User login
Risk assessment first urged for fragility fracture screening
A new Canadian guideline on screening for the primary prevention of fragility fractures recommends risk assessment first, before bone mineral density (BMD) testing, for women aged 65 and older. For younger women and men aged 40 and older, screening is not recommended.
To develop the guideline, a writing group from Canadian Task Force on Preventive Health Care commissioned systematic reviews of studies on the benefits and harms of fragility fracture screenings; the predictive accuracy of current risk-assessment tools; patient acceptability; and benefits of treatment. Treatment harms were analyzed via a rapid overview of reviews.
The guideline, published online in the Canadian Medical Association Journal, is aimed at primary care practitioners for their community-dwelling patients aged 40 and older. The recommendations do not apply to people already taking preventive drugs.
Nondrug treatments were beyond the scope of the current guideline, but guidelines on the prevention of falls and other strategies are planned, Roland Grad, MD, a guideline author and associate professor at McGill University in Montreal, told this news organization.
The new guideline says that women aged 65 and older may be able to avoid fracture through screening and preventive medication. An individual’s fracture risk can be estimated with a new Fragility Fractures Decision Aid, which uses the Canadian FRAX risk-assessment tool.
“A risk assessment–first approach promotes shared decision-making with the patient, based on best medical evidence,” Dr. Grad said.
“To help clinicians, we have created an infographic with visuals to communicate the time spent on BMD vs risk assessment first.”
New evidence
“At least three things motivated this new guideline,” Dr. Grad said. “When we started work on this prior to the pandemic, we saw a need for updated guidance on screening to prevent fragility fractures. We were also aware of new evidence from the publication of screening trials in females older than 65.”
To conduct the risk assessment in older women, clinicians are advised to do the following:
- Use the decision aid (which patients can also use on their own).
- Use the 10-year absolute risk of major osteoporotic fracture to facilitate shared decision-making about possible benefits and harms of preventive pharmacotherapy.
- If pharmacotherapy is being considered, request a BMD using DXA of the femoral neck, then reestimate the fracture risk by adding the BMD T-score into the FRAX.
Potential harms associated with various treatments, with varying levels of evidence, include the following: with alendronate and denosumab, nonserious gastrointestinal adverse events; with denosumab, rash, eczema, and infections; with zoledronic acid, nonserious events, such as headache and flulike symptoms; and with alendronate and bisphosphonates, rare but serious harms of atypical femoral fracture and osteonecrosis of the jaw.
“These recommendations emphasize the importance of good clinical practice, where clinicians are alert to changes in physical health and patient well-being,” the authors wrote. “Clinicians should also be aware of the importance of secondary prevention (i.e., after fracture) and manage patients accordingly.”
“This is an important topic,” Dr. Grad said. “Fragility fractures are consequential for individuals and for our publicly funded health care system. We anticipate questions from clinicians about the time needed to screen with the risk assessment–first strategy. Our modeling work suggests time savings with [this] strategy compared to a strategy of BMD testing first. Following our recommendations may lead to a reduction in BMD testing.”
To promote the guideline, the CMAJ has recorded a podcast and will use other strategies to increase awareness, Dr. Grad said. “The Canadian Task Force has a communications strategy that includes outreach to primary care, stakeholder webinars, social media, partnerships, and other tactics. The College of Family Physicians of Canada has endorsed the guideline and will help promote to its members.”
Other at-risk groups?
Aliya Khan, MD, FRCPC, FACP, FACE, professor in the divisions of endocrinology and metabolism and geriatrics and director of the fellowship in metabolic bone diseases at McMaster University in Hamilton, Ont., told this news organization she agrees with the strategy of evaluating women aged 65 and older for fracture risk.
“The decision aid is useful, but I would like to see it expanded to other circumstances and situations,” she said.
For example, Dr. Khan would like to see recommendations for younger women and for men of all ages regarding secondary causes of osteoporosis or medications known to have a detrimental effect on bone health. By not addressing these patients, she said, “we may miss patients who would benefit from a fracture risk assessment and potentially treatment to prevent low-trauma fractures.”
A recommendation for younger postmenopausal women was included in the most recent Society of Obstetricians and Gynaecologists Canada guideline, she noted.
Overall, she said, “I believe these recommendations will reduce the excess or inappropriate use of BMD testing and that is welcome.”
Funding for the Canadian Task Force on Preventive Health Care is provided by the Public Health Agency of Canada. The task force members report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new Canadian guideline on screening for the primary prevention of fragility fractures recommends risk assessment first, before bone mineral density (BMD) testing, for women aged 65 and older. For younger women and men aged 40 and older, screening is not recommended.
To develop the guideline, a writing group from Canadian Task Force on Preventive Health Care commissioned systematic reviews of studies on the benefits and harms of fragility fracture screenings; the predictive accuracy of current risk-assessment tools; patient acceptability; and benefits of treatment. Treatment harms were analyzed via a rapid overview of reviews.
The guideline, published online in the Canadian Medical Association Journal, is aimed at primary care practitioners for their community-dwelling patients aged 40 and older. The recommendations do not apply to people already taking preventive drugs.
Nondrug treatments were beyond the scope of the current guideline, but guidelines on the prevention of falls and other strategies are planned, Roland Grad, MD, a guideline author and associate professor at McGill University in Montreal, told this news organization.
The new guideline says that women aged 65 and older may be able to avoid fracture through screening and preventive medication. An individual’s fracture risk can be estimated with a new Fragility Fractures Decision Aid, which uses the Canadian FRAX risk-assessment tool.
“A risk assessment–first approach promotes shared decision-making with the patient, based on best medical evidence,” Dr. Grad said.
“To help clinicians, we have created an infographic with visuals to communicate the time spent on BMD vs risk assessment first.”
New evidence
“At least three things motivated this new guideline,” Dr. Grad said. “When we started work on this prior to the pandemic, we saw a need for updated guidance on screening to prevent fragility fractures. We were also aware of new evidence from the publication of screening trials in females older than 65.”
To conduct the risk assessment in older women, clinicians are advised to do the following:
- Use the decision aid (which patients can also use on their own).
- Use the 10-year absolute risk of major osteoporotic fracture to facilitate shared decision-making about possible benefits and harms of preventive pharmacotherapy.
- If pharmacotherapy is being considered, request a BMD using DXA of the femoral neck, then reestimate the fracture risk by adding the BMD T-score into the FRAX.
Potential harms associated with various treatments, with varying levels of evidence, include the following: with alendronate and denosumab, nonserious gastrointestinal adverse events; with denosumab, rash, eczema, and infections; with zoledronic acid, nonserious events, such as headache and flulike symptoms; and with alendronate and bisphosphonates, rare but serious harms of atypical femoral fracture and osteonecrosis of the jaw.
“These recommendations emphasize the importance of good clinical practice, where clinicians are alert to changes in physical health and patient well-being,” the authors wrote. “Clinicians should also be aware of the importance of secondary prevention (i.e., after fracture) and manage patients accordingly.”
“This is an important topic,” Dr. Grad said. “Fragility fractures are consequential for individuals and for our publicly funded health care system. We anticipate questions from clinicians about the time needed to screen with the risk assessment–first strategy. Our modeling work suggests time savings with [this] strategy compared to a strategy of BMD testing first. Following our recommendations may lead to a reduction in BMD testing.”
To promote the guideline, the CMAJ has recorded a podcast and will use other strategies to increase awareness, Dr. Grad said. “The Canadian Task Force has a communications strategy that includes outreach to primary care, stakeholder webinars, social media, partnerships, and other tactics. The College of Family Physicians of Canada has endorsed the guideline and will help promote to its members.”
Other at-risk groups?
Aliya Khan, MD, FRCPC, FACP, FACE, professor in the divisions of endocrinology and metabolism and geriatrics and director of the fellowship in metabolic bone diseases at McMaster University in Hamilton, Ont., told this news organization she agrees with the strategy of evaluating women aged 65 and older for fracture risk.
“The decision aid is useful, but I would like to see it expanded to other circumstances and situations,” she said.
For example, Dr. Khan would like to see recommendations for younger women and for men of all ages regarding secondary causes of osteoporosis or medications known to have a detrimental effect on bone health. By not addressing these patients, she said, “we may miss patients who would benefit from a fracture risk assessment and potentially treatment to prevent low-trauma fractures.”
A recommendation for younger postmenopausal women was included in the most recent Society of Obstetricians and Gynaecologists Canada guideline, she noted.
Overall, she said, “I believe these recommendations will reduce the excess or inappropriate use of BMD testing and that is welcome.”
Funding for the Canadian Task Force on Preventive Health Care is provided by the Public Health Agency of Canada. The task force members report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new Canadian guideline on screening for the primary prevention of fragility fractures recommends risk assessment first, before bone mineral density (BMD) testing, for women aged 65 and older. For younger women and men aged 40 and older, screening is not recommended.
To develop the guideline, a writing group from Canadian Task Force on Preventive Health Care commissioned systematic reviews of studies on the benefits and harms of fragility fracture screenings; the predictive accuracy of current risk-assessment tools; patient acceptability; and benefits of treatment. Treatment harms were analyzed via a rapid overview of reviews.
The guideline, published online in the Canadian Medical Association Journal, is aimed at primary care practitioners for their community-dwelling patients aged 40 and older. The recommendations do not apply to people already taking preventive drugs.
Nondrug treatments were beyond the scope of the current guideline, but guidelines on the prevention of falls and other strategies are planned, Roland Grad, MD, a guideline author and associate professor at McGill University in Montreal, told this news organization.
The new guideline says that women aged 65 and older may be able to avoid fracture through screening and preventive medication. An individual’s fracture risk can be estimated with a new Fragility Fractures Decision Aid, which uses the Canadian FRAX risk-assessment tool.
“A risk assessment–first approach promotes shared decision-making with the patient, based on best medical evidence,” Dr. Grad said.
“To help clinicians, we have created an infographic with visuals to communicate the time spent on BMD vs risk assessment first.”
New evidence
“At least three things motivated this new guideline,” Dr. Grad said. “When we started work on this prior to the pandemic, we saw a need for updated guidance on screening to prevent fragility fractures. We were also aware of new evidence from the publication of screening trials in females older than 65.”
To conduct the risk assessment in older women, clinicians are advised to do the following:
- Use the decision aid (which patients can also use on their own).
- Use the 10-year absolute risk of major osteoporotic fracture to facilitate shared decision-making about possible benefits and harms of preventive pharmacotherapy.
- If pharmacotherapy is being considered, request a BMD using DXA of the femoral neck, then reestimate the fracture risk by adding the BMD T-score into the FRAX.
Potential harms associated with various treatments, with varying levels of evidence, include the following: with alendronate and denosumab, nonserious gastrointestinal adverse events; with denosumab, rash, eczema, and infections; with zoledronic acid, nonserious events, such as headache and flulike symptoms; and with alendronate and bisphosphonates, rare but serious harms of atypical femoral fracture and osteonecrosis of the jaw.
“These recommendations emphasize the importance of good clinical practice, where clinicians are alert to changes in physical health and patient well-being,” the authors wrote. “Clinicians should also be aware of the importance of secondary prevention (i.e., after fracture) and manage patients accordingly.”
“This is an important topic,” Dr. Grad said. “Fragility fractures are consequential for individuals and for our publicly funded health care system. We anticipate questions from clinicians about the time needed to screen with the risk assessment–first strategy. Our modeling work suggests time savings with [this] strategy compared to a strategy of BMD testing first. Following our recommendations may lead to a reduction in BMD testing.”
To promote the guideline, the CMAJ has recorded a podcast and will use other strategies to increase awareness, Dr. Grad said. “The Canadian Task Force has a communications strategy that includes outreach to primary care, stakeholder webinars, social media, partnerships, and other tactics. The College of Family Physicians of Canada has endorsed the guideline and will help promote to its members.”
Other at-risk groups?
Aliya Khan, MD, FRCPC, FACP, FACE, professor in the divisions of endocrinology and metabolism and geriatrics and director of the fellowship in metabolic bone diseases at McMaster University in Hamilton, Ont., told this news organization she agrees with the strategy of evaluating women aged 65 and older for fracture risk.
“The decision aid is useful, but I would like to see it expanded to other circumstances and situations,” she said.
For example, Dr. Khan would like to see recommendations for younger women and for men of all ages regarding secondary causes of osteoporosis or medications known to have a detrimental effect on bone health. By not addressing these patients, she said, “we may miss patients who would benefit from a fracture risk assessment and potentially treatment to prevent low-trauma fractures.”
A recommendation for younger postmenopausal women was included in the most recent Society of Obstetricians and Gynaecologists Canada guideline, she noted.
Overall, she said, “I believe these recommendations will reduce the excess or inappropriate use of BMD testing and that is welcome.”
Funding for the Canadian Task Force on Preventive Health Care is provided by the Public Health Agency of Canada. The task force members report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Can this tool forecast peanut allergies?
Pediatricians may have a new aid to better predict peanut allergies among infants with atopic dermatitis.
Their study of the implementation of the scorecard was presented at the Pediatric Academic Societies annual meeting.
Infants with atopic dermatitis or eczema are six times more likely to have an egg allergy and eleven times more likely to have a peanut allergy at age 12 months than are infants without atopic dermatitis.
The scorecard reflects recent directives from the National Institute of Allergy and Infectious Diseases to help combat the public health problem.
“When the NIAID prevention of peanut allergy guidelines first came out, it asked pediatricians to serve as frontline practitioners in implementing them by identifying children at risk for peanut allergy and guiding families on what to do next,” said Waheeda Samady, MD, professor of pediatrics at Northwestern University, Chicago. “The impetus for the study was to further support pediatricians in this role.”
Although pediatricians are trained to identify and even treat mild to moderate cases of atopic dermatitis, little emphasis has gone to categorizing the condition on the basis of severity and to correlating peanut allergy risk.
The predictive scorecard captures 14 images from one infant of mixed race, two White infants, two Black infants, and two Hispanic infants.
To create the card, two in-house pediatric dermatologists assessed 58 images from 13 children and categorized images from 0 (no signs of atopic dermatitis) to 4 (severe signs of atopic dermatitis). After a first pass on categorization, the doctors agreed on 84% of images.
Of 189 pediatricians who used the card, fewer than half reported that they “sometimes,” “very often,” or “always” used the scorecard for atopic dermatitis evaluation. A little fewer than three-quarters reported that their ability to diagnose and categorize atopic dermatitis improved.
“Severity staging of atopic dermatitis is not something that the general pediatrician necessarily performs on a day-to-day basis,” said Kawaljit Brar, MD, professor of pediatrics in the division of allergy and immunology at Hassenfeld Children’s Hospital in New York.
Dr. Brar explained that children who are identified as being at high risk are often referred to specialists such as her, who then perform allergy screenings and can determine whether introduction of food at home is safe or whether office feedings supervised by an allergist are necessary. Researchers have found that early introduction to peanuts for children with moderate to severe atopic dermatitis could prevent peanut allergy.
“This represents a wonderful initiative to educate pediatricians so that they understand which patients require screening for peanut allergy and which patients don’t and can just get introduced to peanuts at home,” Dr. Brar said.
The atopic dermatitis scorecard reflects a growing recognition that varying skin tones show levels of severity incongruously.
“Many of us in clinical practice have recognized that our education has not always been inclusive of patients with varying skin tones,” Dr. Samady said. “When we looked for photos of patients with different skin tones, we simply could not find any that we thought were appropriate. So we decided to take some ourselves, and we’re currently continuing to take photos in order to improve the scorecard we currently have.”
The study was funded by the National Institute of Health and Food Allergy Research and Education. Dr. Samady and Dr. Brar reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pediatricians may have a new aid to better predict peanut allergies among infants with atopic dermatitis.
Their study of the implementation of the scorecard was presented at the Pediatric Academic Societies annual meeting.
Infants with atopic dermatitis or eczema are six times more likely to have an egg allergy and eleven times more likely to have a peanut allergy at age 12 months than are infants without atopic dermatitis.
The scorecard reflects recent directives from the National Institute of Allergy and Infectious Diseases to help combat the public health problem.
“When the NIAID prevention of peanut allergy guidelines first came out, it asked pediatricians to serve as frontline practitioners in implementing them by identifying children at risk for peanut allergy and guiding families on what to do next,” said Waheeda Samady, MD, professor of pediatrics at Northwestern University, Chicago. “The impetus for the study was to further support pediatricians in this role.”
Although pediatricians are trained to identify and even treat mild to moderate cases of atopic dermatitis, little emphasis has gone to categorizing the condition on the basis of severity and to correlating peanut allergy risk.
The predictive scorecard captures 14 images from one infant of mixed race, two White infants, two Black infants, and two Hispanic infants.
To create the card, two in-house pediatric dermatologists assessed 58 images from 13 children and categorized images from 0 (no signs of atopic dermatitis) to 4 (severe signs of atopic dermatitis). After a first pass on categorization, the doctors agreed on 84% of images.
Of 189 pediatricians who used the card, fewer than half reported that they “sometimes,” “very often,” or “always” used the scorecard for atopic dermatitis evaluation. A little fewer than three-quarters reported that their ability to diagnose and categorize atopic dermatitis improved.
