User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Three genes could predict congenital Zika infection susceptibility
Dr. Irene Rivero-Calle, MD, shared at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year.
ZIKV, an emerging flavivirus, is responsible for one the most critical pandemic emergencies of the last decade and has been associated with severe neonatal brain disabilities, declared Dr. Rivero-Calle, of the Hospital Clínico Universitario de Santiago de Compostela in Santiago de Compostela, Spain. “We think that understanding the genomic background could explain some of the most relevant symptoms of congenital Zika syndrome (CZS) and could be essential to better comprehend this disease.”
To achieve this understanding, Dr. Rivero-Calle and her colleagues conducted a study aiming to analyze any genetic factors that could explain the variation in phenotypes in newborns from mothers who had a Zika infection during their pregnancy. Additionally, they strove to “elucidate if the possible genetic association is specific to mothers or their newborns, and to check if this genomic background or any genomic ancestry pattern could be related with the phenotype,” she explained.
In their study, Dr. Rivero-Calle and her team analyzed 80 samples, comprising 40 samples from mothers who had been infected by ZIKV during their pregnancy and 40 from their newborns. Of those descendants, 20 were asymptomatic and 20 were symptomatic (13 had CZS, 3 had microcephaly, 2 had a pathologic MRI, 1 had hearing loss, and 1 was born preterm).
Population stratification, which Dr. Rivero-Calle explained “lets us know if the population is African, European, or Native American looking at the genes,” did not show any relation with the phenotype. We had a mixture of population genomics among all samples.”
Dr. Rivero-Calle and her team then performed three analyses: genotype analysis, an allelic test, and gene analysis. The allelic test and gene-collapsing method highlighted three genes (PANO1, PIDD1, and SLC25A22) as potential determinants of the varying phenotypes in the newborns from ZIKV-infected mothers. Overrepresentation analysis of gene ontology terms shows that PIDD1 and PANO1 are related to apoptosis and cell death, which is closely related to early infantile epilepsy. This could explain the most severe complications of CZS: seizures, brain damage, microcephaly, and detrimental neurodevelopmental growth. Regarding reactome and KEGG analysis, gene PIID1 is related with p53 pathway, which correlates with cell’s death and apoptosis, and with microcephaly, a typical phenotypic feature of CZS.
“So, in conclusion, we found three genes which could predict susceptibility to congenital Zika infection; we saw that the functionality of these genes seems to be deeply related with mechanisms which could explain the different phenotypes; and we saw that these three genes only appear in the children’s cohort, so there is no candidate gene in the mother’s genomic background which can help predict the phenotype of the newborn,” Dr. Rivero-Calle declared. “Finally, there is no ancestry pattern associated with disabilities caused by Zika infection.”
Dr. Rivero-Calle reported that this project (ZikAction) has received funding from the European Union’s Horizon 2020 research and innovation program, under grant agreement 734857.
Dr. Irene Rivero-Calle, MD, shared at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year.
ZIKV, an emerging flavivirus, is responsible for one the most critical pandemic emergencies of the last decade and has been associated with severe neonatal brain disabilities, declared Dr. Rivero-Calle, of the Hospital Clínico Universitario de Santiago de Compostela in Santiago de Compostela, Spain. “We think that understanding the genomic background could explain some of the most relevant symptoms of congenital Zika syndrome (CZS) and could be essential to better comprehend this disease.”
To achieve this understanding, Dr. Rivero-Calle and her colleagues conducted a study aiming to analyze any genetic factors that could explain the variation in phenotypes in newborns from mothers who had a Zika infection during their pregnancy. Additionally, they strove to “elucidate if the possible genetic association is specific to mothers or their newborns, and to check if this genomic background or any genomic ancestry pattern could be related with the phenotype,” she explained.
In their study, Dr. Rivero-Calle and her team analyzed 80 samples, comprising 40 samples from mothers who had been infected by ZIKV during their pregnancy and 40 from their newborns. Of those descendants, 20 were asymptomatic and 20 were symptomatic (13 had CZS, 3 had microcephaly, 2 had a pathologic MRI, 1 had hearing loss, and 1 was born preterm).
Population stratification, which Dr. Rivero-Calle explained “lets us know if the population is African, European, or Native American looking at the genes,” did not show any relation with the phenotype. We had a mixture of population genomics among all samples.”
Dr. Rivero-Calle and her team then performed three analyses: genotype analysis, an allelic test, and gene analysis. The allelic test and gene-collapsing method highlighted three genes (PANO1, PIDD1, and SLC25A22) as potential determinants of the varying phenotypes in the newborns from ZIKV-infected mothers. Overrepresentation analysis of gene ontology terms shows that PIDD1 and PANO1 are related to apoptosis and cell death, which is closely related to early infantile epilepsy. This could explain the most severe complications of CZS: seizures, brain damage, microcephaly, and detrimental neurodevelopmental growth. Regarding reactome and KEGG analysis, gene PIID1 is related with p53 pathway, which correlates with cell’s death and apoptosis, and with microcephaly, a typical phenotypic feature of CZS.
“So, in conclusion, we found three genes which could predict susceptibility to congenital Zika infection; we saw that the functionality of these genes seems to be deeply related with mechanisms which could explain the different phenotypes; and we saw that these three genes only appear in the children’s cohort, so there is no candidate gene in the mother’s genomic background which can help predict the phenotype of the newborn,” Dr. Rivero-Calle declared. “Finally, there is no ancestry pattern associated with disabilities caused by Zika infection.”
Dr. Rivero-Calle reported that this project (ZikAction) has received funding from the European Union’s Horizon 2020 research and innovation program, under grant agreement 734857.
Dr. Irene Rivero-Calle, MD, shared at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year.
ZIKV, an emerging flavivirus, is responsible for one the most critical pandemic emergencies of the last decade and has been associated with severe neonatal brain disabilities, declared Dr. Rivero-Calle, of the Hospital Clínico Universitario de Santiago de Compostela in Santiago de Compostela, Spain. “We think that understanding the genomic background could explain some of the most relevant symptoms of congenital Zika syndrome (CZS) and could be essential to better comprehend this disease.”
To achieve this understanding, Dr. Rivero-Calle and her colleagues conducted a study aiming to analyze any genetic factors that could explain the variation in phenotypes in newborns from mothers who had a Zika infection during their pregnancy. Additionally, they strove to “elucidate if the possible genetic association is specific to mothers or their newborns, and to check if this genomic background or any genomic ancestry pattern could be related with the phenotype,” she explained.
In their study, Dr. Rivero-Calle and her team analyzed 80 samples, comprising 40 samples from mothers who had been infected by ZIKV during their pregnancy and 40 from their newborns. Of those descendants, 20 were asymptomatic and 20 were symptomatic (13 had CZS, 3 had microcephaly, 2 had a pathologic MRI, 1 had hearing loss, and 1 was born preterm).
Population stratification, which Dr. Rivero-Calle explained “lets us know if the population is African, European, or Native American looking at the genes,” did not show any relation with the phenotype. We had a mixture of population genomics among all samples.”
Dr. Rivero-Calle and her team then performed three analyses: genotype analysis, an allelic test, and gene analysis. The allelic test and gene-collapsing method highlighted three genes (PANO1, PIDD1, and SLC25A22) as potential determinants of the varying phenotypes in the newborns from ZIKV-infected mothers. Overrepresentation analysis of gene ontology terms shows that PIDD1 and PANO1 are related to apoptosis and cell death, which is closely related to early infantile epilepsy. This could explain the most severe complications of CZS: seizures, brain damage, microcephaly, and detrimental neurodevelopmental growth. Regarding reactome and KEGG analysis, gene PIID1 is related with p53 pathway, which correlates with cell’s death and apoptosis, and with microcephaly, a typical phenotypic feature of CZS.
“So, in conclusion, we found three genes which could predict susceptibility to congenital Zika infection; we saw that the functionality of these genes seems to be deeply related with mechanisms which could explain the different phenotypes; and we saw that these three genes only appear in the children’s cohort, so there is no candidate gene in the mother’s genomic background which can help predict the phenotype of the newborn,” Dr. Rivero-Calle declared. “Finally, there is no ancestry pattern associated with disabilities caused by Zika infection.”
Dr. Rivero-Calle reported that this project (ZikAction) has received funding from the European Union’s Horizon 2020 research and innovation program, under grant agreement 734857.
FROM ESPID 2020
Medical societies waive fees, weigh other options during pandemic
COVID-19’s toll on member facilities pushed the American Academy of Sleep Medicine (AASM) recently to take a sizable gamble.
AASM announced in September that it would waive facility fees at all 2,648 AASM-accredited sleep facilities for 2021.
At $1,800-$2,600 for each facility, that will mean lost revenue of between $4.8 million and $6.9 million, but it’s a risk the academy felt it had to take.
AASM President Kannan Ramar, MBBS, MD, said in an interview that they are betting on the future of the field.
An internal survey of members, he said, found that nearly half (46%) of the 551 respondents thought they might have to close by the end of the year.
In addition, 66% reported a lower patient volume in the past month, and 36% reported that their practice or facility had to apply for loans or other financial assistance because of COVID-19, AASM said in its press release.
“We are hoping that if we help our members through this, they will be there for our patients,” Dr. Ramar said.
Other medical societies also are weighing options, straddling the line between needing income to provide resources for members but being acutely aware of the financial toll the pandemic is taking, according to one sampling.
As previously reported, primary care practices are projected to lose more than $68,000 in revenue per full-time physician in 2020, after steep drops in office visits and the collection of fees from March to May, according to a study led by researchers in the Blavatnik Institute at Harvard Medical School, Boston.
Those losses were calculated without considering a potential second wave of COVID-19 this year, the authors noted.
‘We can survive this’
Although AASM waived fees for its member facilities, individual physician fees have not been reduced so far. But the group is looking for more ways to help lower the economic burden on members, Dr. Ramar said.
“I don’t think we’ve ever been in this situation in the 45 years of the academy. This is a once-in-a-lifetime event for challenges we’re going through,” he said. “The board and the leadership realized that, if we’re going to do something, this is the time to do it.”
In addition to waiving the fees, AASM and the AASM Foundation are offering relief funding to state and regional sleep societies and research award recipients through programs created in response to COVID-19.
Some societies said they are not making changes to their dues or fees, some are forgoing cost-of-living fee increases, and some are waiving registration fees for annual meetings.
The American College of Allergy, Asthma and Immunology (ACAAI) waived most members’ registration fees for its annual meeting in November. Typically, that fee would be $500-$800 per member, plus charges for some premium sessions, Michael Blaiss, MD, ACAAI executive medical director, said.
Dr. Blaiss said in an interview that the college thought offering its 6,000 members essentially 25 free hours of CME would benefit them more than waiving annual membership dues, which are about $425 for physicians in the United States.
If the pandemic stretches through 2021, Dr. Blaiss said, “We can survive this. I’m not worried about that at all.”
But he acknowledged the painful effect on medical societies.
“I don’t think any organization would tell you it’s not having an effect on their income,” he said. “I know it is for us and for virtually any medical organization. A high percentage of income comes from the annual meeting.”
Waiving dues has not been a high priority among members in communications so far, Blaiss said.
American Academy of Dermatology President Bruce H. Thiers, MD, said in an interview that there will be no cost-of-living increase for 2021 dues, and AAD members can request a reduction in dues, which will be considered on a case-by-case basis.
“We understand that many members will have to make tough financial decisions,” he said.
In addition, AAD, which has more than 20,000 members, is exploring payment options to help members spread out the cost of membership.
ACP extends membership
The American College of Physicians, whose membership cycle starts in July, did not reduce dues but extended membership at no cost for 3 months through September to its 163,000 members, Phil Masters, MD, ACP’s vice president of membership, said in an interview.
It also expanded its educational offerings related to the pandemic, including webinars on physician wellness and issues regarding telemedicine.
He said expanding educational resources rather than waiving dues was an intentional decision after much discussion because “we’re primarily a services resource organization.”
Membership data are still being calculated, but early indications are that membership is not increasing this year, after seeing annual growth of about 2%-2.5%, Dr. Masters said. He noted that income is down “by several percent.” Annual membership dues average about $500 for physicians who have been practicing for 10 years.
“We’re well positioned to tolerate the ups and downs,” he said, but he acknowledged that “there’s no question the financial impact has been devastating on some practices.”
Like some other associations, ACP decided to cancel this year’s annual meeting, which had been planned for April. The 2021 annual meeting will be conducted online from April 29 to May 1.
Smaller organizations that rely heavily on income from the annual meeting will be severely challenged the longer the pandemic continues, Dr. Masters said.
The decision is not as simple as whether to reduce or eliminate dues, he noted. Organizations will have to reexamine their missions and structure their fees and offerings according to the needs of members.
“It’s a balance in doing things for the community at large and balancing the need to be sensitive to financial implications,” Dr. Masters said.
This article first appeared on Medscape.com.
COVID-19’s toll on member facilities pushed the American Academy of Sleep Medicine (AASM) recently to take a sizable gamble.
AASM announced in September that it would waive facility fees at all 2,648 AASM-accredited sleep facilities for 2021.
At $1,800-$2,600 for each facility, that will mean lost revenue of between $4.8 million and $6.9 million, but it’s a risk the academy felt it had to take.
AASM President Kannan Ramar, MBBS, MD, said in an interview that they are betting on the future of the field.
An internal survey of members, he said, found that nearly half (46%) of the 551 respondents thought they might have to close by the end of the year.
In addition, 66% reported a lower patient volume in the past month, and 36% reported that their practice or facility had to apply for loans or other financial assistance because of COVID-19, AASM said in its press release.
“We are hoping that if we help our members through this, they will be there for our patients,” Dr. Ramar said.
Other medical societies also are weighing options, straddling the line between needing income to provide resources for members but being acutely aware of the financial toll the pandemic is taking, according to one sampling.
As previously reported, primary care practices are projected to lose more than $68,000 in revenue per full-time physician in 2020, after steep drops in office visits and the collection of fees from March to May, according to a study led by researchers in the Blavatnik Institute at Harvard Medical School, Boston.
Those losses were calculated without considering a potential second wave of COVID-19 this year, the authors noted.
‘We can survive this’
Although AASM waived fees for its member facilities, individual physician fees have not been reduced so far. But the group is looking for more ways to help lower the economic burden on members, Dr. Ramar said.
“I don’t think we’ve ever been in this situation in the 45 years of the academy. This is a once-in-a-lifetime event for challenges we’re going through,” he said. “The board and the leadership realized that, if we’re going to do something, this is the time to do it.”
In addition to waiving the fees, AASM and the AASM Foundation are offering relief funding to state and regional sleep societies and research award recipients through programs created in response to COVID-19.
Some societies said they are not making changes to their dues or fees, some are forgoing cost-of-living fee increases, and some are waiving registration fees for annual meetings.
The American College of Allergy, Asthma and Immunology (ACAAI) waived most members’ registration fees for its annual meeting in November. Typically, that fee would be $500-$800 per member, plus charges for some premium sessions, Michael Blaiss, MD, ACAAI executive medical director, said.
Dr. Blaiss said in an interview that the college thought offering its 6,000 members essentially 25 free hours of CME would benefit them more than waiving annual membership dues, which are about $425 for physicians in the United States.
