User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Long COVID symptoms linked to effects on vagus nerve
Several long COVID symptoms could be linked to the effects of the coronavirus on a vital central nerve, according to new research being released in the spring.
The vagus nerve, which runs from the brain into the body, connects to the heart, lungs, intestines, and several muscles involved with swallowing. It plays a role in several body functions that control heart rate, speech, the gag reflex, sweating, and digestion.
Those with long COVID and vagus nerve problems could face long-term issues with their voice, a hard time swallowing, dizziness, a high heart rate, low blood pressure, and diarrhea, the study authors found.
Their findings will be presented at the 2022 European Congress of Clinical Microbiology and Infectious Diseases in late April.
“Most long COVID subjects with vagus nerve dysfunction symptoms had a range of significant, clinically relevant, structural and/or functional alterations in their vagus nerve, including nerve thickening, trouble swallowing, and symptoms of impaired breathing,” the study authors wrote. “Our findings so far thus point at vagus nerve dysfunction as a central pathophysiological feature of long COVID.”
Researchers from the University Hospital Germans Trias i Pujol in Barcelona performed a study to look at vagus nerve functioning in long COVID patients. Among 348 patients, about 66% had at least one symptom that suggested vagus nerve dysfunction. The researchers did a broad evaluation with imaging and functional tests for 22 patients in the university’s Long COVID Clinic from March to June 2021.
Of the 22 patients, 20 were women, and the median age was 44. The most frequent symptoms related to vagus nerve dysfunction were diarrhea (73%), high heart rates (59%), dizziness (45%), swallowing problems (45%), voice problems (45%), and low blood pressure (14%).
Almost all (19 of 22 patients) had three or more symptoms related to vagus nerve dysfunction. The average length of symptoms was 14 months.
Of 22 patients, 6 had a change in the vagus nerve in the neck, which the researchers observed by ultrasound. They had a thickening of the vagus nerve and increased “echogenicity,” which suggests inflammation.
What’s more, 10 of 22 patients had flattened “diaphragmatic curves” during a thoracic ultrasound, which means the diaphragm doesn’t move as well as it should during breathing, and abnormal breathing. In another assessment, 10 of 16 patients had lower maximum inspiration pressures, suggesting a weakness in breathing muscles.
Eating and digestion were also impaired in some patients, with 13 reporting trouble with swallowing. During a gastric and bowel function assessment, eight patients couldn’t move food from the esophagus to the stomach as well as they should, while nine patients had acid reflux. Three patients had a hiatal hernia, which happens when the upper part of the stomach bulges through the diaphragm into the chest cavity.
The voices of some patients changed as well. Eight patients had an abnormal voice handicap index 30 test, which is a standard way to measure voice function. Among those, seven patients had dysphonia, or persistent voice problems.
The study is ongoing, and the research team is continuing to recruit patients to study the links between long COVID and the vagus nerve. The full paper isn’t yet available, and the research hasn’t yet been peer reviewed.
“The study appears to add to a growing collection of data suggesting at least some of the symptoms of long COVID is mediated through a direct impact on the nervous system,” David Strain, MD, a clinical senior lecturer at the University of Exeter (England), told the Science Media Centre.
“Establishing vagal nerve damage is useful information, as there are recognized, albeit not perfect, treatments for other causes of vagal nerve dysfunction that may be extrapolated to be beneficial for people with this type of long COVID,” he said.
A version of this article first appeared on WebMD.com.
Several long COVID symptoms could be linked to the effects of the coronavirus on a vital central nerve, according to new research being released in the spring.
The vagus nerve, which runs from the brain into the body, connects to the heart, lungs, intestines, and several muscles involved with swallowing. It plays a role in several body functions that control heart rate, speech, the gag reflex, sweating, and digestion.
Those with long COVID and vagus nerve problems could face long-term issues with their voice, a hard time swallowing, dizziness, a high heart rate, low blood pressure, and diarrhea, the study authors found.
Their findings will be presented at the 2022 European Congress of Clinical Microbiology and Infectious Diseases in late April.
“Most long COVID subjects with vagus nerve dysfunction symptoms had a range of significant, clinically relevant, structural and/or functional alterations in their vagus nerve, including nerve thickening, trouble swallowing, and symptoms of impaired breathing,” the study authors wrote. “Our findings so far thus point at vagus nerve dysfunction as a central pathophysiological feature of long COVID.”
Researchers from the University Hospital Germans Trias i Pujol in Barcelona performed a study to look at vagus nerve functioning in long COVID patients. Among 348 patients, about 66% had at least one symptom that suggested vagus nerve dysfunction. The researchers did a broad evaluation with imaging and functional tests for 22 patients in the university’s Long COVID Clinic from March to June 2021.
Of the 22 patients, 20 were women, and the median age was 44. The most frequent symptoms related to vagus nerve dysfunction were diarrhea (73%), high heart rates (59%), dizziness (45%), swallowing problems (45%), voice problems (45%), and low blood pressure (14%).
Almost all (19 of 22 patients) had three or more symptoms related to vagus nerve dysfunction. The average length of symptoms was 14 months.
Of 22 patients, 6 had a change in the vagus nerve in the neck, which the researchers observed by ultrasound. They had a thickening of the vagus nerve and increased “echogenicity,” which suggests inflammation.
What’s more, 10 of 22 patients had flattened “diaphragmatic curves” during a thoracic ultrasound, which means the diaphragm doesn’t move as well as it should during breathing, and abnormal breathing. In another assessment, 10 of 16 patients had lower maximum inspiration pressures, suggesting a weakness in breathing muscles.
Eating and digestion were also impaired in some patients, with 13 reporting trouble with swallowing. During a gastric and bowel function assessment, eight patients couldn’t move food from the esophagus to the stomach as well as they should, while nine patients had acid reflux. Three patients had a hiatal hernia, which happens when the upper part of the stomach bulges through the diaphragm into the chest cavity.
The voices of some patients changed as well. Eight patients had an abnormal voice handicap index 30 test, which is a standard way to measure voice function. Among those, seven patients had dysphonia, or persistent voice problems.
The study is ongoing, and the research team is continuing to recruit patients to study the links between long COVID and the vagus nerve. The full paper isn’t yet available, and the research hasn’t yet been peer reviewed.
“The study appears to add to a growing collection of data suggesting at least some of the symptoms of long COVID is mediated through a direct impact on the nervous system,” David Strain, MD, a clinical senior lecturer at the University of Exeter (England), told the Science Media Centre.
“Establishing vagal nerve damage is useful information, as there are recognized, albeit not perfect, treatments for other causes of vagal nerve dysfunction that may be extrapolated to be beneficial for people with this type of long COVID,” he said.
A version of this article first appeared on WebMD.com.
Several long COVID symptoms could be linked to the effects of the coronavirus on a vital central nerve, according to new research being released in the spring.
The vagus nerve, which runs from the brain into the body, connects to the heart, lungs, intestines, and several muscles involved with swallowing. It plays a role in several body functions that control heart rate, speech, the gag reflex, sweating, and digestion.
Those with long COVID and vagus nerve problems could face long-term issues with their voice, a hard time swallowing, dizziness, a high heart rate, low blood pressure, and diarrhea, the study authors found.
Their findings will be presented at the 2022 European Congress of Clinical Microbiology and Infectious Diseases in late April.
“Most long COVID subjects with vagus nerve dysfunction symptoms had a range of significant, clinically relevant, structural and/or functional alterations in their vagus nerve, including nerve thickening, trouble swallowing, and symptoms of impaired breathing,” the study authors wrote. “Our findings so far thus point at vagus nerve dysfunction as a central pathophysiological feature of long COVID.”
Researchers from the University Hospital Germans Trias i Pujol in Barcelona performed a study to look at vagus nerve functioning in long COVID patients. Among 348 patients, about 66% had at least one symptom that suggested vagus nerve dysfunction. The researchers did a broad evaluation with imaging and functional tests for 22 patients in the university’s Long COVID Clinic from March to June 2021.
Of the 22 patients, 20 were women, and the median age was 44. The most frequent symptoms related to vagus nerve dysfunction were diarrhea (73%), high heart rates (59%), dizziness (45%), swallowing problems (45%), voice problems (45%), and low blood pressure (14%).
Almost all (19 of 22 patients) had three or more symptoms related to vagus nerve dysfunction. The average length of symptoms was 14 months.
Of 22 patients, 6 had a change in the vagus nerve in the neck, which the researchers observed by ultrasound. They had a thickening of the vagus nerve and increased “echogenicity,” which suggests inflammation.
What’s more, 10 of 22 patients had flattened “diaphragmatic curves” during a thoracic ultrasound, which means the diaphragm doesn’t move as well as it should during breathing, and abnormal breathing. In another assessment, 10 of 16 patients had lower maximum inspiration pressures, suggesting a weakness in breathing muscles.
Eating and digestion were also impaired in some patients, with 13 reporting trouble with swallowing. During a gastric and bowel function assessment, eight patients couldn’t move food from the esophagus to the stomach as well as they should, while nine patients had acid reflux. Three patients had a hiatal hernia, which happens when the upper part of the stomach bulges through the diaphragm into the chest cavity.
The voices of some patients changed as well. Eight patients had an abnormal voice handicap index 30 test, which is a standard way to measure voice function. Among those, seven patients had dysphonia, or persistent voice problems.
The study is ongoing, and the research team is continuing to recruit patients to study the links between long COVID and the vagus nerve. The full paper isn’t yet available, and the research hasn’t yet been peer reviewed.
“The study appears to add to a growing collection of data suggesting at least some of the symptoms of long COVID is mediated through a direct impact on the nervous system,” David Strain, MD, a clinical senior lecturer at the University of Exeter (England), told the Science Media Centre.
“Establishing vagal nerve damage is useful information, as there are recognized, albeit not perfect, treatments for other causes of vagal nerve dysfunction that may be extrapolated to be beneficial for people with this type of long COVID,” he said.
A version of this article first appeared on WebMD.com.
Ear tubes not recommended for recurrent AOM without effusion, ENTs maintain
A practice guideline update from the ENT community on tympanostomy tubes in children reaffirms that tube insertion should not be considered in cases of otitis media with effusion (OME) lasting less than 3 months, or in children with recurrent acute otitis media (AOM) without middle ear effusion at the time of assessment for the procedure.
New in the update from the American Academy of Otolaryngology–Head and Neck Surgery Foundation (AAO-HNSF) is a strong recommendation for timely follow-up after surgery and recommendations against both routine use of prophylactic antibiotic ear drops after surgery and the initial use of long-term tubes except when there are specific reasons for doing so.
The update also expands the list of risk factors that place children with OME at increased risk of developmental difficulties – and often in need of timely ear tube placement – to include intellectual disability, learning disorder, and attention-deficit/hyperactivity disorder.
“Most of what we said in the 2013 [original] guideline was good and still valid ... and [important for] pediatricians, who are the key players” in managing otitis media, Jesse Hackell, MD, one of two general pediatricians who served on the Academy’s guideline update committee, said in an interview.
OME spontaneously clears up to 90% of the time within 3 months, said Dr. Hackell, of Pomona (New York) Pediatrics, and chair of the American Academy of Pediatrics (AAP) Committee on Practice and Ambulatory Medicine.
The updated guideline, for children 6 months to 12 years, reaffirms a recommendation that tube insertion be offered to children with “bilateral OME for 3 months or longer AND documented hearing difficulties.”
It also reaffirms “options” (a lesser quality of evidence) that in the absence of hearing difficulties, surgery may be performed for children with chronic OME (3 months or longer) in one or both ears if 1) they are at increased risk of developmental difficulties from OME or 2) effusion is likely contributing to balance problems, poor school performance, behavioral problems, ear discomfort, or reduced quality of life.
Children with chronic OME who do not undergo surgery should be reevaluated at 3- to 6-month intervals and monitored until effusion is no longer present, significant hearing loss is detected, or structural abnormalities of the tympanic membrane or middle ear are detected, the update again recommends.
Tympanostomy tube placement is the most common ambulatory surgery performed on children in the United States, the guideline authors say. In 2014, about 9% of children had undergone the surgery, they wrote, noting also that “tubes were placed in 25%-30% of children with frequent ear infections.”
Recurrent AOM
The AAO-HNSF guidance regarding tympanostomy tubes for OME is similar overall to management guidance issued by the AAP in its clinical practice guideline on OME.
The organizations differ, however, on their guidance for tube insertion for recurrent AOM. In its 2013 clinical practice guideline on AOM, the AAP recommends that clinicians may offer tube insertion for recurrent AOM, with no mention of the presence or absence of persistent fluid as a consideration.
According to the AAO-HNSF update, grade A evidence, including some research published since its original 2013 guideline, has shown little benefit to tube insertion in reducing the incidence of AOM in otherwise healthy children who don’t have middle ear effusion.
One study published in 2019 assessed outcomes after watchful waiting and found that only one-third of 123 children eventually went on to tympanostomy tube placement, noted Richard M. Rosenfeld, MD, distinguished professor and chairman of otolaryngology at SUNY Downstate Health Sciences University in Brooklyn, N.Y., and lead author of the original and updated guidelines.
In practice, “the real question [for the ENT] is the future. If the ears are perfectly clear, will tubes really reduce the frequency of infections going forward?” Dr. Rosenfeld said in an interview. “All the evidence seems to say no, it doesn’t make much of a difference.”
Dr. Hackell said he’s confident that the question “is settled enough.” While there “could be stronger research and higher quality studies, the evidence is still pretty good to suggest you gain little to no benefit with tubes when you’re dealing with recurrent AOM without effusion,” he said.
Asked to comment on the ENT update and its guidance on tympanostomy tubes for children with recurrent AOM, an AAP spokesperson said the “issue is under review” and that the AAP did not currently have a statement.
At-risk children
The AAO-HNSF update renews a recommendation to evaluate children with either recurrent AOM or OME of any duration for increased risk for speech, language, or learning problems from OME because of baseline factors (sensory, physical, cognitive, or behavioral).
When OME becomes chronic – or when a tympanogram gives a flat-line reading – OME is likely to persist, and families of at-risk children especially should be encouraged to pursue tube placement, Dr. Rosenfeld said.
Despite prior guidance to this effect, he said, ear tubes are being underutilized in at-risk children, with effusion being missed in primary care and with ENTs not expediting tube placement upon referral.
“These children have learning issues, cognitive issues, developmental issues,” he said in the interview. “It’s a population that does very poorly with ears full of fluid ... and despite guidance suggesting these children should be prioritized with tubes, it doesn’t seem to be happening enough.”
Formulating guidelines for at-risk children is challenging because they are often excluded from trials, Dr. Rosenfeld said, which limits evidence about the benefits of tubes and limits the strength of recommendations.
The addition of attention-deficit/hyperactivity disorder, intellectual disability, and learning disorder to the list of risk factors is notable, Dr. Hackell said. (The list includes autism spectrum disorder, developmental delay, and suspected or confirmed speech and language delay or disorder.)
“We know that kids with ADHD take in and process information a little differently ... it may be harder to get their attention with auditory stimulation,” he said. “So anything that would impact the taking in of information even for a short period of time increases their risk.”
Surgical practice
ENTs are advised in the new guidance to use long-term tubes and perioperative antibiotic ear drops more judiciously. “Long-term tubes have a role, but there are some doctors who routinely use them, even for a first-time surgery,” said Dr. Rosenfeld.
Overuse of long-term tubes results in a higher incidence of tympanic membrane perforation, chronic drainage, and other complications, as well as greater need for long-term follow-up. “There needs to be a reason – something to justify the need for prolonged ventilation,” he said.
Perioperative antibiotic ear drops are often administered during surgery and then prescribed routinely for all children afterward, but research has shown that saline irrigation during surgery and a single application of antibiotic/steroid drops is similarly efficacious in preventing otorrhea, the guideline says. Antibiotic ear drops are also “expensive,” noted Dr. Hackell. “There’s not enough benefit to justify it.”
The update also more explicitly advises selective use of adenoidectomy. A new option says that clinicians may perform the procedure as an adjunct to tube insertion for children 4 years or older to potentially reduce the future incidence of recurrent OME or the need for repeat surgery.
However, in younger children, it should not be offered unless there are symptoms directly related to adenoid infection or nasal obstruction. “Under 4 years, there’s no primary benefit for the ears,” said Dr. Rosenfeld.
Follow-up with the surgeon after tympanostomy tube insertion should occur within 3 months to assess outcomes and educate the family, the update strongly recommends.
And pediatricians should know, Dr. Hackell notes, that clinical evidence continues to show that earplugs and other water precautions are not routinely needed for children who have tubes in place. A good approach, the guideline says, is to “first avoid water precautions and instead reserve them for children with recurrent or persistent tympanostomy tube otorrhea.”
Asked to comment on the guideline update, Tim Joos, MD, MPH, who practices combined internal medicine/pediatrics in Seattle and is an editorial advisory board member of Pediatric News, noted the inclusion of patient information sheets with frequently asked questions – resources that can be useful for guiding parents through what’s often a shared decision-making process.
Neither Dr. Rosenfeld nor Dr. Hackell reported any disclosures. Other members of the guideline update committee reported various book royalties, consulting fees, and other disclosures. Dr. Joos reported he has no connections to the guideline authors.
A practice guideline update from the ENT community on tympanostomy tubes in children reaffirms that tube insertion should not be considered in cases of otitis media with effusion (OME) lasting less than 3 months, or in children with recurrent acute otitis media (AOM) without middle ear effusion at the time of assessment for the procedure.
New in the update from the American Academy of Otolaryngology–Head and Neck Surgery Foundation (AAO-HNSF) is a strong recommendation for timely follow-up after surgery and recommendations against both routine use of prophylactic antibiotic ear drops after surgery and the initial use of long-term tubes except when there are specific reasons for doing so.
The update also expands the list of risk factors that place children with OME at increased risk of developmental difficulties – and often in need of timely ear tube placement – to include intellectual disability, learning disorder, and attention-deficit/hyperactivity disorder.
“Most of what we said in the 2013 [original] guideline was good and still valid ... and [important for] pediatricians, who are the key players” in managing otitis media, Jesse Hackell, MD, one of two general pediatricians who served on the Academy’s guideline update committee, said in an interview.
OME spontaneously clears up to 90% of the time within 3 months, said Dr. Hackell, of Pomona (New York) Pediatrics, and chair of the American Academy of Pediatrics (AAP) Committee on Practice and Ambulatory Medicine.
The updated guideline, for children 6 months to 12 years, reaffirms a recommendation that tube insertion be offered to children with “bilateral OME for 3 months or longer AND documented hearing difficulties.”
It also reaffirms “options” (a lesser quality of evidence) that in the absence of hearing difficulties, surgery may be performed for children with chronic OME (3 months or longer) in one or both ears if 1) they are at increased risk of developmental difficulties from OME or 2) effusion is likely contributing to balance problems, poor school performance, behavioral problems, ear discomfort, or reduced quality of life.
Children with chronic OME who do not undergo surgery should be reevaluated at 3- to 6-month intervals and monitored until effusion is no longer present, significant hearing loss is detected, or structural abnormalities of the tympanic membrane or middle ear are detected, the update again recommends.
Tympanostomy tube placement is the most common ambulatory surgery performed on children in the United States, the guideline authors say. In 2014, about 9% of children had undergone the surgery, they wrote, noting also that “tubes were placed in 25%-30% of children with frequent ear infections.”
Recurrent AOM
The AAO-HNSF guidance regarding tympanostomy tubes for OME is similar overall to management guidance issued by the AAP in its clinical practice guideline on OME.
