User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Stimulants may not improve academic learning in children with ADHD
Extended-release methylphenidate (Concerta) had no effect on learning academic material taught in a small group of children with attention-deficit/hyperactivity disorder (ADHD), a controlled crossover study found.
As in previous studies, however, the stimulant did improve seat work productivity and classroom behavior, but these benefits did not translate into better learning of individual academic learning units, according to William E. Pelham Jr., PhD, of the department of psychology at Florida International University in Miami, and colleagues.
The results were published online in the Journal of Consulting and Clinical Psychology.
The authors said the finding raises questions about how stimulant medication leads to improved academic achievement over time. “This is important given that many parents and pediatricians believe that medication will improve academic achievement; parents are more likely to pursue medication (vs. other treatment options) when they identify academic achievement as a primary goal for treatment. The current findings suggest this emphasis may be misguided,” they wrote.
In their view, efforts to improve learning in children with ADHD should focus on delivering effective academic instruction and support such as individualized educational plans rather than stimulant therapy.
The study
The study cohort consisted of 173 children aged 7-12 (77% male, 86% Hispanic) who met Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, criteria for ADHD and were participating in a therapeutic summer camp classroom.
The experimental design was a triple-masked, within-subject, AB/BA crossover trial. Children completed two consecutive phases of daily, 25-minute instruction in both subject-area content (science and social studies) and vocabulary. Each phase was a standard instructional unit lasting for 3 weeks and lessons were given by credentialed teachers via small-group, evidence-based instruction.
Each child was randomized to receive daily osmotic-release oral system methylphenidate (OROS-MPH) during either the first or second instructional phase and to receive placebo during the other.
Seat work referred to the amount of work a pupil completed in a fixed duration of independent work time, and classroom behavior referred to the frequency of violating classroom rules. Learning was measured by tests, and multilevel models were fit separately to the subject and vocabulary test scores, with four observations per child: pretest and posttest in the two academic subject areas.
The results showed that medication had large, salutary, statistically significant effects on children’s academic seat work productivity and classroom behavior on every single day of the instructional period.
Pupils completed 37% more arithmetic problems per minute when taking OROS-MPH and committed 53% fewer rule violations per hour. In terms of learning the material taught during instruction, however, tests showed that children learned the same amount of subject-area and vocabulary content whether they were taking OROS-MPH or placebo during the instructional period.
Consistent with previous studies, medication slightly helped to improve test scores when taken on the day of a test, but not enough to boost most children’s grades. For example, medication helped children increase on average 1.7 percentage points out of 100 on science and social studies tests.
“This finding has relevance for parents deciding whether to medicate their child for occasions such as a psychoeducational evaluation or high-stakes academic testing – while the effect size was small, findings suggest being medicated would improve scores,” the investigators wrote.
Sharing his perspective on the study but not involved in it, Herschel R. Lessin, MD, a pediatrician at The Children’s Medical Group in Poughkeepsie, N.Y., and coauthor of the American Academy of Pediatrics (AAP) guidelines on ADHD, said, “If you ignore the sensationalized headlines, this study is an interesting but preliminary first step, and justifies further research on the topic. It also has several potential defects, which the authors in fact address in the supplements.” The cohort size was small, for example, the doses of medication were very low, and the study took place in a controlled therapeutic setting – not the everyday classroom.
Furthermore, Dr. Lessin added, the study’s conclusions “are contrary to my 40 years of experience in treating ADHD. If they had used standard measures of assessment, as in previous studies, they would have found medication did impact learning. More research is clearly needed.”
In other comments, Holly K. Harris, MD, assistant professor of pediatrics-development at Baylor College of Medicine and Texas Children’s Hospital in Houston, said the core symptoms of ADHD are primarily behavioral in nature, not academic learning related.
“Stimulant medications are targeting these core behavioral symptoms of ADHD ... but the goal of treatment is more than just the reduction of symptoms; it is to improve a child’s overall functioning so that they succeed at what is expected of them and avoid developing even more impairments,” Dr. Harris said, adding that symptom improvement can sometimes allow a child to learn better in the classroom and achieve more academically.
Children with ADHD may have diagnosed or undiagnosed comorbid learning disabilities, with one 2013 study suggesting a rate of 31%-45%.
With such learning disabilities being distinct from core behavioral symptoms, stimulant medications would not be expected to address a child’s learning disability. “In fact, best practice is for a child with ADHD who is not responding to stimulant medication (doctors might refer to this as complex ADHD) to undergo full individual evaluations either through the school system or an outside psychological assessment to assess for potential learning disabilities or other comorbid developmental/learning or psychiatric diagnosis,” Dr. Harris said.
Rather than changing prescribing patterns, she continued, pediatricians could consider advising parents to request learning evaluations through the school system if the child continues to struggle academically with no change in learning outcomes despite improvement in some behavioral outcomes.
As a reference, Dr. Harris recommended the Society for Developmental and Behavioral Pediatrics guidelines for complex ADHD.
This study was funded by the National Institute on Mental Health with additional support from the National Institute on Alcohol Abuse and Alcoholism, the National Institute on Drug Abuse, and the Institute of Education Sciences. Coauthor James Waxmonsky, MD, has received research funding from the National Institutes of Health, Supernus, and Pfizer and served on the advisory board for Iron Shore, NLS Pharma, and Purdue Pharma.
Extended-release methylphenidate (Concerta) had no effect on learning academic material taught in a small group of children with attention-deficit/hyperactivity disorder (ADHD), a controlled crossover study found.
As in previous studies, however, the stimulant did improve seat work productivity and classroom behavior, but these benefits did not translate into better learning of individual academic learning units, according to William E. Pelham Jr., PhD, of the department of psychology at Florida International University in Miami, and colleagues.
The results were published online in the Journal of Consulting and Clinical Psychology.
The authors said the finding raises questions about how stimulant medication leads to improved academic achievement over time. “This is important given that many parents and pediatricians believe that medication will improve academic achievement; parents are more likely to pursue medication (vs. other treatment options) when they identify academic achievement as a primary goal for treatment. The current findings suggest this emphasis may be misguided,” they wrote.
In their view, efforts to improve learning in children with ADHD should focus on delivering effective academic instruction and support such as individualized educational plans rather than stimulant therapy.
The study
The study cohort consisted of 173 children aged 7-12 (77% male, 86% Hispanic) who met Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, criteria for ADHD and were participating in a therapeutic summer camp classroom.
The experimental design was a triple-masked, within-subject, AB/BA crossover trial. Children completed two consecutive phases of daily, 25-minute instruction in both subject-area content (science and social studies) and vocabulary. Each phase was a standard instructional unit lasting for 3 weeks and lessons were given by credentialed teachers via small-group, evidence-based instruction.
Each child was randomized to receive daily osmotic-release oral system methylphenidate (OROS-MPH) during either the first or second instructional phase and to receive placebo during the other.
Seat work referred to the amount of work a pupil completed in a fixed duration of independent work time, and classroom behavior referred to the frequency of violating classroom rules. Learning was measured by tests, and multilevel models were fit separately to the subject and vocabulary test scores, with four observations per child: pretest and posttest in the two academic subject areas.
The results showed that medication had large, salutary, statistically significant effects on children’s academic seat work productivity and classroom behavior on every single day of the instructional period.
Pupils completed 37% more arithmetic problems per minute when taking OROS-MPH and committed 53% fewer rule violations per hour. In terms of learning the material taught during instruction, however, tests showed that children learned the same amount of subject-area and vocabulary content whether they were taking OROS-MPH or placebo during the instructional period.
Consistent with previous studies, medication slightly helped to improve test scores when taken on the day of a test, but not enough to boost most children’s grades. For example, medication helped children increase on average 1.7 percentage points out of 100 on science and social studies tests.
“This finding has relevance for parents deciding whether to medicate their child for occasions such as a psychoeducational evaluation or high-stakes academic testing – while the effect size was small, findings suggest being medicated would improve scores,” the investigators wrote.
Sharing his perspective on the study but not involved in it, Herschel R. Lessin, MD, a pediatrician at The Children’s Medical Group in Poughkeepsie, N.Y., and coauthor of the American Academy of Pediatrics (AAP) guidelines on ADHD, said, “If you ignore the sensationalized headlines, this study is an interesting but preliminary first step, and justifies further research on the topic. It also has several potential defects, which the authors in fact address in the supplements.” The cohort size was small, for example, the doses of medication were very low, and the study took place in a controlled therapeutic setting – not the everyday classroom.
Furthermore, Dr. Lessin added, the study’s conclusions “are contrary to my 40 years of experience in treating ADHD. If they had used standard measures of assessment, as in previous studies, they would have found medication did impact learning. More research is clearly needed.”
In other comments, Holly K. Harris, MD, assistant professor of pediatrics-development at Baylor College of Medicine and Texas Children’s Hospital in Houston, said the core symptoms of ADHD are primarily behavioral in nature, not academic learning related.
“Stimulant medications are targeting these core behavioral symptoms of ADHD ... but the goal of treatment is more than just the reduction of symptoms; it is to improve a child’s overall functioning so that they succeed at what is expected of them and avoid developing even more impairments,” Dr. Harris said, adding that symptom improvement can sometimes allow a child to learn better in the classroom and achieve more academically.
Children with ADHD may have diagnosed or undiagnosed comorbid learning disabilities, with one 2013 study suggesting a rate of 31%-45%.
With such learning disabilities being distinct from core behavioral symptoms, stimulant medications would not be expected to address a child’s learning disability. “In fact, best practice is for a child with ADHD who is not responding to stimulant medication (doctors might refer to this as complex ADHD) to undergo full individual evaluations either through the school system or an outside psychological assessment to assess for potential learning disabilities or other comorbid developmental/learning or psychiatric diagnosis,” Dr. Harris said.
Rather than changing prescribing patterns, she continued, pediatricians could consider advising parents to request learning evaluations through the school system if the child continues to struggle academically with no change in learning outcomes despite improvement in some behavioral outcomes.
As a reference, Dr. Harris recommended the Society for Developmental and Behavioral Pediatrics guidelines for complex ADHD.
This study was funded by the National Institute on Mental Health with additional support from the National Institute on Alcohol Abuse and Alcoholism, the National Institute on Drug Abuse, and the Institute of Education Sciences. Coauthor James Waxmonsky, MD, has received research funding from the National Institutes of Health, Supernus, and Pfizer and served on the advisory board for Iron Shore, NLS Pharma, and Purdue Pharma.
Extended-release methylphenidate (Concerta) had no effect on learning academic material taught in a small group of children with attention-deficit/hyperactivity disorder (ADHD), a controlled crossover study found.
As in previous studies, however, the stimulant did improve seat work productivity and classroom behavior, but these benefits did not translate into better learning of individual academic learning units, according to William E. Pelham Jr., PhD, of the department of psychology at Florida International University in Miami, and colleagues.
The results were published online in the Journal of Consulting and Clinical Psychology.
The authors said the finding raises questions about how stimulant medication leads to improved academic achievement over time. “This is important given that many parents and pediatricians believe that medication will improve academic achievement; parents are more likely to pursue medication (vs. other treatment options) when they identify academic achievement as a primary goal for treatment. The current findings suggest this emphasis may be misguided,” they wrote.
In their view, efforts to improve learning in children with ADHD should focus on delivering effective academic instruction and support such as individualized educational plans rather than stimulant therapy.
The study
The study cohort consisted of 173 children aged 7-12 (77% male, 86% Hispanic) who met Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, criteria for ADHD and were participating in a therapeutic summer camp classroom.
The experimental design was a triple-masked, within-subject, AB/BA crossover trial. Children completed two consecutive phases of daily, 25-minute instruction in both subject-area content (science and social studies) and vocabulary. Each phase was a standard instructional unit lasting for 3 weeks and lessons were given by credentialed teachers via small-group, evidence-based instruction.
Each child was randomized to receive daily osmotic-release oral system methylphenidate (OROS-MPH) during either the first or second instructional phase and to receive placebo during the other.
Seat work referred to the amount of work a pupil completed in a fixed duration of independent work time, and classroom behavior referred to the frequency of violating classroom rules. Learning was measured by tests, and multilevel models were fit separately to the subject and vocabulary test scores, with four observations per child: pretest and posttest in the two academic subject areas.
The results showed that medication had large, salutary, statistically significant effects on children’s academic seat work productivity and classroom behavior on every single day of the instructional period.
Pupils completed 37% more arithmetic problems per minute when taking OROS-MPH and committed 53% fewer rule violations per hour. In terms of learning the material taught during instruction, however, tests showed that children learned the same amount of subject-area and vocabulary content whether they were taking OROS-MPH or placebo during the instructional period.
Consistent with previous studies, medication slightly helped to improve test scores when taken on the day of a test, but not enough to boost most children’s grades. For example, medication helped children increase on average 1.7 percentage points out of 100 on science and social studies tests.
“This finding has relevance for parents deciding whether to medicate their child for occasions such as a psychoeducational evaluation or high-stakes academic testing – while the effect size was small, findings suggest being medicated would improve scores,” the investigators wrote.
Sharing his perspective on the study but not involved in it, Herschel R. Lessin, MD, a pediatrician at The Children’s Medical Group in Poughkeepsie, N.Y., and coauthor of the American Academy of Pediatrics (AAP) guidelines on ADHD, said, “If you ignore the sensationalized headlines, this study is an interesting but preliminary first step, and justifies further research on the topic. It also has several potential defects, which the authors in fact address in the supplements.” The cohort size was small, for example, the doses of medication were very low, and the study took place in a controlled therapeutic setting – not the everyday classroom.
Furthermore, Dr. Lessin added, the study’s conclusions “are contrary to my 40 years of experience in treating ADHD. If they had used standard measures of assessment, as in previous studies, they would have found medication did impact learning. More research is clearly needed.”
In other comments, Holly K. Harris, MD, assistant professor of pediatrics-development at Baylor College of Medicine and Texas Children’s Hospital in Houston, said the core symptoms of ADHD are primarily behavioral in nature, not academic learning related.
“Stimulant medications are targeting these core behavioral symptoms of ADHD ... but the goal of treatment is more than just the reduction of symptoms; it is to improve a child’s overall functioning so that they succeed at what is expected of them and avoid developing even more impairments,” Dr. Harris said, adding that symptom improvement can sometimes allow a child to learn better in the classroom and achieve more academically.
Children with ADHD may have diagnosed or undiagnosed comorbid learning disabilities, with one 2013 study suggesting a rate of 31%-45%.
With such learning disabilities being distinct from core behavioral symptoms, stimulant medications would not be expected to address a child’s learning disability. “In fact, best practice is for a child with ADHD who is not responding to stimulant medication (doctors might refer to this as complex ADHD) to undergo full individual evaluations either through the school system or an outside psychological assessment to assess for potential learning disabilities or other comorbid developmental/learning or psychiatric diagnosis,” Dr. Harris said.
Rather than changing prescribing patterns, she continued, pediatricians could consider advising parents to request learning evaluations through the school system if the child continues to struggle academically with no change in learning outcomes despite improvement in some behavioral outcomes.
As a reference, Dr. Harris recommended the Society for Developmental and Behavioral Pediatrics guidelines for complex ADHD.
This study was funded by the National Institute on Mental Health with additional support from the National Institute on Alcohol Abuse and Alcoholism, the National Institute on Drug Abuse, and the Institute of Education Sciences. Coauthor James Waxmonsky, MD, has received research funding from the National Institutes of Health, Supernus, and Pfizer and served on the advisory board for Iron Shore, NLS Pharma, and Purdue Pharma.
FROM JOURNAL OF CONSULTING AND CLINICAL PSYCHOLOGY
A prescription for de-diagnosing
In 2016, Gupta and Cahill challenged the field of psychiatry to reexamine prescribing patterns.1 They warned against the use of polypharmacy when not attached to improved patient functioning. They were concerned with the limited evidence for polypharmacy as well as DSM diagnostic criteria. In their inspiring article, they described a process of deprescribing.
In an effort to study and practice their recommendations, we have noticed a lack of literature examining the elimination of diagnostic labels. While there have been some studies looking at comorbidity, especially with substance use disorders,2 there is a paucity of scientific evidence on patients with numerous diagnoses. Yet our practices are filled with patients who have been labeled with multiple conflicting or redundant diagnoses throughout their lives depending on the setting or the orientation of the practitioner.
The DSM-5 warns against diagnosing disorders when “the occurrence … is not better explained by” another disorder.3 A mix of diagnoses creates confusion for patients as well as clinicians trying to sort through their reported psychiatric histories.
A routine example would include a patient presenting for an initial evaluation and stating “I’ve been diagnosed as manic-depressive, high anxiety, split personality, posttraumatic stress, insomnia, ADD, and depression.” A review of the medical record will reveal a list of diagnoses, including bipolar II, generalized anxiety disorder, borderline personality disorder, posttraumatic stress disorder, unspecified insomnia, attention-deficit/hyperactivity disorder, and major depressive disorder. The medication list includes lamotrigine, valproic acid, citalopram, bupropion, buspirone, prazosin, methylphenidate, clonazepam, hydroxyzine, and low-dose quetiapine at night as needed.
This is an example of polypharmacy treating multiple, and at times conflicting, diagnoses. While an extreme case, in our experience, cases like this are not uncommon. It was actually in our efforts to examine deprescribing that we noticed this quandary. When inquiring about patients on many psychotropic medications, we often receive this retort: the patient is only prescribed one medication per disorder. Some providers have the belief that multiple disorders justify multiple medications, and that this tautological thinking legitimizes polypharmacy.
A patient who has varying moods, some fears, a fluctuating temperament, past traumas, occasional difficulty sleeping, intermittent inattention, and some sadness may be given all the diagnoses listed above and the resulting medication list. The multiplication of diagnoses, “polydiagnosing,” is a convenient justification for future polypharmacy. A lack of careful assessment and thinking in the application of new diagnoses permits the use of increasing numbers of pharmacological agents. A constellation of symptoms of anxiety, concentration deficits, affective dysregulation, and psychosis may justify the combination of benzodiazepines, stimulants, mood stabilizers, and antipsychotics, while a patient with “just” schizophrenia who is sometimes sad, scared, or distracted is more likely to be kept on just one medication, likely an antipsychotic.
Contrary to most medical disorders (for example, tuberculosis) but similar to others (for example, chronic pain), psychiatric disorders are based on the opinion of a “modest number of ‘expert’ classifications.”4 While the broad categories of disorders are justifiable, individual diagnoses are burdened with high rates of comorbidity; lack of treatment specificity; and evidence that distinct syndromes share a genetic basis. Those concerns were exemplified in the study examining the inter-rater reliability of DSM-5 diagnoses, where many disorders were found to have questionable validity.5
A psychiatric diagnosis should be based on biological, psychological, and social factors, which align with our understanding of the natural course of an illness. A patient presenting with transient symptoms of sadness in the context of significant social factors like homelessness and/or significant biological factors associated with schizophrenia should not reflexively receive an additional diagnosis of a depressive disorder. A patient reporting poor concentration in the context of a manic episode should not receive an additional diagnosis of attention-deficit disorder. An older patient with depression on multiple antipsychotics for adjunctive treatment should not necessarily receive a diagnosis of cognitive disorder at the first sign of memory problems.
The cavalier and inconsistent use of diagnoses renders the patients with no clear narrative of who they are. They end up integrating the varying providers’ opinions as a cacophony of labels of unclear significance. Many patients have contradictory diagnoses like major depressive disorder and bipolar disorder, or schizophrenia and schizoaffective disorder. Those inaccurate diagnoses could not only lead to treatment mistakes, but also psychological harm.6
A clearer diagnostic picture is not only more scientifically sound but also more coherent to the patient. This in turn can lead to an improved treatment alliance and buy-in from the patient.
How should a provider practice de-diagnosing? Based on the work of Reeve, et al.,7 on the principles crucial to deprescribing, and subsequent research by Gupta and Cahill,8 we compiled a list of considerations for practitioners wishing to engage in this type of work with their patients.
Choose the right time. While insurance companies require diagnostic findings from the first visit, abrupt de-diagnosing for the sake of simplifying the record from that first visit could be detrimental. Patients can become attached to and find meaning in their diagnostic labels. This was exemplified with the removal of Asperger’s syndrome from the DSM-5.9 Acute symptomatology may be an opportune time to revisit the core pathology of a patient, or a poor time for a patient to have this discussion.
Compile a list of all the patient’s diagnoses. Our initial visits are often illuminated when patients enumerate the vast number of diagnoses they have been given by different providers. Patients will often list half a dozen diagnoses. The patterns often follow life courses with ADHD, conduct disorder, and learning disability in childhood; with anxiety, depression, and/or bipolar disorder in early adulthood; to complicated grief, depression with pseudodementia, and neurocognitive disorders in older adults. Yet patients rarely appreciate the temporary or episodic nature of mental disorders and instead accumulate diagnoses at each change of provider.
