User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Youth killed by guns in U.S. equals classroom a day
according to the American Academy of Pediatrics.
Preventing firearm-related injuries and deaths in children and youth “demands a public safety approach like regulation of motor vehicles,” the group said.
The organization on Oct. 8 released an updated policy statement and technical report about gun violence and children at its 2022 annual meeting in Anaheim, Calif. The reports were published in the journal Pediatrics, and the authors plan to discuss them during the conference.
“Each day, 28 U.S. children and teens – the equivalent of a high school classroom – die from gun violence, making it the No. 1 killer of youth through age 24,” the AAP said in a statement about the reports. “The national death rate is significantly higher than all other high-income countries combined, largely due to an alarming increase in suicides and homicides that do not make national headlines.”
Firearms have become the leading cause of death among children in the United States.
In 2020, guns caused 10,197 deaths of Americans younger than 24, according to the Society for Adolescent Health and Medicine.
In 2015, more than 7,200 American youth were killed by firearms. That same year in 28 other high-income countries – which combined would have had a population twice that of the United States – just 685 youth were killed by firearms, according to the AAP.
Separately at the AAP conference, physicians are presenting new research about gun violence and children. And on Oct. 10, a pediatrician who was at Uvalde Memorial Hospital in Texas after the deadly school shooting in May is scheduled to address attendees. The doctor, Roy Guerrero, MD, testified on Capitol Hill to advocate for gun control after the shooting at Robb Elementary School, which killed 19 children and two adults.
“This is not a simple problem, and it cannot be fixed with a simple solution,” Lois K. Lee, MD, MPH, said in the AAP news release. Dr. Lee chairs the AAP Council on Injury, Violence, and Poison Prevention that wrote the new reports. “Pediatricians as a start can offer families guidance and education on more safely storing guns. AAP also calls for supporting legislation that, much like the common-sense requirements for obtaining a driver’s license, would improve gun ownership safety.”
Many deaths occur at home
The rate of homicide from firearms in U.S. youth, especially those aged 15-24 years, increased by 14% during the past decade, and the rate of suicide from firearms increased by 39%, according to the AAP.
Homicides account for 58% of youth firearm deaths, whereas suicides account for 37%. Another 2% of youth firearm deaths are unintentional, and 1% result from law enforcement actions, the group said.
Among children 12 years old and younger, about 85% of firearm deaths occur at home. Teen firearm deaths are about as likely to occur at home (39%) as on the street or sidewalk (38%), according to research based on 2014 data.
“School shootings represent a relatively new phenomenon over the last half-century, and the United States has the highest rate of school shootings in the world,” the AAP technical report noted. Between 1966 and 2008, according to the group, 44 such shootings occurred in the United States, or an average of about one per year. Fast forward a few years and the violence became dramatically worse: Between 2013 and 2015, officials counted 154 school shootings – or about one per week.
Still, school shootings are responsible for less than 1% of all firearm deaths among children 17 years or younger in the United States. While school shootings “receive a tremendous amount of attention,” the report stated, other child firearm deaths may be less likely to make national headlines.
“Many firearm tragedies escape public attention because they occur in a home, sometimes in a child’s own home or at a friend’s house, or their neighbor’s or grandparent’s residence,” Eric W. Fleegler, MD, MPH, Boston Children’s Hospital, a co-author of the new reports, said in a statement from AAP. “Research tells us that families tend to underestimate how children will behave when they encounter a gun and miscalculate the risks. Suicide risks are also a huge concern, especially in families where teens are struggling with their mental health.”
AAP-recommended actions include:
- Mental health screenings and safe gun storage education provided by clinicians as part of routine patient visits
- Increased funding for violence intervention programs in hospital and community settings
- Regulation of firearms like other consumer products, with national requirements that address training, licensing, insurance coverage, registration of individuals purchasing firearms, and safe storage
- The use of technology that allows only authorized users to pull the trigger
- Universal background checks that use federal databases and information from local police before all gun purchases
- Extreme risk protection order laws, or “red flag laws,” that prohibit individuals at risk for harming themselves or others from purchasing or owning a firearm
- More funding for firearm injury and prevention research.
A noticeable increase in the ED
Irma Ugalde, MD, associate professor and director of pediatric emergency medicine research at McGovern Medical School at UTHealth Houston, noticed that firearm-related injuries in children at her hospital were more common during the COVID-19 pandemic, even as pediatric emergency department visits decreased overall.
She and her colleagues studied the trends and reported their findings at the AAP meeting.
“We saw a drop in pediatric admissions overall,” Dr. Ugalde said in a statement about the study. “But what was really noticeable was that trauma was still very prevalent – in fact probably more so – and we were seeing more firearm injuries.”
The researchers found that firearm injuries in children rose from 88 cases in 2019 to 118 in 2020. The number of incidents remained elevated in 2021, with 115 cases.
In addition, the researchers found an initial increase in injuries occurring at home where the shooter was a known family member or friend, and in cases involving firearms that were not properly stored.
By comparison, pediatric ED visits overall decreased by 34.2% from 2019 to 2020, and by 11.8% from 2019 to 2021.
The increase in firearm injuries coincided with an increase in gun sales in the United States, the researchers noted.
“National and statewide initiatives to mitigate the risk of firearm-related injury and death are necessary,” Dr. Ugalde’s group said. “We recommend that health care workers remain vigilant about screening for potential risk factors and safe storage of firearms.”
Accidental injuries
Daniel D. Guzman, MD, with Cook Children’s Health Care Center, Fort Worth, Tex., conducted a study focused on unintentional firearm injuries in children. Dr. Guzman’s group analyzed data from 204 patients younger than age 19 seen at Cook Children’s from January 2015 to June 2021.
Dr. Guzman and his colleagues examined outcomes for injuries caused by powder guns – shotguns, rifles, and handguns – and air-power guns that shoot BBs and pellets.
The researchers found that 29% of the unintentional firearm injuries occurred with powder guns and 71% with air-power weapons, often BB guns.
“It is important that all firearms, powdered and air-powered, be stored safely in a lock box or safe,” Dr. Guzman said in a statement. To that end, Cook Children’s has developed a program called Aim for Safety to teach children and parents about the dangers of unsupervised play with BB guns and pellet guns, as well as the importance of storing all firearms unloaded and in a locked safe.
A version of this article first appeared on Medscape.com.
according to the American Academy of Pediatrics.
Preventing firearm-related injuries and deaths in children and youth “demands a public safety approach like regulation of motor vehicles,” the group said.
The organization on Oct. 8 released an updated policy statement and technical report about gun violence and children at its 2022 annual meeting in Anaheim, Calif. The reports were published in the journal Pediatrics, and the authors plan to discuss them during the conference.
“Each day, 28 U.S. children and teens – the equivalent of a high school classroom – die from gun violence, making it the No. 1 killer of youth through age 24,” the AAP said in a statement about the reports. “The national death rate is significantly higher than all other high-income countries combined, largely due to an alarming increase in suicides and homicides that do not make national headlines.”
Firearms have become the leading cause of death among children in the United States.
In 2020, guns caused 10,197 deaths of Americans younger than 24, according to the Society for Adolescent Health and Medicine.
In 2015, more than 7,200 American youth were killed by firearms. That same year in 28 other high-income countries – which combined would have had a population twice that of the United States – just 685 youth were killed by firearms, according to the AAP.
Separately at the AAP conference, physicians are presenting new research about gun violence and children. And on Oct. 10, a pediatrician who was at Uvalde Memorial Hospital in Texas after the deadly school shooting in May is scheduled to address attendees. The doctor, Roy Guerrero, MD, testified on Capitol Hill to advocate for gun control after the shooting at Robb Elementary School, which killed 19 children and two adults.
“This is not a simple problem, and it cannot be fixed with a simple solution,” Lois K. Lee, MD, MPH, said in the AAP news release. Dr. Lee chairs the AAP Council on Injury, Violence, and Poison Prevention that wrote the new reports. “Pediatricians as a start can offer families guidance and education on more safely storing guns. AAP also calls for supporting legislation that, much like the common-sense requirements for obtaining a driver’s license, would improve gun ownership safety.”
Many deaths occur at home
The rate of homicide from firearms in U.S. youth, especially those aged 15-24 years, increased by 14% during the past decade, and the rate of suicide from firearms increased by 39%, according to the AAP.
Homicides account for 58% of youth firearm deaths, whereas suicides account for 37%. Another 2% of youth firearm deaths are unintentional, and 1% result from law enforcement actions, the group said.
Among children 12 years old and younger, about 85% of firearm deaths occur at home. Teen firearm deaths are about as likely to occur at home (39%) as on the street or sidewalk (38%), according to research based on 2014 data.
“School shootings represent a relatively new phenomenon over the last half-century, and the United States has the highest rate of school shootings in the world,” the AAP technical report noted. Between 1966 and 2008, according to the group, 44 such shootings occurred in the United States, or an average of about one per year. Fast forward a few years and the violence became dramatically worse: Between 2013 and 2015, officials counted 154 school shootings – or about one per week.
Still, school shootings are responsible for less than 1% of all firearm deaths among children 17 years or younger in the United States. While school shootings “receive a tremendous amount of attention,” the report stated, other child firearm deaths may be less likely to make national headlines.
“Many firearm tragedies escape public attention because they occur in a home, sometimes in a child’s own home or at a friend’s house, or their neighbor’s or grandparent’s residence,” Eric W. Fleegler, MD, MPH, Boston Children’s Hospital, a co-author of the new reports, said in a statement from AAP. “Research tells us that families tend to underestimate how children will behave when they encounter a gun and miscalculate the risks. Suicide risks are also a huge concern, especially in families where teens are struggling with their mental health.”
AAP-recommended actions include:
- Mental health screenings and safe gun storage education provided by clinicians as part of routine patient visits
- Increased funding for violence intervention programs in hospital and community settings
- Regulation of firearms like other consumer products, with national requirements that address training, licensing, insurance coverage, registration of individuals purchasing firearms, and safe storage
- The use of technology that allows only authorized users to pull the trigger
- Universal background checks that use federal databases and information from local police before all gun purchases
- Extreme risk protection order laws, or “red flag laws,” that prohibit individuals at risk for harming themselves or others from purchasing or owning a firearm
- More funding for firearm injury and prevention research.
A noticeable increase in the ED
Irma Ugalde, MD, associate professor and director of pediatric emergency medicine research at McGovern Medical School at UTHealth Houston, noticed that firearm-related injuries in children at her hospital were more common during the COVID-19 pandemic, even as pediatric emergency department visits decreased overall.
She and her colleagues studied the trends and reported their findings at the AAP meeting.
“We saw a drop in pediatric admissions overall,” Dr. Ugalde said in a statement about the study. “But what was really noticeable was that trauma was still very prevalent – in fact probably more so – and we were seeing more firearm injuries.”
The researchers found that firearm injuries in children rose from 88 cases in 2019 to 118 in 2020. The number of incidents remained elevated in 2021, with 115 cases.
In addition, the researchers found an initial increase in injuries occurring at home where the shooter was a known family member or friend, and in cases involving firearms that were not properly stored.
By comparison, pediatric ED visits overall decreased by 34.2% from 2019 to 2020, and by 11.8% from 2019 to 2021.
The increase in firearm injuries coincided with an increase in gun sales in the United States, the researchers noted.
“National and statewide initiatives to mitigate the risk of firearm-related injury and death are necessary,” Dr. Ugalde’s group said. “We recommend that health care workers remain vigilant about screening for potential risk factors and safe storage of firearms.”
Accidental injuries
Daniel D. Guzman, MD, with Cook Children’s Health Care Center, Fort Worth, Tex., conducted a study focused on unintentional firearm injuries in children. Dr. Guzman’s group analyzed data from 204 patients younger than age 19 seen at Cook Children’s from January 2015 to June 2021.
Dr. Guzman and his colleagues examined outcomes for injuries caused by powder guns – shotguns, rifles, and handguns – and air-power guns that shoot BBs and pellets.
The researchers found that 29% of the unintentional firearm injuries occurred with powder guns and 71% with air-power weapons, often BB guns.
“It is important that all firearms, powdered and air-powered, be stored safely in a lock box or safe,” Dr. Guzman said in a statement. To that end, Cook Children’s has developed a program called Aim for Safety to teach children and parents about the dangers of unsupervised play with BB guns and pellet guns, as well as the importance of storing all firearms unloaded and in a locked safe.
A version of this article first appeared on Medscape.com.
according to the American Academy of Pediatrics.
Preventing firearm-related injuries and deaths in children and youth “demands a public safety approach like regulation of motor vehicles,” the group said.
The organization on Oct. 8 released an updated policy statement and technical report about gun violence and children at its 2022 annual meeting in Anaheim, Calif. The reports were published in the journal Pediatrics, and the authors plan to discuss them during the conference.
“Each day, 28 U.S. children and teens – the equivalent of a high school classroom – die from gun violence, making it the No. 1 killer of youth through age 24,” the AAP said in a statement about the reports. “The national death rate is significantly higher than all other high-income countries combined, largely due to an alarming increase in suicides and homicides that do not make national headlines.”
Firearms have become the leading cause of death among children in the United States.
In 2020, guns caused 10,197 deaths of Americans younger than 24, according to the Society for Adolescent Health and Medicine.
In 2015, more than 7,200 American youth were killed by firearms. That same year in 28 other high-income countries – which combined would have had a population twice that of the United States – just 685 youth were killed by firearms, according to the AAP.
Separately at the AAP conference, physicians are presenting new research about gun violence and children. And on Oct. 10, a pediatrician who was at Uvalde Memorial Hospital in Texas after the deadly school shooting in May is scheduled to address attendees. The doctor, Roy Guerrero, MD, testified on Capitol Hill to advocate for gun control after the shooting at Robb Elementary School, which killed 19 children and two adults.
“This is not a simple problem, and it cannot be fixed with a simple solution,” Lois K. Lee, MD, MPH, said in the AAP news release. Dr. Lee chairs the AAP Council on Injury, Violence, and Poison Prevention that wrote the new reports. “Pediatricians as a start can offer families guidance and education on more safely storing guns. AAP also calls for supporting legislation that, much like the common-sense requirements for obtaining a driver’s license, would improve gun ownership safety.”
Many deaths occur at home
The rate of homicide from firearms in U.S. youth, especially those aged 15-24 years, increased by 14% during the past decade, and the rate of suicide from firearms increased by 39%, according to the AAP.
Homicides account for 58% of youth firearm deaths, whereas suicides account for 37%. Another 2% of youth firearm deaths are unintentional, and 1% result from law enforcement actions, the group said.
Among children 12 years old and younger, about 85% of firearm deaths occur at home. Teen firearm deaths are about as likely to occur at home (39%) as on the street or sidewalk (38%), according to research based on 2014 data.
“School shootings represent a relatively new phenomenon over the last half-century, and the United States has the highest rate of school shootings in the world,” the AAP technical report noted. Between 1966 and 2008, according to the group, 44 such shootings occurred in the United States, or an average of about one per year. Fast forward a few years and the violence became dramatically worse: Between 2013 and 2015, officials counted 154 school shootings – or about one per week.
Still, school shootings are responsible for less than 1% of all firearm deaths among children 17 years or younger in the United States. While school shootings “receive a tremendous amount of attention,” the report stated, other child firearm deaths may be less likely to make national headlines.
“Many firearm tragedies escape public attention because they occur in a home, sometimes in a child’s own home or at a friend’s house, or their neighbor’s or grandparent’s residence,” Eric W. Fleegler, MD, MPH, Boston Children’s Hospital, a co-author of the new reports, said in a statement from AAP. “Research tells us that families tend to underestimate how children will behave when they encounter a gun and miscalculate the risks. Suicide risks are also a huge concern, especially in families where teens are struggling with their mental health.”
AAP-recommended actions include:
- Mental health screenings and safe gun storage education provided by clinicians as part of routine patient visits
- Increased funding for violence intervention programs in hospital and community settings
- Regulation of firearms like other consumer products, with national requirements that address training, licensing, insurance coverage, registration of individuals purchasing firearms, and safe storage
- The use of technology that allows only authorized users to pull the trigger
- Universal background checks that use federal databases and information from local police before all gun purchases
- Extreme risk protection order laws, or “red flag laws,” that prohibit individuals at risk for harming themselves or others from purchasing or owning a firearm
- More funding for firearm injury and prevention research.
A noticeable increase in the ED
Irma Ugalde, MD, associate professor and director of pediatric emergency medicine research at McGovern Medical School at UTHealth Houston, noticed that firearm-related injuries in children at her hospital were more common during the COVID-19 pandemic, even as pediatric emergency department visits decreased overall.
She and her colleagues studied the trends and reported their findings at the AAP meeting.
“We saw a drop in pediatric admissions overall,” Dr. Ugalde said in a statement about the study. “But what was really noticeable was that trauma was still very prevalent – in fact probably more so – and we were seeing more firearm injuries.”
The researchers found that firearm injuries in children rose from 88 cases in 2019 to 118 in 2020. The number of incidents remained elevated in 2021, with 115 cases.
In addition, the researchers found an initial increase in injuries occurring at home where the shooter was a known family member or friend, and in cases involving firearms that were not properly stored.
By comparison, pediatric ED visits overall decreased by 34.2% from 2019 to 2020, and by 11.8% from 2019 to 2021.
The increase in firearm injuries coincided with an increase in gun sales in the United States, the researchers noted.
“National and statewide initiatives to mitigate the risk of firearm-related injury and death are necessary,” Dr. Ugalde’s group said. “We recommend that health care workers remain vigilant about screening for potential risk factors and safe storage of firearms.”
Accidental injuries
Daniel D. Guzman, MD, with Cook Children’s Health Care Center, Fort Worth, Tex., conducted a study focused on unintentional firearm injuries in children. Dr. Guzman’s group analyzed data from 204 patients younger than age 19 seen at Cook Children’s from January 2015 to June 2021.
Dr. Guzman and his colleagues examined outcomes for injuries caused by powder guns – shotguns, rifles, and handguns – and air-power guns that shoot BBs and pellets.
The researchers found that 29% of the unintentional firearm injuries occurred with powder guns and 71% with air-power weapons, often BB guns.
“It is important that all firearms, powdered and air-powered, be stored safely in a lock box or safe,” Dr. Guzman said in a statement. To that end, Cook Children’s has developed a program called Aim for Safety to teach children and parents about the dangers of unsupervised play with BB guns and pellet guns, as well as the importance of storing all firearms unloaded and in a locked safe.
A version of this article first appeared on Medscape.com.
FROM PEDIATRICS
Physicians speak out: Why they love or hate incentive bonuses
Incentive bonuses have long been part and parcel of many physicians’ compensation packages. They allow doctors in some specialties to boost their compensation by tens of thousands of dollars.
Often tied to metrics that doctors must hit,
A recent Medscape poll asked what physicians think about incentive bonuses and whether or not tying metrics to salary is an outdated practice that interferes with the integrity of a physician’s job or contributes to excellence in patient care and increased productivity.
Here is what 406 physicians who answered the poll, which ran from Aug. 17 to Sept. 1, had to say about incentive bonuses:
More than half the physicians polled (58%) received an incentive bonus in 2021. Of those who received a bonus, 44% received up to $25,000. Almost 30% received $25,001-$50,000 in incentive bonus money. Only 14% received more than $100,000.
When we asked physicians which metrics they prefer their bonus to be based on, a large majority (64%) agreed quality of care was most relevant. Other metrics that respondents think appropriate included professionalism (40%), patient outcomes (40%), patient satisfaction (34%), patient volume (26%), market expansion (7%), and other (3%).
The problem with bonuses
Once thought to improve quality and consistency of care, incentive bonuses may be falling out of favor. Developing, administrating, and tracking them may be cumbersome for the institutions that advocate for them. For instance, determining who gave quality care and how to measure that care can be difficult.
What’s more, some top health care employers, Mayo Clinic and Kaiser Permanente, have switched from the incentive bonus model to straight salaries. Data show that the number of tests patients have and the number of treatments they try decreases when doctors receive straight salaries.
In fact, 74% of the polled physicians think that bonuses can result in consequences like unnecessary tests and higher patient costs. Three-fourths of respondents don’t think incentives improve patient care either.
