a pertussislike syndrome with prolonged cough, and enteric adenoviruses, especially types 40 and 41, cause gastroenteritis that mimics norovirus or rotavirus infection.
Testing for adenovirus is not readily available or routine in most pediatricians’ offices, and while many hospitals and reference labs offer adenovirus polymerase chain reaction testing as part of a comprehensive respiratory virus panel, the test can be expensive and unlikely to change management in most ambulatory patients. This makes it difficult to count the number of adenoviruses annually.
This winter though, adenovirus was in the news ... repeatedly. In November 2018, CBS News reported that a University of Maryland freshman had died of an adenovirus-related illness. The family of Olivia Paregol told reporters that she was being treated for Crohn’s disease. Immune suppression is one recognized risk factor for more severe adenoviral disease; underlying heart and lung disease are others. Testing at the Centers for Disease Control and Prevention revealed that the student and several others on campus were infected with adenovirus type 7, a strain that has been associated with outbreaks of acute, severe respiratory illness in military recruits. As of Jan. 24, 2019, university officials reported 42 confirmed cases of adenovirus in University of Maryland students, 13 of which were confirmed as adenovirus 7.
Adenovirus type 7 also caused an outbreak at a pediatric long-term care facility in New Jersey late last year. Between Sept. 26 and Nov. 11, 2018, 36 residents and 1 staff member became ill. Eleven individuals died. In an unrelated outbreak at a second pediatric long-term care facility, 17 residents were affected between Oct. 20 and Dec. 10, 2018. Adenovirus 3 was identified and all children recovered.
Between October 2013 and July 2014, public health officials in Oregon identified an increase in adenoviral infections in people with respiratory illness. Sixty-nine percent were hospitalized (136/198), 31% needed intensive care, and 18% were mechanically ventilated. Multiple types of adenovirus were recovered but the most common was adenovirus 7 (Emerg Infect Dis. 2016. doi: 10.3201/eid2206.151898).
Depending on your perspective, measures to prevent the spread of adenovirus are elegantly simple, evidence-based, public health intervention or maddeningly little more than common sense. Wash your hands often with soap and water. Avoid touching your eyes, mouth, and nose with unwashed hands. Avoid close contact with people who are sick. The latter is easier if those who are sick stay home. Prior to the start of the most recent academic semester at the University of Maryland, university officials urged students who were sick not to return to campus but to stay at home to rest and recover. Those who fell ill on campus were urged to return home via nonpublic transportation if possible. Those who stayed on campus were advised to stay in their living spaces and clean high-touch surfaces with bleach. Like other nonenveloped viruses, adenovirus is not easily destroyed by many commonly used disinfectants. Under ideal conditions, it can survive on surfaces – remaining infectious – for up to 3 months.
Back at the pediatrician’s office, “We need an adenovirus vaccine,” the mother said as she picked up her child and headed for the door.
There is, in fact, a live oral vaccine that protects against adenovirus types 4 and 7. It is only approved for use in United States military personnel aged 17-50 years and it is given to all recruits as soon as they enter basic training. It works too. Before vaccine was available, up to 80% of recruits became infected during their initial training, half of those developing significant illness and a quarter being hospitalized. When the current vaccine was introduced in 2011, there was a 100-fold decrease in adenovirus-related disease burden (from 5.8 to 0.02 cases per 1,000 person-weeks, P less than .0001). That translates to 1 death, 1,100-2,700 hospitalizations and 13,000 febrile illnesses prevented each year (Clin Infect Dis. 2014 Oct 1. doi: 10.1093/cid/ciu507).
Some experts have suggested that adenovirus vaccine could be useful in civilian populations, too, but I question what the public reception would be. We have safe influenza vaccines that reduce the need for hospitalization and reduce mortality from influenza, but we still can’t convince some people to immunize themselves and their children. In the last 4 years, flu vaccination rates among children have remained just shy of 60% and adult rates are even lower. Collectively, we don’t seem to be ready to relinquish – or at least diminish – the annual suffering that goes with flu. I have to wonder if the same would be true for adenovirus.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
The mother of three looked tired and little worried. She wasn’t one to bring her kids to the pediatrician’s office with every minor illness, but her youngest had 3 days of fever, runny nose, cough, and little of her normal energy.
The pediatrician entered the room and smiled sympathetically.
“We ran tests for flu and RSV [respiratory syncytial virus] and it’s neither of those so. ...”
“So it’s just a virus that we don’t routinely test for and it’s going to need to run its course,” the mother finished his sentence. She knew the drill.
Before the doctor could leave the room though, the mother had one more question. “You don’t think it could be adenovirus do you?”
