User login
US Preventive Services Task Force lowers diabetes screening age for overweight
The United States Preventive Services Task Force has updated its recommendation on the age of screening for prediabetes and type 2 diabetes in the primary care setting – lowering the age from 40 to 35 years for asymptomatic patients who are overweight or obese and encouraging greater interventions when patients do show a risk.
“The USPSTF concludes with moderate certainty that screening for prediabetes and type 2 diabetes and offering or referring patients with prediabetes to effective preventive interventions has a moderate net benefit,” the task force concludes in its recommendation, published Aug. 24 in JAMA.
“Clinicians should offer or refer patients with prediabetes to effective preventive interventions,” they write.
Experts commenting on the issue strongly emphasize that it’s not just the screening, but the subsequent intervention that is needed to make a difference.
“If young adults newly identified with abnormal glucose metabolism do not receive the needed intensive behavioral change support, screening may provide no benefit,” write Richard W. Grant, MD, MPH, and colleagues in an editorial published with the recommendation.
“Given the role of our obesogenic and physically inactive society in the shift toward earlier onset of diabetes, efforts to increase screening and recognition of abnormal glucose metabolism must be coupled with robust public health measures to address the underlying contributors.”
BMI cutoff lower for at-risk ethnic populations
The recommendation, which updates the task force’s 2015 guideline, carries a “B” classification, meaning the USPSTF has high certainty that the net benefit is moderate. It now specifies screening from age 35to 70 for persons classified as overweight (body mass index at least 25) or obese (BMI at least 30) and recommends referral to preventive interventions when patients are found to have prediabetes.
In addition to recommendations of lifestyle changes, such as diet and physical activity, the task force also endorses the diabetes drug metformin as a beneficial intervention in the prevention or delay of diabetes, while noting fewer overall health benefits from metformin than from the lifestyle changes.
A lower BMI cutoff of at least 23 is recommended for diabetes screening of Asian Americans, and, importantly, screening for prediabetes and diabetes should be considered at an even earlier age if the patient is from a population with a disproportionately high prevalence of diabetes, including American Indian/Alaska Native, Black, Hawaiian/Pacific Islander, Hispanic/Latino, the task force recommends.
Screening tests should include fasting plasma glucose, hemoglobin A1c, or an oral glucose tolerance test. Although screening every 3 years “may be a reasonable approach for adults with normal blood glucose levels,” the task force adds that “the optimal screening interval for adults with an initial normal glucose test result is uncertain.”
Data review: Few with prediabetes know they have it
The need for the update was prompted by troubling data showing increasing diabetes rates despite early signs that can and should be identified and acted upon in the primary care setting to prevent disease progression.
Data from the Centers for Disease Control and Prevention, for instance, show that while 13% of all U.S. adults 18 years or older have diabetes and 35% meet criteria for prediabetes, as many as 21% of those with diabetes were not aware of or did not report having the disease. Furthermore, only a small fraction – 15% of those with prediabetes – said they had been told by a health professional that they had this condition, the task force notes.
The task force’s final recommendation was based on a systematic review of evidence regarding the screening of asymptomatic, nonpregnant adults and the harms and benefits of interventions, such as physical activity, behavioral counseling, or pharmacotherapy.
Among key evidence supporting the lower age was a 2014 study showing that the number of people necessary to obtain one positive test for diabetes with screening sharply drops from 80 among those aged 30-34 years to just 31 among those aged 36-39.
Opportunistic universal screening of eligible people aged 35 and older would yield a ratio of 1 out of just 15 to spot a positive test, the authors of that study reported.
In addition, a large cohort study in more than 77,000 people with prediabetes strongly links the risk of developing diabetes with increases in A1c level and with increasing BMI.
ADA recommendations differ
The new recommendations differ from American Diabetes Association guidelines, which call for diabetes screening at all ages for people who are overweight or obese and who have one or more risk factors, such as physical inactivity or a first-degree relative with diabetes. If results are normal, repeat screening at least every 3 years is recommended.
The ADA further recommends universal screening for all adults 45 years and older, regardless of their risk factors.
For the screening of adults over 45, the ADA recommends using a fasting plasma glucose level, 2-hour plasma glucose level during a 75-g oral glucose tolerance test, or A1c level, regardless of risk factors.
The American Association of Clinical Endocrinology also recommends universal screening for prediabetes and diabetes for all adults 45 years or older, regardless of risk factors, and also advises screening those who have risk factors for diabetes regardless of age.
Screening of little benefit without behavior change support
In an interview, Dr. Grant added that broad efforts are essential as those at the practice level have clearly not succeeded.
“The medical model of individual counseling and referral has not really been effective, and so we really need to think in terms of large-scale public health action,” said Dr. Grant, of the division of research, Kaiser Permanente Northern California, Oakland.
His editorial details the sweeping, multifactorial efforts that are needed.
“To turn this recommendation into action – that is, to translate screening activities into improved clinical outcomes – change is needed at the patient-clinician level (recognizing and encouraging eligible individuals to be screened), health care system level (reducing screening barriers and ensuring access to robust lifestyle programs), and societal level (applying effective public health interventions to reduce obesity and increase exercise),” they write.
A top priority has to be a focus on individuals of diverse backgrounds and issues such as access to healthy programs in minority communities, Dr. Grant noted.
“Newly diagnosed adults are more likely to be African-American and Latinx,” he said.
“We really need to invest in healthier communities for low-income, non-White communities to reverse the persistent health care disparities in these communities.”
While the challenges may appear daunting, history shows they are not necessarily insurmountable – as evidenced in the campaign to discourage tobacco smoking.
“National smoking cessation efforts are one example of a mostly successful public health campaign that has made a difference in health behaviors,” Grant noted.
The recommendation is also posted on the USPSTF web site .
Dr. Grant reports receiving grants from the National Institutes of Health and the Patient-Centered Outcomes Research Institute.
The United States Preventive Services Task Force has updated its recommendation on the age of screening for prediabetes and type 2 diabetes in the primary care setting – lowering the age from 40 to 35 years for asymptomatic patients who are overweight or obese and encouraging greater interventions when patients do show a risk.
“The USPSTF concludes with moderate certainty that screening for prediabetes and type 2 diabetes and offering or referring patients with prediabetes to effective preventive interventions has a moderate net benefit,” the task force concludes in its recommendation, published Aug. 24 in JAMA.
“Clinicians should offer or refer patients with prediabetes to effective preventive interventions,” they write.
Experts commenting on the issue strongly emphasize that it’s not just the screening, but the subsequent intervention that is needed to make a difference.
“If young adults newly identified with abnormal glucose metabolism do not receive the needed intensive behavioral change support, screening may provide no benefit,” write Richard W. Grant, MD, MPH, and colleagues in an editorial published with the recommendation.
“Given the role of our obesogenic and physically inactive society in the shift toward earlier onset of diabetes, efforts to increase screening and recognition of abnormal glucose metabolism must be coupled with robust public health measures to address the underlying contributors.”
BMI cutoff lower for at-risk ethnic populations
The recommendation, which updates the task force’s 2015 guideline, carries a “B” classification, meaning the USPSTF has high certainty that the net benefit is moderate. It now specifies screening from age 35to 70 for persons classified as overweight (body mass index at least 25) or obese (BMI at least 30) and recommends referral to preventive interventions when patients are found to have prediabetes.
In addition to recommendations of lifestyle changes, such as diet and physical activity, the task force also endorses the diabetes drug metformin as a beneficial intervention in the prevention or delay of diabetes, while noting fewer overall health benefits from metformin than from the lifestyle changes.
A lower BMI cutoff of at least 23 is recommended for diabetes screening of Asian Americans, and, importantly, screening for prediabetes and diabetes should be considered at an even earlier age if the patient is from a population with a disproportionately high prevalence of diabetes, including American Indian/Alaska Native, Black, Hawaiian/Pacific Islander, Hispanic/Latino, the task force recommends.
Screening tests should include fasting plasma glucose, hemoglobin A1c, or an oral glucose tolerance test. Although screening every 3 years “may be a reasonable approach for adults with normal blood glucose levels,” the task force adds that “the optimal screening interval for adults with an initial normal glucose test result is uncertain.”
Data review: Few with prediabetes know they have it
The need for the update was prompted by troubling data showing increasing diabetes rates despite early signs that can and should be identified and acted upon in the primary care setting to prevent disease progression.
Data from the Centers for Disease Control and Prevention, for instance, show that while 13% of all U.S. adults 18 years or older have diabetes and 35% meet criteria for prediabetes, as many as 21% of those with diabetes were not aware of or did not report having the disease. Furthermore, only a small fraction – 15% of those with prediabetes – said they had been told by a health professional that they had this condition, the task force notes.
The task force’s final recommendation was based on a systematic review of evidence regarding the screening of asymptomatic, nonpregnant adults and the harms and benefits of interventions, such as physical activity, behavioral counseling, or pharmacotherapy.
Among key evidence supporting the lower age was a 2014 study showing that the number of people necessary to obtain one positive test for diabetes with screening sharply drops from 80 among those aged 30-34 years to just 31 among those aged 36-39.
Opportunistic universal screening of eligible people aged 35 and older would yield a ratio of 1 out of just 15 to spot a positive test, the authors of that study reported.
In addition, a large cohort study in more than 77,000 people with prediabetes strongly links the risk of developing diabetes with increases in A1c level and with increasing BMI.
ADA recommendations differ
The new recommendations differ from American Diabetes Association guidelines, which call for diabetes screening at all ages for people who are overweight or obese and who have one or more risk factors, such as physical inactivity or a first-degree relative with diabetes. If results are normal, repeat screening at least every 3 years is recommended.
The ADA further recommends universal screening for all adults 45 years and older, regardless of their risk factors.
For the screening of adults over 45, the ADA recommends using a fasting plasma glucose level, 2-hour plasma glucose level during a 75-g oral glucose tolerance test, or A1c level, regardless of risk factors.
The American Association of Clinical Endocrinology also recommends universal screening for prediabetes and diabetes for all adults 45 years or older, regardless of risk factors, and also advises screening those who have risk factors for diabetes regardless of age.
Screening of little benefit without behavior change support
In an interview, Dr. Grant added that broad efforts are essential as those at the practice level have clearly not succeeded.
“The medical model of individual counseling and referral has not really been effective, and so we really need to think in terms of large-scale public health action,” said Dr. Grant, of the division of research, Kaiser Permanente Northern California, Oakland.
His editorial details the sweeping, multifactorial efforts that are needed.
“To turn this recommendation into action – that is, to translate screening activities into improved clinical outcomes – change is needed at the patient-clinician level (recognizing and encouraging eligible individuals to be screened), health care system level (reducing screening barriers and ensuring access to robust lifestyle programs), and societal level (applying effective public health interventions to reduce obesity and increase exercise),” they write.
A top priority has to be a focus on individuals of diverse backgrounds and issues such as access to healthy programs in minority communities, Dr. Grant noted.
“Newly diagnosed adults are more likely to be African-American and Latinx,” he said.
“We really need to invest in healthier communities for low-income, non-White communities to reverse the persistent health care disparities in these communities.”
While the challenges may appear daunting, history shows they are not necessarily insurmountable – as evidenced in the campaign to discourage tobacco smoking.
“National smoking cessation efforts are one example of a mostly successful public health campaign that has made a difference in health behaviors,” Grant noted.
The recommendation is also posted on the USPSTF web site .
Dr. Grant reports receiving grants from the National Institutes of Health and the Patient-Centered Outcomes Research Institute.
The United States Preventive Services Task Force has updated its recommendation on the age of screening for prediabetes and type 2 diabetes in the primary care setting – lowering the age from 40 to 35 years for asymptomatic patients who are overweight or obese and encouraging greater interventions when patients do show a risk.
“The USPSTF concludes with moderate certainty that screening for prediabetes and type 2 diabetes and offering or referring patients with prediabetes to effective preventive interventions has a moderate net benefit,” the task force concludes in its recommendation, published Aug. 24 in JAMA.
“Clinicians should offer or refer patients with prediabetes to effective preventive interventions,” they write.
Experts commenting on the issue strongly emphasize that it’s not just the screening, but the subsequent intervention that is needed to make a difference.
“If young adults newly identified with abnormal glucose metabolism do not receive the needed intensive behavioral change support, screening may provide no benefit,” write Richard W. Grant, MD, MPH, and colleagues in an editorial published with the recommendation.
“Given the role of our obesogenic and physically inactive society in the shift toward earlier onset of diabetes, efforts to increase screening and recognition of abnormal glucose metabolism must be coupled with robust public health measures to address the underlying contributors.”
BMI cutoff lower for at-risk ethnic populations
The recommendation, which updates the task force’s 2015 guideline, carries a “B” classification, meaning the USPSTF has high certainty that the net benefit is moderate. It now specifies screening from age 35to 70 for persons classified as overweight (body mass index at least 25) or obese (BMI at least 30) and recommends referral to preventive interventions when patients are found to have prediabetes.
In addition to recommendations of lifestyle changes, such as diet and physical activity, the task force also endorses the diabetes drug metformin as a beneficial intervention in the prevention or delay of diabetes, while noting fewer overall health benefits from metformin than from the lifestyle changes.
A lower BMI cutoff of at least 23 is recommended for diabetes screening of Asian Americans, and, importantly, screening for prediabetes and diabetes should be considered at an even earlier age if the patient is from a population with a disproportionately high prevalence of diabetes, including American Indian/Alaska Native, Black, Hawaiian/Pacific Islander, Hispanic/Latino, the task force recommends.
Screening tests should include fasting plasma glucose, hemoglobin A1c, or an oral glucose tolerance test. Although screening every 3 years “may be a reasonable approach for adults with normal blood glucose levels,” the task force adds that “the optimal screening interval for adults with an initial normal glucose test result is uncertain.”
Data review: Few with prediabetes know they have it
The need for the update was prompted by troubling data showing increasing diabetes rates despite early signs that can and should be identified and acted upon in the primary care setting to prevent disease progression.
Data from the Centers for Disease Control and Prevention, for instance, show that while 13% of all U.S. adults 18 years or older have diabetes and 35% meet criteria for prediabetes, as many as 21% of those with diabetes were not aware of or did not report having the disease. Furthermore, only a small fraction – 15% of those with prediabetes – said they had been told by a health professional that they had this condition, the task force notes.
The task force’s final recommendation was based on a systematic review of evidence regarding the screening of asymptomatic, nonpregnant adults and the harms and benefits of interventions, such as physical activity, behavioral counseling, or pharmacotherapy.
Among key evidence supporting the lower age was a 2014 study showing that the number of people necessary to obtain one positive test for diabetes with screening sharply drops from 80 among those aged 30-34 years to just 31 among those aged 36-39.
Opportunistic universal screening of eligible people aged 35 and older would yield a ratio of 1 out of just 15 to spot a positive test, the authors of that study reported.
In addition, a large cohort study in more than 77,000 people with prediabetes strongly links the risk of developing diabetes with increases in A1c level and with increasing BMI.
ADA recommendations differ
The new recommendations differ from American Diabetes Association guidelines, which call for diabetes screening at all ages for people who are overweight or obese and who have one or more risk factors, such as physical inactivity or a first-degree relative with diabetes. If results are normal, repeat screening at least every 3 years is recommended.
The ADA further recommends universal screening for all adults 45 years and older, regardless of their risk factors.
For the screening of adults over 45, the ADA recommends using a fasting plasma glucose level, 2-hour plasma glucose level during a 75-g oral glucose tolerance test, or A1c level, regardless of risk factors.
The American Association of Clinical Endocrinology also recommends universal screening for prediabetes and diabetes for all adults 45 years or older, regardless of risk factors, and also advises screening those who have risk factors for diabetes regardless of age.
Screening of little benefit without behavior change support
In an interview, Dr. Grant added that broad efforts are essential as those at the practice level have clearly not succeeded.
“The medical model of individual counseling and referral has not really been effective, and so we really need to think in terms of large-scale public health action,” said Dr. Grant, of the division of research, Kaiser Permanente Northern California, Oakland.
His editorial details the sweeping, multifactorial efforts that are needed.
“To turn this recommendation into action – that is, to translate screening activities into improved clinical outcomes – change is needed at the patient-clinician level (recognizing and encouraging eligible individuals to be screened), health care system level (reducing screening barriers and ensuring access to robust lifestyle programs), and societal level (applying effective public health interventions to reduce obesity and increase exercise),” they write.
A top priority has to be a focus on individuals of diverse backgrounds and issues such as access to healthy programs in minority communities, Dr. Grant noted.
“Newly diagnosed adults are more likely to be African-American and Latinx,” he said.
“We really need to invest in healthier communities for low-income, non-White communities to reverse the persistent health care disparities in these communities.”
While the challenges may appear daunting, history shows they are not necessarily insurmountable – as evidenced in the campaign to discourage tobacco smoking.
“National smoking cessation efforts are one example of a mostly successful public health campaign that has made a difference in health behaviors,” Grant noted.
The recommendation is also posted on the USPSTF web site .
Dr. Grant reports receiving grants from the National Institutes of Health and the Patient-Centered Outcomes Research Institute.
FROM JAMA
AGA Clinical Practice Update: Expert Review on colonoscopy quality improvement
The American Gastroenterological Association recently issued a clinical practice update expert review outlining tenets of high-quality colonoscopy screening and surveillance.
The update includes 15 best practice advice statements aimed at the endoscopist and/or endoscopy unit, reported lead author Rajesh N. Keswani, MD, of Northwestern University, Chicago, and colleagues.
“The efficacy of colonoscopy varies widely among endoscopists, and lower-quality colonoscopies are associated with higher interval CRC [colorectal cancer] incidence and mortality,” the investigators wrote in Gastroenterology.
According to Dr. Keswani and colleagues, quality of colonoscopy screening and surveillance is shaped by three parameters: safety, effectiveness, and value. Some metrics may be best measured at a unit level, they noted, while others are more clinician specific.
“For uncommon outcomes (e.g., adverse events) or metrics that reflect system-based practice (e.g., bowel preparation quality), measurement of aggregate unit-level performance is best,” the investigators wrote. “In contrast, for metrics that primarily reflect colonoscopist skill (e.g., adenoma detection rate), endoscopist-level measurement is preferred to enable individual feedback.”
Endoscopy unit best practice advice
According to the update, endoscopy units should prepare patients for, and monitor, adverse events. Prior to the procedure, patients should be informed about possible adverse events and warning symptoms, and emergency contact information should be recorded. Following the procedure, systematic monitoring of delayed adverse events may be considered, including “postprocedure bleeding, perforation, hospital readmission, 30-day mortality, and/or interval colorectal cancer cases,” with rates reported at the unit level.
Ensuring high-quality bowel preparation is also the responsibility of the endoscopy unit, according to Dr. Keswani and colleagues, and should be measured at least annually. Units should aim for a Boston Bowel Preparation Scale score of at least 6, with each segment scoring at least 2, in at least 90% of colonoscopies. The update provides best practice advice on split-dose bowel prep, with patient instructions written at a sixth-grade level in their native language. If routine quality measurement reveals suboptimal bowel prep quality, instruction revision may be needed, as well as further patient education and support.
During the actual procedure, a high-definition colonoscope should be used, the expert panel wrote. They called for measurement of endoscopist performance via four parameters: cecal intubation rate, which should be at least 90%; mean withdrawal time, which should be at least 6 minutes (aspirational, ≥9 minutes); adenoma detection rate, measured annually or when a given endoscopist has accrued 250 screening colonoscopies; and serrated lesion detection rate.
Endoscopist best practice advice
Both adenoma detection rate and serrated lesion detection rate should also be measured at an endoscopist level, with rates of at least 30% for adenomas and at least 7% for serrated lesions (aspirational, ≥35% and ≥10%, respectively).
“If rates are low, improvement efforts should be oriented toward both colonoscopists and pathologists,” the investigators noted.
A variety of strategies are advised to improve outcomes at the endoscopist level, including a second look at the right colon to detect polyps, either in forward or retroflexed view; use of cold-snare polypectomy for nonpedunculated polyps 3-9 mm in size and avoidance of forceps in polyps greater than 2 mm in size; evaluation by an expert in polypectomy with attempted resection for patients with complex polyps lacking “overt malignant endoscopic features or pathology consistent with invasive adenocarcinoma”; and thorough documentation of all findings.
More broadly, the update advises endoscopists to follow guideline-recommended intervals for screening and surveillance, including repeat colonoscopy in 3 years for all patients with advanced adenomas versus a 10-year interval for patients with normal risk or “only distal hyperplastic polyps.”
Resource-limited institutions and a look ahead
Dr. Keswani and colleagues concluded the clinical practice update with a nod to the challenges of real-world practice, noting that some institutions may not have the resources to comply with all the best practice advice statements.
“If limited resources are available, measurement of cecal intubation rates, bowel preparation quality, and adenoma detection rate should be prioritized,” they wrote.
They also offered a succinct summary of outstanding research needs, saying “we anticipate future work to clarify optimal polyp resection techniques, refine surveillance intervals based on provider skill and patient risk, and highlight the benefits of artificial intelligence in improving colonoscopy quality.”
This clinical practice update was commissioned and approved by the AGA Institute Clinical Practice Updates Committee and the AGA Governing Board. Dr. Keswani consults for Boston Scientific. The other authors had no disclosures.
This article was updated Aug. 20, 2021.
The American Gastroenterological Association recently issued a clinical practice update expert review outlining tenets of high-quality colonoscopy screening and surveillance.
The update includes 15 best practice advice statements aimed at the endoscopist and/or endoscopy unit, reported lead author Rajesh N. Keswani, MD, of Northwestern University, Chicago, and colleagues.
“The efficacy of colonoscopy varies widely among endoscopists, and lower-quality colonoscopies are associated with higher interval CRC [colorectal cancer] incidence and mortality,” the investigators wrote in Gastroenterology.
According to Dr. Keswani and colleagues, quality of colonoscopy screening and surveillance is shaped by three parameters: safety, effectiveness, and value. Some metrics may be best measured at a unit level, they noted, while others are more clinician specific.
“For uncommon outcomes (e.g., adverse events) or metrics that reflect system-based practice (e.g., bowel preparation quality), measurement of aggregate unit-level performance is best,” the investigators wrote. “In contrast, for metrics that primarily reflect colonoscopist skill (e.g., adenoma detection rate), endoscopist-level measurement is preferred to enable individual feedback.”
Endoscopy unit best practice advice
According to the update, endoscopy units should prepare patients for, and monitor, adverse events. Prior to the procedure, patients should be informed about possible adverse events and warning symptoms, and emergency contact information should be recorded. Following the procedure, systematic monitoring of delayed adverse events may be considered, including “postprocedure bleeding, perforation, hospital readmission, 30-day mortality, and/or interval colorectal cancer cases,” with rates reported at the unit level.
Ensuring high-quality bowel preparation is also the responsibility of the endoscopy unit, according to Dr. Keswani and colleagues, and should be measured at least annually. Units should aim for a Boston Bowel Preparation Scale score of at least 6, with each segment scoring at least 2, in at least 90% of colonoscopies. The update provides best practice advice on split-dose bowel prep, with patient instructions written at a sixth-grade level in their native language. If routine quality measurement reveals suboptimal bowel prep quality, instruction revision may be needed, as well as further patient education and support.
During the actual procedure, a high-definition colonoscope should be used, the expert panel wrote. They called for measurement of endoscopist performance via four parameters: cecal intubation rate, which should be at least 90%; mean withdrawal time, which should be at least 6 minutes (aspirational, ≥9 minutes); adenoma detection rate, measured annually or when a given endoscopist has accrued 250 screening colonoscopies; and serrated lesion detection rate.
Endoscopist best practice advice
Both adenoma detection rate and serrated lesion detection rate should also be measured at an endoscopist level, with rates of at least 30% for adenomas and at least 7% for serrated lesions (aspirational, ≥35% and ≥10%, respectively).
“If rates are low, improvement efforts should be oriented toward both colonoscopists and pathologists,” the investigators noted.