Physicians have long thought incentive bonuses can also have unintended consequences. For example, tying a physician’s monetary reward to metrics such as patient outcomes, like adherence to treatment protocols, may mean that noncompliant patients can jeopardize your metrics and prevent physicians from getting bonuses.
A Merritt Hawkins’ 2019 Review of Physician and Advanced Practitioner Recruiting Incentives found that 56% of bonuses are based in whole or in part on metrics like a patient’s adherence.
Additionally, tying monetary rewards to patient volume encourages some physicians to overbook patients, work more and longer hours, and risk burnout to meet their bonus criteria.
When we asked how hard it was to meet metrics in the Medscape poll, 45% of respondents who receive incentive bonuses said it was somewhat or very difficult. Only 9% consider it very easy. And 71% of physicians say their bonus is at risk because of not meeting their metrics.
Not surprisingly, large pay-for-performance bonuses are only offered to certain specialists and physician specialties in high demand. An orthopedist, for example, can earn up to an average of $126,000 in incentive bonuses, while a pediatrician brings in an average of $28,000, according to the Medscape Physician Compensation Report 2022.
Yet physicians are still torn
Despite these negatives, physicians are split about whether bonuses are good for doctors. The poll shows 51% said no, and 49% said yes. Further, physicians were split 50-50 on whether the bonus makes physicians more productive. Interestingly though, 76% think the bonus compensation method should be phased out in favor of straight salaries.
But many physicians may welcome the “lump sum” nature of receiving large bonuses at certain times of the year to help pay off student loan debt or other expenses, or are just comfortable having a bonus.
Financially speaking
If you have the choice, you may fare better by taking a higher salary and eliminating a bonus. Receiving your pay throughout the year may be preferable to receiving large lump sums only at certain times. Another thing to remember about your incentive bonus is that they are sometimes taxed more heavily based on “supplemental income.” The IRS considers bonuses supplemental to your income, so they may have a higher withholding rate, which can feel penalizing. You may have noticed the extra withholding in your last bonus check.
A version of this article first appeared on Medscape.com.
Incentive bonuses have long been part and parcel of many physicians’ compensation packages. They allow doctors in some specialties to boost their compensation by tens of thousands of dollars.
Often tied to metrics that doctors must hit,
A recent Medscape poll asked what physicians think about incentive bonuses and whether or not tying metrics to salary is an outdated practice that interferes with the integrity of a physician’s job or contributes to excellence in patient care and increased productivity.
Here is what 406 physicians who answered the poll, which ran from Aug. 17 to Sept. 1, had to say about incentive bonuses:
More than half the physicians polled (58%) received an incentive bonus in 2021. Of those who received a bonus, 44% received up to $25,000. Almost 30% received $25,001-$50,000 in incentive bonus money. Only 14% received more than $100,000.
When we asked physicians which metrics they prefer their bonus to be based on, a large majority (64%) agreed quality of care was most relevant. Other metrics that respondents think appropriate included professionalism (40%), patient outcomes (40%), patient satisfaction (34%), patient volume (26%), market expansion (7%), and other (3%).
The problem with bonuses
Once thought to improve quality and consistency of care, incentive bonuses may be falling out of favor. Developing, administrating, and tracking them may be cumbersome for the institutions that advocate for them. For instance, determining who gave quality care and how to measure that care can be difficult.
What’s more, some top health care employers, Mayo Clinic and Kaiser Permanente, have switched from the incentive bonus model to straight salaries. Data show that the number of tests patients have and the number of treatments they try decreases when doctors receive straight salaries.
In fact, 74% of the polled physicians think that bonuses can result in consequences like unnecessary tests and higher patient costs. Three-fourths of respondents don’t think incentives improve patient care either.
Physicians have long thought incentive bonuses can also have unintended consequences. For example, tying a physician’s monetary reward to metrics such as patient outcomes, like adherence to treatment protocols, may mean that noncompliant patients can jeopardize your metrics and prevent physicians from getting bonuses.
A Merritt Hawkins’ 2019 Review of Physician and Advanced Practitioner Recruiting Incentives found that 56% of bonuses are based in whole or in part on metrics like a patient’s adherence.
Additionally, tying monetary rewards to patient volume encourages some physicians to overbook patients, work more and longer hours, and risk burnout to meet their bonus criteria.
When we asked how hard it was to meet metrics in the Medscape poll, 45% of respondents who receive incentive bonuses said it was somewhat or very difficult. Only 9% consider it very easy. And 71% of physicians say their bonus is at risk because of not meeting their metrics.
Not surprisingly, large pay-for-performance bonuses are only offered to certain specialists and physician specialties in high demand. An orthopedist, for example, can earn up to an average of $126,000 in incentive bonuses, while a pediatrician brings in an average of $28,000, according to the Medscape Physician Compensation Report 2022.
Yet physicians are still torn
Despite these negatives, physicians are split about whether bonuses are good for doctors. The poll shows 51% said no, and 49% said yes. Further, physicians were split 50-50 on whether the bonus makes physicians more productive. Interestingly though, 76% think the bonus compensation method should be phased out in favor of straight salaries.
But many physicians may welcome the “lump sum” nature of receiving large bonuses at certain times of the year to help pay off student loan debt or other expenses, or are just comfortable having a bonus.
Financially speaking
If you have the choice, you may fare better by taking a higher salary and eliminating a bonus. Receiving your pay throughout the year may be preferable to receiving large lump sums only at certain times. Another thing to remember about your incentive bonus is that they are sometimes taxed more heavily based on “supplemental income.” The IRS considers bonuses supplemental to your income, so they may have a higher withholding rate, which can feel penalizing. You may have noticed the extra withholding in your last bonus check.
A version of this article first appeared on Medscape.com.
Incentive bonuses have long been part and parcel of many physicians’ compensation packages. They allow doctors in some specialties to boost their compensation by tens of thousands of dollars.
Often tied to metrics that doctors must hit,
A recent Medscape poll asked what physicians think about incentive bonuses and whether or not tying metrics to salary is an outdated practice that interferes with the integrity of a physician’s job or contributes to excellence in patient care and increased productivity.
Here is what 406 physicians who answered the poll, which ran from Aug. 17 to Sept. 1, had to say about incentive bonuses:
More than half the physicians polled (58%) received an incentive bonus in 2021. Of those who received a bonus, 44% received up to $25,000. Almost 30% received $25,001-$50,000 in incentive bonus money. Only 14% received more than $100,000.
When we asked physicians which metrics they prefer their bonus to be based on, a large majority (64%) agreed quality of care was most relevant. Other metrics that respondents think appropriate included professionalism (40%), patient outcomes (40%), patient satisfaction (34%), patient volume (26%), market expansion (7%), and other (3%).
The problem with bonuses
Once thought to improve quality and consistency of care, incentive bonuses may be falling out of favor. Developing, administrating, and tracking them may be cumbersome for the institutions that advocate for them. For instance, determining who gave quality care and how to measure that care can be difficult.
What’s more, some top health care employers, Mayo Clinic and Kaiser Permanente, have switched from the incentive bonus model to straight salaries. Data show that the number of tests patients have and the number of treatments they try decreases when doctors receive straight salaries.
In fact, 74% of the polled physicians think that bonuses can result in consequences like unnecessary tests and higher patient costs. Three-fourths of respondents don’t think incentives improve patient care either.
Physicians have long thought incentive bonuses can also have unintended consequences. For example, tying a physician’s monetary reward to metrics such as patient outcomes, like adherence to treatment protocols, may mean that noncompliant patients can jeopardize your metrics and prevent physicians from getting bonuses.
A Merritt Hawkins’ 2019 Review of Physician and Advanced Practitioner Recruiting Incentives found that 56% of bonuses are based in whole or in part on metrics like a patient’s adherence.
Additionally, tying monetary rewards to patient volume encourages some physicians to overbook patients, work more and longer hours, and risk burnout to meet their bonus criteria.
When we asked how hard it was to meet metrics in the Medscape poll, 45% of respondents who receive incentive bonuses said it was somewhat or very difficult. Only 9% consider it very easy. And 71% of physicians say their bonus is at risk because of not meeting their metrics.
Not surprisingly, large pay-for-performance bonuses are only offered to certain specialists and physician specialties in high demand. An orthopedist, for example, can earn up to an average of $126,000 in incentive bonuses, while a pediatrician brings in an average of $28,000, according to the Medscape Physician Compensation Report 2022.
Yet physicians are still torn
Despite these negatives, physicians are split about whether bonuses are good for doctors. The poll shows 51% said no, and 49% said yes. Further, physicians were split 50-50 on whether the bonus makes physicians more productive. Interestingly though, 76% think the bonus compensation method should be phased out in favor of straight salaries.
But many physicians may welcome the “lump sum” nature of receiving large bonuses at certain times of the year to help pay off student loan debt or other expenses, or are just comfortable having a bonus.
Financially speaking
If you have the choice, you may fare better by taking a higher salary and eliminating a bonus. Receiving your pay throughout the year may be preferable to receiving large lump sums only at certain times. Another thing to remember about your incentive bonus is that they are sometimes taxed more heavily based on “supplemental income.” The IRS considers bonuses supplemental to your income, so they may have a higher withholding rate, which can feel penalizing. You may have noticed the extra withholding in your last bonus check.
A version of this article first appeared on Medscape.com.
Three COVID scenarios that could spell trouble for the fall
As the United States enters a third fall with COVID-19, the virus for many is seemingly gone – or at least out of mind. But for those keeping watch, it is far from forgotten as deaths and infections continue to mount at a lower but steady pace.
What does that mean for the upcoming months? Experts predict different scenarios, some more dire than others – with one more encouraging.
In the United States, more than 300 people still die every day from COVID and more than 44,000 new daily cases are reported, according to the Centers for Disease Control and Prevention.
But progress is undeniable. The stark daily death tolls of 2020 have plummeted. Vaccines and treatments have dramatically reduced severe illness, and mask requirements have mostly turned to personal preference.
among them more-resistant variants coupled with waning immunity, the potential for a “twindemic” with a flu/COVID onslaught, and underuse of lifesaving vaccines and treatments.
Variants loom/waning immunity
Omicron variant BA.5 still makes up about 80% of infections in the United States, followed by BA4.6, according to the CDC, but other subvariants are emerging and showing signs of resistance to current antiviral treatments.
Eric Topol, MD, founder and director of the Scripps Research Translational Institute in San Diego, said about COVID this fall: “There will be another wave, magnitude unknown.”
He said subvariants XBB and BQ.1.1 “have extreme levels of immune evasion and both could pose a challenge,” explaining that XBB is more likely to cause trouble than BQ.1.1 because it is even more resistant to natural or vaccine-induced immunity.
Dr. Topol pointed to new research on those variants in a preprint posted on bioRxiv. The authors’ conclusion: “These results suggest that current herd immunity and BA.5 vaccine boosters may not provide sufficiently broad protection against infection.”
Another variant to watch, some experts say, is Omicron subvariant BA.2.75.2, which has shown resistance to antiviral treatments. It is also growing at a rather alarming rate, says Michael Sweat, PhD, director of the Medical University of South Carolina Center for Global Health in Charleston. That subvariant currently makes up under 2% of U.S. cases but has spread to at least 55 countries and 43 U.S. states after first appearing at the end of last year globally and in mid-June in the United States.
A non–peer-reviewed preprint study from Sweden found that the variant in blood samples was neutralized on average “at titers approximately 6.5 times lower than BA.5, making BA.2.75.2 the most [neutralization-resistant] variant evaluated to date.”
Katelyn Jetelina, PhD, assistant professor in the department of epidemiology at University of Texas Health Science Center, Houston, said in an interview the U.S. waves often follow Europe’s, and Europe has seen a recent spike in cases and hospitalizations not related to Omicron subvariants, but to weather changes, waning immunity, and changes in behavior.
The World Health Organization reported on Oct. 5 that, while cases were down in every other region of the world, Europe’s numbers stand out, with an 8% increase in cases from the week before.
Dr. Jetelina cited events such as Oktoberfest in Germany, which ended in the first week of October after drawing nearly 6 million people over 2 weeks, as a potential contributor, and people heading indoors as weather patterns change in Europe.
Ali Mokdad, PhD, chief strategy officer for population health at the University of Washington, Seattle, said in an interview he is less worried about the documented variants we know about than he is about the potential for a new immune-escape variety yet to emerge.
“Right now we know the Chinese are gearing up to open up the country, and because they have low immunity and little infection, we expect in China there will be a lot of spread of Omicron,” he said. “It’s possible because of the number of infections we could see a new variant.”
Dr. Mokdad said waning immunity could also leave populations vulnerable to variants.
“Even if you get infected, after about 5 months, you’re susceptible again. Remember, most of the infections from Omicron happened in January or February 2022, and we had two waves after that,” he said.
The new bivalent vaccines tweaked to target some Omicron variants will help, Dr. Mokdad said, but he noted, “people are very reluctant to take it.”
Jennifer Nuzzo, DrPH, professor of epidemiology and director of the Pandemic Center at Brown University, Providence, R.I., worries that in the United States we have less ability this year to track variants as funding has receded for testing kits and testing sites. Most people are testing at home – which doesn’t show up in the numbers – and the United States is relying more on other countries’ data to spot trends.
“I think we’re just going to have less visibility into the circulation of this virus,” she said in an interview.
‘Twindemic’: COVID and flu
Dr. Jetelina noted Australia and New Zealand just wrapped up a flu season that saw flu numbers returning to normal after a sharp drop in the last 2 years, and North America typically follows suit.
“We do expect flu will be here in the United States and probably at levels that we saw prepandemic. We’re all holding our breath to see how our health systems hold up with COVID-19 and flu. We haven’t really experienced that yet,” she said.
There is some disagreement, however, about the possibility of a so-called “twindemic” of influenza and COVID.
Richard Webby, PhD, an infectious disease specialist at St. Jude Children’s Research Hospital in Memphis, said in an interview he thinks the possibility of both viruses spiking at the same time is unlikely.
“That’s not to say we won’t get flu and COVID activity in the same winter,” he explained, “but I think both roaring at the same time is unlikely.”
As an indicator, he said, at the beginning of the flu season last year in the Northern Hemisphere, flu activity started to pick up, but when the Omicron variant came along, “flu just wasn’t able to compete in that same environment and flu numbers dropped right off.” Previous literature suggests that when one virus is spiking it’s hard for another respiratory virus to take hold.
Vaccine, treatment underuse
Another threat is vaccines, boosters, and treatments sitting on shelves.
Dr. Sweat referred to frustration with vaccine uptake that seems to be “frozen in amber.”
As of Oct. 4, only 5.3% of people in the United States who were eligible had received the updated booster launched in early September.
Dr. Nuzzo said boosters for people at least 65 years old will be key to severity of COVID this season.
“I think that’s probably the biggest factor going into the fall and winter,” she said.
Only 38% of people at least 50 years old and 45% of those at least 65 years old had gotten a second booster as of early October.
“If we do nothing else, we have to increase booster uptake in that group,” Dr. Nuzzo said.
She said the treatment nirmatrelvir/ritonavir (Paxlovid, Pfizer) for treating mild to moderate COVID-19 in patients at high risk for severe disease is greatly underused, often because providers aren’t prescribing it because they don’t think it helps, are worried about drug interactions, or are worried about its “rebound” effect.
Dr. Nuzzo urged greater use of the drug and education on how to manage drug interactions.
“We have very strong data that it does help keep people out of hospital. Sure, there may be a rebound, but that pales in comparison to the risk of being hospitalized,” she said.
Calm COVID season?
Not all predictions are dire. There is another little-talked-about scenario, Dr. Sweat said – that we could be in for a calm COVID season, and those who seem to be only mildly concerned about COVID may find those thoughts justified in the numbers.
Omicron blew through with such strength, he noted, that it may have left wide immunity in its wake. Because variants seem to be staying in the Omicron family, that may signal optimism.
“If the next variant is a descendant of the Omicron lineage, I would suspect that all these people who just got infected will have some protection, not perfect, but quite a bit of protection,” Dr. Sweat said.
Dr. Topol, Dr. Nuzzo, Dr. Sweat, Dr. Webby, Dr. Mokdad, and Dr. Jetelina reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As the United States enters a third fall with COVID-19, the virus for many is seemingly gone – or at least out of mind. But for those keeping watch, it is far from forgotten as deaths and infections continue to mount at a lower but steady pace.
What does that mean for the upcoming months? Experts predict different scenarios, some more dire than others – with one more encouraging.
In the United States, more than 300 people still die every day from COVID and more than 44,000 new daily cases are reported, according to the Centers for Disease Control and Prevention.
But progress is undeniable. The stark daily death tolls of 2020 have plummeted. Vaccines and treatments have dramatically reduced severe illness, and mask requirements have mostly turned to personal preference.
among them more-resistant variants coupled with waning immunity, the potential for a “twindemic” with a flu/COVID onslaught, and underuse of lifesaving vaccines and treatments.
Variants loom/waning immunity
Omicron variant BA.5 still makes up about 80% of infections in the United States, followed by BA4.6, according to the CDC, but other subvariants are emerging and showing signs of resistance to current antiviral treatments.
Eric Topol, MD, founder and director of the Scripps Research Translational Institute in San Diego, said about COVID this fall: “There will be another wave, magnitude unknown.”
He said subvariants XBB and BQ.1.1 “have extreme levels of immune evasion and both could pose a challenge,” explaining that XBB is more likely to cause trouble than BQ.1.1 because it is even more resistant to natural or vaccine-induced immunity.
Dr. Topol pointed to new research on those variants in a preprint posted on bioRxiv. The authors’ conclusion: “These results suggest that current herd immunity and BA.5 vaccine boosters may not provide sufficiently broad protection against infection.”
Another variant to watch, some experts say, is Omicron subvariant BA.2.75.2, which has shown resistance to antiviral treatments. It is also growing at a rather alarming rate, says Michael Sweat, PhD, director of the Medical University of South Carolina Center for Global Health in Charleston. That subvariant currently makes up under 2% of U.S. cases but has spread to at least 55 countries and 43 U.S. states after first appearing at the end of last year globally and in mid-June in the United States.
A non–peer-reviewed preprint study from Sweden found that the variant in blood samples was neutralized on average “at titers approximately 6.5 times lower than BA.5, making BA.2.75.2 the most [neutralization-resistant] variant evaluated to date.”
Katelyn Jetelina, PhD, assistant professor in the department of epidemiology at University of Texas Health Science Center, Houston, said in an interview the U.S. waves often follow Europe’s, and Europe has seen a recent spike in cases and hospitalizations not related to Omicron subvariants, but to weather changes, waning immunity, and changes in behavior.
The World Health Organization reported on Oct. 5 that, while cases were down in every other region of the world, Europe’s numbers stand out, with an 8% increase in cases from the week before.
Dr. Jetelina cited events such as Oktoberfest in Germany, which ended in the first week of October after drawing nearly 6 million people over 2 weeks, as a potential contributor, and people heading indoors as weather patterns change in Europe.
Ali Mokdad, PhD, chief strategy officer for population health at the University of Washington, Seattle, said in an interview he is less worried about the documented variants we know about than he is about the potential for a new immune-escape variety yet to emerge.
“Right now we know the Chinese are gearing up to open up the country, and because they have low immunity and little infection, we expect in China there will be a lot of spread of Omicron,” he said. “It’s possible because of the number of infections we could see a new variant.”
Dr. Mokdad said waning immunity could also leave populations vulnerable to variants.
“Even if you get infected, after about 5 months, you’re susceptible again. Remember, most of the infections from Omicron happened in January or February 2022, and we had two waves after that,” he said.
The new bivalent vaccines tweaked to target some Omicron variants will help, Dr. Mokdad said, but he noted, “people are very reluctant to take it.”
Jennifer Nuzzo, DrPH, professor of epidemiology and director of the Pandemic Center at Brown University, Providence, R.I., worries that in the United States we have less ability this year to track variants as funding has receded for testing kits and testing sites. Most people are testing at home – which doesn’t show up in the numbers – and the United States is relying more on other countries’ data to spot trends.
“I think we’re just going to have less visibility into the circulation of this virus,” she said in an interview.