“Severity staging of atopic dermatitis is not something that the general pediatrician necessarily performs on a day-to-day basis,” said Kawaljit Brar, MD, professor of pediatrics in the division of allergy and immunology at Hassenfeld Children’s Hospital in New York.
Dr. Brar explained that children who are identified as being at high risk are often referred to specialists such as her, who then perform allergy screenings and can determine whether introduction of food at home is safe or whether office feedings supervised by an allergist are necessary. Researchers have found that early introduction to peanuts for children with moderate to severe atopic dermatitis could prevent peanut allergy.
“This represents a wonderful initiative to educate pediatricians so that they understand which patients require screening for peanut allergy and which patients don’t and can just get introduced to peanuts at home,” Dr. Brar said.
The atopic dermatitis scorecard reflects a growing recognition that varying skin tones show levels of severity incongruously.
“Many of us in clinical practice have recognized that our education has not always been inclusive of patients with varying skin tones,” Dr. Samady said. “When we looked for photos of patients with different skin tones, we simply could not find any that we thought were appropriate. So we decided to take some ourselves, and we’re currently continuing to take photos in order to improve the scorecard we currently have.”
The study was funded by the National Institute of Health and Food Allergy Research and Education. Dr. Samady and Dr. Brar reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pediatricians may have a new aid to better predict peanut allergies among infants with atopic dermatitis.
Their study of the implementation of the scorecard was presented at the Pediatric Academic Societies annual meeting.
Infants with atopic dermatitis or eczema are six times more likely to have an egg allergy and eleven times more likely to have a peanut allergy at age 12 months than are infants without atopic dermatitis.
The scorecard reflects recent directives from the National Institute of Allergy and Infectious Diseases to help combat the public health problem.
“When the NIAID prevention of peanut allergy guidelines first came out, it asked pediatricians to serve as frontline practitioners in implementing them by identifying children at risk for peanut allergy and guiding families on what to do next,” said Waheeda Samady, MD, professor of pediatrics at Northwestern University, Chicago. “The impetus for the study was to further support pediatricians in this role.”
Although pediatricians are trained to identify and even treat mild to moderate cases of atopic dermatitis, little emphasis has gone to categorizing the condition on the basis of severity and to correlating peanut allergy risk.
The predictive scorecard captures 14 images from one infant of mixed race, two White infants, two Black infants, and two Hispanic infants.
To create the card, two in-house pediatric dermatologists assessed 58 images from 13 children and categorized images from 0 (no signs of atopic dermatitis) to 4 (severe signs of atopic dermatitis). After a first pass on categorization, the doctors agreed on 84% of images.
Of 189 pediatricians who used the card, fewer than half reported that they “sometimes,” “very often,” or “always” used the scorecard for atopic dermatitis evaluation. A little fewer than three-quarters reported that their ability to diagnose and categorize atopic dermatitis improved.
“Severity staging of atopic dermatitis is not something that the general pediatrician necessarily performs on a day-to-day basis,” said Kawaljit Brar, MD, professor of pediatrics in the division of allergy and immunology at Hassenfeld Children’s Hospital in New York.
Dr. Brar explained that children who are identified as being at high risk are often referred to specialists such as her, who then perform allergy screenings and can determine whether introduction of food at home is safe or whether office feedings supervised by an allergist are necessary. Researchers have found that early introduction to peanuts for children with moderate to severe atopic dermatitis could prevent peanut allergy.
“This represents a wonderful initiative to educate pediatricians so that they understand which patients require screening for peanut allergy and which patients don’t and can just get introduced to peanuts at home,” Dr. Brar said.
The atopic dermatitis scorecard reflects a growing recognition that varying skin tones show levels of severity incongruously.
“Many of us in clinical practice have recognized that our education has not always been inclusive of patients with varying skin tones,” Dr. Samady said. “When we looked for photos of patients with different skin tones, we simply could not find any that we thought were appropriate. So we decided to take some ourselves, and we’re currently continuing to take photos in order to improve the scorecard we currently have.”
The study was funded by the National Institute of Health and Food Allergy Research and Education. Dr. Samady and Dr. Brar reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PAS 2023
Medical students gain momentum in effort to ban legacy admissions
, which they say offer preferential treatment to applicants based on their association with donors or alumni.
While an estimated 25% of public colleges and universities still use legacy admissions, a growing list of top medical schools have moved away from the practice over the last decade, including Johns Hopkins University, Baltimore, and Tufts University, Medford, Mass.
Legacy admissions contradict schools’ more inclusive policies, Senila Yasmin, MPH, a second-year medical student at Tufts University, said in an interview. While Tufts maintains legacy admissions for its undergraduate applicants, the medical school stopped the practice in 2021, said Ms. Yasmin, a member of a student group that lobbied against the school’s legacy preferences.
Describing herself as a low-income, first-generation Muslim-Pakistani American, Ms. Yasmin wants to use her experience at Tufts to improve accessibility for students like herself.
As a member of the American Medical Association (AMA) Medical Student Section, she coauthored a resolution stating that legacy admissions go against the AMA’s strategic plan to advance racial justice and health equity. The Student Section passed the resolution in November, and in June, the AMA House of Delegates will vote on whether to adopt the policy.
Along with a Supreme Court decision that could strike down race-conscious college admissions, an AMA policy could convince medical schools to rethink legacy admissions and how to maintain diverse student bodies. In June, the court is expected to issue a decision in the Students for Fair Admissions lawsuit against Harvard University, Cambridge, Mass., and the University of North Carolina, Chapel Hill, which alleges that considering race in holistic admissions constitutes racial discrimination and violates the Equal Protection Clause.
Opponents of legacy admissions, like Ms. Yasmin, say it penalizes students from racial minorities and lower socioeconomic backgrounds, hampering a fair and equitable admissions process that attracts diverse medical school admissions.
Diversity of medical applicants
Diversity in medical schools continued to increase last year with more Black, Hispanic, and female students applying and enrolling, according to a recent report by the Association of American Medical Colleges (AAMC). However, universities often include nonacademic criteria in their admission assessments to improve educational access for underrepresented minorities.
Medical schools carefully consider each applicant’s background “to yield a diverse class of students,” Geoffrey Young, PhD, AAMC’s senior director of transforming the health care workforce, told this news organization.
Some schools, such as Morehouse School of Medicine, Atlanta, the University of Virginia School of Medicine, Charlottesville, and the University of Arizona College of Medicine, Tucson, perform a thorough review of candidates while offering admissions practices designed specifically for legacy applicants. The schools assert that legacy designation doesn’t factor into the student’s likelihood of acceptance.
The arrangement may show that schools want to commit to equity and fairness but have trouble moving away from entrenched traditions, two professors from Penn State College of Medicine, Hershey, Pa., who sit on separate medical admissions subcommittees, wrote last year in Bioethics Today.
Legislation may hasten legacies’ end
In December, Ms. Yasmin and a group of Massachusetts Medical Society student-members presented another resolution to the state medical society, which adopted it.
The society’s new policy opposes the use of legacy status in medical school admissions and supports mechanisms to eliminate its inclusion from the application process, Theodore Calianos II, MD, FACS, president of the Massachusetts Medical Society, said in an interview.
“Legacy preferences limit racial and socioeconomic diversity on campuses, so we asked, ‘What can we do so that everyone has equal access to medical education?’ It is exciting to see the students and young physicians – the future of medicine – become involved in policymaking.”
Proposed laws may also hasten the end of legacy admissions. Last year, the U.S. Senate began considering a bill prohibiting colleges receiving federal financial aid from giving preferential treatment to students based on their relations to donors or alumni. However, the bill allows the Department of Education to make exceptions for institutions serving historically underrepresented groups.
The New York State Senate and the New York State Assembly also are reviewing bills that ban legacy and early admissions policies at public and private universities. Connecticut announced similar legislation last year. Massachusetts legislators are considering two bills: one that would ban the practice at the state’s public universities and another that would require all schools using legacy status to pay a “public service fee” equal to a percentage of its endowment. Colleges with endowment assets exceeding $2 billion must pay at least $2 million, according to the bill’s text.
At schools like Harvard, whose endowment surpasses $50 billion, the option to pay the penalty will make the law moot, Michael Walls, DO, MPH, president of the American Medical Student Association (AMSA), said in an interview. “Smaller schools wouldn’t be able to afford the fine and are less likely to be doing [legacy admissions] anyway,” he said. “The schools that want to continue doing it could just pay the fine.”
Dr. Walls said AMSA supports race-conscious admissions processes and anything that increases fairness for medical school applicants. “Whatever [fair] means is up for interpretation, but it would be great to eliminate legacy admissions,” he said.
A version of this article originally appeared on Medscape.com.
, which they say offer preferential treatment to applicants based on their association with donors or alumni.
While an estimated 25% of public colleges and universities still use legacy admissions, a growing list of top medical schools have moved away from the practice over the last decade, including Johns Hopkins University, Baltimore, and Tufts University, Medford, Mass.
Legacy admissions contradict schools’ more inclusive policies, Senila Yasmin, MPH, a second-year medical student at Tufts University, said in an interview. While Tufts maintains legacy admissions for its undergraduate applicants, the medical school stopped the practice in 2021, said Ms. Yasmin, a member of a student group that lobbied against the school’s legacy preferences.
Describing herself as a low-income, first-generation Muslim-Pakistani American, Ms. Yasmin wants to use her experience at Tufts to improve accessibility for students like herself.
As a member of the American Medical Association (AMA) Medical Student Section, she coauthored a resolution stating that legacy admissions go against the AMA’s strategic plan to advance racial justice and health equity. The Student Section passed the resolution in November, and in June, the AMA House of Delegates will vote on whether to adopt the policy.
Along with a Supreme Court decision that could strike down race-conscious college admissions, an AMA policy could convince medical schools to rethink legacy admissions and how to maintain diverse student bodies. In June, the court is expected to issue a decision in the Students for Fair Admissions lawsuit against Harvard University, Cambridge, Mass., and the University of North Carolina, Chapel Hill, which alleges that considering race in holistic admissions constitutes racial discrimination and violates the Equal Protection Clause.
Opponents of legacy admissions, like Ms. Yasmin, say it penalizes students from racial minorities and lower socioeconomic backgrounds, hampering a fair and equitable admissions process that attracts diverse medical school admissions.
Diversity of medical applicants
Diversity in medical schools continued to increase last year with more Black, Hispanic, and female students applying and enrolling, according to a recent report by the Association of American Medical Colleges (AAMC). However, universities often include nonacademic criteria in their admission assessments to improve educational access for underrepresented minorities.
Medical schools carefully consider each applicant’s background “to yield a diverse class of students,” Geoffrey Young, PhD, AAMC’s senior director of transforming the health care workforce, told this news organization.
Some schools, such as Morehouse School of Medicine, Atlanta, the University of Virginia School of Medicine, Charlottesville, and the University of Arizona College of Medicine, Tucson, perform a thorough review of candidates while offering admissions practices designed specifically for legacy applicants. The schools assert that legacy designation doesn’t factor into the student’s likelihood of acceptance.
The arrangement may show that schools want to commit to equity and fairness but have trouble moving away from entrenched traditions, two professors from Penn State College of Medicine, Hershey, Pa., who sit on separate medical admissions subcommittees, wrote last year in Bioethics Today.
Legislation may hasten legacies’ end
In December, Ms. Yasmin and a group of Massachusetts Medical Society student-members presented another resolution to the state medical society, which adopted it.
The society’s new policy opposes the use of legacy status in medical school admissions and supports mechanisms to eliminate its inclusion from the application process, Theodore Calianos II, MD, FACS, president of the Massachusetts Medical Society, said in an interview.
“Legacy preferences limit racial and socioeconomic diversity on campuses, so we asked, ‘What can we do so that everyone has equal access to medical education?’ It is exciting to see the students and young physicians – the future of medicine – become involved in policymaking.”
Proposed laws may also hasten the end of legacy admissions. Last year, the U.S. Senate began considering a bill prohibiting colleges receiving federal financial aid from giving preferential treatment to students based on their relations to donors or alumni. However, the bill allows the Department of Education to make exceptions for institutions serving historically underrepresented groups.
The New York State Senate and the New York State Assembly also are reviewing bills that ban legacy and early admissions policies at public and private universities. Connecticut announced similar legislation last year. Massachusetts legislators are considering two bills: one that would ban the practice at the state’s public universities and another that would require all schools using legacy status to pay a “public service fee” equal to a percentage of its endowment. Colleges with endowment assets exceeding $2 billion must pay at least $2 million, according to the bill’s text.
At schools like Harvard, whose endowment surpasses $50 billion, the option to pay the penalty will make the law moot, Michael Walls, DO, MPH, president of the American Medical Student Association (AMSA), said in an interview. “Smaller schools wouldn’t be able to afford the fine and are less likely to be doing [legacy admissions] anyway,” he said. “The schools that want to continue doing it could just pay the fine.”
Dr. Walls said AMSA supports race-conscious admissions processes and anything that increases fairness for medical school applicants. “Whatever [fair] means is up for interpretation, but it would be great to eliminate legacy admissions,” he said.
A version of this article originally appeared on Medscape.com.
, which they say offer preferential treatment to applicants based on their association with donors or alumni.
While an estimated 25% of public colleges and universities still use legacy admissions, a growing list of top medical schools have moved away from the practice over the last decade, including Johns Hopkins University, Baltimore, and Tufts University, Medford, Mass.
Legacy admissions contradict schools’ more inclusive policies, Senila Yasmin, MPH, a second-year medical student at Tufts University, said in an interview. While Tufts maintains legacy admissions for its undergraduate applicants, the medical school stopped the practice in 2021, said Ms. Yasmin, a member of a student group that lobbied against the school’s legacy preferences.
Describing herself as a low-income, first-generation Muslim-Pakistani American, Ms. Yasmin wants to use her experience at Tufts to improve accessibility for students like herself.
As a member of the American Medical Association (AMA) Medical Student Section, she coauthored a resolution stating that legacy admissions go against the AMA’s strategic plan to advance racial justice and health equity. The Student Section passed the resolution in November, and in June, the AMA House of Delegates will vote on whether to adopt the policy.
Along with a Supreme Court decision that could strike down race-conscious college admissions, an AMA policy could convince medical schools to rethink legacy admissions and how to maintain diverse student bodies. In June, the court is expected to issue a decision in the Students for Fair Admissions lawsuit against Harvard University, Cambridge, Mass., and the University of North Carolina, Chapel Hill, which alleges that considering race in holistic admissions constitutes racial discrimination and violates the Equal Protection Clause.
Opponents of legacy admissions, like Ms. Yasmin, say it penalizes students from racial minorities and lower socioeconomic backgrounds, hampering a fair and equitable admissions process that attracts diverse medical school admissions.
Diversity of medical applicants
Diversity in medical schools continued to increase last year with more Black, Hispanic, and female students applying and enrolling, according to a recent report by the Association of American Medical Colleges (AAMC). However, universities often include nonacademic criteria in their admission assessments to improve educational access for underrepresented minorities.
Medical schools carefully consider each applicant’s background “to yield a diverse class of students,” Geoffrey Young, PhD, AAMC’s senior director of transforming the health care workforce, told this news organization.
Some schools, such as Morehouse School of Medicine, Atlanta, the University of Virginia School of Medicine, Charlottesville, and the University of Arizona College of Medicine, Tucson, perform a thorough review of candidates while offering admissions practices designed specifically for legacy applicants. The schools assert that legacy designation doesn’t factor into the student’s likelihood of acceptance.
The arrangement may show that schools want to commit to equity and fairness but have trouble moving away from entrenched traditions, two professors from Penn State College of Medicine, Hershey, Pa., who sit on separate medical admissions subcommittees, wrote last year in Bioethics Today.
Legislation may hasten legacies’ end
In December, Ms. Yasmin and a group of Massachusetts Medical Society student-members presented another resolution to the state medical society, which adopted it.
The society’s new policy opposes the use of legacy status in medical school admissions and supports mechanisms to eliminate its inclusion from the application process, Theodore Calianos II, MD, FACS, president of the Massachusetts Medical Society, said in an interview.
“Legacy preferences limit racial and socioeconomic diversity on campuses, so we asked, ‘What can we do so that everyone has equal access to medical education?’ It is exciting to see the students and young physicians – the future of medicine – become involved in policymaking.”
Proposed laws may also hasten the end of legacy admissions. Last year, the U.S. Senate began considering a bill prohibiting colleges receiving federal financial aid from giving preferential treatment to students based on their relations to donors or alumni. However, the bill allows the Department of Education to make exceptions for institutions serving historically underrepresented groups.
The New York State Senate and the New York State Assembly also are reviewing bills that ban legacy and early admissions policies at public and private universities. Connecticut announced similar legislation last year. Massachusetts legislators are considering two bills: one that would ban the practice at the state’s public universities and another that would require all schools using legacy status to pay a “public service fee” equal to a percentage of its endowment. Colleges with endowment assets exceeding $2 billion must pay at least $2 million, according to the bill’s text.
