User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Daily Recap: FDA revokes emergency use of hydroxychloroquine; Hardest hit specialties ranked in financial report
Here are the stories our MDedge editors across specialties think you need to know about today:
It’s official: COVID-19 is bad for your health care business
For the months of March and April 2020, use of medical professional services dropped by 65% and 68%, respectively, compared with last year, and estimated revenue fell by 45% and 48%, FAIR Health, a nonprofit organization that manages a database of 31 billion claim records, said in a new report.
Of the seven specialties included in the study, oral surgery was hit the hardest, followed by gastroenterology, cardiology, orthopedics, dermatology, adult primary care, and pediatric primary care, FAIR Health said.
“Even when medical practices have continued to function via telehealth, many have experienced lower reimbursements for telehealth visits than for in-person visits and more time educating patients on how to use the technology,” according to the report. Read more.
FDA revokes emergency use of hydroxychloroquine
The FDA revoked its decision from March 28 allowing use of hydroxychloroquine and chloroquine to treat people hospitalized with COVID-19 under an emergency use authorization (EUA).
"Based on its ongoing analysis of the EUA and emerging scientific data, the FDA determined that chloroquine and hydroxychloroquine are unlikely to be effective in treating COVID-19," the agency announced in a June 15 statement.
"In light of ongoing serious cardiac adverse events and other potential serious side effects, the known and potential benefits of chloroquine and hydroxychloroquine no longer outweigh the known and potential risks for the authorized use," noted the FDA. Read more.
Secondary infections common in COVID-19, implications unclear
Secondary respiratory infections appear to be highly prevalent among patients with severe COVID-19, but at this point, most physicians aren’t sure what to make of this understudied phenomenon.
“We really do not understand the implications of secondary infections on outcomes in COVID-19 patients,” David L. Bowton, MD, FCCP, said in an interview. “In most early reports the incidence of secondary infections was much higher in patients dying from COVID-19, compared to survivors, but it isn’t clear whether this indicates that the secondary infection itself led to excess mortality or was more a marker of the severity of the COVID-19 infection."
An early retrospective cohort study including 191 COVID-19 patients in Wuhan, China found that of the 54 who died in hospital, half had secondary bacterial lung infections (Lancet. 2020 Mar 28;395[10229]:1054-62). That comes as no surprise to U.S. physicians, who learned in training that many deaths during the so-called Spanish influenza epidemic were actually caused by secondary pneumonia involving Staphylococcus aureus, commented Daniel L. Ouellette, MD, FCCP. Read more.
Automated insulin delivery system ‘getting better and better’
Medtronic’s next-generation automated insulin delivery system offers significant improvements over the currently available model, particularly in young people with type 1 diabetes, new data suggest.
Data from three trials of such systems using Medtronic’s advanced hybrid closed-loop (AHCL) algorithm (trade name SmartGuard) were presented during the virtual American Diabetes Association (ADA) 80th Scientific Sessions.
Taken together, the data from the three trials showed that the AHCL-based system improved glycemic time-in-range with no increased risk for hypoglycemia, including in children and teenagers, with high patient-reported satisfaction.
“None of these devices is perfect, but they are a substantial improvement over what we’ve had ... They might make the quality of [patient] lives better. That’s really underappreciated,” session moderator Timothy S. Bailey, MD, commented. Read more.
Access more top news from the ADA virtual meeting.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
It’s official: COVID-19 is bad for your health care business
For the months of March and April 2020, use of medical professional services dropped by 65% and 68%, respectively, compared with last year, and estimated revenue fell by 45% and 48%, FAIR Health, a nonprofit organization that manages a database of 31 billion claim records, said in a new report.
Of the seven specialties included in the study, oral surgery was hit the hardest, followed by gastroenterology, cardiology, orthopedics, dermatology, adult primary care, and pediatric primary care, FAIR Health said.
“Even when medical practices have continued to function via telehealth, many have experienced lower reimbursements for telehealth visits than for in-person visits and more time educating patients on how to use the technology,” according to the report. Read more.
FDA revokes emergency use of hydroxychloroquine
The FDA revoked its decision from March 28 allowing use of hydroxychloroquine and chloroquine to treat people hospitalized with COVID-19 under an emergency use authorization (EUA).
"Based on its ongoing analysis of the EUA and emerging scientific data, the FDA determined that chloroquine and hydroxychloroquine are unlikely to be effective in treating COVID-19," the agency announced in a June 15 statement.
"In light of ongoing serious cardiac adverse events and other potential serious side effects, the known and potential benefits of chloroquine and hydroxychloroquine no longer outweigh the known and potential risks for the authorized use," noted the FDA. Read more.
Secondary infections common in COVID-19, implications unclear
Secondary respiratory infections appear to be highly prevalent among patients with severe COVID-19, but at this point, most physicians aren’t sure what to make of this understudied phenomenon.
“We really do not understand the implications of secondary infections on outcomes in COVID-19 patients,” David L. Bowton, MD, FCCP, said in an interview. “In most early reports the incidence of secondary infections was much higher in patients dying from COVID-19, compared to survivors, but it isn’t clear whether this indicates that the secondary infection itself led to excess mortality or was more a marker of the severity of the COVID-19 infection."
An early retrospective cohort study including 191 COVID-19 patients in Wuhan, China found that of the 54 who died in hospital, half had secondary bacterial lung infections (Lancet. 2020 Mar 28;395[10229]:1054-62). That comes as no surprise to U.S. physicians, who learned in training that many deaths during the so-called Spanish influenza epidemic were actually caused by secondary pneumonia involving Staphylococcus aureus, commented Daniel L. Ouellette, MD, FCCP. Read more.
Automated insulin delivery system ‘getting better and better’
Medtronic’s next-generation automated insulin delivery system offers significant improvements over the currently available model, particularly in young people with type 1 diabetes, new data suggest.
Data from three trials of such systems using Medtronic’s advanced hybrid closed-loop (AHCL) algorithm (trade name SmartGuard) were presented during the virtual American Diabetes Association (ADA) 80th Scientific Sessions.
Taken together, the data from the three trials showed that the AHCL-based system improved glycemic time-in-range with no increased risk for hypoglycemia, including in children and teenagers, with high patient-reported satisfaction.
“None of these devices is perfect, but they are a substantial improvement over what we’ve had ... They might make the quality of [patient] lives better. That’s really underappreciated,” session moderator Timothy S. Bailey, MD, commented. Read more.
Access more top news from the ADA virtual meeting.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
It’s official: COVID-19 is bad for your health care business
For the months of March and April 2020, use of medical professional services dropped by 65% and 68%, respectively, compared with last year, and estimated revenue fell by 45% and 48%, FAIR Health, a nonprofit organization that manages a database of 31 billion claim records, said in a new report.
Of the seven specialties included in the study, oral surgery was hit the hardest, followed by gastroenterology, cardiology, orthopedics, dermatology, adult primary care, and pediatric primary care, FAIR Health said.
“Even when medical practices have continued to function via telehealth, many have experienced lower reimbursements for telehealth visits than for in-person visits and more time educating patients on how to use the technology,” according to the report. Read more.
FDA revokes emergency use of hydroxychloroquine
The FDA revoked its decision from March 28 allowing use of hydroxychloroquine and chloroquine to treat people hospitalized with COVID-19 under an emergency use authorization (EUA).
"Based on its ongoing analysis of the EUA and emerging scientific data, the FDA determined that chloroquine and hydroxychloroquine are unlikely to be effective in treating COVID-19," the agency announced in a June 15 statement.
"In light of ongoing serious cardiac adverse events and other potential serious side effects, the known and potential benefits of chloroquine and hydroxychloroquine no longer outweigh the known and potential risks for the authorized use," noted the FDA. Read more.
Secondary infections common in COVID-19, implications unclear
Secondary respiratory infections appear to be highly prevalent among patients with severe COVID-19, but at this point, most physicians aren’t sure what to make of this understudied phenomenon.
“We really do not understand the implications of secondary infections on outcomes in COVID-19 patients,” David L. Bowton, MD, FCCP, said in an interview. “In most early reports the incidence of secondary infections was much higher in patients dying from COVID-19, compared to survivors, but it isn’t clear whether this indicates that the secondary infection itself led to excess mortality or was more a marker of the severity of the COVID-19 infection."
An early retrospective cohort study including 191 COVID-19 patients in Wuhan, China found that of the 54 who died in hospital, half had secondary bacterial lung infections (Lancet. 2020 Mar 28;395[10229]:1054-62). That comes as no surprise to U.S. physicians, who learned in training that many deaths during the so-called Spanish influenza epidemic were actually caused by secondary pneumonia involving Staphylococcus aureus, commented Daniel L. Ouellette, MD, FCCP. Read more.
Automated insulin delivery system ‘getting better and better’
Medtronic’s next-generation automated insulin delivery system offers significant improvements over the currently available model, particularly in young people with type 1 diabetes, new data suggest.
Data from three trials of such systems using Medtronic’s advanced hybrid closed-loop (AHCL) algorithm (trade name SmartGuard) were presented during the virtual American Diabetes Association (ADA) 80th Scientific Sessions.
Taken together, the data from the three trials showed that the AHCL-based system improved glycemic time-in-range with no increased risk for hypoglycemia, including in children and teenagers, with high patient-reported satisfaction.
“None of these devices is perfect, but they are a substantial improvement over what we’ve had ... They might make the quality of [patient] lives better. That’s really underappreciated,” session moderator Timothy S. Bailey, MD, commented. Read more.
Access more top news from the ADA virtual meeting.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
It’s official: COVID-19 was bad for the health care business
COVID-19 took a huge cut of clinicians’ business in March and April
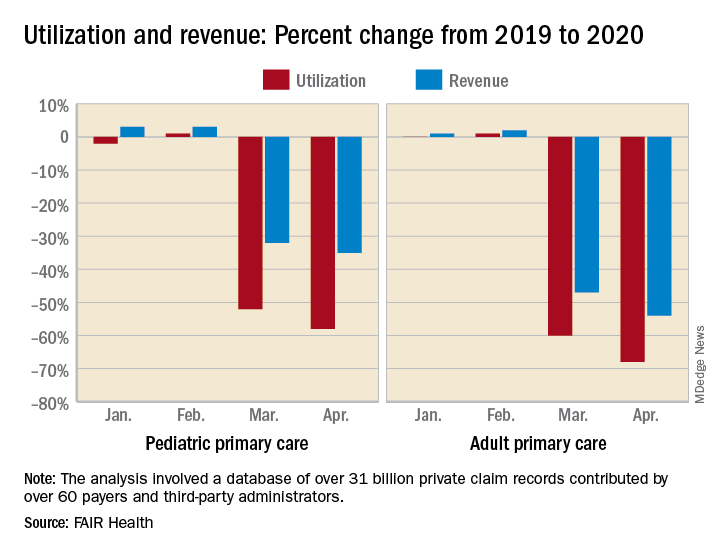
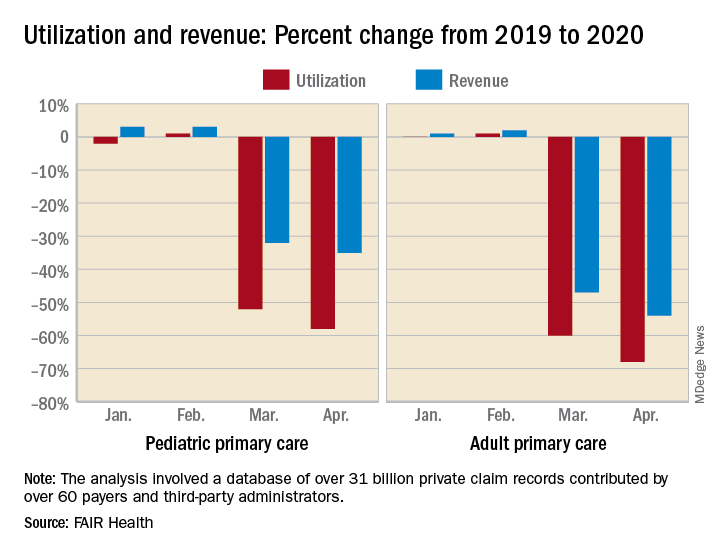
In the first 2 months of the COVID-19 pandemic, health care professionals experienced sharp drops in both utilization and revenue, according to an analysis of the nation’s largest collection of private health care claims data.
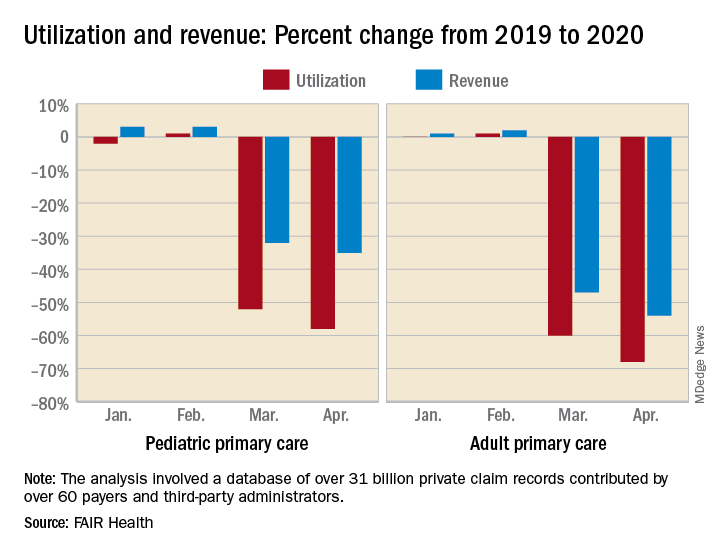
For the months of March and April 2020, use of medical professional services dropped by 65% and 68%, respectively, compared with last year, and estimated revenue fell by 45% and 48%, FAIR Health, a nonprofit organization that manages a database of 31 billion claim records, said in a new report.
For the Northeast states – the epicenter of the pandemic in March and April – patient volume was down by 60% in March and 80% in April, while revenue fell by 55% in March and 79% in April, the organization said.
For this analysis, “a professional service was defined as any service provided by an individual (e.g., physician, nurse, nurse practitioner, physician assistant) instead of being billed by a facility,” FAIR Health noted. Figures for 2019 were adjusted using the Consumer Price Index.
