User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Depression screens do not reduce suicidal acts in teens: Study
Screening adolescents for signs of depression does not reduce their emergency department visits, hospitalizations, or treatment for suicidal behaviors, according to research published in Preventive Medicine. Adolescents who underwent a depression screening were just as likely to need these services as those who did not.
In 2016, the U.S. Preventive Services Task Force recommended that adolescents aged 12-18 years be screened for major depressive disorder, provided that effective treatment options and follow-up strategies are in place.
“The main goal of depression screening is really to reduce adverse psychiatric outcomes. But I think a collateral hope is that, in reducing these adverse psychiatric outcomes, you would also reduce avoidable health services use,” such as ED visits or hospitalizations, said Kira Riehm, PhD, a postdoctoral fellow in epidemiology at Columbia University, New York, who led the research. Dr. Riehm designed the new study, which was part of her doctoral work at Johns Hopkins University, Baltimore, to test this premise.
Dr. Riehm and colleagues compared 14,433 adolescents aged 12-18 years who were screened for depression at least once during a wellness visit from 2014 to 2017 to 43,299 adolescents who were not screened for depression during such visits. Depression screenings were interspersed among a total of 281,463 adolescent wellness visits from 2014 to 2017, which represented 5% of all visits.
The researchers used diagnostic codes from a database of insurance claims to determine who had undergone depression screening. They then compared use of ED services, inpatient hospitalizations, and the number of treatments for suicidal behaviors between the two groups for the 2 years following the wellness visit.
The average age of the adolescents who underwent screening was 13-14 years, as was the average age of adolescents who were not screened. Both groups were evenly matched with respect to being male or female.
The researchers estimated that a high majority of adolescents in the sample were White (83%). Black persons represented 7% of the sample; Hispanic/Latino, 5%; and Asian, 3%. Insurance claims don’t always include racial and ethnicity data, Dr. Riehm said, so her group statistically imputed these proportions. The claims data also do not include details about which type of screening tool was used or the results of the screening, such as whether a teen exhibited mild or severe depression.
Adolescents in both groups were just as likely to go to the ED for any reason, be admitted to the hospital for any reason, or undergo treatment for suicidal behaviors. The researchers observed a slight association between being screened for depression and going to the ED specifically for a mental health reason (relative risk, 1.16; 95% confidence interval, 1.00-1.33). The sex of the adolescents had no bearing on whether they used these services.
“I think people think of [depression screening] as one event. But in reality, screening is a series of different events that all have to be happening in order for a screening program to work,” Dr. Riehm told this news organization.
These events could include ensuring that adolescents who exhibit signs of depression receive a proper assessment, receive medications if needed, and have access to psychotherapists who can help them. Without these supports in place, she said, a one-off depression screening may have limited benefit.
“There’s a lot of places where people could drop out of that care continuum,” Dr. Riehm said.
“One-time screening may not be enough,” said Trân Đoàn, PhD, MPH, a postdoctoral researcher in the University of Pittsburgh department of pediatrics.
Dr. Đoàn, who was not involved in the research, noted that the American Academy of Pediatrics recommends annual screening of all adolescents for depressive symptoms. Given that only 5% of the visits in this sample included any kind of depression screening, Dr. Đoàn said, some pediatric practices may not have felt they had the resources to adequately address positive screenings for depression.
Both Dr. Riehm and Dr. Đoàn are focusing on the link between depression screening and health outcomes. In her own doctoral work at the University of Michigan, Dr. Đoàn modeled the effects of universal annual depression screening in primary care settings on the health status of people aged 12-22 years. She is currently preparing this work for publication.
“I did find that, over the long term, there is improvement in health outcomes if we were to screen on an annual basis,” provided improved screening is coupled with comprehensive treatment plans, Dr. Đoàn said. The model’s health outcomes measures included an increase in life expectancy as well as a greater proportion of depression-free days among adolescents who receive appropriate treatment.
Dr. Riehm and Dr. Đoàn disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Screening adolescents for signs of depression does not reduce their emergency department visits, hospitalizations, or treatment for suicidal behaviors, according to research published in Preventive Medicine. Adolescents who underwent a depression screening were just as likely to need these services as those who did not.
In 2016, the U.S. Preventive Services Task Force recommended that adolescents aged 12-18 years be screened for major depressive disorder, provided that effective treatment options and follow-up strategies are in place.
“The main goal of depression screening is really to reduce adverse psychiatric outcomes. But I think a collateral hope is that, in reducing these adverse psychiatric outcomes, you would also reduce avoidable health services use,” such as ED visits or hospitalizations, said Kira Riehm, PhD, a postdoctoral fellow in epidemiology at Columbia University, New York, who led the research. Dr. Riehm designed the new study, which was part of her doctoral work at Johns Hopkins University, Baltimore, to test this premise.
Dr. Riehm and colleagues compared 14,433 adolescents aged 12-18 years who were screened for depression at least once during a wellness visit from 2014 to 2017 to 43,299 adolescents who were not screened for depression during such visits. Depression screenings were interspersed among a total of 281,463 adolescent wellness visits from 2014 to 2017, which represented 5% of all visits.
The researchers used diagnostic codes from a database of insurance claims to determine who had undergone depression screening. They then compared use of ED services, inpatient hospitalizations, and the number of treatments for suicidal behaviors between the two groups for the 2 years following the wellness visit.
The average age of the adolescents who underwent screening was 13-14 years, as was the average age of adolescents who were not screened. Both groups were evenly matched with respect to being male or female.
The researchers estimated that a high majority of adolescents in the sample were White (83%). Black persons represented 7% of the sample; Hispanic/Latino, 5%; and Asian, 3%. Insurance claims don’t always include racial and ethnicity data, Dr. Riehm said, so her group statistically imputed these proportions. The claims data also do not include details about which type of screening tool was used or the results of the screening, such as whether a teen exhibited mild or severe depression.
Adolescents in both groups were just as likely to go to the ED for any reason, be admitted to the hospital for any reason, or undergo treatment for suicidal behaviors. The researchers observed a slight association between being screened for depression and going to the ED specifically for a mental health reason (relative risk, 1.16; 95% confidence interval, 1.00-1.33). The sex of the adolescents had no bearing on whether they used these services.
“I think people think of [depression screening] as one event. But in reality, screening is a series of different events that all have to be happening in order for a screening program to work,” Dr. Riehm told this news organization.
These events could include ensuring that adolescents who exhibit signs of depression receive a proper assessment, receive medications if needed, and have access to psychotherapists who can help them. Without these supports in place, she said, a one-off depression screening may have limited benefit.
“There’s a lot of places where people could drop out of that care continuum,” Dr. Riehm said.
“One-time screening may not be enough,” said Trân Đoàn, PhD, MPH, a postdoctoral researcher in the University of Pittsburgh department of pediatrics.
Dr. Đoàn, who was not involved in the research, noted that the American Academy of Pediatrics recommends annual screening of all adolescents for depressive symptoms. Given that only 5% of the visits in this sample included any kind of depression screening, Dr. Đoàn said, some pediatric practices may not have felt they had the resources to adequately address positive screenings for depression.
Both Dr. Riehm and Dr. Đoàn are focusing on the link between depression screening and health outcomes. In her own doctoral work at the University of Michigan, Dr. Đoàn modeled the effects of universal annual depression screening in primary care settings on the health status of people aged 12-22 years. She is currently preparing this work for publication.
“I did find that, over the long term, there is improvement in health outcomes if we were to screen on an annual basis,” provided improved screening is coupled with comprehensive treatment plans, Dr. Đoàn said. The model’s health outcomes measures included an increase in life expectancy as well as a greater proportion of depression-free days among adolescents who receive appropriate treatment.
Dr. Riehm and Dr. Đoàn disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Screening adolescents for signs of depression does not reduce their emergency department visits, hospitalizations, or treatment for suicidal behaviors, according to research published in Preventive Medicine. Adolescents who underwent a depression screening were just as likely to need these services as those who did not.
In 2016, the U.S. Preventive Services Task Force recommended that adolescents aged 12-18 years be screened for major depressive disorder, provided that effective treatment options and follow-up strategies are in place.
“The main goal of depression screening is really to reduce adverse psychiatric outcomes. But I think a collateral hope is that, in reducing these adverse psychiatric outcomes, you would also reduce avoidable health services use,” such as ED visits or hospitalizations, said Kira Riehm, PhD, a postdoctoral fellow in epidemiology at Columbia University, New York, who led the research. Dr. Riehm designed the new study, which was part of her doctoral work at Johns Hopkins University, Baltimore, to test this premise.
Dr. Riehm and colleagues compared 14,433 adolescents aged 12-18 years who were screened for depression at least once during a wellness visit from 2014 to 2017 to 43,299 adolescents who were not screened for depression during such visits. Depression screenings were interspersed among a total of 281,463 adolescent wellness visits from 2014 to 2017, which represented 5% of all visits.
The researchers used diagnostic codes from a database of insurance claims to determine who had undergone depression screening. They then compared use of ED services, inpatient hospitalizations, and the number of treatments for suicidal behaviors between the two groups for the 2 years following the wellness visit.
The average age of the adolescents who underwent screening was 13-14 years, as was the average age of adolescents who were not screened. Both groups were evenly matched with respect to being male or female.
The researchers estimated that a high majority of adolescents in the sample were White (83%). Black persons represented 7% of the sample; Hispanic/Latino, 5%; and Asian, 3%. Insurance claims don’t always include racial and ethnicity data, Dr. Riehm said, so her group statistically imputed these proportions. The claims data also do not include details about which type of screening tool was used or the results of the screening, such as whether a teen exhibited mild or severe depression.
Adolescents in both groups were just as likely to go to the ED for any reason, be admitted to the hospital for any reason, or undergo treatment for suicidal behaviors. The researchers observed a slight association between being screened for depression and going to the ED specifically for a mental health reason (relative risk, 1.16; 95% confidence interval, 1.00-1.33). The sex of the adolescents had no bearing on whether they used these services.
“I think people think of [depression screening] as one event. But in reality, screening is a series of different events that all have to be happening in order for a screening program to work,” Dr. Riehm told this news organization.
These events could include ensuring that adolescents who exhibit signs of depression receive a proper assessment, receive medications if needed, and have access to psychotherapists who can help them. Without these supports in place, she said, a one-off depression screening may have limited benefit.
“There’s a lot of places where people could drop out of that care continuum,” Dr. Riehm said.
“One-time screening may not be enough,” said Trân Đoàn, PhD, MPH, a postdoctoral researcher in the University of Pittsburgh department of pediatrics.
Dr. Đoàn, who was not involved in the research, noted that the American Academy of Pediatrics recommends annual screening of all adolescents for depressive symptoms. Given that only 5% of the visits in this sample included any kind of depression screening, Dr. Đoàn said, some pediatric practices may not have felt they had the resources to adequately address positive screenings for depression.
Both Dr. Riehm and Dr. Đoàn are focusing on the link between depression screening and health outcomes. In her own doctoral work at the University of Michigan, Dr. Đoàn modeled the effects of universal annual depression screening in primary care settings on the health status of people aged 12-22 years. She is currently preparing this work for publication.
“I did find that, over the long term, there is improvement in health outcomes if we were to screen on an annual basis,” provided improved screening is coupled with comprehensive treatment plans, Dr. Đoàn said. The model’s health outcomes measures included an increase in life expectancy as well as a greater proportion of depression-free days among adolescents who receive appropriate treatment.
Dr. Riehm and Dr. Đoàn disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PREVENTIVE MEDICINE
Sleep-deprived physicians less empathetic to patient pain?
new research suggests.
In the first of two studies, resident physicians were presented with two hypothetical scenarios involving a patient who complains of pain. They were asked about their likelihood of prescribing pain medication. The test was given to one group of residents who were just starting their day and to another group who were at the end of their night shift after being on call for 26 hours.
Results showed that the night shift residents were less likely than their daytime counterparts to say they would prescribe pain medication to the patients.
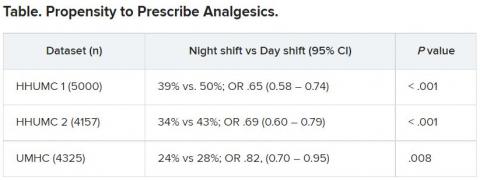
In further analysis of discharge notes from more than 13,000 electronic records of patients presenting with pain complaints at hospitals in Israel and the United States, the likelihood of an analgesic being prescribed during the night shift was 11% lower in Israel and 9% lower in the United States, compared with the day shift.
“Pain management is a major challenge, and a doctor’s perception of a patient’s subjective pain is susceptible to bias,” coinvestigator David Gozal, MD, the Marie M. and Harry L. Smith Endowed Chair of Child Health, University of Missouri–Columbia, said in a press release.
“This study demonstrated that night shift work is an important and previously unrecognized source of bias in pain management, likely stemming from impaired perception of pain,” Dr. Gozal added.
The findings were published online in the Proceedings of the National Academy of Sciences.
‘Directional’ differences
Senior investigator Alex Gileles-Hillel, MD, senior pediatric pulmonologist and sleep researcher at Hadassah University Medical Center, Jerusalem, said in an interview that physicians must make “complex assessments of patients’ subjective pain experience” – and the “subjective nature of pain management decisions can give rise to various biases.”
Dr. Gileles-Hillel has previously researched the cognitive toll of night shift work on physicians.
“It’s pretty established, for example, not to drive when sleep deprived because cognition is impaired,” he said. The current study explored whether sleep deprivation could affect areas other than cognition, including emotions and empathy.
The researchers used “two complementary approaches.” First, they administered tests to measure empathy and pain management decisions in 67 resident physicians at Hadassah Medical Centers either following a 26-hour night shift that began at 8:00 a.m. the day before (n = 36) or immediately before starting the workday (n = 31).
There were no significant differences in demographic, sleep, or burnout measures between the two groups, except that night shift physicians had slept less than those in the daytime group (2.93 vs. 5.96 hours).
Participants completed two tasks. In the empathy-for-pain task, they rated their emotional reactions to pictures of individuals in pain. In the empathy accuracy task, they were asked to assess the feelings of videotaped individuals telling emotional stories.
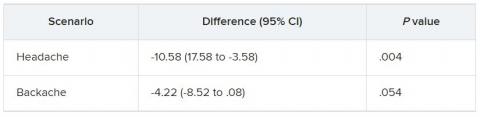
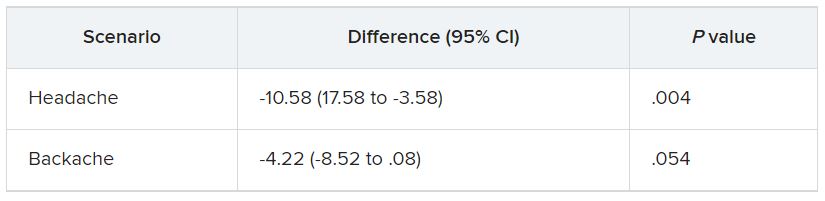
They were then presented with two clinical scenarios: a female patient with a headache and a male patient with a backache. Following that, they were asked to assess the magnitude of the patients’ pain and how likely they would be to prescribe pain medication.
In the empathy-for-pain task, physicians’ empathy scores were significantly lower in the night shift group than in the day group (difference, –0.83; 95% CI, –1.55 to –0.10; P = .026). There were no significant differences between the groups in the empathy accuracy task.
In both scenarios, physicians in the night shift group assessed the patient’s pain as weaker in comparison with physicians in the day group. There was a statistically significant difference in the headache scenario but not the backache scenario.
In the headache scenario, the propensity of the physicians to prescribe analgesics was “directionally lower” but did not reach statistical significance. In the backache scenario, there was no significant difference between the groups’ prescribing propensities.
In both scenarios, pain assessment was positively correlated with the propensity to prescribe analgesics.
Despite the lack of statistical significance, the findings “documented a negative effect of night shift work on physician empathy for pain and a positive association between physician assessment of patient pain and the propensity to prescribe analgesics,” the investigators wrote.
Need for naps?
The researchers then analyzed analgesic prescription patterns drawn from three datasets of discharge notes of patients presenting to the emergency department with pain complaints (n = 13,482) at two branches of Hadassah-Hebrew University Medical Center and the University of Missouri Health Center.
The researchers collected data, including discharge time, medications patients were prescribed upon discharge, and patients’ subjective pain rating on a scale of 0-10 on a visual analogue scale (VAS).
Although patients’ VAS scores did not differ with respect to time or shift, patients were discharged with significantly less prescribed analgesics during the night shift in comparison with the day shift.
No similar differences in prescriptions between night shifts and day shifts were found for nonanalgesic medications, such as for diabetes or blood pressure. This suggests “the effect was specific to pain,” Dr. Gileles-Hillel said.
The pattern remained significant after controlling for potential confounders, including patient and physician variables and emergency department characteristics.
In addition, patients seen during night shifts received fewer analgesics, particularly opioids, than recommended by the World Health Organization for pain management.
