User login
Modified Atkins diet beneficial in drug-resistant epilepsy
, new research shows.
In a randomized prospective study, the number of seizures per month dropped by more than half in one-quarter of patients following the high-fat, low-carb diet; and 5% of the group were free from all seizure activity after 6 months.
Both adults and adolescents reported benefits from the diet, which is a less strict version of a traditional ketogenic diet that many patients find difficult to follow. The modified Atkins diet includes foods such as leafy green vegetables and eggs, chicken, fish, bacon, and other animal proteins.
“The use of an exchange list and recipe booklet with local recipes and spices helped in the initiation of modified Atkins diet with the flexibility of meal choices and ease of administration,” said coinvestigator Manjari Tripathi, MD, DM, department of neurology, All India Institute of Medical Science, New Delhi.
“As items were everyday household ingredients in proportion to the requirement of the modified Atkins diet, this diet is possible in low-income countries also,” Dr. Tripathi added.
The findings were published online in the journal Neurology.
Low carbs, high benefit
The modified Atkins diet includes around 65% fat, 25% protein, and 10% carbohydrates. Unlike a traditional ketogenic diet, the modified Atkins diet includes no restrictions on protein, calories, or fluids.
Researchers have long known that ketogenic and Atkins diets are associated with reduced seizure activity in adolescents with epilepsy. But previous studies were small, and many were retrospective analyses.
The current investigators enrolled 160 patients (80 adults, 80 adolescents) aged 10-55 years whose epilepsy was not controlled despite using at least three antiseizure medications at maximum tolerated doses.
The intervention group received training in the modified Atkins diet and were given a food exchange list, sample menu, and recipe booklet. Carbohydrate intake was restricted to 20 grams per day.
Participants took supplemental multivitamins and minerals, kept a food diary, logged seizure activity, and measured urine ketone levels three times a day. They also received weekly check-up phone calls to ensure diet adherence.
The control group received a normal diet with no carbohydrate restrictions. All participants continued their prescribed antiseizure therapy throughout the trial.
Primary outcome met
The primary study outcome was a reduction in seizures of more than 50%. At 6 months, 26.2% of the intervention group had reached that goal, compared with just 2.5% of the control group (P < .001).
When the median number of seizures in the modified Atkins diet group was analyzed, the frequency dropped in the intervention group from 37.5 per month at baseline to 27.5 per month after 3 months of the modified Atkins diet and to 21.5 per month after 6 months.
Adding the modified Atkins diet had a larger effect on seizure activity in adults than in adolescents. At the end of 6 months, 36% of adolescents on the modified Atkins diet had more than a 50% reduction in seizures, while 57.1% of adults on the diet reached that level.
Quality-of-life scores were also higher in the intervention group.
By the end of the trial, 5% of patients on the modified Atkins diet had no seizure activity at all versus none of the control group. In fact, the median number of seizures increased in the control group during the study.
The mean morning and evening levels of urine ketosis in the intervention group were 58.3 ± 8.0 mg/dL and 62.2 ± 22.6 mg/dL, respectively, suggesting satisfactory diet adherence. There was no significant difference between groups in weight loss.
Dr. Tripathi noted that 33% of participants did not complete the study because of poor tolerance of the diet, lack of benefit, or the inability to follow up – in part due to COVID-19. However, she said tolerance of the modified Atkins diet was better than what has been reported with the ketogenic diet.
“Though the exact mechanism by which such a diet protects against seizures is unknown, there is evidence that it causes effects on intermediary metabolism that influences the dynamics of the major inhibitory and excitatory neurotransmitter systems in the brain,” Dr. Tripathi said.
Benefits outweigh cost
Commenting on the research findings, Mackenzie Cervenka, MD, professor of neurology and director of the Adult Epilepsy Diet Center at Johns Hopkins University, Baltimore, noted that the study is the first randomized controlled trial of this size to demonstrate a benefit from adding the modified Atkins diet to standard antiseizure therapy in treatment-resistant epilepsy.
“Importantly, the study also showed improvement in quality of life and behavior over standard-of-care therapies without significant adverse effects,” said Dr. Cervenka, who was not part of the research.
The investigators noted that the flexibility of the modified Atkins diet allows more variation in menu options and a greater intake of protein, making it easier to follow than a traditional ketogenic diet.
One area of debate, however, is whether these diets are manageable for individuals with low income. Poultry, meat, and fish, all of which are staples of a modified Atkins diet, can be more expensive than other high-carb options such as pasta and rice.
“While some of the foods such as protein sources that patients purchase when they are on a ketogenic diet therapy can be more expensive, if you take into account the cost of antiseizure medications and other antiseizure treatments, hospital visits, and missed work related to seizures, et cetera, the overall financial benefits of seizure reduction with incorporating a ketogenic diet therapy may outweigh these costs,” Dr. Cervenka said.
“There are also low-cost foods that can be used since there is a great deal of flexibility with a modified Atkins diet,” she added.
The study was funded by the Centre of Excellence for Epilepsy, which is funded by the Department of Biotechnology, Government of India. Dr. Tripathi and Dr. Cervenka report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research shows.
In a randomized prospective study, the number of seizures per month dropped by more than half in one-quarter of patients following the high-fat, low-carb diet; and 5% of the group were free from all seizure activity after 6 months.
Both adults and adolescents reported benefits from the diet, which is a less strict version of a traditional ketogenic diet that many patients find difficult to follow. The modified Atkins diet includes foods such as leafy green vegetables and eggs, chicken, fish, bacon, and other animal proteins.
“The use of an exchange list and recipe booklet with local recipes and spices helped in the initiation of modified Atkins diet with the flexibility of meal choices and ease of administration,” said coinvestigator Manjari Tripathi, MD, DM, department of neurology, All India Institute of Medical Science, New Delhi.
“As items were everyday household ingredients in proportion to the requirement of the modified Atkins diet, this diet is possible in low-income countries also,” Dr. Tripathi added.
The findings were published online in the journal Neurology.
Low carbs, high benefit
The modified Atkins diet includes around 65% fat, 25% protein, and 10% carbohydrates. Unlike a traditional ketogenic diet, the modified Atkins diet includes no restrictions on protein, calories, or fluids.
Researchers have long known that ketogenic and Atkins diets are associated with reduced seizure activity in adolescents with epilepsy. But previous studies were small, and many were retrospective analyses.
The current investigators enrolled 160 patients (80 adults, 80 adolescents) aged 10-55 years whose epilepsy was not controlled despite using at least three antiseizure medications at maximum tolerated doses.
The intervention group received training in the modified Atkins diet and were given a food exchange list, sample menu, and recipe booklet. Carbohydrate intake was restricted to 20 grams per day.
Participants took supplemental multivitamins and minerals, kept a food diary, logged seizure activity, and measured urine ketone levels three times a day. They also received weekly check-up phone calls to ensure diet adherence.
The control group received a normal diet with no carbohydrate restrictions. All participants continued their prescribed antiseizure therapy throughout the trial.
Primary outcome met
The primary study outcome was a reduction in seizures of more than 50%. At 6 months, 26.2% of the intervention group had reached that goal, compared with just 2.5% of the control group (P < .001).
When the median number of seizures in the modified Atkins diet group was analyzed, the frequency dropped in the intervention group from 37.5 per month at baseline to 27.5 per month after 3 months of the modified Atkins diet and to 21.5 per month after 6 months.
Adding the modified Atkins diet had a larger effect on seizure activity in adults than in adolescents. At the end of 6 months, 36% of adolescents on the modified Atkins diet had more than a 50% reduction in seizures, while 57.1% of adults on the diet reached that level.
Quality-of-life scores were also higher in the intervention group.
By the end of the trial, 5% of patients on the modified Atkins diet had no seizure activity at all versus none of the control group. In fact, the median number of seizures increased in the control group during the study.
The mean morning and evening levels of urine ketosis in the intervention group were 58.3 ± 8.0 mg/dL and 62.2 ± 22.6 mg/dL, respectively, suggesting satisfactory diet adherence. There was no significant difference between groups in weight loss.
Dr. Tripathi noted that 33% of participants did not complete the study because of poor tolerance of the diet, lack of benefit, or the inability to follow up – in part due to COVID-19. However, she said tolerance of the modified Atkins diet was better than what has been reported with the ketogenic diet.
“Though the exact mechanism by which such a diet protects against seizures is unknown, there is evidence that it causes effects on intermediary metabolism that influences the dynamics of the major inhibitory and excitatory neurotransmitter systems in the brain,” Dr. Tripathi said.
Benefits outweigh cost
Commenting on the research findings, Mackenzie Cervenka, MD, professor of neurology and director of the Adult Epilepsy Diet Center at Johns Hopkins University, Baltimore, noted that the study is the first randomized controlled trial of this size to demonstrate a benefit from adding the modified Atkins diet to standard antiseizure therapy in treatment-resistant epilepsy.
“Importantly, the study also showed improvement in quality of life and behavior over standard-of-care therapies without significant adverse effects,” said Dr. Cervenka, who was not part of the research.
The investigators noted that the flexibility of the modified Atkins diet allows more variation in menu options and a greater intake of protein, making it easier to follow than a traditional ketogenic diet.
One area of debate, however, is whether these diets are manageable for individuals with low income. Poultry, meat, and fish, all of which are staples of a modified Atkins diet, can be more expensive than other high-carb options such as pasta and rice.
“While some of the foods such as protein sources that patients purchase when they are on a ketogenic diet therapy can be more expensive, if you take into account the cost of antiseizure medications and other antiseizure treatments, hospital visits, and missed work related to seizures, et cetera, the overall financial benefits of seizure reduction with incorporating a ketogenic diet therapy may outweigh these costs,” Dr. Cervenka said.
“There are also low-cost foods that can be used since there is a great deal of flexibility with a modified Atkins diet,” she added.
The study was funded by the Centre of Excellence for Epilepsy, which is funded by the Department of Biotechnology, Government of India. Dr. Tripathi and Dr. Cervenka report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research shows.
In a randomized prospective study, the number of seizures per month dropped by more than half in one-quarter of patients following the high-fat, low-carb diet; and 5% of the group were free from all seizure activity after 6 months.
Both adults and adolescents reported benefits from the diet, which is a less strict version of a traditional ketogenic diet that many patients find difficult to follow. The modified Atkins diet includes foods such as leafy green vegetables and eggs, chicken, fish, bacon, and other animal proteins.
“The use of an exchange list and recipe booklet with local recipes and spices helped in the initiation of modified Atkins diet with the flexibility of meal choices and ease of administration,” said coinvestigator Manjari Tripathi, MD, DM, department of neurology, All India Institute of Medical Science, New Delhi.
“As items were everyday household ingredients in proportion to the requirement of the modified Atkins diet, this diet is possible in low-income countries also,” Dr. Tripathi added.
The findings were published online in the journal Neurology.
Low carbs, high benefit
The modified Atkins diet includes around 65% fat, 25% protein, and 10% carbohydrates. Unlike a traditional ketogenic diet, the modified Atkins diet includes no restrictions on protein, calories, or fluids.
Researchers have long known that ketogenic and Atkins diets are associated with reduced seizure activity in adolescents with epilepsy. But previous studies were small, and many were retrospective analyses.
The current investigators enrolled 160 patients (80 adults, 80 adolescents) aged 10-55 years whose epilepsy was not controlled despite using at least three antiseizure medications at maximum tolerated doses.
The intervention group received training in the modified Atkins diet and were given a food exchange list, sample menu, and recipe booklet. Carbohydrate intake was restricted to 20 grams per day.
Participants took supplemental multivitamins and minerals, kept a food diary, logged seizure activity, and measured urine ketone levels three times a day. They also received weekly check-up phone calls to ensure diet adherence.
The control group received a normal diet with no carbohydrate restrictions. All participants continued their prescribed antiseizure therapy throughout the trial.
Primary outcome met
The primary study outcome was a reduction in seizures of more than 50%. At 6 months, 26.2% of the intervention group had reached that goal, compared with just 2.5% of the control group (P < .001).
When the median number of seizures in the modified Atkins diet group was analyzed, the frequency dropped in the intervention group from 37.5 per month at baseline to 27.5 per month after 3 months of the modified Atkins diet and to 21.5 per month after 6 months.
Adding the modified Atkins diet had a larger effect on seizure activity in adults than in adolescents. At the end of 6 months, 36% of adolescents on the modified Atkins diet had more than a 50% reduction in seizures, while 57.1% of adults on the diet reached that level.
Quality-of-life scores were also higher in the intervention group.
By the end of the trial, 5% of patients on the modified Atkins diet had no seizure activity at all versus none of the control group. In fact, the median number of seizures increased in the control group during the study.
The mean morning and evening levels of urine ketosis in the intervention group were 58.3 ± 8.0 mg/dL and 62.2 ± 22.6 mg/dL, respectively, suggesting satisfactory diet adherence. There was no significant difference between groups in weight loss.
Dr. Tripathi noted that 33% of participants did not complete the study because of poor tolerance of the diet, lack of benefit, or the inability to follow up – in part due to COVID-19. However, she said tolerance of the modified Atkins diet was better than what has been reported with the ketogenic diet.
“Though the exact mechanism by which such a diet protects against seizures is unknown, there is evidence that it causes effects on intermediary metabolism that influences the dynamics of the major inhibitory and excitatory neurotransmitter systems in the brain,” Dr. Tripathi said.
Benefits outweigh cost
Commenting on the research findings, Mackenzie Cervenka, MD, professor of neurology and director of the Adult Epilepsy Diet Center at Johns Hopkins University, Baltimore, noted that the study is the first randomized controlled trial of this size to demonstrate a benefit from adding the modified Atkins diet to standard antiseizure therapy in treatment-resistant epilepsy.
“Importantly, the study also showed improvement in quality of life and behavior over standard-of-care therapies without significant adverse effects,” said Dr. Cervenka, who was not part of the research.
The investigators noted that the flexibility of the modified Atkins diet allows more variation in menu options and a greater intake of protein, making it easier to follow than a traditional ketogenic diet.
One area of debate, however, is whether these diets are manageable for individuals with low income. Poultry, meat, and fish, all of which are staples of a modified Atkins diet, can be more expensive than other high-carb options such as pasta and rice.
“While some of the foods such as protein sources that patients purchase when they are on a ketogenic diet therapy can be more expensive, if you take into account the cost of antiseizure medications and other antiseizure treatments, hospital visits, and missed work related to seizures, et cetera, the overall financial benefits of seizure reduction with incorporating a ketogenic diet therapy may outweigh these costs,” Dr. Cervenka said.
“There are also low-cost foods that can be used since there is a great deal of flexibility with a modified Atkins diet,” she added.
The study was funded by the Centre of Excellence for Epilepsy, which is funded by the Department of Biotechnology, Government of India. Dr. Tripathi and Dr. Cervenka report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
‘Low-value’ prostate cancer screening prevalent in primary care
Yet a new study shows that testing for prostate-specific antigen (PSA) and also digital rectal examinations (DRE) are both carried out frequently in older men, even when there is no indication for such testing.
“As a man ages, the risk for a false-positive result increases,” said lead author Chris Gillette, PhD, associate professor of physician assistant studies at Wake Forest University, Winston-Salem, N.C., in a statement
The study authors looked at primary care visits for men who were age 70 or older, and found that, per 100 visits, there were 6.7 PSA tests and 1.6 DRE performed.
Dr. Gillette and colleagues emphasized the importance of their findings. Whereas prior studies have relied on commercially insured men or patient-reported rates of PSA testing, they used a nationally representative clinical dataset that is much more inclusive, as it includes men who are also uninsured or insured through traditional Medicare.
The study was published online in the Journal of the American Board of Family Medicine.
Screening for prostate cancer has been much debated, and the guidelines have changed in recent years. In the period 2012-2018, the U.S. Preventive Services Task Force recommended against PSA-based screening in all men, but then the guidelines changed, and the USPSTF subsequently endorsed individualized screening in those aged 55-69 years after a shared decision-making discussion. That same 2018 update also recommends against PSA screening in men over the age of 70.
In addition, the American Urological Association has recommended against PSA-based prostate cancer screening for men over the age of 70 since 2013.