Initiate discussion with the patient. It is meaningful to see if patients resonate with the question, “Do you ever feel like every psychiatrist you have seen has given you a different diagnosis?” In our experience, patients’ reactions to this question usually exemplify the problematic nature of the vast array of diagnoses our patients are given. The majority of them are unable to confidently explain the meaning of those diagnoses, the context in which they were given, or their significance. This simple exercise has a powerful effect on raising awareness to patients of the problematic nature of polydiagnosing.
Introduce de-diagnosing. The engagement of patients in the diagnostic process has a significant effect. Reviewing not only diagnostic criteria but also nosology and debates in our understanding of diagnoses can provide patients with further engagement in their care. A simple review of the debate of the bereavement exclusion may permit a patient to not only understand the complexity, but also the changing nature of diagnoses. Suddenly, they are no longer bystanders, but informed participants in their care.
Identify diagnoses most appropriate for removal. Contradictory diagnoses are common in the clinical settings we work in. We routinely see patients carrying multiple mood diagnoses, despite our diagnostic systems not permitting one to have both unipolar and bipolar depression. Superfluous diagnoses are also frequent, with patients receiving depressive, or anxious labels when in an acute state of psychosis or mania. This is exemplified by patients suffering from thought blocking and receiving cognitive or attention-related diagnoses. Concurrent yet different diagnoses are also common in patients with a different list of diagnoses by their primary care provider, their therapist, and their psychiatrist. This is particularly problematic as it forces the patient to alternate their thinking or choose between their providers.
Create a new narrative for the patient. Once diagnoses are explained, clarified, and understood, patients with the help of their providers can reexamine their life story under a new and simplified construct. This process often leads to a less confusing sense of self, an increased dedication to the treatment process, whether behavioral, social, psychological, or pharmacologic.
Consider deprescribing. With a more straightforward and more grounded list of diagnoses (or simply one diagnosis), we find the process of deprescribing to be simpler and more engaging for patients. For example, patients can clearly understand the lack of necessity of an antipsychotic prescription for a resolved substance-induced psychosis. Patients are more engaged in their care, leading to improved medication compliance and less attachment to discontinued medications.
Monitor and adapt. One should of course reevaluate diagnoses as the course of illness provides us with additional information. However, we suggest waiting for a manic episode to emerge prior to diagnosing bipolar rather than suggesting the diagnosis because a patient was wearing red shoes, spoke multiple languages, had multiple degrees and was creative.10 The contextual basis and progression of the symptoms should lead to continual reassessment of diagnoses.
Physicians are aware of the balance between Occam’s razor, which promotes the simplest single explanation for a problem, versus Hickam’s dictum that reminds us that patients can have as many diseases as they please. However, similarly to polypharmacy, “polydiagnosing” has negative effects. While the field of psychiatry’s advancing knowledge may encourage providers to diagnose their patients with the growing number of diagnoses, patients still need and benefit from a coherent and clear medical narrative. Psychiatry would be wise to recognize this concerning trend, in its attempt at rectifying polypharmacy.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest. Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He has no conflicts of interest.
References
1. Gupta S & Cahill JD. A prescription for “deprescribing” in psychiatry. Psychiatr Serv. 2016 Aug 1;67(8):904-7. doi: 10.1176/appi.ps.201500359.
2. Schuckit MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction. 2006 Sep;101 Suppl 1:76-88. doi: 10.1111/j.1360-0443.2006.01592.x.
3. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR). American Psychiatric Association, 2022. https://psychiatry.org/psychiatrists/practice/dsm.
4. Kendler KS. An historical framework for psychiatric nosology. Psychol Med. 2009 Dec;39(12):1935-41. doi: 10.1017/S0033291709005753.
5. Regier DA et al. DSM-5 field trials in the United States and Canada. Am J Psychiatry. 2013 Jan;170(1):59-70. doi: 10.1176/appi.ajp.2012.12070999.
6. Bhattacharya R et al. When good news is bad news: psychological impact of false-positive diagnosis of HIV. AIDS Care. 2008 May;20(5):560-4. doi: 10.1080/09540120701867206.
7. Reeve E et al. Review of deprescribing processes and development of an evidence‐based, patient‐centred deprescribing process. Br J Clin Pharmacol. 2014 Oct;78(4):738-47. doi: 10.1111/bcp.12386.
8. Gupta S and Cahill JD. A prescription for “deprescribing” in psychiatry.
9. Solomon M. “On the appearance and disappearance of Asperger’s syndrome” in Kendler and Parnas (eds.) Philosophical Issues in Psychiatry IV: Classification of Psychiatric Illness. Oxford University Press, 2017. doi: 10.1093/med/9780198796022.003.0023.
10. Akiskal HS. Searching for behavioral indicators of bipolar II in patients presenting with major depressive episodes: The “red sign,” the “rule of three,” and other biographic signs of temperamental extravagance, activation, and hypomania. J Affect Disord. 2005 Feb;84(2-3):279-90. doi: 10.1016/j.jad.2004.06.002.
In 2016, Gupta and Cahill challenged the field of psychiatry to reexamine prescribing patterns.1 They warned against the use of polypharmacy when not attached to improved patient functioning. They were concerned with the limited evidence for polypharmacy as well as DSM diagnostic criteria. In their inspiring article, they described a process of deprescribing.
In an effort to study and practice their recommendations, we have noticed a lack of literature examining the elimination of diagnostic labels. While there have been some studies looking at comorbidity, especially with substance use disorders,2 there is a paucity of scientific evidence on patients with numerous diagnoses. Yet our practices are filled with patients who have been labeled with multiple conflicting or redundant diagnoses throughout their lives depending on the setting or the orientation of the practitioner.
The DSM-5 warns against diagnosing disorders when “the occurrence … is not better explained by” another disorder.3 A mix of diagnoses creates confusion for patients as well as clinicians trying to sort through their reported psychiatric histories.
A routine example would include a patient presenting for an initial evaluation and stating “I’ve been diagnosed as manic-depressive, high anxiety, split personality, posttraumatic stress, insomnia, ADD, and depression.” A review of the medical record will reveal a list of diagnoses, including bipolar II, generalized anxiety disorder, borderline personality disorder, posttraumatic stress disorder, unspecified insomnia, attention-deficit/hyperactivity disorder, and major depressive disorder. The medication list includes lamotrigine, valproic acid, citalopram, bupropion, buspirone, prazosin, methylphenidate, clonazepam, hydroxyzine, and low-dose quetiapine at night as needed.
This is an example of polypharmacy treating multiple, and at times conflicting, diagnoses. While an extreme case, in our experience, cases like this are not uncommon. It was actually in our efforts to examine deprescribing that we noticed this quandary. When inquiring about patients on many psychotropic medications, we often receive this retort: the patient is only prescribed one medication per disorder. Some providers have the belief that multiple disorders justify multiple medications, and that this tautological thinking legitimizes polypharmacy.
A patient who has varying moods, some fears, a fluctuating temperament, past traumas, occasional difficulty sleeping, intermittent inattention, and some sadness may be given all the diagnoses listed above and the resulting medication list. The multiplication of diagnoses, “polydiagnosing,” is a convenient justification for future polypharmacy. A lack of careful assessment and thinking in the application of new diagnoses permits the use of increasing numbers of pharmacological agents. A constellation of symptoms of anxiety, concentration deficits, affective dysregulation, and psychosis may justify the combination of benzodiazepines, stimulants, mood stabilizers, and antipsychotics, while a patient with “just” schizophrenia who is sometimes sad, scared, or distracted is more likely to be kept on just one medication, likely an antipsychotic.
Contrary to most medical disorders (for example, tuberculosis) but similar to others (for example, chronic pain), psychiatric disorders are based on the opinion of a “modest number of ‘expert’ classifications.”4 While the broad categories of disorders are justifiable, individual diagnoses are burdened with high rates of comorbidity; lack of treatment specificity; and evidence that distinct syndromes share a genetic basis. Those concerns were exemplified in the study examining the inter-rater reliability of DSM-5 diagnoses, where many disorders were found to have questionable validity.5
A psychiatric diagnosis should be based on biological, psychological, and social factors, which align with our understanding of the natural course of an illness. A patient presenting with transient symptoms of sadness in the context of significant social factors like homelessness and/or significant biological factors associated with schizophrenia should not reflexively receive an additional diagnosis of a depressive disorder. A patient reporting poor concentration in the context of a manic episode should not receive an additional diagnosis of attention-deficit disorder. An older patient with depression on multiple antipsychotics for adjunctive treatment should not necessarily receive a diagnosis of cognitive disorder at the first sign of memory problems.
The cavalier and inconsistent use of diagnoses renders the patients with no clear narrative of who they are. They end up integrating the varying providers’ opinions as a cacophony of labels of unclear significance. Many patients have contradictory diagnoses like major depressive disorder and bipolar disorder, or schizophrenia and schizoaffective disorder. Those inaccurate diagnoses could not only lead to treatment mistakes, but also psychological harm.6
A clearer diagnostic picture is not only more scientifically sound but also more coherent to the patient. This in turn can lead to an improved treatment alliance and buy-in from the patient.
How should a provider practice de-diagnosing? Based on the work of Reeve, et al.,7 on the principles crucial to deprescribing, and subsequent research by Gupta and Cahill,8 we compiled a list of considerations for practitioners wishing to engage in this type of work with their patients.
Choose the right time. While insurance companies require diagnostic findings from the first visit, abrupt de-diagnosing for the sake of simplifying the record from that first visit could be detrimental. Patients can become attached to and find meaning in their diagnostic labels. This was exemplified with the removal of Asperger’s syndrome from the DSM-5.9 Acute symptomatology may be an opportune time to revisit the core pathology of a patient, or a poor time for a patient to have this discussion.
Compile a list of all the patient’s diagnoses. Our initial visits are often illuminated when patients enumerate the vast number of diagnoses they have been given by different providers. Patients will often list half a dozen diagnoses. The patterns often follow life courses with ADHD, conduct disorder, and learning disability in childhood; with anxiety, depression, and/or bipolar disorder in early adulthood; to complicated grief, depression with pseudodementia, and neurocognitive disorders in older adults. Yet patients rarely appreciate the temporary or episodic nature of mental disorders and instead accumulate diagnoses at each change of provider.
Initiate discussion with the patient. It is meaningful to see if patients resonate with the question, “Do you ever feel like every psychiatrist you have seen has given you a different diagnosis?” In our experience, patients’ reactions to this question usually exemplify the problematic nature of the vast array of diagnoses our patients are given. The majority of them are unable to confidently explain the meaning of those diagnoses, the context in which they were given, or their significance. This simple exercise has a powerful effect on raising awareness to patients of the problematic nature of polydiagnosing.
Introduce de-diagnosing. The engagement of patients in the diagnostic process has a significant effect. Reviewing not only diagnostic criteria but also nosology and debates in our understanding of diagnoses can provide patients with further engagement in their care. A simple review of the debate of the bereavement exclusion may permit a patient to not only understand the complexity, but also the changing nature of diagnoses. Suddenly, they are no longer bystanders, but informed participants in their care.
Identify diagnoses most appropriate for removal. Contradictory diagnoses are common in the clinical settings we work in. We routinely see patients carrying multiple mood diagnoses, despite our diagnostic systems not permitting one to have both unipolar and bipolar depression. Superfluous diagnoses are also frequent, with patients receiving depressive, or anxious labels when in an acute state of psychosis or mania. This is exemplified by patients suffering from thought blocking and receiving cognitive or attention-related diagnoses. Concurrent yet different diagnoses are also common in patients with a different list of diagnoses by their primary care provider, their therapist, and their psychiatrist. This is particularly problematic as it forces the patient to alternate their thinking or choose between their providers.
Create a new narrative for the patient. Once diagnoses are explained, clarified, and understood, patients with the help of their providers can reexamine their life story under a new and simplified construct. This process often leads to a less confusing sense of self, an increased dedication to the treatment process, whether behavioral, social, psychological, or pharmacologic.
Consider deprescribing. With a more straightforward and more grounded list of diagnoses (or simply one diagnosis), we find the process of deprescribing to be simpler and more engaging for patients. For example, patients can clearly understand the lack of necessity of an antipsychotic prescription for a resolved substance-induced psychosis. Patients are more engaged in their care, leading to improved medication compliance and less attachment to discontinued medications.
Monitor and adapt. One should of course reevaluate diagnoses as the course of illness provides us with additional information. However, we suggest waiting for a manic episode to emerge prior to diagnosing bipolar rather than suggesting the diagnosis because a patient was wearing red shoes, spoke multiple languages, had multiple degrees and was creative.10 The contextual basis and progression of the symptoms should lead to continual reassessment of diagnoses.
Physicians are aware of the balance between Occam’s razor, which promotes the simplest single explanation for a problem, versus Hickam’s dictum that reminds us that patients can have as many diseases as they please. However, similarly to polypharmacy, “polydiagnosing” has negative effects. While the field of psychiatry’s advancing knowledge may encourage providers to diagnose their patients with the growing number of diagnoses, patients still need and benefit from a coherent and clear medical narrative. Psychiatry would be wise to recognize this concerning trend, in its attempt at rectifying polypharmacy.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest. Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He has no conflicts of interest.
References
1. Gupta S & Cahill JD. A prescription for “deprescribing” in psychiatry. Psychiatr Serv. 2016 Aug 1;67(8):904-7. doi: 10.1176/appi.ps.201500359.
2. Schuckit MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction. 2006 Sep;101 Suppl 1:76-88. doi: 10.1111/j.1360-0443.2006.01592.x.
3. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR). American Psychiatric Association, 2022. https://psychiatry.org/psychiatrists/practice/dsm.
4. Kendler KS. An historical framework for psychiatric nosology. Psychol Med. 2009 Dec;39(12):1935-41. doi: 10.1017/S0033291709005753.
5. Regier DA et al. DSM-5 field trials in the United States and Canada. Am J Psychiatry. 2013 Jan;170(1):59-70. doi: 10.1176/appi.ajp.2012.12070999.
6. Bhattacharya R et al. When good news is bad news: psychological impact of false-positive diagnosis of HIV. AIDS Care. 2008 May;20(5):560-4. doi: 10.1080/09540120701867206.
7. Reeve E et al. Review of deprescribing processes and development of an evidence‐based, patient‐centred deprescribing process. Br J Clin Pharmacol. 2014 Oct;78(4):738-47. doi: 10.1111/bcp.12386.
8. Gupta S and Cahill JD. A prescription for “deprescribing” in psychiatry.
9. Solomon M. “On the appearance and disappearance of Asperger’s syndrome” in Kendler and Parnas (eds.) Philosophical Issues in Psychiatry IV: Classification of Psychiatric Illness. Oxford University Press, 2017. doi: 10.1093/med/9780198796022.003.0023.
10. Akiskal HS. Searching for behavioral indicators of bipolar II in patients presenting with major depressive episodes: The “red sign,” the “rule of three,” and other biographic signs of temperamental extravagance, activation, and hypomania. J Affect Disord. 2005 Feb;84(2-3):279-90. doi: 10.1016/j.jad.2004.06.002.
In 2016, Gupta and Cahill challenged the field of psychiatry to reexamine prescribing patterns.1 They warned against the use of polypharmacy when not attached to improved patient functioning. They were concerned with the limited evidence for polypharmacy as well as DSM diagnostic criteria. In their inspiring article, they described a process of deprescribing.
In an effort to study and practice their recommendations, we have noticed a lack of literature examining the elimination of diagnostic labels. While there have been some studies looking at comorbidity, especially with substance use disorders,2 there is a paucity of scientific evidence on patients with numerous diagnoses. Yet our practices are filled with patients who have been labeled with multiple conflicting or redundant diagnoses throughout their lives depending on the setting or the orientation of the practitioner.
The DSM-5 warns against diagnosing disorders when “the occurrence … is not better explained by” another disorder.3 A mix of diagnoses creates confusion for patients as well as clinicians trying to sort through their reported psychiatric histories.
A routine example would include a patient presenting for an initial evaluation and stating “I’ve been diagnosed as manic-depressive, high anxiety, split personality, posttraumatic stress, insomnia, ADD, and depression.” A review of the medical record will reveal a list of diagnoses, including bipolar II, generalized anxiety disorder, borderline personality disorder, posttraumatic stress disorder, unspecified insomnia, attention-deficit/hyperactivity disorder, and major depressive disorder. The medication list includes lamotrigine, valproic acid, citalopram, bupropion, buspirone, prazosin, methylphenidate, clonazepam, hydroxyzine, and low-dose quetiapine at night as needed.
This is an example of polypharmacy treating multiple, and at times conflicting, diagnoses. While an extreme case, in our experience, cases like this are not uncommon. It was actually in our efforts to examine deprescribing that we noticed this quandary. When inquiring about patients on many psychotropic medications, we often receive this retort: the patient is only prescribed one medication per disorder. Some providers have the belief that multiple disorders justify multiple medications, and that this tautological thinking legitimizes polypharmacy.
A patient who has varying moods, some fears, a fluctuating temperament, past traumas, occasional difficulty sleeping, intermittent inattention, and some sadness may be given all the diagnoses listed above and the resulting medication list. The multiplication of diagnoses, “polydiagnosing,” is a convenient justification for future polypharmacy. A lack of careful assessment and thinking in the application of new diagnoses permits the use of increasing numbers of pharmacological agents. A constellation of symptoms of anxiety, concentration deficits, affective dysregulation, and psychosis may justify the combination of benzodiazepines, stimulants, mood stabilizers, and antipsychotics, while a patient with “just” schizophrenia who is sometimes sad, scared, or distracted is more likely to be kept on just one medication, likely an antipsychotic.
Contrary to most medical disorders (for example, tuberculosis) but similar to others (for example, chronic pain), psychiatric disorders are based on the opinion of a “modest number of ‘expert’ classifications.”4 While the broad categories of disorders are justifiable, individual diagnoses are burdened with high rates of comorbidity; lack of treatment specificity; and evidence that distinct syndromes share a genetic basis. Those concerns were exemplified in the study examining the inter-rater reliability of DSM-5 diagnoses, where many disorders were found to have questionable validity.5
A psychiatric diagnosis should be based on biological, psychological, and social factors, which align with our understanding of the natural course of an illness. A patient presenting with transient symptoms of sadness in the context of significant social factors like homelessness and/or significant biological factors associated with schizophrenia should not reflexively receive an additional diagnosis of a depressive disorder. A patient reporting poor concentration in the context of a manic episode should not receive an additional diagnosis of attention-deficit disorder. An older patient with depression on multiple antipsychotics for adjunctive treatment should not necessarily receive a diagnosis of cognitive disorder at the first sign of memory problems.
The cavalier and inconsistent use of diagnoses renders the patients with no clear narrative of who they are. They end up integrating the varying providers’ opinions as a cacophony of labels of unclear significance. Many patients have contradictory diagnoses like major depressive disorder and bipolar disorder, or schizophrenia and schizoaffective disorder. Those inaccurate diagnoses could not only lead to treatment mistakes, but also psychological harm.6
A clearer diagnostic picture is not only more scientifically sound but also more coherent to the patient. This in turn can lead to an improved treatment alliance and buy-in from the patient.
How should a provider practice de-diagnosing? Based on the work of Reeve, et al.,7 on the principles crucial to deprescribing, and subsequent research by Gupta and Cahill,8 we compiled a list of considerations for practitioners wishing to engage in this type of work with their patients.
Choose the right time. While insurance companies require diagnostic findings from the first visit, abrupt de-diagnosing for the sake of simplifying the record from that first visit could be detrimental. Patients can become attached to and find meaning in their diagnostic labels. This was exemplified with the removal of Asperger’s syndrome from the DSM-5.9 Acute symptomatology may be an opportune time to revisit the core pathology of a patient, or a poor time for a patient to have this discussion.
Compile a list of all the patient’s diagnoses. Our initial visits are often illuminated when patients enumerate the vast number of diagnoses they have been given by different providers. Patients will often list half a dozen diagnoses. The patterns often follow life courses with ADHD, conduct disorder, and learning disability in childhood; with anxiety, depression, and/or bipolar disorder in early adulthood; to complicated grief, depression with pseudodementia, and neurocognitive disorders in older adults. Yet patients rarely appreciate the temporary or episodic nature of mental disorders and instead accumulate diagnoses at each change of provider.
Initiate discussion with the patient. It is meaningful to see if patients resonate with the question, “Do you ever feel like every psychiatrist you have seen has given you a different diagnosis?” In our experience, patients’ reactions to this question usually exemplify the problematic nature of the vast array of diagnoses our patients are given. The majority of them are unable to confidently explain the meaning of those diagnoses, the context in which they were given, or their significance. This simple exercise has a powerful effect on raising awareness to patients of the problematic nature of polydiagnosing.
