User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Powered by CHEST Physician, Clinician Reviews, MDedge Family Medicine, Internal Medicine News, and The Journal of Clinical Outcomes Management.
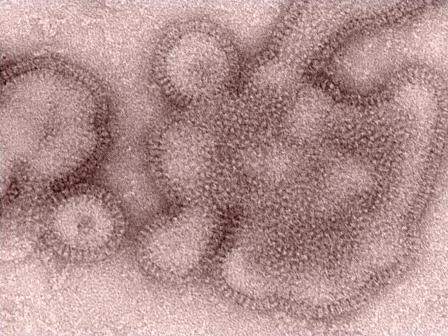
ICEID: TCAD regimen shows promise against H3N2 flu variant
ATLANTA – Triple combination antiviral drug therapy offers a broad-spectrum treatment option for H3N2 variant influenza virus, according to findings from an in vitro study.
The finding suggest that the combination could play an important role in the event of an influenza pandemic, Carrie Sitz reported in a poster at the International Conference on Emerging Infectious Diseases.
After a human infection with the novel A/H3N2 variant was reported in 2011, and trivalent inactivated influenza vaccine was found to be of limited use, as it provided protection against H3N2 but not the H3N2 variant (H3N2v) in ferrets and elicited cross-protection against H3N2 in young adults but not older adults or children, a triple combination antiviral therapy (TCAD) regimen was considered.
Amantadine, oseltamivir carboxylate, and ribavirin each were tested alone and in double and triple combinations against the novel H3N2 variant virus carrying genes from avian, swine, and human origins. Triple therapy achieved a therapeutic effect with lower doses of component drugs, compared with monotherapies of antivirals as single agents, said Ms. Sitz, a microbiology research assistant at the Naval Health Research Center, San Diego.
The agents, which each have different mechanisms of action and which function at distinct points in the virus life cycle, were tested using the various combinations in 96-well plates seeded with Madin-Darby Canine Kidney (MDCK) epithelial cells. They were found to produce synergistic antiviral activity, she noted.
A control experiment in the absence of the drugs also was performed.
Of note, amantadine had no activity as a single agent against H3N2v, even at 100 mcg/mL, the highest dose tested. However, amantadine did contribute to the synergy of the TCAD regimen. This effect was concentration dependent; the potential synergy volume increased steadily and significantly from about 300 to about 450, to about 575, and to about 600 as the amantadine concentration increased from +0.32, to +1.0, to +3.2, to +10, Ms. Sitz noted, adding that this may indicate that amantadine, which is known to have widespread resistance, can still play a therapeutic role in the setting of the TCAD regimen.
Vaccines are usually an effective safeguard against seasonal influenza but may be inadequate in seasons when a novel influenza emerges, resulting in compromised standard of care for treating the emergent viruses, she said, noting that this is especially true in immunocompromised patients.
“These issues point to the likelihood that we may be unprepared for a novel influenza virus displaying both virulence and transmissibility,” she added.
The current findings suggest that TCAD, which has previously been shown to be effective against seasonal and H5 influenza strains, is a broad-spectrum treatment option that could potentially play a role in pandemic preparedness. The mechanism by which oseltamivir carboxylate and ribavirin potentiate amantadine in combination therapy is unknown, and further testing is needed for evaluation, she concluded.
This study was sponsored by the Armed Forces Health Surveillance Center. The authors reported having no conflicts of interest.
ATLANTA – Triple combination antiviral drug therapy offers a broad-spectrum treatment option for H3N2 variant influenza virus, according to findings from an in vitro study.
The finding suggest that the combination could play an important role in the event of an influenza pandemic, Carrie Sitz reported in a poster at the International Conference on Emerging Infectious Diseases.
After a human infection with the novel A/H3N2 variant was reported in 2011, and trivalent inactivated influenza vaccine was found to be of limited use, as it provided protection against H3N2 but not the H3N2 variant (H3N2v) in ferrets and elicited cross-protection against H3N2 in young adults but not older adults or children, a triple combination antiviral therapy (TCAD) regimen was considered.
Amantadine, oseltamivir carboxylate, and ribavirin each were tested alone and in double and triple combinations against the novel H3N2 variant virus carrying genes from avian, swine, and human origins. Triple therapy achieved a therapeutic effect with lower doses of component drugs, compared with monotherapies of antivirals as single agents, said Ms. Sitz, a microbiology research assistant at the Naval Health Research Center, San Diego.
The agents, which each have different mechanisms of action and which function at distinct points in the virus life cycle, were tested using the various combinations in 96-well plates seeded with Madin-Darby Canine Kidney (MDCK) epithelial cells. They were found to produce synergistic antiviral activity, she noted.
A control experiment in the absence of the drugs also was performed.
Of note, amantadine had no activity as a single agent against H3N2v, even at 100 mcg/mL, the highest dose tested. However, amantadine did contribute to the synergy of the TCAD regimen. This effect was concentration dependent; the potential synergy volume increased steadily and significantly from about 300 to about 450, to about 575, and to about 600 as the amantadine concentration increased from +0.32, to +1.0, to +3.2, to +10, Ms. Sitz noted, adding that this may indicate that amantadine, which is known to have widespread resistance, can still play a therapeutic role in the setting of the TCAD regimen.
Vaccines are usually an effective safeguard against seasonal influenza but may be inadequate in seasons when a novel influenza emerges, resulting in compromised standard of care for treating the emergent viruses, she said, noting that this is especially true in immunocompromised patients.
“These issues point to the likelihood that we may be unprepared for a novel influenza virus displaying both virulence and transmissibility,” she added.
The current findings suggest that TCAD, which has previously been shown to be effective against seasonal and H5 influenza strains, is a broad-spectrum treatment option that could potentially play a role in pandemic preparedness. The mechanism by which oseltamivir carboxylate and ribavirin potentiate amantadine in combination therapy is unknown, and further testing is needed for evaluation, she concluded.
This study was sponsored by the Armed Forces Health Surveillance Center. The authors reported having no conflicts of interest.
ATLANTA – Triple combination antiviral drug therapy offers a broad-spectrum treatment option for H3N2 variant influenza virus, according to findings from an in vitro study.
The finding suggest that the combination could play an important role in the event of an influenza pandemic, Carrie Sitz reported in a poster at the International Conference on Emerging Infectious Diseases.
After a human infection with the novel A/H3N2 variant was reported in 2011, and trivalent inactivated influenza vaccine was found to be of limited use, as it provided protection against H3N2 but not the H3N2 variant (H3N2v) in ferrets and elicited cross-protection against H3N2 in young adults but not older adults or children, a triple combination antiviral therapy (TCAD) regimen was considered.
Amantadine, oseltamivir carboxylate, and ribavirin each were tested alone and in double and triple combinations against the novel H3N2 variant virus carrying genes from avian, swine, and human origins. Triple therapy achieved a therapeutic effect with lower doses of component drugs, compared with monotherapies of antivirals as single agents, said Ms. Sitz, a microbiology research assistant at the Naval Health Research Center, San Diego.
The agents, which each have different mechanisms of action and which function at distinct points in the virus life cycle, were tested using the various combinations in 96-well plates seeded with Madin-Darby Canine Kidney (MDCK) epithelial cells. They were found to produce synergistic antiviral activity, she noted.
A control experiment in the absence of the drugs also was performed.
Of note, amantadine had no activity as a single agent against H3N2v, even at 100 mcg/mL, the highest dose tested. However, amantadine did contribute to the synergy of the TCAD regimen. This effect was concentration dependent; the potential synergy volume increased steadily and significantly from about 300 to about 450, to about 575, and to about 600 as the amantadine concentration increased from +0.32, to +1.0, to +3.2, to +10, Ms. Sitz noted, adding that this may indicate that amantadine, which is known to have widespread resistance, can still play a therapeutic role in the setting of the TCAD regimen.
Vaccines are usually an effective safeguard against seasonal influenza but may be inadequate in seasons when a novel influenza emerges, resulting in compromised standard of care for treating the emergent viruses, she said, noting that this is especially true in immunocompromised patients.
“These issues point to the likelihood that we may be unprepared for a novel influenza virus displaying both virulence and transmissibility,” she added.
The current findings suggest that TCAD, which has previously been shown to be effective against seasonal and H5 influenza strains, is a broad-spectrum treatment option that could potentially play a role in pandemic preparedness. The mechanism by which oseltamivir carboxylate and ribavirin potentiate amantadine in combination therapy is unknown, and further testing is needed for evaluation, she concluded.
This study was sponsored by the Armed Forces Health Surveillance Center. The authors reported having no conflicts of interest.
AT ICEID 2015
Key clinical point: Triple combination antiviral drug therapy, or TCAD, offers a broad-spectrum treatment option for H3N2 variant influenza virus.
Major finding: Triple therapy achieved a therapeutic effect with lower doses of component drugs, compared with monotherapies of antivirals as single agents.
Data source: An in vitro study of TCAD for H3N2v.
Disclosures: This study was sponsored by the Armed Forces Health Surveillance Center. The authors reported having no conflicts of interest.
ICEID: Data highlight biofilm role in waterborne illness
ATLANTA – Emerging biofilm-associated pathogens are overtaking those transmitted by the fecal-oral route as the most-common cause of death from waterborne illness in the United States, according to findings from a review of administrative and disease-specific surveillance data.
Between 2003 and 2009, a mean of 2,516 deaths occurred per year as a result of exposure to 1 of more of 14 different waterborne germs or diseases, including campylobacteriosis, cryptosporidiosis, Escherichia coli infections, free-living amoeba, giardiasis, hemolytic uremic syndrome, hepatitis A, Legionnaires’ disease, nontuberculous Mycobacterium, otitis externa, Pseudomonas, salmonellosis, shigellosis, and vibriosis, Julia Gargano, Ph.D., reported in a poster at the International Conference on Emerging Infectious Diseases.
The most commonly documented causes of death, accounting for 88% of deaths, were Pseudomonas pneumonia or P. septicemia, nontuberculosis Mycobacterium, and Legionnaires’ disease – all biofilm pathogens. For those illnesses potentially linked to ingestion of contaminated water – as opposed to those associated with inhalation and contact – the most-commonly documented causes of death were hepatitis A, hemolytic uremic syndrome, and vibriosis, noted Dr. Gargano of the Center for Disease Control and Prevention’s National Center for Emerging and Zoonotic Infectious Diseases, Atlanta.