At schools like Harvard, whose endowment surpasses $50 billion, the option to pay the penalty will make the law moot, Michael Walls, DO, MPH, president of the American Medical Student Association (AMSA), said in an interview. “Smaller schools wouldn’t be able to afford the fine and are less likely to be doing [legacy admissions] anyway,” he said. “The schools that want to continue doing it could just pay the fine.”
Dr. Walls said AMSA supports race-conscious admissions processes and anything that increases fairness for medical school applicants. “Whatever [fair] means is up for interpretation, but it would be great to eliminate legacy admissions,” he said.
A version of this article originally appeared on Medscape.com.
Picosecond laser applications continue to expand
PHOENIX – Ever since PicoSure became the first picosecond laser cleared by the Food and Drug Administration for the treatment of unwanted tattoos and pigmented lesions in 2012, new uses for this technology continue to expand.
Now, These include PicoWay, PicoSure, Enlighten, PicoPlus, PiQo4, and Quanta Pico, among others.
“PicoWay technology has integrated nicely into my practice in Houston, the most ethnically diverse city in the country, with its ability to safely treat a number of various benign, congenital, and acquired epidermal and dermal pigmented lesions with ultrashort pulse duration and low thermal impact, which greatly reduces the risk of postinflammatory hyperpigmentation even in darker skin types,” Paul M. Friedman, MD, director of the Dermatology and Laser Surgery Center, Houston, said at the annual conference of the American Society for Laser Medicine and Surgery.
He emphasized the importance of therapeutic clinical endpoints, noting that with q-switched lasers, “you’re looking for immediate whitening, whereas with picosecond lasers, your endpoint is slight whitening or slight darkening depending on wavelength, indication, and skin type. The ability to fractionate picosecond pulses has also allowed us to utilize this technology for photoaging as well as acne scarring.”
The PicoWay system includes a 730-nm picosecond titanium sapphire handpiece, which is FDA cleared for treatment of benign pigmented lesions and blue and green tattoo removal. Dr. Friedman said that he has seen good clinical results using the handpiece for café-au-lait macules, particularly in skin of color.
In an abstract presented at the ASLMS meeting, he and his colleagues presented a retrospective review of 12 patients with café-au-lait macules with Fitzpatrick skin types III-VI who were treated with the PicoWay 730 nm handpiece between April 2021 and January 2023. Patients received a mean of 3.1 treatments at intervals that ranged from 5 to 40 weeks. Clinical photographs were graded by three board-certified dermatologists using a 5-point visual analogue scale.
Overall, patients were rated to have a mean improvement of 26%-50%. Two patients achieved 100% clearance after four to five treatment sessions. “Café-au-lait macules with smooth borders responded less well to laser treatment, confirming prior studies at our center,” he said. “We often educate parents that café-au-lait macules may recur over time, especially with repeated sun exposure.”
Treating melasma
Dr. Friedman’s go-to devices for melasma include the low-density, low-energy 1,927-nm fractional diode laser; the 1,064 nm picosecond Nd:YAG, the low-fluence 1,064 nm Q-switched Nd:YAG with a nanosecond pulse duration, and the 595-nm pulsed dye laser for lesions exhibiting underlying vascularity. He said that combining therapies that target pigment and vasculature may be ideal to prevent relapses. “Melasma is a multifactorial condition so by improving patient education and expectation alongside advances in laser treatment of melasma, we have ultimately improved our ability to treat this condition,” he said.
“We’re approaching it from all angles, with ultraviolet photography and spectrocolorimetry, behavioral modifications, topical skin-lightening agents, broad spectrum sunscreens with protection against visible light, and oral tranexamic acid in advanced cases. Then, we intervene with these energy-based modalities, and the bottom line is, less energy and density is more, with lengthened treatment intervals. In 2023, we’re better than we’ve ever been in terms of our ability to safely and effectively improve melasma.”
Novel lasers
Dr. Friedman also described the UltraClear, a novel ablative fractional 2,910-nm erbium-doped glass fiber laser that delivers a customized blend of ablation and coagulation based on the patient’s condition, skin type, and tolerability for down time. He provided an overview of the versatility of what he described as highly customizable technology for conditions such as photoaging and dyschromia in patients of various skin types, making it a very versatile platform in his practice.
The AVAVA MIRIA system is a “next generation” laser “where you’re able to use a focal point. Basically, you’re treating the skin from the inside out in a 3D manner and you’re able to focus intradermally up to 1 mm with high energy 1,064 nm or 1,550 nm,” he said. “It’s a unique conical geometry that spares the epidermis, combined with sapphire tip cooling and images the skin at the same time with the potential for personalized treatments of dyschromia and photoaging in all skin types. It’s truly remarkable where the technology is heading.”
Dr. Friedman disclosed that he has received consulting fees from Allergan, Galderma, Acclaro, Merz Aesthetics, Solta Medical, and Cytrellis. He has conducted contracted research for Sofwave and is a member of the speakers bureau for Solta Medical and Candela.
PHOENIX – Ever since PicoSure became the first picosecond laser cleared by the Food and Drug Administration for the treatment of unwanted tattoos and pigmented lesions in 2012, new uses for this technology continue to expand.
Now, These include PicoWay, PicoSure, Enlighten, PicoPlus, PiQo4, and Quanta Pico, among others.
“PicoWay technology has integrated nicely into my practice in Houston, the most ethnically diverse city in the country, with its ability to safely treat a number of various benign, congenital, and acquired epidermal and dermal pigmented lesions with ultrashort pulse duration and low thermal impact, which greatly reduces the risk of postinflammatory hyperpigmentation even in darker skin types,” Paul M. Friedman, MD, director of the Dermatology and Laser Surgery Center, Houston, said at the annual conference of the American Society for Laser Medicine and Surgery.
He emphasized the importance of therapeutic clinical endpoints, noting that with q-switched lasers, “you’re looking for immediate whitening, whereas with picosecond lasers, your endpoint is slight whitening or slight darkening depending on wavelength, indication, and skin type. The ability to fractionate picosecond pulses has also allowed us to utilize this technology for photoaging as well as acne scarring.”
The PicoWay system includes a 730-nm picosecond titanium sapphire handpiece, which is FDA cleared for treatment of benign pigmented lesions and blue and green tattoo removal. Dr. Friedman said that he has seen good clinical results using the handpiece for café-au-lait macules, particularly in skin of color.
In an abstract presented at the ASLMS meeting, he and his colleagues presented a retrospective review of 12 patients with café-au-lait macules with Fitzpatrick skin types III-VI who were treated with the PicoWay 730 nm handpiece between April 2021 and January 2023. Patients received a mean of 3.1 treatments at intervals that ranged from 5 to 40 weeks. Clinical photographs were graded by three board-certified dermatologists using a 5-point visual analogue scale.
Overall, patients were rated to have a mean improvement of 26%-50%. Two patients achieved 100% clearance after four to five treatment sessions. “Café-au-lait macules with smooth borders responded less well to laser treatment, confirming prior studies at our center,” he said. “We often educate parents that café-au-lait macules may recur over time, especially with repeated sun exposure.”
Treating melasma
Dr. Friedman’s go-to devices for melasma include the low-density, low-energy 1,927-nm fractional diode laser; the 1,064 nm picosecond Nd:YAG, the low-fluence 1,064 nm Q-switched Nd:YAG with a nanosecond pulse duration, and the 595-nm pulsed dye laser for lesions exhibiting underlying vascularity. He said that combining therapies that target pigment and vasculature may be ideal to prevent relapses. “Melasma is a multifactorial condition so by improving patient education and expectation alongside advances in laser treatment of melasma, we have ultimately improved our ability to treat this condition,” he said.
“We’re approaching it from all angles, with ultraviolet photography and spectrocolorimetry, behavioral modifications, topical skin-lightening agents, broad spectrum sunscreens with protection against visible light, and oral tranexamic acid in advanced cases. Then, we intervene with these energy-based modalities, and the bottom line is, less energy and density is more, with lengthened treatment intervals. In 2023, we’re better than we’ve ever been in terms of our ability to safely and effectively improve melasma.”
Novel lasers
Dr. Friedman also described the UltraClear, a novel ablative fractional 2,910-nm erbium-doped glass fiber laser that delivers a customized blend of ablation and coagulation based on the patient’s condition, skin type, and tolerability for down time. He provided an overview of the versatility of what he described as highly customizable technology for conditions such as photoaging and dyschromia in patients of various skin types, making it a very versatile platform in his practice.
The AVAVA MIRIA system is a “next generation” laser “where you’re able to use a focal point. Basically, you’re treating the skin from the inside out in a 3D manner and you’re able to focus intradermally up to 1 mm with high energy 1,064 nm or 1,550 nm,” he said. “It’s a unique conical geometry that spares the epidermis, combined with sapphire tip cooling and images the skin at the same time with the potential for personalized treatments of dyschromia and photoaging in all skin types. It’s truly remarkable where the technology is heading.”
Dr. Friedman disclosed that he has received consulting fees from Allergan, Galderma, Acclaro, Merz Aesthetics, Solta Medical, and Cytrellis. He has conducted contracted research for Sofwave and is a member of the speakers bureau for Solta Medical and Candela.
PHOENIX – Ever since PicoSure became the first picosecond laser cleared by the Food and Drug Administration for the treatment of unwanted tattoos and pigmented lesions in 2012, new uses for this technology continue to expand.
Now, These include PicoWay, PicoSure, Enlighten, PicoPlus, PiQo4, and Quanta Pico, among others.
“PicoWay technology has integrated nicely into my practice in Houston, the most ethnically diverse city in the country, with its ability to safely treat a number of various benign, congenital, and acquired epidermal and dermal pigmented lesions with ultrashort pulse duration and low thermal impact, which greatly reduces the risk of postinflammatory hyperpigmentation even in darker skin types,” Paul M. Friedman, MD, director of the Dermatology and Laser Surgery Center, Houston, said at the annual conference of the American Society for Laser Medicine and Surgery.
He emphasized the importance of therapeutic clinical endpoints, noting that with q-switched lasers, “you’re looking for immediate whitening, whereas with picosecond lasers, your endpoint is slight whitening or slight darkening depending on wavelength, indication, and skin type. The ability to fractionate picosecond pulses has also allowed us to utilize this technology for photoaging as well as acne scarring.”
The PicoWay system includes a 730-nm picosecond titanium sapphire handpiece, which is FDA cleared for treatment of benign pigmented lesions and blue and green tattoo removal. Dr. Friedman said that he has seen good clinical results using the handpiece for café-au-lait macules, particularly in skin of color.
In an abstract presented at the ASLMS meeting, he and his colleagues presented a retrospective review of 12 patients with café-au-lait macules with Fitzpatrick skin types III-VI who were treated with the PicoWay 730 nm handpiece between April 2021 and January 2023. Patients received a mean of 3.1 treatments at intervals that ranged from 5 to 40 weeks. Clinical photographs were graded by three board-certified dermatologists using a 5-point visual analogue scale.
Overall, patients were rated to have a mean improvement of 26%-50%. Two patients achieved 100% clearance after four to five treatment sessions. “Café-au-lait macules with smooth borders responded less well to laser treatment, confirming prior studies at our center,” he said. “We often educate parents that café-au-lait macules may recur over time, especially with repeated sun exposure.”
Treating melasma
Dr. Friedman’s go-to devices for melasma include the low-density, low-energy 1,927-nm fractional diode laser; the 1,064 nm picosecond Nd:YAG, the low-fluence 1,064 nm Q-switched Nd:YAG with a nanosecond pulse duration, and the 595-nm pulsed dye laser for lesions exhibiting underlying vascularity. He said that combining therapies that target pigment and vasculature may be ideal to prevent relapses. “Melasma is a multifactorial condition so by improving patient education and expectation alongside advances in laser treatment of melasma, we have ultimately improved our ability to treat this condition,” he said.
“We’re approaching it from all angles, with ultraviolet photography and spectrocolorimetry, behavioral modifications, topical skin-lightening agents, broad spectrum sunscreens with protection against visible light, and oral tranexamic acid in advanced cases. Then, we intervene with these energy-based modalities, and the bottom line is, less energy and density is more, with lengthened treatment intervals. In 2023, we’re better than we’ve ever been in terms of our ability to safely and effectively improve melasma.”
Novel lasers
Dr. Friedman also described the UltraClear, a novel ablative fractional 2,910-nm erbium-doped glass fiber laser that delivers a customized blend of ablation and coagulation based on the patient’s condition, skin type, and tolerability for down time. He provided an overview of the versatility of what he described as highly customizable technology for conditions such as photoaging and dyschromia in patients of various skin types, making it a very versatile platform in his practice.
The AVAVA MIRIA system is a “next generation” laser “where you’re able to use a focal point. Basically, you’re treating the skin from the inside out in a 3D manner and you’re able to focus intradermally up to 1 mm with high energy 1,064 nm or 1,550 nm,” he said. “It’s a unique conical geometry that spares the epidermis, combined with sapphire tip cooling and images the skin at the same time with the potential for personalized treatments of dyschromia and photoaging in all skin types. It’s truly remarkable where the technology is heading.”
Dr. Friedman disclosed that he has received consulting fees from Allergan, Galderma, Acclaro, Merz Aesthetics, Solta Medical, and Cytrellis. He has conducted contracted research for Sofwave and is a member of the speakers bureau for Solta Medical and Candela.
FROM ASLMS 2023
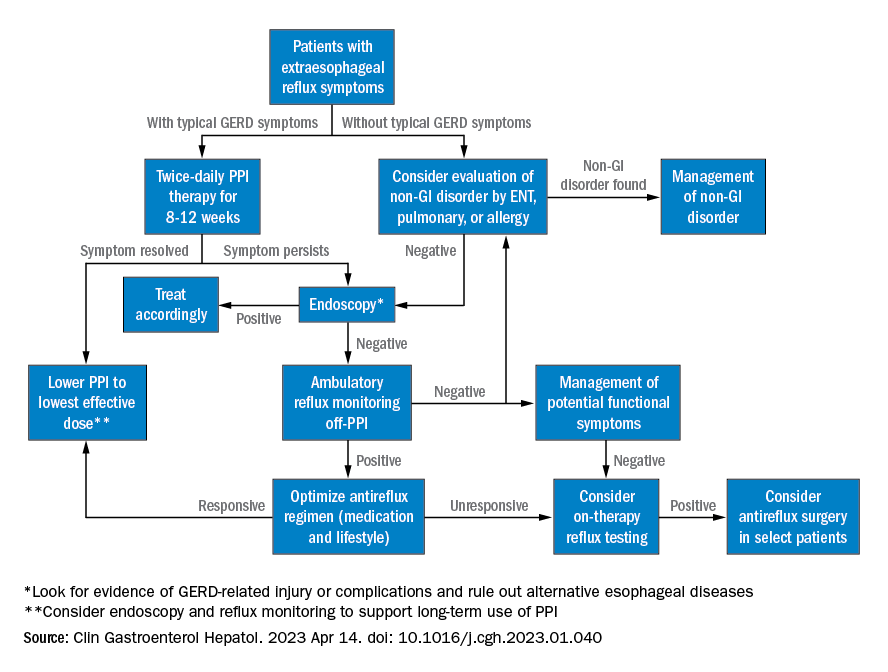
AGA clinical practice update: Extraesophageal gastroesophageal reflux disease
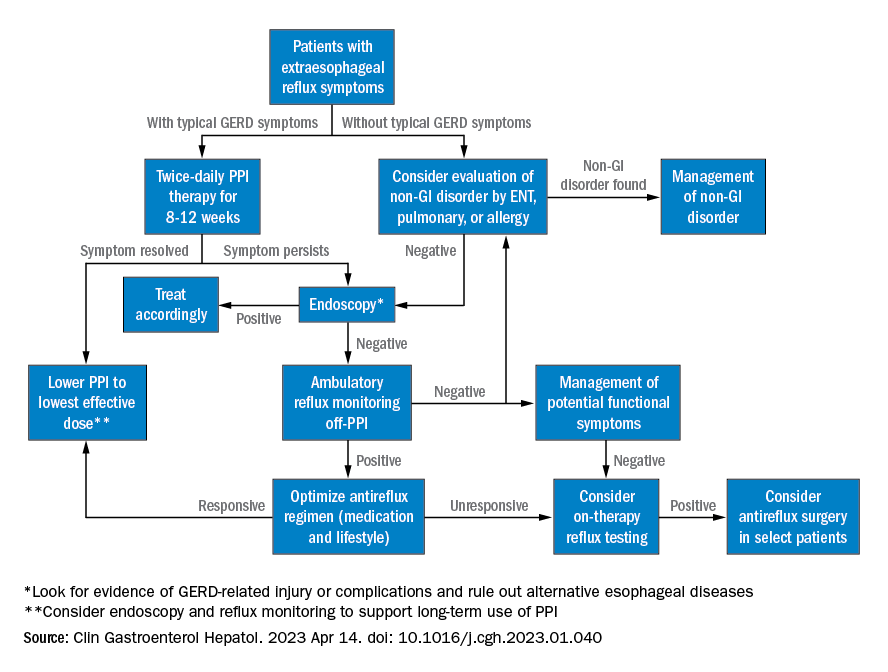
Extraesophageal reflux (EER) symptoms are a subset of gastroesophageal reflux disease (GERD) that can be difficult to diagnose because of its heterogeneous nature and symptoms that overlap with other conditions.