“The first study enabled us to measure empathy for pain directly and examine our hypothesis in a controlled environment, while the second enabled us to test the implications by examining real-life pain management decisions,” Dr. Gileles-Hillel said.
“Physicians need to be aware of this,” he noted. “I try to be aware when I’m taking calls [at night] that I’m less empathetic to others and I might be more brief or angry with others.”
On a “house management level, perhaps institutions should try to schedule naps either before or during overnight call. A nap might give a boost and reboot not only to cognitive but also to emotional resources,” Dr. Gileles-Hillel added.
Compromised safety
In a comment, Eti Ben Simon, PhD, a postdoctoral fellow at the Center for Human Sleep Science, University of California, Berkeley, called the study “an important contribution to a growing list of studies that reveal how long night shifts reduce overall safety” for both patients and clinicians.
“It’s time to abandon the notion that the human brain can function as normal after being deprived of sleep for 24 hours,” said Dr. Ben Simon, who was not involved with the research.
“This is especially true in medicine, where we trust others to take care of us and feel our pain. These functions are simply not possible without adequate sleep,” she added.
Also commenting, Kannan Ramar, MD, president of the American Academy of Sleep Medicine, suggested that being cognizant of these findings “may help providers to mitigate this bias” of underprescribing pain medications when treating their patients.
Dr. Ramar, who is also a critical care specialist, pulmonologist, and sleep medicine specialist at Mayo Clinic, Rochester, Minn., was not involved with the research.
He noted that “further studies that systematically evaluate this further in a prospective and blinded way will be important.”
The research was supported in part by grants from the Israel Science Foundation, Joy Ventures, the Recanati Fund at the Jerusalem School of Business at the Hebrew University, and a fellowship from the Azrieli Foundation and received grant support to various investigators from the NIH, the Leda J. Sears Foundation, and the University of Missouri. The investigators, Ramar, and Ben Simon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
In the first of two studies, resident physicians were presented with two hypothetical scenarios involving a patient who complains of pain. They were asked about their likelihood of prescribing pain medication. The test was given to one group of residents who were just starting their day and to another group who were at the end of their night shift after being on call for 26 hours.
Results showed that the night shift residents were less likely than their daytime counterparts to say they would prescribe pain medication to the patients.
In further analysis of discharge notes from more than 13,000 electronic records of patients presenting with pain complaints at hospitals in Israel and the United States, the likelihood of an analgesic being prescribed during the night shift was 11% lower in Israel and 9% lower in the United States, compared with the day shift.
“Pain management is a major challenge, and a doctor’s perception of a patient’s subjective pain is susceptible to bias,” coinvestigator David Gozal, MD, the Marie M. and Harry L. Smith Endowed Chair of Child Health, University of Missouri–Columbia, said in a press release.
“This study demonstrated that night shift work is an important and previously unrecognized source of bias in pain management, likely stemming from impaired perception of pain,” Dr. Gozal added.
The findings were published online in the Proceedings of the National Academy of Sciences.
‘Directional’ differences
Senior investigator Alex Gileles-Hillel, MD, senior pediatric pulmonologist and sleep researcher at Hadassah University Medical Center, Jerusalem, said in an interview that physicians must make “complex assessments of patients’ subjective pain experience” – and the “subjective nature of pain management decisions can give rise to various biases.”
Dr. Gileles-Hillel has previously researched the cognitive toll of night shift work on physicians.
“It’s pretty established, for example, not to drive when sleep deprived because cognition is impaired,” he said. The current study explored whether sleep deprivation could affect areas other than cognition, including emotions and empathy.
The researchers used “two complementary approaches.” First, they administered tests to measure empathy and pain management decisions in 67 resident physicians at Hadassah Medical Centers either following a 26-hour night shift that began at 8:00 a.m. the day before (n = 36) or immediately before starting the workday (n = 31).
There were no significant differences in demographic, sleep, or burnout measures between the two groups, except that night shift physicians had slept less than those in the daytime group (2.93 vs. 5.96 hours).
Participants completed two tasks. In the empathy-for-pain task, they rated their emotional reactions to pictures of individuals in pain. In the empathy accuracy task, they were asked to assess the feelings of videotaped individuals telling emotional stories.
They were then presented with two clinical scenarios: a female patient with a headache and a male patient with a backache. Following that, they were asked to assess the magnitude of the patients’ pain and how likely they would be to prescribe pain medication.
In the empathy-for-pain task, physicians’ empathy scores were significantly lower in the night shift group than in the day group (difference, –0.83; 95% CI, –1.55 to –0.10; P = .026). There were no significant differences between the groups in the empathy accuracy task.
In both scenarios, physicians in the night shift group assessed the patient’s pain as weaker in comparison with physicians in the day group. There was a statistically significant difference in the headache scenario but not the backache scenario.
In the headache scenario, the propensity of the physicians to prescribe analgesics was “directionally lower” but did not reach statistical significance. In the backache scenario, there was no significant difference between the groups’ prescribing propensities.
In both scenarios, pain assessment was positively correlated with the propensity to prescribe analgesics.
Despite the lack of statistical significance, the findings “documented a negative effect of night shift work on physician empathy for pain and a positive association between physician assessment of patient pain and the propensity to prescribe analgesics,” the investigators wrote.
Need for naps?
The researchers then analyzed analgesic prescription patterns drawn from three datasets of discharge notes of patients presenting to the emergency department with pain complaints (n = 13,482) at two branches of Hadassah-Hebrew University Medical Center and the University of Missouri Health Center.
The researchers collected data, including discharge time, medications patients were prescribed upon discharge, and patients’ subjective pain rating on a scale of 0-10 on a visual analogue scale (VAS).
Although patients’ VAS scores did not differ with respect to time or shift, patients were discharged with significantly less prescribed analgesics during the night shift in comparison with the day shift.
No similar differences in prescriptions between night shifts and day shifts were found for nonanalgesic medications, such as for diabetes or blood pressure. This suggests “the effect was specific to pain,” Dr. Gileles-Hillel said.
The pattern remained significant after controlling for potential confounders, including patient and physician variables and emergency department characteristics.
In addition, patients seen during night shifts received fewer analgesics, particularly opioids, than recommended by the World Health Organization for pain management.
“The first study enabled us to measure empathy for pain directly and examine our hypothesis in a controlled environment, while the second enabled us to test the implications by examining real-life pain management decisions,” Dr. Gileles-Hillel said.
“Physicians need to be aware of this,” he noted. “I try to be aware when I’m taking calls [at night] that I’m less empathetic to others and I might be more brief or angry with others.”
On a “house management level, perhaps institutions should try to schedule naps either before or during overnight call. A nap might give a boost and reboot not only to cognitive but also to emotional resources,” Dr. Gileles-Hillel added.
Compromised safety
In a comment, Eti Ben Simon, PhD, a postdoctoral fellow at the Center for Human Sleep Science, University of California, Berkeley, called the study “an important contribution to a growing list of studies that reveal how long night shifts reduce overall safety” for both patients and clinicians.
“It’s time to abandon the notion that the human brain can function as normal after being deprived of sleep for 24 hours,” said Dr. Ben Simon, who was not involved with the research.
“This is especially true in medicine, where we trust others to take care of us and feel our pain. These functions are simply not possible without adequate sleep,” she added.
Also commenting, Kannan Ramar, MD, president of the American Academy of Sleep Medicine, suggested that being cognizant of these findings “may help providers to mitigate this bias” of underprescribing pain medications when treating their patients.
Dr. Ramar, who is also a critical care specialist, pulmonologist, and sleep medicine specialist at Mayo Clinic, Rochester, Minn., was not involved with the research.
He noted that “further studies that systematically evaluate this further in a prospective and blinded way will be important.”
The research was supported in part by grants from the Israel Science Foundation, Joy Ventures, the Recanati Fund at the Jerusalem School of Business at the Hebrew University, and a fellowship from the Azrieli Foundation and received grant support to various investigators from the NIH, the Leda J. Sears Foundation, and the University of Missouri. The investigators, Ramar, and Ben Simon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
In the first of two studies, resident physicians were presented with two hypothetical scenarios involving a patient who complains of pain. They were asked about their likelihood of prescribing pain medication. The test was given to one group of residents who were just starting their day and to another group who were at the end of their night shift after being on call for 26 hours.
Results showed that the night shift residents were less likely than their daytime counterparts to say they would prescribe pain medication to the patients.
In further analysis of discharge notes from more than 13,000 electronic records of patients presenting with pain complaints at hospitals in Israel and the United States, the likelihood of an analgesic being prescribed during the night shift was 11% lower in Israel and 9% lower in the United States, compared with the day shift.
“Pain management is a major challenge, and a doctor’s perception of a patient’s subjective pain is susceptible to bias,” coinvestigator David Gozal, MD, the Marie M. and Harry L. Smith Endowed Chair of Child Health, University of Missouri–Columbia, said in a press release.
“This study demonstrated that night shift work is an important and previously unrecognized source of bias in pain management, likely stemming from impaired perception of pain,” Dr. Gozal added.
The findings were published online in the Proceedings of the National Academy of Sciences.
‘Directional’ differences
Senior investigator Alex Gileles-Hillel, MD, senior pediatric pulmonologist and sleep researcher at Hadassah University Medical Center, Jerusalem, said in an interview that physicians must make “complex assessments of patients’ subjective pain experience” – and the “subjective nature of pain management decisions can give rise to various biases.”
Dr. Gileles-Hillel has previously researched the cognitive toll of night shift work on physicians.
“It’s pretty established, for example, not to drive when sleep deprived because cognition is impaired,” he said. The current study explored whether sleep deprivation could affect areas other than cognition, including emotions and empathy.
The researchers used “two complementary approaches.” First, they administered tests to measure empathy and pain management decisions in 67 resident physicians at Hadassah Medical Centers either following a 26-hour night shift that began at 8:00 a.m. the day before (n = 36) or immediately before starting the workday (n = 31).
There were no significant differences in demographic, sleep, or burnout measures between the two groups, except that night shift physicians had slept less than those in the daytime group (2.93 vs. 5.96 hours).
Participants completed two tasks. In the empathy-for-pain task, they rated their emotional reactions to pictures of individuals in pain. In the empathy accuracy task, they were asked to assess the feelings of videotaped individuals telling emotional stories.
They were then presented with two clinical scenarios: a female patient with a headache and a male patient with a backache. Following that, they were asked to assess the magnitude of the patients’ pain and how likely they would be to prescribe pain medication.
In the empathy-for-pain task, physicians’ empathy scores were significantly lower in the night shift group than in the day group (difference, –0.83; 95% CI, –1.55 to –0.10; P = .026). There were no significant differences between the groups in the empathy accuracy task.
In both scenarios, physicians in the night shift group assessed the patient’s pain as weaker in comparison with physicians in the day group. There was a statistically significant difference in the headache scenario but not the backache scenario.
In the headache scenario, the propensity of the physicians to prescribe analgesics was “directionally lower” but did not reach statistical significance. In the backache scenario, there was no significant difference between the groups’ prescribing propensities.
In both scenarios, pain assessment was positively correlated with the propensity to prescribe analgesics.
Despite the lack of statistical significance, the findings “documented a negative effect of night shift work on physician empathy for pain and a positive association between physician assessment of patient pain and the propensity to prescribe analgesics,” the investigators wrote.
Need for naps?
The researchers then analyzed analgesic prescription patterns drawn from three datasets of discharge notes of patients presenting to the emergency department with pain complaints (n = 13,482) at two branches of Hadassah-Hebrew University Medical Center and the University of Missouri Health Center.
The researchers collected data, including discharge time, medications patients were prescribed upon discharge, and patients’ subjective pain rating on a scale of 0-10 on a visual analogue scale (VAS).
Although patients’ VAS scores did not differ with respect to time or shift, patients were discharged with significantly less prescribed analgesics during the night shift in comparison with the day shift.
No similar differences in prescriptions between night shifts and day shifts were found for nonanalgesic medications, such as for diabetes or blood pressure. This suggests “the effect was specific to pain,” Dr. Gileles-Hillel said.
The pattern remained significant after controlling for potential confounders, including patient and physician variables and emergency department characteristics.
In addition, patients seen during night shifts received fewer analgesics, particularly opioids, than recommended by the World Health Organization for pain management.
“The first study enabled us to measure empathy for pain directly and examine our hypothesis in a controlled environment, while the second enabled us to test the implications by examining real-life pain management decisions,” Dr. Gileles-Hillel said.
“Physicians need to be aware of this,” he noted. “I try to be aware when I’m taking calls [at night] that I’m less empathetic to others and I might be more brief or angry with others.”
On a “house management level, perhaps institutions should try to schedule naps either before or during overnight call. A nap might give a boost and reboot not only to cognitive but also to emotional resources,” Dr. Gileles-Hillel added.
Compromised safety
In a comment, Eti Ben Simon, PhD, a postdoctoral fellow at the Center for Human Sleep Science, University of California, Berkeley, called the study “an important contribution to a growing list of studies that reveal how long night shifts reduce overall safety” for both patients and clinicians.
“It’s time to abandon the notion that the human brain can function as normal after being deprived of sleep for 24 hours,” said Dr. Ben Simon, who was not involved with the research.
“This is especially true in medicine, where we trust others to take care of us and feel our pain. These functions are simply not possible without adequate sleep,” she added.
Also commenting, Kannan Ramar, MD, president of the American Academy of Sleep Medicine, suggested that being cognizant of these findings “may help providers to mitigate this bias” of underprescribing pain medications when treating their patients.
Dr. Ramar, who is also a critical care specialist, pulmonologist, and sleep medicine specialist at Mayo Clinic, Rochester, Minn., was not involved with the research.
He noted that “further studies that systematically evaluate this further in a prospective and blinded way will be important.”
The research was supported in part by grants from the Israel Science Foundation, Joy Ventures, the Recanati Fund at the Jerusalem School of Business at the Hebrew University, and a fellowship from the Azrieli Foundation and received grant support to various investigators from the NIH, the Leda J. Sears Foundation, and the University of Missouri. The investigators, Ramar, and Ben Simon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCES
Docs reveal perils of giving medical advice to friends and family
Stephen Pribut, DPM, a sports medicine podiatrist based in Washington, has had many friends or family members ask him for medical advice. It’s a scenario every doctor will face at one point or another in their careers, and it’s never an easy one.
Dr. Pribut received a call from a friend about a sore shoulder from swimming, saying that his doctor had dismissed the potential for a rotator cuff injury. “Months later, images revealed it was a rotator cuff tear and he wanted my advice,” says Dr. Pribut.
Not being a shoulder specialist, Dr. Pribut limited his input. “I told him to consider a good physical therapist or a shoulder specialist and gave him some alternative strokes for swimming that hopefully wouldn’t aggravate the injury,” he explains.
But he admits some situations are challenging. “I had a relative asking about a third party with an ankle injury. I advised he hold off on using a balance board until things healed, and to make sure he went to see a specialist. Unfortunately, he went to his general practitioner who likely knows nothing about ankle anatomy,” says Dr. Pribut.
“I finally saw a photo, which revealed swelling higher up on the ankle and no evidence of a hematoma – much lower than we would see in an ankle ligament injury. I would like him to see a sports podiatrist or foot and ankle orthopedist, but now I have to stay calm when the advice isn’t followed,” he says.
When asked, “Do you give medical advice to your friends?” 96% of respondents answered yes.
Yazan Abou-Ismail, MD, assistant professor of medicine in the division of hematology at the University of Utah, Salt Lake City, has often faced questions from friends and family, particularly throughout the COVID-19 pandemic. “How you respond is something all physicians need to analyze carefully,” he says. “I get questions on a regular basis, but this greatly increased with COVID.”
“Sharing general information is okay, and it’s even a requirement that we educate on such topics,” says Dr. Abou-Ismail. “But if someone knows they have COVID, for instance, and wants advice on how to proceed, it’s important to send them to their primary care physician for an evaluation rather than give them instructions on care.”
Dr. Abou-Ismail says that most “curbside consulting” equates to lack of an ethical follow-up. “If you gave medical advice without having assessed them, you’re lacking the medical history, a physical exam, and you should not be giving advice,” he says. “This applies to follow-ups, too.”
Throughout the pandemic, Dr. Abou-Ismail’s requests for advice on COVID even extended to online inquiries, often from strangers. “This is not a place to do a formal assessment,” he reminds. “But there are certain types of advice you can offer appropriately.”
Dr. Abou-Ismail considers safe advice to be simple public health messages that stay far out of specifics. Things like “don’t smoke,” or “eat a healthy diet,” and “get enough sleep,” fall into this safety zone. Even, “What is XYZ disease?” or “How do COVID vaccines work?” are topics he says he answers comfortably.
“But telling someone you need a specific treatment for a condition is inappropriate,” he explains. “This is a general way of practicing medicine – your advice should never venture into the potential of doing harm.”
