User login
J&J pauses production of COVID vaccine
Johnson & Johnson stopped making its COVID-19 vaccine at a key facility in the Netherlands.
The Johnson & Johnson shot is seen as a critical vaccine for poorer countries. , people familiar with the decision told The New York Times.
The plant, located in Leiden, has been making an experimental but potentially more profitable vaccine instead. The experimental vaccine is for an unrelated virus -- respiratory syncytial virus, or RSV -- that will be used for a clinical trial.
The pause is said to be temporary. The Leiden plant is expected to restart production of the COVID-19 vaccine next month. The company has said that it has millions of COVID-19 doses in inventory, though it’s unclear whether the pause has affected vaccine supplies.
The interruption could reduce the supply of Johnson & Johnson’s COVID-19 vaccine by a few hundred million doses, one of the sources told the newspaper, since the doses made from renewed production won’t likely ship until May or June. Other facilities have been hired to produce the vaccine but aren’t running yet or haven’t received regulatory approval to ship doses for packaging.
Jake Sargent, a spokesman for Johnson & Johnson, told the Times that the company is “focused on ensuring our vaccine is available where people are in need” and that its global production network “is working day and night.” He said that the company has millions of doses in inventory and is continuing to deliver vaccine batches to facilities that package doses.
The pause has surprised officials at two main recipients of the Johnson & Johnson shots -- the African Union and Covax, the organization that coordinates COVID-19 vaccines for poorer countries. Leaders of the two organizations learned about the halt in production from reporters at the Times.
“This is not the time to be switching production lines of anything, when the lives of people across the developing world hang in the balance,” Ayoade Alakija, coleader of the African Union’s vaccine delivery program, told the newspaper.
Poorer countries rely on Johnson & Johnson’s vaccine because it doesn’t require ultracold refrigeration. The vaccine is also less expensive than others and easy to provide to hard-to-reach populations.
“In many low- and middle-income countries, our vaccine is the most important and sometimes only option,” Penny Heaton, MD, a Johnson & Johnson executive, said in December during a meeting with the CDC’s vaccine advisory committee.
“We have a global vaccine, and the world is depending on us,” she said.
A version of this article first appeared on WebMD.com.
Johnson & Johnson stopped making its COVID-19 vaccine at a key facility in the Netherlands.
The Johnson & Johnson shot is seen as a critical vaccine for poorer countries. , people familiar with the decision told The New York Times.
The plant, located in Leiden, has been making an experimental but potentially more profitable vaccine instead. The experimental vaccine is for an unrelated virus -- respiratory syncytial virus, or RSV -- that will be used for a clinical trial.
The pause is said to be temporary. The Leiden plant is expected to restart production of the COVID-19 vaccine next month. The company has said that it has millions of COVID-19 doses in inventory, though it’s unclear whether the pause has affected vaccine supplies.
The interruption could reduce the supply of Johnson & Johnson’s COVID-19 vaccine by a few hundred million doses, one of the sources told the newspaper, since the doses made from renewed production won’t likely ship until May or June. Other facilities have been hired to produce the vaccine but aren’t running yet or haven’t received regulatory approval to ship doses for packaging.
Jake Sargent, a spokesman for Johnson & Johnson, told the Times that the company is “focused on ensuring our vaccine is available where people are in need” and that its global production network “is working day and night.” He said that the company has millions of doses in inventory and is continuing to deliver vaccine batches to facilities that package doses.
The pause has surprised officials at two main recipients of the Johnson & Johnson shots -- the African Union and Covax, the organization that coordinates COVID-19 vaccines for poorer countries. Leaders of the two organizations learned about the halt in production from reporters at the Times.
“This is not the time to be switching production lines of anything, when the lives of people across the developing world hang in the balance,” Ayoade Alakija, coleader of the African Union’s vaccine delivery program, told the newspaper.
Poorer countries rely on Johnson & Johnson’s vaccine because it doesn’t require ultracold refrigeration. The vaccine is also less expensive than others and easy to provide to hard-to-reach populations.
“In many low- and middle-income countries, our vaccine is the most important and sometimes only option,” Penny Heaton, MD, a Johnson & Johnson executive, said in December during a meeting with the CDC’s vaccine advisory committee.
“We have a global vaccine, and the world is depending on us,” she said.
A version of this article first appeared on WebMD.com.
Johnson & Johnson stopped making its COVID-19 vaccine at a key facility in the Netherlands.
The Johnson & Johnson shot is seen as a critical vaccine for poorer countries. , people familiar with the decision told The New York Times.
The plant, located in Leiden, has been making an experimental but potentially more profitable vaccine instead. The experimental vaccine is for an unrelated virus -- respiratory syncytial virus, or RSV -- that will be used for a clinical trial.
The pause is said to be temporary. The Leiden plant is expected to restart production of the COVID-19 vaccine next month. The company has said that it has millions of COVID-19 doses in inventory, though it’s unclear whether the pause has affected vaccine supplies.
The interruption could reduce the supply of Johnson & Johnson’s COVID-19 vaccine by a few hundred million doses, one of the sources told the newspaper, since the doses made from renewed production won’t likely ship until May or June. Other facilities have been hired to produce the vaccine but aren’t running yet or haven’t received regulatory approval to ship doses for packaging.
Jake Sargent, a spokesman for Johnson & Johnson, told the Times that the company is “focused on ensuring our vaccine is available where people are in need” and that its global production network “is working day and night.” He said that the company has millions of doses in inventory and is continuing to deliver vaccine batches to facilities that package doses.
The pause has surprised officials at two main recipients of the Johnson & Johnson shots -- the African Union and Covax, the organization that coordinates COVID-19 vaccines for poorer countries. Leaders of the two organizations learned about the halt in production from reporters at the Times.
“This is not the time to be switching production lines of anything, when the lives of people across the developing world hang in the balance,” Ayoade Alakija, coleader of the African Union’s vaccine delivery program, told the newspaper.
Poorer countries rely on Johnson & Johnson’s vaccine because it doesn’t require ultracold refrigeration. The vaccine is also less expensive than others and easy to provide to hard-to-reach populations.
“In many low- and middle-income countries, our vaccine is the most important and sometimes only option,” Penny Heaton, MD, a Johnson & Johnson executive, said in December during a meeting with the CDC’s vaccine advisory committee.
“We have a global vaccine, and the world is depending on us,” she said.
A version of this article first appeared on WebMD.com.
Agreement reached for research definition of ‘long COVID’ in children and young people
Long COVID can affect adults, young people, and children, and now for the first time, in a landmark study accepted for publication in the Archives of Disease in Childhood, formal agreement has been made on a research definition for post–acute COVID-19, or “long COVID” as it is commonly known, in children and young people.
The researchers charged themselves with a single objective – to derive a research definition for long COVID (post–acute COVID-19) in children and young people to allow comparisons between research studies. Specifically, so studies on prevalence, course, and outcome of long COVID in this age group can be reliably compared, because to date there has been no consensus. In fact, the authors pointed out how the “slew of definitions” currently used all differ in number, type, and duration of symptoms, which hampers research efforts. In addition, the lack of definition consensus has contributed to very wide reported variations in the estimated prevalence of long COVID in children of 1%-51%, with the authors saying that a “consistently applied definition of long COVID will help reduce the variability of prevalence estimates.”
Statements sequentially whittled down
“Using robust consensus methodology,” the authors said, “we derived a research definition for long COVID in children and young people.”
To achieve the definition consensus, a three-phase online Delphi process was used, followed by a virtual consensus meeting. The 123 participants registered to take part in the study included 23 people (19%) in a lived experience panel, 50 (42%) in the researcher or researcher/service delivery combined panel and 47 (39%) in the service delivery panel. Of 120 registered participants, 105 (88%) completed phase 1, 86 eligible participants (82% of those completing phase 1) completed phase 2 and 77 eligible participants (90% of those completing phase 2) completed phase 3. Seventeen participants attended and voted at the consensus meeting – 4 (23%) from the service delivery panel, 11 (65%) from the researcher panel, and 2 (12%) from the lived experience panel.
Presented with 49 statements in each phase, participants scored these from 1-9 based on how important they were perceived to be with regards inclusion in the research definition of long COVID in children and young people. Having been sequentially whittled down in three phases, 10 statements were discussed at the consensus meeting, and a panel of eight 11- to 17-year-olds affected by long COVID also reviewed the statements to reach a final agreement.
Five of the statements were agreed to be included in the definition, which stated that long COVID in children and young people is a condition in which a child or young person has symptoms (at least one of which is a physical symptom) that have continued or developed after a diagnosis of COVID-19 (confirmed with one or more positive COVID tests); impact their physical, mental, or social well-being; are interfering with some aspect of daily living (for example, school, work, home, or relationships); and persist for a minimum duration of 12 weeks after initial testing for COVID-19 (even if symptoms have waxed and waned over that period).
David Strain, MBChB, MD, chair of the BMA board of science and clinical senior lecturer and honorary consultant, University of Exeter (England), told the Science Media Centre: “A Delphi study builds a consensus from the world’s experts by presenting a series of statements and continuing to refine them until there is agreement as to what the definition of pediatric long COVID should be.” He added: “This is vitally important in order to align the global research effort into long COVID.”
Reassuringly similar
From the agreed five statements, a further research definition was proposed to align with the World Health Organization definition for adults: “Post–COVID-19 condition occurs in young people with a history of confirmed SARS CoV-2 infection, with at least one persisting physical symptom for a minimum duration of 12 weeks after initial testing that cannot be explained by an alternative diagnosis. The symptoms have an impact on everyday functioning, may continue or develop after COVID-19 infection, and may fluctuate or relapse over time.”
The authors concluded: “This is the first research definition of long COVID (post–COVID-19 condition) in children and young people and complements the clinical case definition in adults proposed by WHO,” adding that the two definitions are “reassuringly similar.”
They reiterated how widespread adoption of this definition would allow comparisons between studies such that a core outcome set can be developed and the prevalence, course and outcome of long COVID in children and young people can be reliably evaluated, which “will substantially help strengthen the evidence base on this debilitating condition.”
In addition, the authors said that a consistently applied definition of long COVID will help to provide a “more accurate picture on the true impact of the condition.”
The researchers emphasized the need to differentiate between a clinical case definition and a research definition of long COVID and explained: “It is understandable that the patient groups representing people with long COVID are concerned about a definition that could restrict access to services that are needed.”
They went on to say that in their view the decision whether a child or young person can see a health care professional, access any support needed, or be referred, investigated, or treated for long COVID should be a “shared decision involving the young person, their carers, and clinicians.”
Dr. Strain reinforced that it was important that the definition was a research one and not a clinical one, pointing out that the 12-week period in the research definition “does not necessarily mean that a child or young person should need to wait 3 months before being offered help or assistance from their health care team, indeed a 3-month delay in offering support to a child or young person, at this vitally important period of their educational development, could have lasting long-term impacts.”
A version of this article first appeared on Medscape.co.uk.
Long COVID can affect adults, young people, and children, and now for the first time, in a landmark study accepted for publication in the Archives of Disease in Childhood, formal agreement has been made on a research definition for post–acute COVID-19, or “long COVID” as it is commonly known, in children and young people.
The researchers charged themselves with a single objective – to derive a research definition for long COVID (post–acute COVID-19) in children and young people to allow comparisons between research studies. Specifically, so studies on prevalence, course, and outcome of long COVID in this age group can be reliably compared, because to date there has been no consensus. In fact, the authors pointed out how the “slew of definitions” currently used all differ in number, type, and duration of symptoms, which hampers research efforts. In addition, the lack of definition consensus has contributed to very wide reported variations in the estimated prevalence of long COVID in children of 1%-51%, with the authors saying that a “consistently applied definition of long COVID will help reduce the variability of prevalence estimates.”
Statements sequentially whittled down
“Using robust consensus methodology,” the authors said, “we derived a research definition for long COVID in children and young people.”
To achieve the definition consensus, a three-phase online Delphi process was used, followed by a virtual consensus meeting. The 123 participants registered to take part in the study included 23 people (19%) in a lived experience panel, 50 (42%) in the researcher or researcher/service delivery combined panel and 47 (39%) in the service delivery panel. Of 120 registered participants, 105 (88%) completed phase 1, 86 eligible participants (82% of those completing phase 1) completed phase 2 and 77 eligible participants (90% of those completing phase 2) completed phase 3. Seventeen participants attended and voted at the consensus meeting – 4 (23%) from the service delivery panel, 11 (65%) from the researcher panel, and 2 (12%) from the lived experience panel.
Presented with 49 statements in each phase, participants scored these from 1-9 based on how important they were perceived to be with regards inclusion in the research definition of long COVID in children and young people. Having been sequentially whittled down in three phases, 10 statements were discussed at the consensus meeting, and a panel of eight 11- to 17-year-olds affected by long COVID also reviewed the statements to reach a final agreement.
Five of the statements were agreed to be included in the definition, which stated that long COVID in children and young people is a condition in which a child or young person has symptoms (at least one of which is a physical symptom) that have continued or developed after a diagnosis of COVID-19 (confirmed with one or more positive COVID tests); impact their physical, mental, or social well-being; are interfering with some aspect of daily living (for example, school, work, home, or relationships); and persist for a minimum duration of 12 weeks after initial testing for COVID-19 (even if symptoms have waxed and waned over that period).
David Strain, MBChB, MD, chair of the BMA board of science and clinical senior lecturer and honorary consultant, University of Exeter (England), told the Science Media Centre: “A Delphi study builds a consensus from the world’s experts by presenting a series of statements and continuing to refine them until there is agreement as to what the definition of pediatric long COVID should be.” He added: “This is vitally important in order to align the global research effort into long COVID.”
Reassuringly similar
From the agreed five statements, a further research definition was proposed to align with the World Health Organization definition for adults: “Post–COVID-19 condition occurs in young people with a history of confirmed SARS CoV-2 infection, with at least one persisting physical symptom for a minimum duration of 12 weeks after initial testing that cannot be explained by an alternative diagnosis. The symptoms have an impact on everyday functioning, may continue or develop after COVID-19 infection, and may fluctuate or relapse over time.”
The authors concluded: “This is the first research definition of long COVID (post–COVID-19 condition) in children and young people and complements the clinical case definition in adults proposed by WHO,” adding that the two definitions are “reassuringly similar.”
They reiterated how widespread adoption of this definition would allow comparisons between studies such that a core outcome set can be developed and the prevalence, course and outcome of long COVID in children and young people can be reliably evaluated, which “will substantially help strengthen the evidence base on this debilitating condition.”
In addition, the authors said that a consistently applied definition of long COVID will help to provide a “more accurate picture on the true impact of the condition.”
The researchers emphasized the need to differentiate between a clinical case definition and a research definition of long COVID and explained: “It is understandable that the patient groups representing people with long COVID are concerned about a definition that could restrict access to services that are needed.”
They went on to say that in their view the decision whether a child or young person can see a health care professional, access any support needed, or be referred, investigated, or treated for long COVID should be a “shared decision involving the young person, their carers, and clinicians.”
Dr. Strain reinforced that it was important that the definition was a research one and not a clinical one, pointing out that the 12-week period in the research definition “does not necessarily mean that a child or young person should need to wait 3 months before being offered help or assistance from their health care team, indeed a 3-month delay in offering support to a child or young person, at this vitally important period of their educational development, could have lasting long-term impacts.”
A version of this article first appeared on Medscape.co.uk.
Long COVID can affect adults, young people, and children, and now for the first time, in a landmark study accepted for publication in the Archives of Disease in Childhood, formal agreement has been made on a research definition for post–acute COVID-19, or “long COVID” as it is commonly known, in children and young people.
The researchers charged themselves with a single objective – to derive a research definition for long COVID (post–acute COVID-19) in children and young people to allow comparisons between research studies. Specifically, so studies on prevalence, course, and outcome of long COVID in this age group can be reliably compared, because to date there has been no consensus. In fact, the authors pointed out how the “slew of definitions” currently used all differ in number, type, and duration of symptoms, which hampers research efforts. In addition, the lack of definition consensus has contributed to very wide reported variations in the estimated prevalence of long COVID in children of 1%-51%, with the authors saying that a “consistently applied definition of long COVID will help reduce the variability of prevalence estimates.”
Statements sequentially whittled down
“Using robust consensus methodology,” the authors said, “we derived a research definition for long COVID in children and young people.”
To achieve the definition consensus, a three-phase online Delphi process was used, followed by a virtual consensus meeting. The 123 participants registered to take part in the study included 23 people (19%) in a lived experience panel, 50 (42%) in the researcher or researcher/service delivery combined panel and 47 (39%) in the service delivery panel. Of 120 registered participants, 105 (88%) completed phase 1, 86 eligible participants (82% of those completing phase 1) completed phase 2 and 77 eligible participants (90% of those completing phase 2) completed phase 3. Seventeen participants attended and voted at the consensus meeting – 4 (23%) from the service delivery panel, 11 (65%) from the researcher panel, and 2 (12%) from the lived experience panel.