‘Twindemic’: COVID and flu
Dr. Jetelina noted Australia and New Zealand just wrapped up a flu season that saw flu numbers returning to normal after a sharp drop in the last 2 years, and North America typically follows suit.
“We do expect flu will be here in the United States and probably at levels that we saw prepandemic. We’re all holding our breath to see how our health systems hold up with COVID-19 and flu. We haven’t really experienced that yet,” she said.
There is some disagreement, however, about the possibility of a so-called “twindemic” of influenza and COVID.
Richard Webby, PhD, an infectious disease specialist at St. Jude Children’s Research Hospital in Memphis, said in an interview he thinks the possibility of both viruses spiking at the same time is unlikely.
“That’s not to say we won’t get flu and COVID activity in the same winter,” he explained, “but I think both roaring at the same time is unlikely.”
As an indicator, he said, at the beginning of the flu season last year in the Northern Hemisphere, flu activity started to pick up, but when the Omicron variant came along, “flu just wasn’t able to compete in that same environment and flu numbers dropped right off.” Previous literature suggests that when one virus is spiking it’s hard for another respiratory virus to take hold.
Vaccine, treatment underuse
Another threat is vaccines, boosters, and treatments sitting on shelves.
Dr. Sweat referred to frustration with vaccine uptake that seems to be “frozen in amber.”
As of Oct. 4, only 5.3% of people in the United States who were eligible had received the updated booster launched in early September.
Dr. Nuzzo said boosters for people at least 65 years old will be key to severity of COVID this season.
“I think that’s probably the biggest factor going into the fall and winter,” she said.
Only 38% of people at least 50 years old and 45% of those at least 65 years old had gotten a second booster as of early October.
“If we do nothing else, we have to increase booster uptake in that group,” Dr. Nuzzo said.
She said the treatment nirmatrelvir/ritonavir (Paxlovid, Pfizer) for treating mild to moderate COVID-19 in patients at high risk for severe disease is greatly underused, often because providers aren’t prescribing it because they don’t think it helps, are worried about drug interactions, or are worried about its “rebound” effect.
Dr. Nuzzo urged greater use of the drug and education on how to manage drug interactions.
“We have very strong data that it does help keep people out of hospital. Sure, there may be a rebound, but that pales in comparison to the risk of being hospitalized,” she said.
Calm COVID season?
Not all predictions are dire. There is another little-talked-about scenario, Dr. Sweat said – that we could be in for a calm COVID season, and those who seem to be only mildly concerned about COVID may find those thoughts justified in the numbers.
Omicron blew through with such strength, he noted, that it may have left wide immunity in its wake. Because variants seem to be staying in the Omicron family, that may signal optimism.
“If the next variant is a descendant of the Omicron lineage, I would suspect that all these people who just got infected will have some protection, not perfect, but quite a bit of protection,” Dr. Sweat said.
Dr. Topol, Dr. Nuzzo, Dr. Sweat, Dr. Webby, Dr. Mokdad, and Dr. Jetelina reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As the United States enters a third fall with COVID-19, the virus for many is seemingly gone – or at least out of mind. But for those keeping watch, it is far from forgotten as deaths and infections continue to mount at a lower but steady pace.
What does that mean for the upcoming months? Experts predict different scenarios, some more dire than others – with one more encouraging.
In the United States, more than 300 people still die every day from COVID and more than 44,000 new daily cases are reported, according to the Centers for Disease Control and Prevention.
But progress is undeniable. The stark daily death tolls of 2020 have plummeted. Vaccines and treatments have dramatically reduced severe illness, and mask requirements have mostly turned to personal preference.
among them more-resistant variants coupled with waning immunity, the potential for a “twindemic” with a flu/COVID onslaught, and underuse of lifesaving vaccines and treatments.
Variants loom/waning immunity
Omicron variant BA.5 still makes up about 80% of infections in the United States, followed by BA4.6, according to the CDC, but other subvariants are emerging and showing signs of resistance to current antiviral treatments.
Eric Topol, MD, founder and director of the Scripps Research Translational Institute in San Diego, said about COVID this fall: “There will be another wave, magnitude unknown.”
He said subvariants XBB and BQ.1.1 “have extreme levels of immune evasion and both could pose a challenge,” explaining that XBB is more likely to cause trouble than BQ.1.1 because it is even more resistant to natural or vaccine-induced immunity.
Dr. Topol pointed to new research on those variants in a preprint posted on bioRxiv. The authors’ conclusion: “These results suggest that current herd immunity and BA.5 vaccine boosters may not provide sufficiently broad protection against infection.”
Another variant to watch, some experts say, is Omicron subvariant BA.2.75.2, which has shown resistance to antiviral treatments. It is also growing at a rather alarming rate, says Michael Sweat, PhD, director of the Medical University of South Carolina Center for Global Health in Charleston. That subvariant currently makes up under 2% of U.S. cases but has spread to at least 55 countries and 43 U.S. states after first appearing at the end of last year globally and in mid-June in the United States.
A non–peer-reviewed preprint study from Sweden found that the variant in blood samples was neutralized on average “at titers approximately 6.5 times lower than BA.5, making BA.2.75.2 the most [neutralization-resistant] variant evaluated to date.”
Katelyn Jetelina, PhD, assistant professor in the department of epidemiology at University of Texas Health Science Center, Houston, said in an interview the U.S. waves often follow Europe’s, and Europe has seen a recent spike in cases and hospitalizations not related to Omicron subvariants, but to weather changes, waning immunity, and changes in behavior.
The World Health Organization reported on Oct. 5 that, while cases were down in every other region of the world, Europe’s numbers stand out, with an 8% increase in cases from the week before.
Dr. Jetelina cited events such as Oktoberfest in Germany, which ended in the first week of October after drawing nearly 6 million people over 2 weeks, as a potential contributor, and people heading indoors as weather patterns change in Europe.
Ali Mokdad, PhD, chief strategy officer for population health at the University of Washington, Seattle, said in an interview he is less worried about the documented variants we know about than he is about the potential for a new immune-escape variety yet to emerge.
“Right now we know the Chinese are gearing up to open up the country, and because they have low immunity and little infection, we expect in China there will be a lot of spread of Omicron,” he said. “It’s possible because of the number of infections we could see a new variant.”
Dr. Mokdad said waning immunity could also leave populations vulnerable to variants.
“Even if you get infected, after about 5 months, you’re susceptible again. Remember, most of the infections from Omicron happened in January or February 2022, and we had two waves after that,” he said.
The new bivalent vaccines tweaked to target some Omicron variants will help, Dr. Mokdad said, but he noted, “people are very reluctant to take it.”
Jennifer Nuzzo, DrPH, professor of epidemiology and director of the Pandemic Center at Brown University, Providence, R.I., worries that in the United States we have less ability this year to track variants as funding has receded for testing kits and testing sites. Most people are testing at home – which doesn’t show up in the numbers – and the United States is relying more on other countries’ data to spot trends.
“I think we’re just going to have less visibility into the circulation of this virus,” she said in an interview.
‘Twindemic’: COVID and flu
Dr. Jetelina noted Australia and New Zealand just wrapped up a flu season that saw flu numbers returning to normal after a sharp drop in the last 2 years, and North America typically follows suit.
“We do expect flu will be here in the United States and probably at levels that we saw prepandemic. We’re all holding our breath to see how our health systems hold up with COVID-19 and flu. We haven’t really experienced that yet,” she said.
There is some disagreement, however, about the possibility of a so-called “twindemic” of influenza and COVID.
Richard Webby, PhD, an infectious disease specialist at St. Jude Children’s Research Hospital in Memphis, said in an interview he thinks the possibility of both viruses spiking at the same time is unlikely.
“That’s not to say we won’t get flu and COVID activity in the same winter,” he explained, “but I think both roaring at the same time is unlikely.”
As an indicator, he said, at the beginning of the flu season last year in the Northern Hemisphere, flu activity started to pick up, but when the Omicron variant came along, “flu just wasn’t able to compete in that same environment and flu numbers dropped right off.” Previous literature suggests that when one virus is spiking it’s hard for another respiratory virus to take hold.
Vaccine, treatment underuse
Another threat is vaccines, boosters, and treatments sitting on shelves.
Dr. Sweat referred to frustration with vaccine uptake that seems to be “frozen in amber.”
As of Oct. 4, only 5.3% of people in the United States who were eligible had received the updated booster launched in early September.
Dr. Nuzzo said boosters for people at least 65 years old will be key to severity of COVID this season.
“I think that’s probably the biggest factor going into the fall and winter,” she said.
Only 38% of people at least 50 years old and 45% of those at least 65 years old had gotten a second booster as of early October.
“If we do nothing else, we have to increase booster uptake in that group,” Dr. Nuzzo said.
She said the treatment nirmatrelvir/ritonavir (Paxlovid, Pfizer) for treating mild to moderate COVID-19 in patients at high risk for severe disease is greatly underused, often because providers aren’t prescribing it because they don’t think it helps, are worried about drug interactions, or are worried about its “rebound” effect.
Dr. Nuzzo urged greater use of the drug and education on how to manage drug interactions.
“We have very strong data that it does help keep people out of hospital. Sure, there may be a rebound, but that pales in comparison to the risk of being hospitalized,” she said.
Calm COVID season?
Not all predictions are dire. There is another little-talked-about scenario, Dr. Sweat said – that we could be in for a calm COVID season, and those who seem to be only mildly concerned about COVID may find those thoughts justified in the numbers.
Omicron blew through with such strength, he noted, that it may have left wide immunity in its wake. Because variants seem to be staying in the Omicron family, that may signal optimism.
“If the next variant is a descendant of the Omicron lineage, I would suspect that all these people who just got infected will have some protection, not perfect, but quite a bit of protection,” Dr. Sweat said.
Dr. Topol, Dr. Nuzzo, Dr. Sweat, Dr. Webby, Dr. Mokdad, and Dr. Jetelina reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FDA: Newborns protected by whooping cough vaccine
The Food and Drug Administration has approved a whooping cough vaccine that protects newborns under 2 months of age.
The vaccine, manufactured by GlaxoSmithKline, was previously approved among pregnant people for their own protection.
“Infants younger than 2 months of age are too young to be protected by the childhood pertussis vaccine series,” Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said in a press release. “This is the first vaccine approved specifically for use during pregnancy to prevent a disease in young infants whose mothers are vaccinated during pregnancy.”
Pertussis is a highly contagious respiratory tract infection caused by the bacterium Bordetella pertussis. Most cases that result in hospitalizations and death are among infants within 2 months of birth.
The FDA said its decision was based on data from observational studies, which included 108 cases of pertussis in infants younger than 2 months old. According to data evaluated by the agency, the vaccine was 78% effective in preventing whooping cough.
Boostrix is administered as a single 0.5-mL dose.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved a whooping cough vaccine that protects newborns under 2 months of age.
The vaccine, manufactured by GlaxoSmithKline, was previously approved among pregnant people for their own protection.
“Infants younger than 2 months of age are too young to be protected by the childhood pertussis vaccine series,” Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said in a press release. “This is the first vaccine approved specifically for use during pregnancy to prevent a disease in young infants whose mothers are vaccinated during pregnancy.”
Pertussis is a highly contagious respiratory tract infection caused by the bacterium Bordetella pertussis. Most cases that result in hospitalizations and death are among infants within 2 months of birth.
The FDA said its decision was based on data from observational studies, which included 108 cases of pertussis in infants younger than 2 months old. According to data evaluated by the agency, the vaccine was 78% effective in preventing whooping cough.
Boostrix is administered as a single 0.5-mL dose.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved a whooping cough vaccine that protects newborns under 2 months of age.
The vaccine, manufactured by GlaxoSmithKline, was previously approved among pregnant people for their own protection.
“Infants younger than 2 months of age are too young to be protected by the childhood pertussis vaccine series,” Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said in a press release. “This is the first vaccine approved specifically for use during pregnancy to prevent a disease in young infants whose mothers are vaccinated during pregnancy.”
Pertussis is a highly contagious respiratory tract infection caused by the bacterium Bordetella pertussis. Most cases that result in hospitalizations and death are among infants within 2 months of birth.
The FDA said its decision was based on data from observational studies, which included 108 cases of pertussis in infants younger than 2 months old. According to data evaluated by the agency, the vaccine was 78% effective in preventing whooping cough.
Boostrix is administered as a single 0.5-mL dose.
A version of this article first appeared on Medscape.com.
Dupilumab study outlines benefits, safety profile in infants, preschoolers with atopic dermatitis
at 31 treatment centers in North America and Europe.
Children younger than 6 years with moderate to severe AD have few options if their symptoms are uncontrolled with topical therapies, and persistent itchiness has a negative impact on quality of life for patients and families, Amy S. Paller, MD, professor and chair of dermatology, and professor of pediatrics at Northwestern University, Chicago, and colleagues wrote in the study, published in the Lancet.
The study was the basis of the Food and Drug Administration expanded approval of dupilumab in June 2022, to include children aged 6 months to 5 years with moderate to severe AD, whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable. Regulatory submission for this age group is under review by the European Medicines Agency, and by regulatory authorities in other countries, according to the manufacturers.
Dupilumab (Dupixent), which inhibits the signaling of the interleukin-4 and IL-13 pathways, was first approved in 2017 for treating adults with moderate to severe AD.
“There has not been a biologic approved before at such a young age, and for such a common disease,” Dr. Paller said in an interview. “This is the drug that has revolutionized care of the most common inflammatory skin disease in children, and this is the pivotal study that brought it to market for the youngest children who suffer from the severe forms.”
The study also sets a precedent for a lower threshold for starting systemic medication in young children for treating moderate to severe disease given the absence of severe side effects and no need for lab monitoring, Dr. Paller noted. However, dupilumab will also be closely watched “for both impact on the developing immune system and the possibility that it will alter the long-term course of the eczema and the development of allergic comorbidities, such as lowering the risk of developing asthma, GI, allergy, and possibly other conditions.”
In the study, the researchers randomized 83 children aged 6 months up to 6 years to treatment with dupilumab, administered subcutaneously, and 79 to placebo every 4 weeks for 16 weeks; both groups also received topical corticosteroids. Dosage of dupilumab was based on body weight; those with a body weight of 5-15 kg received 200 mg, while those with a body weight of 15-30 kg received 300 mg. The primary endpoint was the proportion of patients with clear or almost clear skin at 16 weeks, defined as scores of 0 or 1 on the Investigator’s Global Assessment.
After 16 weeks, 28% of dupilumab patients met the primary endpoint versus 4% of those on placebo (P < .0001). In addition, 53% of dupilumab patients met the key secondary endpoint of a 75% improvement from baseline in Eczema Area and Severity Index, compared with 11% of patients on placebo (P < .0001). Treatment with dupilumab also resulted in significantly greater improvements in pruritus and skin pain, and sleep quality, as well as improved quality of life for patients and their caregivers, the authors reported.
Overall, adverse event rates were slightly lower in the dupilumab-treated patients, compared with patients on placebo (64% vs. 74%); there were no adverse events related to dupilumab that were serious or resulted in treatment discontinuation. Treatment-emergent adverse effects that were reported in 3% or more of patients and affected more of those on dupilumab than those on placebo included molluscum contagiosum (5% vs. 3%), viral gastroenteritis (4% vs. 0), rhinorrhea (5% vs. 1%), dental caries (5% vs. 0), and conjunctivitis (4% vs 0).
The rate of skin infections among the children on dupilumab was 12% vs. 24% among those on placebo.
Severe and treatment-related adverse events also were similar in both subgroups of body weight.
The findings were limited by the small number of patients younger than 2 years and the lack of study sites outside of North America and Europe, the researchers noted. However, the results were strengthened by the randomized, double-blind design and use of background topical therapy to provide a real-world safety and efficacy assessment in a very young population.
Overcoming injection issues
The safety profile for dupilumab, which is of the highest importance, “did not surprise me at all,” Dr. Paller said in an interview. “My only surprise is that the placebo injections actually led to more injection site reactions than [with] dupilumab, but numbers were quite low in both groups.” (Rates were 2% among those on dupilumab and 3% among those on placebo.)
The major barrier to the use of dupilumab in clinical practice is the requirement for injection, which, she explained, can be “unbearable for some young children, and thus becomes impossible for parents because of lack of cooperation and their intensified concern about giving the injection,” because of their child’s response.
“We like to administer the first dose in the office, allowing us to teach parents a few tricks related to proper technique,” including audio and visual distraction, tactile stimulation before and during the injection, use of topical anesthetic if helpful, “and making sure that the medication is at room temperature before administration,” she said. Cost is another potential barrier; however, even public insurance has been covering the medication, often after optimized use of topical medications has been unsuccessful.
Future research questions
As for additional research, the current study had a relatively small number of patients younger than 2 years, and more data are needed for this age group, said Dr. Paller. “We also need better understanding of the safety of dupilumab administration when live vaccines are administered. Finally, we certainly want to know what additional effects dupilumab may have beyond just the efficacy for treating eczema.”
In particular, these questions include whether dupilumab modifies the long-term course of the disease, possibly reducing the risk of persistence of disease with advancing age, or even cures the disease if started at a young age, she said. In addition, research has yet to show whether dupilumab might reduce the risk of other atopic disorders, such as asthma, food allergy, and allergic rhinitis.
“Ongoing studies and real-life experiences in the next several years will help us to answer these questions,” Dr. Paller said.
Data support safety, efficacy, quality of life
AD is associated with immense quality of life impairment, Raj Chovatiya, MD, of Northwestern University, Chicago, said in an interview. Most AD is initially diagnosed in early childhood, but previous treatment options for those with moderate to severe disease have been limited by safety concerns, which adds to the burden on infants and young children, and their parents and caregivers, said Dr. Chovatiya, who was not involved in the study.
“This phase 3 study showed that dupilumab, a fully human monoclonal antibody that selectively inhibits IL-4 and IL-13 mediated type 2 inflammatory signaling, provided both meaningful and statistically significant improvement in AD severity, extent of disease, and itch in patients,” he said. Dupilumab also improved children’s sleep quality and the overall quality of life in both patients and caregivers.
“These findings were quite similar to those described in older children and adults, where dupilumab is already approved for the treatment of moderate-severe AD and has demonstrated real-world safety and efficacy,” said Dr. Chovatiya. However, “the current study was limited to only a short-term analysis of 16 weeks, an ongoing open-label study should further address long-term treatment responses.”
The study was supported by Sanofi and Regeneron Pharmaceuticals. In addition to being an investigator for Regeneron, and several other pharmaceutical companies, Dr. Paller has been a consultant with honorarium for Regeneron, Sanofi, and multiple other companies. Dr. Chovatiya disclosed serving as a consultant and speaker for Regeneron and Sanofi, but was not involved in the current study.
at 31 treatment centers in North America and Europe.
Children younger than 6 years with moderate to severe AD have few options if their symptoms are uncontrolled with topical therapies, and persistent itchiness has a negative impact on quality of life for patients and families, Amy S. Paller, MD, professor and chair of dermatology, and professor of pediatrics at Northwestern University, Chicago, and colleagues wrote in the study, published in the Lancet.
The study was the basis of the Food and Drug Administration expanded approval of dupilumab in June 2022, to include children aged 6 months to 5 years with moderate to severe AD, whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable. Regulatory submission for this age group is under review by the European Medicines Agency, and by regulatory authorities in other countries, according to the manufacturers.
Dupilumab (Dupixent), which inhibits the signaling of the interleukin-4 and IL-13 pathways, was first approved in 2017 for treating adults with moderate to severe AD.
“There has not been a biologic approved before at such a young age, and for such a common disease,” Dr. Paller said in an interview. “This is the drug that has revolutionized care of the most common inflammatory skin disease in children, and this is the pivotal study that brought it to market for the youngest children who suffer from the severe forms.”
The study also sets a precedent for a lower threshold for starting systemic medication in young children for treating moderate to severe disease given the absence of severe side effects and no need for lab monitoring, Dr. Paller noted. However, dupilumab will also be closely watched “for both impact on the developing immune system and the possibility that it will alter the long-term course of the eczema and the development of allergic comorbidities, such as lowering the risk of developing asthma, GI, allergy, and possibly other conditions.”