That puts the onus on physicians to take all symptoms into account and work across disciplines to diagnose, manage, and treat the condition, according to a new clinical practice update from the American Gastroenterological Association, which was published in Clinical Gastroenterology and Hepatology.
GERD is becoming increasingly common, which in turn has led to greater awareness and consideration of EER symptoms. EER symptoms can present a challenge because they may vary considerably and are not unique to GERD. The symptoms often do not respond well to proton pump inhibitor (PPI) therapy.
EER symptoms can include cough, laryngeal hoarseness, dysphonia, pulmonary fibrosis, asthma, dental erosions/caries, sinus disease, ear disease, postnasal drip, and throat clearing. Some patients with EER symptoms do not report heartburn or regurgitation, which leaves it up to the physician to determine if acid reflux is present and contributing to symptoms.
“The concept of extraesophageal symptoms secondary to GERD is complex and often controversial, leading to diagnostic and therapeutic challenges. Several extraesophageal symptoms have been associated with GERD, although the strength of evidence to support a causal relation varies,” wrote the authors, who were led by Joan W. Chen, MD, MS, a gastroenterologist with the University of Michigan, Ann Arbor.
There is also debate over whether fluid refluxate is the source of damage that causes EER symptoms, and if so, whether it is sufficient that the fluid be acidic or that pepsin be present, or if the cause is related to neurogenic signaling and resulting inflammation. Because of these questions, a PPI trial will not necessarily provide insight into the role of acid reflux in EER symptoms.
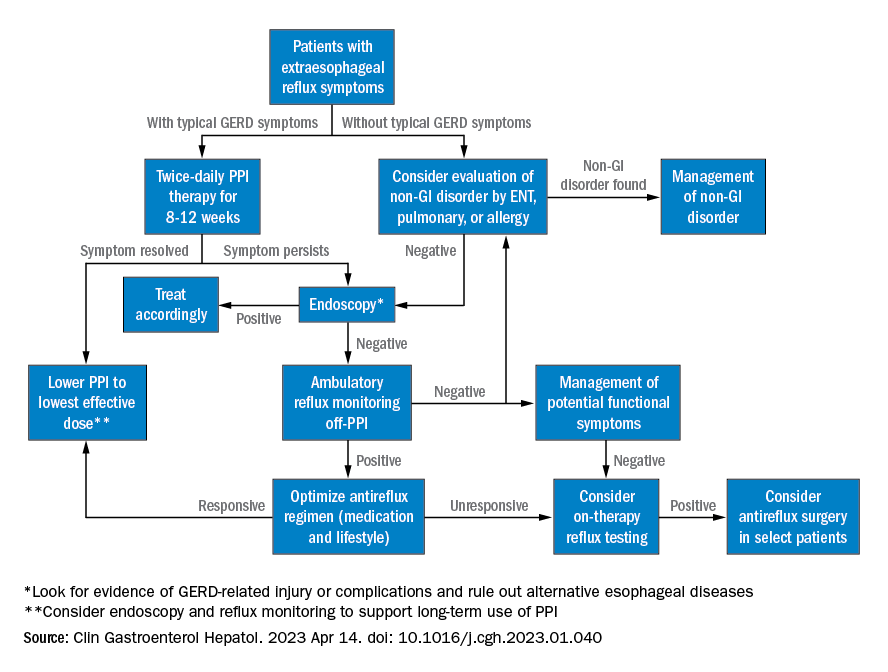
Best practice advice 1: The authors emphasized that gastroenterologists need to be aware of the potential extraesophageal symptoms of GERD. They should inquire with GERD patients to determine if laryngitis, chronic cough, asthma, and dental erosions are present.
Best practice advice 2: Consider a multidisciplinary approach to EER manifestations. Cases may require input from non-GI specialties. Tests performed by other specialists, such as bronchoscopy, thoracic imaging, or laryngoscopy, should be taken into account, since patients will also seek out multiple specialists to address their symptoms.
Best practice advice 3: There is no specific diagnostic test available to determine if GER is the cause of EER symptoms. Instead, physicians should interpret patient symptoms, response to GER therapy, and input from endoscopy and reflux tests.
Best practice advice 4: Rather than subject the patient to the cost and potential for even rare adverse events of a PPI trial, physicians should first consider conducting reflux testing. A PPI trial has clinical value but is insufficient on its own to help diagnose or manage EER. Initial single-dose PPI trial, titrating up to twice daily in those with typical GERD symptoms, is reasonable.
Best practice advice 5: The inconsistent therapeutic response to PPI therapy means that positive effects of PPI therapy on EER symptoms can’t confirm a GERD diagnosis because a placebo effect may be involved, and because symptom improvement can occur through mechanisms other than acid suppression. A meta-analysis found that a PPI trial has a sensitivity of 71%-78% and a specificity of 41%-54% with typical symptoms of heartburn and regurgitation. “Considering the greater variation expected with PPI response for extraesophageal symptoms, the diagnostic performance of empiric PPI trial for a diagnosis of EER would be anticipated to be substantially lower,” the authors wrote.
Best practice advice 6: When EER symptoms related to GERD are suspected and a PPI trial of up to 12 weeks does not lead to adequate improvement, the physician should consider testing for pathologic GER. Additional trials employing other PPIs are unlikely to succeed.
Best practice advice 7: Initial testing to evaluate for reflux should be tailored to patients’ clinical presentation. Potential methods to evaluate reflux include upper endoscopy and ambulatory reflux monitoring studies of acid suppressive therapy, which can assist with a GERD diagnosis, particularly when nonerosive reflux is present.
Best practice advice 8: About 50%-60% of patients with EER symptoms will not have GERD. Testing can be considered for those with an established objective diagnosis of GERD who do not respond well to high doses of acid suppression. Cost-effectiveness studies have confirmed the value of starting with ambulatory reflux monitoring, which can include a catheter-based pH sensor, pH impedance, or wireless pH capsule.
Ambulatory esophageal pH monitoring can also assist in making a GERD diagnosis, but it does not indicate whether GERD may be contributing to EER symptoms.
“Whichever the reflux testing modality, the strongest confidence for EER is achieved after ambulatory reflux testing showing pathologic acid exposure and a positive symptom-reflux association for EER symptoms,” the authors wrote. They also pointed out that ambulatory reflux monitoring in EER patients should be done in the absence of acid suppression unless there is already objective evidence for the presence of GERD.
Best practice advice 9: Aside from acid suppression, EER symptoms can also be managed through other means, including lifestyle modifications, such as eating avoidance prior to lying down, elevation of the head of the bed, sleeping on the left side, and weight loss. Or, alginate containing antacids, external upper esophageal sphincter compression device, cognitive behavioral therapy, and neuromodulators.
Best practice advice 10: In cases where the EER patient has objectively defined evidence of GERD, physicians should employ shared decision-making before considering anti-reflux surgery. If the patient did not respond to PPI therapy, this predicts a lack of response to antireflux surgery.
All four authors reported financial ties to multiple pharmaceutical companies.
Extraesophageal reflux (EER) symptoms are a subset of gastroesophageal reflux disease (GERD) that can be difficult to diagnose because of its heterogeneous nature and symptoms that overlap with other conditions.
That puts the onus on physicians to take all symptoms into account and work across disciplines to diagnose, manage, and treat the condition, according to a new clinical practice update from the American Gastroenterological Association, which was published in Clinical Gastroenterology and Hepatology.
GERD is becoming increasingly common, which in turn has led to greater awareness and consideration of EER symptoms. EER symptoms can present a challenge because they may vary considerably and are not unique to GERD. The symptoms often do not respond well to proton pump inhibitor (PPI) therapy.
EER symptoms can include cough, laryngeal hoarseness, dysphonia, pulmonary fibrosis, asthma, dental erosions/caries, sinus disease, ear disease, postnasal drip, and throat clearing. Some patients with EER symptoms do not report heartburn or regurgitation, which leaves it up to the physician to determine if acid reflux is present and contributing to symptoms.
“The concept of extraesophageal symptoms secondary to GERD is complex and often controversial, leading to diagnostic and therapeutic challenges. Several extraesophageal symptoms have been associated with GERD, although the strength of evidence to support a causal relation varies,” wrote the authors, who were led by Joan W. Chen, MD, MS, a gastroenterologist with the University of Michigan, Ann Arbor.
There is also debate over whether fluid refluxate is the source of damage that causes EER symptoms, and if so, whether it is sufficient that the fluid be acidic or that pepsin be present, or if the cause is related to neurogenic signaling and resulting inflammation. Because of these questions, a PPI trial will not necessarily provide insight into the role of acid reflux in EER symptoms.
Best practice advice 1: The authors emphasized that gastroenterologists need to be aware of the potential extraesophageal symptoms of GERD. They should inquire with GERD patients to determine if laryngitis, chronic cough, asthma, and dental erosions are present.
Best practice advice 2: Consider a multidisciplinary approach to EER manifestations. Cases may require input from non-GI specialties. Tests performed by other specialists, such as bronchoscopy, thoracic imaging, or laryngoscopy, should be taken into account, since patients will also seek out multiple specialists to address their symptoms.
Best practice advice 3: There is no specific diagnostic test available to determine if GER is the cause of EER symptoms. Instead, physicians should interpret patient symptoms, response to GER therapy, and input from endoscopy and reflux tests.
Best practice advice 4: Rather than subject the patient to the cost and potential for even rare adverse events of a PPI trial, physicians should first consider conducting reflux testing. A PPI trial has clinical value but is insufficient on its own to help diagnose or manage EER. Initial single-dose PPI trial, titrating up to twice daily in those with typical GERD symptoms, is reasonable.
Best practice advice 5: The inconsistent therapeutic response to PPI therapy means that positive effects of PPI therapy on EER symptoms can’t confirm a GERD diagnosis because a placebo effect may be involved, and because symptom improvement can occur through mechanisms other than acid suppression. A meta-analysis found that a PPI trial has a sensitivity of 71%-78% and a specificity of 41%-54% with typical symptoms of heartburn and regurgitation. “Considering the greater variation expected with PPI response for extraesophageal symptoms, the diagnostic performance of empiric PPI trial for a diagnosis of EER would be anticipated to be substantially lower,” the authors wrote.
Best practice advice 6: When EER symptoms related to GERD are suspected and a PPI trial of up to 12 weeks does not lead to adequate improvement, the physician should consider testing for pathologic GER. Additional trials employing other PPIs are unlikely to succeed.
Best practice advice 7: Initial testing to evaluate for reflux should be tailored to patients’ clinical presentation. Potential methods to evaluate reflux include upper endoscopy and ambulatory reflux monitoring studies of acid suppressive therapy, which can assist with a GERD diagnosis, particularly when nonerosive reflux is present.
Best practice advice 8: About 50%-60% of patients with EER symptoms will not have GERD. Testing can be considered for those with an established objective diagnosis of GERD who do not respond well to high doses of acid suppression. Cost-effectiveness studies have confirmed the value of starting with ambulatory reflux monitoring, which can include a catheter-based pH sensor, pH impedance, or wireless pH capsule.
Ambulatory esophageal pH monitoring can also assist in making a GERD diagnosis, but it does not indicate whether GERD may be contributing to EER symptoms.
“Whichever the reflux testing modality, the strongest confidence for EER is achieved after ambulatory reflux testing showing pathologic acid exposure and a positive symptom-reflux association for EER symptoms,” the authors wrote. They also pointed out that ambulatory reflux monitoring in EER patients should be done in the absence of acid suppression unless there is already objective evidence for the presence of GERD.
Best practice advice 9: Aside from acid suppression, EER symptoms can also be managed through other means, including lifestyle modifications, such as eating avoidance prior to lying down, elevation of the head of the bed, sleeping on the left side, and weight loss. Or, alginate containing antacids, external upper esophageal sphincter compression device, cognitive behavioral therapy, and neuromodulators.
Best practice advice 10: In cases where the EER patient has objectively defined evidence of GERD, physicians should employ shared decision-making before considering anti-reflux surgery. If the patient did not respond to PPI therapy, this predicts a lack of response to antireflux surgery.
All four authors reported financial ties to multiple pharmaceutical companies.
Extraesophageal reflux (EER) symptoms are a subset of gastroesophageal reflux disease (GERD) that can be difficult to diagnose because of its heterogeneous nature and symptoms that overlap with other conditions.
That puts the onus on physicians to take all symptoms into account and work across disciplines to diagnose, manage, and treat the condition, according to a new clinical practice update from the American Gastroenterological Association, which was published in Clinical Gastroenterology and Hepatology.
GERD is becoming increasingly common, which in turn has led to greater awareness and consideration of EER symptoms. EER symptoms can present a challenge because they may vary considerably and are not unique to GERD. The symptoms often do not respond well to proton pump inhibitor (PPI) therapy.
EER symptoms can include cough, laryngeal hoarseness, dysphonia, pulmonary fibrosis, asthma, dental erosions/caries, sinus disease, ear disease, postnasal drip, and throat clearing. Some patients with EER symptoms do not report heartburn or regurgitation, which leaves it up to the physician to determine if acid reflux is present and contributing to symptoms.
“The concept of extraesophageal symptoms secondary to GERD is complex and often controversial, leading to diagnostic and therapeutic challenges. Several extraesophageal symptoms have been associated with GERD, although the strength of evidence to support a causal relation varies,” wrote the authors, who were led by Joan W. Chen, MD, MS, a gastroenterologist with the University of Michigan, Ann Arbor.
There is also debate over whether fluid refluxate is the source of damage that causes EER symptoms, and if so, whether it is sufficient that the fluid be acidic or that pepsin be present, or if the cause is related to neurogenic signaling and resulting inflammation. Because of these questions, a PPI trial will not necessarily provide insight into the role of acid reflux in EER symptoms.
Best practice advice 1: The authors emphasized that gastroenterologists need to be aware of the potential extraesophageal symptoms of GERD. They should inquire with GERD patients to determine if laryngitis, chronic cough, asthma, and dental erosions are present.
Best practice advice 2: Consider a multidisciplinary approach to EER manifestations. Cases may require input from non-GI specialties. Tests performed by other specialists, such as bronchoscopy, thoracic imaging, or laryngoscopy, should be taken into account, since patients will also seek out multiple specialists to address their symptoms.
Best practice advice 3: There is no specific diagnostic test available to determine if GER is the cause of EER symptoms. Instead, physicians should interpret patient symptoms, response to GER therapy, and input from endoscopy and reflux tests.
Best practice advice 4: Rather than subject the patient to the cost and potential for even rare adverse events of a PPI trial, physicians should first consider conducting reflux testing. A PPI trial has clinical value but is insufficient on its own to help diagnose or manage EER. Initial single-dose PPI trial, titrating up to twice daily in those with typical GERD symptoms, is reasonable.
Best practice advice 5: The inconsistent therapeutic response to PPI therapy means that positive effects of PPI therapy on EER symptoms can’t confirm a GERD diagnosis because a placebo effect may be involved, and because symptom improvement can occur through mechanisms other than acid suppression. A meta-analysis found that a PPI trial has a sensitivity of 71%-78% and a specificity of 41%-54% with typical symptoms of heartburn and regurgitation. “Considering the greater variation expected with PPI response for extraesophageal symptoms, the diagnostic performance of empiric PPI trial for a diagnosis of EER would be anticipated to be substantially lower,” the authors wrote.
Best practice advice 6: When EER symptoms related to GERD are suspected and a PPI trial of up to 12 weeks does not lead to adequate improvement, the physician should consider testing for pathologic GER. Additional trials employing other PPIs are unlikely to succeed.
Best practice advice 7: Initial testing to evaluate for reflux should be tailored to patients’ clinical presentation. Potential methods to evaluate reflux include upper endoscopy and ambulatory reflux monitoring studies of acid suppressive therapy, which can assist with a GERD diagnosis, particularly when nonerosive reflux is present.
Best practice advice 8: About 50%-60% of patients with EER symptoms will not have GERD. Testing can be considered for those with an established objective diagnosis of GERD who do not respond well to high doses of acid suppression. Cost-effectiveness studies have confirmed the value of starting with ambulatory reflux monitoring, which can include a catheter-based pH sensor, pH impedance, or wireless pH capsule.
Ambulatory esophageal pH monitoring can also assist in making a GERD diagnosis, but it does not indicate whether GERD may be contributing to EER symptoms.
“Whichever the reflux testing modality, the strongest confidence for EER is achieved after ambulatory reflux testing showing pathologic acid exposure and a positive symptom-reflux association for EER symptoms,” the authors wrote. They also pointed out that ambulatory reflux monitoring in EER patients should be done in the absence of acid suppression unless there is already objective evidence for the presence of GERD.
Best practice advice 9: Aside from acid suppression, EER symptoms can also be managed through other means, including lifestyle modifications, such as eating avoidance prior to lying down, elevation of the head of the bed, sleeping on the left side, and weight loss. Or, alginate containing antacids, external upper esophageal sphincter compression device, cognitive behavioral therapy, and neuromodulators.
