User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Study: Majority of research on homeopathic remedies unpublished or unregistered
Homeopathy is a form of alternative medicine based on the concept that increasing dilution of a substance leads to a stronger treatment effect.
The authors of the new paper, published in BMJ Evidence-Based Medicine, also found that a quarter of the 90 randomized published trials on homeopathic remedies they analyzed changed their results before publication.
The benefits of homeopathy touted in studies may be greatly exaggerated, suggest the authors, Gerald Gartlehner, MD, of Danube University, Krems, Austria, and colleagues.
The results raise awareness that published homeopathy trials represent a limited proportion of research, skewed toward favorable results, they wrote.
“This likely affects the validity of the body of evidence of homeopathic literature and may substantially overestimate the true treatment effect of homeopathic remedies,” they concluded.
Homeopathy as practiced today was developed approximately 200 years ago in Germany, and despite ongoing debate about its effectiveness, it remains a popular alternative to conventional medicine in many developed countries, the authors noted.
According to the National Institutes of Health, homeopathy is based on the idea of “like cures like,” meaning that a disease can be cured with a substance that produces similar symptoms in healthy people, and the “law of minimum dose,” meaning that a lower dose of medication will be more effective. “Many homeopathic products are so diluted that no molecules of the original substance remain,” according to the NIH.
Homeopathy is not subject to most regulatory requirements, so assessment of effectiveness of homeopathic remedies is limited to published data, the researchers said. “When no information is publicly available about the majority of homeopathic trials, sound conclusions about the efficacy and the risks of using homeopathic medicinal products for treating health conditions are impossible,” they wrote.
Study methods and findings
The researchers examined 17 trial registries for studies involving homeopathic remedies conducted since 2002.
The registries included clinicaltrials.gov, the EU Clinical Trials Register, and the International Clinical Trials Registry Platform up to April 2019 to identify registered homeopathy trials.
To determine whether registered trials were published and to identify trials that were published but unregistered, the researchers examined PubMed, the Allied and Complementary Medicine Database, Embase, and Google Scholar up to April 2021.
They found that approximately 38% of registered trials of homeopathy were never published, and 53% of the published randomized, controlled trials (RCTs) were not registered. Notably, 25% of the trials that were registered and published showed primary outcomes that were changed compared with the registry.
The number of registered homeopathy trials increased significantly over the past 5 years, but approximately one-third (30%) of trials published during the last 5 years were not registered, they said. In a meta-analysis, unregistered RCTs showed significantly greater treatment effects than registered RCTs, with standardized mean differences of –0.53 and –0.14, respectively.
The study findings were limited by several factors including the potential for missed records of studies not covered by the registries searched. Other limitations include the analysis of pooled data from homeopathic treatments that may not generalize to personalized homeopathy, and the exclusion of trials labeled as terminated or suspended.
Proceed with caution before recommending use of homeopathic remedies, says expert
Linda Girgis, MD, noted that prior to reading this report she had known that most homeopathic remedies didn’t have any evidence of being effective, and that, therefore, the results validated her understanding of the findings of studies of homeopathy.
The study is especially important at this time in the wake of the COVID-19 pandemic, Dr. Girgis, a family physician in private practice in South River, N.J., said in an interview.
“Many people are promoting treatments that don’t have any evidence that they are effective, and more people are turning to homeopathic treatments not knowing the risks and assuming they are safe,” she continued. “Many people are taking advantage of this and trying to cash in on this with ill-proven remedies.”
Homeopathic remedies become especially harmful when patients think they can use them instead of traditional medicine, she added.
Noting that some homeopathic remedies have been studied and show some evidence that they work, Dr. Girgis said there may be a role for certain ones in primary care.
“An example would be black cohosh or primrose oil for perimenopausal hot flashes. This could be a good alternative when you want to avoid hormonal supplements,” she said.
At the same time, Dr. Girgis advised clinicians to be cautious about suggesting homeopathic remedies to patients.
“Homeopathy seems to be a good money maker if you sell these products. However, you are not protected from liability and can be found more liable for prescribing off-label treatments or those not [Food and Drug Administration] approved,” Dr. Girgis said. Her general message to clinicians: Stick with evidence-based medicine.
Her message to patients who might want to pursue homeopathic remedies is that just because something is “homeopathic” or natural doesn’t mean that it is safe.
“There are some [homeopathic] products that have caused liver damage or other problems,” she explained. “Also, these remedies can interact with other medications.”
The study received no outside funding. The researchers and Dr. Girgis had no financial conflicts to disclose.
Homeopathy is a form of alternative medicine based on the concept that increasing dilution of a substance leads to a stronger treatment effect.
The authors of the new paper, published in BMJ Evidence-Based Medicine, also found that a quarter of the 90 randomized published trials on homeopathic remedies they analyzed changed their results before publication.
The benefits of homeopathy touted in studies may be greatly exaggerated, suggest the authors, Gerald Gartlehner, MD, of Danube University, Krems, Austria, and colleagues.
The results raise awareness that published homeopathy trials represent a limited proportion of research, skewed toward favorable results, they wrote.
“This likely affects the validity of the body of evidence of homeopathic literature and may substantially overestimate the true treatment effect of homeopathic remedies,” they concluded.
Homeopathy as practiced today was developed approximately 200 years ago in Germany, and despite ongoing debate about its effectiveness, it remains a popular alternative to conventional medicine in many developed countries, the authors noted.
According to the National Institutes of Health, homeopathy is based on the idea of “like cures like,” meaning that a disease can be cured with a substance that produces similar symptoms in healthy people, and the “law of minimum dose,” meaning that a lower dose of medication will be more effective. “Many homeopathic products are so diluted that no molecules of the original substance remain,” according to the NIH.
Homeopathy is not subject to most regulatory requirements, so assessment of effectiveness of homeopathic remedies is limited to published data, the researchers said. “When no information is publicly available about the majority of homeopathic trials, sound conclusions about the efficacy and the risks of using homeopathic medicinal products for treating health conditions are impossible,” they wrote.
Study methods and findings
The researchers examined 17 trial registries for studies involving homeopathic remedies conducted since 2002.
The registries included clinicaltrials.gov, the EU Clinical Trials Register, and the International Clinical Trials Registry Platform up to April 2019 to identify registered homeopathy trials.
To determine whether registered trials were published and to identify trials that were published but unregistered, the researchers examined PubMed, the Allied and Complementary Medicine Database, Embase, and Google Scholar up to April 2021.
They found that approximately 38% of registered trials of homeopathy were never published, and 53% of the published randomized, controlled trials (RCTs) were not registered. Notably, 25% of the trials that were registered and published showed primary outcomes that were changed compared with the registry.
The number of registered homeopathy trials increased significantly over the past 5 years, but approximately one-third (30%) of trials published during the last 5 years were not registered, they said. In a meta-analysis, unregistered RCTs showed significantly greater treatment effects than registered RCTs, with standardized mean differences of –0.53 and –0.14, respectively.
The study findings were limited by several factors including the potential for missed records of studies not covered by the registries searched. Other limitations include the analysis of pooled data from homeopathic treatments that may not generalize to personalized homeopathy, and the exclusion of trials labeled as terminated or suspended.
Proceed with caution before recommending use of homeopathic remedies, says expert
Linda Girgis, MD, noted that prior to reading this report she had known that most homeopathic remedies didn’t have any evidence of being effective, and that, therefore, the results validated her understanding of the findings of studies of homeopathy.
The study is especially important at this time in the wake of the COVID-19 pandemic, Dr. Girgis, a family physician in private practice in South River, N.J., said in an interview.
“Many people are promoting treatments that don’t have any evidence that they are effective, and more people are turning to homeopathic treatments not knowing the risks and assuming they are safe,” she continued. “Many people are taking advantage of this and trying to cash in on this with ill-proven remedies.”
Homeopathic remedies become especially harmful when patients think they can use them instead of traditional medicine, she added.
Noting that some homeopathic remedies have been studied and show some evidence that they work, Dr. Girgis said there may be a role for certain ones in primary care.
“An example would be black cohosh or primrose oil for perimenopausal hot flashes. This could be a good alternative when you want to avoid hormonal supplements,” she said.
At the same time, Dr. Girgis advised clinicians to be cautious about suggesting homeopathic remedies to patients.
“Homeopathy seems to be a good money maker if you sell these products. However, you are not protected from liability and can be found more liable for prescribing off-label treatments or those not [Food and Drug Administration] approved,” Dr. Girgis said. Her general message to clinicians: Stick with evidence-based medicine.
Her message to patients who might want to pursue homeopathic remedies is that just because something is “homeopathic” or natural doesn’t mean that it is safe.
“There are some [homeopathic] products that have caused liver damage or other problems,” she explained. “Also, these remedies can interact with other medications.”
The study received no outside funding. The researchers and Dr. Girgis had no financial conflicts to disclose.
Homeopathy is a form of alternative medicine based on the concept that increasing dilution of a substance leads to a stronger treatment effect.
The authors of the new paper, published in BMJ Evidence-Based Medicine, also found that a quarter of the 90 randomized published trials on homeopathic remedies they analyzed changed their results before publication.
The benefits of homeopathy touted in studies may be greatly exaggerated, suggest the authors, Gerald Gartlehner, MD, of Danube University, Krems, Austria, and colleagues.
The results raise awareness that published homeopathy trials represent a limited proportion of research, skewed toward favorable results, they wrote.
“This likely affects the validity of the body of evidence of homeopathic literature and may substantially overestimate the true treatment effect of homeopathic remedies,” they concluded.
Homeopathy as practiced today was developed approximately 200 years ago in Germany, and despite ongoing debate about its effectiveness, it remains a popular alternative to conventional medicine in many developed countries, the authors noted.
According to the National Institutes of Health, homeopathy is based on the idea of “like cures like,” meaning that a disease can be cured with a substance that produces similar symptoms in healthy people, and the “law of minimum dose,” meaning that a lower dose of medication will be more effective. “Many homeopathic products are so diluted that no molecules of the original substance remain,” according to the NIH.
Homeopathy is not subject to most regulatory requirements, so assessment of effectiveness of homeopathic remedies is limited to published data, the researchers said. “When no information is publicly available about the majority of homeopathic trials, sound conclusions about the efficacy and the risks of using homeopathic medicinal products for treating health conditions are impossible,” they wrote.
Study methods and findings
The researchers examined 17 trial registries for studies involving homeopathic remedies conducted since 2002.
The registries included clinicaltrials.gov, the EU Clinical Trials Register, and the International Clinical Trials Registry Platform up to April 2019 to identify registered homeopathy trials.
To determine whether registered trials were published and to identify trials that were published but unregistered, the researchers examined PubMed, the Allied and Complementary Medicine Database, Embase, and Google Scholar up to April 2021.
They found that approximately 38% of registered trials of homeopathy were never published, and 53% of the published randomized, controlled trials (RCTs) were not registered. Notably, 25% of the trials that were registered and published showed primary outcomes that were changed compared with the registry.
The number of registered homeopathy trials increased significantly over the past 5 years, but approximately one-third (30%) of trials published during the last 5 years were not registered, they said. In a meta-analysis, unregistered RCTs showed significantly greater treatment effects than registered RCTs, with standardized mean differences of –0.53 and –0.14, respectively.
The study findings were limited by several factors including the potential for missed records of studies not covered by the registries searched. Other limitations include the analysis of pooled data from homeopathic treatments that may not generalize to personalized homeopathy, and the exclusion of trials labeled as terminated or suspended.
Proceed with caution before recommending use of homeopathic remedies, says expert
Linda Girgis, MD, noted that prior to reading this report she had known that most homeopathic remedies didn’t have any evidence of being effective, and that, therefore, the results validated her understanding of the findings of studies of homeopathy.
The study is especially important at this time in the wake of the COVID-19 pandemic, Dr. Girgis, a family physician in private practice in South River, N.J., said in an interview.
“Many people are promoting treatments that don’t have any evidence that they are effective, and more people are turning to homeopathic treatments not knowing the risks and assuming they are safe,” she continued. “Many people are taking advantage of this and trying to cash in on this with ill-proven remedies.”
Homeopathic remedies become especially harmful when patients think they can use them instead of traditional medicine, she added.
Noting that some homeopathic remedies have been studied and show some evidence that they work, Dr. Girgis said there may be a role for certain ones in primary care.
“An example would be black cohosh or primrose oil for perimenopausal hot flashes. This could be a good alternative when you want to avoid hormonal supplements,” she said.
At the same time, Dr. Girgis advised clinicians to be cautious about suggesting homeopathic remedies to patients.
“Homeopathy seems to be a good money maker if you sell these products. However, you are not protected from liability and can be found more liable for prescribing off-label treatments or those not [Food and Drug Administration] approved,” Dr. Girgis said. Her general message to clinicians: Stick with evidence-based medicine.
Her message to patients who might want to pursue homeopathic remedies is that just because something is “homeopathic” or natural doesn’t mean that it is safe.
“There are some [homeopathic] products that have caused liver damage or other problems,” she explained. “Also, these remedies can interact with other medications.”
The study received no outside funding. The researchers and Dr. Girgis had no financial conflicts to disclose.
FROM BMJ EVIDENCE BASED MEDICINE
Norovirus vaccine candidates employ different approaches
Scientists are trying different approaches to developing vaccines against norovirus, seeking to replicate the success seen in developing shots against rotavirus.
Speaking at the 12th World Congress of the World Society for Pediatric Infectious Diseases (WSPID), Miguel O’Ryan, MD, of the University of Chile, Santiago, presented an overview of candidate vaccines. Dr. O’Ryan has been involved for many years with research on rotavirus vaccines and has branched into work with the somewhat similar norovirus.
With advances in preventing rotavirus, norovirus has emerged in recent years as a leading cause of acute gastroenteritis (AGE) in most countries worldwide. It’s associated with almost 20% of all acute diarrheal cases globally and with an estimated 685 million episodes and 212,000 deaths annually, Dr. O’Ryan and coauthors reported in a review in the journal Viruses.
If successful, norovirus vaccines may be used someday to prevent outbreaks among military personnel, as this contagious virus has the potential to disrupt missions, Dr. O’Ryan and coauthors wrote. They also said people might consider getting norovirus vaccines ahead of trips to prevent traveler’s diarrhea. But most importantly, these kinds of vaccines could reduce diarrhea-associated hospitalizations and deaths of children.
Takeda Pharmaceutical Company, for whom Dr. O’Ryan has done consulting, last year announced a collaboration with Frazier Healthcare Partners to launch HilleVax. Based in Boston, the company is intended to commercialize Takeda’s norovirus vaccine candidate.
The Takeda-HilleVax candidate vaccine injection has advanced as far as phase 2 studies, including a test done over two winter seasons in U.S. Navy recruits. Takeda and U.S. Navy scientists reported in 2020 in the journal Vaccine that the primary efficacy outcome for this test could not be evaluated due to an unexpectedly low number of cases of norovirus. Still, data taken from this study indicate that the vaccine induces a broad immune response, the scientists reported.
In his WSPID presentation, Dr. O’Ryan also mentioned an oral norovirus vaccine candidate that the company Vaxart is developing, referring to this as a “very interesting approach.”
Betting on the gut
Based in South San Francisco, California, Vaxart is pursuing a theory that a vaccine designed to generate mucosal antibodies locally in the intestine, in addition to systemic antibodies in the blood, may better protect against norovirus infection than an injectable vaccine.
“A key ability to protect against norovirus needs to come from an intestinal immune response, and injected vaccines don’t give those very well,” Sean Tucker, PhD, the founder and chief scientific officer of Vaxart, told this news organization in an interview. “We think that’s one of the reasons why our oral approaches can have significant advantages.”
