User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Check biases when caring for children with obesity
Counting calories should not be the focus of weight-loss strategies for children with obesity, according to an expert who said pediatricians need to change the way they discuss weight with their patients.
During a plenary session of the American Academy of Pediatrics National Conference, Joseph A. Skelton, MD, professor of pediatrics at Wake Forest University School of Medicine, Winston-Salem, N.C., said pediatricians should recognize the behavioral, physical, environmental, and genetic factors that contribute to obesity. For instance, food deserts are on the rise, and they undermine the ability of parents to feed their children healthy meals. In addition, more children are less physically active.
“Obesity is a lot more complex than calories in, calories out,” Dr. Skelton said. “We choose to treat issues of obesity as personal responsibility – ‘you did this to yourself’ – but when you look at how we move around and live our lives, our food systems, our policies, the social and environmental changes have caused shifts in our behavior.”
According to Dr. Skelton, bias against children with obesity can harm their self-image and weaken their motivations for losing weight. In addition, doctors may change how they deliver care on the basis of stereotypes regarding obese children. These stereotypes are often reinforced in media portrayals, Dr. Skelton said.
“When children or when adults who have excess weight or obesity are portrayed, they are portrayed typically in a negative fashion,” Dr. Skelton said. “There’s increasing evidence that weight bias and weight discrimination are increasing the morbidity we see in patients who develop obesity.”
For many children with obesity, visits to the pediatrician often center on weight, regardless of the reason for the appointment. Weight stigma and bias on the part of health care providers can increase stress, as well as adverse health outcomes in children, according to a 2019 study (Curr Opin Endocrinol Diabetes Obes. 2019 Feb 1. doi: 10.1097/MED.0000000000000453). Dr. Skelton recommended that pediatricians listen to their patients’ concerns and make a personalized care plan.
Dr. Skelton said doctors can pull from projects such as Health at Every Size, which offers templates for personalized health plans for children with obesity. It has a heavy focus on a weight-neutral approach to pediatric health.
“There are various ways to manage weight in a healthy and safe way,” Dr. Skelton said.
Evidence-based methods of treating obesity include focusing on health and healthy behaviors rather than weight and using the body mass index as a screening tool for further conversations about overall health, rather than as an indicator of health based on weight.
Dr. Skelton also encouraged pediatricians to be on the alert for indicators of disordered eating, which can include dieting, teasing, or talking excessively about weight at home and can involve reading misinformation about dieting online.
“Your job is to educate people on the dangers of following unscientific information online,” Dr. Skelton said. “We can address issues of weight health in a way that is patient centered and is very safe, without unintended consequences.” Brooke Sweeney, MD, professor of internal medicine and pediatrics at University of Missouri–Kansas City, said problems with weight bias in society and in clinical practice can lead to false assumptions about people who have obesity.
“It’s normal to gain adipose, or fat tissue, at different times in life, during puberty or pregnancy, and some people normally gain more weight than others,” Dr. Sweeney said.
The body will try to maintain a weight set point. That set point is influenced by many factors, such as genetics, environment, and lifestyle.
“When you lose weight, your body tries to get you back to the set point, decreasing energy expenditure and increasing hunger and reward pathways,” she said. “We have gained so much knowledge through research to better understand the pathophysiology of obesity, and we are making good progress on improving advanced treatments for increased weight in children.”
Dr. Skelton reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Counting calories should not be the focus of weight-loss strategies for children with obesity, according to an expert who said pediatricians need to change the way they discuss weight with their patients.
During a plenary session of the American Academy of Pediatrics National Conference, Joseph A. Skelton, MD, professor of pediatrics at Wake Forest University School of Medicine, Winston-Salem, N.C., said pediatricians should recognize the behavioral, physical, environmental, and genetic factors that contribute to obesity. For instance, food deserts are on the rise, and they undermine the ability of parents to feed their children healthy meals. In addition, more children are less physically active.
“Obesity is a lot more complex than calories in, calories out,” Dr. Skelton said. “We choose to treat issues of obesity as personal responsibility – ‘you did this to yourself’ – but when you look at how we move around and live our lives, our food systems, our policies, the social and environmental changes have caused shifts in our behavior.”
According to Dr. Skelton, bias against children with obesity can harm their self-image and weaken their motivations for losing weight. In addition, doctors may change how they deliver care on the basis of stereotypes regarding obese children. These stereotypes are often reinforced in media portrayals, Dr. Skelton said.
“When children or when adults who have excess weight or obesity are portrayed, they are portrayed typically in a negative fashion,” Dr. Skelton said. “There’s increasing evidence that weight bias and weight discrimination are increasing the morbidity we see in patients who develop obesity.”
For many children with obesity, visits to the pediatrician often center on weight, regardless of the reason for the appointment. Weight stigma and bias on the part of health care providers can increase stress, as well as adverse health outcomes in children, according to a 2019 study (Curr Opin Endocrinol Diabetes Obes. 2019 Feb 1. doi: 10.1097/MED.0000000000000453). Dr. Skelton recommended that pediatricians listen to their patients’ concerns and make a personalized care plan.
Dr. Skelton said doctors can pull from projects such as Health at Every Size, which offers templates for personalized health plans for children with obesity. It has a heavy focus on a weight-neutral approach to pediatric health.
“There are various ways to manage weight in a healthy and safe way,” Dr. Skelton said.
Evidence-based methods of treating obesity include focusing on health and healthy behaviors rather than weight and using the body mass index as a screening tool for further conversations about overall health, rather than as an indicator of health based on weight.
Dr. Skelton also encouraged pediatricians to be on the alert for indicators of disordered eating, which can include dieting, teasing, or talking excessively about weight at home and can involve reading misinformation about dieting online.
“Your job is to educate people on the dangers of following unscientific information online,” Dr. Skelton said. “We can address issues of weight health in a way that is patient centered and is very safe, without unintended consequences.” Brooke Sweeney, MD, professor of internal medicine and pediatrics at University of Missouri–Kansas City, said problems with weight bias in society and in clinical practice can lead to false assumptions about people who have obesity.
“It’s normal to gain adipose, or fat tissue, at different times in life, during puberty or pregnancy, and some people normally gain more weight than others,” Dr. Sweeney said.
The body will try to maintain a weight set point. That set point is influenced by many factors, such as genetics, environment, and lifestyle.
“When you lose weight, your body tries to get you back to the set point, decreasing energy expenditure and increasing hunger and reward pathways,” she said. “We have gained so much knowledge through research to better understand the pathophysiology of obesity, and we are making good progress on improving advanced treatments for increased weight in children.”
Dr. Skelton reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Counting calories should not be the focus of weight-loss strategies for children with obesity, according to an expert who said pediatricians need to change the way they discuss weight with their patients.
During a plenary session of the American Academy of Pediatrics National Conference, Joseph A. Skelton, MD, professor of pediatrics at Wake Forest University School of Medicine, Winston-Salem, N.C., said pediatricians should recognize the behavioral, physical, environmental, and genetic factors that contribute to obesity. For instance, food deserts are on the rise, and they undermine the ability of parents to feed their children healthy meals. In addition, more children are less physically active.
“Obesity is a lot more complex than calories in, calories out,” Dr. Skelton said. “We choose to treat issues of obesity as personal responsibility – ‘you did this to yourself’ – but when you look at how we move around and live our lives, our food systems, our policies, the social and environmental changes have caused shifts in our behavior.”
According to Dr. Skelton, bias against children with obesity can harm their self-image and weaken their motivations for losing weight. In addition, doctors may change how they deliver care on the basis of stereotypes regarding obese children. These stereotypes are often reinforced in media portrayals, Dr. Skelton said.
“When children or when adults who have excess weight or obesity are portrayed, they are portrayed typically in a negative fashion,” Dr. Skelton said. “There’s increasing evidence that weight bias and weight discrimination are increasing the morbidity we see in patients who develop obesity.”
For many children with obesity, visits to the pediatrician often center on weight, regardless of the reason for the appointment. Weight stigma and bias on the part of health care providers can increase stress, as well as adverse health outcomes in children, according to a 2019 study (Curr Opin Endocrinol Diabetes Obes. 2019 Feb 1. doi: 10.1097/MED.0000000000000453). Dr. Skelton recommended that pediatricians listen to their patients’ concerns and make a personalized care plan.
Dr. Skelton said doctors can pull from projects such as Health at Every Size, which offers templates for personalized health plans for children with obesity. It has a heavy focus on a weight-neutral approach to pediatric health.
“There are various ways to manage weight in a healthy and safe way,” Dr. Skelton said.
Evidence-based methods of treating obesity include focusing on health and healthy behaviors rather than weight and using the body mass index as a screening tool for further conversations about overall health, rather than as an indicator of health based on weight.
Dr. Skelton also encouraged pediatricians to be on the alert for indicators of disordered eating, which can include dieting, teasing, or talking excessively about weight at home and can involve reading misinformation about dieting online.
“Your job is to educate people on the dangers of following unscientific information online,” Dr. Skelton said. “We can address issues of weight health in a way that is patient centered and is very safe, without unintended consequences.” Brooke Sweeney, MD, professor of internal medicine and pediatrics at University of Missouri–Kansas City, said problems with weight bias in society and in clinical practice can lead to false assumptions about people who have obesity.
“It’s normal to gain adipose, or fat tissue, at different times in life, during puberty or pregnancy, and some people normally gain more weight than others,” Dr. Sweeney said.
The body will try to maintain a weight set point. That set point is influenced by many factors, such as genetics, environment, and lifestyle.
“When you lose weight, your body tries to get you back to the set point, decreasing energy expenditure and increasing hunger and reward pathways,” she said. “We have gained so much knowledge through research to better understand the pathophysiology of obesity, and we are making good progress on improving advanced treatments for increased weight in children.”
Dr. Skelton reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AAP 2022
Pediatricians urged to check for vision problems after concussion
Pediatricians should consider screening children suspected of having a concussion for resulting vision problems that are often overlooked, according to the American Academy of Pediatrics.
Christina Master, MD, a pediatrician and sports medicine specialist at the Children’s Hospital of Philadelphia, said many doctors don’t think of vision problems when examining children who’ve experienced a head injury. But the issues are common and can significantly affect a child’s performance in school and sports, and disrupt daily life.
Dr. Master led a team of sports medicine and vision specialists who wrote an AAP policy statement on vision and concussion. She summarized the new recommendations during a plenary session Oct. 9 at the American Academy of Pediatrics National Conference.
Dr. Master told this news organization that the vast majority of the estimated 1.4 million U.S. children and adolescents who have concussions annually are treated in pediatricians’ offices.
Up to 40% of young patients experience symptoms such as blurred vision, light sensitivity, and double vision following a concussion, the panel said. In addition, children with vision problems are more likely to have prolonged recoveries and delays in returning to school than children who have concussions but don’t have similar eyesight issues.
Concussions affect neurologic pathways of the visual system and disturb basic functions such as the ability of the eyes to change focus from a distant object to a near one.
Dr. Master said most pediatricians do not routinely check for vision problems following a concussion, and children themselves may not recognize that they have vision deficits “unless you ask them very specifically.”
In addition to asking children about their vision, the policy statement recommends pediatricians conduct a thorough exam to assess ocular alignment, the ability to track a moving object, and the ability to maintain focus on an image while moving.
Dr. Master said that an assessment of vision and balance, which is described in an accompanying clinical report, lasts about 5 minutes and is easy for pediatricians to learn.
