User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
New insight into the growing problem of gaming disorder
A team of international researchers led by Orsolya Király, PhD, of the Institute of Psychology, Eötvös Loránd University, Budapest, reviewed the characteristics and etiology of GD. They concluded that its genesis arises from the interaction of environmental factors, game-specific factors and individual factors, including personality traits, comorbid psychopathology, and genetic predisposition.
“The development of GD is a complex process and we identified three major factors involved,” study coauthor Mark Griffiths, PhD, distinguished professor of behavioral addiction and director of the international gaming research unit, psychology department, Nottingham (England) Trent University, said in an interview. Because of this complexity, “prevention and intervention in GD require multiprofessional action.”
The review was published in Comprehensive Psychiatry.
In a second paper, published online in Frontiers in Psychiatry, Chinese investigators reviewing randomized controlled trials (RCTs) presented “compelling evidence” to support four effective interventions for GD: group counseling, acceptance and cognitive restructuring intervention program (ACRIP), short-term cognitive-behavioral therapy (CBT), and craving behavioral intervention (CBI).
A third paper, published online in the Journal of Behavioral Addictions, in which researchers analyzed close to 50 studies of GD, found that the concept of “recovery” is rarely mentioned in GD research. Lead author Belle Gavriel-Fried, PhD, senior professor, Bob Shapell School of Social Work, Tel Aviv University, said in an interview that recovery is a “holistic concept that taps into many aspects of life.”
Understanding the “differences in the impact and availability” of negative and positive human resources and their effect on recovery “can help clinicians to customize treatment,” she said.
Complex interplay
GD is garnering increasing attention in the clinical community, especially since 2019, when the World Health Organization included it in the ICD-11.
“Although for most individuals, gaming is a recreational activity or even a passion, a small group of gamers experiences negative symptoms which impact their mental and physical health and cause functional impairment,” wrote Dr. Király and colleagues.
Dr. Griffiths explained that his team wanted to provide an “up-to-date primer – a ‘one-stop shop’ – on all things etiologic concerning gaming disorder for academics and practitioners” as well as others, such as health policy makers, teachers, and individuals in the gaming industry.
The researchers identified three factors that increase the risk of developing GD, the first being gaming-related factors, which make video games “addictive in a way that vulnerable individuals may develop GD.”
For example, GD is more prevalent among online versus offline game players, possibly because online multiplayer games “provide safe environments in which players can fulfill their social needs while remaining invisible and anonymous.”
Game genre also matters, with massively multiplayer online role-playing games, first-person/third-person shooter games, real-time strategy games, and multiplayer online battle arena games most implicated in problematic gaming. Moreover, the “monetization techniques” of certain games also increase their addictive potential.
The researchers point to individual factors that increase the risk of developing GD, including male sex and younger age, personality traits like impulsivity and sensation-seeking, and comorbidities including ADHD, anxiety, and depression.
Poor self-esteem and lack of social competencies make gaming “an easy and efficient way to compensate for these deficiencies, which in turn, heightens the risk for developing GD,” they add. Neurobiological processes and genetic predisposition also play a role.
Lastly, the authors mentioned environmental factors, including family and peer-group issues, problems at work or school, and cultural factors.
“The take-home messages are that problematic gaming has had a long history of empirical research; that the psychiatric community now views GD as a legitimate mental health issue; and that the reasons for GD are complex, with many different factors involved in the acquisition, development, and maintenance of GD,” said Dr. Griffiths.
Beneficial behavioral therapies
Yuzhou Chen and colleagues, Southwest University, Chongqing, China, conducted a systematic review of RCTs investigating interventions for treating GD. Despite the “large number of intervention approaches developed over the past decade, as yet, there are no authoritative guidelines for what makes an effective GD intervention,” they wrote.
Few studies have focused specifically on GD but instead have focused on a combination of internet addiction and GD. But the interventions used to treat internet addiction may not apply to GD. And few studies have utilized an RCT design. The researchers therefore set out to review studies that specifically used an RCT design to investigate interventions for GD.
They searched six databases to identify RCTs that tested GD interventions from the inception of each database until the end of 2021. To be included, participants had to be diagnosed with GD and receive either a “complete and systematic intervention” or be in a comparator control group receiving no intervention or placebo.
Seven studies met the inclusion criteria (n = 332 participants). The studies tested five interventions:
- Group counseling with three different themes (interpersonal interaction, acceptance and commitment, cognition and behavior)
- CBI, which addresses cravings
- Transcranial direct current stimulation (tDCS)
- ACRIP with the main objectives of reducing GD symptoms and improving psychological well-being
- Short-term CBT, which addresses maladaptive cognitions
The mean duration of the interventions ranged from 3 to 15 weeks.
The primary outcome was GD severity, with secondary outcomes including depression, anxiety, cognition, game time, self-esteem, self-compassion, shyness, impulsivity, and psychological well-being.
Group counseling, CBI, ACRIP, and short-term CBT interventions had “a significant effect on decreasing the severity of GD,” while tDCS had “no significant effect.”
Behavioral therapy “exerts its effect on the behavioral mechanism of GD; for example, by reducing the association between game-related stimuli and the game player’s response to them,” the authors suggested.
Behavioral therapy “exerts its effect on the behavioral mechanism of GD; for example, by reducing the association between game-related stimuli and the game-player’s response to them,” the authors suggested.
Recovery vs. pathology
Recovery “traditionally represents the transition from trauma and illness to health,” Dr. Gavriel-Fried and colleagues noted.
Two paradigms of recovery are “deficit based” and “strength based.” The first assesses recovery in terms of abstinence, sobriety, and symptom reduction; and the second focuses on “growth, rather than a reduction in pathology.”
But although recovery is “embedded within mental health addiction policies and practice,” the concept has received “scant attention” in GD research.
The researchers therefore aimed to “map and summarize the state of the art on recovery from GD,” defining “recovery” as the “ability to handle conflicting feelings and emotions without external mediation.”
They conducted a scoping review of all literature regarding GD or internet GD published before February 2022 (47 studies, 2,924 participants with GD; mean age range, 13-26 years).
Most studies (n = 32) consisted of exclusively male subjects. Only 10 included both sexes, and female participants were in the minority.
Most studies (n = 42) did not address the concept of recovery, although all studies did report significant improvements in gaming-related pathology. Typical terminology used to describe changes in participants’ GD were “reduction” and/or “decrease” in symptom severity.
Although 18 studies mentioned the word “recovery,” only 5 actually discussed issues related to the notion of recovery, and only 5 used the term “abstinence.”
In addition, only 13 studies examined positive components of life in patients with GD, such as increased psychological well-being, life satisfaction, quality of life, improved emotional state, relational skills, and executive control, as well as improved self-care, hygiene, sleep, and interest in school studies.
“As a person and researcher who believes that words shape the way we perceive things, I think we should use the word ‘recovery’ rather than ‘pathology’ much more in research, therapy, and policy,” said Dr. Gavriel-Fried.
She noted that, because GD is a “relatively new behavioral addictive disorder, theories are still being developed and definitions of the symptoms are still being fine-tuned.”
“The field as a whole will benefit from future theoretical work that will lead to practical solutions for treating GD and ways to identify the risk factors,” Dr. Gavriel-Fried said.
Filling a research gap
In a comment, David Greenfield, MD, founder and medical director of the Connecticut-based Center for Internet and Technology Addiction, noted that 3 decades ago, there was almost no research into this area.
“The fact that we have these reviews and studies is good because all of the research adds to the science providing more data about an area we still don’t know that much about, where research is still in its infancy,” said Dr. Greenfield, who was not involved with the present study.
“Although we have definitions, there’s no complete agreement about the definitions of GD, and we do not yet have a unified approach,” continued Dr. Greenfield, who wrote the books Overcoming Internet Addiction for Dummies and Virtual Addiction.
He suggested that “recovery” is rarely used as a concept in GD research perhaps because there’s a “bifurcation in the field of addiction medicine in which behavioral addictions are not seen as equivalent to substance addictions,” and, particularly with GD, the principles of “recovery” have not yet matured.
“Recovery means meaningful life away from the screen, not just abstinence from the screen,” said Dr. Greenfield.
The study by Mr. Chen and colleagues was supported by grants from the National Social Science Foundation of China, the Chongqing Research Program of Basic Research and Frontier Technology, and the Fundamental Research Funds for the Central Universities. Dr. Griffiths has reported receiving research funding from Norsk Tipping (the gambling operator owned by the Norwegian government). The study by Dr. Király and colleagues received support from the Hungarian National Research Development and Innovation Office and the Janos Bolyai Research Scholarship Academy of Sciences to individual investigators. The study by Dr. Gavriel-Fried and colleagues received support from the Hungarian National Research Development and Innovation Office and the Janos Bolyai Research Scholarship Academy of Sciences to individual investigators. Dr. Gavriel-Fried has reported receiving grants from the Israel National Insurance Institute and the Committee for Independent Studies of the Israel Lottery. Dr. Greenfield reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A team of international researchers led by Orsolya Király, PhD, of the Institute of Psychology, Eötvös Loránd University, Budapest, reviewed the characteristics and etiology of GD. They concluded that its genesis arises from the interaction of environmental factors, game-specific factors and individual factors, including personality traits, comorbid psychopathology, and genetic predisposition.
“The development of GD is a complex process and we identified three major factors involved,” study coauthor Mark Griffiths, PhD, distinguished professor of behavioral addiction and director of the international gaming research unit, psychology department, Nottingham (England) Trent University, said in an interview. Because of this complexity, “prevention and intervention in GD require multiprofessional action.”
The review was published in Comprehensive Psychiatry.
In a second paper, published online in Frontiers in Psychiatry, Chinese investigators reviewing randomized controlled trials (RCTs) presented “compelling evidence” to support four effective interventions for GD: group counseling, acceptance and cognitive restructuring intervention program (ACRIP), short-term cognitive-behavioral therapy (CBT), and craving behavioral intervention (CBI).
A third paper, published online in the Journal of Behavioral Addictions, in which researchers analyzed close to 50 studies of GD, found that the concept of “recovery” is rarely mentioned in GD research. Lead author Belle Gavriel-Fried, PhD, senior professor, Bob Shapell School of Social Work, Tel Aviv University, said in an interview that recovery is a “holistic concept that taps into many aspects of life.”
Understanding the “differences in the impact and availability” of negative and positive human resources and their effect on recovery “can help clinicians to customize treatment,” she said.
Complex interplay
GD is garnering increasing attention in the clinical community, especially since 2019, when the World Health Organization included it in the ICD-11.
“Although for most individuals, gaming is a recreational activity or even a passion, a small group of gamers experiences negative symptoms which impact their mental and physical health and cause functional impairment,” wrote Dr. Király and colleagues.
Dr. Griffiths explained that his team wanted to provide an “up-to-date primer – a ‘one-stop shop’ – on all things etiologic concerning gaming disorder for academics and practitioners” as well as others, such as health policy makers, teachers, and individuals in the gaming industry.
The researchers identified three factors that increase the risk of developing GD, the first being gaming-related factors, which make video games “addictive in a way that vulnerable individuals may develop GD.”
For example, GD is more prevalent among online versus offline game players, possibly because online multiplayer games “provide safe environments in which players can fulfill their social needs while remaining invisible and anonymous.”
Game genre also matters, with massively multiplayer online role-playing games, first-person/third-person shooter games, real-time strategy games, and multiplayer online battle arena games most implicated in problematic gaming. Moreover, the “monetization techniques” of certain games also increase their addictive potential.
The researchers point to individual factors that increase the risk of developing GD, including male sex and younger age, personality traits like impulsivity and sensation-seeking, and comorbidities including ADHD, anxiety, and depression.
Poor self-esteem and lack of social competencies make gaming “an easy and efficient way to compensate for these deficiencies, which in turn, heightens the risk for developing GD,” they add. Neurobiological processes and genetic predisposition also play a role.
Lastly, the authors mentioned environmental factors, including family and peer-group issues, problems at work or school, and cultural factors.
“The take-home messages are that problematic gaming has had a long history of empirical research; that the psychiatric community now views GD as a legitimate mental health issue; and that the reasons for GD are complex, with many different factors involved in the acquisition, development, and maintenance of GD,” said Dr. Griffiths.
Beneficial behavioral therapies
Yuzhou Chen and colleagues, Southwest University, Chongqing, China, conducted a systematic review of RCTs investigating interventions for treating GD. Despite the “large number of intervention approaches developed over the past decade, as yet, there are no authoritative guidelines for what makes an effective GD intervention,” they wrote.
Few studies have focused specifically on GD but instead have focused on a combination of internet addiction and GD. But the interventions used to treat internet addiction may not apply to GD. And few studies have utilized an RCT design. The researchers therefore set out to review studies that specifically used an RCT design to investigate interventions for GD.
They searched six databases to identify RCTs that tested GD interventions from the inception of each database until the end of 2021. To be included, participants had to be diagnosed with GD and receive either a “complete and systematic intervention” or be in a comparator control group receiving no intervention or placebo.
Seven studies met the inclusion criteria (n = 332 participants). The studies tested five interventions:
- Group counseling with three different themes (interpersonal interaction, acceptance and commitment, cognition and behavior)
- CBI, which addresses cravings
- Transcranial direct current stimulation (tDCS)
- ACRIP with the main objectives of reducing GD symptoms and improving psychological well-being
- Short-term CBT, which addresses maladaptive cognitions
The mean duration of the interventions ranged from 3 to 15 weeks.
The primary outcome was GD severity, with secondary outcomes including depression, anxiety, cognition, game time, self-esteem, self-compassion, shyness, impulsivity, and psychological well-being.
Group counseling, CBI, ACRIP, and short-term CBT interventions had “a significant effect on decreasing the severity of GD,” while tDCS had “no significant effect.”
Behavioral therapy “exerts its effect on the behavioral mechanism of GD; for example, by reducing the association between game-related stimuli and the game player’s response to them,” the authors suggested.
Behavioral therapy “exerts its effect on the behavioral mechanism of GD; for example, by reducing the association between game-related stimuli and the game-player’s response to them,” the authors suggested.
Recovery vs. pathology
Recovery “traditionally represents the transition from trauma and illness to health,” Dr. Gavriel-Fried and colleagues noted.
Two paradigms of recovery are “deficit based” and “strength based.” The first assesses recovery in terms of abstinence, sobriety, and symptom reduction; and the second focuses on “growth, rather than a reduction in pathology.”
But although recovery is “embedded within mental health addiction policies and practice,” the concept has received “scant attention” in GD research.
The researchers therefore aimed to “map and summarize the state of the art on recovery from GD,” defining “recovery” as the “ability to handle conflicting feelings and emotions without external mediation.”
They conducted a scoping review of all literature regarding GD or internet GD published before February 2022 (47 studies, 2,924 participants with GD; mean age range, 13-26 years).
Most studies (n = 32) consisted of exclusively male subjects. Only 10 included both sexes, and female participants were in the minority.
Most studies (n = 42) did not address the concept of recovery, although all studies did report significant improvements in gaming-related pathology. Typical terminology used to describe changes in participants’ GD were “reduction” and/or “decrease” in symptom severity.
Although 18 studies mentioned the word “recovery,” only 5 actually discussed issues related to the notion of recovery, and only 5 used the term “abstinence.”
In addition, only 13 studies examined positive components of life in patients with GD, such as increased psychological well-being, life satisfaction, quality of life, improved emotional state, relational skills, and executive control, as well as improved self-care, hygiene, sleep, and interest in school studies.
“As a person and researcher who believes that words shape the way we perceive things, I think we should use the word ‘recovery’ rather than ‘pathology’ much more in research, therapy, and policy,” said Dr. Gavriel-Fried.
She noted that, because GD is a “relatively new behavioral addictive disorder, theories are still being developed and definitions of the symptoms are still being fine-tuned.”
“The field as a whole will benefit from future theoretical work that will lead to practical solutions for treating GD and ways to identify the risk factors,” Dr. Gavriel-Fried said.
Filling a research gap
In a comment, David Greenfield, MD, founder and medical director of the Connecticut-based Center for Internet and Technology Addiction, noted that 3 decades ago, there was almost no research into this area.
“The fact that we have these reviews and studies is good because all of the research adds to the science providing more data about an area we still don’t know that much about, where research is still in its infancy,” said Dr. Greenfield, who was not involved with the present study.
“Although we have definitions, there’s no complete agreement about the definitions of GD, and we do not yet have a unified approach,” continued Dr. Greenfield, who wrote the books Overcoming Internet Addiction for Dummies and Virtual Addiction.
He suggested that “recovery” is rarely used as a concept in GD research perhaps because there’s a “bifurcation in the field of addiction medicine in which behavioral addictions are not seen as equivalent to substance addictions,” and, particularly with GD, the principles of “recovery” have not yet matured.
“Recovery means meaningful life away from the screen, not just abstinence from the screen,” said Dr. Greenfield.
The study by Mr. Chen and colleagues was supported by grants from the National Social Science Foundation of China, the Chongqing Research Program of Basic Research and Frontier Technology, and the Fundamental Research Funds for the Central Universities. Dr. Griffiths has reported receiving research funding from Norsk Tipping (the gambling operator owned by the Norwegian government). The study by Dr. Király and colleagues received support from the Hungarian National Research Development and Innovation Office and the Janos Bolyai Research Scholarship Academy of Sciences to individual investigators. The study by Dr. Gavriel-Fried and colleagues received support from the Hungarian National Research Development and Innovation Office and the Janos Bolyai Research Scholarship Academy of Sciences to individual investigators. Dr. Gavriel-Fried has reported receiving grants from the Israel National Insurance Institute and the Committee for Independent Studies of the Israel Lottery. Dr. Greenfield reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A team of international researchers led by Orsolya Király, PhD, of the Institute of Psychology, Eötvös Loránd University, Budapest, reviewed the characteristics and etiology of GD. They concluded that its genesis arises from the interaction of environmental factors, game-specific factors and individual factors, including personality traits, comorbid psychopathology, and genetic predisposition.
“The development of GD is a complex process and we identified three major factors involved,” study coauthor Mark Griffiths, PhD, distinguished professor of behavioral addiction and director of the international gaming research unit, psychology department, Nottingham (England) Trent University, said in an interview. Because of this complexity, “prevention and intervention in GD require multiprofessional action.”
The review was published in Comprehensive Psychiatry.
In a second paper, published online in Frontiers in Psychiatry, Chinese investigators reviewing randomized controlled trials (RCTs) presented “compelling evidence” to support four effective interventions for GD: group counseling, acceptance and cognitive restructuring intervention program (ACRIP), short-term cognitive-behavioral therapy (CBT), and craving behavioral intervention (CBI).
A third paper, published online in the Journal of Behavioral Addictions, in which researchers analyzed close to 50 studies of GD, found that the concept of “recovery” is rarely mentioned in GD research. Lead author Belle Gavriel-Fried, PhD, senior professor, Bob Shapell School of Social Work, Tel Aviv University, said in an interview that recovery is a “holistic concept that taps into many aspects of life.”
Understanding the “differences in the impact and availability” of negative and positive human resources and their effect on recovery “can help clinicians to customize treatment,” she said.
Complex interplay
GD is garnering increasing attention in the clinical community, especially since 2019, when the World Health Organization included it in the ICD-11.
“Although for most individuals, gaming is a recreational activity or even a passion, a small group of gamers experiences negative symptoms which impact their mental and physical health and cause functional impairment,” wrote Dr. Király and colleagues.
Dr. Griffiths explained that his team wanted to provide an “up-to-date primer – a ‘one-stop shop’ – on all things etiologic concerning gaming disorder for academics and practitioners” as well as others, such as health policy makers, teachers, and individuals in the gaming industry.
The researchers identified three factors that increase the risk of developing GD, the first being gaming-related factors, which make video games “addictive in a way that vulnerable individuals may develop GD.”
For example, GD is more prevalent among online versus offline game players, possibly because online multiplayer games “provide safe environments in which players can fulfill their social needs while remaining invisible and anonymous.”
Game genre also matters, with massively multiplayer online role-playing games, first-person/third-person shooter games, real-time strategy games, and multiplayer online battle arena games most implicated in problematic gaming. Moreover, the “monetization techniques” of certain games also increase their addictive potential.
The researchers point to individual factors that increase the risk of developing GD, including male sex and younger age, personality traits like impulsivity and sensation-seeking, and comorbidities including ADHD, anxiety, and depression.
Poor self-esteem and lack of social competencies make gaming “an easy and efficient way to compensate for these deficiencies, which in turn, heightens the risk for developing GD,” they add. Neurobiological processes and genetic predisposition also play a role.
Lastly, the authors mentioned environmental factors, including family and peer-group issues, problems at work or school, and cultural factors.
