User login
FDA approves new treatment for hospital-acquired, ventilator-associated bacterial pneumonia
authorizing it for the treatment of both hospital-acquired and ventilator-associated bacterial pneumonia.
The new indication is for patients 18 years and older. It was based on results of a multinational, double-blind study that compared Zerbaxa with a different antibacterial drug in 726 patients hospitalized with hospital-acquired/ventilator-associated bacterial pneumonia. Mortality and cure rates were similar in the Zerbaxa and comparator groups.
The most common adverse events observed in the trial were elevated liver enzyme levels, renal impairment or failure, and diarrhea. Patients with hypersensitivity to beta-lactam drugs should not be receive Zerbaxa.
“A key global challenge we face as a public health agency is addressing the threat of antimicrobial-resistant infections. Hospital-acquired and ventilator-associated bacterial pneumonia are serious infections that can result in death in some patients. ... That’s why, among our other efforts to address antimicrobial resistance, we’re focused on facilitating the development of safe and effective new treatments to give patients more options to fight life-threatening infections,” said Amy Abernethy, MD, PhD, the FDA’s principal deputy commissioner.
Zerbaxa was initially approved in 2014 for treatment of complicated intra-abdominal and urinary tract infections.
Find the full press release on the FDA website.
authorizing it for the treatment of both hospital-acquired and ventilator-associated bacterial pneumonia.
The new indication is for patients 18 years and older. It was based on results of a multinational, double-blind study that compared Zerbaxa with a different antibacterial drug in 726 patients hospitalized with hospital-acquired/ventilator-associated bacterial pneumonia. Mortality and cure rates were similar in the Zerbaxa and comparator groups.
The most common adverse events observed in the trial were elevated liver enzyme levels, renal impairment or failure, and diarrhea. Patients with hypersensitivity to beta-lactam drugs should not be receive Zerbaxa.
“A key global challenge we face as a public health agency is addressing the threat of antimicrobial-resistant infections. Hospital-acquired and ventilator-associated bacterial pneumonia are serious infections that can result in death in some patients. ... That’s why, among our other efforts to address antimicrobial resistance, we’re focused on facilitating the development of safe and effective new treatments to give patients more options to fight life-threatening infections,” said Amy Abernethy, MD, PhD, the FDA’s principal deputy commissioner.
Zerbaxa was initially approved in 2014 for treatment of complicated intra-abdominal and urinary tract infections.
Find the full press release on the FDA website.
authorizing it for the treatment of both hospital-acquired and ventilator-associated bacterial pneumonia.
The new indication is for patients 18 years and older. It was based on results of a multinational, double-blind study that compared Zerbaxa with a different antibacterial drug in 726 patients hospitalized with hospital-acquired/ventilator-associated bacterial pneumonia. Mortality and cure rates were similar in the Zerbaxa and comparator groups.
The most common adverse events observed in the trial were elevated liver enzyme levels, renal impairment or failure, and diarrhea. Patients with hypersensitivity to beta-lactam drugs should not be receive Zerbaxa.
“A key global challenge we face as a public health agency is addressing the threat of antimicrobial-resistant infections. Hospital-acquired and ventilator-associated bacterial pneumonia are serious infections that can result in death in some patients. ... That’s why, among our other efforts to address antimicrobial resistance, we’re focused on facilitating the development of safe and effective new treatments to give patients more options to fight life-threatening infections,” said Amy Abernethy, MD, PhD, the FDA’s principal deputy commissioner.
Zerbaxa was initially approved in 2014 for treatment of complicated intra-abdominal and urinary tract infections.
Find the full press release on the FDA website.
Hospitalists can help alleviate rising drug costs
Four key actions providers can take
Because of the increasing costs of prescription drugs and medical therapies, many patients are unable to afford the treatment they need that could improve their health or even save their lives. In the United States, drug manufacturers can set their own prices – a policy that has resulted in overall medicine costs being far higher than in other places around the globe. Increasingly, insurers are passing the costs along to patients through higher deductibles, and pharmaceutical companies are making record profits.
Something needs to change in order to achieve the right balance between maintaining pharmaceutical innovation and ensuring patients have proper access to treatments they need. Waiting for legislation, regulation, or the courts is not an effective short-term solution. Instead, hospitalists can take immediate actions to help by alleviating the costs for as many patients possible.
Historical context
Many might be wondering how prescription costs became so imbalanced in the first place. Here are a few important factors that played a role in the dramatic price increase of pharmaceuticals:
Entrance of generic drugs: Around 2012 the entrance of generic drugs caused major unexpected competition in the medical industry. During this time, many insurers were promoting the generic drugs and not allowing brand names to be covered when a generic substitute was available.
“Orphan drugs” and manufacturer pricing: In 2014, 33 new brand-name drugs were launched in the United States, and only 8 had a direct price competitor at the time they were introduced. In addition, manufacturers were free to set their prices. Over the past decade, introductory prices for brand name drugs have reached unprecedented levels. Furthermore, manufacturers use the patent protections to increase their prices every year, even when no significant improvements have been made to the drug.
Expiring patents: According to research, there are 182 drugs that no longer have patent protection or any associated generics available. This creates opportunities for manufacturers to maintain patent-era pricing or even engage in price gouging.
Lack of robust competition: Several high-priced blockbuster drugs hit the market to treat serious diseases, most of which do not have generic brand substitutes, which leaves only one option for patients – and it’s usually not affordable. According to research, more than 500 drugs have only one marketed generic. In addition, manufacturer mergers and acquisitions have occurred, which has led to a more concentrated and less competitive market for pricing.
Stricter Food and Drug Administration policies: American consumers have access to the safest and most advanced pharmaceutical system in the world, which requires several trials and testing before the drug can be approved and brought to the market. Despite the benefits of these strict procedures, the downside means higher costs for the brand and manufacturer that they will want to recoup through the price of the drug on the market.
Number of new drugs allowed to enter the market: New drugs that enter the market in the United States do so more quickly than in most other countries. Research shows the U.S. pharmaceutical market contributes to 45% of the global pharmaceutical market. The $76 billion in research and development that pharmaceutical companies claim overlooks the ways that U.S. employers and taxpayers pay for at least 44% through tax subsidies and credits. What makes it worse is that research shows most corporate research and development is directed at minimally innovative new drugs, using the system to secure patents and charge monopoly prices.
Compared with other high-income countries, the United States spends the most per capita on prescription drugs. While insured U.S. patients often pay little or nothing for generic prescriptions, they can be billed tens of thousands of dollars for certain high-priced medicines. The United States has the highest rate of insured patients skipping or not filling prescriptions because of cost. For example, the price of EpiPens, a drug delivery system that is crucial for persons experiencing life-threatening allergic reactions, has increased more than $500 in just 9 years.
How to alleviate rising drug costs
The good news is that hospitalists can do something about the high costs of pharmaceuticals.
Understand and offer alternative ways for drug intake: Many patients admitted to a hospital with severe infections are initially started with intravenous medications. Although conversion from intravenous to oral therapy is inappropriate for a patient who is critically ill or has an inability to absorb oral medications, every hospital will have a certain number of patients who are eligible for a switch from intravenous to oral therapy.
The World Health Organization (WHO) reports that the irrational use of medicines is a major problem worldwide, including antibiotics. Switching from IV to oral enables one to select a cheaper or older antibiotic that is as effective as the IV antibiotic. However, this requires breaking the belief that many physicians still have that IV medications’ bioavailability is stronger and creates less susceptibility to the illness reoccurring in the patient. For many medications, essentially the same amount of drug is found in the blood when given intravenously or orally. In addition, research has shown several benefits beyond cost reduction for oral over IV, such as earlier discharge and reduced risk of infections.
Limit unnecessary antibiotic prescriptions and consider antibiotics stewardship programs: The Center for Disease Control reports that one in three (47 million) antibiotic prescriptions are unnecessary. Most of these unnecessary antibiotics are prescribed for respiratory conditions caused by viruses including common colds, viral sore throats, bronchitis, and sinus and ear infections that do not respond to antibiotics. Although the White House released The National Action Plan for Combating Antibiotic-Resistant Bacteria (CARB) in 2015, which set a goal of reducing inappropriate outpatient antibiotic use by at least half by 2020, hospitalists can still do more by being extremely cautious with prescribing drugs to patients. Use appropriate consultants whenever necessary to suggest the right drug. For example, consider an infectious disease specialist to suggest the appropriate type and length of time for an antibiotic. In addition, hospital-based programs dedicated to improving antibiotic use, known as antibiotic stewardship programs (ASPs), have been shown to optimize the treatment of infections and reduce adverse events associated with antibiotic use.
Review labs and vitals carefully and encourage a higher level of patient care beyond the digital tools available: Studies have shown an oversight in an exam (a “miss”) can result in real consequences, including death. Our $3.4 trillion health care system is responsible for more than a quarter of a million deaths per year because of medical error. Much of that is a result of poorly coordinated care, poor communication, patients falling through the cracks, or knowledge not being transferred. “True clinical judgment is more than addressing the avalanche of blood work, imaging, and lab tests; it is about using human skills to understand where the patient is in the trajectory of a life and the disease, what the nature of the patient’s family and social circumstances is, and how much they want done,” wrote Dr. Abraham Verghese in the New York Times in 2018 (“How Tech Can Turn Doctors into Clerical Workers”). This also means understanding whether the patient is on any other type of medication and, as a result, having knowledge of possible consequences for drug interactions. Always look for safe medications or discontinue the use of any unnecessary drugs the patient is currently taking.
Allow pharmacies to automatically substitute less expensive equivalent drugs: When prescribing pharmaceuticals for patients, determine if there are any substitutes that can help alleviate costs while delivering equivalent care to the patient. This requires excellent ongoing communication with pharmacists and understanding the substitutes available, as well as any side effects or consequences.
Hospitalists can make a difference
There are many variables that play a role in rising pharmaceutical costs in the United States. One of the most significant is that there are no strategies in place to control pricing of drugs and the profits made by the pharmaceutical companies.
Although finding new drugs that can cure major life-threatening diseases or illnesses is important, so is ensuring that more patients have access to such drugs at a reasonable cost. While there are several ways that the government can and should help with enabling and supporting this balance, it most likely requires such large changes that it will take a long time. As a result, it is important for hospitalists to find effective short-term solutions that can be implemented right away to alleviate the rising costs of pharmaceuticals and provide proper patient care regardless of their economic status – all of which requires better research, analysis, and comparison before prescribing treatment to patients.
Dr. Kasarla is a hospitalist with APOGEE Physicians at Wise Surgical at Parkway in Fort Worth, Tex. He did his internal medicine residency at Mercy Hospital & Medical Center, Chicago. Contact him at [email protected]. Dr. Devireddy is a hospitalist based at Sri Ramachandra Medical Centre, Porur, Tamilnadu, India. Contact her at [email protected].
FURTHER READING
Olson and Sheiner (2017). “The Hutchins Center Explains: Prescription drug spending” Brooking.edu
Lo, Chris (2018). “Cost control: drug pricing policies around the world,” Pharmaceutical-Technology.com
Center for Disease Control and Prevention. (2016). 1 in 3 antibiotic prescriptions unnecessary. Retrieved Jan 31, 2019, from https://www.cdc.gov/media/releases/2016/p0503-unnecessary-prescriptions.html
Verghese, Abraham (2018). “How Tech Can Turn Doctors Into Clerical Workers” NYTimes.Com
Waxman, Corr, Martin et al (2017). “Getting to the Root of High Prescription Drug Prices” Commonwealthfund.org
American Council on Science and Health. (2018). Government Is The Big Reason EpiPen And Other Generics Are So Expensive. Retrieved Jan 31, 2019, from https://www.acsh.org/news/2018/06/23/government-big-reason-epipen-and-other-generics-are-so-expensive-13114
Statista. (2018). U.S. Pharmaceutical Industry – Statistics & Facts. Retrieved Jan 31, 2019, from https://www.statista.com/topics/1719/pharmaceutical-industry/
Four key actions providers can take
Four key actions providers can take
Because of the increasing costs of prescription drugs and medical therapies, many patients are unable to afford the treatment they need that could improve their health or even save their lives. In the United States, drug manufacturers can set their own prices – a policy that has resulted in overall medicine costs being far higher than in other places around the globe. Increasingly, insurers are passing the costs along to patients through higher deductibles, and pharmaceutical companies are making record profits.
Something needs to change in order to achieve the right balance between maintaining pharmaceutical innovation and ensuring patients have proper access to treatments they need. Waiting for legislation, regulation, or the courts is not an effective short-term solution. Instead, hospitalists can take immediate actions to help by alleviating the costs for as many patients possible.
Historical context
Many might be wondering how prescription costs became so imbalanced in the first place. Here are a few important factors that played a role in the dramatic price increase of pharmaceuticals:
Entrance of generic drugs: Around 2012 the entrance of generic drugs caused major unexpected competition in the medical industry. During this time, many insurers were promoting the generic drugs and not allowing brand names to be covered when a generic substitute was available.