Previous studies have shown that clinicians are not adhering to the guidelines. An analysis conducted in March 2022 found that about one in four accredited U.S. cancer centers fails to follow national guidelines for PSA testing to screen for prostate cancer. Contrary to national guidelines, which advocate shared decision-making, 22% of centers recommend all men universally initiate PSA screening at either age 50 or 55 and another 4% of centers recommend this before age 50, earlier than the guidelines advise.
In the current study, Dr. Gillette and colleagues conducted a secondary analysis of the National Ambulatory Medical Care Survey datasets from 2013 to 2016 and 2018. The dataset is a nationally representative sample of visits to nonfederal, office-based physician clinics. This analysis was restricted to male patients aged 70 years and older who visited a primary care clinic.
The team found that health care professionals who order a lot of tests are more likely to order low-value screening such as PSA and DRE.
The data also showed that when there were a higher number of services ordered/provided, the patients were significantly more likely to receive a low-value PSA (odds ratio, 1.49) and a low-value DRE (OR, 1.37). In contrast, patients who had more previous visits to the clinician were less likely to receive a low-value DRE (OR, 0.92).
Overall, there a decline in low-value PSA screening after 2014, but this trend was not seen for DRE during primary care visits.
Speculating as to why these low-value tests are being carried out, Dr. Gillette suggested that health care professionals might be responding to patient requests when ordering these screening tests, or they may be using what’s known as a “shotgun” approach to medical testing where all possible tests are ordered during a medical visit.
“However, as health care systems move toward a more value-based care system – where the benefit of services provided outweighs any risks – clinicians need to engage patients in these discussions on the complexity of this testing,” he commented. “Ultimately, when and if to screen is a decision best left between a provider and the patient.”
There was no outside funding and the authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Yet a new study shows that testing for prostate-specific antigen (PSA) and also digital rectal examinations (DRE) are both carried out frequently in older men, even when there is no indication for such testing.
“As a man ages, the risk for a false-positive result increases,” said lead author Chris Gillette, PhD, associate professor of physician assistant studies at Wake Forest University, Winston-Salem, N.C., in a statement
The study authors looked at primary care visits for men who were age 70 or older, and found that, per 100 visits, there were 6.7 PSA tests and 1.6 DRE performed.
Dr. Gillette and colleagues emphasized the importance of their findings. Whereas prior studies have relied on commercially insured men or patient-reported rates of PSA testing, they used a nationally representative clinical dataset that is much more inclusive, as it includes men who are also uninsured or insured through traditional Medicare.
The study was published online in the Journal of the American Board of Family Medicine.
Screening for prostate cancer has been much debated, and the guidelines have changed in recent years. In the period 2012-2018, the U.S. Preventive Services Task Force recommended against PSA-based screening in all men, but then the guidelines changed, and the USPSTF subsequently endorsed individualized screening in those aged 55-69 years after a shared decision-making discussion. That same 2018 update also recommends against PSA screening in men over the age of 70.
In addition, the American Urological Association has recommended against PSA-based prostate cancer screening for men over the age of 70 since 2013.
Previous studies have shown that clinicians are not adhering to the guidelines. An analysis conducted in March 2022 found that about one in four accredited U.S. cancer centers fails to follow national guidelines for PSA testing to screen for prostate cancer. Contrary to national guidelines, which advocate shared decision-making, 22% of centers recommend all men universally initiate PSA screening at either age 50 or 55 and another 4% of centers recommend this before age 50, earlier than the guidelines advise.
In the current study, Dr. Gillette and colleagues conducted a secondary analysis of the National Ambulatory Medical Care Survey datasets from 2013 to 2016 and 2018. The dataset is a nationally representative sample of visits to nonfederal, office-based physician clinics. This analysis was restricted to male patients aged 70 years and older who visited a primary care clinic.
The team found that health care professionals who order a lot of tests are more likely to order low-value screening such as PSA and DRE.
The data also showed that when there were a higher number of services ordered/provided, the patients were significantly more likely to receive a low-value PSA (odds ratio, 1.49) and a low-value DRE (OR, 1.37). In contrast, patients who had more previous visits to the clinician were less likely to receive a low-value DRE (OR, 0.92).
Overall, there a decline in low-value PSA screening after 2014, but this trend was not seen for DRE during primary care visits.
Speculating as to why these low-value tests are being carried out, Dr. Gillette suggested that health care professionals might be responding to patient requests when ordering these screening tests, or they may be using what’s known as a “shotgun” approach to medical testing where all possible tests are ordered during a medical visit.
“However, as health care systems move toward a more value-based care system – where the benefit of services provided outweighs any risks – clinicians need to engage patients in these discussions on the complexity of this testing,” he commented. “Ultimately, when and if to screen is a decision best left between a provider and the patient.”
There was no outside funding and the authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Yet a new study shows that testing for prostate-specific antigen (PSA) and also digital rectal examinations (DRE) are both carried out frequently in older men, even when there is no indication for such testing.
“As a man ages, the risk for a false-positive result increases,” said lead author Chris Gillette, PhD, associate professor of physician assistant studies at Wake Forest University, Winston-Salem, N.C., in a statement
The study authors looked at primary care visits for men who were age 70 or older, and found that, per 100 visits, there were 6.7 PSA tests and 1.6 DRE performed.
Dr. Gillette and colleagues emphasized the importance of their findings. Whereas prior studies have relied on commercially insured men or patient-reported rates of PSA testing, they used a nationally representative clinical dataset that is much more inclusive, as it includes men who are also uninsured or insured through traditional Medicare.
The study was published online in the Journal of the American Board of Family Medicine.
Screening for prostate cancer has been much debated, and the guidelines have changed in recent years. In the period 2012-2018, the U.S. Preventive Services Task Force recommended against PSA-based screening in all men, but then the guidelines changed, and the USPSTF subsequently endorsed individualized screening in those aged 55-69 years after a shared decision-making discussion. That same 2018 update also recommends against PSA screening in men over the age of 70.
In addition, the American Urological Association has recommended against PSA-based prostate cancer screening for men over the age of 70 since 2013.
Previous studies have shown that clinicians are not adhering to the guidelines. An analysis conducted in March 2022 found that about one in four accredited U.S. cancer centers fails to follow national guidelines for PSA testing to screen for prostate cancer. Contrary to national guidelines, which advocate shared decision-making, 22% of centers recommend all men universally initiate PSA screening at either age 50 or 55 and another 4% of centers recommend this before age 50, earlier than the guidelines advise.
In the current study, Dr. Gillette and colleagues conducted a secondary analysis of the National Ambulatory Medical Care Survey datasets from 2013 to 2016 and 2018. The dataset is a nationally representative sample of visits to nonfederal, office-based physician clinics. This analysis was restricted to male patients aged 70 years and older who visited a primary care clinic.
The team found that health care professionals who order a lot of tests are more likely to order low-value screening such as PSA and DRE.
The data also showed that when there were a higher number of services ordered/provided, the patients were significantly more likely to receive a low-value PSA (odds ratio, 1.49) and a low-value DRE (OR, 1.37). In contrast, patients who had more previous visits to the clinician were less likely to receive a low-value DRE (OR, 0.92).
Overall, there a decline in low-value PSA screening after 2014, but this trend was not seen for DRE during primary care visits.
Speculating as to why these low-value tests are being carried out, Dr. Gillette suggested that health care professionals might be responding to patient requests when ordering these screening tests, or they may be using what’s known as a “shotgun” approach to medical testing where all possible tests are ordered during a medical visit.
“However, as health care systems move toward a more value-based care system – where the benefit of services provided outweighs any risks – clinicians need to engage patients in these discussions on the complexity of this testing,” he commented. “Ultimately, when and if to screen is a decision best left between a provider and the patient.”
There was no outside funding and the authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN BOARD OF FAMILY MEDICINE
FDA approves second antiamyloid for Alzheimer’s disease
Like its controversial cousin aducanumab (Aduhelm, Biogen/Eisai), lecanemab was approved under the FDA’s accelerated approval pathway, which can be used to fast-track a drug that provides a meaningful therapeutic advantage over existing treatments for a serious or life-threatening illness.
Unlike aducanumab, however, there was no formal FDA advisory committee meeting on lecanemab prior to approval.
“Alzheimer’s disease immeasurably incapacitates the lives of those who suffer from it and has devastating effects on their loved ones,” Billy Dunn, MD, director of the Office of Neuroscience in the FDA’s Center for Drug Evaluation and Research, said in a press release.
“This treatment option is the latest therapy to target and affect the underlying disease process of Alzheimer’s, instead of only treating the symptoms of the disease,” Dr. Dunn added.
Eisai has reported that lecanemab will cost $26,500 a year.
Modest benefit, adverse events
The FDA noted, “The labeling states that treatment with Leqembi should be initiated in patients with mild cognitive impairment or mild dementia stage of disease, the population in which treatment was studied in clinical trials.”
The agency approved the treatment on the basis of findings from the CLARITY AD trial, which showed modest cognitive benefit for patients with early AD – but at a cost of increased risk for amyloid-related edema and effusions.
The trial enrolled 1,795 adults with mild cognitive impairment or early Alzheimer’s disease in whom amyloid pathology in the brain had been confirmed. Treatment consisted of lecanemab 10 mg/kg biweekly or matching placebo.
After 18 months of treatment, lecanemab slowed cognitive decline by 27%, compared with placebo, as measured by the Clinical Dementia Rating–Sum of Boxes (CDR-SB). This was an absolute difference of 0.45 points (change from baseline, 1.21 for lecanemab vs. 1.66 with placebo; P < .001).
While the results are “welcome news,” a 0.45-point difference on the CDR-SB might not be clinically meaningful, authors of a recent editorial in The Lancet cautioned.
Amyloid-related imaging abnormalities that manifest as edema or microhemorrhages also occurred in one in five patients taking lecanemab.
In addition, a newly published case report in The New England Journal of Medicine describes a patient with Alzheimer’s disease who was taking lecanemab and who died after experiencing numerous intracerebral hemorrhages during treatment with tissue plasminogen activator (tPA) for acute ischemic stroke.
“The findings raise the possibility of cerebral hemorrhages and necrotizing vasculopathy associated with tPA infusion in a patient with cerebrovascular amyloid who had received lecanemab,” the authors wrote.
Alzheimer’s Association reaction
Still, in anticipation of accelerated approval of lecanemab and the antiamyloid drug donanemab (Eli Lilly), which the FDA has also fast-tracked, the Alzheimer’s Association filed a formal request last month with the Centers for Medicare & Medicaid Services asking that it provide full and unrestricted coverage for FDA-approved Alzheimer’s disease treatments.
In a letter addressed to CMS administrator Chiquita Brooks-LaSure, the association asked the agency to remove the requirements for “coverage with evidence development” in its national coverage determination for FDA-approved antiamyloid monoclonal antibodies.
“Each day matters when it comes to slowing the progression of this disease,” Joanne Pike, DrPH, president and CEO for the Alzheimer’s Association, noted in a news release at the time.
“The current CMS policy to severely limit access to these treatments eliminates people’s options, is resulting in continued irreversible disease progression, and contributes to greater health inequities. That’s not acceptable,” Dr. Pike added.
After news of today’s approval was released, Dr. Pike noted in a new release, “The Alzheimer’s Association welcomes and celebrates this action by the FDA. We now have a second approved treatment that changes the course of Alzheimer’s disease in a meaningful way for people in the early stages of the disease.”
Maria C. Carrillo, PhD, chief science officer at the Alzheimer’s Association, called today’s approval “a milestone achievement.”
“The progress we’ve seen in not only this class of treatments but also in the diversification of treatment types and targets over the past few years is exciting and provides real hope to those impacted by this devastating disease,” Dr. Carrillo said.
Critical issues
Commenting on the approval, Alvaro Pascual-Leone, MD, PhD, professor of neurology at Harvard Medical School, Boston, and chief medical officer at Linus Health, said FDA approval of lecanemab and its adoption in the clinic represent a “very exciting development and prospect; but arguably some critical issues need to be considered.”
He noted that the health care system “is not currently prepared to cope with the challenges and demands of lecanemab,” as well as future pharmacologic agents.
“First, we need better workflows to identify suitable patients who can most benefit from this treatment,” said Dr. Pascual-Leone. He added that beyond identification of cognitive difficulties, amyloid status will need to be determined.
“Presently, this requires expensive and invasive tests,” such as positron-emission tomography scans or lumbar punctures for cerebrospinal fluid analysis. However, these are not fully covered by insurance companies and would be challenging to fully scale, he noted.
“In addition to screening, health systems will need to resolve the logistics challenges around the administration of lecanemab with twice-monthly infusions and the need for careful longitudinal evaluations for potential side effects,” said Dr. Pascual-Leone.
“While lecanemab may represent the first disease-modifying therapy widely available for early Alzheimer’s disease, the likely more promising approach is the addition of other therapies to lecanemab as part of a multi-intervention strategy combining pharmacologic and nonpharmacologic interventions,” he added.
Dr. Pascual-Leone has served as a paid member on scientific advisory boards for Neuroelectrics, Magstim, TetraNeuron, Skin2Neuron, MedRhythms, and Hearts Radiant and is a cofounder of TI Solutions and Linus Health.
A version of this article first appeared on Medscape.com.
This article was updated 1/9/23.
Like its controversial cousin aducanumab (Aduhelm, Biogen/Eisai), lecanemab was approved under the FDA’s accelerated approval pathway, which can be used to fast-track a drug that provides a meaningful therapeutic advantage over existing treatments for a serious or life-threatening illness.
Unlike aducanumab, however, there was no formal FDA advisory committee meeting on lecanemab prior to approval.
“Alzheimer’s disease immeasurably incapacitates the lives of those who suffer from it and has devastating effects on their loved ones,” Billy Dunn, MD, director of the Office of Neuroscience in the FDA’s Center for Drug Evaluation and Research, said in a press release.
“This treatment option is the latest therapy to target and affect the underlying disease process of Alzheimer’s, instead of only treating the symptoms of the disease,” Dr. Dunn added.
Eisai has reported that lecanemab will cost $26,500 a year.
Modest benefit, adverse events
The FDA noted, “The labeling states that treatment with Leqembi should be initiated in patients with mild cognitive impairment or mild dementia stage of disease, the population in which treatment was studied in clinical trials.”
The agency approved the treatment on the basis of findings from the CLARITY AD trial, which showed modest cognitive benefit for patients with early AD – but at a cost of increased risk for amyloid-related edema and effusions.
The trial enrolled 1,795 adults with mild cognitive impairment or early Alzheimer’s disease in whom amyloid pathology in the brain had been confirmed. Treatment consisted of lecanemab 10 mg/kg biweekly or matching placebo.
After 18 months of treatment, lecanemab slowed cognitive decline by 27%, compared with placebo, as measured by the Clinical Dementia Rating–Sum of Boxes (CDR-SB). This was an absolute difference of 0.45 points (change from baseline, 1.21 for lecanemab vs. 1.66 with placebo; P < .001).
While the results are “welcome news,” a 0.45-point difference on the CDR-SB might not be clinically meaningful, authors of a recent editorial in The Lancet cautioned.
Amyloid-related imaging abnormalities that manifest as edema or microhemorrhages also occurred in one in five patients taking lecanemab.
In addition, a newly published case report in The New England Journal of Medicine describes a patient with Alzheimer’s disease who was taking lecanemab and who died after experiencing numerous intracerebral hemorrhages during treatment with tissue plasminogen activator (tPA) for acute ischemic stroke.
“The findings raise the possibility of cerebral hemorrhages and necrotizing vasculopathy associated with tPA infusion in a patient with cerebrovascular amyloid who had received lecanemab,” the authors wrote.
Alzheimer’s Association reaction
Still, in anticipation of accelerated approval of lecanemab and the antiamyloid drug donanemab (Eli Lilly), which the FDA has also fast-tracked, the Alzheimer’s Association filed a formal request last month with the Centers for Medicare & Medicaid Services asking that it provide full and unrestricted coverage for FDA-approved Alzheimer’s disease treatments.
In a letter addressed to CMS administrator Chiquita Brooks-LaSure, the association asked the agency to remove the requirements for “coverage with evidence development” in its national coverage determination for FDA-approved antiamyloid monoclonal antibodies.
