User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Mosquitoes and the vicious circle that’s gone viral
These viruses want mosquitoes with good taste
Taste can be a pretty subjective sense. Not everyone agrees on what tastes good and what tastes bad. Most people would agree that freshly baked cookies taste good, but what about lima beans? And what about mosquitoes? What tastes good to a mosquito?
The answer? Blood. Blood tastes good to a mosquito. That really wasn’t a very hard question, was it? You did know the answer, didn’t you? They don’t care about cookies, and they certainly don’t care about lima beans. It’s blood that they love.
That brings us back to subjectivity, because it is possible for blood to taste even better. The secret ingredient is dengue … and Zika.
A study just published in Cell demonstrates that mice infected with dengue and Zika viruses release a volatile compound called acetophenone. “We found that flavivirus [like dengue and Zika] can utilize the increased release of acetophenone to help itself achieve its lifecycles more effectively by making their hosts more attractive to mosquito vectors,” senior author Gong Cheng of Tsinghua University, Beijing, said in a written statement.
How do they do it? The viruses, he explained, promote the proliferation of acetophenone-producing skin bacteria. “As a result, some bacteria overreplicate and produce more acetophenone. Suddenly, these sick individuals smell as delicious to mosquitoes as a tray of freshly baked cookies to a group of five-year-old children,” the statement said.
And how do you stop a group of tiny, flying 5-year-olds? That’s right, with acne medication. Really? You knew that one but not the blood one before? The investigators fed isotretinoin to the infected mice, which led to reduced acetophenone release from skin bacteria and made the animals no more attractive to the mosquitoes than their uninfected counterparts.
The investigators are planning to take the next step – feeding isotretinoin to people with dengue and Zika – having gotten the official fictional taste-test approval of celebrity chef Gordon Ramsay, who said, “You’re going to feed this #$^% to sick people? ARE YOU &%*$@#& KIDDING ME?”
Okay, so maybe approval isn’t quite the right word.
Welcome to bladders of the rich and famous!
Don’t you hate it when you’re driving out to your multimillion-dollar second home in the Hamptons and traffic is so bad you absolutely have to find a place to “rest” along the way? But wouldn’t you know it, there just isn’t anywhere to stop! Geez, how do we live?
That’s where David Shusterman, MD, a urologist in New York City and a true American hero, comes in. He’s identified a market and positioned himself as the king of both bladder surgery and “bladder Botox” for the wealthy New Yorkers who regularly make long journeys from the city out to their second homes in the Hamptons. Traffic has increased dramatically on Long Island roads in recent years, and the journey can now taking upward of 4 hours. Some people just can’t make it that long without a bathroom break, and there are very few places to stop along the way.
Dr. Shusterman understands the plight of the Hamptons vacationer, as he told Insider.com: “I can’t tell you how many arguments I personally get into – I’ve lost three friends because I’m the driver and refuse to stop for them.” A tragedy worthy of Shakespeare himself.
During the summer season, Dr. Shusterman performs about 10 prostate artery embolizations a week, an hour-long procedure that shrinks the prostate, which is great for 50- to 60-year-old men with enlarged prostates that cause more frequent bathroom trips. He also performs Botox injections into the bladder once or twice a week for women, which reduces the need to urinate for roughly 6 months. The perfect amount of time to get them through the summer season.
These procedures are sometimes covered by insurance but can cost as much as $20,000 if paid out of pocket. That’s a lot of money to us, but if you’re the sort of person who has a second home in the Hamptons, $20,000 is chump change, especially if it means you won’t have to go 2 entire minutes out of your way to use a gas-station bathroom. Then again, having seen a more than a few gas-station bathrooms in our time, maybe they have a point.
Ditch the apples. Go for the avocados
We’ve all heard about “an apple a day,” but instead of apples you might want to go with avocados.
Avocados are generally thought to be a healthy fat. A study just published in the Journal of the American Heart Association proves that they actually don’t do anything for your waistline but will work wonders on your cholesterol level. The study involved 923 participants who were considered overweight/obese split into two groups: One was asked to consume an avocado a day, and the other continued their usual diets and were asked to consume fewer than two avocados a month.
At the end of the 6 months, the researchers found total cholesterol decreased by an additional 2.9 mg/dL and LDL cholesterol by 2.5 mg/dL in those who ate one avocado every day, compared with the usual-diet group. And even though avocados have a lot of calories, there was no clinical evidence that it impacted weight gain or any cardiometabolic risk factors, according to a statement from Penn State University.
Avocados, then, can be considered a guilt-free food. The findings from this study suggest it can give a substantial boost to your overall quality of diet, in turn lessening your risk of developing type 2 diabetes and some cancers, Kristina Peterson, PhD, assistant professor of nutritional sciences at Texas Tech University, said in the statement.
So get creative with your avocado recipes. You can only eat so much guacamole.
Your nose knows a good friend for you
You’ve probably noticed how dogs sniff other dogs and people before becoming friends. It would be pretty comical if people did the same thing, right? Just walked up to strangers and started sniffing them like dogs?
Well, apparently humans do go by smell when it comes to making friends, and they prefer people who smell like them. Maybe you’ve noticed that your friends look like you, share your values, and think the same way as you. You’re probably right, seeing as previous research has pointed to this.
For the current study, done to show how smell affects human behavior, researchers recruited people who befriended each other quickly, before knowing much about each other. They assumed that the relationships between these same-sex, nonromantic “click friends” relied more on physiological traits, including smell. After collecting samples from the click friends, researchers used an eNose to scan chemical signatures. In another experiment, human volunteers sniffed samples to determine if any were similar. Both experiments showed that click friends had more similar smells than pairs of random people.
“This is not to say that we act like goats or shrews – humans likely rely on other, far more dominant cues in their social decision-making. Nevertheless, our study’s results do suggest that our nose plays a bigger role than previously thought in our choice of friends,” said senior author Noam Sobel, PhD, of the Weizmann Institute of Science in Rehovot, Israel.
Lead author Inbal Ravreby, a graduate student at the institute, put it this way: “These results imply that, as the saying goes, there is chemistry in social chemistry.”
These viruses want mosquitoes with good taste
Taste can be a pretty subjective sense. Not everyone agrees on what tastes good and what tastes bad. Most people would agree that freshly baked cookies taste good, but what about lima beans? And what about mosquitoes? What tastes good to a mosquito?
The answer? Blood. Blood tastes good to a mosquito. That really wasn’t a very hard question, was it? You did know the answer, didn’t you? They don’t care about cookies, and they certainly don’t care about lima beans. It’s blood that they love.
That brings us back to subjectivity, because it is possible for blood to taste even better. The secret ingredient is dengue … and Zika.
A study just published in Cell demonstrates that mice infected with dengue and Zika viruses release a volatile compound called acetophenone. “We found that flavivirus [like dengue and Zika] can utilize the increased release of acetophenone to help itself achieve its lifecycles more effectively by making their hosts more attractive to mosquito vectors,” senior author Gong Cheng of Tsinghua University, Beijing, said in a written statement.
How do they do it? The viruses, he explained, promote the proliferation of acetophenone-producing skin bacteria. “As a result, some bacteria overreplicate and produce more acetophenone. Suddenly, these sick individuals smell as delicious to mosquitoes as a tray of freshly baked cookies to a group of five-year-old children,” the statement said.
And how do you stop a group of tiny, flying 5-year-olds? That’s right, with acne medication. Really? You knew that one but not the blood one before? The investigators fed isotretinoin to the infected mice, which led to reduced acetophenone release from skin bacteria and made the animals no more attractive to the mosquitoes than their uninfected counterparts.
The investigators are planning to take the next step – feeding isotretinoin to people with dengue and Zika – having gotten the official fictional taste-test approval of celebrity chef Gordon Ramsay, who said, “You’re going to feed this #$^% to sick people? ARE YOU &%*$@#& KIDDING ME?”
Okay, so maybe approval isn’t quite the right word.
Welcome to bladders of the rich and famous!
Don’t you hate it when you’re driving out to your multimillion-dollar second home in the Hamptons and traffic is so bad you absolutely have to find a place to “rest” along the way? But wouldn’t you know it, there just isn’t anywhere to stop! Geez, how do we live?
That’s where David Shusterman, MD, a urologist in New York City and a true American hero, comes in. He’s identified a market and positioned himself as the king of both bladder surgery and “bladder Botox” for the wealthy New Yorkers who regularly make long journeys from the city out to their second homes in the Hamptons. Traffic has increased dramatically on Long Island roads in recent years, and the journey can now taking upward of 4 hours. Some people just can’t make it that long without a bathroom break, and there are very few places to stop along the way.
Dr. Shusterman understands the plight of the Hamptons vacationer, as he told Insider.com: “I can’t tell you how many arguments I personally get into – I’ve lost three friends because I’m the driver and refuse to stop for them.” A tragedy worthy of Shakespeare himself.
During the summer season, Dr. Shusterman performs about 10 prostate artery embolizations a week, an hour-long procedure that shrinks the prostate, which is great for 50- to 60-year-old men with enlarged prostates that cause more frequent bathroom trips. He also performs Botox injections into the bladder once or twice a week for women, which reduces the need to urinate for roughly 6 months. The perfect amount of time to get them through the summer season.
These procedures are sometimes covered by insurance but can cost as much as $20,000 if paid out of pocket. That’s a lot of money to us, but if you’re the sort of person who has a second home in the Hamptons, $20,000 is chump change, especially if it means you won’t have to go 2 entire minutes out of your way to use a gas-station bathroom. Then again, having seen a more than a few gas-station bathrooms in our time, maybe they have a point.
Ditch the apples. Go for the avocados
We’ve all heard about “an apple a day,” but instead of apples you might want to go with avocados.
Avocados are generally thought to be a healthy fat. A study just published in the Journal of the American Heart Association proves that they actually don’t do anything for your waistline but will work wonders on your cholesterol level. The study involved 923 participants who were considered overweight/obese split into two groups: One was asked to consume an avocado a day, and the other continued their usual diets and were asked to consume fewer than two avocados a month.
At the end of the 6 months, the researchers found total cholesterol decreased by an additional 2.9 mg/dL and LDL cholesterol by 2.5 mg/dL in those who ate one avocado every day, compared with the usual-diet group. And even though avocados have a lot of calories, there was no clinical evidence that it impacted weight gain or any cardiometabolic risk factors, according to a statement from Penn State University.
Avocados, then, can be considered a guilt-free food. The findings from this study suggest it can give a substantial boost to your overall quality of diet, in turn lessening your risk of developing type 2 diabetes and some cancers, Kristina Peterson, PhD, assistant professor of nutritional sciences at Texas Tech University, said in the statement.
So get creative with your avocado recipes. You can only eat so much guacamole.
Your nose knows a good friend for you
You’ve probably noticed how dogs sniff other dogs and people before becoming friends. It would be pretty comical if people did the same thing, right? Just walked up to strangers and started sniffing them like dogs?
Well, apparently humans do go by smell when it comes to making friends, and they prefer people who smell like them. Maybe you’ve noticed that your friends look like you, share your values, and think the same way as you. You’re probably right, seeing as previous research has pointed to this.
For the current study, done to show how smell affects human behavior, researchers recruited people who befriended each other quickly, before knowing much about each other. They assumed that the relationships between these same-sex, nonromantic “click friends” relied more on physiological traits, including smell. After collecting samples from the click friends, researchers used an eNose to scan chemical signatures. In another experiment, human volunteers sniffed samples to determine if any were similar. Both experiments showed that click friends had more similar smells than pairs of random people.
“This is not to say that we act like goats or shrews – humans likely rely on other, far more dominant cues in their social decision-making. Nevertheless, our study’s results do suggest that our nose plays a bigger role than previously thought in our choice of friends,” said senior author Noam Sobel, PhD, of the Weizmann Institute of Science in Rehovot, Israel.
Lead author Inbal Ravreby, a graduate student at the institute, put it this way: “These results imply that, as the saying goes, there is chemistry in social chemistry.”
These viruses want mosquitoes with good taste
Taste can be a pretty subjective sense. Not everyone agrees on what tastes good and what tastes bad. Most people would agree that freshly baked cookies taste good, but what about lima beans? And what about mosquitoes? What tastes good to a mosquito?
The answer? Blood. Blood tastes good to a mosquito. That really wasn’t a very hard question, was it? You did know the answer, didn’t you? They don’t care about cookies, and they certainly don’t care about lima beans. It’s blood that they love.
That brings us back to subjectivity, because it is possible for blood to taste even better. The secret ingredient is dengue … and Zika.
A study just published in Cell demonstrates that mice infected with dengue and Zika viruses release a volatile compound called acetophenone. “We found that flavivirus [like dengue and Zika] can utilize the increased release of acetophenone to help itself achieve its lifecycles more effectively by making their hosts more attractive to mosquito vectors,” senior author Gong Cheng of Tsinghua University, Beijing, said in a written statement.
How do they do it? The viruses, he explained, promote the proliferation of acetophenone-producing skin bacteria. “As a result, some bacteria overreplicate and produce more acetophenone. Suddenly, these sick individuals smell as delicious to mosquitoes as a tray of freshly baked cookies to a group of five-year-old children,” the statement said.
And how do you stop a group of tiny, flying 5-year-olds? That’s right, with acne medication. Really? You knew that one but not the blood one before? The investigators fed isotretinoin to the infected mice, which led to reduced acetophenone release from skin bacteria and made the animals no more attractive to the mosquitoes than their uninfected counterparts.
The investigators are planning to take the next step – feeding isotretinoin to people with dengue and Zika – having gotten the official fictional taste-test approval of celebrity chef Gordon Ramsay, who said, “You’re going to feed this #$^% to sick people? ARE YOU &%*$@#& KIDDING ME?”
Okay, so maybe approval isn’t quite the right word.
Welcome to bladders of the rich and famous!
Don’t you hate it when you’re driving out to your multimillion-dollar second home in the Hamptons and traffic is so bad you absolutely have to find a place to “rest” along the way? But wouldn’t you know it, there just isn’t anywhere to stop! Geez, how do we live?
That’s where David Shusterman, MD, a urologist in New York City and a true American hero, comes in. He’s identified a market and positioned himself as the king of both bladder surgery and “bladder Botox” for the wealthy New Yorkers who regularly make long journeys from the city out to their second homes in the Hamptons. Traffic has increased dramatically on Long Island roads in recent years, and the journey can now taking upward of 4 hours. Some people just can’t make it that long without a bathroom break, and there are very few places to stop along the way.
Dr. Shusterman understands the plight of the Hamptons vacationer, as he told Insider.com: “I can’t tell you how many arguments I personally get into – I’ve lost three friends because I’m the driver and refuse to stop for them.” A tragedy worthy of Shakespeare himself.
During the summer season, Dr. Shusterman performs about 10 prostate artery embolizations a week, an hour-long procedure that shrinks the prostate, which is great for 50- to 60-year-old men with enlarged prostates that cause more frequent bathroom trips. He also performs Botox injections into the bladder once or twice a week for women, which reduces the need to urinate for roughly 6 months. The perfect amount of time to get them through the summer season.
These procedures are sometimes covered by insurance but can cost as much as $20,000 if paid out of pocket. That’s a lot of money to us, but if you’re the sort of person who has a second home in the Hamptons, $20,000 is chump change, especially if it means you won’t have to go 2 entire minutes out of your way to use a gas-station bathroom. Then again, having seen a more than a few gas-station bathrooms in our time, maybe they have a point.
Ditch the apples. Go for the avocados
We’ve all heard about “an apple a day,” but instead of apples you might want to go with avocados.
Avocados are generally thought to be a healthy fat. A study just published in the Journal of the American Heart Association proves that they actually don’t do anything for your waistline but will work wonders on your cholesterol level. The study involved 923 participants who were considered overweight/obese split into two groups: One was asked to consume an avocado a day, and the other continued their usual diets and were asked to consume fewer than two avocados a month.
At the end of the 6 months, the researchers found total cholesterol decreased by an additional 2.9 mg/dL and LDL cholesterol by 2.5 mg/dL in those who ate one avocado every day, compared with the usual-diet group. And even though avocados have a lot of calories, there was no clinical evidence that it impacted weight gain or any cardiometabolic risk factors, according to a statement from Penn State University.
Avocados, then, can be considered a guilt-free food. The findings from this study suggest it can give a substantial boost to your overall quality of diet, in turn lessening your risk of developing type 2 diabetes and some cancers, Kristina Peterson, PhD, assistant professor of nutritional sciences at Texas Tech University, said in the statement.
So get creative with your avocado recipes. You can only eat so much guacamole.
Your nose knows a good friend for you
You’ve probably noticed how dogs sniff other dogs and people before becoming friends. It would be pretty comical if people did the same thing, right? Just walked up to strangers and started sniffing them like dogs?
Well, apparently humans do go by smell when it comes to making friends, and they prefer people who smell like them. Maybe you’ve noticed that your friends look like you, share your values, and think the same way as you. You’re probably right, seeing as previous research has pointed to this.
For the current study, done to show how smell affects human behavior, researchers recruited people who befriended each other quickly, before knowing much about each other. They assumed that the relationships between these same-sex, nonromantic “click friends” relied more on physiological traits, including smell. After collecting samples from the click friends, researchers used an eNose to scan chemical signatures. In another experiment, human volunteers sniffed samples to determine if any were similar. Both experiments showed that click friends had more similar smells than pairs of random people.
“This is not to say that we act like goats or shrews – humans likely rely on other, far more dominant cues in their social decision-making. Nevertheless, our study’s results do suggest that our nose plays a bigger role than previously thought in our choice of friends,” said senior author Noam Sobel, PhD, of the Weizmann Institute of Science in Rehovot, Israel.
Lead author Inbal Ravreby, a graduate student at the institute, put it this way: “These results imply that, as the saying goes, there is chemistry in social chemistry.”
Are social networks threatening adolescents’ mental health?
When it comes to the link between mental health and social networks, be careful of jumping to conclusions. This warning came from Margot Morgiève, PhD, sociology researcher at the French National Institute of Health and Medical Research and the Center for Research in Medicine, Science, Health, Mental Health, and Society (Inserm-Cermes 3). She delivered her remarks at the opening session of the Pediatric Societies Congress organized by the French Society of Pediatrics, based on an increasing amount of scientific literature on the subject.
In 2021, 4.2 billion people, or more than half the world’s population, used social networks, and 80.3% of French citizens had a social network account.
‘Facebook depression’
Between those who condemn social networks for causing problems in adolescents and those who, in contrast, view it as a lifeline, what do we really know about their impact on the mental health of young people?
Although several studies have found a significant association between the heavy use of social networks and anxiety, depressive symptoms, and stress, there have also been reports of decreased life satisfaction, as well as reduced general well-being and self-esteem.
“Due to an increased [concurrence] between mood disorders or depression and the use of social networks, researchers wanted to establish a new disorder: ‘Facebook Depression,’ ” commented Dr. Morgiève, who is also a clinical psychologist and coordinator of the chat and social network unit for the French national suicide prevention hotline 3114.
“But they quickly realized that it would be wrong to recognize it as a characterized disorder, because it would appear that the harmful effects of social networks on mental health are not linked to the social network itself, but rather to problematic social network use.”
Teens’ fantasy life
There are three major categories of problematic social network use, the first being social comparison. This refers to the spontaneous tendency of social beings to compare themselves to individuals who appear to be more attractive than them.
This is nothing new, but it is exacerbated on social networks. Users emphasize the positive aspects of their life and present themselves as balanced, popular, and satisfied.
However, this leads to strong normative constraints, which result in a negative self-assessment, thereby lowering self-esteem and promoting the emergence of depressive symptoms. “Thus, it isn’t the social network that creates depression, but rather the phenomenon of comparison, which it pushes to the extreme,” said Dr. Morgiève.
The second problem associated with social networks is their propensity to promote addictive behavior through [observational learning], which can give rise to compulsive and uncontrolled behavior, as illustrated by “FOMO,” or fear of missing out.
Hence the idea of defining a specific entity called “social network addiction,” which was also quickly abandoned. It is the very features of social networks that generate this fear and thus this tendency, just like news feeds (constant updating of a personalized news list).
“Substitutive” use is the third major category. This is when time spent in the online environment replaces that spent offline. Excessive users report a feeling of loneliness and an awareness of a lack of intimate connections.
Language of distress
Initial studies using artificial intelligence and machine learning tend to show that a digital language of distress exists. Authors noticed that themes associated with self-loathing, loneliness, suicide, death, and self-harm correlated with users who exhibited the highest levels of depression.
The very structure of the language (more words, more use of “I,” more references to death, and fewer verbs) correlated with users in distress.
According to the authors, the typical social network practice of vaguebooking – writing a post that may incite worry, such as “better days are coming” – is a significant predictive factor of suicidal ideation. A visual language of distress also reportedly exists – for example, the use of darker shades, like the black-and-white inkwell filter with no enhancements in Instagram.
Internet risks and dangers
Digital environments entail many risks and dangers. Suicide pacts and online suicides (like the suicide of a young girl on Periscope in 2016) remain rare but go viral. The same is true of challenges. In 2015, the Blue Whale Challenge consisted of a list of 50 challenges ranging from the benign to the dramatic, with the final challenge being to “hang yourself.”
Its huge media coverage might well have added to its viral success had the social networks not quickly reacted in a positive manner.
Trolling, for its part, consists of posting provocative content with the intent of either sparking conflict or causing distress.
Cyberbullying, the most common online risk adolescents face, is the repeated spreading of false, embarrassing, or hostile information.
A growing danger is sexting (sending, receiving, or passing on sexually explicit photographs, messages, or images). The serious potential consequences of sexting include revenge porn or cyber rape, which is defined as the distribution of illicit content without consent, the practice of which has been linked to depression and involvement in risky behavior.
The risk of suicide exposure should no longer be overlooked, in view of the hypothesis that some online content relating to suicide may produce a suggestive effect with respect to the idea or the method of suicide, as well as precipitating suicide attempts.
“People who post suicidal comments are in communities that are closely connected by bonds of affiliation (memberships, friendships) and activities (retweets, likes, comments),” explained Dr. Morgiève.
But in these communities, emotionally charged information that spreads rapidly and repetitively could promote corumination, hence the concept of “suicidocosme [suicide world]», developed in 2017 by Charles-Edouard Notredame, MD, of the child and adolescent psychiatry department at Lille (France) University Hospital. This, in turn, can produce and increase the suicide contagion based on the Werther effect model.
Just one of many examples is Marilyn Monroe’s suicide in 1962, which increased the suicide rate by 40% in Los Angeles. The Werther effect is especially significant because two biases are present: the prestige bias (identification with the person one admires) and similarity bias (identification with the person who resembles me).
Similarity bias is the most decisive in adolescence. It should be noted that the positive counterpart to the Werther effect is the Papageno effect. The Belgian singer-songwriter Stromae’s TV appearances earlier this year, in which he spoke about his suicidal ideations, enabling young people to recognize their suffering and seek help, is an example of the Papageno effect.
Support on social networks?
Social networks can increase connectedness, for example, the feeling of being connected to something meaningful outside oneself. Connectedness promotes psychological well-being and quality of life.
The very characteristics of social networks can enhance elements of connectedness, both objectively by increasing users’ social sphere, and subjectively by reinforcing the feeling of social belonging and subjective well-being.
