User login
Part-time physician: Is it a viable career choice?
On average, physicians reported in the Medscape Physician Compensation Report 2023 that they worked 50 hours per week. Five specialties, including critical care, cardiology, and general surgery reported working 55 or more hours weekly.
In 2011, The New England Journal of Medicine reported that part-time physician careers were rising. At the time, part-time doctors made up 21% of the physician workforce, up from 13% in 2005.
In a more recent survey from the California Health Care Foundation, only 12% of California physicians said they devoted 20-29 hours a week to patient care.
Amy Knoup, a senior recruitment adviser with Provider Solutions & Development), has been helping doctors find jobs for over a decade, and she’s noticed a trend.
“Not only are more physicians seeking part-time roles than they were 10 years ago, but more large health care systems are also offering part time or per diem as well,” said Ms. Knoup.
Who’s working part time, and why?
Ten years ago, the fastest growing segment of part-timers were men nearing retirement and early- to mid-career women.
Pediatricians led the part-time pack in 2002, according to an American Academy of Pediatrics study. At the time, 15% of pediatricians reported their hours as part time. However, the numbers may have increased over the years. For example, a 2021 study by the department of pediatrics, Boston Medical Center, and Boston University found that almost 30% of graduating pediatricians sought part-time work at the end of their training.
At PS&D, Ms. Knoup said she has noticed a trend toward part-timers among primary care, behavioral health, and outpatient specialties such as endocrinology. “We’re also seeing it with the inpatient side in roles that are more shift based like hospitalists, radiologists, and critical care and ER doctors.”
Another trend Ms. Knoup has noticed is with early-career doctors. “They have a different mindset,” she said. “Younger generations are acutely aware of burnout. They may have experienced it in residency or during the pandemic. They’ve had a taste of that and don’t want to go down that road again, so they’re seeking part-time roles. It’s an intentional choice.”
Tracey O’Connell, MD, a radiologist, always knew that she wanted to work part time. “I had a baby as a resident, and I was pregnant with my second child as a fellow,” she said. “I was already feeling overwhelmed with medical training and having a family.”
Dr. O’Connell worked in private practice for 16 years on Mondays, Wednesdays, and Fridays, with no nights or weekends.
“I still found it completely overwhelming,” she said. “Even though I had more days not working than working, I felt like the demands of medical life had advanced faster than human beings could adapt, and I still feel that way.”
Today she runs a part-time teleradiology practice from home but spends more time on her second career as a life coach. “Most of my clients are physicians looking for more fulfillment and sustainable ways of practicing medicine while maintaining their own identity as human beings, not just the all-consuming identity of ‘doctor,’ ” she said.
On the other end of the career spectrum is Lois Goodman, MD, an ob.gyn. in her late 70s. After 42 years in a group practice, she started her solo practice at 72, seeing patients 3 days per week. “I’m just happy to be working. That’s a tremendous payoff for me. I need to keep working for my mental health.”
How does part-time work affect physician shortages and care delivery?
Reducing clinical effort is one of the strategies physicians use to scale down overload. Still, it’s not viable as a long-term solution, said Christine Sinsky, MD, AMA’s vice president of professional satisfaction and a nationally regarded researcher on physician burnout.
“If all the physicians in a community went from working 100% FTE clinical to 50% FTE clinical, then the people in that community would have half the access to care that they had,” said Dr. Sinsky. “There’s less capacity in the system to care for patients.”
Some could argue, then, that part-time physician work may contribute to physician shortage predictions. An Association of American Medical Colleges report estimates there will be a shortage of 37,800 to 124,000 physicians by 2034.
But physicians working part-time express a contrasting point of view. “I don’t believe that part-time workers are responsible for the health care shortage but rather, a great solution,” said Dr. O’Connell. “Because in order to continue working for a long time rather than quitting when the demands exceed human capacity, working part time is a great compromise to offer a life of more sustainable well-being and longevity as a physician, and still live a wholehearted life.”
Pros and cons of being a part-time physician
Pros
Less burnout: The American Medical Association has tracked burnout rates for 22 years. By the end of 2021, nearly 63% of physicians reported burnout symptoms, compared with 38% the year before. Going part time appears to reduce burnout, suggests a study published in Mayo Clinic Proceedings.
Better work-life balance: Rachel Miller, MD, an ob.gyn., worked 60-70 hours weekly for 9 years. In 2022, she went to work as an OB hospitalist for a health care system that welcomes part-time clinicians. Since then, she has achieved a better work-life balance, putting in 26-28 hours a week. Dr. Miller now spends more time with her kids and in her additional role as an executive coach to leaders in the medical field.
More focus: “When I’m at work, I’m 100% mentally in and focused,” said Dr. Miller. “My interactions with patients are different because I’m not burned out. My demeanor and my willingness to connect are stronger.”
Better health: Mehmet Cilingiroglu, MD, with CardioSolution, traded full-time work for part time when health issues and a kidney transplant sidelined his 30-year career in 2018. “Despite my significant health issues, I’ve been able to continue working at a pace that suits me rather than having to retire,” he said. “Part-time physicians can still enjoy patient care, research, innovation, education, and training while balancing that with other areas of life.”
Errin Weisman, a DO who gave up full-time work in 2016, said cutting back makes her feel healthier, happier, and more energized. “Part-time work helps me to bring my A game each day I work and deliver the best care.” She’s also a life coach encouraging other physicians to find balance in their professional and personal lives.
Cons
Cut in pay: Obviously, the No. 1 con is you’ll make less working part time, so adjusting to a salary decrease can be a huge issue, especially if you don’t have other sources of income. Physicians paying off student loans, those caring for children or elderly parents, or those in their prime earning years needing to save for retirement may not be able to go part time.
Diminished career: The chance for promotions or being well known in your field can be diminished, as well as a loss of proficiency if you’re only performing surgery or procedures part time. In some specialties, working part time and not keeping up with (or being able to practice) newer technology developments can harm your career or reputation in the long run.
Missing out: While working part time has many benefits, physicians also experience a wide range of drawbacks. Dr. Goodman, for example, said she misses delivering babies and doing surgeries. Dr. Miller said she gave up some aspects of her specialty, like performing hysterectomies, participating in complex cases, and no longer having an office like she did as a full-time ob.gyn.
Loss of fellowship: Dr. O’Connell said she missed the camaraderie and sense of belonging when she scaled back her hours. “I felt like a fish out of water, that my values didn’t align with the group’s values,” she said. This led to self-doubt, frustrated colleagues, and a reduction in benefits.
Lost esteem: Dr. O’Connell also felt she was expected to work overtime without additional pay and was no longer eligible for bonuses. “I was treated as a team player when I was needed, but not when it came to perks and benefits and insider privilege,” she said. There may be a loss of esteem among colleagues and supervisors.
Overcoming stigma: Because part-time physician work is still not prevalent among colleagues, some may resist the idea, have less respect for it, perceive it as not being serious about your career as a physician, or associate it with being lazy or entitled.
Summing it up
Every physician must weigh the value and drawbacks of part-time work, but the more physicians who go this route, the more part-time medicine gains traction and the more physicians can learn about its values versus its drawbacks.
A version of this article first appeared on Medscape.com.
On average, physicians reported in the Medscape Physician Compensation Report 2023 that they worked 50 hours per week. Five specialties, including critical care, cardiology, and general surgery reported working 55 or more hours weekly.
In 2011, The New England Journal of Medicine reported that part-time physician careers were rising. At the time, part-time doctors made up 21% of the physician workforce, up from 13% in 2005.
In a more recent survey from the California Health Care Foundation, only 12% of California physicians said they devoted 20-29 hours a week to patient care.
Amy Knoup, a senior recruitment adviser with Provider Solutions & Development), has been helping doctors find jobs for over a decade, and she’s noticed a trend.
“Not only are more physicians seeking part-time roles than they were 10 years ago, but more large health care systems are also offering part time or per diem as well,” said Ms. Knoup.
Who’s working part time, and why?
Ten years ago, the fastest growing segment of part-timers were men nearing retirement and early- to mid-career women.
Pediatricians led the part-time pack in 2002, according to an American Academy of Pediatrics study. At the time, 15% of pediatricians reported their hours as part time. However, the numbers may have increased over the years. For example, a 2021 study by the department of pediatrics, Boston Medical Center, and Boston University found that almost 30% of graduating pediatricians sought part-time work at the end of their training.
At PS&D, Ms. Knoup said she has noticed a trend toward part-timers among primary care, behavioral health, and outpatient specialties such as endocrinology. “We’re also seeing it with the inpatient side in roles that are more shift based like hospitalists, radiologists, and critical care and ER doctors.”
Another trend Ms. Knoup has noticed is with early-career doctors. “They have a different mindset,” she said. “Younger generations are acutely aware of burnout. They may have experienced it in residency or during the pandemic. They’ve had a taste of that and don’t want to go down that road again, so they’re seeking part-time roles. It’s an intentional choice.”
Tracey O’Connell, MD, a radiologist, always knew that she wanted to work part time. “I had a baby as a resident, and I was pregnant with my second child as a fellow,” she said. “I was already feeling overwhelmed with medical training and having a family.”
Dr. O’Connell worked in private practice for 16 years on Mondays, Wednesdays, and Fridays, with no nights or weekends.
“I still found it completely overwhelming,” she said. “Even though I had more days not working than working, I felt like the demands of medical life had advanced faster than human beings could adapt, and I still feel that way.”
Today she runs a part-time teleradiology practice from home but spends more time on her second career as a life coach. “Most of my clients are physicians looking for more fulfillment and sustainable ways of practicing medicine while maintaining their own identity as human beings, not just the all-consuming identity of ‘doctor,’ ” she said.
On the other end of the career spectrum is Lois Goodman, MD, an ob.gyn. in her late 70s. After 42 years in a group practice, she started her solo practice at 72, seeing patients 3 days per week. “I’m just happy to be working. That’s a tremendous payoff for me. I need to keep working for my mental health.”
How does part-time work affect physician shortages and care delivery?
Reducing clinical effort is one of the strategies physicians use to scale down overload. Still, it’s not viable as a long-term solution, said Christine Sinsky, MD, AMA’s vice president of professional satisfaction and a nationally regarded researcher on physician burnout.
“If all the physicians in a community went from working 100% FTE clinical to 50% FTE clinical, then the people in that community would have half the access to care that they had,” said Dr. Sinsky. “There’s less capacity in the system to care for patients.”
Some could argue, then, that part-time physician work may contribute to physician shortage predictions. An Association of American Medical Colleges report estimates there will be a shortage of 37,800 to 124,000 physicians by 2034.
But physicians working part-time express a contrasting point of view. “I don’t believe that part-time workers are responsible for the health care shortage but rather, a great solution,” said Dr. O’Connell. “Because in order to continue working for a long time rather than quitting when the demands exceed human capacity, working part time is a great compromise to offer a life of more sustainable well-being and longevity as a physician, and still live a wholehearted life.”
Pros and cons of being a part-time physician
Pros
Less burnout: The American Medical Association has tracked burnout rates for 22 years. By the end of 2021, nearly 63% of physicians reported burnout symptoms, compared with 38% the year before. Going part time appears to reduce burnout, suggests a study published in Mayo Clinic Proceedings.
Better work-life balance: Rachel Miller, MD, an ob.gyn., worked 60-70 hours weekly for 9 years. In 2022, she went to work as an OB hospitalist for a health care system that welcomes part-time clinicians. Since then, she has achieved a better work-life balance, putting in 26-28 hours a week. Dr. Miller now spends more time with her kids and in her additional role as an executive coach to leaders in the medical field.
More focus: “When I’m at work, I’m 100% mentally in and focused,” said Dr. Miller. “My interactions with patients are different because I’m not burned out. My demeanor and my willingness to connect are stronger.”
Better health: Mehmet Cilingiroglu, MD, with CardioSolution, traded full-time work for part time when health issues and a kidney transplant sidelined his 30-year career in 2018. “Despite my significant health issues, I’ve been able to continue working at a pace that suits me rather than having to retire,” he said. “Part-time physicians can still enjoy patient care, research, innovation, education, and training while balancing that with other areas of life.”
Errin Weisman, a DO who gave up full-time work in 2016, said cutting back makes her feel healthier, happier, and more energized. “Part-time work helps me to bring my A game each day I work and deliver the best care.” She’s also a life coach encouraging other physicians to find balance in their professional and personal lives.
Cons
Cut in pay: Obviously, the No. 1 con is you’ll make less working part time, so adjusting to a salary decrease can be a huge issue, especially if you don’t have other sources of income. Physicians paying off student loans, those caring for children or elderly parents, or those in their prime earning years needing to save for retirement may not be able to go part time.
Diminished career: The chance for promotions or being well known in your field can be diminished, as well as a loss of proficiency if you’re only performing surgery or procedures part time. In some specialties, working part time and not keeping up with (or being able to practice) newer technology developments can harm your career or reputation in the long run.
Missing out: While working part time has many benefits, physicians also experience a wide range of drawbacks. Dr. Goodman, for example, said she misses delivering babies and doing surgeries. Dr. Miller said she gave up some aspects of her specialty, like performing hysterectomies, participating in complex cases, and no longer having an office like she did as a full-time ob.gyn.
Loss of fellowship: Dr. O’Connell said she missed the camaraderie and sense of belonging when she scaled back her hours. “I felt like a fish out of water, that my values didn’t align with the group’s values,” she said. This led to self-doubt, frustrated colleagues, and a reduction in benefits.
Lost esteem: Dr. O’Connell also felt she was expected to work overtime without additional pay and was no longer eligible for bonuses. “I was treated as a team player when I was needed, but not when it came to perks and benefits and insider privilege,” she said. There may be a loss of esteem among colleagues and supervisors.
Overcoming stigma: Because part-time physician work is still not prevalent among colleagues, some may resist the idea, have less respect for it, perceive it as not being serious about your career as a physician, or associate it with being lazy or entitled.
Summing it up
Every physician must weigh the value and drawbacks of part-time work, but the more physicians who go this route, the more part-time medicine gains traction and the more physicians can learn about its values versus its drawbacks.
A version of this article first appeared on Medscape.com.
On average, physicians reported in the Medscape Physician Compensation Report 2023 that they worked 50 hours per week. Five specialties, including critical care, cardiology, and general surgery reported working 55 or more hours weekly.
In 2011, The New England Journal of Medicine reported that part-time physician careers were rising. At the time, part-time doctors made up 21% of the physician workforce, up from 13% in 2005.
In a more recent survey from the California Health Care Foundation, only 12% of California physicians said they devoted 20-29 hours a week to patient care.
Amy Knoup, a senior recruitment adviser with Provider Solutions & Development), has been helping doctors find jobs for over a decade, and she’s noticed a trend.
“Not only are more physicians seeking part-time roles than they were 10 years ago, but more large health care systems are also offering part time or per diem as well,” said Ms. Knoup.
Who’s working part time, and why?
Ten years ago, the fastest growing segment of part-timers were men nearing retirement and early- to mid-career women.
Pediatricians led the part-time pack in 2002, according to an American Academy of Pediatrics study. At the time, 15% of pediatricians reported their hours as part time. However, the numbers may have increased over the years. For example, a 2021 study by the department of pediatrics, Boston Medical Center, and Boston University found that almost 30% of graduating pediatricians sought part-time work at the end of their training.
At PS&D, Ms. Knoup said she has noticed a trend toward part-timers among primary care, behavioral health, and outpatient specialties such as endocrinology. “We’re also seeing it with the inpatient side in roles that are more shift based like hospitalists, radiologists, and critical care and ER doctors.”
Another trend Ms. Knoup has noticed is with early-career doctors. “They have a different mindset,” she said. “Younger generations are acutely aware of burnout. They may have experienced it in residency or during the pandemic. They’ve had a taste of that and don’t want to go down that road again, so they’re seeking part-time roles. It’s an intentional choice.”
Tracey O’Connell, MD, a radiologist, always knew that she wanted to work part time. “I had a baby as a resident, and I was pregnant with my second child as a fellow,” she said. “I was already feeling overwhelmed with medical training and having a family.”
Dr. O’Connell worked in private practice for 16 years on Mondays, Wednesdays, and Fridays, with no nights or weekends.
“I still found it completely overwhelming,” she said. “Even though I had more days not working than working, I felt like the demands of medical life had advanced faster than human beings could adapt, and I still feel that way.”
Today she runs a part-time teleradiology practice from home but spends more time on her second career as a life coach. “Most of my clients are physicians looking for more fulfillment and sustainable ways of practicing medicine while maintaining their own identity as human beings, not just the all-consuming identity of ‘doctor,’ ” she said.
On the other end of the career spectrum is Lois Goodman, MD, an ob.gyn. in her late 70s. After 42 years in a group practice, she started her solo practice at 72, seeing patients 3 days per week. “I’m just happy to be working. That’s a tremendous payoff for me. I need to keep working for my mental health.”
How does part-time work affect physician shortages and care delivery?
Reducing clinical effort is one of the strategies physicians use to scale down overload. Still, it’s not viable as a long-term solution, said Christine Sinsky, MD, AMA’s vice president of professional satisfaction and a nationally regarded researcher on physician burnout.
“If all the physicians in a community went from working 100% FTE clinical to 50% FTE clinical, then the people in that community would have half the access to care that they had,” said Dr. Sinsky. “There’s less capacity in the system to care for patients.”
Some could argue, then, that part-time physician work may contribute to physician shortage predictions. An Association of American Medical Colleges report estimates there will be a shortage of 37,800 to 124,000 physicians by 2034.
But physicians working part-time express a contrasting point of view. “I don’t believe that part-time workers are responsible for the health care shortage but rather, a great solution,” said Dr. O’Connell. “Because in order to continue working for a long time rather than quitting when the demands exceed human capacity, working part time is a great compromise to offer a life of more sustainable well-being and longevity as a physician, and still live a wholehearted life.”
Pros and cons of being a part-time physician
Pros
Less burnout: The American Medical Association has tracked burnout rates for 22 years. By the end of 2021, nearly 63% of physicians reported burnout symptoms, compared with 38% the year before. Going part time appears to reduce burnout, suggests a study published in Mayo Clinic Proceedings.
Better work-life balance: Rachel Miller, MD, an ob.gyn., worked 60-70 hours weekly for 9 years. In 2022, she went to work as an OB hospitalist for a health care system that welcomes part-time clinicians. Since then, she has achieved a better work-life balance, putting in 26-28 hours a week. Dr. Miller now spends more time with her kids and in her additional role as an executive coach to leaders in the medical field.
More focus: “When I’m at work, I’m 100% mentally in and focused,” said Dr. Miller. “My interactions with patients are different because I’m not burned out. My demeanor and my willingness to connect are stronger.”
