User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Health care in America: Let that tapeworm grow
In my most recent column, “ ‘They All Laughed When I Spoke of Greedy Doctors,’ ” I attempted to provide a global understanding of some of the economic forces that have made American medicine what it is, how that happened, and why it is still happening.
I did not propose a fix. I have been proposing fixes for more than 30 years, on the pages of JAMA until 1999 and then for this news organization, most recently in 2019 with “Healthcare for All in a Land of Special Interests.”
Where you stand depends a lot on where you sit.
Is this good news or bad news? When William Hubbard was the dean of the University of Michigan School of Medicine in 1969, he said that “an academic medical center is the most efficient energy and resource trapping device that has ever been created” (personal communication, 1969).
To me as a faculty member of an academic medical center for many years, that was great news. We could grow faculty, erect buildings, take the best care of sick people, churn out research papers, mint new physicians and specialists, and get paid well in the process for doing “the Lord’s work.” What’s not to like? At that time, the proportion of the country’s gross national product expended for medical and health care was about 7%. And the predicted life span of an American at birth was 70.5 years.
Is this good news or bad news? In 2021, the proportion of our annual gross domestic product (GDP) consumed by health care was 18.3%, totaling $4.3 trillion, or $12,914 per person. For perspective, in 2021, the median income per capita was $37,638. Because quite a few Americans have very high incomes, the mean income per capita is much higher: $63,444. Predicted life span in 2021 was 76.4 years.
Thus, in a span of 53 years (1969-2022), only 5.9 years of life were gained per person born, for how many trillions of dollars expended? To me as a tax-paying citizen and payer of medical insurance premiums, that is bad news.
Is this good news or bad news? If we compare developed societies globally, our medical system does a whole lot of things very well indeed. But we spend a great deal more than any other country for health care and objectively achieve poorer outcomes. Thus, we are neither efficient nor effective. We keep a lot of workers very busy doing stuff, and they are generally well paid. As a worker, that’s good news; as a manager who values efficiency, it’s bad news indeed.
Is this good news or bad news? We’re the leader at finding money to pay people to do “health care work.” More Americans work in health care than any other field. In 2019, the United States employed some 21,000,000 people doing “health care and social assistance.” Among others, these occupations include physicians, dentists, dental hygienists and assistants, pharmacists, registered nurses, LVNs/LPNs, nursing aides, technologists and technicians, home health aides, respiratory therapists, occupational and speech therapists, social workers, childcare workers, and personal and home care aides. For a patient, parent, grandparent, and great-grandparent, it is good news to have all those folks available to take care of us when we need it.
So, while I have cringed at the frequent exposés from Roy Poses of what seem to me to be massive societal betrayals by American health care industry giants, it doesn’t have to be that way. Might it still be possible to do well while doing good?
A jobs program
Consider such common medical procedures as coronary artery stents or bypass grafts for stable angina (when optimal medical therapy is as good, or better than, and much less expensive); PSAs on asymptomatic men followed by unnecessary surgery for localized cancer; excess surgery for low back pain; and the jobs created by managing the people caught up in medical complications of the obesity epidemic.
Don’t forget the number of people employed simply to “follow the money” within our byzantine cockamamie medical billing system. In 2009, this prompted me to describe the bloated system as a “health care bubble” not unlike Enron, the submarket real estate financing debacle, or the dot-com boom and bust. I warned of the downside of bursting that bubble, particularly lost jobs.
The Affordable Care Act (ACA) provided health insurance to some 35 million Americans who had been uninsured. It retarded health care inflation. But it did nothing to trim administrative costs or very high pay for nonclinical executives, or shareholder profits in those companies that were for-profit, or drug and device prices. Without the support of all those groups, the ACA would never have passed Congress. The ACA has clearly been a mixed blessing.
If any large American constituency were ever serious about reducing the percentage of our GDP expended on health care, we have excellent ways to do that while improving the health and well-being of the American people. But remember, one person’s liability (unnecessary work) is another person’s asset (needed job).
The MBAization of medicine
Meanwhile, back at Dean Hubbard’s voracious academic medical center, the high intellect and driven nature of those who are attracted to medicine as a career has had other effects. The resulting organizations reflect not only the glorious calling of caring for the sick and the availability of lots of money to recruit and compensate leaders, but also the necessity to develop strong executive types who won’t be “eaten alive” by the high-powered workforce of demanding physicians and the surrounding environment.
Thus, it came as no great surprise that in its 2021 determination of America’s top 25 Best Large Employers, Forbes included five health care organizations and seven universities. Beating out such giants as NASA, Cisco, Microsoft, Netflix, and Google, the University of Alabama Birmingham Hospital was ranked first. Mayo Clinic and Yale University came in third and fifth, respectively, and at the other end of the list were Duke (23), MIT (24), and MD Anderson (25).
My goodness! Well done.
Yet, as a country attempting to be balanced, Warren Buffett’s descriptive entreaty on the 2021 failure of Haven, the Amazon-Chase-Berkshire Hathaway joint initiative, remains troubling. Calling upon Haven to change the U.S. health care system, Buffet said, “We learned a lot about the difficulty of changing around an industry that’s 17% of the GDP. We were fighting a tapeworm in the American economy, and the tapeworm won.” They had failed to tame the American health care cost beast.
I am on record as despising the “MBAization” of American medicine. Unfairly, I blamed a professional and technical discipline for what I considered misuse. I hereby repent and renounce my earlier condemnations.
Take it all over?
Here’s an idea: If you can’t beat them, join them.
Medical care is important, especially for acute illnesses and injuries, early cancer therapy, and many chronic conditions. But the real determinants of health writ large are social: wealth, education, housing, nutritious food, childcare, climate, clean air and water, meaningful employment, safety from violence, exercise schemes, vaccinations, and so on.
Why doesn’t the American medical-industrial complex simply bestow the label of “health care” on all health-related social determinants? Take it all over. Good “health care” jobs for everyone. Medical professionals will still be blamed for the low health quality and poor outcome scores, the main social determinants of health over which we have no control or influence.
Let that tapeworm grow to encompass all social determinants of health, and measure results by length and quality of life, national human happiness, and, of course, jobs. We can do it. Let that bubble glow. Party time.
And that’s the way it is. That’s my opinion.
George Lundberg, MD, is editor-in-chief at Cancer Commons, president of the Lundberg Institute, executive advisor at Cureus, and a clinical professor of pathology at Northwestern University. Previously, he served as editor-in-chief of JAMA (including 10 specialty journals), American Medical News, and Medscape.
A version of this article first appeared on Medscape.com.
In my most recent column, “ ‘They All Laughed When I Spoke of Greedy Doctors,’ ” I attempted to provide a global understanding of some of the economic forces that have made American medicine what it is, how that happened, and why it is still happening.
I did not propose a fix. I have been proposing fixes for more than 30 years, on the pages of JAMA until 1999 and then for this news organization, most recently in 2019 with “Healthcare for All in a Land of Special Interests.”
Where you stand depends a lot on where you sit.
Is this good news or bad news? When William Hubbard was the dean of the University of Michigan School of Medicine in 1969, he said that “an academic medical center is the most efficient energy and resource trapping device that has ever been created” (personal communication, 1969).
To me as a faculty member of an academic medical center for many years, that was great news. We could grow faculty, erect buildings, take the best care of sick people, churn out research papers, mint new physicians and specialists, and get paid well in the process for doing “the Lord’s work.” What’s not to like? At that time, the proportion of the country’s gross national product expended for medical and health care was about 7%. And the predicted life span of an American at birth was 70.5 years.
Is this good news or bad news? In 2021, the proportion of our annual gross domestic product (GDP) consumed by health care was 18.3%, totaling $4.3 trillion, or $12,914 per person. For perspective, in 2021, the median income per capita was $37,638. Because quite a few Americans have very high incomes, the mean income per capita is much higher: $63,444. Predicted life span in 2021 was 76.4 years.
Thus, in a span of 53 years (1969-2022), only 5.9 years of life were gained per person born, for how many trillions of dollars expended? To me as a tax-paying citizen and payer of medical insurance premiums, that is bad news.
Is this good news or bad news? If we compare developed societies globally, our medical system does a whole lot of things very well indeed. But we spend a great deal more than any other country for health care and objectively achieve poorer outcomes. Thus, we are neither efficient nor effective. We keep a lot of workers very busy doing stuff, and they are generally well paid. As a worker, that’s good news; as a manager who values efficiency, it’s bad news indeed.
Is this good news or bad news? We’re the leader at finding money to pay people to do “health care work.” More Americans work in health care than any other field. In 2019, the United States employed some 21,000,000 people doing “health care and social assistance.” Among others, these occupations include physicians, dentists, dental hygienists and assistants, pharmacists, registered nurses, LVNs/LPNs, nursing aides, technologists and technicians, home health aides, respiratory therapists, occupational and speech therapists, social workers, childcare workers, and personal and home care aides. For a patient, parent, grandparent, and great-grandparent, it is good news to have all those folks available to take care of us when we need it.
So, while I have cringed at the frequent exposés from Roy Poses of what seem to me to be massive societal betrayals by American health care industry giants, it doesn’t have to be that way. Might it still be possible to do well while doing good?
A jobs program
Consider such common medical procedures as coronary artery stents or bypass grafts for stable angina (when optimal medical therapy is as good, or better than, and much less expensive); PSAs on asymptomatic men followed by unnecessary surgery for localized cancer; excess surgery for low back pain; and the jobs created by managing the people caught up in medical complications of the obesity epidemic.
Don’t forget the number of people employed simply to “follow the money” within our byzantine cockamamie medical billing system. In 2009, this prompted me to describe the bloated system as a “health care bubble” not unlike Enron, the submarket real estate financing debacle, or the dot-com boom and bust. I warned of the downside of bursting that bubble, particularly lost jobs.
The Affordable Care Act (ACA) provided health insurance to some 35 million Americans who had been uninsured. It retarded health care inflation. But it did nothing to trim administrative costs or very high pay for nonclinical executives, or shareholder profits in those companies that were for-profit, or drug and device prices. Without the support of all those groups, the ACA would never have passed Congress. The ACA has clearly been a mixed blessing.
If any large American constituency were ever serious about reducing the percentage of our GDP expended on health care, we have excellent ways to do that while improving the health and well-being of the American people. But remember, one person’s liability (unnecessary work) is another person’s asset (needed job).
The MBAization of medicine
Meanwhile, back at Dean Hubbard’s voracious academic medical center, the high intellect and driven nature of those who are attracted to medicine as a career has had other effects. The resulting organizations reflect not only the glorious calling of caring for the sick and the availability of lots of money to recruit and compensate leaders, but also the necessity to develop strong executive types who won’t be “eaten alive” by the high-powered workforce of demanding physicians and the surrounding environment.
Thus, it came as no great surprise that in its 2021 determination of America’s top 25 Best Large Employers, Forbes included five health care organizations and seven universities. Beating out such giants as NASA, Cisco, Microsoft, Netflix, and Google, the University of Alabama Birmingham Hospital was ranked first. Mayo Clinic and Yale University came in third and fifth, respectively, and at the other end of the list were Duke (23), MIT (24), and MD Anderson (25).
My goodness! Well done.
Yet, as a country attempting to be balanced, Warren Buffett’s descriptive entreaty on the 2021 failure of Haven, the Amazon-Chase-Berkshire Hathaway joint initiative, remains troubling. Calling upon Haven to change the U.S. health care system, Buffet said, “We learned a lot about the difficulty of changing around an industry that’s 17% of the GDP. We were fighting a tapeworm in the American economy, and the tapeworm won.” They had failed to tame the American health care cost beast.
I am on record as despising the “MBAization” of American medicine. Unfairly, I blamed a professional and technical discipline for what I considered misuse. I hereby repent and renounce my earlier condemnations.
Take it all over?
Here’s an idea: If you can’t beat them, join them.
Medical care is important, especially for acute illnesses and injuries, early cancer therapy, and many chronic conditions. But the real determinants of health writ large are social: wealth, education, housing, nutritious food, childcare, climate, clean air and water, meaningful employment, safety from violence, exercise schemes, vaccinations, and so on.
Why doesn’t the American medical-industrial complex simply bestow the label of “health care” on all health-related social determinants? Take it all over. Good “health care” jobs for everyone. Medical professionals will still be blamed for the low health quality and poor outcome scores, the main social determinants of health over which we have no control or influence.
Let that tapeworm grow to encompass all social determinants of health, and measure results by length and quality of life, national human happiness, and, of course, jobs. We can do it. Let that bubble glow. Party time.
And that’s the way it is. That’s my opinion.
George Lundberg, MD, is editor-in-chief at Cancer Commons, president of the Lundberg Institute, executive advisor at Cureus, and a clinical professor of pathology at Northwestern University. Previously, he served as editor-in-chief of JAMA (including 10 specialty journals), American Medical News, and Medscape.
A version of this article first appeared on Medscape.com.
In my most recent column, “ ‘They All Laughed When I Spoke of Greedy Doctors,’ ” I attempted to provide a global understanding of some of the economic forces that have made American medicine what it is, how that happened, and why it is still happening.
I did not propose a fix. I have been proposing fixes for more than 30 years, on the pages of JAMA until 1999 and then for this news organization, most recently in 2019 with “Healthcare for All in a Land of Special Interests.”
Where you stand depends a lot on where you sit.
Is this good news or bad news? When William Hubbard was the dean of the University of Michigan School of Medicine in 1969, he said that “an academic medical center is the most efficient energy and resource trapping device that has ever been created” (personal communication, 1969).
To me as a faculty member of an academic medical center for many years, that was great news. We could grow faculty, erect buildings, take the best care of sick people, churn out research papers, mint new physicians and specialists, and get paid well in the process for doing “the Lord’s work.” What’s not to like? At that time, the proportion of the country’s gross national product expended for medical and health care was about 7%. And the predicted life span of an American at birth was 70.5 years.
Is this good news or bad news? In 2021, the proportion of our annual gross domestic product (GDP) consumed by health care was 18.3%, totaling $4.3 trillion, or $12,914 per person. For perspective, in 2021, the median income per capita was $37,638. Because quite a few Americans have very high incomes, the mean income per capita is much higher: $63,444. Predicted life span in 2021 was 76.4 years.
Thus, in a span of 53 years (1969-2022), only 5.9 years of life were gained per person born, for how many trillions of dollars expended? To me as a tax-paying citizen and payer of medical insurance premiums, that is bad news.
Is this good news or bad news? If we compare developed societies globally, our medical system does a whole lot of things very well indeed. But we spend a great deal more than any other country for health care and objectively achieve poorer outcomes. Thus, we are neither efficient nor effective. We keep a lot of workers very busy doing stuff, and they are generally well paid. As a worker, that’s good news; as a manager who values efficiency, it’s bad news indeed.
Is this good news or bad news? We’re the leader at finding money to pay people to do “health care work.” More Americans work in health care than any other field. In 2019, the United States employed some 21,000,000 people doing “health care and social assistance.” Among others, these occupations include physicians, dentists, dental hygienists and assistants, pharmacists, registered nurses, LVNs/LPNs, nursing aides, technologists and technicians, home health aides, respiratory therapists, occupational and speech therapists, social workers, childcare workers, and personal and home care aides. For a patient, parent, grandparent, and great-grandparent, it is good news to have all those folks available to take care of us when we need it.
So, while I have cringed at the frequent exposés from Roy Poses of what seem to me to be massive societal betrayals by American health care industry giants, it doesn’t have to be that way. Might it still be possible to do well while doing good?
A jobs program
Consider such common medical procedures as coronary artery stents or bypass grafts for stable angina (when optimal medical therapy is as good, or better than, and much less expensive); PSAs on asymptomatic men followed by unnecessary surgery for localized cancer; excess surgery for low back pain; and the jobs created by managing the people caught up in medical complications of the obesity epidemic.
Don’t forget the number of people employed simply to “follow the money” within our byzantine cockamamie medical billing system. In 2009, this prompted me to describe the bloated system as a “health care bubble” not unlike Enron, the submarket real estate financing debacle, or the dot-com boom and bust. I warned of the downside of bursting that bubble, particularly lost jobs.
The Affordable Care Act (ACA) provided health insurance to some 35 million Americans who had been uninsured. It retarded health care inflation. But it did nothing to trim administrative costs or very high pay for nonclinical executives, or shareholder profits in those companies that were for-profit, or drug and device prices. Without the support of all those groups, the ACA would never have passed Congress. The ACA has clearly been a mixed blessing.
If any large American constituency were ever serious about reducing the percentage of our GDP expended on health care, we have excellent ways to do that while improving the health and well-being of the American people. But remember, one person’s liability (unnecessary work) is another person’s asset (needed job).
The MBAization of medicine
Meanwhile, back at Dean Hubbard’s voracious academic medical center, the high intellect and driven nature of those who are attracted to medicine as a career has had other effects. The resulting organizations reflect not only the glorious calling of caring for the sick and the availability of lots of money to recruit and compensate leaders, but also the necessity to develop strong executive types who won’t be “eaten alive” by the high-powered workforce of demanding physicians and the surrounding environment.
Thus, it came as no great surprise that in its 2021 determination of America’s top 25 Best Large Employers, Forbes included five health care organizations and seven universities. Beating out such giants as NASA, Cisco, Microsoft, Netflix, and Google, the University of Alabama Birmingham Hospital was ranked first. Mayo Clinic and Yale University came in third and fifth, respectively, and at the other end of the list were Duke (23), MIT (24), and MD Anderson (25).
My goodness! Well done.
Yet, as a country attempting to be balanced, Warren Buffett’s descriptive entreaty on the 2021 failure of Haven, the Amazon-Chase-Berkshire Hathaway joint initiative, remains troubling. Calling upon Haven to change the U.S. health care system, Buffet said, “We learned a lot about the difficulty of changing around an industry that’s 17% of the GDP. We were fighting a tapeworm in the American economy, and the tapeworm won.” They had failed to tame the American health care cost beast.