Taking Facebook and its “anniversary” feature as an example, it has been shown that the greater the number of Facebook friends, the more individuals saw themselves as being connected to a community.
“Millennials, or people born between the beginning of the 1980s and the end of the 1990s, are thus more likely to take advantage of the digital social environment to establish a new relationship with psychological suffering and its attempts to ease it,” said Dr. Morgiève.
They are also more likely to naturally turn to the digital space to look for help. More and more of them are searching the Internet for information on mental health and sharing experiences to get support.”
An example is the It Gets Better Project, which is a good illustration of the structure of online peer communities, with stories from LGBTQ+ individuals who describe how they succeeded in coping with adversity during their adolescence. In this way, social media seems to help identify peers and positive resources that are usually unavailable outside of the digital space. As a result, thanks to normative models on extremely strong social networks that are easy to conform to, these online peer-support communities have the potential to facilitate social interactions and reinforce a feeling both of hope and of belonging to a group.”
Promoting access to care
In Dr. Morgiève’s opinion, “access to care, particularly in the area of adolescent mental health, is extremely critical, given the lack of support precisely when they need it the most, as [evidenced] by the number of suicide attempts.
“There are two types of barriers to seeking help which can explain this. The first is structural barriers: help is too expensive or too far away or the wait is too long. The second refers to personal barriers, including denying the need for help, which may involve a self-sufficiency bias, the feeling that one cannot be helped, refusal to bother close friends and family, fear of being stigmatized, and a feeling of shame.”
These types of barriers are particularly difficult to overcome because the beliefs regarding care and caregivers are limiting (doubts about caregiver confidentiality, reliability, and competence). This is observed especially in adolescents because of the desire for emancipation and development of identity. So [the help relationship] may be experienced as subordination or alienation.
On a positive note, it is the very properties of social networks that will enable these obstacles to seeking help to be overcome. The fact that they are available everywhere makes up for young people’s lack of mobility and regional disparities. In addition, it ensures discretion and freedom of use, while reducing inhibitions.
The fact that social networks are free of charge overcomes structural obstacles, such as financial and organizational costs, as well as personal obstacles, thereby facilitating engagement and lessening the motivational cost. The dissociative pseudonymity or anonymity reduces the feeling of vulnerability associated with revealing oneself, as well as fears of a breach of confidentiality.
Dr. Morgiève summed it up by saying: “While offline life is silent because young people don’t talk about their suicidal ideations, online life truly removes inhibitions about speaking, relationships, and sharing experiences. Thus, the internet offers adolescents new opportunities to express themselves, which they’re not doing in real life.”
Professionals go digital
France records one suicide every hour (8,885 deaths a year) and one suicide attempt every 4 minutes. Since the 1950s, government-funded telehealth prevention and assistance programs, such as S.O.S. Amitié, Suicide Écoute, SOS Suicide Phénix, etc., have been developed. Their values and principles are anonymity, nondirectivity, nonjudgment, and neutrality. In addition to these nonprofit offerings, a professional teleprevention program, the confidential suicide prevention hotline 3114 – with professionals who are available to listen 24 hours a day, 7 days a week – was launched by the Ministry of Health and Prevention in October 2021.
Its values and principles include confidentiality, proactivity, concern, and caring for others. To date, 13 of 17 centers have opened. In the space of 6 months, they have received 50,000 calls, with an average of 400-500 calls a day. The dedicated chat application was codesigned with users (suicide attempters). And now social networks are joining in. For example, the hotline number 3114 appears whenever a TikTok user types the word “suicide.”
Dr. Morgiève said she has no conflicts of interest regarding the subject presented.
This article was translated from the Medscape French edition. A version of this article first appeared on Medscape.com.
When it comes to the link between mental health and social networks, be careful of jumping to conclusions. This warning came from Margot Morgiève, PhD, sociology researcher at the French National Institute of Health and Medical Research and the Center for Research in Medicine, Science, Health, Mental Health, and Society (Inserm-Cermes 3). She delivered her remarks at the opening session of the Pediatric Societies Congress organized by the French Society of Pediatrics, based on an increasing amount of scientific literature on the subject.
In 2021, 4.2 billion people, or more than half the world’s population, used social networks, and 80.3% of French citizens had a social network account.
‘Facebook depression’
Between those who condemn social networks for causing problems in adolescents and those who, in contrast, view it as a lifeline, what do we really know about their impact on the mental health of young people?
Although several studies have found a significant association between the heavy use of social networks and anxiety, depressive symptoms, and stress, there have also been reports of decreased life satisfaction, as well as reduced general well-being and self-esteem.
“Due to an increased [concurrence] between mood disorders or depression and the use of social networks, researchers wanted to establish a new disorder: ‘Facebook Depression,’ ” commented Dr. Morgiève, who is also a clinical psychologist and coordinator of the chat and social network unit for the French national suicide prevention hotline 3114.
“But they quickly realized that it would be wrong to recognize it as a characterized disorder, because it would appear that the harmful effects of social networks on mental health are not linked to the social network itself, but rather to problematic social network use.”
Teens’ fantasy life
There are three major categories of problematic social network use, the first being social comparison. This refers to the spontaneous tendency of social beings to compare themselves to individuals who appear to be more attractive than them.
This is nothing new, but it is exacerbated on social networks. Users emphasize the positive aspects of their life and present themselves as balanced, popular, and satisfied.
However, this leads to strong normative constraints, which result in a negative self-assessment, thereby lowering self-esteem and promoting the emergence of depressive symptoms. “Thus, it isn’t the social network that creates depression, but rather the phenomenon of comparison, which it pushes to the extreme,” said Dr. Morgiève.
The second problem associated with social networks is their propensity to promote addictive behavior through [observational learning], which can give rise to compulsive and uncontrolled behavior, as illustrated by “FOMO,” or fear of missing out.
Hence the idea of defining a specific entity called “social network addiction,” which was also quickly abandoned. It is the very features of social networks that generate this fear and thus this tendency, just like news feeds (constant updating of a personalized news list).
“Substitutive” use is the third major category. This is when time spent in the online environment replaces that spent offline. Excessive users report a feeling of loneliness and an awareness of a lack of intimate connections.
Language of distress
Initial studies using artificial intelligence and machine learning tend to show that a digital language of distress exists. Authors noticed that themes associated with self-loathing, loneliness, suicide, death, and self-harm correlated with users who exhibited the highest levels of depression.
The very structure of the language (more words, more use of “I,” more references to death, and fewer verbs) correlated with users in distress.
According to the authors, the typical social network practice of vaguebooking – writing a post that may incite worry, such as “better days are coming” – is a significant predictive factor of suicidal ideation. A visual language of distress also reportedly exists – for example, the use of darker shades, like the black-and-white inkwell filter with no enhancements in Instagram.
Internet risks and dangers
Digital environments entail many risks and dangers. Suicide pacts and online suicides (like the suicide of a young girl on Periscope in 2016) remain rare but go viral. The same is true of challenges. In 2015, the Blue Whale Challenge consisted of a list of 50 challenges ranging from the benign to the dramatic, with the final challenge being to “hang yourself.”
Its huge media coverage might well have added to its viral success had the social networks not quickly reacted in a positive manner.
Trolling, for its part, consists of posting provocative content with the intent of either sparking conflict or causing distress.
Cyberbullying, the most common online risk adolescents face, is the repeated spreading of false, embarrassing, or hostile information.
A growing danger is sexting (sending, receiving, or passing on sexually explicit photographs, messages, or images). The serious potential consequences of sexting include revenge porn or cyber rape, which is defined as the distribution of illicit content without consent, the practice of which has been linked to depression and involvement in risky behavior.
The risk of suicide exposure should no longer be overlooked, in view of the hypothesis that some online content relating to suicide may produce a suggestive effect with respect to the idea or the method of suicide, as well as precipitating suicide attempts.
“People who post suicidal comments are in communities that are closely connected by bonds of affiliation (memberships, friendships) and activities (retweets, likes, comments),” explained Dr. Morgiève.
But in these communities, emotionally charged information that spreads rapidly and repetitively could promote corumination, hence the concept of “suicidocosme [suicide world]», developed in 2017 by Charles-Edouard Notredame, MD, of the child and adolescent psychiatry department at Lille (France) University Hospital. This, in turn, can produce and increase the suicide contagion based on the Werther effect model.
Just one of many examples is Marilyn Monroe’s suicide in 1962, which increased the suicide rate by 40% in Los Angeles. The Werther effect is especially significant because two biases are present: the prestige bias (identification with the person one admires) and similarity bias (identification with the person who resembles me).
Similarity bias is the most decisive in adolescence. It should be noted that the positive counterpart to the Werther effect is the Papageno effect. The Belgian singer-songwriter Stromae’s TV appearances earlier this year, in which he spoke about his suicidal ideations, enabling young people to recognize their suffering and seek help, is an example of the Papageno effect.
Support on social networks?
Social networks can increase connectedness, for example, the feeling of being connected to something meaningful outside oneself. Connectedness promotes psychological well-being and quality of life.
The very characteristics of social networks can enhance elements of connectedness, both objectively by increasing users’ social sphere, and subjectively by reinforcing the feeling of social belonging and subjective well-being.
Taking Facebook and its “anniversary” feature as an example, it has been shown that the greater the number of Facebook friends, the more individuals saw themselves as being connected to a community.
“Millennials, or people born between the beginning of the 1980s and the end of the 1990s, are thus more likely to take advantage of the digital social environment to establish a new relationship with psychological suffering and its attempts to ease it,” said Dr. Morgiève.
They are also more likely to naturally turn to the digital space to look for help. More and more of them are searching the Internet for information on mental health and sharing experiences to get support.”
An example is the It Gets Better Project, which is a good illustration of the structure of online peer communities, with stories from LGBTQ+ individuals who describe how they succeeded in coping with adversity during their adolescence. In this way, social media seems to help identify peers and positive resources that are usually unavailable outside of the digital space. As a result, thanks to normative models on extremely strong social networks that are easy to conform to, these online peer-support communities have the potential to facilitate social interactions and reinforce a feeling both of hope and of belonging to a group.”
Promoting access to care
In Dr. Morgiève’s opinion, “access to care, particularly in the area of adolescent mental health, is extremely critical, given the lack of support precisely when they need it the most, as [evidenced] by the number of suicide attempts.
“There are two types of barriers to seeking help which can explain this. The first is structural barriers: help is too expensive or too far away or the wait is too long. The second refers to personal barriers, including denying the need for help, which may involve a self-sufficiency bias, the feeling that one cannot be helped, refusal to bother close friends and family, fear of being stigmatized, and a feeling of shame.”
These types of barriers are particularly difficult to overcome because the beliefs regarding care and caregivers are limiting (doubts about caregiver confidentiality, reliability, and competence). This is observed especially in adolescents because of the desire for emancipation and development of identity. So [the help relationship] may be experienced as subordination or alienation.
On a positive note, it is the very properties of social networks that will enable these obstacles to seeking help to be overcome. The fact that they are available everywhere makes up for young people’s lack of mobility and regional disparities. In addition, it ensures discretion and freedom of use, while reducing inhibitions.
The fact that social networks are free of charge overcomes structural obstacles, such as financial and organizational costs, as well as personal obstacles, thereby facilitating engagement and lessening the motivational cost. The dissociative pseudonymity or anonymity reduces the feeling of vulnerability associated with revealing oneself, as well as fears of a breach of confidentiality.
Dr. Morgiève summed it up by saying: “While offline life is silent because young people don’t talk about their suicidal ideations, online life truly removes inhibitions about speaking, relationships, and sharing experiences. Thus, the internet offers adolescents new opportunities to express themselves, which they’re not doing in real life.”
Professionals go digital
France records one suicide every hour (8,885 deaths a year) and one suicide attempt every 4 minutes. Since the 1950s, government-funded telehealth prevention and assistance programs, such as S.O.S. Amitié, Suicide Écoute, SOS Suicide Phénix, etc., have been developed. Their values and principles are anonymity, nondirectivity, nonjudgment, and neutrality. In addition to these nonprofit offerings, a professional teleprevention program, the confidential suicide prevention hotline 3114 – with professionals who are available to listen 24 hours a day, 7 days a week – was launched by the Ministry of Health and Prevention in October 2021.
Its values and principles include confidentiality, proactivity, concern, and caring for others. To date, 13 of 17 centers have opened. In the space of 6 months, they have received 50,000 calls, with an average of 400-500 calls a day. The dedicated chat application was codesigned with users (suicide attempters). And now social networks are joining in. For example, the hotline number 3114 appears whenever a TikTok user types the word “suicide.”
Dr. Morgiève said she has no conflicts of interest regarding the subject presented.
This article was translated from the Medscape French edition. A version of this article first appeared on Medscape.com.
When it comes to the link between mental health and social networks, be careful of jumping to conclusions. This warning came from Margot Morgiève, PhD, sociology researcher at the French National Institute of Health and Medical Research and the Center for Research in Medicine, Science, Health, Mental Health, and Society (Inserm-Cermes 3). She delivered her remarks at the opening session of the Pediatric Societies Congress organized by the French Society of Pediatrics, based on an increasing amount of scientific literature on the subject.
In 2021, 4.2 billion people, or more than half the world’s population, used social networks, and 80.3% of French citizens had a social network account.
‘Facebook depression’
Between those who condemn social networks for causing problems in adolescents and those who, in contrast, view it as a lifeline, what do we really know about their impact on the mental health of young people?
Although several studies have found a significant association between the heavy use of social networks and anxiety, depressive symptoms, and stress, there have also been reports of decreased life satisfaction, as well as reduced general well-being and self-esteem.
“Due to an increased [concurrence] between mood disorders or depression and the use of social networks, researchers wanted to establish a new disorder: ‘Facebook Depression,’ ” commented Dr. Morgiève, who is also a clinical psychologist and coordinator of the chat and social network unit for the French national suicide prevention hotline 3114.
“But they quickly realized that it would be wrong to recognize it as a characterized disorder, because it would appear that the harmful effects of social networks on mental health are not linked to the social network itself, but rather to problematic social network use.”
Teens’ fantasy life
There are three major categories of problematic social network use, the first being social comparison. This refers to the spontaneous tendency of social beings to compare themselves to individuals who appear to be more attractive than them.
This is nothing new, but it is exacerbated on social networks. Users emphasize the positive aspects of their life and present themselves as balanced, popular, and satisfied.
However, this leads to strong normative constraints, which result in a negative self-assessment, thereby lowering self-esteem and promoting the emergence of depressive symptoms. “Thus, it isn’t the social network that creates depression, but rather the phenomenon of comparison, which it pushes to the extreme,” said Dr. Morgiève.
The second problem associated with social networks is their propensity to promote addictive behavior through [observational learning], which can give rise to compulsive and uncontrolled behavior, as illustrated by “FOMO,” or fear of missing out.
Hence the idea of defining a specific entity called “social network addiction,” which was also quickly abandoned. It is the very features of social networks that generate this fear and thus this tendency, just like news feeds (constant updating of a personalized news list).
“Substitutive” use is the third major category. This is when time spent in the online environment replaces that spent offline. Excessive users report a feeling of loneliness and an awareness of a lack of intimate connections.
Language of distress
Initial studies using artificial intelligence and machine learning tend to show that a digital language of distress exists. Authors noticed that themes associated with self-loathing, loneliness, suicide, death, and self-harm correlated with users who exhibited the highest levels of depression.
The very structure of the language (more words, more use of “I,” more references to death, and fewer verbs) correlated with users in distress.
According to the authors, the typical social network practice of vaguebooking – writing a post that may incite worry, such as “better days are coming” – is a significant predictive factor of suicidal ideation. A visual language of distress also reportedly exists – for example, the use of darker shades, like the black-and-white inkwell filter with no enhancements in Instagram.
Internet risks and dangers
Digital environments entail many risks and dangers. Suicide pacts and online suicides (like the suicide of a young girl on Periscope in 2016) remain rare but go viral. The same is true of challenges. In 2015, the Blue Whale Challenge consisted of a list of 50 challenges ranging from the benign to the dramatic, with the final challenge being to “hang yourself.”
Its huge media coverage might well have added to its viral success had the social networks not quickly reacted in a positive manner.
Trolling, for its part, consists of posting provocative content with the intent of either sparking conflict or causing distress.
Cyberbullying, the most common online risk adolescents face, is the repeated spreading of false, embarrassing, or hostile information.
A growing danger is sexting (sending, receiving, or passing on sexually explicit photographs, messages, or images). The serious potential consequences of sexting include revenge porn or cyber rape, which is defined as the distribution of illicit content without consent, the practice of which has been linked to depression and involvement in risky behavior.
The risk of suicide exposure should no longer be overlooked, in view of the hypothesis that some online content relating to suicide may produce a suggestive effect with respect to the idea or the method of suicide, as well as precipitating suicide attempts.
“People who post suicidal comments are in communities that are closely connected by bonds of affiliation (memberships, friendships) and activities (retweets, likes, comments),” explained Dr. Morgiève.
But in these communities, emotionally charged information that spreads rapidly and repetitively could promote corumination, hence the concept of “suicidocosme [suicide world]», developed in 2017 by Charles-Edouard Notredame, MD, of the child and adolescent psychiatry department at Lille (France) University Hospital. This, in turn, can produce and increase the suicide contagion based on the Werther effect model.
Just one of many examples is Marilyn Monroe’s suicide in 1962, which increased the suicide rate by 40% in Los Angeles. The Werther effect is especially significant because two biases are present: the prestige bias (identification with the person one admires) and similarity bias (identification with the person who resembles me).
Similarity bias is the most decisive in adolescence. It should be noted that the positive counterpart to the Werther effect is the Papageno effect. The Belgian singer-songwriter Stromae’s TV appearances earlier this year, in which he spoke about his suicidal ideations, enabling young people to recognize their suffering and seek help, is an example of the Papageno effect.
Support on social networks?
Social networks can increase connectedness, for example, the feeling of being connected to something meaningful outside oneself. Connectedness promotes psychological well-being and quality of life.
The very characteristics of social networks can enhance elements of connectedness, both objectively by increasing users’ social sphere, and subjectively by reinforcing the feeling of social belonging and subjective well-being.
Taking Facebook and its “anniversary” feature as an example, it has been shown that the greater the number of Facebook friends, the more individuals saw themselves as being connected to a community.
“Millennials, or people born between the beginning of the 1980s and the end of the 1990s, are thus more likely to take advantage of the digital social environment to establish a new relationship with psychological suffering and its attempts to ease it,” said Dr. Morgiève.
They are also more likely to naturally turn to the digital space to look for help. More and more of them are searching the Internet for information on mental health and sharing experiences to get support.”
An example is the It Gets Better Project, which is a good illustration of the structure of online peer communities, with stories from LGBTQ+ individuals who describe how they succeeded in coping with adversity during their adolescence. In this way, social media seems to help identify peers and positive resources that are usually unavailable outside of the digital space. As a result, thanks to normative models on extremely strong social networks that are easy to conform to, these online peer-support communities have the potential to facilitate social interactions and reinforce a feeling both of hope and of belonging to a group.”
Promoting access to care
In Dr. Morgiève’s opinion, “access to care, particularly in the area of adolescent mental health, is extremely critical, given the lack of support precisely when they need it the most, as [evidenced] by the number of suicide attempts.
“There are two types of barriers to seeking help which can explain this. The first is structural barriers: help is too expensive or too far away or the wait is too long. The second refers to personal barriers, including denying the need for help, which may involve a self-sufficiency bias, the feeling that one cannot be helped, refusal to bother close friends and family, fear of being stigmatized, and a feeling of shame.”
These types of barriers are particularly difficult to overcome because the beliefs regarding care and caregivers are limiting (doubts about caregiver confidentiality, reliability, and competence). This is observed especially in adolescents because of the desire for emancipation and development of identity. So [the help relationship] may be experienced as subordination or alienation.
On a positive note, it is the very properties of social networks that will enable these obstacles to seeking help to be overcome. The fact that they are available everywhere makes up for young people’s lack of mobility and regional disparities. In addition, it ensures discretion and freedom of use, while reducing inhibitions.
The fact that social networks are free of charge overcomes structural obstacles, such as financial and organizational costs, as well as personal obstacles, thereby facilitating engagement and lessening the motivational cost. The dissociative pseudonymity or anonymity reduces the feeling of vulnerability associated with revealing oneself, as well as fears of a breach of confidentiality.
Dr. Morgiève summed it up by saying: “While offline life is silent because young people don’t talk about their suicidal ideations, online life truly removes inhibitions about speaking, relationships, and sharing experiences. Thus, the internet offers adolescents new opportunities to express themselves, which they’re not doing in real life.”
Professionals go digital
France records one suicide every hour (8,885 deaths a year) and one suicide attempt every 4 minutes. Since the 1950s, government-funded telehealth prevention and assistance programs, such as S.O.S. Amitié, Suicide Écoute, SOS Suicide Phénix, etc., have been developed. Their values and principles are anonymity, nondirectivity, nonjudgment, and neutrality. In addition to these nonprofit offerings, a professional teleprevention program, the confidential suicide prevention hotline 3114 – with professionals who are available to listen 24 hours a day, 7 days a week – was launched by the Ministry of Health and Prevention in October 2021.
Its values and principles include confidentiality, proactivity, concern, and caring for others. To date, 13 of 17 centers have opened. In the space of 6 months, they have received 50,000 calls, with an average of 400-500 calls a day. The dedicated chat application was codesigned with users (suicide attempters). And now social networks are joining in. For example, the hotline number 3114 appears whenever a TikTok user types the word “suicide.”
Dr. Morgiève said she has no conflicts of interest regarding the subject presented.
This article was translated from the Medscape French edition. A version of this article first appeared on Medscape.com.
What is palliative care and what’s new in practicing this type of medicine?
The World Health Organization defines palliative care as “an approach that improves the quality of life of patients (adults and children) and their families who are facing problems associated with life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment, and treatment of pain and other problems, whether physical, psychosocial or spiritual.”1
The common misperception is that palliative care is only for those at end of life or only in the advanced stages of their illness. However, palliative care is ideally most helpful following individuals from diagnosis through their illness trajectory. Another misperception is that palliative care and hospice are the same thing. Though all hospice is palliative care, all palliative care is not hospice. Both palliative care and hospice provide care for individuals facing a serious illness and focus on the same philosophy of care, but palliative care can be initiated at any stage of illness, even if the goal is to pursue curative and life-prolonging therapies/interventions.
In contrast, hospice is considered for those who are at the end of life and are usually not pursuing life-prolonging therapies or interventions, instead focusing on comfort, symptom management, and optimization of quality of life.
Though there is a growing need for palliative care, there is a shortage of specialist palliative care providers. Much of the palliative care needs can be met by all providers who can offer basic symptom management, identification surrounding goals of care and discussions of advance care planning, and understanding of illness/prognosis and treatment options, which is called primary palliative care.2 In fact, two-thirds of patients with a serious illness other than cancer prefer discussion of end-of-life care or advance care planning with their primary care providers.3
Referral to specialty palliative care should be considered when there are more complexities to symptom/pain management and goals of care/end of life, transition to hospice, or complex communication dynamics.4
Though specialty palliative care was shown to be more comprehensive, both primary palliative care and specialty palliative care have led to improvements in the quality of life in individuals living with serious illness.5 Early integration of palliative care into routine care has been shown to improve symptom burden, mood, quality of life, survival, and health care costs.6
Updates in alternative and complementary therapies to palliative care
There are several alternative and complementary therapies to palliative care, including cannabis and psychedelics. These therapies are becoming or may become a familiar part of medical therapies that are listed in a patient’s history as part of their medical regimen, especially as more states continue to legalize and/or decriminalize the use of these alternative therapies for recreational or medicinal use.