Better health: Mehmet Cilingiroglu, MD, with CardioSolution, traded full-time work for part time when health issues and a kidney transplant sidelined his 30-year career in 2018. “Despite my significant health issues, I’ve been able to continue working at a pace that suits me rather than having to retire,” he said. “Part-time physicians can still enjoy patient care, research, innovation, education, and training while balancing that with other areas of life.”
Errin Weisman, a DO who gave up full-time work in 2016, said cutting back makes her feel healthier, happier, and more energized. “Part-time work helps me to bring my A game each day I work and deliver the best care.” She’s also a life coach encouraging other physicians to find balance in their professional and personal lives.
Cons
Cut in pay: Obviously, the No. 1 con is you’ll make less working part time, so adjusting to a salary decrease can be a huge issue, especially if you don’t have other sources of income. Physicians paying off student loans, those caring for children or elderly parents, or those in their prime earning years needing to save for retirement may not be able to go part time.
Diminished career: The chance for promotions or being well known in your field can be diminished, as well as a loss of proficiency if you’re only performing surgery or procedures part time. In some specialties, working part time and not keeping up with (or being able to practice) newer technology developments can harm your career or reputation in the long run.
Missing out: While working part time has many benefits, physicians also experience a wide range of drawbacks. Dr. Goodman, for example, said she misses delivering babies and doing surgeries. Dr. Miller said she gave up some aspects of her specialty, like performing hysterectomies, participating in complex cases, and no longer having an office like she did as a full-time ob.gyn.
Loss of fellowship: Dr. O’Connell said she missed the camaraderie and sense of belonging when she scaled back her hours. “I felt like a fish out of water, that my values didn’t align with the group’s values,” she said. This led to self-doubt, frustrated colleagues, and a reduction in benefits.
Lost esteem: Dr. O’Connell also felt she was expected to work overtime without additional pay and was no longer eligible for bonuses. “I was treated as a team player when I was needed, but not when it came to perks and benefits and insider privilege,” she said. There may be a loss of esteem among colleagues and supervisors.
Overcoming stigma: Because part-time physician work is still not prevalent among colleagues, some may resist the idea, have less respect for it, perceive it as not being serious about your career as a physician, or associate it with being lazy or entitled.
Summing it up
Every physician must weigh the value and drawbacks of part-time work, but the more physicians who go this route, the more part-time medicine gains traction and the more physicians can learn about its values versus its drawbacks.
A version of this article first appeared on Medscape.com.
Mohs surgery improves survival in early-stage Merkel cell carcinoma
SEATTLE – The use of
Compared with conventional wide local excision, survival was significantly improved among patients treated with Mohs, and a subgroup analysis showed that the survival benefit remained for patients with risk factors.
“At 10 years, overall survival was about 21% higher for those treated with Mohs surgery versus those treated with conventional surgery,” said lead author Shayan Cheraghlou, MD, a dermatology resident at the New York University School of Medicine. “On multivariable analysis, which controlled for tumor and patient factors, Mohs was associated with an over 40% reduction in the hazard for death.”
The findings were presented at the annual meeting of the American College of Mohs Surgery.
MCC is a rare, aggressive, neuroendocrine cutaneous malignancy that carries a high mortality rate. The estimated 5-year survival for patients with localized disease is about 50%, Dr. Cheraghlou noted. “That extrapolates to about 55% for T1 tumors and down to about 30% for T4 tumors.”
Although it’s considered to be a rare cancer, the incidence of MCC has been rapidly rising, and in fact it doubled during the period from the 1990s to the 2010s.
Most commonly treated with wide local excision with or without adjuvant radiation therapy, Mohs as monotherapy may offer an alternative treatment option for patients with MCC. It is generally accepted that the optimal treatment for tumors without regional lymph node involvement is surgical, but the data regarding the optimal surgical approach are mixed. Current National Comprehensive Cancer Network guidelines state that either Mohs surgery or wide local excision can be used.
“However, these guidelines do not indicate a preference for one modality over the other,” said Dr. Cheraghlou, “and present them as interchangeable treatment options.”
A growing body of literature supports Mohs surgery for many types of rare tumors, including MCC. For example, as previously reported at the 2021 ACMS meeting, one study found that Mohs surgery compared favorably with the standard treatment approach when it came to recurrence rates for patients with MCC. The 5-year disease-specific survival rate was 91.2% for patients with stage I disease and 68.6% for patients with stage IIa. These rates were comparable with rates for historical control patients who were treated with wide local excision, with or without radiation (81%-87% for stage I disease, and 63%-67% for stage II).
Study details
In the current study, Dr. Cheraghlou and colleagues sought to evaluate the association of the type of surgical approach with patient survival after excision of early-stage MCC. They conducted a retrospective cohort study using the National Cancer Database to identify cases of MCC with T1/T2 tumors. A total of 2,313 patients who were diagnosed from 2004 to 2018 with pathologically confirmed negative lymph node involvement and who were treated with Mohs surgery or wide lesion excision were included in the analysis.
“About 90% were T1 tumors, about 40% were located on the head and neck, and the vast majority – about 60% – were treated with wide local excision,” he explained. “Only about 5% received Mohs surgery for treatment of the primary tumor.”
But when the researchers assessed survival outcomes, they found that treatment with Mohs surgery was associated with significantly improved overall survival.
The unadjusted 3-, 5-, and 10-year survival rates for patients treated with Mohs was 87.4% (SE: 3.4%), 84.5% (SE: 3.9%), and 81.8% (SE: 4.6%), respectively, while for wide lesion excision, the rates were 86.1% (SE: 0.9%), 76.9% (SE: 1.2%), and 60.9% (SE: 2.0%), respectively.
For patients who underwent treatment with narrow margin excision, survival rates were similar as for those treated with wide lesion excision, with 3-, 5-, and 10-year survival rates of 84.8% (SE: 1.4%), 78.3% (SE: 1.7%), and 60.8% (SE: 3.6%), respectively.
On multivariable survival analysis, Mohs surgery was associated with significantly improved survival, compared with wide lesion excision (hazard ratio, 0.594; P = .038). This was also true after multivariable analysis for patients who had one or more NCCN risk factors, for whom improved survival was also seen with Mohs (HR, 0.530; P = .026).
The results did not differ after a sensitivity analysis that included T3 and T4 tumors.
Given that the use of Mohs was so infrequent, compared with standard surgery, the researchers investigated the factors that were associated with the use of Mohs. High-volume MCC centers were significantly more likely to utilize Mohs than wide lesion excision (odds ratio, 1.993; P < .001), compared with other facilities.
“This study has important implications going forward,” Dr. Cheraghlou concluded. “We think it’s important how few patients were treated with Mohs for Merkel cell, and it was slightly more likely to happen in a high-volume center.”
The reasoning for that may be that high-volume centers are more likely to have a surgeon trained to perform Mohs surgery for MCC. “Or perhaps they are more attuned to the benefits of this procedure,” he said. “We can’t tell that from our data, but its notable that it’s such a small proportion of patients – especially when we consider that it is associated with improved survival for the patients who receive it.”
He added that efforts to increase the utilization of Mohs may yield improved local control and overall survival for these patients. “And perhaps with more data, future versions of guidelines may indicate a preference for Mohs over conventional incisions.”
No changes to current practice
Asked to comment on the study, Anthony J. Olszanski, RPh, MD, associate professor, department of hematology/oncology, Fox Chase Cancer Center, Philadelphia, noted that while the results are intriguing, they must be interpreted with caution.
“This study was retrospective in nature, and unrecognized biases can influence results,” he said. “Additionally, given the relative rarity of Merkel cell carcinoma, the sample size is expectantly small.”
But importantly, Dr. Olszanski emphasized, Mohs may more often have been recommended for patients with lesions that appear less aggressive. “Many patients undergoing wide lesion excision may have been referred by Mohs surgeons secondary to features or characteristics of lesions which were worrisome,” he explained. “The results of this study do not opine on why Mohs would impact overall survival over wide lesion excision, a point worthy of consideration. Presently, both modalities can be considered for patients with T1/T2 MCC. The results of this study should not change current practice and would lend themselves to a more robust study.”
No external funding of the study was reported. Dr. Cheraghlou has disclosed no relevant financial relationships. Dr. Olszanski has received financial support from Merck and BMS for participated on advisory boards.
A version of this article originally appeared on Medscape.com.
SEATTLE – The use of
Compared with conventional wide local excision, survival was significantly improved among patients treated with Mohs, and a subgroup analysis showed that the survival benefit remained for patients with risk factors.
“At 10 years, overall survival was about 21% higher for those treated with Mohs surgery versus those treated with conventional surgery,” said lead author Shayan Cheraghlou, MD, a dermatology resident at the New York University School of Medicine. “On multivariable analysis, which controlled for tumor and patient factors, Mohs was associated with an over 40% reduction in the hazard for death.”
The findings were presented at the annual meeting of the American College of Mohs Surgery.
MCC is a rare, aggressive, neuroendocrine cutaneous malignancy that carries a high mortality rate. The estimated 5-year survival for patients with localized disease is about 50%, Dr. Cheraghlou noted. “That extrapolates to about 55% for T1 tumors and down to about 30% for T4 tumors.”
Although it’s considered to be a rare cancer, the incidence of MCC has been rapidly rising, and in fact it doubled during the period from the 1990s to the 2010s.
Most commonly treated with wide local excision with or without adjuvant radiation therapy, Mohs as monotherapy may offer an alternative treatment option for patients with MCC. It is generally accepted that the optimal treatment for tumors without regional lymph node involvement is surgical, but the data regarding the optimal surgical approach are mixed. Current National Comprehensive Cancer Network guidelines state that either Mohs surgery or wide local excision can be used.
“However, these guidelines do not indicate a preference for one modality over the other,” said Dr. Cheraghlou, “and present them as interchangeable treatment options.”
A growing body of literature supports Mohs surgery for many types of rare tumors, including MCC. For example, as previously reported at the 2021 ACMS meeting, one study found that Mohs surgery compared favorably with the standard treatment approach when it came to recurrence rates for patients with MCC. The 5-year disease-specific survival rate was 91.2% for patients with stage I disease and 68.6% for patients with stage IIa. These rates were comparable with rates for historical control patients who were treated with wide local excision, with or without radiation (81%-87% for stage I disease, and 63%-67% for stage II).
Study details
In the current study, Dr. Cheraghlou and colleagues sought to evaluate the association of the type of surgical approach with patient survival after excision of early-stage MCC. They conducted a retrospective cohort study using the National Cancer Database to identify cases of MCC with T1/T2 tumors. A total of 2,313 patients who were diagnosed from 2004 to 2018 with pathologically confirmed negative lymph node involvement and who were treated with Mohs surgery or wide lesion excision were included in the analysis.
“About 90% were T1 tumors, about 40% were located on the head and neck, and the vast majority – about 60% – were treated with wide local excision,” he explained. “Only about 5% received Mohs surgery for treatment of the primary tumor.”
But when the researchers assessed survival outcomes, they found that treatment with Mohs surgery was associated with significantly improved overall survival.
The unadjusted 3-, 5-, and 10-year survival rates for patients treated with Mohs was 87.4% (SE: 3.4%), 84.5% (SE: 3.9%), and 81.8% (SE: 4.6%), respectively, while for wide lesion excision, the rates were 86.1% (SE: 0.9%), 76.9% (SE: 1.2%), and 60.9% (SE: 2.0%), respectively.
For patients who underwent treatment with narrow margin excision, survival rates were similar as for those treated with wide lesion excision, with 3-, 5-, and 10-year survival rates of 84.8% (SE: 1.4%), 78.3% (SE: 1.7%), and 60.8% (SE: 3.6%), respectively.
On multivariable survival analysis, Mohs surgery was associated with significantly improved survival, compared with wide lesion excision (hazard ratio, 0.594; P = .038). This was also true after multivariable analysis for patients who had one or more NCCN risk factors, for whom improved survival was also seen with Mohs (HR, 0.530; P = .026).
The results did not differ after a sensitivity analysis that included T3 and T4 tumors.
Given that the use of Mohs was so infrequent, compared with standard surgery, the researchers investigated the factors that were associated with the use of Mohs. High-volume MCC centers were significantly more likely to utilize Mohs than wide lesion excision (odds ratio, 1.993; P < .001), compared with other facilities.
“This study has important implications going forward,” Dr. Cheraghlou concluded. “We think it’s important how few patients were treated with Mohs for Merkel cell, and it was slightly more likely to happen in a high-volume center.”
The reasoning for that may be that high-volume centers are more likely to have a surgeon trained to perform Mohs surgery for MCC. “Or perhaps they are more attuned to the benefits of this procedure,” he said. “We can’t tell that from our data, but its notable that it’s such a small proportion of patients – especially when we consider that it is associated with improved survival for the patients who receive it.”
He added that efforts to increase the utilization of Mohs may yield improved local control and overall survival for these patients. “And perhaps with more data, future versions of guidelines may indicate a preference for Mohs over conventional incisions.”
No changes to current practice
Asked to comment on the study, Anthony J. Olszanski, RPh, MD, associate professor, department of hematology/oncology, Fox Chase Cancer Center, Philadelphia, noted that while the results are intriguing, they must be interpreted with caution.
“This study was retrospective in nature, and unrecognized biases can influence results,” he said. “Additionally, given the relative rarity of Merkel cell carcinoma, the sample size is expectantly small.”
But importantly, Dr. Olszanski emphasized, Mohs may more often have been recommended for patients with lesions that appear less aggressive. “Many patients undergoing wide lesion excision may have been referred by Mohs surgeons secondary to features or characteristics of lesions which were worrisome,” he explained. “The results of this study do not opine on why Mohs would impact overall survival over wide lesion excision, a point worthy of consideration. Presently, both modalities can be considered for patients with T1/T2 MCC. The results of this study should not change current practice and would lend themselves to a more robust study.”
No external funding of the study was reported. Dr. Cheraghlou has disclosed no relevant financial relationships. Dr. Olszanski has received financial support from Merck and BMS for participated on advisory boards.
A version of this article originally appeared on Medscape.com.
SEATTLE – The use of
Compared with conventional wide local excision, survival was significantly improved among patients treated with Mohs, and a subgroup analysis showed that the survival benefit remained for patients with risk factors.
“At 10 years, overall survival was about 21% higher for those treated with Mohs surgery versus those treated with conventional surgery,” said lead author Shayan Cheraghlou, MD, a dermatology resident at the New York University School of Medicine. “On multivariable analysis, which controlled for tumor and patient factors, Mohs was associated with an over 40% reduction in the hazard for death.”
The findings were presented at the annual meeting of the American College of Mohs Surgery.
MCC is a rare, aggressive, neuroendocrine cutaneous malignancy that carries a high mortality rate. The estimated 5-year survival for patients with localized disease is about 50%, Dr. Cheraghlou noted. “That extrapolates to about 55% for T1 tumors and down to about 30% for T4 tumors.”
Although it’s considered to be a rare cancer, the incidence of MCC has been rapidly rising, and in fact it doubled during the period from the 1990s to the 2010s.
Most commonly treated with wide local excision with or without adjuvant radiation therapy, Mohs as monotherapy may offer an alternative treatment option for patients with MCC. It is generally accepted that the optimal treatment for tumors without regional lymph node involvement is surgical, but the data regarding the optimal surgical approach are mixed. Current National Comprehensive Cancer Network guidelines state that either Mohs surgery or wide local excision can be used.
“However, these guidelines do not indicate a preference for one modality over the other,” said Dr. Cheraghlou, “and present them as interchangeable treatment options.”
A growing body of literature supports Mohs surgery for many types of rare tumors, including MCC. For example, as previously reported at the 2021 ACMS meeting, one study found that Mohs surgery compared favorably with the standard treatment approach when it came to recurrence rates for patients with MCC. The 5-year disease-specific survival rate was 91.2% for patients with stage I disease and 68.6% for patients with stage IIa. These rates were comparable with rates for historical control patients who were treated with wide local excision, with or without radiation (81%-87% for stage I disease, and 63%-67% for stage II).
Study details
In the current study, Dr. Cheraghlou and colleagues sought to evaluate the association of the type of surgical approach with patient survival after excision of early-stage MCC. They conducted a retrospective cohort study using the National Cancer Database to identify cases of MCC with T1/T2 tumors. A total of 2,313 patients who were diagnosed from 2004 to 2018 with pathologically confirmed negative lymph node involvement and who were treated with Mohs surgery or wide lesion excision were included in the analysis.
“About 90% were T1 tumors, about 40% were located on the head and neck, and the vast majority – about 60% – were treated with wide local excision,” he explained. “Only about 5% received Mohs surgery for treatment of the primary tumor.”
But when the researchers assessed survival outcomes, they found that treatment with Mohs surgery was associated with significantly improved overall survival.
The unadjusted 3-, 5-, and 10-year survival rates for patients treated with Mohs was 87.4% (SE: 3.4%), 84.5% (SE: 3.9%), and 81.8% (SE: 4.6%), respectively, while for wide lesion excision, the rates were 86.1% (SE: 0.9%), 76.9% (SE: 1.2%), and 60.9% (SE: 2.0%), respectively.
For patients who underwent treatment with narrow margin excision, survival rates were similar as for those treated with wide lesion excision, with 3-, 5-, and 10-year survival rates of 84.8% (SE: 1.4%), 78.3% (SE: 1.7%), and 60.8% (SE: 3.6%), respectively.
On multivariable survival analysis, Mohs surgery was associated with significantly improved survival, compared with wide lesion excision (hazard ratio, 0.594; P = .038). This was also true after multivariable analysis for patients who had one or more NCCN risk factors, for whom improved survival was also seen with Mohs (HR, 0.530; P = .026).
The results did not differ after a sensitivity analysis that included T3 and T4 tumors.
Given that the use of Mohs was so infrequent, compared with standard surgery, the researchers investigated the factors that were associated with the use of Mohs. High-volume MCC centers were significantly more likely to utilize Mohs than wide lesion excision (odds ratio, 1.993; P < .001), compared with other facilities.
“This study has important implications going forward,” Dr. Cheraghlou concluded. “We think it’s important how few patients were treated with Mohs for Merkel cell, and it was slightly more likely to happen in a high-volume center.”
The reasoning for that may be that high-volume centers are more likely to have a surgeon trained to perform Mohs surgery for MCC. “Or perhaps they are more attuned to the benefits of this procedure,” he said. “We can’t tell that from our data, but its notable that it’s such a small proportion of patients – especially when we consider that it is associated with improved survival for the patients who receive it.”
He added that efforts to increase the utilization of Mohs may yield improved local control and overall survival for these patients. “And perhaps with more data, future versions of guidelines may indicate a preference for Mohs over conventional incisions.”
No changes to current practice
Asked to comment on the study, Anthony J. Olszanski, RPh, MD, associate professor, department of hematology/oncology, Fox Chase Cancer Center, Philadelphia, noted that while the results are intriguing, they must be interpreted with caution.