The findings were obtained from U.S. death certificates, the Nationwide Inpatient Sample, and disease-specific surveillance.
Although surveillance data consistently show that transmission of waterborne diarrheal diseases continue, such diseases are rarely fatal in the United States. Further, advances in water treatment and sanitation have reduced the burden of such diseases.
The findings of this study demonstrate that the burden of mortality has shifted.
“This is the first time the annual number of deaths due to potentially waterborne disease has been calculated, and [the findings] highlight the emerging trend in biofilm-related illness,” she wrote.
Dr. Gargano reported having no financial disclosures.
ATLANTA – Emerging biofilm-associated pathogens are overtaking those transmitted by the fecal-oral route as the most-common cause of death from waterborne illness in the United States, according to findings from a review of administrative and disease-specific surveillance data.
Between 2003 and 2009, a mean of 2,516 deaths occurred per year as a result of exposure to 1 of more of 14 different waterborne germs or diseases, including campylobacteriosis, cryptosporidiosis, Escherichia coli infections, free-living amoeba, giardiasis, hemolytic uremic syndrome, hepatitis A, Legionnaires’ disease, nontuberculous Mycobacterium, otitis externa, Pseudomonas, salmonellosis, shigellosis, and vibriosis, Julia Gargano, Ph.D., reported in a poster at the International Conference on Emerging Infectious Diseases.
The most commonly documented causes of death, accounting for 88% of deaths, were Pseudomonas pneumonia or P. septicemia, nontuberculosis Mycobacterium, and Legionnaires’ disease – all biofilm pathogens. For those illnesses potentially linked to ingestion of contaminated water – as opposed to those associated with inhalation and contact – the most-commonly documented causes of death were hepatitis A, hemolytic uremic syndrome, and vibriosis, noted Dr. Gargano of the Center for Disease Control and Prevention’s National Center for Emerging and Zoonotic Infectious Diseases, Atlanta.
The findings were obtained from U.S. death certificates, the Nationwide Inpatient Sample, and disease-specific surveillance.
Although surveillance data consistently show that transmission of waterborne diarrheal diseases continue, such diseases are rarely fatal in the United States. Further, advances in water treatment and sanitation have reduced the burden of such diseases.
The findings of this study demonstrate that the burden of mortality has shifted.
“This is the first time the annual number of deaths due to potentially waterborne disease has been calculated, and [the findings] highlight the emerging trend in biofilm-related illness,” she wrote.
Dr. Gargano reported having no financial disclosures.
ATLANTA – Emerging biofilm-associated pathogens are overtaking those transmitted by the fecal-oral route as the most-common cause of death from waterborne illness in the United States, according to findings from a review of administrative and disease-specific surveillance data.
Between 2003 and 2009, a mean of 2,516 deaths occurred per year as a result of exposure to 1 of more of 14 different waterborne germs or diseases, including campylobacteriosis, cryptosporidiosis, Escherichia coli infections, free-living amoeba, giardiasis, hemolytic uremic syndrome, hepatitis A, Legionnaires’ disease, nontuberculous Mycobacterium, otitis externa, Pseudomonas, salmonellosis, shigellosis, and vibriosis, Julia Gargano, Ph.D., reported in a poster at the International Conference on Emerging Infectious Diseases.
The most commonly documented causes of death, accounting for 88% of deaths, were Pseudomonas pneumonia or P. septicemia, nontuberculosis Mycobacterium, and Legionnaires’ disease – all biofilm pathogens. For those illnesses potentially linked to ingestion of contaminated water – as opposed to those associated with inhalation and contact – the most-commonly documented causes of death were hepatitis A, hemolytic uremic syndrome, and vibriosis, noted Dr. Gargano of the Center for Disease Control and Prevention’s National Center for Emerging and Zoonotic Infectious Diseases, Atlanta.
The findings were obtained from U.S. death certificates, the Nationwide Inpatient Sample, and disease-specific surveillance.
Although surveillance data consistently show that transmission of waterborne diarrheal diseases continue, such diseases are rarely fatal in the United States. Further, advances in water treatment and sanitation have reduced the burden of such diseases.
The findings of this study demonstrate that the burden of mortality has shifted.
“This is the first time the annual number of deaths due to potentially waterborne disease has been calculated, and [the findings] highlight the emerging trend in biofilm-related illness,” she wrote.
Dr. Gargano reported having no financial disclosures.
AT ICEID 2015
Key clinical point: Emerging biofilm-associated pathogens are overtaking those transmitted by the fecal-oral route as the most-common cause of death from waterborne illness in the United States.
Major finding: 88% of deaths resulted from Pseudomonas pneumonia or P. septicemia, nontuberculosis Mycobacterium, and Legionnaires’ disease – all biofilm pathogens.
Data source: A review of administrative and disease-specific surveillance data.
Disclosures: Dr. Gargano reported having no financial disclosures.
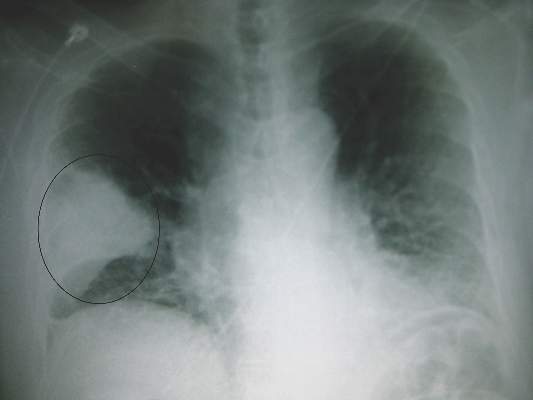
Share of lung cancer patients who never smoked is rising
DENVER – An increasing share of patients with lung cancer report that they have never smoked, according to a pair of retrospective cohort studies reported at a world conference on lung cancer.
At three U.S. institutions serving geographically and racially diverse populations, the proportion of never-smokers rose from 9% to 15% over a 24-year period among patients with non–small-cell lung cancer (NSCLC), but did not change among those with small-cell lung cancer (SCLC). At a U.K. tertiary care institution, the proportion of never-smokers rose from 13% to 27% over a 7-year period among patients undergoing surgery for lung cancer.
Data further suggested that these trends were due at least in part to an increase in the absolute number of never-smokers with lung cancer, and not simply to a decline in the proportion of smokers with lung cancer, or to earlier, incidental detection of tumors resulting from better imaging technology.
More research will be needed to determine the specific factors driving this increase, according to Dr. Everett E. Vokes, cochair of the conference, moderator of a related press conference, and the John E. Ultmann Professor and Chair, department of medicine, University of Chicago.
“What is causing this, for me, would be very, very speculative,” he said. “Secondhand smoke is still there, and radon is mentioned. That shouldn’t necessarily justify an increase, because those are either constant or also decreasing [like smoking]. And of course it could be pollution and factors that have to do with small particles and carcinogens in the air.”
In the first study, investigators led by Dr. Lorraine Pelosof of UT Southwestern Medical Center in Dallas used registries at three institutions – UT Southwestern Medical Center, Parkland Hospital in Dallas, and Vanderbilt University in Nashville, Tenn. – to identify patients who were diagnosed with lung cancer between 1990 and 2013.
Analyses were based on 10,593 patients with NSCLC and 1,510 patients with SCLC. The latter serve as an internal control given that cancer’s tight link with smoking, Dr. Pelosof noted.
In adjusted analyses, the proportion in the NSCLC group who reported never smoking increased from 9% to 15% during the study period (P less than .0001). In contrast, the proportion in the SCLC group held steady at roughly 2%.
Among patients with NSCLC, never-smokers were on average younger and more likely to be female compared with smokers, Dr. Pelosof reported at the conference, which was sponsored by the International Association for the Study of Lung Cancer.
In teasing out the cause for the rise in never-smokers with NSCLC, analyses showed that the absolute numbers of patients with NSCLC increased during the study period.
Preliminary data suggested that earlier, incidental detection did not explain the trend, as rates of stage I, II, and III disease in never-smokers were stable or decreased, while the rate of stage IV disease increased.
In addition, the trend did not appear to be explained by an influx to the institutions of patients with mutations seeking targeted therapies on clinical trials, as the trend persisted after adjustment for race/ethnicity, which was used as a surrogate for mutational status.
The investigators plan several avenues of additional research to sort this out, Dr. Pelosof said.
“We want to look at possibly other institutions that are geographically and demographically diverse. Additional institutions would be helpful,” she said. “And then to get at some of the mechanisms, [looking at] mutational status and biology I think would be very important.”
In the second study, Dr. Eric Lim, a consultant thoracic surgeon at Royal Brompton Hospital, and a senior lecturer and reader in thoracic surgery at the National Heart and Lung Institute, Imperial College, London, and colleagues assessed smoking status among 2,170 patients who underwent surgery for lung cancer at the hospital between 2008 and 2014.
Overall, 20% of the patients in the cohort were never-smokers. Their mean age at presentation was 60 years, and two-thirds were women. The predominant tumor types were adenocarcinoma, seen in 54%, and carcinoid, seen in 27%.
The proportion who were never-smokers more than doubled during the study period, from 13% to 27%. The absolute annual number of such patients also rose, from about 60 to nearly 100.
Fully 52% of the never-smokers presented with only nonspecific symptoms of cough or chest infection, while 11% had hemoptysis. In the remaining 36%, the cancer was identified as an incidental finding on imaging done for other reasons.
“Nonsmoking lung cancer is increasing and now a significant proportion of the workload for surgeons across the United Kingdom,” concluded Dr. Lim. “Early detection in this group is challenging because they have no clear-cut symptoms, and serious symptoms were only present in a minority,” he said.
“Clearly it’s not going to be cost-effective to screen the entire population of nonsmokers for lung cancer,” he added. Since these patients “do not have established risk factors, research into early detection, ideally by noninvasive or molecular screening, is urgently required to identify early lung cancer in nonsmokers.”
Dr. Pelosof and Dr. Lim reported having no conflicts of interest.
DENVER – An increasing share of patients with lung cancer report that they have never smoked, according to a pair of retrospective cohort studies reported at a world conference on lung cancer.
