User login
Expanded hospital testing improves respiratory pathogen detection
SAN DIEGO – Systematic testing of acute respiratory illness patients can increase the likelihood of finding relevant pathogens, according to a study presented at an annual scientific meeting on infectious diseases.
Currently, hospitals conduct either nonroutine assessments or rely heavily on clinical laboratory testing among severe acute respiratory illness patients, which can lead to missing clinically key viruses.
Systematic testing expands on tests ordered and carried out at hospitals, expanding on them by testing for influenza, respiratory syncytial virus (RSV), human metapneumovirus, rhinovirus and enterovirus, adenovirus, coronavirus, and parainfluenza viruses 1-4. To test the efficacy of systematic testing, investigators studied 2,216 severe acute respiratory illness patients hospitalized in one of three hospitals in Minnesota during September 2015-August 2016. Patients were predominantly younger than 5 years old (57%) and had one or more chronic medical condition (63%).
Detection of at least one virus increased from 1,062 patients (48%) to 1,600 patients (72%) when comparing clinically ordered tests against expanded, systematic RT-PCR testing conducted through the Minnesota Health Department (MDH).
By patient age, viral detection increased by 27%, 24%, 18%, and 21% for patients aged younger than 5 years, 5-17 years, 18-64 years, and 65 years and older, respectively. Except for influenza viruses and RSV, the proportions of viruses identified, regardless of age, were all lower in hospital testing, compared with MDH testing.
“RSV targeting was almost systematic among children less than 5 years, but [accounted for] only 28% of RSV detection,” said Dr. Steffen in her presentation. “A smaller proportion of other respiratory viruses, including the human metapneumovirus, were detected at the hospital, and this was especially true for adults.”
Patients with rhinovirus and enterovirus saw a difference between hospital and expanded testing, increasing from a little over 300 patients detected, to nearly 800 patients.
“Patients admitted to the ICU were less likely to have a pathogen detection than those not admitted to the ICU, and those with one or more chronic medical condition had lower viral detection than those without,” Dr. Steffens said. “While testing at MDH did increase the percent of patients in each category, trends remained consistent and significant.”
Since testing information was only collected for patients with positive test results at the hospital, investigators were not able to compare testing practices between patients with and without viruses. This study may also have underrepresented pathogens detected through means other than the hospital laboratory, like rapid tests in emergency departments. The study was also limited by the short time frame of only 1 year.
The presenters reported no relevant financial disclosures.
SOURCE: Steffens A et al. Abstract 885.
SAN DIEGO – Systematic testing of acute respiratory illness patients can increase the likelihood of finding relevant pathogens, according to a study presented at an annual scientific meeting on infectious diseases.
Currently, hospitals conduct either nonroutine assessments or rely heavily on clinical laboratory testing among severe acute respiratory illness patients, which can lead to missing clinically key viruses.
Systematic testing expands on tests ordered and carried out at hospitals, expanding on them by testing for influenza, respiratory syncytial virus (RSV), human metapneumovirus, rhinovirus and enterovirus, adenovirus, coronavirus, and parainfluenza viruses 1-4. To test the efficacy of systematic testing, investigators studied 2,216 severe acute respiratory illness patients hospitalized in one of three hospitals in Minnesota during September 2015-August 2016. Patients were predominantly younger than 5 years old (57%) and had one or more chronic medical condition (63%).
Detection of at least one virus increased from 1,062 patients (48%) to 1,600 patients (72%) when comparing clinically ordered tests against expanded, systematic RT-PCR testing conducted through the Minnesota Health Department (MDH).
By patient age, viral detection increased by 27%, 24%, 18%, and 21% for patients aged younger than 5 years, 5-17 years, 18-64 years, and 65 years and older, respectively. Except for influenza viruses and RSV, the proportions of viruses identified, regardless of age, were all lower in hospital testing, compared with MDH testing.
“RSV targeting was almost systematic among children less than 5 years, but [accounted for] only 28% of RSV detection,” said Dr. Steffen in her presentation. “A smaller proportion of other respiratory viruses, including the human metapneumovirus, were detected at the hospital, and this was especially true for adults.”
Patients with rhinovirus and enterovirus saw a difference between hospital and expanded testing, increasing from a little over 300 patients detected, to nearly 800 patients.
“Patients admitted to the ICU were less likely to have a pathogen detection than those not admitted to the ICU, and those with one or more chronic medical condition had lower viral detection than those without,” Dr. Steffens said. “While testing at MDH did increase the percent of patients in each category, trends remained consistent and significant.”
Since testing information was only collected for patients with positive test results at the hospital, investigators were not able to compare testing practices between patients with and without viruses. This study may also have underrepresented pathogens detected through means other than the hospital laboratory, like rapid tests in emergency departments. The study was also limited by the short time frame of only 1 year.
The presenters reported no relevant financial disclosures.
SOURCE: Steffens A et al. Abstract 885.
SAN DIEGO – Systematic testing of acute respiratory illness patients can increase the likelihood of finding relevant pathogens, according to a study presented at an annual scientific meeting on infectious diseases.
Currently, hospitals conduct either nonroutine assessments or rely heavily on clinical laboratory testing among severe acute respiratory illness patients, which can lead to missing clinically key viruses.
Systematic testing expands on tests ordered and carried out at hospitals, expanding on them by testing for influenza, respiratory syncytial virus (RSV), human metapneumovirus, rhinovirus and enterovirus, adenovirus, coronavirus, and parainfluenza viruses 1-4. To test the efficacy of systematic testing, investigators studied 2,216 severe acute respiratory illness patients hospitalized in one of three hospitals in Minnesota during September 2015-August 2016. Patients were predominantly younger than 5 years old (57%) and had one or more chronic medical condition (63%).
Detection of at least one virus increased from 1,062 patients (48%) to 1,600 patients (72%) when comparing clinically ordered tests against expanded, systematic RT-PCR testing conducted through the Minnesota Health Department (MDH).
By patient age, viral detection increased by 27%, 24%, 18%, and 21% for patients aged younger than 5 years, 5-17 years, 18-64 years, and 65 years and older, respectively. Except for influenza viruses and RSV, the proportions of viruses identified, regardless of age, were all lower in hospital testing, compared with MDH testing.
“RSV targeting was almost systematic among children less than 5 years, but [accounted for] only 28% of RSV detection,” said Dr. Steffen in her presentation. “A smaller proportion of other respiratory viruses, including the human metapneumovirus, were detected at the hospital, and this was especially true for adults.”
Patients with rhinovirus and enterovirus saw a difference between hospital and expanded testing, increasing from a little over 300 patients detected, to nearly 800 patients.
“Patients admitted to the ICU were less likely to have a pathogen detection than those not admitted to the ICU, and those with one or more chronic medical condition had lower viral detection than those without,” Dr. Steffens said. “While testing at MDH did increase the percent of patients in each category, trends remained consistent and significant.”
Since testing information was only collected for patients with positive test results at the hospital, investigators were not able to compare testing practices between patients with and without viruses. This study may also have underrepresented pathogens detected through means other than the hospital laboratory, like rapid tests in emergency departments. The study was also limited by the short time frame of only 1 year.
The presenters reported no relevant financial disclosures.
SOURCE: Steffens A et al. Abstract 885.
REPORTING FROM ID WEEK 2017
Key clinical point:
Major finding: Among 2,216 patients studied, 1,600 (72%) were found to have at least one respiratory virus through expanded testing, compared with 1,062 (48%) patients tested through clincian-directed testing.
Study details: 2,351 severe acute respiratory illness patients hospitalized in one of three hospitals in Minnesota.
Disclosures: The presenter reported no relevant financial disclosures.
Source: Steffens A et al. Abstract 885.
Managing mental health care at the hospital
The numbers tell a grim story. Nationwide, 43.7 million adult Americans experienced a mental health condition during 2016 – an increase of 1.2 million over the previous year. Mental health issues send almost 5.5 million people to emergency departments each year; nearly 60% of adults with a mental illness received no treatment at all.
If that massive – and growing – need is one side of the story, shrinking resources are the other. Mental health resources had already been diminishing for decades before the recession hit – and hit them especially hard. Between 2009 and 2012, states cut $5 billion in mental health services; during that time, at least 4,500 public psychiatric hospital beds nationwide disappeared – nearly 10% of the total supply. The bulk of those resources have never been restored.
Provider numbers also are falling. “Psychiatry is probably the top manpower shortage among all specialties,” said Joe Parks, MD, medical director of the National Council for Behavioral Health. “We have about a third the number of psychiatrists that most estimates say we need, and the number per capita is decreasing.” A significant percentage of psychiatrists – more than 50% – only accept cash, bypassing the low reimbursement rates even private insurance typically offers.
Hospitals, of course, feel those financial disincentives too, which discourage them from investments of their own. “It’s a difficult population to manage, and it’s difficult to manage the financial realities of mental health as well,” said John McHugh, PhD, assistant professor of health policy at Columbia University, New York. “If you were a hospital administrator looking to invest your last dollar and you have the option of investing it in a new heart institute or in behavioral health service, more likely than not, you’re going to invest it in the more profitable cardiovascular service line.”
Providers of last resort
But much of the burden of caring for this population ends up falling on hospitals by default. At Denver Health, Melanie Rylander, MD, medical director of the inpatient psychiatric unit, reports seeing this manifest in three categories of patients. First, there is an influx of people coming into the emergency department with primary mental health issues.
“We’re also seeing an influx of people coming in with physical problems, and upon assessment it becomes very clear very quickly that the real issue is an underlying mental health issue,” she said. Then there are the people coming in for the same physical problems over and over – maybe decompensated heart failure or COPD exacerbations – because mental health issues are impeding their ability to take care of themselves.
Some hospitalists say they feel ill equipped to care for these patients. “We don’t have the facility or the resources many times to properly care for their psychiatric needs when they’re in the hospital. It’s not really part of an internist’s training to be familiar with a lot of the medications,” said Atashi Mandal, MD, a hospitalist and pediatrician in Los Angeles. “Sometimes they get improperly medicated because we don’t know what else to do and the patient’s behavioral issues are escalating, so it’s really a difficult position.”
It’s a dispiriting experience for a hospitalist. “It really bothers me when I am trying to care for a patient who has psychiatric needs, and I feel I’m not able to do it, and I can’t find resources, and I feel that this patient’s needs are being neglected – not because we don’t care, and not because of a lack of effort by the staff. It’s just set up to fail,” Dr. Mandal said.
Ending the silo mentality
Encouraging a more holistic view of health across health care would be an important step to begin to address the problem – after all, the mind and the body are not separate.
“We work in silos, and we really have to stop doing that because these are intertwined,” said Corey Karlin-Zysman, MD, FHM, FACP, chief of the division of hospital medicine at Northwell Health. “A schizophrenic will become worse when they’re medically ill. That illness will be harder to treat if their psychiatric illness is active.” This is starting to happen in the outpatient setting, evidenced by the expansion of the integrated care model, where a primary care doctor is the lead physician working in combination with psychologists, psychiatrists, and social workers. Communication among providers becomes simpler, and patients don’t fall through the cracks as often while trying to navigate the system.
That idea of integration is also making its way into the hospital setting in various ways. In their efforts to bring the care to the patient, rather than the other way around, Dr. Karlin-Zysman’s hospital embedded two hospitalists in the neighboring inpatient psychiatric hospital; when patients need medical treatment, they can receive it without interrupting their behavioral health treatment. As a result, patients who used to end up in their emergency department don’t anymore, and their 30-day readmission rate has fallen by 50%.
But at its foundation, care integration is more of an attitude than a system; it begins with a mindset.
“We talk so much today about system reform, integrated systems, blah, blah,” said Lisa Rosenbaum, MD, a cardiologist at Brigham and Women’s Hospital, Boston. “I don’t want to make it seem like it’s not going to work, but what does it mean for the patient who is psychotic and has 10 problems, with whom you have 15 minutes? Taking good care of these patients means you have to take a deep breath and put in a lot of time and deal with all these things that have nothing to do with the health system under which you practice. There’s this ‘only so much you can do’ feeling that is a problem in itself, because there’s actually a lot we can do.”
Hospitals and communities
It’s axiomatic to say that a better approach to mental health would be based around prevention and early intervention, rather than the less crisis-oriented system we have now. Some efforts are being made in that direction, and they involve, and require, outreach outside the hospital.
“The best hospitals doing work in mental health are going beyond the hospital walls; they’re really looking at their community,” Dr. Nguyen said. “You have hospitals, like Accountable Care Organizations, who are trying to move earlier and think about mental health from a pediatric standpoint: How can we support parents and children during critical phases of brain growth? How can we provide prevention services?” Ultimately, those efforts should help lower future admission rates to EDs and hospitals.
That forward-looking approach may be necessary, but it’s also a challenge. “As a hospital administrator, I would think that you look out at the community and see this problem is not going away – in fact, it is likely going to get worse,” Dr. McHugh said. “A health system may look at themselves and say we have to take the lead on this.” The difficulty is that thinking of it in a sense of value to the community, and making the requisite investments, will have a very long period of payout; a health system that’s struggling may not be able to do it. “It’s the large [health systems] that tend to be more integrated … that are thinking about this much differently,” he said.
Still, the reality is that’s where the root of the problem lies, Dr. Rylander said – not in the hospital, but in the larger community. “In the absence of very basic needs – stable housing, food, heating – it’s really not reasonable to expect that people are going to take care of their physical needs,” she said. “It’s a much larger social issue: how to get resources so that these people can have stable places to live, they can get to and from appointments, that type of thing.”
Those needs are ongoing, of course. Many of these patients suffer from chronic conditions, meaning people will continue to need services and support, said Ron Honberg, JD, senior policy adviser for the National Alliance on Mental Illness. Often, people need services from different systems. “There are complexities in terms of navigating those systems and getting those systems to work well together. Until we make inroads in solving those things, or at least improving those things, the burdens are going to fall on the providers of last resort, and that includes hospitals,” he said.
A collaborative effort may be needed, but hospitals can still be active participants and even leaders.
“If hospitals really want to address these problems, they need to be part of the discussions taking place in communities among the various systems and providers and advocates,” Mr. Honberg said. “Ultimately, we need to develop a better community-based system of care, and a better way of handing people off from inpatient to community-based treatment, and some accountability in terms of requiring that people get services, so they don’t get rehospitalized quickly. You’re increasingly seeing accountability now with other health conditions; we’re measuring things in Medicare like rehospitalization rates and the like. We need to be doing that with mental health treatment as well.”
What a hospitalist can do
One thing hospitalists might consider is starting that practice at their own hospitals, measuring, recording, and sharing that kind of information.
“Hospitalists should measure systematically, and in a very neutral manner, the total burden and frequency of the problem and report it consistently to management, along with their assessment that this impairs the quality of care and creates patient risk,” Dr. Parks said. That information can help hospitalists lobby for access to psychiatric personnel, be that in person or through telemedicine. “We don’t have to lay hands on you. There’s no excuse for any hospital not having a contract in place for on-demand consultation in the ER and on the floors.”
Track outcomes, too, Dr. Mandal suggests. With access to the right personnel, are you getting patients out of the ED faster? Are you having fewer negative outcomes while these patients are in the hospital, such as having to use restraints or get security involved? “Hopefully you can get some data in terms of how much money you’ve saved by decreasing the length of stays and decreasing inadvertent adverse effects because the patients weren’t receiving the proper care,” he said.
As this challenge seems likely to continue to grow, hospitalists might consider finding more training in mental health issues themselves so they are more comfortable handling these issues, Dr. Parks said. “The average mini-psych rotation from medical school is only 4 weeks,” he noted. “The ob.gyn. is at least 8 weeks and often 12 weeks, and if you don’t go into ob.gyn., you’re going to see a lot more mentally ill people through the rest of your practice, no matter what you do, than you are going to see pregnant women.”
Just starting these conversations – with patients, with colleagues, with family and friends – might be the most important change of all. “Even though nobody is above these issues afflicting them, this is still something that is not part of an open dialogue, and this is something that affects our own colleagues,” Dr. Mandal said. “I don’t know how many more trainees jumping out of windows it will take, or colleagues going through depression and feeling that it’s a sign of weakness to even talk about it.
“We need to create safe harbors within our own medical communities and acknowledge that we ourselves can be prone to this,” he said. “Perhaps by doing that, we will develop more empathy and become more comfortable, not just with ourselves and our colleagues but also helping these patients. People get overwhelmed and throw their hands up because it is just such a difficult issue. I don’t want people to give up, both from the medical community and our society as a whole – we can’t give up.”
A med-psych unit pilot project
Med-psych units can be a good model to take on these challenges. At Long Island Jewish Medical Center, they launched a pilot project to see how one would work in their community and summarized the results in an SHM abstract.
The hospital shares a campus with a 200-bed inpatient psych hospital, and doctors were seeing a lot of back and forth between the two institutions, said Corey Karlin-Zysman, MD, FHM, FACP, chief of the division of hospital medicine at Northwell Health. “Patients would come into the hospital because they had an active medical issue, but because of their behavioral issues, they’d have to have continuous observation. It would not be uncommon for us to have sometimes close to 30 patients who needed 24-hour continuous observation to make sure they were not hurting themselves.” These PCAs or nurse’s assistants were doing 8-hour shifts, so each patient needed three. “The math is staggering – and with not any better outcomes.”
So the hospital created a 15-bed closed med-psych unit for medically ill patients with behavioral health disorders. They staffed it with a dedicated hospitalist, a nurse practitioner, a psychologist, and a nurse manager.
The number of patients requiring continuous observation fell to single digits. Once in their own unit, these patients caused less disruption and stress on the medical units. They had a lower length of stay compared to their previous admissions in other units, and this became one of the hospital’s highest performing units in terms of patient experience.
The biggest secret of their success, Dr. Karlin-Zysman said, is cohorting. “Instead of them going to the next open bed, wherever it may be, you get the patients all in one place geographically, with a team trained to manage those patients.” Another factor: it’s a hospitalist-run unit. “You can’t have 20 different doctors taking care of the patients; it’s one or two hospitalists running this unit.”
Care models like this can be a true win-win, and her hospital is using them more and more.
“I have a care model that’s a stroke unit; I have a care model that’s an onc unit and one that’s a pulmonary unit,” she said. “We’re creating these true teams, which I think hospitalists really like being part of. What’s that thing that makes them want to come to work every day? Things like this: running a care model, becoming specialized in something.” There are research and abstract opportunities for hospitalists on these units too, which also helps keep them engaged, she said. “I’ve used this care model and things like that to reduce burnout and keep people excited.”
The persistent mortality gap
Patients with mental illness tend to receive worse medical care than people without, studies have shown; they die an average of 25 years earlier, largely from preventable or treatable conditions such as cardiovascular disease and diabetes. The World Health Organization has called the problem “a hidden human rights emergency.”
In one in a series of articles on mental health, Lisa Rosenbaum, MD, a cardiologist at Brigham and Women’s Hospital, Boston, raises the question: Might physician attitudes toward mentally ill people contribute to this mortality gap, and if so, can we change them?
She recognizes the many obstacles physicians face in treating these patients. “The medicines we have are good but not great and can cause obesity and diabetes, which contributes to cardiovascular morbidity and mortality,” Dr. Rosenbaum said. “We have the adherence challenge for the psychiatric medications and for medications for chronic disease. It’s hard enough for anyone to take a medicine every day, and to do that if you’re homeless or you don’t have insight into the need for it, it’s really hard.”
Also, certain behaviors that are more common among people with serious mental illness – smoking, substance abuse, physical inactivity – increase their risk for chronic diseases.
These hurdles may foster a sense of helplessness among hospitalists who have just a small amount of time to spend with a patient, and attitudes may be hard to change.
“Negotiating more effectively about care refusals, more adeptly assessing capacity, and recognizing when our efforts to orchestrate care have been inadequate seem feasible,” Dr. Rosenbaum writes. “Far harder is overcoming any collective belief that what mentally ill people truly need is not something we can offer.” That’s why a truly honest examination of attitudes and biases is a necessary place to start.
She tells the story of one mentally ill patient she learned of in her research, who, after decades as the quintessential frequent flier in the ER, was living stably in the community. “No one could have known how many tries it would take to help him get there,” she writes. His doctor told her, “Let’s say 10 attempts are necessary. Someone needs to be number 2, 3 and 7. You just never know which number you are.”
Education for physicians
A course created by the National Alliance on Mental Illness addresses mental illness issues from a provider perspective.
“Although the description states that the course is intended for mental health professionals, it can be and has been used to educate and inform other healthcare professionals as well,” said Ron Honberg, JD, senior policy advisor for the National Alliance on Mental Illness. The standard course takes 15 hours; there is an abbreviated 4-hour alternative as well. More information can be found at http://www.nami.org/Find-Support/NAMI-Programs/NAMI-Provider-Education.
Sources
1. Szabo L. Cost of Not Caring: Nowhere to Go. USA Today. https://www.usatoday.com/story/news/nation/2014/05/12/mental-health-system-crisis/7746535/. Accessed March 10, 2017.
2. Mental Health America. The State of Mental Health in America. http://www.mentalhealthamerica.net/issues/state-mental-health-america. Accessed March 30, 2017.
3. Karlin-Zysman C, Lerner K, Warner-Cohen J. Creating a Hybrid Medicine and Psychiatric Unit to Manage Medically Ill Patients with Behavioral Health Disorders [abstract]. Journal of Hospital Medicine. 2015; 10 (suppl 2). http://www.shmabstracts.com/abstract/creating-a-hybrid-medicine-and-psychiatric-unit-to-manage-medically-ill-patients-with-behavioral-health-disorders/. Accessed March 19, 2017.
4. Garey J. When Doctors Discriminate. New York Times. http://www.nytimes.com/2013/08/11/opinion/sunday/when-doctors-discriminate.html. August 10, 2013. Accessed March 15, 2017.
5. Rosenbaum L. Closing the Mortality Gap – Mental Illness and Medical Care. N Engl J Med. 2016; 375:1585-1589. doi: 10.1056/NEJMms1610125.