Introduce de-diagnosing. The engagement of patients in the diagnostic process has a significant effect. Reviewing not only diagnostic criteria but also nosology and debates in our understanding of diagnoses can provide patients with further engagement in their care. A simple review of the debate of the bereavement exclusion may permit a patient to not only understand the complexity, but also the changing nature of diagnoses. Suddenly, they are no longer bystanders, but informed participants in their care.
Identify diagnoses most appropriate for removal. Contradictory diagnoses are common in the clinical settings we work in. We routinely see patients carrying multiple mood diagnoses, despite our diagnostic systems not permitting one to have both unipolar and bipolar depression. Superfluous diagnoses are also frequent, with patients receiving depressive, or anxious labels when in an acute state of psychosis or mania. This is exemplified by patients suffering from thought blocking and receiving cognitive or attention-related diagnoses. Concurrent yet different diagnoses are also common in patients with a different list of diagnoses by their primary care provider, their therapist, and their psychiatrist. This is particularly problematic as it forces the patient to alternate their thinking or choose between their providers.
Create a new narrative for the patient. Once diagnoses are explained, clarified, and understood, patients with the help of their providers can reexamine their life story under a new and simplified construct. This process often leads to a less confusing sense of self, an increased dedication to the treatment process, whether behavioral, social, psychological, or pharmacologic.
Consider deprescribing. With a more straightforward and more grounded list of diagnoses (or simply one diagnosis), we find the process of deprescribing to be simpler and more engaging for patients. For example, patients can clearly understand the lack of necessity of an antipsychotic prescription for a resolved substance-induced psychosis. Patients are more engaged in their care, leading to improved medication compliance and less attachment to discontinued medications.
Monitor and adapt. One should of course reevaluate diagnoses as the course of illness provides us with additional information. However, we suggest waiting for a manic episode to emerge prior to diagnosing bipolar rather than suggesting the diagnosis because a patient was wearing red shoes, spoke multiple languages, had multiple degrees and was creative.10 The contextual basis and progression of the symptoms should lead to continual reassessment of diagnoses.
Physicians are aware of the balance between Occam’s razor, which promotes the simplest single explanation for a problem, versus Hickam’s dictum that reminds us that patients can have as many diseases as they please. However, similarly to polypharmacy, “polydiagnosing” has negative effects. While the field of psychiatry’s advancing knowledge may encourage providers to diagnose their patients with the growing number of diagnoses, patients still need and benefit from a coherent and clear medical narrative. Psychiatry would be wise to recognize this concerning trend, in its attempt at rectifying polypharmacy.
Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. He has no conflicts of interest. Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He has no conflicts of interest.
References
1. Gupta S & Cahill JD. A prescription for “deprescribing” in psychiatry. Psychiatr Serv. 2016 Aug 1;67(8):904-7. doi: 10.1176/appi.ps.201500359.
2. Schuckit MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction. 2006 Sep;101 Suppl 1:76-88. doi: 10.1111/j.1360-0443.2006.01592.x.
3. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR). American Psychiatric Association, 2022. https://psychiatry.org/psychiatrists/practice/dsm.
4. Kendler KS. An historical framework for psychiatric nosology. Psychol Med. 2009 Dec;39(12):1935-41. doi: 10.1017/S0033291709005753.
5. Regier DA et al. DSM-5 field trials in the United States and Canada. Am J Psychiatry. 2013 Jan;170(1):59-70. doi: 10.1176/appi.ajp.2012.12070999.
6. Bhattacharya R et al. When good news is bad news: psychological impact of false-positive diagnosis of HIV. AIDS Care. 2008 May;20(5):560-4. doi: 10.1080/09540120701867206.
7. Reeve E et al. Review of deprescribing processes and development of an evidence‐based, patient‐centred deprescribing process. Br J Clin Pharmacol. 2014 Oct;78(4):738-47. doi: 10.1111/bcp.12386.
8. Gupta S and Cahill JD. A prescription for “deprescribing” in psychiatry.
9. Solomon M. “On the appearance and disappearance of Asperger’s syndrome” in Kendler and Parnas (eds.) Philosophical Issues in Psychiatry IV: Classification of Psychiatric Illness. Oxford University Press, 2017. doi: 10.1093/med/9780198796022.003.0023.
10. Akiskal HS. Searching for behavioral indicators of bipolar II in patients presenting with major depressive episodes: The “red sign,” the “rule of three,” and other biographic signs of temperamental extravagance, activation, and hypomania. J Affect Disord. 2005 Feb;84(2-3):279-90. doi: 10.1016/j.jad.2004.06.002.
ECT may reduce all-cause mortality in major depression
In an analysis of data from a large database of inpatients across the United States, use of ECT for those with resistant MDD was associated with significantly lower in-hospital mortality compared with those who did not receive ECT.
This held true even after the researchers controlled for demographics and loss of function due to comorbid medical conditions.
“I think the risks of ECT are far less than the benefits in this population,” coinvestigator Nagy A. Youssef, MD, PhD, professor of psychiatry and director of clinical research, The Ohio State University, Columbus, told this news organization.
“My hope is that providers will not be afraid to refer appropriate cases for ECT. If meds and other therapeutics are not working, you should start discussing ECT as a second or third line,” he said.
The findings were presented at the American Society of Clinical Psychopharmacology annual meeting.
Lower mortality
Dr. Youssef, a brain stimulation researcher who uses ECT in his clinical practice, said that in his experience, it is a highly effective therapy for resistant depression.
“I see great responses in patients who have tried everything else. Most of the time, it works very well, and results are very rewarding.”
For the study, the investigators used a large, national insurance claims database that included 949,394 adult inpatients with MDD across the United States from 2012 to 2014. The cohort represented over 4,000 hospitals across the country.
The investigators used logistic regression to determine the odds ratio for in-hospital all-cause mortality for the 25,535 MDD patients who were treated with ECT in comparison with 923,859 patients with MDD who were not treated with ECT.
Results showed that ECT use was significantly higher among older patients (mean age, 56.9 years), women (64%), and White patients (86.9%). In addition, patients in the ECT group were physically sicker than were their peers in the non-ECT group.
A higher proportion of patients in the ECT group in comparison with the non-ECT group had experienced major loss of physical function (37% vs. 5%, respectively) and extreme loss of physical function (63% vs. 0.2%).
“By loss of function, I mean the degree of impairment caused by medical disease,” said Dr. Youssef.
He added that patients with MDD are more likely to care less for their health and do things that are not good for their well-being, such as drinking alcohol or using drugs, and are less likely to adhere to prescribed medication regimens or seek medical attention for physical illness.
“Also, there is probably a biological component where depression, by dysregulation of the hypothalamus and pituitary regions of the brain, can increase the likelihood of physical illness or disease,” Dr. Youssef said.
After adjusting for demographics and extreme loss of function because of medical conditions, the investigators found that in-hospital mortality was significantly lower in the ECT group (odds ratio [OR], 0.05; 95% confidence interval [CI], 0.02-0.11; P < .001).
In-hospital mortality was numerically but not statistically significantly lower in the ECT group (OR, 0.7; 95% CI, 0.41-1.50; P < .47) when adjusted for demographics and major loss of function.
“While this was not statistically significant with marked loss of function, it is clinically important and meaningful. With extreme loss of function, the decrease in mortality was statistically significant,” Dr. Youssef noted.
Designations of extreme and major loss of function were derived from ICD codes.
“This is a complex grading system that takes into account how sick the patient is and includes medical disease severity and comorbidities assessed by the clinician,” he said.
A lifesaving treatment
Commenting on the study, Jair C. Soares, MD, PhD, professor and chair, Pat Rutherford Chair in Psychiatry, UT Houston Medical School, Texas, said, “These are interesting results in a very large national sample suggesting some potential benefits of ECT.
“For the most severely ill patients with major depression who do not respond to currently available medications, ECT is still the most efficacious treatment and indeed a lifesaving treatment modality for many patients,” said Dr. Soares, who was not part of the study.
He noted that ECT is not right for everyone, but “as administered these days, with careful patient selection, it is indeed a safe treatment that can save many lives,” Dr. Soares said.
Dr. Youssef reports a financial relationship with Mecta. Dr. Soares reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In an analysis of data from a large database of inpatients across the United States, use of ECT for those with resistant MDD was associated with significantly lower in-hospital mortality compared with those who did not receive ECT.
This held true even after the researchers controlled for demographics and loss of function due to comorbid medical conditions.
“I think the risks of ECT are far less than the benefits in this population,” coinvestigator Nagy A. Youssef, MD, PhD, professor of psychiatry and director of clinical research, The Ohio State University, Columbus, told this news organization.
“My hope is that providers will not be afraid to refer appropriate cases for ECT. If meds and other therapeutics are not working, you should start discussing ECT as a second or third line,” he said.
The findings were presented at the American Society of Clinical Psychopharmacology annual meeting.
Lower mortality
Dr. Youssef, a brain stimulation researcher who uses ECT in his clinical practice, said that in his experience, it is a highly effective therapy for resistant depression.
“I see great responses in patients who have tried everything else. Most of the time, it works very well, and results are very rewarding.”
For the study, the investigators used a large, national insurance claims database that included 949,394 adult inpatients with MDD across the United States from 2012 to 2014. The cohort represented over 4,000 hospitals across the country.
The investigators used logistic regression to determine the odds ratio for in-hospital all-cause mortality for the 25,535 MDD patients who were treated with ECT in comparison with 923,859 patients with MDD who were not treated with ECT.
Results showed that ECT use was significantly higher among older patients (mean age, 56.9 years), women (64%), and White patients (86.9%). In addition, patients in the ECT group were physically sicker than were their peers in the non-ECT group.
A higher proportion of patients in the ECT group in comparison with the non-ECT group had experienced major loss of physical function (37% vs. 5%, respectively) and extreme loss of physical function (63% vs. 0.2%).
“By loss of function, I mean the degree of impairment caused by medical disease,” said Dr. Youssef.
He added that patients with MDD are more likely to care less for their health and do things that are not good for their well-being, such as drinking alcohol or using drugs, and are less likely to adhere to prescribed medication regimens or seek medical attention for physical illness.
“Also, there is probably a biological component where depression, by dysregulation of the hypothalamus and pituitary regions of the brain, can increase the likelihood of physical illness or disease,” Dr. Youssef said.
After adjusting for demographics and extreme loss of function because of medical conditions, the investigators found that in-hospital mortality was significantly lower in the ECT group (odds ratio [OR], 0.05; 95% confidence interval [CI], 0.02-0.11; P < .001).
In-hospital mortality was numerically but not statistically significantly lower in the ECT group (OR, 0.7; 95% CI, 0.41-1.50; P < .47) when adjusted for demographics and major loss of function.
“While this was not statistically significant with marked loss of function, it is clinically important and meaningful. With extreme loss of function, the decrease in mortality was statistically significant,” Dr. Youssef noted.
Designations of extreme and major loss of function were derived from ICD codes.
“This is a complex grading system that takes into account how sick the patient is and includes medical disease severity and comorbidities assessed by the clinician,” he said.
A lifesaving treatment
Commenting on the study, Jair C. Soares, MD, PhD, professor and chair, Pat Rutherford Chair in Psychiatry, UT Houston Medical School, Texas, said, “These are interesting results in a very large national sample suggesting some potential benefits of ECT.
“For the most severely ill patients with major depression who do not respond to currently available medications, ECT is still the most efficacious treatment and indeed a lifesaving treatment modality for many patients,” said Dr. Soares, who was not part of the study.
He noted that ECT is not right for everyone, but “as administered these days, with careful patient selection, it is indeed a safe treatment that can save many lives,” Dr. Soares said.
Dr. Youssef reports a financial relationship with Mecta. Dr. Soares reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In an analysis of data from a large database of inpatients across the United States, use of ECT for those with resistant MDD was associated with significantly lower in-hospital mortality compared with those who did not receive ECT.
This held true even after the researchers controlled for demographics and loss of function due to comorbid medical conditions.
“I think the risks of ECT are far less than the benefits in this population,” coinvestigator Nagy A. Youssef, MD, PhD, professor of psychiatry and director of clinical research, The Ohio State University, Columbus, told this news organization.
“My hope is that providers will not be afraid to refer appropriate cases for ECT. If meds and other therapeutics are not working, you should start discussing ECT as a second or third line,” he said.
The findings were presented at the American Society of Clinical Psychopharmacology annual meeting.
Lower mortality
Dr. Youssef, a brain stimulation researcher who uses ECT in his clinical practice, said that in his experience, it is a highly effective therapy for resistant depression.
“I see great responses in patients who have tried everything else. Most of the time, it works very well, and results are very rewarding.”
For the study, the investigators used a large, national insurance claims database that included 949,394 adult inpatients with MDD across the United States from 2012 to 2014. The cohort represented over 4,000 hospitals across the country.
The investigators used logistic regression to determine the odds ratio for in-hospital all-cause mortality for the 25,535 MDD patients who were treated with ECT in comparison with 923,859 patients with MDD who were not treated with ECT.
Results showed that ECT use was significantly higher among older patients (mean age, 56.9 years), women (64%), and White patients (86.9%). In addition, patients in the ECT group were physically sicker than were their peers in the non-ECT group.
A higher proportion of patients in the ECT group in comparison with the non-ECT group had experienced major loss of physical function (37% vs. 5%, respectively) and extreme loss of physical function (63% vs. 0.2%).
“By loss of function, I mean the degree of impairment caused by medical disease,” said Dr. Youssef.
He added that patients with MDD are more likely to care less for their health and do things that are not good for their well-being, such as drinking alcohol or using drugs, and are less likely to adhere to prescribed medication regimens or seek medical attention for physical illness.
“Also, there is probably a biological component where depression, by dysregulation of the hypothalamus and pituitary regions of the brain, can increase the likelihood of physical illness or disease,” Dr. Youssef said.
After adjusting for demographics and extreme loss of function because of medical conditions, the investigators found that in-hospital mortality was significantly lower in the ECT group (odds ratio [OR], 0.05; 95% confidence interval [CI], 0.02-0.11; P < .001).
In-hospital mortality was numerically but not statistically significantly lower in the ECT group (OR, 0.7; 95% CI, 0.41-1.50; P < .47) when adjusted for demographics and major loss of function.
“While this was not statistically significant with marked loss of function, it is clinically important and meaningful. With extreme loss of function, the decrease in mortality was statistically significant,” Dr. Youssef noted.
Designations of extreme and major loss of function were derived from ICD codes.
“This is a complex grading system that takes into account how sick the patient is and includes medical disease severity and comorbidities assessed by the clinician,” he said.
A lifesaving treatment
Commenting on the study, Jair C. Soares, MD, PhD, professor and chair, Pat Rutherford Chair in Psychiatry, UT Houston Medical School, Texas, said, “These are interesting results in a very large national sample suggesting some potential benefits of ECT.
“For the most severely ill patients with major depression who do not respond to currently available medications, ECT is still the most efficacious treatment and indeed a lifesaving treatment modality for many patients,” said Dr. Soares, who was not part of the study.
He noted that ECT is not right for everyone, but “as administered these days, with careful patient selection, it is indeed a safe treatment that can save many lives,” Dr. Soares said.
Dr. Youssef reports a financial relationship with Mecta. Dr. Soares reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ASCP 2022
Surprising link between herpes zoster and dementia
Herpes zoster does not appear to increase dementia risk – on the contrary, the viral infection may offer some protection, a large population-based study suggests.
“We were surprised by these results [and] the reasons for the decreased risk are unclear,” study author Sigrun Alba Johannesdottir Schmidt, MD, PhD, with Aarhus (Denmark) University Hospital, said in a news release.
The study was published online in Neurology.
Conflicting findings
Herpes zoster (HZ) is an acute, cutaneous viral infection caused by the reactivation of varicella-zoster virus (VZV). Previous population-based studies have reported both decreased and increased risks of dementia after having HZ.
It’s thought that HZ may contribute to the development of dementia through neuroinflammation, cerebral vasculopathy, or direct neural damage, but epidemiologic evidence is limited.
To investigate further, Dr. Schmidt and colleagues used Danish medical registries to identify 247,305 people who had visited a hospital for HZ or were prescribed antiviral medication for HZ over a 20-year period and matched them to 1,235,890 people who did not have HZ. For both cohorts, the median age was 64 years, and 61% were women.
Dementia was diagnosed in 9.7% of zoster patients and 10.3% of matched control persons during up to 21 years of follow-up.
Contrary to the researchers’ expectation, HZ was associated with a small (7%) decreased relative risk of all-cause dementia during follow-up (hazard ratio, 0.93; 95% confidence interval, 0.90-0.95).
There was no increased long-term risk of dementia in subgroup analyses, except possibly among those with HZ that involved the central nervous system (HR, 1.94; 95% CI, 0.78-4.80), which has been shown before.
However, the population attributable fraction of dementia caused by this rare complication is low (< 1%), suggesting that universal vaccination against VZV in the elderly has limited potential to reduce dementia risk, the investigators noted.
Nonetheless, Dr. Schmidt said shingles vaccination should be encouraged in older people because it can prevent complications from the disease.
The research team admitted that the slightly decreased long-term risk of dementia, including Alzheimer’s disease, was “unexpected.” The reasons for this decreased risk are unclear, they say, and could be explained by missed diagnoses of shingles in people with undiagnosed dementia.
They were not able to examine whether antiviral treatment modifies the association between HZ and dementia and said that this topic merits further research.
The study was supported by the Edel and Wilhelm Daubenmerkls Charitable Foundation. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Herpes zoster does not appear to increase dementia risk – on the contrary, the viral infection may offer some protection, a large population-based study suggests.
“We were surprised by these results [and] the reasons for the decreased risk are unclear,” study author Sigrun Alba Johannesdottir Schmidt, MD, PhD, with Aarhus (Denmark) University Hospital, said in a news release.
The study was published online in Neurology.
Conflicting findings
Herpes zoster (HZ) is an acute, cutaneous viral infection caused by the reactivation of varicella-zoster virus (VZV). Previous population-based studies have reported both decreased and increased risks of dementia after having HZ.
It’s thought that HZ may contribute to the development of dementia through neuroinflammation, cerebral vasculopathy, or direct neural damage, but epidemiologic evidence is limited.
To investigate further, Dr. Schmidt and colleagues used Danish medical registries to identify 247,305 people who had visited a hospital for HZ or were prescribed antiviral medication for HZ over a 20-year period and matched them to 1,235,890 people who did not have HZ. For both cohorts, the median age was 64 years, and 61% were women.
Dementia was diagnosed in 9.7% of zoster patients and 10.3% of matched control persons during up to 21 years of follow-up.
Contrary to the researchers’ expectation, HZ was associated with a small (7%) decreased relative risk of all-cause dementia during follow-up (hazard ratio, 0.93; 95% confidence interval, 0.90-0.95).
There was no increased long-term risk of dementia in subgroup analyses, except possibly among those with HZ that involved the central nervous system (HR, 1.94; 95% CI, 0.78-4.80), which has been shown before.
However, the population attributable fraction of dementia caused by this rare complication is low (< 1%), suggesting that universal vaccination against VZV in the elderly has limited potential to reduce dementia risk, the investigators noted.
Nonetheless, Dr. Schmidt said shingles vaccination should be encouraged in older people because it can prevent complications from the disease.
The research team admitted that the slightly decreased long-term risk of dementia, including Alzheimer’s disease, was “unexpected.” The reasons for this decreased risk are unclear, they say, and could be explained by missed diagnoses of shingles in people with undiagnosed dementia.
They were not able to examine whether antiviral treatment modifies the association between HZ and dementia and said that this topic merits further research.
The study was supported by the Edel and Wilhelm Daubenmerkls Charitable Foundation. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Herpes zoster does not appear to increase dementia risk – on the contrary, the viral infection may offer some protection, a large population-based study suggests.
“We were surprised by these results [and] the reasons for the decreased risk are unclear,” study author Sigrun Alba Johannesdottir Schmidt, MD, PhD, with Aarhus (Denmark) University Hospital, said in a news release.
The study was published online in Neurology.
Conflicting findings
Herpes zoster (HZ) is an acute, cutaneous viral infection caused by the reactivation of varicella-zoster virus (VZV). Previous population-based studies have reported both decreased and increased risks of dementia after having HZ.
It’s thought that HZ may contribute to the development of dementia through neuroinflammation, cerebral vasculopathy, or direct neural damage, but epidemiologic evidence is limited.
To investigate further, Dr. Schmidt and colleagues used Danish medical registries to identify 247,305 people who had visited a hospital for HZ or were prescribed antiviral medication for HZ over a 20-year period and matched them to 1,235,890 people who did not have HZ. For both cohorts, the median age was 64 years, and 61% were women.