I am on record as despising the “MBAization” of American medicine. Unfairly, I blamed a professional and technical discipline for what I considered misuse. I hereby repent and renounce my earlier condemnations.
Take it all over?
Here’s an idea: If you can’t beat them, join them.
Medical care is important, especially for acute illnesses and injuries, early cancer therapy, and many chronic conditions. But the real determinants of health writ large are social: wealth, education, housing, nutritious food, childcare, climate, clean air and water, meaningful employment, safety from violence, exercise schemes, vaccinations, and so on.
Why doesn’t the American medical-industrial complex simply bestow the label of “health care” on all health-related social determinants? Take it all over. Good “health care” jobs for everyone. Medical professionals will still be blamed for the low health quality and poor outcome scores, the main social determinants of health over which we have no control or influence.
Let that tapeworm grow to encompass all social determinants of health, and measure results by length and quality of life, national human happiness, and, of course, jobs. We can do it. Let that bubble glow. Party time.
And that’s the way it is. That’s my opinion.
George Lundberg, MD, is editor-in-chief at Cancer Commons, president of the Lundberg Institute, executive advisor at Cureus, and a clinical professor of pathology at Northwestern University. Previously, he served as editor-in-chief of JAMA (including 10 specialty journals), American Medical News, and Medscape.
A version of this article first appeared on Medscape.com.
Previously unknown viral families hide in the darnedest places
You and me and baby makes 10,003
If you were a virus hunter, looking for your next big virus discovery, where would you go? The wholesale seafood market in Wuhan? A gathering of unmasked anti-vaxxers in the heartland of America? The frozen snot fields of northwest Siberia?
How about babies? Well, it’s too late now, because that’s what Dennis Sandris Nielsen, PhD, of the University of Copenhagen, and his associates did, and they hit the mother lode. Actually, it was more like the infant load, if we’re being honest here.
“We found an exceptional number of unknown viruses in the faeces of these babies,” Dr. Nielsen said in a written statement from the university. (The study was published in Nature Microbiology, so we get the English spelling of feces.)
The investigators mapped the gut “viromes” of 647 healthy Danish 1-year-old children over the course of 5 years and found 10,000 species of viruses distributed across 248 different viral families, of which only 16 were already known. Incredible stuff, but then things took a turn for the cute. “The researchers named the remaining 232 unknown viral families after the children whose diapers made the study possible. As a result, new viral families include names like Sylvesterviridae, Rigmorviridae and Tristanviridae,” the university said.
About 90% of the viruses found in the feces are bacterial viruses, aka bacteriophages, which have bacteria as their hosts and don’t attack the children’s cells, so they don’t cause disease. The other 10%, however, are eukaryotic: They use human cells as hosts, so they can be either friend or foe. “It is thought-provoking that all children run around with 10-20 of these virus types that infect human cells. So, there is a constant viral infection taking place, which apparently doesn’t make them sick,” Dr. Nielsen said.
Doesn’t make them sick? Riiiight. The thought that this gives rise to now? People love babies. Everyone wants to pick up the baby. Now we know why. Because the viruses want us to! Well, those cute little faces aren’t fooling us anymore. No more babies for us. Everyone should stay away from babies and their evil little eukaryotic viruses. STOP THE BABIES!
[Editor’s note: After a short timeout, we explained to the staff that the human species actually needs babies for its survival. They calmed down, picked up their crayons, and quietly went back to work.]
Fooled them. Stop the babies!
At least someone out there appreciates hospital food
Life in Alaska is not for the meek. It’s dark half the year. Summer is 3 weeks in July. And somehow, there’s a moose in line ahead of you at the doctor’s office. To make matters worse, it’s arguing about insurance. “What do you mean, you’ve heard the Moo Cross Moo Shield joke before?”
One might expect that Providence Alaska Health Park, located near downtown Anchorage, the largest city in Alaska by a massive margin, might be safe from ungulate invasion. Nope. In recent days, a young moose has taken to hanging around Providence campus, and it just could not find anything to eat. Remember, it may be early April, but this is Alaska. It’s still winter there. The ground’s still covered in snow.
Eventually, the gears in our young moose friend’s mind turned and it settled on a course of action: “Hey, those are some nice-looking plants behind that door over there. …” And that’s how Providence Alaska Health ended up with a moose munching on decorative potted plants in the hospital lobby.
Funnily enough, the moose didn’t even make a big scene. It just walked through the automatic doors and started chowing down. Security only found out because a tenant called them. Naturally though, once security made the announcement that a massive wild animal had been spotted in the building, the lobby was evacuated. … What do you mean, half the hospital came around to see it? Apparently, even though Alaskans have to fight moose herds on their daily commute, a lot of people wanted to see our moose friend do its thing.
“That’s crazy,” a woman in scrubs said in a video as she snapped a photo with her phone.
“This is the best. Like, what’s the code for this?” asked another bystander.
Despite security’s best efforts to shoo the moose out with barricades and offers of tasty branches, our furry friend left of its own volition, presumably irritated that his breakfast had become a spectator sport. But it didn’t go far. It hung around the front drive for a while, then went around the back of the building for a nap. What has four hooves and still doesn’t give a crap? Bob Moose-o! How you doing?
That click sounded stressed
How can people tell that you’re stressed? Maybe you get irritable and a little snappy. Some people have an inability to concentrate or focus. Eating that muffin when you weren’t really hungry could be a sign you’re not relaxed.
Did you know that your computer can be an indicator of your stress levels?
We tend to be working when we’re using computers, right? That can be a stressor in itself. Well, some researchers at ETH Zürich decided to have a look at the situation. Surprisingly, at least to us, one in three Swiss employees experience workplace stress, which makes us wonder what the percentage is in this country.
The Swiss researchers developed a model that tells how stressed someone is just by the way they use their computer mouse or type. The results of their study showed that those who were stressed clicked and tapped differently than participants who were more relaxed.
Stressed people click “more often and less precisely and cover longer distances on the screen,” while the relaxed take “shorter, more direct routes to reach their destination and take more time doing so,” study author Mara Nägelin explained in a written statement from ETH (Eidgenössische Technische Hochschule, or Swiss Federal Institute of Technology) Zürich.
Ever find when you’re frustrated and in a rush you end up making more mistakes? Same deal. Coauthor Jasmine Kerr noted that “increased levels of stress negatively impact our brain’s ability to process information.” Which totally is going to affect how we move.
Hopefully, these results can give insight to companies on how stressed their employees are and the effect it has on their work performance, eventually leading to, guess what, more research on how to alleviate workplace stress in general, which can benefit us all.
So if you find yourself in the office working on your computer like it’s a game of Perfection and time is running out, take a beat. Maybe try a stress-relieving breathing technique. Nonstressed people, according to the study, take fewer and longer pauses on their computers. Perfection on the job may mean relaxing first.
You and me and baby makes 10,003
If you were a virus hunter, looking for your next big virus discovery, where would you go? The wholesale seafood market in Wuhan? A gathering of unmasked anti-vaxxers in the heartland of America? The frozen snot fields of northwest Siberia?
How about babies? Well, it’s too late now, because that’s what Dennis Sandris Nielsen, PhD, of the University of Copenhagen, and his associates did, and they hit the mother lode. Actually, it was more like the infant load, if we’re being honest here.
“We found an exceptional number of unknown viruses in the faeces of these babies,” Dr. Nielsen said in a written statement from the university. (The study was published in Nature Microbiology, so we get the English spelling of feces.)
The investigators mapped the gut “viromes” of 647 healthy Danish 1-year-old children over the course of 5 years and found 10,000 species of viruses distributed across 248 different viral families, of which only 16 were already known. Incredible stuff, but then things took a turn for the cute. “The researchers named the remaining 232 unknown viral families after the children whose diapers made the study possible. As a result, new viral families include names like Sylvesterviridae, Rigmorviridae and Tristanviridae,” the university said.
About 90% of the viruses found in the feces are bacterial viruses, aka bacteriophages, which have bacteria as their hosts and don’t attack the children’s cells, so they don’t cause disease. The other 10%, however, are eukaryotic: They use human cells as hosts, so they can be either friend or foe. “It is thought-provoking that all children run around with 10-20 of these virus types that infect human cells. So, there is a constant viral infection taking place, which apparently doesn’t make them sick,” Dr. Nielsen said.
Doesn’t make them sick? Riiiight. The thought that this gives rise to now? People love babies. Everyone wants to pick up the baby. Now we know why. Because the viruses want us to! Well, those cute little faces aren’t fooling us anymore. No more babies for us. Everyone should stay away from babies and their evil little eukaryotic viruses. STOP THE BABIES!
[Editor’s note: After a short timeout, we explained to the staff that the human species actually needs babies for its survival. They calmed down, picked up their crayons, and quietly went back to work.]
Fooled them. Stop the babies!
At least someone out there appreciates hospital food
Life in Alaska is not for the meek. It’s dark half the year. Summer is 3 weeks in July. And somehow, there’s a moose in line ahead of you at the doctor’s office. To make matters worse, it’s arguing about insurance. “What do you mean, you’ve heard the Moo Cross Moo Shield joke before?”
One might expect that Providence Alaska Health Park, located near downtown Anchorage, the largest city in Alaska by a massive margin, might be safe from ungulate invasion. Nope. In recent days, a young moose has taken to hanging around Providence campus, and it just could not find anything to eat. Remember, it may be early April, but this is Alaska. It’s still winter there. The ground’s still covered in snow.
Eventually, the gears in our young moose friend’s mind turned and it settled on a course of action: “Hey, those are some nice-looking plants behind that door over there. …” And that’s how Providence Alaska Health ended up with a moose munching on decorative potted plants in the hospital lobby.
Funnily enough, the moose didn’t even make a big scene. It just walked through the automatic doors and started chowing down. Security only found out because a tenant called them. Naturally though, once security made the announcement that a massive wild animal had been spotted in the building, the lobby was evacuated. … What do you mean, half the hospital came around to see it? Apparently, even though Alaskans have to fight moose herds on their daily commute, a lot of people wanted to see our moose friend do its thing.
“That’s crazy,” a woman in scrubs said in a video as she snapped a photo with her phone.
“This is the best. Like, what’s the code for this?” asked another bystander.
Despite security’s best efforts to shoo the moose out with barricades and offers of tasty branches, our furry friend left of its own volition, presumably irritated that his breakfast had become a spectator sport. But it didn’t go far. It hung around the front drive for a while, then went around the back of the building for a nap. What has four hooves and still doesn’t give a crap? Bob Moose-o! How you doing?
That click sounded stressed
How can people tell that you’re stressed? Maybe you get irritable and a little snappy. Some people have an inability to concentrate or focus. Eating that muffin when you weren’t really hungry could be a sign you’re not relaxed.
Did you know that your computer can be an indicator of your stress levels?
We tend to be working when we’re using computers, right? That can be a stressor in itself. Well, some researchers at ETH Zürich decided to have a look at the situation. Surprisingly, at least to us, one in three Swiss employees experience workplace stress, which makes us wonder what the percentage is in this country.
The Swiss researchers developed a model that tells how stressed someone is just by the way they use their computer mouse or type. The results of their study showed that those who were stressed clicked and tapped differently than participants who were more relaxed.
Stressed people click “more often and less precisely and cover longer distances on the screen,” while the relaxed take “shorter, more direct routes to reach their destination and take more time doing so,” study author Mara Nägelin explained in a written statement from ETH (Eidgenössische Technische Hochschule, or Swiss Federal Institute of Technology) Zürich.
Ever find when you’re frustrated and in a rush you end up making more mistakes? Same deal. Coauthor Jasmine Kerr noted that “increased levels of stress negatively impact our brain’s ability to process information.” Which totally is going to affect how we move.
Hopefully, these results can give insight to companies on how stressed their employees are and the effect it has on their work performance, eventually leading to, guess what, more research on how to alleviate workplace stress in general, which can benefit us all.
So if you find yourself in the office working on your computer like it’s a game of Perfection and time is running out, take a beat. Maybe try a stress-relieving breathing technique. Nonstressed people, according to the study, take fewer and longer pauses on their computers. Perfection on the job may mean relaxing first.
You and me and baby makes 10,003
If you were a virus hunter, looking for your next big virus discovery, where would you go? The wholesale seafood market in Wuhan? A gathering of unmasked anti-vaxxers in the heartland of America? The frozen snot fields of northwest Siberia?
How about babies? Well, it’s too late now, because that’s what Dennis Sandris Nielsen, PhD, of the University of Copenhagen, and his associates did, and they hit the mother lode. Actually, it was more like the infant load, if we’re being honest here.
“We found an exceptional number of unknown viruses in the faeces of these babies,” Dr. Nielsen said in a written statement from the university. (The study was published in Nature Microbiology, so we get the English spelling of feces.)
The investigators mapped the gut “viromes” of 647 healthy Danish 1-year-old children over the course of 5 years and found 10,000 species of viruses distributed across 248 different viral families, of which only 16 were already known. Incredible stuff, but then things took a turn for the cute. “The researchers named the remaining 232 unknown viral families after the children whose diapers made the study possible. As a result, new viral families include names like Sylvesterviridae, Rigmorviridae and Tristanviridae,” the university said.
About 90% of the viruses found in the feces are bacterial viruses, aka bacteriophages, which have bacteria as their hosts and don’t attack the children’s cells, so they don’t cause disease. The other 10%, however, are eukaryotic: They use human cells as hosts, so they can be either friend or foe. “It is thought-provoking that all children run around with 10-20 of these virus types that infect human cells. So, there is a constant viral infection taking place, which apparently doesn’t make them sick,” Dr. Nielsen said.
Doesn’t make them sick? Riiiight. The thought that this gives rise to now? People love babies. Everyone wants to pick up the baby. Now we know why. Because the viruses want us to! Well, those cute little faces aren’t fooling us anymore. No more babies for us. Everyone should stay away from babies and their evil little eukaryotic viruses. STOP THE BABIES!
[Editor’s note: After a short timeout, we explained to the staff that the human species actually needs babies for its survival. They calmed down, picked up their crayons, and quietly went back to work.]
Fooled them. Stop the babies!
At least someone out there appreciates hospital food
Life in Alaska is not for the meek. It’s dark half the year. Summer is 3 weeks in July. And somehow, there’s a moose in line ahead of you at the doctor’s office. To make matters worse, it’s arguing about insurance. “What do you mean, you’ve heard the Moo Cross Moo Shield joke before?”
One might expect that Providence Alaska Health Park, located near downtown Anchorage, the largest city in Alaska by a massive margin, might be safe from ungulate invasion. Nope. In recent days, a young moose has taken to hanging around Providence campus, and it just could not find anything to eat. Remember, it may be early April, but this is Alaska. It’s still winter there. The ground’s still covered in snow.
Eventually, the gears in our young moose friend’s mind turned and it settled on a course of action: “Hey, those are some nice-looking plants behind that door over there. …” And that’s how Providence Alaska Health ended up with a moose munching on decorative potted plants in the hospital lobby.
Funnily enough, the moose didn’t even make a big scene. It just walked through the automatic doors and started chowing down. Security only found out because a tenant called them. Naturally though, once security made the announcement that a massive wild animal had been spotted in the building, the lobby was evacuated. … What do you mean, half the hospital came around to see it? Apparently, even though Alaskans have to fight moose herds on their daily commute, a lot of people wanted to see our moose friend do its thing.
“That’s crazy,” a woman in scrubs said in a video as she snapped a photo with her phone.
“This is the best. Like, what’s the code for this?” asked another bystander.
Despite security’s best efforts to shoo the moose out with barricades and offers of tasty branches, our furry friend left of its own volition, presumably irritated that his breakfast had become a spectator sport. But it didn’t go far. It hung around the front drive for a while, then went around the back of the building for a nap. What has four hooves and still doesn’t give a crap? Bob Moose-o! How you doing?
That click sounded stressed
How can people tell that you’re stressed? Maybe you get irritable and a little snappy. Some people have an inability to concentrate or focus. Eating that muffin when you weren’t really hungry could be a sign you’re not relaxed.
Did you know that your computer can be an indicator of your stress levels?
We tend to be working when we’re using computers, right? That can be a stressor in itself. Well, some researchers at ETH Zürich decided to have a look at the situation. Surprisingly, at least to us, one in three Swiss employees experience workplace stress, which makes us wonder what the percentage is in this country.
The Swiss researchers developed a model that tells how stressed someone is just by the way they use their computer mouse or type. The results of their study showed that those who were stressed clicked and tapped differently than participants who were more relaxed.
Stressed people click “more often and less precisely and cover longer distances on the screen,” while the relaxed take “shorter, more direct routes to reach their destination and take more time doing so,” study author Mara Nägelin explained in a written statement from ETH (Eidgenössische Technische Hochschule, or Swiss Federal Institute of Technology) Zürich.
Ever find when you’re frustrated and in a rush you end up making more mistakes? Same deal. Coauthor Jasmine Kerr noted that “increased levels of stress negatively impact our brain’s ability to process information.” Which totally is going to affect how we move.
Hopefully, these results can give insight to companies on how stressed their employees are and the effect it has on their work performance, eventually leading to, guess what, more research on how to alleviate workplace stress in general, which can benefit us all.
So if you find yourself in the office working on your computer like it’s a game of Perfection and time is running out, take a beat. Maybe try a stress-relieving breathing technique. Nonstressed people, according to the study, take fewer and longer pauses on their computers. Perfection on the job may mean relaxing first.
Anger in adults a red flag for childhood trauma
PARIS –
Investigators examined data on more than 2,250 individuals who were asked about trauma during childhood and a subsequent tendency toward anger or angry outbursts 4 years later.
Results showed that emotional neglect during childhood was associated with approximately a 40% increased likelihood of subsequent anger, while psychological abuse was linked to a 30% increased likelihood.