In the study, the researchers randomized 83 children aged 6 months up to 6 years to treatment with dupilumab, administered subcutaneously, and 79 to placebo every 4 weeks for 16 weeks; both groups also received topical corticosteroids. Dosage of dupilumab was based on body weight; those with a body weight of 5-15 kg received 200 mg, while those with a body weight of 15-30 kg received 300 mg. The primary endpoint was the proportion of patients with clear or almost clear skin at 16 weeks, defined as scores of 0 or 1 on the Investigator’s Global Assessment.
After 16 weeks, 28% of dupilumab patients met the primary endpoint versus 4% of those on placebo (P < .0001). In addition, 53% of dupilumab patients met the key secondary endpoint of a 75% improvement from baseline in Eczema Area and Severity Index, compared with 11% of patients on placebo (P < .0001). Treatment with dupilumab also resulted in significantly greater improvements in pruritus and skin pain, and sleep quality, as well as improved quality of life for patients and their caregivers, the authors reported.
Overall, adverse event rates were slightly lower in the dupilumab-treated patients, compared with patients on placebo (64% vs. 74%); there were no adverse events related to dupilumab that were serious or resulted in treatment discontinuation. Treatment-emergent adverse effects that were reported in 3% or more of patients and affected more of those on dupilumab than those on placebo included molluscum contagiosum (5% vs. 3%), viral gastroenteritis (4% vs. 0), rhinorrhea (5% vs. 1%), dental caries (5% vs. 0), and conjunctivitis (4% vs 0).
The rate of skin infections among the children on dupilumab was 12% vs. 24% among those on placebo.
Severe and treatment-related adverse events also were similar in both subgroups of body weight.
The findings were limited by the small number of patients younger than 2 years and the lack of study sites outside of North America and Europe, the researchers noted. However, the results were strengthened by the randomized, double-blind design and use of background topical therapy to provide a real-world safety and efficacy assessment in a very young population.
Overcoming injection issues
The safety profile for dupilumab, which is of the highest importance, “did not surprise me at all,” Dr. Paller said in an interview. “My only surprise is that the placebo injections actually led to more injection site reactions than [with] dupilumab, but numbers were quite low in both groups.” (Rates were 2% among those on dupilumab and 3% among those on placebo.)
The major barrier to the use of dupilumab in clinical practice is the requirement for injection, which, she explained, can be “unbearable for some young children, and thus becomes impossible for parents because of lack of cooperation and their intensified concern about giving the injection,” because of their child’s response.
“We like to administer the first dose in the office, allowing us to teach parents a few tricks related to proper technique,” including audio and visual distraction, tactile stimulation before and during the injection, use of topical anesthetic if helpful, “and making sure that the medication is at room temperature before administration,” she said. Cost is another potential barrier; however, even public insurance has been covering the medication, often after optimized use of topical medications has been unsuccessful.
Future research questions
As for additional research, the current study had a relatively small number of patients younger than 2 years, and more data are needed for this age group, said Dr. Paller. “We also need better understanding of the safety of dupilumab administration when live vaccines are administered. Finally, we certainly want to know what additional effects dupilumab may have beyond just the efficacy for treating eczema.”
In particular, these questions include whether dupilumab modifies the long-term course of the disease, possibly reducing the risk of persistence of disease with advancing age, or even cures the disease if started at a young age, she said. In addition, research has yet to show whether dupilumab might reduce the risk of other atopic disorders, such as asthma, food allergy, and allergic rhinitis.
“Ongoing studies and real-life experiences in the next several years will help us to answer these questions,” Dr. Paller said.
Data support safety, efficacy, quality of life
AD is associated with immense quality of life impairment, Raj Chovatiya, MD, of Northwestern University, Chicago, said in an interview. Most AD is initially diagnosed in early childhood, but previous treatment options for those with moderate to severe disease have been limited by safety concerns, which adds to the burden on infants and young children, and their parents and caregivers, said Dr. Chovatiya, who was not involved in the study.
“This phase 3 study showed that dupilumab, a fully human monoclonal antibody that selectively inhibits IL-4 and IL-13 mediated type 2 inflammatory signaling, provided both meaningful and statistically significant improvement in AD severity, extent of disease, and itch in patients,” he said. Dupilumab also improved children’s sleep quality and the overall quality of life in both patients and caregivers.
“These findings were quite similar to those described in older children and adults, where dupilumab is already approved for the treatment of moderate-severe AD and has demonstrated real-world safety and efficacy,” said Dr. Chovatiya. However, “the current study was limited to only a short-term analysis of 16 weeks, an ongoing open-label study should further address long-term treatment responses.”
The study was supported by Sanofi and Regeneron Pharmaceuticals. In addition to being an investigator for Regeneron, and several other pharmaceutical companies, Dr. Paller has been a consultant with honorarium for Regeneron, Sanofi, and multiple other companies. Dr. Chovatiya disclosed serving as a consultant and speaker for Regeneron and Sanofi, but was not involved in the current study.
at 31 treatment centers in North America and Europe.
Children younger than 6 years with moderate to severe AD have few options if their symptoms are uncontrolled with topical therapies, and persistent itchiness has a negative impact on quality of life for patients and families, Amy S. Paller, MD, professor and chair of dermatology, and professor of pediatrics at Northwestern University, Chicago, and colleagues wrote in the study, published in the Lancet.
The study was the basis of the Food and Drug Administration expanded approval of dupilumab in June 2022, to include children aged 6 months to 5 years with moderate to severe AD, whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable. Regulatory submission for this age group is under review by the European Medicines Agency, and by regulatory authorities in other countries, according to the manufacturers.
Dupilumab (Dupixent), which inhibits the signaling of the interleukin-4 and IL-13 pathways, was first approved in 2017 for treating adults with moderate to severe AD.
“There has not been a biologic approved before at such a young age, and for such a common disease,” Dr. Paller said in an interview. “This is the drug that has revolutionized care of the most common inflammatory skin disease in children, and this is the pivotal study that brought it to market for the youngest children who suffer from the severe forms.”
The study also sets a precedent for a lower threshold for starting systemic medication in young children for treating moderate to severe disease given the absence of severe side effects and no need for lab monitoring, Dr. Paller noted. However, dupilumab will also be closely watched “for both impact on the developing immune system and the possibility that it will alter the long-term course of the eczema and the development of allergic comorbidities, such as lowering the risk of developing asthma, GI, allergy, and possibly other conditions.”
In the study, the researchers randomized 83 children aged 6 months up to 6 years to treatment with dupilumab, administered subcutaneously, and 79 to placebo every 4 weeks for 16 weeks; both groups also received topical corticosteroids. Dosage of dupilumab was based on body weight; those with a body weight of 5-15 kg received 200 mg, while those with a body weight of 15-30 kg received 300 mg. The primary endpoint was the proportion of patients with clear or almost clear skin at 16 weeks, defined as scores of 0 or 1 on the Investigator’s Global Assessment.
After 16 weeks, 28% of dupilumab patients met the primary endpoint versus 4% of those on placebo (P < .0001). In addition, 53% of dupilumab patients met the key secondary endpoint of a 75% improvement from baseline in Eczema Area and Severity Index, compared with 11% of patients on placebo (P < .0001). Treatment with dupilumab also resulted in significantly greater improvements in pruritus and skin pain, and sleep quality, as well as improved quality of life for patients and their caregivers, the authors reported.
Overall, adverse event rates were slightly lower in the dupilumab-treated patients, compared with patients on placebo (64% vs. 74%); there were no adverse events related to dupilumab that were serious or resulted in treatment discontinuation. Treatment-emergent adverse effects that were reported in 3% or more of patients and affected more of those on dupilumab than those on placebo included molluscum contagiosum (5% vs. 3%), viral gastroenteritis (4% vs. 0), rhinorrhea (5% vs. 1%), dental caries (5% vs. 0), and conjunctivitis (4% vs 0).
The rate of skin infections among the children on dupilumab was 12% vs. 24% among those on placebo.
Severe and treatment-related adverse events also were similar in both subgroups of body weight.
The findings were limited by the small number of patients younger than 2 years and the lack of study sites outside of North America and Europe, the researchers noted. However, the results were strengthened by the randomized, double-blind design and use of background topical therapy to provide a real-world safety and efficacy assessment in a very young population.
Overcoming injection issues
The safety profile for dupilumab, which is of the highest importance, “did not surprise me at all,” Dr. Paller said in an interview. “My only surprise is that the placebo injections actually led to more injection site reactions than [with] dupilumab, but numbers were quite low in both groups.” (Rates were 2% among those on dupilumab and 3% among those on placebo.)
The major barrier to the use of dupilumab in clinical practice is the requirement for injection, which, she explained, can be “unbearable for some young children, and thus becomes impossible for parents because of lack of cooperation and their intensified concern about giving the injection,” because of their child’s response.
“We like to administer the first dose in the office, allowing us to teach parents a few tricks related to proper technique,” including audio and visual distraction, tactile stimulation before and during the injection, use of topical anesthetic if helpful, “and making sure that the medication is at room temperature before administration,” she said. Cost is another potential barrier; however, even public insurance has been covering the medication, often after optimized use of topical medications has been unsuccessful.
Future research questions
As for additional research, the current study had a relatively small number of patients younger than 2 years, and more data are needed for this age group, said Dr. Paller. “We also need better understanding of the safety of dupilumab administration when live vaccines are administered. Finally, we certainly want to know what additional effects dupilumab may have beyond just the efficacy for treating eczema.”
In particular, these questions include whether dupilumab modifies the long-term course of the disease, possibly reducing the risk of persistence of disease with advancing age, or even cures the disease if started at a young age, she said. In addition, research has yet to show whether dupilumab might reduce the risk of other atopic disorders, such as asthma, food allergy, and allergic rhinitis.
“Ongoing studies and real-life experiences in the next several years will help us to answer these questions,” Dr. Paller said.
Data support safety, efficacy, quality of life
AD is associated with immense quality of life impairment, Raj Chovatiya, MD, of Northwestern University, Chicago, said in an interview. Most AD is initially diagnosed in early childhood, but previous treatment options for those with moderate to severe disease have been limited by safety concerns, which adds to the burden on infants and young children, and their parents and caregivers, said Dr. Chovatiya, who was not involved in the study.
“This phase 3 study showed that dupilumab, a fully human monoclonal antibody that selectively inhibits IL-4 and IL-13 mediated type 2 inflammatory signaling, provided both meaningful and statistically significant improvement in AD severity, extent of disease, and itch in patients,” he said. Dupilumab also improved children’s sleep quality and the overall quality of life in both patients and caregivers.
“These findings were quite similar to those described in older children and adults, where dupilumab is already approved for the treatment of moderate-severe AD and has demonstrated real-world safety and efficacy,” said Dr. Chovatiya. However, “the current study was limited to only a short-term analysis of 16 weeks, an ongoing open-label study should further address long-term treatment responses.”
The study was supported by Sanofi and Regeneron Pharmaceuticals. In addition to being an investigator for Regeneron, and several other pharmaceutical companies, Dr. Paller has been a consultant with honorarium for Regeneron, Sanofi, and multiple other companies. Dr. Chovatiya disclosed serving as a consultant and speaker for Regeneron and Sanofi, but was not involved in the current study.
FROM THE LANCET
Ultra-processed food intake by moms linked with childhood obesity
A mother’s consumption of ultra-processed foods appears to be related to an increased risk of overweight or obesity in her children, according to new research.
Among the 19,958 mother-child pairs studied, 12.4% of children developed obesity or overweight in the full analytic study group, and the offspring of those mothers who ate the most ultra-processed foods had a 26% higher risk of obesity/overweight (12.1 servings/day), compared with those with the lowest consumption (3.4 servings/day), report Andrew T. Chan, MD, MPH, professor of medicine at Harvard Medical School, Boston, and colleagues.
This study demonstrates the possible advantages of restricting ultra-processed food consumption among women and mothers who are in their reproductive years to potentially lower the risk of childhood obesity, the investigators note.
“These data support the importance of refining dietary recommendations and the development of programs to improve nutrition for women of reproductive age to promote offspring health,” they write in their article, published in BMJ.
“As a medical and public health community, we have to understand that the period of time in which a woman is carrying a child or ... the time when she is raising her children represents a unique opportunity to potentially intervene to affect both the health of the mother and also the health of the children,” Dr. Chan said in an interview.
It is important to address these trends both on an individual clinician level and on a societal level, noted Dr. Chan.
“This is a good opportunity to counsel patients about the potential linkage between their consumption of ultra-processed food for not just themselves but also their kids, and I think that added counseling and awareness may motivate individuals to think about their diets in a more favorable way,” he added.
But ultra-processed foods are affordable and convenient, and many communities are not able to easily access fresh and healthy foods, so “it is incumbent upon [clinicians] to make it a priority and to break down those social and economic barriers, which make it difficult to have healthy and less processed food,” Dr. Chan elaborated.
Assessment of maternal junk food intake during peri-pregnancy and childhood
Modern Western diets frequently include ultra-processed foods – such as packaged baked goods and snacks, fizzy drinks, and sugary cereals – which are linked to adult weight increase. The relationship between parental consumption of highly processed meals and offspring weight is, however, unclear across generations, the researchers note.
Hence, they set out to determine whether eating ultra-processed foods during peri-pregnancy and while raising children increased the risk of being overweight or having obesity among children and teens.
The study team assessed 14,553 mothers and their 19,958 children from the Growing Up Today Study (GUTS I and II) and Nurses’ Health Study II (NHS II) in the United States. Males accounted for 45% of the children in the study, and the children’s ages ranged from 7 to 17 years.
The NHS II is a continuing investigation following the lifestyle and health choices of over 100,000 female registered nurses in the United States in 1989, while the GUTS I involved about 17,000 children of the nurses in the NHS II. Participants in GUTS I filled out an initial lifestyle and health survey and were evaluated annually between 1997 and 2001 and every 2 years thereafter.
Roughly 11,000 children from the NHS II were included in the GUTS II. The children were further evaluated in 2006, 2008, and 2011, as well as every 2 years thereafter.
Participants were followed until the children reached 18 years of age or experienced obesity and overweight onset. A subcohort consisted of 2,925 mother-child pairs with data on peri-pregnancy eating patterns.
Maternal intake of ultra-processed foods while raising children was linked with obesity or overweight in children. Moreover, compared with the lowest consumption cohort (3.4 servings/day), there was a 26% greater risk for the greatest maternal ultra-processed food intake cohort (12.1 servings/day) after adjusting for child’s sedentary time, ultra-processed food intake, physical activity, and established maternal risk factors.
Even though rates were elevated, ultra-processed food intake during pregnancy was not significantly linked to a higher risk of obesity or overweight in children (P for trend = .07).
Sex, birth weight, age, gestational age, or maternal body weight had no effect on these correlations either.
The study’s limitations include the fact that some of the children in the pairs were lost during follow-up; there may have been data misreporting, as the weight and diet measures were provided via self-reported questionnaires; and potential residual confounding given the observational study design, the researchers note.
Other limitations include that the mothers involved in the study came from similar socioeconomic backgrounds, had similar personal and familial educational statuses, and were primarily White, which limits the generalizability of these data to other ethnic groups, the authors add.
“Further studies are warranted to investigate specific biological mechanisms and socioeconomic determinants underlying the observed associations between maternal ultra-processed food intake and offspring overweight and obesity,” the researchers conclude.
A version of this article first appeared on Medscape.com.
A mother’s consumption of ultra-processed foods appears to be related to an increased risk of overweight or obesity in her children, according to new research.
Among the 19,958 mother-child pairs studied, 12.4% of children developed obesity or overweight in the full analytic study group, and the offspring of those mothers who ate the most ultra-processed foods had a 26% higher risk of obesity/overweight (12.1 servings/day), compared with those with the lowest consumption (3.4 servings/day), report Andrew T. Chan, MD, MPH, professor of medicine at Harvard Medical School, Boston, and colleagues.
This study demonstrates the possible advantages of restricting ultra-processed food consumption among women and mothers who are in their reproductive years to potentially lower the risk of childhood obesity, the investigators note.
“These data support the importance of refining dietary recommendations and the development of programs to improve nutrition for women of reproductive age to promote offspring health,” they write in their article, published in BMJ.
“As a medical and public health community, we have to understand that the period of time in which a woman is carrying a child or ... the time when she is raising her children represents a unique opportunity to potentially intervene to affect both the health of the mother and also the health of the children,” Dr. Chan said in an interview.
It is important to address these trends both on an individual clinician level and on a societal level, noted Dr. Chan.
“This is a good opportunity to counsel patients about the potential linkage between their consumption of ultra-processed food for not just themselves but also their kids, and I think that added counseling and awareness may motivate individuals to think about their diets in a more favorable way,” he added.
But ultra-processed foods are affordable and convenient, and many communities are not able to easily access fresh and healthy foods, so “it is incumbent upon [clinicians] to make it a priority and to break down those social and economic barriers, which make it difficult to have healthy and less processed food,” Dr. Chan elaborated.
Assessment of maternal junk food intake during peri-pregnancy and childhood
Modern Western diets frequently include ultra-processed foods – such as packaged baked goods and snacks, fizzy drinks, and sugary cereals – which are linked to adult weight increase. The relationship between parental consumption of highly processed meals and offspring weight is, however, unclear across generations, the researchers note.
Hence, they set out to determine whether eating ultra-processed foods during peri-pregnancy and while raising children increased the risk of being overweight or having obesity among children and teens.
The study team assessed 14,553 mothers and their 19,958 children from the Growing Up Today Study (GUTS I and II) and Nurses’ Health Study II (NHS II) in the United States. Males accounted for 45% of the children in the study, and the children’s ages ranged from 7 to 17 years.
The NHS II is a continuing investigation following the lifestyle and health choices of over 100,000 female registered nurses in the United States in 1989, while the GUTS I involved about 17,000 children of the nurses in the NHS II. Participants in GUTS I filled out an initial lifestyle and health survey and were evaluated annually between 1997 and 2001 and every 2 years thereafter.
Roughly 11,000 children from the NHS II were included in the GUTS II. The children were further evaluated in 2006, 2008, and 2011, as well as every 2 years thereafter.
Participants were followed until the children reached 18 years of age or experienced obesity and overweight onset. A subcohort consisted of 2,925 mother-child pairs with data on peri-pregnancy eating patterns.
Maternal intake of ultra-processed foods while raising children was linked with obesity or overweight in children. Moreover, compared with the lowest consumption cohort (3.4 servings/day), there was a 26% greater risk for the greatest maternal ultra-processed food intake cohort (12.1 servings/day) after adjusting for child’s sedentary time, ultra-processed food intake, physical activity, and established maternal risk factors.
Even though rates were elevated, ultra-processed food intake during pregnancy was not significantly linked to a higher risk of obesity or overweight in children (P for trend = .07).
Sex, birth weight, age, gestational age, or maternal body weight had no effect on these correlations either.
The study’s limitations include the fact that some of the children in the pairs were lost during follow-up; there may have been data misreporting, as the weight and diet measures were provided via self-reported questionnaires; and potential residual confounding given the observational study design, the researchers note.
Other limitations include that the mothers involved in the study came from similar socioeconomic backgrounds, had similar personal and familial educational statuses, and were primarily White, which limits the generalizability of these data to other ethnic groups, the authors add.
“Further studies are warranted to investigate specific biological mechanisms and socioeconomic determinants underlying the observed associations between maternal ultra-processed food intake and offspring overweight and obesity,” the researchers conclude.
A version of this article first appeared on Medscape.com.
A mother’s consumption of ultra-processed foods appears to be related to an increased risk of overweight or obesity in her children, according to new research.
Among the 19,958 mother-child pairs studied, 12.4% of children developed obesity or overweight in the full analytic study group, and the offspring of those mothers who ate the most ultra-processed foods had a 26% higher risk of obesity/overweight (12.1 servings/day), compared with those with the lowest consumption (3.4 servings/day), report Andrew T. Chan, MD, MPH, professor of medicine at Harvard Medical School, Boston, and colleagues.
This study demonstrates the possible advantages of restricting ultra-processed food consumption among women and mothers who are in their reproductive years to potentially lower the risk of childhood obesity, the investigators note.