“Each day matters when it comes to slowing the progression of this disease,” Joanne Pike, DrPH, president and CEO for the Alzheimer’s Association, noted in a news release at the time.
“The current CMS policy to severely limit access to these treatments eliminates people’s options, is resulting in continued irreversible disease progression, and contributes to greater health inequities. That’s not acceptable,” Dr. Pike added.
After news of today’s approval was released, Dr. Pike noted in a new release, “The Alzheimer’s Association welcomes and celebrates this action by the FDA. We now have a second approved treatment that changes the course of Alzheimer’s disease in a meaningful way for people in the early stages of the disease.”
Maria C. Carrillo, PhD, chief science officer at the Alzheimer’s Association, called today’s approval “a milestone achievement.”
“The progress we’ve seen in not only this class of treatments but also in the diversification of treatment types and targets over the past few years is exciting and provides real hope to those impacted by this devastating disease,” Dr. Carrillo said.
Critical issues
Commenting on the approval, Alvaro Pascual-Leone, MD, PhD, professor of neurology at Harvard Medical School, Boston, and chief medical officer at Linus Health, said FDA approval of lecanemab and its adoption in the clinic represent a “very exciting development and prospect; but arguably some critical issues need to be considered.”
He noted that the health care system “is not currently prepared to cope with the challenges and demands of lecanemab,” as well as future pharmacologic agents.
“First, we need better workflows to identify suitable patients who can most benefit from this treatment,” said Dr. Pascual-Leone. He added that beyond identification of cognitive difficulties, amyloid status will need to be determined.
“Presently, this requires expensive and invasive tests,” such as positron-emission tomography scans or lumbar punctures for cerebrospinal fluid analysis. However, these are not fully covered by insurance companies and would be challenging to fully scale, he noted.
“In addition to screening, health systems will need to resolve the logistics challenges around the administration of lecanemab with twice-monthly infusions and the need for careful longitudinal evaluations for potential side effects,” said Dr. Pascual-Leone.
“While lecanemab may represent the first disease-modifying therapy widely available for early Alzheimer’s disease, the likely more promising approach is the addition of other therapies to lecanemab as part of a multi-intervention strategy combining pharmacologic and nonpharmacologic interventions,” he added.
Dr. Pascual-Leone has served as a paid member on scientific advisory boards for Neuroelectrics, Magstim, TetraNeuron, Skin2Neuron, MedRhythms, and Hearts Radiant and is a cofounder of TI Solutions and Linus Health.
A version of this article first appeared on Medscape.com.
This article was updated 1/9/23.
Like its controversial cousin aducanumab (Aduhelm, Biogen/Eisai), lecanemab was approved under the FDA’s accelerated approval pathway, which can be used to fast-track a drug that provides a meaningful therapeutic advantage over existing treatments for a serious or life-threatening illness.
Unlike aducanumab, however, there was no formal FDA advisory committee meeting on lecanemab prior to approval.
“Alzheimer’s disease immeasurably incapacitates the lives of those who suffer from it and has devastating effects on their loved ones,” Billy Dunn, MD, director of the Office of Neuroscience in the FDA’s Center for Drug Evaluation and Research, said in a press release.
“This treatment option is the latest therapy to target and affect the underlying disease process of Alzheimer’s, instead of only treating the symptoms of the disease,” Dr. Dunn added.
Eisai has reported that lecanemab will cost $26,500 a year.
Modest benefit, adverse events
The FDA noted, “The labeling states that treatment with Leqembi should be initiated in patients with mild cognitive impairment or mild dementia stage of disease, the population in which treatment was studied in clinical trials.”
The agency approved the treatment on the basis of findings from the CLARITY AD trial, which showed modest cognitive benefit for patients with early AD – but at a cost of increased risk for amyloid-related edema and effusions.
The trial enrolled 1,795 adults with mild cognitive impairment or early Alzheimer’s disease in whom amyloid pathology in the brain had been confirmed. Treatment consisted of lecanemab 10 mg/kg biweekly or matching placebo.
After 18 months of treatment, lecanemab slowed cognitive decline by 27%, compared with placebo, as measured by the Clinical Dementia Rating–Sum of Boxes (CDR-SB). This was an absolute difference of 0.45 points (change from baseline, 1.21 for lecanemab vs. 1.66 with placebo; P < .001).
While the results are “welcome news,” a 0.45-point difference on the CDR-SB might not be clinically meaningful, authors of a recent editorial in The Lancet cautioned.
Amyloid-related imaging abnormalities that manifest as edema or microhemorrhages also occurred in one in five patients taking lecanemab.
In addition, a newly published case report in The New England Journal of Medicine describes a patient with Alzheimer’s disease who was taking lecanemab and who died after experiencing numerous intracerebral hemorrhages during treatment with tissue plasminogen activator (tPA) for acute ischemic stroke.
“The findings raise the possibility of cerebral hemorrhages and necrotizing vasculopathy associated with tPA infusion in a patient with cerebrovascular amyloid who had received lecanemab,” the authors wrote.
Alzheimer’s Association reaction
Still, in anticipation of accelerated approval of lecanemab and the antiamyloid drug donanemab (Eli Lilly), which the FDA has also fast-tracked, the Alzheimer’s Association filed a formal request last month with the Centers for Medicare & Medicaid Services asking that it provide full and unrestricted coverage for FDA-approved Alzheimer’s disease treatments.
In a letter addressed to CMS administrator Chiquita Brooks-LaSure, the association asked the agency to remove the requirements for “coverage with evidence development” in its national coverage determination for FDA-approved antiamyloid monoclonal antibodies.
“Each day matters when it comes to slowing the progression of this disease,” Joanne Pike, DrPH, president and CEO for the Alzheimer’s Association, noted in a news release at the time.
“The current CMS policy to severely limit access to these treatments eliminates people’s options, is resulting in continued irreversible disease progression, and contributes to greater health inequities. That’s not acceptable,” Dr. Pike added.
After news of today’s approval was released, Dr. Pike noted in a new release, “The Alzheimer’s Association welcomes and celebrates this action by the FDA. We now have a second approved treatment that changes the course of Alzheimer’s disease in a meaningful way for people in the early stages of the disease.”
Maria C. Carrillo, PhD, chief science officer at the Alzheimer’s Association, called today’s approval “a milestone achievement.”
“The progress we’ve seen in not only this class of treatments but also in the diversification of treatment types and targets over the past few years is exciting and provides real hope to those impacted by this devastating disease,” Dr. Carrillo said.
Critical issues
Commenting on the approval, Alvaro Pascual-Leone, MD, PhD, professor of neurology at Harvard Medical School, Boston, and chief medical officer at Linus Health, said FDA approval of lecanemab and its adoption in the clinic represent a “very exciting development and prospect; but arguably some critical issues need to be considered.”
He noted that the health care system “is not currently prepared to cope with the challenges and demands of lecanemab,” as well as future pharmacologic agents.
“First, we need better workflows to identify suitable patients who can most benefit from this treatment,” said Dr. Pascual-Leone. He added that beyond identification of cognitive difficulties, amyloid status will need to be determined.
“Presently, this requires expensive and invasive tests,” such as positron-emission tomography scans or lumbar punctures for cerebrospinal fluid analysis. However, these are not fully covered by insurance companies and would be challenging to fully scale, he noted.
“In addition to screening, health systems will need to resolve the logistics challenges around the administration of lecanemab with twice-monthly infusions and the need for careful longitudinal evaluations for potential side effects,” said Dr. Pascual-Leone.
“While lecanemab may represent the first disease-modifying therapy widely available for early Alzheimer’s disease, the likely more promising approach is the addition of other therapies to lecanemab as part of a multi-intervention strategy combining pharmacologic and nonpharmacologic interventions,” he added.
Dr. Pascual-Leone has served as a paid member on scientific advisory boards for Neuroelectrics, Magstim, TetraNeuron, Skin2Neuron, MedRhythms, and Hearts Radiant and is a cofounder of TI Solutions and Linus Health.
A version of this article first appeared on Medscape.com.
This article was updated 1/9/23.
IV ketamine a promising option for resistant depression in older adults
Results showed nearly 50% of participants responded to ketamine and 25% achieved complete remission from TRD, as measured by scores on the Montgomery-Asberg Depression Rating Scale (MADRS).
“Our pilot study suggests that IV ketamine is well-tolerated, safe, and associated with improvement in late-life TRD,” co-investigator Marie Anne Gebara, MD, assistant professor of psychiatry at the University of Pittsburgh, told this news organization.
Dr. Gebara pointed out the treatment “may not be appropriate for all patients with TRD,” such as those with a history of psychotic symptoms or uncontrolled hypertension; but “it appears to be a promising option.”
The findings were published online in the American Journal of Geriatric Psychiatry.
Lack of data in seniors
Although ketamine has been shown in prior research to rapidly reduce suicidal ideation in adults, there has been a lack of data on its efficacy and safety in older adults, the current investigators note.
“Almost 50% of older adults suffering from depression have TRD, which is a leading cause of disability, excess mortality from suicide, and dementia,” Dr. Gebara said.
She added that after two failed trials of antidepressants, “older adults have few evidence-based choices: aripiprazole or bupropion augmentation, transcranial magnetic stimulation, or electroconvulsive therapy. Novel treatments with rapid benefit are needed as long-term outcomes are poor and recurrence rates are high.”
Dr. Gebara and colleagues at five sites (Columbia University, New York State Psychiatric Institute, University of Toronto, University of Pittsburgh, and Washington University in St. Louis) each enrolled five participants aged 60 and older into the pilot study between October 2020 and November 2021, for a total of 25 participants (mean age, 71 years).
Each participant was recruited from patient registries or referred by behavioral health or primary care providers and diagnosed with TRD, which was defined as an episode of major depressive disorder without psychotic features that persisted despite two or more trials of antidepressants including at least one evidence-based second-line treatment.
Participants had to take an oral antidepressant dosage for at least 1 month prior to the start of the IV ketamine infusions, and continue their antidepressant for the length of the trial.
They received IV ketamine twice weekly for 4 weeks. The dosage was weight-dependent.
At the end of the 4 weeks, participants who achieved a MADRS total score of less than 10 or had a 30% or greater reduction from their baseline MADRS score entered another 4-week phase of the trial. This phase consisted of once-weekly administration of IV ketamine.
Larger plans
Results showed 15 of the 25 participants (60%) experienced a 30% or higher reduction in MADRS scores in the first phase of the study. The mean change in MADRS total score from the beginning to the end of the first phase was a decrease of 9.4 points (P < .01).
At the end of the continuation phase, half (48%) met criteria for response and 27% met criteria for remission.
After ketamine administration, the researchers also found an improvement in Fluid Cognition Composite Score (Cohen’s d value = .61), indicating a medium to large effect size, and in three measures of executive function.
Overall, adverse events were rare and did not keep patients from participating in the study, the investigators note. Five of the 25 participants reported infusion-induced hypertension that was transient.
Study limitations cited include the small sample size and the absence of randomization and placebo control or comparison treatment.
“We were very pleased with these findings because they establish the safety of this novel intervention in older adults,” Dr. Gebara said.
“After establishing safety and tolerability, we can plan for larger, randomized controlled trials that will allow us to determine the effectiveness of IV ketamine for older adults with TRD,” she added.
Multiple mechanisms
In a comment, Gerard Sanacora, MD, PhD, professor of psychiatry at Yale University and director of the Yale Depression Research Program, New Haven, Conn., noted multiple mechanisms likely contribute to the antidepressant effects of ketamine.
Dr. Sanacora has independently researched the effects of ketamine but was not involved with the current study.
“Much of the work to date has focused on the drug’s proximal effects on the glutamatergic neurotransmitter system and the resulting enhancement of adaptive neuroplasticity in several brain regions,” he said.
“However, there is also evidence to suggest other neurotransmitter systems and possibly even neuroinflammatory regulators are also contributing to the effect,” Dr. Sanacora added.
He noted that these mechanisms are also likely amplified by the “hope, optimism, expectations, and improved medical management overall that are known to be associated with treatments that require close monitoring and follow-up with health care providers.”
Dr. Gebara noted that “internal/department funds at each site” were used to support the study. She also reported receiving support from Otsuka US. Disclosures for the other investigators are listed in the original article. Dr. Sanacora has reported having “no major direct conflicts” with the study.
A version of this article first appeared on Medscape.com.
Results showed nearly 50% of participants responded to ketamine and 25% achieved complete remission from TRD, as measured by scores on the Montgomery-Asberg Depression Rating Scale (MADRS).
“Our pilot study suggests that IV ketamine is well-tolerated, safe, and associated with improvement in late-life TRD,” co-investigator Marie Anne Gebara, MD, assistant professor of psychiatry at the University of Pittsburgh, told this news organization.
Dr. Gebara pointed out the treatment “may not be appropriate for all patients with TRD,” such as those with a history of psychotic symptoms or uncontrolled hypertension; but “it appears to be a promising option.”
The findings were published online in the American Journal of Geriatric Psychiatry.
Lack of data in seniors
Although ketamine has been shown in prior research to rapidly reduce suicidal ideation in adults, there has been a lack of data on its efficacy and safety in older adults, the current investigators note.
“Almost 50% of older adults suffering from depression have TRD, which is a leading cause of disability, excess mortality from suicide, and dementia,” Dr. Gebara said.
She added that after two failed trials of antidepressants, “older adults have few evidence-based choices: aripiprazole or bupropion augmentation, transcranial magnetic stimulation, or electroconvulsive therapy. Novel treatments with rapid benefit are needed as long-term outcomes are poor and recurrence rates are high.”
Dr. Gebara and colleagues at five sites (Columbia University, New York State Psychiatric Institute, University of Toronto, University of Pittsburgh, and Washington University in St. Louis) each enrolled five participants aged 60 and older into the pilot study between October 2020 and November 2021, for a total of 25 participants (mean age, 71 years).
Each participant was recruited from patient registries or referred by behavioral health or primary care providers and diagnosed with TRD, which was defined as an episode of major depressive disorder without psychotic features that persisted despite two or more trials of antidepressants including at least one evidence-based second-line treatment.
Participants had to take an oral antidepressant dosage for at least 1 month prior to the start of the IV ketamine infusions, and continue their antidepressant for the length of the trial.
They received IV ketamine twice weekly for 4 weeks. The dosage was weight-dependent.
At the end of the 4 weeks, participants who achieved a MADRS total score of less than 10 or had a 30% or greater reduction from their baseline MADRS score entered another 4-week phase of the trial. This phase consisted of once-weekly administration of IV ketamine.
Larger plans
Results showed 15 of the 25 participants (60%) experienced a 30% or higher reduction in MADRS scores in the first phase of the study. The mean change in MADRS total score from the beginning to the end of the first phase was a decrease of 9.4 points (P < .01).
At the end of the continuation phase, half (48%) met criteria for response and 27% met criteria for remission.
After ketamine administration, the researchers also found an improvement in Fluid Cognition Composite Score (Cohen’s d value = .61), indicating a medium to large effect size, and in three measures of executive function.
Overall, adverse events were rare and did not keep patients from participating in the study, the investigators note. Five of the 25 participants reported infusion-induced hypertension that was transient.
Study limitations cited include the small sample size and the absence of randomization and placebo control or comparison treatment.
“We were very pleased with these findings because they establish the safety of this novel intervention in older adults,” Dr. Gebara said.
“After establishing safety and tolerability, we can plan for larger, randomized controlled trials that will allow us to determine the effectiveness of IV ketamine for older adults with TRD,” she added.
Multiple mechanisms
In a comment, Gerard Sanacora, MD, PhD, professor of psychiatry at Yale University and director of the Yale Depression Research Program, New Haven, Conn., noted multiple mechanisms likely contribute to the antidepressant effects of ketamine.
Dr. Sanacora has independently researched the effects of ketamine but was not involved with the current study.
“Much of the work to date has focused on the drug’s proximal effects on the glutamatergic neurotransmitter system and the resulting enhancement of adaptive neuroplasticity in several brain regions,” he said.
“However, there is also evidence to suggest other neurotransmitter systems and possibly even neuroinflammatory regulators are also contributing to the effect,” Dr. Sanacora added.