Childhood physical abuse was also significantly associated with anger in adults, with an increased risk of approximately 40%. The researchers found no link between childhood sexual abuse and adult anger.
“We can’t definitively say that the trauma causes the anger, but the link is clear,” study investigator Nienke De Bles, PhD student, department of psychiatry, Leiden (the Netherlands) University Medical Center, said in a news release.
“Being easily angered can have several consequences,” she continued. “It can make personal interactions more difficult, and it can have consequences for your mental health and well-being, but people who get angry easily also have a greater tendency to discontinue psychiatric treatment, so this anger may mean that it reduces their chances of a better life,” she added.
Ms. De Bles believes that “it should be standard practice to ask depression and anxiety sufferers about anger and past trauma, even if the patient is not exhibiting current anger.”
The findings were presented at the European Psychiatric Association 2023 Congress.
A ‘red flag’ for abuse
“Psychiatric treatments for past trauma may differ from treatments for depression, so psychiatrists need to try to understand the cause so that they can offer the correct treatment to each patient,” said Ms. De Bles.
Ms. De Bles noted that childhood trauma has many negative consequences later in life and that it is associated with a higher prevalence of adult depression and anxiety.
“There are several potential mechanisms for psychopathology in the context of childhood trauma, and emotion regulation seems to be one of the key mechanisms,” she said.
The researchers previously found that anger was highly prevalent among patients with affective disorders. It was present in 30% of those with current anxiety or depressive disorder and in 40% of those with comorbid depression and anxiety with a tendency toward anger versus 5% of healthy control persons.
Other studies have shown that anger is associated with poor treatment outcomes and dropping out of treatment.
To further investigate the link between childhood trauma and anger in adulthood, the researchers examined data on 2,271 participants in the Netherlands Study of Depression and Anxiety (NESDA).
Childhood trauma was assessed at baseline using the semistructured Childhood Trauma Interview. Anger was measured at a 4-year follow-up using the Spielberger Trait Anger Subscale, the Anger Attacks Questionnaire, and the borderline and antisocial subscales of the Personality Disorder Questionnaire 4 to identify cluster B personality traits.
Results showed that emotional neglect during childhood was significantly associated with trait anger in adulthood, at an adjusted odds ratio of 1.42 (P < .001), anger attacks (OR, 1.35; P = .004), and borderline (OR, 1.76; P < .001) and antisocial (OR, 1.88; P = .001) personality traits.
Childhood psychological abuse was also significantly associated with later trait anger (OR, 1.28; P = .002), anger attacks (OR, 1.31; P = .024), and borderline (OR, 1.77; P < .001) and antisocial (OR, 1.69; P = .011) traits.
There was also a significant association between childhood psychical abuse and trait anger in adulthood (OR, 1.37; P < .001), anger attacks (OR, 1.48; P = .004), and borderline (OR, 1.71; P < .001) and antisocial (OR, 1.98; P = .002) traits.
There was no significant association between sexual abuse experienced in childhood and later anger or personality traits.
Ms. De Bles said the findings suggest “there is indeed a relationship between childhood trauma and anger in adulthood, and this is something that might be interesting for clinicians, as anger could be a red flag for a history of childhood trauma.”
She said in an interview that anger is a “very normal human emotion” but that it has not been as widely studied as sadness and anxiety.
She suggested that future research could examine the use of trauma-based therapies for patients with a history of childhood trauma and anger.
Overlooked, neglected
Commenting on the findings, Nur Hani Zainal, PhD, department of healthcare policy, Harvard Medical School, Boston, said the findings are “very consistent with the current biopsychosocial models in psychiatry and clinical psychology.”
Dr. Zainal, who was coauthor of a recent study that showed that anger appears to mediate the relationship between childhood trauma and adult psychopathology, said the current study offers a “good, incremental contribution” to the literature.
She noted there are “good uses” for the emotion of anger, as “sometimes we need anger to set healthy boundaries for ourselves.” However, she agreed that, as an aspect of depression, anxiety, and posttraumatic stress disorder, it is often “overlooked.”
Dr. Zainal said that the findings reinforce the importance of thoroughly evaluating adult patients’ experiences during childhood.
Julian Beezhold, MD, secretary general of the EPA and a consultant psychiatrist with the Norwich (England) Medical School, University of East Anglia, commented in the release that anger is a “somewhat neglected symptom.
“The findings are in line with what we see in day-to-day clinical practice and will hopefully help increase the awareness of the importance of both anger and associated childhood trauma.”
The infrastructure for the NESDA study is funded through the Geestkracht program of the Netherlands Organization for Health Research and Development and financial contributions by participating universities and mental health care organizations. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
PARIS –
Investigators examined data on more than 2,250 individuals who were asked about trauma during childhood and a subsequent tendency toward anger or angry outbursts 4 years later.
Results showed that emotional neglect during childhood was associated with approximately a 40% increased likelihood of subsequent anger, while psychological abuse was linked to a 30% increased likelihood.
Childhood physical abuse was also significantly associated with anger in adults, with an increased risk of approximately 40%. The researchers found no link between childhood sexual abuse and adult anger.
“We can’t definitively say that the trauma causes the anger, but the link is clear,” study investigator Nienke De Bles, PhD student, department of psychiatry, Leiden (the Netherlands) University Medical Center, said in a news release.
“Being easily angered can have several consequences,” she continued. “It can make personal interactions more difficult, and it can have consequences for your mental health and well-being, but people who get angry easily also have a greater tendency to discontinue psychiatric treatment, so this anger may mean that it reduces their chances of a better life,” she added.
Ms. De Bles believes that “it should be standard practice to ask depression and anxiety sufferers about anger and past trauma, even if the patient is not exhibiting current anger.”
The findings were presented at the European Psychiatric Association 2023 Congress.
A ‘red flag’ for abuse
“Psychiatric treatments for past trauma may differ from treatments for depression, so psychiatrists need to try to understand the cause so that they can offer the correct treatment to each patient,” said Ms. De Bles.
Ms. De Bles noted that childhood trauma has many negative consequences later in life and that it is associated with a higher prevalence of adult depression and anxiety.
“There are several potential mechanisms for psychopathology in the context of childhood trauma, and emotion regulation seems to be one of the key mechanisms,” she said.
The researchers previously found that anger was highly prevalent among patients with affective disorders. It was present in 30% of those with current anxiety or depressive disorder and in 40% of those with comorbid depression and anxiety with a tendency toward anger versus 5% of healthy control persons.
Other studies have shown that anger is associated with poor treatment outcomes and dropping out of treatment.
To further investigate the link between childhood trauma and anger in adulthood, the researchers examined data on 2,271 participants in the Netherlands Study of Depression and Anxiety (NESDA).
Childhood trauma was assessed at baseline using the semistructured Childhood Trauma Interview. Anger was measured at a 4-year follow-up using the Spielberger Trait Anger Subscale, the Anger Attacks Questionnaire, and the borderline and antisocial subscales of the Personality Disorder Questionnaire 4 to identify cluster B personality traits.
Results showed that emotional neglect during childhood was significantly associated with trait anger in adulthood, at an adjusted odds ratio of 1.42 (P < .001), anger attacks (OR, 1.35; P = .004), and borderline (OR, 1.76; P < .001) and antisocial (OR, 1.88; P = .001) personality traits.
Childhood psychological abuse was also significantly associated with later trait anger (OR, 1.28; P = .002), anger attacks (OR, 1.31; P = .024), and borderline (OR, 1.77; P < .001) and antisocial (OR, 1.69; P = .011) traits.
There was also a significant association between childhood psychical abuse and trait anger in adulthood (OR, 1.37; P < .001), anger attacks (OR, 1.48; P = .004), and borderline (OR, 1.71; P < .001) and antisocial (OR, 1.98; P = .002) traits.
There was no significant association between sexual abuse experienced in childhood and later anger or personality traits.
Ms. De Bles said the findings suggest “there is indeed a relationship between childhood trauma and anger in adulthood, and this is something that might be interesting for clinicians, as anger could be a red flag for a history of childhood trauma.”
She said in an interview that anger is a “very normal human emotion” but that it has not been as widely studied as sadness and anxiety.
She suggested that future research could examine the use of trauma-based therapies for patients with a history of childhood trauma and anger.
Overlooked, neglected
Commenting on the findings, Nur Hani Zainal, PhD, department of healthcare policy, Harvard Medical School, Boston, said the findings are “very consistent with the current biopsychosocial models in psychiatry and clinical psychology.”
Dr. Zainal, who was coauthor of a recent study that showed that anger appears to mediate the relationship between childhood trauma and adult psychopathology, said the current study offers a “good, incremental contribution” to the literature.
She noted there are “good uses” for the emotion of anger, as “sometimes we need anger to set healthy boundaries for ourselves.” However, she agreed that, as an aspect of depression, anxiety, and posttraumatic stress disorder, it is often “overlooked.”
Dr. Zainal said that the findings reinforce the importance of thoroughly evaluating adult patients’ experiences during childhood.
Julian Beezhold, MD, secretary general of the EPA and a consultant psychiatrist with the Norwich (England) Medical School, University of East Anglia, commented in the release that anger is a “somewhat neglected symptom.
“The findings are in line with what we see in day-to-day clinical practice and will hopefully help increase the awareness of the importance of both anger and associated childhood trauma.”
The infrastructure for the NESDA study is funded through the Geestkracht program of the Netherlands Organization for Health Research and Development and financial contributions by participating universities and mental health care organizations. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
PARIS –
Investigators examined data on more than 2,250 individuals who were asked about trauma during childhood and a subsequent tendency toward anger or angry outbursts 4 years later.
Results showed that emotional neglect during childhood was associated with approximately a 40% increased likelihood of subsequent anger, while psychological abuse was linked to a 30% increased likelihood.
Childhood physical abuse was also significantly associated with anger in adults, with an increased risk of approximately 40%. The researchers found no link between childhood sexual abuse and adult anger.
“We can’t definitively say that the trauma causes the anger, but the link is clear,” study investigator Nienke De Bles, PhD student, department of psychiatry, Leiden (the Netherlands) University Medical Center, said in a news release.
“Being easily angered can have several consequences,” she continued. “It can make personal interactions more difficult, and it can have consequences for your mental health and well-being, but people who get angry easily also have a greater tendency to discontinue psychiatric treatment, so this anger may mean that it reduces their chances of a better life,” she added.
Ms. De Bles believes that “it should be standard practice to ask depression and anxiety sufferers about anger and past trauma, even if the patient is not exhibiting current anger.”
The findings were presented at the European Psychiatric Association 2023 Congress.
A ‘red flag’ for abuse
“Psychiatric treatments for past trauma may differ from treatments for depression, so psychiatrists need to try to understand the cause so that they can offer the correct treatment to each patient,” said Ms. De Bles.
Ms. De Bles noted that childhood trauma has many negative consequences later in life and that it is associated with a higher prevalence of adult depression and anxiety.
“There are several potential mechanisms for psychopathology in the context of childhood trauma, and emotion regulation seems to be one of the key mechanisms,” she said.
The researchers previously found that anger was highly prevalent among patients with affective disorders. It was present in 30% of those with current anxiety or depressive disorder and in 40% of those with comorbid depression and anxiety with a tendency toward anger versus 5% of healthy control persons.
Other studies have shown that anger is associated with poor treatment outcomes and dropping out of treatment.
To further investigate the link between childhood trauma and anger in adulthood, the researchers examined data on 2,271 participants in the Netherlands Study of Depression and Anxiety (NESDA).
Childhood trauma was assessed at baseline using the semistructured Childhood Trauma Interview. Anger was measured at a 4-year follow-up using the Spielberger Trait Anger Subscale, the Anger Attacks Questionnaire, and the borderline and antisocial subscales of the Personality Disorder Questionnaire 4 to identify cluster B personality traits.
Results showed that emotional neglect during childhood was significantly associated with trait anger in adulthood, at an adjusted odds ratio of 1.42 (P < .001), anger attacks (OR, 1.35; P = .004), and borderline (OR, 1.76; P < .001) and antisocial (OR, 1.88; P = .001) personality traits.
Childhood psychological abuse was also significantly associated with later trait anger (OR, 1.28; P = .002), anger attacks (OR, 1.31; P = .024), and borderline (OR, 1.77; P < .001) and antisocial (OR, 1.69; P = .011) traits.
There was also a significant association between childhood psychical abuse and trait anger in adulthood (OR, 1.37; P < .001), anger attacks (OR, 1.48; P = .004), and borderline (OR, 1.71; P < .001) and antisocial (OR, 1.98; P = .002) traits.
There was no significant association between sexual abuse experienced in childhood and later anger or personality traits.
Ms. De Bles said the findings suggest “there is indeed a relationship between childhood trauma and anger in adulthood, and this is something that might be interesting for clinicians, as anger could be a red flag for a history of childhood trauma.”
She said in an interview that anger is a “very normal human emotion” but that it has not been as widely studied as sadness and anxiety.
She suggested that future research could examine the use of trauma-based therapies for patients with a history of childhood trauma and anger.
Overlooked, neglected
Commenting on the findings, Nur Hani Zainal, PhD, department of healthcare policy, Harvard Medical School, Boston, said the findings are “very consistent with the current biopsychosocial models in psychiatry and clinical psychology.”
Dr. Zainal, who was coauthor of a recent study that showed that anger appears to mediate the relationship between childhood trauma and adult psychopathology, said the current study offers a “good, incremental contribution” to the literature.
She noted there are “good uses” for the emotion of anger, as “sometimes we need anger to set healthy boundaries for ourselves.” However, she agreed that, as an aspect of depression, anxiety, and posttraumatic stress disorder, it is often “overlooked.”
Dr. Zainal said that the findings reinforce the importance of thoroughly evaluating adult patients’ experiences during childhood.
Julian Beezhold, MD, secretary general of the EPA and a consultant psychiatrist with the Norwich (England) Medical School, University of East Anglia, commented in the release that anger is a “somewhat neglected symptom.
“The findings are in line with what we see in day-to-day clinical practice and will hopefully help increase the awareness of the importance of both anger and associated childhood trauma.”
The infrastructure for the NESDA study is funded through the Geestkracht program of the Netherlands Organization for Health Research and Development and financial contributions by participating universities and mental health care organizations. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT EPA 2023
Urban green and blue spaces linked to less psychological distress
The findings of the study, which was released ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology, build on a growing understanding of the relationship between types and qualities of urban environments and dementia risk.
Adithya Vegaraju, a student at Washington State University, Spokane, led the study, which looked at data from the Washington State Behavioral Risk Factor Surveillance System to assess prevalence of serious psychological distress among 42,980 Washington state residents aged 65 and over.
The data, collected between 2011 and 2019, used a self-reported questionnaire to determine serious psychological distress, which is defined as a level of mental distress considered debilitating enough to warrant treatment.
Mr. Vegaraju and his coauthor Solmaz Amiri, DDes, also of Washington State University, used ZIP codes, along with U.S. census data, to approximate the urban adults’ proximity to green and blue spaces.
After controlling for potential confounders of age, sex, ethnicity, education, and marital status, the investigators found that people living within half a mile of green or blue spaces had a 17% lower risk of experiencing serious psychological distress, compared with people living farther from these spaces, the investigators said in a news release.
Implications for cognitive decline and dementia?
Psychological distress in adults has been linked in population-based longitudinal studies to later cognitive decline and dementia. One study in older adults found the risk of dementia to be more than 50% higher among adults aged 50-70 with persistent depression. Blue and green spaces have also been investigated in relation to neurodegenerative disease among older adults; a 2022 study looking at data from some 62 million Medicare beneficiaries found those living in areas with more vegetation saw lower risk of hospitalizations for Alzheimer’s disease and related dementias.
“Since we lack effective prevention methods or treatments for mild cognitive impairment and dementia, we need to get creative in how we look at these issues,” Dr. Amiri commented in a press statement about her and Mr. Vegaraju’s findings. “Our hope is that this study showing better mental health among people living close to parks and water will trigger other studies about how these benefits work and whether this proximity can help prevent or delay mild cognitive impairment and dementia.”
The investigators acknowledged that their findings were limited by reliance on a self-reported measure of psychological distress.
A bidirectional connection with depression and dementia
In a comment, Anjum Hajat, PhD, an epidemiologist at University of Washington School of Public Health in Seattle who has also studied the relationship between green space and dementia risk in older adults, noted some further apparent limitations of the new study, for which only an abstract was available at publication.
“It has been shown that people with depression are at higher risk for dementia, but the opposite is also true,” Dr. Hajat commented. “Those with dementia are more likely to develop depression. This bidirectionality makes this study abstract difficult to interpret since the study is based on cross-sectional data: Individuals are not followed over time to see which develops first, dementia or depression.”
Additionally, Dr. Hajat noted, the data used to determine proximity to green and blue spaces did not allow for the calculation of precise distances between subjects’ homes and these spaces.
Mr. Vegaraju and Dr. Amiri’s study had no outside support, and the investigators declared no conflicts of interest. Dr. Hajat declared no conflicts of interest.
The findings of the study, which was released ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology, build on a growing understanding of the relationship between types and qualities of urban environments and dementia risk.
Adithya Vegaraju, a student at Washington State University, Spokane, led the study, which looked at data from the Washington State Behavioral Risk Factor Surveillance System to assess prevalence of serious psychological distress among 42,980 Washington state residents aged 65 and over.
The data, collected between 2011 and 2019, used a self-reported questionnaire to determine serious psychological distress, which is defined as a level of mental distress considered debilitating enough to warrant treatment.
Mr. Vegaraju and his coauthor Solmaz Amiri, DDes, also of Washington State University, used ZIP codes, along with U.S. census data, to approximate the urban adults’ proximity to green and blue spaces.
After controlling for potential confounders of age, sex, ethnicity, education, and marital status, the investigators found that people living within half a mile of green or blue spaces had a 17% lower risk of experiencing serious psychological distress, compared with people living farther from these spaces, the investigators said in a news release.
