User login
Magnesium-rich diet linked to lower dementia risk
Investigators studied more than 6,000 cognitively healthy individuals, aged 40-73, and found that those who consumed more than 550 mg of magnesium daily had a brain age approximately 1 year younger by age 55 years, compared with a person who consumed a normal magnesium intake (~360 mg per day).
“This research highlights the potential benefits of a diet high in magnesium and the role it plays in promoting good brain health,” lead author Khawlah Alateeq, a PhD candidate in neuroscience at Australian National University’s National Centre for Epidemiology and Population Health, said in an interview.
Clinicians “can use [the findings] to counsel patients on the benefits of increasing magnesium intake through a healthy diet and monitoring magnesium levels to prevent deficiencies,” she stated.
The study was published online in the European Journal of Nutrition.
Promising target
The researchers were motivated to conduct the study because of “the growing concern over the increasing prevalence of dementia,” Ms. Alateeq said.
“Since there is no cure for dementia, and the development of pharmacological treatment for dementia has been unsuccessful over the last 30 years, prevention has been suggested as an effective approach to address the issue,” she added.
Nutrition, Ms. Alateeq said, is a “modifiable risk factor that can influence brain health and is highly amenable to scalable and cost-effective interventions.” It represents “a promising target” for risk reduction at a population level.
Previous research shows individuals with lower magnesium levels are at higher risk for AD, while those with higher dietary magnesium intake may be at lower risk of progressing from normal aging to cognitive impairment.
Most previous studies, however, included participants older than age 60 years, and it’s “unclear when the neuroprotective effects of dietary magnesium become detectable,” the researchers note.
Moreover, dietary patterns change and fluctuate, potentially leading to changes in magnesium intake over time. These changes may have as much impact as absolute magnesium at any point in time.
In light of the “current lack of understanding of when and to what extent dietary magnesium exerts its protective effects on the brain,” the researchers examined the association between magnesium trajectories over time, brain matter, and white matter lesions.
They also examined the association between magnesium and several different blood pressure measures (mean arterial pressure, systolic blood pressure, diastolic blood pressure, and pulse pressure).
Since cardiovascular health, neurodegeneration, and brain shrinkage patterns differ between men and women, the researchers stratified their analyses by sex.
Brain volume differences
The researchers analyzed the dietary magnesium intake of 6,001 individuals (mean age, 55.3 years) selected from the UK Biobank – a prospective cohort study of participants aged 37-73 at baseline, who were assessed between 2005 and 2023.
For the current study, only participants with baseline DBP and SBP measurements and structural MRI scans were included. Participants were also required to be free of neurologic disorders and to have an available record of dietary magnesium intake.
Covariates included age, sex, education, health conditions, smoking status, body mass index, amount of physical activity, smoking status, and alcohol intake.
Over a 16-month period, participants completed an online questionnaire five times. Their responses were used to calculate daily magnesium intake. Foods of particular interest included leafy green vegetables, legumes, nuts, seeds, and whole grains, all of which are magnesium rich.
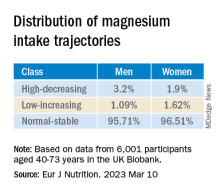
They used latent class analysis (LCA) to “identify mutually exclusive subgroup (classes) of magnesium intake trajectory separately for men and women.”
Men had a slightly higher prevalence of BP medication and diabetes, compared with women, and postmenopausal women had a higher prevalence of BP medication and diabetes, compared with premenopausal women.
Compared with lower baseline magnesium intake, higher baseline dietary intake of magnesium was associated with larger brain volumes in several regions in both men and women.
The latent class analysis identified three classes of magnesium intake:
In women in particular, the “high-decreasing” trajectory was significantly associated with larger brain volumes, compared with the “normal-stable” trajectory, while the “low-increasing” trajectory was associated with smaller brain volumes.
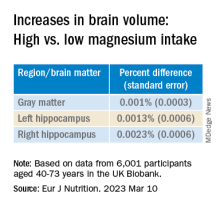
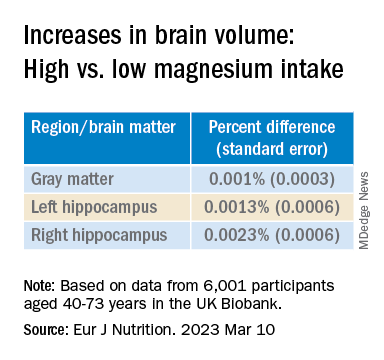
Even an increase of 1 mg of magnesium per day (above 350 mg/day) made a difference in brain volume, especially in women. The changes associated with every 1-mg increase are found in the table below:
Associations between magnesium and BP measures were “mostly nonsignificant,” the researchers say, and the neuroprotective effect of higher magnesium intake in the high-decreasing trajectory was greater in postmenopausal versus premenopausal women.
“Our models indicate that compared to somebody with a normal magnesium intake (~350 mg per day), somebody in the top quartile of magnesium intake (≥ 550 mg per day) would be predicted to have a ~0.20% larger GM and ~0.46% larger RHC,” the authors summarize.
“In a population with an average age of 55 years, this effect corresponds to ~1 year of typical aging,” they note. “In other words, if this effect is generalizable to other populations, a 41% increase in magnesium intake may lead to significantly better brain health.”
Although the exact mechanisms underlying magnesium’s protective effects are “not yet clearly understood, there’s considerable evidence that magnesium levels are related to better cardiovascular health. Magnesium supplementation has been found to decrease blood pressure – and high blood pressure is a well-established risk factor for dementia,” said Ms. Alateeq.
Association, not causation
Yuko Hara, PhD, director of Aging and Prevention, Alzheimer’s Drug Discovery Foundation, noted that the study is observational and therefore shows an association, not causation.
“People eating a high-magnesium diet may also be eating a brain-healthy diet and getting high levels of nutrients/minerals other than magnesium alone,” suggested Dr. Hara, who was not involved with the study.
She noted that many foods are good sources of magnesium, including spinach, almonds, cashews, legumes, yogurt, brown rice, and avocados.
“Eating a brain-healthy diet (for example, the Mediterranean diet) is one of the Seven Steps to Protect Your Cognitive Vitality that ADDF’s Cognitive Vitality promotes,” she said.
Open Access funding was enabled and organized by the Council of Australian University Librarians and its Member Institutions. Ms. Alateeq, her co-authors, and Dr. Hara declare no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Investigators studied more than 6,000 cognitively healthy individuals, aged 40-73, and found that those who consumed more than 550 mg of magnesium daily had a brain age approximately 1 year younger by age 55 years, compared with a person who consumed a normal magnesium intake (~360 mg per day).
“This research highlights the potential benefits of a diet high in magnesium and the role it plays in promoting good brain health,” lead author Khawlah Alateeq, a PhD candidate in neuroscience at Australian National University’s National Centre for Epidemiology and Population Health, said in an interview.
Clinicians “can use [the findings] to counsel patients on the benefits of increasing magnesium intake through a healthy diet and monitoring magnesium levels to prevent deficiencies,” she stated.
The study was published online in the European Journal of Nutrition.
Promising target
The researchers were motivated to conduct the study because of “the growing concern over the increasing prevalence of dementia,” Ms. Alateeq said.
“Since there is no cure for dementia, and the development of pharmacological treatment for dementia has been unsuccessful over the last 30 years, prevention has been suggested as an effective approach to address the issue,” she added.
Nutrition, Ms. Alateeq said, is a “modifiable risk factor that can influence brain health and is highly amenable to scalable and cost-effective interventions.” It represents “a promising target” for risk reduction at a population level.
Previous research shows individuals with lower magnesium levels are at higher risk for AD, while those with higher dietary magnesium intake may be at lower risk of progressing from normal aging to cognitive impairment.
Most previous studies, however, included participants older than age 60 years, and it’s “unclear when the neuroprotective effects of dietary magnesium become detectable,” the researchers note.
Moreover, dietary patterns change and fluctuate, potentially leading to changes in magnesium intake over time. These changes may have as much impact as absolute magnesium at any point in time.
In light of the “current lack of understanding of when and to what extent dietary magnesium exerts its protective effects on the brain,” the researchers examined the association between magnesium trajectories over time, brain matter, and white matter lesions.
They also examined the association between magnesium and several different blood pressure measures (mean arterial pressure, systolic blood pressure, diastolic blood pressure, and pulse pressure).
Since cardiovascular health, neurodegeneration, and brain shrinkage patterns differ between men and women, the researchers stratified their analyses by sex.
Brain volume differences
The researchers analyzed the dietary magnesium intake of 6,001 individuals (mean age, 55.3 years) selected from the UK Biobank – a prospective cohort study of participants aged 37-73 at baseline, who were assessed between 2005 and 2023.
For the current study, only participants with baseline DBP and SBP measurements and structural MRI scans were included. Participants were also required to be free of neurologic disorders and to have an available record of dietary magnesium intake.
Covariates included age, sex, education, health conditions, smoking status, body mass index, amount of physical activity, smoking status, and alcohol intake.
Over a 16-month period, participants completed an online questionnaire five times. Their responses were used to calculate daily magnesium intake. Foods of particular interest included leafy green vegetables, legumes, nuts, seeds, and whole grains, all of which are magnesium rich.
They used latent class analysis (LCA) to “identify mutually exclusive subgroup (classes) of magnesium intake trajectory separately for men and women.”
Men had a slightly higher prevalence of BP medication and diabetes, compared with women, and postmenopausal women had a higher prevalence of BP medication and diabetes, compared with premenopausal women.
Compared with lower baseline magnesium intake, higher baseline dietary intake of magnesium was associated with larger brain volumes in several regions in both men and women.
The latent class analysis identified three classes of magnesium intake:
In women in particular, the “high-decreasing” trajectory was significantly associated with larger brain volumes, compared with the “normal-stable” trajectory, while the “low-increasing” trajectory was associated with smaller brain volumes.
Even an increase of 1 mg of magnesium per day (above 350 mg/day) made a difference in brain volume, especially in women. The changes associated with every 1-mg increase are found in the table below:
Associations between magnesium and BP measures were “mostly nonsignificant,” the researchers say, and the neuroprotective effect of higher magnesium intake in the high-decreasing trajectory was greater in postmenopausal versus premenopausal women.
“Our models indicate that compared to somebody with a normal magnesium intake (~350 mg per day), somebody in the top quartile of magnesium intake (≥ 550 mg per day) would be predicted to have a ~0.20% larger GM and ~0.46% larger RHC,” the authors summarize.
“In a population with an average age of 55 years, this effect corresponds to ~1 year of typical aging,” they note. “In other words, if this effect is generalizable to other populations, a 41% increase in magnesium intake may lead to significantly better brain health.”
Although the exact mechanisms underlying magnesium’s protective effects are “not yet clearly understood, there’s considerable evidence that magnesium levels are related to better cardiovascular health. Magnesium supplementation has been found to decrease blood pressure – and high blood pressure is a well-established risk factor for dementia,” said Ms. Alateeq.
Association, not causation
Yuko Hara, PhD, director of Aging and Prevention, Alzheimer’s Drug Discovery Foundation, noted that the study is observational and therefore shows an association, not causation.
“People eating a high-magnesium diet may also be eating a brain-healthy diet and getting high levels of nutrients/minerals other than magnesium alone,” suggested Dr. Hara, who was not involved with the study.
She noted that many foods are good sources of magnesium, including spinach, almonds, cashews, legumes, yogurt, brown rice, and avocados.
“Eating a brain-healthy diet (for example, the Mediterranean diet) is one of the Seven Steps to Protect Your Cognitive Vitality that ADDF’s Cognitive Vitality promotes,” she said.
Open Access funding was enabled and organized by the Council of Australian University Librarians and its Member Institutions. Ms. Alateeq, her co-authors, and Dr. Hara declare no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Investigators studied more than 6,000 cognitively healthy individuals, aged 40-73, and found that those who consumed more than 550 mg of magnesium daily had a brain age approximately 1 year younger by age 55 years, compared with a person who consumed a normal magnesium intake (~360 mg per day).
“This research highlights the potential benefits of a diet high in magnesium and the role it plays in promoting good brain health,” lead author Khawlah Alateeq, a PhD candidate in neuroscience at Australian National University’s National Centre for Epidemiology and Population Health, said in an interview.
Clinicians “can use [the findings] to counsel patients on the benefits of increasing magnesium intake through a healthy diet and monitoring magnesium levels to prevent deficiencies,” she stated.
The study was published online in the European Journal of Nutrition.
Promising target
The researchers were motivated to conduct the study because of “the growing concern over the increasing prevalence of dementia,” Ms. Alateeq said.
“Since there is no cure for dementia, and the development of pharmacological treatment for dementia has been unsuccessful over the last 30 years, prevention has been suggested as an effective approach to address the issue,” she added.
Nutrition, Ms. Alateeq said, is a “modifiable risk factor that can influence brain health and is highly amenable to scalable and cost-effective interventions.” It represents “a promising target” for risk reduction at a population level.
Previous research shows individuals with lower magnesium levels are at higher risk for AD, while those with higher dietary magnesium intake may be at lower risk of progressing from normal aging to cognitive impairment.
Most previous studies, however, included participants older than age 60 years, and it’s “unclear when the neuroprotective effects of dietary magnesium become detectable,” the researchers note.
Moreover, dietary patterns change and fluctuate, potentially leading to changes in magnesium intake over time. These changes may have as much impact as absolute magnesium at any point in time.
In light of the “current lack of understanding of when and to what extent dietary magnesium exerts its protective effects on the brain,” the researchers examined the association between magnesium trajectories over time, brain matter, and white matter lesions.
They also examined the association between magnesium and several different blood pressure measures (mean arterial pressure, systolic blood pressure, diastolic blood pressure, and pulse pressure).
Since cardiovascular health, neurodegeneration, and brain shrinkage patterns differ between men and women, the researchers stratified their analyses by sex.
Brain volume differences
The researchers analyzed the dietary magnesium intake of 6,001 individuals (mean age, 55.3 years) selected from the UK Biobank – a prospective cohort study of participants aged 37-73 at baseline, who were assessed between 2005 and 2023.
For the current study, only participants with baseline DBP and SBP measurements and structural MRI scans were included. Participants were also required to be free of neurologic disorders and to have an available record of dietary magnesium intake.
Covariates included age, sex, education, health conditions, smoking status, body mass index, amount of physical activity, smoking status, and alcohol intake.
Over a 16-month period, participants completed an online questionnaire five times. Their responses were used to calculate daily magnesium intake. Foods of particular interest included leafy green vegetables, legumes, nuts, seeds, and whole grains, all of which are magnesium rich.
They used latent class analysis (LCA) to “identify mutually exclusive subgroup (classes) of magnesium intake trajectory separately for men and women.”
Men had a slightly higher prevalence of BP medication and diabetes, compared with women, and postmenopausal women had a higher prevalence of BP medication and diabetes, compared with premenopausal women.
Compared with lower baseline magnesium intake, higher baseline dietary intake of magnesium was associated with larger brain volumes in several regions in both men and women.