“These data support the importance of refining dietary recommendations and the development of programs to improve nutrition for women of reproductive age to promote offspring health,” they write in their article, published in BMJ.
“As a medical and public health community, we have to understand that the period of time in which a woman is carrying a child or ... the time when she is raising her children represents a unique opportunity to potentially intervene to affect both the health of the mother and also the health of the children,” Dr. Chan said in an interview.
It is important to address these trends both on an individual clinician level and on a societal level, noted Dr. Chan.
“This is a good opportunity to counsel patients about the potential linkage between their consumption of ultra-processed food for not just themselves but also their kids, and I think that added counseling and awareness may motivate individuals to think about their diets in a more favorable way,” he added.
But ultra-processed foods are affordable and convenient, and many communities are not able to easily access fresh and healthy foods, so “it is incumbent upon [clinicians] to make it a priority and to break down those social and economic barriers, which make it difficult to have healthy and less processed food,” Dr. Chan elaborated.
Assessment of maternal junk food intake during peri-pregnancy and childhood
Modern Western diets frequently include ultra-processed foods – such as packaged baked goods and snacks, fizzy drinks, and sugary cereals – which are linked to adult weight increase. The relationship between parental consumption of highly processed meals and offspring weight is, however, unclear across generations, the researchers note.
Hence, they set out to determine whether eating ultra-processed foods during peri-pregnancy and while raising children increased the risk of being overweight or having obesity among children and teens.
The study team assessed 14,553 mothers and their 19,958 children from the Growing Up Today Study (GUTS I and II) and Nurses’ Health Study II (NHS II) in the United States. Males accounted for 45% of the children in the study, and the children’s ages ranged from 7 to 17 years.
The NHS II is a continuing investigation following the lifestyle and health choices of over 100,000 female registered nurses in the United States in 1989, while the GUTS I involved about 17,000 children of the nurses in the NHS II. Participants in GUTS I filled out an initial lifestyle and health survey and were evaluated annually between 1997 and 2001 and every 2 years thereafter.
Roughly 11,000 children from the NHS II were included in the GUTS II. The children were further evaluated in 2006, 2008, and 2011, as well as every 2 years thereafter.
Participants were followed until the children reached 18 years of age or experienced obesity and overweight onset. A subcohort consisted of 2,925 mother-child pairs with data on peri-pregnancy eating patterns.
Maternal intake of ultra-processed foods while raising children was linked with obesity or overweight in children. Moreover, compared with the lowest consumption cohort (3.4 servings/day), there was a 26% greater risk for the greatest maternal ultra-processed food intake cohort (12.1 servings/day) after adjusting for child’s sedentary time, ultra-processed food intake, physical activity, and established maternal risk factors.
Even though rates were elevated, ultra-processed food intake during pregnancy was not significantly linked to a higher risk of obesity or overweight in children (P for trend = .07).
Sex, birth weight, age, gestational age, or maternal body weight had no effect on these correlations either.
The study’s limitations include the fact that some of the children in the pairs were lost during follow-up; there may have been data misreporting, as the weight and diet measures were provided via self-reported questionnaires; and potential residual confounding given the observational study design, the researchers note.
Other limitations include that the mothers involved in the study came from similar socioeconomic backgrounds, had similar personal and familial educational statuses, and were primarily White, which limits the generalizability of these data to other ethnic groups, the authors add.
“Further studies are warranted to investigate specific biological mechanisms and socioeconomic determinants underlying the observed associations between maternal ultra-processed food intake and offspring overweight and obesity,” the researchers conclude.
A version of this article first appeared on Medscape.com.
Too old to practice medicine?
Unlike for many other professions, there is no age limit for practicing medicine. According to international standards, airplane pilots, for example, who are responsible for the safety of many human lives, must retire by the age of 60 if they work alone, or 65 if they have a copilot. In Brazil, however, this age limit does not exist for pilots or physicians.
The only restriction on professional practice within the medical context is the mandatory retirement imposed on medical professors who teach at public (state and federal) universities, starting at the age of 75. Nevertheless, these professionals can continue practicing administrative and research-related activities. After “expulsion,” as this mandatory retirement is often called, professors who stood out or contributed to the institution and science may receive the title of professor emeritus.
In the private sector, age limits are not formally set, but the hiring of middle-aged professionals is limited.
At the Heart Institute of the University of São Paulo (Brazil) School of Medicine Clinical Hospital (InCor/HCFMUSP), one of the world’s largest teaching and research centers for cardiovascular and pulmonary diseases, several octogenarian specialists lead studies and teams. One of these is Noedir Stolf, MD, an 82-year-old cardiovascular surgeon who operates almost every day and coordinates studies on transplants, mechanical circulatory support, and aortic surgery. There is also Protásio Lemos da Luz, MD, an 82-year-old clinical cardiologist who guides research on subjects including atherosclerosis, the endothelium, microbiota, and diabetes. The protective effect of wine on atherosclerosis is one of his best-known studies.
No longer working is also not in the cards for Angelita Habr-Gama, MD, who, at 89 years old, is one of the oldest physicians in current practice. With a career spanning more than 7 decades, she is a world reference in coloproctology. She was the first woman to become a surgical resident at the HCFMUSP, where she later founded the coloproctology specialty and created the first residency program for the specialty. In April 2022, Dr. Habr-Gama joined the ranks of the 100 most influential scientists in the world, nominated by researchers at Stanford (Calif.) University, and published in PLOS Biology.
In 2020, she was sedated, intubated, and hospitalized in the intensive care unit of the Oswaldo Cruz German Hospital for 54 days because of a SARS-CoV-2 infection. After her discharge, she went back to work in less than 10 days – and added chess classes to her routine. “To get up and go to work makes me very happy. Work is my greatest hobby. No one has ever heard me complain about my life,” Dr. Habr-Gama told this news organization after having rescheduled the interview twice because of emergency surgeries.
“Doctors have a professional longevity that does not exist for other professions in which the person retires and stops practicing their profession or goes on to do something else for entertainment. Doctors can retire from one place of employment or public practice and continue practicing medicine in the office as an administrator or consultant,” Ângelo Vattimo, first secretary of the state of São Paulo Regional Board of Medicine (CREMESP), stated. The board regularly organizes a ceremony to honor professionals who have been practicing for 50 years, awarding them a certificate and engraved medal. “Many of them are around 80 years old, working and teaching. This always makes us very happy. What profession has such exceptional compliance for so long?” said Mr. Vattimo.
In the medical field, the older the age range, the smaller the number of women. According to the 2020 Medical Demographics in Brazil survey, only 2 out of 10 practicing professionals older than 70 are women.
Not everyone over 80 has Dr. Habr-Gama’s vitality, because the impact of aging is not equal. “If you look at a group of 80-year-olds, there will be much more variability than within a group of 40-year-olds,” stated Mark Katlic, MD, chief of surgery at LifeBridge Health System in the United States, who has dedicated his life to studying the subject. Dr. Katlic spoke on the subject in an interview that was published in the article “How Old Is Too Old to Work as a Doctor?” published by this news organization in April of 2022. The article discusses the evaluations of elderly physicians’ skills and competences that U.S. companies conduct. The subject has been leading to profound debate.
Dr. Katlic defends screening programs for elderly physicians, which already are in effect at the company for which he works, LifeBridge Health, and various others in the United States. “We do [screen elderly physicians at LifeBridge Health], and so do a few dozen other [U.S. institutions], but there are hundreds [of health care institutions] that do not conduct this screening,” he pointed out.
Age-related assessment faces great resistance in the United States. One physician who is against the initiative is Frank Stockdale, MD, PhD, an 86-year-old practicing oncologist affiliated with Stanford (Calif.) University Health. “It’s age discrimination ... Physicians [in the United States] receive assessments throughout their careers as part of the accreditation process – there’s no need to change that as physicians reach a certain age,” Dr. Stockdale told this news organization.
The U.S. initiative of instituting physician assessment programs for those of a certain age has even been tested in court. According to an article published in Medscape, “in New Haven, Connecticut, for instance, the U.S. Equal Employment Opportunity Commission (EEOC) filed a suit in 2020 on behalf of the Yale New Haven Hospital staff, alleging a discriminatory late career practitioner policy.”
Also, according to the article, a similar case in Minnesota reached a settlement in 2021, providing monetary relief to staff impacted by out-of-pocket costs for the assessment, in addition to requiring that the hospital in question report to the EEOC any complaints related to age discrimination.
In Brazil, the subject is of interest to more than 34,571 physicians between 65 and 69 years of age and 34,237 physicians older than 70. In all, this population represents approximately 14.3% of the country’s active workforce, according to the 2020 Medical Demographics in Brazil survey.
The significant participation of health care professionals over age 50 in a survey conducted by this news organization to learn what physicians think about the age limit for practicing their professions is evidence that the subject is a present concern. Of a total of 1,641 participants, 57% were age 60 or older, 17% were between 50 and 59 years, and 12% were between 40 and 49 years. Among all participants, 51% were against these limitations, 17% approved of the idea for all specialties, and 32% believed the restriction was appropriate only for some specialties. Regarding the possibility of older physicians undergoing regular assessments, the opinions were divided: Thirty-one percent thought they should be assessed in all specialties. Furthermore, 31% believed that cognitive abilities should be regularly tested in all specialties, 31% thought this should take place for some specialties, and 38% were against this approach.
Professionals want to know, for example, how (and whether) advanced age can interfere with performance, what are the competences required to practice their activities, and if the criteria vary by specialty. “A psychiatrist doesn’t have to have perfect visual acuity, as required from a dermatologist, but it is important that they have good hearing, for example,” argued Clóvis Constantino, MD, former president of the São Paulo Regional Medical Board (CRM-SP) and former vice president of the Brazilian Federal Medical Board (CFM). “However, a surgeon has to stand for several hours in positions that may be uncomfortable. It’s not easy,” he told this news organization.
In the opinion of 82-year-old Henrique Klajner, MD, the oldest pediatrician in practice at the Albert Einstein Israeli Hospital in São Paulo, the physician cannot be subjected to the types of evaluations that have been applied in the United States. “Physicians should conduct constant self-evaluations to see if they have the competences and skills needed to practice their profession ... Moreover, this is not a matter of age. It is a matter of ethics,” said Dr. Klajner.
The ability to adapt to change and implement innovation is critical to professional longevity, he said. “Nowadays, when I admit patients, I no longer do hospital rounds, which requires a mobility equal to physical abuse for me. Therefore, I work with physicians who take care of my hospitalized patients.”
Dr. Klajner also feels there is a distinction between innovations learned through studies and what can be offered safely to patients. “If I have to care for a hospitalized patient with severe pneumonia, for example, since I am not up to date in this specialty, I am going to call upon a pulmonologist I trust and forgo my honorarium for this admission. But I will remain on the team, monitoring the patient’s progression,” he said.
During the COVID-19 pandemic, Dr. Klajner stopped seeing patients in person under the recommendation of his son, Sidney Klajner, MD, also a physician. The elder Dr. Klajner began exploring telemedicine, which opened a whole new world of possibilities. “I have conducted several online visits to provide educational instruction to mothers returning home post delivery, for example,” he told this news organization. The time to stop is not something that concerns Dr. Klajner. “I’m only going to stop when I have a really important reason to do so. For example, if I can no longer write or study, reading and rereading an article without being able to understand what is being said. At this time, none of that is happening.”
In the United States, as well as in Brazil, physicians rarely provide information to human resources departments on colleagues showing signs of cognitive or motor decline affecting their professional performance. “The expectation is that health care professionals will report colleagues with cognitive impairments, but that often does not happen,” Dr. Katlic said.
It is also not common for professionals to report their own deficits to their institutions. In large part, this is caused by a lack of well-defined policies for dealing with this issue. This news organization sought out several public and private hospitals in Brazil to see if there is any guidance on professional longevity: Most said that there is not. Only the A. C. Camargo Cancer Center reported, through its public relations team, that a committee is discussing the subject but that it is still in the early stages.
Brazilian specialist associations do not offer guidelines or instructions on the various aspects of professional longevity. Dr. Constantino tried to put the subject on the agenda during the years in which he was an administrator with the CFM. “We tried to open up discussions regarding truly elderly physicians, but the subject was not well received. I believe that it is precisely because there is a tradition of physicians working until they are no longer able that this is more difficult in Brazil ... No one exactly knows what to do in this respect.” Dr. Constantino is against the use of age as a criterion for quitting practice.
“Of course, this is a point that has to be considered, but I always defended the need for regular assessment of physicians, regardless of age range. And, although assessments are always welcome, in any profession, I also believe this would not be well received in Brazil.” He endorses an assessment of one’s knowledge and not of physical abilities, which are generally assessed through investigation when needed.
The absence of guidelines increases individual responsibility, as well as vulnerability. “Consciously, physicians will not put patients at risk if they do not have the competence to care for them or to perform a surgical procedure,” said Clystenes Odyr Soares Silva, MD, PhD, adjunct professor of pulmonology of the Federal University of São Paulo (Brazil) School of Medicine (UNIFESP). “Your peers will tell you if you are no longer able,” he added. The problem is that physicians rarely admit to or talk about their colleagues’ deficits, especially if they are in the spotlight because of advanced age. In this situation, the observation and opinion of family members regarding the health care professional’s competences and skills will hold more weight.
In case of health-related physical impairment, such as partial loss of hand movement, for example, “it is expected that this will set off an ethical warning in the person,” said Dr. Constantino. When this warning does not occur naturally, patients or colleagues can report the professional, and this may lead to the opening of an administrative investigation. If the report is found to be true, this investigation is used to suspend physicians who do not have the physical or mental ability to continue practicing medicine.
“If it’s something very serious, the physician’s license can be temporarily suspended while [the physician] is treated by a psychiatrist, with follow-up by the professional board. When discharged, the physician will get his or her [professional] license back and can go back to work,” Dr. Constantino explained. If an expert evaluation is needed, the physician will then be assessed by a forensic psychiatrist. One of the most in-demand forensic psychiatrists in Brazil is Guido Arturo Palomba, MD, 73 years old. “I have assessed some physicians for actions reported to see if they were normal people or not, but never for circumstances related to age,” Dr. Palomba said.
In practice, Brazilian medical entities do not have policies or programs to guide physicians who wish to grow old while they work or those who have started to notice they are not performing as they used to. “We have never lived as long; therefore, the quality of life in old age, as well as the concept of aging, are some of the most relevant questions of our time. These are subjects requiring additional discussion, broadening understanding and awareness in this regard,” observed Mr. Vattimo.
Dr. Constantino and Dr. Silva, who are completely against age-based assessments, believe that recertification of the specialist license every 5 years is the best path to confirming whether the physician is still able to practice. “A knowledge-based test every 5 years to recertify the specialist license has often been a topic of conversation. I think it’s an excellent idea. The person would provide a dossier of all they have done in terms of courses, conferences, and other activities, present it, and receive a score,” said Dr. Silva.
In practice, recertification of the specialist license is a topic of discussion that has been raised for years, and it is an idea that the Brazilian Medical Association (AMB) defends. In conjunction with the CFM, the association is studying a way to best implement this assessment. “It’s important to emphasize that this measure would not be retroactive at first. Instead, it would only be in effect for professionals licensed after the recertification requirement is established,” the AMB pointed out in a note sent to this news organization. Even so, the measure has faced significant resistance from a faction of the profession, and its enactment does not seem to be imminent.
The debate regarding professional longevity is taking place in various countries. In 2021, the American Medical Association Council on Medical Education released a report with a set of guidelines for the screening and assessment of physicians. The document is the product of a committee created in 2015 to study the subject. The AMA recommends that the assessment of elderly physicians be based on evidence and ethical, relevant, fair, equitable, transparent, verifiable, nonexhaustive principles, contemplating support and protecting against legal proceedings. In April of this year, a new AMA document highlighted the same principles.
Also in the United States, one of oldest initiatives created to support physicians in the process of recycling, the University of California San Diego Physician Assessment and Clinical Education Program (PACE), has a section focusing on the extended practice of medicine (Practicing Medicine Longer). For those wanting to learn more about discussions on this subject, there are online presentations on experiences in Quebec and Ontario with assessing aging physicians, neuropsychological perspectives on the aging medical population, and what to expect of healthy aging, among other subjects.
Created in 1996, PACE mostly provides services to physicians who need to address requirements of the state medical boards. Few physicians enroll on their own.
The first part of the program assesses knowledge and skills over approximately 2 days. In the second phase, the physician participates in a series of activities in a corresponding residency program. Depending on the results, the physician may have to go through a remedial program with varying activities to deal with performance deficiencies to clinical experiences at the residency level.
A version of this article first appeared on Medscape.com.
Unlike for many other professions, there is no age limit for practicing medicine. According to international standards, airplane pilots, for example, who are responsible for the safety of many human lives, must retire by the age of 60 if they work alone, or 65 if they have a copilot. In Brazil, however, this age limit does not exist for pilots or physicians.
The only restriction on professional practice within the medical context is the mandatory retirement imposed on medical professors who teach at public (state and federal) universities, starting at the age of 75. Nevertheless, these professionals can continue practicing administrative and research-related activities. After “expulsion,” as this mandatory retirement is often called, professors who stood out or contributed to the institution and science may receive the title of professor emeritus.
In the private sector, age limits are not formally set, but the hiring of middle-aged professionals is limited.
At the Heart Institute of the University of São Paulo (Brazil) School of Medicine Clinical Hospital (InCor/HCFMUSP), one of the world’s largest teaching and research centers for cardiovascular and pulmonary diseases, several octogenarian specialists lead studies and teams. One of these is Noedir Stolf, MD, an 82-year-old cardiovascular surgeon who operates almost every day and coordinates studies on transplants, mechanical circulatory support, and aortic surgery. There is also Protásio Lemos da Luz, MD, an 82-year-old clinical cardiologist who guides research on subjects including atherosclerosis, the endothelium, microbiota, and diabetes. The protective effect of wine on atherosclerosis is one of his best-known studies.
No longer working is also not in the cards for Angelita Habr-Gama, MD, who, at 89 years old, is one of the oldest physicians in current practice. With a career spanning more than 7 decades, she is a world reference in coloproctology. She was the first woman to become a surgical resident at the HCFMUSP, where she later founded the coloproctology specialty and created the first residency program for the specialty. In April 2022, Dr. Habr-Gama joined the ranks of the 100 most influential scientists in the world, nominated by researchers at Stanford (Calif.) University, and published in PLOS Biology.
In 2020, she was sedated, intubated, and hospitalized in the intensive care unit of the Oswaldo Cruz German Hospital for 54 days because of a SARS-CoV-2 infection. After her discharge, she went back to work in less than 10 days – and added chess classes to her routine. “To get up and go to work makes me very happy. Work is my greatest hobby. No one has ever heard me complain about my life,” Dr. Habr-Gama told this news organization after having rescheduled the interview twice because of emergency surgeries.
“Doctors have a professional longevity that does not exist for other professions in which the person retires and stops practicing their profession or goes on to do something else for entertainment. Doctors can retire from one place of employment or public practice and continue practicing medicine in the office as an administrator or consultant,” Ângelo Vattimo, first secretary of the state of São Paulo Regional Board of Medicine (CREMESP), stated. The board regularly organizes a ceremony to honor professionals who have been practicing for 50 years, awarding them a certificate and engraved medal. “Many of them are around 80 years old, working and teaching. This always makes us very happy. What profession has such exceptional compliance for so long?” said Mr. Vattimo.
In the medical field, the older the age range, the smaller the number of women. According to the 2020 Medical Demographics in Brazil survey, only 2 out of 10 practicing professionals older than 70 are women.
Not everyone over 80 has Dr. Habr-Gama’s vitality, because the impact of aging is not equal. “If you look at a group of 80-year-olds, there will be much more variability than within a group of 40-year-olds,” stated Mark Katlic, MD, chief of surgery at LifeBridge Health System in the United States, who has dedicated his life to studying the subject. Dr. Katlic spoke on the subject in an interview that was published in the article “How Old Is Too Old to Work as a Doctor?” published by this news organization in April of 2022. The article discusses the evaluations of elderly physicians’ skills and competences that U.S. companies conduct. The subject has been leading to profound debate.