Managing vision problems
Pediatricians can guide parents in talking to their child’s school about accommodations such as extra time on classroom tasks, creating materials with enlarged fonts, and using preprinted or audio notes, the statement said.
At school, vision deficits can interfere with reading by causing children to skip words, lose their place, become fatigued, or lose interest, according to the statement.
Children can also take breaks from visual stressors such as bright lights and screens, and use prescription glasses temporarily to correct blurred vision, the panel noted.
Although most children will recover from a concussion on their own within 4 weeks, up to one-third will have persistent symptoms and may benefit from seeing a specialist who can provide treatment such as rehabilitative exercises. While evidence suggests that referring some children to specialty care within a week of a concussion improves outcomes, the signs of who would benefit are not always clear, according to the panel.
Specialties such as sports medicine, neurology, physiatry, otorhinolaryngology, and occupational therapy may provide care for prolonged symptoms, Dr. Master said.
The panel noted that more study is needed on treatment options such as rehabilitation exercises, which have been shown to help with balance and dizziness.
Dr. Master said the panel did not recommend that pediatricians provide a home exercise program to treat concussion, as she does in her practice, explaining that “it’s not clear that it’s necessary for all kids.”
One author of the policy statement, Ankoor Shah, MD, PhD, reported an intellectual property relationship with Rebion involving a patent application for a pediatric vision screener. Others, including Dr. Master, reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pediatricians should consider screening children suspected of having a concussion for resulting vision problems that are often overlooked, according to the American Academy of Pediatrics.
Christina Master, MD, a pediatrician and sports medicine specialist at the Children’s Hospital of Philadelphia, said many doctors don’t think of vision problems when examining children who’ve experienced a head injury. But the issues are common and can significantly affect a child’s performance in school and sports, and disrupt daily life.
Dr. Master led a team of sports medicine and vision specialists who wrote an AAP policy statement on vision and concussion. She summarized the new recommendations during a plenary session Oct. 9 at the American Academy of Pediatrics National Conference.
Dr. Master told this news organization that the vast majority of the estimated 1.4 million U.S. children and adolescents who have concussions annually are treated in pediatricians’ offices.
Up to 40% of young patients experience symptoms such as blurred vision, light sensitivity, and double vision following a concussion, the panel said. In addition, children with vision problems are more likely to have prolonged recoveries and delays in returning to school than children who have concussions but don’t have similar eyesight issues.
Concussions affect neurologic pathways of the visual system and disturb basic functions such as the ability of the eyes to change focus from a distant object to a near one.
Dr. Master said most pediatricians do not routinely check for vision problems following a concussion, and children themselves may not recognize that they have vision deficits “unless you ask them very specifically.”
In addition to asking children about their vision, the policy statement recommends pediatricians conduct a thorough exam to assess ocular alignment, the ability to track a moving object, and the ability to maintain focus on an image while moving.
Dr. Master said that an assessment of vision and balance, which is described in an accompanying clinical report, lasts about 5 minutes and is easy for pediatricians to learn.
Managing vision problems
Pediatricians can guide parents in talking to their child’s school about accommodations such as extra time on classroom tasks, creating materials with enlarged fonts, and using preprinted or audio notes, the statement said.
At school, vision deficits can interfere with reading by causing children to skip words, lose their place, become fatigued, or lose interest, according to the statement.
Children can also take breaks from visual stressors such as bright lights and screens, and use prescription glasses temporarily to correct blurred vision, the panel noted.
Although most children will recover from a concussion on their own within 4 weeks, up to one-third will have persistent symptoms and may benefit from seeing a specialist who can provide treatment such as rehabilitative exercises. While evidence suggests that referring some children to specialty care within a week of a concussion improves outcomes, the signs of who would benefit are not always clear, according to the panel.
Specialties such as sports medicine, neurology, physiatry, otorhinolaryngology, and occupational therapy may provide care for prolonged symptoms, Dr. Master said.
The panel noted that more study is needed on treatment options such as rehabilitation exercises, which have been shown to help with balance and dizziness.
Dr. Master said the panel did not recommend that pediatricians provide a home exercise program to treat concussion, as she does in her practice, explaining that “it’s not clear that it’s necessary for all kids.”
One author of the policy statement, Ankoor Shah, MD, PhD, reported an intellectual property relationship with Rebion involving a patent application for a pediatric vision screener. Others, including Dr. Master, reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pediatricians should consider screening children suspected of having a concussion for resulting vision problems that are often overlooked, according to the American Academy of Pediatrics.
Christina Master, MD, a pediatrician and sports medicine specialist at the Children’s Hospital of Philadelphia, said many doctors don’t think of vision problems when examining children who’ve experienced a head injury. But the issues are common and can significantly affect a child’s performance in school and sports, and disrupt daily life.
Dr. Master led a team of sports medicine and vision specialists who wrote an AAP policy statement on vision and concussion. She summarized the new recommendations during a plenary session Oct. 9 at the American Academy of Pediatrics National Conference.
Dr. Master told this news organization that the vast majority of the estimated 1.4 million U.S. children and adolescents who have concussions annually are treated in pediatricians’ offices.
Up to 40% of young patients experience symptoms such as blurred vision, light sensitivity, and double vision following a concussion, the panel said. In addition, children with vision problems are more likely to have prolonged recoveries and delays in returning to school than children who have concussions but don’t have similar eyesight issues.
Concussions affect neurologic pathways of the visual system and disturb basic functions such as the ability of the eyes to change focus from a distant object to a near one.
Dr. Master said most pediatricians do not routinely check for vision problems following a concussion, and children themselves may not recognize that they have vision deficits “unless you ask them very specifically.”
In addition to asking children about their vision, the policy statement recommends pediatricians conduct a thorough exam to assess ocular alignment, the ability to track a moving object, and the ability to maintain focus on an image while moving.
Dr. Master said that an assessment of vision and balance, which is described in an accompanying clinical report, lasts about 5 minutes and is easy for pediatricians to learn.
Managing vision problems
Pediatricians can guide parents in talking to their child’s school about accommodations such as extra time on classroom tasks, creating materials with enlarged fonts, and using preprinted or audio notes, the statement said.
At school, vision deficits can interfere with reading by causing children to skip words, lose their place, become fatigued, or lose interest, according to the statement.
Children can also take breaks from visual stressors such as bright lights and screens, and use prescription glasses temporarily to correct blurred vision, the panel noted.
Although most children will recover from a concussion on their own within 4 weeks, up to one-third will have persistent symptoms and may benefit from seeing a specialist who can provide treatment such as rehabilitative exercises. While evidence suggests that referring some children to specialty care within a week of a concussion improves outcomes, the signs of who would benefit are not always clear, according to the panel.
Specialties such as sports medicine, neurology, physiatry, otorhinolaryngology, and occupational therapy may provide care for prolonged symptoms, Dr. Master said.
The panel noted that more study is needed on treatment options such as rehabilitation exercises, which have been shown to help with balance and dizziness.
Dr. Master said the panel did not recommend that pediatricians provide a home exercise program to treat concussion, as she does in her practice, explaining that “it’s not clear that it’s necessary for all kids.”
One author of the policy statement, Ankoor Shah, MD, PhD, reported an intellectual property relationship with Rebion involving a patent application for a pediatric vision screener. Others, including Dr. Master, reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AAP 2022
With sleuth work, pediatricians can identify genetic disorders
Jennifer Kalish, MD, PhD, fields as many as 10 inquiries a month from pediatricians who spot an unusual feature during a clinical exam, and wonder if they should refer the family to a geneticist.
“There are hundreds of rare disorders, and for a pediatrician, they can be hard to recognize,” Dr. Kalish said. “That’s why we’re here as geneticists – to partner so that we can help.”
Pediatricians play a key role in spotting signs of rare genetic diseases, but may need guidance for recognizing the more subtle presentations of a disorder, according to Dr. Kalish, a geneticist and director of the Beckwith-Wiedemann Syndrome Clinic at Children’s Hospital of Philadelphia, who spoke at the American Academy of Pediatrics National Conference.
Spectrums of disease
Pediatricians may struggle with deciding whether to make a referral, in part because genetic syndromes “do not always look like the textbook,” she said.
With many conditions, “we’re starting to understand that there’s really a spectrum of how affected versus less affected one can be,” by genetic and epigenetic changes, which have led to recognition that many cases are more subtle and harder to diagnose, she said.
Beckwith-Wiedemann syndrome is a prime example. The overgrowth disorder affects an estimated 1 in 10,340 infants, and is associated with a heightened risk of Wilms tumors, a form of kidney cancer, and hepatoblastomas. Children diagnosed with these conditions typically undergo frequent screenings to detect tumors to jumpstart treatment.
Some researchers believe Beckwith-Wiedemann syndrome is underdiagnosed because it can present in many different ways because of variations in the distributions of affected cells in the body, known as mosaicism.
To address the complexity, Dr. Kalish guided development of a scoring system for determining whether molecular testing is warranted. Primary features such as an enlarged tongue and lateralized overgrowth carry more points, whereas suggestive features like ear creases or large birth weight carry fewer points.
Diagnostic advances have occurred for other syndromes, as well. For example, researchers have created a scoring system for Russell-Silver syndrome, a less common disorder characterized by slow growth before and after birth, in which mosaicism is also present.
Early diagnosis and intervention of Russell-Silver syndrome can ensure that patients grow to their maximum potential and address problems such as feeding issues.
Spotting a “compilation of features”
Although tools are available, Dr. Kalish said pediatricians don’t need to make a diagnosis, and instead can refer patients to a geneticist after recognizing clinical features that hint at a genetic etiology.
For pediatricians, the process of deciding whether to refer a patient to a geneticist may entail ruling out nongenetic causes, considering patient and family history, and ultimately deciding whether there is a “compilation of features” that falls outside the norm, she said. Unfortunately, she added, there’s “not a simple list I could just hand out saying, ‘If you see these things, call me.’ ”
Dr. Kalish said pediatricians should be aware that two children with similar features can have different syndromes. She presented case studies of two infants, who both had enlarged tongues and older mothers.
One child had hallmarks that pointed to Beckwith-Wiedemann syndrome: conception with in vitro fertilization, length in the 98th percentile, a long umbilical cord, nevus simplex birthmarks, and labial and leg asymmetry.
The other baby had features aligned with Down syndrome: a heart murmur, upward slanting eyes, and a single crease on the palm.
In some cases, isolated features such as the shape, slant, or spacing of eyes, or the presence of creases on the ears, may simply be familial or inherited traits, Dr. Kalish said.
She noted that “there’s been a lot of work in genetics in the past few years to show what syndromes look like” in diverse populations. The American Journal of Medical Genetics Part A has published a series of reports on the topic.
Dr. Kalish reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Jennifer Kalish, MD, PhD, fields as many as 10 inquiries a month from pediatricians who spot an unusual feature during a clinical exam, and wonder if they should refer the family to a geneticist.
“There are hundreds of rare disorders, and for a pediatrician, they can be hard to recognize,” Dr. Kalish said. “That’s why we’re here as geneticists – to partner so that we can help.”
Pediatricians play a key role in spotting signs of rare genetic diseases, but may need guidance for recognizing the more subtle presentations of a disorder, according to Dr. Kalish, a geneticist and director of the Beckwith-Wiedemann Syndrome Clinic at Children’s Hospital of Philadelphia, who spoke at the American Academy of Pediatrics National Conference.