Challenges to developing a norovirus vaccine have included a lack of good animal models to use in research and a lack of an ability to grow the virus well in cell culture, Dr. Tucker said.
Vaxart experienced disruptions in its research during the early stages of the pandemic but has since picked up the pace of its efforts to develop its oral vaccine, Dr. Tucker said during the interview.
In a recent filing with the Securities and Exchange Commission, Vaxart said in early 2021 it resumed its norovirus vaccine program by initiating three clinical studies. These included a phase 1b placebo-controlled dose ranging study in healthy elderly adults aged 55-80. Data from these trials may be unveiled in the coming months.
Vaxart said that this year it has already initiated a phase 2 norovirus challenge study, which will evaluate safety, immunogenicity, and clinical efficacy of a vaccine candidate against placebo.
A version of this article first appeared on Medscape.com.
Scientists are trying different approaches to developing vaccines against norovirus, seeking to replicate the success seen in developing shots against rotavirus.
Speaking at the 12th World Congress of the World Society for Pediatric Infectious Diseases (WSPID), Miguel O’Ryan, MD, of the University of Chile, Santiago, presented an overview of candidate vaccines. Dr. O’Ryan has been involved for many years with research on rotavirus vaccines and has branched into work with the somewhat similar norovirus.
With advances in preventing rotavirus, norovirus has emerged in recent years as a leading cause of acute gastroenteritis (AGE) in most countries worldwide. It’s associated with almost 20% of all acute diarrheal cases globally and with an estimated 685 million episodes and 212,000 deaths annually, Dr. O’Ryan and coauthors reported in a review in the journal Viruses.
If successful, norovirus vaccines may be used someday to prevent outbreaks among military personnel, as this contagious virus has the potential to disrupt missions, Dr. O’Ryan and coauthors wrote. They also said people might consider getting norovirus vaccines ahead of trips to prevent traveler’s diarrhea. But most importantly, these kinds of vaccines could reduce diarrhea-associated hospitalizations and deaths of children.
Takeda Pharmaceutical Company, for whom Dr. O’Ryan has done consulting, last year announced a collaboration with Frazier Healthcare Partners to launch HilleVax. Based in Boston, the company is intended to commercialize Takeda’s norovirus vaccine candidate.
The Takeda-HilleVax candidate vaccine injection has advanced as far as phase 2 studies, including a test done over two winter seasons in U.S. Navy recruits. Takeda and U.S. Navy scientists reported in 2020 in the journal Vaccine that the primary efficacy outcome for this test could not be evaluated due to an unexpectedly low number of cases of norovirus. Still, data taken from this study indicate that the vaccine induces a broad immune response, the scientists reported.
In his WSPID presentation, Dr. O’Ryan also mentioned an oral norovirus vaccine candidate that the company Vaxart is developing, referring to this as a “very interesting approach.”
Betting on the gut
Based in South San Francisco, California, Vaxart is pursuing a theory that a vaccine designed to generate mucosal antibodies locally in the intestine, in addition to systemic antibodies in the blood, may better protect against norovirus infection than an injectable vaccine.
“A key ability to protect against norovirus needs to come from an intestinal immune response, and injected vaccines don’t give those very well,” Sean Tucker, PhD, the founder and chief scientific officer of Vaxart, told this news organization in an interview. “We think that’s one of the reasons why our oral approaches can have significant advantages.”
Challenges to developing a norovirus vaccine have included a lack of good animal models to use in research and a lack of an ability to grow the virus well in cell culture, Dr. Tucker said.
Vaxart experienced disruptions in its research during the early stages of the pandemic but has since picked up the pace of its efforts to develop its oral vaccine, Dr. Tucker said during the interview.
In a recent filing with the Securities and Exchange Commission, Vaxart said in early 2021 it resumed its norovirus vaccine program by initiating three clinical studies. These included a phase 1b placebo-controlled dose ranging study in healthy elderly adults aged 55-80. Data from these trials may be unveiled in the coming months.
Vaxart said that this year it has already initiated a phase 2 norovirus challenge study, which will evaluate safety, immunogenicity, and clinical efficacy of a vaccine candidate against placebo.
A version of this article first appeared on Medscape.com.
Scientists are trying different approaches to developing vaccines against norovirus, seeking to replicate the success seen in developing shots against rotavirus.
Speaking at the 12th World Congress of the World Society for Pediatric Infectious Diseases (WSPID), Miguel O’Ryan, MD, of the University of Chile, Santiago, presented an overview of candidate vaccines. Dr. O’Ryan has been involved for many years with research on rotavirus vaccines and has branched into work with the somewhat similar norovirus.
With advances in preventing rotavirus, norovirus has emerged in recent years as a leading cause of acute gastroenteritis (AGE) in most countries worldwide. It’s associated with almost 20% of all acute diarrheal cases globally and with an estimated 685 million episodes and 212,000 deaths annually, Dr. O’Ryan and coauthors reported in a review in the journal Viruses.
If successful, norovirus vaccines may be used someday to prevent outbreaks among military personnel, as this contagious virus has the potential to disrupt missions, Dr. O’Ryan and coauthors wrote. They also said people might consider getting norovirus vaccines ahead of trips to prevent traveler’s diarrhea. But most importantly, these kinds of vaccines could reduce diarrhea-associated hospitalizations and deaths of children.
Takeda Pharmaceutical Company, for whom Dr. O’Ryan has done consulting, last year announced a collaboration with Frazier Healthcare Partners to launch HilleVax. Based in Boston, the company is intended to commercialize Takeda’s norovirus vaccine candidate.
The Takeda-HilleVax candidate vaccine injection has advanced as far as phase 2 studies, including a test done over two winter seasons in U.S. Navy recruits. Takeda and U.S. Navy scientists reported in 2020 in the journal Vaccine that the primary efficacy outcome for this test could not be evaluated due to an unexpectedly low number of cases of norovirus. Still, data taken from this study indicate that the vaccine induces a broad immune response, the scientists reported.
In his WSPID presentation, Dr. O’Ryan also mentioned an oral norovirus vaccine candidate that the company Vaxart is developing, referring to this as a “very interesting approach.”
Betting on the gut
Based in South San Francisco, California, Vaxart is pursuing a theory that a vaccine designed to generate mucosal antibodies locally in the intestine, in addition to systemic antibodies in the blood, may better protect against norovirus infection than an injectable vaccine.
“A key ability to protect against norovirus needs to come from an intestinal immune response, and injected vaccines don’t give those very well,” Sean Tucker, PhD, the founder and chief scientific officer of Vaxart, told this news organization in an interview. “We think that’s one of the reasons why our oral approaches can have significant advantages.”
Challenges to developing a norovirus vaccine have included a lack of good animal models to use in research and a lack of an ability to grow the virus well in cell culture, Dr. Tucker said.
Vaxart experienced disruptions in its research during the early stages of the pandemic but has since picked up the pace of its efforts to develop its oral vaccine, Dr. Tucker said during the interview.
In a recent filing with the Securities and Exchange Commission, Vaxart said in early 2021 it resumed its norovirus vaccine program by initiating three clinical studies. These included a phase 1b placebo-controlled dose ranging study in healthy elderly adults aged 55-80. Data from these trials may be unveiled in the coming months.
Vaxart said that this year it has already initiated a phase 2 norovirus challenge study, which will evaluate safety, immunogenicity, and clinical efficacy of a vaccine candidate against placebo.
A version of this article first appeared on Medscape.com.
TB treatment can be shortened for most children: study
The World Health Organization is expected to recommend truncating treatment of children with mild tuberculosis by 2 months – from 6 months to 4 – after a randomized trial found similar outcomes with the shorter regimen.
An international team of investigators found the abbreviated course of antibiotics was no less effective or safe than conventional treatment and saved an average of $17.34 per child – money that could be used to mitigate the toll of TB, which is estimated to sicken 1.1 million children worldwide each year.
The findings come as deaths from TB are rising as a result of the COVID-19 pandemic, which has hindered efforts to find and treat patients. In 2020, according to the WHO, an estimated 1.5 million people died from TB, the first year-over-year increase in such deaths since 2005.
Nearly a quarter of children with TB die, primarily because they go undiagnosed, according to the researchers, who published the study in the New England Journal of Medicine. Shorter treatment “translates into very large cost savings that could be used to improve screening and diagnosis to address the current case detection gap,” first author Anna Turkova, MD, of University College London, told this news organization.
The standard TB regimen is based on trials in adults with severe respiratory disease. However, about two-thirds of children have nonsevere infections.
For the study, Dr. Turkova and colleagues assigned 1,204 children with TB in four countries – Uganda, Zambia, South Africa, and India – to either a 4- or 6-month regimen with first-line medications rifampin, isoniazid, pyrazinamide, and ethambutol. Participants were aged 2 months to 15 years and had symptomatic nonsevere lung or lymph node infections with a negative test on a sputum smear microscopy. Eleven percent also had HIV.
After 18 months, 16 participants in the group that received the shortened treatment and 18 in the standard treatment group had experienced an unfavorable outcome – defined as treatment failure, recurrence of TB, loss to follow-up, or death (adjusted difference, -0.4 percentage points; 95% confidence interval, -2.2 to 1.5).
Similar numbers – 47 in the 4-month group and 48 in the 6-month group – experienced severe or life-threatening adverse events, most commonly chest infections, such as pneumonia, and liver problems, during treatment or up to 30 days after the last dose.
New guidelines coming soon
The WHO plans to issue new guidelines and a handbook for TB management in children and adolescents on March 24, World Tuberculosis Day, a spokesman for the agency told Medscape.
Anna Mandalakas, MD, PhD, director of the Global Tuberculosis Program at Baylor College of Medicine, department of pediatrics, Houston, said the shorter regimen should enable more children to successfully complete TB treatment.
“It can be challenging to convince young children to take medications on a regular basis for 6 months,” Dr. Mandalakas, a member of a WHO guidelines development group that reviewed the study, told this news organization. “Despite best intentions, parents often become fatigued and give up the medicine battle.”
Leo Martinez, PhD, an epidemiologist at Boston University School of Public Health who studies pediatric TB, noted that study’s cost-effectiveness analysis applies only to health care costs. Families often suffer financially through lost wages, transportation to health care facilities, and lost employment, fueling a cycle of poverty and disease in low-income countries, he said.
A WHO statement noted that long treatment regimens can add toxicity and risk of drug interactions for children with HIV.
Separate efforts have been underway to hasten TB treatment in different groups of patients. A study published in NEJM showed that 4 months of the potent antibiotic rifapentine, along with another antibiotic, moxifloxacin, was non-inferior to the standard 6-month regimen in patients aged 12 and older. According to the editorial accompanying that study, the research illustrated the potential for shorter treatment courses that would be cheaper and less cumbersome, although that particular combination poses hurdles such as adherence issues and potential bacterial resistance.
Experts agreed that improved diagnostic procedures are critical to significantly reducing TB pediatric deaths – an issue that Dr. Turkova said will be addressed in WHO’s forthcoming handbook.
Because no gold-standard test exists for TB, and symptoms often overlap with other infections, widespread screening of children in households where adults have been diagnosed with TB has been found to improve detection of the disease. “Training of health care workers, easy-to-implement diagnostic algorithms, and widely accessible training materials on chest radiography in childhood TB should also improve case finding and treatment initiation,” she said.
The trial was supported by U.K. government and charitable research funders. Dr. Turkova and Dr. Martinez reported no financial disclosures. Dr. Mandalakas reported honoraria from WHO to support the preparation of diagnostics and treatment chapters in the operational handbook, for providing lectures for Medscape, and for serving on a data safety monitoring board for Janssen Pharmaceuticals.
A version of this article first appeared on Medscape.com.
The World Health Organization is expected to recommend truncating treatment of children with mild tuberculosis by 2 months – from 6 months to 4 – after a randomized trial found similar outcomes with the shorter regimen.
An international team of investigators found the abbreviated course of antibiotics was no less effective or safe than conventional treatment and saved an average of $17.34 per child – money that could be used to mitigate the toll of TB, which is estimated to sicken 1.1 million children worldwide each year.
The findings come as deaths from TB are rising as a result of the COVID-19 pandemic, which has hindered efforts to find and treat patients. In 2020, according to the WHO, an estimated 1.5 million people died from TB, the first year-over-year increase in such deaths since 2005.
Nearly a quarter of children with TB die, primarily because they go undiagnosed, according to the researchers, who published the study in the New England Journal of Medicine. Shorter treatment “translates into very large cost savings that could be used to improve screening and diagnosis to address the current case detection gap,” first author Anna Turkova, MD, of University College London, told this news organization.
The standard TB regimen is based on trials in adults with severe respiratory disease. However, about two-thirds of children have nonsevere infections.
For the study, Dr. Turkova and colleagues assigned 1,204 children with TB in four countries – Uganda, Zambia, South Africa, and India – to either a 4- or 6-month regimen with first-line medications rifampin, isoniazid, pyrazinamide, and ethambutol. Participants were aged 2 months to 15 years and had symptomatic nonsevere lung or lymph node infections with a negative test on a sputum smear microscopy. Eleven percent also had HIV.
After 18 months, 16 participants in the group that received the shortened treatment and 18 in the standard treatment group had experienced an unfavorable outcome – defined as treatment failure, recurrence of TB, loss to follow-up, or death (adjusted difference, -0.4 percentage points; 95% confidence interval, -2.2 to 1.5).
Similar numbers – 47 in the 4-month group and 48 in the 6-month group – experienced severe or life-threatening adverse events, most commonly chest infections, such as pneumonia, and liver problems, during treatment or up to 30 days after the last dose.
New guidelines coming soon
The WHO plans to issue new guidelines and a handbook for TB management in children and adolescents on March 24, World Tuberculosis Day, a spokesman for the agency told Medscape.
Anna Mandalakas, MD, PhD, director of the Global Tuberculosis Program at Baylor College of Medicine, department of pediatrics, Houston, said the shorter regimen should enable more children to successfully complete TB treatment.
“It can be challenging to convince young children to take medications on a regular basis for 6 months,” Dr. Mandalakas, a member of a WHO guidelines development group that reviewed the study, told this news organization. “Despite best intentions, parents often become fatigued and give up the medicine battle.”
Leo Martinez, PhD, an epidemiologist at Boston University School of Public Health who studies pediatric TB, noted that study’s cost-effectiveness analysis applies only to health care costs. Families often suffer financially through lost wages, transportation to health care facilities, and lost employment, fueling a cycle of poverty and disease in low-income countries, he said.
A WHO statement noted that long treatment regimens can add toxicity and risk of drug interactions for children with HIV.
Separate efforts have been underway to hasten TB treatment in different groups of patients. A study published in NEJM showed that 4 months of the potent antibiotic rifapentine, along with another antibiotic, moxifloxacin, was non-inferior to the standard 6-month regimen in patients aged 12 and older. According to the editorial accompanying that study, the research illustrated the potential for shorter treatment courses that would be cheaper and less cumbersome, although that particular combination poses hurdles such as adherence issues and potential bacterial resistance.
Experts agreed that improved diagnostic procedures are critical to significantly reducing TB pediatric deaths – an issue that Dr. Turkova said will be addressed in WHO’s forthcoming handbook.
Because no gold-standard test exists for TB, and symptoms often overlap with other infections, widespread screening of children in households where adults have been diagnosed with TB has been found to improve detection of the disease. “Training of health care workers, easy-to-implement diagnostic algorithms, and widely accessible training materials on chest radiography in childhood TB should also improve case finding and treatment initiation,” she said.
The trial was supported by U.K. government and charitable research funders. Dr. Turkova and Dr. Martinez reported no financial disclosures. Dr. Mandalakas reported honoraria from WHO to support the preparation of diagnostics and treatment chapters in the operational handbook, for providing lectures for Medscape, and for serving on a data safety monitoring board for Janssen Pharmaceuticals.