The organizations differ, however, on their guidance for tube insertion for recurrent AOM. In its 2013 clinical practice guideline on AOM, the AAP recommends that clinicians may offer tube insertion for recurrent AOM, with no mention of the presence or absence of persistent fluid as a consideration.
According to the AAO-HNSF update, grade A evidence, including some research published since its original 2013 guideline, has shown little benefit to tube insertion in reducing the incidence of AOM in otherwise healthy children who don’t have middle ear effusion.
One study published in 2019 assessed outcomes after watchful waiting and found that only one-third of 123 children eventually went on to tympanostomy tube placement, noted Richard M. Rosenfeld, MD, distinguished professor and chairman of otolaryngology at SUNY Downstate Health Sciences University in Brooklyn, N.Y., and lead author of the original and updated guidelines.
In practice, “the real question [for the ENT] is the future. If the ears are perfectly clear, will tubes really reduce the frequency of infections going forward?” Dr. Rosenfeld said in an interview. “All the evidence seems to say no, it doesn’t make much of a difference.”
Dr. Hackell said he’s confident that the question “is settled enough.” While there “could be stronger research and higher quality studies, the evidence is still pretty good to suggest you gain little to no benefit with tubes when you’re dealing with recurrent AOM without effusion,” he said.
Asked to comment on the ENT update and its guidance on tympanostomy tubes for children with recurrent AOM, an AAP spokesperson said the “issue is under review” and that the AAP did not currently have a statement.
At-risk children
The AAO-HNSF update renews a recommendation to evaluate children with either recurrent AOM or OME of any duration for increased risk for speech, language, or learning problems from OME because of baseline factors (sensory, physical, cognitive, or behavioral).
When OME becomes chronic – or when a tympanogram gives a flat-line reading – OME is likely to persist, and families of at-risk children especially should be encouraged to pursue tube placement, Dr. Rosenfeld said.
Despite prior guidance to this effect, he said, ear tubes are being underutilized in at-risk children, with effusion being missed in primary care and with ENTs not expediting tube placement upon referral.
“These children have learning issues, cognitive issues, developmental issues,” he said in the interview. “It’s a population that does very poorly with ears full of fluid ... and despite guidance suggesting these children should be prioritized with tubes, it doesn’t seem to be happening enough.”
Formulating guidelines for at-risk children is challenging because they are often excluded from trials, Dr. Rosenfeld said, which limits evidence about the benefits of tubes and limits the strength of recommendations.
The addition of attention-deficit/hyperactivity disorder, intellectual disability, and learning disorder to the list of risk factors is notable, Dr. Hackell said. (The list includes autism spectrum disorder, developmental delay, and suspected or confirmed speech and language delay or disorder.)
“We know that kids with ADHD take in and process information a little differently ... it may be harder to get their attention with auditory stimulation,” he said. “So anything that would impact the taking in of information even for a short period of time increases their risk.”
Surgical practice
ENTs are advised in the new guidance to use long-term tubes and perioperative antibiotic ear drops more judiciously. “Long-term tubes have a role, but there are some doctors who routinely use them, even for a first-time surgery,” said Dr. Rosenfeld.
Overuse of long-term tubes results in a higher incidence of tympanic membrane perforation, chronic drainage, and other complications, as well as greater need for long-term follow-up. “There needs to be a reason – something to justify the need for prolonged ventilation,” he said.
Perioperative antibiotic ear drops are often administered during surgery and then prescribed routinely for all children afterward, but research has shown that saline irrigation during surgery and a single application of antibiotic/steroid drops is similarly efficacious in preventing otorrhea, the guideline says. Antibiotic ear drops are also “expensive,” noted Dr. Hackell. “There’s not enough benefit to justify it.”
The update also more explicitly advises selective use of adenoidectomy. A new option says that clinicians may perform the procedure as an adjunct to tube insertion for children 4 years or older to potentially reduce the future incidence of recurrent OME or the need for repeat surgery.
However, in younger children, it should not be offered unless there are symptoms directly related to adenoid infection or nasal obstruction. “Under 4 years, there’s no primary benefit for the ears,” said Dr. Rosenfeld.
Follow-up with the surgeon after tympanostomy tube insertion should occur within 3 months to assess outcomes and educate the family, the update strongly recommends.
And pediatricians should know, Dr. Hackell notes, that clinical evidence continues to show that earplugs and other water precautions are not routinely needed for children who have tubes in place. A good approach, the guideline says, is to “first avoid water precautions and instead reserve them for children with recurrent or persistent tympanostomy tube otorrhea.”
Asked to comment on the guideline update, Tim Joos, MD, MPH, who practices combined internal medicine/pediatrics in Seattle and is an editorial advisory board member of Pediatric News, noted the inclusion of patient information sheets with frequently asked questions – resources that can be useful for guiding parents through what’s often a shared decision-making process.
Neither Dr. Rosenfeld nor Dr. Hackell reported any disclosures. Other members of the guideline update committee reported various book royalties, consulting fees, and other disclosures. Dr. Joos reported he has no connections to the guideline authors.
A practice guideline update from the ENT community on tympanostomy tubes in children reaffirms that tube insertion should not be considered in cases of otitis media with effusion (OME) lasting less than 3 months, or in children with recurrent acute otitis media (AOM) without middle ear effusion at the time of assessment for the procedure.
New in the update from the American Academy of Otolaryngology–Head and Neck Surgery Foundation (AAO-HNSF) is a strong recommendation for timely follow-up after surgery and recommendations against both routine use of prophylactic antibiotic ear drops after surgery and the initial use of long-term tubes except when there are specific reasons for doing so.
The update also expands the list of risk factors that place children with OME at increased risk of developmental difficulties – and often in need of timely ear tube placement – to include intellectual disability, learning disorder, and attention-deficit/hyperactivity disorder.
“Most of what we said in the 2013 [original] guideline was good and still valid ... and [important for] pediatricians, who are the key players” in managing otitis media, Jesse Hackell, MD, one of two general pediatricians who served on the Academy’s guideline update committee, said in an interview.
OME spontaneously clears up to 90% of the time within 3 months, said Dr. Hackell, of Pomona (New York) Pediatrics, and chair of the American Academy of Pediatrics (AAP) Committee on Practice and Ambulatory Medicine.
The updated guideline, for children 6 months to 12 years, reaffirms a recommendation that tube insertion be offered to children with “bilateral OME for 3 months or longer AND documented hearing difficulties.”
It also reaffirms “options” (a lesser quality of evidence) that in the absence of hearing difficulties, surgery may be performed for children with chronic OME (3 months or longer) in one or both ears if 1) they are at increased risk of developmental difficulties from OME or 2) effusion is likely contributing to balance problems, poor school performance, behavioral problems, ear discomfort, or reduced quality of life.
Children with chronic OME who do not undergo surgery should be reevaluated at 3- to 6-month intervals and monitored until effusion is no longer present, significant hearing loss is detected, or structural abnormalities of the tympanic membrane or middle ear are detected, the update again recommends.
Tympanostomy tube placement is the most common ambulatory surgery performed on children in the United States, the guideline authors say. In 2014, about 9% of children had undergone the surgery, they wrote, noting also that “tubes were placed in 25%-30% of children with frequent ear infections.”
Recurrent AOM
The AAO-HNSF guidance regarding tympanostomy tubes for OME is similar overall to management guidance issued by the AAP in its clinical practice guideline on OME.
The organizations differ, however, on their guidance for tube insertion for recurrent AOM. In its 2013 clinical practice guideline on AOM, the AAP recommends that clinicians may offer tube insertion for recurrent AOM, with no mention of the presence or absence of persistent fluid as a consideration.
According to the AAO-HNSF update, grade A evidence, including some research published since its original 2013 guideline, has shown little benefit to tube insertion in reducing the incidence of AOM in otherwise healthy children who don’t have middle ear effusion.
One study published in 2019 assessed outcomes after watchful waiting and found that only one-third of 123 children eventually went on to tympanostomy tube placement, noted Richard M. Rosenfeld, MD, distinguished professor and chairman of otolaryngology at SUNY Downstate Health Sciences University in Brooklyn, N.Y., and lead author of the original and updated guidelines.
In practice, “the real question [for the ENT] is the future. If the ears are perfectly clear, will tubes really reduce the frequency of infections going forward?” Dr. Rosenfeld said in an interview. “All the evidence seems to say no, it doesn’t make much of a difference.”
Dr. Hackell said he’s confident that the question “is settled enough.” While there “could be stronger research and higher quality studies, the evidence is still pretty good to suggest you gain little to no benefit with tubes when you’re dealing with recurrent AOM without effusion,” he said.
Asked to comment on the ENT update and its guidance on tympanostomy tubes for children with recurrent AOM, an AAP spokesperson said the “issue is under review” and that the AAP did not currently have a statement.
At-risk children
The AAO-HNSF update renews a recommendation to evaluate children with either recurrent AOM or OME of any duration for increased risk for speech, language, or learning problems from OME because of baseline factors (sensory, physical, cognitive, or behavioral).
When OME becomes chronic – or when a tympanogram gives a flat-line reading – OME is likely to persist, and families of at-risk children especially should be encouraged to pursue tube placement, Dr. Rosenfeld said.
Despite prior guidance to this effect, he said, ear tubes are being underutilized in at-risk children, with effusion being missed in primary care and with ENTs not expediting tube placement upon referral.
“These children have learning issues, cognitive issues, developmental issues,” he said in the interview. “It’s a population that does very poorly with ears full of fluid ... and despite guidance suggesting these children should be prioritized with tubes, it doesn’t seem to be happening enough.”
Formulating guidelines for at-risk children is challenging because they are often excluded from trials, Dr. Rosenfeld said, which limits evidence about the benefits of tubes and limits the strength of recommendations.
The addition of attention-deficit/hyperactivity disorder, intellectual disability, and learning disorder to the list of risk factors is notable, Dr. Hackell said. (The list includes autism spectrum disorder, developmental delay, and suspected or confirmed speech and language delay or disorder.)
“We know that kids with ADHD take in and process information a little differently ... it may be harder to get their attention with auditory stimulation,” he said. “So anything that would impact the taking in of information even for a short period of time increases their risk.”
Surgical practice
ENTs are advised in the new guidance to use long-term tubes and perioperative antibiotic ear drops more judiciously. “Long-term tubes have a role, but there are some doctors who routinely use them, even for a first-time surgery,” said Dr. Rosenfeld.
Overuse of long-term tubes results in a higher incidence of tympanic membrane perforation, chronic drainage, and other complications, as well as greater need for long-term follow-up. “There needs to be a reason – something to justify the need for prolonged ventilation,” he said.
Perioperative antibiotic ear drops are often administered during surgery and then prescribed routinely for all children afterward, but research has shown that saline irrigation during surgery and a single application of antibiotic/steroid drops is similarly efficacious in preventing otorrhea, the guideline says. Antibiotic ear drops are also “expensive,” noted Dr. Hackell. “There’s not enough benefit to justify it.”
The update also more explicitly advises selective use of adenoidectomy. A new option says that clinicians may perform the procedure as an adjunct to tube insertion for children 4 years or older to potentially reduce the future incidence of recurrent OME or the need for repeat surgery.
However, in younger children, it should not be offered unless there are symptoms directly related to adenoid infection or nasal obstruction. “Under 4 years, there’s no primary benefit for the ears,” said Dr. Rosenfeld.
Follow-up with the surgeon after tympanostomy tube insertion should occur within 3 months to assess outcomes and educate the family, the update strongly recommends.
And pediatricians should know, Dr. Hackell notes, that clinical evidence continues to show that earplugs and other water precautions are not routinely needed for children who have tubes in place. A good approach, the guideline says, is to “first avoid water precautions and instead reserve them for children with recurrent or persistent tympanostomy tube otorrhea.”
Asked to comment on the guideline update, Tim Joos, MD, MPH, who practices combined internal medicine/pediatrics in Seattle and is an editorial advisory board member of Pediatric News, noted the inclusion of patient information sheets with frequently asked questions – resources that can be useful for guiding parents through what’s often a shared decision-making process.
Neither Dr. Rosenfeld nor Dr. Hackell reported any disclosures. Other members of the guideline update committee reported various book royalties, consulting fees, and other disclosures. Dr. Joos reported he has no connections to the guideline authors.
FROM OTOLARYNGOLOGY HEAD AND NECK SURGERY
PCOS common in adolescent girls with type 2 diabetes
Polycystic ovary syndrome is common in girls with type 2 diabetes, findings of a new study suggest, and authors say screening for PCOS is critical in this group.
In a systematic review and meta-analysis involving 470 girls (average age 12.9-16.1 years) with type 2 diabetes in six studies, the prevalence of PCOS was nearly 1 in 5 (19.58%; 95% confidence interval, 12.02%-27.14%; P = .002), substantially higher than that of PCOS in the general adolescent population.
PCOS, a complex endocrine disorder, occurs in 1.14%-11.04% of adolescent girls globally, according to the paper published online in JAMA Network Open.
The secondary outcome studied links to prevalence of PCOS with race and obesity.
Insulin resistance and compensatory hyperinsulinemia are present in 44%-70% of women with PCOS, suggesting that they are more likely to develop type 2 diabetes, according to the researchers led by Milena Cioana, BHSc, with the department of pediatrics, McMaster University, Hamilton, Ont.
Kelly A. Curran, MD, an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center in Oklahoma City, where she practices adolescent medicine, said in an interview that it has been known that women with PCOS have higher rates of diabetes and many in the field have suspected the relationship is bidirectional.
“In my clinical practice, I’ve seen a high percentage of women with type 2 diabetes present with irregular menses, some of whom have gone on to be diagnosed with PCOS,” said Dr. Curran, who was not involved with the study.
However, she said, she was surprised the prevalence of PCOS reported in this paper – nearly one in five – was so high. Early diagnosis is important for PCOS to prevent complications such as hypertension, hyperglycemia, and dyslipidemia.
Psychiatric conditions are also prevalent in patients with PCOS, including anxiety (18%), depression (16%), and ADHD (9%).
Dr. Curran agreed there is a need to screen for PCOS and to evaluate for other causes of irregular periods in patients with type 2 diabetes.
“Menstrual irregularities are often overlooked in young women without further work-up, especially in patients who have chronic illnesses,” she noted.
Results come with a caveat
However, the authors said, results should be viewed with caution because “studies including the larger numbers of girls did not report the criteria used to diagnose PCOS, which is a challenge during adolescence.”
Diagnostic criteria for PCOS during adolescence include the combination of menstrual irregularities according to time since their first period and clinical or biochemical hyperandrogenism after excluding other potential causes.
Dr. Curran explained that PCOS symptoms include irregular periods and acne which can overlap with normal changes in puberty. In her experience, PCOS is often diagnosed without patients meeting full criteria. She agreed further research with standardized criteria is urgently needed.
The European Society of Human Reproduction and Embryology/American Society of Reproductive Medicine, the Pediatric Endocrine Society, and the International Consortium of Paediatric Endocrinology guidelines suggest that using ultrasound to check the size of ovaries could help diagnose PCOS, but other guidelines are more conservative, the authors noted.
They added that “there is a need for a consensus to establish the pediatric criteria for diagnosing PCOS in adolescents to ensure accurate diagnosis and lower the misclassification rates.”
Assessing links to obesity and race
Still unclear, the authors wrote, is whether and how obesity and race affect prevalence of PCOS among girls with type 2 diabetes.
The authors wrote: “Although earlier studies suggested that obesity-related insulin resistance and hyperinsulinemia can contribute to PCOS pathogenesis, insulin resistance in patients with PCOS may be present independently of [body mass index]. Obesity seems to increase the risk of PCOS only slightly and might represent a referral bias for PCOS.”
Few studies included in the meta-analysis had race-specific data, so the authors were limited in assessing associations between race and PCOS prevalence.
“However,” they wrote, “our data demonstrate that Indian girls had the highest prevalence, followed by White girls, and then Indigenous girls in Canada.”
Further studies are needed to help define at-risk subgroups and evaluate treatment strategies, the authors noted.
They reported having no relevant financial relationships. Dr. Curran had no conflicts of interest.
Polycystic ovary syndrome is common in girls with type 2 diabetes, findings of a new study suggest, and authors say screening for PCOS is critical in this group.
In a systematic review and meta-analysis involving 470 girls (average age 12.9-16.1 years) with type 2 diabetes in six studies, the prevalence of PCOS was nearly 1 in 5 (19.58%; 95% confidence interval, 12.02%-27.14%; P = .002), substantially higher than that of PCOS in the general adolescent population.
PCOS, a complex endocrine disorder, occurs in 1.14%-11.04% of adolescent girls globally, according to the paper published online in JAMA Network Open.
The secondary outcome studied links to prevalence of PCOS with race and obesity.
Insulin resistance and compensatory hyperinsulinemia are present in 44%-70% of women with PCOS, suggesting that they are more likely to develop type 2 diabetes, according to the researchers led by Milena Cioana, BHSc, with the department of pediatrics, McMaster University, Hamilton, Ont.
Kelly A. Curran, MD, an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center in Oklahoma City, where she practices adolescent medicine, said in an interview that it has been known that women with PCOS have higher rates of diabetes and many in the field have suspected the relationship is bidirectional.
“In my clinical practice, I’ve seen a high percentage of women with type 2 diabetes present with irregular menses, some of whom have gone on to be diagnosed with PCOS,” said Dr. Curran, who was not involved with the study.
However, she said, she was surprised the prevalence of PCOS reported in this paper – nearly one in five – was so high. Early diagnosis is important for PCOS to prevent complications such as hypertension, hyperglycemia, and dyslipidemia.
Psychiatric conditions are also prevalent in patients with PCOS, including anxiety (18%), depression (16%), and ADHD (9%).
Dr. Curran agreed there is a need to screen for PCOS and to evaluate for other causes of irregular periods in patients with type 2 diabetes.
“Menstrual irregularities are often overlooked in young women without further work-up, especially in patients who have chronic illnesses,” she noted.
Results come with a caveat
However, the authors said, results should be viewed with caution because “studies including the larger numbers of girls did not report the criteria used to diagnose PCOS, which is a challenge during adolescence.”
Diagnostic criteria for PCOS during adolescence include the combination of menstrual irregularities according to time since their first period and clinical or biochemical hyperandrogenism after excluding other potential causes.
Dr. Curran explained that PCOS symptoms include irregular periods and acne which can overlap with normal changes in puberty. In her experience, PCOS is often diagnosed without patients meeting full criteria. She agreed further research with standardized criteria is urgently needed.
The European Society of Human Reproduction and Embryology/American Society of Reproductive Medicine, the Pediatric Endocrine Society, and the International Consortium of Paediatric Endocrinology guidelines suggest that using ultrasound to check the size of ovaries could help diagnose PCOS, but other guidelines are more conservative, the authors noted.
They added that “there is a need for a consensus to establish the pediatric criteria for diagnosing PCOS in adolescents to ensure accurate diagnosis and lower the misclassification rates.”
Assessing links to obesity and race
Still unclear, the authors wrote, is whether and how obesity and race affect prevalence of PCOS among girls with type 2 diabetes.
The authors wrote: “Although earlier studies suggested that obesity-related insulin resistance and hyperinsulinemia can contribute to PCOS pathogenesis, insulin resistance in patients with PCOS may be present independently of [body mass index]. Obesity seems to increase the risk of PCOS only slightly and might represent a referral bias for PCOS.”
Few studies included in the meta-analysis had race-specific data, so the authors were limited in assessing associations between race and PCOS prevalence.
“However,” they wrote, “our data demonstrate that Indian girls had the highest prevalence, followed by White girls, and then Indigenous girls in Canada.”