Dr. Katlic defends screening programs for elderly physicians, which already are in effect at the company for which he works, LifeBridge Health, and various others in the United States. “We do [screen elderly physicians at LifeBridge Health], and so do a few dozen other [U.S. institutions], but there are hundreds [of health care institutions] that do not conduct this screening,” he pointed out.
Age-related assessment faces great resistance in the United States. One physician who is against the initiative is Frank Stockdale, MD, PhD, an 86-year-old practicing oncologist affiliated with Stanford (Calif.) University Health. “It’s age discrimination ... Physicians [in the United States] receive assessments throughout their careers as part of the accreditation process – there’s no need to change that as physicians reach a certain age,” Dr. Stockdale told this news organization.
The U.S. initiative of instituting physician assessment programs for those of a certain age has even been tested in court. According to an article published in Medscape, “in New Haven, Connecticut, for instance, the U.S. Equal Employment Opportunity Commission (EEOC) filed a suit in 2020 on behalf of the Yale New Haven Hospital staff, alleging a discriminatory late career practitioner policy.”
Also, according to the article, a similar case in Minnesota reached a settlement in 2021, providing monetary relief to staff impacted by out-of-pocket costs for the assessment, in addition to requiring that the hospital in question report to the EEOC any complaints related to age discrimination.
In Brazil, the subject is of interest to more than 34,571 physicians between 65 and 69 years of age and 34,237 physicians older than 70. In all, this population represents approximately 14.3% of the country’s active workforce, according to the 2020 Medical Demographics in Brazil survey.
The significant participation of health care professionals over age 50 in a survey conducted by this news organization to learn what physicians think about the age limit for practicing their professions is evidence that the subject is a present concern. Of a total of 1,641 participants, 57% were age 60 or older, 17% were between 50 and 59 years, and 12% were between 40 and 49 years. Among all participants, 51% were against these limitations, 17% approved of the idea for all specialties, and 32% believed the restriction was appropriate only for some specialties. Regarding the possibility of older physicians undergoing regular assessments, the opinions were divided: Thirty-one percent thought they should be assessed in all specialties. Furthermore, 31% believed that cognitive abilities should be regularly tested in all specialties, 31% thought this should take place for some specialties, and 38% were against this approach.
Professionals want to know, for example, how (and whether) advanced age can interfere with performance, what are the competences required to practice their activities, and if the criteria vary by specialty. “A psychiatrist doesn’t have to have perfect visual acuity, as required from a dermatologist, but it is important that they have good hearing, for example,” argued Clóvis Constantino, MD, former president of the São Paulo Regional Medical Board (CRM-SP) and former vice president of the Brazilian Federal Medical Board (CFM). “However, a surgeon has to stand for several hours in positions that may be uncomfortable. It’s not easy,” he told this news organization.
In the opinion of 82-year-old Henrique Klajner, MD, the oldest pediatrician in practice at the Albert Einstein Israeli Hospital in São Paulo, the physician cannot be subjected to the types of evaluations that have been applied in the United States. “Physicians should conduct constant self-evaluations to see if they have the competences and skills needed to practice their profession ... Moreover, this is not a matter of age. It is a matter of ethics,” said Dr. Klajner.
The ability to adapt to change and implement innovation is critical to professional longevity, he said. “Nowadays, when I admit patients, I no longer do hospital rounds, which requires a mobility equal to physical abuse for me. Therefore, I work with physicians who take care of my hospitalized patients.”
Dr. Klajner also feels there is a distinction between innovations learned through studies and what can be offered safely to patients. “If I have to care for a hospitalized patient with severe pneumonia, for example, since I am not up to date in this specialty, I am going to call upon a pulmonologist I trust and forgo my honorarium for this admission. But I will remain on the team, monitoring the patient’s progression,” he said.
During the COVID-19 pandemic, Dr. Klajner stopped seeing patients in person under the recommendation of his son, Sidney Klajner, MD, also a physician. The elder Dr. Klajner began exploring telemedicine, which opened a whole new world of possibilities. “I have conducted several online visits to provide educational instruction to mothers returning home post delivery, for example,” he told this news organization. The time to stop is not something that concerns Dr. Klajner. “I’m only going to stop when I have a really important reason to do so. For example, if I can no longer write or study, reading and rereading an article without being able to understand what is being said. At this time, none of that is happening.”
In the United States, as well as in Brazil, physicians rarely provide information to human resources departments on colleagues showing signs of cognitive or motor decline affecting their professional performance. “The expectation is that health care professionals will report colleagues with cognitive impairments, but that often does not happen,” Dr. Katlic said.
It is also not common for professionals to report their own deficits to their institutions. In large part, this is caused by a lack of well-defined policies for dealing with this issue. This news organization sought out several public and private hospitals in Brazil to see if there is any guidance on professional longevity: Most said that there is not. Only the A. C. Camargo Cancer Center reported, through its public relations team, that a committee is discussing the subject but that it is still in the early stages.
Brazilian specialist associations do not offer guidelines or instructions on the various aspects of professional longevity. Dr. Constantino tried to put the subject on the agenda during the years in which he was an administrator with the CFM. “We tried to open up discussions regarding truly elderly physicians, but the subject was not well received. I believe that it is precisely because there is a tradition of physicians working until they are no longer able that this is more difficult in Brazil ... No one exactly knows what to do in this respect.” Dr. Constantino is against the use of age as a criterion for quitting practice.
“Of course, this is a point that has to be considered, but I always defended the need for regular assessment of physicians, regardless of age range. And, although assessments are always welcome, in any profession, I also believe this would not be well received in Brazil.” He endorses an assessment of one’s knowledge and not of physical abilities, which are generally assessed through investigation when needed.
The absence of guidelines increases individual responsibility, as well as vulnerability. “Consciously, physicians will not put patients at risk if they do not have the competence to care for them or to perform a surgical procedure,” said Clystenes Odyr Soares Silva, MD, PhD, adjunct professor of pulmonology of the Federal University of São Paulo (Brazil) School of Medicine (UNIFESP). “Your peers will tell you if you are no longer able,” he added. The problem is that physicians rarely admit to or talk about their colleagues’ deficits, especially if they are in the spotlight because of advanced age. In this situation, the observation and opinion of family members regarding the health care professional’s competences and skills will hold more weight.
In case of health-related physical impairment, such as partial loss of hand movement, for example, “it is expected that this will set off an ethical warning in the person,” said Dr. Constantino. When this warning does not occur naturally, patients or colleagues can report the professional, and this may lead to the opening of an administrative investigation. If the report is found to be true, this investigation is used to suspend physicians who do not have the physical or mental ability to continue practicing medicine.
“If it’s something very serious, the physician’s license can be temporarily suspended while [the physician] is treated by a psychiatrist, with follow-up by the professional board. When discharged, the physician will get his or her [professional] license back and can go back to work,” Dr. Constantino explained. If an expert evaluation is needed, the physician will then be assessed by a forensic psychiatrist. One of the most in-demand forensic psychiatrists in Brazil is Guido Arturo Palomba, MD, 73 years old. “I have assessed some physicians for actions reported to see if they were normal people or not, but never for circumstances related to age,” Dr. Palomba said.
In practice, Brazilian medical entities do not have policies or programs to guide physicians who wish to grow old while they work or those who have started to notice they are not performing as they used to. “We have never lived as long; therefore, the quality of life in old age, as well as the concept of aging, are some of the most relevant questions of our time. These are subjects requiring additional discussion, broadening understanding and awareness in this regard,” observed Mr. Vattimo.
Dr. Constantino and Dr. Silva, who are completely against age-based assessments, believe that recertification of the specialist license every 5 years is the best path to confirming whether the physician is still able to practice. “A knowledge-based test every 5 years to recertify the specialist license has often been a topic of conversation. I think it’s an excellent idea. The person would provide a dossier of all they have done in terms of courses, conferences, and other activities, present it, and receive a score,” said Dr. Silva.
In practice, recertification of the specialist license is a topic of discussion that has been raised for years, and it is an idea that the Brazilian Medical Association (AMB) defends. In conjunction with the CFM, the association is studying a way to best implement this assessment. “It’s important to emphasize that this measure would not be retroactive at first. Instead, it would only be in effect for professionals licensed after the recertification requirement is established,” the AMB pointed out in a note sent to this news organization. Even so, the measure has faced significant resistance from a faction of the profession, and its enactment does not seem to be imminent.
The debate regarding professional longevity is taking place in various countries. In 2021, the American Medical Association Council on Medical Education released a report with a set of guidelines for the screening and assessment of physicians. The document is the product of a committee created in 2015 to study the subject. The AMA recommends that the assessment of elderly physicians be based on evidence and ethical, relevant, fair, equitable, transparent, verifiable, nonexhaustive principles, contemplating support and protecting against legal proceedings. In April of this year, a new AMA document highlighted the same principles.
Also in the United States, one of oldest initiatives created to support physicians in the process of recycling, the University of California San Diego Physician Assessment and Clinical Education Program (PACE), has a section focusing on the extended practice of medicine (Practicing Medicine Longer). For those wanting to learn more about discussions on this subject, there are online presentations on experiences in Quebec and Ontario with assessing aging physicians, neuropsychological perspectives on the aging medical population, and what to expect of healthy aging, among other subjects.
Created in 1996, PACE mostly provides services to physicians who need to address requirements of the state medical boards. Few physicians enroll on their own.
The first part of the program assesses knowledge and skills over approximately 2 days. In the second phase, the physician participates in a series of activities in a corresponding residency program. Depending on the results, the physician may have to go through a remedial program with varying activities to deal with performance deficiencies to clinical experiences at the residency level.
A version of this article first appeared on Medscape.com.
Unlike for many other professions, there is no age limit for practicing medicine. According to international standards, airplane pilots, for example, who are responsible for the safety of many human lives, must retire by the age of 60 if they work alone, or 65 if they have a copilot. In Brazil, however, this age limit does not exist for pilots or physicians.
The only restriction on professional practice within the medical context is the mandatory retirement imposed on medical professors who teach at public (state and federal) universities, starting at the age of 75. Nevertheless, these professionals can continue practicing administrative and research-related activities. After “expulsion,” as this mandatory retirement is often called, professors who stood out or contributed to the institution and science may receive the title of professor emeritus.
In the private sector, age limits are not formally set, but the hiring of middle-aged professionals is limited.
At the Heart Institute of the University of São Paulo (Brazil) School of Medicine Clinical Hospital (InCor/HCFMUSP), one of the world’s largest teaching and research centers for cardiovascular and pulmonary diseases, several octogenarian specialists lead studies and teams. One of these is Noedir Stolf, MD, an 82-year-old cardiovascular surgeon who operates almost every day and coordinates studies on transplants, mechanical circulatory support, and aortic surgery. There is also Protásio Lemos da Luz, MD, an 82-year-old clinical cardiologist who guides research on subjects including atherosclerosis, the endothelium, microbiota, and diabetes. The protective effect of wine on atherosclerosis is one of his best-known studies.
No longer working is also not in the cards for Angelita Habr-Gama, MD, who, at 89 years old, is one of the oldest physicians in current practice. With a career spanning more than 7 decades, she is a world reference in coloproctology. She was the first woman to become a surgical resident at the HCFMUSP, where she later founded the coloproctology specialty and created the first residency program for the specialty. In April 2022, Dr. Habr-Gama joined the ranks of the 100 most influential scientists in the world, nominated by researchers at Stanford (Calif.) University, and published in PLOS Biology.
In 2020, she was sedated, intubated, and hospitalized in the intensive care unit of the Oswaldo Cruz German Hospital for 54 days because of a SARS-CoV-2 infection. After her discharge, she went back to work in less than 10 days – and added chess classes to her routine. “To get up and go to work makes me very happy. Work is my greatest hobby. No one has ever heard me complain about my life,” Dr. Habr-Gama told this news organization after having rescheduled the interview twice because of emergency surgeries.
“Doctors have a professional longevity that does not exist for other professions in which the person retires and stops practicing their profession or goes on to do something else for entertainment. Doctors can retire from one place of employment or public practice and continue practicing medicine in the office as an administrator or consultant,” Ângelo Vattimo, first secretary of the state of São Paulo Regional Board of Medicine (CREMESP), stated. The board regularly organizes a ceremony to honor professionals who have been practicing for 50 years, awarding them a certificate and engraved medal. “Many of them are around 80 years old, working and teaching. This always makes us very happy. What profession has such exceptional compliance for so long?” said Mr. Vattimo.
In the medical field, the older the age range, the smaller the number of women. According to the 2020 Medical Demographics in Brazil survey, only 2 out of 10 practicing professionals older than 70 are women.
Not everyone over 80 has Dr. Habr-Gama’s vitality, because the impact of aging is not equal. “If you look at a group of 80-year-olds, there will be much more variability than within a group of 40-year-olds,” stated Mark Katlic, MD, chief of surgery at LifeBridge Health System in the United States, who has dedicated his life to studying the subject. Dr. Katlic spoke on the subject in an interview that was published in the article “How Old Is Too Old to Work as a Doctor?” published by this news organization in April of 2022. The article discusses the evaluations of elderly physicians’ skills and competences that U.S. companies conduct. The subject has been leading to profound debate.
Dr. Katlic defends screening programs for elderly physicians, which already are in effect at the company for which he works, LifeBridge Health, and various others in the United States. “We do [screen elderly physicians at LifeBridge Health], and so do a few dozen other [U.S. institutions], but there are hundreds [of health care institutions] that do not conduct this screening,” he pointed out.
Age-related assessment faces great resistance in the United States. One physician who is against the initiative is Frank Stockdale, MD, PhD, an 86-year-old practicing oncologist affiliated with Stanford (Calif.) University Health. “It’s age discrimination ... Physicians [in the United States] receive assessments throughout their careers as part of the accreditation process – there’s no need to change that as physicians reach a certain age,” Dr. Stockdale told this news organization.
The U.S. initiative of instituting physician assessment programs for those of a certain age has even been tested in court. According to an article published in Medscape, “in New Haven, Connecticut, for instance, the U.S. Equal Employment Opportunity Commission (EEOC) filed a suit in 2020 on behalf of the Yale New Haven Hospital staff, alleging a discriminatory late career practitioner policy.”
Also, according to the article, a similar case in Minnesota reached a settlement in 2021, providing monetary relief to staff impacted by out-of-pocket costs for the assessment, in addition to requiring that the hospital in question report to the EEOC any complaints related to age discrimination.
In Brazil, the subject is of interest to more than 34,571 physicians between 65 and 69 years of age and 34,237 physicians older than 70. In all, this population represents approximately 14.3% of the country’s active workforce, according to the 2020 Medical Demographics in Brazil survey.
The significant participation of health care professionals over age 50 in a survey conducted by this news organization to learn what physicians think about the age limit for practicing their professions is evidence that the subject is a present concern. Of a total of 1,641 participants, 57% were age 60 or older, 17% were between 50 and 59 years, and 12% were between 40 and 49 years. Among all participants, 51% were against these limitations, 17% approved of the idea for all specialties, and 32% believed the restriction was appropriate only for some specialties. Regarding the possibility of older physicians undergoing regular assessments, the opinions were divided: Thirty-one percent thought they should be assessed in all specialties. Furthermore, 31% believed that cognitive abilities should be regularly tested in all specialties, 31% thought this should take place for some specialties, and 38% were against this approach.
Professionals want to know, for example, how (and whether) advanced age can interfere with performance, what are the competences required to practice their activities, and if the criteria vary by specialty. “A psychiatrist doesn’t have to have perfect visual acuity, as required from a dermatologist, but it is important that they have good hearing, for example,” argued Clóvis Constantino, MD, former president of the São Paulo Regional Medical Board (CRM-SP) and former vice president of the Brazilian Federal Medical Board (CFM). “However, a surgeon has to stand for several hours in positions that may be uncomfortable. It’s not easy,” he told this news organization.
In the opinion of 82-year-old Henrique Klajner, MD, the oldest pediatrician in practice at the Albert Einstein Israeli Hospital in São Paulo, the physician cannot be subjected to the types of evaluations that have been applied in the United States. “Physicians should conduct constant self-evaluations to see if they have the competences and skills needed to practice their profession ... Moreover, this is not a matter of age. It is a matter of ethics,” said Dr. Klajner.
The ability to adapt to change and implement innovation is critical to professional longevity, he said. “Nowadays, when I admit patients, I no longer do hospital rounds, which requires a mobility equal to physical abuse for me. Therefore, I work with physicians who take care of my hospitalized patients.”
Dr. Klajner also feels there is a distinction between innovations learned through studies and what can be offered safely to patients. “If I have to care for a hospitalized patient with severe pneumonia, for example, since I am not up to date in this specialty, I am going to call upon a pulmonologist I trust and forgo my honorarium for this admission. But I will remain on the team, monitoring the patient’s progression,” he said.
During the COVID-19 pandemic, Dr. Klajner stopped seeing patients in person under the recommendation of his son, Sidney Klajner, MD, also a physician. The elder Dr. Klajner began exploring telemedicine, which opened a whole new world of possibilities. “I have conducted several online visits to provide educational instruction to mothers returning home post delivery, for example,” he told this news organization. The time to stop is not something that concerns Dr. Klajner. “I’m only going to stop when I have a really important reason to do so. For example, if I can no longer write or study, reading and rereading an article without being able to understand what is being said. At this time, none of that is happening.”
In the United States, as well as in Brazil, physicians rarely provide information to human resources departments on colleagues showing signs of cognitive or motor decline affecting their professional performance. “The expectation is that health care professionals will report colleagues with cognitive impairments, but that often does not happen,” Dr. Katlic said.
It is also not common for professionals to report their own deficits to their institutions. In large part, this is caused by a lack of well-defined policies for dealing with this issue. This news organization sought out several public and private hospitals in Brazil to see if there is any guidance on professional longevity: Most said that there is not. Only the A. C. Camargo Cancer Center reported, through its public relations team, that a committee is discussing the subject but that it is still in the early stages.
Brazilian specialist associations do not offer guidelines or instructions on the various aspects of professional longevity. Dr. Constantino tried to put the subject on the agenda during the years in which he was an administrator with the CFM. “We tried to open up discussions regarding truly elderly physicians, but the subject was not well received. I believe that it is precisely because there is a tradition of physicians working until they are no longer able that this is more difficult in Brazil ... No one exactly knows what to do in this respect.” Dr. Constantino is against the use of age as a criterion for quitting practice.
“Of course, this is a point that has to be considered, but I always defended the need for regular assessment of physicians, regardless of age range. And, although assessments are always welcome, in any profession, I also believe this would not be well received in Brazil.” He endorses an assessment of one’s knowledge and not of physical abilities, which are generally assessed through investigation when needed.
The absence of guidelines increases individual responsibility, as well as vulnerability. “Consciously, physicians will not put patients at risk if they do not have the competence to care for them or to perform a surgical procedure,” said Clystenes Odyr Soares Silva, MD, PhD, adjunct professor of pulmonology of the Federal University of São Paulo (Brazil) School of Medicine (UNIFESP). “Your peers will tell you if you are no longer able,” he added. The problem is that physicians rarely admit to or talk about their colleagues’ deficits, especially if they are in the spotlight because of advanced age. In this situation, the observation and opinion of family members regarding the health care professional’s competences and skills will hold more weight.
In case of health-related physical impairment, such as partial loss of hand movement, for example, “it is expected that this will set off an ethical warning in the person,” said Dr. Constantino. When this warning does not occur naturally, patients or colleagues can report the professional, and this may lead to the opening of an administrative investigation. If the report is found to be true, this investigation is used to suspend physicians who do not have the physical or mental ability to continue practicing medicine.
“If it’s something very serious, the physician’s license can be temporarily suspended while [the physician] is treated by a psychiatrist, with follow-up by the professional board. When discharged, the physician will get his or her [professional] license back and can go back to work,” Dr. Constantino explained. If an expert evaluation is needed, the physician will then be assessed by a forensic psychiatrist. One of the most in-demand forensic psychiatrists in Brazil is Guido Arturo Palomba, MD, 73 years old. “I have assessed some physicians for actions reported to see if they were normal people or not, but never for circumstances related to age,” Dr. Palomba said.