A version of this article first appeared on Medscape.com.
The World Health Organization is expected to recommend truncating treatment of children with mild tuberculosis by 2 months – from 6 months to 4 – after a randomized trial found similar outcomes with the shorter regimen.
An international team of investigators found the abbreviated course of antibiotics was no less effective or safe than conventional treatment and saved an average of $17.34 per child – money that could be used to mitigate the toll of TB, which is estimated to sicken 1.1 million children worldwide each year.
The findings come as deaths from TB are rising as a result of the COVID-19 pandemic, which has hindered efforts to find and treat patients. In 2020, according to the WHO, an estimated 1.5 million people died from TB, the first year-over-year increase in such deaths since 2005.
Nearly a quarter of children with TB die, primarily because they go undiagnosed, according to the researchers, who published the study in the New England Journal of Medicine. Shorter treatment “translates into very large cost savings that could be used to improve screening and diagnosis to address the current case detection gap,” first author Anna Turkova, MD, of University College London, told this news organization.
The standard TB regimen is based on trials in adults with severe respiratory disease. However, about two-thirds of children have nonsevere infections.
For the study, Dr. Turkova and colleagues assigned 1,204 children with TB in four countries – Uganda, Zambia, South Africa, and India – to either a 4- or 6-month regimen with first-line medications rifampin, isoniazid, pyrazinamide, and ethambutol. Participants were aged 2 months to 15 years and had symptomatic nonsevere lung or lymph node infections with a negative test on a sputum smear microscopy. Eleven percent also had HIV.
After 18 months, 16 participants in the group that received the shortened treatment and 18 in the standard treatment group had experienced an unfavorable outcome – defined as treatment failure, recurrence of TB, loss to follow-up, or death (adjusted difference, -0.4 percentage points; 95% confidence interval, -2.2 to 1.5).
Similar numbers – 47 in the 4-month group and 48 in the 6-month group – experienced severe or life-threatening adverse events, most commonly chest infections, such as pneumonia, and liver problems, during treatment or up to 30 days after the last dose.
New guidelines coming soon
The WHO plans to issue new guidelines and a handbook for TB management in children and adolescents on March 24, World Tuberculosis Day, a spokesman for the agency told Medscape.
Anna Mandalakas, MD, PhD, director of the Global Tuberculosis Program at Baylor College of Medicine, department of pediatrics, Houston, said the shorter regimen should enable more children to successfully complete TB treatment.
“It can be challenging to convince young children to take medications on a regular basis for 6 months,” Dr. Mandalakas, a member of a WHO guidelines development group that reviewed the study, told this news organization. “Despite best intentions, parents often become fatigued and give up the medicine battle.”
Leo Martinez, PhD, an epidemiologist at Boston University School of Public Health who studies pediatric TB, noted that study’s cost-effectiveness analysis applies only to health care costs. Families often suffer financially through lost wages, transportation to health care facilities, and lost employment, fueling a cycle of poverty and disease in low-income countries, he said.
A WHO statement noted that long treatment regimens can add toxicity and risk of drug interactions for children with HIV.
Separate efforts have been underway to hasten TB treatment in different groups of patients. A study published in NEJM showed that 4 months of the potent antibiotic rifapentine, along with another antibiotic, moxifloxacin, was non-inferior to the standard 6-month regimen in patients aged 12 and older. According to the editorial accompanying that study, the research illustrated the potential for shorter treatment courses that would be cheaper and less cumbersome, although that particular combination poses hurdles such as adherence issues and potential bacterial resistance.
Experts agreed that improved diagnostic procedures are critical to significantly reducing TB pediatric deaths – an issue that Dr. Turkova said will be addressed in WHO’s forthcoming handbook.
Because no gold-standard test exists for TB, and symptoms often overlap with other infections, widespread screening of children in households where adults have been diagnosed with TB has been found to improve detection of the disease. “Training of health care workers, easy-to-implement diagnostic algorithms, and widely accessible training materials on chest radiography in childhood TB should also improve case finding and treatment initiation,” she said.
The trial was supported by U.K. government and charitable research funders. Dr. Turkova and Dr. Martinez reported no financial disclosures. Dr. Mandalakas reported honoraria from WHO to support the preparation of diagnostics and treatment chapters in the operational handbook, for providing lectures for Medscape, and for serving on a data safety monitoring board for Janssen Pharmaceuticals.
A version of this article first appeared on Medscape.com.
‘Bigorexia’: Why teenage boys are obsessed with bulking up
Why are teenage boys obsessed with bulking up?
While the effects of Instagram on girls’ body image has long been documented – an article in The Wall Street Journal that was published this fall reported that Facebook knew Instagram was toxic for teen girls – teenage boys are under just as much pressure.
For adolescent boys, the goal is often to get superhero-size buff – and this is leading to anxiety, stress, excessive selfies, and, often, obsessive staring in the mirror to assess their “pec” progress.
So-called “bigorexia” – or extreme gym time, excessive focus on protein diets, and intense muscle-building goals – has hit new and concerning levels, according to a recent New York Times report.
Whether it’s the pandemic or TikTok that’s to blame, teen boys are pushing hard to achieve six-pack abs, with one-third of them in the U.S. trying to bulk up, according to a study published in the Journal of Adolescent Health. What’s more, 22% reported they’re engaging in muscle-enhancing behavior, including excess exercise, taking supplements or steroids, or eating more to bulk up, according to a study published in the International Journal of Eating Disorders.
“The pandemic and social media have been a perfect storm for eating disorders and body image issues for all teens, but this has been under-recognized in boys,” says Jason Nagata, MD, a pediatrician who specializes in adolescent medicine at the University of California, San Francisco. “Both are directly connected to an increase in muscle dysmorphia.”
While “bigorexia” is a newer term coined by mental health professionals, the concept of muscular dysmorphia isn’t, says Jennifer Bahrman, PhD, a licensed psychologist with McGovern Medical School at UTHealth Houston. This may be why about a third of boys ages 11-18 reported that they aren’t enamored with their bodies, according to a small survey published in 2019 in the Californian Journal of Health Promotion.
“When we think of dysmorphia, we think of girls having it, since we see it more in females,” says Dr. Bahrman, who works extensively with adolescents and athletes. “The interesting thing about muscular dysmorphia is that it’s the only body dysmorphic disorder that’s almost exclusively present in males.”
Social media’s role
Unlike other things in boys’ lives, like movies, TV, or even the uber-buff GI Joe doll, social media has created opportunities for young men to put their bodies on display – and become an influencer or get followers because of it.
“An everyday teen can become a celebrity,” Dr. Nagata says. “Then, thanks to social media algorithms, if a teenage boy likes or interacts with a post that features a muscular guy or is all about fitness, they’ll start getting all sorts of related content. They’ll get bombarded with tons of ads for protein shakes, for example, as well as bodybuilding equipment, and that will further distort reality.”
Before-and-after photos are also known to be quite misleading.
“Some of the most popular Instagram posts among teens feature people who have experienced a massive body transformation,” Dr. Nagata says. “It’s usually someone who lost a lot of weight or someone who was scrawny and then got muscular. The most drastic changes tend to get the most likes and are perpetuated the most and shared the most often with friends.”
But as many are aware, photos posted to social media are selected to tell the best story – with the best filters, lighting, and angles possible, however exaggerated.
“A guy will post his worst picture out of a thousand for his before shot and then post the best photo out of a thousand,” Dr. Nagata says. “This, in itself, can really confuse a teenager, because the story of this person’s changed body looks so realistic.”
Worse, these images tend to be damaging to your teenager’s self-esteem.
“When you see images of people you’re aspiring to look like, it can be very upsetting,” Dr. Bahrman says. “After all, it’s easy to think, ‘I’m doing all of these pushups, and I don’t look like this.’ From there, it’s easy to begin internalizing that something is wrong with you.”
Red flags to watch out for
If you’ve noticed that your son is obsessed with his appearance, weight, food, or exercise, take note. Also, notice if he’s asking you to buy protein powder or is spending more time at the gym than with his friends.
“Pay attention if he is withdrawing from friends and family because of his concerns about his appearance,” Dr. Nagata says. “For example, we often hear that a teenager will no longer eat family meals or at a restaurant because the protein content isn’t high enough or the food is too fatty.”
If you’re concerned, always make sure to discuss this with your son’s pediatrician.
“Ultimately, you want to make sure you share your concerns before your teen son becomes even more body-image obsessed,” Dr. Nagata says.
A version of this article first appeared on WebMD.com.
Why are teenage boys obsessed with bulking up?
While the effects of Instagram on girls’ body image has long been documented – an article in The Wall Street Journal that was published this fall reported that Facebook knew Instagram was toxic for teen girls – teenage boys are under just as much pressure.
For adolescent boys, the goal is often to get superhero-size buff – and this is leading to anxiety, stress, excessive selfies, and, often, obsessive staring in the mirror to assess their “pec” progress.
So-called “bigorexia” – or extreme gym time, excessive focus on protein diets, and intense muscle-building goals – has hit new and concerning levels, according to a recent New York Times report.
Whether it’s the pandemic or TikTok that’s to blame, teen boys are pushing hard to achieve six-pack abs, with one-third of them in the U.S. trying to bulk up, according to a study published in the Journal of Adolescent Health. What’s more, 22% reported they’re engaging in muscle-enhancing behavior, including excess exercise, taking supplements or steroids, or eating more to bulk up, according to a study published in the International Journal of Eating Disorders.
“The pandemic and social media have been a perfect storm for eating disorders and body image issues for all teens, but this has been under-recognized in boys,” says Jason Nagata, MD, a pediatrician who specializes in adolescent medicine at the University of California, San Francisco. “Both are directly connected to an increase in muscle dysmorphia.”
While “bigorexia” is a newer term coined by mental health professionals, the concept of muscular dysmorphia isn’t, says Jennifer Bahrman, PhD, a licensed psychologist with McGovern Medical School at UTHealth Houston. This may be why about a third of boys ages 11-18 reported that they aren’t enamored with their bodies, according to a small survey published in 2019 in the Californian Journal of Health Promotion.
“When we think of dysmorphia, we think of girls having it, since we see it more in females,” says Dr. Bahrman, who works extensively with adolescents and athletes. “The interesting thing about muscular dysmorphia is that it’s the only body dysmorphic disorder that’s almost exclusively present in males.”
Social media’s role
Unlike other things in boys’ lives, like movies, TV, or even the uber-buff GI Joe doll, social media has created opportunities for young men to put their bodies on display – and become an influencer or get followers because of it.
“An everyday teen can become a celebrity,” Dr. Nagata says. “Then, thanks to social media algorithms, if a teenage boy likes or interacts with a post that features a muscular guy or is all about fitness, they’ll start getting all sorts of related content. They’ll get bombarded with tons of ads for protein shakes, for example, as well as bodybuilding equipment, and that will further distort reality.”
Before-and-after photos are also known to be quite misleading.
“Some of the most popular Instagram posts among teens feature people who have experienced a massive body transformation,” Dr. Nagata says. “It’s usually someone who lost a lot of weight or someone who was scrawny and then got muscular. The most drastic changes tend to get the most likes and are perpetuated the most and shared the most often with friends.”
But as many are aware, photos posted to social media are selected to tell the best story – with the best filters, lighting, and angles possible, however exaggerated.
“A guy will post his worst picture out of a thousand for his before shot and then post the best photo out of a thousand,” Dr. Nagata says. “This, in itself, can really confuse a teenager, because the story of this person’s changed body looks so realistic.”
Worse, these images tend to be damaging to your teenager’s self-esteem.
“When you see images of people you’re aspiring to look like, it can be very upsetting,” Dr. Bahrman says. “After all, it’s easy to think, ‘I’m doing all of these pushups, and I don’t look like this.’ From there, it’s easy to begin internalizing that something is wrong with you.”
Red flags to watch out for
If you’ve noticed that your son is obsessed with his appearance, weight, food, or exercise, take note. Also, notice if he’s asking you to buy protein powder or is spending more time at the gym than with his friends.
“Pay attention if he is withdrawing from friends and family because of his concerns about his appearance,” Dr. Nagata says. “For example, we often hear that a teenager will no longer eat family meals or at a restaurant because the protein content isn’t high enough or the food is too fatty.”
If you’re concerned, always make sure to discuss this with your son’s pediatrician.
“Ultimately, you want to make sure you share your concerns before your teen son becomes even more body-image obsessed,” Dr. Nagata says.
A version of this article first appeared on WebMD.com.
Why are teenage boys obsessed with bulking up?
While the effects of Instagram on girls’ body image has long been documented – an article in The Wall Street Journal that was published this fall reported that Facebook knew Instagram was toxic for teen girls – teenage boys are under just as much pressure.
For adolescent boys, the goal is often to get superhero-size buff – and this is leading to anxiety, stress, excessive selfies, and, often, obsessive staring in the mirror to assess their “pec” progress.
So-called “bigorexia” – or extreme gym time, excessive focus on protein diets, and intense muscle-building goals – has hit new and concerning levels, according to a recent New York Times report.
Whether it’s the pandemic or TikTok that’s to blame, teen boys are pushing hard to achieve six-pack abs, with one-third of them in the U.S. trying to bulk up, according to a study published in the Journal of Adolescent Health. What’s more, 22% reported they’re engaging in muscle-enhancing behavior, including excess exercise, taking supplements or steroids, or eating more to bulk up, according to a study published in the International Journal of Eating Disorders.
“The pandemic and social media have been a perfect storm for eating disorders and body image issues for all teens, but this has been under-recognized in boys,” says Jason Nagata, MD, a pediatrician who specializes in adolescent medicine at the University of California, San Francisco. “Both are directly connected to an increase in muscle dysmorphia.”
While “bigorexia” is a newer term coined by mental health professionals, the concept of muscular dysmorphia isn’t, says Jennifer Bahrman, PhD, a licensed psychologist with McGovern Medical School at UTHealth Houston. This may be why about a third of boys ages 11-18 reported that they aren’t enamored with their bodies, according to a small survey published in 2019 in the Californian Journal of Health Promotion.
“When we think of dysmorphia, we think of girls having it, since we see it more in females,” says Dr. Bahrman, who works extensively with adolescents and athletes. “The interesting thing about muscular dysmorphia is that it’s the only body dysmorphic disorder that’s almost exclusively present in males.”
Social media’s role
Unlike other things in boys’ lives, like movies, TV, or even the uber-buff GI Joe doll, social media has created opportunities for young men to put their bodies on display – and become an influencer or get followers because of it.
“An everyday teen can become a celebrity,” Dr. Nagata says. “Then, thanks to social media algorithms, if a teenage boy likes or interacts with a post that features a muscular guy or is all about fitness, they’ll start getting all sorts of related content. They’ll get bombarded with tons of ads for protein shakes, for example, as well as bodybuilding equipment, and that will further distort reality.”
Before-and-after photos are also known to be quite misleading.
“Some of the most popular Instagram posts among teens feature people who have experienced a massive body transformation,” Dr. Nagata says. “It’s usually someone who lost a lot of weight or someone who was scrawny and then got muscular. The most drastic changes tend to get the most likes and are perpetuated the most and shared the most often with friends.”
But as many are aware, photos posted to social media are selected to tell the best story – with the best filters, lighting, and angles possible, however exaggerated.
“A guy will post his worst picture out of a thousand for his before shot and then post the best photo out of a thousand,” Dr. Nagata says. “This, in itself, can really confuse a teenager, because the story of this person’s changed body looks so realistic.”
Worse, these images tend to be damaging to your teenager’s self-esteem.