This approach is exactly in line with legal advice, according to Jeff Caesar Chukwuma, founder and senior partner at Chukwuma Law Group, Miami. “It doesn’t mean that doctors should never give medical advice to friends or family, but if they do, they should make sure to take several precautions to protect both themselves and their family and friends,” he says.
When the request for medical advice from an acquaintance migrates into areas in which a physician is not a specialist, sharing recommendations gets even trickier – and more ethically questionable.
Says Mr. Chukwuma, “Doctors should avoid giving advice in areas outside their area of expertise to lower the possibility of providing erroneous or harmful information,” he says.
How to stay safe when asked for advice
The American Medical Association has weighed in on the topic. In the Code of Medical Ethics Opinion 1.2.1, the AMA states that, “Treating oneself or a member of one’s own family poses several challenges for physicians, including concerns about professional objectivity, patient autonomy, and informed consent.”
What about friends or acquaintances, however?
Even so, some respondents voiced their concerns with the scenario. Responses like, “Due to ethics, I would prefer they go and get first, second, and third opinions,” and “Usually the medical advice is very basic first aid (often mental health first aid), and if it’s anything remotely more complicated, I direct them to the appropriate provider.”
The AMA places advising friends in the same basket as advising and treating family members or oneself. In an article appearing in the AMA Journal of Ethics, Horacio Hojman, MD, of Tufts University School of Medicine, Boston, weighed in: “First and foremost, patients deserve objectivity from their doctors. When a physician is emotionally involved with a patient, that physician’s objectivity can be called into question.”
Why is medical advice so thorny when dealing with friends or relatives?
In some cases, a physician might not ask a friend relevant personal questions about his or her medical history, for instance. Or the friend might not want to share details with the doctor. In either case, the lack of information exchange can lead to improper advice.
The issue of giving medical advice to friends, family, and acquaintances can also wade into legal territory. “Personally or professionally, trust is the decisive factor that puts us at ease with the people we surround ourselves with,” says Mr. Chukwuma. “Nowhere is this truer than in medicine, where we approach doctors with some of the most sensitive matters in our lives and entrust our care to them, especially when the physician in question is a close friend or family member.”
Mr. Chukwuma points out that, while there are few strict legal prohibitions against doctors providing care or advice to family and friends, the AMA’s code of ethics states that such action should be reserved for rare situations, such as emergency settings or isolated settings where there is no other qualified physician available, or for minor, not long-term problems.
This was part of the equation for Dr. Pribut when helping his mother navigate her treatment for breast cancer. “With close relatives, offering advice and help can be very hard,” he says.
“This is to protect both patients and doctors,” says Mr. Chukwuma. “Although seeking advice from a family member or friend who is a doctor may be more convenient for a patient, they run the risk of receiving inadequate care by not going in for a formal medical visit complete with tests, medical examination, and follow-up care.”
Mr. Chukwuma offers guidance on how to share medical advice ethically and legally with family, friends, and acquaintances. “First, as much as possible, speak to general medical facts and knowledge rather than comment directly on the patient’s particular situation,” he says. “In the absence of thorough examination and tests, the doctor’s knowledge of a patient’s condition is limited, therefore, you should take care not to provide seemingly definitive answers on that patient’s unique condition in situations where they can’t rely on data to back up their advice and recommendations.”
The AMA’s Journal of Ethics article shares these tips for staying on the right side of the ethical line when dealing with friends and family members:
- Politely decline.
- Offer other forms of assistance – this might help a friend find the right qualified physician – as Dr. Pribut tends to do. Maybe help in navigating the sometimes-confusing health care system.
- Don’t hesitate in an emergency – the old “is there a doctor on board,” scenario on a plane when someone is in distress is a perfectly acceptable, and recommended, time to step in, even if it is a friend or family member.
Dr. Pribut, a long-time veteran of the tricky medical waters involving friends and family, has this to offer: “Be cautious and always stay in the realm of what you know,” he says. “Always encourage people to seek an opinion from a qualified doctor. Help them find a reputable doctor if that’s useful.”
Mr. Chukwuma adds also that doctors should stand firm when pushed by a friend or family member, especially when offering advice, even if it’s in the form of general education. “The doctor should make it clear to the family member or friend that their advice in no way takes the place of actual treatment or examination by a medical professional and that, if need be, the patient should seek formal medical help from another doctor, ideally one not related to or friends with the patient,” he says.
A version of this article first appeared on Medscape.com.
Stephen Pribut, DPM, a sports medicine podiatrist based in Washington, has had many friends or family members ask him for medical advice. It’s a scenario every doctor will face at one point or another in their careers, and it’s never an easy one.
Dr. Pribut received a call from a friend about a sore shoulder from swimming, saying that his doctor had dismissed the potential for a rotator cuff injury. “Months later, images revealed it was a rotator cuff tear and he wanted my advice,” says Dr. Pribut.
Not being a shoulder specialist, Dr. Pribut limited his input. “I told him to consider a good physical therapist or a shoulder specialist and gave him some alternative strokes for swimming that hopefully wouldn’t aggravate the injury,” he explains.
But he admits some situations are challenging. “I had a relative asking about a third party with an ankle injury. I advised he hold off on using a balance board until things healed, and to make sure he went to see a specialist. Unfortunately, he went to his general practitioner who likely knows nothing about ankle anatomy,” says Dr. Pribut.
“I finally saw a photo, which revealed swelling higher up on the ankle and no evidence of a hematoma – much lower than we would see in an ankle ligament injury. I would like him to see a sports podiatrist or foot and ankle orthopedist, but now I have to stay calm when the advice isn’t followed,” he says.
When asked, “Do you give medical advice to your friends?” 96% of respondents answered yes.
Yazan Abou-Ismail, MD, assistant professor of medicine in the division of hematology at the University of Utah, Salt Lake City, has often faced questions from friends and family, particularly throughout the COVID-19 pandemic. “How you respond is something all physicians need to analyze carefully,” he says. “I get questions on a regular basis, but this greatly increased with COVID.”
“Sharing general information is okay, and it’s even a requirement that we educate on such topics,” says Dr. Abou-Ismail. “But if someone knows they have COVID, for instance, and wants advice on how to proceed, it’s important to send them to their primary care physician for an evaluation rather than give them instructions on care.”
Dr. Abou-Ismail says that most “curbside consulting” equates to lack of an ethical follow-up. “If you gave medical advice without having assessed them, you’re lacking the medical history, a physical exam, and you should not be giving advice,” he says. “This applies to follow-ups, too.”
Throughout the pandemic, Dr. Abou-Ismail’s requests for advice on COVID even extended to online inquiries, often from strangers. “This is not a place to do a formal assessment,” he reminds. “But there are certain types of advice you can offer appropriately.”
Dr. Abou-Ismail considers safe advice to be simple public health messages that stay far out of specifics. Things like “don’t smoke,” or “eat a healthy diet,” and “get enough sleep,” fall into this safety zone. Even, “What is XYZ disease?” or “How do COVID vaccines work?” are topics he says he answers comfortably.
“But telling someone you need a specific treatment for a condition is inappropriate,” he explains. “This is a general way of practicing medicine – your advice should never venture into the potential of doing harm.”
This approach is exactly in line with legal advice, according to Jeff Caesar Chukwuma, founder and senior partner at Chukwuma Law Group, Miami. “It doesn’t mean that doctors should never give medical advice to friends or family, but if they do, they should make sure to take several precautions to protect both themselves and their family and friends,” he says.
When the request for medical advice from an acquaintance migrates into areas in which a physician is not a specialist, sharing recommendations gets even trickier – and more ethically questionable.
Says Mr. Chukwuma, “Doctors should avoid giving advice in areas outside their area of expertise to lower the possibility of providing erroneous or harmful information,” he says.
How to stay safe when asked for advice
The American Medical Association has weighed in on the topic. In the Code of Medical Ethics Opinion 1.2.1, the AMA states that, “Treating oneself or a member of one’s own family poses several challenges for physicians, including concerns about professional objectivity, patient autonomy, and informed consent.”
What about friends or acquaintances, however?
Even so, some respondents voiced their concerns with the scenario. Responses like, “Due to ethics, I would prefer they go and get first, second, and third opinions,” and “Usually the medical advice is very basic first aid (often mental health first aid), and if it’s anything remotely more complicated, I direct them to the appropriate provider.”
The AMA places advising friends in the same basket as advising and treating family members or oneself. In an article appearing in the AMA Journal of Ethics, Horacio Hojman, MD, of Tufts University School of Medicine, Boston, weighed in: “First and foremost, patients deserve objectivity from their doctors. When a physician is emotionally involved with a patient, that physician’s objectivity can be called into question.”
Why is medical advice so thorny when dealing with friends or relatives?
In some cases, a physician might not ask a friend relevant personal questions about his or her medical history, for instance. Or the friend might not want to share details with the doctor. In either case, the lack of information exchange can lead to improper advice.
The issue of giving medical advice to friends, family, and acquaintances can also wade into legal territory. “Personally or professionally, trust is the decisive factor that puts us at ease with the people we surround ourselves with,” says Mr. Chukwuma. “Nowhere is this truer than in medicine, where we approach doctors with some of the most sensitive matters in our lives and entrust our care to them, especially when the physician in question is a close friend or family member.”
Mr. Chukwuma points out that, while there are few strict legal prohibitions against doctors providing care or advice to family and friends, the AMA’s code of ethics states that such action should be reserved for rare situations, such as emergency settings or isolated settings where there is no other qualified physician available, or for minor, not long-term problems.
This was part of the equation for Dr. Pribut when helping his mother navigate her treatment for breast cancer. “With close relatives, offering advice and help can be very hard,” he says.
“This is to protect both patients and doctors,” says Mr. Chukwuma. “Although seeking advice from a family member or friend who is a doctor may be more convenient for a patient, they run the risk of receiving inadequate care by not going in for a formal medical visit complete with tests, medical examination, and follow-up care.”
Mr. Chukwuma offers guidance on how to share medical advice ethically and legally with family, friends, and acquaintances. “First, as much as possible, speak to general medical facts and knowledge rather than comment directly on the patient’s particular situation,” he says. “In the absence of thorough examination and tests, the doctor’s knowledge of a patient’s condition is limited, therefore, you should take care not to provide seemingly definitive answers on that patient’s unique condition in situations where they can’t rely on data to back up their advice and recommendations.”
The AMA’s Journal of Ethics article shares these tips for staying on the right side of the ethical line when dealing with friends and family members:
- Politely decline.
- Offer other forms of assistance – this might help a friend find the right qualified physician – as Dr. Pribut tends to do. Maybe help in navigating the sometimes-confusing health care system.
- Don’t hesitate in an emergency – the old “is there a doctor on board,” scenario on a plane when someone is in distress is a perfectly acceptable, and recommended, time to step in, even if it is a friend or family member.
Dr. Pribut, a long-time veteran of the tricky medical waters involving friends and family, has this to offer: “Be cautious and always stay in the realm of what you know,” he says. “Always encourage people to seek an opinion from a qualified doctor. Help them find a reputable doctor if that’s useful.”
Mr. Chukwuma adds also that doctors should stand firm when pushed by a friend or family member, especially when offering advice, even if it’s in the form of general education. “The doctor should make it clear to the family member or friend that their advice in no way takes the place of actual treatment or examination by a medical professional and that, if need be, the patient should seek formal medical help from another doctor, ideally one not related to or friends with the patient,” he says.
A version of this article first appeared on Medscape.com.
Stephen Pribut, DPM, a sports medicine podiatrist based in Washington, has had many friends or family members ask him for medical advice. It’s a scenario every doctor will face at one point or another in their careers, and it’s never an easy one.
Dr. Pribut received a call from a friend about a sore shoulder from swimming, saying that his doctor had dismissed the potential for a rotator cuff injury. “Months later, images revealed it was a rotator cuff tear and he wanted my advice,” says Dr. Pribut.
Not being a shoulder specialist, Dr. Pribut limited his input. “I told him to consider a good physical therapist or a shoulder specialist and gave him some alternative strokes for swimming that hopefully wouldn’t aggravate the injury,” he explains.
But he admits some situations are challenging. “I had a relative asking about a third party with an ankle injury. I advised he hold off on using a balance board until things healed, and to make sure he went to see a specialist. Unfortunately, he went to his general practitioner who likely knows nothing about ankle anatomy,” says Dr. Pribut.
“I finally saw a photo, which revealed swelling higher up on the ankle and no evidence of a hematoma – much lower than we would see in an ankle ligament injury. I would like him to see a sports podiatrist or foot and ankle orthopedist, but now I have to stay calm when the advice isn’t followed,” he says.
When asked, “Do you give medical advice to your friends?” 96% of respondents answered yes.
Yazan Abou-Ismail, MD, assistant professor of medicine in the division of hematology at the University of Utah, Salt Lake City, has often faced questions from friends and family, particularly throughout the COVID-19 pandemic. “How you respond is something all physicians need to analyze carefully,” he says. “I get questions on a regular basis, but this greatly increased with COVID.”
“Sharing general information is okay, and it’s even a requirement that we educate on such topics,” says Dr. Abou-Ismail. “But if someone knows they have COVID, for instance, and wants advice on how to proceed, it’s important to send them to their primary care physician for an evaluation rather than give them instructions on care.”
Dr. Abou-Ismail says that most “curbside consulting” equates to lack of an ethical follow-up. “If you gave medical advice without having assessed them, you’re lacking the medical history, a physical exam, and you should not be giving advice,” he says. “This applies to follow-ups, too.”
Throughout the pandemic, Dr. Abou-Ismail’s requests for advice on COVID even extended to online inquiries, often from strangers. “This is not a place to do a formal assessment,” he reminds. “But there are certain types of advice you can offer appropriately.”
Dr. Abou-Ismail considers safe advice to be simple public health messages that stay far out of specifics. Things like “don’t smoke,” or “eat a healthy diet,” and “get enough sleep,” fall into this safety zone. Even, “What is XYZ disease?” or “How do COVID vaccines work?” are topics he says he answers comfortably.
“But telling someone you need a specific treatment for a condition is inappropriate,” he explains. “This is a general way of practicing medicine – your advice should never venture into the potential of doing harm.”
This approach is exactly in line with legal advice, according to Jeff Caesar Chukwuma, founder and senior partner at Chukwuma Law Group, Miami. “It doesn’t mean that doctors should never give medical advice to friends or family, but if they do, they should make sure to take several precautions to protect both themselves and their family and friends,” he says.
When the request for medical advice from an acquaintance migrates into areas in which a physician is not a specialist, sharing recommendations gets even trickier – and more ethically questionable.
Says Mr. Chukwuma, “Doctors should avoid giving advice in areas outside their area of expertise to lower the possibility of providing erroneous or harmful information,” he says.
How to stay safe when asked for advice
The American Medical Association has weighed in on the topic. In the Code of Medical Ethics Opinion 1.2.1, the AMA states that, “Treating oneself or a member of one’s own family poses several challenges for physicians, including concerns about professional objectivity, patient autonomy, and informed consent.”
What about friends or acquaintances, however?
Even so, some respondents voiced their concerns with the scenario. Responses like, “Due to ethics, I would prefer they go and get first, second, and third opinions,” and “Usually the medical advice is very basic first aid (often mental health first aid), and if it’s anything remotely more complicated, I direct them to the appropriate provider.”
The AMA places advising friends in the same basket as advising and treating family members or oneself. In an article appearing in the AMA Journal of Ethics, Horacio Hojman, MD, of Tufts University School of Medicine, Boston, weighed in: “First and foremost, patients deserve objectivity from their doctors. When a physician is emotionally involved with a patient, that physician’s objectivity can be called into question.”
Why is medical advice so thorny when dealing with friends or relatives?
In some cases, a physician might not ask a friend relevant personal questions about his or her medical history, for instance. Or the friend might not want to share details with the doctor. In either case, the lack of information exchange can lead to improper advice.
The issue of giving medical advice to friends, family, and acquaintances can also wade into legal territory. “Personally or professionally, trust is the decisive factor that puts us at ease with the people we surround ourselves with,” says Mr. Chukwuma. “Nowhere is this truer than in medicine, where we approach doctors with some of the most sensitive matters in our lives and entrust our care to them, especially when the physician in question is a close friend or family member.”
Mr. Chukwuma points out that, while there are few strict legal prohibitions against doctors providing care or advice to family and friends, the AMA’s code of ethics states that such action should be reserved for rare situations, such as emergency settings or isolated settings where there is no other qualified physician available, or for minor, not long-term problems.
This was part of the equation for Dr. Pribut when helping his mother navigate her treatment for breast cancer. “With close relatives, offering advice and help can be very hard,” he says.
“This is to protect both patients and doctors,” says Mr. Chukwuma. “Although seeking advice from a family member or friend who is a doctor may be more convenient for a patient, they run the risk of receiving inadequate care by not going in for a formal medical visit complete with tests, medical examination, and follow-up care.”