The latent class analysis identified three classes of magnesium intake:
In women in particular, the “high-decreasing” trajectory was significantly associated with larger brain volumes, compared with the “normal-stable” trajectory, while the “low-increasing” trajectory was associated with smaller brain volumes.
Even an increase of 1 mg of magnesium per day (above 350 mg/day) made a difference in brain volume, especially in women. The changes associated with every 1-mg increase are found in the table below:
Associations between magnesium and BP measures were “mostly nonsignificant,” the researchers say, and the neuroprotective effect of higher magnesium intake in the high-decreasing trajectory was greater in postmenopausal versus premenopausal women.
“Our models indicate that compared to somebody with a normal magnesium intake (~350 mg per day), somebody in the top quartile of magnesium intake (≥ 550 mg per day) would be predicted to have a ~0.20% larger GM and ~0.46% larger RHC,” the authors summarize.
“In a population with an average age of 55 years, this effect corresponds to ~1 year of typical aging,” they note. “In other words, if this effect is generalizable to other populations, a 41% increase in magnesium intake may lead to significantly better brain health.”
Although the exact mechanisms underlying magnesium’s protective effects are “not yet clearly understood, there’s considerable evidence that magnesium levels are related to better cardiovascular health. Magnesium supplementation has been found to decrease blood pressure – and high blood pressure is a well-established risk factor for dementia,” said Ms. Alateeq.
Association, not causation
Yuko Hara, PhD, director of Aging and Prevention, Alzheimer’s Drug Discovery Foundation, noted that the study is observational and therefore shows an association, not causation.
“People eating a high-magnesium diet may also be eating a brain-healthy diet and getting high levels of nutrients/minerals other than magnesium alone,” suggested Dr. Hara, who was not involved with the study.
She noted that many foods are good sources of magnesium, including spinach, almonds, cashews, legumes, yogurt, brown rice, and avocados.
“Eating a brain-healthy diet (for example, the Mediterranean diet) is one of the Seven Steps to Protect Your Cognitive Vitality that ADDF’s Cognitive Vitality promotes,” she said.
Open Access funding was enabled and organized by the Council of Australian University Librarians and its Member Institutions. Ms. Alateeq, her co-authors, and Dr. Hara declare no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM EUROPEAN JOURNAL OF NUTRITION
Children ate more fruits and vegetables during longer meals: Study
Adding 10 minutes to family mealtimes increased children’s consumption of fruits and vegetables by approximately one portion, based on data from 50 parent-child dyads.
Family meals are known to affect children’s food choices and preferences and can be an effective setting for improving children’s nutrition, wrote Mattea Dallacker, PhD, of the University of Mannheim, Germany, and colleagues.
However, the effect of extending meal duration on increasing fruit and vegetable intake in particular has not been examined, they said.
In a study published in JAMA Network Open, the researchers provided two free evening meals to 50 parent-child dyads under each of two different conditions. The control condition was defined by the families as a regular family mealtime duration (an average meal was 20.83 minutes), while the intervention was an average meal time 10 minutes (50%) longer. The age of the parents ranged from 22 to 55 years, with a mean of 43 years; 72% of the parent participants were mothers. The children’s ages ranged from 6 to 11 years, with a mean of 8 years, with approximately equal numbers of boys and girls.
The study was conducted in a family meal laboratory setting in Berlin, and groups were randomized to the longer or shorter meal setting first. The primary outcome was the total number of pieces of fruit and vegetables eaten by the child as part of each of the two meals.
Both meals were the “typical German evening meal of sliced bread, cold cuts of cheese and meat, and bite-sized pieces of fruits and vegetables,” followed by a dessert course of chocolate pudding or fruit yogurt and cookies, the researchers wrote. Beverages were water and one sugar-sweetened beverage; the specific foods and beverages were based on the child’s preferences, reported in an online preassessment, and the foods were consistent for the longer and shorter meals. All participants were asked not to eat for 2 hours prior to arriving for their meals at the laboratory.
During longer meals, children ate an average of seven additional bite-sized pieces of fruits and vegetables, which translates to approximately a full portion (defined as 100 g, such as a medium apple), the researchers wrote. The difference was significant compared with the shorter meals for fruits (P = .01) and vegetables (P < .001).
A piece of fruit was approximately 10 grams (6-10 g for grapes and tangerine segments; 10-14 g for cherry tomatoes; and 9-11 g for apple, banana, carrot, or cucumber). Other foods served with the meals included cheese, meats, butter, and sweet spreads.
Children also ate more slowly (defined as fewer bites per minute) during the longer meals, and they reported significantly greater satiety after the longer meals (P < .001 for both). The consumption of bread and cold cuts was similar for the two meal settings.
“Higher intake of fruits and vegetables during longer meals cannot be explained by longer exposure to food alone; otherwise, an increased intake of bread and cold cuts would have occurred,” the researchers wrote in their discussion. “One possible explanation is that the fruits and vegetables were cut into bite-sized pieces, making them convenient to eat.”
Further analysis showed that during the longer meals, more fruits and vegetables were consumed overall, but more vegetables were eaten from the start of the meal, while the additional fruit was eaten during the additional time at the end.
The findings were limited by several factors, primarily use of a laboratory setting that does not generalize to natural eating environments, the researchers noted. Other potential limitations included the effect of a video cameras on desirable behaviors and the limited ethnic and socioeconomic diversity of the study population, they said. The results were strengthened by the within-dyad study design that allowed for control of factors such as video observation, but more research is needed with more diverse groups and across longer time frames, the researchers said.
However, the results suggest that adding 10 minutes to a family mealtime can yield significant improvements in children’s diets, they said. They suggested strategies including playing music chosen by the child/children and setting rules that everyone must remain at the table for a certain length of time, with fruits and vegetables available on the table.
“If the effects of this simple, inexpensive, and low-threshold intervention prove stable over time, it could contribute to addressing a major public health problem,” the researchers concluded.
Findings intriguing, more data needed
The current study is important because food and vegetable intake in the majority of children falls below the recommended daily allowance, Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview.
The key take-home message for clinicians is the continued need to stress the importance of family meals, said Dr. Kinsella. “Many children continue to be overbooked with activities, and it may be rare for many families to sit down together for a meal for any length of time.”
Don’t discount the potential effect of a longer school lunch on children’s fruit and vegetable consumption as well, she added. “Advocating for longer lunch time is important, as many kids report not being able to finish their lunch at school.”
The current study was limited by being conducted in a lab setting, which may have influenced children’s desire for different foods, “also they had fewer distractions, and were being offered favorite foods,” said Dr. Kinsella.
Looking ahead, “it would be interesting to see if this result carried over to nonpreferred fruits and veggies and made any difference for picky eaters,” she said.
The study received no outside funding. The open-access publication of the study (but not the study itself) was supported by the Max Planck Institute for Human Development Library Open Access Fund. The researchers had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
Adding 10 minutes to family mealtimes increased children’s consumption of fruits and vegetables by approximately one portion, based on data from 50 parent-child dyads.
Family meals are known to affect children’s food choices and preferences and can be an effective setting for improving children’s nutrition, wrote Mattea Dallacker, PhD, of the University of Mannheim, Germany, and colleagues.
However, the effect of extending meal duration on increasing fruit and vegetable intake in particular has not been examined, they said.
In a study published in JAMA Network Open, the researchers provided two free evening meals to 50 parent-child dyads under each of two different conditions. The control condition was defined by the families as a regular family mealtime duration (an average meal was 20.83 minutes), while the intervention was an average meal time 10 minutes (50%) longer. The age of the parents ranged from 22 to 55 years, with a mean of 43 years; 72% of the parent participants were mothers. The children’s ages ranged from 6 to 11 years, with a mean of 8 years, with approximately equal numbers of boys and girls.
The study was conducted in a family meal laboratory setting in Berlin, and groups were randomized to the longer or shorter meal setting first. The primary outcome was the total number of pieces of fruit and vegetables eaten by the child as part of each of the two meals.
Both meals were the “typical German evening meal of sliced bread, cold cuts of cheese and meat, and bite-sized pieces of fruits and vegetables,” followed by a dessert course of chocolate pudding or fruit yogurt and cookies, the researchers wrote. Beverages were water and one sugar-sweetened beverage; the specific foods and beverages were based on the child’s preferences, reported in an online preassessment, and the foods were consistent for the longer and shorter meals. All participants were asked not to eat for 2 hours prior to arriving for their meals at the laboratory.
During longer meals, children ate an average of seven additional bite-sized pieces of fruits and vegetables, which translates to approximately a full portion (defined as 100 g, such as a medium apple), the researchers wrote. The difference was significant compared with the shorter meals for fruits (P = .01) and vegetables (P < .001).
A piece of fruit was approximately 10 grams (6-10 g for grapes and tangerine segments; 10-14 g for cherry tomatoes; and 9-11 g for apple, banana, carrot, or cucumber). Other foods served with the meals included cheese, meats, butter, and sweet spreads.
Children also ate more slowly (defined as fewer bites per minute) during the longer meals, and they reported significantly greater satiety after the longer meals (P < .001 for both). The consumption of bread and cold cuts was similar for the two meal settings.
“Higher intake of fruits and vegetables during longer meals cannot be explained by longer exposure to food alone; otherwise, an increased intake of bread and cold cuts would have occurred,” the researchers wrote in their discussion. “One possible explanation is that the fruits and vegetables were cut into bite-sized pieces, making them convenient to eat.”
Further analysis showed that during the longer meals, more fruits and vegetables were consumed overall, but more vegetables were eaten from the start of the meal, while the additional fruit was eaten during the additional time at the end.
The findings were limited by several factors, primarily use of a laboratory setting that does not generalize to natural eating environments, the researchers noted. Other potential limitations included the effect of a video cameras on desirable behaviors and the limited ethnic and socioeconomic diversity of the study population, they said. The results were strengthened by the within-dyad study design that allowed for control of factors such as video observation, but more research is needed with more diverse groups and across longer time frames, the researchers said.
However, the results suggest that adding 10 minutes to a family mealtime can yield significant improvements in children’s diets, they said. They suggested strategies including playing music chosen by the child/children and setting rules that everyone must remain at the table for a certain length of time, with fruits and vegetables available on the table.
“If the effects of this simple, inexpensive, and low-threshold intervention prove stable over time, it could contribute to addressing a major public health problem,” the researchers concluded.
Findings intriguing, more data needed
The current study is important because food and vegetable intake in the majority of children falls below the recommended daily allowance, Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview.
The key take-home message for clinicians is the continued need to stress the importance of family meals, said Dr. Kinsella. “Many children continue to be overbooked with activities, and it may be rare for many families to sit down together for a meal for any length of time.”
Don’t discount the potential effect of a longer school lunch on children’s fruit and vegetable consumption as well, she added. “Advocating for longer lunch time is important, as many kids report not being able to finish their lunch at school.”
The current study was limited by being conducted in a lab setting, which may have influenced children’s desire for different foods, “also they had fewer distractions, and were being offered favorite foods,” said Dr. Kinsella.
Looking ahead, “it would be interesting to see if this result carried over to nonpreferred fruits and veggies and made any difference for picky eaters,” she said.
The study received no outside funding. The open-access publication of the study (but not the study itself) was supported by the Max Planck Institute for Human Development Library Open Access Fund. The researchers had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
Adding 10 minutes to family mealtimes increased children’s consumption of fruits and vegetables by approximately one portion, based on data from 50 parent-child dyads.
Family meals are known to affect children’s food choices and preferences and can be an effective setting for improving children’s nutrition, wrote Mattea Dallacker, PhD, of the University of Mannheim, Germany, and colleagues.
However, the effect of extending meal duration on increasing fruit and vegetable intake in particular has not been examined, they said.
In a study published in JAMA Network Open, the researchers provided two free evening meals to 50 parent-child dyads under each of two different conditions. The control condition was defined by the families as a regular family mealtime duration (an average meal was 20.83 minutes), while the intervention was an average meal time 10 minutes (50%) longer. The age of the parents ranged from 22 to 55 years, with a mean of 43 years; 72% of the parent participants were mothers. The children’s ages ranged from 6 to 11 years, with a mean of 8 years, with approximately equal numbers of boys and girls.
The study was conducted in a family meal laboratory setting in Berlin, and groups were randomized to the longer or shorter meal setting first. The primary outcome was the total number of pieces of fruit and vegetables eaten by the child as part of each of the two meals.
Both meals were the “typical German evening meal of sliced bread, cold cuts of cheese and meat, and bite-sized pieces of fruits and vegetables,” followed by a dessert course of chocolate pudding or fruit yogurt and cookies, the researchers wrote. Beverages were water and one sugar-sweetened beverage; the specific foods and beverages were based on the child’s preferences, reported in an online preassessment, and the foods were consistent for the longer and shorter meals. All participants were asked not to eat for 2 hours prior to arriving for their meals at the laboratory.
During longer meals, children ate an average of seven additional bite-sized pieces of fruits and vegetables, which translates to approximately a full portion (defined as 100 g, such as a medium apple), the researchers wrote. The difference was significant compared with the shorter meals for fruits (P = .01) and vegetables (P < .001).
A piece of fruit was approximately 10 grams (6-10 g for grapes and tangerine segments; 10-14 g for cherry tomatoes; and 9-11 g for apple, banana, carrot, or cucumber). Other foods served with the meals included cheese, meats, butter, and sweet spreads.
Children also ate more slowly (defined as fewer bites per minute) during the longer meals, and they reported significantly greater satiety after the longer meals (P < .001 for both). The consumption of bread and cold cuts was similar for the two meal settings.
“Higher intake of fruits and vegetables during longer meals cannot be explained by longer exposure to food alone; otherwise, an increased intake of bread and cold cuts would have occurred,” the researchers wrote in their discussion. “One possible explanation is that the fruits and vegetables were cut into bite-sized pieces, making them convenient to eat.”
Further analysis showed that during the longer meals, more fruits and vegetables were consumed overall, but more vegetables were eaten from the start of the meal, while the additional fruit was eaten during the additional time at the end.
The findings were limited by several factors, primarily use of a laboratory setting that does not generalize to natural eating environments, the researchers noted. Other potential limitations included the effect of a video cameras on desirable behaviors and the limited ethnic and socioeconomic diversity of the study population, they said. The results were strengthened by the within-dyad study design that allowed for control of factors such as video observation, but more research is needed with more diverse groups and across longer time frames, the researchers said.
However, the results suggest that adding 10 minutes to a family mealtime can yield significant improvements in children’s diets, they said. They suggested strategies including playing music chosen by the child/children and setting rules that everyone must remain at the table for a certain length of time, with fruits and vegetables available on the table.
“If the effects of this simple, inexpensive, and low-threshold intervention prove stable over time, it could contribute to addressing a major public health problem,” the researchers concluded.
Findings intriguing, more data needed
The current study is important because food and vegetable intake in the majority of children falls below the recommended daily allowance, Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview.
The key take-home message for clinicians is the continued need to stress the importance of family meals, said Dr. Kinsella. “Many children continue to be overbooked with activities, and it may be rare for many families to sit down together for a meal for any length of time.”
Don’t discount the potential effect of a longer school lunch on children’s fruit and vegetable consumption as well, she added. “Advocating for longer lunch time is important, as many kids report not being able to finish their lunch at school.”