“Orphan drugs” and manufacturer pricing: In 2014, 33 new brand-name drugs were launched in the United States, and only 8 had a direct price competitor at the time they were introduced. In addition, manufacturers were free to set their prices. Over the past decade, introductory prices for brand name drugs have reached unprecedented levels. Furthermore, manufacturers use the patent protections to increase their prices every year, even when no significant improvements have been made to the drug.
Expiring patents: According to research, there are 182 drugs that no longer have patent protection or any associated generics available. This creates opportunities for manufacturers to maintain patent-era pricing or even engage in price gouging.
Lack of robust competition: Several high-priced blockbuster drugs hit the market to treat serious diseases, most of which do not have generic brand substitutes, which leaves only one option for patients – and it’s usually not affordable. According to research, more than 500 drugs have only one marketed generic. In addition, manufacturer mergers and acquisitions have occurred, which has led to a more concentrated and less competitive market for pricing.
Stricter Food and Drug Administration policies: American consumers have access to the safest and most advanced pharmaceutical system in the world, which requires several trials and testing before the drug can be approved and brought to the market. Despite the benefits of these strict procedures, the downside means higher costs for the brand and manufacturer that they will want to recoup through the price of the drug on the market.
Number of new drugs allowed to enter the market: New drugs that enter the market in the United States do so more quickly than in most other countries. Research shows the U.S. pharmaceutical market contributes to 45% of the global pharmaceutical market. The $76 billion in research and development that pharmaceutical companies claim overlooks the ways that U.S. employers and taxpayers pay for at least 44% through tax subsidies and credits. What makes it worse is that research shows most corporate research and development is directed at minimally innovative new drugs, using the system to secure patents and charge monopoly prices.
Compared with other high-income countries, the United States spends the most per capita on prescription drugs. While insured U.S. patients often pay little or nothing for generic prescriptions, they can be billed tens of thousands of dollars for certain high-priced medicines. The United States has the highest rate of insured patients skipping or not filling prescriptions because of cost. For example, the price of EpiPens, a drug delivery system that is crucial for persons experiencing life-threatening allergic reactions, has increased more than $500 in just 9 years.
How to alleviate rising drug costs
The good news is that hospitalists can do something about the high costs of pharmaceuticals.
Understand and offer alternative ways for drug intake: Many patients admitted to a hospital with severe infections are initially started with intravenous medications. Although conversion from intravenous to oral therapy is inappropriate for a patient who is critically ill or has an inability to absorb oral medications, every hospital will have a certain number of patients who are eligible for a switch from intravenous to oral therapy.
The World Health Organization (WHO) reports that the irrational use of medicines is a major problem worldwide, including antibiotics. Switching from IV to oral enables one to select a cheaper or older antibiotic that is as effective as the IV antibiotic. However, this requires breaking the belief that many physicians still have that IV medications’ bioavailability is stronger and creates less susceptibility to the illness reoccurring in the patient. For many medications, essentially the same amount of drug is found in the blood when given intravenously or orally. In addition, research has shown several benefits beyond cost reduction for oral over IV, such as earlier discharge and reduced risk of infections.
Limit unnecessary antibiotic prescriptions and consider antibiotics stewardship programs: The Center for Disease Control reports that one in three (47 million) antibiotic prescriptions are unnecessary. Most of these unnecessary antibiotics are prescribed for respiratory conditions caused by viruses including common colds, viral sore throats, bronchitis, and sinus and ear infections that do not respond to antibiotics. Although the White House released The National Action Plan for Combating Antibiotic-Resistant Bacteria (CARB) in 2015, which set a goal of reducing inappropriate outpatient antibiotic use by at least half by 2020, hospitalists can still do more by being extremely cautious with prescribing drugs to patients. Use appropriate consultants whenever necessary to suggest the right drug. For example, consider an infectious disease specialist to suggest the appropriate type and length of time for an antibiotic. In addition, hospital-based programs dedicated to improving antibiotic use, known as antibiotic stewardship programs (ASPs), have been shown to optimize the treatment of infections and reduce adverse events associated with antibiotic use.
Review labs and vitals carefully and encourage a higher level of patient care beyond the digital tools available: Studies have shown an oversight in an exam (a “miss”) can result in real consequences, including death. Our $3.4 trillion health care system is responsible for more than a quarter of a million deaths per year because of medical error. Much of that is a result of poorly coordinated care, poor communication, patients falling through the cracks, or knowledge not being transferred. “True clinical judgment is more than addressing the avalanche of blood work, imaging, and lab tests; it is about using human skills to understand where the patient is in the trajectory of a life and the disease, what the nature of the patient’s family and social circumstances is, and how much they want done,” wrote Dr. Abraham Verghese in the New York Times in 2018 (“How Tech Can Turn Doctors into Clerical Workers”). This also means understanding whether the patient is on any other type of medication and, as a result, having knowledge of possible consequences for drug interactions. Always look for safe medications or discontinue the use of any unnecessary drugs the patient is currently taking.
Allow pharmacies to automatically substitute less expensive equivalent drugs: When prescribing pharmaceuticals for patients, determine if there are any substitutes that can help alleviate costs while delivering equivalent care to the patient. This requires excellent ongoing communication with pharmacists and understanding the substitutes available, as well as any side effects or consequences.
Hospitalists can make a difference
There are many variables that play a role in rising pharmaceutical costs in the United States. One of the most significant is that there are no strategies in place to control pricing of drugs and the profits made by the pharmaceutical companies.
Although finding new drugs that can cure major life-threatening diseases or illnesses is important, so is ensuring that more patients have access to such drugs at a reasonable cost. While there are several ways that the government can and should help with enabling and supporting this balance, it most likely requires such large changes that it will take a long time. As a result, it is important for hospitalists to find effective short-term solutions that can be implemented right away to alleviate the rising costs of pharmaceuticals and provide proper patient care regardless of their economic status – all of which requires better research, analysis, and comparison before prescribing treatment to patients.
Dr. Kasarla is a hospitalist with APOGEE Physicians at Wise Surgical at Parkway in Fort Worth, Tex. He did his internal medicine residency at Mercy Hospital & Medical Center, Chicago. Contact him at [email protected]. Dr. Devireddy is a hospitalist based at Sri Ramachandra Medical Centre, Porur, Tamilnadu, India. Contact her at [email protected].
FURTHER READING
Olson and Sheiner (2017). “The Hutchins Center Explains: Prescription drug spending” Brooking.edu
Lo, Chris (2018). “Cost control: drug pricing policies around the world,” Pharmaceutical-Technology.com
Center for Disease Control and Prevention. (2016). 1 in 3 antibiotic prescriptions unnecessary. Retrieved Jan 31, 2019, from https://www.cdc.gov/media/releases/2016/p0503-unnecessary-prescriptions.html
Verghese, Abraham (2018). “How Tech Can Turn Doctors Into Clerical Workers” NYTimes.Com
Waxman, Corr, Martin et al (2017). “Getting to the Root of High Prescription Drug Prices” Commonwealthfund.org
American Council on Science and Health. (2018). Government Is The Big Reason EpiPen And Other Generics Are So Expensive. Retrieved Jan 31, 2019, from https://www.acsh.org/news/2018/06/23/government-big-reason-epipen-and-other-generics-are-so-expensive-13114
Statista. (2018). U.S. Pharmaceutical Industry – Statistics & Facts. Retrieved Jan 31, 2019, from https://www.statista.com/topics/1719/pharmaceutical-industry/
Because of the increasing costs of prescription drugs and medical therapies, many patients are unable to afford the treatment they need that could improve their health or even save their lives. In the United States, drug manufacturers can set their own prices – a policy that has resulted in overall medicine costs being far higher than in other places around the globe. Increasingly, insurers are passing the costs along to patients through higher deductibles, and pharmaceutical companies are making record profits.
Something needs to change in order to achieve the right balance between maintaining pharmaceutical innovation and ensuring patients have proper access to treatments they need. Waiting for legislation, regulation, or the courts is not an effective short-term solution. Instead, hospitalists can take immediate actions to help by alleviating the costs for as many patients possible.
Historical context
Many might be wondering how prescription costs became so imbalanced in the first place. Here are a few important factors that played a role in the dramatic price increase of pharmaceuticals:
Entrance of generic drugs: Around 2012 the entrance of generic drugs caused major unexpected competition in the medical industry. During this time, many insurers were promoting the generic drugs and not allowing brand names to be covered when a generic substitute was available.
“Orphan drugs” and manufacturer pricing: In 2014, 33 new brand-name drugs were launched in the United States, and only 8 had a direct price competitor at the time they were introduced. In addition, manufacturers were free to set their prices. Over the past decade, introductory prices for brand name drugs have reached unprecedented levels. Furthermore, manufacturers use the patent protections to increase their prices every year, even when no significant improvements have been made to the drug.
Expiring patents: According to research, there are 182 drugs that no longer have patent protection or any associated generics available. This creates opportunities for manufacturers to maintain patent-era pricing or even engage in price gouging.
Lack of robust competition: Several high-priced blockbuster drugs hit the market to treat serious diseases, most of which do not have generic brand substitutes, which leaves only one option for patients – and it’s usually not affordable. According to research, more than 500 drugs have only one marketed generic. In addition, manufacturer mergers and acquisitions have occurred, which has led to a more concentrated and less competitive market for pricing.
Stricter Food and Drug Administration policies: American consumers have access to the safest and most advanced pharmaceutical system in the world, which requires several trials and testing before the drug can be approved and brought to the market. Despite the benefits of these strict procedures, the downside means higher costs for the brand and manufacturer that they will want to recoup through the price of the drug on the market.
Number of new drugs allowed to enter the market: New drugs that enter the market in the United States do so more quickly than in most other countries. Research shows the U.S. pharmaceutical market contributes to 45% of the global pharmaceutical market. The $76 billion in research and development that pharmaceutical companies claim overlooks the ways that U.S. employers and taxpayers pay for at least 44% through tax subsidies and credits. What makes it worse is that research shows most corporate research and development is directed at minimally innovative new drugs, using the system to secure patents and charge monopoly prices.
Compared with other high-income countries, the United States spends the most per capita on prescription drugs. While insured U.S. patients often pay little or nothing for generic prescriptions, they can be billed tens of thousands of dollars for certain high-priced medicines. The United States has the highest rate of insured patients skipping or not filling prescriptions because of cost. For example, the price of EpiPens, a drug delivery system that is crucial for persons experiencing life-threatening allergic reactions, has increased more than $500 in just 9 years.
How to alleviate rising drug costs
The good news is that hospitalists can do something about the high costs of pharmaceuticals.
Understand and offer alternative ways for drug intake: Many patients admitted to a hospital with severe infections are initially started with intravenous medications. Although conversion from intravenous to oral therapy is inappropriate for a patient who is critically ill or has an inability to absorb oral medications, every hospital will have a certain number of patients who are eligible for a switch from intravenous to oral therapy.
The World Health Organization (WHO) reports that the irrational use of medicines is a major problem worldwide, including antibiotics. Switching from IV to oral enables one to select a cheaper or older antibiotic that is as effective as the IV antibiotic. However, this requires breaking the belief that many physicians still have that IV medications’ bioavailability is stronger and creates less susceptibility to the illness reoccurring in the patient. For many medications, essentially the same amount of drug is found in the blood when given intravenously or orally. In addition, research has shown several benefits beyond cost reduction for oral over IV, such as earlier discharge and reduced risk of infections.
Limit unnecessary antibiotic prescriptions and consider antibiotics stewardship programs: The Center for Disease Control reports that one in three (47 million) antibiotic prescriptions are unnecessary. Most of these unnecessary antibiotics are prescribed for respiratory conditions caused by viruses including common colds, viral sore throats, bronchitis, and sinus and ear infections that do not respond to antibiotics. Although the White House released The National Action Plan for Combating Antibiotic-Resistant Bacteria (CARB) in 2015, which set a goal of reducing inappropriate outpatient antibiotic use by at least half by 2020, hospitalists can still do more by being extremely cautious with prescribing drugs to patients. Use appropriate consultants whenever necessary to suggest the right drug. For example, consider an infectious disease specialist to suggest the appropriate type and length of time for an antibiotic. In addition, hospital-based programs dedicated to improving antibiotic use, known as antibiotic stewardship programs (ASPs), have been shown to optimize the treatment of infections and reduce adverse events associated with antibiotic use.
Review labs and vitals carefully and encourage a higher level of patient care beyond the digital tools available: Studies have shown an oversight in an exam (a “miss”) can result in real consequences, including death. Our $3.4 trillion health care system is responsible for more than a quarter of a million deaths per year because of medical error. Much of that is a result of poorly coordinated care, poor communication, patients falling through the cracks, or knowledge not being transferred. “True clinical judgment is more than addressing the avalanche of blood work, imaging, and lab tests; it is about using human skills to understand where the patient is in the trajectory of a life and the disease, what the nature of the patient’s family and social circumstances is, and how much they want done,” wrote Dr. Abraham Verghese in the New York Times in 2018 (“How Tech Can Turn Doctors into Clerical Workers”). This also means understanding whether the patient is on any other type of medication and, as a result, having knowledge of possible consequences for drug interactions. Always look for safe medications or discontinue the use of any unnecessary drugs the patient is currently taking.