The size of the pandemic-related decreases in utilization and income varied by specialty. Of the seven specialties included in the study, oral surgery was hit the hardest, followed by gastroenterology, cardiology, orthopedics, dermatology, adult primary care, and pediatric primary care, FAIR Health said.
After experiencing a 2% drop in utilization this January and an increase of 4% in February, compared with 2019, gastroenterology saw corresponding drops of 73% in March and 77% in April. Estimated revenue for the specialty was flat in January and rose by 10% in February, but plummeted by 75% in March and 80% in April, the FAIR Health data show.
In cardiology, patient volume from 2019 to 2020 looked like this: Down by 4% in January, up 5% in February, down by 62% in March, and down by 71% in April. The earnings numbers tell a similar story: Down by 2% in January, up by 15% in February, down by 57% in March, and down by 73% in April, the organization reported.
Dermatology did the best among the non–primary care specialties, but that was just a relative success. Utilization still dropped by 62% and 68% in March and April of 2020, compared with last year, and revenue declined by 50% in March and 59% in April, FAIR Health said.
For adult primary care, the utilization numbers were similar, but revenue took a somewhat smaller hit. Patient volume from 2019 to 2020 was fairly steady in January and February, then nosedived in March (down 60%) and April (down 68%). Earnings were up initially, rising 1% in January and 2% in February, but fell 47% in March and 54% in April, FAIR Health said.
Pediatric primary care, it appears, may have been buoyed somewhat by its younger patients. The specialty as a whole saw utilization tumble by 52% in March and 58% in April, but revenue dropped by just 32% and 35%, respectively, according to the report.
A little extra data diving showed that the figures for preventive care visits for patients aged 0-4 years in March and April were –2% and 0% for volume and –2% and 1% for revenue. Meanwhile, the volume of immunizations only dropped by 14% and 10% and vaccine-related revenue slipped by just 7% and 2%, FAIR Health noted.
“Across many specialties from January to April 2020, office or other outpatient [evaluation and management] visits became more common relative to other procedures. ... This may have been due in part to the fact that many of these E&M services could be rendered via telehealth,” FAIR Health said.
Telehealth, however, was no panacea, the report explained: “Even when medical practices have continued to function via telehealth, many have experienced lower reimbursements for telehealth visits than for in-person visits and more time educating patients on how to use the technology.”
COVID-19 took a huge cut of clinicians’ business in March and April
COVID-19 took a huge cut of clinicians’ business in March and April
In the first 2 months of the COVID-19 pandemic, health care professionals experienced sharp drops in both utilization and revenue, according to an analysis of the nation’s largest collection of private health care claims data.
For the months of March and April 2020, use of medical professional services dropped by 65% and 68%, respectively, compared with last year, and estimated revenue fell by 45% and 48%, FAIR Health, a nonprofit organization that manages a database of 31 billion claim records, said in a new report.
For the Northeast states – the epicenter of the pandemic in March and April – patient volume was down by 60% in March and 80% in April, while revenue fell by 55% in March and 79% in April, the organization said.
For this analysis, “a professional service was defined as any service provided by an individual (e.g., physician, nurse, nurse practitioner, physician assistant) instead of being billed by a facility,” FAIR Health noted. Figures for 2019 were adjusted using the Consumer Price Index.
The size of the pandemic-related decreases in utilization and income varied by specialty. Of the seven specialties included in the study, oral surgery was hit the hardest, followed by gastroenterology, cardiology, orthopedics, dermatology, adult primary care, and pediatric primary care, FAIR Health said.
After experiencing a 2% drop in utilization this January and an increase of 4% in February, compared with 2019, gastroenterology saw corresponding drops of 73% in March and 77% in April. Estimated revenue for the specialty was flat in January and rose by 10% in February, but plummeted by 75% in March and 80% in April, the FAIR Health data show.
In cardiology, patient volume from 2019 to 2020 looked like this: Down by 4% in January, up 5% in February, down by 62% in March, and down by 71% in April. The earnings numbers tell a similar story: Down by 2% in January, up by 15% in February, down by 57% in March, and down by 73% in April, the organization reported.
Dermatology did the best among the non–primary care specialties, but that was just a relative success. Utilization still dropped by 62% and 68% in March and April of 2020, compared with last year, and revenue declined by 50% in March and 59% in April, FAIR Health said.
For adult primary care, the utilization numbers were similar, but revenue took a somewhat smaller hit. Patient volume from 2019 to 2020 was fairly steady in January and February, then nosedived in March (down 60%) and April (down 68%). Earnings were up initially, rising 1% in January and 2% in February, but fell 47% in March and 54% in April, FAIR Health said.
Pediatric primary care, it appears, may have been buoyed somewhat by its younger patients. The specialty as a whole saw utilization tumble by 52% in March and 58% in April, but revenue dropped by just 32% and 35%, respectively, according to the report.
A little extra data diving showed that the figures for preventive care visits for patients aged 0-4 years in March and April were –2% and 0% for volume and –2% and 1% for revenue. Meanwhile, the volume of immunizations only dropped by 14% and 10% and vaccine-related revenue slipped by just 7% and 2%, FAIR Health noted.
“Across many specialties from January to April 2020, office or other outpatient [evaluation and management] visits became more common relative to other procedures. ... This may have been due in part to the fact that many of these E&M services could be rendered via telehealth,” FAIR Health said.
Telehealth, however, was no panacea, the report explained: “Even when medical practices have continued to function via telehealth, many have experienced lower reimbursements for telehealth visits than for in-person visits and more time educating patients on how to use the technology.”
In the first 2 months of the COVID-19 pandemic, health care professionals experienced sharp drops in both utilization and revenue, according to an analysis of the nation’s largest collection of private health care claims data.
For the months of March and April 2020, use of medical professional services dropped by 65% and 68%, respectively, compared with last year, and estimated revenue fell by 45% and 48%, FAIR Health, a nonprofit organization that manages a database of 31 billion claim records, said in a new report.
For the Northeast states – the epicenter of the pandemic in March and April – patient volume was down by 60% in March and 80% in April, while revenue fell by 55% in March and 79% in April, the organization said.
For this analysis, “a professional service was defined as any service provided by an individual (e.g., physician, nurse, nurse practitioner, physician assistant) instead of being billed by a facility,” FAIR Health noted. Figures for 2019 were adjusted using the Consumer Price Index.
The size of the pandemic-related decreases in utilization and income varied by specialty. Of the seven specialties included in the study, oral surgery was hit the hardest, followed by gastroenterology, cardiology, orthopedics, dermatology, adult primary care, and pediatric primary care, FAIR Health said.
After experiencing a 2% drop in utilization this January and an increase of 4% in February, compared with 2019, gastroenterology saw corresponding drops of 73% in March and 77% in April. Estimated revenue for the specialty was flat in January and rose by 10% in February, but plummeted by 75% in March and 80% in April, the FAIR Health data show.
In cardiology, patient volume from 2019 to 2020 looked like this: Down by 4% in January, up 5% in February, down by 62% in March, and down by 71% in April. The earnings numbers tell a similar story: Down by 2% in January, up by 15% in February, down by 57% in March, and down by 73% in April, the organization reported.
Dermatology did the best among the non–primary care specialties, but that was just a relative success. Utilization still dropped by 62% and 68% in March and April of 2020, compared with last year, and revenue declined by 50% in March and 59% in April, FAIR Health said.
For adult primary care, the utilization numbers were similar, but revenue took a somewhat smaller hit. Patient volume from 2019 to 2020 was fairly steady in January and February, then nosedived in March (down 60%) and April (down 68%). Earnings were up initially, rising 1% in January and 2% in February, but fell 47% in March and 54% in April, FAIR Health said.
Pediatric primary care, it appears, may have been buoyed somewhat by its younger patients. The specialty as a whole saw utilization tumble by 52% in March and 58% in April, but revenue dropped by just 32% and 35%, respectively, according to the report.
A little extra data diving showed that the figures for preventive care visits for patients aged 0-4 years in March and April were –2% and 0% for volume and –2% and 1% for revenue. Meanwhile, the volume of immunizations only dropped by 14% and 10% and vaccine-related revenue slipped by just 7% and 2%, FAIR Health noted.
“Across many specialties from January to April 2020, office or other outpatient [evaluation and management] visits became more common relative to other procedures. ... This may have been due in part to the fact that many of these E&M services could be rendered via telehealth,” FAIR Health said.
Telehealth, however, was no panacea, the report explained: “Even when medical practices have continued to function via telehealth, many have experienced lower reimbursements for telehealth visits than for in-person visits and more time educating patients on how to use the technology.”
Pediatric Dermatology: A Supplement to Pediatric News & Dermatology News
Content includes:
- Early onset of atopic dermatitis linked to poorer control, could signify more persistent disease
- Patients with actopic dermatitis should be routinely asked about conjunctivitis
- Hope on the horizon: New cantharidin formulation alleviates molluscum contagiosum in pivotal trials
- Patch testing in atopic dermatitis: When and how
- Topical calcineurin inhibitors are an effective treatment option for periorificial dermatitis
- Psychology consults for children’s skin issues can boost adherence, wellness
Content includes:
- Early onset of atopic dermatitis linked to poorer control, could signify more persistent disease
- Patients with actopic dermatitis should be routinely asked about conjunctivitis
- Hope on the horizon: New cantharidin formulation alleviates molluscum contagiosum in pivotal trials
- Patch testing in atopic dermatitis: When and how
- Topical calcineurin inhibitors are an effective treatment option for periorificial dermatitis
- Psychology consults for children’s skin issues can boost adherence, wellness
Content includes:
- Early onset of atopic dermatitis linked to poorer control, could signify more persistent disease
- Patients with actopic dermatitis should be routinely asked about conjunctivitis
- Hope on the horizon: New cantharidin formulation alleviates molluscum contagiosum in pivotal trials
- Patch testing in atopic dermatitis: When and how
- Topical calcineurin inhibitors are an effective treatment option for periorificial dermatitis
- Psychology consults for children’s skin issues can boost adherence, wellness
For COVID-19 plus diabetes, glycemic control tops treatment list
Optimizing glycemic control “is the key to overall treatment in people with diabetes and COVID-19,” said Antonio Ceriello, MD, during a June 5 webinar sponsored by Harvard Medical School, Boston.
Dr. Ceriello, a research consultant with the Italian Ministry of Health, IRCCS Multi-Medica, Milan, highlighted a recent study that examined the association of blood glucose control and outcomes in COVID-19 patients with preexisting type 2 diabetes.
Among 7,000 cases of COVID-19, type 2 diabetes correlated with a higher death rate. However, those with well-controlled blood glucose (upper limit ≤10 mmol/L) had a survival rate of 98.9%, compared with just 11% among those with poorly controlled blood glucose (upper limit >10 mmol/L), a reduction in risk of 86% (adjusted hazard ratio, 0.14; Cell Metab. 2020 May 1. doi: 10.1016/j.cmet.2020.04.021).
Clinicians should also consider the possible side effects of hypoglycemic agents in the evolution of this disease. This is true of all patients, not just diabetes patients, Dr. Ceriello said. “We have data showing that ... hyperglycemia contributes directly to worsening the prognosis of COVID-19 independent of the presence of diabetes.”
One study found that the glycosylation of ACE-2 played an important role in allowing cellular entry of the virus (Am J Physiol Endocrinol Metab. 2020 Mar 31;318:E736-41). “This is something that could be related to hyperglycemia,” he added.
Another risk factor is thrombosis, a clear contributor to death rates in COVID-19. Research on thrombosis incidence in COVID-19 patients with diabetes reported higher levels of D-dimer levels in people with diabetes, especially among those who couldn’t manage their disease.
Tying all of these factors together, Dr. Ceriello discussed how ACE-2 glycosylation, in combination with other factors in SARS-CoV-2 infection, could lead to hyperglycemia, thrombosis, and subsequently multiorgan damage in diabetes patients.
Other research has associated higher HbA1c levels (mean HbA1c, 7.5%) with higher mortality risk in COVID-19 patients, said another speaker, Linong Ji, MD, director for endocrinology and metabolism at Peking University People’s Hospital, Beijing, and director of Peking University’s Diabetes Center. Proper guidance is key to ensuring early detection of hyperglycemic crisis in people with diabetes, advised Dr. Ji.
Global management of diabetes in SARS-CoV-2 patients is “quite challenging,” given that most patients don’t have their diabetes under control, said host and moderator A. Enrique Caballero, MD, an endocrinologist/investigator in the division of endocrinology, diabetes, and hypertension and division of global health equity at Brigham and Women’s Hospital, Boston. “They are not meeting treatment targets for cholesterol or glucose control. So we’re not managing optimal care. And now on top of this, we have COVID-19.”
Optimizing glycemic control “is the key to overall treatment in people with diabetes and COVID-19,” said Antonio Ceriello, MD, during a June 5 webinar sponsored by Harvard Medical School, Boston.
Dr. Ceriello, a research consultant with the Italian Ministry of Health, IRCCS Multi-Medica, Milan, highlighted a recent study that examined the association of blood glucose control and outcomes in COVID-19 patients with preexisting type 2 diabetes.
Among 7,000 cases of COVID-19, type 2 diabetes correlated with a higher death rate. However, those with well-controlled blood glucose (upper limit ≤10 mmol/L) had a survival rate of 98.9%, compared with just 11% among those with poorly controlled blood glucose (upper limit >10 mmol/L), a reduction in risk of 86% (adjusted hazard ratio, 0.14; Cell Metab. 2020 May 1. doi: 10.1016/j.cmet.2020.04.021).
Clinicians should also consider the possible side effects of hypoglycemic agents in the evolution of this disease. This is true of all patients, not just diabetes patients, Dr. Ceriello said. “We have data showing that ... hyperglycemia contributes directly to worsening the prognosis of COVID-19 independent of the presence of diabetes.”
One study found that the glycosylation of ACE-2 played an important role in allowing cellular entry of the virus (Am J Physiol Endocrinol Metab. 2020 Mar 31;318:E736-41). “This is something that could be related to hyperglycemia,” he added.
Another risk factor is thrombosis, a clear contributor to death rates in COVID-19. Research on thrombosis incidence in COVID-19 patients with diabetes reported higher levels of D-dimer levels in people with diabetes, especially among those who couldn’t manage their disease.
