User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Analysis boosts fluvoxamine for COVID, but what’s the evidence?
a new systematic review and meta-analysis has found. But outside experts differ over whether the evidence from just three studies is strong enough to warrant adding the drug to the COVID-19 armamentarium.
The report, published online in JAMA Network Open, looked at three studies and estimated that the drug could reduce the relative risk of hospitalization by around 25% (likelihood of moderate effect, 81.6%-91.8%), depending on the type of analysis used.
“This research might be valuable, but the jury remains out until several other adequately powered and designed trials are completed,” said infectious disease specialist Carl J. Fichtenbaum, MD, of the University of Cincinnati, who’s familiar with the findings. “I’m not sure how useful this is given we have several antiviral agents available. Why would we choose this over Paxlovid, remdesivir, or molnupiravir?”
According to Dr. Fichtenbaum, researchers began focusing on fluvoxamine after case reports about patients improving while on the medication. This led to further interest, he said, boosted by the drug’s known ability to dampen the immune system.
A Silicon Valley investor and antivaccine activist named Steve Kirsch has been pushing the drug along with the debunked treatment hydroxychloroquine. He’s accused the government of a cover-up of fluvoxamine’s worth, according to MIT Technology Review, and he wrote a commentary that referred to the drug as “the fast, easy, safe, simple, low-cost solution to COVID that works 100% of the time that nobody wants to talk about.”
For the new analysis, researchers examined three randomized clinical trials with a total of 2,196 participants. The most extensive trial, the TOGETHER study in Brazil (n = 1,497), focused on an unusual outcome: It linked the drug to a 32% reduction in relative risk of patients with COVID-19 being hospitalized in an ED for fewer than 6 hours or transferred to a tertiary hospital because of the disease.
Another study, the STOP COVID 2 trial in the United States and Canada (n = 547), was stopped because too few patients could be recruited to provide useful results. The initial phase of this trial, STOP COVID 1 (n = 152), was also included in the analysis.
All participants in the three studies were unvaccinated. Their median age was 46-50 years, 55%-72% were women, and 44%-56% were obese. Most were multiracial due to the high number of participants from Brazil.
“In the Bayesian analyses, the pooled risk ratio in favor of fluvoxamine was 0.78 (95% confidence interval, 0.58-1.08) for the weakly neutral prior and 0.73 (95% CI, 0.53-1.01) for the moderately optimistic prior,” the researchers reported, referring to a reduction in risk of hospitalization. “In the frequentist meta-analysis, the pooled risk ratio in favor of fluvoxamine was 0.75 (95% CI, 0.58-0.97; I2, 0.2%).”
Two of the authors of the new analysis were also coauthors of the TOGETHER trial and both STOP COVID trials.
Corresponding author Emily G. McDonald, MD, division of experimental medicine at McGill University, Montreal, said in an interview that the findings show fluvoxamine “very likely reduces hospitalization in high-risk outpatient adults with COVID-19. This effect varies depending on your baseline risk of developing complications in the first place.”
Dr. McDonald added that “fluvoxamine is an option to reduce hospitalizations in high-risk adults. It is likely effective, is inexpensive, and has a long safety track record.” She also noted that “not all countries have access to Paxlovid, and some people have drug interactions that preclude its use. Existing monoclonals are not effective with newer variants.”
The drug’s apparent anti-inflammatory properties seem to be key, she said. According to her, the next steps should be “testing lower doses to see if they remain effective, following patients long term to see what impact there is on long COVID symptoms, testing related medications in the drug class to see if they also show an effect, and testing in vaccinated people and with newer variants.”
In an interview, biostatistician James Watson, PhD, of the Mahidol Oxford Tropical Medicine Research Unit, Bangkok, Thailand, and Nuffield department of medicine, University of Oxford, England, said the findings of the analysis are “not overwhelming data.”
He noted the TOGETHER study’s unusual focus on ED visits that latest fewer than 6 hours, which he described as “not a very objective endpoint.” The new meta-analysis focused instead on “outcome data on emergency department visits lasting more than 24 hours and used this as a more representative proxy for hospital admission than an ED visit alone.”
Dr. Fichtenbaum also highlighted the odd endpoint. “Most of us would have chosen something like use of oxygen, requirement for ventilation, or death,” he said. “There are many reasons why people go to the ED. This endpoint is not very strong.”
He also noted that the three studies “are very different in design and endpoints.”
Jeffrey S. Morris, PhD, a biostatistician at the University of Pennsylvania, Philadelphia, offered a different perspective about the findings in an interview. “There’s good evidence that it helps some,” he said, and may reduce hospitalizations by 10%. “If the pill is super cheap and toxicity is very acceptable, it’s not adding additional risk. Most clinicians would say that: ‘If I’m reducing risk by 10%, it’s worthwhile.’ ”
No funding was reported. Two authors report having a patent application filed by Washington University for methods of treating COVID-19 during the conduct of the study. Dr. Watson is an investigator for studies analyzing antiviral drugs and Prozac as COVID-19 treatments. Dr. Fichtenbaum and Dr. Morris disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
a new systematic review and meta-analysis has found. But outside experts differ over whether the evidence from just three studies is strong enough to warrant adding the drug to the COVID-19 armamentarium.
The report, published online in JAMA Network Open, looked at three studies and estimated that the drug could reduce the relative risk of hospitalization by around 25% (likelihood of moderate effect, 81.6%-91.8%), depending on the type of analysis used.
“This research might be valuable, but the jury remains out until several other adequately powered and designed trials are completed,” said infectious disease specialist Carl J. Fichtenbaum, MD, of the University of Cincinnati, who’s familiar with the findings. “I’m not sure how useful this is given we have several antiviral agents available. Why would we choose this over Paxlovid, remdesivir, or molnupiravir?”
According to Dr. Fichtenbaum, researchers began focusing on fluvoxamine after case reports about patients improving while on the medication. This led to further interest, he said, boosted by the drug’s known ability to dampen the immune system.
A Silicon Valley investor and antivaccine activist named Steve Kirsch has been pushing the drug along with the debunked treatment hydroxychloroquine. He’s accused the government of a cover-up of fluvoxamine’s worth, according to MIT Technology Review, and he wrote a commentary that referred to the drug as “the fast, easy, safe, simple, low-cost solution to COVID that works 100% of the time that nobody wants to talk about.”
For the new analysis, researchers examined three randomized clinical trials with a total of 2,196 participants. The most extensive trial, the TOGETHER study in Brazil (n = 1,497), focused on an unusual outcome: It linked the drug to a 32% reduction in relative risk of patients with COVID-19 being hospitalized in an ED for fewer than 6 hours or transferred to a tertiary hospital because of the disease.
Another study, the STOP COVID 2 trial in the United States and Canada (n = 547), was stopped because too few patients could be recruited to provide useful results. The initial phase of this trial, STOP COVID 1 (n = 152), was also included in the analysis.
All participants in the three studies were unvaccinated. Their median age was 46-50 years, 55%-72% were women, and 44%-56% were obese. Most were multiracial due to the high number of participants from Brazil.
“In the Bayesian analyses, the pooled risk ratio in favor of fluvoxamine was 0.78 (95% confidence interval, 0.58-1.08) for the weakly neutral prior and 0.73 (95% CI, 0.53-1.01) for the moderately optimistic prior,” the researchers reported, referring to a reduction in risk of hospitalization. “In the frequentist meta-analysis, the pooled risk ratio in favor of fluvoxamine was 0.75 (95% CI, 0.58-0.97; I2, 0.2%).”
Two of the authors of the new analysis were also coauthors of the TOGETHER trial and both STOP COVID trials.
Corresponding author Emily G. McDonald, MD, division of experimental medicine at McGill University, Montreal, said in an interview that the findings show fluvoxamine “very likely reduces hospitalization in high-risk outpatient adults with COVID-19. This effect varies depending on your baseline risk of developing complications in the first place.”
Dr. McDonald added that “fluvoxamine is an option to reduce hospitalizations in high-risk adults. It is likely effective, is inexpensive, and has a long safety track record.” She also noted that “not all countries have access to Paxlovid, and some people have drug interactions that preclude its use. Existing monoclonals are not effective with newer variants.”
The drug’s apparent anti-inflammatory properties seem to be key, she said. According to her, the next steps should be “testing lower doses to see if they remain effective, following patients long term to see what impact there is on long COVID symptoms, testing related medications in the drug class to see if they also show an effect, and testing in vaccinated people and with newer variants.”
In an interview, biostatistician James Watson, PhD, of the Mahidol Oxford Tropical Medicine Research Unit, Bangkok, Thailand, and Nuffield department of medicine, University of Oxford, England, said the findings of the analysis are “not overwhelming data.”
He noted the TOGETHER study’s unusual focus on ED visits that latest fewer than 6 hours, which he described as “not a very objective endpoint.” The new meta-analysis focused instead on “outcome data on emergency department visits lasting more than 24 hours and used this as a more representative proxy for hospital admission than an ED visit alone.”
Dr. Fichtenbaum also highlighted the odd endpoint. “Most of us would have chosen something like use of oxygen, requirement for ventilation, or death,” he said. “There are many reasons why people go to the ED. This endpoint is not very strong.”
He also noted that the three studies “are very different in design and endpoints.”
Jeffrey S. Morris, PhD, a biostatistician at the University of Pennsylvania, Philadelphia, offered a different perspective about the findings in an interview. “There’s good evidence that it helps some,” he said, and may reduce hospitalizations by 10%. “If the pill is super cheap and toxicity is very acceptable, it’s not adding additional risk. Most clinicians would say that: ‘If I’m reducing risk by 10%, it’s worthwhile.’ ”
No funding was reported. Two authors report having a patent application filed by Washington University for methods of treating COVID-19 during the conduct of the study. Dr. Watson is an investigator for studies analyzing antiviral drugs and Prozac as COVID-19 treatments. Dr. Fichtenbaum and Dr. Morris disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
a new systematic review and meta-analysis has found. But outside experts differ over whether the evidence from just three studies is strong enough to warrant adding the drug to the COVID-19 armamentarium.
The report, published online in JAMA Network Open, looked at three studies and estimated that the drug could reduce the relative risk of hospitalization by around 25% (likelihood of moderate effect, 81.6%-91.8%), depending on the type of analysis used.
“This research might be valuable, but the jury remains out until several other adequately powered and designed trials are completed,” said infectious disease specialist Carl J. Fichtenbaum, MD, of the University of Cincinnati, who’s familiar with the findings. “I’m not sure how useful this is given we have several antiviral agents available. Why would we choose this over Paxlovid, remdesivir, or molnupiravir?”
According to Dr. Fichtenbaum, researchers began focusing on fluvoxamine after case reports about patients improving while on the medication. This led to further interest, he said, boosted by the drug’s known ability to dampen the immune system.
A Silicon Valley investor and antivaccine activist named Steve Kirsch has been pushing the drug along with the debunked treatment hydroxychloroquine. He’s accused the government of a cover-up of fluvoxamine’s worth, according to MIT Technology Review, and he wrote a commentary that referred to the drug as “the fast, easy, safe, simple, low-cost solution to COVID that works 100% of the time that nobody wants to talk about.”
For the new analysis, researchers examined three randomized clinical trials with a total of 2,196 participants. The most extensive trial, the TOGETHER study in Brazil (n = 1,497), focused on an unusual outcome: It linked the drug to a 32% reduction in relative risk of patients with COVID-19 being hospitalized in an ED for fewer than 6 hours or transferred to a tertiary hospital because of the disease.
Another study, the STOP COVID 2 trial in the United States and Canada (n = 547), was stopped because too few patients could be recruited to provide useful results. The initial phase of this trial, STOP COVID 1 (n = 152), was also included in the analysis.
All participants in the three studies were unvaccinated. Their median age was 46-50 years, 55%-72% were women, and 44%-56% were obese. Most were multiracial due to the high number of participants from Brazil.
“In the Bayesian analyses, the pooled risk ratio in favor of fluvoxamine was 0.78 (95% confidence interval, 0.58-1.08) for the weakly neutral prior and 0.73 (95% CI, 0.53-1.01) for the moderately optimistic prior,” the researchers reported, referring to a reduction in risk of hospitalization. “In the frequentist meta-analysis, the pooled risk ratio in favor of fluvoxamine was 0.75 (95% CI, 0.58-0.97; I2, 0.2%).”
Two of the authors of the new analysis were also coauthors of the TOGETHER trial and both STOP COVID trials.
Corresponding author Emily G. McDonald, MD, division of experimental medicine at McGill University, Montreal, said in an interview that the findings show fluvoxamine “very likely reduces hospitalization in high-risk outpatient adults with COVID-19. This effect varies depending on your baseline risk of developing complications in the first place.”
Dr. McDonald added that “fluvoxamine is an option to reduce hospitalizations in high-risk adults. It is likely effective, is inexpensive, and has a long safety track record.” She also noted that “not all countries have access to Paxlovid, and some people have drug interactions that preclude its use. Existing monoclonals are not effective with newer variants.”
The drug’s apparent anti-inflammatory properties seem to be key, she said. According to her, the next steps should be “testing lower doses to see if they remain effective, following patients long term to see what impact there is on long COVID symptoms, testing related medications in the drug class to see if they also show an effect, and testing in vaccinated people and with newer variants.”
In an interview, biostatistician James Watson, PhD, of the Mahidol Oxford Tropical Medicine Research Unit, Bangkok, Thailand, and Nuffield department of medicine, University of Oxford, England, said the findings of the analysis are “not overwhelming data.”
He noted the TOGETHER study’s unusual focus on ED visits that latest fewer than 6 hours, which he described as “not a very objective endpoint.” The new meta-analysis focused instead on “outcome data on emergency department visits lasting more than 24 hours and used this as a more representative proxy for hospital admission than an ED visit alone.”
Dr. Fichtenbaum also highlighted the odd endpoint. “Most of us would have chosen something like use of oxygen, requirement for ventilation, or death,” he said. “There are many reasons why people go to the ED. This endpoint is not very strong.”
He also noted that the three studies “are very different in design and endpoints.”
Jeffrey S. Morris, PhD, a biostatistician at the University of Pennsylvania, Philadelphia, offered a different perspective about the findings in an interview. “There’s good evidence that it helps some,” he said, and may reduce hospitalizations by 10%. “If the pill is super cheap and toxicity is very acceptable, it’s not adding additional risk. Most clinicians would say that: ‘If I’m reducing risk by 10%, it’s worthwhile.’ ”
No funding was reported. Two authors report having a patent application filed by Washington University for methods of treating COVID-19 during the conduct of the study. Dr. Watson is an investigator for studies analyzing antiviral drugs and Prozac as COVID-19 treatments. Dr. Fichtenbaum and Dr. Morris disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
COVID cases rising in about half of states
About half the states have reported increases in COVID cases fueled by the Omicron subvariant, Axios reported. Alaska, Vermont, and Rhode Island had the highest increases, with more than 20 new cases per 100,000 people.
Nationally, the statistics are encouraging, with the 7-day average of daily cases around 26,000 on April 6, down from around 41,000 on March 6, according to the Centers for Disease Control and Prevention. The number of deaths has dropped to an average of around 600 a day, down 34% from 2 weeks ago.
National health officials have said some spots would have a lot of COVID cases.
“Looking across the country, we see that 95% of counties are reporting low COVID-19 community levels, which represent over 97% of the U.S. population,” CDC Director Rochelle Walensky, MD, said April 5 at a White House news briefing.
“If we look more closely at the local level, we find a handful of counties where we are seeing increases in both cases and markers of more severe disease, like hospitalizations and in-patient bed capacity, which have resulted in an increased COVID-19 community level in some areas.”
Meanwhile, the Commonwealth Fund issued a report April 8 saying the U.S. vaccine program had prevented an estimated 2.2 million deaths and 17 million hospitalizations.
If the vaccine program didn’t exist, the United States would have had another 66 million COVID infections and spent about $900 billion more on health care, the foundation said.
The United States has reported about 982,000 COVID-related deaths so far with about 80 million COVID cases, according to the CDC.
“Our findings highlight the profound and ongoing impact of the vaccination program in reducing infections, hospitalizations, and deaths,” the Commonwealth Fund said.
“Investing in vaccination programs also has produced substantial cost savings – approximately the size of one-fifth of annual national health expenditures – by dramatically reducing the amount spent on COVID-19 hospitalizations.”
A version of this article first appeared on WebMD.com.
About half the states have reported increases in COVID cases fueled by the Omicron subvariant, Axios reported. Alaska, Vermont, and Rhode Island had the highest increases, with more than 20 new cases per 100,000 people.
Nationally, the statistics are encouraging, with the 7-day average of daily cases around 26,000 on April 6, down from around 41,000 on March 6, according to the Centers for Disease Control and Prevention. The number of deaths has dropped to an average of around 600 a day, down 34% from 2 weeks ago.
National health officials have said some spots would have a lot of COVID cases.
“Looking across the country, we see that 95% of counties are reporting low COVID-19 community levels, which represent over 97% of the U.S. population,” CDC Director Rochelle Walensky, MD, said April 5 at a White House news briefing.
“If we look more closely at the local level, we find a handful of counties where we are seeing increases in both cases and markers of more severe disease, like hospitalizations and in-patient bed capacity, which have resulted in an increased COVID-19 community level in some areas.”
Meanwhile, the Commonwealth Fund issued a report April 8 saying the U.S. vaccine program had prevented an estimated 2.2 million deaths and 17 million hospitalizations.
If the vaccine program didn’t exist, the United States would have had another 66 million COVID infections and spent about $900 billion more on health care, the foundation said.
The United States has reported about 982,000 COVID-related deaths so far with about 80 million COVID cases, according to the CDC.
“Our findings highlight the profound and ongoing impact of the vaccination program in reducing infections, hospitalizations, and deaths,” the Commonwealth Fund said.
“Investing in vaccination programs also has produced substantial cost savings – approximately the size of one-fifth of annual national health expenditures – by dramatically reducing the amount spent on COVID-19 hospitalizations.”
A version of this article first appeared on WebMD.com.
About half the states have reported increases in COVID cases fueled by the Omicron subvariant, Axios reported. Alaska, Vermont, and Rhode Island had the highest increases, with more than 20 new cases per 100,000 people.