Dementia was diagnosed in 9.7% of zoster patients and 10.3% of matched control persons during up to 21 years of follow-up.
Contrary to the researchers’ expectation, HZ was associated with a small (7%) decreased relative risk of all-cause dementia during follow-up (hazard ratio, 0.93; 95% confidence interval, 0.90-0.95).
There was no increased long-term risk of dementia in subgroup analyses, except possibly among those with HZ that involved the central nervous system (HR, 1.94; 95% CI, 0.78-4.80), which has been shown before.
However, the population attributable fraction of dementia caused by this rare complication is low (< 1%), suggesting that universal vaccination against VZV in the elderly has limited potential to reduce dementia risk, the investigators noted.
Nonetheless, Dr. Schmidt said shingles vaccination should be encouraged in older people because it can prevent complications from the disease.
The research team admitted that the slightly decreased long-term risk of dementia, including Alzheimer’s disease, was “unexpected.” The reasons for this decreased risk are unclear, they say, and could be explained by missed diagnoses of shingles in people with undiagnosed dementia.
They were not able to examine whether antiviral treatment modifies the association between HZ and dementia and said that this topic merits further research.
The study was supported by the Edel and Wilhelm Daubenmerkls Charitable Foundation. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Analysis shows predictive capabilities of sleep EEG
CHARLOTTE, N.C. – , a researcher reported at the annual meeting of the Associated Professional Sleep Societies. “Sleep EEGs contain decodable information about the risk of unfavorable outcomes,” said Haoqi Sun, PhD, an instructor of neurology at Massachusetts General Hospital, Boston, and lead study author. “The results suggest that it’s feasible to use sleep to identify people with high risk of unfavorable outcomes and it strengthens the concept of sleep as a window into brain and general health.”
The researchers performed a quantitative analysis of sleep data collected on 8,673 adults who had diagnostic sleep studies that included polysomnography (PSG). The analysis used ICD codes to consider these 11 health outcomes: dementia, mild cognitive impairment (MCI) or dementia, ischemic stroke, intracranial hemorrhage, atrial fibrillation, myocardial infarction, type 2 diabetes, hypertension, bipolar disorder, depression, and mortality.
Then, Dr. Sun explained, they extracted 86 spectral and time-domain features of REM and non-REM sleep from sleep EEG recordings, and analyzed that data by adjusting for eight covariates including age, sex, body mass index, and use of benzodiazepines, antidepressants, sedatives, antiseizure drugs, and stimulants.
Participants were partitioned into three sleep-quality groups: poor, average, and good. The outcome-wise mean prediction difference in 10-year cumulative incidence was 2.3% for the poor sleep group, 0.5% for the average sleep group, and 1.3% for the good sleep group.
The outcomes with the three greatest poor to average risk ratios were dementia (6.2; 95% confidence interval, 4.5-9.3), mortality (5.7; 95% CI, 5-7.5) and MCI or dementia (4; 95% CI, 3.2-4.9).
Ready for the clinic?
In an interview, Dr. Sun said the results demonstrated the potential of using EEG brain wave data to predict health outcomes on an individual basis, although he acknowledged that most of the 86 sleep features the researchers used are not readily available in the clinic.
He noted the spectral features used in the study can be captured through software compatible with PSG. “From there you can identify the various bands, the different frequency ranges, and then you can easily see within this range whether a person has a higher power or lower power,” he said. However, the spindle and slow-oscillation features that researchers used in the study are beyond the reach of most clinics.
Next steps
This research is in its early stage, Dr. Sun said, but at some point the data collected from sleep studies could be paired with machine learning to make the model workable for evaluating individual patients. “Our goal is to first make this individualized,” he said. “We want to minimize the noise in the recording and minimize the night-to-night variability in the findings. There is some clinical-informed approach and there is also some algorithm-informed approach where you can minimize the variation over time.”
The model also has the potential to predict outcomes, particularly with chronic diseases such as diabetes and dementia, well before a diagnosis is made, he said.
‘Fascinating’ and ‘provocative’
Donald Bliwise, PhD, professor of neurology at Emory Sleep Center in Atlanta, said the study was “fascinating; it’s provocative; it’s exciting and interesting,” but added, “Sleep is vital for health. That’s abundantly clear in a study like that, but trying to push it a little bit further with all of these 86 measurements of the EEG, I think it becomes complicated.”
The study methodology, particularly the use of cumulative incidence of various diseases, was laudable, he said, and the use of simpler EEG-measured sleep features, such as alpha band power, “make intuitive sense.”
But it’s less clear on how the more sophisticated features the study model used – for example, kurtosis of theta frequency or coupling between spindle and slow oscillation – rank on sleep quality, he said, adding that the researchers have most likely done that but couldn’t add that into the format of the presentation.
“Kurtosis of the theta frequency band we don’t get on everyone in the sleep lab,” Dr. Bliwise said. “We might be able to, but I don’t know how to quite plug that into a turnkey model.”
The clinical components of the study were conducted by M. Brandon Westover, MD, PhD, at Massachusetts General Hospital, and Robert J. Thomas, MD, at Beth Israel Deaconess Medical Center, both in Boston. The study received support from the American Academy of Sleep Medicine Foundation. Dr. Sun has no relevant disclosures. Dr. Bliwise has no disclosures.
CHARLOTTE, N.C. – , a researcher reported at the annual meeting of the Associated Professional Sleep Societies. “Sleep EEGs contain decodable information about the risk of unfavorable outcomes,” said Haoqi Sun, PhD, an instructor of neurology at Massachusetts General Hospital, Boston, and lead study author. “The results suggest that it’s feasible to use sleep to identify people with high risk of unfavorable outcomes and it strengthens the concept of sleep as a window into brain and general health.”
The researchers performed a quantitative analysis of sleep data collected on 8,673 adults who had diagnostic sleep studies that included polysomnography (PSG). The analysis used ICD codes to consider these 11 health outcomes: dementia, mild cognitive impairment (MCI) or dementia, ischemic stroke, intracranial hemorrhage, atrial fibrillation, myocardial infarction, type 2 diabetes, hypertension, bipolar disorder, depression, and mortality.
Then, Dr. Sun explained, they extracted 86 spectral and time-domain features of REM and non-REM sleep from sleep EEG recordings, and analyzed that data by adjusting for eight covariates including age, sex, body mass index, and use of benzodiazepines, antidepressants, sedatives, antiseizure drugs, and stimulants.
Participants were partitioned into three sleep-quality groups: poor, average, and good. The outcome-wise mean prediction difference in 10-year cumulative incidence was 2.3% for the poor sleep group, 0.5% for the average sleep group, and 1.3% for the good sleep group.
The outcomes with the three greatest poor to average risk ratios were dementia (6.2; 95% confidence interval, 4.5-9.3), mortality (5.7; 95% CI, 5-7.5) and MCI or dementia (4; 95% CI, 3.2-4.9).
Ready for the clinic?
In an interview, Dr. Sun said the results demonstrated the potential of using EEG brain wave data to predict health outcomes on an individual basis, although he acknowledged that most of the 86 sleep features the researchers used are not readily available in the clinic.
He noted the spectral features used in the study can be captured through software compatible with PSG. “From there you can identify the various bands, the different frequency ranges, and then you can easily see within this range whether a person has a higher power or lower power,” he said. However, the spindle and slow-oscillation features that researchers used in the study are beyond the reach of most clinics.
Next steps
This research is in its early stage, Dr. Sun said, but at some point the data collected from sleep studies could be paired with machine learning to make the model workable for evaluating individual patients. “Our goal is to first make this individualized,” he said. “We want to minimize the noise in the recording and minimize the night-to-night variability in the findings. There is some clinical-informed approach and there is also some algorithm-informed approach where you can minimize the variation over time.”
The model also has the potential to predict outcomes, particularly with chronic diseases such as diabetes and dementia, well before a diagnosis is made, he said.
‘Fascinating’ and ‘provocative’
Donald Bliwise, PhD, professor of neurology at Emory Sleep Center in Atlanta, said the study was “fascinating; it’s provocative; it’s exciting and interesting,” but added, “Sleep is vital for health. That’s abundantly clear in a study like that, but trying to push it a little bit further with all of these 86 measurements of the EEG, I think it becomes complicated.”
The study methodology, particularly the use of cumulative incidence of various diseases, was laudable, he said, and the use of simpler EEG-measured sleep features, such as alpha band power, “make intuitive sense.”
But it’s less clear on how the more sophisticated features the study model used – for example, kurtosis of theta frequency or coupling between spindle and slow oscillation – rank on sleep quality, he said, adding that the researchers have most likely done that but couldn’t add that into the format of the presentation.
“Kurtosis of the theta frequency band we don’t get on everyone in the sleep lab,” Dr. Bliwise said. “We might be able to, but I don’t know how to quite plug that into a turnkey model.”
The clinical components of the study were conducted by M. Brandon Westover, MD, PhD, at Massachusetts General Hospital, and Robert J. Thomas, MD, at Beth Israel Deaconess Medical Center, both in Boston. The study received support from the American Academy of Sleep Medicine Foundation. Dr. Sun has no relevant disclosures. Dr. Bliwise has no disclosures.
CHARLOTTE, N.C. – , a researcher reported at the annual meeting of the Associated Professional Sleep Societies. “Sleep EEGs contain decodable information about the risk of unfavorable outcomes,” said Haoqi Sun, PhD, an instructor of neurology at Massachusetts General Hospital, Boston, and lead study author. “The results suggest that it’s feasible to use sleep to identify people with high risk of unfavorable outcomes and it strengthens the concept of sleep as a window into brain and general health.”
The researchers performed a quantitative analysis of sleep data collected on 8,673 adults who had diagnostic sleep studies that included polysomnography (PSG). The analysis used ICD codes to consider these 11 health outcomes: dementia, mild cognitive impairment (MCI) or dementia, ischemic stroke, intracranial hemorrhage, atrial fibrillation, myocardial infarction, type 2 diabetes, hypertension, bipolar disorder, depression, and mortality.
Then, Dr. Sun explained, they extracted 86 spectral and time-domain features of REM and non-REM sleep from sleep EEG recordings, and analyzed that data by adjusting for eight covariates including age, sex, body mass index, and use of benzodiazepines, antidepressants, sedatives, antiseizure drugs, and stimulants.
Participants were partitioned into three sleep-quality groups: poor, average, and good. The outcome-wise mean prediction difference in 10-year cumulative incidence was 2.3% for the poor sleep group, 0.5% for the average sleep group, and 1.3% for the good sleep group.
The outcomes with the three greatest poor to average risk ratios were dementia (6.2; 95% confidence interval, 4.5-9.3), mortality (5.7; 95% CI, 5-7.5) and MCI or dementia (4; 95% CI, 3.2-4.9).
Ready for the clinic?
In an interview, Dr. Sun said the results demonstrated the potential of using EEG brain wave data to predict health outcomes on an individual basis, although he acknowledged that most of the 86 sleep features the researchers used are not readily available in the clinic.
He noted the spectral features used in the study can be captured through software compatible with PSG. “From there you can identify the various bands, the different frequency ranges, and then you can easily see within this range whether a person has a higher power or lower power,” he said. However, the spindle and slow-oscillation features that researchers used in the study are beyond the reach of most clinics.
Next steps
This research is in its early stage, Dr. Sun said, but at some point the data collected from sleep studies could be paired with machine learning to make the model workable for evaluating individual patients. “Our goal is to first make this individualized,” he said. “We want to minimize the noise in the recording and minimize the night-to-night variability in the findings. There is some clinical-informed approach and there is also some algorithm-informed approach where you can minimize the variation over time.”
The model also has the potential to predict outcomes, particularly with chronic diseases such as diabetes and dementia, well before a diagnosis is made, he said.
‘Fascinating’ and ‘provocative’
Donald Bliwise, PhD, professor of neurology at Emory Sleep Center in Atlanta, said the study was “fascinating; it’s provocative; it’s exciting and interesting,” but added, “Sleep is vital for health. That’s abundantly clear in a study like that, but trying to push it a little bit further with all of these 86 measurements of the EEG, I think it becomes complicated.”
The study methodology, particularly the use of cumulative incidence of various diseases, was laudable, he said, and the use of simpler EEG-measured sleep features, such as alpha band power, “make intuitive sense.”
But it’s less clear on how the more sophisticated features the study model used – for example, kurtosis of theta frequency or coupling between spindle and slow oscillation – rank on sleep quality, he said, adding that the researchers have most likely done that but couldn’t add that into the format of the presentation.
“Kurtosis of the theta frequency band we don’t get on everyone in the sleep lab,” Dr. Bliwise said. “We might be able to, but I don’t know how to quite plug that into a turnkey model.”
The clinical components of the study were conducted by M. Brandon Westover, MD, PhD, at Massachusetts General Hospital, and Robert J. Thomas, MD, at Beth Israel Deaconess Medical Center, both in Boston. The study received support from the American Academy of Sleep Medicine Foundation. Dr. Sun has no relevant disclosures. Dr. Bliwise has no disclosures.
AT SLEEP 2022
‘My malpractice insurance doubled!’ Why, when fewer patients are suing?
Angela Intili, MD, an ob.gyn., was used to seeing her medical malpractice insurance premium rise slightly every couple of years. But she was shocked by the drastic rise she recently experienced.
In the last 2 years, Dr. Intili’s premiums shot from $60,000 to $130,000, she said.
“After 30 years of practice, this is the first time I’ve asked myself if I can even afford to continue practicing obstetrics and gynecology,” said Dr. Intili, 62, of Joliet, Ill. “It’s gotten very difficult to make ends meet as far as overhead because of the liability costs. I still love what I’m doing but I don’t know if I can afford to do it anymore.”
Even more frustrating for Dr. Intili was learning that claims in Illinois have sharply declined. From 2016 to 2020, tort filings in Illinois decreased by 43%, according to a state report.
“If claims are going down, I don’t understand why premium payments are going up,” she said.
Physicians across the country are experiencing a similar paradox. Claims are down, yet premiums are rising.
Medscape’s Malpractice Report 2021 found that 42% of primary care physicians were sued in 2020 through mid-2021, down from 52% in 2019. Fifty-six percent of specialists were sued in 2020 through mid-2021 compared with 62% in 2019, the report found. The pandemic was undoubtedly behind the decrease in suits, according to legal experts.
Yet, physicians paid higher premiums in 2021 and are on track for increases again in 2022, according to data and analysts.
According to Conning, direct premiums written for physicians increased 7.0% in 2021 (from $5.01 billion to $5.36 billion). Conning, an investment management firm that serves the insurance industry, analyzes annual financial reports filed by insurers to state insurance departments. The Medical Liability Monitor’s 2021 report found that premiums for internists, surgeons, and ob.gyns. in states without Patient Compensation Funds rose by an average of 2% in 2021.
The disparities raise questions about why physicians are paying higher premiums when having fewer claims is likely saving insurers’ money. Shouldn’t physicians’ rates reflect the reduction in claims?
Cases plummet during pandemic
During the pandemic, the volume of new medical malpractice claims dwindled to nearly nothing, said Michael Matray, editor of the Medical Liability Monitor, a national publication that analyzes medical liability insurance premiums.
“The court system closed for a while,” he said. “No elective procedures were being done in 2020 and the early parts of 2021. If you have no treatment, you have no malpractice, so of course, claims frequency tumbled down to a trickle.”
The number of large awards also decreased during the pandemic, noted Bill Burns, a director of insurance research at Conning.
“For claims that were already in the system, many of them could not be resolved because of the court closures, inability to take statements and depositions, etc.,” he said. “This resulted in a drop in verdicts.”
In 2021, there were 16 medical malpractice verdicts of $10 million or more in the United States, according to TransRe, an international reinsurance company that tracks large verdicts. In 2020, there were six verdicts of $10 million or more, TransRe research found. This is down from 52 verdicts of $10 million or more in 2019 and 46 verdicts of $10 million or more in 2018.
But although the pandemic lowered claims and decreased the number of payouts, one important aspect was untouched by the COVID era, said Richard E. Anderson, MD, chairman and CEO for The Doctors Company, a national medical liability insurer, and TDC Group.
“It’s a fair question: If claims are down, why are premiums continuing to go up?” Dr. Anderson said. “The answer is severity.”
High-dollar verdicts pave expensive path
The upward trend in severity has continued for about 6 years and has not slowed, Dr. Anderson said. Severity refers to high-dollar verdicts and settlements.
“We’re seeing record-high verdicts all over the country,” he said. “We used to have maps that showed the top 10 medical malpractice verdicts or awards, and they would be clustered where you’d expect them to be, New York, Florida, Illinois, and so forth. Now, if you look at those top 10 verdicts, they could be anywhere in the country.”
In Minnesota for instance, a jury awarded a record $111 million in damages to a college student in May after finding a hospital and an orthopedic surgeon negligent in treating his broken leg. In April, a Kansas City jury awarded a family $25 million after finding that an ob.gyn. and hospital failed to properly treat a mother in labor, causing brain damage to her infant.
Such record payouts factor into premium costs, said Ned Rand Jr., CEO for ProAssurance, a national medical liability insurer. Though only a minority of claims reach that level, when a high award occurs, it puts pressure on the ultimate cost to resolve claims, he said. The frequency of claims filed is also expected to soon rebound, he noted.
“As we price the product sitting here today, we have to factor both of those in,” Mr. Rand said. “That’s why we, as an industry, continue to see, by and large, rates going up. And we fell behind. Some of this severity, in particular, as an industry, we weren’t pricing fully for, so we’ve been playing catch-up.”
High-dollar awards – also called nuclear verdicts – set the arena for future settlements in similar cases, Dr. Anderson added.
“If it was an orthopedic case for instance, and there was a similar injury in another case, that’s the trial lawyers’ starting point for the award,” he said. “Now, they’re not going to get it, but it distorts the negotiations. As we have more and more nuclear verdicts, it becomes harder to settle claims for reasonable amounts.”
What does 2022 have in store?
Analysts say the backlog of malpractice claims in the court system could prove calamitous for premiums and the liability landscape.
Courts are slogging through the pileup caused by the pandemic, but it’s estimated that there is still about a one-third larger case backlog than normal, according to Mr. Matray.
Such delayed claims may end up costing more because of social inflation, said Mr. Burns.
“People look at the world differently than they did 2 years ago,” he said. “A jury may have awarded $5 million for a claim a few years ago. But then the pandemic hits, and we have the George Floyd incident, and we have people out of work and a shortage in baby formula. Yet, companies are still making a lot of money and many insurance companies are turning record profits. Today, that jury may look at a sympathetic malpractice victim and award $10 million for the same claim.”
Concerns also exist about a potential surge of new malpractice claims. Mr. Rand compares the possible wave to a large bubble.
“I liken it to a cartoon, when one character grabs the hose and a big bubble forms as the water builds up,” he said. “Then the character releases, and water comes flooding out. As an industry, we wait, wondering: Is there going to be this flood of claims as the court systems reopen and the statute of limitations approach around some of these claims? That’s an ongoing concern.”
As for impending premiums, physicians can expect rises in 2022 and again in 2023, according to Chris Wojciechowski, a partner at TigerRisk Partners, a reinsurance broker.
“In general, there is a lot of uncertainty around the state of the economy, the tort environment, litigation post COVID, and overall volatility across the capital markets,” he said. “Furthermore, thanks to social and financial inflation, the potential for very severe verdicts has increased dramatically, and as courthouses reopen, the trends are not looking favorable. While many of the physician carriers have strong balance sheets, they can’t lose money on an underwriting basis forever.”
For Dr. Intili, the Illinois ob.gyn., news of another impending increase in 2022 is distressing. She expects another 10%-20% rise in 2022, she said. If she were younger and earlier in her career, she might’ve considered moving, she said, but her family lives in Illinois and she cares for her older parents.
“I’m not ready to retire,” Dr. Intili said. “I’m looking into options, possibly becoming a hospitalist or doing locum tenens work. I’ve been a solo practitioner for 27 years and I love the autonomy. But these high premiums are making it almost impossible to continue.”
A version of this article first appeared on Medscape.com.
Angela Intili, MD, an ob.gyn., was used to seeing her medical malpractice insurance premium rise slightly every couple of years. But she was shocked by the drastic rise she recently experienced.
In the last 2 years, Dr. Intili’s premiums shot from $60,000 to $130,000, she said.
“After 30 years of practice, this is the first time I’ve asked myself if I can even afford to continue practicing obstetrics and gynecology,” said Dr. Intili, 62, of Joliet, Ill. “It’s gotten very difficult to make ends meet as far as overhead because of the liability costs. I still love what I’m doing but I don’t know if I can afford to do it anymore.”
Even more frustrating for Dr. Intili was learning that claims in Illinois have sharply declined. From 2016 to 2020, tort filings in Illinois decreased by 43%, according to a state report.