“The take-home messages are that problematic gaming has had a long history of empirical research; that the psychiatric community now views GD as a legitimate mental health issue; and that the reasons for GD are complex, with many different factors involved in the acquisition, development, and maintenance of GD,” said Dr. Griffiths.
Beneficial behavioral therapies
Yuzhou Chen and colleagues, Southwest University, Chongqing, China, conducted a systematic review of RCTs investigating interventions for treating GD. Despite the “large number of intervention approaches developed over the past decade, as yet, there are no authoritative guidelines for what makes an effective GD intervention,” they wrote.
Few studies have focused specifically on GD but instead have focused on a combination of internet addiction and GD. But the interventions used to treat internet addiction may not apply to GD. And few studies have utilized an RCT design. The researchers therefore set out to review studies that specifically used an RCT design to investigate interventions for GD.
They searched six databases to identify RCTs that tested GD interventions from the inception of each database until the end of 2021. To be included, participants had to be diagnosed with GD and receive either a “complete and systematic intervention” or be in a comparator control group receiving no intervention or placebo.
Seven studies met the inclusion criteria (n = 332 participants). The studies tested five interventions:
- Group counseling with three different themes (interpersonal interaction, acceptance and commitment, cognition and behavior)
- CBI, which addresses cravings
- Transcranial direct current stimulation (tDCS)
- ACRIP with the main objectives of reducing GD symptoms and improving psychological well-being
- Short-term CBT, which addresses maladaptive cognitions
The mean duration of the interventions ranged from 3 to 15 weeks.
The primary outcome was GD severity, with secondary outcomes including depression, anxiety, cognition, game time, self-esteem, self-compassion, shyness, impulsivity, and psychological well-being.
Group counseling, CBI, ACRIP, and short-term CBT interventions had “a significant effect on decreasing the severity of GD,” while tDCS had “no significant effect.”
Behavioral therapy “exerts its effect on the behavioral mechanism of GD; for example, by reducing the association between game-related stimuli and the game player’s response to them,” the authors suggested.
Behavioral therapy “exerts its effect on the behavioral mechanism of GD; for example, by reducing the association between game-related stimuli and the game-player’s response to them,” the authors suggested.
Recovery vs. pathology
Recovery “traditionally represents the transition from trauma and illness to health,” Dr. Gavriel-Fried and colleagues noted.
Two paradigms of recovery are “deficit based” and “strength based.” The first assesses recovery in terms of abstinence, sobriety, and symptom reduction; and the second focuses on “growth, rather than a reduction in pathology.”
But although recovery is “embedded within mental health addiction policies and practice,” the concept has received “scant attention” in GD research.
The researchers therefore aimed to “map and summarize the state of the art on recovery from GD,” defining “recovery” as the “ability to handle conflicting feelings and emotions without external mediation.”
They conducted a scoping review of all literature regarding GD or internet GD published before February 2022 (47 studies, 2,924 participants with GD; mean age range, 13-26 years).
Most studies (n = 32) consisted of exclusively male subjects. Only 10 included both sexes, and female participants were in the minority.
Most studies (n = 42) did not address the concept of recovery, although all studies did report significant improvements in gaming-related pathology. Typical terminology used to describe changes in participants’ GD were “reduction” and/or “decrease” in symptom severity.
Although 18 studies mentioned the word “recovery,” only 5 actually discussed issues related to the notion of recovery, and only 5 used the term “abstinence.”
In addition, only 13 studies examined positive components of life in patients with GD, such as increased psychological well-being, life satisfaction, quality of life, improved emotional state, relational skills, and executive control, as well as improved self-care, hygiene, sleep, and interest in school studies.
“As a person and researcher who believes that words shape the way we perceive things, I think we should use the word ‘recovery’ rather than ‘pathology’ much more in research, therapy, and policy,” said Dr. Gavriel-Fried.
She noted that, because GD is a “relatively new behavioral addictive disorder, theories are still being developed and definitions of the symptoms are still being fine-tuned.”
“The field as a whole will benefit from future theoretical work that will lead to practical solutions for treating GD and ways to identify the risk factors,” Dr. Gavriel-Fried said.
Filling a research gap
In a comment, David Greenfield, MD, founder and medical director of the Connecticut-based Center for Internet and Technology Addiction, noted that 3 decades ago, there was almost no research into this area.
“The fact that we have these reviews and studies is good because all of the research adds to the science providing more data about an area we still don’t know that much about, where research is still in its infancy,” said Dr. Greenfield, who was not involved with the present study.
“Although we have definitions, there’s no complete agreement about the definitions of GD, and we do not yet have a unified approach,” continued Dr. Greenfield, who wrote the books Overcoming Internet Addiction for Dummies and Virtual Addiction.
He suggested that “recovery” is rarely used as a concept in GD research perhaps because there’s a “bifurcation in the field of addiction medicine in which behavioral addictions are not seen as equivalent to substance addictions,” and, particularly with GD, the principles of “recovery” have not yet matured.
“Recovery means meaningful life away from the screen, not just abstinence from the screen,” said Dr. Greenfield.
The study by Mr. Chen and colleagues was supported by grants from the National Social Science Foundation of China, the Chongqing Research Program of Basic Research and Frontier Technology, and the Fundamental Research Funds for the Central Universities. Dr. Griffiths has reported receiving research funding from Norsk Tipping (the gambling operator owned by the Norwegian government). The study by Dr. Király and colleagues received support from the Hungarian National Research Development and Innovation Office and the Janos Bolyai Research Scholarship Academy of Sciences to individual investigators. The study by Dr. Gavriel-Fried and colleagues received support from the Hungarian National Research Development and Innovation Office and the Janos Bolyai Research Scholarship Academy of Sciences to individual investigators. Dr. Gavriel-Fried has reported receiving grants from the Israel National Insurance Institute and the Committee for Independent Studies of the Israel Lottery. Dr. Greenfield reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New guidelines for cannabis in chronic pain management released
New clinical practice guidelines for cannabis in chronic pain management have been released.
Developed by a group of Canadian researchers, clinicians, and patients, the guidelines note that cannabinoid-based medicines (CBM) may help clinicians offer an effective, less addictive, alternative to opioids in patients with chronic noncancer pain and comorbid conditions.
“We don’t recommend using CBM first line for anything pretty much because there are other alternatives that may be more effective and also offer fewer side effects,” lead guideline author Alan Bell, MD, assistant professor of family and community medicine at the University of Toronto, told this news organization.
“But I would strongly argue that I would use cannabis-based medicine over opioids every time. Why would you use a high potency-high toxicity agent when there’s a low potency-low toxicity alternative?” he said.
The guidelines were published online in the journal Cannabis and Cannabinoid Research.
Examining the evidence
A consistent criticism of CBM has been the lack of quality research supporting its therapeutic utility. To develop the current recommendations, the task force reviewed 47 pain management studies enrolling more than 11,000 patients. Almost half of the studies (n = 22) were randomized controlled trials (RCTs) and 12 of the 19 included systematic reviews focused solely on RCTs.
Overall, 38 of the 47 included studies demonstrated that CBM provided at least moderate benefits for chronic pain, resulting in a “strong” recommendation – mostly as an adjunct or replacement treatment in individuals living with chronic pain.
Overall, the guidelines place a high value on improving chronic pain and functionality, and addressing co-occurring conditions such as insomnia, anxiety and depression, mobility, and inflammation. They also provide practical dosing and formulation tips to support the use of CBM in the clinical setting.
When it comes to chronic pain, CBM is not a panacea. However, prior research suggests cannabinoids and opioids share several pharmacologic properties, including independent but possibly related mechanisms for antinociception, making them an intriguing combination.
In the current guidelines, all of the four studies specifically addressing combined opioids and vaporized cannabis flower demonstrated further pain reduction, reinforcing the conclusion that the benefits of CBM for improving pain control in patients taking opioids outweigh the risk of nonserious adverse events (AEs), such as dry mouth, dizziness, increased appetite, sedation, and concentration difficulties.
The recommendations also highlighted evidence demonstrating that a majority of participants were able to reduce use of routine pain medications with concomitant CBM/opioid administration, while simultaneously offering secondary benefits such as improved sleep, anxiety, and mood, as well as prevention of opioid tolerance and dose escalation.
Importantly, the guidelines offer an evidence-based algorithm with a clear framework for tapering patients off opioids, especially those who are on > 50 mg MED, which places them with a twofold greater risk for fatal overdose.
An effective alternative
Commenting on the new guidelines, Mark Wallace, MD, who has extensive experience researching and treating pain patients with medical cannabis, said the genesis of his interest in medical cannabis mirrors the guidelines’ focus.
“What got me interested in medical cannabis was trying to get patients off of opioids,” said Dr. Wallace, professor of anesthesiology and chief of the division of pain medicine in the department of anesthesiology at the University of California, San Diego. Dr. Wallace, who was not involved in the guidelines’ development study, said that he’s “titrated hundreds of patients off of opioids using cannabis.”
Dr. Wallace said he found the guidelines’ dosing recommendations helpful.
“If you stay within the 1- to 5-mg dosing range, the risks are so incredibly low, you’re not going to harm the patient.”
While there are patients who abuse cannabis and CBMs, Dr. Wallace noted that he has seen only one patient in the past 20 years who was overusing the medical cannabis. He added that his patient population does not use medical cannabis to get high and, in fact, wants to avoid doses that produce that effect at all costs.
Also commenting on the guidelines, Christopher Gilligan, MD, MBA, associate chief medical officer and a pain medicine physician at Brigham and Women’s Hospital in Boston, who was not involved in the guidelines’ development, points to the risks.
“When we have an opportunity to use cannabinoids in place of opioids for our patients, I think that that’s a positive thing ... and a wise choice in terms of risk benefit,” Dr. Gilligan said.
On the other hand, he cautioned that “freely prescribing” cannabinoids for chronic pain in patients who aren’t on opioids is not good practice.
“We have to take seriously the potential adverse effects of [cannabis], including marijuana use disorder, interference with learning, memory impairment, and psychotic breakthroughs,” said Dr. Gilligan.
Given the current climate, it would appear that CBM is a long way from being endorsed by the Food and Drug Administration, but for clinicians interested in trying CBM for chronic pain patients, the guidelines may offer a roadmap for initiation and an alternative to prescribing opioids.
Dr. Bell, Dr. Gilligan, and Dr. Wallace report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New clinical practice guidelines for cannabis in chronic pain management have been released.
Developed by a group of Canadian researchers, clinicians, and patients, the guidelines note that cannabinoid-based medicines (CBM) may help clinicians offer an effective, less addictive, alternative to opioids in patients with chronic noncancer pain and comorbid conditions.
“We don’t recommend using CBM first line for anything pretty much because there are other alternatives that may be more effective and also offer fewer side effects,” lead guideline author Alan Bell, MD, assistant professor of family and community medicine at the University of Toronto, told this news organization.
“But I would strongly argue that I would use cannabis-based medicine over opioids every time. Why would you use a high potency-high toxicity agent when there’s a low potency-low toxicity alternative?” he said.
The guidelines were published online in the journal Cannabis and Cannabinoid Research.
Examining the evidence
A consistent criticism of CBM has been the lack of quality research supporting its therapeutic utility. To develop the current recommendations, the task force reviewed 47 pain management studies enrolling more than 11,000 patients. Almost half of the studies (n = 22) were randomized controlled trials (RCTs) and 12 of the 19 included systematic reviews focused solely on RCTs.
Overall, 38 of the 47 included studies demonstrated that CBM provided at least moderate benefits for chronic pain, resulting in a “strong” recommendation – mostly as an adjunct or replacement treatment in individuals living with chronic pain.
Overall, the guidelines place a high value on improving chronic pain and functionality, and addressing co-occurring conditions such as insomnia, anxiety and depression, mobility, and inflammation. They also provide practical dosing and formulation tips to support the use of CBM in the clinical setting.
When it comes to chronic pain, CBM is not a panacea. However, prior research suggests cannabinoids and opioids share several pharmacologic properties, including independent but possibly related mechanisms for antinociception, making them an intriguing combination.
In the current guidelines, all of the four studies specifically addressing combined opioids and vaporized cannabis flower demonstrated further pain reduction, reinforcing the conclusion that the benefits of CBM for improving pain control in patients taking opioids outweigh the risk of nonserious adverse events (AEs), such as dry mouth, dizziness, increased appetite, sedation, and concentration difficulties.
The recommendations also highlighted evidence demonstrating that a majority of participants were able to reduce use of routine pain medications with concomitant CBM/opioid administration, while simultaneously offering secondary benefits such as improved sleep, anxiety, and mood, as well as prevention of opioid tolerance and dose escalation.
Importantly, the guidelines offer an evidence-based algorithm with a clear framework for tapering patients off opioids, especially those who are on > 50 mg MED, which places them with a twofold greater risk for fatal overdose.
An effective alternative
Commenting on the new guidelines, Mark Wallace, MD, who has extensive experience researching and treating pain patients with medical cannabis, said the genesis of his interest in medical cannabis mirrors the guidelines’ focus.
“What got me interested in medical cannabis was trying to get patients off of opioids,” said Dr. Wallace, professor of anesthesiology and chief of the division of pain medicine in the department of anesthesiology at the University of California, San Diego. Dr. Wallace, who was not involved in the guidelines’ development study, said that he’s “titrated hundreds of patients off of opioids using cannabis.”
Dr. Wallace said he found the guidelines’ dosing recommendations helpful.
“If you stay within the 1- to 5-mg dosing range, the risks are so incredibly low, you’re not going to harm the patient.”
While there are patients who abuse cannabis and CBMs, Dr. Wallace noted that he has seen only one patient in the past 20 years who was overusing the medical cannabis. He added that his patient population does not use medical cannabis to get high and, in fact, wants to avoid doses that produce that effect at all costs.
Also commenting on the guidelines, Christopher Gilligan, MD, MBA, associate chief medical officer and a pain medicine physician at Brigham and Women’s Hospital in Boston, who was not involved in the guidelines’ development, points to the risks.
“When we have an opportunity to use cannabinoids in place of opioids for our patients, I think that that’s a positive thing ... and a wise choice in terms of risk benefit,” Dr. Gilligan said.
On the other hand, he cautioned that “freely prescribing” cannabinoids for chronic pain in patients who aren’t on opioids is not good practice.
“We have to take seriously the potential adverse effects of [cannabis], including marijuana use disorder, interference with learning, memory impairment, and psychotic breakthroughs,” said Dr. Gilligan.
Given the current climate, it would appear that CBM is a long way from being endorsed by the Food and Drug Administration, but for clinicians interested in trying CBM for chronic pain patients, the guidelines may offer a roadmap for initiation and an alternative to prescribing opioids.
Dr. Bell, Dr. Gilligan, and Dr. Wallace report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New clinical practice guidelines for cannabis in chronic pain management have been released.
Developed by a group of Canadian researchers, clinicians, and patients, the guidelines note that cannabinoid-based medicines (CBM) may help clinicians offer an effective, less addictive, alternative to opioids in patients with chronic noncancer pain and comorbid conditions.
“We don’t recommend using CBM first line for anything pretty much because there are other alternatives that may be more effective and also offer fewer side effects,” lead guideline author Alan Bell, MD, assistant professor of family and community medicine at the University of Toronto, told this news organization.
“But I would strongly argue that I would use cannabis-based medicine over opioids every time. Why would you use a high potency-high toxicity agent when there’s a low potency-low toxicity alternative?” he said.
The guidelines were published online in the journal Cannabis and Cannabinoid Research.
Examining the evidence
A consistent criticism of CBM has been the lack of quality research supporting its therapeutic utility. To develop the current recommendations, the task force reviewed 47 pain management studies enrolling more than 11,000 patients. Almost half of the studies (n = 22) were randomized controlled trials (RCTs) and 12 of the 19 included systematic reviews focused solely on RCTs.
Overall, 38 of the 47 included studies demonstrated that CBM provided at least moderate benefits for chronic pain, resulting in a “strong” recommendation – mostly as an adjunct or replacement treatment in individuals living with chronic pain.
Overall, the guidelines place a high value on improving chronic pain and functionality, and addressing co-occurring conditions such as insomnia, anxiety and depression, mobility, and inflammation. They also provide practical dosing and formulation tips to support the use of CBM in the clinical setting.
When it comes to chronic pain, CBM is not a panacea. However, prior research suggests cannabinoids and opioids share several pharmacologic properties, including independent but possibly related mechanisms for antinociception, making them an intriguing combination.
In the current guidelines, all of the four studies specifically addressing combined opioids and vaporized cannabis flower demonstrated further pain reduction, reinforcing the conclusion that the benefits of CBM for improving pain control in patients taking opioids outweigh the risk of nonserious adverse events (AEs), such as dry mouth, dizziness, increased appetite, sedation, and concentration difficulties.
The recommendations also highlighted evidence demonstrating that a majority of participants were able to reduce use of routine pain medications with concomitant CBM/opioid administration, while simultaneously offering secondary benefits such as improved sleep, anxiety, and mood, as well as prevention of opioid tolerance and dose escalation.
Importantly, the guidelines offer an evidence-based algorithm with a clear framework for tapering patients off opioids, especially those who are on > 50 mg MED, which places them with a twofold greater risk for fatal overdose.
An effective alternative
Commenting on the new guidelines, Mark Wallace, MD, who has extensive experience researching and treating pain patients with medical cannabis, said the genesis of his interest in medical cannabis mirrors the guidelines’ focus.
“What got me interested in medical cannabis was trying to get patients off of opioids,” said Dr. Wallace, professor of anesthesiology and chief of the division of pain medicine in the department of anesthesiology at the University of California, San Diego. Dr. Wallace, who was not involved in the guidelines’ development study, said that he’s “titrated hundreds of patients off of opioids using cannabis.”
Dr. Wallace said he found the guidelines’ dosing recommendations helpful.
“If you stay within the 1- to 5-mg dosing range, the risks are so incredibly low, you’re not going to harm the patient.”
While there are patients who abuse cannabis and CBMs, Dr. Wallace noted that he has seen only one patient in the past 20 years who was overusing the medical cannabis. He added that his patient population does not use medical cannabis to get high and, in fact, wants to avoid doses that produce that effect at all costs.
Also commenting on the guidelines, Christopher Gilligan, MD, MBA, associate chief medical officer and a pain medicine physician at Brigham and Women’s Hospital in Boston, who was not involved in the guidelines’ development, points to the risks.
“When we have an opportunity to use cannabinoids in place of opioids for our patients, I think that that’s a positive thing ... and a wise choice in terms of risk benefit,” Dr. Gilligan said.
On the other hand, he cautioned that “freely prescribing” cannabinoids for chronic pain in patients who aren’t on opioids is not good practice.
“We have to take seriously the potential adverse effects of [cannabis], including marijuana use disorder, interference with learning, memory impairment, and psychotic breakthroughs,” said Dr. Gilligan.
Given the current climate, it would appear that CBM is a long way from being endorsed by the Food and Drug Administration, but for clinicians interested in trying CBM for chronic pain patients, the guidelines may offer a roadmap for initiation and an alternative to prescribing opioids.
Dr. Bell, Dr. Gilligan, and Dr. Wallace report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CANNABIS AND CANNABINOID RESEARCH
Four PTSD blood biomarkers identified
“More accurate means of predicting or screening for PTSD could help to overcome the disorder by identifying individuals at high risk of developing PTSD and providing them with early intervention or prevention strategies,” said study investigator Stacy-Ann Miller, MS.
She also noted that the biomarkers could be used to monitor treatment for PTSD, identify subtypes of PTSD, and lead to a new understanding of the mechanisms underlying PTSD.
The findings were presented at Discover BMB, the annual meeting of the American Society for Biochemistry and Molecular Biology.
Toward better clinical assessment
The findings originated from research conducted by the Department of Defense–initiated PTSD Systems Biology Consortium. The consortium’s goals include developing a reproducible panel of blood-based biomarkers with high sensitivity and specificity for PTSD diagnosis and is made up of about 45 researchers, led by Marti Jett, PhD, Charles Marmar, MD, and Francis J. Doyle III, PhD.
The researchers analyzed blood samples from 1,000 active-duty Army personnel from the 101st Airborne at Fort Campbell, Ky. Participants were assessed before and after deployment to Afghanistan in February 2014 and are referred to as the Fort Campbell Cohort (FCC). Participants’ age ranged from 25 to 30 and approximately 6% were female.
Investigators collected blood samples from the service members and looked for four biomarkers: glycolytic ratio, arginine, serotonin, and glutamate. The team then divided the participants into four groups – those with PTSD (PTSD Checklist score above 30), those who were subthreshold for PTSD (PTSD Checklist score 15-30), those who had high resilience, and those who had low levels of resilience.
