User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Screening tool may help better predict suicide attempts in adolescents
Researchers have developed a proprietary computer adaptive screening tool that may help emergency departments more accurately predict suicide attempts in adolescents, according to a recent study in JAMA Psychiatry.
The computerized adaptive screen for suicidal youth (CASSY) had an area under the curve (AUC) of 0.87 in an independent validation cohort that predicted an adolescent suicide attempt within 3 months, according to Cheryl A. King, PhD, of the department of psychiatry at the University of Michigan in Ann Arbor, and colleagues. CASSY’s adaptive design, which presents different questions based on a respondent’s answers, means “an individual’s initial item responses are used to determine a provisional estimate of their standing on the measured trait,” the researchers said.
Dr. King and colleagues evaluated the CASSY algorithm in a first study that consisted of 2,845 adolescents who were mean 15.1 years old, mostly girls (63%) enrolled from 13 different emergency departments across the United States within the Pediatric Emergency Care Applied Research Network (PECARN) between June 2015 and July 2016. To develop the CASSY algorithm, the participants received a 92-item self-report survey at baseline with three “anchor” questions from the Ask Suicide-Screening Questions (ASQ) and Columbia–Suicide Severity Rating Scale (C-SSRS). Based on the answers to the baseline survey, the researchers categorized participants as being at low, medium, or high risk for a suicide attempt, and followed participants for 3 months to record suicide attempts reported by a patient or parent.
Retention of participants at 3 months was 72.9%, leaving data available for 2,075 adolescents for review. The researchers found that the AUC was 0.89 (95% confidence interval, 0.85-0.91) in the first study, with a sensitivity of 82.4% and a specificity of 80%. Participants answered a mean number of 11 items during an assessment (range, 5-21 items) administered in a median time of 1 minute, 24 seconds.
In a second study consisting of a validation cohort, 4,050 adolescents from 14 PECARN emergency departments and 1 Indian Health Service hospital were followed, with a retention of 2,754 participants (69.5%) at the end of 3 months. Of the adolescents available at the end of 3 months, 62.1% were girls with a mean age of 15.0 years. The AUC for this validation group was 0.87 (95% CI, 0.85-0.89). Of these participants, 71.5% reported no previous suicide attempts, 9% reported one prior attempt, 18.2% reported multiple attempts, and 1.2% had an unknown number of suicide attempts. During the 3-month window of the second study, 6.0% of participants had at least one suicide attempt.
The researchers said that while the CASSY instrument may be advantageous for some emergency departments, “a standard screen such as the ASQ, which consists of fewer items, may be preferred in some settings, particularly those in which the cost and technical setup of a computerized adaptive screen poses too high a barrier.”
Dr. King and colleagues concluded.
Climbing adolescent suicide rate
In an interview, Igor Galynker, MD, PhD, professor in the department of psychiatry, and director of the suicide lab and the Zirinsky Center for Bipolar Disorder at the Icahn School of Medicine at Mount Sinai, New York, said the study by Dr. King and colleagues is important during a time when the suicide rate for adolescents is substantially increasing.
According to data from the CDC’s Web-based Injury Statistics Query and Reporting System, 1,750 adolescents died of suicide in 2018, and the rate of deaths by suicide has increased by 62% since the year 2000. “The issue really needs to be addressed,” said Dr. Galynker, who was not involved with the study.
Some methods of screening suicidal ideation that open with a direct question can miss suicide attempts in individuals who do not express these suicidal ideations, he explained, and the problem can be magnified in adolescent patients. “This is particularly difficult with adolescents because they’re notoriously poor historians. They cannot describe their feelings as well. It’s even more important to have methods that work for suicide prevention for adolescents and to support those predictors which do not rely on self-report,” he said.
Dr. Galynker said that CASSY is innovative because asking whether the patient is suicidal is not the “gateway question” and does not categorize people into groups determined to be at low, medium, or high risk for a suicide attempt.
“When you categorize people – adolescents in this particular case – you remove clinical judgment from [the] clinician. You deprive [the] clinician of exercising their clinical judgment in terms of somebody is or is not likely to die by suicide. That’s a serious problem,” he said, noting it may be one reason why these screening tools have difficulty identifying patients at risk of suicide.
Regarding limitations, the 3-month follow-up window for patients in the study may be too long to be clinically meaningful.
“If somebody is in treatment, 3 months is a long time. You want to know whether somebody is going to attempt suicide before the next time you see them, which is usually a month or a week,” he said.
But a strength of the CASSY instrument, Dr. Galynker said, is its ability to capture the patient’s mental state in the moment, as opposed to relying only a patient’s electronic medical record. The study also demonstrates “it should be possible to introduce detailed suicide risk assessment in the emergency rooms, and [it] should be done,” he said.
This study was funded with support from the Health Resources and Services Administration, the Maternal and Child Health Bureau, and the Emergency Medical Services for Children Network Development Demonstration Program, and a grant by the National Institute of Mental Health for the Emergency Department Screen for Teens at Risk for Suicide. Twelve authors reported personal and institutional relationships in the form of fees, grants, consultancies, royalties, copyrighted work, founding of technologies, and scientific council memberships for a variety of agencies, societies, foundations, and other organizations inside and outside of the study. Dr. Galynker reported his work unrelated to the study is supported by the National Institute of Mental Health and the American Foundation for Suicide Prevention. But he has no proprietary interests.
Researchers have developed a proprietary computer adaptive screening tool that may help emergency departments more accurately predict suicide attempts in adolescents, according to a recent study in JAMA Psychiatry.
The computerized adaptive screen for suicidal youth (CASSY) had an area under the curve (AUC) of 0.87 in an independent validation cohort that predicted an adolescent suicide attempt within 3 months, according to Cheryl A. King, PhD, of the department of psychiatry at the University of Michigan in Ann Arbor, and colleagues. CASSY’s adaptive design, which presents different questions based on a respondent’s answers, means “an individual’s initial item responses are used to determine a provisional estimate of their standing on the measured trait,” the researchers said.
Dr. King and colleagues evaluated the CASSY algorithm in a first study that consisted of 2,845 adolescents who were mean 15.1 years old, mostly girls (63%) enrolled from 13 different emergency departments across the United States within the Pediatric Emergency Care Applied Research Network (PECARN) between June 2015 and July 2016. To develop the CASSY algorithm, the participants received a 92-item self-report survey at baseline with three “anchor” questions from the Ask Suicide-Screening Questions (ASQ) and Columbia–Suicide Severity Rating Scale (C-SSRS). Based on the answers to the baseline survey, the researchers categorized participants as being at low, medium, or high risk for a suicide attempt, and followed participants for 3 months to record suicide attempts reported by a patient or parent.
Retention of participants at 3 months was 72.9%, leaving data available for 2,075 adolescents for review. The researchers found that the AUC was 0.89 (95% confidence interval, 0.85-0.91) in the first study, with a sensitivity of 82.4% and a specificity of 80%. Participants answered a mean number of 11 items during an assessment (range, 5-21 items) administered in a median time of 1 minute, 24 seconds.
In a second study consisting of a validation cohort, 4,050 adolescents from 14 PECARN emergency departments and 1 Indian Health Service hospital were followed, with a retention of 2,754 participants (69.5%) at the end of 3 months. Of the adolescents available at the end of 3 months, 62.1% were girls with a mean age of 15.0 years. The AUC for this validation group was 0.87 (95% CI, 0.85-0.89). Of these participants, 71.5% reported no previous suicide attempts, 9% reported one prior attempt, 18.2% reported multiple attempts, and 1.2% had an unknown number of suicide attempts. During the 3-month window of the second study, 6.0% of participants had at least one suicide attempt.
The researchers said that while the CASSY instrument may be advantageous for some emergency departments, “a standard screen such as the ASQ, which consists of fewer items, may be preferred in some settings, particularly those in which the cost and technical setup of a computerized adaptive screen poses too high a barrier.”
Dr. King and colleagues concluded.
Climbing adolescent suicide rate
In an interview, Igor Galynker, MD, PhD, professor in the department of psychiatry, and director of the suicide lab and the Zirinsky Center for Bipolar Disorder at the Icahn School of Medicine at Mount Sinai, New York, said the study by Dr. King and colleagues is important during a time when the suicide rate for adolescents is substantially increasing.
According to data from the CDC’s Web-based Injury Statistics Query and Reporting System, 1,750 adolescents died of suicide in 2018, and the rate of deaths by suicide has increased by 62% since the year 2000. “The issue really needs to be addressed,” said Dr. Galynker, who was not involved with the study.
Some methods of screening suicidal ideation that open with a direct question can miss suicide attempts in individuals who do not express these suicidal ideations, he explained, and the problem can be magnified in adolescent patients. “This is particularly difficult with adolescents because they’re notoriously poor historians. They cannot describe their feelings as well. It’s even more important to have methods that work for suicide prevention for adolescents and to support those predictors which do not rely on self-report,” he said.
Dr. Galynker said that CASSY is innovative because asking whether the patient is suicidal is not the “gateway question” and does not categorize people into groups determined to be at low, medium, or high risk for a suicide attempt.
“When you categorize people – adolescents in this particular case – you remove clinical judgment from [the] clinician. You deprive [the] clinician of exercising their clinical judgment in terms of somebody is or is not likely to die by suicide. That’s a serious problem,” he said, noting it may be one reason why these screening tools have difficulty identifying patients at risk of suicide.
Regarding limitations, the 3-month follow-up window for patients in the study may be too long to be clinically meaningful.
“If somebody is in treatment, 3 months is a long time. You want to know whether somebody is going to attempt suicide before the next time you see them, which is usually a month or a week,” he said.
But a strength of the CASSY instrument, Dr. Galynker said, is its ability to capture the patient’s mental state in the moment, as opposed to relying only a patient’s electronic medical record. The study also demonstrates “it should be possible to introduce detailed suicide risk assessment in the emergency rooms, and [it] should be done,” he said.
This study was funded with support from the Health Resources and Services Administration, the Maternal and Child Health Bureau, and the Emergency Medical Services for Children Network Development Demonstration Program, and a grant by the National Institute of Mental Health for the Emergency Department Screen for Teens at Risk for Suicide. Twelve authors reported personal and institutional relationships in the form of fees, grants, consultancies, royalties, copyrighted work, founding of technologies, and scientific council memberships for a variety of agencies, societies, foundations, and other organizations inside and outside of the study. Dr. Galynker reported his work unrelated to the study is supported by the National Institute of Mental Health and the American Foundation for Suicide Prevention. But he has no proprietary interests.
Researchers have developed a proprietary computer adaptive screening tool that may help emergency departments more accurately predict suicide attempts in adolescents, according to a recent study in JAMA Psychiatry.
The computerized adaptive screen for suicidal youth (CASSY) had an area under the curve (AUC) of 0.87 in an independent validation cohort that predicted an adolescent suicide attempt within 3 months, according to Cheryl A. King, PhD, of the department of psychiatry at the University of Michigan in Ann Arbor, and colleagues. CASSY’s adaptive design, which presents different questions based on a respondent’s answers, means “an individual’s initial item responses are used to determine a provisional estimate of their standing on the measured trait,” the researchers said.
Dr. King and colleagues evaluated the CASSY algorithm in a first study that consisted of 2,845 adolescents who were mean 15.1 years old, mostly girls (63%) enrolled from 13 different emergency departments across the United States within the Pediatric Emergency Care Applied Research Network (PECARN) between June 2015 and July 2016. To develop the CASSY algorithm, the participants received a 92-item self-report survey at baseline with three “anchor” questions from the Ask Suicide-Screening Questions (ASQ) and Columbia–Suicide Severity Rating Scale (C-SSRS). Based on the answers to the baseline survey, the researchers categorized participants as being at low, medium, or high risk for a suicide attempt, and followed participants for 3 months to record suicide attempts reported by a patient or parent.
Retention of participants at 3 months was 72.9%, leaving data available for 2,075 adolescents for review. The researchers found that the AUC was 0.89 (95% confidence interval, 0.85-0.91) in the first study, with a sensitivity of 82.4% and a specificity of 80%. Participants answered a mean number of 11 items during an assessment (range, 5-21 items) administered in a median time of 1 minute, 24 seconds.
In a second study consisting of a validation cohort, 4,050 adolescents from 14 PECARN emergency departments and 1 Indian Health Service hospital were followed, with a retention of 2,754 participants (69.5%) at the end of 3 months. Of the adolescents available at the end of 3 months, 62.1% were girls with a mean age of 15.0 years. The AUC for this validation group was 0.87 (95% CI, 0.85-0.89). Of these participants, 71.5% reported no previous suicide attempts, 9% reported one prior attempt, 18.2% reported multiple attempts, and 1.2% had an unknown number of suicide attempts. During the 3-month window of the second study, 6.0% of participants had at least one suicide attempt.
The researchers said that while the CASSY instrument may be advantageous for some emergency departments, “a standard screen such as the ASQ, which consists of fewer items, may be preferred in some settings, particularly those in which the cost and technical setup of a computerized adaptive screen poses too high a barrier.”
Dr. King and colleagues concluded.
Climbing adolescent suicide rate
In an interview, Igor Galynker, MD, PhD, professor in the department of psychiatry, and director of the suicide lab and the Zirinsky Center for Bipolar Disorder at the Icahn School of Medicine at Mount Sinai, New York, said the study by Dr. King and colleagues is important during a time when the suicide rate for adolescents is substantially increasing.
According to data from the CDC’s Web-based Injury Statistics Query and Reporting System, 1,750 adolescents died of suicide in 2018, and the rate of deaths by suicide has increased by 62% since the year 2000. “The issue really needs to be addressed,” said Dr. Galynker, who was not involved with the study.
Some methods of screening suicidal ideation that open with a direct question can miss suicide attempts in individuals who do not express these suicidal ideations, he explained, and the problem can be magnified in adolescent patients. “This is particularly difficult with adolescents because they’re notoriously poor historians. They cannot describe their feelings as well. It’s even more important to have methods that work for suicide prevention for adolescents and to support those predictors which do not rely on self-report,” he said.
Dr. Galynker said that CASSY is innovative because asking whether the patient is suicidal is not the “gateway question” and does not categorize people into groups determined to be at low, medium, or high risk for a suicide attempt.
“When you categorize people – adolescents in this particular case – you remove clinical judgment from [the] clinician. You deprive [the] clinician of exercising their clinical judgment in terms of somebody is or is not likely to die by suicide. That’s a serious problem,” he said, noting it may be one reason why these screening tools have difficulty identifying patients at risk of suicide.
Regarding limitations, the 3-month follow-up window for patients in the study may be too long to be clinically meaningful.
“If somebody is in treatment, 3 months is a long time. You want to know whether somebody is going to attempt suicide before the next time you see them, which is usually a month or a week,” he said.
But a strength of the CASSY instrument, Dr. Galynker said, is its ability to capture the patient’s mental state in the moment, as opposed to relying only a patient’s electronic medical record. The study also demonstrates “it should be possible to introduce detailed suicide risk assessment in the emergency rooms, and [it] should be done,” he said.
This study was funded with support from the Health Resources and Services Administration, the Maternal and Child Health Bureau, and the Emergency Medical Services for Children Network Development Demonstration Program, and a grant by the National Institute of Mental Health for the Emergency Department Screen for Teens at Risk for Suicide. Twelve authors reported personal and institutional relationships in the form of fees, grants, consultancies, royalties, copyrighted work, founding of technologies, and scientific council memberships for a variety of agencies, societies, foundations, and other organizations inside and outside of the study. Dr. Galynker reported his work unrelated to the study is supported by the National Institute of Mental Health and the American Foundation for Suicide Prevention. But he has no proprietary interests.
FROM JAMA PSYCHIATRY
COVID and schools: A pediatrician's case for a return to class
In a time when this country is struggling to find topics on which we can achieve broad consensus, the question of whether in-class learning is important stands as an outlier. Parents, teachers, students, and pediatricians all agree that having children learn in a social, face-to-face environment is critical to their education and mental health. Because school has become a de facto daycare source for many families, employers have joined in the chorus supporting a return to in-class education.
Of course, beyond that basic point of agreement the myriad of questions relating to when and how that return to the educational norm can be achieved we divide into groups with almost as many answers as there are questions. Part of the problem stems from the national leadership vacuum that fed the confusion. In this void the topic of school reopening has become politicized.
On Jan. 5, 2021, the American Academy of Pediatrics released an updated interim COVID-19 Guidance for Safe Schools at services.aap.org. It is a thorough and well thought out document that should function as a roadmap for communities and pediatricians who serve as official and unofficial advisers to their local school departments. At the very outset it reminds us that “school transmission mirrors but does not drive community transmission.”