Mr. Chukwuma offers guidance on how to share medical advice ethically and legally with family, friends, and acquaintances. “First, as much as possible, speak to general medical facts and knowledge rather than comment directly on the patient’s particular situation,” he says. “In the absence of thorough examination and tests, the doctor’s knowledge of a patient’s condition is limited, therefore, you should take care not to provide seemingly definitive answers on that patient’s unique condition in situations where they can’t rely on data to back up their advice and recommendations.”
The AMA’s Journal of Ethics article shares these tips for staying on the right side of the ethical line when dealing with friends and family members:
- Politely decline.
- Offer other forms of assistance – this might help a friend find the right qualified physician – as Dr. Pribut tends to do. Maybe help in navigating the sometimes-confusing health care system.
- Don’t hesitate in an emergency – the old “is there a doctor on board,” scenario on a plane when someone is in distress is a perfectly acceptable, and recommended, time to step in, even if it is a friend or family member.
Dr. Pribut, a long-time veteran of the tricky medical waters involving friends and family, has this to offer: “Be cautious and always stay in the realm of what you know,” he says. “Always encourage people to seek an opinion from a qualified doctor. Help them find a reputable doctor if that’s useful.”
Mr. Chukwuma adds also that doctors should stand firm when pushed by a friend or family member, especially when offering advice, even if it’s in the form of general education. “The doctor should make it clear to the family member or friend that their advice in no way takes the place of actual treatment or examination by a medical professional and that, if need be, the patient should seek formal medical help from another doctor, ideally one not related to or friends with the patient,” he says.
A version of this article first appeared on Medscape.com.
Compulsivity contributes to poor outcomes in body-focused repetitive behaviors
Although body-focused repetitive behaviors (BFRBs), specifically trichotillomania and skin-picking disorder, are similar in clinical presentation to aspects of obsessive-compulsive disorder (OCD), the role of compulsivity in TTM and SPD has not been well studied, wrote Jon E. Grant, MD, of the University of Chicago and colleagues.
In a study published in the Journal of Psychiatric Research, the authors recruited 69 women and 22 men who met DSM-5 criteria for TTM and SPD. Participants completed diagnostic interviews, symptom inventories, and measures of disability/functioning. Compulsivity was measured using the 15-item Cambridge-Chicago Compulsivity Trait Scale (CHI-T). The average age of the participants was 30.9 years; 48 had TTM, 37 had SPD, and 2 had both conditions.
Overall, total CHI-T scores were significantly correlated with worse disability and quality of life, based on the Quality of Life Inventory (P = .0278) and the Sheehan Disability Scale (P = .0085) but not with severity of TTM or SPD symptoms. TTM and SPD symptoms were assessed using the Massachusetts General Hospital Hair Pulling Scale and the Skin Picking Symptom Symptom Assessment Scale.
“In the current study, we did not find a link between conventional symptom severity measures for BFRBs and disability or quality of life, whereas trans-diagnostic compulsivity did correlate with these clinically important parameters,” the researchers wrote in their discussion. “These findings might suggest the current symptom measures for BFRBs are not including an important aspect of the disease and that a fuller understanding of these symptoms requires measurement of compulsivity. Including validated measures of compulsivity in clinical trials of therapy or medication would also seem to be important for future work,” they said.
The study findings were limited by several factors including the use of a community sample that may not generalize to a clinical setting, the researchers noted. Other limitations include the cross-sectional design, which prevents conclusions about causality, the lack of a control group, and the relatively small sample size, they said.
However, the study is the first known to use a validated compulsivity measure to assess BFRBs, and the results suggest a clinically relevant impact of compulsivity on both psychosocial dysfunction and poor quality of life in this patient population, with possible implications for treatment, the researchers wrote.
The study received no outside funding. Lead author Dr. Grant disclosed research grants from Otsuka and Biohaven Pharmaceuticals, yearly compensation from Springer Publishing for acting as editor in chief of the Journal of Gambling Studies, and royalties from Oxford University Press, American Psychiatric Publishing, Norton Press, and McGraw Hill.
Although body-focused repetitive behaviors (BFRBs), specifically trichotillomania and skin-picking disorder, are similar in clinical presentation to aspects of obsessive-compulsive disorder (OCD), the role of compulsivity in TTM and SPD has not been well studied, wrote Jon E. Grant, MD, of the University of Chicago and colleagues.
In a study published in the Journal of Psychiatric Research, the authors recruited 69 women and 22 men who met DSM-5 criteria for TTM and SPD. Participants completed diagnostic interviews, symptom inventories, and measures of disability/functioning. Compulsivity was measured using the 15-item Cambridge-Chicago Compulsivity Trait Scale (CHI-T). The average age of the participants was 30.9 years; 48 had TTM, 37 had SPD, and 2 had both conditions.
Overall, total CHI-T scores were significantly correlated with worse disability and quality of life, based on the Quality of Life Inventory (P = .0278) and the Sheehan Disability Scale (P = .0085) but not with severity of TTM or SPD symptoms. TTM and SPD symptoms were assessed using the Massachusetts General Hospital Hair Pulling Scale and the Skin Picking Symptom Symptom Assessment Scale.
“In the current study, we did not find a link between conventional symptom severity measures for BFRBs and disability or quality of life, whereas trans-diagnostic compulsivity did correlate with these clinically important parameters,” the researchers wrote in their discussion. “These findings might suggest the current symptom measures for BFRBs are not including an important aspect of the disease and that a fuller understanding of these symptoms requires measurement of compulsivity. Including validated measures of compulsivity in clinical trials of therapy or medication would also seem to be important for future work,” they said.
The study findings were limited by several factors including the use of a community sample that may not generalize to a clinical setting, the researchers noted. Other limitations include the cross-sectional design, which prevents conclusions about causality, the lack of a control group, and the relatively small sample size, they said.
However, the study is the first known to use a validated compulsivity measure to assess BFRBs, and the results suggest a clinically relevant impact of compulsivity on both psychosocial dysfunction and poor quality of life in this patient population, with possible implications for treatment, the researchers wrote.
The study received no outside funding. Lead author Dr. Grant disclosed research grants from Otsuka and Biohaven Pharmaceuticals, yearly compensation from Springer Publishing for acting as editor in chief of the Journal of Gambling Studies, and royalties from Oxford University Press, American Psychiatric Publishing, Norton Press, and McGraw Hill.
Although body-focused repetitive behaviors (BFRBs), specifically trichotillomania and skin-picking disorder, are similar in clinical presentation to aspects of obsessive-compulsive disorder (OCD), the role of compulsivity in TTM and SPD has not been well studied, wrote Jon E. Grant, MD, of the University of Chicago and colleagues.
In a study published in the Journal of Psychiatric Research, the authors recruited 69 women and 22 men who met DSM-5 criteria for TTM and SPD. Participants completed diagnostic interviews, symptom inventories, and measures of disability/functioning. Compulsivity was measured using the 15-item Cambridge-Chicago Compulsivity Trait Scale (CHI-T). The average age of the participants was 30.9 years; 48 had TTM, 37 had SPD, and 2 had both conditions.
Overall, total CHI-T scores were significantly correlated with worse disability and quality of life, based on the Quality of Life Inventory (P = .0278) and the Sheehan Disability Scale (P = .0085) but not with severity of TTM or SPD symptoms. TTM and SPD symptoms were assessed using the Massachusetts General Hospital Hair Pulling Scale and the Skin Picking Symptom Symptom Assessment Scale.
“In the current study, we did not find a link between conventional symptom severity measures for BFRBs and disability or quality of life, whereas trans-diagnostic compulsivity did correlate with these clinically important parameters,” the researchers wrote in their discussion. “These findings might suggest the current symptom measures for BFRBs are not including an important aspect of the disease and that a fuller understanding of these symptoms requires measurement of compulsivity. Including validated measures of compulsivity in clinical trials of therapy or medication would also seem to be important for future work,” they said.
The study findings were limited by several factors including the use of a community sample that may not generalize to a clinical setting, the researchers noted. Other limitations include the cross-sectional design, which prevents conclusions about causality, the lack of a control group, and the relatively small sample size, they said.
However, the study is the first known to use a validated compulsivity measure to assess BFRBs, and the results suggest a clinically relevant impact of compulsivity on both psychosocial dysfunction and poor quality of life in this patient population, with possible implications for treatment, the researchers wrote.
The study received no outside funding. Lead author Dr. Grant disclosed research grants from Otsuka and Biohaven Pharmaceuticals, yearly compensation from Springer Publishing for acting as editor in chief of the Journal of Gambling Studies, and royalties from Oxford University Press, American Psychiatric Publishing, Norton Press, and McGraw Hill.
FROM THE JOURNAL OF PSYCHIATRIC RESEARCH
Early childhood allergies linked with ADHD and ASD
, according to a large retrospective study.
“Our study provides strong evidence for the association between allergic disorders in early childhood and the development of ADHD,” Shay Nemet, MD, of the Kaplan Medical Center, Rehovot, Israel, and colleagues write in Pediatric Allergy and Immunology. “The risk of those children to develop ASD was less significant.”
The researchers analyzed data from 117,022 consecutive children diagnosed with at least one allergic disorder – asthma, conjunctivitis, rhinitis, and drug, food, or skin allergy – and 116,968 children without allergies in the Clalit Health Services pediatric database. The children had been treated from 2000 to 2018; the mean follow-up period was 11 years.
The children who were diagnosed with one or more allergies (mean age, 4.5 years) were significantly more likely to develop ADHD (odds ratio, 2.45; 95% confidence interval, 2.39-2.51), ASD (OR, 1.17; 95% CI, 1.08-1.27), or both ADHD and ASD (OR, 1.56; 95% CI, 1.35-1.79) than were the control children who did not have allergies.
Children diagnosed with rhinitis (OR, 3.96; 95% CI, 3.80-4.12) and conjunctivitis (OR, 3.63; 95% CI, 3.53-3.74) were the most likely to develop ADHD.
Allergy correlation with ADHD and ASD
Cy B. Nadler, PhD, a clinical psychologist and the director of Autism Services at Children’s Mercy Kansas City, Missouri, told this news organization that children and adults with neurodevelopmental differences are also more likely to have other health problems.
“Clinicians practicing in subspecialties such as allergy and immunology may have opportunities to help psychologists identify developmental and behavioral concerns early in childhood,” he added.
“Studies like this can’t be accomplished without large health care databases, but this approach has drawbacks, too,” Dr. Nadler said in an email. “Without more information about these patients’ co-occurring medical and behavioral conditions, we are almost certainly missing important contributors to the observed associations.”
Dr. Nadler, who was not involved in the study, noted that in the multivariable analysis that controlled for age at study entry, gender, and number of annual visits, the link between allergy and ASD diagnosis was not significant.
“It is important to remember not to interpret these study results as causal,” he added.
Desha M. Jordan, MD, FAAP, an assistant professor of pediatrics at UPMC Children’s Hospital of Pittsburgh, called the study “an interesting new area that has been speculated about for some time” and “one of the first I have seen with statistically significant correlations found between ADHD, ASD, and allergic conditions.”
More questions for future studies
Health care providers need to understand the potential sequelae of allergic conditions so that they can manage their patients appropriately, she advised.
Although symptoms and diagnoses were confirmed for all patients, the study’s retrospective design and the possibility of recall bias were limitations, said Dr. Jordan in an email. She also was not involved in the study.
“For example, the family of a child diagnosed with ADHD or ASD may have been more mindful of anything out of the norm in that child’s past, while the family of a child without these conditions may not have recalled allergic symptoms as important,” she explained.
Another question that arises is whether some patients were treated and managed well while others were not and whether this disparity in care affected the development or severity of ADHD or ASD, she added.
“Is a patient with a well-controlled allergic condition less likely to develop ADHD or ASD than a patient with an uncontrolled allergic condition? Does a well-controlled patient ever return to the same probability of getting ADHD or ASD as a nonallergic patient?”
“While this study expands our understanding of these conditions and their interrelationships, it also brings up many additional questions and opens a new segment of research,” Dr. Jordan said. “More studies in this area are necessary to confirm the findings of this paper.”
The study was partially funded by the Israel Ambulatory Pediatric Association. The authors, Dr. Nadler, and Dr. Jordan report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to a large retrospective study.
“Our study provides strong evidence for the association between allergic disorders in early childhood and the development of ADHD,” Shay Nemet, MD, of the Kaplan Medical Center, Rehovot, Israel, and colleagues write in Pediatric Allergy and Immunology. “The risk of those children to develop ASD was less significant.”
The researchers analyzed data from 117,022 consecutive children diagnosed with at least one allergic disorder – asthma, conjunctivitis, rhinitis, and drug, food, or skin allergy – and 116,968 children without allergies in the Clalit Health Services pediatric database. The children had been treated from 2000 to 2018; the mean follow-up period was 11 years.
The children who were diagnosed with one or more allergies (mean age, 4.5 years) were significantly more likely to develop ADHD (odds ratio, 2.45; 95% confidence interval, 2.39-2.51), ASD (OR, 1.17; 95% CI, 1.08-1.27), or both ADHD and ASD (OR, 1.56; 95% CI, 1.35-1.79) than were the control children who did not have allergies.
Children diagnosed with rhinitis (OR, 3.96; 95% CI, 3.80-4.12) and conjunctivitis (OR, 3.63; 95% CI, 3.53-3.74) were the most likely to develop ADHD.
Allergy correlation with ADHD and ASD
Cy B. Nadler, PhD, a clinical psychologist and the director of Autism Services at Children’s Mercy Kansas City, Missouri, told this news organization that children and adults with neurodevelopmental differences are also more likely to have other health problems.
“Clinicians practicing in subspecialties such as allergy and immunology may have opportunities to help psychologists identify developmental and behavioral concerns early in childhood,” he added.
“Studies like this can’t be accomplished without large health care databases, but this approach has drawbacks, too,” Dr. Nadler said in an email. “Without more information about these patients’ co-occurring medical and behavioral conditions, we are almost certainly missing important contributors to the observed associations.”
Dr. Nadler, who was not involved in the study, noted that in the multivariable analysis that controlled for age at study entry, gender, and number of annual visits, the link between allergy and ASD diagnosis was not significant.
“It is important to remember not to interpret these study results as causal,” he added.
Desha M. Jordan, MD, FAAP, an assistant professor of pediatrics at UPMC Children’s Hospital of Pittsburgh, called the study “an interesting new area that has been speculated about for some time” and “one of the first I have seen with statistically significant correlations found between ADHD, ASD, and allergic conditions.”
More questions for future studies
Health care providers need to understand the potential sequelae of allergic conditions so that they can manage their patients appropriately, she advised.
Although symptoms and diagnoses were confirmed for all patients, the study’s retrospective design and the possibility of recall bias were limitations, said Dr. Jordan in an email. She also was not involved in the study.
“For example, the family of a child diagnosed with ADHD or ASD may have been more mindful of anything out of the norm in that child’s past, while the family of a child without these conditions may not have recalled allergic symptoms as important,” she explained.
Another question that arises is whether some patients were treated and managed well while others were not and whether this disparity in care affected the development or severity of ADHD or ASD, she added.
“Is a patient with a well-controlled allergic condition less likely to develop ADHD or ASD than a patient with an uncontrolled allergic condition? Does a well-controlled patient ever return to the same probability of getting ADHD or ASD as a nonallergic patient?”
“While this study expands our understanding of these conditions and their interrelationships, it also brings up many additional questions and opens a new segment of research,” Dr. Jordan said. “More studies in this area are necessary to confirm the findings of this paper.”
The study was partially funded by the Israel Ambulatory Pediatric Association. The authors, Dr. Nadler, and Dr. Jordan report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to a large retrospective study.
“Our study provides strong evidence for the association between allergic disorders in early childhood and the development of ADHD,” Shay Nemet, MD, of the Kaplan Medical Center, Rehovot, Israel, and colleagues write in Pediatric Allergy and Immunology. “The risk of those children to develop ASD was less significant.”
The researchers analyzed data from 117,022 consecutive children diagnosed with at least one allergic disorder – asthma, conjunctivitis, rhinitis, and drug, food, or skin allergy – and 116,968 children without allergies in the Clalit Health Services pediatric database. The children had been treated from 2000 to 2018; the mean follow-up period was 11 years.
The children who were diagnosed with one or more allergies (mean age, 4.5 years) were significantly more likely to develop ADHD (odds ratio, 2.45; 95% confidence interval, 2.39-2.51), ASD (OR, 1.17; 95% CI, 1.08-1.27), or both ADHD and ASD (OR, 1.56; 95% CI, 1.35-1.79) than were the control children who did not have allergies.
Children diagnosed with rhinitis (OR, 3.96; 95% CI, 3.80-4.12) and conjunctivitis (OR, 3.63; 95% CI, 3.53-3.74) were the most likely to develop ADHD.
Allergy correlation with ADHD and ASD
Cy B. Nadler, PhD, a clinical psychologist and the director of Autism Services at Children’s Mercy Kansas City, Missouri, told this news organization that children and adults with neurodevelopmental differences are also more likely to have other health problems.