“This study was retrospective in nature, and unrecognized biases can influence results,” he said. “Additionally, given the relative rarity of Merkel cell carcinoma, the sample size is expectantly small.”
But importantly, Dr. Olszanski emphasized, Mohs may more often have been recommended for patients with lesions that appear less aggressive. “Many patients undergoing wide lesion excision may have been referred by Mohs surgeons secondary to features or characteristics of lesions which were worrisome,” he explained. “The results of this study do not opine on why Mohs would impact overall survival over wide lesion excision, a point worthy of consideration. Presently, both modalities can be considered for patients with T1/T2 MCC. The results of this study should not change current practice and would lend themselves to a more robust study.”
No external funding of the study was reported. Dr. Cheraghlou has disclosed no relevant financial relationships. Dr. Olszanski has received financial support from Merck and BMS for participated on advisory boards.
A version of this article originally appeared on Medscape.com.
AT ACMS 2023
Surprisingly more nonsustained VT shown in HCM using extended ECG monitoring
BARCELONA – , suggests a study that questions current risk stratification practices in HCM.
In the registry study, such arrythmias were observed in about six times as many HCM patients during 30 days of ambulatory electrocardiographic monitoring as would have been identified based on the first 24 hours of the monitoring period: 65% vs. 11% of the cohort.
Also, about 62% of the patients showed NSVT at “extended” 30-day monitoring, compared with an 8% prevalence of the arrhythmia based on the more conventional ECG monitoring period of 24 hours.
Nonsustained ventricular tachycardia, an important arrhythmia used every day in clinical practice to make decisions, is “much, much more prevalent than we thought” in patients with HCM, Juan Caro Codón, MD, the study’s principal investigator, said in an interview. “We should invest in further research regarding extended ECG monitoring in these patients.”
Dr. Caro Codón, of La Paz University Hospital, Madrid, presented the findings from the TEMPO-HCM study at the European Heart Rhythm Association 2023 Congress, held in Barcelona and virtually.
Its results, he said, have implications for stratifying HCM patients according to their risk for sudden cardiac death in deciding who should be offered an implantable cardioverter-defibrillator (ICD).
The life-incidence of atrial fibrillation (AF) in patients like those in the current analysis has previously been found to be about 20%, and the life-prevalence of NSVT about 20%-30%, using traditional 24- or 48-hour Holter monitoring, Dr. Caro Codón said.
“These arrhythmias are clinically relevant events because they are linked to very meaningful clinical endpoints,” including stroke and thromboembolism, he said, “but also for sudden cardiac death.”
Extended ECG monitoring has been shown useful in the setting of cryptogenic stroke and after AF ablation, but similar findings have been scarce in HCM. Patients using personal wearable monitors such as smart watches, Dr. Caro Codón said, have come to his clinic with concerns that the devices may have signaled a problem. But the lack of relevant data leaves them without a sufficient answer.
In other findings, invited discussant Isabelle van Gelder, MD, PhD, observed after Dr. Caro Codón’s presentation that the number of patients with AF almost doubled based on extended monitoring, compared with the first 24 hours of monitoring.
Based on European Society of Cardiology guidelines from 2020, “Once clinical AF has been documented, there is a class IIA recommendation to start anticoagulation,” said Dr. van Gelder, University of Groningen, the Netherlands. “Therefore, your data really are a call for more data on screening for AF in hypertrophic cardiomyopathy patients.”
Prospective multicenter registry
The TEMPO-HCM registry includes patients with HCM and a clinical indication for standard Holter monitoring at five hospitals in Spain. It excludes patients with an HCM-like phenotype but who lack the telltale genotype, as well as those already implanted with an ICD.
Those in the current analysis underwent 30-day ECG monitoring with a small, wearable device that Dr. Caro Codón described as about 7 cm long, worn in what is essentially a T-shirt with a pocket. Patients could remove the shirt and device to bathe or go swimming, for example, and still be monitored for most of the day.
The analysis included the registry’s first 100 patients (mean age, 57 years; 78% male). Hypertension was present in 47%, 58% were on beta-blockers, 16% had prior AF or atrial flutter, and 19% were taking anticoagulants. Only 8% were on antiarrhythmic drugs, Dr. Caro Codón reported.
The patients had good functional status (68% and 29% were in NYHA class 1 and 2, respectively) and their left ventricular ejection fraction averaged 66%. Of the 71 patients who underwent MRI, 28.2% showed late gadolinium enhancement suggesting myocardial scarring.
More arrhythmias on 30-day monitoring
The primary endpoint of clinically relevant arrhythmia (AF, atrial flutter, or NSVT) was identified during the first 24 hours of monitoring in 11% of patients. The prevalence rose to 65% (P < .001) based on 30-day monitoring.
Similarly, prevalences of the composite primary endpoint components grew on extended monitoring, but the increases reached statistical significance only for NSVT; its prevalence went from 8% to 62% (P < .001). Prevalences rose nonsignificantly from 6% to 10% for AF and 0% to 1% for sustained ventricular tachycardia.
The incidence of NSVT during monitoring climbed fastest from day 0 through about day 19 and then rose more slowly through day 30, Dr. Caro Codón said. “It actually didn’t reach a plateau during this time period, so there is the possibility that if we had continued monitoring patients, the difference between both periods may have been even higher.”
Three variables predicted the incidence of nonsustained VT during monitoring, he said: age, atrial wall thickness, and whether there was late gadolinium enhancement at MRI.
An exploratory analysis looked at the 5-year risk of sudden cardiac death using the European Society of Cardiology HCM-SCD risk calculator recommended in guidelines. Risk assessment based on the 30-day extended monitoring period, compared with the first 24 hours of monitoring alone, predicted a significantly higher 5-year risk of sudden death, Dr. Caro Codón said.
“Even more importantly,” he added, “over 20%” of patients would have been reclassified into a higher-risk group and possibly considered for an ICD based on extended monitoring, compared to 24-hour monitoring.
However, given that more than 50% of patients were found to have NSVT during extended monitoring, Dr. Caro Codón proposed that decisions on whether to implant an ICD should not be so “binary” based on the presence or absence of symptoms, and proposed further investigations be conducted into the complete phenotype of these arrhythmias.
The study has limitations, he observed, including a relatively small size; but it was able to detect important differences between 24-hour and 30-day monitoring outcomes even with only 100 patients. It was also limited by a lack of clinical follow-up for information on endpoints like stroke, thromboembolism, and sudden cardiac death.
Extended monitoring detected more cases of NSVT in the study’s relatively low-risk HCM patients who would not generally have an indication for ICD implantation, observed Dr. van Gelder. Also, at present the prognostic value of NSVT for SCD “seems to be more important at younger age” – that is, younger than 30 years – in patients with HCM.
Dr. van Gelder echoed Dr. Caro Codón’s call for more data from prolonged monitoring to help stratify patients according to risk; she proposed NSVT frequency, duration, and rate as possible targets.
The study was supported by an unrestricted grant from Nuubo, which provided the ECG monitoring systems. Dr. Caro Codón and Dr. van Gelder reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BARCELONA – , suggests a study that questions current risk stratification practices in HCM.
In the registry study, such arrythmias were observed in about six times as many HCM patients during 30 days of ambulatory electrocardiographic monitoring as would have been identified based on the first 24 hours of the monitoring period: 65% vs. 11% of the cohort.
Also, about 62% of the patients showed NSVT at “extended” 30-day monitoring, compared with an 8% prevalence of the arrhythmia based on the more conventional ECG monitoring period of 24 hours.
Nonsustained ventricular tachycardia, an important arrhythmia used every day in clinical practice to make decisions, is “much, much more prevalent than we thought” in patients with HCM, Juan Caro Codón, MD, the study’s principal investigator, said in an interview. “We should invest in further research regarding extended ECG monitoring in these patients.”
Dr. Caro Codón, of La Paz University Hospital, Madrid, presented the findings from the TEMPO-HCM study at the European Heart Rhythm Association 2023 Congress, held in Barcelona and virtually.
Its results, he said, have implications for stratifying HCM patients according to their risk for sudden cardiac death in deciding who should be offered an implantable cardioverter-defibrillator (ICD).
The life-incidence of atrial fibrillation (AF) in patients like those in the current analysis has previously been found to be about 20%, and the life-prevalence of NSVT about 20%-30%, using traditional 24- or 48-hour Holter monitoring, Dr. Caro Codón said.
“These arrhythmias are clinically relevant events because they are linked to very meaningful clinical endpoints,” including stroke and thromboembolism, he said, “but also for sudden cardiac death.”
Extended ECG monitoring has been shown useful in the setting of cryptogenic stroke and after AF ablation, but similar findings have been scarce in HCM. Patients using personal wearable monitors such as smart watches, Dr. Caro Codón said, have come to his clinic with concerns that the devices may have signaled a problem. But the lack of relevant data leaves them without a sufficient answer.
In other findings, invited discussant Isabelle van Gelder, MD, PhD, observed after Dr. Caro Codón’s presentation that the number of patients with AF almost doubled based on extended monitoring, compared with the first 24 hours of monitoring.
Based on European Society of Cardiology guidelines from 2020, “Once clinical AF has been documented, there is a class IIA recommendation to start anticoagulation,” said Dr. van Gelder, University of Groningen, the Netherlands. “Therefore, your data really are a call for more data on screening for AF in hypertrophic cardiomyopathy patients.”
Prospective multicenter registry
The TEMPO-HCM registry includes patients with HCM and a clinical indication for standard Holter monitoring at five hospitals in Spain. It excludes patients with an HCM-like phenotype but who lack the telltale genotype, as well as those already implanted with an ICD.
Those in the current analysis underwent 30-day ECG monitoring with a small, wearable device that Dr. Caro Codón described as about 7 cm long, worn in what is essentially a T-shirt with a pocket. Patients could remove the shirt and device to bathe or go swimming, for example, and still be monitored for most of the day.
The analysis included the registry’s first 100 patients (mean age, 57 years; 78% male). Hypertension was present in 47%, 58% were on beta-blockers, 16% had prior AF or atrial flutter, and 19% were taking anticoagulants. Only 8% were on antiarrhythmic drugs, Dr. Caro Codón reported.
The patients had good functional status (68% and 29% were in NYHA class 1 and 2, respectively) and their left ventricular ejection fraction averaged 66%. Of the 71 patients who underwent MRI, 28.2% showed late gadolinium enhancement suggesting myocardial scarring.
More arrhythmias on 30-day monitoring
The primary endpoint of clinically relevant arrhythmia (AF, atrial flutter, or NSVT) was identified during the first 24 hours of monitoring in 11% of patients. The prevalence rose to 65% (P < .001) based on 30-day monitoring.
Similarly, prevalences of the composite primary endpoint components grew on extended monitoring, but the increases reached statistical significance only for NSVT; its prevalence went from 8% to 62% (P < .001). Prevalences rose nonsignificantly from 6% to 10% for AF and 0% to 1% for sustained ventricular tachycardia.
The incidence of NSVT during monitoring climbed fastest from day 0 through about day 19 and then rose more slowly through day 30, Dr. Caro Codón said. “It actually didn’t reach a plateau during this time period, so there is the possibility that if we had continued monitoring patients, the difference between both periods may have been even higher.”
Three variables predicted the incidence of nonsustained VT during monitoring, he said: age, atrial wall thickness, and whether there was late gadolinium enhancement at MRI.
An exploratory analysis looked at the 5-year risk of sudden cardiac death using the European Society of Cardiology HCM-SCD risk calculator recommended in guidelines. Risk assessment based on the 30-day extended monitoring period, compared with the first 24 hours of monitoring alone, predicted a significantly higher 5-year risk of sudden death, Dr. Caro Codón said.
“Even more importantly,” he added, “over 20%” of patients would have been reclassified into a higher-risk group and possibly considered for an ICD based on extended monitoring, compared to 24-hour monitoring.
However, given that more than 50% of patients were found to have NSVT during extended monitoring, Dr. Caro Codón proposed that decisions on whether to implant an ICD should not be so “binary” based on the presence or absence of symptoms, and proposed further investigations be conducted into the complete phenotype of these arrhythmias.
The study has limitations, he observed, including a relatively small size; but it was able to detect important differences between 24-hour and 30-day monitoring outcomes even with only 100 patients. It was also limited by a lack of clinical follow-up for information on endpoints like stroke, thromboembolism, and sudden cardiac death.
Extended monitoring detected more cases of NSVT in the study’s relatively low-risk HCM patients who would not generally have an indication for ICD implantation, observed Dr. van Gelder. Also, at present the prognostic value of NSVT for SCD “seems to be more important at younger age” – that is, younger than 30 years – in patients with HCM.
Dr. van Gelder echoed Dr. Caro Codón’s call for more data from prolonged monitoring to help stratify patients according to risk; she proposed NSVT frequency, duration, and rate as possible targets.
The study was supported by an unrestricted grant from Nuubo, which provided the ECG monitoring systems. Dr. Caro Codón and Dr. van Gelder reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BARCELONA – , suggests a study that questions current risk stratification practices in HCM.
In the registry study, such arrythmias were observed in about six times as many HCM patients during 30 days of ambulatory electrocardiographic monitoring as would have been identified based on the first 24 hours of the monitoring period: 65% vs. 11% of the cohort.
Also, about 62% of the patients showed NSVT at “extended” 30-day monitoring, compared with an 8% prevalence of the arrhythmia based on the more conventional ECG monitoring period of 24 hours.
Nonsustained ventricular tachycardia, an important arrhythmia used every day in clinical practice to make decisions, is “much, much more prevalent than we thought” in patients with HCM, Juan Caro Codón, MD, the study’s principal investigator, said in an interview. “We should invest in further research regarding extended ECG monitoring in these patients.”
Dr. Caro Codón, of La Paz University Hospital, Madrid, presented the findings from the TEMPO-HCM study at the European Heart Rhythm Association 2023 Congress, held in Barcelona and virtually.
Its results, he said, have implications for stratifying HCM patients according to their risk for sudden cardiac death in deciding who should be offered an implantable cardioverter-defibrillator (ICD).
The life-incidence of atrial fibrillation (AF) in patients like those in the current analysis has previously been found to be about 20%, and the life-prevalence of NSVT about 20%-30%, using traditional 24- or 48-hour Holter monitoring, Dr. Caro Codón said.
“These arrhythmias are clinically relevant events because they are linked to very meaningful clinical endpoints,” including stroke and thromboembolism, he said, “but also for sudden cardiac death.”
Extended ECG monitoring has been shown useful in the setting of cryptogenic stroke and after AF ablation, but similar findings have been scarce in HCM. Patients using personal wearable monitors such as smart watches, Dr. Caro Codón said, have come to his clinic with concerns that the devices may have signaled a problem. But the lack of relevant data leaves them without a sufficient answer.
In other findings, invited discussant Isabelle van Gelder, MD, PhD, observed after Dr. Caro Codón’s presentation that the number of patients with AF almost doubled based on extended monitoring, compared with the first 24 hours of monitoring.
Based on European Society of Cardiology guidelines from 2020, “Once clinical AF has been documented, there is a class IIA recommendation to start anticoagulation,” said Dr. van Gelder, University of Groningen, the Netherlands. “Therefore, your data really are a call for more data on screening for AF in hypertrophic cardiomyopathy patients.”
Prospective multicenter registry
The TEMPO-HCM registry includes patients with HCM and a clinical indication for standard Holter monitoring at five hospitals in Spain. It excludes patients with an HCM-like phenotype but who lack the telltale genotype, as well as those already implanted with an ICD.
Those in the current analysis underwent 30-day ECG monitoring with a small, wearable device that Dr. Caro Codón described as about 7 cm long, worn in what is essentially a T-shirt with a pocket. Patients could remove the shirt and device to bathe or go swimming, for example, and still be monitored for most of the day.
The analysis included the registry’s first 100 patients (mean age, 57 years; 78% male). Hypertension was present in 47%, 58% were on beta-blockers, 16% had prior AF or atrial flutter, and 19% were taking anticoagulants. Only 8% were on antiarrhythmic drugs, Dr. Caro Codón reported.
The patients had good functional status (68% and 29% were in NYHA class 1 and 2, respectively) and their left ventricular ejection fraction averaged 66%. Of the 71 patients who underwent MRI, 28.2% showed late gadolinium enhancement suggesting myocardial scarring.
More arrhythmias on 30-day monitoring
The primary endpoint of clinically relevant arrhythmia (AF, atrial flutter, or NSVT) was identified during the first 24 hours of monitoring in 11% of patients. The prevalence rose to 65% (P < .001) based on 30-day monitoring.
Similarly, prevalences of the composite primary endpoint components grew on extended monitoring, but the increases reached statistical significance only for NSVT; its prevalence went from 8% to 62% (P < .001). Prevalences rose nonsignificantly from 6% to 10% for AF and 0% to 1% for sustained ventricular tachycardia.
The incidence of NSVT during monitoring climbed fastest from day 0 through about day 19 and then rose more slowly through day 30, Dr. Caro Codón said. “It actually didn’t reach a plateau during this time period, so there is the possibility that if we had continued monitoring patients, the difference between both periods may have been even higher.”
Three variables predicted the incidence of nonsustained VT during monitoring, he said: age, atrial wall thickness, and whether there was late gadolinium enhancement at MRI.
An exploratory analysis looked at the 5-year risk of sudden cardiac death using the European Society of Cardiology HCM-SCD risk calculator recommended in guidelines. Risk assessment based on the 30-day extended monitoring period, compared with the first 24 hours of monitoring alone, predicted a significantly higher 5-year risk of sudden death, Dr. Caro Codón said.
“Even more importantly,” he added, “over 20%” of patients would have been reclassified into a higher-risk group and possibly considered for an ICD based on extended monitoring, compared to 24-hour monitoring.
However, given that more than 50% of patients were found to have NSVT during extended monitoring, Dr. Caro Codón proposed that decisions on whether to implant an ICD should not be so “binary” based on the presence or absence of symptoms, and proposed further investigations be conducted into the complete phenotype of these arrhythmias.
The study has limitations, he observed, including a relatively small size; but it was able to detect important differences between 24-hour and 30-day monitoring outcomes even with only 100 patients. It was also limited by a lack of clinical follow-up for information on endpoints like stroke, thromboembolism, and sudden cardiac death.
Extended monitoring detected more cases of NSVT in the study’s relatively low-risk HCM patients who would not generally have an indication for ICD implantation, observed Dr. van Gelder. Also, at present the prognostic value of NSVT for SCD “seems to be more important at younger age” – that is, younger than 30 years – in patients with HCM.
Dr. van Gelder echoed Dr. Caro Codón’s call for more data from prolonged monitoring to help stratify patients according to risk; she proposed NSVT frequency, duration, and rate as possible targets.