Further studies are needed to help define at-risk subgroups and evaluate treatment strategies, the authors noted.
They reported having no relevant financial relationships. Dr. Curran had no conflicts of interest.
Polycystic ovary syndrome is common in girls with type 2 diabetes, findings of a new study suggest, and authors say screening for PCOS is critical in this group.
In a systematic review and meta-analysis involving 470 girls (average age 12.9-16.1 years) with type 2 diabetes in six studies, the prevalence of PCOS was nearly 1 in 5 (19.58%; 95% confidence interval, 12.02%-27.14%; P = .002), substantially higher than that of PCOS in the general adolescent population.
PCOS, a complex endocrine disorder, occurs in 1.14%-11.04% of adolescent girls globally, according to the paper published online in JAMA Network Open.
The secondary outcome studied links to prevalence of PCOS with race and obesity.
Insulin resistance and compensatory hyperinsulinemia are present in 44%-70% of women with PCOS, suggesting that they are more likely to develop type 2 diabetes, according to the researchers led by Milena Cioana, BHSc, with the department of pediatrics, McMaster University, Hamilton, Ont.
Kelly A. Curran, MD, an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center in Oklahoma City, where she practices adolescent medicine, said in an interview that it has been known that women with PCOS have higher rates of diabetes and many in the field have suspected the relationship is bidirectional.
“In my clinical practice, I’ve seen a high percentage of women with type 2 diabetes present with irregular menses, some of whom have gone on to be diagnosed with PCOS,” said Dr. Curran, who was not involved with the study.
However, she said, she was surprised the prevalence of PCOS reported in this paper – nearly one in five – was so high. Early diagnosis is important for PCOS to prevent complications such as hypertension, hyperglycemia, and dyslipidemia.
Psychiatric conditions are also prevalent in patients with PCOS, including anxiety (18%), depression (16%), and ADHD (9%).
Dr. Curran agreed there is a need to screen for PCOS and to evaluate for other causes of irregular periods in patients with type 2 diabetes.
“Menstrual irregularities are often overlooked in young women without further work-up, especially in patients who have chronic illnesses,” she noted.
Results come with a caveat
However, the authors said, results should be viewed with caution because “studies including the larger numbers of girls did not report the criteria used to diagnose PCOS, which is a challenge during adolescence.”
Diagnostic criteria for PCOS during adolescence include the combination of menstrual irregularities according to time since their first period and clinical or biochemical hyperandrogenism after excluding other potential causes.
Dr. Curran explained that PCOS symptoms include irregular periods and acne which can overlap with normal changes in puberty. In her experience, PCOS is often diagnosed without patients meeting full criteria. She agreed further research with standardized criteria is urgently needed.
The European Society of Human Reproduction and Embryology/American Society of Reproductive Medicine, the Pediatric Endocrine Society, and the International Consortium of Paediatric Endocrinology guidelines suggest that using ultrasound to check the size of ovaries could help diagnose PCOS, but other guidelines are more conservative, the authors noted.
They added that “there is a need for a consensus to establish the pediatric criteria for diagnosing PCOS in adolescents to ensure accurate diagnosis and lower the misclassification rates.”
Assessing links to obesity and race
Still unclear, the authors wrote, is whether and how obesity and race affect prevalence of PCOS among girls with type 2 diabetes.
The authors wrote: “Although earlier studies suggested that obesity-related insulin resistance and hyperinsulinemia can contribute to PCOS pathogenesis, insulin resistance in patients with PCOS may be present independently of [body mass index]. Obesity seems to increase the risk of PCOS only slightly and might represent a referral bias for PCOS.”
Few studies included in the meta-analysis had race-specific data, so the authors were limited in assessing associations between race and PCOS prevalence.
“However,” they wrote, “our data demonstrate that Indian girls had the highest prevalence, followed by White girls, and then Indigenous girls in Canada.”
Further studies are needed to help define at-risk subgroups and evaluate treatment strategies, the authors noted.
They reported having no relevant financial relationships. Dr. Curran had no conflicts of interest.
FROM JAMA NETWORK OPEN
Medical students help dispel kids’ fears with teddy bear clinics
In December 2021, 26 medical students at Florida State University (FSU) waltzed into the FSU Child Care and Early Learning Center loaded with armfuls of plushy, cute teddy bears. For the first time in several years, the Pediatric Interest Group opened the doors to their teddy bear clinic – an annual event that gives students an opportunity to practice their leadership skills while also helping to demystify trips to the doctor for the young participants.
At the clinic, children aged 2-4 emulate basic medical practices on their fuzzy patients under the guidance of the students.
Teddy bear clinics were started by FSU’s College of Medicine Family Medicine Interest Group in 2018, but it slowed to a halt until second-year medical student Taylor Posey approached the Pediatric Interest Group during her tenure as the group’s president about reinstating a similar program. At FSU, interest groups allow students who are not quite sure which field of medicine they’d like to pursue to gain experience in any they have interest in.
“Pediatrics is the reason I wanted to go to medical school,” Ms. Posey told this news organization. “So it was great that working on this project really solidified the thought that I did the right thing. It’s great to watch the volunteers and children interact together.”
The clinic divides the children into three groups: 2-year-old toddlers, 3-year-old “tweens,” and 4-year-old pre-K children.
The toddlers paint white handprints on black construction paper to “create” x-rays and learn about them. The tweens are given medical equipment such as paper stethoscopes, thermometers, Band Aids, cotton balls, and Q-Tips to put into their very own doctor bags, which are really just folders with the emblematic red plus sign sticker attached to the front. The Pre-K kids are tasked with giving their teddy bears medical exams under the watchful eye of the medical students. Together, they examine the teddy bear’s eyes, heart, and lungs.
“There’s growing research out there that says medical play – which can be defined as children playing as if they were the parents of the teddy bear, learning about a diagnosis, and treating it – decreases the anxiety in children when they go to visit a doctor. Having real medical equipment that the children can manipulate as opposed to plastic toys really makes a big difference,” Ms. Posey said.
One of Ms. Posey’s peers worked with her to create developmentally appropriate activities for the children. Ms. Posey said that some of the ideas for the clinic came from Pinterest boards.
“The planning of it worked really well. I was expecting things to fall through, but they didn’t,” Ms. Posey said. “It can be tough working with young children and trying to do activities with them so that you’re not doing too much but also not having too low of expectations.”
“It was really a massive success on all fronts,” said Mary P. Norton, MD, an assistant professor of pediatrics and faculty Pediatric Interest Group advisor for the clinic. “The ability to be in the community and get hands-on experience has been really cut down by the pandemic, and this allowed for our students to be able to go out in person and apply what they learned in the classroom with the age group they want to work with, which is fantastic.”
Perhaps the most impactful aspect of the clinic is its ability to help ease children’s fears about visits to the doctor. “We want to allow children to have a voice and give them a space to be a part of their treatment plan,” Dr. Norton said. “We want to say, ‘Your voice matters, you’re not a passive being,’ so that they’re a part of that relationship and show them that their experience is important. We hope these clinics aid in forming a partnership between parents, children, and doctors.”
Currently, the Pediatric Interest Group is hoping to have an annual teddy bear clinic. In the future, they hope to increase it to one a semester.
“These registered student organizations are 100% student run – student ideas, student volunteers, connections, and partnerships,” Dr. Norton said. “This clinic was all Taylor and all of the students. I can’t say how proud she is [to be] taking the time out of her busy medical student schedule to organize this for herself, her peers, and for these children.”
A version of this article first appeared on Medscape.com.
In December 2021, 26 medical students at Florida State University (FSU) waltzed into the FSU Child Care and Early Learning Center loaded with armfuls of plushy, cute teddy bears. For the first time in several years, the Pediatric Interest Group opened the doors to their teddy bear clinic – an annual event that gives students an opportunity to practice their leadership skills while also helping to demystify trips to the doctor for the young participants.
At the clinic, children aged 2-4 emulate basic medical practices on their fuzzy patients under the guidance of the students.
Teddy bear clinics were started by FSU’s College of Medicine Family Medicine Interest Group in 2018, but it slowed to a halt until second-year medical student Taylor Posey approached the Pediatric Interest Group during her tenure as the group’s president about reinstating a similar program. At FSU, interest groups allow students who are not quite sure which field of medicine they’d like to pursue to gain experience in any they have interest in.
“Pediatrics is the reason I wanted to go to medical school,” Ms. Posey told this news organization. “So it was great that working on this project really solidified the thought that I did the right thing. It’s great to watch the volunteers and children interact together.”
The clinic divides the children into three groups: 2-year-old toddlers, 3-year-old “tweens,” and 4-year-old pre-K children.
The toddlers paint white handprints on black construction paper to “create” x-rays and learn about them. The tweens are given medical equipment such as paper stethoscopes, thermometers, Band Aids, cotton balls, and Q-Tips to put into their very own doctor bags, which are really just folders with the emblematic red plus sign sticker attached to the front. The Pre-K kids are tasked with giving their teddy bears medical exams under the watchful eye of the medical students. Together, they examine the teddy bear’s eyes, heart, and lungs.
“There’s growing research out there that says medical play – which can be defined as children playing as if they were the parents of the teddy bear, learning about a diagnosis, and treating it – decreases the anxiety in children when they go to visit a doctor. Having real medical equipment that the children can manipulate as opposed to plastic toys really makes a big difference,” Ms. Posey said.
One of Ms. Posey’s peers worked with her to create developmentally appropriate activities for the children. Ms. Posey said that some of the ideas for the clinic came from Pinterest boards.
“The planning of it worked really well. I was expecting things to fall through, but they didn’t,” Ms. Posey said. “It can be tough working with young children and trying to do activities with them so that you’re not doing too much but also not having too low of expectations.”
“It was really a massive success on all fronts,” said Mary P. Norton, MD, an assistant professor of pediatrics and faculty Pediatric Interest Group advisor for the clinic. “The ability to be in the community and get hands-on experience has been really cut down by the pandemic, and this allowed for our students to be able to go out in person and apply what they learned in the classroom with the age group they want to work with, which is fantastic.”
Perhaps the most impactful aspect of the clinic is its ability to help ease children’s fears about visits to the doctor. “We want to allow children to have a voice and give them a space to be a part of their treatment plan,” Dr. Norton said. “We want to say, ‘Your voice matters, you’re not a passive being,’ so that they’re a part of that relationship and show them that their experience is important. We hope these clinics aid in forming a partnership between parents, children, and doctors.”
Currently, the Pediatric Interest Group is hoping to have an annual teddy bear clinic. In the future, they hope to increase it to one a semester.
“These registered student organizations are 100% student run – student ideas, student volunteers, connections, and partnerships,” Dr. Norton said. “This clinic was all Taylor and all of the students. I can’t say how proud she is [to be] taking the time out of her busy medical student schedule to organize this for herself, her peers, and for these children.”
A version of this article first appeared on Medscape.com.
In December 2021, 26 medical students at Florida State University (FSU) waltzed into the FSU Child Care and Early Learning Center loaded with armfuls of plushy, cute teddy bears. For the first time in several years, the Pediatric Interest Group opened the doors to their teddy bear clinic – an annual event that gives students an opportunity to practice their leadership skills while also helping to demystify trips to the doctor for the young participants.
At the clinic, children aged 2-4 emulate basic medical practices on their fuzzy patients under the guidance of the students.
Teddy bear clinics were started by FSU’s College of Medicine Family Medicine Interest Group in 2018, but it slowed to a halt until second-year medical student Taylor Posey approached the Pediatric Interest Group during her tenure as the group’s president about reinstating a similar program. At FSU, interest groups allow students who are not quite sure which field of medicine they’d like to pursue to gain experience in any they have interest in.
“Pediatrics is the reason I wanted to go to medical school,” Ms. Posey told this news organization. “So it was great that working on this project really solidified the thought that I did the right thing. It’s great to watch the volunteers and children interact together.”
The clinic divides the children into three groups: 2-year-old toddlers, 3-year-old “tweens,” and 4-year-old pre-K children.
The toddlers paint white handprints on black construction paper to “create” x-rays and learn about them. The tweens are given medical equipment such as paper stethoscopes, thermometers, Band Aids, cotton balls, and Q-Tips to put into their very own doctor bags, which are really just folders with the emblematic red plus sign sticker attached to the front. The Pre-K kids are tasked with giving their teddy bears medical exams under the watchful eye of the medical students. Together, they examine the teddy bear’s eyes, heart, and lungs.
“There’s growing research out there that says medical play – which can be defined as children playing as if they were the parents of the teddy bear, learning about a diagnosis, and treating it – decreases the anxiety in children when they go to visit a doctor. Having real medical equipment that the children can manipulate as opposed to plastic toys really makes a big difference,” Ms. Posey said.
One of Ms. Posey’s peers worked with her to create developmentally appropriate activities for the children. Ms. Posey said that some of the ideas for the clinic came from Pinterest boards.
“The planning of it worked really well. I was expecting things to fall through, but they didn’t,” Ms. Posey said. “It can be tough working with young children and trying to do activities with them so that you’re not doing too much but also not having too low of expectations.”
“It was really a massive success on all fronts,” said Mary P. Norton, MD, an assistant professor of pediatrics and faculty Pediatric Interest Group advisor for the clinic. “The ability to be in the community and get hands-on experience has been really cut down by the pandemic, and this allowed for our students to be able to go out in person and apply what they learned in the classroom with the age group they want to work with, which is fantastic.”
Perhaps the most impactful aspect of the clinic is its ability to help ease children’s fears about visits to the doctor. “We want to allow children to have a voice and give them a space to be a part of their treatment plan,” Dr. Norton said. “We want to say, ‘Your voice matters, you’re not a passive being,’ so that they’re a part of that relationship and show them that their experience is important. We hope these clinics aid in forming a partnership between parents, children, and doctors.”
Currently, the Pediatric Interest Group is hoping to have an annual teddy bear clinic. In the future, they hope to increase it to one a semester.
“These registered student organizations are 100% student run – student ideas, student volunteers, connections, and partnerships,” Dr. Norton said. “This clinic was all Taylor and all of the students. I can’t say how proud she is [to be] taking the time out of her busy medical student schedule to organize this for herself, her peers, and for these children.”
A version of this article first appeared on Medscape.com.
Treatment duration for acute otitis media – so many choices
Twenty years ago, the dilemma in treating acute otitis media (AOM) was which among 10-plus antibiotics to prescribe. A recent column discussed the evolving pathogen distribution in AOM and its effects on antibiotic choices.1 But here we consider treatment duration. Until the past decade, AOM treatment (except azithromycin) involved 10-day courses. But lately, 10-day antibiotic regimens for uncomplicated infections are disappearing. Shorter-course recommendations are the new norm because of the evolving clinical data showing that an appropriately chosen antibiotic (in partnership with host defenses and source control) resolves infection faster than was previously thought. Shorter courses make sense because of fewer adverse effects, less distortion of normal flora, and less likely induction of pathogen resistance. Table 4.12 in the newest 2021-2024 SOID Redbook lists three antibiotic durations for AOM, and actually there are more than that.
Why so many duration options? Clinical data show that not all AOM is alike and short courses work for subsets of AOM because, besides antibiotics, key elements in AOM resolution are host anatomy and immunity. Bacterial AOM results from a combination of refluxed pathogens in the middle ear being trapped when the eustachian tube malfunctions (infection occurs when middle ear plumbing gets stopped up). If the eustachian tube spontaneously drains and the host immune response slows/stops pathogen growth, no antibiotics are needed. Indeed, a sizable proportion of mild/moderate AOM episodes spontaneously resolve, particularly in children over 2 years old. So a high likelihood of spontaneous remission allows an initial 0-days duration option (watchful waiting) or delayed antibiotics (rescue prescriptions) for older children.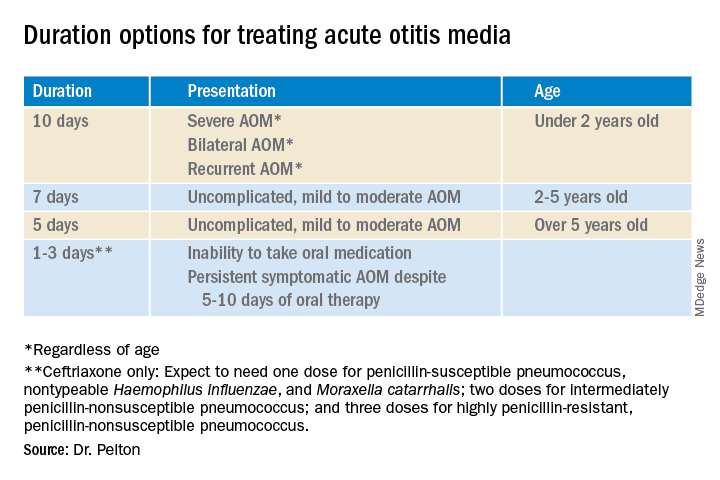
That said, when one chooses to initially prescribe antibiotics for AOM, different durations are recommended. Table 1 has my suggestions.
Data that gave me better microbiological understanding of why oral AOM trials less than 10 days were successful involved purulent AOM drainage from children who had pressure-equalizing (PE) tubes.2 The authors randomized children to either standard-dose amoxicillin-clavulanate or placebo. Of note, 95% of pathogens were susceptible to the antibiotic; 5% were pneumococcus intermediately resistant to penicillin. The authors sampled ear drainage daily for 7 days. Figure 1 shows that cultures remained positive in only around 5% of children by day 3-5 of antibiotics, but viable bacteria persisted through 7 days in over half of placebo recipients. Remember, both groups benefited from a form of source control (drainage of the middle ear via PE tubes). So, if antibiotics can do the job in 3-5 days, why continue antibiotics beyond 5 days?
Anatomy and severity. In children over 5 years old (reasonably mature eustachian tube anatomy) with nonrecurrent (no AOM in past month), nonsevere (no otalgia or high fever) AOM, 5 days is enough. But 2- to 5-year-olds (less mature anatomy) need 7 days and those <2 years old (least mature plumbing) need 10 days. Likewise, severe AOM usually warrants 10 days. Some experts recommend 10 days for bilateral AOM as well.
These age/severity differences make sense because failures are more frequent with:
1. Younger age.3 While not proven, my hypothesis is that “natural” source control (spontaneous internal draining the middle ear into the nasopharynx [NP]) is less frequent in younger children because they have less mature eustachian tube systems. Further, reflux of persisting NP organisms could restart a new AOM episode even if the original pathogen was eliminated by a short 5-day course.
2. Severe AOM. A rationale for longer courses in severe AOM (ear pain, high fever) is that high middle-ear pressures (indicated by degree of tympanic membrane bulging and ear pain) could impede antibiotic penetration, or that high initial bacterial loads (perhaps indicated by systemic fever) require more antibiotic. And finally, return to baseline eustachian tube function may take longer if severe AOM caused enhanced inflammation.
3. Recurrent AOM. (AOM within 1 prior month) – With recurrent AOM, the second “hit” to the eustachian tube may lead to more dysfunction, so a longer antibiotic course may be required to allow more complete source control and more time for more complete functional recovery after a repeated inflammatory injury.