Implications for cognitive decline and dementia?
Psychological distress in adults has been linked in population-based longitudinal studies to later cognitive decline and dementia. One study in older adults found the risk of dementia to be more than 50% higher among adults aged 50-70 with persistent depression. Blue and green spaces have also been investigated in relation to neurodegenerative disease among older adults; a 2022 study looking at data from some 62 million Medicare beneficiaries found those living in areas with more vegetation saw lower risk of hospitalizations for Alzheimer’s disease and related dementias.
“Since we lack effective prevention methods or treatments for mild cognitive impairment and dementia, we need to get creative in how we look at these issues,” Dr. Amiri commented in a press statement about her and Mr. Vegaraju’s findings. “Our hope is that this study showing better mental health among people living close to parks and water will trigger other studies about how these benefits work and whether this proximity can help prevent or delay mild cognitive impairment and dementia.”
The investigators acknowledged that their findings were limited by reliance on a self-reported measure of psychological distress.
A bidirectional connection with depression and dementia
In a comment, Anjum Hajat, PhD, an epidemiologist at University of Washington School of Public Health in Seattle who has also studied the relationship between green space and dementia risk in older adults, noted some further apparent limitations of the new study, for which only an abstract was available at publication.
“It has been shown that people with depression are at higher risk for dementia, but the opposite is also true,” Dr. Hajat commented. “Those with dementia are more likely to develop depression. This bidirectionality makes this study abstract difficult to interpret since the study is based on cross-sectional data: Individuals are not followed over time to see which develops first, dementia or depression.”
Additionally, Dr. Hajat noted, the data used to determine proximity to green and blue spaces did not allow for the calculation of precise distances between subjects’ homes and these spaces.
Mr. Vegaraju and Dr. Amiri’s study had no outside support, and the investigators declared no conflicts of interest. Dr. Hajat declared no conflicts of interest.
The findings of the study, which was released ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology, build on a growing understanding of the relationship between types and qualities of urban environments and dementia risk.
Adithya Vegaraju, a student at Washington State University, Spokane, led the study, which looked at data from the Washington State Behavioral Risk Factor Surveillance System to assess prevalence of serious psychological distress among 42,980 Washington state residents aged 65 and over.
The data, collected between 2011 and 2019, used a self-reported questionnaire to determine serious psychological distress, which is defined as a level of mental distress considered debilitating enough to warrant treatment.
Mr. Vegaraju and his coauthor Solmaz Amiri, DDes, also of Washington State University, used ZIP codes, along with U.S. census data, to approximate the urban adults’ proximity to green and blue spaces.
After controlling for potential confounders of age, sex, ethnicity, education, and marital status, the investigators found that people living within half a mile of green or blue spaces had a 17% lower risk of experiencing serious psychological distress, compared with people living farther from these spaces, the investigators said in a news release.
Implications for cognitive decline and dementia?
Psychological distress in adults has been linked in population-based longitudinal studies to later cognitive decline and dementia. One study in older adults found the risk of dementia to be more than 50% higher among adults aged 50-70 with persistent depression. Blue and green spaces have also been investigated in relation to neurodegenerative disease among older adults; a 2022 study looking at data from some 62 million Medicare beneficiaries found those living in areas with more vegetation saw lower risk of hospitalizations for Alzheimer’s disease and related dementias.
“Since we lack effective prevention methods or treatments for mild cognitive impairment and dementia, we need to get creative in how we look at these issues,” Dr. Amiri commented in a press statement about her and Mr. Vegaraju’s findings. “Our hope is that this study showing better mental health among people living close to parks and water will trigger other studies about how these benefits work and whether this proximity can help prevent or delay mild cognitive impairment and dementia.”
The investigators acknowledged that their findings were limited by reliance on a self-reported measure of psychological distress.
A bidirectional connection with depression and dementia
In a comment, Anjum Hajat, PhD, an epidemiologist at University of Washington School of Public Health in Seattle who has also studied the relationship between green space and dementia risk in older adults, noted some further apparent limitations of the new study, for which only an abstract was available at publication.
“It has been shown that people with depression are at higher risk for dementia, but the opposite is also true,” Dr. Hajat commented. “Those with dementia are more likely to develop depression. This bidirectionality makes this study abstract difficult to interpret since the study is based on cross-sectional data: Individuals are not followed over time to see which develops first, dementia or depression.”
Additionally, Dr. Hajat noted, the data used to determine proximity to green and blue spaces did not allow for the calculation of precise distances between subjects’ homes and these spaces.
Mr. Vegaraju and Dr. Amiri’s study had no outside support, and the investigators declared no conflicts of interest. Dr. Hajat declared no conflicts of interest.
FROM AAN 2023
Bad sleep cuts years off life, but exercise can save us
Experts recommend that most adults get 7-9 hours of sleep a night.
Plenty of research points to sleep and physical activity as crucial factors affecting life expectancy. Regular exercise can lengthen life, while too little or too much sleep may cut it short.
But evidence is growing that exercise may counteract the negative effects of poor sleep. A 2022 study found that being physically active for at least 25 minutes a day can erase the risk of early death associated with too much sleep or trouble falling asleep. And a 2021 study found that lower levels of physical activity may exacerbate the impact of poor sleep on early death, heart disease, and cancer.
The latest such study, published in the European Journal of Preventive Cardiology, suggests that higher volumes of exercise can virtually eliminate the risk of early death associated with sleeping too little or too long.
This study is unique, the researchers say, because it used accelerometers (motion-tracking sensors) to quantify sleep and physical activity. Other studies asked participants to report their own data, opening the door to false reports and mistakes.
Some 92,000 participants in the United Kingdom (mean age, 62 years; 56% women) wore the activity trackers for a week to measure how much they moved and slept. In the following 7 years, 3,080 participants died, mostly from cardiovascular disease or cancer.
As one might expect, the participants who were least likely to die also exercised the most and slept the “normal” amount (6-8 hours a night, as defined by the study).
Compared with that group, those who exercised the least and slept less than 6 hours were 2.5 times more likely to die during those 7 years (P < .001). Less active persons who got the recommended sleep were 79% more likely to die (P < .001). The risk was slightly higher than that for those who logged more than 8 hours a night.
But those risks disappeared for short- or long-sleeping participants who logged at least 150 minutes a week of moderate to vigorous activity.
“Exercise fights inflammatory and metabolic dysregulations and abnormal sympathetic nervous system activity,” said study author Jihui Zhang, PhD, of the Affiliated Brain Hospital of Guangzhou (China). Those problems are associated with cardiovascular diseases and other potentially fatal conditions.
More objective data – with tech
A study’s findings are only as good as the data it relies on. That’s why obtaining objective data not influenced by individual perception is key.
“Self-report questionnaires are prone to misperception, or recall or response bias,” Dr. Zhang explains.
Take sleep, for example. Research reveals that several factors can affect how we judge our sleep. When people have to sleep at irregular times, they often underestimate how many hours they sleep but overestimate how long they nap, found a study in the Journal of Clinical Sleep Medicine.
Another study showed that when people are under a lot of stress, they’ll report more sleep problems than they actually have, as revealed by an Actiheart monitor.
With exercise, participants often report doing more exercise, and doing it at a higher intensity, than objective measurements show they did. At the same time, self-reports typically don’t account for much of the unplanned, low-effort movement people do throughout the day.
Staying active when you’re tired
The study raises a practical question: If you don’t get the proper amount of sleep, how are you supposed to find the time, energy, and motivation to exercise?
The solution is to use one to fix the other.
Exercise and sleep have “a robust directional relationship,” Dr. Zhang said. Exercise improves sleep, while better sleep makes it easier to stick with an exercise program.
Ideally, that program will include a mix of cardio and resistance exercise, said Mitch Duncan, PhD, a professor of public health at the University of Newcastle, Australia.
As Dr. Duncan and his co-authors showed in a recent study, “the largest benefits to health occur when people do a combination of both aerobic and muscle-strengthening activity,” Dr. Duncan said.
“In terms of benefits to sleep, there doesn’t seem to be consistent evidence that favors either as being most effective.”
The timing or intensity of exercise doesn’t seem to matter much, either.
“But there is evidence that a greater duration contributes to larger improvements in sleep,” Dr. Duncan said.
In other words, longer workouts are generally better, but they don’t necessarily have to be super-intense.
The strongest evidence of all, however, shows that recent and regular exercise offer the biggest benefits at bedtime.
Today’s workout will improve tonight’s sleep. And the better you sleep tonight, the more likely you are to stick with the program.
A version of this article first appeared on WebMD.com.
Experts recommend that most adults get 7-9 hours of sleep a night.
Plenty of research points to sleep and physical activity as crucial factors affecting life expectancy. Regular exercise can lengthen life, while too little or too much sleep may cut it short.
But evidence is growing that exercise may counteract the negative effects of poor sleep. A 2022 study found that being physically active for at least 25 minutes a day can erase the risk of early death associated with too much sleep or trouble falling asleep. And a 2021 study found that lower levels of physical activity may exacerbate the impact of poor sleep on early death, heart disease, and cancer.
The latest such study, published in the European Journal of Preventive Cardiology, suggests that higher volumes of exercise can virtually eliminate the risk of early death associated with sleeping too little or too long.
This study is unique, the researchers say, because it used accelerometers (motion-tracking sensors) to quantify sleep and physical activity. Other studies asked participants to report their own data, opening the door to false reports and mistakes.
Some 92,000 participants in the United Kingdom (mean age, 62 years; 56% women) wore the activity trackers for a week to measure how much they moved and slept. In the following 7 years, 3,080 participants died, mostly from cardiovascular disease or cancer.
As one might expect, the participants who were least likely to die also exercised the most and slept the “normal” amount (6-8 hours a night, as defined by the study).
Compared with that group, those who exercised the least and slept less than 6 hours were 2.5 times more likely to die during those 7 years (P < .001). Less active persons who got the recommended sleep were 79% more likely to die (P < .001). The risk was slightly higher than that for those who logged more than 8 hours a night.
But those risks disappeared for short- or long-sleeping participants who logged at least 150 minutes a week of moderate to vigorous activity.
“Exercise fights inflammatory and metabolic dysregulations and abnormal sympathetic nervous system activity,” said study author Jihui Zhang, PhD, of the Affiliated Brain Hospital of Guangzhou (China). Those problems are associated with cardiovascular diseases and other potentially fatal conditions.
More objective data – with tech
A study’s findings are only as good as the data it relies on. That’s why obtaining objective data not influenced by individual perception is key.
“Self-report questionnaires are prone to misperception, or recall or response bias,” Dr. Zhang explains.
Take sleep, for example. Research reveals that several factors can affect how we judge our sleep. When people have to sleep at irregular times, they often underestimate how many hours they sleep but overestimate how long they nap, found a study in the Journal of Clinical Sleep Medicine.
Another study showed that when people are under a lot of stress, they’ll report more sleep problems than they actually have, as revealed by an Actiheart monitor.
With exercise, participants often report doing more exercise, and doing it at a higher intensity, than objective measurements show they did. At the same time, self-reports typically don’t account for much of the unplanned, low-effort movement people do throughout the day.
Staying active when you’re tired
The study raises a practical question: If you don’t get the proper amount of sleep, how are you supposed to find the time, energy, and motivation to exercise?
The solution is to use one to fix the other.
Exercise and sleep have “a robust directional relationship,” Dr. Zhang said. Exercise improves sleep, while better sleep makes it easier to stick with an exercise program.
Ideally, that program will include a mix of cardio and resistance exercise, said Mitch Duncan, PhD, a professor of public health at the University of Newcastle, Australia.
As Dr. Duncan and his co-authors showed in a recent study, “the largest benefits to health occur when people do a combination of both aerobic and muscle-strengthening activity,” Dr. Duncan said.
“In terms of benefits to sleep, there doesn’t seem to be consistent evidence that favors either as being most effective.”
The timing or intensity of exercise doesn’t seem to matter much, either.
“But there is evidence that a greater duration contributes to larger improvements in sleep,” Dr. Duncan said.
In other words, longer workouts are generally better, but they don’t necessarily have to be super-intense.
The strongest evidence of all, however, shows that recent and regular exercise offer the biggest benefits at bedtime.
Today’s workout will improve tonight’s sleep. And the better you sleep tonight, the more likely you are to stick with the program.
A version of this article first appeared on WebMD.com.
Experts recommend that most adults get 7-9 hours of sleep a night.
Plenty of research points to sleep and physical activity as crucial factors affecting life expectancy. Regular exercise can lengthen life, while too little or too much sleep may cut it short.
But evidence is growing that exercise may counteract the negative effects of poor sleep. A 2022 study found that being physically active for at least 25 minutes a day can erase the risk of early death associated with too much sleep or trouble falling asleep. And a 2021 study found that lower levels of physical activity may exacerbate the impact of poor sleep on early death, heart disease, and cancer.
The latest such study, published in the European Journal of Preventive Cardiology, suggests that higher volumes of exercise can virtually eliminate the risk of early death associated with sleeping too little or too long.
This study is unique, the researchers say, because it used accelerometers (motion-tracking sensors) to quantify sleep and physical activity. Other studies asked participants to report their own data, opening the door to false reports and mistakes.
Some 92,000 participants in the United Kingdom (mean age, 62 years; 56% women) wore the activity trackers for a week to measure how much they moved and slept. In the following 7 years, 3,080 participants died, mostly from cardiovascular disease or cancer.
As one might expect, the participants who were least likely to die also exercised the most and slept the “normal” amount (6-8 hours a night, as defined by the study).
Compared with that group, those who exercised the least and slept less than 6 hours were 2.5 times more likely to die during those 7 years (P < .001). Less active persons who got the recommended sleep were 79% more likely to die (P < .001). The risk was slightly higher than that for those who logged more than 8 hours a night.
But those risks disappeared for short- or long-sleeping participants who logged at least 150 minutes a week of moderate to vigorous activity.
“Exercise fights inflammatory and metabolic dysregulations and abnormal sympathetic nervous system activity,” said study author Jihui Zhang, PhD, of the Affiliated Brain Hospital of Guangzhou (China). Those problems are associated with cardiovascular diseases and other potentially fatal conditions.
More objective data – with tech
A study’s findings are only as good as the data it relies on. That’s why obtaining objective data not influenced by individual perception is key.
“Self-report questionnaires are prone to misperception, or recall or response bias,” Dr. Zhang explains.
Take sleep, for example. Research reveals that several factors can affect how we judge our sleep. When people have to sleep at irregular times, they often underestimate how many hours they sleep but overestimate how long they nap, found a study in the Journal of Clinical Sleep Medicine.
Another study showed that when people are under a lot of stress, they’ll report more sleep problems than they actually have, as revealed by an Actiheart monitor.
With exercise, participants often report doing more exercise, and doing it at a higher intensity, than objective measurements show they did. At the same time, self-reports typically don’t account for much of the unplanned, low-effort movement people do throughout the day.
Staying active when you’re tired
The study raises a practical question: If you don’t get the proper amount of sleep, how are you supposed to find the time, energy, and motivation to exercise?
The solution is to use one to fix the other.
Exercise and sleep have “a robust directional relationship,” Dr. Zhang said. Exercise improves sleep, while better sleep makes it easier to stick with an exercise program.
Ideally, that program will include a mix of cardio and resistance exercise, said Mitch Duncan, PhD, a professor of public health at the University of Newcastle, Australia.
As Dr. Duncan and his co-authors showed in a recent study, “the largest benefits to health occur when people do a combination of both aerobic and muscle-strengthening activity,” Dr. Duncan said.
“In terms of benefits to sleep, there doesn’t seem to be consistent evidence that favors either as being most effective.”
The timing or intensity of exercise doesn’t seem to matter much, either.
“But there is evidence that a greater duration contributes to larger improvements in sleep,” Dr. Duncan said.
In other words, longer workouts are generally better, but they don’t necessarily have to be super-intense.
The strongest evidence of all, however, shows that recent and regular exercise offer the biggest benefits at bedtime.
Today’s workout will improve tonight’s sleep. And the better you sleep tonight, the more likely you are to stick with the program.
A version of this article first appeared on WebMD.com.
FROM EUROPEAN JOURNAL OF PREVENTIVE CARDIOLOGY
Single-dose psilocybin promising for resistant depression
PARIS –
Known as COMP360, the synthetic agent, a proprietary, purified form of psilocybin, improved symptoms related to mood and anhedonia while leaving aspects such as appetite and weight changes unaffected, reported investigators led by Guy M. Goodwin, PhD, emeritus professor of psychiatry, University of Oxford, England, and chief medical officer, COMPASS Pathways.
The study was presented at the European Psychiatric Association (EPA) 2023 Congress.
100 million affected
Affecting up to 100 million people globally, TRD is “not an official diagnosis,” although it is often defined as the failure to elicit a response with at least two antidepressant treatments, said Dr. Goodwin.
Compared to their counterparts with non-TRD, those with TRD experience higher relapse rates, higher rates of suicidal behavior, and more residual symptoms even when they do respond to treatment.
Previous results from the study known as P-TRD indicated that a single 25-mg dose of COMP360 significantly reduced depression scores for up to 12 weeks when given along with psychological support, although a later analysis suggested the effect subsequently dropped off.
The vast majority of the patients in the trial were naive to psychedelics, and so, Dr. Goodwin explained, they undergo a preparation phase during which they receive psychoeducation and have at least two visits with a therapist, who then stays with them during administration of the drug to offer support if they experience psychological distress.
Following the psilocybin session, participants go through a process known as integration, which involves two sessions with a therapist within 2 weeks.
“That, in our view, is essentially about safety, and about identifying problems that have arisen as a result of taking the drug,” said Dr. Goodwin.
The phase 2b trial examined changes in specific depression symptoms after psilocybin treatment in 233 patients with TRD. Participants were a mean age of 39.8 years and 59% were women. They were randomized to receive one of three doses of the drug: a 1-mg dose (n = 79), a 10-mg dose (n = 75), or a 25-mg dose (n = 79).