Presented with 49 statements in each phase, participants scored these from 1-9 based on how important they were perceived to be with regards inclusion in the research definition of long COVID in children and young people. Having been sequentially whittled down in three phases, 10 statements were discussed at the consensus meeting, and a panel of eight 11- to 17-year-olds affected by long COVID also reviewed the statements to reach a final agreement.
Five of the statements were agreed to be included in the definition, which stated that long COVID in children and young people is a condition in which a child or young person has symptoms (at least one of which is a physical symptom) that have continued or developed after a diagnosis of COVID-19 (confirmed with one or more positive COVID tests); impact their physical, mental, or social well-being; are interfering with some aspect of daily living (for example, school, work, home, or relationships); and persist for a minimum duration of 12 weeks after initial testing for COVID-19 (even if symptoms have waxed and waned over that period).
David Strain, MBChB, MD, chair of the BMA board of science and clinical senior lecturer and honorary consultant, University of Exeter (England), told the Science Media Centre: “A Delphi study builds a consensus from the world’s experts by presenting a series of statements and continuing to refine them until there is agreement as to what the definition of pediatric long COVID should be.” He added: “This is vitally important in order to align the global research effort into long COVID.”
Reassuringly similar
From the agreed five statements, a further research definition was proposed to align with the World Health Organization definition for adults: “Post–COVID-19 condition occurs in young people with a history of confirmed SARS CoV-2 infection, with at least one persisting physical symptom for a minimum duration of 12 weeks after initial testing that cannot be explained by an alternative diagnosis. The symptoms have an impact on everyday functioning, may continue or develop after COVID-19 infection, and may fluctuate or relapse over time.”
The authors concluded: “This is the first research definition of long COVID (post–COVID-19 condition) in children and young people and complements the clinical case definition in adults proposed by WHO,” adding that the two definitions are “reassuringly similar.”
They reiterated how widespread adoption of this definition would allow comparisons between studies such that a core outcome set can be developed and the prevalence, course and outcome of long COVID in children and young people can be reliably evaluated, which “will substantially help strengthen the evidence base on this debilitating condition.”
In addition, the authors said that a consistently applied definition of long COVID will help to provide a “more accurate picture on the true impact of the condition.”
The researchers emphasized the need to differentiate between a clinical case definition and a research definition of long COVID and explained: “It is understandable that the patient groups representing people with long COVID are concerned about a definition that could restrict access to services that are needed.”
They went on to say that in their view the decision whether a child or young person can see a health care professional, access any support needed, or be referred, investigated, or treated for long COVID should be a “shared decision involving the young person, their carers, and clinicians.”
Dr. Strain reinforced that it was important that the definition was a research one and not a clinical one, pointing out that the 12-week period in the research definition “does not necessarily mean that a child or young person should need to wait 3 months before being offered help or assistance from their health care team, indeed a 3-month delay in offering support to a child or young person, at this vitally important period of their educational development, could have lasting long-term impacts.”
A version of this article first appeared on Medscape.co.uk.
FROM THE ARCHIVES OF DISEASE IN CHILDHOOD
Promising leads to crack long COVID discovered
It’s a story of promise at a time of urgent need.
They proposed many theories on what might be driving long COVID. A role for a virus “cryptic reservoir” that could reactivate at any time, “viral remnants” that trigger chronic inflammation, and action by “autoimmune antibodies” that cause ongoing symptoms are possibilities.
In fact, it’s likely that research will show long COVID is a condition with more than one cause, the experts said during a recent webinar.
People might experience post-infection problems, including organ damage that takes time to heal after initial COVID-19 illness. Or they may be living with post-immune factors, including ongoing immune system responses triggered by autoantibodies.
Determining the cause or causes of long COVID is essential for treatment. For example, if one person’s symptoms persist because of an overactive immune system, “we need to provide immunosuppressant therapies,” Akiko Iwasaki, PhD, said. “But we don’t want to give that to someone who has a persistent virus reservoir,” meaning remnants of the virus remain in their bodies.
Interestingly, a study preprint, which has not been peer reviewed, found dogs were accurate more than half the time in sniffing out long COVID, said Dr. Iwasaki, professor of immunobiology and developmental biology at Yale University, New Haven, Conn.
The dogs were tasked with identifying 45 people with long COVID versus 188 people without it. The findings suggest the presence of a unique chemical in the sweat of people with long COVID that could someday lead to a diagnostic test.
Viral persistence possible
If one of the main theories holds, it could be that the coronavirus somehow remains in the body in some form for some people after COVID-19.
Mady Hornig, MD, agreed this is a possibility that needs to be investigated further.
“A weakened immune response to an infection may mean that you have cryptic reservoirs of virus that are continuing to cause symptoms,” she said during the briefing. Dr. Hornig is a doctor-scientist specializing in epidemiology at Columbia University, New York.
“That may explain why some patients with long COVID feel better after vaccination,” because the vaccine creates a strong antibody response to fight COVID-19, Dr. Iwasaki said.
Researchers are unearthing additional potential factors contributing to long COVID.
Viral persistence could also reactivate other dormant viruses in the body, such as Epstein-Barr virus (EBV), said Lawrence Purpura, MD, MPH, an infectious disease specialist at New York Presbyterian/Columbia University. Reactivation of Epstein-Barr is one of four identifying signs of long COVID revealed in a Jan. 25 study published in the journal Cell.
Immune overactivation also possible?
For other people with long COVID, it’s not the virus sticking around but the body’s reaction that’s the issue.
Investigators suggest autoimmunity plays a role, and they point to the presence of autoantibodies, for example.
When these autoantibodies persist, they can cause tissue and organ damage over time.
Other investigators are proposing “immune exhaustion” in long COVID because of similarities to chronic fatigue syndrome, Dr. Hornig said.
“It should be ‘all hands on deck’ for research into long COVID,” she said. “The number of disabled individuals who will likely qualify for a diagnosis of [chronic fatigue syndrome] is growing by the second.”
Forging ahead on future research
It’s clear there is more work to do. There are investigators working on banking tissue samples from people with long COVID to learn more, for example.
Also, finding a biomarker unique to long COVID could vastly improve the precision of diagnosing long COVID, especially if the dog sniffing option does not pan out.
Of the thousands of biomarker possibilities, Dr. Hornig said, “maybe that’s one or two that ultimately make a real impact on patient care. So it’s going to be critical to find those quickly, translate them, and make them available.”
In the meantime, some answers might come from a large study sponsored by the National Institutes of Health. The NIH is funding the “Researching COVID to Enhance Recovery” project using $470 million from the American Rescue Plan. Investigators at NYU Langone Health are leading the effort and plan to share the wealth by funding more than 100 researchers at more than 30 institutions to create a “metacohort” to study long COVID. More information is available at recovercovid.org.
“Fortunately, through the global research effort, we are now really starting to expand our understanding of how long COVID manifests, how common it is, and what the underlying mechanisms may be,” Dr. Purpura said.
A version of this article first appeared on WebMD.com.
It’s a story of promise at a time of urgent need.
They proposed many theories on what might be driving long COVID. A role for a virus “cryptic reservoir” that could reactivate at any time, “viral remnants” that trigger chronic inflammation, and action by “autoimmune antibodies” that cause ongoing symptoms are possibilities.
In fact, it’s likely that research will show long COVID is a condition with more than one cause, the experts said during a recent webinar.
People might experience post-infection problems, including organ damage that takes time to heal after initial COVID-19 illness. Or they may be living with post-immune factors, including ongoing immune system responses triggered by autoantibodies.
Determining the cause or causes of long COVID is essential for treatment. For example, if one person’s symptoms persist because of an overactive immune system, “we need to provide immunosuppressant therapies,” Akiko Iwasaki, PhD, said. “But we don’t want to give that to someone who has a persistent virus reservoir,” meaning remnants of the virus remain in their bodies.
Interestingly, a study preprint, which has not been peer reviewed, found dogs were accurate more than half the time in sniffing out long COVID, said Dr. Iwasaki, professor of immunobiology and developmental biology at Yale University, New Haven, Conn.
The dogs were tasked with identifying 45 people with long COVID versus 188 people without it. The findings suggest the presence of a unique chemical in the sweat of people with long COVID that could someday lead to a diagnostic test.
Viral persistence possible
If one of the main theories holds, it could be that the coronavirus somehow remains in the body in some form for some people after COVID-19.
Mady Hornig, MD, agreed this is a possibility that needs to be investigated further.
“A weakened immune response to an infection may mean that you have cryptic reservoirs of virus that are continuing to cause symptoms,” she said during the briefing. Dr. Hornig is a doctor-scientist specializing in epidemiology at Columbia University, New York.
“That may explain why some patients with long COVID feel better after vaccination,” because the vaccine creates a strong antibody response to fight COVID-19, Dr. Iwasaki said.
Researchers are unearthing additional potential factors contributing to long COVID.
Viral persistence could also reactivate other dormant viruses in the body, such as Epstein-Barr virus (EBV), said Lawrence Purpura, MD, MPH, an infectious disease specialist at New York Presbyterian/Columbia University. Reactivation of Epstein-Barr is one of four identifying signs of long COVID revealed in a Jan. 25 study published in the journal Cell.
Immune overactivation also possible?
For other people with long COVID, it’s not the virus sticking around but the body’s reaction that’s the issue.
Investigators suggest autoimmunity plays a role, and they point to the presence of autoantibodies, for example.
When these autoantibodies persist, they can cause tissue and organ damage over time.
Other investigators are proposing “immune exhaustion” in long COVID because of similarities to chronic fatigue syndrome, Dr. Hornig said.
“It should be ‘all hands on deck’ for research into long COVID,” she said. “The number of disabled individuals who will likely qualify for a diagnosis of [chronic fatigue syndrome] is growing by the second.”
Forging ahead on future research
It’s clear there is more work to do. There are investigators working on banking tissue samples from people with long COVID to learn more, for example.
Also, finding a biomarker unique to long COVID could vastly improve the precision of diagnosing long COVID, especially if the dog sniffing option does not pan out.
Of the thousands of biomarker possibilities, Dr. Hornig said, “maybe that’s one or two that ultimately make a real impact on patient care. So it’s going to be critical to find those quickly, translate them, and make them available.”
In the meantime, some answers might come from a large study sponsored by the National Institutes of Health. The NIH is funding the “Researching COVID to Enhance Recovery” project using $470 million from the American Rescue Plan. Investigators at NYU Langone Health are leading the effort and plan to share the wealth by funding more than 100 researchers at more than 30 institutions to create a “metacohort” to study long COVID. More information is available at recovercovid.org.
“Fortunately, through the global research effort, we are now really starting to expand our understanding of how long COVID manifests, how common it is, and what the underlying mechanisms may be,” Dr. Purpura said.
A version of this article first appeared on WebMD.com.
It’s a story of promise at a time of urgent need.
They proposed many theories on what might be driving long COVID. A role for a virus “cryptic reservoir” that could reactivate at any time, “viral remnants” that trigger chronic inflammation, and action by “autoimmune antibodies” that cause ongoing symptoms are possibilities.
In fact, it’s likely that research will show long COVID is a condition with more than one cause, the experts said during a recent webinar.
People might experience post-infection problems, including organ damage that takes time to heal after initial COVID-19 illness. Or they may be living with post-immune factors, including ongoing immune system responses triggered by autoantibodies.
Determining the cause or causes of long COVID is essential for treatment. For example, if one person’s symptoms persist because of an overactive immune system, “we need to provide immunosuppressant therapies,” Akiko Iwasaki, PhD, said. “But we don’t want to give that to someone who has a persistent virus reservoir,” meaning remnants of the virus remain in their bodies.
Interestingly, a study preprint, which has not been peer reviewed, found dogs were accurate more than half the time in sniffing out long COVID, said Dr. Iwasaki, professor of immunobiology and developmental biology at Yale University, New Haven, Conn.
The dogs were tasked with identifying 45 people with long COVID versus 188 people without it. The findings suggest the presence of a unique chemical in the sweat of people with long COVID that could someday lead to a diagnostic test.
Viral persistence possible
If one of the main theories holds, it could be that the coronavirus somehow remains in the body in some form for some people after COVID-19.
Mady Hornig, MD, agreed this is a possibility that needs to be investigated further.
“A weakened immune response to an infection may mean that you have cryptic reservoirs of virus that are continuing to cause symptoms,” she said during the briefing. Dr. Hornig is a doctor-scientist specializing in epidemiology at Columbia University, New York.
“That may explain why some patients with long COVID feel better after vaccination,” because the vaccine creates a strong antibody response to fight COVID-19, Dr. Iwasaki said.
Researchers are unearthing additional potential factors contributing to long COVID.
Viral persistence could also reactivate other dormant viruses in the body, such as Epstein-Barr virus (EBV), said Lawrence Purpura, MD, MPH, an infectious disease specialist at New York Presbyterian/Columbia University. Reactivation of Epstein-Barr is one of four identifying signs of long COVID revealed in a Jan. 25 study published in the journal Cell.
Immune overactivation also possible?
For other people with long COVID, it’s not the virus sticking around but the body’s reaction that’s the issue.
Investigators suggest autoimmunity plays a role, and they point to the presence of autoantibodies, for example.
When these autoantibodies persist, they can cause tissue and organ damage over time.
Other investigators are proposing “immune exhaustion” in long COVID because of similarities to chronic fatigue syndrome, Dr. Hornig said.
“It should be ‘all hands on deck’ for research into long COVID,” she said. “The number of disabled individuals who will likely qualify for a diagnosis of [chronic fatigue syndrome] is growing by the second.”
Forging ahead on future research
It’s clear there is more work to do. There are investigators working on banking tissue samples from people with long COVID to learn more, for example.
Also, finding a biomarker unique to long COVID could vastly improve the precision of diagnosing long COVID, especially if the dog sniffing option does not pan out.
Of the thousands of biomarker possibilities, Dr. Hornig said, “maybe that’s one or two that ultimately make a real impact on patient care. So it’s going to be critical to find those quickly, translate them, and make them available.”
In the meantime, some answers might come from a large study sponsored by the National Institutes of Health. The NIH is funding the “Researching COVID to Enhance Recovery” project using $470 million from the American Rescue Plan. Investigators at NYU Langone Health are leading the effort and plan to share the wealth by funding more than 100 researchers at more than 30 institutions to create a “metacohort” to study long COVID. More information is available at recovercovid.org.
“Fortunately, through the global research effort, we are now really starting to expand our understanding of how long COVID manifests, how common it is, and what the underlying mechanisms may be,” Dr. Purpura said.
A version of this article first appeared on WebMD.com.
Children and COVID: New cases down again, but still ‘extremely high’
The indication of an Omicron decline has become a trend: New cases of COVID-19 in children were down for a second consecutive week in the United States, according to the American Academy of Pediatrics and the Children’s Hospital Association.
but the nearly 632,000 cases reported were down by 22% from the previous week and by 45% from what appears to be the peak of the Omicron surge during the week of Jan. 14-20, the AAP/CHA data show.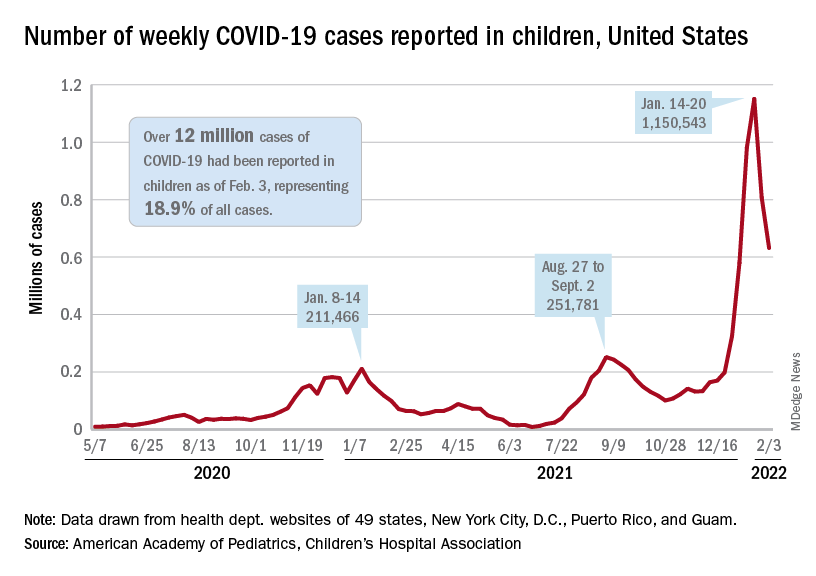
To put the effect of the Delta and Omicron variants into some sort of perspective, the total number of COVID-19 cases among children passed 5 million at the beginning of September 2021, about a year and a half into the pandemic. In the last 5 months, the cumulative count has more than doubled and now stands at 12 million, the AAP and CHA said in their weekly COVID report.
Hospital admissions and emergency department visits followed the same downward trend over the last week. The rate of new hospitalizations fell to 0.81 per 100,000 children aged 0-17 years as of Feb. 2 (down from a peak of 1.25 per 100,000 on Jan. 15), and ED visits with diagnosed COVID-19 dropped to 1.8% (peak was 14.1%), 1.9% (peak was 14.3%), and 3.4% (peak was 14%) of all visits for children aged 16-17, 12-15, and 0-11 years, respectively, the Centers for Disease Control and Prevention reported.