4. Bilateral AOM. Two independent but infected sites mean twice the chance for failure. So, a longer course could allow more time for both sites to undergo “natural” source control.4
More bacteria – more antibiotic? So, is more antibiotic really needed for a higher bacterial load? In vitro this is known as the “inoculum effect,” particularly for beta-lactam drugs, for example, amoxicillin and cephalosporins. Laboratory susceptibility testing is performed with a specifically defined quantity of bacteria (105 bacteria/mL) and the minimum inhibitory concentration (MIC) is the lowest antibiotic concentration that stops bacterial growth. We know that drugs will likely fail if the MIC exceeds the achievable antibiotic concentration at the infection site. But is it as simple as just exceeding the MIC at the infection site? No, pharmacodynamics tell us that overall antibiotic exposure is also important. For example, to be successful, beta-lactam concentrations need to be above the MIC for 40%-50% of the day.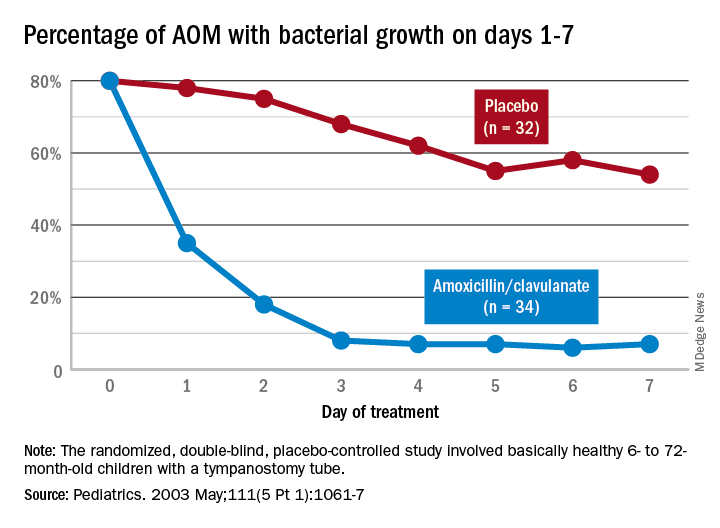
Higher MIC with higher bacterial load. Particularly for beta-lactams, testing with a quantity of bacteria >105/mL produces a higher MIC in vitro. This suggests that clinical failure could occur, even when our in vivo dosing leads to 40%-50% above the “standard” MIC that was obtained from testing the lab standard of 105/mL bacteria, when the infected site’s (middle ear) bacterial load is >105/mL (such higher bacterial loads occur in up to 30% of AOM).5 One way to negate inoculum effect is source control (drain the abscess or debridement), which reduces the bacterial load as well as allowing better antibiotic penetration– both favoring infection resolution. But with suboptimal source control, for example, the middle ear is not drained externally or internally, longer courses (more antibiotic exposure) could aid resolution. Whether the exposure can be administered as higher doses in fewer days or standard doses for more days is debatable but consider that a single parenteral dose of ceftriaxone successfully resolves AOM not attributable to penicillin-nonsusceptible pneumococcus.6Bottom line: Even though the number of potential antibiotics has contracted in the past 20 years, the need to individualize AOM treatment remains important and duration choices are more complex. Indeed, AOM comes in different flavors with patient age, clinical presentation, and episode frequency dictating the choice of duration.
Dr. Christopher J. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics in Kansas City, Mo. Email him at [email protected].
References
1. Pichichero ME. MDedge. 2022 Jan 11.
2. Ruohola A et al. Pediatrics. 2003;111(5):1061-7.
3. Hoberman A et al. N Engl J Med. 2016;375(25):2446-56.
4. Pichichero ME et al. Otolaryngol Head Neck Surg. 2001;124(4):381-7.
5. Harrison CJ et al. Pediatr Infect Dis. 1985;4(6):641-6.
6. Leibovitz E et al. Pediatr Infect Dis. 2000;19(11):1040-5.
Twenty years ago, the dilemma in treating acute otitis media (AOM) was which among 10-plus antibiotics to prescribe. A recent column discussed the evolving pathogen distribution in AOM and its effects on antibiotic choices.1 But here we consider treatment duration. Until the past decade, AOM treatment (except azithromycin) involved 10-day courses. But lately, 10-day antibiotic regimens for uncomplicated infections are disappearing. Shorter-course recommendations are the new norm because of the evolving clinical data showing that an appropriately chosen antibiotic (in partnership with host defenses and source control) resolves infection faster than was previously thought. Shorter courses make sense because of fewer adverse effects, less distortion of normal flora, and less likely induction of pathogen resistance. Table 4.12 in the newest 2021-2024 SOID Redbook lists three antibiotic durations for AOM, and actually there are more than that.
Why so many duration options? Clinical data show that not all AOM is alike and short courses work for subsets of AOM because, besides antibiotics, key elements in AOM resolution are host anatomy and immunity. Bacterial AOM results from a combination of refluxed pathogens in the middle ear being trapped when the eustachian tube malfunctions (infection occurs when middle ear plumbing gets stopped up). If the eustachian tube spontaneously drains and the host immune response slows/stops pathogen growth, no antibiotics are needed. Indeed, a sizable proportion of mild/moderate AOM episodes spontaneously resolve, particularly in children over 2 years old. So a high likelihood of spontaneous remission allows an initial 0-days duration option (watchful waiting) or delayed antibiotics (rescue prescriptions) for older children.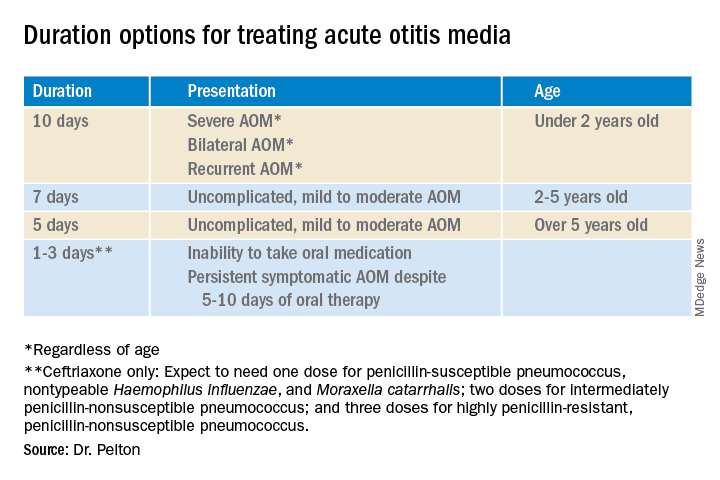
That said, when one chooses to initially prescribe antibiotics for AOM, different durations are recommended. Table 1 has my suggestions.
Data that gave me better microbiological understanding of why oral AOM trials less than 10 days were successful involved purulent AOM drainage from children who had pressure-equalizing (PE) tubes.2 The authors randomized children to either standard-dose amoxicillin-clavulanate or placebo. Of note, 95% of pathogens were susceptible to the antibiotic; 5% were pneumococcus intermediately resistant to penicillin. The authors sampled ear drainage daily for 7 days. Figure 1 shows that cultures remained positive in only around 5% of children by day 3-5 of antibiotics, but viable bacteria persisted through 7 days in over half of placebo recipients. Remember, both groups benefited from a form of source control (drainage of the middle ear via PE tubes). So, if antibiotics can do the job in 3-5 days, why continue antibiotics beyond 5 days?
Anatomy and severity. In children over 5 years old (reasonably mature eustachian tube anatomy) with nonrecurrent (no AOM in past month), nonsevere (no otalgia or high fever) AOM, 5 days is enough. But 2- to 5-year-olds (less mature anatomy) need 7 days and those <2 years old (least mature plumbing) need 10 days. Likewise, severe AOM usually warrants 10 days. Some experts recommend 10 days for bilateral AOM as well.
These age/severity differences make sense because failures are more frequent with:
1. Younger age.3 While not proven, my hypothesis is that “natural” source control (spontaneous internal draining the middle ear into the nasopharynx [NP]) is less frequent in younger children because they have less mature eustachian tube systems. Further, reflux of persisting NP organisms could restart a new AOM episode even if the original pathogen was eliminated by a short 5-day course.
2. Severe AOM. A rationale for longer courses in severe AOM (ear pain, high fever) is that high middle-ear pressures (indicated by degree of tympanic membrane bulging and ear pain) could impede antibiotic penetration, or that high initial bacterial loads (perhaps indicated by systemic fever) require more antibiotic. And finally, return to baseline eustachian tube function may take longer if severe AOM caused enhanced inflammation.
3. Recurrent AOM. (AOM within 1 prior month) – With recurrent AOM, the second “hit” to the eustachian tube may lead to more dysfunction, so a longer antibiotic course may be required to allow more complete source control and more time for more complete functional recovery after a repeated inflammatory injury.
4. Bilateral AOM. Two independent but infected sites mean twice the chance for failure. So, a longer course could allow more time for both sites to undergo “natural” source control.4
More bacteria – more antibiotic? So, is more antibiotic really needed for a higher bacterial load? In vitro this is known as the “inoculum effect,” particularly for beta-lactam drugs, for example, amoxicillin and cephalosporins. Laboratory susceptibility testing is performed with a specifically defined quantity of bacteria (105 bacteria/mL) and the minimum inhibitory concentration (MIC) is the lowest antibiotic concentration that stops bacterial growth. We know that drugs will likely fail if the MIC exceeds the achievable antibiotic concentration at the infection site. But is it as simple as just exceeding the MIC at the infection site? No, pharmacodynamics tell us that overall antibiotic exposure is also important. For example, to be successful, beta-lactam concentrations need to be above the MIC for 40%-50% of the day.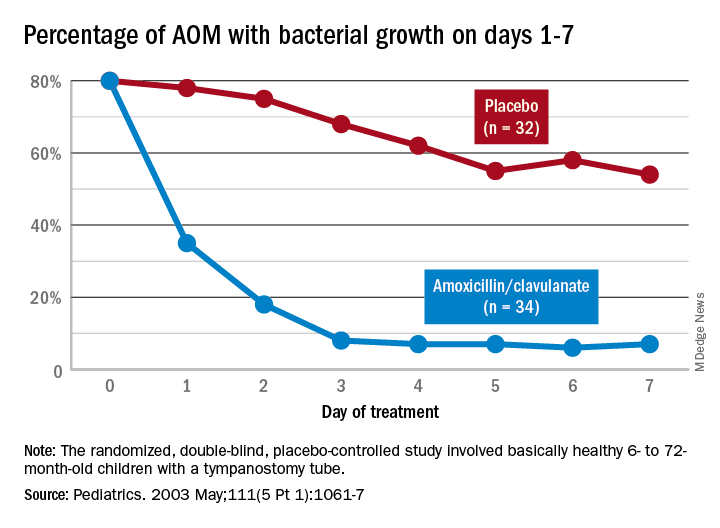
Higher MIC with higher bacterial load. Particularly for beta-lactams, testing with a quantity of bacteria >105/mL produces a higher MIC in vitro. This suggests that clinical failure could occur, even when our in vivo dosing leads to 40%-50% above the “standard” MIC that was obtained from testing the lab standard of 105/mL bacteria, when the infected site’s (middle ear) bacterial load is >105/mL (such higher bacterial loads occur in up to 30% of AOM).5 One way to negate inoculum effect is source control (drain the abscess or debridement), which reduces the bacterial load as well as allowing better antibiotic penetration– both favoring infection resolution. But with suboptimal source control, for example, the middle ear is not drained externally or internally, longer courses (more antibiotic exposure) could aid resolution. Whether the exposure can be administered as higher doses in fewer days or standard doses for more days is debatable but consider that a single parenteral dose of ceftriaxone successfully resolves AOM not attributable to penicillin-nonsusceptible pneumococcus.6Bottom line: Even though the number of potential antibiotics has contracted in the past 20 years, the need to individualize AOM treatment remains important and duration choices are more complex. Indeed, AOM comes in different flavors with patient age, clinical presentation, and episode frequency dictating the choice of duration.
Dr. Christopher J. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics in Kansas City, Mo. Email him at [email protected].
References
1. Pichichero ME. MDedge. 2022 Jan 11.
2. Ruohola A et al. Pediatrics. 2003;111(5):1061-7.
3. Hoberman A et al. N Engl J Med. 2016;375(25):2446-56.
4. Pichichero ME et al. Otolaryngol Head Neck Surg. 2001;124(4):381-7.
5. Harrison CJ et al. Pediatr Infect Dis. 1985;4(6):641-6.
6. Leibovitz E et al. Pediatr Infect Dis. 2000;19(11):1040-5.
Twenty years ago, the dilemma in treating acute otitis media (AOM) was which among 10-plus antibiotics to prescribe. A recent column discussed the evolving pathogen distribution in AOM and its effects on antibiotic choices.1 But here we consider treatment duration. Until the past decade, AOM treatment (except azithromycin) involved 10-day courses. But lately, 10-day antibiotic regimens for uncomplicated infections are disappearing. Shorter-course recommendations are the new norm because of the evolving clinical data showing that an appropriately chosen antibiotic (in partnership with host defenses and source control) resolves infection faster than was previously thought. Shorter courses make sense because of fewer adverse effects, less distortion of normal flora, and less likely induction of pathogen resistance. Table 4.12 in the newest 2021-2024 SOID Redbook lists three antibiotic durations for AOM, and actually there are more than that.
Why so many duration options? Clinical data show that not all AOM is alike and short courses work for subsets of AOM because, besides antibiotics, key elements in AOM resolution are host anatomy and immunity. Bacterial AOM results from a combination of refluxed pathogens in the middle ear being trapped when the eustachian tube malfunctions (infection occurs when middle ear plumbing gets stopped up). If the eustachian tube spontaneously drains and the host immune response slows/stops pathogen growth, no antibiotics are needed. Indeed, a sizable proportion of mild/moderate AOM episodes spontaneously resolve, particularly in children over 2 years old. So a high likelihood of spontaneous remission allows an initial 0-days duration option (watchful waiting) or delayed antibiotics (rescue prescriptions) for older children.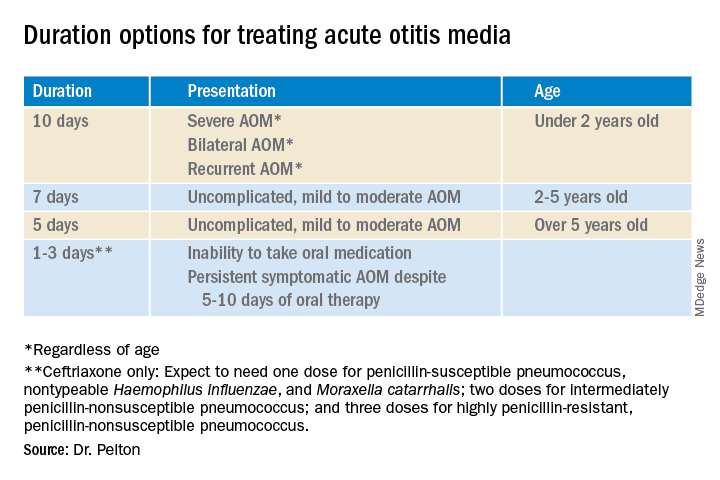
That said, when one chooses to initially prescribe antibiotics for AOM, different durations are recommended. Table 1 has my suggestions.
Data that gave me better microbiological understanding of why oral AOM trials less than 10 days were successful involved purulent AOM drainage from children who had pressure-equalizing (PE) tubes.2 The authors randomized children to either standard-dose amoxicillin-clavulanate or placebo. Of note, 95% of pathogens were susceptible to the antibiotic; 5% were pneumococcus intermediately resistant to penicillin. The authors sampled ear drainage daily for 7 days. Figure 1 shows that cultures remained positive in only around 5% of children by day 3-5 of antibiotics, but viable bacteria persisted through 7 days in over half of placebo recipients. Remember, both groups benefited from a form of source control (drainage of the middle ear via PE tubes). So, if antibiotics can do the job in 3-5 days, why continue antibiotics beyond 5 days?
Anatomy and severity. In children over 5 years old (reasonably mature eustachian tube anatomy) with nonrecurrent (no AOM in past month), nonsevere (no otalgia or high fever) AOM, 5 days is enough. But 2- to 5-year-olds (less mature anatomy) need 7 days and those <2 years old (least mature plumbing) need 10 days. Likewise, severe AOM usually warrants 10 days. Some experts recommend 10 days for bilateral AOM as well.
These age/severity differences make sense because failures are more frequent with:
1. Younger age.3 While not proven, my hypothesis is that “natural” source control (spontaneous internal draining the middle ear into the nasopharynx [NP]) is less frequent in younger children because they have less mature eustachian tube systems. Further, reflux of persisting NP organisms could restart a new AOM episode even if the original pathogen was eliminated by a short 5-day course.
2. Severe AOM. A rationale for longer courses in severe AOM (ear pain, high fever) is that high middle-ear pressures (indicated by degree of tympanic membrane bulging and ear pain) could impede antibiotic penetration, or that high initial bacterial loads (perhaps indicated by systemic fever) require more antibiotic. And finally, return to baseline eustachian tube function may take longer if severe AOM caused enhanced inflammation.
3. Recurrent AOM. (AOM within 1 prior month) – With recurrent AOM, the second “hit” to the eustachian tube may lead to more dysfunction, so a longer antibiotic course may be required to allow more complete source control and more time for more complete functional recovery after a repeated inflammatory injury.
4. Bilateral AOM. Two independent but infected sites mean twice the chance for failure. So, a longer course could allow more time for both sites to undergo “natural” source control.4
More bacteria – more antibiotic? So, is more antibiotic really needed for a higher bacterial load? In vitro this is known as the “inoculum effect,” particularly for beta-lactam drugs, for example, amoxicillin and cephalosporins. Laboratory susceptibility testing is performed with a specifically defined quantity of bacteria (105 bacteria/mL) and the minimum inhibitory concentration (MIC) is the lowest antibiotic concentration that stops bacterial growth. We know that drugs will likely fail if the MIC exceeds the achievable antibiotic concentration at the infection site. But is it as simple as just exceeding the MIC at the infection site? No, pharmacodynamics tell us that overall antibiotic exposure is also important. For example, to be successful, beta-lactam concentrations need to be above the MIC for 40%-50% of the day.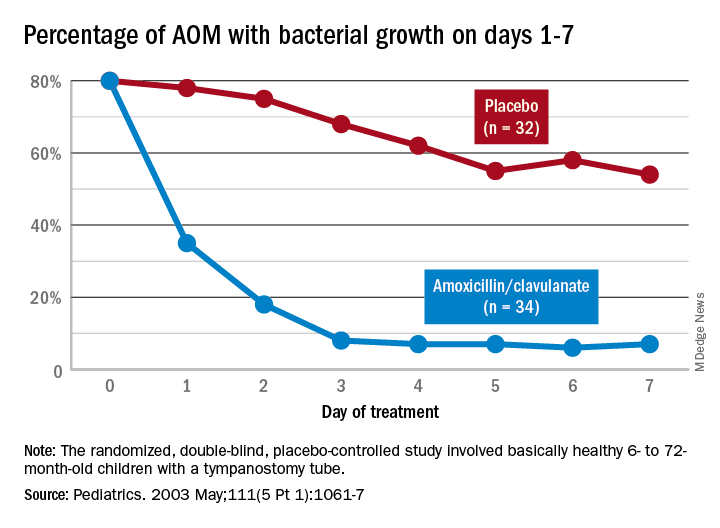
Higher MIC with higher bacterial load. Particularly for beta-lactams, testing with a quantity of bacteria >105/mL produces a higher MIC in vitro. This suggests that clinical failure could occur, even when our in vivo dosing leads to 40%-50% above the “standard” MIC that was obtained from testing the lab standard of 105/mL bacteria, when the infected site’s (middle ear) bacterial load is >105/mL (such higher bacterial loads occur in up to 30% of AOM).5 One way to negate inoculum effect is source control (drain the abscess or debridement), which reduces the bacterial load as well as allowing better antibiotic penetration– both favoring infection resolution. But with suboptimal source control, for example, the middle ear is not drained externally or internally, longer courses (more antibiotic exposure) could aid resolution. Whether the exposure can be administered as higher doses in fewer days or standard doses for more days is debatable but consider that a single parenteral dose of ceftriaxone successfully resolves AOM not attributable to penicillin-nonsusceptible pneumococcus.6Bottom line: Even though the number of potential antibiotics has contracted in the past 20 years, the need to individualize AOM treatment remains important and duration choices are more complex. Indeed, AOM comes in different flavors with patient age, clinical presentation, and episode frequency dictating the choice of duration.