A variety of strategies are advised to improve outcomes at the endoscopist level, including a second look at the right colon to detect polyps, either in forward or retroflexed view; use of cold-snare polypectomy for nonpedunculated polyps 3-9 mm in size and avoidance of forceps in polyps greater than 2 mm in size; evaluation by an expert in polypectomy with attempted resection for patients with complex polyps lacking “overt malignant endoscopic features or pathology consistent with invasive adenocarcinoma”; and thorough documentation of all findings.
More broadly, the update advises endoscopists to follow guideline-recommended intervals for screening and surveillance, including repeat colonoscopy in 3 years for all patients with advanced adenomas versus a 10-year interval for patients with normal risk or “only distal hyperplastic polyps.”
Resource-limited institutions and a look ahead
Dr. Keswani and colleagues concluded the clinical practice update with a nod to the challenges of real-world practice, noting that some institutions may not have the resources to comply with all the best practice advice statements.
“If limited resources are available, measurement of cecal intubation rates, bowel preparation quality, and adenoma detection rate should be prioritized,” they wrote.
They also offered a succinct summary of outstanding research needs, saying “we anticipate future work to clarify optimal polyp resection techniques, refine surveillance intervals based on provider skill and patient risk, and highlight the benefits of artificial intelligence in improving colonoscopy quality.”
This clinical practice update was commissioned and approved by the AGA Institute Clinical Practice Updates Committee and the AGA Governing Board. Dr. Keswani consults for Boston Scientific. The other authors had no disclosures.
This article was updated Aug. 20, 2021.
The American Gastroenterological Association recently issued a clinical practice update expert review outlining tenets of high-quality colonoscopy screening and surveillance.
The update includes 15 best practice advice statements aimed at the endoscopist and/or endoscopy unit, reported lead author Rajesh N. Keswani, MD, of Northwestern University, Chicago, and colleagues.
“The efficacy of colonoscopy varies widely among endoscopists, and lower-quality colonoscopies are associated with higher interval CRC [colorectal cancer] incidence and mortality,” the investigators wrote in Gastroenterology.
According to Dr. Keswani and colleagues, quality of colonoscopy screening and surveillance is shaped by three parameters: safety, effectiveness, and value. Some metrics may be best measured at a unit level, they noted, while others are more clinician specific.
“For uncommon outcomes (e.g., adverse events) or metrics that reflect system-based practice (e.g., bowel preparation quality), measurement of aggregate unit-level performance is best,” the investigators wrote. “In contrast, for metrics that primarily reflect colonoscopist skill (e.g., adenoma detection rate), endoscopist-level measurement is preferred to enable individual feedback.”
Endoscopy unit best practice advice
According to the update, endoscopy units should prepare patients for, and monitor, adverse events. Prior to the procedure, patients should be informed about possible adverse events and warning symptoms, and emergency contact information should be recorded. Following the procedure, systematic monitoring of delayed adverse events may be considered, including “postprocedure bleeding, perforation, hospital readmission, 30-day mortality, and/or interval colorectal cancer cases,” with rates reported at the unit level.
Ensuring high-quality bowel preparation is also the responsibility of the endoscopy unit, according to Dr. Keswani and colleagues, and should be measured at least annually. Units should aim for a Boston Bowel Preparation Scale score of at least 6, with each segment scoring at least 2, in at least 90% of colonoscopies. The update provides best practice advice on split-dose bowel prep, with patient instructions written at a sixth-grade level in their native language. If routine quality measurement reveals suboptimal bowel prep quality, instruction revision may be needed, as well as further patient education and support.
During the actual procedure, a high-definition colonoscope should be used, the expert panel wrote. They called for measurement of endoscopist performance via four parameters: cecal intubation rate, which should be at least 90%; mean withdrawal time, which should be at least 6 minutes (aspirational, ≥9 minutes); adenoma detection rate, measured annually or when a given endoscopist has accrued 250 screening colonoscopies; and serrated lesion detection rate.
Endoscopist best practice advice
Both adenoma detection rate and serrated lesion detection rate should also be measured at an endoscopist level, with rates of at least 30% for adenomas and at least 7% for serrated lesions (aspirational, ≥35% and ≥10%, respectively).
“If rates are low, improvement efforts should be oriented toward both colonoscopists and pathologists,” the investigators noted.
A variety of strategies are advised to improve outcomes at the endoscopist level, including a second look at the right colon to detect polyps, either in forward or retroflexed view; use of cold-snare polypectomy for nonpedunculated polyps 3-9 mm in size and avoidance of forceps in polyps greater than 2 mm in size; evaluation by an expert in polypectomy with attempted resection for patients with complex polyps lacking “overt malignant endoscopic features or pathology consistent with invasive adenocarcinoma”; and thorough documentation of all findings.
More broadly, the update advises endoscopists to follow guideline-recommended intervals for screening and surveillance, including repeat colonoscopy in 3 years for all patients with advanced adenomas versus a 10-year interval for patients with normal risk or “only distal hyperplastic polyps.”
Resource-limited institutions and a look ahead
Dr. Keswani and colleagues concluded the clinical practice update with a nod to the challenges of real-world practice, noting that some institutions may not have the resources to comply with all the best practice advice statements.
“If limited resources are available, measurement of cecal intubation rates, bowel preparation quality, and adenoma detection rate should be prioritized,” they wrote.
They also offered a succinct summary of outstanding research needs, saying “we anticipate future work to clarify optimal polyp resection techniques, refine surveillance intervals based on provider skill and patient risk, and highlight the benefits of artificial intelligence in improving colonoscopy quality.”
This clinical practice update was commissioned and approved by the AGA Institute Clinical Practice Updates Committee and the AGA Governing Board. Dr. Keswani consults for Boston Scientific. The other authors had no disclosures.
This article was updated Aug. 20, 2021.
FROM GASTROENTEROLOGY
Task force affirms routine gestational diabetes testing
Asymptomatic pregnant women with no previous diagnosis of type 1 or 2 diabetes should be screened for gestational diabetes at 24 weeks’ gestation or later, according to an updated recommendation from the U.S. Preventive Services Task Force.
Pregnant individuals who develop gestational diabetes are at increased risk for complications including preeclampsia, fetal macrosomia, and neonatal hypoglycemia, as well as negative long-term outcomes for themselves and their children, wrote lead author Karina W. Davidson, PhD, of Feinstein Institute for Medical Research, Manhasset, N.Y., and colleagues. The statement was published online in JAMA.
The B recommendation and I statement reflect “moderate certainty” that current evidence supports the recommendation in terms of harms versus benefits, and is consistent with the 2014 USPSTF recommendation.
The statement calls for a one-time screening using a glucose tolerance test at or after 24 weeks’ gestation. Although most screening in the United States takes place prior to 28 weeks’ gestation, it can be performed later in patients who begin prenatal care after 28 weeks’ gestation, according to the statement. Data on the harms and benefits of gestational diabetes screening prior to 24 weeks’ gestation are limited, the authors noted. Gestational diabetes was defined as diabetes that develops during pregnancy that is not clearly overt diabetes.
To update the 2014 recommendation, the USPSTF commissioned a systematic review. In 45 prospective studies on the accuracy of gestational diabetes screening, several tests, included oral glucose challenge test, oral glucose tolerance test, and fasting plasma glucose using either a one- or two-step approach were accurate detectors of gestational diabetes; therefore, the USPSTF does not recommend a specific test.
In 13 trials on the impact of treating gestational diabetes on intermediate and health outcomes, treatment was associated with a reduced risk of outcomes, including primary cesarean delivery (but not total cesarean delivery) and preterm delivery, but not with a reduced risk of outcomes including preeclampsia, emergency cesarean delivery, induction of labor, or maternal birth trauma.
The task force also reviewed seven studies of harms associated with screening for gestational diabetes, including three on psychosocial harms, three on hospital experiences, and one of the odds of cesarean delivery after a diagnosis of gestational diabetes. No increase in anxiety or depression occurred following a positive diagnosis or false-positive test result, but data suggested that a gestational diabetes diagnosis may be associated with higher rates of cesarean delivery.
A total of 13 trials evaluated the harms associated with treatment of gestational diabetes, and found no association between treatment and increased risk of several outcomes including severe maternal hypoglycemia, low birth weight, and small for gestational age, and no effect was noted on the number of cesarean deliveries.
Evidence gaps that require additional research include randomized, controlled trials on the effects of gestational diabetes screening on health outcomes, as well as benefits versus harms of screening for pregnant individuals prior to 24 weeks, and studies on the effects of screening in subpopulations of race/ethnicity, age, and socioeconomic factors, according to the task force. Additional research also is needed in areas of maternal health outcomes, long-term outcomes, and the effect on outcomes of one-step versus two-step screening, the USPSTF said.
However, “screening for and detecting gestational diabetes provides a potential opportunity to control blood glucose levels (through lifestyle changes, pharmacological interventions, or both) and reduce the risk of macrosomia and LGA [large for gestational age] infants,” the task force wrote. “In turn, this can prevent associated complications such as primary cesarean delivery, shoulder dystocia, and [neonatal] ICU admissions.”
Support screening with counseling on risk reduction
The USPSTF recommendation is important at this time because “the prevalence of gestational diabetes is increasing secondary to rising rates of obesity,” Iris Krishna, MD, of Emory University, Atlanta, said in an interview.
“In 2014, based on a systematic review of literature, the USPSTF recommended screening all asymptomatic pregnant women for gestational diabetes mellitus [GDM] starting at 24 weeks’ gestation. The recommended gestational age for screening coincides with increasing insulin resistance during pregnancy with advancing gestational age,” Dr. Krishna said.
“An updated systematic review by the USPSTF concluded that existing literature continues to affirm current recommendations of universal screening for GDM at 24 weeks gestation or later. There continues, however, to be no consensus on the optimal approach to screening,” she noted.
“Screening can be performed as a two-step or one-step approach,” said Dr. Krishna. “The two-step approach is commonly used in the United States, and all pregnant women are first screened with a 50-gram oral glucose solution followed by a diagnostic test if they have a positive initial screening.
“Women with risk factors for diabetes, such as prior GDM, obesity, strong family history of diabetes, or history of fetal macrosomia, should be screened early in pregnancy for GDM and have the GDM screen repeated at 24 weeks’ gestation or later if normal in early pregnancy,” Dr. Krishna said. “Pregnant women should be counseled on the importance of diet and exercise and appropriate weight gain in pregnancy to reduce the risk of GDM. Overall, timely diagnosis of gestational diabetes is crucial to improving maternal and fetal pregnancy outcomes.”
The full recommendation statement is also available on the USPSTF website. The research was supported by the Agency for Healthcare Research and Quality. The researchers had no financial conflicts to disclose. Dr. Krishna had no disclosures, but serves on the editorial advisory board of Ob.Gyn News.
Asymptomatic pregnant women with no previous diagnosis of type 1 or 2 diabetes should be screened for gestational diabetes at 24 weeks’ gestation or later, according to an updated recommendation from the U.S. Preventive Services Task Force.
Pregnant individuals who develop gestational diabetes are at increased risk for complications including preeclampsia, fetal macrosomia, and neonatal hypoglycemia, as well as negative long-term outcomes for themselves and their children, wrote lead author Karina W. Davidson, PhD, of Feinstein Institute for Medical Research, Manhasset, N.Y., and colleagues. The statement was published online in JAMA.
The B recommendation and I statement reflect “moderate certainty” that current evidence supports the recommendation in terms of harms versus benefits, and is consistent with the 2014 USPSTF recommendation.
The statement calls for a one-time screening using a glucose tolerance test at or after 24 weeks’ gestation. Although most screening in the United States takes place prior to 28 weeks’ gestation, it can be performed later in patients who begin prenatal care after 28 weeks’ gestation, according to the statement. Data on the harms and benefits of gestational diabetes screening prior to 24 weeks’ gestation are limited, the authors noted. Gestational diabetes was defined as diabetes that develops during pregnancy that is not clearly overt diabetes.
To update the 2014 recommendation, the USPSTF commissioned a systematic review. In 45 prospective studies on the accuracy of gestational diabetes screening, several tests, included oral glucose challenge test, oral glucose tolerance test, and fasting plasma glucose using either a one- or two-step approach were accurate detectors of gestational diabetes; therefore, the USPSTF does not recommend a specific test.
In 13 trials on the impact of treating gestational diabetes on intermediate and health outcomes, treatment was associated with a reduced risk of outcomes, including primary cesarean delivery (but not total cesarean delivery) and preterm delivery, but not with a reduced risk of outcomes including preeclampsia, emergency cesarean delivery, induction of labor, or maternal birth trauma.
The task force also reviewed seven studies of harms associated with screening for gestational diabetes, including three on psychosocial harms, three on hospital experiences, and one of the odds of cesarean delivery after a diagnosis of gestational diabetes. No increase in anxiety or depression occurred following a positive diagnosis or false-positive test result, but data suggested that a gestational diabetes diagnosis may be associated with higher rates of cesarean delivery.
A total of 13 trials evaluated the harms associated with treatment of gestational diabetes, and found no association between treatment and increased risk of several outcomes including severe maternal hypoglycemia, low birth weight, and small for gestational age, and no effect was noted on the number of cesarean deliveries.
Evidence gaps that require additional research include randomized, controlled trials on the effects of gestational diabetes screening on health outcomes, as well as benefits versus harms of screening for pregnant individuals prior to 24 weeks, and studies on the effects of screening in subpopulations of race/ethnicity, age, and socioeconomic factors, according to the task force. Additional research also is needed in areas of maternal health outcomes, long-term outcomes, and the effect on outcomes of one-step versus two-step screening, the USPSTF said.
However, “screening for and detecting gestational diabetes provides a potential opportunity to control blood glucose levels (through lifestyle changes, pharmacological interventions, or both) and reduce the risk of macrosomia and LGA [large for gestational age] infants,” the task force wrote. “In turn, this can prevent associated complications such as primary cesarean delivery, shoulder dystocia, and [neonatal] ICU admissions.”
Support screening with counseling on risk reduction
The USPSTF recommendation is important at this time because “the prevalence of gestational diabetes is increasing secondary to rising rates of obesity,” Iris Krishna, MD, of Emory University, Atlanta, said in an interview.
“In 2014, based on a systematic review of literature, the USPSTF recommended screening all asymptomatic pregnant women for gestational diabetes mellitus [GDM] starting at 24 weeks’ gestation. The recommended gestational age for screening coincides with increasing insulin resistance during pregnancy with advancing gestational age,” Dr. Krishna said.
“An updated systematic review by the USPSTF concluded that existing literature continues to affirm current recommendations of universal screening for GDM at 24 weeks gestation or later. There continues, however, to be no consensus on the optimal approach to screening,” she noted.
“Screening can be performed as a two-step or one-step approach,” said Dr. Krishna. “The two-step approach is commonly used in the United States, and all pregnant women are first screened with a 50-gram oral glucose solution followed by a diagnostic test if they have a positive initial screening.
“Women with risk factors for diabetes, such as prior GDM, obesity, strong family history of diabetes, or history of fetal macrosomia, should be screened early in pregnancy for GDM and have the GDM screen repeated at 24 weeks’ gestation or later if normal in early pregnancy,” Dr. Krishna said. “Pregnant women should be counseled on the importance of diet and exercise and appropriate weight gain in pregnancy to reduce the risk of GDM. Overall, timely diagnosis of gestational diabetes is crucial to improving maternal and fetal pregnancy outcomes.”
The full recommendation statement is also available on the USPSTF website. The research was supported by the Agency for Healthcare Research and Quality. The researchers had no financial conflicts to disclose. Dr. Krishna had no disclosures, but serves on the editorial advisory board of Ob.Gyn News.
Asymptomatic pregnant women with no previous diagnosis of type 1 or 2 diabetes should be screened for gestational diabetes at 24 weeks’ gestation or later, according to an updated recommendation from the U.S. Preventive Services Task Force.
Pregnant individuals who develop gestational diabetes are at increased risk for complications including preeclampsia, fetal macrosomia, and neonatal hypoglycemia, as well as negative long-term outcomes for themselves and their children, wrote lead author Karina W. Davidson, PhD, of Feinstein Institute for Medical Research, Manhasset, N.Y., and colleagues. The statement was published online in JAMA.
The B recommendation and I statement reflect “moderate certainty” that current evidence supports the recommendation in terms of harms versus benefits, and is consistent with the 2014 USPSTF recommendation.
The statement calls for a one-time screening using a glucose tolerance test at or after 24 weeks’ gestation. Although most screening in the United States takes place prior to 28 weeks’ gestation, it can be performed later in patients who begin prenatal care after 28 weeks’ gestation, according to the statement. Data on the harms and benefits of gestational diabetes screening prior to 24 weeks’ gestation are limited, the authors noted. Gestational diabetes was defined as diabetes that develops during pregnancy that is not clearly overt diabetes.
To update the 2014 recommendation, the USPSTF commissioned a systematic review. In 45 prospective studies on the accuracy of gestational diabetes screening, several tests, included oral glucose challenge test, oral glucose tolerance test, and fasting plasma glucose using either a one- or two-step approach were accurate detectors of gestational diabetes; therefore, the USPSTF does not recommend a specific test.
In 13 trials on the impact of treating gestational diabetes on intermediate and health outcomes, treatment was associated with a reduced risk of outcomes, including primary cesarean delivery (but not total cesarean delivery) and preterm delivery, but not with a reduced risk of outcomes including preeclampsia, emergency cesarean delivery, induction of labor, or maternal birth trauma.
The task force also reviewed seven studies of harms associated with screening for gestational diabetes, including three on psychosocial harms, three on hospital experiences, and one of the odds of cesarean delivery after a diagnosis of gestational diabetes. No increase in anxiety or depression occurred following a positive diagnosis or false-positive test result, but data suggested that a gestational diabetes diagnosis may be associated with higher rates of cesarean delivery.
A total of 13 trials evaluated the harms associated with treatment of gestational diabetes, and found no association between treatment and increased risk of several outcomes including severe maternal hypoglycemia, low birth weight, and small for gestational age, and no effect was noted on the number of cesarean deliveries.
Evidence gaps that require additional research include randomized, controlled trials on the effects of gestational diabetes screening on health outcomes, as well as benefits versus harms of screening for pregnant individuals prior to 24 weeks, and studies on the effects of screening in subpopulations of race/ethnicity, age, and socioeconomic factors, according to the task force. Additional research also is needed in areas of maternal health outcomes, long-term outcomes, and the effect on outcomes of one-step versus two-step screening, the USPSTF said.
However, “screening for and detecting gestational diabetes provides a potential opportunity to control blood glucose levels (through lifestyle changes, pharmacological interventions, or both) and reduce the risk of macrosomia and LGA [large for gestational age] infants,” the task force wrote. “In turn, this can prevent associated complications such as primary cesarean delivery, shoulder dystocia, and [neonatal] ICU admissions.”
Support screening with counseling on risk reduction
The USPSTF recommendation is important at this time because “the prevalence of gestational diabetes is increasing secondary to rising rates of obesity,” Iris Krishna, MD, of Emory University, Atlanta, said in an interview.
“In 2014, based on a systematic review of literature, the USPSTF recommended screening all asymptomatic pregnant women for gestational diabetes mellitus [GDM] starting at 24 weeks’ gestation. The recommended gestational age for screening coincides with increasing insulin resistance during pregnancy with advancing gestational age,” Dr. Krishna said.
“An updated systematic review by the USPSTF concluded that existing literature continues to affirm current recommendations of universal screening for GDM at 24 weeks gestation or later. There continues, however, to be no consensus on the optimal approach to screening,” she noted.
“Screening can be performed as a two-step or one-step approach,” said Dr. Krishna. “The two-step approach is commonly used in the United States, and all pregnant women are first screened with a 50-gram oral glucose solution followed by a diagnostic test if they have a positive initial screening.
“Women with risk factors for diabetes, such as prior GDM, obesity, strong family history of diabetes, or history of fetal macrosomia, should be screened early in pregnancy for GDM and have the GDM screen repeated at 24 weeks’ gestation or later if normal in early pregnancy,” Dr. Krishna said. “Pregnant women should be counseled on the importance of diet and exercise and appropriate weight gain in pregnancy to reduce the risk of GDM. Overall, timely diagnosis of gestational diabetes is crucial to improving maternal and fetal pregnancy outcomes.”
The full recommendation statement is also available on the USPSTF website. The research was supported by the Agency for Healthcare Research and Quality. The researchers had no financial conflicts to disclose. Dr. Krishna had no disclosures, but serves on the editorial advisory board of Ob.Gyn News.
FROM JAMA
AGA Clinical Practice Update Expert Review: Management of malignant alimentary tract obstruction
The American Gastroenterological Association published a clinical practice update expert review for managing malignant alimentary tract obstructions (MATOs) that includes 14 best practice advice statements, ranging from general principles to specific clinical choices.
“There are many options available for the management of MATOs, with the addition of new modalities as interventional endoscopy continues to evolve,” Osman Ahmed, MD, of the University of Toronto and colleagues wrote in Clinical Gastroenterology and Hepatology. “The important concept to understand for any physician managing MATOs is that there is no longer a ‘one-size-fits-all’ approach that can be applied to all patients.”
First, the investigators called for an individualized, multidisciplinary approach that includes oncologists, surgeons, and endoscopists. They advised physicians to “take into account the characteristics of the obstruction, patient’s expectations, prognosis, expected subsequent therapies, and functional status.”
The remaining advice statements are organized by site of obstruction, with various management approaches based on candidacy for resection and other patient factors.
Esophageal obstruction
For patients with esophageal obstruction who are candidates for resection or chemoradiation, Dr. Ahmed and colleagues advised against routine use of self-expanding metal stents (SEMS) due to “high rates of stent migration, higher morbidity and mortality, and potentially lower R0 (microscopically negative margins) resection rates.”
If such patients are at risk of malnutrition, an enteral feeding tube may be considered, although patients should be counseled about associated procedural risks, such as abdominal wall tumor seeding.
Among patients with esophageal obstruction who are not candidates for resection, SEMS insertion or brachytherapy may be used separately or in combination, according to the investigators.
“Clinicians should not consider the use of laser therapy or photodynamic therapy because of the lack of evidence of better outcomes and superior alternatives,” the investigators noted.
If SEMS placement is elected, Dr. Ahmed and colleagues noted there remains ongoing debate. For this expert review, the authors advised using a fully covered stent, based on potentially higher risk for tumor ingrowth and reinterventions with uncovered SEMS.
Gastric outlet obstruction
According to the update, patients with gastric outlet obstruction who have good functional status and a life expectancy greater than 2 months should undergo surgical gastrojejunostomy, ideally via a laparoscopic approach instead of an open approach because of shorter hospital stays and less blood loss. If a sufficiently experienced endoscopist is available, an endoscopic ultrasound-guided gastrojejunostomy may be performed, although Dr. Ahmed and colleagues noted that no devices have been approved by the Food and Drug Administration for this technique.
For patients who are not candidates for gastrojejunostomy, enteral stent insertion should be considered; however, they should not be used in patients with severely impaired gastric motility or multiple luminal obstructions “because of limited benefit in these scenarios.” Instead, a venting gastrostomy may be elected.
Colonic obstruction
For patients with malignant colonic obstruction, SEMS may be considered as a “bridge to surgery,” wrote Dr. Ahmed and colleagues, and in the case of proximal or right-sided malignant obstruction, as a bridge to surgery or a palliative measure, keeping in mind “the technical challenges of SEMS insertion in those areas.”
Extracolonic obstruction
Finally, the expert panel suggested that SEMS may be appropriate for selective extracolonic malignancy if patients are not surgical candidates, noting that SEMS placement in this scenario “is more technically challenging, clinical success rates are more variable, and complications (including stent migration) are more frequent.”
The investigators concluded by advising clinicians to remain within the realm of their abilities when managing MATOs, and to refer when needed.
“[I]t is important for physicians to understand their limits and expertise and recognize when cases are best managed at experienced high-volume centers,” they wrote.
The clinical practice update expert review was commissioned and approved by the AGA Institute Clinical Practice Updates Committee and the AGA Governing Board. Dr. Lee disclosed a relationship with Boston Scientific.
The American Gastroenterological Association published a clinical practice update expert review for managing malignant alimentary tract obstructions (MATOs) that includes 14 best practice advice statements, ranging from general principles to specific clinical choices.