The vaccination response
The surge of infections brought about by the Omicron variant, however, did not translate into increased vaccination, at least for the youngest eligible children. Vaccine initiation rose slightly among children aged 5-11 in early and mid-January but, by early February, new vaccinations had declined to their lowest point since approval in early November of 2021, the AAP said in its weekly COVID vaccination report.
As a result, the 5- to 11-year-olds are well behind the pace set by those aged 12-15 for the first 3 months of their vaccination experience. Through the first 13 weeks after the COVID vaccine was approved for children aged 12-15 in early May, 44.5% had received at least one dose and 32.3% were fully vaccinated. Among children aged 5-11, the corresponding figures through 13 weeks were 31% and 22.5%, according to CDC data.
The vaccination reaction to Omicron was somewhat more robust for children aged 12-17, compared with the younger group, but initiations dropped at the same time that new cases began to decline. In terms of total volume, the response among 12- to 17-year-olds was much smaller than that seen in July and August of 2021 as the Delta surge was hitting the United States, the AAP vaccination report shows.
All those vaccinations add up to this: Over 16.8 million children aged 12-17 and almost 9 million aged 5-11 had received at least one dose of vaccine as of Feb. 7, which works out to 66.6% of the older group and 31.2% of the younger cohort. Almost 14.3 million (56.4%) of those aged 12-17 are fully vaccinated, as are 6.6 million (22.9%) of the 5- to 11-year-olds, the CDC said on its COVID Data Tracker.
The indication of an Omicron decline has become a trend: New cases of COVID-19 in children were down for a second consecutive week in the United States, according to the American Academy of Pediatrics and the Children’s Hospital Association.
but the nearly 632,000 cases reported were down by 22% from the previous week and by 45% from what appears to be the peak of the Omicron surge during the week of Jan. 14-20, the AAP/CHA data show.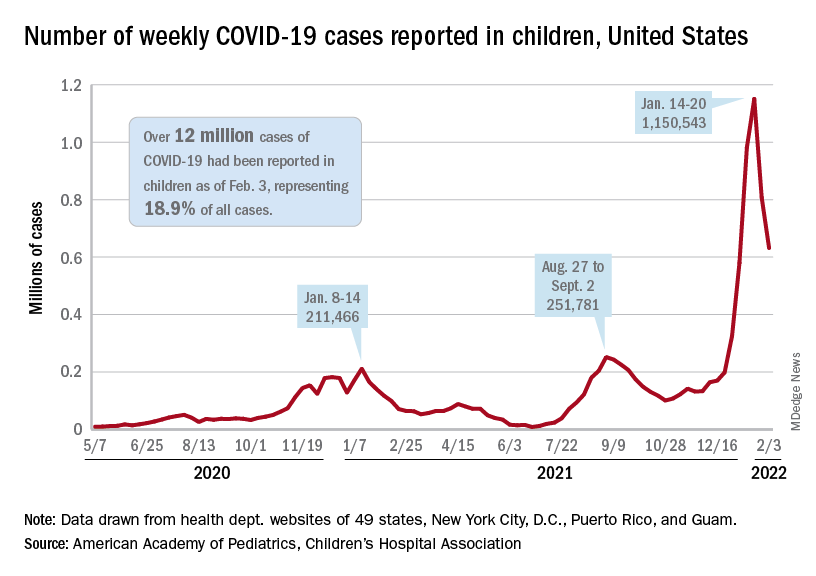
To put the effect of the Delta and Omicron variants into some sort of perspective, the total number of COVID-19 cases among children passed 5 million at the beginning of September 2021, about a year and a half into the pandemic. In the last 5 months, the cumulative count has more than doubled and now stands at 12 million, the AAP and CHA said in their weekly COVID report.
Hospital admissions and emergency department visits followed the same downward trend over the last week. The rate of new hospitalizations fell to 0.81 per 100,000 children aged 0-17 years as of Feb. 2 (down from a peak of 1.25 per 100,000 on Jan. 15), and ED visits with diagnosed COVID-19 dropped to 1.8% (peak was 14.1%), 1.9% (peak was 14.3%), and 3.4% (peak was 14%) of all visits for children aged 16-17, 12-15, and 0-11 years, respectively, the Centers for Disease Control and Prevention reported.
The vaccination response
The surge of infections brought about by the Omicron variant, however, did not translate into increased vaccination, at least for the youngest eligible children. Vaccine initiation rose slightly among children aged 5-11 in early and mid-January but, by early February, new vaccinations had declined to their lowest point since approval in early November of 2021, the AAP said in its weekly COVID vaccination report.
As a result, the 5- to 11-year-olds are well behind the pace set by those aged 12-15 for the first 3 months of their vaccination experience. Through the first 13 weeks after the COVID vaccine was approved for children aged 12-15 in early May, 44.5% had received at least one dose and 32.3% were fully vaccinated. Among children aged 5-11, the corresponding figures through 13 weeks were 31% and 22.5%, according to CDC data.
The vaccination reaction to Omicron was somewhat more robust for children aged 12-17, compared with the younger group, but initiations dropped at the same time that new cases began to decline. In terms of total volume, the response among 12- to 17-year-olds was much smaller than that seen in July and August of 2021 as the Delta surge was hitting the United States, the AAP vaccination report shows.
All those vaccinations add up to this: Over 16.8 million children aged 12-17 and almost 9 million aged 5-11 had received at least one dose of vaccine as of Feb. 7, which works out to 66.6% of the older group and 31.2% of the younger cohort. Almost 14.3 million (56.4%) of those aged 12-17 are fully vaccinated, as are 6.6 million (22.9%) of the 5- to 11-year-olds, the CDC said on its COVID Data Tracker.
The indication of an Omicron decline has become a trend: New cases of COVID-19 in children were down for a second consecutive week in the United States, according to the American Academy of Pediatrics and the Children’s Hospital Association.
but the nearly 632,000 cases reported were down by 22% from the previous week and by 45% from what appears to be the peak of the Omicron surge during the week of Jan. 14-20, the AAP/CHA data show.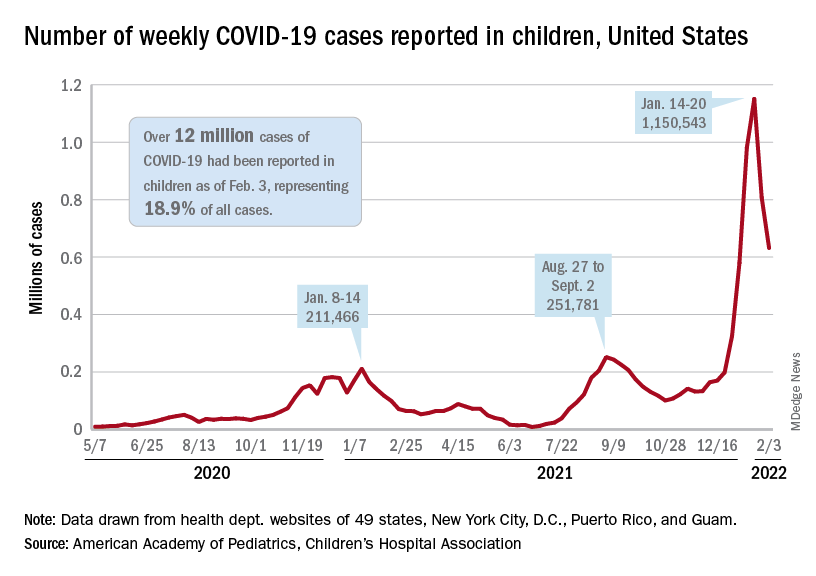
To put the effect of the Delta and Omicron variants into some sort of perspective, the total number of COVID-19 cases among children passed 5 million at the beginning of September 2021, about a year and a half into the pandemic. In the last 5 months, the cumulative count has more than doubled and now stands at 12 million, the AAP and CHA said in their weekly COVID report.
Hospital admissions and emergency department visits followed the same downward trend over the last week. The rate of new hospitalizations fell to 0.81 per 100,000 children aged 0-17 years as of Feb. 2 (down from a peak of 1.25 per 100,000 on Jan. 15), and ED visits with diagnosed COVID-19 dropped to 1.8% (peak was 14.1%), 1.9% (peak was 14.3%), and 3.4% (peak was 14%) of all visits for children aged 16-17, 12-15, and 0-11 years, respectively, the Centers for Disease Control and Prevention reported.
The vaccination response
The surge of infections brought about by the Omicron variant, however, did not translate into increased vaccination, at least for the youngest eligible children. Vaccine initiation rose slightly among children aged 5-11 in early and mid-January but, by early February, new vaccinations had declined to their lowest point since approval in early November of 2021, the AAP said in its weekly COVID vaccination report.
As a result, the 5- to 11-year-olds are well behind the pace set by those aged 12-15 for the first 3 months of their vaccination experience. Through the first 13 weeks after the COVID vaccine was approved for children aged 12-15 in early May, 44.5% had received at least one dose and 32.3% were fully vaccinated. Among children aged 5-11, the corresponding figures through 13 weeks were 31% and 22.5%, according to CDC data.
The vaccination reaction to Omicron was somewhat more robust for children aged 12-17, compared with the younger group, but initiations dropped at the same time that new cases began to decline. In terms of total volume, the response among 12- to 17-year-olds was much smaller than that seen in July and August of 2021 as the Delta surge was hitting the United States, the AAP vaccination report shows.
All those vaccinations add up to this: Over 16.8 million children aged 12-17 and almost 9 million aged 5-11 had received at least one dose of vaccine as of Feb. 7, which works out to 66.6% of the older group and 31.2% of the younger cohort. Almost 14.3 million (56.4%) of those aged 12-17 are fully vaccinated, as are 6.6 million (22.9%) of the 5- to 11-year-olds, the CDC said on its COVID Data Tracker.
Enough is enough: the pandemic and loss of female oncologists
Imagine this: As a young girl, you decide you want to become a doctor when you grow up. You spend countless hours studying, researching, and volunteering to eventually make it into medical school. Four years later, you graduate top of your class and match into your first-choice residency program. You are so proud of yourself!
During your last year of residency, a pandemic takes the entire world by storm. You persevere through your last 14 months of residency that included additional time in the ICU, not seeing your colleagues, and interviewing for your new job all from your own living room. After all of this, you finally get to start doing what you have been waiting to do for the past decade: train with the brilliant minds in hematology and oncology.
All of a sudden, You start to question: If these incredible women have decided that the sacrifice this career requires is too much, then (1) How will I survive? and (2) Did I make a huge mistake in my career decision? Spoiler alert: This girl is me.
The World Health Organization defines burnout as a “syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed. It is characterized by energy depletion or exhaustion, increased mental distance from one’s job, and reduced professional efficacy.”
We know that 33% of oncologists are feeling burned out right now, according to the Medscape National Physician Burnout & Suicide Report 2021. Of the 51% of female physicians that are burned out, work-life balance has been identified as the biggest workplace concern to them. Research has shown that hours per week devoted to direct patient care is the dominant predictor of burnout for practicing oncologists. But in academic oncology, that is followed by grant deadlines, manuscript rejections, and the constant reminders that you are a new face in oncology, a specialty that was previously male-dominated.
In less than a year, we have had several key female oncologists leave our cancer center. While some made the decision to retire early, two of them chose to pivot their careers and leave clinical medicine to assist with drug development and clinical trials. Although this is extremely important work for cancer care, I was shocked to hear that these amazing and successful clinicians were choosing to remove all direct patient care from their practice, when for many of them, patient care was what motivated them to pursue medicine in the first place. They were loved by their patients, respected as researchers, and well known as educators within the division.
One shared that she no longer felt like she could be a good mother, wife, or daughter with what was currently being demanded of her to have a successful academic career. In hearing this news, I was saddened to have to say goodbye to a mentor of mine and immediately started second-guessing my career choice. I felt that my goal of having an impactful career and prosperous home life was not only unattainable but potentially unrealistic.
While we know that female physicians already experience a greater degree of burnout, the pandemic has only added fuel to the fire. This is especially true in cancer care. It has been estimated that new cancer diagnosis have decreased by as much as 23% since the beginning of the pandemic. This delay in diagnosis will lead to patients presenting with more advanced disease, busier clinic schedules, and worsened clinical outcomes for years to come. With no end in sight, I worry what this will mean for women currently in oncology, in addition to those in training or deciding if they should pursue this as a career.
Extrapolating evidence from prior epidemics, physicians are at increased risk for burnout due to immediate and long-term effects from this pandemic. We need to act now to not only continue addressing previously existing individual and organizational causes of burnout but also develop strategies to provide support for the COVID-19–specific impacts on oncologists’ well-being. An editorial published by the American Society of Clinical Oncology provides helpful suggestions on how to do this.
A recent cross-sectional survey found that 22% of academic female oncologists were likely or very likely to pursue a career outside of academia in the next 5 years. Losing these women would be detrimental to the field. This would mean a significant number of patients losing their long-term oncologists with whom they have years of care, trainees losing their professional and research mentors to guide and help mold them into successful independent practitioners and researchers, and arguably most important, little girls losing role models to show them that regardless of their gender, they can become an oncologist.Dr. Poterala is a current hematology and oncology fellow at the University of Wisconsin Carbone Cancer Center, Madison. She disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Imagine this: As a young girl, you decide you want to become a doctor when you grow up. You spend countless hours studying, researching, and volunteering to eventually make it into medical school. Four years later, you graduate top of your class and match into your first-choice residency program. You are so proud of yourself!
During your last year of residency, a pandemic takes the entire world by storm. You persevere through your last 14 months of residency that included additional time in the ICU, not seeing your colleagues, and interviewing for your new job all from your own living room. After all of this, you finally get to start doing what you have been waiting to do for the past decade: train with the brilliant minds in hematology and oncology.
All of a sudden, You start to question: If these incredible women have decided that the sacrifice this career requires is too much, then (1) How will I survive? and (2) Did I make a huge mistake in my career decision? Spoiler alert: This girl is me.
The World Health Organization defines burnout as a “syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed. It is characterized by energy depletion or exhaustion, increased mental distance from one’s job, and reduced professional efficacy.”
We know that 33% of oncologists are feeling burned out right now, according to the Medscape National Physician Burnout & Suicide Report 2021. Of the 51% of female physicians that are burned out, work-life balance has been identified as the biggest workplace concern to them. Research has shown that hours per week devoted to direct patient care is the dominant predictor of burnout for practicing oncologists. But in academic oncology, that is followed by grant deadlines, manuscript rejections, and the constant reminders that you are a new face in oncology, a specialty that was previously male-dominated.
In less than a year, we have had several key female oncologists leave our cancer center. While some made the decision to retire early, two of them chose to pivot their careers and leave clinical medicine to assist with drug development and clinical trials. Although this is extremely important work for cancer care, I was shocked to hear that these amazing and successful clinicians were choosing to remove all direct patient care from their practice, when for many of them, patient care was what motivated them to pursue medicine in the first place. They were loved by their patients, respected as researchers, and well known as educators within the division.
One shared that she no longer felt like she could be a good mother, wife, or daughter with what was currently being demanded of her to have a successful academic career. In hearing this news, I was saddened to have to say goodbye to a mentor of mine and immediately started second-guessing my career choice. I felt that my goal of having an impactful career and prosperous home life was not only unattainable but potentially unrealistic.
While we know that female physicians already experience a greater degree of burnout, the pandemic has only added fuel to the fire. This is especially true in cancer care. It has been estimated that new cancer diagnosis have decreased by as much as 23% since the beginning of the pandemic. This delay in diagnosis will lead to patients presenting with more advanced disease, busier clinic schedules, and worsened clinical outcomes for years to come. With no end in sight, I worry what this will mean for women currently in oncology, in addition to those in training or deciding if they should pursue this as a career.
Extrapolating evidence from prior epidemics, physicians are at increased risk for burnout due to immediate and long-term effects from this pandemic. We need to act now to not only continue addressing previously existing individual and organizational causes of burnout but also develop strategies to provide support for the COVID-19–specific impacts on oncologists’ well-being. An editorial published by the American Society of Clinical Oncology provides helpful suggestions on how to do this.
A recent cross-sectional survey found that 22% of academic female oncologists were likely or very likely to pursue a career outside of academia in the next 5 years. Losing these women would be detrimental to the field. This would mean a significant number of patients losing their long-term oncologists with whom they have years of care, trainees losing their professional and research mentors to guide and help mold them into successful independent practitioners and researchers, and arguably most important, little girls losing role models to show them that regardless of their gender, they can become an oncologist.Dr. Poterala is a current hematology and oncology fellow at the University of Wisconsin Carbone Cancer Center, Madison. She disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Imagine this: As a young girl, you decide you want to become a doctor when you grow up. You spend countless hours studying, researching, and volunteering to eventually make it into medical school. Four years later, you graduate top of your class and match into your first-choice residency program. You are so proud of yourself!