Dr. Christopher J. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics in Kansas City, Mo. Email him at [email protected].
References
1. Pichichero ME. MDedge. 2022 Jan 11.
2. Ruohola A et al. Pediatrics. 2003;111(5):1061-7.
3. Hoberman A et al. N Engl J Med. 2016;375(25):2446-56.
4. Pichichero ME et al. Otolaryngol Head Neck Surg. 2001;124(4):381-7.
5. Harrison CJ et al. Pediatr Infect Dis. 1985;4(6):641-6.
6. Leibovitz E et al. Pediatr Infect Dis. 2000;19(11):1040-5.
CDC, AAP issues new guidelines to better define developmental milestones
The Centers for Disease Control and Prevention and the American Academy of Pediatrics recently issued revised milestone guidelines for their developmental surveillance campaign, Learn the Signs, Act Early (LTSAE).
The new guidelines, published in Pediatrics, were drafted in “easy-to-understand” language and identify the behaviors that 75% or more of children should exhibit at certain ages based on developmental resources, existing data, and clinician experience. The previous milestone checklists, developed in 2004, used 50th percentile or average-age milestones.
The CDC, in collaboration with the AAP, convened a group of eight subject matter experts in various fields of child development, including a developmental pediatrician and researcher from Kennedy Krieger Institute, to develop new and clearer guidelines.
“The goals of the group were to identify evidence-informed milestones to include in CDC checklists, clarify when most children can be expected to reach a milestone (to discourage a wait-and-see approach), and support clinical judgment regarding screening between recommended ages,” wrote lead author Jennifer M. Zubler, MD, of the National Center on Birth Defects and Developmental Disabilities in Atlanta, and colleagues.
Key changes
The experts established 11 criteria for CDC surveillance milestones and tools, including milestones most children (75% or more) would be expected to reach by defined health supervision visit ages and those that are easily recognized in natural settings.
Criteria for developmental milestones and surveillance tools:
- Milestones are included at the age most (≥75%) children would be expected to demonstrate the milestone.
- Eliminate “warning signs.”
- Are easy for families of different social, cultural, and ethnic backgrounds to observe and use.
- Are able to be answered with yes, not yet, or not sure.
- Use plain language, avoiding vague terms like may, can, and begins.
- Are organized in developmental domains.
- Show progression of skills with age, when possible.
- Milestones are not repeated across checklists.
- Include open-ended questions.
- Include information for developmental promotion.
- Include information on how to act early if there are concerns.
The previous guidelines were critiqued by some clinicians as being “not helpful to individual families who had concerns about their child’s development,” and in some cases, led to delays in diagnoses as decision-makers opted for a “wait-and-see approach.”
“The earlier a child is identified with a developmental delay the better, as treatment as well as learning interventions can begin,” Paul Lipkin, MD, an associate professor of pediatrics at the Johns Hopkins University, Baltimore, said in an accompanying press release. “Revising the guidelines with expertise and data from clinicians in the field accomplishes these goals.”
Additional changes included new checklists for children between the ages of 15 and 30 months, additional social and emotional milestones, as well as the removal of complex language and duplicate milestones. The experts also developed new, open-ended questions to aid discussions with families.
“Review of a child’s development with these milestones opens up a continuous dialogue between a parent and the health care provider about their child’s present and future development,” said Dr. Lipkin.
Originally pioneered in 2005, the LTSAE awareness campaign provides free resources to clinicians and families to support early detection of children with developmental delays and disabilities. After the new guidelines were drafted, they were presented to parents of various racial groups, income levels, and educational backgrounds to confirm ease of use and understandability.
“These criteria and revised checklists can be used to support developmental surveillance, clinical judgment regarding additional developmental screening, and research in developmental surveillance processes,” wrote Dr. Zubler.
Expert perspective
“These new guidelines will allow us to catch more children with developmental delays as they raise the threshold to 75% of children achieving those milestones at that particular age,” Karalyn Kinsella, MD, a pediatrician in Cheshire, Conn., said in an interview.
Dr. Kinsella added that the new guidelines simplify the milestones and reduce redundancy across different developmental domains. “Most importantly, it gave me the opportunity to see just how great the CDC milestone tracker app is – I think parents would really like it.”
This project was supported by the CDC and Prevention of the Department of Health & Human Services. One author is a developer of the Ages & Stages Questionnaires and receives royalties from Brookes Publishing, the company that publishes this tool; the other authors have indicated they have no relevant conflicts of interest to disclose.
The Centers for Disease Control and Prevention and the American Academy of Pediatrics recently issued revised milestone guidelines for their developmental surveillance campaign, Learn the Signs, Act Early (LTSAE).
The new guidelines, published in Pediatrics, were drafted in “easy-to-understand” language and identify the behaviors that 75% or more of children should exhibit at certain ages based on developmental resources, existing data, and clinician experience. The previous milestone checklists, developed in 2004, used 50th percentile or average-age milestones.
The CDC, in collaboration with the AAP, convened a group of eight subject matter experts in various fields of child development, including a developmental pediatrician and researcher from Kennedy Krieger Institute, to develop new and clearer guidelines.
“The goals of the group were to identify evidence-informed milestones to include in CDC checklists, clarify when most children can be expected to reach a milestone (to discourage a wait-and-see approach), and support clinical judgment regarding screening between recommended ages,” wrote lead author Jennifer M. Zubler, MD, of the National Center on Birth Defects and Developmental Disabilities in Atlanta, and colleagues.
Key changes
The experts established 11 criteria for CDC surveillance milestones and tools, including milestones most children (75% or more) would be expected to reach by defined health supervision visit ages and those that are easily recognized in natural settings.
Criteria for developmental milestones and surveillance tools:
- Milestones are included at the age most (≥75%) children would be expected to demonstrate the milestone.
- Eliminate “warning signs.”
- Are easy for families of different social, cultural, and ethnic backgrounds to observe and use.
- Are able to be answered with yes, not yet, or not sure.
- Use plain language, avoiding vague terms like may, can, and begins.
- Are organized in developmental domains.
- Show progression of skills with age, when possible.
- Milestones are not repeated across checklists.
- Include open-ended questions.
- Include information for developmental promotion.
- Include information on how to act early if there are concerns.
The previous guidelines were critiqued by some clinicians as being “not helpful to individual families who had concerns about their child’s development,” and in some cases, led to delays in diagnoses as decision-makers opted for a “wait-and-see approach.”
“The earlier a child is identified with a developmental delay the better, as treatment as well as learning interventions can begin,” Paul Lipkin, MD, an associate professor of pediatrics at the Johns Hopkins University, Baltimore, said in an accompanying press release. “Revising the guidelines with expertise and data from clinicians in the field accomplishes these goals.”
Additional changes included new checklists for children between the ages of 15 and 30 months, additional social and emotional milestones, as well as the removal of complex language and duplicate milestones. The experts also developed new, open-ended questions to aid discussions with families.
“Review of a child’s development with these milestones opens up a continuous dialogue between a parent and the health care provider about their child’s present and future development,” said Dr. Lipkin.
Originally pioneered in 2005, the LTSAE awareness campaign provides free resources to clinicians and families to support early detection of children with developmental delays and disabilities. After the new guidelines were drafted, they were presented to parents of various racial groups, income levels, and educational backgrounds to confirm ease of use and understandability.
“These criteria and revised checklists can be used to support developmental surveillance, clinical judgment regarding additional developmental screening, and research in developmental surveillance processes,” wrote Dr. Zubler.
Expert perspective
“These new guidelines will allow us to catch more children with developmental delays as they raise the threshold to 75% of children achieving those milestones at that particular age,” Karalyn Kinsella, MD, a pediatrician in Cheshire, Conn., said in an interview.
Dr. Kinsella added that the new guidelines simplify the milestones and reduce redundancy across different developmental domains. “Most importantly, it gave me the opportunity to see just how great the CDC milestone tracker app is – I think parents would really like it.”
This project was supported by the CDC and Prevention of the Department of Health & Human Services. One author is a developer of the Ages & Stages Questionnaires and receives royalties from Brookes Publishing, the company that publishes this tool; the other authors have indicated they have no relevant conflicts of interest to disclose.
The Centers for Disease Control and Prevention and the American Academy of Pediatrics recently issued revised milestone guidelines for their developmental surveillance campaign, Learn the Signs, Act Early (LTSAE).
The new guidelines, published in Pediatrics, were drafted in “easy-to-understand” language and identify the behaviors that 75% or more of children should exhibit at certain ages based on developmental resources, existing data, and clinician experience. The previous milestone checklists, developed in 2004, used 50th percentile or average-age milestones.
The CDC, in collaboration with the AAP, convened a group of eight subject matter experts in various fields of child development, including a developmental pediatrician and researcher from Kennedy Krieger Institute, to develop new and clearer guidelines.
“The goals of the group were to identify evidence-informed milestones to include in CDC checklists, clarify when most children can be expected to reach a milestone (to discourage a wait-and-see approach), and support clinical judgment regarding screening between recommended ages,” wrote lead author Jennifer M. Zubler, MD, of the National Center on Birth Defects and Developmental Disabilities in Atlanta, and colleagues.
Key changes
The experts established 11 criteria for CDC surveillance milestones and tools, including milestones most children (75% or more) would be expected to reach by defined health supervision visit ages and those that are easily recognized in natural settings.
Criteria for developmental milestones and surveillance tools:
- Milestones are included at the age most (≥75%) children would be expected to demonstrate the milestone.
- Eliminate “warning signs.”
- Are easy for families of different social, cultural, and ethnic backgrounds to observe and use.
- Are able to be answered with yes, not yet, or not sure.
- Use plain language, avoiding vague terms like may, can, and begins.
- Are organized in developmental domains.
- Show progression of skills with age, when possible.
- Milestones are not repeated across checklists.
- Include open-ended questions.
- Include information for developmental promotion.
- Include information on how to act early if there are concerns.
The previous guidelines were critiqued by some clinicians as being “not helpful to individual families who had concerns about their child’s development,” and in some cases, led to delays in diagnoses as decision-makers opted for a “wait-and-see approach.”
“The earlier a child is identified with a developmental delay the better, as treatment as well as learning interventions can begin,” Paul Lipkin, MD, an associate professor of pediatrics at the Johns Hopkins University, Baltimore, said in an accompanying press release. “Revising the guidelines with expertise and data from clinicians in the field accomplishes these goals.”
Additional changes included new checklists for children between the ages of 15 and 30 months, additional social and emotional milestones, as well as the removal of complex language and duplicate milestones. The experts also developed new, open-ended questions to aid discussions with families.
“Review of a child’s development with these milestones opens up a continuous dialogue between a parent and the health care provider about their child’s present and future development,” said Dr. Lipkin.
Originally pioneered in 2005, the LTSAE awareness campaign provides free resources to clinicians and families to support early detection of children with developmental delays and disabilities. After the new guidelines were drafted, they were presented to parents of various racial groups, income levels, and educational backgrounds to confirm ease of use and understandability.
“These criteria and revised checklists can be used to support developmental surveillance, clinical judgment regarding additional developmental screening, and research in developmental surveillance processes,” wrote Dr. Zubler.
Expert perspective
“These new guidelines will allow us to catch more children with developmental delays as they raise the threshold to 75% of children achieving those milestones at that particular age,” Karalyn Kinsella, MD, a pediatrician in Cheshire, Conn., said in an interview.
Dr. Kinsella added that the new guidelines simplify the milestones and reduce redundancy across different developmental domains. “Most importantly, it gave me the opportunity to see just how great the CDC milestone tracker app is – I think parents would really like it.”
This project was supported by the CDC and Prevention of the Department of Health & Human Services. One author is a developer of the Ages & Stages Questionnaires and receives royalties from Brookes Publishing, the company that publishes this tool; the other authors have indicated they have no relevant conflicts of interest to disclose.
FROM PEDIATRICS
Autism, ADHD linked to increased mortality risk
All-cause mortality is significantly higher for individuals with autism spectrum disorder or attention-deficit/hyperactivity disorder than for the general population, based on data from more than 600,000 individuals.
Studies of individuals with mental disorders have suggested an increased mortality risk, compared with the general population, but similar studies of individuals with autism spectrum disorder (ASD) or ADHD have yielded inconsistent results, Ferrán Catalá-López, PhD, of the Institute of Health Carlos III, Madrid, and colleagues wrote.
In a systematic review and meta-analysis published in JAMA Pediatrics, the researchers examined 27 studies including 642,260 individuals; 154,238 with ASD and 396,488 with ADHD. The studies were published up to April 1, 2021, and included deaths from natural causes (such as respiratory illness or cancer) and unnatural (external) causes, such as accident, injury, or poisoning. The proportion of females in the studies ranged from 14% to 100%; the follow-up ranged from 3 to 33 years; and three studies included first-degree relatives.
Overall, all-cause mortality was significantly higher among individuals with ASD (rate ratio, 2.37) and ADHD (RR, 2.13), compared with the general population. Among individuals with ASD, deaths from natural causes and unnatural causes were significantly increased, compared with the general population (RR, 3.80 and RR, 2.50, respectively). Among individuals with ADHD, deaths from natural causes were not significantly increased (RR, 1.62), but deaths from unnatural causes were significantly increased, compared with the general population (RR, 2.81).
Potential mechanisms to explain the excess mortality among individuals with ASD and ADHD include health determinants and biological pathways, but the complex nature of the associations make the establishment of causality a challenge, the researchers wrote in their discussion of the findings. In general, “severe mental and behavioral disorders appear to be associated with reduced life expectancy, both in terms of mortality from external causes and mortality from other medical conditions or diseases.” With regard to ASD/ADHD in particular, these individuals often experience emotional and social problems as they enter adulthood. “Behaviors such as impulsivity and/or inattention can be contributing factors for injuries and unintentional incidents in children with ASD/ADHD,” they added.
The study findings were limited by several factors including the possible omission of studies and the use of study-level data rather than individual participant data, as well as the limitation of electronic health records, the researchers noted. Also, the studies were mostly conducted in Western countries and the results may not be generalizable to other countries.
Although ASD and ADHD were associated with a significant increased risk of all-cause mortality, “the results should be interpreted with caution because there was evidence of heterogeneity between study estimates of the mortality risks,” the researchers said. However, the results were strengthened by the large study sample, and offer a comprehensive look at the evidence supporting increased mortality risk among individuals with ASD or ADHD, and highlight the need to identify modifiable risk factors.
“Understanding the mechanisms of these associations may lead to targeted strategies to prevent avoidable deaths in high-risk groups of children and young people as an approach to improve public health,” they said.
Recent research support associations
The study was important because ASD and ADHD may persist into adulthood, but data from previous epidemiological studies on the impact of these disorders on mortality are inconsistent, lead author Dr. Catalá-López said in an interview.
“We conducted a systematic review and meta-analysis to evaluate all available studies of mortality associations in people with these disorders, which provide the most updated and evidence-based approach,” he explained. “Our study has only become possible in the past few years because several large population-based epidemiological studies have been available reporting similar mortality-related outcomes.”
Dr. Catalá-López said that the study findings have value in clinical practice. “We found that people with autism or attention-deficit/hyperactivity disorders would have an increased risk of mortality when compared to the general population. In our opinion, understanding the causes and mechanisms of these associations can lead to specific strategies to prevent avoidable deaths.
“Autism and attention-hyperactivity/deficit disorder are problems that can be managed with adequate and concrete programs at an early age, and most premature deaths, at least deaths from unnatural causes, can be prevented,” Dr. Catalá-López said.
“Furthermore, we believe that these results may shed some light for future research. For example, more prospective studies would be needed, particularly to examine cause-specific mortality, in larger populations of children and youth with autism/attention-deficit/hyperactivity disorder, including some of the more common comorbidities,” Dr. Catalá-López added.
Findings support need for screening and prevention strategies
The clear message that individuals with ASD or ADHD often die of preventable or unnatural causes demands attention and “demands widespread recognition and the implementation of systematic screening and preventive approaches,” Russell A. Barkley, PhD, of Virginia Commonwealth University, Richmond, and Geraldine Dawson, PhD, of Duke University, Durham, N.C., wrote in an accompanying editorial.
The studies included in the review also demonstrate that ADHD is associated with more than a twofold risk of early mortality in children and a more than a fourfold risk in mortality by age 45 years, they said.
The editorialists noted that the increased mortality risk may explain the ongoing conundrum among clinicians as to why the prevalence of ADHD seems to decline with age, “such that 5%-8% of children may meet diagnostic criteria for ADHD while that figure falls to 4%-5% of adults and 2%-3% of older adults,” despite evidence that a majority of childhood cases will be rediagnosed in adulthood. However, the current study offers an alternative. “This systematic review and meta-analysis and the studies included within it make plain that another explanation is the greater loss of individuals with these conditions from the population over time owing to heightened mortality, compared with typical peers,” they said.
“In addition to ADHD diagnosis, ASD diagnosis is also associated with other psychiatric comorbidities that are correlated with increased risk for mortality, including anxiety and affective disorders,” the editorialists noted. Other considerations for increased mortality among individuals with ASD include different protective and risk factors associated with suicide risk, compared with the general population, as well as poorer social and daily living skills compared to the general population.
The study findings “argue for individuals with ADHD and individuals with ASD being viewed through a public health lens with screening and prevention strategies offered beginning in early childhood. These findings should also give impetus to efforts to try to reduce the first order risk factors that are predisposing to reduced life expectancy, such as obesity, substance use, poor diet, poor sleep, and limited exercise among children and adults with ASD and ADHD,” they said.
“A preventive strategy would necessitate primary care physicians becoming more aware of the linkage between both ASD diagnosis and ADHD diagnosis and early mortality as well as their link to reduced [estimated life expectancy],” and such an approach could potentially reduce the higher mortality risk identified in the current review, they concluded.
Dr. Barkley reported speaking and other fees from Takeda, Medice Pharmaceutical, and AstraZeneca; book royalties from Guilford Publications and the American Psychological Association; and course royalties from ContiningEdCourses.net and Premier Educational Seminars. Dr. Dawson reported grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Institute of Mental Health during the submitted work and personal fees from Apple. Dr. Dawson also disclosed a patent for license to Apple, and Dr. Dawson and Duke University have benefited financially from technology and data that have been licensed to Apple. The study was supported by the Institute of Health Carlos III and Generalitat Valenciana. Researchers including lead author Dr. Catalá-López received funding from sources including the Centro de Investigación Biomédica en Red de Salud Mental; one coauthor received support from an Australian Research Council Discovery Early Career Researcher Award, a new investigator award from the Canadian Institutes of Health Research and the Drug Safety and Effectiveness Network, the Spanish Health Services Research on Chronic Patients Network, and Institute of Health Carlos III. The researchers had no financial conflicts to disclose.
All-cause mortality is significantly higher for individuals with autism spectrum disorder or attention-deficit/hyperactivity disorder than for the general population, based on data from more than 600,000 individuals.
Studies of individuals with mental disorders have suggested an increased mortality risk, compared with the general population, but similar studies of individuals with autism spectrum disorder (ASD) or ADHD have yielded inconsistent results, Ferrán Catalá-López, PhD, of the Institute of Health Carlos III, Madrid, and colleagues wrote.
