User login
The psychiatric clinic of the future
Despite the tremendous advances in psychiatry in recent years, the current clinical practice of psychiatry continues to rely on data from intermittent assessments along with subjective and unquantifiable accounts from patients and caregivers. Furthermore, there continues to be significant diagnostic variations among practitioners. Fortunately, technology to address these issues appears to be on the horizon.
How might the psychiatric clinic of the future look? What changes could we envision? These 4 critical factors may soon bring about dynamic changes in the way we practice psychiatry:
- precision psychiatry
- digital psychiatry
- technology-enhanced psychotherapy
- electronic health record (EHR) reforms.
In this article, we review how advances in each of these areas might lead to improved care for our patients.
Precision psychiatry
Precision psychiatry takes into account each patient’s variability in genes, environment, and lifestyle to determine individualized treatment and prevention strategies. It relies on pharmacogenomic testing as the primary tool. Pharmacogenomics is the study of variability in drug response due to heredity.
Emerging data on the clinical utility and cost-effectiveness of pharmacogenomic testing are encouraging, but its routine use is not well supported by current evidence.2 One limit to using pharmacogenomic testing is that many genes simultaneously exert an effect on the structure and function of neurons and associated pathophysiology. According to the International Society of Psychiatric Genetics, no single genetic variant is sufficient to cause psychiatric disorders such as depression, bipolar disorder, substance dependence, or schizophrenia. This limits the possibility of using genetic tests to establish a diagnosis.3
In the future, better algorithms could promote more accurate pharmacogenomics profiles for individual patients, which could influence treatment.
Precision psychiatry could lead to:
- identification of novel targets for new medications
- pharmacogenetic profiling of the patient to predict disease susceptibility and medication response
- personalized therapy: the right drug at the right dose for the right patient.
- improved efficacy and fewer adverse medication reactions.
Continue to: Digital psychiatry
Digital psychiatry
Integrating computer-based technology into psychiatric practice has given birth to a new frontier that could be called digital psychiatry. This might encompass the following:
- telepsychiatry
- social media with a mental health focus
- web-based applications/devices
- artificial intelligence (AI).
Telepsychiatry. Videoconferencing is the most widely used form of telepsychiatry. It provides patients with easier access to mental health treatment.4 Telepsychiatry has the potential to match patients and clinicians with similar cultural backgrounds, thus minimizing cultural gaps and misunderstandings. Most importantly, it is comparable to face-to-face interviews in terms of the reliability of assessment and treatment outcomes.5
Telepsychiatry might be particularly helpful for patients with restricted mobility, such as those who live in remote areas, nursing homes, or correctional facilities. In correctional settings, transferring prisoners is expensive and carries the risk of escape. In a small study (N = 86) conducted in Hong Kong, Chen et al6 found that using videoconferencing to conduct clinical interviews of inmates was cost-efficient and scored high in terms of patient acceptability.
Social media. Social media could be a powerful platform for early detection of mental illness. Staying connected with patients on social media could allow psychiatrists to be more aware of their patient’s mood fluctuations, which might lead to more timely assessments. Physicians could be automatically notified about changes in their patients’ social media activity that indicate changes in mental state, which could solicit immediate intervention and treatment. On the other hand, such use of social media could blur professional boundaries. Psychiatrists also could use social media to promote awareness of mental health and educate the public on ways to improve or maintain their mental well-being.7
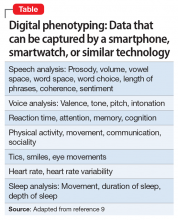
Web-based applications/devices. Real-time monitoring through applications or internet-based smart devices creates a new avenue for patients to receive personalized assessments, treatment, and intervention.8 Smartwatches with internet connectivity may offer a glimpse of the wearer’s sleep architecture and duration, thus providing real-time data on patients who have insomnia. We can now passively collect objective data from devices, such as smartphones and laptops, to phenotype an individual’s mood and mental state, a process called digital phenotyping. The Table9 lists examples of the types of mental health–related metrics that can be captured by smartphones, smartwatches, and similar technology. Information from these devices can be accumulated to create a database that can be used to predict symptoms.10 For example, the way people use a smartphone’s keyboard, including latency time between space and character types, can be used to generate variables for data. This type of information is being studied for use in screening depression and passively assessing mood in real time.11
Continue to: Artificial intelligence
Artificial intelligence—the development of computer systems able to perform tasks that normally require human intelligence—is being increasingly used in psychiatry. Some studies have suggested AI can be used to identify patients’ risk of suicide12-15 or psychosis.16,17 Kalanderian and Nasrallah18 reviewed several of these studies in
Other researchers have found clinical uses for machine learning, a subset of AI that uses methods to automatically detect patterns and make predictions based on those patterns. In one study, a machine learning analysis of functional MRI scans was able to identify 4 distinct subtypes of depression.19 In another study, a machine learning model was able to predict with 60% accuracy which patients with depression would respond to antidepressants.20
In the future, AI might be used to change mental health classification systems. Because many mental health disorders share similar symptom clusters, machine learning can help to identify associations between symptoms, behavior, brain function, and real-world function across different diagnoses, potentially affecting how we will classify mental disorders.21
Technology-enhanced psychotherapy
In the future, it might be common for psychotherapy to be provided by a computer, or “virtual therapist.” Several studies have evaluated the use of technology-enhanced psychotherapy.
Lucas et al22 investigated patients’ interactions with a virtual therapist. Participants were interviewed by an avatar named Ellie, who they saw on a TV screen. Half of the participants were told Ellie was not human, and half were told Ellie was being controlled remotely by a human. Three psychologists who were blinded to group allocations analyzed transcripts of the interviews and video recordings of participants’ facial expressions to quantify the participants’ fear, sadness, and other emotional responses during the interviews, as well as their openness to the questions. Participants who believed Ellie was fully automated reported significantly lower fear of self-disclosure and impression management (attempts to control how others perceive them) than participants who were told that Ellie was operated by a human. Additionally, participants who believed they were interacting with a computer were more open during the interview.22
Continue to: Researchers at the University of Southern California...
Researchers at the University of Southern California developed software that assessed 74 acoustic features, including pitch, volume, quality, shimmer, jitter, and prosody, to predict outcomes among patients receiving couples therapy. This software was able to predict marital discord at least as well as human therapists.23
Many mental health apps purport to implement specific components of psychotherapy. Many of these apps focus on cognitive-behavioral therapy worksheets, mindfulness exercises, and/or mood tracking. The features provided by such apps emulate the tasks and intended outcomes of traditional psychotherapy, but in an entirely decentralized venue.24
Some have expressed concern that an increased use of virtual therapists powered by AI might lead to a dehumanization of psychiatry (Box25,26).
Box
Whether there are aspects of the psychiatric patient encounter that cannot be managed by a “virtual clinician” created by artificial intelligence (AI) remains to be determined. Some of the benefits of using AI in this manner may be difficult to anticipate, or may be specific to an individual’s relationship with his/her clinician.25
On the other hand, AI systems blur previously assumed boundaries between reality and fiction, and this could have complex effects on patients. Similar to therapeutic relationships with a human clinician, there is the risk of transference of emotions, thoughts, and feelings to a virtual therapist powered by AI. Unlike with a psychiatrist or therapist, however, there is no person on the other side of this transference. Whether virtual clinicians will be able to manage such transference remains to be seen.
In Deep Medicine,26 cardiologist Eric Topol, MD, emphasizes a crucial component of a patient encounter that AI will be unlikely able to provide: empathy. Virtual therapists powered by AI will inherit the tasks best done by machines, leaving humans more time to do what they do best—providing empathy and being “present” for patients.
Electronic health record reforms
Although many clinicians find EHRs to be onerous and time-consuming, EHR technology is constantly improving, and EHRs have revolutionized documentation and order implementation. Several potential advances could improve clinical practice. For example, EHRs could incorporate a clinical decision support system that uses AI-based algorithms to assist psychiatrists with diagnosis, monitoring, and treatment.27 In the future, EHRs might have the ability to monitor and learn from errors and adverse events, and automatically design an algorithm to avoid them.28 They should be designed to better manage analysis of pharmacogenetic test results, which is challenging due to the amount and complexity of the data.29 Future EHRs should eliminate the non-intuitive and multi-click interfaces and cumbersome data searches of today’s EHRs.30
Technology brings new ethical considerations
Mental health interventions based on AI typically work with algorithms, and algorithms bring ethical issues. Mental health devices or systems that use AI could contain biases that have the potential to harm in unintended ways, such as a data-driven sexist or racist bias.31 This may require investing additional time to explain to patients (and their families) what an algorithm is and how it works in relation to the therapy provided.
Continue to: Another concern is patient...
Another concern is patient autonomy.32 For example, it would be ethically problematic if a patient were to assume that there was a human physician “at the other end” of a virtual therapist or other technology who is communicating or reviewing his/her messages. Similarly, an older adult or a patient with intellectual disabilities may not be able to understand advanced technology or what it does when it is installed in their home to monitor the patient’s activities. This would increase the risk of privacy violations, manipulation, or even coercion if the requirements for informed consent are not satisfied.
A flowchart for the future
Although current research and innovations typically target specific areas of psychiatry, these advances can be integrated by devising algorithms and protocols that will change the current practice of psychiatry. The Figure provides a glimpse of how the psychiatry clinic of the future might work. A maxim of management is that “the best way to predict the future is to create it.” However, the mere conception of a vision is not enough—working towards it is essential.
Bottom Line
With advances in technology, psychiatric practice will soon be radically different from what it is today. The expanded use of telepsychiatry, social media, artificial intelligence, and web-based applications/devices holds great promise for psychiatric assessment, diagnosis, and treatment, although certain ethical and privacy concerns need to be adequately addressed.
Related Resources
- National Institute of Mental Health. Technology and the future of mental health treatment. www.nimh.nih.gov/health/topics/technology-and-the-future-of-mental-health-treatment/index.shtml. Revised September 2019.
- Hays R, Farrell HM, Touros J. Mobile apps and mental health: using technology to quantify real-time clinical risk. Current Psychiatry. 2019;18(6):37-41.
- Torous J, Luo J, Chan SR. Mental health apps: what to tell patients. Current Psychiatry. 2018;17(3):21-25.
1. Pirmohamed M. Pharmacogenetics and pharmacogenomics. Br J Clin Pharmacol. 2001;52(4):345-347.
2. Benitez J, Cool CL, Scotti DJ. Use of combinatorial pharmacogenomic guidance in treating psychiatric disorders. Per Med. 2018;15(6):481-494.
3. Cannon TD. Candidate gene studies in the GWAS era: the MET proto-oncogene, neurocognition, and schizophrenia. Am J Psychiatry. 2010;167(4):4,369-372.
4. Greenwood J, Chamberlain C, Parker G. Evaluation of a rural telepsychiatry service. Australas Psychiatry. 2004;12(3):268-272.
5. Hubley S, Lynch SB, Schneck C, et al. Review of key telepsychiatry outcomes. World J Psychiatry. 2016;6(2):269-282.
6. Cheng KM, Siu BW, Yeung CC, et al. Telepsychiatry for stable Chinese psychiatric out-patients in custody in Hong Kong: a case-control pilot study. Hong Kong Med J. 2018;24(4):378-383.
7. Frankish K, Ryan C, Harris A. Psychiatry and online social media: potential, pitfalls and ethical guidelines for psychiatrists and trainees. Australasian Psychiatry. 2012;20(3):181-187.
8. de la Torre Díez I, Alonso SG, Hamrioui S, et al. IoT-based services and applications for mental health in the literature. J Med Syst. 2019;43(1):4-9.
9. Topol E. Deep Medicine. New York, NY: Basic Books; 2019:168.
10. Adams RA, Huys QJM, Roiser JP. Computational Psychiatry: towards a mathematically informed understanding of mental illness. J Neurol Neurosurg Psychiatry. 2016;87(1):53-63.
11. Insel TR. Bending the curve for mental health: technology for a public health approach. Am J Public Health. 2019;109(suppl 3):S168-S170.
12. Just MA, Pan L, Cherkassky VL, et al. Machine learning of neural representations of suicide and emotion concepts identifies suicidal youth. Nat Hum Behav. 2017;1:911-919.
13. Pestian J, Nasrallah H, Matykiewicz P, et al. Suicide note classification using natural language processing: a content analysis. Biomed Inform Insights. 2010;2010(3):19-28.
14. Walsh CG, Ribeiro JD, Franklin JC. Predicting risk of suicide attempts over time through machine learning. Clinical Psychological Science. 2017;5(3):457-469.
15. Pestian JP, Sorter M, Connolly B, et al; STM Research Group. A machine learning approach to identifying the thought markers of suicidal subjects: a prospective multicenter trial. Suicide Life Threat Behav. 2017;47(1):112-121.
16. Corcoran CM, Carrillo F, Fernández-Slezak D, et al. Prediction of psychosis across protocols and risk cohorts using automated language analysis. World Psychiatry. 2018;17(1):67-75.
17. Bedi G, Carrillo F, Cecchi GA, et al. Automated analysis of free speech predicts psychosis onset in high-risk youths. NPJ Schizophr. 2015;1:15030. doi: 10.1038/npjschz.2015.30.
18. Kalanderian H, Nasrallah HA. Artificial intelligence in psychiatry. Current Psychiatry. 2019;18(8):33-38.
19. Drysdale AT, Grosenick L, Downar J, et al. Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nat Med. 2017;23(1):28-38.
20. Chekroud AM, Zotti RJ, Shehzad Z, et al. Cross-trial prediction of treatment outcome in depression: a machine learning approach. Lancet Psychiatry. 2016;3(3):243-250.
21. Grisanzio KA, Goldstein-Piekarski AN, Wang MY, et al. Transdiagnostic symptom clusters and associations with brain, behavior, and daily function in mood, anxiety, and trauma disorders. JAMA Psychiatry. 2018;75(2):201-209.
22. Lucas G, Gratch J, King A, et al. It’s only a computer: virtual humans increase willingness to disclose. Computers in Human Behavior. 2014;37:94-100.
23. Nasir M, Baucom BR, Georgiou P, et al. Predicting couple therapy outcomes based on speech acoustic features. PLoS One. 2017;12(9):e0185123. doi: 10.1371/journal.pone.0185123.
24. Huguet A, Rao S, McGrath PJ, et al. A systematic review of cognitive behavioral therapy and behavioral activation apps for depression. PLoS One. 2016;11(5):e0154248. doi: 10.1371/journal.pone.0154248.
25. Scholten MR, Kelders SM, Van Gemert-Pijnen JE. Self-guided web-based interventions: scoping review on user needs and the potential of embodied conversational agents to address them. J Med Internet Res. 2017;19(11):e383.
26. Topol E. Deep Medicine. New York, NY: Basic Books; 2019:283-310.
27. Abramson EL, McGinnis S, Edwards A, et al. Electronic health record adoption and health information exchange among hospitals in New York State. J Eval Clin Pract. 2012;18(6):1156-1162.
28. Meeks DW, Smith MW, Taylor L, et al. An analysis of electronic health record-related patient safety concerns. J Am Med Inform Assoc. 2014;21(6):1053-1059.
29. Kho AN, Rasmussen LV, Connolly JJ, et al. Practical challenges in integrating genomic data into the electronic health record. Genet Med. 2013;15(10):772-778.
30. Ornstein SM, Oates RB, Fox GN. The computer-based medical record: current status. J Fam Pract. 1992;35(5):556-565.
31. Corea F. Machine ethics and artificial moral agents. In: Applied artificial intelligence: where AI can be used in business. Basel, Switzerland: Springer; 2019:33-41.
32. Beauchamp T, Childress J. Principles of biomedical ethics. 7th ed. New York, NY: Oxford University Press; 2012:44.
Despite the tremendous advances in psychiatry in recent years, the current clinical practice of psychiatry continues to rely on data from intermittent assessments along with subjective and unquantifiable accounts from patients and caregivers. Furthermore, there continues to be significant diagnostic variations among practitioners. Fortunately, technology to address these issues appears to be on the horizon.
How might the psychiatric clinic of the future look? What changes could we envision? These 4 critical factors may soon bring about dynamic changes in the way we practice psychiatry:
- precision psychiatry
- digital psychiatry
- technology-enhanced psychotherapy
- electronic health record (EHR) reforms.
In this article, we review how advances in each of these areas might lead to improved care for our patients.
Precision psychiatry
Precision psychiatry takes into account each patient’s variability in genes, environment, and lifestyle to determine individualized treatment and prevention strategies. It relies on pharmacogenomic testing as the primary tool. Pharmacogenomics is the study of variability in drug response due to heredity.
Emerging data on the clinical utility and cost-effectiveness of pharmacogenomic testing are encouraging, but its routine use is not well supported by current evidence.2 One limit to using pharmacogenomic testing is that many genes simultaneously exert an effect on the structure and function of neurons and associated pathophysiology. According to the International Society of Psychiatric Genetics, no single genetic variant is sufficient to cause psychiatric disorders such as depression, bipolar disorder, substance dependence, or schizophrenia. This limits the possibility of using genetic tests to establish a diagnosis.3
In the future, better algorithms could promote more accurate pharmacogenomics profiles for individual patients, which could influence treatment.
Precision psychiatry could lead to:
- identification of novel targets for new medications
- pharmacogenetic profiling of the patient to predict disease susceptibility and medication response
- personalized therapy: the right drug at the right dose for the right patient.
- improved efficacy and fewer adverse medication reactions.
Continue to: Digital psychiatry
Digital psychiatry
Integrating computer-based technology into psychiatric practice has given birth to a new frontier that could be called digital psychiatry. This might encompass the following:
- telepsychiatry
- social media with a mental health focus
- web-based applications/devices
- artificial intelligence (AI).
Telepsychiatry. Videoconferencing is the most widely used form of telepsychiatry. It provides patients with easier access to mental health treatment.4 Telepsychiatry has the potential to match patients and clinicians with similar cultural backgrounds, thus minimizing cultural gaps and misunderstandings. Most importantly, it is comparable to face-to-face interviews in terms of the reliability of assessment and treatment outcomes.5
Telepsychiatry might be particularly helpful for patients with restricted mobility, such as those who live in remote areas, nursing homes, or correctional facilities. In correctional settings, transferring prisoners is expensive and carries the risk of escape. In a small study (N = 86) conducted in Hong Kong, Chen et al6 found that using videoconferencing to conduct clinical interviews of inmates was cost-efficient and scored high in terms of patient acceptability.
Social media. Social media could be a powerful platform for early detection of mental illness. Staying connected with patients on social media could allow psychiatrists to be more aware of their patient’s mood fluctuations, which might lead to more timely assessments. Physicians could be automatically notified about changes in their patients’ social media activity that indicate changes in mental state, which could solicit immediate intervention and treatment. On the other hand, such use of social media could blur professional boundaries. Psychiatrists also could use social media to promote awareness of mental health and educate the public on ways to improve or maintain their mental well-being.7
Web-based applications/devices. Real-time monitoring through applications or internet-based smart devices creates a new avenue for patients to receive personalized assessments, treatment, and intervention.8 Smartwatches with internet connectivity may offer a glimpse of the wearer’s sleep architecture and duration, thus providing real-time data on patients who have insomnia. We can now passively collect objective data from devices, such as smartphones and laptops, to phenotype an individual’s mood and mental state, a process called digital phenotyping. The Table9 lists examples of the types of mental health–related metrics that can be captured by smartphones, smartwatches, and similar technology. Information from these devices can be accumulated to create a database that can be used to predict symptoms.10 For example, the way people use a smartphone’s keyboard, including latency time between space and character types, can be used to generate variables for data. This type of information is being studied for use in screening depression and passively assessing mood in real time.11
Continue to: Artificial intelligence
Artificial intelligence—the development of computer systems able to perform tasks that normally require human intelligence—is being increasingly used in psychiatry. Some studies have suggested AI can be used to identify patients’ risk of suicide12-15 or psychosis.16,17 Kalanderian and Nasrallah18 reviewed several of these studies in
Other researchers have found clinical uses for machine learning, a subset of AI that uses methods to automatically detect patterns and make predictions based on those patterns. In one study, a machine learning analysis of functional MRI scans was able to identify 4 distinct subtypes of depression.19 In another study, a machine learning model was able to predict with 60% accuracy which patients with depression would respond to antidepressants.20
In the future, AI might be used to change mental health classification systems. Because many mental health disorders share similar symptom clusters, machine learning can help to identify associations between symptoms, behavior, brain function, and real-world function across different diagnoses, potentially affecting how we will classify mental disorders.21
Technology-enhanced psychotherapy
In the future, it might be common for psychotherapy to be provided by a computer, or “virtual therapist.” Several studies have evaluated the use of technology-enhanced psychotherapy.
Lucas et al22 investigated patients’ interactions with a virtual therapist. Participants were interviewed by an avatar named Ellie, who they saw on a TV screen. Half of the participants were told Ellie was not human, and half were told Ellie was being controlled remotely by a human. Three psychologists who were blinded to group allocations analyzed transcripts of the interviews and video recordings of participants’ facial expressions to quantify the participants’ fear, sadness, and other emotional responses during the interviews, as well as their openness to the questions. Participants who believed Ellie was fully automated reported significantly lower fear of self-disclosure and impression management (attempts to control how others perceive them) than participants who were told that Ellie was operated by a human. Additionally, participants who believed they were interacting with a computer were more open during the interview.22
Continue to: Researchers at the University of Southern California...
Researchers at the University of Southern California developed software that assessed 74 acoustic features, including pitch, volume, quality, shimmer, jitter, and prosody, to predict outcomes among patients receiving couples therapy. This software was able to predict marital discord at least as well as human therapists.23
Many mental health apps purport to implement specific components of psychotherapy. Many of these apps focus on cognitive-behavioral therapy worksheets, mindfulness exercises, and/or mood tracking. The features provided by such apps emulate the tasks and intended outcomes of traditional psychotherapy, but in an entirely decentralized venue.24
Some have expressed concern that an increased use of virtual therapists powered by AI might lead to a dehumanization of psychiatry (Box25,26).
Box
Whether there are aspects of the psychiatric patient encounter that cannot be managed by a “virtual clinician” created by artificial intelligence (AI) remains to be determined. Some of the benefits of using AI in this manner may be difficult to anticipate, or may be specific to an individual’s relationship with his/her clinician.25
On the other hand, AI systems blur previously assumed boundaries between reality and fiction, and this could have complex effects on patients. Similar to therapeutic relationships with a human clinician, there is the risk of transference of emotions, thoughts, and feelings to a virtual therapist powered by AI. Unlike with a psychiatrist or therapist, however, there is no person on the other side of this transference. Whether virtual clinicians will be able to manage such transference remains to be seen.
In Deep Medicine,26 cardiologist Eric Topol, MD, emphasizes a crucial component of a patient encounter that AI will be unlikely able to provide: empathy. Virtual therapists powered by AI will inherit the tasks best done by machines, leaving humans more time to do what they do best—providing empathy and being “present” for patients.