6. Rosenbaum L. Unlearning Our Helplessness – Coexisting Serious Mental and Medical Illness. N Engl J Med. 2016;375:1690-4. doi: 10.1056/NEJMms1610127.
The numbers tell a grim story. Nationwide, 43.7 million adult Americans experienced a mental health condition during 2016 – an increase of 1.2 million over the previous year. Mental health issues send almost 5.5 million people to emergency departments each year; nearly 60% of adults with a mental illness received no treatment at all.
If that massive – and growing – need is one side of the story, shrinking resources are the other. Mental health resources had already been diminishing for decades before the recession hit – and hit them especially hard. Between 2009 and 2012, states cut $5 billion in mental health services; during that time, at least 4,500 public psychiatric hospital beds nationwide disappeared – nearly 10% of the total supply. The bulk of those resources have never been restored.
Provider numbers also are falling. “Psychiatry is probably the top manpower shortage among all specialties,” said Joe Parks, MD, medical director of the National Council for Behavioral Health. “We have about a third the number of psychiatrists that most estimates say we need, and the number per capita is decreasing.” A significant percentage of psychiatrists – more than 50% – only accept cash, bypassing the low reimbursement rates even private insurance typically offers.
Hospitals, of course, feel those financial disincentives too, which discourage them from investments of their own. “It’s a difficult population to manage, and it’s difficult to manage the financial realities of mental health as well,” said John McHugh, PhD, assistant professor of health policy at Columbia University, New York. “If you were a hospital administrator looking to invest your last dollar and you have the option of investing it in a new heart institute or in behavioral health service, more likely than not, you’re going to invest it in the more profitable cardiovascular service line.”
Providers of last resort
But much of the burden of caring for this population ends up falling on hospitals by default. At Denver Health, Melanie Rylander, MD, medical director of the inpatient psychiatric unit, reports seeing this manifest in three categories of patients. First, there is an influx of people coming into the emergency department with primary mental health issues.
“We’re also seeing an influx of people coming in with physical problems, and upon assessment it becomes very clear very quickly that the real issue is an underlying mental health issue,” she said. Then there are the people coming in for the same physical problems over and over – maybe decompensated heart failure or COPD exacerbations – because mental health issues are impeding their ability to take care of themselves.
Some hospitalists say they feel ill equipped to care for these patients. “We don’t have the facility or the resources many times to properly care for their psychiatric needs when they’re in the hospital. It’s not really part of an internist’s training to be familiar with a lot of the medications,” said Atashi Mandal, MD, a hospitalist and pediatrician in Los Angeles. “Sometimes they get improperly medicated because we don’t know what else to do and the patient’s behavioral issues are escalating, so it’s really a difficult position.”
It’s a dispiriting experience for a hospitalist. “It really bothers me when I am trying to care for a patient who has psychiatric needs, and I feel I’m not able to do it, and I can’t find resources, and I feel that this patient’s needs are being neglected – not because we don’t care, and not because of a lack of effort by the staff. It’s just set up to fail,” Dr. Mandal said.
Ending the silo mentality
Encouraging a more holistic view of health across health care would be an important step to begin to address the problem – after all, the mind and the body are not separate.
“We work in silos, and we really have to stop doing that because these are intertwined,” said Corey Karlin-Zysman, MD, FHM, FACP, chief of the division of hospital medicine at Northwell Health. “A schizophrenic will become worse when they’re medically ill. That illness will be harder to treat if their psychiatric illness is active.” This is starting to happen in the outpatient setting, evidenced by the expansion of the integrated care model, where a primary care doctor is the lead physician working in combination with psychologists, psychiatrists, and social workers. Communication among providers becomes simpler, and patients don’t fall through the cracks as often while trying to navigate the system.
That idea of integration is also making its way into the hospital setting in various ways. In their efforts to bring the care to the patient, rather than the other way around, Dr. Karlin-Zysman’s hospital embedded two hospitalists in the neighboring inpatient psychiatric hospital; when patients need medical treatment, they can receive it without interrupting their behavioral health treatment. As a result, patients who used to end up in their emergency department don’t anymore, and their 30-day readmission rate has fallen by 50%.
But at its foundation, care integration is more of an attitude than a system; it begins with a mindset.
“We talk so much today about system reform, integrated systems, blah, blah,” said Lisa Rosenbaum, MD, a cardiologist at Brigham and Women’s Hospital, Boston. “I don’t want to make it seem like it’s not going to work, but what does it mean for the patient who is psychotic and has 10 problems, with whom you have 15 minutes? Taking good care of these patients means you have to take a deep breath and put in a lot of time and deal with all these things that have nothing to do with the health system under which you practice. There’s this ‘only so much you can do’ feeling that is a problem in itself, because there’s actually a lot we can do.”
Hospitals and communities
It’s axiomatic to say that a better approach to mental health would be based around prevention and early intervention, rather than the less crisis-oriented system we have now. Some efforts are being made in that direction, and they involve, and require, outreach outside the hospital.
“The best hospitals doing work in mental health are going beyond the hospital walls; they’re really looking at their community,” Dr. Nguyen said. “You have hospitals, like Accountable Care Organizations, who are trying to move earlier and think about mental health from a pediatric standpoint: How can we support parents and children during critical phases of brain growth? How can we provide prevention services?” Ultimately, those efforts should help lower future admission rates to EDs and hospitals.
That forward-looking approach may be necessary, but it’s also a challenge. “As a hospital administrator, I would think that you look out at the community and see this problem is not going away – in fact, it is likely going to get worse,” Dr. McHugh said. “A health system may look at themselves and say we have to take the lead on this.” The difficulty is that thinking of it in a sense of value to the community, and making the requisite investments, will have a very long period of payout; a health system that’s struggling may not be able to do it. “It’s the large [health systems] that tend to be more integrated … that are thinking about this much differently,” he said.
Still, the reality is that’s where the root of the problem lies, Dr. Rylander said – not in the hospital, but in the larger community. “In the absence of very basic needs – stable housing, food, heating – it’s really not reasonable to expect that people are going to take care of their physical needs,” she said. “It’s a much larger social issue: how to get resources so that these people can have stable places to live, they can get to and from appointments, that type of thing.”
Those needs are ongoing, of course. Many of these patients suffer from chronic conditions, meaning people will continue to need services and support, said Ron Honberg, JD, senior policy adviser for the National Alliance on Mental Illness. Often, people need services from different systems. “There are complexities in terms of navigating those systems and getting those systems to work well together. Until we make inroads in solving those things, or at least improving those things, the burdens are going to fall on the providers of last resort, and that includes hospitals,” he said.
A collaborative effort may be needed, but hospitals can still be active participants and even leaders.
“If hospitals really want to address these problems, they need to be part of the discussions taking place in communities among the various systems and providers and advocates,” Mr. Honberg said. “Ultimately, we need to develop a better community-based system of care, and a better way of handing people off from inpatient to community-based treatment, and some accountability in terms of requiring that people get services, so they don’t get rehospitalized quickly. You’re increasingly seeing accountability now with other health conditions; we’re measuring things in Medicare like rehospitalization rates and the like. We need to be doing that with mental health treatment as well.”
What a hospitalist can do
One thing hospitalists might consider is starting that practice at their own hospitals, measuring, recording, and sharing that kind of information.
“Hospitalists should measure systematically, and in a very neutral manner, the total burden and frequency of the problem and report it consistently to management, along with their assessment that this impairs the quality of care and creates patient risk,” Dr. Parks said. That information can help hospitalists lobby for access to psychiatric personnel, be that in person or through telemedicine. “We don’t have to lay hands on you. There’s no excuse for any hospital not having a contract in place for on-demand consultation in the ER and on the floors.”
Track outcomes, too, Dr. Mandal suggests. With access to the right personnel, are you getting patients out of the ED faster? Are you having fewer negative outcomes while these patients are in the hospital, such as having to use restraints or get security involved? “Hopefully you can get some data in terms of how much money you’ve saved by decreasing the length of stays and decreasing inadvertent adverse effects because the patients weren’t receiving the proper care,” he said.
As this challenge seems likely to continue to grow, hospitalists might consider finding more training in mental health issues themselves so they are more comfortable handling these issues, Dr. Parks said. “The average mini-psych rotation from medical school is only 4 weeks,” he noted. “The ob.gyn. is at least 8 weeks and often 12 weeks, and if you don’t go into ob.gyn., you’re going to see a lot more mentally ill people through the rest of your practice, no matter what you do, than you are going to see pregnant women.”
Just starting these conversations – with patients, with colleagues, with family and friends – might be the most important change of all. “Even though nobody is above these issues afflicting them, this is still something that is not part of an open dialogue, and this is something that affects our own colleagues,” Dr. Mandal said. “I don’t know how many more trainees jumping out of windows it will take, or colleagues going through depression and feeling that it’s a sign of weakness to even talk about it.
“We need to create safe harbors within our own medical communities and acknowledge that we ourselves can be prone to this,” he said. “Perhaps by doing that, we will develop more empathy and become more comfortable, not just with ourselves and our colleagues but also helping these patients. People get overwhelmed and throw their hands up because it is just such a difficult issue. I don’t want people to give up, both from the medical community and our society as a whole – we can’t give up.”
A med-psych unit pilot project
Med-psych units can be a good model to take on these challenges. At Long Island Jewish Medical Center, they launched a pilot project to see how one would work in their community and summarized the results in an SHM abstract.
The hospital shares a campus with a 200-bed inpatient psych hospital, and doctors were seeing a lot of back and forth between the two institutions, said Corey Karlin-Zysman, MD, FHM, FACP, chief of the division of hospital medicine at Northwell Health. “Patients would come into the hospital because they had an active medical issue, but because of their behavioral issues, they’d have to have continuous observation. It would not be uncommon for us to have sometimes close to 30 patients who needed 24-hour continuous observation to make sure they were not hurting themselves.” These PCAs or nurse’s assistants were doing 8-hour shifts, so each patient needed three. “The math is staggering – and with not any better outcomes.”
So the hospital created a 15-bed closed med-psych unit for medically ill patients with behavioral health disorders. They staffed it with a dedicated hospitalist, a nurse practitioner, a psychologist, and a nurse manager.
The number of patients requiring continuous observation fell to single digits. Once in their own unit, these patients caused less disruption and stress on the medical units. They had a lower length of stay compared to their previous admissions in other units, and this became one of the hospital’s highest performing units in terms of patient experience.
The biggest secret of their success, Dr. Karlin-Zysman said, is cohorting. “Instead of them going to the next open bed, wherever it may be, you get the patients all in one place geographically, with a team trained to manage those patients.” Another factor: it’s a hospitalist-run unit. “You can’t have 20 different doctors taking care of the patients; it’s one or two hospitalists running this unit.”
Care models like this can be a true win-win, and her hospital is using them more and more.
“I have a care model that’s a stroke unit; I have a care model that’s an onc unit and one that’s a pulmonary unit,” she said. “We’re creating these true teams, which I think hospitalists really like being part of. What’s that thing that makes them want to come to work every day? Things like this: running a care model, becoming specialized in something.” There are research and abstract opportunities for hospitalists on these units too, which also helps keep them engaged, she said. “I’ve used this care model and things like that to reduce burnout and keep people excited.”
The persistent mortality gap
Patients with mental illness tend to receive worse medical care than people without, studies have shown; they die an average of 25 years earlier, largely from preventable or treatable conditions such as cardiovascular disease and diabetes. The World Health Organization has called the problem “a hidden human rights emergency.”
In one in a series of articles on mental health, Lisa Rosenbaum, MD, a cardiologist at Brigham and Women’s Hospital, Boston, raises the question: Might physician attitudes toward mentally ill people contribute to this mortality gap, and if so, can we change them?
She recognizes the many obstacles physicians face in treating these patients. “The medicines we have are good but not great and can cause obesity and diabetes, which contributes to cardiovascular morbidity and mortality,” Dr. Rosenbaum said. “We have the adherence challenge for the psychiatric medications and for medications for chronic disease. It’s hard enough for anyone to take a medicine every day, and to do that if you’re homeless or you don’t have insight into the need for it, it’s really hard.”
Also, certain behaviors that are more common among people with serious mental illness – smoking, substance abuse, physical inactivity – increase their risk for chronic diseases.
These hurdles may foster a sense of helplessness among hospitalists who have just a small amount of time to spend with a patient, and attitudes may be hard to change.
“Negotiating more effectively about care refusals, more adeptly assessing capacity, and recognizing when our efforts to orchestrate care have been inadequate seem feasible,” Dr. Rosenbaum writes. “Far harder is overcoming any collective belief that what mentally ill people truly need is not something we can offer.” That’s why a truly honest examination of attitudes and biases is a necessary place to start.
She tells the story of one mentally ill patient she learned of in her research, who, after decades as the quintessential frequent flier in the ER, was living stably in the community. “No one could have known how many tries it would take to help him get there,” she writes. His doctor told her, “Let’s say 10 attempts are necessary. Someone needs to be number 2, 3 and 7. You just never know which number you are.”
Education for physicians
A course created by the National Alliance on Mental Illness addresses mental illness issues from a provider perspective.
“Although the description states that the course is intended for mental health professionals, it can be and has been used to educate and inform other healthcare professionals as well,” said Ron Honberg, JD, senior policy advisor for the National Alliance on Mental Illness. The standard course takes 15 hours; there is an abbreviated 4-hour alternative as well. More information can be found at http://www.nami.org/Find-Support/NAMI-Programs/NAMI-Provider-Education.
Sources
1. Szabo L. Cost of Not Caring: Nowhere to Go. USA Today. https://www.usatoday.com/story/news/nation/2014/05/12/mental-health-system-crisis/7746535/. Accessed March 10, 2017.
2. Mental Health America. The State of Mental Health in America. http://www.mentalhealthamerica.net/issues/state-mental-health-america. Accessed March 30, 2017.
3. Karlin-Zysman C, Lerner K, Warner-Cohen J. Creating a Hybrid Medicine and Psychiatric Unit to Manage Medically Ill Patients with Behavioral Health Disorders [abstract]. Journal of Hospital Medicine. 2015; 10 (suppl 2). http://www.shmabstracts.com/abstract/creating-a-hybrid-medicine-and-psychiatric-unit-to-manage-medically-ill-patients-with-behavioral-health-disorders/. Accessed March 19, 2017.
4. Garey J. When Doctors Discriminate. New York Times. http://www.nytimes.com/2013/08/11/opinion/sunday/when-doctors-discriminate.html. August 10, 2013. Accessed March 15, 2017.
5. Rosenbaum L. Closing the Mortality Gap – Mental Illness and Medical Care. N Engl J Med. 2016; 375:1585-1589. doi: 10.1056/NEJMms1610125.
6. Rosenbaum L. Unlearning Our Helplessness – Coexisting Serious Mental and Medical Illness. N Engl J Med. 2016;375:1690-4. doi: 10.1056/NEJMms1610127.
The numbers tell a grim story. Nationwide, 43.7 million adult Americans experienced a mental health condition during 2016 – an increase of 1.2 million over the previous year. Mental health issues send almost 5.5 million people to emergency departments each year; nearly 60% of adults with a mental illness received no treatment at all.
If that massive – and growing – need is one side of the story, shrinking resources are the other. Mental health resources had already been diminishing for decades before the recession hit – and hit them especially hard. Between 2009 and 2012, states cut $5 billion in mental health services; during that time, at least 4,500 public psychiatric hospital beds nationwide disappeared – nearly 10% of the total supply. The bulk of those resources have never been restored.
Provider numbers also are falling. “Psychiatry is probably the top manpower shortage among all specialties,” said Joe Parks, MD, medical director of the National Council for Behavioral Health. “We have about a third the number of psychiatrists that most estimates say we need, and the number per capita is decreasing.” A significant percentage of psychiatrists – more than 50% – only accept cash, bypassing the low reimbursement rates even private insurance typically offers.
Hospitals, of course, feel those financial disincentives too, which discourage them from investments of their own. “It’s a difficult population to manage, and it’s difficult to manage the financial realities of mental health as well,” said John McHugh, PhD, assistant professor of health policy at Columbia University, New York. “If you were a hospital administrator looking to invest your last dollar and you have the option of investing it in a new heart institute or in behavioral health service, more likely than not, you’re going to invest it in the more profitable cardiovascular service line.”
Providers of last resort
But much of the burden of caring for this population ends up falling on hospitals by default. At Denver Health, Melanie Rylander, MD, medical director of the inpatient psychiatric unit, reports seeing this manifest in three categories of patients. First, there is an influx of people coming into the emergency department with primary mental health issues.
“We’re also seeing an influx of people coming in with physical problems, and upon assessment it becomes very clear very quickly that the real issue is an underlying mental health issue,” she said. Then there are the people coming in for the same physical problems over and over – maybe decompensated heart failure or COPD exacerbations – because mental health issues are impeding their ability to take care of themselves.
Some hospitalists say they feel ill equipped to care for these patients. “We don’t have the facility or the resources many times to properly care for their psychiatric needs when they’re in the hospital. It’s not really part of an internist’s training to be familiar with a lot of the medications,” said Atashi Mandal, MD, a hospitalist and pediatrician in Los Angeles. “Sometimes they get improperly medicated because we don’t know what else to do and the patient’s behavioral issues are escalating, so it’s really a difficult position.”
It’s a dispiriting experience for a hospitalist. “It really bothers me when I am trying to care for a patient who has psychiatric needs, and I feel I’m not able to do it, and I can’t find resources, and I feel that this patient’s needs are being neglected – not because we don’t care, and not because of a lack of effort by the staff. It’s just set up to fail,” Dr. Mandal said.
Ending the silo mentality
Encouraging a more holistic view of health across health care would be an important step to begin to address the problem – after all, the mind and the body are not separate.
“We work in silos, and we really have to stop doing that because these are intertwined,” said Corey Karlin-Zysman, MD, FHM, FACP, chief of the division of hospital medicine at Northwell Health. “A schizophrenic will become worse when they’re medically ill. That illness will be harder to treat if their psychiatric illness is active.” This is starting to happen in the outpatient setting, evidenced by the expansion of the integrated care model, where a primary care doctor is the lead physician working in combination with psychologists, psychiatrists, and social workers. Communication among providers becomes simpler, and patients don’t fall through the cracks as often while trying to navigate the system.
That idea of integration is also making its way into the hospital setting in various ways. In their efforts to bring the care to the patient, rather than the other way around, Dr. Karlin-Zysman’s hospital embedded two hospitalists in the neighboring inpatient psychiatric hospital; when patients need medical treatment, they can receive it without interrupting their behavioral health treatment. As a result, patients who used to end up in their emergency department don’t anymore, and their 30-day readmission rate has fallen by 50%.
But at its foundation, care integration is more of an attitude than a system; it begins with a mindset.
“We talk so much today about system reform, integrated systems, blah, blah,” said Lisa Rosenbaum, MD, a cardiologist at Brigham and Women’s Hospital, Boston. “I don’t want to make it seem like it’s not going to work, but what does it mean for the patient who is psychotic and has 10 problems, with whom you have 15 minutes? Taking good care of these patients means you have to take a deep breath and put in a lot of time and deal with all these things that have nothing to do with the health system under which you practice. There’s this ‘only so much you can do’ feeling that is a problem in itself, because there’s actually a lot we can do.”
Hospitals and communities
It’s axiomatic to say that a better approach to mental health would be based around prevention and early intervention, rather than the less crisis-oriented system we have now. Some efforts are being made in that direction, and they involve, and require, outreach outside the hospital.
“The best hospitals doing work in mental health are going beyond the hospital walls; they’re really looking at their community,” Dr. Nguyen said. “You have hospitals, like Accountable Care Organizations, who are trying to move earlier and think about mental health from a pediatric standpoint: How can we support parents and children during critical phases of brain growth? How can we provide prevention services?” Ultimately, those efforts should help lower future admission rates to EDs and hospitals.
That forward-looking approach may be necessary, but it’s also a challenge. “As a hospital administrator, I would think that you look out at the community and see this problem is not going away – in fact, it is likely going to get worse,” Dr. McHugh said. “A health system may look at themselves and say we have to take the lead on this.” The difficulty is that thinking of it in a sense of value to the community, and making the requisite investments, will have a very long period of payout; a health system that’s struggling may not be able to do it. “It’s the large [health systems] that tend to be more integrated … that are thinking about this much differently,” he said.
Still, the reality is that’s where the root of the problem lies, Dr. Rylander said – not in the hospital, but in the larger community. “In the absence of very basic needs – stable housing, food, heating – it’s really not reasonable to expect that people are going to take care of their physical needs,” she said. “It’s a much larger social issue: how to get resources so that these people can have stable places to live, they can get to and from appointments, that type of thing.”
Those needs are ongoing, of course. Many of these patients suffer from chronic conditions, meaning people will continue to need services and support, said Ron Honberg, JD, senior policy adviser for the National Alliance on Mental Illness. Often, people need services from different systems. “There are complexities in terms of navigating those systems and getting those systems to work well together. Until we make inroads in solving those things, or at least improving those things, the burdens are going to fall on the providers of last resort, and that includes hospitals,” he said.
A collaborative effort may be needed, but hospitals can still be active participants and even leaders.
“If hospitals really want to address these problems, they need to be part of the discussions taking place in communities among the various systems and providers and advocates,” Mr. Honberg said. “Ultimately, we need to develop a better community-based system of care, and a better way of handing people off from inpatient to community-based treatment, and some accountability in terms of requiring that people get services, so they don’t get rehospitalized quickly. You’re increasingly seeing accountability now with other health conditions; we’re measuring things in Medicare like rehospitalization rates and the like. We need to be doing that with mental health treatment as well.”
What a hospitalist can do
One thing hospitalists might consider is starting that practice at their own hospitals, measuring, recording, and sharing that kind of information.
“Hospitalists should measure systematically, and in a very neutral manner, the total burden and frequency of the problem and report it consistently to management, along with their assessment that this impairs the quality of care and creates patient risk,” Dr. Parks said. That information can help hospitalists lobby for access to psychiatric personnel, be that in person or through telemedicine. “We don’t have to lay hands on you. There’s no excuse for any hospital not having a contract in place for on-demand consultation in the ER and on the floors.”