He noted that these mechanisms are also likely amplified by the “hope, optimism, expectations, and improved medical management overall that are known to be associated with treatments that require close monitoring and follow-up with health care providers.”
Dr. Gebara noted that “internal/department funds at each site” were used to support the study. She also reported receiving support from Otsuka US. Disclosures for the other investigators are listed in the original article. Dr. Sanacora has reported having “no major direct conflicts” with the study.
A version of this article first appeared on Medscape.com.
Results showed nearly 50% of participants responded to ketamine and 25% achieved complete remission from TRD, as measured by scores on the Montgomery-Asberg Depression Rating Scale (MADRS).
“Our pilot study suggests that IV ketamine is well-tolerated, safe, and associated with improvement in late-life TRD,” co-investigator Marie Anne Gebara, MD, assistant professor of psychiatry at the University of Pittsburgh, told this news organization.
Dr. Gebara pointed out the treatment “may not be appropriate for all patients with TRD,” such as those with a history of psychotic symptoms or uncontrolled hypertension; but “it appears to be a promising option.”
The findings were published online in the American Journal of Geriatric Psychiatry.
Lack of data in seniors
Although ketamine has been shown in prior research to rapidly reduce suicidal ideation in adults, there has been a lack of data on its efficacy and safety in older adults, the current investigators note.
“Almost 50% of older adults suffering from depression have TRD, which is a leading cause of disability, excess mortality from suicide, and dementia,” Dr. Gebara said.
She added that after two failed trials of antidepressants, “older adults have few evidence-based choices: aripiprazole or bupropion augmentation, transcranial magnetic stimulation, or electroconvulsive therapy. Novel treatments with rapid benefit are needed as long-term outcomes are poor and recurrence rates are high.”
Dr. Gebara and colleagues at five sites (Columbia University, New York State Psychiatric Institute, University of Toronto, University of Pittsburgh, and Washington University in St. Louis) each enrolled five participants aged 60 and older into the pilot study between October 2020 and November 2021, for a total of 25 participants (mean age, 71 years).
Each participant was recruited from patient registries or referred by behavioral health or primary care providers and diagnosed with TRD, which was defined as an episode of major depressive disorder without psychotic features that persisted despite two or more trials of antidepressants including at least one evidence-based second-line treatment.
Participants had to take an oral antidepressant dosage for at least 1 month prior to the start of the IV ketamine infusions, and continue their antidepressant for the length of the trial.
They received IV ketamine twice weekly for 4 weeks. The dosage was weight-dependent.
At the end of the 4 weeks, participants who achieved a MADRS total score of less than 10 or had a 30% or greater reduction from their baseline MADRS score entered another 4-week phase of the trial. This phase consisted of once-weekly administration of IV ketamine.
Larger plans
Results showed 15 of the 25 participants (60%) experienced a 30% or higher reduction in MADRS scores in the first phase of the study. The mean change in MADRS total score from the beginning to the end of the first phase was a decrease of 9.4 points (P < .01).
At the end of the continuation phase, half (48%) met criteria for response and 27% met criteria for remission.
After ketamine administration, the researchers also found an improvement in Fluid Cognition Composite Score (Cohen’s d value = .61), indicating a medium to large effect size, and in three measures of executive function.
Overall, adverse events were rare and did not keep patients from participating in the study, the investigators note. Five of the 25 participants reported infusion-induced hypertension that was transient.
Study limitations cited include the small sample size and the absence of randomization and placebo control or comparison treatment.
“We were very pleased with these findings because they establish the safety of this novel intervention in older adults,” Dr. Gebara said.
“After establishing safety and tolerability, we can plan for larger, randomized controlled trials that will allow us to determine the effectiveness of IV ketamine for older adults with TRD,” she added.
Multiple mechanisms
In a comment, Gerard Sanacora, MD, PhD, professor of psychiatry at Yale University and director of the Yale Depression Research Program, New Haven, Conn., noted multiple mechanisms likely contribute to the antidepressant effects of ketamine.
Dr. Sanacora has independently researched the effects of ketamine but was not involved with the current study.
“Much of the work to date has focused on the drug’s proximal effects on the glutamatergic neurotransmitter system and the resulting enhancement of adaptive neuroplasticity in several brain regions,” he said.
“However, there is also evidence to suggest other neurotransmitter systems and possibly even neuroinflammatory regulators are also contributing to the effect,” Dr. Sanacora added.
He noted that these mechanisms are also likely amplified by the “hope, optimism, expectations, and improved medical management overall that are known to be associated with treatments that require close monitoring and follow-up with health care providers.”
Dr. Gebara noted that “internal/department funds at each site” were used to support the study. She also reported receiving support from Otsuka US. Disclosures for the other investigators are listed in the original article. Dr. Sanacora has reported having “no major direct conflicts” with the study.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF GERIATRIC PSYCHIATRY
Small study finds high dose vitamin D relieved toxic erythema of chemotherapy
seen on an inpatient dermatology consultative service.
Currently, chemotherapy cessation, delay, or dose modification are the “only reliable methods of resolving TEC,” and supportive agents such as topical corticosteroids, topical keratolytics, and pain control are associated with variable and “relatively slow improvement involving 2 to 4 weeks of recovery after chemotherapy interruption,” Cuong V. Nguyen, MD, of the department of dermatology at Northwestern University, Chicago, and colleagues, wrote in a research letter.
Onset of TEC in the six patients occurred a mean of 8.5 days after chemotherapy. Vitamin D – 50,000 IU for one patient and 100,000 IU for the others – was administered a mean of 4.3 days from rash onset and again in 7 days. Triamcinolone, 0.1%, or clobetasol, 0.05%, ointments were also prescribed.
All patients experienced symptomatic improvement in pain, pruritus, or swelling within a day of the first vitamin D treatment, and improvement in redness within 1 to 4 days, the authors said. The second treatment was administered for residual symptoms.
Adam Friedman, MD, professor and chair of dermatology and director of the supportive oncodermatology clinic at George Washington University, Washington, said that supporting patients through the “expected, disabling and often treatment-limiting side effects of oncologic therapies” is an area that is “in its infancy” and is characterized by limited evidence-based approaches.
“Creativity is therefore a must,” he said, commenting on the research letter. “Practice starts with anecdote, and this is certainly an exciting finding ... I look forward to trialing this with our patients at GW.”
Five of the six patients had a hematologic condition that required induction chemotherapy before hematopoietic stem cell transplant, and one was receiving regorafenib for treatment of glioblastoma multiforme. Diagnosis of TEC was established by clinical presentation, and five of the six patients underwent a biopsy. Biopsy findings were consistent with a TEC diagnosis in three patients, and showed nonspecific perivascular dermatitis in two, the investigators reported.
Further research is needed to determine optimal dosing, “delineate safety concerns and potential role in cancer treatment, and establish whether a durable response in patients with continuous chemotherapy, such as in an outpatient setting, is possible,” they said.
Dr. Nguyen and his coauthors reported no conflict of interest disclosures.
seen on an inpatient dermatology consultative service.
Currently, chemotherapy cessation, delay, or dose modification are the “only reliable methods of resolving TEC,” and supportive agents such as topical corticosteroids, topical keratolytics, and pain control are associated with variable and “relatively slow improvement involving 2 to 4 weeks of recovery after chemotherapy interruption,” Cuong V. Nguyen, MD, of the department of dermatology at Northwestern University, Chicago, and colleagues, wrote in a research letter.
Onset of TEC in the six patients occurred a mean of 8.5 days after chemotherapy. Vitamin D – 50,000 IU for one patient and 100,000 IU for the others – was administered a mean of 4.3 days from rash onset and again in 7 days. Triamcinolone, 0.1%, or clobetasol, 0.05%, ointments were also prescribed.
All patients experienced symptomatic improvement in pain, pruritus, or swelling within a day of the first vitamin D treatment, and improvement in redness within 1 to 4 days, the authors said. The second treatment was administered for residual symptoms.
Adam Friedman, MD, professor and chair of dermatology and director of the supportive oncodermatology clinic at George Washington University, Washington, said that supporting patients through the “expected, disabling and often treatment-limiting side effects of oncologic therapies” is an area that is “in its infancy” and is characterized by limited evidence-based approaches.
“Creativity is therefore a must,” he said, commenting on the research letter. “Practice starts with anecdote, and this is certainly an exciting finding ... I look forward to trialing this with our patients at GW.”
Five of the six patients had a hematologic condition that required induction chemotherapy before hematopoietic stem cell transplant, and one was receiving regorafenib for treatment of glioblastoma multiforme. Diagnosis of TEC was established by clinical presentation, and five of the six patients underwent a biopsy. Biopsy findings were consistent with a TEC diagnosis in three patients, and showed nonspecific perivascular dermatitis in two, the investigators reported.
Further research is needed to determine optimal dosing, “delineate safety concerns and potential role in cancer treatment, and establish whether a durable response in patients with continuous chemotherapy, such as in an outpatient setting, is possible,” they said.
Dr. Nguyen and his coauthors reported no conflict of interest disclosures.
seen on an inpatient dermatology consultative service.
Currently, chemotherapy cessation, delay, or dose modification are the “only reliable methods of resolving TEC,” and supportive agents such as topical corticosteroids, topical keratolytics, and pain control are associated with variable and “relatively slow improvement involving 2 to 4 weeks of recovery after chemotherapy interruption,” Cuong V. Nguyen, MD, of the department of dermatology at Northwestern University, Chicago, and colleagues, wrote in a research letter.
Onset of TEC in the six patients occurred a mean of 8.5 days after chemotherapy. Vitamin D – 50,000 IU for one patient and 100,000 IU for the others – was administered a mean of 4.3 days from rash onset and again in 7 days. Triamcinolone, 0.1%, or clobetasol, 0.05%, ointments were also prescribed.
All patients experienced symptomatic improvement in pain, pruritus, or swelling within a day of the first vitamin D treatment, and improvement in redness within 1 to 4 days, the authors said. The second treatment was administered for residual symptoms.
Adam Friedman, MD, professor and chair of dermatology and director of the supportive oncodermatology clinic at George Washington University, Washington, said that supporting patients through the “expected, disabling and often treatment-limiting side effects of oncologic therapies” is an area that is “in its infancy” and is characterized by limited evidence-based approaches.
“Creativity is therefore a must,” he said, commenting on the research letter. “Practice starts with anecdote, and this is certainly an exciting finding ... I look forward to trialing this with our patients at GW.”
Five of the six patients had a hematologic condition that required induction chemotherapy before hematopoietic stem cell transplant, and one was receiving regorafenib for treatment of glioblastoma multiforme. Diagnosis of TEC was established by clinical presentation, and five of the six patients underwent a biopsy. Biopsy findings were consistent with a TEC diagnosis in three patients, and showed nonspecific perivascular dermatitis in two, the investigators reported.
Further research is needed to determine optimal dosing, “delineate safety concerns and potential role in cancer treatment, and establish whether a durable response in patients with continuous chemotherapy, such as in an outpatient setting, is possible,” they said.
Dr. Nguyen and his coauthors reported no conflict of interest disclosures.
FROM JAMA DERMATOLOGY
Science reveals link between gut health and exercise motivation
Researchers at the University of Pennsylvania, Philadelphia recently explored this topic when they wanted to find out why some lab mice seem to love their exercise wheel, while others mostly ignore it.
To start, the researchers used a machine-learning algorithm to look for biological traits that could explain the differences in activity levels among mice. And what they found surprised them: Genetics seemed to have little to do with it, but differences in gut bacteria appeared to matter more. A handful of studies backed that up: Thriving gut microbiomes have been linked with optimal muscle function in mice.
Sure enough, when the researchers dosed mice with broad-spectrum antibiotics, killing off their gut bacteria, the distance the rodents were able to run dropped by half. But off the antibiotics, the mice mostly regained their previous performance levels.
The findings, published in the journal Nature, suggest that the gut microbiome may help regulate the desire to exercise.
If confirmed in humans, this hypothesis could help explain why so many Americans fail to get the recommended amount of physical activity. Some may blame lack of time, energy, or interest. But perhaps the reason could come down to the trillions of microbes living in their gut.
This line of research could also lead to microbiome-based ways to get sedentary people off the couch or optimize athletic performance.
But how could one’s microbiome impact the motivation to move? To find the answer, the researchers zeroed in on the brain.
The gut-brain connection
After treating the mice with antibiotics, the researchers sequenced RNA in the rodents’ striatum (the part of the brain responsible for motivation). They found reduced gene expression in the cells’ dopamine receptors – which release the neurochemical dopamine, making one feel like they’ve accomplished something good. In other words: Mice treated with antibiotics were getting less of a dopamine hit after their run.
“Only when we started focusing on the brain did we understand that the microbiome’s effect on exercise capacity was mediated by the central and peripheral nervous systems,” said study author Christoph Thaiss, PhD, a microbiologist at the University of Pennsylvania. “This realization completely changed the trajectory of the project.”
To find out how, exactly, bacteria in the colon were signaling the brain, the researchers performed a series of experiments over several years. They identified two types of bacteria, Eubacterium rectale and Coprococcus eutactus. These strains produce compounds called fatty acid amides that interact with endocannabinoid receptors in the gut.
Those endocannabinoid receptors signal the brain to cut back its production of monoamine oxidase, the compound that breaks down dopamine. With less of this dopamine-clearing compound in the brain, more dopamine could build up after a long run, making the mice feel good and eager to hit the exercise wheel again soon.
This gut-brain pathway “may have evolved to couple the initiation of prolonged physical activity to the nutritional status of the gastrointestinal tract,” Dr. Thaiss said. Gut bacteria monitor what’s in your colon and tell your brain whether you have enough food to fuel a workout.
The colon, or gut, hosts trillions of microbes with potentially hundreds of different bacteria strains. These strains are determined by the food we eat and the environment we occupy.
“The genetic impact on the microbiome is rather minor,” Dr. Thaiss said, “but lifestyle factors strongly impact the composition of the gut microbiome.”
He hopes to develop nutritional interventions to encourage the growth of the motivating types of bacteria, the kind that make a person want to go for a 5-mile run.
What’s next?
Moving forward, the researchers need to find out whether the gut affects motivation in humans, too. To do that, they’re analyzing the gut microbiomes of people with varying levels of exercise motivation.
“With enough samples, we could potentially correlate species of microbiota that exist in exercise-motivated individuals,” said study coauthor Nicholas Betley, PhD, a biologist at the University of Pennsylvania.
Variations in the gut microbiome could help explain the “runner’s high” that some people have in a long-distance race. The research could also help promote weight training or sports participation.
“Imagine if a sports team could optimally motivate the athletes on the team to exercise,” said Dr. Betley. The lab is investigating the microbiome’s impact on high-intensity interval training.
Signals from the gut to the brain could be affecting body processes in other ways too, the researchers speculated.
“There are so many possibilities for how these signals may change physiology and impact health,” Dr. Betley said. “A new set of studies may well establish a whole new branch of exercise physiology.”
A version of this article first appeared on WebMD.com.
Researchers at the University of Pennsylvania, Philadelphia recently explored this topic when they wanted to find out why some lab mice seem to love their exercise wheel, while others mostly ignore it.
To start, the researchers used a machine-learning algorithm to look for biological traits that could explain the differences in activity levels among mice. And what they found surprised them: Genetics seemed to have little to do with it, but differences in gut bacteria appeared to matter more. A handful of studies backed that up: Thriving gut microbiomes have been linked with optimal muscle function in mice.
Sure enough, when the researchers dosed mice with broad-spectrum antibiotics, killing off their gut bacteria, the distance the rodents were able to run dropped by half. But off the antibiotics, the mice mostly regained their previous performance levels.
The findings, published in the journal Nature, suggest that the gut microbiome may help regulate the desire to exercise.
If confirmed in humans, this hypothesis could help explain why so many Americans fail to get the recommended amount of physical activity. Some may blame lack of time, energy, or interest. But perhaps the reason could come down to the trillions of microbes living in their gut.
This line of research could also lead to microbiome-based ways to get sedentary people off the couch or optimize athletic performance.
But how could one’s microbiome impact the motivation to move? To find the answer, the researchers zeroed in on the brain.