“Clinicians practicing in subspecialties such as allergy and immunology may have opportunities to help psychologists identify developmental and behavioral concerns early in childhood,” he added.
“Studies like this can’t be accomplished without large health care databases, but this approach has drawbacks, too,” Dr. Nadler said in an email. “Without more information about these patients’ co-occurring medical and behavioral conditions, we are almost certainly missing important contributors to the observed associations.”
Dr. Nadler, who was not involved in the study, noted that in the multivariable analysis that controlled for age at study entry, gender, and number of annual visits, the link between allergy and ASD diagnosis was not significant.
“It is important to remember not to interpret these study results as causal,” he added.
Desha M. Jordan, MD, FAAP, an assistant professor of pediatrics at UPMC Children’s Hospital of Pittsburgh, called the study “an interesting new area that has been speculated about for some time” and “one of the first I have seen with statistically significant correlations found between ADHD, ASD, and allergic conditions.”
More questions for future studies
Health care providers need to understand the potential sequelae of allergic conditions so that they can manage their patients appropriately, she advised.
Although symptoms and diagnoses were confirmed for all patients, the study’s retrospective design and the possibility of recall bias were limitations, said Dr. Jordan in an email. She also was not involved in the study.
“For example, the family of a child diagnosed with ADHD or ASD may have been more mindful of anything out of the norm in that child’s past, while the family of a child without these conditions may not have recalled allergic symptoms as important,” she explained.
Another question that arises is whether some patients were treated and managed well while others were not and whether this disparity in care affected the development or severity of ADHD or ASD, she added.
“Is a patient with a well-controlled allergic condition less likely to develop ADHD or ASD than a patient with an uncontrolled allergic condition? Does a well-controlled patient ever return to the same probability of getting ADHD or ASD as a nonallergic patient?”
“While this study expands our understanding of these conditions and their interrelationships, it also brings up many additional questions and opens a new segment of research,” Dr. Jordan said. “More studies in this area are necessary to confirm the findings of this paper.”
The study was partially funded by the Israel Ambulatory Pediatric Association. The authors, Dr. Nadler, and Dr. Jordan report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PEDIATRIC ALLERGY AND IMMUNOLOGY
Telemental health linked with improvements in key outcomes
, new research suggests.
In a nationwide study, researchers drew on Medicare data from nearly 3,000 counties covering the period from 2000 to 2018. Results show that counties in which there was greater use of telemental health services reported higher increases of clinical visits and better follow-up after hospitalization among patients with bipolar 1 disorder and schizophrenia or other psychotic disorders.
In the study, “clinical visits” referred to both in-person and telemental health visits.
“These findings really support the idea that telemental health can be safe and effective and beneficial for in-person care for people with severe mental illness,” coinvestigator Haiden Huskamp, PhD, professor of health care policy at Harvard Medical School, Boston, said in an interview.
The findings were published online in JAMA Network Open.
Continuing trend?
Past studies have pointed to a sharp increase in the use of telepsychiatry services for patients with SMI. As reported by this news organization, this is a trend some clinicians say is likely to continue after the pandemic.
Use of telemedicine during the pandemic received a boost by the temporary suspension of certain Medicare rules that restrict telehealth use. Debate continues at the federal and state levels on whether to make that suspension permanent. Dr. Huskamp said more information is needed about the efficacy and accessibility of telemental health.
To investigate, researchers used Medicare fee-for-service data from 118,170 patients in 2,916 counties. More than two-thirds of the patients were aged 65 years or younger.
During the study period, telemental health service increased from 0.03 visits per patient with SMI in 2010 to 0.19 visits per patient in 2018. This increase was broad, with the number of counties reporting high use of telemental health increasing from 2% in 2010 to 17% in 2018.
Compared with counties in which there was no telemental health services, those with high use were less densely populated and had fewer health care professionals and hospital beds.
The number of overall visits with a mental health professional increased slightly in high-use counties compared to no-use counties, from 4.65 visits in 2010 to 4.79 visits in 2018. The number of in-person visits during that period declined from 4.55 visits in 2010 to 3.73 visits in 2018, which suggests that the overall increase was due to higher use of telemental health.
In the high-use group, the number of patients who had at least four mental health care visits increased 8%, and the number of patients who had a follow-up visit within 30 days of a hospitalization increased 20.4%.
A ‘helpful option’
“Telemedicine doesn’t address the national shortage of providers, but it definitely helps in underserved areas [and] rural areas,” Dr. Huskamp said.
“We need more mental health providers and need to develop new models of care that can leverage the providers we have in the best way possible. This is at least a helpful option, especially when you’re thinking about the maldistribution of providers across the country,” she added.
The study results showed that there was no difference in medication adherence between low- and high-use counties.
There was greater contact with mental health care providers in counties with high use of telemental health, and patients in the high-use group were 7.6% more likely to be hospitalized within a year compared with their peers in counties that had no telemental health use.
“We did see modest increases in inpatient use in counties that shifted the most to telemental health services, but that’s not typically viewed as a measure of quality because it can mean so many different things,” Dr. Huskamp said.
For example, it could mean that counties with greater telemental health use did a better job of identifying and responding to patients’ need for acute care, she noted. It could also be a reflection of the loss of psychiatric inpatient care in low-use communities.
Another tool
Commenting on the findings, Robert Caudill, MD, director of Telemedicine and Information Technology Programs at the University of Louisville (Ky.), called the increase in hospitalization in high-use counties “surprising.” However, he noted it might be a reflection of the need to fine-tune telemental health for patients with SMI.
“I think that more time and experience with telehealth will further normalize the practice and help to narrow, if not close, the gap,” said Dr. Caudill, who was not involved with the research.
“There are so many side benefits to doing things via telehealth,” he added. “It is a simple matter of continuing to learn how to do those things better.”
A multidisciplinary approach that includes psychiatric care and case management is generally considered to be the gold standard in treating patients with the types of mental illness included in this study, Dr. Caudill said.
While some of that care can be delivered effectively via telemedicine, it is possible other aspects, such as case management, are better handled in person, he added.
“I don’t think it is the role of telehealth to make in-person care obsolete. It is simply a tool to be used when appropriate,” said Dr. Caudill, past chair of the American Telemedicine Association’s Telemental Health Special Interest Group.
“Surgeons did not abandon scalpels when laser surgery became possible,” he said.
The study was funded by the National Institutes of Mental Health. Dr. Huskamp and Dr. Caudill report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
In a nationwide study, researchers drew on Medicare data from nearly 3,000 counties covering the period from 2000 to 2018. Results show that counties in which there was greater use of telemental health services reported higher increases of clinical visits and better follow-up after hospitalization among patients with bipolar 1 disorder and schizophrenia or other psychotic disorders.
In the study, “clinical visits” referred to both in-person and telemental health visits.
“These findings really support the idea that telemental health can be safe and effective and beneficial for in-person care for people with severe mental illness,” coinvestigator Haiden Huskamp, PhD, professor of health care policy at Harvard Medical School, Boston, said in an interview.
The findings were published online in JAMA Network Open.
Continuing trend?
Past studies have pointed to a sharp increase in the use of telepsychiatry services for patients with SMI. As reported by this news organization, this is a trend some clinicians say is likely to continue after the pandemic.
Use of telemedicine during the pandemic received a boost by the temporary suspension of certain Medicare rules that restrict telehealth use. Debate continues at the federal and state levels on whether to make that suspension permanent. Dr. Huskamp said more information is needed about the efficacy and accessibility of telemental health.
To investigate, researchers used Medicare fee-for-service data from 118,170 patients in 2,916 counties. More than two-thirds of the patients were aged 65 years or younger.
During the study period, telemental health service increased from 0.03 visits per patient with SMI in 2010 to 0.19 visits per patient in 2018. This increase was broad, with the number of counties reporting high use of telemental health increasing from 2% in 2010 to 17% in 2018.
Compared with counties in which there was no telemental health services, those with high use were less densely populated and had fewer health care professionals and hospital beds.
The number of overall visits with a mental health professional increased slightly in high-use counties compared to no-use counties, from 4.65 visits in 2010 to 4.79 visits in 2018. The number of in-person visits during that period declined from 4.55 visits in 2010 to 3.73 visits in 2018, which suggests that the overall increase was due to higher use of telemental health.
In the high-use group, the number of patients who had at least four mental health care visits increased 8%, and the number of patients who had a follow-up visit within 30 days of a hospitalization increased 20.4%.
A ‘helpful option’
“Telemedicine doesn’t address the national shortage of providers, but it definitely helps in underserved areas [and] rural areas,” Dr. Huskamp said.
“We need more mental health providers and need to develop new models of care that can leverage the providers we have in the best way possible. This is at least a helpful option, especially when you’re thinking about the maldistribution of providers across the country,” she added.
The study results showed that there was no difference in medication adherence between low- and high-use counties.
There was greater contact with mental health care providers in counties with high use of telemental health, and patients in the high-use group were 7.6% more likely to be hospitalized within a year compared with their peers in counties that had no telemental health use.
“We did see modest increases in inpatient use in counties that shifted the most to telemental health services, but that’s not typically viewed as a measure of quality because it can mean so many different things,” Dr. Huskamp said.
For example, it could mean that counties with greater telemental health use did a better job of identifying and responding to patients’ need for acute care, she noted. It could also be a reflection of the loss of psychiatric inpatient care in low-use communities.
Another tool
Commenting on the findings, Robert Caudill, MD, director of Telemedicine and Information Technology Programs at the University of Louisville (Ky.), called the increase in hospitalization in high-use counties “surprising.” However, he noted it might be a reflection of the need to fine-tune telemental health for patients with SMI.
“I think that more time and experience with telehealth will further normalize the practice and help to narrow, if not close, the gap,” said Dr. Caudill, who was not involved with the research.
“There are so many side benefits to doing things via telehealth,” he added. “It is a simple matter of continuing to learn how to do those things better.”
A multidisciplinary approach that includes psychiatric care and case management is generally considered to be the gold standard in treating patients with the types of mental illness included in this study, Dr. Caudill said.
While some of that care can be delivered effectively via telemedicine, it is possible other aspects, such as case management, are better handled in person, he added.
“I don’t think it is the role of telehealth to make in-person care obsolete. It is simply a tool to be used when appropriate,” said Dr. Caudill, past chair of the American Telemedicine Association’s Telemental Health Special Interest Group.
“Surgeons did not abandon scalpels when laser surgery became possible,” he said.
The study was funded by the National Institutes of Mental Health. Dr. Huskamp and Dr. Caudill report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
In a nationwide study, researchers drew on Medicare data from nearly 3,000 counties covering the period from 2000 to 2018. Results show that counties in which there was greater use of telemental health services reported higher increases of clinical visits and better follow-up after hospitalization among patients with bipolar 1 disorder and schizophrenia or other psychotic disorders.
In the study, “clinical visits” referred to both in-person and telemental health visits.
“These findings really support the idea that telemental health can be safe and effective and beneficial for in-person care for people with severe mental illness,” coinvestigator Haiden Huskamp, PhD, professor of health care policy at Harvard Medical School, Boston, said in an interview.
The findings were published online in JAMA Network Open.
Continuing trend?
Past studies have pointed to a sharp increase in the use of telepsychiatry services for patients with SMI. As reported by this news organization, this is a trend some clinicians say is likely to continue after the pandemic.
Use of telemedicine during the pandemic received a boost by the temporary suspension of certain Medicare rules that restrict telehealth use. Debate continues at the federal and state levels on whether to make that suspension permanent. Dr. Huskamp said more information is needed about the efficacy and accessibility of telemental health.
To investigate, researchers used Medicare fee-for-service data from 118,170 patients in 2,916 counties. More than two-thirds of the patients were aged 65 years or younger.
During the study period, telemental health service increased from 0.03 visits per patient with SMI in 2010 to 0.19 visits per patient in 2018. This increase was broad, with the number of counties reporting high use of telemental health increasing from 2% in 2010 to 17% in 2018.
Compared with counties in which there was no telemental health services, those with high use were less densely populated and had fewer health care professionals and hospital beds.
The number of overall visits with a mental health professional increased slightly in high-use counties compared to no-use counties, from 4.65 visits in 2010 to 4.79 visits in 2018. The number of in-person visits during that period declined from 4.55 visits in 2010 to 3.73 visits in 2018, which suggests that the overall increase was due to higher use of telemental health.
In the high-use group, the number of patients who had at least four mental health care visits increased 8%, and the number of patients who had a follow-up visit within 30 days of a hospitalization increased 20.4%.
A ‘helpful option’
“Telemedicine doesn’t address the national shortage of providers, but it definitely helps in underserved areas [and] rural areas,” Dr. Huskamp said.
“We need more mental health providers and need to develop new models of care that can leverage the providers we have in the best way possible. This is at least a helpful option, especially when you’re thinking about the maldistribution of providers across the country,” she added.
The study results showed that there was no difference in medication adherence between low- and high-use counties.
There was greater contact with mental health care providers in counties with high use of telemental health, and patients in the high-use group were 7.6% more likely to be hospitalized within a year compared with their peers in counties that had no telemental health use.
“We did see modest increases in inpatient use in counties that shifted the most to telemental health services, but that’s not typically viewed as a measure of quality because it can mean so many different things,” Dr. Huskamp said.
For example, it could mean that counties with greater telemental health use did a better job of identifying and responding to patients’ need for acute care, she noted. It could also be a reflection of the loss of psychiatric inpatient care in low-use communities.
Another tool
Commenting on the findings, Robert Caudill, MD, director of Telemedicine and Information Technology Programs at the University of Louisville (Ky.), called the increase in hospitalization in high-use counties “surprising.” However, he noted it might be a reflection of the need to fine-tune telemental health for patients with SMI.
“I think that more time and experience with telehealth will further normalize the practice and help to narrow, if not close, the gap,” said Dr. Caudill, who was not involved with the research.
“There are so many side benefits to doing things via telehealth,” he added. “It is a simple matter of continuing to learn how to do those things better.”
A multidisciplinary approach that includes psychiatric care and case management is generally considered to be the gold standard in treating patients with the types of mental illness included in this study, Dr. Caudill said.
While some of that care can be delivered effectively via telemedicine, it is possible other aspects, such as case management, are better handled in person, he added.
“I don’t think it is the role of telehealth to make in-person care obsolete. It is simply a tool to be used when appropriate,” said Dr. Caudill, past chair of the American Telemedicine Association’s Telemental Health Special Interest Group.
“Surgeons did not abandon scalpels when laser surgery became possible,” he said.
The study was funded by the National Institutes of Mental Health. Dr. Huskamp and Dr. Caudill report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
U.K. survey: Dermatologists want training in prescribing antipsychotics for delusional infestation
GLASGOW – that also indicated there is a clear demand for training in prescribing these drugs.
Delusional infestation is a rare disorder characterized by an individual’s belief that his or her skin, body, or immediate environment is infested by small, living pathogens, despite a lack of any medical evidence. Most of these patients require antipsychotic medication to alleviate symptoms.
The survey of almost 80 dermatologists found that almost 90% had not prescribed antipsychotics in the previous month for patients with psychodermatology conditions and that the most common barrier to prescribing was lack of experience with the drugs.
This was reflected in only 10% of survey respondents who said they were “happy to” prescribe antipsychotics without consulting either dermatology or psychiatric colleagues, and less than half having attended a related course.
Yet the research, presented at the annual meeting of the British Association of Dermatologists, indicated that more than 75% of respondents would attend such a course to increase their confidence.
This finding, said study presenter Ling Li, MD, Churchill Hospital, Oxford (England) University Hospitals NHS Foundation Trust, shows that there is a “clear demand for training, particularly among all the registrars [residents] who we surveyed.”
Dr. Li noted that the UK’s Joint Royal Colleges of Physicians Training Board’s latest curriculum for dermatology training highlights psychocutaneous medicine as a key area, and “that will include antipsychotic medication.”
The BAD also recently published guidelines for the management of adults with delusional infestation, which includes a recommendation to conduct a survey on attitudes toward antipsychotic prescribing for the condition among U.K. dermatologists.
Heeding that call, Dr. Li and colleagues sent an email containing a 10-question online survey to members of the BAD and the British Society for Medical Dermatology. Questions covered familiarity with antipsychotics and frequency of prescribing, confidence around antipsychotics, and current training and future needs. Responses were received between February through April 2021.
Among the 79 respondents, 51 (65%) were consultants and 20 (25%) were dermatology registrars, with the remainder dermatology clinical fellows, foundation doctors, or other doctors. A total of 31 respondents had an average of more than 50 visits with patients per week, 18 had an average of 41-50 patient visits, and 13 had an average of 31-40 visits per week; the remainder had an average of 11-30 visits per week.
Most of the respondents (39) said they had seen 2-5 patients with psychodermatology conditions in the last 6 months, while 17 said they had seen 1 patient, 13 said they had seen more than 10 patients, and 6 said they had seen 6-10 patients (4 had seen none and 1 could not remember).