Allow pharmacies to automatically substitute less expensive equivalent drugs: When prescribing pharmaceuticals for patients, determine if there are any substitutes that can help alleviate costs while delivering equivalent care to the patient. This requires excellent ongoing communication with pharmacists and understanding the substitutes available, as well as any side effects or consequences.
Hospitalists can make a difference
There are many variables that play a role in rising pharmaceutical costs in the United States. One of the most significant is that there are no strategies in place to control pricing of drugs and the profits made by the pharmaceutical companies.
Although finding new drugs that can cure major life-threatening diseases or illnesses is important, so is ensuring that more patients have access to such drugs at a reasonable cost. While there are several ways that the government can and should help with enabling and supporting this balance, it most likely requires such large changes that it will take a long time. As a result, it is important for hospitalists to find effective short-term solutions that can be implemented right away to alleviate the rising costs of pharmaceuticals and provide proper patient care regardless of their economic status – all of which requires better research, analysis, and comparison before prescribing treatment to patients.
Dr. Kasarla is a hospitalist with APOGEE Physicians at Wise Surgical at Parkway in Fort Worth, Tex. He did his internal medicine residency at Mercy Hospital & Medical Center, Chicago. Contact him at [email protected]. Dr. Devireddy is a hospitalist based at Sri Ramachandra Medical Centre, Porur, Tamilnadu, India. Contact her at [email protected].
FURTHER READING
Olson and Sheiner (2017). “The Hutchins Center Explains: Prescription drug spending” Brooking.edu
Lo, Chris (2018). “Cost control: drug pricing policies around the world,” Pharmaceutical-Technology.com
Center for Disease Control and Prevention. (2016). 1 in 3 antibiotic prescriptions unnecessary. Retrieved Jan 31, 2019, from https://www.cdc.gov/media/releases/2016/p0503-unnecessary-prescriptions.html
Verghese, Abraham (2018). “How Tech Can Turn Doctors Into Clerical Workers” NYTimes.Com
Waxman, Corr, Martin et al (2017). “Getting to the Root of High Prescription Drug Prices” Commonwealthfund.org
American Council on Science and Health. (2018). Government Is The Big Reason EpiPen And Other Generics Are So Expensive. Retrieved Jan 31, 2019, from https://www.acsh.org/news/2018/06/23/government-big-reason-epipen-and-other-generics-are-so-expensive-13114
Statista. (2018). U.S. Pharmaceutical Industry – Statistics & Facts. Retrieved Jan 31, 2019, from https://www.statista.com/topics/1719/pharmaceutical-industry/
Subsegmental PEs overtreated despite link with patient harm
Background: CT pulmonary angiography (CTPA) often detects distal, subsegmental pulmonary embolisms (SSPE) for which there is unclear clinical significance. For these isolated SSPEs, the 2016 CHEST guidelines recommend clinical surveillance in lieu of treatment. Such clinical surveillance has not been associated with an increased recurrence of venous thromboembolism (VTE) over 3 months.
Study design: Retrospective review.
Setting: Tertiary care center in Quebec.
Synopsis: A review of all CTPAs at McGill University in Montreal, from 2014-2016 yielded 222 acute pulmonary emboli (PEs), 71 of which were SSPEs without associated Doppler imaging positive for deep vein thrombosis. Of those 71, 62 (87%) were systemically anticoagulated, compared with 135/143 (94%) of the more proximal PEs. The adverse events of both groups of anticoagulated patients were common and similar. Over the following 3 months, 26 patients in the SSPE group visited the ED or were readmitted (42%; 95% confidence interval, 30%-55%), 21 had a drop in hemoglobin level of 2 g/dL or greater and/or received a blood transfusion (34%; 95% CI, 22%-47%), and 10 died from causes unrelated to VTE (16%; 95% CI, 8%-28%). Limitations of this study included the small number of participants and short time to follow-up.
Bottom line: Although SSPEs have unknown clinical significance, they are being treated with systemic anticoagulation at a similar rate to more proximal PEs and are associated with patient harm.
Citation: Raslan IA et al. Rates of overtreatment and treatment-related adverse effects among patients with subsegmental pulmonary embolism. JAMA Intern Med. 2018 Sep 1;178(9):1272-4.
Dr. Shaw is an assistant professor in the division of hospital medicine, University of New Mexico.
Background: CT pulmonary angiography (CTPA) often detects distal, subsegmental pulmonary embolisms (SSPE) for which there is unclear clinical significance. For these isolated SSPEs, the 2016 CHEST guidelines recommend clinical surveillance in lieu of treatment. Such clinical surveillance has not been associated with an increased recurrence of venous thromboembolism (VTE) over 3 months.
Study design: Retrospective review.
Setting: Tertiary care center in Quebec.
Synopsis: A review of all CTPAs at McGill University in Montreal, from 2014-2016 yielded 222 acute pulmonary emboli (PEs), 71 of which were SSPEs without associated Doppler imaging positive for deep vein thrombosis. Of those 71, 62 (87%) were systemically anticoagulated, compared with 135/143 (94%) of the more proximal PEs. The adverse events of both groups of anticoagulated patients were common and similar. Over the following 3 months, 26 patients in the SSPE group visited the ED or were readmitted (42%; 95% confidence interval, 30%-55%), 21 had a drop in hemoglobin level of 2 g/dL or greater and/or received a blood transfusion (34%; 95% CI, 22%-47%), and 10 died from causes unrelated to VTE (16%; 95% CI, 8%-28%). Limitations of this study included the small number of participants and short time to follow-up.
Bottom line: Although SSPEs have unknown clinical significance, they are being treated with systemic anticoagulation at a similar rate to more proximal PEs and are associated with patient harm.
Citation: Raslan IA et al. Rates of overtreatment and treatment-related adverse effects among patients with subsegmental pulmonary embolism. JAMA Intern Med. 2018 Sep 1;178(9):1272-4.
Dr. Shaw is an assistant professor in the division of hospital medicine, University of New Mexico.
Background: CT pulmonary angiography (CTPA) often detects distal, subsegmental pulmonary embolisms (SSPE) for which there is unclear clinical significance. For these isolated SSPEs, the 2016 CHEST guidelines recommend clinical surveillance in lieu of treatment. Such clinical surveillance has not been associated with an increased recurrence of venous thromboembolism (VTE) over 3 months.
Study design: Retrospective review.
Setting: Tertiary care center in Quebec.
Synopsis: A review of all CTPAs at McGill University in Montreal, from 2014-2016 yielded 222 acute pulmonary emboli (PEs), 71 of which were SSPEs without associated Doppler imaging positive for deep vein thrombosis. Of those 71, 62 (87%) were systemically anticoagulated, compared with 135/143 (94%) of the more proximal PEs. The adverse events of both groups of anticoagulated patients were common and similar. Over the following 3 months, 26 patients in the SSPE group visited the ED or were readmitted (42%; 95% confidence interval, 30%-55%), 21 had a drop in hemoglobin level of 2 g/dL or greater and/or received a blood transfusion (34%; 95% CI, 22%-47%), and 10 died from causes unrelated to VTE (16%; 95% CI, 8%-28%). Limitations of this study included the small number of participants and short time to follow-up.
Bottom line: Although SSPEs have unknown clinical significance, they are being treated with systemic anticoagulation at a similar rate to more proximal PEs and are associated with patient harm.
Citation: Raslan IA et al. Rates of overtreatment and treatment-related adverse effects among patients with subsegmental pulmonary embolism. JAMA Intern Med. 2018 Sep 1;178(9):1272-4.
Dr. Shaw is an assistant professor in the division of hospital medicine, University of New Mexico.
When is electroconvulsive therapy (ECT) indicated?
Know the general work-up and contraindications
Case
A 56-year-old female comes to the hospitalist service for presumed sepsis with acute renal insufficiency. She has a history of steadily progressive Parkinson’s disease. Vital signs show a temperature of 104° F; heart rate,135; BP, 100/70; respiratory rate, 20; oxygen saturation, 100% on room air. She is rigid on exam with creatine kinase, 2450 IU/L, and serum creatinine, 2.2. History reveals the patient’s levodopa was increased to 1,200 mg/day recently, then stopped by the family after she became paranoid. A diagnosis of neuroleptic malignant syndrome (NMS) is made.
Background
Electroconvulsive therapy (ECT) has been the gold standard for treatment of refractory psychiatric disease for decades. While it has proven beneficial for both medical and psychiatric disorders, it remains surrounded in controversy. Additionally, there is a significant degree of discomfort among nonpsychiatric providers on when to consider ECT, as well as how to evaluate the patient and manage their comorbidities before and during the procedure1.
Hospitalists should be familiar with the relative contraindications and general work-up for ECT, which can expedite both psychiatric and anesthesia evaluations and minimize adverse outcomes.
While the mechanism of action still is not known, ECT exerts a variety of effects in the brain and periphery. The dominant theory is that ECT increases neurotransmitter activity throughout the brain. Studies have shown increased GABA transmission, normalized glutamate transmission, and resetting of the hypothalamic-pituitary axis, as well as activation of downstream signal transduction pathways leading to increased synaptic connectivity in the brain. Many of ECT’s results may be caused by combinations of the above mechanisms2.
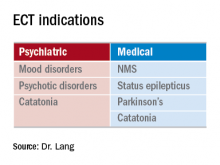
ECT principally is indicated for refractory mood and psychotic disorders. These include schizophrenia, bipolar disorder, and major depression. ECT-responsive patients typically have failed multiple appropriate medication trials and often have prolonged hospitalizations. What is less known are the medical indications for this procedure. Examples include Parkinson’s disease (especially with on/off phenomenon), status epilepticus, and neuroleptic malignant syndrome. Additionally, ECT has been shown to be beneficial for slow-to-resolve delirium and catatonia (regardless of etiology).
A psychiatrist also may take into consideration factors such as past response to ECT or the level of urgency to the patient’s presentation. A general work-up includes basic comprehensive metabolic panel, complete blood count, chest x-ray, EKG, and other testing based on history, physical, and past medical history.
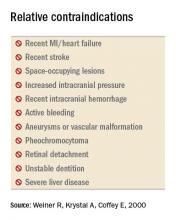
While there are no absolute contraindications to ECT, several relative contraindications exist. These include recent MI or stroke (generally within the last 30 days), increased intracranial pressure, active bleeding (especially from the central nervous system), retinal detachment, and unstable dentition. Apart from making sure the technique is medically indicated, an ECT consultant also evaluates the medical comorbidities. The patient may require treatment, such as removal of unstable dentition prior to the procedure, if clinical urgency does not preclude a delay.
Select patients require more detailed consultation prior to the onset of anesthesia. Examples would include patients with pseudocholinesterase deficiency, myasthenia gravis, or pregnancy. Pregnancy often is considered a contraindication, but ECT has no notable effect on labor & delivery, fetal injury, or development. It would be a preferred modality over medications, especially in unstable mothers during the first trimester. ECT exerts little effect on the fetus, as the amount of current that actually gets to the fetus is negligible6.
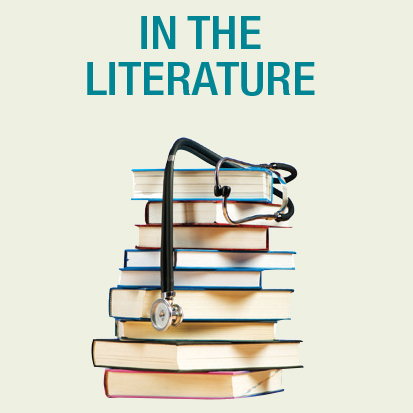
Outside the central nervous system, ECT exerts the most influence over the cardiovascular system. During the tonic phase of a seizure, increased vagal tone can depress the heart rate to asystole in some patients (see chart below). This may last for 3-4 seconds until the clonic phase occurs (with a noradrenergic surge), whereupon the heart rate can accelerate to the 140s. Unless unstable cardiac disease is present, patients typically tolerate this extremely well without any adverse sequela7. Studies involving patients who have severe aortic stenosis and pacemakers/defibrillators show overall excellent tolerability8,9.
Medications can have an impact on the onset, quality, and duration of seizures. Thus, a careful medication review is needed. A consultant will look first for medications such as benzodiazepines or anticonvulsants that would raise the seizure threshold. Ideally, the medications would be stopped, but if not feasible, they can be held the night before (or the day before in the case of such long half-life agents as diazepam) to minimize their impact.
As for anticonvulsants, the doses can be reduced, along with modest increases in energy settings to facilitate seizure. If used for mood stabilization only, one could consider stopping them completely, but this is usually not required (it is not recommended to stop them if used for epilepsy). Lithium can lead to prolonged neuromuscular blockade, prolonged seizures, or postictal delirium. However, discontinuation of lithium also has a risk-benefit consideration, so usually, doses are reduced and/or decreased doses of neuromuscular blockade are employed. Theophylline can induce extended seizures or status epilepticus so it is usually held prior to ECT.