Nationally, the statistics are encouraging, with the 7-day average of daily cases around 26,000 on April 6, down from around 41,000 on March 6, according to the Centers for Disease Control and Prevention. The number of deaths has dropped to an average of around 600 a day, down 34% from 2 weeks ago.
National health officials have said some spots would have a lot of COVID cases.
“Looking across the country, we see that 95% of counties are reporting low COVID-19 community levels, which represent over 97% of the U.S. population,” CDC Director Rochelle Walensky, MD, said April 5 at a White House news briefing.
“If we look more closely at the local level, we find a handful of counties where we are seeing increases in both cases and markers of more severe disease, like hospitalizations and in-patient bed capacity, which have resulted in an increased COVID-19 community level in some areas.”
Meanwhile, the Commonwealth Fund issued a report April 8 saying the U.S. vaccine program had prevented an estimated 2.2 million deaths and 17 million hospitalizations.
If the vaccine program didn’t exist, the United States would have had another 66 million COVID infections and spent about $900 billion more on health care, the foundation said.
The United States has reported about 982,000 COVID-related deaths so far with about 80 million COVID cases, according to the CDC.
“Our findings highlight the profound and ongoing impact of the vaccination program in reducing infections, hospitalizations, and deaths,” the Commonwealth Fund said.
“Investing in vaccination programs also has produced substantial cost savings – approximately the size of one-fifth of annual national health expenditures – by dramatically reducing the amount spent on COVID-19 hospitalizations.”
A version of this article first appeared on WebMD.com.
Transgender youth: Bringing evidence to the political debates
In 2021, state lawmakers introduced a record number of bills that would affect transgender and gender-diverse people. The vast majority were focused on transgender and gender-diverse youth in particular. We’ve seen bills that would take away gender-affirming medical care for minors, ones that would force trans kids to play on sports teams that don’t match their gender identity, and others that would ban trans kids from public facilities like bathrooms that match their gender identities.
These bills aren’t particularly new, but state lawmakers are putting more energy into them than ever. In response, some public figures have started pushing back. Ariana Grande just pledged to match up to 1.5 million dollars in donations to combat anti–trans youth legislative initiatives. However, doctors have been underrepresented in the political discourse.
Sadly, much of the discussion in this area has been driven by wild speculation and emotional rhetoric. It’s rare that we see actual data brought to the table. As clinicians and scientists, we have a responsibility to highlight the data relevant to these legislative debates, and to share them with our representatives. I’m going to break down what we know quantitatively about each of these issues, so that you’ll feel empowered to bring that information to these debates. My hope is that we can move toward evidence-based public policy instead of rhetoric-based public policy, so that we can ensure the best health possible for young people around the country.
Bathroom bills
Though they’ve been less of a focus recently, politicians for years have argued that trans people should be forced to use bathrooms and other public facilities that match their sex assigned at birth, not their gender identity. Their central argument is that trans-inclusive public facility policies will result in higher rates of assault. Published peer-review data show this isn’t true. A 2019 study in Sexuality Research and Social Policy examined the impacts of trans-inclusive public facility policies and found they resulted in no increase in assaults among the general (mostly cisgender) population. Another 2019 study in Pediatrics found that trans-inclusive facility policies were associated with lower odds of sexual assault victimization against transgender youth. The myth that trans-inclusive public facilities increase assault risk is simply that: a myth. All existing data indicate that trans-inclusive policies will improve public safety.
Sports bills
One of the hottest debates recently involves whether transgender girls should be allowed to participate in girls’ sports teams. Those in favor of these bills argue that transgender girls have an innate biological sports advantage over cisgender girls, and if allowed to compete in girls’ sports leagues, they will dominate the events, and cisgender girls will no longer win sports titles. The bills feed into longstanding assumptions – those who were assigned male at birth are strong, and those who were assigned female at birth are weak.
But evidence doesn’t show that trans women dominate female sports leagues. It turns out, there are shockingly few transgender athletes competing in sports leagues around the United States, and even fewer winning major titles. When the Associated Press conducted an investigation asking lawmakers introducing such sports bills to name trans athletes in their states, most couldn’t point to a single one. After Utah state legislators passed a trans sports ban, Governor Spencer Cox vetoed it, pointing out that, of 75,000 high school kids participating in sports in Utah, there was only a single transgender girl (the state legislature overrode the veto anyway).
California has explicitly protected the rights of trans athletes to compete on sports teams that match their gender identity since 2013. There’s still an underrepresentation of trans athletes in sports participation and titles. This is likely because the deck is stacked against these young people in so many other ways that are unrelated to testosterone levels. Trans youth suffer from high rates of harassment, discrimination, and subsequent anxiety and depression that make it difficult to compete in and excel in sports.
Medical bills
State legislators have introduced bills around the country that would criminalize the provision of gender-affirming medical care for transgender youth. Though such bills are opposed by all major medical organizations (including the American Medical Association, the American Academy of Pediatrics, the American Academy of Child & Adolescent Psychiatry, and the American Psychiatric Association), misinformation continues to spread, and in some instances the bills have become law (though none are currently active due to legal challenges).
Clinicians should be aware that there have been sixteen studies to date, each with unique study designs, that have overall linked gender-affirming medical care for transgender youth to better mental health outcomes. While these interventions do (as with all medications) carry some risks (like delayed bone mineralization with pubertal suppression), the risks must be weighed against potential benefits. Unfortunately, these risks and benefits have not been accurately portrayed in state legislative debates. Politicians have spread a great deal of misinformation about gender-affirming medical care for transgender youth, including false assertions that puberty blockers cause infertility and that most transgender adolescents will grow up to identify as cisgender and regret gender-affirming medical interventions.
Minority stress
These bills have direct consequences for pediatric patients. For example, trans-inclusive bathroom policies are associated with lower rates of sexual assault. However, there are also important indirect effects to consider. The gender minority stress framework explains the ways in which stigmatizing national discourse drives higher rates of anxiety, depression, and suicidality among transgender youth. Under this model, so-called “distal factors” like the recent conversations at the national level that marginalize trans young people, are expected to drive higher rates of adverse mental health outcomes. As transgender youth hear high-profile politicians argue that they’re dangerous to their peers in bathrooms and on sports teams, it’s difficult to imagine their mental health would not worsen. Over time, such “distal factors” also lead to “proximal factors” like internalized transphobia in which youth begin to believe the negative things that are said about them. These dangerous processes can have dramatic negative impacts on self-esteem and emotional development. There is strong precedence that public policies have strong indirect mental health effects on LGBTQ youth.
We’ve entered a dangerous era in which politicians are legislating medical care and other aspects of public policy with the potential to hurt the mental health of our young patients. It’s imperative that clinicians and scientists contact their legislators to make sure they are voting for public policy based on data and fact, not misinformation and political rhetoric. The health of American children depends on it.
Dr. Turban (twitter.com/jack_turban) is a chief fellow in child and adolescent psychiatry at Stanford (Calif.) University.
In 2021, state lawmakers introduced a record number of bills that would affect transgender and gender-diverse people. The vast majority were focused on transgender and gender-diverse youth in particular. We’ve seen bills that would take away gender-affirming medical care for minors, ones that would force trans kids to play on sports teams that don’t match their gender identity, and others that would ban trans kids from public facilities like bathrooms that match their gender identities.
These bills aren’t particularly new, but state lawmakers are putting more energy into them than ever. In response, some public figures have started pushing back. Ariana Grande just pledged to match up to 1.5 million dollars in donations to combat anti–trans youth legislative initiatives. However, doctors have been underrepresented in the political discourse.
Sadly, much of the discussion in this area has been driven by wild speculation and emotional rhetoric. It’s rare that we see actual data brought to the table. As clinicians and scientists, we have a responsibility to highlight the data relevant to these legislative debates, and to share them with our representatives. I’m going to break down what we know quantitatively about each of these issues, so that you’ll feel empowered to bring that information to these debates. My hope is that we can move toward evidence-based public policy instead of rhetoric-based public policy, so that we can ensure the best health possible for young people around the country.
Bathroom bills
Though they’ve been less of a focus recently, politicians for years have argued that trans people should be forced to use bathrooms and other public facilities that match their sex assigned at birth, not their gender identity. Their central argument is that trans-inclusive public facility policies will result in higher rates of assault. Published peer-review data show this isn’t true. A 2019 study in Sexuality Research and Social Policy examined the impacts of trans-inclusive public facility policies and found they resulted in no increase in assaults among the general (mostly cisgender) population. Another 2019 study in Pediatrics found that trans-inclusive facility policies were associated with lower odds of sexual assault victimization against transgender youth. The myth that trans-inclusive public facilities increase assault risk is simply that: a myth. All existing data indicate that trans-inclusive policies will improve public safety.
Sports bills
One of the hottest debates recently involves whether transgender girls should be allowed to participate in girls’ sports teams. Those in favor of these bills argue that transgender girls have an innate biological sports advantage over cisgender girls, and if allowed to compete in girls’ sports leagues, they will dominate the events, and cisgender girls will no longer win sports titles. The bills feed into longstanding assumptions – those who were assigned male at birth are strong, and those who were assigned female at birth are weak.
But evidence doesn’t show that trans women dominate female sports leagues. It turns out, there are shockingly few transgender athletes competing in sports leagues around the United States, and even fewer winning major titles. When the Associated Press conducted an investigation asking lawmakers introducing such sports bills to name trans athletes in their states, most couldn’t point to a single one. After Utah state legislators passed a trans sports ban, Governor Spencer Cox vetoed it, pointing out that, of 75,000 high school kids participating in sports in Utah, there was only a single transgender girl (the state legislature overrode the veto anyway).
California has explicitly protected the rights of trans athletes to compete on sports teams that match their gender identity since 2013. There’s still an underrepresentation of trans athletes in sports participation and titles. This is likely because the deck is stacked against these young people in so many other ways that are unrelated to testosterone levels. Trans youth suffer from high rates of harassment, discrimination, and subsequent anxiety and depression that make it difficult to compete in and excel in sports.
Medical bills
State legislators have introduced bills around the country that would criminalize the provision of gender-affirming medical care for transgender youth. Though such bills are opposed by all major medical organizations (including the American Medical Association, the American Academy of Pediatrics, the American Academy of Child & Adolescent Psychiatry, and the American Psychiatric Association), misinformation continues to spread, and in some instances the bills have become law (though none are currently active due to legal challenges).
Clinicians should be aware that there have been sixteen studies to date, each with unique study designs, that have overall linked gender-affirming medical care for transgender youth to better mental health outcomes. While these interventions do (as with all medications) carry some risks (like delayed bone mineralization with pubertal suppression), the risks must be weighed against potential benefits. Unfortunately, these risks and benefits have not been accurately portrayed in state legislative debates. Politicians have spread a great deal of misinformation about gender-affirming medical care for transgender youth, including false assertions that puberty blockers cause infertility and that most transgender adolescents will grow up to identify as cisgender and regret gender-affirming medical interventions.
Minority stress
These bills have direct consequences for pediatric patients. For example, trans-inclusive bathroom policies are associated with lower rates of sexual assault. However, there are also important indirect effects to consider. The gender minority stress framework explains the ways in which stigmatizing national discourse drives higher rates of anxiety, depression, and suicidality among transgender youth. Under this model, so-called “distal factors” like the recent conversations at the national level that marginalize trans young people, are expected to drive higher rates of adverse mental health outcomes. As transgender youth hear high-profile politicians argue that they’re dangerous to their peers in bathrooms and on sports teams, it’s difficult to imagine their mental health would not worsen. Over time, such “distal factors” also lead to “proximal factors” like internalized transphobia in which youth begin to believe the negative things that are said about them. These dangerous processes can have dramatic negative impacts on self-esteem and emotional development. There is strong precedence that public policies have strong indirect mental health effects on LGBTQ youth.
We’ve entered a dangerous era in which politicians are legislating medical care and other aspects of public policy with the potential to hurt the mental health of our young patients. It’s imperative that clinicians and scientists contact their legislators to make sure they are voting for public policy based on data and fact, not misinformation and political rhetoric. The health of American children depends on it.
Dr. Turban (twitter.com/jack_turban) is a chief fellow in child and adolescent psychiatry at Stanford (Calif.) University.
In 2021, state lawmakers introduced a record number of bills that would affect transgender and gender-diverse people. The vast majority were focused on transgender and gender-diverse youth in particular. We’ve seen bills that would take away gender-affirming medical care for minors, ones that would force trans kids to play on sports teams that don’t match their gender identity, and others that would ban trans kids from public facilities like bathrooms that match their gender identities.
These bills aren’t particularly new, but state lawmakers are putting more energy into them than ever. In response, some public figures have started pushing back. Ariana Grande just pledged to match up to 1.5 million dollars in donations to combat anti–trans youth legislative initiatives. However, doctors have been underrepresented in the political discourse.
Sadly, much of the discussion in this area has been driven by wild speculation and emotional rhetoric. It’s rare that we see actual data brought to the table. As clinicians and scientists, we have a responsibility to highlight the data relevant to these legislative debates, and to share them with our representatives. I’m going to break down what we know quantitatively about each of these issues, so that you’ll feel empowered to bring that information to these debates. My hope is that we can move toward evidence-based public policy instead of rhetoric-based public policy, so that we can ensure the best health possible for young people around the country.
Bathroom bills
Though they’ve been less of a focus recently, politicians for years have argued that trans people should be forced to use bathrooms and other public facilities that match their sex assigned at birth, not their gender identity. Their central argument is that trans-inclusive public facility policies will result in higher rates of assault. Published peer-review data show this isn’t true. A 2019 study in Sexuality Research and Social Policy examined the impacts of trans-inclusive public facility policies and found they resulted in no increase in assaults among the general (mostly cisgender) population. Another 2019 study in Pediatrics found that trans-inclusive facility policies were associated with lower odds of sexual assault victimization against transgender youth. The myth that trans-inclusive public facilities increase assault risk is simply that: a myth. All existing data indicate that trans-inclusive policies will improve public safety.
Sports bills
One of the hottest debates recently involves whether transgender girls should be allowed to participate in girls’ sports teams. Those in favor of these bills argue that transgender girls have an innate biological sports advantage over cisgender girls, and if allowed to compete in girls’ sports leagues, they will dominate the events, and cisgender girls will no longer win sports titles. The bills feed into longstanding assumptions – those who were assigned male at birth are strong, and those who were assigned female at birth are weak.
But evidence doesn’t show that trans women dominate female sports leagues. It turns out, there are shockingly few transgender athletes competing in sports leagues around the United States, and even fewer winning major titles. When the Associated Press conducted an investigation asking lawmakers introducing such sports bills to name trans athletes in their states, most couldn’t point to a single one. After Utah state legislators passed a trans sports ban, Governor Spencer Cox vetoed it, pointing out that, of 75,000 high school kids participating in sports in Utah, there was only a single transgender girl (the state legislature overrode the veto anyway).
California has explicitly protected the rights of trans athletes to compete on sports teams that match their gender identity since 2013. There’s still an underrepresentation of trans athletes in sports participation and titles. This is likely because the deck is stacked against these young people in so many other ways that are unrelated to testosterone levels. Trans youth suffer from high rates of harassment, discrimination, and subsequent anxiety and depression that make it difficult to compete in and excel in sports.
Medical bills
State legislators have introduced bills around the country that would criminalize the provision of gender-affirming medical care for transgender youth. Though such bills are opposed by all major medical organizations (including the American Medical Association, the American Academy of Pediatrics, the American Academy of Child & Adolescent Psychiatry, and the American Psychiatric Association), misinformation continues to spread, and in some instances the bills have become law (though none are currently active due to legal challenges).
Clinicians should be aware that there have been sixteen studies to date, each with unique study designs, that have overall linked gender-affirming medical care for transgender youth to better mental health outcomes. While these interventions do (as with all medications) carry some risks (like delayed bone mineralization with pubertal suppression), the risks must be weighed against potential benefits. Unfortunately, these risks and benefits have not been accurately portrayed in state legislative debates. Politicians have spread a great deal of misinformation about gender-affirming medical care for transgender youth, including false assertions that puberty blockers cause infertility and that most transgender adolescents will grow up to identify as cisgender and regret gender-affirming medical interventions.
Minority stress
These bills have direct consequences for pediatric patients. For example, trans-inclusive bathroom policies are associated with lower rates of sexual assault. However, there are also important indirect effects to consider. The gender minority stress framework explains the ways in which stigmatizing national discourse drives higher rates of anxiety, depression, and suicidality among transgender youth. Under this model, so-called “distal factors” like the recent conversations at the national level that marginalize trans young people, are expected to drive higher rates of adverse mental health outcomes. As transgender youth hear high-profile politicians argue that they’re dangerous to their peers in bathrooms and on sports teams, it’s difficult to imagine their mental health would not worsen. Over time, such “distal factors” also lead to “proximal factors” like internalized transphobia in which youth begin to believe the negative things that are said about them. These dangerous processes can have dramatic negative impacts on self-esteem and emotional development. There is strong precedence that public policies have strong indirect mental health effects on LGBTQ youth.
We’ve entered a dangerous era in which politicians are legislating medical care and other aspects of public policy with the potential to hurt the mental health of our young patients. It’s imperative that clinicians and scientists contact their legislators to make sure they are voting for public policy based on data and fact, not misinformation and political rhetoric. The health of American children depends on it.
Dr. Turban (twitter.com/jack_turban) is a chief fellow in child and adolescent psychiatry at Stanford (Calif.) University.
Metacognitive training an effective, durable treatment for schizophrenia
Metacognitive training (MCT) is effective in reducing positive and negative symptoms of schizophrenia, new research suggests.
MCT for psychosis is a brief intervention that “combines psychoeducation, cognitive bias modification, and strategy teaching but does not directly target psychosis symptoms.”
Additionally, MCT led to improvement in self-esteem and functioning, and all benefits were maintained up to 1 year post intervention.
“Our study demonstrates the effectiveness and durability of a brief, nonconfrontational intervention in the reduction of serious and debilitating symptoms of schizophrenia,” study investigator Danielle Penney, a doctoral candidate at the University of Montreal, told this news organization.
“Our results were observed in several treatment contexts and suggest that MCT can be successfully delivered by a variety of mental health practitioners [and] provide solid evidence to consider MCT in international treatment guidelines for schizophrenia spectrum disorders,” Ms. Penney said.
The findings were published online in JAMA Psychiatry.