The most commonly prescribed antipsychotics for psychodermatology patients in the past 6 months were risperidone (Risperdal; prescribed by five respondents), followed by olanzapine (Zyprexa; by four respondents). Seventy respondents had not prescribed any antipsychotics.
Asked about how confident they felt about prescribing antipsychotic medication for patients with delusional infestation, 8 (10%) said they were happy to prescribe independently, while 42 (54%) said they were not at all confident. Another 10 (13%) respondents said they would be happy to prescribe the medications after liaising with a dermatology colleague, while 17 (22%) said they would prefer to consult with the psychiatry team.
The most common barrier to prescribing antipsychotic medications was a lack of experience with the drugs, cited by 66 respondents, followed by concerns over drug monitoring, cited by 43 respondents.
In addition, 42 respondents highlighted concerns over adverse effects, 36 cited lack of experience in psychodermatology clinics, and 19 cited lack of experience in discussing psychodermatologic conditions with patients. Other barriers mentioned by the respondents included difficulties with patient acceptance of a psychiatric medication prescribed by a dermatologist.
An audience member went further, saying that clinicians have been told not to “confront” such patients and that the temptation is therefore to cloak the discussion of antipsychotics in nonthreatening language so that it is more acceptable to the patient.
However, under the U.K. system, a letter with the results of the consultation, including information that an antipsychotic has been prescribed, must be sent to the patient’s family doctor along with a copy that goes to the patient. “The situation is almost impossible,” the audience member said, adding that there “must be some arrangement where in certain circumstances dermatologists could be allowed not to write to the patient” or alternatively, “write an entirely different letter” to the family doctor.
Session cochair Susannah Baron, MD, a consultant dermatologist at St. John’s Institute of Dermatology, Guy’s and St. Thomas’ Hospital, London, said that, in these situations, it is “really helpful to talk about doses” with patients.
She explained that she uses the analogy of aspirin, which has different effects depending on the dose given, giving pain relief at high doses but primarily an antiplatelet effect at low doses.
In the case of an antipsychotic, it is helpful to explain to the patient that “you don’t think they’re psychotic, and you’re prescribing it in a very low dose, because what it can do is help with their symptoms,” Dr. Baron added. “You have to be very open because if you’re not, they go to the pharmacy, and the pharmacist says: ‘Why are you on an antipsychotic?’ ”
Further results from the survey revealed that 56 (71%) respondents did not have access to a specialist psychodermatology clinic, whereas 36 (46%) had not yet attended a psychodermatology course.
Despite these responses, 60 (77%) respondents said they would be interested in attending a training course for prescribing antipsychotics, which included all 20 of the registrars who took part in the survey. a psychodermatologist at Frimley Health Foundation Trust, Windsor, England, and lead author of the BAD guidelines, commented from the audience that the survey results were “sort of what we expected.”
She explained that the intention of the authors when developing the guidelines “was to be able to help our junior colleagues and our peers to be able to feel competent to discuss antipsychotics with patients with delusional infestation and also initiate management.”
Dr. Ahmed added: “Why we’re encouraging our colleagues to prescribe antipsychotics is the longer you leave this type of psychotic illness untreated, the worse the prognosis.”
No funding or relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
GLASGOW – that also indicated there is a clear demand for training in prescribing these drugs.
Delusional infestation is a rare disorder characterized by an individual’s belief that his or her skin, body, or immediate environment is infested by small, living pathogens, despite a lack of any medical evidence. Most of these patients require antipsychotic medication to alleviate symptoms.
The survey of almost 80 dermatologists found that almost 90% had not prescribed antipsychotics in the previous month for patients with psychodermatology conditions and that the most common barrier to prescribing was lack of experience with the drugs.
This was reflected in only 10% of survey respondents who said they were “happy to” prescribe antipsychotics without consulting either dermatology or psychiatric colleagues, and less than half having attended a related course.
Yet the research, presented at the annual meeting of the British Association of Dermatologists, indicated that more than 75% of respondents would attend such a course to increase their confidence.
This finding, said study presenter Ling Li, MD, Churchill Hospital, Oxford (England) University Hospitals NHS Foundation Trust, shows that there is a “clear demand for training, particularly among all the registrars [residents] who we surveyed.”
Dr. Li noted that the UK’s Joint Royal Colleges of Physicians Training Board’s latest curriculum for dermatology training highlights psychocutaneous medicine as a key area, and “that will include antipsychotic medication.”
The BAD also recently published guidelines for the management of adults with delusional infestation, which includes a recommendation to conduct a survey on attitudes toward antipsychotic prescribing for the condition among U.K. dermatologists.
Heeding that call, Dr. Li and colleagues sent an email containing a 10-question online survey to members of the BAD and the British Society for Medical Dermatology. Questions covered familiarity with antipsychotics and frequency of prescribing, confidence around antipsychotics, and current training and future needs. Responses were received between February through April 2021.
Among the 79 respondents, 51 (65%) were consultants and 20 (25%) were dermatology registrars, with the remainder dermatology clinical fellows, foundation doctors, or other doctors. A total of 31 respondents had an average of more than 50 visits with patients per week, 18 had an average of 41-50 patient visits, and 13 had an average of 31-40 visits per week; the remainder had an average of 11-30 visits per week.
Most of the respondents (39) said they had seen 2-5 patients with psychodermatology conditions in the last 6 months, while 17 said they had seen 1 patient, 13 said they had seen more than 10 patients, and 6 said they had seen 6-10 patients (4 had seen none and 1 could not remember).
The most commonly prescribed antipsychotics for psychodermatology patients in the past 6 months were risperidone (Risperdal; prescribed by five respondents), followed by olanzapine (Zyprexa; by four respondents). Seventy respondents had not prescribed any antipsychotics.
Asked about how confident they felt about prescribing antipsychotic medication for patients with delusional infestation, 8 (10%) said they were happy to prescribe independently, while 42 (54%) said they were not at all confident. Another 10 (13%) respondents said they would be happy to prescribe the medications after liaising with a dermatology colleague, while 17 (22%) said they would prefer to consult with the psychiatry team.
The most common barrier to prescribing antipsychotic medications was a lack of experience with the drugs, cited by 66 respondents, followed by concerns over drug monitoring, cited by 43 respondents.
In addition, 42 respondents highlighted concerns over adverse effects, 36 cited lack of experience in psychodermatology clinics, and 19 cited lack of experience in discussing psychodermatologic conditions with patients. Other barriers mentioned by the respondents included difficulties with patient acceptance of a psychiatric medication prescribed by a dermatologist.
An audience member went further, saying that clinicians have been told not to “confront” such patients and that the temptation is therefore to cloak the discussion of antipsychotics in nonthreatening language so that it is more acceptable to the patient.
However, under the U.K. system, a letter with the results of the consultation, including information that an antipsychotic has been prescribed, must be sent to the patient’s family doctor along with a copy that goes to the patient. “The situation is almost impossible,” the audience member said, adding that there “must be some arrangement where in certain circumstances dermatologists could be allowed not to write to the patient” or alternatively, “write an entirely different letter” to the family doctor.
Session cochair Susannah Baron, MD, a consultant dermatologist at St. John’s Institute of Dermatology, Guy’s and St. Thomas’ Hospital, London, said that, in these situations, it is “really helpful to talk about doses” with patients.
She explained that she uses the analogy of aspirin, which has different effects depending on the dose given, giving pain relief at high doses but primarily an antiplatelet effect at low doses.
In the case of an antipsychotic, it is helpful to explain to the patient that “you don’t think they’re psychotic, and you’re prescribing it in a very low dose, because what it can do is help with their symptoms,” Dr. Baron added. “You have to be very open because if you’re not, they go to the pharmacy, and the pharmacist says: ‘Why are you on an antipsychotic?’ ”
Further results from the survey revealed that 56 (71%) respondents did not have access to a specialist psychodermatology clinic, whereas 36 (46%) had not yet attended a psychodermatology course.
Despite these responses, 60 (77%) respondents said they would be interested in attending a training course for prescribing antipsychotics, which included all 20 of the registrars who took part in the survey. a psychodermatologist at Frimley Health Foundation Trust, Windsor, England, and lead author of the BAD guidelines, commented from the audience that the survey results were “sort of what we expected.”
She explained that the intention of the authors when developing the guidelines “was to be able to help our junior colleagues and our peers to be able to feel competent to discuss antipsychotics with patients with delusional infestation and also initiate management.”
Dr. Ahmed added: “Why we’re encouraging our colleagues to prescribe antipsychotics is the longer you leave this type of psychotic illness untreated, the worse the prognosis.”
No funding or relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
GLASGOW – that also indicated there is a clear demand for training in prescribing these drugs.
Delusional infestation is a rare disorder characterized by an individual’s belief that his or her skin, body, or immediate environment is infested by small, living pathogens, despite a lack of any medical evidence. Most of these patients require antipsychotic medication to alleviate symptoms.
The survey of almost 80 dermatologists found that almost 90% had not prescribed antipsychotics in the previous month for patients with psychodermatology conditions and that the most common barrier to prescribing was lack of experience with the drugs.
This was reflected in only 10% of survey respondents who said they were “happy to” prescribe antipsychotics without consulting either dermatology or psychiatric colleagues, and less than half having attended a related course.
Yet the research, presented at the annual meeting of the British Association of Dermatologists, indicated that more than 75% of respondents would attend such a course to increase their confidence.
This finding, said study presenter Ling Li, MD, Churchill Hospital, Oxford (England) University Hospitals NHS Foundation Trust, shows that there is a “clear demand for training, particularly among all the registrars [residents] who we surveyed.”
Dr. Li noted that the UK’s Joint Royal Colleges of Physicians Training Board’s latest curriculum for dermatology training highlights psychocutaneous medicine as a key area, and “that will include antipsychotic medication.”
The BAD also recently published guidelines for the management of adults with delusional infestation, which includes a recommendation to conduct a survey on attitudes toward antipsychotic prescribing for the condition among U.K. dermatologists.
Heeding that call, Dr. Li and colleagues sent an email containing a 10-question online survey to members of the BAD and the British Society for Medical Dermatology. Questions covered familiarity with antipsychotics and frequency of prescribing, confidence around antipsychotics, and current training and future needs. Responses were received between February through April 2021.
Among the 79 respondents, 51 (65%) were consultants and 20 (25%) were dermatology registrars, with the remainder dermatology clinical fellows, foundation doctors, or other doctors. A total of 31 respondents had an average of more than 50 visits with patients per week, 18 had an average of 41-50 patient visits, and 13 had an average of 31-40 visits per week; the remainder had an average of 11-30 visits per week.
Most of the respondents (39) said they had seen 2-5 patients with psychodermatology conditions in the last 6 months, while 17 said they had seen 1 patient, 13 said they had seen more than 10 patients, and 6 said they had seen 6-10 patients (4 had seen none and 1 could not remember).
The most commonly prescribed antipsychotics for psychodermatology patients in the past 6 months were risperidone (Risperdal; prescribed by five respondents), followed by olanzapine (Zyprexa; by four respondents). Seventy respondents had not prescribed any antipsychotics.
Asked about how confident they felt about prescribing antipsychotic medication for patients with delusional infestation, 8 (10%) said they were happy to prescribe independently, while 42 (54%) said they were not at all confident. Another 10 (13%) respondents said they would be happy to prescribe the medications after liaising with a dermatology colleague, while 17 (22%) said they would prefer to consult with the psychiatry team.
The most common barrier to prescribing antipsychotic medications was a lack of experience with the drugs, cited by 66 respondents, followed by concerns over drug monitoring, cited by 43 respondents.
In addition, 42 respondents highlighted concerns over adverse effects, 36 cited lack of experience in psychodermatology clinics, and 19 cited lack of experience in discussing psychodermatologic conditions with patients. Other barriers mentioned by the respondents included difficulties with patient acceptance of a psychiatric medication prescribed by a dermatologist.
An audience member went further, saying that clinicians have been told not to “confront” such patients and that the temptation is therefore to cloak the discussion of antipsychotics in nonthreatening language so that it is more acceptable to the patient.
However, under the U.K. system, a letter with the results of the consultation, including information that an antipsychotic has been prescribed, must be sent to the patient’s family doctor along with a copy that goes to the patient. “The situation is almost impossible,” the audience member said, adding that there “must be some arrangement where in certain circumstances dermatologists could be allowed not to write to the patient” or alternatively, “write an entirely different letter” to the family doctor.
Session cochair Susannah Baron, MD, a consultant dermatologist at St. John’s Institute of Dermatology, Guy’s and St. Thomas’ Hospital, London, said that, in these situations, it is “really helpful to talk about doses” with patients.
She explained that she uses the analogy of aspirin, which has different effects depending on the dose given, giving pain relief at high doses but primarily an antiplatelet effect at low doses.
In the case of an antipsychotic, it is helpful to explain to the patient that “you don’t think they’re psychotic, and you’re prescribing it in a very low dose, because what it can do is help with their symptoms,” Dr. Baron added. “You have to be very open because if you’re not, they go to the pharmacy, and the pharmacist says: ‘Why are you on an antipsychotic?’ ”
Further results from the survey revealed that 56 (71%) respondents did not have access to a specialist psychodermatology clinic, whereas 36 (46%) had not yet attended a psychodermatology course.
Despite these responses, 60 (77%) respondents said they would be interested in attending a training course for prescribing antipsychotics, which included all 20 of the registrars who took part in the survey. a psychodermatologist at Frimley Health Foundation Trust, Windsor, England, and lead author of the BAD guidelines, commented from the audience that the survey results were “sort of what we expected.”
She explained that the intention of the authors when developing the guidelines “was to be able to help our junior colleagues and our peers to be able to feel competent to discuss antipsychotics with patients with delusional infestation and also initiate management.”
Dr. Ahmed added: “Why we’re encouraging our colleagues to prescribe antipsychotics is the longer you leave this type of psychotic illness untreated, the worse the prognosis.”
No funding or relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
AT BAD 2022
How to manage cancer pain when patients misuse opioids
Opioids remain a staple in pain management for cancer, but there is little guidance around how to treat patients who have a history of opioid misuse.
Recently,
“There is a tendency to ignore treatment of opioid use disorder in advanced cancer patients because people think: ‘Oh, this person has bigger fish to fry,’ but that’s not a very patient-centric way of looking at things,” senior author Jessica Merlin, MD, PhD, with the University of Pittsburgh, said in a news release.
“We know that opioid use disorder is a really important factor in quality of life, so addressing opioid addiction and prescription opioid misuse in people with advanced cancer is really critical,” Dr. Merlin added.
The study was published online in JAMA Oncology.
To improve care for people with advanced cancer and cancer-related pain, the researchers first assessed how clinicians currently treat patients with opioid complexity.
Using an online Delphi platform, the team invited 120 clinicians with expertise in palliative care, pain management, and addiction medicine to weigh in on three common clinical scenarios – a patient with a recent history of untreated opioid use disorder, a patient taking more opioids than prescribed, and a patient using nonprescribed benzodiazepines.
For a patient with cancer and a recent history of untreated opioid use disorder, regardless of prognosis, the panel deemed it appropriate to begin treatment with buprenorphine/naloxone for pain but inappropriate to refer the patient to a methadone clinic. The panel felt that going to a methadone clinic would be too burdensome for a patient with advanced cancer and not possible for those with limited prognoses.
“This underscores the importance of access to [opioid use disorder] treatment in cancer treatment settings, including non–addiction specialists waivered to prescribe buprenorphine/naloxone and addiction specialists for more complex cases,” the authors wrote.
For a patient with untreated opioid use disorder, the panel deemed split-dose methadone (two to three times daily) appropriate in those with limited prognosis of weeks to months but was uncertain about the suitability of this approach for patients with longer prognoses of a year or longer.
The appropriateness of initiating treatment with a full-agonist opioid was considered uncertain for a patient with limited prognosis and inappropriate for a patient with longer prognosis.
For a patient with cancer pain and no medical history of opioid use disorder but taking more opioids than prescribed, regardless of prognosis, the panel felt it was appropriate to increase monitoring and inappropriate to taper opioids. The panel was not certain about whether to increase opioids based on the patient’s account of what they need or transition to buprenorphine/naloxone.
For a patient with no history of opioid use disorder who was prescribed traditional opioids for pain and had a positive urine drug test for nonprescribed benzodiazepines, regardless of prognosis, the panel felt it was appropriate to continue opioids with close monitoring and inappropriate to taper opioids or transition to buprenorphine/naloxone.
The researchers said that improving education around buprenorphine and cancer pain management in the context of opioid use disorder or misuse is needed.
In a related editorial, two experts noted that the patients considered in this “important article” require considerable time and expertise from an interdisciplinary team.
“It is important that cancer centers establish and fund such teams mainly as a safety measure for these patients and also as a major contribution to the care of all patients with cancer,” wrote Joseph Arthur, MD, and Eduardo Bruera, MD, with the University of Texas MD Anderson Cancer Center, Houston.