Tying all of these factors together, Dr. Ceriello discussed how ACE-2 glycosylation, in combination with other factors in SARS-CoV-2 infection, could lead to hyperglycemia, thrombosis, and subsequently multiorgan damage in diabetes patients.
Other research has associated higher HbA1c levels (mean HbA1c, 7.5%) with higher mortality risk in COVID-19 patients, said another speaker, Linong Ji, MD, director for endocrinology and metabolism at Peking University People’s Hospital, Beijing, and director of Peking University’s Diabetes Center. Proper guidance is key to ensuring early detection of hyperglycemic crisis in people with diabetes, advised Dr. Ji.
Global management of diabetes in SARS-CoV-2 patients is “quite challenging,” given that most patients don’t have their diabetes under control, said host and moderator A. Enrique Caballero, MD, an endocrinologist/investigator in the division of endocrinology, diabetes, and hypertension and division of global health equity at Brigham and Women’s Hospital, Boston. “They are not meeting treatment targets for cholesterol or glucose control. So we’re not managing optimal care. And now on top of this, we have COVID-19.”
Optimizing glycemic control “is the key to overall treatment in people with diabetes and COVID-19,” said Antonio Ceriello, MD, during a June 5 webinar sponsored by Harvard Medical School, Boston.
Dr. Ceriello, a research consultant with the Italian Ministry of Health, IRCCS Multi-Medica, Milan, highlighted a recent study that examined the association of blood glucose control and outcomes in COVID-19 patients with preexisting type 2 diabetes.
Among 7,000 cases of COVID-19, type 2 diabetes correlated with a higher death rate. However, those with well-controlled blood glucose (upper limit ≤10 mmol/L) had a survival rate of 98.9%, compared with just 11% among those with poorly controlled blood glucose (upper limit >10 mmol/L), a reduction in risk of 86% (adjusted hazard ratio, 0.14; Cell Metab. 2020 May 1. doi: 10.1016/j.cmet.2020.04.021).
Clinicians should also consider the possible side effects of hypoglycemic agents in the evolution of this disease. This is true of all patients, not just diabetes patients, Dr. Ceriello said. “We have data showing that ... hyperglycemia contributes directly to worsening the prognosis of COVID-19 independent of the presence of diabetes.”
One study found that the glycosylation of ACE-2 played an important role in allowing cellular entry of the virus (Am J Physiol Endocrinol Metab. 2020 Mar 31;318:E736-41). “This is something that could be related to hyperglycemia,” he added.
Another risk factor is thrombosis, a clear contributor to death rates in COVID-19. Research on thrombosis incidence in COVID-19 patients with diabetes reported higher levels of D-dimer levels in people with diabetes, especially among those who couldn’t manage their disease.
Tying all of these factors together, Dr. Ceriello discussed how ACE-2 glycosylation, in combination with other factors in SARS-CoV-2 infection, could lead to hyperglycemia, thrombosis, and subsequently multiorgan damage in diabetes patients.
Other research has associated higher HbA1c levels (mean HbA1c, 7.5%) with higher mortality risk in COVID-19 patients, said another speaker, Linong Ji, MD, director for endocrinology and metabolism at Peking University People’s Hospital, Beijing, and director of Peking University’s Diabetes Center. Proper guidance is key to ensuring early detection of hyperglycemic crisis in people with diabetes, advised Dr. Ji.
Global management of diabetes in SARS-CoV-2 patients is “quite challenging,” given that most patients don’t have their diabetes under control, said host and moderator A. Enrique Caballero, MD, an endocrinologist/investigator in the division of endocrinology, diabetes, and hypertension and division of global health equity at Brigham and Women’s Hospital, Boston. “They are not meeting treatment targets for cholesterol or glucose control. So we’re not managing optimal care. And now on top of this, we have COVID-19.”
Secondary infections common in COVID-19, implications unclear
but at this point, most pulmonologists aren’t sure what to make of this understudied phenomenon.
“We really do not understand the implications of secondary infections on outcomes in COVID-19 patients,” David L. Bowton, MD, FCCP, said in an interview. “In most early reports the incidence of secondary infections was much higher in patients dying from COVID-19, compared to survivors, but it isn’t clear whether this indicates that the secondary infection itself led to excess mortality or was more a marker of the severity of the COVID-19 infection.
“Further, details of the diagnostic criteria used, the microbiology, and the appropriateness of treatment of these secondary infections has not generally been included in these reports,” added Dr. Bowton, a pulmonologist and professor emeritus of critical care anesthesiology at Wake Forest University, Winston-Salem, N.C.
One such early retrospective cohort study included 191 COVID-19 patients in Wuhan, China. Of the 54 who died in hospital, half had secondary bacterial lung infections (Lancet. 2020 Mar 28;395[10229]:1054-62). That comes as no surprise to U.S. pulmonologists, who learned back in their training that many deaths during the so-called Spanish influenza epidemic of 1918-1920 were actually caused by secondary pneumonia involving Staphylococcus aureus, commented Daniel L. Ouellette, MD, FCCP, associate director of medical critical care at Henry Ford Hospital, Detroit.
“Critically ill patients are highly susceptible to secondary infections regardless of the cause of the patient’s critical illness,” he noted in an interview. “Recent reports of secondary infections in patients critically ill from COVID-19 are interesting but should be considered in this context. To confirm that COVID-19 patients have a different, or increased, risk of infection at specific sites or from specific agents will require careful study.”
That will be no easy matter given the challenges of obtaining bronchoalveolar lavage samples in mechanically ventilated patients with COVID-19, according to Eric J. Gartman, MD, FCCP, a pulmonologist at Brown University, Providence, R.I., and director of the pulmonary function laboratory at the Providence Veterans Affairs Medical Center.
“Unfortunately, many of the invasive modalities that are typically employed to help diagnose secondary infections in critically ill patients are being severely limited or even prohibited in COVID-19 patients due to infection control measures,” he said. As a result, Dr. Gartman noted, intensivists are often resorting to empiric broad-spectrum antimicrobial therapy in patients with severe COVID-19 and are without ready access to the bacterial cultures which might otherwise permit later treatment de-escalation or retargeting.
Among the myriad areas of uncertainty regarding COVID-19 is the proportion of bacterial coinfections that are hospital acquired. Given the lengthy duration of invasive mechanical ventilation in patients with severe COVID-19 – a mean of 9.1 days in the United Kingdom – the chances of hospital-acquired infection are likely substantial. Moreover, a recent single-center U.K. study involving microbiologic testing in 195 consecutive patients newly hospitalized for COVID-19 reported that community-acquired bacterial infection was uncommon: Just 4% of patients had pneumococcal coinfection at hospital admission, and S. aureus wasn’t detected in anyone (Lancet. 2020;1:362. doi:10.1016/S2666-5247[20]30036-7). French investigators have reported detecting putative invasive pulmonary aspergillosis in nearly one-third of a small series of 27 consecutive mechanically ventilated COVID-19 patients (Lancet Resp Med. 2020; 8[6]:e48-9). Dr. Gartman said the diagnostic testing methods utilized in this and similar reports haven’t been prospectively validated in COVID-19. The testing methods may not indicate invasive Aspergillus infection in this population with a high degree of certainty, since they have previously been performed mainly in patients with hematologic malignancies.
“Although there is nothing definitive regarding this research, as a practicing critical care doctor one should respect these findings and consider this secondary diagnosis if the supporting clinical data is positive, especially given that the mortality risk in this population is high,” he advised.
Dr. Bowton said that he and his fellow intensivists at Wake Forest Baptist Health don’t routinely screen COVID-19 patients for secondary bacterial or fungal infections. And in talking with colleagues around the country, it’s his impression that most have similarly elected not to do so.
“However, our clinical index of suspicion for secondary infections is heightened and, if triggered, will initiate a search for and treatment of these secondary infections,” Dr. Bowton said.
but at this point, most pulmonologists aren’t sure what to make of this understudied phenomenon.
“We really do not understand the implications of secondary infections on outcomes in COVID-19 patients,” David L. Bowton, MD, FCCP, said in an interview. “In most early reports the incidence of secondary infections was much higher in patients dying from COVID-19, compared to survivors, but it isn’t clear whether this indicates that the secondary infection itself led to excess mortality or was more a marker of the severity of the COVID-19 infection.
“Further, details of the diagnostic criteria used, the microbiology, and the appropriateness of treatment of these secondary infections has not generally been included in these reports,” added Dr. Bowton, a pulmonologist and professor emeritus of critical care anesthesiology at Wake Forest University, Winston-Salem, N.C.
One such early retrospective cohort study included 191 COVID-19 patients in Wuhan, China. Of the 54 who died in hospital, half had secondary bacterial lung infections (Lancet. 2020 Mar 28;395[10229]:1054-62). That comes as no surprise to U.S. pulmonologists, who learned back in their training that many deaths during the so-called Spanish influenza epidemic of 1918-1920 were actually caused by secondary pneumonia involving Staphylococcus aureus, commented Daniel L. Ouellette, MD, FCCP, associate director of medical critical care at Henry Ford Hospital, Detroit.
“Critically ill patients are highly susceptible to secondary infections regardless of the cause of the patient’s critical illness,” he noted in an interview. “Recent reports of secondary infections in patients critically ill from COVID-19 are interesting but should be considered in this context. To confirm that COVID-19 patients have a different, or increased, risk of infection at specific sites or from specific agents will require careful study.”
That will be no easy matter given the challenges of obtaining bronchoalveolar lavage samples in mechanically ventilated patients with COVID-19, according to Eric J. Gartman, MD, FCCP, a pulmonologist at Brown University, Providence, R.I., and director of the pulmonary function laboratory at the Providence Veterans Affairs Medical Center.
“Unfortunately, many of the invasive modalities that are typically employed to help diagnose secondary infections in critically ill patients are being severely limited or even prohibited in COVID-19 patients due to infection control measures,” he said. As a result, Dr. Gartman noted, intensivists are often resorting to empiric broad-spectrum antimicrobial therapy in patients with severe COVID-19 and are without ready access to the bacterial cultures which might otherwise permit later treatment de-escalation or retargeting.
Among the myriad areas of uncertainty regarding COVID-19 is the proportion of bacterial coinfections that are hospital acquired. Given the lengthy duration of invasive mechanical ventilation in patients with severe COVID-19 – a mean of 9.1 days in the United Kingdom – the chances of hospital-acquired infection are likely substantial. Moreover, a recent single-center U.K. study involving microbiologic testing in 195 consecutive patients newly hospitalized for COVID-19 reported that community-acquired bacterial infection was uncommon: Just 4% of patients had pneumococcal coinfection at hospital admission, and S. aureus wasn’t detected in anyone (Lancet. 2020;1:362. doi:10.1016/S2666-5247[20]30036-7). French investigators have reported detecting putative invasive pulmonary aspergillosis in nearly one-third of a small series of 27 consecutive mechanically ventilated COVID-19 patients (Lancet Resp Med. 2020; 8[6]:e48-9). Dr. Gartman said the diagnostic testing methods utilized in this and similar reports haven’t been prospectively validated in COVID-19. The testing methods may not indicate invasive Aspergillus infection in this population with a high degree of certainty, since they have previously been performed mainly in patients with hematologic malignancies.
“Although there is nothing definitive regarding this research, as a practicing critical care doctor one should respect these findings and consider this secondary diagnosis if the supporting clinical data is positive, especially given that the mortality risk in this population is high,” he advised.
Dr. Bowton said that he and his fellow intensivists at Wake Forest Baptist Health don’t routinely screen COVID-19 patients for secondary bacterial or fungal infections. And in talking with colleagues around the country, it’s his impression that most have similarly elected not to do so.
“However, our clinical index of suspicion for secondary infections is heightened and, if triggered, will initiate a search for and treatment of these secondary infections,” Dr. Bowton said.
but at this point, most pulmonologists aren’t sure what to make of this understudied phenomenon.
“We really do not understand the implications of secondary infections on outcomes in COVID-19 patients,” David L. Bowton, MD, FCCP, said in an interview. “In most early reports the incidence of secondary infections was much higher in patients dying from COVID-19, compared to survivors, but it isn’t clear whether this indicates that the secondary infection itself led to excess mortality or was more a marker of the severity of the COVID-19 infection.
“Further, details of the diagnostic criteria used, the microbiology, and the appropriateness of treatment of these secondary infections has not generally been included in these reports,” added Dr. Bowton, a pulmonologist and professor emeritus of critical care anesthesiology at Wake Forest University, Winston-Salem, N.C.
One such early retrospective cohort study included 191 COVID-19 patients in Wuhan, China. Of the 54 who died in hospital, half had secondary bacterial lung infections (Lancet. 2020 Mar 28;395[10229]:1054-62). That comes as no surprise to U.S. pulmonologists, who learned back in their training that many deaths during the so-called Spanish influenza epidemic of 1918-1920 were actually caused by secondary pneumonia involving Staphylococcus aureus, commented Daniel L. Ouellette, MD, FCCP, associate director of medical critical care at Henry Ford Hospital, Detroit.
“Critically ill patients are highly susceptible to secondary infections regardless of the cause of the patient’s critical illness,” he noted in an interview. “Recent reports of secondary infections in patients critically ill from COVID-19 are interesting but should be considered in this context. To confirm that COVID-19 patients have a different, or increased, risk of infection at specific sites or from specific agents will require careful study.”
That will be no easy matter given the challenges of obtaining bronchoalveolar lavage samples in mechanically ventilated patients with COVID-19, according to Eric J. Gartman, MD, FCCP, a pulmonologist at Brown University, Providence, R.I., and director of the pulmonary function laboratory at the Providence Veterans Affairs Medical Center.
“Unfortunately, many of the invasive modalities that are typically employed to help diagnose secondary infections in critically ill patients are being severely limited or even prohibited in COVID-19 patients due to infection control measures,” he said. As a result, Dr. Gartman noted, intensivists are often resorting to empiric broad-spectrum antimicrobial therapy in patients with severe COVID-19 and are without ready access to the bacterial cultures which might otherwise permit later treatment de-escalation or retargeting.