During your last year of residency, a pandemic takes the entire world by storm. You persevere through your last 14 months of residency that included additional time in the ICU, not seeing your colleagues, and interviewing for your new job all from your own living room. After all of this, you finally get to start doing what you have been waiting to do for the past decade: train with the brilliant minds in hematology and oncology.
All of a sudden, You start to question: If these incredible women have decided that the sacrifice this career requires is too much, then (1) How will I survive? and (2) Did I make a huge mistake in my career decision? Spoiler alert: This girl is me.
The World Health Organization defines burnout as a “syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed. It is characterized by energy depletion or exhaustion, increased mental distance from one’s job, and reduced professional efficacy.”
We know that 33% of oncologists are feeling burned out right now, according to the Medscape National Physician Burnout & Suicide Report 2021. Of the 51% of female physicians that are burned out, work-life balance has been identified as the biggest workplace concern to them. Research has shown that hours per week devoted to direct patient care is the dominant predictor of burnout for practicing oncologists. But in academic oncology, that is followed by grant deadlines, manuscript rejections, and the constant reminders that you are a new face in oncology, a specialty that was previously male-dominated.
In less than a year, we have had several key female oncologists leave our cancer center. While some made the decision to retire early, two of them chose to pivot their careers and leave clinical medicine to assist with drug development and clinical trials. Although this is extremely important work for cancer care, I was shocked to hear that these amazing and successful clinicians were choosing to remove all direct patient care from their practice, when for many of them, patient care was what motivated them to pursue medicine in the first place. They were loved by their patients, respected as researchers, and well known as educators within the division.
One shared that she no longer felt like she could be a good mother, wife, or daughter with what was currently being demanded of her to have a successful academic career. In hearing this news, I was saddened to have to say goodbye to a mentor of mine and immediately started second-guessing my career choice. I felt that my goal of having an impactful career and prosperous home life was not only unattainable but potentially unrealistic.
While we know that female physicians already experience a greater degree of burnout, the pandemic has only added fuel to the fire. This is especially true in cancer care. It has been estimated that new cancer diagnosis have decreased by as much as 23% since the beginning of the pandemic. This delay in diagnosis will lead to patients presenting with more advanced disease, busier clinic schedules, and worsened clinical outcomes for years to come. With no end in sight, I worry what this will mean for women currently in oncology, in addition to those in training or deciding if they should pursue this as a career.
Extrapolating evidence from prior epidemics, physicians are at increased risk for burnout due to immediate and long-term effects from this pandemic. We need to act now to not only continue addressing previously existing individual and organizational causes of burnout but also develop strategies to provide support for the COVID-19–specific impacts on oncologists’ well-being. An editorial published by the American Society of Clinical Oncology provides helpful suggestions on how to do this.
A recent cross-sectional survey found that 22% of academic female oncologists were likely or very likely to pursue a career outside of academia in the next 5 years. Losing these women would be detrimental to the field. This would mean a significant number of patients losing their long-term oncologists with whom they have years of care, trainees losing their professional and research mentors to guide and help mold them into successful independent practitioners and researchers, and arguably most important, little girls losing role models to show them that regardless of their gender, they can become an oncologist.Dr. Poterala is a current hematology and oncology fellow at the University of Wisconsin Carbone Cancer Center, Madison. She disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Q&A: Long COVID symptoms, management, and where we’re headed
Long COVID continues to be a moving target – continuously evolving and still surprising doctors and patients who have sometimes incapacitating long-term symptoms.
Little about the disorder seems predictable at this point. People can have long COVID after asymptomatic, mild, or severe COVID-19, for example. And when a person gets long COVID – also known as long-haul COVID – symptoms can vary widely.
To address all the uncertainty, the New York State Department of Health gathered experts in primary care, pediatrics, physical medicine, rehabilitation, and pulmonology to answer some pressing questions.
New York in 2020 was the first epicenter of the pandemic in the United States, making it also the center of the long COVID epidemic, says Emily Lutterloh, MD, director of the Division of Epidemiology at the New York State Department of Health.
What do you do when you’re seeing a patient with long COVID for the first time?
The first exam varies because there are so many different ways long COVID presents itself, says Benjamin Abramoff, MD, a physical medicine and rehabilitation specialist at Penn Medicine in Philadelphia.
I’ve now been seriously ill with #LongCovid for 11 months. I was never hospitalized. I didn’t even have a “mild” covid case. Instead, I developed Long Covid from an asymptomatic infection.
I’m far from unique. Up to 1/5 of asymptomatic patients go on to have long-term symptoms.
— Ravi Veriah Jacques (@RaviHVJ) February 3, 2022
Assessing their previous and current care also helps to direct their ongoing management, says Zijian Chen, MD, medical director of the Center for Post-COVID Care at Mount Sinai Health System in New York.
Can vaccination help people with long COVID?
Anything that we can do to help prevent people from being critically ill or being hospitalized with COVID-19 is helpful to prevent long COVID, says Dr. Abramoff, who is also director of the long COVID clinic at the University of Pennsylvania, Philadelphia.
“So that’s something I always discuss with patients. In some research, sometimes patients do feel better after the vaccine,” he says.
What kind of therapies do you find helpful for your patients?
Rehabilitation is a key part of recovery from long COVID, Dr. Abramoff says. “It is very important to make this very patient-specific.”
“We have patients that are working. They’re already going to the gym in some cases but don’t feel like they have the same endurance,” he says. “And then we have patients who are so crippled by their fatigue that they can’t get out of bed.”
1/ What is #LongCOVID?!
A disabling malady from ongoing inflammation, autoimmunity, & potential viral reservoirs (GI, brain?)
NEW DATA: The Lungs “light up” on special MRI Scans 3 to 9 months later in patients never hospitalized for COVID.https://t.co/I2kyZ4cK5F pic.twitter.com/dL1P67L2DK
— WesElyMD (@WesElyMD) February 2, 2022
An exercise program can help people who have long COVID.
“There’s a big role for therapy services in the recovery of these patients,” says John Baratta, MD, of the department of physical medicine and rehabilitation at the University of North Carolina at Chapel Hill.
But the limited number of long COVID clinics can mean some people are unable to get to therapists trained on the needs of patients with lingering COVID symptoms. Educating community physical and occupational therapists is one solution.
How long does it take for people with long COVID to recover and get back to 100% if they can?
Specific numbers aren’t really available, Dr. Baratta says.
“But I can tell you the general trend that I see is that a lot of patients have a gradual improvement of symptoms. The slow but steady improvement with time may be the body’s natural healing process, a result of medical interventions, or both.”
It can help to reassure people with long COVID that they will not be discharged from care until they feel they’ve maximized their health, says Sharagim Kemp, DO, medical director of the COVID Recovery Program for Nuvance Health, a health system in New York and Connecticut.
It’s essential to set realistic recovery expectations and tell patients that not everyone will return to 100% of their pre-COVID functioning, she says.
“Once we are able to help them reset their expectations, there’s almost an accelerated recovery because they are not putting that pressure on themselves anymore,” Dr. Kemp says.
What are the most common symptoms you’re seeing in long COVID?
It’s helpful to think of long COVID as a very broad umbrella term, Dr. Abramoff says.
Echoing what many others have observed, fatigue, cognitive dysfunction or “brain fog,“ and shortness of breath or troubled breathing appear to be the most common symptoms, he says.
Some reported vague symptoms, Dr. Kemp says.
People may go to the doctor “not even realizing that they had COVID. That’s one of the important points here – to have a high index of suspicion for patients who come in with multiple symptoms,” she says.
For this reason, patients can report symptoms that don’t necessarily fit into any specialty, says Sarah J. Ryan, MD, an internal medicine doctor at Columbia University Irving Medical Center in New York. People say they are “just not themselves” or they are tired after their COVID-19 recovery.
Is there a connection between severe COVID cases and severe long COVID?
“It’s not like that at all. I would say that more than 80% of the patients that we see had mild to moderate illness and they were not hospitalized,” Dr. Baratta says.
Long COVID is a bit different in children and teenagers, says Ixsy Ramirez, MD, a pediatric pulmonologist at University of Michigan Health, Ann Arbor. Most patients in the long COVID clinic at the University of Michigan were previously healthy, and not children with asthma or other lung conditions as one might expect. In fact, many are student athletes, or were before they had long COVID.
In this population, shortness of breath is most common, followed by chest pain and fatigue. Unfortunately, the symptoms are so serious for many kids that their performance is limited, even if they can return to competitive play.
Are there defined criteria you use to diagnose long COVID? How do you give someone a diagnosis?
That’s an ever-evolving question, Dr. Kemp says. The generally accepted definition centers on persistent or new symptoms 4 weeks or more after the original COVID-19 illness, but there are exceptions.
Researchers are working on lab tests to help confirm the diagnosis. But without a definitive blood biomarker, getting to the diagnosis requires “some thorough detective work,” Dr. Ryan says.
Do you bring in mental health providers to help with treatment?
“We focus on mental health quite a bit actually,” says, Dr. Chen, cofounder of his institution’s COVID recovery clinic. Mount Sinai offers one-on-one and group mental health services, for example.
“Personally, I’ve seen patients that I did not expect to have such severe mental health changes” with long COVID.
One of the most powerful accounts and testimonies I have seen on what most #LongCovid patients experience when interacting with their doctors.
“I did not fit in a box, so they chose not to see me, even worse they made me feel like it was my fault for not fitting in their box” pic.twitter.com/7GQLBucuO5
— charlos (@loscharlos) February 3, 2022
Examples include severe depression, cases of acute psychosis, hallucinations, and other problems “that are really unexpected after a viral illness.”
Stony Brook University Hospital in New York has a long COVID clinic staffed by multiple primary care doctors who do exams and refer patients to services. A bonus of offering psychological services to all post-COVID patients is doctors get a more complete picture of each person and a better understanding of what they are going through, says Abigail Chua, MD, a pulmonologist at Stony Brook.
Some empathy is essential, Dr. Baratta says. “It’s important to recognize that a lot of these patients present with a sense of grief or loss for their prior life.”
What does the future hold?
A simple test to diagnose long COVID, combined with an effective treatment that helps people feel better within a week, would be ideal, Dr. Abramoff says.
“That would be lovely. But you know, we’re just not at that point.”
And it would be helpful to start identifying subtypes of long COVID so diagnosis and treatment can be more targeted, Dr. Abramoff says. Otherwise, “It’s going to be a very challenging approach to try to treat all of our patients with long COVID symptoms the same way.”
Good clinical trials likewise are needed to address all the subtleties of long COVID.
A number of long COVID centers are collaborating on research to find out more, Dr. Chen says. Actions include setting up a bank of tissue samples from people with long COVID so researchers can continue to figure out the condition.
One goal, Dr. Chen says, would be the ability to treat long COVID rather than just its symptoms.
Long COVID emphasizes the need to prevent people from getting COVID in the first place, Dr. Ramirez says. This will continue to be important, particularly when some people dismiss the seriousness of COVID, comparing it to a cold if they get it. That attitude discounts the large number of people who unfortunately go on to develop long-term, often debilitating, symptoms.
A version of this article first appeared on WebMD.com.
Long COVID continues to be a moving target – continuously evolving and still surprising doctors and patients who have sometimes incapacitating long-term symptoms.
Little about the disorder seems predictable at this point. People can have long COVID after asymptomatic, mild, or severe COVID-19, for example. And when a person gets long COVID – also known as long-haul COVID – symptoms can vary widely.
To address all the uncertainty, the New York State Department of Health gathered experts in primary care, pediatrics, physical medicine, rehabilitation, and pulmonology to answer some pressing questions.
New York in 2020 was the first epicenter of the pandemic in the United States, making it also the center of the long COVID epidemic, says Emily Lutterloh, MD, director of the Division of Epidemiology at the New York State Department of Health.
What do you do when you’re seeing a patient with long COVID for the first time?
The first exam varies because there are so many different ways long COVID presents itself, says Benjamin Abramoff, MD, a physical medicine and rehabilitation specialist at Penn Medicine in Philadelphia.
I’ve now been seriously ill with #LongCovid for 11 months. I was never hospitalized. I didn’t even have a “mild” covid case. Instead, I developed Long Covid from an asymptomatic infection.
I’m far from unique. Up to 1/5 of asymptomatic patients go on to have long-term symptoms.
— Ravi Veriah Jacques (@RaviHVJ) February 3, 2022
Assessing their previous and current care also helps to direct their ongoing management, says Zijian Chen, MD, medical director of the Center for Post-COVID Care at Mount Sinai Health System in New York.
Can vaccination help people with long COVID?
Anything that we can do to help prevent people from being critically ill or being hospitalized with COVID-19 is helpful to prevent long COVID, says Dr. Abramoff, who is also director of the long COVID clinic at the University of Pennsylvania, Philadelphia.
“So that’s something I always discuss with patients. In some research, sometimes patients do feel better after the vaccine,” he says.
What kind of therapies do you find helpful for your patients?
Rehabilitation is a key part of recovery from long COVID, Dr. Abramoff says. “It is very important to make this very patient-specific.”
“We have patients that are working. They’re already going to the gym in some cases but don’t feel like they have the same endurance,” he says. “And then we have patients who are so crippled by their fatigue that they can’t get out of bed.”
1/ What is #LongCOVID?!
A disabling malady from ongoing inflammation, autoimmunity, & potential viral reservoirs (GI, brain?)
NEW DATA: The Lungs “light up” on special MRI Scans 3 to 9 months later in patients never hospitalized for COVID.https://t.co/I2kyZ4cK5F pic.twitter.com/dL1P67L2DK
— WesElyMD (@WesElyMD) February 2, 2022
An exercise program can help people who have long COVID.
“There’s a big role for therapy services in the recovery of these patients,” says John Baratta, MD, of the department of physical medicine and rehabilitation at the University of North Carolina at Chapel Hill.
But the limited number of long COVID clinics can mean some people are unable to get to therapists trained on the needs of patients with lingering COVID symptoms. Educating community physical and occupational therapists is one solution.
How long does it take for people with long COVID to recover and get back to 100% if they can?
Specific numbers aren’t really available, Dr. Baratta says.
“But I can tell you the general trend that I see is that a lot of patients have a gradual improvement of symptoms. The slow but steady improvement with time may be the body’s natural healing process, a result of medical interventions, or both.”
It can help to reassure people with long COVID that they will not be discharged from care until they feel they’ve maximized their health, says Sharagim Kemp, DO, medical director of the COVID Recovery Program for Nuvance Health, a health system in New York and Connecticut.
It’s essential to set realistic recovery expectations and tell patients that not everyone will return to 100% of their pre-COVID functioning, she says.
“Once we are able to help them reset their expectations, there’s almost an accelerated recovery because they are not putting that pressure on themselves anymore,” Dr. Kemp says.
What are the most common symptoms you’re seeing in long COVID?
It’s helpful to think of long COVID as a very broad umbrella term, Dr. Abramoff says.
Echoing what many others have observed, fatigue, cognitive dysfunction or “brain fog,“ and shortness of breath or troubled breathing appear to be the most common symptoms, he says.
Some reported vague symptoms, Dr. Kemp says.
People may go to the doctor “not even realizing that they had COVID. That’s one of the important points here – to have a high index of suspicion for patients who come in with multiple symptoms,” she says.
For this reason, patients can report symptoms that don’t necessarily fit into any specialty, says Sarah J. Ryan, MD, an internal medicine doctor at Columbia University Irving Medical Center in New York. People say they are “just not themselves” or they are tired after their COVID-19 recovery.
Is there a connection between severe COVID cases and severe long COVID?
“It’s not like that at all. I would say that more than 80% of the patients that we see had mild to moderate illness and they were not hospitalized,” Dr. Baratta says.
Long COVID is a bit different in children and teenagers, says Ixsy Ramirez, MD, a pediatric pulmonologist at University of Michigan Health, Ann Arbor. Most patients in the long COVID clinic at the University of Michigan were previously healthy, and not children with asthma or other lung conditions as one might expect. In fact, many are student athletes, or were before they had long COVID.
In this population, shortness of breath is most common, followed by chest pain and fatigue. Unfortunately, the symptoms are so serious for many kids that their performance is limited, even if they can return to competitive play.
Are there defined criteria you use to diagnose long COVID? How do you give someone a diagnosis?
That’s an ever-evolving question, Dr. Kemp says. The generally accepted definition centers on persistent or new symptoms 4 weeks or more after the original COVID-19 illness, but there are exceptions.
Researchers are working on lab tests to help confirm the diagnosis. But without a definitive blood biomarker, getting to the diagnosis requires “some thorough detective work,” Dr. Ryan says.
Do you bring in mental health providers to help with treatment?
“We focus on mental health quite a bit actually,” says, Dr. Chen, cofounder of his institution’s COVID recovery clinic. Mount Sinai offers one-on-one and group mental health services, for example.
“Personally, I’ve seen patients that I did not expect to have such severe mental health changes” with long COVID.
One of the most powerful accounts and testimonies I have seen on what most #LongCovid patients experience when interacting with their doctors.