‘Novel contribution’
MCT is a brief intervention consisting of eight to 16 modules that can be delivered in a group setting or on an individual basis. Instead of directly targeting psychotic symptoms, it uses an “indirect approach by promoting awareness of cognitive biases,” the investigators note.
Such biases include maladaptive thinking styles common to psychosis, such as jumping to conclusions, belief inflexibility, and overconfidence in judgments.
It is hypothesized that these biases “contribute to the formation and maintenance of positive symptoms, particularly delusions,” the researchers write.
MCT “aims to plant doubt in delusional beliefs through raising awareness of cognitive biases and aims to raise service engagement by proposing work on this less-confrontational objective first, which is likely to facilitate the therapeutic alliance and more direct work on psychotic symptoms,” they add.
Previous studies of MCT for psychosis yielded inconsistent results. Of the eight previous meta-analyses that analyzed MCT for psychosis, “none investigated the long-term effects of the intervention on directly targeted treatment outcomes,” such as delusions and cognitive biases, Ms. Penney said.
She added that “to our knowledge, no meta-analysis has examined the effectiveness of important indirectly targeted outcomes,” including self-esteem and functioning.
“These important gaps in the literature,” along with a large increase in recently conducted MCT efficacy trials, “provided the motivation for the current study,” said Ms. Penney.
To investigate, the researchers searched 11 databases, beginning with data from 2007, which was when the first report of MCT was published. Studies included participants with schizophrenia spectrum and related psychotic disorders.
Outcomes for the current review and meta-analysis were organized according to a “proximal-distal framework.” Proximal outcomes were those directly targeted by MCT, while distal outcomes were those not directly targeted by MCT but that were associated with improvement in proximal outcomes, either directly or indirectly.
The investigators examined these outcomes quantitatively and qualitatively from preintervention to postintervention and follow-up, “which, to our knowledge, is a novel contribution,” they write.
The review included 43 studies, of which 30 (70%) were randomized controlled trials (RCTs), 11 (25%) were non-RCTs, and two (5%) were quantitative descriptive studies. Of these, 40 reports (n = 1,816 participants) were included in the meta-analysis, and six were included in the narrative review.
Transdiagnostic treatment?
Results showed a “small to moderate” effect size (ES) in global proximal outcomes (g = .39; 95% confidence interval, .25-.53; P < .001; 38 reports).
When proximal outcomes were analyzed separately, the largest ES was found for delusions; smaller ES values were found for hallucinations and cognitive biases.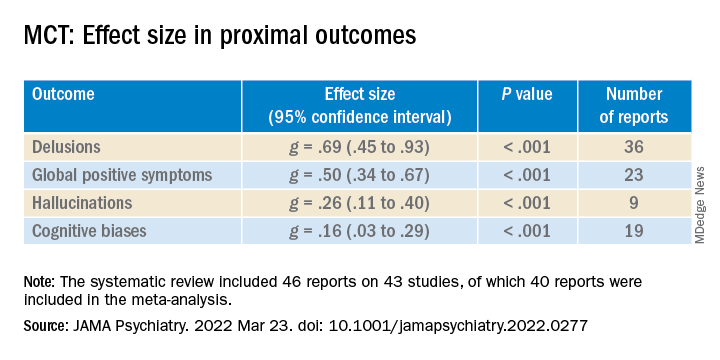
Newer studies reported higher ES values for hallucinations, compared with older studies (β = .04; 95% CI, .00-.07).
ES was small to moderate for distal outcomes (g = .31; 95% CI, .19-.44; P < .001; 26 reports). “Small but significant” ES values were shown for self-esteem and negative symptoms, small to moderate for functioning, and small but nonsignificant for quality of life (QOL).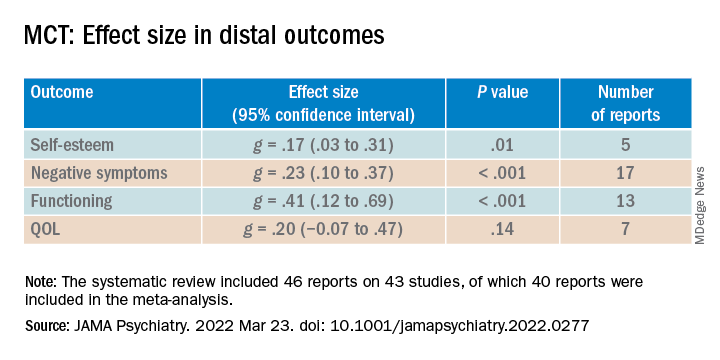
The researchers also analyzed RCTs by comparing differences between the treatment and control groups in scores from follow-up to post-treatment. Although the therapeutic gains made by the experimental group were “steadily maintained, the ES values were “small” and nonsignificant.
When the difference in scores between follow-up and baseline were compared in both groups, small to moderate ES values were found for proximal as well as distal outcomes.
“These results further indicate that net therapeutic gains remain significant even 1 year following MCT,” the investigators note.
Lower-quality studies showed significantly lower ES values for distal (between-group comparison, P = .05) but not proximal outcomes.
Overall, the findings suggest that MCT is a “beneficial and durable low-threshold intervention that can be flexibly delivered at minimal cost in a variety of contexts to individuals with psychotic disorders,” the researchers write.
They note that MCT has also been associated with positive outcomes in other patient populations, including patients with borderline personality disorder, depression, and obsessive-compulsive disorder. Future research “might consider investigating MCT as a transdiagnostic treatment,” they add.
Consistent beneficial effects
Commenting on the study, Philip Harvey, PhD, Leonard M. Miller Professor of Psychiatry and Behavioral Sciences and director of the Division of Psychology, University of Miami Miller School of Medicine, noted that self-awareness and self-assessment are critically important features in patients with serious mental illness.
Impairments in these areas “can actually have a greater impact on everyday functioning than cognitive deficits,” said Dr. Harvey, who is also the editor-in-chief of Schizophrenia Research: Cognition. He was not involved with the current meta-analysis.
He noted that the current results show that “MCT has consistent beneficial effects.”
“This is an intervention that should be considered for most people with serious mental illness, with a specific focus on those with specific types of delusions and more global challenges in self-assessment,” Dr. Harvey concluded.
Funding was provided by the Canada First Research Excellence Fund, awarded through the Healthy Brains, Healthy Lives initiative at McGill University. Ms. Penney reported no relevant financial relationships. Disclosures for the other investigators are listed in the original article. Dr. Harvey reported being a reviewer of the article but that he was not involved in its authorship.
A version of this article first appeared on Medscape.com.
Metacognitive training (MCT) is effective in reducing positive and negative symptoms of schizophrenia, new research suggests.
MCT for psychosis is a brief intervention that “combines psychoeducation, cognitive bias modification, and strategy teaching but does not directly target psychosis symptoms.”
Additionally, MCT led to improvement in self-esteem and functioning, and all benefits were maintained up to 1 year post intervention.
“Our study demonstrates the effectiveness and durability of a brief, nonconfrontational intervention in the reduction of serious and debilitating symptoms of schizophrenia,” study investigator Danielle Penney, a doctoral candidate at the University of Montreal, told this news organization.
“Our results were observed in several treatment contexts and suggest that MCT can be successfully delivered by a variety of mental health practitioners [and] provide solid evidence to consider MCT in international treatment guidelines for schizophrenia spectrum disorders,” Ms. Penney said.
The findings were published online in JAMA Psychiatry.
‘Novel contribution’
MCT is a brief intervention consisting of eight to 16 modules that can be delivered in a group setting or on an individual basis. Instead of directly targeting psychotic symptoms, it uses an “indirect approach by promoting awareness of cognitive biases,” the investigators note.
Such biases include maladaptive thinking styles common to psychosis, such as jumping to conclusions, belief inflexibility, and overconfidence in judgments.
It is hypothesized that these biases “contribute to the formation and maintenance of positive symptoms, particularly delusions,” the researchers write.
MCT “aims to plant doubt in delusional beliefs through raising awareness of cognitive biases and aims to raise service engagement by proposing work on this less-confrontational objective first, which is likely to facilitate the therapeutic alliance and more direct work on psychotic symptoms,” they add.
Previous studies of MCT for psychosis yielded inconsistent results. Of the eight previous meta-analyses that analyzed MCT for psychosis, “none investigated the long-term effects of the intervention on directly targeted treatment outcomes,” such as delusions and cognitive biases, Ms. Penney said.
She added that “to our knowledge, no meta-analysis has examined the effectiveness of important indirectly targeted outcomes,” including self-esteem and functioning.
“These important gaps in the literature,” along with a large increase in recently conducted MCT efficacy trials, “provided the motivation for the current study,” said Ms. Penney.
To investigate, the researchers searched 11 databases, beginning with data from 2007, which was when the first report of MCT was published. Studies included participants with schizophrenia spectrum and related psychotic disorders.
Outcomes for the current review and meta-analysis were organized according to a “proximal-distal framework.” Proximal outcomes were those directly targeted by MCT, while distal outcomes were those not directly targeted by MCT but that were associated with improvement in proximal outcomes, either directly or indirectly.
The investigators examined these outcomes quantitatively and qualitatively from preintervention to postintervention and follow-up, “which, to our knowledge, is a novel contribution,” they write.
The review included 43 studies, of which 30 (70%) were randomized controlled trials (RCTs), 11 (25%) were non-RCTs, and two (5%) were quantitative descriptive studies. Of these, 40 reports (n = 1,816 participants) were included in the meta-analysis, and six were included in the narrative review.
Transdiagnostic treatment?
Results showed a “small to moderate” effect size (ES) in global proximal outcomes (g = .39; 95% confidence interval, .25-.53; P < .001; 38 reports).
When proximal outcomes were analyzed separately, the largest ES was found for delusions; smaller ES values were found for hallucinations and cognitive biases.
Newer studies reported higher ES values for hallucinations, compared with older studies (β = .04; 95% CI, .00-.07).
ES was small to moderate for distal outcomes (g = .31; 95% CI, .19-.44; P < .001; 26 reports). “Small but significant” ES values were shown for self-esteem and negative symptoms, small to moderate for functioning, and small but nonsignificant for quality of life (QOL).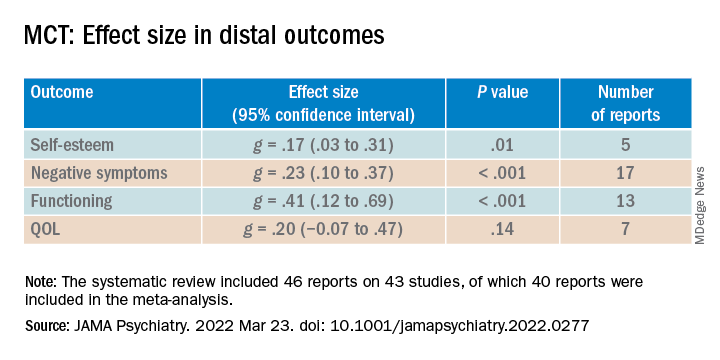
The researchers also analyzed RCTs by comparing differences between the treatment and control groups in scores from follow-up to post-treatment. Although the therapeutic gains made by the experimental group were “steadily maintained, the ES values were “small” and nonsignificant.
When the difference in scores between follow-up and baseline were compared in both groups, small to moderate ES values were found for proximal as well as distal outcomes.
“These results further indicate that net therapeutic gains remain significant even 1 year following MCT,” the investigators note.
Lower-quality studies showed significantly lower ES values for distal (between-group comparison, P = .05) but not proximal outcomes.
Overall, the findings suggest that MCT is a “beneficial and durable low-threshold intervention that can be flexibly delivered at minimal cost in a variety of contexts to individuals with psychotic disorders,” the researchers write.
They note that MCT has also been associated with positive outcomes in other patient populations, including patients with borderline personality disorder, depression, and obsessive-compulsive disorder. Future research “might consider investigating MCT as a transdiagnostic treatment,” they add.
Consistent beneficial effects
Commenting on the study, Philip Harvey, PhD, Leonard M. Miller Professor of Psychiatry and Behavioral Sciences and director of the Division of Psychology, University of Miami Miller School of Medicine, noted that self-awareness and self-assessment are critically important features in patients with serious mental illness.
Impairments in these areas “can actually have a greater impact on everyday functioning than cognitive deficits,” said Dr. Harvey, who is also the editor-in-chief of Schizophrenia Research: Cognition. He was not involved with the current meta-analysis.
He noted that the current results show that “MCT has consistent beneficial effects.”
“This is an intervention that should be considered for most people with serious mental illness, with a specific focus on those with specific types of delusions and more global challenges in self-assessment,” Dr. Harvey concluded.
Funding was provided by the Canada First Research Excellence Fund, awarded through the Healthy Brains, Healthy Lives initiative at McGill University. Ms. Penney reported no relevant financial relationships. Disclosures for the other investigators are listed in the original article. Dr. Harvey reported being a reviewer of the article but that he was not involved in its authorship.
A version of this article first appeared on Medscape.com.
Metacognitive training (MCT) is effective in reducing positive and negative symptoms of schizophrenia, new research suggests.
MCT for psychosis is a brief intervention that “combines psychoeducation, cognitive bias modification, and strategy teaching but does not directly target psychosis symptoms.”
Additionally, MCT led to improvement in self-esteem and functioning, and all benefits were maintained up to 1 year post intervention.
“Our study demonstrates the effectiveness and durability of a brief, nonconfrontational intervention in the reduction of serious and debilitating symptoms of schizophrenia,” study investigator Danielle Penney, a doctoral candidate at the University of Montreal, told this news organization.
“Our results were observed in several treatment contexts and suggest that MCT can be successfully delivered by a variety of mental health practitioners [and] provide solid evidence to consider MCT in international treatment guidelines for schizophrenia spectrum disorders,” Ms. Penney said.
The findings were published online in JAMA Psychiatry.
‘Novel contribution’
MCT is a brief intervention consisting of eight to 16 modules that can be delivered in a group setting or on an individual basis. Instead of directly targeting psychotic symptoms, it uses an “indirect approach by promoting awareness of cognitive biases,” the investigators note.
Such biases include maladaptive thinking styles common to psychosis, such as jumping to conclusions, belief inflexibility, and overconfidence in judgments.
It is hypothesized that these biases “contribute to the formation and maintenance of positive symptoms, particularly delusions,” the researchers write.
MCT “aims to plant doubt in delusional beliefs through raising awareness of cognitive biases and aims to raise service engagement by proposing work on this less-confrontational objective first, which is likely to facilitate the therapeutic alliance and more direct work on psychotic symptoms,” they add.
Previous studies of MCT for psychosis yielded inconsistent results. Of the eight previous meta-analyses that analyzed MCT for psychosis, “none investigated the long-term effects of the intervention on directly targeted treatment outcomes,” such as delusions and cognitive biases, Ms. Penney said.
She added that “to our knowledge, no meta-analysis has examined the effectiveness of important indirectly targeted outcomes,” including self-esteem and functioning.
“These important gaps in the literature,” along with a large increase in recently conducted MCT efficacy trials, “provided the motivation for the current study,” said Ms. Penney.
To investigate, the researchers searched 11 databases, beginning with data from 2007, which was when the first report of MCT was published. Studies included participants with schizophrenia spectrum and related psychotic disorders.
Outcomes for the current review and meta-analysis were organized according to a “proximal-distal framework.” Proximal outcomes were those directly targeted by MCT, while distal outcomes were those not directly targeted by MCT but that were associated with improvement in proximal outcomes, either directly or indirectly.
The investigators examined these outcomes quantitatively and qualitatively from preintervention to postintervention and follow-up, “which, to our knowledge, is a novel contribution,” they write.
The review included 43 studies, of which 30 (70%) were randomized controlled trials (RCTs), 11 (25%) were non-RCTs, and two (5%) were quantitative descriptive studies. Of these, 40 reports (n = 1,816 participants) were included in the meta-analysis, and six were included in the narrative review.
Transdiagnostic treatment?
Results showed a “small to moderate” effect size (ES) in global proximal outcomes (g = .39; 95% confidence interval, .25-.53; P < .001; 38 reports).
When proximal outcomes were analyzed separately, the largest ES was found for delusions; smaller ES values were found for hallucinations and cognitive biases.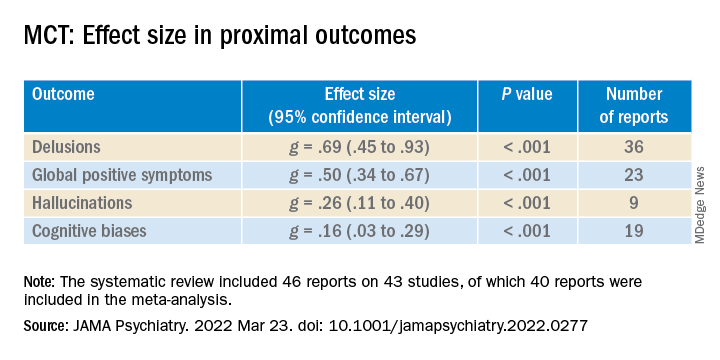
Newer studies reported higher ES values for hallucinations, compared with older studies (β = .04; 95% CI, .00-.07).
ES was small to moderate for distal outcomes (g = .31; 95% CI, .19-.44; P < .001; 26 reports). “Small but significant” ES values were shown for self-esteem and negative symptoms, small to moderate for functioning, and small but nonsignificant for quality of life (QOL).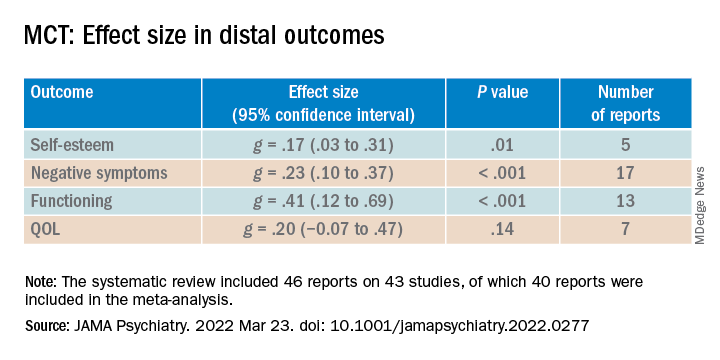
The researchers also analyzed RCTs by comparing differences between the treatment and control groups in scores from follow-up to post-treatment. Although the therapeutic gains made by the experimental group were “steadily maintained, the ES values were “small” and nonsignificant.