“When you see images of people you’re aspiring to look like, it can be very upsetting,” Dr. Bahrman says. “After all, it’s easy to think, ‘I’m doing all of these pushups, and I don’t look like this.’ From there, it’s easy to begin internalizing that something is wrong with you.”
Red flags to watch out for
If you’ve noticed that your son is obsessed with his appearance, weight, food, or exercise, take note. Also, notice if he’s asking you to buy protein powder or is spending more time at the gym than with his friends.
“Pay attention if he is withdrawing from friends and family because of his concerns about his appearance,” Dr. Nagata says. “For example, we often hear that a teenager will no longer eat family meals or at a restaurant because the protein content isn’t high enough or the food is too fatty.”
If you’re concerned, always make sure to discuss this with your son’s pediatrician.
“Ultimately, you want to make sure you share your concerns before your teen son becomes even more body-image obsessed,” Dr. Nagata says.
A version of this article first appeared on WebMD.com.
Food insecurity linked to metabolic syndrome in Hispanic/Latino youth
Severe food insecurity was associated with metabolic syndrome and unfavorable cardiometabolic markers in Hispanic/Latino youth, researchers report.
The findings, published March 16 in Pediatrics, highlight the need to investigate interventions that address food insecurity among Hispanic/Latino youth, a segment of the U.S. population at high risk of cardiometabolic complications.
“Among Hispanic/Latino youth, no study, to our knowledge has evaluated food insecurity’s role in metabolic syndrome and metabolic syndrome–relevant cardiometabolic markers in this population,” lead author Luis E. Maldonado, PhD, of the University of North Carolina at Chapel Hill, and colleagues explained.
The researchers conducted a cross-sectional study to evaluate the associations between lower household and child food security and metabolic syndrome, as well as clinically measured cardiometabolic markers, including fasting plasma glucose, waist circumference, triglycerides, systolic and diastolic blood pressure, and high-density lipoprotein cholesterol (HDL-C).
Household food security (high, marginal, low, very low) and child food security (high, marginal, low/very low) measures were evaluated separately, and were adjusted for participant age, sex, site, parental education, and poverty-income ratio.
Data were obtained from the Hispanic Community Children’s Health Study/Study of Latino Youth, a study of offspring of adults enrolled in the Hispanic Community Health Survey/Study of Latinos.
Results
The study cohort included 1,325 Hispanic/Latino youth aged 8-16 years. For both household food security and child food security, youth in the lowest food security category had significantly lower HDL-C compared with youth with high food security (household food security, –3.17; 95% confidence interval, –5.65 to –0.70; child food security, –1.81; 95% CI, –3.54 to –0.09).
In addition, low/very low compared with high child food security was associated with higher triglycerides (beta, 8.68; 95% CI, 1.75-15.61), higher fasting plasma glucose (beta, 1.37; 95% CI, 0.08-2.65), and metabolic syndrome composite variable expected log counts (beta, 2.12; 95% CI, 0.02-0.45).
Furthermore, the researchers found statistically significant interactions between each of the two food security measures and receipt of any food assistance in the previous year in models of triglycerides (P for interactions: household food security, .03 and child food security, .005) and HDL-C (P for interactions: household food security, .01 and child food security, .04).
After evaluating the effect of parental place of birth, they found a statistically significant association for triglycerides only (P for interactions: household food security, .05 and child food security, .008).
“Our study is among the first to document adverse associations between household and child food security measures with a metabolic syndrome score variable and several metabolic syndrome–relevant cardiometabolic markers among US Hispanic/Latino youth,” the researchers wrote.
The researchers acknowledged that the cross-sectional nature of the study was a key limitation; thus, causality could not be inferred.
“In the future, we plan to conduct more qualitative work to better understand how Hispanic/Latino families respond to food insecurity, which may identify the factors that shape their response,” study author Sandra S. Albrecht, PhD, of Columbia University, New York, NY, said in an interview.
Recommendations for pediatricians
Food insecurity researcher Yankun Wang, PhD candidate at Indiana University, Bloomington, commented: “I would recommend pediatricians pay more attention to children from low-income households since they are more likely to have mental and physical health issues due to food insecurity.
“It can be very helpful if pediatricians could help families obtain SNAP benefits, enroll youth in the school breakfast and lunch programs, and promote nutrition education in schools,” Mr. Wang added.
This study was supported by grant funding from the National Heart, Lung, and Blood Institute. The authors reported no relevant disclosures.
Severe food insecurity was associated with metabolic syndrome and unfavorable cardiometabolic markers in Hispanic/Latino youth, researchers report.
The findings, published March 16 in Pediatrics, highlight the need to investigate interventions that address food insecurity among Hispanic/Latino youth, a segment of the U.S. population at high risk of cardiometabolic complications.
“Among Hispanic/Latino youth, no study, to our knowledge has evaluated food insecurity’s role in metabolic syndrome and metabolic syndrome–relevant cardiometabolic markers in this population,” lead author Luis E. Maldonado, PhD, of the University of North Carolina at Chapel Hill, and colleagues explained.
The researchers conducted a cross-sectional study to evaluate the associations between lower household and child food security and metabolic syndrome, as well as clinically measured cardiometabolic markers, including fasting plasma glucose, waist circumference, triglycerides, systolic and diastolic blood pressure, and high-density lipoprotein cholesterol (HDL-C).
Household food security (high, marginal, low, very low) and child food security (high, marginal, low/very low) measures were evaluated separately, and were adjusted for participant age, sex, site, parental education, and poverty-income ratio.
Data were obtained from the Hispanic Community Children’s Health Study/Study of Latino Youth, a study of offspring of adults enrolled in the Hispanic Community Health Survey/Study of Latinos.
Results
The study cohort included 1,325 Hispanic/Latino youth aged 8-16 years. For both household food security and child food security, youth in the lowest food security category had significantly lower HDL-C compared with youth with high food security (household food security, –3.17; 95% confidence interval, –5.65 to –0.70; child food security, –1.81; 95% CI, –3.54 to –0.09).
In addition, low/very low compared with high child food security was associated with higher triglycerides (beta, 8.68; 95% CI, 1.75-15.61), higher fasting plasma glucose (beta, 1.37; 95% CI, 0.08-2.65), and metabolic syndrome composite variable expected log counts (beta, 2.12; 95% CI, 0.02-0.45).
Furthermore, the researchers found statistically significant interactions between each of the two food security measures and receipt of any food assistance in the previous year in models of triglycerides (P for interactions: household food security, .03 and child food security, .005) and HDL-C (P for interactions: household food security, .01 and child food security, .04).
After evaluating the effect of parental place of birth, they found a statistically significant association for triglycerides only (P for interactions: household food security, .05 and child food security, .008).
“Our study is among the first to document adverse associations between household and child food security measures with a metabolic syndrome score variable and several metabolic syndrome–relevant cardiometabolic markers among US Hispanic/Latino youth,” the researchers wrote.
The researchers acknowledged that the cross-sectional nature of the study was a key limitation; thus, causality could not be inferred.
“In the future, we plan to conduct more qualitative work to better understand how Hispanic/Latino families respond to food insecurity, which may identify the factors that shape their response,” study author Sandra S. Albrecht, PhD, of Columbia University, New York, NY, said in an interview.
Recommendations for pediatricians
Food insecurity researcher Yankun Wang, PhD candidate at Indiana University, Bloomington, commented: “I would recommend pediatricians pay more attention to children from low-income households since they are more likely to have mental and physical health issues due to food insecurity.
“It can be very helpful if pediatricians could help families obtain SNAP benefits, enroll youth in the school breakfast and lunch programs, and promote nutrition education in schools,” Mr. Wang added.
This study was supported by grant funding from the National Heart, Lung, and Blood Institute. The authors reported no relevant disclosures.
Severe food insecurity was associated with metabolic syndrome and unfavorable cardiometabolic markers in Hispanic/Latino youth, researchers report.
The findings, published March 16 in Pediatrics, highlight the need to investigate interventions that address food insecurity among Hispanic/Latino youth, a segment of the U.S. population at high risk of cardiometabolic complications.
“Among Hispanic/Latino youth, no study, to our knowledge has evaluated food insecurity’s role in metabolic syndrome and metabolic syndrome–relevant cardiometabolic markers in this population,” lead author Luis E. Maldonado, PhD, of the University of North Carolina at Chapel Hill, and colleagues explained.
The researchers conducted a cross-sectional study to evaluate the associations between lower household and child food security and metabolic syndrome, as well as clinically measured cardiometabolic markers, including fasting plasma glucose, waist circumference, triglycerides, systolic and diastolic blood pressure, and high-density lipoprotein cholesterol (HDL-C).
Household food security (high, marginal, low, very low) and child food security (high, marginal, low/very low) measures were evaluated separately, and were adjusted for participant age, sex, site, parental education, and poverty-income ratio.
Data were obtained from the Hispanic Community Children’s Health Study/Study of Latino Youth, a study of offspring of adults enrolled in the Hispanic Community Health Survey/Study of Latinos.
Results
The study cohort included 1,325 Hispanic/Latino youth aged 8-16 years. For both household food security and child food security, youth in the lowest food security category had significantly lower HDL-C compared with youth with high food security (household food security, –3.17; 95% confidence interval, –5.65 to –0.70; child food security, –1.81; 95% CI, –3.54 to –0.09).
In addition, low/very low compared with high child food security was associated with higher triglycerides (beta, 8.68; 95% CI, 1.75-15.61), higher fasting plasma glucose (beta, 1.37; 95% CI, 0.08-2.65), and metabolic syndrome composite variable expected log counts (beta, 2.12; 95% CI, 0.02-0.45).
Furthermore, the researchers found statistically significant interactions between each of the two food security measures and receipt of any food assistance in the previous year in models of triglycerides (P for interactions: household food security, .03 and child food security, .005) and HDL-C (P for interactions: household food security, .01 and child food security, .04).
After evaluating the effect of parental place of birth, they found a statistically significant association for triglycerides only (P for interactions: household food security, .05 and child food security, .008).
“Our study is among the first to document adverse associations between household and child food security measures with a metabolic syndrome score variable and several metabolic syndrome–relevant cardiometabolic markers among US Hispanic/Latino youth,” the researchers wrote.
The researchers acknowledged that the cross-sectional nature of the study was a key limitation; thus, causality could not be inferred.
“In the future, we plan to conduct more qualitative work to better understand how Hispanic/Latino families respond to food insecurity, which may identify the factors that shape their response,” study author Sandra S. Albrecht, PhD, of Columbia University, New York, NY, said in an interview.
Recommendations for pediatricians
Food insecurity researcher Yankun Wang, PhD candidate at Indiana University, Bloomington, commented: “I would recommend pediatricians pay more attention to children from low-income households since they are more likely to have mental and physical health issues due to food insecurity.
“It can be very helpful if pediatricians could help families obtain SNAP benefits, enroll youth in the school breakfast and lunch programs, and promote nutrition education in schools,” Mr. Wang added.
This study was supported by grant funding from the National Heart, Lung, and Blood Institute. The authors reported no relevant disclosures.
FROM PEDIATRICS
New guidance on palliative care for neurologic disorders
Palliative care includes much more than hospice services, lead author of the new position statement Lynne P. Taylor, MD, University of Washington, Seattle, and a fellow of the AAN, said in a press release.
“Neurologists provide palliative care to people living with life-altering neurologic illnesses not just at the end of life but throughout the course of a disease, improving their lives with symptom control,” Dr. Taylor added.
The position paper, developed by a joint committee of the AAN, American Neurological Association, and Child Neurology Society, was published online March 8 in Neurology.
Guidance across the lifespan
The new paper, an update of previous position statements, includes palliative care guidance for different neurologic disorders across the lifespan. For example, neuropalliative care for neonates deserves “extra consideration,” because one-third of pediatric deaths occur during the neonatal period, most often in the neonatal intensive care unit, and after withdrawal of life-sustaining interventions, the authors note.
For older children, neuropalliative care consultation benefits families trying to maximize the quality of the remainder of their child’s life. Decisionmaking must consider the child’s cognitive abilities, the diagnosis, the perceived level of suffering, parental values, and the family’s understanding of the prognosis, the authors note.
They note that discussions about prognosis are often difficult but critical. Previous research “supports that patients desire prognostic information even when prognosis is uncertain and appreciate when their physicians disclose the presence of that uncertainty,” the authors note.
Also important is engaging in shared decisionmaking with patients and families. “This approach requires the physician to elicit a patient’s goals, make recommendations based on whether medical treatments are likely to achieve those goals, and work with patients and families to finalize a treatment plan,” according to the new guidance.
Ethical considerations
When treatments are physiologically futile, clinicians need to explain why interventions that may cause harm and have no benefit are not offered.
The authors cite cardiopulmonary resuscitation in the setting of cardiac arrest from irreversible herniation as an example of futility in the context of neurologic disease.
When life-prolonging care is no longer an option, clinicians have an obligation to shift the focus of care to preserving quality of life and comfort as much as possible, they add.
Hospices, which provide comfort-focused medical care as well as psychosocial and spiritual support, are reserved for patients believed to be in the last 6 months of their life if their disease follows the expected course.
The investigators also broached ethical considerations for individual neurologic conditions. Concerns for disorders of consciousness include misdiagnosis or inaccurate prognostication, and serial examinations are needed to re-evaluate levels of cognition, psychological state, decisionmaking capacity, and disease trajectory.
In patients with locked-in syndrome, a state of irreversible paralysis, often with respiratory and vocal paralysis, consciousness may range from a chronic minimally conscious state to intact cognition.
Without careful examination, patients with preserved consciousness may be mistaken as having a disorder of consciousness and risk their decisional capacity being ignored, the researchers note.
These patients may need assistance from speech pathologists to identify techniques to enhance communication, such as careful “yes/no” questioning, communication boards, or advanced eye-gaze technology, they add.
Stroke, dementia, Parkinson’s guidance
For stroke, the guidance suggests neurologists encourage patients with retained decisionmaking capacity to complete advance care planning given the risk of recurrent stroke and loss of capacity in the future.
For dementia, a proper and timely diagnosis can help patients and their families prepare for the consequences of cognitive dysfunction and loss of autonomy while respecting their identified values, the authors write.
They note that for Parkinson’s disease, which is marked by slow functional and cognitive decline, neurologists must aim to anticipate and treat symptoms, address psychosocial and spiritual distress and caregiver burden, and engage patients and families in advance care planning before onset of cognitive impairment.
For patients with amyotrophic lateral sclerosis (ALS) and related disorders, clinicians should aim to document goals and treatment preferences prior to extreme weakness and aphonia.
It is also important to anticipate patient preferences for future disability-specific decisions, such as those related to feeding tubes and mechanical ventilation, and to identify the patient’s minimal acceptable outcome from these life-sustaining interventions.
On the topic of withdrawal of treatment, the paper notes that competent patients have the right to refuse life-prolonging therapies, including artificial nutrition, hydration, mechanical ventilation, and antibiotics. If physicians have a moral objection to removing life-support systems, they are obligated to transfer the care of the patient to another physician, the authors add.
Once a decision is made to forgo life-sustaining treatment, physicians should minimize subsequent suffering. The investigators note most symptoms at the end of life can be managed without sedation.
In broaching the “gap” in neurology training programs, the statement referred to a survey of 49 neurology residency programs. Results showed that 42% of respondents reported being dissatisfied with their palliative care education.
Well-timed update
Kate T. Brizzi, MD, a Boston neurologist with experience in hospice and palliative care, said the updated position statement is “well-timed” as neuropalliative care has evolved dramatically over the last decade.
“In the last several years, I’ve witnessed a significant increase in trainee interest in the field, and there is growing recognition of how a palliative care approach can improve patient care and hopefully outcomes,” said Dr. Brizzi.