Unfortunately, timing is everything and while the document’s salient points received some media attention it was mostly buried by the tsunami of press coverage in the wake of the storming of the Capitol the next day and the postinauguration reshuffling of the federal government. Even if it had been released on one of those seldom seen quiet news days, I fear the document’s message encouraging the return to in-class learning would have still not received the attention it deserved.
The lack of a high-visibility celebrity spokesperson and a system of short-tenure presidencies puts the AAP at a disadvantage when it comes to getting its message across to a national audience. The advocacy role filters down to those of us in our own communities who must convince school boards that not only is in-class learning critical but there are safe ways to do it.
In some communities the timing of return to in-class learning may pit pediatricians against teachers. Usually, these two groups share an enthusiastic advocacy for children. However, facing what has up to this point been a poorly defined health risk, teachers are understandably resistant to return to the classroom although they acknowledge its importance.
Armed with the AAP’s guidance document, pediatricians should encourage school boards and state and local health departments to look closely at the epidemiologic evidence and consider creative ways to prioritize teachers for what currently are limited and erratic vaccine supplies. Strategies might include offering vaccines to teachers based strictly on their age and/or health status. However, teachers and in-class education are so critical to the educational process and the national economy that an open offer to all teachers makes more sense.
While some states have already prioritized teachers for vaccines, the AAP must continue to speak loudly that in-class education is critical and urge all states to do what is necessary to make teachers feel safe to return to the classroom.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
In a time when this country is struggling to find topics on which we can achieve broad consensus, the question of whether in-class learning is important stands as an outlier. Parents, teachers, students, and pediatricians all agree that having children learn in a social, face-to-face environment is critical to their education and mental health. Because school has become a de facto daycare source for many families, employers have joined in the chorus supporting a return to in-class education.
Of course, beyond that basic point of agreement the myriad of questions relating to when and how that return to the educational norm can be achieved we divide into groups with almost as many answers as there are questions. Part of the problem stems from the national leadership vacuum that fed the confusion. In this void the topic of school reopening has become politicized.
On Jan. 5, 2021, the American Academy of Pediatrics released an updated interim COVID-19 Guidance for Safe Schools at services.aap.org. It is a thorough and well thought out document that should function as a roadmap for communities and pediatricians who serve as official and unofficial advisers to their local school departments. At the very outset it reminds us that “school transmission mirrors but does not drive community transmission.”
Unfortunately, timing is everything and while the document’s salient points received some media attention it was mostly buried by the tsunami of press coverage in the wake of the storming of the Capitol the next day and the postinauguration reshuffling of the federal government. Even if it had been released on one of those seldom seen quiet news days, I fear the document’s message encouraging the return to in-class learning would have still not received the attention it deserved.
The lack of a high-visibility celebrity spokesperson and a system of short-tenure presidencies puts the AAP at a disadvantage when it comes to getting its message across to a national audience. The advocacy role filters down to those of us in our own communities who must convince school boards that not only is in-class learning critical but there are safe ways to do it.
In some communities the timing of return to in-class learning may pit pediatricians against teachers. Usually, these two groups share an enthusiastic advocacy for children. However, facing what has up to this point been a poorly defined health risk, teachers are understandably resistant to return to the classroom although they acknowledge its importance.
Armed with the AAP’s guidance document, pediatricians should encourage school boards and state and local health departments to look closely at the epidemiologic evidence and consider creative ways to prioritize teachers for what currently are limited and erratic vaccine supplies. Strategies might include offering vaccines to teachers based strictly on their age and/or health status. However, teachers and in-class education are so critical to the educational process and the national economy that an open offer to all teachers makes more sense.
While some states have already prioritized teachers for vaccines, the AAP must continue to speak loudly that in-class education is critical and urge all states to do what is necessary to make teachers feel safe to return to the classroom.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
In a time when this country is struggling to find topics on which we can achieve broad consensus, the question of whether in-class learning is important stands as an outlier. Parents, teachers, students, and pediatricians all agree that having children learn in a social, face-to-face environment is critical to their education and mental health. Because school has become a de facto daycare source for many families, employers have joined in the chorus supporting a return to in-class education.
Of course, beyond that basic point of agreement the myriad of questions relating to when and how that return to the educational norm can be achieved we divide into groups with almost as many answers as there are questions. Part of the problem stems from the national leadership vacuum that fed the confusion. In this void the topic of school reopening has become politicized.
On Jan. 5, 2021, the American Academy of Pediatrics released an updated interim COVID-19 Guidance for Safe Schools at services.aap.org. It is a thorough and well thought out document that should function as a roadmap for communities and pediatricians who serve as official and unofficial advisers to their local school departments. At the very outset it reminds us that “school transmission mirrors but does not drive community transmission.”
Unfortunately, timing is everything and while the document’s salient points received some media attention it was mostly buried by the tsunami of press coverage in the wake of the storming of the Capitol the next day and the postinauguration reshuffling of the federal government. Even if it had been released on one of those seldom seen quiet news days, I fear the document’s message encouraging the return to in-class learning would have still not received the attention it deserved.
The lack of a high-visibility celebrity spokesperson and a system of short-tenure presidencies puts the AAP at a disadvantage when it comes to getting its message across to a national audience. The advocacy role filters down to those of us in our own communities who must convince school boards that not only is in-class learning critical but there are safe ways to do it.
In some communities the timing of return to in-class learning may pit pediatricians against teachers. Usually, these two groups share an enthusiastic advocacy for children. However, facing what has up to this point been a poorly defined health risk, teachers are understandably resistant to return to the classroom although they acknowledge its importance.
Armed with the AAP’s guidance document, pediatricians should encourage school boards and state and local health departments to look closely at the epidemiologic evidence and consider creative ways to prioritize teachers for what currently are limited and erratic vaccine supplies. Strategies might include offering vaccines to teachers based strictly on their age and/or health status. However, teachers and in-class education are so critical to the educational process and the national economy that an open offer to all teachers makes more sense.
While some states have already prioritized teachers for vaccines, the AAP must continue to speak loudly that in-class education is critical and urge all states to do what is necessary to make teachers feel safe to return to the classroom.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Safety profiles of hemophilia agents vary widely
Despite their similar functions, each current and emerging therapy for treating hemophilia has a unique safety profile, and each needs to be weighed apart from agents both within and outside its pharmacologic class, a hemophilia specialist said.
“My view is that each new molecule coming to the hemophilia space, including variant factor molecules, needs to be scrutinized separately, without class assumptions or extrapolations, and it’s clear that thrombosis risk has become a priority safety consideration,” said Dan Hart, MBChB, MRCP, FRCPath, PhD, from Barts and the London School of Medicine and Dentistry.
He reviewed the comparative safety of standard and novel therapies for hemophilia at the annual congress of the European Association for Haemophilia and Allied Disorders.
Factor inhibitors
Inhibitors occur in both hemophilia A and hemophilia B, and are primarily seen in patients with childhood exposure to factor concentrates. Inhibitors, which include anti–factor VIII and factor IX alloantibodies, are more common among patients with severe hemophilia and those with more disruptive factor VIII and factor IX mutations.
“There can be transient vs. persistent inhibitors, and arguably the more you look, the more you find, but clinically we never miss high-titer inhibitors that have a big impact on individuals and the subsequent decisions about management,” he said.
Hamster vs. human
It’s currently unclear whether there is an immunologic advantage for previously untreated patients to be started on factor VIII concentrates derived from recombinant human cells lines, or from products derived from Chinese hamster ovary (CHO) or baby hamster kidney (BHK) cell lines, Dr. Hart said.
“We need to ensure that we’re not selective about comparator choice for new products in the absence of head-to-head studies,” he said.
Route of administration matters
Inhibitors appear to be a more common occurrence among patients who received factor concentrates subcutaneously, compared with intravenously, Dr. Hart noted, pointing to a 2011 study indicating a background annual risk of 5 cases of inhibitor development per 1,000 treatment years in previously treated patients who received intravenous therapy (Blood. 2011 Jun 9;117[23]:6367-70).
In contrast, in a phase 1 trial of subcutaneous turoctocog alfa pegol, 5 out of 26 patients had detectable N8-GP–binding antibodies after 42-91 exposure days. Of these patients, one developed an inhibitor to factor VIII, and anti–N8-GP antibody appearance was associated with a decline in factor VIII plasma activity in four of the five patients. In addition, five patients reported a total of nine bleeding episodes requiring treatment during prophylaxis. As a result of this trial, further clinical development of the subcutaneous version was suspended. (J Thromb Haemost. 2020 Feb;18[2]:341-51).
Other subcutaneously administered factors are currently in development, Dr. Hart noted.
Nonfactor inhibitors?
“The nonfactor agents do have the risk of generating antibodies: Monoclonal antibodies outside the hemophilia setting provoke antidrug antibodies,” he said.
Although there is no consensus regarding which assay can best monitor antidrug antibodies (ADA), enzyme-linked immunosorbent assay (ELISA) can detect neutralizing antibodies and other antibodies.
In the hemophilia setting, surrogate markers for loss of drug efficacy include longer activated partial thromboplastin time (ATTP) or a drop in serum drug levels. Worsening bleeding phenotype can also be a marker for loss of efficacy, albeit an imperfect one.
Emicizumab (Hemlibara), the first nonfactor monoclonal agent to make it to market, has the largest dataset available, and evidence suggests a rate of neutralizing antibodies with this agent of less than 1% in the HAVEN clinical trial series, but 5.2% in the single-arm STASEY trial.
“We shouldn’t assume that other biophenotypics will have a similar ADA rate, and this needs to be evaluated for each molecule, as it will need to be for other monoclonals” such as anti–tissue factor pathway (TFPI) antibodies, Dr. Hart emphasized.
Pegylation
Pegylated compounds include polyethylene glycol, an inert polymer, covalently bound to the therapeutic protein to extend its half-life, and theoretically, reduce immunogenicity.
Many patients may already have exposure to pegylated products in the form of peginterferon to treat hepatitis C, consumer products such as toothpaste, cough medicine, and cosmetics, and, more recently, in vaccines against COVID-19.
Safety considerations with pegylated agents in hemophilia include concerns about accumulation of polyethylene glycol (PEG), although “some of the preclinical models looking at excretion of PEG are difficult to interpret in my view, and people debate about whether studies are long enough, but it’s undoubtedly the case that toxicology dosing is order of magnitude higher than the routine dosing in hemophilia,” he said.
After more than 5 years of experience with pegylated products there is no clinical evidence of concern, although “it’s not clear, actually, what we’re looking for, whether it’s a clinical parameter, or imaging or histological parameter.”
Patients may also not have lifelong exposure to pegylated products, as it is unlikely that they will stay on the same product for decades, Dr. Hart said.
Thrombosis
As of June 30, 2020, more than 7,200 persons with hemophilia have received emicizumab, and there have been 23 reported thrombotic events, 19 of which occurred in the postmarketing period. Of the reported cases, six patients had a myocardial infarction, and all of these patients had at least one cardiovascular risk factor.
The antithrombin agent fitusiran was associated with one fatal thrombotic event in a phase 2, open-label extension trial, leading to a pause and resumption with mitigation protocols, but that trial has since been paused again because of additional, nonfatal thrombotic events.
Nonfatal thrombotic events have also occurred in clinical trials for the investigational anti-TFPI monoclonal antibodies BAY 1093884 and concizumab, but none have thus far been reported in phase 3 trial of marstacimab.
“We need renewed efforts for prospective reporting and independent review of all adverse events of all agents, old and new: This will need some guidance nationally and internationally, and I think the relevant trial [serious adverse events] need to be reported in peer review literature, and clinicaltrials.gov updated in a timely manner, regardless of whether that strategy was successful or unsuccessful,” Dr. Hart said.
Risk with longer-acting agents?
In the question and answer following his presentation, Christoph Königs, MD, PhD, from University Hospital Frankfurt, asked whether there was potential for increased thrombosis risk with second-generation extended half-life (EHL) molecules in clinical trials.
“As we edge towards normalization of hemostasis, clearly the other non–hemophilia dependent issues of thrombosis risk come into play,” Dr. Hart acknowledged. “I think it will be an inevitability that there will be events, and we need to understand what the denominators are – hence my pitch for there being a renewed effort to try and collate sufficient data that we can really define events happening with people treated with standard half-life [products] through into the novel agents,” he said.
Dr. Hart disclosed grant/research support and speaker bureau activities for Bayer, Octapharma, Takeda, and others. Dr. Königs has reported no relevant disclosures.
Despite their similar functions, each current and emerging therapy for treating hemophilia has a unique safety profile, and each needs to be weighed apart from agents both within and outside its pharmacologic class, a hemophilia specialist said.
“My view is that each new molecule coming to the hemophilia space, including variant factor molecules, needs to be scrutinized separately, without class assumptions or extrapolations, and it’s clear that thrombosis risk has become a priority safety consideration,” said Dan Hart, MBChB, MRCP, FRCPath, PhD, from Barts and the London School of Medicine and Dentistry.
He reviewed the comparative safety of standard and novel therapies for hemophilia at the annual congress of the European Association for Haemophilia and Allied Disorders.
Factor inhibitors
Inhibitors occur in both hemophilia A and hemophilia B, and are primarily seen in patients with childhood exposure to factor concentrates. Inhibitors, which include anti–factor VIII and factor IX alloantibodies, are more common among patients with severe hemophilia and those with more disruptive factor VIII and factor IX mutations.
“There can be transient vs. persistent inhibitors, and arguably the more you look, the more you find, but clinically we never miss high-titer inhibitors that have a big impact on individuals and the subsequent decisions about management,” he said.
Hamster vs. human
It’s currently unclear whether there is an immunologic advantage for previously untreated patients to be started on factor VIII concentrates derived from recombinant human cells lines, or from products derived from Chinese hamster ovary (CHO) or baby hamster kidney (BHK) cell lines, Dr. Hart said.
“We need to ensure that we’re not selective about comparator choice for new products in the absence of head-to-head studies,” he said.
Route of administration matters
Inhibitors appear to be a more common occurrence among patients who received factor concentrates subcutaneously, compared with intravenously, Dr. Hart noted, pointing to a 2011 study indicating a background annual risk of 5 cases of inhibitor development per 1,000 treatment years in previously treated patients who received intravenous therapy (Blood. 2011 Jun 9;117[23]:6367-70).
In contrast, in a phase 1 trial of subcutaneous turoctocog alfa pegol, 5 out of 26 patients had detectable N8-GP–binding antibodies after 42-91 exposure days. Of these patients, one developed an inhibitor to factor VIII, and anti–N8-GP antibody appearance was associated with a decline in factor VIII plasma activity in four of the five patients. In addition, five patients reported a total of nine bleeding episodes requiring treatment during prophylaxis. As a result of this trial, further clinical development of the subcutaneous version was suspended. (J Thromb Haemost. 2020 Feb;18[2]:341-51).
Other subcutaneously administered factors are currently in development, Dr. Hart noted.
Nonfactor inhibitors?
“The nonfactor agents do have the risk of generating antibodies: Monoclonal antibodies outside the hemophilia setting provoke antidrug antibodies,” he said.
Although there is no consensus regarding which assay can best monitor antidrug antibodies (ADA), enzyme-linked immunosorbent assay (ELISA) can detect neutralizing antibodies and other antibodies.
In the hemophilia setting, surrogate markers for loss of drug efficacy include longer activated partial thromboplastin time (ATTP) or a drop in serum drug levels. Worsening bleeding phenotype can also be a marker for loss of efficacy, albeit an imperfect one.
Emicizumab (Hemlibara), the first nonfactor monoclonal agent to make it to market, has the largest dataset available, and evidence suggests a rate of neutralizing antibodies with this agent of less than 1% in the HAVEN clinical trial series, but 5.2% in the single-arm STASEY trial.
“We shouldn’t assume that other biophenotypics will have a similar ADA rate, and this needs to be evaluated for each molecule, as it will need to be for other monoclonals” such as anti–tissue factor pathway (TFPI) antibodies, Dr. Hart emphasized.
Pegylation
Pegylated compounds include polyethylene glycol, an inert polymer, covalently bound to the therapeutic protein to extend its half-life, and theoretically, reduce immunogenicity.
Many patients may already have exposure to pegylated products in the form of peginterferon to treat hepatitis C, consumer products such as toothpaste, cough medicine, and cosmetics, and, more recently, in vaccines against COVID-19.
Safety considerations with pegylated agents in hemophilia include concerns about accumulation of polyethylene glycol (PEG), although “some of the preclinical models looking at excretion of PEG are difficult to interpret in my view, and people debate about whether studies are long enough, but it’s undoubtedly the case that toxicology dosing is order of magnitude higher than the routine dosing in hemophilia,” he said.