Both cannabis and psychedelics have a longstanding history of therapeutic and holistic use. Cannabis has been used to manage symptoms such as pain since the 16th and 17th century.7 In palliative care, more patients may turn to various forms of cannabis as a source of relief from symptoms and suffering as their focus shifts more to quality of life.
Even with the increasing popularity of the use of cannabis among seriously ill patients, there is still a lack of evidence of the benefits of medical cannabis use in palliative care, and there is a lack of standardization of type of cannabis used and state regulations regarding their use.7
A recent systematic review found that despite the reported positive treatment effects of cannabis in palliative care, the results of the studies were conflicting. This highlights the need for further high-quality research to determine whether cannabis products are an effective treatment in palliative care patients.8
One limitation to note is that the majority of the included studies focused on cannabis use in patients with cancer for cancer-related symptoms. Few studies included patients with other serious conditions.
Psychedelics
There is evidence that psychedelic assisted therapy (PAT) is a safe and effective treatment for individuals with refractory depression, posttraumatic stress disorder, and substance use disorder.9 Plus, there have been ample studies providing support that PAT improves symptoms such as refractory anxiety/depression, demoralization, and existential distress in seriously ill patients, thus improving their quality of life and overall well-being.9
Nine U.S. cities and the State of Oregon have decriminalized or legalized the psychedelic psilocybin, based on the medical benefits patients have experienced evidenced from using it.10
In light of the increasing interest in PAT, Dr. Ira Byock provided the following points on what “all clinicians should know as they enter this uncharted territory”:
- Psychedelics have been around for a long time.
- Psychedelic-assisted therapies’ therapeutic effects are experiential.
- There are a variety of terms for specific categories of psychedelic compounds.
- Some palliative care teams are already caring for patients who undergo psychedelic experiences.
- Use of psychedelics should be well-observed by a skilled clinician with expertise.
I am hoping this provides a general refresher on palliative care and an overview of updates to alternative and complementary therapies for patients living with serious illness.9
Dr. Kang is a geriatrician and palliative care provider at the University of Washington, Seattle in the division of geriatrics and gerontology. She has no conflicts related to the content of this piece.
References
1. World Health Organization. Palliative care. 2020 Aug 5..
2. Weissman DE and Meier DE. Identifying patients in need of a palliative care assessment in the hospital setting a consensus report from the center to advance palliative care. J Palliat Med. 2011;14(1):17-23.
3. Sherry D et al. Is primary care physician involvement associated with earlier advance care planning? A study of patients in an academic primary care setting. J Palliat Med. 2022;25(1):75-80.
4. Quill TE and Abernethy AP. Generalist plus specialist palliative care-creating a more sustainable model. N Engl J Med. 2013;368:1173-75.
5. Ernecoff NC et al. Comparing specialty and primary palliative care interventions: Analysis of a systematic review. J Palliat Med. 2020;23(3):389-96.
6. Temmel JS et al. Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med. 2011;363:733-42.
7. Kogan M and Sexton M. Medical cannabis: A new old tool for palliative care. J Altern Complement Med . 2020 Sep;26(9):776-8.
8. Doppen M et al. Cannabis in palliative care: A systematic review of the current evidence. J Pain Symptom Manage. 2022 Jun 12;S0885-3924(22)00760-6.
9. Byock I. Psychedelics for serious illness: Five things clinicians need to know. The Center to Advance Palliative Care. Psychedelics for Serious Illness, Palliative in Practice, Center to Advance Palliative Care (capc.org). June 13, 2022.
10. Marks M. A strategy for rescheduling psilocybin. Scientific American. Oct. 11, 2021.
The World Health Organization defines palliative care as “an approach that improves the quality of life of patients (adults and children) and their families who are facing problems associated with life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment, and treatment of pain and other problems, whether physical, psychosocial or spiritual.”1
The common misperception is that palliative care is only for those at end of life or only in the advanced stages of their illness. However, palliative care is ideally most helpful following individuals from diagnosis through their illness trajectory. Another misperception is that palliative care and hospice are the same thing. Though all hospice is palliative care, all palliative care is not hospice. Both palliative care and hospice provide care for individuals facing a serious illness and focus on the same philosophy of care, but palliative care can be initiated at any stage of illness, even if the goal is to pursue curative and life-prolonging therapies/interventions.
In contrast, hospice is considered for those who are at the end of life and are usually not pursuing life-prolonging therapies or interventions, instead focusing on comfort, symptom management, and optimization of quality of life.
Though there is a growing need for palliative care, there is a shortage of specialist palliative care providers. Much of the palliative care needs can be met by all providers who can offer basic symptom management, identification surrounding goals of care and discussions of advance care planning, and understanding of illness/prognosis and treatment options, which is called primary palliative care.2 In fact, two-thirds of patients with a serious illness other than cancer prefer discussion of end-of-life care or advance care planning with their primary care providers.3
Referral to specialty palliative care should be considered when there are more complexities to symptom/pain management and goals of care/end of life, transition to hospice, or complex communication dynamics.4
Though specialty palliative care was shown to be more comprehensive, both primary palliative care and specialty palliative care have led to improvements in the quality of life in individuals living with serious illness.5 Early integration of palliative care into routine care has been shown to improve symptom burden, mood, quality of life, survival, and health care costs.6
Updates in alternative and complementary therapies to palliative care
There are several alternative and complementary therapies to palliative care, including cannabis and psychedelics. These therapies are becoming or may become a familiar part of medical therapies that are listed in a patient’s history as part of their medical regimen, especially as more states continue to legalize and/or decriminalize the use of these alternative therapies for recreational or medicinal use.
Both cannabis and psychedelics have a longstanding history of therapeutic and holistic use. Cannabis has been used to manage symptoms such as pain since the 16th and 17th century.7 In palliative care, more patients may turn to various forms of cannabis as a source of relief from symptoms and suffering as their focus shifts more to quality of life.
Even with the increasing popularity of the use of cannabis among seriously ill patients, there is still a lack of evidence of the benefits of medical cannabis use in palliative care, and there is a lack of standardization of type of cannabis used and state regulations regarding their use.7
A recent systematic review found that despite the reported positive treatment effects of cannabis in palliative care, the results of the studies were conflicting. This highlights the need for further high-quality research to determine whether cannabis products are an effective treatment in palliative care patients.8
One limitation to note is that the majority of the included studies focused on cannabis use in patients with cancer for cancer-related symptoms. Few studies included patients with other serious conditions.
Psychedelics
There is evidence that psychedelic assisted therapy (PAT) is a safe and effective treatment for individuals with refractory depression, posttraumatic stress disorder, and substance use disorder.9 Plus, there have been ample studies providing support that PAT improves symptoms such as refractory anxiety/depression, demoralization, and existential distress in seriously ill patients, thus improving their quality of life and overall well-being.9
Nine U.S. cities and the State of Oregon have decriminalized or legalized the psychedelic psilocybin, based on the medical benefits patients have experienced evidenced from using it.10
In light of the increasing interest in PAT, Dr. Ira Byock provided the following points on what “all clinicians should know as they enter this uncharted territory”:
- Psychedelics have been around for a long time.
- Psychedelic-assisted therapies’ therapeutic effects are experiential.
- There are a variety of terms for specific categories of psychedelic compounds.
- Some palliative care teams are already caring for patients who undergo psychedelic experiences.
- Use of psychedelics should be well-observed by a skilled clinician with expertise.
I am hoping this provides a general refresher on palliative care and an overview of updates to alternative and complementary therapies for patients living with serious illness.9
Dr. Kang is a geriatrician and palliative care provider at the University of Washington, Seattle in the division of geriatrics and gerontology. She has no conflicts related to the content of this piece.
References
1. World Health Organization. Palliative care. 2020 Aug 5..
2. Weissman DE and Meier DE. Identifying patients in need of a palliative care assessment in the hospital setting a consensus report from the center to advance palliative care. J Palliat Med. 2011;14(1):17-23.
3. Sherry D et al. Is primary care physician involvement associated with earlier advance care planning? A study of patients in an academic primary care setting. J Palliat Med. 2022;25(1):75-80.
4. Quill TE and Abernethy AP. Generalist plus specialist palliative care-creating a more sustainable model. N Engl J Med. 2013;368:1173-75.
5. Ernecoff NC et al. Comparing specialty and primary palliative care interventions: Analysis of a systematic review. J Palliat Med. 2020;23(3):389-96.
6. Temmel JS et al. Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med. 2011;363:733-42.
7. Kogan M and Sexton M. Medical cannabis: A new old tool for palliative care. J Altern Complement Med . 2020 Sep;26(9):776-8.
8. Doppen M et al. Cannabis in palliative care: A systematic review of the current evidence. J Pain Symptom Manage. 2022 Jun 12;S0885-3924(22)00760-6.
9. Byock I. Psychedelics for serious illness: Five things clinicians need to know. The Center to Advance Palliative Care. Psychedelics for Serious Illness, Palliative in Practice, Center to Advance Palliative Care (capc.org). June 13, 2022.
10. Marks M. A strategy for rescheduling psilocybin. Scientific American. Oct. 11, 2021.
The World Health Organization defines palliative care as “an approach that improves the quality of life of patients (adults and children) and their families who are facing problems associated with life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment, and treatment of pain and other problems, whether physical, psychosocial or spiritual.”1
The common misperception is that palliative care is only for those at end of life or only in the advanced stages of their illness. However, palliative care is ideally most helpful following individuals from diagnosis through their illness trajectory. Another misperception is that palliative care and hospice are the same thing. Though all hospice is palliative care, all palliative care is not hospice. Both palliative care and hospice provide care for individuals facing a serious illness and focus on the same philosophy of care, but palliative care can be initiated at any stage of illness, even if the goal is to pursue curative and life-prolonging therapies/interventions.
In contrast, hospice is considered for those who are at the end of life and are usually not pursuing life-prolonging therapies or interventions, instead focusing on comfort, symptom management, and optimization of quality of life.
Though there is a growing need for palliative care, there is a shortage of specialist palliative care providers. Much of the palliative care needs can be met by all providers who can offer basic symptom management, identification surrounding goals of care and discussions of advance care planning, and understanding of illness/prognosis and treatment options, which is called primary palliative care.2 In fact, two-thirds of patients with a serious illness other than cancer prefer discussion of end-of-life care or advance care planning with their primary care providers.3
Referral to specialty palliative care should be considered when there are more complexities to symptom/pain management and goals of care/end of life, transition to hospice, or complex communication dynamics.4
Though specialty palliative care was shown to be more comprehensive, both primary palliative care and specialty palliative care have led to improvements in the quality of life in individuals living with serious illness.5 Early integration of palliative care into routine care has been shown to improve symptom burden, mood, quality of life, survival, and health care costs.6
Updates in alternative and complementary therapies to palliative care
There are several alternative and complementary therapies to palliative care, including cannabis and psychedelics. These therapies are becoming or may become a familiar part of medical therapies that are listed in a patient’s history as part of their medical regimen, especially as more states continue to legalize and/or decriminalize the use of these alternative therapies for recreational or medicinal use.
Both cannabis and psychedelics have a longstanding history of therapeutic and holistic use. Cannabis has been used to manage symptoms such as pain since the 16th and 17th century.7 In palliative care, more patients may turn to various forms of cannabis as a source of relief from symptoms and suffering as their focus shifts more to quality of life.
Even with the increasing popularity of the use of cannabis among seriously ill patients, there is still a lack of evidence of the benefits of medical cannabis use in palliative care, and there is a lack of standardization of type of cannabis used and state regulations regarding their use.7
A recent systematic review found that despite the reported positive treatment effects of cannabis in palliative care, the results of the studies were conflicting. This highlights the need for further high-quality research to determine whether cannabis products are an effective treatment in palliative care patients.8
One limitation to note is that the majority of the included studies focused on cannabis use in patients with cancer for cancer-related symptoms. Few studies included patients with other serious conditions.
Psychedelics
There is evidence that psychedelic assisted therapy (PAT) is a safe and effective treatment for individuals with refractory depression, posttraumatic stress disorder, and substance use disorder.9 Plus, there have been ample studies providing support that PAT improves symptoms such as refractory anxiety/depression, demoralization, and existential distress in seriously ill patients, thus improving their quality of life and overall well-being.9
Nine U.S. cities and the State of Oregon have decriminalized or legalized the psychedelic psilocybin, based on the medical benefits patients have experienced evidenced from using it.10
In light of the increasing interest in PAT, Dr. Ira Byock provided the following points on what “all clinicians should know as they enter this uncharted territory”:
- Psychedelics have been around for a long time.
- Psychedelic-assisted therapies’ therapeutic effects are experiential.
- There are a variety of terms for specific categories of psychedelic compounds.
- Some palliative care teams are already caring for patients who undergo psychedelic experiences.
- Use of psychedelics should be well-observed by a skilled clinician with expertise.
I am hoping this provides a general refresher on palliative care and an overview of updates to alternative and complementary therapies for patients living with serious illness.9
Dr. Kang is a geriatrician and palliative care provider at the University of Washington, Seattle in the division of geriatrics and gerontology. She has no conflicts related to the content of this piece.
References
1. World Health Organization. Palliative care. 2020 Aug 5..
2. Weissman DE and Meier DE. Identifying patients in need of a palliative care assessment in the hospital setting a consensus report from the center to advance palliative care. J Palliat Med. 2011;14(1):17-23.
3. Sherry D et al. Is primary care physician involvement associated with earlier advance care planning? A study of patients in an academic primary care setting. J Palliat Med. 2022;25(1):75-80.
4. Quill TE and Abernethy AP. Generalist plus specialist palliative care-creating a more sustainable model. N Engl J Med. 2013;368:1173-75.
5. Ernecoff NC et al. Comparing specialty and primary palliative care interventions: Analysis of a systematic review. J Palliat Med. 2020;23(3):389-96.
6. Temmel JS et al. Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med. 2011;363:733-42.
7. Kogan M and Sexton M. Medical cannabis: A new old tool for palliative care. J Altern Complement Med . 2020 Sep;26(9):776-8.
8. Doppen M et al. Cannabis in palliative care: A systematic review of the current evidence. J Pain Symptom Manage. 2022 Jun 12;S0885-3924(22)00760-6.
9. Byock I. Psychedelics for serious illness: Five things clinicians need to know. The Center to Advance Palliative Care. Psychedelics for Serious Illness, Palliative in Practice, Center to Advance Palliative Care (capc.org). June 13, 2022.
10. Marks M. A strategy for rescheduling psilocybin. Scientific American. Oct. 11, 2021.
Physicians react: Compensation isn’t worth the hassles. What’s the solution?
How satisfied are physicians that they are fairly compensated for their dedication, skills, and time? That’s a subject that seems to steer many physicians to heated emotions and to a variety of issues with today’s medical field – not all of which directly affect their pay.
Medscape’s Physician Compensation Report 2022: “Incomes Gain, Pay Gaps Remain” generally shows encouraging trends. Physician income rose from a year earlier, when it stagnated as COVID-19 restrictions led patients to stay home and medical practices to cut hours or close. And for the first time in Medscape’s 11 years of reporting on physician compensation, average income rose for every medical specialty surveyed.
Heartening findings, right? Yet the tone of comments to the report was anything but peppy. One physician even complained his plumber earns more than he does.
A family physician lamented that he has “made less in the past 3 years, with more hassles and work” and he “can’t wait to retire next year.” Meanwhile, he complained, the U.S. health system is “the costliest, yet wasteful, with worse outcomes; reactive, not preventative; and has the costliest drugs and social issues.”
Do NPs and PAs encroach on your income?
The conversation about fair compensation launched some commenters into a discussion about competition from nurse practitioners (NPs) and physician assistants (PAs). Some physicians expressed wariness at best, and anger at worst, about NPs and PAs evolving beyond traditional doctor support roles into certain direct patient support.
One-fourth of respondents in the compensation report said their income was negatively affected by competition from NPs, PAs, and other nonphysician providers. For example, with states like Arkansas expanding independent practice for certified registered nurse anesthetists (CRNAs), one commenter complained, “we are no longer needed.”
Added another physician, “primary care, especially internal medicine, is just going away for doctors. We wasted, by all accounts, 4 full years of our working lives because NPs are ‘just as good.’ ”
Greater independence for NPs and PAs strengthens the hands of health insurers and “will end up hastening the demise of primary care as we have known it,” another reader predicted. Other physicians’ takes: “For the institution, it’s much cheaper to hire NPs than to hire doctors” and “overall, physician negotiating power will decrease in the future.”
Medicare reimbursement rates grate
Although 7 in 10 respondents in the compensation report said they would continue to accept new Medicare or Medicaid patients, comments reveal resentment about the practical need to work with Medicare and its resentment rates.
“An open question to Medicare: Are you doing the dumbest thing possible by paying low wages and giving huge administrative burdens for internal medicine on purpose?” one physician wrote. “Or are you really that short-sighted?”
Another reader cited an analysis from the American College of Surgeons of Medicare’s 1998 surgical CPT codes. If Medicare had left those codes alone beyond annual inflation adjustments, the study found, reimbursement rates by 2019 would be half of what they became.
Another way of looking at the code reimbursement increases is a 50% pay cut over 20 years for doctors and medical practices, that reader insisted. “The rising cost of employee wages, particularly of the last two-and-a-half years of COVID-19, combined with the effective pay cuts over the last 20 years, equals time to quit!”
Another commenter concurred. “In the 1990s, most full-time docs were making almost double what you see [in the report], and everything cost almost half of what it does now. So, MD purchasing power is between half and one-quarter of what it was in the early 1990s.”
Are self-pay models better?
Do physicians have a better chance at consistently fair income under a self-pay practice that avoids dealing with insurance companies?
One commenter hypothesized that psychiatrists once trailed internists in income but today earn more because many “quit working for insurance and went to a cash business 15 years ago.” Many family physicians did something similar by switching to a direct primary care model, he said.
This physician said he has done the same “with great results” for patients as well: shorter office visits, faster booking of appointments, no deductibles owed. Best of all, “I love practicing medicine again, and my patients love the great health care they receive.”
Another commenter agreed. “Two words: cash practice.” But another objected, “I guess only the very rich can afford to cover your business costs.”
Regardless of the payment model, another physician argued for private practice over employed positions. “Save on the bureaucratic expenses. Go back to private practice and get rid of electronic records.”
A version of this article first appeared on Medscape.com.
How satisfied are physicians that they are fairly compensated for their dedication, skills, and time? That’s a subject that seems to steer many physicians to heated emotions and to a variety of issues with today’s medical field – not all of which directly affect their pay.
Medscape’s Physician Compensation Report 2022: “Incomes Gain, Pay Gaps Remain” generally shows encouraging trends. Physician income rose from a year earlier, when it stagnated as COVID-19 restrictions led patients to stay home and medical practices to cut hours or close. And for the first time in Medscape’s 11 years of reporting on physician compensation, average income rose for every medical specialty surveyed.
Heartening findings, right? Yet the tone of comments to the report was anything but peppy. One physician even complained his plumber earns more than he does.
A family physician lamented that he has “made less in the past 3 years, with more hassles and work” and he “can’t wait to retire next year.” Meanwhile, he complained, the U.S. health system is “the costliest, yet wasteful, with worse outcomes; reactive, not preventative; and has the costliest drugs and social issues.”
Do NPs and PAs encroach on your income?
The conversation about fair compensation launched some commenters into a discussion about competition from nurse practitioners (NPs) and physician assistants (PAs). Some physicians expressed wariness at best, and anger at worst, about NPs and PAs evolving beyond traditional doctor support roles into certain direct patient support.
One-fourth of respondents in the compensation report said their income was negatively affected by competition from NPs, PAs, and other nonphysician providers. For example, with states like Arkansas expanding independent practice for certified registered nurse anesthetists (CRNAs), one commenter complained, “we are no longer needed.”
Added another physician, “primary care, especially internal medicine, is just going away for doctors. We wasted, by all accounts, 4 full years of our working lives because NPs are ‘just as good.’ ”
Greater independence for NPs and PAs strengthens the hands of health insurers and “will end up hastening the demise of primary care as we have known it,” another reader predicted. Other physicians’ takes: “For the institution, it’s much cheaper to hire NPs than to hire doctors” and “overall, physician negotiating power will decrease in the future.”
Medicare reimbursement rates grate
Although 7 in 10 respondents in the compensation report said they would continue to accept new Medicare or Medicaid patients, comments reveal resentment about the practical need to work with Medicare and its resentment rates.
“An open question to Medicare: Are you doing the dumbest thing possible by paying low wages and giving huge administrative burdens for internal medicine on purpose?” one physician wrote. “Or are you really that short-sighted?”
Another reader cited an analysis from the American College of Surgeons of Medicare’s 1998 surgical CPT codes. If Medicare had left those codes alone beyond annual inflation adjustments, the study found, reimbursement rates by 2019 would be half of what they became.
Another way of looking at the code reimbursement increases is a 50% pay cut over 20 years for doctors and medical practices, that reader insisted. “The rising cost of employee wages, particularly of the last two-and-a-half years of COVID-19, combined with the effective pay cuts over the last 20 years, equals time to quit!”
Another commenter concurred. “In the 1990s, most full-time docs were making almost double what you see [in the report], and everything cost almost half of what it does now. So, MD purchasing power is between half and one-quarter of what it was in the early 1990s.”
Are self-pay models better?
Do physicians have a better chance at consistently fair income under a self-pay practice that avoids dealing with insurance companies?
One commenter hypothesized that psychiatrists once trailed internists in income but today earn more because many “quit working for insurance and went to a cash business 15 years ago.” Many family physicians did something similar by switching to a direct primary care model, he said.
This physician said he has done the same “with great results” for patients as well: shorter office visits, faster booking of appointments, no deductibles owed. Best of all, “I love practicing medicine again, and my patients love the great health care they receive.”
Another commenter agreed. “Two words: cash practice.” But another objected, “I guess only the very rich can afford to cover your business costs.”
Regardless of the payment model, another physician argued for private practice over employed positions. “Save on the bureaucratic expenses. Go back to private practice and get rid of electronic records.”
A version of this article first appeared on Medscape.com.
How satisfied are physicians that they are fairly compensated for their dedication, skills, and time? That’s a subject that seems to steer many physicians to heated emotions and to a variety of issues with today’s medical field – not all of which directly affect their pay.
Medscape’s Physician Compensation Report 2022: “Incomes Gain, Pay Gaps Remain” generally shows encouraging trends. Physician income rose from a year earlier, when it stagnated as COVID-19 restrictions led patients to stay home and medical practices to cut hours or close. And for the first time in Medscape’s 11 years of reporting on physician compensation, average income rose for every medical specialty surveyed.