At three U.S. institutions serving geographically and racially diverse populations, the proportion of never-smokers rose from 9% to 15% over a 24-year period among patients with non–small-cell lung cancer (NSCLC), but did not change among those with small-cell lung cancer (SCLC). At a U.K. tertiary care institution, the proportion of never-smokers rose from 13% to 27% over a 7-year period among patients undergoing surgery for lung cancer.
Data further suggested that these trends were due at least in part to an increase in the absolute number of never-smokers with lung cancer, and not simply to a decline in the proportion of smokers with lung cancer, or to earlier, incidental detection of tumors resulting from better imaging technology.
More research will be needed to determine the specific factors driving this increase, according to Dr. Everett E. Vokes, cochair of the conference, moderator of a related press conference, and the John E. Ultmann Professor and Chair, department of medicine, University of Chicago.
“What is causing this, for me, would be very, very speculative,” he said. “Secondhand smoke is still there, and radon is mentioned. That shouldn’t necessarily justify an increase, because those are either constant or also decreasing [like smoking]. And of course it could be pollution and factors that have to do with small particles and carcinogens in the air.”
In the first study, investigators led by Dr. Lorraine Pelosof of UT Southwestern Medical Center in Dallas used registries at three institutions – UT Southwestern Medical Center, Parkland Hospital in Dallas, and Vanderbilt University in Nashville, Tenn. – to identify patients who were diagnosed with lung cancer between 1990 and 2013.
Analyses were based on 10,593 patients with NSCLC and 1,510 patients with SCLC. The latter serve as an internal control given that cancer’s tight link with smoking, Dr. Pelosof noted.
In adjusted analyses, the proportion in the NSCLC group who reported never smoking increased from 9% to 15% during the study period (P less than .0001). In contrast, the proportion in the SCLC group held steady at roughly 2%.
Among patients with NSCLC, never-smokers were on average younger and more likely to be female compared with smokers, Dr. Pelosof reported at the conference, which was sponsored by the International Association for the Study of Lung Cancer.
In teasing out the cause for the rise in never-smokers with NSCLC, analyses showed that the absolute numbers of patients with NSCLC increased during the study period.
Preliminary data suggested that earlier, incidental detection did not explain the trend, as rates of stage I, II, and III disease in never-smokers were stable or decreased, while the rate of stage IV disease increased.
In addition, the trend did not appear to be explained by an influx to the institutions of patients with mutations seeking targeted therapies on clinical trials, as the trend persisted after adjustment for race/ethnicity, which was used as a surrogate for mutational status.
The investigators plan several avenues of additional research to sort this out, Dr. Pelosof said.
“We want to look at possibly other institutions that are geographically and demographically diverse. Additional institutions would be helpful,” she said. “And then to get at some of the mechanisms, [looking at] mutational status and biology I think would be very important.”
In the second study, Dr. Eric Lim, a consultant thoracic surgeon at Royal Brompton Hospital, and a senior lecturer and reader in thoracic surgery at the National Heart and Lung Institute, Imperial College, London, and colleagues assessed smoking status among 2,170 patients who underwent surgery for lung cancer at the hospital between 2008 and 2014.
Overall, 20% of the patients in the cohort were never-smokers. Their mean age at presentation was 60 years, and two-thirds were women. The predominant tumor types were adenocarcinoma, seen in 54%, and carcinoid, seen in 27%.
The proportion who were never-smokers more than doubled during the study period, from 13% to 27%. The absolute annual number of such patients also rose, from about 60 to nearly 100.
Fully 52% of the never-smokers presented with only nonspecific symptoms of cough or chest infection, while 11% had hemoptysis. In the remaining 36%, the cancer was identified as an incidental finding on imaging done for other reasons.
“Nonsmoking lung cancer is increasing and now a significant proportion of the workload for surgeons across the United Kingdom,” concluded Dr. Lim. “Early detection in this group is challenging because they have no clear-cut symptoms, and serious symptoms were only present in a minority,” he said.
“Clearly it’s not going to be cost-effective to screen the entire population of nonsmokers for lung cancer,” he added. Since these patients “do not have established risk factors, research into early detection, ideally by noninvasive or molecular screening, is urgently required to identify early lung cancer in nonsmokers.”
Dr. Pelosof and Dr. Lim reported having no conflicts of interest.
DENVER – An increasing share of patients with lung cancer report that they have never smoked, according to a pair of retrospective cohort studies reported at a world conference on lung cancer.
At three U.S. institutions serving geographically and racially diverse populations, the proportion of never-smokers rose from 9% to 15% over a 24-year period among patients with non–small-cell lung cancer (NSCLC), but did not change among those with small-cell lung cancer (SCLC). At a U.K. tertiary care institution, the proportion of never-smokers rose from 13% to 27% over a 7-year period among patients undergoing surgery for lung cancer.
Data further suggested that these trends were due at least in part to an increase in the absolute number of never-smokers with lung cancer, and not simply to a decline in the proportion of smokers with lung cancer, or to earlier, incidental detection of tumors resulting from better imaging technology.
More research will be needed to determine the specific factors driving this increase, according to Dr. Everett E. Vokes, cochair of the conference, moderator of a related press conference, and the John E. Ultmann Professor and Chair, department of medicine, University of Chicago.
“What is causing this, for me, would be very, very speculative,” he said. “Secondhand smoke is still there, and radon is mentioned. That shouldn’t necessarily justify an increase, because those are either constant or also decreasing [like smoking]. And of course it could be pollution and factors that have to do with small particles and carcinogens in the air.”
In the first study, investigators led by Dr. Lorraine Pelosof of UT Southwestern Medical Center in Dallas used registries at three institutions – UT Southwestern Medical Center, Parkland Hospital in Dallas, and Vanderbilt University in Nashville, Tenn. – to identify patients who were diagnosed with lung cancer between 1990 and 2013.
Analyses were based on 10,593 patients with NSCLC and 1,510 patients with SCLC. The latter serve as an internal control given that cancer’s tight link with smoking, Dr. Pelosof noted.
In adjusted analyses, the proportion in the NSCLC group who reported never smoking increased from 9% to 15% during the study period (P less than .0001). In contrast, the proportion in the SCLC group held steady at roughly 2%.
Among patients with NSCLC, never-smokers were on average younger and more likely to be female compared with smokers, Dr. Pelosof reported at the conference, which was sponsored by the International Association for the Study of Lung Cancer.
In teasing out the cause for the rise in never-smokers with NSCLC, analyses showed that the absolute numbers of patients with NSCLC increased during the study period.
Preliminary data suggested that earlier, incidental detection did not explain the trend, as rates of stage I, II, and III disease in never-smokers were stable or decreased, while the rate of stage IV disease increased.
In addition, the trend did not appear to be explained by an influx to the institutions of patients with mutations seeking targeted therapies on clinical trials, as the trend persisted after adjustment for race/ethnicity, which was used as a surrogate for mutational status.
The investigators plan several avenues of additional research to sort this out, Dr. Pelosof said.
“We want to look at possibly other institutions that are geographically and demographically diverse. Additional institutions would be helpful,” she said. “And then to get at some of the mechanisms, [looking at] mutational status and biology I think would be very important.”
In the second study, Dr. Eric Lim, a consultant thoracic surgeon at Royal Brompton Hospital, and a senior lecturer and reader in thoracic surgery at the National Heart and Lung Institute, Imperial College, London, and colleagues assessed smoking status among 2,170 patients who underwent surgery for lung cancer at the hospital between 2008 and 2014.
Overall, 20% of the patients in the cohort were never-smokers. Their mean age at presentation was 60 years, and two-thirds were women. The predominant tumor types were adenocarcinoma, seen in 54%, and carcinoid, seen in 27%.
The proportion who were never-smokers more than doubled during the study period, from 13% to 27%. The absolute annual number of such patients also rose, from about 60 to nearly 100.
Fully 52% of the never-smokers presented with only nonspecific symptoms of cough or chest infection, while 11% had hemoptysis. In the remaining 36%, the cancer was identified as an incidental finding on imaging done for other reasons.
“Nonsmoking lung cancer is increasing and now a significant proportion of the workload for surgeons across the United Kingdom,” concluded Dr. Lim. “Early detection in this group is challenging because they have no clear-cut symptoms, and serious symptoms were only present in a minority,” he said.
“Clearly it’s not going to be cost-effective to screen the entire population of nonsmokers for lung cancer,” he added. Since these patients “do not have established risk factors, research into early detection, ideally by noninvasive or molecular screening, is urgently required to identify early lung cancer in nonsmokers.”
Dr. Pelosof and Dr. Lim reported having no conflicts of interest.
AT THE IASLC WORLD CONFERENCE
Key clinical point: The proportion of patients with lung cancer who have never smoked has risen in recent decades.
Major finding: Between 1990 and 2013 in the United States, the proportion with NSCLC who never smoked rose from 9% to 15%. Between 2008 and 2014 in the United Kingdom, the proportion undergoing surgery for lung cancer who never smoked rose from 13% to 27%.
Data source: A pair of retrospective cohort studies of 12,103 U.S. patients and 2,170 U.K. patients with lung cancer.
Disclosures: Dr. Pelosof and Dr. Lim reported having no conflicts of interest.
Peripartum probiotics linked to lower atopic dermatitis risk in offspring
Peripartum consumption of probiotic milk was associated with a decline in the incidence of atopic dermatitis in offspring, but other allergy-related diseases were not reduced in the children, the results of a randomized study indicate.
In a randomized study, 415 pregnant women drank eiher probiotic or placebo milk from 36 weeks’ gestation to 3 months postpartum. At 6 years follow-up, there was a lower cumulative incidence of AD in the probiotic group compared with the placebo group (OR = 0.64; 95% CI 0.39-1.07; p = .086; NNT = 10), Dr. Melanie Rae Simpson and coauthors from the Department of Public Health and General Practice Faculty of Medicine at the Norwegian University of Science and Technology in Trondheim, reported.
The children’s incidence of other allergy related diseases, including asthma, atopic sensitization, and allergic rhinoconjunctivitis, were not significantly changed by probiotic use, the investigators said in the report.
The findings suggest that perinatal probiotics prevent, rather than merely delay, the onset of childhood atopic dermatitis, the authors concluded.