The gut-brain connection
After treating the mice with antibiotics, the researchers sequenced RNA in the rodents’ striatum (the part of the brain responsible for motivation). They found reduced gene expression in the cells’ dopamine receptors – which release the neurochemical dopamine, making one feel like they’ve accomplished something good. In other words: Mice treated with antibiotics were getting less of a dopamine hit after their run.
“Only when we started focusing on the brain did we understand that the microbiome’s effect on exercise capacity was mediated by the central and peripheral nervous systems,” said study author Christoph Thaiss, PhD, a microbiologist at the University of Pennsylvania. “This realization completely changed the trajectory of the project.”
To find out how, exactly, bacteria in the colon were signaling the brain, the researchers performed a series of experiments over several years. They identified two types of bacteria, Eubacterium rectale and Coprococcus eutactus. These strains produce compounds called fatty acid amides that interact with endocannabinoid receptors in the gut.
Those endocannabinoid receptors signal the brain to cut back its production of monoamine oxidase, the compound that breaks down dopamine. With less of this dopamine-clearing compound in the brain, more dopamine could build up after a long run, making the mice feel good and eager to hit the exercise wheel again soon.
This gut-brain pathway “may have evolved to couple the initiation of prolonged physical activity to the nutritional status of the gastrointestinal tract,” Dr. Thaiss said. Gut bacteria monitor what’s in your colon and tell your brain whether you have enough food to fuel a workout.
The colon, or gut, hosts trillions of microbes with potentially hundreds of different bacteria strains. These strains are determined by the food we eat and the environment we occupy.
“The genetic impact on the microbiome is rather minor,” Dr. Thaiss said, “but lifestyle factors strongly impact the composition of the gut microbiome.”
He hopes to develop nutritional interventions to encourage the growth of the motivating types of bacteria, the kind that make a person want to go for a 5-mile run.
What’s next?
Moving forward, the researchers need to find out whether the gut affects motivation in humans, too. To do that, they’re analyzing the gut microbiomes of people with varying levels of exercise motivation.
“With enough samples, we could potentially correlate species of microbiota that exist in exercise-motivated individuals,” said study coauthor Nicholas Betley, PhD, a biologist at the University of Pennsylvania.
Variations in the gut microbiome could help explain the “runner’s high” that some people have in a long-distance race. The research could also help promote weight training or sports participation.
“Imagine if a sports team could optimally motivate the athletes on the team to exercise,” said Dr. Betley. The lab is investigating the microbiome’s impact on high-intensity interval training.
Signals from the gut to the brain could be affecting body processes in other ways too, the researchers speculated.
“There are so many possibilities for how these signals may change physiology and impact health,” Dr. Betley said. “A new set of studies may well establish a whole new branch of exercise physiology.”
A version of this article first appeared on WebMD.com.
Researchers at the University of Pennsylvania, Philadelphia recently explored this topic when they wanted to find out why some lab mice seem to love their exercise wheel, while others mostly ignore it.
To start, the researchers used a machine-learning algorithm to look for biological traits that could explain the differences in activity levels among mice. And what they found surprised them: Genetics seemed to have little to do with it, but differences in gut bacteria appeared to matter more. A handful of studies backed that up: Thriving gut microbiomes have been linked with optimal muscle function in mice.
Sure enough, when the researchers dosed mice with broad-spectrum antibiotics, killing off their gut bacteria, the distance the rodents were able to run dropped by half. But off the antibiotics, the mice mostly regained their previous performance levels.
The findings, published in the journal Nature, suggest that the gut microbiome may help regulate the desire to exercise.
If confirmed in humans, this hypothesis could help explain why so many Americans fail to get the recommended amount of physical activity. Some may blame lack of time, energy, or interest. But perhaps the reason could come down to the trillions of microbes living in their gut.
This line of research could also lead to microbiome-based ways to get sedentary people off the couch or optimize athletic performance.
But how could one’s microbiome impact the motivation to move? To find the answer, the researchers zeroed in on the brain.
The gut-brain connection
After treating the mice with antibiotics, the researchers sequenced RNA in the rodents’ striatum (the part of the brain responsible for motivation). They found reduced gene expression in the cells’ dopamine receptors – which release the neurochemical dopamine, making one feel like they’ve accomplished something good. In other words: Mice treated with antibiotics were getting less of a dopamine hit after their run.
“Only when we started focusing on the brain did we understand that the microbiome’s effect on exercise capacity was mediated by the central and peripheral nervous systems,” said study author Christoph Thaiss, PhD, a microbiologist at the University of Pennsylvania. “This realization completely changed the trajectory of the project.”
To find out how, exactly, bacteria in the colon were signaling the brain, the researchers performed a series of experiments over several years. They identified two types of bacteria, Eubacterium rectale and Coprococcus eutactus. These strains produce compounds called fatty acid amides that interact with endocannabinoid receptors in the gut.
Those endocannabinoid receptors signal the brain to cut back its production of monoamine oxidase, the compound that breaks down dopamine. With less of this dopamine-clearing compound in the brain, more dopamine could build up after a long run, making the mice feel good and eager to hit the exercise wheel again soon.
This gut-brain pathway “may have evolved to couple the initiation of prolonged physical activity to the nutritional status of the gastrointestinal tract,” Dr. Thaiss said. Gut bacteria monitor what’s in your colon and tell your brain whether you have enough food to fuel a workout.
The colon, or gut, hosts trillions of microbes with potentially hundreds of different bacteria strains. These strains are determined by the food we eat and the environment we occupy.
“The genetic impact on the microbiome is rather minor,” Dr. Thaiss said, “but lifestyle factors strongly impact the composition of the gut microbiome.”
He hopes to develop nutritional interventions to encourage the growth of the motivating types of bacteria, the kind that make a person want to go for a 5-mile run.
What’s next?
Moving forward, the researchers need to find out whether the gut affects motivation in humans, too. To do that, they’re analyzing the gut microbiomes of people with varying levels of exercise motivation.
“With enough samples, we could potentially correlate species of microbiota that exist in exercise-motivated individuals,” said study coauthor Nicholas Betley, PhD, a biologist at the University of Pennsylvania.
Variations in the gut microbiome could help explain the “runner’s high” that some people have in a long-distance race. The research could also help promote weight training or sports participation.
“Imagine if a sports team could optimally motivate the athletes on the team to exercise,” said Dr. Betley. The lab is investigating the microbiome’s impact on high-intensity interval training.
Signals from the gut to the brain could be affecting body processes in other ways too, the researchers speculated.
“There are so many possibilities for how these signals may change physiology and impact health,” Dr. Betley said. “A new set of studies may well establish a whole new branch of exercise physiology.”
A version of this article first appeared on WebMD.com.
FROM NATURE
Lifestyle changes may reduce colorectal cancer risk
Changes regarding smoking, drinking, body weight, and physical activity may alter the risk for colorectal cancer (CRC), the results of a study on a large European cohort suggest.
“This is a clear message that practicing clinicians and gastroenterologists could give to their patients and to CRC screening participants to improve CRC prevention,” write Edoardo Botteri, PhD, Cancer Registry of Norway, Oslo, and colleagues in an article published in the American Journal of Gastroenterology.
Previous studies have shown a correlation between cancer in general and unhealthy lifestyle factors. They have also shown an association between weight gain and an increased risk for CRC and a reduced risk with smoking cessation. But Dr. Botteri and colleagues could not find any published research on the association of other lifestyle factors and the risk for CRC specifically, they write.
To help fill this gap, they followed 295,865 people who participated in the European Prospective Investigation into Cancer (EPIC) for a median of 7.8 years. The participants were mostly aged from 35 to 70 years and lived in Denmark, France, Germany, Greece, Italy, the Netherlands, Norway, Spain, Sweden, and the United Kingdom.
The researchers calculated a healthy lifestyle index (HLI) score on the basis of smoking status, alcohol consumption, body mass index, and physical activity. The median time between baseline and the follow-up questionnaire was 5.7 years.
They awarded points as indicated in the following table.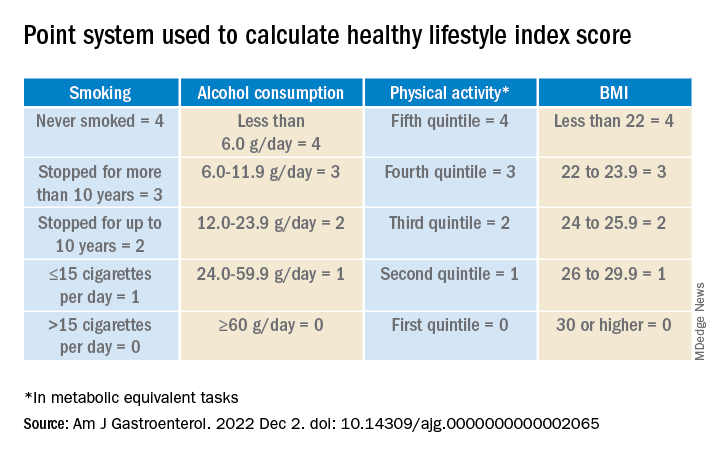
Participants’ scores ranged from 0 to 16. At baseline, the mean HLI score was 10.04. It dipped slightly to 9.95 at follow-up.
Men had more favorable changes than women, and the associations between the HLI score and CRC risk were only statistically significant among men.
Overall, a 1-unit increase in the HLI score was associated with a 3% lower risk for CRC.
When the HLI scores were grouped into tertiles, improvements from an “unfavorable lifestyle” (0-9) to a “favorable lifestyle” (12-16) were associated with a 23% lower risk for CRC (compared with no change). Likewise, a decline from a “favorable lifestyle” to an “unfavorable lifestyle” was associated with a 34% higher risk.
Changes in the BMI score from baseline showed a trend toward an association with CRC risk.
Decreases in alcohol consumption were significantly associated with a reduction in CRC risk among participants aged 55 years or younger at baseline.
Increases in physical activity were significantly associated with a lower risk for proximal colon cancer, especially in younger participants.
On the other hand, reductions in smoking were associated with an increase in CRC risk. This correlation might be the result of “inverse causation,” the researchers note; that is, people may have quit smoking because they experienced early symptoms of CRC. Smoking had only a marginal influence on the HLI calculations in this study because only a small proportion of participants changed their smoking rates.
Information on diet was collected only at baseline, so changes in this factor could not be measured. The researchers adjusted their analysis for diet at baseline, but they acknowledge that their inability to incorporate diet into the HLI score was a limitation of the study.
Similarly, they used education as a marker of socioeconomic status but acknowledge that this is only a proxy.
“The HLI score may therefore not accurately capture the complex relationship between lifestyle habits and risk for CRC,” they write.
Still, if the results of this observational study are confirmed by other research, the findings could provide evidence to design intervention studies to prevent CRC, they conclude.
The study was supported by the grant LIBERTY from the French Institut National du Cancer. Financial supporters of the national cohorts and the coordination of EPIC are listed in the published study. The researchers reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Changes regarding smoking, drinking, body weight, and physical activity may alter the risk for colorectal cancer (CRC), the results of a study on a large European cohort suggest.
“This is a clear message that practicing clinicians and gastroenterologists could give to their patients and to CRC screening participants to improve CRC prevention,” write Edoardo Botteri, PhD, Cancer Registry of Norway, Oslo, and colleagues in an article published in the American Journal of Gastroenterology.
Previous studies have shown a correlation between cancer in general and unhealthy lifestyle factors. They have also shown an association between weight gain and an increased risk for CRC and a reduced risk with smoking cessation. But Dr. Botteri and colleagues could not find any published research on the association of other lifestyle factors and the risk for CRC specifically, they write.
To help fill this gap, they followed 295,865 people who participated in the European Prospective Investigation into Cancer (EPIC) for a median of 7.8 years. The participants were mostly aged from 35 to 70 years and lived in Denmark, France, Germany, Greece, Italy, the Netherlands, Norway, Spain, Sweden, and the United Kingdom.
The researchers calculated a healthy lifestyle index (HLI) score on the basis of smoking status, alcohol consumption, body mass index, and physical activity. The median time between baseline and the follow-up questionnaire was 5.7 years.
They awarded points as indicated in the following table.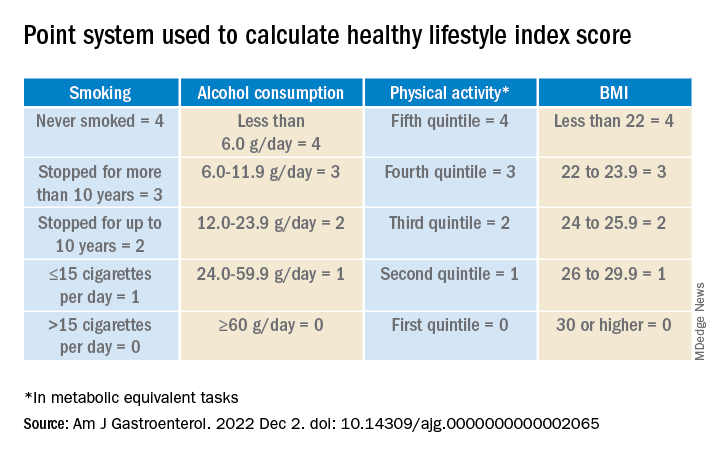
Participants’ scores ranged from 0 to 16. At baseline, the mean HLI score was 10.04. It dipped slightly to 9.95 at follow-up.
Men had more favorable changes than women, and the associations between the HLI score and CRC risk were only statistically significant among men.
Overall, a 1-unit increase in the HLI score was associated with a 3% lower risk for CRC.
When the HLI scores were grouped into tertiles, improvements from an “unfavorable lifestyle” (0-9) to a “favorable lifestyle” (12-16) were associated with a 23% lower risk for CRC (compared with no change). Likewise, a decline from a “favorable lifestyle” to an “unfavorable lifestyle” was associated with a 34% higher risk.
Changes in the BMI score from baseline showed a trend toward an association with CRC risk.
Decreases in alcohol consumption were significantly associated with a reduction in CRC risk among participants aged 55 years or younger at baseline.
Increases in physical activity were significantly associated with a lower risk for proximal colon cancer, especially in younger participants.
On the other hand, reductions in smoking were associated with an increase in CRC risk. This correlation might be the result of “inverse causation,” the researchers note; that is, people may have quit smoking because they experienced early symptoms of CRC. Smoking had only a marginal influence on the HLI calculations in this study because only a small proportion of participants changed their smoking rates.
Information on diet was collected only at baseline, so changes in this factor could not be measured. The researchers adjusted their analysis for diet at baseline, but they acknowledge that their inability to incorporate diet into the HLI score was a limitation of the study.
Similarly, they used education as a marker of socioeconomic status but acknowledge that this is only a proxy.
“The HLI score may therefore not accurately capture the complex relationship between lifestyle habits and risk for CRC,” they write.
Still, if the results of this observational study are confirmed by other research, the findings could provide evidence to design intervention studies to prevent CRC, they conclude.
The study was supported by the grant LIBERTY from the French Institut National du Cancer. Financial supporters of the national cohorts and the coordination of EPIC are listed in the published study. The researchers reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Changes regarding smoking, drinking, body weight, and physical activity may alter the risk for colorectal cancer (CRC), the results of a study on a large European cohort suggest.
“This is a clear message that practicing clinicians and gastroenterologists could give to their patients and to CRC screening participants to improve CRC prevention,” write Edoardo Botteri, PhD, Cancer Registry of Norway, Oslo, and colleagues in an article published in the American Journal of Gastroenterology.
Previous studies have shown a correlation between cancer in general and unhealthy lifestyle factors. They have also shown an association between weight gain and an increased risk for CRC and a reduced risk with smoking cessation. But Dr. Botteri and colleagues could not find any published research on the association of other lifestyle factors and the risk for CRC specifically, they write.
To help fill this gap, they followed 295,865 people who participated in the European Prospective Investigation into Cancer (EPIC) for a median of 7.8 years. The participants were mostly aged from 35 to 70 years and lived in Denmark, France, Germany, Greece, Italy, the Netherlands, Norway, Spain, Sweden, and the United Kingdom.
The researchers calculated a healthy lifestyle index (HLI) score on the basis of smoking status, alcohol consumption, body mass index, and physical activity. The median time between baseline and the follow-up questionnaire was 5.7 years.