She praised the authors for doing “an excellent job” in highlighting the ethical challenges facing the neurology provider, particularly as it relates to prognostication in an uncertain setting.
Dr. Brizzi noted communication tools that help facilitate discussions around shared decisionmaking “have enhanced our ability to meet the palliative care needs of our patients and can be incorporated by any provider.”
However, she added that the paper only briefly comments on the role of the neurologist in “lawful physician-hastened death.”
“I anticipate that this will be an area of further discussion in the neurology and palliative care community in the future, as requests for hastened death are frequently encountered from patients with serious neurologic illness,” she said.
Dr. Brizzi also noted the importance of understanding the reasons behind the request – and addressing patient worries related to end-of-life care, which can frequently help alleviate distress.
There was no targeted funding for this paper. Coauthor Salvador Cruz-Flores, MD, department of neurology, Texas Tech University Center, El Paso, reported participation on member adjudication committees for clinical trials for Novo Nordisk, Sunovion, and Galapagos. The remaining authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Palliative care includes much more than hospice services, lead author of the new position statement Lynne P. Taylor, MD, University of Washington, Seattle, and a fellow of the AAN, said in a press release.
“Neurologists provide palliative care to people living with life-altering neurologic illnesses not just at the end of life but throughout the course of a disease, improving their lives with symptom control,” Dr. Taylor added.
The position paper, developed by a joint committee of the AAN, American Neurological Association, and Child Neurology Society, was published online March 8 in Neurology.
Guidance across the lifespan
The new paper, an update of previous position statements, includes palliative care guidance for different neurologic disorders across the lifespan. For example, neuropalliative care for neonates deserves “extra consideration,” because one-third of pediatric deaths occur during the neonatal period, most often in the neonatal intensive care unit, and after withdrawal of life-sustaining interventions, the authors note.
For older children, neuropalliative care consultation benefits families trying to maximize the quality of the remainder of their child’s life. Decisionmaking must consider the child’s cognitive abilities, the diagnosis, the perceived level of suffering, parental values, and the family’s understanding of the prognosis, the authors note.
They note that discussions about prognosis are often difficult but critical. Previous research “supports that patients desire prognostic information even when prognosis is uncertain and appreciate when their physicians disclose the presence of that uncertainty,” the authors note.
Also important is engaging in shared decisionmaking with patients and families. “This approach requires the physician to elicit a patient’s goals, make recommendations based on whether medical treatments are likely to achieve those goals, and work with patients and families to finalize a treatment plan,” according to the new guidance.
Ethical considerations
When treatments are physiologically futile, clinicians need to explain why interventions that may cause harm and have no benefit are not offered.
The authors cite cardiopulmonary resuscitation in the setting of cardiac arrest from irreversible herniation as an example of futility in the context of neurologic disease.
When life-prolonging care is no longer an option, clinicians have an obligation to shift the focus of care to preserving quality of life and comfort as much as possible, they add.
Hospices, which provide comfort-focused medical care as well as psychosocial and spiritual support, are reserved for patients believed to be in the last 6 months of their life if their disease follows the expected course.
The investigators also broached ethical considerations for individual neurologic conditions. Concerns for disorders of consciousness include misdiagnosis or inaccurate prognostication, and serial examinations are needed to re-evaluate levels of cognition, psychological state, decisionmaking capacity, and disease trajectory.
In patients with locked-in syndrome, a state of irreversible paralysis, often with respiratory and vocal paralysis, consciousness may range from a chronic minimally conscious state to intact cognition.
Without careful examination, patients with preserved consciousness may be mistaken as having a disorder of consciousness and risk their decisional capacity being ignored, the researchers note.
These patients may need assistance from speech pathologists to identify techniques to enhance communication, such as careful “yes/no” questioning, communication boards, or advanced eye-gaze technology, they add.
Stroke, dementia, Parkinson’s guidance
For stroke, the guidance suggests neurologists encourage patients with retained decisionmaking capacity to complete advance care planning given the risk of recurrent stroke and loss of capacity in the future.
For dementia, a proper and timely diagnosis can help patients and their families prepare for the consequences of cognitive dysfunction and loss of autonomy while respecting their identified values, the authors write.
They note that for Parkinson’s disease, which is marked by slow functional and cognitive decline, neurologists must aim to anticipate and treat symptoms, address psychosocial and spiritual distress and caregiver burden, and engage patients and families in advance care planning before onset of cognitive impairment.
For patients with amyotrophic lateral sclerosis (ALS) and related disorders, clinicians should aim to document goals and treatment preferences prior to extreme weakness and aphonia.
It is also important to anticipate patient preferences for future disability-specific decisions, such as those related to feeding tubes and mechanical ventilation, and to identify the patient’s minimal acceptable outcome from these life-sustaining interventions.
On the topic of withdrawal of treatment, the paper notes that competent patients have the right to refuse life-prolonging therapies, including artificial nutrition, hydration, mechanical ventilation, and antibiotics. If physicians have a moral objection to removing life-support systems, they are obligated to transfer the care of the patient to another physician, the authors add.
Once a decision is made to forgo life-sustaining treatment, physicians should minimize subsequent suffering. The investigators note most symptoms at the end of life can be managed without sedation.
In broaching the “gap” in neurology training programs, the statement referred to a survey of 49 neurology residency programs. Results showed that 42% of respondents reported being dissatisfied with their palliative care education.
Well-timed update
Kate T. Brizzi, MD, a Boston neurologist with experience in hospice and palliative care, said the updated position statement is “well-timed” as neuropalliative care has evolved dramatically over the last decade.
“In the last several years, I’ve witnessed a significant increase in trainee interest in the field, and there is growing recognition of how a palliative care approach can improve patient care and hopefully outcomes,” said Dr. Brizzi.
She praised the authors for doing “an excellent job” in highlighting the ethical challenges facing the neurology provider, particularly as it relates to prognostication in an uncertain setting.
Dr. Brizzi noted communication tools that help facilitate discussions around shared decisionmaking “have enhanced our ability to meet the palliative care needs of our patients and can be incorporated by any provider.”
However, she added that the paper only briefly comments on the role of the neurologist in “lawful physician-hastened death.”
“I anticipate that this will be an area of further discussion in the neurology and palliative care community in the future, as requests for hastened death are frequently encountered from patients with serious neurologic illness,” she said.
Dr. Brizzi also noted the importance of understanding the reasons behind the request – and addressing patient worries related to end-of-life care, which can frequently help alleviate distress.
There was no targeted funding for this paper. Coauthor Salvador Cruz-Flores, MD, department of neurology, Texas Tech University Center, El Paso, reported participation on member adjudication committees for clinical trials for Novo Nordisk, Sunovion, and Galapagos. The remaining authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Palliative care includes much more than hospice services, lead author of the new position statement Lynne P. Taylor, MD, University of Washington, Seattle, and a fellow of the AAN, said in a press release.
“Neurologists provide palliative care to people living with life-altering neurologic illnesses not just at the end of life but throughout the course of a disease, improving their lives with symptom control,” Dr. Taylor added.
The position paper, developed by a joint committee of the AAN, American Neurological Association, and Child Neurology Society, was published online March 8 in Neurology.
Guidance across the lifespan
The new paper, an update of previous position statements, includes palliative care guidance for different neurologic disorders across the lifespan. For example, neuropalliative care for neonates deserves “extra consideration,” because one-third of pediatric deaths occur during the neonatal period, most often in the neonatal intensive care unit, and after withdrawal of life-sustaining interventions, the authors note.
For older children, neuropalliative care consultation benefits families trying to maximize the quality of the remainder of their child’s life. Decisionmaking must consider the child’s cognitive abilities, the diagnosis, the perceived level of suffering, parental values, and the family’s understanding of the prognosis, the authors note.
They note that discussions about prognosis are often difficult but critical. Previous research “supports that patients desire prognostic information even when prognosis is uncertain and appreciate when their physicians disclose the presence of that uncertainty,” the authors note.
Also important is engaging in shared decisionmaking with patients and families. “This approach requires the physician to elicit a patient’s goals, make recommendations based on whether medical treatments are likely to achieve those goals, and work with patients and families to finalize a treatment plan,” according to the new guidance.
Ethical considerations
When treatments are physiologically futile, clinicians need to explain why interventions that may cause harm and have no benefit are not offered.
The authors cite cardiopulmonary resuscitation in the setting of cardiac arrest from irreversible herniation as an example of futility in the context of neurologic disease.
When life-prolonging care is no longer an option, clinicians have an obligation to shift the focus of care to preserving quality of life and comfort as much as possible, they add.
Hospices, which provide comfort-focused medical care as well as psychosocial and spiritual support, are reserved for patients believed to be in the last 6 months of their life if their disease follows the expected course.
The investigators also broached ethical considerations for individual neurologic conditions. Concerns for disorders of consciousness include misdiagnosis or inaccurate prognostication, and serial examinations are needed to re-evaluate levels of cognition, psychological state, decisionmaking capacity, and disease trajectory.
In patients with locked-in syndrome, a state of irreversible paralysis, often with respiratory and vocal paralysis, consciousness may range from a chronic minimally conscious state to intact cognition.
Without careful examination, patients with preserved consciousness may be mistaken as having a disorder of consciousness and risk their decisional capacity being ignored, the researchers note.
These patients may need assistance from speech pathologists to identify techniques to enhance communication, such as careful “yes/no” questioning, communication boards, or advanced eye-gaze technology, they add.
Stroke, dementia, Parkinson’s guidance
For stroke, the guidance suggests neurologists encourage patients with retained decisionmaking capacity to complete advance care planning given the risk of recurrent stroke and loss of capacity in the future.
For dementia, a proper and timely diagnosis can help patients and their families prepare for the consequences of cognitive dysfunction and loss of autonomy while respecting their identified values, the authors write.
They note that for Parkinson’s disease, which is marked by slow functional and cognitive decline, neurologists must aim to anticipate and treat symptoms, address psychosocial and spiritual distress and caregiver burden, and engage patients and families in advance care planning before onset of cognitive impairment.
For patients with amyotrophic lateral sclerosis (ALS) and related disorders, clinicians should aim to document goals and treatment preferences prior to extreme weakness and aphonia.
It is also important to anticipate patient preferences for future disability-specific decisions, such as those related to feeding tubes and mechanical ventilation, and to identify the patient’s minimal acceptable outcome from these life-sustaining interventions.
On the topic of withdrawal of treatment, the paper notes that competent patients have the right to refuse life-prolonging therapies, including artificial nutrition, hydration, mechanical ventilation, and antibiotics. If physicians have a moral objection to removing life-support systems, they are obligated to transfer the care of the patient to another physician, the authors add.
Once a decision is made to forgo life-sustaining treatment, physicians should minimize subsequent suffering. The investigators note most symptoms at the end of life can be managed without sedation.
In broaching the “gap” in neurology training programs, the statement referred to a survey of 49 neurology residency programs. Results showed that 42% of respondents reported being dissatisfied with their palliative care education.
Well-timed update
Kate T. Brizzi, MD, a Boston neurologist with experience in hospice and palliative care, said the updated position statement is “well-timed” as neuropalliative care has evolved dramatically over the last decade.
“In the last several years, I’ve witnessed a significant increase in trainee interest in the field, and there is growing recognition of how a palliative care approach can improve patient care and hopefully outcomes,” said Dr. Brizzi.
She praised the authors for doing “an excellent job” in highlighting the ethical challenges facing the neurology provider, particularly as it relates to prognostication in an uncertain setting.
Dr. Brizzi noted communication tools that help facilitate discussions around shared decisionmaking “have enhanced our ability to meet the palliative care needs of our patients and can be incorporated by any provider.”
However, she added that the paper only briefly comments on the role of the neurologist in “lawful physician-hastened death.”
“I anticipate that this will be an area of further discussion in the neurology and palliative care community in the future, as requests for hastened death are frequently encountered from patients with serious neurologic illness,” she said.
Dr. Brizzi also noted the importance of understanding the reasons behind the request – and addressing patient worries related to end-of-life care, which can frequently help alleviate distress.
There was no targeted funding for this paper. Coauthor Salvador Cruz-Flores, MD, department of neurology, Texas Tech University Center, El Paso, reported participation on member adjudication committees for clinical trials for Novo Nordisk, Sunovion, and Galapagos. The remaining authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
From Neurology
Surveillance program highly predictive for early autism
A population-based developmental surveillance program showed high diagnostic accuracy in identifying autism in a community-based sample of infants, toddlers, and preschoolers, according to new data published online in JAMA Network Open.
Researchers, led by Josephine Barbaro, PhD, of Olga Tennison Autism Research Centre at La Trobe University, Bundoora, Australia, said their findings indicate the benefit of using early autism developmental surveillance from infancy to the preschool period rather than one-time screening.
For the study, maternal and child health nurses in Melbourne were trained to use the Social Attention and Communication Surveillance–Revised (SACS-R) and SACS-Preschool (SACS-PR) tools during well-child checkups at 11-30 months of age and at follow-up (42 months of age). Dr. Barbaro helped develop the SACS tools.
Children identified as being at high likelihood for autism (1-2 years of age: n = 327; 42 months of age: n = 168) and at low likelihood for autism plus concerns (42 months of age: n = 28) were referred by their nurse for diagnostic assessment by the researchers.
Diagnostic accuracy of the SACS-R and SACS-PR was determined by comparing likelihood for autism with children’s diagnostic outcome using clinical judgment based on standard autism assessments.
Researchers included 13,511 children ages 11 months to 42 months. Results indicated the SACS-R with SACS-PR (SACS-R+PR) had very high diagnostic accuracy for early autism detection.
According to the paper, SACS-R showed 83% positive predictive value (95% confidence interval, 0.77-0.87) and 99% estimated negative predictive value (95% CI, 0.01-0.02). Specificity (99.6%; 95% CI, 0.99-1.00) was high, with modest sensitivity (62%; 95% CI, 0.57-0.66). When the SACS-PR 42-month assessment was added, estimated sensitivity grew to 96% (95% CI, 0.94-0.98).
“Its greater accuracy, compared with psychometrics of commonly used autism screening tools when used in community-based samples, suggests that the SACS-R+PR can be used universally for the early identification of autism,” the authors wrote.
According to La Trobe University, the tool is used in 10 other countries around the world – among them China, Singapore, Poland, Japan, New Zealand, Nepal, and Bangladesh.
Early identification is crucial for children on the autism spectrum and their families because it facilitates early diagnosis and can help families get access to supports and services.
About 2% of the world’s population is on the autism spectrum. Some studies report prevalence of 4% or higher, the authors noted.
The authors called attention to a systematic review of universal autism screening in primary care, including the Infant-Toddler Checklist and the Modified Checklist for Autism in Toddlers and various versions. The authors of the review noted that few studies had enough participants to establish population sensitivity, specificity, and positive predictive value. Also, psychometric properties reported were modest and/or wide ranging, putting into question the diagnostic accuracy of the tools.
Dr. Barbaro and colleagues highlighted an advantage the current study offers. “A critical difference in this study was the use of a community-based sample rather than a clinical or high-likelihood sibling sample, which may not be representative of the general population of children on the autism spectrum because child outcomes, cognition, and autism prevalence vary by ascertainment strategy and multiplex or simplex status.”
The authors explained that, in the United States, The U.S. Preventive Services Task Force has said there is not enough evidence to recommend universal autism screening and instead recommends routine general developmental surveillance. The American Academy of Pediatrics recommends developmental surveillance between 9 and 30 months and autism-specific screening at 18 and 24 months because of the benefits of early supports and services.
Karen Pierce, PhD, codirector of the Autism Center of Excellence at University of California, San Diego, said in an interview that she was pleased to see that the researchers were able to identify a high percentage of children on the autism spectrum.