If the pandemic stretches through 2021, Dr. Blaiss said, “We can survive this. I’m not worried about that at all.”
But he acknowledged the painful effect on medical societies.
“I don’t think any organization would tell you it’s not having an effect on their income,” he said. “I know it is for us and for virtually any medical organization. A high percentage of income comes from the annual meeting.”
Waiving dues has not been a high priority among members in communications so far, Blaiss said.
American Academy of Dermatology President Bruce H. Thiers, MD, said in an interview that there will be no cost-of-living increase for 2021 dues, and AAD members can request a reduction in dues, which will be considered on a case-by-case basis.
“We understand that many members will have to make tough financial decisions,” he said.
In addition, AAD, which has more than 20,000 members, is exploring payment options to help members spread out the cost of membership.
ACP extends membership
The American College of Physicians, whose membership cycle starts in July, did not reduce dues but extended membership at no cost for 3 months through September to its 163,000 members, Phil Masters, MD, ACP’s vice president of membership, said in an interview.
It also expanded its educational offerings related to the pandemic, including webinars on physician wellness and issues regarding telemedicine.
He said expanding educational resources rather than waiving dues was an intentional decision after much discussion because “we’re primarily a services resource organization.”
Membership data are still being calculated, but early indications are that membership is not increasing this year, after seeing annual growth of about 2%-2.5%, Dr. Masters said. He noted that income is down “by several percent.” Annual membership dues average about $500 for physicians who have been practicing for 10 years.
“We’re well positioned to tolerate the ups and downs,” he said, but he acknowledged that “there’s no question the financial impact has been devastating on some practices.”
Like some other associations, ACP decided to cancel this year’s annual meeting, which had been planned for April. The 2021 annual meeting will be conducted online from April 29 to May 1.
Smaller organizations that rely heavily on income from the annual meeting will be severely challenged the longer the pandemic continues, Dr. Masters said.
The decision is not as simple as whether to reduce or eliminate dues, he noted. Organizations will have to reexamine their missions and structure their fees and offerings according to the needs of members.
“It’s a balance in doing things for the community at large and balancing the need to be sensitive to financial implications,” Dr. Masters said.
This article first appeared on Medscape.com.
COVID-19’s toll on member facilities pushed the American Academy of Sleep Medicine (AASM) recently to take a sizable gamble.
AASM announced in September that it would waive facility fees at all 2,648 AASM-accredited sleep facilities for 2021.
At $1,800-$2,600 for each facility, that will mean lost revenue of between $4.8 million and $6.9 million, but it’s a risk the academy felt it had to take.
AASM President Kannan Ramar, MBBS, MD, said in an interview that they are betting on the future of the field.
An internal survey of members, he said, found that nearly half (46%) of the 551 respondents thought they might have to close by the end of the year.
In addition, 66% reported a lower patient volume in the past month, and 36% reported that their practice or facility had to apply for loans or other financial assistance because of COVID-19, AASM said in its press release.
“We are hoping that if we help our members through this, they will be there for our patients,” Dr. Ramar said.
Other medical societies also are weighing options, straddling the line between needing income to provide resources for members but being acutely aware of the financial toll the pandemic is taking, according to one sampling.
As previously reported, primary care practices are projected to lose more than $68,000 in revenue per full-time physician in 2020, after steep drops in office visits and the collection of fees from March to May, according to a study led by researchers in the Blavatnik Institute at Harvard Medical School, Boston.
Those losses were calculated without considering a potential second wave of COVID-19 this year, the authors noted.
‘We can survive this’
Although AASM waived fees for its member facilities, individual physician fees have not been reduced so far. But the group is looking for more ways to help lower the economic burden on members, Dr. Ramar said.
“I don’t think we’ve ever been in this situation in the 45 years of the academy. This is a once-in-a-lifetime event for challenges we’re going through,” he said. “The board and the leadership realized that, if we’re going to do something, this is the time to do it.”
In addition to waiving the fees, AASM and the AASM Foundation are offering relief funding to state and regional sleep societies and research award recipients through programs created in response to COVID-19.
Some societies said they are not making changes to their dues or fees, some are forgoing cost-of-living fee increases, and some are waiving registration fees for annual meetings.
The American College of Allergy, Asthma and Immunology (ACAAI) waived most members’ registration fees for its annual meeting in November. Typically, that fee would be $500-$800 per member, plus charges for some premium sessions, Michael Blaiss, MD, ACAAI executive medical director, said.
Dr. Blaiss said in an interview that the college thought offering its 6,000 members essentially 25 free hours of CME would benefit them more than waiving annual membership dues, which are about $425 for physicians in the United States.
If the pandemic stretches through 2021, Dr. Blaiss said, “We can survive this. I’m not worried about that at all.”
But he acknowledged the painful effect on medical societies.
“I don’t think any organization would tell you it’s not having an effect on their income,” he said. “I know it is for us and for virtually any medical organization. A high percentage of income comes from the annual meeting.”
Waiving dues has not been a high priority among members in communications so far, Blaiss said.
American Academy of Dermatology President Bruce H. Thiers, MD, said in an interview that there will be no cost-of-living increase for 2021 dues, and AAD members can request a reduction in dues, which will be considered on a case-by-case basis.
“We understand that many members will have to make tough financial decisions,” he said.
In addition, AAD, which has more than 20,000 members, is exploring payment options to help members spread out the cost of membership.
ACP extends membership
The American College of Physicians, whose membership cycle starts in July, did not reduce dues but extended membership at no cost for 3 months through September to its 163,000 members, Phil Masters, MD, ACP’s vice president of membership, said in an interview.
It also expanded its educational offerings related to the pandemic, including webinars on physician wellness and issues regarding telemedicine.
He said expanding educational resources rather than waiving dues was an intentional decision after much discussion because “we’re primarily a services resource organization.”
Membership data are still being calculated, but early indications are that membership is not increasing this year, after seeing annual growth of about 2%-2.5%, Dr. Masters said. He noted that income is down “by several percent.” Annual membership dues average about $500 for physicians who have been practicing for 10 years.
“We’re well positioned to tolerate the ups and downs,” he said, but he acknowledged that “there’s no question the financial impact has been devastating on some practices.”
Like some other associations, ACP decided to cancel this year’s annual meeting, which had been planned for April. The 2021 annual meeting will be conducted online from April 29 to May 1.
Smaller organizations that rely heavily on income from the annual meeting will be severely challenged the longer the pandemic continues, Dr. Masters said.
The decision is not as simple as whether to reduce or eliminate dues, he noted. Organizations will have to reexamine their missions and structure their fees and offerings according to the needs of members.
“It’s a balance in doing things for the community at large and balancing the need to be sensitive to financial implications,” Dr. Masters said.
This article first appeared on Medscape.com.
Meningococcal transmission risk appears low among pediatric health care professionals
at a university – lower than expected for all age groups, Lisa-Maria Steurer, MD, said regarding study findings reported at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year.
“This implicates that the risk of horizontal meningococcal transmission via this health care professional cohort seems to be low,” said Dr. Steurer, of the Medical University of Vienna.
Her data were based on a survey conducted between April and October 2018 at the department of paediatrics and adolescent medicine at the tertiary university pediatric hospital. The study aimed to determine colonization rates of Neisseria meningitidis and the serogroup distribution of carried meningococcal isolates in asymptomatic health care professionals employed there, reported Dr. Steurer. Her research team also sought to identify what factors increased risk of N. meningitidis carriage.
“We who work in pediatrics and adolescent medicine are exposed to those patient cohorts with the highest risk for meningococcal carriage, but also to those patients who have the highest risk for serious, invasive meningococcal disease, which peaks at the extremities of age,” declared Dr. Steurer. “But currently, there is no surveillance of asymptomatic carriers in this health care professional cohort.”
A total of 437 oropharyngeal swabs were collected from enrolled nurses, pediatricians, and medical students working in the department and immediately plated onto selective agar plates. Conventional culture was used to identify bacteria, and meningococcal isolates were characterized further through whole-genome sequencing. Sociodemographic data and information on participants’ vaccination status were collected via questionnaire.
The main finding was an overall meningococcal prevalence of 1.14%. Among the participants, the median age was 33 years, and the highest rate of carriage, 4.4%, was observed in those aged 18-25 years. None of the carriers were older than 35 years. There was a negative association found between carriage and participants’ age and time employed in the field, Dr. Steurer said.
“Risk-factor analysis found an inverse correlation with meningococcal carriage for age and timespan working in pediatrics. On the contrary, no correlations with carriage could be found for all other factors evaluated,” she said. These factors included recent contact with an immunodeficient patient, respiratory tract infection, smoking, vaccination against any meningococcal serogroup, different professions, main work settings, month of swab collection, and living with children or adolescents in the same household.
Of the study population, 29% reported that they had been vaccinated against at least one meningococcal serogroup. “Interestingly, while more than 50% of doctors and medical students had a vaccination against at least one meningococcal serogroup, only 17% of nurses were vaccinated,” Dr. Steurer remarked.
The study was financially supported by Pfizer. Dr. Steurer had no other relevant financial disclosures.
at a university – lower than expected for all age groups, Lisa-Maria Steurer, MD, said regarding study findings reported at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year.
“This implicates that the risk of horizontal meningococcal transmission via this health care professional cohort seems to be low,” said Dr. Steurer, of the Medical University of Vienna.
Her data were based on a survey conducted between April and October 2018 at the department of paediatrics and adolescent medicine at the tertiary university pediatric hospital. The study aimed to determine colonization rates of Neisseria meningitidis and the serogroup distribution of carried meningococcal isolates in asymptomatic health care professionals employed there, reported Dr. Steurer. Her research team also sought to identify what factors increased risk of N. meningitidis carriage.
“We who work in pediatrics and adolescent medicine are exposed to those patient cohorts with the highest risk for meningococcal carriage, but also to those patients who have the highest risk for serious, invasive meningococcal disease, which peaks at the extremities of age,” declared Dr. Steurer. “But currently, there is no surveillance of asymptomatic carriers in this health care professional cohort.”
A total of 437 oropharyngeal swabs were collected from enrolled nurses, pediatricians, and medical students working in the department and immediately plated onto selective agar plates. Conventional culture was used to identify bacteria, and meningococcal isolates were characterized further through whole-genome sequencing. Sociodemographic data and information on participants’ vaccination status were collected via questionnaire.
The main finding was an overall meningococcal prevalence of 1.14%. Among the participants, the median age was 33 years, and the highest rate of carriage, 4.4%, was observed in those aged 18-25 years. None of the carriers were older than 35 years. There was a negative association found between carriage and participants’ age and time employed in the field, Dr. Steurer said.
“Risk-factor analysis found an inverse correlation with meningococcal carriage for age and timespan working in pediatrics. On the contrary, no correlations with carriage could be found for all other factors evaluated,” she said. These factors included recent contact with an immunodeficient patient, respiratory tract infection, smoking, vaccination against any meningococcal serogroup, different professions, main work settings, month of swab collection, and living with children or adolescents in the same household.
Of the study population, 29% reported that they had been vaccinated against at least one meningococcal serogroup. “Interestingly, while more than 50% of doctors and medical students had a vaccination against at least one meningococcal serogroup, only 17% of nurses were vaccinated,” Dr. Steurer remarked.
The study was financially supported by Pfizer. Dr. Steurer had no other relevant financial disclosures.
at a university – lower than expected for all age groups, Lisa-Maria Steurer, MD, said regarding study findings reported at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year.
“This implicates that the risk of horizontal meningococcal transmission via this health care professional cohort seems to be low,” said Dr. Steurer, of the Medical University of Vienna.
Her data were based on a survey conducted between April and October 2018 at the department of paediatrics and adolescent medicine at the tertiary university pediatric hospital. The study aimed to determine colonization rates of Neisseria meningitidis and the serogroup distribution of carried meningococcal isolates in asymptomatic health care professionals employed there, reported Dr. Steurer. Her research team also sought to identify what factors increased risk of N. meningitidis carriage.
“We who work in pediatrics and adolescent medicine are exposed to those patient cohorts with the highest risk for meningococcal carriage, but also to those patients who have the highest risk for serious, invasive meningococcal disease, which peaks at the extremities of age,” declared Dr. Steurer. “But currently, there is no surveillance of asymptomatic carriers in this health care professional cohort.”
A total of 437 oropharyngeal swabs were collected from enrolled nurses, pediatricians, and medical students working in the department and immediately plated onto selective agar plates. Conventional culture was used to identify bacteria, and meningococcal isolates were characterized further through whole-genome sequencing. Sociodemographic data and information on participants’ vaccination status were collected via questionnaire.
The main finding was an overall meningococcal prevalence of 1.14%. Among the participants, the median age was 33 years, and the highest rate of carriage, 4.4%, was observed in those aged 18-25 years. None of the carriers were older than 35 years. There was a negative association found between carriage and participants’ age and time employed in the field, Dr. Steurer said.
“Risk-factor analysis found an inverse correlation with meningococcal carriage for age and timespan working in pediatrics. On the contrary, no correlations with carriage could be found for all other factors evaluated,” she said. These factors included recent contact with an immunodeficient patient, respiratory tract infection, smoking, vaccination against any meningococcal serogroup, different professions, main work settings, month of swab collection, and living with children or adolescents in the same household.
Of the study population, 29% reported that they had been vaccinated against at least one meningococcal serogroup. “Interestingly, while more than 50% of doctors and medical students had a vaccination against at least one meningococcal serogroup, only 17% of nurses were vaccinated,” Dr. Steurer remarked.
The study was financially supported by Pfizer. Dr. Steurer had no other relevant financial disclosures.
FROM ESPID 2020
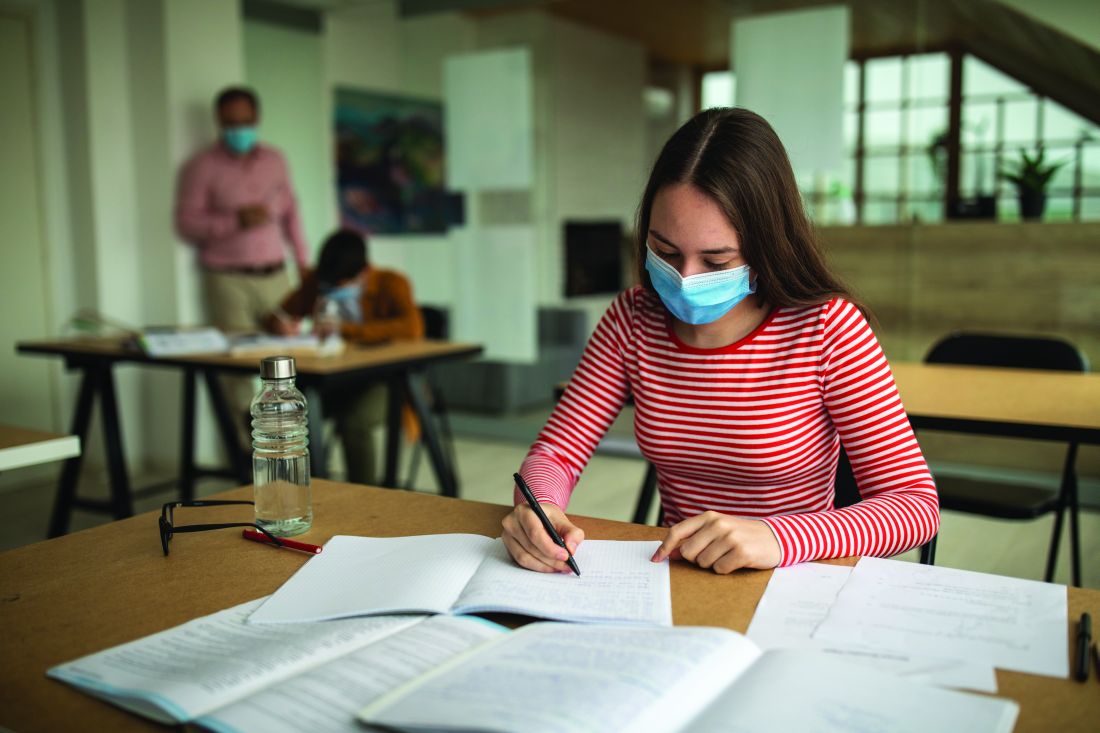
Children and school during the pandemic: What’s the answer?