Back to the case
Given the patient’s severe Parkinson’s disease and concurrent NMS, ECT was initiated. By the second treatment, fever and tachycardia resolved. By the sixth treatment, all NMS symptoms and associated paranoia had completely resolved and her Parkinson’s disease rating scale score went from 142 to 42. Her levodopa dose was reduced from 1,200 to 300 mg/day. She remained stable for years afterward.
Bottom line
ECT is both effective and well tolerated in patients who have received appropriate medical evaluation.
Dr. Lang is clinical associate professor in the departments of psychiatry and internal medicine and director of the electroconvulsive therapy and transcranial magnetic stimulation programs at East Carolina University, Greenville, N.C.
Key points
- ECT is indicated for psychotic and depressive disorders, with high efficacy and rapid response.
- ECT also has proven benefits for NMS, catatonia, delirium, status epilepticus, and Parkinson’s disease.
- Evaluation and focused treatment of relative contraindications maximizes both safety and tolerability of ECT.
References
1. Weiner R et al. “Electroconvulsive therapy in the medical & neurologic patient” in A Stoudemire, BS Fogel & D Greenberg (eds) Psychiatric Care of the Medical Patient, 2nd ed., New York, Oxford Univ Press. 2000:419-28. (Second edition is out of print.)
2. Baghai T et al. Electroconvulsive therapy and its different indications. Dialogues Clin Neurosci. Mar 2008;10(1):105-17.
3. Ozer F et al. Electroconvulsive therapy in drug-induced psychiatric states and neuroleptic malignant syndrome. J ECT. 2005 Jun;21(2):125-7.
4. Taylor S. Electroconvulsive therapy: A review of history, patient selection, technique, and medication management. South Med J. 2007 May;100(5):494-8.
5. The Practice of Electroconvulsive Therapy, 2nd edition. A Task Force Report of the American Psychiatric Association. 2001. pp. 84-85.
6. Miller LJ. Use of electroconvulsive therapy during pregnancy. Hosp Community Psychiatry. 1994 May;45(5):444-50.
7. Miller R et al. ECT: Physiologic Effects. Miller’s Anesthesia. 7th Edition. 2009.
8. Mueller PS et al. The Safety of electroconvulsive therapy in patients with severe aortic stenosis. Mayo Clin Proc. 2007 Nov;82(11):1360-3.
9. Dolenc TJ et al. Electroconvulsive therapy in patients with cardiac pacemakers & implantable cardioverter defibrillators. Pacing Clin Electrophysiol. 2004 Sep;27(9):1257-63.
Suggested readings
The practice of electroconvulsive therapy: Recommendations for treatment, training, and privileging (A Task Force Report of the American Psychiatric Association), 2nd Edition. APA Publishing. 2001.
Weiner R et al. “Electroconvulsive therapy in the medical & neurologic patient” in A Stoudemire, BS Fogel & D Greenberg (eds) Psychiatric Care of the Medical Patient, 2nd ed., New York, Oxford Univ Press. 2000:419-28. (Second edition is out of print.)
Rosenquist P et al. Charting the course of electroconvulsive therapy: Where have we been and where are we headed? J Psychosoc Nurs Ment Health Serv. 2016 Dec 1;54(12):39-43.
QUIZ
1. All of the following are indications for ECT except?
A. Schizophrenia.
B. Panic attacks.
C. Bipolar mania.
D. Catatonia.
Answer: B. Panic attacks. ECT is not effective for anxiety disorders including panic, generalized anxiety, PTSD, or OCD.
2. The most commonly accepted mechanism of action for ECT is?
A. Reduction in glutamate levels.
B. Altering signal transduction pathways.
C. Increased neurotransmitter activity.
D. Increased cerebral blood flow.
Answer: C. Increased neurotransmitter activity. There are data to support all, but neurotransmitter flow is most accepted thus far.
3. Which of the following is a common side effect of ECT?
A. Bronchospasm.
B. Diarrhea.
C. Delirium.
D. Visual changes.
Answer: C. Delirium. The rest are rare or not noted.
4. Which of the following is a relative contraindication for ECT?
A. Pregnancy.
B. Epilepsy.
C. Advanced age.
D. Increased intracranial pressure.
Answer: D. Increased intracranial pressure.
Know the general work-up and contraindications
Know the general work-up and contraindications
Case
A 56-year-old female comes to the hospitalist service for presumed sepsis with acute renal insufficiency. She has a history of steadily progressive Parkinson’s disease. Vital signs show a temperature of 104° F; heart rate,135; BP, 100/70; respiratory rate, 20; oxygen saturation, 100% on room air. She is rigid on exam with creatine kinase, 2450 IU/L, and serum creatinine, 2.2. History reveals the patient’s levodopa was increased to 1,200 mg/day recently, then stopped by the family after she became paranoid. A diagnosis of neuroleptic malignant syndrome (NMS) is made.
Background
Electroconvulsive therapy (ECT) has been the gold standard for treatment of refractory psychiatric disease for decades. While it has proven beneficial for both medical and psychiatric disorders, it remains surrounded in controversy. Additionally, there is a significant degree of discomfort among nonpsychiatric providers on when to consider ECT, as well as how to evaluate the patient and manage their comorbidities before and during the procedure1.
Hospitalists should be familiar with the relative contraindications and general work-up for ECT, which can expedite both psychiatric and anesthesia evaluations and minimize adverse outcomes.
While the mechanism of action still is not known, ECT exerts a variety of effects in the brain and periphery. The dominant theory is that ECT increases neurotransmitter activity throughout the brain. Studies have shown increased GABA transmission, normalized glutamate transmission, and resetting of the hypothalamic-pituitary axis, as well as activation of downstream signal transduction pathways leading to increased synaptic connectivity in the brain. Many of ECT’s results may be caused by combinations of the above mechanisms2.
ECT principally is indicated for refractory mood and psychotic disorders. These include schizophrenia, bipolar disorder, and major depression. ECT-responsive patients typically have failed multiple appropriate medication trials and often have prolonged hospitalizations. What is less known are the medical indications for this procedure. Examples include Parkinson’s disease (especially with on/off phenomenon), status epilepticus, and neuroleptic malignant syndrome. Additionally, ECT has been shown to be beneficial for slow-to-resolve delirium and catatonia (regardless of etiology).
A psychiatrist also may take into consideration factors such as past response to ECT or the level of urgency to the patient’s presentation. A general work-up includes basic comprehensive metabolic panel, complete blood count, chest x-ray, EKG, and other testing based on history, physical, and past medical history.
While there are no absolute contraindications to ECT, several relative contraindications exist. These include recent MI or stroke (generally within the last 30 days), increased intracranial pressure, active bleeding (especially from the central nervous system), retinal detachment, and unstable dentition. Apart from making sure the technique is medically indicated, an ECT consultant also evaluates the medical comorbidities. The patient may require treatment, such as removal of unstable dentition prior to the procedure, if clinical urgency does not preclude a delay.
Select patients require more detailed consultation prior to the onset of anesthesia. Examples would include patients with pseudocholinesterase deficiency, myasthenia gravis, or pregnancy. Pregnancy often is considered a contraindication, but ECT has no notable effect on labor & delivery, fetal injury, or development. It would be a preferred modality over medications, especially in unstable mothers during the first trimester. ECT exerts little effect on the fetus, as the amount of current that actually gets to the fetus is negligible6.
Outside the central nervous system, ECT exerts the most influence over the cardiovascular system. During the tonic phase of a seizure, increased vagal tone can depress the heart rate to asystole in some patients (see chart below). This may last for 3-4 seconds until the clonic phase occurs (with a noradrenergic surge), whereupon the heart rate can accelerate to the 140s. Unless unstable cardiac disease is present, patients typically tolerate this extremely well without any adverse sequela7. Studies involving patients who have severe aortic stenosis and pacemakers/defibrillators show overall excellent tolerability8,9.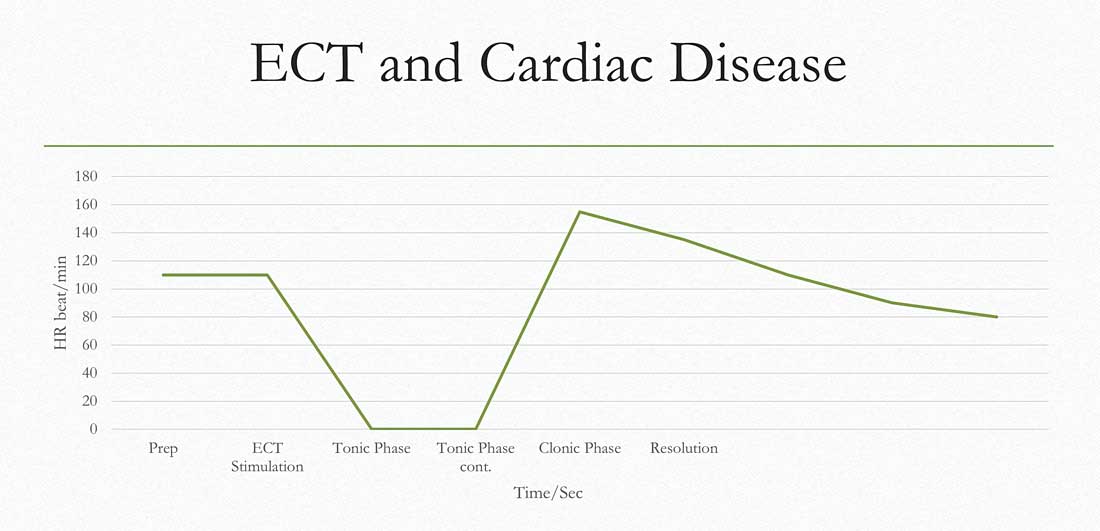
Medications can have an impact on the onset, quality, and duration of seizures. Thus, a careful medication review is needed. A consultant will look first for medications such as benzodiazepines or anticonvulsants that would raise the seizure threshold. Ideally, the medications would be stopped, but if not feasible, they can be held the night before (or the day before in the case of such long half-life agents as diazepam) to minimize their impact.
As for anticonvulsants, the doses can be reduced, along with modest increases in energy settings to facilitate seizure. If used for mood stabilization only, one could consider stopping them completely, but this is usually not required (it is not recommended to stop them if used for epilepsy). Lithium can lead to prolonged neuromuscular blockade, prolonged seizures, or postictal delirium. However, discontinuation of lithium also has a risk-benefit consideration, so usually, doses are reduced and/or decreased doses of neuromuscular blockade are employed. Theophylline can induce extended seizures or status epilepticus so it is usually held prior to ECT.
Back to the case
Given the patient’s severe Parkinson’s disease and concurrent NMS, ECT was initiated. By the second treatment, fever and tachycardia resolved. By the sixth treatment, all NMS symptoms and associated paranoia had completely resolved and her Parkinson’s disease rating scale score went from 142 to 42. Her levodopa dose was reduced from 1,200 to 300 mg/day. She remained stable for years afterward.
Bottom line
ECT is both effective and well tolerated in patients who have received appropriate medical evaluation.
Dr. Lang is clinical associate professor in the departments of psychiatry and internal medicine and director of the electroconvulsive therapy and transcranial magnetic stimulation programs at East Carolina University, Greenville, N.C.
Key points
- ECT is indicated for psychotic and depressive disorders, with high efficacy and rapid response.
- ECT also has proven benefits for NMS, catatonia, delirium, status epilepticus, and Parkinson’s disease.
- Evaluation and focused treatment of relative contraindications maximizes both safety and tolerability of ECT.
References
1. Weiner R et al. “Electroconvulsive therapy in the medical & neurologic patient” in A Stoudemire, BS Fogel & D Greenberg (eds) Psychiatric Care of the Medical Patient, 2nd ed., New York, Oxford Univ Press. 2000:419-28. (Second edition is out of print.)
2. Baghai T et al. Electroconvulsive therapy and its different indications. Dialogues Clin Neurosci. Mar 2008;10(1):105-17.
3. Ozer F et al. Electroconvulsive therapy in drug-induced psychiatric states and neuroleptic malignant syndrome. J ECT. 2005 Jun;21(2):125-7.
4. Taylor S. Electroconvulsive therapy: A review of history, patient selection, technique, and medication management. South Med J. 2007 May;100(5):494-8.
5. The Practice of Electroconvulsive Therapy, 2nd edition. A Task Force Report of the American Psychiatric Association. 2001. pp. 84-85.
6. Miller LJ. Use of electroconvulsive therapy during pregnancy. Hosp Community Psychiatry. 1994 May;45(5):444-50.
7. Miller R et al. ECT: Physiologic Effects. Miller’s Anesthesia. 7th Edition. 2009.
8. Mueller PS et al. The Safety of electroconvulsive therapy in patients with severe aortic stenosis. Mayo Clin Proc. 2007 Nov;82(11):1360-3.
9. Dolenc TJ et al. Electroconvulsive therapy in patients with cardiac pacemakers & implantable cardioverter defibrillators. Pacing Clin Electrophysiol. 2004 Sep;27(9):1257-63.
Suggested readings
The practice of electroconvulsive therapy: Recommendations for treatment, training, and privileging (A Task Force Report of the American Psychiatric Association), 2nd Edition. APA Publishing. 2001.