Spectrums of disease
Pediatricians may struggle with deciding whether to make a referral, in part because genetic syndromes “do not always look like the textbook,” she said.
With many conditions, “we’re starting to understand that there’s really a spectrum of how affected versus less affected one can be,” by genetic and epigenetic changes, which have led to recognition that many cases are more subtle and harder to diagnose, she said.
Beckwith-Wiedemann syndrome is a prime example. The overgrowth disorder affects an estimated 1 in 10,340 infants, and is associated with a heightened risk of Wilms tumors, a form of kidney cancer, and hepatoblastomas. Children diagnosed with these conditions typically undergo frequent screenings to detect tumors to jumpstart treatment.
Some researchers believe Beckwith-Wiedemann syndrome is underdiagnosed because it can present in many different ways because of variations in the distributions of affected cells in the body, known as mosaicism.
To address the complexity, Dr. Kalish guided development of a scoring system for determining whether molecular testing is warranted. Primary features such as an enlarged tongue and lateralized overgrowth carry more points, whereas suggestive features like ear creases or large birth weight carry fewer points.
Diagnostic advances have occurred for other syndromes, as well. For example, researchers have created a scoring system for Russell-Silver syndrome, a less common disorder characterized by slow growth before and after birth, in which mosaicism is also present.
Early diagnosis and intervention of Russell-Silver syndrome can ensure that patients grow to their maximum potential and address problems such as feeding issues.
Spotting a “compilation of features”
Although tools are available, Dr. Kalish said pediatricians don’t need to make a diagnosis, and instead can refer patients to a geneticist after recognizing clinical features that hint at a genetic etiology.
For pediatricians, the process of deciding whether to refer a patient to a geneticist may entail ruling out nongenetic causes, considering patient and family history, and ultimately deciding whether there is a “compilation of features” that falls outside the norm, she said. Unfortunately, she added, there’s “not a simple list I could just hand out saying, ‘If you see these things, call me.’ ”
Dr. Kalish said pediatricians should be aware that two children with similar features can have different syndromes. She presented case studies of two infants, who both had enlarged tongues and older mothers.
One child had hallmarks that pointed to Beckwith-Wiedemann syndrome: conception with in vitro fertilization, length in the 98th percentile, a long umbilical cord, nevus simplex birthmarks, and labial and leg asymmetry.
The other baby had features aligned with Down syndrome: a heart murmur, upward slanting eyes, and a single crease on the palm.
In some cases, isolated features such as the shape, slant, or spacing of eyes, or the presence of creases on the ears, may simply be familial or inherited traits, Dr. Kalish said.
She noted that “there’s been a lot of work in genetics in the past few years to show what syndromes look like” in diverse populations. The American Journal of Medical Genetics Part A has published a series of reports on the topic.
Dr. Kalish reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Jennifer Kalish, MD, PhD, fields as many as 10 inquiries a month from pediatricians who spot an unusual feature during a clinical exam, and wonder if they should refer the family to a geneticist.
“There are hundreds of rare disorders, and for a pediatrician, they can be hard to recognize,” Dr. Kalish said. “That’s why we’re here as geneticists – to partner so that we can help.”
Pediatricians play a key role in spotting signs of rare genetic diseases, but may need guidance for recognizing the more subtle presentations of a disorder, according to Dr. Kalish, a geneticist and director of the Beckwith-Wiedemann Syndrome Clinic at Children’s Hospital of Philadelphia, who spoke at the American Academy of Pediatrics National Conference.
Spectrums of disease
Pediatricians may struggle with deciding whether to make a referral, in part because genetic syndromes “do not always look like the textbook,” she said.
With many conditions, “we’re starting to understand that there’s really a spectrum of how affected versus less affected one can be,” by genetic and epigenetic changes, which have led to recognition that many cases are more subtle and harder to diagnose, she said.
Beckwith-Wiedemann syndrome is a prime example. The overgrowth disorder affects an estimated 1 in 10,340 infants, and is associated with a heightened risk of Wilms tumors, a form of kidney cancer, and hepatoblastomas. Children diagnosed with these conditions typically undergo frequent screenings to detect tumors to jumpstart treatment.
Some researchers believe Beckwith-Wiedemann syndrome is underdiagnosed because it can present in many different ways because of variations in the distributions of affected cells in the body, known as mosaicism.
To address the complexity, Dr. Kalish guided development of a scoring system for determining whether molecular testing is warranted. Primary features such as an enlarged tongue and lateralized overgrowth carry more points, whereas suggestive features like ear creases or large birth weight carry fewer points.
Diagnostic advances have occurred for other syndromes, as well. For example, researchers have created a scoring system for Russell-Silver syndrome, a less common disorder characterized by slow growth before and after birth, in which mosaicism is also present.
Early diagnosis and intervention of Russell-Silver syndrome can ensure that patients grow to their maximum potential and address problems such as feeding issues.
Spotting a “compilation of features”
Although tools are available, Dr. Kalish said pediatricians don’t need to make a diagnosis, and instead can refer patients to a geneticist after recognizing clinical features that hint at a genetic etiology.
For pediatricians, the process of deciding whether to refer a patient to a geneticist may entail ruling out nongenetic causes, considering patient and family history, and ultimately deciding whether there is a “compilation of features” that falls outside the norm, she said. Unfortunately, she added, there’s “not a simple list I could just hand out saying, ‘If you see these things, call me.’ ”
Dr. Kalish said pediatricians should be aware that two children with similar features can have different syndromes. She presented case studies of two infants, who both had enlarged tongues and older mothers.
One child had hallmarks that pointed to Beckwith-Wiedemann syndrome: conception with in vitro fertilization, length in the 98th percentile, a long umbilical cord, nevus simplex birthmarks, and labial and leg asymmetry.
The other baby had features aligned with Down syndrome: a heart murmur, upward slanting eyes, and a single crease on the palm.
In some cases, isolated features such as the shape, slant, or spacing of eyes, or the presence of creases on the ears, may simply be familial or inherited traits, Dr. Kalish said.
She noted that “there’s been a lot of work in genetics in the past few years to show what syndromes look like” in diverse populations. The American Journal of Medical Genetics Part A has published a series of reports on the topic.
Dr. Kalish reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AAP 2022
Congenital syphilis: It’s still a significant public health problem
You’re rounding in the nursery and informed of the following about one of your new patients: He’s a 38-week-old infant delivered to a mother diagnosed with syphilis at 12 weeks’ gestation at her initial prenatal visit. Her rapid plasma reagin (RPR) was 1:64 and the fluorescent treponemal antibody–absorption (FTA-ABS) test was positive. By report she was appropriately treated. Maternal RPRs obtained at 18 and 28 weeks’ gestation were 1:16 and 1:4, respectively. Maternal RPR at delivery and the infant’s RPR obtained shortly after birth were both 1:4. The mother wants to know if her baby is infected.
One result of syphilis during pregnancy is intrauterine infection and resultant congenital disease in the infant. Before you answer this mother, let’s discuss syphilis.
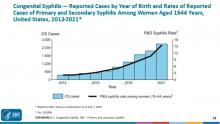
Congenital syphilis is a significant public health problem. In 2021, there were a total of 2,677 cases reported for a rate of 74.1 per 100,000 live births. Between 2020 and 2021, the number of cases of congenital syphilis increased 24.1% (2,158-2,677 cases), concurrent with a 45.8% increase (10.7-15.6 per 100,000) in the rate of primary and secondary syphilis in women aged 15-44 years. Between 2012 and 2021, the number of cases of congenital syphilis increased 701.5% (334-2,677 cases) and the increase in rates of primary and secondary syphilis in women aged 15-44 was 642.9% over the same period.
Why are the rates of congenital syphilis increasing? Most cases result from a lack of prenatal care and thus no testing for syphilis. The next most common cause is inadequate maternal treatment.
Congenital syphilis usually is acquired through transplacental transmission of spirochetes in the maternal bloodstream. Occasionally, it occurs at delivery via direct contact with maternal lesions. It is not transmitted in breast milk. Transmission of syphilis:
- Can occur any time during pregnancy.
- Is more likely to occur in women with untreated primary or secondary disease (60%-100%).
- Is approximately 40% in those with early latent syphilis and less than 8% in mothers with late latent syphilis.
- Is higher in women coinfected with HIV since they more frequently receive no prenatal care and their disease is inadequately treated.
Coinfection with syphilis may also increase the rate of mother-to-child transmission of HIV.
Untreated early syphilis during pregnancy results in spontaneous abortion, stillbirth, or perinatal death in up to 40% of cases. Infected newborns with early congenital syphilis can be asymptomatic or have evidence of hepatosplenomegaly, generalized lymphadenopathy, nasal discharge that is occasionally bloody, rash, and skeletal abnormalities (osteochondritis and periostitis). Other manifestations include edema, hemolytic anemia, jaundice, pneumonia, pseudoparalysis, and thrombocytopenia. Asymptomatic infants may have abnormal cerebrospinal fluid findings including elevated CSF white cell count, elevated protein, and a reactive venereal disease research laboratory test.
Late congenital syphilis, defined as the onset of symptoms after 2 years of age is secondary to scarring or persistent inflammation and gumma formation in a variety of tissues. It occurs in up to 40% of cases of untreated maternal disease. Most cases can be prevented by maternal treatment and treatment of the infant within the first 3 months of life. Common clinical manifestations include interstitial keratitis, sensorineural hearing loss, frontal bossing, saddle nose, Hutchinson teeth, mulberry molars, perforation of the hard palate, anterior bowing of the tibia (saber shins), and other skeletal abnormalities.
Diagnostic tests. Maternal diagnosis is dependent upon knowing the results of both a nontreponemal (RPR, VDRL) and a confirmatory treponemal test (TP-PA, TP-EIA, TP-CIA, FTA-ABS,) before or at delivery. TP-PA is the preferred test. When maternal disease is confirmed, the newborn should have the same quantitative nontreponemal test as the mother. A confirmatory treponemal test is not required
Evaluation and treatment. It’s imperative that children born to mothers with a reactive test, regardless of their treatment status, have a thorough exam performed before hospital discharge. The provider must determine what additional interventions should be performed.
The American Academy of Pediatrics and the Centers for Disease Control and Prevention (www.cdc.gov/std/treatment-guidelines/congenital-syphilis.htm) have developed standard algorithms for the diagnostic approach and treatment of infants born to mothers with reactive serologic tests for syphilis. It is available in the Red Book for AAP members (https://publications.aap.org/redbook). Recommendations based on various scenarios for neonates up to 1 month of age include proven or highly probable congenital syphilis, possible congenital syphilis, congenital syphilis less likely, and congenital syphilis unlikely. It is beyond the scope of this article to list the criteria and evaluation for each scenario. The reader is referred to the algorithm.
If syphilis is suspected in infants or children older than 1 month, the challenge is to determine if it is untreated congenital syphilis or acquired syphilis. Maternal syphilis status should be determined. Evaluation for congenital syphilis in this age group includes CSF analysis for VDRL, cell count and protein, CBC with differential and platelets, hepatic panel, abdominal ultrasound, long-bone radiographs, chest radiograph, neuroimaging, auditory brain stem response, and HIV testing.