Read the full article in BMC Dermatology.
Peripartum consumption of probiotic milk was associated with a decline in the incidence of atopic dermatitis in offspring, but other allergy-related diseases were not reduced in the children, the results of a randomized study indicate.
In a randomized study, 415 pregnant women drank eiher probiotic or placebo milk from 36 weeks’ gestation to 3 months postpartum. At 6 years follow-up, there was a lower cumulative incidence of AD in the probiotic group compared with the placebo group (OR = 0.64; 95% CI 0.39-1.07; p = .086; NNT = 10), Dr. Melanie Rae Simpson and coauthors from the Department of Public Health and General Practice Faculty of Medicine at the Norwegian University of Science and Technology in Trondheim, reported.
The children’s incidence of other allergy related diseases, including asthma, atopic sensitization, and allergic rhinoconjunctivitis, were not significantly changed by probiotic use, the investigators said in the report.
The findings suggest that perinatal probiotics prevent, rather than merely delay, the onset of childhood atopic dermatitis, the authors concluded.
Read the full article in BMC Dermatology.
Peripartum consumption of probiotic milk was associated with a decline in the incidence of atopic dermatitis in offspring, but other allergy-related diseases were not reduced in the children, the results of a randomized study indicate.
In a randomized study, 415 pregnant women drank eiher probiotic or placebo milk from 36 weeks’ gestation to 3 months postpartum. At 6 years follow-up, there was a lower cumulative incidence of AD in the probiotic group compared with the placebo group (OR = 0.64; 95% CI 0.39-1.07; p = .086; NNT = 10), Dr. Melanie Rae Simpson and coauthors from the Department of Public Health and General Practice Faculty of Medicine at the Norwegian University of Science and Technology in Trondheim, reported.
The children’s incidence of other allergy related diseases, including asthma, atopic sensitization, and allergic rhinoconjunctivitis, were not significantly changed by probiotic use, the investigators said in the report.
The findings suggest that perinatal probiotics prevent, rather than merely delay, the onset of childhood atopic dermatitis, the authors concluded.
Read the full article in BMC Dermatology.
IASLC issues new tobacco declaration
DENVER – The International Association for the Study of Lung Cancer (IASLC) this week released an updated Tobacco Control and Smoking Cessation declaration that outlines a set of measures aimed at reducing smoking and lung cancer.
The declaration could be viewed as a vaccine of sorts, according to Kenneth Michael Cummings, PhD, a professor at the Hollings Cancer Center, Medical University of South Carolina, and Co-Chair of IASLC’s Tobacco Control and Smoking Cessation Committee.
“How about a vaccine to prevent 80% of lung cancer deaths worldwide? We have it: get rid of cigarettes,” he said in a press conference at the World Congress on Lung Cancer, where the declaration was released.
The previous declaration, released in 2008, focused heavily on giving the Food and Drug Administration (FDA) the authority to regulate tobacco in the United States, which it now has. Since then, the economics of tobacco have evolved rapidly, and new products such as e-cigarettes have become available.
Also, 180 countries have ratified the World Health Organization’s Framework Convention on Tobacco Control (FCTC) treaty, allowing them to implement evidence-based policies such as smoke-free environments, warning labels, advertising bans, and taxation.
Nevertheless, lung cancer still accounts for nearly 2 million cases and 1.6 million lives lost each year. And at least 80% of those deaths are directly attributable to smoking, Dr. Cummings said.
In some parts of the world, cigarette consumption has declined, but “that’s not happening everywhere,” he said. “In parts of Asia, such as China, Japan, and Southeast Asia, and in Latin America, we are still seeing a rapid increase in lung cancer deaths. And in parts of the world which have not taken up smoking but are the targets of the industry, such as Africa and Indonesia, we are likely going to see an epidemic there, which can be prevented, which is really the point of our new statement.”
The 2015 declaration has five components that address tobacco control and smoking cessation.
The first component calls for forceful implementation of the FCTC treaty, especially through higher cigarette prices via taxation. “This is…the most important component of our ‘vaccine,’ for every member of this organization to really advocate for raising the cigarette prices to a level where it makes it unaffordable for young people to take up the behavior,” Dr. Cummings said. In low- and middle-income countries, where cigarettes remain relatively inexpensive, imposing a tax of at least 70% of the retail price would immediately cut consumption by about a third (N Engl J Med. 2014;370:60-8).
Trade policies and tobacco interference are related issues, he noted. “Our organization has been strong in trying to keep tobacco out of trade agreements.” Some countries, such as Malaysia, have refused to allow tobacco to be part of the Trans-Pacific Partnership agreement now under negotiation. “We need to support that (stance) because if tobacco is in there, we have countries being sued under trade agreements for doing the right things in terms of implementing policies.”
The declaration’s second component calls for holding cigarette companies civilly and criminally accountable for their actions. While Philip Morris International has stated that they support evidence-based regulation of tobacco, “I think our organization can help (by taking) cigarettes off the shelf today,” Dr. Cummings said. Holding manufacturers accountable in courts is another way to raise the price of cigarettes and thereby reduce consumption, he added.
The third component of the declaration is to support policies that keep young people from starting to smoke, such as raising the legal age of use to 21. “The neurobiology is very clear: the younger you are when you get exposed to an addictive substance, the more likely it is you are going to find it hard to quit at the end. So raising the legal age is certainly something we ought to do,” Dr. Cummings asserted, adding that 21 “is sort of a compromise” as the brain continues to develop until the age of 25.
Ensuring provision of tobacco-cessation services to all smokers, the declaration’s fourth component, is important no matter what a patient’s status. “Even in our cancer patients, it’s not too late. It has a big effect on their outcomes,” he said.
The fifth component is support for policies that address alternatives for nicotine delivery that are likely safer than cigarettes. “I don’t really care if companies make money selling something, but they don’t have to kill one out of two of their consumers to do it,” Dr. Cummings commented.
These alternatives might include e-cigarettes, provided evidence supports their inclusion. “I think that’s the problem we have with e-cigarettes today,” he said, noting that much less is known about them as compared with standard cigarettes, and that the products and manufacturers change monthly.
These factors have made it difficult for the FDA to address e-cigarettes. “They have done one thing I would have recommended they do: they have proposed deeming authority to take into account a whole variety of [tobacco] products,” he said. Although e-cigarettes contain a nicotine nebulizer with an electronic device, and as such could potentially have been regulated as medical devices just like nicotine patches and gum, courts have instead ruled that they are tobacco products.
“It’s a complex issue, but I’m all for getting people off of cigarettes, and there are alternative nicotine delivery devices,” Dr. Cummings concluded. “I think they need to be shown to be safe and effective.”
DENVER – The International Association for the Study of Lung Cancer (IASLC) this week released an updated Tobacco Control and Smoking Cessation declaration that outlines a set of measures aimed at reducing smoking and lung cancer.
The declaration could be viewed as a vaccine of sorts, according to Kenneth Michael Cummings, PhD, a professor at the Hollings Cancer Center, Medical University of South Carolina, and Co-Chair of IASLC’s Tobacco Control and Smoking Cessation Committee.
“How about a vaccine to prevent 80% of lung cancer deaths worldwide? We have it: get rid of cigarettes,” he said in a press conference at the World Congress on Lung Cancer, where the declaration was released.
The previous declaration, released in 2008, focused heavily on giving the Food and Drug Administration (FDA) the authority to regulate tobacco in the United States, which it now has. Since then, the economics of tobacco have evolved rapidly, and new products such as e-cigarettes have become available.
Also, 180 countries have ratified the World Health Organization’s Framework Convention on Tobacco Control (FCTC) treaty, allowing them to implement evidence-based policies such as smoke-free environments, warning labels, advertising bans, and taxation.
Nevertheless, lung cancer still accounts for nearly 2 million cases and 1.6 million lives lost each year. And at least 80% of those deaths are directly attributable to smoking, Dr. Cummings said.
In some parts of the world, cigarette consumption has declined, but “that’s not happening everywhere,” he said. “In parts of Asia, such as China, Japan, and Southeast Asia, and in Latin America, we are still seeing a rapid increase in lung cancer deaths. And in parts of the world which have not taken up smoking but are the targets of the industry, such as Africa and Indonesia, we are likely going to see an epidemic there, which can be prevented, which is really the point of our new statement.”
The 2015 declaration has five components that address tobacco control and smoking cessation.
The first component calls for forceful implementation of the FCTC treaty, especially through higher cigarette prices via taxation. “This is…the most important component of our ‘vaccine,’ for every member of this organization to really advocate for raising the cigarette prices to a level where it makes it unaffordable for young people to take up the behavior,” Dr. Cummings said. In low- and middle-income countries, where cigarettes remain relatively inexpensive, imposing a tax of at least 70% of the retail price would immediately cut consumption by about a third (N Engl J Med. 2014;370:60-8).
Trade policies and tobacco interference are related issues, he noted. “Our organization has been strong in trying to keep tobacco out of trade agreements.” Some countries, such as Malaysia, have refused to allow tobacco to be part of the Trans-Pacific Partnership agreement now under negotiation. “We need to support that (stance) because if tobacco is in there, we have countries being sued under trade agreements for doing the right things in terms of implementing policies.”
The declaration’s second component calls for holding cigarette companies civilly and criminally accountable for their actions. While Philip Morris International has stated that they support evidence-based regulation of tobacco, “I think our organization can help (by taking) cigarettes off the shelf today,” Dr. Cummings said. Holding manufacturers accountable in courts is another way to raise the price of cigarettes and thereby reduce consumption, he added.
The third component of the declaration is to support policies that keep young people from starting to smoke, such as raising the legal age of use to 21. “The neurobiology is very clear: the younger you are when you get exposed to an addictive substance, the more likely it is you are going to find it hard to quit at the end. So raising the legal age is certainly something we ought to do,” Dr. Cummings asserted, adding that 21 “is sort of a compromise” as the brain continues to develop until the age of 25.
Ensuring provision of tobacco-cessation services to all smokers, the declaration’s fourth component, is important no matter what a patient’s status. “Even in our cancer patients, it’s not too late. It has a big effect on their outcomes,” he said.