“If claims are going down, I don’t understand why premium payments are going up,” she said.
Physicians across the country are experiencing a similar paradox. Claims are down, yet premiums are rising.
Medscape’s Malpractice Report 2021 found that 42% of primary care physicians were sued in 2020 through mid-2021, down from 52% in 2019. Fifty-six percent of specialists were sued in 2020 through mid-2021 compared with 62% in 2019, the report found. The pandemic was undoubtedly behind the decrease in suits, according to legal experts.
Yet, physicians paid higher premiums in 2021 and are on track for increases again in 2022, according to data and analysts.
According to Conning, direct premiums written for physicians increased 7.0% in 2021 (from $5.01 billion to $5.36 billion). Conning, an investment management firm that serves the insurance industry, analyzes annual financial reports filed by insurers to state insurance departments. The Medical Liability Monitor’s 2021 report found that premiums for internists, surgeons, and ob.gyns. in states without Patient Compensation Funds rose by an average of 2% in 2021.
The disparities raise questions about why physicians are paying higher premiums when having fewer claims is likely saving insurers’ money. Shouldn’t physicians’ rates reflect the reduction in claims?
Cases plummet during pandemic
During the pandemic, the volume of new medical malpractice claims dwindled to nearly nothing, said Michael Matray, editor of the Medical Liability Monitor, a national publication that analyzes medical liability insurance premiums.
“The court system closed for a while,” he said. “No elective procedures were being done in 2020 and the early parts of 2021. If you have no treatment, you have no malpractice, so of course, claims frequency tumbled down to a trickle.”
The number of large awards also decreased during the pandemic, noted Bill Burns, a director of insurance research at Conning.
“For claims that were already in the system, many of them could not be resolved because of the court closures, inability to take statements and depositions, etc.,” he said. “This resulted in a drop in verdicts.”
In 2021, there were 16 medical malpractice verdicts of $10 million or more in the United States, according to TransRe, an international reinsurance company that tracks large verdicts. In 2020, there were six verdicts of $10 million or more, TransRe research found. This is down from 52 verdicts of $10 million or more in 2019 and 46 verdicts of $10 million or more in 2018.
But although the pandemic lowered claims and decreased the number of payouts, one important aspect was untouched by the COVID era, said Richard E. Anderson, MD, chairman and CEO for The Doctors Company, a national medical liability insurer, and TDC Group.
“It’s a fair question: If claims are down, why are premiums continuing to go up?” Dr. Anderson said. “The answer is severity.”
High-dollar verdicts pave expensive path
The upward trend in severity has continued for about 6 years and has not slowed, Dr. Anderson said. Severity refers to high-dollar verdicts and settlements.
“We’re seeing record-high verdicts all over the country,” he said. “We used to have maps that showed the top 10 medical malpractice verdicts or awards, and they would be clustered where you’d expect them to be, New York, Florida, Illinois, and so forth. Now, if you look at those top 10 verdicts, they could be anywhere in the country.”
In Minnesota for instance, a jury awarded a record $111 million in damages to a college student in May after finding a hospital and an orthopedic surgeon negligent in treating his broken leg. In April, a Kansas City jury awarded a family $25 million after finding that an ob.gyn. and hospital failed to properly treat a mother in labor, causing brain damage to her infant.
Such record payouts factor into premium costs, said Ned Rand Jr., CEO for ProAssurance, a national medical liability insurer. Though only a minority of claims reach that level, when a high award occurs, it puts pressure on the ultimate cost to resolve claims, he said. The frequency of claims filed is also expected to soon rebound, he noted.
“As we price the product sitting here today, we have to factor both of those in,” Mr. Rand said. “That’s why we, as an industry, continue to see, by and large, rates going up. And we fell behind. Some of this severity, in particular, as an industry, we weren’t pricing fully for, so we’ve been playing catch-up.”
High-dollar awards – also called nuclear verdicts – set the arena for future settlements in similar cases, Dr. Anderson added.
“If it was an orthopedic case for instance, and there was a similar injury in another case, that’s the trial lawyers’ starting point for the award,” he said. “Now, they’re not going to get it, but it distorts the negotiations. As we have more and more nuclear verdicts, it becomes harder to settle claims for reasonable amounts.”
What does 2022 have in store?
Analysts say the backlog of malpractice claims in the court system could prove calamitous for premiums and the liability landscape.
Courts are slogging through the pileup caused by the pandemic, but it’s estimated that there is still about a one-third larger case backlog than normal, according to Mr. Matray.
Such delayed claims may end up costing more because of social inflation, said Mr. Burns.
“People look at the world differently than they did 2 years ago,” he said. “A jury may have awarded $5 million for a claim a few years ago. But then the pandemic hits, and we have the George Floyd incident, and we have people out of work and a shortage in baby formula. Yet, companies are still making a lot of money and many insurance companies are turning record profits. Today, that jury may look at a sympathetic malpractice victim and award $10 million for the same claim.”
Concerns also exist about a potential surge of new malpractice claims. Mr. Rand compares the possible wave to a large bubble.
“I liken it to a cartoon, when one character grabs the hose and a big bubble forms as the water builds up,” he said. “Then the character releases, and water comes flooding out. As an industry, we wait, wondering: Is there going to be this flood of claims as the court systems reopen and the statute of limitations approach around some of these claims? That’s an ongoing concern.”
As for impending premiums, physicians can expect rises in 2022 and again in 2023, according to Chris Wojciechowski, a partner at TigerRisk Partners, a reinsurance broker.
“In general, there is a lot of uncertainty around the state of the economy, the tort environment, litigation post COVID, and overall volatility across the capital markets,” he said. “Furthermore, thanks to social and financial inflation, the potential for very severe verdicts has increased dramatically, and as courthouses reopen, the trends are not looking favorable. While many of the physician carriers have strong balance sheets, they can’t lose money on an underwriting basis forever.”
For Dr. Intili, the Illinois ob.gyn., news of another impending increase in 2022 is distressing. She expects another 10%-20% rise in 2022, she said. If she were younger and earlier in her career, she might’ve considered moving, she said, but her family lives in Illinois and she cares for her older parents.
“I’m not ready to retire,” Dr. Intili said. “I’m looking into options, possibly becoming a hospitalist or doing locum tenens work. I’ve been a solo practitioner for 27 years and I love the autonomy. But these high premiums are making it almost impossible to continue.”
A version of this article first appeared on Medscape.com.
Angela Intili, MD, an ob.gyn., was used to seeing her medical malpractice insurance premium rise slightly every couple of years. But she was shocked by the drastic rise she recently experienced.
In the last 2 years, Dr. Intili’s premiums shot from $60,000 to $130,000, she said.
“After 30 years of practice, this is the first time I’ve asked myself if I can even afford to continue practicing obstetrics and gynecology,” said Dr. Intili, 62, of Joliet, Ill. “It’s gotten very difficult to make ends meet as far as overhead because of the liability costs. I still love what I’m doing but I don’t know if I can afford to do it anymore.”
Even more frustrating for Dr. Intili was learning that claims in Illinois have sharply declined. From 2016 to 2020, tort filings in Illinois decreased by 43%, according to a state report.
“If claims are going down, I don’t understand why premium payments are going up,” she said.
Physicians across the country are experiencing a similar paradox. Claims are down, yet premiums are rising.
Medscape’s Malpractice Report 2021 found that 42% of primary care physicians were sued in 2020 through mid-2021, down from 52% in 2019. Fifty-six percent of specialists were sued in 2020 through mid-2021 compared with 62% in 2019, the report found. The pandemic was undoubtedly behind the decrease in suits, according to legal experts.
Yet, physicians paid higher premiums in 2021 and are on track for increases again in 2022, according to data and analysts.
According to Conning, direct premiums written for physicians increased 7.0% in 2021 (from $5.01 billion to $5.36 billion). Conning, an investment management firm that serves the insurance industry, analyzes annual financial reports filed by insurers to state insurance departments. The Medical Liability Monitor’s 2021 report found that premiums for internists, surgeons, and ob.gyns. in states without Patient Compensation Funds rose by an average of 2% in 2021.
The disparities raise questions about why physicians are paying higher premiums when having fewer claims is likely saving insurers’ money. Shouldn’t physicians’ rates reflect the reduction in claims?
Cases plummet during pandemic
During the pandemic, the volume of new medical malpractice claims dwindled to nearly nothing, said Michael Matray, editor of the Medical Liability Monitor, a national publication that analyzes medical liability insurance premiums.
“The court system closed for a while,” he said. “No elective procedures were being done in 2020 and the early parts of 2021. If you have no treatment, you have no malpractice, so of course, claims frequency tumbled down to a trickle.”
The number of large awards also decreased during the pandemic, noted Bill Burns, a director of insurance research at Conning.
“For claims that were already in the system, many of them could not be resolved because of the court closures, inability to take statements and depositions, etc.,” he said. “This resulted in a drop in verdicts.”
In 2021, there were 16 medical malpractice verdicts of $10 million or more in the United States, according to TransRe, an international reinsurance company that tracks large verdicts. In 2020, there were six verdicts of $10 million or more, TransRe research found. This is down from 52 verdicts of $10 million or more in 2019 and 46 verdicts of $10 million or more in 2018.
But although the pandemic lowered claims and decreased the number of payouts, one important aspect was untouched by the COVID era, said Richard E. Anderson, MD, chairman and CEO for The Doctors Company, a national medical liability insurer, and TDC Group.
“It’s a fair question: If claims are down, why are premiums continuing to go up?” Dr. Anderson said. “The answer is severity.”
High-dollar verdicts pave expensive path
The upward trend in severity has continued for about 6 years and has not slowed, Dr. Anderson said. Severity refers to high-dollar verdicts and settlements.
“We’re seeing record-high verdicts all over the country,” he said. “We used to have maps that showed the top 10 medical malpractice verdicts or awards, and they would be clustered where you’d expect them to be, New York, Florida, Illinois, and so forth. Now, if you look at those top 10 verdicts, they could be anywhere in the country.”
In Minnesota for instance, a jury awarded a record $111 million in damages to a college student in May after finding a hospital and an orthopedic surgeon negligent in treating his broken leg. In April, a Kansas City jury awarded a family $25 million after finding that an ob.gyn. and hospital failed to properly treat a mother in labor, causing brain damage to her infant.
Such record payouts factor into premium costs, said Ned Rand Jr., CEO for ProAssurance, a national medical liability insurer. Though only a minority of claims reach that level, when a high award occurs, it puts pressure on the ultimate cost to resolve claims, he said. The frequency of claims filed is also expected to soon rebound, he noted.
“As we price the product sitting here today, we have to factor both of those in,” Mr. Rand said. “That’s why we, as an industry, continue to see, by and large, rates going up. And we fell behind. Some of this severity, in particular, as an industry, we weren’t pricing fully for, so we’ve been playing catch-up.”
High-dollar awards – also called nuclear verdicts – set the arena for future settlements in similar cases, Dr. Anderson added.
“If it was an orthopedic case for instance, and there was a similar injury in another case, that’s the trial lawyers’ starting point for the award,” he said. “Now, they’re not going to get it, but it distorts the negotiations. As we have more and more nuclear verdicts, it becomes harder to settle claims for reasonable amounts.”
What does 2022 have in store?
Analysts say the backlog of malpractice claims in the court system could prove calamitous for premiums and the liability landscape.
Courts are slogging through the pileup caused by the pandemic, but it’s estimated that there is still about a one-third larger case backlog than normal, according to Mr. Matray.
Such delayed claims may end up costing more because of social inflation, said Mr. Burns.
“People look at the world differently than they did 2 years ago,” he said. “A jury may have awarded $5 million for a claim a few years ago. But then the pandemic hits, and we have the George Floyd incident, and we have people out of work and a shortage in baby formula. Yet, companies are still making a lot of money and many insurance companies are turning record profits. Today, that jury may look at a sympathetic malpractice victim and award $10 million for the same claim.”
Concerns also exist about a potential surge of new malpractice claims. Mr. Rand compares the possible wave to a large bubble.
“I liken it to a cartoon, when one character grabs the hose and a big bubble forms as the water builds up,” he said. “Then the character releases, and water comes flooding out. As an industry, we wait, wondering: Is there going to be this flood of claims as the court systems reopen and the statute of limitations approach around some of these claims? That’s an ongoing concern.”
As for impending premiums, physicians can expect rises in 2022 and again in 2023, according to Chris Wojciechowski, a partner at TigerRisk Partners, a reinsurance broker.
“In general, there is a lot of uncertainty around the state of the economy, the tort environment, litigation post COVID, and overall volatility across the capital markets,” he said. “Furthermore, thanks to social and financial inflation, the potential for very severe verdicts has increased dramatically, and as courthouses reopen, the trends are not looking favorable. While many of the physician carriers have strong balance sheets, they can’t lose money on an underwriting basis forever.”
For Dr. Intili, the Illinois ob.gyn., news of another impending increase in 2022 is distressing. She expects another 10%-20% rise in 2022, she said. If she were younger and earlier in her career, she might’ve considered moving, she said, but her family lives in Illinois and she cares for her older parents.
“I’m not ready to retire,” Dr. Intili said. “I’m looking into options, possibly becoming a hospitalist or doing locum tenens work. I’ve been a solo practitioner for 27 years and I love the autonomy. But these high premiums are making it almost impossible to continue.”
A version of this article first appeared on Medscape.com.
Opioid use in the elderly a dementia risk factor?
in new findings that suggest exposure to these drugs may be another modifiable risk factor for dementia.
“Clinicians and others may want to consider that opioid exposure in those aged 75-80 increases dementia risk, and to balance the potential benefits of opioid use in old age with adverse side effects,” said Stephen Z. Levine, PhD, professor, department of community mental health, University of Haifa (Israel).
The study was published online in the American Journal of Geriatric Psychiatry.
Widespread use
Evidence points to a relatively high rate of opioid prescriptions among older adults. A Morbidity and Mortality Weekly Report noted 19.2% of the U.S. adult population filled an opioid prescription in 2018, with the rate in those over 65 double that of adults aged 20-24 years (25% vs. 11.2%).
Disorders and illnesses for which opioids might be prescribed, including cancer and some pain conditions, “are far more prevalent in old age than at a younger age,” said Dr. Levine.
This high rate of opioid use underscores the need to consider the risks of opioid use in old age, said Dr. Levine. “Unfortunately, studies of the association between opioid use and dementia risk in old age are few, and their results are inconsistent.”
The study included 91,307 Israeli citizens aged 60 and over without dementia who were enrolled in the Meuhedet Healthcare Services, a nonprofit health maintenance organization (HMO) serving 14% of the country’s population. Meuhedet has maintained an up-to-date dementia registry since 2002.
The average age of the study sample was 68.29 years at the start of the study (in 2012).
In Israel, opioids are prescribed for a 30-day period. In this study, opioid exposure was defined as opioid medication fills covering 60 days (or two prescriptions) within a 120-day interval.
The primary outcome was incident dementia during follow-up from Jan. 1, 2013 to Oct. 30, 2017. The analysis controlled for a number of factors, including age, sex, smoking status, health conditions such as arthritis, depression, diabetes, osteoporosis, cognitive decline, vitamin deficiencies, cancer, cardiovascular conditions, and hospitalizations for falls.
Researchers also accounted for the competing risk of mortality.
During the study, 3.1% of subjects were exposed to opioids at a mean age of 73.94 years, and 5.8% of subjects developed dementia at an average age of 78.07 years.
Increased dementia risk
The risk of incident dementia was significantly increased in those exposed to opioids versus unexposed individuals in the 75- to 80-year age group (adjusted hazard ratio, 1.39; 95% confidence interval, 1.01-1.92; z statistic = 2.02; P < .05).
The authors noted the effect size for opioid exposure in this elderly age group is like other potentially modifiable risk factors for dementia, including body mass index and smoking.
The current study could not determine the biological explanation for the increased dementia risk among older opioid users. “Causal notions are challenging in observational studies and should be viewed with caution,” Dr. Levine noted.
However, a plausible mechanism highlighted in the literature is that opioids promote apoptosis of microglia and neurons that contribute to neurodegenerative diseases, he said.
The study included 14 sensitivity analyses, including those that looked at females, subjects older than 70, smokers, and groups with and without comorbid health conditions. The only sensitivity analysis that didn’t have similar findings to the primary analysis looked at dementia risk restricted to subjects without a vitamin deficiency.
“It’s reassuring that 13 or 14 sensitivity analyses found a significant association between opioid exposure and dementia risk,” said Dr. Levine.
Some prior studies did not show an association between opioid exposure and dementia risk. One possible reason for the discrepancy with the current findings is that the previous research didn’t account for age-specific opioid use effects, or the competing risk of mortality, said Dr. Levine.
Clinicians have a number of potential alternatives to opioids to treat various conditions including acetaminophen, non-steroidal anti-inflammatory drugs, amine reuptake inhibitors (ARIs), membrane stabilizers, muscle relaxants, topical capsaicin, botulinum toxin, cannabinoids, and steroids.
A limitation of the study was that it didn’t adjust for all possible comorbid health conditions, including vascular conditions, or for use of benzodiazepines, and surgical procedures.
In addition, since up to 50% of dementia cases are undetected, it’s possible some in the unexposed opioid group may actually have undiagnosed dementia, thereby reducing the effect sizes in the results.
Reverse causality is also a possibility as the neuropathological process associated with dementia could have started prior to opioid exposure. In addition, the results are limited to prolonged opioid exposure.
Interpret with caution
Commenting on the study, David Knopman, MD, a neurologist at Mayo Clinic in Rochester, Minn., whose research involves late-life cognitive disorders, was skeptical.
“On the face of it, the fact that an association was seen only in one narrow age range – 75+ to 80 years – ought to raise serious suspicion about the reliability and validity of the claim that opioid use is a risk factor for dementia, he said.
Although the researchers performed several sensitivity analyses, including accounting for mortality, “pharmacoepidemiological studies are terribly sensitive to residual biases” related to physician and patient choices related to medication use, added Dr. Knopman.
The claim that opioids are a dementia risk “should be viewed with great caution” and should not influence use of opioids where they’re truly indicated, he said.
“It would be a great pity if patients with pain requiring opioids avoid them because of fears about dementia based on the dubious relationship between age and opioid use.”
Dr. Levine and Dr. Knopman report no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
in new findings that suggest exposure to these drugs may be another modifiable risk factor for dementia.
“Clinicians and others may want to consider that opioid exposure in those aged 75-80 increases dementia risk, and to balance the potential benefits of opioid use in old age with adverse side effects,” said Stephen Z. Levine, PhD, professor, department of community mental health, University of Haifa (Israel).
The study was published online in the American Journal of Geriatric Psychiatry.
Widespread use
Evidence points to a relatively high rate of opioid prescriptions among older adults. A Morbidity and Mortality Weekly Report noted 19.2% of the U.S. adult population filled an opioid prescription in 2018, with the rate in those over 65 double that of adults aged 20-24 years (25% vs. 11.2%).
Disorders and illnesses for which opioids might be prescribed, including cancer and some pain conditions, “are far more prevalent in old age than at a younger age,” said Dr. Levine.
This high rate of opioid use underscores the need to consider the risks of opioid use in old age, said Dr. Levine. “Unfortunately, studies of the association between opioid use and dementia risk in old age are few, and their results are inconsistent.”
The study included 91,307 Israeli citizens aged 60 and over without dementia who were enrolled in the Meuhedet Healthcare Services, a nonprofit health maintenance organization (HMO) serving 14% of the country’s population. Meuhedet has maintained an up-to-date dementia registry since 2002.
The average age of the study sample was 68.29 years at the start of the study (in 2012).
In Israel, opioids are prescribed for a 30-day period. In this study, opioid exposure was defined as opioid medication fills covering 60 days (or two prescriptions) within a 120-day interval.
The primary outcome was incident dementia during follow-up from Jan. 1, 2013 to Oct. 30, 2017. The analysis controlled for a number of factors, including age, sex, smoking status, health conditions such as arthritis, depression, diabetes, osteoporosis, cognitive decline, vitamin deficiencies, cancer, cardiovascular conditions, and hospitalizations for falls.
Researchers also accounted for the competing risk of mortality.
During the study, 3.1% of subjects were exposed to opioids at a mean age of 73.94 years, and 5.8% of subjects developed dementia at an average age of 78.07 years.
Increased dementia risk
The risk of incident dementia was significantly increased in those exposed to opioids versus unexposed individuals in the 75- to 80-year age group (adjusted hazard ratio, 1.39; 95% confidence interval, 1.01-1.92; z statistic = 2.02; P < .05).
The authors noted the effect size for opioid exposure in this elderly age group is like other potentially modifiable risk factors for dementia, including body mass index and smoking.