Weiner R et al. “Electroconvulsive therapy in the medical & neurologic patient” in A Stoudemire, BS Fogel & D Greenberg (eds) Psychiatric Care of the Medical Patient, 2nd ed., New York, Oxford Univ Press. 2000:419-28. (Second edition is out of print.)
Rosenquist P et al. Charting the course of electroconvulsive therapy: Where have we been and where are we headed? J Psychosoc Nurs Ment Health Serv. 2016 Dec 1;54(12):39-43.
QUIZ
1. All of the following are indications for ECT except?
A. Schizophrenia.
B. Panic attacks.
C. Bipolar mania.
D. Catatonia.
Answer: B. Panic attacks. ECT is not effective for anxiety disorders including panic, generalized anxiety, PTSD, or OCD.
2. The most commonly accepted mechanism of action for ECT is?
A. Reduction in glutamate levels.
B. Altering signal transduction pathways.
C. Increased neurotransmitter activity.
D. Increased cerebral blood flow.
Answer: C. Increased neurotransmitter activity. There are data to support all, but neurotransmitter flow is most accepted thus far.
3. Which of the following is a common side effect of ECT?
A. Bronchospasm.
B. Diarrhea.
C. Delirium.
D. Visual changes.
Answer: C. Delirium. The rest are rare or not noted.
4. Which of the following is a relative contraindication for ECT?
A. Pregnancy.
B. Epilepsy.
C. Advanced age.
D. Increased intracranial pressure.
Answer: D. Increased intracranial pressure.
Case
A 56-year-old female comes to the hospitalist service for presumed sepsis with acute renal insufficiency. She has a history of steadily progressive Parkinson’s disease. Vital signs show a temperature of 104° F; heart rate,135; BP, 100/70; respiratory rate, 20; oxygen saturation, 100% on room air. She is rigid on exam with creatine kinase, 2450 IU/L, and serum creatinine, 2.2. History reveals the patient’s levodopa was increased to 1,200 mg/day recently, then stopped by the family after she became paranoid. A diagnosis of neuroleptic malignant syndrome (NMS) is made.
Background
Electroconvulsive therapy (ECT) has been the gold standard for treatment of refractory psychiatric disease for decades. While it has proven beneficial for both medical and psychiatric disorders, it remains surrounded in controversy. Additionally, there is a significant degree of discomfort among nonpsychiatric providers on when to consider ECT, as well as how to evaluate the patient and manage their comorbidities before and during the procedure1.
Hospitalists should be familiar with the relative contraindications and general work-up for ECT, which can expedite both psychiatric and anesthesia evaluations and minimize adverse outcomes.
While the mechanism of action still is not known, ECT exerts a variety of effects in the brain and periphery. The dominant theory is that ECT increases neurotransmitter activity throughout the brain. Studies have shown increased GABA transmission, normalized glutamate transmission, and resetting of the hypothalamic-pituitary axis, as well as activation of downstream signal transduction pathways leading to increased synaptic connectivity in the brain. Many of ECT’s results may be caused by combinations of the above mechanisms2.
ECT principally is indicated for refractory mood and psychotic disorders. These include schizophrenia, bipolar disorder, and major depression. ECT-responsive patients typically have failed multiple appropriate medication trials and often have prolonged hospitalizations. What is less known are the medical indications for this procedure. Examples include Parkinson’s disease (especially with on/off phenomenon), status epilepticus, and neuroleptic malignant syndrome. Additionally, ECT has been shown to be beneficial for slow-to-resolve delirium and catatonia (regardless of etiology).
A psychiatrist also may take into consideration factors such as past response to ECT or the level of urgency to the patient’s presentation. A general work-up includes basic comprehensive metabolic panel, complete blood count, chest x-ray, EKG, and other testing based on history, physical, and past medical history.
While there are no absolute contraindications to ECT, several relative contraindications exist. These include recent MI or stroke (generally within the last 30 days), increased intracranial pressure, active bleeding (especially from the central nervous system), retinal detachment, and unstable dentition. Apart from making sure the technique is medically indicated, an ECT consultant also evaluates the medical comorbidities. The patient may require treatment, such as removal of unstable dentition prior to the procedure, if clinical urgency does not preclude a delay.
Select patients require more detailed consultation prior to the onset of anesthesia. Examples would include patients with pseudocholinesterase deficiency, myasthenia gravis, or pregnancy. Pregnancy often is considered a contraindication, but ECT has no notable effect on labor & delivery, fetal injury, or development. It would be a preferred modality over medications, especially in unstable mothers during the first trimester. ECT exerts little effect on the fetus, as the amount of current that actually gets to the fetus is negligible6.
Outside the central nervous system, ECT exerts the most influence over the cardiovascular system. During the tonic phase of a seizure, increased vagal tone can depress the heart rate to asystole in some patients (see chart below). This may last for 3-4 seconds until the clonic phase occurs (with a noradrenergic surge), whereupon the heart rate can accelerate to the 140s. Unless unstable cardiac disease is present, patients typically tolerate this extremely well without any adverse sequela7. Studies involving patients who have severe aortic stenosis and pacemakers/defibrillators show overall excellent tolerability8,9.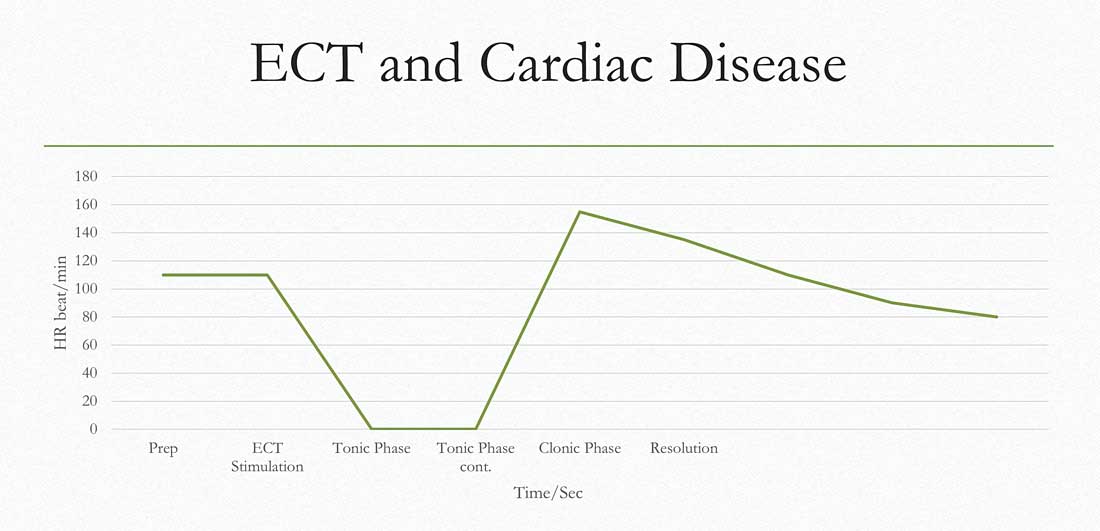
Medications can have an impact on the onset, quality, and duration of seizures. Thus, a careful medication review is needed. A consultant will look first for medications such as benzodiazepines or anticonvulsants that would raise the seizure threshold. Ideally, the medications would be stopped, but if not feasible, they can be held the night before (or the day before in the case of such long half-life agents as diazepam) to minimize their impact.
As for anticonvulsants, the doses can be reduced, along with modest increases in energy settings to facilitate seizure. If used for mood stabilization only, one could consider stopping them completely, but this is usually not required (it is not recommended to stop them if used for epilepsy). Lithium can lead to prolonged neuromuscular blockade, prolonged seizures, or postictal delirium. However, discontinuation of lithium also has a risk-benefit consideration, so usually, doses are reduced and/or decreased doses of neuromuscular blockade are employed. Theophylline can induce extended seizures or status epilepticus so it is usually held prior to ECT.
Back to the case
Given the patient’s severe Parkinson’s disease and concurrent NMS, ECT was initiated. By the second treatment, fever and tachycardia resolved. By the sixth treatment, all NMS symptoms and associated paranoia had completely resolved and her Parkinson’s disease rating scale score went from 142 to 42. Her levodopa dose was reduced from 1,200 to 300 mg/day. She remained stable for years afterward.
Bottom line
ECT is both effective and well tolerated in patients who have received appropriate medical evaluation.
Dr. Lang is clinical associate professor in the departments of psychiatry and internal medicine and director of the electroconvulsive therapy and transcranial magnetic stimulation programs at East Carolina University, Greenville, N.C.
Key points
- ECT is indicated for psychotic and depressive disorders, with high efficacy and rapid response.
- ECT also has proven benefits for NMS, catatonia, delirium, status epilepticus, and Parkinson’s disease.
- Evaluation and focused treatment of relative contraindications maximizes both safety and tolerability of ECT.
References
1. Weiner R et al. “Electroconvulsive therapy in the medical & neurologic patient” in A Stoudemire, BS Fogel & D Greenberg (eds) Psychiatric Care of the Medical Patient, 2nd ed., New York, Oxford Univ Press. 2000:419-28. (Second edition is out of print.)
2. Baghai T et al. Electroconvulsive therapy and its different indications. Dialogues Clin Neurosci. Mar 2008;10(1):105-17.
3. Ozer F et al. Electroconvulsive therapy in drug-induced psychiatric states and neuroleptic malignant syndrome. J ECT. 2005 Jun;21(2):125-7.
4. Taylor S. Electroconvulsive therapy: A review of history, patient selection, technique, and medication management. South Med J. 2007 May;100(5):494-8.
5. The Practice of Electroconvulsive Therapy, 2nd edition. A Task Force Report of the American Psychiatric Association. 2001. pp. 84-85.
6. Miller LJ. Use of electroconvulsive therapy during pregnancy. Hosp Community Psychiatry. 1994 May;45(5):444-50.
7. Miller R et al. ECT: Physiologic Effects. Miller’s Anesthesia. 7th Edition. 2009.
8. Mueller PS et al. The Safety of electroconvulsive therapy in patients with severe aortic stenosis. Mayo Clin Proc. 2007 Nov;82(11):1360-3.
9. Dolenc TJ et al. Electroconvulsive therapy in patients with cardiac pacemakers & implantable cardioverter defibrillators. Pacing Clin Electrophysiol. 2004 Sep;27(9):1257-63.
Suggested readings
The practice of electroconvulsive therapy: Recommendations for treatment, training, and privileging (A Task Force Report of the American Psychiatric Association), 2nd Edition. APA Publishing. 2001.
Weiner R et al. “Electroconvulsive therapy in the medical & neurologic patient” in A Stoudemire, BS Fogel & D Greenberg (eds) Psychiatric Care of the Medical Patient, 2nd ed., New York, Oxford Univ Press. 2000:419-28. (Second edition is out of print.)
Rosenquist P et al. Charting the course of electroconvulsive therapy: Where have we been and where are we headed? J Psychosoc Nurs Ment Health Serv. 2016 Dec 1;54(12):39-43.
QUIZ
1. All of the following are indications for ECT except?
A. Schizophrenia.
B. Panic attacks.
C. Bipolar mania.
D. Catatonia.
Answer: B. Panic attacks. ECT is not effective for anxiety disorders including panic, generalized anxiety, PTSD, or OCD.
2. The most commonly accepted mechanism of action for ECT is?
A. Reduction in glutamate levels.
B. Altering signal transduction pathways.
C. Increased neurotransmitter activity.
D. Increased cerebral blood flow.
Answer: C. Increased neurotransmitter activity. There are data to support all, but neurotransmitter flow is most accepted thus far.
3. Which of the following is a common side effect of ECT?
A. Bronchospasm.
B. Diarrhea.
C. Delirium.
D. Visual changes.
Answer: C. Delirium. The rest are rare or not noted.
4. Which of the following is a relative contraindication for ECT?
A. Pregnancy.
B. Epilepsy.
C. Advanced age.
D. Increased intracranial pressure.
Answer: D. Increased intracranial pressure.
By the numbers: Readmissions for skin conditions
Almost 10% of patients
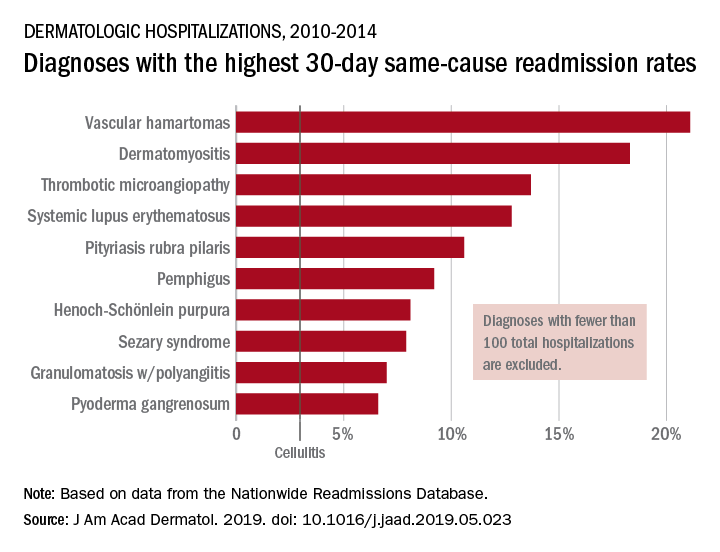
Data from the Nationwide Readmissions Database also showed that the same-cause readmission rate was 3.3% after 30 days and 7.8% within the calendar year (CY) over the 5-year study period of 2010-2014, Myron Zhang, MD, of the department of dermatology at Weill Cornell Medicine, New York, and his associates reported in the Journal of the American Academy of Dermatology.