They awarded points as indicated in the following table.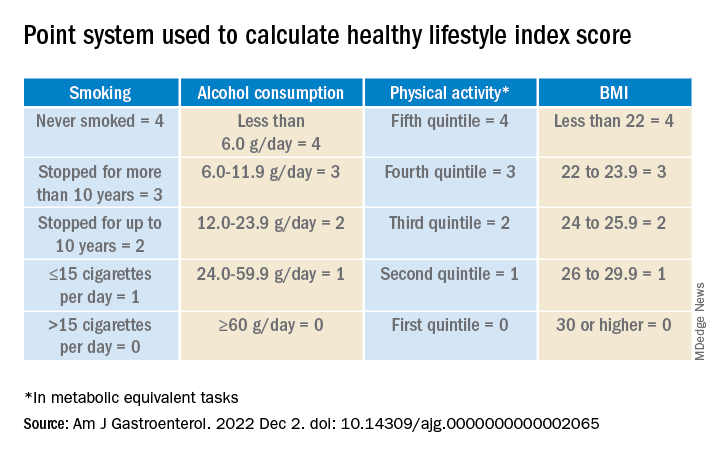
Participants’ scores ranged from 0 to 16. At baseline, the mean HLI score was 10.04. It dipped slightly to 9.95 at follow-up.
Men had more favorable changes than women, and the associations between the HLI score and CRC risk were only statistically significant among men.
Overall, a 1-unit increase in the HLI score was associated with a 3% lower risk for CRC.
When the HLI scores were grouped into tertiles, improvements from an “unfavorable lifestyle” (0-9) to a “favorable lifestyle” (12-16) were associated with a 23% lower risk for CRC (compared with no change). Likewise, a decline from a “favorable lifestyle” to an “unfavorable lifestyle” was associated with a 34% higher risk.
Changes in the BMI score from baseline showed a trend toward an association with CRC risk.
Decreases in alcohol consumption were significantly associated with a reduction in CRC risk among participants aged 55 years or younger at baseline.
Increases in physical activity were significantly associated with a lower risk for proximal colon cancer, especially in younger participants.
On the other hand, reductions in smoking were associated with an increase in CRC risk. This correlation might be the result of “inverse causation,” the researchers note; that is, people may have quit smoking because they experienced early symptoms of CRC. Smoking had only a marginal influence on the HLI calculations in this study because only a small proportion of participants changed their smoking rates.
Information on diet was collected only at baseline, so changes in this factor could not be measured. The researchers adjusted their analysis for diet at baseline, but they acknowledge that their inability to incorporate diet into the HLI score was a limitation of the study.
Similarly, they used education as a marker of socioeconomic status but acknowledge that this is only a proxy.
“The HLI score may therefore not accurately capture the complex relationship between lifestyle habits and risk for CRC,” they write.
Still, if the results of this observational study are confirmed by other research, the findings could provide evidence to design intervention studies to prevent CRC, they conclude.
The study was supported by the grant LIBERTY from the French Institut National du Cancer. Financial supporters of the national cohorts and the coordination of EPIC are listed in the published study. The researchers reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF GASTROENTEROLOGY
Long COVID clinical trials may offer shortcut to new treatments
With no proven treatments for long COVID, millions of Americans struggling with debilitating symptoms may be wondering whether it’s worth it to try something they’ve never considered before: a clinical trial.
But it may take years for these trials to prove which drugs, devices, and behavioral therapies are safe and effective.
“We’re not in warp speed,” said Kanecia Zimmerman, MD, a principal investigator at the Duke Clinical Research Institute in Durham, N.C., who is overseeing long COVID trials for the NIH. Operation Warp Speed – the 2020-2021 federal effort to get COVID vaccines designed, tested, authorized and distributed – benefited from existing scientific knowledge about other coronaviruses and about vaccines in general. But there’s no similar foundation of scientific knowledge about long COVID.
“We are in a place of not really knowing anything,” Dr. Zimmerman said.
But some glimmers of hope are emerging. A Veterans Affairs study recently found the antiviral Paxlovid might help prevent long COVID. A small case study at Yale found the ADHD drug guanfacine may ease brain fog from long COVID. And preliminary results from an NIH-funded study suggest COVID vaccines might help children with a rare but serious inflammatory condition known as multisystem inflammatory syndrome (MIS-C).
More results are expected very soon from the trial for kids with MIS-C, which can strike suddenly long after a COVID infection clears up. While the exact causes aren’t yet clear, MIS-C can cause dangerous inflammation in the heart, lungs, kidneys, brain, skin, eyes, or gastrointestinal system.
Because the virus often triggered a delayed response of MIS-C in kids who had few if any symptoms of acute COVID-19, scientists wondered whether children infected with the virus might respond to a vaccine dose to prevent MIS-C from developing, Gary Gibbons, MD, director of the National Heart, Lung, and Blood Institute, said during a Dec. 9 presentation at the NIH. It’s not yet clear if vaccination helps, but it doesn’t harm the children, Dr. Gibbons said.
“Indeed, the studies suggest with some relief that yes, these children could be vaccinated safely,” he said.
Several new trials are also testing Paxlovid against long COVID, including one late-stage study that may have results in about a year.
“We already know that Paxlovid reduces the risk of developing long COVID, but it would be a game changer if it can improve long COVID symptoms as well,” said Surendra Barshikar, MD, an associate professor and medical director of the COVID Recover program at the University of Texas Southwestern Medical Center, Dallas.
In other studies, researchers are looking at a wide variety of previously approved and experimental drugs and devices. For example, scientists in New York are testing the mood stabilizer lithium to treat brain fog and fatigue. And researchers in Illinois are investigating efgartigimod, a drug approved for the rare muscle-weakening autoimmune disorder myasthenia gravis, to see if it helps ease a long COVID complication known as POTS that can cause a sudden rapid heart rate and chronic fatigue.
“The good news is that enrollment will proceed quickly, given the vast number of patients,” said Kristin Englund, MD, director of the reCOVer Center of Excellence at the Cleveland Clinic.
This is all encouraging because roughly one in five American adults who have acute COVID infections develop persistent symptoms of long COVID, also known as post–acute sequelae of SARS-CoV-2 (PASC). And many of these long COVID patients have complex, overlapping clusters of symptoms that make traditional treatment approaches largely ineffective against this new, formidable disease.
But not every patient living with long COVID will qualify for trials or find it easy to take part even if they do. Patients should consider how severe their symptoms are, the potential risks of any experimental treatments, and the many challenges they may have with getting to and from clinical trial sites that are largely concentrated around major cities and might be far from home.
While this holds true for any type of trial, it’s essential for long COVID patients, who may have fatigue, muscle weakness, and other symptoms that make distance an impossible factor to ignore, said Aaron Friedberg, MD, clinical colead of the post–COVID-19 recovery program at the Ohio State University Wexner Medical Center, Columbus.
“I think it is a personal decision, since the fatigue and pain that patients with PASC can experience can make it very challenging to travel long distances,” Dr. Friedberg said. “I would recommend calling or messaging ahead to find out exactly what type of travel might be required because there may be steps that can be completed by email or video, which could make it easier to participate, and some trials may be entirely remote.”
Even when patients feel up to the travel, they still might not be a good fit for a clinical trial. Scientists often look for people who didn’t have pre-existing health problems before they got long COVID, Dr. Barshikar noted. Patients taking medications may also be unable to participate in drug trials, particularly for experimental treatments because of concerns about unknown side effects from drug interactions.
When clinical trials do seem like a good option, patients may want to consider seeking treatment at an academic medical center that is already doing long COVID research, particularly if their symptoms are too complex or severe to manage only through their primary care provider, said Jonathan Whiteson, MD, who helped draft long COVID treatment guidelines for the American Academy of Physical Medicine and Rehabilitation. He also serves as codirector of the New York University Langone Health post–COVID care program.
Many health care professionals on the front lines treating long COVID patients are optimistic that the sheer number of trials and the vast number of patients taking part should ultimately produce some better treatment options than people have right now. It’s just not going to happen overnight.
“I suspect that while we will see some new treatments coming in the next 1-2 years, it may be several years before targets can be identified and full trials conducted to see results,” Dr. Friedberg said. “Getting good data takes time.”
A version of this article first appeared on WebMD.com.
With no proven treatments for long COVID, millions of Americans struggling with debilitating symptoms may be wondering whether it’s worth it to try something they’ve never considered before: a clinical trial.
But it may take years for these trials to prove which drugs, devices, and behavioral therapies are safe and effective.
“We’re not in warp speed,” said Kanecia Zimmerman, MD, a principal investigator at the Duke Clinical Research Institute in Durham, N.C., who is overseeing long COVID trials for the NIH. Operation Warp Speed – the 2020-2021 federal effort to get COVID vaccines designed, tested, authorized and distributed – benefited from existing scientific knowledge about other coronaviruses and about vaccines in general. But there’s no similar foundation of scientific knowledge about long COVID.
“We are in a place of not really knowing anything,” Dr. Zimmerman said.
But some glimmers of hope are emerging. A Veterans Affairs study recently found the antiviral Paxlovid might help prevent long COVID. A small case study at Yale found the ADHD drug guanfacine may ease brain fog from long COVID. And preliminary results from an NIH-funded study suggest COVID vaccines might help children with a rare but serious inflammatory condition known as multisystem inflammatory syndrome (MIS-C).
More results are expected very soon from the trial for kids with MIS-C, which can strike suddenly long after a COVID infection clears up. While the exact causes aren’t yet clear, MIS-C can cause dangerous inflammation in the heart, lungs, kidneys, brain, skin, eyes, or gastrointestinal system.
Because the virus often triggered a delayed response of MIS-C in kids who had few if any symptoms of acute COVID-19, scientists wondered whether children infected with the virus might respond to a vaccine dose to prevent MIS-C from developing, Gary Gibbons, MD, director of the National Heart, Lung, and Blood Institute, said during a Dec. 9 presentation at the NIH. It’s not yet clear if vaccination helps, but it doesn’t harm the children, Dr. Gibbons said.
“Indeed, the studies suggest with some relief that yes, these children could be vaccinated safely,” he said.
Several new trials are also testing Paxlovid against long COVID, including one late-stage study that may have results in about a year.
“We already know that Paxlovid reduces the risk of developing long COVID, but it would be a game changer if it can improve long COVID symptoms as well,” said Surendra Barshikar, MD, an associate professor and medical director of the COVID Recover program at the University of Texas Southwestern Medical Center, Dallas.
In other studies, researchers are looking at a wide variety of previously approved and experimental drugs and devices. For example, scientists in New York are testing the mood stabilizer lithium to treat brain fog and fatigue. And researchers in Illinois are investigating efgartigimod, a drug approved for the rare muscle-weakening autoimmune disorder myasthenia gravis, to see if it helps ease a long COVID complication known as POTS that can cause a sudden rapid heart rate and chronic fatigue.
“The good news is that enrollment will proceed quickly, given the vast number of patients,” said Kristin Englund, MD, director of the reCOVer Center of Excellence at the Cleveland Clinic.
This is all encouraging because roughly one in five American adults who have acute COVID infections develop persistent symptoms of long COVID, also known as post–acute sequelae of SARS-CoV-2 (PASC). And many of these long COVID patients have complex, overlapping clusters of symptoms that make traditional treatment approaches largely ineffective against this new, formidable disease.
But not every patient living with long COVID will qualify for trials or find it easy to take part even if they do. Patients should consider how severe their symptoms are, the potential risks of any experimental treatments, and the many challenges they may have with getting to and from clinical trial sites that are largely concentrated around major cities and might be far from home.
While this holds true for any type of trial, it’s essential for long COVID patients, who may have fatigue, muscle weakness, and other symptoms that make distance an impossible factor to ignore, said Aaron Friedberg, MD, clinical colead of the post–COVID-19 recovery program at the Ohio State University Wexner Medical Center, Columbus.
“I think it is a personal decision, since the fatigue and pain that patients with PASC can experience can make it very challenging to travel long distances,” Dr. Friedberg said. “I would recommend calling or messaging ahead to find out exactly what type of travel might be required because there may be steps that can be completed by email or video, which could make it easier to participate, and some trials may be entirely remote.”
Even when patients feel up to the travel, they still might not be a good fit for a clinical trial. Scientists often look for people who didn’t have pre-existing health problems before they got long COVID, Dr. Barshikar noted. Patients taking medications may also be unable to participate in drug trials, particularly for experimental treatments because of concerns about unknown side effects from drug interactions.
When clinical trials do seem like a good option, patients may want to consider seeking treatment at an academic medical center that is already doing long COVID research, particularly if their symptoms are too complex or severe to manage only through their primary care provider, said Jonathan Whiteson, MD, who helped draft long COVID treatment guidelines for the American Academy of Physical Medicine and Rehabilitation. He also serves as codirector of the New York University Langone Health post–COVID care program.
Many health care professionals on the front lines treating long COVID patients are optimistic that the sheer number of trials and the vast number of patients taking part should ultimately produce some better treatment options than people have right now. It’s just not going to happen overnight.
“I suspect that while we will see some new treatments coming in the next 1-2 years, it may be several years before targets can be identified and full trials conducted to see results,” Dr. Friedberg said. “Getting good data takes time.”
A version of this article first appeared on WebMD.com.
With no proven treatments for long COVID, millions of Americans struggling with debilitating symptoms may be wondering whether it’s worth it to try something they’ve never considered before: a clinical trial.
But it may take years for these trials to prove which drugs, devices, and behavioral therapies are safe and effective.
“We’re not in warp speed,” said Kanecia Zimmerman, MD, a principal investigator at the Duke Clinical Research Institute in Durham, N.C., who is overseeing long COVID trials for the NIH. Operation Warp Speed – the 2020-2021 federal effort to get COVID vaccines designed, tested, authorized and distributed – benefited from existing scientific knowledge about other coronaviruses and about vaccines in general. But there’s no similar foundation of scientific knowledge about long COVID.
“We are in a place of not really knowing anything,” Dr. Zimmerman said.
But some glimmers of hope are emerging. A Veterans Affairs study recently found the antiviral Paxlovid might help prevent long COVID. A small case study at Yale found the ADHD drug guanfacine may ease brain fog from long COVID. And preliminary results from an NIH-funded study suggest COVID vaccines might help children with a rare but serious inflammatory condition known as multisystem inflammatory syndrome (MIS-C).
More results are expected very soon from the trial for kids with MIS-C, which can strike suddenly long after a COVID infection clears up. While the exact causes aren’t yet clear, MIS-C can cause dangerous inflammation in the heart, lungs, kidneys, brain, skin, eyes, or gastrointestinal system.
Because the virus often triggered a delayed response of MIS-C in kids who had few if any symptoms of acute COVID-19, scientists wondered whether children infected with the virus might respond to a vaccine dose to prevent MIS-C from developing, Gary Gibbons, MD, director of the National Heart, Lung, and Blood Institute, said during a Dec. 9 presentation at the NIH. It’s not yet clear if vaccination helps, but it doesn’t harm the children, Dr. Gibbons said.
“Indeed, the studies suggest with some relief that yes, these children could be vaccinated safely,” he said.
Several new trials are also testing Paxlovid against long COVID, including one late-stage study that may have results in about a year.
“We already know that Paxlovid reduces the risk of developing long COVID, but it would be a game changer if it can improve long COVID symptoms as well,” said Surendra Barshikar, MD, an associate professor and medical director of the COVID Recover program at the University of Texas Southwestern Medical Center, Dallas.
In other studies, researchers are looking at a wide variety of previously approved and experimental drugs and devices. For example, scientists in New York are testing the mood stabilizer lithium to treat brain fog and fatigue. And researchers in Illinois are investigating efgartigimod, a drug approved for the rare muscle-weakening autoimmune disorder myasthenia gravis, to see if it helps ease a long COVID complication known as POTS that can cause a sudden rapid heart rate and chronic fatigue.
“The good news is that enrollment will proceed quickly, given the vast number of patients,” said Kristin Englund, MD, director of the reCOVer Center of Excellence at the Cleveland Clinic.