The current study was limited by being conducted in a lab setting, which may have influenced children’s desire for different foods, “also they had fewer distractions, and were being offered favorite foods,” said Dr. Kinsella.
Looking ahead, “it would be interesting to see if this result carried over to nonpreferred fruits and veggies and made any difference for picky eaters,” she said.
The study received no outside funding. The open-access publication of the study (but not the study itself) was supported by the Max Planck Institute for Human Development Library Open Access Fund. The researchers had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
FROM JAMA NETWORK OPEN
Likely cause of mysterious hepatitis outbreak in children identified
Coinfection with AAV2 and a human adenovirus (HAdV), in particular, appears to leave some children more vulnerable to this acute hepatitis of unknown origin, researchers reported in three studies published online in Nature. Coinfection with Epstein-Barr virus (EBV), herpes, and enterovirus also were found. Adeno-associated viruses are not considered pathogenic on their own and require a “helper” virus for productive infection.
“I am quite confident that we have identified the key viruses involved because we used a comprehensive metagenomic sequencing approach to look for potential infections from any virus or non-viral pathogen,” Charles Chiu, MD, PhD, senior author and professor of laboratory medicine and medicine/infectious diseases at the University of California, San Francisco, said in an interview.
Dr. Chiu and colleagues propose that lockdowns and social isolation during the COVID-19 pandemic left more children susceptible. A major aspect of immunity in childhood is the adaptive immune response – both cell-mediated and humoral – shaped in part by exposure to viruses and other pathogens early in life, Dr. Chiu said.
“Due to COVID-19, a large population of children did not experience this, so it is possible once restrictions were lifted, they were suddenly exposed over a short period of time to multiple viruses that, in a poorly trained immune system, would have increased their risk of developing severe disease,” he said.
This theory has been popular, especially because cases of unexplained acute hepatitis peaked during the height of the COVID-19 pandemic when isolation was common, William F. Balistreri, MD, who was not affiliated with the study, told this news organization. Dr. Balistreri is professor of pediatrics and director emeritus of the Pediatric Liver Care Center at Cincinnati Children’s Hospital Medical Center.
Identifying the culprits
Determining what factors might be involved was the main aim of the etiology study by Dr. Chiu and colleagues published online in Nature.
The journal simultaneously published a genomic study confirming the presence of AAV2 and other suspected viruses and a genomic and laboratory study further corroborating the results.
More than 1,000 children worldwide had been diagnosed with unexplained acute pediatric hepatitis as of August 2022. In the United States, there have been 358 cases, including 22 in which the child required a liver transplant and 13 in which the child died.
This new form of hepatitis, first detected in October 2021, does not fit into existing classifications of types A through E, so some researchers refer to the condition as acute non–A-E hepatitis of unknown etiology.
The investigators started with an important clue based on previous research: the role adenovirus might play. Dr. Chiu and colleagues assessed 27 blood, stool, and other samples from 16 affected children who each previously tested positive for adenoviruses. The researchers included cases of the condition identified up until May 22, 2022. The median age was 3 years, and approximately half were boys.
They compared viruses present in these children with those in 113 controls without the mysterious hepatitis. The control group consisted of 15 children who were hospitalized with a nonhepatitis inflammatory condition, 27 with a noninflammatory condition, 30 with acute hepatitis of known origin, 12 with acute gastroenteritis and an HAdV-positive stool sample, and 11 with acute gastroenteritis and an HAdV-negative stool sample, as well as 18 blood donors. The median age was 7 years.
The researchers assessed samples using multiple technologies, including metagenomic sequencing, tiling multiplex polymerase chain reaction (PCR) amplicon sequencing, metagenomic sequencing with probe capture viral enrichment, and virus-specific PCR. Many of these advanced techniques were not even available 5-10 years ago, Dr. Chiu said.
Key findings
Blood samples were available for 14 of the 16 children with acute hepatitis of unknown origin. Among this study group, AAV2 was found in 13 (93%). No other adeno-associated viruses were found. HAdV was detected in all 14 children: HAdV-41 in 11 children and HAdV-40, HAdV-2, and an untypeable strain in one child each. This finding was not intuitive because HAdVs are not commonly associated with hepatitis, according to the study.
AAV2 was much less common in the control group. For example, it was found in none of the children with hepatitis of known origin and in only four children (3.5%) with acute gastroenteritis and HAdV-positive stool. Of note, neither AAV2 nor HAdV-41 was detected among the 30 pediatric controls with acute hepatitis of defined etiology nor 42 of the hospitalized children without hepatitis, the researchers wrote.
In the search for other viruses in the study group, metagenomic sequencing detected EBV, also known as human herpesvirus (HHV)–4, in two children, cytomegalovirus (CMV) in one child, and HAdV type C in one child.
Analysis of whole blood revealed enterovirus A71 in one patient. HAdV type C also was detected in one child on the basis of a nasopharyngeal swab, and picobirnavirus was found in a stool sample from another patient.
Researchers conducted virus-specific PCR tests on both patient groups to identify additional viruses that may be associated with the unexplained acute hepatitis. EBV/HHV-4 was detected in 11 children (79%) in the study group vs. in 1 child (0.88%) in the control group. HHV-6 was detected in seven children (50%) in the study group, compared with one case in the control group. CMV was not detected in any of the children in the study group versus vs. two children (1.8%) in the control group.
“Although we found significant differences in the relative proportions of EBV and HHV-6 in cases compared to controls, we do not believe that these viruses are the primary cause of acute severe hepatitis,” the researchers wrote. The viral load of the two herpes viruses were very low, so the positive results could represent integrated proviral DNA rather than bona fide low-level herpesvirus. In addition, herpesvirus can be reactivated by an inflammatory condition.
“Nevertheless, it is striking that among the 16 cases (in the study group), dual, triple, or quadruple infections with AAV2, adenovirus, and one or both herpesviruses were detected in whole blood from at least 12 cases (75%),” the researchers wrote.
Management of suspected hepatitis
The study’s key messages for parents and health care providers “are awareness and reassurance,” Dr. Balistreri said in an interview.
Vigilance also is warranted if a child develops prodromal symptoms including respiratory and/or gastrointestinal signs such as nausea, vomiting, diarrhea, and abdomen pain, he said. If jaundice or scleral icterus is noted, then hepatitis should be suspected.
Some patients need hospitalization and quickly recover. In very rare instances, the inflammation may progress to liver failure and transplantation, Dr. Balistreri said.
“Reassurance is based on the good news that most children with acute hepatitis get better. If a case arises, it is good practice to keep the child well hydrated, offer a normal diet, and avoid medications that may be cleared by the liver,” Dr. Balistreri added.
“Of course, COVID-19 vaccination is strongly suggested,” he said.
Some existing treatments could help against unexplained acute hepatitis, Dr. Chiu said. “The findings suggest that antiviral therapy might be effective in these cases.”
Cidofovir can be effective against adenovirus, according to a report in The Lancet . Similarly, ganciclovir or valganciclovir may have activity against EBV/HHV-4 or HHV-6, Dr. Chiu said. “However, antiviral therapy is not available for AAV2.”
The three studies published in Nature “offer compelling evidence, from disparate centers, of a linkage of outbreak cases to infection by AAV2,” Dr. Balistreri said. The studies also suggest that liver injury was related to abnormal immune responses. This is an important clinical distinction, indicating a potential therapeutic approach to future cases – immunosuppression rather than anti-adenoviral agents, he said.
“We await further studies of this important concept,” Dr. Balistreri said.
Many unanswered questions remain about the condition’s etiology, he added. Is there a synergy or shared susceptibility related to SARS-CoV-2? Is the COVID-19 virus helping to trigger these infections, or does it increase the risk once infected? Also, are other epigenetic factors or viruses involved?
Moving forward
The next steps in the research could go beyond identifying presence of these different viruses and determining which one(s) are contributing the most to the acute pediatric hepatitis, Dr. Chiu said.
The researchers also would like to test early results from the United Kingdom that identified a potential association of acute severe hepatitis with the presence of human leukocyte antigen genotype DRB1*04:01, he added.
They also might investigate other unintended potential clinical consequences of the COVID-19 pandemic, including long COVID and resurgence of infections from other viruses, such as respiratory syncytial virus, influenza, and enterovirus D68.
The study was supported by the Centers for Disease Control and Prevention, the National Institutes of Health, the Department of Homeland Security, and other grants. Dr. Chiu is a founder of Delve Bio and on the scientific advisory board for Delve Bio, Mammoth Biosciences, BiomeSense, and Poppy Health. Dr. Balistreri had no relevant disclosures.
A version of this article first appeared on Medscape.com.
Coinfection with AAV2 and a human adenovirus (HAdV), in particular, appears to leave some children more vulnerable to this acute hepatitis of unknown origin, researchers reported in three studies published online in Nature. Coinfection with Epstein-Barr virus (EBV), herpes, and enterovirus also were found. Adeno-associated viruses are not considered pathogenic on their own and require a “helper” virus for productive infection.
“I am quite confident that we have identified the key viruses involved because we used a comprehensive metagenomic sequencing approach to look for potential infections from any virus or non-viral pathogen,” Charles Chiu, MD, PhD, senior author and professor of laboratory medicine and medicine/infectious diseases at the University of California, San Francisco, said in an interview.
Dr. Chiu and colleagues propose that lockdowns and social isolation during the COVID-19 pandemic left more children susceptible. A major aspect of immunity in childhood is the adaptive immune response – both cell-mediated and humoral – shaped in part by exposure to viruses and other pathogens early in life, Dr. Chiu said.
“Due to COVID-19, a large population of children did not experience this, so it is possible once restrictions were lifted, they were suddenly exposed over a short period of time to multiple viruses that, in a poorly trained immune system, would have increased their risk of developing severe disease,” he said.
This theory has been popular, especially because cases of unexplained acute hepatitis peaked during the height of the COVID-19 pandemic when isolation was common, William F. Balistreri, MD, who was not affiliated with the study, told this news organization. Dr. Balistreri is professor of pediatrics and director emeritus of the Pediatric Liver Care Center at Cincinnati Children’s Hospital Medical Center.
Identifying the culprits
Determining what factors might be involved was the main aim of the etiology study by Dr. Chiu and colleagues published online in Nature.
The journal simultaneously published a genomic study confirming the presence of AAV2 and other suspected viruses and a genomic and laboratory study further corroborating the results.
More than 1,000 children worldwide had been diagnosed with unexplained acute pediatric hepatitis as of August 2022. In the United States, there have been 358 cases, including 22 in which the child required a liver transplant and 13 in which the child died.
This new form of hepatitis, first detected in October 2021, does not fit into existing classifications of types A through E, so some researchers refer to the condition as acute non–A-E hepatitis of unknown etiology.
The investigators started with an important clue based on previous research: the role adenovirus might play. Dr. Chiu and colleagues assessed 27 blood, stool, and other samples from 16 affected children who each previously tested positive for adenoviruses. The researchers included cases of the condition identified up until May 22, 2022. The median age was 3 years, and approximately half were boys.
They compared viruses present in these children with those in 113 controls without the mysterious hepatitis. The control group consisted of 15 children who were hospitalized with a nonhepatitis inflammatory condition, 27 with a noninflammatory condition, 30 with acute hepatitis of known origin, 12 with acute gastroenteritis and an HAdV-positive stool sample, and 11 with acute gastroenteritis and an HAdV-negative stool sample, as well as 18 blood donors. The median age was 7 years.
The researchers assessed samples using multiple technologies, including metagenomic sequencing, tiling multiplex polymerase chain reaction (PCR) amplicon sequencing, metagenomic sequencing with probe capture viral enrichment, and virus-specific PCR. Many of these advanced techniques were not even available 5-10 years ago, Dr. Chiu said.
Key findings
Blood samples were available for 14 of the 16 children with acute hepatitis of unknown origin. Among this study group, AAV2 was found in 13 (93%). No other adeno-associated viruses were found. HAdV was detected in all 14 children: HAdV-41 in 11 children and HAdV-40, HAdV-2, and an untypeable strain in one child each. This finding was not intuitive because HAdVs are not commonly associated with hepatitis, according to the study.
AAV2 was much less common in the control group. For example, it was found in none of the children with hepatitis of known origin and in only four children (3.5%) with acute gastroenteritis and HAdV-positive stool. Of note, neither AAV2 nor HAdV-41 was detected among the 30 pediatric controls with acute hepatitis of defined etiology nor 42 of the hospitalized children without hepatitis, the researchers wrote.
In the search for other viruses in the study group, metagenomic sequencing detected EBV, also known as human herpesvirus (HHV)–4, in two children, cytomegalovirus (CMV) in one child, and HAdV type C in one child.
Analysis of whole blood revealed enterovirus A71 in one patient. HAdV type C also was detected in one child on the basis of a nasopharyngeal swab, and picobirnavirus was found in a stool sample from another patient.
Researchers conducted virus-specific PCR tests on both patient groups to identify additional viruses that may be associated with the unexplained acute hepatitis. EBV/HHV-4 was detected in 11 children (79%) in the study group vs. in 1 child (0.88%) in the control group. HHV-6 was detected in seven children (50%) in the study group, compared with one case in the control group. CMV was not detected in any of the children in the study group versus vs. two children (1.8%) in the control group.
“Although we found significant differences in the relative proportions of EBV and HHV-6 in cases compared to controls, we do not believe that these viruses are the primary cause of acute severe hepatitis,” the researchers wrote. The viral load of the two herpes viruses were very low, so the positive results could represent integrated proviral DNA rather than bona fide low-level herpesvirus. In addition, herpesvirus can be reactivated by an inflammatory condition.
“Nevertheless, it is striking that among the 16 cases (in the study group), dual, triple, or quadruple infections with AAV2, adenovirus, and one or both herpesviruses were detected in whole blood from at least 12 cases (75%),” the researchers wrote.
Management of suspected hepatitis
The study’s key messages for parents and health care providers “are awareness and reassurance,” Dr. Balistreri said in an interview.
Vigilance also is warranted if a child develops prodromal symptoms including respiratory and/or gastrointestinal signs such as nausea, vomiting, diarrhea, and abdomen pain, he said. If jaundice or scleral icterus is noted, then hepatitis should be suspected.
Some patients need hospitalization and quickly recover. In very rare instances, the inflammation may progress to liver failure and transplantation, Dr. Balistreri said.
“Reassurance is based on the good news that most children with acute hepatitis get better. If a case arises, it is good practice to keep the child well hydrated, offer a normal diet, and avoid medications that may be cleared by the liver,” Dr. Balistreri added.
“Of course, COVID-19 vaccination is strongly suggested,” he said.
Some existing treatments could help against unexplained acute hepatitis, Dr. Chiu said. “The findings suggest that antiviral therapy might be effective in these cases.”
Cidofovir can be effective against adenovirus, according to a report in The Lancet . Similarly, ganciclovir or valganciclovir may have activity against EBV/HHV-4 or HHV-6, Dr. Chiu said. “However, antiviral therapy is not available for AAV2.”