The resilience groups were determined based on answers to the Generalized Anxiety Disorder Questionnaire, Patient Health Questionnaire, Pittsburgh Sleep Quality Index, Intensive Combat Exposure (DRRI-D), the number of deployments, whether they had moderate or severe traumatic brain injury, and scores on the Alcohol Use Disorders Identification Test.
Those who scored in the high range at current or prior time points or who were PTSD/subthreshold at prior time points were placed in the low resilience group.
Ms. Miller noted that those in the PTSD group had more severe symptoms than those in the PTSD subthreshold group based on the longitudinal clinical assessment at 3-6 months, 5 years, and longer post deployment. The low resilience group had a much higher rate of PTSD post deployment than the high resilience group.
Investigators found participants with PTSD or subthreshold PTSD had significantly higher glycolic ratios and lower arginine than those with high resilience. They also found that those with PTSD had significantly lower serotonin and higher glutamate levels versus those with high resilience. These associations were independent of factors such as sex, age, body mass index, smoking, and caffeine consumption.
Ms. Miller said that the study results require further validation by the consortium’s labs and third-party labs.
“We are also interested in determining the most appropriate time to screen soldiers for PTSD, as it has been noted that the time period where we see the most psychological issues is around 2-3 months post return from deployment and when the soldier is preparing for their next assignment, perhaps a next deployment,” she said.
She added that previous studies have identified several promising biomarkers of PTSD. “However, like much of the research data, the study sample was comprised mainly of combat-exposed males. With more women serving on the front lines, the military faces new challenges in how combat affects females in the military,” including sex-specific biomarkers that will improve clinical assessment for female soldiers.
Eventually, the team would also like to be able to apply their research to the civilian population experiencing PTSD.
“Our research is anticipated to be useful in helping the medical provider select appropriate therapeutic interventions,” Ms. Miller said.
A version of this article first appeared on Medscape.com.
“More accurate means of predicting or screening for PTSD could help to overcome the disorder by identifying individuals at high risk of developing PTSD and providing them with early intervention or prevention strategies,” said study investigator Stacy-Ann Miller, MS.
She also noted that the biomarkers could be used to monitor treatment for PTSD, identify subtypes of PTSD, and lead to a new understanding of the mechanisms underlying PTSD.
The findings were presented at Discover BMB, the annual meeting of the American Society for Biochemistry and Molecular Biology.
Toward better clinical assessment
The findings originated from research conducted by the Department of Defense–initiated PTSD Systems Biology Consortium. The consortium’s goals include developing a reproducible panel of blood-based biomarkers with high sensitivity and specificity for PTSD diagnosis and is made up of about 45 researchers, led by Marti Jett, PhD, Charles Marmar, MD, and Francis J. Doyle III, PhD.
The researchers analyzed blood samples from 1,000 active-duty Army personnel from the 101st Airborne at Fort Campbell, Ky. Participants were assessed before and after deployment to Afghanistan in February 2014 and are referred to as the Fort Campbell Cohort (FCC). Participants’ age ranged from 25 to 30 and approximately 6% were female.
Investigators collected blood samples from the service members and looked for four biomarkers: glycolytic ratio, arginine, serotonin, and glutamate. The team then divided the participants into four groups – those with PTSD (PTSD Checklist score above 30), those who were subthreshold for PTSD (PTSD Checklist score 15-30), those who had high resilience, and those who had low levels of resilience.
The resilience groups were determined based on answers to the Generalized Anxiety Disorder Questionnaire, Patient Health Questionnaire, Pittsburgh Sleep Quality Index, Intensive Combat Exposure (DRRI-D), the number of deployments, whether they had moderate or severe traumatic brain injury, and scores on the Alcohol Use Disorders Identification Test.
Those who scored in the high range at current or prior time points or who were PTSD/subthreshold at prior time points were placed in the low resilience group.
Ms. Miller noted that those in the PTSD group had more severe symptoms than those in the PTSD subthreshold group based on the longitudinal clinical assessment at 3-6 months, 5 years, and longer post deployment. The low resilience group had a much higher rate of PTSD post deployment than the high resilience group.
Investigators found participants with PTSD or subthreshold PTSD had significantly higher glycolic ratios and lower arginine than those with high resilience. They also found that those with PTSD had significantly lower serotonin and higher glutamate levels versus those with high resilience. These associations were independent of factors such as sex, age, body mass index, smoking, and caffeine consumption.
Ms. Miller said that the study results require further validation by the consortium’s labs and third-party labs.
“We are also interested in determining the most appropriate time to screen soldiers for PTSD, as it has been noted that the time period where we see the most psychological issues is around 2-3 months post return from deployment and when the soldier is preparing for their next assignment, perhaps a next deployment,” she said.
She added that previous studies have identified several promising biomarkers of PTSD. “However, like much of the research data, the study sample was comprised mainly of combat-exposed males. With more women serving on the front lines, the military faces new challenges in how combat affects females in the military,” including sex-specific biomarkers that will improve clinical assessment for female soldiers.
Eventually, the team would also like to be able to apply their research to the civilian population experiencing PTSD.
“Our research is anticipated to be useful in helping the medical provider select appropriate therapeutic interventions,” Ms. Miller said.
A version of this article first appeared on Medscape.com.
“More accurate means of predicting or screening for PTSD could help to overcome the disorder by identifying individuals at high risk of developing PTSD and providing them with early intervention or prevention strategies,” said study investigator Stacy-Ann Miller, MS.
She also noted that the biomarkers could be used to monitor treatment for PTSD, identify subtypes of PTSD, and lead to a new understanding of the mechanisms underlying PTSD.
The findings were presented at Discover BMB, the annual meeting of the American Society for Biochemistry and Molecular Biology.
Toward better clinical assessment
The findings originated from research conducted by the Department of Defense–initiated PTSD Systems Biology Consortium. The consortium’s goals include developing a reproducible panel of blood-based biomarkers with high sensitivity and specificity for PTSD diagnosis and is made up of about 45 researchers, led by Marti Jett, PhD, Charles Marmar, MD, and Francis J. Doyle III, PhD.
The researchers analyzed blood samples from 1,000 active-duty Army personnel from the 101st Airborne at Fort Campbell, Ky. Participants were assessed before and after deployment to Afghanistan in February 2014 and are referred to as the Fort Campbell Cohort (FCC). Participants’ age ranged from 25 to 30 and approximately 6% were female.
Investigators collected blood samples from the service members and looked for four biomarkers: glycolytic ratio, arginine, serotonin, and glutamate. The team then divided the participants into four groups – those with PTSD (PTSD Checklist score above 30), those who were subthreshold for PTSD (PTSD Checklist score 15-30), those who had high resilience, and those who had low levels of resilience.
The resilience groups were determined based on answers to the Generalized Anxiety Disorder Questionnaire, Patient Health Questionnaire, Pittsburgh Sleep Quality Index, Intensive Combat Exposure (DRRI-D), the number of deployments, whether they had moderate or severe traumatic brain injury, and scores on the Alcohol Use Disorders Identification Test.
Those who scored in the high range at current or prior time points or who were PTSD/subthreshold at prior time points were placed in the low resilience group.
Ms. Miller noted that those in the PTSD group had more severe symptoms than those in the PTSD subthreshold group based on the longitudinal clinical assessment at 3-6 months, 5 years, and longer post deployment. The low resilience group had a much higher rate of PTSD post deployment than the high resilience group.
Investigators found participants with PTSD or subthreshold PTSD had significantly higher glycolic ratios and lower arginine than those with high resilience. They also found that those with PTSD had significantly lower serotonin and higher glutamate levels versus those with high resilience. These associations were independent of factors such as sex, age, body mass index, smoking, and caffeine consumption.
Ms. Miller said that the study results require further validation by the consortium’s labs and third-party labs.
“We are also interested in determining the most appropriate time to screen soldiers for PTSD, as it has been noted that the time period where we see the most psychological issues is around 2-3 months post return from deployment and when the soldier is preparing for their next assignment, perhaps a next deployment,” she said.
She added that previous studies have identified several promising biomarkers of PTSD. “However, like much of the research data, the study sample was comprised mainly of combat-exposed males. With more women serving on the front lines, the military faces new challenges in how combat affects females in the military,” including sex-specific biomarkers that will improve clinical assessment for female soldiers.
Eventually, the team would also like to be able to apply their research to the civilian population experiencing PTSD.
“Our research is anticipated to be useful in helping the medical provider select appropriate therapeutic interventions,” Ms. Miller said.
A version of this article first appeared on Medscape.com.
FROM DISCOVER BMB
Lack of food for thought: Starve a bacterium, feed an infection
A whole new, tiny level of hangry
Ever been so hungry that everything just got on your nerves? Maybe you feel a little snappy right now? Like you’ll just lash out unless you get something to eat? Been there. And so have bacteria.
New research shows that some bacteria go into a full-on Hulk smash if they’re not getting the nutrients they need by releasing toxins into the body. Sounds like a bacterial temper tantrum.
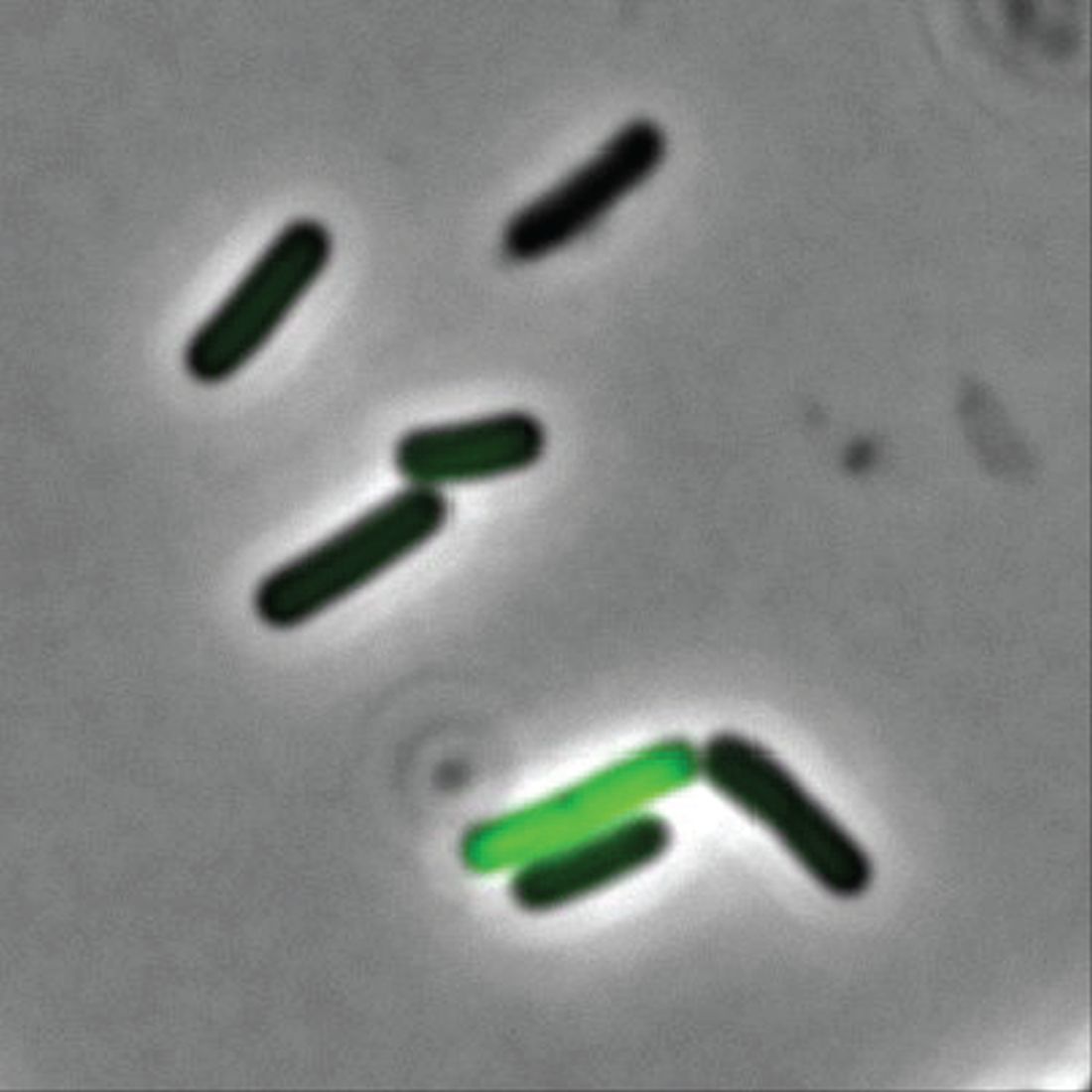
Even though two cells may be genetically identical, they don’t always behave the same in a bacterial community. Some do their job and stay in line, but some evil twins rage out and make people sick by releasing toxins into the environment, Adam Rosenthal, PhD, of the University of North Carolina and his colleagues discovered.
To figure out why some cells were all business as usual while others were not, the investigators looked at Clostridium perfringens, a bacterium found in the intestines of humans and other vertebrates. When the C. perfringens cells were fed a little acetate to munch on, the hangry cells calmed down faster than a kid with a bag of fruit snacks, reducing toxin levels. Some cells even disappeared, falling in line with their model-citizen counterparts.
So what does this really mean? More research, duh. Now that we know nutrients play a role in toxicity, it may open the door to finding a way to fight against antibiotic resistance in humans and reduce antibiotic use in the food industry.
So think to yourself. Are you bothered for no reason? Getting a little testy with your friends and coworkers? Maybe you just haven’t eaten in a while. You’re literally not alone. Even a single-cell organism can behave based on its hunger levels.
Now go have a snack. Your bacteria are getting restless.
The very hangry iguana?
Imagine yourself on a warm, sunny tropical beach. You are enjoying a piece of cake as you take in the slow beat of the waves lapping against the shore. Life is as good as it could be.
Then you feel a presence nearby. Hostility. Hunger. A set of feral, covetous eyes in the nearby jungle. A reptilian beast stalks you, and its all-encompassing sweet tooth desires your cake.
Wait, hold on, what?
As an unfortunate 3-year-old on vacation in Costa Rica found out, there’s at least one iguana in the world out there with a taste for sugar (better than a taste for blood, we suppose).
While out on the beach, the lizard darted out of nowhere, bit the girl on the back of the hand, and stole her cake. Still not the worst party guest ever. The child was taken to a local clinic, where the wound was cleaned and a 5-day antibiotic treatment (lizards carry salmonella) was provided. Things seemed fine, and the girl returned home without incident.
But of course, that’s not the end of the story. Five months later, the girl’s parents noticed a red bump at the wound site. Over the next 3 months, the surrounding skin grew red and painful. A trip to the hospital in California revealed that she had a ganglion cyst and a discharge of pus. Turns out our cake-obsessed lizard friend did give the little girl a gift: the first known human case of Mycobacterium marinum infection following an iguana bite on record.
M. marinum, which causes a disease similar to tuberculosis, typically infects fish but can infect humans if skin wounds are exposed to contaminated water. It’s also resistant to most antibiotics, which is why the first round didn’t clear up the infection. A second round of more-potent antibiotics seems to be working well.
So, to sum up, this poor child got bitten by a lizard, had her cake stolen, and contracted a rare illness in exchange. For a 3-year-old, that’s gotta be in the top-10 worst days ever. Unless, of course, we’re actually living in the Marvel universe (sorry, multiverse at this point). Then we’re totally going to see the emergence of the new superhero Iguana Girl in 15 years or so. Keep your eyes open.
No allergies? Let them give up cake
Allergy season is already here – starting earlier every year, it seems – and many people are not happy about it. So unhappy, actually, that there’s a list of things they would be willing to give up for a year to get rid of their of allergies, according to a survey conducted by OnePoll on behalf of Flonase.
Nearly 40% of 2,000 respondents with allergies would go a year without eating cake or chocolate or playing video games in exchange for allergy-free status, the survey results show. Almost as many would forgo coffee (38%) or pizza (37%) for a year, while 36% would stay off social media and 31% would take a pay cut or give up their smartphones, the Independent reported.
More than half of the allergic Americans – 54%, to be exact – who were polled this past winter – Feb. 24 to March 1, to be exact – consider allergy symptoms to be the most frustrating part of the spring. Annoying things that were less frustrating to the group included mosquitoes (41%), filing tax returns (38%), and daylight savings time (37%).
The Trump arraignment circus, of course, occurred too late to make the list, as did the big “We’re going back to the office! No wait, we’re closing the office forever!” email extravaganza and emotional roller coaster. That second one, however, did not get nearly as much media coverage.
A whole new, tiny level of hangry
Ever been so hungry that everything just got on your nerves? Maybe you feel a little snappy right now? Like you’ll just lash out unless you get something to eat? Been there. And so have bacteria.
New research shows that some bacteria go into a full-on Hulk smash if they’re not getting the nutrients they need by releasing toxins into the body. Sounds like a bacterial temper tantrum.
Even though two cells may be genetically identical, they don’t always behave the same in a bacterial community. Some do their job and stay in line, but some evil twins rage out and make people sick by releasing toxins into the environment, Adam Rosenthal, PhD, of the University of North Carolina and his colleagues discovered.
To figure out why some cells were all business as usual while others were not, the investigators looked at Clostridium perfringens, a bacterium found in the intestines of humans and other vertebrates. When the C. perfringens cells were fed a little acetate to munch on, the hangry cells calmed down faster than a kid with a bag of fruit snacks, reducing toxin levels. Some cells even disappeared, falling in line with their model-citizen counterparts.
So what does this really mean? More research, duh. Now that we know nutrients play a role in toxicity, it may open the door to finding a way to fight against antibiotic resistance in humans and reduce antibiotic use in the food industry.
So think to yourself. Are you bothered for no reason? Getting a little testy with your friends and coworkers? Maybe you just haven’t eaten in a while. You’re literally not alone. Even a single-cell organism can behave based on its hunger levels.
Now go have a snack. Your bacteria are getting restless.
The very hangry iguana?
Imagine yourself on a warm, sunny tropical beach. You are enjoying a piece of cake as you take in the slow beat of the waves lapping against the shore. Life is as good as it could be.
Then you feel a presence nearby. Hostility. Hunger. A set of feral, covetous eyes in the nearby jungle. A reptilian beast stalks you, and its all-encompassing sweet tooth desires your cake.
Wait, hold on, what?
As an unfortunate 3-year-old on vacation in Costa Rica found out, there’s at least one iguana in the world out there with a taste for sugar (better than a taste for blood, we suppose).
While out on the beach, the lizard darted out of nowhere, bit the girl on the back of the hand, and stole her cake. Still not the worst party guest ever. The child was taken to a local clinic, where the wound was cleaned and a 5-day antibiotic treatment (lizards carry salmonella) was provided. Things seemed fine, and the girl returned home without incident.
But of course, that’s not the end of the story. Five months later, the girl’s parents noticed a red bump at the wound site. Over the next 3 months, the surrounding skin grew red and painful. A trip to the hospital in California revealed that she had a ganglion cyst and a discharge of pus. Turns out our cake-obsessed lizard friend did give the little girl a gift: the first known human case of Mycobacterium marinum infection following an iguana bite on record.
M. marinum, which causes a disease similar to tuberculosis, typically infects fish but can infect humans if skin wounds are exposed to contaminated water. It’s also resistant to most antibiotics, which is why the first round didn’t clear up the infection. A second round of more-potent antibiotics seems to be working well.
So, to sum up, this poor child got bitten by a lizard, had her cake stolen, and contracted a rare illness in exchange. For a 3-year-old, that’s gotta be in the top-10 worst days ever. Unless, of course, we’re actually living in the Marvel universe (sorry, multiverse at this point). Then we’re totally going to see the emergence of the new superhero Iguana Girl in 15 years or so. Keep your eyes open.
No allergies? Let them give up cake
Allergy season is already here – starting earlier every year, it seems – and many people are not happy about it. So unhappy, actually, that there’s a list of things they would be willing to give up for a year to get rid of their of allergies, according to a survey conducted by OnePoll on behalf of Flonase.
Nearly 40% of 2,000 respondents with allergies would go a year without eating cake or chocolate or playing video games in exchange for allergy-free status, the survey results show. Almost as many would forgo coffee (38%) or pizza (37%) for a year, while 36% would stay off social media and 31% would take a pay cut or give up their smartphones, the Independent reported.
More than half of the allergic Americans – 54%, to be exact – who were polled this past winter – Feb. 24 to March 1, to be exact – consider allergy symptoms to be the most frustrating part of the spring. Annoying things that were less frustrating to the group included mosquitoes (41%), filing tax returns (38%), and daylight savings time (37%).