In the wider context, Dr. Arthur and Dr. Bruera highlighted how treatments for patients with advanced cancer have evolved over the past 3 decades, yet patients have continued to be given opioids to address cancer-related pain. Developing more sophisticated drugs that relieve pain without significant side effects or addictive properties is imperative.
Dr. Arthur and Dr. Bruera said the study authors “appropriately emphasize the value of delivering compassionate and expert care for these particularly complex cases and the importance of conducting research on the best ways to alleviate the suffering in this rapidly growing patient population.”
This research was supported by Cambia Health Foundation and the National Institute of Nursing Research. Dr. Merlin, Dr. Arthur, and Dr. Bruera reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Opioids remain a staple in pain management for cancer, but there is little guidance around how to treat patients who have a history of opioid misuse.
Recently,
“There is a tendency to ignore treatment of opioid use disorder in advanced cancer patients because people think: ‘Oh, this person has bigger fish to fry,’ but that’s not a very patient-centric way of looking at things,” senior author Jessica Merlin, MD, PhD, with the University of Pittsburgh, said in a news release.
“We know that opioid use disorder is a really important factor in quality of life, so addressing opioid addiction and prescription opioid misuse in people with advanced cancer is really critical,” Dr. Merlin added.
The study was published online in JAMA Oncology.
To improve care for people with advanced cancer and cancer-related pain, the researchers first assessed how clinicians currently treat patients with opioid complexity.
Using an online Delphi platform, the team invited 120 clinicians with expertise in palliative care, pain management, and addiction medicine to weigh in on three common clinical scenarios – a patient with a recent history of untreated opioid use disorder, a patient taking more opioids than prescribed, and a patient using nonprescribed benzodiazepines.
For a patient with cancer and a recent history of untreated opioid use disorder, regardless of prognosis, the panel deemed it appropriate to begin treatment with buprenorphine/naloxone for pain but inappropriate to refer the patient to a methadone clinic. The panel felt that going to a methadone clinic would be too burdensome for a patient with advanced cancer and not possible for those with limited prognoses.
“This underscores the importance of access to [opioid use disorder] treatment in cancer treatment settings, including non–addiction specialists waivered to prescribe buprenorphine/naloxone and addiction specialists for more complex cases,” the authors wrote.
For a patient with untreated opioid use disorder, the panel deemed split-dose methadone (two to three times daily) appropriate in those with limited prognosis of weeks to months but was uncertain about the suitability of this approach for patients with longer prognoses of a year or longer.
The appropriateness of initiating treatment with a full-agonist opioid was considered uncertain for a patient with limited prognosis and inappropriate for a patient with longer prognosis.
For a patient with cancer pain and no medical history of opioid use disorder but taking more opioids than prescribed, regardless of prognosis, the panel felt it was appropriate to increase monitoring and inappropriate to taper opioids. The panel was not certain about whether to increase opioids based on the patient’s account of what they need or transition to buprenorphine/naloxone.
For a patient with no history of opioid use disorder who was prescribed traditional opioids for pain and had a positive urine drug test for nonprescribed benzodiazepines, regardless of prognosis, the panel felt it was appropriate to continue opioids with close monitoring and inappropriate to taper opioids or transition to buprenorphine/naloxone.
The researchers said that improving education around buprenorphine and cancer pain management in the context of opioid use disorder or misuse is needed.
In a related editorial, two experts noted that the patients considered in this “important article” require considerable time and expertise from an interdisciplinary team.
“It is important that cancer centers establish and fund such teams mainly as a safety measure for these patients and also as a major contribution to the care of all patients with cancer,” wrote Joseph Arthur, MD, and Eduardo Bruera, MD, with the University of Texas MD Anderson Cancer Center, Houston.
In the wider context, Dr. Arthur and Dr. Bruera highlighted how treatments for patients with advanced cancer have evolved over the past 3 decades, yet patients have continued to be given opioids to address cancer-related pain. Developing more sophisticated drugs that relieve pain without significant side effects or addictive properties is imperative.
Dr. Arthur and Dr. Bruera said the study authors “appropriately emphasize the value of delivering compassionate and expert care for these particularly complex cases and the importance of conducting research on the best ways to alleviate the suffering in this rapidly growing patient population.”
This research was supported by Cambia Health Foundation and the National Institute of Nursing Research. Dr. Merlin, Dr. Arthur, and Dr. Bruera reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Opioids remain a staple in pain management for cancer, but there is little guidance around how to treat patients who have a history of opioid misuse.
Recently,
“There is a tendency to ignore treatment of opioid use disorder in advanced cancer patients because people think: ‘Oh, this person has bigger fish to fry,’ but that’s not a very patient-centric way of looking at things,” senior author Jessica Merlin, MD, PhD, with the University of Pittsburgh, said in a news release.
“We know that opioid use disorder is a really important factor in quality of life, so addressing opioid addiction and prescription opioid misuse in people with advanced cancer is really critical,” Dr. Merlin added.
The study was published online in JAMA Oncology.
To improve care for people with advanced cancer and cancer-related pain, the researchers first assessed how clinicians currently treat patients with opioid complexity.
Using an online Delphi platform, the team invited 120 clinicians with expertise in palliative care, pain management, and addiction medicine to weigh in on three common clinical scenarios – a patient with a recent history of untreated opioid use disorder, a patient taking more opioids than prescribed, and a patient using nonprescribed benzodiazepines.
For a patient with cancer and a recent history of untreated opioid use disorder, regardless of prognosis, the panel deemed it appropriate to begin treatment with buprenorphine/naloxone for pain but inappropriate to refer the patient to a methadone clinic. The panel felt that going to a methadone clinic would be too burdensome for a patient with advanced cancer and not possible for those with limited prognoses.
“This underscores the importance of access to [opioid use disorder] treatment in cancer treatment settings, including non–addiction specialists waivered to prescribe buprenorphine/naloxone and addiction specialists for more complex cases,” the authors wrote.
For a patient with untreated opioid use disorder, the panel deemed split-dose methadone (two to three times daily) appropriate in those with limited prognosis of weeks to months but was uncertain about the suitability of this approach for patients with longer prognoses of a year or longer.
The appropriateness of initiating treatment with a full-agonist opioid was considered uncertain for a patient with limited prognosis and inappropriate for a patient with longer prognosis.
For a patient with cancer pain and no medical history of opioid use disorder but taking more opioids than prescribed, regardless of prognosis, the panel felt it was appropriate to increase monitoring and inappropriate to taper opioids. The panel was not certain about whether to increase opioids based on the patient’s account of what they need or transition to buprenorphine/naloxone.
For a patient with no history of opioid use disorder who was prescribed traditional opioids for pain and had a positive urine drug test for nonprescribed benzodiazepines, regardless of prognosis, the panel felt it was appropriate to continue opioids with close monitoring and inappropriate to taper opioids or transition to buprenorphine/naloxone.
The researchers said that improving education around buprenorphine and cancer pain management in the context of opioid use disorder or misuse is needed.
In a related editorial, two experts noted that the patients considered in this “important article” require considerable time and expertise from an interdisciplinary team.
“It is important that cancer centers establish and fund such teams mainly as a safety measure for these patients and also as a major contribution to the care of all patients with cancer,” wrote Joseph Arthur, MD, and Eduardo Bruera, MD, with the University of Texas MD Anderson Cancer Center, Houston.
In the wider context, Dr. Arthur and Dr. Bruera highlighted how treatments for patients with advanced cancer have evolved over the past 3 decades, yet patients have continued to be given opioids to address cancer-related pain. Developing more sophisticated drugs that relieve pain without significant side effects or addictive properties is imperative.
Dr. Arthur and Dr. Bruera said the study authors “appropriately emphasize the value of delivering compassionate and expert care for these particularly complex cases and the importance of conducting research on the best ways to alleviate the suffering in this rapidly growing patient population.”
This research was supported by Cambia Health Foundation and the National Institute of Nursing Research. Dr. Merlin, Dr. Arthur, and Dr. Bruera reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM JAMA ONCOLOGY
Mosquitoes and the vicious circle that’s gone viral
These viruses want mosquitoes with good taste
Taste can be a pretty subjective sense. Not everyone agrees on what tastes good and what tastes bad. Most people would agree that freshly baked cookies taste good, but what about lima beans? And what about mosquitoes? What tastes good to a mosquito?
The answer? Blood. Blood tastes good to a mosquito. That really wasn’t a very hard question, was it? You did know the answer, didn’t you? They don’t care about cookies, and they certainly don’t care about lima beans. It’s blood that they love.
That brings us back to subjectivity, because it is possible for blood to taste even better. The secret ingredient is dengue … and Zika.
A study just published in Cell demonstrates that mice infected with dengue and Zika viruses release a volatile compound called acetophenone. “We found that flavivirus [like dengue and Zika] can utilize the increased release of acetophenone to help itself achieve its lifecycles more effectively by making their hosts more attractive to mosquito vectors,” senior author Gong Cheng of Tsinghua University, Beijing, said in a written statement.
How do they do it? The viruses, he explained, promote the proliferation of acetophenone-producing skin bacteria. “As a result, some bacteria overreplicate and produce more acetophenone. Suddenly, these sick individuals smell as delicious to mosquitoes as a tray of freshly baked cookies to a group of five-year-old children,” the statement said.
And how do you stop a group of tiny, flying 5-year-olds? That’s right, with acne medication. Really? You knew that one but not the blood one before? The investigators fed isotretinoin to the infected mice, which led to reduced acetophenone release from skin bacteria and made the animals no more attractive to the mosquitoes than their uninfected counterparts.
The investigators are planning to take the next step – feeding isotretinoin to people with dengue and Zika – having gotten the official fictional taste-test approval of celebrity chef Gordon Ramsay, who said, “You’re going to feed this #$^% to sick people? ARE YOU &%*$@#& KIDDING ME?”
Okay, so maybe approval isn’t quite the right word.
Welcome to bladders of the rich and famous!
Don’t you hate it when you’re driving out to your multimillion-dollar second home in the Hamptons and traffic is so bad you absolutely have to find a place to “rest” along the way? But wouldn’t you know it, there just isn’t anywhere to stop! Geez, how do we live?
That’s where David Shusterman, MD, a urologist in New York City and a true American hero, comes in. He’s identified a market and positioned himself as the king of both bladder surgery and “bladder Botox” for the wealthy New Yorkers who regularly make long journeys from the city out to their second homes in the Hamptons. Traffic has increased dramatically on Long Island roads in recent years, and the journey can now taking upward of 4 hours. Some people just can’t make it that long without a bathroom break, and there are very few places to stop along the way.
Dr. Shusterman understands the plight of the Hamptons vacationer, as he told Insider.com: “I can’t tell you how many arguments I personally get into – I’ve lost three friends because I’m the driver and refuse to stop for them.” A tragedy worthy of Shakespeare himself.
During the summer season, Dr. Shusterman performs about 10 prostate artery embolizations a week, an hour-long procedure that shrinks the prostate, which is great for 50- to 60-year-old men with enlarged prostates that cause more frequent bathroom trips. He also performs Botox injections into the bladder once or twice a week for women, which reduces the need to urinate for roughly 6 months. The perfect amount of time to get them through the summer season.
These procedures are sometimes covered by insurance but can cost as much as $20,000 if paid out of pocket. That’s a lot of money to us, but if you’re the sort of person who has a second home in the Hamptons, $20,000 is chump change, especially if it means you won’t have to go 2 entire minutes out of your way to use a gas-station bathroom. Then again, having seen a more than a few gas-station bathrooms in our time, maybe they have a point.
Ditch the apples. Go for the avocados
We’ve all heard about “an apple a day,” but instead of apples you might want to go with avocados.
Avocados are generally thought to be a healthy fat. A study just published in the Journal of the American Heart Association proves that they actually don’t do anything for your waistline but will work wonders on your cholesterol level. The study involved 923 participants who were considered overweight/obese split into two groups: One was asked to consume an avocado a day, and the other continued their usual diets and were asked to consume fewer than two avocados a month.
At the end of the 6 months, the researchers found total cholesterol decreased by an additional 2.9 mg/dL and LDL cholesterol by 2.5 mg/dL in those who ate one avocado every day, compared with the usual-diet group. And even though avocados have a lot of calories, there was no clinical evidence that it impacted weight gain or any cardiometabolic risk factors, according to a statement from Penn State University.
Avocados, then, can be considered a guilt-free food. The findings from this study suggest it can give a substantial boost to your overall quality of diet, in turn lessening your risk of developing type 2 diabetes and some cancers, Kristina Peterson, PhD, assistant professor of nutritional sciences at Texas Tech University, said in the statement.
So get creative with your avocado recipes. You can only eat so much guacamole.
Your nose knows a good friend for you
You’ve probably noticed how dogs sniff other dogs and people before becoming friends. It would be pretty comical if people did the same thing, right? Just walked up to strangers and started sniffing them like dogs?
Well, apparently humans do go by smell when it comes to making friends, and they prefer people who smell like them. Maybe you’ve noticed that your friends look like you, share your values, and think the same way as you. You’re probably right, seeing as previous research has pointed to this.
For the current study, done to show how smell affects human behavior, researchers recruited people who befriended each other quickly, before knowing much about each other. They assumed that the relationships between these same-sex, nonromantic “click friends” relied more on physiological traits, including smell. After collecting samples from the click friends, researchers used an eNose to scan chemical signatures. In another experiment, human volunteers sniffed samples to determine if any were similar. Both experiments showed that click friends had more similar smells than pairs of random people.
“This is not to say that we act like goats or shrews – humans likely rely on other, far more dominant cues in their social decision-making. Nevertheless, our study’s results do suggest that our nose plays a bigger role than previously thought in our choice of friends,” said senior author Noam Sobel, PhD, of the Weizmann Institute of Science in Rehovot, Israel.
Lead author Inbal Ravreby, a graduate student at the institute, put it this way: “These results imply that, as the saying goes, there is chemistry in social chemistry.”
These viruses want mosquitoes with good taste
Taste can be a pretty subjective sense. Not everyone agrees on what tastes good and what tastes bad. Most people would agree that freshly baked cookies taste good, but what about lima beans? And what about mosquitoes? What tastes good to a mosquito?
The answer? Blood. Blood tastes good to a mosquito. That really wasn’t a very hard question, was it? You did know the answer, didn’t you? They don’t care about cookies, and they certainly don’t care about lima beans. It’s blood that they love.
That brings us back to subjectivity, because it is possible for blood to taste even better. The secret ingredient is dengue … and Zika.
A study just published in Cell demonstrates that mice infected with dengue and Zika viruses release a volatile compound called acetophenone. “We found that flavivirus [like dengue and Zika] can utilize the increased release of acetophenone to help itself achieve its lifecycles more effectively by making their hosts more attractive to mosquito vectors,” senior author Gong Cheng of Tsinghua University, Beijing, said in a written statement.
How do they do it? The viruses, he explained, promote the proliferation of acetophenone-producing skin bacteria. “As a result, some bacteria overreplicate and produce more acetophenone. Suddenly, these sick individuals smell as delicious to mosquitoes as a tray of freshly baked cookies to a group of five-year-old children,” the statement said.
And how do you stop a group of tiny, flying 5-year-olds? That’s right, with acne medication. Really? You knew that one but not the blood one before? The investigators fed isotretinoin to the infected mice, which led to reduced acetophenone release from skin bacteria and made the animals no more attractive to the mosquitoes than their uninfected counterparts.
The investigators are planning to take the next step – feeding isotretinoin to people with dengue and Zika – having gotten the official fictional taste-test approval of celebrity chef Gordon Ramsay, who said, “You’re going to feed this #$^% to sick people? ARE YOU &%*$@#& KIDDING ME?”
Okay, so maybe approval isn’t quite the right word.
Welcome to bladders of the rich and famous!
Don’t you hate it when you’re driving out to your multimillion-dollar second home in the Hamptons and traffic is so bad you absolutely have to find a place to “rest” along the way? But wouldn’t you know it, there just isn’t anywhere to stop! Geez, how do we live?
That’s where David Shusterman, MD, a urologist in New York City and a true American hero, comes in. He’s identified a market and positioned himself as the king of both bladder surgery and “bladder Botox” for the wealthy New Yorkers who regularly make long journeys from the city out to their second homes in the Hamptons. Traffic has increased dramatically on Long Island roads in recent years, and the journey can now taking upward of 4 hours. Some people just can’t make it that long without a bathroom break, and there are very few places to stop along the way.
Dr. Shusterman understands the plight of the Hamptons vacationer, as he told Insider.com: “I can’t tell you how many arguments I personally get into – I’ve lost three friends because I’m the driver and refuse to stop for them.” A tragedy worthy of Shakespeare himself.
During the summer season, Dr. Shusterman performs about 10 prostate artery embolizations a week, an hour-long procedure that shrinks the prostate, which is great for 50- to 60-year-old men with enlarged prostates that cause more frequent bathroom trips. He also performs Botox injections into the bladder once or twice a week for women, which reduces the need to urinate for roughly 6 months. The perfect amount of time to get them through the summer season.