Electronic health record reforms
Although many clinicians find EHRs to be onerous and time-consuming, EHR technology is constantly improving, and EHRs have revolutionized documentation and order implementation. Several potential advances could improve clinical practice. For example, EHRs could incorporate a clinical decision support system that uses AI-based algorithms to assist psychiatrists with diagnosis, monitoring, and treatment.27 In the future, EHRs might have the ability to monitor and learn from errors and adverse events, and automatically design an algorithm to avoid them.28 They should be designed to better manage analysis of pharmacogenetic test results, which is challenging due to the amount and complexity of the data.29 Future EHRs should eliminate the non-intuitive and multi-click interfaces and cumbersome data searches of today’s EHRs.30
Technology brings new ethical considerations
Mental health interventions based on AI typically work with algorithms, and algorithms bring ethical issues. Mental health devices or systems that use AI could contain biases that have the potential to harm in unintended ways, such as a data-driven sexist or racist bias.31 This may require investing additional time to explain to patients (and their families) what an algorithm is and how it works in relation to the therapy provided.
Continue to: Another concern is patient...
Another concern is patient autonomy.32 For example, it would be ethically problematic if a patient were to assume that there was a human physician “at the other end” of a virtual therapist or other technology who is communicating or reviewing his/her messages. Similarly, an older adult or a patient with intellectual disabilities may not be able to understand advanced technology or what it does when it is installed in their home to monitor the patient’s activities. This would increase the risk of privacy violations, manipulation, or even coercion if the requirements for informed consent are not satisfied.
A flowchart for the future
Although current research and innovations typically target specific areas of psychiatry, these advances can be integrated by devising algorithms and protocols that will change the current practice of psychiatry. The Figure provides a glimpse of how the psychiatry clinic of the future might work. A maxim of management is that “the best way to predict the future is to create it.” However, the mere conception of a vision is not enough—working towards it is essential.
Bottom Line
With advances in technology, psychiatric practice will soon be radically different from what it is today. The expanded use of telepsychiatry, social media, artificial intelligence, and web-based applications/devices holds great promise for psychiatric assessment, diagnosis, and treatment, although certain ethical and privacy concerns need to be adequately addressed.
Related Resources
- National Institute of Mental Health. Technology and the future of mental health treatment. www.nimh.nih.gov/health/topics/technology-and-the-future-of-mental-health-treatment/index.shtml. Revised September 2019.
- Hays R, Farrell HM, Touros J. Mobile apps and mental health: using technology to quantify real-time clinical risk. Current Psychiatry. 2019;18(6):37-41.
- Torous J, Luo J, Chan SR. Mental health apps: what to tell patients. Current Psychiatry. 2018;17(3):21-25.
Despite the tremendous advances in psychiatry in recent years, the current clinical practice of psychiatry continues to rely on data from intermittent assessments along with subjective and unquantifiable accounts from patients and caregivers. Furthermore, there continues to be significant diagnostic variations among practitioners. Fortunately, technology to address these issues appears to be on the horizon.
How might the psychiatric clinic of the future look? What changes could we envision? These 4 critical factors may soon bring about dynamic changes in the way we practice psychiatry:
- precision psychiatry
- digital psychiatry
- technology-enhanced psychotherapy
- electronic health record (EHR) reforms.
In this article, we review how advances in each of these areas might lead to improved care for our patients.
Precision psychiatry
Precision psychiatry takes into account each patient’s variability in genes, environment, and lifestyle to determine individualized treatment and prevention strategies. It relies on pharmacogenomic testing as the primary tool. Pharmacogenomics is the study of variability in drug response due to heredity.
Emerging data on the clinical utility and cost-effectiveness of pharmacogenomic testing are encouraging, but its routine use is not well supported by current evidence.2 One limit to using pharmacogenomic testing is that many genes simultaneously exert an effect on the structure and function of neurons and associated pathophysiology. According to the International Society of Psychiatric Genetics, no single genetic variant is sufficient to cause psychiatric disorders such as depression, bipolar disorder, substance dependence, or schizophrenia. This limits the possibility of using genetic tests to establish a diagnosis.3
In the future, better algorithms could promote more accurate pharmacogenomics profiles for individual patients, which could influence treatment.
Precision psychiatry could lead to:
- identification of novel targets for new medications
- pharmacogenetic profiling of the patient to predict disease susceptibility and medication response
- personalized therapy: the right drug at the right dose for the right patient.
- improved efficacy and fewer adverse medication reactions.
Continue to: Digital psychiatry
Digital psychiatry
Integrating computer-based technology into psychiatric practice has given birth to a new frontier that could be called digital psychiatry. This might encompass the following:
- telepsychiatry
- social media with a mental health focus
- web-based applications/devices
- artificial intelligence (AI).
Telepsychiatry. Videoconferencing is the most widely used form of telepsychiatry. It provides patients with easier access to mental health treatment.4 Telepsychiatry has the potential to match patients and clinicians with similar cultural backgrounds, thus minimizing cultural gaps and misunderstandings. Most importantly, it is comparable to face-to-face interviews in terms of the reliability of assessment and treatment outcomes.5
Telepsychiatry might be particularly helpful for patients with restricted mobility, such as those who live in remote areas, nursing homes, or correctional facilities. In correctional settings, transferring prisoners is expensive and carries the risk of escape. In a small study (N = 86) conducted in Hong Kong, Chen et al6 found that using videoconferencing to conduct clinical interviews of inmates was cost-efficient and scored high in terms of patient acceptability.
Social media. Social media could be a powerful platform for early detection of mental illness. Staying connected with patients on social media could allow psychiatrists to be more aware of their patient’s mood fluctuations, which might lead to more timely assessments. Physicians could be automatically notified about changes in their patients’ social media activity that indicate changes in mental state, which could solicit immediate intervention and treatment. On the other hand, such use of social media could blur professional boundaries. Psychiatrists also could use social media to promote awareness of mental health and educate the public on ways to improve or maintain their mental well-being.7
Web-based applications/devices. Real-time monitoring through applications or internet-based smart devices creates a new avenue for patients to receive personalized assessments, treatment, and intervention.8 Smartwatches with internet connectivity may offer a glimpse of the wearer’s sleep architecture and duration, thus providing real-time data on patients who have insomnia. We can now passively collect objective data from devices, such as smartphones and laptops, to phenotype an individual’s mood and mental state, a process called digital phenotyping. The Table9 lists examples of the types of mental health–related metrics that can be captured by smartphones, smartwatches, and similar technology. Information from these devices can be accumulated to create a database that can be used to predict symptoms.10 For example, the way people use a smartphone’s keyboard, including latency time between space and character types, can be used to generate variables for data. This type of information is being studied for use in screening depression and passively assessing mood in real time.11
Continue to: Artificial intelligence
Artificial intelligence—the development of computer systems able to perform tasks that normally require human intelligence—is being increasingly used in psychiatry. Some studies have suggested AI can be used to identify patients’ risk of suicide12-15 or psychosis.16,17 Kalanderian and Nasrallah18 reviewed several of these studies in
Other researchers have found clinical uses for machine learning, a subset of AI that uses methods to automatically detect patterns and make predictions based on those patterns. In one study, a machine learning analysis of functional MRI scans was able to identify 4 distinct subtypes of depression.19 In another study, a machine learning model was able to predict with 60% accuracy which patients with depression would respond to antidepressants.20
In the future, AI might be used to change mental health classification systems. Because many mental health disorders share similar symptom clusters, machine learning can help to identify associations between symptoms, behavior, brain function, and real-world function across different diagnoses, potentially affecting how we will classify mental disorders.21
Technology-enhanced psychotherapy
In the future, it might be common for psychotherapy to be provided by a computer, or “virtual therapist.” Several studies have evaluated the use of technology-enhanced psychotherapy.
Lucas et al22 investigated patients’ interactions with a virtual therapist. Participants were interviewed by an avatar named Ellie, who they saw on a TV screen. Half of the participants were told Ellie was not human, and half were told Ellie was being controlled remotely by a human. Three psychologists who were blinded to group allocations analyzed transcripts of the interviews and video recordings of participants’ facial expressions to quantify the participants’ fear, sadness, and other emotional responses during the interviews, as well as their openness to the questions. Participants who believed Ellie was fully automated reported significantly lower fear of self-disclosure and impression management (attempts to control how others perceive them) than participants who were told that Ellie was operated by a human. Additionally, participants who believed they were interacting with a computer were more open during the interview.22
Continue to: Researchers at the University of Southern California...
Researchers at the University of Southern California developed software that assessed 74 acoustic features, including pitch, volume, quality, shimmer, jitter, and prosody, to predict outcomes among patients receiving couples therapy. This software was able to predict marital discord at least as well as human therapists.23
Many mental health apps purport to implement specific components of psychotherapy. Many of these apps focus on cognitive-behavioral therapy worksheets, mindfulness exercises, and/or mood tracking. The features provided by such apps emulate the tasks and intended outcomes of traditional psychotherapy, but in an entirely decentralized venue.24
Some have expressed concern that an increased use of virtual therapists powered by AI might lead to a dehumanization of psychiatry (Box25,26).
Box
Whether there are aspects of the psychiatric patient encounter that cannot be managed by a “virtual clinician” created by artificial intelligence (AI) remains to be determined. Some of the benefits of using AI in this manner may be difficult to anticipate, or may be specific to an individual’s relationship with his/her clinician.25
On the other hand, AI systems blur previously assumed boundaries between reality and fiction, and this could have complex effects on patients. Similar to therapeutic relationships with a human clinician, there is the risk of transference of emotions, thoughts, and feelings to a virtual therapist powered by AI. Unlike with a psychiatrist or therapist, however, there is no person on the other side of this transference. Whether virtual clinicians will be able to manage such transference remains to be seen.
In Deep Medicine,26 cardiologist Eric Topol, MD, emphasizes a crucial component of a patient encounter that AI will be unlikely able to provide: empathy. Virtual therapists powered by AI will inherit the tasks best done by machines, leaving humans more time to do what they do best—providing empathy and being “present” for patients.
Electronic health record reforms
Although many clinicians find EHRs to be onerous and time-consuming, EHR technology is constantly improving, and EHRs have revolutionized documentation and order implementation. Several potential advances could improve clinical practice. For example, EHRs could incorporate a clinical decision support system that uses AI-based algorithms to assist psychiatrists with diagnosis, monitoring, and treatment.27 In the future, EHRs might have the ability to monitor and learn from errors and adverse events, and automatically design an algorithm to avoid them.28 They should be designed to better manage analysis of pharmacogenetic test results, which is challenging due to the amount and complexity of the data.29 Future EHRs should eliminate the non-intuitive and multi-click interfaces and cumbersome data searches of today’s EHRs.30
Technology brings new ethical considerations
Mental health interventions based on AI typically work with algorithms, and algorithms bring ethical issues. Mental health devices or systems that use AI could contain biases that have the potential to harm in unintended ways, such as a data-driven sexist or racist bias.31 This may require investing additional time to explain to patients (and their families) what an algorithm is and how it works in relation to the therapy provided.
Continue to: Another concern is patient...
Another concern is patient autonomy.32 For example, it would be ethically problematic if a patient were to assume that there was a human physician “at the other end” of a virtual therapist or other technology who is communicating or reviewing his/her messages. Similarly, an older adult or a patient with intellectual disabilities may not be able to understand advanced technology or what it does when it is installed in their home to monitor the patient’s activities. This would increase the risk of privacy violations, manipulation, or even coercion if the requirements for informed consent are not satisfied.
A flowchart for the future
Although current research and innovations typically target specific areas of psychiatry, these advances can be integrated by devising algorithms and protocols that will change the current practice of psychiatry. The Figure provides a glimpse of how the psychiatry clinic of the future might work. A maxim of management is that “the best way to predict the future is to create it.” However, the mere conception of a vision is not enough—working towards it is essential.
Bottom Line
With advances in technology, psychiatric practice will soon be radically different from what it is today. The expanded use of telepsychiatry, social media, artificial intelligence, and web-based applications/devices holds great promise for psychiatric assessment, diagnosis, and treatment, although certain ethical and privacy concerns need to be adequately addressed.
Related Resources
- National Institute of Mental Health. Technology and the future of mental health treatment. www.nimh.nih.gov/health/topics/technology-and-the-future-of-mental-health-treatment/index.shtml. Revised September 2019.
- Hays R, Farrell HM, Touros J. Mobile apps and mental health: using technology to quantify real-time clinical risk. Current Psychiatry. 2019;18(6):37-41.
- Torous J, Luo J, Chan SR. Mental health apps: what to tell patients. Current Psychiatry. 2018;17(3):21-25.
1. Pirmohamed M. Pharmacogenetics and pharmacogenomics. Br J Clin Pharmacol. 2001;52(4):345-347.
2. Benitez J, Cool CL, Scotti DJ. Use of combinatorial pharmacogenomic guidance in treating psychiatric disorders. Per Med. 2018;15(6):481-494.
3. Cannon TD. Candidate gene studies in the GWAS era: the MET proto-oncogene, neurocognition, and schizophrenia. Am J Psychiatry. 2010;167(4):4,369-372.
4. Greenwood J, Chamberlain C, Parker G. Evaluation of a rural telepsychiatry service. Australas Psychiatry. 2004;12(3):268-272.
5. Hubley S, Lynch SB, Schneck C, et al. Review of key telepsychiatry outcomes. World J Psychiatry. 2016;6(2):269-282.
6. Cheng KM, Siu BW, Yeung CC, et al. Telepsychiatry for stable Chinese psychiatric out-patients in custody in Hong Kong: a case-control pilot study. Hong Kong Med J. 2018;24(4):378-383.
7. Frankish K, Ryan C, Harris A. Psychiatry and online social media: potential, pitfalls and ethical guidelines for psychiatrists and trainees. Australasian Psychiatry. 2012;20(3):181-187.
8. de la Torre Díez I, Alonso SG, Hamrioui S, et al. IoT-based services and applications for mental health in the literature. J Med Syst. 2019;43(1):4-9.
9. Topol E. Deep Medicine. New York, NY: Basic Books; 2019:168.
10. Adams RA, Huys QJM, Roiser JP. Computational Psychiatry: towards a mathematically informed understanding of mental illness. J Neurol Neurosurg Psychiatry. 2016;87(1):53-63.
11. Insel TR. Bending the curve for mental health: technology for a public health approach. Am J Public Health. 2019;109(suppl 3):S168-S170.
12. Just MA, Pan L, Cherkassky VL, et al. Machine learning of neural representations of suicide and emotion concepts identifies suicidal youth. Nat Hum Behav. 2017;1:911-919.
13. Pestian J, Nasrallah H, Matykiewicz P, et al. Suicide note classification using natural language processing: a content analysis. Biomed Inform Insights. 2010;2010(3):19-28.
14. Walsh CG, Ribeiro JD, Franklin JC. Predicting risk of suicide attempts over time through machine learning. Clinical Psychological Science. 2017;5(3):457-469.
15. Pestian JP, Sorter M, Connolly B, et al; STM Research Group. A machine learning approach to identifying the thought markers of suicidal subjects: a prospective multicenter trial. Suicide Life Threat Behav. 2017;47(1):112-121.
16. Corcoran CM, Carrillo F, Fernández-Slezak D, et al. Prediction of psychosis across protocols and risk cohorts using automated language analysis. World Psychiatry. 2018;17(1):67-75.
17. Bedi G, Carrillo F, Cecchi GA, et al. Automated analysis of free speech predicts psychosis onset in high-risk youths. NPJ Schizophr. 2015;1:15030. doi: 10.1038/npjschz.2015.30.
18. Kalanderian H, Nasrallah HA. Artificial intelligence in psychiatry. Current Psychiatry. 2019;18(8):33-38.
19. Drysdale AT, Grosenick L, Downar J, et al. Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nat Med. 2017;23(1):28-38.
20. Chekroud AM, Zotti RJ, Shehzad Z, et al. Cross-trial prediction of treatment outcome in depression: a machine learning approach. Lancet Psychiatry. 2016;3(3):243-250.
21. Grisanzio KA, Goldstein-Piekarski AN, Wang MY, et al. Transdiagnostic symptom clusters and associations with brain, behavior, and daily function in mood, anxiety, and trauma disorders. JAMA Psychiatry. 2018;75(2):201-209.
22. Lucas G, Gratch J, King A, et al. It’s only a computer: virtual humans increase willingness to disclose. Computers in Human Behavior. 2014;37:94-100.
23. Nasir M, Baucom BR, Georgiou P, et al. Predicting couple therapy outcomes based on speech acoustic features. PLoS One. 2017;12(9):e0185123. doi: 10.1371/journal.pone.0185123.
24. Huguet A, Rao S, McGrath PJ, et al. A systematic review of cognitive behavioral therapy and behavioral activation apps for depression. PLoS One. 2016;11(5):e0154248. doi: 10.1371/journal.pone.0154248.
25. Scholten MR, Kelders SM, Van Gemert-Pijnen JE. Self-guided web-based interventions: scoping review on user needs and the potential of embodied conversational agents to address them. J Med Internet Res. 2017;19(11):e383.
26. Topol E. Deep Medicine. New York, NY: Basic Books; 2019:283-310.
27. Abramson EL, McGinnis S, Edwards A, et al. Electronic health record adoption and health information exchange among hospitals in New York State. J Eval Clin Pract. 2012;18(6):1156-1162.
28. Meeks DW, Smith MW, Taylor L, et al. An analysis of electronic health record-related patient safety concerns. J Am Med Inform Assoc. 2014;21(6):1053-1059.
29. Kho AN, Rasmussen LV, Connolly JJ, et al. Practical challenges in integrating genomic data into the electronic health record. Genet Med. 2013;15(10):772-778.
30. Ornstein SM, Oates RB, Fox GN. The computer-based medical record: current status. J Fam Pract. 1992;35(5):556-565.
31. Corea F. Machine ethics and artificial moral agents. In: Applied artificial intelligence: where AI can be used in business. Basel, Switzerland: Springer; 2019:33-41.
32. Beauchamp T, Childress J. Principles of biomedical ethics. 7th ed. New York, NY: Oxford University Press; 2012:44.
1. Pirmohamed M. Pharmacogenetics and pharmacogenomics. Br J Clin Pharmacol. 2001;52(4):345-347.
2. Benitez J, Cool CL, Scotti DJ. Use of combinatorial pharmacogenomic guidance in treating psychiatric disorders. Per Med. 2018;15(6):481-494.
3. Cannon TD. Candidate gene studies in the GWAS era: the MET proto-oncogene, neurocognition, and schizophrenia. Am J Psychiatry. 2010;167(4):4,369-372.
4. Greenwood J, Chamberlain C, Parker G. Evaluation of a rural telepsychiatry service. Australas Psychiatry. 2004;12(3):268-272.
5. Hubley S, Lynch SB, Schneck C, et al. Review of key telepsychiatry outcomes. World J Psychiatry. 2016;6(2):269-282.
6. Cheng KM, Siu BW, Yeung CC, et al. Telepsychiatry for stable Chinese psychiatric out-patients in custody in Hong Kong: a case-control pilot study. Hong Kong Med J. 2018;24(4):378-383.
7. Frankish K, Ryan C, Harris A. Psychiatry and online social media: potential, pitfalls and ethical guidelines for psychiatrists and trainees. Australasian Psychiatry. 2012;20(3):181-187.
8. de la Torre Díez I, Alonso SG, Hamrioui S, et al. IoT-based services and applications for mental health in the literature. J Med Syst. 2019;43(1):4-9.
9. Topol E. Deep Medicine. New York, NY: Basic Books; 2019:168.
10. Adams RA, Huys QJM, Roiser JP. Computational Psychiatry: towards a mathematically informed understanding of mental illness. J Neurol Neurosurg Psychiatry. 2016;87(1):53-63.
11. Insel TR. Bending the curve for mental health: technology for a public health approach. Am J Public Health. 2019;109(suppl 3):S168-S170.
12. Just MA, Pan L, Cherkassky VL, et al. Machine learning of neural representations of suicide and emotion concepts identifies suicidal youth. Nat Hum Behav. 2017;1:911-919.
13. Pestian J, Nasrallah H, Matykiewicz P, et al. Suicide note classification using natural language processing: a content analysis. Biomed Inform Insights. 2010;2010(3):19-28.
14. Walsh CG, Ribeiro JD, Franklin JC. Predicting risk of suicide attempts over time through machine learning. Clinical Psychological Science. 2017;5(3):457-469.
15. Pestian JP, Sorter M, Connolly B, et al; STM Research Group. A machine learning approach to identifying the thought markers of suicidal subjects: a prospective multicenter trial. Suicide Life Threat Behav. 2017;47(1):112-121.
16. Corcoran CM, Carrillo F, Fernández-Slezak D, et al. Prediction of psychosis across protocols and risk cohorts using automated language analysis. World Psychiatry. 2018;17(1):67-75.
17. Bedi G, Carrillo F, Cecchi GA, et al. Automated analysis of free speech predicts psychosis onset in high-risk youths. NPJ Schizophr. 2015;1:15030. doi: 10.1038/npjschz.2015.30.
18. Kalanderian H, Nasrallah HA. Artificial intelligence in psychiatry. Current Psychiatry. 2019;18(8):33-38.
19. Drysdale AT, Grosenick L, Downar J, et al. Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nat Med. 2017;23(1):28-38.
20. Chekroud AM, Zotti RJ, Shehzad Z, et al. Cross-trial prediction of treatment outcome in depression: a machine learning approach. Lancet Psychiatry. 2016;3(3):243-250.
21. Grisanzio KA, Goldstein-Piekarski AN, Wang MY, et al. Transdiagnostic symptom clusters and associations with brain, behavior, and daily function in mood, anxiety, and trauma disorders. JAMA Psychiatry. 2018;75(2):201-209.
22. Lucas G, Gratch J, King A, et al. It’s only a computer: virtual humans increase willingness to disclose. Computers in Human Behavior. 2014;37:94-100.
23. Nasir M, Baucom BR, Georgiou P, et al. Predicting couple therapy outcomes based on speech acoustic features. PLoS One. 2017;12(9):e0185123. doi: 10.1371/journal.pone.0185123.
24. Huguet A, Rao S, McGrath PJ, et al. A systematic review of cognitive behavioral therapy and behavioral activation apps for depression. PLoS One. 2016;11(5):e0154248. doi: 10.1371/journal.pone.0154248.
25. Scholten MR, Kelders SM, Van Gemert-Pijnen JE. Self-guided web-based interventions: scoping review on user needs and the potential of embodied conversational agents to address them. J Med Internet Res. 2017;19(11):e383.
26. Topol E. Deep Medicine. New York, NY: Basic Books; 2019:283-310.
27. Abramson EL, McGinnis S, Edwards A, et al. Electronic health record adoption and health information exchange among hospitals in New York State. J Eval Clin Pract. 2012;18(6):1156-1162.
28. Meeks DW, Smith MW, Taylor L, et al. An analysis of electronic health record-related patient safety concerns. J Am Med Inform Assoc. 2014;21(6):1053-1059.
29. Kho AN, Rasmussen LV, Connolly JJ, et al. Practical challenges in integrating genomic data into the electronic health record. Genet Med. 2013;15(10):772-778.