After more than 5 years of experience with pegylated products there is no clinical evidence of concern, although “it’s not clear, actually, what we’re looking for, whether it’s a clinical parameter, or imaging or histological parameter.”
Patients may also not have lifelong exposure to pegylated products, as it is unlikely that they will stay on the same product for decades, Dr. Hart said.
Thrombosis
As of June 30, 2020, more than 7,200 persons with hemophilia have received emicizumab, and there have been 23 reported thrombotic events, 19 of which occurred in the postmarketing period. Of the reported cases, six patients had a myocardial infarction, and all of these patients had at least one cardiovascular risk factor.
The antithrombin agent fitusiran was associated with one fatal thrombotic event in a phase 2, open-label extension trial, leading to a pause and resumption with mitigation protocols, but that trial has since been paused again because of additional, nonfatal thrombotic events.
Nonfatal thrombotic events have also occurred in clinical trials for the investigational anti-TFPI monoclonal antibodies BAY 1093884 and concizumab, but none have thus far been reported in phase 3 trial of marstacimab.
“We need renewed efforts for prospective reporting and independent review of all adverse events of all agents, old and new: This will need some guidance nationally and internationally, and I think the relevant trial [serious adverse events] need to be reported in peer review literature, and clinicaltrials.gov updated in a timely manner, regardless of whether that strategy was successful or unsuccessful,” Dr. Hart said.
Risk with longer-acting agents?
In the question and answer following his presentation, Christoph Königs, MD, PhD, from University Hospital Frankfurt, asked whether there was potential for increased thrombosis risk with second-generation extended half-life (EHL) molecules in clinical trials.
“As we edge towards normalization of hemostasis, clearly the other non–hemophilia dependent issues of thrombosis risk come into play,” Dr. Hart acknowledged. “I think it will be an inevitability that there will be events, and we need to understand what the denominators are – hence my pitch for there being a renewed effort to try and collate sufficient data that we can really define events happening with people treated with standard half-life [products] through into the novel agents,” he said.
Dr. Hart disclosed grant/research support and speaker bureau activities for Bayer, Octapharma, Takeda, and others. Dr. Königs has reported no relevant disclosures.
Despite their similar functions, each current and emerging therapy for treating hemophilia has a unique safety profile, and each needs to be weighed apart from agents both within and outside its pharmacologic class, a hemophilia specialist said.
“My view is that each new molecule coming to the hemophilia space, including variant factor molecules, needs to be scrutinized separately, without class assumptions or extrapolations, and it’s clear that thrombosis risk has become a priority safety consideration,” said Dan Hart, MBChB, MRCP, FRCPath, PhD, from Barts and the London School of Medicine and Dentistry.
He reviewed the comparative safety of standard and novel therapies for hemophilia at the annual congress of the European Association for Haemophilia and Allied Disorders.
Factor inhibitors
Inhibitors occur in both hemophilia A and hemophilia B, and are primarily seen in patients with childhood exposure to factor concentrates. Inhibitors, which include anti–factor VIII and factor IX alloantibodies, are more common among patients with severe hemophilia and those with more disruptive factor VIII and factor IX mutations.
“There can be transient vs. persistent inhibitors, and arguably the more you look, the more you find, but clinically we never miss high-titer inhibitors that have a big impact on individuals and the subsequent decisions about management,” he said.
Hamster vs. human
It’s currently unclear whether there is an immunologic advantage for previously untreated patients to be started on factor VIII concentrates derived from recombinant human cells lines, or from products derived from Chinese hamster ovary (CHO) or baby hamster kidney (BHK) cell lines, Dr. Hart said.
“We need to ensure that we’re not selective about comparator choice for new products in the absence of head-to-head studies,” he said.
Route of administration matters
Inhibitors appear to be a more common occurrence among patients who received factor concentrates subcutaneously, compared with intravenously, Dr. Hart noted, pointing to a 2011 study indicating a background annual risk of 5 cases of inhibitor development per 1,000 treatment years in previously treated patients who received intravenous therapy (Blood. 2011 Jun 9;117[23]:6367-70).
In contrast, in a phase 1 trial of subcutaneous turoctocog alfa pegol, 5 out of 26 patients had detectable N8-GP–binding antibodies after 42-91 exposure days. Of these patients, one developed an inhibitor to factor VIII, and anti–N8-GP antibody appearance was associated with a decline in factor VIII plasma activity in four of the five patients. In addition, five patients reported a total of nine bleeding episodes requiring treatment during prophylaxis. As a result of this trial, further clinical development of the subcutaneous version was suspended. (J Thromb Haemost. 2020 Feb;18[2]:341-51).
Other subcutaneously administered factors are currently in development, Dr. Hart noted.
Nonfactor inhibitors?
“The nonfactor agents do have the risk of generating antibodies: Monoclonal antibodies outside the hemophilia setting provoke antidrug antibodies,” he said.
Although there is no consensus regarding which assay can best monitor antidrug antibodies (ADA), enzyme-linked immunosorbent assay (ELISA) can detect neutralizing antibodies and other antibodies.
In the hemophilia setting, surrogate markers for loss of drug efficacy include longer activated partial thromboplastin time (ATTP) or a drop in serum drug levels. Worsening bleeding phenotype can also be a marker for loss of efficacy, albeit an imperfect one.
Emicizumab (Hemlibara), the first nonfactor monoclonal agent to make it to market, has the largest dataset available, and evidence suggests a rate of neutralizing antibodies with this agent of less than 1% in the HAVEN clinical trial series, but 5.2% in the single-arm STASEY trial.
“We shouldn’t assume that other biophenotypics will have a similar ADA rate, and this needs to be evaluated for each molecule, as it will need to be for other monoclonals” such as anti–tissue factor pathway (TFPI) antibodies, Dr. Hart emphasized.
Pegylation
Pegylated compounds include polyethylene glycol, an inert polymer, covalently bound to the therapeutic protein to extend its half-life, and theoretically, reduce immunogenicity.
Many patients may already have exposure to pegylated products in the form of peginterferon to treat hepatitis C, consumer products such as toothpaste, cough medicine, and cosmetics, and, more recently, in vaccines against COVID-19.
Safety considerations with pegylated agents in hemophilia include concerns about accumulation of polyethylene glycol (PEG), although “some of the preclinical models looking at excretion of PEG are difficult to interpret in my view, and people debate about whether studies are long enough, but it’s undoubtedly the case that toxicology dosing is order of magnitude higher than the routine dosing in hemophilia,” he said.
After more than 5 years of experience with pegylated products there is no clinical evidence of concern, although “it’s not clear, actually, what we’re looking for, whether it’s a clinical parameter, or imaging or histological parameter.”
Patients may also not have lifelong exposure to pegylated products, as it is unlikely that they will stay on the same product for decades, Dr. Hart said.
Thrombosis
As of June 30, 2020, more than 7,200 persons with hemophilia have received emicizumab, and there have been 23 reported thrombotic events, 19 of which occurred in the postmarketing period. Of the reported cases, six patients had a myocardial infarction, and all of these patients had at least one cardiovascular risk factor.
The antithrombin agent fitusiran was associated with one fatal thrombotic event in a phase 2, open-label extension trial, leading to a pause and resumption with mitigation protocols, but that trial has since been paused again because of additional, nonfatal thrombotic events.
Nonfatal thrombotic events have also occurred in clinical trials for the investigational anti-TFPI monoclonal antibodies BAY 1093884 and concizumab, but none have thus far been reported in phase 3 trial of marstacimab.
“We need renewed efforts for prospective reporting and independent review of all adverse events of all agents, old and new: This will need some guidance nationally and internationally, and I think the relevant trial [serious adverse events] need to be reported in peer review literature, and clinicaltrials.gov updated in a timely manner, regardless of whether that strategy was successful or unsuccessful,” Dr. Hart said.
Risk with longer-acting agents?
In the question and answer following his presentation, Christoph Königs, MD, PhD, from University Hospital Frankfurt, asked whether there was potential for increased thrombosis risk with second-generation extended half-life (EHL) molecules in clinical trials.
“As we edge towards normalization of hemostasis, clearly the other non–hemophilia dependent issues of thrombosis risk come into play,” Dr. Hart acknowledged. “I think it will be an inevitability that there will be events, and we need to understand what the denominators are – hence my pitch for there being a renewed effort to try and collate sufficient data that we can really define events happening with people treated with standard half-life [products] through into the novel agents,” he said.
Dr. Hart disclosed grant/research support and speaker bureau activities for Bayer, Octapharma, Takeda, and others. Dr. Königs has reported no relevant disclosures.
FROM EAHAD 2021
Strep A and tic worsening: Final word?
Exposure to Group A streptococcus (GAS) does not appear to worsen symptoms of Tourette syndrome and other chronic tic disorders (CTDs) in children and adolescents, new research suggests.
Investigators studied over 700 children and teenagers with CTDs, one-third of whom also had attention deficit hyperactivity disorder and one-third who had obsessive-compulsive disorder (OCD).
The youngsters were followed for an average of 16 months and evaluated at 4-month intervals to see if they were infected with GAS. Tic severity was monitored through telephone interviews, in-person visits, and parental reports.
A little less than half the children experienced worsening of tics during the study period, but the researchers found no association between these exacerbations and GAS exposure.
There was also no link between GAS and worsening OCD. However, researchers did find an association between GAS exposure and an increase in hyperactivity and impulsivity in patients with ADHD.
“This study does not support GAS exposures as contributing factors for tic exacerbations in children with CTD,” the authors note.
“Specific work-up or active management of GAS infections is unlikely to help modifying the course of tics in CTD and is therefore not recommended,” they conclude.
The study was published online in Neurology.
‘Intense debate’
The association between GAS and CTD stems from the description of Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infection (PANDAS) – a condition that is now incorporated in the pediatric acute neuropsychiatric syndromes (PANS), the authors note. Tics constitute an “accompanying feature” of this condition.
However, neither population-based nor longitudinal clinical studies “could definitely establish if tic exacerbations in CTD are associated with GAS infections,” they note.
“The link between streptococcus and tics in children is still a matter of intense debate,” said study author Davide Martino, MD, PhD, director of the Movement Disorders Program at the University of Calgary (Alta.), in a press release.
“We wanted to look at that question, as well as a possible link between strep and behavioral symptoms like obsessive-compulsive disorder and attention deficit hyperactivity disorder,” he said.
The researchers followed 715 children with CTD (mean age 10.7 years, 76.8% male) who were drawn from 16 specialist clinics in nine countries. Almost all (90.8%) had a diagnosis of Tourette syndrome (TS); 31.7% had OCD, and 36.1% had ADHD.
Participants received a throat swab at baseline, and of these, 8.4% tested positive for GAS.
Participants were evaluated over a 16- to 18-month period, consisting of:
- Face-to-face interviews and collection of throat swabs and serum at 4-month intervals.
- Telephone interviews at 4-month intervals, which took place at 2 months between study visit.
- Weekly diaries: Parents were asked to indicate any worsening of tics and focus on detecting the earliest possible tic exacerbation.
Beyond the regularly scheduled visits, parents were instructed to report, by phone or email, any noticeable increase in tic severity and then attend an in-person visit.
Tic exacerbations were defined as an increase of greater than or equal to 6 points on the Yale Global Tic Severity Scale-Total Tic Severity Score (YGTSS-TTS), compared with the previous assessment.
OCD and ADHD symptoms were assessed according to the Yale-Brown Obsessive-Compulsive Scale and the parent-reported Swanson, Nolan, and Pelham-IV (SNAP-IV) questionnaire.
The researchers divided GAS exposures into four categories: new definite exposure; new possible exposure; ongoing definite exposure; and ongoing possible exposure.
Unlikely trigger
During the follow-up period, 43.1% (n = 308) of participants experienced tic exacerbations. Of these, 218 participants experienced one exacerbation, while 90 participants experienced two, three, or four exacerbations.
The researchers did not find a significant association between GAS exposure status and tic exacerbation.
Participants who did develop a GAS-associated exacerbation (n = 49) were younger at study exit (9.63 vs. 11.4 years, P < .0001) and were more likely to be male (46/49 vs. 210/259, Fisher’s = .035), compared with participants who developed a non-GAS-associated tic exacerbation (n = 259).
Additional analyses were adjusted for sex, age at onset, exposure to psychotropic medications, exposures to antibiotics, geographical regions, and number of visits in the time interval of interest. These analyses continued to yield no significant association between new or ongoing concurrent GAS exposure episodes and tic exacerbation events.
Of the children in the study, 103 had a positive throat swab, indicating a new definite GAS exposure, whereas 46 had a positive throat swab indicating an ongoing definite exposure (n = 149 visits). Of these visits, only 20 corresponded to tic exacerbations.
There was also no association between GAS exposure and OCD symptom severity. However, it was associated with longitudinal changes (between 17% and 21%, depending on GAS exposure definition) in the severity of hyperactivity-impulsivity symptoms in children with ADHD.
“It is known that immune activation may concur with tic severity in youth with CTDs and that psychosocial stress levels may predict short-term future tic severity in these patients,” the authors write.
“Our findings suggest that GAS is unlikely to be the main trigger for immune activation in these patients,” they add.
Brick or cornerstone?
Commenting on the study for this news organization, Margo Thienemann, MD, clinical professor of psychiatry, Stanford (Calif.) University, said that in the clinic population they treat, GAS, other pathogens, and other stresses can “each be associated with PANS symptom exacerbations.”
However, these “would not be likely to cause PANS symptoms exacerbations in the vast majority of individuals, only individuals with genetic backgrounds and immunologic dysfunctions creating susceptibility,” said Dr. Thienemann, who also directs the Pediatric Acute-Onset Neuropsychiatric Syndrome (PANS) Clinic at Stanford Children’s Health. She was not involved with the study.
In an accompanying editorial, Andrea Cavanna, MD, PhD, honorary reader in neuropsychiatry, Birmingham (England) Medical School and Keith Coffman, MD, director, Tourette Syndrome Center of Excellence, Children’s Mercy Hospital, Kansas City, Mo., suggest that perhaps the “interaction of psychosocial stress and GAS infections contributes more to tic exacerbation than psychosocial stress alone.”
“Time will tell whether this study stands as another brick – a cornerstone? – in the wall that separates streptococcus from tics,” they write.
The study was supported by the European Union’s Seventh Framework Program. Dr. Martino has received honoraria for lecturing from the Movement Disorders Society, Tourette Syndrome Association of America, and Dystonia Medical Research Foundation Canada; research funding support from Dystonia Medical Research Foundation Canada, the University of Calgary (Alta.), the Michael P. Smith Family, the Owerko Foundation, Ipsen Corporate, the Parkinson Association of Alberta, and the Canadian Institutes for Health Research; and royalties from Springer-Verlag. The other authors’ disclosures are listed in the original article. Dr. Cavanna, Dr. Coffman, and Dr. Thienemann have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Exposure to Group A streptococcus (GAS) does not appear to worsen symptoms of Tourette syndrome and other chronic tic disorders (CTDs) in children and adolescents, new research suggests.
Investigators studied over 700 children and teenagers with CTDs, one-third of whom also had attention deficit hyperactivity disorder and one-third who had obsessive-compulsive disorder (OCD).
The youngsters were followed for an average of 16 months and evaluated at 4-month intervals to see if they were infected with GAS. Tic severity was monitored through telephone interviews, in-person visits, and parental reports.
A little less than half the children experienced worsening of tics during the study period, but the researchers found no association between these exacerbations and GAS exposure.
There was also no link between GAS and worsening OCD. However, researchers did find an association between GAS exposure and an increase in hyperactivity and impulsivity in patients with ADHD.
“This study does not support GAS exposures as contributing factors for tic exacerbations in children with CTD,” the authors note.
“Specific work-up or active management of GAS infections is unlikely to help modifying the course of tics in CTD and is therefore not recommended,” they conclude.
The study was published online in Neurology.
‘Intense debate’
The association between GAS and CTD stems from the description of Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infection (PANDAS) – a condition that is now incorporated in the pediatric acute neuropsychiatric syndromes (PANS), the authors note. Tics constitute an “accompanying feature” of this condition.
However, neither population-based nor longitudinal clinical studies “could definitely establish if tic exacerbations in CTD are associated with GAS infections,” they note.
“The link between streptococcus and tics in children is still a matter of intense debate,” said study author Davide Martino, MD, PhD, director of the Movement Disorders Program at the University of Calgary (Alta.), in a press release.
“We wanted to look at that question, as well as a possible link between strep and behavioral symptoms like obsessive-compulsive disorder and attention deficit hyperactivity disorder,” he said.
The researchers followed 715 children with CTD (mean age 10.7 years, 76.8% male) who were drawn from 16 specialist clinics in nine countries. Almost all (90.8%) had a diagnosis of Tourette syndrome (TS); 31.7% had OCD, and 36.1% had ADHD.