Best practice advice 10: In cases where the EER patient has objectively defined evidence of GERD, physicians should employ shared decision-making before considering anti-reflux surgery. If the patient did not respond to PPI therapy, this predicts a lack of response to antireflux surgery.
All four authors reported financial ties to multiple pharmaceutical companies.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Two phase 3 trials show benefits of dupilumab for prurigo nodularis
The results, which were published online in Nature Medicine, were the basis for the FDA approval of dupilumab (Dupixent) for adults with PN in September 2022, the first treatment approved for treating PN in the United States.
“These positive studies support the involvement of type 2 cytokines in driving PN disease pathogenesis and the targeting of the [interleukin]-4/IL-13 axis as a novel therapeutic paradigm for patients with PN,” wrote the researchers, who were led by principal investigator Gil Yosipovitch, MD, professor of dermatology at the University of Miami, Fla. Dupilumab, an IL-4 receptor alpha antagonist, blocks the shared receptor component (IL-4R alpha) for IL-4 and IL-13.
For the two phase 3 trials, which were called LIBERTY-PN PRIME and PRIME2 and were sponsored by Sanofi and Regeneron Pharmaceuticals, researchers randomized adults with PN with 20 or more nodules and severe itch uncontrolled with topical therapies 1:1 to 300 mg dupilumab or placebo subcutaneously every 2 weeks for 24 weeks. The primary endpoint was pruritus improvement, which was measured by the proportion of patients with a 4-point or greater reduction in Worst Itch Numeric Rating Scale (WI-NRS) from baseline at week 24 (PRIME) or week 12 (PRIME2). Key secondary endpoints included a reduction in the number of nodules to 5 or fewer at week 24.
PRIME and PRIME2 enrolled 151 and 160 patients, respectively. In PRIME, 60% of patients in the dupilumab arm achieved a 4-point or greater reduction in the WI-NRS at week 24, compared with 18.4% of patients in the placebo arm (P < .001). In PRIME2, 37.2% of patients in the dupilumab arm achieved a 4-point or greater reduction in the WI-NRS at week 12, compared with 22% of patients in the placebo arm (P = .022).
The researchers also reported that, from an initial baseline of 20 to greater than 100 nodules, 32.0% of dupilumab-treated patients in PRIME and 25.6% in PRIME2 showed a reduction to 5 nodules or fewer, which corresponded to a response of “clear” or “almost clear” skin at week 12, compared with 11.8% and 12.2% of placebo-treated patients, respectively. This treatment effect on skin lesions continued to improve after week 12, with 48% of dupilumab-treated patients in PRIME and 44.9% in PRIME2 having five nodules or fewer at week 24, compared with 18.4% and 15.9% of placebo-treated patients, respectively. Safety was consistent with the known dupilumab safety profile.
“Validation is the first success of this paper,” said Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington, who was asked to comment on the study. “While both the safety and efficacy of dupilumab in these two phase 3 programs is the meat of the matter, nuanced highlights for me include the rigid nature of the exclusion criteria to ensure a study population that truly has PN as a stand-alone disease, rather than a secondary finding as we once believed to be the entire story. I think it’s important for us to recognize that it’s not one or the other, rather there is both ‘primary’ prurigo nodularis, and then there is secondary prurigo nodularis associated with something else [a wide range of underlying medical conditions], just like we divide primary and secondary hyperhidrosis.”
Dr. Yosipovitch reported having competing interests with several pharmaceutical companies, including Regeneron and Sanofi. Dr. Friedman disclosed that he is a consultant to and a speaker for Regeneron.
The results, which were published online in Nature Medicine, were the basis for the FDA approval of dupilumab (Dupixent) for adults with PN in September 2022, the first treatment approved for treating PN in the United States.
“These positive studies support the involvement of type 2 cytokines in driving PN disease pathogenesis and the targeting of the [interleukin]-4/IL-13 axis as a novel therapeutic paradigm for patients with PN,” wrote the researchers, who were led by principal investigator Gil Yosipovitch, MD, professor of dermatology at the University of Miami, Fla. Dupilumab, an IL-4 receptor alpha antagonist, blocks the shared receptor component (IL-4R alpha) for IL-4 and IL-13.
For the two phase 3 trials, which were called LIBERTY-PN PRIME and PRIME2 and were sponsored by Sanofi and Regeneron Pharmaceuticals, researchers randomized adults with PN with 20 or more nodules and severe itch uncontrolled with topical therapies 1:1 to 300 mg dupilumab or placebo subcutaneously every 2 weeks for 24 weeks. The primary endpoint was pruritus improvement, which was measured by the proportion of patients with a 4-point or greater reduction in Worst Itch Numeric Rating Scale (WI-NRS) from baseline at week 24 (PRIME) or week 12 (PRIME2). Key secondary endpoints included a reduction in the number of nodules to 5 or fewer at week 24.
PRIME and PRIME2 enrolled 151 and 160 patients, respectively. In PRIME, 60% of patients in the dupilumab arm achieved a 4-point or greater reduction in the WI-NRS at week 24, compared with 18.4% of patients in the placebo arm (P < .001). In PRIME2, 37.2% of patients in the dupilumab arm achieved a 4-point or greater reduction in the WI-NRS at week 12, compared with 22% of patients in the placebo arm (P = .022).
The researchers also reported that, from an initial baseline of 20 to greater than 100 nodules, 32.0% of dupilumab-treated patients in PRIME and 25.6% in PRIME2 showed a reduction to 5 nodules or fewer, which corresponded to a response of “clear” or “almost clear” skin at week 12, compared with 11.8% and 12.2% of placebo-treated patients, respectively. This treatment effect on skin lesions continued to improve after week 12, with 48% of dupilumab-treated patients in PRIME and 44.9% in PRIME2 having five nodules or fewer at week 24, compared with 18.4% and 15.9% of placebo-treated patients, respectively. Safety was consistent with the known dupilumab safety profile.
“Validation is the first success of this paper,” said Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington, who was asked to comment on the study. “While both the safety and efficacy of dupilumab in these two phase 3 programs is the meat of the matter, nuanced highlights for me include the rigid nature of the exclusion criteria to ensure a study population that truly has PN as a stand-alone disease, rather than a secondary finding as we once believed to be the entire story. I think it’s important for us to recognize that it’s not one or the other, rather there is both ‘primary’ prurigo nodularis, and then there is secondary prurigo nodularis associated with something else [a wide range of underlying medical conditions], just like we divide primary and secondary hyperhidrosis.”
Dr. Yosipovitch reported having competing interests with several pharmaceutical companies, including Regeneron and Sanofi. Dr. Friedman disclosed that he is a consultant to and a speaker for Regeneron.
The results, which were published online in Nature Medicine, were the basis for the FDA approval of dupilumab (Dupixent) for adults with PN in September 2022, the first treatment approved for treating PN in the United States.
“These positive studies support the involvement of type 2 cytokines in driving PN disease pathogenesis and the targeting of the [interleukin]-4/IL-13 axis as a novel therapeutic paradigm for patients with PN,” wrote the researchers, who were led by principal investigator Gil Yosipovitch, MD, professor of dermatology at the University of Miami, Fla. Dupilumab, an IL-4 receptor alpha antagonist, blocks the shared receptor component (IL-4R alpha) for IL-4 and IL-13.
For the two phase 3 trials, which were called LIBERTY-PN PRIME and PRIME2 and were sponsored by Sanofi and Regeneron Pharmaceuticals, researchers randomized adults with PN with 20 or more nodules and severe itch uncontrolled with topical therapies 1:1 to 300 mg dupilumab or placebo subcutaneously every 2 weeks for 24 weeks. The primary endpoint was pruritus improvement, which was measured by the proportion of patients with a 4-point or greater reduction in Worst Itch Numeric Rating Scale (WI-NRS) from baseline at week 24 (PRIME) or week 12 (PRIME2). Key secondary endpoints included a reduction in the number of nodules to 5 or fewer at week 24.
PRIME and PRIME2 enrolled 151 and 160 patients, respectively. In PRIME, 60% of patients in the dupilumab arm achieved a 4-point or greater reduction in the WI-NRS at week 24, compared with 18.4% of patients in the placebo arm (P < .001). In PRIME2, 37.2% of patients in the dupilumab arm achieved a 4-point or greater reduction in the WI-NRS at week 12, compared with 22% of patients in the placebo arm (P = .022).
The researchers also reported that, from an initial baseline of 20 to greater than 100 nodules, 32.0% of dupilumab-treated patients in PRIME and 25.6% in PRIME2 showed a reduction to 5 nodules or fewer, which corresponded to a response of “clear” or “almost clear” skin at week 12, compared with 11.8% and 12.2% of placebo-treated patients, respectively. This treatment effect on skin lesions continued to improve after week 12, with 48% of dupilumab-treated patients in PRIME and 44.9% in PRIME2 having five nodules or fewer at week 24, compared with 18.4% and 15.9% of placebo-treated patients, respectively. Safety was consistent with the known dupilumab safety profile.
“Validation is the first success of this paper,” said Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington, who was asked to comment on the study. “While both the safety and efficacy of dupilumab in these two phase 3 programs is the meat of the matter, nuanced highlights for me include the rigid nature of the exclusion criteria to ensure a study population that truly has PN as a stand-alone disease, rather than a secondary finding as we once believed to be the entire story. I think it’s important for us to recognize that it’s not one or the other, rather there is both ‘primary’ prurigo nodularis, and then there is secondary prurigo nodularis associated with something else [a wide range of underlying medical conditions], just like we divide primary and secondary hyperhidrosis.”
Dr. Yosipovitch reported having competing interests with several pharmaceutical companies, including Regeneron and Sanofi. Dr. Friedman disclosed that he is a consultant to and a speaker for Regeneron.
FROM NATURE MEDICINE
Bundled strategy increased preteen lipid screening
WASHINGTON – A bundled intervention combining point-of-care testing, electronic medical record support, and provider education significantly improved lipid screening rates in children aged 9-11 years, according to data from approximately 100 monthly visits over a 3-year period.
Guidelines from the National Heart, Lung, and Blood Institute currently recommend universal lipid screening for children aged 9-11 years, but screening rates in clinical practice remain low, according to Ruth E. Gardner, MD, of Penn State University, Hershey, and colleagues.
In a poster presented at the Pediatric Academic Societies annual meeting, Dr. Gardner and colleagues shared results of the implementation of a bundled testing protocol designed to improve screening.
The researchers reviewed data on lipid testing within 30 days for all 9- to 11-year-old well child visits at a single center between May 2019 and February 2022. The bundled intervention was introduced in May 2021.
The bundled protocol included in-office capillary testing and provider education. In addition, electronic medical record templates were modified to include prompts for lipid screening at relevant ages, and EMR orders were adjusted to include lipid testing. The researchers also collected targeted provider feedback on individualized screening rates in February 2022.
Screening rates were plotted monthly. For the period from May 2019 through May 2021, the rates averaged 6.5%. However, after the introduction of the bundled intervention, the rate increased to 29.9%. Following targeted provider feedback in February 2022, the researchers found an additional shift to 52.1% through March and April 2022.
The findings were limited by the use of data from a single center, and the researchers used an extended study period to account for disruptions to well-child care in the spring of 2020 related to the COVID-19 pandemic.
However, the results support the effectiveness of a bundled intervention for improving lipid screening rates in children aged 9-11 years, the researchers said, and targeted provider feedback and education could yield additional improvements, they concluded.
Preteen years are an optimal time for screening
“The current study is important because atherosclerosis begins in childhood, and screening at ages 9-11 is an optimal time to begin lifestyle changes to improve overall health and reduce risks of heart disease,” said Margaret Thew, DNP, FNP-BC, of the Medical College of Wisconsin, Milwaukee, in an interview.
Ms. Thew, who was not involved in the study, said, “The number of recommended and required screening items needed in pediatrics is vast, so many providers have to select which items to focus on for their health screenings with these ages.”
Overall, “I was impressed with the improvements that were made in this quality improvement study,” said Ms. Thew.
Barriers to lipid screening in this population include the reduced number of health screenings and immunizations recommended for this age group; the consequence is that access is limited to discuss preventive care opportunities, said Ms. Thew in an interview. Steps to overcome these barriers could include the use of many of the screening tools introduced in the current study, such as point-of-care testing in the office, use of the EMR to remind providers of testing, which can be done during well visits or school physicals, and educating providers about the current guidelines, she noted.
Other strategies to increase screening include moving the immunization series to provide more frequent appointments to children aged 9-11 years to offer education and preventive care, Ms. Thew added.
The study received no outside funding. The researchers had no financial conflicts to disclose. Ms. Thew had no financial conflicts to disclose and serves on the Editorial Advisory Board of Pediatric News.
WASHINGTON – A bundled intervention combining point-of-care testing, electronic medical record support, and provider education significantly improved lipid screening rates in children aged 9-11 years, according to data from approximately 100 monthly visits over a 3-year period.
Guidelines from the National Heart, Lung, and Blood Institute currently recommend universal lipid screening for children aged 9-11 years, but screening rates in clinical practice remain low, according to Ruth E. Gardner, MD, of Penn State University, Hershey, and colleagues.
In a poster presented at the Pediatric Academic Societies annual meeting, Dr. Gardner and colleagues shared results of the implementation of a bundled testing protocol designed to improve screening.
The researchers reviewed data on lipid testing within 30 days for all 9- to 11-year-old well child visits at a single center between May 2019 and February 2022. The bundled intervention was introduced in May 2021.
The bundled protocol included in-office capillary testing and provider education. In addition, electronic medical record templates were modified to include prompts for lipid screening at relevant ages, and EMR orders were adjusted to include lipid testing. The researchers also collected targeted provider feedback on individualized screening rates in February 2022.
Screening rates were plotted monthly. For the period from May 2019 through May 2021, the rates averaged 6.5%. However, after the introduction of the bundled intervention, the rate increased to 29.9%. Following targeted provider feedback in February 2022, the researchers found an additional shift to 52.1% through March and April 2022.
The findings were limited by the use of data from a single center, and the researchers used an extended study period to account for disruptions to well-child care in the spring of 2020 related to the COVID-19 pandemic.
However, the results support the effectiveness of a bundled intervention for improving lipid screening rates in children aged 9-11 years, the researchers said, and targeted provider feedback and education could yield additional improvements, they concluded.
Preteen years are an optimal time for screening
“The current study is important because atherosclerosis begins in childhood, and screening at ages 9-11 is an optimal time to begin lifestyle changes to improve overall health and reduce risks of heart disease,” said Margaret Thew, DNP, FNP-BC, of the Medical College of Wisconsin, Milwaukee, in an interview.
Ms. Thew, who was not involved in the study, said, “The number of recommended and required screening items needed in pediatrics is vast, so many providers have to select which items to focus on for their health screenings with these ages.”
Overall, “I was impressed with the improvements that were made in this quality improvement study,” said Ms. Thew.
Barriers to lipid screening in this population include the reduced number of health screenings and immunizations recommended for this age group; the consequence is that access is limited to discuss preventive care opportunities, said Ms. Thew in an interview. Steps to overcome these barriers could include the use of many of the screening tools introduced in the current study, such as point-of-care testing in the office, use of the EMR to remind providers of testing, which can be done during well visits or school physicals, and educating providers about the current guidelines, she noted.
Other strategies to increase screening include moving the immunization series to provide more frequent appointments to children aged 9-11 years to offer education and preventive care, Ms. Thew added.
The study received no outside funding. The researchers had no financial conflicts to disclose. Ms. Thew had no financial conflicts to disclose and serves on the Editorial Advisory Board of Pediatric News.
WASHINGTON – A bundled intervention combining point-of-care testing, electronic medical record support, and provider education significantly improved lipid screening rates in children aged 9-11 years, according to data from approximately 100 monthly visits over a 3-year period.
Guidelines from the National Heart, Lung, and Blood Institute currently recommend universal lipid screening for children aged 9-11 years, but screening rates in clinical practice remain low, according to Ruth E. Gardner, MD, of Penn State University, Hershey, and colleagues.
In a poster presented at the Pediatric Academic Societies annual meeting, Dr. Gardner and colleagues shared results of the implementation of a bundled testing protocol designed to improve screening.
The researchers reviewed data on lipid testing within 30 days for all 9- to 11-year-old well child visits at a single center between May 2019 and February 2022. The bundled intervention was introduced in May 2021.
The bundled protocol included in-office capillary testing and provider education. In addition, electronic medical record templates were modified to include prompts for lipid screening at relevant ages, and EMR orders were adjusted to include lipid testing. The researchers also collected targeted provider feedback on individualized screening rates in February 2022.
Screening rates were plotted monthly. For the period from May 2019 through May 2021, the rates averaged 6.5%. However, after the introduction of the bundled intervention, the rate increased to 29.9%. Following targeted provider feedback in February 2022, the researchers found an additional shift to 52.1% through March and April 2022.
The findings were limited by the use of data from a single center, and the researchers used an extended study period to account for disruptions to well-child care in the spring of 2020 related to the COVID-19 pandemic.