30. Ornstein SM, Oates RB, Fox GN. The computer-based medical record: current status. J Fam Pract. 1992;35(5):556-565.
31. Corea F. Machine ethics and artificial moral agents. In: Applied artificial intelligence: where AI can be used in business. Basel, Switzerland: Springer; 2019:33-41.
32. Beauchamp T, Childress J. Principles of biomedical ethics. 7th ed. New York, NY: Oxford University Press; 2012:44.
In the Phoenix area, we are in a lull before the coronavirus storm
“There is no sound save the throb of the blowers and the vibration of the hard-driven engines. There is little motion as the gun crews man their guns and the fire-control details stand with heads bent and their hands clapped over their headphones. Somewhere out there are the enemy planes.”
That’s from one of my favorite WW2 histories, “Torpedo Junction,” by Robert J. Casey. He was a reporter stationed on board the cruiser USS Salt Lake City. The entry is from a day in February 1942 when the ship was part of a force that bombarded the Japanese encampment on Wake Island. The excerpt describes the scene later that afternoon, as they awaited a counterattack from Japanese planes.
For some reason that paragraph kept going through my mind this past Sunday afternoon, in the comparatively mundane situation of sitting in the hospital library signing off on my dictations and reviewing test results. I certainly was in no danger of being bombed or strafed, yet ...
Around me, the hospital was preparing for battle. As I rounded, most of the beds were empty and many of the floors above me were shut down and darkened. Waiting rooms were empty. If you hadn’t read the news you’d think there was a sudden lull in the health care world.
But the real truth is that it’s the calm before an anticipated storm. The elective procedures have all been canceled. Nonurgent outpatient tests are on hold. Only the sickest are being admitted, and they’re being sent out as soon as possible. Every bed possible is being kept open for the feared onslaught of coronavirus patients in the coming weeks. Protective equipment, already in short supply, is being stockpiled as it becomes available. Plans have been made to erect triage tents in the parking lots.
I sit in the library and think of this. It’s quiet except for the soft hum of the air conditioning blowers as Phoenix starts to warm up for another summer. The muted purr of the computer’s hard drive as I click away on the keys. On the floors above me the nurses and respiratory techs and doctors go about their daily business of patient care, wondering when the real battle will begin (probably 2-3 weeks from the time of this writing, if not sooner).
These are scary times. I’d be lying if I said I wasn’t frightened about what might happen to me, my family, my friends, my coworkers, my patients.
The people working in the hospital above me are in the same boat, all nervous about what’s going to happen. None of them is any more immune to coronavirus than the people they’ll be treating.
But, like the crew of the USS Salt Lake City, they’re ready to do their jobs. Because it’s part of what drove each of us into our own part of this field. Because we care and want to help. And health care doesn’t work unless the whole team does.
I respect them all for it. I always have and always will, and now more than ever.
Good luck.
Dr. Block has a solo neurology practice in Scottsdale, Ariz. He has no relevant disclosures.
“There is no sound save the throb of the blowers and the vibration of the hard-driven engines. There is little motion as the gun crews man their guns and the fire-control details stand with heads bent and their hands clapped over their headphones. Somewhere out there are the enemy planes.”
That’s from one of my favorite WW2 histories, “Torpedo Junction,” by Robert J. Casey. He was a reporter stationed on board the cruiser USS Salt Lake City. The entry is from a day in February 1942 when the ship was part of a force that bombarded the Japanese encampment on Wake Island. The excerpt describes the scene later that afternoon, as they awaited a counterattack from Japanese planes.
For some reason that paragraph kept going through my mind this past Sunday afternoon, in the comparatively mundane situation of sitting in the hospital library signing off on my dictations and reviewing test results. I certainly was in no danger of being bombed or strafed, yet ...
Around me, the hospital was preparing for battle. As I rounded, most of the beds were empty and many of the floors above me were shut down and darkened. Waiting rooms were empty. If you hadn’t read the news you’d think there was a sudden lull in the health care world.
But the real truth is that it’s the calm before an anticipated storm. The elective procedures have all been canceled. Nonurgent outpatient tests are on hold. Only the sickest are being admitted, and they’re being sent out as soon as possible. Every bed possible is being kept open for the feared onslaught of coronavirus patients in the coming weeks. Protective equipment, already in short supply, is being stockpiled as it becomes available. Plans have been made to erect triage tents in the parking lots.
I sit in the library and think of this. It’s quiet except for the soft hum of the air conditioning blowers as Phoenix starts to warm up for another summer. The muted purr of the computer’s hard drive as I click away on the keys. On the floors above me the nurses and respiratory techs and doctors go about their daily business of patient care, wondering when the real battle will begin (probably 2-3 weeks from the time of this writing, if not sooner).
These are scary times. I’d be lying if I said I wasn’t frightened about what might happen to me, my family, my friends, my coworkers, my patients.
The people working in the hospital above me are in the same boat, all nervous about what’s going to happen. None of them is any more immune to coronavirus than the people they’ll be treating.
But, like the crew of the USS Salt Lake City, they’re ready to do their jobs. Because it’s part of what drove each of us into our own part of this field. Because we care and want to help. And health care doesn’t work unless the whole team does.
I respect them all for it. I always have and always will, and now more than ever.
Good luck.
Dr. Block has a solo neurology practice in Scottsdale, Ariz. He has no relevant disclosures.
“There is no sound save the throb of the blowers and the vibration of the hard-driven engines. There is little motion as the gun crews man their guns and the fire-control details stand with heads bent and their hands clapped over their headphones. Somewhere out there are the enemy planes.”
That’s from one of my favorite WW2 histories, “Torpedo Junction,” by Robert J. Casey. He was a reporter stationed on board the cruiser USS Salt Lake City. The entry is from a day in February 1942 when the ship was part of a force that bombarded the Japanese encampment on Wake Island. The excerpt describes the scene later that afternoon, as they awaited a counterattack from Japanese planes.
For some reason that paragraph kept going through my mind this past Sunday afternoon, in the comparatively mundane situation of sitting in the hospital library signing off on my dictations and reviewing test results. I certainly was in no danger of being bombed or strafed, yet ...
Around me, the hospital was preparing for battle. As I rounded, most of the beds were empty and many of the floors above me were shut down and darkened. Waiting rooms were empty. If you hadn’t read the news you’d think there was a sudden lull in the health care world.
But the real truth is that it’s the calm before an anticipated storm. The elective procedures have all been canceled. Nonurgent outpatient tests are on hold. Only the sickest are being admitted, and they’re being sent out as soon as possible. Every bed possible is being kept open for the feared onslaught of coronavirus patients in the coming weeks. Protective equipment, already in short supply, is being stockpiled as it becomes available. Plans have been made to erect triage tents in the parking lots.
I sit in the library and think of this. It’s quiet except for the soft hum of the air conditioning blowers as Phoenix starts to warm up for another summer. The muted purr of the computer’s hard drive as I click away on the keys. On the floors above me the nurses and respiratory techs and doctors go about their daily business of patient care, wondering when the real battle will begin (probably 2-3 weeks from the time of this writing, if not sooner).
These are scary times. I’d be lying if I said I wasn’t frightened about what might happen to me, my family, my friends, my coworkers, my patients.
The people working in the hospital above me are in the same boat, all nervous about what’s going to happen. None of them is any more immune to coronavirus than the people they’ll be treating.
But, like the crew of the USS Salt Lake City, they’re ready to do their jobs. Because it’s part of what drove each of us into our own part of this field. Because we care and want to help. And health care doesn’t work unless the whole team does.
I respect them all for it. I always have and always will, and now more than ever.
Good luck.
Dr. Block has a solo neurology practice in Scottsdale, Ariz. He has no relevant disclosures.
Do we need another vital sign?
If you haven’t already found out that activity is a critical component in the physical and mental health of your patients, or if you’re trying to convince an influential person or group it deserves their attention and investment, I suggest you chase down this clinical report from the American Academy of Pediatrics. Representing the AAP’s Council on Sports Medicine and Fitness and Section on Obesity, the authors quite thoroughly make the case that anyone concerned about the health of this nation and its children should make promotion of physical activity a top priority.
I suspect that, like many of the position papers that come from the AAP, this clinical report is another example of preaching to the choir. However, I understand that the academy also hopes to convince a broader audience of nonphysician decision makers by laying out all of the evidence they can muster.
With their voluminous supporting evidence on the table, the authors move on to getting those of us in clinical practice to make our approach to this more systematic – including the addition of a Physical Activity Vital Sign (PAVS) in our patients’ health records. And here is where the authors begin to drift into the hazy dream world of unreality. They admit that “pediatricians will need efficient workflows to incorporate physical activity assessment, counseling and referral in the clinical visit.” Although there is no pediatrician more convinced of the importance of physical activity, I would find it very difficult to include a detailed assessment of my patients’ daily activity in their charts in the manner that the council members envision. Clunky EHRs, limited support staff, and a crowd of advocates already clamoring for my attention on their favorite health issue (nutrition, gun safety, parental depression, dental health to name just a few) all make creating an “efficient workflow” difficult on a good day and impossible on many days.
But, as I have said, I am a strong advocate of physical activity. So here’s a more nuanced suggestion based on a combination of my practical experience and the council’s recommendations.
If you provide good continuity of care to the families in your practice and have been asking good “getting to know you” questions at each visit, you probably already know which of your patients are sufficiently active. You don’t need to ask them how many hours a week they are doing something active. You should be able to just check a box that says “active.”
For patients that you haven’t seen before or suspect are too sedentary from looking at their biometrics and listening to their complaints you need only ask “What do you and your family like to do for fun?” The simple follow-up question of how many hours are spent watching TV, looking at smart phones or tablets, and playing video games in each day completes the survey. You don’t need to chart the depressing details because, as we know, relying on patient or parental recall is unlikely to provide the actual numbers. Just simply check the box that says “not active enough.” What you do with this crude assessment activity is another story and will be the topic for the next Letters from Maine.
This clinical report from the AAP is an excellent and exhaustive discussion of the importance of physical activity, but I hope that it doesn’t spark further cluttering of our already challenged EHR systems. Most of us don’t have the time to be data collectors and quantifiers. Let’s leave that to the clinical researchers. We already know activity is important and that most of our sedentary families aren’t going to be impressed by more science. Our challenge is to get them moving.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
If you haven’t already found out that activity is a critical component in the physical and mental health of your patients, or if you’re trying to convince an influential person or group it deserves their attention and investment, I suggest you chase down this clinical report from the American Academy of Pediatrics. Representing the AAP’s Council on Sports Medicine and Fitness and Section on Obesity, the authors quite thoroughly make the case that anyone concerned about the health of this nation and its children should make promotion of physical activity a top priority.
I suspect that, like many of the position papers that come from the AAP, this clinical report is another example of preaching to the choir. However, I understand that the academy also hopes to convince a broader audience of nonphysician decision makers by laying out all of the evidence they can muster.
With their voluminous supporting evidence on the table, the authors move on to getting those of us in clinical practice to make our approach to this more systematic – including the addition of a Physical Activity Vital Sign (PAVS) in our patients’ health records. And here is where the authors begin to drift into the hazy dream world of unreality. They admit that “pediatricians will need efficient workflows to incorporate physical activity assessment, counseling and referral in the clinical visit.” Although there is no pediatrician more convinced of the importance of physical activity, I would find it very difficult to include a detailed assessment of my patients’ daily activity in their charts in the manner that the council members envision. Clunky EHRs, limited support staff, and a crowd of advocates already clamoring for my attention on their favorite health issue (nutrition, gun safety, parental depression, dental health to name just a few) all make creating an “efficient workflow” difficult on a good day and impossible on many days.
But, as I have said, I am a strong advocate of physical activity. So here’s a more nuanced suggestion based on a combination of my practical experience and the council’s recommendations.
If you provide good continuity of care to the families in your practice and have been asking good “getting to know you” questions at each visit, you probably already know which of your patients are sufficiently active. You don’t need to ask them how many hours a week they are doing something active. You should be able to just check a box that says “active.”
For patients that you haven’t seen before or suspect are too sedentary from looking at their biometrics and listening to their complaints you need only ask “What do you and your family like to do for fun?” The simple follow-up question of how many hours are spent watching TV, looking at smart phones or tablets, and playing video games in each day completes the survey. You don’t need to chart the depressing details because, as we know, relying on patient or parental recall is unlikely to provide the actual numbers. Just simply check the box that says “not active enough.” What you do with this crude assessment activity is another story and will be the topic for the next Letters from Maine.
This clinical report from the AAP is an excellent and exhaustive discussion of the importance of physical activity, but I hope that it doesn’t spark further cluttering of our already challenged EHR systems. Most of us don’t have the time to be data collectors and quantifiers. Let’s leave that to the clinical researchers. We already know activity is important and that most of our sedentary families aren’t going to be impressed by more science. Our challenge is to get them moving.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
If you haven’t already found out that activity is a critical component in the physical and mental health of your patients, or if you’re trying to convince an influential person or group it deserves their attention and investment, I suggest you chase down this clinical report from the American Academy of Pediatrics. Representing the AAP’s Council on Sports Medicine and Fitness and Section on Obesity, the authors quite thoroughly make the case that anyone concerned about the health of this nation and its children should make promotion of physical activity a top priority.
I suspect that, like many of the position papers that come from the AAP, this clinical report is another example of preaching to the choir. However, I understand that the academy also hopes to convince a broader audience of nonphysician decision makers by laying out all of the evidence they can muster.
With their voluminous supporting evidence on the table, the authors move on to getting those of us in clinical practice to make our approach to this more systematic – including the addition of a Physical Activity Vital Sign (PAVS) in our patients’ health records. And here is where the authors begin to drift into the hazy dream world of unreality. They admit that “pediatricians will need efficient workflows to incorporate physical activity assessment, counseling and referral in the clinical visit.” Although there is no pediatrician more convinced of the importance of physical activity, I would find it very difficult to include a detailed assessment of my patients’ daily activity in their charts in the manner that the council members envision. Clunky EHRs, limited support staff, and a crowd of advocates already clamoring for my attention on their favorite health issue (nutrition, gun safety, parental depression, dental health to name just a few) all make creating an “efficient workflow” difficult on a good day and impossible on many days.
But, as I have said, I am a strong advocate of physical activity. So here’s a more nuanced suggestion based on a combination of my practical experience and the council’s recommendations.
If you provide good continuity of care to the families in your practice and have been asking good “getting to know you” questions at each visit, you probably already know which of your patients are sufficiently active. You don’t need to ask them how many hours a week they are doing something active. You should be able to just check a box that says “active.”
For patients that you haven’t seen before or suspect are too sedentary from looking at their biometrics and listening to their complaints you need only ask “What do you and your family like to do for fun?” The simple follow-up question of how many hours are spent watching TV, looking at smart phones or tablets, and playing video games in each day completes the survey. You don’t need to chart the depressing details because, as we know, relying on patient or parental recall is unlikely to provide the actual numbers. Just simply check the box that says “not active enough.” What you do with this crude assessment activity is another story and will be the topic for the next Letters from Maine.
This clinical report from the AAP is an excellent and exhaustive discussion of the importance of physical activity, but I hope that it doesn’t spark further cluttering of our already challenged EHR systems. Most of us don’t have the time to be data collectors and quantifiers. Let’s leave that to the clinical researchers. We already know activity is important and that most of our sedentary families aren’t going to be impressed by more science. Our challenge is to get them moving.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
‘Impressive’ SOLO3 results should influence practice
In this edition of “Applying research to practice,” I highlight a study suggesting olaparib is helpful in patients BRCA mutations experiencing multiple relapses of ovarian cancer.
SOLO3 was the first phase 3 trial comparing the oral PARP inhibitor olaparib (OLA; 300 mg twice daily) with physician’s choice of intravenous single-agent chemotherapy (TPC) in relapsed high-grade serous or endometroid ovarian, fallopian tube, or primary peritoneal cancer (J Clin Oncol. 2020 Feb 19. doi: 10.1200/JCO.19.02745).
The trial involved 266 BRCA-mutated patients who had received two (approximately 50%) or more lines of platinum-based TPC. All patients were required to be completely platinum sensitive (progression beyond 12 months from last platinum exposure) or partially platinum sensitive (progression within 6-12 months).
Women were randomized to receive either OLA or nonplatinum TPC (pegylated liposomal doxorubicin, paclitaxel, gemcitabine, or topotecan). After an amendment to the study in 2017, the primary endpoint was objective response rate, determined by blinded independent central review, with a variety of secondary endpoints.
Among 223 patients with measurable disease, the objective response rate was 72.2% with OLA and 51.4% with TPC (odds ratio, 2.53; P = .002). Across all patients, the median progression-free survival was significantly better with OLA (13.4 months) than with TPC (9.2 months; P = .013). Overall survival data were immature.
The superiority of OLA for the primary endpoint was maintained in multiple subgroups of patients, including those who had received only two prior lines of therapy (OR, 3.44) and those who had three or more prior lines (OR, 2.21). Time to first subsequent therapy (HR, 0.48) and time to treatment discontinuation or death (HR, 0.17) were significantly longer for OLA than for TPC.
Adverse events were consistent with the established safety profiles of OLA and chemotherapy. The most common grade 3 or higher adverse events were anemia (21.3%) with OLA and neutropenia (15.8%) and hand-foot syndrome (11.8%) with TPC.
However, median treatment durations were substantially and consistently longer for OLA than for TPC, and there were fewer treatment discontinuations because of toxicity for OLA than for TPC. At the time of data cutoff, 43 patients in the OLA group and 1 patient in the TPC cohort remained on treatment.
How these results influence practice
The results of the SOLO3 trial are clear: Treatment with OLA is a reasonable alternative to nonplatinum-containing chemotherapy for women with BRCA mutations and platinum-sensitive ovarian cancer. OLA is a “chemotherapy-free” option for these patients in the second- and later-line settings.
Less clear are the following:
- How many patients with BRCA mutations will not have already received a PARP inhibitor in the frontline maintenance setting in the future? SOLO3 required modification in the accrual target and endpoint because of challenges in patient recruitment from the entry of PARP inhibitors into routine clinical practice.
- Would OLA be superior to a carboplatin doublet rather than a nonplatinum single agent in patients with two prior relapses of platinum-sensitive ovarian cancer? Standard practice would be for patients in the second-line setting to receive a platinum doublet.
- Is extending the platinum-free interval a worthwhile objective, or would some patients prefer a finite interval of a platinum doublet over an indefinite period of treatment with OLA?
All phase 3 clinical trials have limitations since they require years to complete and the applicability of the results are challenged by intercurrent advances in treatment options and diagnostic tests.
However, overall, the results of SOLO3 are impressive and should influence clinical practice for the subset of relapsed ovarian cancer patients who would have qualified to participate in it. OLA represents an important treatment advance for a group of patients who are trying to string together remission after remission, with limited negative impact on quality of life.
Dr. Lyss was an oncologist and researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
In this edition of “Applying research to practice,” I highlight a study suggesting olaparib is helpful in patients BRCA mutations experiencing multiple relapses of ovarian cancer.
SOLO3 was the first phase 3 trial comparing the oral PARP inhibitor olaparib (OLA; 300 mg twice daily) with physician’s choice of intravenous single-agent chemotherapy (TPC) in relapsed high-grade serous or endometroid ovarian, fallopian tube, or primary peritoneal cancer (J Clin Oncol. 2020 Feb 19. doi: 10.1200/JCO.19.02745).
The trial involved 266 BRCA-mutated patients who had received two (approximately 50%) or more lines of platinum-based TPC. All patients were required to be completely platinum sensitive (progression beyond 12 months from last platinum exposure) or partially platinum sensitive (progression within 6-12 months).
Women were randomized to receive either OLA or nonplatinum TPC (pegylated liposomal doxorubicin, paclitaxel, gemcitabine, or topotecan). After an amendment to the study in 2017, the primary endpoint was objective response rate, determined by blinded independent central review, with a variety of secondary endpoints.
Among 223 patients with measurable disease, the objective response rate was 72.2% with OLA and 51.4% with TPC (odds ratio, 2.53; P = .002). Across all patients, the median progression-free survival was significantly better with OLA (13.4 months) than with TPC (9.2 months; P = .013). Overall survival data were immature.
The superiority of OLA for the primary endpoint was maintained in multiple subgroups of patients, including those who had received only two prior lines of therapy (OR, 3.44) and those who had three or more prior lines (OR, 2.21). Time to first subsequent therapy (HR, 0.48) and time to treatment discontinuation or death (HR, 0.17) were significantly longer for OLA than for TPC.
Adverse events were consistent with the established safety profiles of OLA and chemotherapy. The most common grade 3 or higher adverse events were anemia (21.3%) with OLA and neutropenia (15.8%) and hand-foot syndrome (11.8%) with TPC.
However, median treatment durations were substantially and consistently longer for OLA than for TPC, and there were fewer treatment discontinuations because of toxicity for OLA than for TPC. At the time of data cutoff, 43 patients in the OLA group and 1 patient in the TPC cohort remained on treatment.
How these results influence practice
The results of the SOLO3 trial are clear: Treatment with OLA is a reasonable alternative to nonplatinum-containing chemotherapy for women with BRCA mutations and platinum-sensitive ovarian cancer. OLA is a “chemotherapy-free” option for these patients in the second- and later-line settings.
Less clear are the following:
- How many patients with BRCA mutations will not have already received a PARP inhibitor in the frontline maintenance setting in the future? SOLO3 required modification in the accrual target and endpoint because of challenges in patient recruitment from the entry of PARP inhibitors into routine clinical practice.
- Would OLA be superior to a carboplatin doublet rather than a nonplatinum single agent in patients with two prior relapses of platinum-sensitive ovarian cancer? Standard practice would be for patients in the second-line setting to receive a platinum doublet.
- Is extending the platinum-free interval a worthwhile objective, or would some patients prefer a finite interval of a platinum doublet over an indefinite period of treatment with OLA?
All phase 3 clinical trials have limitations since they require years to complete and the applicability of the results are challenged by intercurrent advances in treatment options and diagnostic tests.
However, overall, the results of SOLO3 are impressive and should influence clinical practice for the subset of relapsed ovarian cancer patients who would have qualified to participate in it. OLA represents an important treatment advance for a group of patients who are trying to string together remission after remission, with limited negative impact on quality of life.
Dr. Lyss was an oncologist and researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
In this edition of “Applying research to practice,” I highlight a study suggesting olaparib is helpful in patients BRCA mutations experiencing multiple relapses of ovarian cancer.
SOLO3 was the first phase 3 trial comparing the oral PARP inhibitor olaparib (OLA; 300 mg twice daily) with physician’s choice of intravenous single-agent chemotherapy (TPC) in relapsed high-grade serous or endometroid ovarian, fallopian tube, or primary peritoneal cancer (J Clin Oncol. 2020 Feb 19. doi: 10.1200/JCO.19.02745).
The trial involved 266 BRCA-mutated patients who had received two (approximately 50%) or more lines of platinum-based TPC. All patients were required to be completely platinum sensitive (progression beyond 12 months from last platinum exposure) or partially platinum sensitive (progression within 6-12 months).