“I did not fit in a box, so they chose not to see me, even worse they made me feel like it was my fault for not fitting in their box” pic.twitter.com/7GQLBucuO5
— charlos (@loscharlos) February 3, 2022
Examples include severe depression, cases of acute psychosis, hallucinations, and other problems “that are really unexpected after a viral illness.”
Stony Brook University Hospital in New York has a long COVID clinic staffed by multiple primary care doctors who do exams and refer patients to services. A bonus of offering psychological services to all post-COVID patients is doctors get a more complete picture of each person and a better understanding of what they are going through, says Abigail Chua, MD, a pulmonologist at Stony Brook.
Some empathy is essential, Dr. Baratta says. “It’s important to recognize that a lot of these patients present with a sense of grief or loss for their prior life.”
What does the future hold?
A simple test to diagnose long COVID, combined with an effective treatment that helps people feel better within a week, would be ideal, Dr. Abramoff says.
“That would be lovely. But you know, we’re just not at that point.”
And it would be helpful to start identifying subtypes of long COVID so diagnosis and treatment can be more targeted, Dr. Abramoff says. Otherwise, “It’s going to be a very challenging approach to try to treat all of our patients with long COVID symptoms the same way.”
Good clinical trials likewise are needed to address all the subtleties of long COVID.
A number of long COVID centers are collaborating on research to find out more, Dr. Chen says. Actions include setting up a bank of tissue samples from people with long COVID so researchers can continue to figure out the condition.
One goal, Dr. Chen says, would be the ability to treat long COVID rather than just its symptoms.
Long COVID emphasizes the need to prevent people from getting COVID in the first place, Dr. Ramirez says. This will continue to be important, particularly when some people dismiss the seriousness of COVID, comparing it to a cold if they get it. That attitude discounts the large number of people who unfortunately go on to develop long-term, often debilitating, symptoms.
A version of this article first appeared on WebMD.com.
Long COVID continues to be a moving target – continuously evolving and still surprising doctors and patients who have sometimes incapacitating long-term symptoms.
Little about the disorder seems predictable at this point. People can have long COVID after asymptomatic, mild, or severe COVID-19, for example. And when a person gets long COVID – also known as long-haul COVID – symptoms can vary widely.
To address all the uncertainty, the New York State Department of Health gathered experts in primary care, pediatrics, physical medicine, rehabilitation, and pulmonology to answer some pressing questions.
New York in 2020 was the first epicenter of the pandemic in the United States, making it also the center of the long COVID epidemic, says Emily Lutterloh, MD, director of the Division of Epidemiology at the New York State Department of Health.
What do you do when you’re seeing a patient with long COVID for the first time?
The first exam varies because there are so many different ways long COVID presents itself, says Benjamin Abramoff, MD, a physical medicine and rehabilitation specialist at Penn Medicine in Philadelphia.
I’ve now been seriously ill with #LongCovid for 11 months. I was never hospitalized. I didn’t even have a “mild” covid case. Instead, I developed Long Covid from an asymptomatic infection.
I’m far from unique. Up to 1/5 of asymptomatic patients go on to have long-term symptoms.
— Ravi Veriah Jacques (@RaviHVJ) February 3, 2022
Assessing their previous and current care also helps to direct their ongoing management, says Zijian Chen, MD, medical director of the Center for Post-COVID Care at Mount Sinai Health System in New York.
Can vaccination help people with long COVID?
Anything that we can do to help prevent people from being critically ill or being hospitalized with COVID-19 is helpful to prevent long COVID, says Dr. Abramoff, who is also director of the long COVID clinic at the University of Pennsylvania, Philadelphia.
“So that’s something I always discuss with patients. In some research, sometimes patients do feel better after the vaccine,” he says.
What kind of therapies do you find helpful for your patients?
Rehabilitation is a key part of recovery from long COVID, Dr. Abramoff says. “It is very important to make this very patient-specific.”
“We have patients that are working. They’re already going to the gym in some cases but don’t feel like they have the same endurance,” he says. “And then we have patients who are so crippled by their fatigue that they can’t get out of bed.”
1/ What is #LongCOVID?!
A disabling malady from ongoing inflammation, autoimmunity, & potential viral reservoirs (GI, brain?)
NEW DATA: The Lungs “light up” on special MRI Scans 3 to 9 months later in patients never hospitalized for COVID.https://t.co/I2kyZ4cK5F pic.twitter.com/dL1P67L2DK
— WesElyMD (@WesElyMD) February 2, 2022
An exercise program can help people who have long COVID.
“There’s a big role for therapy services in the recovery of these patients,” says John Baratta, MD, of the department of physical medicine and rehabilitation at the University of North Carolina at Chapel Hill.
But the limited number of long COVID clinics can mean some people are unable to get to therapists trained on the needs of patients with lingering COVID symptoms. Educating community physical and occupational therapists is one solution.
How long does it take for people with long COVID to recover and get back to 100% if they can?
Specific numbers aren’t really available, Dr. Baratta says.
“But I can tell you the general trend that I see is that a lot of patients have a gradual improvement of symptoms. The slow but steady improvement with time may be the body’s natural healing process, a result of medical interventions, or both.”
It can help to reassure people with long COVID that they will not be discharged from care until they feel they’ve maximized their health, says Sharagim Kemp, DO, medical director of the COVID Recovery Program for Nuvance Health, a health system in New York and Connecticut.
It’s essential to set realistic recovery expectations and tell patients that not everyone will return to 100% of their pre-COVID functioning, she says.
“Once we are able to help them reset their expectations, there’s almost an accelerated recovery because they are not putting that pressure on themselves anymore,” Dr. Kemp says.
What are the most common symptoms you’re seeing in long COVID?
It’s helpful to think of long COVID as a very broad umbrella term, Dr. Abramoff says.
Echoing what many others have observed, fatigue, cognitive dysfunction or “brain fog,“ and shortness of breath or troubled breathing appear to be the most common symptoms, he says.
Some reported vague symptoms, Dr. Kemp says.
People may go to the doctor “not even realizing that they had COVID. That’s one of the important points here – to have a high index of suspicion for patients who come in with multiple symptoms,” she says.
For this reason, patients can report symptoms that don’t necessarily fit into any specialty, says Sarah J. Ryan, MD, an internal medicine doctor at Columbia University Irving Medical Center in New York. People say they are “just not themselves” or they are tired after their COVID-19 recovery.
Is there a connection between severe COVID cases and severe long COVID?
“It’s not like that at all. I would say that more than 80% of the patients that we see had mild to moderate illness and they were not hospitalized,” Dr. Baratta says.
Long COVID is a bit different in children and teenagers, says Ixsy Ramirez, MD, a pediatric pulmonologist at University of Michigan Health, Ann Arbor. Most patients in the long COVID clinic at the University of Michigan were previously healthy, and not children with asthma or other lung conditions as one might expect. In fact, many are student athletes, or were before they had long COVID.
In this population, shortness of breath is most common, followed by chest pain and fatigue. Unfortunately, the symptoms are so serious for many kids that their performance is limited, even if they can return to competitive play.
Are there defined criteria you use to diagnose long COVID? How do you give someone a diagnosis?
That’s an ever-evolving question, Dr. Kemp says. The generally accepted definition centers on persistent or new symptoms 4 weeks or more after the original COVID-19 illness, but there are exceptions.
Researchers are working on lab tests to help confirm the diagnosis. But without a definitive blood biomarker, getting to the diagnosis requires “some thorough detective work,” Dr. Ryan says.
Do you bring in mental health providers to help with treatment?
“We focus on mental health quite a bit actually,” says, Dr. Chen, cofounder of his institution’s COVID recovery clinic. Mount Sinai offers one-on-one and group mental health services, for example.
“Personally, I’ve seen patients that I did not expect to have such severe mental health changes” with long COVID.
One of the most powerful accounts and testimonies I have seen on what most #LongCovid patients experience when interacting with their doctors.
“I did not fit in a box, so they chose not to see me, even worse they made me feel like it was my fault for not fitting in their box” pic.twitter.com/7GQLBucuO5
— charlos (@loscharlos) February 3, 2022
Examples include severe depression, cases of acute psychosis, hallucinations, and other problems “that are really unexpected after a viral illness.”
Stony Brook University Hospital in New York has a long COVID clinic staffed by multiple primary care doctors who do exams and refer patients to services. A bonus of offering psychological services to all post-COVID patients is doctors get a more complete picture of each person and a better understanding of what they are going through, says Abigail Chua, MD, a pulmonologist at Stony Brook.
Some empathy is essential, Dr. Baratta says. “It’s important to recognize that a lot of these patients present with a sense of grief or loss for their prior life.”
What does the future hold?
A simple test to diagnose long COVID, combined with an effective treatment that helps people feel better within a week, would be ideal, Dr. Abramoff says.
“That would be lovely. But you know, we’re just not at that point.”
And it would be helpful to start identifying subtypes of long COVID so diagnosis and treatment can be more targeted, Dr. Abramoff says. Otherwise, “It’s going to be a very challenging approach to try to treat all of our patients with long COVID symptoms the same way.”
Good clinical trials likewise are needed to address all the subtleties of long COVID.
A number of long COVID centers are collaborating on research to find out more, Dr. Chen says. Actions include setting up a bank of tissue samples from people with long COVID so researchers can continue to figure out the condition.
One goal, Dr. Chen says, would be the ability to treat long COVID rather than just its symptoms.
Long COVID emphasizes the need to prevent people from getting COVID in the first place, Dr. Ramirez says. This will continue to be important, particularly when some people dismiss the seriousness of COVID, comparing it to a cold if they get it. That attitude discounts the large number of people who unfortunately go on to develop long-term, often debilitating, symptoms.
A version of this article first appeared on WebMD.com.
No COVID vax, no transplant: Unfair or good medicine?
Right now, more than 106,600 people in the United States are on the national transplant waiting list, each hoping to hear soon that a lung, kidney, heart, or other vital organ has been found for them. It’s the promise not just of a new organ, but a new life.
Well before they are placed on that list, transplant candidates, as they’re known, are evaluated with a battery of tests and exams to be sure they are infection free, their other organs are healthy, and that all their vaccinations are up to date.
In January, a 31-year-old Boston father of two declined to get the COVID-19 vaccine, and Brigham and Women’s Hospital officials removed him from the heart transplant waiting list. And in North Carolina, a 38-year-old man in need of a kidney transplant said he, too, was denied the organ when he declined to get the vaccination.
Those are just two of the most recent cases. The decisions by the transplant centers to remove the candidates from the waiting list have set off a national debate among ethicists, family members, doctors, patients, and others.
On social media and in conversation, the question persists: Is removing them from the list unfair and cruel, or simply business as usual to keep the patient as healthy as possible and the transplant as successful as possible?
Two recent tweets sum up the debate.
“The people responsible for this should be charged with attempted homicide,” one Twitter user said, while another suggested that the more accurate way to headline the news about a transplant candidate refusing the COVID-19 vaccine would be: “Patient voluntarily forfeits donor organ.”
Doctors and ethics experts, as well as other patients on the waiting list, say it’s simply good medicine to require the COVID vaccine, along with a host of other pretransplant requirements.
Transplant protocols
“Transplant medicine has always been a strong promoter of vaccination,” said Silas Prescod Norman, MD, a clinical associate professor of nephrology and internal medicine at the University of Michigan, Ann Arbor. He is a kidney specialist who works in the university’s transplant clinic.
Requiring the COVID vaccine is in line with requirements to get numerous other vaccines, he said.“Promoting the COVID vaccine among our transplant candidates and recipients is just an extension of our usual practice.
“In transplantation, first and foremost is patient safety,” Dr. Norman said. “And we know that solid organ transplant patients are at substantially higher risk of contracting COVID than nontransplant patients.”
After the transplant, they are placed on immunosuppressant drugs, that weaken the immune system while also decreasing the body’s ability to reject the new organ.
“We know now, because there is good data about the vaccine to show that people who are on transplant medications are less likely to make detectable antibodies after vaccination,” said Dr. Norman, who’s also a medical adviser for the American Kidney Fund, a nonprofit that provides kidney health information and financial assistance for dialysis.
And this is not a surprise because of the immunosuppressive effects, he said. “So it only makes sense to get people vaccinated before transplantation.”
Researchers compared the cases of more than 17,000 people who had received organ transplants and were hospitalized from April to November 2020, either for COVID (1,682 of them) or other health issues. Those who had COVID were more likely to have complications and to die in the hospital than those who did not have it.
Vaccination guidelines, policies
Federal COVID-19 treatment guidelines from the National Institutes of Health state that transplant patients on immunosuppressant drugs used after the procedure should be considered at a higher risk of getting severe COVID if infected.
In a joint statement from the American Society of Transplant Surgeons, the American Society of Transplantation, and the International Society for Heart and Lung Transplantation, the organizations say they “strongly recommend that all eligible children and adult transplant candidates and recipients be vaccinated with a COVID-19 vaccine [and booster] that is approved or authorized in their jurisdiction. Whenever possible, vaccination should occur prior to transplantation.” Ideally, it should be completed at least 2 weeks before the transplant.
The organizations also “support the development of institutional policies regarding pretransplant vaccination. We believe that this is in the best interest of the transplant candidate, optimizing their chances of getting through the perioperative and posttransplant periods without severe COVID-19 disease, especially at times of greater infection prevalence.”
Officials at Brigham and Women’s Hospital, where the 31-year-old father was removed from the list, issued a statement that reads, in part: “Our Mass General Brigham health care system requires several [Centers for Disease Control and Prevention]-recommended vaccines, including the COVID-19 vaccine, and lifestyle behaviors for transplant candidates to create both the best chance for a successful operation and to optimize the patient’s survival after transplantation, given that their immune system is drastically suppressed. Patients are not active on the wait list without this.”
Ethics amid organ shortage
“Organs are scarce,” said Arthur L. Caplan, PhD, director of the division of medical ethics at New York University Langone Medical Center. That makes the goal of choosing the very best candidates for success even more crucial.
“You try to maximize the chance the organ will work,” he said. Pretransplant vaccination is one way.
The shortage is most severe for kidney transplants. In 2020, according to federal statistics, more than 91,000 kidney transplants were needed, but fewer than 23,000 were received. During 2021, 41,354 transplants were done, an increase of nearly 6% over the previous year. The total includes kidneys, hearts, lungs, and other organs, with kidneys accounting for more than 24,000 of the total.
Even with the rise in transplant numbers, supply does not meet demand. According to federal statistics, 17 people in the United States die each day waiting for an organ transplant. Every 9 minutes, someone is added to the waiting list.
“This isn’t and it shouldn’t be a fight about the COVID vaccine,” Dr. Caplan said. “This isn’t an issue about punishing non-COVID vaccinators. It’s deciding who is going to get a scarce organ.”
“A lot of people [opposed to removing the nonvaccinated from the list] think: ‘Oh, they are just killing those people who won’t take a COVID vaccine.’ That’s not what is going on.”
The transplant candidate must be in the best possible shape overall, Dr. Caplan and doctors agreed. Someone who is smoking, drinking heavily, or abusing drugs isn’t going to the top of the list either. And for other procedures, such as bariatric surgery or knee surgery, some patients are told first to lose weight before a surgeon will operate.
The worry about side effects from the vaccine, which some patients have cited as a concern, is misplaced, Dr. Caplan said. What transplant candidates who refuse the COVID vaccine may not be thinking about is that they are facing a serious operation and will be on numerous anti-rejection drugs, with side effects, after the surgery.
“So to be worried about the side effects of a COVID vaccine is irrational,” he said.
Transplants: The process
The patients who were recently removed from the transplant list could seek care and a transplant at an alternate center, said Anne Paschke, a spokesperson for the United Network for Organ Sharing, a nonprofit group that is under contract with the federal government and operates the national Organ Procurement and Transplantation Network (OPTN).
“Transplant hospitals decide which patients to add to the wait list based on their own criteria and medical judgment to create the best chance for a positive transplant outcome,” she said. That’s done with the understanding that patients will help with their medical care.
So, if one program won’t accept a patient, another may. But, if a patient turned down at one center due to refusing to get the COVID vaccine tries another center, the requirements at that hospital may be the same, she said.
OPTN maintains a list of transplant centers. As of Jan. 28, there were 251 transplant centers, according to UNOS, which manages the waiting list, matches donors and recipients, and strives for equity, among other duties.
Pretransplant refusers not typical
“The cases we are seeing are outliers,” Dr. Caplan said of the handful of known candidates who have refused the vaccine. Most ask their doctor exactly what they need to do to live and follow those instructions.
Dr. Norman agreed. Most of the kidney patients he cares for who are hoping for a transplant have been on dialysis, “which they do not like. They are doing whatever they can to make sure they don’t go back on dialysis. As a group, they tend to be very adherent, very safety conscious because they understand their risk and they understand the gift they have received [or will receive] through transplantation. They want to do everything they can to respect and protect that gift.”