The three studies published in Nature “offer compelling evidence, from disparate centers, of a linkage of outbreak cases to infection by AAV2,” Dr. Balistreri said. The studies also suggest that liver injury was related to abnormal immune responses. This is an important clinical distinction, indicating a potential therapeutic approach to future cases – immunosuppression rather than anti-adenoviral agents, he said.
“We await further studies of this important concept,” Dr. Balistreri said.
Many unanswered questions remain about the condition’s etiology, he added. Is there a synergy or shared susceptibility related to SARS-CoV-2? Is the COVID-19 virus helping to trigger these infections, or does it increase the risk once infected? Also, are other epigenetic factors or viruses involved?
Moving forward
The next steps in the research could go beyond identifying presence of these different viruses and determining which one(s) are contributing the most to the acute pediatric hepatitis, Dr. Chiu said.
The researchers also would like to test early results from the United Kingdom that identified a potential association of acute severe hepatitis with the presence of human leukocyte antigen genotype DRB1*04:01, he added.
They also might investigate other unintended potential clinical consequences of the COVID-19 pandemic, including long COVID and resurgence of infections from other viruses, such as respiratory syncytial virus, influenza, and enterovirus D68.
The study was supported by the Centers for Disease Control and Prevention, the National Institutes of Health, the Department of Homeland Security, and other grants. Dr. Chiu is a founder of Delve Bio and on the scientific advisory board for Delve Bio, Mammoth Biosciences, BiomeSense, and Poppy Health. Dr. Balistreri had no relevant disclosures.
A version of this article first appeared on Medscape.com.
Coinfection with AAV2 and a human adenovirus (HAdV), in particular, appears to leave some children more vulnerable to this acute hepatitis of unknown origin, researchers reported in three studies published online in Nature. Coinfection with Epstein-Barr virus (EBV), herpes, and enterovirus also were found. Adeno-associated viruses are not considered pathogenic on their own and require a “helper” virus for productive infection.
“I am quite confident that we have identified the key viruses involved because we used a comprehensive metagenomic sequencing approach to look for potential infections from any virus or non-viral pathogen,” Charles Chiu, MD, PhD, senior author and professor of laboratory medicine and medicine/infectious diseases at the University of California, San Francisco, said in an interview.
Dr. Chiu and colleagues propose that lockdowns and social isolation during the COVID-19 pandemic left more children susceptible. A major aspect of immunity in childhood is the adaptive immune response – both cell-mediated and humoral – shaped in part by exposure to viruses and other pathogens early in life, Dr. Chiu said.
“Due to COVID-19, a large population of children did not experience this, so it is possible once restrictions were lifted, they were suddenly exposed over a short period of time to multiple viruses that, in a poorly trained immune system, would have increased their risk of developing severe disease,” he said.
This theory has been popular, especially because cases of unexplained acute hepatitis peaked during the height of the COVID-19 pandemic when isolation was common, William F. Balistreri, MD, who was not affiliated with the study, told this news organization. Dr. Balistreri is professor of pediatrics and director emeritus of the Pediatric Liver Care Center at Cincinnati Children’s Hospital Medical Center.
Identifying the culprits
Determining what factors might be involved was the main aim of the etiology study by Dr. Chiu and colleagues published online in Nature.
The journal simultaneously published a genomic study confirming the presence of AAV2 and other suspected viruses and a genomic and laboratory study further corroborating the results.
More than 1,000 children worldwide had been diagnosed with unexplained acute pediatric hepatitis as of August 2022. In the United States, there have been 358 cases, including 22 in which the child required a liver transplant and 13 in which the child died.
This new form of hepatitis, first detected in October 2021, does not fit into existing classifications of types A through E, so some researchers refer to the condition as acute non–A-E hepatitis of unknown etiology.
The investigators started with an important clue based on previous research: the role adenovirus might play. Dr. Chiu and colleagues assessed 27 blood, stool, and other samples from 16 affected children who each previously tested positive for adenoviruses. The researchers included cases of the condition identified up until May 22, 2022. The median age was 3 years, and approximately half were boys.
They compared viruses present in these children with those in 113 controls without the mysterious hepatitis. The control group consisted of 15 children who were hospitalized with a nonhepatitis inflammatory condition, 27 with a noninflammatory condition, 30 with acute hepatitis of known origin, 12 with acute gastroenteritis and an HAdV-positive stool sample, and 11 with acute gastroenteritis and an HAdV-negative stool sample, as well as 18 blood donors. The median age was 7 years.
The researchers assessed samples using multiple technologies, including metagenomic sequencing, tiling multiplex polymerase chain reaction (PCR) amplicon sequencing, metagenomic sequencing with probe capture viral enrichment, and virus-specific PCR. Many of these advanced techniques were not even available 5-10 years ago, Dr. Chiu said.
Key findings
Blood samples were available for 14 of the 16 children with acute hepatitis of unknown origin. Among this study group, AAV2 was found in 13 (93%). No other adeno-associated viruses were found. HAdV was detected in all 14 children: HAdV-41 in 11 children and HAdV-40, HAdV-2, and an untypeable strain in one child each. This finding was not intuitive because HAdVs are not commonly associated with hepatitis, according to the study.
AAV2 was much less common in the control group. For example, it was found in none of the children with hepatitis of known origin and in only four children (3.5%) with acute gastroenteritis and HAdV-positive stool. Of note, neither AAV2 nor HAdV-41 was detected among the 30 pediatric controls with acute hepatitis of defined etiology nor 42 of the hospitalized children without hepatitis, the researchers wrote.
In the search for other viruses in the study group, metagenomic sequencing detected EBV, also known as human herpesvirus (HHV)–4, in two children, cytomegalovirus (CMV) in one child, and HAdV type C in one child.
Analysis of whole blood revealed enterovirus A71 in one patient. HAdV type C also was detected in one child on the basis of a nasopharyngeal swab, and picobirnavirus was found in a stool sample from another patient.
Researchers conducted virus-specific PCR tests on both patient groups to identify additional viruses that may be associated with the unexplained acute hepatitis. EBV/HHV-4 was detected in 11 children (79%) in the study group vs. in 1 child (0.88%) in the control group. HHV-6 was detected in seven children (50%) in the study group, compared with one case in the control group. CMV was not detected in any of the children in the study group versus vs. two children (1.8%) in the control group.
“Although we found significant differences in the relative proportions of EBV and HHV-6 in cases compared to controls, we do not believe that these viruses are the primary cause of acute severe hepatitis,” the researchers wrote. The viral load of the two herpes viruses were very low, so the positive results could represent integrated proviral DNA rather than bona fide low-level herpesvirus. In addition, herpesvirus can be reactivated by an inflammatory condition.
“Nevertheless, it is striking that among the 16 cases (in the study group), dual, triple, or quadruple infections with AAV2, adenovirus, and one or both herpesviruses were detected in whole blood from at least 12 cases (75%),” the researchers wrote.
Management of suspected hepatitis
The study’s key messages for parents and health care providers “are awareness and reassurance,” Dr. Balistreri said in an interview.
Vigilance also is warranted if a child develops prodromal symptoms including respiratory and/or gastrointestinal signs such as nausea, vomiting, diarrhea, and abdomen pain, he said. If jaundice or scleral icterus is noted, then hepatitis should be suspected.
Some patients need hospitalization and quickly recover. In very rare instances, the inflammation may progress to liver failure and transplantation, Dr. Balistreri said.
“Reassurance is based on the good news that most children with acute hepatitis get better. If a case arises, it is good practice to keep the child well hydrated, offer a normal diet, and avoid medications that may be cleared by the liver,” Dr. Balistreri added.
“Of course, COVID-19 vaccination is strongly suggested,” he said.
Some existing treatments could help against unexplained acute hepatitis, Dr. Chiu said. “The findings suggest that antiviral therapy might be effective in these cases.”
Cidofovir can be effective against adenovirus, according to a report in The Lancet . Similarly, ganciclovir or valganciclovir may have activity against EBV/HHV-4 or HHV-6, Dr. Chiu said. “However, antiviral therapy is not available for AAV2.”
The three studies published in Nature “offer compelling evidence, from disparate centers, of a linkage of outbreak cases to infection by AAV2,” Dr. Balistreri said. The studies also suggest that liver injury was related to abnormal immune responses. This is an important clinical distinction, indicating a potential therapeutic approach to future cases – immunosuppression rather than anti-adenoviral agents, he said.
“We await further studies of this important concept,” Dr. Balistreri said.
Many unanswered questions remain about the condition’s etiology, he added. Is there a synergy or shared susceptibility related to SARS-CoV-2? Is the COVID-19 virus helping to trigger these infections, or does it increase the risk once infected? Also, are other epigenetic factors or viruses involved?
Moving forward
The next steps in the research could go beyond identifying presence of these different viruses and determining which one(s) are contributing the most to the acute pediatric hepatitis, Dr. Chiu said.
The researchers also would like to test early results from the United Kingdom that identified a potential association of acute severe hepatitis with the presence of human leukocyte antigen genotype DRB1*04:01, he added.
They also might investigate other unintended potential clinical consequences of the COVID-19 pandemic, including long COVID and resurgence of infections from other viruses, such as respiratory syncytial virus, influenza, and enterovirus D68.
The study was supported by the Centers for Disease Control and Prevention, the National Institutes of Health, the Department of Homeland Security, and other grants. Dr. Chiu is a founder of Delve Bio and on the scientific advisory board for Delve Bio, Mammoth Biosciences, BiomeSense, and Poppy Health. Dr. Balistreri had no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM NATURE
Is vaping a gateway to cigarettes for kids?
Vaping may not be a gateway to long-term cigarette use for adolescents, a new study published in JAMA Network Open suggests.
Many studies have found that youth who vape are more likely to take up cigarette smoking, but whether that new habit lasts for a month or a lifetime has been unclear.
The percentage of adolescents who move on to smoking after starting to vape remains low, and those who do start smoking are unlikely to continue doing so for a long time, the new research shows.
“If they simply experiment with smoking but do not continue, their risks of smoking-related adverse health outcomes are low,” said Ruoyan Sun, PhD, assistant professor with the department of health policy and organization at the University of Alabama at Birmingham and the study’s lead author. “But if they do become regular or established smokers, then the risks can be substantial.”
Dr. Sun and her colleagues analyzed data from several waves of the longitudinal Population Assessment of Tobacco and Health study. Participants included 8,671 children and adolescents aged 12-17 years. Among teens who had ever vaped, 6% began smoking cigarettes and continued to smoke in the subsequent 3 years, the researchers found (95% confidence interval, 4.5%-8.0%), compared with 1.1% among teens who never vaped (95% CI, 0.8%-1.3%).
“The real concern is whether vaping is inducing significant numbers of young people to become confirmed smokers,” said Dr. Sun. “The answer is that it does not.”
Previous studies using PATH data have suggested that adolescents who use e-cigarettes are up to 3.5 times more likely than nonusers to start smoking tobacco cigarettes and that they may continue to use both products.
But in the new study, despite the low overall number of cigarette smokers, those in the group who used e-cigarettes were 81% more likely to continue smoking tobacco cigarettes after 3 years, compared with those who did not use e-cigarettes, researchers found (95% CI, 1.03-3.18).
Rachel Boykan, MD, clinical professor of pediatrics and attending physician at Stony Brook (N.Y.) Children’s Hospital, said that despite the findings, the overall messaging to patients remains the same: Vaping is linked to smoking.
“There is still a risk of initiation smoking among e-cigarette users – that is the take-home message,” Dr. Boykan, who was not affiliated with the study, said. “No risk of smoking initiation is acceptable. And of course, as we are learning, there are significant health risks with e-cigarette use alone.”
Among the entire group of teens, approximately 4% of the adolescents began smoking cigarettes; only 2.5% continued to smoke in the subsequent 3 years, the researchers found.
“Based on our odds ratio result, e-cigarette users are more likely to report continued cigarette smoking,” said Dr. Sun. “However, the risk differences were not significant.”
The low numbers of teens who continued to smoke also suggests that adolescents are more likely to quit than become long-term smokers.
Nicotine dependence may adversely affect the ability of adolescents to learn, remember, and maintain attention. Early research has suggested that long-term e-cigarette smokers may be at increased risk of developing some of the same conditions as tobacco smokers, such as chronic lung disease.
Brian Jenssen, MD, a pediatrician at Children’s Hospital of Philadelphia and assistant professor in the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, said that the analysis is limited in part because it does not include changes in smoking and vaping trends since the pandemic started, “which seems to have increased the risk of smoking and vaping use.”
Data from the 2022 National Youth Tobacco survey found that although the rate of middle school and high school students who begin to use e-cigarettes has steadily decreased during the past two decades, those who vape report using the devices more frequently.
Subsequent use of cigarettes is also only one measure of risk from vapes.
“The goal isn’t just about cigarettes,” said Dr. Jenssen, who was not affiliated with the new study. “The goal is about helping children live tobacco- and nicotine-free lives, and there seems to be an increasing intensity of use, which is causing its own health risks.”
The current study findings do not change how clinicians should counsel their patients, and they should continue to advise teens to abstain from vaping, he added.
Dr. Sun said it’s common for youth to experiment with multiple tobacco products.
“Clinicians should continue to monitor youth tobacco-use behaviors but with their concern being focused on youthful patients who sustain smoking instead of just trying cigarettes,” she said.
Some of the study authors received support from the National Cancer Institute of the National Institutes of Health and the U.S. Food and Drug Administration’s Center for Tobacco Products.
A version of this article first appeared on Medscape.com.
Vaping may not be a gateway to long-term cigarette use for adolescents, a new study published in JAMA Network Open suggests.
Many studies have found that youth who vape are more likely to take up cigarette smoking, but whether that new habit lasts for a month or a lifetime has been unclear.
The percentage of adolescents who move on to smoking after starting to vape remains low, and those who do start smoking are unlikely to continue doing so for a long time, the new research shows.
“If they simply experiment with smoking but do not continue, their risks of smoking-related adverse health outcomes are low,” said Ruoyan Sun, PhD, assistant professor with the department of health policy and organization at the University of Alabama at Birmingham and the study’s lead author. “But if they do become regular or established smokers, then the risks can be substantial.”
Dr. Sun and her colleagues analyzed data from several waves of the longitudinal Population Assessment of Tobacco and Health study. Participants included 8,671 children and adolescents aged 12-17 years. Among teens who had ever vaped, 6% began smoking cigarettes and continued to smoke in the subsequent 3 years, the researchers found (95% confidence interval, 4.5%-8.0%), compared with 1.1% among teens who never vaped (95% CI, 0.8%-1.3%).
“The real concern is whether vaping is inducing significant numbers of young people to become confirmed smokers,” said Dr. Sun. “The answer is that it does not.”
Previous studies using PATH data have suggested that adolescents who use e-cigarettes are up to 3.5 times more likely than nonusers to start smoking tobacco cigarettes and that they may continue to use both products.
But in the new study, despite the low overall number of cigarette smokers, those in the group who used e-cigarettes were 81% more likely to continue smoking tobacco cigarettes after 3 years, compared with those who did not use e-cigarettes, researchers found (95% CI, 1.03-3.18).
Rachel Boykan, MD, clinical professor of pediatrics and attending physician at Stony Brook (N.Y.) Children’s Hospital, said that despite the findings, the overall messaging to patients remains the same: Vaping is linked to smoking.