When the difference in scores between follow-up and baseline were compared in both groups, small to moderate ES values were found for proximal as well as distal outcomes.
“These results further indicate that net therapeutic gains remain significant even 1 year following MCT,” the investigators note.
Lower-quality studies showed significantly lower ES values for distal (between-group comparison, P = .05) but not proximal outcomes.
Overall, the findings suggest that MCT is a “beneficial and durable low-threshold intervention that can be flexibly delivered at minimal cost in a variety of contexts to individuals with psychotic disorders,” the researchers write.
They note that MCT has also been associated with positive outcomes in other patient populations, including patients with borderline personality disorder, depression, and obsessive-compulsive disorder. Future research “might consider investigating MCT as a transdiagnostic treatment,” they add.
Consistent beneficial effects
Commenting on the study, Philip Harvey, PhD, Leonard M. Miller Professor of Psychiatry and Behavioral Sciences and director of the Division of Psychology, University of Miami Miller School of Medicine, noted that self-awareness and self-assessment are critically important features in patients with serious mental illness.
Impairments in these areas “can actually have a greater impact on everyday functioning than cognitive deficits,” said Dr. Harvey, who is also the editor-in-chief of Schizophrenia Research: Cognition. He was not involved with the current meta-analysis.
He noted that the current results show that “MCT has consistent beneficial effects.”
“This is an intervention that should be considered for most people with serious mental illness, with a specific focus on those with specific types of delusions and more global challenges in self-assessment,” Dr. Harvey concluded.
Funding was provided by the Canada First Research Excellence Fund, awarded through the Healthy Brains, Healthy Lives initiative at McGill University. Ms. Penney reported no relevant financial relationships. Disclosures for the other investigators are listed in the original article. Dr. Harvey reported being a reviewer of the article but that he was not involved in its authorship.
A version of this article first appeared on Medscape.com.
Study: Physical fitness in children linked with concentration, quality of life
The findings of the German study involving more than 6,500 kids emphasize the importance of cardiorespiratory health in childhood, and support physical fitness initiatives in schools, according to lead author Katharina Köble, MSc, of the Technical University of Munich (Germany), and colleagues.
“Recent studies show that only a few children meet the recommendations of physical activity,” the investigators wrote in Journal of Clinical Medicine.
While the health benefits of physical activity are clearly documented, Ms. Köble and colleagues noted that typical measures of activity, such as accelerometers or self-reported questionnaires, are suboptimal research tools.
“Physical fitness is a more objective parameter to quantify when evaluating health promotion,” the investigators wrote. “Furthermore, cardiorespiratory fitness as part of physical fitness is more strongly related to risk factors of cardiovascular disease than physical activity.”
According to the investigators, physical fitness has also been linked with better concentration and HRQOL, but never in the same population of children.
The new study aimed to address this knowledge gap by assessing 6,533 healthy children aged 6-10 years, approximately half boys and half girls. Associations between physical fitness, concentration, and HRQOL were evaluated using multiple linear regression analysis in participants aged 9-10 years.
Physical fitness was measured using a series of challenges, including curl-ups (pull-ups with palms facing body), push-ups, standing long jump, handgrip strength measurement, and Progressive Aerobic Cardiovascular Endurance Run (PACER). Performing the multistage shuttle run, PACER, “requires participants to maintain the pace set by an audio signal, which progressively increases the intensity every minute.” Results of the PACER test were used to estimate VO2max.
Concentration was measured using the d2-R test, “a paper-pencil cancellation test, where subjects have to cross out all ‘d’ letters with two dashes under a time limit.”
HRQOL was evaluated with the KINDL questionnaire, which covers emotional well-being, physical well-being, everyday functioning (school), friends, family, and self-esteem.
Analysis showed that physical fitness improved with age (P < .001), except for VO2max in girls (P = .129). Concentration also improved with age (P < .001), while HRQOL did not (P = .179).
Among children aged 9-10 years, VO2max scores were strongly associated with both HRQOL (P < .001) and concentration (P < .001).
“VO2max was found to be one of the main factors influencing concentration levels and HRQOL dimensions in primary school children,” the investigators wrote. “Physical fitness, especially cardiorespiratory performance, should therefore be promoted more specifically in school settings to support the promotion of an overall healthy lifestyle in children and adolescents.”
Findings are having a real-word impact, according to researcher
In an interview, Ms. Köble noted that the findings are already having a real-world impact.
“We continued data assessment in the long-term and specifically adapted prevention programs in school to the needs of the school children we identified in our study,” she said. “Schools are partially offering specific movement and nutrition classes now.”
In addition, Ms. Köble and colleagues plan on educating teachers about the “urgent need for sufficient physical activity.”
“Academic performance should be considered as an additional health factor in future studies, as well as screen time and eating patterns, as all those variables showed interactions with physical fitness and concentration. In a subanalysis, we showed that children with better physical fitness and concentration values were those who usually went to higher education secondary schools,” they wrote.
VO2max did not correlate with BMI
Gregory Weaver, MD, a pediatrician at Cleveland Clinic Children’s, voiced some concerns about the reliability of the findings. He noted that VO2max did not correlate with body mass index or other measures of physical fitness, and that using the PACER test to estimate VO2max may have skewed the association between physical fitness and concentration.
“It is quite conceivable that children who can maintain the focus to perform maximally on this test will also do well on other tests of attention/concentration,” Dr. Weaver said. “Most children I know would have a very difficult time performing a physical fitness test which requires them to match a recorded pace that slowly increases overtime. I’m not an expert in the area, but it is my understanding that usually VO2max tests involve a treadmill which allows investigators to have complete control over pace.”
Dr. Weaver concluded that more work is needed to determine if physical fitness interventions can have a positive impact on HRQOL and concentration.
“I think the authors of this study attempted to ask an important question about the possible association between physical fitness and concentration among school aged children,” Dr. Weaver said in an interview. “But what is even more vital are studies demonstrating that a change in modifiable health factors like nutrition, physical fitness, or the built environment can improve quality of life. I was hoping the authors would show that an improvement in VO2max over time resulted in an improvement in concentration. Frustratingly, that is not what this article demonstrates.”
The investigators and Dr. Weaver reported no conflicts of interest.
The findings of the German study involving more than 6,500 kids emphasize the importance of cardiorespiratory health in childhood, and support physical fitness initiatives in schools, according to lead author Katharina Köble, MSc, of the Technical University of Munich (Germany), and colleagues.
“Recent studies show that only a few children meet the recommendations of physical activity,” the investigators wrote in Journal of Clinical Medicine.
While the health benefits of physical activity are clearly documented, Ms. Köble and colleagues noted that typical measures of activity, such as accelerometers or self-reported questionnaires, are suboptimal research tools.
“Physical fitness is a more objective parameter to quantify when evaluating health promotion,” the investigators wrote. “Furthermore, cardiorespiratory fitness as part of physical fitness is more strongly related to risk factors of cardiovascular disease than physical activity.”
According to the investigators, physical fitness has also been linked with better concentration and HRQOL, but never in the same population of children.
The new study aimed to address this knowledge gap by assessing 6,533 healthy children aged 6-10 years, approximately half boys and half girls. Associations between physical fitness, concentration, and HRQOL were evaluated using multiple linear regression analysis in participants aged 9-10 years.
Physical fitness was measured using a series of challenges, including curl-ups (pull-ups with palms facing body), push-ups, standing long jump, handgrip strength measurement, and Progressive Aerobic Cardiovascular Endurance Run (PACER). Performing the multistage shuttle run, PACER, “requires participants to maintain the pace set by an audio signal, which progressively increases the intensity every minute.” Results of the PACER test were used to estimate VO2max.
Concentration was measured using the d2-R test, “a paper-pencil cancellation test, where subjects have to cross out all ‘d’ letters with two dashes under a time limit.”
HRQOL was evaluated with the KINDL questionnaire, which covers emotional well-being, physical well-being, everyday functioning (school), friends, family, and self-esteem.
Analysis showed that physical fitness improved with age (P < .001), except for VO2max in girls (P = .129). Concentration also improved with age (P < .001), while HRQOL did not (P = .179).
Among children aged 9-10 years, VO2max scores were strongly associated with both HRQOL (P < .001) and concentration (P < .001).
“VO2max was found to be one of the main factors influencing concentration levels and HRQOL dimensions in primary school children,” the investigators wrote. “Physical fitness, especially cardiorespiratory performance, should therefore be promoted more specifically in school settings to support the promotion of an overall healthy lifestyle in children and adolescents.”
Findings are having a real-word impact, according to researcher
In an interview, Ms. Köble noted that the findings are already having a real-world impact.
“We continued data assessment in the long-term and specifically adapted prevention programs in school to the needs of the school children we identified in our study,” she said. “Schools are partially offering specific movement and nutrition classes now.”
In addition, Ms. Köble and colleagues plan on educating teachers about the “urgent need for sufficient physical activity.”
“Academic performance should be considered as an additional health factor in future studies, as well as screen time and eating patterns, as all those variables showed interactions with physical fitness and concentration. In a subanalysis, we showed that children with better physical fitness and concentration values were those who usually went to higher education secondary schools,” they wrote.
VO2max did not correlate with BMI
Gregory Weaver, MD, a pediatrician at Cleveland Clinic Children’s, voiced some concerns about the reliability of the findings. He noted that VO2max did not correlate with body mass index or other measures of physical fitness, and that using the PACER test to estimate VO2max may have skewed the association between physical fitness and concentration.
“It is quite conceivable that children who can maintain the focus to perform maximally on this test will also do well on other tests of attention/concentration,” Dr. Weaver said. “Most children I know would have a very difficult time performing a physical fitness test which requires them to match a recorded pace that slowly increases overtime. I’m not an expert in the area, but it is my understanding that usually VO2max tests involve a treadmill which allows investigators to have complete control over pace.”
Dr. Weaver concluded that more work is needed to determine if physical fitness interventions can have a positive impact on HRQOL and concentration.
“I think the authors of this study attempted to ask an important question about the possible association between physical fitness and concentration among school aged children,” Dr. Weaver said in an interview. “But what is even more vital are studies demonstrating that a change in modifiable health factors like nutrition, physical fitness, or the built environment can improve quality of life. I was hoping the authors would show that an improvement in VO2max over time resulted in an improvement in concentration. Frustratingly, that is not what this article demonstrates.”
The investigators and Dr. Weaver reported no conflicts of interest.
The findings of the German study involving more than 6,500 kids emphasize the importance of cardiorespiratory health in childhood, and support physical fitness initiatives in schools, according to lead author Katharina Köble, MSc, of the Technical University of Munich (Germany), and colleagues.
“Recent studies show that only a few children meet the recommendations of physical activity,” the investigators wrote in Journal of Clinical Medicine.
While the health benefits of physical activity are clearly documented, Ms. Köble and colleagues noted that typical measures of activity, such as accelerometers or self-reported questionnaires, are suboptimal research tools.
“Physical fitness is a more objective parameter to quantify when evaluating health promotion,” the investigators wrote. “Furthermore, cardiorespiratory fitness as part of physical fitness is more strongly related to risk factors of cardiovascular disease than physical activity.”
According to the investigators, physical fitness has also been linked with better concentration and HRQOL, but never in the same population of children.
The new study aimed to address this knowledge gap by assessing 6,533 healthy children aged 6-10 years, approximately half boys and half girls. Associations between physical fitness, concentration, and HRQOL were evaluated using multiple linear regression analysis in participants aged 9-10 years.
Physical fitness was measured using a series of challenges, including curl-ups (pull-ups with palms facing body), push-ups, standing long jump, handgrip strength measurement, and Progressive Aerobic Cardiovascular Endurance Run (PACER). Performing the multistage shuttle run, PACER, “requires participants to maintain the pace set by an audio signal, which progressively increases the intensity every minute.” Results of the PACER test were used to estimate VO2max.
Concentration was measured using the d2-R test, “a paper-pencil cancellation test, where subjects have to cross out all ‘d’ letters with two dashes under a time limit.”
HRQOL was evaluated with the KINDL questionnaire, which covers emotional well-being, physical well-being, everyday functioning (school), friends, family, and self-esteem.
Analysis showed that physical fitness improved with age (P < .001), except for VO2max in girls (P = .129). Concentration also improved with age (P < .001), while HRQOL did not (P = .179).
Among children aged 9-10 years, VO2max scores were strongly associated with both HRQOL (P < .001) and concentration (P < .001).
“VO2max was found to be one of the main factors influencing concentration levels and HRQOL dimensions in primary school children,” the investigators wrote. “Physical fitness, especially cardiorespiratory performance, should therefore be promoted more specifically in school settings to support the promotion of an overall healthy lifestyle in children and adolescents.”
Findings are having a real-word impact, according to researcher
In an interview, Ms. Köble noted that the findings are already having a real-world impact.
“We continued data assessment in the long-term and specifically adapted prevention programs in school to the needs of the school children we identified in our study,” she said. “Schools are partially offering specific movement and nutrition classes now.”
In addition, Ms. Köble and colleagues plan on educating teachers about the “urgent need for sufficient physical activity.”
“Academic performance should be considered as an additional health factor in future studies, as well as screen time and eating patterns, as all those variables showed interactions with physical fitness and concentration. In a subanalysis, we showed that children with better physical fitness and concentration values were those who usually went to higher education secondary schools,” they wrote.
VO2max did not correlate with BMI
Gregory Weaver, MD, a pediatrician at Cleveland Clinic Children’s, voiced some concerns about the reliability of the findings. He noted that VO2max did not correlate with body mass index or other measures of physical fitness, and that using the PACER test to estimate VO2max may have skewed the association between physical fitness and concentration.
“It is quite conceivable that children who can maintain the focus to perform maximally on this test will also do well on other tests of attention/concentration,” Dr. Weaver said. “Most children I know would have a very difficult time performing a physical fitness test which requires them to match a recorded pace that slowly increases overtime. I’m not an expert in the area, but it is my understanding that usually VO2max tests involve a treadmill which allows investigators to have complete control over pace.”
Dr. Weaver concluded that more work is needed to determine if physical fitness interventions can have a positive impact on HRQOL and concentration.
“I think the authors of this study attempted to ask an important question about the possible association between physical fitness and concentration among school aged children,” Dr. Weaver said in an interview. “But what is even more vital are studies demonstrating that a change in modifiable health factors like nutrition, physical fitness, or the built environment can improve quality of life. I was hoping the authors would show that an improvement in VO2max over time resulted in an improvement in concentration. Frustratingly, that is not what this article demonstrates.”
The investigators and Dr. Weaver reported no conflicts of interest.
FROM THE JOURNAL OF CLINICAL MEDICINE
Trichotillomania: What you should know about this common hair-pulling disorder
Trichotillomania is a chronic psychiatric disorder that causes people to repeatedly pull out their own hair. Not only does it result in alopecia with no other underlying causes but it can have significant psychosocial ramifications and rare, but serious, complications. Though the reported prevalence rates are up to approximately 2%, it’s probable that you’ll come upon a patient suffering with this disorder at your practice, if you haven’t already.
To find out more about the best methods for diagnosing and treating this disorder, we spoke with Jon E. Grant, JD, MD, MPH, a leading trichotillomania researcher and part of the department of psychiatry and behavioral neuroscience at the University of Chicago.
Defining trichotillomania
What were the earliest descriptions of trichotillomania in medical literature?
The first real discussion of it probably goes back to Hippocrates, but from a modern medical perspective, discussion began in the 19th century with reports from the French dermatologist François Hallopeau.
They didn’t really call them disorders then – it was long before the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) – but they described this in young men who kept pulling their hair for unclear reasons. These early case reports don’t provide a lot of psychological perspective, but they seem consistent with what we see now.
What are the diagnostic criteria for trichotillomania?
The current DSM-5 criteria are recurrent pulling out of hair, an inability to stop it, the pulling resulting in some noticeable thinning or hair loss, and that it causes some level of distress or some type of impairment in functioning.
At what age do most people experience an onset of symptoms?
Generally speaking, it’s in early adolescence, post puberty, around 12-15 years of age. Having said that, we do see children as young as 1-2 years who are pulling their hair, and we occasionally see somebody far older who is doing it for the first time, a sort of geriatric onset.
Overlap and differences with other disorders
You’ve written that although trichotillomania is grouped with obsessive-compulsive disorder (OCD) in the DSM-5, the thinking around that has recently shifted. Why is that?
At first, it was noticed that many of these people pulled their hair repetitively in an almost ritualized manner, perhaps every night before bed. That looked like a compulsion of OCD.
When DSM-5 came out in 2013, they grouped it with OCD. Yet people shifted to thinking that it’s kind of a cousin of OCD because it has this compulsive quality but doesn’t really have obsessive thinking that drives it. Many people just pull their hair. They’re not even always aware of it: sometimes yes, sometimes no.
We know that it has some links to OCD. You’ll see more OCD in folks with trichotillomania, but it clearly is not just the same as OCD. One of the biggest pieces of evidence for that is that our first-line treatment for OCD – a selective serotonin reuptake inhibitor antidepressant – does not really help hair pulling.
Having said that, if people are looking for help with trichotillomania, they often are best served by therapists and doctors who have a familiarity with OCD and have kept it on their radar over the past couple of decades.
How does trichotillomania overlap with skin picking disorder, which is another condition that you’ve closely researched?
It does have some overlap with skin picking in the sense that it often seems familial. For example, the mother may pull her hair and child picks their skin.
It also has a fair amount of comorbidity with skin picking. Many people who pull will pick a little bit or did at some point. Many people who pick pulled their hair at some point. It seems closely related to nail biting as well.
Studies have also shown that one of the things that runs in the histories of most families of people with trichotillomania might be substance abuse – alcohol or drug addiction.
All of this has led people to believe that there might be subtypes of trichotillomania: one that’s more like an OCD and one that’s more like an addiction. That’s similar to the debate with other mental health conditions, that there are probably multiple types of depression, multiple types of schizophrenia.
Is there a component of this that could be defined as self-harm?
That’s been its own debate. It doesn’t seem to have the same developmental trajectory that we see with self-harm, or even some of the personality features.
However, there may be a small segment of folks with trichotillomania that might more appropriately fit that category. For example, those with family histories of trauma, higher rates of posttraumatic stress disorder, or borderline personality. But it wouldn’t be the majority.