The Trump arraignment circus, of course, occurred too late to make the list, as did the big “We’re going back to the office! No wait, we’re closing the office forever!” email extravaganza and emotional roller coaster. That second one, however, did not get nearly as much media coverage.
A whole new, tiny level of hangry
Ever been so hungry that everything just got on your nerves? Maybe you feel a little snappy right now? Like you’ll just lash out unless you get something to eat? Been there. And so have bacteria.
New research shows that some bacteria go into a full-on Hulk smash if they’re not getting the nutrients they need by releasing toxins into the body. Sounds like a bacterial temper tantrum.
Even though two cells may be genetically identical, they don’t always behave the same in a bacterial community. Some do their job and stay in line, but some evil twins rage out and make people sick by releasing toxins into the environment, Adam Rosenthal, PhD, of the University of North Carolina and his colleagues discovered.
To figure out why some cells were all business as usual while others were not, the investigators looked at Clostridium perfringens, a bacterium found in the intestines of humans and other vertebrates. When the C. perfringens cells were fed a little acetate to munch on, the hangry cells calmed down faster than a kid with a bag of fruit snacks, reducing toxin levels. Some cells even disappeared, falling in line with their model-citizen counterparts.
So what does this really mean? More research, duh. Now that we know nutrients play a role in toxicity, it may open the door to finding a way to fight against antibiotic resistance in humans and reduce antibiotic use in the food industry.
So think to yourself. Are you bothered for no reason? Getting a little testy with your friends and coworkers? Maybe you just haven’t eaten in a while. You’re literally not alone. Even a single-cell organism can behave based on its hunger levels.
Now go have a snack. Your bacteria are getting restless.
The very hangry iguana?
Imagine yourself on a warm, sunny tropical beach. You are enjoying a piece of cake as you take in the slow beat of the waves lapping against the shore. Life is as good as it could be.
Then you feel a presence nearby. Hostility. Hunger. A set of feral, covetous eyes in the nearby jungle. A reptilian beast stalks you, and its all-encompassing sweet tooth desires your cake.
Wait, hold on, what?
As an unfortunate 3-year-old on vacation in Costa Rica found out, there’s at least one iguana in the world out there with a taste for sugar (better than a taste for blood, we suppose).
While out on the beach, the lizard darted out of nowhere, bit the girl on the back of the hand, and stole her cake. Still not the worst party guest ever. The child was taken to a local clinic, where the wound was cleaned and a 5-day antibiotic treatment (lizards carry salmonella) was provided. Things seemed fine, and the girl returned home without incident.
But of course, that’s not the end of the story. Five months later, the girl’s parents noticed a red bump at the wound site. Over the next 3 months, the surrounding skin grew red and painful. A trip to the hospital in California revealed that she had a ganglion cyst and a discharge of pus. Turns out our cake-obsessed lizard friend did give the little girl a gift: the first known human case of Mycobacterium marinum infection following an iguana bite on record.
M. marinum, which causes a disease similar to tuberculosis, typically infects fish but can infect humans if skin wounds are exposed to contaminated water. It’s also resistant to most antibiotics, which is why the first round didn’t clear up the infection. A second round of more-potent antibiotics seems to be working well.
So, to sum up, this poor child got bitten by a lizard, had her cake stolen, and contracted a rare illness in exchange. For a 3-year-old, that’s gotta be in the top-10 worst days ever. Unless, of course, we’re actually living in the Marvel universe (sorry, multiverse at this point). Then we’re totally going to see the emergence of the new superhero Iguana Girl in 15 years or so. Keep your eyes open.
No allergies? Let them give up cake
Allergy season is already here – starting earlier every year, it seems – and many people are not happy about it. So unhappy, actually, that there’s a list of things they would be willing to give up for a year to get rid of their of allergies, according to a survey conducted by OnePoll on behalf of Flonase.
Nearly 40% of 2,000 respondents with allergies would go a year without eating cake or chocolate or playing video games in exchange for allergy-free status, the survey results show. Almost as many would forgo coffee (38%) or pizza (37%) for a year, while 36% would stay off social media and 31% would take a pay cut or give up their smartphones, the Independent reported.
More than half of the allergic Americans – 54%, to be exact – who were polled this past winter – Feb. 24 to March 1, to be exact – consider allergy symptoms to be the most frustrating part of the spring. Annoying things that were less frustrating to the group included mosquitoes (41%), filing tax returns (38%), and daylight savings time (37%).
The Trump arraignment circus, of course, occurred too late to make the list, as did the big “We’re going back to the office! No wait, we’re closing the office forever!” email extravaganza and emotional roller coaster. That second one, however, did not get nearly as much media coverage.
Kidney disease skews Alzheimer’s biomarker testing
New research provides more evidence that
In a cross-sectional study of adults with and those without cognitive impairment, chronic kidney disease was associated with increased plasma concentrations of phosphorylated tau (p-tau) 217 and 181.
However, there were no associations between chronic kidney disease and the ratio of p-tau217 to unphosphorylated tau 217 (pT217/T217), and the associations with p-tau181 to unphosphorylated tau 181 (pT181/T181) were attenuated in patients with cognitive impairment.
“These novel findings suggest that plasma measures of the phosphorylated to unphosphorylated tau ratios are more accurate than p-tau forms alone as they correlate less with individual difference in glomerular filtration rate or impaired kidney function,” reported an investigative team led by Oskar Hansson, MD, PhD, with Lund University in Sweden.
“Thus, to mitigate the effects of non-Alzheimer’s–related comorbidities like chronic kidney disease on the performance of plasma Alzheimer’s disease biomarkers, certain tau ratios, and specifically pT217/T217, should be considered for implementation in clinical practice and drug trials,” they added.
The study was published online in JAMA Neurology to coincide with a presentation at the International Conference on Alzheimer’s and Parkinson’s Diseases in Gothenburg, Sweden.
Skewed tau levels
Plasma biomarkers of amyloid-beta (Abeta) and tau pathologies, and in particular variants in p-tau217 and p-tau181, have shown promise for use in Alzheimer’s disease diagnosis and prognosis. However, previous reports have suggested that chronic kidney disease might influence plasma p-tau217 and p-tau181 concentrations, potentially decreasing their usefulness in the diagnostic workup of dementia.
Researchers investigated associations of chronic kidney disease with plasma ratios of p-tau217 and p-tau181 to the corresponding unphosphorylated peptides in Alzheimer’s disease.
The data came from 473 older adults, with and without cognitive impairment, from the Swedish BioFinder-2 study who had plasma tau assessments and chronic kidney disease status established within 6 months of plasma collection.
The researchers found that lower estimated glomerular filtration rate levels (indicative of kidney dysfunction) were associated with higher plasma concentrations of phosphorylated and unphosphorylated tau peptides measured simultaneously using the tau immunoprecipitation mass spectrometry assay.
However, the correlations with estimated glomerular filtration rate were nonsignificant for the pT217/T217 ratio in individuals with cognitive impairment and were significantly attenuated for pT217/T217 in cognitively unimpaired individuals and for pT181/T181 in both cognitively unimpaired and impaired individuals.
“Importantly, we demonstrate that there were no significant associations between chronic kidney disease and the pT217/T217 ratio and changes in plasma pT181/T181 associated with chronic kidney disease were small or nonsignificant,” the researchers noted.
“Our results indicate that by using p-tau/tau ratios we may be able to reduce the variability in plasma p-tau levels driven by impaired kidney function and consequently such ratios are more robust measures of brain p-tau pathology in individuals with both early- and later-stage Alzheimer’s disease,” they added.
The researchers believe this is likely true for the ratios of other related proteins – a view that is supported by findings of attenuated associations of chronic kidney disease with Abeta42/40, compared with Abeta42 and Abeta40 in the current study and in previous studies.
Important clinical implications
Reached for comment, Rebecca Edelmayer, PhD, Alzheimer’s Association senior director of scientific engagement, noted that research continues to indicate that blood biomarkers have “promise for improving, and possibly even redefining, the clinical workup for Alzheimer’s disease.
“Many of the Alzheimer’s blood tests in development today have focused on core blood biomarkers associated with amyloid accumulation and tau tangle formation in the brain,” Dr. Edelmayer said.
“Before these tests can be used more broadly in the clinic, we need to understand all of the variables that may impact the results of various blood biomarkers, including differences that may be driven by race, ethnicity, sex, and underlying health conditions, such as chronic kidney disease.
“This study corroborates other research suggesting that some Alzheimer’s-associated markers can be affected by chronic kidney disease, but by using ratios of amyloid or tau markers, we may be able to minimize these differences in results caused by underlying disease,” Dr. Edelmayer said.
Howard Fillit, MD, cofounder and chief science officer at the Alzheimer’s Drug Discovery Foundation, said, “Using these ratios makes a lot of sense because the ratios wouldn’t change with kidney function. I think this is an important advance in clinical utilization of these tests.”
Dr. Fillit noted that older people often have declining kidney function, which can be easily measured by glomerular filtration rate. Changes in blood levels of these markers with declining kidney function are “not unexpected, but [it’s] important that it’s been demonstrated.
“As we go forward, maybe the future utilization of these tests will be not only recording the ratios but also reporting the ratios in the context of somebody’s glomerular filtration rate. You could imagine a scenario where when the test is done, it’s automatically done alongside of glomerular filtration rate,” Dr. Fillit said in an interview.
The study was supported by Coins for Alzheimer’s Research Trust, the Tracy Family Stable Isotope Labeling Quantitation Center, and the National Institute of Neurological Disorders and Stroke. Dr. Hansson has received support to his institution from ADx, AVID Radiopharmaceuticals, Biogen, Eli Lilly, Eisai, Fujirebio, GE Healthcare, Pfizer, and Roche; consultancy/speaker fees from Amylyx, Alzpath, Biogen, Cerveau, Fujirebio, Genentech, Novartis, Roche, and Siemens; and personal fees from Eli Lilly, Eisai, Bioarctic, and Biogen outside the submitted work. Dr. Edelmayer and Dr. Fillit have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New research provides more evidence that
In a cross-sectional study of adults with and those without cognitive impairment, chronic kidney disease was associated with increased plasma concentrations of phosphorylated tau (p-tau) 217 and 181.
However, there were no associations between chronic kidney disease and the ratio of p-tau217 to unphosphorylated tau 217 (pT217/T217), and the associations with p-tau181 to unphosphorylated tau 181 (pT181/T181) were attenuated in patients with cognitive impairment.
“These novel findings suggest that plasma measures of the phosphorylated to unphosphorylated tau ratios are more accurate than p-tau forms alone as they correlate less with individual difference in glomerular filtration rate or impaired kidney function,” reported an investigative team led by Oskar Hansson, MD, PhD, with Lund University in Sweden.
“Thus, to mitigate the effects of non-Alzheimer’s–related comorbidities like chronic kidney disease on the performance of plasma Alzheimer’s disease biomarkers, certain tau ratios, and specifically pT217/T217, should be considered for implementation in clinical practice and drug trials,” they added.
The study was published online in JAMA Neurology to coincide with a presentation at the International Conference on Alzheimer’s and Parkinson’s Diseases in Gothenburg, Sweden.
Skewed tau levels
Plasma biomarkers of amyloid-beta (Abeta) and tau pathologies, and in particular variants in p-tau217 and p-tau181, have shown promise for use in Alzheimer’s disease diagnosis and prognosis. However, previous reports have suggested that chronic kidney disease might influence plasma p-tau217 and p-tau181 concentrations, potentially decreasing their usefulness in the diagnostic workup of dementia.
Researchers investigated associations of chronic kidney disease with plasma ratios of p-tau217 and p-tau181 to the corresponding unphosphorylated peptides in Alzheimer’s disease.
The data came from 473 older adults, with and without cognitive impairment, from the Swedish BioFinder-2 study who had plasma tau assessments and chronic kidney disease status established within 6 months of plasma collection.
The researchers found that lower estimated glomerular filtration rate levels (indicative of kidney dysfunction) were associated with higher plasma concentrations of phosphorylated and unphosphorylated tau peptides measured simultaneously using the tau immunoprecipitation mass spectrometry assay.
However, the correlations with estimated glomerular filtration rate were nonsignificant for the pT217/T217 ratio in individuals with cognitive impairment and were significantly attenuated for pT217/T217 in cognitively unimpaired individuals and for pT181/T181 in both cognitively unimpaired and impaired individuals.
“Importantly, we demonstrate that there were no significant associations between chronic kidney disease and the pT217/T217 ratio and changes in plasma pT181/T181 associated with chronic kidney disease were small or nonsignificant,” the researchers noted.
“Our results indicate that by using p-tau/tau ratios we may be able to reduce the variability in plasma p-tau levels driven by impaired kidney function and consequently such ratios are more robust measures of brain p-tau pathology in individuals with both early- and later-stage Alzheimer’s disease,” they added.
The researchers believe this is likely true for the ratios of other related proteins – a view that is supported by findings of attenuated associations of chronic kidney disease with Abeta42/40, compared with Abeta42 and Abeta40 in the current study and in previous studies.
Important clinical implications
Reached for comment, Rebecca Edelmayer, PhD, Alzheimer’s Association senior director of scientific engagement, noted that research continues to indicate that blood biomarkers have “promise for improving, and possibly even redefining, the clinical workup for Alzheimer’s disease.
“Many of the Alzheimer’s blood tests in development today have focused on core blood biomarkers associated with amyloid accumulation and tau tangle formation in the brain,” Dr. Edelmayer said.
“Before these tests can be used more broadly in the clinic, we need to understand all of the variables that may impact the results of various blood biomarkers, including differences that may be driven by race, ethnicity, sex, and underlying health conditions, such as chronic kidney disease.
“This study corroborates other research suggesting that some Alzheimer’s-associated markers can be affected by chronic kidney disease, but by using ratios of amyloid or tau markers, we may be able to minimize these differences in results caused by underlying disease,” Dr. Edelmayer said.
Howard Fillit, MD, cofounder and chief science officer at the Alzheimer’s Drug Discovery Foundation, said, “Using these ratios makes a lot of sense because the ratios wouldn’t change with kidney function. I think this is an important advance in clinical utilization of these tests.”
Dr. Fillit noted that older people often have declining kidney function, which can be easily measured by glomerular filtration rate. Changes in blood levels of these markers with declining kidney function are “not unexpected, but [it’s] important that it’s been demonstrated.
“As we go forward, maybe the future utilization of these tests will be not only recording the ratios but also reporting the ratios in the context of somebody’s glomerular filtration rate. You could imagine a scenario where when the test is done, it’s automatically done alongside of glomerular filtration rate,” Dr. Fillit said in an interview.
The study was supported by Coins for Alzheimer’s Research Trust, the Tracy Family Stable Isotope Labeling Quantitation Center, and the National Institute of Neurological Disorders and Stroke. Dr. Hansson has received support to his institution from ADx, AVID Radiopharmaceuticals, Biogen, Eli Lilly, Eisai, Fujirebio, GE Healthcare, Pfizer, and Roche; consultancy/speaker fees from Amylyx, Alzpath, Biogen, Cerveau, Fujirebio, Genentech, Novartis, Roche, and Siemens; and personal fees from Eli Lilly, Eisai, Bioarctic, and Biogen outside the submitted work. Dr. Edelmayer and Dr. Fillit have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New research provides more evidence that
In a cross-sectional study of adults with and those without cognitive impairment, chronic kidney disease was associated with increased plasma concentrations of phosphorylated tau (p-tau) 217 and 181.
However, there were no associations between chronic kidney disease and the ratio of p-tau217 to unphosphorylated tau 217 (pT217/T217), and the associations with p-tau181 to unphosphorylated tau 181 (pT181/T181) were attenuated in patients with cognitive impairment.
“These novel findings suggest that plasma measures of the phosphorylated to unphosphorylated tau ratios are more accurate than p-tau forms alone as they correlate less with individual difference in glomerular filtration rate or impaired kidney function,” reported an investigative team led by Oskar Hansson, MD, PhD, with Lund University in Sweden.
“Thus, to mitigate the effects of non-Alzheimer’s–related comorbidities like chronic kidney disease on the performance of plasma Alzheimer’s disease biomarkers, certain tau ratios, and specifically pT217/T217, should be considered for implementation in clinical practice and drug trials,” they added.
The study was published online in JAMA Neurology to coincide with a presentation at the International Conference on Alzheimer’s and Parkinson’s Diseases in Gothenburg, Sweden.
Skewed tau levels
Plasma biomarkers of amyloid-beta (Abeta) and tau pathologies, and in particular variants in p-tau217 and p-tau181, have shown promise for use in Alzheimer’s disease diagnosis and prognosis. However, previous reports have suggested that chronic kidney disease might influence plasma p-tau217 and p-tau181 concentrations, potentially decreasing their usefulness in the diagnostic workup of dementia.
Researchers investigated associations of chronic kidney disease with plasma ratios of p-tau217 and p-tau181 to the corresponding unphosphorylated peptides in Alzheimer’s disease.
The data came from 473 older adults, with and without cognitive impairment, from the Swedish BioFinder-2 study who had plasma tau assessments and chronic kidney disease status established within 6 months of plasma collection.
The researchers found that lower estimated glomerular filtration rate levels (indicative of kidney dysfunction) were associated with higher plasma concentrations of phosphorylated and unphosphorylated tau peptides measured simultaneously using the tau immunoprecipitation mass spectrometry assay.
However, the correlations with estimated glomerular filtration rate were nonsignificant for the pT217/T217 ratio in individuals with cognitive impairment and were significantly attenuated for pT217/T217 in cognitively unimpaired individuals and for pT181/T181 in both cognitively unimpaired and impaired individuals.
“Importantly, we demonstrate that there were no significant associations between chronic kidney disease and the pT217/T217 ratio and changes in plasma pT181/T181 associated with chronic kidney disease were small or nonsignificant,” the researchers noted.
“Our results indicate that by using p-tau/tau ratios we may be able to reduce the variability in plasma p-tau levels driven by impaired kidney function and consequently such ratios are more robust measures of brain p-tau pathology in individuals with both early- and later-stage Alzheimer’s disease,” they added.
The researchers believe this is likely true for the ratios of other related proteins – a view that is supported by findings of attenuated associations of chronic kidney disease with Abeta42/40, compared with Abeta42 and Abeta40 in the current study and in previous studies.
Important clinical implications
Reached for comment, Rebecca Edelmayer, PhD, Alzheimer’s Association senior director of scientific engagement, noted that research continues to indicate that blood biomarkers have “promise for improving, and possibly even redefining, the clinical workup for Alzheimer’s disease.
“Many of the Alzheimer’s blood tests in development today have focused on core blood biomarkers associated with amyloid accumulation and tau tangle formation in the brain,” Dr. Edelmayer said.
“Before these tests can be used more broadly in the clinic, we need to understand all of the variables that may impact the results of various blood biomarkers, including differences that may be driven by race, ethnicity, sex, and underlying health conditions, such as chronic kidney disease.
“This study corroborates other research suggesting that some Alzheimer’s-associated markers can be affected by chronic kidney disease, but by using ratios of amyloid or tau markers, we may be able to minimize these differences in results caused by underlying disease,” Dr. Edelmayer said.
Howard Fillit, MD, cofounder and chief science officer at the Alzheimer’s Drug Discovery Foundation, said, “Using these ratios makes a lot of sense because the ratios wouldn’t change with kidney function. I think this is an important advance in clinical utilization of these tests.”
Dr. Fillit noted that older people often have declining kidney function, which can be easily measured by glomerular filtration rate. Changes in blood levels of these markers with declining kidney function are “not unexpected, but [it’s] important that it’s been demonstrated.
“As we go forward, maybe the future utilization of these tests will be not only recording the ratios but also reporting the ratios in the context of somebody’s glomerular filtration rate. You could imagine a scenario where when the test is done, it’s automatically done alongside of glomerular filtration rate,” Dr. Fillit said in an interview.
The study was supported by Coins for Alzheimer’s Research Trust, the Tracy Family Stable Isotope Labeling Quantitation Center, and the National Institute of Neurological Disorders and Stroke. Dr. Hansson has received support to his institution from ADx, AVID Radiopharmaceuticals, Biogen, Eli Lilly, Eisai, Fujirebio, GE Healthcare, Pfizer, and Roche; consultancy/speaker fees from Amylyx, Alzpath, Biogen, Cerveau, Fujirebio, Genentech, Novartis, Roche, and Siemens; and personal fees from Eli Lilly, Eisai, Bioarctic, and Biogen outside the submitted work. Dr. Edelmayer and Dr. Fillit have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AD/PD 2023
Mindfulness-based CBT an ‘important’ option for moderate depression
The findings suggest that “offering practitioner-supported MBCT-SH as an intervention for mild to moderate depression would improve outcomes and save money compared with practitioner-supported CBT-SH,” noted the investigators, led by Clara Strauss, PhD, DClinPsy, with the University of Sussex School of Psychology in England.