Not surprisingly, some on the transplant list who are vaccinated have strong opinions about those who refuse to get the vaccine. Dana J. Ufkes, 61, a Seattle realtor, has been on the kidney transplant list – this time – since 2003, hoping for her third transplant. When asked if potential recipients should be removed from the list if they refuse the COVID vaccine, her answer was immediate: “Absolutely.”
At age 17, Ms. Ufkes got a serious kidney infection that went undiagnosed and untreated. Her kidney health worsened, and she needed a transplant. She got her first one in 1986, then again in 1992.
“They last longer than they used to,” she said. But not forever. (According to the American Kidney Fund, transplants from a living kidney donor last about 15-20 years; from a deceased donor, 10-15.)
The decision to decline the vaccine is, of course, each person’s choice, Ms. Ufkes said. But “if they don’t want to be vaccinated [and still want to be on the list], I think that’s BS.”
Citing the lack of organs, “it’s not like they are handing these out like jellybeans.”
A version of this article first appeared on WebMD.com.
Right now, more than 106,600 people in the United States are on the national transplant waiting list, each hoping to hear soon that a lung, kidney, heart, or other vital organ has been found for them. It’s the promise not just of a new organ, but a new life.
Well before they are placed on that list, transplant candidates, as they’re known, are evaluated with a battery of tests and exams to be sure they are infection free, their other organs are healthy, and that all their vaccinations are up to date.
In January, a 31-year-old Boston father of two declined to get the COVID-19 vaccine, and Brigham and Women’s Hospital officials removed him from the heart transplant waiting list. And in North Carolina, a 38-year-old man in need of a kidney transplant said he, too, was denied the organ when he declined to get the vaccination.
Those are just two of the most recent cases. The decisions by the transplant centers to remove the candidates from the waiting list have set off a national debate among ethicists, family members, doctors, patients, and others.
On social media and in conversation, the question persists: Is removing them from the list unfair and cruel, or simply business as usual to keep the patient as healthy as possible and the transplant as successful as possible?
Two recent tweets sum up the debate.
“The people responsible for this should be charged with attempted homicide,” one Twitter user said, while another suggested that the more accurate way to headline the news about a transplant candidate refusing the COVID-19 vaccine would be: “Patient voluntarily forfeits donor organ.”
Doctors and ethics experts, as well as other patients on the waiting list, say it’s simply good medicine to require the COVID vaccine, along with a host of other pretransplant requirements.
Transplant protocols
“Transplant medicine has always been a strong promoter of vaccination,” said Silas Prescod Norman, MD, a clinical associate professor of nephrology and internal medicine at the University of Michigan, Ann Arbor. He is a kidney specialist who works in the university’s transplant clinic.
Requiring the COVID vaccine is in line with requirements to get numerous other vaccines, he said.“Promoting the COVID vaccine among our transplant candidates and recipients is just an extension of our usual practice.
“In transplantation, first and foremost is patient safety,” Dr. Norman said. “And we know that solid organ transplant patients are at substantially higher risk of contracting COVID than nontransplant patients.”
After the transplant, they are placed on immunosuppressant drugs, that weaken the immune system while also decreasing the body’s ability to reject the new organ.
“We know now, because there is good data about the vaccine to show that people who are on transplant medications are less likely to make detectable antibodies after vaccination,” said Dr. Norman, who’s also a medical adviser for the American Kidney Fund, a nonprofit that provides kidney health information and financial assistance for dialysis.
And this is not a surprise because of the immunosuppressive effects, he said. “So it only makes sense to get people vaccinated before transplantation.”
Researchers compared the cases of more than 17,000 people who had received organ transplants and were hospitalized from April to November 2020, either for COVID (1,682 of them) or other health issues. Those who had COVID were more likely to have complications and to die in the hospital than those who did not have it.
Vaccination guidelines, policies
Federal COVID-19 treatment guidelines from the National Institutes of Health state that transplant patients on immunosuppressant drugs used after the procedure should be considered at a higher risk of getting severe COVID if infected.
In a joint statement from the American Society of Transplant Surgeons, the American Society of Transplantation, and the International Society for Heart and Lung Transplantation, the organizations say they “strongly recommend that all eligible children and adult transplant candidates and recipients be vaccinated with a COVID-19 vaccine [and booster] that is approved or authorized in their jurisdiction. Whenever possible, vaccination should occur prior to transplantation.” Ideally, it should be completed at least 2 weeks before the transplant.
The organizations also “support the development of institutional policies regarding pretransplant vaccination. We believe that this is in the best interest of the transplant candidate, optimizing their chances of getting through the perioperative and posttransplant periods without severe COVID-19 disease, especially at times of greater infection prevalence.”
Officials at Brigham and Women’s Hospital, where the 31-year-old father was removed from the list, issued a statement that reads, in part: “Our Mass General Brigham health care system requires several [Centers for Disease Control and Prevention]-recommended vaccines, including the COVID-19 vaccine, and lifestyle behaviors for transplant candidates to create both the best chance for a successful operation and to optimize the patient’s survival after transplantation, given that their immune system is drastically suppressed. Patients are not active on the wait list without this.”
Ethics amid organ shortage
“Organs are scarce,” said Arthur L. Caplan, PhD, director of the division of medical ethics at New York University Langone Medical Center. That makes the goal of choosing the very best candidates for success even more crucial.
“You try to maximize the chance the organ will work,” he said. Pretransplant vaccination is one way.
The shortage is most severe for kidney transplants. In 2020, according to federal statistics, more than 91,000 kidney transplants were needed, but fewer than 23,000 were received. During 2021, 41,354 transplants were done, an increase of nearly 6% over the previous year. The total includes kidneys, hearts, lungs, and other organs, with kidneys accounting for more than 24,000 of the total.
Even with the rise in transplant numbers, supply does not meet demand. According to federal statistics, 17 people in the United States die each day waiting for an organ transplant. Every 9 minutes, someone is added to the waiting list.
“This isn’t and it shouldn’t be a fight about the COVID vaccine,” Dr. Caplan said. “This isn’t an issue about punishing non-COVID vaccinators. It’s deciding who is going to get a scarce organ.”
“A lot of people [opposed to removing the nonvaccinated from the list] think: ‘Oh, they are just killing those people who won’t take a COVID vaccine.’ That’s not what is going on.”
The transplant candidate must be in the best possible shape overall, Dr. Caplan and doctors agreed. Someone who is smoking, drinking heavily, or abusing drugs isn’t going to the top of the list either. And for other procedures, such as bariatric surgery or knee surgery, some patients are told first to lose weight before a surgeon will operate.
The worry about side effects from the vaccine, which some patients have cited as a concern, is misplaced, Dr. Caplan said. What transplant candidates who refuse the COVID vaccine may not be thinking about is that they are facing a serious operation and will be on numerous anti-rejection drugs, with side effects, after the surgery.
“So to be worried about the side effects of a COVID vaccine is irrational,” he said.
Transplants: The process
The patients who were recently removed from the transplant list could seek care and a transplant at an alternate center, said Anne Paschke, a spokesperson for the United Network for Organ Sharing, a nonprofit group that is under contract with the federal government and operates the national Organ Procurement and Transplantation Network (OPTN).
“Transplant hospitals decide which patients to add to the wait list based on their own criteria and medical judgment to create the best chance for a positive transplant outcome,” she said. That’s done with the understanding that patients will help with their medical care.
So, if one program won’t accept a patient, another may. But, if a patient turned down at one center due to refusing to get the COVID vaccine tries another center, the requirements at that hospital may be the same, she said.
OPTN maintains a list of transplant centers. As of Jan. 28, there were 251 transplant centers, according to UNOS, which manages the waiting list, matches donors and recipients, and strives for equity, among other duties.
Pretransplant refusers not typical
“The cases we are seeing are outliers,” Dr. Caplan said of the handful of known candidates who have refused the vaccine. Most ask their doctor exactly what they need to do to live and follow those instructions.
Dr. Norman agreed. Most of the kidney patients he cares for who are hoping for a transplant have been on dialysis, “which they do not like. They are doing whatever they can to make sure they don’t go back on dialysis. As a group, they tend to be very adherent, very safety conscious because they understand their risk and they understand the gift they have received [or will receive] through transplantation. They want to do everything they can to respect and protect that gift.”
Not surprisingly, some on the transplant list who are vaccinated have strong opinions about those who refuse to get the vaccine. Dana J. Ufkes, 61, a Seattle realtor, has been on the kidney transplant list – this time – since 2003, hoping for her third transplant. When asked if potential recipients should be removed from the list if they refuse the COVID vaccine, her answer was immediate: “Absolutely.”
At age 17, Ms. Ufkes got a serious kidney infection that went undiagnosed and untreated. Her kidney health worsened, and she needed a transplant. She got her first one in 1986, then again in 1992.
“They last longer than they used to,” she said. But not forever. (According to the American Kidney Fund, transplants from a living kidney donor last about 15-20 years; from a deceased donor, 10-15.)
The decision to decline the vaccine is, of course, each person’s choice, Ms. Ufkes said. But “if they don’t want to be vaccinated [and still want to be on the list], I think that’s BS.”
Citing the lack of organs, “it’s not like they are handing these out like jellybeans.”
A version of this article first appeared on WebMD.com.
Right now, more than 106,600 people in the United States are on the national transplant waiting list, each hoping to hear soon that a lung, kidney, heart, or other vital organ has been found for them. It’s the promise not just of a new organ, but a new life.
Well before they are placed on that list, transplant candidates, as they’re known, are evaluated with a battery of tests and exams to be sure they are infection free, their other organs are healthy, and that all their vaccinations are up to date.
In January, a 31-year-old Boston father of two declined to get the COVID-19 vaccine, and Brigham and Women’s Hospital officials removed him from the heart transplant waiting list. And in North Carolina, a 38-year-old man in need of a kidney transplant said he, too, was denied the organ when he declined to get the vaccination.
Those are just two of the most recent cases. The decisions by the transplant centers to remove the candidates from the waiting list have set off a national debate among ethicists, family members, doctors, patients, and others.
On social media and in conversation, the question persists: Is removing them from the list unfair and cruel, or simply business as usual to keep the patient as healthy as possible and the transplant as successful as possible?
Two recent tweets sum up the debate.
“The people responsible for this should be charged with attempted homicide,” one Twitter user said, while another suggested that the more accurate way to headline the news about a transplant candidate refusing the COVID-19 vaccine would be: “Patient voluntarily forfeits donor organ.”
Doctors and ethics experts, as well as other patients on the waiting list, say it’s simply good medicine to require the COVID vaccine, along with a host of other pretransplant requirements.
Transplant protocols
“Transplant medicine has always been a strong promoter of vaccination,” said Silas Prescod Norman, MD, a clinical associate professor of nephrology and internal medicine at the University of Michigan, Ann Arbor. He is a kidney specialist who works in the university’s transplant clinic.
Requiring the COVID vaccine is in line with requirements to get numerous other vaccines, he said.“Promoting the COVID vaccine among our transplant candidates and recipients is just an extension of our usual practice.
“In transplantation, first and foremost is patient safety,” Dr. Norman said. “And we know that solid organ transplant patients are at substantially higher risk of contracting COVID than nontransplant patients.”
After the transplant, they are placed on immunosuppressant drugs, that weaken the immune system while also decreasing the body’s ability to reject the new organ.
“We know now, because there is good data about the vaccine to show that people who are on transplant medications are less likely to make detectable antibodies after vaccination,” said Dr. Norman, who’s also a medical adviser for the American Kidney Fund, a nonprofit that provides kidney health information and financial assistance for dialysis.
And this is not a surprise because of the immunosuppressive effects, he said. “So it only makes sense to get people vaccinated before transplantation.”
Researchers compared the cases of more than 17,000 people who had received organ transplants and were hospitalized from April to November 2020, either for COVID (1,682 of them) or other health issues. Those who had COVID were more likely to have complications and to die in the hospital than those who did not have it.
Vaccination guidelines, policies
Federal COVID-19 treatment guidelines from the National Institutes of Health state that transplant patients on immunosuppressant drugs used after the procedure should be considered at a higher risk of getting severe COVID if infected.
In a joint statement from the American Society of Transplant Surgeons, the American Society of Transplantation, and the International Society for Heart and Lung Transplantation, the organizations say they “strongly recommend that all eligible children and adult transplant candidates and recipients be vaccinated with a COVID-19 vaccine [and booster] that is approved or authorized in their jurisdiction. Whenever possible, vaccination should occur prior to transplantation.” Ideally, it should be completed at least 2 weeks before the transplant.
The organizations also “support the development of institutional policies regarding pretransplant vaccination. We believe that this is in the best interest of the transplant candidate, optimizing their chances of getting through the perioperative and posttransplant periods without severe COVID-19 disease, especially at times of greater infection prevalence.”
Officials at Brigham and Women’s Hospital, where the 31-year-old father was removed from the list, issued a statement that reads, in part: “Our Mass General Brigham health care system requires several [Centers for Disease Control and Prevention]-recommended vaccines, including the COVID-19 vaccine, and lifestyle behaviors for transplant candidates to create both the best chance for a successful operation and to optimize the patient’s survival after transplantation, given that their immune system is drastically suppressed. Patients are not active on the wait list without this.”
Ethics amid organ shortage
“Organs are scarce,” said Arthur L. Caplan, PhD, director of the division of medical ethics at New York University Langone Medical Center. That makes the goal of choosing the very best candidates for success even more crucial.
“You try to maximize the chance the organ will work,” he said. Pretransplant vaccination is one way.
The shortage is most severe for kidney transplants. In 2020, according to federal statistics, more than 91,000 kidney transplants were needed, but fewer than 23,000 were received. During 2021, 41,354 transplants were done, an increase of nearly 6% over the previous year. The total includes kidneys, hearts, lungs, and other organs, with kidneys accounting for more than 24,000 of the total.
Even with the rise in transplant numbers, supply does not meet demand. According to federal statistics, 17 people in the United States die each day waiting for an organ transplant. Every 9 minutes, someone is added to the waiting list.
“This isn’t and it shouldn’t be a fight about the COVID vaccine,” Dr. Caplan said. “This isn’t an issue about punishing non-COVID vaccinators. It’s deciding who is going to get a scarce organ.”
“A lot of people [opposed to removing the nonvaccinated from the list] think: ‘Oh, they are just killing those people who won’t take a COVID vaccine.’ That’s not what is going on.”
The transplant candidate must be in the best possible shape overall, Dr. Caplan and doctors agreed. Someone who is smoking, drinking heavily, or abusing drugs isn’t going to the top of the list either. And for other procedures, such as bariatric surgery or knee surgery, some patients are told first to lose weight before a surgeon will operate.
The worry about side effects from the vaccine, which some patients have cited as a concern, is misplaced, Dr. Caplan said. What transplant candidates who refuse the COVID vaccine may not be thinking about is that they are facing a serious operation and will be on numerous anti-rejection drugs, with side effects, after the surgery.
“So to be worried about the side effects of a COVID vaccine is irrational,” he said.
Transplants: The process
The patients who were recently removed from the transplant list could seek care and a transplant at an alternate center, said Anne Paschke, a spokesperson for the United Network for Organ Sharing, a nonprofit group that is under contract with the federal government and operates the national Organ Procurement and Transplantation Network (OPTN).
“Transplant hospitals decide which patients to add to the wait list based on their own criteria and medical judgment to create the best chance for a positive transplant outcome,” she said. That’s done with the understanding that patients will help with their medical care.
So, if one program won’t accept a patient, another may. But, if a patient turned down at one center due to refusing to get the COVID vaccine tries another center, the requirements at that hospital may be the same, she said.
OPTN maintains a list of transplant centers. As of Jan. 28, there were 251 transplant centers, according to UNOS, which manages the waiting list, matches donors and recipients, and strives for equity, among other duties.
Pretransplant refusers not typical
“The cases we are seeing are outliers,” Dr. Caplan said of the handful of known candidates who have refused the vaccine. Most ask their doctor exactly what they need to do to live and follow those instructions.
Dr. Norman agreed. Most of the kidney patients he cares for who are hoping for a transplant have been on dialysis, “which they do not like. They are doing whatever they can to make sure they don’t go back on dialysis. As a group, they tend to be very adherent, very safety conscious because they understand their risk and they understand the gift they have received [or will receive] through transplantation. They want to do everything they can to respect and protect that gift.”
Not surprisingly, some on the transplant list who are vaccinated have strong opinions about those who refuse to get the vaccine. Dana J. Ufkes, 61, a Seattle realtor, has been on the kidney transplant list – this time – since 2003, hoping for her third transplant. When asked if potential recipients should be removed from the list if they refuse the COVID vaccine, her answer was immediate: “Absolutely.”
At age 17, Ms. Ufkes got a serious kidney infection that went undiagnosed and untreated. Her kidney health worsened, and she needed a transplant. She got her first one in 1986, then again in 1992.
“They last longer than they used to,” she said. But not forever. (According to the American Kidney Fund, transplants from a living kidney donor last about 15-20 years; from a deceased donor, 10-15.)
The decision to decline the vaccine is, of course, each person’s choice, Ms. Ufkes said. But “if they don’t want to be vaccinated [and still want to be on the list], I think that’s BS.”