Heartening findings, right? Yet the tone of comments to the report was anything but peppy. One physician even complained his plumber earns more than he does.
A family physician lamented that he has “made less in the past 3 years, with more hassles and work” and he “can’t wait to retire next year.” Meanwhile, he complained, the U.S. health system is “the costliest, yet wasteful, with worse outcomes; reactive, not preventative; and has the costliest drugs and social issues.”
Do NPs and PAs encroach on your income?
The conversation about fair compensation launched some commenters into a discussion about competition from nurse practitioners (NPs) and physician assistants (PAs). Some physicians expressed wariness at best, and anger at worst, about NPs and PAs evolving beyond traditional doctor support roles into certain direct patient support.
One-fourth of respondents in the compensation report said their income was negatively affected by competition from NPs, PAs, and other nonphysician providers. For example, with states like Arkansas expanding independent practice for certified registered nurse anesthetists (CRNAs), one commenter complained, “we are no longer needed.”
Added another physician, “primary care, especially internal medicine, is just going away for doctors. We wasted, by all accounts, 4 full years of our working lives because NPs are ‘just as good.’ ”
Greater independence for NPs and PAs strengthens the hands of health insurers and “will end up hastening the demise of primary care as we have known it,” another reader predicted. Other physicians’ takes: “For the institution, it’s much cheaper to hire NPs than to hire doctors” and “overall, physician negotiating power will decrease in the future.”
Medicare reimbursement rates grate
Although 7 in 10 respondents in the compensation report said they would continue to accept new Medicare or Medicaid patients, comments reveal resentment about the practical need to work with Medicare and its resentment rates.
“An open question to Medicare: Are you doing the dumbest thing possible by paying low wages and giving huge administrative burdens for internal medicine on purpose?” one physician wrote. “Or are you really that short-sighted?”
Another reader cited an analysis from the American College of Surgeons of Medicare’s 1998 surgical CPT codes. If Medicare had left those codes alone beyond annual inflation adjustments, the study found, reimbursement rates by 2019 would be half of what they became.
Another way of looking at the code reimbursement increases is a 50% pay cut over 20 years for doctors and medical practices, that reader insisted. “The rising cost of employee wages, particularly of the last two-and-a-half years of COVID-19, combined with the effective pay cuts over the last 20 years, equals time to quit!”
Another commenter concurred. “In the 1990s, most full-time docs were making almost double what you see [in the report], and everything cost almost half of what it does now. So, MD purchasing power is between half and one-quarter of what it was in the early 1990s.”
Are self-pay models better?
Do physicians have a better chance at consistently fair income under a self-pay practice that avoids dealing with insurance companies?
One commenter hypothesized that psychiatrists once trailed internists in income but today earn more because many “quit working for insurance and went to a cash business 15 years ago.” Many family physicians did something similar by switching to a direct primary care model, he said.
This physician said he has done the same “with great results” for patients as well: shorter office visits, faster booking of appointments, no deductibles owed. Best of all, “I love practicing medicine again, and my patients love the great health care they receive.”
Another commenter agreed. “Two words: cash practice.” But another objected, “I guess only the very rich can afford to cover your business costs.”
Regardless of the payment model, another physician argued for private practice over employed positions. “Save on the bureaucratic expenses. Go back to private practice and get rid of electronic records.”
A version of this article first appeared on Medscape.com.
Caring for the young elite athlete
Concerns about the potential harm resulting from overzealous training regimens and performance schedules for young elite athletes seems to come in cycles much like the Olympics. But, more recently, the media attention has become more intense fueled by the very visible psychological vulnerabilities of some young gymnasts, tennis players, and figure skaters. Accusations of physical and psychological abuse by team physicians and coaches continue to surface with troubling regularity.
A recent article in the Wall St. Journal explores a variety of initiatives aimed at redefining the relationship between youth sports and the physical and mental health of its elite athletes. (Louise Radnofsky, The Wall Street Journal, June 9, 2022).
An example of the new awareness is the recent invitation of Peter Donnelly, PhD, an emeritus professor at the University of Toronto and long-time advocate for regulatory protections for youth athletes, to deliver a paper at a global conference in South Africa devoted to the elimination of child labor. Referring to youth sports, Dr. Donnelly observes “What if McDonalds had the same accident rate? ... There would be huge commissions of inquiry, regulations, and policies.” He suggests that the United Nations Convention on the Rights of the Child might be a mechanism to address the problem.
Writing in the Marquette University Sports Law Review in 2015, Kristin Hoffman, a law student at the time, suggested that the federal Fair Labor Standards Act or state child labor laws could be used to restructure sports like gymnastics or figure skating with tarnished histories. California law prohibits child actors from working more than 5 hours a day on school days and 7 hours on nonschool days but says little about child athletes. On paper, the National Collegiate Athletic Association limits college athletes to 20 hours participation per week but teenagers on club teams are not limited and may sometimes practice 30 hours or more.
Regulation in any form is a tough sell in this country. Coaches, parents, and athletes caught up in the myth that more repetitions and more touches on the ball are always the ticket to success will argue that most elite athletes are self-motivated and don’t view the long hours as a hardship.
Exactly how many are self-driven and how many are being pushed by parents and coaches is unknown. Across the street from us lived a young girl who, despite not having the obvious physical gifts, was clearly committed to excel in sports. She begged her parents to set up lights to allow her to practice well into the evening. She went on to have a good college career as a player and a very successful career as a Division I coach. Now in retirement, she is very open about her mental health history that in large part explains her inner drive and her subsequent troubles.
We need to be realistic in our hope for regulating the current state of youth sports out of its current situation. State laws that put reasonable limits on the hourly commitment to sports much like the California child actor laws feel like a reasonable goal. However, as physicians for these young athletes we must take each child – and we must remind ourselves that they are still children – as an individual.
When faced with patients who are clearly on the elite sport pathway, our goal is to protect their health – both physical and mental. If they are having symptoms of overuse we need to help them find alternative activities that will rest their injuries but still allow them to satisfy their competitive zeal. However, we must be ever alert to the risk that what appears to be unusual self-motivation may be instead a warning that pathologic obsession and compulsion lurk below the surface.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Concerns about the potential harm resulting from overzealous training regimens and performance schedules for young elite athletes seems to come in cycles much like the Olympics. But, more recently, the media attention has become more intense fueled by the very visible psychological vulnerabilities of some young gymnasts, tennis players, and figure skaters. Accusations of physical and psychological abuse by team physicians and coaches continue to surface with troubling regularity.
A recent article in the Wall St. Journal explores a variety of initiatives aimed at redefining the relationship between youth sports and the physical and mental health of its elite athletes. (Louise Radnofsky, The Wall Street Journal, June 9, 2022).
An example of the new awareness is the recent invitation of Peter Donnelly, PhD, an emeritus professor at the University of Toronto and long-time advocate for regulatory protections for youth athletes, to deliver a paper at a global conference in South Africa devoted to the elimination of child labor. Referring to youth sports, Dr. Donnelly observes “What if McDonalds had the same accident rate? ... There would be huge commissions of inquiry, regulations, and policies.” He suggests that the United Nations Convention on the Rights of the Child might be a mechanism to address the problem.
Writing in the Marquette University Sports Law Review in 2015, Kristin Hoffman, a law student at the time, suggested that the federal Fair Labor Standards Act or state child labor laws could be used to restructure sports like gymnastics or figure skating with tarnished histories. California law prohibits child actors from working more than 5 hours a day on school days and 7 hours on nonschool days but says little about child athletes. On paper, the National Collegiate Athletic Association limits college athletes to 20 hours participation per week but teenagers on club teams are not limited and may sometimes practice 30 hours or more.
Regulation in any form is a tough sell in this country. Coaches, parents, and athletes caught up in the myth that more repetitions and more touches on the ball are always the ticket to success will argue that most elite athletes are self-motivated and don’t view the long hours as a hardship.
Exactly how many are self-driven and how many are being pushed by parents and coaches is unknown. Across the street from us lived a young girl who, despite not having the obvious physical gifts, was clearly committed to excel in sports. She begged her parents to set up lights to allow her to practice well into the evening. She went on to have a good college career as a player and a very successful career as a Division I coach. Now in retirement, she is very open about her mental health history that in large part explains her inner drive and her subsequent troubles.
We need to be realistic in our hope for regulating the current state of youth sports out of its current situation. State laws that put reasonable limits on the hourly commitment to sports much like the California child actor laws feel like a reasonable goal. However, as physicians for these young athletes we must take each child – and we must remind ourselves that they are still children – as an individual.
When faced with patients who are clearly on the elite sport pathway, our goal is to protect their health – both physical and mental. If they are having symptoms of overuse we need to help them find alternative activities that will rest their injuries but still allow them to satisfy their competitive zeal. However, we must be ever alert to the risk that what appears to be unusual self-motivation may be instead a warning that pathologic obsession and compulsion lurk below the surface.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Concerns about the potential harm resulting from overzealous training regimens and performance schedules for young elite athletes seems to come in cycles much like the Olympics. But, more recently, the media attention has become more intense fueled by the very visible psychological vulnerabilities of some young gymnasts, tennis players, and figure skaters. Accusations of physical and psychological abuse by team physicians and coaches continue to surface with troubling regularity.
A recent article in the Wall St. Journal explores a variety of initiatives aimed at redefining the relationship between youth sports and the physical and mental health of its elite athletes. (Louise Radnofsky, The Wall Street Journal, June 9, 2022).
An example of the new awareness is the recent invitation of Peter Donnelly, PhD, an emeritus professor at the University of Toronto and long-time advocate for regulatory protections for youth athletes, to deliver a paper at a global conference in South Africa devoted to the elimination of child labor. Referring to youth sports, Dr. Donnelly observes “What if McDonalds had the same accident rate? ... There would be huge commissions of inquiry, regulations, and policies.” He suggests that the United Nations Convention on the Rights of the Child might be a mechanism to address the problem.
Writing in the Marquette University Sports Law Review in 2015, Kristin Hoffman, a law student at the time, suggested that the federal Fair Labor Standards Act or state child labor laws could be used to restructure sports like gymnastics or figure skating with tarnished histories. California law prohibits child actors from working more than 5 hours a day on school days and 7 hours on nonschool days but says little about child athletes. On paper, the National Collegiate Athletic Association limits college athletes to 20 hours participation per week but teenagers on club teams are not limited and may sometimes practice 30 hours or more.
Regulation in any form is a tough sell in this country. Coaches, parents, and athletes caught up in the myth that more repetitions and more touches on the ball are always the ticket to success will argue that most elite athletes are self-motivated and don’t view the long hours as a hardship.
Exactly how many are self-driven and how many are being pushed by parents and coaches is unknown. Across the street from us lived a young girl who, despite not having the obvious physical gifts, was clearly committed to excel in sports. She begged her parents to set up lights to allow her to practice well into the evening. She went on to have a good college career as a player and a very successful career as a Division I coach. Now in retirement, she is very open about her mental health history that in large part explains her inner drive and her subsequent troubles.
We need to be realistic in our hope for regulating the current state of youth sports out of its current situation. State laws that put reasonable limits on the hourly commitment to sports much like the California child actor laws feel like a reasonable goal. However, as physicians for these young athletes we must take each child – and we must remind ourselves that they are still children – as an individual.
When faced with patients who are clearly on the elite sport pathway, our goal is to protect their health – both physical and mental. If they are having symptoms of overuse we need to help them find alternative activities that will rest their injuries but still allow them to satisfy their competitive zeal. However, we must be ever alert to the risk that what appears to be unusual self-motivation may be instead a warning that pathologic obsession and compulsion lurk below the surface.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
How racist is your algorithm?
Every time Nathan Chomilo, MD, uses a clinical decision support tool, he tells his patients they have a choice: He can input their race or keep that field blank.
Until recently, many clinicians didn’t question the use of race as a datapoint in tools used to make decisions about diagnosis and care. But that is changing.
“I’ve almost universally had patients appreciate that someone actually told them that their kidney function was being scored differently because of the color of their skin or how they were identified in the medical chart along lines of race,” Dr. Chomilo, an adjunct assistant professor of pediatrics at the University of Minnesota Medical School, Minneapolis, said.
Dr. Chomilo is referring to the estimated glomerular filtration rate (eGFR), which combines results from a blood test with factors such as age, sex, and race to calculate kidney function.
The eGFR weighed an input of “African American” as automatically indicating a higher concentration of serum creatinine than a non African American patient on the basis of the unsubstantiated idea that Black people have more creatinine in their blood at baseline.
The calculator creates a picture of a Black patient who is not as sick as a White patient with the same levels of kidney failure. But race is based on the color of a patient’s skin, not on genetics or other clinical datapoints.
“I often use my own example of being a biracial Black man: My father’s family is from Cameroon, my mother’s family is from Norway. Are you going to assign my kidneys or my lungs to my mom’s side or my dad’s side? That’s not clear at all in the way we use race in medicine,” Dr. Chomilo, an executive committee member on the section on minority health equity and inclusion at the American Academy of Pediatrics (AAP), said.
Long before the COVID-19 pandemic so publicly exposed the depths of inequality in morbidity and mortality in the United States, health advocates had been pointing out these disparities in tools used by medical professionals. But efforts to recognize that race is a poor proxy for genetics is in its infancy.
In May, the AAP published a policy statement that kicked off its examination of clinical guidelines and policies that include race as a biological proxy. A committee for the society is combing through each guideline or calculator, evaluating the scientific basis for the use of race, and examining whether a stronger datapoint could be used instead.
The eGFR is perhaps the best example of a calculator that’s gone through the process: Health care stakeholders questioned the use of race, and investigators went back to study whether race was really a good datapoint. It wasn’t, and Dr. Chamilo’s hospital joined many others in retiring the calculator.
But the eGFR is one of countless clinical tools – from rudimentary algorithms to sophisticated machine-learning instruments – that change the course of care in part on the basis of race in the same way datapoints such as weight, age, and height are used to inform decisions about patient management. But unlike race, height, weight, and age can be objectively measured. A physician either makes a guess, or a patient enters their race on a form. And while that can be useful on a population level, race does not equal genetics or any other measurable datapoint.
In a study published in JAMA Pediatrics, researchers reviewed 414 clinical practice guidelines from sources such as PubMed and MetaLib.gov. Almost 1 in 6 guidelines included race in an inappropriate way, such as by conflating race as a biological risk factor or establishing testing or treatment thresholds using race.
Waiting for alternatives
The University of Maryland Medical System last year embarked on a project similar to the AAP initiative but within its own system. The first use of race to be eliminated was in the eGFR. The health system also recently removed the variable from a tool for diagnosing urinary tract infections (UTIs) in children younger than 2 years.
Part of that tool includes deciding to perform a catheterized urine test. If a doctor chose “White” as the race, the tool would recommend the test. If the doctor chose “Black,” the tool would recommend to not test. Joseph Wright, MD, MPH, chief health equity officer at University of Maryland Medical System, said this step in the tool is based on the unproven assumption that young Black children had a lower likelihood of UTIs than their White peers.
“We simply want folks to not by default lob race in as a decisionmaking point when we have, with a little bit more scientific diligence, the ability to include better clinical variables,” Dr. Wright, who is also an adjunct professor of health policy and management at the University of Maryland School of Public Health, College Park, said.
The developers of the UTI tool recently released a revised version that removes race in favor of two new medical datapoints: whether the patient has had a fever for over 48 hours, and whether the patient has previously had a UTI.
The process of re-examining tools, coming up with new datapoints, and implementing changes is not simple, according to Dr. Wright.
“This is just the baby step to fix the algorithms, because we’re all going to have to examine our own house, where these calculators live, whether it’s in a textbook, whether it’s in an electronic health record, and that’s the heavy lift,” he said. “All sources of clinical guidance have to be scrutinized, and it’s going to literally take years to unroot.”
Electronic medical record vendor Cerner said it generally revises its algorithms after medical societies make changes, then communicates those fixes to providers.
Rebecca C. Winokur, MD, MPH, lead physician executive and health equity service line leader at Cerner, explained that if doctors ordered an eGFR a year ago and then another today, the results might be different because of the new code that eliminates race.
“The numbers are so different, how do you know that the patient may or may not have the same function?” Dr. Winokur said.
Dr. Winokur said the company is trying to determine at which point a message should pop up in the records workflow that would inform clinicians that they may be comparing apples to cherries. The company also is reconsidering the use of race in tools that estimate the probability of a successful vaginal birth after prior cesarean delivery, a calculator that predicts the risk of urethral stones in patients with flank pain, and another that measures lung function to help diagnose pulmonary disease.
In addition to managing the logistics of removing race, health institutions also need buy-in from clinicians. At Mass General Brigham, Boston, Thomas Sequist, MD, MPH, chief medical officer, is leading a project to examine how the system uses race in calculators.
“People struggle mainly with, well, if we shouldn’t use this calculator, what should we use, because we need a calculator. And that’s a legitimate question,” Dr. Sequist said in an interview. “If we’re going to stop using this race-based calculator, I still need to know what dose of medication I give my patient. We’re not going to pull any of these calculators until we have a safe and reliable alternative.”
For each calculator, relevant specialty chiefs come to the table with Dr. Sequist and his team; current projects include examining bone density screenings and cardiac risk scores. A large part of the work is communicating the lack of science behind the inclusion of race as a variable.
“It’s hard because these tools have been in existence for decades, and people are used to using them,” Dr. Sequist said. “So this is a big-change management project.”
Some clinicians also have difficulty discerning why their health system may stratify patient outcomes by race while providers are being told that race is being removed from the calculators they use every day. The key difference is that stratifying outcomes by race illuminates systemic problems that can be targeted by a health system.
For instance, if readmission rates are higher for Black patients overall after surgery, the reason might be that nurses are not delivering the same level of care to them as they are to non-Black patients, possibly because of hidden bias. Or, perhaps Black patients at a hospital have less access to transportation for follow-up appointments after surgery. The potential reasons can be investigated, and solutions can be created.
“If you look at a population level, what you’re looking for is not for the evidence of race as a biological construct,” Dr. Chomilo said. “You’re looking for the impact of racism on populations, and that’s the difference: It’s racism, not race.”
A version of this article first appeared on Medscape.com.
Every time Nathan Chomilo, MD, uses a clinical decision support tool, he tells his patients they have a choice: He can input their race or keep that field blank.
Until recently, many clinicians didn’t question the use of race as a datapoint in tools used to make decisions about diagnosis and care. But that is changing.
“I’ve almost universally had patients appreciate that someone actually told them that their kidney function was being scored differently because of the color of their skin or how they were identified in the medical chart along lines of race,” Dr. Chomilo, an adjunct assistant professor of pediatrics at the University of Minnesota Medical School, Minneapolis, said.
Dr. Chomilo is referring to the estimated glomerular filtration rate (eGFR), which combines results from a blood test with factors such as age, sex, and race to calculate kidney function.
The eGFR weighed an input of “African American” as automatically indicating a higher concentration of serum creatinine than a non African American patient on the basis of the unsubstantiated idea that Black people have more creatinine in their blood at baseline.
The calculator creates a picture of a Black patient who is not as sick as a White patient with the same levels of kidney failure. But race is based on the color of a patient’s skin, not on genetics or other clinical datapoints.
“I often use my own example of being a biracial Black man: My father’s family is from Cameroon, my mother’s family is from Norway. Are you going to assign my kidneys or my lungs to my mom’s side or my dad’s side? That’s not clear at all in the way we use race in medicine,” Dr. Chomilo, an executive committee member on the section on minority health equity and inclusion at the American Academy of Pediatrics (AAP), said.
Long before the COVID-19 pandemic so publicly exposed the depths of inequality in morbidity and mortality in the United States, health advocates had been pointing out these disparities in tools used by medical professionals. But efforts to recognize that race is a poor proxy for genetics is in its infancy.
In May, the AAP published a policy statement that kicked off its examination of clinical guidelines and policies that include race as a biological proxy. A committee for the society is combing through each guideline or calculator, evaluating the scientific basis for the use of race, and examining whether a stronger datapoint could be used instead.
The eGFR is perhaps the best example of a calculator that’s gone through the process: Health care stakeholders questioned the use of race, and investigators went back to study whether race was really a good datapoint. It wasn’t, and Dr. Chamilo’s hospital joined many others in retiring the calculator.
But the eGFR is one of countless clinical tools – from rudimentary algorithms to sophisticated machine-learning instruments – that change the course of care in part on the basis of race in the same way datapoints such as weight, age, and height are used to inform decisions about patient management. But unlike race, height, weight, and age can be objectively measured. A physician either makes a guess, or a patient enters their race on a form. And while that can be useful on a population level, race does not equal genetics or any other measurable datapoint.
In a study published in JAMA Pediatrics, researchers reviewed 414 clinical practice guidelines from sources such as PubMed and MetaLib.gov. Almost 1 in 6 guidelines included race in an inappropriate way, such as by conflating race as a biological risk factor or establishing testing or treatment thresholds using race.
Waiting for alternatives
The University of Maryland Medical System last year embarked on a project similar to the AAP initiative but within its own system. The first use of race to be eliminated was in the eGFR. The health system also recently removed the variable from a tool for diagnosing urinary tract infections (UTIs) in children younger than 2 years.
Part of that tool includes deciding to perform a catheterized urine test. If a doctor chose “White” as the race, the tool would recommend the test. If the doctor chose “Black,” the tool would recommend to not test. Joseph Wright, MD, MPH, chief health equity officer at University of Maryland Medical System, said this step in the tool is based on the unproven assumption that young Black children had a lower likelihood of UTIs than their White peers.
“We simply want folks to not by default lob race in as a decisionmaking point when we have, with a little bit more scientific diligence, the ability to include better clinical variables,” Dr. Wright, who is also an adjunct professor of health policy and management at the University of Maryland School of Public Health, College Park, said.
The developers of the UTI tool recently released a revised version that removes race in favor of two new medical datapoints: whether the patient has had a fever for over 48 hours, and whether the patient has previously had a UTI.
The process of re-examining tools, coming up with new datapoints, and implementing changes is not simple, according to Dr. Wright.
“This is just the baby step to fix the algorithms, because we’re all going to have to examine our own house, where these calculators live, whether it’s in a textbook, whether it’s in an electronic health record, and that’s the heavy lift,” he said. “All sources of clinical guidance have to be scrutinized, and it’s going to literally take years to unroot.”
Electronic medical record vendor Cerner said it generally revises its algorithms after medical societies make changes, then communicates those fixes to providers.
Rebecca C. Winokur, MD, MPH, lead physician executive and health equity service line leader at Cerner, explained that if doctors ordered an eGFR a year ago and then another today, the results might be different because of the new code that eliminates race.
“The numbers are so different, how do you know that the patient may or may not have the same function?” Dr. Winokur said.
Dr. Winokur said the company is trying to determine at which point a message should pop up in the records workflow that would inform clinicians that they may be comparing apples to cherries. The company also is reconsidering the use of race in tools that estimate the probability of a successful vaginal birth after prior cesarean delivery, a calculator that predicts the risk of urethral stones in patients with flank pain, and another that measures lung function to help diagnose pulmonary disease.
In addition to managing the logistics of removing race, health institutions also need buy-in from clinicians. At Mass General Brigham, Boston, Thomas Sequist, MD, MPH, chief medical officer, is leading a project to examine how the system uses race in calculators.