The fifth component is support for policies that address alternatives for nicotine delivery that are likely safer than cigarettes. “I don’t really care if companies make money selling something, but they don’t have to kill one out of two of their consumers to do it,” Dr. Cummings commented.
These alternatives might include e-cigarettes, provided evidence supports their inclusion. “I think that’s the problem we have with e-cigarettes today,” he said, noting that much less is known about them as compared with standard cigarettes, and that the products and manufacturers change monthly.
These factors have made it difficult for the FDA to address e-cigarettes. “They have done one thing I would have recommended they do: they have proposed deeming authority to take into account a whole variety of [tobacco] products,” he said. Although e-cigarettes contain a nicotine nebulizer with an electronic device, and as such could potentially have been regulated as medical devices just like nicotine patches and gum, courts have instead ruled that they are tobacco products.
“It’s a complex issue, but I’m all for getting people off of cigarettes, and there are alternative nicotine delivery devices,” Dr. Cummings concluded. “I think they need to be shown to be safe and effective.”
DENVER – The International Association for the Study of Lung Cancer (IASLC) this week released an updated Tobacco Control and Smoking Cessation declaration that outlines a set of measures aimed at reducing smoking and lung cancer.
The declaration could be viewed as a vaccine of sorts, according to Kenneth Michael Cummings, PhD, a professor at the Hollings Cancer Center, Medical University of South Carolina, and Co-Chair of IASLC’s Tobacco Control and Smoking Cessation Committee.
“How about a vaccine to prevent 80% of lung cancer deaths worldwide? We have it: get rid of cigarettes,” he said in a press conference at the World Congress on Lung Cancer, where the declaration was released.
The previous declaration, released in 2008, focused heavily on giving the Food and Drug Administration (FDA) the authority to regulate tobacco in the United States, which it now has. Since then, the economics of tobacco have evolved rapidly, and new products such as e-cigarettes have become available.
Also, 180 countries have ratified the World Health Organization’s Framework Convention on Tobacco Control (FCTC) treaty, allowing them to implement evidence-based policies such as smoke-free environments, warning labels, advertising bans, and taxation.
Nevertheless, lung cancer still accounts for nearly 2 million cases and 1.6 million lives lost each year. And at least 80% of those deaths are directly attributable to smoking, Dr. Cummings said.
In some parts of the world, cigarette consumption has declined, but “that’s not happening everywhere,” he said. “In parts of Asia, such as China, Japan, and Southeast Asia, and in Latin America, we are still seeing a rapid increase in lung cancer deaths. And in parts of the world which have not taken up smoking but are the targets of the industry, such as Africa and Indonesia, we are likely going to see an epidemic there, which can be prevented, which is really the point of our new statement.”
The 2015 declaration has five components that address tobacco control and smoking cessation.
The first component calls for forceful implementation of the FCTC treaty, especially through higher cigarette prices via taxation. “This is…the most important component of our ‘vaccine,’ for every member of this organization to really advocate for raising the cigarette prices to a level where it makes it unaffordable for young people to take up the behavior,” Dr. Cummings said. In low- and middle-income countries, where cigarettes remain relatively inexpensive, imposing a tax of at least 70% of the retail price would immediately cut consumption by about a third (N Engl J Med. 2014;370:60-8).
Trade policies and tobacco interference are related issues, he noted. “Our organization has been strong in trying to keep tobacco out of trade agreements.” Some countries, such as Malaysia, have refused to allow tobacco to be part of the Trans-Pacific Partnership agreement now under negotiation. “We need to support that (stance) because if tobacco is in there, we have countries being sued under trade agreements for doing the right things in terms of implementing policies.”
The declaration’s second component calls for holding cigarette companies civilly and criminally accountable for their actions. While Philip Morris International has stated that they support evidence-based regulation of tobacco, “I think our organization can help (by taking) cigarettes off the shelf today,” Dr. Cummings said. Holding manufacturers accountable in courts is another way to raise the price of cigarettes and thereby reduce consumption, he added.
The third component of the declaration is to support policies that keep young people from starting to smoke, such as raising the legal age of use to 21. “The neurobiology is very clear: the younger you are when you get exposed to an addictive substance, the more likely it is you are going to find it hard to quit at the end. So raising the legal age is certainly something we ought to do,” Dr. Cummings asserted, adding that 21 “is sort of a compromise” as the brain continues to develop until the age of 25.
Ensuring provision of tobacco-cessation services to all smokers, the declaration’s fourth component, is important no matter what a patient’s status. “Even in our cancer patients, it’s not too late. It has a big effect on their outcomes,” he said.
The fifth component is support for policies that address alternatives for nicotine delivery that are likely safer than cigarettes. “I don’t really care if companies make money selling something, but they don’t have to kill one out of two of their consumers to do it,” Dr. Cummings commented.
These alternatives might include e-cigarettes, provided evidence supports their inclusion. “I think that’s the problem we have with e-cigarettes today,” he said, noting that much less is known about them as compared with standard cigarettes, and that the products and manufacturers change monthly.
These factors have made it difficult for the FDA to address e-cigarettes. “They have done one thing I would have recommended they do: they have proposed deeming authority to take into account a whole variety of [tobacco] products,” he said. Although e-cigarettes contain a nicotine nebulizer with an electronic device, and as such could potentially have been regulated as medical devices just like nicotine patches and gum, courts have instead ruled that they are tobacco products.
“It’s a complex issue, but I’m all for getting people off of cigarettes, and there are alternative nicotine delivery devices,” Dr. Cummings concluded. “I think they need to be shown to be safe and effective.”
AT THE WORLD CONGRESS ON LUNG CANCER
Physicians rarely talk to teens about e-cigarettes
Although 86% of physicians surveyed reported routinely screening adolescent patients for cigarette smoking, only 14% routinely screened for electronic cigarette (e-cigarette) use; in fact, only 34% of physicians reported having ever discussed e-cigarettes during an adolescent’s visit, a survey-based study revealed.
As reported in the Journal of Adolescent Health, Jessica K. Pepper, Ph.D., of the University of North Carolina, Chapel Hill and her associates emailed invitations to complete a brief survey to 2,368 U.S. physician panel members with pediatric or family medicine specialties, of whom 776 (53% pediatricians, 47% family medicine physicians) were eligible and completed the survey.
Family medicine physicians had higher odds of engaging in prevention of e-cigarette use than pediatricians (26% vs. 18%; adjusted odds ratio, 1.57). Among the 34% of physicians who had conversations on e-cigarettes with adolescents during a clinical encounter, the most frequent topics of conversation were the potential health harms of using e-cigarettes (77%), discussions on not starting to use e-cigarettes (65%), whether e-cigarette use helps smokers quit (49%), and whether using e-cigarettes leads to smoking (42%). Also of note, 40% of physicians said they would, if asked, tell their patients that e-cigarettes are less harmful than cigarettes, and 24% would recommend e-cigarettes to adolescents for smoking cessation.
“The results of the present study suggest a need to improve routine screening and counseling for e-cigarette use among adolescents, and provide educational resources to physicians. Incorporating e-cigarettes into existing practice guidelines about tobacco use could boost prevention efforts and possibly prevent recommendation of e-cigarettes as smoking cessation tools for adolescents until there is conclusive evidence among youth,” the authors wrote.
Read the full article at the Journal of Adolescent Health.
Although 86% of physicians surveyed reported routinely screening adolescent patients for cigarette smoking, only 14% routinely screened for electronic cigarette (e-cigarette) use; in fact, only 34% of physicians reported having ever discussed e-cigarettes during an adolescent’s visit, a survey-based study revealed.
As reported in the Journal of Adolescent Health, Jessica K. Pepper, Ph.D., of the University of North Carolina, Chapel Hill and her associates emailed invitations to complete a brief survey to 2,368 U.S. physician panel members with pediatric or family medicine specialties, of whom 776 (53% pediatricians, 47% family medicine physicians) were eligible and completed the survey.
Family medicine physicians had higher odds of engaging in prevention of e-cigarette use than pediatricians (26% vs. 18%; adjusted odds ratio, 1.57). Among the 34% of physicians who had conversations on e-cigarettes with adolescents during a clinical encounter, the most frequent topics of conversation were the potential health harms of using e-cigarettes (77%), discussions on not starting to use e-cigarettes (65%), whether e-cigarette use helps smokers quit (49%), and whether using e-cigarettes leads to smoking (42%). Also of note, 40% of physicians said they would, if asked, tell their patients that e-cigarettes are less harmful than cigarettes, and 24% would recommend e-cigarettes to adolescents for smoking cessation.
“The results of the present study suggest a need to improve routine screening and counseling for e-cigarette use among adolescents, and provide educational resources to physicians. Incorporating e-cigarettes into existing practice guidelines about tobacco use could boost prevention efforts and possibly prevent recommendation of e-cigarettes as smoking cessation tools for adolescents until there is conclusive evidence among youth,” the authors wrote.
Read the full article at the Journal of Adolescent Health.
Although 86% of physicians surveyed reported routinely screening adolescent patients for cigarette smoking, only 14% routinely screened for electronic cigarette (e-cigarette) use; in fact, only 34% of physicians reported having ever discussed e-cigarettes during an adolescent’s visit, a survey-based study revealed.
As reported in the Journal of Adolescent Health, Jessica K. Pepper, Ph.D., of the University of North Carolina, Chapel Hill and her associates emailed invitations to complete a brief survey to 2,368 U.S. physician panel members with pediatric or family medicine specialties, of whom 776 (53% pediatricians, 47% family medicine physicians) were eligible and completed the survey.
Family medicine physicians had higher odds of engaging in prevention of e-cigarette use than pediatricians (26% vs. 18%; adjusted odds ratio, 1.57). Among the 34% of physicians who had conversations on e-cigarettes with adolescents during a clinical encounter, the most frequent topics of conversation were the potential health harms of using e-cigarettes (77%), discussions on not starting to use e-cigarettes (65%), whether e-cigarette use helps smokers quit (49%), and whether using e-cigarettes leads to smoking (42%). Also of note, 40% of physicians said they would, if asked, tell their patients that e-cigarettes are less harmful than cigarettes, and 24% would recommend e-cigarettes to adolescents for smoking cessation.