Among the myriad areas of uncertainty regarding COVID-19 is the proportion of bacterial coinfections that are hospital acquired. Given the lengthy duration of invasive mechanical ventilation in patients with severe COVID-19 – a mean of 9.1 days in the United Kingdom – the chances of hospital-acquired infection are likely substantial. Moreover, a recent single-center U.K. study involving microbiologic testing in 195 consecutive patients newly hospitalized for COVID-19 reported that community-acquired bacterial infection was uncommon: Just 4% of patients had pneumococcal coinfection at hospital admission, and S. aureus wasn’t detected in anyone (Lancet. 2020;1:362. doi:10.1016/S2666-5247[20]30036-7). French investigators have reported detecting putative invasive pulmonary aspergillosis in nearly one-third of a small series of 27 consecutive mechanically ventilated COVID-19 patients (Lancet Resp Med. 2020; 8[6]:e48-9). Dr. Gartman said the diagnostic testing methods utilized in this and similar reports haven’t been prospectively validated in COVID-19. The testing methods may not indicate invasive Aspergillus infection in this population with a high degree of certainty, since they have previously been performed mainly in patients with hematologic malignancies.
“Although there is nothing definitive regarding this research, as a practicing critical care doctor one should respect these findings and consider this secondary diagnosis if the supporting clinical data is positive, especially given that the mortality risk in this population is high,” he advised.
Dr. Bowton said that he and his fellow intensivists at Wake Forest Baptist Health don’t routinely screen COVID-19 patients for secondary bacterial or fungal infections. And in talking with colleagues around the country, it’s his impression that most have similarly elected not to do so.
“However, our clinical index of suspicion for secondary infections is heightened and, if triggered, will initiate a search for and treatment of these secondary infections,” Dr. Bowton said.
CDC emphasizes pandemic not over, need to avoid large gatherings
Robert Redfield, MD, Director, CDC, and Jay C. Butler, MD, Deputy Director of Infectious Diseases and COVID-19 Response Incident Manager, CDC, discussed two new sets of CDC guidance on deciding to go out and attending group gatherings.
“We recognize that we’re all getting tired of staying at home; people long for the life that they had back in December, and as we head into the summer months, we know that Americans will be looking forward to reconnecting with family and friends and being able to attend events, and we want that to occur as safely as possible,” Butler said.
“Our recommendations evolved based on new information that becomes available, but it continues to be extremely important that we embrace the recommendations of social distancing, handwashing, and wearing a face covering when we’re in public as some of the key defenses that we have against this virus,” Redfield explained.
“The pandemic is not over and it’s important to recognize that. While COVID-19 is still making headlines everywhere, we know the pandemic hasn’t affected everyone everywhere in the same way,” Butler said.
He noted that it is important to prepare for next fall and winter, when we can expect influenza season to complicate matters. “If anything, we must be overly-prepared for what we might face later this year,” he continued, adding that it is important to get vaccinated against influenza. “[F]lu and COVID-19 could be circulating together as we move into the fall and winter months,” he concluded.
Americans Mostly Following Guidelines
The agency also presented data from an article published online June 12 in Morbidity and Mortality Weekly Report that “underscores the fact that American people have taken mitigation efforts seriously…and it demonstrates our collective spirit in responding to the pandemic,” Butler said.
In it, the researchers describe representative panel surveys conducted among 4042 adults aged 18 years or older in New York City and Los Angeles — the two most populous cities in the United States — and “broadly across the United States” during May 5 to May 12, 2020.
Most respondents supported stay-at-home orders and nonessential business closures (United States, 79.5%; New York City, 86.7%; Los Angeles, 81.5%) and always or often wore cloth face coverings in public (United States, 74.1%; New York City, 89.6%; Los Angeles, 89.8%). Respondents also agreed that nonessential workers should remain at home (United States, 67.3%; New York City, 76.6%; Los Angeles, 69.1%), report Mark É. Czeisler, from Monash University and Austin Health, both in Melbourne, Australia, and colleagues.
There was wide support with public health guidelines: more than 87% of individuals in each area agreed that individuals should keep six feet of distance between themselves and others, and more than 82% in each area said that people should limit gatherings to fewer than 10 individuals.
At the time the survey was conducted, most were against indoor dining at restaurants (United States, 66.6%; New York City, 81.5%; Los Angeles, 71.8%).
Adherence “Widespread,” Survey Finds
Most respondents said they were adhering to COVID-19 mitigation guidance, including self-isolating (United States, 77.3%; New York City, 84.6%; Los Angeles, 83.0%) and “always or often” kept at least six feet between themselves and others (New York City, 85.7%; Los Angeles, 82.6%).
More than 85% of respondents in each of the three cohorts said they always or often avoided groups of 10 or more individuals.
About 90% of respondents said they had been in a public area during the last week, with 74.1% of those saying they always or often covered their face in public; respondents in New York City (89.6%) and Los Angeles (89.8%) had higher percentages of this behavior compared with respondents from the United States overall.
Most respondents felt that restrictions in their state were balanced or too lax (United States, 84.3%; New York City, 89.7%; Los Angeles, 79.7%) and said they would feel unsafe if restrictions were eased nationwide at that time (United States, 74.3%; New York City, 81.5%; Los Angeles, 73.4%). However, some individuals who said they would feel unsafe still wanted community mitigation strategies eased and were willing to accept risks resulting from lifting restrictions (United States, 17.1%; New York City, 12.6%; Los Angeles, 12.7%).
“Reported prevalence of self-isolation and feeling safe if community mitigation strategies were lifted differed significantly by age, employment status, and essential worker status among adults in the U.S. survey cohort,” the authors write.
Reports of self-isolation were highest among persons aged 18 to 24 years (92.3%) and lowest among those aged 45 to 54 years (71.5%). Yet, young adults aged 18 to 24 years (43.1%) were more than twice as likely to say they would feel safe if community mitigation strategies were eased, compared with adults aged 65 years or older (19.2%).
Almost half (47.2%) of employed respondents in the US cohort were essential workers; essential workers were “significantly less likely” to report self-isolating when compared with nonessential workers (63.1% vs 80.6%). Some 37.7% of essential workers said they would feel safe if community mitigation strategies were eased, compared with 23.7% of nonessential workers.
“Respondents who were male, employed, or essential workers were significantly more likely to report having been in public areas in the past week. Among respondents who had been in public areas during the preceding week, significantly higher percentages of women, adults aged ≥ 65 years, retired persons, and those living in urban areas reported wearing cloth face coverings,” the authors explain.
The findings are subject to several limitations, including self-reporting and the fact that some respondents may have known someone who tested positive for COVID-19 or died from it, the authors note. Respondents were not representative of the US population and the findings may not be generalizable.
This article first appeared on Medscape.com.
Robert Redfield, MD, Director, CDC, and Jay C. Butler, MD, Deputy Director of Infectious Diseases and COVID-19 Response Incident Manager, CDC, discussed two new sets of CDC guidance on deciding to go out and attending group gatherings.
“We recognize that we’re all getting tired of staying at home; people long for the life that they had back in December, and as we head into the summer months, we know that Americans will be looking forward to reconnecting with family and friends and being able to attend events, and we want that to occur as safely as possible,” Butler said.
“Our recommendations evolved based on new information that becomes available, but it continues to be extremely important that we embrace the recommendations of social distancing, handwashing, and wearing a face covering when we’re in public as some of the key defenses that we have against this virus,” Redfield explained.
“The pandemic is not over and it’s important to recognize that. While COVID-19 is still making headlines everywhere, we know the pandemic hasn’t affected everyone everywhere in the same way,” Butler said.
He noted that it is important to prepare for next fall and winter, when we can expect influenza season to complicate matters. “If anything, we must be overly-prepared for what we might face later this year,” he continued, adding that it is important to get vaccinated against influenza. “[F]lu and COVID-19 could be circulating together as we move into the fall and winter months,” he concluded.
Americans Mostly Following Guidelines
The agency also presented data from an article published online June 12 in Morbidity and Mortality Weekly Report that “underscores the fact that American people have taken mitigation efforts seriously…and it demonstrates our collective spirit in responding to the pandemic,” Butler said.
In it, the researchers describe representative panel surveys conducted among 4042 adults aged 18 years or older in New York City and Los Angeles — the two most populous cities in the United States — and “broadly across the United States” during May 5 to May 12, 2020.
Most respondents supported stay-at-home orders and nonessential business closures (United States, 79.5%; New York City, 86.7%; Los Angeles, 81.5%) and always or often wore cloth face coverings in public (United States, 74.1%; New York City, 89.6%; Los Angeles, 89.8%). Respondents also agreed that nonessential workers should remain at home (United States, 67.3%; New York City, 76.6%; Los Angeles, 69.1%), report Mark É. Czeisler, from Monash University and Austin Health, both in Melbourne, Australia, and colleagues.
There was wide support with public health guidelines: more than 87% of individuals in each area agreed that individuals should keep six feet of distance between themselves and others, and more than 82% in each area said that people should limit gatherings to fewer than 10 individuals.
At the time the survey was conducted, most were against indoor dining at restaurants (United States, 66.6%; New York City, 81.5%; Los Angeles, 71.8%).
Adherence “Widespread,” Survey Finds
Most respondents said they were adhering to COVID-19 mitigation guidance, including self-isolating (United States, 77.3%; New York City, 84.6%; Los Angeles, 83.0%) and “always or often” kept at least six feet between themselves and others (New York City, 85.7%; Los Angeles, 82.6%).
More than 85% of respondents in each of the three cohorts said they always or often avoided groups of 10 or more individuals.
About 90% of respondents said they had been in a public area during the last week, with 74.1% of those saying they always or often covered their face in public; respondents in New York City (89.6%) and Los Angeles (89.8%) had higher percentages of this behavior compared with respondents from the United States overall.
Most respondents felt that restrictions in their state were balanced or too lax (United States, 84.3%; New York City, 89.7%; Los Angeles, 79.7%) and said they would feel unsafe if restrictions were eased nationwide at that time (United States, 74.3%; New York City, 81.5%; Los Angeles, 73.4%). However, some individuals who said they would feel unsafe still wanted community mitigation strategies eased and were willing to accept risks resulting from lifting restrictions (United States, 17.1%; New York City, 12.6%; Los Angeles, 12.7%).
“Reported prevalence of self-isolation and feeling safe if community mitigation strategies were lifted differed significantly by age, employment status, and essential worker status among adults in the U.S. survey cohort,” the authors write.
Reports of self-isolation were highest among persons aged 18 to 24 years (92.3%) and lowest among those aged 45 to 54 years (71.5%). Yet, young adults aged 18 to 24 years (43.1%) were more than twice as likely to say they would feel safe if community mitigation strategies were eased, compared with adults aged 65 years or older (19.2%).
Almost half (47.2%) of employed respondents in the US cohort were essential workers; essential workers were “significantly less likely” to report self-isolating when compared with nonessential workers (63.1% vs 80.6%). Some 37.7% of essential workers said they would feel safe if community mitigation strategies were eased, compared with 23.7% of nonessential workers.
“Respondents who were male, employed, or essential workers were significantly more likely to report having been in public areas in the past week. Among respondents who had been in public areas during the preceding week, significantly higher percentages of women, adults aged ≥ 65 years, retired persons, and those living in urban areas reported wearing cloth face coverings,” the authors explain.
The findings are subject to several limitations, including self-reporting and the fact that some respondents may have known someone who tested positive for COVID-19 or died from it, the authors note. Respondents were not representative of the US population and the findings may not be generalizable.
This article first appeared on Medscape.com.
Robert Redfield, MD, Director, CDC, and Jay C. Butler, MD, Deputy Director of Infectious Diseases and COVID-19 Response Incident Manager, CDC, discussed two new sets of CDC guidance on deciding to go out and attending group gatherings.
“We recognize that we’re all getting tired of staying at home; people long for the life that they had back in December, and as we head into the summer months, we know that Americans will be looking forward to reconnecting with family and friends and being able to attend events, and we want that to occur as safely as possible,” Butler said.
“Our recommendations evolved based on new information that becomes available, but it continues to be extremely important that we embrace the recommendations of social distancing, handwashing, and wearing a face covering when we’re in public as some of the key defenses that we have against this virus,” Redfield explained.
“The pandemic is not over and it’s important to recognize that. While COVID-19 is still making headlines everywhere, we know the pandemic hasn’t affected everyone everywhere in the same way,” Butler said.
He noted that it is important to prepare for next fall and winter, when we can expect influenza season to complicate matters. “If anything, we must be overly-prepared for what we might face later this year,” he continued, adding that it is important to get vaccinated against influenza. “[F]lu and COVID-19 could be circulating together as we move into the fall and winter months,” he concluded.
Americans Mostly Following Guidelines
The agency also presented data from an article published online June 12 in Morbidity and Mortality Weekly Report that “underscores the fact that American people have taken mitigation efforts seriously…and it demonstrates our collective spirit in responding to the pandemic,” Butler said.
In it, the researchers describe representative panel surveys conducted among 4042 adults aged 18 years or older in New York City and Los Angeles — the two most populous cities in the United States — and “broadly across the United States” during May 5 to May 12, 2020.
Most respondents supported stay-at-home orders and nonessential business closures (United States, 79.5%; New York City, 86.7%; Los Angeles, 81.5%) and always or often wore cloth face coverings in public (United States, 74.1%; New York City, 89.6%; Los Angeles, 89.8%). Respondents also agreed that nonessential workers should remain at home (United States, 67.3%; New York City, 76.6%; Los Angeles, 69.1%), report Mark É. Czeisler, from Monash University and Austin Health, both in Melbourne, Australia, and colleagues.
There was wide support with public health guidelines: more than 87% of individuals in each area agreed that individuals should keep six feet of distance between themselves and others, and more than 82% in each area said that people should limit gatherings to fewer than 10 individuals.
At the time the survey was conducted, most were against indoor dining at restaurants (United States, 66.6%; New York City, 81.5%; Los Angeles, 71.8%).
Adherence “Widespread,” Survey Finds
Most respondents said they were adhering to COVID-19 mitigation guidance, including self-isolating (United States, 77.3%; New York City, 84.6%; Los Angeles, 83.0%) and “always or often” kept at least six feet between themselves and others (New York City, 85.7%; Los Angeles, 82.6%).
More than 85% of respondents in each of the three cohorts said they always or often avoided groups of 10 or more individuals.
About 90% of respondents said they had been in a public area during the last week, with 74.1% of those saying they always or often covered their face in public; respondents in New York City (89.6%) and Los Angeles (89.8%) had higher percentages of this behavior compared with respondents from the United States overall.