Women were randomized to receive either OLA or nonplatinum TPC (pegylated liposomal doxorubicin, paclitaxel, gemcitabine, or topotecan). After an amendment to the study in 2017, the primary endpoint was objective response rate, determined by blinded independent central review, with a variety of secondary endpoints.
Among 223 patients with measurable disease, the objective response rate was 72.2% with OLA and 51.4% with TPC (odds ratio, 2.53; P = .002). Across all patients, the median progression-free survival was significantly better with OLA (13.4 months) than with TPC (9.2 months; P = .013). Overall survival data were immature.
The superiority of OLA for the primary endpoint was maintained in multiple subgroups of patients, including those who had received only two prior lines of therapy (OR, 3.44) and those who had three or more prior lines (OR, 2.21). Time to first subsequent therapy (HR, 0.48) and time to treatment discontinuation or death (HR, 0.17) were significantly longer for OLA than for TPC.
Adverse events were consistent with the established safety profiles of OLA and chemotherapy. The most common grade 3 or higher adverse events were anemia (21.3%) with OLA and neutropenia (15.8%) and hand-foot syndrome (11.8%) with TPC.
However, median treatment durations were substantially and consistently longer for OLA than for TPC, and there were fewer treatment discontinuations because of toxicity for OLA than for TPC. At the time of data cutoff, 43 patients in the OLA group and 1 patient in the TPC cohort remained on treatment.
How these results influence practice
The results of the SOLO3 trial are clear: Treatment with OLA is a reasonable alternative to nonplatinum-containing chemotherapy for women with BRCA mutations and platinum-sensitive ovarian cancer. OLA is a “chemotherapy-free” option for these patients in the second- and later-line settings.
Less clear are the following:
- How many patients with BRCA mutations will not have already received a PARP inhibitor in the frontline maintenance setting in the future? SOLO3 required modification in the accrual target and endpoint because of challenges in patient recruitment from the entry of PARP inhibitors into routine clinical practice.
- Would OLA be superior to a carboplatin doublet rather than a nonplatinum single agent in patients with two prior relapses of platinum-sensitive ovarian cancer? Standard practice would be for patients in the second-line setting to receive a platinum doublet.
- Is extending the platinum-free interval a worthwhile objective, or would some patients prefer a finite interval of a platinum doublet over an indefinite period of treatment with OLA?
All phase 3 clinical trials have limitations since they require years to complete and the applicability of the results are challenged by intercurrent advances in treatment options and diagnostic tests.
However, overall, the results of SOLO3 are impressive and should influence clinical practice for the subset of relapsed ovarian cancer patients who would have qualified to participate in it. OLA represents an important treatment advance for a group of patients who are trying to string together remission after remission, with limited negative impact on quality of life.
Dr. Lyss was an oncologist and researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
The power and promise of person-generated health data (Part II)
In Part I of our discussion we introduced the concept of person-generated health data (PGHD), defined as wellness and/or health-related data created, recorded, or gathered by individuals.
Such rich, longitudinal information is now being used in combination with traditional clinical information to predict, diagnose, and formulate treatment plans for diseases, as well as understand the safety and effectiveness of medical interventions.
Identifying a disease early
One novel example of digital technologies being used for early identification of disease was a promising 2019 study by Eli Lilly (in collaboration with Apple and Evidation Health) called the Lilly Exploratory Digital Assessment Study.
In this study, the feasibility of using PGHD for identifying physiological and behavioral signatures of cognitive impairment was examined for the purpose of seeking new methods to detect mild cognitive impairment (MCI) in a timely and cost-effective manner. The study enrolled 31 study participants with cognitive impairment and 82 without cognitive impairment. It used consumer-grade sensor technologies (the iPhone, Apple Watch, iPad, and Beddit sleep monitor) to continuously and unobtrusively collect data. Among the information the researchers collected were interaction with the phone keyboard, accelerometer data from the Apple Watch, volume of messages sent/received, and sleep cycles.1

A total of 16 terabytes of data were collected over the course of 12 weeks. Data were organized into a behaviorgram (See Figure 1) that gives a holistic picture of a day in a patient’s life. A machine learning model was used to distinguish between behaviorgrams of symptomatic versus healthy controls, identifying typing speed, circadian rhythm shifts, and reliance on helper apps, among other things, as differentiating cognitively impaired from healthy controls. These behaviorgrams may someday serve as “fingerprints” of different diseases, with specific diseases displaying predictable patterns. In the near future, digital measures like the ones investigated in this study are likely to be used to help clinicians predict and diagnose disease, as well as to better understand disease progression and treatment response.
Leading to better health outcomes
The potential of PGHD to detect diseases early and lead to better health outcomes is being investigated in the Heartline study, a collaboration between Johnson & Johnson and Apple, which is supported by Evidation.2
This study aims to enroll 150,000 adults age 65 years and over to analyze the impact of Apple Watch–based early detection of irregular heart rhythms consistent with atrial fibrillation (AFib). The researchers’ hypothesis is that jointly detecting atrial fibrillation early and providing cardiovascular health programs to new AFib patients, will lead to patients being treated by a medical provider for AFib that otherwise would not have been detected. This, in turn, would lead to these AFib patients decreasing their risks of stroke and other serious cardiovascular events, including death, the study authors speculated.
Presenting new challenges
While PGHD has the potential to help people, it also presents new challenges. It is highly sensitive and personal – it can be as identifying as DNA.3
The vast amount of data that PGHD can collect from interaction with consumer wearable devices poses serious privacy risks if done improperly. To address those risks, companies like Evidation have built in protections. Evidation has an app, Achievement, that has enlisted a connected population of more than 3.5 million members who earn rewards for performing health-related actions, as tracked by wearables devices and apps. Through the Achievement app (See Figure 2.), members are provided opportunities to join research studies. As part of these studies, data collected from sensors and apps is used by permission of the member so that it is clear how their data are contributing to specific research questions or use cases.
This is a collaborative model of data collection built upon trust and permission and is substantially different than the collection of data from electronic health records (EHRs) – which is typically aggregated, deidentified, and commercialized, often without the patients’ knowledge or consent. Stringent protections, explicit permission, and transparency are absolutely imperative until privacy frameworks for data outside of HIPAA regulation catches up and protects patients from discrimination and unintended uses of their data.
Large connected cohorts can help advance our understanding of public health. In one study run on Achievement during the 2017-2018 flu season, a survey was sent to the Achievement population every week asking about symptoms of influenza-like illness and requesting permission to access historical data from their wearable around the influenza-like illness event.4 With the data, it was possible to analyze patterns of activity, sleep, and resting heart rate change around flu events. Resting heart rate, in particular, is shown to increase during fever and at the population level. In fact, through the use of PGHD, it is possible to use the fraction of people with resting heart rate above their usual baseline as a proxy to quantify the number of infected people in a region.5 This resting heart rate–informed flu surveillance method, if refined to increased accuracy, can work in near real time. This means it may be able detect influenza outbreaks days earlier than current epidemiological methods.
Health data generated by connected populations are in the early stages of development. It is clear that it will yield novel insights into health and disease. Only time will tell if it will be able to help clinicians and patients better predict, diagnose, and formulate treatment plans for disease.
Neil Skolnik, M.D. is a professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, and associate director of the Family Medicine Residency Program at Abington Jefferson Health. Luca Foschini PhD, is co-founder & chief data scientist at Evidation Health. Bray Patrick-Lake, MFS, is a patient thought leader and director of strategic partnerships at Evidation Health.
References
1. Chen R et al. Developing measures of cognitive impairment in the real world from consumer-grade multimodal sensor streams. KDD ’19. August 4–8, 2019 Aug 4-8.
2. The Heartline Study. https://www.heartline.com.
3. Foschini L. Privacy of Wearable and Sensors Data (or, the Lack Thereof?). Data Driven Investor, Medium. 2019.
4. Bradshaw B et al. Influenza surveillance using wearable mobile health devices. Online J Public Health Inform. 2019;11(1):e249.
5. Radin JM et al. Harnessing wearable device data to improve state-level real-time surveillance of influenza-like illness in the USA: a population-based study. Lancet Digital Health. 2020. doi: 10.1016/S2589-7500(19)30222-5.
In Part I of our discussion we introduced the concept of person-generated health data (PGHD), defined as wellness and/or health-related data created, recorded, or gathered by individuals.
Such rich, longitudinal information is now being used in combination with traditional clinical information to predict, diagnose, and formulate treatment plans for diseases, as well as understand the safety and effectiveness of medical interventions.
Identifying a disease early
One novel example of digital technologies being used for early identification of disease was a promising 2019 study by Eli Lilly (in collaboration with Apple and Evidation Health) called the Lilly Exploratory Digital Assessment Study.
In this study, the feasibility of using PGHD for identifying physiological and behavioral signatures of cognitive impairment was examined for the purpose of seeking new methods to detect mild cognitive impairment (MCI) in a timely and cost-effective manner. The study enrolled 31 study participants with cognitive impairment and 82 without cognitive impairment. It used consumer-grade sensor technologies (the iPhone, Apple Watch, iPad, and Beddit sleep monitor) to continuously and unobtrusively collect data. Among the information the researchers collected were interaction with the phone keyboard, accelerometer data from the Apple Watch, volume of messages sent/received, and sleep cycles.1

A total of 16 terabytes of data were collected over the course of 12 weeks. Data were organized into a behaviorgram (See Figure 1) that gives a holistic picture of a day in a patient’s life. A machine learning model was used to distinguish between behaviorgrams of symptomatic versus healthy controls, identifying typing speed, circadian rhythm shifts, and reliance on helper apps, among other things, as differentiating cognitively impaired from healthy controls. These behaviorgrams may someday serve as “fingerprints” of different diseases, with specific diseases displaying predictable patterns. In the near future, digital measures like the ones investigated in this study are likely to be used to help clinicians predict and diagnose disease, as well as to better understand disease progression and treatment response.
Leading to better health outcomes
The potential of PGHD to detect diseases early and lead to better health outcomes is being investigated in the Heartline study, a collaboration between Johnson & Johnson and Apple, which is supported by Evidation.2
This study aims to enroll 150,000 adults age 65 years and over to analyze the impact of Apple Watch–based early detection of irregular heart rhythms consistent with atrial fibrillation (AFib). The researchers’ hypothesis is that jointly detecting atrial fibrillation early and providing cardiovascular health programs to new AFib patients, will lead to patients being treated by a medical provider for AFib that otherwise would not have been detected. This, in turn, would lead to these AFib patients decreasing their risks of stroke and other serious cardiovascular events, including death, the study authors speculated.
Presenting new challenges
While PGHD has the potential to help people, it also presents new challenges. It is highly sensitive and personal – it can be as identifying as DNA.3
The vast amount of data that PGHD can collect from interaction with consumer wearable devices poses serious privacy risks if done improperly. To address those risks, companies like Evidation have built in protections. Evidation has an app, Achievement, that has enlisted a connected population of more than 3.5 million members who earn rewards for performing health-related actions, as tracked by wearables devices and apps. Through the Achievement app (See Figure 2.), members are provided opportunities to join research studies. As part of these studies, data collected from sensors and apps is used by permission of the member so that it is clear how their data are contributing to specific research questions or use cases.
This is a collaborative model of data collection built upon trust and permission and is substantially different than the collection of data from electronic health records (EHRs) – which is typically aggregated, deidentified, and commercialized, often without the patients’ knowledge or consent. Stringent protections, explicit permission, and transparency are absolutely imperative until privacy frameworks for data outside of HIPAA regulation catches up and protects patients from discrimination and unintended uses of their data.
Large connected cohorts can help advance our understanding of public health. In one study run on Achievement during the 2017-2018 flu season, a survey was sent to the Achievement population every week asking about symptoms of influenza-like illness and requesting permission to access historical data from their wearable around the influenza-like illness event.4 With the data, it was possible to analyze patterns of activity, sleep, and resting heart rate change around flu events. Resting heart rate, in particular, is shown to increase during fever and at the population level. In fact, through the use of PGHD, it is possible to use the fraction of people with resting heart rate above their usual baseline as a proxy to quantify the number of infected people in a region.5 This resting heart rate–informed flu surveillance method, if refined to increased accuracy, can work in near real time. This means it may be able detect influenza outbreaks days earlier than current epidemiological methods.
Health data generated by connected populations are in the early stages of development. It is clear that it will yield novel insights into health and disease. Only time will tell if it will be able to help clinicians and patients better predict, diagnose, and formulate treatment plans for disease.
Neil Skolnik, M.D. is a professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, and associate director of the Family Medicine Residency Program at Abington Jefferson Health. Luca Foschini PhD, is co-founder & chief data scientist at Evidation Health. Bray Patrick-Lake, MFS, is a patient thought leader and director of strategic partnerships at Evidation Health.
References
1. Chen R et al. Developing measures of cognitive impairment in the real world from consumer-grade multimodal sensor streams. KDD ’19. August 4–8, 2019 Aug 4-8.
2. The Heartline Study. https://www.heartline.com.
3. Foschini L. Privacy of Wearable and Sensors Data (or, the Lack Thereof?). Data Driven Investor, Medium. 2019.
4. Bradshaw B et al. Influenza surveillance using wearable mobile health devices. Online J Public Health Inform. 2019;11(1):e249.
5. Radin JM et al. Harnessing wearable device data to improve state-level real-time surveillance of influenza-like illness in the USA: a population-based study. Lancet Digital Health. 2020. doi: 10.1016/S2589-7500(19)30222-5.
In Part I of our discussion we introduced the concept of person-generated health data (PGHD), defined as wellness and/or health-related data created, recorded, or gathered by individuals.
Such rich, longitudinal information is now being used in combination with traditional clinical information to predict, diagnose, and formulate treatment plans for diseases, as well as understand the safety and effectiveness of medical interventions.
Identifying a disease early
One novel example of digital technologies being used for early identification of disease was a promising 2019 study by Eli Lilly (in collaboration with Apple and Evidation Health) called the Lilly Exploratory Digital Assessment Study.
In this study, the feasibility of using PGHD for identifying physiological and behavioral signatures of cognitive impairment was examined for the purpose of seeking new methods to detect mild cognitive impairment (MCI) in a timely and cost-effective manner. The study enrolled 31 study participants with cognitive impairment and 82 without cognitive impairment. It used consumer-grade sensor technologies (the iPhone, Apple Watch, iPad, and Beddit sleep monitor) to continuously and unobtrusively collect data. Among the information the researchers collected were interaction with the phone keyboard, accelerometer data from the Apple Watch, volume of messages sent/received, and sleep cycles.1

A total of 16 terabytes of data were collected over the course of 12 weeks. Data were organized into a behaviorgram (See Figure 1) that gives a holistic picture of a day in a patient’s life. A machine learning model was used to distinguish between behaviorgrams of symptomatic versus healthy controls, identifying typing speed, circadian rhythm shifts, and reliance on helper apps, among other things, as differentiating cognitively impaired from healthy controls. These behaviorgrams may someday serve as “fingerprints” of different diseases, with specific diseases displaying predictable patterns. In the near future, digital measures like the ones investigated in this study are likely to be used to help clinicians predict and diagnose disease, as well as to better understand disease progression and treatment response.
Leading to better health outcomes
The potential of PGHD to detect diseases early and lead to better health outcomes is being investigated in the Heartline study, a collaboration between Johnson & Johnson and Apple, which is supported by Evidation.2
This study aims to enroll 150,000 adults age 65 years and over to analyze the impact of Apple Watch–based early detection of irregular heart rhythms consistent with atrial fibrillation (AFib). The researchers’ hypothesis is that jointly detecting atrial fibrillation early and providing cardiovascular health programs to new AFib patients, will lead to patients being treated by a medical provider for AFib that otherwise would not have been detected. This, in turn, would lead to these AFib patients decreasing their risks of stroke and other serious cardiovascular events, including death, the study authors speculated.
Presenting new challenges
While PGHD has the potential to help people, it also presents new challenges. It is highly sensitive and personal – it can be as identifying as DNA.3
The vast amount of data that PGHD can collect from interaction with consumer wearable devices poses serious privacy risks if done improperly. To address those risks, companies like Evidation have built in protections. Evidation has an app, Achievement, that has enlisted a connected population of more than 3.5 million members who earn rewards for performing health-related actions, as tracked by wearables devices and apps. Through the Achievement app (See Figure 2.), members are provided opportunities to join research studies. As part of these studies, data collected from sensors and apps is used by permission of the member so that it is clear how their data are contributing to specific research questions or use cases.
This is a collaborative model of data collection built upon trust and permission and is substantially different than the collection of data from electronic health records (EHRs) – which is typically aggregated, deidentified, and commercialized, often without the patients’ knowledge or consent. Stringent protections, explicit permission, and transparency are absolutely imperative until privacy frameworks for data outside of HIPAA regulation catches up and protects patients from discrimination and unintended uses of their data.
Large connected cohorts can help advance our understanding of public health. In one study run on Achievement during the 2017-2018 flu season, a survey was sent to the Achievement population every week asking about symptoms of influenza-like illness and requesting permission to access historical data from their wearable around the influenza-like illness event.4 With the data, it was possible to analyze patterns of activity, sleep, and resting heart rate change around flu events. Resting heart rate, in particular, is shown to increase during fever and at the population level. In fact, through the use of PGHD, it is possible to use the fraction of people with resting heart rate above their usual baseline as a proxy to quantify the number of infected people in a region.5 This resting heart rate–informed flu surveillance method, if refined to increased accuracy, can work in near real time. This means it may be able detect influenza outbreaks days earlier than current epidemiological methods.
Health data generated by connected populations are in the early stages of development. It is clear that it will yield novel insights into health and disease. Only time will tell if it will be able to help clinicians and patients better predict, diagnose, and formulate treatment plans for disease.
Neil Skolnik, M.D. is a professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, and associate director of the Family Medicine Residency Program at Abington Jefferson Health. Luca Foschini PhD, is co-founder & chief data scientist at Evidation Health. Bray Patrick-Lake, MFS, is a patient thought leader and director of strategic partnerships at Evidation Health.
References
1. Chen R et al. Developing measures of cognitive impairment in the real world from consumer-grade multimodal sensor streams. KDD ’19. August 4–8, 2019 Aug 4-8.
2. The Heartline Study. https://www.heartline.com.
3. Foschini L. Privacy of Wearable and Sensors Data (or, the Lack Thereof?). Data Driven Investor, Medium. 2019.
4. Bradshaw B et al. Influenza surveillance using wearable mobile health devices. Online J Public Health Inform. 2019;11(1):e249.
5. Radin JM et al. Harnessing wearable device data to improve state-level real-time surveillance of influenza-like illness in the USA: a population-based study. Lancet Digital Health. 2020. doi: 10.1016/S2589-7500(19)30222-5.
Novel drugs approved in 2019
In 2019, the Food and Drug Administration approved 42 drugs, 6 of which will not be discussed here because of space limitations: recarbrio, a three-drug combination, containing imipenem, cilastatin, and relebactam; polatuzumab (Polivy) combined with bendamustine and a rituximab product; pretomanid combined with bedaquiline and linezolid; romosozumab (Evenity) for postmenopausal women; and alpelisib (Piqray) for postmenopausal women. In addition, darolutamide (Nubeqa) will not be included because it is indicated for the treatment of patients with prostate cancer. The remaining 36 agents are listed alphabetically below with the trade names in parentheses.
The molecular weights (if available), rounded to the nearest whole number, are shown in parentheses.
Air polymer-type a intrauterine foam (ExEm Foam), an ultrasound contrast agent, is indicated for sonohysterosalpingography to assess fallopian tube patency in women with known or suspected infertility. Animal studies have not been conducted, and the agent is contraindicated in pregnancy.
Afamelanotide implant (Scenesse) (1,647) is a melanocortin 1 receptor agonist that is indicated to increase pain-free light exposure in adult patients with a history of phototoxic reactions from erythropoietic protoporphyria. The drug caused no embryofetal toxicity in two species of rats. The molecular weight suggests that it will not cross the placenta, at least early in pregnancy.
Alpelisib (Piqray) (441) is a kinase inhibitor that is combined with fulvestrant for the treatment of advanced breast cancer in women and men. The molecular weight suggests that it can cross the human placenta. It is contraindicated in pregnancy because it can cause embryofetal toxicity.
Bremelanotide (Vyleesi) (1,025) is indicated for the treatment of premenopausal women with hypoactive sexual disorder. The drug caused fetal harm in dogs and mice. If a pregnant woman is exposed to the drug, health care providers are encouraged to call the VYLEESI Pregnancy Exposure Registry at 877-411-2510.
Brolucizumab (Beovu) (26,000) is a human vascular endothelial growth factor that is indicated for the treatment of neovascular age-related macular degeneration. In animals, it caused malformations, embryofetal resorption, and decreased fetal weight. Other adverse effects were follicular development, corpus luteum function, and fertility.
Caplacizumab (Cablivi) (28,000) is indicated for the treatment of adult patients with acquired thrombotic thrombocytopenia purpura, in combination with plasma exchange and immunosuppressive therapy. If used in pregnancy, there is a risk of hemorrhage in the mother and fetus. In guinea pigs given intramuscular doses of the drug, there was no evidence of adverse developmental outcomes.
Cefiderocol (Fetroja) (3,044) is an IV cephalosporin antibiotic indicated for the treatment of urinary tract infections, including pyelonephritis. The manufacturer states that it should be used in patients 18 years of age or older who have limited or no alternative treatment options. Consistent with other cephalosporins, no developmental adverse effects were observed in rats and mice.
Cenobamate (Xcopri) (268) is indicated for the treatment of partial-onset seizures in adults. In pregnant animals given the drug, there was increased embryo-fetal mortality, decreased fetal and offspring body weight, and neurobehavioral and reproductive impairment in offspring. If a pregnant woman receives this drug, encourage her to enroll in the North American Antiepileptic Drug Pregnancy Registry by calling the toll-free number 1-888-233-2334.
Crizanlizumab (Adakveo) (146,000) is indicated to reduce the frequency of vaso-occlusive crises in patients with sickle cell disease. In monkeys given doses slightly higher than those given to humans, there was increased fetal loss (abortions/stillbirths).
Entrectinib (Rozlytrek) (561) is a kinase inhibitor indicated for the treatment of cancer. The drug was teratogenic in rats. It is contraindicated in pregnancy because it can cause embryo-fetal toxicity.
Erdafitinib (Balversa) (447), a kinase inhibitor, is indicated for the treatment of locally advanced or metastatic urothelial carcinoma. In rats given doses during organogenesis with maternal exposures less than human exposures, the drug was teratogenic and caused embryofetal death. The manufacturer states that women of reproductive potential should use effective contraception during treatment and for 1 month after the last dose. The same advice was provided for male patients with female partners of reproductive potential. It is contraindicated in pregnancy because it can cause embryofetal toxicity.