“The results of the present study suggest a need to improve routine screening and counseling for e-cigarette use among adolescents, and provide educational resources to physicians. Incorporating e-cigarettes into existing practice guidelines about tobacco use could boost prevention efforts and possibly prevent recommendation of e-cigarettes as smoking cessation tools for adolescents until there is conclusive evidence among youth,” the authors wrote.
Read the full article at the Journal of Adolescent Health.
FROM THE JOURNAL OF ADOLESCENT HEALTH
Adolescents’ unsupervised time with peers correlated with substance use
Adolescents’ unsupervised time with peers and participation in sports were significantly associated with substance use at the end of high school, according to a study.
The researchers examined longitudinal data on 766 adolescents from 10 locations across the United States. All of the research subjects’ participation in out-of-school time (OST) activities (unsupervised time with peers, sports, and other organized activities, such as band; and paid employment) and use of alcohol, marijuana, and tobacco were measured when they were 15 years old and when they were finishing high school.
More unsupervised time was correlated with higher amounts of all three types of substance use the researchers examined; for cigarette use (r = 0.19), for alcohol use (r = 0.23), and for marijuana use (r = 0.24). More involvement in paid employment also was related to higher amounts of cigarette (r = 0.10) and alcohol use (r = 0.08), but not marijuana use. More participation in sports was positively correlated only with more alcohol use (r = 0.10). In fact, greater participation in sports actually was associated with lower amounts of cigarette (r = –0.17) and marijuana use (r = –0.08).
“Consistent with predictions of Routine Activity Theory and with prior empirical research, more unsupervised time with peers was found to increase both the odds and amount of substance use reported by adolescents at the end of high school,” according to Kenneth T.H. Lee and Deborah Lowe Vandell, Ph.D., of the University of California, Irvine. “That these relations were found, even when time in other OST contexts were controlled, suggests that lack of adult supervision, the presence of peers, and minimal structure are important processes for influencing substance use in adolescence. Other forms of OST also appeared to be linked to substance use in adolescence, suggesting that these relations were not simply artifacts of a confounding with unsupervised time.”
Among this study’s unique findings are that participation in sports appeared to be a protective factor for marijuana and tobacco use, and that participation in other organized activities did not seem to play a significant protective role against substance use, according to the researchers.
Areas that were not addressed in this study include the amount of participation in different types of OST non-sports, organized activities, and paid employment, and the efficacy of reducing the amount of unsupervised time that adolescents spend with peers at preventing substance use and abuse.
Read the full study in the Journal of Adolescent Health (doi: 10.1016/j.jadohealth.2015.07.003).
Adolescents’ unsupervised time with peers and participation in sports were significantly associated with substance use at the end of high school, according to a study.
The researchers examined longitudinal data on 766 adolescents from 10 locations across the United States. All of the research subjects’ participation in out-of-school time (OST) activities (unsupervised time with peers, sports, and other organized activities, such as band; and paid employment) and use of alcohol, marijuana, and tobacco were measured when they were 15 years old and when they were finishing high school.
More unsupervised time was correlated with higher amounts of all three types of substance use the researchers examined; for cigarette use (r = 0.19), for alcohol use (r = 0.23), and for marijuana use (r = 0.24). More involvement in paid employment also was related to higher amounts of cigarette (r = 0.10) and alcohol use (r = 0.08), but not marijuana use. More participation in sports was positively correlated only with more alcohol use (r = 0.10). In fact, greater participation in sports actually was associated with lower amounts of cigarette (r = –0.17) and marijuana use (r = –0.08).
“Consistent with predictions of Routine Activity Theory and with prior empirical research, more unsupervised time with peers was found to increase both the odds and amount of substance use reported by adolescents at the end of high school,” according to Kenneth T.H. Lee and Deborah Lowe Vandell, Ph.D., of the University of California, Irvine. “That these relations were found, even when time in other OST contexts were controlled, suggests that lack of adult supervision, the presence of peers, and minimal structure are important processes for influencing substance use in adolescence. Other forms of OST also appeared to be linked to substance use in adolescence, suggesting that these relations were not simply artifacts of a confounding with unsupervised time.”
Among this study’s unique findings are that participation in sports appeared to be a protective factor for marijuana and tobacco use, and that participation in other organized activities did not seem to play a significant protective role against substance use, according to the researchers.
Areas that were not addressed in this study include the amount of participation in different types of OST non-sports, organized activities, and paid employment, and the efficacy of reducing the amount of unsupervised time that adolescents spend with peers at preventing substance use and abuse.
Read the full study in the Journal of Adolescent Health (doi: 10.1016/j.jadohealth.2015.07.003).
Adolescents’ unsupervised time with peers and participation in sports were significantly associated with substance use at the end of high school, according to a study.
The researchers examined longitudinal data on 766 adolescents from 10 locations across the United States. All of the research subjects’ participation in out-of-school time (OST) activities (unsupervised time with peers, sports, and other organized activities, such as band; and paid employment) and use of alcohol, marijuana, and tobacco were measured when they were 15 years old and when they were finishing high school.
More unsupervised time was correlated with higher amounts of all three types of substance use the researchers examined; for cigarette use (r = 0.19), for alcohol use (r = 0.23), and for marijuana use (r = 0.24). More involvement in paid employment also was related to higher amounts of cigarette (r = 0.10) and alcohol use (r = 0.08), but not marijuana use. More participation in sports was positively correlated only with more alcohol use (r = 0.10). In fact, greater participation in sports actually was associated with lower amounts of cigarette (r = –0.17) and marijuana use (r = –0.08).
“Consistent with predictions of Routine Activity Theory and with prior empirical research, more unsupervised time with peers was found to increase both the odds and amount of substance use reported by adolescents at the end of high school,” according to Kenneth T.H. Lee and Deborah Lowe Vandell, Ph.D., of the University of California, Irvine. “That these relations were found, even when time in other OST contexts were controlled, suggests that lack of adult supervision, the presence of peers, and minimal structure are important processes for influencing substance use in adolescence. Other forms of OST also appeared to be linked to substance use in adolescence, suggesting that these relations were not simply artifacts of a confounding with unsupervised time.”
Among this study’s unique findings are that participation in sports appeared to be a protective factor for marijuana and tobacco use, and that participation in other organized activities did not seem to play a significant protective role against substance use, according to the researchers.
Areas that were not addressed in this study include the amount of participation in different types of OST non-sports, organized activities, and paid employment, and the efficacy of reducing the amount of unsupervised time that adolescents spend with peers at preventing substance use and abuse.
Read the full study in the Journal of Adolescent Health (doi: 10.1016/j.jadohealth.2015.07.003).
FROM THE JOURNAL OF ADOLESCENT HEALTH
Extremes of sleep linked with early signs of CVD
Extremely short or extremely long sleep was associated with increased incidence of preclinical signs of cardiovascular disease in a large cross-sectional study of healthy and relatively young adults. Poor subjective sleep quality was also associated with early signs of CVD.
Dr. Chan-Won Kim of the Sungkyunkwan University in Seoul, South Korea, and his coinvestigators gathered self-reports of sleep quality and sleep duration from 47,309 healthy adults who underwent regularly scheduled physical examinations. Of those, 29,203 adults, 81% of whom were male, had measurement of coronary artery calcification (CAC); while 18,106 patients, 69% of whom were male, underwent brachial-ankle pulse wave velocity (baPWV) measurement. The patients were relatively young, with a mean age of 42 years for the CAC cohort and 46 for the baPWV cohort.
Coronary artery calcification and distal arterial stiffness are considered to be markers for preclinical CVD; by measuring these markers in a relatively young cohort, the investigators sought to avoid the many confounders that complicate the association between CVD and sleep in older patients with more comorbidities.
The study used multivariable analysis to control for factors such as smoking and alcohol use, marital status and education attainment, and physiologic variables including blood pressure, body mass index, and cholesterol.
Overall, more than 80% of subjects reported good subjective sleep quality, regardless of duration. However, women who reported poor sleep had a higher incidence of CAC, and men with poor sleep had a higher mean baPWV.
For sleep duration, Dr. Kim, Dr. Chang, and their colleagues found a U-shaped association between sleep duration and CAC and baPWV. Compared with individuals who slept 7 hours per night, individuals who reported sleeping less than 5 hours nightly had a CAC score ratio of 1.50, and an increase in baPWV of 6.7 cm/sec. At the other extreme, those who slept 9 or more hours per night had a CAC score ratio of 1.72 and an increase in baPWV of 9.6cm/sec. All these differences were statistically significant (Arterioscler Thromb Vasc Biol. 2015 Sept 10; doi: 10.1161/ATVBAHA.115.306110.).
The results help clarify that the previously known associations between sleep duration, quality, and CVD risk are not fully attributable to the comorbidities that can affect both sleep and heart health, said Dr. Kim and associates. Though they encourage further study to delineate sleep’s contribution to CVD, their results “underscore the importance of adequate sleep quantity and quality, and support the need for considering subjects with extreme duration or poor subjective quality of sleep at high risk for CVD,” they said.
On Twitter @karioakes
Extremely short or extremely long sleep was associated with increased incidence of preclinical signs of cardiovascular disease in a large cross-sectional study of healthy and relatively young adults. Poor subjective sleep quality was also associated with early signs of CVD.
Dr. Chan-Won Kim of the Sungkyunkwan University in Seoul, South Korea, and his coinvestigators gathered self-reports of sleep quality and sleep duration from 47,309 healthy adults who underwent regularly scheduled physical examinations. Of those, 29,203 adults, 81% of whom were male, had measurement of coronary artery calcification (CAC); while 18,106 patients, 69% of whom were male, underwent brachial-ankle pulse wave velocity (baPWV) measurement. The patients were relatively young, with a mean age of 42 years for the CAC cohort and 46 for the baPWV cohort.
Coronary artery calcification and distal arterial stiffness are considered to be markers for preclinical CVD; by measuring these markers in a relatively young cohort, the investigators sought to avoid the many confounders that complicate the association between CVD and sleep in older patients with more comorbidities.
The study used multivariable analysis to control for factors such as smoking and alcohol use, marital status and education attainment, and physiologic variables including blood pressure, body mass index, and cholesterol.
Overall, more than 80% of subjects reported good subjective sleep quality, regardless of duration. However, women who reported poor sleep had a higher incidence of CAC, and men with poor sleep had a higher mean baPWV.