The problem is, if you look at some of the pediatrician data, they often group picking, pulling, and cutting. I think that’s far too all-inclusive.
A gap in clinician education
Are adolescent patients likely to self-report this behavior, or is it something that physicians need to suss out for themselves?
Clearly, if child psychologists, psychiatrists, or pediatricians see young people with patches of alopecia – eyebrows or eyelashes missing, head hair with spots – in addition to a dermatologic assessment, they should simply ask, “Do you pull your hair?”
But it’s interesting that with the internet, young people are much more likely to disclose and actually come forward and tell their parents that they think they have trichotillomania.
I also hear from a lot of the adolescents that they have to educate their doctors about trichotillomania because so often physicians don’t know much about it and will assume that it’s self-injury or just a symptom of anxiety. It’s a little bit of a flip from what we might have seen 20 years ago.
I’ve seen several patients who’ve said, basically, “I’m tired of no professionals seeming to know about this. I shouldn’t have to be educating my doctors about this.” I tell them that I completely agree. It’s a shame because if a doctor doesn’t know about it, then how can they get the appropriate care?
What are the complications that accompany trichotillomania?
A small percentage, maybe about 10%, will ingest their hair, much like people who bite and swallow their fingernails. The concern there is that because hair is nondigestible, it could create an intestinal plug that could rupture and be potentially life-threatening. That makes it all the more important to ask those who pull their hair what they do with the hair once they pull it.
However, with most people, the real problem is with self-esteem. Young people may not want to socialize, go on dates, or do other things they would normally do because of it. In adults, you may find that they’re far more educated than their job allows but don’t want to go to an interview because they don’t want to have somebody sit there and look at them and notice that perhaps they don’t have any eyebrows, or that they’re wearing a wig. Those psychosocial implications are huge for so many people.
Treatment options
In a 2021 study, you showed that nearly one-quarter of people with trichotillomania do naturally recover from it. What characteristics do they seem to have?
It’s interesting because we see natural recovery across many mental health problems: alcohol addition, gambling, OCD. The question then becomes why is that some people can seemingly just stop doing a behavior? Can we learn from those people?
We did see that those who naturally recovered were less likely to have some other mental health comorbidities. It seems like when you have other things such as skin picking or OCD plus trichotillomania, that it probably speaks to something that perhaps synergistically is keeping it going. But this is just a first study; learning how to harness and understand it is the next step.
What’s the goal of treating trichotillomania?
The desired goal is zero pulling. The realistic goal is more likely significantly reduced pulling that then leads to greater function in life, greater quality-of-life.
One doesn’t have to go from 100 to 0 in order to do that. I always tell people that maybe every now and then, every few months, when something is going on in life, you might find yourself pulling a hair or two. That’s okay. If you’re not pulling every day and it’s significantly reduced, we’ll call that a success. I think that setting reasonable goals at this point is really important.
And what would the treatment pathway look like for most patients?
The standard approach is probably some type of habit-reversal therapy, of which there have been many variants over the years. It involves doing something different with your hand, identifying the triggers that may set you off, and then doing something in response to those triggers that is not pulling and might neutralize whatever that anxious or stressed feeling is. That could be different with each person.
At this point, there is no drug approved by the U.S. Food and Drug Administration for trichotillomania. Our best approaches have included N-acetylcysteine, a glutamate modulator, which we’ve done research in.
That’s kind of a go-to option for people because its side-effect profile is generally innocuous. The data show that it could be beneficial in many people with very few, if any, side effects. That would be one “medication,” although it’s actually an over-the-counter vitamin. But we’re constantly looking for better and better treatments.
Do you have any final advice for clinicians or researchers?
Given how common it is, I don’t think clinicians should just see it as an innocuous little habit that people should be able to stop on their own. Clinicians should educate themselves about trichotillomania and know where the person should get the appropriate care.
From the research perspective, given the fact that we see this in animals of multiple species – that they overgroom – this seems to be deeply ingrained in us as animals. So when it comes to the underlying neuroscience, people should pay more attention because it probably has a lot to do with our understanding of habit and compulsive behaviors. It arguably can cut across a lot of different behaviors.
A version of this article first appeared on Medscape.com.
Trichotillomania is a chronic psychiatric disorder that causes people to repeatedly pull out their own hair. Not only does it result in alopecia with no other underlying causes but it can have significant psychosocial ramifications and rare, but serious, complications. Though the reported prevalence rates are up to approximately 2%, it’s probable that you’ll come upon a patient suffering with this disorder at your practice, if you haven’t already.
To find out more about the best methods for diagnosing and treating this disorder, we spoke with Jon E. Grant, JD, MD, MPH, a leading trichotillomania researcher and part of the department of psychiatry and behavioral neuroscience at the University of Chicago.
Defining trichotillomania
What were the earliest descriptions of trichotillomania in medical literature?
The first real discussion of it probably goes back to Hippocrates, but from a modern medical perspective, discussion began in the 19th century with reports from the French dermatologist François Hallopeau.
They didn’t really call them disorders then – it was long before the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) – but they described this in young men who kept pulling their hair for unclear reasons. These early case reports don’t provide a lot of psychological perspective, but they seem consistent with what we see now.
What are the diagnostic criteria for trichotillomania?
The current DSM-5 criteria are recurrent pulling out of hair, an inability to stop it, the pulling resulting in some noticeable thinning or hair loss, and that it causes some level of distress or some type of impairment in functioning.
At what age do most people experience an onset of symptoms?
Generally speaking, it’s in early adolescence, post puberty, around 12-15 years of age. Having said that, we do see children as young as 1-2 years who are pulling their hair, and we occasionally see somebody far older who is doing it for the first time, a sort of geriatric onset.
Overlap and differences with other disorders
You’ve written that although trichotillomania is grouped with obsessive-compulsive disorder (OCD) in the DSM-5, the thinking around that has recently shifted. Why is that?
At first, it was noticed that many of these people pulled their hair repetitively in an almost ritualized manner, perhaps every night before bed. That looked like a compulsion of OCD.
When DSM-5 came out in 2013, they grouped it with OCD. Yet people shifted to thinking that it’s kind of a cousin of OCD because it has this compulsive quality but doesn’t really have obsessive thinking that drives it. Many people just pull their hair. They’re not even always aware of it: sometimes yes, sometimes no.
We know that it has some links to OCD. You’ll see more OCD in folks with trichotillomania, but it clearly is not just the same as OCD. One of the biggest pieces of evidence for that is that our first-line treatment for OCD – a selective serotonin reuptake inhibitor antidepressant – does not really help hair pulling.
Having said that, if people are looking for help with trichotillomania, they often are best served by therapists and doctors who have a familiarity with OCD and have kept it on their radar over the past couple of decades.
How does trichotillomania overlap with skin picking disorder, which is another condition that you’ve closely researched?
It does have some overlap with skin picking in the sense that it often seems familial. For example, the mother may pull her hair and child picks their skin.
It also has a fair amount of comorbidity with skin picking. Many people who pull will pick a little bit or did at some point. Many people who pick pulled their hair at some point. It seems closely related to nail biting as well.
Studies have also shown that one of the things that runs in the histories of most families of people with trichotillomania might be substance abuse – alcohol or drug addiction.
All of this has led people to believe that there might be subtypes of trichotillomania: one that’s more like an OCD and one that’s more like an addiction. That’s similar to the debate with other mental health conditions, that there are probably multiple types of depression, multiple types of schizophrenia.
Is there a component of this that could be defined as self-harm?
That’s been its own debate. It doesn’t seem to have the same developmental trajectory that we see with self-harm, or even some of the personality features.
However, there may be a small segment of folks with trichotillomania that might more appropriately fit that category. For example, those with family histories of trauma, higher rates of posttraumatic stress disorder, or borderline personality. But it wouldn’t be the majority.
The problem is, if you look at some of the pediatrician data, they often group picking, pulling, and cutting. I think that’s far too all-inclusive.
A gap in clinician education
Are adolescent patients likely to self-report this behavior, or is it something that physicians need to suss out for themselves?
Clearly, if child psychologists, psychiatrists, or pediatricians see young people with patches of alopecia – eyebrows or eyelashes missing, head hair with spots – in addition to a dermatologic assessment, they should simply ask, “Do you pull your hair?”
But it’s interesting that with the internet, young people are much more likely to disclose and actually come forward and tell their parents that they think they have trichotillomania.
I also hear from a lot of the adolescents that they have to educate their doctors about trichotillomania because so often physicians don’t know much about it and will assume that it’s self-injury or just a symptom of anxiety. It’s a little bit of a flip from what we might have seen 20 years ago.
I’ve seen several patients who’ve said, basically, “I’m tired of no professionals seeming to know about this. I shouldn’t have to be educating my doctors about this.” I tell them that I completely agree. It’s a shame because if a doctor doesn’t know about it, then how can they get the appropriate care?
What are the complications that accompany trichotillomania?
A small percentage, maybe about 10%, will ingest their hair, much like people who bite and swallow their fingernails. The concern there is that because hair is nondigestible, it could create an intestinal plug that could rupture and be potentially life-threatening. That makes it all the more important to ask those who pull their hair what they do with the hair once they pull it.
However, with most people, the real problem is with self-esteem. Young people may not want to socialize, go on dates, or do other things they would normally do because of it. In adults, you may find that they’re far more educated than their job allows but don’t want to go to an interview because they don’t want to have somebody sit there and look at them and notice that perhaps they don’t have any eyebrows, or that they’re wearing a wig. Those psychosocial implications are huge for so many people.
Treatment options
In a 2021 study, you showed that nearly one-quarter of people with trichotillomania do naturally recover from it. What characteristics do they seem to have?
It’s interesting because we see natural recovery across many mental health problems: alcohol addition, gambling, OCD. The question then becomes why is that some people can seemingly just stop doing a behavior? Can we learn from those people?
We did see that those who naturally recovered were less likely to have some other mental health comorbidities. It seems like when you have other things such as skin picking or OCD plus trichotillomania, that it probably speaks to something that perhaps synergistically is keeping it going. But this is just a first study; learning how to harness and understand it is the next step.
What’s the goal of treating trichotillomania?
The desired goal is zero pulling. The realistic goal is more likely significantly reduced pulling that then leads to greater function in life, greater quality-of-life.
One doesn’t have to go from 100 to 0 in order to do that. I always tell people that maybe every now and then, every few months, when something is going on in life, you might find yourself pulling a hair or two. That’s okay. If you’re not pulling every day and it’s significantly reduced, we’ll call that a success. I think that setting reasonable goals at this point is really important.
And what would the treatment pathway look like for most patients?
The standard approach is probably some type of habit-reversal therapy, of which there have been many variants over the years. It involves doing something different with your hand, identifying the triggers that may set you off, and then doing something in response to those triggers that is not pulling and might neutralize whatever that anxious or stressed feeling is. That could be different with each person.
At this point, there is no drug approved by the U.S. Food and Drug Administration for trichotillomania. Our best approaches have included N-acetylcysteine, a glutamate modulator, which we’ve done research in.
That’s kind of a go-to option for people because its side-effect profile is generally innocuous. The data show that it could be beneficial in many people with very few, if any, side effects. That would be one “medication,” although it’s actually an over-the-counter vitamin. But we’re constantly looking for better and better treatments.
Do you have any final advice for clinicians or researchers?
Given how common it is, I don’t think clinicians should just see it as an innocuous little habit that people should be able to stop on their own. Clinicians should educate themselves about trichotillomania and know where the person should get the appropriate care.
From the research perspective, given the fact that we see this in animals of multiple species – that they overgroom – this seems to be deeply ingrained in us as animals. So when it comes to the underlying neuroscience, people should pay more attention because it probably has a lot to do with our understanding of habit and compulsive behaviors. It arguably can cut across a lot of different behaviors.
A version of this article first appeared on Medscape.com.
Trichotillomania is a chronic psychiatric disorder that causes people to repeatedly pull out their own hair. Not only does it result in alopecia with no other underlying causes but it can have significant psychosocial ramifications and rare, but serious, complications. Though the reported prevalence rates are up to approximately 2%, it’s probable that you’ll come upon a patient suffering with this disorder at your practice, if you haven’t already.
To find out more about the best methods for diagnosing and treating this disorder, we spoke with Jon E. Grant, JD, MD, MPH, a leading trichotillomania researcher and part of the department of psychiatry and behavioral neuroscience at the University of Chicago.
Defining trichotillomania
What were the earliest descriptions of trichotillomania in medical literature?
The first real discussion of it probably goes back to Hippocrates, but from a modern medical perspective, discussion began in the 19th century with reports from the French dermatologist François Hallopeau.
They didn’t really call them disorders then – it was long before the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) – but they described this in young men who kept pulling their hair for unclear reasons. These early case reports don’t provide a lot of psychological perspective, but they seem consistent with what we see now.
What are the diagnostic criteria for trichotillomania?
The current DSM-5 criteria are recurrent pulling out of hair, an inability to stop it, the pulling resulting in some noticeable thinning or hair loss, and that it causes some level of distress or some type of impairment in functioning.
At what age do most people experience an onset of symptoms?
Generally speaking, it’s in early adolescence, post puberty, around 12-15 years of age. Having said that, we do see children as young as 1-2 years who are pulling their hair, and we occasionally see somebody far older who is doing it for the first time, a sort of geriatric onset.
Overlap and differences with other disorders
You’ve written that although trichotillomania is grouped with obsessive-compulsive disorder (OCD) in the DSM-5, the thinking around that has recently shifted. Why is that?
At first, it was noticed that many of these people pulled their hair repetitively in an almost ritualized manner, perhaps every night before bed. That looked like a compulsion of OCD.
When DSM-5 came out in 2013, they grouped it with OCD. Yet people shifted to thinking that it’s kind of a cousin of OCD because it has this compulsive quality but doesn’t really have obsessive thinking that drives it. Many people just pull their hair. They’re not even always aware of it: sometimes yes, sometimes no.
We know that it has some links to OCD. You’ll see more OCD in folks with trichotillomania, but it clearly is not just the same as OCD. One of the biggest pieces of evidence for that is that our first-line treatment for OCD – a selective serotonin reuptake inhibitor antidepressant – does not really help hair pulling.
Having said that, if people are looking for help with trichotillomania, they often are best served by therapists and doctors who have a familiarity with OCD and have kept it on their radar over the past couple of decades.
How does trichotillomania overlap with skin picking disorder, which is another condition that you’ve closely researched?
It does have some overlap with skin picking in the sense that it often seems familial. For example, the mother may pull her hair and child picks their skin.
It also has a fair amount of comorbidity with skin picking. Many people who pull will pick a little bit or did at some point. Many people who pick pulled their hair at some point. It seems closely related to nail biting as well.
Studies have also shown that one of the things that runs in the histories of most families of people with trichotillomania might be substance abuse – alcohol or drug addiction.
All of this has led people to believe that there might be subtypes of trichotillomania: one that’s more like an OCD and one that’s more like an addiction. That’s similar to the debate with other mental health conditions, that there are probably multiple types of depression, multiple types of schizophrenia.
Is there a component of this that could be defined as self-harm?
That’s been its own debate. It doesn’t seem to have the same developmental trajectory that we see with self-harm, or even some of the personality features.
However, there may be a small segment of folks with trichotillomania that might more appropriately fit that category. For example, those with family histories of trauma, higher rates of posttraumatic stress disorder, or borderline personality. But it wouldn’t be the majority.
The problem is, if you look at some of the pediatrician data, they often group picking, pulling, and cutting. I think that’s far too all-inclusive.
A gap in clinician education
Are adolescent patients likely to self-report this behavior, or is it something that physicians need to suss out for themselves?
Clearly, if child psychologists, psychiatrists, or pediatricians see young people with patches of alopecia – eyebrows or eyelashes missing, head hair with spots – in addition to a dermatologic assessment, they should simply ask, “Do you pull your hair?”
But it’s interesting that with the internet, young people are much more likely to disclose and actually come forward and tell their parents that they think they have trichotillomania.
I also hear from a lot of the adolescents that they have to educate their doctors about trichotillomania because so often physicians don’t know much about it and will assume that it’s self-injury or just a symptom of anxiety. It’s a little bit of a flip from what we might have seen 20 years ago.
I’ve seen several patients who’ve said, basically, “I’m tired of no professionals seeming to know about this. I shouldn’t have to be educating my doctors about this.” I tell them that I completely agree. It’s a shame because if a doctor doesn’t know about it, then how can they get the appropriate care?
What are the complications that accompany trichotillomania?
A small percentage, maybe about 10%, will ingest their hair, much like people who bite and swallow their fingernails. The concern there is that because hair is nondigestible, it could create an intestinal plug that could rupture and be potentially life-threatening. That makes it all the more important to ask those who pull their hair what they do with the hair once they pull it.
However, with most people, the real problem is with self-esteem. Young people may not want to socialize, go on dates, or do other things they would normally do because of it. In adults, you may find that they’re far more educated than their job allows but don’t want to go to an interview because they don’t want to have somebody sit there and look at them and notice that perhaps they don’t have any eyebrows, or that they’re wearing a wig. Those psychosocial implications are huge for so many people.
Treatment options
In a 2021 study, you showed that nearly one-quarter of people with trichotillomania do naturally recover from it. What characteristics do they seem to have?
It’s interesting because we see natural recovery across many mental health problems: alcohol addition, gambling, OCD. The question then becomes why is that some people can seemingly just stop doing a behavior? Can we learn from those people?
We did see that those who naturally recovered were less likely to have some other mental health comorbidities. It seems like when you have other things such as skin picking or OCD plus trichotillomania, that it probably speaks to something that perhaps synergistically is keeping it going. But this is just a first study; learning how to harness and understand it is the next step.
What’s the goal of treating trichotillomania?
The desired goal is zero pulling. The realistic goal is more likely significantly reduced pulling that then leads to greater function in life, greater quality-of-life.
One doesn’t have to go from 100 to 0 in order to do that. I always tell people that maybe every now and then, every few months, when something is going on in life, you might find yourself pulling a hair or two. That’s okay. If you’re not pulling every day and it’s significantly reduced, we’ll call that a success. I think that setting reasonable goals at this point is really important.
And what would the treatment pathway look like for most patients?