Let’s go back to your patient. The mother was diagnosed with syphilis during pregnancy. You confirm that she was treated with benzathine penicillin G, and the course was completed at least 4 weeks before delivery. Treatment with any other drug during pregnancy is not appropriate. The RPR has declined, and the infant’s titer is equal to or less than four times the maternal titer. The exam is significant for generalized adenopathy and slightly bloody nasal discharge. This infant has two findings consistent with congenital syphilis regardless of RPR titer or treatment status. This places him in the proven or highly probable congenital syphilis group. Management includes CSF analysis (VDRL, cell count, and protein), CBC with differential and platelet count, and treatment with penicillin G for 10 days. Additional tests as clinically indicated include: long-bone radiograph, chest radiography, aspartate aminotranferase and alanine aminotransferase levels, neuroimaging, ophthalmologic exam, and auditory brain stem response. Despite maternal treatment, this newborn has congenital syphilis. The same nontreponemal test should be obtained every 2-3 months until it is nonreactive. It should be nonreactive by 6 months. If the infection persists to 6-12 months post treatment, reevaluation including CSF analysis and retreatment may be indicated.
Congenital syphilis can be prevented by maternal screening, diagnosis, and treatment. When that fails it is up to us to diagnosis and adequately treat our patients.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at [email protected].
You’re rounding in the nursery and informed of the following about one of your new patients: He’s a 38-week-old infant delivered to a mother diagnosed with syphilis at 12 weeks’ gestation at her initial prenatal visit. Her rapid plasma reagin (RPR) was 1:64 and the fluorescent treponemal antibody–absorption (FTA-ABS) test was positive. By report she was appropriately treated. Maternal RPRs obtained at 18 and 28 weeks’ gestation were 1:16 and 1:4, respectively. Maternal RPR at delivery and the infant’s RPR obtained shortly after birth were both 1:4. The mother wants to know if her baby is infected.
One result of syphilis during pregnancy is intrauterine infection and resultant congenital disease in the infant. Before you answer this mother, let’s discuss syphilis.
Congenital syphilis is a significant public health problem. In 2021, there were a total of 2,677 cases reported for a rate of 74.1 per 100,000 live births. Between 2020 and 2021, the number of cases of congenital syphilis increased 24.1% (2,158-2,677 cases), concurrent with a 45.8% increase (10.7-15.6 per 100,000) in the rate of primary and secondary syphilis in women aged 15-44 years. Between 2012 and 2021, the number of cases of congenital syphilis increased 701.5% (334-2,677 cases) and the increase in rates of primary and secondary syphilis in women aged 15-44 was 642.9% over the same period.
Why are the rates of congenital syphilis increasing? Most cases result from a lack of prenatal care and thus no testing for syphilis. The next most common cause is inadequate maternal treatment.
Congenital syphilis usually is acquired through transplacental transmission of spirochetes in the maternal bloodstream. Occasionally, it occurs at delivery via direct contact with maternal lesions. It is not transmitted in breast milk. Transmission of syphilis:
- Can occur any time during pregnancy.
- Is more likely to occur in women with untreated primary or secondary disease (60%-100%).
- Is approximately 40% in those with early latent syphilis and less than 8% in mothers with late latent syphilis.
- Is higher in women coinfected with HIV since they more frequently receive no prenatal care and their disease is inadequately treated.
Coinfection with syphilis may also increase the rate of mother-to-child transmission of HIV.
Untreated early syphilis during pregnancy results in spontaneous abortion, stillbirth, or perinatal death in up to 40% of cases. Infected newborns with early congenital syphilis can be asymptomatic or have evidence of hepatosplenomegaly, generalized lymphadenopathy, nasal discharge that is occasionally bloody, rash, and skeletal abnormalities (osteochondritis and periostitis). Other manifestations include edema, hemolytic anemia, jaundice, pneumonia, pseudoparalysis, and thrombocytopenia. Asymptomatic infants may have abnormal cerebrospinal fluid findings including elevated CSF white cell count, elevated protein, and a reactive venereal disease research laboratory test.
Late congenital syphilis, defined as the onset of symptoms after 2 years of age is secondary to scarring or persistent inflammation and gumma formation in a variety of tissues. It occurs in up to 40% of cases of untreated maternal disease. Most cases can be prevented by maternal treatment and treatment of the infant within the first 3 months of life. Common clinical manifestations include interstitial keratitis, sensorineural hearing loss, frontal bossing, saddle nose, Hutchinson teeth, mulberry molars, perforation of the hard palate, anterior bowing of the tibia (saber shins), and other skeletal abnormalities.
Diagnostic tests. Maternal diagnosis is dependent upon knowing the results of both a nontreponemal (RPR, VDRL) and a confirmatory treponemal test (TP-PA, TP-EIA, TP-CIA, FTA-ABS,) before or at delivery. TP-PA is the preferred test. When maternal disease is confirmed, the newborn should have the same quantitative nontreponemal test as the mother. A confirmatory treponemal test is not required
Evaluation and treatment. It’s imperative that children born to mothers with a reactive test, regardless of their treatment status, have a thorough exam performed before hospital discharge. The provider must determine what additional interventions should be performed.
The American Academy of Pediatrics and the Centers for Disease Control and Prevention (www.cdc.gov/std/treatment-guidelines/congenital-syphilis.htm) have developed standard algorithms for the diagnostic approach and treatment of infants born to mothers with reactive serologic tests for syphilis. It is available in the Red Book for AAP members (https://publications.aap.org/redbook). Recommendations based on various scenarios for neonates up to 1 month of age include proven or highly probable congenital syphilis, possible congenital syphilis, congenital syphilis less likely, and congenital syphilis unlikely. It is beyond the scope of this article to list the criteria and evaluation for each scenario. The reader is referred to the algorithm.
If syphilis is suspected in infants or children older than 1 month, the challenge is to determine if it is untreated congenital syphilis or acquired syphilis. Maternal syphilis status should be determined. Evaluation for congenital syphilis in this age group includes CSF analysis for VDRL, cell count and protein, CBC with differential and platelets, hepatic panel, abdominal ultrasound, long-bone radiographs, chest radiograph, neuroimaging, auditory brain stem response, and HIV testing.
Let’s go back to your patient. The mother was diagnosed with syphilis during pregnancy. You confirm that she was treated with benzathine penicillin G, and the course was completed at least 4 weeks before delivery. Treatment with any other drug during pregnancy is not appropriate. The RPR has declined, and the infant’s titer is equal to or less than four times the maternal titer. The exam is significant for generalized adenopathy and slightly bloody nasal discharge. This infant has two findings consistent with congenital syphilis regardless of RPR titer or treatment status. This places him in the proven or highly probable congenital syphilis group. Management includes CSF analysis (VDRL, cell count, and protein), CBC with differential and platelet count, and treatment with penicillin G for 10 days. Additional tests as clinically indicated include: long-bone radiograph, chest radiography, aspartate aminotranferase and alanine aminotransferase levels, neuroimaging, ophthalmologic exam, and auditory brain stem response. Despite maternal treatment, this newborn has congenital syphilis. The same nontreponemal test should be obtained every 2-3 months until it is nonreactive. It should be nonreactive by 6 months. If the infection persists to 6-12 months post treatment, reevaluation including CSF analysis and retreatment may be indicated.
Congenital syphilis can be prevented by maternal screening, diagnosis, and treatment. When that fails it is up to us to diagnosis and adequately treat our patients.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at [email protected].
You’re rounding in the nursery and informed of the following about one of your new patients: He’s a 38-week-old infant delivered to a mother diagnosed with syphilis at 12 weeks’ gestation at her initial prenatal visit. Her rapid plasma reagin (RPR) was 1:64 and the fluorescent treponemal antibody–absorption (FTA-ABS) test was positive. By report she was appropriately treated. Maternal RPRs obtained at 18 and 28 weeks’ gestation were 1:16 and 1:4, respectively. Maternal RPR at delivery and the infant’s RPR obtained shortly after birth were both 1:4. The mother wants to know if her baby is infected.
One result of syphilis during pregnancy is intrauterine infection and resultant congenital disease in the infant. Before you answer this mother, let’s discuss syphilis.
Congenital syphilis is a significant public health problem. In 2021, there were a total of 2,677 cases reported for a rate of 74.1 per 100,000 live births. Between 2020 and 2021, the number of cases of congenital syphilis increased 24.1% (2,158-2,677 cases), concurrent with a 45.8% increase (10.7-15.6 per 100,000) in the rate of primary and secondary syphilis in women aged 15-44 years. Between 2012 and 2021, the number of cases of congenital syphilis increased 701.5% (334-2,677 cases) and the increase in rates of primary and secondary syphilis in women aged 15-44 was 642.9% over the same period.
Why are the rates of congenital syphilis increasing? Most cases result from a lack of prenatal care and thus no testing for syphilis. The next most common cause is inadequate maternal treatment.
Congenital syphilis usually is acquired through transplacental transmission of spirochetes in the maternal bloodstream. Occasionally, it occurs at delivery via direct contact with maternal lesions. It is not transmitted in breast milk. Transmission of syphilis:
- Can occur any time during pregnancy.
- Is more likely to occur in women with untreated primary or secondary disease (60%-100%).
- Is approximately 40% in those with early latent syphilis and less than 8% in mothers with late latent syphilis.
- Is higher in women coinfected with HIV since they more frequently receive no prenatal care and their disease is inadequately treated.
Coinfection with syphilis may also increase the rate of mother-to-child transmission of HIV.
Untreated early syphilis during pregnancy results in spontaneous abortion, stillbirth, or perinatal death in up to 40% of cases. Infected newborns with early congenital syphilis can be asymptomatic or have evidence of hepatosplenomegaly, generalized lymphadenopathy, nasal discharge that is occasionally bloody, rash, and skeletal abnormalities (osteochondritis and periostitis). Other manifestations include edema, hemolytic anemia, jaundice, pneumonia, pseudoparalysis, and thrombocytopenia. Asymptomatic infants may have abnormal cerebrospinal fluid findings including elevated CSF white cell count, elevated protein, and a reactive venereal disease research laboratory test.
Late congenital syphilis, defined as the onset of symptoms after 2 years of age is secondary to scarring or persistent inflammation and gumma formation in a variety of tissues. It occurs in up to 40% of cases of untreated maternal disease. Most cases can be prevented by maternal treatment and treatment of the infant within the first 3 months of life. Common clinical manifestations include interstitial keratitis, sensorineural hearing loss, frontal bossing, saddle nose, Hutchinson teeth, mulberry molars, perforation of the hard palate, anterior bowing of the tibia (saber shins), and other skeletal abnormalities.
Diagnostic tests. Maternal diagnosis is dependent upon knowing the results of both a nontreponemal (RPR, VDRL) and a confirmatory treponemal test (TP-PA, TP-EIA, TP-CIA, FTA-ABS,) before or at delivery. TP-PA is the preferred test. When maternal disease is confirmed, the newborn should have the same quantitative nontreponemal test as the mother. A confirmatory treponemal test is not required
Evaluation and treatment. It’s imperative that children born to mothers with a reactive test, regardless of their treatment status, have a thorough exam performed before hospital discharge. The provider must determine what additional interventions should be performed.