Countries across the world are in the process of closing and reopening schools to contain the spread of COVID-19. Should there be universal testing and quarantining of sick school children and their classmates?
In a lively debate at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year, Andreea M. Panciu, MD, from the National Institute of Infectious Diseases in Bucharest, argued for routine testing and quarantining of all school children. Her opposite number, Danilo Buonsenso, MD, from the Centre for Global Health Research and Studies, Fondazione Policlinico Universitario Agostino Gemelli Istituto di Ricovero e Cura a Carattere Scientifico, Rome, made the case for a more selective approach.
Should children be sent to school?
stated Dr. Panciu as she started the debate by explaining the challenges faced by schools in adhering to key mitigation strategies. The U.S. Centers for Disease Control and Prevention recommends that students keep 1.8 m (6 feet) distance from one another. “In many school settings this is not feasible without drastically limiting the number of students,” she explained. “This is a massive challenge for many schools that are already overcrowded.”
The use of facemasks also is a challenge in classrooms. Children have a lower tolerance or may not be able to use the mask properly. There also are concerns regarding impaired learning, speech development, social development, and facial recognition. “We need to look at the evidence; preventive measures work,” responded Dr. Buonsenso. If distance can be implemented, the more distance the lower the transmission of infection, with 1.5-2 meters having the best effects. “Distance can be difficult when school buildings do not allow it, however, governments have had time to plan, and this should not be a limitation to education for kids.”
A recent review clearly showed that children and adolescents aged under 20 years have a much lower risk of susceptibility to COVID-19 infection, compared with adults. This is especially the case for children younger than 14 years. “There is no excuse, let’s bring the children back to school,” argued Dr. Buonsenso.
Dr. Panciu responded with several studies that have tried to quantify the amount of SARS-CoV-2 virus that is carried by infected children. Viral load in the nasopharynx in children under 5 years with mild to moderate COVID-19 symptoms was higher than that of both children over 5 as well as adults. The viral load in young children did not seem to differ by age or symptom severity. “There doesn’t appear to be a significant difference in viral load between symptomatic children and symptomatic adults,” she stated.
“But the question is: ‘How infectious are children?’ ” reacted Dr. Buonsenso. Data from South Korea showed that, for children, particularly those under 10 years, the number of secondary cases of contacts was very low, suggesting that children are rarely spreading the virus.
Dr. Buonsenso and colleagues assessed 30 households containing children aged under 18 years where an adult had been infected with COVID-19 in Rome during the peak of the pandemic. In no cases was it found that a child was the index case. This was supported by data from China, also obtained during the peak of the pandemic, which showed that the number of children infected was very low, but more importantly the number of secondary attacks from contact with children was also very low.
What about children who are sick at school?
The debate moved to discussing what should be done when a child is sick at school. Dr. Panciu clarified recommendations by the CDC regarding what steps to take if a student displays signs of infection consistent with COVID-19: Should they test positive, they are to stay at home for 10 days from the time signs and symptoms first appeared. Further, any teachers or students identified as close contacts are advised to stay at home for 14 days. (Since the ESPID meeting, the CDC has made changes in quarantine times for COVID-19. People can now quarantine for 10 days without a COVID-19 test if they have no symptoms. Alternatively, a quarantine can end after 7 days for someone with a negative test and no symptoms. The agency recommends a polymerase chain reaction test or an antigen assay within 48 hours before the end of a quarantine.)
A significant problem is the overlap between COVID-19 symptoms and those associated with other common illnesses because of a range of viruses. This is particularly true in younger children who often suffer from viral infections. “It is common for children to have up to eight respiratory illnesses a year,” explained Dr. Panciu, “and some may have symptoms so mild that they don’t notice them.”
“We need to be a little bit more children focused, otherwise we are going to be isolating children all the time,” said Dr. Buonsenso. The Royal College of Paediatrics and Child Health state that a child with a simple runny nose or sporadic cough without a fever, who would have attended school in other times, should not be tested for COVID-19. He moved on to then cite several studies that show little or no evidence of COVID-19 transmission between school children. This included a prospective cohort study in Australia showing that child-to-child transmission occurred in 0.3%. “To date, the advantages from routine quarantine and over testing seem too low to balance the social consequences on children and families,” he concluded.
As the debate drew to a close, Dr. Panciu reported several studies that did demonstrate transmission between school-age children. Data from an overnight camp in Georgia where the median age was 12 years showed the attack rate was 44% for ages 11-17 years and 51% for ages 6-10 years. Similar conclusions were reached in an Israeli study looking at a large COVID-19 outbreak in a school. This occurred 10 days after reopening, in spite of preventive measures being in place. “Opening safely isn’t just about the adjustments a school makes,” she said, “it’s also about how much of the virus is circulating in the community, which affects the likelihood that students and staff will bring COVID-19 into their classrooms.”
Damian Roland, consultant and honorary associate professor in pediatric emergency medicine at the University of Leicester (England), commented: “Maximizing educational potential while reducing the spread of COVID19 is a challenge laden with scientific equipoise while simultaneously infused with emotion. The evidence of transmission between, and infectivity from, children is not complete, as this debate has demonstrated. It is important scientists, clinicians, educators, and policy makers make collaborative decisions, aware there is not one perfect answer, and willing to understand and incorporate others views and objectives rather than holding onto single beliefs or approaches.”
No financial conflicts of interest were declared.
Countries across the world are in the process of closing and reopening schools to contain the spread of COVID-19. Should there be universal testing and quarantining of sick school children and their classmates?
In a lively debate at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year, Andreea M. Panciu, MD, from the National Institute of Infectious Diseases in Bucharest, argued for routine testing and quarantining of all school children. Her opposite number, Danilo Buonsenso, MD, from the Centre for Global Health Research and Studies, Fondazione Policlinico Universitario Agostino Gemelli Istituto di Ricovero e Cura a Carattere Scientifico, Rome, made the case for a more selective approach.
Should children be sent to school?
stated Dr. Panciu as she started the debate by explaining the challenges faced by schools in adhering to key mitigation strategies. The U.S. Centers for Disease Control and Prevention recommends that students keep 1.8 m (6 feet) distance from one another. “In many school settings this is not feasible without drastically limiting the number of students,” she explained. “This is a massive challenge for many schools that are already overcrowded.”
The use of facemasks also is a challenge in classrooms. Children have a lower tolerance or may not be able to use the mask properly. There also are concerns regarding impaired learning, speech development, social development, and facial recognition. “We need to look at the evidence; preventive measures work,” responded Dr. Buonsenso. If distance can be implemented, the more distance the lower the transmission of infection, with 1.5-2 meters having the best effects. “Distance can be difficult when school buildings do not allow it, however, governments have had time to plan, and this should not be a limitation to education for kids.”
A recent review clearly showed that children and adolescents aged under 20 years have a much lower risk of susceptibility to COVID-19 infection, compared with adults. This is especially the case for children younger than 14 years. “There is no excuse, let’s bring the children back to school,” argued Dr. Buonsenso.
Dr. Panciu responded with several studies that have tried to quantify the amount of SARS-CoV-2 virus that is carried by infected children. Viral load in the nasopharynx in children under 5 years with mild to moderate COVID-19 symptoms was higher than that of both children over 5 as well as adults. The viral load in young children did not seem to differ by age or symptom severity. “There doesn’t appear to be a significant difference in viral load between symptomatic children and symptomatic adults,” she stated.
“But the question is: ‘How infectious are children?’ ” reacted Dr. Buonsenso. Data from South Korea showed that, for children, particularly those under 10 years, the number of secondary cases of contacts was very low, suggesting that children are rarely spreading the virus.
Dr. Buonsenso and colleagues assessed 30 households containing children aged under 18 years where an adult had been infected with COVID-19 in Rome during the peak of the pandemic. In no cases was it found that a child was the index case. This was supported by data from China, also obtained during the peak of the pandemic, which showed that the number of children infected was very low, but more importantly the number of secondary attacks from contact with children was also very low.
What about children who are sick at school?
The debate moved to discussing what should be done when a child is sick at school. Dr. Panciu clarified recommendations by the CDC regarding what steps to take if a student displays signs of infection consistent with COVID-19: Should they test positive, they are to stay at home for 10 days from the time signs and symptoms first appeared. Further, any teachers or students identified as close contacts are advised to stay at home for 14 days. (Since the ESPID meeting, the CDC has made changes in quarantine times for COVID-19. People can now quarantine for 10 days without a COVID-19 test if they have no symptoms. Alternatively, a quarantine can end after 7 days for someone with a negative test and no symptoms. The agency recommends a polymerase chain reaction test or an antigen assay within 48 hours before the end of a quarantine.)
A significant problem is the overlap between COVID-19 symptoms and those associated with other common illnesses because of a range of viruses. This is particularly true in younger children who often suffer from viral infections. “It is common for children to have up to eight respiratory illnesses a year,” explained Dr. Panciu, “and some may have symptoms so mild that they don’t notice them.”
“We need to be a little bit more children focused, otherwise we are going to be isolating children all the time,” said Dr. Buonsenso. The Royal College of Paediatrics and Child Health state that a child with a simple runny nose or sporadic cough without a fever, who would have attended school in other times, should not be tested for COVID-19. He moved on to then cite several studies that show little or no evidence of COVID-19 transmission between school children. This included a prospective cohort study in Australia showing that child-to-child transmission occurred in 0.3%. “To date, the advantages from routine quarantine and over testing seem too low to balance the social consequences on children and families,” he concluded.
As the debate drew to a close, Dr. Panciu reported several studies that did demonstrate transmission between school-age children. Data from an overnight camp in Georgia where the median age was 12 years showed the attack rate was 44% for ages 11-17 years and 51% for ages 6-10 years. Similar conclusions were reached in an Israeli study looking at a large COVID-19 outbreak in a school. This occurred 10 days after reopening, in spite of preventive measures being in place. “Opening safely isn’t just about the adjustments a school makes,” she said, “it’s also about how much of the virus is circulating in the community, which affects the likelihood that students and staff will bring COVID-19 into their classrooms.”
Damian Roland, consultant and honorary associate professor in pediatric emergency medicine at the University of Leicester (England), commented: “Maximizing educational potential while reducing the spread of COVID19 is a challenge laden with scientific equipoise while simultaneously infused with emotion. The evidence of transmission between, and infectivity from, children is not complete, as this debate has demonstrated. It is important scientists, clinicians, educators, and policy makers make collaborative decisions, aware there is not one perfect answer, and willing to understand and incorporate others views and objectives rather than holding onto single beliefs or approaches.”
No financial conflicts of interest were declared.
Countries across the world are in the process of closing and reopening schools to contain the spread of COVID-19. Should there be universal testing and quarantining of sick school children and their classmates?
In a lively debate at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year, Andreea M. Panciu, MD, from the National Institute of Infectious Diseases in Bucharest, argued for routine testing and quarantining of all school children. Her opposite number, Danilo Buonsenso, MD, from the Centre for Global Health Research and Studies, Fondazione Policlinico Universitario Agostino Gemelli Istituto di Ricovero e Cura a Carattere Scientifico, Rome, made the case for a more selective approach.
Should children be sent to school?
stated Dr. Panciu as she started the debate by explaining the challenges faced by schools in adhering to key mitigation strategies. The U.S. Centers for Disease Control and Prevention recommends that students keep 1.8 m (6 feet) distance from one another. “In many school settings this is not feasible without drastically limiting the number of students,” she explained. “This is a massive challenge for many schools that are already overcrowded.”
The use of facemasks also is a challenge in classrooms. Children have a lower tolerance or may not be able to use the mask properly. There also are concerns regarding impaired learning, speech development, social development, and facial recognition. “We need to look at the evidence; preventive measures work,” responded Dr. Buonsenso. If distance can be implemented, the more distance the lower the transmission of infection, with 1.5-2 meters having the best effects. “Distance can be difficult when school buildings do not allow it, however, governments have had time to plan, and this should not be a limitation to education for kids.”
A recent review clearly showed that children and adolescents aged under 20 years have a much lower risk of susceptibility to COVID-19 infection, compared with adults. This is especially the case for children younger than 14 years. “There is no excuse, let’s bring the children back to school,” argued Dr. Buonsenso.
Dr. Panciu responded with several studies that have tried to quantify the amount of SARS-CoV-2 virus that is carried by infected children. Viral load in the nasopharynx in children under 5 years with mild to moderate COVID-19 symptoms was higher than that of both children over 5 as well as adults. The viral load in young children did not seem to differ by age or symptom severity. “There doesn’t appear to be a significant difference in viral load between symptomatic children and symptomatic adults,” she stated.
“But the question is: ‘How infectious are children?’ ” reacted Dr. Buonsenso. Data from South Korea showed that, for children, particularly those under 10 years, the number of secondary cases of contacts was very low, suggesting that children are rarely spreading the virus.
Dr. Buonsenso and colleagues assessed 30 households containing children aged under 18 years where an adult had been infected with COVID-19 in Rome during the peak of the pandemic. In no cases was it found that a child was the index case. This was supported by data from China, also obtained during the peak of the pandemic, which showed that the number of children infected was very low, but more importantly the number of secondary attacks from contact with children was also very low.
What about children who are sick at school?
The debate moved to discussing what should be done when a child is sick at school. Dr. Panciu clarified recommendations by the CDC regarding what steps to take if a student displays signs of infection consistent with COVID-19: Should they test positive, they are to stay at home for 10 days from the time signs and symptoms first appeared. Further, any teachers or students identified as close contacts are advised to stay at home for 14 days. (Since the ESPID meeting, the CDC has made changes in quarantine times for COVID-19. People can now quarantine for 10 days without a COVID-19 test if they have no symptoms. Alternatively, a quarantine can end after 7 days for someone with a negative test and no symptoms. The agency recommends a polymerase chain reaction test or an antigen assay within 48 hours before the end of a quarantine.)
A significant problem is the overlap between COVID-19 symptoms and those associated with other common illnesses because of a range of viruses. This is particularly true in younger children who often suffer from viral infections. “It is common for children to have up to eight respiratory illnesses a year,” explained Dr. Panciu, “and some may have symptoms so mild that they don’t notice them.”