Participants received a throat swab at baseline, and of these, 8.4% tested positive for GAS.
Participants were evaluated over a 16- to 18-month period, consisting of:
- Face-to-face interviews and collection of throat swabs and serum at 4-month intervals.
- Telephone interviews at 4-month intervals, which took place at 2 months between study visit.
- Weekly diaries: Parents were asked to indicate any worsening of tics and focus on detecting the earliest possible tic exacerbation.
Beyond the regularly scheduled visits, parents were instructed to report, by phone or email, any noticeable increase in tic severity and then attend an in-person visit.
Tic exacerbations were defined as an increase of greater than or equal to 6 points on the Yale Global Tic Severity Scale-Total Tic Severity Score (YGTSS-TTS), compared with the previous assessment.
OCD and ADHD symptoms were assessed according to the Yale-Brown Obsessive-Compulsive Scale and the parent-reported Swanson, Nolan, and Pelham-IV (SNAP-IV) questionnaire.
The researchers divided GAS exposures into four categories: new definite exposure; new possible exposure; ongoing definite exposure; and ongoing possible exposure.
Unlikely trigger
During the follow-up period, 43.1% (n = 308) of participants experienced tic exacerbations. Of these, 218 participants experienced one exacerbation, while 90 participants experienced two, three, or four exacerbations.
The researchers did not find a significant association between GAS exposure status and tic exacerbation.
Participants who did develop a GAS-associated exacerbation (n = 49) were younger at study exit (9.63 vs. 11.4 years, P < .0001) and were more likely to be male (46/49 vs. 210/259, Fisher’s = .035), compared with participants who developed a non-GAS-associated tic exacerbation (n = 259).
Additional analyses were adjusted for sex, age at onset, exposure to psychotropic medications, exposures to antibiotics, geographical regions, and number of visits in the time interval of interest. These analyses continued to yield no significant association between new or ongoing concurrent GAS exposure episodes and tic exacerbation events.
Of the children in the study, 103 had a positive throat swab, indicating a new definite GAS exposure, whereas 46 had a positive throat swab indicating an ongoing definite exposure (n = 149 visits). Of these visits, only 20 corresponded to tic exacerbations.
There was also no association between GAS exposure and OCD symptom severity. However, it was associated with longitudinal changes (between 17% and 21%, depending on GAS exposure definition) in the severity of hyperactivity-impulsivity symptoms in children with ADHD.
“It is known that immune activation may concur with tic severity in youth with CTDs and that psychosocial stress levels may predict short-term future tic severity in these patients,” the authors write.
“Our findings suggest that GAS is unlikely to be the main trigger for immune activation in these patients,” they add.
Brick or cornerstone?
Commenting on the study for this news organization, Margo Thienemann, MD, clinical professor of psychiatry, Stanford (Calif.) University, said that in the clinic population they treat, GAS, other pathogens, and other stresses can “each be associated with PANS symptom exacerbations.”
However, these “would not be likely to cause PANS symptoms exacerbations in the vast majority of individuals, only individuals with genetic backgrounds and immunologic dysfunctions creating susceptibility,” said Dr. Thienemann, who also directs the Pediatric Acute-Onset Neuropsychiatric Syndrome (PANS) Clinic at Stanford Children’s Health. She was not involved with the study.
In an accompanying editorial, Andrea Cavanna, MD, PhD, honorary reader in neuropsychiatry, Birmingham (England) Medical School and Keith Coffman, MD, director, Tourette Syndrome Center of Excellence, Children’s Mercy Hospital, Kansas City, Mo., suggest that perhaps the “interaction of psychosocial stress and GAS infections contributes more to tic exacerbation than psychosocial stress alone.”
“Time will tell whether this study stands as another brick – a cornerstone? – in the wall that separates streptococcus from tics,” they write.
The study was supported by the European Union’s Seventh Framework Program. Dr. Martino has received honoraria for lecturing from the Movement Disorders Society, Tourette Syndrome Association of America, and Dystonia Medical Research Foundation Canada; research funding support from Dystonia Medical Research Foundation Canada, the University of Calgary (Alta.), the Michael P. Smith Family, the Owerko Foundation, Ipsen Corporate, the Parkinson Association of Alberta, and the Canadian Institutes for Health Research; and royalties from Springer-Verlag. The other authors’ disclosures are listed in the original article. Dr. Cavanna, Dr. Coffman, and Dr. Thienemann have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Exposure to Group A streptococcus (GAS) does not appear to worsen symptoms of Tourette syndrome and other chronic tic disorders (CTDs) in children and adolescents, new research suggests.
Investigators studied over 700 children and teenagers with CTDs, one-third of whom also had attention deficit hyperactivity disorder and one-third who had obsessive-compulsive disorder (OCD).
The youngsters were followed for an average of 16 months and evaluated at 4-month intervals to see if they were infected with GAS. Tic severity was monitored through telephone interviews, in-person visits, and parental reports.
A little less than half the children experienced worsening of tics during the study period, but the researchers found no association between these exacerbations and GAS exposure.
There was also no link between GAS and worsening OCD. However, researchers did find an association between GAS exposure and an increase in hyperactivity and impulsivity in patients with ADHD.
“This study does not support GAS exposures as contributing factors for tic exacerbations in children with CTD,” the authors note.
“Specific work-up or active management of GAS infections is unlikely to help modifying the course of tics in CTD and is therefore not recommended,” they conclude.
The study was published online in Neurology.
‘Intense debate’
The association between GAS and CTD stems from the description of Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infection (PANDAS) – a condition that is now incorporated in the pediatric acute neuropsychiatric syndromes (PANS), the authors note. Tics constitute an “accompanying feature” of this condition.
However, neither population-based nor longitudinal clinical studies “could definitely establish if tic exacerbations in CTD are associated with GAS infections,” they note.
“The link between streptococcus and tics in children is still a matter of intense debate,” said study author Davide Martino, MD, PhD, director of the Movement Disorders Program at the University of Calgary (Alta.), in a press release.
“We wanted to look at that question, as well as a possible link between strep and behavioral symptoms like obsessive-compulsive disorder and attention deficit hyperactivity disorder,” he said.
The researchers followed 715 children with CTD (mean age 10.7 years, 76.8% male) who were drawn from 16 specialist clinics in nine countries. Almost all (90.8%) had a diagnosis of Tourette syndrome (TS); 31.7% had OCD, and 36.1% had ADHD.
Participants received a throat swab at baseline, and of these, 8.4% tested positive for GAS.
Participants were evaluated over a 16- to 18-month period, consisting of:
- Face-to-face interviews and collection of throat swabs and serum at 4-month intervals.
- Telephone interviews at 4-month intervals, which took place at 2 months between study visit.
- Weekly diaries: Parents were asked to indicate any worsening of tics and focus on detecting the earliest possible tic exacerbation.
Beyond the regularly scheduled visits, parents were instructed to report, by phone or email, any noticeable increase in tic severity and then attend an in-person visit.
Tic exacerbations were defined as an increase of greater than or equal to 6 points on the Yale Global Tic Severity Scale-Total Tic Severity Score (YGTSS-TTS), compared with the previous assessment.
OCD and ADHD symptoms were assessed according to the Yale-Brown Obsessive-Compulsive Scale and the parent-reported Swanson, Nolan, and Pelham-IV (SNAP-IV) questionnaire.
The researchers divided GAS exposures into four categories: new definite exposure; new possible exposure; ongoing definite exposure; and ongoing possible exposure.
Unlikely trigger
During the follow-up period, 43.1% (n = 308) of participants experienced tic exacerbations. Of these, 218 participants experienced one exacerbation, while 90 participants experienced two, three, or four exacerbations.
The researchers did not find a significant association between GAS exposure status and tic exacerbation.
Participants who did develop a GAS-associated exacerbation (n = 49) were younger at study exit (9.63 vs. 11.4 years, P < .0001) and were more likely to be male (46/49 vs. 210/259, Fisher’s = .035), compared with participants who developed a non-GAS-associated tic exacerbation (n = 259).
Additional analyses were adjusted for sex, age at onset, exposure to psychotropic medications, exposures to antibiotics, geographical regions, and number of visits in the time interval of interest. These analyses continued to yield no significant association between new or ongoing concurrent GAS exposure episodes and tic exacerbation events.
Of the children in the study, 103 had a positive throat swab, indicating a new definite GAS exposure, whereas 46 had a positive throat swab indicating an ongoing definite exposure (n = 149 visits). Of these visits, only 20 corresponded to tic exacerbations.
There was also no association between GAS exposure and OCD symptom severity. However, it was associated with longitudinal changes (between 17% and 21%, depending on GAS exposure definition) in the severity of hyperactivity-impulsivity symptoms in children with ADHD.
“It is known that immune activation may concur with tic severity in youth with CTDs and that psychosocial stress levels may predict short-term future tic severity in these patients,” the authors write.
“Our findings suggest that GAS is unlikely to be the main trigger for immune activation in these patients,” they add.
Brick or cornerstone?
Commenting on the study for this news organization, Margo Thienemann, MD, clinical professor of psychiatry, Stanford (Calif.) University, said that in the clinic population they treat, GAS, other pathogens, and other stresses can “each be associated with PANS symptom exacerbations.”
However, these “would not be likely to cause PANS symptoms exacerbations in the vast majority of individuals, only individuals with genetic backgrounds and immunologic dysfunctions creating susceptibility,” said Dr. Thienemann, who also directs the Pediatric Acute-Onset Neuropsychiatric Syndrome (PANS) Clinic at Stanford Children’s Health. She was not involved with the study.
In an accompanying editorial, Andrea Cavanna, MD, PhD, honorary reader in neuropsychiatry, Birmingham (England) Medical School and Keith Coffman, MD, director, Tourette Syndrome Center of Excellence, Children’s Mercy Hospital, Kansas City, Mo., suggest that perhaps the “interaction of psychosocial stress and GAS infections contributes more to tic exacerbation than psychosocial stress alone.”
“Time will tell whether this study stands as another brick – a cornerstone? – in the wall that separates streptococcus from tics,” they write.
The study was supported by the European Union’s Seventh Framework Program. Dr. Martino has received honoraria for lecturing from the Movement Disorders Society, Tourette Syndrome Association of America, and Dystonia Medical Research Foundation Canada; research funding support from Dystonia Medical Research Foundation Canada, the University of Calgary (Alta.), the Michael P. Smith Family, the Owerko Foundation, Ipsen Corporate, the Parkinson Association of Alberta, and the Canadian Institutes for Health Research; and royalties from Springer-Verlag. The other authors’ disclosures are listed in the original article. Dr. Cavanna, Dr. Coffman, and Dr. Thienemann have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
7 key changes: The 2021 child and adolescent immunization schedules
Each February, the Centers for Disease Control and Prevention, along with multiple professional organizations, releases an updated Recommended Child and Adolescent Immunization Schedule.
Recent years have seen fewer changes in the vaccine schedule, mostly with adjustments based on products coming on or off the market, and sometimes with slight changes in recommendations. This year is no different, with mostly minor changes in store. As most practitioners know, having quick access to the tables that accompany the recommendations is always handy. Table 1 contains the typical, recommended immunization schedule. Table 2 contains the catch-up provisions, and Table 3 provides guidance on vaccines for special circumstances and for children with specific medical conditions.
2021 childhood and adolescent immunization schedule
One update is a recommendation that patients with egg allergies who had symptoms more extensive than hives should receive the influenza vaccine in a medical setting where severe allergic reactions or anaphylaxis can be recognized and treated, with the exclusion of two specific preparations, Flublok and Flucelvax.
In regard to the live attenuated influenza vaccine (LAIV), there are several points of reinforcement. First, the nomenclature has generally been changed to “LAIV4” throughout the document because only quadrivalent preparations are available. There are specific recommendations that patients should not receive LAIV4 if they recently took antiviral medication for influenza, with “lockout” periods lasting from 2 days to 17 days, depending on the antiviral preparation used. In addition, there is an emphasis on not using LAIV4 for children younger than 2 years.
Two updates to the meningococcal group B vaccine are worth reviewing. The first is that children aged 10 years or older with complement deficiency, complement inhibitor use, or asplenia should receive a meningitis B booster dose beginning 1 year after completion of the primary series, with boosters thereafter every 2 or 3 years as long as that patient remains at greater risk. Another recommendation for patients 10 years or older is that, even if they have received a primary series of meningitis B vaccines, they should receive a booster dose in the setting of an outbreak if it has been 1 year or more since completion of their primary series.
Recommendations have generally been relaxed for tetanus prophylaxis in older children, indicating that individuals requiring tetanus prophylaxis or their 10-year tetanus booster after receipt of at least one Tdap vaccine can receive either tetanus-diphtheria toxoid or Tdap.
COVID-19 vaccines
Although childhood vaccination against COVID-19 is still currently limited to adolescents involved in clinical trials, pediatricians surely are getting peppered with questions from parents about whether they should be vaccinated and what to make of the recent reports about allergic reactions. Fortunately, there are several resources for pediatricians. First, two reports point out that true anaphylactic reactions to COVID-19 vaccines appear quite rare. The reported data on Pfizer-developed mRNA vaccine demonstrated an anaphylaxis rate of approximately 2 cases per 1 million doses administered. Among the 21 recipients who experienced anaphylaxis (out of over 11 million total doses administered), fully one third had a history of anaphylaxis episodes. The report also reviews vaccine reactions that were reported but were not classified as anaphylaxis, pointing out that when reporting vaccine reactions, we should be very careful in the nomenclature we use.
Reporting on the Moderna mRNA vaccine showed anaphylaxis rates of about 2.5 per 1 million doses, with 50% of the recipients who experienced true anaphylaxis having a history of anaphylaxis. Most of those who experienced anaphylaxis (90% in the Moderna group and 86% in the Pfizer group) exhibited symptoms of anaphylaxis within 30 minutes of receiving the vaccine. The take-home point, and the current CDC recommendation, is that many individuals, even those with a history of anaphylaxis, can still receive COVID-19 vaccines. The rates of observed anaphylaxis after COVID vaccination are far below population rates of a history of allergy or severe allergic reactions. When coupled with an estimated mortality rate of 0.5%-1% for SARS-CoV-2 disease, that CDC recommends that we encourage people, even those with severe allergies, to get vaccinated.
One clear caveat is that individuals with a history of severe anaphylaxis, and even those concerned about allergies, should be observed for a longer period after vaccination (at least 30 minutes) than the 15 minutes recommended for the general population. In addition, individuals with a specific anaphylactic reaction or severe allergic reaction to any injectable vaccine should confer with an immunologist before considering vaccination.
Another useful resource is a column published by the American Medical Association that walks through some talking points for providers when discussing whether a patient should receive COVID-19 vaccination. Advice is offered on answering patient questions about which preparation to get, what side effects to watch for, and how to report an adverse reaction. Providers are reminded to urge patients to complete whichever series they begin (get that second dose!), and that they currently should not have to pay for a vaccine. FAQ resource pages are available for patients and health care providers.
More vaccine news: HPV and influenza
Meanwhile, published vaccine reports provide evidence from the field to demonstrate the benefits of vaccination. A study published in the New England Journal of Medicine reported on the effectiveness of human papillomavirus (HPV) vaccine in a Swedish cohort. The report evaluated females aged between 10 and 30 years beginning in 2006 and followed them through 2017, comparing rates of invasive cervical cancer among the group who received one or more HPV vaccine doses with the group who receive none. Even without adjustment, the raw rate of invasive cervical cancer in the vaccinated group was half of that in the unvaccinated group. After full adjustment, some populations experienced incident rate ratios that were greater than 80% reduced. The largest reduction, and therefore the biggest benefit, was among those who received the HPV vaccine before age 17.
A report from the United States looking at the 2018-2019 influenza season demonstrated a vaccine effectiveness rate against hospitalization of 41% and 51% against any ED visit related to influenza. The authors note that there was considerable drift in the influenza A type that appeared late in the influenza season, reducing the overall effectiveness, but that the vaccine was still largely effective.
William T. Basco Jr, MD, MS, is a professor of pediatrics at the Medical University of South Carolina, Charleston, and director of the division of general pediatrics. He is an active health services researcher and has published more than 60 manuscripts in the peer-reviewed literature.
A version of this article first appeared on Medscape.com.
Each February, the Centers for Disease Control and Prevention, along with multiple professional organizations, releases an updated Recommended Child and Adolescent Immunization Schedule.
Recent years have seen fewer changes in the vaccine schedule, mostly with adjustments based on products coming on or off the market, and sometimes with slight changes in recommendations. This year is no different, with mostly minor changes in store. As most practitioners know, having quick access to the tables that accompany the recommendations is always handy. Table 1 contains the typical, recommended immunization schedule. Table 2 contains the catch-up provisions, and Table 3 provides guidance on vaccines for special circumstances and for children with specific medical conditions.