Fedratinib (Inrebic) (616), a kinase inhibitor, is indicated for patients with intermediate-2 or high-risk primary or secondary myelofibrosis. The drug was teratogenic in rats when doses that were about 0.1 times the human exposure based on AUC (area under the curve) at the recommended daily dose during organogenesis. It is contraindicated in pregnancy because it can cause embryofetal toxicity.
Fluorodopa f18 (214) is a radioactive diagnostic agent. It is indicated for use in positron emission tomography to visualize dopaminergic nerve terminals in the striatum for evaluation of adult patients with suspected parkinsonian syndromes. The potential for adverse pregnant outcomes is based on the radiation dose and the gestational timing of exposure.
Givosiran sodium (Givlaari) (17,2460) is an aminolevulinate synthase 1-directed small interfering RNA given subcutaneously. It is indicated for the treatment of adults with acute hepatic porphyria. Doses less than 10 times the human dose in rats and rabbits produced maternal toxicity. In rats there was increased postimplantation loss, and in rats there was skeletal variation (incomplete ossification of pubes).
Golodirsen (Vyondys 53) (8,647) is indicated for the treatment of Duchenne muscular dystrophy given intravenously. There are no human or animal data available to assess the use of this drug during pregnancy.
Istradefylline (Nourianz) (384) is an adenosine receptor antagonist given orally. It is indicated as adjunctive treatment to levodopa/carbidopa in patients with Parkinson’s disease experiencing “off” episodes. In pregnant rats and rabbits, the drug was related to teratogenicity, embryo-fetal and offspring mortality, and growth deficits at clinically relevant exposures.
Lasmiditan (Reyvow) (436), a serotonin receptor agonist, is indicated for acute treatment of migraine with or without aura. In animals, the drug caused increased incidences of fetal defects, increased embryo-fetal and offspring mortality, and decreased fetal body weight at maternal exposures less than (rabbits) or greater than (rat) those observed clinically.
Lefamulin (Xenleta) (568) is an antibacterial agent available for oral and IV administration. They are indicated for the treatment of community-acquired bacterial pneumonia. The drug was teratogenic in rats at systemic exposures lower than those in humans, an increased incidence of post-implantation fetal loss and stillbirths, and decreased fetal body weights and ossification. There was also an apparent delay in sexual maturation in rats.
Luspatercept (Reblozyl) (76,000) is given subcutaneously for the treatment of anemia in patients with beta thalassemia who require regular red blood cell transfusions. In rats and rabbits, the drug cause increased embryo-fetal mortality, alteration to growth, and structural defects at exposures (based on AUC) that were about 13 times (rats) and 18 times (rabbits) the maximum recommended human dose.
Pexidartinib (Turalio) (454) is an oral kinase inhibitor that is indicated for the treatment of symptomatic tenosynovial giant cell tumor associated with severe morbidity or functional limitations and not amenable with surgery. In rats and rabbits, the drug caused malformations, increased post-implantation loss, and abortion at exposures nearly equal to the human exposure. It is contraindicated in pregnancy because it can cause embryo-fetal toxicity.
Pitolisant HCl (Wakix) (296) is an histamine-3 receptor antagonist/inverse agonist indicated for the treatment of excessive daytime sleepiness in patients with narcolepsy. The drug has caused maternal and embryofetal toxicity in rats and rabbits at doses greater than and equal to 13 times and greater than 4 times the maximum human dose, respectively. The manufacturer has a pregnancy exposure registry that patients can contact at 1-800-833-7460.
Prabotulinum toxin A (Jeuveau) (900,000) is an acetylcholine release inhibitor and a neuromuscular blocking agent indicated for the temporary improvement in the appearance of moderate to severe glabellar lines associated with corrugator and/or procerus muscle activity. The drug caused no adverse embryo-fetal in rats with doses up to 12 times the human dose.
Risankizumab-rzaa (Skyrizi) (molecular weight unknown), an interleukin-23 antagonist, is used for the treatment of moderate-to-severe plaque psoriasis. In pregnant monkeys, doses that were 20 times the maximum human dose increased fetal/infant loss.
Selinexor (Xpovio) (443) is an oral nuclear export inhibitor given in combination with dexamethasone for the treatment of relapsed or refractory myeloma. At doses lower than those used clinically, the drug caused structural abnormalities and alterations to growth in fetal rats.
Siponimod (Mayzent) (1,149) is an oral sphingosine 1-phosphate receptor modulator. It is indicated for the treatment of relapsing forms of multiple sclerosis. At low doses, the drug caused embryotoxicity and fetotoxicity in rats and rabbits including embryofetal deaths and abortions. The drug was teratogenic in both species.
Solriamfetol (Sunosi) (231) is an oral dopamine and norepinephrine reuptake inhibitor that is indicated to improve wakefulness in adult patients with excessive daytime sleepiness associated with narcolepsy or obstructive sleep apnea. The drug caused maternal and fetal toxicities in rats and rabbits and was teratogenic. The manufacturer has a pregnancy exposure registry to monitor pregnancy outcomes. Health care providers or patients can enroll in the program by calling 1-877-283-6220 or contacting the company.
Tafamidis meglumine (Vyndaqel) (503) and tafamidis (Vyndamax) (308) are indicated for the treatment of the cardiomyopathy of wild type or hereditary transthyretin-mediated amyloidosis to reduce cardiovascular mortality and cardiovascular-related hospitalization. In rabbits and rats, use of the drugs during pregnancy caused birth defects, embryo-fetal mortality, and fetal body weight reduction. Limited available data with Vyndaqel use in human pregnancy at a dose of 20 mg/day have not identified any drug-associated risks for major birth defects, miscarriage, or adverse maternal or fetal outcomes (see package insert).
Tenapanor (Ibsrela) (1,218) is indicated for the treatment of irritable bowel syndrome with constipation. The drug is minimally absorbed systemically, with plasma concentrations below the limit of quantification. No adverse maternal or fetal outcomes in rats or rabbits were observed. As reported by the manufacturer, in a small number of pregnant women, no drug-induced adverse maternal or fetal outcomes were identified.
Triclabendazole (Egaten) (360), an oral anthelmintic, is indicated for the treatment of fascioliasis. The drug was not teratogenic in mice and rabbits.
Trifarotene (Aklief) (460) cream is a retinoid that is indicated for the topical treatment of acne vulgaris. Animal data was related to oral retinoids and it not applicable to this agent. The manufacturer reported that available data from the use of the cream in pregnant women have not identified a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes.
Upadacitinib (Rinvoq) (389) is an oral Janus inhibitor. It is indicated for the treatment of moderate to severe active rheumatoid arthritis in patients who have had an inadequate response or intolerance to methotrexate. The drug caused increases in fetal malformations when given to rats and rabbits during organogenesis.
Voxelotor (Oxbryta) (337) is an oral hemoglobin S polymerization inhibitor indicated for the treatment of sickle cell disease. In rats and rabbits, there was no evidence of adverse developmental outcomes.
Zanubrutinib (Brukinsa) (472), an oral kinase inhibitor, is indicated for the treatment of mantle cell lymphoma. The drug caused embryofetal toxicity in pregnant rats, including malformations. It is contraindicated in pregnancy because it can cause embryo-fetal toxicity.
Breastfeeding
Brexanolone (Zulresso) (319) is indicated for the treatment of postpartum depression. It is given as a continuous IV infusion over 60 hours. The drug, at exposures close to those seen in humans, did not cause structural defects in rabbits and rats, but did cause fetal toxicity. Because patients are at risk of excessive sedation or sudden loss of consciousness when receiving the drug, it is only available through a restricted program called the ZULRESSO REMS. Health care providers are encouraged to register patients by calling the National Pregnancy Registry for Antidepressants at 844-405-6185. To obtain a list of health care facilities enrolled in the program call 844-472-4379.
Nearly all of the above drugs will cross into a woman’s colostrum during the first 48 hours post partum. These amounts should be very small, but not breastfeeding is the best choice.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
In 2019, the Food and Drug Administration approved 42 drugs, 6 of which will not be discussed here because of space limitations: recarbrio, a three-drug combination, containing imipenem, cilastatin, and relebactam; polatuzumab (Polivy) combined with bendamustine and a rituximab product; pretomanid combined with bedaquiline and linezolid; romosozumab (Evenity) for postmenopausal women; and alpelisib (Piqray) for postmenopausal women. In addition, darolutamide (Nubeqa) will not be included because it is indicated for the treatment of patients with prostate cancer. The remaining 36 agents are listed alphabetically below with the trade names in parentheses.
The molecular weights (if available), rounded to the nearest whole number, are shown in parentheses.
Air polymer-type a intrauterine foam (ExEm Foam), an ultrasound contrast agent, is indicated for sonohysterosalpingography to assess fallopian tube patency in women with known or suspected infertility. Animal studies have not been conducted, and the agent is contraindicated in pregnancy.
Afamelanotide implant (Scenesse) (1,647) is a melanocortin 1 receptor agonist that is indicated to increase pain-free light exposure in adult patients with a history of phototoxic reactions from erythropoietic protoporphyria. The drug caused no embryofetal toxicity in two species of rats. The molecular weight suggests that it will not cross the placenta, at least early in pregnancy.
Alpelisib (Piqray) (441) is a kinase inhibitor that is combined with fulvestrant for the treatment of advanced breast cancer in women and men. The molecular weight suggests that it can cross the human placenta. It is contraindicated in pregnancy because it can cause embryofetal toxicity.
Bremelanotide (Vyleesi) (1,025) is indicated for the treatment of premenopausal women with hypoactive sexual disorder. The drug caused fetal harm in dogs and mice. If a pregnant woman is exposed to the drug, health care providers are encouraged to call the VYLEESI Pregnancy Exposure Registry at 877-411-2510.
Brolucizumab (Beovu) (26,000) is a human vascular endothelial growth factor that is indicated for the treatment of neovascular age-related macular degeneration. In animals, it caused malformations, embryofetal resorption, and decreased fetal weight. Other adverse effects were follicular development, corpus luteum function, and fertility.
Caplacizumab (Cablivi) (28,000) is indicated for the treatment of adult patients with acquired thrombotic thrombocytopenia purpura, in combination with plasma exchange and immunosuppressive therapy. If used in pregnancy, there is a risk of hemorrhage in the mother and fetus. In guinea pigs given intramuscular doses of the drug, there was no evidence of adverse developmental outcomes.
Cefiderocol (Fetroja) (3,044) is an IV cephalosporin antibiotic indicated for the treatment of urinary tract infections, including pyelonephritis. The manufacturer states that it should be used in patients 18 years of age or older who have limited or no alternative treatment options. Consistent with other cephalosporins, no developmental adverse effects were observed in rats and mice.
Cenobamate (Xcopri) (268) is indicated for the treatment of partial-onset seizures in adults. In pregnant animals given the drug, there was increased embryo-fetal mortality, decreased fetal and offspring body weight, and neurobehavioral and reproductive impairment in offspring. If a pregnant woman receives this drug, encourage her to enroll in the North American Antiepileptic Drug Pregnancy Registry by calling the toll-free number 1-888-233-2334.
Crizanlizumab (Adakveo) (146,000) is indicated to reduce the frequency of vaso-occlusive crises in patients with sickle cell disease. In monkeys given doses slightly higher than those given to humans, there was increased fetal loss (abortions/stillbirths).
Entrectinib (Rozlytrek) (561) is a kinase inhibitor indicated for the treatment of cancer. The drug was teratogenic in rats. It is contraindicated in pregnancy because it can cause embryo-fetal toxicity.
Erdafitinib (Balversa) (447), a kinase inhibitor, is indicated for the treatment of locally advanced or metastatic urothelial carcinoma. In rats given doses during organogenesis with maternal exposures less than human exposures, the drug was teratogenic and caused embryofetal death. The manufacturer states that women of reproductive potential should use effective contraception during treatment and for 1 month after the last dose. The same advice was provided for male patients with female partners of reproductive potential. It is contraindicated in pregnancy because it can cause embryofetal toxicity.
Fedratinib (Inrebic) (616), a kinase inhibitor, is indicated for patients with intermediate-2 or high-risk primary or secondary myelofibrosis. The drug was teratogenic in rats when doses that were about 0.1 times the human exposure based on AUC (area under the curve) at the recommended daily dose during organogenesis. It is contraindicated in pregnancy because it can cause embryofetal toxicity.
Fluorodopa f18 (214) is a radioactive diagnostic agent. It is indicated for use in positron emission tomography to visualize dopaminergic nerve terminals in the striatum for evaluation of adult patients with suspected parkinsonian syndromes. The potential for adverse pregnant outcomes is based on the radiation dose and the gestational timing of exposure.
Givosiran sodium (Givlaari) (17,2460) is an aminolevulinate synthase 1-directed small interfering RNA given subcutaneously. It is indicated for the treatment of adults with acute hepatic porphyria. Doses less than 10 times the human dose in rats and rabbits produced maternal toxicity. In rats there was increased postimplantation loss, and in rats there was skeletal variation (incomplete ossification of pubes).
Golodirsen (Vyondys 53) (8,647) is indicated for the treatment of Duchenne muscular dystrophy given intravenously. There are no human or animal data available to assess the use of this drug during pregnancy.
Istradefylline (Nourianz) (384) is an adenosine receptor antagonist given orally. It is indicated as adjunctive treatment to levodopa/carbidopa in patients with Parkinson’s disease experiencing “off” episodes. In pregnant rats and rabbits, the drug was related to teratogenicity, embryo-fetal and offspring mortality, and growth deficits at clinically relevant exposures.
Lasmiditan (Reyvow) (436), a serotonin receptor agonist, is indicated for acute treatment of migraine with or without aura. In animals, the drug caused increased incidences of fetal defects, increased embryo-fetal and offspring mortality, and decreased fetal body weight at maternal exposures less than (rabbits) or greater than (rat) those observed clinically.
Lefamulin (Xenleta) (568) is an antibacterial agent available for oral and IV administration. They are indicated for the treatment of community-acquired bacterial pneumonia. The drug was teratogenic in rats at systemic exposures lower than those in humans, an increased incidence of post-implantation fetal loss and stillbirths, and decreased fetal body weights and ossification. There was also an apparent delay in sexual maturation in rats.
Luspatercept (Reblozyl) (76,000) is given subcutaneously for the treatment of anemia in patients with beta thalassemia who require regular red blood cell transfusions. In rats and rabbits, the drug cause increased embryo-fetal mortality, alteration to growth, and structural defects at exposures (based on AUC) that were about 13 times (rats) and 18 times (rabbits) the maximum recommended human dose.
Pexidartinib (Turalio) (454) is an oral kinase inhibitor that is indicated for the treatment of symptomatic tenosynovial giant cell tumor associated with severe morbidity or functional limitations and not amenable with surgery. In rats and rabbits, the drug caused malformations, increased post-implantation loss, and abortion at exposures nearly equal to the human exposure. It is contraindicated in pregnancy because it can cause embryo-fetal toxicity.
Pitolisant HCl (Wakix) (296) is an histamine-3 receptor antagonist/inverse agonist indicated for the treatment of excessive daytime sleepiness in patients with narcolepsy. The drug has caused maternal and embryofetal toxicity in rats and rabbits at doses greater than and equal to 13 times and greater than 4 times the maximum human dose, respectively. The manufacturer has a pregnancy exposure registry that patients can contact at 1-800-833-7460.
Prabotulinum toxin A (Jeuveau) (900,000) is an acetylcholine release inhibitor and a neuromuscular blocking agent indicated for the temporary improvement in the appearance of moderate to severe glabellar lines associated with corrugator and/or procerus muscle activity. The drug caused no adverse embryo-fetal in rats with doses up to 12 times the human dose.
Risankizumab-rzaa (Skyrizi) (molecular weight unknown), an interleukin-23 antagonist, is used for the treatment of moderate-to-severe plaque psoriasis. In pregnant monkeys, doses that were 20 times the maximum human dose increased fetal/infant loss.
Selinexor (Xpovio) (443) is an oral nuclear export inhibitor given in combination with dexamethasone for the treatment of relapsed or refractory myeloma. At doses lower than those used clinically, the drug caused structural abnormalities and alterations to growth in fetal rats.
Siponimod (Mayzent) (1,149) is an oral sphingosine 1-phosphate receptor modulator. It is indicated for the treatment of relapsing forms of multiple sclerosis. At low doses, the drug caused embryotoxicity and fetotoxicity in rats and rabbits including embryofetal deaths and abortions. The drug was teratogenic in both species.
Solriamfetol (Sunosi) (231) is an oral dopamine and norepinephrine reuptake inhibitor that is indicated to improve wakefulness in adult patients with excessive daytime sleepiness associated with narcolepsy or obstructive sleep apnea. The drug caused maternal and fetal toxicities in rats and rabbits and was teratogenic. The manufacturer has a pregnancy exposure registry to monitor pregnancy outcomes. Health care providers or patients can enroll in the program by calling 1-877-283-6220 or contacting the company.
Tafamidis meglumine (Vyndaqel) (503) and tafamidis (Vyndamax) (308) are indicated for the treatment of the cardiomyopathy of wild type or hereditary transthyretin-mediated amyloidosis to reduce cardiovascular mortality and cardiovascular-related hospitalization. In rabbits and rats, use of the drugs during pregnancy caused birth defects, embryo-fetal mortality, and fetal body weight reduction. Limited available data with Vyndaqel use in human pregnancy at a dose of 20 mg/day have not identified any drug-associated risks for major birth defects, miscarriage, or adverse maternal or fetal outcomes (see package insert).
Tenapanor (Ibsrela) (1,218) is indicated for the treatment of irritable bowel syndrome with constipation. The drug is minimally absorbed systemically, with plasma concentrations below the limit of quantification. No adverse maternal or fetal outcomes in rats or rabbits were observed. As reported by the manufacturer, in a small number of pregnant women, no drug-induced adverse maternal or fetal outcomes were identified.
Triclabendazole (Egaten) (360), an oral anthelmintic, is indicated for the treatment of fascioliasis. The drug was not teratogenic in mice and rabbits.
Trifarotene (Aklief) (460) cream is a retinoid that is indicated for the topical treatment of acne vulgaris. Animal data was related to oral retinoids and it not applicable to this agent. The manufacturer reported that available data from the use of the cream in pregnant women have not identified a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes.
Upadacitinib (Rinvoq) (389) is an oral Janus inhibitor. It is indicated for the treatment of moderate to severe active rheumatoid arthritis in patients who have had an inadequate response or intolerance to methotrexate. The drug caused increases in fetal malformations when given to rats and rabbits during organogenesis.
Voxelotor (Oxbryta) (337) is an oral hemoglobin S polymerization inhibitor indicated for the treatment of sickle cell disease. In rats and rabbits, there was no evidence of adverse developmental outcomes.
Zanubrutinib (Brukinsa) (472), an oral kinase inhibitor, is indicated for the treatment of mantle cell lymphoma. The drug caused embryofetal toxicity in pregnant rats, including malformations. It is contraindicated in pregnancy because it can cause embryo-fetal toxicity.
Breastfeeding
Brexanolone (Zulresso) (319) is indicated for the treatment of postpartum depression. It is given as a continuous IV infusion over 60 hours. The drug, at exposures close to those seen in humans, did not cause structural defects in rabbits and rats, but did cause fetal toxicity. Because patients are at risk of excessive sedation or sudden loss of consciousness when receiving the drug, it is only available through a restricted program called the ZULRESSO REMS. Health care providers are encouraged to register patients by calling the National Pregnancy Registry for Antidepressants at 844-405-6185. To obtain a list of health care facilities enrolled in the program call 844-472-4379.
Nearly all of the above drugs will cross into a woman’s colostrum during the first 48 hours post partum. These amounts should be very small, but not breastfeeding is the best choice.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
In 2019, the Food and Drug Administration approved 42 drugs, 6 of which will not be discussed here because of space limitations: recarbrio, a three-drug combination, containing imipenem, cilastatin, and relebactam; polatuzumab (Polivy) combined with bendamustine and a rituximab product; pretomanid combined with bedaquiline and linezolid; romosozumab (Evenity) for postmenopausal women; and alpelisib (Piqray) for postmenopausal women. In addition, darolutamide (Nubeqa) will not be included because it is indicated for the treatment of patients with prostate cancer. The remaining 36 agents are listed alphabetically below with the trade names in parentheses.
The molecular weights (if available), rounded to the nearest whole number, are shown in parentheses.
Air polymer-type a intrauterine foam (ExEm Foam), an ultrasound contrast agent, is indicated for sonohysterosalpingography to assess fallopian tube patency in women with known or suspected infertility. Animal studies have not been conducted, and the agent is contraindicated in pregnancy.
Afamelanotide implant (Scenesse) (1,647) is a melanocortin 1 receptor agonist that is indicated to increase pain-free light exposure in adult patients with a history of phototoxic reactions from erythropoietic protoporphyria. The drug caused no embryofetal toxicity in two species of rats. The molecular weight suggests that it will not cross the placenta, at least early in pregnancy.
Alpelisib (Piqray) (441) is a kinase inhibitor that is combined with fulvestrant for the treatment of advanced breast cancer in women and men. The molecular weight suggests that it can cross the human placenta. It is contraindicated in pregnancy because it can cause embryofetal toxicity.
Bremelanotide (Vyleesi) (1,025) is indicated for the treatment of premenopausal women with hypoactive sexual disorder. The drug caused fetal harm in dogs and mice. If a pregnant woman is exposed to the drug, health care providers are encouraged to call the VYLEESI Pregnancy Exposure Registry at 877-411-2510.
Brolucizumab (Beovu) (26,000) is a human vascular endothelial growth factor that is indicated for the treatment of neovascular age-related macular degeneration. In animals, it caused malformations, embryofetal resorption, and decreased fetal weight. Other adverse effects were follicular development, corpus luteum function, and fertility.
Caplacizumab (Cablivi) (28,000) is indicated for the treatment of adult patients with acquired thrombotic thrombocytopenia purpura, in combination with plasma exchange and immunosuppressive therapy. If used in pregnancy, there is a risk of hemorrhage in the mother and fetus. In guinea pigs given intramuscular doses of the drug, there was no evidence of adverse developmental outcomes.
Cefiderocol (Fetroja) (3,044) is an IV cephalosporin antibiotic indicated for the treatment of urinary tract infections, including pyelonephritis. The manufacturer states that it should be used in patients 18 years of age or older who have limited or no alternative treatment options. Consistent with other cephalosporins, no developmental adverse effects were observed in rats and mice.
Cenobamate (Xcopri) (268) is indicated for the treatment of partial-onset seizures in adults. In pregnant animals given the drug, there was increased embryo-fetal mortality, decreased fetal and offspring body weight, and neurobehavioral and reproductive impairment in offspring. If a pregnant woman receives this drug, encourage her to enroll in the North American Antiepileptic Drug Pregnancy Registry by calling the toll-free number 1-888-233-2334.
Crizanlizumab (Adakveo) (146,000) is indicated to reduce the frequency of vaso-occlusive crises in patients with sickle cell disease. In monkeys given doses slightly higher than those given to humans, there was increased fetal loss (abortions/stillbirths).
Entrectinib (Rozlytrek) (561) is a kinase inhibitor indicated for the treatment of cancer. The drug was teratogenic in rats. It is contraindicated in pregnancy because it can cause embryo-fetal toxicity.