“People struggle mainly with, well, if we shouldn’t use this calculator, what should we use, because we need a calculator. And that’s a legitimate question,” Dr. Sequist said in an interview. “If we’re going to stop using this race-based calculator, I still need to know what dose of medication I give my patient. We’re not going to pull any of these calculators until we have a safe and reliable alternative.”
For each calculator, relevant specialty chiefs come to the table with Dr. Sequist and his team; current projects include examining bone density screenings and cardiac risk scores. A large part of the work is communicating the lack of science behind the inclusion of race as a variable.
“It’s hard because these tools have been in existence for decades, and people are used to using them,” Dr. Sequist said. “So this is a big-change management project.”
Some clinicians also have difficulty discerning why their health system may stratify patient outcomes by race while providers are being told that race is being removed from the calculators they use every day. The key difference is that stratifying outcomes by race illuminates systemic problems that can be targeted by a health system.
For instance, if readmission rates are higher for Black patients overall after surgery, the reason might be that nurses are not delivering the same level of care to them as they are to non-Black patients, possibly because of hidden bias. Or, perhaps Black patients at a hospital have less access to transportation for follow-up appointments after surgery. The potential reasons can be investigated, and solutions can be created.
“If you look at a population level, what you’re looking for is not for the evidence of race as a biological construct,” Dr. Chomilo said. “You’re looking for the impact of racism on populations, and that’s the difference: It’s racism, not race.”
A version of this article first appeared on Medscape.com.
Every time Nathan Chomilo, MD, uses a clinical decision support tool, he tells his patients they have a choice: He can input their race or keep that field blank.
Until recently, many clinicians didn’t question the use of race as a datapoint in tools used to make decisions about diagnosis and care. But that is changing.
“I’ve almost universally had patients appreciate that someone actually told them that their kidney function was being scored differently because of the color of their skin or how they were identified in the medical chart along lines of race,” Dr. Chomilo, an adjunct assistant professor of pediatrics at the University of Minnesota Medical School, Minneapolis, said.
Dr. Chomilo is referring to the estimated glomerular filtration rate (eGFR), which combines results from a blood test with factors such as age, sex, and race to calculate kidney function.
The eGFR weighed an input of “African American” as automatically indicating a higher concentration of serum creatinine than a non African American patient on the basis of the unsubstantiated idea that Black people have more creatinine in their blood at baseline.
The calculator creates a picture of a Black patient who is not as sick as a White patient with the same levels of kidney failure. But race is based on the color of a patient’s skin, not on genetics or other clinical datapoints.
“I often use my own example of being a biracial Black man: My father’s family is from Cameroon, my mother’s family is from Norway. Are you going to assign my kidneys or my lungs to my mom’s side or my dad’s side? That’s not clear at all in the way we use race in medicine,” Dr. Chomilo, an executive committee member on the section on minority health equity and inclusion at the American Academy of Pediatrics (AAP), said.
Long before the COVID-19 pandemic so publicly exposed the depths of inequality in morbidity and mortality in the United States, health advocates had been pointing out these disparities in tools used by medical professionals. But efforts to recognize that race is a poor proxy for genetics is in its infancy.
In May, the AAP published a policy statement that kicked off its examination of clinical guidelines and policies that include race as a biological proxy. A committee for the society is combing through each guideline or calculator, evaluating the scientific basis for the use of race, and examining whether a stronger datapoint could be used instead.
The eGFR is perhaps the best example of a calculator that’s gone through the process: Health care stakeholders questioned the use of race, and investigators went back to study whether race was really a good datapoint. It wasn’t, and Dr. Chamilo’s hospital joined many others in retiring the calculator.
But the eGFR is one of countless clinical tools – from rudimentary algorithms to sophisticated machine-learning instruments – that change the course of care in part on the basis of race in the same way datapoints such as weight, age, and height are used to inform decisions about patient management. But unlike race, height, weight, and age can be objectively measured. A physician either makes a guess, or a patient enters their race on a form. And while that can be useful on a population level, race does not equal genetics or any other measurable datapoint.
In a study published in JAMA Pediatrics, researchers reviewed 414 clinical practice guidelines from sources such as PubMed and MetaLib.gov. Almost 1 in 6 guidelines included race in an inappropriate way, such as by conflating race as a biological risk factor or establishing testing or treatment thresholds using race.
Waiting for alternatives
The University of Maryland Medical System last year embarked on a project similar to the AAP initiative but within its own system. The first use of race to be eliminated was in the eGFR. The health system also recently removed the variable from a tool for diagnosing urinary tract infections (UTIs) in children younger than 2 years.
Part of that tool includes deciding to perform a catheterized urine test. If a doctor chose “White” as the race, the tool would recommend the test. If the doctor chose “Black,” the tool would recommend to not test. Joseph Wright, MD, MPH, chief health equity officer at University of Maryland Medical System, said this step in the tool is based on the unproven assumption that young Black children had a lower likelihood of UTIs than their White peers.
“We simply want folks to not by default lob race in as a decisionmaking point when we have, with a little bit more scientific diligence, the ability to include better clinical variables,” Dr. Wright, who is also an adjunct professor of health policy and management at the University of Maryland School of Public Health, College Park, said.
The developers of the UTI tool recently released a revised version that removes race in favor of two new medical datapoints: whether the patient has had a fever for over 48 hours, and whether the patient has previously had a UTI.
The process of re-examining tools, coming up with new datapoints, and implementing changes is not simple, according to Dr. Wright.
“This is just the baby step to fix the algorithms, because we’re all going to have to examine our own house, where these calculators live, whether it’s in a textbook, whether it’s in an electronic health record, and that’s the heavy lift,” he said. “All sources of clinical guidance have to be scrutinized, and it’s going to literally take years to unroot.”
Electronic medical record vendor Cerner said it generally revises its algorithms after medical societies make changes, then communicates those fixes to providers.
Rebecca C. Winokur, MD, MPH, lead physician executive and health equity service line leader at Cerner, explained that if doctors ordered an eGFR a year ago and then another today, the results might be different because of the new code that eliminates race.
“The numbers are so different, how do you know that the patient may or may not have the same function?” Dr. Winokur said.
Dr. Winokur said the company is trying to determine at which point a message should pop up in the records workflow that would inform clinicians that they may be comparing apples to cherries. The company also is reconsidering the use of race in tools that estimate the probability of a successful vaginal birth after prior cesarean delivery, a calculator that predicts the risk of urethral stones in patients with flank pain, and another that measures lung function to help diagnose pulmonary disease.
In addition to managing the logistics of removing race, health institutions also need buy-in from clinicians. At Mass General Brigham, Boston, Thomas Sequist, MD, MPH, chief medical officer, is leading a project to examine how the system uses race in calculators.
“People struggle mainly with, well, if we shouldn’t use this calculator, what should we use, because we need a calculator. And that’s a legitimate question,” Dr. Sequist said in an interview. “If we’re going to stop using this race-based calculator, I still need to know what dose of medication I give my patient. We’re not going to pull any of these calculators until we have a safe and reliable alternative.”
For each calculator, relevant specialty chiefs come to the table with Dr. Sequist and his team; current projects include examining bone density screenings and cardiac risk scores. A large part of the work is communicating the lack of science behind the inclusion of race as a variable.
“It’s hard because these tools have been in existence for decades, and people are used to using them,” Dr. Sequist said. “So this is a big-change management project.”
Some clinicians also have difficulty discerning why their health system may stratify patient outcomes by race while providers are being told that race is being removed from the calculators they use every day. The key difference is that stratifying outcomes by race illuminates systemic problems that can be targeted by a health system.
For instance, if readmission rates are higher for Black patients overall after surgery, the reason might be that nurses are not delivering the same level of care to them as they are to non-Black patients, possibly because of hidden bias. Or, perhaps Black patients at a hospital have less access to transportation for follow-up appointments after surgery. The potential reasons can be investigated, and solutions can be created.
“If you look at a population level, what you’re looking for is not for the evidence of race as a biological construct,” Dr. Chomilo said. “You’re looking for the impact of racism on populations, and that’s the difference: It’s racism, not race.”
A version of this article first appeared on Medscape.com.
Erythematous Pedunculated Plaque on the Dorsal Aspect of the Foot
The Diagnosis: Molluscum Contagiosum
A tangential shave removal with electrocautery was performed. Histopathology demonstrated numerous eosinophilic intracytoplasmic inclusion bodies (Figure), confirming a diagnosis of molluscum contagiosum (MC).
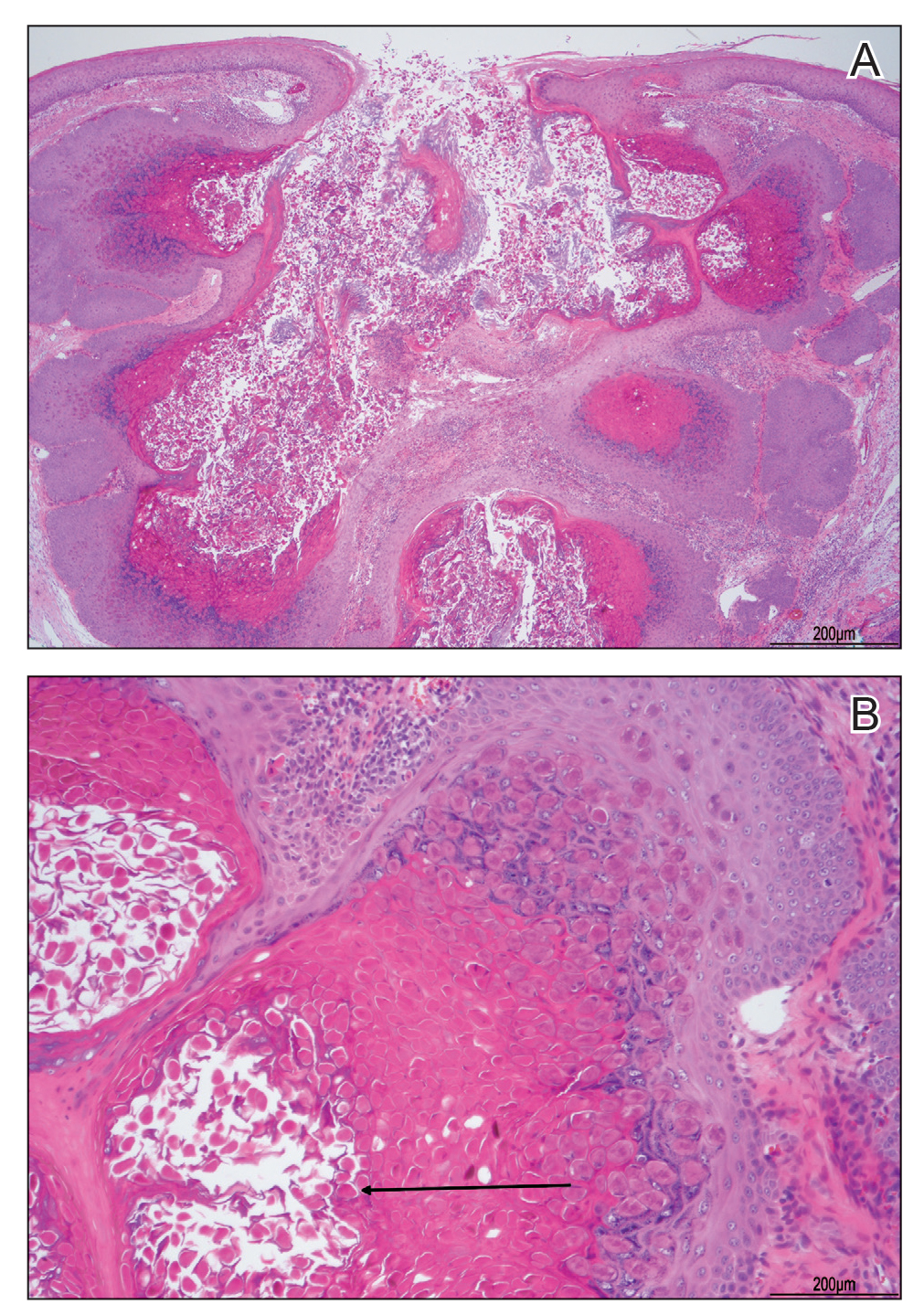
Molluscum contagiosum is a common poxvirus infection that is transmitted through fomites, contact, or self-inoculation.1 This infection most frequently occurs in school-aged children younger than 8 years1-3; peak incidence is 6 years of age.2,3 The worldwide estimated prevalence in children is 5.1% to 11.5%.1,3 In children cohabitating with others infected by MC, approximately 40% of households experienced a spread of infection; the risk of transmission is not associated with greater number of lesions.4 In adults, infection most commonly occurs in the setting of immunodeficiency or as a sexually transmitted infection in immunocompetent patients.3 Molluscum contagiosum infection classically presents as 1- to 3-mm, flesh- or white-colored, dome-shaped, smooth papules with central umbilication.1 Lesions often occur in clusters or lines, indicating local spread. The trunk, extremities, and face are areas that frequently are involved.2,3
Atypical presentations of MC infection can occur, as demonstrated by our case. Involvement of hair follicles by the infection can result in follicular induction.1,5 Secondary infection can mimic abscess formation.1 Inflamed MC lesions demonstrating the “beginning of the end” sign often are mistaken for primary infection, which is thought to be an inflammatory immune response to the virus.6 Lesions located on the eye or eyelid can present as unilateral conjunctivitis, conjunctival or corneal nodules, eyelid abscesses, or chalazions.1 Giant MC is a nodular variant of this infection measuring larger than 1 cm in size that can present similar to epidermoid cysts, condyloma acuminatum, or verruca vulgaris.1,7 Other reported mimicked conditions include basal cell carcinoma, trichoepithelioma, appendageal tumors, keratoacanthoma, foreign body granulomas, nevus sebaceous, or ecthyma.1,3 Molluscum contagiosum also has been reported to present as large ulcerative growths.8 In immunocompromised patients, deep fungal infection is another mimicker.1 Lesions on the plantar surfaces of the feet often are misdiagnosed as plantar verruca and present with pain during ambulation.9
The diagnosis of MC is clinical, with additional diagnostic tools reserved for more challenging situations.1 In cases with atypical presentations, dermoscopy may aid diagnosis through visualization of orifices and vascular patterns including crown, radial, and punctiform vessels.10 Biopsy or fine-needle aspiration also can be utilized as a diagnostic tool. Histopathology often reveals pathognomonic intracytoplasmic inclusions or Henderson-Paterson bodies.8,10 The appearance of MC can mimic other conditions that should be included in the differential diagnosis. Pyogenic granuloma often presents as a benign red papule that may grow rapidly and become pedunculated, sometimes with bleeding and crusting, though histology reveals groups of proliferating capillaries.11 More than half of amelanotic melanomas present in the papulonodular form as vascular or ulcerated nodules, and others may appear as erythematous macules. Diagnosis of amelanotic melanoma is made through histologic examination, which reveals atypical melanocytes in nests or cords, in conjunction with immunohistochemical stains such as S-100.12 Spitz nevi often appear as round, dome-shaped papules that most commonly are red, pink, or fleshcolored. They appear histologically similar to melanoma with nests of atypical melanocytes and nuclear atypia.13
A variety of treatment modalities can be used for MC including cantharidin, curettage, and cryotherapy.14 Imiquimod no longer is recommended due to a lack of demonstrated superiority over placebo in recent studies as well as its adverse effects.3 Topical retinoids have been recommended; however, their use frequently is limited by local irritation.3,14 Cantharidin is the most frequently utilized treatment by pediatric dermatologists. Most health care providers report subjective satisfaction with its results and efficacy, though some side effects may occur including discomfort and temporary changes in pigmentation. Treatment for MC is not required, as the condition is self-limiting.14 Therapy often is reserved for those with extensive disease, complications from lesions, cosmetic or psychological concerns, or genital involvement given the potential for sexual transmission.3 Time to resolution without treatment varies and is more prolonged in immunocompromised patients. Mean time to resolution in immunocompetent hosts has been reported as 13.3 months, but most infections are noted to clear within 2 to 4 years.1,4 Although resolution without treatment occurs, transmission to others and negative impact on quality of life (QOL) can occur and support the need for treatment. Greater impact on QOL was observed in females, those with more lesions, and patients with a longer duration of symptoms. Moderate impact on QOL was reported in 28% of patients (n=301), and severe effects were reported in 11%.4
In conclusion, MC is a common, benign, treatable cutaneous viral infection that often presents as small, flesh-colored papules in children. Its appearance can mimic a variety of other conditions. In cases with abnormal presentations, definitive diagnosis with pathology can be important to differentiate MC from more dangerous etiologies that may require further treatment.
- Brown J, Janniger CK, Schwartz RA, et al. Childhood molluscum contagiosum. Int J Dermatol. 2006;45:93-99. doi:10.1111 /j.1365-4632.2006.02737.x
- Dohil MA, Lin P, Lee J, et al. The epidemiology of molluscum contagiosum in children. J Am Acad Dermatol. 2006;54:47-54. doi:10.1016/j.jaad.2005.08.035
- Robinson G, Townsend S, Jahnke MN. Molluscum contagiosum: review and update on clinical presentation, diagnosis, risk, prevention, and treatment. Curr Derm Rep. 2020;9:83-92.
- Olsen JR, Gallacher J, Finlay AY, et al. Time to resolution and effect on quality of life of molluscum contagiosum in children in the UK: a prospective community cohort study. Lancet Infect Dis. 2015;15:190-195. doi:10.1016/S1473-3099(14)71053-9
- Davey J, Biswas A. Follicular induction in a case of molluscum contagiosum: possible link with secondary anetoderma-like changes? Am J Dermatopathol. 2014;36:E19-E21. doi:10.1097/DAD.0b013e31828bc7c7
- Butala N, Siegfried E, Weissler A. Molluscum BOTE sign: a predictor of imminent resolution. Pediatrics. 2013;131:E1650-E1653. doi:10.1542/peds.2012-2933
- Uzuncakmak TK, Kuru BC, Zemheri EI, et al. Isolated giant molluscum contagiosum mimicking epidermoid cyst. Dermatol Pract Concept. 2016;6:71-73. doi:10.5826/dpc.0603a15
- Singh S, Swain M, Shukla S, et al. An unusual presentation of giant molluscum contagiosum diagnosed on cytology. Diagn Cytopathol. 2018;46:794-796. doi:10.1002/dc.23964
- Cohen PR, Tschen JA. Plantar molluscum contagiosum: a case report of molluscum contagiosum occurring on the sole of the foot and a review of the world literature. Cutis. 2012;90:35-41.
- Megalla M, Bronsnick T, Noor O, et al. Dermoscopic, confocal microscopic, and histologic characteristics of an atypical presentation of molluscum contagiosum. Ann Clin Pathol. 2014;2:1038.
- Patrice SJ, Wiss K, Mulliken JB. Pyogenic granuloma (lobular capillary hemangioma): a clinicopathologic study of 178 cases. Pediatr Dermatol. 1991;8:267-276. doi:10.1111/j.1525-1470.1991.tb00931.x
- Gong H-Z, Zheng H-Y, Li J. Amelanotic melanoma. Melanoma Res. 2019;29:221-230. doi:10.1097/CMR.0000000000000571
- Casso EM, Grin-Jorgensen CM, Grant-Kels JM. Spitz nevi. J Am Acad Dermatol. 1992;27(6 pt 1):901-913. doi:10.1016/0190-9622(92)70286-o
- Coloe J, Morrell DS. Cantharidin use among pediatric dermatologists in the treatment of molluscum contagiosum. Pediatr Dermatol. 2009;26:405-408.
The Diagnosis: Molluscum Contagiosum
A tangential shave removal with electrocautery was performed. Histopathology demonstrated numerous eosinophilic intracytoplasmic inclusion bodies (Figure), confirming a diagnosis of molluscum contagiosum (MC).