The current study could not determine the biological explanation for the increased dementia risk among older opioid users. “Causal notions are challenging in observational studies and should be viewed with caution,” Dr. Levine noted.
However, a plausible mechanism highlighted in the literature is that opioids promote apoptosis of microglia and neurons that contribute to neurodegenerative diseases, he said.
The study included 14 sensitivity analyses, including those that looked at females, subjects older than 70, smokers, and groups with and without comorbid health conditions. The only sensitivity analysis that didn’t have similar findings to the primary analysis looked at dementia risk restricted to subjects without a vitamin deficiency.
“It’s reassuring that 13 or 14 sensitivity analyses found a significant association between opioid exposure and dementia risk,” said Dr. Levine.
Some prior studies did not show an association between opioid exposure and dementia risk. One possible reason for the discrepancy with the current findings is that the previous research didn’t account for age-specific opioid use effects, or the competing risk of mortality, said Dr. Levine.
Clinicians have a number of potential alternatives to opioids to treat various conditions including acetaminophen, non-steroidal anti-inflammatory drugs, amine reuptake inhibitors (ARIs), membrane stabilizers, muscle relaxants, topical capsaicin, botulinum toxin, cannabinoids, and steroids.
A limitation of the study was that it didn’t adjust for all possible comorbid health conditions, including vascular conditions, or for use of benzodiazepines, and surgical procedures.
In addition, since up to 50% of dementia cases are undetected, it’s possible some in the unexposed opioid group may actually have undiagnosed dementia, thereby reducing the effect sizes in the results.
Reverse causality is also a possibility as the neuropathological process associated with dementia could have started prior to opioid exposure. In addition, the results are limited to prolonged opioid exposure.
Interpret with caution
Commenting on the study, David Knopman, MD, a neurologist at Mayo Clinic in Rochester, Minn., whose research involves late-life cognitive disorders, was skeptical.
“On the face of it, the fact that an association was seen only in one narrow age range – 75+ to 80 years – ought to raise serious suspicion about the reliability and validity of the claim that opioid use is a risk factor for dementia, he said.
Although the researchers performed several sensitivity analyses, including accounting for mortality, “pharmacoepidemiological studies are terribly sensitive to residual biases” related to physician and patient choices related to medication use, added Dr. Knopman.
The claim that opioids are a dementia risk “should be viewed with great caution” and should not influence use of opioids where they’re truly indicated, he said.
“It would be a great pity if patients with pain requiring opioids avoid them because of fears about dementia based on the dubious relationship between age and opioid use.”
Dr. Levine and Dr. Knopman report no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
in new findings that suggest exposure to these drugs may be another modifiable risk factor for dementia.
“Clinicians and others may want to consider that opioid exposure in those aged 75-80 increases dementia risk, and to balance the potential benefits of opioid use in old age with adverse side effects,” said Stephen Z. Levine, PhD, professor, department of community mental health, University of Haifa (Israel).
The study was published online in the American Journal of Geriatric Psychiatry.
Widespread use
Evidence points to a relatively high rate of opioid prescriptions among older adults. A Morbidity and Mortality Weekly Report noted 19.2% of the U.S. adult population filled an opioid prescription in 2018, with the rate in those over 65 double that of adults aged 20-24 years (25% vs. 11.2%).
Disorders and illnesses for which opioids might be prescribed, including cancer and some pain conditions, “are far more prevalent in old age than at a younger age,” said Dr. Levine.
This high rate of opioid use underscores the need to consider the risks of opioid use in old age, said Dr. Levine. “Unfortunately, studies of the association between opioid use and dementia risk in old age are few, and their results are inconsistent.”
The study included 91,307 Israeli citizens aged 60 and over without dementia who were enrolled in the Meuhedet Healthcare Services, a nonprofit health maintenance organization (HMO) serving 14% of the country’s population. Meuhedet has maintained an up-to-date dementia registry since 2002.
The average age of the study sample was 68.29 years at the start of the study (in 2012).
In Israel, opioids are prescribed for a 30-day period. In this study, opioid exposure was defined as opioid medication fills covering 60 days (or two prescriptions) within a 120-day interval.
The primary outcome was incident dementia during follow-up from Jan. 1, 2013 to Oct. 30, 2017. The analysis controlled for a number of factors, including age, sex, smoking status, health conditions such as arthritis, depression, diabetes, osteoporosis, cognitive decline, vitamin deficiencies, cancer, cardiovascular conditions, and hospitalizations for falls.
Researchers also accounted for the competing risk of mortality.
During the study, 3.1% of subjects were exposed to opioids at a mean age of 73.94 years, and 5.8% of subjects developed dementia at an average age of 78.07 years.
Increased dementia risk
The risk of incident dementia was significantly increased in those exposed to opioids versus unexposed individuals in the 75- to 80-year age group (adjusted hazard ratio, 1.39; 95% confidence interval, 1.01-1.92; z statistic = 2.02; P < .05).
The authors noted the effect size for opioid exposure in this elderly age group is like other potentially modifiable risk factors for dementia, including body mass index and smoking.
The current study could not determine the biological explanation for the increased dementia risk among older opioid users. “Causal notions are challenging in observational studies and should be viewed with caution,” Dr. Levine noted.
However, a plausible mechanism highlighted in the literature is that opioids promote apoptosis of microglia and neurons that contribute to neurodegenerative diseases, he said.
The study included 14 sensitivity analyses, including those that looked at females, subjects older than 70, smokers, and groups with and without comorbid health conditions. The only sensitivity analysis that didn’t have similar findings to the primary analysis looked at dementia risk restricted to subjects without a vitamin deficiency.
“It’s reassuring that 13 or 14 sensitivity analyses found a significant association between opioid exposure and dementia risk,” said Dr. Levine.
Some prior studies did not show an association between opioid exposure and dementia risk. One possible reason for the discrepancy with the current findings is that the previous research didn’t account for age-specific opioid use effects, or the competing risk of mortality, said Dr. Levine.
Clinicians have a number of potential alternatives to opioids to treat various conditions including acetaminophen, non-steroidal anti-inflammatory drugs, amine reuptake inhibitors (ARIs), membrane stabilizers, muscle relaxants, topical capsaicin, botulinum toxin, cannabinoids, and steroids.
A limitation of the study was that it didn’t adjust for all possible comorbid health conditions, including vascular conditions, or for use of benzodiazepines, and surgical procedures.
In addition, since up to 50% of dementia cases are undetected, it’s possible some in the unexposed opioid group may actually have undiagnosed dementia, thereby reducing the effect sizes in the results.
Reverse causality is also a possibility as the neuropathological process associated with dementia could have started prior to opioid exposure. In addition, the results are limited to prolonged opioid exposure.
Interpret with caution
Commenting on the study, David Knopman, MD, a neurologist at Mayo Clinic in Rochester, Minn., whose research involves late-life cognitive disorders, was skeptical.
“On the face of it, the fact that an association was seen only in one narrow age range – 75+ to 80 years – ought to raise serious suspicion about the reliability and validity of the claim that opioid use is a risk factor for dementia, he said.
Although the researchers performed several sensitivity analyses, including accounting for mortality, “pharmacoepidemiological studies are terribly sensitive to residual biases” related to physician and patient choices related to medication use, added Dr. Knopman.
The claim that opioids are a dementia risk “should be viewed with great caution” and should not influence use of opioids where they’re truly indicated, he said.
“It would be a great pity if patients with pain requiring opioids avoid them because of fears about dementia based on the dubious relationship between age and opioid use.”
Dr. Levine and Dr. Knopman report no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
FROM AMERICAN JOURNAL OF GERIATRIC PSYCHIATRY
Asian American teens have highest rate of suicidal ideation
NEW ORLEANS – In an unexpected finding, researchers discovered that According to a weighted analysis, 24% of Asian Americans reported thinking about or planning suicide vs. 22% of Whites and Blacks and 20% of Hispanics (P < .01).
“We were shocked,” said study lead author Esha Hansoti, MD, who conducted the research at UT Southwestern Medical Center, Dallas, and is now a psychiatry resident at Zucker Hillside Hospital Northwell/Hofstra in Glen Oaks, NY. The findings were released at the annual meeting of the American Psychiatric Association.
Dr. Hansoti and colleagues launched the analysis in light of sparse research into Asian American mental health, she said. Even within this population, she said, mental illness “tends to be overlooked” and discussion of the topic may be considered taboo.
For the new study, researchers analyzed the 2019 Youth Risk Behavior Survey, conducted biennially by the Centers for Disease Control and Prevention, which had more than 13,000 participants in grades 9-12.
A weighted bivariate analysis of 618 Asian American adolescents – adjusted for age, sex, and depressive symptoms – found no statistically significant impact on suicidal ideation by gender, age, substance use, sexual/physical dating violence, or fluency in English.
However, several groups had a statistically significant higher risk, including victims of forced sexual intercourse and those who were threatened or bullied at school.
Those who didn’t get mostly A grades were also at high risk: Adolescents with mostly Ds and Fs were more likely to have acknowledged suicidal ideation than those with mostly As (adjusted odds ratio [AOR] = 3.2).
Gays and lesbians (AOR = 7.9 vs. heterosexuals), and bisexuals (AOR = 5.2 vs. heterosexuals) also showed sharply higher rates of suicidal ideation.
It’s not clear why Asian American adolescents may be at higher risk of suicidal ideation. The survey was completed prior to the COVID-19 pandemic, which spawned bigotry against people of Asian descent and an ongoing outbreak of high-profile violence against Asian Americans across the country.
Dr. Hansoti noted that Asian Americans face the pressures to live up to the standards of being a “model minority.” In addition, “very few Asian American adolescents are taken to a therapist, and few mental health providers are Asian Americans.”
She urged fellow psychiatrists “to remember that our perceptions of Asian Americans might hinder some of the diagnoses we could be making. Be thoughtful about how their ethnicity and race affects their presentation and their own perception of their illness.”
She added that Asian Americans may experience mental illness and anxiety “more somatically and physically than emotionally.”
In an interview, Anne Saw, PhD, associate professor of clinical-community psychology at DePaul University, Chicago, said the findings are “helpful for corroborating other studies identifying risk factors of suicidal ideation among Asian American adolescents. Since this research utilizes the Youth Risk Behavior Survey, these findings can be compared with risk factors of suicidal ideation among adolescents from other racial/ethnic backgrounds to pinpoint general as well as specific risk factors, thus informing how we can tailor interventions for specific groups.”
According to Dr. Saw, while it’s clear that suicide is a leading cause of death among Asian American adolescents, it’s still unknown which specific subgroups other than girls and LGBTIA+ individuals are especially vulnerable and which culturally tailored interventions are most effective for decreasing suicide risk.
“Psychiatrists should understand that risk and protective factors for suicidal behavior in Asian American adolescents are multifaceted and require careful attention and intervention across different environments,” she said.
No funding and no disclosures were reported.
NEW ORLEANS – In an unexpected finding, researchers discovered that According to a weighted analysis, 24% of Asian Americans reported thinking about or planning suicide vs. 22% of Whites and Blacks and 20% of Hispanics (P < .01).
“We were shocked,” said study lead author Esha Hansoti, MD, who conducted the research at UT Southwestern Medical Center, Dallas, and is now a psychiatry resident at Zucker Hillside Hospital Northwell/Hofstra in Glen Oaks, NY. The findings were released at the annual meeting of the American Psychiatric Association.
Dr. Hansoti and colleagues launched the analysis in light of sparse research into Asian American mental health, she said. Even within this population, she said, mental illness “tends to be overlooked” and discussion of the topic may be considered taboo.
For the new study, researchers analyzed the 2019 Youth Risk Behavior Survey, conducted biennially by the Centers for Disease Control and Prevention, which had more than 13,000 participants in grades 9-12.
A weighted bivariate analysis of 618 Asian American adolescents – adjusted for age, sex, and depressive symptoms – found no statistically significant impact on suicidal ideation by gender, age, substance use, sexual/physical dating violence, or fluency in English.
However, several groups had a statistically significant higher risk, including victims of forced sexual intercourse and those who were threatened or bullied at school.
Those who didn’t get mostly A grades were also at high risk: Adolescents with mostly Ds and Fs were more likely to have acknowledged suicidal ideation than those with mostly As (adjusted odds ratio [AOR] = 3.2).
Gays and lesbians (AOR = 7.9 vs. heterosexuals), and bisexuals (AOR = 5.2 vs. heterosexuals) also showed sharply higher rates of suicidal ideation.
It’s not clear why Asian American adolescents may be at higher risk of suicidal ideation. The survey was completed prior to the COVID-19 pandemic, which spawned bigotry against people of Asian descent and an ongoing outbreak of high-profile violence against Asian Americans across the country.
Dr. Hansoti noted that Asian Americans face the pressures to live up to the standards of being a “model minority.” In addition, “very few Asian American adolescents are taken to a therapist, and few mental health providers are Asian Americans.”
She urged fellow psychiatrists “to remember that our perceptions of Asian Americans might hinder some of the diagnoses we could be making. Be thoughtful about how their ethnicity and race affects their presentation and their own perception of their illness.”
She added that Asian Americans may experience mental illness and anxiety “more somatically and physically than emotionally.”
In an interview, Anne Saw, PhD, associate professor of clinical-community psychology at DePaul University, Chicago, said the findings are “helpful for corroborating other studies identifying risk factors of suicidal ideation among Asian American adolescents. Since this research utilizes the Youth Risk Behavior Survey, these findings can be compared with risk factors of suicidal ideation among adolescents from other racial/ethnic backgrounds to pinpoint general as well as specific risk factors, thus informing how we can tailor interventions for specific groups.”
According to Dr. Saw, while it’s clear that suicide is a leading cause of death among Asian American adolescents, it’s still unknown which specific subgroups other than girls and LGBTIA+ individuals are especially vulnerable and which culturally tailored interventions are most effective for decreasing suicide risk.
“Psychiatrists should understand that risk and protective factors for suicidal behavior in Asian American adolescents are multifaceted and require careful attention and intervention across different environments,” she said.
No funding and no disclosures were reported.
NEW ORLEANS – In an unexpected finding, researchers discovered that According to a weighted analysis, 24% of Asian Americans reported thinking about or planning suicide vs. 22% of Whites and Blacks and 20% of Hispanics (P < .01).
“We were shocked,” said study lead author Esha Hansoti, MD, who conducted the research at UT Southwestern Medical Center, Dallas, and is now a psychiatry resident at Zucker Hillside Hospital Northwell/Hofstra in Glen Oaks, NY. The findings were released at the annual meeting of the American Psychiatric Association.
Dr. Hansoti and colleagues launched the analysis in light of sparse research into Asian American mental health, she said. Even within this population, she said, mental illness “tends to be overlooked” and discussion of the topic may be considered taboo.
For the new study, researchers analyzed the 2019 Youth Risk Behavior Survey, conducted biennially by the Centers for Disease Control and Prevention, which had more than 13,000 participants in grades 9-12.
A weighted bivariate analysis of 618 Asian American adolescents – adjusted for age, sex, and depressive symptoms – found no statistically significant impact on suicidal ideation by gender, age, substance use, sexual/physical dating violence, or fluency in English.
However, several groups had a statistically significant higher risk, including victims of forced sexual intercourse and those who were threatened or bullied at school.
Those who didn’t get mostly A grades were also at high risk: Adolescents with mostly Ds and Fs were more likely to have acknowledged suicidal ideation than those with mostly As (adjusted odds ratio [AOR] = 3.2).
Gays and lesbians (AOR = 7.9 vs. heterosexuals), and bisexuals (AOR = 5.2 vs. heterosexuals) also showed sharply higher rates of suicidal ideation.
It’s not clear why Asian American adolescents may be at higher risk of suicidal ideation. The survey was completed prior to the COVID-19 pandemic, which spawned bigotry against people of Asian descent and an ongoing outbreak of high-profile violence against Asian Americans across the country.
Dr. Hansoti noted that Asian Americans face the pressures to live up to the standards of being a “model minority.” In addition, “very few Asian American adolescents are taken to a therapist, and few mental health providers are Asian Americans.”
She urged fellow psychiatrists “to remember that our perceptions of Asian Americans might hinder some of the diagnoses we could be making. Be thoughtful about how their ethnicity and race affects their presentation and their own perception of their illness.”
She added that Asian Americans may experience mental illness and anxiety “more somatically and physically than emotionally.”
In an interview, Anne Saw, PhD, associate professor of clinical-community psychology at DePaul University, Chicago, said the findings are “helpful for corroborating other studies identifying risk factors of suicidal ideation among Asian American adolescents. Since this research utilizes the Youth Risk Behavior Survey, these findings can be compared with risk factors of suicidal ideation among adolescents from other racial/ethnic backgrounds to pinpoint general as well as specific risk factors, thus informing how we can tailor interventions for specific groups.”
According to Dr. Saw, while it’s clear that suicide is a leading cause of death among Asian American adolescents, it’s still unknown which specific subgroups other than girls and LGBTIA+ individuals are especially vulnerable and which culturally tailored interventions are most effective for decreasing suicide risk.
“Psychiatrists should understand that risk and protective factors for suicidal behavior in Asian American adolescents are multifaceted and require careful attention and intervention across different environments,” she said.
No funding and no disclosures were reported.
AT APA 2022
Youth with bipolar disorder at high risk of eating disorders
Investigators studied close to 200 youth with BD and found that more than 25% had a lifetime ED, which included anorexia nervosa (AN), bulimia nervosa (BN), and an ED not otherwise specified (NOS).
Those with comorbid EDs were more likely to be female and to have BD-II subtype. Their presentations were also more complicated and included a history of suicidality, additional psychiatric conditions, smoking, and a history of sexual abuse, as well as more severe depression and emotional instability.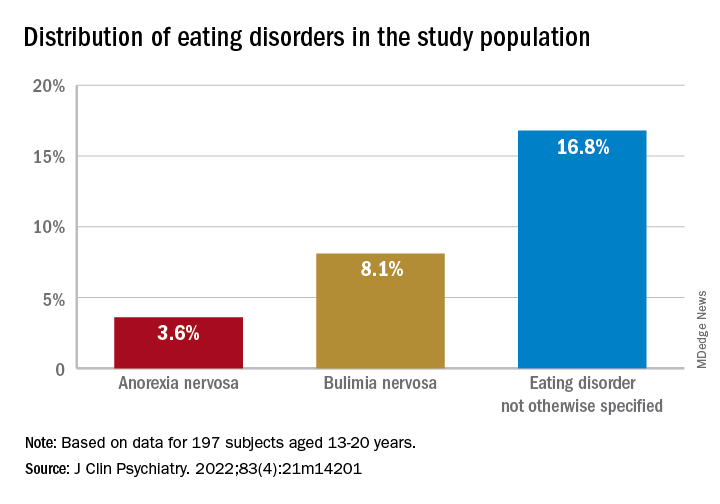
“We think the take-home message is that, in addition to other more recognized psychiatric comorbidities, youth with BD are also vulnerable to developing EDs. Thus, clinicians should be routinely monitoring for eating, appetite, and body image disturbances when working with this population,” lead author Diana Khoubaeva, research analyst at the Centre for Youth Bipolar Disorder, Centre for Addiction and Mental Health, Toronto, and senior author Benjamin Goldstein, MD, PhD, director of the Centre for Youth Bipolar Disorder, wrote in an e-mail to this news organization.
“Given the more complicated clinical picture of youth with co-occurring BD and EDs, this combination warrants careful attention,” the investigators note.
The study was published online May 11 in the Journal of Clinical Psychiatry.
Lack of research
“From the existing literature, we learned that EDs are not uncommon in individuals with BD, and that they are often associated with a more severe clinical profile,” say the researchers. “However, the majority of these studies have been limited to adult samples, and there was a real scarcity of studies that examined this co-occurrence in youth.”
This is “surprising” because EDs often have their onset in adolescence, so the researchers decided to explore the issue in their “fairly large sample of youth with BD.”
To investigate the issue, the researchers studied 197 youth (aged 13-20 years) with a diagnosis of BD (BD-I, BD-II, or BD-NOS) who were recruited between 2009 and 2017 (mean [standard deviation] age, 16.69 [1.50] years; 67.5% female).
ED diagnoses included both current and lifetime AN, BN, and ED-NOS. The researchers used the Kiddie Schedule for Affective Disorders and Schizophrenia for School Age Children, Present and Lifetime Version (K-SADS-PL) to determine the diagnosis of BD.
They also collected information about comorbid psychiatric disorders, as well as substance use disorders and cigarette smoking. The Life Problems Inventory (LPI) was used to identify dimensional borderline personality traits.
Information about physical and sexual abuse, suicidal ideation, nonsuicidal self-injury (NSSI), and affect regulation were obtained from other measurement tools. Participants’ height and weight were measured to calculate body mass index.