Practitioner-supported CBT-SH is recommended in U.K. national treatment guidelines for mild to moderate depression. However, some patients’ conditions don’t respond, and dropout rates are high.
The Low-Intensity Guided Help Through Mindfulness (LIGHTMind) trial tested practitioner-supported MBCT-SH as an alternative.
The findings have “important implications” for the more than 100,000 people currently offered CBT-SH for depression in the Improving Access to Psychological Therapies (IAPT) program each year and in publicly funded services elsewhere, the researchers noted.
If translated into routine practice, “this would see many more people recovering from depression while costing health services less money,” they added.
The study was published online in JAMA Psychiatry .
Practice changing?
The trial included 410 adults (mean age, 32 years; 62% women) with mild to moderate depression who were recruited from 10 publicly funded psychological therapy services in England as part of the IAPT program.
Participants were given one of two established self-help workbooks – The Mindful Way Workbook: An 8-Week Program to Free Yourself from Depression and Emotional Distress, written by the pioneers of MBCT, or Overcoming Depression and Low Mood, 3rd Edition: A Five Areas Approach, which is a CBT-SH program widely used in IAPT.
Use of the self-help books was supported by six structured phone or in-person sessions with a trained psychological well-being practitioner.
The primary outcome was depression symptom severity at 16 weeks, which was determined on the basis of Patient Health Questionnaire 9 (PHQ-9) score.
At 16 weeks following randomization, MBCT-SH led to significantly greater reductions in depression symptom severity compared with CBT-SH (mean PHQ-9 score, 7.2 vs. 8.6; between-group difference, 1.5 points; P = .009; d = −0.36).
MBCT-SH also had superior effects on anxiety symptom severity at 16 weeks.
At the 42-week follow-up, between-group effects on depression and anxiety symptom severity remained in the hypothesized direction but were nonsignificant.
This could be due in part by the greater postintervention psychological therapy accessed by participants in the CBT-SH group, the investigators noted.
Practitioner-supported MBCT-SH was more cost-effective than supported CBT-SH.
On average, the CBT-SH intervention cost health services £526 ($631) more per participant than the MBCT-SH intervention over the 42-week follow-up. The probability of MBCT-SH being cost-effective compared with CBT-SH exceeded 95%, the researchers noted.
Useful model for the United States
Commenting for this news organization, Zindel Segal, PhD, professor of psychology, University of Toronto, Scarborough, cautioned against making too much of the differences between the groups, because CBT-SH “trended positive and had a pretty healthy effect size, it just never reached significance.
“I wouldn’t say mindfulness drastically outperformed cognitive therapy. But cognitive therapy is a robust treatment in its own right, and so doing a little bit better is significant,” Dr. Segal said.
He also noted that, appropriately, the trial enrolled adults who were experiencing moderate depression and were not acutely ill. “That’s one of the rationales for self-help compared to providing patients with a more resource-intensive group treatment.
“If you look at the needs of people with moderate depression, what you find is that for cognitive therapy to work, negative thoughts and feelings need to be pervasive in order to make use of the techniques,” Dr. Segal explained.
“With mindfulness, you don’t need any to have constant negative thoughts or feelings. Anything that arises in your experience serves as grist for mill in terms of concentration and focus,” Dr. Segal said.
He also noted that mindfulness-based intervention is “more optimized” for people who are experiencing some measure of recovery or remission.
“It’s well suited for that, as it trends towards the wellness spectrum. But for people who might have greater levels of acuity or severity, cognitive-behavioral therapy might be indicated,” said Dr. Segal.
He also said the U.K. study findings are relevant to U.S. patients with depression.
“While it’s not disseminated in the same way through any kind of national program, the self-help books that are used are widely available, and the support that people were offered, either in person, telephone, or email, could be easily delivered. This would be a very useful model,” Dr. Segal said.
The LIGHTMind trial was funded by the National Institute for Health and Care Research and the Brighton and Sussex Clinical Trials Unit. Dr. Strauss has received grants from Headspace, is research lead for Sussex Mindfulness Centre, and has been chief investigator on National Institute for Health and Care Research. Dr. Segal is one of the authors of the MBCT-SH workbooks used in the study.
A version of this article first appeared on Medscape.com.
The findings suggest that “offering practitioner-supported MBCT-SH as an intervention for mild to moderate depression would improve outcomes and save money compared with practitioner-supported CBT-SH,” noted the investigators, led by Clara Strauss, PhD, DClinPsy, with the University of Sussex School of Psychology in England.
Practitioner-supported CBT-SH is recommended in U.K. national treatment guidelines for mild to moderate depression. However, some patients’ conditions don’t respond, and dropout rates are high.
The Low-Intensity Guided Help Through Mindfulness (LIGHTMind) trial tested practitioner-supported MBCT-SH as an alternative.
The findings have “important implications” for the more than 100,000 people currently offered CBT-SH for depression in the Improving Access to Psychological Therapies (IAPT) program each year and in publicly funded services elsewhere, the researchers noted.
If translated into routine practice, “this would see many more people recovering from depression while costing health services less money,” they added.
The study was published online in JAMA Psychiatry .
Practice changing?
The trial included 410 adults (mean age, 32 years; 62% women) with mild to moderate depression who were recruited from 10 publicly funded psychological therapy services in England as part of the IAPT program.
Participants were given one of two established self-help workbooks – The Mindful Way Workbook: An 8-Week Program to Free Yourself from Depression and Emotional Distress, written by the pioneers of MBCT, or Overcoming Depression and Low Mood, 3rd Edition: A Five Areas Approach, which is a CBT-SH program widely used in IAPT.
Use of the self-help books was supported by six structured phone or in-person sessions with a trained psychological well-being practitioner.
The primary outcome was depression symptom severity at 16 weeks, which was determined on the basis of Patient Health Questionnaire 9 (PHQ-9) score.
At 16 weeks following randomization, MBCT-SH led to significantly greater reductions in depression symptom severity compared with CBT-SH (mean PHQ-9 score, 7.2 vs. 8.6; between-group difference, 1.5 points; P = .009; d = −0.36).
MBCT-SH also had superior effects on anxiety symptom severity at 16 weeks.
At the 42-week follow-up, between-group effects on depression and anxiety symptom severity remained in the hypothesized direction but were nonsignificant.
This could be due in part by the greater postintervention psychological therapy accessed by participants in the CBT-SH group, the investigators noted.
Practitioner-supported MBCT-SH was more cost-effective than supported CBT-SH.
On average, the CBT-SH intervention cost health services £526 ($631) more per participant than the MBCT-SH intervention over the 42-week follow-up. The probability of MBCT-SH being cost-effective compared with CBT-SH exceeded 95%, the researchers noted.
Useful model for the United States
Commenting for this news organization, Zindel Segal, PhD, professor of psychology, University of Toronto, Scarborough, cautioned against making too much of the differences between the groups, because CBT-SH “trended positive and had a pretty healthy effect size, it just never reached significance.
“I wouldn’t say mindfulness drastically outperformed cognitive therapy. But cognitive therapy is a robust treatment in its own right, and so doing a little bit better is significant,” Dr. Segal said.
He also noted that, appropriately, the trial enrolled adults who were experiencing moderate depression and were not acutely ill. “That’s one of the rationales for self-help compared to providing patients with a more resource-intensive group treatment.
“If you look at the needs of people with moderate depression, what you find is that for cognitive therapy to work, negative thoughts and feelings need to be pervasive in order to make use of the techniques,” Dr. Segal explained.
“With mindfulness, you don’t need any to have constant negative thoughts or feelings. Anything that arises in your experience serves as grist for mill in terms of concentration and focus,” Dr. Segal said.
He also noted that mindfulness-based intervention is “more optimized” for people who are experiencing some measure of recovery or remission.
“It’s well suited for that, as it trends towards the wellness spectrum. But for people who might have greater levels of acuity or severity, cognitive-behavioral therapy might be indicated,” said Dr. Segal.
He also said the U.K. study findings are relevant to U.S. patients with depression.
“While it’s not disseminated in the same way through any kind of national program, the self-help books that are used are widely available, and the support that people were offered, either in person, telephone, or email, could be easily delivered. This would be a very useful model,” Dr. Segal said.
The LIGHTMind trial was funded by the National Institute for Health and Care Research and the Brighton and Sussex Clinical Trials Unit. Dr. Strauss has received grants from Headspace, is research lead for Sussex Mindfulness Centre, and has been chief investigator on National Institute for Health and Care Research. Dr. Segal is one of the authors of the MBCT-SH workbooks used in the study.
A version of this article first appeared on Medscape.com.
The findings suggest that “offering practitioner-supported MBCT-SH as an intervention for mild to moderate depression would improve outcomes and save money compared with practitioner-supported CBT-SH,” noted the investigators, led by Clara Strauss, PhD, DClinPsy, with the University of Sussex School of Psychology in England.
Practitioner-supported CBT-SH is recommended in U.K. national treatment guidelines for mild to moderate depression. However, some patients’ conditions don’t respond, and dropout rates are high.
The Low-Intensity Guided Help Through Mindfulness (LIGHTMind) trial tested practitioner-supported MBCT-SH as an alternative.
The findings have “important implications” for the more than 100,000 people currently offered CBT-SH for depression in the Improving Access to Psychological Therapies (IAPT) program each year and in publicly funded services elsewhere, the researchers noted.
If translated into routine practice, “this would see many more people recovering from depression while costing health services less money,” they added.
The study was published online in JAMA Psychiatry .
Practice changing?
The trial included 410 adults (mean age, 32 years; 62% women) with mild to moderate depression who were recruited from 10 publicly funded psychological therapy services in England as part of the IAPT program.
Participants were given one of two established self-help workbooks – The Mindful Way Workbook: An 8-Week Program to Free Yourself from Depression and Emotional Distress, written by the pioneers of MBCT, or Overcoming Depression and Low Mood, 3rd Edition: A Five Areas Approach, which is a CBT-SH program widely used in IAPT.
Use of the self-help books was supported by six structured phone or in-person sessions with a trained psychological well-being practitioner.
The primary outcome was depression symptom severity at 16 weeks, which was determined on the basis of Patient Health Questionnaire 9 (PHQ-9) score.
At 16 weeks following randomization, MBCT-SH led to significantly greater reductions in depression symptom severity compared with CBT-SH (mean PHQ-9 score, 7.2 vs. 8.6; between-group difference, 1.5 points; P = .009; d = −0.36).
MBCT-SH also had superior effects on anxiety symptom severity at 16 weeks.
At the 42-week follow-up, between-group effects on depression and anxiety symptom severity remained in the hypothesized direction but were nonsignificant.
This could be due in part by the greater postintervention psychological therapy accessed by participants in the CBT-SH group, the investigators noted.
Practitioner-supported MBCT-SH was more cost-effective than supported CBT-SH.
On average, the CBT-SH intervention cost health services £526 ($631) more per participant than the MBCT-SH intervention over the 42-week follow-up. The probability of MBCT-SH being cost-effective compared with CBT-SH exceeded 95%, the researchers noted.
Useful model for the United States
Commenting for this news organization, Zindel Segal, PhD, professor of psychology, University of Toronto, Scarborough, cautioned against making too much of the differences between the groups, because CBT-SH “trended positive and had a pretty healthy effect size, it just never reached significance.
“I wouldn’t say mindfulness drastically outperformed cognitive therapy. But cognitive therapy is a robust treatment in its own right, and so doing a little bit better is significant,” Dr. Segal said.
He also noted that, appropriately, the trial enrolled adults who were experiencing moderate depression and were not acutely ill. “That’s one of the rationales for self-help compared to providing patients with a more resource-intensive group treatment.
“If you look at the needs of people with moderate depression, what you find is that for cognitive therapy to work, negative thoughts and feelings need to be pervasive in order to make use of the techniques,” Dr. Segal explained.
“With mindfulness, you don’t need any to have constant negative thoughts or feelings. Anything that arises in your experience serves as grist for mill in terms of concentration and focus,” Dr. Segal said.
He also noted that mindfulness-based intervention is “more optimized” for people who are experiencing some measure of recovery or remission.
“It’s well suited for that, as it trends towards the wellness spectrum. But for people who might have greater levels of acuity or severity, cognitive-behavioral therapy might be indicated,” said Dr. Segal.
He also said the U.K. study findings are relevant to U.S. patients with depression.
“While it’s not disseminated in the same way through any kind of national program, the self-help books that are used are widely available, and the support that people were offered, either in person, telephone, or email, could be easily delivered. This would be a very useful model,” Dr. Segal said.
The LIGHTMind trial was funded by the National Institute for Health and Care Research and the Brighton and Sussex Clinical Trials Unit. Dr. Strauss has received grants from Headspace, is research lead for Sussex Mindfulness Centre, and has been chief investigator on National Institute for Health and Care Research. Dr. Segal is one of the authors of the MBCT-SH workbooks used in the study.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Too high: Can you ID pot-induced psychosis?
The youngest patient with cannabis-induced psychosis (CIP) whom Karen Randall, DO, has treated was a 7-year-old boy. She remembers the screaming, the yelling, the uncontrollable rage.
Dr. Randall is an emergency medicine physician at Southern Colorado Emergency Medicine Associates, a group practice in Pueblo, Colo. She treats youth for cannabis-related medical problems in the emergency department an average of two or three times per shift, she said.
Colorado legalized the recreational use of cannabis for adults older than 21 in 2012. Since then, Dr. Randall said, she has noticed an uptick in cannabis use among youth, as well as an increase in CIP, a syndrome that can be indistinguishable from other psychiatric disorders such as schizophrenia in the emergency department. But the two conditions require different approaches to care.
“You can’t differentiate unless you know the patient,” Dr. Randall said in an interview.
In 2019, 37% of high school students in the United States reported ever using marijuana, and 22% reported use in the past 30 days. Rates remained steady in 2020 following increases in 2018 and 2019, according to the Centers for Disease Control and Prevention.
The CDC also found that 8% of 8th graders, 19% of 10th graders, and 22% of 12th graders reported vaping marijuana in the past year.
Clinicians in states where recreational marijuana has been legalized say they have noticed an increase in young patients with psychiatric problems – especially after consumption of cannabis products in high doses., which often begin to present in adolescence.
How to differentiate
CIP is characterized by delusions and hallucinations and sometimes anxiety, disorganized thoughts, paranoia, dissociation, and changes in mood and behavior. Symptoms typically last for a couple hours and do not require specific treatment, although they can persist, depending on a patient’s tolerance and the dose of tetrahydrocannabinol (THC) they have consumed. Research suggests that the higher the dose and concentration of the drug consumed, the more likely a person will develop symptoms of psychosis.
Diagnosis requires gathering information on previous bipolar disorder or schizophrenia diagnosis, prescriptions for mental illness indications, whether there is a family history of mental illness, and whether the patient recently started using marijuana. In some cases, marijuana use might exacerbate or unmask mental illness.
If symptoms of CIP resolve, and usually they do, clinicians can recommend that patients abstain from cannabis going forward, and psychosis would not need further treatment, according to Divya Singh, MD, a psychiatrist at Banner Behavioral Health Hospital in Scottsdale, Ariz., where recreational cannabis became legal in 2020.
“When I have limited information, especially in the first couple of days, I err on the side of safety,” Dr. Singh said.
Psychosis is the combination of symptoms, including delusions, hallucinations, and disorganized behavior, but it is not a disorder in itself. Rather, it is the primary symptom of schizophrenia and other chronic psychiatric illnesses.
Schizophrenia can be diagnosed only after a patient presents with signs of disturbance for at least 6 months, according to guidelines in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Dr. Singh said a diagnosis of schizophrenia cannot be made in a one-off interaction.
If the patient is younger than 24 years and has no family history of mental illness, a full recovery is likely if the patient abstains from marijuana, he said. But if the patient does have a family history, “the chances of them having a full-blown mental illness is very high,” Dr. Singh said.
If a patient reports that he or she has recently started using marijuana and was previously diagnosed with bipolar disorder or schizophrenia, Dr. Singh said he generally prescribes medications such as lithium or quetiapine and refers the patient to services such as cognitive-behavioral therapy. He also advises against continuing use of cannabis.
“Cannabis can result in people requiring a higher dose of medication than they took before,” Dr. Singh said. “If they were stable on 600 mg of lithium before, they might need more and may never be able to lower the dose in some cases, even after the acute episode.”
The science of cannabis
As of March 2023, 21 states and the District of Columbia permit the recreational use of marijuana, according to the Congressional Research Service. Thirty-seven states and the District of Columbia allow medicinal use of marijuana, and 10 states allow “limited access to medical cannabis,” defined as low-THC cannabis or cannabidiol (CBD) oil.
THC is the main psychoactive compound in cannabis. It creates a high feeling after binding with receptors in the brain that control pain and mood. CBD is another chemical found in cannabis, but it does not create a high.
Some research suggests cannabinoids may help reduce anxiety, reduce inflammation, relieve pain, control nausea, reduce cancer cells, slow the growth of tumor cells, relax tight muscles, and stimulate appetite.
The drug also carries risks, according to Mayo Clinic. Use of marijuana is linked to mental health problems in teens and adults, such as depression, social anxiety, and temporary psychosis, and long-lasting mental disorders, such as schizophrenia.
In the worst cases, CIP can persist for weeks or months – long after a negative drug test – and sometimes does not subside at all, according to Ken Finn, MD, president and founder of Springs Rehabilitation, PC, a pain medicine practice in Colorado Springs, Colo.
Dr. Finn, the co–vice president of the International Academy on the Science and Impact of Cannabis, which opposes making the drug more accessible, said educating health care providers is an urgent need.
Studies are mixed on whether the legalization of cannabis has led to more cases of CIP.
A 2021 study found that experiences of psychosis among users of cannabis jumped 2.5-fold between 2001 and 2013. But a study published earlier this year of more than 63 million medical claims from 2003 to 2017 found no statistically significant difference in rates of psychosis-related diagnoses or prescribed antipsychotics in states that have legalized medical or recreational cannabis compared with states where cannabis is still illegal. However, a secondary analysis did find that rates of psychosis-related diagnoses increased significantly among men, people aged 55-64 years, and Asian adults in states where recreational marijuana has been legalized.
Complicating matters, researchers say, is the question of causality. Cannabis may exacerbate or trigger psychosis, but people with an underlying psychological illness may also be more likely to use cannabis.
Dr. Finn said clinicians in Colorado and other states with legalization laws are seeing more patients with CIP. As more states consider legalizing recreational marijuana, he expects the data will reflect what doctors experience on the ground.
Cannabis-induced “psychosis is complicated and likely underdiagnosed,” Dr. Finn said.
Talking to teens
Clinicians outside the emergency department can play a role in aiding young people at risk for CIP. Primary care physicians, for instance, might explain to young patients that the brain only becomes fully developed at roughly age 26, after which the long-term health consequences of using cannabis become less likely. According to the CDC, using cannabis before age 18 can change how the brain builds connections and can impair attention, memory, and learning.
Dr. Singh takes a harm reduction approach when he engages with a patient who is forthcoming about substance use.
“If I see an 18-year-old, I tell them to abstain,” he said. “I tell them if they are ever going to use it, to use it after 26.”
Clinicians also should understand dosages to provide the optimal guidance to their patients who use cannabis.
“People often have no idea how much cannabis they are taking,” especially when using vape cartridges, Dr. Singh said. “If you don’t know, you can’t tell patients about the harms – and if you tell them the wrong information, they will write you off.”
Dr. Singh said he advises his patients to avoid using cannabis vapes or dabbing pens. Both can contain much higher levels of THC than dried flower or edible forms of the drug. He also says patients should stick with low concentrations and use products that contain CBD, which some studies have shown has a protective effect against CIP, although other studies have found that CBD can induce anxiety.
He also tells patients to buy from legal dispensaries and to avoid buying street products that may have methamphetamine or fentanyl mixed in.
Despite the risks, Dr. Singh said legalization can reduce the stigma associated with cannabis use and may prompt patients to be honest with their clinicians. Dr. Singh recalled a 28-year-old patient who was using cannabis to alleviate her arthritic pain. She also was taking a transplant medication, which carried potential side effects of delirium, generalized anxiety disorder, and hallucinosis. After doubling her THC dose, the patient experienced severe anxiety and paranoia.
Dr. Singh’s patient paid him a visit and asked for help. Dr. Singh told her to reduce the dose and to keep track of how she felt. If she continued to feel anxious and paranoid, he recommended that she switch to CBD instead.