The standard approach is probably some type of habit-reversal therapy, of which there have been many variants over the years. It involves doing something different with your hand, identifying the triggers that may set you off, and then doing something in response to those triggers that is not pulling and might neutralize whatever that anxious or stressed feeling is. That could be different with each person.
At this point, there is no drug approved by the U.S. Food and Drug Administration for trichotillomania. Our best approaches have included N-acetylcysteine, a glutamate modulator, which we’ve done research in.
That’s kind of a go-to option for people because its side-effect profile is generally innocuous. The data show that it could be beneficial in many people with very few, if any, side effects. That would be one “medication,” although it’s actually an over-the-counter vitamin. But we’re constantly looking for better and better treatments.
Do you have any final advice for clinicians or researchers?
Given how common it is, I don’t think clinicians should just see it as an innocuous little habit that people should be able to stop on their own. Clinicians should educate themselves about trichotillomania and know where the person should get the appropriate care.
From the research perspective, given the fact that we see this in animals of multiple species – that they overgroom – this seems to be deeply ingrained in us as animals. So when it comes to the underlying neuroscience, people should pay more attention because it probably has a lot to do with our understanding of habit and compulsive behaviors. It arguably can cut across a lot of different behaviors.
A version of this article first appeared on Medscape.com.
Restless legs syndrome occurs often in X-linked adrenoleukodystrophy
Patients with X-linked adrenoleukodystrophy (ALD), a neurodegenerative disease, often experience gait and balance problems, as well as leg discomfort, sleep disturbances, and pain, wrote John W. Winkelman, MD, of Massachusetts General Hospital, Boston, and colleagues. Restless legs syndrome (RLS) has been associated with neurological conditions including Parkinson’s disease, but the prevalence of RLS in ALD patients has not been examined, they said.
In a pilot study published in Sleep Medicine, the researchers identified 21 women and 11 men with ALD who were treated at a single center. The median age of the patients was 45.9 years. Twenty-seven patients had symptoms of myelopathy, with a median age of onset of 34 years.
The researchers assessed RLS severity using questionnaires and the Hopkins Telephone Diagnostic Interview (HTDI), a validated RLS assessment tool. They also reviewed patients’ charts for data on neurological examinations, functional gait measures, and laboratory assessments. Functional gait assessments included the 25-Foot Walk test (25-FW), the Timed Up and Go test (TUG), and Six Minute Walk test (6MW).
Thirteen patients (10 women and 3 men) met criteria for RLS based on the HTDI. The median age of RLS onset was 35 years. Six RLS patients (46.2%) reported using medication to relieve symptoms, and eight RLS patients had a history of antidepressant use.
In addition, six patients with RLS reported a history of anemia or iron deficiency. Ferritin levels were available for 14 patients: 8 women with RLS and 4 women and 2 men without RLS; the mean ferritin levels were 74.0 mcg/L in RLS patients and 99.5 mcg/L in those without RLS.
Of the seven ALD patients with brain lesions, all were men, only two were diagnosed with RLS, and all seven cases were mild, the researchers noted.
Overall, patients with RLS had more neurological signs and symptoms than those without RLS; the most significant were pain and gait difficulty. However, patients with RLS also were more likely than were those without RLS to report spasticity, muscle weakness, impaired coordination, hyperreflexia, impaired sensation, and paraesthesia, as well as bladder, bowel, and erectile dysfunction.
The 40.6% prevalence of RLS in patients with ALD is notably higher than that of the general population, in which the prevalence of RLS is 5%-10%, the researchers wrote in their discussion.
“Consistent with patterns observed in the general population, risk factors for RLS in this cohort of adults with ALD included female gender, increased age, lower iron indices, and use of serotonergic antidepressants,” they said.
The study findings were limited by several factors including the small size and the possible contribution of antidepressant use to the high rate of RLS, the researchers noted.
“Awareness of RLS in patients with ALD would allow for its effective treatment, which may improve the functional impairments as well as quality of life, mood, and anxiety issues in those with ALD,” they concluded.
The study received no outside funding.
Dr. Winkelman disclosed ties with Advance Medical, Avadel, Disc Medicine, Eisai, Emalex, Idorsia, Noctrix, UpToDate, and Merck Pharmaceuticals, as well as research support from the National Institute on Drug Abuse and the Baszucki Brain Research Foundation. The study also was supported by grants from the National Institute of Neurological Disorders and Stroke, the European Leukodystrophy Association, the Arrivederci Foundation, the Leblang Foundation, and the Hammer Family Fund Journal Preproof for ALD Research and Therapies for Women.
Patients with X-linked adrenoleukodystrophy (ALD), a neurodegenerative disease, often experience gait and balance problems, as well as leg discomfort, sleep disturbances, and pain, wrote John W. Winkelman, MD, of Massachusetts General Hospital, Boston, and colleagues. Restless legs syndrome (RLS) has been associated with neurological conditions including Parkinson’s disease, but the prevalence of RLS in ALD patients has not been examined, they said.
In a pilot study published in Sleep Medicine, the researchers identified 21 women and 11 men with ALD who were treated at a single center. The median age of the patients was 45.9 years. Twenty-seven patients had symptoms of myelopathy, with a median age of onset of 34 years.
The researchers assessed RLS severity using questionnaires and the Hopkins Telephone Diagnostic Interview (HTDI), a validated RLS assessment tool. They also reviewed patients’ charts for data on neurological examinations, functional gait measures, and laboratory assessments. Functional gait assessments included the 25-Foot Walk test (25-FW), the Timed Up and Go test (TUG), and Six Minute Walk test (6MW).
Thirteen patients (10 women and 3 men) met criteria for RLS based on the HTDI. The median age of RLS onset was 35 years. Six RLS patients (46.2%) reported using medication to relieve symptoms, and eight RLS patients had a history of antidepressant use.
In addition, six patients with RLS reported a history of anemia or iron deficiency. Ferritin levels were available for 14 patients: 8 women with RLS and 4 women and 2 men without RLS; the mean ferritin levels were 74.0 mcg/L in RLS patients and 99.5 mcg/L in those without RLS.
Of the seven ALD patients with brain lesions, all were men, only two were diagnosed with RLS, and all seven cases were mild, the researchers noted.
Overall, patients with RLS had more neurological signs and symptoms than those without RLS; the most significant were pain and gait difficulty. However, patients with RLS also were more likely than were those without RLS to report spasticity, muscle weakness, impaired coordination, hyperreflexia, impaired sensation, and paraesthesia, as well as bladder, bowel, and erectile dysfunction.
The 40.6% prevalence of RLS in patients with ALD is notably higher than that of the general population, in which the prevalence of RLS is 5%-10%, the researchers wrote in their discussion.
“Consistent with patterns observed in the general population, risk factors for RLS in this cohort of adults with ALD included female gender, increased age, lower iron indices, and use of serotonergic antidepressants,” they said.
The study findings were limited by several factors including the small size and the possible contribution of antidepressant use to the high rate of RLS, the researchers noted.
“Awareness of RLS in patients with ALD would allow for its effective treatment, which may improve the functional impairments as well as quality of life, mood, and anxiety issues in those with ALD,” they concluded.
The study received no outside funding.
Dr. Winkelman disclosed ties with Advance Medical, Avadel, Disc Medicine, Eisai, Emalex, Idorsia, Noctrix, UpToDate, and Merck Pharmaceuticals, as well as research support from the National Institute on Drug Abuse and the Baszucki Brain Research Foundation. The study also was supported by grants from the National Institute of Neurological Disorders and Stroke, the European Leukodystrophy Association, the Arrivederci Foundation, the Leblang Foundation, and the Hammer Family Fund Journal Preproof for ALD Research and Therapies for Women.
Patients with X-linked adrenoleukodystrophy (ALD), a neurodegenerative disease, often experience gait and balance problems, as well as leg discomfort, sleep disturbances, and pain, wrote John W. Winkelman, MD, of Massachusetts General Hospital, Boston, and colleagues. Restless legs syndrome (RLS) has been associated with neurological conditions including Parkinson’s disease, but the prevalence of RLS in ALD patients has not been examined, they said.
In a pilot study published in Sleep Medicine, the researchers identified 21 women and 11 men with ALD who were treated at a single center. The median age of the patients was 45.9 years. Twenty-seven patients had symptoms of myelopathy, with a median age of onset of 34 years.
The researchers assessed RLS severity using questionnaires and the Hopkins Telephone Diagnostic Interview (HTDI), a validated RLS assessment tool. They also reviewed patients’ charts for data on neurological examinations, functional gait measures, and laboratory assessments. Functional gait assessments included the 25-Foot Walk test (25-FW), the Timed Up and Go test (TUG), and Six Minute Walk test (6MW).
Thirteen patients (10 women and 3 men) met criteria for RLS based on the HTDI. The median age of RLS onset was 35 years. Six RLS patients (46.2%) reported using medication to relieve symptoms, and eight RLS patients had a history of antidepressant use.
In addition, six patients with RLS reported a history of anemia or iron deficiency. Ferritin levels were available for 14 patients: 8 women with RLS and 4 women and 2 men without RLS; the mean ferritin levels were 74.0 mcg/L in RLS patients and 99.5 mcg/L in those without RLS.
Of the seven ALD patients with brain lesions, all were men, only two were diagnosed with RLS, and all seven cases were mild, the researchers noted.
Overall, patients with RLS had more neurological signs and symptoms than those without RLS; the most significant were pain and gait difficulty. However, patients with RLS also were more likely than were those without RLS to report spasticity, muscle weakness, impaired coordination, hyperreflexia, impaired sensation, and paraesthesia, as well as bladder, bowel, and erectile dysfunction.
The 40.6% prevalence of RLS in patients with ALD is notably higher than that of the general population, in which the prevalence of RLS is 5%-10%, the researchers wrote in their discussion.
“Consistent with patterns observed in the general population, risk factors for RLS in this cohort of adults with ALD included female gender, increased age, lower iron indices, and use of serotonergic antidepressants,” they said.
The study findings were limited by several factors including the small size and the possible contribution of antidepressant use to the high rate of RLS, the researchers noted.
“Awareness of RLS in patients with ALD would allow for its effective treatment, which may improve the functional impairments as well as quality of life, mood, and anxiety issues in those with ALD,” they concluded.
The study received no outside funding.
Dr. Winkelman disclosed ties with Advance Medical, Avadel, Disc Medicine, Eisai, Emalex, Idorsia, Noctrix, UpToDate, and Merck Pharmaceuticals, as well as research support from the National Institute on Drug Abuse and the Baszucki Brain Research Foundation. The study also was supported by grants from the National Institute of Neurological Disorders and Stroke, the European Leukodystrophy Association, the Arrivederci Foundation, the Leblang Foundation, and the Hammer Family Fund Journal Preproof for ALD Research and Therapies for Women.
FROM SLEEP MEDICINE
About 19% of COVID-19 headaches become chronic
Approximately one in five patients who presented with headache during the acute phase of COVID-19 developed chronic daily headache, according to a study published in Cephalalgia. The greater the headache’s intensity during the acute phase, the greater the likelihood that it would persist.
The research, carried out by members of the Headache Study Group of the Spanish Society of Neurology, evaluated the evolution of headache in more than 900 Spanish patients. Because they found that headache intensity during the acute phase was associated with a more prolonged duration of headache, the team stressed the importance of promptly evaluating patients who have had COVID-19 and who then experience persistent headache.
Long-term evolution unknown
Headache is a common symptom of COVID-19, but its long-term evolution remains unknown. The objective of this study was to evaluate the long-term duration of headache in patients who presented with this symptom during the acute phase of the disease.
Recruitment for this multicenter study took place in March and April 2020. The 905 patients who were enrolled came from six level 3 hospitals in Spain. All completed 9 months of neurologic follow-up.
Their median age was 51 years, 66.5% were women, and more than half (52.7%) had a history of primary headache. About half of the patients required hospitalization (50.5%); the rest were treated as outpatients. The most common headache phenotype was holocranial (67.8%) of severe intensity (50.6%).
Persistent headache common
In the 96.6% cases for which data were available, the median duration of headache was 14 days. The headache persisted at 1 month in 31.1% of patients, at 2 months in 21.5%, at 3 months in 19%, at 6 months in 16.8%, and at 9 months in 16.0%.
“The median duration of COVID-19 headache is around 2 weeks,” David García Azorín, MD, PhD, a member of the Spanish Society of Neurology and one of the coauthors of the study, said in an interview. “However, almost 20% of patients experience it for longer than that. When still present at 2 months, the headache is more likely to follow a chronic daily pattern.” Dr. García Azorín is a neurologist and clinical researcher at the headache unit of the Hospital Clínico Universitario in Valladolid, Spain.
“So, if the headache isn’t letting up, it’s important to make the most of that window of opportunity and provide treatment in that period of 6-12 weeks,” he continued. “To do this, the best option is to carry out preventive treatment so that the patient will have a better chance of recovering.”
Study participants whose headache persisted at 9 months were older and were mostly women. They were less likely to have had pneumonia or to have experienced stabbing pain, photophobia, or phonophobia. They reported that the headache got worse when they engaged in physical activity but less frequently manifested as a throbbing headache.
Secondary tension headaches
On the other hand, Jaime Rodríguez Vico, MD, head of the headache unit at the Jiménez Díaz Foundation Hospital in Madrid, said in an interview that, according to his case studies, the most striking characteristics of post–COVID-19 headaches “in general are secondary, with similarities to tension headaches that patients are able to differentiate from other clinical types of headache. In patients with migraine, very often we see that we’re dealing with a trigger. In other words, more migraines – and more intense ones at that – are brought about.”
He added: “Generally, post–COVID-19 headache usually lasts 1-2 weeks, but we have cases of it lasting several months and even over a year with persistent daily headache. These more persistent cases are probably connected to another type of pathology that makes them more susceptible to becoming chronic, something that occurs in another type of primary headache known as new daily persistent headache.”
Primary headache exacerbation
Dr. García Azorín pointed out that it’s not uncommon that among people who already have primary headache, their condition worsens after they become infected with SARS-CoV-2. However, many people differentiate the headache associated with the infection from their usual headache because after becoming infected, their headache is predominantly frontal, oppressive, and chronic.
“Having a prior history of headache is one of the factors that can increase the likelihood that a headache experienced while suffering from COVID-19 will become chronic,” he noted.
This study also found that, more often than not, patients with persistent headache at 9 months had migraine-like pain.
As for headaches in these patients beyond 9 months, “based on our research, the evolution is quite variable,” said Dr. Rodríguez Vico. “Our unit’s numbers are skewed due to the high number of migraine cases that we follow, and therefore our high volume of migraine patients who’ve gotten worse. The same thing happens with COVID-19 vaccines. Migraine is a polygenic disorder with multiple variants and a pathophysiology that we are just beginning to describe. This is why one patient is completely different from another. It’s a real challenge.”
Infections are a common cause of acute and chronic headache. The persistence of a headache after an infection may be caused by the infection becoming chronic, as happens in some types of chronic meningitis, such as tuberculous meningitis. It may also be caused by the persistence of a certain response and activation of the immune system or to the uncovering or worsening of a primary headache coincident with the infection, added Dr. García Azorín.
“Likewise, there are other people who have a biological predisposition to headache as a multifactorial disorder and polygenic disorder, such that a particular stimulus – from trauma or an infection to alcohol consumption – can cause them to develop a headache very similar to a migraine,” he said.
Providing prognosis and treatment
Certain factors can give an idea of how long the headache might last. The study’s univariate analysis showed that age, female sex, headache intensity, pressure-like quality, the presence of photophobia/phonophobia, and worsening with physical activity were associated with headache of longer duration. But in the multivariate analysis, only headache intensity during the acute phase remained statistically significant (hazard ratio, 0.655; 95% confidence interval, 0.582-0.737; P < .001).
When asked whether they planned to continue the study, Dr. García Azorín commented, “The main questions that have arisen from this study have been, above all: ‘Why does this headache happen?’ and ‘How can it be treated or avoided?’ To answer them, we’re looking into pain: which factors could predispose a person to it and which changes may be associated with its presence.”
In addition, different treatments that may improve patient outcomes are being evaluated, because to date, treatment has been empirical and based on the predominant pain phenotype.
In any case, most doctors currently treat post–COVID-19 headache on the basis of how similar the symptoms are to those of other primary headaches. “Given the impact that headache has on patients’ quality of life, there’s a pressing need for controlled studies on possible treatments and their effectiveness,” noted Patricia Pozo Rosich, MD, PhD, one of the coauthors of the study.
“We at the Spanish Society of Neurology truly believe that if these patients were to have this symptom correctly addressed from the start, they could avoid many of the problems that arise in the situation becoming chronic,” she concluded.
Dr. García Azorín and Dr. Rodríguez Vico disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Approximately one in five patients who presented with headache during the acute phase of COVID-19 developed chronic daily headache, according to a study published in Cephalalgia. The greater the headache’s intensity during the acute phase, the greater the likelihood that it would persist.
The research, carried out by members of the Headache Study Group of the Spanish Society of Neurology, evaluated the evolution of headache in more than 900 Spanish patients. Because they found that headache intensity during the acute phase was associated with a more prolonged duration of headache, the team stressed the importance of promptly evaluating patients who have had COVID-19 and who then experience persistent headache.
Long-term evolution unknown
Headache is a common symptom of COVID-19, but its long-term evolution remains unknown. The objective of this study was to evaluate the long-term duration of headache in patients who presented with this symptom during the acute phase of the disease.
Recruitment for this multicenter study took place in March and April 2020. The 905 patients who were enrolled came from six level 3 hospitals in Spain. All completed 9 months of neurologic follow-up.
Their median age was 51 years, 66.5% were women, and more than half (52.7%) had a history of primary headache. About half of the patients required hospitalization (50.5%); the rest were treated as outpatients. The most common headache phenotype was holocranial (67.8%) of severe intensity (50.6%).
Persistent headache common
In the 96.6% cases for which data were available, the median duration of headache was 14 days. The headache persisted at 1 month in 31.1% of patients, at 2 months in 21.5%, at 3 months in 19%, at 6 months in 16.8%, and at 9 months in 16.0%.
“The median duration of COVID-19 headache is around 2 weeks,” David García Azorín, MD, PhD, a member of the Spanish Society of Neurology and one of the coauthors of the study, said in an interview. “However, almost 20% of patients experience it for longer than that. When still present at 2 months, the headache is more likely to follow a chronic daily pattern.” Dr. García Azorín is a neurologist and clinical researcher at the headache unit of the Hospital Clínico Universitario in Valladolid, Spain.