The primary outcome was changes in individual items on the Montgomery-Åsberg Depression Rating Scale (MADRS) and 16-item Quick Inventory of Depressive Symptomatology–Self Report (QIDS-SR-16) scale.
While the effect on overall depression scores is important, said Dr. Goodwin, many of the items included in the depression assessment scales are “uninformative.”
Reduction in ‘core’ symptoms
Participants were assessed by a blinded rater at baseline, day 1, day 2, and at 1, 2, 3, 6, 9, and 12 weeks after administration of COMP360. The primary endpoint was a reduction in individual items on MADRS and scores from baseline to 3 weeks. Individual items on the QIDS-SR-16 were rated by participants at the same time points.
Investigators found the largest mean changes from baseline were on reported and apparent sadness, lassitude, inability to feel, and concentration difficulties, with “very nice and clear dose-related differences,” Dr. Goodwin said.
The results indicate that the significant benefit with the largest dose at 3 weeks versus baseline was confined to items such as inability to feel and reported and apparent sadness on the MADRS and feeling sad and general interest on the QIDS-SR-16 (Table 1).
The results suggest the effect of COMP360 is “on the core symptoms of depression,” said Dr. Goodwin.
Results were similar for individual items on the QIDS-SR-16, with the greatest changes in items including feeling sad, general interest, energy level, falling asleep, view of myself, concentration/decision-making, and feeling down.
Other scale items, such as decreased appetite, feel restless, and weight changes, showed negligible changes in response to COMP360 therapy and were described by Dr. Goodwin as “inconsequential.”
“Essentially, these items are contributing nothing but noise to the signal,” he said.
He added the results of the study need to be replicated and that plans for phase 3 trials are underway. These studies, he said, are designed to convince the Food and Drug Administration that “this is not just a recreational drug, it’s a medicine.”
Enthusiasm running ahead of the data
Commenting on the findings, Bertha K. Madras, PhD, professor of psychobiology, department of psychiatry, Harvard Medical School, Boston, who was not involved in the study, said “hallucinogens are an intriguing class of drugs and I support ongoing high-quality research in this area.”
However, she told this news organization that the “breathtaking endorsement of this drug is far ahead of scientific data.”
She cited concerns such as the “narrow demographics” of participants, their previous experience with and expectations of hallucinogens, the “potential for symptom fluidity of enrollees,” such as depression evolving into psychosis, and the “undefined role” of the therapist during a hallucinogenic session.
“Finally, I am concerned that enthusiasm for therapeutic potential has been, and will continue to be, preempted and directed towards legalization and widespread access for vulnerable populations,” Dr. Madras said.
This, she said, “is occurring at breakneck speed in the U.S., with scant resistance or skepticism from the investigators engaged in therapeutic assessment.”
The study was funded by COMPASS Pathways. Dr. Goodwin has reported relationships with COMPASS Pathways, Buckley Psytech, Boehringer Ingelheim, Clerkenwell Health, EVA Pharma, Lundbeck, Janssen Global Services, Novartis, Ocean Neurosciences, P1vital, Sage Therapeutics, Servier, Takeda, and WebMD.
A version of this article first appeared on Medscape.com.
PARIS –
Known as COMP360, the synthetic agent, a proprietary, purified form of psilocybin, improved symptoms related to mood and anhedonia while leaving aspects such as appetite and weight changes unaffected, reported investigators led by Guy M. Goodwin, PhD, emeritus professor of psychiatry, University of Oxford, England, and chief medical officer, COMPASS Pathways.
The study was presented at the European Psychiatric Association (EPA) 2023 Congress.
100 million affected
Affecting up to 100 million people globally, TRD is “not an official diagnosis,” although it is often defined as the failure to elicit a response with at least two antidepressant treatments, said Dr. Goodwin.
Compared to their counterparts with non-TRD, those with TRD experience higher relapse rates, higher rates of suicidal behavior, and more residual symptoms even when they do respond to treatment.
Previous results from the study known as P-TRD indicated that a single 25-mg dose of COMP360 significantly reduced depression scores for up to 12 weeks when given along with psychological support, although a later analysis suggested the effect subsequently dropped off.
The vast majority of the patients in the trial were naive to psychedelics, and so, Dr. Goodwin explained, they undergo a preparation phase during which they receive psychoeducation and have at least two visits with a therapist, who then stays with them during administration of the drug to offer support if they experience psychological distress.
Following the psilocybin session, participants go through a process known as integration, which involves two sessions with a therapist within 2 weeks.
“That, in our view, is essentially about safety, and about identifying problems that have arisen as a result of taking the drug,” said Dr. Goodwin.
The phase 2b trial examined changes in specific depression symptoms after psilocybin treatment in 233 patients with TRD. Participants were a mean age of 39.8 years and 59% were women. They were randomized to receive one of three doses of the drug: a 1-mg dose (n = 79), a 10-mg dose (n = 75), or a 25-mg dose (n = 79).
The primary outcome was changes in individual items on the Montgomery-Åsberg Depression Rating Scale (MADRS) and 16-item Quick Inventory of Depressive Symptomatology–Self Report (QIDS-SR-16) scale.
While the effect on overall depression scores is important, said Dr. Goodwin, many of the items included in the depression assessment scales are “uninformative.”
Reduction in ‘core’ symptoms
Participants were assessed by a blinded rater at baseline, day 1, day 2, and at 1, 2, 3, 6, 9, and 12 weeks after administration of COMP360. The primary endpoint was a reduction in individual items on MADRS and scores from baseline to 3 weeks. Individual items on the QIDS-SR-16 were rated by participants at the same time points.
Investigators found the largest mean changes from baseline were on reported and apparent sadness, lassitude, inability to feel, and concentration difficulties, with “very nice and clear dose-related differences,” Dr. Goodwin said.
The results indicate that the significant benefit with the largest dose at 3 weeks versus baseline was confined to items such as inability to feel and reported and apparent sadness on the MADRS and feeling sad and general interest on the QIDS-SR-16 (Table 1).
The results suggest the effect of COMP360 is “on the core symptoms of depression,” said Dr. Goodwin.
Results were similar for individual items on the QIDS-SR-16, with the greatest changes in items including feeling sad, general interest, energy level, falling asleep, view of myself, concentration/decision-making, and feeling down.
Other scale items, such as decreased appetite, feel restless, and weight changes, showed negligible changes in response to COMP360 therapy and were described by Dr. Goodwin as “inconsequential.”
“Essentially, these items are contributing nothing but noise to the signal,” he said.
He added the results of the study need to be replicated and that plans for phase 3 trials are underway. These studies, he said, are designed to convince the Food and Drug Administration that “this is not just a recreational drug, it’s a medicine.”
Enthusiasm running ahead of the data
Commenting on the findings, Bertha K. Madras, PhD, professor of psychobiology, department of psychiatry, Harvard Medical School, Boston, who was not involved in the study, said “hallucinogens are an intriguing class of drugs and I support ongoing high-quality research in this area.”
However, she told this news organization that the “breathtaking endorsement of this drug is far ahead of scientific data.”
She cited concerns such as the “narrow demographics” of participants, their previous experience with and expectations of hallucinogens, the “potential for symptom fluidity of enrollees,” such as depression evolving into psychosis, and the “undefined role” of the therapist during a hallucinogenic session.
“Finally, I am concerned that enthusiasm for therapeutic potential has been, and will continue to be, preempted and directed towards legalization and widespread access for vulnerable populations,” Dr. Madras said.
This, she said, “is occurring at breakneck speed in the U.S., with scant resistance or skepticism from the investigators engaged in therapeutic assessment.”
The study was funded by COMPASS Pathways. Dr. Goodwin has reported relationships with COMPASS Pathways, Buckley Psytech, Boehringer Ingelheim, Clerkenwell Health, EVA Pharma, Lundbeck, Janssen Global Services, Novartis, Ocean Neurosciences, P1vital, Sage Therapeutics, Servier, Takeda, and WebMD.
A version of this article first appeared on Medscape.com.
PARIS –
Known as COMP360, the synthetic agent, a proprietary, purified form of psilocybin, improved symptoms related to mood and anhedonia while leaving aspects such as appetite and weight changes unaffected, reported investigators led by Guy M. Goodwin, PhD, emeritus professor of psychiatry, University of Oxford, England, and chief medical officer, COMPASS Pathways.
The study was presented at the European Psychiatric Association (EPA) 2023 Congress.
100 million affected
Affecting up to 100 million people globally, TRD is “not an official diagnosis,” although it is often defined as the failure to elicit a response with at least two antidepressant treatments, said Dr. Goodwin.
Compared to their counterparts with non-TRD, those with TRD experience higher relapse rates, higher rates of suicidal behavior, and more residual symptoms even when they do respond to treatment.
Previous results from the study known as P-TRD indicated that a single 25-mg dose of COMP360 significantly reduced depression scores for up to 12 weeks when given along with psychological support, although a later analysis suggested the effect subsequently dropped off.
The vast majority of the patients in the trial were naive to psychedelics, and so, Dr. Goodwin explained, they undergo a preparation phase during which they receive psychoeducation and have at least two visits with a therapist, who then stays with them during administration of the drug to offer support if they experience psychological distress.
Following the psilocybin session, participants go through a process known as integration, which involves two sessions with a therapist within 2 weeks.
“That, in our view, is essentially about safety, and about identifying problems that have arisen as a result of taking the drug,” said Dr. Goodwin.
The phase 2b trial examined changes in specific depression symptoms after psilocybin treatment in 233 patients with TRD. Participants were a mean age of 39.8 years and 59% were women. They were randomized to receive one of three doses of the drug: a 1-mg dose (n = 79), a 10-mg dose (n = 75), or a 25-mg dose (n = 79).
The primary outcome was changes in individual items on the Montgomery-Åsberg Depression Rating Scale (MADRS) and 16-item Quick Inventory of Depressive Symptomatology–Self Report (QIDS-SR-16) scale.
While the effect on overall depression scores is important, said Dr. Goodwin, many of the items included in the depression assessment scales are “uninformative.”
Reduction in ‘core’ symptoms
Participants were assessed by a blinded rater at baseline, day 1, day 2, and at 1, 2, 3, 6, 9, and 12 weeks after administration of COMP360. The primary endpoint was a reduction in individual items on MADRS and scores from baseline to 3 weeks. Individual items on the QIDS-SR-16 were rated by participants at the same time points.
Investigators found the largest mean changes from baseline were on reported and apparent sadness, lassitude, inability to feel, and concentration difficulties, with “very nice and clear dose-related differences,” Dr. Goodwin said.
The results indicate that the significant benefit with the largest dose at 3 weeks versus baseline was confined to items such as inability to feel and reported and apparent sadness on the MADRS and feeling sad and general interest on the QIDS-SR-16 (Table 1).
The results suggest the effect of COMP360 is “on the core symptoms of depression,” said Dr. Goodwin.
Results were similar for individual items on the QIDS-SR-16, with the greatest changes in items including feeling sad, general interest, energy level, falling asleep, view of myself, concentration/decision-making, and feeling down.
Other scale items, such as decreased appetite, feel restless, and weight changes, showed negligible changes in response to COMP360 therapy and were described by Dr. Goodwin as “inconsequential.”
“Essentially, these items are contributing nothing but noise to the signal,” he said.
He added the results of the study need to be replicated and that plans for phase 3 trials are underway. These studies, he said, are designed to convince the Food and Drug Administration that “this is not just a recreational drug, it’s a medicine.”
Enthusiasm running ahead of the data
Commenting on the findings, Bertha K. Madras, PhD, professor of psychobiology, department of psychiatry, Harvard Medical School, Boston, who was not involved in the study, said “hallucinogens are an intriguing class of drugs and I support ongoing high-quality research in this area.”
However, she told this news organization that the “breathtaking endorsement of this drug is far ahead of scientific data.”
She cited concerns such as the “narrow demographics” of participants, their previous experience with and expectations of hallucinogens, the “potential for symptom fluidity of enrollees,” such as depression evolving into psychosis, and the “undefined role” of the therapist during a hallucinogenic session.
“Finally, I am concerned that enthusiasm for therapeutic potential has been, and will continue to be, preempted and directed towards legalization and widespread access for vulnerable populations,” Dr. Madras said.
This, she said, “is occurring at breakneck speed in the U.S., with scant resistance or skepticism from the investigators engaged in therapeutic assessment.”
The study was funded by COMPASS Pathways. Dr. Goodwin has reported relationships with COMPASS Pathways, Buckley Psytech, Boehringer Ingelheim, Clerkenwell Health, EVA Pharma, Lundbeck, Janssen Global Services, Novartis, Ocean Neurosciences, P1vital, Sage Therapeutics, Servier, Takeda, and WebMD.
A version of this article first appeared on Medscape.com.
AT EPA 2023
Seven ‘simple’ cardiovascular health measures linked to reduced dementia risk in women
according to results of a study that was released early, ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology.
Epidemiologist Pamela M. Rist, ScD, assistant professor of medicine at Harvard Medical School and associate epidemiologist at Brigham and Women’s Hospital, both in Boston, and colleagues, used data from 13,720 women whose mean age was 54 when they enrolled in the Harvard-based Women’s Health Study between 1992 and 1995. Subjects in that study were followed up in 2004.
Putting ‘Life’s Simple 7’ to the test
Dr. Rist and colleagues used the Harvard data to discern how well closely women conformed, during the initial study period and at 10-year follow up, to what the American Heart Association describes as “Life’s Simple 7,” a list of behavioral and biometric measures that indicate and predict cardiovascular health. The measures include four modifiable behaviors – not smoking, healthy weight, a healthy diet, and being physically active – along with three biometric measures of blood pressure, cholesterol, and blood sugar (AHA has since added a sleep component).
Researchers assigned women one point for each desirable habit or measure on the list, with subjects’ average Simple 7 score at baseline 4.3, and 4.2 at 10 years’ follow-up.
The investigators then looked at Medicare data for the study subjects from 2011 to 2018 – approximately 20 years after their enrollment in the Women’s Health Study – seeking dementia diagnoses. Some 13% of the study cohort (n = 1,771) had gone on to develop dementia.
Each point on the Simple 7 score at baseline corresponded with a 6% reduction in later dementia risk, Dr. Rist and her colleagues found after adjusting for variables including age and education (odds ratio per one unit change in score, 0.94; 95% CI, 0.90-0.98). This effect was similar for Simple 7 scores measured at 10 years of follow-up (OR, 0.95; 95% CI, 0.91-1.00).
“It can be empowering for people to know that by taking steps such as exercising for a half an hour a day or keeping their blood pressure under control, they can reduce their risk of dementia,” Dr. Rist said in a statement on the findings.
‘A simple take-home message’
Reached for comment, Andrew E. Budson, MD, chief of cognitive-behavioral neurology at the VA Boston Healthcare System, praised Dr. Rist and colleagues’ study as one that “builds on existing knowledge to provide a simple take-home message that empowers women to take control of their dementia risk.”
Each of the seven known risk factors – being active, eating better, maintaining a healthy weight, not smoking, maintaining a healthy blood pressure, controlling cholesterol, and having low blood sugar – “was associated with a 6% reduced risk of dementia,” Dr. Budson continued. “So, women who work to address all seven risk factors can reduce their risk of developing dementia by 42%: a huge amount. Moreover, although this study only looked at women, I am confident that if men follow this same advice they will also be able to reduce their risk of dementia, although we don’t know if the size of the effect will be the same.”
Dr. Rist and colleagues’ study was supported by the National Institutes of Health. None of the study authors reported conflicts of interest. Dr. Budson has reported receiving past compensation as a speaker for Eli Lilly.
according to results of a study that was released early, ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology.
Epidemiologist Pamela M. Rist, ScD, assistant professor of medicine at Harvard Medical School and associate epidemiologist at Brigham and Women’s Hospital, both in Boston, and colleagues, used data from 13,720 women whose mean age was 54 when they enrolled in the Harvard-based Women’s Health Study between 1992 and 1995. Subjects in that study were followed up in 2004.
Putting ‘Life’s Simple 7’ to the test
Dr. Rist and colleagues used the Harvard data to discern how well closely women conformed, during the initial study period and at 10-year follow up, to what the American Heart Association describes as “Life’s Simple 7,” a list of behavioral and biometric measures that indicate and predict cardiovascular health. The measures include four modifiable behaviors – not smoking, healthy weight, a healthy diet, and being physically active – along with three biometric measures of blood pressure, cholesterol, and blood sugar (AHA has since added a sleep component).
Researchers assigned women one point for each desirable habit or measure on the list, with subjects’ average Simple 7 score at baseline 4.3, and 4.2 at 10 years’ follow-up.
The investigators then looked at Medicare data for the study subjects from 2011 to 2018 – approximately 20 years after their enrollment in the Women’s Health Study – seeking dementia diagnoses. Some 13% of the study cohort (n = 1,771) had gone on to develop dementia.
Each point on the Simple 7 score at baseline corresponded with a 6% reduction in later dementia risk, Dr. Rist and her colleagues found after adjusting for variables including age and education (odds ratio per one unit change in score, 0.94; 95% CI, 0.90-0.98). This effect was similar for Simple 7 scores measured at 10 years of follow-up (OR, 0.95; 95% CI, 0.91-1.00).
“It can be empowering for people to know that by taking steps such as exercising for a half an hour a day or keeping their blood pressure under control, they can reduce their risk of dementia,” Dr. Rist said in a statement on the findings.
‘A simple take-home message’
Reached for comment, Andrew E. Budson, MD, chief of cognitive-behavioral neurology at the VA Boston Healthcare System, praised Dr. Rist and colleagues’ study as one that “builds on existing knowledge to provide a simple take-home message that empowers women to take control of their dementia risk.”