Most respondents felt that restrictions in their state were balanced or too lax (United States, 84.3%; New York City, 89.7%; Los Angeles, 79.7%) and said they would feel unsafe if restrictions were eased nationwide at that time (United States, 74.3%; New York City, 81.5%; Los Angeles, 73.4%). However, some individuals who said they would feel unsafe still wanted community mitigation strategies eased and were willing to accept risks resulting from lifting restrictions (United States, 17.1%; New York City, 12.6%; Los Angeles, 12.7%).
“Reported prevalence of self-isolation and feeling safe if community mitigation strategies were lifted differed significantly by age, employment status, and essential worker status among adults in the U.S. survey cohort,” the authors write.
Reports of self-isolation were highest among persons aged 18 to 24 years (92.3%) and lowest among those aged 45 to 54 years (71.5%). Yet, young adults aged 18 to 24 years (43.1%) were more than twice as likely to say they would feel safe if community mitigation strategies were eased, compared with adults aged 65 years or older (19.2%).
Almost half (47.2%) of employed respondents in the US cohort were essential workers; essential workers were “significantly less likely” to report self-isolating when compared with nonessential workers (63.1% vs 80.6%). Some 37.7% of essential workers said they would feel safe if community mitigation strategies were eased, compared with 23.7% of nonessential workers.
“Respondents who were male, employed, or essential workers were significantly more likely to report having been in public areas in the past week. Among respondents who had been in public areas during the preceding week, significantly higher percentages of women, adults aged ≥ 65 years, retired persons, and those living in urban areas reported wearing cloth face coverings,” the authors explain.
The findings are subject to several limitations, including self-reporting and the fact that some respondents may have known someone who tested positive for COVID-19 or died from it, the authors note. Respondents were not representative of the US population and the findings may not be generalizable.
This article first appeared on Medscape.com.
Daily Recap: Stressed out primary care docs, ‘hospital at home’ for cancer patients
Here are the stories our MDedge editors across specialties think you need to know about today:
Racism, COVID-19 lead to sky-high stress levels
Primary care clinicians, already experiencing all-time high stress levels related to COVID-19, are now struggling to cope with the fallout from racism and the death of George Floyd, according to a survey conducted June 5-8.
When asked how the situation has affected their practices, 12% of the survey’s 586 respondents “drew clear connections between the current racial unrest and the health of their patients,” the Larry A. Green Center said in a recent statement. One-third of the clinicians also said that recent racism-related events have had a negative effect on their own well-being.
In a related survey of 1,111 patients conducted June 8 about 65% of patients said that racism affected emotional, psychological, and behavioral health.
“The fact that so many patients and clinicians agree that racism is a driver of health points to the incredible role primary care plays in creating safe spaces to process deep societal and personal issues,” said Christine Bechtel, cofounder of 3rd Conversation, a community of patients and providers. Read more.
Medical teams take to the streets
They stanched bleeding wounds and plucked disoriented teenagers from clouds of gas, entering dangerous corners where on-duty emergency health responders may fear to go. Many are medical professionals who see parallels between the front lines of COVID-19, where they confront stark racial imbalances among those stricken by the coronavirus, and what they see as racialized police brutality.
Iris Butler, a 21-year-old certified nursing assistant who works in a nursing home, decided to offer her skills after seeing a man injured by a rubber bullet on her first night at the Denver protests. She showed up as a medic every night thereafter. “I am working full time and basically being at the protest after getting straight off of work,” said Ms. Butler, who is black. That’s tiring, she added, but so is being a black woman in America. Read more.
At-home management of type 1 diabetes, COVID-19
Although hyperglycemia and diabetic ketoacidosis are common in people with type 1 diabetes who develop COVID-19, many are still able to manage the illness at home and overall mortality is relatively low.
These new findings are still preliminary and were published online June 5 in Diabetes Care by Osagie A. Ebekozien, MD, vice president, quality improvement and population health at the T1D Exchange, and colleagues.
The published study includes data as of May 5 on 64 individuals from a total of 64 US sites. Since the paper was submitted, there are now 220 patients from 68 sites. There were two deaths in the preliminary report, Dr. Ebekozien said. There have been a few more deaths in the larger dataset, but the mortality rate remains relatively low.
Overall, 34.9% of patients were able to manage COVID-19 entirely at home. At the other extreme, 22.2% of patients overall were admitted to the intensive care unit. Including the small proportion of patients sent home after being seen in emergency or urgent care, overall roughly half were not admitted to the hospital. “Even in this preliminary study, half were managed at home via telemedicine with an endocrinologist and infectious disease specialist ... I think it continues to be a case-by-case clinical decision between the patient and their provider,” Dr. Ebekozien said. Read more.
‘Hospital at home’ for cancer patients
Visits to the emergency department (ED) and hospitalizations are often frequent occurrences for cancer patients, but what if the “hospital” could be brought into the home instead?
A new American cohort study provides evidence that this can be a workable option for cancer patients. The authors report improved patient outcomes, with 56% lower odds of unplanned hospitalizations, 45% lower odds of ED visits, and 50% lower cumulative charges, as compared with patients who received usual care.
“The oncology hospital-at-home model of care that extends acute-level care to the patient at home offers promise in addressing a long-term gap in cancer care service delivery,” said lead author Kathi Mooney, PhD, RN, distinguished professor of nursing at the University of Utah, Salt Lake City. “In light of the current global pandemic, we are compelled to consider new ways to provide cancer care, and the oncology hospital-at-home model is on point to address critical elements of an improved cancer care delivery system.”
Dr. Mooney presented the findings during the virtual scientific program of the American Society of Clinical Oncology 2020 annual meeting (abstract 7000). Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Racism, COVID-19 lead to sky-high stress levels
Primary care clinicians, already experiencing all-time high stress levels related to COVID-19, are now struggling to cope with the fallout from racism and the death of George Floyd, according to a survey conducted June 5-8.
When asked how the situation has affected their practices, 12% of the survey’s 586 respondents “drew clear connections between the current racial unrest and the health of their patients,” the Larry A. Green Center said in a recent statement. One-third of the clinicians also said that recent racism-related events have had a negative effect on their own well-being.
In a related survey of 1,111 patients conducted June 8 about 65% of patients said that racism affected emotional, psychological, and behavioral health.
“The fact that so many patients and clinicians agree that racism is a driver of health points to the incredible role primary care plays in creating safe spaces to process deep societal and personal issues,” said Christine Bechtel, cofounder of 3rd Conversation, a community of patients and providers. Read more.
Medical teams take to the streets
They stanched bleeding wounds and plucked disoriented teenagers from clouds of gas, entering dangerous corners where on-duty emergency health responders may fear to go. Many are medical professionals who see parallels between the front lines of COVID-19, where they confront stark racial imbalances among those stricken by the coronavirus, and what they see as racialized police brutality.
Iris Butler, a 21-year-old certified nursing assistant who works in a nursing home, decided to offer her skills after seeing a man injured by a rubber bullet on her first night at the Denver protests. She showed up as a medic every night thereafter. “I am working full time and basically being at the protest after getting straight off of work,” said Ms. Butler, who is black. That’s tiring, she added, but so is being a black woman in America. Read more.
At-home management of type 1 diabetes, COVID-19
Although hyperglycemia and diabetic ketoacidosis are common in people with type 1 diabetes who develop COVID-19, many are still able to manage the illness at home and overall mortality is relatively low.
These new findings are still preliminary and were published online June 5 in Diabetes Care by Osagie A. Ebekozien, MD, vice president, quality improvement and population health at the T1D Exchange, and colleagues.
The published study includes data as of May 5 on 64 individuals from a total of 64 US sites. Since the paper was submitted, there are now 220 patients from 68 sites. There were two deaths in the preliminary report, Dr. Ebekozien said. There have been a few more deaths in the larger dataset, but the mortality rate remains relatively low.
Overall, 34.9% of patients were able to manage COVID-19 entirely at home. At the other extreme, 22.2% of patients overall were admitted to the intensive care unit. Including the small proportion of patients sent home after being seen in emergency or urgent care, overall roughly half were not admitted to the hospital. “Even in this preliminary study, half were managed at home via telemedicine with an endocrinologist and infectious disease specialist ... I think it continues to be a case-by-case clinical decision between the patient and their provider,” Dr. Ebekozien said. Read more.
‘Hospital at home’ for cancer patients
Visits to the emergency department (ED) and hospitalizations are often frequent occurrences for cancer patients, but what if the “hospital” could be brought into the home instead?
A new American cohort study provides evidence that this can be a workable option for cancer patients. The authors report improved patient outcomes, with 56% lower odds of unplanned hospitalizations, 45% lower odds of ED visits, and 50% lower cumulative charges, as compared with patients who received usual care.
“The oncology hospital-at-home model of care that extends acute-level care to the patient at home offers promise in addressing a long-term gap in cancer care service delivery,” said lead author Kathi Mooney, PhD, RN, distinguished professor of nursing at the University of Utah, Salt Lake City. “In light of the current global pandemic, we are compelled to consider new ways to provide cancer care, and the oncology hospital-at-home model is on point to address critical elements of an improved cancer care delivery system.”
Dr. Mooney presented the findings during the virtual scientific program of the American Society of Clinical Oncology 2020 annual meeting (abstract 7000). Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Racism, COVID-19 lead to sky-high stress levels
Primary care clinicians, already experiencing all-time high stress levels related to COVID-19, are now struggling to cope with the fallout from racism and the death of George Floyd, according to a survey conducted June 5-8.
When asked how the situation has affected their practices, 12% of the survey’s 586 respondents “drew clear connections between the current racial unrest and the health of their patients,” the Larry A. Green Center said in a recent statement. One-third of the clinicians also said that recent racism-related events have had a negative effect on their own well-being.
In a related survey of 1,111 patients conducted June 8 about 65% of patients said that racism affected emotional, psychological, and behavioral health.
“The fact that so many patients and clinicians agree that racism is a driver of health points to the incredible role primary care plays in creating safe spaces to process deep societal and personal issues,” said Christine Bechtel, cofounder of 3rd Conversation, a community of patients and providers. Read more.
Medical teams take to the streets
They stanched bleeding wounds and plucked disoriented teenagers from clouds of gas, entering dangerous corners where on-duty emergency health responders may fear to go. Many are medical professionals who see parallels between the front lines of COVID-19, where they confront stark racial imbalances among those stricken by the coronavirus, and what they see as racialized police brutality.
Iris Butler, a 21-year-old certified nursing assistant who works in a nursing home, decided to offer her skills after seeing a man injured by a rubber bullet on her first night at the Denver protests. She showed up as a medic every night thereafter. “I am working full time and basically being at the protest after getting straight off of work,” said Ms. Butler, who is black. That’s tiring, she added, but so is being a black woman in America. Read more.
At-home management of type 1 diabetes, COVID-19
Although hyperglycemia and diabetic ketoacidosis are common in people with type 1 diabetes who develop COVID-19, many are still able to manage the illness at home and overall mortality is relatively low.
These new findings are still preliminary and were published online June 5 in Diabetes Care by Osagie A. Ebekozien, MD, vice president, quality improvement and population health at the T1D Exchange, and colleagues.
The published study includes data as of May 5 on 64 individuals from a total of 64 US sites. Since the paper was submitted, there are now 220 patients from 68 sites. There were two deaths in the preliminary report, Dr. Ebekozien said. There have been a few more deaths in the larger dataset, but the mortality rate remains relatively low.
Overall, 34.9% of patients were able to manage COVID-19 entirely at home. At the other extreme, 22.2% of patients overall were admitted to the intensive care unit. Including the small proportion of patients sent home after being seen in emergency or urgent care, overall roughly half were not admitted to the hospital. “Even in this preliminary study, half were managed at home via telemedicine with an endocrinologist and infectious disease specialist ... I think it continues to be a case-by-case clinical decision between the patient and their provider,” Dr. Ebekozien said. Read more.
‘Hospital at home’ for cancer patients
Visits to the emergency department (ED) and hospitalizations are often frequent occurrences for cancer patients, but what if the “hospital” could be brought into the home instead?
A new American cohort study provides evidence that this can be a workable option for cancer patients. The authors report improved patient outcomes, with 56% lower odds of unplanned hospitalizations, 45% lower odds of ED visits, and 50% lower cumulative charges, as compared with patients who received usual care.
“The oncology hospital-at-home model of care that extends acute-level care to the patient at home offers promise in addressing a long-term gap in cancer care service delivery,” said lead author Kathi Mooney, PhD, RN, distinguished professor of nursing at the University of Utah, Salt Lake City. “In light of the current global pandemic, we are compelled to consider new ways to provide cancer care, and the oncology hospital-at-home model is on point to address critical elements of an improved cancer care delivery system.”
Dr. Mooney presented the findings during the virtual scientific program of the American Society of Clinical Oncology 2020 annual meeting (abstract 7000). Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Many COVID patients shed virus in feces, even without GI symptoms
Even without GI symptoms, many patients with COVID-19 shed viral RNA in feces, suggesting that stool testing and prevention of fecal-oral transmission may be needed to combat the ongoing pandemic, according to investigators.
A meta-analysis of 29 studies showed that 12% of patients with COVID-19 developed nausea, diarrhea, or vomiting, while 41% shed viral RNA in feces, reported lead author Sravanthi Parasa, MD, of Swedish Medical Center, Seattle.Writing in JAMA Network Open, Dr. Parasa and colleagues emphasized that respiratory symptoms remain the predominant form of disease; however, GI symptoms can occur.
“In fact, the first reported patient with COVID-19 in the U.S. reported GI symptoms of loose bowel movements and abdominal discomfort,” the investigators wrote, noting that the patient went on to test positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in both respiratory and stool specimens.
“This raises the question of inadvertent human-to-human transmission via the fecal route despite public health emphasis on droplet transmission and precautions for contact with respiratory secretions,” the investigators wrote.
To address this question, the investigators conducted a systematic review and meta-analysis involving 23 published and 6 preprint studies involving a total of 4,805 patients, all of whom tested positive for SARS-CoV-2 based on PCR results from nasopharyngeal swabs. Dr. Parasa and colleagues noted that most of the studies “scored between 8 and 10 on the MINORS quality assessment,” suggesting moderate quality.