In practice, Brazilian medical entities do not have policies or programs to guide physicians who wish to grow old while they work or those who have started to notice they are not performing as they used to. “We have never lived as long; therefore, the quality of life in old age, as well as the concept of aging, are some of the most relevant questions of our time. These are subjects requiring additional discussion, broadening understanding and awareness in this regard,” observed Mr. Vattimo.
Dr. Constantino and Dr. Silva, who are completely against age-based assessments, believe that recertification of the specialist license every 5 years is the best path to confirming whether the physician is still able to practice. “A knowledge-based test every 5 years to recertify the specialist license has often been a topic of conversation. I think it’s an excellent idea. The person would provide a dossier of all they have done in terms of courses, conferences, and other activities, present it, and receive a score,” said Dr. Silva.
In practice, recertification of the specialist license is a topic of discussion that has been raised for years, and it is an idea that the Brazilian Medical Association (AMB) defends. In conjunction with the CFM, the association is studying a way to best implement this assessment. “It’s important to emphasize that this measure would not be retroactive at first. Instead, it would only be in effect for professionals licensed after the recertification requirement is established,” the AMB pointed out in a note sent to this news organization. Even so, the measure has faced significant resistance from a faction of the profession, and its enactment does not seem to be imminent.
The debate regarding professional longevity is taking place in various countries. In 2021, the American Medical Association Council on Medical Education released a report with a set of guidelines for the screening and assessment of physicians. The document is the product of a committee created in 2015 to study the subject. The AMA recommends that the assessment of elderly physicians be based on evidence and ethical, relevant, fair, equitable, transparent, verifiable, nonexhaustive principles, contemplating support and protecting against legal proceedings. In April of this year, a new AMA document highlighted the same principles.
Also in the United States, one of oldest initiatives created to support physicians in the process of recycling, the University of California San Diego Physician Assessment and Clinical Education Program (PACE), has a section focusing on the extended practice of medicine (Practicing Medicine Longer). For those wanting to learn more about discussions on this subject, there are online presentations on experiences in Quebec and Ontario with assessing aging physicians, neuropsychological perspectives on the aging medical population, and what to expect of healthy aging, among other subjects.
Created in 1996, PACE mostly provides services to physicians who need to address requirements of the state medical boards. Few physicians enroll on their own.
The first part of the program assesses knowledge and skills over approximately 2 days. In the second phase, the physician participates in a series of activities in a corresponding residency program. Depending on the results, the physician may have to go through a remedial program with varying activities to deal with performance deficiencies to clinical experiences at the residency level.
A version of this article first appeared on Medscape.com.
Malaria vaccine gets special delivery by tiny health personnel
Don’t like needles? Have we got a vaccine for you
Here’s a quick question: How do you turn the most annoying thing ever into something positive?
No, we’re not talking about politicians this time. No, not Elon Musk, either. Infomercials? Guess again. Humidity? Nope, even more annoying than that.
Give up? The most annoying thing ever is mosquitoes. This time, however, NPR reports that mosquitoes have been used to deliver a vaccine for the very disease they’ve been transmitting to their human food sources all these years.
In a recent proof-of-concept trial, investigators used CRISPR technology to genetically modify malaria-causing Plasmodium falciparum sporozoites, which just happen to live in the salivary glands of Anopheles mosquitoes. And since the Plasmodium parasites are already in the mosquitoes, it made sense to use the buzzy little critters as the delivery device for the vaccine.
More sense than a syringe, you ask? Have you ever tried to poke a syringe into the salivary gland of a mosquito? No, we thought not. Well, we can tell you from experience that it’s really, really hard. Never mind how we know. We just do.
The 14 study volunteers – who were paid $4,100 for their participation – were first exposed to hundreds of mosquitoes carrying the altered Plasmodium parasites. Then, to test the vaccine, they were exposed to mosquitoes that had actual, malaria-carrying Plasmodium. Half of the subjects got malaria, so the vaccine was only 50% effective, meaning there’s still work to do.
Meanwhile, the scientists here at LOTMEco are all over this mosquito-delivery business, working on a vaccine to prevent Elon Musk. Plan B involves some sort of really big swatter.
Climate change: Sleeping your life away
It’s no secret that climate change is raising the temperature on everything. You may think you’re getting relief when the sun goes down, but in some places it’s still hot. A new survey conducted in central Japan shows how bad it can be and how higher nighttime temperatures can have a serious impact on people’s health.
That online survey, the Sleep Quality Index for Daily Sleep, enabled the investigators to correlate sleep quality with daily temperature for 1,284 adults in 2011 and 2012 who completed the survey over 10 days.
Not only was there a significant difference in sleep disturbance among younger men (higher) versus older men, but the prevalence of sleep disturbance went up when the daytime temperature was above 24.8° C. They also found that disability-adjusted life-years (DALYs), which measure time lost through premature death and time lived in certain conditions that put one’s health at risk, were 81.8 years for the city of Nagoya (population, 2.2 million) in 2012.
The damage to health from sleep disorders caused by daily temperatures higher than 25° C “is comparable to that of heatstroke and must be addressed,” lead author Tomohiko Ihara of the University of Tokyo said in a written statement.
The researchers hope that this information will help sway legislators to consider the impact of higher nighttime temperatures and that it can be used to provide guidance for better sleep. The solution for now? Sleep with the air conditioner on. Your energy bill might increase, but just think about those DALYs. If using the AC lowers DALYs and increases time lived, then we say it’s worth it.
Maybe it would have been a dragon WITH cancer
If you ask a random person on the street to tell you all they know about the country of Wales, they’ll probably mention two things: One, the contorted collection of jumbled-up letters that is the Welsh language (looking at you, Llanfairpwllgwyngyllgogerychwyrndrobwllllantysiliogogogoch) and, two, the association with dragons. The Welsh flag even has a dragon on it.
With that in mind, take a guess as to what sort of statue art dealer Simon Wingett wanted to build in the Welsh town of Wrexham. No, not a monument to the second-longest place name in the world. Try again. His dragon would not be some piddly little thing either; he wanted a virtual kaiju overlooking the town, with the whole statue to stand about 60 meters high. That’s taller than the original 1954 Godzilla.
Artistic masterpieces may sell for frankly insane prices, but art dealers themselves are not the wealthiest of individuals, so Mr. Wingett needed money to fund his dragon-based dream. Lucky for him, he also happened to be the manager of a cancer charity – initially set up by Mr. Wingett’s father, who had throat cancer – which nominally aimed to provide equipment and resources to cancer patients in the Wrexham area.
Yes, this is going precisely where you think it’s going. From 2011 to 2018, when the charity closed, Mr. Wingett used the charity’s donations to fund his dragon statue – which never actually got built, by the way – to the tune of over 400,000 pounds. Of course, Mr. Wingett came under scrutiny when people started to notice that his cancer charity hadn’t actually done anything charitable since 2011, and he was recently banned by the Welsh High Court from serving as trustee of any charity for 10 years. Oh no, tragedy and horror! Truly a punishment worse than death itself.
Okay fine, he also has to pay back 117,000 pounds to actual legitimate cancer charities. The astute mathematicians out there may notice that 117,000 is a lot less than 400,000. But it’s just as the old saying goes: One-quarter of crime doesn’t pay. You can keep three-quarters of it, though, that’s completely fine.
Don’t like needles? Have we got a vaccine for you
Here’s a quick question: How do you turn the most annoying thing ever into something positive?
No, we’re not talking about politicians this time. No, not Elon Musk, either. Infomercials? Guess again. Humidity? Nope, even more annoying than that.
Give up? The most annoying thing ever is mosquitoes. This time, however, NPR reports that mosquitoes have been used to deliver a vaccine for the very disease they’ve been transmitting to their human food sources all these years.
In a recent proof-of-concept trial, investigators used CRISPR technology to genetically modify malaria-causing Plasmodium falciparum sporozoites, which just happen to live in the salivary glands of Anopheles mosquitoes. And since the Plasmodium parasites are already in the mosquitoes, it made sense to use the buzzy little critters as the delivery device for the vaccine.
More sense than a syringe, you ask? Have you ever tried to poke a syringe into the salivary gland of a mosquito? No, we thought not. Well, we can tell you from experience that it’s really, really hard. Never mind how we know. We just do.
The 14 study volunteers – who were paid $4,100 for their participation – were first exposed to hundreds of mosquitoes carrying the altered Plasmodium parasites. Then, to test the vaccine, they were exposed to mosquitoes that had actual, malaria-carrying Plasmodium. Half of the subjects got malaria, so the vaccine was only 50% effective, meaning there’s still work to do.
Meanwhile, the scientists here at LOTMEco are all over this mosquito-delivery business, working on a vaccine to prevent Elon Musk. Plan B involves some sort of really big swatter.
Climate change: Sleeping your life away
It’s no secret that climate change is raising the temperature on everything. You may think you’re getting relief when the sun goes down, but in some places it’s still hot. A new survey conducted in central Japan shows how bad it can be and how higher nighttime temperatures can have a serious impact on people’s health.
That online survey, the Sleep Quality Index for Daily Sleep, enabled the investigators to correlate sleep quality with daily temperature for 1,284 adults in 2011 and 2012 who completed the survey over 10 days.
Not only was there a significant difference in sleep disturbance among younger men (higher) versus older men, but the prevalence of sleep disturbance went up when the daytime temperature was above 24.8° C. They also found that disability-adjusted life-years (DALYs), which measure time lost through premature death and time lived in certain conditions that put one’s health at risk, were 81.8 years for the city of Nagoya (population, 2.2 million) in 2012.
The damage to health from sleep disorders caused by daily temperatures higher than 25° C “is comparable to that of heatstroke and must be addressed,” lead author Tomohiko Ihara of the University of Tokyo said in a written statement.
The researchers hope that this information will help sway legislators to consider the impact of higher nighttime temperatures and that it can be used to provide guidance for better sleep. The solution for now? Sleep with the air conditioner on. Your energy bill might increase, but just think about those DALYs. If using the AC lowers DALYs and increases time lived, then we say it’s worth it.
Maybe it would have been a dragon WITH cancer
If you ask a random person on the street to tell you all they know about the country of Wales, they’ll probably mention two things: One, the contorted collection of jumbled-up letters that is the Welsh language (looking at you, Llanfairpwllgwyngyllgogerychwyrndrobwllllantysiliogogogoch) and, two, the association with dragons. The Welsh flag even has a dragon on it.
With that in mind, take a guess as to what sort of statue art dealer Simon Wingett wanted to build in the Welsh town of Wrexham. No, not a monument to the second-longest place name in the world. Try again. His dragon would not be some piddly little thing either; he wanted a virtual kaiju overlooking the town, with the whole statue to stand about 60 meters high. That’s taller than the original 1954 Godzilla.
Artistic masterpieces may sell for frankly insane prices, but art dealers themselves are not the wealthiest of individuals, so Mr. Wingett needed money to fund his dragon-based dream. Lucky for him, he also happened to be the manager of a cancer charity – initially set up by Mr. Wingett’s father, who had throat cancer – which nominally aimed to provide equipment and resources to cancer patients in the Wrexham area.
Yes, this is going precisely where you think it’s going. From 2011 to 2018, when the charity closed, Mr. Wingett used the charity’s donations to fund his dragon statue – which never actually got built, by the way – to the tune of over 400,000 pounds. Of course, Mr. Wingett came under scrutiny when people started to notice that his cancer charity hadn’t actually done anything charitable since 2011, and he was recently banned by the Welsh High Court from serving as trustee of any charity for 10 years. Oh no, tragedy and horror! Truly a punishment worse than death itself.
Okay fine, he also has to pay back 117,000 pounds to actual legitimate cancer charities. The astute mathematicians out there may notice that 117,000 is a lot less than 400,000. But it’s just as the old saying goes: One-quarter of crime doesn’t pay. You can keep three-quarters of it, though, that’s completely fine.
Don’t like needles? Have we got a vaccine for you
Here’s a quick question: How do you turn the most annoying thing ever into something positive?
No, we’re not talking about politicians this time. No, not Elon Musk, either. Infomercials? Guess again. Humidity? Nope, even more annoying than that.
Give up? The most annoying thing ever is mosquitoes. This time, however, NPR reports that mosquitoes have been used to deliver a vaccine for the very disease they’ve been transmitting to their human food sources all these years.
In a recent proof-of-concept trial, investigators used CRISPR technology to genetically modify malaria-causing Plasmodium falciparum sporozoites, which just happen to live in the salivary glands of Anopheles mosquitoes. And since the Plasmodium parasites are already in the mosquitoes, it made sense to use the buzzy little critters as the delivery device for the vaccine.
More sense than a syringe, you ask? Have you ever tried to poke a syringe into the salivary gland of a mosquito? No, we thought not. Well, we can tell you from experience that it’s really, really hard. Never mind how we know. We just do.
The 14 study volunteers – who were paid $4,100 for their participation – were first exposed to hundreds of mosquitoes carrying the altered Plasmodium parasites. Then, to test the vaccine, they were exposed to mosquitoes that had actual, malaria-carrying Plasmodium. Half of the subjects got malaria, so the vaccine was only 50% effective, meaning there’s still work to do.
Meanwhile, the scientists here at LOTMEco are all over this mosquito-delivery business, working on a vaccine to prevent Elon Musk. Plan B involves some sort of really big swatter.
Climate change: Sleeping your life away
It’s no secret that climate change is raising the temperature on everything. You may think you’re getting relief when the sun goes down, but in some places it’s still hot. A new survey conducted in central Japan shows how bad it can be and how higher nighttime temperatures can have a serious impact on people’s health.
That online survey, the Sleep Quality Index for Daily Sleep, enabled the investigators to correlate sleep quality with daily temperature for 1,284 adults in 2011 and 2012 who completed the survey over 10 days.
Not only was there a significant difference in sleep disturbance among younger men (higher) versus older men, but the prevalence of sleep disturbance went up when the daytime temperature was above 24.8° C. They also found that disability-adjusted life-years (DALYs), which measure time lost through premature death and time lived in certain conditions that put one’s health at risk, were 81.8 years for the city of Nagoya (population, 2.2 million) in 2012.
The damage to health from sleep disorders caused by daily temperatures higher than 25° C “is comparable to that of heatstroke and must be addressed,” lead author Tomohiko Ihara of the University of Tokyo said in a written statement.
The researchers hope that this information will help sway legislators to consider the impact of higher nighttime temperatures and that it can be used to provide guidance for better sleep. The solution for now? Sleep with the air conditioner on. Your energy bill might increase, but just think about those DALYs. If using the AC lowers DALYs and increases time lived, then we say it’s worth it.
Maybe it would have been a dragon WITH cancer
If you ask a random person on the street to tell you all they know about the country of Wales, they’ll probably mention two things: One, the contorted collection of jumbled-up letters that is the Welsh language (looking at you, Llanfairpwllgwyngyllgogerychwyrndrobwllllantysiliogogogoch) and, two, the association with dragons. The Welsh flag even has a dragon on it.
With that in mind, take a guess as to what sort of statue art dealer Simon Wingett wanted to build in the Welsh town of Wrexham. No, not a monument to the second-longest place name in the world. Try again. His dragon would not be some piddly little thing either; he wanted a virtual kaiju overlooking the town, with the whole statue to stand about 60 meters high. That’s taller than the original 1954 Godzilla.
Artistic masterpieces may sell for frankly insane prices, but art dealers themselves are not the wealthiest of individuals, so Mr. Wingett needed money to fund his dragon-based dream. Lucky for him, he also happened to be the manager of a cancer charity – initially set up by Mr. Wingett’s father, who had throat cancer – which nominally aimed to provide equipment and resources to cancer patients in the Wrexham area.
Yes, this is going precisely where you think it’s going. From 2011 to 2018, when the charity closed, Mr. Wingett used the charity’s donations to fund his dragon statue – which never actually got built, by the way – to the tune of over 400,000 pounds. Of course, Mr. Wingett came under scrutiny when people started to notice that his cancer charity hadn’t actually done anything charitable since 2011, and he was recently banned by the Welsh High Court from serving as trustee of any charity for 10 years. Oh no, tragedy and horror! Truly a punishment worse than death itself.
Okay fine, he also has to pay back 117,000 pounds to actual legitimate cancer charities. The astute mathematicians out there may notice that 117,000 is a lot less than 400,000. But it’s just as the old saying goes: One-quarter of crime doesn’t pay. You can keep three-quarters of it, though, that’s completely fine.
Children and COVID: Weekly cases dropped by 57% in September
The last full week of September brought a 4th straight week of declines in the number of new COVID-19 cases reported among children, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, with the month of September bringing a decline of about 57% in reported cases for the 45 states and territories that are still releasing pediatric COVID data on their health department websites, the AAP and CHA said in their joint weekly report.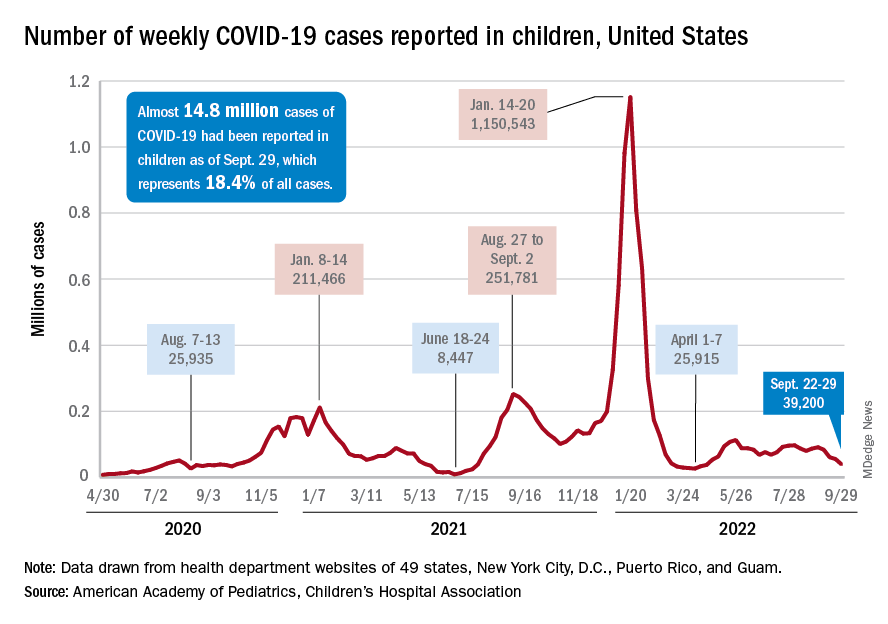
New cases dropped in all four regions after the Northeast and West had seen increases the previous week, and the distribution of cases for the latest week was fairly even, with the Midwest and Northeast right around 10,000, the South slightly over 10,000, and the West under 10,000 by about the same amount. At the state level, the largest increases – around 1.5% – over the last 2 weeks occurred in Kentucky and Nevada, the AAP/CHA data show.
The cumulative number of COVID-19 cases in children was almost 14.8 million as of Sept. 29, with children representing 18.4% of all cases since the pandemic began, the AAP and CHA said. The Centers for Disease Control and Prevention, which is able to use a uniform age range of 0-17 years, puts total cases at 15.2 million and the proportion of child cases at 17.4%. Total deaths in children from COVID as of Oct. 3 were 1,745, the CDC reported.
New vaccinations, in the meantime, are being added in numbers only slightly higher than new cases. Initial COVID vaccinations for the week of Sept. 22-28 were about 44,000 for children under 5 years of age (down from 51,000 the week before), 24,000 for children aged 5-11 years (down from 28,000), and 17,000 for those aged 12-17 (down from 18,000), the AAP said in its weekly vaccination report.
To look at it another way, the total proportion of children under 5 years of age who had received at least one dose of COVID vaccine as of Sept. 28 was 6.5%, compared with 6.4% on Sept. 21, while the corresponding rates for children aged 5-11 and 12-17 were unchanged at 38.5% and 70.9%. The 12- to 17-year-olds, in fact, have been stuck at 70.9% since Sept. 13, according to data from the CDC.
In a recent study published in Vaccine, investigators attributed the discrepancies between age groups at least partly to the acceptance of misinformation about vaccine safety in general and the COVID-19 vaccines in particular.