“There are many options available for the management of MATOs, with the addition of new modalities as interventional endoscopy continues to evolve,” Osman Ahmed, MD, of the University of Toronto and colleagues wrote in Clinical Gastroenterology and Hepatology. “The important concept to understand for any physician managing MATOs is that there is no longer a ‘one-size-fits-all’ approach that can be applied to all patients.”
First, the investigators called for an individualized, multidisciplinary approach that includes oncologists, surgeons, and endoscopists. They advised physicians to “take into account the characteristics of the obstruction, patient’s expectations, prognosis, expected subsequent therapies, and functional status.”
The remaining advice statements are organized by site of obstruction, with various management approaches based on candidacy for resection and other patient factors.
Esophageal obstruction
For patients with esophageal obstruction who are candidates for resection or chemoradiation, Dr. Ahmed and colleagues advised against routine use of self-expanding metal stents (SEMS) due to “high rates of stent migration, higher morbidity and mortality, and potentially lower R0 (microscopically negative margins) resection rates.”
If such patients are at risk of malnutrition, an enteral feeding tube may be considered, although patients should be counseled about associated procedural risks, such as abdominal wall tumor seeding.
Among patients with esophageal obstruction who are not candidates for resection, SEMS insertion or brachytherapy may be used separately or in combination, according to the investigators.
“Clinicians should not consider the use of laser therapy or photodynamic therapy because of the lack of evidence of better outcomes and superior alternatives,” the investigators noted.
If SEMS placement is elected, Dr. Ahmed and colleagues noted there remains ongoing debate. For this expert review, the authors advised using a fully covered stent, based on potentially higher risk for tumor ingrowth and reinterventions with uncovered SEMS.
Gastric outlet obstruction
According to the update, patients with gastric outlet obstruction who have good functional status and a life expectancy greater than 2 months should undergo surgical gastrojejunostomy, ideally via a laparoscopic approach instead of an open approach because of shorter hospital stays and less blood loss. If a sufficiently experienced endoscopist is available, an endoscopic ultrasound-guided gastrojejunostomy may be performed, although Dr. Ahmed and colleagues noted that no devices have been approved by the Food and Drug Administration for this technique.
For patients who are not candidates for gastrojejunostomy, enteral stent insertion should be considered; however, they should not be used in patients with severely impaired gastric motility or multiple luminal obstructions “because of limited benefit in these scenarios.” Instead, a venting gastrostomy may be elected.
Colonic obstruction
For patients with malignant colonic obstruction, SEMS may be considered as a “bridge to surgery,” wrote Dr. Ahmed and colleagues, and in the case of proximal or right-sided malignant obstruction, as a bridge to surgery or a palliative measure, keeping in mind “the technical challenges of SEMS insertion in those areas.”
Extracolonic obstruction
Finally, the expert panel suggested that SEMS may be appropriate for selective extracolonic malignancy if patients are not surgical candidates, noting that SEMS placement in this scenario “is more technically challenging, clinical success rates are more variable, and complications (including stent migration) are more frequent.”
The investigators concluded by advising clinicians to remain within the realm of their abilities when managing MATOs, and to refer when needed.
“[I]t is important for physicians to understand their limits and expertise and recognize when cases are best managed at experienced high-volume centers,” they wrote.
The clinical practice update expert review was commissioned and approved by the AGA Institute Clinical Practice Updates Committee and the AGA Governing Board. Dr. Lee disclosed a relationship with Boston Scientific.
The American Gastroenterological Association published a clinical practice update expert review for managing malignant alimentary tract obstructions (MATOs) that includes 14 best practice advice statements, ranging from general principles to specific clinical choices.
“There are many options available for the management of MATOs, with the addition of new modalities as interventional endoscopy continues to evolve,” Osman Ahmed, MD, of the University of Toronto and colleagues wrote in Clinical Gastroenterology and Hepatology. “The important concept to understand for any physician managing MATOs is that there is no longer a ‘one-size-fits-all’ approach that can be applied to all patients.”
First, the investigators called for an individualized, multidisciplinary approach that includes oncologists, surgeons, and endoscopists. They advised physicians to “take into account the characteristics of the obstruction, patient’s expectations, prognosis, expected subsequent therapies, and functional status.”
The remaining advice statements are organized by site of obstruction, with various management approaches based on candidacy for resection and other patient factors.
Esophageal obstruction
For patients with esophageal obstruction who are candidates for resection or chemoradiation, Dr. Ahmed and colleagues advised against routine use of self-expanding metal stents (SEMS) due to “high rates of stent migration, higher morbidity and mortality, and potentially lower R0 (microscopically negative margins) resection rates.”
If such patients are at risk of malnutrition, an enteral feeding tube may be considered, although patients should be counseled about associated procedural risks, such as abdominal wall tumor seeding.
Among patients with esophageal obstruction who are not candidates for resection, SEMS insertion or brachytherapy may be used separately or in combination, according to the investigators.
“Clinicians should not consider the use of laser therapy or photodynamic therapy because of the lack of evidence of better outcomes and superior alternatives,” the investigators noted.
If SEMS placement is elected, Dr. Ahmed and colleagues noted there remains ongoing debate. For this expert review, the authors advised using a fully covered stent, based on potentially higher risk for tumor ingrowth and reinterventions with uncovered SEMS.
Gastric outlet obstruction
According to the update, patients with gastric outlet obstruction who have good functional status and a life expectancy greater than 2 months should undergo surgical gastrojejunostomy, ideally via a laparoscopic approach instead of an open approach because of shorter hospital stays and less blood loss. If a sufficiently experienced endoscopist is available, an endoscopic ultrasound-guided gastrojejunostomy may be performed, although Dr. Ahmed and colleagues noted that no devices have been approved by the Food and Drug Administration for this technique.
For patients who are not candidates for gastrojejunostomy, enteral stent insertion should be considered; however, they should not be used in patients with severely impaired gastric motility or multiple luminal obstructions “because of limited benefit in these scenarios.” Instead, a venting gastrostomy may be elected.
Colonic obstruction
For patients with malignant colonic obstruction, SEMS may be considered as a “bridge to surgery,” wrote Dr. Ahmed and colleagues, and in the case of proximal or right-sided malignant obstruction, as a bridge to surgery or a palliative measure, keeping in mind “the technical challenges of SEMS insertion in those areas.”
Extracolonic obstruction
Finally, the expert panel suggested that SEMS may be appropriate for selective extracolonic malignancy if patients are not surgical candidates, noting that SEMS placement in this scenario “is more technically challenging, clinical success rates are more variable, and complications (including stent migration) are more frequent.”
The investigators concluded by advising clinicians to remain within the realm of their abilities when managing MATOs, and to refer when needed.
“[I]t is important for physicians to understand their limits and expertise and recognize when cases are best managed at experienced high-volume centers,” they wrote.
The clinical practice update expert review was commissioned and approved by the AGA Institute Clinical Practice Updates Committee and the AGA Governing Board. Dr. Lee disclosed a relationship with Boston Scientific.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
ESC heart failure guideline to integrate bounty of new meds
Today there are so many evidence-based drug therapies for heart failure with reduced ejection fraction (HFrEF) that physicians treating HF patients almost don’t know what to do them.
It’s an exciting new age that way, but to many vexingly unclear how best to merge the shiny new options with mainstay regimens based on time-honored renin-angiotensin system (RAS) inhibitors and beta-blockers.
To impart some clarity, the authors of a new HF guideline document recently took center stage at the Heart Failure Association of the European Society of Cardiology (ESC-HFA) annual meeting to preview their updated recommendations, with novel twists based on recent major trials, for the new age of HF pharmacotherapeutics.
The guideline committee considered the evidence base that existed “up until the end of March of this year,” Theresa A. McDonagh, MD, King’s College London, said during the presentation. The document “is now finalized, it’s with the publishers, and it will be presented in full with simultaneous publication at the ESC meeting” that starts August 27.
It describes a game plan, already followed by some clinicians in practice without official guidance, for initiating drugs from each of four classes in virtually all patients with HFrEF.
New indicated drugs, new perspective for HFrEF
Three of the drug categories are old acquaintances. Among them are the RAS inhibitors, which include angiotensin-receptor/neprilysin inhibitors, beta-blockers, and the mineralocorticoid receptor antagonists. The latter drugs are gaining new respect after having been underplayed in HF prescribing despite longstanding evidence of efficacy.
Completing the quartet of first-line HFrEF drug classes is a recent arrival to the HF arena, the sodium-glucose cotransporter 2 inhibitors.
“We now have new data and a simplified treatment algorithm for heart failure with reduced ejection fraction based on the early administration of the four major classes of drugs,” said Marco Metra, MD, University of Brescia (Italy), previewing the medical-therapy portions of the new guideline at the ESC-HFA sessions, which launched virtually and live in Florence, Italy, on July 29.
The new game plan offers a simple answer to a once-common but complex question: How and in what order are the different drug classes initiated in patients with HFrEF? In the new document, the stated goal is to get them all on board expeditiously and safely, by any means possible.
The guideline writers did not specify a sequence, preferring to leave that decision to physicians, said Dr. Metra, who stated only two guiding principles. The first is to consider the patient’s unique circumstances. The order in which the drugs are introduced might vary, depending on, for example, whether the patient has low or high blood pressure or renal dysfunction.
Second, “it is very important that we try to give all four classes of drugs to the patient in the shortest time possible, because this saves lives,” he said.
That there is no recommendation on sequencing the drugs has led some to the wrong interpretation that all should be started at once, observed coauthor Javed Butler, MD, MPH, University of Mississippi, Jackson, as a panelist during the presentation. Far from it, he said. “The doctor with the patient in front of you can make the best decision. The idea here is to get all the therapies on as soon as possible, as safely as possible.”
“The order in which they are introduced is not really important,” agreed Vijay Chopra, MD, Max Super Specialty Hospital Saket, New Delhi, another coauthor on the panel. “The important thing is that at least some dose of all the four drugs needs to be introduced in the first 4-6 weeks, and then up-titrated.”
Other medical therapy can be more tailored, Dr. Metra noted, such as loop diuretics for patients with congestion, iron for those with iron deficiency, and other drugs depending on whether there is, for example, atrial fibrillation or coronary disease.
Adoption of emerging definitions
The document adopts the emerging characterization of HFrEF by a left ventricular ejection fraction (LVEF) up to 40%.
And it will leverage an expanding evidence base for medication in a segment of patients once said to have HF with preserved ejection fraction (HFpEF), who had therefore lacked specific, guideline-directed medical therapies. Now, patients with an LVEF of 41%-49% will be said to have HF with mildly reduced ejection fraction (HFmrEF), a tweak to the recently introduced HF with “mid-range” LVEF that is designed to assert its nature as something to treat. The new document’s HFmrEF recommendations come with various class and level-of-evidence ratings.
That leaves HFpEF to be characterized by an LVEF of 50% in combination with structural or functional abnormalities associated with LV diastolic dysfunction or raised LV filling pressures, including raised natriuretic peptide levels.
The definitions are consistent with those proposed internationally by the ESC-HFA, the Heart Failure Society of America, and other groups in a statement published in March.
Expanded HFrEF med landscape
Since the 2016 ESC guideline on HF therapy, Dr. McDonagh said, “there’s been no substantial change in the evidence for many of the classical drugs that we use in heart failure. However, we had a lot of new and exciting evidence to consider,” especially in support of the SGLT2 inhibitors as one of the core medications in HFrEF.
The new data came from two controlled trials in particular. In DAPA-HF, patients with HFrEF who were initially without diabetes and who went on dapagliflozin (Farxiga, AstraZeneca) showed a 27% drop in cardiovascular (CV) death or worsening-HF events over a median of 18 months.
“That was followed up with very concordant results with empagliflozin [Jardiance, Boehringer Ingelheim/Eli Lilly] in HFrEF in the EMPEROR-Reduced trial,” Dr. McDonagh said. In that trial, comparable patients who took empagliflozin showed a 25% drop in a primary endpoint similar to that in DAPA-HF over the median 16-month follow-up.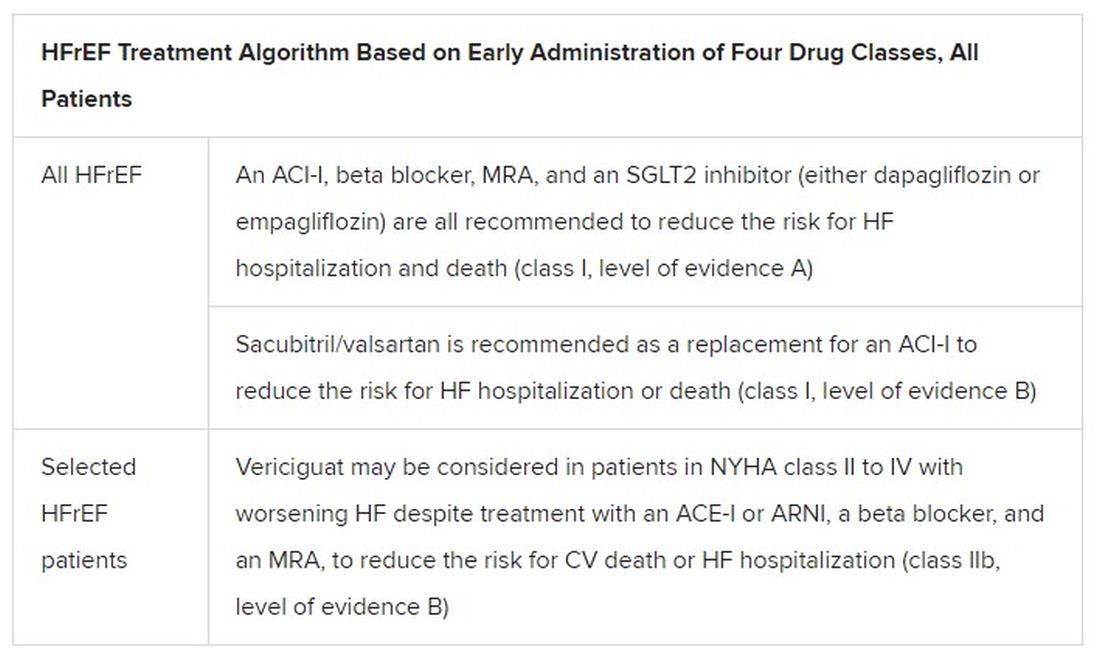
Other HFrEF recommendations are for selected patients. They include ivabradine, already in the guidelines, for patients in sinus rhythm with an elevated resting heart rate who can’t take beta-blockers for whatever reason. But, Dr. McDonagh noted, “we had some new classes of drugs to consider as well.”
In particular, the oral soluble guanylate-cyclase receptor stimulator vericiguat (Verquvo) emerged about a year ago from the VICTORIA trial as a modest success for patients with HFrEF and a previous HF hospitalization. In the trial with more than 5,000 patients, treatment with vericiguat atop standard drug and device therapy was followed by a significant 10% drop in risk for CV death or HF hospitalization.
Available now or likely to be available in the United States, the European Union, Japan, and other countries, vericiguat is recommended in the new guideline for VICTORIA-like patients who don’t adequately respond to other indicated medications.
Little for HFpEF as newly defined
“Almost nothing is new” in the guidelines for HFpEF, Dr. Metra said. The document recommends screening for and treatment of any underlying disorder and comorbidities, plus diuretics for any congestion. “That’s what we have to date.”
But that evidence base might soon change. The new HFpEF recommendations could possibly be up-staged at the ESC sessions by the August 27 scheduled presentation of EMPEROR-Preserved, a randomized test of empagliflozin in HFpEF and – it could be said – HFmrEF. The trial entered patients with chronic HF and an LVEF greater than 40%.
Eli Lilly and Boehringer Ingelheim offered the world a peek at the results, which suggest the SGLT2 inhibitor had a positive impact on the primary endpoint of CV death or HF hospitalization. They announced the cursory top-line outcomes in early July as part of its regulatory obligations, noting that the trial had “met” its primary endpoint.
But many unknowns remain, including the degree of benefit and whether it varied among subgroups, and especially whether outcomes were different for HFmrEF than for HFpEF.
Upgrades for familiar agents
Still, HFmrEF gets noteworthy attention in the document. “For the first time, we have recommendations for these patients,” Dr. Metra said. “We already knew that diuretics are indicated for the treatment of congestion. But now, ACE inhibitors, ARBs, beta-blockers, mineralocorticoid antagonists, as well as sacubitril/valsartan, may be considered to improve outcomes in these patients.” Their upgrades in the new guidelines were based on review of trials in the CHARM program and of TOPCAT and PARAGON-HF, among others, he said.
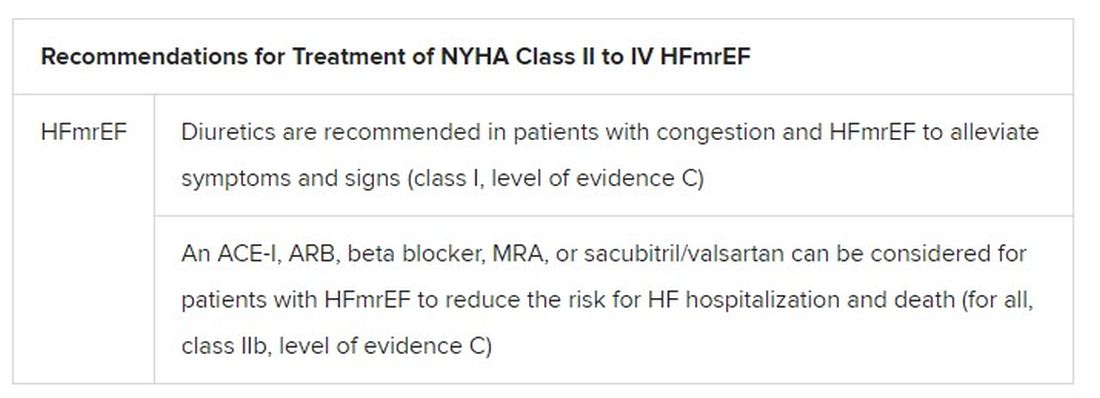
The new document also includes “treatment algorithms based on phenotypes”; that is, comorbidities and less common HF precipitants. For example, “assessment of iron status is now mandated in all patients with heart failure,” Dr. Metra said.
AFFIRM-HF is the key trial in this arena, with its more than 1,100 iron-deficient patients with LVEF less than 50% who had been recently hospitalized for HF. A year of treatment with ferric carboxymaltose (Ferinject/Injectafer, Vifor) led to a 26% drop in risk for HF hospitalization, but without affecting mortality.
For those who are iron deficient, Dr. Metra said, “ferric carboxymaltose intravenously should be considered not only in patients with low ejection fraction and outpatients, but also in patients recently hospitalized for acute heart failure.”
The SGLT2 inhibitors are recommended in HFrEF patients with type 2 diabetes. And treatment with tafamidis (Vyndaqel, Pfizer) in patients with genetic or wild-type transthyretin cardiac amyloidosis gets a class I recommendation based on survival gains seen in the ATTR-ACT trial.
Also recommended is a full CV assessment for patients with cancer who are on cardiotoxic agents or otherwise might be at risk for chemotherapy cardiotoxicity. “Beta-blockers and ACE inhibitors should be considered in those who develop left ventricular systolic dysfunction after anticancer therapy,” Dr. Metra said.
The ongoing pandemic made its mark on the document’s genesis, as it has with most everything else. “For better or worse, we were a ‘COVID guideline,’ ” Dr. McDonagh said. The writing committee consisted of “a large task force of 31 individuals, including two patients,” and there were “only two face-to-face meetings prior to the first wave of COVID hitting Europe.”
The committee voted on each of the recommendations, “and we had to have agreement of more than 75% of the task force to assign a class of recommendation or level of evidence,” she said. “I think we did the best we could in the circumstances. We had the benefit of many discussions over Zoom, and I think at the end of the day we have achieved a consensus.”
With such a large body of participants and the 75% threshold for agreement, “you end up with perhaps a conservative guideline. But that’s not a bad thing for clinical practice, for guidelines to be conservative,” Dr. McDonagh said. “They’re mainly concerned with looking at evidence and safety.”
A version of this article first appeared on Medscape.com.
Today there are so many evidence-based drug therapies for heart failure with reduced ejection fraction (HFrEF) that physicians treating HF patients almost don’t know what to do them.
It’s an exciting new age that way, but to many vexingly unclear how best to merge the shiny new options with mainstay regimens based on time-honored renin-angiotensin system (RAS) inhibitors and beta-blockers.
To impart some clarity, the authors of a new HF guideline document recently took center stage at the Heart Failure Association of the European Society of Cardiology (ESC-HFA) annual meeting to preview their updated recommendations, with novel twists based on recent major trials, for the new age of HF pharmacotherapeutics.
The guideline committee considered the evidence base that existed “up until the end of March of this year,” Theresa A. McDonagh, MD, King’s College London, said during the presentation. The document “is now finalized, it’s with the publishers, and it will be presented in full with simultaneous publication at the ESC meeting” that starts August 27.
It describes a game plan, already followed by some clinicians in practice without official guidance, for initiating drugs from each of four classes in virtually all patients with HFrEF.
New indicated drugs, new perspective for HFrEF
Three of the drug categories are old acquaintances. Among them are the RAS inhibitors, which include angiotensin-receptor/neprilysin inhibitors, beta-blockers, and the mineralocorticoid receptor antagonists. The latter drugs are gaining new respect after having been underplayed in HF prescribing despite longstanding evidence of efficacy.
Completing the quartet of first-line HFrEF drug classes is a recent arrival to the HF arena, the sodium-glucose cotransporter 2 inhibitors.
“We now have new data and a simplified treatment algorithm for heart failure with reduced ejection fraction based on the early administration of the four major classes of drugs,” said Marco Metra, MD, University of Brescia (Italy), previewing the medical-therapy portions of the new guideline at the ESC-HFA sessions, which launched virtually and live in Florence, Italy, on July 29.
The new game plan offers a simple answer to a once-common but complex question: How and in what order are the different drug classes initiated in patients with HFrEF? In the new document, the stated goal is to get them all on board expeditiously and safely, by any means possible.
The guideline writers did not specify a sequence, preferring to leave that decision to physicians, said Dr. Metra, who stated only two guiding principles. The first is to consider the patient’s unique circumstances. The order in which the drugs are introduced might vary, depending on, for example, whether the patient has low or high blood pressure or renal dysfunction.
Second, “it is very important that we try to give all four classes of drugs to the patient in the shortest time possible, because this saves lives,” he said.
That there is no recommendation on sequencing the drugs has led some to the wrong interpretation that all should be started at once, observed coauthor Javed Butler, MD, MPH, University of Mississippi, Jackson, as a panelist during the presentation. Far from it, he said. “The doctor with the patient in front of you can make the best decision. The idea here is to get all the therapies on as soon as possible, as safely as possible.”
“The order in which they are introduced is not really important,” agreed Vijay Chopra, MD, Max Super Specialty Hospital Saket, New Delhi, another coauthor on the panel. “The important thing is that at least some dose of all the four drugs needs to be introduced in the first 4-6 weeks, and then up-titrated.”
Other medical therapy can be more tailored, Dr. Metra noted, such as loop diuretics for patients with congestion, iron for those with iron deficiency, and other drugs depending on whether there is, for example, atrial fibrillation or coronary disease.
Adoption of emerging definitions
The document adopts the emerging characterization of HFrEF by a left ventricular ejection fraction (LVEF) up to 40%.
And it will leverage an expanding evidence base for medication in a segment of patients once said to have HF with preserved ejection fraction (HFpEF), who had therefore lacked specific, guideline-directed medical therapies. Now, patients with an LVEF of 41%-49% will be said to have HF with mildly reduced ejection fraction (HFmrEF), a tweak to the recently introduced HF with “mid-range” LVEF that is designed to assert its nature as something to treat. The new document’s HFmrEF recommendations come with various class and level-of-evidence ratings.
That leaves HFpEF to be characterized by an LVEF of 50% in combination with structural or functional abnormalities associated with LV diastolic dysfunction or raised LV filling pressures, including raised natriuretic peptide levels.