Track outcomes, too, Dr. Mandal suggests. With access to the right personnel, are you getting patients out of the ED faster? Are you having fewer negative outcomes while these patients are in the hospital, such as having to use restraints or get security involved? “Hopefully you can get some data in terms of how much money you’ve saved by decreasing the length of stays and decreasing inadvertent adverse effects because the patients weren’t receiving the proper care,” he said.
As this challenge seems likely to continue to grow, hospitalists might consider finding more training in mental health issues themselves so they are more comfortable handling these issues, Dr. Parks said. “The average mini-psych rotation from medical school is only 4 weeks,” he noted. “The ob.gyn. is at least 8 weeks and often 12 weeks, and if you don’t go into ob.gyn., you’re going to see a lot more mentally ill people through the rest of your practice, no matter what you do, than you are going to see pregnant women.”
Just starting these conversations – with patients, with colleagues, with family and friends – might be the most important change of all. “Even though nobody is above these issues afflicting them, this is still something that is not part of an open dialogue, and this is something that affects our own colleagues,” Dr. Mandal said. “I don’t know how many more trainees jumping out of windows it will take, or colleagues going through depression and feeling that it’s a sign of weakness to even talk about it.
“We need to create safe harbors within our own medical communities and acknowledge that we ourselves can be prone to this,” he said. “Perhaps by doing that, we will develop more empathy and become more comfortable, not just with ourselves and our colleagues but also helping these patients. People get overwhelmed and throw their hands up because it is just such a difficult issue. I don’t want people to give up, both from the medical community and our society as a whole – we can’t give up.”
A med-psych unit pilot project
Med-psych units can be a good model to take on these challenges. At Long Island Jewish Medical Center, they launched a pilot project to see how one would work in their community and summarized the results in an SHM abstract.
The hospital shares a campus with a 200-bed inpatient psych hospital, and doctors were seeing a lot of back and forth between the two institutions, said Corey Karlin-Zysman, MD, FHM, FACP, chief of the division of hospital medicine at Northwell Health. “Patients would come into the hospital because they had an active medical issue, but because of their behavioral issues, they’d have to have continuous observation. It would not be uncommon for us to have sometimes close to 30 patients who needed 24-hour continuous observation to make sure they were not hurting themselves.” These PCAs or nurse’s assistants were doing 8-hour shifts, so each patient needed three. “The math is staggering – and with not any better outcomes.”
So the hospital created a 15-bed closed med-psych unit for medically ill patients with behavioral health disorders. They staffed it with a dedicated hospitalist, a nurse practitioner, a psychologist, and a nurse manager.
The number of patients requiring continuous observation fell to single digits. Once in their own unit, these patients caused less disruption and stress on the medical units. They had a lower length of stay compared to their previous admissions in other units, and this became one of the hospital’s highest performing units in terms of patient experience.
The biggest secret of their success, Dr. Karlin-Zysman said, is cohorting. “Instead of them going to the next open bed, wherever it may be, you get the patients all in one place geographically, with a team trained to manage those patients.” Another factor: it’s a hospitalist-run unit. “You can’t have 20 different doctors taking care of the patients; it’s one or two hospitalists running this unit.”
Care models like this can be a true win-win, and her hospital is using them more and more.
“I have a care model that’s a stroke unit; I have a care model that’s an onc unit and one that’s a pulmonary unit,” she said. “We’re creating these true teams, which I think hospitalists really like being part of. What’s that thing that makes them want to come to work every day? Things like this: running a care model, becoming specialized in something.” There are research and abstract opportunities for hospitalists on these units too, which also helps keep them engaged, she said. “I’ve used this care model and things like that to reduce burnout and keep people excited.”
The persistent mortality gap
Patients with mental illness tend to receive worse medical care than people without, studies have shown; they die an average of 25 years earlier, largely from preventable or treatable conditions such as cardiovascular disease and diabetes. The World Health Organization has called the problem “a hidden human rights emergency.”
In one in a series of articles on mental health, Lisa Rosenbaum, MD, a cardiologist at Brigham and Women’s Hospital, Boston, raises the question: Might physician attitudes toward mentally ill people contribute to this mortality gap, and if so, can we change them?
She recognizes the many obstacles physicians face in treating these patients. “The medicines we have are good but not great and can cause obesity and diabetes, which contributes to cardiovascular morbidity and mortality,” Dr. Rosenbaum said. “We have the adherence challenge for the psychiatric medications and for medications for chronic disease. It’s hard enough for anyone to take a medicine every day, and to do that if you’re homeless or you don’t have insight into the need for it, it’s really hard.”
Also, certain behaviors that are more common among people with serious mental illness – smoking, substance abuse, physical inactivity – increase their risk for chronic diseases.
These hurdles may foster a sense of helplessness among hospitalists who have just a small amount of time to spend with a patient, and attitudes may be hard to change.
“Negotiating more effectively about care refusals, more adeptly assessing capacity, and recognizing when our efforts to orchestrate care have been inadequate seem feasible,” Dr. Rosenbaum writes. “Far harder is overcoming any collective belief that what mentally ill people truly need is not something we can offer.” That’s why a truly honest examination of attitudes and biases is a necessary place to start.
She tells the story of one mentally ill patient she learned of in her research, who, after decades as the quintessential frequent flier in the ER, was living stably in the community. “No one could have known how many tries it would take to help him get there,” she writes. His doctor told her, “Let’s say 10 attempts are necessary. Someone needs to be number 2, 3 and 7. You just never know which number you are.”
Education for physicians
A course created by the National Alliance on Mental Illness addresses mental illness issues from a provider perspective.
“Although the description states that the course is intended for mental health professionals, it can be and has been used to educate and inform other healthcare professionals as well,” said Ron Honberg, JD, senior policy advisor for the National Alliance on Mental Illness. The standard course takes 15 hours; there is an abbreviated 4-hour alternative as well. More information can be found at http://www.nami.org/Find-Support/NAMI-Programs/NAMI-Provider-Education.
Sources
1. Szabo L. Cost of Not Caring: Nowhere to Go. USA Today. https://www.usatoday.com/story/news/nation/2014/05/12/mental-health-system-crisis/7746535/. Accessed March 10, 2017.
2. Mental Health America. The State of Mental Health in America. http://www.mentalhealthamerica.net/issues/state-mental-health-america. Accessed March 30, 2017.
3. Karlin-Zysman C, Lerner K, Warner-Cohen J. Creating a Hybrid Medicine and Psychiatric Unit to Manage Medically Ill Patients with Behavioral Health Disorders [abstract]. Journal of Hospital Medicine. 2015; 10 (suppl 2). http://www.shmabstracts.com/abstract/creating-a-hybrid-medicine-and-psychiatric-unit-to-manage-medically-ill-patients-with-behavioral-health-disorders/. Accessed March 19, 2017.
4. Garey J. When Doctors Discriminate. New York Times. http://www.nytimes.com/2013/08/11/opinion/sunday/when-doctors-discriminate.html. August 10, 2013. Accessed March 15, 2017.
5. Rosenbaum L. Closing the Mortality Gap – Mental Illness and Medical Care. N Engl J Med. 2016; 375:1585-1589. doi: 10.1056/NEJMms1610125.
6. Rosenbaum L. Unlearning Our Helplessness – Coexisting Serious Mental and Medical Illness. N Engl J Med. 2016;375:1690-4. doi: 10.1056/NEJMms1610127.
Pharmacomechanical thrombolysis does not reduce post-thrombotic syndrome risk
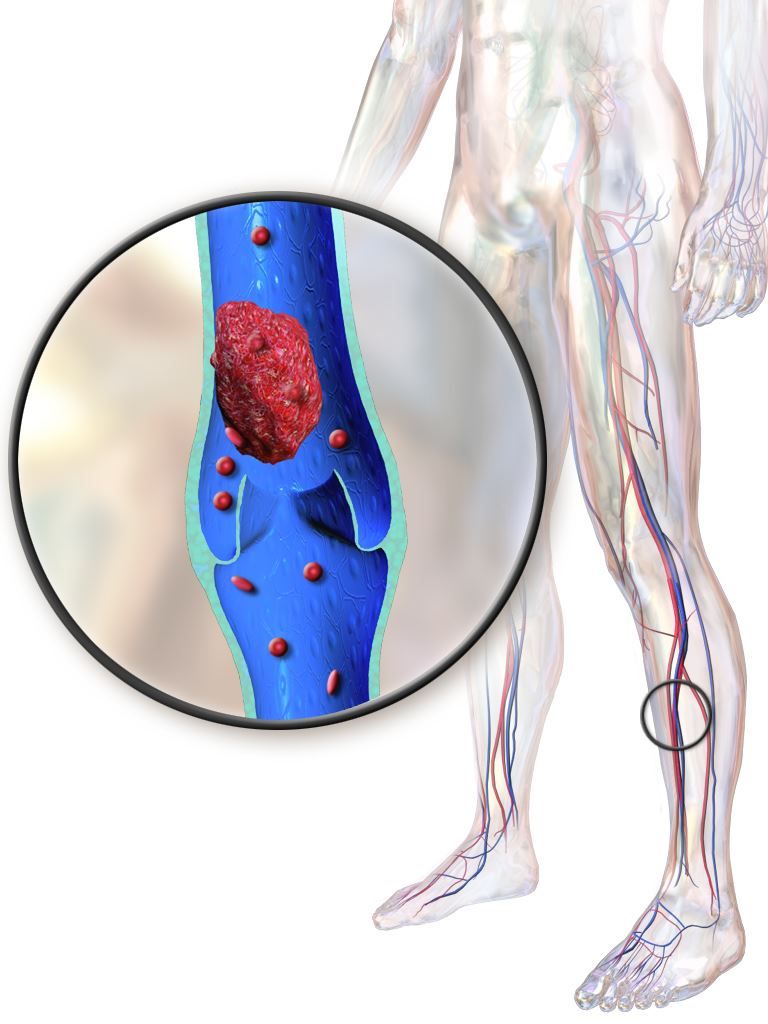
In patients with acute proximal deep vein thrombosis who were undergoing anticoagulation, adding pharmacomechanical catheter-directed thrombolysis did not reduce risk of the post-thrombotic syndrome, according to results of a phase 3, randomized, controlled trial.
Moreover, addition of pharmacomechanical thrombolysis increased risk of major bleeding risk, investigators wrote in a report published online Dec. 6 in the New England Journal of Medicine.
“Our trial, for uncertain reasons, did not confirm these findings,” wrote Suresh Vedantham, MD of Washington University, St. Louis, and his coauthors.
Post-thrombotic syndrome is associated with chronic limb swelling and pain, and can lead to leg ulcers, impaired quality of life, and major disability. About half of patients with proximal deep vein thrombosis (DVT) will develop the post-thrombotic syndrome within 2 years, despite use of anticoagulation therapy, Dr. Vedantham and his colleagues noted.
Pharmacomechanical thrombosis is the catheter-directed delivery of a fibrinolytic agent into the thrombus, along with aspiration or maceration of the thrombus. The goal of the treatment is to reduce the burden of thrombus, which in turn might reduce risk of the post-thrombotic syndrome.
However, in their randomized trial known as ATTRACT, which included 692 patients with an acute proximal DVT, rates of post-thrombotic syndrome between 6 to 24 months after intervention were 47% in the pharmacomechanical thrombolysis group and 48% in the control group (risk ratio, 0.96; 95% CI, 0.82-1.11; P = .56), according to the report (N Engl J Med. 2017;377:2240-52). Control group patients received no procedural intervention.
Major bleeds within 10 days of the intervention were 1.7% and 0.3% for the pharmacomechanical thrombolysis and control groups, respectively (P = .049).
By contrast, in the CAVENT trial, catheter-directed thrombolysis reduced the risk of the post-thrombotic syndrome over 5 years of follow-up (Lancet Haematol. 2016;3[2]:e64-71). Dr. Vedantham and his coauthors suggested that factors potentially explaining the difference in outcomes include the number of patients enrolled (692 in ATTRACT, versus 209 in CAVENT), or the greater use of mechanical therapies in ATTRACT versus longer recombinant tissue plasminogen activator infusions in CAVENT.
The study was supported by multiple sources, including the National Heart, Lung and Blood Institute (NHLBI), Boston Scientific, Covidien (now Medtronic), Genentech, and others. Dr. Vedantham reported receiving grant support from Cook Medical and Volcano. Some of the other authors reported financial ties to Abbott Vascular, Boston Scientific, Medtronic, and other pharmaceutical and device companies.
In patients with acute proximal deep vein thrombosis who were undergoing anticoagulation, adding pharmacomechanical catheter-directed thrombolysis did not reduce risk of the post-thrombotic syndrome, according to results of a phase 3, randomized, controlled trial.
Moreover, addition of pharmacomechanical thrombolysis increased risk of major bleeding risk, investigators wrote in a report published online Dec. 6 in the New England Journal of Medicine.
“Our trial, for uncertain reasons, did not confirm these findings,” wrote Suresh Vedantham, MD of Washington University, St. Louis, and his coauthors.
Post-thrombotic syndrome is associated with chronic limb swelling and pain, and can lead to leg ulcers, impaired quality of life, and major disability. About half of patients with proximal deep vein thrombosis (DVT) will develop the post-thrombotic syndrome within 2 years, despite use of anticoagulation therapy, Dr. Vedantham and his colleagues noted.
Pharmacomechanical thrombosis is the catheter-directed delivery of a fibrinolytic agent into the thrombus, along with aspiration or maceration of the thrombus. The goal of the treatment is to reduce the burden of thrombus, which in turn might reduce risk of the post-thrombotic syndrome.
However, in their randomized trial known as ATTRACT, which included 692 patients with an acute proximal DVT, rates of post-thrombotic syndrome between 6 to 24 months after intervention were 47% in the pharmacomechanical thrombolysis group and 48% in the control group (risk ratio, 0.96; 95% CI, 0.82-1.11; P = .56), according to the report (N Engl J Med. 2017;377:2240-52). Control group patients received no procedural intervention.
Major bleeds within 10 days of the intervention were 1.7% and 0.3% for the pharmacomechanical thrombolysis and control groups, respectively (P = .049).
By contrast, in the CAVENT trial, catheter-directed thrombolysis reduced the risk of the post-thrombotic syndrome over 5 years of follow-up (Lancet Haematol. 2016;3[2]:e64-71). Dr. Vedantham and his coauthors suggested that factors potentially explaining the difference in outcomes include the number of patients enrolled (692 in ATTRACT, versus 209 in CAVENT), or the greater use of mechanical therapies in ATTRACT versus longer recombinant tissue plasminogen activator infusions in CAVENT.
The study was supported by multiple sources, including the National Heart, Lung and Blood Institute (NHLBI), Boston Scientific, Covidien (now Medtronic), Genentech, and others. Dr. Vedantham reported receiving grant support from Cook Medical and Volcano. Some of the other authors reported financial ties to Abbott Vascular, Boston Scientific, Medtronic, and other pharmaceutical and device companies.
In patients with acute proximal deep vein thrombosis who were undergoing anticoagulation, adding pharmacomechanical catheter-directed thrombolysis did not reduce risk of the post-thrombotic syndrome, according to results of a phase 3, randomized, controlled trial.
Moreover, addition of pharmacomechanical thrombolysis increased risk of major bleeding risk, investigators wrote in a report published online Dec. 6 in the New England Journal of Medicine.
“Our trial, for uncertain reasons, did not confirm these findings,” wrote Suresh Vedantham, MD of Washington University, St. Louis, and his coauthors.
Post-thrombotic syndrome is associated with chronic limb swelling and pain, and can lead to leg ulcers, impaired quality of life, and major disability. About half of patients with proximal deep vein thrombosis (DVT) will develop the post-thrombotic syndrome within 2 years, despite use of anticoagulation therapy, Dr. Vedantham and his colleagues noted.
Pharmacomechanical thrombosis is the catheter-directed delivery of a fibrinolytic agent into the thrombus, along with aspiration or maceration of the thrombus. The goal of the treatment is to reduce the burden of thrombus, which in turn might reduce risk of the post-thrombotic syndrome.
However, in their randomized trial known as ATTRACT, which included 692 patients with an acute proximal DVT, rates of post-thrombotic syndrome between 6 to 24 months after intervention were 47% in the pharmacomechanical thrombolysis group and 48% in the control group (risk ratio, 0.96; 95% CI, 0.82-1.11; P = .56), according to the report (N Engl J Med. 2017;377:2240-52). Control group patients received no procedural intervention.
Major bleeds within 10 days of the intervention were 1.7% and 0.3% for the pharmacomechanical thrombolysis and control groups, respectively (P = .049).
By contrast, in the CAVENT trial, catheter-directed thrombolysis reduced the risk of the post-thrombotic syndrome over 5 years of follow-up (Lancet Haematol. 2016;3[2]:e64-71). Dr. Vedantham and his coauthors suggested that factors potentially explaining the difference in outcomes include the number of patients enrolled (692 in ATTRACT, versus 209 in CAVENT), or the greater use of mechanical therapies in ATTRACT versus longer recombinant tissue plasminogen activator infusions in CAVENT.
The study was supported by multiple sources, including the National Heart, Lung and Blood Institute (NHLBI), Boston Scientific, Covidien (now Medtronic), Genentech, and others. Dr. Vedantham reported receiving grant support from Cook Medical and Volcano. Some of the other authors reported financial ties to Abbott Vascular, Boston Scientific, Medtronic, and other pharmaceutical and device companies.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: Rates of post-thrombotic syndrome were 47% in the pharmacomechanical thrombolysis group, and 48% in the control group (risk ratio, 0.96; 95% CI, 0.82-1.11; P = .56).
Data source: A phase 3, multicenter, randomized, open-label, assessor-blinded, controlled clinical trial, including 692 patients with acute proximal deep vein thrombosis.
Disclosures: The study was supported by multiple sources, including the National Heart, Lung and Blood Institute (NHLBI), Boston Scientific, Covidien (now Medtronic), Genentech, and others. First author Suresh Vedantham, MD, reported receiving grant support from Cook Medical and Volcano. Some of the other authors reported financial ties to Abbott Vascular, Boston Scientific, Medtronic, and other pharmaceutical and device companies.
Alarm reductions don’t improve ICU response times
TORONTO – It will take more than a reduction in alarms to address the issue of alarm fatigue in the ICU; a change in the ICU staff culture is needed, suggests new research.
“It may take years to recondition clinicians [to realize] that alarms are actionable and must get a response,” Afua Kunadu, MD, said during her presentation on the study at the CHEST annual meeting. Results from prior studies had suggested that as many as 99% of clinical alarms do not result in clinical intervention, noted Dr. Kunadu, an internal medicine physician at Harlem Hospital Center in New York.
She described the program, which started in the 20-bed adult ICU of Harlem Hospital Center, following a 2014 National Patient Safety Goal issued by The Joint Commission to improve the safety of clinical alarm systems by reducing unneeded alarms and alarm fatigue. The Harlem Hospital task force that ran the program began with an audit of alarms that went off in the ICU and used the results to identify the three most common alarms: bedside cardiac monitors, infusion pumps, and mechanical ventilators. The task force arranged to reset the default settings on these devices to decrease alarm frequency and boost the clinical importance of each alarm that still sounded. Concurrently, they ran educational sessions about the new alarm thresholds, the anticipated drop in alarm number, and the increased urgency to respond to the remaining alarms very quickly for the ICU staff.
The raised thresholds effectively cut the number of alarms. The average number of alarms per patient per hour fell from 4.5 at baseline during September 2016 to about 2 after 1 month, during December 2016. Then the rate further declined to reach a steady nadir that stayed at about 1.3 alarms per patient per hour 4 months into the program.
But timely responses, measured as the percentage of alarm responses occurring within 60 seconds after the alarm went off, fell from 60% at 1 month into the program down to 12% after 4 months, Dr. Kunadu reported.
She had no disclosures.
[email protected]
On Twitter @mitchelzoler
TORONTO – It will take more than a reduction in alarms to address the issue of alarm fatigue in the ICU; a change in the ICU staff culture is needed, suggests new research.
“It may take years to recondition clinicians [to realize] that alarms are actionable and must get a response,” Afua Kunadu, MD, said during her presentation on the study at the CHEST annual meeting. Results from prior studies had suggested that as many as 99% of clinical alarms do not result in clinical intervention, noted Dr. Kunadu, an internal medicine physician at Harlem Hospital Center in New York.
She described the program, which started in the 20-bed adult ICU of Harlem Hospital Center, following a 2014 National Patient Safety Goal issued by The Joint Commission to improve the safety of clinical alarm systems by reducing unneeded alarms and alarm fatigue. The Harlem Hospital task force that ran the program began with an audit of alarms that went off in the ICU and used the results to identify the three most common alarms: bedside cardiac monitors, infusion pumps, and mechanical ventilators. The task force arranged to reset the default settings on these devices to decrease alarm frequency and boost the clinical importance of each alarm that still sounded. Concurrently, they ran educational sessions about the new alarm thresholds, the anticipated drop in alarm number, and the increased urgency to respond to the remaining alarms very quickly for the ICU staff.
The raised thresholds effectively cut the number of alarms. The average number of alarms per patient per hour fell from 4.5 at baseline during September 2016 to about 2 after 1 month, during December 2016. Then the rate further declined to reach a steady nadir that stayed at about 1.3 alarms per patient per hour 4 months into the program.
But timely responses, measured as the percentage of alarm responses occurring within 60 seconds after the alarm went off, fell from 60% at 1 month into the program down to 12% after 4 months, Dr. Kunadu reported.
She had no disclosures.
[email protected]
On Twitter @mitchelzoler
TORONTO – It will take more than a reduction in alarms to address the issue of alarm fatigue in the ICU; a change in the ICU staff culture is needed, suggests new research.
“It may take years to recondition clinicians [to realize] that alarms are actionable and must get a response,” Afua Kunadu, MD, said during her presentation on the study at the CHEST annual meeting. Results from prior studies had suggested that as many as 99% of clinical alarms do not result in clinical intervention, noted Dr. Kunadu, an internal medicine physician at Harlem Hospital Center in New York.