“I think education and knowledge is liberating,” Dr. Singh said. “Legalization and frank conversations help people understand how to use a product – and right now, I think that’s lacking.”
A version of this article first appeared on Medscape.com.
The youngest patient with cannabis-induced psychosis (CIP) whom Karen Randall, DO, has treated was a 7-year-old boy. She remembers the screaming, the yelling, the uncontrollable rage.
Dr. Randall is an emergency medicine physician at Southern Colorado Emergency Medicine Associates, a group practice in Pueblo, Colo. She treats youth for cannabis-related medical problems in the emergency department an average of two or three times per shift, she said.
Colorado legalized the recreational use of cannabis for adults older than 21 in 2012. Since then, Dr. Randall said, she has noticed an uptick in cannabis use among youth, as well as an increase in CIP, a syndrome that can be indistinguishable from other psychiatric disorders such as schizophrenia in the emergency department. But the two conditions require different approaches to care.
“You can’t differentiate unless you know the patient,” Dr. Randall said in an interview.
In 2019, 37% of high school students in the United States reported ever using marijuana, and 22% reported use in the past 30 days. Rates remained steady in 2020 following increases in 2018 and 2019, according to the Centers for Disease Control and Prevention.
The CDC also found that 8% of 8th graders, 19% of 10th graders, and 22% of 12th graders reported vaping marijuana in the past year.
Clinicians in states where recreational marijuana has been legalized say they have noticed an increase in young patients with psychiatric problems – especially after consumption of cannabis products in high doses., which often begin to present in adolescence.
How to differentiate
CIP is characterized by delusions and hallucinations and sometimes anxiety, disorganized thoughts, paranoia, dissociation, and changes in mood and behavior. Symptoms typically last for a couple hours and do not require specific treatment, although they can persist, depending on a patient’s tolerance and the dose of tetrahydrocannabinol (THC) they have consumed. Research suggests that the higher the dose and concentration of the drug consumed, the more likely a person will develop symptoms of psychosis.
Diagnosis requires gathering information on previous bipolar disorder or schizophrenia diagnosis, prescriptions for mental illness indications, whether there is a family history of mental illness, and whether the patient recently started using marijuana. In some cases, marijuana use might exacerbate or unmask mental illness.
If symptoms of CIP resolve, and usually they do, clinicians can recommend that patients abstain from cannabis going forward, and psychosis would not need further treatment, according to Divya Singh, MD, a psychiatrist at Banner Behavioral Health Hospital in Scottsdale, Ariz., where recreational cannabis became legal in 2020.
“When I have limited information, especially in the first couple of days, I err on the side of safety,” Dr. Singh said.
Psychosis is the combination of symptoms, including delusions, hallucinations, and disorganized behavior, but it is not a disorder in itself. Rather, it is the primary symptom of schizophrenia and other chronic psychiatric illnesses.
Schizophrenia can be diagnosed only after a patient presents with signs of disturbance for at least 6 months, according to guidelines in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Dr. Singh said a diagnosis of schizophrenia cannot be made in a one-off interaction.
If the patient is younger than 24 years and has no family history of mental illness, a full recovery is likely if the patient abstains from marijuana, he said. But if the patient does have a family history, “the chances of them having a full-blown mental illness is very high,” Dr. Singh said.
If a patient reports that he or she has recently started using marijuana and was previously diagnosed with bipolar disorder or schizophrenia, Dr. Singh said he generally prescribes medications such as lithium or quetiapine and refers the patient to services such as cognitive-behavioral therapy. He also advises against continuing use of cannabis.
“Cannabis can result in people requiring a higher dose of medication than they took before,” Dr. Singh said. “If they were stable on 600 mg of lithium before, they might need more and may never be able to lower the dose in some cases, even after the acute episode.”
The science of cannabis
As of March 2023, 21 states and the District of Columbia permit the recreational use of marijuana, according to the Congressional Research Service. Thirty-seven states and the District of Columbia allow medicinal use of marijuana, and 10 states allow “limited access to medical cannabis,” defined as low-THC cannabis or cannabidiol (CBD) oil.
THC is the main psychoactive compound in cannabis. It creates a high feeling after binding with receptors in the brain that control pain and mood. CBD is another chemical found in cannabis, but it does not create a high.
Some research suggests cannabinoids may help reduce anxiety, reduce inflammation, relieve pain, control nausea, reduce cancer cells, slow the growth of tumor cells, relax tight muscles, and stimulate appetite.
The drug also carries risks, according to Mayo Clinic. Use of marijuana is linked to mental health problems in teens and adults, such as depression, social anxiety, and temporary psychosis, and long-lasting mental disorders, such as schizophrenia.
In the worst cases, CIP can persist for weeks or months – long after a negative drug test – and sometimes does not subside at all, according to Ken Finn, MD, president and founder of Springs Rehabilitation, PC, a pain medicine practice in Colorado Springs, Colo.
Dr. Finn, the co–vice president of the International Academy on the Science and Impact of Cannabis, which opposes making the drug more accessible, said educating health care providers is an urgent need.
Studies are mixed on whether the legalization of cannabis has led to more cases of CIP.
A 2021 study found that experiences of psychosis among users of cannabis jumped 2.5-fold between 2001 and 2013. But a study published earlier this year of more than 63 million medical claims from 2003 to 2017 found no statistically significant difference in rates of psychosis-related diagnoses or prescribed antipsychotics in states that have legalized medical or recreational cannabis compared with states where cannabis is still illegal. However, a secondary analysis did find that rates of psychosis-related diagnoses increased significantly among men, people aged 55-64 years, and Asian adults in states where recreational marijuana has been legalized.
Complicating matters, researchers say, is the question of causality. Cannabis may exacerbate or trigger psychosis, but people with an underlying psychological illness may also be more likely to use cannabis.
Dr. Finn said clinicians in Colorado and other states with legalization laws are seeing more patients with CIP. As more states consider legalizing recreational marijuana, he expects the data will reflect what doctors experience on the ground.
Cannabis-induced “psychosis is complicated and likely underdiagnosed,” Dr. Finn said.
Talking to teens
Clinicians outside the emergency department can play a role in aiding young people at risk for CIP. Primary care physicians, for instance, might explain to young patients that the brain only becomes fully developed at roughly age 26, after which the long-term health consequences of using cannabis become less likely. According to the CDC, using cannabis before age 18 can change how the brain builds connections and can impair attention, memory, and learning.
Dr. Singh takes a harm reduction approach when he engages with a patient who is forthcoming about substance use.
“If I see an 18-year-old, I tell them to abstain,” he said. “I tell them if they are ever going to use it, to use it after 26.”
Clinicians also should understand dosages to provide the optimal guidance to their patients who use cannabis.
“People often have no idea how much cannabis they are taking,” especially when using vape cartridges, Dr. Singh said. “If you don’t know, you can’t tell patients about the harms – and if you tell them the wrong information, they will write you off.”
Dr. Singh said he advises his patients to avoid using cannabis vapes or dabbing pens. Both can contain much higher levels of THC than dried flower or edible forms of the drug. He also says patients should stick with low concentrations and use products that contain CBD, which some studies have shown has a protective effect against CIP, although other studies have found that CBD can induce anxiety.
He also tells patients to buy from legal dispensaries and to avoid buying street products that may have methamphetamine or fentanyl mixed in.
Despite the risks, Dr. Singh said legalization can reduce the stigma associated with cannabis use and may prompt patients to be honest with their clinicians. Dr. Singh recalled a 28-year-old patient who was using cannabis to alleviate her arthritic pain. She also was taking a transplant medication, which carried potential side effects of delirium, generalized anxiety disorder, and hallucinosis. After doubling her THC dose, the patient experienced severe anxiety and paranoia.
Dr. Singh’s patient paid him a visit and asked for help. Dr. Singh told her to reduce the dose and to keep track of how she felt. If she continued to feel anxious and paranoid, he recommended that she switch to CBD instead.
“I think education and knowledge is liberating,” Dr. Singh said. “Legalization and frank conversations help people understand how to use a product – and right now, I think that’s lacking.”
A version of this article first appeared on Medscape.com.
The youngest patient with cannabis-induced psychosis (CIP) whom Karen Randall, DO, has treated was a 7-year-old boy. She remembers the screaming, the yelling, the uncontrollable rage.
Dr. Randall is an emergency medicine physician at Southern Colorado Emergency Medicine Associates, a group practice in Pueblo, Colo. She treats youth for cannabis-related medical problems in the emergency department an average of two or three times per shift, she said.
Colorado legalized the recreational use of cannabis for adults older than 21 in 2012. Since then, Dr. Randall said, she has noticed an uptick in cannabis use among youth, as well as an increase in CIP, a syndrome that can be indistinguishable from other psychiatric disorders such as schizophrenia in the emergency department. But the two conditions require different approaches to care.
“You can’t differentiate unless you know the patient,” Dr. Randall said in an interview.
In 2019, 37% of high school students in the United States reported ever using marijuana, and 22% reported use in the past 30 days. Rates remained steady in 2020 following increases in 2018 and 2019, according to the Centers for Disease Control and Prevention.
The CDC also found that 8% of 8th graders, 19% of 10th graders, and 22% of 12th graders reported vaping marijuana in the past year.
Clinicians in states where recreational marijuana has been legalized say they have noticed an increase in young patients with psychiatric problems – especially after consumption of cannabis products in high doses., which often begin to present in adolescence.
How to differentiate
CIP is characterized by delusions and hallucinations and sometimes anxiety, disorganized thoughts, paranoia, dissociation, and changes in mood and behavior. Symptoms typically last for a couple hours and do not require specific treatment, although they can persist, depending on a patient’s tolerance and the dose of tetrahydrocannabinol (THC) they have consumed. Research suggests that the higher the dose and concentration of the drug consumed, the more likely a person will develop symptoms of psychosis.
Diagnosis requires gathering information on previous bipolar disorder or schizophrenia diagnosis, prescriptions for mental illness indications, whether there is a family history of mental illness, and whether the patient recently started using marijuana. In some cases, marijuana use might exacerbate or unmask mental illness.
If symptoms of CIP resolve, and usually they do, clinicians can recommend that patients abstain from cannabis going forward, and psychosis would not need further treatment, according to Divya Singh, MD, a psychiatrist at Banner Behavioral Health Hospital in Scottsdale, Ariz., where recreational cannabis became legal in 2020.
“When I have limited information, especially in the first couple of days, I err on the side of safety,” Dr. Singh said.
Psychosis is the combination of symptoms, including delusions, hallucinations, and disorganized behavior, but it is not a disorder in itself. Rather, it is the primary symptom of schizophrenia and other chronic psychiatric illnesses.
Schizophrenia can be diagnosed only after a patient presents with signs of disturbance for at least 6 months, according to guidelines in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Dr. Singh said a diagnosis of schizophrenia cannot be made in a one-off interaction.
If the patient is younger than 24 years and has no family history of mental illness, a full recovery is likely if the patient abstains from marijuana, he said. But if the patient does have a family history, “the chances of them having a full-blown mental illness is very high,” Dr. Singh said.
If a patient reports that he or she has recently started using marijuana and was previously diagnosed with bipolar disorder or schizophrenia, Dr. Singh said he generally prescribes medications such as lithium or quetiapine and refers the patient to services such as cognitive-behavioral therapy. He also advises against continuing use of cannabis.
“Cannabis can result in people requiring a higher dose of medication than they took before,” Dr. Singh said. “If they were stable on 600 mg of lithium before, they might need more and may never be able to lower the dose in some cases, even after the acute episode.”
The science of cannabis
As of March 2023, 21 states and the District of Columbia permit the recreational use of marijuana, according to the Congressional Research Service. Thirty-seven states and the District of Columbia allow medicinal use of marijuana, and 10 states allow “limited access to medical cannabis,” defined as low-THC cannabis or cannabidiol (CBD) oil.
THC is the main psychoactive compound in cannabis. It creates a high feeling after binding with receptors in the brain that control pain and mood. CBD is another chemical found in cannabis, but it does not create a high.
Some research suggests cannabinoids may help reduce anxiety, reduce inflammation, relieve pain, control nausea, reduce cancer cells, slow the growth of tumor cells, relax tight muscles, and stimulate appetite.
The drug also carries risks, according to Mayo Clinic. Use of marijuana is linked to mental health problems in teens and adults, such as depression, social anxiety, and temporary psychosis, and long-lasting mental disorders, such as schizophrenia.
In the worst cases, CIP can persist for weeks or months – long after a negative drug test – and sometimes does not subside at all, according to Ken Finn, MD, president and founder of Springs Rehabilitation, PC, a pain medicine practice in Colorado Springs, Colo.
Dr. Finn, the co–vice president of the International Academy on the Science and Impact of Cannabis, which opposes making the drug more accessible, said educating health care providers is an urgent need.
Studies are mixed on whether the legalization of cannabis has led to more cases of CIP.
A 2021 study found that experiences of psychosis among users of cannabis jumped 2.5-fold between 2001 and 2013. But a study published earlier this year of more than 63 million medical claims from 2003 to 2017 found no statistically significant difference in rates of psychosis-related diagnoses or prescribed antipsychotics in states that have legalized medical or recreational cannabis compared with states where cannabis is still illegal. However, a secondary analysis did find that rates of psychosis-related diagnoses increased significantly among men, people aged 55-64 years, and Asian adults in states where recreational marijuana has been legalized.
Complicating matters, researchers say, is the question of causality. Cannabis may exacerbate or trigger psychosis, but people with an underlying psychological illness may also be more likely to use cannabis.
Dr. Finn said clinicians in Colorado and other states with legalization laws are seeing more patients with CIP. As more states consider legalizing recreational marijuana, he expects the data will reflect what doctors experience on the ground.
Cannabis-induced “psychosis is complicated and likely underdiagnosed,” Dr. Finn said.
Talking to teens
Clinicians outside the emergency department can play a role in aiding young people at risk for CIP. Primary care physicians, for instance, might explain to young patients that the brain only becomes fully developed at roughly age 26, after which the long-term health consequences of using cannabis become less likely. According to the CDC, using cannabis before age 18 can change how the brain builds connections and can impair attention, memory, and learning.
Dr. Singh takes a harm reduction approach when he engages with a patient who is forthcoming about substance use.
“If I see an 18-year-old, I tell them to abstain,” he said. “I tell them if they are ever going to use it, to use it after 26.”
Clinicians also should understand dosages to provide the optimal guidance to their patients who use cannabis.
“People often have no idea how much cannabis they are taking,” especially when using vape cartridges, Dr. Singh said. “If you don’t know, you can’t tell patients about the harms – and if you tell them the wrong information, they will write you off.”
Dr. Singh said he advises his patients to avoid using cannabis vapes or dabbing pens. Both can contain much higher levels of THC than dried flower or edible forms of the drug. He also says patients should stick with low concentrations and use products that contain CBD, which some studies have shown has a protective effect against CIP, although other studies have found that CBD can induce anxiety.
He also tells patients to buy from legal dispensaries and to avoid buying street products that may have methamphetamine or fentanyl mixed in.
Despite the risks, Dr. Singh said legalization can reduce the stigma associated with cannabis use and may prompt patients to be honest with their clinicians. Dr. Singh recalled a 28-year-old patient who was using cannabis to alleviate her arthritic pain. She also was taking a transplant medication, which carried potential side effects of delirium, generalized anxiety disorder, and hallucinosis. After doubling her THC dose, the patient experienced severe anxiety and paranoia.
Dr. Singh’s patient paid him a visit and asked for help. Dr. Singh told her to reduce the dose and to keep track of how she felt. If she continued to feel anxious and paranoid, he recommended that she switch to CBD instead.
“I think education and knowledge is liberating,” Dr. Singh said. “Legalization and frank conversations help people understand how to use a product – and right now, I think that’s lacking.”
A version of this article first appeared on Medscape.com.
Clozapine may curb schizophrenia’s ‘most dreaded outcome’
Investigators reviewed over 53,000 autopsy records, including over 600 from individuals whose autopsies revealed the presence of the antipsychotics clozapine or olanzapine, and found that those who took clozapine were significantly less likely to have died by suicide, compared with their counterparts who were taking olanzapine.
“Clozapine is an important and effective antisuicide medicine and should be strongly considered for treatment-resistant psychotic disorders, especially when the patient may be at risk for suicide,” study investigator Paul Nestadt, MD, associate professor, department of psychiatry and behavioral sciences, Johns Hopkins School of Medicine, Baltimore, told this news organization.
The study was published online in The Journal of Clinical Psychiatry.
Underutilized medication
Clozapine is the only medication indicated for treatment-resistant schizophrenia and is considered “the most efficacious antipsychotic,” the investigators note. Unfortunately, it has “long been underutilized” for several reasons, including prescriber hesitancy and concerns about side effects.
The authors note that its mechanism of action and the basis for superior efficacy are “still poorly understood” but “may extend beyond neurotransmitter receptor binding.”
Importantly, it may have a beneficial impact on domains other than positive symptoms of schizophrenia, including suicidality. Several studies have shown that it’s beneficial in this regard, but it is “unclear whether the unique antisuicidal properties of clozapine are related to better symptom control ... or to the closer monitoring and follow-up mandated for clozapine use,” they note.
A previous trial, the International Suicide Prevention Trial (InterSePT), demonstrated that clozapine is associated with a greater reduction in suicidality, and the findings “led to an FDA indication for clozapine in reducing the risk of recurrent suicidal behavior.”
However, the authors note, “in the severely ill populations in these studies, it is difficult to be certain about patients’ adherence to prescribed clozapine.”
“Other studies, such as InterSePT, have shown some evidence of clozapine working to reduce suicide-related outcomes, such as attempts or suicidal ideation, but few have been sufficiently powered to measure an effect on actual suicide deaths,” said Dr. Nestadt.
“As a suicidologist, I feel it is very important that we understand what treatments and interventions can actually prevent suicide deaths, as most suicides are not associated with past attempts or ideation, with suicide decedents usually looking very different from characteristic nonfatal attempters, from a clinical or epidemiological standpoint,” he added.
“If we could show that clozapine actually decreases the likelihood of suicide deaths in our patients, it gives us more reason to choose it over less effective neuroleptics in our clinics – especially for patients at high risk of suicide,” he said.
For the study, the researchers reviewed 19-year state-wide autopsy records of Maryland’s Office of the Chief Medical Examiner, which “performs uniquely comprehensive death investigations.” Data included in these investigations are full toxicologic panels with postmortem blood levels of antipsychotics.
The researchers compared decedents who tested positive for clozapine and decedents who tested positive for olanzapine. They evaluated demographics, clinical features, and manner-of-death outcomes.
‘Untapped resource’
Of 53,133 decedents, olanzapine or clozapine was detected in the blood of 621 persons (n = 571 and n = 50, respectively).
There were no significant differences in age, sex, race, or urban residence between the decedents who were treated with olanzapine and those who received clozapine.
The odds of a death by suicide in those treated with clozapine were less than half of the odds among decedents who had been treated with olanzapine (odds ratio, 0.47; 95% confidence interval, 0.26-0.84; P = .011).
In sensitivity analyses, the investigators reanalyzed the data to compare clozapine with other antipsychotics, including chlorpromazine, thioridazine, quetiapine, and olanzapine, and the results were similar. The odds of suicide (compared with accident) in those taking clozapine were much lower than in those taking any other tested antipsychotics individually or in combination (OR, 0.42; 95% CI, 0.24-0.73; P = .002).
Dr. Nestadt outlined several hypotheses regarding the mechanism of clozapine’s antisuicidal properties.
“Most theories stem from the differences in its receptor affinity, compared [with] the other neuroleptics,” he said. “In addition to the more typical dopaminergic blockade seen in neuroleptics, clozapine enhances serotonin release and greatly increases peripheral norepinephrine.”
This has been shown to “grant clozapine a greater antidepressant effect than other neuroleptics while also potentially decreasing aggression and impulsivity, which are both strongly associated with suicide risk,” he said.
Clozapine may also “work to reduce the inflammation-triggered activation of the kynurenine pathway, which otherwise contributes to serotonin depletion,” he added.
He noted that some studies have shown that as many as 1 in 10 patients with schizophrenia die by suicide, “so addressing this risk is paramount,” and that clozapine can play an important role in this.
The authors note that the findings “also highlight the utility of state-wide autopsy records, an untapped resource for investigating the potential protective effect of psychiatric medications on suicide at a population level.
“Importantly, we can be certain that this was not an issue of nonadherence to treatment in either group, which is a common issue in the use of these drugs because, instead of prescription records or self-report, we used actual measurements of drug presence in decedents’ blood at death,” said Dr. Nestadt.