Most years, influenza and RSV command center stage, and adenovirus is relegated to the wings. It is not so much lack of disease or morbidity, but rather lack of recognition. Yes, we all learned in medical school that it is a cause of epidemic keratoconjunctivitis, but many adenoviral infections are clinically indistinguishable from infections caused by other viruses. Common symptoms – fever, cough, sore throat, and malaise – overlap with those caused by influenza. Like rhinovirus, adenovirus can cause common cold symptoms. Like RSV, it can cause bronchiolitis. Just like parainfluenza, it can cause croup. It can cause a pertussislike syndrome with prolonged cough, and enteric adenoviruses, especially types 40 and 41, cause gastroenteritis that mimics norovirus or rotavirus infection.
Testing for adenovirus is not readily available or routine in most pediatricians’ offices, and while many hospitals and reference labs offer adenovirus polymerase chain reaction testing as part of a comprehensive respiratory virus panel, the test can be expensive and unlikely to change management in most ambulatory patients. This makes it difficult to count the number of adenoviruses annually.
This winter though, adenovirus was in the news ... repeatedly. In November 2018, CBS News reported that a University of Maryland freshman had died of an adenovirus-related illness. The family of Olivia Paregol told reporters that she was being treated for Crohn’s disease. Immune suppression is one recognized risk factor for more severe adenoviral disease; underlying heart and lung disease are others. Testing at the Centers for Disease Control and Prevention revealed that the student and several others on campus were infected with adenovirus type 7, a strain that has been associated with outbreaks of acute, severe respiratory illness in military recruits. As of Jan. 24, 2019, university officials reported 42 confirmed cases of adenovirus in University of Maryland students, 13 of which were confirmed as adenovirus 7.
Adenovirus type 7 also caused an outbreak at a pediatric long-term care facility in New Jersey late last year. Between Sept. 26 and Nov. 11, 2018, 36 residents and 1 staff member became ill. Eleven individuals died. In an unrelated outbreak at a second pediatric long-term care facility, 17 residents were affected between Oct. 20 and Dec. 10, 2018. Adenovirus 3 was identified and all children recovered.
Between October 2013 and July 2014, public health officials in Oregon identified an increase in adenoviral infections in people with respiratory illness. Sixty-nine percent were hospitalized (136/198), 31% needed intensive care, and 18% were mechanically ventilated. Multiple types of adenovirus were recovered but the most common was adenovirus 7 (Emerg Infect Dis. 2016. doi: 10.3201/eid2206.151898).
Depending on your perspective, measures to prevent the spread of adenovirus are elegantly simple, evidence-based, public health intervention or maddeningly little more than common sense. Wash your hands often with soap and water. Avoid touching your eyes, mouth, and nose with unwashed hands. Avoid close contact with people who are sick. The latter is easier if those who are sick stay home. Prior to the start of the most recent academic semester at the University of Maryland, university officials urged students who were sick not to return to campus but to stay at home to rest and recover. Those who fell ill on campus were urged to return home via nonpublic transportation if possible. Those who stayed on campus were advised to stay in their living spaces and clean high-touch surfaces with bleach. Like other nonenveloped viruses, adenovirus is not easily destroyed by many commonly used disinfectants. Under ideal conditions, it can survive on surfaces – remaining infectious – for up to 3 months.
Back at the pediatrician’s office, “We need an adenovirus vaccine,” the mother said as she picked up her child and headed for the door.
There is, in fact, a live oral vaccine that protects against adenovirus types 4 and 7. It is only approved for use in United States military personnel aged 17-50 years and it is given to all recruits as soon as they enter basic training. It works too. Before vaccine was available, up to 80% of recruits became infected during their initial training, half of those developing significant illness and a quarter being hospitalized. When the current vaccine was introduced in 2011, there was a 100-fold decrease in adenovirus-related disease burden (from 5.8 to 0.02 cases per 1,000 person-weeks, P less than .0001). That translates to 1 death, 1,100-2,700 hospitalizations and 13,000 febrile illnesses prevented each year (Clin Infect Dis. 2014 Oct 1. doi: 10.1093/cid/ciu507).
Some experts have suggested that adenovirus vaccine could be useful in civilian populations, too, but I question what the public reception would be. We have safe influenza vaccines that reduce the need for hospitalization and reduce mortality from influenza, but we still can’t convince some people to immunize themselves and their children. In the last 4 years, flu vaccination rates among children have remained just shy of 60% and adult rates are even lower. Collectively, we don’t seem to be ready to relinquish – or at least diminish – the annual suffering that goes with flu. I have to wonder if the same would be true for adenovirus.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
The mother of three looked tired and little worried. She wasn’t one to bring her kids to the pediatrician’s office with every minor illness, but her youngest had 3 days of fever, runny nose, cough, and little of her normal energy.
The pediatrician entered the room and smiled sympathetically.
“We ran tests for flu and RSV [respiratory syncytial virus] and it’s neither of those so. ...”