The American Academy of Pediatrics and the Centers for Disease Control and Prevention (www.cdc.gov/std/treatment-guidelines/congenital-syphilis.htm) have developed standard algorithms for the diagnostic approach and treatment of infants born to mothers with reactive serologic tests for syphilis. It is available in the Red Book for AAP members (https://publications.aap.org/redbook). Recommendations based on various scenarios for neonates up to 1 month of age include proven or highly probable congenital syphilis, possible congenital syphilis, congenital syphilis less likely, and congenital syphilis unlikely. It is beyond the scope of this article to list the criteria and evaluation for each scenario. The reader is referred to the algorithm.
If syphilis is suspected in infants or children older than 1 month, the challenge is to determine if it is untreated congenital syphilis or acquired syphilis. Maternal syphilis status should be determined. Evaluation for congenital syphilis in this age group includes CSF analysis for VDRL, cell count and protein, CBC with differential and platelets, hepatic panel, abdominal ultrasound, long-bone radiographs, chest radiograph, neuroimaging, auditory brain stem response, and HIV testing.
Let’s go back to your patient. The mother was diagnosed with syphilis during pregnancy. You confirm that she was treated with benzathine penicillin G, and the course was completed at least 4 weeks before delivery. Treatment with any other drug during pregnancy is not appropriate. The RPR has declined, and the infant’s titer is equal to or less than four times the maternal titer. The exam is significant for generalized adenopathy and slightly bloody nasal discharge. This infant has two findings consistent with congenital syphilis regardless of RPR titer or treatment status. This places him in the proven or highly probable congenital syphilis group. Management includes CSF analysis (VDRL, cell count, and protein), CBC with differential and platelet count, and treatment with penicillin G for 10 days. Additional tests as clinically indicated include: long-bone radiograph, chest radiography, aspartate aminotranferase and alanine aminotransferase levels, neuroimaging, ophthalmologic exam, and auditory brain stem response. Despite maternal treatment, this newborn has congenital syphilis. The same nontreponemal test should be obtained every 2-3 months until it is nonreactive. It should be nonreactive by 6 months. If the infection persists to 6-12 months post treatment, reevaluation including CSF analysis and retreatment may be indicated.
Congenital syphilis can be prevented by maternal screening, diagnosis, and treatment. When that fails it is up to us to diagnosis and adequately treat our patients.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at [email protected].
Digital mental health training acceptable to boarding teens
ANAHEIM, CALIF. – A modular digital intervention to teach mental health skills to youth awaiting transfer to psychiatric care appeared feasible to implement and acceptable to teens and their parents, according to a study presented at the American Academy of Pediatrics National Conference.
“This program has the potential to teach evidence-based mental health skills to youth during boarding, providing a head start on recovery prior to psychiatric hospitalization,” study coauthor Samantha House, DO, MPH, section chief of pediatric hospital medicine at Dartmouth Hitchcock Medical Center, Lebanon, N.H., told attendees.
Mental health boarding has become increasingly common as psychiatric care resources have been stretched by a crisis in pediatric mental health that began even before the COVID pandemic. Since youth often don’t receive evidence-based therapies while boarding, Dr. House and her coauthor, JoAnna K. Leyenaar, MD, PhD, MPH, developed a pilot program called I-CARE, which stands for Improving Care, Accelerating Recovery and Education.
I-CARE is a digital health intervention that combines videos on a tablet with workbook exercises that teach mental health skills. The seven modules include an introduction and one each on schedule-making, safety planning, psychoeducation, behavioral activation, relaxation skills, and mindfulness skills. Licensed nursing assistants who have received a 6-hour training from a clinical psychologist administer the program and provide safety supervision during boarding.
“I-CARE was designed to be largely self-directed, supported by ‘coaches’ who are not mental health professionals,” Dr. Leyenaar, vice chair of research in the department of pediatrics and an associate professor of pediatrics at Geisel School of Medicine at Dartmouth, Hanover, N.H., said in an interview. With this model, the program requires minimal additional resources beyond the tablets and workbooks, and is designed for implementation in settings with few or no mental health professionals, she said.
Cora Breuner, MD, MPH, a professor of pediatrics at the University of Washington, Seattle, and an attending physician at Seattle Children’s Hospital, was not involved in the study but was excited to see it.
“I think it’s a really good idea, and I like that it’s being studied,” Dr. Breuner said in an interview. She said the health care and public health system has let down an entire population who data had shown were experiencing mental health problems.
“We knew before the pandemic that behavioral health issues were creeping up slowly with anxiety, depression, suicidal ideation, and, of course, substance use disorders and eating disorders, and not a lot was being done about it,” Dr. Breuner said, and the pandemic exacerbated those issues. ”I don’t know why no one realized that this was going to be the downstream effect of having no socialization for kids for 18 months and limited resources for those who we need desperately to provide care for,” especially BIPOC [Black, Indigenous, and people of color] kids and underresourced kids.
That sentiment is exactly what inspired the creation of the program, according to Dr. Leyenaar.
The I-CARE program was implemented at Dartmouth Hitchcock Medical Center in November 2021 for adolescents aged 12-17 who were boarding because of suicidality or self-harm. The program and study excluded youth with psychosis and other cognitive or behavioral conditions that didn’t fit with the skills taught by the module training.
The researchers qualitatively evaluated the I-CARE program in youth who were offered at least two I-CARE modules and with parents present during boarding.
Twenty-four youth, with a median age of 14, were offered the I-CARE program between November 2021 and April 2022 while boarding for a median 8 days. Most of the patients were female (79%), and a third were transgender or gender diverse. Most were White (83%), and about two-thirds had Medicaid (62.5%). The most common diagnoses among the participants were major depressive disorder (71%) and generalized anxiety disorder (46%). Others included PTSD (29%), restrictive eating disorder (21%), and bipolar disorder (12.5%).
All offered the program completed the first module, and 79% participated in additional modules. The main reason for discontinuation was transfer to another facility, but a few youth either refused to engage with the program or felt they knew the material well enough that they weren’t benefiting from it.
The evaluation involved 16 youth, seven parents, and 17 clinicians. On a Likert scale, the composite score for the program’s appropriateness – suitability, applicability, and meeting needs – was an average 3.7, with a higher rating from clinicians (4.3) and caregivers (3.5) than youth (2.8).
“Some youth felt the intervention was better suited for a younger audience or those with less familiarity with mental health skills, but they acknowledged that the intervention would be helpful and appropriate for others,” Dr. House, who is also an assistant professor of pediatrics at Geisel School of Medicine, said.
Youth rated the acceptability of the program more highly (3.6) and all three groups found it easy to use, with an average feasibility score of 4 across the board. The program’s acceptability received an average score of 4 from parents and clinicians.
”Teens seem to particularly value the psychoeducation module that explains the relationship between thoughts and feelings, as well as the opportunity to develop a personalized safety plan,” Dr. Leyenaar said.
Among the challenges expressed by the participating teens were that the loud sounds and beeping in the hospital made it difficult to practice mindfulness and that they often had to wait for staff to be available to do I-CARE.
“I feel like not many people have been trained yet,” one teen said, “so to have more nurses available to do I-CARE would be helpful.”
Another participant found the coaches helpful. “Sometimes they were my nurse, sometimes they were someone I never met before. … and also, they were all really, really nice,” the teen said.
Another teen regarded the material as “really surface-level mental health stuff” that they thought “could be helpful to other people who are here for the first time.” But others found the content more beneficial.
“The videos were helpful. … I was worried that they weren’t going to be very informative, but they did make sense to me,” one participant said. “They weren’t overcomplicating things. … They weren’t saying anything I didn’t understand, so that was good.”
The researchers next plan to conduct a multisite study to determine the program’s effectiveness in improving health outcomes and reducing suicidal ideation. Dr. House and Dr. Leyenaar are looking at ways to refine the program.
”We may narrow the age range for participants, with an upper age limit of 16, since some older teens said that the modules were best suited for a younger audience,” Dr. Leyenaar said. “We are also discussing how to best support youth who are readmitted to our hospital and have participated in I-CARE previously.”
Dr. Breuner said she would be interested to see, in future studies of the program, whether it reduced the likelihood of inpatient psychiatric stay, the length of psychiatric stay after admission, or the risk of readmission. She also wondered if the program might be offered in languages other than English, whether a version might be specifically designed for BIPOC youth, and whether the researchers had considered offering the intervention to caregivers as well.
The modules are teaching the kids but should they also be teaching the parents? Dr. Breuner wondered. A lot of times, she said, the parents are bringing these kids in because they don’t know what to do and can’t deal with them anymore. Offering modules on the same skills to caregivers would also enable the caregivers to reinforce and reteach the skills to their children, especially if the youth struggled to really take in what the modules were trying to teach.
Dr. Leyenaar said she expects buy-in for a program like this would be high at other institutions, but it’s premature to scale it up until they’ve conducted at least another clinical trial on its effectiveness. The biggest potential barrier to buy-in that Dr. Breuner perceived would be cost.
“It’s always difficult when it costs money” since the hospital needs to train the clinicians who provide the care, Dr. Breuner said, but it’s possible those costs could be offset if the program reduces the risk of readmission or return to the emergency department.
While the overall risk of harms from the intervention are low, Dr. Breuner said it is important to be conscious that the intervention may not necessarily be appropriate for all youth.
“There’s always risk when there’s a trauma background, and you have to be very careful, especially with mindfulness training,” Dr. Breuner said. For those with a history of abuse or other adverse childhood experiences “for someone to get into a very calm, still place can actually be counterproductive.”
Dr. Breuner especially appreciated that the researchers involved the youth and caregivers in the evaluation process. “That the parents expressed positive attitudes is really incredible,” she said.
Dr. House, Dr. Leyenaar, and Dr. Breuner had no disclosures. No external funding was noted for the study.
ANAHEIM, CALIF. – A modular digital intervention to teach mental health skills to youth awaiting transfer to psychiatric care appeared feasible to implement and acceptable to teens and their parents, according to a study presented at the American Academy of Pediatrics National Conference.
“This program has the potential to teach evidence-based mental health skills to youth during boarding, providing a head start on recovery prior to psychiatric hospitalization,” study coauthor Samantha House, DO, MPH, section chief of pediatric hospital medicine at Dartmouth Hitchcock Medical Center, Lebanon, N.H., told attendees.
Mental health boarding has become increasingly common as psychiatric care resources have been stretched by a crisis in pediatric mental health that began even before the COVID pandemic. Since youth often don’t receive evidence-based therapies while boarding, Dr. House and her coauthor, JoAnna K. Leyenaar, MD, PhD, MPH, developed a pilot program called I-CARE, which stands for Improving Care, Accelerating Recovery and Education.
I-CARE is a digital health intervention that combines videos on a tablet with workbook exercises that teach mental health skills. The seven modules include an introduction and one each on schedule-making, safety planning, psychoeducation, behavioral activation, relaxation skills, and mindfulness skills. Licensed nursing assistants who have received a 6-hour training from a clinical psychologist administer the program and provide safety supervision during boarding.
“I-CARE was designed to be largely self-directed, supported by ‘coaches’ who are not mental health professionals,” Dr. Leyenaar, vice chair of research in the department of pediatrics and an associate professor of pediatrics at Geisel School of Medicine at Dartmouth, Hanover, N.H., said in an interview. With this model, the program requires minimal additional resources beyond the tablets and workbooks, and is designed for implementation in settings with few or no mental health professionals, she said.
Cora Breuner, MD, MPH, a professor of pediatrics at the University of Washington, Seattle, and an attending physician at Seattle Children’s Hospital, was not involved in the study but was excited to see it.