However, the results support the effectiveness of a bundled intervention for improving lipid screening rates in children aged 9-11 years, the researchers said, and targeted provider feedback and education could yield additional improvements, they concluded.
Preteen years are an optimal time for screening
“The current study is important because atherosclerosis begins in childhood, and screening at ages 9-11 is an optimal time to begin lifestyle changes to improve overall health and reduce risks of heart disease,” said Margaret Thew, DNP, FNP-BC, of the Medical College of Wisconsin, Milwaukee, in an interview.
Ms. Thew, who was not involved in the study, said, “The number of recommended and required screening items needed in pediatrics is vast, so many providers have to select which items to focus on for their health screenings with these ages.”
Overall, “I was impressed with the improvements that were made in this quality improvement study,” said Ms. Thew.
Barriers to lipid screening in this population include the reduced number of health screenings and immunizations recommended for this age group; the consequence is that access is limited to discuss preventive care opportunities, said Ms. Thew in an interview. Steps to overcome these barriers could include the use of many of the screening tools introduced in the current study, such as point-of-care testing in the office, use of the EMR to remind providers of testing, which can be done during well visits or school physicals, and educating providers about the current guidelines, she noted.
Other strategies to increase screening include moving the immunization series to provide more frequent appointments to children aged 9-11 years to offer education and preventive care, Ms. Thew added.
The study received no outside funding. The researchers had no financial conflicts to disclose. Ms. Thew had no financial conflicts to disclose and serves on the Editorial Advisory Board of Pediatric News.
FROM PAS 2023
Mental health promotion
May is Mental Health Awareness Month, providing us a chance to go beyond discussing the screening, diagnosis, and evidence-based treatments for the mental illnesses of youth. The World Health Organization defines good mental health as “a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her own community.” While the science of mental health promotion and disease prevention in childhood and adolescence is relatively young, there are several discrete domains in which you can follow and support your patient’s developing mental health. This begins with the well-being of new parents, and then moves into how parents are helping their children to develop skills to manage their basic daily needs and impulses, their thoughts and feelings, their stresses and their relationships. With a little support from you, parents can confidently help their children develop the foundations for good mental health.
First year of life: Parental mental health
Perhaps the strongest risk factor for serious mental illness in childhood and adulthood is parental neglect during the first year of life, and neglect in the first several months of life is the most commonly reported form of child abuse. Infant neglect is associated with parental depression (and other mental illnesses), parental substance use, and a parent’s own experience of childhood abuse or neglect. Neglect is more common with teenaged parents and parents living in poverty. Pediatricians are uniquely connected to families during the first year of a child’s life. The American Academy of Pediatrics recommends screening new mothers for depression at 1-, 2-, 4-, and 6-month infant check-ups with the Edinburgh Postnatal Depression Screen. Even without a positive screen, new parents may need the fortifications of extra community support to adapt to the changes parenthood brings.
At checkups, ask (both) parents how they are managing the stresses of a new baby. Are they getting restful sleep? Do they have social supports? Are they connected to a community (friends, extended family, faith) or isolated? Are they developing confidence as parents or feeling overwhelmed? Simple guidance, such as “sleep when the baby sleeps” and reassurance that taking good care of themselves is taking good care of the baby is always helpful. Sometimes you will need to refer for treatment or to community supports. Have your list of online and in-person resources at the ready to provide parents with these prescriptions. Supporting parental mental health and adjustment in the first year of life is possibly the most important building block for their child’s future mental health.
Toddlers and up: Emotional literacy
Emotional literacy (sometimes called “emotional intelligence”) is the capacity to recognize, identify, and manage feelings in oneself and in others. This skill begins to develop in infancy when parents respond to their baby’s cries with attunement, feeding or changing them if needed, and at other times simply reflecting their feelings and soothing them with movement, singing, or quiet talking. As children grow, so does their range of feelings, and their (cognitive) capacity to identify and manage them. Parents support this development by being available whenever their young children experience strong emotions, calmly listening, and acknowledging their discomfort. Parents can offer words for describing those feelings, and even be curious with their young children where in their bodies they are feeling them, how they can stay patient while the feeling passes or things they might be able to do to feel better. Parents may want to remove their child’s distress, but staying calm, curious, and present while helping their child to manage it will build their child’s emotional health. Parents can nurture this development in a less intense way by reading books about feelings together and noticing and identifying feelings in other children or in cartoon characters.
School-age children: Adding mindfulness
While a child’s cognitive development unfolds naturally, school-age children can cultivate awareness of their thoughts. This becomes possible after awareness of feelings and parents can help their older children consider whether something they are experiencing is a thought, a feeling, or a fact. They do so in the same way they helped their child develop emotional literacy: By responding with calm, curiosity, and confidence every time their child comes to them in distress (especially mild distress, like boredom!) or with a challenge or a question. With a difficult situation, parents start by helping their child to identify thoughts and feelings before impulsively acting on them. Parents can help children identify what’s in their control, try different approaches, and be flexible if their first efforts don’t work. Children need to learn that failing at things is how we learn and grow. Just like learning to ride a bike, it builds their frustration tolerance, their knowledge that they can do difficult things, and that distress subsides. These are critical building blocks for adolescence, when the challenges become greater and they manage them more independently.
Learning “mindfulness” (a practice that cultivates nonjudgmental awareness of one’s own thoughts, feelings, and sensations) can help children (and parents) to cultivate quiet self-awareness outside of moments of difficulty. “Stop, Breathe, and Think” and “Mindful gNATs” are two free apps that are recommended by the American Academy of Child and Adolescent Psychiatry for children (and their parents) to use to practice this awareness of thoughts and feelings.
Early and later adolescence: Stress management skills
Building on this awareness of thoughts and emotions, adolescents develop adaptive coping skills by facing challenges with the support of their parents nearby. Parents should still be ready to respond to charged emotional moments with calm and curiosity, validating their child’s distress while helping them to consider healthy responses. Helping their teenager to describe their experience, differentiating feelings from thoughts (and facts), and considering different choices within their control is foundational to resilience in adulthood. Parents also help their teenagers by reminding them of the need for good self-care (sleep, exercise, nutrition), nourishing social relationships, and protecting time for rest and recharging activities. Sometimes, parents will think with their teenager about why they are engaged in an activity that is stressful, whether it is authentically important to them, and why. Adolescents should be deepening their sense of identity, interests, talents, and even values, and stressful moments are rich opportunities to do so, with the support of caring adults. Without intentionally building these skills, adolescents will be more prone to managing stress with avoidance or unhealthy coping, such as excessive eating, video gaming, drugs, or alcohol.
Infancy and up: Behavioral healthy habits (sleep, physical activity, nutrition, and screen time)
Healthy habits sound simple, but establishing them is not always easy. The idea of a habit is that it makes managing something challenging or important more automatic, and thus easier and more reliable. Many of the same habits that promote physical health in adulthood also promote mental health: adequate, restful sleep; daily physical activity; a nutritious diet and a healthy relationship with food; and managing screen time in a developmentally appropriate way. Infants depend entirely on their parents for regulation of these behaviors. As their children grow, parents will adapt these routines so that their children are gradually regulating these needs and activities more independently. In each of these areas, children need clear expectations and routines, consistent consequences and positive feedback, and the modeling and patient support of their parents. Educate parents about what good sleep hygiene looks like at each age. Discuss ways to support regular physical activity, especially as a family. Ask the parents about nutrition, including how they manage picky eating; how many family meals they enjoy together; and whether food is ever used to manage boredom or distress. Finally, talk with parents about a developmentally appropriate approach to rules and expectations around screen time and the importance of using family-based rules. Establishing expectations and routines during early childhood means children learn how good it feels to have restful sleep, regular exercise, and happy, healthy family meals. In adolescence, parents can then focus on helping their children to manage temptation, challenge, disappointment, and frustration more independently.
Infancy and up: Relational health
Children develop the skills needed for healthy relationships at home, and they are connected to all of the skills described above. Children need attuned, responsive, and reliable parenting to build a capacity for trust of others, to learn how to communicate honestly and effectively, to learn to expect and offer compassion and respect, and to learn how to handle disagreement and conflict. They learn these skills by watching their parents and by developing the emotional, cognitive, and behavioral healthy habits with their parents’ help. They need a consistently safe and responsive environment at home. They need parents who are attuned and flexible, while maintaining routines and high expectations. They need parents who make time for them when they are sad or struggling, and make time for joy, play, and mindless fun. While a detailed assessment of how the family is functioning may go beyond a check-up, you can ask about those routines that build healthy habits (family mealtime, sleep routines, screen time rules), communication style, and what the family enjoys doing together. Learning about how a family is building these healthy habits and how connected they are to one another can give you a clear snapshot of how well a child may be doing on their mental health growth curve, and what areas might benefit from more active guidance and support.
Dr. Swick is physician in chief at Ohana Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
May is Mental Health Awareness Month, providing us a chance to go beyond discussing the screening, diagnosis, and evidence-based treatments for the mental illnesses of youth. The World Health Organization defines good mental health as “a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her own community.” While the science of mental health promotion and disease prevention in childhood and adolescence is relatively young, there are several discrete domains in which you can follow and support your patient’s developing mental health. This begins with the well-being of new parents, and then moves into how parents are helping their children to develop skills to manage their basic daily needs and impulses, their thoughts and feelings, their stresses and their relationships. With a little support from you, parents can confidently help their children develop the foundations for good mental health.
First year of life: Parental mental health
Perhaps the strongest risk factor for serious mental illness in childhood and adulthood is parental neglect during the first year of life, and neglect in the first several months of life is the most commonly reported form of child abuse. Infant neglect is associated with parental depression (and other mental illnesses), parental substance use, and a parent’s own experience of childhood abuse or neglect. Neglect is more common with teenaged parents and parents living in poverty. Pediatricians are uniquely connected to families during the first year of a child’s life. The American Academy of Pediatrics recommends screening new mothers for depression at 1-, 2-, 4-, and 6-month infant check-ups with the Edinburgh Postnatal Depression Screen. Even without a positive screen, new parents may need the fortifications of extra community support to adapt to the changes parenthood brings.
At checkups, ask (both) parents how they are managing the stresses of a new baby. Are they getting restful sleep? Do they have social supports? Are they connected to a community (friends, extended family, faith) or isolated? Are they developing confidence as parents or feeling overwhelmed? Simple guidance, such as “sleep when the baby sleeps” and reassurance that taking good care of themselves is taking good care of the baby is always helpful. Sometimes you will need to refer for treatment or to community supports. Have your list of online and in-person resources at the ready to provide parents with these prescriptions. Supporting parental mental health and adjustment in the first year of life is possibly the most important building block for their child’s future mental health.
Toddlers and up: Emotional literacy
Emotional literacy (sometimes called “emotional intelligence”) is the capacity to recognize, identify, and manage feelings in oneself and in others. This skill begins to develop in infancy when parents respond to their baby’s cries with attunement, feeding or changing them if needed, and at other times simply reflecting their feelings and soothing them with movement, singing, or quiet talking. As children grow, so does their range of feelings, and their (cognitive) capacity to identify and manage them. Parents support this development by being available whenever their young children experience strong emotions, calmly listening, and acknowledging their discomfort. Parents can offer words for describing those feelings, and even be curious with their young children where in their bodies they are feeling them, how they can stay patient while the feeling passes or things they might be able to do to feel better. Parents may want to remove their child’s distress, but staying calm, curious, and present while helping their child to manage it will build their child’s emotional health. Parents can nurture this development in a less intense way by reading books about feelings together and noticing and identifying feelings in other children or in cartoon characters.
School-age children: Adding mindfulness
While a child’s cognitive development unfolds naturally, school-age children can cultivate awareness of their thoughts. This becomes possible after awareness of feelings and parents can help their older children consider whether something they are experiencing is a thought, a feeling, or a fact. They do so in the same way they helped their child develop emotional literacy: By responding with calm, curiosity, and confidence every time their child comes to them in distress (especially mild distress, like boredom!) or with a challenge or a question. With a difficult situation, parents start by helping their child to identify thoughts and feelings before impulsively acting on them. Parents can help children identify what’s in their control, try different approaches, and be flexible if their first efforts don’t work. Children need to learn that failing at things is how we learn and grow. Just like learning to ride a bike, it builds their frustration tolerance, their knowledge that they can do difficult things, and that distress subsides. These are critical building blocks for adolescence, when the challenges become greater and they manage them more independently.
Learning “mindfulness” (a practice that cultivates nonjudgmental awareness of one’s own thoughts, feelings, and sensations) can help children (and parents) to cultivate quiet self-awareness outside of moments of difficulty. “Stop, Breathe, and Think” and “Mindful gNATs” are two free apps that are recommended by the American Academy of Child and Adolescent Psychiatry for children (and their parents) to use to practice this awareness of thoughts and feelings.
Early and later adolescence: Stress management skills
Building on this awareness of thoughts and emotions, adolescents develop adaptive coping skills by facing challenges with the support of their parents nearby. Parents should still be ready to respond to charged emotional moments with calm and curiosity, validating their child’s distress while helping them to consider healthy responses. Helping their teenager to describe their experience, differentiating feelings from thoughts (and facts), and considering different choices within their control is foundational to resilience in adulthood. Parents also help their teenagers by reminding them of the need for good self-care (sleep, exercise, nutrition), nourishing social relationships, and protecting time for rest and recharging activities. Sometimes, parents will think with their teenager about why they are engaged in an activity that is stressful, whether it is authentically important to them, and why. Adolescents should be deepening their sense of identity, interests, talents, and even values, and stressful moments are rich opportunities to do so, with the support of caring adults. Without intentionally building these skills, adolescents will be more prone to managing stress with avoidance or unhealthy coping, such as excessive eating, video gaming, drugs, or alcohol.
Infancy and up: Behavioral healthy habits (sleep, physical activity, nutrition, and screen time)
Healthy habits sound simple, but establishing them is not always easy. The idea of a habit is that it makes managing something challenging or important more automatic, and thus easier and more reliable. Many of the same habits that promote physical health in adulthood also promote mental health: adequate, restful sleep; daily physical activity; a nutritious diet and a healthy relationship with food; and managing screen time in a developmentally appropriate way. Infants depend entirely on their parents for regulation of these behaviors. As their children grow, parents will adapt these routines so that their children are gradually regulating these needs and activities more independently. In each of these areas, children need clear expectations and routines, consistent consequences and positive feedback, and the modeling and patient support of their parents. Educate parents about what good sleep hygiene looks like at each age. Discuss ways to support regular physical activity, especially as a family. Ask the parents about nutrition, including how they manage picky eating; how many family meals they enjoy together; and whether food is ever used to manage boredom or distress. Finally, talk with parents about a developmentally appropriate approach to rules and expectations around screen time and the importance of using family-based rules. Establishing expectations and routines during early childhood means children learn how good it feels to have restful sleep, regular exercise, and happy, healthy family meals. In adolescence, parents can then focus on helping their children to manage temptation, challenge, disappointment, and frustration more independently.
Infancy and up: Relational health
Children develop the skills needed for healthy relationships at home, and they are connected to all of the skills described above. Children need attuned, responsive, and reliable parenting to build a capacity for trust of others, to learn how to communicate honestly and effectively, to learn to expect and offer compassion and respect, and to learn how to handle disagreement and conflict. They learn these skills by watching their parents and by developing the emotional, cognitive, and behavioral healthy habits with their parents’ help. They need a consistently safe and responsive environment at home. They need parents who are attuned and flexible, while maintaining routines and high expectations. They need parents who make time for them when they are sad or struggling, and make time for joy, play, and mindless fun. While a detailed assessment of how the family is functioning may go beyond a check-up, you can ask about those routines that build healthy habits (family mealtime, sleep routines, screen time rules), communication style, and what the family enjoys doing together. Learning about how a family is building these healthy habits and how connected they are to one another can give you a clear snapshot of how well a child may be doing on their mental health growth curve, and what areas might benefit from more active guidance and support.
Dr. Swick is physician in chief at Ohana Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
May is Mental Health Awareness Month, providing us a chance to go beyond discussing the screening, diagnosis, and evidence-based treatments for the mental illnesses of youth. The World Health Organization defines good mental health as “a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her own community.” While the science of mental health promotion and disease prevention in childhood and adolescence is relatively young, there are several discrete domains in which you can follow and support your patient’s developing mental health. This begins with the well-being of new parents, and then moves into how parents are helping their children to develop skills to manage their basic daily needs and impulses, their thoughts and feelings, their stresses and their relationships. With a little support from you, parents can confidently help their children develop the foundations for good mental health.
First year of life: Parental mental health
Perhaps the strongest risk factor for serious mental illness in childhood and adulthood is parental neglect during the first year of life, and neglect in the first several months of life is the most commonly reported form of child abuse. Infant neglect is associated with parental depression (and other mental illnesses), parental substance use, and a parent’s own experience of childhood abuse or neglect. Neglect is more common with teenaged parents and parents living in poverty. Pediatricians are uniquely connected to families during the first year of a child’s life. The American Academy of Pediatrics recommends screening new mothers for depression at 1-, 2-, 4-, and 6-month infant check-ups with the Edinburgh Postnatal Depression Screen. Even without a positive screen, new parents may need the fortifications of extra community support to adapt to the changes parenthood brings.