She said, however, that the system proposed in this paper involves a substantial amount of time for training the nurses.
The authors acknowledged that, saying, “there may be instances in which this could be impractical.”
Dr. Pierce said that, in the United States, parent questionnaires are combined with clinical judgment to decide which kids are at risk.
“It doesn’t take very much time to fill out these questionnaires,” she said. “That’s the sticking point. I’m not saying necessarily that it shouldn’t be adopted. It would be very hard, I think, to incorporate into current pediatric practice.”
She said a benefit of the SACS program is more hands-on observation of the child, beyond the parent report, which sometimes can reflect more emotionally how the parent is feeling about the child.
She pointed out it was impressive that the Australian team found virtually no false positives.
The researchers also identified an additional 168 children using the preschool version at 42 months who had actually passed at the earlier checkpoint, using the regular SACS-R.
“This underscores a supercritical point,” Dr. Pierce said. “Just because your child may have gotten screened at 12, 18, 24 months and they pass and everything’s looking great, it doesn’t necessarily mean at some point early in development around age 3 that there [wouldn’t] be some clearer signs of autism.”
She said in her own study, published in JAMA Pediatrics, 24% of their sample tested fine at first but were later identified as having autism.
“It underscores the need for repeat screening,” Dr. Pierce said. “That was a striking finding in this study.”
She also pointed out that the authors talk about the “false dichotomy” between screening and surveillance. “They are saying it doesn’t have to be that way. It can be a combined effort. We can have parents filling out screening tools and we can have more observational sessions with kids during checkups. It doesn’t have to be this rigid line between screening and surveillance. I would completely agree with that.”
Dr. Barbaro reported receiving grants from the Sir Robert Menzies Foundation and the Cooperative Research Centre for Living with Autism (Autism CRC) during the study. Funds are partially distributed to Dr. Barbaro for the background intellectual property. One coauthor reported grants from the Menzies Foundation and Autism CRC during the study. Another coauthor reported receiving salary from Autism CRC during the study. No other disclosures were reported. This work was supported by an Allied Health Sciences start-up grant from the Menzies Foundation and the Cooperative Research Centre for Living with Autism, established and supported under the Australian Government’s Cooperative Research Centres Program. Dr. Pierce reports no relevant financial relationships.
A population-based developmental surveillance program showed high diagnostic accuracy in identifying autism in a community-based sample of infants, toddlers, and preschoolers, according to new data published online in JAMA Network Open.
Researchers, led by Josephine Barbaro, PhD, of Olga Tennison Autism Research Centre at La Trobe University, Bundoora, Australia, said their findings indicate the benefit of using early autism developmental surveillance from infancy to the preschool period rather than one-time screening.
For the study, maternal and child health nurses in Melbourne were trained to use the Social Attention and Communication Surveillance–Revised (SACS-R) and SACS-Preschool (SACS-PR) tools during well-child checkups at 11-30 months of age and at follow-up (42 months of age). Dr. Barbaro helped develop the SACS tools.
Children identified as being at high likelihood for autism (1-2 years of age: n = 327; 42 months of age: n = 168) and at low likelihood for autism plus concerns (42 months of age: n = 28) were referred by their nurse for diagnostic assessment by the researchers.
Diagnostic accuracy of the SACS-R and SACS-PR was determined by comparing likelihood for autism with children’s diagnostic outcome using clinical judgment based on standard autism assessments.
Researchers included 13,511 children ages 11 months to 42 months. Results indicated the SACS-R with SACS-PR (SACS-R+PR) had very high diagnostic accuracy for early autism detection.
According to the paper, SACS-R showed 83% positive predictive value (95% confidence interval, 0.77-0.87) and 99% estimated negative predictive value (95% CI, 0.01-0.02). Specificity (99.6%; 95% CI, 0.99-1.00) was high, with modest sensitivity (62%; 95% CI, 0.57-0.66). When the SACS-PR 42-month assessment was added, estimated sensitivity grew to 96% (95% CI, 0.94-0.98).
“Its greater accuracy, compared with psychometrics of commonly used autism screening tools when used in community-based samples, suggests that the SACS-R+PR can be used universally for the early identification of autism,” the authors wrote.
According to La Trobe University, the tool is used in 10 other countries around the world – among them China, Singapore, Poland, Japan, New Zealand, Nepal, and Bangladesh.
Early identification is crucial for children on the autism spectrum and their families because it facilitates early diagnosis and can help families get access to supports and services.
About 2% of the world’s population is on the autism spectrum. Some studies report prevalence of 4% or higher, the authors noted.
The authors called attention to a systematic review of universal autism screening in primary care, including the Infant-Toddler Checklist and the Modified Checklist for Autism in Toddlers and various versions. The authors of the review noted that few studies had enough participants to establish population sensitivity, specificity, and positive predictive value. Also, psychometric properties reported were modest and/or wide ranging, putting into question the diagnostic accuracy of the tools.
Dr. Barbaro and colleagues highlighted an advantage the current study offers. “A critical difference in this study was the use of a community-based sample rather than a clinical or high-likelihood sibling sample, which may not be representative of the general population of children on the autism spectrum because child outcomes, cognition, and autism prevalence vary by ascertainment strategy and multiplex or simplex status.”
The authors explained that, in the United States, The U.S. Preventive Services Task Force has said there is not enough evidence to recommend universal autism screening and instead recommends routine general developmental surveillance. The American Academy of Pediatrics recommends developmental surveillance between 9 and 30 months and autism-specific screening at 18 and 24 months because of the benefits of early supports and services.
Karen Pierce, PhD, codirector of the Autism Center of Excellence at University of California, San Diego, said in an interview that she was pleased to see that the researchers were able to identify a high percentage of children on the autism spectrum.
She said, however, that the system proposed in this paper involves a substantial amount of time for training the nurses.
The authors acknowledged that, saying, “there may be instances in which this could be impractical.”
Dr. Pierce said that, in the United States, parent questionnaires are combined with clinical judgment to decide which kids are at risk.
“It doesn’t take very much time to fill out these questionnaires,” she said. “That’s the sticking point. I’m not saying necessarily that it shouldn’t be adopted. It would be very hard, I think, to incorporate into current pediatric practice.”
She said a benefit of the SACS program is more hands-on observation of the child, beyond the parent report, which sometimes can reflect more emotionally how the parent is feeling about the child.
She pointed out it was impressive that the Australian team found virtually no false positives.
The researchers also identified an additional 168 children using the preschool version at 42 months who had actually passed at the earlier checkpoint, using the regular SACS-R.
“This underscores a supercritical point,” Dr. Pierce said. “Just because your child may have gotten screened at 12, 18, 24 months and they pass and everything’s looking great, it doesn’t necessarily mean at some point early in development around age 3 that there [wouldn’t] be some clearer signs of autism.”
She said in her own study, published in JAMA Pediatrics, 24% of their sample tested fine at first but were later identified as having autism.
“It underscores the need for repeat screening,” Dr. Pierce said. “That was a striking finding in this study.”
She also pointed out that the authors talk about the “false dichotomy” between screening and surveillance. “They are saying it doesn’t have to be that way. It can be a combined effort. We can have parents filling out screening tools and we can have more observational sessions with kids during checkups. It doesn’t have to be this rigid line between screening and surveillance. I would completely agree with that.”
Dr. Barbaro reported receiving grants from the Sir Robert Menzies Foundation and the Cooperative Research Centre for Living with Autism (Autism CRC) during the study. Funds are partially distributed to Dr. Barbaro for the background intellectual property. One coauthor reported grants from the Menzies Foundation and Autism CRC during the study. Another coauthor reported receiving salary from Autism CRC during the study. No other disclosures were reported. This work was supported by an Allied Health Sciences start-up grant from the Menzies Foundation and the Cooperative Research Centre for Living with Autism, established and supported under the Australian Government’s Cooperative Research Centres Program. Dr. Pierce reports no relevant financial relationships.
A population-based developmental surveillance program showed high diagnostic accuracy in identifying autism in a community-based sample of infants, toddlers, and preschoolers, according to new data published online in JAMA Network Open.
Researchers, led by Josephine Barbaro, PhD, of Olga Tennison Autism Research Centre at La Trobe University, Bundoora, Australia, said their findings indicate the benefit of using early autism developmental surveillance from infancy to the preschool period rather than one-time screening.
For the study, maternal and child health nurses in Melbourne were trained to use the Social Attention and Communication Surveillance–Revised (SACS-R) and SACS-Preschool (SACS-PR) tools during well-child checkups at 11-30 months of age and at follow-up (42 months of age). Dr. Barbaro helped develop the SACS tools.
Children identified as being at high likelihood for autism (1-2 years of age: n = 327; 42 months of age: n = 168) and at low likelihood for autism plus concerns (42 months of age: n = 28) were referred by their nurse for diagnostic assessment by the researchers.
Diagnostic accuracy of the SACS-R and SACS-PR was determined by comparing likelihood for autism with children’s diagnostic outcome using clinical judgment based on standard autism assessments.
Researchers included 13,511 children ages 11 months to 42 months. Results indicated the SACS-R with SACS-PR (SACS-R+PR) had very high diagnostic accuracy for early autism detection.
According to the paper, SACS-R showed 83% positive predictive value (95% confidence interval, 0.77-0.87) and 99% estimated negative predictive value (95% CI, 0.01-0.02). Specificity (99.6%; 95% CI, 0.99-1.00) was high, with modest sensitivity (62%; 95% CI, 0.57-0.66). When the SACS-PR 42-month assessment was added, estimated sensitivity grew to 96% (95% CI, 0.94-0.98).
“Its greater accuracy, compared with psychometrics of commonly used autism screening tools when used in community-based samples, suggests that the SACS-R+PR can be used universally for the early identification of autism,” the authors wrote.
According to La Trobe University, the tool is used in 10 other countries around the world – among them China, Singapore, Poland, Japan, New Zealand, Nepal, and Bangladesh.
Early identification is crucial for children on the autism spectrum and their families because it facilitates early diagnosis and can help families get access to supports and services.
About 2% of the world’s population is on the autism spectrum. Some studies report prevalence of 4% or higher, the authors noted.
The authors called attention to a systematic review of universal autism screening in primary care, including the Infant-Toddler Checklist and the Modified Checklist for Autism in Toddlers and various versions. The authors of the review noted that few studies had enough participants to establish population sensitivity, specificity, and positive predictive value. Also, psychometric properties reported were modest and/or wide ranging, putting into question the diagnostic accuracy of the tools.
Dr. Barbaro and colleagues highlighted an advantage the current study offers. “A critical difference in this study was the use of a community-based sample rather than a clinical or high-likelihood sibling sample, which may not be representative of the general population of children on the autism spectrum because child outcomes, cognition, and autism prevalence vary by ascertainment strategy and multiplex or simplex status.”
The authors explained that, in the United States, The U.S. Preventive Services Task Force has said there is not enough evidence to recommend universal autism screening and instead recommends routine general developmental surveillance. The American Academy of Pediatrics recommends developmental surveillance between 9 and 30 months and autism-specific screening at 18 and 24 months because of the benefits of early supports and services.
Karen Pierce, PhD, codirector of the Autism Center of Excellence at University of California, San Diego, said in an interview that she was pleased to see that the researchers were able to identify a high percentage of children on the autism spectrum.
She said, however, that the system proposed in this paper involves a substantial amount of time for training the nurses.
The authors acknowledged that, saying, “there may be instances in which this could be impractical.”
Dr. Pierce said that, in the United States, parent questionnaires are combined with clinical judgment to decide which kids are at risk.
“It doesn’t take very much time to fill out these questionnaires,” she said. “That’s the sticking point. I’m not saying necessarily that it shouldn’t be adopted. It would be very hard, I think, to incorporate into current pediatric practice.”
She said a benefit of the SACS program is more hands-on observation of the child, beyond the parent report, which sometimes can reflect more emotionally how the parent is feeling about the child.
She pointed out it was impressive that the Australian team found virtually no false positives.
The researchers also identified an additional 168 children using the preschool version at 42 months who had actually passed at the earlier checkpoint, using the regular SACS-R.
“This underscores a supercritical point,” Dr. Pierce said. “Just because your child may have gotten screened at 12, 18, 24 months and they pass and everything’s looking great, it doesn’t necessarily mean at some point early in development around age 3 that there [wouldn’t] be some clearer signs of autism.”
She said in her own study, published in JAMA Pediatrics, 24% of their sample tested fine at first but were later identified as having autism.
“It underscores the need for repeat screening,” Dr. Pierce said. “That was a striking finding in this study.”
She also pointed out that the authors talk about the “false dichotomy” between screening and surveillance. “They are saying it doesn’t have to be that way. It can be a combined effort. We can have parents filling out screening tools and we can have more observational sessions with kids during checkups. It doesn’t have to be this rigid line between screening and surveillance. I would completely agree with that.”
Dr. Barbaro reported receiving grants from the Sir Robert Menzies Foundation and the Cooperative Research Centre for Living with Autism (Autism CRC) during the study. Funds are partially distributed to Dr. Barbaro for the background intellectual property. One coauthor reported grants from the Menzies Foundation and Autism CRC during the study. Another coauthor reported receiving salary from Autism CRC during the study. No other disclosures were reported. This work was supported by an Allied Health Sciences start-up grant from the Menzies Foundation and the Cooperative Research Centre for Living with Autism, established and supported under the Australian Government’s Cooperative Research Centres Program. Dr. Pierce reports no relevant financial relationships.
FROM JAMA NETWORK OPEN
Selling your practice
My previous column on practice valuation prompted a number of questions on the mechanics of selling a private practice. As usual, I cannot hope to cover this complex topic comprehensively in only 750 words, but here are the basics.
A generation ago, the sale of a medical practice was much like the sale of any other business: A retiring physician would sell his or her practice to a young doctor and the practice would continue on as before. Occasionally, that still happens, but changes in the business of medicine – most significantly the growth of managed care – have had a big impact on the way medical practices are bought and sold.
For one thing, there are far fewer solo practitioners these days, and polls indicate that most young physicians intend to continue that trend. .
For another, because the rules governing such sales have become so numbingly complex, the services of expert (and expensive) third parties are essential.
While these issues may complicate matters, there is still a market for the sale of medical practices. However, you must do everything possible to ensure you identify the best possible buyer and structure the best deal.
The first hurdle is the accurate valuation of your practice, which was covered in some detail in my last column. Briefly, for the protection of both parties, it is important that the appraisal be done by an experienced and neutral financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation be supplied to support the conclusions reached.
Keep in mind that the valuation will not necessarily equal the purchase price; other factors may need to be considered before a final price can be agreed upon. Keep in mind, too, that there may be legal constraints on the purchase price. For example, if the buyer is a nonprofit corporation such as a hospital or HMO, by law it cannot pay in excess of fair market value for the practice – which may rule out any valuation of “good will.” In some states, the purchase of private practices by hospitals is prohibited altogether – so you might need to consider a long-term lease rather than a sale.
Once a value has been agreed upon, you must consider how the transaction will be structured. The most popular structures include purchase of assets, purchase of corporate stock, and merger.
Many buyers prefer to purchase assets, because it allows them to pick and choose only those items that have value to them. This can leave you with a bunch of “odd lot” assets to dispose of. But depending on the circumstances, an asset sale may still be to your advantage.
Sellers typically prefer to sell stock, because it allows them to sell their entire practice, which is often worth more than the sum of its parts, and often provides tax advantages.
The third option, merger, continues to grow in popularity and is a column subject in itself, and I will address it separately next month.
Tax issues must always be considered. Most private practices are corporations, and the sale of corporate stock will result in a long-term capital gain that will be taxed – currently at 15%-20%. As the saying goes, it’s not what you earn, it’s what you keep. So it may benefit you to accept a slightly lower price if the sale can be structured to provide significantly lower tax treatment. However, any gain that does not qualify as a long-term capital gain will be taxed as regular income – currently in the 32%-37% percent range – plus a Social Security tax of about 15%.