The study was supported by an unrestricted grant from Nuubo, which provided the ECG monitoring systems. Dr. Caro Codón and Dr. van Gelder reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM EHRA
Colchicine’s 2010 price spike had major impact on gout care
A large price increase for colchicine in 2010 led to a significant falloff in its use for gout that persisted for the next decade while emergency and rheumatology visits for gout rose, suggesting poorer disease control, a retrospective cohort study reported.
The price of colchicine, commonly prescribed for acute gout attacks, climbed from $11.25 per prescription in 2009 to $190.49 in 2011, with the average out-of-pocket cost more than quadrupling, from $7.37 to $29.42, the study noted. Colchicine prescriptions for gout declined 27% over the next decade, according to adjusted analyses that the study authors performed.
“A roughly 16-fold increase in colchicine prices appeared to have lowered colchicine use over the next decade,” senior author Zirui Song, MD, PhD, an associate professor of health care policy and medicine at Harvard Medical School and an internist at Massachusetts General Hospital in Boston, told this news organization in written comments. “Over the same period, patients with gout used more of other medications that could treat gout. They also had more emergency department visits for gout and rheumatologist visits for gout, which potentially signals poorer disease control.”
The study, published online in JAMA Internal Medicine, examined MarketScan data from a longitudinal cohort of patients who had employer-sponsored health insurance and a diagnosis of gout from 2007 to 2019. MarketScan is an IBM database of medical and drug data from employers and health plans. The study examined more than 2.7 million patient-year observations over the 13-year period.
How the price increase happened
After 2011, a large percentage of patients shifted to less effective but more affordable drugs to treat gout. Prescriptions for allopurinol increased 32% (P < .001) and oral corticosteroids 8.3% over the decade. “These are imperfect substitutes,” Dr. Song said. “Allopurinol is used to prevent gout, while oral corticosteroids can be used to treat a gout flare.”
At the same time, visits for gout-related complaints to emergency departments and rheumatology offices increased through the ensuing years: 39.8% and 10.5% on an adjusted analysis, respectively (P < .001 for both).
Colchicine is actually a drug that predates the creation of the U.S. Food and Drug Administration in 1938 and had been grandfathered under its Unapproved Drug Initiative. Then in 2009, the FDA determined that colchicine was effective for treating arthritis-related gout flares after the manufacturer, URL Pharma, presented results of a randomized, controlled trial of 185 patients with gout.
The next year, the FDA granted URL Pharma 3 years of market exclusivity for the drug under the brand name Colcrys, now trademarked by Takeda Pharmaceuticals.
The latest study noted that longer-term analysis of the impact of the FDA’s decision had been lacking. The goal, said Dr. Song, was “to better understand the long-run implications of large drug price increases in the U.S. by studying the case of colchicine.”
He added, “For drugs that lack competition, large price increases can have large economic and clinical consequences over many years.”
Absorbing the cost
Lead author Dan P. Ly, MD, PhD, MPP, assistant professor at the University of California, Los Angeles, added, “Our study has large implications [for] when generic medications or other medications experience large price increases. Use of the medication in question drops or patients have to pay more out of pocket, and patient health can suffer as a result.”
The dropoff in colchicine use in this patient population could have been worse, Dr. Song said. “Despite colchicine use decreasing by 27% over nearly a decade, the fact that it did not decline more suggests that for patients with gout, the large price increase was mostly absorbed by their insurers, employers, or themselves – e.g., passed through to higher premiums, lower wages, or higher cost-sharing.”
Aaron Kesselheim, MD, JD, MPH, a professor at Harvard Medical School, Boston, reported previously on the price consequences of colchicine early on after the FDA granted the manufacturer market exclusivity.
“In our past research, we looked at how the massive increase in the price of colchicine increased spending on the drug and reduced use in a relatively short time period after the price hike,” said Dr. Kesselheim, who was not involved in this current study by Dr. Ly, Dr. Song, and Mia Giuriato, BBA, MA, from Harvard Medical School. “This study evaluated the experiences of patients with gout over multiple years and showed that the reductions in use persisted and were associated with increases in ED and rheumatology visits, suggesting worsening control of gout due to the relative inaccessibility of the drug at the new high price.”
The latest findings have public policy implications, Dr. Kesselheim said. “In the case of colchicine, the FDA made a bad pitch, leading to a home run for the manufacturer and a shutout for patients.”
“The FDA needs to make sure to take into account the quite predictable patient effects that can result from disruptions to competition when it considers taking steps like it did in the colchicine case to disrupt the market and create an artificial monopoly, even if the FDA acted in the best of intentions in this case,” Dr. Kesselheim added.
Dr. Song received funding for the study from the National Institutes of Health and Arnold Ventures. He also disclosed receiving personal fees from the Research Triangle Institute, Google Ventures, VBID Health, and the International Foundation of Employee Benefit Plans. Dr. Ly, Ms. Giuriato, and Dr. Kesselheim report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A large price increase for colchicine in 2010 led to a significant falloff in its use for gout that persisted for the next decade while emergency and rheumatology visits for gout rose, suggesting poorer disease control, a retrospective cohort study reported.
The price of colchicine, commonly prescribed for acute gout attacks, climbed from $11.25 per prescription in 2009 to $190.49 in 2011, with the average out-of-pocket cost more than quadrupling, from $7.37 to $29.42, the study noted. Colchicine prescriptions for gout declined 27% over the next decade, according to adjusted analyses that the study authors performed.
“A roughly 16-fold increase in colchicine prices appeared to have lowered colchicine use over the next decade,” senior author Zirui Song, MD, PhD, an associate professor of health care policy and medicine at Harvard Medical School and an internist at Massachusetts General Hospital in Boston, told this news organization in written comments. “Over the same period, patients with gout used more of other medications that could treat gout. They also had more emergency department visits for gout and rheumatologist visits for gout, which potentially signals poorer disease control.”
The study, published online in JAMA Internal Medicine, examined MarketScan data from a longitudinal cohort of patients who had employer-sponsored health insurance and a diagnosis of gout from 2007 to 2019. MarketScan is an IBM database of medical and drug data from employers and health plans. The study examined more than 2.7 million patient-year observations over the 13-year period.
How the price increase happened
After 2011, a large percentage of patients shifted to less effective but more affordable drugs to treat gout. Prescriptions for allopurinol increased 32% (P < .001) and oral corticosteroids 8.3% over the decade. “These are imperfect substitutes,” Dr. Song said. “Allopurinol is used to prevent gout, while oral corticosteroids can be used to treat a gout flare.”
At the same time, visits for gout-related complaints to emergency departments and rheumatology offices increased through the ensuing years: 39.8% and 10.5% on an adjusted analysis, respectively (P < .001 for both).
Colchicine is actually a drug that predates the creation of the U.S. Food and Drug Administration in 1938 and had been grandfathered under its Unapproved Drug Initiative. Then in 2009, the FDA determined that colchicine was effective for treating arthritis-related gout flares after the manufacturer, URL Pharma, presented results of a randomized, controlled trial of 185 patients with gout.
The next year, the FDA granted URL Pharma 3 years of market exclusivity for the drug under the brand name Colcrys, now trademarked by Takeda Pharmaceuticals.
The latest study noted that longer-term analysis of the impact of the FDA’s decision had been lacking. The goal, said Dr. Song, was “to better understand the long-run implications of large drug price increases in the U.S. by studying the case of colchicine.”
He added, “For drugs that lack competition, large price increases can have large economic and clinical consequences over many years.”
Absorbing the cost
Lead author Dan P. Ly, MD, PhD, MPP, assistant professor at the University of California, Los Angeles, added, “Our study has large implications [for] when generic medications or other medications experience large price increases. Use of the medication in question drops or patients have to pay more out of pocket, and patient health can suffer as a result.”
The dropoff in colchicine use in this patient population could have been worse, Dr. Song said. “Despite colchicine use decreasing by 27% over nearly a decade, the fact that it did not decline more suggests that for patients with gout, the large price increase was mostly absorbed by their insurers, employers, or themselves – e.g., passed through to higher premiums, lower wages, or higher cost-sharing.”
Aaron Kesselheim, MD, JD, MPH, a professor at Harvard Medical School, Boston, reported previously on the price consequences of colchicine early on after the FDA granted the manufacturer market exclusivity.
“In our past research, we looked at how the massive increase in the price of colchicine increased spending on the drug and reduced use in a relatively short time period after the price hike,” said Dr. Kesselheim, who was not involved in this current study by Dr. Ly, Dr. Song, and Mia Giuriato, BBA, MA, from Harvard Medical School. “This study evaluated the experiences of patients with gout over multiple years and showed that the reductions in use persisted and were associated with increases in ED and rheumatology visits, suggesting worsening control of gout due to the relative inaccessibility of the drug at the new high price.”
The latest findings have public policy implications, Dr. Kesselheim said. “In the case of colchicine, the FDA made a bad pitch, leading to a home run for the manufacturer and a shutout for patients.”
“The FDA needs to make sure to take into account the quite predictable patient effects that can result from disruptions to competition when it considers taking steps like it did in the colchicine case to disrupt the market and create an artificial monopoly, even if the FDA acted in the best of intentions in this case,” Dr. Kesselheim added.
Dr. Song received funding for the study from the National Institutes of Health and Arnold Ventures. He also disclosed receiving personal fees from the Research Triangle Institute, Google Ventures, VBID Health, and the International Foundation of Employee Benefit Plans. Dr. Ly, Ms. Giuriato, and Dr. Kesselheim report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A large price increase for colchicine in 2010 led to a significant falloff in its use for gout that persisted for the next decade while emergency and rheumatology visits for gout rose, suggesting poorer disease control, a retrospective cohort study reported.
The price of colchicine, commonly prescribed for acute gout attacks, climbed from $11.25 per prescription in 2009 to $190.49 in 2011, with the average out-of-pocket cost more than quadrupling, from $7.37 to $29.42, the study noted. Colchicine prescriptions for gout declined 27% over the next decade, according to adjusted analyses that the study authors performed.
“A roughly 16-fold increase in colchicine prices appeared to have lowered colchicine use over the next decade,” senior author Zirui Song, MD, PhD, an associate professor of health care policy and medicine at Harvard Medical School and an internist at Massachusetts General Hospital in Boston, told this news organization in written comments. “Over the same period, patients with gout used more of other medications that could treat gout. They also had more emergency department visits for gout and rheumatologist visits for gout, which potentially signals poorer disease control.”
The study, published online in JAMA Internal Medicine, examined MarketScan data from a longitudinal cohort of patients who had employer-sponsored health insurance and a diagnosis of gout from 2007 to 2019. MarketScan is an IBM database of medical and drug data from employers and health plans. The study examined more than 2.7 million patient-year observations over the 13-year period.
How the price increase happened
After 2011, a large percentage of patients shifted to less effective but more affordable drugs to treat gout. Prescriptions for allopurinol increased 32% (P < .001) and oral corticosteroids 8.3% over the decade. “These are imperfect substitutes,” Dr. Song said. “Allopurinol is used to prevent gout, while oral corticosteroids can be used to treat a gout flare.”
At the same time, visits for gout-related complaints to emergency departments and rheumatology offices increased through the ensuing years: 39.8% and 10.5% on an adjusted analysis, respectively (P < .001 for both).
Colchicine is actually a drug that predates the creation of the U.S. Food and Drug Administration in 1938 and had been grandfathered under its Unapproved Drug Initiative. Then in 2009, the FDA determined that colchicine was effective for treating arthritis-related gout flares after the manufacturer, URL Pharma, presented results of a randomized, controlled trial of 185 patients with gout.
The next year, the FDA granted URL Pharma 3 years of market exclusivity for the drug under the brand name Colcrys, now trademarked by Takeda Pharmaceuticals.
The latest study noted that longer-term analysis of the impact of the FDA’s decision had been lacking. The goal, said Dr. Song, was “to better understand the long-run implications of large drug price increases in the U.S. by studying the case of colchicine.”
He added, “For drugs that lack competition, large price increases can have large economic and clinical consequences over many years.”
Absorbing the cost
Lead author Dan P. Ly, MD, PhD, MPP, assistant professor at the University of California, Los Angeles, added, “Our study has large implications [for] when generic medications or other medications experience large price increases. Use of the medication in question drops or patients have to pay more out of pocket, and patient health can suffer as a result.”
The dropoff in colchicine use in this patient population could have been worse, Dr. Song said. “Despite colchicine use decreasing by 27% over nearly a decade, the fact that it did not decline more suggests that for patients with gout, the large price increase was mostly absorbed by their insurers, employers, or themselves – e.g., passed through to higher premiums, lower wages, or higher cost-sharing.”
Aaron Kesselheim, MD, JD, MPH, a professor at Harvard Medical School, Boston, reported previously on the price consequences of colchicine early on after the FDA granted the manufacturer market exclusivity.
“In our past research, we looked at how the massive increase in the price of colchicine increased spending on the drug and reduced use in a relatively short time period after the price hike,” said Dr. Kesselheim, who was not involved in this current study by Dr. Ly, Dr. Song, and Mia Giuriato, BBA, MA, from Harvard Medical School. “This study evaluated the experiences of patients with gout over multiple years and showed that the reductions in use persisted and were associated with increases in ED and rheumatology visits, suggesting worsening control of gout due to the relative inaccessibility of the drug at the new high price.”
The latest findings have public policy implications, Dr. Kesselheim said. “In the case of colchicine, the FDA made a bad pitch, leading to a home run for the manufacturer and a shutout for patients.”
“The FDA needs to make sure to take into account the quite predictable patient effects that can result from disruptions to competition when it considers taking steps like it did in the colchicine case to disrupt the market and create an artificial monopoly, even if the FDA acted in the best of intentions in this case,” Dr. Kesselheim added.
Dr. Song received funding for the study from the National Institutes of Health and Arnold Ventures. He also disclosed receiving personal fees from the Research Triangle Institute, Google Ventures, VBID Health, and the International Foundation of Employee Benefit Plans. Dr. Ly, Ms. Giuriato, and Dr. Kesselheim report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Watching feasible for asymptomatic kidney stones
Many patients with asymptomatic renal stones can qualify for an active surveillance program, Swiss researchers report at the American Urological Association 2023 Annual Meeting.
Kevin Stritt, MD, chief resident in the urology department at Lausanne University Hospital, said kidney stones often pass without symptoms. But until now, data on the frequency of asymptomatic, spontaneous passage of stones have been lacking.
The new data come from the NOSTONE trial, a prospective, multicenter, double-blind, placebo-controlled randomized trial to assess the efficacy of hydrochlorothiazide in the prevention of recurrence in patients with recurrent calcium-containing kidney stones.
Dr. Stritt and colleagues evaluated the natural history of asymptomatic renal stones during a median follow-up of 35 months. “We found for the first time that a relevant number of kidney stone passages [39%] were asymptomatic, spontaneous stone passages,” Dr. Stritt told this news organization.
All asymptomatic spontaneous stone passages were analyzed in a comparison of the total number of kidney stones on low-dose, nonintravenous contrast CT imaging at the beginning and end of the 3-year follow-up.
Of the 403 stones passed spontaneously, 61% (245) were symptomatic stone passages and 39% (158) were asymptomatic stone passages, Dr. Stritt told this news organization.
Asymptomatic stones were a median size of 2.4 mm, and symptomatic stones were 2.15 mm, which was not significantly different (P = .366), according to the researchers. Dr. Stritt said the spontaneous passage of asymptomatic stones was largely influenced by a higher number of stones on CT imaging at randomization (P = .001) and a lower total stone volume (P = .001).
Ephrem Olweny, MD, an assistant professor of urology and section chief of endourology at Rush University Medical Center in Chicago, said previous studies have found that the rate of spontaneous passage of kidney stones ranges from 3% to 29%.
“But this secondary analysis of data from a prior multicenter prospective randomized trial offers higher-quality data that will be of value in guiding patient counseling,” Dr. Olweny said.
“Observation should be initially offered to these patients. However, patients should be informed that 52% are likely to develop symptoms, and some may indeed opt for preemptive surgical removal,” he added.
David Schulsinger, MD, an associate professor in the department of urology at Stony Brook (N.Y.) University Hospital, said the incidence of kidney stones has been increasing worldwide, affecting approximately 12% of men and 6% of women. Dehydration and diets high in sodium and calcium are major factors, he said.
Patients with a history of stones have a 50% risk of recurrence in the next 5 years, and an 80% risk in their lifetime, he added.
Dr. Schulsinger said the message from the Swiss study is that urologists can be “comfortable” watching small stones, those averaging 2.4 mm or less in size. “But if a patient has a 7- or 8-mm stone, you might be more inclined to manage that patient a little bit more aggressively.”
Roughly half of patients with stones less than 2 mm will pass it in about 8 days, he said.
Dr. Olweny noted that the study was a secondary analysis of data from a randomized controlled trial that evaluated the efficacy of thiazides in preventing the recurrence of calcium stones. “The original study was not specifically designed to look at asymptomatic stone passage rates for small renal stones, and therefore, the observed rates may not reflect the most precise estimates,” he said.
Dr. Stritt said his group has not studied the size limit of stones that pass spontaneously without symptoms. “This study could serve to construct recurrence prediction models based on medical history and stone burden on CT imaging. More well-designed research on this topic is urgently needed,” he said. “These results should encourage urologists to counsel patients about the possibility of an active surveillance strategy when smaller kidney stones are present.”
The author and independent commentators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Many patients with asymptomatic renal stones can qualify for an active surveillance program, Swiss researchers report at the American Urological Association 2023 Annual Meeting.
Kevin Stritt, MD, chief resident in the urology department at Lausanne University Hospital, said kidney stones often pass without symptoms. But until now, data on the frequency of asymptomatic, spontaneous passage of stones have been lacking.
The new data come from the NOSTONE trial, a prospective, multicenter, double-blind, placebo-controlled randomized trial to assess the efficacy of hydrochlorothiazide in the prevention of recurrence in patients with recurrent calcium-containing kidney stones.
Dr. Stritt and colleagues evaluated the natural history of asymptomatic renal stones during a median follow-up of 35 months. “We found for the first time that a relevant number of kidney stone passages [39%] were asymptomatic, spontaneous stone passages,” Dr. Stritt told this news organization.
All asymptomatic spontaneous stone passages were analyzed in a comparison of the total number of kidney stones on low-dose, nonintravenous contrast CT imaging at the beginning and end of the 3-year follow-up.
Of the 403 stones passed spontaneously, 61% (245) were symptomatic stone passages and 39% (158) were asymptomatic stone passages, Dr. Stritt told this news organization.
Asymptomatic stones were a median size of 2.4 mm, and symptomatic stones were 2.15 mm, which was not significantly different (P = .366), according to the researchers. Dr. Stritt said the spontaneous passage of asymptomatic stones was largely influenced by a higher number of stones on CT imaging at randomization (P = .001) and a lower total stone volume (P = .001).
Ephrem Olweny, MD, an assistant professor of urology and section chief of endourology at Rush University Medical Center in Chicago, said previous studies have found that the rate of spontaneous passage of kidney stones ranges from 3% to 29%.