Citing the lack of organs, “it’s not like they are handing these out like jellybeans.”
A version of this article first appeared on WebMD.com.
Updated guidance for COVID vaccination in rheumatology patients arrives amid continued hesitancy
As rheumatologists contend with vaccine hesitancy among certain subsets of patients, the American College of Rheumatology has released updated clinical guidelines on COVID-19 vaccination for patients with rheumatic and musculoskeletal diseases (RMDs), including new recommendations on supplemental and booster doses.
The revised guidance from this fifth version of the ACR guidelines includes strongly recommending that all RMD patients receive a booster after their primary vaccine series, regardless of whether they have been naturally infected with COVID-19. In addition, they strongly recommend third supplemental doses for patients with autoimmune inflammatory rheumatic diseases (AIIRDs) who likely mounted an inadequate vaccine response, which would then be followed by a fourth booster dose as advised by the Centers for Disease Control and Prevention for immunocompromised individuals.
Other recommendations include pre-exposure prophylaxis monoclonal antibody treatment for high-risk AIIRD patients, defined as those with moderate to severely compromised immune systems who may not mount an adequate immune response to COVID-19 vaccination, when it is available and authorized for emergency use by the Food and Drug Administration, as well as monoclonal antibody therapy for postexposure prophylaxis of asymptomatic, recently exposed high-risk AIIRD patients or as treatment for newly symptomatic, high-risk AIIRD patients. The ACR guidance notes that, currently, neither the monoclonal antibodies bamlanivimab and etesevimab (administered together) nor casirivimab and imdevimab (REGEN-COV), are licensed or available under an emergency use authorization given their lack of activity against the Omicron variant, the dominant strain of SARS-CoV-2 circulating in the United States.
Finally, the guidance clarified that the timing of intravenous immunoglobulin doses does not need to be modified around the administration of COVID vaccine doses, based on moderate consensus among task force members.
Vaccine hesitancy in community rheumatology practices
The revised guidelines were released just as Arthritis & Rheumatology published a new study that assessed vaccine hesitancy among rheumatology patients on immunomodulatory therapies. A three-item electronic survey was conducted at 101 offices within a community practice–based rheumatology research network and ultimately collected responses from 58,529 patients, 20,987 of whom had an AIIRD and were receiving targeted therapies like biologics or Janus kinase inhibitors.
Of the total respondents, 77% (n = 43,675) had been vaccinated, 16.9% were not vaccinated and did not plan to be, and 6.1% were not vaccinated but planned to be. However, AIIRD patients were 16% less likely to be vaccinated, compared with the other patients, such as those with osteoarthritis or osteoporosis who were not receiving disease-modifying antirheumatic drugs (76.9% vs. 87%; odds ratio, 0.84; 95% confidence interval, 0.77-0.92; P < .001). Multivariable analysis also found that older patients (OR, 1.49 per 10 years) and Asians (OR, 2.42; 95% CI, 1.77-3.33) were more likely to be vaccinated.
“Rheumatologists need to be asking their patients more than just: ‘Are you vaccinated?’ ” Jeffrey Curtis, MD, MPH, head of the ACR COVID-19 vaccine task force and a coauthor of the vaccine hesitancy study, said in an interview. “A year ago, that was a fine approach, but now they need to be asking whether you’ve been vaccinated, and with what, and how many times, and how recently. There are a whole lot of subtleties there; ‘vaccinated: yes or no’ is just the tip of the iceberg.”
His research into the vaccine hesitant includes recent anecdotal data from thousands of patients treated in local rheumatology community practices, many of whom cited long-term safety data and potential side effects as reasons why they were unwilling to get vaccinated. But despite their on-paper responses, he cautioned rheumatologists to think critically when determining which patients may truly be open to vaccination.
“If you’re designing strategies to affect vaccine hesitancy, you may be wasting your time with some people,” said Dr. Curtis, professor of medicine at the University of Alabama at Birmingham. “A critical need is to figure out who are the patients who may be amendable to more information or an intervention or a little bit more time and care, and who are the people where you know, this is a lost cause: You don’t get a flu shot, you haven’t been vaccinated for shingles, [and] you’re not going to get this one either.
“In terms of a research agenda, how do we develop efficient, simple, short screening tools?” he added. “Something with a few helpful questions, on a patient portal or an iPad, that will do a good job identifying your patients at risk who haven’t had vaccination but that you might be able to spend time with, intervene, and actually change their mind. If you spend gobs of time with everyone, you’ll help some people, but clinicians don’t have an infinite amount of time.”
One of the authors of the vaccine hesitancy study acknowledged being employed by the rheumatology research network that hosted the survey. Several others, including Dr. Curtis, reported receiving grants and consulting fees from various pharmaceutical companies.
As rheumatologists contend with vaccine hesitancy among certain subsets of patients, the American College of Rheumatology has released updated clinical guidelines on COVID-19 vaccination for patients with rheumatic and musculoskeletal diseases (RMDs), including new recommendations on supplemental and booster doses.
The revised guidance from this fifth version of the ACR guidelines includes strongly recommending that all RMD patients receive a booster after their primary vaccine series, regardless of whether they have been naturally infected with COVID-19. In addition, they strongly recommend third supplemental doses for patients with autoimmune inflammatory rheumatic diseases (AIIRDs) who likely mounted an inadequate vaccine response, which would then be followed by a fourth booster dose as advised by the Centers for Disease Control and Prevention for immunocompromised individuals.
Other recommendations include pre-exposure prophylaxis monoclonal antibody treatment for high-risk AIIRD patients, defined as those with moderate to severely compromised immune systems who may not mount an adequate immune response to COVID-19 vaccination, when it is available and authorized for emergency use by the Food and Drug Administration, as well as monoclonal antibody therapy for postexposure prophylaxis of asymptomatic, recently exposed high-risk AIIRD patients or as treatment for newly symptomatic, high-risk AIIRD patients. The ACR guidance notes that, currently, neither the monoclonal antibodies bamlanivimab and etesevimab (administered together) nor casirivimab and imdevimab (REGEN-COV), are licensed or available under an emergency use authorization given their lack of activity against the Omicron variant, the dominant strain of SARS-CoV-2 circulating in the United States.
Finally, the guidance clarified that the timing of intravenous immunoglobulin doses does not need to be modified around the administration of COVID vaccine doses, based on moderate consensus among task force members.
Vaccine hesitancy in community rheumatology practices
The revised guidelines were released just as Arthritis & Rheumatology published a new study that assessed vaccine hesitancy among rheumatology patients on immunomodulatory therapies. A three-item electronic survey was conducted at 101 offices within a community practice–based rheumatology research network and ultimately collected responses from 58,529 patients, 20,987 of whom had an AIIRD and were receiving targeted therapies like biologics or Janus kinase inhibitors.
Of the total respondents, 77% (n = 43,675) had been vaccinated, 16.9% were not vaccinated and did not plan to be, and 6.1% were not vaccinated but planned to be. However, AIIRD patients were 16% less likely to be vaccinated, compared with the other patients, such as those with osteoarthritis or osteoporosis who were not receiving disease-modifying antirheumatic drugs (76.9% vs. 87%; odds ratio, 0.84; 95% confidence interval, 0.77-0.92; P < .001). Multivariable analysis also found that older patients (OR, 1.49 per 10 years) and Asians (OR, 2.42; 95% CI, 1.77-3.33) were more likely to be vaccinated.
“Rheumatologists need to be asking their patients more than just: ‘Are you vaccinated?’ ” Jeffrey Curtis, MD, MPH, head of the ACR COVID-19 vaccine task force and a coauthor of the vaccine hesitancy study, said in an interview. “A year ago, that was a fine approach, but now they need to be asking whether you’ve been vaccinated, and with what, and how many times, and how recently. There are a whole lot of subtleties there; ‘vaccinated: yes or no’ is just the tip of the iceberg.”
His research into the vaccine hesitant includes recent anecdotal data from thousands of patients treated in local rheumatology community practices, many of whom cited long-term safety data and potential side effects as reasons why they were unwilling to get vaccinated. But despite their on-paper responses, he cautioned rheumatologists to think critically when determining which patients may truly be open to vaccination.
“If you’re designing strategies to affect vaccine hesitancy, you may be wasting your time with some people,” said Dr. Curtis, professor of medicine at the University of Alabama at Birmingham. “A critical need is to figure out who are the patients who may be amendable to more information or an intervention or a little bit more time and care, and who are the people where you know, this is a lost cause: You don’t get a flu shot, you haven’t been vaccinated for shingles, [and] you’re not going to get this one either.
“In terms of a research agenda, how do we develop efficient, simple, short screening tools?” he added. “Something with a few helpful questions, on a patient portal or an iPad, that will do a good job identifying your patients at risk who haven’t had vaccination but that you might be able to spend time with, intervene, and actually change their mind. If you spend gobs of time with everyone, you’ll help some people, but clinicians don’t have an infinite amount of time.”
One of the authors of the vaccine hesitancy study acknowledged being employed by the rheumatology research network that hosted the survey. Several others, including Dr. Curtis, reported receiving grants and consulting fees from various pharmaceutical companies.
As rheumatologists contend with vaccine hesitancy among certain subsets of patients, the American College of Rheumatology has released updated clinical guidelines on COVID-19 vaccination for patients with rheumatic and musculoskeletal diseases (RMDs), including new recommendations on supplemental and booster doses.
The revised guidance from this fifth version of the ACR guidelines includes strongly recommending that all RMD patients receive a booster after their primary vaccine series, regardless of whether they have been naturally infected with COVID-19. In addition, they strongly recommend third supplemental doses for patients with autoimmune inflammatory rheumatic diseases (AIIRDs) who likely mounted an inadequate vaccine response, which would then be followed by a fourth booster dose as advised by the Centers for Disease Control and Prevention for immunocompromised individuals.
Other recommendations include pre-exposure prophylaxis monoclonal antibody treatment for high-risk AIIRD patients, defined as those with moderate to severely compromised immune systems who may not mount an adequate immune response to COVID-19 vaccination, when it is available and authorized for emergency use by the Food and Drug Administration, as well as monoclonal antibody therapy for postexposure prophylaxis of asymptomatic, recently exposed high-risk AIIRD patients or as treatment for newly symptomatic, high-risk AIIRD patients. The ACR guidance notes that, currently, neither the monoclonal antibodies bamlanivimab and etesevimab (administered together) nor casirivimab and imdevimab (REGEN-COV), are licensed or available under an emergency use authorization given their lack of activity against the Omicron variant, the dominant strain of SARS-CoV-2 circulating in the United States.
Finally, the guidance clarified that the timing of intravenous immunoglobulin doses does not need to be modified around the administration of COVID vaccine doses, based on moderate consensus among task force members.
Vaccine hesitancy in community rheumatology practices
The revised guidelines were released just as Arthritis & Rheumatology published a new study that assessed vaccine hesitancy among rheumatology patients on immunomodulatory therapies. A three-item electronic survey was conducted at 101 offices within a community practice–based rheumatology research network and ultimately collected responses from 58,529 patients, 20,987 of whom had an AIIRD and were receiving targeted therapies like biologics or Janus kinase inhibitors.
Of the total respondents, 77% (n = 43,675) had been vaccinated, 16.9% were not vaccinated and did not plan to be, and 6.1% were not vaccinated but planned to be. However, AIIRD patients were 16% less likely to be vaccinated, compared with the other patients, such as those with osteoarthritis or osteoporosis who were not receiving disease-modifying antirheumatic drugs (76.9% vs. 87%; odds ratio, 0.84; 95% confidence interval, 0.77-0.92; P < .001). Multivariable analysis also found that older patients (OR, 1.49 per 10 years) and Asians (OR, 2.42; 95% CI, 1.77-3.33) were more likely to be vaccinated.
“Rheumatologists need to be asking their patients more than just: ‘Are you vaccinated?’ ” Jeffrey Curtis, MD, MPH, head of the ACR COVID-19 vaccine task force and a coauthor of the vaccine hesitancy study, said in an interview. “A year ago, that was a fine approach, but now they need to be asking whether you’ve been vaccinated, and with what, and how many times, and how recently. There are a whole lot of subtleties there; ‘vaccinated: yes or no’ is just the tip of the iceberg.”
His research into the vaccine hesitant includes recent anecdotal data from thousands of patients treated in local rheumatology community practices, many of whom cited long-term safety data and potential side effects as reasons why they were unwilling to get vaccinated. But despite their on-paper responses, he cautioned rheumatologists to think critically when determining which patients may truly be open to vaccination.
“If you’re designing strategies to affect vaccine hesitancy, you may be wasting your time with some people,” said Dr. Curtis, professor of medicine at the University of Alabama at Birmingham. “A critical need is to figure out who are the patients who may be amendable to more information or an intervention or a little bit more time and care, and who are the people where you know, this is a lost cause: You don’t get a flu shot, you haven’t been vaccinated for shingles, [and] you’re not going to get this one either.
“In terms of a research agenda, how do we develop efficient, simple, short screening tools?” he added. “Something with a few helpful questions, on a patient portal or an iPad, that will do a good job identifying your patients at risk who haven’t had vaccination but that you might be able to spend time with, intervene, and actually change their mind. If you spend gobs of time with everyone, you’ll help some people, but clinicians don’t have an infinite amount of time.”
One of the authors of the vaccine hesitancy study acknowledged being employed by the rheumatology research network that hosted the survey. Several others, including Dr. Curtis, reported receiving grants and consulting fees from various pharmaceutical companies.
FROM ARTHRITIS & RHEUMATOLOGY
Boosted Americans 97 times less likely to die of COVID-19 than unvaccinated
according to a new update from the CDC.
In addition, fully vaccinated Americans — meaning those with up to two doses, but no booster — are 14 times less likely to die from COVID-19 than unvaccinated people.
“These data confirm that vaccination and boosting continues to protect against severe illness and hospitalization, even during the Omicron surge,” Rochelle Walensky, MD, director of the CDC, said during a briefing by the White House COVID-19 Response Team.
“If you are not up to date on your COVID-19 vaccinations, you have not optimized your protection against severe disease and death, and you should get vaccinated and boosted if you are eligible,” she said.
Dr. Walensky presented the latest numbers on Feb. 2 based on reports from 25 jurisdictions in early December. The number of average weekly deaths for those who were unvaccinated was 9.7 per 100,000 people, as compared with 0.7 of those who were vaccinated and 0.1 of those who had received a booster.
“The data are really stunningly obvious why a booster is really very important,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said during the briefing.
Dr. Fauci also encouraged vaccination for those who are pregnant and couples who may want to conceive in the near feature. He highlighted two recent studies that found vaccination in either partner didn’t affect fertility, including in vitro fertilization.
Meanwhile, fertility fell temporarily among men who were infected with the coronavirus. Couples were 18% less likely to conceive if the male partner had contracted the coronavirus within 60 days before a menstrual cycle.
“New data adds to previous studies that indicate that COVID-19 vaccination does not negatively impact fertility,” Dr. Fauci said. “Vaccination is recommended for people who are trying to get pregnant now or might become pregnant in the future, as well as their partners.”
About 80% of eligible Americans have received at least one vaccine dose, and 68% are fully vaccinated, according to the latest CDC data. About 51% of those who are eligible for a booster dose have received one.
The FDA could authorize the Pfizer vaccine for children under age 5 later this month. When that happens, about 18 million children will qualify for a shot, Jeff Zients, coordinator of the White House COVID-19 Response Team, said during the briefing. The Biden administration is already working on distribution plans for the shot for young kids, he added.
“We’ll be ready to start getting shots in arms soon after FDA and CDC make their decisions,” he said.
A version of this article first appeared on WebMD.com.
according to a new update from the CDC.
In addition, fully vaccinated Americans — meaning those with up to two doses, but no booster — are 14 times less likely to die from COVID-19 than unvaccinated people.
“These data confirm that vaccination and boosting continues to protect against severe illness and hospitalization, even during the Omicron surge,” Rochelle Walensky, MD, director of the CDC, said during a briefing by the White House COVID-19 Response Team.
“If you are not up to date on your COVID-19 vaccinations, you have not optimized your protection against severe disease and death, and you should get vaccinated and boosted if you are eligible,” she said.
Dr. Walensky presented the latest numbers on Feb. 2 based on reports from 25 jurisdictions in early December. The number of average weekly deaths for those who were unvaccinated was 9.7 per 100,000 people, as compared with 0.7 of those who were vaccinated and 0.1 of those who had received a booster.
“The data are really stunningly obvious why a booster is really very important,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said during the briefing.
Dr. Fauci also encouraged vaccination for those who are pregnant and couples who may want to conceive in the near feature. He highlighted two recent studies that found vaccination in either partner didn’t affect fertility, including in vitro fertilization.
Meanwhile, fertility fell temporarily among men who were infected with the coronavirus. Couples were 18% less likely to conceive if the male partner had contracted the coronavirus within 60 days before a menstrual cycle.