For sleep duration, Dr. Kim, Dr. Chang, and their colleagues found a U-shaped association between sleep duration and CAC and baPWV. Compared with individuals who slept 7 hours per night, individuals who reported sleeping less than 5 hours nightly had a CAC score ratio of 1.50, and an increase in baPWV of 6.7 cm/sec. At the other extreme, those who slept 9 or more hours per night had a CAC score ratio of 1.72 and an increase in baPWV of 9.6cm/sec. All these differences were statistically significant (Arterioscler Thromb Vasc Biol. 2015 Sept 10; doi: 10.1161/ATVBAHA.115.306110.).
The results help clarify that the previously known associations between sleep duration, quality, and CVD risk are not fully attributable to the comorbidities that can affect both sleep and heart health, said Dr. Kim and associates. Though they encourage further study to delineate sleep’s contribution to CVD, their results “underscore the importance of adequate sleep quantity and quality, and support the need for considering subjects with extreme duration or poor subjective quality of sleep at high risk for CVD,” they said.
On Twitter @karioakes
Extremely short or extremely long sleep was associated with increased incidence of preclinical signs of cardiovascular disease in a large cross-sectional study of healthy and relatively young adults. Poor subjective sleep quality was also associated with early signs of CVD.
Dr. Chan-Won Kim of the Sungkyunkwan University in Seoul, South Korea, and his coinvestigators gathered self-reports of sleep quality and sleep duration from 47,309 healthy adults who underwent regularly scheduled physical examinations. Of those, 29,203 adults, 81% of whom were male, had measurement of coronary artery calcification (CAC); while 18,106 patients, 69% of whom were male, underwent brachial-ankle pulse wave velocity (baPWV) measurement. The patients were relatively young, with a mean age of 42 years for the CAC cohort and 46 for the baPWV cohort.
Coronary artery calcification and distal arterial stiffness are considered to be markers for preclinical CVD; by measuring these markers in a relatively young cohort, the investigators sought to avoid the many confounders that complicate the association between CVD and sleep in older patients with more comorbidities.
The study used multivariable analysis to control for factors such as smoking and alcohol use, marital status and education attainment, and physiologic variables including blood pressure, body mass index, and cholesterol.
Overall, more than 80% of subjects reported good subjective sleep quality, regardless of duration. However, women who reported poor sleep had a higher incidence of CAC, and men with poor sleep had a higher mean baPWV.
For sleep duration, Dr. Kim, Dr. Chang, and their colleagues found a U-shaped association between sleep duration and CAC and baPWV. Compared with individuals who slept 7 hours per night, individuals who reported sleeping less than 5 hours nightly had a CAC score ratio of 1.50, and an increase in baPWV of 6.7 cm/sec. At the other extreme, those who slept 9 or more hours per night had a CAC score ratio of 1.72 and an increase in baPWV of 9.6cm/sec. All these differences were statistically significant (Arterioscler Thromb Vasc Biol. 2015 Sept 10; doi: 10.1161/ATVBAHA.115.306110.).
The results help clarify that the previously known associations between sleep duration, quality, and CVD risk are not fully attributable to the comorbidities that can affect both sleep and heart health, said Dr. Kim and associates. Though they encourage further study to delineate sleep’s contribution to CVD, their results “underscore the importance of adequate sleep quantity and quality, and support the need for considering subjects with extreme duration or poor subjective quality of sleep at high risk for CVD,” they said.
On Twitter @karioakes
FROM ARTERIOSCLEROSIS, THROMBOSIS, AND VASCULAR BIOLOGY
Key clinical point: Individuals with very long or short sleep, or poor sleep quality, showed signs of early cardiovascular disease.
Major finding: Extremely short and extremely long sleep duration were associated with significantly increased levels of coronary artery calcification (CAC) and increased brachial-ankle pulse wave velocity (baPWV).
Data source: Cross-sectional study of more than 47,000 healthy adult men and women who reported sleep duration and quality, and underwent either measurement of CAC.
Disclosures: The funding source was not reported. The authors reported no disclosures.
VIDEO: Patients use CardioMEMS feedback to improve self-management
Some of the highly selected heart failure patients who have received the CardioMEMS device at Brigham and Women’s Hospital in Boston have shown clinically meaningful behavior changes in response to the feedback they receive on fluctuations in their pulmonary artery pressures. This feedback has prompted patients to change things like their salt and fluid intake so that they have fewer spikes in their pulmonary-artery diastolic pressure, an important step toward reducing their need for hospitalization because of acute decompensation episodes and possibly improving their long-term outcomes, Dr. Eldrin F. Lewis said in an interview.
“In our clinical practice we notice that when patients get feedback on their pulmonary-artery pressure they often change their behavior. In some patients their pulmonary-artery pressures normalized and stayed in the normal range more consistently,” said Dr. Lewis, a heart failure cardiologist at Brigham and Women’s. This apparent effect of daily monitoring of pulmonary artery pressure using CardioMEMS on patient behavior had not previously been assessed in the device’s clinical trials.
Those trials documented that diligent monitoring of pulmonary artery pressures and tweaking therapy to optimize those pressures led to significant reduction in heart failure hospitalizations, but Dr. Lewis and other heart failure specialists speculate that patients may reap other benefits.
“If we can dramatically reduce heart failure hospitalization rates in these patients, that should eventually translate into improved survival, and I think that by keeping fluid levels down it should also improve exercise capacity and quality of life,” he said.
The CardioMEMS monitoring system is marketed by St. Jude Medical. Dr. Lewis has no disclosures that involve St. Jude. He has received research grants from Amgen, Novartis, and Sanofi.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
Some of the highly selected heart failure patients who have received the CardioMEMS device at Brigham and Women’s Hospital in Boston have shown clinically meaningful behavior changes in response to the feedback they receive on fluctuations in their pulmonary artery pressures. This feedback has prompted patients to change things like their salt and fluid intake so that they have fewer spikes in their pulmonary-artery diastolic pressure, an important step toward reducing their need for hospitalization because of acute decompensation episodes and possibly improving their long-term outcomes, Dr. Eldrin F. Lewis said in an interview.
“In our clinical practice we notice that when patients get feedback on their pulmonary-artery pressure they often change their behavior. In some patients their pulmonary-artery pressures normalized and stayed in the normal range more consistently,” said Dr. Lewis, a heart failure cardiologist at Brigham and Women’s. This apparent effect of daily monitoring of pulmonary artery pressure using CardioMEMS on patient behavior had not previously been assessed in the device’s clinical trials.
Those trials documented that diligent monitoring of pulmonary artery pressures and tweaking therapy to optimize those pressures led to significant reduction in heart failure hospitalizations, but Dr. Lewis and other heart failure specialists speculate that patients may reap other benefits.
“If we can dramatically reduce heart failure hospitalization rates in these patients, that should eventually translate into improved survival, and I think that by keeping fluid levels down it should also improve exercise capacity and quality of life,” he said.
The CardioMEMS monitoring system is marketed by St. Jude Medical. Dr. Lewis has no disclosures that involve St. Jude. He has received research grants from Amgen, Novartis, and Sanofi.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
Some of the highly selected heart failure patients who have received the CardioMEMS device at Brigham and Women’s Hospital in Boston have shown clinically meaningful behavior changes in response to the feedback they receive on fluctuations in their pulmonary artery pressures. This feedback has prompted patients to change things like their salt and fluid intake so that they have fewer spikes in their pulmonary-artery diastolic pressure, an important step toward reducing their need for hospitalization because of acute decompensation episodes and possibly improving their long-term outcomes, Dr. Eldrin F. Lewis said in an interview.
“In our clinical practice we notice that when patients get feedback on their pulmonary-artery pressure they often change their behavior. In some patients their pulmonary-artery pressures normalized and stayed in the normal range more consistently,” said Dr. Lewis, a heart failure cardiologist at Brigham and Women’s. This apparent effect of daily monitoring of pulmonary artery pressure using CardioMEMS on patient behavior had not previously been assessed in the device’s clinical trials.
Those trials documented that diligent monitoring of pulmonary artery pressures and tweaking therapy to optimize those pressures led to significant reduction in heart failure hospitalizations, but Dr. Lewis and other heart failure specialists speculate that patients may reap other benefits.
“If we can dramatically reduce heart failure hospitalization rates in these patients, that should eventually translate into improved survival, and I think that by keeping fluid levels down it should also improve exercise capacity and quality of life,” he said.
The CardioMEMS monitoring system is marketed by St. Jude Medical. Dr. Lewis has no disclosures that involve St. Jude. He has received research grants from Amgen, Novartis, and Sanofi.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
Workshop tackles finer points of lung cancer screening
DENVER – In its third CT Screening Workshop, the Strategic Screening Advisory Committee of the International Association for the Study of Lung Cancer discussed the finer points of using this technology to screen for lung cancer, including issues such as metrics, quality control, and cost-effectiveness.
“Lung cancer is the major problem of all cancers,” committee chair Dr. John K. Field maintained in press conference at the annual World Conference on Lung Cancer, which was held in conjunction with the workshop. This cancer still causes more deaths than all of those from breast, colon, and prostate cancer combined.
“However, the good news is that the future does lie in early detection,” he said. The National Lung Screening Trial established that low-dose CT screening reduces the risk of lung cancer death by 20% compared with plain chest radiographic screening (N Engl J Med. 2011;365:395-409).
“That was the first time anybody had actually demonstrated such a mortality advantage with anything in lung cancer, so it led to an enormous stage shift in our thinking,” noted Dr. Field, who is also Personal Clinical Chair in Molecular Oncology at the University of Liverpool, England.
In the workshop, committee members reviewed new guidelines on managing screen-detected nodules from the ongoing NELSON (Dutch Belgian Randomised Lung Cancer Screening Trial) (Lancet Oncol. 2014;15:1332-41) and from the British Thoracic Society (Thorax. 2015;70:794-8). Main results from NELSON, as well as from the similar U.K. Lung Cancer Screening Trial, are expected shortly.
“We also looked at quality control for future screening programs. It’s extremely important that if we do have screening in place, that we have the necessary quality control behind it,” Dr. Field asserted.
Another topic discussed was whether CT screening is cost-effective. “Cost-effectiveness is going to be a major issue, especially in Europe,” where policy makers are awaiting results from the two trials before implementing screening, he said. “At this moment in time, it looks as though we will be cost-effective.”