She described the program, which started in the 20-bed adult ICU of Harlem Hospital Center, following a 2014 National Patient Safety Goal issued by The Joint Commission to improve the safety of clinical alarm systems by reducing unneeded alarms and alarm fatigue. The Harlem Hospital task force that ran the program began with an audit of alarms that went off in the ICU and used the results to identify the three most common alarms: bedside cardiac monitors, infusion pumps, and mechanical ventilators. The task force arranged to reset the default settings on these devices to decrease alarm frequency and boost the clinical importance of each alarm that still sounded. Concurrently, they ran educational sessions about the new alarm thresholds, the anticipated drop in alarm number, and the increased urgency to respond to the remaining alarms very quickly for the ICU staff.
The raised thresholds effectively cut the number of alarms. The average number of alarms per patient per hour fell from 4.5 at baseline during September 2016 to about 2 after 1 month, during December 2016. Then the rate further declined to reach a steady nadir that stayed at about 1.3 alarms per patient per hour 4 months into the program.
But timely responses, measured as the percentage of alarm responses occurring within 60 seconds after the alarm went off, fell from 60% at 1 month into the program down to 12% after 4 months, Dr. Kunadu reported.
She had no disclosures.
[email protected]
On Twitter @mitchelzoler
AT CHEST 2017
Key clinical point:
Major finding: Average alarms/patient/hour fell from 4.5 to 1.3, but the percentage of responses in less than 60 seconds fell from 60% to 12%.
Data source: An observational study at a single adult ICU in the United States.
Disclosures: Dr. Kunadu had no disclosures.
Underlying peripheral arterial or venous disease in patients with lower extremity SSTIs
Clinical case
A 56-year-old woman with type 2 diabetes, morbid obesity, and hypertension presents with right lower extremity erythema, weeping, and exquisite tenderness associated with chills. She reports a 2-year history of chronic lower extremity swelling and cramps with a more recent development of scaling and two superficial ulcers on lower third of her leg. For 1 month, she has noted significant pain circumferentially around the ankles with focal tautness and pallor of the skin. She has tried acetaminophen and oxycodone with little relief.
Over the past week, she noted foul smelling discharge from one of the superficial ulcers with redness extending up to the knee prompting presentation to the emergency department. She had a fever to 101.2° F, tachycardia to 105 beats per minute, and leukocytosis to 14.7. She is admitted to the hospitalist service for sepsis secondary to right lower extremity cellulitis.
Introduction
Skin and soft tissue infections (SSTIs) remain among the most common inpatient diagnoses cared for by hospitalists. Most patients admitted to a hospitalist service with an SSTI meet the criteria for either moderate or severe infection as outlined by the Infectious Disease Society of America – systemic signs of infection by SIRS criteria or a high likelihood of an immunocompromised state, methicillin-resistant Staphylococcus aureus infection, trauma, or wounds.1
Often these patients have several comorbid conditions such as diabetes, morbid obesity, or peripheral arterial and venous disease. Though most hospitalists are adept at managing diabetes, blood pressure, and other comorbidities, the ability to recognize and manage peripheral vascular disease can be challenging. This article will discuss ways to help providers better identify and manage underlying peripheral arterial disease (PAD) and/or chronic venous insufficiency (CVI) in patients admitted with lower extremity SSTIs.
1. In addition to an infection, could there also be underlying peripheral arterial or venous disease?
Patients with peripheral edema and vascular disease are predisposed to recurrent lower extremity SSTIs. When assessing for vascular disease, it is important to consider PAD and CVI separately.
CVI refers to the spectrum of syndromes caused by venous valvular incompetency, venous obstruction, or decreased muscle contraction. Veins cannot maximally deliver venous blood back to the heart resulting in venous pooling in the lower extremities. The exact mechanism of the skin changes that accompany venous insufficiency is unknown but may be related to cytokine cascades that result in perivascular inflammation and a weakening of the dermal barrier. Over time, this can develop into spontaneous ulceration of the skin.2,3
PAD refers to atherosclerosis of the noncerebral, noncoronary arteries, which leads to ischemic symptoms and atrophy of the supplied territory. Ulceration usually results from mild trauma due to poor wound healing.4,5 A thorough history, assessment of risk factors, and physical exam are essential to identifying these two potential diagnoses in patients admitted with SSTIs.
First, the provider should assess risk factors for underlying vascular disease. For PAD, these include risk factors similar to those of coronary artery disease (CAD): hypertension, hyperlipidemia, history of smoking, and poorly-controlled diabetes. Chronic kidney disease and family history are also associated with PAD. Since PAD and CAD share similar risk factors, it is often common for patients with CAD (as well as patients with cerebrovascular disease) to have PAD. Risk factors for CVI include obesity, chronic sedentary lifestyle, multiple pregnancies, family history, and prior superficial or deep venous thrombosis.2,4
Next, the provider should ask the patient about symptoms experienced prior to the onset of the current SSTI. Patients with either arterial or venous disease will typically report lower extremity symptoms that have been occurring for months to years, long before the acute SSTI. The classic symptom for PAD is claudication – leg pain or cramping that occurs on exertion and improves with rest. This is due to decreased arterial blood flow to the affected limb, felt most acutely during exercise. Other symptoms include numbness, a cool lower extremity, and lower extremity hair loss. As PAD progresses, a patient may also have rest pain, which may indicate more critical ischemia, as well nonhealing wounds after mild trauma.
In contrast, symptoms of CVI present more variably. CVI can be associated with heaviness, cramping, and pain that are usually worse in the dependent position and relieved with elevation. Patients may also report dry skin, edema, pruritus, scaling, skin tightness, and indolent ulcers at advanced stages.2-6
The physical exam can help the provider distinguish between venous and arterial disease. Patients with PAD often have diminished or nonpalpable distal pulses, bruits in proximal arteries, pallor, hair loss, nail thickening, decreased capillary refill time, and ulceration of the toes. CVI shares some common characteristics but can be distinguished by evidence of varicose veins, telangiectasia, edema (which spares the foot), lipodermatosclerosis, and atrophie blanche (white scarring around the ankle). Patients with venous disease tend to have warm lower extremities and palpable pulses. Often, there is hyperpigmentation, especially around the ankles, and associated eczematous changes with scaling, erythema, and weeping. CVI can also present with ulcers. In addition, if the SSTI is not responding to appropriate antibiotics in the typical time frame, this may be a clue that there is an underlying vascular issue.2-6
Ulcers, whether arterial or venous, comprise a break in the skin’s protective barrier and give bacteria a point of entry. Thus, ulcers often get superinfected, leading to an SSTI rather than SSTIs causing ulcers. The anatomic location can help differentiate between venous and arterial ulcers. Arterial ulcers tend to occur on the toes, heels, and lateral and medial malleoli. Venous ulcers are classically present above the medial malleolus but can occur anywhere on the medial lower third of the leg. Venous ulcers are more superficial and have an irregular shape, while arterial ulcers are deeper, have smoother edges and a “punched-out” shape. Both arterial and venous ulcers can be exudative though venous ulcers are rarely necrotic. Both arterial and venous ulcers can be painful.7-9
2. There are signs and symptoms of underlying vascular disease in a patient with a lower extremity SSTI. Now what?
Neither PAD nor CVI is a clinical diagnosis, thus further work-up is required to confirm the diagnosis and accurately classify disease severity. The timing of this work-up is of unique interest to hospitalists.
Most patients who are hospitalized with cellulitis or a superficial wound infection do not need urgent inpatient work-up of suspected peripheral arterial or venous disease. The one notable exception to this is patients with diabetic foot infections or infected arterial ulcers that need prompt evaluation for possible critical limb ischemia. Barring cases of critical limb ischemia, the main objective of identifying PAD or CVI in patients hospitalized for SSTIs is to appropriately arrange testing and follow-up after discharge.
To address specific management strategies, it is useful to stratify patients by symptom and exam severity as follows: mild/moderate PAD symptoms without ulcer; infected ulcer with PAD features; mild/moderate CVI symptoms without ulcer; and infected ulcer with CVI features. As specific guidelines for the inpatient work-up and management of suspected peripheral arterial and venous disease are sparse, we rely on guidelines and best practices used in the outpatient setting and adapt them to these potential inpatient presentations.
Mild/Moderate PAD symptoms with superimposed cellulitis but no ulceration
In a patient admitted for cellulitis without open wounds, history and review of systems might reveal the presence of claudication or other symptoms suspicious for PAD. While the U.S. Preventative Services Task Force and American College of Cardiology discourages the routine screening of asymptomatic patients for PAD, patients with risk factors who endorse symptoms should undergo initial testing for PAD with an ankle-brachial index (ABI).10
The ABI is the ratio of ankle blood pressure to arm blood pressure, and is measured via sphygmomanometry with a Doppler probe. The ABI remains the simplest, most inexpensive first-line test for PAD. An ABI value of less than 0.9 is considered diagnostic for PAD and has been found to be more than 95% specific for arterial stenoses of greater than 50% on angiography across multiple studies.11
In an inpatient with risk factors for PAD and claudication symptoms, referral for outpatient ABIs with subsequent follow-up by a primary care physician should be arranged. If a diagnosis of PAD is made via ABI, the PCP should reinforce risk factor modification (tobacco cessation, diet, exercise, and aggressive lipid, blood pressure and blood glucose control) and start medical management with a single anti-platelet agent to reduce the risk of MI, stroke, or “vascular death.” The most recent ACC guidelines recommend either aspirin or clopidogrel as an acceptable anti-platelet agent (grade 1A).12 Cilostazol may be considered if claudication symptoms are significantly interfering with lifestyle. If this management fails, the patient may be referred to a vascular specialist for consideration of revascularization.
Infected ulcer with PAD features
Unlike cellulitis, arterial ulcers are a direct sequela of arterial insufficiency and represent the far end of the spectrum of disease severity and in certain cases treatment failure. Patients who present with advanced ischemic and/or diabetic foot ulcers may have never been evaluated for PAD as an outpatient. Prompt work-up and management is required given the high degree of morbidity and mortality associated with arterial ulcers. Whether an urgent inpatient evaluation is indicated depends on the clinical evaluation.
The first step is to determine the depth of the ulceration. Critical limb ischemia may be present if the ulcer is deep, gangrenous, overlies a bony prominence, or is associated with systemic signs of sepsis. A physical exam should include an assessment of the pulses including femoral, popliteal, PT and DP, preferably with bedside Doppler ultrasound. If pulses are absent, urgent vascular surgery evaluation is warranted to prevent loss of limb; the work-up generally involves imaging such as computed tomography angiography or magnetic resonance angiography to identify culprit lesions, or if sufficiently suspicious, immediate invasive angiogram with the potential for endovascular intervention.
While palpable pulses can be reassuring and raise the possibility of a nonarterial etiology of ulceration – such as a microvascular, neuropathic or venous disease – it is important to remember that pulse exams are often unreliable and provider dependent.13 Moreover, the presence of pulses does not effectively exclude severe PAD or critical limb ischemia in patients with a high pretest probability.14 Thus, in cases of deep, complex lower extremity and foot ulcers, it is prudent to obtain urgent evaluation by a surgical wound specialist, which depending on the institution may be podiatry, vascular surgery, or wound care. This may lead to a better clinical assessment of the wound and clearer recommendations regarding the need for additional testing, such as imaging, to rule out osteomyelitis, surgical debridement, or amputation.
Inpatient ABIs in this situation may help diagnose and quantify the severity of PAD. Newer classification schemes such as the Society of Vascular Surgery Wound Ischemia Foot Infection score take into account clinical findings as well as ABI scores to better prognosticate limb loss and select patients for intervention.15 If the clinical picture is deemed sufficiently suspicious for critical limb ischemia, the patient may be taken directly for invasive testing with possible intervention.
If an infected ulcer is superficial, shows no signs of gangrene, and has been present for less than 30 days, further work-up for suspected PAD can generally be deferred to an outpatient setting after resolution of the acute infection. Management of the wound is highly institution dependent. When available, a wound care specialist (physician or nurse) or a plastic surgeon can be consulted as an inpatient to give specific recommendations that can range anywhere from enzymatic debridement to simple dressing. If this service is unavailable, we recommend dressing the wound with moist nonocclusive dressings with frequent changes. Referrals for ABI testing and follow up in podiatry, wound care, or vascular clinic should be arranged. Finally, educating the patient on what to expect can increase compliance with the outpatient treatment plan.
Mild to moderate CVI symptoms with superimposed cellulitis but no ulceration
Chronic venous insufficiency is a syndrome that has variable presentations based on the location and degree of valvular incompetence in the superficial or, less commonly, deep venous systems. For a patient with cellulitis and CVI, the clinical exam findings may be associated with venous hypertension syndrome – in which there is deep axial reflux and possible obstruction – and could also represent complex varicose disease which is usually caused by superficial reflux of the greater saphenous vein.3 The lack of advanced skin changes and ulceration raises the suspicion of mild to moderate CVI.
Guidelines from the American Venous Forum and the Society for Vascular Surgery recommend that all patients with suspected CVI, regardless of severity, undergo venous duplex ultrasound scanning as a first diagnostic test (grade 1A) to accurately classify the disease according to the Clinical Etiological Anatomical Pathophysiology (CEAP) system (Table 1).16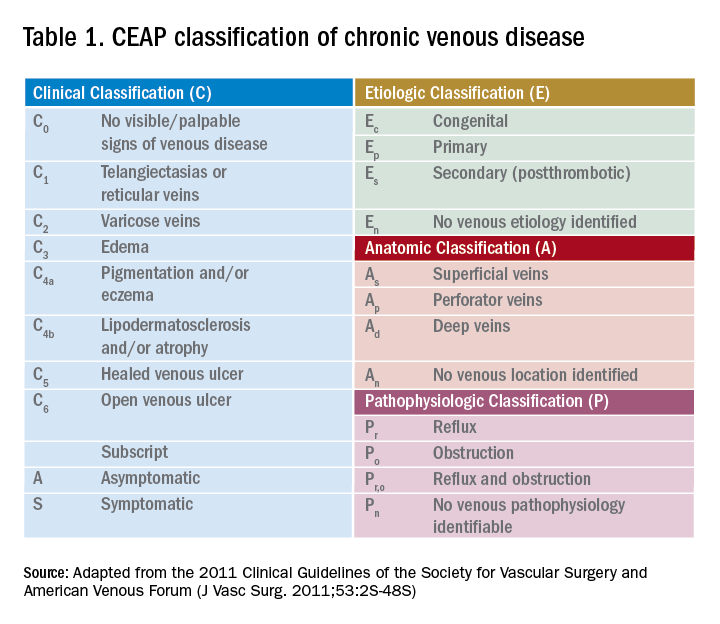
Compression therapy is commonly accepted as a noninvasive treatment option for all levels of CVI, yet most of the evidence comes from secondary prevention studies in patients with advanced CVI with venous ulcers.18 Strong evidence for the role of compression stockings in mild to moderate CVI is lacking. In fact, recent guidelines from the Society of Vascular Surgery, reviewed by the American Heart Association, do not recommend compression therapy as a primary treatment modality in patients with symptomatic varicose veins (without ulcers) if the patient is a candidate for saphenous vein ablation.19 This recommendation is based on clinical trial data that showed greater efficacy and cost-effectiveness of surgery versus conservative management in patients with CEAP2 (low severity) CVI as well as studies noting noncompliance with compression therapy as high as 75%.20-21
However, determining a patient’s candidacy for ablative or surgical therapy requires ultrasound data for accurate CEAP scoring, which is often not achieved as an inpatient. Given the potential benefit and lack of severe adverse effects, hospitalists can consider initiating compression therapy at the time of discharge in a patient with mild to moderate signs of CVI and a low risk profile for severe PAD. The prescription should specify knee-length elastic stockings with graduated compression between 20 to 30 mm Hg.22 The patient should also be encouraged to complete the outpatient duplex ultrasound testing prior to the PCP visit so that he or she can be referred to a vascular specialist appropriately.
Infected ulcer with CVI features
If the patient’s exam is suspicious for advanced venous disease with ulceration, the clinician should evaluate for the presence of scarring. This would indicate that there has been long-standing venous disease with recurrent ulceration. This patient should be asked about a previous diagnosis of CVI, prior compression therapy, and barriers to compliance with compression therapy such as poor fit or difficulty of use due to obesity or immobility. It is important to note that mixed ulcers are present in up to 20% of patients; a careful assessment of risk factors for PAD, pulse exam, and referral for outpatient ABI testing is warranted to rule out arterial insufficiency in this patient with likely venous ulcer.23
The AHA recommends prompt specialist evaluation for CEAP scores greater than or equal to 4; based on physical exam alone, this patient’s active venous ulcer yields the highest possible score of 6.2 If not previously done, this patient with advanced CVI and ulceration should be referred for an outpatient venous duplex ultrasound as well as urgent follow-up with a vascular specialist soon after discharge.
There is significant consensus in the literature that multilayer compression therapy between 30 and 40 mm Hg is the first-line treatment in patients with venous ulcers as it has been shown to promote ulcer healing and prevent recurrence.24-25 In addition, superficial venous surgery, including minimally invasive ablation, can reduce the recurrence of ulcers if used as adjunctive therapy in selected patients.26 However, compressive therapy should generally not be prescribed in patients with venous ulcers until PAD has been ruled out.
If ABI results are available, the clinician can consider compression at 30-40 mm Hg for ABI values greater than 0.8 and reduced compression at 20-30 mm Hg for values of 0.5-0.8; compression is contraindicated if the ABI is less than 0.5. Prompt follow-up with a vascular specialist can help direct compressive and/or surgical therapy. Wound care consultation as an inpatient can assist with dressing recommendations, though the evidence has not shown that dressings of any type worn under compressive garments improve ulcer healing.27
Bottom line
Hospitalists are in a unique position to identify patients with underlying peripheral arterial and venous disease when they are admitted for lower extremity skin and soft tissue infections. A focused history and physical exam can yield significant clinical clues and should prompt either inpatient or outpatient work-up.
In patients with deep ulcers and concern for critical limb ischemia, inpatient consultation should be sought. In patients with superficial venous or arterial ulcers, referral for outpatient ABI, color duplex ultrasound, or both should be made; most of these patients should also be directly referred to a vascular and/or wound specialist. Patients with more benign forms of disease who endorse chronic symptoms suspicious for mild to moderate PAD or CVI can be seen by a PCP for further management. All patients should be educated about the importance of follow-up as it remains their best chance to curb the progression of disease, reduce the risks for recurrent infection, and improve overall quality of life.
Back to the original case
Our patient’s lower extremity erythema, fever, and leukocytosis improved with 3 days of IV vancomycin treatment. Her wound was kept clean with moist dressings and showed no signs of deep infection; with elevation, her bilateral lower extremity edema also improved. Her physical exam findings and clinical history were highly suspicious for long-standing CVI. She was discharged with oral antibiotics and a referral to wound care for ongoing management of her superficial ulcers. An outpatient venous duplex ultrasound and ABI were scheduled prior to her vascular surgery appointment to effectively rule out PAD before consideration of further therapy for severe CVI.
Key Points
- Hospitalists are in a unique position to identify patients with peripheral vascular disease when they are admitted with SSTIs.
- When assessing patients, it is important to consider peripheral arterial disease (PAD) and chronic venous insufficiency (CVI) separately.
- The classic symptom for PAD is claudication. In contrast, symptoms of CVI present more variably.
- Barring cases of critical limb ischemia, the main objective of identifying PAD or CVI is to arrange testing and follow-up after discharge.
References
1. Stevens, DL, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2014;59(2):147-59.
2. Eberhardt, RT, et al. Chronic venous insufficiency. Circulation. 2014;130:333-46.
3. Raju, S, et al. Chronic venous insufficiency and varicose veins. N Engl J Med. 2009;360:2319-27.
4. Kullo, IJ, et al. Peripheral artery disease. N Engl J Med. 2016;374(9):861-71.
5. Hennion D, et al. Diagnosis and treatment of peripheral arterial disease. Am Fam Physician. 2013 Sep 1;88(5):306-10.
6. Henke P, et al. ACP Observer Extra: Peripheral arterial disease. June 2007.
7. Vivas A. Venous leg ulcers. Ann Intern Med. 2016;165(3):ITC17-32.
8. Sumpio BE. Foot ulcers. N Engl J Med. 2000;343(11):787-93.
9. Bazari H, et al. Case 7–2007. 59-year-old woman with diabetic renal disease and nonhealing skin ulcers. N Engl J Med. 2007 Mar 8; 356(10):1049-57.
10. Moyer VA. Screening for peripheral artery disease and cardiovascular disease risk assessment with the ankle-brachial index in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013 Sep 3.159(5):342-8.
11. Khan TH, et al. Critical review of the ankle brachial index. Curr Cardiol Rev. 2008 May;4(2):101-6.
12. Gerhard-Herman MD, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease. A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. 2016.
13. Brearley S, et al. Peripheral pulse palpation: An unreliable physical sign. Ann R Coll Surg Engl. 1992;74:169-71.
14. Khan NA, et al. Does the clinical examination predict lower extremity peripheral arterial disease? JAMA. 2006;295(5):536-46.
15. Mills JL Sr., et al. The Society for Vascular Surgery Lower Extremity Threatened Limb Classification System: Risk stratification based on wound, ischemia, and foot infection (WIfI). J Vasc Surg. 2014 Jan;59(1):220-34.e1-2.
16. Gloviczki P, et al. The care of patients with varicose veins and associated chronic venous diseases: Clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2011;53(5, Suppl):2S-48S.
17. Hamper UM,et al. Ultrasound evaluation of the lower extremity veins. Radiol Clin North Am. 2007 May;45(3):525-47.
18. Vivas A. Venous leg ulcers. Ann Intern Med. 2016;165(3):ITC17-32.
19. Gloviczki P, et al. The care of patients with varicose veins and associated chronic venous diseases: Clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2011;53(5, Suppl):2S-48S.
20. Michaels JA, et al. Randomized clinical trial comparing surgery with conservative treatment for uncomplicated varicose veins. Br J Surg. 2006 Feb;93(2):175-81.