The total cost of the CY readmissions was $2.54 billion, which works out to $508 million per year or $8,995 per visit. The most common dermatologic diagnosis – cellulitis made up 83.6% of all hospitalizations – was also the most expensive in terms of readmissions, resulting in $1.9 billion in CY costs, Dr. Zhang and associates wrote.
Overall readmission rates for cellulitis were not provided, but annual rates ranged from 9.1% to 9.3% (30-day all cause), from 7.7% to 8.1% (CY same cause), and from 3.1% to 3.3% (30-day same cause), they wrote.
The dermatologic diagnosis with the highest 30-day same-cause readmission rate was vascular hamartomas at 21.1%, followed by dermatomyositis (18.3%) and thrombotic microangiopathy (13.7%). Dermatomyositis had the highest CY same-cause readmission rate (30.8%) and mycosis fungoides had the highest 30-day all-cause rate (32.3%), according to the investigators.
“Diseases, characteristics, and comorbidities associated with high readmission rates should trigger hospitals to consider dermatology consultation, coordinate outpatient follow-up, and support underinsured outpatient access. These measures have been shown to reduce readmissions or hospital visits in general dermatologic settings, but outcomes in individual diseases are not well studied,” Dr. Zhang and associates wrote. They noted that there have been “very few prior studies of readmissions for skin diseases.”
[email protected]
SOURCE: Zhang M et al. J Am Acad. Dermatol. 2019. doi: 10.1016/j.jaad.2019.05.023. .
Almost 10% of patients
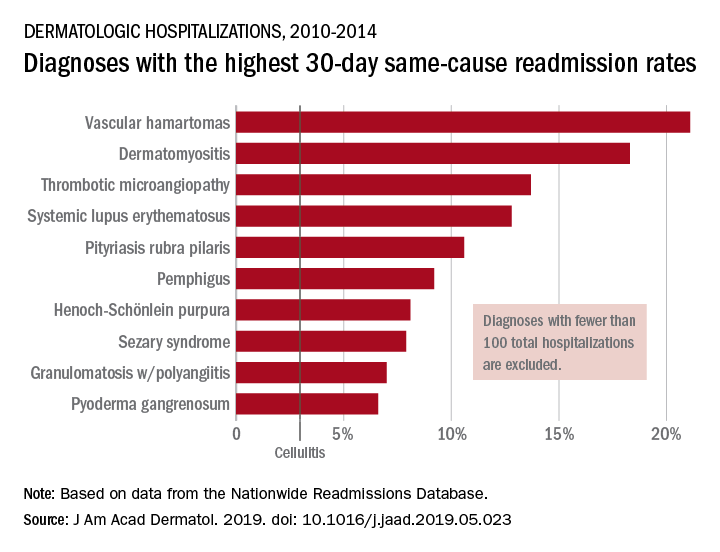
Data from the Nationwide Readmissions Database also showed that the same-cause readmission rate was 3.3% after 30 days and 7.8% within the calendar year (CY) over the 5-year study period of 2010-2014, Myron Zhang, MD, of the department of dermatology at Weill Cornell Medicine, New York, and his associates reported in the Journal of the American Academy of Dermatology.
The total cost of the CY readmissions was $2.54 billion, which works out to $508 million per year or $8,995 per visit. The most common dermatologic diagnosis – cellulitis made up 83.6% of all hospitalizations – was also the most expensive in terms of readmissions, resulting in $1.9 billion in CY costs, Dr. Zhang and associates wrote.
Overall readmission rates for cellulitis were not provided, but annual rates ranged from 9.1% to 9.3% (30-day all cause), from 7.7% to 8.1% (CY same cause), and from 3.1% to 3.3% (30-day same cause), they wrote.
The dermatologic diagnosis with the highest 30-day same-cause readmission rate was vascular hamartomas at 21.1%, followed by dermatomyositis (18.3%) and thrombotic microangiopathy (13.7%). Dermatomyositis had the highest CY same-cause readmission rate (30.8%) and mycosis fungoides had the highest 30-day all-cause rate (32.3%), according to the investigators.
“Diseases, characteristics, and comorbidities associated with high readmission rates should trigger hospitals to consider dermatology consultation, coordinate outpatient follow-up, and support underinsured outpatient access. These measures have been shown to reduce readmissions or hospital visits in general dermatologic settings, but outcomes in individual diseases are not well studied,” Dr. Zhang and associates wrote. They noted that there have been “very few prior studies of readmissions for skin diseases.”
[email protected]
SOURCE: Zhang M et al. J Am Acad. Dermatol. 2019. doi: 10.1016/j.jaad.2019.05.023. .
Almost 10% of patients
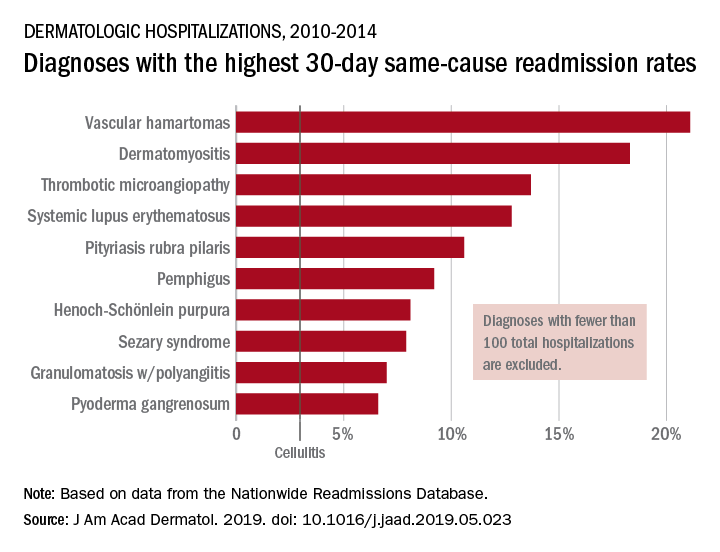
Data from the Nationwide Readmissions Database also showed that the same-cause readmission rate was 3.3% after 30 days and 7.8% within the calendar year (CY) over the 5-year study period of 2010-2014, Myron Zhang, MD, of the department of dermatology at Weill Cornell Medicine, New York, and his associates reported in the Journal of the American Academy of Dermatology.
The total cost of the CY readmissions was $2.54 billion, which works out to $508 million per year or $8,995 per visit. The most common dermatologic diagnosis – cellulitis made up 83.6% of all hospitalizations – was also the most expensive in terms of readmissions, resulting in $1.9 billion in CY costs, Dr. Zhang and associates wrote.
Overall readmission rates for cellulitis were not provided, but annual rates ranged from 9.1% to 9.3% (30-day all cause), from 7.7% to 8.1% (CY same cause), and from 3.1% to 3.3% (30-day same cause), they wrote.
The dermatologic diagnosis with the highest 30-day same-cause readmission rate was vascular hamartomas at 21.1%, followed by dermatomyositis (18.3%) and thrombotic microangiopathy (13.7%). Dermatomyositis had the highest CY same-cause readmission rate (30.8%) and mycosis fungoides had the highest 30-day all-cause rate (32.3%), according to the investigators.
“Diseases, characteristics, and comorbidities associated with high readmission rates should trigger hospitals to consider dermatology consultation, coordinate outpatient follow-up, and support underinsured outpatient access. These measures have been shown to reduce readmissions or hospital visits in general dermatologic settings, but outcomes in individual diseases are not well studied,” Dr. Zhang and associates wrote. They noted that there have been “very few prior studies of readmissions for skin diseases.”
[email protected]
SOURCE: Zhang M et al. J Am Acad. Dermatol. 2019. doi: 10.1016/j.jaad.2019.05.023. .
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Restrictive transfusion strategy in cardiac surgery remains noninferior
Clinical question: Does using a restrictive transfusion strategy with patients undergoing cardiac surgery affect long-term outcomes?
Background: Using a restrictive transfusion strategy in patients undergoing cardiac surgery is known to use fewer units of allogeneic red cells, compared with a liberal strategy, while still having noninferior short-term clinical outcomes. At this time, little is known about such a strategy’s long-term effects.
Study design: Randomized, open-label, noninferiority trial.
Setting: 74 hospitals in 19 countries.
Synopsis: 5,243 adults undergoing nontransplant cardiac surgeries and having at least a moderate predicted risk for death were randomly divided into a liberal or restrictive transfusion strategy. Restrictive-strategy participants received a transfusion when hemoglobin was less than 7.5 g/dL, compared with either a hemoglobin of 8.5 g/dL on the floor or 9.5 g/dL in the ICU for the liberal-strategy group. During the hospitalization, the restrictive group received fewer U of red cells and had a lower mean predischarge hemoglobin. At 6 months, the groups were compared for the primary outcomes of death, MI, stroke, or renal failure requiring dialysis, finding an occurrence of such in 402/2,317 in the restrictive-strategy group and 402/2,347 in the liberal-strategy group (P = .006 for noninferiority). Limitations include the study being a noninferiority trial and the very specific patient population selected.
Bottom line: In patients undergoing cardiac surgery, a restrictive transfusion strategy is noninferior to a liberal strategy with respect to death from any cause, MI, stroke, and new renal failure requiring dialysis at 6 months postop.
Citation: Mazer CD et al. Six-month outcomes after restrictive or liberal transfusion for cardiac surgery. N Eng J Med. 2018 Sep 27;379(13):1224-33.
Dr. Shaw is an assistant professor in the division of hospital medicine,University of New Mexico.
Clinical question: Does using a restrictive transfusion strategy with patients undergoing cardiac surgery affect long-term outcomes?
Background: Using a restrictive transfusion strategy in patients undergoing cardiac surgery is known to use fewer units of allogeneic red cells, compared with a liberal strategy, while still having noninferior short-term clinical outcomes. At this time, little is known about such a strategy’s long-term effects.
Study design: Randomized, open-label, noninferiority trial.
Setting: 74 hospitals in 19 countries.
Synopsis: 5,243 adults undergoing nontransplant cardiac surgeries and having at least a moderate predicted risk for death were randomly divided into a liberal or restrictive transfusion strategy. Restrictive-strategy participants received a transfusion when hemoglobin was less than 7.5 g/dL, compared with either a hemoglobin of 8.5 g/dL on the floor or 9.5 g/dL in the ICU for the liberal-strategy group. During the hospitalization, the restrictive group received fewer U of red cells and had a lower mean predischarge hemoglobin. At 6 months, the groups were compared for the primary outcomes of death, MI, stroke, or renal failure requiring dialysis, finding an occurrence of such in 402/2,317 in the restrictive-strategy group and 402/2,347 in the liberal-strategy group (P = .006 for noninferiority). Limitations include the study being a noninferiority trial and the very specific patient population selected.
Bottom line: In patients undergoing cardiac surgery, a restrictive transfusion strategy is noninferior to a liberal strategy with respect to death from any cause, MI, stroke, and new renal failure requiring dialysis at 6 months postop.
Citation: Mazer CD et al. Six-month outcomes after restrictive or liberal transfusion for cardiac surgery. N Eng J Med. 2018 Sep 27;379(13):1224-33.
Dr. Shaw is an assistant professor in the division of hospital medicine,University of New Mexico.
Clinical question: Does using a restrictive transfusion strategy with patients undergoing cardiac surgery affect long-term outcomes?
Background: Using a restrictive transfusion strategy in patients undergoing cardiac surgery is known to use fewer units of allogeneic red cells, compared with a liberal strategy, while still having noninferior short-term clinical outcomes. At this time, little is known about such a strategy’s long-term effects.
Study design: Randomized, open-label, noninferiority trial.
Setting: 74 hospitals in 19 countries.
Synopsis: 5,243 adults undergoing nontransplant cardiac surgeries and having at least a moderate predicted risk for death were randomly divided into a liberal or restrictive transfusion strategy. Restrictive-strategy participants received a transfusion when hemoglobin was less than 7.5 g/dL, compared with either a hemoglobin of 8.5 g/dL on the floor or 9.5 g/dL in the ICU for the liberal-strategy group. During the hospitalization, the restrictive group received fewer U of red cells and had a lower mean predischarge hemoglobin. At 6 months, the groups were compared for the primary outcomes of death, MI, stroke, or renal failure requiring dialysis, finding an occurrence of such in 402/2,317 in the restrictive-strategy group and 402/2,347 in the liberal-strategy group (P = .006 for noninferiority). Limitations include the study being a noninferiority trial and the very specific patient population selected.