“So, if the headache isn’t letting up, it’s important to make the most of that window of opportunity and provide treatment in that period of 6-12 weeks,” he continued. “To do this, the best option is to carry out preventive treatment so that the patient will have a better chance of recovering.”
Study participants whose headache persisted at 9 months were older and were mostly women. They were less likely to have had pneumonia or to have experienced stabbing pain, photophobia, or phonophobia. They reported that the headache got worse when they engaged in physical activity but less frequently manifested as a throbbing headache.
Secondary tension headaches
On the other hand, Jaime Rodríguez Vico, MD, head of the headache unit at the Jiménez Díaz Foundation Hospital in Madrid, said in an interview that, according to his case studies, the most striking characteristics of post–COVID-19 headaches “in general are secondary, with similarities to tension headaches that patients are able to differentiate from other clinical types of headache. In patients with migraine, very often we see that we’re dealing with a trigger. In other words, more migraines – and more intense ones at that – are brought about.”
He added: “Generally, post–COVID-19 headache usually lasts 1-2 weeks, but we have cases of it lasting several months and even over a year with persistent daily headache. These more persistent cases are probably connected to another type of pathology that makes them more susceptible to becoming chronic, something that occurs in another type of primary headache known as new daily persistent headache.”
Primary headache exacerbation
Dr. García Azorín pointed out that it’s not uncommon that among people who already have primary headache, their condition worsens after they become infected with SARS-CoV-2. However, many people differentiate the headache associated with the infection from their usual headache because after becoming infected, their headache is predominantly frontal, oppressive, and chronic.
“Having a prior history of headache is one of the factors that can increase the likelihood that a headache experienced while suffering from COVID-19 will become chronic,” he noted.
This study also found that, more often than not, patients with persistent headache at 9 months had migraine-like pain.
As for headaches in these patients beyond 9 months, “based on our research, the evolution is quite variable,” said Dr. Rodríguez Vico. “Our unit’s numbers are skewed due to the high number of migraine cases that we follow, and therefore our high volume of migraine patients who’ve gotten worse. The same thing happens with COVID-19 vaccines. Migraine is a polygenic disorder with multiple variants and a pathophysiology that we are just beginning to describe. This is why one patient is completely different from another. It’s a real challenge.”
Infections are a common cause of acute and chronic headache. The persistence of a headache after an infection may be caused by the infection becoming chronic, as happens in some types of chronic meningitis, such as tuberculous meningitis. It may also be caused by the persistence of a certain response and activation of the immune system or to the uncovering or worsening of a primary headache coincident with the infection, added Dr. García Azorín.
“Likewise, there are other people who have a biological predisposition to headache as a multifactorial disorder and polygenic disorder, such that a particular stimulus – from trauma or an infection to alcohol consumption – can cause them to develop a headache very similar to a migraine,” he said.
Providing prognosis and treatment
Certain factors can give an idea of how long the headache might last. The study’s univariate analysis showed that age, female sex, headache intensity, pressure-like quality, the presence of photophobia/phonophobia, and worsening with physical activity were associated with headache of longer duration. But in the multivariate analysis, only headache intensity during the acute phase remained statistically significant (hazard ratio, 0.655; 95% confidence interval, 0.582-0.737; P < .001).
When asked whether they planned to continue the study, Dr. García Azorín commented, “The main questions that have arisen from this study have been, above all: ‘Why does this headache happen?’ and ‘How can it be treated or avoided?’ To answer them, we’re looking into pain: which factors could predispose a person to it and which changes may be associated with its presence.”
In addition, different treatments that may improve patient outcomes are being evaluated, because to date, treatment has been empirical and based on the predominant pain phenotype.
In any case, most doctors currently treat post–COVID-19 headache on the basis of how similar the symptoms are to those of other primary headaches. “Given the impact that headache has on patients’ quality of life, there’s a pressing need for controlled studies on possible treatments and their effectiveness,” noted Patricia Pozo Rosich, MD, PhD, one of the coauthors of the study.
“We at the Spanish Society of Neurology truly believe that if these patients were to have this symptom correctly addressed from the start, they could avoid many of the problems that arise in the situation becoming chronic,” she concluded.
Dr. García Azorín and Dr. Rodríguez Vico disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Approximately one in five patients who presented with headache during the acute phase of COVID-19 developed chronic daily headache, according to a study published in Cephalalgia. The greater the headache’s intensity during the acute phase, the greater the likelihood that it would persist.
The research, carried out by members of the Headache Study Group of the Spanish Society of Neurology, evaluated the evolution of headache in more than 900 Spanish patients. Because they found that headache intensity during the acute phase was associated with a more prolonged duration of headache, the team stressed the importance of promptly evaluating patients who have had COVID-19 and who then experience persistent headache.
Long-term evolution unknown
Headache is a common symptom of COVID-19, but its long-term evolution remains unknown. The objective of this study was to evaluate the long-term duration of headache in patients who presented with this symptom during the acute phase of the disease.
Recruitment for this multicenter study took place in March and April 2020. The 905 patients who were enrolled came from six level 3 hospitals in Spain. All completed 9 months of neurologic follow-up.
Their median age was 51 years, 66.5% were women, and more than half (52.7%) had a history of primary headache. About half of the patients required hospitalization (50.5%); the rest were treated as outpatients. The most common headache phenotype was holocranial (67.8%) of severe intensity (50.6%).
Persistent headache common
In the 96.6% cases for which data were available, the median duration of headache was 14 days. The headache persisted at 1 month in 31.1% of patients, at 2 months in 21.5%, at 3 months in 19%, at 6 months in 16.8%, and at 9 months in 16.0%.
“The median duration of COVID-19 headache is around 2 weeks,” David García Azorín, MD, PhD, a member of the Spanish Society of Neurology and one of the coauthors of the study, said in an interview. “However, almost 20% of patients experience it for longer than that. When still present at 2 months, the headache is more likely to follow a chronic daily pattern.” Dr. García Azorín is a neurologist and clinical researcher at the headache unit of the Hospital Clínico Universitario in Valladolid, Spain.
“So, if the headache isn’t letting up, it’s important to make the most of that window of opportunity and provide treatment in that period of 6-12 weeks,” he continued. “To do this, the best option is to carry out preventive treatment so that the patient will have a better chance of recovering.”
Study participants whose headache persisted at 9 months were older and were mostly women. They were less likely to have had pneumonia or to have experienced stabbing pain, photophobia, or phonophobia. They reported that the headache got worse when they engaged in physical activity but less frequently manifested as a throbbing headache.
Secondary tension headaches
On the other hand, Jaime Rodríguez Vico, MD, head of the headache unit at the Jiménez Díaz Foundation Hospital in Madrid, said in an interview that, according to his case studies, the most striking characteristics of post–COVID-19 headaches “in general are secondary, with similarities to tension headaches that patients are able to differentiate from other clinical types of headache. In patients with migraine, very often we see that we’re dealing with a trigger. In other words, more migraines – and more intense ones at that – are brought about.”
He added: “Generally, post–COVID-19 headache usually lasts 1-2 weeks, but we have cases of it lasting several months and even over a year with persistent daily headache. These more persistent cases are probably connected to another type of pathology that makes them more susceptible to becoming chronic, something that occurs in another type of primary headache known as new daily persistent headache.”
Primary headache exacerbation
Dr. García Azorín pointed out that it’s not uncommon that among people who already have primary headache, their condition worsens after they become infected with SARS-CoV-2. However, many people differentiate the headache associated with the infection from their usual headache because after becoming infected, their headache is predominantly frontal, oppressive, and chronic.
“Having a prior history of headache is one of the factors that can increase the likelihood that a headache experienced while suffering from COVID-19 will become chronic,” he noted.
This study also found that, more often than not, patients with persistent headache at 9 months had migraine-like pain.
As for headaches in these patients beyond 9 months, “based on our research, the evolution is quite variable,” said Dr. Rodríguez Vico. “Our unit’s numbers are skewed due to the high number of migraine cases that we follow, and therefore our high volume of migraine patients who’ve gotten worse. The same thing happens with COVID-19 vaccines. Migraine is a polygenic disorder with multiple variants and a pathophysiology that we are just beginning to describe. This is why one patient is completely different from another. It’s a real challenge.”
Infections are a common cause of acute and chronic headache. The persistence of a headache after an infection may be caused by the infection becoming chronic, as happens in some types of chronic meningitis, such as tuberculous meningitis. It may also be caused by the persistence of a certain response and activation of the immune system or to the uncovering or worsening of a primary headache coincident with the infection, added Dr. García Azorín.
“Likewise, there are other people who have a biological predisposition to headache as a multifactorial disorder and polygenic disorder, such that a particular stimulus – from trauma or an infection to alcohol consumption – can cause them to develop a headache very similar to a migraine,” he said.
Providing prognosis and treatment
Certain factors can give an idea of how long the headache might last. The study’s univariate analysis showed that age, female sex, headache intensity, pressure-like quality, the presence of photophobia/phonophobia, and worsening with physical activity were associated with headache of longer duration. But in the multivariate analysis, only headache intensity during the acute phase remained statistically significant (hazard ratio, 0.655; 95% confidence interval, 0.582-0.737; P < .001).
When asked whether they planned to continue the study, Dr. García Azorín commented, “The main questions that have arisen from this study have been, above all: ‘Why does this headache happen?’ and ‘How can it be treated or avoided?’ To answer them, we’re looking into pain: which factors could predispose a person to it and which changes may be associated with its presence.”
In addition, different treatments that may improve patient outcomes are being evaluated, because to date, treatment has been empirical and based on the predominant pain phenotype.
In any case, most doctors currently treat post–COVID-19 headache on the basis of how similar the symptoms are to those of other primary headaches. “Given the impact that headache has on patients’ quality of life, there’s a pressing need for controlled studies on possible treatments and their effectiveness,” noted Patricia Pozo Rosich, MD, PhD, one of the coauthors of the study.
“We at the Spanish Society of Neurology truly believe that if these patients were to have this symptom correctly addressed from the start, they could avoid many of the problems that arise in the situation becoming chronic,” she concluded.
Dr. García Azorín and Dr. Rodríguez Vico disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CEPHALALGIA
Abnormal growth of the amygdala in infants tied to autism
A new study suggests that overgrowth of the amygdala in infants during the first 6-12 months of life is tied to a later diagnosis of autism spectrum disorder (ASD).
“The faster the amygdala grew in infancy, the more social difficulties the child showed when diagnosed with autism a year later,” first author Mark Shen, PhD, assistant professor of psychiatry and neuroscience, University of North Carolina, Chapel Hill, told this news organization.
The study was published online in the American Journal of Psychiatry.
Unique to autism
The amygdala plays a key role in processing memory, emotional responses, and decisionmaking.
It’s long been known that the amygdala is abnormally large in school-aged children with ASD, but until now, it was not known precisely when aberrant amygdala growth happens, what the clinical consequences may be, and whether amygdala overgrowth is unique to autism.
To investigate, Dr. Shen and colleagues evaluated 1,099 longitudinal MRI scans obtained during natural sleep at 6, 12, and 24 months of age in 408 infants in the Infant Brain Imaging Study (IBIS) Network.
The cohort included 58 infants at high likelihood of developing ASD who were later diagnosed with the disorder, 212 infants at high likelihood of ASD who did not develop ASD, 109 typically-developing control infants, and 29 infants with fragile X syndrome.
At 6 months, infants who developed ASD had typically sized amygdala volumes but showed significantly faster amygdala growth between 6 and 24 months, such that by 12 months the ASD group had significantly larger amygdala volume (Cohen’s d = 0.56), compared with all other groups.
Amygdala growth rate between 6 and 12 months was significantly associated with greater social deficits at 24 months when the children were diagnosed with ASD.
“We found that the amygdala grows too rapidly between 6 and 12 months of age, during a presymptomatic period in autism, prior to when the diagnostic symptoms of autism (social difficulties and repetitive behaviors) are evident and lead to the later diagnosis of autism,” Dr. Shen said in an interview.
This brain growth pattern appears to be unique to autism, as babies with the genetic disorder fragile X syndrome – another neurodevelopmental condition – showed a markedly different brain growth pattern: no differences in amygdala growth but enlargement of a different brain structure, the caudate, which was linked to increased repetitive behaviors, the investigators found.
Earlier intervention
Prior research has shown that children who are later diagnosed with ASD often display problems in infancy with how they attend to visual stimuli in their surroundings.
These early problems with processing visual and sensory information may put increased stress on the amygdala, potentially leading to amygdala hyperactivity, deficits in pruning dendritic connections, and overgrowth, Dr. Shen and colleagues hypothesize.
Amygdala overgrowth has also been linked to chronic stress in studies of other psychiatric conditions, such as depression and anxiety, and may provide a clue to understanding this observation in infants who later develop autism.
“This research suggests that an optimal time to begin supports for children who are at the highest likelihood of developing autism may be during the first year of life: to improve early precursors to social development, such as sensory processing, in babies even before social difficulties arise,” Dr. Shen said.
Cyrus A. Raji, MD, PhD, assistant professor of radiology and neurology, Washington University, St. Louis, said, “What makes this study important is the finding of abnormally increased amygdala growth rate in autism using a longitudinal design that focuses on earlier development.”
“While we are typically used to understanding brain structure as abnormally decreasing over time in certain disorders like Alzheimer’s disease, this study challenges us to understand that too much brain volume growth can also be abnormal in specific conditions,” Dr. Raji added.
This research was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute of Environmental Health Sciences, and National Institute of Mental Health, along with Autism Speaks and the Simons Foundation. Dr. Shen and Dr. Raji have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study suggests that overgrowth of the amygdala in infants during the first 6-12 months of life is tied to a later diagnosis of autism spectrum disorder (ASD).
“The faster the amygdala grew in infancy, the more social difficulties the child showed when diagnosed with autism a year later,” first author Mark Shen, PhD, assistant professor of psychiatry and neuroscience, University of North Carolina, Chapel Hill, told this news organization.
The study was published online in the American Journal of Psychiatry.
Unique to autism
The amygdala plays a key role in processing memory, emotional responses, and decisionmaking.
It’s long been known that the amygdala is abnormally large in school-aged children with ASD, but until now, it was not known precisely when aberrant amygdala growth happens, what the clinical consequences may be, and whether amygdala overgrowth is unique to autism.
To investigate, Dr. Shen and colleagues evaluated 1,099 longitudinal MRI scans obtained during natural sleep at 6, 12, and 24 months of age in 408 infants in the Infant Brain Imaging Study (IBIS) Network.
The cohort included 58 infants at high likelihood of developing ASD who were later diagnosed with the disorder, 212 infants at high likelihood of ASD who did not develop ASD, 109 typically-developing control infants, and 29 infants with fragile X syndrome.
At 6 months, infants who developed ASD had typically sized amygdala volumes but showed significantly faster amygdala growth between 6 and 24 months, such that by 12 months the ASD group had significantly larger amygdala volume (Cohen’s d = 0.56), compared with all other groups.
Amygdala growth rate between 6 and 12 months was significantly associated with greater social deficits at 24 months when the children were diagnosed with ASD.
“We found that the amygdala grows too rapidly between 6 and 12 months of age, during a presymptomatic period in autism, prior to when the diagnostic symptoms of autism (social difficulties and repetitive behaviors) are evident and lead to the later diagnosis of autism,” Dr. Shen said in an interview.
This brain growth pattern appears to be unique to autism, as babies with the genetic disorder fragile X syndrome – another neurodevelopmental condition – showed a markedly different brain growth pattern: no differences in amygdala growth but enlargement of a different brain structure, the caudate, which was linked to increased repetitive behaviors, the investigators found.
Earlier intervention
Prior research has shown that children who are later diagnosed with ASD often display problems in infancy with how they attend to visual stimuli in their surroundings.
These early problems with processing visual and sensory information may put increased stress on the amygdala, potentially leading to amygdala hyperactivity, deficits in pruning dendritic connections, and overgrowth, Dr. Shen and colleagues hypothesize.
Amygdala overgrowth has also been linked to chronic stress in studies of other psychiatric conditions, such as depression and anxiety, and may provide a clue to understanding this observation in infants who later develop autism.
“This research suggests that an optimal time to begin supports for children who are at the highest likelihood of developing autism may be during the first year of life: to improve early precursors to social development, such as sensory processing, in babies even before social difficulties arise,” Dr. Shen said.
Cyrus A. Raji, MD, PhD, assistant professor of radiology and neurology, Washington University, St. Louis, said, “What makes this study important is the finding of abnormally increased amygdala growth rate in autism using a longitudinal design that focuses on earlier development.”
“While we are typically used to understanding brain structure as abnormally decreasing over time in certain disorders like Alzheimer’s disease, this study challenges us to understand that too much brain volume growth can also be abnormal in specific conditions,” Dr. Raji added.
This research was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute of Environmental Health Sciences, and National Institute of Mental Health, along with Autism Speaks and the Simons Foundation. Dr. Shen and Dr. Raji have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study suggests that overgrowth of the amygdala in infants during the first 6-12 months of life is tied to a later diagnosis of autism spectrum disorder (ASD).
“The faster the amygdala grew in infancy, the more social difficulties the child showed when diagnosed with autism a year later,” first author Mark Shen, PhD, assistant professor of psychiatry and neuroscience, University of North Carolina, Chapel Hill, told this news organization.
The study was published online in the American Journal of Psychiatry.
Unique to autism
The amygdala plays a key role in processing memory, emotional responses, and decisionmaking.
It’s long been known that the amygdala is abnormally large in school-aged children with ASD, but until now, it was not known precisely when aberrant amygdala growth happens, what the clinical consequences may be, and whether amygdala overgrowth is unique to autism.
To investigate, Dr. Shen and colleagues evaluated 1,099 longitudinal MRI scans obtained during natural sleep at 6, 12, and 24 months of age in 408 infants in the Infant Brain Imaging Study (IBIS) Network.
The cohort included 58 infants at high likelihood of developing ASD who were later diagnosed with the disorder, 212 infants at high likelihood of ASD who did not develop ASD, 109 typically-developing control infants, and 29 infants with fragile X syndrome.