Neurobiological and environmental factors
Of the total sample, 24.84% had received a diagnosis of ED in their lifetime.
Moreover, 28.9% had a lifetime history of binge eating. Of these, 17.7% also had been diagnosed with an ED.
Participants with BD-II were significantly more likely than those with BD-I to report both current and lifetime BN. There were no significant differences by BD subtype in AN, ED-NOS, or binge eating.
Higher correlates of clinical characteristics, psychiatric morbidity, treatment history, and dimensional traits in those with vs. those without an ED are detailed in the accompanying table.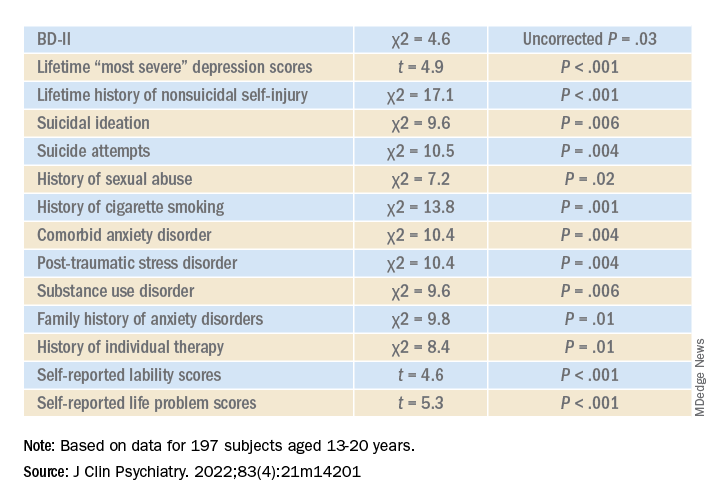
The ED group scored significantly higher on all LPI scores, including impulsivity, emotional dysregulation, identity confusion, and interpersonal problems, compared to those without an ED. They also were less likely to report lifetime lithium use (chi2 = 7.9, P = .01).
Multivariate analysis revealed that lifetime EDs were significantly associated with female sex, history of cigarette smoking, history of individual therapy, family history of anxiety, and LPI total score and were negatively associated with BD-I subtype.
“The comorbidity [between EDs and BD] could be driven by both neurobiological and environmental factors,” Dr. Khoubaeva and Dr. Goldstein noted. EDs and BD “are both illnesses that are fundamentally linked with dysfunction in reward systems – that is, there are imbalances in terms of too much or too little reward seeking.”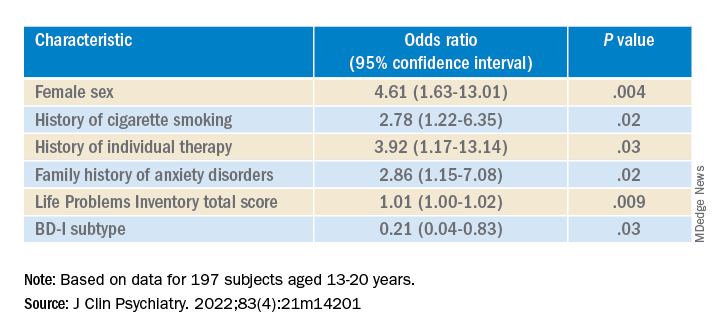
They added that individuals affected by these conditions have “ongoing challenges with instability of emotions and ability to manage emotions; and eating too much or too little can be a manifestation of coping with emotions.”
In addition, medications commonly used to treat BD “are known to have side effects such as weight/appetite/metabolic changes, which may make it harder to regulate eating, and which may exacerbate preexisting body image challenges.”
The researchers recommend implementing trauma-informed care, assessing and addressing suicidality and self-injury, and prioritizing therapies that target emotional dysregulation, such as dialectical behavioral therapy.
‘Clarion call’
Commenting on the study, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the Mood Disorders Psychopharmacology Unit, said the study is “the first of its kind to comprehensively characterize the prevalence of ED in youth living with BD.
“It could be hypothesized that EDs have overlapping domain disturbances of cognitive dysfunction, such as executive function and impulse control, as well as cognitive reward processes,” said Dr. McIntyre, who is the chairman and executive director of the Brain and Cognitive Discover Foundation, Toronto, and was not involved with the study.
“The data are a clarion call for clinicians to routinely screen for EDs in youth with BD and, when present, to be aware of the greater complexity, severity, and risk in this patient subpopulation. The higher prevalence of ED in youth with BD-II is an additional reminder of the severity, morbidity, and complexity of BD-II,” Dr. McIntyre said.
The study received no direct funding. It was supported by philanthropic donations to the Centre for Youth Bipolar Disorder and the CAMH Discovery Fund. Dr. Goldstein reports grant support from Brain Canada, Canadian Institutes of Health Research, Heart and Stroke Foundation, National Institute of Mental Health, and the departments of psychiatry at the University of Toronto and Sunnybrook Health Sciences Centre. He also acknowledges his position as RBC investments chair in Children›s Mental Health and Developmental Psychopathology at CAMH, a joint Hospital-University chair among the University of Toronto, CAMH, and the CAMH Foundation. Ms. Khoubaeva reports no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China (NSFC); speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Abbvie, and Atai Life Sciences. Dr. McIntyre is a CEO of Braxia Scientific.
A version of this article first appeared on Medscape.com.
Investigators studied close to 200 youth with BD and found that more than 25% had a lifetime ED, which included anorexia nervosa (AN), bulimia nervosa (BN), and an ED not otherwise specified (NOS).
Those with comorbid EDs were more likely to be female and to have BD-II subtype. Their presentations were also more complicated and included a history of suicidality, additional psychiatric conditions, smoking, and a history of sexual abuse, as well as more severe depression and emotional instability.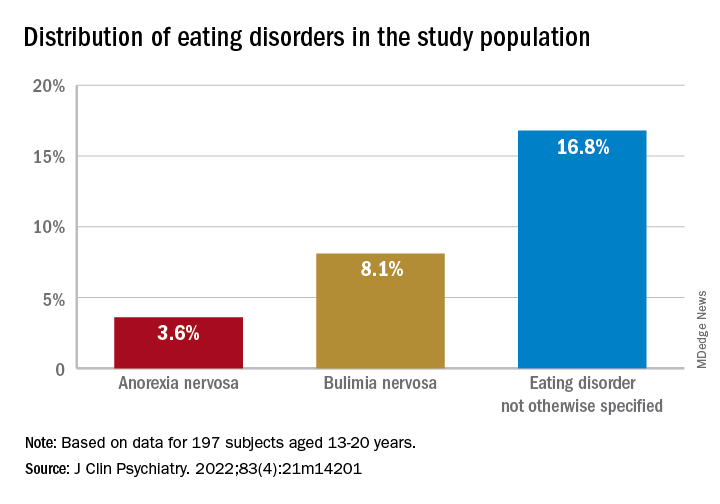
“We think the take-home message is that, in addition to other more recognized psychiatric comorbidities, youth with BD are also vulnerable to developing EDs. Thus, clinicians should be routinely monitoring for eating, appetite, and body image disturbances when working with this population,” lead author Diana Khoubaeva, research analyst at the Centre for Youth Bipolar Disorder, Centre for Addiction and Mental Health, Toronto, and senior author Benjamin Goldstein, MD, PhD, director of the Centre for Youth Bipolar Disorder, wrote in an e-mail to this news organization.
“Given the more complicated clinical picture of youth with co-occurring BD and EDs, this combination warrants careful attention,” the investigators note.
The study was published online May 11 in the Journal of Clinical Psychiatry.
Lack of research
“From the existing literature, we learned that EDs are not uncommon in individuals with BD, and that they are often associated with a more severe clinical profile,” say the researchers. “However, the majority of these studies have been limited to adult samples, and there was a real scarcity of studies that examined this co-occurrence in youth.”
This is “surprising” because EDs often have their onset in adolescence, so the researchers decided to explore the issue in their “fairly large sample of youth with BD.”
To investigate the issue, the researchers studied 197 youth (aged 13-20 years) with a diagnosis of BD (BD-I, BD-II, or BD-NOS) who were recruited between 2009 and 2017 (mean [standard deviation] age, 16.69 [1.50] years; 67.5% female).
ED diagnoses included both current and lifetime AN, BN, and ED-NOS. The researchers used the Kiddie Schedule for Affective Disorders and Schizophrenia for School Age Children, Present and Lifetime Version (K-SADS-PL) to determine the diagnosis of BD.
They also collected information about comorbid psychiatric disorders, as well as substance use disorders and cigarette smoking. The Life Problems Inventory (LPI) was used to identify dimensional borderline personality traits.
Information about physical and sexual abuse, suicidal ideation, nonsuicidal self-injury (NSSI), and affect regulation were obtained from other measurement tools. Participants’ height and weight were measured to calculate body mass index.
Neurobiological and environmental factors
Of the total sample, 24.84% had received a diagnosis of ED in their lifetime.
Moreover, 28.9% had a lifetime history of binge eating. Of these, 17.7% also had been diagnosed with an ED.
Participants with BD-II were significantly more likely than those with BD-I to report both current and lifetime BN. There were no significant differences by BD subtype in AN, ED-NOS, or binge eating.
Higher correlates of clinical characteristics, psychiatric morbidity, treatment history, and dimensional traits in those with vs. those without an ED are detailed in the accompanying table.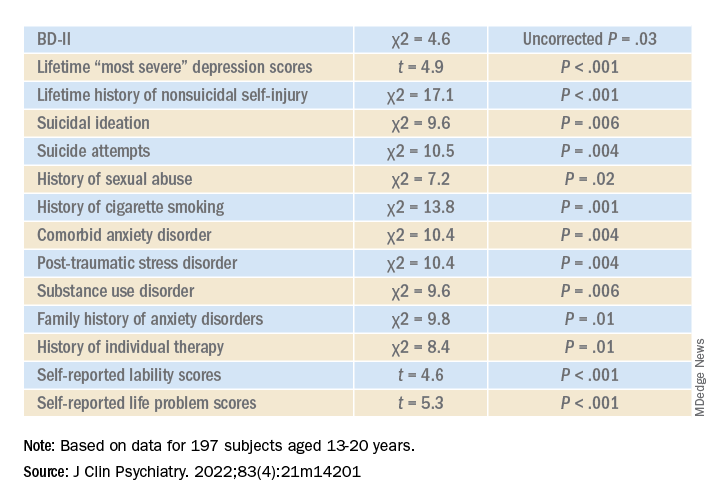
The ED group scored significantly higher on all LPI scores, including impulsivity, emotional dysregulation, identity confusion, and interpersonal problems, compared to those without an ED. They also were less likely to report lifetime lithium use (chi2 = 7.9, P = .01).
Multivariate analysis revealed that lifetime EDs were significantly associated with female sex, history of cigarette smoking, history of individual therapy, family history of anxiety, and LPI total score and were negatively associated with BD-I subtype.
“The comorbidity [between EDs and BD] could be driven by both neurobiological and environmental factors,” Dr. Khoubaeva and Dr. Goldstein noted. EDs and BD “are both illnesses that are fundamentally linked with dysfunction in reward systems – that is, there are imbalances in terms of too much or too little reward seeking.”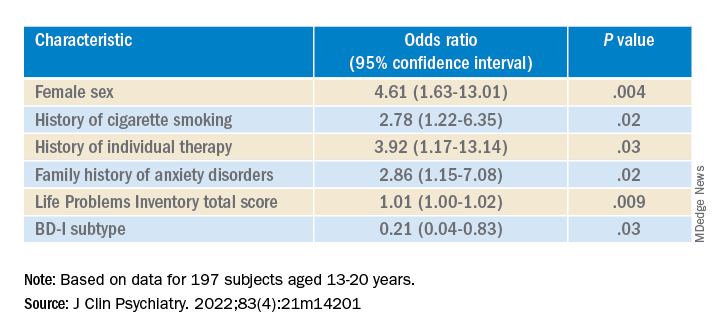
They added that individuals affected by these conditions have “ongoing challenges with instability of emotions and ability to manage emotions; and eating too much or too little can be a manifestation of coping with emotions.”
In addition, medications commonly used to treat BD “are known to have side effects such as weight/appetite/metabolic changes, which may make it harder to regulate eating, and which may exacerbate preexisting body image challenges.”
The researchers recommend implementing trauma-informed care, assessing and addressing suicidality and self-injury, and prioritizing therapies that target emotional dysregulation, such as dialectical behavioral therapy.
‘Clarion call’
Commenting on the study, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the Mood Disorders Psychopharmacology Unit, said the study is “the first of its kind to comprehensively characterize the prevalence of ED in youth living with BD.
“It could be hypothesized that EDs have overlapping domain disturbances of cognitive dysfunction, such as executive function and impulse control, as well as cognitive reward processes,” said Dr. McIntyre, who is the chairman and executive director of the Brain and Cognitive Discover Foundation, Toronto, and was not involved with the study.
“The data are a clarion call for clinicians to routinely screen for EDs in youth with BD and, when present, to be aware of the greater complexity, severity, and risk in this patient subpopulation. The higher prevalence of ED in youth with BD-II is an additional reminder of the severity, morbidity, and complexity of BD-II,” Dr. McIntyre said.
The study received no direct funding. It was supported by philanthropic donations to the Centre for Youth Bipolar Disorder and the CAMH Discovery Fund. Dr. Goldstein reports grant support from Brain Canada, Canadian Institutes of Health Research, Heart and Stroke Foundation, National Institute of Mental Health, and the departments of psychiatry at the University of Toronto and Sunnybrook Health Sciences Centre. He also acknowledges his position as RBC investments chair in Children›s Mental Health and Developmental Psychopathology at CAMH, a joint Hospital-University chair among the University of Toronto, CAMH, and the CAMH Foundation. Ms. Khoubaeva reports no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China (NSFC); speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Abbvie, and Atai Life Sciences. Dr. McIntyre is a CEO of Braxia Scientific.
A version of this article first appeared on Medscape.com.
Investigators studied close to 200 youth with BD and found that more than 25% had a lifetime ED, which included anorexia nervosa (AN), bulimia nervosa (BN), and an ED not otherwise specified (NOS).
Those with comorbid EDs were more likely to be female and to have BD-II subtype. Their presentations were also more complicated and included a history of suicidality, additional psychiatric conditions, smoking, and a history of sexual abuse, as well as more severe depression and emotional instability.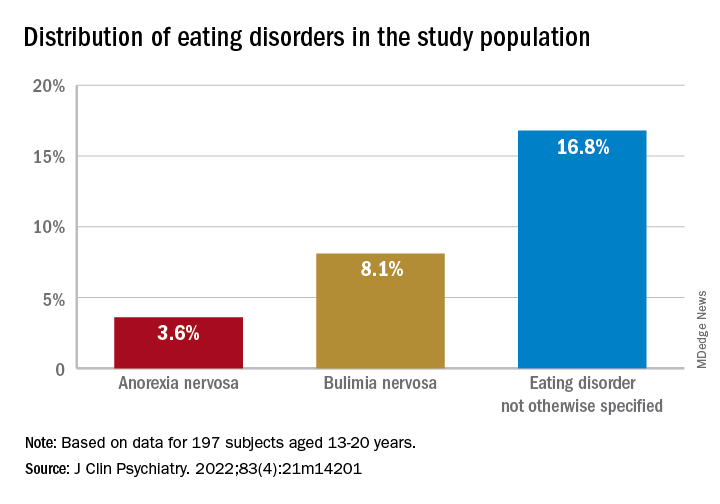
“We think the take-home message is that, in addition to other more recognized psychiatric comorbidities, youth with BD are also vulnerable to developing EDs. Thus, clinicians should be routinely monitoring for eating, appetite, and body image disturbances when working with this population,” lead author Diana Khoubaeva, research analyst at the Centre for Youth Bipolar Disorder, Centre for Addiction and Mental Health, Toronto, and senior author Benjamin Goldstein, MD, PhD, director of the Centre for Youth Bipolar Disorder, wrote in an e-mail to this news organization.
“Given the more complicated clinical picture of youth with co-occurring BD and EDs, this combination warrants careful attention,” the investigators note.
The study was published online May 11 in the Journal of Clinical Psychiatry.
Lack of research
“From the existing literature, we learned that EDs are not uncommon in individuals with BD, and that they are often associated with a more severe clinical profile,” say the researchers. “However, the majority of these studies have been limited to adult samples, and there was a real scarcity of studies that examined this co-occurrence in youth.”
This is “surprising” because EDs often have their onset in adolescence, so the researchers decided to explore the issue in their “fairly large sample of youth with BD.”
To investigate the issue, the researchers studied 197 youth (aged 13-20 years) with a diagnosis of BD (BD-I, BD-II, or BD-NOS) who were recruited between 2009 and 2017 (mean [standard deviation] age, 16.69 [1.50] years; 67.5% female).
ED diagnoses included both current and lifetime AN, BN, and ED-NOS. The researchers used the Kiddie Schedule for Affective Disorders and Schizophrenia for School Age Children, Present and Lifetime Version (K-SADS-PL) to determine the diagnosis of BD.
They also collected information about comorbid psychiatric disorders, as well as substance use disorders and cigarette smoking. The Life Problems Inventory (LPI) was used to identify dimensional borderline personality traits.
Information about physical and sexual abuse, suicidal ideation, nonsuicidal self-injury (NSSI), and affect regulation were obtained from other measurement tools. Participants’ height and weight were measured to calculate body mass index.
Neurobiological and environmental factors
Of the total sample, 24.84% had received a diagnosis of ED in their lifetime.
Moreover, 28.9% had a lifetime history of binge eating. Of these, 17.7% also had been diagnosed with an ED.
Participants with BD-II were significantly more likely than those with BD-I to report both current and lifetime BN. There were no significant differences by BD subtype in AN, ED-NOS, or binge eating.
Higher correlates of clinical characteristics, psychiatric morbidity, treatment history, and dimensional traits in those with vs. those without an ED are detailed in the accompanying table.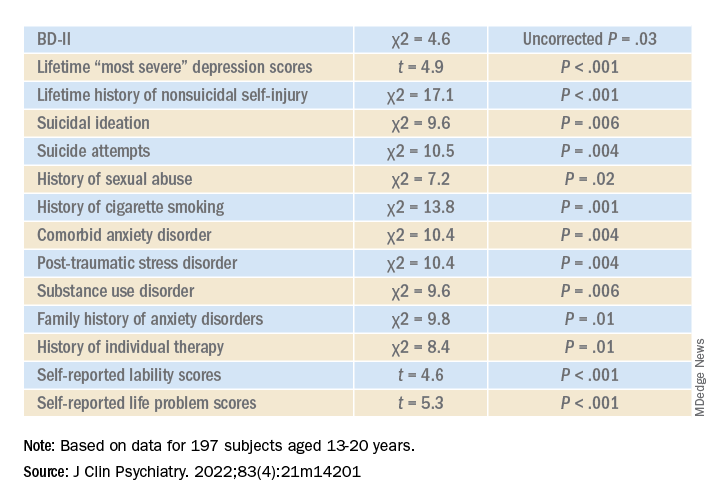
The ED group scored significantly higher on all LPI scores, including impulsivity, emotional dysregulation, identity confusion, and interpersonal problems, compared to those without an ED. They also were less likely to report lifetime lithium use (chi2 = 7.9, P = .01).
Multivariate analysis revealed that lifetime EDs were significantly associated with female sex, history of cigarette smoking, history of individual therapy, family history of anxiety, and LPI total score and were negatively associated with BD-I subtype.
“The comorbidity [between EDs and BD] could be driven by both neurobiological and environmental factors,” Dr. Khoubaeva and Dr. Goldstein noted. EDs and BD “are both illnesses that are fundamentally linked with dysfunction in reward systems – that is, there are imbalances in terms of too much or too little reward seeking.”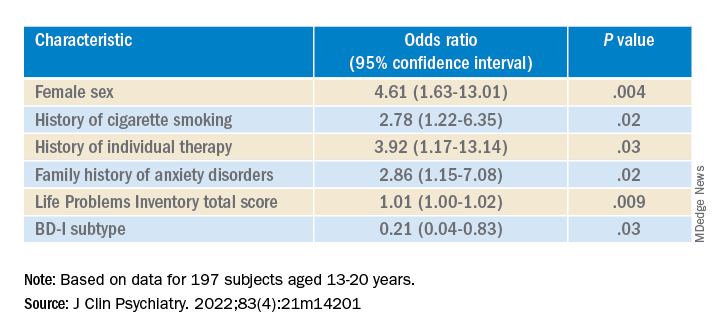
They added that individuals affected by these conditions have “ongoing challenges with instability of emotions and ability to manage emotions; and eating too much or too little can be a manifestation of coping with emotions.”