“But this secondary analysis of data from a prior multicenter prospective randomized trial offers higher-quality data that will be of value in guiding patient counseling,” Dr. Olweny said.
“Observation should be initially offered to these patients. However, patients should be informed that 52% are likely to develop symptoms, and some may indeed opt for preemptive surgical removal,” he added.
David Schulsinger, MD, an associate professor in the department of urology at Stony Brook (N.Y.) University Hospital, said the incidence of kidney stones has been increasing worldwide, affecting approximately 12% of men and 6% of women. Dehydration and diets high in sodium and calcium are major factors, he said.
Patients with a history of stones have a 50% risk of recurrence in the next 5 years, and an 80% risk in their lifetime, he added.
Dr. Schulsinger said the message from the Swiss study is that urologists can be “comfortable” watching small stones, those averaging 2.4 mm or less in size. “But if a patient has a 7- or 8-mm stone, you might be more inclined to manage that patient a little bit more aggressively.”
Roughly half of patients with stones less than 2 mm will pass it in about 8 days, he said.
Dr. Olweny noted that the study was a secondary analysis of data from a randomized controlled trial that evaluated the efficacy of thiazides in preventing the recurrence of calcium stones. “The original study was not specifically designed to look at asymptomatic stone passage rates for small renal stones, and therefore, the observed rates may not reflect the most precise estimates,” he said.
Dr. Stritt said his group has not studied the size limit of stones that pass spontaneously without symptoms. “This study could serve to construct recurrence prediction models based on medical history and stone burden on CT imaging. More well-designed research on this topic is urgently needed,” he said. “These results should encourage urologists to counsel patients about the possibility of an active surveillance strategy when smaller kidney stones are present.”
The author and independent commentators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Many patients with asymptomatic renal stones can qualify for an active surveillance program, Swiss researchers report at the American Urological Association 2023 Annual Meeting.
Kevin Stritt, MD, chief resident in the urology department at Lausanne University Hospital, said kidney stones often pass without symptoms. But until now, data on the frequency of asymptomatic, spontaneous passage of stones have been lacking.
The new data come from the NOSTONE trial, a prospective, multicenter, double-blind, placebo-controlled randomized trial to assess the efficacy of hydrochlorothiazide in the prevention of recurrence in patients with recurrent calcium-containing kidney stones.
Dr. Stritt and colleagues evaluated the natural history of asymptomatic renal stones during a median follow-up of 35 months. “We found for the first time that a relevant number of kidney stone passages [39%] were asymptomatic, spontaneous stone passages,” Dr. Stritt told this news organization.
All asymptomatic spontaneous stone passages were analyzed in a comparison of the total number of kidney stones on low-dose, nonintravenous contrast CT imaging at the beginning and end of the 3-year follow-up.
Of the 403 stones passed spontaneously, 61% (245) were symptomatic stone passages and 39% (158) were asymptomatic stone passages, Dr. Stritt told this news organization.
Asymptomatic stones were a median size of 2.4 mm, and symptomatic stones were 2.15 mm, which was not significantly different (P = .366), according to the researchers. Dr. Stritt said the spontaneous passage of asymptomatic stones was largely influenced by a higher number of stones on CT imaging at randomization (P = .001) and a lower total stone volume (P = .001).
Ephrem Olweny, MD, an assistant professor of urology and section chief of endourology at Rush University Medical Center in Chicago, said previous studies have found that the rate of spontaneous passage of kidney stones ranges from 3% to 29%.
“But this secondary analysis of data from a prior multicenter prospective randomized trial offers higher-quality data that will be of value in guiding patient counseling,” Dr. Olweny said.
“Observation should be initially offered to these patients. However, patients should be informed that 52% are likely to develop symptoms, and some may indeed opt for preemptive surgical removal,” he added.
David Schulsinger, MD, an associate professor in the department of urology at Stony Brook (N.Y.) University Hospital, said the incidence of kidney stones has been increasing worldwide, affecting approximately 12% of men and 6% of women. Dehydration and diets high in sodium and calcium are major factors, he said.
Patients with a history of stones have a 50% risk of recurrence in the next 5 years, and an 80% risk in their lifetime, he added.
Dr. Schulsinger said the message from the Swiss study is that urologists can be “comfortable” watching small stones, those averaging 2.4 mm or less in size. “But if a patient has a 7- or 8-mm stone, you might be more inclined to manage that patient a little bit more aggressively.”
Roughly half of patients with stones less than 2 mm will pass it in about 8 days, he said.
Dr. Olweny noted that the study was a secondary analysis of data from a randomized controlled trial that evaluated the efficacy of thiazides in preventing the recurrence of calcium stones. “The original study was not specifically designed to look at asymptomatic stone passage rates for small renal stones, and therefore, the observed rates may not reflect the most precise estimates,” he said.
Dr. Stritt said his group has not studied the size limit of stones that pass spontaneously without symptoms. “This study could serve to construct recurrence prediction models based on medical history and stone burden on CT imaging. More well-designed research on this topic is urgently needed,” he said. “These results should encourage urologists to counsel patients about the possibility of an active surveillance strategy when smaller kidney stones are present.”
The author and independent commentators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Study of hospitalizations in Canada quantifies benefit of COVID-19 vaccine to reduce death, ICU admissions
A cohort study of more than 1.5 million hospital admissions in Canada through the first 2 years of the COVID-19 pandemic has quantified the benefit of vaccinations. Unvaccinated patients were found to be up to 15 times more likely to die from COVID-19 than fully vaccinated patients.
Investigators analyzed 1.513 million admissions at 155 hospitals across Canada from March 15, 2020, to May 28, 2022. The study included 51,679 adult admissions and 4,035 pediatric admissions for COVID-19. Although the share of COVID-19 admissions increased in the fifth and sixth waves, from Dec. 26, 2021, to March 19, 2022 – after the full vaccine rollout – to 7.73% from 2.47% in the previous four waves, the proportion of adults admitted to the intensive care unit was significantly lower, at 8.7% versus 21.8% (odds ratio, 0.35; 95% confidence interval, 0.32-0.36).
“The good thing about waves five and six was we were able to show the COVID cases tended to be less severe, but on the other hand, because the disease in the community was so much higher, the demands on the health care system were much higher than the previous waves,” study author Charles Frenette, MD, director of infection prevention and control at McGill University, Montreal, and chair of the study’s adult subgroup, said in an interview. “But here we were able to show the benefit of vaccinations, particularly the boosting dose, in protecting against those severe outcomes.”
The study, published in JAMA Network Open, used the Canadian Nosocomial Infection Surveillance Program database, which collects hospital data across Canada. It was activated in March 2020 to collect details on all COVID-19 admissions, co-author Nisha Thampi, MD, chair of the study’s pediatric subgroup, told this news organization.
“We’re now over 3 years into the pandemic, and CNISP continues to monitor COVID-19 as well as other pathogens in near real time,” said Dr. Thampi, an associate professor and infectious disease specialist at Children’s Hospital of Eastern Ontario.
“That’s a particular strength of this surveillance program as well. We would see this data on a biweekly basis, and that allows for [us] to implement timely protection and action.”
Tracing trends over six waves
The study tracked COVID-19 hospitalizations during six waves. The first lasted from March 15 to August 31, 2020, and the second lasted from Sept. 1, 2020, to Feb. 28, 2021. The wild-type variant was dominant during both waves. The third wave lasted from March 1 to June 30, 2021, and was marked by the mixed Alpha, Beta, and Gamma variants. The fourth wave lasted from July 1 to Dec. 25, 2021, when the Alpha variant was dominant. The Omicron variant dominated during waves five (Dec. 26, 2021, to March 19, 2022) and six (March 20 to May 28, 2022).
Hospitalizations reached a peak of 14,461 in wave five. ICU admissions, however, peaked at 2,164 during wave four, and all-cause deaths peaked at 1,663 during wave two.
The investigators also analyzed how unvaccinated patients fared, compared with the fully vaccinated and the fully vaccinated-plus (that is, patients with one or more additional doses). During waves five and six, unvaccinated patients were 4.3 times more likely to end up in the ICU than fully vaccinated patients and were 12.2 times more likely than fully vaccinated-plus patients. Likewise, the rate for all-cause in-hospital death for unvaccinated patients was 3.9 times greater than that for fully vaccinated patients and 15.1 times greater than that for fully vaccinated-plus patients.
The effect of vaccines emerged in waves three and four, said Dr. Frenette. “We started to see really, really significant protection and benefit from the vaccine, not only in incidence of admission but also in the incidence of complications of ICU care, ventilation, and mortality.”
Results for pediatric patients were similar to those for adults, Dr. Thampi noted. During waves five and six, overall admissions peaked, but the share of ICU admissions decreased to 9.4% from 18.1%, which was the rate during the previous four waves (OR, 0.47).
“What’s important is how pediatric hospitalizations changed over the course of the various waves,” said Dr. Thampi.
“Where we saw the highest admissions during the early Omicron dominance, we actually had the lowest numbers of hospitalizations with death and admissions into ICUs.”
Doing more with the data
David Fisman, MD, MPH, a professor of epidemiology at the University of Toronto, said, “This is a study that shows us how tremendously dramatic the effects of the COVID-19 vaccine were in terms of saving lives during the pandemic.” Dr. Fisman was not involved in the study.
But CNISP, which receives funding from Public Health Agency of Canada, could do more with the data it collects to better protect the public from COVID-19 and other nosocomial infections, Dr. Fisman said.
“The first problematic thing about this paper is that Canadians are paying for a surveillance system that looks at risks of acquiring infections, including COVID-19 infections, in the hospital, but that data is not fed back to the people paying for its production,” he said.
“So, Canadians don’t have the ability to really understand in real time how much risk they’re experiencing via going to the hospital for some other reason.”
The study was independently supported. Dr. Frenette and Dr. Thampi report no relevant financial relationships. Dr. Fisman has disclosed financial relationships with Pfizer, AstraZeneca, Sanofi, Seqirus, Merck, the Ontario Nurses Association, and the Elementary Teachers’ Federation of Ontario.
A version of this article first appeared on Medscape.com.
A cohort study of more than 1.5 million hospital admissions in Canada through the first 2 years of the COVID-19 pandemic has quantified the benefit of vaccinations. Unvaccinated patients were found to be up to 15 times more likely to die from COVID-19 than fully vaccinated patients.
Investigators analyzed 1.513 million admissions at 155 hospitals across Canada from March 15, 2020, to May 28, 2022. The study included 51,679 adult admissions and 4,035 pediatric admissions for COVID-19. Although the share of COVID-19 admissions increased in the fifth and sixth waves, from Dec. 26, 2021, to March 19, 2022 – after the full vaccine rollout – to 7.73% from 2.47% in the previous four waves, the proportion of adults admitted to the intensive care unit was significantly lower, at 8.7% versus 21.8% (odds ratio, 0.35; 95% confidence interval, 0.32-0.36).
“The good thing about waves five and six was we were able to show the COVID cases tended to be less severe, but on the other hand, because the disease in the community was so much higher, the demands on the health care system were much higher than the previous waves,” study author Charles Frenette, MD, director of infection prevention and control at McGill University, Montreal, and chair of the study’s adult subgroup, said in an interview. “But here we were able to show the benefit of vaccinations, particularly the boosting dose, in protecting against those severe outcomes.”
The study, published in JAMA Network Open, used the Canadian Nosocomial Infection Surveillance Program database, which collects hospital data across Canada. It was activated in March 2020 to collect details on all COVID-19 admissions, co-author Nisha Thampi, MD, chair of the study’s pediatric subgroup, told this news organization.
“We’re now over 3 years into the pandemic, and CNISP continues to monitor COVID-19 as well as other pathogens in near real time,” said Dr. Thampi, an associate professor and infectious disease specialist at Children’s Hospital of Eastern Ontario.
“That’s a particular strength of this surveillance program as well. We would see this data on a biweekly basis, and that allows for [us] to implement timely protection and action.”
Tracing trends over six waves
The study tracked COVID-19 hospitalizations during six waves. The first lasted from March 15 to August 31, 2020, and the second lasted from Sept. 1, 2020, to Feb. 28, 2021. The wild-type variant was dominant during both waves. The third wave lasted from March 1 to June 30, 2021, and was marked by the mixed Alpha, Beta, and Gamma variants. The fourth wave lasted from July 1 to Dec. 25, 2021, when the Alpha variant was dominant. The Omicron variant dominated during waves five (Dec. 26, 2021, to March 19, 2022) and six (March 20 to May 28, 2022).
Hospitalizations reached a peak of 14,461 in wave five. ICU admissions, however, peaked at 2,164 during wave four, and all-cause deaths peaked at 1,663 during wave two.
The investigators also analyzed how unvaccinated patients fared, compared with the fully vaccinated and the fully vaccinated-plus (that is, patients with one or more additional doses). During waves five and six, unvaccinated patients were 4.3 times more likely to end up in the ICU than fully vaccinated patients and were 12.2 times more likely than fully vaccinated-plus patients. Likewise, the rate for all-cause in-hospital death for unvaccinated patients was 3.9 times greater than that for fully vaccinated patients and 15.1 times greater than that for fully vaccinated-plus patients.
The effect of vaccines emerged in waves three and four, said Dr. Frenette. “We started to see really, really significant protection and benefit from the vaccine, not only in incidence of admission but also in the incidence of complications of ICU care, ventilation, and mortality.”
Results for pediatric patients were similar to those for adults, Dr. Thampi noted. During waves five and six, overall admissions peaked, but the share of ICU admissions decreased to 9.4% from 18.1%, which was the rate during the previous four waves (OR, 0.47).
“What’s important is how pediatric hospitalizations changed over the course of the various waves,” said Dr. Thampi.
“Where we saw the highest admissions during the early Omicron dominance, we actually had the lowest numbers of hospitalizations with death and admissions into ICUs.”
Doing more with the data
David Fisman, MD, MPH, a professor of epidemiology at the University of Toronto, said, “This is a study that shows us how tremendously dramatic the effects of the COVID-19 vaccine were in terms of saving lives during the pandemic.” Dr. Fisman was not involved in the study.
But CNISP, which receives funding from Public Health Agency of Canada, could do more with the data it collects to better protect the public from COVID-19 and other nosocomial infections, Dr. Fisman said.
“The first problematic thing about this paper is that Canadians are paying for a surveillance system that looks at risks of acquiring infections, including COVID-19 infections, in the hospital, but that data is not fed back to the people paying for its production,” he said.
“So, Canadians don’t have the ability to really understand in real time how much risk they’re experiencing via going to the hospital for some other reason.”
The study was independently supported. Dr. Frenette and Dr. Thampi report no relevant financial relationships. Dr. Fisman has disclosed financial relationships with Pfizer, AstraZeneca, Sanofi, Seqirus, Merck, the Ontario Nurses Association, and the Elementary Teachers’ Federation of Ontario.
A version of this article first appeared on Medscape.com.
A cohort study of more than 1.5 million hospital admissions in Canada through the first 2 years of the COVID-19 pandemic has quantified the benefit of vaccinations. Unvaccinated patients were found to be up to 15 times more likely to die from COVID-19 than fully vaccinated patients.
Investigators analyzed 1.513 million admissions at 155 hospitals across Canada from March 15, 2020, to May 28, 2022. The study included 51,679 adult admissions and 4,035 pediatric admissions for COVID-19. Although the share of COVID-19 admissions increased in the fifth and sixth waves, from Dec. 26, 2021, to March 19, 2022 – after the full vaccine rollout – to 7.73% from 2.47% in the previous four waves, the proportion of adults admitted to the intensive care unit was significantly lower, at 8.7% versus 21.8% (odds ratio, 0.35; 95% confidence interval, 0.32-0.36).
“The good thing about waves five and six was we were able to show the COVID cases tended to be less severe, but on the other hand, because the disease in the community was so much higher, the demands on the health care system were much higher than the previous waves,” study author Charles Frenette, MD, director of infection prevention and control at McGill University, Montreal, and chair of the study’s adult subgroup, said in an interview. “But here we were able to show the benefit of vaccinations, particularly the boosting dose, in protecting against those severe outcomes.”
The study, published in JAMA Network Open, used the Canadian Nosocomial Infection Surveillance Program database, which collects hospital data across Canada. It was activated in March 2020 to collect details on all COVID-19 admissions, co-author Nisha Thampi, MD, chair of the study’s pediatric subgroup, told this news organization.
“We’re now over 3 years into the pandemic, and CNISP continues to monitor COVID-19 as well as other pathogens in near real time,” said Dr. Thampi, an associate professor and infectious disease specialist at Children’s Hospital of Eastern Ontario.
“That’s a particular strength of this surveillance program as well. We would see this data on a biweekly basis, and that allows for [us] to implement timely protection and action.”
Tracing trends over six waves
The study tracked COVID-19 hospitalizations during six waves. The first lasted from March 15 to August 31, 2020, and the second lasted from Sept. 1, 2020, to Feb. 28, 2021. The wild-type variant was dominant during both waves. The third wave lasted from March 1 to June 30, 2021, and was marked by the mixed Alpha, Beta, and Gamma variants. The fourth wave lasted from July 1 to Dec. 25, 2021, when the Alpha variant was dominant. The Omicron variant dominated during waves five (Dec. 26, 2021, to March 19, 2022) and six (March 20 to May 28, 2022).
Hospitalizations reached a peak of 14,461 in wave five. ICU admissions, however, peaked at 2,164 during wave four, and all-cause deaths peaked at 1,663 during wave two.
The investigators also analyzed how unvaccinated patients fared, compared with the fully vaccinated and the fully vaccinated-plus (that is, patients with one or more additional doses). During waves five and six, unvaccinated patients were 4.3 times more likely to end up in the ICU than fully vaccinated patients and were 12.2 times more likely than fully vaccinated-plus patients. Likewise, the rate for all-cause in-hospital death for unvaccinated patients was 3.9 times greater than that for fully vaccinated patients and 15.1 times greater than that for fully vaccinated-plus patients.
The effect of vaccines emerged in waves three and four, said Dr. Frenette. “We started to see really, really significant protection and benefit from the vaccine, not only in incidence of admission but also in the incidence of complications of ICU care, ventilation, and mortality.”
Results for pediatric patients were similar to those for adults, Dr. Thampi noted. During waves five and six, overall admissions peaked, but the share of ICU admissions decreased to 9.4% from 18.1%, which was the rate during the previous four waves (OR, 0.47).
“What’s important is how pediatric hospitalizations changed over the course of the various waves,” said Dr. Thampi.
“Where we saw the highest admissions during the early Omicron dominance, we actually had the lowest numbers of hospitalizations with death and admissions into ICUs.”
Doing more with the data
David Fisman, MD, MPH, a professor of epidemiology at the University of Toronto, said, “This is a study that shows us how tremendously dramatic the effects of the COVID-19 vaccine were in terms of saving lives during the pandemic.” Dr. Fisman was not involved in the study.