The definitions are consistent with those proposed internationally by the ESC-HFA, the Heart Failure Society of America, and other groups in a statement published in March.
Expanded HFrEF med landscape
Since the 2016 ESC guideline on HF therapy, Dr. McDonagh said, “there’s been no substantial change in the evidence for many of the classical drugs that we use in heart failure. However, we had a lot of new and exciting evidence to consider,” especially in support of the SGLT2 inhibitors as one of the core medications in HFrEF.
The new data came from two controlled trials in particular. In DAPA-HF, patients with HFrEF who were initially without diabetes and who went on dapagliflozin (Farxiga, AstraZeneca) showed a 27% drop in cardiovascular (CV) death or worsening-HF events over a median of 18 months.
“That was followed up with very concordant results with empagliflozin [Jardiance, Boehringer Ingelheim/Eli Lilly] in HFrEF in the EMPEROR-Reduced trial,” Dr. McDonagh said. In that trial, comparable patients who took empagliflozin showed a 25% drop in a primary endpoint similar to that in DAPA-HF over the median 16-month follow-up.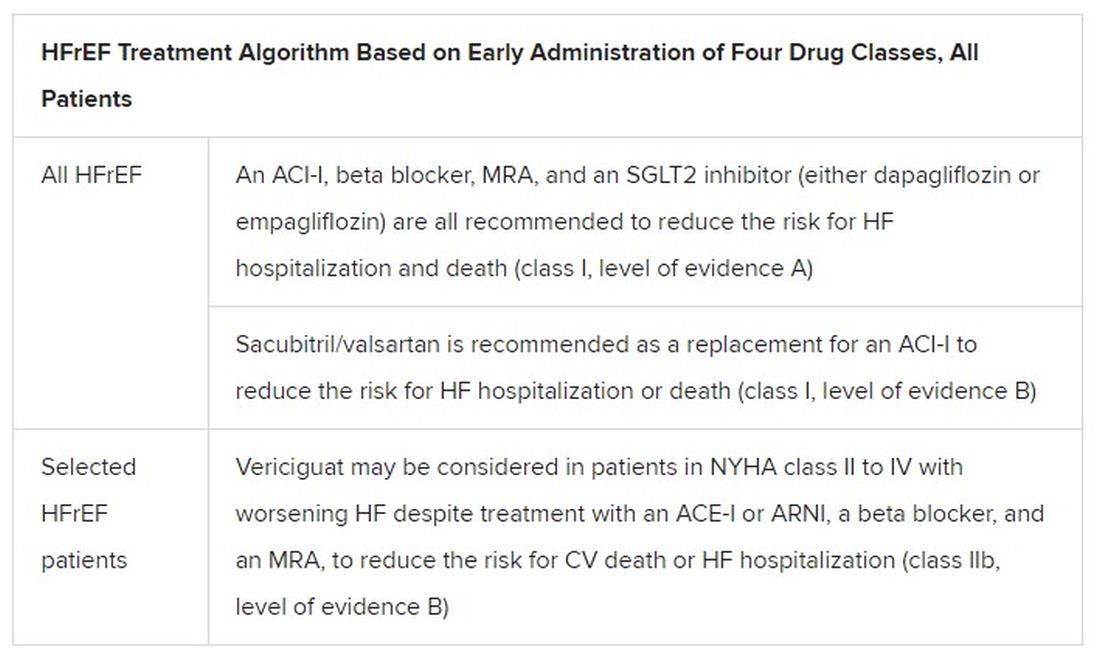
Other HFrEF recommendations are for selected patients. They include ivabradine, already in the guidelines, for patients in sinus rhythm with an elevated resting heart rate who can’t take beta-blockers for whatever reason. But, Dr. McDonagh noted, “we had some new classes of drugs to consider as well.”
In particular, the oral soluble guanylate-cyclase receptor stimulator vericiguat (Verquvo) emerged about a year ago from the VICTORIA trial as a modest success for patients with HFrEF and a previous HF hospitalization. In the trial with more than 5,000 patients, treatment with vericiguat atop standard drug and device therapy was followed by a significant 10% drop in risk for CV death or HF hospitalization.
Available now or likely to be available in the United States, the European Union, Japan, and other countries, vericiguat is recommended in the new guideline for VICTORIA-like patients who don’t adequately respond to other indicated medications.
Little for HFpEF as newly defined
“Almost nothing is new” in the guidelines for HFpEF, Dr. Metra said. The document recommends screening for and treatment of any underlying disorder and comorbidities, plus diuretics for any congestion. “That’s what we have to date.”
But that evidence base might soon change. The new HFpEF recommendations could possibly be up-staged at the ESC sessions by the August 27 scheduled presentation of EMPEROR-Preserved, a randomized test of empagliflozin in HFpEF and – it could be said – HFmrEF. The trial entered patients with chronic HF and an LVEF greater than 40%.
Eli Lilly and Boehringer Ingelheim offered the world a peek at the results, which suggest the SGLT2 inhibitor had a positive impact on the primary endpoint of CV death or HF hospitalization. They announced the cursory top-line outcomes in early July as part of its regulatory obligations, noting that the trial had “met” its primary endpoint.
But many unknowns remain, including the degree of benefit and whether it varied among subgroups, and especially whether outcomes were different for HFmrEF than for HFpEF.
Upgrades for familiar agents
Still, HFmrEF gets noteworthy attention in the document. “For the first time, we have recommendations for these patients,” Dr. Metra said. “We already knew that diuretics are indicated for the treatment of congestion. But now, ACE inhibitors, ARBs, beta-blockers, mineralocorticoid antagonists, as well as sacubitril/valsartan, may be considered to improve outcomes in these patients.” Their upgrades in the new guidelines were based on review of trials in the CHARM program and of TOPCAT and PARAGON-HF, among others, he said.
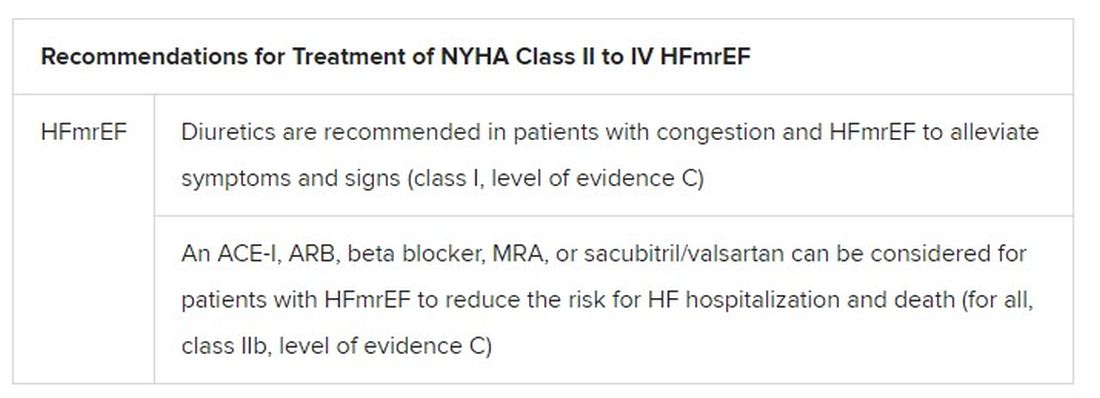
The new document also includes “treatment algorithms based on phenotypes”; that is, comorbidities and less common HF precipitants. For example, “assessment of iron status is now mandated in all patients with heart failure,” Dr. Metra said.
AFFIRM-HF is the key trial in this arena, with its more than 1,100 iron-deficient patients with LVEF less than 50% who had been recently hospitalized for HF. A year of treatment with ferric carboxymaltose (Ferinject/Injectafer, Vifor) led to a 26% drop in risk for HF hospitalization, but without affecting mortality.
For those who are iron deficient, Dr. Metra said, “ferric carboxymaltose intravenously should be considered not only in patients with low ejection fraction and outpatients, but also in patients recently hospitalized for acute heart failure.”
The SGLT2 inhibitors are recommended in HFrEF patients with type 2 diabetes. And treatment with tafamidis (Vyndaqel, Pfizer) in patients with genetic or wild-type transthyretin cardiac amyloidosis gets a class I recommendation based on survival gains seen in the ATTR-ACT trial.
Also recommended is a full CV assessment for patients with cancer who are on cardiotoxic agents or otherwise might be at risk for chemotherapy cardiotoxicity. “Beta-blockers and ACE inhibitors should be considered in those who develop left ventricular systolic dysfunction after anticancer therapy,” Dr. Metra said.
The ongoing pandemic made its mark on the document’s genesis, as it has with most everything else. “For better or worse, we were a ‘COVID guideline,’ ” Dr. McDonagh said. The writing committee consisted of “a large task force of 31 individuals, including two patients,” and there were “only two face-to-face meetings prior to the first wave of COVID hitting Europe.”
The committee voted on each of the recommendations, “and we had to have agreement of more than 75% of the task force to assign a class of recommendation or level of evidence,” she said. “I think we did the best we could in the circumstances. We had the benefit of many discussions over Zoom, and I think at the end of the day we have achieved a consensus.”
With such a large body of participants and the 75% threshold for agreement, “you end up with perhaps a conservative guideline. But that’s not a bad thing for clinical practice, for guidelines to be conservative,” Dr. McDonagh said. “They’re mainly concerned with looking at evidence and safety.”
A version of this article first appeared on Medscape.com.
Today there are so many evidence-based drug therapies for heart failure with reduced ejection fraction (HFrEF) that physicians treating HF patients almost don’t know what to do them.
It’s an exciting new age that way, but to many vexingly unclear how best to merge the shiny new options with mainstay regimens based on time-honored renin-angiotensin system (RAS) inhibitors and beta-blockers.
To impart some clarity, the authors of a new HF guideline document recently took center stage at the Heart Failure Association of the European Society of Cardiology (ESC-HFA) annual meeting to preview their updated recommendations, with novel twists based on recent major trials, for the new age of HF pharmacotherapeutics.
The guideline committee considered the evidence base that existed “up until the end of March of this year,” Theresa A. McDonagh, MD, King’s College London, said during the presentation. The document “is now finalized, it’s with the publishers, and it will be presented in full with simultaneous publication at the ESC meeting” that starts August 27.
It describes a game plan, already followed by some clinicians in practice without official guidance, for initiating drugs from each of four classes in virtually all patients with HFrEF.
New indicated drugs, new perspective for HFrEF
Three of the drug categories are old acquaintances. Among them are the RAS inhibitors, which include angiotensin-receptor/neprilysin inhibitors, beta-blockers, and the mineralocorticoid receptor antagonists. The latter drugs are gaining new respect after having been underplayed in HF prescribing despite longstanding evidence of efficacy.
Completing the quartet of first-line HFrEF drug classes is a recent arrival to the HF arena, the sodium-glucose cotransporter 2 inhibitors.
“We now have new data and a simplified treatment algorithm for heart failure with reduced ejection fraction based on the early administration of the four major classes of drugs,” said Marco Metra, MD, University of Brescia (Italy), previewing the medical-therapy portions of the new guideline at the ESC-HFA sessions, which launched virtually and live in Florence, Italy, on July 29.
The new game plan offers a simple answer to a once-common but complex question: How and in what order are the different drug classes initiated in patients with HFrEF? In the new document, the stated goal is to get them all on board expeditiously and safely, by any means possible.
The guideline writers did not specify a sequence, preferring to leave that decision to physicians, said Dr. Metra, who stated only two guiding principles. The first is to consider the patient’s unique circumstances. The order in which the drugs are introduced might vary, depending on, for example, whether the patient has low or high blood pressure or renal dysfunction.
Second, “it is very important that we try to give all four classes of drugs to the patient in the shortest time possible, because this saves lives,” he said.
That there is no recommendation on sequencing the drugs has led some to the wrong interpretation that all should be started at once, observed coauthor Javed Butler, MD, MPH, University of Mississippi, Jackson, as a panelist during the presentation. Far from it, he said. “The doctor with the patient in front of you can make the best decision. The idea here is to get all the therapies on as soon as possible, as safely as possible.”
“The order in which they are introduced is not really important,” agreed Vijay Chopra, MD, Max Super Specialty Hospital Saket, New Delhi, another coauthor on the panel. “The important thing is that at least some dose of all the four drugs needs to be introduced in the first 4-6 weeks, and then up-titrated.”
Other medical therapy can be more tailored, Dr. Metra noted, such as loop diuretics for patients with congestion, iron for those with iron deficiency, and other drugs depending on whether there is, for example, atrial fibrillation or coronary disease.
Adoption of emerging definitions
The document adopts the emerging characterization of HFrEF by a left ventricular ejection fraction (LVEF) up to 40%.
And it will leverage an expanding evidence base for medication in a segment of patients once said to have HF with preserved ejection fraction (HFpEF), who had therefore lacked specific, guideline-directed medical therapies. Now, patients with an LVEF of 41%-49% will be said to have HF with mildly reduced ejection fraction (HFmrEF), a tweak to the recently introduced HF with “mid-range” LVEF that is designed to assert its nature as something to treat. The new document’s HFmrEF recommendations come with various class and level-of-evidence ratings.
That leaves HFpEF to be characterized by an LVEF of 50% in combination with structural or functional abnormalities associated with LV diastolic dysfunction or raised LV filling pressures, including raised natriuretic peptide levels.
The definitions are consistent with those proposed internationally by the ESC-HFA, the Heart Failure Society of America, and other groups in a statement published in March.
Expanded HFrEF med landscape
Since the 2016 ESC guideline on HF therapy, Dr. McDonagh said, “there’s been no substantial change in the evidence for many of the classical drugs that we use in heart failure. However, we had a lot of new and exciting evidence to consider,” especially in support of the SGLT2 inhibitors as one of the core medications in HFrEF.
The new data came from two controlled trials in particular. In DAPA-HF, patients with HFrEF who were initially without diabetes and who went on dapagliflozin (Farxiga, AstraZeneca) showed a 27% drop in cardiovascular (CV) death or worsening-HF events over a median of 18 months.
“That was followed up with very concordant results with empagliflozin [Jardiance, Boehringer Ingelheim/Eli Lilly] in HFrEF in the EMPEROR-Reduced trial,” Dr. McDonagh said. In that trial, comparable patients who took empagliflozin showed a 25% drop in a primary endpoint similar to that in DAPA-HF over the median 16-month follow-up.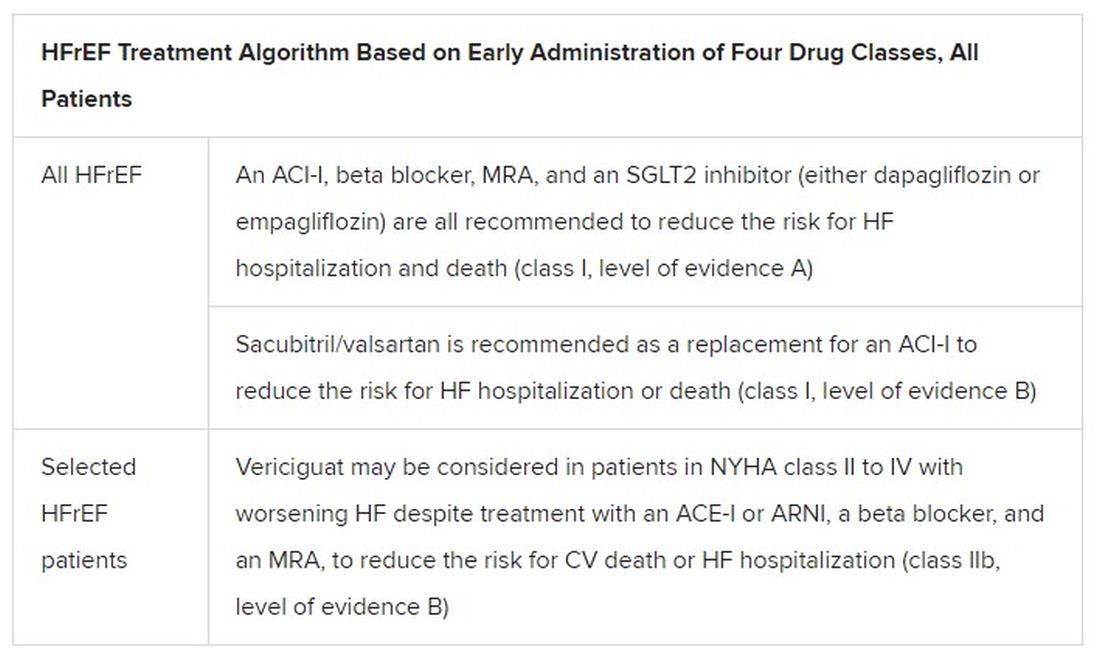
Other HFrEF recommendations are for selected patients. They include ivabradine, already in the guidelines, for patients in sinus rhythm with an elevated resting heart rate who can’t take beta-blockers for whatever reason. But, Dr. McDonagh noted, “we had some new classes of drugs to consider as well.”
In particular, the oral soluble guanylate-cyclase receptor stimulator vericiguat (Verquvo) emerged about a year ago from the VICTORIA trial as a modest success for patients with HFrEF and a previous HF hospitalization. In the trial with more than 5,000 patients, treatment with vericiguat atop standard drug and device therapy was followed by a significant 10% drop in risk for CV death or HF hospitalization.
Available now or likely to be available in the United States, the European Union, Japan, and other countries, vericiguat is recommended in the new guideline for VICTORIA-like patients who don’t adequately respond to other indicated medications.
Little for HFpEF as newly defined
“Almost nothing is new” in the guidelines for HFpEF, Dr. Metra said. The document recommends screening for and treatment of any underlying disorder and comorbidities, plus diuretics for any congestion. “That’s what we have to date.”
But that evidence base might soon change. The new HFpEF recommendations could possibly be up-staged at the ESC sessions by the August 27 scheduled presentation of EMPEROR-Preserved, a randomized test of empagliflozin in HFpEF and – it could be said – HFmrEF. The trial entered patients with chronic HF and an LVEF greater than 40%.
Eli Lilly and Boehringer Ingelheim offered the world a peek at the results, which suggest the SGLT2 inhibitor had a positive impact on the primary endpoint of CV death or HF hospitalization. They announced the cursory top-line outcomes in early July as part of its regulatory obligations, noting that the trial had “met” its primary endpoint.
But many unknowns remain, including the degree of benefit and whether it varied among subgroups, and especially whether outcomes were different for HFmrEF than for HFpEF.
Upgrades for familiar agents
Still, HFmrEF gets noteworthy attention in the document. “For the first time, we have recommendations for these patients,” Dr. Metra said. “We already knew that diuretics are indicated for the treatment of congestion. But now, ACE inhibitors, ARBs, beta-blockers, mineralocorticoid antagonists, as well as sacubitril/valsartan, may be considered to improve outcomes in these patients.” Their upgrades in the new guidelines were based on review of trials in the CHARM program and of TOPCAT and PARAGON-HF, among others, he said.
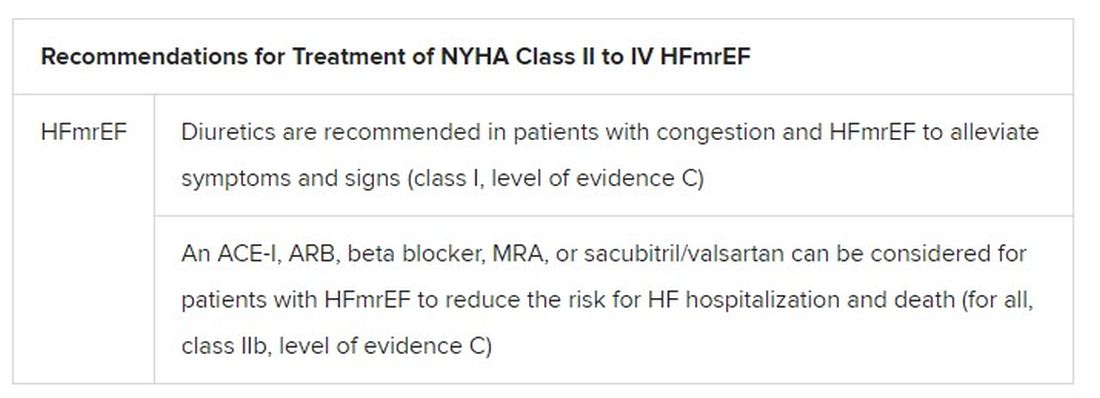
The new document also includes “treatment algorithms based on phenotypes”; that is, comorbidities and less common HF precipitants. For example, “assessment of iron status is now mandated in all patients with heart failure,” Dr. Metra said.
AFFIRM-HF is the key trial in this arena, with its more than 1,100 iron-deficient patients with LVEF less than 50% who had been recently hospitalized for HF. A year of treatment with ferric carboxymaltose (Ferinject/Injectafer, Vifor) led to a 26% drop in risk for HF hospitalization, but without affecting mortality.
For those who are iron deficient, Dr. Metra said, “ferric carboxymaltose intravenously should be considered not only in patients with low ejection fraction and outpatients, but also in patients recently hospitalized for acute heart failure.”
The SGLT2 inhibitors are recommended in HFrEF patients with type 2 diabetes. And treatment with tafamidis (Vyndaqel, Pfizer) in patients with genetic or wild-type transthyretin cardiac amyloidosis gets a class I recommendation based on survival gains seen in the ATTR-ACT trial.
Also recommended is a full CV assessment for patients with cancer who are on cardiotoxic agents or otherwise might be at risk for chemotherapy cardiotoxicity. “Beta-blockers and ACE inhibitors should be considered in those who develop left ventricular systolic dysfunction after anticancer therapy,” Dr. Metra said.
The ongoing pandemic made its mark on the document’s genesis, as it has with most everything else. “For better or worse, we were a ‘COVID guideline,’ ” Dr. McDonagh said. The writing committee consisted of “a large task force of 31 individuals, including two patients,” and there were “only two face-to-face meetings prior to the first wave of COVID hitting Europe.”
The committee voted on each of the recommendations, “and we had to have agreement of more than 75% of the task force to assign a class of recommendation or level of evidence,” she said. “I think we did the best we could in the circumstances. We had the benefit of many discussions over Zoom, and I think at the end of the day we have achieved a consensus.”
With such a large body of participants and the 75% threshold for agreement, “you end up with perhaps a conservative guideline. But that’s not a bad thing for clinical practice, for guidelines to be conservative,” Dr. McDonagh said. “They’re mainly concerned with looking at evidence and safety.”
A version of this article first appeared on Medscape.com.
ACC issues decision pathway for hypertriglyceridemia management
A new decision pathway for the management of hypertriglyceridemia, prompted by a large and growing body of evidence that elevated triglycerides to a targetable risk factor for atherosclerotic cardiovascular disease (ASCVD), has been issued by the American College of Cardiology.
According to the chairman of the writing committee, Salim S. Virani, MD, PhD, the recommendations amplify and update more than alter the hypertriglyceridemia treatment recommendations in the 2018 joint multisociety blood cholesterol guidelines issued in 2018.
This decision pathway, however, is focused on triglycerides alone.
“The previous guidelines included a section on strategies for addressing hypertriglyceridemia to reduce ASCVD risk, but this new decision pathway builds on the recommendations with more details and with additional information,” explained Dr. Virani, professor of medicine in the section of cardiovascular research, Baylor College of Medicine, Houston.
Within this newly published document, the definitions of hypertriglyceridemia and rationale for treatment are followed by detailed algorithms for four specific patient groups with varying triglyceride levels:
- Adults with ASCVD.
- Adults at least 40 years of age with diabetes but no ASCVD.
- Adults at least 20 years of age with no ASCVD or diabetes.
- Adults at least 20 years of age with severe hypertriglyceridemia.
“In the design of these algorithms, we made an active effort to make them suitable for use by primary care physicians as well as specialists,” said Dr. Virani. Despite “lots of boxes and arrows,” the flowcharts for each of these patient groups permit clinicians to follow the decision pathway without having to reread the text.