The committee also assessed the potential of lung cancer biomarkers. “If we can actually improve the CT screening by using a particular biomarker, that would help us identify individuals easier. But also, once we undertake the CT, we are sometimes left with a gray situation of nodules that may become malignant but are not large enough to actually undertake any surgical intervention. And if we had a biomarker that would tell us if it was an aggressive tumor, that would be an enormous advantage,” Dr. Field elaborated.
Finally, the committee reviewed the status of national plans for implementing lung cancer CT screening around the world. Implementation is a multistep process requiring clinical experts and policy makers to hammer out a variety of issues, he noted (Lancet. 2013;382:732-41).
These issues include how best to identify individuals at high risk, typically accomplished with the LLP (Liverpool Lung Project) risk model in the United Kingdom and the PLCO (Prostate, Lung, Colorectal, and Ovarian) risk model in the United States. Screening age must also be considered. “In the U.K., our recommendation would probably be 60-75, but in the U.S. it would be 55-80, which came from the U.S. Preventive Services Task Force,” Dr. Field noted.
Another issue is whether nodules identified on CT are better measured by their maximal diameter (used in the National Lung Screening Trial) or their volume (used in the ongoing NELSON and U.K. trials). “There are advantages and disadvantages of both. We feel that volume is the way forward,” he said.
The nature of any subsequent work-up, including whether a biopsy is performed and additional tests, is also a consideration, as is the management of small nodules, including whether patients should undergo video-assisted thoracoscopic surgery.
Similarly, clinical experts and policy makers must decide on the optimal screening interval, whether every year or every 2 years, as well as the age at which to stop screening, he noted. And cost-effectiveness will be a critical point.
Workshop attendees from around the world shared current screening practices in their countries. “It’s quite clear that we all have different approaches, but we all have one objective: to identify high-risk individuals early. And we know if we identify them early, successful surgery will actually give them a long life,” Dr. Field said.
“Therefore, we feel that the future is through screening and we need to implement it. At this moment in time, the funding is there within the U.S., we are moving towards implementing it. In Europe, we are still waiting for the NELSON trial, but we are looking at an 18-month or 2-year period where that decision hopefully will be made,” he concluded.
Dr. Field disclosed no relevant conflicts of interest.
DENVER – In its third CT Screening Workshop, the Strategic Screening Advisory Committee of the International Association for the Study of Lung Cancer discussed the finer points of using this technology to screen for lung cancer, including issues such as metrics, quality control, and cost-effectiveness.
“Lung cancer is the major problem of all cancers,” committee chair Dr. John K. Field maintained in press conference at the annual World Conference on Lung Cancer, which was held in conjunction with the workshop. This cancer still causes more deaths than all of those from breast, colon, and prostate cancer combined.
“However, the good news is that the future does lie in early detection,” he said. The National Lung Screening Trial established that low-dose CT screening reduces the risk of lung cancer death by 20% compared with plain chest radiographic screening (N Engl J Med. 2011;365:395-409).
“That was the first time anybody had actually demonstrated such a mortality advantage with anything in lung cancer, so it led to an enormous stage shift in our thinking,” noted Dr. Field, who is also Personal Clinical Chair in Molecular Oncology at the University of Liverpool, England.
In the workshop, committee members reviewed new guidelines on managing screen-detected nodules from the ongoing NELSON (Dutch Belgian Randomised Lung Cancer Screening Trial) (Lancet Oncol. 2014;15:1332-41) and from the British Thoracic Society (Thorax. 2015;70:794-8). Main results from NELSON, as well as from the similar U.K. Lung Cancer Screening Trial, are expected shortly.
“We also looked at quality control for future screening programs. It’s extremely important that if we do have screening in place, that we have the necessary quality control behind it,” Dr. Field asserted.
Another topic discussed was whether CT screening is cost-effective. “Cost-effectiveness is going to be a major issue, especially in Europe,” where policy makers are awaiting results from the two trials before implementing screening, he said. “At this moment in time, it looks as though we will be cost-effective.”
The committee also assessed the potential of lung cancer biomarkers. “If we can actually improve the CT screening by using a particular biomarker, that would help us identify individuals easier. But also, once we undertake the CT, we are sometimes left with a gray situation of nodules that may become malignant but are not large enough to actually undertake any surgical intervention. And if we had a biomarker that would tell us if it was an aggressive tumor, that would be an enormous advantage,” Dr. Field elaborated.
Finally, the committee reviewed the status of national plans for implementing lung cancer CT screening around the world. Implementation is a multistep process requiring clinical experts and policy makers to hammer out a variety of issues, he noted (Lancet. 2013;382:732-41).
These issues include how best to identify individuals at high risk, typically accomplished with the LLP (Liverpool Lung Project) risk model in the United Kingdom and the PLCO (Prostate, Lung, Colorectal, and Ovarian) risk model in the United States. Screening age must also be considered. “In the U.K., our recommendation would probably be 60-75, but in the U.S. it would be 55-80, which came from the U.S. Preventive Services Task Force,” Dr. Field noted.
Another issue is whether nodules identified on CT are better measured by their maximal diameter (used in the National Lung Screening Trial) or their volume (used in the ongoing NELSON and U.K. trials). “There are advantages and disadvantages of both. We feel that volume is the way forward,” he said.
The nature of any subsequent work-up, including whether a biopsy is performed and additional tests, is also a consideration, as is the management of small nodules, including whether patients should undergo video-assisted thoracoscopic surgery.
Similarly, clinical experts and policy makers must decide on the optimal screening interval, whether every year or every 2 years, as well as the age at which to stop screening, he noted. And cost-effectiveness will be a critical point.
Workshop attendees from around the world shared current screening practices in their countries. “It’s quite clear that we all have different approaches, but we all have one objective: to identify high-risk individuals early. And we know if we identify them early, successful surgery will actually give them a long life,” Dr. Field said.
“Therefore, we feel that the future is through screening and we need to implement it. At this moment in time, the funding is there within the U.S., we are moving towards implementing it. In Europe, we are still waiting for the NELSON trial, but we are looking at an 18-month or 2-year period where that decision hopefully will be made,” he concluded.
Dr. Field disclosed no relevant conflicts of interest.
DENVER – In its third CT Screening Workshop, the Strategic Screening Advisory Committee of the International Association for the Study of Lung Cancer discussed the finer points of using this technology to screen for lung cancer, including issues such as metrics, quality control, and cost-effectiveness.
“Lung cancer is the major problem of all cancers,” committee chair Dr. John K. Field maintained in press conference at the annual World Conference on Lung Cancer, which was held in conjunction with the workshop. This cancer still causes more deaths than all of those from breast, colon, and prostate cancer combined.
“However, the good news is that the future does lie in early detection,” he said. The National Lung Screening Trial established that low-dose CT screening reduces the risk of lung cancer death by 20% compared with plain chest radiographic screening (N Engl J Med. 2011;365:395-409).
“That was the first time anybody had actually demonstrated such a mortality advantage with anything in lung cancer, so it led to an enormous stage shift in our thinking,” noted Dr. Field, who is also Personal Clinical Chair in Molecular Oncology at the University of Liverpool, England.
In the workshop, committee members reviewed new guidelines on managing screen-detected nodules from the ongoing NELSON (Dutch Belgian Randomised Lung Cancer Screening Trial) (Lancet Oncol. 2014;15:1332-41) and from the British Thoracic Society (Thorax. 2015;70:794-8). Main results from NELSON, as well as from the similar U.K. Lung Cancer Screening Trial, are expected shortly.
“We also looked at quality control for future screening programs. It’s extremely important that if we do have screening in place, that we have the necessary quality control behind it,” Dr. Field asserted.
Another topic discussed was whether CT screening is cost-effective. “Cost-effectiveness is going to be a major issue, especially in Europe,” where policy makers are awaiting results from the two trials before implementing screening, he said. “At this moment in time, it looks as though we will be cost-effective.”
The committee also assessed the potential of lung cancer biomarkers. “If we can actually improve the CT screening by using a particular biomarker, that would help us identify individuals easier. But also, once we undertake the CT, we are sometimes left with a gray situation of nodules that may become malignant but are not large enough to actually undertake any surgical intervention. And if we had a biomarker that would tell us if it was an aggressive tumor, that would be an enormous advantage,” Dr. Field elaborated.
Finally, the committee reviewed the status of national plans for implementing lung cancer CT screening around the world. Implementation is a multistep process requiring clinical experts and policy makers to hammer out a variety of issues, he noted (Lancet. 2013;382:732-41).
These issues include how best to identify individuals at high risk, typically accomplished with the LLP (Liverpool Lung Project) risk model in the United Kingdom and the PLCO (Prostate, Lung, Colorectal, and Ovarian) risk model in the United States. Screening age must also be considered. “In the U.K., our recommendation would probably be 60-75, but in the U.S. it would be 55-80, which came from the U.S. Preventive Services Task Force,” Dr. Field noted.
Another issue is whether nodules identified on CT are better measured by their maximal diameter (used in the National Lung Screening Trial) or their volume (used in the ongoing NELSON and U.K. trials). “There are advantages and disadvantages of both. We feel that volume is the way forward,” he said.
The nature of any subsequent work-up, including whether a biopsy is performed and additional tests, is also a consideration, as is the management of small nodules, including whether patients should undergo video-assisted thoracoscopic surgery.
Similarly, clinical experts and policy makers must decide on the optimal screening interval, whether every year or every 2 years, as well as the age at which to stop screening, he noted. And cost-effectiveness will be a critical point.
Workshop attendees from around the world shared current screening practices in their countries. “It’s quite clear that we all have different approaches, but we all have one objective: to identify high-risk individuals early. And we know if we identify them early, successful surgery will actually give them a long life,” Dr. Field said.
“Therefore, we feel that the future is through screening and we need to implement it. At this moment in time, the funding is there within the U.S., we are moving towards implementing it. In Europe, we are still waiting for the NELSON trial, but we are looking at an 18-month or 2-year period where that decision hopefully will be made,” he concluded.
Dr. Field disclosed no relevant conflicts of interest.
EXPERT ANALYSIS FROM THE IASLC WORLD CONFERENCE