“I think it’s a really good idea, and I like that it’s being studied,” Dr. Breuner said in an interview. She said the health care and public health system has let down an entire population who data had shown were experiencing mental health problems.
“We knew before the pandemic that behavioral health issues were creeping up slowly with anxiety, depression, suicidal ideation, and, of course, substance use disorders and eating disorders, and not a lot was being done about it,” Dr. Breuner said, and the pandemic exacerbated those issues. ”I don’t know why no one realized that this was going to be the downstream effect of having no socialization for kids for 18 months and limited resources for those who we need desperately to provide care for,” especially BIPOC [Black, Indigenous, and people of color] kids and underresourced kids.
That sentiment is exactly what inspired the creation of the program, according to Dr. Leyenaar.
The I-CARE program was implemented at Dartmouth Hitchcock Medical Center in November 2021 for adolescents aged 12-17 who were boarding because of suicidality or self-harm. The program and study excluded youth with psychosis and other cognitive or behavioral conditions that didn’t fit with the skills taught by the module training.
The researchers qualitatively evaluated the I-CARE program in youth who were offered at least two I-CARE modules and with parents present during boarding.
Twenty-four youth, with a median age of 14, were offered the I-CARE program between November 2021 and April 2022 while boarding for a median 8 days. Most of the patients were female (79%), and a third were transgender or gender diverse. Most were White (83%), and about two-thirds had Medicaid (62.5%). The most common diagnoses among the participants were major depressive disorder (71%) and generalized anxiety disorder (46%). Others included PTSD (29%), restrictive eating disorder (21%), and bipolar disorder (12.5%).
All offered the program completed the first module, and 79% participated in additional modules. The main reason for discontinuation was transfer to another facility, but a few youth either refused to engage with the program or felt they knew the material well enough that they weren’t benefiting from it.
The evaluation involved 16 youth, seven parents, and 17 clinicians. On a Likert scale, the composite score for the program’s appropriateness – suitability, applicability, and meeting needs – was an average 3.7, with a higher rating from clinicians (4.3) and caregivers (3.5) than youth (2.8).
“Some youth felt the intervention was better suited for a younger audience or those with less familiarity with mental health skills, but they acknowledged that the intervention would be helpful and appropriate for others,” Dr. House, who is also an assistant professor of pediatrics at Geisel School of Medicine, said.
Youth rated the acceptability of the program more highly (3.6) and all three groups found it easy to use, with an average feasibility score of 4 across the board. The program’s acceptability received an average score of 4 from parents and clinicians.
”Teens seem to particularly value the psychoeducation module that explains the relationship between thoughts and feelings, as well as the opportunity to develop a personalized safety plan,” Dr. Leyenaar said.
Among the challenges expressed by the participating teens were that the loud sounds and beeping in the hospital made it difficult to practice mindfulness and that they often had to wait for staff to be available to do I-CARE.
“I feel like not many people have been trained yet,” one teen said, “so to have more nurses available to do I-CARE would be helpful.”
Another participant found the coaches helpful. “Sometimes they were my nurse, sometimes they were someone I never met before. … and also, they were all really, really nice,” the teen said.
Another teen regarded the material as “really surface-level mental health stuff” that they thought “could be helpful to other people who are here for the first time.” But others found the content more beneficial.
“The videos were helpful. … I was worried that they weren’t going to be very informative, but they did make sense to me,” one participant said. “They weren’t overcomplicating things. … They weren’t saying anything I didn’t understand, so that was good.”
The researchers next plan to conduct a multisite study to determine the program’s effectiveness in improving health outcomes and reducing suicidal ideation. Dr. House and Dr. Leyenaar are looking at ways to refine the program.
”We may narrow the age range for participants, with an upper age limit of 16, since some older teens said that the modules were best suited for a younger audience,” Dr. Leyenaar said. “We are also discussing how to best support youth who are readmitted to our hospital and have participated in I-CARE previously.”
Dr. Breuner said she would be interested to see, in future studies of the program, whether it reduced the likelihood of inpatient psychiatric stay, the length of psychiatric stay after admission, or the risk of readmission. She also wondered if the program might be offered in languages other than English, whether a version might be specifically designed for BIPOC youth, and whether the researchers had considered offering the intervention to caregivers as well.
The modules are teaching the kids but should they also be teaching the parents? Dr. Breuner wondered. A lot of times, she said, the parents are bringing these kids in because they don’t know what to do and can’t deal with them anymore. Offering modules on the same skills to caregivers would also enable the caregivers to reinforce and reteach the skills to their children, especially if the youth struggled to really take in what the modules were trying to teach.
Dr. Leyenaar said she expects buy-in for a program like this would be high at other institutions, but it’s premature to scale it up until they’ve conducted at least another clinical trial on its effectiveness. The biggest potential barrier to buy-in that Dr. Breuner perceived would be cost.
“It’s always difficult when it costs money” since the hospital needs to train the clinicians who provide the care, Dr. Breuner said, but it’s possible those costs could be offset if the program reduces the risk of readmission or return to the emergency department.
While the overall risk of harms from the intervention are low, Dr. Breuner said it is important to be conscious that the intervention may not necessarily be appropriate for all youth.
“There’s always risk when there’s a trauma background, and you have to be very careful, especially with mindfulness training,” Dr. Breuner said. For those with a history of abuse or other adverse childhood experiences “for someone to get into a very calm, still place can actually be counterproductive.”
Dr. Breuner especially appreciated that the researchers involved the youth and caregivers in the evaluation process. “That the parents expressed positive attitudes is really incredible,” she said.
Dr. House, Dr. Leyenaar, and Dr. Breuner had no disclosures. No external funding was noted for the study.
ANAHEIM, CALIF. – A modular digital intervention to teach mental health skills to youth awaiting transfer to psychiatric care appeared feasible to implement and acceptable to teens and their parents, according to a study presented at the American Academy of Pediatrics National Conference.
“This program has the potential to teach evidence-based mental health skills to youth during boarding, providing a head start on recovery prior to psychiatric hospitalization,” study coauthor Samantha House, DO, MPH, section chief of pediatric hospital medicine at Dartmouth Hitchcock Medical Center, Lebanon, N.H., told attendees.
Mental health boarding has become increasingly common as psychiatric care resources have been stretched by a crisis in pediatric mental health that began even before the COVID pandemic. Since youth often don’t receive evidence-based therapies while boarding, Dr. House and her coauthor, JoAnna K. Leyenaar, MD, PhD, MPH, developed a pilot program called I-CARE, which stands for Improving Care, Accelerating Recovery and Education.
I-CARE is a digital health intervention that combines videos on a tablet with workbook exercises that teach mental health skills. The seven modules include an introduction and one each on schedule-making, safety planning, psychoeducation, behavioral activation, relaxation skills, and mindfulness skills. Licensed nursing assistants who have received a 6-hour training from a clinical psychologist administer the program and provide safety supervision during boarding.
“I-CARE was designed to be largely self-directed, supported by ‘coaches’ who are not mental health professionals,” Dr. Leyenaar, vice chair of research in the department of pediatrics and an associate professor of pediatrics at Geisel School of Medicine at Dartmouth, Hanover, N.H., said in an interview. With this model, the program requires minimal additional resources beyond the tablets and workbooks, and is designed for implementation in settings with few or no mental health professionals, she said.
Cora Breuner, MD, MPH, a professor of pediatrics at the University of Washington, Seattle, and an attending physician at Seattle Children’s Hospital, was not involved in the study but was excited to see it.
“I think it’s a really good idea, and I like that it’s being studied,” Dr. Breuner said in an interview. She said the health care and public health system has let down an entire population who data had shown were experiencing mental health problems.
“We knew before the pandemic that behavioral health issues were creeping up slowly with anxiety, depression, suicidal ideation, and, of course, substance use disorders and eating disorders, and not a lot was being done about it,” Dr. Breuner said, and the pandemic exacerbated those issues. ”I don’t know why no one realized that this was going to be the downstream effect of having no socialization for kids for 18 months and limited resources for those who we need desperately to provide care for,” especially BIPOC [Black, Indigenous, and people of color] kids and underresourced kids.
That sentiment is exactly what inspired the creation of the program, according to Dr. Leyenaar.
The I-CARE program was implemented at Dartmouth Hitchcock Medical Center in November 2021 for adolescents aged 12-17 who were boarding because of suicidality or self-harm. The program and study excluded youth with psychosis and other cognitive or behavioral conditions that didn’t fit with the skills taught by the module training.
The researchers qualitatively evaluated the I-CARE program in youth who were offered at least two I-CARE modules and with parents present during boarding.
Twenty-four youth, with a median age of 14, were offered the I-CARE program between November 2021 and April 2022 while boarding for a median 8 days. Most of the patients were female (79%), and a third were transgender or gender diverse. Most were White (83%), and about two-thirds had Medicaid (62.5%). The most common diagnoses among the participants were major depressive disorder (71%) and generalized anxiety disorder (46%). Others included PTSD (29%), restrictive eating disorder (21%), and bipolar disorder (12.5%).
All offered the program completed the first module, and 79% participated in additional modules. The main reason for discontinuation was transfer to another facility, but a few youth either refused to engage with the program or felt they knew the material well enough that they weren’t benefiting from it.
The evaluation involved 16 youth, seven parents, and 17 clinicians. On a Likert scale, the composite score for the program’s appropriateness – suitability, applicability, and meeting needs – was an average 3.7, with a higher rating from clinicians (4.3) and caregivers (3.5) than youth (2.8).
“Some youth felt the intervention was better suited for a younger audience or those with less familiarity with mental health skills, but they acknowledged that the intervention would be helpful and appropriate for others,” Dr. House, who is also an assistant professor of pediatrics at Geisel School of Medicine, said.
Youth rated the acceptability of the program more highly (3.6) and all three groups found it easy to use, with an average feasibility score of 4 across the board. The program’s acceptability received an average score of 4 from parents and clinicians.
”Teens seem to particularly value the psychoeducation module that explains the relationship between thoughts and feelings, as well as the opportunity to develop a personalized safety plan,” Dr. Leyenaar said.
Among the challenges expressed by the participating teens were that the loud sounds and beeping in the hospital made it difficult to practice mindfulness and that they often had to wait for staff to be available to do I-CARE.
“I feel like not many people have been trained yet,” one teen said, “so to have more nurses available to do I-CARE would be helpful.”
Another participant found the coaches helpful. “Sometimes they were my nurse, sometimes they were someone I never met before. … and also, they were all really, really nice,” the teen said.
Another teen regarded the material as “really surface-level mental health stuff” that they thought “could be helpful to other people who are here for the first time.” But others found the content more beneficial.
“The videos were helpful. … I was worried that they weren’t going to be very informative, but they did make sense to me,” one participant said. “They weren’t overcomplicating things. … They weren’t saying anything I didn’t understand, so that was good.”
The researchers next plan to conduct a multisite study to determine the program’s effectiveness in improving health outcomes and reducing suicidal ideation. Dr. House and Dr. Leyenaar are looking at ways to refine the program.
”We may narrow the age range for participants, with an upper age limit of 16, since some older teens said that the modules were best suited for a younger audience,” Dr. Leyenaar said. “We are also discussing how to best support youth who are readmitted to our hospital and have participated in I-CARE previously.”