Payment in installments is a popular way to defer taxes, since they are incurred on each installment as it is paid; but such payments may be mistaken by the IRS for payments for referrals, which is illegal. And there is always the problem of making certain all payments are eventually made.
You may wish to continue working at the practice as an employee for an agreed-upon period of time, and this is often to the buyer’s advantage as well. Transitioning to new ownership in stages often maximizes the value of the business by improving patient retention, and allows patients to become accustomed to the transition. However, care must be taken, with the aid of good legal advice, to structure such an arrangement in a way that minimizes concerns of fraud and abuse.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
My previous column on practice valuation prompted a number of questions on the mechanics of selling a private practice. As usual, I cannot hope to cover this complex topic comprehensively in only 750 words, but here are the basics.
A generation ago, the sale of a medical practice was much like the sale of any other business: A retiring physician would sell his or her practice to a young doctor and the practice would continue on as before. Occasionally, that still happens, but changes in the business of medicine – most significantly the growth of managed care – have had a big impact on the way medical practices are bought and sold.
For one thing, there are far fewer solo practitioners these days, and polls indicate that most young physicians intend to continue that trend. .
For another, because the rules governing such sales have become so numbingly complex, the services of expert (and expensive) third parties are essential.
While these issues may complicate matters, there is still a market for the sale of medical practices. However, you must do everything possible to ensure you identify the best possible buyer and structure the best deal.
The first hurdle is the accurate valuation of your practice, which was covered in some detail in my last column. Briefly, for the protection of both parties, it is important that the appraisal be done by an experienced and neutral financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation be supplied to support the conclusions reached.
Keep in mind that the valuation will not necessarily equal the purchase price; other factors may need to be considered before a final price can be agreed upon. Keep in mind, too, that there may be legal constraints on the purchase price. For example, if the buyer is a nonprofit corporation such as a hospital or HMO, by law it cannot pay in excess of fair market value for the practice – which may rule out any valuation of “good will.” In some states, the purchase of private practices by hospitals is prohibited altogether – so you might need to consider a long-term lease rather than a sale.
Once a value has been agreed upon, you must consider how the transaction will be structured. The most popular structures include purchase of assets, purchase of corporate stock, and merger.
Many buyers prefer to purchase assets, because it allows them to pick and choose only those items that have value to them. This can leave you with a bunch of “odd lot” assets to dispose of. But depending on the circumstances, an asset sale may still be to your advantage.
Sellers typically prefer to sell stock, because it allows them to sell their entire practice, which is often worth more than the sum of its parts, and often provides tax advantages.
The third option, merger, continues to grow in popularity and is a column subject in itself, and I will address it separately next month.
Tax issues must always be considered. Most private practices are corporations, and the sale of corporate stock will result in a long-term capital gain that will be taxed – currently at 15%-20%. As the saying goes, it’s not what you earn, it’s what you keep. So it may benefit you to accept a slightly lower price if the sale can be structured to provide significantly lower tax treatment. However, any gain that does not qualify as a long-term capital gain will be taxed as regular income – currently in the 32%-37% percent range – plus a Social Security tax of about 15%.
Payment in installments is a popular way to defer taxes, since they are incurred on each installment as it is paid; but such payments may be mistaken by the IRS for payments for referrals, which is illegal. And there is always the problem of making certain all payments are eventually made.
You may wish to continue working at the practice as an employee for an agreed-upon period of time, and this is often to the buyer’s advantage as well. Transitioning to new ownership in stages often maximizes the value of the business by improving patient retention, and allows patients to become accustomed to the transition. However, care must be taken, with the aid of good legal advice, to structure such an arrangement in a way that minimizes concerns of fraud and abuse.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
My previous column on practice valuation prompted a number of questions on the mechanics of selling a private practice. As usual, I cannot hope to cover this complex topic comprehensively in only 750 words, but here are the basics.
A generation ago, the sale of a medical practice was much like the sale of any other business: A retiring physician would sell his or her practice to a young doctor and the practice would continue on as before. Occasionally, that still happens, but changes in the business of medicine – most significantly the growth of managed care – have had a big impact on the way medical practices are bought and sold.
For one thing, there are far fewer solo practitioners these days, and polls indicate that most young physicians intend to continue that trend. .
For another, because the rules governing such sales have become so numbingly complex, the services of expert (and expensive) third parties are essential.
While these issues may complicate matters, there is still a market for the sale of medical practices. However, you must do everything possible to ensure you identify the best possible buyer and structure the best deal.
The first hurdle is the accurate valuation of your practice, which was covered in some detail in my last column. Briefly, for the protection of both parties, it is important that the appraisal be done by an experienced and neutral financial consultant, that all techniques used in the valuation be divulged and explained, and that documentation be supplied to support the conclusions reached.
Keep in mind that the valuation will not necessarily equal the purchase price; other factors may need to be considered before a final price can be agreed upon. Keep in mind, too, that there may be legal constraints on the purchase price. For example, if the buyer is a nonprofit corporation such as a hospital or HMO, by law it cannot pay in excess of fair market value for the practice – which may rule out any valuation of “good will.” In some states, the purchase of private practices by hospitals is prohibited altogether – so you might need to consider a long-term lease rather than a sale.
Once a value has been agreed upon, you must consider how the transaction will be structured. The most popular structures include purchase of assets, purchase of corporate stock, and merger.
Many buyers prefer to purchase assets, because it allows them to pick and choose only those items that have value to them. This can leave you with a bunch of “odd lot” assets to dispose of. But depending on the circumstances, an asset sale may still be to your advantage.
Sellers typically prefer to sell stock, because it allows them to sell their entire practice, which is often worth more than the sum of its parts, and often provides tax advantages.
The third option, merger, continues to grow in popularity and is a column subject in itself, and I will address it separately next month.
Tax issues must always be considered. Most private practices are corporations, and the sale of corporate stock will result in a long-term capital gain that will be taxed – currently at 15%-20%. As the saying goes, it’s not what you earn, it’s what you keep. So it may benefit you to accept a slightly lower price if the sale can be structured to provide significantly lower tax treatment. However, any gain that does not qualify as a long-term capital gain will be taxed as regular income – currently in the 32%-37% percent range – plus a Social Security tax of about 15%.
Payment in installments is a popular way to defer taxes, since they are incurred on each installment as it is paid; but such payments may be mistaken by the IRS for payments for referrals, which is illegal. And there is always the problem of making certain all payments are eventually made.
You may wish to continue working at the practice as an employee for an agreed-upon period of time, and this is often to the buyer’s advantage as well. Transitioning to new ownership in stages often maximizes the value of the business by improving patient retention, and allows patients to become accustomed to the transition. However, care must be taken, with the aid of good legal advice, to structure such an arrangement in a way that minimizes concerns of fraud and abuse.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Children and COVID: Decline in new cases reaches 7th week
New cases of COVID-19 in U.S. children have fallen to their lowest level since the beginning of the Delta surge in July of 2021, according to the American Academy of Pediatrics and the Children’s Hospital Association.
. Over those 7 weeks, new cases dropped over 96% from the 1.15 million reported for Jan. 14-20, based on data collected by the AAP and CHA from state and territorial health departments.
The last time that the weekly count was below 42,000 was July 16-22, 2021, when almost 39,000 cases were reported in the midst of the Delta upsurge. That was shortly after cases had reached their lowest point, 8,447, since the early stages of the pandemic in 2020, the AAP/CHA data show.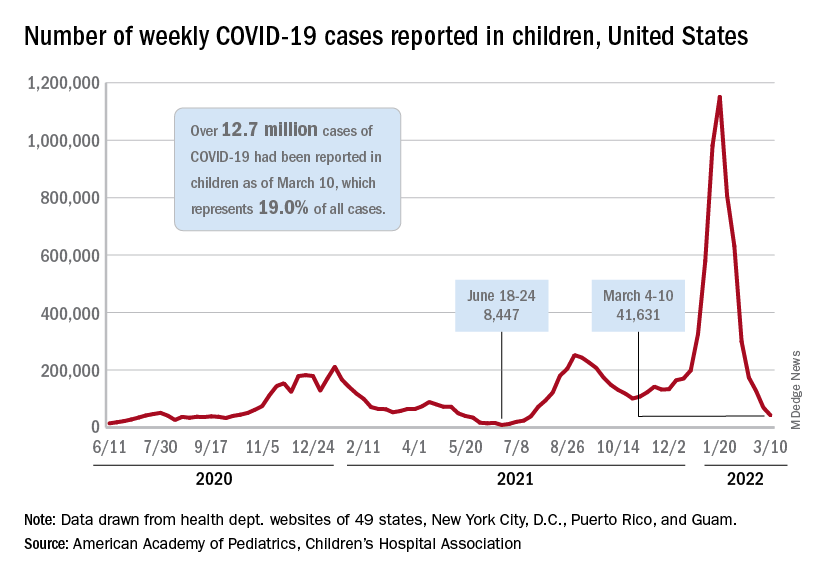
The cumulative number of pediatric cases is now up to 12.7 million, while the overall proportion of cases occurring in children held steady at 19.0% for the 4th week in a row, the AAP and CHA said in their weekly COVID-19 report. The Centers for Disease Control and Prevention, using an age range of 0-18 versus the states’ variety of ages, puts total cases at 11.7 million and deaths at 1,656 as of March 14.
Data from the CDC’s COVID-19–Associated Hospitalization Surveillance Network show that hospitalizations with laboratory-confirmed infection were down by 50% in children aged 0-4 years, by 63% among 5- to 11-year-olds, and by 58% in those aged 12-17 years for the week of Feb. 27 to March 5, compared with the week before.
The pace of vaccination continues to follow a similar trend, as the declines seen through February have continued into March. Cumulatively, 33.7% of children aged 5-11 have received at least one dose, and 26.8% are fully vaccinated, with corresponding numbers of 68.0% and 58.0% for children aged 12-17, the CDC reported on its COVID Data Tracker.
State-level data show that children aged 5-11 in Vermont, with a rate of 65%, are the most likely to have received at least one dose of COVID vaccine, while just 15% of 5- to 11-year-olds in Alabama, Louisiana, and Mississippi have gotten their first dose. Among children aged 12-17, that rate ranges from 40% in Wyoming to 94% in Hawaii, Massachusetts, and Rhode Island, the AAP said in a separate report based on CDC data.
In a recent report involving 1,364 children aged 5-15 years, two doses of the COVID-19 vaccine reduced the risk of infection from the Omicron variant by 31% in children aged 5-11 years and by 59% among children aged 12-15 years, said Ashley L. Fowlkes, ScD, of the CDC’s COVID-19 Emergency Response Team, and associates (MMWR 2022 Mar 11;71).
New cases of COVID-19 in U.S. children have fallen to their lowest level since the beginning of the Delta surge in July of 2021, according to the American Academy of Pediatrics and the Children’s Hospital Association.
. Over those 7 weeks, new cases dropped over 96% from the 1.15 million reported for Jan. 14-20, based on data collected by the AAP and CHA from state and territorial health departments.
The last time that the weekly count was below 42,000 was July 16-22, 2021, when almost 39,000 cases were reported in the midst of the Delta upsurge. That was shortly after cases had reached their lowest point, 8,447, since the early stages of the pandemic in 2020, the AAP/CHA data show.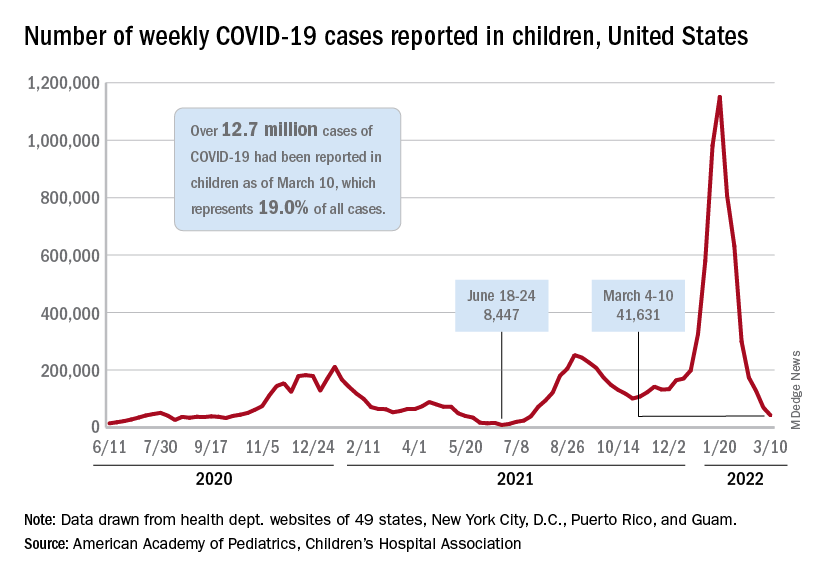
The cumulative number of pediatric cases is now up to 12.7 million, while the overall proportion of cases occurring in children held steady at 19.0% for the 4th week in a row, the AAP and CHA said in their weekly COVID-19 report. The Centers for Disease Control and Prevention, using an age range of 0-18 versus the states’ variety of ages, puts total cases at 11.7 million and deaths at 1,656 as of March 14.
Data from the CDC’s COVID-19–Associated Hospitalization Surveillance Network show that hospitalizations with laboratory-confirmed infection were down by 50% in children aged 0-4 years, by 63% among 5- to 11-year-olds, and by 58% in those aged 12-17 years for the week of Feb. 27 to March 5, compared with the week before.
The pace of vaccination continues to follow a similar trend, as the declines seen through February have continued into March. Cumulatively, 33.7% of children aged 5-11 have received at least one dose, and 26.8% are fully vaccinated, with corresponding numbers of 68.0% and 58.0% for children aged 12-17, the CDC reported on its COVID Data Tracker.
State-level data show that children aged 5-11 in Vermont, with a rate of 65%, are the most likely to have received at least one dose of COVID vaccine, while just 15% of 5- to 11-year-olds in Alabama, Louisiana, and Mississippi have gotten their first dose. Among children aged 12-17, that rate ranges from 40% in Wyoming to 94% in Hawaii, Massachusetts, and Rhode Island, the AAP said in a separate report based on CDC data.
In a recent report involving 1,364 children aged 5-15 years, two doses of the COVID-19 vaccine reduced the risk of infection from the Omicron variant by 31% in children aged 5-11 years and by 59% among children aged 12-15 years, said Ashley L. Fowlkes, ScD, of the CDC’s COVID-19 Emergency Response Team, and associates (MMWR 2022 Mar 11;71).
New cases of COVID-19 in U.S. children have fallen to their lowest level since the beginning of the Delta surge in July of 2021, according to the American Academy of Pediatrics and the Children’s Hospital Association.
. Over those 7 weeks, new cases dropped over 96% from the 1.15 million reported for Jan. 14-20, based on data collected by the AAP and CHA from state and territorial health departments.