But CNISP, which receives funding from Public Health Agency of Canada, could do more with the data it collects to better protect the public from COVID-19 and other nosocomial infections, Dr. Fisman said.
“The first problematic thing about this paper is that Canadians are paying for a surveillance system that looks at risks of acquiring infections, including COVID-19 infections, in the hospital, but that data is not fed back to the people paying for its production,” he said.
“So, Canadians don’t have the ability to really understand in real time how much risk they’re experiencing via going to the hospital for some other reason.”
The study was independently supported. Dr. Frenette and Dr. Thampi report no relevant financial relationships. Dr. Fisman has disclosed financial relationships with Pfizer, AstraZeneca, Sanofi, Seqirus, Merck, the Ontario Nurses Association, and the Elementary Teachers’ Federation of Ontario.
A version of this article first appeared on Medscape.com.
Study shifts burden of IgG4-related disease to women
The incidence and prevalence of IgG4-related disease each rose considerably from 2015 to 2019 in the United States, and the risk of death in those with the immune-mediated condition is about 2.5 times higher than those who are not affected, based on an analysis of claims data from commercially insured adults.
The first population-based study of IgG4-RD incidence, prevalence, and mortality establishes “key benchmarks for informing the diagnosis and management of patients” with a condition “that causes fibrosing inflammatory lesions at nearly any anatomic site,” and wasn’t initially described until 2001, Zachary S. Wallace, MD, and associates said in Annals of the Rheumatic Diseases.
The increases in incidence and prevalence likely reflected increased disease awareness, they suggested. Overall U.S. incidence was 1.2 per 100,000 person-years for the 5-year period of 2015-2019, rising 86% from 0.78 per 100,000 person-years to 1.45 in 2018 before dropping to 1.39 in 2019. The change in prevalence was even greater, increasing 122% from 2.41 per 100,000 persons in 2015 to 5.34 per 100,000 in 2019, the investigators said.
Previous studies had indicated that the majority of patients with IgG4-RD were male, but the current study, using Optum’s Clinformatics Data Mart, which includes commercial health plan and Medicare Advantage members in all 50 states, showed that both incidence and prevalence (see graph) were higher among women, noted Dr. Wallace of Massachusetts General Hospital, Boston, and associates. They identified 524 patients (57.6% female) in the database who met the criteria for IgG4-RD from Jan. 1, 2010, to Dec. 31, 2019.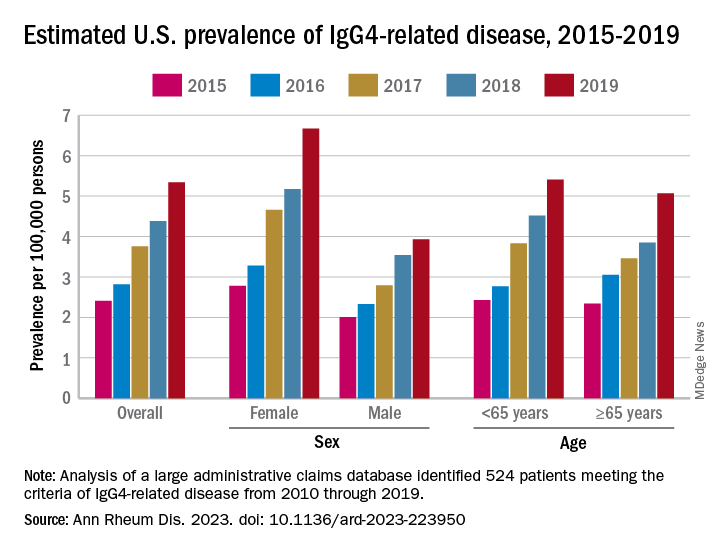
Incidence over the course of the study “was similar in patients identified as Asian or White but lower in those identified as Black or Hispanic,” they noted, adding that “the prevalence of IgG4-RD during this period reflected similar trends.” A jump in prevalence from 2018 to 2019, however, left White patients with a much higher rate (6.13 per 100,000 persons) than Asian patients (4.54 per 100,000), Black patients (3.42), and Hispanic patients (3.02).
For the mortality analysis, 516 patients with IgG4-RD were age-, sex-, and race-matched with 5,160 patients without IgG4-RD. Mortality was 3.42 and 1.46 per 100 person-years, respectively, over the 5.5 years of follow-up, so IgG4-RD was associated with a 2.5-fold higher risk of death. “The association of IgG4-RD with a higher risk of death was observed across the age spectrum and among both male and female patients,” the researchers said.
“Clinicians across specialties should be aware of IgG4-RD given the incidence, prevalence, and excess risk of death associated with this condition. ... Additional studies are urgently needed to define optimal management strategies to improve survival,” they wrote.
The study was supported by a grant to Massachusetts General Hospital from Sanofi, and Dr. Wallace received funding from the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases, and the Rheumatology Research Foundation. He has received research support and consulting fees from several companies, and four coinvestigators are employees of Sanofi.
The incidence and prevalence of IgG4-related disease each rose considerably from 2015 to 2019 in the United States, and the risk of death in those with the immune-mediated condition is about 2.5 times higher than those who are not affected, based on an analysis of claims data from commercially insured adults.
The first population-based study of IgG4-RD incidence, prevalence, and mortality establishes “key benchmarks for informing the diagnosis and management of patients” with a condition “that causes fibrosing inflammatory lesions at nearly any anatomic site,” and wasn’t initially described until 2001, Zachary S. Wallace, MD, and associates said in Annals of the Rheumatic Diseases.
The increases in incidence and prevalence likely reflected increased disease awareness, they suggested. Overall U.S. incidence was 1.2 per 100,000 person-years for the 5-year period of 2015-2019, rising 86% from 0.78 per 100,000 person-years to 1.45 in 2018 before dropping to 1.39 in 2019. The change in prevalence was even greater, increasing 122% from 2.41 per 100,000 persons in 2015 to 5.34 per 100,000 in 2019, the investigators said.
Previous studies had indicated that the majority of patients with IgG4-RD were male, but the current study, using Optum’s Clinformatics Data Mart, which includes commercial health plan and Medicare Advantage members in all 50 states, showed that both incidence and prevalence (see graph) were higher among women, noted Dr. Wallace of Massachusetts General Hospital, Boston, and associates. They identified 524 patients (57.6% female) in the database who met the criteria for IgG4-RD from Jan. 1, 2010, to Dec. 31, 2019.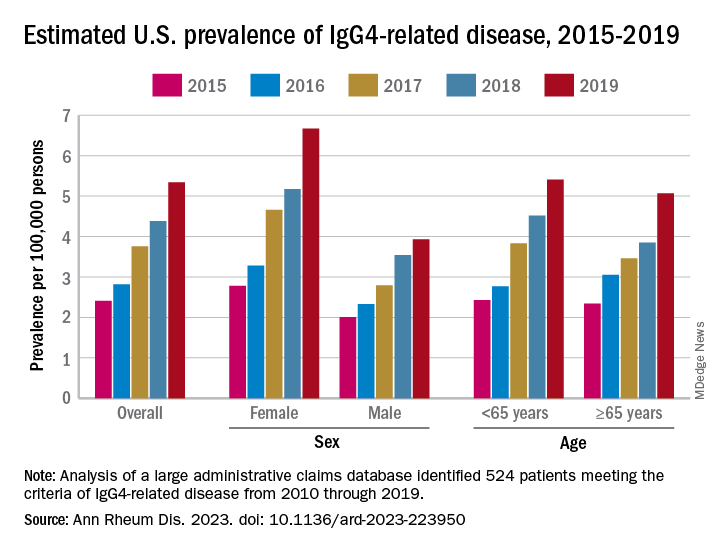
Incidence over the course of the study “was similar in patients identified as Asian or White but lower in those identified as Black or Hispanic,” they noted, adding that “the prevalence of IgG4-RD during this period reflected similar trends.” A jump in prevalence from 2018 to 2019, however, left White patients with a much higher rate (6.13 per 100,000 persons) than Asian patients (4.54 per 100,000), Black patients (3.42), and Hispanic patients (3.02).
For the mortality analysis, 516 patients with IgG4-RD were age-, sex-, and race-matched with 5,160 patients without IgG4-RD. Mortality was 3.42 and 1.46 per 100 person-years, respectively, over the 5.5 years of follow-up, so IgG4-RD was associated with a 2.5-fold higher risk of death. “The association of IgG4-RD with a higher risk of death was observed across the age spectrum and among both male and female patients,” the researchers said.
“Clinicians across specialties should be aware of IgG4-RD given the incidence, prevalence, and excess risk of death associated with this condition. ... Additional studies are urgently needed to define optimal management strategies to improve survival,” they wrote.
The study was supported by a grant to Massachusetts General Hospital from Sanofi, and Dr. Wallace received funding from the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases, and the Rheumatology Research Foundation. He has received research support and consulting fees from several companies, and four coinvestigators are employees of Sanofi.
The incidence and prevalence of IgG4-related disease each rose considerably from 2015 to 2019 in the United States, and the risk of death in those with the immune-mediated condition is about 2.5 times higher than those who are not affected, based on an analysis of claims data from commercially insured adults.
The first population-based study of IgG4-RD incidence, prevalence, and mortality establishes “key benchmarks for informing the diagnosis and management of patients” with a condition “that causes fibrosing inflammatory lesions at nearly any anatomic site,” and wasn’t initially described until 2001, Zachary S. Wallace, MD, and associates said in Annals of the Rheumatic Diseases.
The increases in incidence and prevalence likely reflected increased disease awareness, they suggested. Overall U.S. incidence was 1.2 per 100,000 person-years for the 5-year period of 2015-2019, rising 86% from 0.78 per 100,000 person-years to 1.45 in 2018 before dropping to 1.39 in 2019. The change in prevalence was even greater, increasing 122% from 2.41 per 100,000 persons in 2015 to 5.34 per 100,000 in 2019, the investigators said.
Previous studies had indicated that the majority of patients with IgG4-RD were male, but the current study, using Optum’s Clinformatics Data Mart, which includes commercial health plan and Medicare Advantage members in all 50 states, showed that both incidence and prevalence (see graph) were higher among women, noted Dr. Wallace of Massachusetts General Hospital, Boston, and associates. They identified 524 patients (57.6% female) in the database who met the criteria for IgG4-RD from Jan. 1, 2010, to Dec. 31, 2019.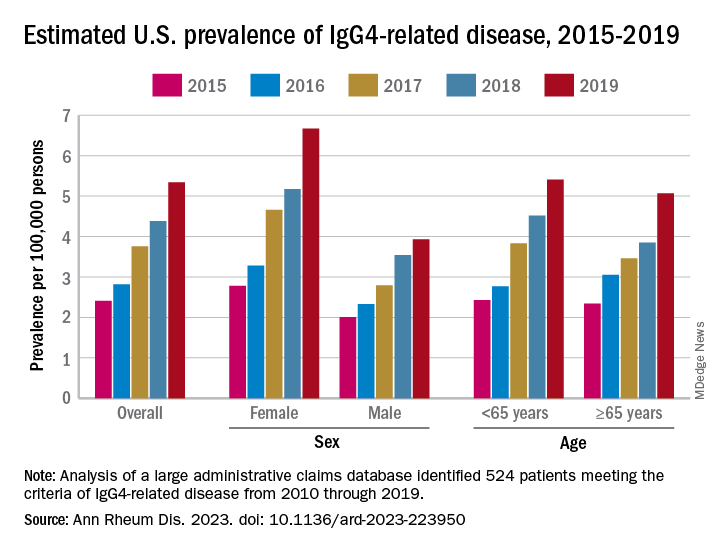
Incidence over the course of the study “was similar in patients identified as Asian or White but lower in those identified as Black or Hispanic,” they noted, adding that “the prevalence of IgG4-RD during this period reflected similar trends.” A jump in prevalence from 2018 to 2019, however, left White patients with a much higher rate (6.13 per 100,000 persons) than Asian patients (4.54 per 100,000), Black patients (3.42), and Hispanic patients (3.02).
For the mortality analysis, 516 patients with IgG4-RD were age-, sex-, and race-matched with 5,160 patients without IgG4-RD. Mortality was 3.42 and 1.46 per 100 person-years, respectively, over the 5.5 years of follow-up, so IgG4-RD was associated with a 2.5-fold higher risk of death. “The association of IgG4-RD with a higher risk of death was observed across the age spectrum and among both male and female patients,” the researchers said.
“Clinicians across specialties should be aware of IgG4-RD given the incidence, prevalence, and excess risk of death associated with this condition. ... Additional studies are urgently needed to define optimal management strategies to improve survival,” they wrote.
The study was supported by a grant to Massachusetts General Hospital from Sanofi, and Dr. Wallace received funding from the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases, and the Rheumatology Research Foundation. He has received research support and consulting fees from several companies, and four coinvestigators are employees of Sanofi.
FROM ANNALS OF THE RHEUMATIC DISEASES
New USPSTF draft suggests mammography start at 40, not 50
The major change: USPSTF proposed reducing the recommended start age for routine screening mammograms from age 50 to age 40. The latest recommendation, which carries a B grade, also calls for screening every other year and sets a cutoff age of 74.
The task force’s A and B ratings indicate strong confidence in the evidence for benefit, meaning that clinicians should encourage their patients to get these services as appropriate.
The influential federal advisory panel last updated these recommendations in 2016. At the time, USPSTF recommended routine screening mammograms starting at age 50, and gave a C grade to starting before that.
In the 2016 recommendations, “we felt a woman could start screening in her 40s depending on how she feels about the harms and benefits in an individualized personal decision,” USPSTF member John Wong, MD, chief of clinical decision making and a primary care physician at Tufts Medical Center in Boston, said in an interview. “In this draft recommendation, we now recommend that all women get screened starting at age 40.”
Two major factors prompted the change, explained Dr. Wong. One is that more women are being diagnosed with breast cancer in their 40s. The other is that a growing body of evidence showing that Black women get breast cancer younger, are more likely to die of breast cancer, and would benefit from earlier screening.
“It is now clear that screening every other year starting at age 40 has the potential to save about 20% more lives among all women and there is even greater potential benefit for Black women, who are much more likely to die from breast cancer,” Dr. Wong said.
The American Cancer Society (ACS) called the draft recommendations a “significant positive change,” while noting that the task force recommendations only apply to women at average risk for breast cancer.
The American College of Radiology (ACR) already recommends yearly mammograms for average risk women starting at age 40. Its latest guidelines on mammography call for women at higher-than-average risk for breast cancer to undergo a risk assessment by age 25 to determine if screening before age 40 is needed.
When asked about the differing views, Debra Monticciolo, MD, division chief for breast imaging at Massachusetts General Hospital, said annual screenings that follow ACR recommendations would save more lives than the every-other-year approach backed by the task force. Dr. Monticciolo also highlighted that the available scientific evidence supports earlier assessment as well as augmented and earlier-than-age-40 screening of many women – particularly Black women.
“These evidence-based updates should spur more-informed doctor–patient conversations and help providers save more lives,” Dr. Monticciolo said in a press release.
Insurance access
Typically, upgrading a USPSTF recommendation from C to B leads to better access and insurance coverage for patients. The Affordable Care Act (ACA) of 2010 requires insurers to cover the cost of services that get A and B recommendations from the USPSTF without charging copays – a mandate intended to promote greater use for highly regarded services.
But Congress created a special workaround that effectively makes the ACA mandate apply to the 2002 task force recommendations on mammography. In those recommendations, the task force gave a B grade to screening mammograms every 1 or 2 years starting at age 40 without an age limit.
Federal lawmakers have sought to provide copay-free access to mammograms for this entire population even when the USPSTF recommendations in 2009 and 2016 gave a C grade to routine screening for women under 50.
Still, “it is important to note that our recommendation is based solely on the science of what works to prevent breast cancer and it is not a recommendation for or against insurance coverage,” the task force acknowledged when unveiling the new draft update. “Coverage decisions involve considerations beyond the evidence about clinical benefit, and in the end, these decisions are the responsibility of payors, regulators, and legislators.”
Uncertainties persist
The new draft recommendations also highlight the persistent gaps in knowledge about the uses of mammography, despite years of widespread use of this screening tool.
The updated draft recommendations emphasize the lack of sufficient evidence to address major areas of concern related to screening and treating Black women, older women, women with dense breasts, and those with ductal carcinoma in situ (DCIS).
The task force called for more research addressing the underlying causes of elevated breast cancer mortality rates among Black women.
The USPSTF also issued an ‘I’ statement for providing women with dense breasts additional screening with breast ultrasound or MRI and for screening women older than 75 for breast cancer. Such statements indicate that the available evidence is lacking, poor quality, or conflicting, and thus the USPSTF can’t assess the benefits and harms or make a recommendation for or against providing the preventive service.
“Nearly half of all women have dense breasts, which increases their risk for breast cancer and means that mammograms may not work as well for them. We need to know more about whether and how additional screening might help women with dense breasts stay healthy,” the task force explained.
The task force also called for more research on approaches to reduce the risk for overdiagnosis and overtreatment for breast lesions, such as DCIS, which are identified through screening.
One analysis – the COMET study – is currently underway to assess whether women could be spared surgery for DCIS and opt for watchful waiting instead.
“If we can find that monitoring them carefully, either with or without some sort of endocrine therapy, is just as effective in keeping patients free of invasive cancer as surgery, then I think we could help to de-escalate treatment for this very low-risk group of patients,” Shelley Hwang, MD, MPH, principal investigator of the COMET study, told this news organization in December.
The task force will accept comments from the public on this draft update through June 5.
A version of this article first appeared on Medscape.com.
The major change: USPSTF proposed reducing the recommended start age for routine screening mammograms from age 50 to age 40. The latest recommendation, which carries a B grade, also calls for screening every other year and sets a cutoff age of 74.
The task force’s A and B ratings indicate strong confidence in the evidence for benefit, meaning that clinicians should encourage their patients to get these services as appropriate.
The influential federal advisory panel last updated these recommendations in 2016. At the time, USPSTF recommended routine screening mammograms starting at age 50, and gave a C grade to starting before that.
In the 2016 recommendations, “we felt a woman could start screening in her 40s depending on how she feels about the harms and benefits in an individualized personal decision,” USPSTF member John Wong, MD, chief of clinical decision making and a primary care physician at Tufts Medical Center in Boston, said in an interview. “In this draft recommendation, we now recommend that all women get screened starting at age 40.”
Two major factors prompted the change, explained Dr. Wong. One is that more women are being diagnosed with breast cancer in their 40s. The other is that a growing body of evidence showing that Black women get breast cancer younger, are more likely to die of breast cancer, and would benefit from earlier screening.
“It is now clear that screening every other year starting at age 40 has the potential to save about 20% more lives among all women and there is even greater potential benefit for Black women, who are much more likely to die from breast cancer,” Dr. Wong said.