21. Raju S, et al. Use of compression stockings in chronic venous disease: Patient compliance and efficacy. Ann Vasc Surg. 2007 Nov;21(6):790-5.
22. Gloviczki P, et al. The care of patients with varicose veins and associated chronic venous diseases: Clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2011;53(5, Suppl):2S-48S.
23. Humphreys ML, et al. Management of mixed arterial and venous leg ulcers. Br J Surg. 2007 Sep;94(9):1104-7.
24. O’Meara S, et al. Compression for venous leg ulcers. Cochrane Database Syst Rev. 2012 Nov 14;11:CD000265.
25. Dolibog P, et al. A comparative clinical study on five types of compression therapy in patients with venous leg ulcers. Int J Med Sci. 2013;11(1):34-43.
26. Gohel MS, et al. Long term results of compression therapy alone versus compression plus surgery in chronic venous ulceration (ESCHAR): Randomised controlled trial. BMJ. 2007 Jul 14;335(7610):83.
27. Palfreyman S, et al. Dressings for venous leg ulcers: systematic review and meta-analysis. BMJ. 2007 Aug 4;335(7613):244.
Clinical case
A 56-year-old woman with type 2 diabetes, morbid obesity, and hypertension presents with right lower extremity erythema, weeping, and exquisite tenderness associated with chills. She reports a 2-year history of chronic lower extremity swelling and cramps with a more recent development of scaling and two superficial ulcers on lower third of her leg. For 1 month, she has noted significant pain circumferentially around the ankles with focal tautness and pallor of the skin. She has tried acetaminophen and oxycodone with little relief.
Over the past week, she noted foul smelling discharge from one of the superficial ulcers with redness extending up to the knee prompting presentation to the emergency department. She had a fever to 101.2° F, tachycardia to 105 beats per minute, and leukocytosis to 14.7. She is admitted to the hospitalist service for sepsis secondary to right lower extremity cellulitis.
Introduction
Skin and soft tissue infections (SSTIs) remain among the most common inpatient diagnoses cared for by hospitalists. Most patients admitted to a hospitalist service with an SSTI meet the criteria for either moderate or severe infection as outlined by the Infectious Disease Society of America – systemic signs of infection by SIRS criteria or a high likelihood of an immunocompromised state, methicillin-resistant Staphylococcus aureus infection, trauma, or wounds.1
Often these patients have several comorbid conditions such as diabetes, morbid obesity, or peripheral arterial and venous disease. Though most hospitalists are adept at managing diabetes, blood pressure, and other comorbidities, the ability to recognize and manage peripheral vascular disease can be challenging. This article will discuss ways to help providers better identify and manage underlying peripheral arterial disease (PAD) and/or chronic venous insufficiency (CVI) in patients admitted with lower extremity SSTIs.
1. In addition to an infection, could there also be underlying peripheral arterial or venous disease?
Patients with peripheral edema and vascular disease are predisposed to recurrent lower extremity SSTIs. When assessing for vascular disease, it is important to consider PAD and CVI separately.
CVI refers to the spectrum of syndromes caused by venous valvular incompetency, venous obstruction, or decreased muscle contraction. Veins cannot maximally deliver venous blood back to the heart resulting in venous pooling in the lower extremities. The exact mechanism of the skin changes that accompany venous insufficiency is unknown but may be related to cytokine cascades that result in perivascular inflammation and a weakening of the dermal barrier. Over time, this can develop into spontaneous ulceration of the skin.2,3
PAD refers to atherosclerosis of the noncerebral, noncoronary arteries, which leads to ischemic symptoms and atrophy of the supplied territory. Ulceration usually results from mild trauma due to poor wound healing.4,5 A thorough history, assessment of risk factors, and physical exam are essential to identifying these two potential diagnoses in patients admitted with SSTIs.
First, the provider should assess risk factors for underlying vascular disease. For PAD, these include risk factors similar to those of coronary artery disease (CAD): hypertension, hyperlipidemia, history of smoking, and poorly-controlled diabetes. Chronic kidney disease and family history are also associated with PAD. Since PAD and CAD share similar risk factors, it is often common for patients with CAD (as well as patients with cerebrovascular disease) to have PAD. Risk factors for CVI include obesity, chronic sedentary lifestyle, multiple pregnancies, family history, and prior superficial or deep venous thrombosis.2,4
Next, the provider should ask the patient about symptoms experienced prior to the onset of the current SSTI. Patients with either arterial or venous disease will typically report lower extremity symptoms that have been occurring for months to years, long before the acute SSTI. The classic symptom for PAD is claudication – leg pain or cramping that occurs on exertion and improves with rest. This is due to decreased arterial blood flow to the affected limb, felt most acutely during exercise. Other symptoms include numbness, a cool lower extremity, and lower extremity hair loss. As PAD progresses, a patient may also have rest pain, which may indicate more critical ischemia, as well nonhealing wounds after mild trauma.
In contrast, symptoms of CVI present more variably. CVI can be associated with heaviness, cramping, and pain that are usually worse in the dependent position and relieved with elevation. Patients may also report dry skin, edema, pruritus, scaling, skin tightness, and indolent ulcers at advanced stages.2-6
The physical exam can help the provider distinguish between venous and arterial disease. Patients with PAD often have diminished or nonpalpable distal pulses, bruits in proximal arteries, pallor, hair loss, nail thickening, decreased capillary refill time, and ulceration of the toes. CVI shares some common characteristics but can be distinguished by evidence of varicose veins, telangiectasia, edema (which spares the foot), lipodermatosclerosis, and atrophie blanche (white scarring around the ankle). Patients with venous disease tend to have warm lower extremities and palpable pulses. Often, there is hyperpigmentation, especially around the ankles, and associated eczematous changes with scaling, erythema, and weeping. CVI can also present with ulcers. In addition, if the SSTI is not responding to appropriate antibiotics in the typical time frame, this may be a clue that there is an underlying vascular issue.2-6
Ulcers, whether arterial or venous, comprise a break in the skin’s protective barrier and give bacteria a point of entry. Thus, ulcers often get superinfected, leading to an SSTI rather than SSTIs causing ulcers. The anatomic location can help differentiate between venous and arterial ulcers. Arterial ulcers tend to occur on the toes, heels, and lateral and medial malleoli. Venous ulcers are classically present above the medial malleolus but can occur anywhere on the medial lower third of the leg. Venous ulcers are more superficial and have an irregular shape, while arterial ulcers are deeper, have smoother edges and a “punched-out” shape. Both arterial and venous ulcers can be exudative though venous ulcers are rarely necrotic. Both arterial and venous ulcers can be painful.7-9
2. There are signs and symptoms of underlying vascular disease in a patient with a lower extremity SSTI. Now what?
Neither PAD nor CVI is a clinical diagnosis, thus further work-up is required to confirm the diagnosis and accurately classify disease severity. The timing of this work-up is of unique interest to hospitalists.
Most patients who are hospitalized with cellulitis or a superficial wound infection do not need urgent inpatient work-up of suspected peripheral arterial or venous disease. The one notable exception to this is patients with diabetic foot infections or infected arterial ulcers that need prompt evaluation for possible critical limb ischemia. Barring cases of critical limb ischemia, the main objective of identifying PAD or CVI in patients hospitalized for SSTIs is to appropriately arrange testing and follow-up after discharge.
To address specific management strategies, it is useful to stratify patients by symptom and exam severity as follows: mild/moderate PAD symptoms without ulcer; infected ulcer with PAD features; mild/moderate CVI symptoms without ulcer; and infected ulcer with CVI features. As specific guidelines for the inpatient work-up and management of suspected peripheral arterial and venous disease are sparse, we rely on guidelines and best practices used in the outpatient setting and adapt them to these potential inpatient presentations.
Mild/Moderate PAD symptoms with superimposed cellulitis but no ulceration
In a patient admitted for cellulitis without open wounds, history and review of systems might reveal the presence of claudication or other symptoms suspicious for PAD. While the U.S. Preventative Services Task Force and American College of Cardiology discourages the routine screening of asymptomatic patients for PAD, patients with risk factors who endorse symptoms should undergo initial testing for PAD with an ankle-brachial index (ABI).10
The ABI is the ratio of ankle blood pressure to arm blood pressure, and is measured via sphygmomanometry with a Doppler probe. The ABI remains the simplest, most inexpensive first-line test for PAD. An ABI value of less than 0.9 is considered diagnostic for PAD and has been found to be more than 95% specific for arterial stenoses of greater than 50% on angiography across multiple studies.11
In an inpatient with risk factors for PAD and claudication symptoms, referral for outpatient ABIs with subsequent follow-up by a primary care physician should be arranged. If a diagnosis of PAD is made via ABI, the PCP should reinforce risk factor modification (tobacco cessation, diet, exercise, and aggressive lipid, blood pressure and blood glucose control) and start medical management with a single anti-platelet agent to reduce the risk of MI, stroke, or “vascular death.” The most recent ACC guidelines recommend either aspirin or clopidogrel as an acceptable anti-platelet agent (grade 1A).12 Cilostazol may be considered if claudication symptoms are significantly interfering with lifestyle. If this management fails, the patient may be referred to a vascular specialist for consideration of revascularization.
Infected ulcer with PAD features
Unlike cellulitis, arterial ulcers are a direct sequela of arterial insufficiency and represent the far end of the spectrum of disease severity and in certain cases treatment failure. Patients who present with advanced ischemic and/or diabetic foot ulcers may have never been evaluated for PAD as an outpatient. Prompt work-up and management is required given the high degree of morbidity and mortality associated with arterial ulcers. Whether an urgent inpatient evaluation is indicated depends on the clinical evaluation.
The first step is to determine the depth of the ulceration. Critical limb ischemia may be present if the ulcer is deep, gangrenous, overlies a bony prominence, or is associated with systemic signs of sepsis. A physical exam should include an assessment of the pulses including femoral, popliteal, PT and DP, preferably with bedside Doppler ultrasound. If pulses are absent, urgent vascular surgery evaluation is warranted to prevent loss of limb; the work-up generally involves imaging such as computed tomography angiography or magnetic resonance angiography to identify culprit lesions, or if sufficiently suspicious, immediate invasive angiogram with the potential for endovascular intervention.
While palpable pulses can be reassuring and raise the possibility of a nonarterial etiology of ulceration – such as a microvascular, neuropathic or venous disease – it is important to remember that pulse exams are often unreliable and provider dependent.13 Moreover, the presence of pulses does not effectively exclude severe PAD or critical limb ischemia in patients with a high pretest probability.14 Thus, in cases of deep, complex lower extremity and foot ulcers, it is prudent to obtain urgent evaluation by a surgical wound specialist, which depending on the institution may be podiatry, vascular surgery, or wound care. This may lead to a better clinical assessment of the wound and clearer recommendations regarding the need for additional testing, such as imaging, to rule out osteomyelitis, surgical debridement, or amputation.
Inpatient ABIs in this situation may help diagnose and quantify the severity of PAD. Newer classification schemes such as the Society of Vascular Surgery Wound Ischemia Foot Infection score take into account clinical findings as well as ABI scores to better prognosticate limb loss and select patients for intervention.15 If the clinical picture is deemed sufficiently suspicious for critical limb ischemia, the patient may be taken directly for invasive testing with possible intervention.
If an infected ulcer is superficial, shows no signs of gangrene, and has been present for less than 30 days, further work-up for suspected PAD can generally be deferred to an outpatient setting after resolution of the acute infection. Management of the wound is highly institution dependent. When available, a wound care specialist (physician or nurse) or a plastic surgeon can be consulted as an inpatient to give specific recommendations that can range anywhere from enzymatic debridement to simple dressing. If this service is unavailable, we recommend dressing the wound with moist nonocclusive dressings with frequent changes. Referrals for ABI testing and follow up in podiatry, wound care, or vascular clinic should be arranged. Finally, educating the patient on what to expect can increase compliance with the outpatient treatment plan.
Mild to moderate CVI symptoms with superimposed cellulitis but no ulceration
Chronic venous insufficiency is a syndrome that has variable presentations based on the location and degree of valvular incompetence in the superficial or, less commonly, deep venous systems. For a patient with cellulitis and CVI, the clinical exam findings may be associated with venous hypertension syndrome – in which there is deep axial reflux and possible obstruction – and could also represent complex varicose disease which is usually caused by superficial reflux of the greater saphenous vein.3 The lack of advanced skin changes and ulceration raises the suspicion of mild to moderate CVI.
Guidelines from the American Venous Forum and the Society for Vascular Surgery recommend that all patients with suspected CVI, regardless of severity, undergo venous duplex ultrasound scanning as a first diagnostic test (grade 1A) to accurately classify the disease according to the Clinical Etiological Anatomical Pathophysiology (CEAP) system (Table 1).16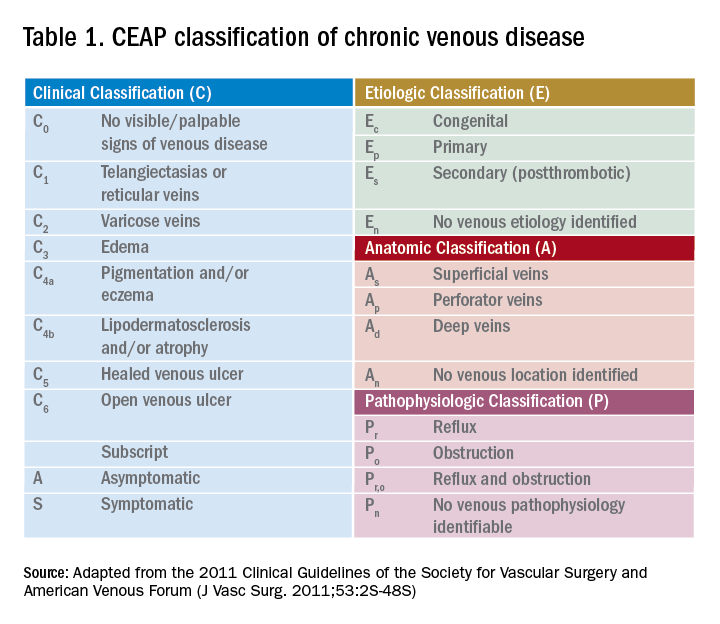
Compression therapy is commonly accepted as a noninvasive treatment option for all levels of CVI, yet most of the evidence comes from secondary prevention studies in patients with advanced CVI with venous ulcers.18 Strong evidence for the role of compression stockings in mild to moderate CVI is lacking. In fact, recent guidelines from the Society of Vascular Surgery, reviewed by the American Heart Association, do not recommend compression therapy as a primary treatment modality in patients with symptomatic varicose veins (without ulcers) if the patient is a candidate for saphenous vein ablation.19 This recommendation is based on clinical trial data that showed greater efficacy and cost-effectiveness of surgery versus conservative management in patients with CEAP2 (low severity) CVI as well as studies noting noncompliance with compression therapy as high as 75%.20-21
However, determining a patient’s candidacy for ablative or surgical therapy requires ultrasound data for accurate CEAP scoring, which is often not achieved as an inpatient. Given the potential benefit and lack of severe adverse effects, hospitalists can consider initiating compression therapy at the time of discharge in a patient with mild to moderate signs of CVI and a low risk profile for severe PAD. The prescription should specify knee-length elastic stockings with graduated compression between 20 to 30 mm Hg.22 The patient should also be encouraged to complete the outpatient duplex ultrasound testing prior to the PCP visit so that he or she can be referred to a vascular specialist appropriately.
Infected ulcer with CVI features
If the patient’s exam is suspicious for advanced venous disease with ulceration, the clinician should evaluate for the presence of scarring. This would indicate that there has been long-standing venous disease with recurrent ulceration. This patient should be asked about a previous diagnosis of CVI, prior compression therapy, and barriers to compliance with compression therapy such as poor fit or difficulty of use due to obesity or immobility. It is important to note that mixed ulcers are present in up to 20% of patients; a careful assessment of risk factors for PAD, pulse exam, and referral for outpatient ABI testing is warranted to rule out arterial insufficiency in this patient with likely venous ulcer.23
The AHA recommends prompt specialist evaluation for CEAP scores greater than or equal to 4; based on physical exam alone, this patient’s active venous ulcer yields the highest possible score of 6.2 If not previously done, this patient with advanced CVI and ulceration should be referred for an outpatient venous duplex ultrasound as well as urgent follow-up with a vascular specialist soon after discharge.
There is significant consensus in the literature that multilayer compression therapy between 30 and 40 mm Hg is the first-line treatment in patients with venous ulcers as it has been shown to promote ulcer healing and prevent recurrence.24-25 In addition, superficial venous surgery, including minimally invasive ablation, can reduce the recurrence of ulcers if used as adjunctive therapy in selected patients.26 However, compressive therapy should generally not be prescribed in patients with venous ulcers until PAD has been ruled out.
If ABI results are available, the clinician can consider compression at 30-40 mm Hg for ABI values greater than 0.8 and reduced compression at 20-30 mm Hg for values of 0.5-0.8; compression is contraindicated if the ABI is less than 0.5. Prompt follow-up with a vascular specialist can help direct compressive and/or surgical therapy. Wound care consultation as an inpatient can assist with dressing recommendations, though the evidence has not shown that dressings of any type worn under compressive garments improve ulcer healing.27
Bottom line
Hospitalists are in a unique position to identify patients with underlying peripheral arterial and venous disease when they are admitted for lower extremity skin and soft tissue infections. A focused history and physical exam can yield significant clinical clues and should prompt either inpatient or outpatient work-up.
In patients with deep ulcers and concern for critical limb ischemia, inpatient consultation should be sought. In patients with superficial venous or arterial ulcers, referral for outpatient ABI, color duplex ultrasound, or both should be made; most of these patients should also be directly referred to a vascular and/or wound specialist. Patients with more benign forms of disease who endorse chronic symptoms suspicious for mild to moderate PAD or CVI can be seen by a PCP for further management. All patients should be educated about the importance of follow-up as it remains their best chance to curb the progression of disease, reduce the risks for recurrent infection, and improve overall quality of life.
Back to the original case
Our patient’s lower extremity erythema, fever, and leukocytosis improved with 3 days of IV vancomycin treatment. Her wound was kept clean with moist dressings and showed no signs of deep infection; with elevation, her bilateral lower extremity edema also improved. Her physical exam findings and clinical history were highly suspicious for long-standing CVI. She was discharged with oral antibiotics and a referral to wound care for ongoing management of her superficial ulcers. An outpatient venous duplex ultrasound and ABI were scheduled prior to her vascular surgery appointment to effectively rule out PAD before consideration of further therapy for severe CVI.
Key Points
- Hospitalists are in a unique position to identify patients with peripheral vascular disease when they are admitted with SSTIs.
- When assessing patients, it is important to consider peripheral arterial disease (PAD) and chronic venous insufficiency (CVI) separately.
- The classic symptom for PAD is claudication. In contrast, symptoms of CVI present more variably.
- Barring cases of critical limb ischemia, the main objective of identifying PAD or CVI is to arrange testing and follow-up after discharge.
References
1. Stevens, DL, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2014;59(2):147-59.
2. Eberhardt, RT, et al. Chronic venous insufficiency. Circulation. 2014;130:333-46.
3. Raju, S, et al. Chronic venous insufficiency and varicose veins. N Engl J Med. 2009;360:2319-27.
4. Kullo, IJ, et al. Peripheral artery disease. N Engl J Med. 2016;374(9):861-71.
5. Hennion D, et al. Diagnosis and treatment of peripheral arterial disease. Am Fam Physician. 2013 Sep 1;88(5):306-10.
6. Henke P, et al. ACP Observer Extra: Peripheral arterial disease. June 2007.
7. Vivas A. Venous leg ulcers. Ann Intern Med. 2016;165(3):ITC17-32.
8. Sumpio BE. Foot ulcers. N Engl J Med. 2000;343(11):787-93.
9. Bazari H, et al. Case 7–2007. 59-year-old woman with diabetic renal disease and nonhealing skin ulcers. N Engl J Med. 2007 Mar 8; 356(10):1049-57.
10. Moyer VA. Screening for peripheral artery disease and cardiovascular disease risk assessment with the ankle-brachial index in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013 Sep 3.159(5):342-8.
11. Khan TH, et al. Critical review of the ankle brachial index. Curr Cardiol Rev. 2008 May;4(2):101-6.
12. Gerhard-Herman MD, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease. A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. 2016.
13. Brearley S, et al. Peripheral pulse palpation: An unreliable physical sign. Ann R Coll Surg Engl. 1992;74:169-71.
14. Khan NA, et al. Does the clinical examination predict lower extremity peripheral arterial disease? JAMA. 2006;295(5):536-46.
15. Mills JL Sr., et al. The Society for Vascular Surgery Lower Extremity Threatened Limb Classification System: Risk stratification based on wound, ischemia, and foot infection (WIfI). J Vasc Surg. 2014 Jan;59(1):220-34.e1-2.
16. Gloviczki P, et al. The care of patients with varicose veins and associated chronic venous diseases: Clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2011;53(5, Suppl):2S-48S.
17. Hamper UM,et al. Ultrasound evaluation of the lower extremity veins. Radiol Clin North Am. 2007 May;45(3):525-47.
18. Vivas A. Venous leg ulcers. Ann Intern Med. 2016;165(3):ITC17-32.
19. Gloviczki P, et al. The care of patients with varicose veins and associated chronic venous diseases: Clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2011;53(5, Suppl):2S-48S.
20. Michaels JA, et al. Randomized clinical trial comparing surgery with conservative treatment for uncomplicated varicose veins. Br J Surg. 2006 Feb;93(2):175-81.
21. Raju S, et al. Use of compression stockings in chronic venous disease: Patient compliance and efficacy. Ann Vasc Surg. 2007 Nov;21(6):790-5.
22. Gloviczki P, et al. The care of patients with varicose veins and associated chronic venous diseases: Clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2011;53(5, Suppl):2S-48S.