“So it’s just a virus that we don’t routinely test for and it’s going to need to run its course,” the mother finished his sentence. She knew the drill.
Before the doctor could leave the room though, the mother had one more question. “You don’t think it could be adenovirus do you?”
Most years, influenza and RSV command center stage, and adenovirus is relegated to the wings. It is not so much lack of disease or morbidity, but rather lack of recognition. Yes, we all learned in medical school that it is a cause of epidemic keratoconjunctivitis, but many adenoviral infections are clinically indistinguishable from infections caused by other viruses. Common symptoms – fever, cough, sore throat, and malaise – overlap with those caused by influenza. Like rhinovirus, adenovirus can cause common cold symptoms. Like RSV, it can cause bronchiolitis. Just like parainfluenza, it can cause croup. It can cause a pertussislike syndrome with prolonged cough, and enteric adenoviruses, especially types 40 and 41, cause gastroenteritis that mimics norovirus or rotavirus infection.
Testing for adenovirus is not readily available or routine in most pediatricians’ offices, and while many hospitals and reference labs offer adenovirus polymerase chain reaction testing as part of a comprehensive respiratory virus panel, the test can be expensive and unlikely to change management in most ambulatory patients. This makes it difficult to count the number of adenoviruses annually.
This winter though, adenovirus was in the news ... repeatedly. In November 2018, CBS News reported that a University of Maryland freshman had died of an adenovirus-related illness. The family of Olivia Paregol told reporters that she was being treated for Crohn’s disease. Immune suppression is one recognized risk factor for more severe adenoviral disease; underlying heart and lung disease are others. Testing at the Centers for Disease Control and Prevention revealed that the student and several others on campus were infected with adenovirus type 7, a strain that has been associated with outbreaks of acute, severe respiratory illness in military recruits. As of Jan. 24, 2019, university officials reported 42 confirmed cases of adenovirus in University of Maryland students, 13 of which were confirmed as adenovirus 7.
Adenovirus type 7 also caused an outbreak at a pediatric long-term care facility in New Jersey late last year. Between Sept. 26 and Nov. 11, 2018, 36 residents and 1 staff member became ill. Eleven individuals died. In an unrelated outbreak at a second pediatric long-term care facility, 17 residents were affected between Oct. 20 and Dec. 10, 2018. Adenovirus 3 was identified and all children recovered.
Between October 2013 and July 2014, public health officials in Oregon identified an increase in adenoviral infections in people with respiratory illness. Sixty-nine percent were hospitalized (136/198), 31% needed intensive care, and 18% were mechanically ventilated. Multiple types of adenovirus were recovered but the most common was adenovirus 7 (Emerg Infect Dis. 2016. doi: 10.3201/eid2206.151898).
Depending on your perspective, measures to prevent the spread of adenovirus are elegantly simple, evidence-based, public health intervention or maddeningly little more than common sense. Wash your hands often with soap and water. Avoid touching your eyes, mouth, and nose with unwashed hands. Avoid close contact with people who are sick. The latter is easier if those who are sick stay home. Prior to the start of the most recent academic semester at the University of Maryland, university officials urged students who were sick not to return to campus but to stay at home to rest and recover. Those who fell ill on campus were urged to return home via nonpublic transportation if possible. Those who stayed on campus were advised to stay in their living spaces and clean high-touch surfaces with bleach. Like other nonenveloped viruses, adenovirus is not easily destroyed by many commonly used disinfectants. Under ideal conditions, it can survive on surfaces – remaining infectious – for up to 3 months.
Back at the pediatrician’s office, “We need an adenovirus vaccine,” the mother said as she picked up her child and headed for the door.
There is, in fact, a live oral vaccine that protects against adenovirus types 4 and 7. It is only approved for use in United States military personnel aged 17-50 years and it is given to all recruits as soon as they enter basic training. It works too. Before vaccine was available, up to 80% of recruits became infected during their initial training, half of those developing significant illness and a quarter being hospitalized. When the current vaccine was introduced in 2011, there was a 100-fold decrease in adenovirus-related disease burden (from 5.8 to 0.02 cases per 1,000 person-weeks, P less than .0001). That translates to 1 death, 1,100-2,700 hospitalizations and 13,000 febrile illnesses prevented each year (Clin Infect Dis. 2014 Oct 1. doi: 10.1093/cid/ciu507).
Some experts have suggested that adenovirus vaccine could be useful in civilian populations, too, but I question what the public reception would be. We have safe influenza vaccines that reduce the need for hospitalization and reduce mortality from influenza, but we still can’t convince some people to immunize themselves and their children. In the last 4 years, flu vaccination rates among children have remained just shy of 60% and adult rates are even lower. Collectively, we don’t seem to be ready to relinquish – or at least diminish – the annual suffering that goes with flu. I have to wonder if the same would be true for adenovirus.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].