These procedures are sometimes covered by insurance but can cost as much as $20,000 if paid out of pocket. That’s a lot of money to us, but if you’re the sort of person who has a second home in the Hamptons, $20,000 is chump change, especially if it means you won’t have to go 2 entire minutes out of your way to use a gas-station bathroom. Then again, having seen a more than a few gas-station bathrooms in our time, maybe they have a point.
Ditch the apples. Go for the avocados
We’ve all heard about “an apple a day,” but instead of apples you might want to go with avocados.
Avocados are generally thought to be a healthy fat. A study just published in the Journal of the American Heart Association proves that they actually don’t do anything for your waistline but will work wonders on your cholesterol level. The study involved 923 participants who were considered overweight/obese split into two groups: One was asked to consume an avocado a day, and the other continued their usual diets and were asked to consume fewer than two avocados a month.
At the end of the 6 months, the researchers found total cholesterol decreased by an additional 2.9 mg/dL and LDL cholesterol by 2.5 mg/dL in those who ate one avocado every day, compared with the usual-diet group. And even though avocados have a lot of calories, there was no clinical evidence that it impacted weight gain or any cardiometabolic risk factors, according to a statement from Penn State University.
Avocados, then, can be considered a guilt-free food. The findings from this study suggest it can give a substantial boost to your overall quality of diet, in turn lessening your risk of developing type 2 diabetes and some cancers, Kristina Peterson, PhD, assistant professor of nutritional sciences at Texas Tech University, said in the statement.
So get creative with your avocado recipes. You can only eat so much guacamole.
Your nose knows a good friend for you
You’ve probably noticed how dogs sniff other dogs and people before becoming friends. It would be pretty comical if people did the same thing, right? Just walked up to strangers and started sniffing them like dogs?
Well, apparently humans do go by smell when it comes to making friends, and they prefer people who smell like them. Maybe you’ve noticed that your friends look like you, share your values, and think the same way as you. You’re probably right, seeing as previous research has pointed to this.
For the current study, done to show how smell affects human behavior, researchers recruited people who befriended each other quickly, before knowing much about each other. They assumed that the relationships between these same-sex, nonromantic “click friends” relied more on physiological traits, including smell. After collecting samples from the click friends, researchers used an eNose to scan chemical signatures. In another experiment, human volunteers sniffed samples to determine if any were similar. Both experiments showed that click friends had more similar smells than pairs of random people.
“This is not to say that we act like goats or shrews – humans likely rely on other, far more dominant cues in their social decision-making. Nevertheless, our study’s results do suggest that our nose plays a bigger role than previously thought in our choice of friends,” said senior author Noam Sobel, PhD, of the Weizmann Institute of Science in Rehovot, Israel.
Lead author Inbal Ravreby, a graduate student at the institute, put it this way: “These results imply that, as the saying goes, there is chemistry in social chemistry.”
These viruses want mosquitoes with good taste
Taste can be a pretty subjective sense. Not everyone agrees on what tastes good and what tastes bad. Most people would agree that freshly baked cookies taste good, but what about lima beans? And what about mosquitoes? What tastes good to a mosquito?
The answer? Blood. Blood tastes good to a mosquito. That really wasn’t a very hard question, was it? You did know the answer, didn’t you? They don’t care about cookies, and they certainly don’t care about lima beans. It’s blood that they love.
That brings us back to subjectivity, because it is possible for blood to taste even better. The secret ingredient is dengue … and Zika.
A study just published in Cell demonstrates that mice infected with dengue and Zika viruses release a volatile compound called acetophenone. “We found that flavivirus [like dengue and Zika] can utilize the increased release of acetophenone to help itself achieve its lifecycles more effectively by making their hosts more attractive to mosquito vectors,” senior author Gong Cheng of Tsinghua University, Beijing, said in a written statement.
How do they do it? The viruses, he explained, promote the proliferation of acetophenone-producing skin bacteria. “As a result, some bacteria overreplicate and produce more acetophenone. Suddenly, these sick individuals smell as delicious to mosquitoes as a tray of freshly baked cookies to a group of five-year-old children,” the statement said.
And how do you stop a group of tiny, flying 5-year-olds? That’s right, with acne medication. Really? You knew that one but not the blood one before? The investigators fed isotretinoin to the infected mice, which led to reduced acetophenone release from skin bacteria and made the animals no more attractive to the mosquitoes than their uninfected counterparts.
The investigators are planning to take the next step – feeding isotretinoin to people with dengue and Zika – having gotten the official fictional taste-test approval of celebrity chef Gordon Ramsay, who said, “You’re going to feed this #$^% to sick people? ARE YOU &%*$@#& KIDDING ME?”
Okay, so maybe approval isn’t quite the right word.
Welcome to bladders of the rich and famous!
Don’t you hate it when you’re driving out to your multimillion-dollar second home in the Hamptons and traffic is so bad you absolutely have to find a place to “rest” along the way? But wouldn’t you know it, there just isn’t anywhere to stop! Geez, how do we live?
That’s where David Shusterman, MD, a urologist in New York City and a true American hero, comes in. He’s identified a market and positioned himself as the king of both bladder surgery and “bladder Botox” for the wealthy New Yorkers who regularly make long journeys from the city out to their second homes in the Hamptons. Traffic has increased dramatically on Long Island roads in recent years, and the journey can now taking upward of 4 hours. Some people just can’t make it that long without a bathroom break, and there are very few places to stop along the way.
Dr. Shusterman understands the plight of the Hamptons vacationer, as he told Insider.com: “I can’t tell you how many arguments I personally get into – I’ve lost three friends because I’m the driver and refuse to stop for them.” A tragedy worthy of Shakespeare himself.
During the summer season, Dr. Shusterman performs about 10 prostate artery embolizations a week, an hour-long procedure that shrinks the prostate, which is great for 50- to 60-year-old men with enlarged prostates that cause more frequent bathroom trips. He also performs Botox injections into the bladder once or twice a week for women, which reduces the need to urinate for roughly 6 months. The perfect amount of time to get them through the summer season.
These procedures are sometimes covered by insurance but can cost as much as $20,000 if paid out of pocket. That’s a lot of money to us, but if you’re the sort of person who has a second home in the Hamptons, $20,000 is chump change, especially if it means you won’t have to go 2 entire minutes out of your way to use a gas-station bathroom. Then again, having seen a more than a few gas-station bathrooms in our time, maybe they have a point.
Ditch the apples. Go for the avocados
We’ve all heard about “an apple a day,” but instead of apples you might want to go with avocados.
Avocados are generally thought to be a healthy fat. A study just published in the Journal of the American Heart Association proves that they actually don’t do anything for your waistline but will work wonders on your cholesterol level. The study involved 923 participants who were considered overweight/obese split into two groups: One was asked to consume an avocado a day, and the other continued their usual diets and were asked to consume fewer than two avocados a month.
At the end of the 6 months, the researchers found total cholesterol decreased by an additional 2.9 mg/dL and LDL cholesterol by 2.5 mg/dL in those who ate one avocado every day, compared with the usual-diet group. And even though avocados have a lot of calories, there was no clinical evidence that it impacted weight gain or any cardiometabolic risk factors, according to a statement from Penn State University.
Avocados, then, can be considered a guilt-free food. The findings from this study suggest it can give a substantial boost to your overall quality of diet, in turn lessening your risk of developing type 2 diabetes and some cancers, Kristina Peterson, PhD, assistant professor of nutritional sciences at Texas Tech University, said in the statement.
So get creative with your avocado recipes. You can only eat so much guacamole.
Your nose knows a good friend for you
You’ve probably noticed how dogs sniff other dogs and people before becoming friends. It would be pretty comical if people did the same thing, right? Just walked up to strangers and started sniffing them like dogs?
Well, apparently humans do go by smell when it comes to making friends, and they prefer people who smell like them. Maybe you’ve noticed that your friends look like you, share your values, and think the same way as you. You’re probably right, seeing as previous research has pointed to this.
For the current study, done to show how smell affects human behavior, researchers recruited people who befriended each other quickly, before knowing much about each other. They assumed that the relationships between these same-sex, nonromantic “click friends” relied more on physiological traits, including smell. After collecting samples from the click friends, researchers used an eNose to scan chemical signatures. In another experiment, human volunteers sniffed samples to determine if any were similar. Both experiments showed that click friends had more similar smells than pairs of random people.
“This is not to say that we act like goats or shrews – humans likely rely on other, far more dominant cues in their social decision-making. Nevertheless, our study’s results do suggest that our nose plays a bigger role than previously thought in our choice of friends,” said senior author Noam Sobel, PhD, of the Weizmann Institute of Science in Rehovot, Israel.
Lead author Inbal Ravreby, a graduate student at the institute, put it this way: “These results imply that, as the saying goes, there is chemistry in social chemistry.”
Book Review: Quality improvement in mental health care
Sunil Khushalani and Antonio DePaolo,
“Transforming Mental Healthcare: Applying Performance Improvement Methods to Mental Healthcare”
(London: Routledge, Taylor & Francis, 2022)
Since the publication of our book, “Lean Behavioral Health: The Kings County Hospital Story” (Oxford, England: Oxford University Press, 2014) almost a decade ago, “Transforming Mental Healthcare” is the first major book published about the use of a system for quality improvement across the health care continuum. That it has taken this long is probably surprising to those of us who have spent careers on trying to improve what is universally described as a system that is “broken” and in need of a major overhaul.
Every news cycle that reports mass violence typically spends a good bit of time talking about the failures of the mental health care system. One important lesson I learned when taking over the beleaguered Kings County (N.Y.) psychiatry service in 2009 (a department that has made extraordinary improvements over the years and is now exclaimed by the U.S. Department of Justice as “a model program”), is that the employees on the front line are often erroneously blamed for such failures.
The failure is systemic and usually starts at the top of the table of organization, not at the bottom. Dr. Khushalani and Dr. DePaolo have produced an excellent volume that should be purchased by every mental health care CEO and given “with thanks” to the local leaders overseeing the direct care of some of our nation’s most vulnerable patient populations.
The first part of “Transforming Mental Healthcare” provides an excellent overview of the current state of our mental health care system and its too numerous to name problems. This section could be a primer for all our legislators so their eyes can be opened to the failures on the ground that require their help in correcting. Many of the “failures” of our mental health care are societal failures – lack of affordable housing, access to care, reimbursement for care, gun access, etc. – and cannot be “fixed” by providers of care. Such problems are societal problems that call for societal and governmental solutions, and not only at the local level but from coast to coast.
The remainder of this easy to read and follow text provides many rich resources for the deliverers of mental health care. (e.g., plan-do-act, standard work, and A3 thinking).
The closing section focuses on leadership and culture – often overlooked to the detriment of any organization that doesn’t pay close attention to supporting both. Culture is cultivated and nourished by the organization’s leaders. Culture empowers staff to become problem solvers and agents of improvement. Empowered staff support and enrich their culture. Together a workplace that brings out the best of all its people is created, and burnout is held at bay.
“Transforming Mental Healthcare: Applying Performance Improvement Methods to Mental Healthcare” is a welcome and essential addition to the current morass, which is our mental health care delivery system, an oasis in the desert from which perhaps the lotus flower can emerge.
Dr. Merlino is emeritus professor of psychiatry, SUNY Downstate College of Medicine, Rhinebeck, N.Y., and formerly director of psychiatry at Kings County Hospital Center, Brooklyn, NY. He is the coauthor of “Lean Behavioral Health: The Kings County Hospital Story.” .
Sunil Khushalani and Antonio DePaolo,
“Transforming Mental Healthcare: Applying Performance Improvement Methods to Mental Healthcare”
(London: Routledge, Taylor & Francis, 2022)
Since the publication of our book, “Lean Behavioral Health: The Kings County Hospital Story” (Oxford, England: Oxford University Press, 2014) almost a decade ago, “Transforming Mental Healthcare” is the first major book published about the use of a system for quality improvement across the health care continuum. That it has taken this long is probably surprising to those of us who have spent careers on trying to improve what is universally described as a system that is “broken” and in need of a major overhaul.
Every news cycle that reports mass violence typically spends a good bit of time talking about the failures of the mental health care system. One important lesson I learned when taking over the beleaguered Kings County (N.Y.) psychiatry service in 2009 (a department that has made extraordinary improvements over the years and is now exclaimed by the U.S. Department of Justice as “a model program”), is that the employees on the front line are often erroneously blamed for such failures.
The failure is systemic and usually starts at the top of the table of organization, not at the bottom. Dr. Khushalani and Dr. DePaolo have produced an excellent volume that should be purchased by every mental health care CEO and given “with thanks” to the local leaders overseeing the direct care of some of our nation’s most vulnerable patient populations.
The first part of “Transforming Mental Healthcare” provides an excellent overview of the current state of our mental health care system and its too numerous to name problems. This section could be a primer for all our legislators so their eyes can be opened to the failures on the ground that require their help in correcting. Many of the “failures” of our mental health care are societal failures – lack of affordable housing, access to care, reimbursement for care, gun access, etc. – and cannot be “fixed” by providers of care. Such problems are societal problems that call for societal and governmental solutions, and not only at the local level but from coast to coast.
The remainder of this easy to read and follow text provides many rich resources for the deliverers of mental health care. (e.g., plan-do-act, standard work, and A3 thinking).
The closing section focuses on leadership and culture – often overlooked to the detriment of any organization that doesn’t pay close attention to supporting both. Culture is cultivated and nourished by the organization’s leaders. Culture empowers staff to become problem solvers and agents of improvement. Empowered staff support and enrich their culture. Together a workplace that brings out the best of all its people is created, and burnout is held at bay.
“Transforming Mental Healthcare: Applying Performance Improvement Methods to Mental Healthcare” is a welcome and essential addition to the current morass, which is our mental health care delivery system, an oasis in the desert from which perhaps the lotus flower can emerge.
Dr. Merlino is emeritus professor of psychiatry, SUNY Downstate College of Medicine, Rhinebeck, N.Y., and formerly director of psychiatry at Kings County Hospital Center, Brooklyn, NY. He is the coauthor of “Lean Behavioral Health: The Kings County Hospital Story.” .
Sunil Khushalani and Antonio DePaolo,
“Transforming Mental Healthcare: Applying Performance Improvement Methods to Mental Healthcare”
(London: Routledge, Taylor & Francis, 2022)
Since the publication of our book, “Lean Behavioral Health: The Kings County Hospital Story” (Oxford, England: Oxford University Press, 2014) almost a decade ago, “Transforming Mental Healthcare” is the first major book published about the use of a system for quality improvement across the health care continuum. That it has taken this long is probably surprising to those of us who have spent careers on trying to improve what is universally described as a system that is “broken” and in need of a major overhaul.
Every news cycle that reports mass violence typically spends a good bit of time talking about the failures of the mental health care system. One important lesson I learned when taking over the beleaguered Kings County (N.Y.) psychiatry service in 2009 (a department that has made extraordinary improvements over the years and is now exclaimed by the U.S. Department of Justice as “a model program”), is that the employees on the front line are often erroneously blamed for such failures.
The failure is systemic and usually starts at the top of the table of organization, not at the bottom. Dr. Khushalani and Dr. DePaolo have produced an excellent volume that should be purchased by every mental health care CEO and given “with thanks” to the local leaders overseeing the direct care of some of our nation’s most vulnerable patient populations.
The first part of “Transforming Mental Healthcare” provides an excellent overview of the current state of our mental health care system and its too numerous to name problems. This section could be a primer for all our legislators so their eyes can be opened to the failures on the ground that require their help in correcting. Many of the “failures” of our mental health care are societal failures – lack of affordable housing, access to care, reimbursement for care, gun access, etc. – and cannot be “fixed” by providers of care. Such problems are societal problems that call for societal and governmental solutions, and not only at the local level but from coast to coast.
The remainder of this easy to read and follow text provides many rich resources for the deliverers of mental health care. (e.g., plan-do-act, standard work, and A3 thinking).
The closing section focuses on leadership and culture – often overlooked to the detriment of any organization that doesn’t pay close attention to supporting both. Culture is cultivated and nourished by the organization’s leaders. Culture empowers staff to become problem solvers and agents of improvement. Empowered staff support and enrich their culture. Together a workplace that brings out the best of all its people is created, and burnout is held at bay.
“Transforming Mental Healthcare: Applying Performance Improvement Methods to Mental Healthcare” is a welcome and essential addition to the current morass, which is our mental health care delivery system, an oasis in the desert from which perhaps the lotus flower can emerge.
Dr. Merlino is emeritus professor of psychiatry, SUNY Downstate College of Medicine, Rhinebeck, N.Y., and formerly director of psychiatry at Kings County Hospital Center, Brooklyn, NY. He is the coauthor of “Lean Behavioral Health: The Kings County Hospital Story.” .