The common emphasis in all four algorithms is to begin by evaluating patients for secondary causes of hypertriglyceridemia, such as multifactorial chylomicronemia syndrome and other diseases associated with elevated triglycerides. The next steps, also common to all algorithms, are to optimize diet and lifestyle changes that lower triglycerides, optimize glycemic control, and optimize statin therapy.
“Although commonly recognized for their impact on LDL-C, statins also provide a 10%-30% dose-dependent reduction in triglycerides in patients with elevated levels,” the guidelines state. Statins are considered a fundamental step to secondary prevention of ASCVD regardless of triglyceride levels.
Once treatable causes or contributors to hypertriglyceridemia have been addressed, lifestyle interventions and statin therapy have been optimized, pharmacologic therapy directed specifically at control of hypertriglyceridemia “can be considered” in those at highest risk of ASCVD events, but Dr. Virani explained that this is never an early or first step in control of elevated triglycerides.
“The entire working group agreed that lifestyle interventions should be highlighted front and center before considering any other intervention,” Dr. Virani explained.
Pharmacologic therapy for hypertriglyceridemia is not ignored. Prescription omega-3 fatty acid products are preferred over nonprescription dietary supplements, which may vary in quality and purity. But these products, rather than a standalone solution, are best applied within the context of efforts to improve diet, lower body weight, and increase physical activity.
Several trials have associated ethyl ester and carboxylic acid preparations with meaningful reductions in triglycerides, but these drugs, including icosapent ethyl (IPE), are not without adverse events. In the pivotal REDUCE-IT trial, IPE was linked with an increased risk of atrial fibrillation relative to placebo.
IPE is “the best option” and the only therapy with an indication for reduction in ASCVD risk, according to Dr. Virani, but he explained that safety concerns led the authors of the new decision pathway to employ cautious language in regard to its use, suggesting that it be “considered” in high-risk patients after other methods of lowering triglycerides have been optimized.
In the algorithm for the four different risk groups, the decision pathways follow stratifications for different levels of hypertriglyceridemia (defined under fasting and nonfasting conditions) and also for specific levels of LDL cholesterol. ASCVD risk assessment is also a factor in determining the next steps along the decision pathway.
According to Michael Davidson, MD, director of the lipid clinic at the University of Chicago, the emphasis on lifestyle changes for hypertriglyceridemia and the prudent language in regard to pharmacologic therapy is appropriate.
“In light of the controversies regarding the REDUCE-IT trial, the writing committee has done a nice job with providing useful guidance regarding the utilization of icosapent ethyl in higher risk patients,” Dr. Davidson said.
Calling the ACC decision pathway “a welcome enhancement of the 2018 ACC/AHA cholesterol guidelines,” Dr. Davidson praised the way in which the limitations of the evidence regarding pharmacologic therapies were explained.
“Most importantly, this decision pathway helps clinicians appreciate that hypertriglyceridemia can be best managed with lifestyle changes and addressing potential secondary causes,” Dr. Davidson said.
Dr. Virani reports no potential conflicts of interest. Dr. Davidson reports financial relationships with multiple pharmaceutical companies including those making or pursuing therapies for control of hypertriglyceridemia.
A new decision pathway for the management of hypertriglyceridemia, prompted by a large and growing body of evidence that elevated triglycerides to a targetable risk factor for atherosclerotic cardiovascular disease (ASCVD), has been issued by the American College of Cardiology.
According to the chairman of the writing committee, Salim S. Virani, MD, PhD, the recommendations amplify and update more than alter the hypertriglyceridemia treatment recommendations in the 2018 joint multisociety blood cholesterol guidelines issued in 2018.
This decision pathway, however, is focused on triglycerides alone.
“The previous guidelines included a section on strategies for addressing hypertriglyceridemia to reduce ASCVD risk, but this new decision pathway builds on the recommendations with more details and with additional information,” explained Dr. Virani, professor of medicine in the section of cardiovascular research, Baylor College of Medicine, Houston.
Within this newly published document, the definitions of hypertriglyceridemia and rationale for treatment are followed by detailed algorithms for four specific patient groups with varying triglyceride levels:
- Adults with ASCVD.
- Adults at least 40 years of age with diabetes but no ASCVD.
- Adults at least 20 years of age with no ASCVD or diabetes.
- Adults at least 20 years of age with severe hypertriglyceridemia.
“In the design of these algorithms, we made an active effort to make them suitable for use by primary care physicians as well as specialists,” said Dr. Virani. Despite “lots of boxes and arrows,” the flowcharts for each of these patient groups permit clinicians to follow the decision pathway without having to reread the text.
The common emphasis in all four algorithms is to begin by evaluating patients for secondary causes of hypertriglyceridemia, such as multifactorial chylomicronemia syndrome and other diseases associated with elevated triglycerides. The next steps, also common to all algorithms, are to optimize diet and lifestyle changes that lower triglycerides, optimize glycemic control, and optimize statin therapy.
“Although commonly recognized for their impact on LDL-C, statins also provide a 10%-30% dose-dependent reduction in triglycerides in patients with elevated levels,” the guidelines state. Statins are considered a fundamental step to secondary prevention of ASCVD regardless of triglyceride levels.
Once treatable causes or contributors to hypertriglyceridemia have been addressed, lifestyle interventions and statin therapy have been optimized, pharmacologic therapy directed specifically at control of hypertriglyceridemia “can be considered” in those at highest risk of ASCVD events, but Dr. Virani explained that this is never an early or first step in control of elevated triglycerides.
“The entire working group agreed that lifestyle interventions should be highlighted front and center before considering any other intervention,” Dr. Virani explained.
Pharmacologic therapy for hypertriglyceridemia is not ignored. Prescription omega-3 fatty acid products are preferred over nonprescription dietary supplements, which may vary in quality and purity. But these products, rather than a standalone solution, are best applied within the context of efforts to improve diet, lower body weight, and increase physical activity.
Several trials have associated ethyl ester and carboxylic acid preparations with meaningful reductions in triglycerides, but these drugs, including icosapent ethyl (IPE), are not without adverse events. In the pivotal REDUCE-IT trial, IPE was linked with an increased risk of atrial fibrillation relative to placebo.
IPE is “the best option” and the only therapy with an indication for reduction in ASCVD risk, according to Dr. Virani, but he explained that safety concerns led the authors of the new decision pathway to employ cautious language in regard to its use, suggesting that it be “considered” in high-risk patients after other methods of lowering triglycerides have been optimized.
In the algorithm for the four different risk groups, the decision pathways follow stratifications for different levels of hypertriglyceridemia (defined under fasting and nonfasting conditions) and also for specific levels of LDL cholesterol. ASCVD risk assessment is also a factor in determining the next steps along the decision pathway.
According to Michael Davidson, MD, director of the lipid clinic at the University of Chicago, the emphasis on lifestyle changes for hypertriglyceridemia and the prudent language in regard to pharmacologic therapy is appropriate.
“In light of the controversies regarding the REDUCE-IT trial, the writing committee has done a nice job with providing useful guidance regarding the utilization of icosapent ethyl in higher risk patients,” Dr. Davidson said.
Calling the ACC decision pathway “a welcome enhancement of the 2018 ACC/AHA cholesterol guidelines,” Dr. Davidson praised the way in which the limitations of the evidence regarding pharmacologic therapies were explained.
“Most importantly, this decision pathway helps clinicians appreciate that hypertriglyceridemia can be best managed with lifestyle changes and addressing potential secondary causes,” Dr. Davidson said.
Dr. Virani reports no potential conflicts of interest. Dr. Davidson reports financial relationships with multiple pharmaceutical companies including those making or pursuing therapies for control of hypertriglyceridemia.
A new decision pathway for the management of hypertriglyceridemia, prompted by a large and growing body of evidence that elevated triglycerides to a targetable risk factor for atherosclerotic cardiovascular disease (ASCVD), has been issued by the American College of Cardiology.
According to the chairman of the writing committee, Salim S. Virani, MD, PhD, the recommendations amplify and update more than alter the hypertriglyceridemia treatment recommendations in the 2018 joint multisociety blood cholesterol guidelines issued in 2018.
This decision pathway, however, is focused on triglycerides alone.
“The previous guidelines included a section on strategies for addressing hypertriglyceridemia to reduce ASCVD risk, but this new decision pathway builds on the recommendations with more details and with additional information,” explained Dr. Virani, professor of medicine in the section of cardiovascular research, Baylor College of Medicine, Houston.
Within this newly published document, the definitions of hypertriglyceridemia and rationale for treatment are followed by detailed algorithms for four specific patient groups with varying triglyceride levels:
- Adults with ASCVD.
- Adults at least 40 years of age with diabetes but no ASCVD.
- Adults at least 20 years of age with no ASCVD or diabetes.
- Adults at least 20 years of age with severe hypertriglyceridemia.
“In the design of these algorithms, we made an active effort to make them suitable for use by primary care physicians as well as specialists,” said Dr. Virani. Despite “lots of boxes and arrows,” the flowcharts for each of these patient groups permit clinicians to follow the decision pathway without having to reread the text.
The common emphasis in all four algorithms is to begin by evaluating patients for secondary causes of hypertriglyceridemia, such as multifactorial chylomicronemia syndrome and other diseases associated with elevated triglycerides. The next steps, also common to all algorithms, are to optimize diet and lifestyle changes that lower triglycerides, optimize glycemic control, and optimize statin therapy.
“Although commonly recognized for their impact on LDL-C, statins also provide a 10%-30% dose-dependent reduction in triglycerides in patients with elevated levels,” the guidelines state. Statins are considered a fundamental step to secondary prevention of ASCVD regardless of triglyceride levels.
Once treatable causes or contributors to hypertriglyceridemia have been addressed, lifestyle interventions and statin therapy have been optimized, pharmacologic therapy directed specifically at control of hypertriglyceridemia “can be considered” in those at highest risk of ASCVD events, but Dr. Virani explained that this is never an early or first step in control of elevated triglycerides.
“The entire working group agreed that lifestyle interventions should be highlighted front and center before considering any other intervention,” Dr. Virani explained.
Pharmacologic therapy for hypertriglyceridemia is not ignored. Prescription omega-3 fatty acid products are preferred over nonprescription dietary supplements, which may vary in quality and purity. But these products, rather than a standalone solution, are best applied within the context of efforts to improve diet, lower body weight, and increase physical activity.
Several trials have associated ethyl ester and carboxylic acid preparations with meaningful reductions in triglycerides, but these drugs, including icosapent ethyl (IPE), are not without adverse events. In the pivotal REDUCE-IT trial, IPE was linked with an increased risk of atrial fibrillation relative to placebo.
IPE is “the best option” and the only therapy with an indication for reduction in ASCVD risk, according to Dr. Virani, but he explained that safety concerns led the authors of the new decision pathway to employ cautious language in regard to its use, suggesting that it be “considered” in high-risk patients after other methods of lowering triglycerides have been optimized.
In the algorithm for the four different risk groups, the decision pathways follow stratifications for different levels of hypertriglyceridemia (defined under fasting and nonfasting conditions) and also for specific levels of LDL cholesterol. ASCVD risk assessment is also a factor in determining the next steps along the decision pathway.
According to Michael Davidson, MD, director of the lipid clinic at the University of Chicago, the emphasis on lifestyle changes for hypertriglyceridemia and the prudent language in regard to pharmacologic therapy is appropriate.
“In light of the controversies regarding the REDUCE-IT trial, the writing committee has done a nice job with providing useful guidance regarding the utilization of icosapent ethyl in higher risk patients,” Dr. Davidson said.
Calling the ACC decision pathway “a welcome enhancement of the 2018 ACC/AHA cholesterol guidelines,” Dr. Davidson praised the way in which the limitations of the evidence regarding pharmacologic therapies were explained.
“Most importantly, this decision pathway helps clinicians appreciate that hypertriglyceridemia can be best managed with lifestyle changes and addressing potential secondary causes,” Dr. Davidson said.
Dr. Virani reports no potential conflicts of interest. Dr. Davidson reports financial relationships with multiple pharmaceutical companies including those making or pursuing therapies for control of hypertriglyceridemia.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
The febrile infant: New AAP guidance for the first 2 months of life
Sixteen years in the making, the American Academy of Pediatrics just released a new clinical practice guideline (CPG), “Evaluation and Management of Well-Appearing Febrile Infants 8-60 Days Old”. The recommendations were derived from interpretations of sequential studies in young, febrile, but well-appearing infants that covered invasive bacterial infection (IBI) incidence, diagnostic modalities, and treatment during the first 2 months of life, further refining approaches to evaluation and empirical treatment.
Pediatricians have long had solid information to help assess the risk for IBI among febrile infants aged 0-3 months, but there has been an ongoing desire to further refine the suggested evaluation of these very young infants. A study of febrile infants from the Pediatric Research in Office Settings network along with subsequent evidence has identified the first 3 weeks of life as the period of highest risk for IBI, with risk declining in a graded fashion aged between 22 and 56 days.
Critical caveats
First, some caveats. Infants 0-7 days are not addressed in the CPG, and all should be treated as high risk and receive full IBI evaluation according to newborn protocols. Second, the recommendations apply only to “well-appearing” infants. Any ill-appearing infant should be treated as high risk and receive full IBI evaluation and begun on empirical antimicrobials. Third, even though the CPG deals with infants as young as 8-21 days old, the recommendations are to treat all infants in this age group as high risk, even if well-appearing, and complete full IBI evaluation and empirical therapy while awaiting results. Fourth, these guidelines apply only to infants born at 37 weeks’ gestation or more. Finally, the new CPG action statements are meant to be recommendations rather than a standard of medical care, leaving some leeway for clinician interpretation of individual patient scenarios. Where appropriate, parents’ values and preferences should be incorporated as part of shared decision-making.
The CPG divides young, febrile infants into three cohorts based on age:
- 8-21 days old
- 22-28 days old
- 29-60 days old
Age 8-21 days
For well-appearing febrile infants 8-21 days old, the CPG recommends a complete IBI evaluation that includes urine, blood, and cerebrospinal fluid (CSF) for culture, approaching all infants in this cohort as high risk. Inflammatory markers may be obtained, but the evidence is not comprehensive enough to evaluate their role in decision-making for this age group. A two-step urine evaluation method (urine analysis followed by culture if the urine analysis looks concerning) is not recommended for infants aged 8-21 days. Urine samples for culture from these young infants should be obtained by catheterization or suprapubic aspiration.
The CPG recommends drawing blood cultures and CSF by lumbar puncture from this cohort. These infants should be admitted to the hospital, treated empirically with antimicrobials, and actively monitored. However, if the cultures are negative at 24-36 hours, the clinician should discontinue antimicrobials and discharge the infant if there is no other reason for continued hospitalization.
Age 22-28 days
Well-appearing, febrile infants 22-28 days old are in an intermediate-risk zone. The recommendation for infants in this cohort is to obtain a urine specimen by catheterization or suprapubic aspiration for both urine analysis and culture. Clinicians may consider obtaining urine samples for analysis noninvasively (e.g., urine bag) in this cohort, but this is not the preferred method.
Blood culture should be obtained from all infants in this group. Inflammatory markers can help clinicians identify infants at greater risk for IBI, including meningitis. Previous data suggested that inflammatory markers such as serum white blood cell counts greater than 11,000/mcL, a serum absolute neutrophil count of greater than 4,000/mcL, and elevated C-reactive protein and procalcitonin levels could help providers identify febrile infants with true IBI. A 2008 study demonstrated that procalcitonin had the best receiver operating characteristic curve in regard to predicting IBI in young febrile infants. Other research backed up that finding and identified cutoff values for procalcitonin levels greater than 1.0 ng/mL. The CPG recommends considering a procalcitonin value of 0.5 ng/mL or higher as positive, indicating that the infant is at greater risk for IBI and potentially should undergo an expanded IBI workup. Therefore, in infants aged 22-28 days, inflammatory markers can play a role in deciding whether to perform a lumbar puncture.
Many more nuanced recommendations for whether to and how to empirically treat with antimicrobials in this cohort can be found in the CPG, including whether to manage in the hospital or at home. Treatment recommendations vary greatly for this cohort on the basis of the tests obtained and whether tests were positive or negative at the initial evaluation.
Age 29-60 days
The CPG will be most helpful when clinicians are faced with well-appearing, febrile infants in the 29- to 60-day age group. As with the other groups, a urine evaluation is recommended; however, the CPG suggests that the two-step approach – obtaining a urine analysis by a noninvasive method and only obtaining culture if the urine analysis is positive – is reasonable. This means that a bag or free-flowing urine specimen would be appropriate for urinalysis, followed by catheterization/suprapubic aspiration if a culture is necessary. This would save approximately 90% of infants from invasive urine collection. Regardless, only catheter or suprapubic specimens are appropriate for urine culture.
The CPG also recommends that clinicians obtain blood culture on all of these infants. Inflammatory markers should be assessed in this cohort because avoiding lumbar puncture for CSF culture would be appropriate in this cohort if the inflammatory markers are negative. If CSF is obtained in this age cohort, enterovirus testing should be added to the testing regimen. Again, for any infant considered at higher risk for IBI on the basis of screening tests, the CPG recommends a 24- to 36-hour rule-out period with empirical antimicrobial treatment and active monitoring in the hospital.
Summary
The recommended approach for febrile infants 8-21 days old is relatively aggressive, with urine, blood, and CSF evaluation for IBI. Clinicians gain some leeway for infants age 22-28 days, but the guidelines recommend a more flexible approach to evaluating well-appearing, febrile infants age 29-60 days, when a two-step urine evaluation and inflammatory marker assessment can help clinicians and parents have a better discussion about the risk-benefit trade-offs of more aggressive testing and empirical treatment.
The author would like to thank Ken Roberts, MD, for his review and helpful comments on this summary of the CPG highlights. Summary points of the CPG were presented by the writing group at the 2021 Pediatric Academic Societies meeting.
William T. Basco, Jr, MD, MS, is a professor of pediatrics at the Medical University of South Carolina, Charleston, and director of the division of general pediatrics. He is an active health services researcher and has published more than 60 manuscripts in the peer-reviewed literature.
A version of this article first appeared on Medscape.com.
Sixteen years in the making, the American Academy of Pediatrics just released a new clinical practice guideline (CPG), “Evaluation and Management of Well-Appearing Febrile Infants 8-60 Days Old”. The recommendations were derived from interpretations of sequential studies in young, febrile, but well-appearing infants that covered invasive bacterial infection (IBI) incidence, diagnostic modalities, and treatment during the first 2 months of life, further refining approaches to evaluation and empirical treatment.
Pediatricians have long had solid information to help assess the risk for IBI among febrile infants aged 0-3 months, but there has been an ongoing desire to further refine the suggested evaluation of these very young infants. A study of febrile infants from the Pediatric Research in Office Settings network along with subsequent evidence has identified the first 3 weeks of life as the period of highest risk for IBI, with risk declining in a graded fashion aged between 22 and 56 days.
Critical caveats
First, some caveats. Infants 0-7 days are not addressed in the CPG, and all should be treated as high risk and receive full IBI evaluation according to newborn protocols. Second, the recommendations apply only to “well-appearing” infants. Any ill-appearing infant should be treated as high risk and receive full IBI evaluation and begun on empirical antimicrobials. Third, even though the CPG deals with infants as young as 8-21 days old, the recommendations are to treat all infants in this age group as high risk, even if well-appearing, and complete full IBI evaluation and empirical therapy while awaiting results. Fourth, these guidelines apply only to infants born at 37 weeks’ gestation or more. Finally, the new CPG action statements are meant to be recommendations rather than a standard of medical care, leaving some leeway for clinician interpretation of individual patient scenarios. Where appropriate, parents’ values and preferences should be incorporated as part of shared decision-making.
The CPG divides young, febrile infants into three cohorts based on age:
- 8-21 days old
- 22-28 days old
- 29-60 days old
Age 8-21 days
For well-appearing febrile infants 8-21 days old, the CPG recommends a complete IBI evaluation that includes urine, blood, and cerebrospinal fluid (CSF) for culture, approaching all infants in this cohort as high risk. Inflammatory markers may be obtained, but the evidence is not comprehensive enough to evaluate their role in decision-making for this age group. A two-step urine evaluation method (urine analysis followed by culture if the urine analysis looks concerning) is not recommended for infants aged 8-21 days. Urine samples for culture from these young infants should be obtained by catheterization or suprapubic aspiration.
The CPG recommends drawing blood cultures and CSF by lumbar puncture from this cohort. These infants should be admitted to the hospital, treated empirically with antimicrobials, and actively monitored. However, if the cultures are negative at 24-36 hours, the clinician should discontinue antimicrobials and discharge the infant if there is no other reason for continued hospitalization.
Age 22-28 days
Well-appearing, febrile infants 22-28 days old are in an intermediate-risk zone. The recommendation for infants in this cohort is to obtain a urine specimen by catheterization or suprapubic aspiration for both urine analysis and culture. Clinicians may consider obtaining urine samples for analysis noninvasively (e.g., urine bag) in this cohort, but this is not the preferred method.
Blood culture should be obtained from all infants in this group. Inflammatory markers can help clinicians identify infants at greater risk for IBI, including meningitis. Previous data suggested that inflammatory markers such as serum white blood cell counts greater than 11,000/mcL, a serum absolute neutrophil count of greater than 4,000/mcL, and elevated C-reactive protein and procalcitonin levels could help providers identify febrile infants with true IBI. A 2008 study demonstrated that procalcitonin had the best receiver operating characteristic curve in regard to predicting IBI in young febrile infants. Other research backed up that finding and identified cutoff values for procalcitonin levels greater than 1.0 ng/mL. The CPG recommends considering a procalcitonin value of 0.5 ng/mL or higher as positive, indicating that the infant is at greater risk for IBI and potentially should undergo an expanded IBI workup. Therefore, in infants aged 22-28 days, inflammatory markers can play a role in deciding whether to perform a lumbar puncture.
Many more nuanced recommendations for whether to and how to empirically treat with antimicrobials in this cohort can be found in the CPG, including whether to manage in the hospital or at home. Treatment recommendations vary greatly for this cohort on the basis of the tests obtained and whether tests were positive or negative at the initial evaluation.
Age 29-60 days
The CPG will be most helpful when clinicians are faced with well-appearing, febrile infants in the 29- to 60-day age group. As with the other groups, a urine evaluation is recommended; however, the CPG suggests that the two-step approach – obtaining a urine analysis by a noninvasive method and only obtaining culture if the urine analysis is positive – is reasonable. This means that a bag or free-flowing urine specimen would be appropriate for urinalysis, followed by catheterization/suprapubic aspiration if a culture is necessary. This would save approximately 90% of infants from invasive urine collection. Regardless, only catheter or suprapubic specimens are appropriate for urine culture.
The CPG also recommends that clinicians obtain blood culture on all of these infants. Inflammatory markers should be assessed in this cohort because avoiding lumbar puncture for CSF culture would be appropriate in this cohort if the inflammatory markers are negative. If CSF is obtained in this age cohort, enterovirus testing should be added to the testing regimen. Again, for any infant considered at higher risk for IBI on the basis of screening tests, the CPG recommends a 24- to 36-hour rule-out period with empirical antimicrobial treatment and active monitoring in the hospital.
Summary
The recommended approach for febrile infants 8-21 days old is relatively aggressive, with urine, blood, and CSF evaluation for IBI. Clinicians gain some leeway for infants age 22-28 days, but the guidelines recommend a more flexible approach to evaluating well-appearing, febrile infants age 29-60 days, when a two-step urine evaluation and inflammatory marker assessment can help clinicians and parents have a better discussion about the risk-benefit trade-offs of more aggressive testing and empirical treatment.
The author would like to thank Ken Roberts, MD, for his review and helpful comments on this summary of the CPG highlights. Summary points of the CPG were presented by the writing group at the 2021 Pediatric Academic Societies meeting.
William T. Basco, Jr, MD, MS, is a professor of pediatrics at the Medical University of South Carolina, Charleston, and director of the division of general pediatrics. He is an active health services researcher and has published more than 60 manuscripts in the peer-reviewed literature.
A version of this article first appeared on Medscape.com.