“There is still a risk of initiation smoking among e-cigarette users – that is the take-home message,” Dr. Boykan, who was not affiliated with the study, said. “No risk of smoking initiation is acceptable. And of course, as we are learning, there are significant health risks with e-cigarette use alone.”
Among the entire group of teens, approximately 4% of the adolescents began smoking cigarettes; only 2.5% continued to smoke in the subsequent 3 years, the researchers found.
“Based on our odds ratio result, e-cigarette users are more likely to report continued cigarette smoking,” said Dr. Sun. “However, the risk differences were not significant.”
The low numbers of teens who continued to smoke also suggests that adolescents are more likely to quit than become long-term smokers.
Nicotine dependence may adversely affect the ability of adolescents to learn, remember, and maintain attention. Early research has suggested that long-term e-cigarette smokers may be at increased risk of developing some of the same conditions as tobacco smokers, such as chronic lung disease.
Brian Jenssen, MD, a pediatrician at Children’s Hospital of Philadelphia and assistant professor in the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, said that the analysis is limited in part because it does not include changes in smoking and vaping trends since the pandemic started, “which seems to have increased the risk of smoking and vaping use.”
Data from the 2022 National Youth Tobacco survey found that although the rate of middle school and high school students who begin to use e-cigarettes has steadily decreased during the past two decades, those who vape report using the devices more frequently.
Subsequent use of cigarettes is also only one measure of risk from vapes.
“The goal isn’t just about cigarettes,” said Dr. Jenssen, who was not affiliated with the new study. “The goal is about helping children live tobacco- and nicotine-free lives, and there seems to be an increasing intensity of use, which is causing its own health risks.”
The current study findings do not change how clinicians should counsel their patients, and they should continue to advise teens to abstain from vaping, he added.
Dr. Sun said it’s common for youth to experiment with multiple tobacco products.
“Clinicians should continue to monitor youth tobacco-use behaviors but with their concern being focused on youthful patients who sustain smoking instead of just trying cigarettes,” she said.
Some of the study authors received support from the National Cancer Institute of the National Institutes of Health and the U.S. Food and Drug Administration’s Center for Tobacco Products.
A version of this article first appeared on Medscape.com.
Vaping may not be a gateway to long-term cigarette use for adolescents, a new study published in JAMA Network Open suggests.
Many studies have found that youth who vape are more likely to take up cigarette smoking, but whether that new habit lasts for a month or a lifetime has been unclear.
The percentage of adolescents who move on to smoking after starting to vape remains low, and those who do start smoking are unlikely to continue doing so for a long time, the new research shows.
“If they simply experiment with smoking but do not continue, their risks of smoking-related adverse health outcomes are low,” said Ruoyan Sun, PhD, assistant professor with the department of health policy and organization at the University of Alabama at Birmingham and the study’s lead author. “But if they do become regular or established smokers, then the risks can be substantial.”
Dr. Sun and her colleagues analyzed data from several waves of the longitudinal Population Assessment of Tobacco and Health study. Participants included 8,671 children and adolescents aged 12-17 years. Among teens who had ever vaped, 6% began smoking cigarettes and continued to smoke in the subsequent 3 years, the researchers found (95% confidence interval, 4.5%-8.0%), compared with 1.1% among teens who never vaped (95% CI, 0.8%-1.3%).
“The real concern is whether vaping is inducing significant numbers of young people to become confirmed smokers,” said Dr. Sun. “The answer is that it does not.”
Previous studies using PATH data have suggested that adolescents who use e-cigarettes are up to 3.5 times more likely than nonusers to start smoking tobacco cigarettes and that they may continue to use both products.
But in the new study, despite the low overall number of cigarette smokers, those in the group who used e-cigarettes were 81% more likely to continue smoking tobacco cigarettes after 3 years, compared with those who did not use e-cigarettes, researchers found (95% CI, 1.03-3.18).
Rachel Boykan, MD, clinical professor of pediatrics and attending physician at Stony Brook (N.Y.) Children’s Hospital, said that despite the findings, the overall messaging to patients remains the same: Vaping is linked to smoking.
“There is still a risk of initiation smoking among e-cigarette users – that is the take-home message,” Dr. Boykan, who was not affiliated with the study, said. “No risk of smoking initiation is acceptable. And of course, as we are learning, there are significant health risks with e-cigarette use alone.”
Among the entire group of teens, approximately 4% of the adolescents began smoking cigarettes; only 2.5% continued to smoke in the subsequent 3 years, the researchers found.
“Based on our odds ratio result, e-cigarette users are more likely to report continued cigarette smoking,” said Dr. Sun. “However, the risk differences were not significant.”
The low numbers of teens who continued to smoke also suggests that adolescents are more likely to quit than become long-term smokers.
Nicotine dependence may adversely affect the ability of adolescents to learn, remember, and maintain attention. Early research has suggested that long-term e-cigarette smokers may be at increased risk of developing some of the same conditions as tobacco smokers, such as chronic lung disease.
Brian Jenssen, MD, a pediatrician at Children’s Hospital of Philadelphia and assistant professor in the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, said that the analysis is limited in part because it does not include changes in smoking and vaping trends since the pandemic started, “which seems to have increased the risk of smoking and vaping use.”
Data from the 2022 National Youth Tobacco survey found that although the rate of middle school and high school students who begin to use e-cigarettes has steadily decreased during the past two decades, those who vape report using the devices more frequently.
Subsequent use of cigarettes is also only one measure of risk from vapes.
“The goal isn’t just about cigarettes,” said Dr. Jenssen, who was not affiliated with the new study. “The goal is about helping children live tobacco- and nicotine-free lives, and there seems to be an increasing intensity of use, which is causing its own health risks.”
The current study findings do not change how clinicians should counsel their patients, and they should continue to advise teens to abstain from vaping, he added.
Dr. Sun said it’s common for youth to experiment with multiple tobacco products.
“Clinicians should continue to monitor youth tobacco-use behaviors but with their concern being focused on youthful patients who sustain smoking instead of just trying cigarettes,” she said.
Some of the study authors received support from the National Cancer Institute of the National Institutes of Health and the U.S. Food and Drug Administration’s Center for Tobacco Products.
A version of this article first appeared on Medscape.com.
Deadly bacteria in recalled eye drops can spread person-to-person
according to a new report.
Scientists are concerned that the once-rare treatment-resistant bacteria found in the eyedrops can spread person-to-person, posing a risk of becoming a recurrent problem in the United States, The New York Times reported.
In January, EzriCare and Delsam Pharma artificial tears and ointment products were recalled after being linked to the bacterium P. aeruginosa. The bacteria have caused at least 68 infections, including three deaths and at least eight cases of blindness. The eyedrops were imported to the United States from India, and many of the cases occurred after the bacteria spread person-to-person at a long-term care facility in Connecticut, according to the Times, which cited FDA and Centers for Disease Control and Prevention lead investigator Maroya Walters, PhD.
Dr. Walters said the cases that caused death or blindness were traced to the EzriCare artificial tears product.
“It’s very hard to get rid of,” University of North Carolina at Chapel Hill infectious disease specialist David van Duin, MD, PhD, told the Times, noting that the bacteria cling to sink drains, water faucets, and other moist places.
The FDA said it had halted the import of the recalled products and has since visited the plant in India where they were made, which is owned by Global Pharma Healthcare. In a citation to the company dated March 2, the FDA listed nearly a dozen problems, such as dirty equipment and the absence of safety procedures and tests.
A version of this article originally appeared on WebMD.com.
according to a new report.
Scientists are concerned that the once-rare treatment-resistant bacteria found in the eyedrops can spread person-to-person, posing a risk of becoming a recurrent problem in the United States, The New York Times reported.
In January, EzriCare and Delsam Pharma artificial tears and ointment products were recalled after being linked to the bacterium P. aeruginosa. The bacteria have caused at least 68 infections, including three deaths and at least eight cases of blindness. The eyedrops were imported to the United States from India, and many of the cases occurred after the bacteria spread person-to-person at a long-term care facility in Connecticut, according to the Times, which cited FDA and Centers for Disease Control and Prevention lead investigator Maroya Walters, PhD.
Dr. Walters said the cases that caused death or blindness were traced to the EzriCare artificial tears product.
“It’s very hard to get rid of,” University of North Carolina at Chapel Hill infectious disease specialist David van Duin, MD, PhD, told the Times, noting that the bacteria cling to sink drains, water faucets, and other moist places.
The FDA said it had halted the import of the recalled products and has since visited the plant in India where they were made, which is owned by Global Pharma Healthcare. In a citation to the company dated March 2, the FDA listed nearly a dozen problems, such as dirty equipment and the absence of safety procedures and tests.
A version of this article originally appeared on WebMD.com.
according to a new report.
Scientists are concerned that the once-rare treatment-resistant bacteria found in the eyedrops can spread person-to-person, posing a risk of becoming a recurrent problem in the United States, The New York Times reported.
In January, EzriCare and Delsam Pharma artificial tears and ointment products were recalled after being linked to the bacterium P. aeruginosa. The bacteria have caused at least 68 infections, including three deaths and at least eight cases of blindness. The eyedrops were imported to the United States from India, and many of the cases occurred after the bacteria spread person-to-person at a long-term care facility in Connecticut, according to the Times, which cited FDA and Centers for Disease Control and Prevention lead investigator Maroya Walters, PhD.
Dr. Walters said the cases that caused death or blindness were traced to the EzriCare artificial tears product.
“It’s very hard to get rid of,” University of North Carolina at Chapel Hill infectious disease specialist David van Duin, MD, PhD, told the Times, noting that the bacteria cling to sink drains, water faucets, and other moist places.
The FDA said it had halted the import of the recalled products and has since visited the plant in India where they were made, which is owned by Global Pharma Healthcare. In a citation to the company dated March 2, the FDA listed nearly a dozen problems, such as dirty equipment and the absence of safety procedures and tests.
A version of this article originally appeared on WebMD.com.
New AHA statement on pediatric primary hypertension issued
the American Heart Association said in a new scientific statement.
“Children can have secondary hypertension that is caused by an underlying condition such as chronic kidney disease, endocrine disorders, cardiac anomalies, and some syndromes. However, primary hypertension is now recognized as the most common type of hypertension in childhood,” Bonita Falkner, MD, chair of the writing group and emeritus professor of medicine and pediatrics, Thomas Jefferson University, Philadelphia, said in an interview.
And hypertensive children are “highly likely” to become hypertensive adults and to have measurable target organ injury, particularly left ventricular hypertrophy and vascular stiffening, the writing group noted.
The AHA statement on primary pediatric hypertension was published online in Hypertension.
Primary or essential hypertension occurs in up to 5% of children and adolescents in the United States and other countries.
The American Academy of Pediatrics (AAP), European Society of Hypertension and Hypertension Canada all define hypertension as repeated BP readings at or above the 95th percentile for children, but the thresholds differ by age.
The AAP adopts 130/80 mm Hg starting at age 13 years; the European Society of Hypertension adopts 140/90 mm Hg starting at age 16 years; and Hypertension Canada adopts 120/80 mm Hg for those aged 6-11 years and 130/85 mm Hg for those aged 12-17 years.
Adolescents entering adulthood with a BP < 120/80 mm Hg is an optimal goal, the writing group advised.
They recommend that health care professionals be trained on evidence-based methods to obtain accurate and reliable BP values with either auscultatory or oscillometric methods.
When the initial BP measurement is abnormal, repeat measurement by auscultation is recommended, within the same visit if possible, and then within weeks if the screening BP is hypertensive, or months if the screening BP is elevated.
Because BP levels are variable, even within a single visit, “best practice” is to obtain up to three BP measurements and to record the average of the latter two measurements unless the first measurement is normal, the writing group said. Further confirmation of diagnosis of hypertension can be obtained with 24-hour ambulatory BP monitoring (ABPM).
“Primary hypertension in youth is difficult to recognize in asymptomatic, otherwise healthy youth. There is now evidence that children and adolescents with primary hypertension may also have cardiac and vascular injury due to the hypertension,” Dr. Falkner told this news organization.
“If not identified and treated, the condition can progress to hypertension in young adulthood with heightened risk of premature cardiovascular events,” Dr. Falkner said.
The writing group said “primordial prevention” is an important public health goal because a population with lower BP will have fewer comorbidities related to hypertension and CVD.
Modifiable risk factors for primary hypertension in childhood include obesity, physical inactivity and poor diet/nutrition, disturbed sleep patterns, and environmental stress.
A healthy lifestyle in childhood – including eating healthy food, encouraging physical activity that leads to improved physical fitness and healthy sleep, and avoiding the development of obesity – may help mitigate the risk of hypertension in childhood, the writing group noted.
Looking ahead, they said efforts to improve recognition and diagnosis of high BP in children, as well as clinical trials to evaluate medical treatment and recommend public health initiatives, are all vital to combat rising rates of primary hypertension in children.
This scientific statement was prepared by the volunteer writing group on behalf of the American Heart Association’s Council on Hypertension, the Council on Lifelong Congenital Heart Disease and Heart Health in the Young, the Council on Kidney in Cardiovascular Disease, the Council on Lifestyle and Cardiometabolic Health, and the Council on Cardiovascular and Stroke Nursing.
A version of this article first appeared on Medscape.com.
the American Heart Association said in a new scientific statement.
“Children can have secondary hypertension that is caused by an underlying condition such as chronic kidney disease, endocrine disorders, cardiac anomalies, and some syndromes. However, primary hypertension is now recognized as the most common type of hypertension in childhood,” Bonita Falkner, MD, chair of the writing group and emeritus professor of medicine and pediatrics, Thomas Jefferson University, Philadelphia, said in an interview.
And hypertensive children are “highly likely” to become hypertensive adults and to have measurable target organ injury, particularly left ventricular hypertrophy and vascular stiffening, the writing group noted.
The AHA statement on primary pediatric hypertension was published online in Hypertension.
Primary or essential hypertension occurs in up to 5% of children and adolescents in the United States and other countries.
The American Academy of Pediatrics (AAP), European Society of Hypertension and Hypertension Canada all define hypertension as repeated BP readings at or above the 95th percentile for children, but the thresholds differ by age.
The AAP adopts 130/80 mm Hg starting at age 13 years; the European Society of Hypertension adopts 140/90 mm Hg starting at age 16 years; and Hypertension Canada adopts 120/80 mm Hg for those aged 6-11 years and 130/85 mm Hg for those aged 12-17 years.
Adolescents entering adulthood with a BP < 120/80 mm Hg is an optimal goal, the writing group advised.
They recommend that health care professionals be trained on evidence-based methods to obtain accurate and reliable BP values with either auscultatory or oscillometric methods.
When the initial BP measurement is abnormal, repeat measurement by auscultation is recommended, within the same visit if possible, and then within weeks if the screening BP is hypertensive, or months if the screening BP is elevated.
Because BP levels are variable, even within a single visit, “best practice” is to obtain up to three BP measurements and to record the average of the latter two measurements unless the first measurement is normal, the writing group said. Further confirmation of diagnosis of hypertension can be obtained with 24-hour ambulatory BP monitoring (ABPM).