“We need to be a little bit more children focused, otherwise we are going to be isolating children all the time,” said Dr. Buonsenso. The Royal College of Paediatrics and Child Health state that a child with a simple runny nose or sporadic cough without a fever, who would have attended school in other times, should not be tested for COVID-19. He moved on to then cite several studies that show little or no evidence of COVID-19 transmission between school children. This included a prospective cohort study in Australia showing that child-to-child transmission occurred in 0.3%. “To date, the advantages from routine quarantine and over testing seem too low to balance the social consequences on children and families,” he concluded.
As the debate drew to a close, Dr. Panciu reported several studies that did demonstrate transmission between school-age children. Data from an overnight camp in Georgia where the median age was 12 years showed the attack rate was 44% for ages 11-17 years and 51% for ages 6-10 years. Similar conclusions were reached in an Israeli study looking at a large COVID-19 outbreak in a school. This occurred 10 days after reopening, in spite of preventive measures being in place. “Opening safely isn’t just about the adjustments a school makes,” she said, “it’s also about how much of the virus is circulating in the community, which affects the likelihood that students and staff will bring COVID-19 into their classrooms.”
Damian Roland, consultant and honorary associate professor in pediatric emergency medicine at the University of Leicester (England), commented: “Maximizing educational potential while reducing the spread of COVID19 is a challenge laden with scientific equipoise while simultaneously infused with emotion. The evidence of transmission between, and infectivity from, children is not complete, as this debate has demonstrated. It is important scientists, clinicians, educators, and policy makers make collaborative decisions, aware there is not one perfect answer, and willing to understand and incorporate others views and objectives rather than holding onto single beliefs or approaches.”
No financial conflicts of interest were declared.
FROM ESPID 2020
Prioritize COVID-19 vaccination in both types of diabetes, say docs
The risk for increased COVID-19 severity in people with type 1 diabetes appears similar to that of type 2 diabetes, contrary to some official advice from the Centers for Disease Control and Prevention. The new finding indicates that people with both types should be priority for receiving a vaccine, investigators say.
The study is the first to prospectively evaluate both inpatients and outpatients and to examine COVID-19 severity factors in addition to death in people with type 1 and type 2 diabetes separately, and was published online Dec. 2 in Diabetes Care.
Among the patients, who were seen at Vanderbilt University Medical Center in Nashville, Tenn., between March and August of 2020, those with both type 1 and type 2 diabetes had between a three- and fourfold greater risk for COVID-19 hospitalization and greater illness severity compared with people without diabetes after adjustments for age, race, and a number of other risk factors.
This finding is important since as of Dec. 1, 2020, the CDC has classified the diabetes types differently in terms of underlying medical conditions that increase the risk for severe COVID-19.
Adults of any age with type 2 diabetes are considered “at increased risk of severe illness” from the virus that causes COVID-19 whereas the CDC says those with type 1 “might be at an increased risk.”
Lead author of the new paper Justin M. Gregory, MD, said in an interview: “I think this needs revision based on the current evidence. I think the data presented in our study and that of Barron et al. in Lancet Endocrinology 2020 indicate the need to place type 1 diabetes at parity with type 2 diabetes.
“These studies indicate both conditions carry an adjusted odds ratio of three to four when compared with people without diabetes for hospitalization, illness severity, and mortality,” he stressed.
Vaccines look promising for patients with diabetes
There were no phase 3 vaccine data available for the vaccine at the time that Dr. Gregory, of the Ian M. Burr Division of Pediatric Endocrinology and Diabetes, Vanderbilt University, Nashville, Tenn., and colleagues were writing their manuscript in late summer, so the article does not mention this.
But now, Dr. Gregory said, “Based on the initial press releases from Pfizer and Moderna, I am now optimistic that these vaccines might mitigate the excess morbidity and mortality from COVID-19 experienced by patients with diabetes.
“I am eager to see what we learn on December 10 and 17 [the scheduled dates for the meetings of the Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee to review the Pfizer and Moderna vaccines, respectively].”
But with the winter pandemic surge in the meantime, “Our investigation suggests that as COVID-19 hospitalizations rise, patients with both type 1 and 2 diabetes will comprise a disproportionately higher number of those admissions and, once hospitalized, demonstrate a greater degree of illness severity,” he and his colleagues said.
“In light of these data, we call on our colleagues to emphasize the importance of social distancing measures and hand hygiene, with particular emphasis on patients with diabetes, including those in the most vulnerable communities whom our study affirms will face the most severe impact.”
After adjustments, excess severity risk similar for both diabetes types
The new study data came from electronic health records at Vanderbilt University Medical Center, comprising 137 primary care, urgent care, and hospital facilities where patients were tested for SARS-CoV-2 regardless of the reason for their visit.
Between March 17 and August 7, 2020, 6,451 patients tested positive for COVID-19. Of those, 273 had type 2 diabetes and 40 had type 1 diabetes.
Children younger than 18 years accounted for 20% of those with type 1 diabetes and 9.4% of those without diabetes, but none of the type 2 group. The group with type 2 diabetes was considerably older than the type 1 diabetes and no-diabetes groups, 58 years versus 37 and 33 years, respectively.
Before adjustment for baseline characteristics that differed between groups, patients with type 1 diabetes appeared to have a risk for hospitalization and greater illness severity that was intermediate between the group with no diabetes and the group with type 2 diabetes, the researchers said.
But after adjustment for age, race, sex, hypertension, smoking, and body mass index, people with type 1 diabetes had odds ratios of 3.90 for hospitalization and 3.35 for greater illness severity, which was similar to risk in type 2 diabetes (3.36 and 3.42, respectively), compared to those without diabetes.
Deep dive explores COVID-19 severity risk factors in type 1 diabetes
The investigators then conducted a detailed chart review for 37 of the 40 patients with type 1 diabetes and phone surveys with 15 of them.
The majority (28) had not been hospitalized, and only one was hospitalized for diabetic ketoacidosis (DKA) within 14 days of positive SARS-CoV-2 testing.
This contrasts with a report from the T1D Exchange, in which nearly half of 33 patients with type 1 diabetes and COVID-19 had been hospitalized with DKA. The reason for the discrepancy may be that more severe patients would more likely be referred to the T1D Exchange Registry, Dr. Gregory and colleagues hypothesized.
Clinical factors associated with COVID-19 severity (P < .05) in their study included a prior hypertension diagnosis, higher hemoglobin A1c, at least one prior DKA admission in the past year, and not using a continuous glucose monitor (CGM).
Hospitalizations were twice as likely and illness severity nearly twice as great among those with type 1 diabetes who were Black versus White. Just 8% of those with private insurance were hospitalized, compared with 60% of those with public insurance and 67% with no insurance (P = .001).
“Whereas previous reports have indicated proportionally higher rates of hospitalizations from COVID-19 among Black patients and those with public insurance, this study is the first to show a similar finding in the population with type 1 diabetes,” Dr. Gregory and colleagues wrote.
Only 9% of patients using a CGM were hospitalized versus 47% who used blood glucose meters (P < .016). Similarly, hospitalizations occurred in 6% using an insulin pump versus 33% using multiple daily injections (P < .085).
“Our analysis cannot exclude the possibility that greater amounts of diabetes technology use are a surrogate for higher socioeconomic status,” they noted.
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases, JDRF, and the Appleby Foundation. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The risk for increased COVID-19 severity in people with type 1 diabetes appears similar to that of type 2 diabetes, contrary to some official advice from the Centers for Disease Control and Prevention. The new finding indicates that people with both types should be priority for receiving a vaccine, investigators say.
The study is the first to prospectively evaluate both inpatients and outpatients and to examine COVID-19 severity factors in addition to death in people with type 1 and type 2 diabetes separately, and was published online Dec. 2 in Diabetes Care.
Among the patients, who were seen at Vanderbilt University Medical Center in Nashville, Tenn., between March and August of 2020, those with both type 1 and type 2 diabetes had between a three- and fourfold greater risk for COVID-19 hospitalization and greater illness severity compared with people without diabetes after adjustments for age, race, and a number of other risk factors.
This finding is important since as of Dec. 1, 2020, the CDC has classified the diabetes types differently in terms of underlying medical conditions that increase the risk for severe COVID-19.
Adults of any age with type 2 diabetes are considered “at increased risk of severe illness” from the virus that causes COVID-19 whereas the CDC says those with type 1 “might be at an increased risk.”
Lead author of the new paper Justin M. Gregory, MD, said in an interview: “I think this needs revision based on the current evidence. I think the data presented in our study and that of Barron et al. in Lancet Endocrinology 2020 indicate the need to place type 1 diabetes at parity with type 2 diabetes.
“These studies indicate both conditions carry an adjusted odds ratio of three to four when compared with people without diabetes for hospitalization, illness severity, and mortality,” he stressed.
Vaccines look promising for patients with diabetes
There were no phase 3 vaccine data available for the vaccine at the time that Dr. Gregory, of the Ian M. Burr Division of Pediatric Endocrinology and Diabetes, Vanderbilt University, Nashville, Tenn., and colleagues were writing their manuscript in late summer, so the article does not mention this.
But now, Dr. Gregory said, “Based on the initial press releases from Pfizer and Moderna, I am now optimistic that these vaccines might mitigate the excess morbidity and mortality from COVID-19 experienced by patients with diabetes.
“I am eager to see what we learn on December 10 and 17 [the scheduled dates for the meetings of the Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee to review the Pfizer and Moderna vaccines, respectively].”
But with the winter pandemic surge in the meantime, “Our investigation suggests that as COVID-19 hospitalizations rise, patients with both type 1 and 2 diabetes will comprise a disproportionately higher number of those admissions and, once hospitalized, demonstrate a greater degree of illness severity,” he and his colleagues said.
“In light of these data, we call on our colleagues to emphasize the importance of social distancing measures and hand hygiene, with particular emphasis on patients with diabetes, including those in the most vulnerable communities whom our study affirms will face the most severe impact.”
After adjustments, excess severity risk similar for both diabetes types
The new study data came from electronic health records at Vanderbilt University Medical Center, comprising 137 primary care, urgent care, and hospital facilities where patients were tested for SARS-CoV-2 regardless of the reason for their visit.
Between March 17 and August 7, 2020, 6,451 patients tested positive for COVID-19. Of those, 273 had type 2 diabetes and 40 had type 1 diabetes.
Children younger than 18 years accounted for 20% of those with type 1 diabetes and 9.4% of those without diabetes, but none of the type 2 group. The group with type 2 diabetes was considerably older than the type 1 diabetes and no-diabetes groups, 58 years versus 37 and 33 years, respectively.
Before adjustment for baseline characteristics that differed between groups, patients with type 1 diabetes appeared to have a risk for hospitalization and greater illness severity that was intermediate between the group with no diabetes and the group with type 2 diabetes, the researchers said.
But after adjustment for age, race, sex, hypertension, smoking, and body mass index, people with type 1 diabetes had odds ratios of 3.90 for hospitalization and 3.35 for greater illness severity, which was similar to risk in type 2 diabetes (3.36 and 3.42, respectively), compared to those without diabetes.
Deep dive explores COVID-19 severity risk factors in type 1 diabetes
The investigators then conducted a detailed chart review for 37 of the 40 patients with type 1 diabetes and phone surveys with 15 of them.
The majority (28) had not been hospitalized, and only one was hospitalized for diabetic ketoacidosis (DKA) within 14 days of positive SARS-CoV-2 testing.
This contrasts with a report from the T1D Exchange, in which nearly half of 33 patients with type 1 diabetes and COVID-19 had been hospitalized with DKA. The reason for the discrepancy may be that more severe patients would more likely be referred to the T1D Exchange Registry, Dr. Gregory and colleagues hypothesized.
Clinical factors associated with COVID-19 severity (P < .05) in their study included a prior hypertension diagnosis, higher hemoglobin A1c, at least one prior DKA admission in the past year, and not using a continuous glucose monitor (CGM).
Hospitalizations were twice as likely and illness severity nearly twice as great among those with type 1 diabetes who were Black versus White. Just 8% of those with private insurance were hospitalized, compared with 60% of those with public insurance and 67% with no insurance (P = .001).
“Whereas previous reports have indicated proportionally higher rates of hospitalizations from COVID-19 among Black patients and those with public insurance, this study is the first to show a similar finding in the population with type 1 diabetes,” Dr. Gregory and colleagues wrote.
Only 9% of patients using a CGM were hospitalized versus 47% who used blood glucose meters (P < .016). Similarly, hospitalizations occurred in 6% using an insulin pump versus 33% using multiple daily injections (P < .085).
“Our analysis cannot exclude the possibility that greater amounts of diabetes technology use are a surrogate for higher socioeconomic status,” they noted.
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases, JDRF, and the Appleby Foundation. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The risk for increased COVID-19 severity in people with type 1 diabetes appears similar to that of type 2 diabetes, contrary to some official advice from the Centers for Disease Control and Prevention. The new finding indicates that people with both types should be priority for receiving a vaccine, investigators say.
The study is the first to prospectively evaluate both inpatients and outpatients and to examine COVID-19 severity factors in addition to death in people with type 1 and type 2 diabetes separately, and was published online Dec. 2 in Diabetes Care.
Among the patients, who were seen at Vanderbilt University Medical Center in Nashville, Tenn., between March and August of 2020, those with both type 1 and type 2 diabetes had between a three- and fourfold greater risk for COVID-19 hospitalization and greater illness severity compared with people without diabetes after adjustments for age, race, and a number of other risk factors.
This finding is important since as of Dec. 1, 2020, the CDC has classified the diabetes types differently in terms of underlying medical conditions that increase the risk for severe COVID-19.
Adults of any age with type 2 diabetes are considered “at increased risk of severe illness” from the virus that causes COVID-19 whereas the CDC says those with type 1 “might be at an increased risk.”
Lead author of the new paper Justin M. Gregory, MD, said in an interview: “I think this needs revision based on the current evidence. I think the data presented in our study and that of Barron et al. in Lancet Endocrinology 2020 indicate the need to place type 1 diabetes at parity with type 2 diabetes.
“These studies indicate both conditions carry an adjusted odds ratio of three to four when compared with people without diabetes for hospitalization, illness severity, and mortality,” he stressed.
Vaccines look promising for patients with diabetes
There were no phase 3 vaccine data available for the vaccine at the time that Dr. Gregory, of the Ian M. Burr Division of Pediatric Endocrinology and Diabetes, Vanderbilt University, Nashville, Tenn., and colleagues were writing their manuscript in late summer, so the article does not mention this.
But now, Dr. Gregory said, “Based on the initial press releases from Pfizer and Moderna, I am now optimistic that these vaccines might mitigate the excess morbidity and mortality from COVID-19 experienced by patients with diabetes.
“I am eager to see what we learn on December 10 and 17 [the scheduled dates for the meetings of the Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee to review the Pfizer and Moderna vaccines, respectively].”
But with the winter pandemic surge in the meantime, “Our investigation suggests that as COVID-19 hospitalizations rise, patients with both type 1 and 2 diabetes will comprise a disproportionately higher number of those admissions and, once hospitalized, demonstrate a greater degree of illness severity,” he and his colleagues said.
“In light of these data, we call on our colleagues to emphasize the importance of social distancing measures and hand hygiene, with particular emphasis on patients with diabetes, including those in the most vulnerable communities whom our study affirms will face the most severe impact.”