23. Humphreys ML, et al. Management of mixed arterial and venous leg ulcers. Br J Surg. 2007 Sep;94(9):1104-7.
24. O’Meara S, et al. Compression for venous leg ulcers. Cochrane Database Syst Rev. 2012 Nov 14;11:CD000265.
25. Dolibog P, et al. A comparative clinical study on five types of compression therapy in patients with venous leg ulcers. Int J Med Sci. 2013;11(1):34-43.
26. Gohel MS, et al. Long term results of compression therapy alone versus compression plus surgery in chronic venous ulceration (ESCHAR): Randomised controlled trial. BMJ. 2007 Jul 14;335(7610):83.
27. Palfreyman S, et al. Dressings for venous leg ulcers: systematic review and meta-analysis. BMJ. 2007 Aug 4;335(7613):244.
Clinical case
A 56-year-old woman with type 2 diabetes, morbid obesity, and hypertension presents with right lower extremity erythema, weeping, and exquisite tenderness associated with chills. She reports a 2-year history of chronic lower extremity swelling and cramps with a more recent development of scaling and two superficial ulcers on lower third of her leg. For 1 month, she has noted significant pain circumferentially around the ankles with focal tautness and pallor of the skin. She has tried acetaminophen and oxycodone with little relief.
Over the past week, she noted foul smelling discharge from one of the superficial ulcers with redness extending up to the knee prompting presentation to the emergency department. She had a fever to 101.2° F, tachycardia to 105 beats per minute, and leukocytosis to 14.7. She is admitted to the hospitalist service for sepsis secondary to right lower extremity cellulitis.
Introduction
Skin and soft tissue infections (SSTIs) remain among the most common inpatient diagnoses cared for by hospitalists. Most patients admitted to a hospitalist service with an SSTI meet the criteria for either moderate or severe infection as outlined by the Infectious Disease Society of America – systemic signs of infection by SIRS criteria or a high likelihood of an immunocompromised state, methicillin-resistant Staphylococcus aureus infection, trauma, or wounds.1
Often these patients have several comorbid conditions such as diabetes, morbid obesity, or peripheral arterial and venous disease. Though most hospitalists are adept at managing diabetes, blood pressure, and other comorbidities, the ability to recognize and manage peripheral vascular disease can be challenging. This article will discuss ways to help providers better identify and manage underlying peripheral arterial disease (PAD) and/or chronic venous insufficiency (CVI) in patients admitted with lower extremity SSTIs.
1. In addition to an infection, could there also be underlying peripheral arterial or venous disease?
Patients with peripheral edema and vascular disease are predisposed to recurrent lower extremity SSTIs. When assessing for vascular disease, it is important to consider PAD and CVI separately.
CVI refers to the spectrum of syndromes caused by venous valvular incompetency, venous obstruction, or decreased muscle contraction. Veins cannot maximally deliver venous blood back to the heart resulting in venous pooling in the lower extremities. The exact mechanism of the skin changes that accompany venous insufficiency is unknown but may be related to cytokine cascades that result in perivascular inflammation and a weakening of the dermal barrier. Over time, this can develop into spontaneous ulceration of the skin.2,3
PAD refers to atherosclerosis of the noncerebral, noncoronary arteries, which leads to ischemic symptoms and atrophy of the supplied territory. Ulceration usually results from mild trauma due to poor wound healing.4,5 A thorough history, assessment of risk factors, and physical exam are essential to identifying these two potential diagnoses in patients admitted with SSTIs.
First, the provider should assess risk factors for underlying vascular disease. For PAD, these include risk factors similar to those of coronary artery disease (CAD): hypertension, hyperlipidemia, history of smoking, and poorly-controlled diabetes. Chronic kidney disease and family history are also associated with PAD. Since PAD and CAD share similar risk factors, it is often common for patients with CAD (as well as patients with cerebrovascular disease) to have PAD. Risk factors for CVI include obesity, chronic sedentary lifestyle, multiple pregnancies, family history, and prior superficial or deep venous thrombosis.2,4
Next, the provider should ask the patient about symptoms experienced prior to the onset of the current SSTI. Patients with either arterial or venous disease will typically report lower extremity symptoms that have been occurring for months to years, long before the acute SSTI. The classic symptom for PAD is claudication – leg pain or cramping that occurs on exertion and improves with rest. This is due to decreased arterial blood flow to the affected limb, felt most acutely during exercise. Other symptoms include numbness, a cool lower extremity, and lower extremity hair loss. As PAD progresses, a patient may also have rest pain, which may indicate more critical ischemia, as well nonhealing wounds after mild trauma.
In contrast, symptoms of CVI present more variably. CVI can be associated with heaviness, cramping, and pain that are usually worse in the dependent position and relieved with elevation. Patients may also report dry skin, edema, pruritus, scaling, skin tightness, and indolent ulcers at advanced stages.2-6
The physical exam can help the provider distinguish between venous and arterial disease. Patients with PAD often have diminished or nonpalpable distal pulses, bruits in proximal arteries, pallor, hair loss, nail thickening, decreased capillary refill time, and ulceration of the toes. CVI shares some common characteristics but can be distinguished by evidence of varicose veins, telangiectasia, edema (which spares the foot), lipodermatosclerosis, and atrophie blanche (white scarring around the ankle). Patients with venous disease tend to have warm lower extremities and palpable pulses. Often, there is hyperpigmentation, especially around the ankles, and associated eczematous changes with scaling, erythema, and weeping. CVI can also present with ulcers. In addition, if the SSTI is not responding to appropriate antibiotics in the typical time frame, this may be a clue that there is an underlying vascular issue.2-6
Ulcers, whether arterial or venous, comprise a break in the skin’s protective barrier and give bacteria a point of entry. Thus, ulcers often get superinfected, leading to an SSTI rather than SSTIs causing ulcers. The anatomic location can help differentiate between venous and arterial ulcers. Arterial ulcers tend to occur on the toes, heels, and lateral and medial malleoli. Venous ulcers are classically present above the medial malleolus but can occur anywhere on the medial lower third of the leg. Venous ulcers are more superficial and have an irregular shape, while arterial ulcers are deeper, have smoother edges and a “punched-out” shape. Both arterial and venous ulcers can be exudative though venous ulcers are rarely necrotic. Both arterial and venous ulcers can be painful.7-9
2. There are signs and symptoms of underlying vascular disease in a patient with a lower extremity SSTI. Now what?
Neither PAD nor CVI is a clinical diagnosis, thus further work-up is required to confirm the diagnosis and accurately classify disease severity. The timing of this work-up is of unique interest to hospitalists.
Most patients who are hospitalized with cellulitis or a superficial wound infection do not need urgent inpatient work-up of suspected peripheral arterial or venous disease. The one notable exception to this is patients with diabetic foot infections or infected arterial ulcers that need prompt evaluation for possible critical limb ischemia. Barring cases of critical limb ischemia, the main objective of identifying PAD or CVI in patients hospitalized for SSTIs is to appropriately arrange testing and follow-up after discharge.
To address specific management strategies, it is useful to stratify patients by symptom and exam severity as follows: mild/moderate PAD symptoms without ulcer; infected ulcer with PAD features; mild/moderate CVI symptoms without ulcer; and infected ulcer with CVI features. As specific guidelines for the inpatient work-up and management of suspected peripheral arterial and venous disease are sparse, we rely on guidelines and best practices used in the outpatient setting and adapt them to these potential inpatient presentations.
Mild/Moderate PAD symptoms with superimposed cellulitis but no ulceration
In a patient admitted for cellulitis without open wounds, history and review of systems might reveal the presence of claudication or other symptoms suspicious for PAD. While the U.S. Preventative Services Task Force and American College of Cardiology discourages the routine screening of asymptomatic patients for PAD, patients with risk factors who endorse symptoms should undergo initial testing for PAD with an ankle-brachial index (ABI).10
The ABI is the ratio of ankle blood pressure to arm blood pressure, and is measured via sphygmomanometry with a Doppler probe. The ABI remains the simplest, most inexpensive first-line test for PAD. An ABI value of less than 0.9 is considered diagnostic for PAD and has been found to be more than 95% specific for arterial stenoses of greater than 50% on angiography across multiple studies.11
In an inpatient with risk factors for PAD and claudication symptoms, referral for outpatient ABIs with subsequent follow-up by a primary care physician should be arranged. If a diagnosis of PAD is made via ABI, the PCP should reinforce risk factor modification (tobacco cessation, diet, exercise, and aggressive lipid, blood pressure and blood glucose control) and start medical management with a single anti-platelet agent to reduce the risk of MI, stroke, or “vascular death.” The most recent ACC guidelines recommend either aspirin or clopidogrel as an acceptable anti-platelet agent (grade 1A).12 Cilostazol may be considered if claudication symptoms are significantly interfering with lifestyle. If this management fails, the patient may be referred to a vascular specialist for consideration of revascularization.
Infected ulcer with PAD features
Unlike cellulitis, arterial ulcers are a direct sequela of arterial insufficiency and represent the far end of the spectrum of disease severity and in certain cases treatment failure. Patients who present with advanced ischemic and/or diabetic foot ulcers may have never been evaluated for PAD as an outpatient. Prompt work-up and management is required given the high degree of morbidity and mortality associated with arterial ulcers. Whether an urgent inpatient evaluation is indicated depends on the clinical evaluation.
The first step is to determine the depth of the ulceration. Critical limb ischemia may be present if the ulcer is deep, gangrenous, overlies a bony prominence, or is associated with systemic signs of sepsis. A physical exam should include an assessment of the pulses including femoral, popliteal, PT and DP, preferably with bedside Doppler ultrasound. If pulses are absent, urgent vascular surgery evaluation is warranted to prevent loss of limb; the work-up generally involves imaging such as computed tomography angiography or magnetic resonance angiography to identify culprit lesions, or if sufficiently suspicious, immediate invasive angiogram with the potential for endovascular intervention.
While palpable pulses can be reassuring and raise the possibility of a nonarterial etiology of ulceration – such as a microvascular, neuropathic or venous disease – it is important to remember that pulse exams are often unreliable and provider dependent.13 Moreover, the presence of pulses does not effectively exclude severe PAD or critical limb ischemia in patients with a high pretest probability.14 Thus, in cases of deep, complex lower extremity and foot ulcers, it is prudent to obtain urgent evaluation by a surgical wound specialist, which depending on the institution may be podiatry, vascular surgery, or wound care. This may lead to a better clinical assessment of the wound and clearer recommendations regarding the need for additional testing, such as imaging, to rule out osteomyelitis, surgical debridement, or amputation.
Inpatient ABIs in this situation may help diagnose and quantify the severity of PAD. Newer classification schemes such as the Society of Vascular Surgery Wound Ischemia Foot Infection score take into account clinical findings as well as ABI scores to better prognosticate limb loss and select patients for intervention.15 If the clinical picture is deemed sufficiently suspicious for critical limb ischemia, the patient may be taken directly for invasive testing with possible intervention.
If an infected ulcer is superficial, shows no signs of gangrene, and has been present for less than 30 days, further work-up for suspected PAD can generally be deferred to an outpatient setting after resolution of the acute infection. Management of the wound is highly institution dependent. When available, a wound care specialist (physician or nurse) or a plastic surgeon can be consulted as an inpatient to give specific recommendations that can range anywhere from enzymatic debridement to simple dressing. If this service is unavailable, we recommend dressing the wound with moist nonocclusive dressings with frequent changes. Referrals for ABI testing and follow up in podiatry, wound care, or vascular clinic should be arranged. Finally, educating the patient on what to expect can increase compliance with the outpatient treatment plan.
Mild to moderate CVI symptoms with superimposed cellulitis but no ulceration
Chronic venous insufficiency is a syndrome that has variable presentations based on the location and degree of valvular incompetence in the superficial or, less commonly, deep venous systems. For a patient with cellulitis and CVI, the clinical exam findings may be associated with venous hypertension syndrome – in which there is deep axial reflux and possible obstruction – and could also represent complex varicose disease which is usually caused by superficial reflux of the greater saphenous vein.3 The lack of advanced skin changes and ulceration raises the suspicion of mild to moderate CVI.
Guidelines from the American Venous Forum and the Society for Vascular Surgery recommend that all patients with suspected CVI, regardless of severity, undergo venous duplex ultrasound scanning as a first diagnostic test (grade 1A) to accurately classify the disease according to the Clinical Etiological Anatomical Pathophysiology (CEAP) system (Table 1).16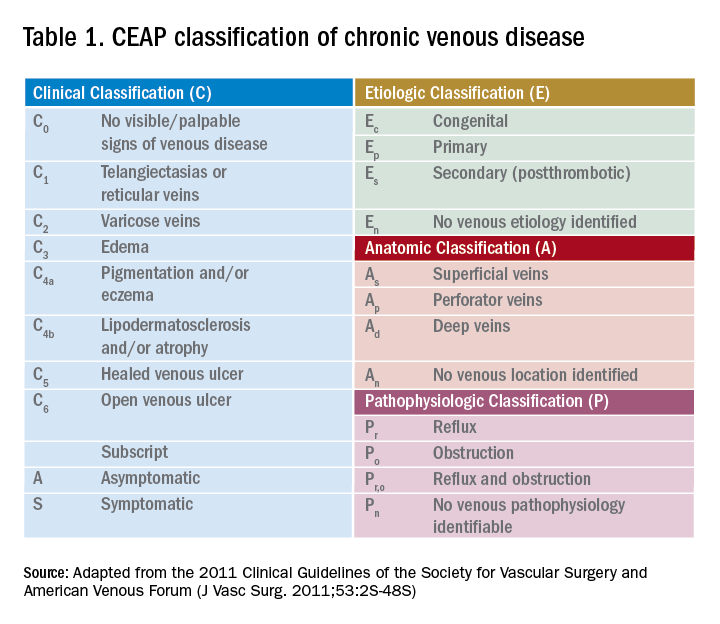
Compression therapy is commonly accepted as a noninvasive treatment option for all levels of CVI, yet most of the evidence comes from secondary prevention studies in patients with advanced CVI with venous ulcers.18 Strong evidence for the role of compression stockings in mild to moderate CVI is lacking. In fact, recent guidelines from the Society of Vascular Surgery, reviewed by the American Heart Association, do not recommend compression therapy as a primary treatment modality in patients with symptomatic varicose veins (without ulcers) if the patient is a candidate for saphenous vein ablation.19 This recommendation is based on clinical trial data that showed greater efficacy and cost-effectiveness of surgery versus conservative management in patients with CEAP2 (low severity) CVI as well as studies noting noncompliance with compression therapy as high as 75%.20-21
However, determining a patient’s candidacy for ablative or surgical therapy requires ultrasound data for accurate CEAP scoring, which is often not achieved as an inpatient. Given the potential benefit and lack of severe adverse effects, hospitalists can consider initiating compression therapy at the time of discharge in a patient with mild to moderate signs of CVI and a low risk profile for severe PAD. The prescription should specify knee-length elastic stockings with graduated compression between 20 to 30 mm Hg.22 The patient should also be encouraged to complete the outpatient duplex ultrasound testing prior to the PCP visit so that he or she can be referred to a vascular specialist appropriately.
Infected ulcer with CVI features
If the patient’s exam is suspicious for advanced venous disease with ulceration, the clinician should evaluate for the presence of scarring. This would indicate that there has been long-standing venous disease with recurrent ulceration. This patient should be asked about a previous diagnosis of CVI, prior compression therapy, and barriers to compliance with compression therapy such as poor fit or difficulty of use due to obesity or immobility. It is important to note that mixed ulcers are present in up to 20% of patients; a careful assessment of risk factors for PAD, pulse exam, and referral for outpatient ABI testing is warranted to rule out arterial insufficiency in this patient with likely venous ulcer.23
The AHA recommends prompt specialist evaluation for CEAP scores greater than or equal to 4; based on physical exam alone, this patient’s active venous ulcer yields the highest possible score of 6.2 If not previously done, this patient with advanced CVI and ulceration should be referred for an outpatient venous duplex ultrasound as well as urgent follow-up with a vascular specialist soon after discharge.
There is significant consensus in the literature that multilayer compression therapy between 30 and 40 mm Hg is the first-line treatment in patients with venous ulcers as it has been shown to promote ulcer healing and prevent recurrence.24-25 In addition, superficial venous surgery, including minimally invasive ablation, can reduce the recurrence of ulcers if used as adjunctive therapy in selected patients.26 However, compressive therapy should generally not be prescribed in patients with venous ulcers until PAD has been ruled out.
If ABI results are available, the clinician can consider compression at 30-40 mm Hg for ABI values greater than 0.8 and reduced compression at 20-30 mm Hg for values of 0.5-0.8; compression is contraindicated if the ABI is less than 0.5. Prompt follow-up with a vascular specialist can help direct compressive and/or surgical therapy. Wound care consultation as an inpatient can assist with dressing recommendations, though the evidence has not shown that dressings of any type worn under compressive garments improve ulcer healing.27
Bottom line
Hospitalists are in a unique position to identify patients with underlying peripheral arterial and venous disease when they are admitted for lower extremity skin and soft tissue infections. A focused history and physical exam can yield significant clinical clues and should prompt either inpatient or outpatient work-up.
In patients with deep ulcers and concern for critical limb ischemia, inpatient consultation should be sought. In patients with superficial venous or arterial ulcers, referral for outpatient ABI, color duplex ultrasound, or both should be made; most of these patients should also be directly referred to a vascular and/or wound specialist. Patients with more benign forms of disease who endorse chronic symptoms suspicious for mild to moderate PAD or CVI can be seen by a PCP for further management. All patients should be educated about the importance of follow-up as it remains their best chance to curb the progression of disease, reduce the risks for recurrent infection, and improve overall quality of life.
Back to the original case
Our patient’s lower extremity erythema, fever, and leukocytosis improved with 3 days of IV vancomycin treatment. Her wound was kept clean with moist dressings and showed no signs of deep infection; with elevation, her bilateral lower extremity edema also improved. Her physical exam findings and clinical history were highly suspicious for long-standing CVI. She was discharged with oral antibiotics and a referral to wound care for ongoing management of her superficial ulcers. An outpatient venous duplex ultrasound and ABI were scheduled prior to her vascular surgery appointment to effectively rule out PAD before consideration of further therapy for severe CVI.
Key Points
- Hospitalists are in a unique position to identify patients with peripheral vascular disease when they are admitted with SSTIs.
- When assessing patients, it is important to consider peripheral arterial disease (PAD) and chronic venous insufficiency (CVI) separately.
- The classic symptom for PAD is claudication. In contrast, symptoms of CVI present more variably.
- Barring cases of critical limb ischemia, the main objective of identifying PAD or CVI is to arrange testing and follow-up after discharge.
References
1. Stevens, DL, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2014;59(2):147-59.
2. Eberhardt, RT, et al. Chronic venous insufficiency. Circulation. 2014;130:333-46.
3. Raju, S, et al. Chronic venous insufficiency and varicose veins. N Engl J Med. 2009;360:2319-27.
4. Kullo, IJ, et al. Peripheral artery disease. N Engl J Med. 2016;374(9):861-71.
5. Hennion D, et al. Diagnosis and treatment of peripheral arterial disease. Am Fam Physician. 2013 Sep 1;88(5):306-10.
6. Henke P, et al. ACP Observer Extra: Peripheral arterial disease. June 2007.
7. Vivas A. Venous leg ulcers. Ann Intern Med. 2016;165(3):ITC17-32.
8. Sumpio BE. Foot ulcers. N Engl J Med. 2000;343(11):787-93.
9. Bazari H, et al. Case 7–2007. 59-year-old woman with diabetic renal disease and nonhealing skin ulcers. N Engl J Med. 2007 Mar 8; 356(10):1049-57.
10. Moyer VA. Screening for peripheral artery disease and cardiovascular disease risk assessment with the ankle-brachial index in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013 Sep 3.159(5):342-8.
11. Khan TH, et al. Critical review of the ankle brachial index. Curr Cardiol Rev. 2008 May;4(2):101-6.
12. Gerhard-Herman MD, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease. A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. 2016.
13. Brearley S, et al. Peripheral pulse palpation: An unreliable physical sign. Ann R Coll Surg Engl. 1992;74:169-71.
14. Khan NA, et al. Does the clinical examination predict lower extremity peripheral arterial disease? JAMA. 2006;295(5):536-46.
15. Mills JL Sr., et al. The Society for Vascular Surgery Lower Extremity Threatened Limb Classification System: Risk stratification based on wound, ischemia, and foot infection (WIfI). J Vasc Surg. 2014 Jan;59(1):220-34.e1-2.
16. Gloviczki P, et al. The care of patients with varicose veins and associated chronic venous diseases: Clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2011;53(5, Suppl):2S-48S.
17. Hamper UM,et al. Ultrasound evaluation of the lower extremity veins. Radiol Clin North Am. 2007 May;45(3):525-47.
18. Vivas A. Venous leg ulcers. Ann Intern Med. 2016;165(3):ITC17-32.
19. Gloviczki P, et al. The care of patients with varicose veins and associated chronic venous diseases: Clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2011;53(5, Suppl):2S-48S.
20. Michaels JA, et al. Randomized clinical trial comparing surgery with conservative treatment for uncomplicated varicose veins. Br J Surg. 2006 Feb;93(2):175-81.
21. Raju S, et al. Use of compression stockings in chronic venous disease: Patient compliance and efficacy. Ann Vasc Surg. 2007 Nov;21(6):790-5.
22. Gloviczki P, et al. The care of patients with varicose veins and associated chronic venous diseases: Clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2011;53(5, Suppl):2S-48S.
23. Humphreys ML, et al. Management of mixed arterial and venous leg ulcers. Br J Surg. 2007 Sep;94(9):1104-7.
24. O’Meara S, et al. Compression for venous leg ulcers. Cochrane Database Syst Rev. 2012 Nov 14;11:CD000265.
25. Dolibog P, et al. A comparative clinical study on five types of compression therapy in patients with venous leg ulcers. Int J Med Sci. 2013;11(1):34-43.
26. Gohel MS, et al. Long term results of compression therapy alone versus compression plus surgery in chronic venous ulceration (ESCHAR): Randomised controlled trial. BMJ. 2007 Jul 14;335(7610):83.