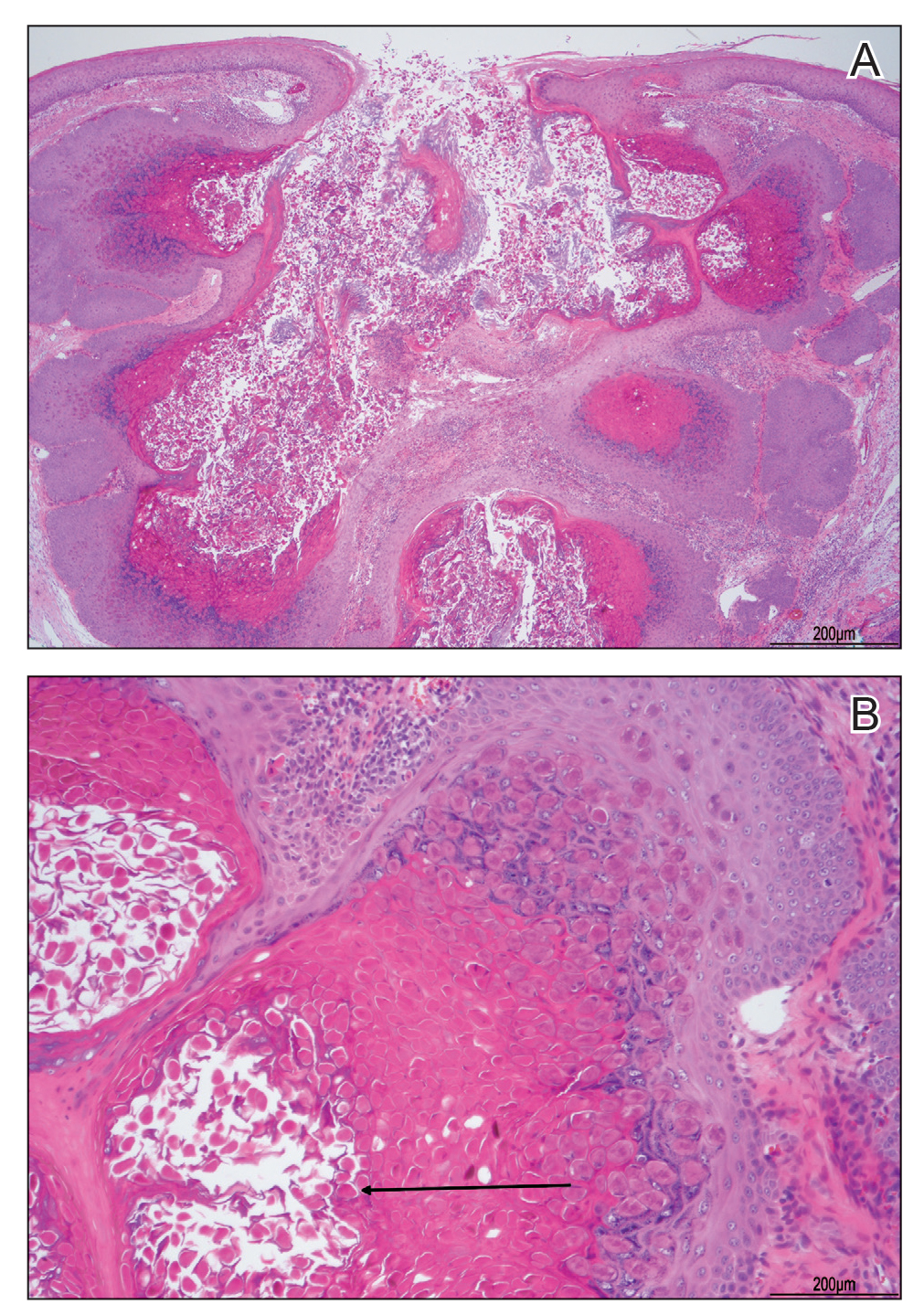
Molluscum contagiosum is a common poxvirus infection that is transmitted through fomites, contact, or self-inoculation.1 This infection most frequently occurs in school-aged children younger than 8 years1-3; peak incidence is 6 years of age.2,3 The worldwide estimated prevalence in children is 5.1% to 11.5%.1,3 In children cohabitating with others infected by MC, approximately 40% of households experienced a spread of infection; the risk of transmission is not associated with greater number of lesions.4 In adults, infection most commonly occurs in the setting of immunodeficiency or as a sexually transmitted infection in immunocompetent patients.3 Molluscum contagiosum infection classically presents as 1- to 3-mm, flesh- or white-colored, dome-shaped, smooth papules with central umbilication.1 Lesions often occur in clusters or lines, indicating local spread. The trunk, extremities, and face are areas that frequently are involved.2,3
Atypical presentations of MC infection can occur, as demonstrated by our case. Involvement of hair follicles by the infection can result in follicular induction.1,5 Secondary infection can mimic abscess formation.1 Inflamed MC lesions demonstrating the “beginning of the end” sign often are mistaken for primary infection, which is thought to be an inflammatory immune response to the virus.6 Lesions located on the eye or eyelid can present as unilateral conjunctivitis, conjunctival or corneal nodules, eyelid abscesses, or chalazions.1 Giant MC is a nodular variant of this infection measuring larger than 1 cm in size that can present similar to epidermoid cysts, condyloma acuminatum, or verruca vulgaris.1,7 Other reported mimicked conditions include basal cell carcinoma, trichoepithelioma, appendageal tumors, keratoacanthoma, foreign body granulomas, nevus sebaceous, or ecthyma.1,3 Molluscum contagiosum also has been reported to present as large ulcerative growths.8 In immunocompromised patients, deep fungal infection is another mimicker.1 Lesions on the plantar surfaces of the feet often are misdiagnosed as plantar verruca and present with pain during ambulation.9
The diagnosis of MC is clinical, with additional diagnostic tools reserved for more challenging situations.1 In cases with atypical presentations, dermoscopy may aid diagnosis through visualization of orifices and vascular patterns including crown, radial, and punctiform vessels.10 Biopsy or fine-needle aspiration also can be utilized as a diagnostic tool. Histopathology often reveals pathognomonic intracytoplasmic inclusions or Henderson-Paterson bodies.8,10 The appearance of MC can mimic other conditions that should be included in the differential diagnosis. Pyogenic granuloma often presents as a benign red papule that may grow rapidly and become pedunculated, sometimes with bleeding and crusting, though histology reveals groups of proliferating capillaries.11 More than half of amelanotic melanomas present in the papulonodular form as vascular or ulcerated nodules, and others may appear as erythematous macules. Diagnosis of amelanotic melanoma is made through histologic examination, which reveals atypical melanocytes in nests or cords, in conjunction with immunohistochemical stains such as S-100.12 Spitz nevi often appear as round, dome-shaped papules that most commonly are red, pink, or fleshcolored. They appear histologically similar to melanoma with nests of atypical melanocytes and nuclear atypia.13
A variety of treatment modalities can be used for MC including cantharidin, curettage, and cryotherapy.14 Imiquimod no longer is recommended due to a lack of demonstrated superiority over placebo in recent studies as well as its adverse effects.3 Topical retinoids have been recommended; however, their use frequently is limited by local irritation.3,14 Cantharidin is the most frequently utilized treatment by pediatric dermatologists. Most health care providers report subjective satisfaction with its results and efficacy, though some side effects may occur including discomfort and temporary changes in pigmentation. Treatment for MC is not required, as the condition is self-limiting.14 Therapy often is reserved for those with extensive disease, complications from lesions, cosmetic or psychological concerns, or genital involvement given the potential for sexual transmission.3 Time to resolution without treatment varies and is more prolonged in immunocompromised patients. Mean time to resolution in immunocompetent hosts has been reported as 13.3 months, but most infections are noted to clear within 2 to 4 years.1,4 Although resolution without treatment occurs, transmission to others and negative impact on quality of life (QOL) can occur and support the need for treatment. Greater impact on QOL was observed in females, those with more lesions, and patients with a longer duration of symptoms. Moderate impact on QOL was reported in 28% of patients (n=301), and severe effects were reported in 11%.4
In conclusion, MC is a common, benign, treatable cutaneous viral infection that often presents as small, flesh-colored papules in children. Its appearance can mimic a variety of other conditions. In cases with abnormal presentations, definitive diagnosis with pathology can be important to differentiate MC from more dangerous etiologies that may require further treatment.
The Diagnosis: Molluscum Contagiosum
A tangential shave removal with electrocautery was performed. Histopathology demonstrated numerous eosinophilic intracytoplasmic inclusion bodies (Figure), confirming a diagnosis of molluscum contagiosum (MC).
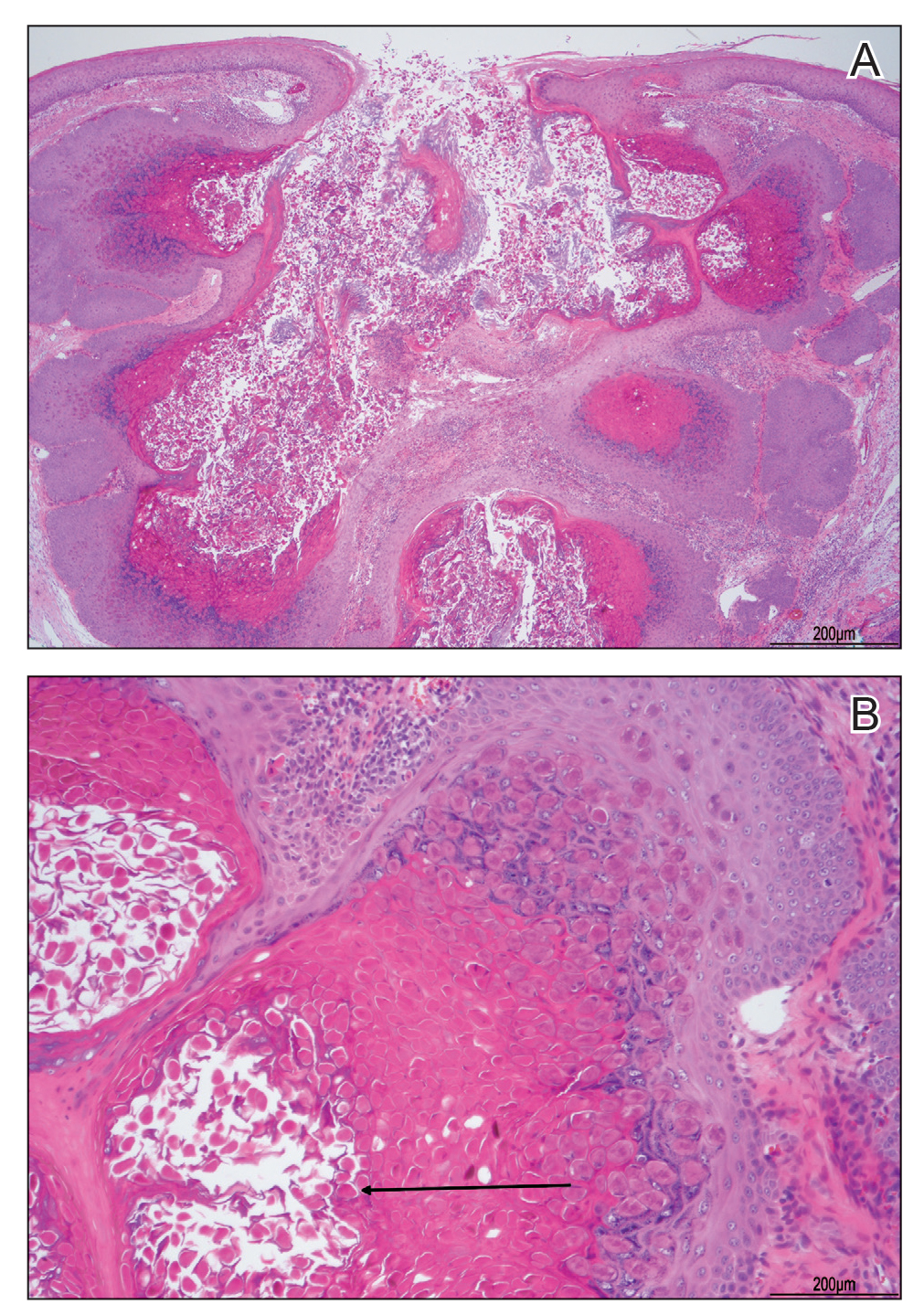
Molluscum contagiosum is a common poxvirus infection that is transmitted through fomites, contact, or self-inoculation.1 This infection most frequently occurs in school-aged children younger than 8 years1-3; peak incidence is 6 years of age.2,3 The worldwide estimated prevalence in children is 5.1% to 11.5%.1,3 In children cohabitating with others infected by MC, approximately 40% of households experienced a spread of infection; the risk of transmission is not associated with greater number of lesions.4 In adults, infection most commonly occurs in the setting of immunodeficiency or as a sexually transmitted infection in immunocompetent patients.3 Molluscum contagiosum infection classically presents as 1- to 3-mm, flesh- or white-colored, dome-shaped, smooth papules with central umbilication.1 Lesions often occur in clusters or lines, indicating local spread. The trunk, extremities, and face are areas that frequently are involved.2,3
Atypical presentations of MC infection can occur, as demonstrated by our case. Involvement of hair follicles by the infection can result in follicular induction.1,5 Secondary infection can mimic abscess formation.1 Inflamed MC lesions demonstrating the “beginning of the end” sign often are mistaken for primary infection, which is thought to be an inflammatory immune response to the virus.6 Lesions located on the eye or eyelid can present as unilateral conjunctivitis, conjunctival or corneal nodules, eyelid abscesses, or chalazions.1 Giant MC is a nodular variant of this infection measuring larger than 1 cm in size that can present similar to epidermoid cysts, condyloma acuminatum, or verruca vulgaris.1,7 Other reported mimicked conditions include basal cell carcinoma, trichoepithelioma, appendageal tumors, keratoacanthoma, foreign body granulomas, nevus sebaceous, or ecthyma.1,3 Molluscum contagiosum also has been reported to present as large ulcerative growths.8 In immunocompromised patients, deep fungal infection is another mimicker.1 Lesions on the plantar surfaces of the feet often are misdiagnosed as plantar verruca and present with pain during ambulation.9
The diagnosis of MC is clinical, with additional diagnostic tools reserved for more challenging situations.1 In cases with atypical presentations, dermoscopy may aid diagnosis through visualization of orifices and vascular patterns including crown, radial, and punctiform vessels.10 Biopsy or fine-needle aspiration also can be utilized as a diagnostic tool. Histopathology often reveals pathognomonic intracytoplasmic inclusions or Henderson-Paterson bodies.8,10 The appearance of MC can mimic other conditions that should be included in the differential diagnosis. Pyogenic granuloma often presents as a benign red papule that may grow rapidly and become pedunculated, sometimes with bleeding and crusting, though histology reveals groups of proliferating capillaries.11 More than half of amelanotic melanomas present in the papulonodular form as vascular or ulcerated nodules, and others may appear as erythematous macules. Diagnosis of amelanotic melanoma is made through histologic examination, which reveals atypical melanocytes in nests or cords, in conjunction with immunohistochemical stains such as S-100.12 Spitz nevi often appear as round, dome-shaped papules that most commonly are red, pink, or fleshcolored. They appear histologically similar to melanoma with nests of atypical melanocytes and nuclear atypia.13
A variety of treatment modalities can be used for MC including cantharidin, curettage, and cryotherapy.14 Imiquimod no longer is recommended due to a lack of demonstrated superiority over placebo in recent studies as well as its adverse effects.3 Topical retinoids have been recommended; however, their use frequently is limited by local irritation.3,14 Cantharidin is the most frequently utilized treatment by pediatric dermatologists. Most health care providers report subjective satisfaction with its results and efficacy, though some side effects may occur including discomfort and temporary changes in pigmentation. Treatment for MC is not required, as the condition is self-limiting.14 Therapy often is reserved for those with extensive disease, complications from lesions, cosmetic or psychological concerns, or genital involvement given the potential for sexual transmission.3 Time to resolution without treatment varies and is more prolonged in immunocompromised patients. Mean time to resolution in immunocompetent hosts has been reported as 13.3 months, but most infections are noted to clear within 2 to 4 years.1,4 Although resolution without treatment occurs, transmission to others and negative impact on quality of life (QOL) can occur and support the need for treatment. Greater impact on QOL was observed in females, those with more lesions, and patients with a longer duration of symptoms. Moderate impact on QOL was reported in 28% of patients (n=301), and severe effects were reported in 11%.4
In conclusion, MC is a common, benign, treatable cutaneous viral infection that often presents as small, flesh-colored papules in children. Its appearance can mimic a variety of other conditions. In cases with abnormal presentations, definitive diagnosis with pathology can be important to differentiate MC from more dangerous etiologies that may require further treatment.
- Brown J, Janniger CK, Schwartz RA, et al. Childhood molluscum contagiosum. Int J Dermatol. 2006;45:93-99. doi:10.1111 /j.1365-4632.2006.02737.x
- Dohil MA, Lin P, Lee J, et al. The epidemiology of molluscum contagiosum in children. J Am Acad Dermatol. 2006;54:47-54. doi:10.1016/j.jaad.2005.08.035
- Robinson G, Townsend S, Jahnke MN. Molluscum contagiosum: review and update on clinical presentation, diagnosis, risk, prevention, and treatment. Curr Derm Rep. 2020;9:83-92.
- Olsen JR, Gallacher J, Finlay AY, et al. Time to resolution and effect on quality of life of molluscum contagiosum in children in the UK: a prospective community cohort study. Lancet Infect Dis. 2015;15:190-195. doi:10.1016/S1473-3099(14)71053-9
- Davey J, Biswas A. Follicular induction in a case of molluscum contagiosum: possible link with secondary anetoderma-like changes? Am J Dermatopathol. 2014;36:E19-E21. doi:10.1097/DAD.0b013e31828bc7c7
- Butala N, Siegfried E, Weissler A. Molluscum BOTE sign: a predictor of imminent resolution. Pediatrics. 2013;131:E1650-E1653. doi:10.1542/peds.2012-2933
- Uzuncakmak TK, Kuru BC, Zemheri EI, et al. Isolated giant molluscum contagiosum mimicking epidermoid cyst. Dermatol Pract Concept. 2016;6:71-73. doi:10.5826/dpc.0603a15
- Singh S, Swain M, Shukla S, et al. An unusual presentation of giant molluscum contagiosum diagnosed on cytology. Diagn Cytopathol. 2018;46:794-796. doi:10.1002/dc.23964
- Cohen PR, Tschen JA. Plantar molluscum contagiosum: a case report of molluscum contagiosum occurring on the sole of the foot and a review of the world literature. Cutis. 2012;90:35-41.
- Megalla M, Bronsnick T, Noor O, et al. Dermoscopic, confocal microscopic, and histologic characteristics of an atypical presentation of molluscum contagiosum. Ann Clin Pathol. 2014;2:1038.
- Patrice SJ, Wiss K, Mulliken JB. Pyogenic granuloma (lobular capillary hemangioma): a clinicopathologic study of 178 cases. Pediatr Dermatol. 1991;8:267-276. doi:10.1111/j.1525-1470.1991.tb00931.x
- Gong H-Z, Zheng H-Y, Li J. Amelanotic melanoma. Melanoma Res. 2019;29:221-230. doi:10.1097/CMR.0000000000000571
- Casso EM, Grin-Jorgensen CM, Grant-Kels JM. Spitz nevi. J Am Acad Dermatol. 1992;27(6 pt 1):901-913. doi:10.1016/0190-9622(92)70286-o
- Coloe J, Morrell DS. Cantharidin use among pediatric dermatologists in the treatment of molluscum contagiosum. Pediatr Dermatol. 2009;26:405-408.
- Brown J, Janniger CK, Schwartz RA, et al. Childhood molluscum contagiosum. Int J Dermatol. 2006;45:93-99. doi:10.1111 /j.1365-4632.2006.02737.x
- Dohil MA, Lin P, Lee J, et al. The epidemiology of molluscum contagiosum in children. J Am Acad Dermatol. 2006;54:47-54. doi:10.1016/j.jaad.2005.08.035
- Robinson G, Townsend S, Jahnke MN. Molluscum contagiosum: review and update on clinical presentation, diagnosis, risk, prevention, and treatment. Curr Derm Rep. 2020;9:83-92.
- Olsen JR, Gallacher J, Finlay AY, et al. Time to resolution and effect on quality of life of molluscum contagiosum in children in the UK: a prospective community cohort study. Lancet Infect Dis. 2015;15:190-195. doi:10.1016/S1473-3099(14)71053-9
- Davey J, Biswas A. Follicular induction in a case of molluscum contagiosum: possible link with secondary anetoderma-like changes? Am J Dermatopathol. 2014;36:E19-E21. doi:10.1097/DAD.0b013e31828bc7c7
- Butala N, Siegfried E, Weissler A. Molluscum BOTE sign: a predictor of imminent resolution. Pediatrics. 2013;131:E1650-E1653. doi:10.1542/peds.2012-2933
- Uzuncakmak TK, Kuru BC, Zemheri EI, et al. Isolated giant molluscum contagiosum mimicking epidermoid cyst. Dermatol Pract Concept. 2016;6:71-73. doi:10.5826/dpc.0603a15
- Singh S, Swain M, Shukla S, et al. An unusual presentation of giant molluscum contagiosum diagnosed on cytology. Diagn Cytopathol. 2018;46:794-796. doi:10.1002/dc.23964
- Cohen PR, Tschen JA. Plantar molluscum contagiosum: a case report of molluscum contagiosum occurring on the sole of the foot and a review of the world literature. Cutis. 2012;90:35-41.
- Megalla M, Bronsnick T, Noor O, et al. Dermoscopic, confocal microscopic, and histologic characteristics of an atypical presentation of molluscum contagiosum. Ann Clin Pathol. 2014;2:1038.
- Patrice SJ, Wiss K, Mulliken JB. Pyogenic granuloma (lobular capillary hemangioma): a clinicopathologic study of 178 cases. Pediatr Dermatol. 1991;8:267-276. doi:10.1111/j.1525-1470.1991.tb00931.x
- Gong H-Z, Zheng H-Y, Li J. Amelanotic melanoma. Melanoma Res. 2019;29:221-230. doi:10.1097/CMR.0000000000000571
- Casso EM, Grin-Jorgensen CM, Grant-Kels JM. Spitz nevi. J Am Acad Dermatol. 1992;27(6 pt 1):901-913. doi:10.1016/0190-9622(92)70286-o
- Coloe J, Morrell DS. Cantharidin use among pediatric dermatologists in the treatment of molluscum contagiosum. Pediatr Dermatol. 2009;26:405-408.
A 13-year-old adolescent girl presented for evaluation of a lesion on the dorsal aspect of the right foot of 1 week’s duration. She had a history of acne vulgaris and seasonal allergic rhinitis. She previously had noticed a persistent, small, flesh-colored bump of unknown chronicity in the same location, which had been diagnosed as a skin tag at an outside clinic. She denied any prior treatment in this area. Approximately a week prior to presentation, the lesion became painful, larger, and darkened in color before draining yellowish fluid. Due to concern for superinfection, the patient was prescribed cephalexin by her pediatrician. Dermatologic examination revealed a 1-cm, violaceous, pedunculated plaque with hemorrhagic crust on the dorsal aspect of the right foot with surrounding erythema and tenderness.

Pediatricians’ incomes rose faster than most specialties in 2021: Survey
In an unprecedented year when income increased for all specialties, pediatricians did better than most, according to a recent survey by Medscape.
. Medscape also noted that, for the first time in the 11 years it’s been conducting these physician compensation surveys, “all specialties have seen an increase in income.”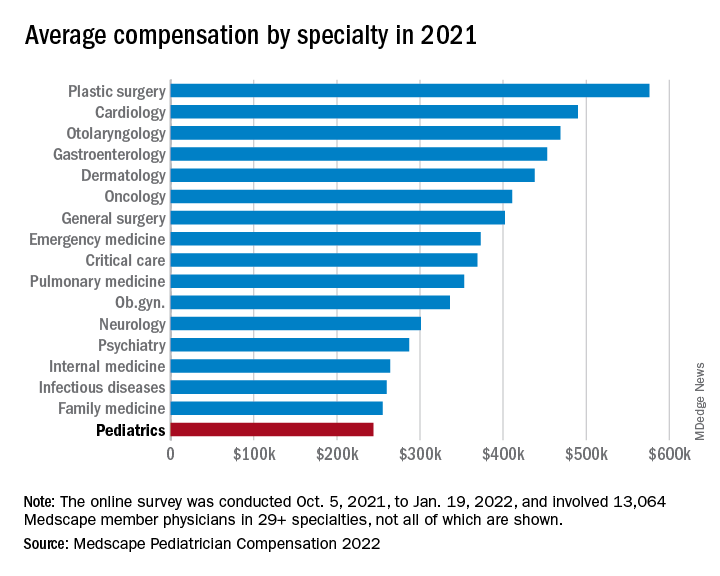
At least some of that positive news can be traced back to the reduced impact of COVID-19. “Compensation for most physicians is trending back up as demand for physicians accelerates. The market for physicians has done a complete 180 over just 7 or 8 months,” James Taylor of AMN Healthcare’s physician and leadership solutions division said in Medscape Pediatrician Compensation Report 2022.
The 10% increase in pediatricians’ income, however, was not enough to reach the average for primary care physicians, $260,000, which was up by 7.4% over 2020. It was enough, though, to move pediatricians from the bottom of the earnings-by-specialty list, where they were last year, to next-to-last this year (public health/preventive medicine, with average earnings of $243,000 in 2021, is not shown in the graph).
The gender gap in earnings left male pediatricians’ income 26% higher than their female counterparts, slightly above the gap of 25% for primary care physicians and 24% for all physicians. For specialists, the gap was 31% in favor of men, based on data from 13,064 Medscape member physicians who participated in the survey, which was conducted online from Oct. 5, 2021, to Jan. 19, 2022. For the record, 57% of the pediatricians who responded were women.
The gaps and low income averages were enough, it seems, to keep pediatricians fairly negative regarding their feelings on compensation. Only 47% think they were fairly compensated in 2021, higher only than diabetes/endocrinology and nephrology. Among the other primary care specialties, internal medicine and ob.gyn. were slightly higher at 49% and family medicine was 55% – still just middle of the pack, compared with public health/preventive medicine at 72%, Medscape said in the report.
Would you do it again?