Bottom line: In patients undergoing cardiac surgery, a restrictive transfusion strategy is noninferior to a liberal strategy with respect to death from any cause, MI, stroke, and new renal failure requiring dialysis at 6 months postop.
Citation: Mazer CD et al. Six-month outcomes after restrictive or liberal transfusion for cardiac surgery. N Eng J Med. 2018 Sep 27;379(13):1224-33.
Dr. Shaw is an assistant professor in the division of hospital medicine,University of New Mexico.
p-TIPS improves outcomes for high-risk variceal bleeding
Background: Acute variceal bleeding remains the most severe and life-threatening complication of portal hypertension in cirrhotic patients. Several small studies have shown improved outcomes with p-TIPS without worsening of hepatic encephalopathy or other adverse events.
Study design: Multicenter, international, observational study.
Setting: One Canadian and 33 European referral centers.
Synopsis: 2,138 patients were registered for analysis, of which 671 were identified as high risk based on Child-Pugh score (either Child class C of less than 14 or Child class B with active bleeding seen on endoscopy). Multiple exclusion criteria were used including Child-Pugh score of 14 or more, renal failure, occlusive portal vein thrombosis, sepsis, heart failure, or hepatocellular carcinoma outside Milan criteria. Each patient underwent initial management with vasoactive medications, antibiotics, and endoscopy with subsequent intervention (p-TIPS vs. standard care) based on provider decision. p-TIPS was defined as TIPS within 72 hours of initial bleed. 31.4% of the cohort was lost to follow-up at 1 year. p-TIPS improved 1-year mortality significantly (78% vs. 62%; P = .014) and did not confer an increased risk of hepatic encephalopathy or other complication. Additionally, the authors found that the effect was significantly greater in the Child-Pugh Class C group (1-year mortality rate of 78% vs. 53%; P = .002). The authors then compared observed mortality with MELD-predicted mortality and found that with standard care, MELD scores matched with predicted mortality, but with p-TIPS, MELD scores predicted a greater mortality than the observed mortality. The authors calculated that the number needed to treat to save one life for 1 year with p-TIPS is 4.2. The major limitation of this study is the observational design and the inherent risk of selection bias. Additionally, almost one-third of patients were lost to follow-up.
Bottom line: Significant improvements in mortality are observed when high-risk patients undergo p-TIPS procedures as opposed to usual care with medications and endoscopy.
Citation: Hernández Gea V et al. Preemptive TIPS improves outcome in high risk variceal bleeding: An observational study. Hepatology. 2018 Jul 16. doi: 10.1002/hep.30182.
Dr. Imber is an assistant professor in the division of hospital medicine, University of New Mexico.
Background: Acute variceal bleeding remains the most severe and life-threatening complication of portal hypertension in cirrhotic patients. Several small studies have shown improved outcomes with p-TIPS without worsening of hepatic encephalopathy or other adverse events.
Study design: Multicenter, international, observational study.
Setting: One Canadian and 33 European referral centers.
Synopsis: 2,138 patients were registered for analysis, of which 671 were identified as high risk based on Child-Pugh score (either Child class C of less than 14 or Child class B with active bleeding seen on endoscopy). Multiple exclusion criteria were used including Child-Pugh score of 14 or more, renal failure, occlusive portal vein thrombosis, sepsis, heart failure, or hepatocellular carcinoma outside Milan criteria. Each patient underwent initial management with vasoactive medications, antibiotics, and endoscopy with subsequent intervention (p-TIPS vs. standard care) based on provider decision. p-TIPS was defined as TIPS within 72 hours of initial bleed. 31.4% of the cohort was lost to follow-up at 1 year. p-TIPS improved 1-year mortality significantly (78% vs. 62%; P = .014) and did not confer an increased risk of hepatic encephalopathy or other complication. Additionally, the authors found that the effect was significantly greater in the Child-Pugh Class C group (1-year mortality rate of 78% vs. 53%; P = .002). The authors then compared observed mortality with MELD-predicted mortality and found that with standard care, MELD scores matched with predicted mortality, but with p-TIPS, MELD scores predicted a greater mortality than the observed mortality. The authors calculated that the number needed to treat to save one life for 1 year with p-TIPS is 4.2. The major limitation of this study is the observational design and the inherent risk of selection bias. Additionally, almost one-third of patients were lost to follow-up.
Bottom line: Significant improvements in mortality are observed when high-risk patients undergo p-TIPS procedures as opposed to usual care with medications and endoscopy.
Citation: Hernández Gea V et al. Preemptive TIPS improves outcome in high risk variceal bleeding: An observational study. Hepatology. 2018 Jul 16. doi: 10.1002/hep.30182.
Dr. Imber is an assistant professor in the division of hospital medicine, University of New Mexico.
Background: Acute variceal bleeding remains the most severe and life-threatening complication of portal hypertension in cirrhotic patients. Several small studies have shown improved outcomes with p-TIPS without worsening of hepatic encephalopathy or other adverse events.
Study design: Multicenter, international, observational study.
Setting: One Canadian and 33 European referral centers.
Synopsis: 2,138 patients were registered for analysis, of which 671 were identified as high risk based on Child-Pugh score (either Child class C of less than 14 or Child class B with active bleeding seen on endoscopy). Multiple exclusion criteria were used including Child-Pugh score of 14 or more, renal failure, occlusive portal vein thrombosis, sepsis, heart failure, or hepatocellular carcinoma outside Milan criteria. Each patient underwent initial management with vasoactive medications, antibiotics, and endoscopy with subsequent intervention (p-TIPS vs. standard care) based on provider decision. p-TIPS was defined as TIPS within 72 hours of initial bleed. 31.4% of the cohort was lost to follow-up at 1 year. p-TIPS improved 1-year mortality significantly (78% vs. 62%; P = .014) and did not confer an increased risk of hepatic encephalopathy or other complication. Additionally, the authors found that the effect was significantly greater in the Child-Pugh Class C group (1-year mortality rate of 78% vs. 53%; P = .002). The authors then compared observed mortality with MELD-predicted mortality and found that with standard care, MELD scores matched with predicted mortality, but with p-TIPS, MELD scores predicted a greater mortality than the observed mortality. The authors calculated that the number needed to treat to save one life for 1 year with p-TIPS is 4.2. The major limitation of this study is the observational design and the inherent risk of selection bias. Additionally, almost one-third of patients were lost to follow-up.
Bottom line: Significant improvements in mortality are observed when high-risk patients undergo p-TIPS procedures as opposed to usual care with medications and endoscopy.
Citation: Hernández Gea V et al. Preemptive TIPS improves outcome in high risk variceal bleeding: An observational study. Hepatology. 2018 Jul 16. doi: 10.1002/hep.30182.
Dr. Imber is an assistant professor in the division of hospital medicine, University of New Mexico.
Posthospitalization thromboprophylaxis with rivaroxaban is unnecessary
Background: Anticoagulation for at-risk medical populations for posthospitalization thromboprophylaxis has been investigated in previous studies demonstrating a benefit in reducing risk of asymptomatic deep-vein thrombosis (DVT) development, but no studies have examined symptomatic DVTs.
Study design: Randomized, double-blind, placebo-controlled, multinational clinical trial.
Setting: 671 multinational hospitals.
Synopsis: 11,962 patients were identified as at-risk patients based on length of hospitalization (3-10 days), diagnosis, and additional risk factors identified by an IMPROVE risk score of greater than 4 or 2-3 with a D-dimer level more than twice the upper limit of normal. Patients were randomly assigned to receive rivaroxaban or placebo for 45 days. Primary outcome was composite of any symptomatic DVT or death related to VTE. Safety outcomes were principally related to bleeding. Symptomatic VTE or death from VTE occurred in 0.83% in the anticoagulation group and 1.1% in the placebo group (95% confidence interval, 0.52-1.09; P = .14). No significant difference was found in safety outcomes. The major limitation of the study was the low incidence of VTE and the need to include lower-risk patients (IMPROVE score 2/3 with elevated D-dimer), which may have decreased the effect of anticoagulation in the high-risk group (IMPROVE score 4 or greater).
Bottom line: No significant improvement in symptomatic VTE complications was found with posthospitalization thromboprophylaxis using rivaroxaban for an at-risk medical population.
Citation: Spyropoulos AC et al. Rivaroxaban for thromboprophylaxis after hospitalization for medical illness. N Eng J Med. 2018 Sep 20;379:1118-27.
Dr. Imber is an assistant professor in the division of hospital medicine, University of New Mexico.
Background: Anticoagulation for at-risk medical populations for posthospitalization thromboprophylaxis has been investigated in previous studies demonstrating a benefit in reducing risk of asymptomatic deep-vein thrombosis (DVT) development, but no studies have examined symptomatic DVTs.
Study design: Randomized, double-blind, placebo-controlled, multinational clinical trial.
Setting: 671 multinational hospitals.
Synopsis: 11,962 patients were identified as at-risk patients based on length of hospitalization (3-10 days), diagnosis, and additional risk factors identified by an IMPROVE risk score of greater than 4 or 2-3 with a D-dimer level more than twice the upper limit of normal. Patients were randomly assigned to receive rivaroxaban or placebo for 45 days. Primary outcome was composite of any symptomatic DVT or death related to VTE. Safety outcomes were principally related to bleeding. Symptomatic VTE or death from VTE occurred in 0.83% in the anticoagulation group and 1.1% in the placebo group (95% confidence interval, 0.52-1.09; P = .14). No significant difference was found in safety outcomes. The major limitation of the study was the low incidence of VTE and the need to include lower-risk patients (IMPROVE score 2/3 with elevated D-dimer), which may have decreased the effect of anticoagulation in the high-risk group (IMPROVE score 4 or greater).
Bottom line: No significant improvement in symptomatic VTE complications was found with posthospitalization thromboprophylaxis using rivaroxaban for an at-risk medical population.
Citation: Spyropoulos AC et al. Rivaroxaban for thromboprophylaxis after hospitalization for medical illness. N Eng J Med. 2018 Sep 20;379:1118-27.
Dr. Imber is an assistant professor in the division of hospital medicine, University of New Mexico.
Background: Anticoagulation for at-risk medical populations for posthospitalization thromboprophylaxis has been investigated in previous studies demonstrating a benefit in reducing risk of asymptomatic deep-vein thrombosis (DVT) development, but no studies have examined symptomatic DVTs.
Study design: Randomized, double-blind, placebo-controlled, multinational clinical trial.
Setting: 671 multinational hospitals.
Synopsis: 11,962 patients were identified as at-risk patients based on length of hospitalization (3-10 days), diagnosis, and additional risk factors identified by an IMPROVE risk score of greater than 4 or 2-3 with a D-dimer level more than twice the upper limit of normal. Patients were randomly assigned to receive rivaroxaban or placebo for 45 days. Primary outcome was composite of any symptomatic DVT or death related to VTE. Safety outcomes were principally related to bleeding. Symptomatic VTE or death from VTE occurred in 0.83% in the anticoagulation group and 1.1% in the placebo group (95% confidence interval, 0.52-1.09; P = .14). No significant difference was found in safety outcomes. The major limitation of the study was the low incidence of VTE and the need to include lower-risk patients (IMPROVE score 2/3 with elevated D-dimer), which may have decreased the effect of anticoagulation in the high-risk group (IMPROVE score 4 or greater).
Bottom line: No significant improvement in symptomatic VTE complications was found with posthospitalization thromboprophylaxis using rivaroxaban for an at-risk medical population.
Citation: Spyropoulos AC et al. Rivaroxaban for thromboprophylaxis after hospitalization for medical illness. N Eng J Med. 2018 Sep 20;379:1118-27.
Dr. Imber is an assistant professor in the division of hospital medicine, University of New Mexico.
HM19: Pediatric sepsis
Improving recognition and treatment
Presenters
Elise van der Jagt, MD, MPH
Workshop title
What you need to know about pediatric sepsis
Session summary
Dr. Elise van der Jagt of the University of Rochester (N.Y.) Medical Center, introduced the topic of pediatric sepsis and its epidemiology with the story of 12-year-old Rory Staunton, who died in 2012 of sepsis. In pediatrics, sepsis is the 10th leading cause of death, with severe sepsis having a mortality rate of 4%-10%. As a response to Rory Staunton’s death from sepsis, New York Governor Andrew Cuomo mandated all hospitals to implement ways to improve recognition and treatment of septic shock, especially in children.
The definition and management of sepsis in pediatrics is complex, and forms a spectrum of disease from sepsis to severe sepsis, and septic shock. Dr. van der Jagt advised not to use the adult sepsis definition in children. Sepsis, stated Dr. van der Jagt, is systemic inflammatory response syndrome in association with suspected or proven infection. Severe sepsis is sepsis with cardiovascular dysfunction, respiratory dysfunction, or dysfunction of two other systems. Septic shock is sepsis with cardiovascular dysfunction that persists despite 40 mL/kg of fluid bolus in 1 hour.