Erdafitinib (Balversa) (447), a kinase inhibitor, is indicated for the treatment of locally advanced or metastatic urothelial carcinoma. In rats given doses during organogenesis with maternal exposures less than human exposures, the drug was teratogenic and caused embryofetal death. The manufacturer states that women of reproductive potential should use effective contraception during treatment and for 1 month after the last dose. The same advice was provided for male patients with female partners of reproductive potential. It is contraindicated in pregnancy because it can cause embryofetal toxicity.
Fedratinib (Inrebic) (616), a kinase inhibitor, is indicated for patients with intermediate-2 or high-risk primary or secondary myelofibrosis. The drug was teratogenic in rats when doses that were about 0.1 times the human exposure based on AUC (area under the curve) at the recommended daily dose during organogenesis. It is contraindicated in pregnancy because it can cause embryofetal toxicity.
Fluorodopa f18 (214) is a radioactive diagnostic agent. It is indicated for use in positron emission tomography to visualize dopaminergic nerve terminals in the striatum for evaluation of adult patients with suspected parkinsonian syndromes. The potential for adverse pregnant outcomes is based on the radiation dose and the gestational timing of exposure.
Givosiran sodium (Givlaari) (17,2460) is an aminolevulinate synthase 1-directed small interfering RNA given subcutaneously. It is indicated for the treatment of adults with acute hepatic porphyria. Doses less than 10 times the human dose in rats and rabbits produced maternal toxicity. In rats there was increased postimplantation loss, and in rats there was skeletal variation (incomplete ossification of pubes).
Golodirsen (Vyondys 53) (8,647) is indicated for the treatment of Duchenne muscular dystrophy given intravenously. There are no human or animal data available to assess the use of this drug during pregnancy.
Istradefylline (Nourianz) (384) is an adenosine receptor antagonist given orally. It is indicated as adjunctive treatment to levodopa/carbidopa in patients with Parkinson’s disease experiencing “off” episodes. In pregnant rats and rabbits, the drug was related to teratogenicity, embryo-fetal and offspring mortality, and growth deficits at clinically relevant exposures.
Lasmiditan (Reyvow) (436), a serotonin receptor agonist, is indicated for acute treatment of migraine with or without aura. In animals, the drug caused increased incidences of fetal defects, increased embryo-fetal and offspring mortality, and decreased fetal body weight at maternal exposures less than (rabbits) or greater than (rat) those observed clinically.
Lefamulin (Xenleta) (568) is an antibacterial agent available for oral and IV administration. They are indicated for the treatment of community-acquired bacterial pneumonia. The drug was teratogenic in rats at systemic exposures lower than those in humans, an increased incidence of post-implantation fetal loss and stillbirths, and decreased fetal body weights and ossification. There was also an apparent delay in sexual maturation in rats.
Luspatercept (Reblozyl) (76,000) is given subcutaneously for the treatment of anemia in patients with beta thalassemia who require regular red blood cell transfusions. In rats and rabbits, the drug cause increased embryo-fetal mortality, alteration to growth, and structural defects at exposures (based on AUC) that were about 13 times (rats) and 18 times (rabbits) the maximum recommended human dose.
Pexidartinib (Turalio) (454) is an oral kinase inhibitor that is indicated for the treatment of symptomatic tenosynovial giant cell tumor associated with severe morbidity or functional limitations and not amenable with surgery. In rats and rabbits, the drug caused malformations, increased post-implantation loss, and abortion at exposures nearly equal to the human exposure. It is contraindicated in pregnancy because it can cause embryo-fetal toxicity.
Pitolisant HCl (Wakix) (296) is an histamine-3 receptor antagonist/inverse agonist indicated for the treatment of excessive daytime sleepiness in patients with narcolepsy. The drug has caused maternal and embryofetal toxicity in rats and rabbits at doses greater than and equal to 13 times and greater than 4 times the maximum human dose, respectively. The manufacturer has a pregnancy exposure registry that patients can contact at 1-800-833-7460.
Prabotulinum toxin A (Jeuveau) (900,000) is an acetylcholine release inhibitor and a neuromuscular blocking agent indicated for the temporary improvement in the appearance of moderate to severe glabellar lines associated with corrugator and/or procerus muscle activity. The drug caused no adverse embryo-fetal in rats with doses up to 12 times the human dose.
Risankizumab-rzaa (Skyrizi) (molecular weight unknown), an interleukin-23 antagonist, is used for the treatment of moderate-to-severe plaque psoriasis. In pregnant monkeys, doses that were 20 times the maximum human dose increased fetal/infant loss.
Selinexor (Xpovio) (443) is an oral nuclear export inhibitor given in combination with dexamethasone for the treatment of relapsed or refractory myeloma. At doses lower than those used clinically, the drug caused structural abnormalities and alterations to growth in fetal rats.
Siponimod (Mayzent) (1,149) is an oral sphingosine 1-phosphate receptor modulator. It is indicated for the treatment of relapsing forms of multiple sclerosis. At low doses, the drug caused embryotoxicity and fetotoxicity in rats and rabbits including embryofetal deaths and abortions. The drug was teratogenic in both species.
Solriamfetol (Sunosi) (231) is an oral dopamine and norepinephrine reuptake inhibitor that is indicated to improve wakefulness in adult patients with excessive daytime sleepiness associated with narcolepsy or obstructive sleep apnea. The drug caused maternal and fetal toxicities in rats and rabbits and was teratogenic. The manufacturer has a pregnancy exposure registry to monitor pregnancy outcomes. Health care providers or patients can enroll in the program by calling 1-877-283-6220 or contacting the company.
Tafamidis meglumine (Vyndaqel) (503) and tafamidis (Vyndamax) (308) are indicated for the treatment of the cardiomyopathy of wild type or hereditary transthyretin-mediated amyloidosis to reduce cardiovascular mortality and cardiovascular-related hospitalization. In rabbits and rats, use of the drugs during pregnancy caused birth defects, embryo-fetal mortality, and fetal body weight reduction. Limited available data with Vyndaqel use in human pregnancy at a dose of 20 mg/day have not identified any drug-associated risks for major birth defects, miscarriage, or adverse maternal or fetal outcomes (see package insert).
Tenapanor (Ibsrela) (1,218) is indicated for the treatment of irritable bowel syndrome with constipation. The drug is minimally absorbed systemically, with plasma concentrations below the limit of quantification. No adverse maternal or fetal outcomes in rats or rabbits were observed. As reported by the manufacturer, in a small number of pregnant women, no drug-induced adverse maternal or fetal outcomes were identified.
Triclabendazole (Egaten) (360), an oral anthelmintic, is indicated for the treatment of fascioliasis. The drug was not teratogenic in mice and rabbits.
Trifarotene (Aklief) (460) cream is a retinoid that is indicated for the topical treatment of acne vulgaris. Animal data was related to oral retinoids and it not applicable to this agent. The manufacturer reported that available data from the use of the cream in pregnant women have not identified a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes.
Upadacitinib (Rinvoq) (389) is an oral Janus inhibitor. It is indicated for the treatment of moderate to severe active rheumatoid arthritis in patients who have had an inadequate response or intolerance to methotrexate. The drug caused increases in fetal malformations when given to rats and rabbits during organogenesis.
Voxelotor (Oxbryta) (337) is an oral hemoglobin S polymerization inhibitor indicated for the treatment of sickle cell disease. In rats and rabbits, there was no evidence of adverse developmental outcomes.
Zanubrutinib (Brukinsa) (472), an oral kinase inhibitor, is indicated for the treatment of mantle cell lymphoma. The drug caused embryofetal toxicity in pregnant rats, including malformations. It is contraindicated in pregnancy because it can cause embryo-fetal toxicity.
Breastfeeding
Brexanolone (Zulresso) (319) is indicated for the treatment of postpartum depression. It is given as a continuous IV infusion over 60 hours. The drug, at exposures close to those seen in humans, did not cause structural defects in rabbits and rats, but did cause fetal toxicity. Because patients are at risk of excessive sedation or sudden loss of consciousness when receiving the drug, it is only available through a restricted program called the ZULRESSO REMS. Health care providers are encouraged to register patients by calling the National Pregnancy Registry for Antidepressants at 844-405-6185. To obtain a list of health care facilities enrolled in the program call 844-472-4379.
Nearly all of the above drugs will cross into a woman’s colostrum during the first 48 hours post partum. These amounts should be very small, but not breastfeeding is the best choice.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
Two decades of leadership
In recognition of Dr. Larry Wellikson’s contributions to SHM
It’s already been a few years since I exited the Society of Hospital Medicine’s Board of Directors (2 years, or maybe 3 – I’ve already lost count), and sitting in my proverbial rocking chair in the Old Hospitalists’ Home, I heard, as many of you did, that Larry Wellikson, MD, MHM, the first and only CEO in the Society’s history, is stepping down soon.
With all the idle time that I find myself with these days, I have had the opportunity to ruminate on what Larry has brought to SHM in his 2 decades of leadership. And among the many answers, two stand out for me.
The first is Larry’s deep appreciation of the value of relationships that he has developed and nurtured, an attribute which he has imprinted on many of us who have worked with him over the years. Although Larry speaks of the camaraderie of the first years of SHM and the bonds that he, Bob Wachter, Win Whitcomb, and John Nelson established, he also has kept in touch with a vast network of hospitalists over the last 20-plus years.
Go to lunch with Larry, and be amazed at how much he knows about the goings-on of many of our colleagues. The fondness that Larry has for the people in his life is without parallel. These aren’t just professional colleagues who have impacted him in some way – for Larry, every one of these is a true lifetime friendship, and he continues to establish new ones every year. He makes each of his friends feel truly special to him.
The second is the critical value of and need for change and disruption. The specialty of hospital medicine was, from its beginning, disruptive, and from his career as a physician executive, Larry understood and has brought to SHM an understanding of the necessity of disruption to encourage growth and fresh thinking. If one steps back and looks at, for example, the composition of the Board over the years, or the Journal of Hospital Medicine’s editorial staff, or of our committees, one sees a pattern – a commitment to continuously bringing on young leaders who are still on the early and ascending part of their career paths.
Other organizations identify Board candidates at the peak of their careers, but at SHM, many of us were elected when we had just enough experience to contribute but then continued to grow in our careers after finishing our terms. I joined the Board in 2012 (I think) and while I would probably be a more seasoned and stately Board member if I joined at this point in my life, I would also have less new and novel to offer – and therefore be less effective for what the Society needs. While SHM respects its past leaders, it does not revere them. Our past is important, but our present and future are more important. Larry brought that mentality to SHM.
Ironically, the one position within SHM which has not, until this year, been subject to that same kind of transition is the CEO position itself. And this year, that domino will fall as well. While transitions are hard, change is good – and I am confident that our Society’s commitment to seeking out new, talented leaders, and making transitions at all levels – Board, committees, chapters, speakers – with the intent of bringing new perspectives and creativity, is firmly entrenched in our culture. And Larry can join me in the rocking chair as we relive our common SHM experiences together – and create new memories as well.
Congratulations Larry, and thank you.
Dr. Harte is a past president of SHM, and president of Cleveland Clinic Akron (Ohio) General and the Southern Region. He formerly served as president of Cleveland Clinic Hillcrest Hospital and Cleveland Clinic South Pointe Hospital.
In recognition of Dr. Larry Wellikson’s contributions to SHM
In recognition of Dr. Larry Wellikson’s contributions to SHM
It’s already been a few years since I exited the Society of Hospital Medicine’s Board of Directors (2 years, or maybe 3 – I’ve already lost count), and sitting in my proverbial rocking chair in the Old Hospitalists’ Home, I heard, as many of you did, that Larry Wellikson, MD, MHM, the first and only CEO in the Society’s history, is stepping down soon.
With all the idle time that I find myself with these days, I have had the opportunity to ruminate on what Larry has brought to SHM in his 2 decades of leadership. And among the many answers, two stand out for me.
The first is Larry’s deep appreciation of the value of relationships that he has developed and nurtured, an attribute which he has imprinted on many of us who have worked with him over the years. Although Larry speaks of the camaraderie of the first years of SHM and the bonds that he, Bob Wachter, Win Whitcomb, and John Nelson established, he also has kept in touch with a vast network of hospitalists over the last 20-plus years.
Go to lunch with Larry, and be amazed at how much he knows about the goings-on of many of our colleagues. The fondness that Larry has for the people in his life is without parallel. These aren’t just professional colleagues who have impacted him in some way – for Larry, every one of these is a true lifetime friendship, and he continues to establish new ones every year. He makes each of his friends feel truly special to him.
The second is the critical value of and need for change and disruption. The specialty of hospital medicine was, from its beginning, disruptive, and from his career as a physician executive, Larry understood and has brought to SHM an understanding of the necessity of disruption to encourage growth and fresh thinking. If one steps back and looks at, for example, the composition of the Board over the years, or the Journal of Hospital Medicine’s editorial staff, or of our committees, one sees a pattern – a commitment to continuously bringing on young leaders who are still on the early and ascending part of their career paths.
Other organizations identify Board candidates at the peak of their careers, but at SHM, many of us were elected when we had just enough experience to contribute but then continued to grow in our careers after finishing our terms. I joined the Board in 2012 (I think) and while I would probably be a more seasoned and stately Board member if I joined at this point in my life, I would also have less new and novel to offer – and therefore be less effective for what the Society needs. While SHM respects its past leaders, it does not revere them. Our past is important, but our present and future are more important. Larry brought that mentality to SHM.
Ironically, the one position within SHM which has not, until this year, been subject to that same kind of transition is the CEO position itself. And this year, that domino will fall as well. While transitions are hard, change is good – and I am confident that our Society’s commitment to seeking out new, talented leaders, and making transitions at all levels – Board, committees, chapters, speakers – with the intent of bringing new perspectives and creativity, is firmly entrenched in our culture. And Larry can join me in the rocking chair as we relive our common SHM experiences together – and create new memories as well.
Congratulations Larry, and thank you.
Dr. Harte is a past president of SHM, and president of Cleveland Clinic Akron (Ohio) General and the Southern Region. He formerly served as president of Cleveland Clinic Hillcrest Hospital and Cleveland Clinic South Pointe Hospital.
It’s already been a few years since I exited the Society of Hospital Medicine’s Board of Directors (2 years, or maybe 3 – I’ve already lost count), and sitting in my proverbial rocking chair in the Old Hospitalists’ Home, I heard, as many of you did, that Larry Wellikson, MD, MHM, the first and only CEO in the Society’s history, is stepping down soon.
With all the idle time that I find myself with these days, I have had the opportunity to ruminate on what Larry has brought to SHM in his 2 decades of leadership. And among the many answers, two stand out for me.
The first is Larry’s deep appreciation of the value of relationships that he has developed and nurtured, an attribute which he has imprinted on many of us who have worked with him over the years. Although Larry speaks of the camaraderie of the first years of SHM and the bonds that he, Bob Wachter, Win Whitcomb, and John Nelson established, he also has kept in touch with a vast network of hospitalists over the last 20-plus years.
Go to lunch with Larry, and be amazed at how much he knows about the goings-on of many of our colleagues. The fondness that Larry has for the people in his life is without parallel. These aren’t just professional colleagues who have impacted him in some way – for Larry, every one of these is a true lifetime friendship, and he continues to establish new ones every year. He makes each of his friends feel truly special to him.
The second is the critical value of and need for change and disruption. The specialty of hospital medicine was, from its beginning, disruptive, and from his career as a physician executive, Larry understood and has brought to SHM an understanding of the necessity of disruption to encourage growth and fresh thinking. If one steps back and looks at, for example, the composition of the Board over the years, or the Journal of Hospital Medicine’s editorial staff, or of our committees, one sees a pattern – a commitment to continuously bringing on young leaders who are still on the early and ascending part of their career paths.
Other organizations identify Board candidates at the peak of their careers, but at SHM, many of us were elected when we had just enough experience to contribute but then continued to grow in our careers after finishing our terms. I joined the Board in 2012 (I think) and while I would probably be a more seasoned and stately Board member if I joined at this point in my life, I would also have less new and novel to offer – and therefore be less effective for what the Society needs. While SHM respects its past leaders, it does not revere them. Our past is important, but our present and future are more important. Larry brought that mentality to SHM.
Ironically, the one position within SHM which has not, until this year, been subject to that same kind of transition is the CEO position itself. And this year, that domino will fall as well. While transitions are hard, change is good – and I am confident that our Society’s commitment to seeking out new, talented leaders, and making transitions at all levels – Board, committees, chapters, speakers – with the intent of bringing new perspectives and creativity, is firmly entrenched in our culture. And Larry can join me in the rocking chair as we relive our common SHM experiences together – and create new memories as well.
Congratulations Larry, and thank you.
Dr. Harte is a past president of SHM, and president of Cleveland Clinic Akron (Ohio) General and the Southern Region. He formerly served as president of Cleveland Clinic Hillcrest Hospital and Cleveland Clinic South Pointe Hospital.
Perspective from the heartland: Cancer care and research during a public health crisis
I have no knowledge of, or experience with, managing a cancer patient during a pandemic. However, from the published and otherwise shared experience of others, we should not allow ourselves to underestimate the voracity of the coronavirus pandemic on our patients, communities, and health care systems.
Data from China suggest cancer patients infected with SARS-CoV-2 face a 3.5 times higher risk of mechanical ventilation, intensive care unit admission, or death, compared with infected patients without cancer (Lancet Oncol 2020;21:335-7).
Health care workers in Seattle have also shared their experiences battling coronavirus infections in cancer patients (J Natl Compr Canc Netw. 2020 Mar 20. doi: 10.6004/jnccn.2020.7560). Masumi Ueda, MD, of Seattle Cancer Care Alliance, and colleagues reviewed their decisions in multiple domains over a 7-week period, during which the state of Washington went from a single case of SARS-CoV-2 infection to nearly 650 cases and 40 deaths.
Making tough treatment decisions
Dr. Ueda and colleagues contrasted their customary resource-rich, innovation-oriented, cancer-combatting environment with their current circumstance, in which they must prioritize treatment for patients for whom the risk-reward balance has tilted substantially toward “risk.”
The authors noted that their most difficult decisions were those regarding delay of cancer treatment. They suggested that plans for potentially curative adjuvant therapy should likely proceed, but, for patients with metastatic disease, the equation is more nuanced.
In some cases, treatment should be delayed or interrupted with recognition of how that could result in worsening performance status and admission for symptom palliation, further stressing inpatient resources.
The authors suggested scenarios for prioritizing cancer surgery. For example, several months of systemic therapy (ideally, low-risk systemic therapy such as hormone therapy for breast or prostate cancer) and surgical delay may be worthwhile, without compromising patient care.
Patients with aggressive hematologic malignancy requiring urgent systemic treatment (potentially stem cell transplantation and cellular immunotherapies) should be treated promptly. However, even in those cases, opportunities should be sought to lessen immunosuppression and transition care as quickly as possible to the outpatient clinic, according to guidelines from the American Society of Transplantation and Cellular Therapy.
See one, do one, teach one
Rendering patient care during a pandemic would be unique for me. However, I, like all physicians, am familiar with feelings of inadequacy at times of professional challenge. On countless occasions, I have started my day or walked into a patient’s room wondering whether I will have the fortitude, knowledge, creativity, or help I need to get through that day or make that patient “better” by any definition of that word.
We all know the formula: “Work hard. Make evidence-based, personalized decisions for those who have entrusted their care to us. Learn from those encounters. Teach from our knowledge and experience – that is, ‘See one, do one, teach one.’ ”
The Seattle oncologists are living the lives of first responders and deserve our admiration for putting pen to paper so we can learn from their considerable, relevant experience.
Similar admiration is due to Giuseppe Curigliano, MD, of the European Institute of Oncology in Milan. In the ASCO Daily News, Dr. Curigliano described an epidemic that, within 3 weeks, overloaded the health care system across northern Italy.
Hospitalization was needed for over 60% of infected patients, and nearly 15% of those patients needed intensive care unit services for respiratory distress. The Italians centralized oncology care in specialized hubs, with spokes of institutions working in parallel to provide cancer-specific care in a COVID-free environment.
To build upon cancer-specific information from Italy and other areas hard-hit by COVID-19, more than 30 cancer centers have joined together to form the COVID-19 and Cancer Consortium. The consortium’s website hosts a survey designed to “capture details related to cancer patients presumed to have COVID-19.”
Calculating deaths and long-term consequences for cancer care delivery
It is proper that the authors from China, Italy, and Seattle did not focus attention on the case fatality rate from the COVID-19 pandemic among cancer patients. To say the least, it would be complicated to tally the direct mortality – either overall or in clinically important subsets of patients, including country-specific cohorts.
What we know from published reports is that, in Italy, cancer patients account for about 20% of deaths from coronavirus. In China, the case-fatality rate for patients with cancer was 5.6% (JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648).
However, we know nothing about the indirect death toll from malignancy (without coronavirus infection) that was untreated or managed less than optimally because of personnel and physical resources that were diverted to COVID-19–associated cases.
Similarly, we cannot begin to estimate indirect consequences of the pandemic to oncology practices, such as accelerated burnout and posttraumatic stress disorder, as well as the long-range effects of economic turmoil on patients, health care workers, and provider organizations.
What happens to cancer trials?
From China, Italy, and Seattle, thus far, there is little information about how the pandemic will affect the vital clinical research endeavor. The Seattle physicians did say they plan to enroll patients on clinical trials only when the trial offers a high chance of benefiting the patient over standard therapy alone.
Fortunately, the National Institutes of Health and Food and Drug Administration have released guidance documents related to clinical trials.
The National Cancer Institute (NCI) has also released guidance documents (March 13 guidance; March 23 guidance) for patients on clinical trials supported by the NCI Cancer Therapy Evaluation Program (CTEP) and the NCI Community Oncology Research Program (NCORP).
CTEP and NCORP are making reasonable accommodations to suspend monitoring visits and audits, allow tele–follow-up visits for patients, and permit local physicians to provide care for patients on study. In addition, with appropriate procedural adherence and documentation, CTEP and NCORP will allow oral investigational medicines to be mailed directly to patients’ homes.
Planned NCI National Clinical Trials Network meetings will be conducted via remote access webinars, conference calls, and similar technology. These adjustments – and probably many more to come – are geared toward facilitating ongoing care to proceed safely and with minimal risk for patients currently receiving investigational therapies and for the sites and investigators engaged in those studies.
Each of us has probably faced a personal “defining professional moment,” when we had to utilize every skill in our arsenal and examine the motivations that led us to a career in oncology. However, it is clear from the forgoing clinical and research processes and guidelines that the COVID-19 pandemic is such a defining professional moment for each of us, in every community we serve.
Critical junctures like this cause more rapid behavior change and innovation than the slow-moving pace that characterizes our idealized preferences. As oncologists who embrace new data and behavioral change, we stand to learn processes that will facilitate more perfected systems of care than the one that preceded this unprecedented crisis, promote more efficient sharing of high-quality information, and improve the outcome for our future patients.