Moving to the less-economic aspects of the survey, respondents also were asked if they would choose medicine again as a career. Once more pediatricians were low on the scale, as only 70% said that they would enter medicine again, down from 77% last year and lower than this year’s average of 73% average for all physicians.
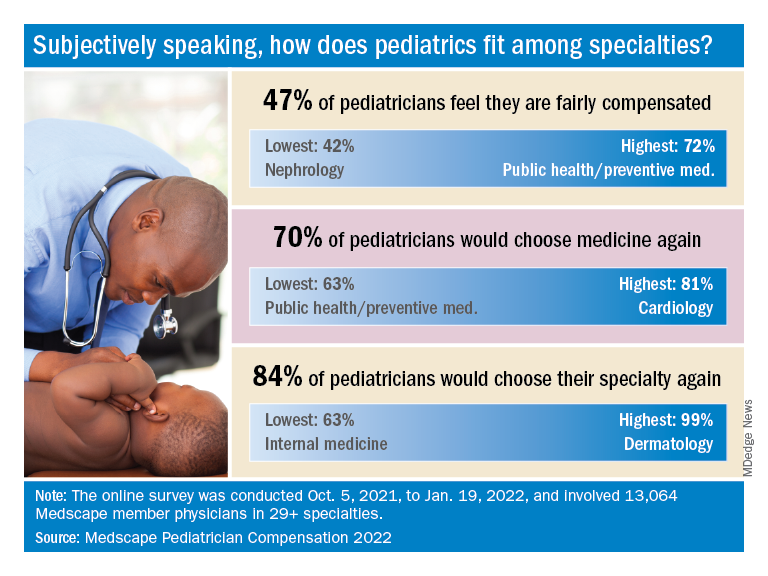
When they were asked if they would choose pediatrics again as a specialty, the response was a bit more positive: 84% said yes. That middle-of-the-pack showing was well ahead of internal medicine (63%) and family medicine (68%), but well below dermatology (99%) and orthopedics (97%), which are “among the top groups in our survey year after year,” Medscape said.
Did the administrative challenges of medical practice have an effect on those answers? Pediatrician respondents said that they spend 14.9 hours per week on paperwork and administration, close to the average of 15.5 hours for all physicians. The internists, who are least likely to choose their original specialty again, spend 18.7 hours on paperwork each week, while dermatologists, the most likely to repeat their first choice, have just 11.9 hours of paperwork per week.
The exact number of pediatricians involved in the survey was not provided, but they made up about 8% of the total cohort, which works out to somewhere between 1,000 and 1,100 individuals. All respondents had to be practicing in the United States, and compensation was analyzed for full-time physicians only. The sampling error is ±0.86% at a 95% confidence level.
In an unprecedented year when income increased for all specialties, pediatricians did better than most, according to a recent survey by Medscape.
. Medscape also noted that, for the first time in the 11 years it’s been conducting these physician compensation surveys, “all specialties have seen an increase in income.”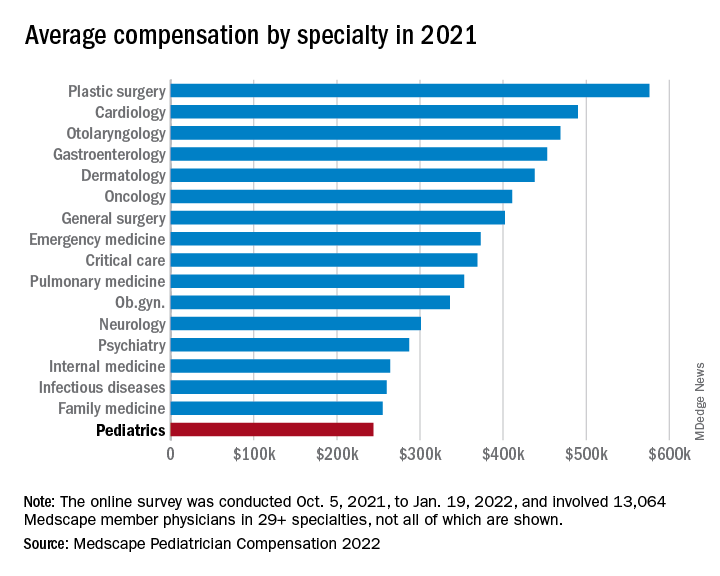
At least some of that positive news can be traced back to the reduced impact of COVID-19. “Compensation for most physicians is trending back up as demand for physicians accelerates. The market for physicians has done a complete 180 over just 7 or 8 months,” James Taylor of AMN Healthcare’s physician and leadership solutions division said in Medscape Pediatrician Compensation Report 2022.
The 10% increase in pediatricians’ income, however, was not enough to reach the average for primary care physicians, $260,000, which was up by 7.4% over 2020. It was enough, though, to move pediatricians from the bottom of the earnings-by-specialty list, where they were last year, to next-to-last this year (public health/preventive medicine, with average earnings of $243,000 in 2021, is not shown in the graph).
The gender gap in earnings left male pediatricians’ income 26% higher than their female counterparts, slightly above the gap of 25% for primary care physicians and 24% for all physicians. For specialists, the gap was 31% in favor of men, based on data from 13,064 Medscape member physicians who participated in the survey, which was conducted online from Oct. 5, 2021, to Jan. 19, 2022. For the record, 57% of the pediatricians who responded were women.
The gaps and low income averages were enough, it seems, to keep pediatricians fairly negative regarding their feelings on compensation. Only 47% think they were fairly compensated in 2021, higher only than diabetes/endocrinology and nephrology. Among the other primary care specialties, internal medicine and ob.gyn. were slightly higher at 49% and family medicine was 55% – still just middle of the pack, compared with public health/preventive medicine at 72%, Medscape said in the report.
Would you do it again?
Moving to the less-economic aspects of the survey, respondents also were asked if they would choose medicine again as a career. Once more pediatricians were low on the scale, as only 70% said that they would enter medicine again, down from 77% last year and lower than this year’s average of 73% average for all physicians.
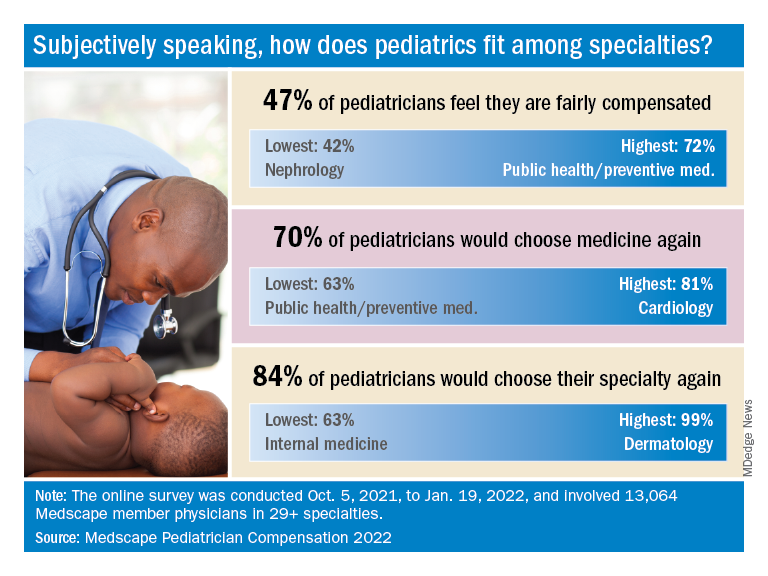
When they were asked if they would choose pediatrics again as a specialty, the response was a bit more positive: 84% said yes. That middle-of-the-pack showing was well ahead of internal medicine (63%) and family medicine (68%), but well below dermatology (99%) and orthopedics (97%), which are “among the top groups in our survey year after year,” Medscape said.
Did the administrative challenges of medical practice have an effect on those answers? Pediatrician respondents said that they spend 14.9 hours per week on paperwork and administration, close to the average of 15.5 hours for all physicians. The internists, who are least likely to choose their original specialty again, spend 18.7 hours on paperwork each week, while dermatologists, the most likely to repeat their first choice, have just 11.9 hours of paperwork per week.
The exact number of pediatricians involved in the survey was not provided, but they made up about 8% of the total cohort, which works out to somewhere between 1,000 and 1,100 individuals. All respondents had to be practicing in the United States, and compensation was analyzed for full-time physicians only. The sampling error is ±0.86% at a 95% confidence level.
In an unprecedented year when income increased for all specialties, pediatricians did better than most, according to a recent survey by Medscape.
. Medscape also noted that, for the first time in the 11 years it’s been conducting these physician compensation surveys, “all specialties have seen an increase in income.”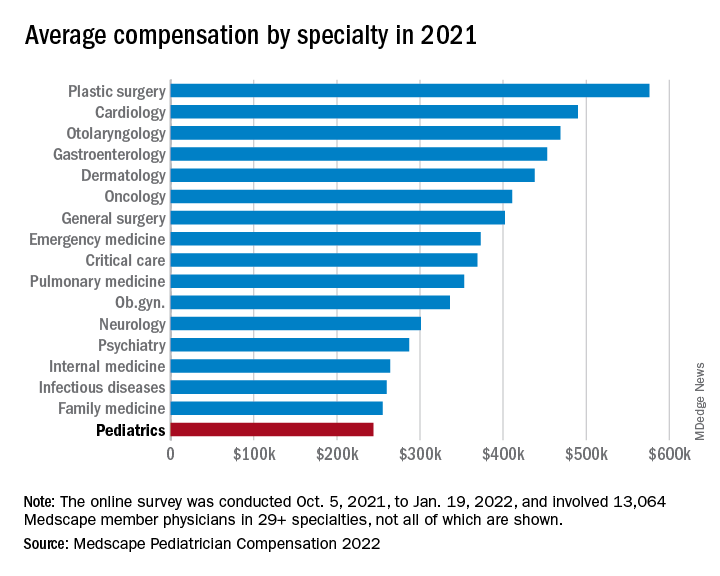
At least some of that positive news can be traced back to the reduced impact of COVID-19. “Compensation for most physicians is trending back up as demand for physicians accelerates. The market for physicians has done a complete 180 over just 7 or 8 months,” James Taylor of AMN Healthcare’s physician and leadership solutions division said in Medscape Pediatrician Compensation Report 2022.
The 10% increase in pediatricians’ income, however, was not enough to reach the average for primary care physicians, $260,000, which was up by 7.4% over 2020. It was enough, though, to move pediatricians from the bottom of the earnings-by-specialty list, where they were last year, to next-to-last this year (public health/preventive medicine, with average earnings of $243,000 in 2021, is not shown in the graph).
The gender gap in earnings left male pediatricians’ income 26% higher than their female counterparts, slightly above the gap of 25% for primary care physicians and 24% for all physicians. For specialists, the gap was 31% in favor of men, based on data from 13,064 Medscape member physicians who participated in the survey, which was conducted online from Oct. 5, 2021, to Jan. 19, 2022. For the record, 57% of the pediatricians who responded were women.
The gaps and low income averages were enough, it seems, to keep pediatricians fairly negative regarding their feelings on compensation. Only 47% think they were fairly compensated in 2021, higher only than diabetes/endocrinology and nephrology. Among the other primary care specialties, internal medicine and ob.gyn. were slightly higher at 49% and family medicine was 55% – still just middle of the pack, compared with public health/preventive medicine at 72%, Medscape said in the report.
Would you do it again?
Moving to the less-economic aspects of the survey, respondents also were asked if they would choose medicine again as a career. Once more pediatricians were low on the scale, as only 70% said that they would enter medicine again, down from 77% last year and lower than this year’s average of 73% average for all physicians.
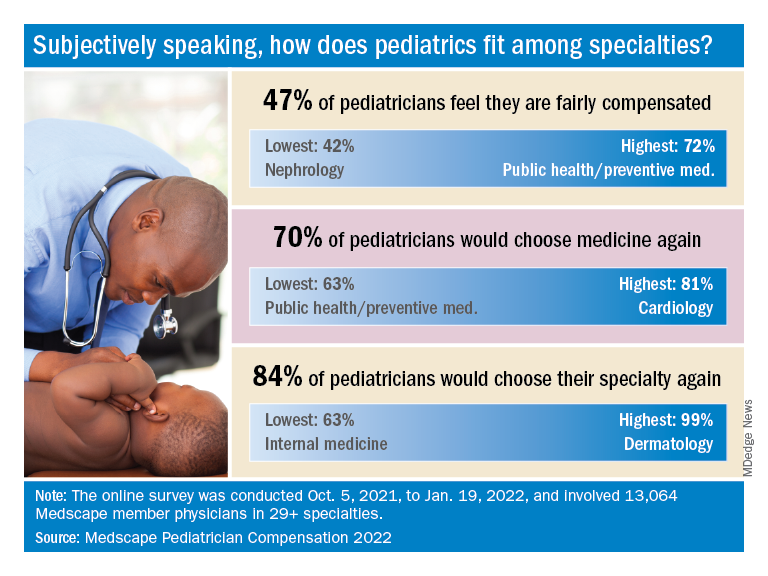
When they were asked if they would choose pediatrics again as a specialty, the response was a bit more positive: 84% said yes. That middle-of-the-pack showing was well ahead of internal medicine (63%) and family medicine (68%), but well below dermatology (99%) and orthopedics (97%), which are “among the top groups in our survey year after year,” Medscape said.
Did the administrative challenges of medical practice have an effect on those answers? Pediatrician respondents said that they spend 14.9 hours per week on paperwork and administration, close to the average of 15.5 hours for all physicians. The internists, who are least likely to choose their original specialty again, spend 18.7 hours on paperwork each week, while dermatologists, the most likely to repeat their first choice, have just 11.9 hours of paperwork per week.
The exact number of pediatricians involved in the survey was not provided, but they made up about 8% of the total cohort, which works out to somewhere between 1,000 and 1,100 individuals. All respondents had to be practicing in the United States, and compensation was analyzed for full-time physicians only. The sampling error is ±0.86% at a 95% confidence level.
Can dietary tweaks improve some skin diseases?
Since 1950, the terms “diet and skin” in the medical literature have markedly increased, said Vivian Shi, MD associate professor of dermatology at the University of Arkansas for Medical Sciences, Little Rock, who talked about nutritional approaches for select skin diseases at MedscapeLive’s Women’s and Pediatric Dermatology Seminar.
Myths abound, but some associations of diet with skin diseases hold water, and she said.
Acne
What’s known, Dr. Shi said, is that the prevalence of acne is substantially lower in non-Westernized countries, and that diets in those countries generally have a low glycemic load, which decreases IGF-1 insulinlike growth factor 1 (IGF-1) concentrations, an accepted risk factor for acne. The Western diet also includes the hormonal effects of cow’s milk products.
Whey protein, which is popular as a supplement, isn’t good for acne, Dr. Shi said. It takes a couple of hours to digest, while casein protein digests more slowly, over 5-7 hours. If casein protein isn’t acceptable, good alternatives to whey protein are hemp seed, plant protein blends (peas, seeds, berries), egg white, brown rice isolate, and soy isolate protein.
Dairy products increase IGF-1 levels, hormonal mediators that can make acne worse. In addition, industrial cow’s milk can contain anabolic steroids and growth factor, leading to sebogenesis, Dr. Shi said. As for the type of milk, skim milk tends to be the most acnegenic and associated with the highest blood levels of IGF-1.
Supplementing with omega-3 fatty acids and gamma-linolenic acid improved mild to moderate acne in a double-blind, controlled study. Researchers randomized 45 patients with mild to moderate acne to an omega-3 fatty acid group (2,000 mg of eicosapentaenoic acid and docosahexaenoic acid), a gamma-linolenic acid group (borage oil with 400 mg gamma-linolenic acid) or a control group. After 10 weeks in both treatment groups, there was a significant reduction in inflammatory and noninflammatory lesions.
Those with acne are more likely to be deficient in Vitamin D, research suggests. Researchers also found that among those who had vitamin D deficiency, supplementing with 1,000 IU daily for 2 months reduced inflammatory lesions by 35% after 8 weeks, compared with a 6% reduction in the control group.
Other research has found that those with a low serum zinc level had more severe acne and that 30-200 mg of zinc orally for 2-4 months reduced inflammatory acne. However, Dr. Shi cautioned that those taking zinc for more than 2 months also need a copper supplement, as zinc reduces the amount of copper absorbed by the body.
Dr. Shi’s “do’s” diet list for acne patients is a follows: Paleolithic and Mediterranean diets, omega-3 fatty acids, gamma-linolenic acids, Vitamin D, zinc, tubers, legumes, vegetables, fruits, and fish.
Unknowns, she said, include chocolate, caffeine, green tea, and high salt.
Hidradenitis suppurativa
Patents with HS who follow a Mediterranean diet most closely have less severe disease, research has found. In this study, those patients with HS with the lowest adherence had a Sartorius HS score of 59.38, while those who followed it the most closely had a score of 39 (of 80).
In another study, patients with HS reported the following foods as exacerbating HS: sweets, bread/pasta/rice, dairy, and high-fat foods. Alleviating foods included vegetables, fruit, chicken, and fish.
Dr. Shi’s dietary recommendations for patients with HS: Follow a Mediterranean diet, avoid high fat foods and highly processed foods, and focus on eating more vegetables, fresh fruit, corn-based cereal, white meat, and fish.
A retrospective study of patients with Hurley stage 1 and 2 found that oral zinc gluconate, 90 mg a day, combined with 2% topical triclosan twice a day, resulted in significantly decreased HS scores and nodules and improved quality of life after 3 months. Expect vitamin D deficiency, she added.
Lastly, Dr. Shi recommended, if necessary, “weight loss to reduce the inflammatory burden.”
Rosacea
Dietary triggers for rosacea are thought to include high-fat foods, dairy foods, spicy foods, hot drinks, cinnamon, and vanilla.
A population-based case-control study in China, which evaluated 1,347 rosacea patients and 1,290 healthy controls, found that a high intake of fatty foods positively correlated with erythematotelangiectatic rosacea (ETR) and phymatous rosacea. High-frequency dairy intake negatively correlated with ETR and papulopustular rosacea, which was a surprise, she said. And in this study, no significant correlations were found between sweets, coffee, and spicy foods. That goes against the traditional thinking, she said, but this was a Chinese cohort and their diet is probably vastly different than those in the United States.
Other rosacea triggers, Dr. Shi said, are niacin-containing foods such as turkey, chicken breast, crustaceans, dried Shiitake mushrooms, peanuts, tuna, and liver, as well as cold drinks, and formalin-containing foods (fish, squid, tofu, wet noodles).
As the field of nutrigenics – how genes affect how the body responds to food – evolves, more answers about the impact of diet on these diseases will be forthcoming, Dr. Shi said.
In an interactive panel discussion, she was asked if she talks about diet with all her patients with acne, rosacea, and HS, or just those not responding to traditional therapy.
“I think it’s an important conversation to have,” Dr. Shi responded. “When I’m done with the medication [instructions], I say: ‘There is something else you can do to augment what I just told you.’ ” That’s when she explains the dietary information. She also has a handout on diet and routinely refers patients for dietary counseling.
MedscapeLive and this news organization are owned by the same parent company. Dr. Shi disclosed consulting, investigative and research funding from several sources, but not directly related to the content of her talk.
Since 1950, the terms “diet and skin” in the medical literature have markedly increased, said Vivian Shi, MD associate professor of dermatology at the University of Arkansas for Medical Sciences, Little Rock, who talked about nutritional approaches for select skin diseases at MedscapeLive’s Women’s and Pediatric Dermatology Seminar.
Myths abound, but some associations of diet with skin diseases hold water, and she said.
Acne
What’s known, Dr. Shi said, is that the prevalence of acne is substantially lower in non-Westernized countries, and that diets in those countries generally have a low glycemic load, which decreases IGF-1 insulinlike growth factor 1 (IGF-1) concentrations, an accepted risk factor for acne. The Western diet also includes the hormonal effects of cow’s milk products.
Whey protein, which is popular as a supplement, isn’t good for acne, Dr. Shi said. It takes a couple of hours to digest, while casein protein digests more slowly, over 5-7 hours. If casein protein isn’t acceptable, good alternatives to whey protein are hemp seed, plant protein blends (peas, seeds, berries), egg white, brown rice isolate, and soy isolate protein.
Dairy products increase IGF-1 levels, hormonal mediators that can make acne worse. In addition, industrial cow’s milk can contain anabolic steroids and growth factor, leading to sebogenesis, Dr. Shi said. As for the type of milk, skim milk tends to be the most acnegenic and associated with the highest blood levels of IGF-1.
Supplementing with omega-3 fatty acids and gamma-linolenic acid improved mild to moderate acne in a double-blind, controlled study. Researchers randomized 45 patients with mild to moderate acne to an omega-3 fatty acid group (2,000 mg of eicosapentaenoic acid and docosahexaenoic acid), a gamma-linolenic acid group (borage oil with 400 mg gamma-linolenic acid) or a control group. After 10 weeks in both treatment groups, there was a significant reduction in inflammatory and noninflammatory lesions.
Those with acne are more likely to be deficient in Vitamin D, research suggests. Researchers also found that among those who had vitamin D deficiency, supplementing with 1,000 IU daily for 2 months reduced inflammatory lesions by 35% after 8 weeks, compared with a 6% reduction in the control group.
Other research has found that those with a low serum zinc level had more severe acne and that 30-200 mg of zinc orally for 2-4 months reduced inflammatory acne. However, Dr. Shi cautioned that those taking zinc for more than 2 months also need a copper supplement, as zinc reduces the amount of copper absorbed by the body.
Dr. Shi’s “do’s” diet list for acne patients is a follows: Paleolithic and Mediterranean diets, omega-3 fatty acids, gamma-linolenic acids, Vitamin D, zinc, tubers, legumes, vegetables, fruits, and fish.
Unknowns, she said, include chocolate, caffeine, green tea, and high salt.
Hidradenitis suppurativa
Patents with HS who follow a Mediterranean diet most closely have less severe disease, research has found. In this study, those patients with HS with the lowest adherence had a Sartorius HS score of 59.38, while those who followed it the most closely had a score of 39 (of 80).
In another study, patients with HS reported the following foods as exacerbating HS: sweets, bread/pasta/rice, dairy, and high-fat foods. Alleviating foods included vegetables, fruit, chicken, and fish.
Dr. Shi’s dietary recommendations for patients with HS: Follow a Mediterranean diet, avoid high fat foods and highly processed foods, and focus on eating more vegetables, fresh fruit, corn-based cereal, white meat, and fish.
A retrospective study of patients with Hurley stage 1 and 2 found that oral zinc gluconate, 90 mg a day, combined with 2% topical triclosan twice a day, resulted in significantly decreased HS scores and nodules and improved quality of life after 3 months. Expect vitamin D deficiency, she added.
Lastly, Dr. Shi recommended, if necessary, “weight loss to reduce the inflammatory burden.”
Rosacea
Dietary triggers for rosacea are thought to include high-fat foods, dairy foods, spicy foods, hot drinks, cinnamon, and vanilla.
A population-based case-control study in China, which evaluated 1,347 rosacea patients and 1,290 healthy controls, found that a high intake of fatty foods positively correlated with erythematotelangiectatic rosacea (ETR) and phymatous rosacea. High-frequency dairy intake negatively correlated with ETR and papulopustular rosacea, which was a surprise, she said. And in this study, no significant correlations were found between sweets, coffee, and spicy foods. That goes against the traditional thinking, she said, but this was a Chinese cohort and their diet is probably vastly different than those in the United States.