The American Cancer Society (ACS) called the draft recommendations a “significant positive change,” while noting that the task force recommendations only apply to women at average risk for breast cancer.
The American College of Radiology (ACR) already recommends yearly mammograms for average risk women starting at age 40. Its latest guidelines on mammography call for women at higher-than-average risk for breast cancer to undergo a risk assessment by age 25 to determine if screening before age 40 is needed.
When asked about the differing views, Debra Monticciolo, MD, division chief for breast imaging at Massachusetts General Hospital, said annual screenings that follow ACR recommendations would save more lives than the every-other-year approach backed by the task force. Dr. Monticciolo also highlighted that the available scientific evidence supports earlier assessment as well as augmented and earlier-than-age-40 screening of many women – particularly Black women.
“These evidence-based updates should spur more-informed doctor–patient conversations and help providers save more lives,” Dr. Monticciolo said in a press release.
Insurance access
Typically, upgrading a USPSTF recommendation from C to B leads to better access and insurance coverage for patients. The Affordable Care Act (ACA) of 2010 requires insurers to cover the cost of services that get A and B recommendations from the USPSTF without charging copays – a mandate intended to promote greater use for highly regarded services.
But Congress created a special workaround that effectively makes the ACA mandate apply to the 2002 task force recommendations on mammography. In those recommendations, the task force gave a B grade to screening mammograms every 1 or 2 years starting at age 40 without an age limit.
Federal lawmakers have sought to provide copay-free access to mammograms for this entire population even when the USPSTF recommendations in 2009 and 2016 gave a C grade to routine screening for women under 50.
Still, “it is important to note that our recommendation is based solely on the science of what works to prevent breast cancer and it is not a recommendation for or against insurance coverage,” the task force acknowledged when unveiling the new draft update. “Coverage decisions involve considerations beyond the evidence about clinical benefit, and in the end, these decisions are the responsibility of payors, regulators, and legislators.”
Uncertainties persist
The new draft recommendations also highlight the persistent gaps in knowledge about the uses of mammography, despite years of widespread use of this screening tool.
The updated draft recommendations emphasize the lack of sufficient evidence to address major areas of concern related to screening and treating Black women, older women, women with dense breasts, and those with ductal carcinoma in situ (DCIS).
The task force called for more research addressing the underlying causes of elevated breast cancer mortality rates among Black women.
The USPSTF also issued an ‘I’ statement for providing women with dense breasts additional screening with breast ultrasound or MRI and for screening women older than 75 for breast cancer. Such statements indicate that the available evidence is lacking, poor quality, or conflicting, and thus the USPSTF can’t assess the benefits and harms or make a recommendation for or against providing the preventive service.
“Nearly half of all women have dense breasts, which increases their risk for breast cancer and means that mammograms may not work as well for them. We need to know more about whether and how additional screening might help women with dense breasts stay healthy,” the task force explained.
The task force also called for more research on approaches to reduce the risk for overdiagnosis and overtreatment for breast lesions, such as DCIS, which are identified through screening.
One analysis – the COMET study – is currently underway to assess whether women could be spared surgery for DCIS and opt for watchful waiting instead.
“If we can find that monitoring them carefully, either with or without some sort of endocrine therapy, is just as effective in keeping patients free of invasive cancer as surgery, then I think we could help to de-escalate treatment for this very low-risk group of patients,” Shelley Hwang, MD, MPH, principal investigator of the COMET study, told this news organization in December.
The task force will accept comments from the public on this draft update through June 5.
A version of this article first appeared on Medscape.com.
The major change: USPSTF proposed reducing the recommended start age for routine screening mammograms from age 50 to age 40. The latest recommendation, which carries a B grade, also calls for screening every other year and sets a cutoff age of 74.
The task force’s A and B ratings indicate strong confidence in the evidence for benefit, meaning that clinicians should encourage their patients to get these services as appropriate.
The influential federal advisory panel last updated these recommendations in 2016. At the time, USPSTF recommended routine screening mammograms starting at age 50, and gave a C grade to starting before that.
In the 2016 recommendations, “we felt a woman could start screening in her 40s depending on how she feels about the harms and benefits in an individualized personal decision,” USPSTF member John Wong, MD, chief of clinical decision making and a primary care physician at Tufts Medical Center in Boston, said in an interview. “In this draft recommendation, we now recommend that all women get screened starting at age 40.”
Two major factors prompted the change, explained Dr. Wong. One is that more women are being diagnosed with breast cancer in their 40s. The other is that a growing body of evidence showing that Black women get breast cancer younger, are more likely to die of breast cancer, and would benefit from earlier screening.
“It is now clear that screening every other year starting at age 40 has the potential to save about 20% more lives among all women and there is even greater potential benefit for Black women, who are much more likely to die from breast cancer,” Dr. Wong said.
The American Cancer Society (ACS) called the draft recommendations a “significant positive change,” while noting that the task force recommendations only apply to women at average risk for breast cancer.
The American College of Radiology (ACR) already recommends yearly mammograms for average risk women starting at age 40. Its latest guidelines on mammography call for women at higher-than-average risk for breast cancer to undergo a risk assessment by age 25 to determine if screening before age 40 is needed.
When asked about the differing views, Debra Monticciolo, MD, division chief for breast imaging at Massachusetts General Hospital, said annual screenings that follow ACR recommendations would save more lives than the every-other-year approach backed by the task force. Dr. Monticciolo also highlighted that the available scientific evidence supports earlier assessment as well as augmented and earlier-than-age-40 screening of many women – particularly Black women.
“These evidence-based updates should spur more-informed doctor–patient conversations and help providers save more lives,” Dr. Monticciolo said in a press release.
Insurance access
Typically, upgrading a USPSTF recommendation from C to B leads to better access and insurance coverage for patients. The Affordable Care Act (ACA) of 2010 requires insurers to cover the cost of services that get A and B recommendations from the USPSTF without charging copays – a mandate intended to promote greater use for highly regarded services.
But Congress created a special workaround that effectively makes the ACA mandate apply to the 2002 task force recommendations on mammography. In those recommendations, the task force gave a B grade to screening mammograms every 1 or 2 years starting at age 40 without an age limit.
Federal lawmakers have sought to provide copay-free access to mammograms for this entire population even when the USPSTF recommendations in 2009 and 2016 gave a C grade to routine screening for women under 50.
Still, “it is important to note that our recommendation is based solely on the science of what works to prevent breast cancer and it is not a recommendation for or against insurance coverage,” the task force acknowledged when unveiling the new draft update. “Coverage decisions involve considerations beyond the evidence about clinical benefit, and in the end, these decisions are the responsibility of payors, regulators, and legislators.”
Uncertainties persist
The new draft recommendations also highlight the persistent gaps in knowledge about the uses of mammography, despite years of widespread use of this screening tool.
The updated draft recommendations emphasize the lack of sufficient evidence to address major areas of concern related to screening and treating Black women, older women, women with dense breasts, and those with ductal carcinoma in situ (DCIS).
The task force called for more research addressing the underlying causes of elevated breast cancer mortality rates among Black women.
The USPSTF also issued an ‘I’ statement for providing women with dense breasts additional screening with breast ultrasound or MRI and for screening women older than 75 for breast cancer. Such statements indicate that the available evidence is lacking, poor quality, or conflicting, and thus the USPSTF can’t assess the benefits and harms or make a recommendation for or against providing the preventive service.
“Nearly half of all women have dense breasts, which increases their risk for breast cancer and means that mammograms may not work as well for them. We need to know more about whether and how additional screening might help women with dense breasts stay healthy,” the task force explained.
The task force also called for more research on approaches to reduce the risk for overdiagnosis and overtreatment for breast lesions, such as DCIS, which are identified through screening.
One analysis – the COMET study – is currently underway to assess whether women could be spared surgery for DCIS and opt for watchful waiting instead.
“If we can find that monitoring them carefully, either with or without some sort of endocrine therapy, is just as effective in keeping patients free of invasive cancer as surgery, then I think we could help to de-escalate treatment for this very low-risk group of patients,” Shelley Hwang, MD, MPH, principal investigator of the COMET study, told this news organization in December.
The task force will accept comments from the public on this draft update through June 5.
A version of this article first appeared on Medscape.com.
Axial spondyloarthritis versus axial psoriatic arthritis: Different entities?
Are there clinically significant differences between axial spondyloarthritis with psoriasis and psoriatic arthritis with axial symptoms? Does it matter?
It all depends on whom you ask, but right now the evidence seems to be tipping in favor of the “splitters” who cite evidence supporting their contention that axial spondyloarthritis (axSpA)/ankylosing spondylitis (AS) with psoriasis and psoriatic arthritis (PsA) with axial symptoms are distinct clinical entities that require more precise diagnosis and treatment.
“Lumpers,” in contrast, argue that they are different points on the same clinical spectrum.
The debate is not just of academic interest, but has real consequences for patients, say specialists on both sides of the aisle.
Overlapping features, different presentations
“Axial SpA and axPsA have overlapping features but also meaningful differences in genetics, clinical presentation, imaging, and immunophenotype. Efforts are underway to develop classification criteria for axPsA to aid research efforts as well as clinical diagnosis and management,” Philip J. Mease, MD, director of rheumatology research at Swedish Medical Center/Providence–St. Joseph Health in Seattle, and colleagues contend.
In an editorial published in the International Journal of Rheumatic Diseases, Dr. Mease and colleagues noted that, although HLA-B*27 is a genetic risk factor for both axPsA and axSpA, some HLA-B alleles are significantly associated with axPsA, whereas other alleles are associated with axSpA.
In addition, while genes in the interleukin-23 and IL-17 pathway are associated with increased risk for axSpA, genes in the IL-13 pathway have been identified as risk markers for axPsA, they noted.
Two cohorts better than one?
Dafna Gladman, MD, professor of medicine at the University of Toronto and senior scientist at the Schroeder Arthritis Institute at Toronto Western Hospital, and colleagues have a unique perspective on the similarities and differences between the disease entities.
Her group’s research uses data on cohorts of patients treated in two separate clinics at Toronto Western Hospital: one for patients with PsA, and one for patients with axial spondyloarthritis, including those with ankylosing spondylitis, nonradiographic axSpA, and spondylitis associated with inflammatory bowel disease.
“Our work has shown that there are differences, and one of the reasons that it’s now important is that the anti–IL-23 medications, both the IL-12/23 inhibitor ustekinumab [Stelara] and the IL-23 inhibitor guselkumab [Tremfya] work for psoriatic arthritis, whereas IL-23 did not work in ankylosing spondylitis, so that provided further impetus to look into the distinction between the two groups,” Dr. Gladman said in an interview.
Dr. Gladman and colleagues published a study in Rheumatology in which they compared clinical presentations and features of patients with AS with or without psoriasis with patients with axPsA.
They found that patients with AS with or without psoriasis tended to be younger, had a higher proportion of males to females, and were more likely to be positive for HLA-B*27. Patients with AS also had more back pain at presentation, worse axial disease activity scores, worse global assessments by physicians, and higher grades of sacroiliitis, and they were more likely to be taking biologic agents.
“What that showed, right off the top, that whether we’re looking at the total group or we’re looking specifically at those patients who have psoriasis or don’t have psoriasis, they are different from those with psoriatic arthritis with axial disease,” she said.
They concluded that “axPsA seems to be a distinct entity.”
Two clinics, same presentation
Because the aforementioned study included all patients with PsA with or without peripheral disease, the investigators decided to filter out some of the background noise and conduct a second study in which they compared patients who presented to the two clinics with the same presentation, either with spinal disease and psoriasis to the spondylitis clinic, or with psoriasis and isolated axial disease to the PsA clinic.
The results, published in Annals of the Rheumatic Diseases, showed that just 2.03% of patients with PsA had isolated axial disease, and an additional 29.38% had axial and peripheral disease.
In this study, “you can see that even in that group there are distinct differences. The patients that are labeled psoriatic spondylitis are different from those that are labeled ankylosing spondylitis with psoriasis,” Dr. Gladman said.
Isolated axial disease in patients with PsA was associated with HLA-B*27 positivity and lower Health Assessment Questionnaire scores. In addition, patients who were HLA-B*27 positive also had a nearly eightfold higher risk for developing peripheral disease over time.
Patients with isolated axial PsA were significantly more likely to be diagnosed at an older age (mean, 37.44 vs. 29.65 years), had higher Psoriasis Area Severity Index scores and a higher likelihood of having psoriatic nail lesions than patients with AS with isolated axial disease and psoriasis.
In contrast, patients with isolated axSpA with psoriasis were more likely to have inflammatory back pain, spinal pain, joint pain/swelling, and areas of localized tenderness, and they had greater severity of morning stiffness.
Dr. Gladman noted that, although AS and PsA are associated with the same gene that encodes for the IL-23 receptor, each condition is associated with a different single-nucleotide polymorphism.
Same disease, different flavors?
But as Mark Twain said, it is difference of opinion that makes horse races, and some specialists in rheumatology say that axSpA amd axPsA are just two sides of the same coin.
“There are always different schools of thought. I believe that they are not different diseases, but a spectrum of diseases,” said Shailendra Singh, MD, a rheumatologist at Unity Health Medical Center in Searcy, Ark., and past president of the Arkansas Rheumatology Association.
In an interview, Dr. Singh said that the spectrum ranges from diseases with primarily axial involvement, such as AS, to those with primarily peripheral involvement, such as reactive arthritis.
He pointed out that these conditions have overlapping symptoms, including enthesitis, dactylitis, and uveitis, and inflammatory arthritis.
Daniel Wendling, MD, PhD, from the Centre Hospitalier Régional Universitaire de Besançon (France), Université de Franche-Comté, and colleagues agreed.
“The criteria currently available for both SpA [ASAS (Assessment of Spondyloarthritis International Society) criteria] and PsA [CASPAR (Classification for Psoriatic Arthritis) criteria] are classification criteria, not diagnostic criteria. They are not very stringent and are not exclusive. Thus, the same patient can easily be classified simultaneously in both entities, making the distinction between axSpA with psoriasis and axPsA theoretical,” they wrote in an editorial published in Joint Bone Spine.
They cited as an example of the allegedly fuzzy criteria a prospective study conducted by the investigators in Bath, England, in which modified New York criteria for AS were met by 24% of patients with AS, and CASPAR criteria for PsA were met by an equal number of patients with AS.
Therapeutic implications
Dr. Wendling and colleagues acknowledge the differences cited in studies by Dr. Gladman, Dr. Mease, and others between patients with axPsA and those with axSpA, but argue that the differences are not that great and not so clear.
“It should also be emphasized that, although some differences between axPsA and axSpA reach statistical significance, they are mostly at the margin, with low odd ratios,” they wrote.
“It is also important to consider the variability in the definition of axPsA, sometimes simply ‘physician reported’ and elsewhere based on the modified New York radiographic criteria; the latter are only present late in the course of the disease, and this may induce bias,” they continued.
Dr. Singh agreed that, as noted by Dr. Gladman, some patients will respond to anti–IL-17, anti–IL-23, and anti–IL-12/23 agents, whereas others will have better responses with tumor necrosis factor (TNF) inhibitors, and still others, such as those with peripheral involvement in the hands and feet may fare better with nonbiologic disease-modifying antirheumatic drugs such as methotrexate.
Answers to come?
Dr. Gladman noted that the information available to date about the efficacy of IL-23 inhibition in axPsA is based on a post hoc analysis of the PSUMMIT 1 and 2 controlled trials in PsA, and is not definitive.
The randomized, controlled STAR trial, currently recruiting patients, is designed to see whether guselkumab can reduce axial symptoms and inflammation in patients with active axPsA.
“What I say is, there is a rationale for [anti–IL-23] to work in psoriatic arthritis, and not work in ankylosing spondylitis,” she said.
In contrast, IL-17 inhibitors, anti-TNF agents, and Janus kinase inhibitors show efficacy against both axPsA and AS. Rituximab is ineffective against PsA, but has shown efficacy against AS, especially in patients with neurologic complications from anti-TNF agents.
“There may be other medications that would work more specifically in axial psoriatic arthritis that don’t work in ankylosing spondylitis, but at least recognizing that there may be some differences, and that therefore a correct diagnosis should be obtained, might be important,” she said.
Ideally, the picture will become clearer with results from the ongoing Axial Involvement in Psoriatic Arthritis cohort, a joint project of ASAS and the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis. The multinational, cross-sectional study is designed “to systematically evaluate clinical and imaging manifestations indicative of axial involvement in patients with PsA and to develop classification criteria and a unified nomenclature for axial involvement in PsA that would allow defining a homogeneous subgroup of patients for research.”
Stay tuned.
Dr. Gladman’s research is supported by a grant from the Krembil Foundation. Dr. Singh disclosed research support from various companies. Funding sources and conflict of interest disclosures from other works cited are contained in their respective references.
Are there clinically significant differences between axial spondyloarthritis with psoriasis and psoriatic arthritis with axial symptoms? Does it matter?
It all depends on whom you ask, but right now the evidence seems to be tipping in favor of the “splitters” who cite evidence supporting their contention that axial spondyloarthritis (axSpA)/ankylosing spondylitis (AS) with psoriasis and psoriatic arthritis (PsA) with axial symptoms are distinct clinical entities that require more precise diagnosis and treatment.
“Lumpers,” in contrast, argue that they are different points on the same clinical spectrum.
The debate is not just of academic interest, but has real consequences for patients, say specialists on both sides of the aisle.
Overlapping features, different presentations
“Axial SpA and axPsA have overlapping features but also meaningful differences in genetics, clinical presentation, imaging, and immunophenotype. Efforts are underway to develop classification criteria for axPsA to aid research efforts as well as clinical diagnosis and management,” Philip J. Mease, MD, director of rheumatology research at Swedish Medical Center/Providence–St. Joseph Health in Seattle, and colleagues contend.
In an editorial published in the International Journal of Rheumatic Diseases, Dr. Mease and colleagues noted that, although HLA-B*27 is a genetic risk factor for both axPsA and axSpA, some HLA-B alleles are significantly associated with axPsA, whereas other alleles are associated with axSpA.
In addition, while genes in the interleukin-23 and IL-17 pathway are associated with increased risk for axSpA, genes in the IL-13 pathway have been identified as risk markers for axPsA, they noted.
Two cohorts better than one?
Dafna Gladman, MD, professor of medicine at the University of Toronto and senior scientist at the Schroeder Arthritis Institute at Toronto Western Hospital, and colleagues have a unique perspective on the similarities and differences between the disease entities.
Her group’s research uses data on cohorts of patients treated in two separate clinics at Toronto Western Hospital: one for patients with PsA, and one for patients with axial spondyloarthritis, including those with ankylosing spondylitis, nonradiographic axSpA, and spondylitis associated with inflammatory bowel disease.