After adjustments, excess severity risk similar for both diabetes types
The new study data came from electronic health records at Vanderbilt University Medical Center, comprising 137 primary care, urgent care, and hospital facilities where patients were tested for SARS-CoV-2 regardless of the reason for their visit.
Between March 17 and August 7, 2020, 6,451 patients tested positive for COVID-19. Of those, 273 had type 2 diabetes and 40 had type 1 diabetes.
Children younger than 18 years accounted for 20% of those with type 1 diabetes and 9.4% of those without diabetes, but none of the type 2 group. The group with type 2 diabetes was considerably older than the type 1 diabetes and no-diabetes groups, 58 years versus 37 and 33 years, respectively.
Before adjustment for baseline characteristics that differed between groups, patients with type 1 diabetes appeared to have a risk for hospitalization and greater illness severity that was intermediate between the group with no diabetes and the group with type 2 diabetes, the researchers said.
But after adjustment for age, race, sex, hypertension, smoking, and body mass index, people with type 1 diabetes had odds ratios of 3.90 for hospitalization and 3.35 for greater illness severity, which was similar to risk in type 2 diabetes (3.36 and 3.42, respectively), compared to those without diabetes.
Deep dive explores COVID-19 severity risk factors in type 1 diabetes
The investigators then conducted a detailed chart review for 37 of the 40 patients with type 1 diabetes and phone surveys with 15 of them.
The majority (28) had not been hospitalized, and only one was hospitalized for diabetic ketoacidosis (DKA) within 14 days of positive SARS-CoV-2 testing.
This contrasts with a report from the T1D Exchange, in which nearly half of 33 patients with type 1 diabetes and COVID-19 had been hospitalized with DKA. The reason for the discrepancy may be that more severe patients would more likely be referred to the T1D Exchange Registry, Dr. Gregory and colleagues hypothesized.
Clinical factors associated with COVID-19 severity (P < .05) in their study included a prior hypertension diagnosis, higher hemoglobin A1c, at least one prior DKA admission in the past year, and not using a continuous glucose monitor (CGM).
Hospitalizations were twice as likely and illness severity nearly twice as great among those with type 1 diabetes who were Black versus White. Just 8% of those with private insurance were hospitalized, compared with 60% of those with public insurance and 67% with no insurance (P = .001).
“Whereas previous reports have indicated proportionally higher rates of hospitalizations from COVID-19 among Black patients and those with public insurance, this study is the first to show a similar finding in the population with type 1 diabetes,” Dr. Gregory and colleagues wrote.
Only 9% of patients using a CGM were hospitalized versus 47% who used blood glucose meters (P < .016). Similarly, hospitalizations occurred in 6% using an insulin pump versus 33% using multiple daily injections (P < .085).
“Our analysis cannot exclude the possibility that greater amounts of diabetes technology use are a surrogate for higher socioeconomic status,” they noted.
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases, JDRF, and the Appleby Foundation. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Emotions, worse attention linked to pain-related health care use in SCD
The cognitive and emotional status of children with sickle cell disease (SCD) appears to have a significant effect on how they cope with pain and use health care resources, investigators have found.
Results of a retrospective study of 112 children and adolescents with SCD, the majority of whom had sickle cell anemia, showed that ED visits and hospitalizations were significantly lower among children with SCD who performed better on an attention task, as well as those who were better able to cope emotionally with having SCD and pain, reported Zaria Williams, a second-year medical student at Howard University, Washington, and colleagues.
“Since I started learning more about sickle cell disease, I’ve been very concerned about the great disease burden that this condition can place on pediatric patients, particularly those who suffer from pain,” Ms. Williams said in an oral abstract presented at the annual meeting of the American Society of Hematology.
Although many children and adolescents with SCD can have their pain effectively managed at home with opioids and other medications, some require ED visits and potentially hospitalizations for pain management.
“There is great variability in health care utilization among patients with sickle cell disease, with some having to come to the ED and be admit to the hospital more than others. In searching for reasons why this might be the case, we thought about cognitive function and emotional differences between children with sickle cell disease as potentially affecting disease management,” she said.
Anxiety and catastrophizing
Children with SCD are known to be susceptible to affective comorbidities such as anxiety and catastrophizing, and to conditions that have the potential for deleterious effects on executive function, attention, and working memory. To determine whether cognitive and emotional factors affect the disease self-management in children and adolescents with SCD, Ms. Williams and coinvestigators looked at a cohort of 112 SCD patients aged 7-16 years treated at Children’s National Hospital in Washington, D.C.
The patients had participated in a previous pilot study of computerized working memory training. The authors reviewed charts for data on health care utilization, focusing on ED visits and hospitalization for pain 1 and 3 years after enrollment in the study.
They collected data on SCD genotype, disease-related variables, psychosocial information, and measures of cognition and emotion from the dataset. The information included socioeconomic status, parent education level, household income, and number of adults in the household.
Cognitive measures included the Weschler Intelligence Scale for Children full scale IQ, and the Cogstate computerized cognitive assessment system, which measures attention, executive function, and working memory.
Emotional measures were captured from the Pediatric Quality of Life Inventory Sickle Cell Disease module, including questions about worrying and emotions such as anger regarding SCD and pain.
The mean age of participants was 10.61 years. Of the 112 children/adolescents in the study, 65 (58%) were female, and 83 (74%) had sickle cell anemia (either HbSS or HbSβ0 thalassemia).
The participants had a median number of ED visits for pain of one within a year of enrollment, and a median of three within 3 years of enrollment,
The median number of hospital admissions for pain was zero and one, respectively.
Attention, emotions linked to higher use
Factors significantly associated with ED visits for pain within the first year were higher (worse) scores for attention (P = .001) and self-reported emotion (P = .049). ED visits within 3 years of enrollment were associated with attention (P = .003) and working memory (P = .039).
Similarly, hospitalizations for pain within the first year were significantly associated with worse attention scores (P = .009) and child-reported emotion (P = .013). Hospitalizations for pain within 3 years of enrollment were also significantly associated with attention deficits (P = .006) and with worse emotional function as reported by a parent (P = .020).
There was no significant effect of SCD genotype or socioeconomic status on either pain-related ED visits or hospitalizations, however.
The investigators theorized that poor attention may make it difficult to distract children from focusing on their pain, and could also hamper disease self-management strategies such as medication adherence and avoiding pain triggers.
Age-related differences?
In the question-and-answer session following her presentation, comoderator Susanna A Curtis, MD, from Yale New Haven (Conn.) Hospital, commented that “some previous work has shown that adolescents and young adults with sickle cell disease have higher utilization as compared to their younger counterparts,” and asked whether the investigators found differences between cognition and utilization among different age groups within the cohort.
“We didn’t find a significant association with age, but I’m also very interested in that as well, especially considering that maybe there is more or less parent involvement, considering how old the child is,” Ms. Williams said.
Dr. Curtis noted that many of the comorbidities of sickle cell disease such as stroke or degree of anemia can affect cognitive function, but can also have an effect on health care utilization as well, asked whether the investigators were able to look at the potential confounding effects of comorbidities.
Ms. Williams said that, although they have not looked at potential confounders as yet, they hope to do so in future research.
Asked by another audience member whether the authors had considered using the Pain Catastrophizing Scale for children and/or their parents, in addition to other markers, Ms. Williams replied that “I definitely have considered it. Under recommendations from my mentors, we just focused on the quality-of-life scale first, but catastrophizing is something I’m very interested in. Especially, I would love to have the parent factors as well, so along the journey I hope to include that.”
The study was sponsored in part by a grant from the Doris Duke Charitable Foundation. Ms Williams is the recipient of an ASH Minority Medical Student Award. Dr. Curtis and Ms. Williams both reported no relevant conflicts of interest to disclose.
SOURCE: Williams Z et al. ASH 2020, Abstract 366
The cognitive and emotional status of children with sickle cell disease (SCD) appears to have a significant effect on how they cope with pain and use health care resources, investigators have found.
Results of a retrospective study of 112 children and adolescents with SCD, the majority of whom had sickle cell anemia, showed that ED visits and hospitalizations were significantly lower among children with SCD who performed better on an attention task, as well as those who were better able to cope emotionally with having SCD and pain, reported Zaria Williams, a second-year medical student at Howard University, Washington, and colleagues.
“Since I started learning more about sickle cell disease, I’ve been very concerned about the great disease burden that this condition can place on pediatric patients, particularly those who suffer from pain,” Ms. Williams said in an oral abstract presented at the annual meeting of the American Society of Hematology.
Although many children and adolescents with SCD can have their pain effectively managed at home with opioids and other medications, some require ED visits and potentially hospitalizations for pain management.
“There is great variability in health care utilization among patients with sickle cell disease, with some having to come to the ED and be admit to the hospital more than others. In searching for reasons why this might be the case, we thought about cognitive function and emotional differences between children with sickle cell disease as potentially affecting disease management,” she said.
Anxiety and catastrophizing
Children with SCD are known to be susceptible to affective comorbidities such as anxiety and catastrophizing, and to conditions that have the potential for deleterious effects on executive function, attention, and working memory. To determine whether cognitive and emotional factors affect the disease self-management in children and adolescents with SCD, Ms. Williams and coinvestigators looked at a cohort of 112 SCD patients aged 7-16 years treated at Children’s National Hospital in Washington, D.C.
The patients had participated in a previous pilot study of computerized working memory training. The authors reviewed charts for data on health care utilization, focusing on ED visits and hospitalization for pain 1 and 3 years after enrollment in the study.
They collected data on SCD genotype, disease-related variables, psychosocial information, and measures of cognition and emotion from the dataset. The information included socioeconomic status, parent education level, household income, and number of adults in the household.
Cognitive measures included the Weschler Intelligence Scale for Children full scale IQ, and the Cogstate computerized cognitive assessment system, which measures attention, executive function, and working memory.
Emotional measures were captured from the Pediatric Quality of Life Inventory Sickle Cell Disease module, including questions about worrying and emotions such as anger regarding SCD and pain.
The mean age of participants was 10.61 years. Of the 112 children/adolescents in the study, 65 (58%) were female, and 83 (74%) had sickle cell anemia (either HbSS or HbSβ0 thalassemia).
The participants had a median number of ED visits for pain of one within a year of enrollment, and a median of three within 3 years of enrollment,
The median number of hospital admissions for pain was zero and one, respectively.
Attention, emotions linked to higher use
Factors significantly associated with ED visits for pain within the first year were higher (worse) scores for attention (P = .001) and self-reported emotion (P = .049). ED visits within 3 years of enrollment were associated with attention (P = .003) and working memory (P = .039).
Similarly, hospitalizations for pain within the first year were significantly associated with worse attention scores (P = .009) and child-reported emotion (P = .013). Hospitalizations for pain within 3 years of enrollment were also significantly associated with attention deficits (P = .006) and with worse emotional function as reported by a parent (P = .020).
There was no significant effect of SCD genotype or socioeconomic status on either pain-related ED visits or hospitalizations, however.
The investigators theorized that poor attention may make it difficult to distract children from focusing on their pain, and could also hamper disease self-management strategies such as medication adherence and avoiding pain triggers.
Age-related differences?
In the question-and-answer session following her presentation, comoderator Susanna A Curtis, MD, from Yale New Haven (Conn.) Hospital, commented that “some previous work has shown that adolescents and young adults with sickle cell disease have higher utilization as compared to their younger counterparts,” and asked whether the investigators found differences between cognition and utilization among different age groups within the cohort.
“We didn’t find a significant association with age, but I’m also very interested in that as well, especially considering that maybe there is more or less parent involvement, considering how old the child is,” Ms. Williams said.
Dr. Curtis noted that many of the comorbidities of sickle cell disease such as stroke or degree of anemia can affect cognitive function, but can also have an effect on health care utilization as well, asked whether the investigators were able to look at the potential confounding effects of comorbidities.
Ms. Williams said that, although they have not looked at potential confounders as yet, they hope to do so in future research.
Asked by another audience member whether the authors had considered using the Pain Catastrophizing Scale for children and/or their parents, in addition to other markers, Ms. Williams replied that “I definitely have considered it. Under recommendations from my mentors, we just focused on the quality-of-life scale first, but catastrophizing is something I’m very interested in. Especially, I would love to have the parent factors as well, so along the journey I hope to include that.”
The study was sponsored in part by a grant from the Doris Duke Charitable Foundation. Ms Williams is the recipient of an ASH Minority Medical Student Award. Dr. Curtis and Ms. Williams both reported no relevant conflicts of interest to disclose.
SOURCE: Williams Z et al. ASH 2020, Abstract 366
The cognitive and emotional status of children with sickle cell disease (SCD) appears to have a significant effect on how they cope with pain and use health care resources, investigators have found.
Results of a retrospective study of 112 children and adolescents with SCD, the majority of whom had sickle cell anemia, showed that ED visits and hospitalizations were significantly lower among children with SCD who performed better on an attention task, as well as those who were better able to cope emotionally with having SCD and pain, reported Zaria Williams, a second-year medical student at Howard University, Washington, and colleagues.
“Since I started learning more about sickle cell disease, I’ve been very concerned about the great disease burden that this condition can place on pediatric patients, particularly those who suffer from pain,” Ms. Williams said in an oral abstract presented at the annual meeting of the American Society of Hematology.
Although many children and adolescents with SCD can have their pain effectively managed at home with opioids and other medications, some require ED visits and potentially hospitalizations for pain management.
“There is great variability in health care utilization among patients with sickle cell disease, with some having to come to the ED and be admit to the hospital more than others. In searching for reasons why this might be the case, we thought about cognitive function and emotional differences between children with sickle cell disease as potentially affecting disease management,” she said.
Anxiety and catastrophizing
Children with SCD are known to be susceptible to affective comorbidities such as anxiety and catastrophizing, and to conditions that have the potential for deleterious effects on executive function, attention, and working memory. To determine whether cognitive and emotional factors affect the disease self-management in children and adolescents with SCD, Ms. Williams and coinvestigators looked at a cohort of 112 SCD patients aged 7-16 years treated at Children’s National Hospital in Washington, D.C.
The patients had participated in a previous pilot study of computerized working memory training. The authors reviewed charts for data on health care utilization, focusing on ED visits and hospitalization for pain 1 and 3 years after enrollment in the study.
They collected data on SCD genotype, disease-related variables, psychosocial information, and measures of cognition and emotion from the dataset. The information included socioeconomic status, parent education level, household income, and number of adults in the household.
Cognitive measures included the Weschler Intelligence Scale for Children full scale IQ, and the Cogstate computerized cognitive assessment system, which measures attention, executive function, and working memory.
Emotional measures were captured from the Pediatric Quality of Life Inventory Sickle Cell Disease module, including questions about worrying and emotions such as anger regarding SCD and pain.
The mean age of participants was 10.61 years. Of the 112 children/adolescents in the study, 65 (58%) were female, and 83 (74%) had sickle cell anemia (either HbSS or HbSβ0 thalassemia).
The participants had a median number of ED visits for pain of one within a year of enrollment, and a median of three within 3 years of enrollment,
The median number of hospital admissions for pain was zero and one, respectively.