Sixteen years in the making, the American Academy of Pediatrics just released a new clinical practice guideline (CPG), “Evaluation and Management of Well-Appearing Febrile Infants 8-60 Days Old”. The recommendations were derived from interpretations of sequential studies in young, febrile, but well-appearing infants that covered invasive bacterial infection (IBI) incidence, diagnostic modalities, and treatment during the first 2 months of life, further refining approaches to evaluation and empirical treatment.
Pediatricians have long had solid information to help assess the risk for IBI among febrile infants aged 0-3 months, but there has been an ongoing desire to further refine the suggested evaluation of these very young infants. A study of febrile infants from the Pediatric Research in Office Settings network along with subsequent evidence has identified the first 3 weeks of life as the period of highest risk for IBI, with risk declining in a graded fashion aged between 22 and 56 days.
Critical caveats
First, some caveats. Infants 0-7 days are not addressed in the CPG, and all should be treated as high risk and receive full IBI evaluation according to newborn protocols. Second, the recommendations apply only to “well-appearing” infants. Any ill-appearing infant should be treated as high risk and receive full IBI evaluation and begun on empirical antimicrobials. Third, even though the CPG deals with infants as young as 8-21 days old, the recommendations are to treat all infants in this age group as high risk, even if well-appearing, and complete full IBI evaluation and empirical therapy while awaiting results. Fourth, these guidelines apply only to infants born at 37 weeks’ gestation or more. Finally, the new CPG action statements are meant to be recommendations rather than a standard of medical care, leaving some leeway for clinician interpretation of individual patient scenarios. Where appropriate, parents’ values and preferences should be incorporated as part of shared decision-making.
The CPG divides young, febrile infants into three cohorts based on age:
- 8-21 days old
- 22-28 days old
- 29-60 days old
Age 8-21 days
For well-appearing febrile infants 8-21 days old, the CPG recommends a complete IBI evaluation that includes urine, blood, and cerebrospinal fluid (CSF) for culture, approaching all infants in this cohort as high risk. Inflammatory markers may be obtained, but the evidence is not comprehensive enough to evaluate their role in decision-making for this age group. A two-step urine evaluation method (urine analysis followed by culture if the urine analysis looks concerning) is not recommended for infants aged 8-21 days. Urine samples for culture from these young infants should be obtained by catheterization or suprapubic aspiration.
The CPG recommends drawing blood cultures and CSF by lumbar puncture from this cohort. These infants should be admitted to the hospital, treated empirically with antimicrobials, and actively monitored. However, if the cultures are negative at 24-36 hours, the clinician should discontinue antimicrobials and discharge the infant if there is no other reason for continued hospitalization.
Age 22-28 days
Well-appearing, febrile infants 22-28 days old are in an intermediate-risk zone. The recommendation for infants in this cohort is to obtain a urine specimen by catheterization or suprapubic aspiration for both urine analysis and culture. Clinicians may consider obtaining urine samples for analysis noninvasively (e.g., urine bag) in this cohort, but this is not the preferred method.
Blood culture should be obtained from all infants in this group. Inflammatory markers can help clinicians identify infants at greater risk for IBI, including meningitis. Previous data suggested that inflammatory markers such as serum white blood cell counts greater than 11,000/mcL, a serum absolute neutrophil count of greater than 4,000/mcL, and elevated C-reactive protein and procalcitonin levels could help providers identify febrile infants with true IBI. A 2008 study demonstrated that procalcitonin had the best receiver operating characteristic curve in regard to predicting IBI in young febrile infants. Other research backed up that finding and identified cutoff values for procalcitonin levels greater than 1.0 ng/mL. The CPG recommends considering a procalcitonin value of 0.5 ng/mL or higher as positive, indicating that the infant is at greater risk for IBI and potentially should undergo an expanded IBI workup. Therefore, in infants aged 22-28 days, inflammatory markers can play a role in deciding whether to perform a lumbar puncture.
Many more nuanced recommendations for whether to and how to empirically treat with antimicrobials in this cohort can be found in the CPG, including whether to manage in the hospital or at home. Treatment recommendations vary greatly for this cohort on the basis of the tests obtained and whether tests were positive or negative at the initial evaluation.
Age 29-60 days
The CPG will be most helpful when clinicians are faced with well-appearing, febrile infants in the 29- to 60-day age group. As with the other groups, a urine evaluation is recommended; however, the CPG suggests that the two-step approach – obtaining a urine analysis by a noninvasive method and only obtaining culture if the urine analysis is positive – is reasonable. This means that a bag or free-flowing urine specimen would be appropriate for urinalysis, followed by catheterization/suprapubic aspiration if a culture is necessary. This would save approximately 90% of infants from invasive urine collection. Regardless, only catheter or suprapubic specimens are appropriate for urine culture.
The CPG also recommends that clinicians obtain blood culture on all of these infants. Inflammatory markers should be assessed in this cohort because avoiding lumbar puncture for CSF culture would be appropriate in this cohort if the inflammatory markers are negative. If CSF is obtained in this age cohort, enterovirus testing should be added to the testing regimen. Again, for any infant considered at higher risk for IBI on the basis of screening tests, the CPG recommends a 24- to 36-hour rule-out period with empirical antimicrobial treatment and active monitoring in the hospital.
Summary
The recommended approach for febrile infants 8-21 days old is relatively aggressive, with urine, blood, and CSF evaluation for IBI. Clinicians gain some leeway for infants age 22-28 days, but the guidelines recommend a more flexible approach to evaluating well-appearing, febrile infants age 29-60 days, when a two-step urine evaluation and inflammatory marker assessment can help clinicians and parents have a better discussion about the risk-benefit trade-offs of more aggressive testing and empirical treatment.
The author would like to thank Ken Roberts, MD, for his review and helpful comments on this summary of the CPG highlights. Summary points of the CPG were presented by the writing group at the 2021 Pediatric Academic Societies meeting.
William T. Basco, Jr, MD, MS, is a professor of pediatrics at the Medical University of South Carolina, Charleston, and director of the division of general pediatrics. He is an active health services researcher and has published more than 60 manuscripts in the peer-reviewed literature.
A version of this article first appeared on Medscape.com.
Three new ACR guidelines recommend treatment for six forms of vasculitis
Three new guidelines from the American College of Rheumatology, in partnership with the Vasculitis Foundation, offer evidence-based recommendations for managing and treating six different forms of systemic vasculitis.
“It’s not unusual for many rheumatologists to have fairly limited experience caring for patients with vasculitis,” coauthor Sharon Chung, MD, director of the Vasculitis Clinic at the University of California, San Francisco, said in an interview. “And with limited experience comes anxiety and concerns about whether or not one is treating patients appropriately. First and foremost, these guidelines are to help rheumatologists who may not have experience treating patients with vasculitides, to provide them with a framework they can use.”
The guidelines – the first to be produced and endorsed by both the ACR and the Vasculitis Foundation – were published July 8 in both Arthritis & Rheumatology and Arthritis Care & Research.
To assess the recent expansion in diagnostic and treatment options for various forms of vasculitis, the ACR assembled a literature review team, an 11-person patient panel, and a voting panel – made up of 9 adult rheumatologists, 5 pediatric rheumatologists, and 2 patients – to evaluate evidence, provide feedback, and formulate and vote on recommendations, respectively. The guidelines cover six types of vasculitis: one focusing on giant cell arteritis (GCA) and Takayasu arteritis (TAK); one on polyarteritis nodosa (PAN), and another on three forms of antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV): granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA).
As with other ACR guidelines, these three were developed via the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology, which was used to rate the quality of the gathered evidence. For a recommendation to be published, it required 70% consensus or greater from the voting panel.
GCA and TAK guideline
Regarding the management and treatment of GCA and TAK, the guideline offers 42 recommendations and three ungraded position statements. Due to the low quality of evidence – “reflecting the paucity of randomized clinical trials in these diseases,” the authors noted – only one of the GCA recommendations and one of the TAK recommendations are strong; the rest are conditional.
For patients with GCA, the guideline strongly recommends long-term clinical monitoring over no clinical monitoring for anyone in apparent clinical remission. Other notable recommendations include favoring oral glucocorticoids (GCs) with tocilizumab (Actemra) over oral glucocorticoids alone in newly diagnosed GCA, adding a non-GC immunosuppressive agent to oral GCs for GCA patients with active extracranial large vessel involvement, and preferring temporary artery biopsy as their “diagnostic test of choice at this time.”
“The Europeans generally are more comfortable relying on temporal artery ultrasound,” Robert F. Spiera, MD, director of the vasculitis and scleroderma program at the Hospital for Special Surgery, New York, said in an interview. “In this country, possibly in part due to less uniform expertise in performing these ultrasounds, we have not had as much success in terms of accuracy.
These ACR guidelines therefore recommended biopsy to establish the diagnosis in patients with cranial presentations, whereas in the EULAR guidelines, ultrasound was felt to be preferable to biopsy.”
“While we have temporal artery ultrasound available in the United States, we just don’t have the expertise at this point to perform or interpret that test like the European rheumatologists do,” Dr. Chung agreed. “But I think we’re all hopeful that experience with temporal artery ultrasound will improve in the future, so we can use that test instead of an invasive biopsy.”
Dr. Spiera, who was not a coauthor on any of the guidelines, also highlighted the conditional recommendation of noninvasive vascular imaging of the large vessels in patients with newly diagnosed GCA.
“It is well recognized that a substantial portion of patients with GCA have unrecognized evidence of large vessel involvement, and patients with GCA in general are at higher risk of aneurysms later in the disease course,” he said. “These guidelines suggest screening even patients with purely cranial presentations for large vessel involvement with imaging to possibly identify the patients at higher risk for those later complications.
“What they didn’t offer were recommendations on how to follow up on that imaging,” he added, “which is an important and as-yet-unanswered question.”
For patients with TAK, the guideline again strongly recommends long-term clinical monitoring over no clinical monitoring for anyone in apparent clinical remission. Other conditional recommendations include choosing a non-GC immunosuppressive agent such as methotrexate or a tumor necrosis factor (TNF) inhibitor over tocilizumab as initial therapy because “the efficacy of tocilizumab in TAK is not established at this time.”
AAV guideline
Regarding the management and treatment of GPA, MPA, and EGPA, the guideline offers 41 recommendations and 10 ungraded position statements. All recommendations were conditional, and many address GPA and MPA together because, as the authors noted, “pivotal trials have enrolled both groups and presented results for these diseases together.”
One notable recommendation is their preference for rituximab over cyclophosphamide for remission induction and for rituximab over methotrexate or azathioprine for remission maintenance in patients with severe GPA or MPA. “I don’t think this is a surprise to people, but I think it reaffirms where our current practice is moving,” Dr. Chung said.
“The literature supports that in patients with relapsing disease, rituximab works better than cyclophosphamide for remission induction,” Dr. Spiera said. “But in these guidelines, even in new disease, rituximab is suggested as the agent of choice to induce remission. I would say that that is reasonable, but you could make an argument that it’s maybe beyond what the literature supports, particularly in patients with advanced renal insufficiency attributable to that initial vasculitis flare.”
Other recommendations include being against routinely adding plasma exchange to remission induction therapy in GPA or MPA patients with active glomerulonephritis – although they added that it should be considered in patients at high risk of end-stage kidney disease – as well as preferring cyclophosphamide or rituximab over mepolizumab for remission induction in patients with severe EGPA.
“We, to the surprise of many, were more supportive for the use of rituximab in EGPA than others were expecting, given the limited evidence,” Dr. Chung said. “One of the reasons for that is the wide experience we’ve had with rituximab in GPA and MPA, and our recognition that there is a population of patients with EGPA who are ANCA positive who do seem to benefit from rituximab therapy.”
And although the voting panel strongly favored treatment with methotrexate or azathioprine over trimethoprim/sulfamethoxazole for GPA patients in remission, they ultimately labeled the recommendation as conditional “due to the lack of sufficient high-quality evidence comparing the two treatments.”
“There has been progress in terms of well-done clinical trials to inform our decision-making, particularly for ANCA-associated vasculitis, both in terms of how to induce and maintain remission,” Dr. Spiera said. “Though the recommendations were conditional, I think there’s very strong data to support many of them.”
PAN guideline
Regarding the management and treatment of PAN, the guideline offers 16 recommendations – all but one are conditional – and one ungraded position statement. Their strong recommendation was for treatment with TNF inhibitors over GCs in patients with clinical manifestations of deficiency of adenosine deaminase 2, which they asked doctors to consider “in the setting of a PAN-like syndrome with strokes.” Other conditional recommendations include treating patients with newly diagnosed, severe PAN with cyclophosphamide and GCs, as well as the use of abdominal vascular imaging and/or a deep-skin biopsy to help establish a diagnosis.
According to the authors, a fourth guideline on treating and managing Kawasaki syndrome will be released in the coming weeks.
The guidelines were supported by the ACR and the Vasculitis Foundation. Several authors acknowledged potential conflicts of interest, including receiving speaking and consulting fees, research grants, and honoraria from various pharmaceutical companies. Dr. Spiera has received grant support or consulting fees from Roche-Genentech, GlaxoSmithKline, Boehringer Ingelheim, Chemocentryx, Corbus, Formation Biologics, InflaRx, Kadmon, AstraZeneca, AbbVie, CSL Behring, Sanofi, and Janssen.
Three new guidelines from the American College of Rheumatology, in partnership with the Vasculitis Foundation, offer evidence-based recommendations for managing and treating six different forms of systemic vasculitis.
“It’s not unusual for many rheumatologists to have fairly limited experience caring for patients with vasculitis,” coauthor Sharon Chung, MD, director of the Vasculitis Clinic at the University of California, San Francisco, said in an interview. “And with limited experience comes anxiety and concerns about whether or not one is treating patients appropriately. First and foremost, these guidelines are to help rheumatologists who may not have experience treating patients with vasculitides, to provide them with a framework they can use.”
The guidelines – the first to be produced and endorsed by both the ACR and the Vasculitis Foundation – were published July 8 in both Arthritis & Rheumatology and Arthritis Care & Research.
To assess the recent expansion in diagnostic and treatment options for various forms of vasculitis, the ACR assembled a literature review team, an 11-person patient panel, and a voting panel – made up of 9 adult rheumatologists, 5 pediatric rheumatologists, and 2 patients – to evaluate evidence, provide feedback, and formulate and vote on recommendations, respectively. The guidelines cover six types of vasculitis: one focusing on giant cell arteritis (GCA) and Takayasu arteritis (TAK); one on polyarteritis nodosa (PAN), and another on three forms of antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV): granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA).
As with other ACR guidelines, these three were developed via the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology, which was used to rate the quality of the gathered evidence. For a recommendation to be published, it required 70% consensus or greater from the voting panel.
GCA and TAK guideline
Regarding the management and treatment of GCA and TAK, the guideline offers 42 recommendations and three ungraded position statements. Due to the low quality of evidence – “reflecting the paucity of randomized clinical trials in these diseases,” the authors noted – only one of the GCA recommendations and one of the TAK recommendations are strong; the rest are conditional.
For patients with GCA, the guideline strongly recommends long-term clinical monitoring over no clinical monitoring for anyone in apparent clinical remission. Other notable recommendations include favoring oral glucocorticoids (GCs) with tocilizumab (Actemra) over oral glucocorticoids alone in newly diagnosed GCA, adding a non-GC immunosuppressive agent to oral GCs for GCA patients with active extracranial large vessel involvement, and preferring temporary artery biopsy as their “diagnostic test of choice at this time.”
“The Europeans generally are more comfortable relying on temporal artery ultrasound,” Robert F. Spiera, MD, director of the vasculitis and scleroderma program at the Hospital for Special Surgery, New York, said in an interview. “In this country, possibly in part due to less uniform expertise in performing these ultrasounds, we have not had as much success in terms of accuracy.
These ACR guidelines therefore recommended biopsy to establish the diagnosis in patients with cranial presentations, whereas in the EULAR guidelines, ultrasound was felt to be preferable to biopsy.”
“While we have temporal artery ultrasound available in the United States, we just don’t have the expertise at this point to perform or interpret that test like the European rheumatologists do,” Dr. Chung agreed. “But I think we’re all hopeful that experience with temporal artery ultrasound will improve in the future, so we can use that test instead of an invasive biopsy.”
Dr. Spiera, who was not a coauthor on any of the guidelines, also highlighted the conditional recommendation of noninvasive vascular imaging of the large vessels in patients with newly diagnosed GCA.
“It is well recognized that a substantial portion of patients with GCA have unrecognized evidence of large vessel involvement, and patients with GCA in general are at higher risk of aneurysms later in the disease course,” he said. “These guidelines suggest screening even patients with purely cranial presentations for large vessel involvement with imaging to possibly identify the patients at higher risk for those later complications.
“What they didn’t offer were recommendations on how to follow up on that imaging,” he added, “which is an important and as-yet-unanswered question.”
For patients with TAK, the guideline again strongly recommends long-term clinical monitoring over no clinical monitoring for anyone in apparent clinical remission. Other conditional recommendations include choosing a non-GC immunosuppressive agent such as methotrexate or a tumor necrosis factor (TNF) inhibitor over tocilizumab as initial therapy because “the efficacy of tocilizumab in TAK is not established at this time.”
AAV guideline
Regarding the management and treatment of GPA, MPA, and EGPA, the guideline offers 41 recommendations and 10 ungraded position statements. All recommendations were conditional, and many address GPA and MPA together because, as the authors noted, “pivotal trials have enrolled both groups and presented results for these diseases together.”
One notable recommendation is their preference for rituximab over cyclophosphamide for remission induction and for rituximab over methotrexate or azathioprine for remission maintenance in patients with severe GPA or MPA. “I don’t think this is a surprise to people, but I think it reaffirms where our current practice is moving,” Dr. Chung said.
“The literature supports that in patients with relapsing disease, rituximab works better than cyclophosphamide for remission induction,” Dr. Spiera said. “But in these guidelines, even in new disease, rituximab is suggested as the agent of choice to induce remission. I would say that that is reasonable, but you could make an argument that it’s maybe beyond what the literature supports, particularly in patients with advanced renal insufficiency attributable to that initial vasculitis flare.”
Other recommendations include being against routinely adding plasma exchange to remission induction therapy in GPA or MPA patients with active glomerulonephritis – although they added that it should be considered in patients at high risk of end-stage kidney disease – as well as preferring cyclophosphamide or rituximab over mepolizumab for remission induction in patients with severe EGPA.
“We, to the surprise of many, were more supportive for the use of rituximab in EGPA than others were expecting, given the limited evidence,” Dr. Chung said. “One of the reasons for that is the wide experience we’ve had with rituximab in GPA and MPA, and our recognition that there is a population of patients with EGPA who are ANCA positive who do seem to benefit from rituximab therapy.”
And although the voting panel strongly favored treatment with methotrexate or azathioprine over trimethoprim/sulfamethoxazole for GPA patients in remission, they ultimately labeled the recommendation as conditional “due to the lack of sufficient high-quality evidence comparing the two treatments.”
“There has been progress in terms of well-done clinical trials to inform our decision-making, particularly for ANCA-associated vasculitis, both in terms of how to induce and maintain remission,” Dr. Spiera said. “Though the recommendations were conditional, I think there’s very strong data to support many of them.”
PAN guideline
Regarding the management and treatment of PAN, the guideline offers 16 recommendations – all but one are conditional – and one ungraded position statement. Their strong recommendation was for treatment with TNF inhibitors over GCs in patients with clinical manifestations of deficiency of adenosine deaminase 2, which they asked doctors to consider “in the setting of a PAN-like syndrome with strokes.” Other conditional recommendations include treating patients with newly diagnosed, severe PAN with cyclophosphamide and GCs, as well as the use of abdominal vascular imaging and/or a deep-skin biopsy to help establish a diagnosis.
According to the authors, a fourth guideline on treating and managing Kawasaki syndrome will be released in the coming weeks.
The guidelines were supported by the ACR and the Vasculitis Foundation. Several authors acknowledged potential conflicts of interest, including receiving speaking and consulting fees, research grants, and honoraria from various pharmaceutical companies. Dr. Spiera has received grant support or consulting fees from Roche-Genentech, GlaxoSmithKline, Boehringer Ingelheim, Chemocentryx, Corbus, Formation Biologics, InflaRx, Kadmon, AstraZeneca, AbbVie, CSL Behring, Sanofi, and Janssen.
Three new guidelines from the American College of Rheumatology, in partnership with the Vasculitis Foundation, offer evidence-based recommendations for managing and treating six different forms of systemic vasculitis.
“It’s not unusual for many rheumatologists to have fairly limited experience caring for patients with vasculitis,” coauthor Sharon Chung, MD, director of the Vasculitis Clinic at the University of California, San Francisco, said in an interview. “And with limited experience comes anxiety and concerns about whether or not one is treating patients appropriately. First and foremost, these guidelines are to help rheumatologists who may not have experience treating patients with vasculitides, to provide them with a framework they can use.”
The guidelines – the first to be produced and endorsed by both the ACR and the Vasculitis Foundation – were published July 8 in both Arthritis & Rheumatology and Arthritis Care & Research.
To assess the recent expansion in diagnostic and treatment options for various forms of vasculitis, the ACR assembled a literature review team, an 11-person patient panel, and a voting panel – made up of 9 adult rheumatologists, 5 pediatric rheumatologists, and 2 patients – to evaluate evidence, provide feedback, and formulate and vote on recommendations, respectively. The guidelines cover six types of vasculitis: one focusing on giant cell arteritis (GCA) and Takayasu arteritis (TAK); one on polyarteritis nodosa (PAN), and another on three forms of antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV): granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA).
As with other ACR guidelines, these three were developed via the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology, which was used to rate the quality of the gathered evidence. For a recommendation to be published, it required 70% consensus or greater from the voting panel.
GCA and TAK guideline
Regarding the management and treatment of GCA and TAK, the guideline offers 42 recommendations and three ungraded position statements. Due to the low quality of evidence – “reflecting the paucity of randomized clinical trials in these diseases,” the authors noted – only one of the GCA recommendations and one of the TAK recommendations are strong; the rest are conditional.
For patients with GCA, the guideline strongly recommends long-term clinical monitoring over no clinical monitoring for anyone in apparent clinical remission. Other notable recommendations include favoring oral glucocorticoids (GCs) with tocilizumab (Actemra) over oral glucocorticoids alone in newly diagnosed GCA, adding a non-GC immunosuppressive agent to oral GCs for GCA patients with active extracranial large vessel involvement, and preferring temporary artery biopsy as their “diagnostic test of choice at this time.”
“The Europeans generally are more comfortable relying on temporal artery ultrasound,” Robert F. Spiera, MD, director of the vasculitis and scleroderma program at the Hospital for Special Surgery, New York, said in an interview. “In this country, possibly in part due to less uniform expertise in performing these ultrasounds, we have not had as much success in terms of accuracy.
These ACR guidelines therefore recommended biopsy to establish the diagnosis in patients with cranial presentations, whereas in the EULAR guidelines, ultrasound was felt to be preferable to biopsy.”
“While we have temporal artery ultrasound available in the United States, we just don’t have the expertise at this point to perform or interpret that test like the European rheumatologists do,” Dr. Chung agreed. “But I think we’re all hopeful that experience with temporal artery ultrasound will improve in the future, so we can use that test instead of an invasive biopsy.”
Dr. Spiera, who was not a coauthor on any of the guidelines, also highlighted the conditional recommendation of noninvasive vascular imaging of the large vessels in patients with newly diagnosed GCA.
“It is well recognized that a substantial portion of patients with GCA have unrecognized evidence of large vessel involvement, and patients with GCA in general are at higher risk of aneurysms later in the disease course,” he said. “These guidelines suggest screening even patients with purely cranial presentations for large vessel involvement with imaging to possibly identify the patients at higher risk for those later complications.
“What they didn’t offer were recommendations on how to follow up on that imaging,” he added, “which is an important and as-yet-unanswered question.”
For patients with TAK, the guideline again strongly recommends long-term clinical monitoring over no clinical monitoring for anyone in apparent clinical remission. Other conditional recommendations include choosing a non-GC immunosuppressive agent such as methotrexate or a tumor necrosis factor (TNF) inhibitor over tocilizumab as initial therapy because “the efficacy of tocilizumab in TAK is not established at this time.”