Pooled data from these studies showed that 4.6% of patients reported nausea or vomiting, while 7.4% reported diarrhea. Such symptoms may serve as an early warning flag for clinicians, the investigators noted.
“[T]he presence of GI symptoms may portend a worse outcome for patients infected with SARS-CoV-2,” they wrote, citing a study by Pan and colleagues, which found that GI symptoms were associated with lower rates of recovery and hospital discharge.
Regardless of GI symptoms, 40.5% of patients in the meta-analysis tested positive for viral RNA in feces (95% confidence interval, 27.4%-55.1%). Duration of viral shedding in feces lasted up to 11 days after symptom onset, or in a single-patient case study, 18 days after hospitalization.
The investigators called these duration figures “particularly concerning,” especially in light of a study published by Xiao and colleagues, which showed that 23.3% of patients with negative respiratory tests were still shedding live virus in feces.
“[T]he fecal-oral route of transmission could be an additional potential source of infection spread,” wrote Dr. Parasa and colleagues. “Our results also suggest that testing of the virus in feces ... could be helpful in disease monitoring and surveillance.”
David A. Johnson, MD, professor of medicine and chief of gastroenterology at Eastern Virginia Medical School in Norfolk, said that the findings confirm what has been suspected for some time: GI disease is relatively common with COVID-19.
“The evidence is clear now that a sizable percentage of patients have GI symptoms,” Dr. Johnson said in an interview.
GI issues may precede respiratory signs, he added, so clinicians should be aware that nausea, vomiting, or diarrhea could be early indicators of COVID-19, and possibly, a worse outcome.
“The other highlight of this study is that stool shedding may be extended beyond respiratory shedding,” Dr. Johnson said.
He suggested that this finding could influence current CDC criteria, which define absence of infectious risk by two consecutive, negative nasopharyngeal swabs. Instead, fecal testing may be needed, he said, along with measures to prevent fecal-oral transmission.
Dr. Johnson expressed particular concern for risk of infection via toilet plume, in which toilet flushing aerosolizes viral particles.
“As much as people try to social distance by 6 feet – you can do that when you walk into a store, or a building, but you can’t necessarily do that when you walk into a public toilet, where the plume may have been expansive for a period of time,” he said. “That toilet may never really get cleaned to a high level of disinfection, and those droplets set up potential for fecal-oral spread.”
Dr. Sharma disclosed relationships with Medtronic, Fujifilm, Boston Scientific, and others. Dr. Johnson disclosed no relevant conflicts of interest.
SOURCE: Parasa S et al. JAMA Network Open. 2020 Jun 11. doi: 10.1001/jamanetworkopen.2020.11335.
Even without GI symptoms, many patients with COVID-19 shed viral RNA in feces, suggesting that stool testing and prevention of fecal-oral transmission may be needed to combat the ongoing pandemic, according to investigators.
A meta-analysis of 29 studies showed that 12% of patients with COVID-19 developed nausea, diarrhea, or vomiting, while 41% shed viral RNA in feces, reported lead author Sravanthi Parasa, MD, of Swedish Medical Center, Seattle.Writing in JAMA Network Open, Dr. Parasa and colleagues emphasized that respiratory symptoms remain the predominant form of disease; however, GI symptoms can occur.
“In fact, the first reported patient with COVID-19 in the U.S. reported GI symptoms of loose bowel movements and abdominal discomfort,” the investigators wrote, noting that the patient went on to test positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in both respiratory and stool specimens.
“This raises the question of inadvertent human-to-human transmission via the fecal route despite public health emphasis on droplet transmission and precautions for contact with respiratory secretions,” the investigators wrote.
To address this question, the investigators conducted a systematic review and meta-analysis involving 23 published and 6 preprint studies involving a total of 4,805 patients, all of whom tested positive for SARS-CoV-2 based on PCR results from nasopharyngeal swabs. Dr. Parasa and colleagues noted that most of the studies “scored between 8 and 10 on the MINORS quality assessment,” suggesting moderate quality.
Pooled data from these studies showed that 4.6% of patients reported nausea or vomiting, while 7.4% reported diarrhea. Such symptoms may serve as an early warning flag for clinicians, the investigators noted.
“[T]he presence of GI symptoms may portend a worse outcome for patients infected with SARS-CoV-2,” they wrote, citing a study by Pan and colleagues, which found that GI symptoms were associated with lower rates of recovery and hospital discharge.
Regardless of GI symptoms, 40.5% of patients in the meta-analysis tested positive for viral RNA in feces (95% confidence interval, 27.4%-55.1%). Duration of viral shedding in feces lasted up to 11 days after symptom onset, or in a single-patient case study, 18 days after hospitalization.
The investigators called these duration figures “particularly concerning,” especially in light of a study published by Xiao and colleagues, which showed that 23.3% of patients with negative respiratory tests were still shedding live virus in feces.
“[T]he fecal-oral route of transmission could be an additional potential source of infection spread,” wrote Dr. Parasa and colleagues. “Our results also suggest that testing of the virus in feces ... could be helpful in disease monitoring and surveillance.”
David A. Johnson, MD, professor of medicine and chief of gastroenterology at Eastern Virginia Medical School in Norfolk, said that the findings confirm what has been suspected for some time: GI disease is relatively common with COVID-19.
“The evidence is clear now that a sizable percentage of patients have GI symptoms,” Dr. Johnson said in an interview.
GI issues may precede respiratory signs, he added, so clinicians should be aware that nausea, vomiting, or diarrhea could be early indicators of COVID-19, and possibly, a worse outcome.
“The other highlight of this study is that stool shedding may be extended beyond respiratory shedding,” Dr. Johnson said.
He suggested that this finding could influence current CDC criteria, which define absence of infectious risk by two consecutive, negative nasopharyngeal swabs. Instead, fecal testing may be needed, he said, along with measures to prevent fecal-oral transmission.
Dr. Johnson expressed particular concern for risk of infection via toilet plume, in which toilet flushing aerosolizes viral particles.
“As much as people try to social distance by 6 feet – you can do that when you walk into a store, or a building, but you can’t necessarily do that when you walk into a public toilet, where the plume may have been expansive for a period of time,” he said. “That toilet may never really get cleaned to a high level of disinfection, and those droplets set up potential for fecal-oral spread.”
Dr. Sharma disclosed relationships with Medtronic, Fujifilm, Boston Scientific, and others. Dr. Johnson disclosed no relevant conflicts of interest.
SOURCE: Parasa S et al. JAMA Network Open. 2020 Jun 11. doi: 10.1001/jamanetworkopen.2020.11335.
Even without GI symptoms, many patients with COVID-19 shed viral RNA in feces, suggesting that stool testing and prevention of fecal-oral transmission may be needed to combat the ongoing pandemic, according to investigators.
A meta-analysis of 29 studies showed that 12% of patients with COVID-19 developed nausea, diarrhea, or vomiting, while 41% shed viral RNA in feces, reported lead author Sravanthi Parasa, MD, of Swedish Medical Center, Seattle.Writing in JAMA Network Open, Dr. Parasa and colleagues emphasized that respiratory symptoms remain the predominant form of disease; however, GI symptoms can occur.
“In fact, the first reported patient with COVID-19 in the U.S. reported GI symptoms of loose bowel movements and abdominal discomfort,” the investigators wrote, noting that the patient went on to test positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in both respiratory and stool specimens.
“This raises the question of inadvertent human-to-human transmission via the fecal route despite public health emphasis on droplet transmission and precautions for contact with respiratory secretions,” the investigators wrote.
To address this question, the investigators conducted a systematic review and meta-analysis involving 23 published and 6 preprint studies involving a total of 4,805 patients, all of whom tested positive for SARS-CoV-2 based on PCR results from nasopharyngeal swabs. Dr. Parasa and colleagues noted that most of the studies “scored between 8 and 10 on the MINORS quality assessment,” suggesting moderate quality.
Pooled data from these studies showed that 4.6% of patients reported nausea or vomiting, while 7.4% reported diarrhea. Such symptoms may serve as an early warning flag for clinicians, the investigators noted.
“[T]he presence of GI symptoms may portend a worse outcome for patients infected with SARS-CoV-2,” they wrote, citing a study by Pan and colleagues, which found that GI symptoms were associated with lower rates of recovery and hospital discharge.
Regardless of GI symptoms, 40.5% of patients in the meta-analysis tested positive for viral RNA in feces (95% confidence interval, 27.4%-55.1%). Duration of viral shedding in feces lasted up to 11 days after symptom onset, or in a single-patient case study, 18 days after hospitalization.
The investigators called these duration figures “particularly concerning,” especially in light of a study published by Xiao and colleagues, which showed that 23.3% of patients with negative respiratory tests were still shedding live virus in feces.
“[T]he fecal-oral route of transmission could be an additional potential source of infection spread,” wrote Dr. Parasa and colleagues. “Our results also suggest that testing of the virus in feces ... could be helpful in disease monitoring and surveillance.”
David A. Johnson, MD, professor of medicine and chief of gastroenterology at Eastern Virginia Medical School in Norfolk, said that the findings confirm what has been suspected for some time: GI disease is relatively common with COVID-19.
“The evidence is clear now that a sizable percentage of patients have GI symptoms,” Dr. Johnson said in an interview.
GI issues may precede respiratory signs, he added, so clinicians should be aware that nausea, vomiting, or diarrhea could be early indicators of COVID-19, and possibly, a worse outcome.
“The other highlight of this study is that stool shedding may be extended beyond respiratory shedding,” Dr. Johnson said.
He suggested that this finding could influence current CDC criteria, which define absence of infectious risk by two consecutive, negative nasopharyngeal swabs. Instead, fecal testing may be needed, he said, along with measures to prevent fecal-oral transmission.
Dr. Johnson expressed particular concern for risk of infection via toilet plume, in which toilet flushing aerosolizes viral particles.
“As much as people try to social distance by 6 feet – you can do that when you walk into a store, or a building, but you can’t necessarily do that when you walk into a public toilet, where the plume may have been expansive for a period of time,” he said. “That toilet may never really get cleaned to a high level of disinfection, and those droplets set up potential for fecal-oral spread.”
Dr. Sharma disclosed relationships with Medtronic, Fujifilm, Boston Scientific, and others. Dr. Johnson disclosed no relevant conflicts of interest.
SOURCE: Parasa S et al. JAMA Network Open. 2020 Jun 11. doi: 10.1001/jamanetworkopen.2020.11335.
FROM JAMA NETWORK OPEN
Half of type 1 diabetes patients with COVID-19 manage at home
New preliminary data from the T1D Exchange suggest that, although hyperglycemia and diabetic ketoacidosis (DKA) are common in people with type 1 diabetes who develop COVID-19, many are still able to manage the illness at home and overall mortality is relatively low.
The new findings – the first US data on individuals with type 1 diabetes and COVID-19 – were published online June 5 in Diabetes Care by Osagie A. Ebekozien, MD, vice president, quality improvement and population health at the T1D Exchange, and colleagues.
Two UK studies are the only prior ones to previously examine the topic.
The newly published study includes data as of May 5 on 64 individuals from a total of 64 US sites, including 15 T1D Exchange member clinics and an additional 49 endocrinology clinics from around the country. Since the paper was submitted, there are now 220 patients from 68 sites. Another publication with a more detailed analysis of risk factors and adjustment for confounders is planned for later this year.
Some of the findings from the preliminary data have shifted, but many aspects remain consistent, Ebekozien told Medscape Medical News.
“One thing still very true, even with the unpublished findings, is the influence of A1c and glycemic management. ...With higher A1c levels, we’re seeing more COVID-19 hospitalizations and worse outcomes,” he said.
And as has been generally reported for COVID-19, high body mass index was a major risk factor in the preliminary dataset – and remains so.
There were two deaths in the preliminary report, both individuals with comorbidities in addition to type 1 diabetes, Ebekozien said. There have been a few more deaths in the larger dataset, but the mortality rate remains relatively low.
Interestingly, females predominate in both cohorts. That may be a reporting phenomenon, another factor that is being analyzed.
Hyperglycemia Remains a Major Risk Factor
The study is specifically being conducted by the T1D Exchange’s Quality Improvement Collaborative, which Ebekozien heads.
Data were obtained for 33 patients with type 1 diabetes who tested positive for COVID-19, and another 31 who were classified as “COVID-19–like” because they had symptoms consistent with COVID-19, as identified by the Centers for Disease Control and Prevention, but hadn’t been tested for the virus.
For all 64 patients, the mean age was 20.9 years and two thirds (65.6%) were aged 18 or younger. A higher proportion of the COVID-19–like patients were pediatric than the confirmed cases. The larger dataset includes more adult patients, Ebekozien told Medscape Medical News.
Overall, 60.9% of patients were female. Nearly half were white, a quarter Hispanic, and 18.8% black. More confirmed COVID-19 cases were black compared with suspected cases (30.3% vs 6.5%).
Median A1c for the overall group (including suspected COVID-19 cases) was 8.0%, but it was 8.5% among confirmed cases. Overall, six patients (9.8%) presented with new-onset type 1 diabetes after they developed COVID-19.
Hyperglycemia was present in half (32) of patients overall. DKA occurred in 19 people (30.2%): 15 of the confirmed COVID-19 cases (45.5%) versus just 4 (13.3%) of the COVID-19–like cases. Nausea was reported in 30.2% of patients overall.
Other symptoms were typical of COVID-19, including fever (41.3%), dry cough (38.1%), and shortness of breath (27.0%). Loss of taste and smell was less common, at just 9.5% overall.
Obesity was present in 39.7% of patients overall, with similar proportions in the confirmed and suspected COVID-19 groups. Hypertension and/or cardiovascular disease were present in 14.3% of patients overall, and the rate was similar between the two subgroups.
One of the two patients who died was a 79-year-old man who had hypertension and a prior stroke in addition to type 1 diabetes. The other was a 19-year-old woman with a history of asthma who developed a pulmonary embolism during the onset of COVID-19. Neither had DKA.
Even in Type 1 Diabetes, COVID-19 Can Be Managed at Home
Overall, 34.9% of patients were able to manage COVID-19 entirely at home, with 27.3% of the confirmed and 43.3% of the suspected cases able to do so.
At the other extreme, 22.2% of patients overall were admitted to the intensive care unit; 30.3% of the confirmed versus 13.3% of suspected cases.