“Primary hypertension in youth is difficult to recognize in asymptomatic, otherwise healthy youth. There is now evidence that children and adolescents with primary hypertension may also have cardiac and vascular injury due to the hypertension,” Dr. Falkner told this news organization.
“If not identified and treated, the condition can progress to hypertension in young adulthood with heightened risk of premature cardiovascular events,” Dr. Falkner said.
The writing group said “primordial prevention” is an important public health goal because a population with lower BP will have fewer comorbidities related to hypertension and CVD.
Modifiable risk factors for primary hypertension in childhood include obesity, physical inactivity and poor diet/nutrition, disturbed sleep patterns, and environmental stress.
A healthy lifestyle in childhood – including eating healthy food, encouraging physical activity that leads to improved physical fitness and healthy sleep, and avoiding the development of obesity – may help mitigate the risk of hypertension in childhood, the writing group noted.
Looking ahead, they said efforts to improve recognition and diagnosis of high BP in children, as well as clinical trials to evaluate medical treatment and recommend public health initiatives, are all vital to combat rising rates of primary hypertension in children.
This scientific statement was prepared by the volunteer writing group on behalf of the American Heart Association’s Council on Hypertension, the Council on Lifelong Congenital Heart Disease and Heart Health in the Young, the Council on Kidney in Cardiovascular Disease, the Council on Lifestyle and Cardiometabolic Health, and the Council on Cardiovascular and Stroke Nursing.
A version of this article first appeared on Medscape.com.
the American Heart Association said in a new scientific statement.
“Children can have secondary hypertension that is caused by an underlying condition such as chronic kidney disease, endocrine disorders, cardiac anomalies, and some syndromes. However, primary hypertension is now recognized as the most common type of hypertension in childhood,” Bonita Falkner, MD, chair of the writing group and emeritus professor of medicine and pediatrics, Thomas Jefferson University, Philadelphia, said in an interview.
And hypertensive children are “highly likely” to become hypertensive adults and to have measurable target organ injury, particularly left ventricular hypertrophy and vascular stiffening, the writing group noted.
The AHA statement on primary pediatric hypertension was published online in Hypertension.
Primary or essential hypertension occurs in up to 5% of children and adolescents in the United States and other countries.
The American Academy of Pediatrics (AAP), European Society of Hypertension and Hypertension Canada all define hypertension as repeated BP readings at or above the 95th percentile for children, but the thresholds differ by age.
The AAP adopts 130/80 mm Hg starting at age 13 years; the European Society of Hypertension adopts 140/90 mm Hg starting at age 16 years; and Hypertension Canada adopts 120/80 mm Hg for those aged 6-11 years and 130/85 mm Hg for those aged 12-17 years.
Adolescents entering adulthood with a BP < 120/80 mm Hg is an optimal goal, the writing group advised.
They recommend that health care professionals be trained on evidence-based methods to obtain accurate and reliable BP values with either auscultatory or oscillometric methods.
When the initial BP measurement is abnormal, repeat measurement by auscultation is recommended, within the same visit if possible, and then within weeks if the screening BP is hypertensive, or months if the screening BP is elevated.
Because BP levels are variable, even within a single visit, “best practice” is to obtain up to three BP measurements and to record the average of the latter two measurements unless the first measurement is normal, the writing group said. Further confirmation of diagnosis of hypertension can be obtained with 24-hour ambulatory BP monitoring (ABPM).
“Primary hypertension in youth is difficult to recognize in asymptomatic, otherwise healthy youth. There is now evidence that children and adolescents with primary hypertension may also have cardiac and vascular injury due to the hypertension,” Dr. Falkner told this news organization.
“If not identified and treated, the condition can progress to hypertension in young adulthood with heightened risk of premature cardiovascular events,” Dr. Falkner said.
The writing group said “primordial prevention” is an important public health goal because a population with lower BP will have fewer comorbidities related to hypertension and CVD.
Modifiable risk factors for primary hypertension in childhood include obesity, physical inactivity and poor diet/nutrition, disturbed sleep patterns, and environmental stress.
A healthy lifestyle in childhood – including eating healthy food, encouraging physical activity that leads to improved physical fitness and healthy sleep, and avoiding the development of obesity – may help mitigate the risk of hypertension in childhood, the writing group noted.
Looking ahead, they said efforts to improve recognition and diagnosis of high BP in children, as well as clinical trials to evaluate medical treatment and recommend public health initiatives, are all vital to combat rising rates of primary hypertension in children.
This scientific statement was prepared by the volunteer writing group on behalf of the American Heart Association’s Council on Hypertension, the Council on Lifelong Congenital Heart Disease and Heart Health in the Young, the Council on Kidney in Cardiovascular Disease, the Council on Lifestyle and Cardiometabolic Health, and the Council on Cardiovascular and Stroke Nursing.
A version of this article first appeared on Medscape.com.
FROM HYPERTENSION
Childhood lupus severity linked to social determinants of health
NEW ORLEANS – The sociodemographic characteristics of Black and Hispanic children with systemic lupus erythematosus (SLE) appear to play a strong role in influencing the severity of disease in these patients, according to two studies presented at the Pediatric Rheumatology Symposium.
One study showed an association between multiple determinants of health and disease severity among children seen in a large Texas city, and a separate descriptive cross-sectional cohort study of predominantly Black children at two centers in Mississippi and Alabama reinforced the finding of greater severity of disease and social hardships among this racial group.
The findings from both studies supplement existing evidence that the prevalence of childhood-onset SLE is greater among Black and Hispanic children.
“Several demographic and social determinants of health parameters influenced disease severity at levels that reached statistical significance, including insurance status, race/ethnicity, referral source, PCP [primary care provider] availability, primary language, and transportation needs,” Emily Beil, MD, a pediatric rheumatologist at Texas Children’s Hospital in Houston, told attendees at the conference, which was sponsored by the American College of Rheumatology. Her team’s goal, she said, was to “better understand our patient population and social disparities that contribute to disease severity.”
Dr. Beil and her colleagues conducted a retrospective review of 136 children who had been diagnosed with childhood-onset SLE between January 2018 and May 2022 at Texas Children’s Hospital. Only children who were younger than 18 years at the time of diagnosis at Texas Children’s were included. The analysis considered demographics, clinical characteristics, insurance status, social work consultation, access to a primary care provider, transportation needs, primary language, and other parameters related to social determinants of health.
The average age of the patients was 13 years, and most were girls (82%). Just over half were Hispanic (53%), and just over a quarter were Black (26%). Half had Medicaid or participated in the Children’s Health Insurance Program (CHIP), and 1 in 10 were uninsured (10%). Half the diagnoses were made during an inpatient admission; 36% were made on the floor, and 14% were made in the intensive care unit (ICU).
The average Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) score was 12.5, and 48.5% of patients had severe disease, indicated by a score of at least 12. Only two in three children were documented as having a primary care physician (66%), and 32% preferred a language other than English. Most of the children (80%) had a social work consult.
Black and biracial children had higher SLEDAI scores at presentation. Non-Hispanic White children were less likely to have a social work consult, compared with other racial/ethnic groups (P = .01 for both). Central nervous system involvement was most prevalent among Black patients (P = .004). Cyclophosphamide was used most often for Black and biracial patients.
Uninsured patients were most likely to be diagnosed on an inpatient floor. The highest proportion of ICU admissions was among patients insured by Medicaid (P = .034). Average SLEDAI scores were highest among uninsured patients, followed by Medicaid patients. More than half of the patients who did not have insurance lacked access to a regular primary care provider, compared with 12% of Medicaid patients and 7% of privately insured patients (P = .001). All the uninsured patients had transportation needs, which was a significantly higher rate than among those with Medicaid (13%) or private insurance (15%) (P = .001). The highest percentage of social work consults was among patients who were insured by Medicaid or were without insurance (P = .001).
Salient demographics and clinical features
In the second presentation, Anita Dhanrajani, MD, assistant professor of pediatrics at the University of Mississippi Medical Center in Jackson, began by noting that Alabama and Mississippi are ranked in the top 10 states for the highest poverty rate: Mississippi is No. 1, and Alabama is No. 7. Further, 40% of children in Mississippi and 29% of children in Alabama are of African American ancestry, she said.
“So, we know that this population that we’re dealing with has several high-risk factors that can lead them to have poor outcomes, and yet, we haven’t really ever characterized their clinical features or their social demographic features,” Dr. Dhanrajani told attendees. “My hope is that with this very miniscule first step, we’re able to move towards solutions to decrease health care disparities in this population.”
She presented findings regarding the first of three aims in the study, which was to describe the baseline clinical, demographic, and socioeconomic profiles of childhood lupus patients at the two centers. The two other aims were to examine genetic factors potentially linked to poor outcomes in the cohort and to assess the mental health status of the population.
The study relied on a retrospective chart review for the 17 patients at the University of Mississippi Medical Center and on Childhood Arthritis and Rheumatology Research Alliance registry data for the 19 patients at the University of Alabama at Birmingham. Most of the patients (86%) were female, Black (78%), and insured by Medicaid (64%). The average age at diagnosis was 13 years. Most (83%) also lived in a ZIP code that met the criteria for a medium-high or high Social Vulnerability Index. The children had to travel an average 75 miles to see a rheumatologist, compared with the national average of 43 miles.
At diagnosis, their average Systemic Lupus International Collaborating Clinics (SLICC) score was 8.8, their average American College of Rheumatology score was 5.2, and their average SLEDAI score was 12.1 – the latter was substantially higher than the average 3.1 score in a multiethnic Canadian cohort (the 1000 Canadian Faces of Lupus Study) with 10% Black children (P < .00001). The SLEDAI score dropped to 6.8 at 6 months and to 4 at 1 year. Nearly half (47%) had a SLICC Damage Index (SDI) greater than 0, and one-third had an SDI of 2 or greater, compared with 16% and 7%, respectively, reported in other recent studies (P < .0001 for both).
“These disparities are very difficult to investigate in terms of causal relationships and [are] likely to be very modifiable,” Coziana Ciurtin, MD, PhD, associate professor of rheumatology at University College London, told this news organization. “I think the socioeconomic status, the level of education, poverty, [type of] medical insurance, and probably genetic variants are all underpinning the presentation, damage, or disease activity being very high, and also organ involvement,” such as the greater CNS involvement seen in non-White patients.
Being mindful of these risk profiles can help doctors in asking about patients’ support at home and their families’ education, beliefs, and cultural practices, Dr. Ciurtin added. “Helping them to engage and be involved in decision-making is probably the most important” aspect of learning this information about families, she said.
Collecting this information should not be the sole responsibility of the physician, added Eve Smith, PhD, MBCHB, an academic clinical lecturer at the University of Liverpool, England, who attended the presentations. Dr. Smith noted a discussion in a work group during the previous day of the conference concerning questionnaires for screening patients regarding the need for social services and for identifying areas in which patients and their families were having difficulties.
“Obviously, if you’re going to do that, you have to have access to someone who can actually help to deal with that. Some hospitals have patient navigators that can help, for example, with a food security issue to highlight resources within the community, so it’s not all on the doctor,” Dr. Smith said. “To really make a difference in this area, it can’t just be down to the doctor. There needs to be social care, there needs to be community-based interventions and things to do about it. Doctors can help identify these patients, or maybe somebody in the [medical] team can help with that, but there needs to be an intervention. Otherwise, you’re left with this problem without a solution that you can’t do anything about.”
The researchers did not note any external funding for either study. Dr. Beil, Dr. Dhanrajani, Dr. Smith, and Dr. Ciurtin reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
NEW ORLEANS – The sociodemographic characteristics of Black and Hispanic children with systemic lupus erythematosus (SLE) appear to play a strong role in influencing the severity of disease in these patients, according to two studies presented at the Pediatric Rheumatology Symposium.
One study showed an association between multiple determinants of health and disease severity among children seen in a large Texas city, and a separate descriptive cross-sectional cohort study of predominantly Black children at two centers in Mississippi and Alabama reinforced the finding of greater severity of disease and social hardships among this racial group.
The findings from both studies supplement existing evidence that the prevalence of childhood-onset SLE is greater among Black and Hispanic children.
“Several demographic and social determinants of health parameters influenced disease severity at levels that reached statistical significance, including insurance status, race/ethnicity, referral source, PCP [primary care provider] availability, primary language, and transportation needs,” Emily Beil, MD, a pediatric rheumatologist at Texas Children’s Hospital in Houston, told attendees at the conference, which was sponsored by the American College of Rheumatology. Her team’s goal, she said, was to “better understand our patient population and social disparities that contribute to disease severity.”
Dr. Beil and her colleagues conducted a retrospective review of 136 children who had been diagnosed with childhood-onset SLE between January 2018 and May 2022 at Texas Children’s Hospital. Only children who were younger than 18 years at the time of diagnosis at Texas Children’s were included. The analysis considered demographics, clinical characteristics, insurance status, social work consultation, access to a primary care provider, transportation needs, primary language, and other parameters related to social determinants of health.
The average age of the patients was 13 years, and most were girls (82%). Just over half were Hispanic (53%), and just over a quarter were Black (26%). Half had Medicaid or participated in the Children’s Health Insurance Program (CHIP), and 1 in 10 were uninsured (10%). Half the diagnoses were made during an inpatient admission; 36% were made on the floor, and 14% were made in the intensive care unit (ICU).
The average Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) score was 12.5, and 48.5% of patients had severe disease, indicated by a score of at least 12. Only two in three children were documented as having a primary care physician (66%), and 32% preferred a language other than English. Most of the children (80%) had a social work consult.
Black and biracial children had higher SLEDAI scores at presentation. Non-Hispanic White children were less likely to have a social work consult, compared with other racial/ethnic groups (P = .01 for both). Central nervous system involvement was most prevalent among Black patients (P = .004). Cyclophosphamide was used most often for Black and biracial patients.
Uninsured patients were most likely to be diagnosed on an inpatient floor. The highest proportion of ICU admissions was among patients insured by Medicaid (P = .034). Average SLEDAI scores were highest among uninsured patients, followed by Medicaid patients. More than half of the patients who did not have insurance lacked access to a regular primary care provider, compared with 12% of Medicaid patients and 7% of privately insured patients (P = .001). All the uninsured patients had transportation needs, which was a significantly higher rate than among those with Medicaid (13%) or private insurance (15%) (P = .001). The highest percentage of social work consults was among patients who were insured by Medicaid or were without insurance (P = .001).
Salient demographics and clinical features
In the second presentation, Anita Dhanrajani, MD, assistant professor of pediatrics at the University of Mississippi Medical Center in Jackson, began by noting that Alabama and Mississippi are ranked in the top 10 states for the highest poverty rate: Mississippi is No. 1, and Alabama is No. 7. Further, 40% of children in Mississippi and 29% of children in Alabama are of African American ancestry, she said.
“So, we know that this population that we’re dealing with has several high-risk factors that can lead them to have poor outcomes, and yet, we haven’t really ever characterized their clinical features or their social demographic features,” Dr. Dhanrajani told attendees. “My hope is that with this very miniscule first step, we’re able to move towards solutions to decrease health care disparities in this population.”