Early recognition and management of sepsis decreases mortality. Early recognition can be improved by initiating a recognition bundle. Multiple trigger tools are available such as pSOFA (Pediatric Sequential Organ Failure Assessment). Any trigger tool, however, must be combined with physician evaluation. This clinician assessment should be initiated within 15 minutes for any patient who screens positive with a trigger tool.
Resuscitation bundles also decrease mortality. A good goal is establishing intravenous or intraosseous access within 5 minutes, fluid administration within 30 minutes, and antibiotics and inotrope administration (if needed) in 60 minutes. Resuscitation bundles could include a sepsis clock, rapid response team, check list, protocol, and order set. Additional studies are needed to determine which of the components of a sepsis bundle is most important. Studies show that mortality increases with delays in initiating fluids and less fluids given. However, giving too much fluid also increases morbidity. It is imperative, stated Dr. van der Jagt, to reassess after fluid boluses. Use of lactate measurement can be problematic in pediatrics, as normal lactate can be seen with florid sepsis.
Stabilization bundles are more common in the ICU setting. They include an arterial line, central venous pressure, cardiopulmonary monitor, urinary catheter, and pulse oximeter. A performance bundle is important to assess adherence to the other bundles. This could include providing debriefing, data review, feedback, and formal quality improvement projects. Assigning a sepsis champion in each area helps to overcome barriers and continue performance bundles.
Key takeaways for HM
- Patients with severe sepsis/septic shock should be rapidly identified with the 2014/2017 American College of Critical Care Medicine consensus criteria.
- Efficient, time-based care should be provided during the first hour after recognizing pediatric severe sepsis/septic shock.
- Overcoming systems barriers to rapid sepsis recognition and treatment requires sepsis champions in each area, continuous data collection and feedback, persistence, and patience.
Dr. Eboh is a pediatric hospitalist at Covenant Children’s Hospital in Lubbock, Texas, and assistant professor of pediatrics at Texas Tech University Health Sciences Center. Dr. Wright is a pediatric hospitalist at Texas Tech University Health Sciences Center.
Improving recognition and treatment
Improving recognition and treatment
Presenters
Elise van der Jagt, MD, MPH
Workshop title
What you need to know about pediatric sepsis
Session summary
Dr. Elise van der Jagt of the University of Rochester (N.Y.) Medical Center, introduced the topic of pediatric sepsis and its epidemiology with the story of 12-year-old Rory Staunton, who died in 2012 of sepsis. In pediatrics, sepsis is the 10th leading cause of death, with severe sepsis having a mortality rate of 4%-10%. As a response to Rory Staunton’s death from sepsis, New York Governor Andrew Cuomo mandated all hospitals to implement ways to improve recognition and treatment of septic shock, especially in children.
The definition and management of sepsis in pediatrics is complex, and forms a spectrum of disease from sepsis to severe sepsis, and septic shock. Dr. van der Jagt advised not to use the adult sepsis definition in children. Sepsis, stated Dr. van der Jagt, is systemic inflammatory response syndrome in association with suspected or proven infection. Severe sepsis is sepsis with cardiovascular dysfunction, respiratory dysfunction, or dysfunction of two other systems. Septic shock is sepsis with cardiovascular dysfunction that persists despite 40 mL/kg of fluid bolus in 1 hour.
Early recognition and management of sepsis decreases mortality. Early recognition can be improved by initiating a recognition bundle. Multiple trigger tools are available such as pSOFA (Pediatric Sequential Organ Failure Assessment). Any trigger tool, however, must be combined with physician evaluation. This clinician assessment should be initiated within 15 minutes for any patient who screens positive with a trigger tool.
Resuscitation bundles also decrease mortality. A good goal is establishing intravenous or intraosseous access within 5 minutes, fluid administration within 30 minutes, and antibiotics and inotrope administration (if needed) in 60 minutes. Resuscitation bundles could include a sepsis clock, rapid response team, check list, protocol, and order set. Additional studies are needed to determine which of the components of a sepsis bundle is most important. Studies show that mortality increases with delays in initiating fluids and less fluids given. However, giving too much fluid also increases morbidity. It is imperative, stated Dr. van der Jagt, to reassess after fluid boluses. Use of lactate measurement can be problematic in pediatrics, as normal lactate can be seen with florid sepsis.
Stabilization bundles are more common in the ICU setting. They include an arterial line, central venous pressure, cardiopulmonary monitor, urinary catheter, and pulse oximeter. A performance bundle is important to assess adherence to the other bundles. This could include providing debriefing, data review, feedback, and formal quality improvement projects. Assigning a sepsis champion in each area helps to overcome barriers and continue performance bundles.
Key takeaways for HM
- Patients with severe sepsis/septic shock should be rapidly identified with the 2014/2017 American College of Critical Care Medicine consensus criteria.
- Efficient, time-based care should be provided during the first hour after recognizing pediatric severe sepsis/septic shock.
- Overcoming systems barriers to rapid sepsis recognition and treatment requires sepsis champions in each area, continuous data collection and feedback, persistence, and patience.
Dr. Eboh is a pediatric hospitalist at Covenant Children’s Hospital in Lubbock, Texas, and assistant professor of pediatrics at Texas Tech University Health Sciences Center. Dr. Wright is a pediatric hospitalist at Texas Tech University Health Sciences Center.
Presenters
Elise van der Jagt, MD, MPH
Workshop title
What you need to know about pediatric sepsis
Session summary
Dr. Elise van der Jagt of the University of Rochester (N.Y.) Medical Center, introduced the topic of pediatric sepsis and its epidemiology with the story of 12-year-old Rory Staunton, who died in 2012 of sepsis. In pediatrics, sepsis is the 10th leading cause of death, with severe sepsis having a mortality rate of 4%-10%. As a response to Rory Staunton’s death from sepsis, New York Governor Andrew Cuomo mandated all hospitals to implement ways to improve recognition and treatment of septic shock, especially in children.
The definition and management of sepsis in pediatrics is complex, and forms a spectrum of disease from sepsis to severe sepsis, and septic shock. Dr. van der Jagt advised not to use the adult sepsis definition in children. Sepsis, stated Dr. van der Jagt, is systemic inflammatory response syndrome in association with suspected or proven infection. Severe sepsis is sepsis with cardiovascular dysfunction, respiratory dysfunction, or dysfunction of two other systems. Septic shock is sepsis with cardiovascular dysfunction that persists despite 40 mL/kg of fluid bolus in 1 hour.
Early recognition and management of sepsis decreases mortality. Early recognition can be improved by initiating a recognition bundle. Multiple trigger tools are available such as pSOFA (Pediatric Sequential Organ Failure Assessment). Any trigger tool, however, must be combined with physician evaluation. This clinician assessment should be initiated within 15 minutes for any patient who screens positive with a trigger tool.
Resuscitation bundles also decrease mortality. A good goal is establishing intravenous or intraosseous access within 5 minutes, fluid administration within 30 minutes, and antibiotics and inotrope administration (if needed) in 60 minutes. Resuscitation bundles could include a sepsis clock, rapid response team, check list, protocol, and order set. Additional studies are needed to determine which of the components of a sepsis bundle is most important. Studies show that mortality increases with delays in initiating fluids and less fluids given. However, giving too much fluid also increases morbidity. It is imperative, stated Dr. van der Jagt, to reassess after fluid boluses. Use of lactate measurement can be problematic in pediatrics, as normal lactate can be seen with florid sepsis.
Stabilization bundles are more common in the ICU setting. They include an arterial line, central venous pressure, cardiopulmonary monitor, urinary catheter, and pulse oximeter. A performance bundle is important to assess adherence to the other bundles. This could include providing debriefing, data review, feedback, and formal quality improvement projects. Assigning a sepsis champion in each area helps to overcome barriers and continue performance bundles.
Key takeaways for HM
- Patients with severe sepsis/septic shock should be rapidly identified with the 2014/2017 American College of Critical Care Medicine consensus criteria.
- Efficient, time-based care should be provided during the first hour after recognizing pediatric severe sepsis/septic shock.
- Overcoming systems barriers to rapid sepsis recognition and treatment requires sepsis champions in each area, continuous data collection and feedback, persistence, and patience.
Dr. Eboh is a pediatric hospitalist at Covenant Children’s Hospital in Lubbock, Texas, and assistant professor of pediatrics at Texas Tech University Health Sciences Center. Dr. Wright is a pediatric hospitalist at Texas Tech University Health Sciences Center.
Short Takes
Evidence is uncertain for benefit of short-stay unit hospitalization
A Cochrane review of 14 randomized trials evaluating short-stay unit hospitalization for internal medicine conditions was unable to ascertain any definite benefit or harm, compared with usual care, with concerns for heterogeneity, bias, and random error in the studies. The authors recommended conducting more trials with low risk of bias and low risk of random errors.
Citation: Strøm C et al. Hospitalisation in short-stay units for adults with internal medicine diseases and conditions. Cochrane Database Syst Rev. 2018;8. CD012370. doi: 10.1002/14651858.CD012370.pub2.
Hospice use among Medicare patients with heart failure
Of the 4% percent of Medicare patients discharged to hospice from a hospitalization for heart failure, 25% died within 72 hours of discharge, leading the authors to conclude that hospice is underutilized and initiated too late in the setting of heart failure.
Citation: Warraich HJ et al. Trends in hospice discharge and relative outcomes among Medicare patients in the Get With The Guidelines–Heart Failure Registry. JAMA Cardiol. 2018 Oct 1;3(10):917-26.
Culprit lesion PCI has similar 1-year mortality to immediate multivessel PCI
This is the follow-up study to CULPRIT-SHOCK trial , which examined percutaneous coronary intervention in culprit lesion only vs. multivessel PCI in the setting of cardiogenic shock. The initial trial showed improved 30-day mortality outcomes with culprit lesion PCI only and the follow-up demonstrated no significant difference in 1-year mortality between the two groups.
Citation: Thiele H et al. One-year outcomes after PCI strategies in cardiogenic shock. N Engl J Med. 2018 Nov 1;379(18):1699-710 .
Evidence is uncertain for benefit of short-stay unit hospitalization
A Cochrane review of 14 randomized trials evaluating short-stay unit hospitalization for internal medicine conditions was unable to ascertain any definite benefit or harm, compared with usual care, with concerns for heterogeneity, bias, and random error in the studies. The authors recommended conducting more trials with low risk of bias and low risk of random errors.
Citation: Strøm C et al. Hospitalisation in short-stay units for adults with internal medicine diseases and conditions. Cochrane Database Syst Rev. 2018;8. CD012370. doi: 10.1002/14651858.CD012370.pub2.
Hospice use among Medicare patients with heart failure
Of the 4% percent of Medicare patients discharged to hospice from a hospitalization for heart failure, 25% died within 72 hours of discharge, leading the authors to conclude that hospice is underutilized and initiated too late in the setting of heart failure.
Citation: Warraich HJ et al. Trends in hospice discharge and relative outcomes among Medicare patients in the Get With The Guidelines–Heart Failure Registry. JAMA Cardiol. 2018 Oct 1;3(10):917-26.
Culprit lesion PCI has similar 1-year mortality to immediate multivessel PCI
This is the follow-up study to CULPRIT-SHOCK trial , which examined percutaneous coronary intervention in culprit lesion only vs. multivessel PCI in the setting of cardiogenic shock. The initial trial showed improved 30-day mortality outcomes with culprit lesion PCI only and the follow-up demonstrated no significant difference in 1-year mortality between the two groups.
Citation: Thiele H et al. One-year outcomes after PCI strategies in cardiogenic shock. N Engl J Med. 2018 Nov 1;379(18):1699-710 .
Evidence is uncertain for benefit of short-stay unit hospitalization
A Cochrane review of 14 randomized trials evaluating short-stay unit hospitalization for internal medicine conditions was unable to ascertain any definite benefit or harm, compared with usual care, with concerns for heterogeneity, bias, and random error in the studies. The authors recommended conducting more trials with low risk of bias and low risk of random errors.
Citation: Strøm C et al. Hospitalisation in short-stay units for adults with internal medicine diseases and conditions. Cochrane Database Syst Rev. 2018;8. CD012370. doi: 10.1002/14651858.CD012370.pub2.
Hospice use among Medicare patients with heart failure
Of the 4% percent of Medicare patients discharged to hospice from a hospitalization for heart failure, 25% died within 72 hours of discharge, leading the authors to conclude that hospice is underutilized and initiated too late in the setting of heart failure.
Citation: Warraich HJ et al. Trends in hospice discharge and relative outcomes among Medicare patients in the Get With The Guidelines–Heart Failure Registry. JAMA Cardiol. 2018 Oct 1;3(10):917-26.
Culprit lesion PCI has similar 1-year mortality to immediate multivessel PCI
This is the follow-up study to CULPRIT-SHOCK trial , which examined percutaneous coronary intervention in culprit lesion only vs. multivessel PCI in the setting of cardiogenic shock. The initial trial showed improved 30-day mortality outcomes with culprit lesion PCI only and the follow-up demonstrated no significant difference in 1-year mortality between the two groups.
Citation: Thiele H et al. One-year outcomes after PCI strategies in cardiogenic shock. N Engl J Med. 2018 Nov 1;379(18):1699-710 .