Dr. Lyss was an oncologist and researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
I have no knowledge of, or experience with, managing a cancer patient during a pandemic. However, from the published and otherwise shared experience of others, we should not allow ourselves to underestimate the voracity of the coronavirus pandemic on our patients, communities, and health care systems.
Data from China suggest cancer patients infected with SARS-CoV-2 face a 3.5 times higher risk of mechanical ventilation, intensive care unit admission, or death, compared with infected patients without cancer (Lancet Oncol 2020;21:335-7).
Health care workers in Seattle have also shared their experiences battling coronavirus infections in cancer patients (J Natl Compr Canc Netw. 2020 Mar 20. doi: 10.6004/jnccn.2020.7560). Masumi Ueda, MD, of Seattle Cancer Care Alliance, and colleagues reviewed their decisions in multiple domains over a 7-week period, during which the state of Washington went from a single case of SARS-CoV-2 infection to nearly 650 cases and 40 deaths.
Making tough treatment decisions
Dr. Ueda and colleagues contrasted their customary resource-rich, innovation-oriented, cancer-combatting environment with their current circumstance, in which they must prioritize treatment for patients for whom the risk-reward balance has tilted substantially toward “risk.”
The authors noted that their most difficult decisions were those regarding delay of cancer treatment. They suggested that plans for potentially curative adjuvant therapy should likely proceed, but, for patients with metastatic disease, the equation is more nuanced.
In some cases, treatment should be delayed or interrupted with recognition of how that could result in worsening performance status and admission for symptom palliation, further stressing inpatient resources.
The authors suggested scenarios for prioritizing cancer surgery. For example, several months of systemic therapy (ideally, low-risk systemic therapy such as hormone therapy for breast or prostate cancer) and surgical delay may be worthwhile, without compromising patient care.
Patients with aggressive hematologic malignancy requiring urgent systemic treatment (potentially stem cell transplantation and cellular immunotherapies) should be treated promptly. However, even in those cases, opportunities should be sought to lessen immunosuppression and transition care as quickly as possible to the outpatient clinic, according to guidelines from the American Society of Transplantation and Cellular Therapy.
See one, do one, teach one
Rendering patient care during a pandemic would be unique for me. However, I, like all physicians, am familiar with feelings of inadequacy at times of professional challenge. On countless occasions, I have started my day or walked into a patient’s room wondering whether I will have the fortitude, knowledge, creativity, or help I need to get through that day or make that patient “better” by any definition of that word.
We all know the formula: “Work hard. Make evidence-based, personalized decisions for those who have entrusted their care to us. Learn from those encounters. Teach from our knowledge and experience – that is, ‘See one, do one, teach one.’ ”
The Seattle oncologists are living the lives of first responders and deserve our admiration for putting pen to paper so we can learn from their considerable, relevant experience.
Similar admiration is due to Giuseppe Curigliano, MD, of the European Institute of Oncology in Milan. In the ASCO Daily News, Dr. Curigliano described an epidemic that, within 3 weeks, overloaded the health care system across northern Italy.
Hospitalization was needed for over 60% of infected patients, and nearly 15% of those patients needed intensive care unit services for respiratory distress. The Italians centralized oncology care in specialized hubs, with spokes of institutions working in parallel to provide cancer-specific care in a COVID-free environment.
To build upon cancer-specific information from Italy and other areas hard-hit by COVID-19, more than 30 cancer centers have joined together to form the COVID-19 and Cancer Consortium. The consortium’s website hosts a survey designed to “capture details related to cancer patients presumed to have COVID-19.”
Calculating deaths and long-term consequences for cancer care delivery
It is proper that the authors from China, Italy, and Seattle did not focus attention on the case fatality rate from the COVID-19 pandemic among cancer patients. To say the least, it would be complicated to tally the direct mortality – either overall or in clinically important subsets of patients, including country-specific cohorts.
What we know from published reports is that, in Italy, cancer patients account for about 20% of deaths from coronavirus. In China, the case-fatality rate for patients with cancer was 5.6% (JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648).
However, we know nothing about the indirect death toll from malignancy (without coronavirus infection) that was untreated or managed less than optimally because of personnel and physical resources that were diverted to COVID-19–associated cases.
Similarly, we cannot begin to estimate indirect consequences of the pandemic to oncology practices, such as accelerated burnout and posttraumatic stress disorder, as well as the long-range effects of economic turmoil on patients, health care workers, and provider organizations.
What happens to cancer trials?
From China, Italy, and Seattle, thus far, there is little information about how the pandemic will affect the vital clinical research endeavor. The Seattle physicians did say they plan to enroll patients on clinical trials only when the trial offers a high chance of benefiting the patient over standard therapy alone.
Fortunately, the National Institutes of Health and Food and Drug Administration have released guidance documents related to clinical trials.
The National Cancer Institute (NCI) has also released guidance documents (March 13 guidance; March 23 guidance) for patients on clinical trials supported by the NCI Cancer Therapy Evaluation Program (CTEP) and the NCI Community Oncology Research Program (NCORP).
CTEP and NCORP are making reasonable accommodations to suspend monitoring visits and audits, allow tele–follow-up visits for patients, and permit local physicians to provide care for patients on study. In addition, with appropriate procedural adherence and documentation, CTEP and NCORP will allow oral investigational medicines to be mailed directly to patients’ homes.
Planned NCI National Clinical Trials Network meetings will be conducted via remote access webinars, conference calls, and similar technology. These adjustments – and probably many more to come – are geared toward facilitating ongoing care to proceed safely and with minimal risk for patients currently receiving investigational therapies and for the sites and investigators engaged in those studies.
Each of us has probably faced a personal “defining professional moment,” when we had to utilize every skill in our arsenal and examine the motivations that led us to a career in oncology. However, it is clear from the forgoing clinical and research processes and guidelines that the COVID-19 pandemic is such a defining professional moment for each of us, in every community we serve.
Critical junctures like this cause more rapid behavior change and innovation than the slow-moving pace that characterizes our idealized preferences. As oncologists who embrace new data and behavioral change, we stand to learn processes that will facilitate more perfected systems of care than the one that preceded this unprecedented crisis, promote more efficient sharing of high-quality information, and improve the outcome for our future patients.
Dr. Lyss was an oncologist and researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
I have no knowledge of, or experience with, managing a cancer patient during a pandemic. However, from the published and otherwise shared experience of others, we should not allow ourselves to underestimate the voracity of the coronavirus pandemic on our patients, communities, and health care systems.
Data from China suggest cancer patients infected with SARS-CoV-2 face a 3.5 times higher risk of mechanical ventilation, intensive care unit admission, or death, compared with infected patients without cancer (Lancet Oncol 2020;21:335-7).
Health care workers in Seattle have also shared their experiences battling coronavirus infections in cancer patients (J Natl Compr Canc Netw. 2020 Mar 20. doi: 10.6004/jnccn.2020.7560). Masumi Ueda, MD, of Seattle Cancer Care Alliance, and colleagues reviewed their decisions in multiple domains over a 7-week period, during which the state of Washington went from a single case of SARS-CoV-2 infection to nearly 650 cases and 40 deaths.
Making tough treatment decisions
Dr. Ueda and colleagues contrasted their customary resource-rich, innovation-oriented, cancer-combatting environment with their current circumstance, in which they must prioritize treatment for patients for whom the risk-reward balance has tilted substantially toward “risk.”
The authors noted that their most difficult decisions were those regarding delay of cancer treatment. They suggested that plans for potentially curative adjuvant therapy should likely proceed, but, for patients with metastatic disease, the equation is more nuanced.
In some cases, treatment should be delayed or interrupted with recognition of how that could result in worsening performance status and admission for symptom palliation, further stressing inpatient resources.
The authors suggested scenarios for prioritizing cancer surgery. For example, several months of systemic therapy (ideally, low-risk systemic therapy such as hormone therapy for breast or prostate cancer) and surgical delay may be worthwhile, without compromising patient care.
Patients with aggressive hematologic malignancy requiring urgent systemic treatment (potentially stem cell transplantation and cellular immunotherapies) should be treated promptly. However, even in those cases, opportunities should be sought to lessen immunosuppression and transition care as quickly as possible to the outpatient clinic, according to guidelines from the American Society of Transplantation and Cellular Therapy.
See one, do one, teach one
Rendering patient care during a pandemic would be unique for me. However, I, like all physicians, am familiar with feelings of inadequacy at times of professional challenge. On countless occasions, I have started my day or walked into a patient’s room wondering whether I will have the fortitude, knowledge, creativity, or help I need to get through that day or make that patient “better” by any definition of that word.
We all know the formula: “Work hard. Make evidence-based, personalized decisions for those who have entrusted their care to us. Learn from those encounters. Teach from our knowledge and experience – that is, ‘See one, do one, teach one.’ ”
The Seattle oncologists are living the lives of first responders and deserve our admiration for putting pen to paper so we can learn from their considerable, relevant experience.
Similar admiration is due to Giuseppe Curigliano, MD, of the European Institute of Oncology in Milan. In the ASCO Daily News, Dr. Curigliano described an epidemic that, within 3 weeks, overloaded the health care system across northern Italy.
Hospitalization was needed for over 60% of infected patients, and nearly 15% of those patients needed intensive care unit services for respiratory distress. The Italians centralized oncology care in specialized hubs, with spokes of institutions working in parallel to provide cancer-specific care in a COVID-free environment.
To build upon cancer-specific information from Italy and other areas hard-hit by COVID-19, more than 30 cancer centers have joined together to form the COVID-19 and Cancer Consortium. The consortium’s website hosts a survey designed to “capture details related to cancer patients presumed to have COVID-19.”
Calculating deaths and long-term consequences for cancer care delivery
It is proper that the authors from China, Italy, and Seattle did not focus attention on the case fatality rate from the COVID-19 pandemic among cancer patients. To say the least, it would be complicated to tally the direct mortality – either overall or in clinically important subsets of patients, including country-specific cohorts.
What we know from published reports is that, in Italy, cancer patients account for about 20% of deaths from coronavirus. In China, the case-fatality rate for patients with cancer was 5.6% (JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648).
However, we know nothing about the indirect death toll from malignancy (without coronavirus infection) that was untreated or managed less than optimally because of personnel and physical resources that were diverted to COVID-19–associated cases.
Similarly, we cannot begin to estimate indirect consequences of the pandemic to oncology practices, such as accelerated burnout and posttraumatic stress disorder, as well as the long-range effects of economic turmoil on patients, health care workers, and provider organizations.
What happens to cancer trials?
From China, Italy, and Seattle, thus far, there is little information about how the pandemic will affect the vital clinical research endeavor. The Seattle physicians did say they plan to enroll patients on clinical trials only when the trial offers a high chance of benefiting the patient over standard therapy alone.
Fortunately, the National Institutes of Health and Food and Drug Administration have released guidance documents related to clinical trials.
The National Cancer Institute (NCI) has also released guidance documents (March 13 guidance; March 23 guidance) for patients on clinical trials supported by the NCI Cancer Therapy Evaluation Program (CTEP) and the NCI Community Oncology Research Program (NCORP).
CTEP and NCORP are making reasonable accommodations to suspend monitoring visits and audits, allow tele–follow-up visits for patients, and permit local physicians to provide care for patients on study. In addition, with appropriate procedural adherence and documentation, CTEP and NCORP will allow oral investigational medicines to be mailed directly to patients’ homes.
Planned NCI National Clinical Trials Network meetings will be conducted via remote access webinars, conference calls, and similar technology. These adjustments – and probably many more to come – are geared toward facilitating ongoing care to proceed safely and with minimal risk for patients currently receiving investigational therapies and for the sites and investigators engaged in those studies.
Each of us has probably faced a personal “defining professional moment,” when we had to utilize every skill in our arsenal and examine the motivations that led us to a career in oncology. However, it is clear from the forgoing clinical and research processes and guidelines that the COVID-19 pandemic is such a defining professional moment for each of us, in every community we serve.
Critical junctures like this cause more rapid behavior change and innovation than the slow-moving pace that characterizes our idealized preferences. As oncologists who embrace new data and behavioral change, we stand to learn processes that will facilitate more perfected systems of care than the one that preceded this unprecedented crisis, promote more efficient sharing of high-quality information, and improve the outcome for our future patients.
Dr. Lyss was an oncologist and researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Psychiatrists deemed ‘essential’ in time of COVID-19
New American Psychiatric Association poll shows depth of anxiety
The coronavirus pandemic weighs heavily on psychiatric patients with conditions such as anxiety, depression and PTSD. Meanwhile, a national poll released March 25 by the American Psychiatric Association shows that almost half of all Americans are anxious about contracting COVID-19 and 40% are anxious about becoming seriously ill or dying from the virus. In light of stressors on patients and nonpatients alike, mental health professionals have a key role in helping to alleviate suffering tied to the public health crisis, according to psychiatrists from across the country.
“There’s so much we can do to help people put order on this chaos,” said Shaili Jain, MD, section chief of outpatient mental health with the Veterans Affairs Palo Alto (Calif.) Health Care System, in an interview. “We are essential workers in this time.”
Dr. Jain, who specializes in treating PTSD, said those patients are especially vulnerable to the stress and disruptions spawned by the pandemic. “When you go to the grocery store and there’s no food, that can be triggering for people who survived situations with a feeling of calamity or panic,” she said. “People are reporting worsening of nightmares and spontaneous panic attacks after having been stable with symptoms for many months. These are the kinds of stories that are starting to filter through.”
To make things even more difficult, she said, shelter-in-place orders are preventing patients from taking advantage of healthy coping strategies, such as working out at the gym or going to support groups. “We have an invaluable role to play in trying to prevent long-term consequences by going into problem-solving modes with patients.” Dr. Jain offered several tips that might help patients who are suffering:
- Use technology to stay in touch with support communities and boost self-care. “How can you be flexible with FaceTime, Skype, or phone even if you might not be able to have that face-to-face time? What are you doing to double down on your efforts at self-care – listening to music, reading, daily meditation, or walks? Double down on what you can do to prevent anxiety and stress levels from building up.”
- Take breaks from the news, which can contribute to hypervigilance and disrupted sleep. “I’m seeing that people are going down these rabbit holes of having the news or social media on 24/7,” Dr. Jain said. “You have to stay informed. But you need to pick trusted news sources and have chunks of time that are free of coronavirus coverage.” Understand that life is going to be difficult for a while. “We’re doing a lot of reassurance and education,” she said, “helping people to know and accept that the next few days, weeks, and months are going to be stressful.”
Dr. Jain cautioned colleagues, however, that “there will be a tsunami” of mental illness when the coronavirus crisis lifts. She is especially concerned about patient populations that are socioeconomically disadvantaged already and how their lives with be affected by lost wages, unemployment, and business failures. “Medical professionals will see the consequences of this in the days and weeks and months after the pandemic has settled,” she predicted.
The APA poll shows that, early in the crisis, more than 60% of people are anxious about family and loved ones contracting COVID-19.
Maintaining ‘reflective space’ essential
At the Austen Riggs Center, a psychiatric residential treatment facility in Stockbridge, Mass., staff and patients are adjusting to new rules that aim to prevent transmission of the novel coronavirus. “Social distancing requirements are having a huge impact,” said Eric M. Plakun, MD, medical director and CEO of Austen Riggs, in an interview. “You can’t have groups in the same way; you can’t have families come in for a family meeting; you can’t have quite the same the freedom to come and go. A lot of management issues are being addressed, but it is crucial also to maintain the ‘reflective space’ essential to do the kind of clinical work we do.” One approach, he said, is virtual meetings with colleagues that address on-the-job management issues, but also leave a space for how staff members are feeling.
“It’s easy to get into crisis-response mode,” he said, “where you’re always managing but never leave a space to talk about vulnerability, helplessness, and fear.”
As the facility’s staff adjusts by embracing teleconference technology and adapting group meetings to the 6-feet-apart rule,
Dr. Plakun said he said, noting that patients have approached staff members to say they want to collaborate about changes. “That’s a credible offer we intend to accept.”
Still, communicating with patients as a whole about the coronavirus can be difficult. As Dr. Plakun noted, it’s now impossible to bring 75 people together into one room for a meeting. “If you have four to five smaller meetings, how do you maintain some congruence in the information that’s presented?”
Dr. Plakun suggested that colleagues find time to engage in the familiar, such as face-to-face clinical work. “That’s been the most reassuring and rewarding part of my day since it feels almost like normal,” he said.
Stocking up on medications
Jessica “Jessi” Gold, MD, MS, an assistant professor at Washington University in St. Louis, often treats college students. Asian students started to worry early in the pandemic, she said in an interview.
“At the beginning, there were a lot of concerns about the public’s view: ‘Did this come from China? Is it China’s fault?’ A lot of our students felt that if they coughed, and they were a white person, they’d be OK. But if they were Asian, everyone would wonder why they were in class and not at home. That got worse over time: the fear about – and anxiety from – stoking racism.”
Later, as classes began to be canceled, Dr. Gold started to see the psychological effects of disruption and uncertainty about the future. “This can lead people to feel like what they knew before is just not there anymore. This can obviously cause anxiety but also has the potential to cause depression.” Patients also might slip into overuse of alcohol and drugs, or they might engage in other kinds of harmful behavior. Eating disorders, for example, “are ways to have control when other things aren’t in control,” she said.
Dr. Gold pointed to research into the mental health after effects of quarantines, such as those imposed during the SARS outbreak. A review of 24 studies published this year found that most “reported negative psychological effects, including post-traumatic stress symptoms, confusion, and anger. Stressors included longer quarantine duration, infection fears, frustration, boredom, inadequate supplies, inadequate information, financial loss, and stigma. Some researchers have suggested long-lasting effects” (Lancet. 2020;395:912-20).
Dr. Gold is urging patients to recall the warning signs that alerted them to psychological downturns in the past: “Try to remember what those warning signs are and pay attention to whether you see them.” And, Dr. Gold said, she asks patients to think about what has helped them get better.
In some cases, she said, patients are already preparing themselves for experiencing mental distress by stocking up on medications. “Some people have a bottle of 10-20 pills that they only use in emergencies and keep as a kind of security blanket,” she said, and she’s seen some of them ask for refills. It seems they’ve either taken the pills recently or want to stash them just in case. This makes sense, since their anxiety is higher, she said.
Dr. Gold cautioned that psychiatrists need to be careful to not overextend themselves when they’re not treating patients. “It is easy to be therapist to friends, family, and colleagues,” she said, “but we need to take care of ourselves, too.”
Dr. Jain is author of “The Unspeakable Mind: Stories of Trauma and Healing From the Frontlines of PTSD Science” (New York: Harper, 2019). She has no other disclosures. Dr. Plakun and Dr. Gold reported no relevant disclosures.
New American Psychiatric Association poll shows depth of anxiety
New American Psychiatric Association poll shows depth of anxiety
The coronavirus pandemic weighs heavily on psychiatric patients with conditions such as anxiety, depression and PTSD. Meanwhile, a national poll released March 25 by the American Psychiatric Association shows that almost half of all Americans are anxious about contracting COVID-19 and 40% are anxious about becoming seriously ill or dying from the virus. In light of stressors on patients and nonpatients alike, mental health professionals have a key role in helping to alleviate suffering tied to the public health crisis, according to psychiatrists from across the country.
“There’s so much we can do to help people put order on this chaos,” said Shaili Jain, MD, section chief of outpatient mental health with the Veterans Affairs Palo Alto (Calif.) Health Care System, in an interview. “We are essential workers in this time.”
Dr. Jain, who specializes in treating PTSD, said those patients are especially vulnerable to the stress and disruptions spawned by the pandemic. “When you go to the grocery store and there’s no food, that can be triggering for people who survived situations with a feeling of calamity or panic,” she said. “People are reporting worsening of nightmares and spontaneous panic attacks after having been stable with symptoms for many months. These are the kinds of stories that are starting to filter through.”
To make things even more difficult, she said, shelter-in-place orders are preventing patients from taking advantage of healthy coping strategies, such as working out at the gym or going to support groups. “We have an invaluable role to play in trying to prevent long-term consequences by going into problem-solving modes with patients.” Dr. Jain offered several tips that might help patients who are suffering:
- Use technology to stay in touch with support communities and boost self-care. “How can you be flexible with FaceTime, Skype, or phone even if you might not be able to have that face-to-face time? What are you doing to double down on your efforts at self-care – listening to music, reading, daily meditation, or walks? Double down on what you can do to prevent anxiety and stress levels from building up.”
- Take breaks from the news, which can contribute to hypervigilance and disrupted sleep. “I’m seeing that people are going down these rabbit holes of having the news or social media on 24/7,” Dr. Jain said. “You have to stay informed. But you need to pick trusted news sources and have chunks of time that are free of coronavirus coverage.” Understand that life is going to be difficult for a while. “We’re doing a lot of reassurance and education,” she said, “helping people to know and accept that the next few days, weeks, and months are going to be stressful.”
Dr. Jain cautioned colleagues, however, that “there will be a tsunami” of mental illness when the coronavirus crisis lifts. She is especially concerned about patient populations that are socioeconomically disadvantaged already and how their lives with be affected by lost wages, unemployment, and business failures. “Medical professionals will see the consequences of this in the days and weeks and months after the pandemic has settled,” she predicted.
The APA poll shows that, early in the crisis, more than 60% of people are anxious about family and loved ones contracting COVID-19.
Maintaining ‘reflective space’ essential
At the Austen Riggs Center, a psychiatric residential treatment facility in Stockbridge, Mass., staff and patients are adjusting to new rules that aim to prevent transmission of the novel coronavirus. “Social distancing requirements are having a huge impact,” said Eric M. Plakun, MD, medical director and CEO of Austen Riggs, in an interview. “You can’t have groups in the same way; you can’t have families come in for a family meeting; you can’t have quite the same the freedom to come and go. A lot of management issues are being addressed, but it is crucial also to maintain the ‘reflective space’ essential to do the kind of clinical work we do.” One approach, he said, is virtual meetings with colleagues that address on-the-job management issues, but also leave a space for how staff members are feeling.
“It’s easy to get into crisis-response mode,” he said, “where you’re always managing but never leave a space to talk about vulnerability, helplessness, and fear.”
As the facility’s staff adjusts by embracing teleconference technology and adapting group meetings to the 6-feet-apart rule,
Dr. Plakun said he said, noting that patients have approached staff members to say they want to collaborate about changes. “That’s a credible offer we intend to accept.”
Still, communicating with patients as a whole about the coronavirus can be difficult. As Dr. Plakun noted, it’s now impossible to bring 75 people together into one room for a meeting. “If you have four to five smaller meetings, how do you maintain some congruence in the information that’s presented?”
Dr. Plakun suggested that colleagues find time to engage in the familiar, such as face-to-face clinical work. “That’s been the most reassuring and rewarding part of my day since it feels almost like normal,” he said.
Stocking up on medications
Jessica “Jessi” Gold, MD, MS, an assistant professor at Washington University in St. Louis, often treats college students. Asian students started to worry early in the pandemic, she said in an interview.