At 6 months, infants who developed ASD had typically sized amygdala volumes but showed significantly faster amygdala growth between 6 and 24 months, such that by 12 months the ASD group had significantly larger amygdala volume (Cohen’s d = 0.56), compared with all other groups.
Amygdala growth rate between 6 and 12 months was significantly associated with greater social deficits at 24 months when the children were diagnosed with ASD.
“We found that the amygdala grows too rapidly between 6 and 12 months of age, during a presymptomatic period in autism, prior to when the diagnostic symptoms of autism (social difficulties and repetitive behaviors) are evident and lead to the later diagnosis of autism,” Dr. Shen said in an interview.
This brain growth pattern appears to be unique to autism, as babies with the genetic disorder fragile X syndrome – another neurodevelopmental condition – showed a markedly different brain growth pattern: no differences in amygdala growth but enlargement of a different brain structure, the caudate, which was linked to increased repetitive behaviors, the investigators found.
Earlier intervention
Prior research has shown that children who are later diagnosed with ASD often display problems in infancy with how they attend to visual stimuli in their surroundings.
These early problems with processing visual and sensory information may put increased stress on the amygdala, potentially leading to amygdala hyperactivity, deficits in pruning dendritic connections, and overgrowth, Dr. Shen and colleagues hypothesize.
Amygdala overgrowth has also been linked to chronic stress in studies of other psychiatric conditions, such as depression and anxiety, and may provide a clue to understanding this observation in infants who later develop autism.
“This research suggests that an optimal time to begin supports for children who are at the highest likelihood of developing autism may be during the first year of life: to improve early precursors to social development, such as sensory processing, in babies even before social difficulties arise,” Dr. Shen said.
Cyrus A. Raji, MD, PhD, assistant professor of radiology and neurology, Washington University, St. Louis, said, “What makes this study important is the finding of abnormally increased amygdala growth rate in autism using a longitudinal design that focuses on earlier development.”
“While we are typically used to understanding brain structure as abnormally decreasing over time in certain disorders like Alzheimer’s disease, this study challenges us to understand that too much brain volume growth can also be abnormal in specific conditions,” Dr. Raji added.
This research was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute of Environmental Health Sciences, and National Institute of Mental Health, along with Autism Speaks and the Simons Foundation. Dr. Shen and Dr. Raji have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Bellies up to the bar, the weight gain is on us
I’d do anything for weight loss (but I won’t do that)
Weight loss isn’t a multibillion-dollar industry for nothing. How many people step onto the scale in the morning and sigh, wishing they could lose that last 10 pounds?
Alcohol also isn’t a multibillion-dollar industry for nothing. If there’s one thing more universal than wishing you could lose weight, it’s drinking to forget your woes about being unable to lose weight.
Naturally, and unfortunately for those of us who rather enjoy a good beer, one of the best ways to lose weight is to stop drinking. Alcohol is almost the definition of empty calories. So, which wins out: The unstoppable force of wanting to lose weight, or the immovable object of alcohol? According to a survey from DrugAbuse.com, it’s alcohol, and it’s not even close.
Even in a state with as health conscious a reputation as California, not only are people not willing to give up alcohol to lose weight, they’re willing to gain a noticeable amount of weight in order to continue drinking. It’s 14 pounds for Californians, which is in the middle of the road for America, which overall averaged 13 pounds to keep drinking. Hawaiians, South Dakotans, Utahns, and Vermonters were at the bottom, willing to add only 8 pounds to keep booze in their diet. At the other end of the scale, willing to add 28 whole pounds to keep the beer flowing, is humble little Rhode Island, followed by Wyoming at 23 pounds, Maryland at 22, and Tennessee at 21.
Obviously, that’s a lot of weight to gain, but to drive home the exact quantity of just how much weight, KRON-TV noted that adding the U.S. average of 13 pounds to your body is the equivalent of strapping 224 slices of bacon to yourself, which, to us, is just the poorest choice of comparison. If there’s one thing we’re less willing to give up than alcohol, it’s probably bacon. Or if you’re feeling especially ambitious, you could go for bacon-scented beer from the Waffle House. Now that’s a drink.
This looks like a job for the ‘magnetic slime robot’
What’s that? While you were in the process of gaining 14 pounds so you could keep drinking alcohol you swallowed something that you shouldn’t have? Did you swallow a lot of aggression?
You swallowed a what? An ear bud? But how did you manage that? No, never mind, we don’t really want to hear about your personal life. Lucky for you, though, today’s LOTME phrase that pays is “magnetic turd” and it’s just the thing for the busy executive/child with a foreign object stuck in their … whatever.
Yes, we said magnetic turd. Or, if you prefer, a “magnetic slime robot.” The black-brown–colored blob/robot/turd in question is an investigational substance that can be controlled magnetically to move through very narrow spaces and encircle small objects that have been accidentally swallowed, its cocreator, Li Zhang of the Chinese University of Hong Kong, told the Guardian.
It’s made by combining the polymer polyvinyl alcohol with borax and particles of neodymium magnet. And since those neodymium particles are not particularly friendly to humans, Dr. Zhang and the research team coated the slime with silica to seal in the toxicity. The slime has the consistency of custard and exhibits “visco-elastic properties,” Dr. Zhang said, meaning that “sometimes it behaves like a solid, sometimes it behaves like a liquid.”
We could go on, telling you about the substance’s self-healing ability and electrical conductivity and how it does look very, very turd-like. Instead, we offer this link to the team’s really freaky video.
We’re going to be seeing that in our nightmares.
Fish: More than meets the fry?
When you think of fish, intelligence isn’t usually the first thing to pop into your head. Their short memory spans, which can be as little as 3 seconds, probably don’t help their cause.
Recently, though, it has become apparent that fish can be trained to do simple math problems like adding and subtracting. Research conducted in Germany has shown that cichlids – tropical fish often found in home aquariums – and stingrays can observe small quantities and know how many things are there without actually counting, kind of like how a human can look at a bowl of apples and know about how many are in it.
Fish, once thought to be not very smart, may be on the same level of intelligence as birds, suggested Vera Schluessel, PhD, of the University of Bonn’s Institute of Zoology, and associates.
“Successful fish showed abilities far above chance level, specifically in the stingrays. Again, this raises the question of what abilities fish may be capable of if being asked the ‘right’ question,” the researchers said in Scientific Reports.
They tried to teach the cichlids and stingrays how to add and subtract by recognizing colors: Blue meant to add one and yellow meant to subtract one. Gates were set up and when the fish chose a correct answer, they were rewarded with food. Although it took many sessions for the fish to completely catch on, they did figure it out eventually.
If fish are smarter than we thought, maybe we can stop paying for math tutors for our kids and just have the family goldfish do it.
For earthworms, not all plastics are created equal
Everything living on the earth has to deal with pollution in some way, including earthworms. Not only have they have adapted to eating plastics found in soil, they have preferences.
The earthworm is a little creature with a big job. The materials and minerals they munch on as they go through the earth get recycled through their tiny bodies to create more fertile soil for things to grow – making them the hidden heroes of every garden. But what about soil that’s full of microscopic plastic pieces? Well, turns out earthworms will eat that too, investigators from Nankai University in Tianjin, China, reported in Environmental Science & Technology.
The researchers looked at how these eating machines were digesting the plastic and found that they actually have preferences. Soils with bio-based polylactic acid (PLA) or petroleum-derived polyethylene terephthalate (PET) particles were a hit. Another test showed that the worms broke the PLA particles down into smaller fragments than the PET ones. So at least the “healthier” option agreed with them more. More work is needed, however, to determine if the worms are being harmed by all the waste they’re digesting.
So what does this mean for the evolution or even survival of this unsung hero of the planet? Scientists still need to dig into that question. No pun intended.
I’d do anything for weight loss (but I won’t do that)
Weight loss isn’t a multibillion-dollar industry for nothing. How many people step onto the scale in the morning and sigh, wishing they could lose that last 10 pounds?
Alcohol also isn’t a multibillion-dollar industry for nothing. If there’s one thing more universal than wishing you could lose weight, it’s drinking to forget your woes about being unable to lose weight.
Naturally, and unfortunately for those of us who rather enjoy a good beer, one of the best ways to lose weight is to stop drinking. Alcohol is almost the definition of empty calories. So, which wins out: The unstoppable force of wanting to lose weight, or the immovable object of alcohol? According to a survey from DrugAbuse.com, it’s alcohol, and it’s not even close.
Even in a state with as health conscious a reputation as California, not only are people not willing to give up alcohol to lose weight, they’re willing to gain a noticeable amount of weight in order to continue drinking. It’s 14 pounds for Californians, which is in the middle of the road for America, which overall averaged 13 pounds to keep drinking. Hawaiians, South Dakotans, Utahns, and Vermonters were at the bottom, willing to add only 8 pounds to keep booze in their diet. At the other end of the scale, willing to add 28 whole pounds to keep the beer flowing, is humble little Rhode Island, followed by Wyoming at 23 pounds, Maryland at 22, and Tennessee at 21.
Obviously, that’s a lot of weight to gain, but to drive home the exact quantity of just how much weight, KRON-TV noted that adding the U.S. average of 13 pounds to your body is the equivalent of strapping 224 slices of bacon to yourself, which, to us, is just the poorest choice of comparison. If there’s one thing we’re less willing to give up than alcohol, it’s probably bacon. Or if you’re feeling especially ambitious, you could go for bacon-scented beer from the Waffle House. Now that’s a drink.
This looks like a job for the ‘magnetic slime robot’
What’s that? While you were in the process of gaining 14 pounds so you could keep drinking alcohol you swallowed something that you shouldn’t have? Did you swallow a lot of aggression?
You swallowed a what? An ear bud? But how did you manage that? No, never mind, we don’t really want to hear about your personal life. Lucky for you, though, today’s LOTME phrase that pays is “magnetic turd” and it’s just the thing for the busy executive/child with a foreign object stuck in their … whatever.
Yes, we said magnetic turd. Or, if you prefer, a “magnetic slime robot.” The black-brown–colored blob/robot/turd in question is an investigational substance that can be controlled magnetically to move through very narrow spaces and encircle small objects that have been accidentally swallowed, its cocreator, Li Zhang of the Chinese University of Hong Kong, told the Guardian.
It’s made by combining the polymer polyvinyl alcohol with borax and particles of neodymium magnet. And since those neodymium particles are not particularly friendly to humans, Dr. Zhang and the research team coated the slime with silica to seal in the toxicity. The slime has the consistency of custard and exhibits “visco-elastic properties,” Dr. Zhang said, meaning that “sometimes it behaves like a solid, sometimes it behaves like a liquid.”
We could go on, telling you about the substance’s self-healing ability and electrical conductivity and how it does look very, very turd-like. Instead, we offer this link to the team’s really freaky video.
We’re going to be seeing that in our nightmares.
Fish: More than meets the fry?
When you think of fish, intelligence isn’t usually the first thing to pop into your head. Their short memory spans, which can be as little as 3 seconds, probably don’t help their cause.
Recently, though, it has become apparent that fish can be trained to do simple math problems like adding and subtracting. Research conducted in Germany has shown that cichlids – tropical fish often found in home aquariums – and stingrays can observe small quantities and know how many things are there without actually counting, kind of like how a human can look at a bowl of apples and know about how many are in it.
Fish, once thought to be not very smart, may be on the same level of intelligence as birds, suggested Vera Schluessel, PhD, of the University of Bonn’s Institute of Zoology, and associates.
“Successful fish showed abilities far above chance level, specifically in the stingrays. Again, this raises the question of what abilities fish may be capable of if being asked the ‘right’ question,” the researchers said in Scientific Reports.
They tried to teach the cichlids and stingrays how to add and subtract by recognizing colors: Blue meant to add one and yellow meant to subtract one. Gates were set up and when the fish chose a correct answer, they were rewarded with food. Although it took many sessions for the fish to completely catch on, they did figure it out eventually.
If fish are smarter than we thought, maybe we can stop paying for math tutors for our kids and just have the family goldfish do it.
For earthworms, not all plastics are created equal
Everything living on the earth has to deal with pollution in some way, including earthworms. Not only have they have adapted to eating plastics found in soil, they have preferences.
The earthworm is a little creature with a big job. The materials and minerals they munch on as they go through the earth get recycled through their tiny bodies to create more fertile soil for things to grow – making them the hidden heroes of every garden. But what about soil that’s full of microscopic plastic pieces? Well, turns out earthworms will eat that too, investigators from Nankai University in Tianjin, China, reported in Environmental Science & Technology.
The researchers looked at how these eating machines were digesting the plastic and found that they actually have preferences. Soils with bio-based polylactic acid (PLA) or petroleum-derived polyethylene terephthalate (PET) particles were a hit. Another test showed that the worms broke the PLA particles down into smaller fragments than the PET ones. So at least the “healthier” option agreed with them more. More work is needed, however, to determine if the worms are being harmed by all the waste they’re digesting.
So what does this mean for the evolution or even survival of this unsung hero of the planet? Scientists still need to dig into that question. No pun intended.
I’d do anything for weight loss (but I won’t do that)
Weight loss isn’t a multibillion-dollar industry for nothing. How many people step onto the scale in the morning and sigh, wishing they could lose that last 10 pounds?
Alcohol also isn’t a multibillion-dollar industry for nothing. If there’s one thing more universal than wishing you could lose weight, it’s drinking to forget your woes about being unable to lose weight.
Naturally, and unfortunately for those of us who rather enjoy a good beer, one of the best ways to lose weight is to stop drinking. Alcohol is almost the definition of empty calories. So, which wins out: The unstoppable force of wanting to lose weight, or the immovable object of alcohol? According to a survey from DrugAbuse.com, it’s alcohol, and it’s not even close.
Even in a state with as health conscious a reputation as California, not only are people not willing to give up alcohol to lose weight, they’re willing to gain a noticeable amount of weight in order to continue drinking. It’s 14 pounds for Californians, which is in the middle of the road for America, which overall averaged 13 pounds to keep drinking. Hawaiians, South Dakotans, Utahns, and Vermonters were at the bottom, willing to add only 8 pounds to keep booze in their diet. At the other end of the scale, willing to add 28 whole pounds to keep the beer flowing, is humble little Rhode Island, followed by Wyoming at 23 pounds, Maryland at 22, and Tennessee at 21.
Obviously, that’s a lot of weight to gain, but to drive home the exact quantity of just how much weight, KRON-TV noted that adding the U.S. average of 13 pounds to your body is the equivalent of strapping 224 slices of bacon to yourself, which, to us, is just the poorest choice of comparison. If there’s one thing we’re less willing to give up than alcohol, it’s probably bacon. Or if you’re feeling especially ambitious, you could go for bacon-scented beer from the Waffle House. Now that’s a drink.
This looks like a job for the ‘magnetic slime robot’
What’s that? While you were in the process of gaining 14 pounds so you could keep drinking alcohol you swallowed something that you shouldn’t have? Did you swallow a lot of aggression?
You swallowed a what? An ear bud? But how did you manage that? No, never mind, we don’t really want to hear about your personal life. Lucky for you, though, today’s LOTME phrase that pays is “magnetic turd” and it’s just the thing for the busy executive/child with a foreign object stuck in their … whatever.
Yes, we said magnetic turd. Or, if you prefer, a “magnetic slime robot.” The black-brown–colored blob/robot/turd in question is an investigational substance that can be controlled magnetically to move through very narrow spaces and encircle small objects that have been accidentally swallowed, its cocreator, Li Zhang of the Chinese University of Hong Kong, told the Guardian.
It’s made by combining the polymer polyvinyl alcohol with borax and particles of neodymium magnet. And since those neodymium particles are not particularly friendly to humans, Dr. Zhang and the research team coated the slime with silica to seal in the toxicity. The slime has the consistency of custard and exhibits “visco-elastic properties,” Dr. Zhang said, meaning that “sometimes it behaves like a solid, sometimes it behaves like a liquid.”
We could go on, telling you about the substance’s self-healing ability and electrical conductivity and how it does look very, very turd-like. Instead, we offer this link to the team’s really freaky video.
We’re going to be seeing that in our nightmares.
Fish: More than meets the fry?
When you think of fish, intelligence isn’t usually the first thing to pop into your head. Their short memory spans, which can be as little as 3 seconds, probably don’t help their cause.
Recently, though, it has become apparent that fish can be trained to do simple math problems like adding and subtracting. Research conducted in Germany has shown that cichlids – tropical fish often found in home aquariums – and stingrays can observe small quantities and know how many things are there without actually counting, kind of like how a human can look at a bowl of apples and know about how many are in it.
Fish, once thought to be not very smart, may be on the same level of intelligence as birds, suggested Vera Schluessel, PhD, of the University of Bonn’s Institute of Zoology, and associates.
“Successful fish showed abilities far above chance level, specifically in the stingrays. Again, this raises the question of what abilities fish may be capable of if being asked the ‘right’ question,” the researchers said in Scientific Reports.
They tried to teach the cichlids and stingrays how to add and subtract by recognizing colors: Blue meant to add one and yellow meant to subtract one. Gates were set up and when the fish chose a correct answer, they were rewarded with food. Although it took many sessions for the fish to completely catch on, they did figure it out eventually.
If fish are smarter than we thought, maybe we can stop paying for math tutors for our kids and just have the family goldfish do it.
For earthworms, not all plastics are created equal
Everything living on the earth has to deal with pollution in some way, including earthworms. Not only have they have adapted to eating plastics found in soil, they have preferences.
The earthworm is a little creature with a big job. The materials and minerals they munch on as they go through the earth get recycled through their tiny bodies to create more fertile soil for things to grow – making them the hidden heroes of every garden. But what about soil that’s full of microscopic plastic pieces? Well, turns out earthworms will eat that too, investigators from Nankai University in Tianjin, China, reported in Environmental Science & Technology.
The researchers looked at how these eating machines were digesting the plastic and found that they actually have preferences. Soils with bio-based polylactic acid (PLA) or petroleum-derived polyethylene terephthalate (PET) particles were a hit. Another test showed that the worms broke the PLA particles down into smaller fragments than the PET ones. So at least the “healthier” option agreed with them more. More work is needed, however, to determine if the worms are being harmed by all the waste they’re digesting.
So what does this mean for the evolution or even survival of this unsung hero of the planet? Scientists still need to dig into that question. No pun intended.