Attention, emotions linked to higher use
Factors significantly associated with ED visits for pain within the first year were higher (worse) scores for attention (P = .001) and self-reported emotion (P = .049). ED visits within 3 years of enrollment were associated with attention (P = .003) and working memory (P = .039).
Similarly, hospitalizations for pain within the first year were significantly associated with worse attention scores (P = .009) and child-reported emotion (P = .013). Hospitalizations for pain within 3 years of enrollment were also significantly associated with attention deficits (P = .006) and with worse emotional function as reported by a parent (P = .020).
There was no significant effect of SCD genotype or socioeconomic status on either pain-related ED visits or hospitalizations, however.
The investigators theorized that poor attention may make it difficult to distract children from focusing on their pain, and could also hamper disease self-management strategies such as medication adherence and avoiding pain triggers.
Age-related differences?
In the question-and-answer session following her presentation, comoderator Susanna A Curtis, MD, from Yale New Haven (Conn.) Hospital, commented that “some previous work has shown that adolescents and young adults with sickle cell disease have higher utilization as compared to their younger counterparts,” and asked whether the investigators found differences between cognition and utilization among different age groups within the cohort.
“We didn’t find a significant association with age, but I’m also very interested in that as well, especially considering that maybe there is more or less parent involvement, considering how old the child is,” Ms. Williams said.
Dr. Curtis noted that many of the comorbidities of sickle cell disease such as stroke or degree of anemia can affect cognitive function, but can also have an effect on health care utilization as well, asked whether the investigators were able to look at the potential confounding effects of comorbidities.
Ms. Williams said that, although they have not looked at potential confounders as yet, they hope to do so in future research.
Asked by another audience member whether the authors had considered using the Pain Catastrophizing Scale for children and/or their parents, in addition to other markers, Ms. Williams replied that “I definitely have considered it. Under recommendations from my mentors, we just focused on the quality-of-life scale first, but catastrophizing is something I’m very interested in. Especially, I would love to have the parent factors as well, so along the journey I hope to include that.”
The study was sponsored in part by a grant from the Doris Duke Charitable Foundation. Ms Williams is the recipient of an ASH Minority Medical Student Award. Dr. Curtis and Ms. Williams both reported no relevant conflicts of interest to disclose.
SOURCE: Williams Z et al. ASH 2020, Abstract 366
FROM ASH 2020
Demand for COVID vaccines expected to get heated – and fast
Americans have made no secret of their skepticism of COVID-19 vaccines this year, with fears of political interference and a “warp speed” timeline blunting confidence in the shots. As recently as September, nearly half of U.S. adults said they didn’t intend to be inoculated.
But with two promising vaccines primed for release, likely within weeks, experts in ethics and immunization behavior say they expect attitudes to shift quickly from widespread hesitancy to urgent, even heated demand.
“People talk about the antivaccine people being able to kind of squelch uptake. I don’t see that happening,” Dr. Paul Offit, MD, a vaccinologist with Children’s Hospital of Philadelphia, told viewers of a recent JAMA Network webinar. “This, to me, is more like the Beanie Baby phenomenon. The attractiveness of a limited edition.”
Reports that vaccines produced by drugmakers Pfizer and BioNTech and Moderna appear to be safe and effective, along with the deliberate emphasis on science-based guidance from the incoming Biden administration, are likely to reverse uncertainty in a big way, said Arthur Caplan, PhD, director of the division of medical ethics at New York University.
“I think that’s going to flip the trust issue,” he said.
The shift is already apparent. A new poll by the Pew Research Center found that by the end of November 60% of Americans said they would get a vaccine for the coronavirus. This month, even as a federal advisory group met to hash out guidelines for vaccine distribution, a long list of advocacy groups – from those representing home-based health workers and community health centers to patients with kidney disease – were lobbying state and federal officials in hopes their constituents would be prioritized for the first scarce doses.
“As we get closer to the vaccine being a reality, there’s a lot of jockeying, to be sure,” said Katie Smith Sloan, chief executive of LeadingAge, a nonprofit organization pushing for staff and patients at long-term care centers to be included in the highest-priority category.
Certainly, some consumers remain wary, said Rupali Limaye, PhD, a social and behavioral health scientist at the Johns Hopkins Bloomberg School of Public Health, Baltimore. Fears that drugmakers and regulators might cut corners to speed a vaccine linger, even as details of the trials become public and the review process is made more transparent. Some health care workers, who are at the front of the line for the shots, are not eager to go first.
“There will be people who will say, ‘I will wait a little bit more for safety data,” Dr. Limaye said.
But those doubts likely will recede once the vaccines are approved for use and begin to circulate broadly, said Dr. Offit, who sits on the Food and Drug Administration advisory panel set to review the requests for emergency authorization Pfizer and Moderna have submitted.
He predicted demand for the COVID vaccines could rival the clamor that occurred in 2004, when production problems caused a severe shortage of flu shots just as influenza season began. That led to long lines, rationed doses and ethical debates over distribution.
“That was a highly desired vaccine,” Dr. Offit said. “I think in many ways that might happen here.”
Initially, vaccine supplies will be tight, with federal officials planning to ship 6.4 million doses within 24 hours of FDA authorization and up to 40 million doses by the end of the year. The CDC panel recommended that the first shots go to the 21 million health care workers in the United States and 3 million nursing home staff and residents, before being rolled out to other groups based on a hierarchy of risk factors.
Even before any vaccine is available, some people are trying to boost their chances of access, said Allison Kempe, MD, a professor of pediatrics at the University of Coloradoat Denver, Aurora, and expert in vaccine dissemination. “People have called me and said, ‘How can I get the vaccine?’” she said. “I think that not everyone will be happy to wait, that’s for sure. I don’t think there will be rioting in the streets, but there may be pressure brought to bear.”
That likely will include emotional debates over how, when, and to whom next doses should be distributed, said Dr. Caplan. Under the CDC recommendations, vulnerable groups next in line include 87 million workers whose jobs are deemed “essential” – a broad and ill-defined category – as well as 53 million adults age 65 and older.
“We’re going to have some fights about high-risk groups,” Dr. Caplan said.
The conversations will be complicated. Should prisoners, who have little control over their COVID exposure, get vaccine priority? How about professional sports teams, whose performance could bolster society’s overall morale? And what about residents of facilities providing care for people with intellectual and developmental disabilities, who are three times more likely to die from COVID-19 than the general population?
Control over vaccination allocation rests with the states, so that’s where the biggest conflicts will occur, Dr. Caplan said. “It’s a short fight, I hope, in the sense in which it gets done in a few months, but I think it will be pretty vocal.”
Once vaccine supplies become more plentiful, perhaps by May or June, another consideration is sure to boost demand: requirements for proof of COVID vaccination for work and travel.
“It’s inevitable that you’re going to see immunity passports or that you’re required to show a certificate on the train, airplane, bus, or subway,” Dr. Caplan predicted. “Probably also to enter certain hospitals, probably to enter certain restaurants and government facilities.”
But with a grueling winter surge ahead, and new predictions that COVID-19 will fell as many as 450,000 Americans by February, the tragic reality of the disease will no doubt fuel ample demand for vaccination.
“People now know someone who has gotten COVID, who has been hospitalized or has unfortunately died,” Dr. Limaye said.
“We’re all seeing this now,” said Dr. Kempe. “Even deniers are beginning to see what this illness can do.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Americans have made no secret of their skepticism of COVID-19 vaccines this year, with fears of political interference and a “warp speed” timeline blunting confidence in the shots. As recently as September, nearly half of U.S. adults said they didn’t intend to be inoculated.
But with two promising vaccines primed for release, likely within weeks, experts in ethics and immunization behavior say they expect attitudes to shift quickly from widespread hesitancy to urgent, even heated demand.
“People talk about the antivaccine people being able to kind of squelch uptake. I don’t see that happening,” Dr. Paul Offit, MD, a vaccinologist with Children’s Hospital of Philadelphia, told viewers of a recent JAMA Network webinar. “This, to me, is more like the Beanie Baby phenomenon. The attractiveness of a limited edition.”
Reports that vaccines produced by drugmakers Pfizer and BioNTech and Moderna appear to be safe and effective, along with the deliberate emphasis on science-based guidance from the incoming Biden administration, are likely to reverse uncertainty in a big way, said Arthur Caplan, PhD, director of the division of medical ethics at New York University.
“I think that’s going to flip the trust issue,” he said.
The shift is already apparent. A new poll by the Pew Research Center found that by the end of November 60% of Americans said they would get a vaccine for the coronavirus. This month, even as a federal advisory group met to hash out guidelines for vaccine distribution, a long list of advocacy groups – from those representing home-based health workers and community health centers to patients with kidney disease – were lobbying state and federal officials in hopes their constituents would be prioritized for the first scarce doses.
“As we get closer to the vaccine being a reality, there’s a lot of jockeying, to be sure,” said Katie Smith Sloan, chief executive of LeadingAge, a nonprofit organization pushing for staff and patients at long-term care centers to be included in the highest-priority category.
Certainly, some consumers remain wary, said Rupali Limaye, PhD, a social and behavioral health scientist at the Johns Hopkins Bloomberg School of Public Health, Baltimore. Fears that drugmakers and regulators might cut corners to speed a vaccine linger, even as details of the trials become public and the review process is made more transparent. Some health care workers, who are at the front of the line for the shots, are not eager to go first.
“There will be people who will say, ‘I will wait a little bit more for safety data,” Dr. Limaye said.
But those doubts likely will recede once the vaccines are approved for use and begin to circulate broadly, said Dr. Offit, who sits on the Food and Drug Administration advisory panel set to review the requests for emergency authorization Pfizer and Moderna have submitted.
He predicted demand for the COVID vaccines could rival the clamor that occurred in 2004, when production problems caused a severe shortage of flu shots just as influenza season began. That led to long lines, rationed doses and ethical debates over distribution.
“That was a highly desired vaccine,” Dr. Offit said. “I think in many ways that might happen here.”
Initially, vaccine supplies will be tight, with federal officials planning to ship 6.4 million doses within 24 hours of FDA authorization and up to 40 million doses by the end of the year. The CDC panel recommended that the first shots go to the 21 million health care workers in the United States and 3 million nursing home staff and residents, before being rolled out to other groups based on a hierarchy of risk factors.
Even before any vaccine is available, some people are trying to boost their chances of access, said Allison Kempe, MD, a professor of pediatrics at the University of Coloradoat Denver, Aurora, and expert in vaccine dissemination. “People have called me and said, ‘How can I get the vaccine?’” she said. “I think that not everyone will be happy to wait, that’s for sure. I don’t think there will be rioting in the streets, but there may be pressure brought to bear.”
That likely will include emotional debates over how, when, and to whom next doses should be distributed, said Dr. Caplan. Under the CDC recommendations, vulnerable groups next in line include 87 million workers whose jobs are deemed “essential” – a broad and ill-defined category – as well as 53 million adults age 65 and older.
“We’re going to have some fights about high-risk groups,” Dr. Caplan said.
The conversations will be complicated. Should prisoners, who have little control over their COVID exposure, get vaccine priority? How about professional sports teams, whose performance could bolster society’s overall morale? And what about residents of facilities providing care for people with intellectual and developmental disabilities, who are three times more likely to die from COVID-19 than the general population?
Control over vaccination allocation rests with the states, so that’s where the biggest conflicts will occur, Dr. Caplan said. “It’s a short fight, I hope, in the sense in which it gets done in a few months, but I think it will be pretty vocal.”
Once vaccine supplies become more plentiful, perhaps by May or June, another consideration is sure to boost demand: requirements for proof of COVID vaccination for work and travel.
“It’s inevitable that you’re going to see immunity passports or that you’re required to show a certificate on the train, airplane, bus, or subway,” Dr. Caplan predicted. “Probably also to enter certain hospitals, probably to enter certain restaurants and government facilities.”
But with a grueling winter surge ahead, and new predictions that COVID-19 will fell as many as 450,000 Americans by February, the tragic reality of the disease will no doubt fuel ample demand for vaccination.
“People now know someone who has gotten COVID, who has been hospitalized or has unfortunately died,” Dr. Limaye said.
“We’re all seeing this now,” said Dr. Kempe. “Even deniers are beginning to see what this illness can do.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Americans have made no secret of their skepticism of COVID-19 vaccines this year, with fears of political interference and a “warp speed” timeline blunting confidence in the shots. As recently as September, nearly half of U.S. adults said they didn’t intend to be inoculated.
But with two promising vaccines primed for release, likely within weeks, experts in ethics and immunization behavior say they expect attitudes to shift quickly from widespread hesitancy to urgent, even heated demand.
“People talk about the antivaccine people being able to kind of squelch uptake. I don’t see that happening,” Dr. Paul Offit, MD, a vaccinologist with Children’s Hospital of Philadelphia, told viewers of a recent JAMA Network webinar. “This, to me, is more like the Beanie Baby phenomenon. The attractiveness of a limited edition.”
Reports that vaccines produced by drugmakers Pfizer and BioNTech and Moderna appear to be safe and effective, along with the deliberate emphasis on science-based guidance from the incoming Biden administration, are likely to reverse uncertainty in a big way, said Arthur Caplan, PhD, director of the division of medical ethics at New York University.
“I think that’s going to flip the trust issue,” he said.
The shift is already apparent. A new poll by the Pew Research Center found that by the end of November 60% of Americans said they would get a vaccine for the coronavirus. This month, even as a federal advisory group met to hash out guidelines for vaccine distribution, a long list of advocacy groups – from those representing home-based health workers and community health centers to patients with kidney disease – were lobbying state and federal officials in hopes their constituents would be prioritized for the first scarce doses.
“As we get closer to the vaccine being a reality, there’s a lot of jockeying, to be sure,” said Katie Smith Sloan, chief executive of LeadingAge, a nonprofit organization pushing for staff and patients at long-term care centers to be included in the highest-priority category.
Certainly, some consumers remain wary, said Rupali Limaye, PhD, a social and behavioral health scientist at the Johns Hopkins Bloomberg School of Public Health, Baltimore. Fears that drugmakers and regulators might cut corners to speed a vaccine linger, even as details of the trials become public and the review process is made more transparent. Some health care workers, who are at the front of the line for the shots, are not eager to go first.
“There will be people who will say, ‘I will wait a little bit more for safety data,” Dr. Limaye said.
But those doubts likely will recede once the vaccines are approved for use and begin to circulate broadly, said Dr. Offit, who sits on the Food and Drug Administration advisory panel set to review the requests for emergency authorization Pfizer and Moderna have submitted.
He predicted demand for the COVID vaccines could rival the clamor that occurred in 2004, when production problems caused a severe shortage of flu shots just as influenza season began. That led to long lines, rationed doses and ethical debates over distribution.
“That was a highly desired vaccine,” Dr. Offit said. “I think in many ways that might happen here.”
Initially, vaccine supplies will be tight, with federal officials planning to ship 6.4 million doses within 24 hours of FDA authorization and up to 40 million doses by the end of the year. The CDC panel recommended that the first shots go to the 21 million health care workers in the United States and 3 million nursing home staff and residents, before being rolled out to other groups based on a hierarchy of risk factors.