Dr. Breuner said she would be interested to see, in future studies of the program, whether it reduced the likelihood of inpatient psychiatric stay, the length of psychiatric stay after admission, or the risk of readmission. She also wondered if the program might be offered in languages other than English, whether a version might be specifically designed for BIPOC youth, and whether the researchers had considered offering the intervention to caregivers as well.
The modules are teaching the kids but should they also be teaching the parents? Dr. Breuner wondered. A lot of times, she said, the parents are bringing these kids in because they don’t know what to do and can’t deal with them anymore. Offering modules on the same skills to caregivers would also enable the caregivers to reinforce and reteach the skills to their children, especially if the youth struggled to really take in what the modules were trying to teach.
Dr. Leyenaar said she expects buy-in for a program like this would be high at other institutions, but it’s premature to scale it up until they’ve conducted at least another clinical trial on its effectiveness. The biggest potential barrier to buy-in that Dr. Breuner perceived would be cost.
“It’s always difficult when it costs money” since the hospital needs to train the clinicians who provide the care, Dr. Breuner said, but it’s possible those costs could be offset if the program reduces the risk of readmission or return to the emergency department.
While the overall risk of harms from the intervention are low, Dr. Breuner said it is important to be conscious that the intervention may not necessarily be appropriate for all youth.
“There’s always risk when there’s a trauma background, and you have to be very careful, especially with mindfulness training,” Dr. Breuner said. For those with a history of abuse or other adverse childhood experiences “for someone to get into a very calm, still place can actually be counterproductive.”
Dr. Breuner especially appreciated that the researchers involved the youth and caregivers in the evaluation process. “That the parents expressed positive attitudes is really incredible,” she said.
Dr. House, Dr. Leyenaar, and Dr. Breuner had no disclosures. No external funding was noted for the study.
AT AAP 2022
Why people lie about COVID
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
Have you ever lied about COVID-19?
Before you get upset, before the “how dare you,” I want you to think carefully.
Did you have COVID-19 (or think you did) and not mention it to someone you were going to be with? Did you tell someone you were taking more COVID precautions than you really were? Did you tell someone you were vaccinated when you weren’t? Have you avoided getting a COVID test even though you knew you should have?
Researchers appreciated the fact that public health interventions in COVID are important but are only as good as the percentage of people who actually abide by them. So, they designed a survey to ask the questions that many people don’t want to hear the answer to.
A total of 1,733 participants – 80% of those invited – responded to the survey. By design, approximately one-third of respondents (477) had already had COVID, one-third (499) were vaccinated and not yet infected, and one-third (509) were unvaccinated and not yet infected.
Of those surveyed, 41.6% admitted that they lied about COVID or didn’t adhere to COVID guidelines - a conservative estimate, if you ask me.
Breaking down some of the results, about 20% of people who previously were infected with COVID said they didn’t mention it when meeting with someone. A similar number said they didn’t tell anyone when they were entering a public place. A bit more concerning to me, roughly 20% reported not disclosing their COVID-positive status when going to a health care provider’s office.
About 10% of those who had not been vaccinated reported lying about their vaccination status. That’s actually less than the 15% of vaccinated people who lied and told someone they weren’t vaccinated.
About 17% of people lied about the need to quarantine, and many more broke quarantine rules.
The authors tried to see if certain personal characteristics predicted people who were more likely to lie about COVID-19–related issues. Turns out there was only one thing that predicted honesty: age.
Older people were more honest about their COVID status and COVID habits. Other factors – gender, education, race, political affiliation, COVID-19 conspiracy beliefs, and where you got your COVID information – did not seem to make much of a difference. Why are older people more honest? Because older people take COVID more seriously. And they should; COVID is more severe in older people.
The problem arises, of course, because people who are at lower risk for COVID complications interact with people at higher risk – and in those situations, honesty matters more.
On the other hand, isn’t lying about COVID stuff inevitable? If you know that a positive test means you can’t go to work, and not going to work means you won’t get paid, might you not be more likely to lie about the test? Or not get the test at all?
The authors explored the reasons for dishonesty and they are fairly broad, ranging from the desire for life to feel normal (more than half of people who lied) to not believing that COVID was real (a whopping 30%). Some of the reasons for lying included:
- Wanted life to feel normal (50%).
- Freedom (45%).
- It’s no one’s business (40%).
- COVID isn’t real (30%).
In the end, though, we need to realize that public health recommendations are not going to be universally followed, and people may tell us they are following them when, in fact, they are not.
What this adds is another data point to a trend we’ve seen across the course of the pandemic, a shift from collective to individual responsibility. If you can’t be sure what others are doing in regard to COVID, you need to focus on protecting yourself. Perhaps that shift was inevitable. Doesn’t mean we have to like it.
A version of this article first appeared on Medscape.com.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
Have you ever lied about COVID-19?
Before you get upset, before the “how dare you,” I want you to think carefully.
Did you have COVID-19 (or think you did) and not mention it to someone you were going to be with? Did you tell someone you were taking more COVID precautions than you really were? Did you tell someone you were vaccinated when you weren’t? Have you avoided getting a COVID test even though you knew you should have?
Researchers appreciated the fact that public health interventions in COVID are important but are only as good as the percentage of people who actually abide by them. So, they designed a survey to ask the questions that many people don’t want to hear the answer to.
A total of 1,733 participants – 80% of those invited – responded to the survey. By design, approximately one-third of respondents (477) had already had COVID, one-third (499) were vaccinated and not yet infected, and one-third (509) were unvaccinated and not yet infected.
Of those surveyed, 41.6% admitted that they lied about COVID or didn’t adhere to COVID guidelines - a conservative estimate, if you ask me.
Breaking down some of the results, about 20% of people who previously were infected with COVID said they didn’t mention it when meeting with someone. A similar number said they didn’t tell anyone when they were entering a public place. A bit more concerning to me, roughly 20% reported not disclosing their COVID-positive status when going to a health care provider’s office.
About 10% of those who had not been vaccinated reported lying about their vaccination status. That’s actually less than the 15% of vaccinated people who lied and told someone they weren’t vaccinated.
About 17% of people lied about the need to quarantine, and many more broke quarantine rules.
The authors tried to see if certain personal characteristics predicted people who were more likely to lie about COVID-19–related issues. Turns out there was only one thing that predicted honesty: age.
Older people were more honest about their COVID status and COVID habits. Other factors – gender, education, race, political affiliation, COVID-19 conspiracy beliefs, and where you got your COVID information – did not seem to make much of a difference. Why are older people more honest? Because older people take COVID more seriously. And they should; COVID is more severe in older people.
The problem arises, of course, because people who are at lower risk for COVID complications interact with people at higher risk – and in those situations, honesty matters more.
On the other hand, isn’t lying about COVID stuff inevitable? If you know that a positive test means you can’t go to work, and not going to work means you won’t get paid, might you not be more likely to lie about the test? Or not get the test at all?
The authors explored the reasons for dishonesty and they are fairly broad, ranging from the desire for life to feel normal (more than half of people who lied) to not believing that COVID was real (a whopping 30%). Some of the reasons for lying included:
- Wanted life to feel normal (50%).
- Freedom (45%).
- It’s no one’s business (40%).
- COVID isn’t real (30%).
In the end, though, we need to realize that public health recommendations are not going to be universally followed, and people may tell us they are following them when, in fact, they are not.
What this adds is another data point to a trend we’ve seen across the course of the pandemic, a shift from collective to individual responsibility. If you can’t be sure what others are doing in regard to COVID, you need to focus on protecting yourself. Perhaps that shift was inevitable. Doesn’t mean we have to like it.
A version of this article first appeared on Medscape.com.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
Have you ever lied about COVID-19?
Before you get upset, before the “how dare you,” I want you to think carefully.
Did you have COVID-19 (or think you did) and not mention it to someone you were going to be with? Did you tell someone you were taking more COVID precautions than you really were? Did you tell someone you were vaccinated when you weren’t? Have you avoided getting a COVID test even though you knew you should have?
Researchers appreciated the fact that public health interventions in COVID are important but are only as good as the percentage of people who actually abide by them. So, they designed a survey to ask the questions that many people don’t want to hear the answer to.
A total of 1,733 participants – 80% of those invited – responded to the survey. By design, approximately one-third of respondents (477) had already had COVID, one-third (499) were vaccinated and not yet infected, and one-third (509) were unvaccinated and not yet infected.
Of those surveyed, 41.6% admitted that they lied about COVID or didn’t adhere to COVID guidelines - a conservative estimate, if you ask me.
Breaking down some of the results, about 20% of people who previously were infected with COVID said they didn’t mention it when meeting with someone. A similar number said they didn’t tell anyone when they were entering a public place. A bit more concerning to me, roughly 20% reported not disclosing their COVID-positive status when going to a health care provider’s office.
About 10% of those who had not been vaccinated reported lying about their vaccination status. That’s actually less than the 15% of vaccinated people who lied and told someone they weren’t vaccinated.
About 17% of people lied about the need to quarantine, and many more broke quarantine rules.
The authors tried to see if certain personal characteristics predicted people who were more likely to lie about COVID-19–related issues. Turns out there was only one thing that predicted honesty: age.
Older people were more honest about their COVID status and COVID habits. Other factors – gender, education, race, political affiliation, COVID-19 conspiracy beliefs, and where you got your COVID information – did not seem to make much of a difference. Why are older people more honest? Because older people take COVID more seriously. And they should; COVID is more severe in older people.
The problem arises, of course, because people who are at lower risk for COVID complications interact with people at higher risk – and in those situations, honesty matters more.
On the other hand, isn’t lying about COVID stuff inevitable? If you know that a positive test means you can’t go to work, and not going to work means you won’t get paid, might you not be more likely to lie about the test? Or not get the test at all?
The authors explored the reasons for dishonesty and they are fairly broad, ranging from the desire for life to feel normal (more than half of people who lied) to not believing that COVID was real (a whopping 30%). Some of the reasons for lying included:
- Wanted life to feel normal (50%).
- Freedom (45%).
- It’s no one’s business (40%).
- COVID isn’t real (30%).
In the end, though, we need to realize that public health recommendations are not going to be universally followed, and people may tell us they are following them when, in fact, they are not.
What this adds is another data point to a trend we’ve seen across the course of the pandemic, a shift from collective to individual responsibility. If you can’t be sure what others are doing in regard to COVID, you need to focus on protecting yourself. Perhaps that shift was inevitable. Doesn’t mean we have to like it.
A version of this article first appeared on Medscape.com.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com.
USPSTF calls for universal anxiety screening in children 8-18, jury out on suicide screening
For the first time, the task force recommended screening for anxiety in children aged 8-18 years who do not have a diagnosed anxiety disorder and are not showing signs or symptoms of anxiety.
This “B” recommendation reflects “moderate certainty” evidence that screening for anxiety in 8- to 18-year-olds has a moderate net benefit, the task force said.
However, the task force found “insufficient” evidence to weigh the balance of benefits and harms of screening for anxiety in children aged 7 and younger and therefore issued an “I” statement.
The task force also recommended screening for children aged 12-18 years for major depressive disorder (“B” recommendation) but said there is insufficient evidence to weigh the balance of benefits and harms of screening for depression in children aged 11 and younger (“I” statement).
These recommendations are in line with the 2016 recommendations on depression screening from the USPSTF.
“Fortunately, screening older children for anxiety and depression can identify these conditions so children and teens can receive the care that they need,” task force member Martha Kubik, PhD, RN, with George Mason University, Fairfax, Va., said in a statement.