In addition, medications commonly used to treat BD “are known to have side effects such as weight/appetite/metabolic changes, which may make it harder to regulate eating, and which may exacerbate preexisting body image challenges.”
The researchers recommend implementing trauma-informed care, assessing and addressing suicidality and self-injury, and prioritizing therapies that target emotional dysregulation, such as dialectical behavioral therapy.
‘Clarion call’
Commenting on the study, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the Mood Disorders Psychopharmacology Unit, said the study is “the first of its kind to comprehensively characterize the prevalence of ED in youth living with BD.
“It could be hypothesized that EDs have overlapping domain disturbances of cognitive dysfunction, such as executive function and impulse control, as well as cognitive reward processes,” said Dr. McIntyre, who is the chairman and executive director of the Brain and Cognitive Discover Foundation, Toronto, and was not involved with the study.
“The data are a clarion call for clinicians to routinely screen for EDs in youth with BD and, when present, to be aware of the greater complexity, severity, and risk in this patient subpopulation. The higher prevalence of ED in youth with BD-II is an additional reminder of the severity, morbidity, and complexity of BD-II,” Dr. McIntyre said.
The study received no direct funding. It was supported by philanthropic donations to the Centre for Youth Bipolar Disorder and the CAMH Discovery Fund. Dr. Goldstein reports grant support from Brain Canada, Canadian Institutes of Health Research, Heart and Stroke Foundation, National Institute of Mental Health, and the departments of psychiatry at the University of Toronto and Sunnybrook Health Sciences Centre. He also acknowledges his position as RBC investments chair in Children›s Mental Health and Developmental Psychopathology at CAMH, a joint Hospital-University chair among the University of Toronto, CAMH, and the CAMH Foundation. Ms. Khoubaeva reports no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China (NSFC); speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Abbvie, and Atai Life Sciences. Dr. McIntyre is a CEO of Braxia Scientific.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL PSYCHIATRY
Genetic testing for best antidepressant accurate, cost effective
new research suggests.
CYP2D6 and CYP2C19, from the cytochrome P450 family, are involved in the metabolism and elimination of various molecules, including medications. Variants in the genes encoding these enzymes affect the speed at which drugs are metabolized, altering their pharmacokinetic profiles.
The researchers studied 125 patients with MDD and used CYP2D6 and CYP2C19 genotyping to determine the presence of actionable phenotypes in line with Food and Drug Administration labeling.
They found that, in many cases, pharmacogenetic testing could have predicted poor response to the initial treatment selection and could have helped guide subsequent choices to improve outcomes.
In addition, a pharmacoeconomic evaluation that combined direct and indirect costs resulting from MDD with the prevalence of CYP2D6 and CYP2C19 phenotypes showed that testing for functional variants in both genes would be cost effective at a national level.
Had psychiatrists who treated patients in the study known about their metabolizing profiles, it “might have contributed to switches in medication” and could have reduced “delays in response,” said lead researcher Alessio Squassina, PhD, associate professor of pharmacology at the University of Cagliari (Italy).
The findings were presented at the European Psychiatric Association 2022 Congress.
Highly variable response rates
Dr. Squassina noted that the response to antidepressants is a “highly variable trait,” and while it is known that genetics play a role, their contribution is “still not completely understood.”
He explained that the use of pharmacogenetics, which leverages genetic information to guide treatment decision-making, has increased significantly.
While regulatory bodies, including the FDA, have been “very active” in defining strict criteria for interpreting the information from pharmacogenetic tests, there remains some “discrepancy” in their clinical utility.
Dr. Squassina said the FDA provides guidance on use of genetic testing on the labels of 34 psychiatric medications. Of these, 79% relate to CYP2D6, 12% relate to CYP2C19, and 9% relate to other genes.
These labels provide guidance on when genetic testing is recommended or required, as well as potentially clinically actionable gene-drug associations in patients with certain functional alleles.
However, Dr. Squassina noted that the distribution of such alleles is not the same across Europe, so it’s possible that a psychiatrist in Italy may be less likely to treat a patient with a phenotype affecting response to treatment or risk of adverse events than one in Norway or Sweden.
For the study, the investigators examined the frequency of CYP2D6 and CYP2C19 phenotypes in psychiatric patients in Sardinia and their relationship with pharmacologic treatment and cost-effectiveness.
They set out to recruit 200 patients with MDD who had a documented 5-year medical and treatment history, including alterations in treatment, adverse events, hospitalizations, suicide, and symptom scores, as well as sociodemographic variables.
An interim analysis of the first 125 patients recruited to the study showed that the most common CYP2D6 phenotype was normal metabolizers (NM), at 60.5%, followed by intermediate metabolizers (IM), at 28.2%, ultrarapid metabolizers (UR), at 8.9%, and poor metabolizers (PM), at 2.4%.
For CYP2C19, the most common phenotype was NM (49%), followed by IM (29.0%), UR (25.0%), and PM (4.0%). While there were differences in the overall European averages, they were not significant.
To highlight the potential impact that pharmacogenetic testing could have had on patient care and outcome, Dr. Squassina highlighted two cases.
The first concerned a patient with a CYP2D6 IM and CYP2C19 UR phenotype, who did not respond to escitalopram. The FDA drug label indicates this phenotype is actionable and recommends an alternative drug.
The patient was subsequently switched to venlafaxine. The FDA drug label on venlafaxine notes that patients with this phenotype are likely to have a suboptimal response to this drug, and again, this patient did not respond to treatment.
Another patient with a CYP2D6 NM and CYP2C19 IM phenotype was also prescribed escitalopram. The FDA label on this drug notes that patients with this phenotype can try venlafaxine but may not respond. Indeed, this patient did not respond and was switched to venlafaxine and started responding.
“The psychiatrists [in these cases] may made have made different [drug] choices if they had known the genotypes in advance,” Dr. Squassina said.
Cost effective?
To determine the cost-effectiveness of screening for CYP2D6 and CYP2C19 phenotypes in patients with MDD, the researchers used real-world data to develop a Markov model with a hypothetical cohort of 2000 MDD patients, half of whom underwent pharmacogenetic testing, to determine the potential impact on outcomes over an 18-week period.
The model included the cost of medications and hospitalization, psychiatric counseling, loss of productivity, and the estimated probability of response and adverse events, adjusted for the patient’s likelihood of having a particular metabolizing phenotype.
Results showed that, for CYP2C19, compared to no testing, pharmacogenetic testing would be cost-effective at an incremental cost-effective ratio (ICER) of €60,000 ($64,000 USD) per quality-adjusted life-year (QALY).
This, Squassina said, is “below the willingness to pay threshold” for health authorities in developed countries.
For CYP2D6, pharmacogenetic testing would become cost-effective at an ICER of approximately €47,000 ($40,000 USD) per QALY.
The team plans to complete recruitment and perform a “detailed evaluation of all the variables, especially those relating to the medication history and changes in dosage, and adverse drug reactions.” The researchers would also like to study genetic phenotypes for other metabolizing enzymes and repeat the pharmacoeconomic analysis with the complete dataset.
A glimpse into the future
Approached for comment, Alessandro Serretti, MD, PhD, department of biomedical and neuromotor sciences, University of Bologna (Italy), who was not involved in the study, said the findings show there is a “small but evident benefit” from CYP profiling, “which makes sense.”
He added that in the Netherlands and other European countries, efforts are already underway to record the CYP status of patients at a national level. “Sooner or later, all Western countries will implement it as a routine,” he said in an interview.
He explained that, when such testing is widely available, electronic health record data will allow physicians to immediately select the optimal antidepressant for an individual patient. This will end the current trial-and-error process that leads to delayed treatment and will help avoid serious consequences, such as suicide.
While reducing a single patient’s treatment by a few weeks with the most appropriate antidepressant choice does not make a large difference in the cost per episode, at a population level, it has the potential to make a significant difference.
Dr. Serretti does not envisage genotyping all 333 million Europeans for the CYP phenotype at this point but imagines that in the future, individuals will undergo whole-genome sequencing to determine risks for cancer, dementia, and heart disease, at which point they will also undergo CYP functional allele profiling, and all these data will be recorded on individuals’ EHR.
“So, every doctor, a psychiatrist or cardiologist, can see everything, whenever they need it,” he said.
The study was funded by Fondazione di Sardegna and Regione Autonoma della Sardegna. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
CYP2D6 and CYP2C19, from the cytochrome P450 family, are involved in the metabolism and elimination of various molecules, including medications. Variants in the genes encoding these enzymes affect the speed at which drugs are metabolized, altering their pharmacokinetic profiles.
The researchers studied 125 patients with MDD and used CYP2D6 and CYP2C19 genotyping to determine the presence of actionable phenotypes in line with Food and Drug Administration labeling.
They found that, in many cases, pharmacogenetic testing could have predicted poor response to the initial treatment selection and could have helped guide subsequent choices to improve outcomes.
In addition, a pharmacoeconomic evaluation that combined direct and indirect costs resulting from MDD with the prevalence of CYP2D6 and CYP2C19 phenotypes showed that testing for functional variants in both genes would be cost effective at a national level.
Had psychiatrists who treated patients in the study known about their metabolizing profiles, it “might have contributed to switches in medication” and could have reduced “delays in response,” said lead researcher Alessio Squassina, PhD, associate professor of pharmacology at the University of Cagliari (Italy).
The findings were presented at the European Psychiatric Association 2022 Congress.
Highly variable response rates
Dr. Squassina noted that the response to antidepressants is a “highly variable trait,” and while it is known that genetics play a role, their contribution is “still not completely understood.”
He explained that the use of pharmacogenetics, which leverages genetic information to guide treatment decision-making, has increased significantly.
While regulatory bodies, including the FDA, have been “very active” in defining strict criteria for interpreting the information from pharmacogenetic tests, there remains some “discrepancy” in their clinical utility.
Dr. Squassina said the FDA provides guidance on use of genetic testing on the labels of 34 psychiatric medications. Of these, 79% relate to CYP2D6, 12% relate to CYP2C19, and 9% relate to other genes.
These labels provide guidance on when genetic testing is recommended or required, as well as potentially clinically actionable gene-drug associations in patients with certain functional alleles.
However, Dr. Squassina noted that the distribution of such alleles is not the same across Europe, so it’s possible that a psychiatrist in Italy may be less likely to treat a patient with a phenotype affecting response to treatment or risk of adverse events than one in Norway or Sweden.
For the study, the investigators examined the frequency of CYP2D6 and CYP2C19 phenotypes in psychiatric patients in Sardinia and their relationship with pharmacologic treatment and cost-effectiveness.
They set out to recruit 200 patients with MDD who had a documented 5-year medical and treatment history, including alterations in treatment, adverse events, hospitalizations, suicide, and symptom scores, as well as sociodemographic variables.
An interim analysis of the first 125 patients recruited to the study showed that the most common CYP2D6 phenotype was normal metabolizers (NM), at 60.5%, followed by intermediate metabolizers (IM), at 28.2%, ultrarapid metabolizers (UR), at 8.9%, and poor metabolizers (PM), at 2.4%.
For CYP2C19, the most common phenotype was NM (49%), followed by IM (29.0%), UR (25.0%), and PM (4.0%). While there were differences in the overall European averages, they were not significant.
To highlight the potential impact that pharmacogenetic testing could have had on patient care and outcome, Dr. Squassina highlighted two cases.
The first concerned a patient with a CYP2D6 IM and CYP2C19 UR phenotype, who did not respond to escitalopram. The FDA drug label indicates this phenotype is actionable and recommends an alternative drug.
The patient was subsequently switched to venlafaxine. The FDA drug label on venlafaxine notes that patients with this phenotype are likely to have a suboptimal response to this drug, and again, this patient did not respond to treatment.
Another patient with a CYP2D6 NM and CYP2C19 IM phenotype was also prescribed escitalopram. The FDA label on this drug notes that patients with this phenotype can try venlafaxine but may not respond. Indeed, this patient did not respond and was switched to venlafaxine and started responding.
“The psychiatrists [in these cases] may made have made different [drug] choices if they had known the genotypes in advance,” Dr. Squassina said.
Cost effective?
To determine the cost-effectiveness of screening for CYP2D6 and CYP2C19 phenotypes in patients with MDD, the researchers used real-world data to develop a Markov model with a hypothetical cohort of 2000 MDD patients, half of whom underwent pharmacogenetic testing, to determine the potential impact on outcomes over an 18-week period.
The model included the cost of medications and hospitalization, psychiatric counseling, loss of productivity, and the estimated probability of response and adverse events, adjusted for the patient’s likelihood of having a particular metabolizing phenotype.
Results showed that, for CYP2C19, compared to no testing, pharmacogenetic testing would be cost-effective at an incremental cost-effective ratio (ICER) of €60,000 ($64,000 USD) per quality-adjusted life-year (QALY).
This, Squassina said, is “below the willingness to pay threshold” for health authorities in developed countries.
For CYP2D6, pharmacogenetic testing would become cost-effective at an ICER of approximately €47,000 ($40,000 USD) per QALY.
The team plans to complete recruitment and perform a “detailed evaluation of all the variables, especially those relating to the medication history and changes in dosage, and adverse drug reactions.” The researchers would also like to study genetic phenotypes for other metabolizing enzymes and repeat the pharmacoeconomic analysis with the complete dataset.
A glimpse into the future
Approached for comment, Alessandro Serretti, MD, PhD, department of biomedical and neuromotor sciences, University of Bologna (Italy), who was not involved in the study, said the findings show there is a “small but evident benefit” from CYP profiling, “which makes sense.”
He added that in the Netherlands and other European countries, efforts are already underway to record the CYP status of patients at a national level. “Sooner or later, all Western countries will implement it as a routine,” he said in an interview.
He explained that, when such testing is widely available, electronic health record data will allow physicians to immediately select the optimal antidepressant for an individual patient. This will end the current trial-and-error process that leads to delayed treatment and will help avoid serious consequences, such as suicide.
While reducing a single patient’s treatment by a few weeks with the most appropriate antidepressant choice does not make a large difference in the cost per episode, at a population level, it has the potential to make a significant difference.
Dr. Serretti does not envisage genotyping all 333 million Europeans for the CYP phenotype at this point but imagines that in the future, individuals will undergo whole-genome sequencing to determine risks for cancer, dementia, and heart disease, at which point they will also undergo CYP functional allele profiling, and all these data will be recorded on individuals’ EHR.
“So, every doctor, a psychiatrist or cardiologist, can see everything, whenever they need it,” he said.
The study was funded by Fondazione di Sardegna and Regione Autonoma della Sardegna. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
CYP2D6 and CYP2C19, from the cytochrome P450 family, are involved in the metabolism and elimination of various molecules, including medications. Variants in the genes encoding these enzymes affect the speed at which drugs are metabolized, altering their pharmacokinetic profiles.
The researchers studied 125 patients with MDD and used CYP2D6 and CYP2C19 genotyping to determine the presence of actionable phenotypes in line with Food and Drug Administration labeling.
They found that, in many cases, pharmacogenetic testing could have predicted poor response to the initial treatment selection and could have helped guide subsequent choices to improve outcomes.
In addition, a pharmacoeconomic evaluation that combined direct and indirect costs resulting from MDD with the prevalence of CYP2D6 and CYP2C19 phenotypes showed that testing for functional variants in both genes would be cost effective at a national level.
Had psychiatrists who treated patients in the study known about their metabolizing profiles, it “might have contributed to switches in medication” and could have reduced “delays in response,” said lead researcher Alessio Squassina, PhD, associate professor of pharmacology at the University of Cagliari (Italy).
The findings were presented at the European Psychiatric Association 2022 Congress.
Highly variable response rates
Dr. Squassina noted that the response to antidepressants is a “highly variable trait,” and while it is known that genetics play a role, their contribution is “still not completely understood.”
He explained that the use of pharmacogenetics, which leverages genetic information to guide treatment decision-making, has increased significantly.
While regulatory bodies, including the FDA, have been “very active” in defining strict criteria for interpreting the information from pharmacogenetic tests, there remains some “discrepancy” in their clinical utility.
Dr. Squassina said the FDA provides guidance on use of genetic testing on the labels of 34 psychiatric medications. Of these, 79% relate to CYP2D6, 12% relate to CYP2C19, and 9% relate to other genes.
These labels provide guidance on when genetic testing is recommended or required, as well as potentially clinically actionable gene-drug associations in patients with certain functional alleles.
However, Dr. Squassina noted that the distribution of such alleles is not the same across Europe, so it’s possible that a psychiatrist in Italy may be less likely to treat a patient with a phenotype affecting response to treatment or risk of adverse events than one in Norway or Sweden.
For the study, the investigators examined the frequency of CYP2D6 and CYP2C19 phenotypes in psychiatric patients in Sardinia and their relationship with pharmacologic treatment and cost-effectiveness.
They set out to recruit 200 patients with MDD who had a documented 5-year medical and treatment history, including alterations in treatment, adverse events, hospitalizations, suicide, and symptom scores, as well as sociodemographic variables.
An interim analysis of the first 125 patients recruited to the study showed that the most common CYP2D6 phenotype was normal metabolizers (NM), at 60.5%, followed by intermediate metabolizers (IM), at 28.2%, ultrarapid metabolizers (UR), at 8.9%, and poor metabolizers (PM), at 2.4%.
For CYP2C19, the most common phenotype was NM (49%), followed by IM (29.0%), UR (25.0%), and PM (4.0%). While there were differences in the overall European averages, they were not significant.
To highlight the potential impact that pharmacogenetic testing could have had on patient care and outcome, Dr. Squassina highlighted two cases.
The first concerned a patient with a CYP2D6 IM and CYP2C19 UR phenotype, who did not respond to escitalopram. The FDA drug label indicates this phenotype is actionable and recommends an alternative drug.
The patient was subsequently switched to venlafaxine. The FDA drug label on venlafaxine notes that patients with this phenotype are likely to have a suboptimal response to this drug, and again, this patient did not respond to treatment.
Another patient with a CYP2D6 NM and CYP2C19 IM phenotype was also prescribed escitalopram. The FDA label on this drug notes that patients with this phenotype can try venlafaxine but may not respond. Indeed, this patient did not respond and was switched to venlafaxine and started responding.
“The psychiatrists [in these cases] may made have made different [drug] choices if they had known the genotypes in advance,” Dr. Squassina said.
Cost effective?
To determine the cost-effectiveness of screening for CYP2D6 and CYP2C19 phenotypes in patients with MDD, the researchers used real-world data to develop a Markov model with a hypothetical cohort of 2000 MDD patients, half of whom underwent pharmacogenetic testing, to determine the potential impact on outcomes over an 18-week period.
The model included the cost of medications and hospitalization, psychiatric counseling, loss of productivity, and the estimated probability of response and adverse events, adjusted for the patient’s likelihood of having a particular metabolizing phenotype.
Results showed that, for CYP2C19, compared to no testing, pharmacogenetic testing would be cost-effective at an incremental cost-effective ratio (ICER) of €60,000 ($64,000 USD) per quality-adjusted life-year (QALY).
This, Squassina said, is “below the willingness to pay threshold” for health authorities in developed countries.
For CYP2D6, pharmacogenetic testing would become cost-effective at an ICER of approximately €47,000 ($40,000 USD) per QALY.
The team plans to complete recruitment and perform a “detailed evaluation of all the variables, especially those relating to the medication history and changes in dosage, and adverse drug reactions.” The researchers would also like to study genetic phenotypes for other metabolizing enzymes and repeat the pharmacoeconomic analysis with the complete dataset.
A glimpse into the future
Approached for comment, Alessandro Serretti, MD, PhD, department of biomedical and neuromotor sciences, University of Bologna (Italy), who was not involved in the study, said the findings show there is a “small but evident benefit” from CYP profiling, “which makes sense.”
He added that in the Netherlands and other European countries, efforts are already underway to record the CYP status of patients at a national level. “Sooner or later, all Western countries will implement it as a routine,” he said in an interview.
He explained that, when such testing is widely available, electronic health record data will allow physicians to immediately select the optimal antidepressant for an individual patient. This will end the current trial-and-error process that leads to delayed treatment and will help avoid serious consequences, such as suicide.
While reducing a single patient’s treatment by a few weeks with the most appropriate antidepressant choice does not make a large difference in the cost per episode, at a population level, it has the potential to make a significant difference.
Dr. Serretti does not envisage genotyping all 333 million Europeans for the CYP phenotype at this point but imagines that in the future, individuals will undergo whole-genome sequencing to determine risks for cancer, dementia, and heart disease, at which point they will also undergo CYP functional allele profiling, and all these data will be recorded on individuals’ EHR.
“So, every doctor, a psychiatrist or cardiologist, can see everything, whenever they need it,” he said.
The study was funded by Fondazione di Sardegna and Regione Autonoma della Sardegna. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM EPA 2022