2021 childhood and adolescent immunization schedule
One update is a recommendation that patients with egg allergies who had symptoms more extensive than hives should receive the influenza vaccine in a medical setting where severe allergic reactions or anaphylaxis can be recognized and treated, with the exclusion of two specific preparations, Flublok and Flucelvax.
In regard to the live attenuated influenza vaccine (LAIV), there are several points of reinforcement. First, the nomenclature has generally been changed to “LAIV4” throughout the document because only quadrivalent preparations are available. There are specific recommendations that patients should not receive LAIV4 if they recently took antiviral medication for influenza, with “lockout” periods lasting from 2 days to 17 days, depending on the antiviral preparation used. In addition, there is an emphasis on not using LAIV4 for children younger than 2 years.
Two updates to the meningococcal group B vaccine are worth reviewing. The first is that children aged 10 years or older with complement deficiency, complement inhibitor use, or asplenia should receive a meningitis B booster dose beginning 1 year after completion of the primary series, with boosters thereafter every 2 or 3 years as long as that patient remains at greater risk. Another recommendation for patients 10 years or older is that, even if they have received a primary series of meningitis B vaccines, they should receive a booster dose in the setting of an outbreak if it has been 1 year or more since completion of their primary series.
Recommendations have generally been relaxed for tetanus prophylaxis in older children, indicating that individuals requiring tetanus prophylaxis or their 10-year tetanus booster after receipt of at least one Tdap vaccine can receive either tetanus-diphtheria toxoid or Tdap.
COVID-19 vaccines
Although childhood vaccination against COVID-19 is still currently limited to adolescents involved in clinical trials, pediatricians surely are getting peppered with questions from parents about whether they should be vaccinated and what to make of the recent reports about allergic reactions. Fortunately, there are several resources for pediatricians. First, two reports point out that true anaphylactic reactions to COVID-19 vaccines appear quite rare. The reported data on Pfizer-developed mRNA vaccine demonstrated an anaphylaxis rate of approximately 2 cases per 1 million doses administered. Among the 21 recipients who experienced anaphylaxis (out of over 11 million total doses administered), fully one third had a history of anaphylaxis episodes. The report also reviews vaccine reactions that were reported but were not classified as anaphylaxis, pointing out that when reporting vaccine reactions, we should be very careful in the nomenclature we use.
Reporting on the Moderna mRNA vaccine showed anaphylaxis rates of about 2.5 per 1 million doses, with 50% of the recipients who experienced true anaphylaxis having a history of anaphylaxis. Most of those who experienced anaphylaxis (90% in the Moderna group and 86% in the Pfizer group) exhibited symptoms of anaphylaxis within 30 minutes of receiving the vaccine. The take-home point, and the current CDC recommendation, is that many individuals, even those with a history of anaphylaxis, can still receive COVID-19 vaccines. The rates of observed anaphylaxis after COVID vaccination are far below population rates of a history of allergy or severe allergic reactions. When coupled with an estimated mortality rate of 0.5%-1% for SARS-CoV-2 disease, that CDC recommends that we encourage people, even those with severe allergies, to get vaccinated.
One clear caveat is that individuals with a history of severe anaphylaxis, and even those concerned about allergies, should be observed for a longer period after vaccination (at least 30 minutes) than the 15 minutes recommended for the general population. In addition, individuals with a specific anaphylactic reaction or severe allergic reaction to any injectable vaccine should confer with an immunologist before considering vaccination.
Another useful resource is a column published by the American Medical Association that walks through some talking points for providers when discussing whether a patient should receive COVID-19 vaccination. Advice is offered on answering patient questions about which preparation to get, what side effects to watch for, and how to report an adverse reaction. Providers are reminded to urge patients to complete whichever series they begin (get that second dose!), and that they currently should not have to pay for a vaccine. FAQ resource pages are available for patients and health care providers.
More vaccine news: HPV and influenza
Meanwhile, published vaccine reports provide evidence from the field to demonstrate the benefits of vaccination. A study published in the New England Journal of Medicine reported on the effectiveness of human papillomavirus (HPV) vaccine in a Swedish cohort. The report evaluated females aged between 10 and 30 years beginning in 2006 and followed them through 2017, comparing rates of invasive cervical cancer among the group who received one or more HPV vaccine doses with the group who receive none. Even without adjustment, the raw rate of invasive cervical cancer in the vaccinated group was half of that in the unvaccinated group. After full adjustment, some populations experienced incident rate ratios that were greater than 80% reduced. The largest reduction, and therefore the biggest benefit, was among those who received the HPV vaccine before age 17.
A report from the United States looking at the 2018-2019 influenza season demonstrated a vaccine effectiveness rate against hospitalization of 41% and 51% against any ED visit related to influenza. The authors note that there was considerable drift in the influenza A type that appeared late in the influenza season, reducing the overall effectiveness, but that the vaccine was still largely effective.
William T. Basco Jr, MD, MS, is a professor of pediatrics at the Medical University of South Carolina, Charleston, and director of the division of general pediatrics. He is an active health services researcher and has published more than 60 manuscripts in the peer-reviewed literature.
A version of this article first appeared on Medscape.com.
Each February, the Centers for Disease Control and Prevention, along with multiple professional organizations, releases an updated Recommended Child and Adolescent Immunization Schedule.
Recent years have seen fewer changes in the vaccine schedule, mostly with adjustments based on products coming on or off the market, and sometimes with slight changes in recommendations. This year is no different, with mostly minor changes in store. As most practitioners know, having quick access to the tables that accompany the recommendations is always handy. Table 1 contains the typical, recommended immunization schedule. Table 2 contains the catch-up provisions, and Table 3 provides guidance on vaccines for special circumstances and for children with specific medical conditions.
2021 childhood and adolescent immunization schedule
One update is a recommendation that patients with egg allergies who had symptoms more extensive than hives should receive the influenza vaccine in a medical setting where severe allergic reactions or anaphylaxis can be recognized and treated, with the exclusion of two specific preparations, Flublok and Flucelvax.
In regard to the live attenuated influenza vaccine (LAIV), there are several points of reinforcement. First, the nomenclature has generally been changed to “LAIV4” throughout the document because only quadrivalent preparations are available. There are specific recommendations that patients should not receive LAIV4 if they recently took antiviral medication for influenza, with “lockout” periods lasting from 2 days to 17 days, depending on the antiviral preparation used. In addition, there is an emphasis on not using LAIV4 for children younger than 2 years.
Two updates to the meningococcal group B vaccine are worth reviewing. The first is that children aged 10 years or older with complement deficiency, complement inhibitor use, or asplenia should receive a meningitis B booster dose beginning 1 year after completion of the primary series, with boosters thereafter every 2 or 3 years as long as that patient remains at greater risk. Another recommendation for patients 10 years or older is that, even if they have received a primary series of meningitis B vaccines, they should receive a booster dose in the setting of an outbreak if it has been 1 year or more since completion of their primary series.
Recommendations have generally been relaxed for tetanus prophylaxis in older children, indicating that individuals requiring tetanus prophylaxis or their 10-year tetanus booster after receipt of at least one Tdap vaccine can receive either tetanus-diphtheria toxoid or Tdap.
COVID-19 vaccines
Although childhood vaccination against COVID-19 is still currently limited to adolescents involved in clinical trials, pediatricians surely are getting peppered with questions from parents about whether they should be vaccinated and what to make of the recent reports about allergic reactions. Fortunately, there are several resources for pediatricians. First, two reports point out that true anaphylactic reactions to COVID-19 vaccines appear quite rare. The reported data on Pfizer-developed mRNA vaccine demonstrated an anaphylaxis rate of approximately 2 cases per 1 million doses administered. Among the 21 recipients who experienced anaphylaxis (out of over 11 million total doses administered), fully one third had a history of anaphylaxis episodes. The report also reviews vaccine reactions that were reported but were not classified as anaphylaxis, pointing out that when reporting vaccine reactions, we should be very careful in the nomenclature we use.
Reporting on the Moderna mRNA vaccine showed anaphylaxis rates of about 2.5 per 1 million doses, with 50% of the recipients who experienced true anaphylaxis having a history of anaphylaxis. Most of those who experienced anaphylaxis (90% in the Moderna group and 86% in the Pfizer group) exhibited symptoms of anaphylaxis within 30 minutes of receiving the vaccine. The take-home point, and the current CDC recommendation, is that many individuals, even those with a history of anaphylaxis, can still receive COVID-19 vaccines. The rates of observed anaphylaxis after COVID vaccination are far below population rates of a history of allergy or severe allergic reactions. When coupled with an estimated mortality rate of 0.5%-1% for SARS-CoV-2 disease, that CDC recommends that we encourage people, even those with severe allergies, to get vaccinated.
One clear caveat is that individuals with a history of severe anaphylaxis, and even those concerned about allergies, should be observed for a longer period after vaccination (at least 30 minutes) than the 15 minutes recommended for the general population. In addition, individuals with a specific anaphylactic reaction or severe allergic reaction to any injectable vaccine should confer with an immunologist before considering vaccination.
Another useful resource is a column published by the American Medical Association that walks through some talking points for providers when discussing whether a patient should receive COVID-19 vaccination. Advice is offered on answering patient questions about which preparation to get, what side effects to watch for, and how to report an adverse reaction. Providers are reminded to urge patients to complete whichever series they begin (get that second dose!), and that they currently should not have to pay for a vaccine. FAQ resource pages are available for patients and health care providers.
More vaccine news: HPV and influenza
Meanwhile, published vaccine reports provide evidence from the field to demonstrate the benefits of vaccination. A study published in the New England Journal of Medicine reported on the effectiveness of human papillomavirus (HPV) vaccine in a Swedish cohort. The report evaluated females aged between 10 and 30 years beginning in 2006 and followed them through 2017, comparing rates of invasive cervical cancer among the group who received one or more HPV vaccine doses with the group who receive none. Even without adjustment, the raw rate of invasive cervical cancer in the vaccinated group was half of that in the unvaccinated group. After full adjustment, some populations experienced incident rate ratios that were greater than 80% reduced. The largest reduction, and therefore the biggest benefit, was among those who received the HPV vaccine before age 17.
A report from the United States looking at the 2018-2019 influenza season demonstrated a vaccine effectiveness rate against hospitalization of 41% and 51% against any ED visit related to influenza. The authors note that there was considerable drift in the influenza A type that appeared late in the influenza season, reducing the overall effectiveness, but that the vaccine was still largely effective.
William T. Basco Jr, MD, MS, is a professor of pediatrics at the Medical University of South Carolina, Charleston, and director of the division of general pediatrics. He is an active health services researcher and has published more than 60 manuscripts in the peer-reviewed literature.
A version of this article first appeared on Medscape.com.
New cases of child COVID-19 drop for fifth straight week
The fifth consecutive week with a decline has the number of new COVID-19 cases in children at its lowest level since late October, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
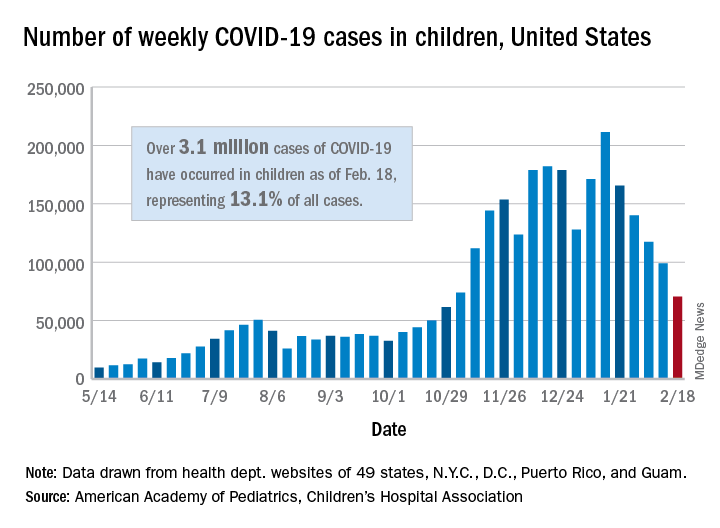
, when 61,000 cases were reported, the AAP and CHA said in their weekly COVID-19 report.
The cumulative number of COVID-19 cases in children is now just over 3.1 million, which represents 13.1% of cases among all ages in the United States, based on data gathered from the health departments of 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
More children in California (439,000) have been infected than in any other state, while Illinois (176,000), Florida (145,000), Tennessee (137,000), Arizona (127,000), Ohio (121,000), and Pennsylvania (111,000) are the only other states with more than 100,000 cases, the AAP/CHA report shows.
Proportionally, the children of Wyoming have been hardest hit: Pediatric cases represent 19.4% of all cases in the state. The other four states with proportions of 18% or more are Alaska, Vermont, South Carolina, and Tennessee. Cumulative rates, however, tell a somewhat different story, as North Dakota leads with just over 8,500 cases per 100,000 children, followed by Tennessee (7,700 per 100,000) and Rhode Island (7,000 per 100,000), the AAP and CHA said.
Deaths in children, which had not been following the trend of fewer new cases over the last few weeks, dropped below double digits for the first time in a month. The six deaths that occurred during the week of Feb. 12-18 bring the total to 247 since the start of the pandemic in the 43 states, along with New York City and Guam, that are reporting such data, according to the report.
The fifth consecutive week with a decline has the number of new COVID-19 cases in children at its lowest level since late October, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
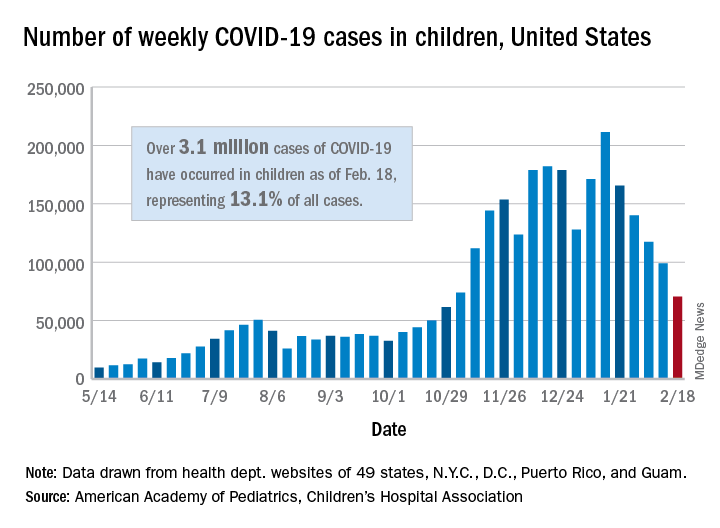
, when 61,000 cases were reported, the AAP and CHA said in their weekly COVID-19 report.
The cumulative number of COVID-19 cases in children is now just over 3.1 million, which represents 13.1% of cases among all ages in the United States, based on data gathered from the health departments of 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
More children in California (439,000) have been infected than in any other state, while Illinois (176,000), Florida (145,000), Tennessee (137,000), Arizona (127,000), Ohio (121,000), and Pennsylvania (111,000) are the only other states with more than 100,000 cases, the AAP/CHA report shows.
Proportionally, the children of Wyoming have been hardest hit: Pediatric cases represent 19.4% of all cases in the state. The other four states with proportions of 18% or more are Alaska, Vermont, South Carolina, and Tennessee. Cumulative rates, however, tell a somewhat different story, as North Dakota leads with just over 8,500 cases per 100,000 children, followed by Tennessee (7,700 per 100,000) and Rhode Island (7,000 per 100,000), the AAP and CHA said.
Deaths in children, which had not been following the trend of fewer new cases over the last few weeks, dropped below double digits for the first time in a month. The six deaths that occurred during the week of Feb. 12-18 bring the total to 247 since the start of the pandemic in the 43 states, along with New York City and Guam, that are reporting such data, according to the report.
The fifth consecutive week with a decline has the number of new COVID-19 cases in children at its lowest level since late October, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
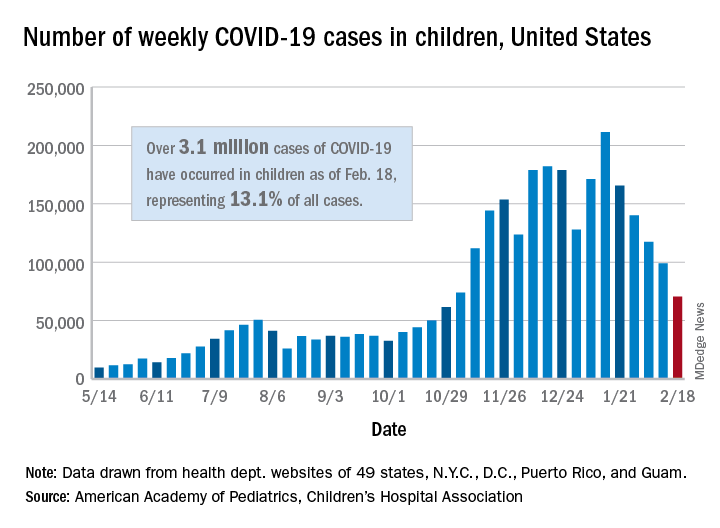
, when 61,000 cases were reported, the AAP and CHA said in their weekly COVID-19 report.