‘Strongly suggestive’ data
Commenting on the study, Maria Oquendo, MD, PhD, Ruth Meltzer Professor and chair of psychiatry, Perelman School of Medicine, University of Pennsylvania, Philadelphia, said most work on antisuicidal psychopharmacologic approaches “focuses on suicidal ideation or suicide attempts, due to the rarity of suicide death, even in high-risk populations.”
“Showing that clozapine may decrease risk for the most dreaded outcome of schizophrenia – suicide – is critically important,” said Dr. Oquendo, past president of the American Psychiatric Association.
Nevertheless, some questions remain, said Dr. Oquendo, who was not involved with the study. “Comparison of suicides to only accidental deaths has limitations. Many individuals who die due to accidents, like many suicides, are not similar to the general population,” she added.
However, she acknowledged, the data are strongly suggestive that clozapine protects against suicide.
“While not definitive, ideally these findings will stimulate changes in prescribing practices which may be lifesaving both literally – in terms of preventing suicides – and figuratively, given the drug’s effect on symptoms that impact quality of life and functioning,” said Dr. Oquendo.
The study received no funding or support. Dr. Nestadt is supported by the American Foundation for Suicide prevention and the National Institute on Drug Abuse. The other authors’ disclosures are listed in the original article. Dr. Oquendo receives royalties from the Research Foundation for Mental Hygiene for the commercial use of the Columbia Suicide Severity Rating Scale. She serves as an advisor to Alkermes, Mind Medicine, Sage Therapeutics, St. George’s University, and Fundacion Jimenez Diaz. Her family owns stock in Bristol-Myers Squibb.
A version of this article first appeared on Medscape.com.
Investigators reviewed over 53,000 autopsy records, including over 600 from individuals whose autopsies revealed the presence of the antipsychotics clozapine or olanzapine, and found that those who took clozapine were significantly less likely to have died by suicide, compared with their counterparts who were taking olanzapine.
“Clozapine is an important and effective antisuicide medicine and should be strongly considered for treatment-resistant psychotic disorders, especially when the patient may be at risk for suicide,” study investigator Paul Nestadt, MD, associate professor, department of psychiatry and behavioral sciences, Johns Hopkins School of Medicine, Baltimore, told this news organization.
The study was published online in The Journal of Clinical Psychiatry.
Underutilized medication
Clozapine is the only medication indicated for treatment-resistant schizophrenia and is considered “the most efficacious antipsychotic,” the investigators note. Unfortunately, it has “long been underutilized” for several reasons, including prescriber hesitancy and concerns about side effects.
The authors note that its mechanism of action and the basis for superior efficacy are “still poorly understood” but “may extend beyond neurotransmitter receptor binding.”
Importantly, it may have a beneficial impact on domains other than positive symptoms of schizophrenia, including suicidality. Several studies have shown that it’s beneficial in this regard, but it is “unclear whether the unique antisuicidal properties of clozapine are related to better symptom control ... or to the closer monitoring and follow-up mandated for clozapine use,” they note.
A previous trial, the International Suicide Prevention Trial (InterSePT), demonstrated that clozapine is associated with a greater reduction in suicidality, and the findings “led to an FDA indication for clozapine in reducing the risk of recurrent suicidal behavior.”
However, the authors note, “in the severely ill populations in these studies, it is difficult to be certain about patients’ adherence to prescribed clozapine.”
“Other studies, such as InterSePT, have shown some evidence of clozapine working to reduce suicide-related outcomes, such as attempts or suicidal ideation, but few have been sufficiently powered to measure an effect on actual suicide deaths,” said Dr. Nestadt.
“As a suicidologist, I feel it is very important that we understand what treatments and interventions can actually prevent suicide deaths, as most suicides are not associated with past attempts or ideation, with suicide decedents usually looking very different from characteristic nonfatal attempters, from a clinical or epidemiological standpoint,” he added.
“If we could show that clozapine actually decreases the likelihood of suicide deaths in our patients, it gives us more reason to choose it over less effective neuroleptics in our clinics – especially for patients at high risk of suicide,” he said.
For the study, the researchers reviewed 19-year state-wide autopsy records of Maryland’s Office of the Chief Medical Examiner, which “performs uniquely comprehensive death investigations.” Data included in these investigations are full toxicologic panels with postmortem blood levels of antipsychotics.
The researchers compared decedents who tested positive for clozapine and decedents who tested positive for olanzapine. They evaluated demographics, clinical features, and manner-of-death outcomes.
‘Untapped resource’
Of 53,133 decedents, olanzapine or clozapine was detected in the blood of 621 persons (n = 571 and n = 50, respectively).
There were no significant differences in age, sex, race, or urban residence between the decedents who were treated with olanzapine and those who received clozapine.
The odds of a death by suicide in those treated with clozapine were less than half of the odds among decedents who had been treated with olanzapine (odds ratio, 0.47; 95% confidence interval, 0.26-0.84; P = .011).
In sensitivity analyses, the investigators reanalyzed the data to compare clozapine with other antipsychotics, including chlorpromazine, thioridazine, quetiapine, and olanzapine, and the results were similar. The odds of suicide (compared with accident) in those taking clozapine were much lower than in those taking any other tested antipsychotics individually or in combination (OR, 0.42; 95% CI, 0.24-0.73; P = .002).
Dr. Nestadt outlined several hypotheses regarding the mechanism of clozapine’s antisuicidal properties.
“Most theories stem from the differences in its receptor affinity, compared [with] the other neuroleptics,” he said. “In addition to the more typical dopaminergic blockade seen in neuroleptics, clozapine enhances serotonin release and greatly increases peripheral norepinephrine.”
This has been shown to “grant clozapine a greater antidepressant effect than other neuroleptics while also potentially decreasing aggression and impulsivity, which are both strongly associated with suicide risk,” he said.
Clozapine may also “work to reduce the inflammation-triggered activation of the kynurenine pathway, which otherwise contributes to serotonin depletion,” he added.
He noted that some studies have shown that as many as 1 in 10 patients with schizophrenia die by suicide, “so addressing this risk is paramount,” and that clozapine can play an important role in this.
The authors note that the findings “also highlight the utility of state-wide autopsy records, an untapped resource for investigating the potential protective effect of psychiatric medications on suicide at a population level.
“Importantly, we can be certain that this was not an issue of nonadherence to treatment in either group, which is a common issue in the use of these drugs because, instead of prescription records or self-report, we used actual measurements of drug presence in decedents’ blood at death,” said Dr. Nestadt.
‘Strongly suggestive’ data
Commenting on the study, Maria Oquendo, MD, PhD, Ruth Meltzer Professor and chair of psychiatry, Perelman School of Medicine, University of Pennsylvania, Philadelphia, said most work on antisuicidal psychopharmacologic approaches “focuses on suicidal ideation or suicide attempts, due to the rarity of suicide death, even in high-risk populations.”
“Showing that clozapine may decrease risk for the most dreaded outcome of schizophrenia – suicide – is critically important,” said Dr. Oquendo, past president of the American Psychiatric Association.
Nevertheless, some questions remain, said Dr. Oquendo, who was not involved with the study. “Comparison of suicides to only accidental deaths has limitations. Many individuals who die due to accidents, like many suicides, are not similar to the general population,” she added.
However, she acknowledged, the data are strongly suggestive that clozapine protects against suicide.
“While not definitive, ideally these findings will stimulate changes in prescribing practices which may be lifesaving both literally – in terms of preventing suicides – and figuratively, given the drug’s effect on symptoms that impact quality of life and functioning,” said Dr. Oquendo.
The study received no funding or support. Dr. Nestadt is supported by the American Foundation for Suicide prevention and the National Institute on Drug Abuse. The other authors’ disclosures are listed in the original article. Dr. Oquendo receives royalties from the Research Foundation for Mental Hygiene for the commercial use of the Columbia Suicide Severity Rating Scale. She serves as an advisor to Alkermes, Mind Medicine, Sage Therapeutics, St. George’s University, and Fundacion Jimenez Diaz. Her family owns stock in Bristol-Myers Squibb.
A version of this article first appeared on Medscape.com.
Investigators reviewed over 53,000 autopsy records, including over 600 from individuals whose autopsies revealed the presence of the antipsychotics clozapine or olanzapine, and found that those who took clozapine were significantly less likely to have died by suicide, compared with their counterparts who were taking olanzapine.
“Clozapine is an important and effective antisuicide medicine and should be strongly considered for treatment-resistant psychotic disorders, especially when the patient may be at risk for suicide,” study investigator Paul Nestadt, MD, associate professor, department of psychiatry and behavioral sciences, Johns Hopkins School of Medicine, Baltimore, told this news organization.
The study was published online in The Journal of Clinical Psychiatry.
Underutilized medication
Clozapine is the only medication indicated for treatment-resistant schizophrenia and is considered “the most efficacious antipsychotic,” the investigators note. Unfortunately, it has “long been underutilized” for several reasons, including prescriber hesitancy and concerns about side effects.
The authors note that its mechanism of action and the basis for superior efficacy are “still poorly understood” but “may extend beyond neurotransmitter receptor binding.”
Importantly, it may have a beneficial impact on domains other than positive symptoms of schizophrenia, including suicidality. Several studies have shown that it’s beneficial in this regard, but it is “unclear whether the unique antisuicidal properties of clozapine are related to better symptom control ... or to the closer monitoring and follow-up mandated for clozapine use,” they note.
A previous trial, the International Suicide Prevention Trial (InterSePT), demonstrated that clozapine is associated with a greater reduction in suicidality, and the findings “led to an FDA indication for clozapine in reducing the risk of recurrent suicidal behavior.”
However, the authors note, “in the severely ill populations in these studies, it is difficult to be certain about patients’ adherence to prescribed clozapine.”
“Other studies, such as InterSePT, have shown some evidence of clozapine working to reduce suicide-related outcomes, such as attempts or suicidal ideation, but few have been sufficiently powered to measure an effect on actual suicide deaths,” said Dr. Nestadt.
“As a suicidologist, I feel it is very important that we understand what treatments and interventions can actually prevent suicide deaths, as most suicides are not associated with past attempts or ideation, with suicide decedents usually looking very different from characteristic nonfatal attempters, from a clinical or epidemiological standpoint,” he added.
“If we could show that clozapine actually decreases the likelihood of suicide deaths in our patients, it gives us more reason to choose it over less effective neuroleptics in our clinics – especially for patients at high risk of suicide,” he said.
For the study, the researchers reviewed 19-year state-wide autopsy records of Maryland’s Office of the Chief Medical Examiner, which “performs uniquely comprehensive death investigations.” Data included in these investigations are full toxicologic panels with postmortem blood levels of antipsychotics.
The researchers compared decedents who tested positive for clozapine and decedents who tested positive for olanzapine. They evaluated demographics, clinical features, and manner-of-death outcomes.
‘Untapped resource’
Of 53,133 decedents, olanzapine or clozapine was detected in the blood of 621 persons (n = 571 and n = 50, respectively).
There were no significant differences in age, sex, race, or urban residence between the decedents who were treated with olanzapine and those who received clozapine.
The odds of a death by suicide in those treated with clozapine were less than half of the odds among decedents who had been treated with olanzapine (odds ratio, 0.47; 95% confidence interval, 0.26-0.84; P = .011).
In sensitivity analyses, the investigators reanalyzed the data to compare clozapine with other antipsychotics, including chlorpromazine, thioridazine, quetiapine, and olanzapine, and the results were similar. The odds of suicide (compared with accident) in those taking clozapine were much lower than in those taking any other tested antipsychotics individually or in combination (OR, 0.42; 95% CI, 0.24-0.73; P = .002).
Dr. Nestadt outlined several hypotheses regarding the mechanism of clozapine’s antisuicidal properties.
“Most theories stem from the differences in its receptor affinity, compared [with] the other neuroleptics,” he said. “In addition to the more typical dopaminergic blockade seen in neuroleptics, clozapine enhances serotonin release and greatly increases peripheral norepinephrine.”
This has been shown to “grant clozapine a greater antidepressant effect than other neuroleptics while also potentially decreasing aggression and impulsivity, which are both strongly associated with suicide risk,” he said.
Clozapine may also “work to reduce the inflammation-triggered activation of the kynurenine pathway, which otherwise contributes to serotonin depletion,” he added.
He noted that some studies have shown that as many as 1 in 10 patients with schizophrenia die by suicide, “so addressing this risk is paramount,” and that clozapine can play an important role in this.
The authors note that the findings “also highlight the utility of state-wide autopsy records, an untapped resource for investigating the potential protective effect of psychiatric medications on suicide at a population level.
“Importantly, we can be certain that this was not an issue of nonadherence to treatment in either group, which is a common issue in the use of these drugs because, instead of prescription records or self-report, we used actual measurements of drug presence in decedents’ blood at death,” said Dr. Nestadt.
‘Strongly suggestive’ data
Commenting on the study, Maria Oquendo, MD, PhD, Ruth Meltzer Professor and chair of psychiatry, Perelman School of Medicine, University of Pennsylvania, Philadelphia, said most work on antisuicidal psychopharmacologic approaches “focuses on suicidal ideation or suicide attempts, due to the rarity of suicide death, even in high-risk populations.”
“Showing that clozapine may decrease risk for the most dreaded outcome of schizophrenia – suicide – is critically important,” said Dr. Oquendo, past president of the American Psychiatric Association.
Nevertheless, some questions remain, said Dr. Oquendo, who was not involved with the study. “Comparison of suicides to only accidental deaths has limitations. Many individuals who die due to accidents, like many suicides, are not similar to the general population,” she added.
However, she acknowledged, the data are strongly suggestive that clozapine protects against suicide.
“While not definitive, ideally these findings will stimulate changes in prescribing practices which may be lifesaving both literally – in terms of preventing suicides – and figuratively, given the drug’s effect on symptoms that impact quality of life and functioning,” said Dr. Oquendo.
The study received no funding or support. Dr. Nestadt is supported by the American Foundation for Suicide prevention and the National Institute on Drug Abuse. The other authors’ disclosures are listed in the original article. Dr. Oquendo receives royalties from the Research Foundation for Mental Hygiene for the commercial use of the Columbia Suicide Severity Rating Scale. She serves as an advisor to Alkermes, Mind Medicine, Sage Therapeutics, St. George’s University, and Fundacion Jimenez Diaz. Her family owns stock in Bristol-Myers Squibb.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL PSYCHIATRY
The sacrifice of orthodoxy: Maintaining collegiality in psychiatry
Psychiatrists practice in a wide array of ways. We approach our work and our patients with beliefs and preconceptions that develop over time. Our training has significant influence, though our own personalities and biases also affect our understanding.
Psychiatrists have philosophical lenses through which they see patients. We can reflect and see some standard archetypes. We are familiar with the reductionistic pharmacologist, the somatic treatment specialist, the psychodynamic ‘guru,’ and the medicolegally paralyzed practitioner. It is without judgment that we lay these out, for our very point is that we have these constituent parts within our own clinical identities. The intensity with which we subscribe to these clinical sensibilities could contribute to a biased orthodoxy.
Orthodoxy can be defined as an accepted theory that stems from an authoritative entity. This is a well-known phenomenon that continues to be visible. For example, one can quickly peruse psychodynamic literature to find one school of thought criticizing another. It is not without some confrontation and even interpersonal rifts that the lineage of psychoanalytic theory has evolved. This has always been of interest to us. A core facet of psychoanalysis is empathy, truly knowing the inner state of a different person. And yet, the very bastions of this clinical sensibility frequently resort to veiled attacks on those in their field who have opposing views. It then begs the question: If even enlightened institutions fail at a nonjudgmental approach toward their colleagues, what hope is there for the rest of us clinicians, mired in the thick of day-to-day clinical practice?
It is our contention that the odds are against us. Even the aforementioned critique of psychoanalytic orthodoxy is just another example of how we humans organize our experience. Even as we write an article in argument against unbridled critique, we find it difficult to do so without engaging in it. For to criticize another is to help shore up our own personal identities. This is especially the case when clinicians deal with issues that we feel strongly about. The human psyche has a need to organize its experience, as “our experience of ourselves is fundamental to how we operate in the world. Our subjective experience is the phenomenology of all that one might be aware of.”1
In this vein, we would like to cite attribution theory. This is a view of human behavior within social psychology. The Austrian psychologist Fritz Heider, PhD, investigated “the domain of social interactions, wondering how people perceive each other in interaction and especially how they make sense of each other’s behavior.”2 Attribution theory suggests that as humans organize our social interactions, we may make two basic assumptions. One is that our own behavior is highly affected by an environment that is beyond our control. The second is that when judging the behavior of others, we are more likely to attribute it to internal traits that they have. A classic example is automobile traffic. When we see someone driving erratically, we are more likely to blame them for being an inherently bad driver. However, if attention is called to our own driving, we are more likely to cite external factors such as rush hour, a bad driver around us, or a faulty vehicle.
We would like to reference one last model of human behavior. It has become customary within the field of neuroscience to view the brain as a predictive organ: “Theories of prediction in perception, action, and learning suggest that the brain serves to reduce the discrepancies between expectation and actual experience, i.e., by reducing the prediction error.”3 Perception itself has recently been described as a controlled hallucination, where the brain makes predictions of what it thinks it is about to see based on past experiences. Visual stimulus ultimately takes time to enter our eyes and be processed in the brain – “predictions would need to preactivate neural representations that would typically be driven by sensory input, before the actual arrival of that input.”4 It thus seems to be an inherent method of the brain to anticipate visual and even social events to help human beings sustain themselves.
Having spoken of a psychoanalytic conceptualization of self-organization, the theory of attribution, and research into social neuroscience, we turn our attention back to the central question that this article would like to address.
When we find ourselves busy in rote clinical practice, we believe the likelihood of intercollegiate mentalization is low; our ability to relate to our peers becomes strained. We ultimately do not practice in a vacuum. Psychiatrists, even those in a solo private practice, are ultimately part of a community of providers who, more or less, follow some emergent ‘standard of care.’ This can be a vague concept; but one that takes on a concrete form in the minds of certain clinicians and certainly in the setting of a medicolegal court. Yet, the psychiatrists that we know all have very stereotyped ways of practice. And at the heart of it, we all think that we are right.
We can use polypharmacy as an example. Imagine that you have a new patient intake, who tells you that they are transferring care from another psychiatrist. They inform you of their medication regimen. This patient presents on eight or more psychotropics. Many of us may have a visceral reaction at this point and, following the aforementioned attribution theory, we may ask ourselves what ‘quack’ of a doctor would do this. Yet some among us would think that a very competent psychopharmacologist was daring enough to use the full armamentarium of psychopharmacology to help this patient, who must be treatment refractory.
When speaking with such a patient, we would be quick to reflect on our own parsimonious use of medications. We would tell ourselves that we are responsible providers and would be quick to recommend discontinuation of medications. This would help us feel better about ourselves, and would of course assuage the ever-present medicolegal ‘big brother’ in our minds. It is through this very process that we affirm our self-identities. For if this patient’s previous physician was a bad psychiatrist, then we are a good psychiatrist. It is through this process that our clinical selves find confirmation.
We do not mean to reduce the complexities of human behavior to quick stereotypes. However, it is our belief that when confronted with clinical or philosophical disputes with our colleagues, the basic rules of human behavior will attempt to dissolve and override efforts at mentalization, collegiality, or interpersonal sensitivity. For to accept a clinical practice view that is different from ours would be akin to giving up the essence of our clinical identities. It could be compared to the fragmentation process of a vulnerable psyche when confronted with a reality that is at odds with preconceived notions and experiences.
While we may be able to appreciate the nuances and sensibilities of another provider, we believe it would be particularly difficult for most of us to actually attempt to practice in a fashion that is not congruent with our own organizers of experience. Whether or not our practice style is ‘perfect,’ it has worked for us. Social neuroscience and our understanding of the organization of the self would predict that we would hold onto our way of practice with all the mind’s defenses. Externalization, denial, and projection could all be called into action in this battle against existential fragmentation.
Do we seek to portray a clinical world where there is no hope for genuine modeling of clinical sensibilities to other psychiatrists? That is not our intention. Yet it seems that many of the theoretical frameworks that we subscribe to argue against this possibility. We would be hypocritical if we did not here state that our own theoretical frameworks are yet other examples of “organizers of experience.” Attribution theory, intersubjectivity, and social neuroscience are simply our ways of organizing the chaos of perceptions, ideas, and intricacies of human behavior.