AAV guideline
Regarding the management and treatment of GPA, MPA, and EGPA, the guideline offers 41 recommendations and 10 ungraded position statements. All recommendations were conditional, and many address GPA and MPA together because, as the authors noted, “pivotal trials have enrolled both groups and presented results for these diseases together.”
One notable recommendation is their preference for rituximab over cyclophosphamide for remission induction and for rituximab over methotrexate or azathioprine for remission maintenance in patients with severe GPA or MPA. “I don’t think this is a surprise to people, but I think it reaffirms where our current practice is moving,” Dr. Chung said.
“The literature supports that in patients with relapsing disease, rituximab works better than cyclophosphamide for remission induction,” Dr. Spiera said. “But in these guidelines, even in new disease, rituximab is suggested as the agent of choice to induce remission. I would say that that is reasonable, but you could make an argument that it’s maybe beyond what the literature supports, particularly in patients with advanced renal insufficiency attributable to that initial vasculitis flare.”
Other recommendations include being against routinely adding plasma exchange to remission induction therapy in GPA or MPA patients with active glomerulonephritis – although they added that it should be considered in patients at high risk of end-stage kidney disease – as well as preferring cyclophosphamide or rituximab over mepolizumab for remission induction in patients with severe EGPA.
“We, to the surprise of many, were more supportive for the use of rituximab in EGPA than others were expecting, given the limited evidence,” Dr. Chung said. “One of the reasons for that is the wide experience we’ve had with rituximab in GPA and MPA, and our recognition that there is a population of patients with EGPA who are ANCA positive who do seem to benefit from rituximab therapy.”
And although the voting panel strongly favored treatment with methotrexate or azathioprine over trimethoprim/sulfamethoxazole for GPA patients in remission, they ultimately labeled the recommendation as conditional “due to the lack of sufficient high-quality evidence comparing the two treatments.”
“There has been progress in terms of well-done clinical trials to inform our decision-making, particularly for ANCA-associated vasculitis, both in terms of how to induce and maintain remission,” Dr. Spiera said. “Though the recommendations were conditional, I think there’s very strong data to support many of them.”
PAN guideline
Regarding the management and treatment of PAN, the guideline offers 16 recommendations – all but one are conditional – and one ungraded position statement. Their strong recommendation was for treatment with TNF inhibitors over GCs in patients with clinical manifestations of deficiency of adenosine deaminase 2, which they asked doctors to consider “in the setting of a PAN-like syndrome with strokes.” Other conditional recommendations include treating patients with newly diagnosed, severe PAN with cyclophosphamide and GCs, as well as the use of abdominal vascular imaging and/or a deep-skin biopsy to help establish a diagnosis.
According to the authors, a fourth guideline on treating and managing Kawasaki syndrome will be released in the coming weeks.
The guidelines were supported by the ACR and the Vasculitis Foundation. Several authors acknowledged potential conflicts of interest, including receiving speaking and consulting fees, research grants, and honoraria from various pharmaceutical companies. Dr. Spiera has received grant support or consulting fees from Roche-Genentech, GlaxoSmithKline, Boehringer Ingelheim, Chemocentryx, Corbus, Formation Biologics, InflaRx, Kadmon, AstraZeneca, AbbVie, CSL Behring, Sanofi, and Janssen.
FROM ARTHRITIS & RHEUMATOLOGY
ADA/EASD draft guidance aims to bring adults with type 1 diabetes out of shadows
A new draft consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes (EASD) addresses diagnosis and management of type 1 diabetes in adults.
The impetus for the document comes from the “highly influential” EASD-ADA consensus report on the management of type 2 diabetes, which led to the realization that a comparable document was needed for adults with type 1 diabetes, said writing panel cochair Anne L. Peters, MD, professor of clinical medicine at the University of Southern California, Los Angeles.
“In recent years, there have been rapid advances in the treatment of type 1 diabetes together with a growing recognition of the psychosocial burden of living with [it],” Dr. Peters said.
She noted that although there is already some guidance available for the management of type 1 diabetes in adults, “this gets admixed into broader guidelines, and many of those are mostly derived from data in people with type 2 diabetes.”
The new draft document was coauthored by 14 content experts in type 1 diabetes, with equal numbers from the United States and Europe.
We want to be helpful to clinicians
Topics covered include diagnosis of type 1 diabetes, goals of therapy and glycemic targets, schedule of care, diabetes self-management education and additional behavioral considerations, glucose monitoring, insulin therapy, hypoglycemia, psychosocial care, diabetic ketoacidosis, pancreas and islet cell transplantation, adjunctive therapies, special populations (including pregnant women, older adults, and inpatient management), and emergent/future perspectives, including beta-cell replacement and immunotherapy.
At the end of the document are tables of glycemic targets for adults with type 1 diabetes, schedule of care, nonglycemic factors that alter A1c levels, standardized continuous glucose meter (CGM) metrics for clinical care, examples of subcutaneous insulin regimens, and the various properties of approved and nonapproved adjunctive therapies for type 1 diabetes, including metformin, pramlintide, GLP-1 agonists, and SGLT2 inhibitors.
Several colorful flowcharts are also provided, including algorithms for diagnosing and managing type 1 diabetes in adults.
Document coauthor M. Sue Kirkman, MD, of the Diabetes Care Center’s Clinical Trials Unit at the University of North Carolina, Chapel Hill, told this news organization: “We want it to be helpful to clinicians who are diagnosing type 1 diabetes in adults or caring for adults with type 1 diabetes, whether diagnosed in childhood or adulthood.”
The authors presented an overview of the document in a symposium on June 28 at the virtual ADA scientific sessions. The final version will be presented Oct. 1 at the EASD 2021 annual meeting.
The draft document and video of the ADA meeting presentation are both available on the ADA website.
New algorithm to reduce misdiagnosis of type 1 diabetes in adults
Misdiagnosis of adult-onset type 1 diabetes is common, occurring in up to 40% of those who develop the condition after age 30 years, said J. Hans de Vries, MD, PhD, medical director, Profil Institute for Metabolic Research, Neuss, Germany.
There are multiple reasons for this, including the fact that obesity and type 2 diabetes are becoming more prevalent at younger ages, C-peptide levels may still be relatively high at the time of clinical type 1 diabetes onset, and islet autoantibodies don’t have 100% positive predictive value.
“No single feature confirms type 1 diabetes in isolation,” Dr. de Vries noted.
The document provides a detailed diagnostic algorithm specifically for adults in whom type 1 diabetes is suspected, starting with autoantibody measurement. If the diagnosis isn’t confirmed that way, the algorithm advises investigating for monogenic diabetes, including use of a maturity-onset diabetes of the young (MODY) calculator and subsequent C-peptide measurement.
Measurement of C-peptide is also recommended if the diabetes type is still uncertain more than 3 years after diabetes onset in those treated with insulin, because by that point it is likely to be <200 pmol/L in people with type 1 diabetes.
Clear statements on diabetes technology, preferred insulins
The draft document clearly states that physiologic insulin replacement using a pump or multiple daily injections, CGM, and analog rather than human insulin are standards of care for adults with type 1 diabetes. Use of hybrid closed-loop insulin delivery systems is advised when available, as they offer the “greatest benefits.”
However, the document also notes that in cases of cost barriers, subcutaneous regimens of human regular and NPH insulin may be used. It cautions, though, that these may result in higher glucose variability, higher risk of hypoglycemia, and less lifestyle flexibility.
Dr. Kirkman told this news organization: “Using human insulins such as NPH and Regular in type 1 diabetes is definitely not preferred, but sometimes due to people’s inability to afford analogs we have to use them. People need to know how to use them safely.”
As for the do-it-yourself insulin delivery systems, which many with type 1 diabetes now use with open-source software algorithms that reverse-engineer older pumps, the document advises that health care providers shouldn’t actively recommend them as they’re not approved by regulatory authorities, but should also “respect the individual’s right to make informed choices and continue to offer support,” Dr. Kirkman said when presenting the insulin therapy section.
Psychosocial aspects of type 1 diabetes ‘underappreciated’
Special emphasis is placed on psychosocial support, which may be overlooked in adults, Dr. Kirkman noted.
“Clinicians probably underappreciate what people with type 1 diabetes go through on a daily basis. A lot of the evidence out there regarding psychosocial issues is in children and families of children with type 1 diabetes, or in adults with type 2 diabetes ... Maximizing quality of life needs to be at the forefront of care, not just focusing on glycemic goals.”
Indeed, between 20% and 40% of people with type 1 diabetes experience diabetes-related emotional distress – including 15% with depression – particularly at the time of diagnosis and when complications develop, noted Frank J. Snoek, PhD, professor of medical psychology at Amsterdam University Medical Center, the Netherlands.
To address this, the draft advises that “self-management difficulties, psychological, and social problems” be screened periodically and monitored using validated screening tools.
“Health care providers should be proficient at asking questions about and discussing emotional health, psychological needs, and social challenges as part of the consultation,” Dr. Snoek said.
Dr. Peters disclosed ties with Abbott Diabetes Care, AstraZeneca, Lilly, Medscape, Novo Nordisk, Vertex, and Zealand, Omada, and Teladoc. Dr. Kirkman has received research support from Novo Nordisk and Bayer. Dr. de Vries disclosed ties with Adocia, Novo Nordisk, Zealand, Eli Lilly, and Afon Technology. Dr. Snoek reported ties with Roche Diabetes, Novo Nordisk, Sanofi, and Eli Lilly.
A version of this article first appeared on Medscape.com.
A new draft consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes (EASD) addresses diagnosis and management of type 1 diabetes in adults.
The impetus for the document comes from the “highly influential” EASD-ADA consensus report on the management of type 2 diabetes, which led to the realization that a comparable document was needed for adults with type 1 diabetes, said writing panel cochair Anne L. Peters, MD, professor of clinical medicine at the University of Southern California, Los Angeles.
“In recent years, there have been rapid advances in the treatment of type 1 diabetes together with a growing recognition of the psychosocial burden of living with [it],” Dr. Peters said.
She noted that although there is already some guidance available for the management of type 1 diabetes in adults, “this gets admixed into broader guidelines, and many of those are mostly derived from data in people with type 2 diabetes.”
The new draft document was coauthored by 14 content experts in type 1 diabetes, with equal numbers from the United States and Europe.
We want to be helpful to clinicians
Topics covered include diagnosis of type 1 diabetes, goals of therapy and glycemic targets, schedule of care, diabetes self-management education and additional behavioral considerations, glucose monitoring, insulin therapy, hypoglycemia, psychosocial care, diabetic ketoacidosis, pancreas and islet cell transplantation, adjunctive therapies, special populations (including pregnant women, older adults, and inpatient management), and emergent/future perspectives, including beta-cell replacement and immunotherapy.
At the end of the document are tables of glycemic targets for adults with type 1 diabetes, schedule of care, nonglycemic factors that alter A1c levels, standardized continuous glucose meter (CGM) metrics for clinical care, examples of subcutaneous insulin regimens, and the various properties of approved and nonapproved adjunctive therapies for type 1 diabetes, including metformin, pramlintide, GLP-1 agonists, and SGLT2 inhibitors.
Several colorful flowcharts are also provided, including algorithms for diagnosing and managing type 1 diabetes in adults.
Document coauthor M. Sue Kirkman, MD, of the Diabetes Care Center’s Clinical Trials Unit at the University of North Carolina, Chapel Hill, told this news organization: “We want it to be helpful to clinicians who are diagnosing type 1 diabetes in adults or caring for adults with type 1 diabetes, whether diagnosed in childhood or adulthood.”
The authors presented an overview of the document in a symposium on June 28 at the virtual ADA scientific sessions. The final version will be presented Oct. 1 at the EASD 2021 annual meeting.
The draft document and video of the ADA meeting presentation are both available on the ADA website.
New algorithm to reduce misdiagnosis of type 1 diabetes in adults
Misdiagnosis of adult-onset type 1 diabetes is common, occurring in up to 40% of those who develop the condition after age 30 years, said J. Hans de Vries, MD, PhD, medical director, Profil Institute for Metabolic Research, Neuss, Germany.
There are multiple reasons for this, including the fact that obesity and type 2 diabetes are becoming more prevalent at younger ages, C-peptide levels may still be relatively high at the time of clinical type 1 diabetes onset, and islet autoantibodies don’t have 100% positive predictive value.
“No single feature confirms type 1 diabetes in isolation,” Dr. de Vries noted.
The document provides a detailed diagnostic algorithm specifically for adults in whom type 1 diabetes is suspected, starting with autoantibody measurement. If the diagnosis isn’t confirmed that way, the algorithm advises investigating for monogenic diabetes, including use of a maturity-onset diabetes of the young (MODY) calculator and subsequent C-peptide measurement.
Measurement of C-peptide is also recommended if the diabetes type is still uncertain more than 3 years after diabetes onset in those treated with insulin, because by that point it is likely to be <200 pmol/L in people with type 1 diabetes.
Clear statements on diabetes technology, preferred insulins
The draft document clearly states that physiologic insulin replacement using a pump or multiple daily injections, CGM, and analog rather than human insulin are standards of care for adults with type 1 diabetes. Use of hybrid closed-loop insulin delivery systems is advised when available, as they offer the “greatest benefits.”
However, the document also notes that in cases of cost barriers, subcutaneous regimens of human regular and NPH insulin may be used. It cautions, though, that these may result in higher glucose variability, higher risk of hypoglycemia, and less lifestyle flexibility.
Dr. Kirkman told this news organization: “Using human insulins such as NPH and Regular in type 1 diabetes is definitely not preferred, but sometimes due to people’s inability to afford analogs we have to use them. People need to know how to use them safely.”
As for the do-it-yourself insulin delivery systems, which many with type 1 diabetes now use with open-source software algorithms that reverse-engineer older pumps, the document advises that health care providers shouldn’t actively recommend them as they’re not approved by regulatory authorities, but should also “respect the individual’s right to make informed choices and continue to offer support,” Dr. Kirkman said when presenting the insulin therapy section.
Psychosocial aspects of type 1 diabetes ‘underappreciated’
Special emphasis is placed on psychosocial support, which may be overlooked in adults, Dr. Kirkman noted.
“Clinicians probably underappreciate what people with type 1 diabetes go through on a daily basis. A lot of the evidence out there regarding psychosocial issues is in children and families of children with type 1 diabetes, or in adults with type 2 diabetes ... Maximizing quality of life needs to be at the forefront of care, not just focusing on glycemic goals.”
Indeed, between 20% and 40% of people with type 1 diabetes experience diabetes-related emotional distress – including 15% with depression – particularly at the time of diagnosis and when complications develop, noted Frank J. Snoek, PhD, professor of medical psychology at Amsterdam University Medical Center, the Netherlands.
To address this, the draft advises that “self-management difficulties, psychological, and social problems” be screened periodically and monitored using validated screening tools.
“Health care providers should be proficient at asking questions about and discussing emotional health, psychological needs, and social challenges as part of the consultation,” Dr. Snoek said.
Dr. Peters disclosed ties with Abbott Diabetes Care, AstraZeneca, Lilly, Medscape, Novo Nordisk, Vertex, and Zealand, Omada, and Teladoc. Dr. Kirkman has received research support from Novo Nordisk and Bayer. Dr. de Vries disclosed ties with Adocia, Novo Nordisk, Zealand, Eli Lilly, and Afon Technology. Dr. Snoek reported ties with Roche Diabetes, Novo Nordisk, Sanofi, and Eli Lilly.
A version of this article first appeared on Medscape.com.
A new draft consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes (EASD) addresses diagnosis and management of type 1 diabetes in adults.
The impetus for the document comes from the “highly influential” EASD-ADA consensus report on the management of type 2 diabetes, which led to the realization that a comparable document was needed for adults with type 1 diabetes, said writing panel cochair Anne L. Peters, MD, professor of clinical medicine at the University of Southern California, Los Angeles.
“In recent years, there have been rapid advances in the treatment of type 1 diabetes together with a growing recognition of the psychosocial burden of living with [it],” Dr. Peters said.
She noted that although there is already some guidance available for the management of type 1 diabetes in adults, “this gets admixed into broader guidelines, and many of those are mostly derived from data in people with type 2 diabetes.”
The new draft document was coauthored by 14 content experts in type 1 diabetes, with equal numbers from the United States and Europe.
We want to be helpful to clinicians
Topics covered include diagnosis of type 1 diabetes, goals of therapy and glycemic targets, schedule of care, diabetes self-management education and additional behavioral considerations, glucose monitoring, insulin therapy, hypoglycemia, psychosocial care, diabetic ketoacidosis, pancreas and islet cell transplantation, adjunctive therapies, special populations (including pregnant women, older adults, and inpatient management), and emergent/future perspectives, including beta-cell replacement and immunotherapy.
At the end of the document are tables of glycemic targets for adults with type 1 diabetes, schedule of care, nonglycemic factors that alter A1c levels, standardized continuous glucose meter (CGM) metrics for clinical care, examples of subcutaneous insulin regimens, and the various properties of approved and nonapproved adjunctive therapies for type 1 diabetes, including metformin, pramlintide, GLP-1 agonists, and SGLT2 inhibitors.
Several colorful flowcharts are also provided, including algorithms for diagnosing and managing type 1 diabetes in adults.
Document coauthor M. Sue Kirkman, MD, of the Diabetes Care Center’s Clinical Trials Unit at the University of North Carolina, Chapel Hill, told this news organization: “We want it to be helpful to clinicians who are diagnosing type 1 diabetes in adults or caring for adults with type 1 diabetes, whether diagnosed in childhood or adulthood.”
The authors presented an overview of the document in a symposium on June 28 at the virtual ADA scientific sessions. The final version will be presented Oct. 1 at the EASD 2021 annual meeting.
The draft document and video of the ADA meeting presentation are both available on the ADA website.
New algorithm to reduce misdiagnosis of type 1 diabetes in adults
Misdiagnosis of adult-onset type 1 diabetes is common, occurring in up to 40% of those who develop the condition after age 30 years, said J. Hans de Vries, MD, PhD, medical director, Profil Institute for Metabolic Research, Neuss, Germany.
There are multiple reasons for this, including the fact that obesity and type 2 diabetes are becoming more prevalent at younger ages, C-peptide levels may still be relatively high at the time of clinical type 1 diabetes onset, and islet autoantibodies don’t have 100% positive predictive value.
“No single feature confirms type 1 diabetes in isolation,” Dr. de Vries noted.
The document provides a detailed diagnostic algorithm specifically for adults in whom type 1 diabetes is suspected, starting with autoantibody measurement. If the diagnosis isn’t confirmed that way, the algorithm advises investigating for monogenic diabetes, including use of a maturity-onset diabetes of the young (MODY) calculator and subsequent C-peptide measurement.
Measurement of C-peptide is also recommended if the diabetes type is still uncertain more than 3 years after diabetes onset in those treated with insulin, because by that point it is likely to be <200 pmol/L in people with type 1 diabetes.
Clear statements on diabetes technology, preferred insulins
The draft document clearly states that physiologic insulin replacement using a pump or multiple daily injections, CGM, and analog rather than human insulin are standards of care for adults with type 1 diabetes. Use of hybrid closed-loop insulin delivery systems is advised when available, as they offer the “greatest benefits.”
However, the document also notes that in cases of cost barriers, subcutaneous regimens of human regular and NPH insulin may be used. It cautions, though, that these may result in higher glucose variability, higher risk of hypoglycemia, and less lifestyle flexibility.
Dr. Kirkman told this news organization: “Using human insulins such as NPH and Regular in type 1 diabetes is definitely not preferred, but sometimes due to people’s inability to afford analogs we have to use them. People need to know how to use them safely.”
As for the do-it-yourself insulin delivery systems, which many with type 1 diabetes now use with open-source software algorithms that reverse-engineer older pumps, the document advises that health care providers shouldn’t actively recommend them as they’re not approved by regulatory authorities, but should also “respect the individual’s right to make informed choices and continue to offer support,” Dr. Kirkman said when presenting the insulin therapy section.
Psychosocial aspects of type 1 diabetes ‘underappreciated’
Special emphasis is placed on psychosocial support, which may be overlooked in adults, Dr. Kirkman noted.
“Clinicians probably underappreciate what people with type 1 diabetes go through on a daily basis. A lot of the evidence out there regarding psychosocial issues is in children and families of children with type 1 diabetes, or in adults with type 2 diabetes ... Maximizing quality of life needs to be at the forefront of care, not just focusing on glycemic goals.”
Indeed, between 20% and 40% of people with type 1 diabetes experience diabetes-related emotional distress – including 15% with depression – particularly at the time of diagnosis and when complications develop, noted Frank J. Snoek, PhD, professor of medical psychology at Amsterdam University Medical Center, the Netherlands.
To address this, the draft advises that “self-management difficulties, psychological, and social problems” be screened periodically and monitored using validated screening tools.
“Health care providers should be proficient at asking questions about and discussing emotional health, psychological needs, and social challenges as part of the consultation,” Dr. Snoek said.
Dr. Peters disclosed ties with Abbott Diabetes Care, AstraZeneca, Lilly, Medscape, Novo Nordisk, Vertex, and Zealand, Omada, and Teladoc. Dr. Kirkman has received research support from Novo Nordisk and Bayer. Dr. de Vries disclosed ties with Adocia, Novo Nordisk, Zealand, Eli Lilly, and Afon Technology. Dr. Snoek reported ties with Roche Diabetes, Novo Nordisk, Sanofi, and Eli Lilly.
A version of this article first appeared on Medscape.com.
South Asian ancestry associated with twice the risk of heart disease
according to the results of a new study.
These findings confirm previous reports and practice guidelines that identify South Asian ancestry as a risk enhancer for atherosclerotic cardiovascular disease (ASCVD), suggesting that earlier heart disease screening and prevention is warranted in this patient population, lead author Aniruddh P. Patel, MD, research fellow at the Center for Genomic Medicine, Massachusetts General Hospital, Boston, and colleagues said.
“Previous studies in multiple countries have estimated a 1.7- to 4-fold higher risk of ASCVD among South Asian individuals, compared with other ancestries, but have important potential limitations,” Dr. Patel and colleagues wrote in the paper on their prospective cohort study, published in Circulation.
The INTERHEART case-control study, for example, which assessed risk factors for acute myocardial infarction among more than 15,000 cases from 52 countries, is now 2 decades old, and “may not reflect recent advances in cardiovascular disease prevention,” the investigators wrote.
Most studies in the area have been small and retrospective, they added, and have not adequately assessed emerging risk factors, such as prediabetes, which appear to play a relatively greater role in the development of heart disease among South Asians.
Methods and results
To address this knowledge gap, Dr. Patel and colleagues analyzed data from the UK Biobank prospective cohort study, including 449,349 middle-aged participants of European ancestry and 8,124 similarly aged participants of South Asian descent who did not have heart disease upon enrollment. Respective rates of incident ASCVD (i.e., MI, ischemic stroke, or coronary revascularization) were analyzed in the context of a variety of lifestyle, anthropometric, and clinical factors.
After a median follow-up of 11.1 years, individuals of South Asian descent had an incident ASCVD rate of 6.8%, compared with 4.4% for individuals of European descent, representing twice the relative risk (adjusted hazard ratio, 2.03; 95% CI, 1.86-2.22; P < .001). Even after accounting for all covariates, risk of ASCVD remained 45% higher for South Asian individuals (aHR, 1.45; 95% CI, 1.28-1.65; P < .001). This elevation in risk was not captured by existing risk calculators, including the American College of Cardiology/American Heart Association Pooled Cohort Equations, or the QRISK3 equations.
The findings were “largely consistent across a range of age, sex, and clinical subgroups,” and “confirm and extend previous reports that hypertension, diabetes, and central adiposity are the leading associations in this observed disparity,” the investigators wrote.
Two diabetes subtypes are more prevalent in South Asians
Hypertension, diabetes, and central adiposity do not fully explain South Asians’ higher risk for ASCVD, wrote Namratha R. Kandula, MD, of Northwestern University Medical Center, Chicago, and Alka M. Kanaya, MD, of the University of California, San Francisco, in an accompanying editorial published in Circulation.