Each of the seven known risk factors – being active, eating better, maintaining a healthy weight, not smoking, maintaining a healthy blood pressure, controlling cholesterol, and having low blood sugar – “was associated with a 6% reduced risk of dementia,” Dr. Budson continued. “So, women who work to address all seven risk factors can reduce their risk of developing dementia by 42%: a huge amount. Moreover, although this study only looked at women, I am confident that if men follow this same advice they will also be able to reduce their risk of dementia, although we don’t know if the size of the effect will be the same.”
Dr. Rist and colleagues’ study was supported by the National Institutes of Health. None of the study authors reported conflicts of interest. Dr. Budson has reported receiving past compensation as a speaker for Eli Lilly.
according to results of a study that was released early, ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology.
Epidemiologist Pamela M. Rist, ScD, assistant professor of medicine at Harvard Medical School and associate epidemiologist at Brigham and Women’s Hospital, both in Boston, and colleagues, used data from 13,720 women whose mean age was 54 when they enrolled in the Harvard-based Women’s Health Study between 1992 and 1995. Subjects in that study were followed up in 2004.
Putting ‘Life’s Simple 7’ to the test
Dr. Rist and colleagues used the Harvard data to discern how well closely women conformed, during the initial study period and at 10-year follow up, to what the American Heart Association describes as “Life’s Simple 7,” a list of behavioral and biometric measures that indicate and predict cardiovascular health. The measures include four modifiable behaviors – not smoking, healthy weight, a healthy diet, and being physically active – along with three biometric measures of blood pressure, cholesterol, and blood sugar (AHA has since added a sleep component).
Researchers assigned women one point for each desirable habit or measure on the list, with subjects’ average Simple 7 score at baseline 4.3, and 4.2 at 10 years’ follow-up.
The investigators then looked at Medicare data for the study subjects from 2011 to 2018 – approximately 20 years after their enrollment in the Women’s Health Study – seeking dementia diagnoses. Some 13% of the study cohort (n = 1,771) had gone on to develop dementia.
Each point on the Simple 7 score at baseline corresponded with a 6% reduction in later dementia risk, Dr. Rist and her colleagues found after adjusting for variables including age and education (odds ratio per one unit change in score, 0.94; 95% CI, 0.90-0.98). This effect was similar for Simple 7 scores measured at 10 years of follow-up (OR, 0.95; 95% CI, 0.91-1.00).
“It can be empowering for people to know that by taking steps such as exercising for a half an hour a day or keeping their blood pressure under control, they can reduce their risk of dementia,” Dr. Rist said in a statement on the findings.
‘A simple take-home message’
Reached for comment, Andrew E. Budson, MD, chief of cognitive-behavioral neurology at the VA Boston Healthcare System, praised Dr. Rist and colleagues’ study as one that “builds on existing knowledge to provide a simple take-home message that empowers women to take control of their dementia risk.”
Each of the seven known risk factors – being active, eating better, maintaining a healthy weight, not smoking, maintaining a healthy blood pressure, controlling cholesterol, and having low blood sugar – “was associated with a 6% reduced risk of dementia,” Dr. Budson continued. “So, women who work to address all seven risk factors can reduce their risk of developing dementia by 42%: a huge amount. Moreover, although this study only looked at women, I am confident that if men follow this same advice they will also be able to reduce their risk of dementia, although we don’t know if the size of the effect will be the same.”
Dr. Rist and colleagues’ study was supported by the National Institutes of Health. None of the study authors reported conflicts of interest. Dr. Budson has reported receiving past compensation as a speaker for Eli Lilly.
FROM AAN 2023
Family violence after COVID: Understanding coercive relationships
Despite the ability of some couples to pull together and manage through the COVID-19 pandemic, other couples and families failed to thrive. Increasing divorce rates have been noted nationwide with many disagreements being specifically about COVID.1
A review of over 1 million tweets, between April 12 and July 16, 2020, found an increase in calls to hotlines and increased reports of a variety of types of family violence. There were also more inquiries about social services for family violence, an increased presence from social movements, and more domestic violence-related news.2
The literature addressing family violence uses a variety of terms, so here are some definitions.
Domestic violence is defined as a pattern of behaviors used to gain or maintain power and control. Broadly speaking, domestic violence includes elder abuse, sibling abuse, child abuse, intimate partner abuse, parent abuse, and can also include people who don’t necessarily live together but who have an intimate relationship. Domestic violence centers use the Power and Control Wheel (see graphic) developed by the Domestic Abuse Intervention Project in Duluth, Minn., to describe how domestic violence occurs.
Intimate partner violence is more specific, referring to violence that happens between people in an ongoing or former intimate or romantic relationship, and is a subcategory of domestic violence.
Coercive control is the use of power for control and compliance. It is a dynamic and systematic process described in the top left corner of the Power and Control Wheel. Overt control occurs with the implication that “if you don’t follow the rules, I’ll kill you.” More subtle control is when obedience is forced through monopolizing resources, dictating preferred choices, microregulating a partner’s behavior, and deprivation of supports needed to exercise independent judgment.
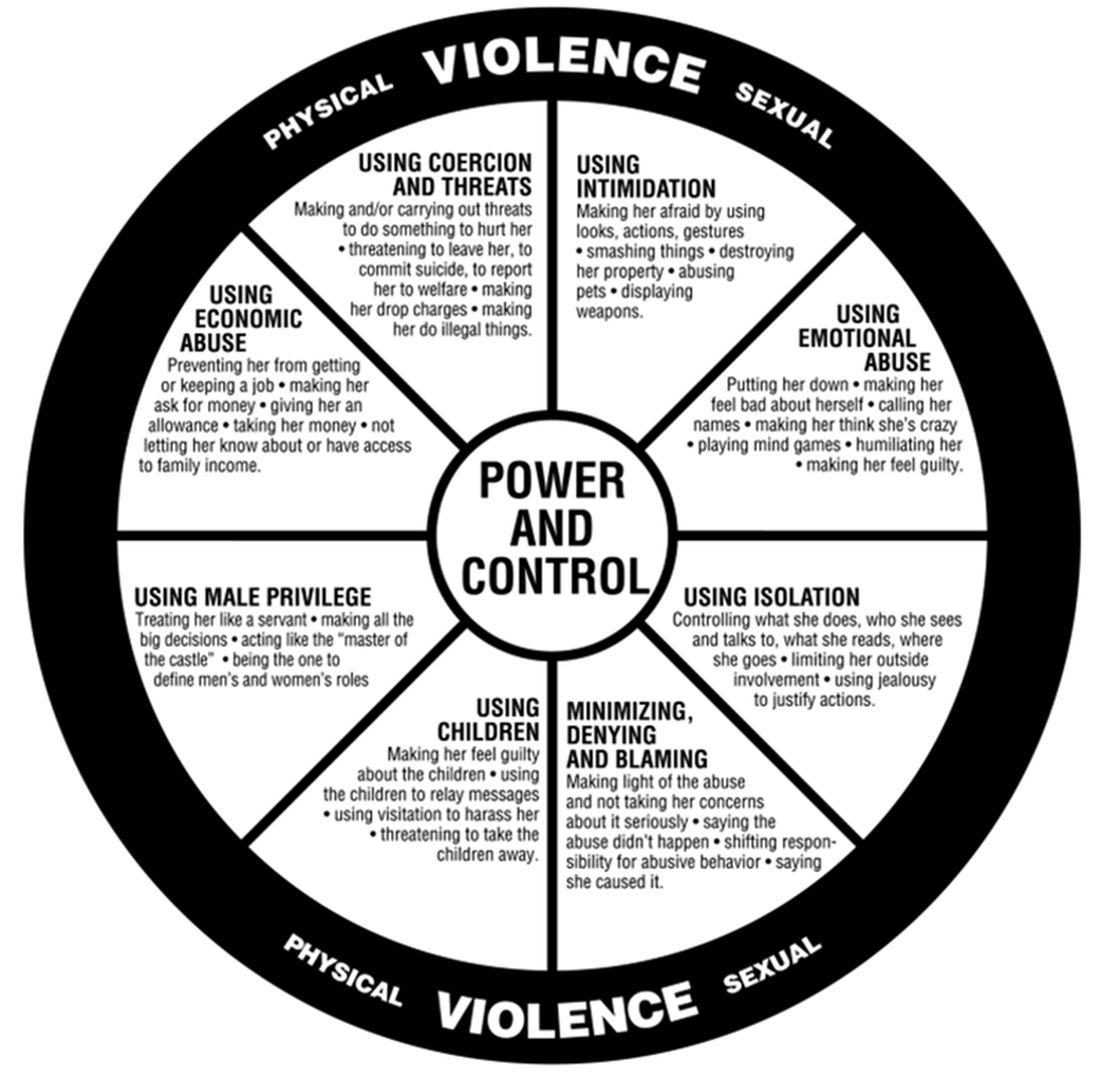
All interpersonal relationships have elements of persuasion and influence; however, the goal of coercive relationships is to maintain power and control. It is a dynamic of the relationship. Coercive control emphasizes the systematic, organized, multifaceted, and patterned nature of this interpersonal dynamic and can be considered to originate in the patriarchal dynamic where men control women.
Most professionals who work in this interdisciplinary area now refer to domestic violence as coercive control. Victimizers target women whom they sense they can control to get their own needs met. They are disinclined to invest in relationships with women who stress their own points of view, who do not readily accept blame when there is a disagreement, and who offer nurturing only when it is reciprocated.
In my office, if I think there are elements of coercion in a relationship, I bring out the Power and Control Wheel and the patient and I go over it. Good education is our responsibility. However, we all have met women who decide to stay in unhealthy relationships.
Assessing people who stay in coercive relationships
Fear
The most important first step is to assess safety. Are they afraid of increased violence if they challenge their partner? Restraining orders or other legal deterrents may not offer solace, as many women are clear that their spouse will come after them, if not tomorrow, then next week, or even next month. They are sure that they will not be safe.
In these cases, I go over safety steps with them so that if they decide to go, they will be prepared. I bring out the “safety box,” which includes the following action steps:
- Memorize important phone numbers of people to call in an emergency.
- If your children are old enough, teach them important phone numbers, including when to dial 911.
- If you can, open your own bank account.
- Stay in touch with friends. Get to know your neighbors. Don’t cut yourself off from people, even if you feel like you want to be alone.
- Rehearse your escape plan until you know it by heart.
- Leave a set of car keys, extra money, a change of clothes and copies of important documents with a trusted friend or relative: your own and your children’s birth certificates, children’s school and medical records, bank books, welfare identification, passport/green card, immigration papers, social security card, lease agreements or mortgage payment books, insurance papers, important addresses, and telephone numbers.
- Keep information about domestic violence in a safe place, where your abuser won’t find it, but where you can get it when you need to review it.
Some women may acknowledge that the risk of physical violence is not the determining factor in their decision to stay and have difficulty explaining why they choose to stay. I suggest that we then consider the following frames that have their origin in the study of the impact of trauma.
Shame
From this lens, abusive events are humiliating experiences, now represented as shame experiences. Humiliation and shame hide hostile feelings that the patient is not able to acknowledge.
“In shame, the self is the failure and others may reject or be critical of this exposed, flawed self.”3 Women will therefore remain attached to an abuser to avoid the exposure of their defective self.
Action steps: Empathic engagement and acknowledgment of shame and humiliation are key. For someone to overcome shame, they must face their sense of their defective self and have strategies to manage these feelings. The development of such strategies is the next step.
Trauma repetition and trauma bonding
Women subjected to domestic violence often respond with incapacitating traumatic syndromes. The concept of “trauma repetition” is suggested as a cause of vulnerability to repeated abuse, and “trauma bonding” is the term for the intense and tenacious bond that can form between abusers and victims.4
Trauma bonding implies that a sense of safety and closeness and secure attachment can only be reached through highly abusive engagement; anything else is experienced as “superficial, cold, or irrelevant.”5 Trauma bonding may have its origins in emotional neglect, according to self reports of 116 women.6Action steps: The literature on trauma is growing and many patients will benefit from good curated sources. Having a good list of books and website on hand is important. Discussion and exploration of the impact of trauma will be needed, and can be provided by someone who is available on a consistent and frequent basis. This work may be time consuming and difficult.
Some asides
1. Some psychiatrists proffer the explanation that these women who stay must be masochistic. The misogynistic concept of masochism still haunts the halls of psychiatry. It is usually offered as a way to dismiss these women’s concerns.
2. One of the obstacles to recognizing chronic mistreatment in relationships is that most abusive men simply “do not seem like abusers.” They have many good qualities, including times of kindness, warmth, and humor, especially in the initial period of a relationship. An abuser’s friends may think the world of him. He may have a successful work life and have no problems with drugs or alcohol. He may simply not fit anyone’s image of a cruel or intimidating person. So, when a woman feels her relationship spinning out of control, it may not occur to her that her partner is an abuser. Even if she does consider her partner to be overly controlling, others may question her perception.
3. Neutrality in family courts is systemic sexism/misogyny. When it comes to domestic violence, family courts tend to split the difference. Stephanie Brandt, MD, notes that The assumption that it is violence alone that matters has formed the basis of much clinical and legal confusion.7 As an analyst, she has gone against the grain of a favored neutrality and become active in the courts, noting the secondary victimization that occurs when a woman enters the legal system.
In summary, psychiatrists must reclaim our expertise in systemic dynamics and point out the role of systemic misogyny. Justices and other court officials need to be educated. Ideally, justice should be based on the equality of men and women in a society free of systemic misogyny. Unfortunately our society has not yet reached this position. In the meanwhile, we must think systemically about interpersonal dynamics. This is our lane. This should not be controversial.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at [email protected]. Dr. Heru would like to thank Dr. Stephanie Brandt for discussing this topic with her and supporting this work.
References
1. Ellyatt H. Arguing with your partner over Covid? You’re not alone, with the pandemic straining many relationships. 2022 Jan 21. https://www.cnbc.com/2022/01/21/covid-has-put-pressures-and-strains-on-relationships.html
2. Xue J et al. J Med Internet Res. 2020 Nov 6;22(11):e24361. doi: 10.2196/24361.
3. Dorahy MJ. J Trauma Dissociation. 2017 May-Jun;18(3):383-96. doi: 10.1080/15299732.2017.1295422.
4. Dutton DG and Painter SL. Victimology. 1981 Jan;6(1):139-55.
5. Sachs A. J Trauma Dissociation. 2017 May-Jun;18(3):319-39. doi: 10.1080/15299732.2017.1295400.
6. Krüger C and Fletcher L. J Trauma Dissociation. 2017 May-Jun;18(3):356-72. doi: 10.1080/15299732.2017.1295420.
7. Brandt S and Rudden M. Int J Appl Psychoanal Studies. 2020 Sept;17(3):215-31. doi: 10.1002/aps.1671.
Despite the ability of some couples to pull together and manage through the COVID-19 pandemic, other couples and families failed to thrive. Increasing divorce rates have been noted nationwide with many disagreements being specifically about COVID.1
A review of over 1 million tweets, between April 12 and July 16, 2020, found an increase in calls to hotlines and increased reports of a variety of types of family violence. There were also more inquiries about social services for family violence, an increased presence from social movements, and more domestic violence-related news.2
The literature addressing family violence uses a variety of terms, so here are some definitions.
Domestic violence is defined as a pattern of behaviors used to gain or maintain power and control. Broadly speaking, domestic violence includes elder abuse, sibling abuse, child abuse, intimate partner abuse, parent abuse, and can also include people who don’t necessarily live together but who have an intimate relationship. Domestic violence centers use the Power and Control Wheel (see graphic) developed by the Domestic Abuse Intervention Project in Duluth, Minn., to describe how domestic violence occurs.
Intimate partner violence is more specific, referring to violence that happens between people in an ongoing or former intimate or romantic relationship, and is a subcategory of domestic violence.
Coercive control is the use of power for control and compliance. It is a dynamic and systematic process described in the top left corner of the Power and Control Wheel. Overt control occurs with the implication that “if you don’t follow the rules, I’ll kill you.” More subtle control is when obedience is forced through monopolizing resources, dictating preferred choices, microregulating a partner’s behavior, and deprivation of supports needed to exercise independent judgment.
All interpersonal relationships have elements of persuasion and influence; however, the goal of coercive relationships is to maintain power and control. It is a dynamic of the relationship. Coercive control emphasizes the systematic, organized, multifaceted, and patterned nature of this interpersonal dynamic and can be considered to originate in the patriarchal dynamic where men control women.
Most professionals who work in this interdisciplinary area now refer to domestic violence as coercive control. Victimizers target women whom they sense they can control to get their own needs met. They are disinclined to invest in relationships with women who stress their own points of view, who do not readily accept blame when there is a disagreement, and who offer nurturing only when it is reciprocated.
In my office, if I think there are elements of coercion in a relationship, I bring out the Power and Control Wheel and the patient and I go over it. Good education is our responsibility. However, we all have met women who decide to stay in unhealthy relationships.
Assessing people who stay in coercive relationships
Fear
The most important first step is to assess safety. Are they afraid of increased violence if they challenge their partner? Restraining orders or other legal deterrents may not offer solace, as many women are clear that their spouse will come after them, if not tomorrow, then next week, or even next month. They are sure that they will not be safe.
In these cases, I go over safety steps with them so that if they decide to go, they will be prepared. I bring out the “safety box,” which includes the following action steps:
- Memorize important phone numbers of people to call in an emergency.
- If your children are old enough, teach them important phone numbers, including when to dial 911.
- If you can, open your own bank account.
- Stay in touch with friends. Get to know your neighbors. Don’t cut yourself off from people, even if you feel like you want to be alone.
- Rehearse your escape plan until you know it by heart.
- Leave a set of car keys, extra money, a change of clothes and copies of important documents with a trusted friend or relative: your own and your children’s birth certificates, children’s school and medical records, bank books, welfare identification, passport/green card, immigration papers, social security card, lease agreements or mortgage payment books, insurance papers, important addresses, and telephone numbers.