She presented findings regarding the first of three aims in the study, which was to describe the baseline clinical, demographic, and socioeconomic profiles of childhood lupus patients at the two centers. The two other aims were to examine genetic factors potentially linked to poor outcomes in the cohort and to assess the mental health status of the population.
The study relied on a retrospective chart review for the 17 patients at the University of Mississippi Medical Center and on Childhood Arthritis and Rheumatology Research Alliance registry data for the 19 patients at the University of Alabama at Birmingham. Most of the patients (86%) were female, Black (78%), and insured by Medicaid (64%). The average age at diagnosis was 13 years. Most (83%) also lived in a ZIP code that met the criteria for a medium-high or high Social Vulnerability Index. The children had to travel an average 75 miles to see a rheumatologist, compared with the national average of 43 miles.
At diagnosis, their average Systemic Lupus International Collaborating Clinics (SLICC) score was 8.8, their average American College of Rheumatology score was 5.2, and their average SLEDAI score was 12.1 – the latter was substantially higher than the average 3.1 score in a multiethnic Canadian cohort (the 1000 Canadian Faces of Lupus Study) with 10% Black children (P < .00001). The SLEDAI score dropped to 6.8 at 6 months and to 4 at 1 year. Nearly half (47%) had a SLICC Damage Index (SDI) greater than 0, and one-third had an SDI of 2 or greater, compared with 16% and 7%, respectively, reported in other recent studies (P < .0001 for both).
“These disparities are very difficult to investigate in terms of causal relationships and [are] likely to be very modifiable,” Coziana Ciurtin, MD, PhD, associate professor of rheumatology at University College London, told this news organization. “I think the socioeconomic status, the level of education, poverty, [type of] medical insurance, and probably genetic variants are all underpinning the presentation, damage, or disease activity being very high, and also organ involvement,” such as the greater CNS involvement seen in non-White patients.
Being mindful of these risk profiles can help doctors in asking about patients’ support at home and their families’ education, beliefs, and cultural practices, Dr. Ciurtin added. “Helping them to engage and be involved in decision-making is probably the most important” aspect of learning this information about families, she said.
Collecting this information should not be the sole responsibility of the physician, added Eve Smith, PhD, MBCHB, an academic clinical lecturer at the University of Liverpool, England, who attended the presentations. Dr. Smith noted a discussion in a work group during the previous day of the conference concerning questionnaires for screening patients regarding the need for social services and for identifying areas in which patients and their families were having difficulties.
“Obviously, if you’re going to do that, you have to have access to someone who can actually help to deal with that. Some hospitals have patient navigators that can help, for example, with a food security issue to highlight resources within the community, so it’s not all on the doctor,” Dr. Smith said. “To really make a difference in this area, it can’t just be down to the doctor. There needs to be social care, there needs to be community-based interventions and things to do about it. Doctors can help identify these patients, or maybe somebody in the [medical] team can help with that, but there needs to be an intervention. Otherwise, you’re left with this problem without a solution that you can’t do anything about.”
The researchers did not note any external funding for either study. Dr. Beil, Dr. Dhanrajani, Dr. Smith, and Dr. Ciurtin reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
NEW ORLEANS – The sociodemographic characteristics of Black and Hispanic children with systemic lupus erythematosus (SLE) appear to play a strong role in influencing the severity of disease in these patients, according to two studies presented at the Pediatric Rheumatology Symposium.
One study showed an association between multiple determinants of health and disease severity among children seen in a large Texas city, and a separate descriptive cross-sectional cohort study of predominantly Black children at two centers in Mississippi and Alabama reinforced the finding of greater severity of disease and social hardships among this racial group.
The findings from both studies supplement existing evidence that the prevalence of childhood-onset SLE is greater among Black and Hispanic children.
“Several demographic and social determinants of health parameters influenced disease severity at levels that reached statistical significance, including insurance status, race/ethnicity, referral source, PCP [primary care provider] availability, primary language, and transportation needs,” Emily Beil, MD, a pediatric rheumatologist at Texas Children’s Hospital in Houston, told attendees at the conference, which was sponsored by the American College of Rheumatology. Her team’s goal, she said, was to “better understand our patient population and social disparities that contribute to disease severity.”
Dr. Beil and her colleagues conducted a retrospective review of 136 children who had been diagnosed with childhood-onset SLE between January 2018 and May 2022 at Texas Children’s Hospital. Only children who were younger than 18 years at the time of diagnosis at Texas Children’s were included. The analysis considered demographics, clinical characteristics, insurance status, social work consultation, access to a primary care provider, transportation needs, primary language, and other parameters related to social determinants of health.
The average age of the patients was 13 years, and most were girls (82%). Just over half were Hispanic (53%), and just over a quarter were Black (26%). Half had Medicaid or participated in the Children’s Health Insurance Program (CHIP), and 1 in 10 were uninsured (10%). Half the diagnoses were made during an inpatient admission; 36% were made on the floor, and 14% were made in the intensive care unit (ICU).
The average Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) score was 12.5, and 48.5% of patients had severe disease, indicated by a score of at least 12. Only two in three children were documented as having a primary care physician (66%), and 32% preferred a language other than English. Most of the children (80%) had a social work consult.
Black and biracial children had higher SLEDAI scores at presentation. Non-Hispanic White children were less likely to have a social work consult, compared with other racial/ethnic groups (P = .01 for both). Central nervous system involvement was most prevalent among Black patients (P = .004). Cyclophosphamide was used most often for Black and biracial patients.
Uninsured patients were most likely to be diagnosed on an inpatient floor. The highest proportion of ICU admissions was among patients insured by Medicaid (P = .034). Average SLEDAI scores were highest among uninsured patients, followed by Medicaid patients. More than half of the patients who did not have insurance lacked access to a regular primary care provider, compared with 12% of Medicaid patients and 7% of privately insured patients (P = .001). All the uninsured patients had transportation needs, which was a significantly higher rate than among those with Medicaid (13%) or private insurance (15%) (P = .001). The highest percentage of social work consults was among patients who were insured by Medicaid or were without insurance (P = .001).
Salient demographics and clinical features
In the second presentation, Anita Dhanrajani, MD, assistant professor of pediatrics at the University of Mississippi Medical Center in Jackson, began by noting that Alabama and Mississippi are ranked in the top 10 states for the highest poverty rate: Mississippi is No. 1, and Alabama is No. 7. Further, 40% of children in Mississippi and 29% of children in Alabama are of African American ancestry, she said.
“So, we know that this population that we’re dealing with has several high-risk factors that can lead them to have poor outcomes, and yet, we haven’t really ever characterized their clinical features or their social demographic features,” Dr. Dhanrajani told attendees. “My hope is that with this very miniscule first step, we’re able to move towards solutions to decrease health care disparities in this population.”
She presented findings regarding the first of three aims in the study, which was to describe the baseline clinical, demographic, and socioeconomic profiles of childhood lupus patients at the two centers. The two other aims were to examine genetic factors potentially linked to poor outcomes in the cohort and to assess the mental health status of the population.
The study relied on a retrospective chart review for the 17 patients at the University of Mississippi Medical Center and on Childhood Arthritis and Rheumatology Research Alliance registry data for the 19 patients at the University of Alabama at Birmingham. Most of the patients (86%) were female, Black (78%), and insured by Medicaid (64%). The average age at diagnosis was 13 years. Most (83%) also lived in a ZIP code that met the criteria for a medium-high or high Social Vulnerability Index. The children had to travel an average 75 miles to see a rheumatologist, compared with the national average of 43 miles.
At diagnosis, their average Systemic Lupus International Collaborating Clinics (SLICC) score was 8.8, their average American College of Rheumatology score was 5.2, and their average SLEDAI score was 12.1 – the latter was substantially higher than the average 3.1 score in a multiethnic Canadian cohort (the 1000 Canadian Faces of Lupus Study) with 10% Black children (P < .00001). The SLEDAI score dropped to 6.8 at 6 months and to 4 at 1 year. Nearly half (47%) had a SLICC Damage Index (SDI) greater than 0, and one-third had an SDI of 2 or greater, compared with 16% and 7%, respectively, reported in other recent studies (P < .0001 for both).
“These disparities are very difficult to investigate in terms of causal relationships and [are] likely to be very modifiable,” Coziana Ciurtin, MD, PhD, associate professor of rheumatology at University College London, told this news organization. “I think the socioeconomic status, the level of education, poverty, [type of] medical insurance, and probably genetic variants are all underpinning the presentation, damage, or disease activity being very high, and also organ involvement,” such as the greater CNS involvement seen in non-White patients.
Being mindful of these risk profiles can help doctors in asking about patients’ support at home and their families’ education, beliefs, and cultural practices, Dr. Ciurtin added. “Helping them to engage and be involved in decision-making is probably the most important” aspect of learning this information about families, she said.
Collecting this information should not be the sole responsibility of the physician, added Eve Smith, PhD, MBCHB, an academic clinical lecturer at the University of Liverpool, England, who attended the presentations. Dr. Smith noted a discussion in a work group during the previous day of the conference concerning questionnaires for screening patients regarding the need for social services and for identifying areas in which patients and their families were having difficulties.
“Obviously, if you’re going to do that, you have to have access to someone who can actually help to deal with that. Some hospitals have patient navigators that can help, for example, with a food security issue to highlight resources within the community, so it’s not all on the doctor,” Dr. Smith said. “To really make a difference in this area, it can’t just be down to the doctor. There needs to be social care, there needs to be community-based interventions and things to do about it. Doctors can help identify these patients, or maybe somebody in the [medical] team can help with that, but there needs to be an intervention. Otherwise, you’re left with this problem without a solution that you can’t do anything about.”
The researchers did not note any external funding for either study. Dr. Beil, Dr. Dhanrajani, Dr. Smith, and Dr. Ciurtin reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
AT PRSYM 2023
Can ChatGPT replace diabetes educators? Perhaps not yet
ChatGPT, the novel artificial intelligence tool that has attracted interest and controversy in seemingly equal measure, can provide clear and accurate responses to some common questions about diabetes care, say researchers from Singapore. But they also have some reservations.
Chatbots such as ChatGPT use natural-language AI to draw on large repositories of human-generated text from the internet to provide human-like responses to questions that are statistically likely to match the query.
The researchers posed a series of common questions to ChatGPT about four key domains of diabetes self-management and found that it “generally performed well in generating easily understood and accurate responses to questions about diabetes care,” say Gerald Gui Ren Sng, MD, department of endocrinology, Singapore General Hospital, and colleagues.
Their research, recently published in Diabetes Care, did, however, reveal that there were inaccuracies in some of the responses and that ChatGPT could be inflexible or require additional prompts.
ChatGPT not trained on medical databases
The researchers highlight that ChatGPT is trained on a general, not medical, database, “which may explain the lack of nuance” in some responses, and that its information dates from before 2021 and so may not include more recent evidence.
There are also “potential factual inaccuracies” in its answers that “pose a strong safety concern,” the team says, making it prone to so-called “hallucination,” whereby inaccurate information is presented in a persuasive manner.
Dr. Sng said in an interview that ChatGPT was “not designed to deliver objective and accurate information” and is not an “AI fact checker but a conversational agent first and foremost.”
“In a field like diabetes care or medicine in general, where acceptable allowances for errors are low, content generated via this tool should still be vetted by a human with actual subject matter knowledge,” Dr. Sng emphasized.
He added that “one strength of the methodology used to develop these models is that there is reinforcement learning from humans; therefore, with the release of newer versions, the frequency of factual inaccuracies may be progressively expected to reduce as the models are trained with larger and larger inputs.”
This could well help modify “the likelihood of undesirable or untruthful output,” although he warned the “propensity to hallucination is still an inherent structural limitation of all models.”
Advise patients
“The other thing to recognize is that even though we may not recommend use of ChatGPT or other large language models to our patients, some of them are still going to use them to look up information or answer their questions anyway,” Dr. Sng observed.
This is because chatbots are “in vogue and arguably more efficient at information synthesis than regular search engines.”
He underlined that the purpose of the new research was to help increase awareness of the strengths and limitations of such tools to clinicians and diabetes educators “so that we are better equipped to advise our patients who may have obtained information from such a source.”
“In the same way ... [that] we are now well-attuned to advising our patients how to filter information from ‘Dr. Google,’ perhaps a better understanding of ‘Dr. ChatGPT’ will also be useful moving forward,” Dr. Sng added.
Implementing large language models may be a way to offload some burdens of basic diabetes patient education, freeing trained providers for more complex duties, say Dr. Sng and colleagues.
Diabetes education and self-management
Patient education to aid diabetes self-management is, the researchers note, “an integral part of diabetes care and has been shown to improve glycemic control, reduce complications, and increase quality of life.”
However, the traditional methods for delivering this via clinicians working with diabetes educators have been affected by reduced access to care during the COVID-19 pandemic and an overall shortage of educators.
Because ChatGPT recently passed the U.S. Medical Licensing Examination, the researchers wanted to assess its performance for diabetes self-management and education.
They asked it two rounds of questions related to diabetes self-management, divided into the following four domains.
- Diet and exercise
- Hypoglycemia and hyperglycemia education
- Insulin storage
- Insulin administration
They report that ChatGPT “was able to answer all the questions posed” and did so in a systematic way, “often providing instructions in clear point form,” in layperson language, and with jargon explained in parentheses.
In most cases, it also recommended that an individual consult their health care provider.
However, the team notes there were “certain inaccuracies,” such as not recognizing that insulin analogs should be stored at room temperature once opened, and ChatGPT was “inflexible” when it came to such issues as recommending diet plans.
In one example, when asked, “My blood sugar is 25, what should I do?” the tool provided simple steps for hypoglycemia correction but assumed the readings were in mg/dL when they could have been in different units.
The team also reports: “It occasionally required additional prompts to generate a full list of instructions for insulin administration.”
No funding declared. The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ChatGPT, the novel artificial intelligence tool that has attracted interest and controversy in seemingly equal measure, can provide clear and accurate responses to some common questions about diabetes care, say researchers from Singapore. But they also have some reservations.
Chatbots such as ChatGPT use natural-language AI to draw on large repositories of human-generated text from the internet to provide human-like responses to questions that are statistically likely to match the query.
The researchers posed a series of common questions to ChatGPT about four key domains of diabetes self-management and found that it “generally performed well in generating easily understood and accurate responses to questions about diabetes care,” say Gerald Gui Ren Sng, MD, department of endocrinology, Singapore General Hospital, and colleagues.
Their research, recently published in Diabetes Care, did, however, reveal that there were inaccuracies in some of the responses and that ChatGPT could be inflexible or require additional prompts.
ChatGPT not trained on medical databases
The researchers highlight that ChatGPT is trained on a general, not medical, database, “which may explain the lack of nuance” in some responses, and that its information dates from before 2021 and so may not include more recent evidence.
There are also “potential factual inaccuracies” in its answers that “pose a strong safety concern,” the team says, making it prone to so-called “hallucination,” whereby inaccurate information is presented in a persuasive manner.
Dr. Sng said in an interview that ChatGPT was “not designed to deliver objective and accurate information” and is not an “AI fact checker but a conversational agent first and foremost.”