Including the small proportion of patients sent home after being seen in emergency or urgent care, overall roughly half were not admitted to hospital.
“Interestingly, even in this preliminary study, half were managed at home via telemedicine with an endocrinologist and infectious disease specialist. ... I think it continues to be a case-by-case clinical decision between the patient and their provider,” Ebekozien said.
“But, we’re seeing a good number of patients who are managed at home and the symptoms resolve in a week or two, and the illness runs its course, and they don’t have to even be seen,” he added.
The research team is also collecting data on barriers to remote care, including challenges with telemedicine and how frontline providers are navigating them.
“Those are all things that our future paper will be able to shed more light on,” he explained.
Endocrinologists around the country are invited to report cases of COVID-19 in patients with type 1 diabetes to the T1D Exchange by emailing [email protected].
And in fact, Ebekozien also requested that clinicians with a large type 1 diabetes population also report if they’ve had no COVID-19 cases.
“Even if they haven’t had a case, that’s very useful information for us to know. One of the things we want to calculate down the line is the incidence ratio. Not all participating sites have had a case.”
Endocrinologists from all the participating sites have formed a dedicated community that meets regularly via webinars to share information, he noted. “It’s been a very selfless effort to work collaboratively as a community to quickly answer critical questions.”
The Helmsley Charitable Trust funds the T1D Exchange Quality Improvement Collaborative. The T1D Exchange received financial support for this study from Abbott Diabetes, Dexcom, JDRF, Insulet Corporation, Lilly, Medtronic, and Tandem Diabetes Care. No other relevant financial relationships were reported.
This article first appeared on Medscape.com.
New preliminary data from the T1D Exchange suggest that, although hyperglycemia and diabetic ketoacidosis (DKA) are common in people with type 1 diabetes who develop COVID-19, many are still able to manage the illness at home and overall mortality is relatively low.
The new findings – the first US data on individuals with type 1 diabetes and COVID-19 – were published online June 5 in Diabetes Care by Osagie A. Ebekozien, MD, vice president, quality improvement and population health at the T1D Exchange, and colleagues.
Two UK studies are the only prior ones to previously examine the topic.
The newly published study includes data as of May 5 on 64 individuals from a total of 64 US sites, including 15 T1D Exchange member clinics and an additional 49 endocrinology clinics from around the country. Since the paper was submitted, there are now 220 patients from 68 sites. Another publication with a more detailed analysis of risk factors and adjustment for confounders is planned for later this year.
Some of the findings from the preliminary data have shifted, but many aspects remain consistent, Ebekozien told Medscape Medical News.
“One thing still very true, even with the unpublished findings, is the influence of A1c and glycemic management. ...With higher A1c levels, we’re seeing more COVID-19 hospitalizations and worse outcomes,” he said.
And as has been generally reported for COVID-19, high body mass index was a major risk factor in the preliminary dataset – and remains so.
There were two deaths in the preliminary report, both individuals with comorbidities in addition to type 1 diabetes, Ebekozien said. There have been a few more deaths in the larger dataset, but the mortality rate remains relatively low.
Interestingly, females predominate in both cohorts. That may be a reporting phenomenon, another factor that is being analyzed.
Hyperglycemia Remains a Major Risk Factor
The study is specifically being conducted by the T1D Exchange’s Quality Improvement Collaborative, which Ebekozien heads.
Data were obtained for 33 patients with type 1 diabetes who tested positive for COVID-19, and another 31 who were classified as “COVID-19–like” because they had symptoms consistent with COVID-19, as identified by the Centers for Disease Control and Prevention, but hadn’t been tested for the virus.
For all 64 patients, the mean age was 20.9 years and two thirds (65.6%) were aged 18 or younger. A higher proportion of the COVID-19–like patients were pediatric than the confirmed cases. The larger dataset includes more adult patients, Ebekozien told Medscape Medical News.
Overall, 60.9% of patients were female. Nearly half were white, a quarter Hispanic, and 18.8% black. More confirmed COVID-19 cases were black compared with suspected cases (30.3% vs 6.5%).
Median A1c for the overall group (including suspected COVID-19 cases) was 8.0%, but it was 8.5% among confirmed cases. Overall, six patients (9.8%) presented with new-onset type 1 diabetes after they developed COVID-19.
Hyperglycemia was present in half (32) of patients overall. DKA occurred in 19 people (30.2%): 15 of the confirmed COVID-19 cases (45.5%) versus just 4 (13.3%) of the COVID-19–like cases. Nausea was reported in 30.2% of patients overall.
Other symptoms were typical of COVID-19, including fever (41.3%), dry cough (38.1%), and shortness of breath (27.0%). Loss of taste and smell was less common, at just 9.5% overall.
Obesity was present in 39.7% of patients overall, with similar proportions in the confirmed and suspected COVID-19 groups. Hypertension and/or cardiovascular disease were present in 14.3% of patients overall, and the rate was similar between the two subgroups.
One of the two patients who died was a 79-year-old man who had hypertension and a prior stroke in addition to type 1 diabetes. The other was a 19-year-old woman with a history of asthma who developed a pulmonary embolism during the onset of COVID-19. Neither had DKA.
Even in Type 1 Diabetes, COVID-19 Can Be Managed at Home
Overall, 34.9% of patients were able to manage COVID-19 entirely at home, with 27.3% of the confirmed and 43.3% of the suspected cases able to do so.
At the other extreme, 22.2% of patients overall were admitted to the intensive care unit; 30.3% of the confirmed versus 13.3% of suspected cases.
Including the small proportion of patients sent home after being seen in emergency or urgent care, overall roughly half were not admitted to hospital.
“Interestingly, even in this preliminary study, half were managed at home via telemedicine with an endocrinologist and infectious disease specialist. ... I think it continues to be a case-by-case clinical decision between the patient and their provider,” Ebekozien said.
“But, we’re seeing a good number of patients who are managed at home and the symptoms resolve in a week or two, and the illness runs its course, and they don’t have to even be seen,” he added.
The research team is also collecting data on barriers to remote care, including challenges with telemedicine and how frontline providers are navigating them.
“Those are all things that our future paper will be able to shed more light on,” he explained.
Endocrinologists around the country are invited to report cases of COVID-19 in patients with type 1 diabetes to the T1D Exchange by emailing [email protected].
And in fact, Ebekozien also requested that clinicians with a large type 1 diabetes population also report if they’ve had no COVID-19 cases.
“Even if they haven’t had a case, that’s very useful information for us to know. One of the things we want to calculate down the line is the incidence ratio. Not all participating sites have had a case.”
Endocrinologists from all the participating sites have formed a dedicated community that meets regularly via webinars to share information, he noted. “It’s been a very selfless effort to work collaboratively as a community to quickly answer critical questions.”
The Helmsley Charitable Trust funds the T1D Exchange Quality Improvement Collaborative. The T1D Exchange received financial support for this study from Abbott Diabetes, Dexcom, JDRF, Insulet Corporation, Lilly, Medtronic, and Tandem Diabetes Care. No other relevant financial relationships were reported.
This article first appeared on Medscape.com.
New preliminary data from the T1D Exchange suggest that, although hyperglycemia and diabetic ketoacidosis (DKA) are common in people with type 1 diabetes who develop COVID-19, many are still able to manage the illness at home and overall mortality is relatively low.
The new findings – the first US data on individuals with type 1 diabetes and COVID-19 – were published online June 5 in Diabetes Care by Osagie A. Ebekozien, MD, vice president, quality improvement and population health at the T1D Exchange, and colleagues.
Two UK studies are the only prior ones to previously examine the topic.
The newly published study includes data as of May 5 on 64 individuals from a total of 64 US sites, including 15 T1D Exchange member clinics and an additional 49 endocrinology clinics from around the country. Since the paper was submitted, there are now 220 patients from 68 sites. Another publication with a more detailed analysis of risk factors and adjustment for confounders is planned for later this year.
Some of the findings from the preliminary data have shifted, but many aspects remain consistent, Ebekozien told Medscape Medical News.
“One thing still very true, even with the unpublished findings, is the influence of A1c and glycemic management. ...With higher A1c levels, we’re seeing more COVID-19 hospitalizations and worse outcomes,” he said.
And as has been generally reported for COVID-19, high body mass index was a major risk factor in the preliminary dataset – and remains so.
There were two deaths in the preliminary report, both individuals with comorbidities in addition to type 1 diabetes, Ebekozien said. There have been a few more deaths in the larger dataset, but the mortality rate remains relatively low.
Interestingly, females predominate in both cohorts. That may be a reporting phenomenon, another factor that is being analyzed.
Hyperglycemia Remains a Major Risk Factor
The study is specifically being conducted by the T1D Exchange’s Quality Improvement Collaborative, which Ebekozien heads.
Data were obtained for 33 patients with type 1 diabetes who tested positive for COVID-19, and another 31 who were classified as “COVID-19–like” because they had symptoms consistent with COVID-19, as identified by the Centers for Disease Control and Prevention, but hadn’t been tested for the virus.
For all 64 patients, the mean age was 20.9 years and two thirds (65.6%) were aged 18 or younger. A higher proportion of the COVID-19–like patients were pediatric than the confirmed cases. The larger dataset includes more adult patients, Ebekozien told Medscape Medical News.
Overall, 60.9% of patients were female. Nearly half were white, a quarter Hispanic, and 18.8% black. More confirmed COVID-19 cases were black compared with suspected cases (30.3% vs 6.5%).
Median A1c for the overall group (including suspected COVID-19 cases) was 8.0%, but it was 8.5% among confirmed cases. Overall, six patients (9.8%) presented with new-onset type 1 diabetes after they developed COVID-19.
Hyperglycemia was present in half (32) of patients overall. DKA occurred in 19 people (30.2%): 15 of the confirmed COVID-19 cases (45.5%) versus just 4 (13.3%) of the COVID-19–like cases. Nausea was reported in 30.2% of patients overall.
Other symptoms were typical of COVID-19, including fever (41.3%), dry cough (38.1%), and shortness of breath (27.0%). Loss of taste and smell was less common, at just 9.5% overall.
Obesity was present in 39.7% of patients overall, with similar proportions in the confirmed and suspected COVID-19 groups. Hypertension and/or cardiovascular disease were present in 14.3% of patients overall, and the rate was similar between the two subgroups.
One of the two patients who died was a 79-year-old man who had hypertension and a prior stroke in addition to type 1 diabetes. The other was a 19-year-old woman with a history of asthma who developed a pulmonary embolism during the onset of COVID-19. Neither had DKA.
Even in Type 1 Diabetes, COVID-19 Can Be Managed at Home
Overall, 34.9% of patients were able to manage COVID-19 entirely at home, with 27.3% of the confirmed and 43.3% of the suspected cases able to do so.
At the other extreme, 22.2% of patients overall were admitted to the intensive care unit; 30.3% of the confirmed versus 13.3% of suspected cases.
Including the small proportion of patients sent home after being seen in emergency or urgent care, overall roughly half were not admitted to hospital.
“Interestingly, even in this preliminary study, half were managed at home via telemedicine with an endocrinologist and infectious disease specialist. ... I think it continues to be a case-by-case clinical decision between the patient and their provider,” Ebekozien said.
“But, we’re seeing a good number of patients who are managed at home and the symptoms resolve in a week or two, and the illness runs its course, and they don’t have to even be seen,” he added.
The research team is also collecting data on barriers to remote care, including challenges with telemedicine and how frontline providers are navigating them.
“Those are all things that our future paper will be able to shed more light on,” he explained.
Endocrinologists around the country are invited to report cases of COVID-19 in patients with type 1 diabetes to the T1D Exchange by emailing [email protected].
And in fact, Ebekozien also requested that clinicians with a large type 1 diabetes population also report if they’ve had no COVID-19 cases.
“Even if they haven’t had a case, that’s very useful information for us to know. One of the things we want to calculate down the line is the incidence ratio. Not all participating sites have had a case.”
Endocrinologists from all the participating sites have formed a dedicated community that meets regularly via webinars to share information, he noted. “It’s been a very selfless effort to work collaboratively as a community to quickly answer critical questions.”
The Helmsley Charitable Trust funds the T1D Exchange Quality Improvement Collaborative. The T1D Exchange received financial support for this study from Abbott Diabetes, Dexcom, JDRF, Insulet Corporation, Lilly, Medtronic, and Tandem Diabetes Care. No other relevant financial relationships were reported.
This article first appeared on Medscape.com.
Fighting COVID and police brutality, medical teams take to streets to treat protesters
Amid clouds of choking tear gas, booming flash-bang grenades and other “riot control agents,” volunteer medics plunged into street protests over the past weeks to help the injured – sometimes rushing to the front lines as soon as their hospital shifts ended.
Known as “street medics,” these unorthodox teams of nursing students, veterinarians, doctors, trauma surgeons, security guards, ski patrollers, nurses, wilderness EMTs, and off-the-clock ambulance workers poured water – not milk – into the eyes of tear-gassed protesters. They stanched bleeding wounds and plucked disoriented teenagers from clouds of gas, entering dangerous corners where on-duty emergency health responders may fear to go.
So donning cloth masks to protect against the virus – plus helmets, makeshift shields and other gear to guard against rubber bullets, projectiles and tear gas – the volunteer medics organized themselves into a web of first responders to care for people on the streets. They showed up early, set up first-aid stations, established transportation networks and covered their arms, helmets and backpacks with crosses made of red duct tape, to signify that they were medics. Some stayed late into the night past curfews until every protester had left.
Iris Butler, a 21-year-old certified nursing assistant who works in a nursing home, decided to offer her skills after seeing a man injured by a rubber bullet on her first night at the Denver protests. She showed up as a medic every night thereafter. She didn’t see it as a choice.
“I am working full time and basically being at the protest after getting straight off of work,” said Butler, who is black. That’s tiring, she added, but so is being a black woman in America.
After going out as a medic on her own, she soon met other volunteers. Together they used text-message chains to organize their efforts. One night, she responded to a man who had been shot with a rubber bullet in the chest; she said his torso had turned blue and purple from the impact. She also provided aid after a shooting near the protest left someone in critical condition.
“It’s hard, but bills need to be paid and justice needs to be served,” she said.