The cumulative number of COVID-19 cases in children is now just over 3.1 million, which represents 13.1% of cases among all ages in the United States, based on data gathered from the health departments of 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
More children in California (439,000) have been infected than in any other state, while Illinois (176,000), Florida (145,000), Tennessee (137,000), Arizona (127,000), Ohio (121,000), and Pennsylvania (111,000) are the only other states with more than 100,000 cases, the AAP/CHA report shows.
Proportionally, the children of Wyoming have been hardest hit: Pediatric cases represent 19.4% of all cases in the state. The other four states with proportions of 18% or more are Alaska, Vermont, South Carolina, and Tennessee. Cumulative rates, however, tell a somewhat different story, as North Dakota leads with just over 8,500 cases per 100,000 children, followed by Tennessee (7,700 per 100,000) and Rhode Island (7,000 per 100,000), the AAP and CHA said.
Deaths in children, which had not been following the trend of fewer new cases over the last few weeks, dropped below double digits for the first time in a month. The six deaths that occurred during the week of Feb. 12-18 bring the total to 247 since the start of the pandemic in the 43 states, along with New York City and Guam, that are reporting such data, according to the report.
Variants spur new FDA guidance on COVID vaccines, tests, drugs
The United States is currently facing three main variant threats, according to the Centers for Disease Control and Prevention: B.1.1.7, which originated in the United Kingdom; B.1.351 from South Africa; and the P.1 variant, which originated in Brazil.
Acting FDA Commissioner Janet Woodcock, MD, said on a telephone press briefing call Feb. 22 that the FDA has already been communicating with individual manufacturers as they assess the variants’ effect on their products, but these guidelines are issued for the sake of transparency and to welcome scientific input.
Tailoring may be necessary
Dr. Woodcock emphasized that, “at this time, available data suggest the FDA-authorized vaccines are effective in protecting circulating strains of SARS-CoV-2.” However, in the event the strains start to show resistance, it may be necessary to tailor the vaccine to the variant.
In that case, effectiveness of a modified vaccine should be determined by data from clinical immunogenicity studies, which would compare a recipient’s immune response with virus variants induced by the modified vaccine against the immune response to the authorized vaccine, the guidance states.
Manufacturers should also study the vaccine in both nonvaccinated people and people fully vaccinated with the authorized vaccine, according to the guidance.
Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said on the call that the clinical immunogenicity data is needed to understand, for instance, whether a new vaccine strain is able to cover the new and old strain or whether it just covers the new strain. Information is also needed to understand whether the modified vaccine, when given to someone fully vaccinated, will still promote a positive response without introducing safety concerns.
Further discussions will be necessary to decide whether future modified vaccines may be authorized without the need for clinical studies.
Variants and testing
The FDA’s updated guidance for test developers, Policy for Evaluating Impact of Viral Mutations on COVID-19 Tests, includes information that test performance can be influenced by the sequence of the variant, prevalence of the variant in the population, or design of the test. For example, molecular tests designed to detect multiple SARS-CoV-2 genetic targets are less susceptible to genetic variants than tests designed to detect a single genetic target.
The FDA already issued a safety alert on Jan. 8 to caution that genetic mutations to the virus in a patient sample can potentially change the performance of a diagnostic test. The FDA identified three tests that had been granted emergency-use authorization (EUA) that are known to be affected.
However, Dr. Woodcock said on the call, “at this time the impact does not appear to be significant.”
Updated guidance for therapeutics
The FDA has issued new guidance on the effect of variants on monoclonal antibody treatments.
“The FDA is aware that some of the monoclonal antibodies that have been authorized are less active against some of the SARS-CoV-2 variants that have emerged,” the FDA noted in its press release. “This guidance provides recommendations on efficient approaches to the generation of ... manufacturing and controls data that could potentially support an EUA for monoclonal antibody products that may be effective against emerging variants.”
While the FDA is monitoring the effects of variants, manufacturers bear a lot of the responsibility as well.
The FDA added: “With these guidances, the FDA is encouraging developers of drugs or biological products targeting SARS-CoV-2 to continuously monitor genomic databases for emerging SARS-CoV-2 variants and evaluate phenotypically any specific variants in the product target that are becoming prevalent or could potentially impact its activity.”
Dr.Woodcock added that “we urge all Americans to continue to get tested, get their vaccines when available, and follow important heath measures such as handwashing, masking, and social distancing.”
A version of this article first appeared on Medscape.com.
The United States is currently facing three main variant threats, according to the Centers for Disease Control and Prevention: B.1.1.7, which originated in the United Kingdom; B.1.351 from South Africa; and the P.1 variant, which originated in Brazil.
Acting FDA Commissioner Janet Woodcock, MD, said on a telephone press briefing call Feb. 22 that the FDA has already been communicating with individual manufacturers as they assess the variants’ effect on their products, but these guidelines are issued for the sake of transparency and to welcome scientific input.
Tailoring may be necessary
Dr. Woodcock emphasized that, “at this time, available data suggest the FDA-authorized vaccines are effective in protecting circulating strains of SARS-CoV-2.” However, in the event the strains start to show resistance, it may be necessary to tailor the vaccine to the variant.
In that case, effectiveness of a modified vaccine should be determined by data from clinical immunogenicity studies, which would compare a recipient’s immune response with virus variants induced by the modified vaccine against the immune response to the authorized vaccine, the guidance states.
Manufacturers should also study the vaccine in both nonvaccinated people and people fully vaccinated with the authorized vaccine, according to the guidance.
Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said on the call that the clinical immunogenicity data is needed to understand, for instance, whether a new vaccine strain is able to cover the new and old strain or whether it just covers the new strain. Information is also needed to understand whether the modified vaccine, when given to someone fully vaccinated, will still promote a positive response without introducing safety concerns.
Further discussions will be necessary to decide whether future modified vaccines may be authorized without the need for clinical studies.
Variants and testing
The FDA’s updated guidance for test developers, Policy for Evaluating Impact of Viral Mutations on COVID-19 Tests, includes information that test performance can be influenced by the sequence of the variant, prevalence of the variant in the population, or design of the test. For example, molecular tests designed to detect multiple SARS-CoV-2 genetic targets are less susceptible to genetic variants than tests designed to detect a single genetic target.
The FDA already issued a safety alert on Jan. 8 to caution that genetic mutations to the virus in a patient sample can potentially change the performance of a diagnostic test. The FDA identified three tests that had been granted emergency-use authorization (EUA) that are known to be affected.
However, Dr. Woodcock said on the call, “at this time the impact does not appear to be significant.”
Updated guidance for therapeutics
The FDA has issued new guidance on the effect of variants on monoclonal antibody treatments.
“The FDA is aware that some of the monoclonal antibodies that have been authorized are less active against some of the SARS-CoV-2 variants that have emerged,” the FDA noted in its press release. “This guidance provides recommendations on efficient approaches to the generation of ... manufacturing and controls data that could potentially support an EUA for monoclonal antibody products that may be effective against emerging variants.”
While the FDA is monitoring the effects of variants, manufacturers bear a lot of the responsibility as well.
The FDA added: “With these guidances, the FDA is encouraging developers of drugs or biological products targeting SARS-CoV-2 to continuously monitor genomic databases for emerging SARS-CoV-2 variants and evaluate phenotypically any specific variants in the product target that are becoming prevalent or could potentially impact its activity.”
Dr.Woodcock added that “we urge all Americans to continue to get tested, get their vaccines when available, and follow important heath measures such as handwashing, masking, and social distancing.”
A version of this article first appeared on Medscape.com.
The United States is currently facing three main variant threats, according to the Centers for Disease Control and Prevention: B.1.1.7, which originated in the United Kingdom; B.1.351 from South Africa; and the P.1 variant, which originated in Brazil.
Acting FDA Commissioner Janet Woodcock, MD, said on a telephone press briefing call Feb. 22 that the FDA has already been communicating with individual manufacturers as they assess the variants’ effect on their products, but these guidelines are issued for the sake of transparency and to welcome scientific input.
Tailoring may be necessary
Dr. Woodcock emphasized that, “at this time, available data suggest the FDA-authorized vaccines are effective in protecting circulating strains of SARS-CoV-2.” However, in the event the strains start to show resistance, it may be necessary to tailor the vaccine to the variant.
In that case, effectiveness of a modified vaccine should be determined by data from clinical immunogenicity studies, which would compare a recipient’s immune response with virus variants induced by the modified vaccine against the immune response to the authorized vaccine, the guidance states.
Manufacturers should also study the vaccine in both nonvaccinated people and people fully vaccinated with the authorized vaccine, according to the guidance.
Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said on the call that the clinical immunogenicity data is needed to understand, for instance, whether a new vaccine strain is able to cover the new and old strain or whether it just covers the new strain. Information is also needed to understand whether the modified vaccine, when given to someone fully vaccinated, will still promote a positive response without introducing safety concerns.
Further discussions will be necessary to decide whether future modified vaccines may be authorized without the need for clinical studies.
Variants and testing
The FDA’s updated guidance for test developers, Policy for Evaluating Impact of Viral Mutations on COVID-19 Tests, includes information that test performance can be influenced by the sequence of the variant, prevalence of the variant in the population, or design of the test. For example, molecular tests designed to detect multiple SARS-CoV-2 genetic targets are less susceptible to genetic variants than tests designed to detect a single genetic target.
The FDA already issued a safety alert on Jan. 8 to caution that genetic mutations to the virus in a patient sample can potentially change the performance of a diagnostic test. The FDA identified three tests that had been granted emergency-use authorization (EUA) that are known to be affected.
However, Dr. Woodcock said on the call, “at this time the impact does not appear to be significant.”
Updated guidance for therapeutics
The FDA has issued new guidance on the effect of variants on monoclonal antibody treatments.
“The FDA is aware that some of the monoclonal antibodies that have been authorized are less active against some of the SARS-CoV-2 variants that have emerged,” the FDA noted in its press release. “This guidance provides recommendations on efficient approaches to the generation of ... manufacturing and controls data that could potentially support an EUA for monoclonal antibody products that may be effective against emerging variants.”
While the FDA is monitoring the effects of variants, manufacturers bear a lot of the responsibility as well.
The FDA added: “With these guidances, the FDA is encouraging developers of drugs or biological products targeting SARS-CoV-2 to continuously monitor genomic databases for emerging SARS-CoV-2 variants and evaluate phenotypically any specific variants in the product target that are becoming prevalent or could potentially impact its activity.”
Dr.Woodcock added that “we urge all Americans to continue to get tested, get their vaccines when available, and follow important heath measures such as handwashing, masking, and social distancing.”
A version of this article first appeared on Medscape.com.
Tips offered for treating co-occurring ADHD and SUDs
When Frances R. Levin, MD, began her clinical psychiatry career in the mid-1990s, she spent a lot of time educating colleagues about the validity of an ADHD diagnosis in adults.
“That’s no longer an issue,” Dr. Levin, the Kennedy-Leavy Professor of Psychiatry at Columbia University, New York, said during an annual psychopharmacology update held by the Nevada Psychiatric Association. “But at the time, we often thought, ‘ADHD is something that’s specific to people who are stimulant users.’ In fact, what we found over the years was that these rates are elevated in a range of substance use populations.”
According to National Comorbidity Survey, a nontreatment sample of more than 3,000 adults, individuals who have SUD have two to three times the risk of having ADHD, while individuals who have ADHD have about three times the rate of having an SUD, compared with those who don’t (Am J Psychiatry. 2006;163[4]:716-23). “When you move to treatment samples, the rates also remain quite high,” said Dr. Levin, who is also chief of the division of substance use disorders at the medical center.
“In the general population, the rates of ADHD are 2%-4%. When we look at people who are coming in specifically for treatment of their SUD, the rates are substantially higher, ranging from 10% to 24%.”
According to a 2014 review of medical literature, potential reasons for the association between ADHD and SUD vary and include underlying biologic deficits, such as parental SUDs and genetics; conduct disorder symptoms, such as defiance, rule breaking, and delinquency; poor performance in school, such as low grades, grade retention, or drop-out; and social difficulties, such as rejection from conventional groups or few quality friendships (Annu Rev Clin Psychol. 2014;10:607-39). Other potential pathways include neurocognitive deficits, stress-negative affect models, impulsive anger, and other underlying traits.
One key reason to treat ADHD in patients with SUDs is that they tend to develop the SUD earlier when the ADHD is present, Dr. Levin said. They’re also less likely to be retained in treatment and have a reduced likelihood of going into remission if dependence develops. “Even when they do achieve remission, it seems to take longer for people to reach remission,” she said. “They have more treatment exposure yet do less well in treatment. This can make it more challenging to treat this population.”
One common assumption from clinicians regarding patients with ADHD and a concomitant SUD is that standard treatments for ADHD do not work in active substance users. Another is that, even if treatments work for ADHD, they do not affect the substance use disorder. “Understandably, there is also concern that active substance abusers will misuse and divert their medications,” she said. “Finally, there are often additional psychiatric comorbidities that may make it harder to effectively treat individuals with ADHD and SUD.”
Since 2002, 15 double-blind outpatient studies using stimulants/atomoxetine to treat substance abusers with ADHD have appeared in the medical literature, Dr. Levin said. Only three have included adolescents. “That’s surprising, because up to 40% of kids who come in for treatment, often for cannabis use disorder, will have ADHD, yet there is very little guidance from empirical studies as to how to best treat them,” she said. “There have been several studies looking at atomoxetine to treat substance abusers with ADHD, but results have been mixed. In the cannabis use populations, atomoxetine has not been shown to be effective in treating the substance use disorder, and results are mixed regarding superiority in reducing ADHD symptoms. There is one study showing that ADHD is more likely to be improved in adults with alcohol use disorders with mixed results regarding the alcohol use.”
Overall, most of the outpatient and inpatient studies conducted in this population have demonstrated some signal in terms of reducing ADHD, she said, while a minority of the outpatient studies suggest some benefit in terms of substance use. “What’s interesting is that when you see a response in terms of the ADHD, you often see an improvement in the substance use as well,” Dr. Levin said. “This potentially suggests that patients may be self-medicating their ADHD symptoms or that if the ADHD responds to treatment, then the patient may benefit from the psychosocial interventions that targets the SUD.”
A separate meta-analysis involving more than 1,000 patients found mixed results from pharmacologic interventions and concluded that, while they modestly improved ADHD symptoms, no beneficial effect was seen on drug abstinence or on treatment discontinuation (J Psychopharmacol. 2015 Jan;29[1]:15-23). “I would argue that you don’t need to be as nihilistic about this as the meta-analysis might suggest, because the devil’s in the details,” said Dr. Levin, whose own research was included in the work.
“First of all, many of the studies had high drop-out rates. The outcome measures were variable, and some of the studies used formulations with poor bioavailability. Also, trials that evaluated atomoxetine or stimulants were combined, which may be problematic given the different mechanisms of action. Further, the meta-analysis did not include two recent placebo-controlled trials in adults with stimulant-use disorders that both found that higher dosing of a long-acting stimulant resulted in greater improvements in ADHD symptoms and stimulant use” (Addict. 2014;109[3]:440-9 and JAMA Psychiatry. 2015;72[6]:593-602).
Dr. Levin went on to note that there are few empirical data to guide treatment for those who have multiple psychiatric disorders, let alone treatment for ADHD and SUDs without additional psychiatric disorders. The challenge is what to treat first and/or how to treat the concomitant conditions safely.
“Generally, if possible, treat what is most clinically impairing first,” she said. “Overall, both stimulants and atomoxetine may work for ADHD even in the presence of additional depression, anxiety disorders, and substance use disorders.”
She cautioned against treating a patient with ADHD medication if there is a preexisting psychosis or bipolar illness. “If you start a stimulant or atomoxetine and psychosis or mania occurs, you clearly want to stop the medication and reassess,” she said. Researchers found that the risk of precipitating mania with a stimulant is uncommon if you alleviate symptoms first with a mood stabilizer. “This is a situation where you probably want to treat the bipolar illness first, but it does not preclude the treatment of ADHD once the mood stabilization has occurred,” she said.