27. Palfreyman S, et al. Dressings for venous leg ulcers: systematic review and meta-analysis. BMJ. 2007 Aug 4;335(7613):244.
Benefit of dabigatran over warfarin persists in AF patient subgroups undergoing PCI
ANAHEIM, CALIF. – The benefit of dabigatran dual therapy versus warfarin triple therapy after percutaneous coronary intervention in patients with atrial fibrillation was consistent whether patients had drug-eluting or bare-metal stents, concomitant treatment with ticagrelor or clopidogrel, or acute coronary syndrome or stable disease as the indication for PCI, according to a subgroup analysis of the RE-DUAL PCI trial.
The trial, presented at the American Heart Association scientific sessions, randomized 2,725 patients to triple therapy with warfarin plus a P2Y12 inhibitor (clopidogrel or ticagrelor) and aspirin – the triple therapy group – or dabigatran 110 mg or 150 mg twice daily plus clopidogrel or ticagrelor – the dual therapy groups (N Engl J Med. 2017 Oct 19;377[16]:1513-24).
After a mean follow-up 14 months, the incidence of the major or clinically relevant nonmajor bleeding was 15.4% in the 110-mg dual-therapy group (hazard ratio, 0.52; 95% CI, 0.42-0.63; P less than .001) and 20.2% in the 150-mg dual-therapy group (HR, 0.72; 95% CI, 0.58-0.88; P less than .001), versus about 26% with triple-therapy.
The incidence of the composite efficacy endpoint – death, unplanned revascularization, myocardial infarction, stroke, or systemic embolism – was 13.7% in the two dual-therapy groups versus 13.4% with triple-therapy (HR, 1.04; 95% CI, 0.84-1.29; P = .005).
The investigators found consistent results when they analyzed their prespecified subgroups.
Drug-eluting stents were placed in 83% of patients; the rest had bare metal stents (BMS). The groups were well-balanced, except BMS patients were again more likely to be new to oral anticoagulation. Bleeding, thromboembolic events, and mortality were consistent with the main results regardless of the stent type, Most of the subjects were on clopidogrel, with just 12% on ticagrelor in both the dabigatran and warfarin groups. Ticagrelor patients were more likely to have ACS as their PCI indication and be new to oral anticoagulation. Ticagrelor patients were also more clinically complex, with a higher bleeding risk. Even so, they had relative bleeding risk reduction and efficacy results with dabigatran that were consistent with the overall finding, Dr. Oldgren said.
Patients were eligible for RE-DUAL PCI (Evaluation of Dual Therapy with Dabigatran vs. Triple Therapy with Warfarin in Patients with AF That Undergo a PCI with Stenting) if they had nonvalvular atrial fibrillation and a successful PCI within 120 hours. Those with bioprosthetic or mechanical heart valves, severe renal insufficiency, or other major comorbidities were excluded.
The trial was funded by Boehringer Ingelheim, the maker of dabigatran. Several investigators were employees. Dr. Oldgren is an adviser to Boehringer Ingelheim. Other authors reported financial ties to the company as well.
ANAHEIM, CALIF. – The benefit of dabigatran dual therapy versus warfarin triple therapy after percutaneous coronary intervention in patients with atrial fibrillation was consistent whether patients had drug-eluting or bare-metal stents, concomitant treatment with ticagrelor or clopidogrel, or acute coronary syndrome or stable disease as the indication for PCI, according to a subgroup analysis of the RE-DUAL PCI trial.
The trial, presented at the American Heart Association scientific sessions, randomized 2,725 patients to triple therapy with warfarin plus a P2Y12 inhibitor (clopidogrel or ticagrelor) and aspirin – the triple therapy group – or dabigatran 110 mg or 150 mg twice daily plus clopidogrel or ticagrelor – the dual therapy groups (N Engl J Med. 2017 Oct 19;377[16]:1513-24).
After a mean follow-up 14 months, the incidence of the major or clinically relevant nonmajor bleeding was 15.4% in the 110-mg dual-therapy group (hazard ratio, 0.52; 95% CI, 0.42-0.63; P less than .001) and 20.2% in the 150-mg dual-therapy group (HR, 0.72; 95% CI, 0.58-0.88; P less than .001), versus about 26% with triple-therapy.
The incidence of the composite efficacy endpoint – death, unplanned revascularization, myocardial infarction, stroke, or systemic embolism – was 13.7% in the two dual-therapy groups versus 13.4% with triple-therapy (HR, 1.04; 95% CI, 0.84-1.29; P = .005).
The investigators found consistent results when they analyzed their prespecified subgroups.
Drug-eluting stents were placed in 83% of patients; the rest had bare metal stents (BMS). The groups were well-balanced, except BMS patients were again more likely to be new to oral anticoagulation. Bleeding, thromboembolic events, and mortality were consistent with the main results regardless of the stent type, Most of the subjects were on clopidogrel, with just 12% on ticagrelor in both the dabigatran and warfarin groups. Ticagrelor patients were more likely to have ACS as their PCI indication and be new to oral anticoagulation. Ticagrelor patients were also more clinically complex, with a higher bleeding risk. Even so, they had relative bleeding risk reduction and efficacy results with dabigatran that were consistent with the overall finding, Dr. Oldgren said.
Patients were eligible for RE-DUAL PCI (Evaluation of Dual Therapy with Dabigatran vs. Triple Therapy with Warfarin in Patients with AF That Undergo a PCI with Stenting) if they had nonvalvular atrial fibrillation and a successful PCI within 120 hours. Those with bioprosthetic or mechanical heart valves, severe renal insufficiency, or other major comorbidities were excluded.
The trial was funded by Boehringer Ingelheim, the maker of dabigatran. Several investigators were employees. Dr. Oldgren is an adviser to Boehringer Ingelheim. Other authors reported financial ties to the company as well.
ANAHEIM, CALIF. – The benefit of dabigatran dual therapy versus warfarin triple therapy after percutaneous coronary intervention in patients with atrial fibrillation was consistent whether patients had drug-eluting or bare-metal stents, concomitant treatment with ticagrelor or clopidogrel, or acute coronary syndrome or stable disease as the indication for PCI, according to a subgroup analysis of the RE-DUAL PCI trial.
The trial, presented at the American Heart Association scientific sessions, randomized 2,725 patients to triple therapy with warfarin plus a P2Y12 inhibitor (clopidogrel or ticagrelor) and aspirin – the triple therapy group – or dabigatran 110 mg or 150 mg twice daily plus clopidogrel or ticagrelor – the dual therapy groups (N Engl J Med. 2017 Oct 19;377[16]:1513-24).
After a mean follow-up 14 months, the incidence of the major or clinically relevant nonmajor bleeding was 15.4% in the 110-mg dual-therapy group (hazard ratio, 0.52; 95% CI, 0.42-0.63; P less than .001) and 20.2% in the 150-mg dual-therapy group (HR, 0.72; 95% CI, 0.58-0.88; P less than .001), versus about 26% with triple-therapy.
The incidence of the composite efficacy endpoint – death, unplanned revascularization, myocardial infarction, stroke, or systemic embolism – was 13.7% in the two dual-therapy groups versus 13.4% with triple-therapy (HR, 1.04; 95% CI, 0.84-1.29; P = .005).
The investigators found consistent results when they analyzed their prespecified subgroups.
Drug-eluting stents were placed in 83% of patients; the rest had bare metal stents (BMS). The groups were well-balanced, except BMS patients were again more likely to be new to oral anticoagulation. Bleeding, thromboembolic events, and mortality were consistent with the main results regardless of the stent type, Most of the subjects were on clopidogrel, with just 12% on ticagrelor in both the dabigatran and warfarin groups. Ticagrelor patients were more likely to have ACS as their PCI indication and be new to oral anticoagulation. Ticagrelor patients were also more clinically complex, with a higher bleeding risk. Even so, they had relative bleeding risk reduction and efficacy results with dabigatran that were consistent with the overall finding, Dr. Oldgren said.
Patients were eligible for RE-DUAL PCI (Evaluation of Dual Therapy with Dabigatran vs. Triple Therapy with Warfarin in Patients with AF That Undergo a PCI with Stenting) if they had nonvalvular atrial fibrillation and a successful PCI within 120 hours. Those with bioprosthetic or mechanical heart valves, severe renal insufficiency, or other major comorbidities were excluded.
The trial was funded by Boehringer Ingelheim, the maker of dabigatran. Several investigators were employees. Dr. Oldgren is an adviser to Boehringer Ingelheim. Other authors reported financial ties to the company as well.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: After a mean follow-up of 14 months, the incidence of major or clinically relevant nonmajor bleeding was 15.4% in the 110-mg dual-therapy group (HR, 0.52; 95% CI, 0.42-0.63, P less than .001) and 20.2% in the 150-mg dual-therapy group (HR, 0.72; 95% CI, 0.58-0.88; P less than .001), versus about 26% with triple-therapy.
Data source: Subgroup analysis of RE-DUAL PCI trial
Disclosures: The trial was funded by Boehringer Ingelheim, the maker of dabigatran. Several investigators were employees. Authors disclosed various financial ties to the company.
Intense urine output monitoring beneficial in ICU
Intense monitoring of urine output could be a useful tool in detecting acute kidney injury (AKI), according to a study conducted at the University of Pittsburgh.
Kui Jin, MD, of the University of Pittsburgh and his associates found that, after adjustment for baseline characteristics, intensive monitoring of urine output (UO) was associated with higher rates of AKI, with an odds ratio of 1.22. Intensive UO monitoring also was strongly associated with improved 30-day survival among patients developing AKI.
This retrospective cohort study included 15,724 adult patients admitted to the center’s ICUs during 2000-2008. All patients had either their UO or serum creatinine (SC) monitored. These patients were then divided into subcohorts that were monitored at one of two different intensities. UO intensive monitoring was defined by hourly recordings, with gaps no greater than 3 hours for the first 48 hours after ICU admission. The group receiving less intensive UO monitoring comprised patients who did not meet intensive monitoring criteria, regardless of their UO in the 7 days following ICU admission. The patients who had their SC intensively monitored had 3 calendar days of samples taken after their ICU admissions. Those who did not meet SC intensive monitoring criteria were placed into the less intensive SC monitoring group.
To understand the effect of the monitoring strategies on detecting the development of AKI, the researchers determined each patient’s baseline, admission, and reference serum creatinine levels. Baseline creatinine was defined as the lowest value in the year prior to hospital admission. Reference creatinine was the baseline creatinine, if available, or the lowest creatinine level recorded within 24 hours after ICU admission. A third method for determining reference creatinine levels was used for some patients, which involved making an estimation based on the Modification of Diet in Renal Disease equation for serum creatinine.
The crude rates of stage 2-3 AKI 7 days after admission to the ICU were similar between patients from both groups that had their UO monitored; 62.5% of intensive and 63.9% of less intensive patients displayed symptoms. After the researchers adjusted for baseline characteristics, however, intensive monitoring of UO was associated with greater rates of stage 2-3 AKI (OR, 1.22; P less than .001). Crude rates were higher in the patients who received intensive monitoring for SC, compared with patients who received less intensive monitoring for SC. Ultimately, Dr. Jin and his associates found that, when caring for patients with or without AKI, fluid management is one of the most important factors. Patients who underwent intensive UO monitoring received less fluid in their first 24 hours (3.6 L) in the ICU, compared with patients who received less intense UO monitoring (4.2 L). Patients who received intensive monitoring of their UO also were less likely to use vasopressors (29.9% vs. 43.3%; P less than .001), suggesting these patients were more hemodynamically stable. Further, the percentage of patients at or above 10% of fluid overload was lower in the group who received intensive monitoring of their UO (2.49% vs. 5.68%; P less than .001), during the first 72 hours in the ICU.
“Our results should help inform clinical decisions and ICU policy around frequency of monitoring of UO, especially for patients at high risk of AKI,” Dr. Jin and his colleagues wrote.
None of the authors had financial disclosures to report. Partial funding was provided by a research grant from C.R. Bard.
Intense monitoring of urine output could be a useful tool in detecting acute kidney injury (AKI), according to a study conducted at the University of Pittsburgh.
Kui Jin, MD, of the University of Pittsburgh and his associates found that, after adjustment for baseline characteristics, intensive monitoring of urine output (UO) was associated with higher rates of AKI, with an odds ratio of 1.22. Intensive UO monitoring also was strongly associated with improved 30-day survival among patients developing AKI.
This retrospective cohort study included 15,724 adult patients admitted to the center’s ICUs during 2000-2008. All patients had either their UO or serum creatinine (SC) monitored. These patients were then divided into subcohorts that were monitored at one of two different intensities. UO intensive monitoring was defined by hourly recordings, with gaps no greater than 3 hours for the first 48 hours after ICU admission. The group receiving less intensive UO monitoring comprised patients who did not meet intensive monitoring criteria, regardless of their UO in the 7 days following ICU admission. The patients who had their SC intensively monitored had 3 calendar days of samples taken after their ICU admissions. Those who did not meet SC intensive monitoring criteria were placed into the less intensive SC monitoring group.
To understand the effect of the monitoring strategies on detecting the development of AKI, the researchers determined each patient’s baseline, admission, and reference serum creatinine levels. Baseline creatinine was defined as the lowest value in the year prior to hospital admission. Reference creatinine was the baseline creatinine, if available, or the lowest creatinine level recorded within 24 hours after ICU admission. A third method for determining reference creatinine levels was used for some patients, which involved making an estimation based on the Modification of Diet in Renal Disease equation for serum creatinine.
The crude rates of stage 2-3 AKI 7 days after admission to the ICU were similar between patients from both groups that had their UO monitored; 62.5% of intensive and 63.9% of less intensive patients displayed symptoms. After the researchers adjusted for baseline characteristics, however, intensive monitoring of UO was associated with greater rates of stage 2-3 AKI (OR, 1.22; P less than .001). Crude rates were higher in the patients who received intensive monitoring for SC, compared with patients who received less intensive monitoring for SC. Ultimately, Dr. Jin and his associates found that, when caring for patients with or without AKI, fluid management is one of the most important factors. Patients who underwent intensive UO monitoring received less fluid in their first 24 hours (3.6 L) in the ICU, compared with patients who received less intense UO monitoring (4.2 L). Patients who received intensive monitoring of their UO also were less likely to use vasopressors (29.9% vs. 43.3%; P less than .001), suggesting these patients were more hemodynamically stable. Further, the percentage of patients at or above 10% of fluid overload was lower in the group who received intensive monitoring of their UO (2.49% vs. 5.68%; P less than .001), during the first 72 hours in the ICU.
“Our results should help inform clinical decisions and ICU policy around frequency of monitoring of UO, especially for patients at high risk of AKI,” Dr. Jin and his colleagues wrote.
None of the authors had financial disclosures to report. Partial funding was provided by a research grant from C.R. Bard.
Intense monitoring of urine output could be a useful tool in detecting acute kidney injury (AKI), according to a study conducted at the University of Pittsburgh.
Kui Jin, MD, of the University of Pittsburgh and his associates found that, after adjustment for baseline characteristics, intensive monitoring of urine output (UO) was associated with higher rates of AKI, with an odds ratio of 1.22. Intensive UO monitoring also was strongly associated with improved 30-day survival among patients developing AKI.
This retrospective cohort study included 15,724 adult patients admitted to the center’s ICUs during 2000-2008. All patients had either their UO or serum creatinine (SC) monitored. These patients were then divided into subcohorts that were monitored at one of two different intensities. UO intensive monitoring was defined by hourly recordings, with gaps no greater than 3 hours for the first 48 hours after ICU admission. The group receiving less intensive UO monitoring comprised patients who did not meet intensive monitoring criteria, regardless of their UO in the 7 days following ICU admission. The patients who had their SC intensively monitored had 3 calendar days of samples taken after their ICU admissions. Those who did not meet SC intensive monitoring criteria were placed into the less intensive SC monitoring group.
To understand the effect of the monitoring strategies on detecting the development of AKI, the researchers determined each patient’s baseline, admission, and reference serum creatinine levels. Baseline creatinine was defined as the lowest value in the year prior to hospital admission. Reference creatinine was the baseline creatinine, if available, or the lowest creatinine level recorded within 24 hours after ICU admission. A third method for determining reference creatinine levels was used for some patients, which involved making an estimation based on the Modification of Diet in Renal Disease equation for serum creatinine.
The crude rates of stage 2-3 AKI 7 days after admission to the ICU were similar between patients from both groups that had their UO monitored; 62.5% of intensive and 63.9% of less intensive patients displayed symptoms. After the researchers adjusted for baseline characteristics, however, intensive monitoring of UO was associated with greater rates of stage 2-3 AKI (OR, 1.22; P less than .001). Crude rates were higher in the patients who received intensive monitoring for SC, compared with patients who received less intensive monitoring for SC. Ultimately, Dr. Jin and his associates found that, when caring for patients with or without AKI, fluid management is one of the most important factors. Patients who underwent intensive UO monitoring received less fluid in their first 24 hours (3.6 L) in the ICU, compared with patients who received less intense UO monitoring (4.2 L). Patients who received intensive monitoring of their UO also were less likely to use vasopressors (29.9% vs. 43.3%; P less than .001), suggesting these patients were more hemodynamically stable. Further, the percentage of patients at or above 10% of fluid overload was lower in the group who received intensive monitoring of their UO (2.49% vs. 5.68%; P less than .001), during the first 72 hours in the ICU.
“Our results should help inform clinical decisions and ICU policy around frequency of monitoring of UO, especially for patients at high risk of AKI,” Dr. Jin and his colleagues wrote.
None of the authors had financial disclosures to report. Partial funding was provided by a research grant from C.R. Bard.
FROM CHEST
Key clinical point:
Major finding: AKI was more likely to be seen in patients who received intensive monitoring of their urine output (OR,1.22; P less than .001).
Data source: Retrospective cohort study at a single academic medical center of 15,724 adult patients admitted to the center’s ICUs during 2000-2008.
Disclosures: None of the authors had financial disclosures to report. Partial funding was provided by a research grant from C.R. Bard.
New buprenorphine formulation approved for medication-assisted treatment
The Food and Drug Administration has approved an extended-release, subcutaneous injection formulation of buprenorphine for use in treating moderate to severe opioid use disorder (OUD), the manufacturer of the drug announced Nov. 30.
The new product, called Sublocade, is a monthly injection intended for use in patients who have already begun treatment of OUD with transmucosal buprenorphine products, followed by a dose adjustment for a minimum of 7 days. Sublocade contains the partial mu-opioid agonist buprenorphine. By administering a consistent level of buprenorphine into the body, it ensures that levels of buprenorphine are delivered to the mu-opioid receptors, diminishing the effects of opioids, including the euphoric sensations associated with opioid use. During the clinical trial program, buprenorphine plasma concentrations of 2-3 ng/mL were found to bind to greater than 70% of mu-opioid receptors.
According to a statement from the FDA, Sublocade will be distributed only to health care providers as part of a Risk Evaluation and Mitigation Strategy to ensure that the product is not distributed directly to patients. Sublocade should be administered only by a health care professional. Self-injection of Sublocade into the blood stream instead of subcutaneously could lead to occlusion of blood vessels and embolism, according to one of the drug’s boxed warnings. It also should be used as part of a complete treatment program that includes counseling and psychosocial support.
The FDA is also requiring the manufacturer to conduct postmarketing studies to assess which patients would benefit from a higher dosing regimen, to determine whether Sublocade can be safely initiated without a dose stabilization period of sublingual buprenorphine, to assess the feasibility of administering Sublocade at a longer inter-dose interval than once monthly, and to determine a process for transitioning patients with long-term stability on a transmucosal buprenorphine dose to a monthly dose of Sublocade without the use of a higher dose for the first 2 months of treatment.
At recent joint meetings of the FDA’s Psychopharmacologic Drugs and Drug Safety and Risk Management advisory committees, panelists voted on Oct. 31 to recommend approval of Sublocade and on Nov. 1 for another subcutaneous buprenorphine injection formulation. These actions have not gone unnoticed by the American Medical Association.
“The AMA enthusiastically supports Food and Drug Administration Commissioner Scott Gottlieb’s efforts to advance policies and actions to treat those suffering from an opioid use disorder,” Patrice Harris, MD, immediate past chair of the American Medical Association Board of Trustees and a member of the AMA Opioid Task Force, said in a statement. “We also second his bold acknowledgment that criminal justice systems should offer [medication-assisted treatment] to those being detained. As he points out, ‘At the very moment when the criminal justice system could be dramatically lowering the risk of overdose, it is creating the conditions of reduced tolerance to opioids that substantially raises the risk of death upon release.’ With his clear explanation of the problem and solution, this situation can be remedied.”
The Food and Drug Administration has approved an extended-release, subcutaneous injection formulation of buprenorphine for use in treating moderate to severe opioid use disorder (OUD), the manufacturer of the drug announced Nov. 30.
The new product, called Sublocade, is a monthly injection intended for use in patients who have already begun treatment of OUD with transmucosal buprenorphine products, followed by a dose adjustment for a minimum of 7 days. Sublocade contains the partial mu-opioid agonist buprenorphine. By administering a consistent level of buprenorphine into the body, it ensures that levels of buprenorphine are delivered to the mu-opioid receptors, diminishing the effects of opioids, including the euphoric sensations associated with opioid use. During the clinical trial program, buprenorphine plasma concentrations of 2-3 ng/mL were found to bind to greater than 70% of mu-opioid receptors.
According to a statement from the FDA, Sublocade will be distributed only to health care providers as part of a Risk Evaluation and Mitigation Strategy to ensure that the product is not distributed directly to patients. Sublocade should be administered only by a health care professional. Self-injection of Sublocade into the blood stream instead of subcutaneously could lead to occlusion of blood vessels and embolism, according to one of the drug’s boxed warnings. It also should be used as part of a complete treatment program that includes counseling and psychosocial support.
The FDA is also requiring the manufacturer to conduct postmarketing studies to assess which patients would benefit from a higher dosing regimen, to determine whether Sublocade can be safely initiated without a dose stabilization period of sublingual buprenorphine, to assess the feasibility of administering Sublocade at a longer inter-dose interval than once monthly, and to determine a process for transitioning patients with long-term stability on a transmucosal buprenorphine dose to a monthly dose of Sublocade without the use of a higher dose for the first 2 months of treatment.