The last time that the weekly count was below 42,000 was July 16-22, 2021, when almost 39,000 cases were reported in the midst of the Delta upsurge. That was shortly after cases had reached their lowest point, 8,447, since the early stages of the pandemic in 2020, the AAP/CHA data show.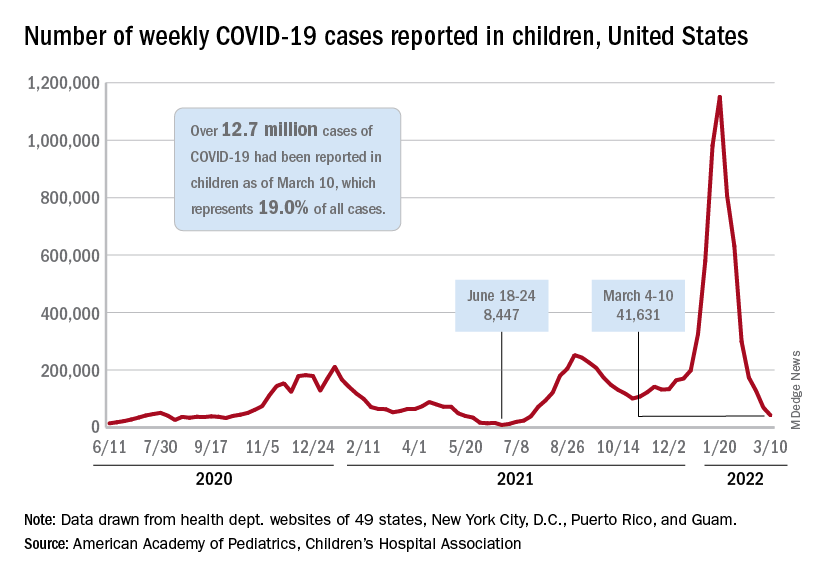
The cumulative number of pediatric cases is now up to 12.7 million, while the overall proportion of cases occurring in children held steady at 19.0% for the 4th week in a row, the AAP and CHA said in their weekly COVID-19 report. The Centers for Disease Control and Prevention, using an age range of 0-18 versus the states’ variety of ages, puts total cases at 11.7 million and deaths at 1,656 as of March 14.
Data from the CDC’s COVID-19–Associated Hospitalization Surveillance Network show that hospitalizations with laboratory-confirmed infection were down by 50% in children aged 0-4 years, by 63% among 5- to 11-year-olds, and by 58% in those aged 12-17 years for the week of Feb. 27 to March 5, compared with the week before.
The pace of vaccination continues to follow a similar trend, as the declines seen through February have continued into March. Cumulatively, 33.7% of children aged 5-11 have received at least one dose, and 26.8% are fully vaccinated, with corresponding numbers of 68.0% and 58.0% for children aged 12-17, the CDC reported on its COVID Data Tracker.
State-level data show that children aged 5-11 in Vermont, with a rate of 65%, are the most likely to have received at least one dose of COVID vaccine, while just 15% of 5- to 11-year-olds in Alabama, Louisiana, and Mississippi have gotten their first dose. Among children aged 12-17, that rate ranges from 40% in Wyoming to 94% in Hawaii, Massachusetts, and Rhode Island, the AAP said in a separate report based on CDC data.
In a recent report involving 1,364 children aged 5-15 years, two doses of the COVID-19 vaccine reduced the risk of infection from the Omicron variant by 31% in children aged 5-11 years and by 59% among children aged 12-15 years, said Ashley L. Fowlkes, ScD, of the CDC’s COVID-19 Emergency Response Team, and associates (MMWR 2022 Mar 11;71).
Air trapping common in patients with long COVID
, according to a prospective study that compared 100 COVID-19 survivors who had persistent symptoms and 106 healthy control persons.
“Something is going on in the distal airways related to either inflammation or fibrosis that is giving us a signal of air trapping,” noted senior author Alejandro P. Comellas, MD, in a press release. The study was stimulated by reports from University of Iowa clinicians noting that many patients with initial SARS-CoV-2 infection who were either hospitalized or were treated in the ambulatory setting later reported shortness of breath and other respiratory symptoms indicative of chronic lung disease.
Study results
Investigators classified patients (mean age, 48 years; 66 women) with post-acute sequelae of COVID-19 according to whether they were ambulatory (67%), hospitalized (17%), or required treatment in the intensive care unit (16%). They then compared CT findings of patients who had COVID-19 and persistent symptoms with those of a healthy control group.
COVID-19 severity did not affect the percentage of cases of lung with air trapping among these patients. Air trapping occurred at rates of 25.4% among ambulatory patients, 34.6% in hospitalized patients, and in 27.3% of those requiring intensive care (P = .10). The percentage of lungs affected by air trapping in ambulatory participants was sharply and significantly higher than in healthy controls (25.4% vs. 7.2%; P < .001). Also, air trapping persisted; it was still present in 8 of 9 participants who underwent imaging more than 200 days post diagnosis.
Qualitative analysis of chest CT images showed that the most common imaging abnormality was air trapping (58%); ground glass opacities (GGOs) were found in 51% (46/91), note Dr. Comellas and coauthors. This suggests ongoing lung inflammation, edema, or fibrosis. These symptoms are often observed during acute COVID-19, frequently in an organizing pneumonia pattern, and have been shown to persist for months after infection in survivors of severe disease. The mean percentage of total lung classified as having regional GGOs on chest CT scans was 13.2% and 28.7%, respectively, in the hospitalized and ICU groups, both very much higher than in the ambulatory group, at 3.7% (P < .001 for both). Among healthy controls, the GGO rate on chest CT was only 0.06% (P < .001).
In addition, air trapping correlated with the ratio of residual volume to total lung capacity (r = 0.6; P < .001) but not with spirometry results. In fact, the investigators did not observe airflow obstruction by spirometry in any group, suggesting that air trapping in these patients involves only small rather than large airways and that these small airways contribute little to total airway resistance. Only when a large percentage, perhaps 75% or more, of all small airways are obstructed will spirometry pick up small airways disease, the authors observe.
Continuing disease
The findings taken together suggest that functional small airways disease and air trapping are a consequence of SARS-CoV-2 infection, according to Dr. Comellas. “If a portion of patients continues to have small airways disease, then we need to think about the mechanisms behind it,” he said. “It could be something related to inflammation that’s reversible, or it may be something related to a scar that is irreversible, and then we need to look at ways to prevent further progression of the disease.” Furthermore, “studies aimed at determining the natural history of functional small airways disease in patients with post-acute sequelae of COVID-19 and the biological mechanisms that underlie these findings are urgently needed to identify therapeutic and preventative interventions,” Dr. Comellas, professor of internal medicine at Carver College of Medicine, University of Iowa, Iowa City, concluded.
The study limitations, the authors state, include the fact that theirs was a single-center study that enrolled participants infected early during the COVID-19 pandemic and did not include patients with Delta or Omicron variants, thus limiting the generalizability of the findings.
The study was published in Radiology.
The reported findings “indicate a long-term impact on bronchiolar obstruction,” states Brett M. Elicker, MD, professor of clinical radiology, University of California, San Francisco, in an accompanying editorial . Because collagen may be absorbed for months after an acute insult, it is not entirely clear whether the abnormalities seen in the current study will be permanent. He said further, “the presence of ground glass opacity and/or fibrosis on CT were most common in the patients admitted to the ICU and likely correspond to post-organizing pneumonia and/or post-diffuse alveolar damage fibrosis.”
Dr. Elicker also pointed out that organizing pneumonia is especially common among patients with COVID-19 and is usually highly steroid-responsive. The opacities improve or resolve with treatment, but sometimes residual fibrosis occurs. “Longer-term studies assessing the clinical and imaging manifestations 1-2 years after the initial infection are needed to fully ascertain the permanent manifestations of post-COVID fibrosis.”
The study was supported by grants from the National Institutes of Health. The authors and Dr. Elicker have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to a prospective study that compared 100 COVID-19 survivors who had persistent symptoms and 106 healthy control persons.
“Something is going on in the distal airways related to either inflammation or fibrosis that is giving us a signal of air trapping,” noted senior author Alejandro P. Comellas, MD, in a press release. The study was stimulated by reports from University of Iowa clinicians noting that many patients with initial SARS-CoV-2 infection who were either hospitalized or were treated in the ambulatory setting later reported shortness of breath and other respiratory symptoms indicative of chronic lung disease.
Study results
Investigators classified patients (mean age, 48 years; 66 women) with post-acute sequelae of COVID-19 according to whether they were ambulatory (67%), hospitalized (17%), or required treatment in the intensive care unit (16%). They then compared CT findings of patients who had COVID-19 and persistent symptoms with those of a healthy control group.
COVID-19 severity did not affect the percentage of cases of lung with air trapping among these patients. Air trapping occurred at rates of 25.4% among ambulatory patients, 34.6% in hospitalized patients, and in 27.3% of those requiring intensive care (P = .10). The percentage of lungs affected by air trapping in ambulatory participants was sharply and significantly higher than in healthy controls (25.4% vs. 7.2%; P < .001). Also, air trapping persisted; it was still present in 8 of 9 participants who underwent imaging more than 200 days post diagnosis.
Qualitative analysis of chest CT images showed that the most common imaging abnormality was air trapping (58%); ground glass opacities (GGOs) were found in 51% (46/91), note Dr. Comellas and coauthors. This suggests ongoing lung inflammation, edema, or fibrosis. These symptoms are often observed during acute COVID-19, frequently in an organizing pneumonia pattern, and have been shown to persist for months after infection in survivors of severe disease. The mean percentage of total lung classified as having regional GGOs on chest CT scans was 13.2% and 28.7%, respectively, in the hospitalized and ICU groups, both very much higher than in the ambulatory group, at 3.7% (P < .001 for both). Among healthy controls, the GGO rate on chest CT was only 0.06% (P < .001).
In addition, air trapping correlated with the ratio of residual volume to total lung capacity (r = 0.6; P < .001) but not with spirometry results. In fact, the investigators did not observe airflow obstruction by spirometry in any group, suggesting that air trapping in these patients involves only small rather than large airways and that these small airways contribute little to total airway resistance. Only when a large percentage, perhaps 75% or more, of all small airways are obstructed will spirometry pick up small airways disease, the authors observe.
Continuing disease
The findings taken together suggest that functional small airways disease and air trapping are a consequence of SARS-CoV-2 infection, according to Dr. Comellas. “If a portion of patients continues to have small airways disease, then we need to think about the mechanisms behind it,” he said. “It could be something related to inflammation that’s reversible, or it may be something related to a scar that is irreversible, and then we need to look at ways to prevent further progression of the disease.” Furthermore, “studies aimed at determining the natural history of functional small airways disease in patients with post-acute sequelae of COVID-19 and the biological mechanisms that underlie these findings are urgently needed to identify therapeutic and preventative interventions,” Dr. Comellas, professor of internal medicine at Carver College of Medicine, University of Iowa, Iowa City, concluded.
The study limitations, the authors state, include the fact that theirs was a single-center study that enrolled participants infected early during the COVID-19 pandemic and did not include patients with Delta or Omicron variants, thus limiting the generalizability of the findings.
The study was published in Radiology.
The reported findings “indicate a long-term impact on bronchiolar obstruction,” states Brett M. Elicker, MD, professor of clinical radiology, University of California, San Francisco, in an accompanying editorial . Because collagen may be absorbed for months after an acute insult, it is not entirely clear whether the abnormalities seen in the current study will be permanent. He said further, “the presence of ground glass opacity and/or fibrosis on CT were most common in the patients admitted to the ICU and likely correspond to post-organizing pneumonia and/or post-diffuse alveolar damage fibrosis.”
Dr. Elicker also pointed out that organizing pneumonia is especially common among patients with COVID-19 and is usually highly steroid-responsive. The opacities improve or resolve with treatment, but sometimes residual fibrosis occurs. “Longer-term studies assessing the clinical and imaging manifestations 1-2 years after the initial infection are needed to fully ascertain the permanent manifestations of post-COVID fibrosis.”
The study was supported by grants from the National Institutes of Health. The authors and Dr. Elicker have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to a prospective study that compared 100 COVID-19 survivors who had persistent symptoms and 106 healthy control persons.
“Something is going on in the distal airways related to either inflammation or fibrosis that is giving us a signal of air trapping,” noted senior author Alejandro P. Comellas, MD, in a press release. The study was stimulated by reports from University of Iowa clinicians noting that many patients with initial SARS-CoV-2 infection who were either hospitalized or were treated in the ambulatory setting later reported shortness of breath and other respiratory symptoms indicative of chronic lung disease.
Study results
Investigators classified patients (mean age, 48 years; 66 women) with post-acute sequelae of COVID-19 according to whether they were ambulatory (67%), hospitalized (17%), or required treatment in the intensive care unit (16%). They then compared CT findings of patients who had COVID-19 and persistent symptoms with those of a healthy control group.
COVID-19 severity did not affect the percentage of cases of lung with air trapping among these patients. Air trapping occurred at rates of 25.4% among ambulatory patients, 34.6% in hospitalized patients, and in 27.3% of those requiring intensive care (P = .10). The percentage of lungs affected by air trapping in ambulatory participants was sharply and significantly higher than in healthy controls (25.4% vs. 7.2%; P < .001). Also, air trapping persisted; it was still present in 8 of 9 participants who underwent imaging more than 200 days post diagnosis.
Qualitative analysis of chest CT images showed that the most common imaging abnormality was air trapping (58%); ground glass opacities (GGOs) were found in 51% (46/91), note Dr. Comellas and coauthors. This suggests ongoing lung inflammation, edema, or fibrosis. These symptoms are often observed during acute COVID-19, frequently in an organizing pneumonia pattern, and have been shown to persist for months after infection in survivors of severe disease. The mean percentage of total lung classified as having regional GGOs on chest CT scans was 13.2% and 28.7%, respectively, in the hospitalized and ICU groups, both very much higher than in the ambulatory group, at 3.7% (P < .001 for both). Among healthy controls, the GGO rate on chest CT was only 0.06% (P < .001).
In addition, air trapping correlated with the ratio of residual volume to total lung capacity (r = 0.6; P < .001) but not with spirometry results. In fact, the investigators did not observe airflow obstruction by spirometry in any group, suggesting that air trapping in these patients involves only small rather than large airways and that these small airways contribute little to total airway resistance. Only when a large percentage, perhaps 75% or more, of all small airways are obstructed will spirometry pick up small airways disease, the authors observe.
Continuing disease
The findings taken together suggest that functional small airways disease and air trapping are a consequence of SARS-CoV-2 infection, according to Dr. Comellas. “If a portion of patients continues to have small airways disease, then we need to think about the mechanisms behind it,” he said. “It could be something related to inflammation that’s reversible, or it may be something related to a scar that is irreversible, and then we need to look at ways to prevent further progression of the disease.” Furthermore, “studies aimed at determining the natural history of functional small airways disease in patients with post-acute sequelae of COVID-19 and the biological mechanisms that underlie these findings are urgently needed to identify therapeutic and preventative interventions,” Dr. Comellas, professor of internal medicine at Carver College of Medicine, University of Iowa, Iowa City, concluded.
The study limitations, the authors state, include the fact that theirs was a single-center study that enrolled participants infected early during the COVID-19 pandemic and did not include patients with Delta or Omicron variants, thus limiting the generalizability of the findings.
The study was published in Radiology.
The reported findings “indicate a long-term impact on bronchiolar obstruction,” states Brett M. Elicker, MD, professor of clinical radiology, University of California, San Francisco, in an accompanying editorial . Because collagen may be absorbed for months after an acute insult, it is not entirely clear whether the abnormalities seen in the current study will be permanent. He said further, “the presence of ground glass opacity and/or fibrosis on CT were most common in the patients admitted to the ICU and likely correspond to post-organizing pneumonia and/or post-diffuse alveolar damage fibrosis.”
Dr. Elicker also pointed out that organizing pneumonia is especially common among patients with COVID-19 and is usually highly steroid-responsive. The opacities improve or resolve with treatment, but sometimes residual fibrosis occurs. “Longer-term studies assessing the clinical and imaging manifestations 1-2 years after the initial infection are needed to fully ascertain the permanent manifestations of post-COVID fibrosis.”
The study was supported by grants from the National Institutes of Health. The authors and Dr. Elicker have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM RADIOLOGY