“New data adds to previous studies that indicate that COVID-19 vaccination does not negatively impact fertility,” Dr. Fauci said. “Vaccination is recommended for people who are trying to get pregnant now or might become pregnant in the future, as well as their partners.”
About 80% of eligible Americans have received at least one vaccine dose, and 68% are fully vaccinated, according to the latest CDC data. About 51% of those who are eligible for a booster dose have received one.
The FDA could authorize the Pfizer vaccine for children under age 5 later this month. When that happens, about 18 million children will qualify for a shot, Jeff Zients, coordinator of the White House COVID-19 Response Team, said during the briefing. The Biden administration is already working on distribution plans for the shot for young kids, he added.
“We’ll be ready to start getting shots in arms soon after FDA and CDC make their decisions,” he said.
A version of this article first appeared on WebMD.com.
according to a new update from the CDC.
In addition, fully vaccinated Americans — meaning those with up to two doses, but no booster — are 14 times less likely to die from COVID-19 than unvaccinated people.
“These data confirm that vaccination and boosting continues to protect against severe illness and hospitalization, even during the Omicron surge,” Rochelle Walensky, MD, director of the CDC, said during a briefing by the White House COVID-19 Response Team.
“If you are not up to date on your COVID-19 vaccinations, you have not optimized your protection against severe disease and death, and you should get vaccinated and boosted if you are eligible,” she said.
Dr. Walensky presented the latest numbers on Feb. 2 based on reports from 25 jurisdictions in early December. The number of average weekly deaths for those who were unvaccinated was 9.7 per 100,000 people, as compared with 0.7 of those who were vaccinated and 0.1 of those who had received a booster.
“The data are really stunningly obvious why a booster is really very important,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said during the briefing.
Dr. Fauci also encouraged vaccination for those who are pregnant and couples who may want to conceive in the near feature. He highlighted two recent studies that found vaccination in either partner didn’t affect fertility, including in vitro fertilization.
Meanwhile, fertility fell temporarily among men who were infected with the coronavirus. Couples were 18% less likely to conceive if the male partner had contracted the coronavirus within 60 days before a menstrual cycle.
“New data adds to previous studies that indicate that COVID-19 vaccination does not negatively impact fertility,” Dr. Fauci said. “Vaccination is recommended for people who are trying to get pregnant now or might become pregnant in the future, as well as their partners.”
About 80% of eligible Americans have received at least one vaccine dose, and 68% are fully vaccinated, according to the latest CDC data. About 51% of those who are eligible for a booster dose have received one.
The FDA could authorize the Pfizer vaccine for children under age 5 later this month. When that happens, about 18 million children will qualify for a shot, Jeff Zients, coordinator of the White House COVID-19 Response Team, said during the briefing. The Biden administration is already working on distribution plans for the shot for young kids, he added.
“We’ll be ready to start getting shots in arms soon after FDA and CDC make their decisions,” he said.
A version of this article first appeared on WebMD.com.
Global pediatric oncology workforce hit hard, but resilient amid pandemic
according to a study that surveyed workers from more than 200 institutions in 79 countries.
A snapshot of the extensive findings reveals that half of participating institutions experienced staffing shortages that had a “major impact” on pediatric cancer care. On the financial front, many respondents pointed to instances of unpaid leave and diminished salary, and others highlighted the psychological toll of providing care, including high rates of burnout and stress. The challenges were evident across high- and low-income countries.
Despite these barriers, pediatric oncology clinicians demonstrated incredible perseverance.
Health care professionals “caring for children with cancer across the world were shown to be incredibly resilient, coming together to continue to provide care even in the direst circumstances,” Elizabeth R. Sniderman, MSN, APRN, of St. Jude Children’s Research Hospital, Memphis, and colleagues concluded.
The findings, published online Jan. 24, 2022, in Cancer, highlight the global impact of COVID-19 on pediatric oncology clinicians early in the pandemic.
The survey, conducted in summer 2020, included responses from 311 pediatric oncology clinicians who completed a 60-item questionnaire about their experiences of clinical care, resources, and support. The investigators also convened 19 multidisciplinary focus groups who answered questions related to teamwork, communication, and changes to care. Respondents practiced in low- to high-income countries, and included pediatric hematologists and oncologists, nurses, and infectious disease physicians.
Overall, the investigators found that just over half of institutions experienced “major” shortages of clinical staff (108 of 213), and two-thirds experienced reductions in staffing availability (141 of 213). Notably, national income was not associated with this reduction; rather, staffing shortages were more likely to occur in countries with greater COVID-19 incidence and mortality rates.
Respondents reported experiencing threats to their physical health, with half pointing to a lack of necessary personal protective equipment. The financial and psychological toll of the pandemic represented another major stressor, with the effects described across all income levels.
One respondent from Belarus commented on financial concerns, noting that “people don’t really want to admit that they don’t feel well ... they know, that if infected, unpaid self-isolation is waiting for them. Either you don’t go to work for 2 weeks, unpaid, or you go to work for 2 weeks, paid, and endanger all of your colleagues with your infection.”
A respondent from Mexico described the psychological stress: “Honestly, I think that sometimes we put aside the mental health of all of us involved, myself included. I think we were all on the verge of collapse ... practically all the residents who were rotating here told us that they had anxiety attacks, panic attacks, they could not sleep, [and] many of them needed psychiatric medicine.”
Others highlighted feelings of guilt about their ability to provide the highest level of care. An oncologist in the United States noted: “This was a major stress for many providers because [we are] feeling unable to provide the same level of care which we used to provide. And this is what eventually takes a toll.”
And despite these pandemic-related challenges, the study authors found that only 46% of institutions (99 of 213) made psychological support available to staff.
Rays of hope
But it was not all bad news.
Participants also described a greater sense of teamwork, communication, and collegiality throughout the pandemic – “stabilizing elements,” which helped mitigate the many physical, psychological, and financial stressors.
An infection-control physician in Belarus highlighted the importance of receiving “support and encouragement” from colleagues: “When a person gets tired and they have no more enthusiasm, it’s easy to give up and say: ‘I can’t do this anymore.’ But when you see a colleague who tries ... to share the work, and help each other, then you get extra strength.”
An oncologist in South Africa agreed, noting that “everyone has got their sleeves rolled up and are doing the work ... and that’s a testament to everyone that we work with. There was no one that shied away from work or used this as an excuse to do less work.”
An oncologist in Spain described practicing during the pandemic being “one of the best experiences I have had,” explaining that “I have been working in this hospital for ... 25 years, [and] I have never had the feeling of being so informed at all levels.”
Overall, the findings paint a picture of a resilient workforce, and offer lessons about preparedness for future crises, the investigators concluded.
“To protect pediatric oncology providers and their patients, organizations must pay attention to interventions that increase physical, psychological, and financial safety,” the authors stressed. For instance, providing adequate personal protective equipment and vaccines, allowing for time off and rest, and setting up professional psychology services as well as access to peer-support programs can help protect staff.
Although this survey took place relatively early in the pandemic, organizations should take heed of the findings, Lorena V. Baroni, MD, of Hospital J P Garrahan, Buenos Aires, and Eric Bouffet, MD, of The Hospital for Sick Children, Toronto, wrote in an accompanying editorial.
“The results presented in this study should not be taken lightly,” Dr. Baroni and Dr. Bouffet wrote. “The most concerning findings are the physical and psychological impact experienced by pediatric oncology providers.” And perhaps most surprisingly, “the survey did not identify any difference based on country income groups. Participants in both low- and high-income countries described similar oncologic care limitations.”
Overall, these findings “reflect a serious risk that can ultimately affect the care of children and compromise the success of their treatment,” Dr. Baroni and Dr. Bouffet wrote.
This study was supported by the American Lebanese Syrian Associated Charities. The study authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a study that surveyed workers from more than 200 institutions in 79 countries.
A snapshot of the extensive findings reveals that half of participating institutions experienced staffing shortages that had a “major impact” on pediatric cancer care. On the financial front, many respondents pointed to instances of unpaid leave and diminished salary, and others highlighted the psychological toll of providing care, including high rates of burnout and stress. The challenges were evident across high- and low-income countries.
Despite these barriers, pediatric oncology clinicians demonstrated incredible perseverance.
Health care professionals “caring for children with cancer across the world were shown to be incredibly resilient, coming together to continue to provide care even in the direst circumstances,” Elizabeth R. Sniderman, MSN, APRN, of St. Jude Children’s Research Hospital, Memphis, and colleagues concluded.
The findings, published online Jan. 24, 2022, in Cancer, highlight the global impact of COVID-19 on pediatric oncology clinicians early in the pandemic.
The survey, conducted in summer 2020, included responses from 311 pediatric oncology clinicians who completed a 60-item questionnaire about their experiences of clinical care, resources, and support. The investigators also convened 19 multidisciplinary focus groups who answered questions related to teamwork, communication, and changes to care. Respondents practiced in low- to high-income countries, and included pediatric hematologists and oncologists, nurses, and infectious disease physicians.
Overall, the investigators found that just over half of institutions experienced “major” shortages of clinical staff (108 of 213), and two-thirds experienced reductions in staffing availability (141 of 213). Notably, national income was not associated with this reduction; rather, staffing shortages were more likely to occur in countries with greater COVID-19 incidence and mortality rates.
Respondents reported experiencing threats to their physical health, with half pointing to a lack of necessary personal protective equipment. The financial and psychological toll of the pandemic represented another major stressor, with the effects described across all income levels.
One respondent from Belarus commented on financial concerns, noting that “people don’t really want to admit that they don’t feel well ... they know, that if infected, unpaid self-isolation is waiting for them. Either you don’t go to work for 2 weeks, unpaid, or you go to work for 2 weeks, paid, and endanger all of your colleagues with your infection.”
A respondent from Mexico described the psychological stress: “Honestly, I think that sometimes we put aside the mental health of all of us involved, myself included. I think we were all on the verge of collapse ... practically all the residents who were rotating here told us that they had anxiety attacks, panic attacks, they could not sleep, [and] many of them needed psychiatric medicine.”
Others highlighted feelings of guilt about their ability to provide the highest level of care. An oncologist in the United States noted: “This was a major stress for many providers because [we are] feeling unable to provide the same level of care which we used to provide. And this is what eventually takes a toll.”
And despite these pandemic-related challenges, the study authors found that only 46% of institutions (99 of 213) made psychological support available to staff.
Rays of hope
But it was not all bad news.
Participants also described a greater sense of teamwork, communication, and collegiality throughout the pandemic – “stabilizing elements,” which helped mitigate the many physical, psychological, and financial stressors.
An infection-control physician in Belarus highlighted the importance of receiving “support and encouragement” from colleagues: “When a person gets tired and they have no more enthusiasm, it’s easy to give up and say: ‘I can’t do this anymore.’ But when you see a colleague who tries ... to share the work, and help each other, then you get extra strength.”
An oncologist in South Africa agreed, noting that “everyone has got their sleeves rolled up and are doing the work ... and that’s a testament to everyone that we work with. There was no one that shied away from work or used this as an excuse to do less work.”
An oncologist in Spain described practicing during the pandemic being “one of the best experiences I have had,” explaining that “I have been working in this hospital for ... 25 years, [and] I have never had the feeling of being so informed at all levels.”
Overall, the findings paint a picture of a resilient workforce, and offer lessons about preparedness for future crises, the investigators concluded.
“To protect pediatric oncology providers and their patients, organizations must pay attention to interventions that increase physical, psychological, and financial safety,” the authors stressed. For instance, providing adequate personal protective equipment and vaccines, allowing for time off and rest, and setting up professional psychology services as well as access to peer-support programs can help protect staff.
Although this survey took place relatively early in the pandemic, organizations should take heed of the findings, Lorena V. Baroni, MD, of Hospital J P Garrahan, Buenos Aires, and Eric Bouffet, MD, of The Hospital for Sick Children, Toronto, wrote in an accompanying editorial.
“The results presented in this study should not be taken lightly,” Dr. Baroni and Dr. Bouffet wrote. “The most concerning findings are the physical and psychological impact experienced by pediatric oncology providers.” And perhaps most surprisingly, “the survey did not identify any difference based on country income groups. Participants in both low- and high-income countries described similar oncologic care limitations.”
Overall, these findings “reflect a serious risk that can ultimately affect the care of children and compromise the success of their treatment,” Dr. Baroni and Dr. Bouffet wrote.
This study was supported by the American Lebanese Syrian Associated Charities. The study authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a study that surveyed workers from more than 200 institutions in 79 countries.
A snapshot of the extensive findings reveals that half of participating institutions experienced staffing shortages that had a “major impact” on pediatric cancer care. On the financial front, many respondents pointed to instances of unpaid leave and diminished salary, and others highlighted the psychological toll of providing care, including high rates of burnout and stress. The challenges were evident across high- and low-income countries.
Despite these barriers, pediatric oncology clinicians demonstrated incredible perseverance.
Health care professionals “caring for children with cancer across the world were shown to be incredibly resilient, coming together to continue to provide care even in the direst circumstances,” Elizabeth R. Sniderman, MSN, APRN, of St. Jude Children’s Research Hospital, Memphis, and colleagues concluded.
The findings, published online Jan. 24, 2022, in Cancer, highlight the global impact of COVID-19 on pediatric oncology clinicians early in the pandemic.
The survey, conducted in summer 2020, included responses from 311 pediatric oncology clinicians who completed a 60-item questionnaire about their experiences of clinical care, resources, and support. The investigators also convened 19 multidisciplinary focus groups who answered questions related to teamwork, communication, and changes to care. Respondents practiced in low- to high-income countries, and included pediatric hematologists and oncologists, nurses, and infectious disease physicians.
Overall, the investigators found that just over half of institutions experienced “major” shortages of clinical staff (108 of 213), and two-thirds experienced reductions in staffing availability (141 of 213). Notably, national income was not associated with this reduction; rather, staffing shortages were more likely to occur in countries with greater COVID-19 incidence and mortality rates.
Respondents reported experiencing threats to their physical health, with half pointing to a lack of necessary personal protective equipment. The financial and psychological toll of the pandemic represented another major stressor, with the effects described across all income levels.
One respondent from Belarus commented on financial concerns, noting that “people don’t really want to admit that they don’t feel well ... they know, that if infected, unpaid self-isolation is waiting for them. Either you don’t go to work for 2 weeks, unpaid, or you go to work for 2 weeks, paid, and endanger all of your colleagues with your infection.”
A respondent from Mexico described the psychological stress: “Honestly, I think that sometimes we put aside the mental health of all of us involved, myself included. I think we were all on the verge of collapse ... practically all the residents who were rotating here told us that they had anxiety attacks, panic attacks, they could not sleep, [and] many of them needed psychiatric medicine.”
Others highlighted feelings of guilt about their ability to provide the highest level of care. An oncologist in the United States noted: “This was a major stress for many providers because [we are] feeling unable to provide the same level of care which we used to provide. And this is what eventually takes a toll.”
And despite these pandemic-related challenges, the study authors found that only 46% of institutions (99 of 213) made psychological support available to staff.
Rays of hope
But it was not all bad news.
Participants also described a greater sense of teamwork, communication, and collegiality throughout the pandemic – “stabilizing elements,” which helped mitigate the many physical, psychological, and financial stressors.
An infection-control physician in Belarus highlighted the importance of receiving “support and encouragement” from colleagues: “When a person gets tired and they have no more enthusiasm, it’s easy to give up and say: ‘I can’t do this anymore.’ But when you see a colleague who tries ... to share the work, and help each other, then you get extra strength.”
An oncologist in South Africa agreed, noting that “everyone has got their sleeves rolled up and are doing the work ... and that’s a testament to everyone that we work with. There was no one that shied away from work or used this as an excuse to do less work.”
An oncologist in Spain described practicing during the pandemic being “one of the best experiences I have had,” explaining that “I have been working in this hospital for ... 25 years, [and] I have never had the feeling of being so informed at all levels.”
Overall, the findings paint a picture of a resilient workforce, and offer lessons about preparedness for future crises, the investigators concluded.
“To protect pediatric oncology providers and their patients, organizations must pay attention to interventions that increase physical, psychological, and financial safety,” the authors stressed. For instance, providing adequate personal protective equipment and vaccines, allowing for time off and rest, and setting up professional psychology services as well as access to peer-support programs can help protect staff.
Although this survey took place relatively early in the pandemic, organizations should take heed of the findings, Lorena V. Baroni, MD, of Hospital J P Garrahan, Buenos Aires, and Eric Bouffet, MD, of The Hospital for Sick Children, Toronto, wrote in an accompanying editorial.
“The results presented in this study should not be taken lightly,” Dr. Baroni and Dr. Bouffet wrote. “The most concerning findings are the physical and psychological impact experienced by pediatric oncology providers.” And perhaps most surprisingly, “the survey did not identify any difference based on country income groups. Participants in both low- and high-income countries described similar oncologic care limitations.”
Overall, these findings “reflect a serious risk that can ultimately affect the care of children and compromise the success of their treatment,” Dr. Baroni and Dr. Bouffet wrote.
This study was supported by the American Lebanese Syrian Associated Charities. The study authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CANCER