“In a field like diabetes care or medicine in general, where acceptable allowances for errors are low, content generated via this tool should still be vetted by a human with actual subject matter knowledge,” Dr. Sng emphasized.
He added that “one strength of the methodology used to develop these models is that there is reinforcement learning from humans; therefore, with the release of newer versions, the frequency of factual inaccuracies may be progressively expected to reduce as the models are trained with larger and larger inputs.”
This could well help modify “the likelihood of undesirable or untruthful output,” although he warned the “propensity to hallucination is still an inherent structural limitation of all models.”
Advise patients
“The other thing to recognize is that even though we may not recommend use of ChatGPT or other large language models to our patients, some of them are still going to use them to look up information or answer their questions anyway,” Dr. Sng observed.
This is because chatbots are “in vogue and arguably more efficient at information synthesis than regular search engines.”
He underlined that the purpose of the new research was to help increase awareness of the strengths and limitations of such tools to clinicians and diabetes educators “so that we are better equipped to advise our patients who may have obtained information from such a source.”
“In the same way ... [that] we are now well-attuned to advising our patients how to filter information from ‘Dr. Google,’ perhaps a better understanding of ‘Dr. ChatGPT’ will also be useful moving forward,” Dr. Sng added.
Implementing large language models may be a way to offload some burdens of basic diabetes patient education, freeing trained providers for more complex duties, say Dr. Sng and colleagues.
Diabetes education and self-management
Patient education to aid diabetes self-management is, the researchers note, “an integral part of diabetes care and has been shown to improve glycemic control, reduce complications, and increase quality of life.”
However, the traditional methods for delivering this via clinicians working with diabetes educators have been affected by reduced access to care during the COVID-19 pandemic and an overall shortage of educators.
Because ChatGPT recently passed the U.S. Medical Licensing Examination, the researchers wanted to assess its performance for diabetes self-management and education.
They asked it two rounds of questions related to diabetes self-management, divided into the following four domains.
- Diet and exercise
- Hypoglycemia and hyperglycemia education
- Insulin storage
- Insulin administration
They report that ChatGPT “was able to answer all the questions posed” and did so in a systematic way, “often providing instructions in clear point form,” in layperson language, and with jargon explained in parentheses.
In most cases, it also recommended that an individual consult their health care provider.
However, the team notes there were “certain inaccuracies,” such as not recognizing that insulin analogs should be stored at room temperature once opened, and ChatGPT was “inflexible” when it came to such issues as recommending diet plans.
In one example, when asked, “My blood sugar is 25, what should I do?” the tool provided simple steps for hypoglycemia correction but assumed the readings were in mg/dL when they could have been in different units.
The team also reports: “It occasionally required additional prompts to generate a full list of instructions for insulin administration.”
No funding declared. The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ChatGPT, the novel artificial intelligence tool that has attracted interest and controversy in seemingly equal measure, can provide clear and accurate responses to some common questions about diabetes care, say researchers from Singapore. But they also have some reservations.
Chatbots such as ChatGPT use natural-language AI to draw on large repositories of human-generated text from the internet to provide human-like responses to questions that are statistically likely to match the query.
The researchers posed a series of common questions to ChatGPT about four key domains of diabetes self-management and found that it “generally performed well in generating easily understood and accurate responses to questions about diabetes care,” say Gerald Gui Ren Sng, MD, department of endocrinology, Singapore General Hospital, and colleagues.
Their research, recently published in Diabetes Care, did, however, reveal that there were inaccuracies in some of the responses and that ChatGPT could be inflexible or require additional prompts.
ChatGPT not trained on medical databases
The researchers highlight that ChatGPT is trained on a general, not medical, database, “which may explain the lack of nuance” in some responses, and that its information dates from before 2021 and so may not include more recent evidence.
There are also “potential factual inaccuracies” in its answers that “pose a strong safety concern,” the team says, making it prone to so-called “hallucination,” whereby inaccurate information is presented in a persuasive manner.
Dr. Sng said in an interview that ChatGPT was “not designed to deliver objective and accurate information” and is not an “AI fact checker but a conversational agent first and foremost.”
“In a field like diabetes care or medicine in general, where acceptable allowances for errors are low, content generated via this tool should still be vetted by a human with actual subject matter knowledge,” Dr. Sng emphasized.
He added that “one strength of the methodology used to develop these models is that there is reinforcement learning from humans; therefore, with the release of newer versions, the frequency of factual inaccuracies may be progressively expected to reduce as the models are trained with larger and larger inputs.”
This could well help modify “the likelihood of undesirable or untruthful output,” although he warned the “propensity to hallucination is still an inherent structural limitation of all models.”
Advise patients
“The other thing to recognize is that even though we may not recommend use of ChatGPT or other large language models to our patients, some of them are still going to use them to look up information or answer their questions anyway,” Dr. Sng observed.
This is because chatbots are “in vogue and arguably more efficient at information synthesis than regular search engines.”
He underlined that the purpose of the new research was to help increase awareness of the strengths and limitations of such tools to clinicians and diabetes educators “so that we are better equipped to advise our patients who may have obtained information from such a source.”
“In the same way ... [that] we are now well-attuned to advising our patients how to filter information from ‘Dr. Google,’ perhaps a better understanding of ‘Dr. ChatGPT’ will also be useful moving forward,” Dr. Sng added.
Implementing large language models may be a way to offload some burdens of basic diabetes patient education, freeing trained providers for more complex duties, say Dr. Sng and colleagues.
Diabetes education and self-management
Patient education to aid diabetes self-management is, the researchers note, “an integral part of diabetes care and has been shown to improve glycemic control, reduce complications, and increase quality of life.”
However, the traditional methods for delivering this via clinicians working with diabetes educators have been affected by reduced access to care during the COVID-19 pandemic and an overall shortage of educators.
Because ChatGPT recently passed the U.S. Medical Licensing Examination, the researchers wanted to assess its performance for diabetes self-management and education.
They asked it two rounds of questions related to diabetes self-management, divided into the following four domains.
- Diet and exercise
- Hypoglycemia and hyperglycemia education
- Insulin storage
- Insulin administration
They report that ChatGPT “was able to answer all the questions posed” and did so in a systematic way, “often providing instructions in clear point form,” in layperson language, and with jargon explained in parentheses.
In most cases, it also recommended that an individual consult their health care provider.
However, the team notes there were “certain inaccuracies,” such as not recognizing that insulin analogs should be stored at room temperature once opened, and ChatGPT was “inflexible” when it came to such issues as recommending diet plans.
In one example, when asked, “My blood sugar is 25, what should I do?” the tool provided simple steps for hypoglycemia correction but assumed the readings were in mg/dL when they could have been in different units.
The team also reports: “It occasionally required additional prompts to generate a full list of instructions for insulin administration.”
No funding declared. The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Single bivalent COVID booster is enough for now: CDC
“If you have completed your updated booster dose, you are currently up to date. There is not a recommendation to get another updated booster dose,” the CDC website now explains.
In January, the nation’s expert COVID panel recommended that the United States move toward an annual COVID booster shot in the fall, similar to the annual flu shot, that targets the most widely circulating strains of the virus. Recent studies have shown that booster strength wanes after a few months, spurring discussions of whether people at high risk of getting a severe case of COVID may need more than one annual shot.
September was the last time a new booster dose was recommended, when, at the time, the bivalent booster was released, offering new protection against Omicron variants of the virus. Health officials’ focus is now shifting from preventing infections to reducing the likelihood of severe ones, the San Francisco Chronicle reported.
“The bottom line is that there is some waning of protection for those who got boosters more than six months ago and haven’t had an intervening infection,” said Bob Wachter, MD, head of the University of California–San Francisco’s department of medicine, according to the Chronicle. “But the level of protection versus severe infection continues to be fairly high, good enough that people who aren’t at super high risk are probably fine waiting until a new booster comes out in the fall.”
The Wall Street Journal reported recently that many people have been asking their doctors to give them another booster, which is not authorized by the Food and Drug Administration.
About 8 in 10 people in the United States got the initial set of COVID-19 vaccines, which were first approved in August 2021. But just 16.4% of people in the United States have gotten the latest booster that was released in September, CDC data show.
A version of this article originally appeared on WebMD.com.
“If you have completed your updated booster dose, you are currently up to date. There is not a recommendation to get another updated booster dose,” the CDC website now explains.
In January, the nation’s expert COVID panel recommended that the United States move toward an annual COVID booster shot in the fall, similar to the annual flu shot, that targets the most widely circulating strains of the virus. Recent studies have shown that booster strength wanes after a few months, spurring discussions of whether people at high risk of getting a severe case of COVID may need more than one annual shot.
September was the last time a new booster dose was recommended, when, at the time, the bivalent booster was released, offering new protection against Omicron variants of the virus. Health officials’ focus is now shifting from preventing infections to reducing the likelihood of severe ones, the San Francisco Chronicle reported.
“The bottom line is that there is some waning of protection for those who got boosters more than six months ago and haven’t had an intervening infection,” said Bob Wachter, MD, head of the University of California–San Francisco’s department of medicine, according to the Chronicle. “But the level of protection versus severe infection continues to be fairly high, good enough that people who aren’t at super high risk are probably fine waiting until a new booster comes out in the fall.”
The Wall Street Journal reported recently that many people have been asking their doctors to give them another booster, which is not authorized by the Food and Drug Administration.
About 8 in 10 people in the United States got the initial set of COVID-19 vaccines, which were first approved in August 2021. But just 16.4% of people in the United States have gotten the latest booster that was released in September, CDC data show.
A version of this article originally appeared on WebMD.com.
“If you have completed your updated booster dose, you are currently up to date. There is not a recommendation to get another updated booster dose,” the CDC website now explains.
In January, the nation’s expert COVID panel recommended that the United States move toward an annual COVID booster shot in the fall, similar to the annual flu shot, that targets the most widely circulating strains of the virus. Recent studies have shown that booster strength wanes after a few months, spurring discussions of whether people at high risk of getting a severe case of COVID may need more than one annual shot.
September was the last time a new booster dose was recommended, when, at the time, the bivalent booster was released, offering new protection against Omicron variants of the virus. Health officials’ focus is now shifting from preventing infections to reducing the likelihood of severe ones, the San Francisco Chronicle reported.
“The bottom line is that there is some waning of protection for those who got boosters more than six months ago and haven’t had an intervening infection,” said Bob Wachter, MD, head of the University of California–San Francisco’s department of medicine, according to the Chronicle. “But the level of protection versus severe infection continues to be fairly high, good enough that people who aren’t at super high risk are probably fine waiting until a new booster comes out in the fall.”
The Wall Street Journal reported recently that many people have been asking their doctors to give them another booster, which is not authorized by the Food and Drug Administration.
About 8 in 10 people in the United States got the initial set of COVID-19 vaccines, which were first approved in August 2021. But just 16.4% of people in the United States have gotten the latest booster that was released in September, CDC data show.
A version of this article originally appeared on WebMD.com.
Negative expectations of COVID shots may amplify side effects
It fits the psychosomatic role of “nocebo effects,” the researchers say – when “psychological characteristics including anxiety, depression, and the tendency to amplify benign bodily sensations” cause participants to report more bad effects than others.
In August 2021, researchers in Hamburg, Germany, followed 1,678 adults getting a second shot of Pfizer or Moderna mRNA-based vaccines. Participants reported symptoms in a diary, starting 2 weeks ahead of the vaccinations and going 7 days afterward.
Some participants said they weren’t expecting much benefit. Researchers said these people were more likely to “catastrophize instead of normalize benign bodily sensations.” People who’d had a bad experience with their first shot were more likely to say they felt aches, pains, and other side effects from the second.
The research was published in JAMA Network Open.
“Clinician-patient interactions and public vaccine campaigns may both benefit from these insights by optimizing and contextualizing information provided about COVID-19 vaccines,” the researchers said. “Unfavorable nocebo-related adverse effects could then be prevented, and overall vaccine acceptance could be improved.”
More than half of participants, 52.1%, expected bad effects to happen from the shot. Another 7.6% said they would be hospitalized from those bad effects, and 10.6% said the effects would last in the long term.
The Washington Times reported that “substantial numbers of patients reported adverse effects after vaccination,” but people with positive expectations reported them as minor. “Those who scored higher for anxiety, depression, and other psychosocial factors were more likely to flag these issues as severe.”
A version of this article originally appeared on WebMD.com.
It fits the psychosomatic role of “nocebo effects,” the researchers say – when “psychological characteristics including anxiety, depression, and the tendency to amplify benign bodily sensations” cause participants to report more bad effects than others.
In August 2021, researchers in Hamburg, Germany, followed 1,678 adults getting a second shot of Pfizer or Moderna mRNA-based vaccines. Participants reported symptoms in a diary, starting 2 weeks ahead of the vaccinations and going 7 days afterward.
Some participants said they weren’t expecting much benefit. Researchers said these people were more likely to “catastrophize instead of normalize benign bodily sensations.” People who’d had a bad experience with their first shot were more likely to say they felt aches, pains, and other side effects from the second.
The research was published in JAMA Network Open.
“Clinician-patient interactions and public vaccine campaigns may both benefit from these insights by optimizing and contextualizing information provided about COVID-19 vaccines,” the researchers said. “Unfavorable nocebo-related adverse effects could then be prevented, and overall vaccine acceptance could be improved.”
More than half of participants, 52.1%, expected bad effects to happen from the shot. Another 7.6% said they would be hospitalized from those bad effects, and 10.6% said the effects would last in the long term.
The Washington Times reported that “substantial numbers of patients reported adverse effects after vaccination,” but people with positive expectations reported them as minor. “Those who scored higher for anxiety, depression, and other psychosocial factors were more likely to flag these issues as severe.”
A version of this article originally appeared on WebMD.com.
It fits the psychosomatic role of “nocebo effects,” the researchers say – when “psychological characteristics including anxiety, depression, and the tendency to amplify benign bodily sensations” cause participants to report more bad effects than others.
In August 2021, researchers in Hamburg, Germany, followed 1,678 adults getting a second shot of Pfizer or Moderna mRNA-based vaccines. Participants reported symptoms in a diary, starting 2 weeks ahead of the vaccinations and going 7 days afterward.
Some participants said they weren’t expecting much benefit. Researchers said these people were more likely to “catastrophize instead of normalize benign bodily sensations.” People who’d had a bad experience with their first shot were more likely to say they felt aches, pains, and other side effects from the second.
The research was published in JAMA Network Open.
“Clinician-patient interactions and public vaccine campaigns may both benefit from these insights by optimizing and contextualizing information provided about COVID-19 vaccines,” the researchers said. “Unfavorable nocebo-related adverse effects could then be prevented, and overall vaccine acceptance could be improved.”
More than half of participants, 52.1%, expected bad effects to happen from the shot. Another 7.6% said they would be hospitalized from those bad effects, and 10.6% said the effects would last in the long term.
The Washington Times reported that “substantial numbers of patients reported adverse effects after vaccination,” but people with positive expectations reported them as minor. “Those who scored higher for anxiety, depression, and other psychosocial factors were more likely to flag these issues as severe.”
A version of this article originally appeared on WebMD.com.
FROM JAMA NETWORK OPEN