Even before any vaccine is available, some people are trying to boost their chances of access, said Allison Kempe, MD, a professor of pediatrics at the University of Coloradoat Denver, Aurora, and expert in vaccine dissemination. “People have called me and said, ‘How can I get the vaccine?’” she said. “I think that not everyone will be happy to wait, that’s for sure. I don’t think there will be rioting in the streets, but there may be pressure brought to bear.”
That likely will include emotional debates over how, when, and to whom next doses should be distributed, said Dr. Caplan. Under the CDC recommendations, vulnerable groups next in line include 87 million workers whose jobs are deemed “essential” – a broad and ill-defined category – as well as 53 million adults age 65 and older.
“We’re going to have some fights about high-risk groups,” Dr. Caplan said.
The conversations will be complicated. Should prisoners, who have little control over their COVID exposure, get vaccine priority? How about professional sports teams, whose performance could bolster society’s overall morale? And what about residents of facilities providing care for people with intellectual and developmental disabilities, who are three times more likely to die from COVID-19 than the general population?
Control over vaccination allocation rests with the states, so that’s where the biggest conflicts will occur, Dr. Caplan said. “It’s a short fight, I hope, in the sense in which it gets done in a few months, but I think it will be pretty vocal.”
Once vaccine supplies become more plentiful, perhaps by May or June, another consideration is sure to boost demand: requirements for proof of COVID vaccination for work and travel.
“It’s inevitable that you’re going to see immunity passports or that you’re required to show a certificate on the train, airplane, bus, or subway,” Dr. Caplan predicted. “Probably also to enter certain hospitals, probably to enter certain restaurants and government facilities.”
But with a grueling winter surge ahead, and new predictions that COVID-19 will fell as many as 450,000 Americans by February, the tragic reality of the disease will no doubt fuel ample demand for vaccination.
“People now know someone who has gotten COVID, who has been hospitalized or has unfortunately died,” Dr. Limaye said.
“We’re all seeing this now,” said Dr. Kempe. “Even deniers are beginning to see what this illness can do.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Rap music mention of mental health topics more than doubles
Mental health distress is rising but often is undertreated among children and young adults in the United States, wrote Alex Kresovich, MA, of the University of North Carolina, Chapel Hill, and colleagues.
“Mental health risk especially is increasing among young Black/ African American male individuals (YBAAM), who are often disproportionately exposed to environmental, economic, and family stressors linked with depression and anxiety,” they said. Adolescents and young adults, especially YBAAM, make up a large part of the audience for rap music.
In recent years, more rap artists have disclosed mental health issues, and they have included mental health topics such as depression and suicidal thoughts into their music, the researchers said.
In a study published in JAMA Pediatrics, the researchers identified 125 songs from the period between 1998 and 2018, then assessed them for references to mental health. The song selections included the top 25 rap songs in 1998, 2003, 2008, 2013, and 2018, based on the Billboard music charts.
The majority of the songs (123) featured lead artists from North America, and 97 of them were Black/African American males. The average age of the artists was 28 years. “Prominent artists captured in the sample included 50 Cent, Drake, Eminem, Kanye West, Jay-Z, and Lil’Wayne, among others,” they said. The researchers divided mental health issues into four categories: anxiety or anxious thinking; depression or depressive thinking; metaphors (such as struggling with mental stability); and suicide or suicidal ideation.
Mental health references rise
Across the study period, 35 songs (28%) mentioned anxiety, 28 (22%) mentioned depression, 8 (6%) mentioned suicide, and 26 (21%) mentioned a mental health metaphor. The proportion of songs with a mental health reference increased in a significant linear trend across the study period for suicide (0%-12%), depression (16%-32%), and mental health metaphors (8%-44%).
All references to suicide or suicidal ideation were found in songs that were popular between 2013 and 2018, the researchers noted.
“This increase is important, given that rap artists serve as role models to their audience, which extends beyond YBAAM to include U.S. young people across strata, constituting a large group with increased risk of mental health issues and underuse of mental health services,” Mr. Kresovich and associates said.
In addition, the researchers found that stressors related to environmental conditions and love were significantly more likely to co-occur with mental health references (adjusted odds ratios 8.1 and 4.8, respectively).
The study findings were limited by several factors including the selection of songs only from the Billboard hot rap songs year-end charts, which “does not fully represent the population of rap music between 1998 and 2018,” the researchers said. In addition, they could not address causation or motivations for the increased mental health references over the study period. “We are also unable to ascertain how U.S. youth interact with this music or are positively or negatively affected by its messages.”
“For example, positively framed references to mental health awareness, treatment, or support may lead to reduced stigma and increased willingness to seek treatment,” Mr. Kresovich and associates wrote. “However, negatively framed references to mental health struggles might lead to negative outcomes, including copycat behavior in which listeners model harmful behavior, such as suicide attempts, if those behaviors are described in lyrics (i.e., the Werther effect),” they added.
Despite these limitations, the results support the need for more research on the impact of rap music as a way to reduce stigma and potentially reduce mental health risk in adolescents and young adults, Mr. Kresovich and associates concluded.
Music may help raise tough topics
The study is important because children and adolescents have more control than ever over the media they consume, Sarah Vinson, MD, founder of the Lorio Psych Group in Atlanta, said in an interview.
“With more and more children with access to their own devices, they spend a great amount of time consuming content, including music,” Dr. Vinson said. “The norms reflected in the lyrics they hear have an impact on their emerging view of themselves, others, and the world.”
The increased recognition of mental health issues by rap musicians as a topic “certainly has the potential to have a positive impact; however, the way that it is discussed can influence [the] nature of that impact,” she explained.
“It is important for people who are dealing with the normal range of human emotions to know that they are not alone. It is even more important for people dealing with suicidality or mental illness to know that,” Dr. Vinson said.
“Validation and sense of connection are human needs, and stigma related to mental illness can be isolating,” she emphasized. “Rappers have a platform and are often people that children and adolescents look up to, for better or for worse.” Through their music, “the rappers are signaling that these topics are worthy of our attention and okay to talk about.”
Unfortunately, many barriers persist for adolescents in need of mental health treatment, said Dr. Vinson. “The children’s mental health workforce, quantitatively, is not enough to meet the current needs,” she said. “Mental health is not reimbursed at the same rate as other kinds of health care, which contributes to healthy systems not prioritizing these services. Additionally, the racial, ethnic, and socioeconomic background of those who are mental health providers is not reflective of the larger population, and mental health training insufficiently incorporates the cultural and structural humility needed to help professionals navigate those differences,” she explained.
“Children at increased risk are those who face many of those environmental barriers that the rappers reference in those lyrics. They are likely to have even poorer access because they are disproportionately impacted by residential segregation, transportation challenges, financial barriers, and structural racism in mental health care,” Dr. Vinson added. A take-home message for clinicians is to find out what their patients are listening to. “One way to understand what is on the hearts and minds of children is to ask them what’s in their playlist,” she said.
Additional research is needed to examine “moderating factors for the impact, good or bad, of increased mental health content in hip hop for young listeners’ mental health awareness, symptoms and/or interest in seeking treatment,” Dr. Vinson concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Dr. Vinson served as chair for a workshop on mental health and hip-hop at the American Psychiatric Association annual meeting. She had no financial conflicts to disclose.
SOURCE: Kresovich A et al. JAMA Pediatr. 2020 Dec 7. doi: 10.1001/jamapediatrics.2020.5155.
This article was updated on December 21, 2020.
Mental health distress is rising but often is undertreated among children and young adults in the United States, wrote Alex Kresovich, MA, of the University of North Carolina, Chapel Hill, and colleagues.
“Mental health risk especially is increasing among young Black/ African American male individuals (YBAAM), who are often disproportionately exposed to environmental, economic, and family stressors linked with depression and anxiety,” they said. Adolescents and young adults, especially YBAAM, make up a large part of the audience for rap music.
In recent years, more rap artists have disclosed mental health issues, and they have included mental health topics such as depression and suicidal thoughts into their music, the researchers said.
In a study published in JAMA Pediatrics, the researchers identified 125 songs from the period between 1998 and 2018, then assessed them for references to mental health. The song selections included the top 25 rap songs in 1998, 2003, 2008, 2013, and 2018, based on the Billboard music charts.
The majority of the songs (123) featured lead artists from North America, and 97 of them were Black/African American males. The average age of the artists was 28 years. “Prominent artists captured in the sample included 50 Cent, Drake, Eminem, Kanye West, Jay-Z, and Lil’Wayne, among others,” they said. The researchers divided mental health issues into four categories: anxiety or anxious thinking; depression or depressive thinking; metaphors (such as struggling with mental stability); and suicide or suicidal ideation.
Mental health references rise
Across the study period, 35 songs (28%) mentioned anxiety, 28 (22%) mentioned depression, 8 (6%) mentioned suicide, and 26 (21%) mentioned a mental health metaphor. The proportion of songs with a mental health reference increased in a significant linear trend across the study period for suicide (0%-12%), depression (16%-32%), and mental health metaphors (8%-44%).
All references to suicide or suicidal ideation were found in songs that were popular between 2013 and 2018, the researchers noted.
“This increase is important, given that rap artists serve as role models to their audience, which extends beyond YBAAM to include U.S. young people across strata, constituting a large group with increased risk of mental health issues and underuse of mental health services,” Mr. Kresovich and associates said.
In addition, the researchers found that stressors related to environmental conditions and love were significantly more likely to co-occur with mental health references (adjusted odds ratios 8.1 and 4.8, respectively).
The study findings were limited by several factors including the selection of songs only from the Billboard hot rap songs year-end charts, which “does not fully represent the population of rap music between 1998 and 2018,” the researchers said. In addition, they could not address causation or motivations for the increased mental health references over the study period. “We are also unable to ascertain how U.S. youth interact with this music or are positively or negatively affected by its messages.”
“For example, positively framed references to mental health awareness, treatment, or support may lead to reduced stigma and increased willingness to seek treatment,” Mr. Kresovich and associates wrote. “However, negatively framed references to mental health struggles might lead to negative outcomes, including copycat behavior in which listeners model harmful behavior, such as suicide attempts, if those behaviors are described in lyrics (i.e., the Werther effect),” they added.
Despite these limitations, the results support the need for more research on the impact of rap music as a way to reduce stigma and potentially reduce mental health risk in adolescents and young adults, Mr. Kresovich and associates concluded.
Music may help raise tough topics
The study is important because children and adolescents have more control than ever over the media they consume, Sarah Vinson, MD, founder of the Lorio Psych Group in Atlanta, said in an interview.
“With more and more children with access to their own devices, they spend a great amount of time consuming content, including music,” Dr. Vinson said. “The norms reflected in the lyrics they hear have an impact on their emerging view of themselves, others, and the world.”
The increased recognition of mental health issues by rap musicians as a topic “certainly has the potential to have a positive impact; however, the way that it is discussed can influence [the] nature of that impact,” she explained.
“It is important for people who are dealing with the normal range of human emotions to know that they are not alone. It is even more important for people dealing with suicidality or mental illness to know that,” Dr. Vinson said.
“Validation and sense of connection are human needs, and stigma related to mental illness can be isolating,” she emphasized. “Rappers have a platform and are often people that children and adolescents look up to, for better or for worse.” Through their music, “the rappers are signaling that these topics are worthy of our attention and okay to talk about.”
Unfortunately, many barriers persist for adolescents in need of mental health treatment, said Dr. Vinson. “The children’s mental health workforce, quantitatively, is not enough to meet the current needs,” she said. “Mental health is not reimbursed at the same rate as other kinds of health care, which contributes to healthy systems not prioritizing these services. Additionally, the racial, ethnic, and socioeconomic background of those who are mental health providers is not reflective of the larger population, and mental health training insufficiently incorporates the cultural and structural humility needed to help professionals navigate those differences,” she explained.
“Children at increased risk are those who face many of those environmental barriers that the rappers reference in those lyrics. They are likely to have even poorer access because they are disproportionately impacted by residential segregation, transportation challenges, financial barriers, and structural racism in mental health care,” Dr. Vinson added. A take-home message for clinicians is to find out what their patients are listening to. “One way to understand what is on the hearts and minds of children is to ask them what’s in their playlist,” she said.
Additional research is needed to examine “moderating factors for the impact, good or bad, of increased mental health content in hip hop for young listeners’ mental health awareness, symptoms and/or interest in seeking treatment,” Dr. Vinson concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Dr. Vinson served as chair for a workshop on mental health and hip-hop at the American Psychiatric Association annual meeting. She had no financial conflicts to disclose.
SOURCE: Kresovich A et al. JAMA Pediatr. 2020 Dec 7. doi: 10.1001/jamapediatrics.2020.5155.
This article was updated on December 21, 2020.
Mental health distress is rising but often is undertreated among children and young adults in the United States, wrote Alex Kresovich, MA, of the University of North Carolina, Chapel Hill, and colleagues.
“Mental health risk especially is increasing among young Black/ African American male individuals (YBAAM), who are often disproportionately exposed to environmental, economic, and family stressors linked with depression and anxiety,” they said. Adolescents and young adults, especially YBAAM, make up a large part of the audience for rap music.
In recent years, more rap artists have disclosed mental health issues, and they have included mental health topics such as depression and suicidal thoughts into their music, the researchers said.
In a study published in JAMA Pediatrics, the researchers identified 125 songs from the period between 1998 and 2018, then assessed them for references to mental health. The song selections included the top 25 rap songs in 1998, 2003, 2008, 2013, and 2018, based on the Billboard music charts.
The majority of the songs (123) featured lead artists from North America, and 97 of them were Black/African American males. The average age of the artists was 28 years. “Prominent artists captured in the sample included 50 Cent, Drake, Eminem, Kanye West, Jay-Z, and Lil’Wayne, among others,” they said. The researchers divided mental health issues into four categories: anxiety or anxious thinking; depression or depressive thinking; metaphors (such as struggling with mental stability); and suicide or suicidal ideation.
Mental health references rise
Across the study period, 35 songs (28%) mentioned anxiety, 28 (22%) mentioned depression, 8 (6%) mentioned suicide, and 26 (21%) mentioned a mental health metaphor. The proportion of songs with a mental health reference increased in a significant linear trend across the study period for suicide (0%-12%), depression (16%-32%), and mental health metaphors (8%-44%).
All references to suicide or suicidal ideation were found in songs that were popular between 2013 and 2018, the researchers noted.
“This increase is important, given that rap artists serve as role models to their audience, which extends beyond YBAAM to include U.S. young people across strata, constituting a large group with increased risk of mental health issues and underuse of mental health services,” Mr. Kresovich and associates said.
In addition, the researchers found that stressors related to environmental conditions and love were significantly more likely to co-occur with mental health references (adjusted odds ratios 8.1 and 4.8, respectively).
The study findings were limited by several factors including the selection of songs only from the Billboard hot rap songs year-end charts, which “does not fully represent the population of rap music between 1998 and 2018,” the researchers said. In addition, they could not address causation or motivations for the increased mental health references over the study period. “We are also unable to ascertain how U.S. youth interact with this music or are positively or negatively affected by its messages.”
“For example, positively framed references to mental health awareness, treatment, or support may lead to reduced stigma and increased willingness to seek treatment,” Mr. Kresovich and associates wrote. “However, negatively framed references to mental health struggles might lead to negative outcomes, including copycat behavior in which listeners model harmful behavior, such as suicide attempts, if those behaviors are described in lyrics (i.e., the Werther effect),” they added.