In patients with ADHD and anxiety, she often treats the ADHD first, “because oftentimes the anxiety is driven by the procrastination and the inability to get things done,” she explained. “It’s important to determine whether the anxiety is an independent disorder rather than symptoms of ADHD. Inner restlessness can be described as anxiety.”
When there are concerns that preclude the use of a controlled medication, there are medications, in addition to atomoxetine, that might be considered. While bupropion is not Food and Drug Administration approved for ADHD, it might be useful in comorbid mood disorders for nicotine dependence. Other off-label medications that may help include guanfacine, modafinil, and tricyclic antidepressants.
“To date, robust dosing of long-acting amphetamine or methylphenidate formulations have been shown to be effective for patients with stimulant-use disorder, but as mentioned earlier, the data only come from two studies,” she said.
In order to determine whether stimulant treatment is yielding a benefit in a patient with co-occurring ADHD and SUD, she recommends carrying out a structured assessment of ADHD symptoms. Monitoring for functional improvement is also key.
“If there is no improvement in social, occupational, or academic settings and the patient is still actively using drugs, then there is no reason to keep prescribing,” she said. Close monitoring for cardiovascular or other psychiatric symptoms are key as well. Further, for those individuals with both ADHD and a substance-use disorder, it is critical that both are targeted for treatment.
Dr. Levin reported that she has received research, training, or salary support from the National Institute on Drug Abuse, New York state, and the Substance Abuse and Mental Health Services Administration. She has also received or currently receives industry support from Indivior and U.S. World Meds and for medication and from Major League Baseball. In addition, Dr. Levin has been an unpaid scientific advisory board member for Alkermes, Indivior, and Novartis.
When Frances R. Levin, MD, began her clinical psychiatry career in the mid-1990s, she spent a lot of time educating colleagues about the validity of an ADHD diagnosis in adults.
“That’s no longer an issue,” Dr. Levin, the Kennedy-Leavy Professor of Psychiatry at Columbia University, New York, said during an annual psychopharmacology update held by the Nevada Psychiatric Association. “But at the time, we often thought, ‘ADHD is something that’s specific to people who are stimulant users.’ In fact, what we found over the years was that these rates are elevated in a range of substance use populations.”
According to National Comorbidity Survey, a nontreatment sample of more than 3,000 adults, individuals who have SUD have two to three times the risk of having ADHD, while individuals who have ADHD have about three times the rate of having an SUD, compared with those who don’t (Am J Psychiatry. 2006;163[4]:716-23). “When you move to treatment samples, the rates also remain quite high,” said Dr. Levin, who is also chief of the division of substance use disorders at the medical center.
“In the general population, the rates of ADHD are 2%-4%. When we look at people who are coming in specifically for treatment of their SUD, the rates are substantially higher, ranging from 10% to 24%.”
According to a 2014 review of medical literature, potential reasons for the association between ADHD and SUD vary and include underlying biologic deficits, such as parental SUDs and genetics; conduct disorder symptoms, such as defiance, rule breaking, and delinquency; poor performance in school, such as low grades, grade retention, or drop-out; and social difficulties, such as rejection from conventional groups or few quality friendships (Annu Rev Clin Psychol. 2014;10:607-39). Other potential pathways include neurocognitive deficits, stress-negative affect models, impulsive anger, and other underlying traits.
One key reason to treat ADHD in patients with SUDs is that they tend to develop the SUD earlier when the ADHD is present, Dr. Levin said. They’re also less likely to be retained in treatment and have a reduced likelihood of going into remission if dependence develops. “Even when they do achieve remission, it seems to take longer for people to reach remission,” she said. “They have more treatment exposure yet do less well in treatment. This can make it more challenging to treat this population.”
One common assumption from clinicians regarding patients with ADHD and a concomitant SUD is that standard treatments for ADHD do not work in active substance users. Another is that, even if treatments work for ADHD, they do not affect the substance use disorder. “Understandably, there is also concern that active substance abusers will misuse and divert their medications,” she said. “Finally, there are often additional psychiatric comorbidities that may make it harder to effectively treat individuals with ADHD and SUD.”
Since 2002, 15 double-blind outpatient studies using stimulants/atomoxetine to treat substance abusers with ADHD have appeared in the medical literature, Dr. Levin said. Only three have included adolescents. “That’s surprising, because up to 40% of kids who come in for treatment, often for cannabis use disorder, will have ADHD, yet there is very little guidance from empirical studies as to how to best treat them,” she said. “There have been several studies looking at atomoxetine to treat substance abusers with ADHD, but results have been mixed. In the cannabis use populations, atomoxetine has not been shown to be effective in treating the substance use disorder, and results are mixed regarding superiority in reducing ADHD symptoms. There is one study showing that ADHD is more likely to be improved in adults with alcohol use disorders with mixed results regarding the alcohol use.”
Overall, most of the outpatient and inpatient studies conducted in this population have demonstrated some signal in terms of reducing ADHD, she said, while a minority of the outpatient studies suggest some benefit in terms of substance use. “What’s interesting is that when you see a response in terms of the ADHD, you often see an improvement in the substance use as well,” Dr. Levin said. “This potentially suggests that patients may be self-medicating their ADHD symptoms or that if the ADHD responds to treatment, then the patient may benefit from the psychosocial interventions that targets the SUD.”
A separate meta-analysis involving more than 1,000 patients found mixed results from pharmacologic interventions and concluded that, while they modestly improved ADHD symptoms, no beneficial effect was seen on drug abstinence or on treatment discontinuation (J Psychopharmacol. 2015 Jan;29[1]:15-23). “I would argue that you don’t need to be as nihilistic about this as the meta-analysis might suggest, because the devil’s in the details,” said Dr. Levin, whose own research was included in the work.
“First of all, many of the studies had high drop-out rates. The outcome measures were variable, and some of the studies used formulations with poor bioavailability. Also, trials that evaluated atomoxetine or stimulants were combined, which may be problematic given the different mechanisms of action. Further, the meta-analysis did not include two recent placebo-controlled trials in adults with stimulant-use disorders that both found that higher dosing of a long-acting stimulant resulted in greater improvements in ADHD symptoms and stimulant use” (Addict. 2014;109[3]:440-9 and JAMA Psychiatry. 2015;72[6]:593-602).
Dr. Levin went on to note that there are few empirical data to guide treatment for those who have multiple psychiatric disorders, let alone treatment for ADHD and SUDs without additional psychiatric disorders. The challenge is what to treat first and/or how to treat the concomitant conditions safely.
“Generally, if possible, treat what is most clinically impairing first,” she said. “Overall, both stimulants and atomoxetine may work for ADHD even in the presence of additional depression, anxiety disorders, and substance use disorders.”
She cautioned against treating a patient with ADHD medication if there is a preexisting psychosis or bipolar illness. “If you start a stimulant or atomoxetine and psychosis or mania occurs, you clearly want to stop the medication and reassess,” she said. Researchers found that the risk of precipitating mania with a stimulant is uncommon if you alleviate symptoms first with a mood stabilizer. “This is a situation where you probably want to treat the bipolar illness first, but it does not preclude the treatment of ADHD once the mood stabilization has occurred,” she said.
In patients with ADHD and anxiety, she often treats the ADHD first, “because oftentimes the anxiety is driven by the procrastination and the inability to get things done,” she explained. “It’s important to determine whether the anxiety is an independent disorder rather than symptoms of ADHD. Inner restlessness can be described as anxiety.”
When there are concerns that preclude the use of a controlled medication, there are medications, in addition to atomoxetine, that might be considered. While bupropion is not Food and Drug Administration approved for ADHD, it might be useful in comorbid mood disorders for nicotine dependence. Other off-label medications that may help include guanfacine, modafinil, and tricyclic antidepressants.
“To date, robust dosing of long-acting amphetamine or methylphenidate formulations have been shown to be effective for patients with stimulant-use disorder, but as mentioned earlier, the data only come from two studies,” she said.
In order to determine whether stimulant treatment is yielding a benefit in a patient with co-occurring ADHD and SUD, she recommends carrying out a structured assessment of ADHD symptoms. Monitoring for functional improvement is also key.
“If there is no improvement in social, occupational, or academic settings and the patient is still actively using drugs, then there is no reason to keep prescribing,” she said. Close monitoring for cardiovascular or other psychiatric symptoms are key as well. Further, for those individuals with both ADHD and a substance-use disorder, it is critical that both are targeted for treatment.
Dr. Levin reported that she has received research, training, or salary support from the National Institute on Drug Abuse, New York state, and the Substance Abuse and Mental Health Services Administration. She has also received or currently receives industry support from Indivior and U.S. World Meds and for medication and from Major League Baseball. In addition, Dr. Levin has been an unpaid scientific advisory board member for Alkermes, Indivior, and Novartis.
When Frances R. Levin, MD, began her clinical psychiatry career in the mid-1990s, she spent a lot of time educating colleagues about the validity of an ADHD diagnosis in adults.
“That’s no longer an issue,” Dr. Levin, the Kennedy-Leavy Professor of Psychiatry at Columbia University, New York, said during an annual psychopharmacology update held by the Nevada Psychiatric Association. “But at the time, we often thought, ‘ADHD is something that’s specific to people who are stimulant users.’ In fact, what we found over the years was that these rates are elevated in a range of substance use populations.”
According to National Comorbidity Survey, a nontreatment sample of more than 3,000 adults, individuals who have SUD have two to three times the risk of having ADHD, while individuals who have ADHD have about three times the rate of having an SUD, compared with those who don’t (Am J Psychiatry. 2006;163[4]:716-23). “When you move to treatment samples, the rates also remain quite high,” said Dr. Levin, who is also chief of the division of substance use disorders at the medical center.
“In the general population, the rates of ADHD are 2%-4%. When we look at people who are coming in specifically for treatment of their SUD, the rates are substantially higher, ranging from 10% to 24%.”
According to a 2014 review of medical literature, potential reasons for the association between ADHD and SUD vary and include underlying biologic deficits, such as parental SUDs and genetics; conduct disorder symptoms, such as defiance, rule breaking, and delinquency; poor performance in school, such as low grades, grade retention, or drop-out; and social difficulties, such as rejection from conventional groups or few quality friendships (Annu Rev Clin Psychol. 2014;10:607-39). Other potential pathways include neurocognitive deficits, stress-negative affect models, impulsive anger, and other underlying traits.
One key reason to treat ADHD in patients with SUDs is that they tend to develop the SUD earlier when the ADHD is present, Dr. Levin said. They’re also less likely to be retained in treatment and have a reduced likelihood of going into remission if dependence develops. “Even when they do achieve remission, it seems to take longer for people to reach remission,” she said. “They have more treatment exposure yet do less well in treatment. This can make it more challenging to treat this population.”
One common assumption from clinicians regarding patients with ADHD and a concomitant SUD is that standard treatments for ADHD do not work in active substance users. Another is that, even if treatments work for ADHD, they do not affect the substance use disorder. “Understandably, there is also concern that active substance abusers will misuse and divert their medications,” she said. “Finally, there are often additional psychiatric comorbidities that may make it harder to effectively treat individuals with ADHD and SUD.”
Since 2002, 15 double-blind outpatient studies using stimulants/atomoxetine to treat substance abusers with ADHD have appeared in the medical literature, Dr. Levin said. Only three have included adolescents. “That’s surprising, because up to 40% of kids who come in for treatment, often for cannabis use disorder, will have ADHD, yet there is very little guidance from empirical studies as to how to best treat them,” she said. “There have been several studies looking at atomoxetine to treat substance abusers with ADHD, but results have been mixed. In the cannabis use populations, atomoxetine has not been shown to be effective in treating the substance use disorder, and results are mixed regarding superiority in reducing ADHD symptoms. There is one study showing that ADHD is more likely to be improved in adults with alcohol use disorders with mixed results regarding the alcohol use.”
Overall, most of the outpatient and inpatient studies conducted in this population have demonstrated some signal in terms of reducing ADHD, she said, while a minority of the outpatient studies suggest some benefit in terms of substance use. “What’s interesting is that when you see a response in terms of the ADHD, you often see an improvement in the substance use as well,” Dr. Levin said. “This potentially suggests that patients may be self-medicating their ADHD symptoms or that if the ADHD responds to treatment, then the patient may benefit from the psychosocial interventions that targets the SUD.”
A separate meta-analysis involving more than 1,000 patients found mixed results from pharmacologic interventions and concluded that, while they modestly improved ADHD symptoms, no beneficial effect was seen on drug abstinence or on treatment discontinuation (J Psychopharmacol. 2015 Jan;29[1]:15-23). “I would argue that you don’t need to be as nihilistic about this as the meta-analysis might suggest, because the devil’s in the details,” said Dr. Levin, whose own research was included in the work.
“First of all, many of the studies had high drop-out rates. The outcome measures were variable, and some of the studies used formulations with poor bioavailability. Also, trials that evaluated atomoxetine or stimulants were combined, which may be problematic given the different mechanisms of action. Further, the meta-analysis did not include two recent placebo-controlled trials in adults with stimulant-use disorders that both found that higher dosing of a long-acting stimulant resulted in greater improvements in ADHD symptoms and stimulant use” (Addict. 2014;109[3]:440-9 and JAMA Psychiatry. 2015;72[6]:593-602).
Dr. Levin went on to note that there are few empirical data to guide treatment for those who have multiple psychiatric disorders, let alone treatment for ADHD and SUDs without additional psychiatric disorders. The challenge is what to treat first and/or how to treat the concomitant conditions safely.
“Generally, if possible, treat what is most clinically impairing first,” she said. “Overall, both stimulants and atomoxetine may work for ADHD even in the presence of additional depression, anxiety disorders, and substance use disorders.”
She cautioned against treating a patient with ADHD medication if there is a preexisting psychosis or bipolar illness. “If you start a stimulant or atomoxetine and psychosis or mania occurs, you clearly want to stop the medication and reassess,” she said. Researchers found that the risk of precipitating mania with a stimulant is uncommon if you alleviate symptoms first with a mood stabilizer. “This is a situation where you probably want to treat the bipolar illness first, but it does not preclude the treatment of ADHD once the mood stabilization has occurred,” she said.
In patients with ADHD and anxiety, she often treats the ADHD first, “because oftentimes the anxiety is driven by the procrastination and the inability to get things done,” she explained. “It’s important to determine whether the anxiety is an independent disorder rather than symptoms of ADHD. Inner restlessness can be described as anxiety.”
When there are concerns that preclude the use of a controlled medication, there are medications, in addition to atomoxetine, that might be considered. While bupropion is not Food and Drug Administration approved for ADHD, it might be useful in comorbid mood disorders for nicotine dependence. Other off-label medications that may help include guanfacine, modafinil, and tricyclic antidepressants.
“To date, robust dosing of long-acting amphetamine or methylphenidate formulations have been shown to be effective for patients with stimulant-use disorder, but as mentioned earlier, the data only come from two studies,” she said.
In order to determine whether stimulant treatment is yielding a benefit in a patient with co-occurring ADHD and SUD, she recommends carrying out a structured assessment of ADHD symptoms. Monitoring for functional improvement is also key.
“If there is no improvement in social, occupational, or academic settings and the patient is still actively using drugs, then there is no reason to keep prescribing,” she said. Close monitoring for cardiovascular or other psychiatric symptoms are key as well. Further, for those individuals with both ADHD and a substance-use disorder, it is critical that both are targeted for treatment.
Dr. Levin reported that she has received research, training, or salary support from the National Institute on Drug Abuse, New York state, and the Substance Abuse and Mental Health Services Administration. She has also received or currently receives industry support from Indivior and U.S. World Meds and for medication and from Major League Baseball. In addition, Dr. Levin has been an unpaid scientific advisory board member for Alkermes, Indivior, and Novartis.
FROM NPA 2021
Oxford launches COVID-19 vaccine study in children
Oxford University is starting a COVID-19 vaccine study with children and young adults aged between 6 and 17 years.
At Oxford and three partner sites in London, Southampton, and Bristol, the phase 2 clinical trial will test whether kids and teens have a good immune response to the AstraZeneca vaccine. Previous trials have shown that the shot is safe in children.
“While most children are relatively unaffected by coronavirus and are unlikely to become unwell with the infection, it is important to establish the safety and immune response to the vaccine in children and young people as some children may benefit from vaccination,” Andrew Pollard, PhD, the chief investigator for the trial and a professor of pediatric infection and immunity at Oxford, said in a statement.
The new trial will enroll 300 volunteers, with up to 240 receiving the vaccine. The control group will receive a meningitis vaccine, which is safe in children and produces similar side effects to the COVID-19 vaccine, such as a sore arm.