Some of the undetected risk may stem from unique diabetes disease factors, Dr. Kandula and Dr. Kanaya added.
“Newer data have demonstrated distinct subtypes of type 2 diabetes, with South Asians having a higher prevalence of both a severe insulin resistant with obesity subtype and a less recognized severe insulin deficient subtype,” they wrote. “Importantly, both of these more prevalent diabetes subtypes in South Asians were associated with a higher incidence of coronary artery calcium, a marker of subclinical atherosclerosis and strong predictor of future ASCVD, compared to other diabetes subtypes.”
Diabetes rate is higher for South Asians in the U.S.
Although the present study was conducted in the United Kingdom, the findings likely apply to individuals of South Asian ancestry living in the United States, according to principal author Amit V. Khera, MD, associate director of the precision medicine unit at the Center for Genomic Medicine, Massachusetts General Hospital.
“There are already more than 5 million individuals of South Asian ancestry in the U.S. and this represents one of the fastest-growing ethnic subgroups,” Dr. Khera said in an interview. “As in our study of individuals in the U.K., South Asians in the U.S. suffer from diabetes at much higher rates – 23% versus 12% – and this often occurs even in the absence of obesity.”
Dr. Khera noted that the 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease identify South Asian ancestry as a risk-enhancing factor, calling this a “stopgap measure.” More work is needed, he said, in the research arena and in the clinic.
Zero South Asians included in studies used to develop risk estimator
“I think the first step is to simply acknowledge that the risk estimators we use in clinical practice have important limitations when it comes to diverse patient populations,” Dr. Khera said in an interview. “We saw this in our study, where – despite a more than doubling of risk – the predicted risk based on the equations used in primary care showed no difference. This risk estimator was developed based on legacy cohort studies, in [which] zero South Asians were included. Despite important differences across race/ethnicity, the current state-of-the-art in the U.S. is to use one equation for Black individuals and another for all other ethnicities.”
Experts suggest steps for reducing heart disease risk
While risk modeling remains suboptimal, Dr. Khera suggested that clinicians can take immediate steps to reduce the risk of heart disease among individuals with South Asian ancestry.
“Despite all of the uncertainty – we still don’t have a complete understanding of why the risk is so high – there are still several things primary care doctors can do for their patients,” Dr. Khera said.
Foremost, he recommended lifestyle and dietary counseling.
“Dietary counseling is particularly effective if put in the context of cultural norms,” Dr. Khera said. “Many South Asians consider fruit juices or white rice to be healthy, when they lead to rapid spikes in blood sugar.”
Dr. Khera also advised earlier heart disease screening, such as coronary calcium scanning “sometime between age 40-50 years,” noting that positive test results may motivate patients to start or adhere to medications, such as cholesterol-lowering therapies. If necessary, clinicians can also refer to heart centers for South Asian patients, which are becoming increasingly common.
According to Cheryl A.M. Anderson, PhD, chair of the AHA’s Council on Epidemiology and Prevention, and professor and dean of the Herbert Wertheim School of Public Health and Human Longevity Science at the University of California, San Diego, the current study suggests that heart disease management strategies for South Asian patients may be lacking.
“We have had a tradition of preventing or trying to treat heart disease in a fashion that doesn’t yet account for the increased risk that might be prevalent in those of South Asian ancestry,” Dr. Anderson said in an interview.
She suggested that improving associated risk-analysis tools could be beneficial, although the tools themselves, in the context of race or ethnicity, may present their own risks.
“We want to be mindful of potential adverse implications from having everything linked to one’s ancestry, which I think this tool doesn’t do,” Dr. Anderson said, referring to the AHA/ACC Pooled Cohort Equations. “But in sort of the bigger picture of things, we always want to expand and refine our toolkit.”
According to Rajesh Dash, MD, PhD, associate professor, cardiologist, and director of the South Asian Translational Heart Initiative (SSATHI) Prevention Clinic and CardioClick Telemedicine Clinic at Stanford (Calif.) HealthCare, the science supports more active risk mitigation strategies for South Asian patients, and the AHA and the ACC “are the two entities that need to lead the way.”
“Certainly the American Heart Association and the American College of Cardiology should be taking a more active leadership role in this,” Dr. Dash said in an interview.
In 2018, the AHA issued a scientific statement about the elevated risk of ASCVD among South Asian individuals, “but it did not rise to the level of specific recommendations, and did not necessarily go as far as to incorporate new screening parameters for that population,” Dr. Dash said. He also noted that the most recent AHA/ACC guideline identifies South Asian ancestry as a risk-enhancing feature, a statement similarly lacking in actionable value.
“That does not definitively lead someone like a primary care physician to a decision to start a statin, or to be more aggressive with a diagnostic workup, like a stress test, for instance, for a patient who they otherwise would not have done one in had they not been South Asian,” Dr. Dash said.
The steps taken by the AHA and the ACC are “a healthy step forward,” he noted, “but not nearly the degree of attention or vigilance that is required, as well as the level of action that is required to change the narrative for the population.”
At the SSATHI Prevention Clinic, Dr. Dash and colleagues aren’t waiting for the narrative to change, and are already taking a more aggressive approach.
The clinic has an average patient age of 41 years, “easily 15 years younger than the average age in most cardiology clinics,” Dr. Dash said, based on the fact that approximately two-thirds of heart attacks in South Asian individuals occur under the age of 55. “We have to look earlier.”
The SSATHI Prevention Clinic screens for both traditional and emerging risk factors, and Dr. Dash suggested that primary care doctors should do the same.
“If you have a South Asian patient as a primary care physician, you should be aggressively looking for risk factors, traditional ones to start, like elevated cholesterol, hypertension, diabetes, or – and I would argue strongly – prediabetes or insulin resistance.”
Dr. Dash also recommended looking into family history, and considering screening for inflammatory biomarkers, the latter of which are commonly elevated at an earlier age among South Asian individuals, and may have a relatively greater prognostic impact.
To encourage broader implementation of this kind of approach, Dr. Dash called for more large-scale studies. Ideally, these would be randomized clinical trials, but, realistically, real-world datasets may be the answer.
The study was supported by the National Heart, Lung, and Blood Institute; the Broad Institute at MIT and Harvard; the National Human Genome Research Institute; and others. The investigators disclosed relationships with IBM Research, Sanofi, Amgen, and others. Dr. Dash disclosed relationships with HealthPals and AstraZeneca. Dr. Anderson reported no relevant conflicts of interest.
according to the results of a new study.
These findings confirm previous reports and practice guidelines that identify South Asian ancestry as a risk enhancer for atherosclerotic cardiovascular disease (ASCVD), suggesting that earlier heart disease screening and prevention is warranted in this patient population, lead author Aniruddh P. Patel, MD, research fellow at the Center for Genomic Medicine, Massachusetts General Hospital, Boston, and colleagues said.
“Previous studies in multiple countries have estimated a 1.7- to 4-fold higher risk of ASCVD among South Asian individuals, compared with other ancestries, but have important potential limitations,” Dr. Patel and colleagues wrote in the paper on their prospective cohort study, published in Circulation.
The INTERHEART case-control study, for example, which assessed risk factors for acute myocardial infarction among more than 15,000 cases from 52 countries, is now 2 decades old, and “may not reflect recent advances in cardiovascular disease prevention,” the investigators wrote.
Most studies in the area have been small and retrospective, they added, and have not adequately assessed emerging risk factors, such as prediabetes, which appear to play a relatively greater role in the development of heart disease among South Asians.
Methods and results
To address this knowledge gap, Dr. Patel and colleagues analyzed data from the UK Biobank prospective cohort study, including 449,349 middle-aged participants of European ancestry and 8,124 similarly aged participants of South Asian descent who did not have heart disease upon enrollment. Respective rates of incident ASCVD (i.e., MI, ischemic stroke, or coronary revascularization) were analyzed in the context of a variety of lifestyle, anthropometric, and clinical factors.
After a median follow-up of 11.1 years, individuals of South Asian descent had an incident ASCVD rate of 6.8%, compared with 4.4% for individuals of European descent, representing twice the relative risk (adjusted hazard ratio, 2.03; 95% CI, 1.86-2.22; P < .001). Even after accounting for all covariates, risk of ASCVD remained 45% higher for South Asian individuals (aHR, 1.45; 95% CI, 1.28-1.65; P < .001). This elevation in risk was not captured by existing risk calculators, including the American College of Cardiology/American Heart Association Pooled Cohort Equations, or the QRISK3 equations.
The findings were “largely consistent across a range of age, sex, and clinical subgroups,” and “confirm and extend previous reports that hypertension, diabetes, and central adiposity are the leading associations in this observed disparity,” the investigators wrote.
Two diabetes subtypes are more prevalent in South Asians
Hypertension, diabetes, and central adiposity do not fully explain South Asians’ higher risk for ASCVD, wrote Namratha R. Kandula, MD, of Northwestern University Medical Center, Chicago, and Alka M. Kanaya, MD, of the University of California, San Francisco, in an accompanying editorial published in Circulation.
Some of the undetected risk may stem from unique diabetes disease factors, Dr. Kandula and Dr. Kanaya added.
“Newer data have demonstrated distinct subtypes of type 2 diabetes, with South Asians having a higher prevalence of both a severe insulin resistant with obesity subtype and a less recognized severe insulin deficient subtype,” they wrote. “Importantly, both of these more prevalent diabetes subtypes in South Asians were associated with a higher incidence of coronary artery calcium, a marker of subclinical atherosclerosis and strong predictor of future ASCVD, compared to other diabetes subtypes.”
Diabetes rate is higher for South Asians in the U.S.
Although the present study was conducted in the United Kingdom, the findings likely apply to individuals of South Asian ancestry living in the United States, according to principal author Amit V. Khera, MD, associate director of the precision medicine unit at the Center for Genomic Medicine, Massachusetts General Hospital.
“There are already more than 5 million individuals of South Asian ancestry in the U.S. and this represents one of the fastest-growing ethnic subgroups,” Dr. Khera said in an interview. “As in our study of individuals in the U.K., South Asians in the U.S. suffer from diabetes at much higher rates – 23% versus 12% – and this often occurs even in the absence of obesity.”
Dr. Khera noted that the 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease identify South Asian ancestry as a risk-enhancing factor, calling this a “stopgap measure.” More work is needed, he said, in the research arena and in the clinic.
Zero South Asians included in studies used to develop risk estimator
“I think the first step is to simply acknowledge that the risk estimators we use in clinical practice have important limitations when it comes to diverse patient populations,” Dr. Khera said in an interview. “We saw this in our study, where – despite a more than doubling of risk – the predicted risk based on the equations used in primary care showed no difference. This risk estimator was developed based on legacy cohort studies, in [which] zero South Asians were included. Despite important differences across race/ethnicity, the current state-of-the-art in the U.S. is to use one equation for Black individuals and another for all other ethnicities.”
Experts suggest steps for reducing heart disease risk
While risk modeling remains suboptimal, Dr. Khera suggested that clinicians can take immediate steps to reduce the risk of heart disease among individuals with South Asian ancestry.
“Despite all of the uncertainty – we still don’t have a complete understanding of why the risk is so high – there are still several things primary care doctors can do for their patients,” Dr. Khera said.
Foremost, he recommended lifestyle and dietary counseling.
“Dietary counseling is particularly effective if put in the context of cultural norms,” Dr. Khera said. “Many South Asians consider fruit juices or white rice to be healthy, when they lead to rapid spikes in blood sugar.”
Dr. Khera also advised earlier heart disease screening, such as coronary calcium scanning “sometime between age 40-50 years,” noting that positive test results may motivate patients to start or adhere to medications, such as cholesterol-lowering therapies. If necessary, clinicians can also refer to heart centers for South Asian patients, which are becoming increasingly common.
According to Cheryl A.M. Anderson, PhD, chair of the AHA’s Council on Epidemiology and Prevention, and professor and dean of the Herbert Wertheim School of Public Health and Human Longevity Science at the University of California, San Diego, the current study suggests that heart disease management strategies for South Asian patients may be lacking.
“We have had a tradition of preventing or trying to treat heart disease in a fashion that doesn’t yet account for the increased risk that might be prevalent in those of South Asian ancestry,” Dr. Anderson said in an interview.
She suggested that improving associated risk-analysis tools could be beneficial, although the tools themselves, in the context of race or ethnicity, may present their own risks.
“We want to be mindful of potential adverse implications from having everything linked to one’s ancestry, which I think this tool doesn’t do,” Dr. Anderson said, referring to the AHA/ACC Pooled Cohort Equations. “But in sort of the bigger picture of things, we always want to expand and refine our toolkit.”
According to Rajesh Dash, MD, PhD, associate professor, cardiologist, and director of the South Asian Translational Heart Initiative (SSATHI) Prevention Clinic and CardioClick Telemedicine Clinic at Stanford (Calif.) HealthCare, the science supports more active risk mitigation strategies for South Asian patients, and the AHA and the ACC “are the two entities that need to lead the way.”
“Certainly the American Heart Association and the American College of Cardiology should be taking a more active leadership role in this,” Dr. Dash said in an interview.
In 2018, the AHA issued a scientific statement about the elevated risk of ASCVD among South Asian individuals, “but it did not rise to the level of specific recommendations, and did not necessarily go as far as to incorporate new screening parameters for that population,” Dr. Dash said. He also noted that the most recent AHA/ACC guideline identifies South Asian ancestry as a risk-enhancing feature, a statement similarly lacking in actionable value.
“That does not definitively lead someone like a primary care physician to a decision to start a statin, or to be more aggressive with a diagnostic workup, like a stress test, for instance, for a patient who they otherwise would not have done one in had they not been South Asian,” Dr. Dash said.
The steps taken by the AHA and the ACC are “a healthy step forward,” he noted, “but not nearly the degree of attention or vigilance that is required, as well as the level of action that is required to change the narrative for the population.”
At the SSATHI Prevention Clinic, Dr. Dash and colleagues aren’t waiting for the narrative to change, and are already taking a more aggressive approach.
The clinic has an average patient age of 41 years, “easily 15 years younger than the average age in most cardiology clinics,” Dr. Dash said, based on the fact that approximately two-thirds of heart attacks in South Asian individuals occur under the age of 55. “We have to look earlier.”
The SSATHI Prevention Clinic screens for both traditional and emerging risk factors, and Dr. Dash suggested that primary care doctors should do the same.
“If you have a South Asian patient as a primary care physician, you should be aggressively looking for risk factors, traditional ones to start, like elevated cholesterol, hypertension, diabetes, or – and I would argue strongly – prediabetes or insulin resistance.”
Dr. Dash also recommended looking into family history, and considering screening for inflammatory biomarkers, the latter of which are commonly elevated at an earlier age among South Asian individuals, and may have a relatively greater prognostic impact.
To encourage broader implementation of this kind of approach, Dr. Dash called for more large-scale studies. Ideally, these would be randomized clinical trials, but, realistically, real-world datasets may be the answer.
The study was supported by the National Heart, Lung, and Blood Institute; the Broad Institute at MIT and Harvard; the National Human Genome Research Institute; and others. The investigators disclosed relationships with IBM Research, Sanofi, Amgen, and others. Dr. Dash disclosed relationships with HealthPals and AstraZeneca. Dr. Anderson reported no relevant conflicts of interest.
according to the results of a new study.
These findings confirm previous reports and practice guidelines that identify South Asian ancestry as a risk enhancer for atherosclerotic cardiovascular disease (ASCVD), suggesting that earlier heart disease screening and prevention is warranted in this patient population, lead author Aniruddh P. Patel, MD, research fellow at the Center for Genomic Medicine, Massachusetts General Hospital, Boston, and colleagues said.
“Previous studies in multiple countries have estimated a 1.7- to 4-fold higher risk of ASCVD among South Asian individuals, compared with other ancestries, but have important potential limitations,” Dr. Patel and colleagues wrote in the paper on their prospective cohort study, published in Circulation.
The INTERHEART case-control study, for example, which assessed risk factors for acute myocardial infarction among more than 15,000 cases from 52 countries, is now 2 decades old, and “may not reflect recent advances in cardiovascular disease prevention,” the investigators wrote.
Most studies in the area have been small and retrospective, they added, and have not adequately assessed emerging risk factors, such as prediabetes, which appear to play a relatively greater role in the development of heart disease among South Asians.
Methods and results
To address this knowledge gap, Dr. Patel and colleagues analyzed data from the UK Biobank prospective cohort study, including 449,349 middle-aged participants of European ancestry and 8,124 similarly aged participants of South Asian descent who did not have heart disease upon enrollment. Respective rates of incident ASCVD (i.e., MI, ischemic stroke, or coronary revascularization) were analyzed in the context of a variety of lifestyle, anthropometric, and clinical factors.
After a median follow-up of 11.1 years, individuals of South Asian descent had an incident ASCVD rate of 6.8%, compared with 4.4% for individuals of European descent, representing twice the relative risk (adjusted hazard ratio, 2.03; 95% CI, 1.86-2.22; P < .001). Even after accounting for all covariates, risk of ASCVD remained 45% higher for South Asian individuals (aHR, 1.45; 95% CI, 1.28-1.65; P < .001). This elevation in risk was not captured by existing risk calculators, including the American College of Cardiology/American Heart Association Pooled Cohort Equations, or the QRISK3 equations.
The findings were “largely consistent across a range of age, sex, and clinical subgroups,” and “confirm and extend previous reports that hypertension, diabetes, and central adiposity are the leading associations in this observed disparity,” the investigators wrote.
Two diabetes subtypes are more prevalent in South Asians
Hypertension, diabetes, and central adiposity do not fully explain South Asians’ higher risk for ASCVD, wrote Namratha R. Kandula, MD, of Northwestern University Medical Center, Chicago, and Alka M. Kanaya, MD, of the University of California, San Francisco, in an accompanying editorial published in Circulation.
Some of the undetected risk may stem from unique diabetes disease factors, Dr. Kandula and Dr. Kanaya added.
“Newer data have demonstrated distinct subtypes of type 2 diabetes, with South Asians having a higher prevalence of both a severe insulin resistant with obesity subtype and a less recognized severe insulin deficient subtype,” they wrote. “Importantly, both of these more prevalent diabetes subtypes in South Asians were associated with a higher incidence of coronary artery calcium, a marker of subclinical atherosclerosis and strong predictor of future ASCVD, compared to other diabetes subtypes.”
Diabetes rate is higher for South Asians in the U.S.
Although the present study was conducted in the United Kingdom, the findings likely apply to individuals of South Asian ancestry living in the United States, according to principal author Amit V. Khera, MD, associate director of the precision medicine unit at the Center for Genomic Medicine, Massachusetts General Hospital.
“There are already more than 5 million individuals of South Asian ancestry in the U.S. and this represents one of the fastest-growing ethnic subgroups,” Dr. Khera said in an interview. “As in our study of individuals in the U.K., South Asians in the U.S. suffer from diabetes at much higher rates – 23% versus 12% – and this often occurs even in the absence of obesity.”
Dr. Khera noted that the 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease identify South Asian ancestry as a risk-enhancing factor, calling this a “stopgap measure.” More work is needed, he said, in the research arena and in the clinic.
Zero South Asians included in studies used to develop risk estimator
“I think the first step is to simply acknowledge that the risk estimators we use in clinical practice have important limitations when it comes to diverse patient populations,” Dr. Khera said in an interview. “We saw this in our study, where – despite a more than doubling of risk – the predicted risk based on the equations used in primary care showed no difference. This risk estimator was developed based on legacy cohort studies, in [which] zero South Asians were included. Despite important differences across race/ethnicity, the current state-of-the-art in the U.S. is to use one equation for Black individuals and another for all other ethnicities.”
Experts suggest steps for reducing heart disease risk
While risk modeling remains suboptimal, Dr. Khera suggested that clinicians can take immediate steps to reduce the risk of heart disease among individuals with South Asian ancestry.
“Despite all of the uncertainty – we still don’t have a complete understanding of why the risk is so high – there are still several things primary care doctors can do for their patients,” Dr. Khera said.
Foremost, he recommended lifestyle and dietary counseling.
“Dietary counseling is particularly effective if put in the context of cultural norms,” Dr. Khera said. “Many South Asians consider fruit juices or white rice to be healthy, when they lead to rapid spikes in blood sugar.”
Dr. Khera also advised earlier heart disease screening, such as coronary calcium scanning “sometime between age 40-50 years,” noting that positive test results may motivate patients to start or adhere to medications, such as cholesterol-lowering therapies. If necessary, clinicians can also refer to heart centers for South Asian patients, which are becoming increasingly common.
According to Cheryl A.M. Anderson, PhD, chair of the AHA’s Council on Epidemiology and Prevention, and professor and dean of the Herbert Wertheim School of Public Health and Human Longevity Science at the University of California, San Diego, the current study suggests that heart disease management strategies for South Asian patients may be lacking.
“We have had a tradition of preventing or trying to treat heart disease in a fashion that doesn’t yet account for the increased risk that might be prevalent in those of South Asian ancestry,” Dr. Anderson said in an interview.
She suggested that improving associated risk-analysis tools could be beneficial, although the tools themselves, in the context of race or ethnicity, may present their own risks.
“We want to be mindful of potential adverse implications from having everything linked to one’s ancestry, which I think this tool doesn’t do,” Dr. Anderson said, referring to the AHA/ACC Pooled Cohort Equations. “But in sort of the bigger picture of things, we always want to expand and refine our toolkit.”
According to Rajesh Dash, MD, PhD, associate professor, cardiologist, and director of the South Asian Translational Heart Initiative (SSATHI) Prevention Clinic and CardioClick Telemedicine Clinic at Stanford (Calif.) HealthCare, the science supports more active risk mitigation strategies for South Asian patients, and the AHA and the ACC “are the two entities that need to lead the way.”
“Certainly the American Heart Association and the American College of Cardiology should be taking a more active leadership role in this,” Dr. Dash said in an interview.
In 2018, the AHA issued a scientific statement about the elevated risk of ASCVD among South Asian individuals, “but it did not rise to the level of specific recommendations, and did not necessarily go as far as to incorporate new screening parameters for that population,” Dr. Dash said. He also noted that the most recent AHA/ACC guideline identifies South Asian ancestry as a risk-enhancing feature, a statement similarly lacking in actionable value.
“That does not definitively lead someone like a primary care physician to a decision to start a statin, or to be more aggressive with a diagnostic workup, like a stress test, for instance, for a patient who they otherwise would not have done one in had they not been South Asian,” Dr. Dash said.
The steps taken by the AHA and the ACC are “a healthy step forward,” he noted, “but not nearly the degree of attention or vigilance that is required, as well as the level of action that is required to change the narrative for the population.”
At the SSATHI Prevention Clinic, Dr. Dash and colleagues aren’t waiting for the narrative to change, and are already taking a more aggressive approach.
The clinic has an average patient age of 41 years, “easily 15 years younger than the average age in most cardiology clinics,” Dr. Dash said, based on the fact that approximately two-thirds of heart attacks in South Asian individuals occur under the age of 55. “We have to look earlier.”
The SSATHI Prevention Clinic screens for both traditional and emerging risk factors, and Dr. Dash suggested that primary care doctors should do the same.
“If you have a South Asian patient as a primary care physician, you should be aggressively looking for risk factors, traditional ones to start, like elevated cholesterol, hypertension, diabetes, or – and I would argue strongly – prediabetes or insulin resistance.”
Dr. Dash also recommended looking into family history, and considering screening for inflammatory biomarkers, the latter of which are commonly elevated at an earlier age among South Asian individuals, and may have a relatively greater prognostic impact.
To encourage broader implementation of this kind of approach, Dr. Dash called for more large-scale studies. Ideally, these would be randomized clinical trials, but, realistically, real-world datasets may be the answer.
The study was supported by the National Heart, Lung, and Blood Institute; the Broad Institute at MIT and Harvard; the National Human Genome Research Institute; and others. The investigators disclosed relationships with IBM Research, Sanofi, Amgen, and others. Dr. Dash disclosed relationships with HealthPals and AstraZeneca. Dr. Anderson reported no relevant conflicts of interest.
FROM CIRCULATION