In a systematic review and meta-analysis published in JAMA Pediatrics, the researchers examined 27 studies including 642,260 individuals; 154,238 with ASD and 396,488 with ADHD. The studies were published up to April 1, 2021, and included deaths from natural causes (such as respiratory illness or cancer) and unnatural (external) causes, such as accident, injury, or poisoning. The proportion of females in the studies ranged from 14% to 100%; the follow-up ranged from 3 to 33 years; and three studies included first-degree relatives.
Overall, all-cause mortality was significantly higher among individuals with ASD (rate ratio, 2.37) and ADHD (RR, 2.13), compared with the general population. Among individuals with ASD, deaths from natural causes and unnatural causes were significantly increased, compared with the general population (RR, 3.80 and RR, 2.50, respectively). Among individuals with ADHD, deaths from natural causes were not significantly increased (RR, 1.62), but deaths from unnatural causes were significantly increased, compared with the general population (RR, 2.81).
Potential mechanisms to explain the excess mortality among individuals with ASD and ADHD include health determinants and biological pathways, but the complex nature of the associations make the establishment of causality a challenge, the researchers wrote in their discussion of the findings. In general, “severe mental and behavioral disorders appear to be associated with reduced life expectancy, both in terms of mortality from external causes and mortality from other medical conditions or diseases.” With regard to ASD/ADHD in particular, these individuals often experience emotional and social problems as they enter adulthood. “Behaviors such as impulsivity and/or inattention can be contributing factors for injuries and unintentional incidents in children with ASD/ADHD,” they added.
The study findings were limited by several factors including the possible omission of studies and the use of study-level data rather than individual participant data, as well as the limitation of electronic health records, the researchers noted. Also, the studies were mostly conducted in Western countries and the results may not be generalizable to other countries.
Although ASD and ADHD were associated with a significant increased risk of all-cause mortality, “the results should be interpreted with caution because there was evidence of heterogeneity between study estimates of the mortality risks,” the researchers said. However, the results were strengthened by the large study sample, and offer a comprehensive look at the evidence supporting increased mortality risk among individuals with ASD or ADHD, and highlight the need to identify modifiable risk factors.
“Understanding the mechanisms of these associations may lead to targeted strategies to prevent avoidable deaths in high-risk groups of children and young people as an approach to improve public health,” they said.
Recent research support associations
The study was important because ASD and ADHD may persist into adulthood, but data from previous epidemiological studies on the impact of these disorders on mortality are inconsistent, lead author Dr. Catalá-López said in an interview.
“We conducted a systematic review and meta-analysis to evaluate all available studies of mortality associations in people with these disorders, which provide the most updated and evidence-based approach,” he explained. “Our study has only become possible in the past few years because several large population-based epidemiological studies have been available reporting similar mortality-related outcomes.”
Dr. Catalá-López said that the study findings have value in clinical practice. “We found that people with autism or attention-deficit/hyperactivity disorders would have an increased risk of mortality when compared to the general population. In our opinion, understanding the causes and mechanisms of these associations can lead to specific strategies to prevent avoidable deaths.
“Autism and attention-hyperactivity/deficit disorder are problems that can be managed with adequate and concrete programs at an early age, and most premature deaths, at least deaths from unnatural causes, can be prevented,” Dr. Catalá-López said.
“Furthermore, we believe that these results may shed some light for future research. For example, more prospective studies would be needed, particularly to examine cause-specific mortality, in larger populations of children and youth with autism/attention-deficit/hyperactivity disorder, including some of the more common comorbidities,” Dr. Catalá-López added.
Findings support need for screening and prevention strategies
The clear message that individuals with ASD or ADHD often die of preventable or unnatural causes demands attention and “demands widespread recognition and the implementation of systematic screening and preventive approaches,” Russell A. Barkley, PhD, of Virginia Commonwealth University, Richmond, and Geraldine Dawson, PhD, of Duke University, Durham, N.C., wrote in an accompanying editorial.
The studies included in the review also demonstrate that ADHD is associated with more than a twofold risk of early mortality in children and a more than a fourfold risk in mortality by age 45 years, they said.
The editorialists noted that the increased mortality risk may explain the ongoing conundrum among clinicians as to why the prevalence of ADHD seems to decline with age, “such that 5%-8% of children may meet diagnostic criteria for ADHD while that figure falls to 4%-5% of adults and 2%-3% of older adults,” despite evidence that a majority of childhood cases will be rediagnosed in adulthood. However, the current study offers an alternative. “This systematic review and meta-analysis and the studies included within it make plain that another explanation is the greater loss of individuals with these conditions from the population over time owing to heightened mortality, compared with typical peers,” they said.
“In addition to ADHD diagnosis, ASD diagnosis is also associated with other psychiatric comorbidities that are correlated with increased risk for mortality, including anxiety and affective disorders,” the editorialists noted. Other considerations for increased mortality among individuals with ASD include different protective and risk factors associated with suicide risk, compared with the general population, as well as poorer social and daily living skills compared to the general population.
The study findings “argue for individuals with ADHD and individuals with ASD being viewed through a public health lens with screening and prevention strategies offered beginning in early childhood. These findings should also give impetus to efforts to try to reduce the first order risk factors that are predisposing to reduced life expectancy, such as obesity, substance use, poor diet, poor sleep, and limited exercise among children and adults with ASD and ADHD,” they said.
“A preventive strategy would necessitate primary care physicians becoming more aware of the linkage between both ASD diagnosis and ADHD diagnosis and early mortality as well as their link to reduced [estimated life expectancy],” and such an approach could potentially reduce the higher mortality risk identified in the current review, they concluded.
Dr. Barkley reported speaking and other fees from Takeda, Medice Pharmaceutical, and AstraZeneca; book royalties from Guilford Publications and the American Psychological Association; and course royalties from ContiningEdCourses.net and Premier Educational Seminars. Dr. Dawson reported grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Institute of Mental Health during the submitted work and personal fees from Apple. Dr. Dawson also disclosed a patent for license to Apple, and Dr. Dawson and Duke University have benefited financially from technology and data that have been licensed to Apple. The study was supported by the Institute of Health Carlos III and Generalitat Valenciana. Researchers including lead author Dr. Catalá-López received funding from sources including the Centro de Investigación Biomédica en Red de Salud Mental; one coauthor received support from an Australian Research Council Discovery Early Career Researcher Award, a new investigator award from the Canadian Institutes of Health Research and the Drug Safety and Effectiveness Network, the Spanish Health Services Research on Chronic Patients Network, and Institute of Health Carlos III. The researchers had no financial conflicts to disclose.
All-cause mortality is significantly higher for individuals with autism spectrum disorder or attention-deficit/hyperactivity disorder than for the general population, based on data from more than 600,000 individuals.
Studies of individuals with mental disorders have suggested an increased mortality risk, compared with the general population, but similar studies of individuals with autism spectrum disorder (ASD) or ADHD have yielded inconsistent results, Ferrán Catalá-López, PhD, of the Institute of Health Carlos III, Madrid, and colleagues wrote.
In a systematic review and meta-analysis published in JAMA Pediatrics, the researchers examined 27 studies including 642,260 individuals; 154,238 with ASD and 396,488 with ADHD. The studies were published up to April 1, 2021, and included deaths from natural causes (such as respiratory illness or cancer) and unnatural (external) causes, such as accident, injury, or poisoning. The proportion of females in the studies ranged from 14% to 100%; the follow-up ranged from 3 to 33 years; and three studies included first-degree relatives.
Overall, all-cause mortality was significantly higher among individuals with ASD (rate ratio, 2.37) and ADHD (RR, 2.13), compared with the general population. Among individuals with ASD, deaths from natural causes and unnatural causes were significantly increased, compared with the general population (RR, 3.80 and RR, 2.50, respectively). Among individuals with ADHD, deaths from natural causes were not significantly increased (RR, 1.62), but deaths from unnatural causes were significantly increased, compared with the general population (RR, 2.81).
Potential mechanisms to explain the excess mortality among individuals with ASD and ADHD include health determinants and biological pathways, but the complex nature of the associations make the establishment of causality a challenge, the researchers wrote in their discussion of the findings. In general, “severe mental and behavioral disorders appear to be associated with reduced life expectancy, both in terms of mortality from external causes and mortality from other medical conditions or diseases.” With regard to ASD/ADHD in particular, these individuals often experience emotional and social problems as they enter adulthood. “Behaviors such as impulsivity and/or inattention can be contributing factors for injuries and unintentional incidents in children with ASD/ADHD,” they added.
The study findings were limited by several factors including the possible omission of studies and the use of study-level data rather than individual participant data, as well as the limitation of electronic health records, the researchers noted. Also, the studies were mostly conducted in Western countries and the results may not be generalizable to other countries.
Although ASD and ADHD were associated with a significant increased risk of all-cause mortality, “the results should be interpreted with caution because there was evidence of heterogeneity between study estimates of the mortality risks,” the researchers said. However, the results were strengthened by the large study sample, and offer a comprehensive look at the evidence supporting increased mortality risk among individuals with ASD or ADHD, and highlight the need to identify modifiable risk factors.
“Understanding the mechanisms of these associations may lead to targeted strategies to prevent avoidable deaths in high-risk groups of children and young people as an approach to improve public health,” they said.
Recent research support associations
The study was important because ASD and ADHD may persist into adulthood, but data from previous epidemiological studies on the impact of these disorders on mortality are inconsistent, lead author Dr. Catalá-López said in an interview.
“We conducted a systematic review and meta-analysis to evaluate all available studies of mortality associations in people with these disorders, which provide the most updated and evidence-based approach,” he explained. “Our study has only become possible in the past few years because several large population-based epidemiological studies have been available reporting similar mortality-related outcomes.”
Dr. Catalá-López said that the study findings have value in clinical practice. “We found that people with autism or attention-deficit/hyperactivity disorders would have an increased risk of mortality when compared to the general population. In our opinion, understanding the causes and mechanisms of these associations can lead to specific strategies to prevent avoidable deaths.
“Autism and attention-hyperactivity/deficit disorder are problems that can be managed with adequate and concrete programs at an early age, and most premature deaths, at least deaths from unnatural causes, can be prevented,” Dr. Catalá-López said.
“Furthermore, we believe that these results may shed some light for future research. For example, more prospective studies would be needed, particularly to examine cause-specific mortality, in larger populations of children and youth with autism/attention-deficit/hyperactivity disorder, including some of the more common comorbidities,” Dr. Catalá-López added.
Findings support need for screening and prevention strategies
The clear message that individuals with ASD or ADHD often die of preventable or unnatural causes demands attention and “demands widespread recognition and the implementation of systematic screening and preventive approaches,” Russell A. Barkley, PhD, of Virginia Commonwealth University, Richmond, and Geraldine Dawson, PhD, of Duke University, Durham, N.C., wrote in an accompanying editorial.
The studies included in the review also demonstrate that ADHD is associated with more than a twofold risk of early mortality in children and a more than a fourfold risk in mortality by age 45 years, they said.
The editorialists noted that the increased mortality risk may explain the ongoing conundrum among clinicians as to why the prevalence of ADHD seems to decline with age, “such that 5%-8% of children may meet diagnostic criteria for ADHD while that figure falls to 4%-5% of adults and 2%-3% of older adults,” despite evidence that a majority of childhood cases will be rediagnosed in adulthood. However, the current study offers an alternative. “This systematic review and meta-analysis and the studies included within it make plain that another explanation is the greater loss of individuals with these conditions from the population over time owing to heightened mortality, compared with typical peers,” they said.
“In addition to ADHD diagnosis, ASD diagnosis is also associated with other psychiatric comorbidities that are correlated with increased risk for mortality, including anxiety and affective disorders,” the editorialists noted. Other considerations for increased mortality among individuals with ASD include different protective and risk factors associated with suicide risk, compared with the general population, as well as poorer social and daily living skills compared to the general population.
The study findings “argue for individuals with ADHD and individuals with ASD being viewed through a public health lens with screening and prevention strategies offered beginning in early childhood. These findings should also give impetus to efforts to try to reduce the first order risk factors that are predisposing to reduced life expectancy, such as obesity, substance use, poor diet, poor sleep, and limited exercise among children and adults with ASD and ADHD,” they said.
“A preventive strategy would necessitate primary care physicians becoming more aware of the linkage between both ASD diagnosis and ADHD diagnosis and early mortality as well as their link to reduced [estimated life expectancy],” and such an approach could potentially reduce the higher mortality risk identified in the current review, they concluded.
Dr. Barkley reported speaking and other fees from Takeda, Medice Pharmaceutical, and AstraZeneca; book royalties from Guilford Publications and the American Psychological Association; and course royalties from ContiningEdCourses.net and Premier Educational Seminars. Dr. Dawson reported grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Institute of Mental Health during the submitted work and personal fees from Apple. Dr. Dawson also disclosed a patent for license to Apple, and Dr. Dawson and Duke University have benefited financially from technology and data that have been licensed to Apple. The study was supported by the Institute of Health Carlos III and Generalitat Valenciana. Researchers including lead author Dr. Catalá-López received funding from sources including the Centro de Investigación Biomédica en Red de Salud Mental; one coauthor received support from an Australian Research Council Discovery Early Career Researcher Award, a new investigator award from the Canadian Institutes of Health Research and the Drug Safety and Effectiveness Network, the Spanish Health Services Research on Chronic Patients Network, and Institute of Health Carlos III. The researchers had no financial conflicts to disclose.
FROM JAMA PEDIATRICS
Strep infection and tics in children: new data
Group A streptococcus (GAS) infection is not associated with new-onset tic disorders in at-risk children, findings from a large prospective study show.
The results mean that if preteens present with a new-onset tic condition, “they’re unlikely to have it as a result of a group A streptococcal throat infection,” study author Anette Eleonore Schrag, MD, PhD, professor, department of clinical neuroscience, Institute of Neurology, University College London, told this news organization.
Therefore, clinicians should not automatically prescribe antibiotics for children with tics, which sometimes occurs, said Dr. Schrag.
The study was published online Feb. 2 in Neurology.
Ongoing controversy
Research shows that genetic and environmental factors contribute to chronic tic disorders (CTDs) and Tourette syndrome (TS). Prenatal exposure to maternal smoking and central nervous system (CNS) stimulants, as well as psychosocial stress, may play a role.
There has been an ongoing controversy regarding the possible role of GAS in tics, with some studies showing an association and others not showing a link. However, previous studies have been retrospective, registry based, or had limited sample size.
This new prospective study is the first in children without a tic disorder but who were at relatively high risk of developing one. The children were followed to assess development of streptococcal infections and tics, said Dr. Schrag.
The study included 259 children aged 3-10 years (mean baseline age, 6.8 years; over half female) who had a first-degree relative such as a parent or sibling with TS or CTD.
The average age at TS onset is 7 years, peaking in prevalence and severity at about 9-12 years. GAS throat infections are common in this age group.
Although study participants did not have tics themselves, they represented “an enriched group,” said Dr. Schrag. “Because they had family history, we knew they were at increased risk for developing tics.”
Participants were evaluated every 2 months, alternating between scheduled hospital visits and telephone interviews. Parents kept a weekly diary and were instructed to bring their child in for assessment if they showed any signs of tics.
The average follow-up period was 1.6 years, but some of the children were followed for up to 48 months. During the study, there were a total of 1,944 assessments, including 939 telephone interviews and 1,005 clinical visits.
More common in boys
Investigators defined tic onset as the first occurrence of any sudden, rapid, recurrent, nonrhythmic involuntary movement and/or vocalization on at least three separate days within a period of 3 weeks.
The investigators assessed GAS exposure using parameters from throat swabs, serum anti-streptolysin O titers, and anti-DNAse B titers.
They used multiple definitions and combinations of GAS exposures “to make sure we weren’t missing any association because we didn’t use the right definition,” said Dr. Schrag. She explained a definitive strep infection is not always clear-cut.
At baseline, 17.0% participants tested positive for GAS, and 78.8% tested negative. No throat swab was available from 4.2% of participants.
During follow-up, the number of confirmed positive GAS exposures was 59, 102, 125, and 138, depending on the definition.
Researchers identified 61 tic cases during the study period. There was no evidence of an association of tic onset with GAS exposure after adjusting for age, sex, and parental education level.
However, there was a strong association between tic onset and sex, with girls being 60% less likely to develop tics than boys (hazard ratio, 0.4; 95% CI, 0.2-0.7; P < .01).
This result wasn’t particularly surprising, as it’s known that more boys develop tics than girls. “We just confirmed that in a prospective way,” said Dr. Schrag.
Results from sensitivity analyses confirmed the results. This was also the case with analyses that excluded visits with missing data on GAS exposure and that further adjusted for clinical site and psychotropic medication use.
Other pathogens?
Although the results showed no association between strep and tics in this population, it does not “close the door completely” on a potential relationship, said Dr. Schrag.
“By and large, the development of tics in children is not associated with group A strep, but differences in small subgroups can never be excluded by a study like this.”
Participants in this study were part of the European Multicentre Tics in Children Studies (EMTICS), a prospective cohort study exploring the role of environmental and genetic factors in pediatric CTD. That project is also looking at immune system factors, “which might play a role in the development of chronic tic disorder and associated conditions,” said Dr. Schrag.
It’s still possible, she added, that other pathogens could play a role in tic development. “That’s going to be the subject of further analysis and future studies,” she said.
Tamara Pringsheim, MD, professor of clinical neurosciences, psychiatry, pediatrics, and community health sciences, University of Calgary (Alta.), praised the research.
“This was a well-designed study, with a large sample of 260 children followed for up to 4 years, using a standardized protocol to assess for group A streptococcal infection and new onset of tics.”
The study, which did not uncover an association between GAS exposure and tic onset, “provides high level evidence that group A streptococcal exposure is not an important risk factor for the new onset of tics in children with a family history of tic disorders.”
The study received funding from the European Union Seventh Framework Program for research technological development and demonstration. Dr. Schrag reports receiving consultancy or advisory board honoraria from Biogen, Abbvie, Bial, and Neurotechnology; research support from the National Institute of Health Research, Parkinsons UK, and the Economic and Social Research Council and the European Commission; and Royalties from Oxford University Press. Dr. Pringsheim reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Group A streptococcus (GAS) infection is not associated with new-onset tic disorders in at-risk children, findings from a large prospective study show.
The results mean that if preteens present with a new-onset tic condition, “they’re unlikely to have it as a result of a group A streptococcal throat infection,” study author Anette Eleonore Schrag, MD, PhD, professor, department of clinical neuroscience, Institute of Neurology, University College London, told this news organization.
Therefore, clinicians should not automatically prescribe antibiotics for children with tics, which sometimes occurs, said Dr. Schrag.
The study was published online Feb. 2 in Neurology.
Ongoing controversy
Research shows that genetic and environmental factors contribute to chronic tic disorders (CTDs) and Tourette syndrome (TS). Prenatal exposure to maternal smoking and central nervous system (CNS) stimulants, as well as psychosocial stress, may play a role.
There has been an ongoing controversy regarding the possible role of GAS in tics, with some studies showing an association and others not showing a link. However, previous studies have been retrospective, registry based, or had limited sample size.
This new prospective study is the first in children without a tic disorder but who were at relatively high risk of developing one. The children were followed to assess development of streptococcal infections and tics, said Dr. Schrag.
The study included 259 children aged 3-10 years (mean baseline age, 6.8 years; over half female) who had a first-degree relative such as a parent or sibling with TS or CTD.
The average age at TS onset is 7 years, peaking in prevalence and severity at about 9-12 years. GAS throat infections are common in this age group.