This is all encouraging because roughly one in five American adults who have acute COVID infections develop persistent symptoms of long COVID, also known as post–acute sequelae of SARS-CoV-2 (PASC). And many of these long COVID patients have complex, overlapping clusters of symptoms that make traditional treatment approaches largely ineffective against this new, formidable disease.
But not every patient living with long COVID will qualify for trials or find it easy to take part even if they do. Patients should consider how severe their symptoms are, the potential risks of any experimental treatments, and the many challenges they may have with getting to and from clinical trial sites that are largely concentrated around major cities and might be far from home.
While this holds true for any type of trial, it’s essential for long COVID patients, who may have fatigue, muscle weakness, and other symptoms that make distance an impossible factor to ignore, said Aaron Friedberg, MD, clinical colead of the post–COVID-19 recovery program at the Ohio State University Wexner Medical Center, Columbus.
“I think it is a personal decision, since the fatigue and pain that patients with PASC can experience can make it very challenging to travel long distances,” Dr. Friedberg said. “I would recommend calling or messaging ahead to find out exactly what type of travel might be required because there may be steps that can be completed by email or video, which could make it easier to participate, and some trials may be entirely remote.”
Even when patients feel up to the travel, they still might not be a good fit for a clinical trial. Scientists often look for people who didn’t have pre-existing health problems before they got long COVID, Dr. Barshikar noted. Patients taking medications may also be unable to participate in drug trials, particularly for experimental treatments because of concerns about unknown side effects from drug interactions.
When clinical trials do seem like a good option, patients may want to consider seeking treatment at an academic medical center that is already doing long COVID research, particularly if their symptoms are too complex or severe to manage only through their primary care provider, said Jonathan Whiteson, MD, who helped draft long COVID treatment guidelines for the American Academy of Physical Medicine and Rehabilitation. He also serves as codirector of the New York University Langone Health post–COVID care program.
Many health care professionals on the front lines treating long COVID patients are optimistic that the sheer number of trials and the vast number of patients taking part should ultimately produce some better treatment options than people have right now. It’s just not going to happen overnight.
“I suspect that while we will see some new treatments coming in the next 1-2 years, it may be several years before targets can be identified and full trials conducted to see results,” Dr. Friedberg said. “Getting good data takes time.”
A version of this article first appeared on WebMD.com.
New osteoporosis guideline says start with a bisphosphonate
This is the first update for 5 years since the previous guidance was published in 2017.
It strongly recommends initial therapy with bisphosphonates for postmenopausal women with osteoporosis, as well as men with osteoporosis, among other recommendations.
However, the author of an accompanying editorial, Susan M. Ott, MD, says: “The decision to start a bisphosphonate is actually not that easy.”
She also queries some of the other recommendations in the guidance.
Her editorial, along with the guideline by Amir Qaseem, MD, PhD, MPH, and colleagues, and systematic review by Chelsea Ayers, MPH, and colleagues, were published in the Annals of Internal Medicine.
Ryan D. Mire, MD, MACP, president of the ACP, gave a brief overview of the new guidance in a video.
Systematic review
The ACP commissioned a review of the evidence because it says new data have emerged on the efficacy of newer medications for osteoporosis and low bone mass, as well as treatment comparisons, and treatment in men.
The review authors identified 34 randomized controlled trials (in 100 publications) and 36 observational studies, which evaluated the following pharmacologic interventions:
- Antiresorptive drugs: four bisphosphonates (alendronate, ibandronate, risedronate, zoledronate) and a RANK ligand inhibitor (denosumab).
- Anabolic drugs: an analog of human parathyroid hormone (PTH)–related protein (abaloparatide), recombinant human PTH (teriparatide), and a sclerostin inhibitor (romosozumab).
- Estrogen agonists: selective estrogen receptor modulators (bazedoxifene, raloxifene).
The authors focused on effectiveness and harms of active drugs compared with placebo or bisphosphonates.
Major changes from 2017 guidelines, some questions
“Though there are many nuanced changes in this [2023 guideline] version, perhaps the major change is the explicit hierarchy of pharmacologic recommendations: bisphosphonates first, then denosumab,” Thomas G. Cooney, MD, senior author of the clinical guideline, explained in an interview.
“Bisphosphonates had the most favorable balance among benefits, harms, patient values and preferences, and cost among the examined drugs in postmenopausal females with primary osteoporosis,” Dr. Cooney, professor of medicine, Oregon Health & Science University, Portland, noted, as is stated in the guideline.
“Denosumab also had a favorable long-term net benefit, but bisphosphonates are much cheaper than other pharmacologic treatments and available in generic formulations,” the document states.
The new guideline suggests use of denosumab as second-line pharmacotherapy in adults who have contraindications to or experience adverse effects with bisphosphonates.
The choice among bisphosphonates (alendronate, risedronate, zoledronic acid) would be based on a patient-centered discussion between physician and patient, addressing costs (often related to insurance), delivery-mode preferences (oral versus intravenous), and “values,” which includes the patient’s priorities, concerns, and expectations regarding their health care, Dr. Cooney explained.
Another update in the new guideline is, “We also clarify the specific, albeit more limited, role of sclerostin inhibitors and recombinant PTH ‘to reduce the risk of fractures only in females with primary osteoporosis with very high-risk of fracture’,” Dr. Cooney noted.
In addition, the guideline now states, “treatment to reduce the risk of fractures in males rather than limiting it to ‘vertebral fracture’ in men,” as in the 2017 guideline.
It also explicitly includes denosumab as second-line therapy for men, Dr. Cooney noted, but as in 2017, the strength of evidence in men remains low.
“Finally, we also clarified that in females over the age of 65 with low bone mass or osteopenia that an individualized approach be taken to treatment (similar to last guideline), but if treatment is initiated, that a bisphosphonate be used (new content),” he said.
The use of estrogen, treatment duration, drug discontinuation, and serial bone mineral density monitoring were not addressed in this guideline, but will likely be evaluated within 2 to 3 years.
‘Osteoporosis treatment: Not easy’ – editorial
In her editorial, Dr. Ott writes: “The data about bisphosphonates may seem overwhelmingly positive, leading to strong recommendations for their use to treat osteoporosis, but the decision to start a bisphosphonate is actually not that easy.”
“A strong recommendation should be given only when future studies are unlikely to change it,” continues Dr. Ott, professor of medicine, University of Washington, Seattle.
“Yet, data already suggest that, in patients with serious osteoporosis, treatment should start with anabolic medications because previous treatment with either bisphosphonates or denosumab will prevent the anabolic response of newer medications.”
“Starting with bisphosphonate will change the bone so it will not respond to the newer medicines, and then a patient will lose the chance for getting the best improvement,” Dr. Ott clarified in an email to this news organization.
But, in fact, the new guidance does suggest that, to reduce the risk of fractures in females with primary osteoporosis at very high risk of fracture, one should consider use of the sclerostin inhibitor romosozumab (moderate-certainty evidence) or recombinant human parathyroid hormone (teriparatide) (low-certainty evidence) followed by a bisphosphonate (conditional recommendation).
Dr. Ott said: “If the [fracture] risk is high, then we should start with an anabolic medication for 1-2 years. If the risk is medium, then use a bisphosphonate for up to 5 years, and then stop and monitor the patient for signs that the medicine is wearing off,” based on blood and urine tests.
‘We need medicines that will stop bone aging’
Osteopenia is defined by an arbitrary bone density measurement, Dr. Ott explained. “About half of women over 65 will have osteopenia, and by age 85 there are hardly any ‘normal’ women left.”
“We need medicines that will stop bone aging, which might sound impossible, but we should still try,” she continued.
“In the meantime, while waiting on new discoveries,” Dr. Ott said, “I would not use bisphosphonates in patients who did not already have a fracture or whose bone density T-score was better than –2.5 because, in the major study, alendronate did not prevent fractures in this group.”
Many people are worried about bisphosphonates because of problems with the jaw or femur. These are real, but they are very rare during the first 5 years of treatment, Dr. Ott noted. Then the risk starts to rise, up to more than 1 in 1,000 after 8 years. So people can get the benefits of these drugs with very low risk for 5 years.
“An immediate [guideline] update is necessary to address the severity of bone loss and the high risk for vertebral fractures after discontinuation of denosumab,” Dr. Ott urged.
“I don’t agree with using denosumab for osteoporosis as a second-line treatment,” she said. “I would use it only in patients who have cancer or unusually high bone resorption. You have to get a dose strictly every 6 months, and if you need to stop, it is recommended to treat with bisphosphonates. Denosumab is a poor choice for somebody who does not want to take a bisphosphonate. Many patients and even too many doctors do not realize how serious it can be to skip a dose.”
“I also think that men could be treated with anabolic medications,” Dr. Ott said. “Clinical trials show they respond the same as women. Many men have osteoporosis as a consequence of low testosterone, and then they can usually be treated with testosterone. Osteoporosis in men is a serious problem that is too often ignored – almost reverse discrimination.”
It is also unfortunate that the review and recommendations do not address estrogen, one of the most effective medications to prevent osteoporotic fractures, according to Dr. Ott.
Clinical considerations in addition to drug types
The new guideline also advises:
- Clinicians treating adults with osteoporosis should encourage adherence to recommended treatments and healthy lifestyle habits, including exercise, and counseling to evaluate and prevent falls.
- All adults with osteopenia or osteoporosis should have adequate calcium and vitamin D intake, as part of fracture prevention.
- Clinicians should assess baseline fracture risk based on bone density, fracture history, fracture risk factors, and response to prior osteoporosis treatments.
- Current evidence suggests that more than 3-5 years of bisphosphonate therapy reduces risk for new vertebral but not other fractures; however, it also increases risk for long-term harms. Therefore, clinicians should consider stopping bisphosphonate treatment after 5 years unless the patient has a strong indication for treatment continuation.
- The decision for a bisphosphonate holiday (temporary discontinuation) and its duration should be based on baseline fracture risk, medication half-life in bone, and benefits and harms.
- Women treated with an anabolic agent who discontinue it should be offered an antiresorptive agent to preserve gains and because of serious risk for rebound and multiple vertebral fractures.
- Adults older than 65 years with osteoporosis may be at increased risk for falls or other adverse events because of drug interactions.
- Transgender persons have variable risk for low bone mass.
The review and guideline were funded by the ACP. Dr. Ott has reported no relevant disclosures. Relevant financial disclosures for other authors are listed with the guideline and review.
A version of this article first appeared on Medscape.com.
This is the first update for 5 years since the previous guidance was published in 2017.
It strongly recommends initial therapy with bisphosphonates for postmenopausal women with osteoporosis, as well as men with osteoporosis, among other recommendations.
However, the author of an accompanying editorial, Susan M. Ott, MD, says: “The decision to start a bisphosphonate is actually not that easy.”
She also queries some of the other recommendations in the guidance.
Her editorial, along with the guideline by Amir Qaseem, MD, PhD, MPH, and colleagues, and systematic review by Chelsea Ayers, MPH, and colleagues, were published in the Annals of Internal Medicine.
Ryan D. Mire, MD, MACP, president of the ACP, gave a brief overview of the new guidance in a video.
Systematic review
The ACP commissioned a review of the evidence because it says new data have emerged on the efficacy of newer medications for osteoporosis and low bone mass, as well as treatment comparisons, and treatment in men.
The review authors identified 34 randomized controlled trials (in 100 publications) and 36 observational studies, which evaluated the following pharmacologic interventions:
- Antiresorptive drugs: four bisphosphonates (alendronate, ibandronate, risedronate, zoledronate) and a RANK ligand inhibitor (denosumab).
- Anabolic drugs: an analog of human parathyroid hormone (PTH)–related protein (abaloparatide), recombinant human PTH (teriparatide), and a sclerostin inhibitor (romosozumab).
- Estrogen agonists: selective estrogen receptor modulators (bazedoxifene, raloxifene).
The authors focused on effectiveness and harms of active drugs compared with placebo or bisphosphonates.
Major changes from 2017 guidelines, some questions
“Though there are many nuanced changes in this [2023 guideline] version, perhaps the major change is the explicit hierarchy of pharmacologic recommendations: bisphosphonates first, then denosumab,” Thomas G. Cooney, MD, senior author of the clinical guideline, explained in an interview.
“Bisphosphonates had the most favorable balance among benefits, harms, patient values and preferences, and cost among the examined drugs in postmenopausal females with primary osteoporosis,” Dr. Cooney, professor of medicine, Oregon Health & Science University, Portland, noted, as is stated in the guideline.
“Denosumab also had a favorable long-term net benefit, but bisphosphonates are much cheaper than other pharmacologic treatments and available in generic formulations,” the document states.
The new guideline suggests use of denosumab as second-line pharmacotherapy in adults who have contraindications to or experience adverse effects with bisphosphonates.
The choice among bisphosphonates (alendronate, risedronate, zoledronic acid) would be based on a patient-centered discussion between physician and patient, addressing costs (often related to insurance), delivery-mode preferences (oral versus intravenous), and “values,” which includes the patient’s priorities, concerns, and expectations regarding their health care, Dr. Cooney explained.
Another update in the new guideline is, “We also clarify the specific, albeit more limited, role of sclerostin inhibitors and recombinant PTH ‘to reduce the risk of fractures only in females with primary osteoporosis with very high-risk of fracture’,” Dr. Cooney noted.
In addition, the guideline now states, “treatment to reduce the risk of fractures in males rather than limiting it to ‘vertebral fracture’ in men,” as in the 2017 guideline.
It also explicitly includes denosumab as second-line therapy for men, Dr. Cooney noted, but as in 2017, the strength of evidence in men remains low.
“Finally, we also clarified that in females over the age of 65 with low bone mass or osteopenia that an individualized approach be taken to treatment (similar to last guideline), but if treatment is initiated, that a bisphosphonate be used (new content),” he said.
The use of estrogen, treatment duration, drug discontinuation, and serial bone mineral density monitoring were not addressed in this guideline, but will likely be evaluated within 2 to 3 years.
‘Osteoporosis treatment: Not easy’ – editorial
In her editorial, Dr. Ott writes: “The data about bisphosphonates may seem overwhelmingly positive, leading to strong recommendations for their use to treat osteoporosis, but the decision to start a bisphosphonate is actually not that easy.”
“A strong recommendation should be given only when future studies are unlikely to change it,” continues Dr. Ott, professor of medicine, University of Washington, Seattle.
“Yet, data already suggest that, in patients with serious osteoporosis, treatment should start with anabolic medications because previous treatment with either bisphosphonates or denosumab will prevent the anabolic response of newer medications.”
“Starting with bisphosphonate will change the bone so it will not respond to the newer medicines, and then a patient will lose the chance for getting the best improvement,” Dr. Ott clarified in an email to this news organization.
But, in fact, the new guidance does suggest that, to reduce the risk of fractures in females with primary osteoporosis at very high risk of fracture, one should consider use of the sclerostin inhibitor romosozumab (moderate-certainty evidence) or recombinant human parathyroid hormone (teriparatide) (low-certainty evidence) followed by a bisphosphonate (conditional recommendation).
Dr. Ott said: “If the [fracture] risk is high, then we should start with an anabolic medication for 1-2 years. If the risk is medium, then use a bisphosphonate for up to 5 years, and then stop and monitor the patient for signs that the medicine is wearing off,” based on blood and urine tests.
‘We need medicines that will stop bone aging’
Osteopenia is defined by an arbitrary bone density measurement, Dr. Ott explained. “About half of women over 65 will have osteopenia, and by age 85 there are hardly any ‘normal’ women left.”
“We need medicines that will stop bone aging, which might sound impossible, but we should still try,” she continued.
“In the meantime, while waiting on new discoveries,” Dr. Ott said, “I would not use bisphosphonates in patients who did not already have a fracture or whose bone density T-score was better than –2.5 because, in the major study, alendronate did not prevent fractures in this group.”
Many people are worried about bisphosphonates because of problems with the jaw or femur. These are real, but they are very rare during the first 5 years of treatment, Dr. Ott noted. Then the risk starts to rise, up to more than 1 in 1,000 after 8 years. So people can get the benefits of these drugs with very low risk for 5 years.
“An immediate [guideline] update is necessary to address the severity of bone loss and the high risk for vertebral fractures after discontinuation of denosumab,” Dr. Ott urged.