“At the beginning, there were a lot of concerns about the public’s view: ‘Did this come from China? Is it China’s fault?’ A lot of our students felt that if they coughed, and they were a white person, they’d be OK. But if they were Asian, everyone would wonder why they were in class and not at home. That got worse over time: the fear about – and anxiety from – stoking racism.”
Later, as classes began to be canceled, Dr. Gold started to see the psychological effects of disruption and uncertainty about the future. “This can lead people to feel like what they knew before is just not there anymore. This can obviously cause anxiety but also has the potential to cause depression.” Patients also might slip into overuse of alcohol and drugs, or they might engage in other kinds of harmful behavior. Eating disorders, for example, “are ways to have control when other things aren’t in control,” she said.
Dr. Gold pointed to research into the mental health after effects of quarantines, such as those imposed during the SARS outbreak. A review of 24 studies published this year found that most “reported negative psychological effects, including post-traumatic stress symptoms, confusion, and anger. Stressors included longer quarantine duration, infection fears, frustration, boredom, inadequate supplies, inadequate information, financial loss, and stigma. Some researchers have suggested long-lasting effects” (Lancet. 2020;395:912-20).
Dr. Gold is urging patients to recall the warning signs that alerted them to psychological downturns in the past: “Try to remember what those warning signs are and pay attention to whether you see them.” And, Dr. Gold said, she asks patients to think about what has helped them get better.
In some cases, she said, patients are already preparing themselves for experiencing mental distress by stocking up on medications. “Some people have a bottle of 10-20 pills that they only use in emergencies and keep as a kind of security blanket,” she said, and she’s seen some of them ask for refills. It seems they’ve either taken the pills recently or want to stash them just in case. This makes sense, since their anxiety is higher, she said.
Dr. Gold cautioned that psychiatrists need to be careful to not overextend themselves when they’re not treating patients. “It is easy to be therapist to friends, family, and colleagues,” she said, “but we need to take care of ourselves, too.”
Dr. Jain is author of “The Unspeakable Mind: Stories of Trauma and Healing From the Frontlines of PTSD Science” (New York: Harper, 2019). She has no other disclosures. Dr. Plakun and Dr. Gold reported no relevant disclosures.
The coronavirus pandemic weighs heavily on psychiatric patients with conditions such as anxiety, depression and PTSD. Meanwhile, a national poll released March 25 by the American Psychiatric Association shows that almost half of all Americans are anxious about contracting COVID-19 and 40% are anxious about becoming seriously ill or dying from the virus. In light of stressors on patients and nonpatients alike, mental health professionals have a key role in helping to alleviate suffering tied to the public health crisis, according to psychiatrists from across the country.
“There’s so much we can do to help people put order on this chaos,” said Shaili Jain, MD, section chief of outpatient mental health with the Veterans Affairs Palo Alto (Calif.) Health Care System, in an interview. “We are essential workers in this time.”
Dr. Jain, who specializes in treating PTSD, said those patients are especially vulnerable to the stress and disruptions spawned by the pandemic. “When you go to the grocery store and there’s no food, that can be triggering for people who survived situations with a feeling of calamity or panic,” she said. “People are reporting worsening of nightmares and spontaneous panic attacks after having been stable with symptoms for many months. These are the kinds of stories that are starting to filter through.”
To make things even more difficult, she said, shelter-in-place orders are preventing patients from taking advantage of healthy coping strategies, such as working out at the gym or going to support groups. “We have an invaluable role to play in trying to prevent long-term consequences by going into problem-solving modes with patients.” Dr. Jain offered several tips that might help patients who are suffering:
- Use technology to stay in touch with support communities and boost self-care. “How can you be flexible with FaceTime, Skype, or phone even if you might not be able to have that face-to-face time? What are you doing to double down on your efforts at self-care – listening to music, reading, daily meditation, or walks? Double down on what you can do to prevent anxiety and stress levels from building up.”
- Take breaks from the news, which can contribute to hypervigilance and disrupted sleep. “I’m seeing that people are going down these rabbit holes of having the news or social media on 24/7,” Dr. Jain said. “You have to stay informed. But you need to pick trusted news sources and have chunks of time that are free of coronavirus coverage.” Understand that life is going to be difficult for a while. “We’re doing a lot of reassurance and education,” she said, “helping people to know and accept that the next few days, weeks, and months are going to be stressful.”
Dr. Jain cautioned colleagues, however, that “there will be a tsunami” of mental illness when the coronavirus crisis lifts. She is especially concerned about patient populations that are socioeconomically disadvantaged already and how their lives with be affected by lost wages, unemployment, and business failures. “Medical professionals will see the consequences of this in the days and weeks and months after the pandemic has settled,” she predicted.
The APA poll shows that, early in the crisis, more than 60% of people are anxious about family and loved ones contracting COVID-19.
Maintaining ‘reflective space’ essential
At the Austen Riggs Center, a psychiatric residential treatment facility in Stockbridge, Mass., staff and patients are adjusting to new rules that aim to prevent transmission of the novel coronavirus. “Social distancing requirements are having a huge impact,” said Eric M. Plakun, MD, medical director and CEO of Austen Riggs, in an interview. “You can’t have groups in the same way; you can’t have families come in for a family meeting; you can’t have quite the same the freedom to come and go. A lot of management issues are being addressed, but it is crucial also to maintain the ‘reflective space’ essential to do the kind of clinical work we do.” One approach, he said, is virtual meetings with colleagues that address on-the-job management issues, but also leave a space for how staff members are feeling.
“It’s easy to get into crisis-response mode,” he said, “where you’re always managing but never leave a space to talk about vulnerability, helplessness, and fear.”
As the facility’s staff adjusts by embracing teleconference technology and adapting group meetings to the 6-feet-apart rule,
Dr. Plakun said he said, noting that patients have approached staff members to say they want to collaborate about changes. “That’s a credible offer we intend to accept.”
Still, communicating with patients as a whole about the coronavirus can be difficult. As Dr. Plakun noted, it’s now impossible to bring 75 people together into one room for a meeting. “If you have four to five smaller meetings, how do you maintain some congruence in the information that’s presented?”
Dr. Plakun suggested that colleagues find time to engage in the familiar, such as face-to-face clinical work. “That’s been the most reassuring and rewarding part of my day since it feels almost like normal,” he said.
Stocking up on medications
Jessica “Jessi” Gold, MD, MS, an assistant professor at Washington University in St. Louis, often treats college students. Asian students started to worry early in the pandemic, she said in an interview.
“At the beginning, there were a lot of concerns about the public’s view: ‘Did this come from China? Is it China’s fault?’ A lot of our students felt that if they coughed, and they were a white person, they’d be OK. But if they were Asian, everyone would wonder why they were in class and not at home. That got worse over time: the fear about – and anxiety from – stoking racism.”
Later, as classes began to be canceled, Dr. Gold started to see the psychological effects of disruption and uncertainty about the future. “This can lead people to feel like what they knew before is just not there anymore. This can obviously cause anxiety but also has the potential to cause depression.” Patients also might slip into overuse of alcohol and drugs, or they might engage in other kinds of harmful behavior. Eating disorders, for example, “are ways to have control when other things aren’t in control,” she said.
Dr. Gold pointed to research into the mental health after effects of quarantines, such as those imposed during the SARS outbreak. A review of 24 studies published this year found that most “reported negative psychological effects, including post-traumatic stress symptoms, confusion, and anger. Stressors included longer quarantine duration, infection fears, frustration, boredom, inadequate supplies, inadequate information, financial loss, and stigma. Some researchers have suggested long-lasting effects” (Lancet. 2020;395:912-20).
Dr. Gold is urging patients to recall the warning signs that alerted them to psychological downturns in the past: “Try to remember what those warning signs are and pay attention to whether you see them.” And, Dr. Gold said, she asks patients to think about what has helped them get better.
In some cases, she said, patients are already preparing themselves for experiencing mental distress by stocking up on medications. “Some people have a bottle of 10-20 pills that they only use in emergencies and keep as a kind of security blanket,” she said, and she’s seen some of them ask for refills. It seems they’ve either taken the pills recently or want to stash them just in case. This makes sense, since their anxiety is higher, she said.
Dr. Gold cautioned that psychiatrists need to be careful to not overextend themselves when they’re not treating patients. “It is easy to be therapist to friends, family, and colleagues,” she said, “but we need to take care of ourselves, too.”
Dr. Jain is author of “The Unspeakable Mind: Stories of Trauma and Healing From the Frontlines of PTSD Science” (New York: Harper, 2019). She has no other disclosures. Dr. Plakun and Dr. Gold reported no relevant disclosures.
Is COVID-19 leading to a mental illness pandemic?
People living through this crisis are experiencing trauma
We are in the midst of an epidemic and possibly pandemic of anxiety and distress. The worry that folks have about themselves, families, finances, and work is overwhelming for millions.
I speak with people who report periods of racing thoughts jumping back in time and thinking of roads not taken. They also talk about their thoughts jumping forward with life plans of what they’ll do to change their lives in the future – if they survive COVID-19.
that is well-controlled with care (and even without care). Those people are suffering even more. Meanwhile, people with obsessive-compulsive disorder that had been under control appear to have worsened with the added stress.
Social distancing has disrupted our everyday routines. For many, there is no work, no spending time with people we care about, no going to movies or shows, no doing discretionary shopping, no going to school. Parents with children at home report frustration about balancing working from home with completing home-schooling packets. Physicians on the front lines of this unprecedented time report not having the proper protective equipment and worrying about the possibility of exposing their families to SARS-CoV-2.
We hear stories about the illness and even deaths of some young and middle-aged people with no underlying conditions, not to mention the loss of older adults. People are bursting into tears, and becoming easily frustrated and angry. Add in nightmares, ongoing anxiety states, insomnia, and decreased concentration.
We are seeing news reports of people stocking up on guns and ammunition and a case of one taking – and dying from – nonpharmaceutical grade chloroquine in an effort to prevent COVID-19.
I spoke with Juliana Tseng, PsyD, a clinical psychologist based in New York, and she said that the hype, half-truths, and false information from some outlets in the popular media are making things worse. Dr. Tseng added that the lack of coordination among local, state, and federal governments also is increasing fear and alienation.
As I see this period in time, my first thoughts are that we are witnessing a national epidemic of trauma. Specifically, what we have here is a clinical picture of PTSD.
PTSD is defined clearly as a traumatic disorder with a real or perceived fracture with life. Isolation (which we are creating as a way to “flatten the curve” or slow the spread of COVID-19), although that strategy is in our best personal and public health interests, is both painful and stressful. Frustration, flashbacks of past life experiences plus flashbacks of being ill are reported in people I’ve spoken with. Avoidance, even though it is planned in this instance, is part of the PTSD complex.
What can we as mental health professionals do to help alleviate this suffering?
First, of course, we must listen to the scientific experts and the data – and tell people to do the same. Most experts will say that COVID-19 is a mild or moderate illness for the vast majority of people. We also must encourage people to observe precautions outlined by the Centers for Disease Control and Prevention, such as distancing from people, hand washing, and avoiding those who are ill. Explain to people that, currently, there is no vaccine to prevent COVID-19. Treatment is mainly supportive, and some medication trials are being explored. However, we can empower people by helping them to develop skills aimed at increasing the ability to relax and focus on more positive aspects of life to break the chain of the stress and tension of anxiety as well as control the PTSD.
For more than 40 years, I have helped people master relaxation techniques and guided imagery. When taught properly, people are able to use these techniques on their own.
To begin, I teach people how to relax, using a simple three-point method:
- Get comfortable in a nice chair, and slowly count from one to three. At the count of one, do one thing: “roll your eyes up to the top of your head.”
- At the count of two, do two things, “close your lids on your eyes and take a deep breath.”
- At three, exhale slowly, relax your eyes, and concentrate on a restful feeling of floating.
- Do this for about 30 seconds to a minute.
- Count backward, from three to two to one and open your eyes.
The person will notice how nice and restful they will feel.
After that exercise, get the person to move to the graduate level and go beyond just relaxation. In the following exercise, people can go into a relaxed state by imagining a movie screen. Tell the person to do two things:
1. Look at the imagined movie screen and project on it any pleasant scene you wish; this is your screen. You will feel yourself becoming more and more relaxed. The person can do this one, two, three or whatever times a day. The exercise can last 1 minute or 5.
2. Incorporate the 1, 2, 3 relaxation described earlier, allowing yourself to float into this restful state and go to your movie screen. Now, on the screen, imagine a thick line down the center, and on the left side, project your worries and anxieties and fears. The idea is to see but not experience them. Then shift to the ride side of the screen, and again, visualize any pleasant scene you wish. Again, do this for 1 minute or 5 minutes, whatever works.
You will notice that the pleasant scene on the right will overcome the anxiety scene on the left, in that pleasantness, in most instances, overcomes anxiety. For many, these techniques have proved very useful – whether the problem is anxiety or fear – or both. In my experience, these techniques are a good beginning for controlling PTSD and successfully treating it.
We are in the midst of what could be the biggest public health crisis that America has faced since the 1918 pandemic, also known as the Spanish flu. The lockdowns, quarantines, and the myriad of other disruptions can lead to alienation. In fact, it would be strange for us not to experience strong emotions under these extreme conditions. Life will get better! In the meantime, let’s encourage people to hope, pray, and use relaxation techniques and guided imagery approaches to help control anxiety, worry, stress, and issues related to PTSD. These approaches can give our minds and bodies periods of relaxation and recovery, and ultimately, they can calm our minds.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
People living through this crisis are experiencing trauma
People living through this crisis are experiencing trauma
We are in the midst of an epidemic and possibly pandemic of anxiety and distress. The worry that folks have about themselves, families, finances, and work is overwhelming for millions.
I speak with people who report periods of racing thoughts jumping back in time and thinking of roads not taken. They also talk about their thoughts jumping forward with life plans of what they’ll do to change their lives in the future – if they survive COVID-19.
that is well-controlled with care (and even without care). Those people are suffering even more. Meanwhile, people with obsessive-compulsive disorder that had been under control appear to have worsened with the added stress.
Social distancing has disrupted our everyday routines. For many, there is no work, no spending time with people we care about, no going to movies or shows, no doing discretionary shopping, no going to school. Parents with children at home report frustration about balancing working from home with completing home-schooling packets. Physicians on the front lines of this unprecedented time report not having the proper protective equipment and worrying about the possibility of exposing their families to SARS-CoV-2.
We hear stories about the illness and even deaths of some young and middle-aged people with no underlying conditions, not to mention the loss of older adults. People are bursting into tears, and becoming easily frustrated and angry. Add in nightmares, ongoing anxiety states, insomnia, and decreased concentration.
We are seeing news reports of people stocking up on guns and ammunition and a case of one taking – and dying from – nonpharmaceutical grade chloroquine in an effort to prevent COVID-19.
I spoke with Juliana Tseng, PsyD, a clinical psychologist based in New York, and she said that the hype, half-truths, and false information from some outlets in the popular media are making things worse. Dr. Tseng added that the lack of coordination among local, state, and federal governments also is increasing fear and alienation.
As I see this period in time, my first thoughts are that we are witnessing a national epidemic of trauma. Specifically, what we have here is a clinical picture of PTSD.
PTSD is defined clearly as a traumatic disorder with a real or perceived fracture with life. Isolation (which we are creating as a way to “flatten the curve” or slow the spread of COVID-19), although that strategy is in our best personal and public health interests, is both painful and stressful. Frustration, flashbacks of past life experiences plus flashbacks of being ill are reported in people I’ve spoken with. Avoidance, even though it is planned in this instance, is part of the PTSD complex.
What can we as mental health professionals do to help alleviate this suffering?
First, of course, we must listen to the scientific experts and the data – and tell people to do the same. Most experts will say that COVID-19 is a mild or moderate illness for the vast majority of people. We also must encourage people to observe precautions outlined by the Centers for Disease Control and Prevention, such as distancing from people, hand washing, and avoiding those who are ill. Explain to people that, currently, there is no vaccine to prevent COVID-19. Treatment is mainly supportive, and some medication trials are being explored. However, we can empower people by helping them to develop skills aimed at increasing the ability to relax and focus on more positive aspects of life to break the chain of the stress and tension of anxiety as well as control the PTSD.
For more than 40 years, I have helped people master relaxation techniques and guided imagery. When taught properly, people are able to use these techniques on their own.
To begin, I teach people how to relax, using a simple three-point method:
- Get comfortable in a nice chair, and slowly count from one to three. At the count of one, do one thing: “roll your eyes up to the top of your head.”
- At the count of two, do two things, “close your lids on your eyes and take a deep breath.”
- At three, exhale slowly, relax your eyes, and concentrate on a restful feeling of floating.
- Do this for about 30 seconds to a minute.
- Count backward, from three to two to one and open your eyes.
The person will notice how nice and restful they will feel.
After that exercise, get the person to move to the graduate level and go beyond just relaxation. In the following exercise, people can go into a relaxed state by imagining a movie screen. Tell the person to do two things:
1. Look at the imagined movie screen and project on it any pleasant scene you wish; this is your screen. You will feel yourself becoming more and more relaxed. The person can do this one, two, three or whatever times a day. The exercise can last 1 minute or 5.
2. Incorporate the 1, 2, 3 relaxation described earlier, allowing yourself to float into this restful state and go to your movie screen. Now, on the screen, imagine a thick line down the center, and on the left side, project your worries and anxieties and fears. The idea is to see but not experience them. Then shift to the ride side of the screen, and again, visualize any pleasant scene you wish. Again, do this for 1 minute or 5 minutes, whatever works.
You will notice that the pleasant scene on the right will overcome the anxiety scene on the left, in that pleasantness, in most instances, overcomes anxiety. For many, these techniques have proved very useful – whether the problem is anxiety or fear – or both. In my experience, these techniques are a good beginning for controlling PTSD and successfully treating it.
We are in the midst of what could be the biggest public health crisis that America has faced since the 1918 pandemic, also known as the Spanish flu. The lockdowns, quarantines, and the myriad of other disruptions can lead to alienation. In fact, it would be strange for us not to experience strong emotions under these extreme conditions. Life will get better! In the meantime, let’s encourage people to hope, pray, and use relaxation techniques and guided imagery approaches to help control anxiety, worry, stress, and issues related to PTSD. These approaches can give our minds and bodies periods of relaxation and recovery, and ultimately, they can calm our minds.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
We are in the midst of an epidemic and possibly pandemic of anxiety and distress. The worry that folks have about themselves, families, finances, and work is overwhelming for millions.
I speak with people who report periods of racing thoughts jumping back in time and thinking of roads not taken. They also talk about their thoughts jumping forward with life plans of what they’ll do to change their lives in the future – if they survive COVID-19.
that is well-controlled with care (and even without care). Those people are suffering even more. Meanwhile, people with obsessive-compulsive disorder that had been under control appear to have worsened with the added stress.
Social distancing has disrupted our everyday routines. For many, there is no work, no spending time with people we care about, no going to movies or shows, no doing discretionary shopping, no going to school. Parents with children at home report frustration about balancing working from home with completing home-schooling packets. Physicians on the front lines of this unprecedented time report not having the proper protective equipment and worrying about the possibility of exposing their families to SARS-CoV-2.
We hear stories about the illness and even deaths of some young and middle-aged people with no underlying conditions, not to mention the loss of older adults. People are bursting into tears, and becoming easily frustrated and angry. Add in nightmares, ongoing anxiety states, insomnia, and decreased concentration.
We are seeing news reports of people stocking up on guns and ammunition and a case of one taking – and dying from – nonpharmaceutical grade chloroquine in an effort to prevent COVID-19.
I spoke with Juliana Tseng, PsyD, a clinical psychologist based in New York, and she said that the hype, half-truths, and false information from some outlets in the popular media are making things worse. Dr. Tseng added that the lack of coordination among local, state, and federal governments also is increasing fear and alienation.
As I see this period in time, my first thoughts are that we are witnessing a national epidemic of trauma. Specifically, what we have here is a clinical picture of PTSD.
PTSD is defined clearly as a traumatic disorder with a real or perceived fracture with life. Isolation (which we are creating as a way to “flatten the curve” or slow the spread of COVID-19), although that strategy is in our best personal and public health interests, is both painful and stressful. Frustration, flashbacks of past life experiences plus flashbacks of being ill are reported in people I’ve spoken with. Avoidance, even though it is planned in this instance, is part of the PTSD complex.
What can we as mental health professionals do to help alleviate this suffering?
First, of course, we must listen to the scientific experts and the data – and tell people to do the same. Most experts will say that COVID-19 is a mild or moderate illness for the vast majority of people. We also must encourage people to observe precautions outlined by the Centers for Disease Control and Prevention, such as distancing from people, hand washing, and avoiding those who are ill. Explain to people that, currently, there is no vaccine to prevent COVID-19. Treatment is mainly supportive, and some medication trials are being explored. However, we can empower people by helping them to develop skills aimed at increasing the ability to relax and focus on more positive aspects of life to break the chain of the stress and tension of anxiety as well as control the PTSD.
For more than 40 years, I have helped people master relaxation techniques and guided imagery. When taught properly, people are able to use these techniques on their own.
To begin, I teach people how to relax, using a simple three-point method:
- Get comfortable in a nice chair, and slowly count from one to three. At the count of one, do one thing: “roll your eyes up to the top of your head.”
- At the count of two, do two things, “close your lids on your eyes and take a deep breath.”
- At three, exhale slowly, relax your eyes, and concentrate on a restful feeling of floating.
- Do this for about 30 seconds to a minute.
- Count backward, from three to two to one and open your eyes.
The person will notice how nice and restful they will feel.
After that exercise, get the person to move to the graduate level and go beyond just relaxation. In the following exercise, people can go into a relaxed state by imagining a movie screen. Tell the person to do two things:
1. Look at the imagined movie screen and project on it any pleasant scene you wish; this is your screen. You will feel yourself becoming more and more relaxed. The person can do this one, two, three or whatever times a day. The exercise can last 1 minute or 5.
2. Incorporate the 1, 2, 3 relaxation described earlier, allowing yourself to float into this restful state and go to your movie screen. Now, on the screen, imagine a thick line down the center, and on the left side, project your worries and anxieties and fears. The idea is to see but not experience them. Then shift to the ride side of the screen, and again, visualize any pleasant scene you wish. Again, do this for 1 minute or 5 minutes, whatever works.
You will notice that the pleasant scene on the right will overcome the anxiety scene on the left, in that pleasantness, in most instances, overcomes anxiety. For many, these techniques have proved very useful – whether the problem is anxiety or fear – or both. In my experience, these techniques are a good beginning for controlling PTSD and successfully treating it.
We are in the midst of what could be the biggest public health crisis that America has faced since the 1918 pandemic, also known as the Spanish flu. The lockdowns, quarantines, and the myriad of other disruptions can lead to alienation. In fact, it would be strange for us not to experience strong emotions under these extreme conditions. Life will get better! In the meantime, let’s encourage people to hope, pray, and use relaxation techniques and guided imagery approaches to help control anxiety, worry, stress, and issues related to PTSD. These approaches can give our minds and bodies periods of relaxation and recovery, and ultimately, they can calm our minds.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.