At checkups, ask (both) parents how they are managing the stresses of a new baby. Are they getting restful sleep? Do they have social supports? Are they connected to a community (friends, extended family, faith) or isolated? Are they developing confidence as parents or feeling overwhelmed? Simple guidance, such as “sleep when the baby sleeps” and reassurance that taking good care of themselves is taking good care of the baby is always helpful. Sometimes you will need to refer for treatment or to community supports. Have your list of online and in-person resources at the ready to provide parents with these prescriptions. Supporting parental mental health and adjustment in the first year of life is possibly the most important building block for their child’s future mental health.
Toddlers and up: Emotional literacy
Emotional literacy (sometimes called “emotional intelligence”) is the capacity to recognize, identify, and manage feelings in oneself and in others. This skill begins to develop in infancy when parents respond to their baby’s cries with attunement, feeding or changing them if needed, and at other times simply reflecting their feelings and soothing them with movement, singing, or quiet talking. As children grow, so does their range of feelings, and their (cognitive) capacity to identify and manage them. Parents support this development by being available whenever their young children experience strong emotions, calmly listening, and acknowledging their discomfort. Parents can offer words for describing those feelings, and even be curious with their young children where in their bodies they are feeling them, how they can stay patient while the feeling passes or things they might be able to do to feel better. Parents may want to remove their child’s distress, but staying calm, curious, and present while helping their child to manage it will build their child’s emotional health. Parents can nurture this development in a less intense way by reading books about feelings together and noticing and identifying feelings in other children or in cartoon characters.
School-age children: Adding mindfulness
While a child’s cognitive development unfolds naturally, school-age children can cultivate awareness of their thoughts. This becomes possible after awareness of feelings and parents can help their older children consider whether something they are experiencing is a thought, a feeling, or a fact. They do so in the same way they helped their child develop emotional literacy: By responding with calm, curiosity, and confidence every time their child comes to them in distress (especially mild distress, like boredom!) or with a challenge or a question. With a difficult situation, parents start by helping their child to identify thoughts and feelings before impulsively acting on them. Parents can help children identify what’s in their control, try different approaches, and be flexible if their first efforts don’t work. Children need to learn that failing at things is how we learn and grow. Just like learning to ride a bike, it builds their frustration tolerance, their knowledge that they can do difficult things, and that distress subsides. These are critical building blocks for adolescence, when the challenges become greater and they manage them more independently.
Learning “mindfulness” (a practice that cultivates nonjudgmental awareness of one’s own thoughts, feelings, and sensations) can help children (and parents) to cultivate quiet self-awareness outside of moments of difficulty. “Stop, Breathe, and Think” and “Mindful gNATs” are two free apps that are recommended by the American Academy of Child and Adolescent Psychiatry for children (and their parents) to use to practice this awareness of thoughts and feelings.
Early and later adolescence: Stress management skills
Building on this awareness of thoughts and emotions, adolescents develop adaptive coping skills by facing challenges with the support of their parents nearby. Parents should still be ready to respond to charged emotional moments with calm and curiosity, validating their child’s distress while helping them to consider healthy responses. Helping their teenager to describe their experience, differentiating feelings from thoughts (and facts), and considering different choices within their control is foundational to resilience in adulthood. Parents also help their teenagers by reminding them of the need for good self-care (sleep, exercise, nutrition), nourishing social relationships, and protecting time for rest and recharging activities. Sometimes, parents will think with their teenager about why they are engaged in an activity that is stressful, whether it is authentically important to them, and why. Adolescents should be deepening their sense of identity, interests, talents, and even values, and stressful moments are rich opportunities to do so, with the support of caring adults. Without intentionally building these skills, adolescents will be more prone to managing stress with avoidance or unhealthy coping, such as excessive eating, video gaming, drugs, or alcohol.
Infancy and up: Behavioral healthy habits (sleep, physical activity, nutrition, and screen time)
Healthy habits sound simple, but establishing them is not always easy. The idea of a habit is that it makes managing something challenging or important more automatic, and thus easier and more reliable. Many of the same habits that promote physical health in adulthood also promote mental health: adequate, restful sleep; daily physical activity; a nutritious diet and a healthy relationship with food; and managing screen time in a developmentally appropriate way. Infants depend entirely on their parents for regulation of these behaviors. As their children grow, parents will adapt these routines so that their children are gradually regulating these needs and activities more independently. In each of these areas, children need clear expectations and routines, consistent consequences and positive feedback, and the modeling and patient support of their parents. Educate parents about what good sleep hygiene looks like at each age. Discuss ways to support regular physical activity, especially as a family. Ask the parents about nutrition, including how they manage picky eating; how many family meals they enjoy together; and whether food is ever used to manage boredom or distress. Finally, talk with parents about a developmentally appropriate approach to rules and expectations around screen time and the importance of using family-based rules. Establishing expectations and routines during early childhood means children learn how good it feels to have restful sleep, regular exercise, and happy, healthy family meals. In adolescence, parents can then focus on helping their children to manage temptation, challenge, disappointment, and frustration more independently.
Infancy and up: Relational health
Children develop the skills needed for healthy relationships at home, and they are connected to all of the skills described above. Children need attuned, responsive, and reliable parenting to build a capacity for trust of others, to learn how to communicate honestly and effectively, to learn to expect and offer compassion and respect, and to learn how to handle disagreement and conflict. They learn these skills by watching their parents and by developing the emotional, cognitive, and behavioral healthy habits with their parents’ help. They need a consistently safe and responsive environment at home. They need parents who are attuned and flexible, while maintaining routines and high expectations. They need parents who make time for them when they are sad or struggling, and make time for joy, play, and mindless fun. While a detailed assessment of how the family is functioning may go beyond a check-up, you can ask about those routines that build healthy habits (family mealtime, sleep routines, screen time rules), communication style, and what the family enjoys doing together. Learning about how a family is building these healthy habits and how connected they are to one another can give you a clear snapshot of how well a child may be doing on their mental health growth curve, and what areas might benefit from more active guidance and support.
Dr. Swick is physician in chief at Ohana Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
New protocol could cut fasting period to detect insulinomas
SEATTLE – , therefore yielding significant hospital cost savings, new data suggest.
Insulinomas are small, rare types of pancreatic tumors that are benign but secrete excess insulin, leading to hypoglycemia. More than 99% of people with insulinomas develop hypoglycemia within 72 hours, hence, the use of a 72-hour fast to detect these tumors.
But most people who are evaluated for hypoglycemia do not have an insulinoma and fasting in hospital for 3 days is burdensome and costly.
As part of a quality improvement project, Cleveland Clinic endocrinology fellow Michelle D. Lundholm, MD, and colleagues modified their hospital’s protocol to include measurement of beta-hydroxybutyrate (BHB), a marker of insulin suppression, every 12 hours with a cutoff of ≥ 2.7mmol/L for stopping the fast if hypoglycemia (venous glucose ≤ 45mg/dL) hasn’t occurred. This intervention cut in half the number of patients who needed to fast for the full 72 hours, without missing any insulinomas.
“We are excited to share how a relatively simple adjustment to our protocol allowed us to successfully reduce the burden of fasting on patients and more effectively utilize hospital resources. We hope that this encourages other centers to consider doing the same,” Dr. Lundholm said in an interview.
“These data support a 48-hour fast. The literature supports that’s sufficient to detect 95% of insulinomas. ... But, given our small insulinoma cohort, we are looking forward to learning from other studies,” she added.
Dr. Lundholm presented the late-breaking oral abstract at the annual scientific & clinical congress of the American Association of Clinical Endocrinology.
Asked to comment, session moderator Jenna Sarvaideo, MD, said: “We’re often steeped in tradition. That’s why this abstract and this quality improvement project is so exciting to me because it challenges the history. … and I think it’s ultimately helping patients.”
Dr. Sarvaideo, of Clement J. Zablocki VA Medical Center, Milwaukee, noted that, typically, although the fast will be stopped before 72 hours if the patient develops hypoglycemia, “often they don’t, so we keep going on and on. If we just paid more attention to the beta-hydroxybutyrate, I think that would be practice changing.”
She added that more data would be optimal, given that there were under 100 patients in the study, “but I do think that devising protocols is … very much still at the hands of the endocrinologists. I think that this work could make groups reevaluate their protocol and change it, maybe even with a small dataset and then move on from there and see what they see.”
Indeed, Dr. Lundholm pointed out that some institutions, such as the Mayo Clinic, already include 6-hour BHB measurements (along with glucose and insulin) in their protocols.
“For any institution that already draws regular BHB levels like this, it would be very easy to implement a new stopping criterion without adding any additional costs,” she said in an interview.
All insulinomas became apparent in less than 48 hours
The first report to look at the value of testing BHB at regular intervals was published by the Mayo Clinic in 2005 after they noticed patients without insulinoma were complaining of ketosis symptoms such as foul breath and digestive problems toward the end of the fast.
However, although BHB testing is used today as part of the evaluation, it’s typically only drawn at the start of the protocol and again at the time of hypoglycemia or at the end of 72 hours because more frequent values hadn’t been thought to be useful for guiding clinical management, Dr. Lundholm explained.
Between January 2018 and June 2020, Dr. Lundholm and colleagues followed 34 Cleveland Clinic patients who completed the usual 72-hour fast protocol. Overall, 71% were female, and 26% had undergone prior bariatric surgery procedures. Eleven (32%) developed hypoglycemia and stopped fasting. The other 23 (68%) fasted for the full 72 hours.
Dr. Lundholm and colleagues determined that the fast could have ended earlier in 35% of patients based on an elevated BHB without missing any insulinomas.
And so, in June 2020 the group revised their protocol to include the BHB ≥ 2.7mmol/L stopping criterion. Of the 30 patients evaluated from June 2020 to January 2023, 87% were female and 17% had undergone a bariatric procedure.
Here, 15 (50%) reached a BHB ≥ 2.7mmol/L and ended their fast at an average of 43.8 hours. Another seven (23%) ended the fast after developing hypoglycemia. Just eight patients (27%) fasted for the full 72 hours.
Overall, this resulted in approximately 376 fewer cumulative hours of inpatient admission than if patients had fasted for the full time.
Of the 64 patients who have completed the fasting protocol since 2018, seven (11%) who did have an insulinoma developed hypoglycemia within 48 hours and with a BHB < 2.7 mmol/L (median, 0.15).
Advantages: cost, adherence
A day in a general medicine bed at Cleveland Clinic was quoted as costing $2,420, based on publicly available information as of Jan. 1, 2023. “If half of patients leave 1 day earlier, this equates to about $1,210 per patient in savings from bed costs alone,” Dr. Lundholm told this news organization.
The revised protocol required an additional two to four blood draws, depending on the length of the fast. “The cost of these extra blood tests varies by lab and by count, but even at its highest does not exceed the amount of savings from bed costs,” she noted.
Patient adherence is another potential benefit of the revised protocol.
“Any study that requires 72 hours of patient cooperation is a challenge, particularly in an uncomfortable position like fasting. When we looked at these adherence numbers, we found that the percentage of patients who prematurely ended their fast decreased from 35% to 17% with the updated protocol,” Dr. Lundholm continued.
“This translates to fewer inconclusive results and fewer readmissions for repeat 72-hour fasting. While this was not our primary outcome, it was another noted benefit of our change,” she said.
Dr. Lundholm and Dr. Sarvaideo have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
SEATTLE – , therefore yielding significant hospital cost savings, new data suggest.
Insulinomas are small, rare types of pancreatic tumors that are benign but secrete excess insulin, leading to hypoglycemia. More than 99% of people with insulinomas develop hypoglycemia within 72 hours, hence, the use of a 72-hour fast to detect these tumors.
But most people who are evaluated for hypoglycemia do not have an insulinoma and fasting in hospital for 3 days is burdensome and costly.
As part of a quality improvement project, Cleveland Clinic endocrinology fellow Michelle D. Lundholm, MD, and colleagues modified their hospital’s protocol to include measurement of beta-hydroxybutyrate (BHB), a marker of insulin suppression, every 12 hours with a cutoff of ≥ 2.7mmol/L for stopping the fast if hypoglycemia (venous glucose ≤ 45mg/dL) hasn’t occurred. This intervention cut in half the number of patients who needed to fast for the full 72 hours, without missing any insulinomas.
“We are excited to share how a relatively simple adjustment to our protocol allowed us to successfully reduce the burden of fasting on patients and more effectively utilize hospital resources. We hope that this encourages other centers to consider doing the same,” Dr. Lundholm said in an interview.
“These data support a 48-hour fast. The literature supports that’s sufficient to detect 95% of insulinomas. ... But, given our small insulinoma cohort, we are looking forward to learning from other studies,” she added.
Dr. Lundholm presented the late-breaking oral abstract at the annual scientific & clinical congress of the American Association of Clinical Endocrinology.
Asked to comment, session moderator Jenna Sarvaideo, MD, said: “We’re often steeped in tradition. That’s why this abstract and this quality improvement project is so exciting to me because it challenges the history. … and I think it’s ultimately helping patients.”
Dr. Sarvaideo, of Clement J. Zablocki VA Medical Center, Milwaukee, noted that, typically, although the fast will be stopped before 72 hours if the patient develops hypoglycemia, “often they don’t, so we keep going on and on. If we just paid more attention to the beta-hydroxybutyrate, I think that would be practice changing.”
She added that more data would be optimal, given that there were under 100 patients in the study, “but I do think that devising protocols is … very much still at the hands of the endocrinologists. I think that this work could make groups reevaluate their protocol and change it, maybe even with a small dataset and then move on from there and see what they see.”
Indeed, Dr. Lundholm pointed out that some institutions, such as the Mayo Clinic, already include 6-hour BHB measurements (along with glucose and insulin) in their protocols.
“For any institution that already draws regular BHB levels like this, it would be very easy to implement a new stopping criterion without adding any additional costs,” she said in an interview.
All insulinomas became apparent in less than 48 hours
The first report to look at the value of testing BHB at regular intervals was published by the Mayo Clinic in 2005 after they noticed patients without insulinoma were complaining of ketosis symptoms such as foul breath and digestive problems toward the end of the fast.
However, although BHB testing is used today as part of the evaluation, it’s typically only drawn at the start of the protocol and again at the time of hypoglycemia or at the end of 72 hours because more frequent values hadn’t been thought to be useful for guiding clinical management, Dr. Lundholm explained.
Between January 2018 and June 2020, Dr. Lundholm and colleagues followed 34 Cleveland Clinic patients who completed the usual 72-hour fast protocol. Overall, 71% were female, and 26% had undergone prior bariatric surgery procedures. Eleven (32%) developed hypoglycemia and stopped fasting. The other 23 (68%) fasted for the full 72 hours.
Dr. Lundholm and colleagues determined that the fast could have ended earlier in 35% of patients based on an elevated BHB without missing any insulinomas.
And so, in June 2020 the group revised their protocol to include the BHB ≥ 2.7mmol/L stopping criterion. Of the 30 patients evaluated from June 2020 to January 2023, 87% were female and 17% had undergone a bariatric procedure.
Here, 15 (50%) reached a BHB ≥ 2.7mmol/L and ended their fast at an average of 43.8 hours. Another seven (23%) ended the fast after developing hypoglycemia. Just eight patients (27%) fasted for the full 72 hours.
Overall, this resulted in approximately 376 fewer cumulative hours of inpatient admission than if patients had fasted for the full time.
Of the 64 patients who have completed the fasting protocol since 2018, seven (11%) who did have an insulinoma developed hypoglycemia within 48 hours and with a BHB < 2.7 mmol/L (median, 0.15).
Advantages: cost, adherence
A day in a general medicine bed at Cleveland Clinic was quoted as costing $2,420, based on publicly available information as of Jan. 1, 2023. “If half of patients leave 1 day earlier, this equates to about $1,210 per patient in savings from bed costs alone,” Dr. Lundholm told this news organization.
The revised protocol required an additional two to four blood draws, depending on the length of the fast. “The cost of these extra blood tests varies by lab and by count, but even at its highest does not exceed the amount of savings from bed costs,” she noted.
Patient adherence is another potential benefit of the revised protocol.
“Any study that requires 72 hours of patient cooperation is a challenge, particularly in an uncomfortable position like fasting. When we looked at these adherence numbers, we found that the percentage of patients who prematurely ended their fast decreased from 35% to 17% with the updated protocol,” Dr. Lundholm continued.
“This translates to fewer inconclusive results and fewer readmissions for repeat 72-hour fasting. While this was not our primary outcome, it was another noted benefit of our change,” she said.
Dr. Lundholm and Dr. Sarvaideo have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
SEATTLE – , therefore yielding significant hospital cost savings, new data suggest.
Insulinomas are small, rare types of pancreatic tumors that are benign but secrete excess insulin, leading to hypoglycemia. More than 99% of people with insulinomas develop hypoglycemia within 72 hours, hence, the use of a 72-hour fast to detect these tumors.