“I don’t agree with using denosumab for osteoporosis as a second-line treatment,” she said. “I would use it only in patients who have cancer or unusually high bone resorption. You have to get a dose strictly every 6 months, and if you need to stop, it is recommended to treat with bisphosphonates. Denosumab is a poor choice for somebody who does not want to take a bisphosphonate. Many patients and even too many doctors do not realize how serious it can be to skip a dose.”
“I also think that men could be treated with anabolic medications,” Dr. Ott said. “Clinical trials show they respond the same as women. Many men have osteoporosis as a consequence of low testosterone, and then they can usually be treated with testosterone. Osteoporosis in men is a serious problem that is too often ignored – almost reverse discrimination.”
It is also unfortunate that the review and recommendations do not address estrogen, one of the most effective medications to prevent osteoporotic fractures, according to Dr. Ott.
Clinical considerations in addition to drug types
The new guideline also advises:
- Clinicians treating adults with osteoporosis should encourage adherence to recommended treatments and healthy lifestyle habits, including exercise, and counseling to evaluate and prevent falls.
- All adults with osteopenia or osteoporosis should have adequate calcium and vitamin D intake, as part of fracture prevention.
- Clinicians should assess baseline fracture risk based on bone density, fracture history, fracture risk factors, and response to prior osteoporosis treatments.
- Current evidence suggests that more than 3-5 years of bisphosphonate therapy reduces risk for new vertebral but not other fractures; however, it also increases risk for long-term harms. Therefore, clinicians should consider stopping bisphosphonate treatment after 5 years unless the patient has a strong indication for treatment continuation.
- The decision for a bisphosphonate holiday (temporary discontinuation) and its duration should be based on baseline fracture risk, medication half-life in bone, and benefits and harms.
- Women treated with an anabolic agent who discontinue it should be offered an antiresorptive agent to preserve gains and because of serious risk for rebound and multiple vertebral fractures.
- Adults older than 65 years with osteoporosis may be at increased risk for falls or other adverse events because of drug interactions.
- Transgender persons have variable risk for low bone mass.
The review and guideline were funded by the ACP. Dr. Ott has reported no relevant disclosures. Relevant financial disclosures for other authors are listed with the guideline and review.
A version of this article first appeared on Medscape.com.
This is the first update for 5 years since the previous guidance was published in 2017.
It strongly recommends initial therapy with bisphosphonates for postmenopausal women with osteoporosis, as well as men with osteoporosis, among other recommendations.
However, the author of an accompanying editorial, Susan M. Ott, MD, says: “The decision to start a bisphosphonate is actually not that easy.”
She also queries some of the other recommendations in the guidance.
Her editorial, along with the guideline by Amir Qaseem, MD, PhD, MPH, and colleagues, and systematic review by Chelsea Ayers, MPH, and colleagues, were published in the Annals of Internal Medicine.
Ryan D. Mire, MD, MACP, president of the ACP, gave a brief overview of the new guidance in a video.
Systematic review
The ACP commissioned a review of the evidence because it says new data have emerged on the efficacy of newer medications for osteoporosis and low bone mass, as well as treatment comparisons, and treatment in men.
The review authors identified 34 randomized controlled trials (in 100 publications) and 36 observational studies, which evaluated the following pharmacologic interventions:
- Antiresorptive drugs: four bisphosphonates (alendronate, ibandronate, risedronate, zoledronate) and a RANK ligand inhibitor (denosumab).
- Anabolic drugs: an analog of human parathyroid hormone (PTH)–related protein (abaloparatide), recombinant human PTH (teriparatide), and a sclerostin inhibitor (romosozumab).
- Estrogen agonists: selective estrogen receptor modulators (bazedoxifene, raloxifene).
The authors focused on effectiveness and harms of active drugs compared with placebo or bisphosphonates.
Major changes from 2017 guidelines, some questions
“Though there are many nuanced changes in this [2023 guideline] version, perhaps the major change is the explicit hierarchy of pharmacologic recommendations: bisphosphonates first, then denosumab,” Thomas G. Cooney, MD, senior author of the clinical guideline, explained in an interview.
“Bisphosphonates had the most favorable balance among benefits, harms, patient values and preferences, and cost among the examined drugs in postmenopausal females with primary osteoporosis,” Dr. Cooney, professor of medicine, Oregon Health & Science University, Portland, noted, as is stated in the guideline.
“Denosumab also had a favorable long-term net benefit, but bisphosphonates are much cheaper than other pharmacologic treatments and available in generic formulations,” the document states.
The new guideline suggests use of denosumab as second-line pharmacotherapy in adults who have contraindications to or experience adverse effects with bisphosphonates.
The choice among bisphosphonates (alendronate, risedronate, zoledronic acid) would be based on a patient-centered discussion between physician and patient, addressing costs (often related to insurance), delivery-mode preferences (oral versus intravenous), and “values,” which includes the patient’s priorities, concerns, and expectations regarding their health care, Dr. Cooney explained.
Another update in the new guideline is, “We also clarify the specific, albeit more limited, role of sclerostin inhibitors and recombinant PTH ‘to reduce the risk of fractures only in females with primary osteoporosis with very high-risk of fracture’,” Dr. Cooney noted.
In addition, the guideline now states, “treatment to reduce the risk of fractures in males rather than limiting it to ‘vertebral fracture’ in men,” as in the 2017 guideline.
It also explicitly includes denosumab as second-line therapy for men, Dr. Cooney noted, but as in 2017, the strength of evidence in men remains low.
“Finally, we also clarified that in females over the age of 65 with low bone mass or osteopenia that an individualized approach be taken to treatment (similar to last guideline), but if treatment is initiated, that a bisphosphonate be used (new content),” he said.
The use of estrogen, treatment duration, drug discontinuation, and serial bone mineral density monitoring were not addressed in this guideline, but will likely be evaluated within 2 to 3 years.
‘Osteoporosis treatment: Not easy’ – editorial
In her editorial, Dr. Ott writes: “The data about bisphosphonates may seem overwhelmingly positive, leading to strong recommendations for their use to treat osteoporosis, but the decision to start a bisphosphonate is actually not that easy.”
“A strong recommendation should be given only when future studies are unlikely to change it,” continues Dr. Ott, professor of medicine, University of Washington, Seattle.
“Yet, data already suggest that, in patients with serious osteoporosis, treatment should start with anabolic medications because previous treatment with either bisphosphonates or denosumab will prevent the anabolic response of newer medications.”
“Starting with bisphosphonate will change the bone so it will not respond to the newer medicines, and then a patient will lose the chance for getting the best improvement,” Dr. Ott clarified in an email to this news organization.
But, in fact, the new guidance does suggest that, to reduce the risk of fractures in females with primary osteoporosis at very high risk of fracture, one should consider use of the sclerostin inhibitor romosozumab (moderate-certainty evidence) or recombinant human parathyroid hormone (teriparatide) (low-certainty evidence) followed by a bisphosphonate (conditional recommendation).
Dr. Ott said: “If the [fracture] risk is high, then we should start with an anabolic medication for 1-2 years. If the risk is medium, then use a bisphosphonate for up to 5 years, and then stop and monitor the patient for signs that the medicine is wearing off,” based on blood and urine tests.
‘We need medicines that will stop bone aging’
Osteopenia is defined by an arbitrary bone density measurement, Dr. Ott explained. “About half of women over 65 will have osteopenia, and by age 85 there are hardly any ‘normal’ women left.”
“We need medicines that will stop bone aging, which might sound impossible, but we should still try,” she continued.
“In the meantime, while waiting on new discoveries,” Dr. Ott said, “I would not use bisphosphonates in patients who did not already have a fracture or whose bone density T-score was better than –2.5 because, in the major study, alendronate did not prevent fractures in this group.”
Many people are worried about bisphosphonates because of problems with the jaw or femur. These are real, but they are very rare during the first 5 years of treatment, Dr. Ott noted. Then the risk starts to rise, up to more than 1 in 1,000 after 8 years. So people can get the benefits of these drugs with very low risk for 5 years.
“An immediate [guideline] update is necessary to address the severity of bone loss and the high risk for vertebral fractures after discontinuation of denosumab,” Dr. Ott urged.
“I don’t agree with using denosumab for osteoporosis as a second-line treatment,” she said. “I would use it only in patients who have cancer or unusually high bone resorption. You have to get a dose strictly every 6 months, and if you need to stop, it is recommended to treat with bisphosphonates. Denosumab is a poor choice for somebody who does not want to take a bisphosphonate. Many patients and even too many doctors do not realize how serious it can be to skip a dose.”
“I also think that men could be treated with anabolic medications,” Dr. Ott said. “Clinical trials show they respond the same as women. Many men have osteoporosis as a consequence of low testosterone, and then they can usually be treated with testosterone. Osteoporosis in men is a serious problem that is too often ignored – almost reverse discrimination.”
It is also unfortunate that the review and recommendations do not address estrogen, one of the most effective medications to prevent osteoporotic fractures, according to Dr. Ott.
Clinical considerations in addition to drug types
The new guideline also advises:
- Clinicians treating adults with osteoporosis should encourage adherence to recommended treatments and healthy lifestyle habits, including exercise, and counseling to evaluate and prevent falls.
- All adults with osteopenia or osteoporosis should have adequate calcium and vitamin D intake, as part of fracture prevention.
- Clinicians should assess baseline fracture risk based on bone density, fracture history, fracture risk factors, and response to prior osteoporosis treatments.
- Current evidence suggests that more than 3-5 years of bisphosphonate therapy reduces risk for new vertebral but not other fractures; however, it also increases risk for long-term harms. Therefore, clinicians should consider stopping bisphosphonate treatment after 5 years unless the patient has a strong indication for treatment continuation.
- The decision for a bisphosphonate holiday (temporary discontinuation) and its duration should be based on baseline fracture risk, medication half-life in bone, and benefits and harms.
- Women treated with an anabolic agent who discontinue it should be offered an antiresorptive agent to preserve gains and because of serious risk for rebound and multiple vertebral fractures.
- Adults older than 65 years with osteoporosis may be at increased risk for falls or other adverse events because of drug interactions.
- Transgender persons have variable risk for low bone mass.
The review and guideline were funded by the ACP. Dr. Ott has reported no relevant disclosures. Relevant financial disclosures for other authors are listed with the guideline and review.
A version of this article first appeared on Medscape.com.
FROM THE ANNALS OF INTERNAL MEDICINE
FDA considers regulating CBD products
The products can have drug-like effects on the body and contain CBD (cannabidiol) and THC (tetrahydrocannabinol). Both CBD and THC can be derived from hemp, which was legalized by Congress in 2018.
“Given what we know about the safety of CBD so far, it raises concerns for FDA about whether these existing regulatory pathways for food and dietary supplements are appropriate for this substance,” FDA Principal Deputy Commissioner Janet Woodcock, MD, told The Wall Street Journal.
A 2021 FDA report valued the CBD market at $4.6 billion and projected it to quadruple by 2026. The only FDA-approved CBD product is an oil called Epidiolex, which can be prescribed for the seizure-associated disease epilepsy. Research on CBD to treat other diseases is ongoing.
Food, beverage, and beauty products containing CBD are sold in stores and online in many forms, including oils, vaporized liquids, and oil-based capsules, but “research supporting the drug’s benefits is still limited,” the Mayo Clinic said.
Recently, investigations have found that many CBD products also contain THC, which can be derived from legal hemp in a form that is referred to as Delta 8 and produces a psychoactive high. The CDC warned in 2022 that people “mistook” THC products for CBD products, which are often sold at the same stores, and experienced “adverse events.”
The Centers for Disease Control and Prevention and FDA warn that much is unknown about CBD and delta-8 products. The CDC says known CBD risks include liver damage; interference with other drugs you are taking, which may lead to injury or serious side effects; drowsiness or sleepiness; diarrhea or changes in appetite; changes in mood, such as crankiness; potential negative effects on fetuses during pregnancy or on babies during breastfeeding; or unintentional poisoning of children when mistaking THC products for CBD products or due to containing other ingredients such as THC or pesticides.
“I don’t think that we can have the perfect be the enemy of the good when we’re looking at such a vast market that is so available and utilized,” Norman Birenbaum, a senior FDA adviser who is working on the regulatory issue, told the Journal. “You’ve got a widely unregulated market.”
A version of this article first appeared on WebMD.com.
The products can have drug-like effects on the body and contain CBD (cannabidiol) and THC (tetrahydrocannabinol). Both CBD and THC can be derived from hemp, which was legalized by Congress in 2018.
“Given what we know about the safety of CBD so far, it raises concerns for FDA about whether these existing regulatory pathways for food and dietary supplements are appropriate for this substance,” FDA Principal Deputy Commissioner Janet Woodcock, MD, told The Wall Street Journal.
A 2021 FDA report valued the CBD market at $4.6 billion and projected it to quadruple by 2026. The only FDA-approved CBD product is an oil called Epidiolex, which can be prescribed for the seizure-associated disease epilepsy. Research on CBD to treat other diseases is ongoing.
Food, beverage, and beauty products containing CBD are sold in stores and online in many forms, including oils, vaporized liquids, and oil-based capsules, but “research supporting the drug’s benefits is still limited,” the Mayo Clinic said.
Recently, investigations have found that many CBD products also contain THC, which can be derived from legal hemp in a form that is referred to as Delta 8 and produces a psychoactive high. The CDC warned in 2022 that people “mistook” THC products for CBD products, which are often sold at the same stores, and experienced “adverse events.”
The Centers for Disease Control and Prevention and FDA warn that much is unknown about CBD and delta-8 products. The CDC says known CBD risks include liver damage; interference with other drugs you are taking, which may lead to injury or serious side effects; drowsiness or sleepiness; diarrhea or changes in appetite; changes in mood, such as crankiness; potential negative effects on fetuses during pregnancy or on babies during breastfeeding; or unintentional poisoning of children when mistaking THC products for CBD products or due to containing other ingredients such as THC or pesticides.
“I don’t think that we can have the perfect be the enemy of the good when we’re looking at such a vast market that is so available and utilized,” Norman Birenbaum, a senior FDA adviser who is working on the regulatory issue, told the Journal. “You’ve got a widely unregulated market.”
A version of this article first appeared on WebMD.com.
The products can have drug-like effects on the body and contain CBD (cannabidiol) and THC (tetrahydrocannabinol). Both CBD and THC can be derived from hemp, which was legalized by Congress in 2018.
“Given what we know about the safety of CBD so far, it raises concerns for FDA about whether these existing regulatory pathways for food and dietary supplements are appropriate for this substance,” FDA Principal Deputy Commissioner Janet Woodcock, MD, told The Wall Street Journal.
A 2021 FDA report valued the CBD market at $4.6 billion and projected it to quadruple by 2026. The only FDA-approved CBD product is an oil called Epidiolex, which can be prescribed for the seizure-associated disease epilepsy. Research on CBD to treat other diseases is ongoing.
Food, beverage, and beauty products containing CBD are sold in stores and online in many forms, including oils, vaporized liquids, and oil-based capsules, but “research supporting the drug’s benefits is still limited,” the Mayo Clinic said.
Recently, investigations have found that many CBD products also contain THC, which can be derived from legal hemp in a form that is referred to as Delta 8 and produces a psychoactive high. The CDC warned in 2022 that people “mistook” THC products for CBD products, which are often sold at the same stores, and experienced “adverse events.”
The Centers for Disease Control and Prevention and FDA warn that much is unknown about CBD and delta-8 products. The CDC says known CBD risks include liver damage; interference with other drugs you are taking, which may lead to injury or serious side effects; drowsiness or sleepiness; diarrhea or changes in appetite; changes in mood, such as crankiness; potential negative effects on fetuses during pregnancy or on babies during breastfeeding; or unintentional poisoning of children when mistaking THC products for CBD products or due to containing other ingredients such as THC or pesticides.
“I don’t think that we can have the perfect be the enemy of the good when we’re looking at such a vast market that is so available and utilized,” Norman Birenbaum, a senior FDA adviser who is working on the regulatory issue, told the Journal. “You’ve got a widely unregulated market.”
A version of this article first appeared on WebMD.com.