“All of the misconceptions we studied focused in one way or another on the safety of vaccination, and that explains why people’s misbeliefs about vaccinating kids are so highly related to their concerns about vaccines in general. Unfortunately, those concerns weigh even more heavily when adults consider vaccinating children,” lead author Dan Romer, PhD, of the University of Pennsylvania, Philadelphia, said in a written statement.
The last full week of September brought a 4th straight week of declines in the number of new COVID-19 cases reported among children, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, with the month of September bringing a decline of about 57% in reported cases for the 45 states and territories that are still releasing pediatric COVID data on their health department websites, the AAP and CHA said in their joint weekly report.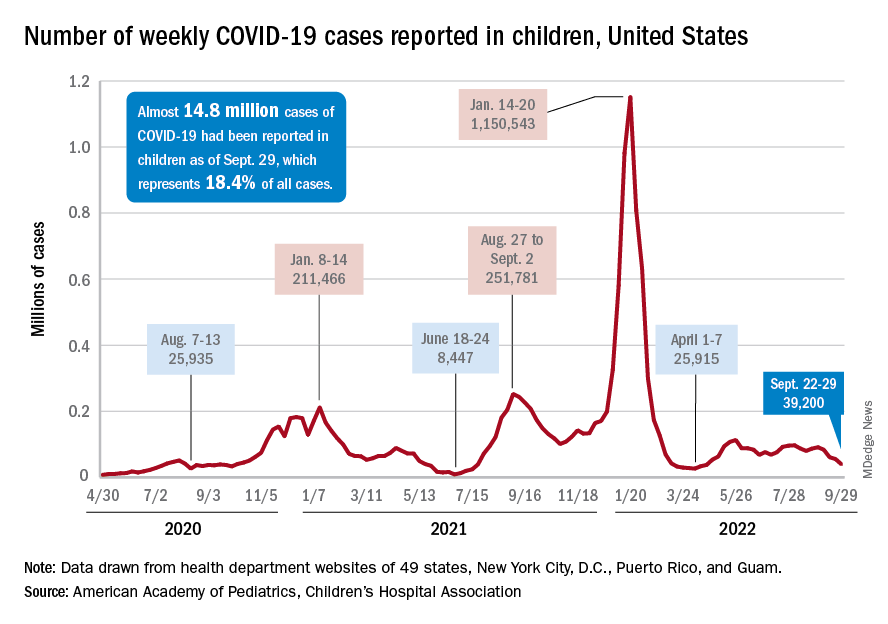
New cases dropped in all four regions after the Northeast and West had seen increases the previous week, and the distribution of cases for the latest week was fairly even, with the Midwest and Northeast right around 10,000, the South slightly over 10,000, and the West under 10,000 by about the same amount. At the state level, the largest increases – around 1.5% – over the last 2 weeks occurred in Kentucky and Nevada, the AAP/CHA data show.
The cumulative number of COVID-19 cases in children was almost 14.8 million as of Sept. 29, with children representing 18.4% of all cases since the pandemic began, the AAP and CHA said. The Centers for Disease Control and Prevention, which is able to use a uniform age range of 0-17 years, puts total cases at 15.2 million and the proportion of child cases at 17.4%. Total deaths in children from COVID as of Oct. 3 were 1,745, the CDC reported.
New vaccinations, in the meantime, are being added in numbers only slightly higher than new cases. Initial COVID vaccinations for the week of Sept. 22-28 were about 44,000 for children under 5 years of age (down from 51,000 the week before), 24,000 for children aged 5-11 years (down from 28,000), and 17,000 for those aged 12-17 (down from 18,000), the AAP said in its weekly vaccination report.
To look at it another way, the total proportion of children under 5 years of age who had received at least one dose of COVID vaccine as of Sept. 28 was 6.5%, compared with 6.4% on Sept. 21, while the corresponding rates for children aged 5-11 and 12-17 were unchanged at 38.5% and 70.9%. The 12- to 17-year-olds, in fact, have been stuck at 70.9% since Sept. 13, according to data from the CDC.
In a recent study published in Vaccine, investigators attributed the discrepancies between age groups at least partly to the acceptance of misinformation about vaccine safety in general and the COVID-19 vaccines in particular.
“All of the misconceptions we studied focused in one way or another on the safety of vaccination, and that explains why people’s misbeliefs about vaccinating kids are so highly related to their concerns about vaccines in general. Unfortunately, those concerns weigh even more heavily when adults consider vaccinating children,” lead author Dan Romer, PhD, of the University of Pennsylvania, Philadelphia, said in a written statement.
The last full week of September brought a 4th straight week of declines in the number of new COVID-19 cases reported among children, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, with the month of September bringing a decline of about 57% in reported cases for the 45 states and territories that are still releasing pediatric COVID data on their health department websites, the AAP and CHA said in their joint weekly report.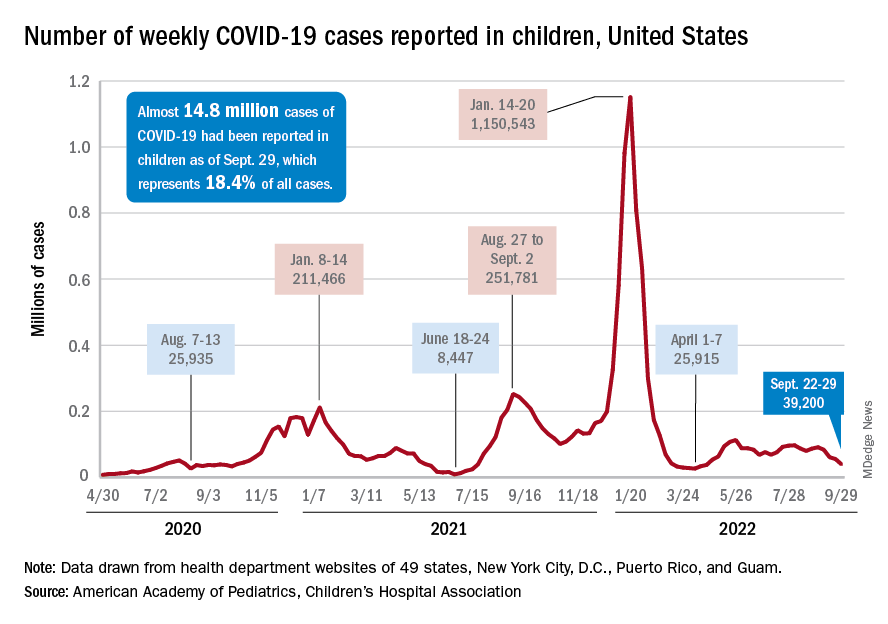
New cases dropped in all four regions after the Northeast and West had seen increases the previous week, and the distribution of cases for the latest week was fairly even, with the Midwest and Northeast right around 10,000, the South slightly over 10,000, and the West under 10,000 by about the same amount. At the state level, the largest increases – around 1.5% – over the last 2 weeks occurred in Kentucky and Nevada, the AAP/CHA data show.
The cumulative number of COVID-19 cases in children was almost 14.8 million as of Sept. 29, with children representing 18.4% of all cases since the pandemic began, the AAP and CHA said. The Centers for Disease Control and Prevention, which is able to use a uniform age range of 0-17 years, puts total cases at 15.2 million and the proportion of child cases at 17.4%. Total deaths in children from COVID as of Oct. 3 were 1,745, the CDC reported.
New vaccinations, in the meantime, are being added in numbers only slightly higher than new cases. Initial COVID vaccinations for the week of Sept. 22-28 were about 44,000 for children under 5 years of age (down from 51,000 the week before), 24,000 for children aged 5-11 years (down from 28,000), and 17,000 for those aged 12-17 (down from 18,000), the AAP said in its weekly vaccination report.
To look at it another way, the total proportion of children under 5 years of age who had received at least one dose of COVID vaccine as of Sept. 28 was 6.5%, compared with 6.4% on Sept. 21, while the corresponding rates for children aged 5-11 and 12-17 were unchanged at 38.5% and 70.9%. The 12- to 17-year-olds, in fact, have been stuck at 70.9% since Sept. 13, according to data from the CDC.
In a recent study published in Vaccine, investigators attributed the discrepancies between age groups at least partly to the acceptance of misinformation about vaccine safety in general and the COVID-19 vaccines in particular.
“All of the misconceptions we studied focused in one way or another on the safety of vaccination, and that explains why people’s misbeliefs about vaccinating kids are so highly related to their concerns about vaccines in general. Unfortunately, those concerns weigh even more heavily when adults consider vaccinating children,” lead author Dan Romer, PhD, of the University of Pennsylvania, Philadelphia, said in a written statement.
Childhood peanut allergy linked with other legume allergies
, a retrospective study reports.
“Among children allergic to peanut, at least two-thirds were sensitized to one other legume, and legume allergy was diagnosed in one-quarter of the sensitized patients,” senior study author Amandine Divaret-Chauveau, MD, of the Centre Hospitalier Universitaire de Nancy in Vandoeuvre-les-Nancy, France, and colleagues reported in Pediatric Allergy and Immunology.
People worldwide are eating more legumes these days, the authors noted. High in protein, low in unsaturated fats, with low production costs, legumes are important components of increasingly vegetarian, healthy, sustainable diets.
Food allergens are the most common childhood triggers of allergic reactions. Among children in France, legumes cause 14.6% of food-related anaphylactic reactions, with peanut as the main allergen, they added.
Dr. Divaret-Chauveau and colleagues assessed the prevalence and relevance of sensitization to legumes among all children and adolescents aged 1-17 years who had peanut allergy and had been admitted to one academic pediatric allergy department over roughly 3 years, beginning in early 2017. For the 195 study participants, peanut allergy had been confirmed, and they had been documented to have consumed or to have sensitization to at least one nonpeanut legume; 69.7% were boys.
The researchers analyzed data on consumption history, skin-prick tests, specific immunoglobulin E status, prior allergic reactions, and oral food challenges for each legume. They found the following:
Among the 195 children with peanut allergy, 98.4% had at least one other atopic disease.
Of the 195 children with peanut allergy, 122 (63.9%) were sensitized to at least one other legume. Of these 122 children, 66.3% were sensitized to fenugreek, 42.2% to lentil, 39.9% to soy, and 34.2% to lupin.
Allergy to one or more legumes was confirmed for 27.9% of the 122 sensitized children, including 4.9% who had multiple legume allergies. Lentil, lupin, and pea were the main allergens.
Of the 118 children also having a nonlegume food allergy, the main food allergens were egg (57.6%), cow’s milk (33.0%), cashew (39.0%), pistachio (23.7%), and hazelnut (30.5%).
50% of allergic reactions to nonpeanut legumes were severe, often showing as asthma. Atopic comorbidities, including asthma, in most participants may have contributed to the severity of allergic reactions, the authors noted.
Allergy awareness needs to grow with plant-based diets
“The high prevalence of legume sensitization reported in our study highlights the need to explore legume consumption in children with PA [peanut allergy], and the need to investigate sensitization in the absence of consumption,” they added.
Jodi A. Shroba, MSN, APRN, CPNP, coordinator for the Food Allergy Program at Children’s Mercy Kansas City (Mo.), said in an interview that few data are available in the literature regarding allergies to legumes other than peanut.
“It was interesting that these authors found such a high legume sensitization in their peanut-allergic patients,” Dr. Shroba, who was not involved in the study, said by email. “As more people are starting to eat plant-based diets, it is important that we better understand their allergenicity and cross-reactivity so we can better help guide patient management and education.”
Deborah Albright, MD, assistant professor of pediatrics at the University of Pittsburgh, agreed.
“As plant-based protein consumption broadens worldwide, awareness of the potential for cross-reactivity and co-allergy amongst legumes will become increasingly important,” she said in a comment.
“However, positive allergy tests do not reliably correlate with true food allergy; therefore, the diagnosis of legume co-allergy should be confirmed by the individual patient’s history, a formal food challenge, or both,” advised Dr. Albright. She was not involved in the study.
“Cross-sensitization to other legumes in patients with a single legume allergy is common; however, true clinical reactivity is often not present,” she added. “Also, legume allergy test sensitization rates and objective reactivity on food challenge can vary by region, depending on diet and pollen aeroallergen exposure.
“Systematic exploration of tolerance versus co-allergy to other legumes should be considered in patients allergic to peanut or other legumes,” Dr. Albright said.
The authors recommend further research and registry data collection of legume anaphylaxis.
Details regarding funding for the study were not provided. The authors, Dr. Shroba, and Dr. Albright report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, a retrospective study reports.
“Among children allergic to peanut, at least two-thirds were sensitized to one other legume, and legume allergy was diagnosed in one-quarter of the sensitized patients,” senior study author Amandine Divaret-Chauveau, MD, of the Centre Hospitalier Universitaire de Nancy in Vandoeuvre-les-Nancy, France, and colleagues reported in Pediatric Allergy and Immunology.
People worldwide are eating more legumes these days, the authors noted. High in protein, low in unsaturated fats, with low production costs, legumes are important components of increasingly vegetarian, healthy, sustainable diets.
Food allergens are the most common childhood triggers of allergic reactions. Among children in France, legumes cause 14.6% of food-related anaphylactic reactions, with peanut as the main allergen, they added.
Dr. Divaret-Chauveau and colleagues assessed the prevalence and relevance of sensitization to legumes among all children and adolescents aged 1-17 years who had peanut allergy and had been admitted to one academic pediatric allergy department over roughly 3 years, beginning in early 2017. For the 195 study participants, peanut allergy had been confirmed, and they had been documented to have consumed or to have sensitization to at least one nonpeanut legume; 69.7% were boys.
The researchers analyzed data on consumption history, skin-prick tests, specific immunoglobulin E status, prior allergic reactions, and oral food challenges for each legume. They found the following:
Among the 195 children with peanut allergy, 98.4% had at least one other atopic disease.
Of the 195 children with peanut allergy, 122 (63.9%) were sensitized to at least one other legume. Of these 122 children, 66.3% were sensitized to fenugreek, 42.2% to lentil, 39.9% to soy, and 34.2% to lupin.
Allergy to one or more legumes was confirmed for 27.9% of the 122 sensitized children, including 4.9% who had multiple legume allergies. Lentil, lupin, and pea were the main allergens.
Of the 118 children also having a nonlegume food allergy, the main food allergens were egg (57.6%), cow’s milk (33.0%), cashew (39.0%), pistachio (23.7%), and hazelnut (30.5%).
50% of allergic reactions to nonpeanut legumes were severe, often showing as asthma. Atopic comorbidities, including asthma, in most participants may have contributed to the severity of allergic reactions, the authors noted.
Allergy awareness needs to grow with plant-based diets
“The high prevalence of legume sensitization reported in our study highlights the need to explore legume consumption in children with PA [peanut allergy], and the need to investigate sensitization in the absence of consumption,” they added.
Jodi A. Shroba, MSN, APRN, CPNP, coordinator for the Food Allergy Program at Children’s Mercy Kansas City (Mo.), said in an interview that few data are available in the literature regarding allergies to legumes other than peanut.
“It was interesting that these authors found such a high legume sensitization in their peanut-allergic patients,” Dr. Shroba, who was not involved in the study, said by email. “As more people are starting to eat plant-based diets, it is important that we better understand their allergenicity and cross-reactivity so we can better help guide patient management and education.”
Deborah Albright, MD, assistant professor of pediatrics at the University of Pittsburgh, agreed.
“As plant-based protein consumption broadens worldwide, awareness of the potential for cross-reactivity and co-allergy amongst legumes will become increasingly important,” she said in a comment.
“However, positive allergy tests do not reliably correlate with true food allergy; therefore, the diagnosis of legume co-allergy should be confirmed by the individual patient’s history, a formal food challenge, or both,” advised Dr. Albright. She was not involved in the study.
“Cross-sensitization to other legumes in patients with a single legume allergy is common; however, true clinical reactivity is often not present,” she added. “Also, legume allergy test sensitization rates and objective reactivity on food challenge can vary by region, depending on diet and pollen aeroallergen exposure.
“Systematic exploration of tolerance versus co-allergy to other legumes should be considered in patients allergic to peanut or other legumes,” Dr. Albright said.
The authors recommend further research and registry data collection of legume anaphylaxis.
Details regarding funding for the study were not provided. The authors, Dr. Shroba, and Dr. Albright report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, a retrospective study reports.
“Among children allergic to peanut, at least two-thirds were sensitized to one other legume, and legume allergy was diagnosed in one-quarter of the sensitized patients,” senior study author Amandine Divaret-Chauveau, MD, of the Centre Hospitalier Universitaire de Nancy in Vandoeuvre-les-Nancy, France, and colleagues reported in Pediatric Allergy and Immunology.
People worldwide are eating more legumes these days, the authors noted. High in protein, low in unsaturated fats, with low production costs, legumes are important components of increasingly vegetarian, healthy, sustainable diets.
Food allergens are the most common childhood triggers of allergic reactions. Among children in France, legumes cause 14.6% of food-related anaphylactic reactions, with peanut as the main allergen, they added.
Dr. Divaret-Chauveau and colleagues assessed the prevalence and relevance of sensitization to legumes among all children and adolescents aged 1-17 years who had peanut allergy and had been admitted to one academic pediatric allergy department over roughly 3 years, beginning in early 2017. For the 195 study participants, peanut allergy had been confirmed, and they had been documented to have consumed or to have sensitization to at least one nonpeanut legume; 69.7% were boys.
The researchers analyzed data on consumption history, skin-prick tests, specific immunoglobulin E status, prior allergic reactions, and oral food challenges for each legume. They found the following:
Among the 195 children with peanut allergy, 98.4% had at least one other atopic disease.
Of the 195 children with peanut allergy, 122 (63.9%) were sensitized to at least one other legume. Of these 122 children, 66.3% were sensitized to fenugreek, 42.2% to lentil, 39.9% to soy, and 34.2% to lupin.
Allergy to one or more legumes was confirmed for 27.9% of the 122 sensitized children, including 4.9% who had multiple legume allergies. Lentil, lupin, and pea were the main allergens.
Of the 118 children also having a nonlegume food allergy, the main food allergens were egg (57.6%), cow’s milk (33.0%), cashew (39.0%), pistachio (23.7%), and hazelnut (30.5%).
50% of allergic reactions to nonpeanut legumes were severe, often showing as asthma. Atopic comorbidities, including asthma, in most participants may have contributed to the severity of allergic reactions, the authors noted.
Allergy awareness needs to grow with plant-based diets
“The high prevalence of legume sensitization reported in our study highlights the need to explore legume consumption in children with PA [peanut allergy], and the need to investigate sensitization in the absence of consumption,” they added.
Jodi A. Shroba, MSN, APRN, CPNP, coordinator for the Food Allergy Program at Children’s Mercy Kansas City (Mo.), said in an interview that few data are available in the literature regarding allergies to legumes other than peanut.
“It was interesting that these authors found such a high legume sensitization in their peanut-allergic patients,” Dr. Shroba, who was not involved in the study, said by email. “As more people are starting to eat plant-based diets, it is important that we better understand their allergenicity and cross-reactivity so we can better help guide patient management and education.”
Deborah Albright, MD, assistant professor of pediatrics at the University of Pittsburgh, agreed.
“As plant-based protein consumption broadens worldwide, awareness of the potential for cross-reactivity and co-allergy amongst legumes will become increasingly important,” she said in a comment.
“However, positive allergy tests do not reliably correlate with true food allergy; therefore, the diagnosis of legume co-allergy should be confirmed by the individual patient’s history, a formal food challenge, or both,” advised Dr. Albright. She was not involved in the study.
“Cross-sensitization to other legumes in patients with a single legume allergy is common; however, true clinical reactivity is often not present,” she added. “Also, legume allergy test sensitization rates and objective reactivity on food challenge can vary by region, depending on diet and pollen aeroallergen exposure.
“Systematic exploration of tolerance versus co-allergy to other legumes should be considered in patients allergic to peanut or other legumes,” Dr. Albright said.
The authors recommend further research and registry data collection of legume anaphylaxis.
Details regarding funding for the study were not provided. The authors, Dr. Shroba, and Dr. Albright report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PEDIATRIC ALLERGY AND IMMUNOLOGY