- Keep information about domestic violence in a safe place, where your abuser won’t find it, but where you can get it when you need to review it.
Some women may acknowledge that the risk of physical violence is not the determining factor in their decision to stay and have difficulty explaining why they choose to stay. I suggest that we then consider the following frames that have their origin in the study of the impact of trauma.
Shame
From this lens, abusive events are humiliating experiences, now represented as shame experiences. Humiliation and shame hide hostile feelings that the patient is not able to acknowledge.
“In shame, the self is the failure and others may reject or be critical of this exposed, flawed self.”3 Women will therefore remain attached to an abuser to avoid the exposure of their defective self.
Action steps: Empathic engagement and acknowledgment of shame and humiliation are key. For someone to overcome shame, they must face their sense of their defective self and have strategies to manage these feelings. The development of such strategies is the next step.
Trauma repetition and trauma bonding
Women subjected to domestic violence often respond with incapacitating traumatic syndromes. The concept of “trauma repetition” is suggested as a cause of vulnerability to repeated abuse, and “trauma bonding” is the term for the intense and tenacious bond that can form between abusers and victims.4
Trauma bonding implies that a sense of safety and closeness and secure attachment can only be reached through highly abusive engagement; anything else is experienced as “superficial, cold, or irrelevant.”5 Trauma bonding may have its origins in emotional neglect, according to self reports of 116 women.6Action steps: The literature on trauma is growing and many patients will benefit from good curated sources. Having a good list of books and website on hand is important. Discussion and exploration of the impact of trauma will be needed, and can be provided by someone who is available on a consistent and frequent basis. This work may be time consuming and difficult.
Some asides
1. Some psychiatrists proffer the explanation that these women who stay must be masochistic. The misogynistic concept of masochism still haunts the halls of psychiatry. It is usually offered as a way to dismiss these women’s concerns.
2. One of the obstacles to recognizing chronic mistreatment in relationships is that most abusive men simply “do not seem like abusers.” They have many good qualities, including times of kindness, warmth, and humor, especially in the initial period of a relationship. An abuser’s friends may think the world of him. He may have a successful work life and have no problems with drugs or alcohol. He may simply not fit anyone’s image of a cruel or intimidating person. So, when a woman feels her relationship spinning out of control, it may not occur to her that her partner is an abuser. Even if she does consider her partner to be overly controlling, others may question her perception.
3. Neutrality in family courts is systemic sexism/misogyny. When it comes to domestic violence, family courts tend to split the difference. Stephanie Brandt, MD, notes that The assumption that it is violence alone that matters has formed the basis of much clinical and legal confusion.7 As an analyst, she has gone against the grain of a favored neutrality and become active in the courts, noting the secondary victimization that occurs when a woman enters the legal system.
In summary, psychiatrists must reclaim our expertise in systemic dynamics and point out the role of systemic misogyny. Justices and other court officials need to be educated. Ideally, justice should be based on the equality of men and women in a society free of systemic misogyny. Unfortunately our society has not yet reached this position. In the meanwhile, we must think systemically about interpersonal dynamics. This is our lane. This should not be controversial.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at [email protected]. Dr. Heru would like to thank Dr. Stephanie Brandt for discussing this topic with her and supporting this work.
References
1. Ellyatt H. Arguing with your partner over Covid? You’re not alone, with the pandemic straining many relationships. 2022 Jan 21. https://www.cnbc.com/2022/01/21/covid-has-put-pressures-and-strains-on-relationships.html
2. Xue J et al. J Med Internet Res. 2020 Nov 6;22(11):e24361. doi: 10.2196/24361.
3. Dorahy MJ. J Trauma Dissociation. 2017 May-Jun;18(3):383-96. doi: 10.1080/15299732.2017.1295422.
4. Dutton DG and Painter SL. Victimology. 1981 Jan;6(1):139-55.
5. Sachs A. J Trauma Dissociation. 2017 May-Jun;18(3):319-39. doi: 10.1080/15299732.2017.1295400.
6. Krüger C and Fletcher L. J Trauma Dissociation. 2017 May-Jun;18(3):356-72. doi: 10.1080/15299732.2017.1295420.
7. Brandt S and Rudden M. Int J Appl Psychoanal Studies. 2020 Sept;17(3):215-31. doi: 10.1002/aps.1671.
Despite the ability of some couples to pull together and manage through the COVID-19 pandemic, other couples and families failed to thrive. Increasing divorce rates have been noted nationwide with many disagreements being specifically about COVID.1
A review of over 1 million tweets, between April 12 and July 16, 2020, found an increase in calls to hotlines and increased reports of a variety of types of family violence. There were also more inquiries about social services for family violence, an increased presence from social movements, and more domestic violence-related news.2
The literature addressing family violence uses a variety of terms, so here are some definitions.
Domestic violence is defined as a pattern of behaviors used to gain or maintain power and control. Broadly speaking, domestic violence includes elder abuse, sibling abuse, child abuse, intimate partner abuse, parent abuse, and can also include people who don’t necessarily live together but who have an intimate relationship. Domestic violence centers use the Power and Control Wheel (see graphic) developed by the Domestic Abuse Intervention Project in Duluth, Minn., to describe how domestic violence occurs.
Intimate partner violence is more specific, referring to violence that happens between people in an ongoing or former intimate or romantic relationship, and is a subcategory of domestic violence.
Coercive control is the use of power for control and compliance. It is a dynamic and systematic process described in the top left corner of the Power and Control Wheel. Overt control occurs with the implication that “if you don’t follow the rules, I’ll kill you.” More subtle control is when obedience is forced through monopolizing resources, dictating preferred choices, microregulating a partner’s behavior, and deprivation of supports needed to exercise independent judgment.
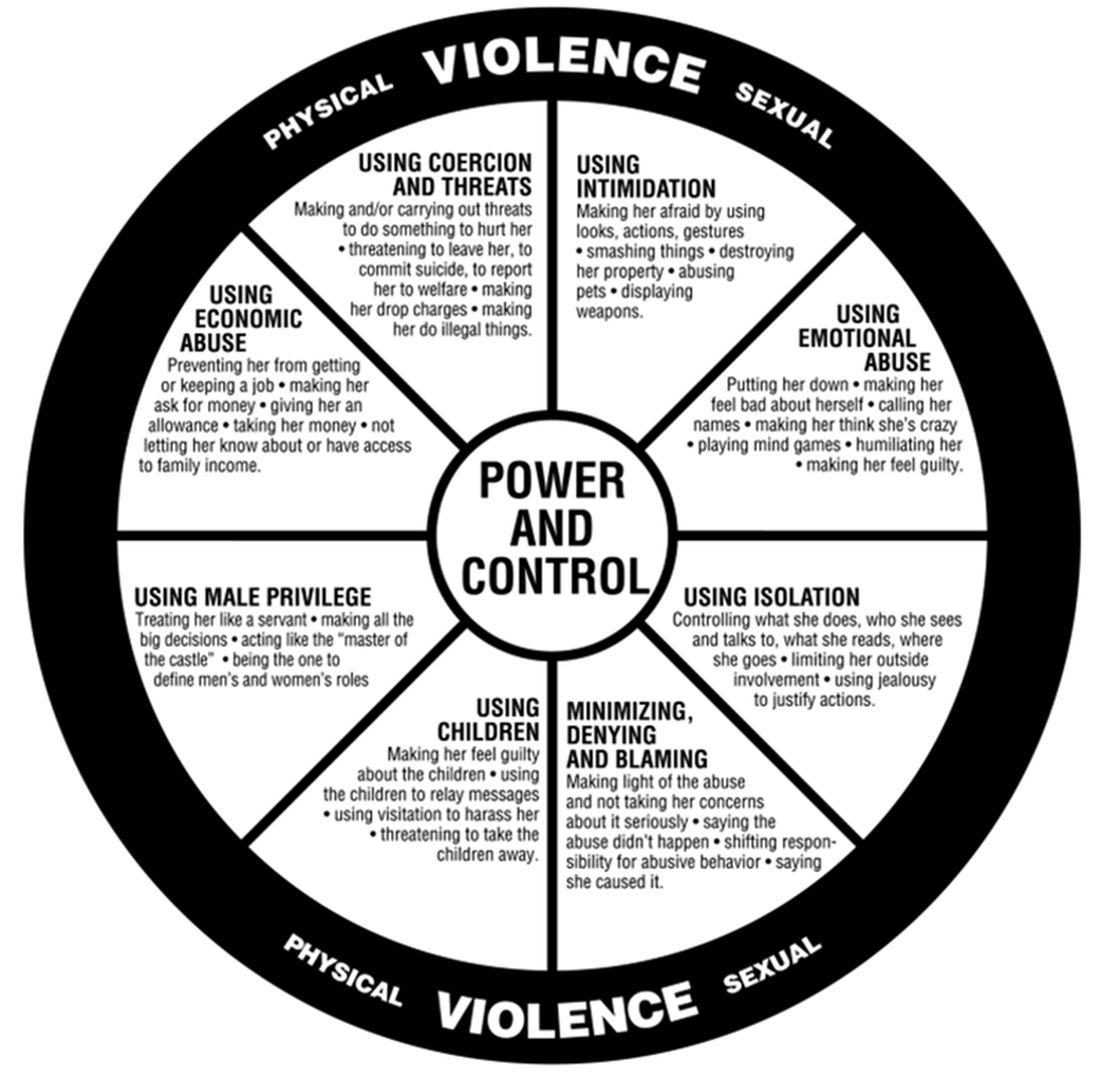
All interpersonal relationships have elements of persuasion and influence; however, the goal of coercive relationships is to maintain power and control. It is a dynamic of the relationship. Coercive control emphasizes the systematic, organized, multifaceted, and patterned nature of this interpersonal dynamic and can be considered to originate in the patriarchal dynamic where men control women.
Most professionals who work in this interdisciplinary area now refer to domestic violence as coercive control. Victimizers target women whom they sense they can control to get their own needs met. They are disinclined to invest in relationships with women who stress their own points of view, who do not readily accept blame when there is a disagreement, and who offer nurturing only when it is reciprocated.
In my office, if I think there are elements of coercion in a relationship, I bring out the Power and Control Wheel and the patient and I go over it. Good education is our responsibility. However, we all have met women who decide to stay in unhealthy relationships.
Assessing people who stay in coercive relationships
Fear
The most important first step is to assess safety. Are they afraid of increased violence if they challenge their partner? Restraining orders or other legal deterrents may not offer solace, as many women are clear that their spouse will come after them, if not tomorrow, then next week, or even next month. They are sure that they will not be safe.
In these cases, I go over safety steps with them so that if they decide to go, they will be prepared. I bring out the “safety box,” which includes the following action steps:
- Memorize important phone numbers of people to call in an emergency.
- If your children are old enough, teach them important phone numbers, including when to dial 911.
- If you can, open your own bank account.
- Stay in touch with friends. Get to know your neighbors. Don’t cut yourself off from people, even if you feel like you want to be alone.
- Rehearse your escape plan until you know it by heart.
- Leave a set of car keys, extra money, a change of clothes and copies of important documents with a trusted friend or relative: your own and your children’s birth certificates, children’s school and medical records, bank books, welfare identification, passport/green card, immigration papers, social security card, lease agreements or mortgage payment books, insurance papers, important addresses, and telephone numbers.
- Keep information about domestic violence in a safe place, where your abuser won’t find it, but where you can get it when you need to review it.
Some women may acknowledge that the risk of physical violence is not the determining factor in their decision to stay and have difficulty explaining why they choose to stay. I suggest that we then consider the following frames that have their origin in the study of the impact of trauma.
Shame
From this lens, abusive events are humiliating experiences, now represented as shame experiences. Humiliation and shame hide hostile feelings that the patient is not able to acknowledge.
“In shame, the self is the failure and others may reject or be critical of this exposed, flawed self.”3 Women will therefore remain attached to an abuser to avoid the exposure of their defective self.
Action steps: Empathic engagement and acknowledgment of shame and humiliation are key. For someone to overcome shame, they must face their sense of their defective self and have strategies to manage these feelings. The development of such strategies is the next step.
Trauma repetition and trauma bonding
Women subjected to domestic violence often respond with incapacitating traumatic syndromes. The concept of “trauma repetition” is suggested as a cause of vulnerability to repeated abuse, and “trauma bonding” is the term for the intense and tenacious bond that can form between abusers and victims.4
Trauma bonding implies that a sense of safety and closeness and secure attachment can only be reached through highly abusive engagement; anything else is experienced as “superficial, cold, or irrelevant.”5 Trauma bonding may have its origins in emotional neglect, according to self reports of 116 women.6Action steps: The literature on trauma is growing and many patients will benefit from good curated sources. Having a good list of books and website on hand is important. Discussion and exploration of the impact of trauma will be needed, and can be provided by someone who is available on a consistent and frequent basis. This work may be time consuming and difficult.
Some asides
1. Some psychiatrists proffer the explanation that these women who stay must be masochistic. The misogynistic concept of masochism still haunts the halls of psychiatry. It is usually offered as a way to dismiss these women’s concerns.
2. One of the obstacles to recognizing chronic mistreatment in relationships is that most abusive men simply “do not seem like abusers.” They have many good qualities, including times of kindness, warmth, and humor, especially in the initial period of a relationship. An abuser’s friends may think the world of him. He may have a successful work life and have no problems with drugs or alcohol. He may simply not fit anyone’s image of a cruel or intimidating person. So, when a woman feels her relationship spinning out of control, it may not occur to her that her partner is an abuser. Even if she does consider her partner to be overly controlling, others may question her perception.
3. Neutrality in family courts is systemic sexism/misogyny. When it comes to domestic violence, family courts tend to split the difference. Stephanie Brandt, MD, notes that The assumption that it is violence alone that matters has formed the basis of much clinical and legal confusion.7 As an analyst, she has gone against the grain of a favored neutrality and become active in the courts, noting the secondary victimization that occurs when a woman enters the legal system.
In summary, psychiatrists must reclaim our expertise in systemic dynamics and point out the role of systemic misogyny. Justices and other court officials need to be educated. Ideally, justice should be based on the equality of men and women in a society free of systemic misogyny. Unfortunately our society has not yet reached this position. In the meanwhile, we must think systemically about interpersonal dynamics. This is our lane. This should not be controversial.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at [email protected]. Dr. Heru would like to thank Dr. Stephanie Brandt for discussing this topic with her and supporting this work.
References
1. Ellyatt H. Arguing with your partner over Covid? You’re not alone, with the pandemic straining many relationships. 2022 Jan 21. https://www.cnbc.com/2022/01/21/covid-has-put-pressures-and-strains-on-relationships.html
2. Xue J et al. J Med Internet Res. 2020 Nov 6;22(11):e24361. doi: 10.2196/24361.
3. Dorahy MJ. J Trauma Dissociation. 2017 May-Jun;18(3):383-96. doi: 10.1080/15299732.2017.1295422.
4. Dutton DG and Painter SL. Victimology. 1981 Jan;6(1):139-55.
5. Sachs A. J Trauma Dissociation. 2017 May-Jun;18(3):319-39. doi: 10.1080/15299732.2017.1295400.
6. Krüger C and Fletcher L. J Trauma Dissociation. 2017 May-Jun;18(3):356-72. doi: 10.1080/15299732.2017.1295420.
7. Brandt S and Rudden M. Int J Appl Psychoanal Studies. 2020 Sept;17(3):215-31. doi: 10.1002/aps.1671.
New Medicare rule streamlines prior authorization in Medicare Advantage plans
A new federal rule seeks to reduce Medicare Advantage insurance plans’ prior authorization burdens on physicians while also ensuring that enrollees have the same access to necessary care that they would receive under traditional fee-for-service Medicare.
The prior authorization changes, announced this week, are part of the Centers for Medicare & Medicaid Services’ 2024 update of policy changes for Medicare Advantage and Part D pharmacy plans
Medicare Advantage plans’ business practices have raised significant concerns in recent years. More than 28 million Americans were enrolled in a Medicare Advantage plan in 2022, which is nearly half of all Medicare enrollees, according to the Kaiser Family Foundation.
Medicare pays a fixed amount per enrollee per year to these privately run managed care plans, in contrast to traditional fee-for-service Medicare. Medicare Advantage plans have been criticized for aggressive marketing, for overbilling the federal government for care, and for using prior authorization to inappropriately deny needed care to patients.
About 13% of prior authorization requests that are denied by Medicare Advantage plans actually met Medicare coverage rules and should have been approved, the Office of the Inspector General at the U.S. Department of Health & Human Services reported in 2022.
The newly finalized rule now requires Medicare Advantage plans to do the following.
- Ensure that a prior authorization approval, once granted, remains valid for as long as medically necessary to avoid disruptions in care.
- Conduct an annual review of utilization management policies.
- Ensure that coverage denials based on medical necessity be reviewed by health care professionals with relevant expertise before a denial can be issued.
Physician groups welcomed the changes. In a statement, the American Medical Association said that an initial reading of the rule suggested CMS had “taken important steps toward right-sizing the prior authorization process.”
The Medical Group Management Association praised CMS in a statement for having limited “dangerous disruptions and delays to necessary patient care” resulting from the cumbersome processes of prior approval. With the new rules, CMS will provide greater consistency across Advantage plans as well as traditional Medicare, said Anders Gilberg, MGMA’s senior vice president of government affairs, in a statement.
Peer consideration
The final rule did disappoint physician groups in one key way. CMS rebuffed requests to have CMS require Advantage plans to use reviewers of the same specialty as treating physicians in handling disputes about prior authorization. CMS said it expects plans to exercise judgment in finding reviewers with “sufficient expertise to make an informed and supportable decision.”
“In some instances, we expect that plans will use a physician or other health care professional of the same specialty or subspecialty as the treating physician,” CMS said. “In other instances, we expect that plans will utilize a reviewer with specialized training, certification, or clinical experience in the applicable field of medicine.”