Although study participants did not have tics themselves, they represented “an enriched group,” said Dr. Schrag. “Because they had family history, we knew they were at increased risk for developing tics.”
Participants were evaluated every 2 months, alternating between scheduled hospital visits and telephone interviews. Parents kept a weekly diary and were instructed to bring their child in for assessment if they showed any signs of tics.
The average follow-up period was 1.6 years, but some of the children were followed for up to 48 months. During the study, there were a total of 1,944 assessments, including 939 telephone interviews and 1,005 clinical visits.
More common in boys
Investigators defined tic onset as the first occurrence of any sudden, rapid, recurrent, nonrhythmic involuntary movement and/or vocalization on at least three separate days within a period of 3 weeks.
The investigators assessed GAS exposure using parameters from throat swabs, serum anti-streptolysin O titers, and anti-DNAse B titers.
They used multiple definitions and combinations of GAS exposures “to make sure we weren’t missing any association because we didn’t use the right definition,” said Dr. Schrag. She explained a definitive strep infection is not always clear-cut.
At baseline, 17.0% participants tested positive for GAS, and 78.8% tested negative. No throat swab was available from 4.2% of participants.
During follow-up, the number of confirmed positive GAS exposures was 59, 102, 125, and 138, depending on the definition.
Researchers identified 61 tic cases during the study period. There was no evidence of an association of tic onset with GAS exposure after adjusting for age, sex, and parental education level.
However, there was a strong association between tic onset and sex, with girls being 60% less likely to develop tics than boys (hazard ratio, 0.4; 95% CI, 0.2-0.7; P < .01).
This result wasn’t particularly surprising, as it’s known that more boys develop tics than girls. “We just confirmed that in a prospective way,” said Dr. Schrag.
Results from sensitivity analyses confirmed the results. This was also the case with analyses that excluded visits with missing data on GAS exposure and that further adjusted for clinical site and psychotropic medication use.
Other pathogens?
Although the results showed no association between strep and tics in this population, it does not “close the door completely” on a potential relationship, said Dr. Schrag.
“By and large, the development of tics in children is not associated with group A strep, but differences in small subgroups can never be excluded by a study like this.”
Participants in this study were part of the European Multicentre Tics in Children Studies (EMTICS), a prospective cohort study exploring the role of environmental and genetic factors in pediatric CTD. That project is also looking at immune system factors, “which might play a role in the development of chronic tic disorder and associated conditions,” said Dr. Schrag.
It’s still possible, she added, that other pathogens could play a role in tic development. “That’s going to be the subject of further analysis and future studies,” she said.
Tamara Pringsheim, MD, professor of clinical neurosciences, psychiatry, pediatrics, and community health sciences, University of Calgary (Alta.), praised the research.
“This was a well-designed study, with a large sample of 260 children followed for up to 4 years, using a standardized protocol to assess for group A streptococcal infection and new onset of tics.”
The study, which did not uncover an association between GAS exposure and tic onset, “provides high level evidence that group A streptococcal exposure is not an important risk factor for the new onset of tics in children with a family history of tic disorders.”
The study received funding from the European Union Seventh Framework Program for research technological development and demonstration. Dr. Schrag reports receiving consultancy or advisory board honoraria from Biogen, Abbvie, Bial, and Neurotechnology; research support from the National Institute of Health Research, Parkinsons UK, and the Economic and Social Research Council and the European Commission; and Royalties from Oxford University Press. Dr. Pringsheim reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Group A streptococcus (GAS) infection is not associated with new-onset tic disorders in at-risk children, findings from a large prospective study show.
The results mean that if preteens present with a new-onset tic condition, “they’re unlikely to have it as a result of a group A streptococcal throat infection,” study author Anette Eleonore Schrag, MD, PhD, professor, department of clinical neuroscience, Institute of Neurology, University College London, told this news organization.
Therefore, clinicians should not automatically prescribe antibiotics for children with tics, which sometimes occurs, said Dr. Schrag.
The study was published online Feb. 2 in Neurology.
Ongoing controversy
Research shows that genetic and environmental factors contribute to chronic tic disorders (CTDs) and Tourette syndrome (TS). Prenatal exposure to maternal smoking and central nervous system (CNS) stimulants, as well as psychosocial stress, may play a role.
There has been an ongoing controversy regarding the possible role of GAS in tics, with some studies showing an association and others not showing a link. However, previous studies have been retrospective, registry based, or had limited sample size.
This new prospective study is the first in children without a tic disorder but who were at relatively high risk of developing one. The children were followed to assess development of streptococcal infections and tics, said Dr. Schrag.
The study included 259 children aged 3-10 years (mean baseline age, 6.8 years; over half female) who had a first-degree relative such as a parent or sibling with TS or CTD.
The average age at TS onset is 7 years, peaking in prevalence and severity at about 9-12 years. GAS throat infections are common in this age group.
Although study participants did not have tics themselves, they represented “an enriched group,” said Dr. Schrag. “Because they had family history, we knew they were at increased risk for developing tics.”
Participants were evaluated every 2 months, alternating between scheduled hospital visits and telephone interviews. Parents kept a weekly diary and were instructed to bring their child in for assessment if they showed any signs of tics.
The average follow-up period was 1.6 years, but some of the children were followed for up to 48 months. During the study, there were a total of 1,944 assessments, including 939 telephone interviews and 1,005 clinical visits.
More common in boys
Investigators defined tic onset as the first occurrence of any sudden, rapid, recurrent, nonrhythmic involuntary movement and/or vocalization on at least three separate days within a period of 3 weeks.
The investigators assessed GAS exposure using parameters from throat swabs, serum anti-streptolysin O titers, and anti-DNAse B titers.
They used multiple definitions and combinations of GAS exposures “to make sure we weren’t missing any association because we didn’t use the right definition,” said Dr. Schrag. She explained a definitive strep infection is not always clear-cut.
At baseline, 17.0% participants tested positive for GAS, and 78.8% tested negative. No throat swab was available from 4.2% of participants.
During follow-up, the number of confirmed positive GAS exposures was 59, 102, 125, and 138, depending on the definition.
Researchers identified 61 tic cases during the study period. There was no evidence of an association of tic onset with GAS exposure after adjusting for age, sex, and parental education level.
However, there was a strong association between tic onset and sex, with girls being 60% less likely to develop tics than boys (hazard ratio, 0.4; 95% CI, 0.2-0.7; P < .01).
This result wasn’t particularly surprising, as it’s known that more boys develop tics than girls. “We just confirmed that in a prospective way,” said Dr. Schrag.
Results from sensitivity analyses confirmed the results. This was also the case with analyses that excluded visits with missing data on GAS exposure and that further adjusted for clinical site and psychotropic medication use.
Other pathogens?
Although the results showed no association between strep and tics in this population, it does not “close the door completely” on a potential relationship, said Dr. Schrag.
“By and large, the development of tics in children is not associated with group A strep, but differences in small subgroups can never be excluded by a study like this.”
Participants in this study were part of the European Multicentre Tics in Children Studies (EMTICS), a prospective cohort study exploring the role of environmental and genetic factors in pediatric CTD. That project is also looking at immune system factors, “which might play a role in the development of chronic tic disorder and associated conditions,” said Dr. Schrag.
It’s still possible, she added, that other pathogens could play a role in tic development. “That’s going to be the subject of further analysis and future studies,” she said.
Tamara Pringsheim, MD, professor of clinical neurosciences, psychiatry, pediatrics, and community health sciences, University of Calgary (Alta.), praised the research.
“This was a well-designed study, with a large sample of 260 children followed for up to 4 years, using a standardized protocol to assess for group A streptococcal infection and new onset of tics.”
The study, which did not uncover an association between GAS exposure and tic onset, “provides high level evidence that group A streptococcal exposure is not an important risk factor for the new onset of tics in children with a family history of tic disorders.”
The study received funding from the European Union Seventh Framework Program for research technological development and demonstration. Dr. Schrag reports receiving consultancy or advisory board honoraria from Biogen, Abbvie, Bial, and Neurotechnology; research support from the National Institute of Health Research, Parkinsons UK, and the Economic and Social Research Council and the European Commission; and Royalties from Oxford University Press. Dr. Pringsheim reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
COVID vaccines open rifts between parents, children
The picture of rebellious teenagers sneaking “shots” has widened beyond breaking into Mom and Dad’s liquor cabinet. For some teens now, it means getting a COVID-19 vaccination without their parents’ consent – and, unlike the cabinet raids for the booze, they have adults willing to endorse the practice.
Since the U.S. Food and Drug Administration first granted emergency use authorization to Pfizer’s COVID-19 vaccine for teenagers in mid-2021, health officials have had to deal with a small subset of vaccine hesitancy where minors want the shot over the objections of their reluctant parents. The split has buoyed groups that were formed initially to convince teenagers to get vaccinated against other diseases.
When 14-year-old Arin Parsa of San Jose, California founded Teens for Vaccines in 2019 after a measles outbreak among unvaccinated children, “hardly anyone was interested,” he said. “Many teens were into climate change and other causes. Then, when the pandemic hit, so many were suddenly aware.”
Heavy toll on teens
Mr. Parsa’s parents fully supported Teens for Vaccines, he said, but he quickly found out how “politicized” COVID shots had become.
“We find people who are sad, angry, and frustrated at this stage of the pandemic,” he told this news organization. “The anti-vax lobby is riding the coat-tails of other movements. It has a very severe effect on their mental health. They can’t go out with their friends and socialize.”
In the pandemic’s initial stages, children were less likely to fall sick with COVID, but the Omicron variant led to a dramatic increase in illnesses among young people. The American Academy of Pediatrics has found that 3.5 million of the 11.4 million pediatric cases of the virus in the United States were reported in January 2022 alone. Meanwhile, vaccination rates for children aged 12-17, which were only 34% in June 2021 and lagged through the fall, are now at about 61% thanks to a sharp uptick during the Omicron surge, according to polling by the Kaiser Family Foundation.
No statistics are available on how many minors have received a COVID vaccine against their parents’ wishes.
“It’s not like there’s a big movement,” said Arthur Caplan, PhD, who heads the Division of Medical Ethics at the NYU Grossman School of Medicine. He said he noticed a divide around the HPV and hepatitis B vaccines. “They were tied up with sexual behavior,” he said, but “there were also some kids whose parents were really antivaxxers.”
Mr. Parsa said his and similar teen-oriented groups, such as VaxTeen, seek to educate their teen cohort, convince family members of the vaccines’ benefits, and to connect them with resources to get a shot. They also strive to change laws to make it easier for teenagers to receive the vaccine.
Consent laws vary from state to state (and within states), and proposed changes are afoot – some to loosen the laws and some to tighten them. Currently a 14-year-old in Alabama may get a COVID shot without parental permission, according to VaxTeen. In California, minors may receive the HPV shot without parental consent but not a COVID vaccine, although groups like Teens for Vaccines are pushing to change that. A bill now before the state legislature, the Teens Choose Vaccines Act (Senate Bill 866), would allow adolescents aged 12 and older to be able receive any FDA-approved vaccine – including COVID vaccines – without parental consent.
A second bill in California, the Keep Schools Open and Safe Act, would add the COVID-19 vaccines to the required list of immunizations needed to attend school in the state as well as eliminate the “personal belief” exemption against immunization.
California Sen. Richard Pan, MD (D-6th District), cowrote both bills with fellow Democrat Sen. Scott Wiener (D-11th District) and teen advocates from Teens for Vaccines and Generation Up, who helped draft the language in consultation with the lawmakers.
“As a pediatrician, I have seen all manner of situations where the requirement for a signed form has prevented teens from being able to get a vaccine that otherwise they and their guardians approved of them getting,” Dr. Pan told this news organization. “As a father, I don’t want to see my kids or any teen that wishes to protect themselves from deadly diseases unable to do so, particularly as we continue to fight off the dangers of the COVID-19 pandemic. I always encourage parents or teens that have questions about vaccines to speak directly with their pediatrician.”
Lawmakers in Philadelphia passed a provision last year to allow anyone age 11 or over to get the COVID vaccine without parental permission, keeping it in line with other vaccinations like hepatitis or HPV. “People from surrounding counties have come into the city, but it hasn’t been a huge rush,” says James Garrow, MPH, a spokesman for the city’s Department of Health.
Strive for collaboration, but listen to the children
Experts say the best solution is to for a doctor to meet with minors and their reluctant parents to get them on board for a COVID shot.
“Physicians are still the trusted messengers,” said Emma Olivera, MD, a pediatrician in suburban Chicago who advises groups that combat COVID misinformation.
Dr. Olivera said she often finds that internet-savvy teenagers have access to more information than older people, including their parents.
Thanks to COVID policies, office meetings are “difficult to do,” NYU’s Dr. Caplan added. In such a meeting, Dr. Caplan said he would try to convince the parents that the shots are needed for their children to stay in school or play sports. In the end, he said minors should get the shot but would also notify the parents before that happens: “My duty is to them.”
If parents take opposite stances, the pro-vaccine side is likely to prevail, even in California, said Patrick Baghdaserians, JD, a family law attorney in Pasadena. Mr. Baghdaserians said he is now representing a father who wants his teenager to get vaccinated but the mother doesn’t. “The court will fall on our side,” he predicted.
A version of this article first appeared on Medscape.com.
The picture of rebellious teenagers sneaking “shots” has widened beyond breaking into Mom and Dad’s liquor cabinet. For some teens now, it means getting a COVID-19 vaccination without their parents’ consent – and, unlike the cabinet raids for the booze, they have adults willing to endorse the practice.
Since the U.S. Food and Drug Administration first granted emergency use authorization to Pfizer’s COVID-19 vaccine for teenagers in mid-2021, health officials have had to deal with a small subset of vaccine hesitancy where minors want the shot over the objections of their reluctant parents. The split has buoyed groups that were formed initially to convince teenagers to get vaccinated against other diseases.
When 14-year-old Arin Parsa of San Jose, California founded Teens for Vaccines in 2019 after a measles outbreak among unvaccinated children, “hardly anyone was interested,” he said. “Many teens were into climate change and other causes. Then, when the pandemic hit, so many were suddenly aware.”
Heavy toll on teens
Mr. Parsa’s parents fully supported Teens for Vaccines, he said, but he quickly found out how “politicized” COVID shots had become.
“We find people who are sad, angry, and frustrated at this stage of the pandemic,” he told this news organization. “The anti-vax lobby is riding the coat-tails of other movements. It has a very severe effect on their mental health. They can’t go out with their friends and socialize.”
In the pandemic’s initial stages, children were less likely to fall sick with COVID, but the Omicron variant led to a dramatic increase in illnesses among young people. The American Academy of Pediatrics has found that 3.5 million of the 11.4 million pediatric cases of the virus in the United States were reported in January 2022 alone. Meanwhile, vaccination rates for children aged 12-17, which were only 34% in June 2021 and lagged through the fall, are now at about 61% thanks to a sharp uptick during the Omicron surge, according to polling by the Kaiser Family Foundation.
No statistics are available on how many minors have received a COVID vaccine against their parents’ wishes.
“It’s not like there’s a big movement,” said Arthur Caplan, PhD, who heads the Division of Medical Ethics at the NYU Grossman School of Medicine. He said he noticed a divide around the HPV and hepatitis B vaccines. “They were tied up with sexual behavior,” he said, but “there were also some kids whose parents were really antivaxxers.”
Mr. Parsa said his and similar teen-oriented groups, such as VaxTeen, seek to educate their teen cohort, convince family members of the vaccines’ benefits, and to connect them with resources to get a shot. They also strive to change laws to make it easier for teenagers to receive the vaccine.
Consent laws vary from state to state (and within states), and proposed changes are afoot – some to loosen the laws and some to tighten them. Currently a 14-year-old in Alabama may get a COVID shot without parental permission, according to VaxTeen. In California, minors may receive the HPV shot without parental consent but not a COVID vaccine, although groups like Teens for Vaccines are pushing to change that. A bill now before the state legislature, the Teens Choose Vaccines Act (Senate Bill 866), would allow adolescents aged 12 and older to be able receive any FDA-approved vaccine – including COVID vaccines – without parental consent.
A second bill in California, the Keep Schools Open and Safe Act, would add the COVID-19 vaccines to the required list of immunizations needed to attend school in the state as well as eliminate the “personal belief” exemption against immunization.
California Sen. Richard Pan, MD (D-6th District), cowrote both bills with fellow Democrat Sen. Scott Wiener (D-11th District) and teen advocates from Teens for Vaccines and Generation Up, who helped draft the language in consultation with the lawmakers.
“As a pediatrician, I have seen all manner of situations where the requirement for a signed form has prevented teens from being able to get a vaccine that otherwise they and their guardians approved of them getting,” Dr. Pan told this news organization. “As a father, I don’t want to see my kids or any teen that wishes to protect themselves from deadly diseases unable to do so, particularly as we continue to fight off the dangers of the COVID-19 pandemic. I always encourage parents or teens that have questions about vaccines to speak directly with their pediatrician.”
Lawmakers in Philadelphia passed a provision last year to allow anyone age 11 or over to get the COVID vaccine without parental permission, keeping it in line with other vaccinations like hepatitis or HPV. “People from surrounding counties have come into the city, but it hasn’t been a huge rush,” says James Garrow, MPH, a spokesman for the city’s Department of Health.
Strive for collaboration, but listen to the children
Experts say the best solution is to for a doctor to meet with minors and their reluctant parents to get them on board for a COVID shot.
“Physicians are still the trusted messengers,” said Emma Olivera, MD, a pediatrician in suburban Chicago who advises groups that combat COVID misinformation.
Dr. Olivera said she often finds that internet-savvy teenagers have access to more information than older people, including their parents.
Thanks to COVID policies, office meetings are “difficult to do,” NYU’s Dr. Caplan added. In such a meeting, Dr. Caplan said he would try to convince the parents that the shots are needed for their children to stay in school or play sports. In the end, he said minors should get the shot but would also notify the parents before that happens: “My duty is to them.”
If parents take opposite stances, the pro-vaccine side is likely to prevail, even in California, said Patrick Baghdaserians, JD, a family law attorney in Pasadena. Mr. Baghdaserians said he is now representing a father who wants his teenager to get vaccinated but the mother doesn’t. “The court will fall on our side,” he predicted.
A version of this article first appeared on Medscape.com.
The picture of rebellious teenagers sneaking “shots” has widened beyond breaking into Mom and Dad’s liquor cabinet. For some teens now, it means getting a COVID-19 vaccination without their parents’ consent – and, unlike the cabinet raids for the booze, they have adults willing to endorse the practice.
Since the U.S. Food and Drug Administration first granted emergency use authorization to Pfizer’s COVID-19 vaccine for teenagers in mid-2021, health officials have had to deal with a small subset of vaccine hesitancy where minors want the shot over the objections of their reluctant parents. The split has buoyed groups that were formed initially to convince teenagers to get vaccinated against other diseases.
When 14-year-old Arin Parsa of San Jose, California founded Teens for Vaccines in 2019 after a measles outbreak among unvaccinated children, “hardly anyone was interested,” he said. “Many teens were into climate change and other causes. Then, when the pandemic hit, so many were suddenly aware.”
Heavy toll on teens
Mr. Parsa’s parents fully supported Teens for Vaccines, he said, but he quickly found out how “politicized” COVID shots had become.
“We find people who are sad, angry, and frustrated at this stage of the pandemic,” he told this news organization. “The anti-vax lobby is riding the coat-tails of other movements. It has a very severe effect on their mental health. They can’t go out with their friends and socialize.”