But most people who are evaluated for hypoglycemia do not have an insulinoma and fasting in hospital for 3 days is burdensome and costly.
As part of a quality improvement project, Cleveland Clinic endocrinology fellow Michelle D. Lundholm, MD, and colleagues modified their hospital’s protocol to include measurement of beta-hydroxybutyrate (BHB), a marker of insulin suppression, every 12 hours with a cutoff of ≥ 2.7mmol/L for stopping the fast if hypoglycemia (venous glucose ≤ 45mg/dL) hasn’t occurred. This intervention cut in half the number of patients who needed to fast for the full 72 hours, without missing any insulinomas.
“We are excited to share how a relatively simple adjustment to our protocol allowed us to successfully reduce the burden of fasting on patients and more effectively utilize hospital resources. We hope that this encourages other centers to consider doing the same,” Dr. Lundholm said in an interview.
“These data support a 48-hour fast. The literature supports that’s sufficient to detect 95% of insulinomas. ... But, given our small insulinoma cohort, we are looking forward to learning from other studies,” she added.
Dr. Lundholm presented the late-breaking oral abstract at the annual scientific & clinical congress of the American Association of Clinical Endocrinology.
Asked to comment, session moderator Jenna Sarvaideo, MD, said: “We’re often steeped in tradition. That’s why this abstract and this quality improvement project is so exciting to me because it challenges the history. … and I think it’s ultimately helping patients.”
Dr. Sarvaideo, of Clement J. Zablocki VA Medical Center, Milwaukee, noted that, typically, although the fast will be stopped before 72 hours if the patient develops hypoglycemia, “often they don’t, so we keep going on and on. If we just paid more attention to the beta-hydroxybutyrate, I think that would be practice changing.”
She added that more data would be optimal, given that there were under 100 patients in the study, “but I do think that devising protocols is … very much still at the hands of the endocrinologists. I think that this work could make groups reevaluate their protocol and change it, maybe even with a small dataset and then move on from there and see what they see.”
Indeed, Dr. Lundholm pointed out that some institutions, such as the Mayo Clinic, already include 6-hour BHB measurements (along with glucose and insulin) in their protocols.
“For any institution that already draws regular BHB levels like this, it would be very easy to implement a new stopping criterion without adding any additional costs,” she said in an interview.
All insulinomas became apparent in less than 48 hours
The first report to look at the value of testing BHB at regular intervals was published by the Mayo Clinic in 2005 after they noticed patients without insulinoma were complaining of ketosis symptoms such as foul breath and digestive problems toward the end of the fast.
However, although BHB testing is used today as part of the evaluation, it’s typically only drawn at the start of the protocol and again at the time of hypoglycemia or at the end of 72 hours because more frequent values hadn’t been thought to be useful for guiding clinical management, Dr. Lundholm explained.
Between January 2018 and June 2020, Dr. Lundholm and colleagues followed 34 Cleveland Clinic patients who completed the usual 72-hour fast protocol. Overall, 71% were female, and 26% had undergone prior bariatric surgery procedures. Eleven (32%) developed hypoglycemia and stopped fasting. The other 23 (68%) fasted for the full 72 hours.
Dr. Lundholm and colleagues determined that the fast could have ended earlier in 35% of patients based on an elevated BHB without missing any insulinomas.
And so, in June 2020 the group revised their protocol to include the BHB ≥ 2.7mmol/L stopping criterion. Of the 30 patients evaluated from June 2020 to January 2023, 87% were female and 17% had undergone a bariatric procedure.
Here, 15 (50%) reached a BHB ≥ 2.7mmol/L and ended their fast at an average of 43.8 hours. Another seven (23%) ended the fast after developing hypoglycemia. Just eight patients (27%) fasted for the full 72 hours.
Overall, this resulted in approximately 376 fewer cumulative hours of inpatient admission than if patients had fasted for the full time.
Of the 64 patients who have completed the fasting protocol since 2018, seven (11%) who did have an insulinoma developed hypoglycemia within 48 hours and with a BHB < 2.7 mmol/L (median, 0.15).
Advantages: cost, adherence
A day in a general medicine bed at Cleveland Clinic was quoted as costing $2,420, based on publicly available information as of Jan. 1, 2023. “If half of patients leave 1 day earlier, this equates to about $1,210 per patient in savings from bed costs alone,” Dr. Lundholm told this news organization.
The revised protocol required an additional two to four blood draws, depending on the length of the fast. “The cost of these extra blood tests varies by lab and by count, but even at its highest does not exceed the amount of savings from bed costs,” she noted.
Patient adherence is another potential benefit of the revised protocol.
“Any study that requires 72 hours of patient cooperation is a challenge, particularly in an uncomfortable position like fasting. When we looked at these adherence numbers, we found that the percentage of patients who prematurely ended their fast decreased from 35% to 17% with the updated protocol,” Dr. Lundholm continued.
“This translates to fewer inconclusive results and fewer readmissions for repeat 72-hour fasting. While this was not our primary outcome, it was another noted benefit of our change,” she said.
Dr. Lundholm and Dr. Sarvaideo have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
AT AACE 2023
Low disease state for childhood lupus approaches validation
MANCHESTER, ENGLAND – An age-appropriate version of the Lupus Low Disease Activity State (LLDAS) has been developed by an international task force that will hopefully enable childhood-onset systemic lupus erythematosus (cSLE) to be treated to target in the near future.
The new childhood LLDAS (cLLDAS) has been purposefully developed to align with that already used for adults, Eve Smith, MBChB, PhD, explained at the annual meeting of the British Society for Rheumatology.
“There’s a lot of compelling data that’s accumulating from adult lupus and increasingly from childhood lupus that [treat to target] might be a good idea,” said Dr. Smith, who is a senior clinical fellow and honorary consultant at the University of Liverpool (England) and Alder Hey Children’s NHS Foundation Trust Hospital, also in Liverpool.
Urgent need to improve childhood lupus outcomes
“We urgently need to do something to try and improve outcomes for children,” Dr. Smith said.
“We know that childhood lupus patients have got higher disease activity as compared to adults; they have a greater medication burden, particularly steroids; and they tend to have more severe organ manifestations,” she added.
Moreover, data show that one-fifth of pediatric patients with lupus have already accrued early damage, and there is much higher mortality associated with childhood lupus than there is with adult lupus.
“So, really we want to use treat to target as a way to try and improve on these aspects,” Dr. Smith said.
The treat-to-target (T2T) approach is not a new idea in lupus, with a lot of work already done in adult patients. One large study of more than 3,300 patients conducted in 13 countries has shown that patients who never achieve LLDAS are more likely to have high levels of damage, greater glucocorticoid use, worse quality of life, and higher mortality than are those who do.
Conversely, data have also shown that achieving a LLDAS is associated with a reduction in the risk for new damage, flares, and hospitalization, as well as reducing health care costs and improving patients’ overall health-related quality of life.
T2T is a recognized approach in European adult SLE guidelines, Dr. Smith said, although the approach has not really been fully realized as of yet, even in adult practice.
The cSLE T2T international task force and cLLDAS definition
With evidence accumulating on the benefits of getting children with SLE to a low disease activity state, Dr. Smith and colleague Michael Beresford, MBChB, PhD, Brough Chair, Professor of Child Health at the University of Liverpool, put out a call to develop a task force to look into the feasibility of a T2T approach.
“We had a really enthusiastic response internationally, which we were really encouraged by,” Dr. Smith said, “and we now lead a task force of 20 experts from across all five continents, and we have really strong patient involvement.”
Through a consensus process, an international cSLE T2T Task Force agreed on overarching principles and points to consider that will “lay the foundation for future T2T approaches in cSLE,” according to the recommendations statement, which was endorsed by the Paediatric Rheumatology European Society.
Next, they looked to develop an age-appropriate definition for low disease activity.
“We’re deliberately wanting to maintain sufficient unity with the adult definition, so that we could facilitate life-course studies,” said Dr. Smith, who presented the results of a literature review and series of Delphi surveys at the meeting.
The conceptual definition of cLLDAS is similar to adults in describing it as a sustained state that is associated with a low likelihood of adverse outcome, Dr. Smith said, but with the added wording of “considering disease activity, damage, and medication toxicity.”
The definition is achieved when the SLE Disease Activity Index-2K is ≤ 4 and there is no activity in major organ systems; there are no new features of lupus disease activity since the last assessment; there is a score of ≤ 1 on Physician Global Assessment; steroid doses are ≤ 0.15 mg/kg/day or a maximum of 7.5 mg/day (whichever is lower); and immunosuppressive treatment is stable, with any changes to medication only because of side effects, adherence, changes in weight, or when in the process of reaching a target dose.
“It’s all very well having a definition, but you need to think about how that will work in practice,” Dr. Smith said. This is something that the task force is thinking about very carefully.
The task force next aims to validate the cLLDAS definition, form an extensive research agenda to inform the T2T methods, and develop innovative methods to apply the approach in practice.
The work is supported by the Wellcome Trust, National Institutes for Health Research, Versus Arthritis, and the University of Liverpool, Alder Hey Children’s NHS Foundation Trust and the Alder Hey Charity. Dr. Smith reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MANCHESTER, ENGLAND – An age-appropriate version of the Lupus Low Disease Activity State (LLDAS) has been developed by an international task force that will hopefully enable childhood-onset systemic lupus erythematosus (cSLE) to be treated to target in the near future.
The new childhood LLDAS (cLLDAS) has been purposefully developed to align with that already used for adults, Eve Smith, MBChB, PhD, explained at the annual meeting of the British Society for Rheumatology.
“There’s a lot of compelling data that’s accumulating from adult lupus and increasingly from childhood lupus that [treat to target] might be a good idea,” said Dr. Smith, who is a senior clinical fellow and honorary consultant at the University of Liverpool (England) and Alder Hey Children’s NHS Foundation Trust Hospital, also in Liverpool.
Urgent need to improve childhood lupus outcomes
“We urgently need to do something to try and improve outcomes for children,” Dr. Smith said.
“We know that childhood lupus patients have got higher disease activity as compared to adults; they have a greater medication burden, particularly steroids; and they tend to have more severe organ manifestations,” she added.
Moreover, data show that one-fifth of pediatric patients with lupus have already accrued early damage, and there is much higher mortality associated with childhood lupus than there is with adult lupus.
“So, really we want to use treat to target as a way to try and improve on these aspects,” Dr. Smith said.
The treat-to-target (T2T) approach is not a new idea in lupus, with a lot of work already done in adult patients. One large study of more than 3,300 patients conducted in 13 countries has shown that patients who never achieve LLDAS are more likely to have high levels of damage, greater glucocorticoid use, worse quality of life, and higher mortality than are those who do.
Conversely, data have also shown that achieving a LLDAS is associated with a reduction in the risk for new damage, flares, and hospitalization, as well as reducing health care costs and improving patients’ overall health-related quality of life.
T2T is a recognized approach in European adult SLE guidelines, Dr. Smith said, although the approach has not really been fully realized as of yet, even in adult practice.
The cSLE T2T international task force and cLLDAS definition
With evidence accumulating on the benefits of getting children with SLE to a low disease activity state, Dr. Smith and colleague Michael Beresford, MBChB, PhD, Brough Chair, Professor of Child Health at the University of Liverpool, put out a call to develop a task force to look into the feasibility of a T2T approach.
“We had a really enthusiastic response internationally, which we were really encouraged by,” Dr. Smith said, “and we now lead a task force of 20 experts from across all five continents, and we have really strong patient involvement.”
Through a consensus process, an international cSLE T2T Task Force agreed on overarching principles and points to consider that will “lay the foundation for future T2T approaches in cSLE,” according to the recommendations statement, which was endorsed by the Paediatric Rheumatology European Society.
Next, they looked to develop an age-appropriate definition for low disease activity.
“We’re deliberately wanting to maintain sufficient unity with the adult definition, so that we could facilitate life-course studies,” said Dr. Smith, who presented the results of a literature review and series of Delphi surveys at the meeting.
The conceptual definition of cLLDAS is similar to adults in describing it as a sustained state that is associated with a low likelihood of adverse outcome, Dr. Smith said, but with the added wording of “considering disease activity, damage, and medication toxicity.”
The definition is achieved when the SLE Disease Activity Index-2K is ≤ 4 and there is no activity in major organ systems; there are no new features of lupus disease activity since the last assessment; there is a score of ≤ 1 on Physician Global Assessment; steroid doses are ≤ 0.15 mg/kg/day or a maximum of 7.5 mg/day (whichever is lower); and immunosuppressive treatment is stable, with any changes to medication only because of side effects, adherence, changes in weight, or when in the process of reaching a target dose.
“It’s all very well having a definition, but you need to think about how that will work in practice,” Dr. Smith said. This is something that the task force is thinking about very carefully.
The task force next aims to validate the cLLDAS definition, form an extensive research agenda to inform the T2T methods, and develop innovative methods to apply the approach in practice.
The work is supported by the Wellcome Trust, National Institutes for Health Research, Versus Arthritis, and the University of Liverpool, Alder Hey Children’s NHS Foundation Trust and the Alder Hey Charity. Dr. Smith reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MANCHESTER, ENGLAND – An age-appropriate version of the Lupus Low Disease Activity State (LLDAS) has been developed by an international task force that will hopefully enable childhood-onset systemic lupus erythematosus (cSLE) to be treated to target in the near future.
The new childhood LLDAS (cLLDAS) has been purposefully developed to align with that already used for adults, Eve Smith, MBChB, PhD, explained at the annual meeting of the British Society for Rheumatology.
“There’s a lot of compelling data that’s accumulating from adult lupus and increasingly from childhood lupus that [treat to target] might be a good idea,” said Dr. Smith, who is a senior clinical fellow and honorary consultant at the University of Liverpool (England) and Alder Hey Children’s NHS Foundation Trust Hospital, also in Liverpool.
Urgent need to improve childhood lupus outcomes
“We urgently need to do something to try and improve outcomes for children,” Dr. Smith said.
“We know that childhood lupus patients have got higher disease activity as compared to adults; they have a greater medication burden, particularly steroids; and they tend to have more severe organ manifestations,” she added.
Moreover, data show that one-fifth of pediatric patients with lupus have already accrued early damage, and there is much higher mortality associated with childhood lupus than there is with adult lupus.
“So, really we want to use treat to target as a way to try and improve on these aspects,” Dr. Smith said.
The treat-to-target (T2T) approach is not a new idea in lupus, with a lot of work already done in adult patients. One large study of more than 3,300 patients conducted in 13 countries has shown that patients who never achieve LLDAS are more likely to have high levels of damage, greater glucocorticoid use, worse quality of life, and higher mortality than are those who do.
Conversely, data have also shown that achieving a LLDAS is associated with a reduction in the risk for new damage, flares, and hospitalization, as well as reducing health care costs and improving patients’ overall health-related quality of life.
T2T is a recognized approach in European adult SLE guidelines, Dr. Smith said, although the approach has not really been fully realized as of yet, even in adult practice.
The cSLE T2T international task force and cLLDAS definition
With evidence accumulating on the benefits of getting children with SLE to a low disease activity state, Dr. Smith and colleague Michael Beresford, MBChB, PhD, Brough Chair, Professor of Child Health at the University of Liverpool, put out a call to develop a task force to look into the feasibility of a T2T approach.
“We had a really enthusiastic response internationally, which we were really encouraged by,” Dr. Smith said, “and we now lead a task force of 20 experts from across all five continents, and we have really strong patient involvement.”
Through a consensus process, an international cSLE T2T Task Force agreed on overarching principles and points to consider that will “lay the foundation for future T2T approaches in cSLE,” according to the recommendations statement, which was endorsed by the Paediatric Rheumatology European Society.
Next, they looked to develop an age-appropriate definition for low disease activity.
“We’re deliberately wanting to maintain sufficient unity with the adult definition, so that we could facilitate life-course studies,” said Dr. Smith, who presented the results of a literature review and series of Delphi surveys at the meeting.
The conceptual definition of cLLDAS is similar to adults in describing it as a sustained state that is associated with a low likelihood of adverse outcome, Dr. Smith said, but with the added wording of “considering disease activity, damage, and medication toxicity.”
The definition is achieved when the SLE Disease Activity Index-2K is ≤ 4 and there is no activity in major organ systems; there are no new features of lupus disease activity since the last assessment; there is a score of ≤ 1 on Physician Global Assessment; steroid doses are ≤ 0.15 mg/kg/day or a maximum of 7.5 mg/day (whichever is lower); and immunosuppressive treatment is stable, with any changes to medication only because of side effects, adherence, changes in weight, or when in the process of reaching a target dose.
“It’s all very well having a definition, but you need to think about how that will work in practice,” Dr. Smith said. This is something that the task force is thinking about very carefully.
The task force next aims to validate the cLLDAS definition, form an extensive research agenda to inform the T2T methods, and develop innovative methods to apply the approach in practice.
The work is supported by the Wellcome Trust, National Institutes for Health Research, Versus Arthritis, and the University of Liverpool, Alder Hey Children’s NHS Foundation Trust and the Alder Hey Charity. Dr. Smith reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT BSR 2023