Other rosacea triggers, Dr. Shi said, are niacin-containing foods such as turkey, chicken breast, crustaceans, dried Shiitake mushrooms, peanuts, tuna, and liver, as well as cold drinks, and formalin-containing foods (fish, squid, tofu, wet noodles).
As the field of nutrigenics – how genes affect how the body responds to food – evolves, more answers about the impact of diet on these diseases will be forthcoming, Dr. Shi said.
In an interactive panel discussion, she was asked if she talks about diet with all her patients with acne, rosacea, and HS, or just those not responding to traditional therapy.
“I think it’s an important conversation to have,” Dr. Shi responded. “When I’m done with the medication [instructions], I say: ‘There is something else you can do to augment what I just told you.’ ” That’s when she explains the dietary information. She also has a handout on diet and routinely refers patients for dietary counseling.
MedscapeLive and this news organization are owned by the same parent company. Dr. Shi disclosed consulting, investigative and research funding from several sources, but not directly related to the content of her talk.
Since 1950, the terms “diet and skin” in the medical literature have markedly increased, said Vivian Shi, MD associate professor of dermatology at the University of Arkansas for Medical Sciences, Little Rock, who talked about nutritional approaches for select skin diseases at MedscapeLive’s Women’s and Pediatric Dermatology Seminar.
Myths abound, but some associations of diet with skin diseases hold water, and she said.
Acne
What’s known, Dr. Shi said, is that the prevalence of acne is substantially lower in non-Westernized countries, and that diets in those countries generally have a low glycemic load, which decreases IGF-1 insulinlike growth factor 1 (IGF-1) concentrations, an accepted risk factor for acne. The Western diet also includes the hormonal effects of cow’s milk products.
Whey protein, which is popular as a supplement, isn’t good for acne, Dr. Shi said. It takes a couple of hours to digest, while casein protein digests more slowly, over 5-7 hours. If casein protein isn’t acceptable, good alternatives to whey protein are hemp seed, plant protein blends (peas, seeds, berries), egg white, brown rice isolate, and soy isolate protein.
Dairy products increase IGF-1 levels, hormonal mediators that can make acne worse. In addition, industrial cow’s milk can contain anabolic steroids and growth factor, leading to sebogenesis, Dr. Shi said. As for the type of milk, skim milk tends to be the most acnegenic and associated with the highest blood levels of IGF-1.
Supplementing with omega-3 fatty acids and gamma-linolenic acid improved mild to moderate acne in a double-blind, controlled study. Researchers randomized 45 patients with mild to moderate acne to an omega-3 fatty acid group (2,000 mg of eicosapentaenoic acid and docosahexaenoic acid), a gamma-linolenic acid group (borage oil with 400 mg gamma-linolenic acid) or a control group. After 10 weeks in both treatment groups, there was a significant reduction in inflammatory and noninflammatory lesions.
Those with acne are more likely to be deficient in Vitamin D, research suggests. Researchers also found that among those who had vitamin D deficiency, supplementing with 1,000 IU daily for 2 months reduced inflammatory lesions by 35% after 8 weeks, compared with a 6% reduction in the control group.
Other research has found that those with a low serum zinc level had more severe acne and that 30-200 mg of zinc orally for 2-4 months reduced inflammatory acne. However, Dr. Shi cautioned that those taking zinc for more than 2 months also need a copper supplement, as zinc reduces the amount of copper absorbed by the body.
Dr. Shi’s “do’s” diet list for acne patients is a follows: Paleolithic and Mediterranean diets, omega-3 fatty acids, gamma-linolenic acids, Vitamin D, zinc, tubers, legumes, vegetables, fruits, and fish.
Unknowns, she said, include chocolate, caffeine, green tea, and high salt.
Hidradenitis suppurativa
Patents with HS who follow a Mediterranean diet most closely have less severe disease, research has found. In this study, those patients with HS with the lowest adherence had a Sartorius HS score of 59.38, while those who followed it the most closely had a score of 39 (of 80).
In another study, patients with HS reported the following foods as exacerbating HS: sweets, bread/pasta/rice, dairy, and high-fat foods. Alleviating foods included vegetables, fruit, chicken, and fish.
Dr. Shi’s dietary recommendations for patients with HS: Follow a Mediterranean diet, avoid high fat foods and highly processed foods, and focus on eating more vegetables, fresh fruit, corn-based cereal, white meat, and fish.
A retrospective study of patients with Hurley stage 1 and 2 found that oral zinc gluconate, 90 mg a day, combined with 2% topical triclosan twice a day, resulted in significantly decreased HS scores and nodules and improved quality of life after 3 months. Expect vitamin D deficiency, she added.
Lastly, Dr. Shi recommended, if necessary, “weight loss to reduce the inflammatory burden.”
Rosacea
Dietary triggers for rosacea are thought to include high-fat foods, dairy foods, spicy foods, hot drinks, cinnamon, and vanilla.
A population-based case-control study in China, which evaluated 1,347 rosacea patients and 1,290 healthy controls, found that a high intake of fatty foods positively correlated with erythematotelangiectatic rosacea (ETR) and phymatous rosacea. High-frequency dairy intake negatively correlated with ETR and papulopustular rosacea, which was a surprise, she said. And in this study, no significant correlations were found between sweets, coffee, and spicy foods. That goes against the traditional thinking, she said, but this was a Chinese cohort and their diet is probably vastly different than those in the United States.
Other rosacea triggers, Dr. Shi said, are niacin-containing foods such as turkey, chicken breast, crustaceans, dried Shiitake mushrooms, peanuts, tuna, and liver, as well as cold drinks, and formalin-containing foods (fish, squid, tofu, wet noodles).
As the field of nutrigenics – how genes affect how the body responds to food – evolves, more answers about the impact of diet on these diseases will be forthcoming, Dr. Shi said.
In an interactive panel discussion, she was asked if she talks about diet with all her patients with acne, rosacea, and HS, or just those not responding to traditional therapy.
“I think it’s an important conversation to have,” Dr. Shi responded. “When I’m done with the medication [instructions], I say: ‘There is something else you can do to augment what I just told you.’ ” That’s when she explains the dietary information. She also has a handout on diet and routinely refers patients for dietary counseling.
MedscapeLive and this news organization are owned by the same parent company. Dr. Shi disclosed consulting, investigative and research funding from several sources, but not directly related to the content of her talk.
FROM MEDSCAPELIVE WOMEN’S & PEDIATRIC DERMATOLOGY SEMINAR
How much health insurers pay for almost everything is about to go public
perhaps helping answer a question that has long dogged those who buy insurance: Are we getting the best deal we can?
As of July 1, health insurers and self-insured employers must post on websites just about every price they’ve negotiated with providers for health care services, item by item. About the only thing excluded are the prices paid for prescription drugs, except those administered in hospitals or doctors’ offices.
The federally required data release could affect future prices or even how employers contract for health care. Many will see for the first time how well their insurers are doing, compared with others.
The new rules are far broader than those that went into effect in 2021 requiring hospitals to post their negotiated rates for the public to see. Now insurers must post the amounts paid for “every physician in network, every hospital, every surgery center, every nursing facility,” said Jeffrey Leibach, a partner at the consulting firm Guidehouse.
“When you start doing the math, you’re talking trillions of records,” he said. The fines the federal government could impose for noncompliance are also heftier than the penalties that hospitals face.
Federal officials learned from the hospital experience and gave insurers more direction on what was expected, said Mr. Leibach. Insurers or self-insured employers could be fined as much as $100 a day for each violation, for each affected enrollee if they fail to provide the data.
“Get your calculator out: All of a sudden you are in the millions pretty fast,” Mr. Leibach said.
Determined consumers, especially those with high-deductible health plans, may try to dig in right away and use the data to try comparing what they will have to pay at different hospitals, clinics, or doctor offices for specific services.
But each database’s enormous size may mean that most people “will find it very hard to use the data in a nuanced way,” said Katherine Baicker, dean of the University of Chicago Harris School of Public Policy.
At least at first.
Entrepreneurs are expected to quickly translate the information into more user-friendly formats so it can be incorporated into new or existing services that estimate costs for patients. And starting Jan. 1, the rules require insurers to provide online tools that will help people get up-front cost estimates for about 500 so-called “shoppable” services, meaning medical care they can schedule ahead of time.
Once those things happen, “you’ll at least have the options in front of you,” said Chris Severn, CEO of Turquoise Health, an online company that has posted price information made available under the rules for hospitals, although many hospitals have yet to comply.
With the addition of the insurers’ data, sites like his will be able to drill down further into cost variation from one place to another or among insurers.
“If you’re going to get an x-ray, you will be able to see that you can do it for $250 at this hospital, $75 at the imaging center down the road, or your specialist can do it in office for $25,” he said.
Everyone will know everyone else’s business: for example, how much insurers Aetna and Humana pay the same surgery center for a knee replacement.
The requirements stem from the Affordable Care Act and a 2019 executive order by then-President Donald Trump.
“These plans are supposed to be acting on behalf of employers in negotiating good rates, and the little insight we have on that shows it has not happened,” said Elizabeth Mitchell, president and CEO of the Purchaser Business Group on Health, an affiliation of employers who offer job-based health benefits to workers. “I do believe the dynamics are going to change.”
Other observers are more circumspect.
“Maybe at best this will reduce the wide variance of prices out there,” said Zack Cooper, director of health policy at the Yale University Institution for Social and Policy Studies, New Haven, Conn. “But it won’t be unleashing a consumer revolution.”
Still, the biggest value of the July data release may well be to shed light on how successful insurers have been at negotiating prices. It comes on the heels of research that has shown tremendous variation in what is paid for health care. A recent study by Rand, for example, shows that employers that offer job-based insurance plans paid, on average, 224% more than Medicare for the same services.
Tens of thousands of employers who buy insurance coverage for their workers will get this more-complete pricing picture – and may not like what they see.
“What we’re learning from the hospital data is that insurers are really bad at negotiating,” said Gerard Anderson, a professor in the department of health policy at the Johns Hopkins Bloomberg, Baltimore, citing research that found that negotiated rates for hospital care can be higher than what the facilities accept from patients who are not using insurance and are paying cash.
That could add to the frustration that Ms. Mitchell and others say employers have with the current health insurance system. More might try to contract with providers directly, only using insurance companies for claims processing.
Other employers may bring their insurers back to the bargaining table.
“For the first time, an employer will be able to go to an insurance company and say: ‘You have not negotiated a good-enough deal, and we know that because we can see the same provider has negotiated a better deal with another company,’ ” said James Gelfand, president of the ERISA Industry Committee, a trade group of self-insured employers.
If that happens, he added, “patients will be able to save money.”
That’s not necessarily a given, however.
Because this kind of public release of pricing data hasn’t been tried widely in health care before, how it will affect future spending remains uncertain. If insurers are pushed back to the bargaining table or providers see where they stand relative to their peers, prices could drop. However, some providers could raise their prices if they see they are charging less than their peers.
“Downward pressure may not be a given,” said Kelley Schultz, vice president of commercial policy for AHIP, the industry’s trade lobby.
Ms. Baicker said that, even after the data is out, rates will continue to be heavily influenced by local conditions, such as the size of an insurer or employer – providers often give bigger discounts, for example, to the insurers or self-insured employers that can send them the most patients. The number of hospitals in a region also matters – if an area has only one, for instance, that usually means the facility can demand higher rates.
Another unknown: Will insurers meet the deadline and provide usable data?
Ms. Schultz, at AHIP, said the industry is well on the way, partly because the original deadline was extended by 6 months. She expects insurers to do better than the hospital industry. “We saw a lot of hospitals that just decided not to post files or make them difficult to find,” she said.
So far, more than 300 noncompliant hospitals received warning letters from the government. But they could face fines of $300 a day fines for failing to comply, which is less than what insurers potentially face, although the federal government has recently upped the ante to up to $5,500 a day for the largest facilities.
Even after the pricing data is public, “I don’t think things will change overnight,” said Mr. Leibach. “Patients are still going to make care decisions based on their doctors and referrals, a lot of reasons other than price.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
perhaps helping answer a question that has long dogged those who buy insurance: Are we getting the best deal we can?
As of July 1, health insurers and self-insured employers must post on websites just about every price they’ve negotiated with providers for health care services, item by item. About the only thing excluded are the prices paid for prescription drugs, except those administered in hospitals or doctors’ offices.
The federally required data release could affect future prices or even how employers contract for health care. Many will see for the first time how well their insurers are doing, compared with others.
The new rules are far broader than those that went into effect in 2021 requiring hospitals to post their negotiated rates for the public to see. Now insurers must post the amounts paid for “every physician in network, every hospital, every surgery center, every nursing facility,” said Jeffrey Leibach, a partner at the consulting firm Guidehouse.
“When you start doing the math, you’re talking trillions of records,” he said. The fines the federal government could impose for noncompliance are also heftier than the penalties that hospitals face.
Federal officials learned from the hospital experience and gave insurers more direction on what was expected, said Mr. Leibach. Insurers or self-insured employers could be fined as much as $100 a day for each violation, for each affected enrollee if they fail to provide the data.
“Get your calculator out: All of a sudden you are in the millions pretty fast,” Mr. Leibach said.
Determined consumers, especially those with high-deductible health plans, may try to dig in right away and use the data to try comparing what they will have to pay at different hospitals, clinics, or doctor offices for specific services.
But each database’s enormous size may mean that most people “will find it very hard to use the data in a nuanced way,” said Katherine Baicker, dean of the University of Chicago Harris School of Public Policy.
At least at first.
Entrepreneurs are expected to quickly translate the information into more user-friendly formats so it can be incorporated into new or existing services that estimate costs for patients. And starting Jan. 1, the rules require insurers to provide online tools that will help people get up-front cost estimates for about 500 so-called “shoppable” services, meaning medical care they can schedule ahead of time.
Once those things happen, “you’ll at least have the options in front of you,” said Chris Severn, CEO of Turquoise Health, an online company that has posted price information made available under the rules for hospitals, although many hospitals have yet to comply.
With the addition of the insurers’ data, sites like his will be able to drill down further into cost variation from one place to another or among insurers.
“If you’re going to get an x-ray, you will be able to see that you can do it for $250 at this hospital, $75 at the imaging center down the road, or your specialist can do it in office for $25,” he said.
Everyone will know everyone else’s business: for example, how much insurers Aetna and Humana pay the same surgery center for a knee replacement.
The requirements stem from the Affordable Care Act and a 2019 executive order by then-President Donald Trump.
“These plans are supposed to be acting on behalf of employers in negotiating good rates, and the little insight we have on that shows it has not happened,” said Elizabeth Mitchell, president and CEO of the Purchaser Business Group on Health, an affiliation of employers who offer job-based health benefits to workers. “I do believe the dynamics are going to change.”
Other observers are more circumspect.
“Maybe at best this will reduce the wide variance of prices out there,” said Zack Cooper, director of health policy at the Yale University Institution for Social and Policy Studies, New Haven, Conn. “But it won’t be unleashing a consumer revolution.”
Still, the biggest value of the July data release may well be to shed light on how successful insurers have been at negotiating prices. It comes on the heels of research that has shown tremendous variation in what is paid for health care. A recent study by Rand, for example, shows that employers that offer job-based insurance plans paid, on average, 224% more than Medicare for the same services.
Tens of thousands of employers who buy insurance coverage for their workers will get this more-complete pricing picture – and may not like what they see.
“What we’re learning from the hospital data is that insurers are really bad at negotiating,” said Gerard Anderson, a professor in the department of health policy at the Johns Hopkins Bloomberg, Baltimore, citing research that found that negotiated rates for hospital care can be higher than what the facilities accept from patients who are not using insurance and are paying cash.
That could add to the frustration that Ms. Mitchell and others say employers have with the current health insurance system. More might try to contract with providers directly, only using insurance companies for claims processing.
Other employers may bring their insurers back to the bargaining table.
“For the first time, an employer will be able to go to an insurance company and say: ‘You have not negotiated a good-enough deal, and we know that because we can see the same provider has negotiated a better deal with another company,’ ” said James Gelfand, president of the ERISA Industry Committee, a trade group of self-insured employers.
If that happens, he added, “patients will be able to save money.”
That’s not necessarily a given, however.
Because this kind of public release of pricing data hasn’t been tried widely in health care before, how it will affect future spending remains uncertain. If insurers are pushed back to the bargaining table or providers see where they stand relative to their peers, prices could drop. However, some providers could raise their prices if they see they are charging less than their peers.
“Downward pressure may not be a given,” said Kelley Schultz, vice president of commercial policy for AHIP, the industry’s trade lobby.
Ms. Baicker said that, even after the data is out, rates will continue to be heavily influenced by local conditions, such as the size of an insurer or employer – providers often give bigger discounts, for example, to the insurers or self-insured employers that can send them the most patients. The number of hospitals in a region also matters – if an area has only one, for instance, that usually means the facility can demand higher rates.
Another unknown: Will insurers meet the deadline and provide usable data?
Ms. Schultz, at AHIP, said the industry is well on the way, partly because the original deadline was extended by 6 months. She expects insurers to do better than the hospital industry. “We saw a lot of hospitals that just decided not to post files or make them difficult to find,” she said.
So far, more than 300 noncompliant hospitals received warning letters from the government. But they could face fines of $300 a day fines for failing to comply, which is less than what insurers potentially face, although the federal government has recently upped the ante to up to $5,500 a day for the largest facilities.
Even after the pricing data is public, “I don’t think things will change overnight,” said Mr. Leibach. “Patients are still going to make care decisions based on their doctors and referrals, a lot of reasons other than price.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
perhaps helping answer a question that has long dogged those who buy insurance: Are we getting the best deal we can?
As of July 1, health insurers and self-insured employers must post on websites just about every price they’ve negotiated with providers for health care services, item by item. About the only thing excluded are the prices paid for prescription drugs, except those administered in hospitals or doctors’ offices.
The federally required data release could affect future prices or even how employers contract for health care. Many will see for the first time how well their insurers are doing, compared with others.
The new rules are far broader than those that went into effect in 2021 requiring hospitals to post their negotiated rates for the public to see. Now insurers must post the amounts paid for “every physician in network, every hospital, every surgery center, every nursing facility,” said Jeffrey Leibach, a partner at the consulting firm Guidehouse.
“When you start doing the math, you’re talking trillions of records,” he said. The fines the federal government could impose for noncompliance are also heftier than the penalties that hospitals face.
Federal officials learned from the hospital experience and gave insurers more direction on what was expected, said Mr. Leibach. Insurers or self-insured employers could be fined as much as $100 a day for each violation, for each affected enrollee if they fail to provide the data.
“Get your calculator out: All of a sudden you are in the millions pretty fast,” Mr. Leibach said.
Determined consumers, especially those with high-deductible health plans, may try to dig in right away and use the data to try comparing what they will have to pay at different hospitals, clinics, or doctor offices for specific services.
But each database’s enormous size may mean that most people “will find it very hard to use the data in a nuanced way,” said Katherine Baicker, dean of the University of Chicago Harris School of Public Policy.
At least at first.
Entrepreneurs are expected to quickly translate the information into more user-friendly formats so it can be incorporated into new or existing services that estimate costs for patients. And starting Jan. 1, the rules require insurers to provide online tools that will help people get up-front cost estimates for about 500 so-called “shoppable” services, meaning medical care they can schedule ahead of time.
Once those things happen, “you’ll at least have the options in front of you,” said Chris Severn, CEO of Turquoise Health, an online company that has posted price information made available under the rules for hospitals, although many hospitals have yet to comply.
With the addition of the insurers’ data, sites like his will be able to drill down further into cost variation from one place to another or among insurers.
“If you’re going to get an x-ray, you will be able to see that you can do it for $250 at this hospital, $75 at the imaging center down the road, or your specialist can do it in office for $25,” he said.
Everyone will know everyone else’s business: for example, how much insurers Aetna and Humana pay the same surgery center for a knee replacement.
The requirements stem from the Affordable Care Act and a 2019 executive order by then-President Donald Trump.
“These plans are supposed to be acting on behalf of employers in negotiating good rates, and the little insight we have on that shows it has not happened,” said Elizabeth Mitchell, president and CEO of the Purchaser Business Group on Health, an affiliation of employers who offer job-based health benefits to workers. “I do believe the dynamics are going to change.”
Other observers are more circumspect.
“Maybe at best this will reduce the wide variance of prices out there,” said Zack Cooper, director of health policy at the Yale University Institution for Social and Policy Studies, New Haven, Conn. “But it won’t be unleashing a consumer revolution.”
Still, the biggest value of the July data release may well be to shed light on how successful insurers have been at negotiating prices. It comes on the heels of research that has shown tremendous variation in what is paid for health care. A recent study by Rand, for example, shows that employers that offer job-based insurance plans paid, on average, 224% more than Medicare for the same services.
Tens of thousands of employers who buy insurance coverage for their workers will get this more-complete pricing picture – and may not like what they see.
“What we’re learning from the hospital data is that insurers are really bad at negotiating,” said Gerard Anderson, a professor in the department of health policy at the Johns Hopkins Bloomberg, Baltimore, citing research that found that negotiated rates for hospital care can be higher than what the facilities accept from patients who are not using insurance and are paying cash.
That could add to the frustration that Ms. Mitchell and others say employers have with the current health insurance system. More might try to contract with providers directly, only using insurance companies for claims processing.
Other employers may bring their insurers back to the bargaining table.
“For the first time, an employer will be able to go to an insurance company and say: ‘You have not negotiated a good-enough deal, and we know that because we can see the same provider has negotiated a better deal with another company,’ ” said James Gelfand, president of the ERISA Industry Committee, a trade group of self-insured employers.
If that happens, he added, “patients will be able to save money.”
That’s not necessarily a given, however.
Because this kind of public release of pricing data hasn’t been tried widely in health care before, how it will affect future spending remains uncertain. If insurers are pushed back to the bargaining table or providers see where they stand relative to their peers, prices could drop. However, some providers could raise their prices if they see they are charging less than their peers.
“Downward pressure may not be a given,” said Kelley Schultz, vice president of commercial policy for AHIP, the industry’s trade lobby.
Ms. Baicker said that, even after the data is out, rates will continue to be heavily influenced by local conditions, such as the size of an insurer or employer – providers often give bigger discounts, for example, to the insurers or self-insured employers that can send them the most patients. The number of hospitals in a region also matters – if an area has only one, for instance, that usually means the facility can demand higher rates.
Another unknown: Will insurers meet the deadline and provide usable data?
Ms. Schultz, at AHIP, said the industry is well on the way, partly because the original deadline was extended by 6 months. She expects insurers to do better than the hospital industry. “We saw a lot of hospitals that just decided not to post files or make them difficult to find,” she said.
So far, more than 300 noncompliant hospitals received warning letters from the government. But they could face fines of $300 a day fines for failing to comply, which is less than what insurers potentially face, although the federal government has recently upped the ante to up to $5,500 a day for the largest facilities.
Even after the pricing data is public, “I don’t think things will change overnight,” said Mr. Leibach. “Patients are still going to make care decisions based on their doctors and referrals, a lot of reasons other than price.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.