In the pandemic’s initial stages, children were less likely to fall sick with COVID, but the Omicron variant led to a dramatic increase in illnesses among young people. The American Academy of Pediatrics has found that 3.5 million of the 11.4 million pediatric cases of the virus in the United States were reported in January 2022 alone. Meanwhile, vaccination rates for children aged 12-17, which were only 34% in June 2021 and lagged through the fall, are now at about 61% thanks to a sharp uptick during the Omicron surge, according to polling by the Kaiser Family Foundation.
No statistics are available on how many minors have received a COVID vaccine against their parents’ wishes.
“It’s not like there’s a big movement,” said Arthur Caplan, PhD, who heads the Division of Medical Ethics at the NYU Grossman School of Medicine. He said he noticed a divide around the HPV and hepatitis B vaccines. “They were tied up with sexual behavior,” he said, but “there were also some kids whose parents were really antivaxxers.”
Mr. Parsa said his and similar teen-oriented groups, such as VaxTeen, seek to educate their teen cohort, convince family members of the vaccines’ benefits, and to connect them with resources to get a shot. They also strive to change laws to make it easier for teenagers to receive the vaccine.
Consent laws vary from state to state (and within states), and proposed changes are afoot – some to loosen the laws and some to tighten them. Currently a 14-year-old in Alabama may get a COVID shot without parental permission, according to VaxTeen. In California, minors may receive the HPV shot without parental consent but not a COVID vaccine, although groups like Teens for Vaccines are pushing to change that. A bill now before the state legislature, the Teens Choose Vaccines Act (Senate Bill 866), would allow adolescents aged 12 and older to be able receive any FDA-approved vaccine – including COVID vaccines – without parental consent.
A second bill in California, the Keep Schools Open and Safe Act, would add the COVID-19 vaccines to the required list of immunizations needed to attend school in the state as well as eliminate the “personal belief” exemption against immunization.
California Sen. Richard Pan, MD (D-6th District), cowrote both bills with fellow Democrat Sen. Scott Wiener (D-11th District) and teen advocates from Teens for Vaccines and Generation Up, who helped draft the language in consultation with the lawmakers.
“As a pediatrician, I have seen all manner of situations where the requirement for a signed form has prevented teens from being able to get a vaccine that otherwise they and their guardians approved of them getting,” Dr. Pan told this news organization. “As a father, I don’t want to see my kids or any teen that wishes to protect themselves from deadly diseases unable to do so, particularly as we continue to fight off the dangers of the COVID-19 pandemic. I always encourage parents or teens that have questions about vaccines to speak directly with their pediatrician.”
Lawmakers in Philadelphia passed a provision last year to allow anyone age 11 or over to get the COVID vaccine without parental permission, keeping it in line with other vaccinations like hepatitis or HPV. “People from surrounding counties have come into the city, but it hasn’t been a huge rush,” says James Garrow, MPH, a spokesman for the city’s Department of Health.
Strive for collaboration, but listen to the children
Experts say the best solution is to for a doctor to meet with minors and their reluctant parents to get them on board for a COVID shot.
“Physicians are still the trusted messengers,” said Emma Olivera, MD, a pediatrician in suburban Chicago who advises groups that combat COVID misinformation.
Dr. Olivera said she often finds that internet-savvy teenagers have access to more information than older people, including their parents.
Thanks to COVID policies, office meetings are “difficult to do,” NYU’s Dr. Caplan added. In such a meeting, Dr. Caplan said he would try to convince the parents that the shots are needed for their children to stay in school or play sports. In the end, he said minors should get the shot but would also notify the parents before that happens: “My duty is to them.”
If parents take opposite stances, the pro-vaccine side is likely to prevail, even in California, said Patrick Baghdaserians, JD, a family law attorney in Pasadena. Mr. Baghdaserians said he is now representing a father who wants his teenager to get vaccinated but the mother doesn’t. “The court will fall on our side,” he predicted.
A version of this article first appeared on Medscape.com.
Caring for suicidal youth: An approach for pediatricians
This month’s column is driven by the recent increase of youth in crisis, and COVID-19–related limitations of higher-level services. Suicide is the second leading cause of death among youth1 and populations who face discrimination are at increased risk.2,3
A pediatrician colleague recently asked me about how to support patients who may be at risk. With inpatient units and emergency departments over capacity, properly allocating resources to patients with the most acute needs is crucial. When appropriate, providing preventive suicide care in primary care similarly saves lives.
Case summary
Cassandra is a 16-year-old Black girl who told a friend on Snapchat that she did not want to be alive. The friend told her parents and Cassandra’s parents brought their daughter to an urgent primary care appointment. Cassandra has had a history of difficulty with large transitions like a family move when she was 13. She spent more time in her room for several months before joining the volleyball team and making new friends. She has always done well academically in school but struggled with insomnia and classwork when her high school shifted to remote learning for the 2020-2021 school year because of the pandemic. This year she attends school in person but is unable to play volleyball because of COVID-19 restrictions. Her parents report that she is again spending more time online in her room. She is passing her classes and doing well in math, but overall, her grades have fallen since the pandemic began. She reports recent difficulties with friends and notes feeling hopeless about a changing climate and race relations in the United States.
Discussion
This case example illustrates some factors pediatricians can consider in determining how to proceed in similar circumstances. What are Cassandra’s immediate risk and treatment needs? In cases like Cassandra’s, the American Academy of Pediatrics recommends the ABCD (Assess, Build hope, Connect, Develop a safety plan) approach.4 Preparing practices to deliver this best possible preventive suicide care is essential.
1. Is this patient at imminent risk of harming herself?
Assess: Screen for suicide risk and assess risk level. Several standardized screening tools exist for gauging a patient’s risk. The Ask Suicide Screening Questionnaire (asQ) is a straightforward screening tool (not to be confused with the ASQ Ages and Stages developmental screening). These questionnaires take only a few minutes and next steps are suggested depending on the score (low, moderate, or high risk) and clinical judgment. What matters most is using a standardized screener to directly ask questions about suicide and then follow up appropriately based on risk.
2. What can be done during the visit to promote a good outcome?
Build hope/reasons for living. Validate that people sometimes feel suicidal when things are difficult, but that the feelings come and go and people go on to live meaningful lives. Tell the patients that you care about keeping them safe when the feelings come up. Motivational interviewing can be helpful to reflect back patient-identified reasons for living. Genuinely tell the patients how much you care about their wellbeing.
3. What can be done outside the visit to promote a good outcome?
Connect: Strengthen connections with protective adults. Make a plan to have the patient connect regularly with parents/trusted adults. She could engage in social action, or connect one-on-one. With more structured social opportunities, she will spend less time online. Medical practices can reach out with postcards and phone calls to show that they care about the patient, an intervention called “Caring Contacts” that has been shown to decrease suicide.
4. Once suicide risk is identified, what are specific tools to use during the visit to keep her safe?
Develop a plan for staying safe: Restrict access to lethal means, develop a safety plan and healthy ways of coping. There is a free 2-hour CALM (Counseling on Access to Lethal Means) training to help providers feel competent in restricting access to lethal means prior to increased risk. This resource provides safety plan templates that help identify triggers, specific ways to stay safe, people to talk to, and suicide prevention resources including lifelines (988) and chat options (text 2 letter state to 741741).
Enacting suicide prevention requires practice readiness and workflow changes. Providers should assess mental health supports in and out of the office, and then rehearse workflow around suicide prevention care. Increasingly, there are embedded case managers or behavioral health providers available. Sometimes local mental health crisis services are the best option. A practice introductory letter to community mental health practitioners can improve later coordination efforts when caring for suicidal youth. Having practice-level support for provider well-being can improve outcomes.
Case follow-up
After interviewing the girl separately, and performing a PHQ-A and an asQ, followed by the Brief Suicide Safety Assessment to screen for acuity, the pediatrician felt confident that Cassandra was suffering from moderate depression and had moderate but not imminent risk of suicide. Options to treat her depression were discussed with Cassandra and her parents, and a referral to therapy was made.
The provider knew that depression care is complementary but not sufficient as standalone suicide prevention. The provider used the asQ pathway to determine next steps. He made a safety plan, and referred her to an outpatient mental health clinician with whom the practice had an established relationship for an urgent mental health evaluation. A follow-up primary care appointment was scheduled within 72 hours to re-check safety and ensure that she had an appointment scheduled to start therapy. A nurse contacted the patient and her family regularly to check on her wellbeing. Her parents made a plan with her volleyball coach to organize outdoor off-season conditioning to help with exercise and socializing. The family removed screens prior to bedtime and sleep improved. At a 3-month follow-up, Cassandra had only mild depressive symptoms and the frequency and intensity of her suicidal ideation had decreased.
Dr. Spottswood is a child psychiatrist practicing in an integrated care clinic at the Community Health Centers of Burlington, Vermont, a Federally Qualified Health Center. She is the medical director of the Vermont Child Psychiatry Access Program and a clinical assistant professor in the department of psychiatry at the University of Vermont.
References
1. National Institute of Mental Health: Suicide.
2. Hottes TS et al. Am J Public Health. 2016 May;106(5):e1-12.
3. Bridge JA et al. JAMA Pediatr. 2018;172(7):697-9.
4. Asarnow JR. SAMHSA Center for Adolescent Suicide and Self-Harm..
This month’s column is driven by the recent increase of youth in crisis, and COVID-19–related limitations of higher-level services. Suicide is the second leading cause of death among youth1 and populations who face discrimination are at increased risk.2,3
A pediatrician colleague recently asked me about how to support patients who may be at risk. With inpatient units and emergency departments over capacity, properly allocating resources to patients with the most acute needs is crucial. When appropriate, providing preventive suicide care in primary care similarly saves lives.
Case summary
Cassandra is a 16-year-old Black girl who told a friend on Snapchat that she did not want to be alive. The friend told her parents and Cassandra’s parents brought their daughter to an urgent primary care appointment. Cassandra has had a history of difficulty with large transitions like a family move when she was 13. She spent more time in her room for several months before joining the volleyball team and making new friends. She has always done well academically in school but struggled with insomnia and classwork when her high school shifted to remote learning for the 2020-2021 school year because of the pandemic. This year she attends school in person but is unable to play volleyball because of COVID-19 restrictions. Her parents report that she is again spending more time online in her room. She is passing her classes and doing well in math, but overall, her grades have fallen since the pandemic began. She reports recent difficulties with friends and notes feeling hopeless about a changing climate and race relations in the United States.
Discussion
This case example illustrates some factors pediatricians can consider in determining how to proceed in similar circumstances. What are Cassandra’s immediate risk and treatment needs? In cases like Cassandra’s, the American Academy of Pediatrics recommends the ABCD (Assess, Build hope, Connect, Develop a safety plan) approach.4 Preparing practices to deliver this best possible preventive suicide care is essential.
1. Is this patient at imminent risk of harming herself?
Assess: Screen for suicide risk and assess risk level. Several standardized screening tools exist for gauging a patient’s risk. The Ask Suicide Screening Questionnaire (asQ) is a straightforward screening tool (not to be confused with the ASQ Ages and Stages developmental screening). These questionnaires take only a few minutes and next steps are suggested depending on the score (low, moderate, or high risk) and clinical judgment. What matters most is using a standardized screener to directly ask questions about suicide and then follow up appropriately based on risk.
2. What can be done during the visit to promote a good outcome?
Build hope/reasons for living. Validate that people sometimes feel suicidal when things are difficult, but that the feelings come and go and people go on to live meaningful lives. Tell the patients that you care about keeping them safe when the feelings come up. Motivational interviewing can be helpful to reflect back patient-identified reasons for living. Genuinely tell the patients how much you care about their wellbeing.
3. What can be done outside the visit to promote a good outcome?
Connect: Strengthen connections with protective adults. Make a plan to have the patient connect regularly with parents/trusted adults. She could engage in social action, or connect one-on-one. With more structured social opportunities, she will spend less time online. Medical practices can reach out with postcards and phone calls to show that they care about the patient, an intervention called “Caring Contacts” that has been shown to decrease suicide.
4. Once suicide risk is identified, what are specific tools to use during the visit to keep her safe?
Develop a plan for staying safe: Restrict access to lethal means, develop a safety plan and healthy ways of coping. There is a free 2-hour CALM (Counseling on Access to Lethal Means) training to help providers feel competent in restricting access to lethal means prior to increased risk. This resource provides safety plan templates that help identify triggers, specific ways to stay safe, people to talk to, and suicide prevention resources including lifelines (988) and chat options (text 2 letter state to 741741).
Enacting suicide prevention requires practice readiness and workflow changes. Providers should assess mental health supports in and out of the office, and then rehearse workflow around suicide prevention care. Increasingly, there are embedded case managers or behavioral health providers available. Sometimes local mental health crisis services are the best option. A practice introductory letter to community mental health practitioners can improve later coordination efforts when caring for suicidal youth. Having practice-level support for provider well-being can improve outcomes.
Case follow-up
After interviewing the girl separately, and performing a PHQ-A and an asQ, followed by the Brief Suicide Safety Assessment to screen for acuity, the pediatrician felt confident that Cassandra was suffering from moderate depression and had moderate but not imminent risk of suicide. Options to treat her depression were discussed with Cassandra and her parents, and a referral to therapy was made.
The provider knew that depression care is complementary but not sufficient as standalone suicide prevention. The provider used the asQ pathway to determine next steps. He made a safety plan, and referred her to an outpatient mental health clinician with whom the practice had an established relationship for an urgent mental health evaluation. A follow-up primary care appointment was scheduled within 72 hours to re-check safety and ensure that she had an appointment scheduled to start therapy. A nurse contacted the patient and her family regularly to check on her wellbeing. Her parents made a plan with her volleyball coach to organize outdoor off-season conditioning to help with exercise and socializing. The family removed screens prior to bedtime and sleep improved. At a 3-month follow-up, Cassandra had only mild depressive symptoms and the frequency and intensity of her suicidal ideation had decreased.
Dr. Spottswood is a child psychiatrist practicing in an integrated care clinic at the Community Health Centers of Burlington, Vermont, a Federally Qualified Health Center. She is the medical director of the Vermont Child Psychiatry Access Program and a clinical assistant professor in the department of psychiatry at the University of Vermont.
References
1. National Institute of Mental Health: Suicide.
2. Hottes TS et al. Am J Public Health. 2016 May;106(5):e1-12.
3. Bridge JA et al. JAMA Pediatr. 2018;172(7):697-9.
4. Asarnow JR. SAMHSA Center for Adolescent Suicide and Self-Harm..
This month’s column is driven by the recent increase of youth in crisis, and COVID-19–related limitations of higher-level services. Suicide is the second leading cause of death among youth1 and populations who face discrimination are at increased risk.2,3
A pediatrician colleague recently asked me about how to support patients who may be at risk. With inpatient units and emergency departments over capacity, properly allocating resources to patients with the most acute needs is crucial. When appropriate, providing preventive suicide care in primary care similarly saves lives.
Case summary
Cassandra is a 16-year-old Black girl who told a friend on Snapchat that she did not want to be alive. The friend told her parents and Cassandra’s parents brought their daughter to an urgent primary care appointment. Cassandra has had a history of difficulty with large transitions like a family move when she was 13. She spent more time in her room for several months before joining the volleyball team and making new friends. She has always done well academically in school but struggled with insomnia and classwork when her high school shifted to remote learning for the 2020-2021 school year because of the pandemic. This year she attends school in person but is unable to play volleyball because of COVID-19 restrictions. Her parents report that she is again spending more time online in her room. She is passing her classes and doing well in math, but overall, her grades have fallen since the pandemic began. She reports recent difficulties with friends and notes feeling hopeless about a changing climate and race relations in the United States.
Discussion
This case example illustrates some factors pediatricians can consider in determining how to proceed in similar circumstances. What are Cassandra’s immediate risk and treatment needs? In cases like Cassandra’s, the American Academy of Pediatrics recommends the ABCD (Assess, Build hope, Connect, Develop a safety plan) approach.4 Preparing practices to deliver this best possible preventive suicide care is essential.
1. Is this patient at imminent risk of harming herself?
Assess: Screen for suicide risk and assess risk level. Several standardized screening tools exist for gauging a patient’s risk. The Ask Suicide Screening Questionnaire (asQ) is a straightforward screening tool (not to be confused with the ASQ Ages and Stages developmental screening). These questionnaires take only a few minutes and next steps are suggested depending on the score (low, moderate, or high risk) and clinical judgment. What matters most is using a standardized screener to directly ask questions about suicide and then follow up appropriately based on risk.
2. What can be done during the visit to promote a good outcome?
Build hope/reasons for living. Validate that people sometimes feel suicidal when things are difficult, but that the feelings come and go and people go on to live meaningful lives. Tell the patients that you care about keeping them safe when the feelings come up. Motivational interviewing can be helpful to reflect back patient-identified reasons for living. Genuinely tell the patients how much you care about their wellbeing.
3. What can be done outside the visit to promote a good outcome?
Connect: Strengthen connections with protective adults. Make a plan to have the patient connect regularly with parents/trusted adults. She could engage in social action, or connect one-on-one. With more structured social opportunities, she will spend less time online. Medical practices can reach out with postcards and phone calls to show that they care about the patient, an intervention called “Caring Contacts” that has been shown to decrease suicide.
4. Once suicide risk is identified, what are specific tools to use during the visit to keep her safe?
Develop a plan for staying safe: Restrict access to lethal means, develop a safety plan and healthy ways of coping. There is a free 2-hour CALM (Counseling on Access to Lethal Means) training to help providers feel competent in restricting access to lethal means prior to increased risk. This resource provides safety plan templates that help identify triggers, specific ways to stay safe, people to talk to, and suicide prevention resources including lifelines (988) and chat options (text 2 letter state to 741741).
Enacting suicide prevention requires practice readiness and workflow changes. Providers should assess mental health supports in and out of the office, and then rehearse workflow around suicide prevention care. Increasingly, there are embedded case managers or behavioral health providers available. Sometimes local mental health crisis services are the best option. A practice introductory letter to community mental health practitioners can improve later coordination efforts when caring for suicidal youth. Having practice-level support for provider well-being can improve outcomes.
Case follow-up
After interviewing the girl separately, and performing a PHQ-A and an asQ, followed by the Brief Suicide Safety Assessment to screen for acuity, the pediatrician felt confident that Cassandra was suffering from moderate depression and had moderate but not imminent risk of suicide. Options to treat her depression were discussed with Cassandra and her parents, and a referral to therapy was made.
The provider knew that depression care is complementary but not sufficient as standalone suicide prevention. The provider used the asQ pathway to determine next steps. He made a safety plan, and referred her to an outpatient mental health clinician with whom the practice had an established relationship for an urgent mental health evaluation. A follow-up primary care appointment was scheduled within 72 hours to re-check safety and ensure that she had an appointment scheduled to start therapy. A nurse contacted the patient and her family regularly to check on her wellbeing. Her parents made a plan with her volleyball coach to organize outdoor off-season conditioning to help with exercise and socializing. The family removed screens prior to bedtime and sleep improved. At a 3-month follow-up, Cassandra had only mild depressive symptoms and the frequency and intensity of her suicidal ideation had decreased.
Dr. Spottswood is a child psychiatrist practicing in an integrated care clinic at the Community Health Centers of Burlington, Vermont, a Federally Qualified Health Center. She is the medical director of the Vermont Child Psychiatry Access Program and a clinical assistant professor in the department of psychiatry at the University of Vermont.
References
1. National Institute of Mental Health: Suicide.
2. Hottes TS et al. Am J Public Health. 2016 May;106(5):e1-12.
3. Bridge JA et al. JAMA Pediatr. 2018;172(7):697-9.
4. Asarnow JR. SAMHSA Center for Adolescent Suicide and Self-Harm..