COVID-19 vaccine trials have included children over age 12, so this marks the youngest group to be tested so far. Pfizer, Moderna, and Janssen have announced plans to start trials in younger children this spring, according to the Washington Post. Widespread vaccination in children likely won’t occur until 2022, the newspaper reported.
The trial launched on Feb. 12, and the first vaccinations are expected by the end of the month. Parents can visit Oxford’s COVID-19 Vaccine Trial website to sign their children up for the study.
“This study will play an important role in helping to protect children in the future,” Grace Li, a pediatric clinical research fellow for the Oxford Vaccine Group, said in the statement.
“We’ve already seen that the vaccine is safe and effective in adults, and our understanding of how children are affected by the coronavirus continues to evolve,” she said.
A version of this article first appeared on WebMD.com.
Oxford University is starting a COVID-19 vaccine study with children and young adults aged between 6 and 17 years.
At Oxford and three partner sites in London, Southampton, and Bristol, the phase 2 clinical trial will test whether kids and teens have a good immune response to the AstraZeneca vaccine. Previous trials have shown that the shot is safe in children.
“While most children are relatively unaffected by coronavirus and are unlikely to become unwell with the infection, it is important to establish the safety and immune response to the vaccine in children and young people as some children may benefit from vaccination,” Andrew Pollard, PhD, the chief investigator for the trial and a professor of pediatric infection and immunity at Oxford, said in a statement.
The new trial will enroll 300 volunteers, with up to 240 receiving the vaccine. The control group will receive a meningitis vaccine, which is safe in children and produces similar side effects to the COVID-19 vaccine, such as a sore arm.
COVID-19 vaccine trials have included children over age 12, so this marks the youngest group to be tested so far. Pfizer, Moderna, and Janssen have announced plans to start trials in younger children this spring, according to the Washington Post. Widespread vaccination in children likely won’t occur until 2022, the newspaper reported.
The trial launched on Feb. 12, and the first vaccinations are expected by the end of the month. Parents can visit Oxford’s COVID-19 Vaccine Trial website to sign their children up for the study.
“This study will play an important role in helping to protect children in the future,” Grace Li, a pediatric clinical research fellow for the Oxford Vaccine Group, said in the statement.
“We’ve already seen that the vaccine is safe and effective in adults, and our understanding of how children are affected by the coronavirus continues to evolve,” she said.
A version of this article first appeared on WebMD.com.
Oxford University is starting a COVID-19 vaccine study with children and young adults aged between 6 and 17 years.
At Oxford and three partner sites in London, Southampton, and Bristol, the phase 2 clinical trial will test whether kids and teens have a good immune response to the AstraZeneca vaccine. Previous trials have shown that the shot is safe in children.
“While most children are relatively unaffected by coronavirus and are unlikely to become unwell with the infection, it is important to establish the safety and immune response to the vaccine in children and young people as some children may benefit from vaccination,” Andrew Pollard, PhD, the chief investigator for the trial and a professor of pediatric infection and immunity at Oxford, said in a statement.
The new trial will enroll 300 volunteers, with up to 240 receiving the vaccine. The control group will receive a meningitis vaccine, which is safe in children and produces similar side effects to the COVID-19 vaccine, such as a sore arm.
COVID-19 vaccine trials have included children over age 12, so this marks the youngest group to be tested so far. Pfizer, Moderna, and Janssen have announced plans to start trials in younger children this spring, according to the Washington Post. Widespread vaccination in children likely won’t occur until 2022, the newspaper reported.
The trial launched on Feb. 12, and the first vaccinations are expected by the end of the month. Parents can visit Oxford’s COVID-19 Vaccine Trial website to sign their children up for the study.
“This study will play an important role in helping to protect children in the future,” Grace Li, a pediatric clinical research fellow for the Oxford Vaccine Group, said in the statement.
“We’ve already seen that the vaccine is safe and effective in adults, and our understanding of how children are affected by the coronavirus continues to evolve,” she said.
A version of this article first appeared on WebMD.com.
Hospitalizations for food anaphylaxis triple, but deaths down in United Kingdom
The rate of hospital admissions in the United Kingdom for food-induced anaphylaxis more than tripled over the 20 years from 1998 to 2018, but the case fatality rate fell by more than half, researchers report in BMJ.
“Cow’s milk is increasingly identified as the culprit allergen for fatal food reactions and is now the commonest cause of fatal anaphylaxis in children,” write Alessia Baseggio Conrado, PhD, a biochemist with the National Heart and Lung Institute at Imperial College London, and colleagues. “More education is needed to highlight the specific risks posed by cow’s milk to people who are allergic to increase awareness among food businesses.”
Whereas recognition of the risks posed by nut allergies has increased, people think milk allergy is mild, says senior author Paul. J. Turner, BMBCh, PhD, an allergist/immunologist at Imperial College. “This is often true in very young children, but school-aged children who still have milk allergy tend to have a more allergic profile, often with other allergies, including asthma,” Dr. Turner told this news organization. “Also, milk is very common in our diet, and you don’t need much milk to achieve a decent dose of allergen.”
During the study period, 101,891 people were hospitalized for anaphylaxis; 30,700 cases (30%) were coded as having been triggered by food.
These food-related admissions represent an increase from 1.23 to 4.04 per 100,000 population per year, for an annual increase of 5.7% (95% confidence interval, 5.5-5.9; P < .001), the authors write.
The largest jump occurred among children younger than 15 years, for whom admissions rose from 2.1 to 9.2 per 100,000 population per year, an annual increase of 6.6% (95% CI, 6.3-7.0). The annual increases were 5.9% (95% CI, 5.6-6.2) among persons aged 15 to 59 years and 2.1% (95% CI, 1.8-3.1) among those aged 60 years and older.
The investigators used data from England, Scotland, Wales, and Northern Ireland to track temporal trends and age and sex distributions for hospital admissions for which the primary diagnosis was anaphylaxis attributable to both food and nonfood triggers. These data were compared with nationally reported fatalities.
Over the 20-year period, 152 deaths were attributed to likely food-induced anaphylaxis. During that time, the case fatality rate for confirmed fatal food anaphylaxis fell from 0.7% to 0.19% (rate ratio, 0.931; 95% CI, 0.904-0.959; P < .001) and declined to 0.30% for suspected fatal food anaphylaxis (rate ratio, 0.970; 95% CI, 0.945-0.996; P = .024).
Between 1992 and 2018, at least 46% of all anaphylactic fatalities were deemed to be triggered by peanut or tree nut. Among school-aged children, 26% of anaphylactic fatalities were attributed to cow’s milk.
Not surprisingly, during the study period, there was an increase of 336% in prescriptions for adrenaline autoinjectors. Such prescriptions increased 11% per year.
Global trend
The data extend findings Dr. Turner and colleagues reported for England and Wales in 2014 regarding the entire United Kingdom population and align with epidemiologic trends in hospital admissions for anaphylaxis in the United States and Australia.
The researchers say better recognition and management of anaphylaxis could partly explain the decrease in fatalities, but the rise in hospitalizations remains puzzling. “Whether a true increase in the prevalence of anaphylaxis has occurred (rather than a reduction in the threshold to admit patients presenting with anaphylaxis) is unclear because evidence is lacking for an increase in prevalence of food allergy in the [United Kingdom] (and elsewhere) over the same time period,” they write.
Ronna L. Campbell, MD, PhD, an emergency physician at the Mayo Clinic in Rochester, Minn., has noted similar trends in the United States. “It may be that anaphylaxis recognition and diagnosis have improved, resulting in earlier administration of epinephrine,” Dr. Campbell said in an interview. “So while cases are increasing, earlier recognition and treatment result in decreased fatalities.” She is unaware of any new guidelines recommending increased hospitalization that would explain the puzzling rise in admissions.
According to the study authors, the clinical criteria used to diagnose anaphylaxis in the United Kingdom did not change during the study period. Although national guidance recommending the hospitalization of children younger than 16 who are suspected of having anaphylaxis was introduced in 2011 and may have boosted admissions, the year-on-year rate of increase has persisted since 2014. “Therefore the increase over the past 5 years cannot be attributed to the impact of the guidance,” they write.
The study was funded by grants from the U.K. Medical Research Council and U.K. Food Standards Agency. Two coauthors have disclosed financial relationships with industry outside of the submitted work. Dr. Conrado has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com
The rate of hospital admissions in the United Kingdom for food-induced anaphylaxis more than tripled over the 20 years from 1998 to 2018, but the case fatality rate fell by more than half, researchers report in BMJ.
“Cow’s milk is increasingly identified as the culprit allergen for fatal food reactions and is now the commonest cause of fatal anaphylaxis in children,” write Alessia Baseggio Conrado, PhD, a biochemist with the National Heart and Lung Institute at Imperial College London, and colleagues. “More education is needed to highlight the specific risks posed by cow’s milk to people who are allergic to increase awareness among food businesses.”
Whereas recognition of the risks posed by nut allergies has increased, people think milk allergy is mild, says senior author Paul. J. Turner, BMBCh, PhD, an allergist/immunologist at Imperial College. “This is often true in very young children, but school-aged children who still have milk allergy tend to have a more allergic profile, often with other allergies, including asthma,” Dr. Turner told this news organization. “Also, milk is very common in our diet, and you don’t need much milk to achieve a decent dose of allergen.”
During the study period, 101,891 people were hospitalized for anaphylaxis; 30,700 cases (30%) were coded as having been triggered by food.
These food-related admissions represent an increase from 1.23 to 4.04 per 100,000 population per year, for an annual increase of 5.7% (95% confidence interval, 5.5-5.9; P < .001), the authors write.
The largest jump occurred among children younger than 15 years, for whom admissions rose from 2.1 to 9.2 per 100,000 population per year, an annual increase of 6.6% (95% CI, 6.3-7.0). The annual increases were 5.9% (95% CI, 5.6-6.2) among persons aged 15 to 59 years and 2.1% (95% CI, 1.8-3.1) among those aged 60 years and older.
The investigators used data from England, Scotland, Wales, and Northern Ireland to track temporal trends and age and sex distributions for hospital admissions for which the primary diagnosis was anaphylaxis attributable to both food and nonfood triggers. These data were compared with nationally reported fatalities.
Over the 20-year period, 152 deaths were attributed to likely food-induced anaphylaxis. During that time, the case fatality rate for confirmed fatal food anaphylaxis fell from 0.7% to 0.19% (rate ratio, 0.931; 95% CI, 0.904-0.959; P < .001) and declined to 0.30% for suspected fatal food anaphylaxis (rate ratio, 0.970; 95% CI, 0.945-0.996; P = .024).
Between 1992 and 2018, at least 46% of all anaphylactic fatalities were deemed to be triggered by peanut or tree nut. Among school-aged children, 26% of anaphylactic fatalities were attributed to cow’s milk.
Not surprisingly, during the study period, there was an increase of 336% in prescriptions for adrenaline autoinjectors. Such prescriptions increased 11% per year.
Global trend
The data extend findings Dr. Turner and colleagues reported for England and Wales in 2014 regarding the entire United Kingdom population and align with epidemiologic trends in hospital admissions for anaphylaxis in the United States and Australia.
The researchers say better recognition and management of anaphylaxis could partly explain the decrease in fatalities, but the rise in hospitalizations remains puzzling. “Whether a true increase in the prevalence of anaphylaxis has occurred (rather than a reduction in the threshold to admit patients presenting with anaphylaxis) is unclear because evidence is lacking for an increase in prevalence of food allergy in the [United Kingdom] (and elsewhere) over the same time period,” they write.
Ronna L. Campbell, MD, PhD, an emergency physician at the Mayo Clinic in Rochester, Minn., has noted similar trends in the United States. “It may be that anaphylaxis recognition and diagnosis have improved, resulting in earlier administration of epinephrine,” Dr. Campbell said in an interview. “So while cases are increasing, earlier recognition and treatment result in decreased fatalities.” She is unaware of any new guidelines recommending increased hospitalization that would explain the puzzling rise in admissions.
According to the study authors, the clinical criteria used to diagnose anaphylaxis in the United Kingdom did not change during the study period. Although national guidance recommending the hospitalization of children younger than 16 who are suspected of having anaphylaxis was introduced in 2011 and may have boosted admissions, the year-on-year rate of increase has persisted since 2014. “Therefore the increase over the past 5 years cannot be attributed to the impact of the guidance,” they write.
The study was funded by grants from the U.K. Medical Research Council and U.K. Food Standards Agency. Two coauthors have disclosed financial relationships with industry outside of the submitted work. Dr. Conrado has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com
The rate of hospital admissions in the United Kingdom for food-induced anaphylaxis more than tripled over the 20 years from 1998 to 2018, but the case fatality rate fell by more than half, researchers report in BMJ.
“Cow’s milk is increasingly identified as the culprit allergen for fatal food reactions and is now the commonest cause of fatal anaphylaxis in children,” write Alessia Baseggio Conrado, PhD, a biochemist with the National Heart and Lung Institute at Imperial College London, and colleagues. “More education is needed to highlight the specific risks posed by cow’s milk to people who are allergic to increase awareness among food businesses.”
Whereas recognition of the risks posed by nut allergies has increased, people think milk allergy is mild, says senior author Paul. J. Turner, BMBCh, PhD, an allergist/immunologist at Imperial College. “This is often true in very young children, but school-aged children who still have milk allergy tend to have a more allergic profile, often with other allergies, including asthma,” Dr. Turner told this news organization. “Also, milk is very common in our diet, and you don’t need much milk to achieve a decent dose of allergen.”
During the study period, 101,891 people were hospitalized for anaphylaxis; 30,700 cases (30%) were coded as having been triggered by food.
These food-related admissions represent an increase from 1.23 to 4.04 per 100,000 population per year, for an annual increase of 5.7% (95% confidence interval, 5.5-5.9; P < .001), the authors write.
The largest jump occurred among children younger than 15 years, for whom admissions rose from 2.1 to 9.2 per 100,000 population per year, an annual increase of 6.6% (95% CI, 6.3-7.0). The annual increases were 5.9% (95% CI, 5.6-6.2) among persons aged 15 to 59 years and 2.1% (95% CI, 1.8-3.1) among those aged 60 years and older.
The investigators used data from England, Scotland, Wales, and Northern Ireland to track temporal trends and age and sex distributions for hospital admissions for which the primary diagnosis was anaphylaxis attributable to both food and nonfood triggers. These data were compared with nationally reported fatalities.
Over the 20-year period, 152 deaths were attributed to likely food-induced anaphylaxis. During that time, the case fatality rate for confirmed fatal food anaphylaxis fell from 0.7% to 0.19% (rate ratio, 0.931; 95% CI, 0.904-0.959; P < .001) and declined to 0.30% for suspected fatal food anaphylaxis (rate ratio, 0.970; 95% CI, 0.945-0.996; P = .024).
Between 1992 and 2018, at least 46% of all anaphylactic fatalities were deemed to be triggered by peanut or tree nut. Among school-aged children, 26% of anaphylactic fatalities were attributed to cow’s milk.
Not surprisingly, during the study period, there was an increase of 336% in prescriptions for adrenaline autoinjectors. Such prescriptions increased 11% per year.
Global trend
The data extend findings Dr. Turner and colleagues reported for England and Wales in 2014 regarding the entire United Kingdom population and align with epidemiologic trends in hospital admissions for anaphylaxis in the United States and Australia.
The researchers say better recognition and management of anaphylaxis could partly explain the decrease in fatalities, but the rise in hospitalizations remains puzzling. “Whether a true increase in the prevalence of anaphylaxis has occurred (rather than a reduction in the threshold to admit patients presenting with anaphylaxis) is unclear because evidence is lacking for an increase in prevalence of food allergy in the [United Kingdom] (and elsewhere) over the same time period,” they write.
Ronna L. Campbell, MD, PhD, an emergency physician at the Mayo Clinic in Rochester, Minn., has noted similar trends in the United States. “It may be that anaphylaxis recognition and diagnosis have improved, resulting in earlier administration of epinephrine,” Dr. Campbell said in an interview. “So while cases are increasing, earlier recognition and treatment result in decreased fatalities.” She is unaware of any new guidelines recommending increased hospitalization that would explain the puzzling rise in admissions.
According to the study authors, the clinical criteria used to diagnose anaphylaxis in the United Kingdom did not change during the study period. Although national guidance recommending the hospitalization of children younger than 16 who are suspected of having anaphylaxis was introduced in 2011 and may have boosted admissions, the year-on-year rate of increase has persisted since 2014. “Therefore the increase over the past 5 years cannot be attributed to the impact of the guidance,” they write.
The study was funded by grants from the U.K. Medical Research Council and U.K. Food Standards Agency. Two coauthors have disclosed financial relationships with industry outside of the submitted work. Dr. Conrado has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com