At recent joint meetings of the FDA’s Psychopharmacologic Drugs and Drug Safety and Risk Management advisory committees, panelists voted on Oct. 31 to recommend approval of Sublocade and on Nov. 1 for another subcutaneous buprenorphine injection formulation. These actions have not gone unnoticed by the American Medical Association.
“The AMA enthusiastically supports Food and Drug Administration Commissioner Scott Gottlieb’s efforts to advance policies and actions to treat those suffering from an opioid use disorder,” Patrice Harris, MD, immediate past chair of the American Medical Association Board of Trustees and a member of the AMA Opioid Task Force, said in a statement. “We also second his bold acknowledgment that criminal justice systems should offer [medication-assisted treatment] to those being detained. As he points out, ‘At the very moment when the criminal justice system could be dramatically lowering the risk of overdose, it is creating the conditions of reduced tolerance to opioids that substantially raises the risk of death upon release.’ With his clear explanation of the problem and solution, this situation can be remedied.”
The Food and Drug Administration has approved an extended-release, subcutaneous injection formulation of buprenorphine for use in treating moderate to severe opioid use disorder (OUD), the manufacturer of the drug announced Nov. 30.
The new product, called Sublocade, is a monthly injection intended for use in patients who have already begun treatment of OUD with transmucosal buprenorphine products, followed by a dose adjustment for a minimum of 7 days. Sublocade contains the partial mu-opioid agonist buprenorphine. By administering a consistent level of buprenorphine into the body, it ensures that levels of buprenorphine are delivered to the mu-opioid receptors, diminishing the effects of opioids, including the euphoric sensations associated with opioid use. During the clinical trial program, buprenorphine plasma concentrations of 2-3 ng/mL were found to bind to greater than 70% of mu-opioid receptors.
According to a statement from the FDA, Sublocade will be distributed only to health care providers as part of a Risk Evaluation and Mitigation Strategy to ensure that the product is not distributed directly to patients. Sublocade should be administered only by a health care professional. Self-injection of Sublocade into the blood stream instead of subcutaneously could lead to occlusion of blood vessels and embolism, according to one of the drug’s boxed warnings. It also should be used as part of a complete treatment program that includes counseling and psychosocial support.
The FDA is also requiring the manufacturer to conduct postmarketing studies to assess which patients would benefit from a higher dosing regimen, to determine whether Sublocade can be safely initiated without a dose stabilization period of sublingual buprenorphine, to assess the feasibility of administering Sublocade at a longer inter-dose interval than once monthly, and to determine a process for transitioning patients with long-term stability on a transmucosal buprenorphine dose to a monthly dose of Sublocade without the use of a higher dose for the first 2 months of treatment.
At recent joint meetings of the FDA’s Psychopharmacologic Drugs and Drug Safety and Risk Management advisory committees, panelists voted on Oct. 31 to recommend approval of Sublocade and on Nov. 1 for another subcutaneous buprenorphine injection formulation. These actions have not gone unnoticed by the American Medical Association.
“The AMA enthusiastically supports Food and Drug Administration Commissioner Scott Gottlieb’s efforts to advance policies and actions to treat those suffering from an opioid use disorder,” Patrice Harris, MD, immediate past chair of the American Medical Association Board of Trustees and a member of the AMA Opioid Task Force, said in a statement. “We also second his bold acknowledgment that criminal justice systems should offer [medication-assisted treatment] to those being detained. As he points out, ‘At the very moment when the criminal justice system could be dramatically lowering the risk of overdose, it is creating the conditions of reduced tolerance to opioids that substantially raises the risk of death upon release.’ With his clear explanation of the problem and solution, this situation can be remedied.”
Pediatric acute appendicitis: Is it time for nonoperative treatment (NOT)?
Clinical question
What are the differences in rates of treatment failure, duration of hospitalization, and cost between nonoperative treatment (NOT) for acute uncomplicated appendicitis versus urgent appendectomy?
Background
Acute appendicitis is found in around 5% of children presenting for urgent or emergent evaluation of abdominal pain. It is the most common illness prompting emergency abdominal surgery in children.
Several trials in adults have shown that urgent surgery may not be necessary, and NOT of uncomplicated appendicitis may be both effective and safe. NOT involves a course of IV antibiotics and careful clinical monitoring while hospitalized, then a course of oral antibiotics after discharge. Regimens vary but include coverage for aerobic and anaerobic gut flora, such as piperacillin-tazobactam followed by amoxicillin. Little is known about the safety and efficacy of NOT in children.
Study design
Meta-analysis.
Search strategy
PubMed, MEDLINE, EMBASE, and Cochrane Library were searched for relevant studies. This search identified 527 potential articles, of which the authors examined the full text of 68 and ultimately identified 5 single-center trials for analysis (4 prospective cohort trials and 1 randomized, controlled trial).
Synopsis
A total of 404 patients with uncomplicated appendicitis were seen in all trials: 168 received NOT and 236 received standard surgical care (urgent appendectomy). In the single randomized, controlled trial, patients were assigned NOT or surgical care randomly. In the other trials parental preference directed therapy.
The heterogeneity of the design, populations, definitions of illness, duration of follow-up, and NOT treatment regimens made the meta-analysis challenging. Antibiotic options for NOT varied by center but included a course of IV antibiotics followed by 7-10 days of oral antibiotics. NOT success was defined as no need for surgery within 48 hours and no recurrence of appendicitis within 1 month. Of the 236 patients who received standard surgical care, all had appendicitis and 1 had a complication requiring repeat operation. Of the NOT group, 16 (9.5%) had treatment failures, including 3 with perforated appendicitis, and 45 (27%) went on to have an appendectomy within the following year, yielding a risk ratio of failure versus standard treatment of 8.9 (95% confidence interval, 2.7-29.8). A subgroup analysis of patients with appendicoliths who received NOT found that these patients experienced a substantially increased risk of treatment failures and recurrent appendicitis with the risk ratio versus NOT without appendicolith of 10.4 (95% CI, 1.5-74). Of the 30 patients who experienced treatment failure with NOT, 15 had appendicoliths. NOT lengthened hospital stays by 14.3 hours (95% CI, 7.5-21.1) but led to lower total costs by $1,310 (95% CI, $920-$1,690).
Bottom line
NOT may be a reasonable alternative to standard surgical management for acute uncomplicated appendicitis without appendicolith in children, with a success rate of greater than 90%. Further larger, randomized prospective studies are required to establish its safety and efficacy.
Citation
Huang L et al. Comparison of antibiotic therapy and appendectomy for acute uncomplicated appendicitis in children: A meta-analysis. JAMA Pediatr. 2017;171(5):426-34.
Dr. Stubblefield is a pediatric hospitalist at Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del., and a clinical assistant professor of pediatrics at Jefferson Medical College in Philadelphia.
Clinical question
What are the differences in rates of treatment failure, duration of hospitalization, and cost between nonoperative treatment (NOT) for acute uncomplicated appendicitis versus urgent appendectomy?
Background
Acute appendicitis is found in around 5% of children presenting for urgent or emergent evaluation of abdominal pain. It is the most common illness prompting emergency abdominal surgery in children.
Several trials in adults have shown that urgent surgery may not be necessary, and NOT of uncomplicated appendicitis may be both effective and safe. NOT involves a course of IV antibiotics and careful clinical monitoring while hospitalized, then a course of oral antibiotics after discharge. Regimens vary but include coverage for aerobic and anaerobic gut flora, such as piperacillin-tazobactam followed by amoxicillin. Little is known about the safety and efficacy of NOT in children.
Study design
Meta-analysis.
Search strategy
PubMed, MEDLINE, EMBASE, and Cochrane Library were searched for relevant studies. This search identified 527 potential articles, of which the authors examined the full text of 68 and ultimately identified 5 single-center trials for analysis (4 prospective cohort trials and 1 randomized, controlled trial).
Synopsis
A total of 404 patients with uncomplicated appendicitis were seen in all trials: 168 received NOT and 236 received standard surgical care (urgent appendectomy). In the single randomized, controlled trial, patients were assigned NOT or surgical care randomly. In the other trials parental preference directed therapy.
The heterogeneity of the design, populations, definitions of illness, duration of follow-up, and NOT treatment regimens made the meta-analysis challenging. Antibiotic options for NOT varied by center but included a course of IV antibiotics followed by 7-10 days of oral antibiotics. NOT success was defined as no need for surgery within 48 hours and no recurrence of appendicitis within 1 month. Of the 236 patients who received standard surgical care, all had appendicitis and 1 had a complication requiring repeat operation. Of the NOT group, 16 (9.5%) had treatment failures, including 3 with perforated appendicitis, and 45 (27%) went on to have an appendectomy within the following year, yielding a risk ratio of failure versus standard treatment of 8.9 (95% confidence interval, 2.7-29.8). A subgroup analysis of patients with appendicoliths who received NOT found that these patients experienced a substantially increased risk of treatment failures and recurrent appendicitis with the risk ratio versus NOT without appendicolith of 10.4 (95% CI, 1.5-74). Of the 30 patients who experienced treatment failure with NOT, 15 had appendicoliths. NOT lengthened hospital stays by 14.3 hours (95% CI, 7.5-21.1) but led to lower total costs by $1,310 (95% CI, $920-$1,690).
Bottom line
NOT may be a reasonable alternative to standard surgical management for acute uncomplicated appendicitis without appendicolith in children, with a success rate of greater than 90%. Further larger, randomized prospective studies are required to establish its safety and efficacy.
Citation
Huang L et al. Comparison of antibiotic therapy and appendectomy for acute uncomplicated appendicitis in children: A meta-analysis. JAMA Pediatr. 2017;171(5):426-34.
Dr. Stubblefield is a pediatric hospitalist at Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del., and a clinical assistant professor of pediatrics at Jefferson Medical College in Philadelphia.
Clinical question
What are the differences in rates of treatment failure, duration of hospitalization, and cost between nonoperative treatment (NOT) for acute uncomplicated appendicitis versus urgent appendectomy?
Background
Acute appendicitis is found in around 5% of children presenting for urgent or emergent evaluation of abdominal pain. It is the most common illness prompting emergency abdominal surgery in children.
Several trials in adults have shown that urgent surgery may not be necessary, and NOT of uncomplicated appendicitis may be both effective and safe. NOT involves a course of IV antibiotics and careful clinical monitoring while hospitalized, then a course of oral antibiotics after discharge. Regimens vary but include coverage for aerobic and anaerobic gut flora, such as piperacillin-tazobactam followed by amoxicillin. Little is known about the safety and efficacy of NOT in children.
Study design
Meta-analysis.
Search strategy
PubMed, MEDLINE, EMBASE, and Cochrane Library were searched for relevant studies. This search identified 527 potential articles, of which the authors examined the full text of 68 and ultimately identified 5 single-center trials for analysis (4 prospective cohort trials and 1 randomized, controlled trial).
Synopsis
A total of 404 patients with uncomplicated appendicitis were seen in all trials: 168 received NOT and 236 received standard surgical care (urgent appendectomy). In the single randomized, controlled trial, patients were assigned NOT or surgical care randomly. In the other trials parental preference directed therapy.
The heterogeneity of the design, populations, definitions of illness, duration of follow-up, and NOT treatment regimens made the meta-analysis challenging. Antibiotic options for NOT varied by center but included a course of IV antibiotics followed by 7-10 days of oral antibiotics. NOT success was defined as no need for surgery within 48 hours and no recurrence of appendicitis within 1 month. Of the 236 patients who received standard surgical care, all had appendicitis and 1 had a complication requiring repeat operation. Of the NOT group, 16 (9.5%) had treatment failures, including 3 with perforated appendicitis, and 45 (27%) went on to have an appendectomy within the following year, yielding a risk ratio of failure versus standard treatment of 8.9 (95% confidence interval, 2.7-29.8). A subgroup analysis of patients with appendicoliths who received NOT found that these patients experienced a substantially increased risk of treatment failures and recurrent appendicitis with the risk ratio versus NOT without appendicolith of 10.4 (95% CI, 1.5-74). Of the 30 patients who experienced treatment failure with NOT, 15 had appendicoliths. NOT lengthened hospital stays by 14.3 hours (95% CI, 7.5-21.1) but led to lower total costs by $1,310 (95% CI, $920-$1,690).
Bottom line
NOT may be a reasonable alternative to standard surgical management for acute uncomplicated appendicitis without appendicolith in children, with a success rate of greater than 90%. Further larger, randomized prospective studies are required to establish its safety and efficacy.
Citation
Huang L et al. Comparison of antibiotic therapy and appendectomy for acute uncomplicated appendicitis in children: A meta-analysis. JAMA Pediatr. 2017;171(5):426-34.
Dr. Stubblefield is a pediatric hospitalist at Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del., and a clinical assistant professor of pediatrics at Jefferson Medical College in Philadelphia.
Observing BP measurement made no difference in SPRINT
ANAHEIM, CALIF. – More than half of the BP measurements of patients in the SPRINT trial were at least partially attended by clinic staff, but those efforts made no difference in outcomes, according to a survey presented by SPRINT investigators at the American Heart Association scientific sessions.
“It really didn’t matter” whether measurements were observed or not; blood pressure control and outcomes – fewer deaths and cardiovascular events when hypertension was treated to below 120 mm Hg instead of below 140 mm Hg – were largely the same either way, said the survey’s lead investigator Karen C. Johnson, MD, professor of women’s health and preventive medicine at the University of Tennessee in Memphis.
What did matter were the other measures SPRINT [Systolic Blood Pressure Intervention Trial] took to ensure accurate blood pressure measurement, including patients resting for 5 minutes; three automated readings taken afterward then averaged; proper cuff size; feet flat on the floor while patients sat; arms at proper level, and no talking, texting, or filling out forms during the reading, Dr. Johnson said (N Engl J Med. 2015 Nov 26;373[22]:2103-16).
“If you do [those things], then it doesn’t matter if somebody is in the room or not; you can treat to the levels we are talking about,” said William Cushman, MD, professor of medicine and physiology at the university, and also a SPRINT investigator.
Although the SPRINT researchers hadn’t addressed the issue before the AHA meeting, it’s been widely thought, and even reported in some places, that blood pressures in the trial were unattended. The misperception has led to anxiety about how to apply SPRINT to everyday practice, since few clinics are set up to have patients sit alone for 5 or 10 minutes for a blood pressure.
To address the concern, the SPRINT team surveyed study sites after the trial ended. It turned out that 4,082 subjects were at sites where patients were usually left alone for both the 5-minute rest period and the three BP readings, and 2,247 were at sites where staff usually attended both; 1,746 were at sites that left patients alone for the rest period only; and 570 were at sites where patients were alone only for the BP readings.
Observation had no impact on blood pressure. In the intensive arm, participants achieved and maintained an average systolic BP of about 120 mm Hg in all four groups. In the standard treatment arm, that average was about 135 mm Hg in all four groups. “When we look at the number of medications used, they were very similar in all four blood pressure groups,” with intensive treatment patients taking an average of one extra drug, Dr. Johnson said.
Intensive treatment, versus standard treatment, reduced cardiovascular events to a similar extent in patients who were alone for the entire blood pressure reading (by 38%) and those who were accompanied throughout (by 36%). For reasons that are not clear, intensive treatment did not significantly reduce risk among subjects who were observed during rest or observed for blood pressure readings. Both groups had lower Framingham 10-year cardiovascular disease risk scores, which may have been a confounder.
Meanwhile, the rate of adverse events and total mortality – lower with intensive treatment – did not vary by observation, Dr. Johnson said.
The survey excluded 716 subjects at 14 study sites who could not be classified into one of the four BP observation categories.
SPRINT was sponsored by the National Institutes of Health. Doctors Johnson and Cushman didn’t have any disclosures.
ANAHEIM, CALIF. – More than half of the BP measurements of patients in the SPRINT trial were at least partially attended by clinic staff, but those efforts made no difference in outcomes, according to a survey presented by SPRINT investigators at the American Heart Association scientific sessions.
“It really didn’t matter” whether measurements were observed or not; blood pressure control and outcomes – fewer deaths and cardiovascular events when hypertension was treated to below 120 mm Hg instead of below 140 mm Hg – were largely the same either way, said the survey’s lead investigator Karen C. Johnson, MD, professor of women’s health and preventive medicine at the University of Tennessee in Memphis.
What did matter were the other measures SPRINT [Systolic Blood Pressure Intervention Trial] took to ensure accurate blood pressure measurement, including patients resting for 5 minutes; three automated readings taken afterward then averaged; proper cuff size; feet flat on the floor while patients sat; arms at proper level, and no talking, texting, or filling out forms during the reading, Dr. Johnson said (N Engl J Med. 2015 Nov 26;373[22]:2103-16).
“If you do [those things], then it doesn’t matter if somebody is in the room or not; you can treat to the levels we are talking about,” said William Cushman, MD, professor of medicine and physiology at the university, and also a SPRINT investigator.
Although the SPRINT researchers hadn’t addressed the issue before the AHA meeting, it’s been widely thought, and even reported in some places, that blood pressures in the trial were unattended. The misperception has led to anxiety about how to apply SPRINT to everyday practice, since few clinics are set up to have patients sit alone for 5 or 10 minutes for a blood pressure.
To address the concern, the SPRINT team surveyed study sites after the trial ended. It turned out that 4,082 subjects were at sites where patients were usually left alone for both the 5-minute rest period and the three BP readings, and 2,247 were at sites where staff usually attended both; 1,746 were at sites that left patients alone for the rest period only; and 570 were at sites where patients were alone only for the BP readings.
Observation had no impact on blood pressure. In the intensive arm, participants achieved and maintained an average systolic BP of about 120 mm Hg in all four groups. In the standard treatment arm, that average was about 135 mm Hg in all four groups. “When we look at the number of medications used, they were very similar in all four blood pressure groups,” with intensive treatment patients taking an average of one extra drug, Dr. Johnson said.
Intensive treatment, versus standard treatment, reduced cardiovascular events to a similar extent in patients who were alone for the entire blood pressure reading (by 38%) and those who were accompanied throughout (by 36%). For reasons that are not clear, intensive treatment did not significantly reduce risk among subjects who were observed during rest or observed for blood pressure readings. Both groups had lower Framingham 10-year cardiovascular disease risk scores, which may have been a confounder.
Meanwhile, the rate of adverse events and total mortality – lower with intensive treatment – did not vary by observation, Dr. Johnson said.
The survey excluded 716 subjects at 14 study sites who could not be classified into one of the four BP observation categories.
SPRINT was sponsored by the National Institutes of Health. Doctors Johnson and Cushman didn’t have any disclosures.
ANAHEIM, CALIF. – More than half of the BP measurements of patients in the SPRINT trial were at least partially attended by clinic staff, but those efforts made no difference in outcomes, according to a survey presented by SPRINT investigators at the American Heart Association scientific sessions.
“It really didn’t matter” whether measurements were observed or not; blood pressure control and outcomes – fewer deaths and cardiovascular events when hypertension was treated to below 120 mm Hg instead of below 140 mm Hg – were largely the same either way, said the survey’s lead investigator Karen C. Johnson, MD, professor of women’s health and preventive medicine at the University of Tennessee in Memphis.
What did matter were the other measures SPRINT [Systolic Blood Pressure Intervention Trial] took to ensure accurate blood pressure measurement, including patients resting for 5 minutes; three automated readings taken afterward then averaged; proper cuff size; feet flat on the floor while patients sat; arms at proper level, and no talking, texting, or filling out forms during the reading, Dr. Johnson said (N Engl J Med. 2015 Nov 26;373[22]:2103-16).
“If you do [those things], then it doesn’t matter if somebody is in the room or not; you can treat to the levels we are talking about,” said William Cushman, MD, professor of medicine and physiology at the university, and also a SPRINT investigator.
Although the SPRINT researchers hadn’t addressed the issue before the AHA meeting, it’s been widely thought, and even reported in some places, that blood pressures in the trial were unattended. The misperception has led to anxiety about how to apply SPRINT to everyday practice, since few clinics are set up to have patients sit alone for 5 or 10 minutes for a blood pressure.
To address the concern, the SPRINT team surveyed study sites after the trial ended. It turned out that 4,082 subjects were at sites where patients were usually left alone for both the 5-minute rest period and the three BP readings, and 2,247 were at sites where staff usually attended both; 1,746 were at sites that left patients alone for the rest period only; and 570 were at sites where patients were alone only for the BP readings.
Observation had no impact on blood pressure. In the intensive arm, participants achieved and maintained an average systolic BP of about 120 mm Hg in all four groups. In the standard treatment arm, that average was about 135 mm Hg in all four groups. “When we look at the number of medications used, they were very similar in all four blood pressure groups,” with intensive treatment patients taking an average of one extra drug, Dr. Johnson said.
Intensive treatment, versus standard treatment, reduced cardiovascular events to a similar extent in patients who were alone for the entire blood pressure reading (by 38%) and those who were accompanied throughout (by 36%). For reasons that are not clear, intensive treatment did not significantly reduce risk among subjects who were observed during rest or observed for blood pressure readings. Both groups had lower Framingham 10-year cardiovascular disease risk scores, which may have been a confounder.
Meanwhile, the rate of adverse events and total mortality – lower with intensive treatment – did not vary by observation, Dr. Johnson said.
The survey excluded 716 subjects at 14 study sites who could not be classified into one of the four BP observation categories.
SPRINT was sponsored by the National Institutes of Health. Doctors Johnson and Cushman didn’t have any disclosures.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: Blood pressure and CV event reductions were similar in the 4,082 subjects at sites where patients were usually left alone for both the 5-minute rest period and the three BP readings, the 2,247 patients at sites where staff usually attended both, the 1,746 at sites that left patients alone for the rest period only, and the 570 at sites where patients were alone only for the BP readings.
Data source: A survey of SPRINT study sites.
Disclosures: SPRINT was sponsored by the National Institutes of Health. The presenter had no disclosures.