The street medic movement traces its roots, in part, to the 1960s protests, as well as the American Indian Movement and the Black Panther Party. Denver Action Medic Network offers a 20-hour training course that prepares them to treat patients in conflicts with police and large crowds; a four-hour session is offered to medical professionals as “bridge” training.
Since the coronavirus pandemic began, the Denver Action Medic Network has added new training guidelines: Don’t go to protests if sick or in contact with those who are infected; wear a mask; give people lots of space and use hand sanitizer. Jordan Garcia, a 39-year-old medic for over 20 years who works with the network of veteran street medics, said they also warn medics about the increased risk of transmission because of protesters coughing from tear gas, and urge them to get tested for the virus after the protests.
The number of volunteer medics swelled after George Floyd’s May 25 killing in Minneapolis. In Denver alone, at least 40 people reached out to the Denver Action Medic Network for training.
On June 3, Dr. Rupa Marya, an associate professor of medicine at the University of California,San Francisco, and the co-founder of the Do No Harm Coalition, which runs street medic training in the Bay Area, hosted a national webinar attended by over 3,000 medical professionals to provide the bridge training to be a street medic. In her online bio, Marya describes the coalition as “an organization of over 450 health workers committed to structural change” in addressing health problems.
“When we see suffering, that’s where we go,” Marya said. “And right now that suffering is happening on the streets.”
In the recent Denver protests, street medics responded to major head, face and eye injuries among protesters from what are sometimes described as “kinetic impact projectiles” or “less-than-lethal” bullets shot at protesters, along with tear-gas and flash-bang stun grenade canisters that either hit them or exploded in their faces.
Garcia, who by day works for an immigrant rights nonprofit, said that these weapons are not designed to be shot directly at people.
“We’re seeing police use these less-lethal weapons in lethal ways, and that is pretty upsetting,” Garcia said about the recent protests.
Denver police Chief Paul Pazen promised to make changes, including banning chokeholds and requiring SWAT teams to turn on their body cameras. Last week, a federal judge also issued a temporary injunction to stop Denver police from using tear gas and other less-than-lethal weapons in response to a class action lawsuit, in which a medic stated he was shot multiple times by police with pepper balls while treating patients. (Last week in North Carolina police were recorded destroying medic stations.)
Denver street medic Kevin Connell, a 30-year-old emergency room nurse, said he was hit with pepper balls in the back of his medic vest – which was clearly marked by red crosses – while treating a patient. He showed up to the Denver protests every night he did not have to work, he said, wearing a Kevlar medic vest, protective goggles and a homemade gas mask fashioned from a water bottle. As a member of the Denver Action Medic Network, Connell also served at the Standing Rock protests in North Dakota in a dispute over the building of the Dakota Access Pipeline.
“I mean, as bad as it sounds, it was only tear gas, pepper balls and rubber bullets that were being fired on us,” Connell said of his recent experience in Denver. “When I was at Standing Rock, they were using high-powered water hoses even when it was, like, freezing cold. … So I think the police here had a little bit more restraint.”
Still, first-time street medic Aj Mossman, a 31-year-old Denver emergency medical technician studying for nursing school, was shocked to be tear-gassed and struck in the back of the leg with a flash grenade while treating a protester on May 30. Mossman still has a large leg bruise.
The following night, Mossman, who uses the pronoun they, brought more protective gear, but said they are still having difficulty processing what felt like a war zone.
“I thought I understood what my black friends went through. I thought I understood what the black community went through,” said Mossman, who is white. “But I had absolutely no idea how violent the police were and how little they cared about who they hurt.”
For Butler, serving as a medic with others from various walks of life was inspiring. “They’re also out there to protect black and brown bodies. And that’s amazing,” she said. “That’s just a beautiful sight.”
This article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Amid clouds of choking tear gas, booming flash-bang grenades and other “riot control agents,” volunteer medics plunged into street protests over the past weeks to help the injured – sometimes rushing to the front lines as soon as their hospital shifts ended.
Known as “street medics,” these unorthodox teams of nursing students, veterinarians, doctors, trauma surgeons, security guards, ski patrollers, nurses, wilderness EMTs, and off-the-clock ambulance workers poured water – not milk – into the eyes of tear-gassed protesters. They stanched bleeding wounds and plucked disoriented teenagers from clouds of gas, entering dangerous corners where on-duty emergency health responders may fear to go.
So donning cloth masks to protect against the virus – plus helmets, makeshift shields and other gear to guard against rubber bullets, projectiles and tear gas – the volunteer medics organized themselves into a web of first responders to care for people on the streets. They showed up early, set up first-aid stations, established transportation networks and covered their arms, helmets and backpacks with crosses made of red duct tape, to signify that they were medics. Some stayed late into the night past curfews until every protester had left.
Iris Butler, a 21-year-old certified nursing assistant who works in a nursing home, decided to offer her skills after seeing a man injured by a rubber bullet on her first night at the Denver protests. She showed up as a medic every night thereafter. She didn’t see it as a choice.
“I am working full time and basically being at the protest after getting straight off of work,” said Butler, who is black. That’s tiring, she added, but so is being a black woman in America.
After going out as a medic on her own, she soon met other volunteers. Together they used text-message chains to organize their efforts. One night, she responded to a man who had been shot with a rubber bullet in the chest; she said his torso had turned blue and purple from the impact. She also provided aid after a shooting near the protest left someone in critical condition.
“It’s hard, but bills need to be paid and justice needs to be served,” she said.
The street medic movement traces its roots, in part, to the 1960s protests, as well as the American Indian Movement and the Black Panther Party. Denver Action Medic Network offers a 20-hour training course that prepares them to treat patients in conflicts with police and large crowds; a four-hour session is offered to medical professionals as “bridge” training.
Since the coronavirus pandemic began, the Denver Action Medic Network has added new training guidelines: Don’t go to protests if sick or in contact with those who are infected; wear a mask; give people lots of space and use hand sanitizer. Jordan Garcia, a 39-year-old medic for over 20 years who works with the network of veteran street medics, said they also warn medics about the increased risk of transmission because of protesters coughing from tear gas, and urge them to get tested for the virus after the protests.
The number of volunteer medics swelled after George Floyd’s May 25 killing in Minneapolis. In Denver alone, at least 40 people reached out to the Denver Action Medic Network for training.
On June 3, Dr. Rupa Marya, an associate professor of medicine at the University of California,San Francisco, and the co-founder of the Do No Harm Coalition, which runs street medic training in the Bay Area, hosted a national webinar attended by over 3,000 medical professionals to provide the bridge training to be a street medic. In her online bio, Marya describes the coalition as “an organization of over 450 health workers committed to structural change” in addressing health problems.
“When we see suffering, that’s where we go,” Marya said. “And right now that suffering is happening on the streets.”
In the recent Denver protests, street medics responded to major head, face and eye injuries among protesters from what are sometimes described as “kinetic impact projectiles” or “less-than-lethal” bullets shot at protesters, along with tear-gas and flash-bang stun grenade canisters that either hit them or exploded in their faces.
Garcia, who by day works for an immigrant rights nonprofit, said that these weapons are not designed to be shot directly at people.
“We’re seeing police use these less-lethal weapons in lethal ways, and that is pretty upsetting,” Garcia said about the recent protests.
Denver police Chief Paul Pazen promised to make changes, including banning chokeholds and requiring SWAT teams to turn on their body cameras. Last week, a federal judge also issued a temporary injunction to stop Denver police from using tear gas and other less-than-lethal weapons in response to a class action lawsuit, in which a medic stated he was shot multiple times by police with pepper balls while treating patients. (Last week in North Carolina police were recorded destroying medic stations.)
Denver street medic Kevin Connell, a 30-year-old emergency room nurse, said he was hit with pepper balls in the back of his medic vest – which was clearly marked by red crosses – while treating a patient. He showed up to the Denver protests every night he did not have to work, he said, wearing a Kevlar medic vest, protective goggles and a homemade gas mask fashioned from a water bottle. As a member of the Denver Action Medic Network, Connell also served at the Standing Rock protests in North Dakota in a dispute over the building of the Dakota Access Pipeline.
“I mean, as bad as it sounds, it was only tear gas, pepper balls and rubber bullets that were being fired on us,” Connell said of his recent experience in Denver. “When I was at Standing Rock, they were using high-powered water hoses even when it was, like, freezing cold. … So I think the police here had a little bit more restraint.”
Still, first-time street medic Aj Mossman, a 31-year-old Denver emergency medical technician studying for nursing school, was shocked to be tear-gassed and struck in the back of the leg with a flash grenade while treating a protester on May 30. Mossman still has a large leg bruise.
The following night, Mossman, who uses the pronoun they, brought more protective gear, but said they are still having difficulty processing what felt like a war zone.
“I thought I understood what my black friends went through. I thought I understood what the black community went through,” said Mossman, who is white. “But I had absolutely no idea how violent the police were and how little they cared about who they hurt.”
For Butler, serving as a medic with others from various walks of life was inspiring. “They’re also out there to protect black and brown bodies. And that’s amazing,” she said. “That’s just a beautiful sight.”
This article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Amid clouds of choking tear gas, booming flash-bang grenades and other “riot control agents,” volunteer medics plunged into street protests over the past weeks to help the injured – sometimes rushing to the front lines as soon as their hospital shifts ended.
Known as “street medics,” these unorthodox teams of nursing students, veterinarians, doctors, trauma surgeons, security guards, ski patrollers, nurses, wilderness EMTs, and off-the-clock ambulance workers poured water – not milk – into the eyes of tear-gassed protesters. They stanched bleeding wounds and plucked disoriented teenagers from clouds of gas, entering dangerous corners where on-duty emergency health responders may fear to go.
So donning cloth masks to protect against the virus – plus helmets, makeshift shields and other gear to guard against rubber bullets, projectiles and tear gas – the volunteer medics organized themselves into a web of first responders to care for people on the streets. They showed up early, set up first-aid stations, established transportation networks and covered their arms, helmets and backpacks with crosses made of red duct tape, to signify that they were medics. Some stayed late into the night past curfews until every protester had left.
Iris Butler, a 21-year-old certified nursing assistant who works in a nursing home, decided to offer her skills after seeing a man injured by a rubber bullet on her first night at the Denver protests. She showed up as a medic every night thereafter. She didn’t see it as a choice.
“I am working full time and basically being at the protest after getting straight off of work,” said Butler, who is black. That’s tiring, she added, but so is being a black woman in America.
After going out as a medic on her own, she soon met other volunteers. Together they used text-message chains to organize their efforts. One night, she responded to a man who had been shot with a rubber bullet in the chest; she said his torso had turned blue and purple from the impact. She also provided aid after a shooting near the protest left someone in critical condition.
“It’s hard, but bills need to be paid and justice needs to be served,” she said.
The street medic movement traces its roots, in part, to the 1960s protests, as well as the American Indian Movement and the Black Panther Party. Denver Action Medic Network offers a 20-hour training course that prepares them to treat patients in conflicts with police and large crowds; a four-hour session is offered to medical professionals as “bridge” training.
Since the coronavirus pandemic began, the Denver Action Medic Network has added new training guidelines: Don’t go to protests if sick or in contact with those who are infected; wear a mask; give people lots of space and use hand sanitizer. Jordan Garcia, a 39-year-old medic for over 20 years who works with the network of veteran street medics, said they also warn medics about the increased risk of transmission because of protesters coughing from tear gas, and urge them to get tested for the virus after the protests.
The number of volunteer medics swelled after George Floyd’s May 25 killing in Minneapolis. In Denver alone, at least 40 people reached out to the Denver Action Medic Network for training.
On June 3, Dr. Rupa Marya, an associate professor of medicine at the University of California,San Francisco, and the co-founder of the Do No Harm Coalition, which runs street medic training in the Bay Area, hosted a national webinar attended by over 3,000 medical professionals to provide the bridge training to be a street medic. In her online bio, Marya describes the coalition as “an organization of over 450 health workers committed to structural change” in addressing health problems.
“When we see suffering, that’s where we go,” Marya said. “And right now that suffering is happening on the streets.”
In the recent Denver protests, street medics responded to major head, face and eye injuries among protesters from what are sometimes described as “kinetic impact projectiles” or “less-than-lethal” bullets shot at protesters, along with tear-gas and flash-bang stun grenade canisters that either hit them or exploded in their faces.
Garcia, who by day works for an immigrant rights nonprofit, said that these weapons are not designed to be shot directly at people.
“We’re seeing police use these less-lethal weapons in lethal ways, and that is pretty upsetting,” Garcia said about the recent protests.
Denver police Chief Paul Pazen promised to make changes, including banning chokeholds and requiring SWAT teams to turn on their body cameras. Last week, a federal judge also issued a temporary injunction to stop Denver police from using tear gas and other less-than-lethal weapons in response to a class action lawsuit, in which a medic stated he was shot multiple times by police with pepper balls while treating patients. (Last week in North Carolina police were recorded destroying medic stations.)
Denver street medic Kevin Connell, a 30-year-old emergency room nurse, said he was hit with pepper balls in the back of his medic vest – which was clearly marked by red crosses – while treating a patient. He showed up to the Denver protests every night he did not have to work, he said, wearing a Kevlar medic vest, protective goggles and a homemade gas mask fashioned from a water bottle. As a member of the Denver Action Medic Network, Connell also served at the Standing Rock protests in North Dakota in a dispute over the building of the Dakota Access Pipeline.
“I mean, as bad as it sounds, it was only tear gas, pepper balls and rubber bullets that were being fired on us,” Connell said of his recent experience in Denver. “When I was at Standing Rock, they were using high-powered water hoses even when it was, like, freezing cold. … So I think the police here had a little bit more restraint.”
Still, first-time street medic Aj Mossman, a 31-year-old Denver emergency medical technician studying for nursing school, was shocked to be tear-gassed and struck in the back of the leg with a flash grenade while treating a protester on May 30. Mossman still has a large leg bruise.
The following night, Mossman, who uses the pronoun they, brought more protective gear, but said they are still having difficulty processing what felt like a war zone.
“I thought I understood what my black friends went through. I thought I understood what the black community went through,” said Mossman, who is white. “But I had absolutely no idea how violent the police were and how little they cared about who they hurt.”
For Butler, serving as a medic with others from various walks of life was inspiring. “They’re also out there to protect black and brown bodies. And that’s amazing,” she said. “That’s just a beautiful sight.”
This article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.