Medicare Advantage marketing ‘sowing confusion’
With this final rule, CMS also sought to protect consumers from “potentially misleading marketing practices” used in promoting Medicare Advantage and Part D prescription drug plans.
The agency said it had received complaints about people who have received official-looking promotional materials for Medicare that directed them not to government sources of information but to Medicare Advantage and Part D plans or their agents and brokers.
Ads now must mention a specific plan name, and they cannot use the Medicare name, CMS logo, Medicare card, or other government information in a misleading way, CMS said.
“CMS can see no value or purpose in a non-governmental entity’s use of the Medicare logo or HHS logo except for the express purpose of sowing confusion and misrepresenting itself as the government,” the agency said.
A version of this article first appeared on Medscape.com.
A new federal rule seeks to reduce Medicare Advantage insurance plans’ prior authorization burdens on physicians while also ensuring that enrollees have the same access to necessary care that they would receive under traditional fee-for-service Medicare.
The prior authorization changes, announced this week, are part of the Centers for Medicare & Medicaid Services’ 2024 update of policy changes for Medicare Advantage and Part D pharmacy plans
Medicare Advantage plans’ business practices have raised significant concerns in recent years. More than 28 million Americans were enrolled in a Medicare Advantage plan in 2022, which is nearly half of all Medicare enrollees, according to the Kaiser Family Foundation.
Medicare pays a fixed amount per enrollee per year to these privately run managed care plans, in contrast to traditional fee-for-service Medicare. Medicare Advantage plans have been criticized for aggressive marketing, for overbilling the federal government for care, and for using prior authorization to inappropriately deny needed care to patients.
About 13% of prior authorization requests that are denied by Medicare Advantage plans actually met Medicare coverage rules and should have been approved, the Office of the Inspector General at the U.S. Department of Health & Human Services reported in 2022.
The newly finalized rule now requires Medicare Advantage plans to do the following.
- Ensure that a prior authorization approval, once granted, remains valid for as long as medically necessary to avoid disruptions in care.
- Conduct an annual review of utilization management policies.
- Ensure that coverage denials based on medical necessity be reviewed by health care professionals with relevant expertise before a denial can be issued.
Physician groups welcomed the changes. In a statement, the American Medical Association said that an initial reading of the rule suggested CMS had “taken important steps toward right-sizing the prior authorization process.”
The Medical Group Management Association praised CMS in a statement for having limited “dangerous disruptions and delays to necessary patient care” resulting from the cumbersome processes of prior approval. With the new rules, CMS will provide greater consistency across Advantage plans as well as traditional Medicare, said Anders Gilberg, MGMA’s senior vice president of government affairs, in a statement.
Peer consideration
The final rule did disappoint physician groups in one key way. CMS rebuffed requests to have CMS require Advantage plans to use reviewers of the same specialty as treating physicians in handling disputes about prior authorization. CMS said it expects plans to exercise judgment in finding reviewers with “sufficient expertise to make an informed and supportable decision.”
“In some instances, we expect that plans will use a physician or other health care professional of the same specialty or subspecialty as the treating physician,” CMS said. “In other instances, we expect that plans will utilize a reviewer with specialized training, certification, or clinical experience in the applicable field of medicine.”
Medicare Advantage marketing ‘sowing confusion’
With this final rule, CMS also sought to protect consumers from “potentially misleading marketing practices” used in promoting Medicare Advantage and Part D prescription drug plans.
The agency said it had received complaints about people who have received official-looking promotional materials for Medicare that directed them not to government sources of information but to Medicare Advantage and Part D plans or their agents and brokers.
Ads now must mention a specific plan name, and they cannot use the Medicare name, CMS logo, Medicare card, or other government information in a misleading way, CMS said.
“CMS can see no value or purpose in a non-governmental entity’s use of the Medicare logo or HHS logo except for the express purpose of sowing confusion and misrepresenting itself as the government,” the agency said.
A version of this article first appeared on Medscape.com.
A new federal rule seeks to reduce Medicare Advantage insurance plans’ prior authorization burdens on physicians while also ensuring that enrollees have the same access to necessary care that they would receive under traditional fee-for-service Medicare.
The prior authorization changes, announced this week, are part of the Centers for Medicare & Medicaid Services’ 2024 update of policy changes for Medicare Advantage and Part D pharmacy plans
Medicare Advantage plans’ business practices have raised significant concerns in recent years. More than 28 million Americans were enrolled in a Medicare Advantage plan in 2022, which is nearly half of all Medicare enrollees, according to the Kaiser Family Foundation.
Medicare pays a fixed amount per enrollee per year to these privately run managed care plans, in contrast to traditional fee-for-service Medicare. Medicare Advantage plans have been criticized for aggressive marketing, for overbilling the federal government for care, and for using prior authorization to inappropriately deny needed care to patients.
About 13% of prior authorization requests that are denied by Medicare Advantage plans actually met Medicare coverage rules and should have been approved, the Office of the Inspector General at the U.S. Department of Health & Human Services reported in 2022.
The newly finalized rule now requires Medicare Advantage plans to do the following.
- Ensure that a prior authorization approval, once granted, remains valid for as long as medically necessary to avoid disruptions in care.
- Conduct an annual review of utilization management policies.
- Ensure that coverage denials based on medical necessity be reviewed by health care professionals with relevant expertise before a denial can be issued.
Physician groups welcomed the changes. In a statement, the American Medical Association said that an initial reading of the rule suggested CMS had “taken important steps toward right-sizing the prior authorization process.”
The Medical Group Management Association praised CMS in a statement for having limited “dangerous disruptions and delays to necessary patient care” resulting from the cumbersome processes of prior approval. With the new rules, CMS will provide greater consistency across Advantage plans as well as traditional Medicare, said Anders Gilberg, MGMA’s senior vice president of government affairs, in a statement.
Peer consideration
The final rule did disappoint physician groups in one key way. CMS rebuffed requests to have CMS require Advantage plans to use reviewers of the same specialty as treating physicians in handling disputes about prior authorization. CMS said it expects plans to exercise judgment in finding reviewers with “sufficient expertise to make an informed and supportable decision.”
“In some instances, we expect that plans will use a physician or other health care professional of the same specialty or subspecialty as the treating physician,” CMS said. “In other instances, we expect that plans will utilize a reviewer with specialized training, certification, or clinical experience in the applicable field of medicine.”
Medicare Advantage marketing ‘sowing confusion’
With this final rule, CMS also sought to protect consumers from “potentially misleading marketing practices” used in promoting Medicare Advantage and Part D prescription drug plans.
The agency said it had received complaints about people who have received official-looking promotional materials for Medicare that directed them not to government sources of information but to Medicare Advantage and Part D plans or their agents and brokers.
Ads now must mention a specific plan name, and they cannot use the Medicare name, CMS logo, Medicare card, or other government information in a misleading way, CMS said.
“CMS can see no value or purpose in a non-governmental entity’s use of the Medicare logo or HHS logo except for the express purpose of sowing confusion and misrepresenting itself as the government,” the agency said.
A version of this article first appeared on Medscape.com.
Glutathione a potential biomarker for postpartum suicide
Approximately 10,000 suicide deaths are recorded in Brazil every year. The suicide risk is highest among patients with depressive disorders, particularly women (> 18% vs. 11% for men).
There are countless people who work to prevent suicide, and the challenges they face are many. But now, on the horizon, there are new tools that could prove invaluable to their efforts – tools such as biomarkers. In a study recently published in the journal Frontiers in Psychiatry, researchers from the Catholic University of Pelotas (UCPel), Brazil, reported an association of glutathione (GSH) with the degree of suicide risk in women at 18 months postpartum. Specifically, they found that reduced serum GSH levels were significantly lower for those with moderate to high suicide risk than for those without suicide risk. Their findings suggest that GSH may be a potential biomarker or etiologic factor among women at risk for suicide, with therapeutic implications.
This was a case-control study nested within a cohort study. From this cohort, 45 women were selected at 18 months postpartum. Thirty of them had mood disorders, such as major depression and bipolar disorder. The other 15 participants, none of whom had a mood disorder, made up the control group.
Depression and the risk for suicide were assessed using the Mini International Neuropsychiatric Interview Plus (MINI-Plus 5.0.0 Brazilian version), module A and module C, respectively. Blood samples were collected to evaluate serum levels of the following oxidative stress biomarkers: reactive oxygen species, superoxide dismutase, and GSH.
The prevalence of suicide risk observed in the women at 18 months postpartum was 24.4%. The prevalence of suicide risk in the mood disorder group was 36.7%.
In addition, the statistical analysis found that women with moderate to high suicide risk had cerebral redox imbalance, resulting in a decrease in blood GSH levels.
The study team was led by neuroscientist Adriano Martimbianco de Assis, PhD, the coordinator of UCPel’s postgraduate program in health and behavior. He said that the correlation identified between GSH serum levels and suicide risk gives rise to two possible applications: using GSH as a biomarker for suicide risk and using GSH therapeutically.
Regarding the former application, Dr. Martimbianco de Assis explained that additional studies are needed to take a step forward. “Although we believe that most of the GSH came from the brain – given that it’s the brain’s main antioxidant – as we analyze blood samples, we’re not yet able to rule out the possibility that it came from other organs,” he said in an interview. So, confirming that hypothesis will require studies that involve imaging brain tissue. According to Dr. Martimbianco de Assis, once there is confirmation, it will be possible to move to using the antioxidant as a biomarker for suicide risk.
He also shared his views about the second application: using GSH therapeutically. “We already know that there are very simple alternatives that can influence GSH levels, [and they] mostly have to do with exercise and [improving the quality of] the food one eats. But there are also drugs: for example, N-acetyl cysteine, which is a precursor of GSH.” Adopting strategies to increase the levels of this antioxidant in the body should reverse the imbalance identified in the study and, as a result, may lead to lowering the risk for suicide. But, he reiterated, “getting to a place where GSH [can be used] in clinical practice hinges on getting that confirmation that it did, in fact, come from the brain. Recall that our study found lower levels of GSH in women at risk for suicide.”
Even though the study evaluated postpartum women, it’s possible that the results can be extrapolated to other populations, said Dr. Martimbianco de Assis. This is because when the data were collected, 18 months had already passed since giving birth. The participants’ physiological condition at that point was more similar to the one prior to becoming pregnant.
The UCPel researchers continue to follow the cohort. “We intend to continue monitoring GSH levels at other times. Forty-eight months have now passed since the women gave birth, and the idea is to continue studying [the patients involved in the study],” said Dr. Martimbianco de Assis, adding that the team also intends to analyze brain tissue from in vitro studies using cell cultures.
This article was translated from the Medscape Portuguese Edition and a version appeared on Medscape.com.
Approximately 10,000 suicide deaths are recorded in Brazil every year. The suicide risk is highest among patients with depressive disorders, particularly women (> 18% vs. 11% for men).
There are countless people who work to prevent suicide, and the challenges they face are many. But now, on the horizon, there are new tools that could prove invaluable to their efforts – tools such as biomarkers. In a study recently published in the journal Frontiers in Psychiatry, researchers from the Catholic University of Pelotas (UCPel), Brazil, reported an association of glutathione (GSH) with the degree of suicide risk in women at 18 months postpartum. Specifically, they found that reduced serum GSH levels were significantly lower for those with moderate to high suicide risk than for those without suicide risk. Their findings suggest that GSH may be a potential biomarker or etiologic factor among women at risk for suicide, with therapeutic implications.
This was a case-control study nested within a cohort study. From this cohort, 45 women were selected at 18 months postpartum. Thirty of them had mood disorders, such as major depression and bipolar disorder. The other 15 participants, none of whom had a mood disorder, made up the control group.
Depression and the risk for suicide were assessed using the Mini International Neuropsychiatric Interview Plus (MINI-Plus 5.0.0 Brazilian version), module A and module C, respectively. Blood samples were collected to evaluate serum levels of the following oxidative stress biomarkers: reactive oxygen species, superoxide dismutase, and GSH.
The prevalence of suicide risk observed in the women at 18 months postpartum was 24.4%. The prevalence of suicide risk in the mood disorder group was 36.7%.
In addition, the statistical analysis found that women with moderate to high suicide risk had cerebral redox imbalance, resulting in a decrease in blood GSH levels.
The study team was led by neuroscientist Adriano Martimbianco de Assis, PhD, the coordinator of UCPel’s postgraduate program in health and behavior. He said that the correlation identified between GSH serum levels and suicide risk gives rise to two possible applications: using GSH as a biomarker for suicide risk and using GSH therapeutically.
Regarding the former application, Dr. Martimbianco de Assis explained that additional studies are needed to take a step forward. “Although we believe that most of the GSH came from the brain – given that it’s the brain’s main antioxidant – as we analyze blood samples, we’re not yet able to rule out the possibility that it came from other organs,” he said in an interview. So, confirming that hypothesis will require studies that involve imaging brain tissue. According to Dr. Martimbianco de Assis, once there is confirmation, it will be possible to move to using the antioxidant as a biomarker for suicide risk.
He also shared his views about the second application: using GSH therapeutically. “We already know that there are very simple alternatives that can influence GSH levels, [and they] mostly have to do with exercise and [improving the quality of] the food one eats. But there are also drugs: for example, N-acetyl cysteine, which is a precursor of GSH.” Adopting strategies to increase the levels of this antioxidant in the body should reverse the imbalance identified in the study and, as a result, may lead to lowering the risk for suicide. But, he reiterated, “getting to a place where GSH [can be used] in clinical practice hinges on getting that confirmation that it did, in fact, come from the brain. Recall that our study found lower levels of GSH in women at risk for suicide.”
Even though the study evaluated postpartum women, it’s possible that the results can be extrapolated to other populations, said Dr. Martimbianco de Assis. This is because when the data were collected, 18 months had already passed since giving birth. The participants’ physiological condition at that point was more similar to the one prior to becoming pregnant.
The UCPel researchers continue to follow the cohort. “We intend to continue monitoring GSH levels at other times. Forty-eight months have now passed since the women gave birth, and the idea is to continue studying [the patients involved in the study],” said Dr. Martimbianco de Assis, adding that the team also intends to analyze brain tissue from in vitro studies using cell cultures.
This article was translated from the Medscape Portuguese Edition and a version appeared on Medscape.com.
Approximately 10,000 suicide deaths are recorded in Brazil every year. The suicide risk is highest among patients with depressive disorders, particularly women (> 18% vs. 11% for men).
There are countless people who work to prevent suicide, and the challenges they face are many. But now, on the horizon, there are new tools that could prove invaluable to their efforts – tools such as biomarkers. In a study recently published in the journal Frontiers in Psychiatry, researchers from the Catholic University of Pelotas (UCPel), Brazil, reported an association of glutathione (GSH) with the degree of suicide risk in women at 18 months postpartum. Specifically, they found that reduced serum GSH levels were significantly lower for those with moderate to high suicide risk than for those without suicide risk. Their findings suggest that GSH may be a potential biomarker or etiologic factor among women at risk for suicide, with therapeutic implications.
This was a case-control study nested within a cohort study. From this cohort, 45 women were selected at 18 months postpartum. Thirty of them had mood disorders, such as major depression and bipolar disorder. The other 15 participants, none of whom had a mood disorder, made up the control group.
Depression and the risk for suicide were assessed using the Mini International Neuropsychiatric Interview Plus (MINI-Plus 5.0.0 Brazilian version), module A and module C, respectively. Blood samples were collected to evaluate serum levels of the following oxidative stress biomarkers: reactive oxygen species, superoxide dismutase, and GSH.
The prevalence of suicide risk observed in the women at 18 months postpartum was 24.4%. The prevalence of suicide risk in the mood disorder group was 36.7%.
In addition, the statistical analysis found that women with moderate to high suicide risk had cerebral redox imbalance, resulting in a decrease in blood GSH levels.
The study team was led by neuroscientist Adriano Martimbianco de Assis, PhD, the coordinator of UCPel’s postgraduate program in health and behavior. He said that the correlation identified between GSH serum levels and suicide risk gives rise to two possible applications: using GSH as a biomarker for suicide risk and using GSH therapeutically.
Regarding the former application, Dr. Martimbianco de Assis explained that additional studies are needed to take a step forward. “Although we believe that most of the GSH came from the brain – given that it’s the brain’s main antioxidant – as we analyze blood samples, we’re not yet able to rule out the possibility that it came from other organs,” he said in an interview. So, confirming that hypothesis will require studies that involve imaging brain tissue. According to Dr. Martimbianco de Assis, once there is confirmation, it will be possible to move to using the antioxidant as a biomarker for suicide risk.
He also shared his views about the second application: using GSH therapeutically. “We already know that there are very simple alternatives that can influence GSH levels, [and they] mostly have to do with exercise and [improving the quality of] the food one eats. But there are also drugs: for example, N-acetyl cysteine, which is a precursor of GSH.” Adopting strategies to increase the levels of this antioxidant in the body should reverse the imbalance identified in the study and, as a result, may lead to lowering the risk for suicide. But, he reiterated, “getting to a place where GSH [can be used] in clinical practice hinges on getting that confirmation that it did, in fact, come from the brain. Recall that our study found lower levels of GSH in women at risk for suicide.”
Even though the study evaluated postpartum women, it’s possible that the results can be extrapolated to other populations, said Dr. Martimbianco de Assis. This is because when the data were collected, 18 months had already passed since giving birth. The participants’ physiological condition at that point was more similar to the one prior to becoming pregnant.
The UCPel researchers continue to follow the cohort. “We intend to continue monitoring GSH levels at other times. Forty-eight months have now passed since the women gave birth, and the idea is to continue studying [the patients involved in the study],” said Dr. Martimbianco de Assis, adding that the team also intends to analyze brain tissue from in vitro studies using cell cultures.
This article was translated from the Medscape Portuguese Edition and a version appeared on Medscape.com.