Despite these limitations, the results support the need for more research on the impact of rap music as a way to reduce stigma and potentially reduce mental health risk in adolescents and young adults, Mr. Kresovich and associates concluded.
Music may help raise tough topics
The study is important because children and adolescents have more control than ever over the media they consume, Sarah Vinson, MD, founder of the Lorio Psych Group in Atlanta, said in an interview.
“With more and more children with access to their own devices, they spend a great amount of time consuming content, including music,” Dr. Vinson said. “The norms reflected in the lyrics they hear have an impact on their emerging view of themselves, others, and the world.”
The increased recognition of mental health issues by rap musicians as a topic “certainly has the potential to have a positive impact; however, the way that it is discussed can influence [the] nature of that impact,” she explained.
“It is important for people who are dealing with the normal range of human emotions to know that they are not alone. It is even more important for people dealing with suicidality or mental illness to know that,” Dr. Vinson said.
“Validation and sense of connection are human needs, and stigma related to mental illness can be isolating,” she emphasized. “Rappers have a platform and are often people that children and adolescents look up to, for better or for worse.” Through their music, “the rappers are signaling that these topics are worthy of our attention and okay to talk about.”
Unfortunately, many barriers persist for adolescents in need of mental health treatment, said Dr. Vinson. “The children’s mental health workforce, quantitatively, is not enough to meet the current needs,” she said. “Mental health is not reimbursed at the same rate as other kinds of health care, which contributes to healthy systems not prioritizing these services. Additionally, the racial, ethnic, and socioeconomic background of those who are mental health providers is not reflective of the larger population, and mental health training insufficiently incorporates the cultural and structural humility needed to help professionals navigate those differences,” she explained.
“Children at increased risk are those who face many of those environmental barriers that the rappers reference in those lyrics. They are likely to have even poorer access because they are disproportionately impacted by residential segregation, transportation challenges, financial barriers, and structural racism in mental health care,” Dr. Vinson added. A take-home message for clinicians is to find out what their patients are listening to. “One way to understand what is on the hearts and minds of children is to ask them what’s in their playlist,” she said.
Additional research is needed to examine “moderating factors for the impact, good or bad, of increased mental health content in hip hop for young listeners’ mental health awareness, symptoms and/or interest in seeking treatment,” Dr. Vinson concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Dr. Vinson served as chair for a workshop on mental health and hip-hop at the American Psychiatric Association annual meeting. She had no financial conflicts to disclose.
SOURCE: Kresovich A et al. JAMA Pediatr. 2020 Dec 7. doi: 10.1001/jamapediatrics.2020.5155.
This article was updated on December 21, 2020.
FROM JAMA PEDIATRICS
New child COVID-19 cases down in last weekly count
A tiny bit of light may have broken though the COVID-19 storm clouds.
The number of new cases in children in the United States did not set a new weekly high for the first time in months and the cumulative proportion of COVID-19 cases occurring in children did not go up for the first time since the pandemic started, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association. 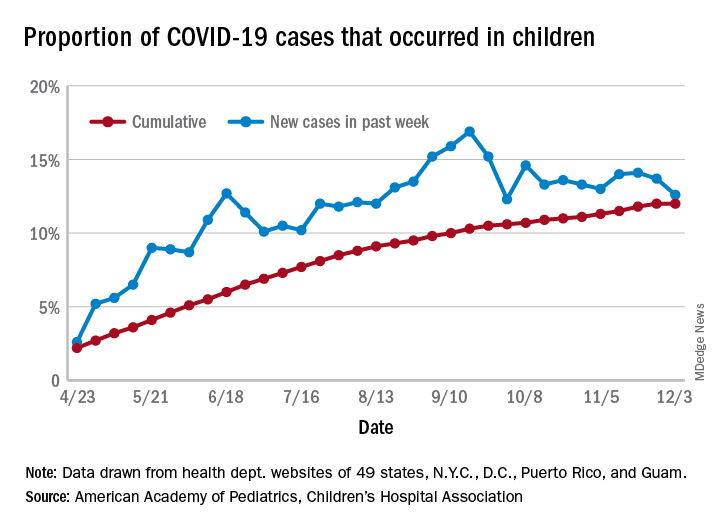
which is the first time since late September that the weekly total has fallen in the United States, the AAP/CHA data show.
Another measure, the cumulative proportion of infected children among all COVID-19 cases, stayed at 12.0% for the second week in a row, and that is the first time there was no increase since the AAP and CHA started tracking health department websites in 49 states (not New York), the District of Columbia, New York City, Puerto Rico, and Guam in April.
For the week ending Dec. 3, those 123,688 children represented 12.6% of all U.S. COVID-19 cases, marking the second consecutive weekly drop in that figure, which has been as high as 16.9% in the previous 3 months, based on data in the AAP/CHA weekly report.
The total number of reported COVID-19 cases in children is now up to 1.46 million, and the overall rate is 1,941 per 100,000 children. Comparable figures for states show that California has the most cumulative cases at over 139,000 and that North Dakota has the highest rate at over 6,800 per 100,000 children. Vermont, the state with the smallest child population, has the fewest cases (687) and the lowest rate (511 per 100,000), the report said.
The total number of COVID-19–related deaths in children has reached 154 in the 44 jurisdictions (43 states and New York City) reporting such data. That number represents 0.06% of all coronavirus deaths, a proportion that has changed little – ranging from 0.04% to 0.07% – over the course of the pandemic, the AAP and CHA said.
A tiny bit of light may have broken though the COVID-19 storm clouds.
The number of new cases in children in the United States did not set a new weekly high for the first time in months and the cumulative proportion of COVID-19 cases occurring in children did not go up for the first time since the pandemic started, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association. 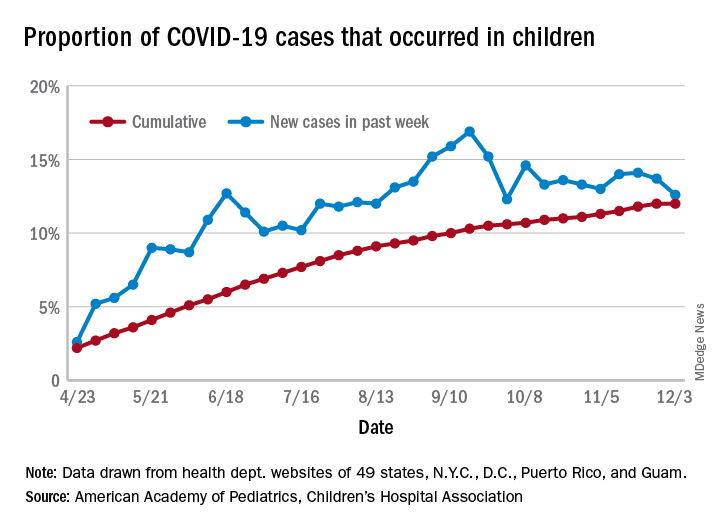
which is the first time since late September that the weekly total has fallen in the United States, the AAP/CHA data show.
Another measure, the cumulative proportion of infected children among all COVID-19 cases, stayed at 12.0% for the second week in a row, and that is the first time there was no increase since the AAP and CHA started tracking health department websites in 49 states (not New York), the District of Columbia, New York City, Puerto Rico, and Guam in April.
For the week ending Dec. 3, those 123,688 children represented 12.6% of all U.S. COVID-19 cases, marking the second consecutive weekly drop in that figure, which has been as high as 16.9% in the previous 3 months, based on data in the AAP/CHA weekly report.
The total number of reported COVID-19 cases in children is now up to 1.46 million, and the overall rate is 1,941 per 100,000 children. Comparable figures for states show that California has the most cumulative cases at over 139,000 and that North Dakota has the highest rate at over 6,800 per 100,000 children. Vermont, the state with the smallest child population, has the fewest cases (687) and the lowest rate (511 per 100,000), the report said.
The total number of COVID-19–related deaths in children has reached 154 in the 44 jurisdictions (43 states and New York City) reporting such data. That number represents 0.06% of all coronavirus deaths, a proportion that has changed little – ranging from 0.04% to 0.07% – over the course of the pandemic, the AAP and CHA said.
A tiny bit of light may have broken though the COVID-19 storm clouds.
The number of new cases in children in the United States did not set a new weekly high for the first time in months and the cumulative proportion of COVID-19 cases occurring in children did not go up for the first time since the pandemic started, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association. 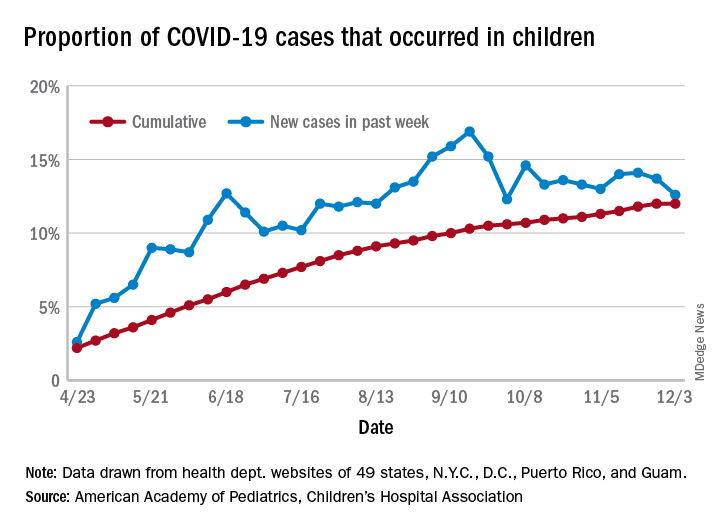
which is the first time since late September that the weekly total has fallen in the United States, the AAP/CHA data show.
Another measure, the cumulative proportion of infected children among all COVID-19 cases, stayed at 12.0% for the second week in a row, and that is the first time there was no increase since the AAP and CHA started tracking health department websites in 49 states (not New York), the District of Columbia, New York City, Puerto Rico, and Guam in April.
For the week ending Dec. 3, those 123,688 children represented 12.6% of all U.S. COVID-19 cases, marking the second consecutive weekly drop in that figure, which has been as high as 16.9% in the previous 3 months, based on data in the AAP/CHA weekly report.
The total number of reported COVID-19 cases in children is now up to 1.46 million, and the overall rate is 1,941 per 100,000 children. Comparable figures for states show that California has the most cumulative cases at over 139,000 and that North Dakota has the highest rate at over 6,800 per 100,000 children. Vermont, the state with the smallest child population, has the fewest cases (687) and the lowest rate (511 per 100,000), the report said.
The total number of COVID-19–related deaths in children has reached 154 in the 44 jurisdictions (43 states and New York City) reporting such data. That number represents 0.06% of all coronavirus deaths, a proportion that has changed little – ranging from 0.04% to 0.07% – over the course of the pandemic, the AAP and CHA said.
New residency matching sets record, says NRMP
beginning in 2021, the NRMP reported.
“Specifically, the 2020 MSMP included 6,847 applicants submitting certified rank order lists (an 8.9% increase), 2042 programs submitting certified rank order lists (a 4.3% increase), 5,734 positions (a 2.8% increase), and 5,208 positions filled (a 6.1% increase),” according to a news release.
The MSMP now includes 14 internal medicine subspecialties and four sub-subspecialties. The MSMP offered 5,734 positions this year, and 5,208 (90.8%) were successfully filled. That represents an increase of almost 3 percentage points, compared with last year’s results.
Among those subspecialties that offered 30 positions or more, the most competitive were allergy and immunology, cardiovascular disease, clinical cardiac electrophysiology, gastroenterology, hematology and oncology, and pulmonary/critical care. Each of those filled at least 95% of available slots. More than half of the positions were filled by U.S. MDs.
By contrast, the least competitive subspecialties were geriatric medicine and nephrology. Programs in these two fields filled less than 75% of positions offered. Less than 45% were filled by U.S. MDs.
More than 76% of the 6,847 applicants who submitted rank order lists (5,208) matched into residency programs.
The number of U.S. MDs in this category increased nearly 7% over last year, with a total of 2,935. The number of DO graduates increased as well, with a total of 855, which was 9.6% more than the previous year.
More U.S. citizens who graduated from international medical schools matched this year as well; 1,087 placed into subspecialty residency, a 9% increase, compared with last year.
A version of this article originally appeared on Medscape.com.
beginning in 2021, the NRMP reported.
“Specifically, the 2020 MSMP included 6,847 applicants submitting certified rank order lists (an 8.9% increase), 2042 programs submitting certified rank order lists (a 4.3% increase), 5,734 positions (a 2.8% increase), and 5,208 positions filled (a 6.1% increase),” according to a news release.
The MSMP now includes 14 internal medicine subspecialties and four sub-subspecialties. The MSMP offered 5,734 positions this year, and 5,208 (90.8%) were successfully filled. That represents an increase of almost 3 percentage points, compared with last year’s results.
Among those subspecialties that offered 30 positions or more, the most competitive were allergy and immunology, cardiovascular disease, clinical cardiac electrophysiology, gastroenterology, hematology and oncology, and pulmonary/critical care. Each of those filled at least 95% of available slots. More than half of the positions were filled by U.S. MDs.
By contrast, the least competitive subspecialties were geriatric medicine and nephrology. Programs in these two fields filled less than 75% of positions offered. Less than 45% were filled by U.S. MDs.
More than 76% of the 6,847 applicants who submitted rank order lists (5,208) matched into residency programs.
The number of U.S. MDs in this category increased nearly 7% over last year, with a total of 2,935. The number of DO graduates increased as well, with a total of 855, which was 9.6% more than the previous year.
More U.S. citizens who graduated from international medical schools matched this year as well; 1,087 placed into subspecialty residency, a 9% increase, compared with last year.
A version of this article originally appeared on Medscape.com.
beginning in 2021, the NRMP reported.
“Specifically, the 2020 MSMP included 6,847 applicants submitting certified rank order lists (an 8.9% increase), 2042 programs submitting certified rank order lists (a 4.3% increase), 5,734 positions (a 2.8% increase), and 5,208 positions filled (a 6.1% increase),” according to a news release.
The MSMP now includes 14 internal medicine subspecialties and four sub-subspecialties. The MSMP offered 5,734 positions this year, and 5,208 (90.8%) were successfully filled. That represents an increase of almost 3 percentage points, compared with last year’s results.
Among those subspecialties that offered 30 positions or more, the most competitive were allergy and immunology, cardiovascular disease, clinical cardiac electrophysiology, gastroenterology, hematology and oncology, and pulmonary/critical care. Each of those filled at least 95% of available slots. More than half of the positions were filled by U.S. MDs.
By contrast, the least competitive subspecialties were geriatric medicine and nephrology. Programs in these two fields filled less than 75% of positions offered. Less than 45% were filled by U.S. MDs.
More than 76% of the 6,847 applicants who submitted rank order lists (5,208) matched into residency programs.
The number of U.S. MDs in this category increased nearly 7% over last year, with a total of 2,935. The number of DO graduates increased as well, with a total of 855, which was 9.6% more than the previous year.
More U.S. citizens who graduated from international medical schools matched this year as well; 1,087 placed into subspecialty residency, a 9% increase, compared with last year.
A version of this article originally appeared on Medscape.com.