If we accept that psychiatrists, like all human beings, are trapped in a subjective experience, then we can be more playful and flexible when interacting with our colleagues. We do not have to be as defensive of our practices and accusatory of others. If we practice daily according to some orthodoxy, then we color our experiences of the patient and of our colleagues’ ways of practice. We automatically start off on the wrong foot. And yet, to give up this orthodoxy would, by definition, be disorganizing and fragmenting to us. For as Nietzsche said, “truth is an illusion without which a certain species could not survive.”5
Dr. Khalafian practices full time as a general outpatient psychiatrist. He trained at the University of California, San Diego, for his psychiatric residency and currently works as a telepsychiatrist, serving an outpatient clinic population in northern California. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. Dr. Badre and Dr. Khalafian have no conflicts of interest.
References
1. Buirski P and Haglund P. Making sense together: The intersubjective approach to psychotherapy. Northvale, NJ: Jason Aronson; 2001.
2. Malle BF. Attribution theories: How people make sense of behavior. In Chadee D (ed.), Theories in social psychology. pp. 72-95. Wiley-Blackwell; 2011.
3. Brown EC and Brune M. The role of prediction in social neuroscience. Front Hum Neurosci. 2012 May 24;6:147. doi: 10.3389/fnhum.2012.00147.
4. Blom T et al. Predictions drive neural representations of visual events ahead of incoming sensory information. Proc Natl Acad Sci USA. 2020 Mar 31;117(13):7510-7515. doi: 10.1073/pnas.1917777117.
5. Yalom I. The Gift of Therapy. Harper Perennial; 2002.
Psychiatrists practice in a wide array of ways. We approach our work and our patients with beliefs and preconceptions that develop over time. Our training has significant influence, though our own personalities and biases also affect our understanding.
Psychiatrists have philosophical lenses through which they see patients. We can reflect and see some standard archetypes. We are familiar with the reductionistic pharmacologist, the somatic treatment specialist, the psychodynamic ‘guru,’ and the medicolegally paralyzed practitioner. It is without judgment that we lay these out, for our very point is that we have these constituent parts within our own clinical identities. The intensity with which we subscribe to these clinical sensibilities could contribute to a biased orthodoxy.
Orthodoxy can be defined as an accepted theory that stems from an authoritative entity. This is a well-known phenomenon that continues to be visible. For example, one can quickly peruse psychodynamic literature to find one school of thought criticizing another. It is not without some confrontation and even interpersonal rifts that the lineage of psychoanalytic theory has evolved. This has always been of interest to us. A core facet of psychoanalysis is empathy, truly knowing the inner state of a different person. And yet, the very bastions of this clinical sensibility frequently resort to veiled attacks on those in their field who have opposing views. It then begs the question: If even enlightened institutions fail at a nonjudgmental approach toward their colleagues, what hope is there for the rest of us clinicians, mired in the thick of day-to-day clinical practice?
It is our contention that the odds are against us. Even the aforementioned critique of psychoanalytic orthodoxy is just another example of how we humans organize our experience. Even as we write an article in argument against unbridled critique, we find it difficult to do so without engaging in it. For to criticize another is to help shore up our own personal identities. This is especially the case when clinicians deal with issues that we feel strongly about. The human psyche has a need to organize its experience, as “our experience of ourselves is fundamental to how we operate in the world. Our subjective experience is the phenomenology of all that one might be aware of.”1
In this vein, we would like to cite attribution theory. This is a view of human behavior within social psychology. The Austrian psychologist Fritz Heider, PhD, investigated “the domain of social interactions, wondering how people perceive each other in interaction and especially how they make sense of each other’s behavior.”2 Attribution theory suggests that as humans organize our social interactions, we may make two basic assumptions. One is that our own behavior is highly affected by an environment that is beyond our control. The second is that when judging the behavior of others, we are more likely to attribute it to internal traits that they have. A classic example is automobile traffic. When we see someone driving erratically, we are more likely to blame them for being an inherently bad driver. However, if attention is called to our own driving, we are more likely to cite external factors such as rush hour, a bad driver around us, or a faulty vehicle.
We would like to reference one last model of human behavior. It has become customary within the field of neuroscience to view the brain as a predictive organ: “Theories of prediction in perception, action, and learning suggest that the brain serves to reduce the discrepancies between expectation and actual experience, i.e., by reducing the prediction error.”3 Perception itself has recently been described as a controlled hallucination, where the brain makes predictions of what it thinks it is about to see based on past experiences. Visual stimulus ultimately takes time to enter our eyes and be processed in the brain – “predictions would need to preactivate neural representations that would typically be driven by sensory input, before the actual arrival of that input.”4 It thus seems to be an inherent method of the brain to anticipate visual and even social events to help human beings sustain themselves.
Having spoken of a psychoanalytic conceptualization of self-organization, the theory of attribution, and research into social neuroscience, we turn our attention back to the central question that this article would like to address.
When we find ourselves busy in rote clinical practice, we believe the likelihood of intercollegiate mentalization is low; our ability to relate to our peers becomes strained. We ultimately do not practice in a vacuum. Psychiatrists, even those in a solo private practice, are ultimately part of a community of providers who, more or less, follow some emergent ‘standard of care.’ This can be a vague concept; but one that takes on a concrete form in the minds of certain clinicians and certainly in the setting of a medicolegal court. Yet, the psychiatrists that we know all have very stereotyped ways of practice. And at the heart of it, we all think that we are right.
We can use polypharmacy as an example. Imagine that you have a new patient intake, who tells you that they are transferring care from another psychiatrist. They inform you of their medication regimen. This patient presents on eight or more psychotropics. Many of us may have a visceral reaction at this point and, following the aforementioned attribution theory, we may ask ourselves what ‘quack’ of a doctor would do this. Yet some among us would think that a very competent psychopharmacologist was daring enough to use the full armamentarium of psychopharmacology to help this patient, who must be treatment refractory.
When speaking with such a patient, we would be quick to reflect on our own parsimonious use of medications. We would tell ourselves that we are responsible providers and would be quick to recommend discontinuation of medications. This would help us feel better about ourselves, and would of course assuage the ever-present medicolegal ‘big brother’ in our minds. It is through this very process that we affirm our self-identities. For if this patient’s previous physician was a bad psychiatrist, then we are a good psychiatrist. It is through this process that our clinical selves find confirmation.
We do not mean to reduce the complexities of human behavior to quick stereotypes. However, it is our belief that when confronted with clinical or philosophical disputes with our colleagues, the basic rules of human behavior will attempt to dissolve and override efforts at mentalization, collegiality, or interpersonal sensitivity. For to accept a clinical practice view that is different from ours would be akin to giving up the essence of our clinical identities. It could be compared to the fragmentation process of a vulnerable psyche when confronted with a reality that is at odds with preconceived notions and experiences.
While we may be able to appreciate the nuances and sensibilities of another provider, we believe it would be particularly difficult for most of us to actually attempt to practice in a fashion that is not congruent with our own organizers of experience. Whether or not our practice style is ‘perfect,’ it has worked for us. Social neuroscience and our understanding of the organization of the self would predict that we would hold onto our way of practice with all the mind’s defenses. Externalization, denial, and projection could all be called into action in this battle against existential fragmentation.
Do we seek to portray a clinical world where there is no hope for genuine modeling of clinical sensibilities to other psychiatrists? That is not our intention. Yet it seems that many of the theoretical frameworks that we subscribe to argue against this possibility. We would be hypocritical if we did not here state that our own theoretical frameworks are yet other examples of “organizers of experience.” Attribution theory, intersubjectivity, and social neuroscience are simply our ways of organizing the chaos of perceptions, ideas, and intricacies of human behavior.
If we accept that psychiatrists, like all human beings, are trapped in a subjective experience, then we can be more playful and flexible when interacting with our colleagues. We do not have to be as defensive of our practices and accusatory of others. If we practice daily according to some orthodoxy, then we color our experiences of the patient and of our colleagues’ ways of practice. We automatically start off on the wrong foot. And yet, to give up this orthodoxy would, by definition, be disorganizing and fragmenting to us. For as Nietzsche said, “truth is an illusion without which a certain species could not survive.”5
Dr. Khalafian practices full time as a general outpatient psychiatrist. He trained at the University of California, San Diego, for his psychiatric residency and currently works as a telepsychiatrist, serving an outpatient clinic population in northern California. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. Dr. Badre and Dr. Khalafian have no conflicts of interest.
References
1. Buirski P and Haglund P. Making sense together: The intersubjective approach to psychotherapy. Northvale, NJ: Jason Aronson; 2001.
2. Malle BF. Attribution theories: How people make sense of behavior. In Chadee D (ed.), Theories in social psychology. pp. 72-95. Wiley-Blackwell; 2011.
3. Brown EC and Brune M. The role of prediction in social neuroscience. Front Hum Neurosci. 2012 May 24;6:147. doi: 10.3389/fnhum.2012.00147.
4. Blom T et al. Predictions drive neural representations of visual events ahead of incoming sensory information. Proc Natl Acad Sci USA. 2020 Mar 31;117(13):7510-7515. doi: 10.1073/pnas.1917777117.
5. Yalom I. The Gift of Therapy. Harper Perennial; 2002.
Psychiatrists practice in a wide array of ways. We approach our work and our patients with beliefs and preconceptions that develop over time. Our training has significant influence, though our own personalities and biases also affect our understanding.
Psychiatrists have philosophical lenses through which they see patients. We can reflect and see some standard archetypes. We are familiar with the reductionistic pharmacologist, the somatic treatment specialist, the psychodynamic ‘guru,’ and the medicolegally paralyzed practitioner. It is without judgment that we lay these out, for our very point is that we have these constituent parts within our own clinical identities. The intensity with which we subscribe to these clinical sensibilities could contribute to a biased orthodoxy.
Orthodoxy can be defined as an accepted theory that stems from an authoritative entity. This is a well-known phenomenon that continues to be visible. For example, one can quickly peruse psychodynamic literature to find one school of thought criticizing another. It is not without some confrontation and even interpersonal rifts that the lineage of psychoanalytic theory has evolved. This has always been of interest to us. A core facet of psychoanalysis is empathy, truly knowing the inner state of a different person. And yet, the very bastions of this clinical sensibility frequently resort to veiled attacks on those in their field who have opposing views. It then begs the question: If even enlightened institutions fail at a nonjudgmental approach toward their colleagues, what hope is there for the rest of us clinicians, mired in the thick of day-to-day clinical practice?
It is our contention that the odds are against us. Even the aforementioned critique of psychoanalytic orthodoxy is just another example of how we humans organize our experience. Even as we write an article in argument against unbridled critique, we find it difficult to do so without engaging in it. For to criticize another is to help shore up our own personal identities. This is especially the case when clinicians deal with issues that we feel strongly about. The human psyche has a need to organize its experience, as “our experience of ourselves is fundamental to how we operate in the world. Our subjective experience is the phenomenology of all that one might be aware of.”1
In this vein, we would like to cite attribution theory. This is a view of human behavior within social psychology. The Austrian psychologist Fritz Heider, PhD, investigated “the domain of social interactions, wondering how people perceive each other in interaction and especially how they make sense of each other’s behavior.”2 Attribution theory suggests that as humans organize our social interactions, we may make two basic assumptions. One is that our own behavior is highly affected by an environment that is beyond our control. The second is that when judging the behavior of others, we are more likely to attribute it to internal traits that they have. A classic example is automobile traffic. When we see someone driving erratically, we are more likely to blame them for being an inherently bad driver. However, if attention is called to our own driving, we are more likely to cite external factors such as rush hour, a bad driver around us, or a faulty vehicle.
We would like to reference one last model of human behavior. It has become customary within the field of neuroscience to view the brain as a predictive organ: “Theories of prediction in perception, action, and learning suggest that the brain serves to reduce the discrepancies between expectation and actual experience, i.e., by reducing the prediction error.”3 Perception itself has recently been described as a controlled hallucination, where the brain makes predictions of what it thinks it is about to see based on past experiences. Visual stimulus ultimately takes time to enter our eyes and be processed in the brain – “predictions would need to preactivate neural representations that would typically be driven by sensory input, before the actual arrival of that input.”4 It thus seems to be an inherent method of the brain to anticipate visual and even social events to help human beings sustain themselves.
Having spoken of a psychoanalytic conceptualization of self-organization, the theory of attribution, and research into social neuroscience, we turn our attention back to the central question that this article would like to address.
When we find ourselves busy in rote clinical practice, we believe the likelihood of intercollegiate mentalization is low; our ability to relate to our peers becomes strained. We ultimately do not practice in a vacuum. Psychiatrists, even those in a solo private practice, are ultimately part of a community of providers who, more or less, follow some emergent ‘standard of care.’ This can be a vague concept; but one that takes on a concrete form in the minds of certain clinicians and certainly in the setting of a medicolegal court. Yet, the psychiatrists that we know all have very stereotyped ways of practice. And at the heart of it, we all think that we are right.
We can use polypharmacy as an example. Imagine that you have a new patient intake, who tells you that they are transferring care from another psychiatrist. They inform you of their medication regimen. This patient presents on eight or more psychotropics. Many of us may have a visceral reaction at this point and, following the aforementioned attribution theory, we may ask ourselves what ‘quack’ of a doctor would do this. Yet some among us would think that a very competent psychopharmacologist was daring enough to use the full armamentarium of psychopharmacology to help this patient, who must be treatment refractory.
When speaking with such a patient, we would be quick to reflect on our own parsimonious use of medications. We would tell ourselves that we are responsible providers and would be quick to recommend discontinuation of medications. This would help us feel better about ourselves, and would of course assuage the ever-present medicolegal ‘big brother’ in our minds. It is through this very process that we affirm our self-identities. For if this patient’s previous physician was a bad psychiatrist, then we are a good psychiatrist. It is through this process that our clinical selves find confirmation.
We do not mean to reduce the complexities of human behavior to quick stereotypes. However, it is our belief that when confronted with clinical or philosophical disputes with our colleagues, the basic rules of human behavior will attempt to dissolve and override efforts at mentalization, collegiality, or interpersonal sensitivity. For to accept a clinical practice view that is different from ours would be akin to giving up the essence of our clinical identities. It could be compared to the fragmentation process of a vulnerable psyche when confronted with a reality that is at odds with preconceived notions and experiences.
While we may be able to appreciate the nuances and sensibilities of another provider, we believe it would be particularly difficult for most of us to actually attempt to practice in a fashion that is not congruent with our own organizers of experience. Whether or not our practice style is ‘perfect,’ it has worked for us. Social neuroscience and our understanding of the organization of the self would predict that we would hold onto our way of practice with all the mind’s defenses. Externalization, denial, and projection could all be called into action in this battle against existential fragmentation.
Do we seek to portray a clinical world where there is no hope for genuine modeling of clinical sensibilities to other psychiatrists? That is not our intention. Yet it seems that many of the theoretical frameworks that we subscribe to argue against this possibility. We would be hypocritical if we did not here state that our own theoretical frameworks are yet other examples of “organizers of experience.” Attribution theory, intersubjectivity, and social neuroscience are simply our ways of organizing the chaos of perceptions, ideas, and intricacies of human behavior.
If we accept that psychiatrists, like all human beings, are trapped in a subjective experience, then we can be more playful and flexible when interacting with our colleagues. We do not have to be as defensive of our practices and accusatory of others. If we practice daily according to some orthodoxy, then we color our experiences of the patient and of our colleagues’ ways of practice. We automatically start off on the wrong foot. And yet, to give up this orthodoxy would, by definition, be disorganizing and fragmenting to us. For as Nietzsche said, “truth is an illusion without which a certain species could not survive.”5
Dr. Khalafian practices full time as a general outpatient psychiatrist. He trained at the University of California, San Diego, for his psychiatric residency and currently works as a telepsychiatrist, serving an outpatient clinic population in northern California. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Dr. Badre can be reached at his website, BadreMD.com. Dr. Badre and Dr. Khalafian have no conflicts of interest.
References
1. Buirski P and Haglund P. Making sense together: The intersubjective approach to psychotherapy. Northvale, NJ: Jason Aronson; 2001.
2. Malle BF. Attribution theories: How people make sense of behavior. In Chadee D (ed.), Theories in social psychology. pp. 72-95. Wiley-Blackwell; 2011.
3. Brown EC and Brune M. The role of prediction in social neuroscience. Front Hum Neurosci. 2012 May 24;6:147. doi: 10.3389/fnhum.2012.00147.
4. Blom T et al. Predictions drive neural representations of visual events ahead of incoming sensory information. Proc Natl Acad Sci USA. 2020 Mar 31;117(13):7510-7515. doi: 10.1073/pnas.1917777117.
5. Yalom I. The Gift of Therapy. Harper Perennial; 2002.
Negative expectations of COVID shots may amplify side effects
It fits the psychosomatic role of “nocebo effects,” the researchers say – when “psychological characteristics including anxiety, depression, and the tendency to amplify benign bodily sensations” cause participants to report more bad effects than others.
In August 2021, researchers in Hamburg, Germany, followed 1,678 adults getting a second shot of Pfizer or Moderna mRNA-based vaccines. Participants reported symptoms in a diary, starting 2 weeks ahead of the vaccinations and going 7 days afterward.
Some participants said they weren’t expecting much benefit. Researchers said these people were more likely to “catastrophize instead of normalize benign bodily sensations.” People who’d had a bad experience with their first shot were more likely to say they felt aches, pains, and other side effects from the second.
The research was published in JAMA Network Open.
“Clinician-patient interactions and public vaccine campaigns may both benefit from these insights by optimizing and contextualizing information provided about COVID-19 vaccines,” the researchers said. “Unfavorable nocebo-related adverse effects could then be prevented, and overall vaccine acceptance could be improved.”
More than half of participants, 52.1%, expected bad effects to happen from the shot. Another 7.6% said they would be hospitalized from those bad effects, and 10.6% said the effects would last in the long term.
The Washington Times reported that “substantial numbers of patients reported adverse effects after vaccination,” but people with positive expectations reported them as minor. “Those who scored higher for anxiety, depression, and other psychosocial factors were more likely to flag these issues as severe.”
A version of this article originally appeared on WebMD.com.
It fits the psychosomatic role of “nocebo effects,” the researchers say – when “psychological characteristics including anxiety, depression, and the tendency to amplify benign bodily sensations” cause participants to report more bad effects than others.
In August 2021, researchers in Hamburg, Germany, followed 1,678 adults getting a second shot of Pfizer or Moderna mRNA-based vaccines. Participants reported symptoms in a diary, starting 2 weeks ahead of the vaccinations and going 7 days afterward.
Some participants said they weren’t expecting much benefit. Researchers said these people were more likely to “catastrophize instead of normalize benign bodily sensations.” People who’d had a bad experience with their first shot were more likely to say they felt aches, pains, and other side effects from the second.
The research was published in JAMA Network Open.
“Clinician-patient interactions and public vaccine campaigns may both benefit from these insights by optimizing and contextualizing information provided about COVID-19 vaccines,” the researchers said. “Unfavorable nocebo-related adverse effects could then be prevented, and overall vaccine acceptance could be improved.”
More than half of participants, 52.1%, expected bad effects to happen from the shot. Another 7.6% said they would be hospitalized from those bad effects, and 10.6% said the effects would last in the long term.
The Washington Times reported that “substantial numbers of patients reported adverse effects after vaccination,” but people with positive expectations reported them as minor. “Those who scored higher for anxiety, depression, and other psychosocial factors were more likely to flag these issues as severe.”
A version of this article originally appeared on WebMD.com.
It fits the psychosomatic role of “nocebo effects,” the researchers say – when “psychological characteristics including anxiety, depression, and the tendency to amplify benign bodily sensations” cause participants to report more bad effects than others.
In August 2021, researchers in Hamburg, Germany, followed 1,678 adults getting a second shot of Pfizer or Moderna mRNA-based vaccines. Participants reported symptoms in a diary, starting 2 weeks ahead of the vaccinations and going 7 days afterward.
Some participants said they weren’t expecting much benefit. Researchers said these people were more likely to “catastrophize instead of normalize benign bodily sensations.” People who’d had a bad experience with their first shot were more likely to say they felt aches, pains, and other side effects from the second.
The research was published in JAMA Network Open.
“Clinician-patient interactions and public vaccine campaigns may both benefit from these insights by optimizing and contextualizing information provided about COVID-19 vaccines,” the researchers said. “Unfavorable nocebo-related adverse effects could then be prevented, and overall vaccine acceptance could be improved.”
More than half of participants, 52.1%, expected bad effects to happen from the shot. Another 7.6% said they would be hospitalized from those bad effects, and 10.6% said the effects would last in the long term.
The Washington Times reported that “substantial numbers of patients reported adverse effects after vaccination,” but people with positive expectations reported them as minor. “Those who scored higher for anxiety, depression, and other psychosocial factors were more likely to flag these issues as severe.”
A version of this article originally appeared on WebMD.com.
FROM JAMA NETWORK OPEN