“Our work has shown that there are differences, and one of the reasons that it’s now important is that the anti–IL-23 medications, both the IL-12/23 inhibitor ustekinumab [Stelara] and the IL-23 inhibitor guselkumab [Tremfya] work for psoriatic arthritis, whereas IL-23 did not work in ankylosing spondylitis, so that provided further impetus to look into the distinction between the two groups,” Dr. Gladman said in an interview.
Dr. Gladman and colleagues published a study in Rheumatology in which they compared clinical presentations and features of patients with AS with or without psoriasis with patients with axPsA.
They found that patients with AS with or without psoriasis tended to be younger, had a higher proportion of males to females, and were more likely to be positive for HLA-B*27. Patients with AS also had more back pain at presentation, worse axial disease activity scores, worse global assessments by physicians, and higher grades of sacroiliitis, and they were more likely to be taking biologic agents.
“What that showed, right off the top, that whether we’re looking at the total group or we’re looking specifically at those patients who have psoriasis or don’t have psoriasis, they are different from those with psoriatic arthritis with axial disease,” she said.
They concluded that “axPsA seems to be a distinct entity.”
Two clinics, same presentation
Because the aforementioned study included all patients with PsA with or without peripheral disease, the investigators decided to filter out some of the background noise and conduct a second study in which they compared patients who presented to the two clinics with the same presentation, either with spinal disease and psoriasis to the spondylitis clinic, or with psoriasis and isolated axial disease to the PsA clinic.
The results, published in Annals of the Rheumatic Diseases, showed that just 2.03% of patients with PsA had isolated axial disease, and an additional 29.38% had axial and peripheral disease.
In this study, “you can see that even in that group there are distinct differences. The patients that are labeled psoriatic spondylitis are different from those that are labeled ankylosing spondylitis with psoriasis,” Dr. Gladman said.
Isolated axial disease in patients with PsA was associated with HLA-B*27 positivity and lower Health Assessment Questionnaire scores. In addition, patients who were HLA-B*27 positive also had a nearly eightfold higher risk for developing peripheral disease over time.
Patients with isolated axial PsA were significantly more likely to be diagnosed at an older age (mean, 37.44 vs. 29.65 years), had higher Psoriasis Area Severity Index scores and a higher likelihood of having psoriatic nail lesions than patients with AS with isolated axial disease and psoriasis.
In contrast, patients with isolated axSpA with psoriasis were more likely to have inflammatory back pain, spinal pain, joint pain/swelling, and areas of localized tenderness, and they had greater severity of morning stiffness.
Dr. Gladman noted that, although AS and PsA are associated with the same gene that encodes for the IL-23 receptor, each condition is associated with a different single-nucleotide polymorphism.
Same disease, different flavors?
But as Mark Twain said, it is difference of opinion that makes horse races, and some specialists in rheumatology say that axSpA amd axPsA are just two sides of the same coin.
“There are always different schools of thought. I believe that they are not different diseases, but a spectrum of diseases,” said Shailendra Singh, MD, a rheumatologist at Unity Health Medical Center in Searcy, Ark., and past president of the Arkansas Rheumatology Association.
In an interview, Dr. Singh said that the spectrum ranges from diseases with primarily axial involvement, such as AS, to those with primarily peripheral involvement, such as reactive arthritis.
He pointed out that these conditions have overlapping symptoms, including enthesitis, dactylitis, and uveitis, and inflammatory arthritis.
Daniel Wendling, MD, PhD, from the Centre Hospitalier Régional Universitaire de Besançon (France), Université de Franche-Comté, and colleagues agreed.
“The criteria currently available for both SpA [ASAS (Assessment of Spondyloarthritis International Society) criteria] and PsA [CASPAR (Classification for Psoriatic Arthritis) criteria] are classification criteria, not diagnostic criteria. They are not very stringent and are not exclusive. Thus, the same patient can easily be classified simultaneously in both entities, making the distinction between axSpA with psoriasis and axPsA theoretical,” they wrote in an editorial published in Joint Bone Spine.
They cited as an example of the allegedly fuzzy criteria a prospective study conducted by the investigators in Bath, England, in which modified New York criteria for AS were met by 24% of patients with AS, and CASPAR criteria for PsA were met by an equal number of patients with AS.
Therapeutic implications
Dr. Wendling and colleagues acknowledge the differences cited in studies by Dr. Gladman, Dr. Mease, and others between patients with axPsA and those with axSpA, but argue that the differences are not that great and not so clear.
“It should also be emphasized that, although some differences between axPsA and axSpA reach statistical significance, they are mostly at the margin, with low odd ratios,” they wrote.
“It is also important to consider the variability in the definition of axPsA, sometimes simply ‘physician reported’ and elsewhere based on the modified New York radiographic criteria; the latter are only present late in the course of the disease, and this may induce bias,” they continued.
Dr. Singh agreed that, as noted by Dr. Gladman, some patients will respond to anti–IL-17, anti–IL-23, and anti–IL-12/23 agents, whereas others will have better responses with tumor necrosis factor (TNF) inhibitors, and still others, such as those with peripheral involvement in the hands and feet may fare better with nonbiologic disease-modifying antirheumatic drugs such as methotrexate.
Answers to come?
Dr. Gladman noted that the information available to date about the efficacy of IL-23 inhibition in axPsA is based on a post hoc analysis of the PSUMMIT 1 and 2 controlled trials in PsA, and is not definitive.
The randomized, controlled STAR trial, currently recruiting patients, is designed to see whether guselkumab can reduce axial symptoms and inflammation in patients with active axPsA.
“What I say is, there is a rationale for [anti–IL-23] to work in psoriatic arthritis, and not work in ankylosing spondylitis,” she said.
In contrast, IL-17 inhibitors, anti-TNF agents, and Janus kinase inhibitors show efficacy against both axPsA and AS. Rituximab is ineffective against PsA, but has shown efficacy against AS, especially in patients with neurologic complications from anti-TNF agents.
“There may be other medications that would work more specifically in axial psoriatic arthritis that don’t work in ankylosing spondylitis, but at least recognizing that there may be some differences, and that therefore a correct diagnosis should be obtained, might be important,” she said.
Ideally, the picture will become clearer with results from the ongoing Axial Involvement in Psoriatic Arthritis cohort, a joint project of ASAS and the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis. The multinational, cross-sectional study is designed “to systematically evaluate clinical and imaging manifestations indicative of axial involvement in patients with PsA and to develop classification criteria and a unified nomenclature for axial involvement in PsA that would allow defining a homogeneous subgroup of patients for research.”
Stay tuned.
Dr. Gladman’s research is supported by a grant from the Krembil Foundation. Dr. Singh disclosed research support from various companies. Funding sources and conflict of interest disclosures from other works cited are contained in their respective references.
Are there clinically significant differences between axial spondyloarthritis with psoriasis and psoriatic arthritis with axial symptoms? Does it matter?
It all depends on whom you ask, but right now the evidence seems to be tipping in favor of the “splitters” who cite evidence supporting their contention that axial spondyloarthritis (axSpA)/ankylosing spondylitis (AS) with psoriasis and psoriatic arthritis (PsA) with axial symptoms are distinct clinical entities that require more precise diagnosis and treatment.
“Lumpers,” in contrast, argue that they are different points on the same clinical spectrum.
The debate is not just of academic interest, but has real consequences for patients, say specialists on both sides of the aisle.
Overlapping features, different presentations
“Axial SpA and axPsA have overlapping features but also meaningful differences in genetics, clinical presentation, imaging, and immunophenotype. Efforts are underway to develop classification criteria for axPsA to aid research efforts as well as clinical diagnosis and management,” Philip J. Mease, MD, director of rheumatology research at Swedish Medical Center/Providence–St. Joseph Health in Seattle, and colleagues contend.
In an editorial published in the International Journal of Rheumatic Diseases, Dr. Mease and colleagues noted that, although HLA-B*27 is a genetic risk factor for both axPsA and axSpA, some HLA-B alleles are significantly associated with axPsA, whereas other alleles are associated with axSpA.
In addition, while genes in the interleukin-23 and IL-17 pathway are associated with increased risk for axSpA, genes in the IL-13 pathway have been identified as risk markers for axPsA, they noted.
Two cohorts better than one?
Dafna Gladman, MD, professor of medicine at the University of Toronto and senior scientist at the Schroeder Arthritis Institute at Toronto Western Hospital, and colleagues have a unique perspective on the similarities and differences between the disease entities.
Her group’s research uses data on cohorts of patients treated in two separate clinics at Toronto Western Hospital: one for patients with PsA, and one for patients with axial spondyloarthritis, including those with ankylosing spondylitis, nonradiographic axSpA, and spondylitis associated with inflammatory bowel disease.
“Our work has shown that there are differences, and one of the reasons that it’s now important is that the anti–IL-23 medications, both the IL-12/23 inhibitor ustekinumab [Stelara] and the IL-23 inhibitor guselkumab [Tremfya] work for psoriatic arthritis, whereas IL-23 did not work in ankylosing spondylitis, so that provided further impetus to look into the distinction between the two groups,” Dr. Gladman said in an interview.
Dr. Gladman and colleagues published a study in Rheumatology in which they compared clinical presentations and features of patients with AS with or without psoriasis with patients with axPsA.
They found that patients with AS with or without psoriasis tended to be younger, had a higher proportion of males to females, and were more likely to be positive for HLA-B*27. Patients with AS also had more back pain at presentation, worse axial disease activity scores, worse global assessments by physicians, and higher grades of sacroiliitis, and they were more likely to be taking biologic agents.
“What that showed, right off the top, that whether we’re looking at the total group or we’re looking specifically at those patients who have psoriasis or don’t have psoriasis, they are different from those with psoriatic arthritis with axial disease,” she said.
They concluded that “axPsA seems to be a distinct entity.”
Two clinics, same presentation
Because the aforementioned study included all patients with PsA with or without peripheral disease, the investigators decided to filter out some of the background noise and conduct a second study in which they compared patients who presented to the two clinics with the same presentation, either with spinal disease and psoriasis to the spondylitis clinic, or with psoriasis and isolated axial disease to the PsA clinic.
The results, published in Annals of the Rheumatic Diseases, showed that just 2.03% of patients with PsA had isolated axial disease, and an additional 29.38% had axial and peripheral disease.
In this study, “you can see that even in that group there are distinct differences. The patients that are labeled psoriatic spondylitis are different from those that are labeled ankylosing spondylitis with psoriasis,” Dr. Gladman said.
Isolated axial disease in patients with PsA was associated with HLA-B*27 positivity and lower Health Assessment Questionnaire scores. In addition, patients who were HLA-B*27 positive also had a nearly eightfold higher risk for developing peripheral disease over time.
Patients with isolated axial PsA were significantly more likely to be diagnosed at an older age (mean, 37.44 vs. 29.65 years), had higher Psoriasis Area Severity Index scores and a higher likelihood of having psoriatic nail lesions than patients with AS with isolated axial disease and psoriasis.
In contrast, patients with isolated axSpA with psoriasis were more likely to have inflammatory back pain, spinal pain, joint pain/swelling, and areas of localized tenderness, and they had greater severity of morning stiffness.
Dr. Gladman noted that, although AS and PsA are associated with the same gene that encodes for the IL-23 receptor, each condition is associated with a different single-nucleotide polymorphism.
Same disease, different flavors?
But as Mark Twain said, it is difference of opinion that makes horse races, and some specialists in rheumatology say that axSpA amd axPsA are just two sides of the same coin.
“There are always different schools of thought. I believe that they are not different diseases, but a spectrum of diseases,” said Shailendra Singh, MD, a rheumatologist at Unity Health Medical Center in Searcy, Ark., and past president of the Arkansas Rheumatology Association.
In an interview, Dr. Singh said that the spectrum ranges from diseases with primarily axial involvement, such as AS, to those with primarily peripheral involvement, such as reactive arthritis.
He pointed out that these conditions have overlapping symptoms, including enthesitis, dactylitis, and uveitis, and inflammatory arthritis.
Daniel Wendling, MD, PhD, from the Centre Hospitalier Régional Universitaire de Besançon (France), Université de Franche-Comté, and colleagues agreed.
“The criteria currently available for both SpA [ASAS (Assessment of Spondyloarthritis International Society) criteria] and PsA [CASPAR (Classification for Psoriatic Arthritis) criteria] are classification criteria, not diagnostic criteria. They are not very stringent and are not exclusive. Thus, the same patient can easily be classified simultaneously in both entities, making the distinction between axSpA with psoriasis and axPsA theoretical,” they wrote in an editorial published in Joint Bone Spine.
They cited as an example of the allegedly fuzzy criteria a prospective study conducted by the investigators in Bath, England, in which modified New York criteria for AS were met by 24% of patients with AS, and CASPAR criteria for PsA were met by an equal number of patients with AS.
Therapeutic implications
Dr. Wendling and colleagues acknowledge the differences cited in studies by Dr. Gladman, Dr. Mease, and others between patients with axPsA and those with axSpA, but argue that the differences are not that great and not so clear.
“It should also be emphasized that, although some differences between axPsA and axSpA reach statistical significance, they are mostly at the margin, with low odd ratios,” they wrote.
“It is also important to consider the variability in the definition of axPsA, sometimes simply ‘physician reported’ and elsewhere based on the modified New York radiographic criteria; the latter are only present late in the course of the disease, and this may induce bias,” they continued.
Dr. Singh agreed that, as noted by Dr. Gladman, some patients will respond to anti–IL-17, anti–IL-23, and anti–IL-12/23 agents, whereas others will have better responses with tumor necrosis factor (TNF) inhibitors, and still others, such as those with peripheral involvement in the hands and feet may fare better with nonbiologic disease-modifying antirheumatic drugs such as methotrexate.
Answers to come?
Dr. Gladman noted that the information available to date about the efficacy of IL-23 inhibition in axPsA is based on a post hoc analysis of the PSUMMIT 1 and 2 controlled trials in PsA, and is not definitive.
The randomized, controlled STAR trial, currently recruiting patients, is designed to see whether guselkumab can reduce axial symptoms and inflammation in patients with active axPsA.
“What I say is, there is a rationale for [anti–IL-23] to work in psoriatic arthritis, and not work in ankylosing spondylitis,” she said.
In contrast, IL-17 inhibitors, anti-TNF agents, and Janus kinase inhibitors show efficacy against both axPsA and AS. Rituximab is ineffective against PsA, but has shown efficacy against AS, especially in patients with neurologic complications from anti-TNF agents.
“There may be other medications that would work more specifically in axial psoriatic arthritis that don’t work in ankylosing spondylitis, but at least recognizing that there may be some differences, and that therefore a correct diagnosis should be obtained, might be important,” she said.
Ideally, the picture will become clearer with results from the ongoing Axial Involvement in Psoriatic Arthritis cohort, a joint project of ASAS and the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis. The multinational, cross-sectional study is designed “to systematically evaluate clinical and imaging manifestations indicative of axial involvement in patients with PsA and to develop classification criteria and a unified nomenclature for axial involvement in PsA that would allow defining a homogeneous subgroup of patients for research.”
Stay tuned.
Dr. Gladman’s research is supported by a grant from the Krembil Foundation. Dr. Singh disclosed research support from various companies. Funding sources and conflict of interest disclosures from other works cited are contained in their respective references.
FDA expands use of dapagliflozin to broader range of HF
– including HF with mildly reduced ejection fraction (HFmrEF) and with preserved ejection fraction (HFpEF).
The sodium-glucose cotransporter 2 (SGLT2) inhibitor was previously approved in the United States for adults with heart failure with reduced ejection fraction (HFrEF).
The expanded indication is based on data from the phase 3 DELIVER trial, which showed clear clinical benefits of the SGLT2 inhibitor for patients with HF regardless of left ventricular function.
In the trial, which included more than 6,200 patients, dapagliflozin led to a statistically significant and clinically meaningful early reduction in the primary composite endpoint of cardiovascular (CV) death or worsening HF for patients with HFmrEF or HFpEFF.
In addition, results of a pooled analysis of the DAPA-HF and DELIVER phase 3 trials showed a consistent benefit from dapagliflozin treatment in significantly reducing the combined endpoint of CV death or HF hospitalization across the range of LVEF.
The European Commission expanded the indication for dapagliflozin (Forxiga) to include HF across the full spectrum of LVEF in February.
The SGLT2 inhibitor is also approved for use by patients with chronic kidney disease. It was first approved in 2014 to improve glycemic control for patients with diabetes mellitus.
A version of this article first appeared on Medscape.com.
– including HF with mildly reduced ejection fraction (HFmrEF) and with preserved ejection fraction (HFpEF).
The sodium-glucose cotransporter 2 (SGLT2) inhibitor was previously approved in the United States for adults with heart failure with reduced ejection fraction (HFrEF).
The expanded indication is based on data from the phase 3 DELIVER trial, which showed clear clinical benefits of the SGLT2 inhibitor for patients with HF regardless of left ventricular function.
In the trial, which included more than 6,200 patients, dapagliflozin led to a statistically significant and clinically meaningful early reduction in the primary composite endpoint of cardiovascular (CV) death or worsening HF for patients with HFmrEF or HFpEFF.
In addition, results of a pooled analysis of the DAPA-HF and DELIVER phase 3 trials showed a consistent benefit from dapagliflozin treatment in significantly reducing the combined endpoint of CV death or HF hospitalization across the range of LVEF.
The European Commission expanded the indication for dapagliflozin (Forxiga) to include HF across the full spectrum of LVEF in February.
The SGLT2 inhibitor is also approved for use by patients with chronic kidney disease. It was first approved in 2014 to improve glycemic control for patients with diabetes mellitus.
A version of this article first appeared on Medscape.com.
– including HF with mildly reduced ejection fraction (HFmrEF) and with preserved ejection fraction (HFpEF).
The sodium-glucose cotransporter 2 (SGLT2) inhibitor was previously approved in the United States for adults with heart failure with reduced ejection fraction (HFrEF).
The expanded indication is based on data from the phase 3 DELIVER trial, which showed clear clinical benefits of the SGLT2 inhibitor for patients with HF regardless of left ventricular function.
In the trial, which included more than 6,200 patients, dapagliflozin led to a statistically significant and clinically meaningful early reduction in the primary composite endpoint of cardiovascular (CV) death or worsening HF for patients with HFmrEF or HFpEFF.
In addition, results of a pooled analysis of the DAPA-HF and DELIVER phase 3 trials showed a consistent benefit from dapagliflozin treatment in significantly reducing the combined endpoint of CV death or HF hospitalization across the range of LVEF.
The European Commission expanded the indication for dapagliflozin (Forxiga) to include HF across the full spectrum of LVEF in February.
The SGLT2 inhibitor is also approved for use by patients with chronic kidney disease. It was first approved in 2014 to improve glycemic control for patients with diabetes mellitus.
A version of this article first appeared on Medscape.com.