“Unfortunately, there are key evidence gaps related to screening for anxiety and depression in younger children and screening for suicide risk in all youth,” added task force member Lori Pbert, PhD, University of Massachusetts, Worcester.
“We are calling for more research in these critical areas so we can provide health care professionals with evidence-based ways to keep their young patients healthy,” Dr. Pbert said.
Suicide screening
Turning to suicide, the task force says there is not enough evidence to recommend for or against screening for suicide risk in children and adolescents, and therefore issued an “I” statement – in line with the 2014 recommendation statement from the task force.
The task force acknowledged that the American Academy of Pediatrics, the American Foundation for Suicide Prevention, and experts from the National Institute of Mental Health have released a “Blueprint for Youth Suicide Prevention” that recommends universal screening for suicide risk in youth 12 years or older, while children aged 8-11 years should be screened as clinically indicated.
The task force’s final recommendation statements and corresponding evidence summaries on screening children and adolescents for anxiety, depression and suicide were published online Oct. 11, 2022, in JAMA and the USPSTF website.
The final recommendations are consistent with the 2022 draft recommendation statements on these topics.
The task force emphasized that screening is only the first step in helping children and adolescents with anxiety and depression. Youth who screen positive need further evaluation to determine if they have anxiety or depression.
After diagnosis, youth should participate in shared decision-making with their parents and healthcare professional to identify the best treatment or combination of treatments.
Only a first step
In an accompanying editorial, John Walkup, MD, with Ann and Robert H. Lurie Children’s Hospital, Chicago, and coauthors made the point that, for the potential of screening for pediatric anxiety disorders to be fully realized, research focused on the process of screening from evaluation to treatment needs to be a priority.
“Perhaps most critical is developing a smart and sophisticated process of screening aligned with evidence-based treatment strategies that brings added value to routine pediatric medical care and that improves physical and mental health outcomes for children and adolescents,” they wrote.
Members of the USPSTF disclosed no relevant financial relationships. Dr. Walkup reported serving as an unpaid member of the scientific council of the Anxiety and Depression Association of America, receiving royalties for anxiety-related continuing medical education activities from Wolters Kluwer and honoraria for anxiety presentations from the American Academy of Child and Adolescent Psychiatry and the American Academy of Pediatrics.
A version of this article first appeared on Medscape.com.
For the first time, the task force recommended screening for anxiety in children aged 8-18 years who do not have a diagnosed anxiety disorder and are not showing signs or symptoms of anxiety.
This “B” recommendation reflects “moderate certainty” evidence that screening for anxiety in 8- to 18-year-olds has a moderate net benefit, the task force said.
However, the task force found “insufficient” evidence to weigh the balance of benefits and harms of screening for anxiety in children aged 7 and younger and therefore issued an “I” statement.
The task force also recommended screening for children aged 12-18 years for major depressive disorder (“B” recommendation) but said there is insufficient evidence to weigh the balance of benefits and harms of screening for depression in children aged 11 and younger (“I” statement).
These recommendations are in line with the 2016 recommendations on depression screening from the USPSTF.
“Fortunately, screening older children for anxiety and depression can identify these conditions so children and teens can receive the care that they need,” task force member Martha Kubik, PhD, RN, with George Mason University, Fairfax, Va., said in a statement.
“Unfortunately, there are key evidence gaps related to screening for anxiety and depression in younger children and screening for suicide risk in all youth,” added task force member Lori Pbert, PhD, University of Massachusetts, Worcester.
“We are calling for more research in these critical areas so we can provide health care professionals with evidence-based ways to keep their young patients healthy,” Dr. Pbert said.
Suicide screening
Turning to suicide, the task force says there is not enough evidence to recommend for or against screening for suicide risk in children and adolescents, and therefore issued an “I” statement – in line with the 2014 recommendation statement from the task force.
The task force acknowledged that the American Academy of Pediatrics, the American Foundation for Suicide Prevention, and experts from the National Institute of Mental Health have released a “Blueprint for Youth Suicide Prevention” that recommends universal screening for suicide risk in youth 12 years or older, while children aged 8-11 years should be screened as clinically indicated.
The task force’s final recommendation statements and corresponding evidence summaries on screening children and adolescents for anxiety, depression and suicide were published online Oct. 11, 2022, in JAMA and the USPSTF website.
The final recommendations are consistent with the 2022 draft recommendation statements on these topics.
The task force emphasized that screening is only the first step in helping children and adolescents with anxiety and depression. Youth who screen positive need further evaluation to determine if they have anxiety or depression.
After diagnosis, youth should participate in shared decision-making with their parents and healthcare professional to identify the best treatment or combination of treatments.
Only a first step
In an accompanying editorial, John Walkup, MD, with Ann and Robert H. Lurie Children’s Hospital, Chicago, and coauthors made the point that, for the potential of screening for pediatric anxiety disorders to be fully realized, research focused on the process of screening from evaluation to treatment needs to be a priority.
“Perhaps most critical is developing a smart and sophisticated process of screening aligned with evidence-based treatment strategies that brings added value to routine pediatric medical care and that improves physical and mental health outcomes for children and adolescents,” they wrote.
Members of the USPSTF disclosed no relevant financial relationships. Dr. Walkup reported serving as an unpaid member of the scientific council of the Anxiety and Depression Association of America, receiving royalties for anxiety-related continuing medical education activities from Wolters Kluwer and honoraria for anxiety presentations from the American Academy of Child and Adolescent Psychiatry and the American Academy of Pediatrics.
A version of this article first appeared on Medscape.com.
For the first time, the task force recommended screening for anxiety in children aged 8-18 years who do not have a diagnosed anxiety disorder and are not showing signs or symptoms of anxiety.
This “B” recommendation reflects “moderate certainty” evidence that screening for anxiety in 8- to 18-year-olds has a moderate net benefit, the task force said.
However, the task force found “insufficient” evidence to weigh the balance of benefits and harms of screening for anxiety in children aged 7 and younger and therefore issued an “I” statement.
The task force also recommended screening for children aged 12-18 years for major depressive disorder (“B” recommendation) but said there is insufficient evidence to weigh the balance of benefits and harms of screening for depression in children aged 11 and younger (“I” statement).
These recommendations are in line with the 2016 recommendations on depression screening from the USPSTF.
“Fortunately, screening older children for anxiety and depression can identify these conditions so children and teens can receive the care that they need,” task force member Martha Kubik, PhD, RN, with George Mason University, Fairfax, Va., said in a statement.
“Unfortunately, there are key evidence gaps related to screening for anxiety and depression in younger children and screening for suicide risk in all youth,” added task force member Lori Pbert, PhD, University of Massachusetts, Worcester.
“We are calling for more research in these critical areas so we can provide health care professionals with evidence-based ways to keep their young patients healthy,” Dr. Pbert said.
Suicide screening
Turning to suicide, the task force says there is not enough evidence to recommend for or against screening for suicide risk in children and adolescents, and therefore issued an “I” statement – in line with the 2014 recommendation statement from the task force.
The task force acknowledged that the American Academy of Pediatrics, the American Foundation for Suicide Prevention, and experts from the National Institute of Mental Health have released a “Blueprint for Youth Suicide Prevention” that recommends universal screening for suicide risk in youth 12 years or older, while children aged 8-11 years should be screened as clinically indicated.
The task force’s final recommendation statements and corresponding evidence summaries on screening children and adolescents for anxiety, depression and suicide were published online Oct. 11, 2022, in JAMA and the USPSTF website.
The final recommendations are consistent with the 2022 draft recommendation statements on these topics.
The task force emphasized that screening is only the first step in helping children and adolescents with anxiety and depression. Youth who screen positive need further evaluation to determine if they have anxiety or depression.
After diagnosis, youth should participate in shared decision-making with their parents and healthcare professional to identify the best treatment or combination of treatments.
Only a first step
In an accompanying editorial, John Walkup, MD, with Ann and Robert H. Lurie Children’s Hospital, Chicago, and coauthors made the point that, for the potential of screening for pediatric anxiety disorders to be fully realized, research focused on the process of screening from evaluation to treatment needs to be a priority.
“Perhaps most critical is developing a smart and sophisticated process of screening aligned with evidence-based treatment strategies that brings added value to routine pediatric medical care and that improves physical and mental health outcomes for children and adolescents,” they wrote.
Members of the USPSTF disclosed no relevant financial relationships. Dr. Walkup reported serving as an unpaid member of the scientific council of the Anxiety and Depression Association of America, receiving royalties for anxiety-related continuing medical education activities from Wolters Kluwer and honoraria for anxiety presentations from the American Academy of Child and Adolescent Psychiatry and the American Academy of Pediatrics.
A version of this article first appeared on Medscape.com.
FROM JAMA
New screening tool identifies asthma risk in toddlers
A symptom-based screening tool can identify 2-year-olds at increased risk of asthma, persistent symptoms of wheeze, and health care burden by the age of 5, according to researchers.
The validated CHILDhood Asthma Risk Tool (CHART) determines high, moderate, or low risk of asthma based on symptoms reported before the age of 3 years. It also recommends follow-up.
Potentially, CHART could be used “to identify children who need monitoring, timely symptom control, and introduction of preventive therapies,” said Padmaja Subbarao, MD, MSc, associate chief of clinical research at the Hospital for Sick Children, Toronto, and colleagues in JAMA Network Open.
“The implementation of CHART as a first-step screening tool in general practice could promote timely treatment control and, in turn, improve quality of life for patients and reduce the clinical and economic burden of asthma,” they wrote.
Dr. Subbarao and colleagues developed CHART using data from parent questionnaires and 3- and 5-year clinic visits in the CHILD study. Children were categorized as “high risk” when they experienced two or more episodes of wheeze annually at both 3 and 5 years of age, concurrent with ED visits, hospitalizations, asthma medication, or frequent dry cough. Children with only cough episodes or with cough episodes plus one episode of wheeze in the past 12 months were categorized as “low risk.”
“Our unique approach to classification of wheeze symptoms is important because it helps busy practitioners identify the smaller subset of children with more frequent or severe wheezing episodes who have a higher probability of continued symptoms and impaired lung function in adult life among most children with infrequent wheeze,” Dr. Sabbarao and coauthors said.
Their diagnostic study to evaluate CHART’s predictive capacity showed that the tool had the highest proportion of true-positive asthma at 5 years (sensitivity, 50.0%), compared with physicians’ diagnosis at 3 years (sensitivity, 43.5%), and positive standardized modified Asthma Predictive Index (mAPI) at 3 years (sensitivity, 24.4%).
CHART also outperformed physician assessments and mAPI for predicting persistent wheeze at 5 years and provided the highest predictive capacity for subsequent health care use at 5 years of age. The study showed that it identified 20% more children with emergency department visits or hospitalizations than the standardized mAPI (sensitivity 45.5% vs. 25.0%), and approximately 10% more at-risk children than physician diagnosis.
“These findings are especially important given that many hospitalizations are avoidable if appropriate treatment and management of asthma are implemented at primary care,” Dr. Subbarao and colleagues wrote.
CHART has been validated in two external cohorts: a general-population cohort of 2,185 children from the Raine Study in Australia at 5 years of age; and the other a high-risk cohort of 349 children from the Canadian Asthma Primary Prevention Study at 7 years of age.
“We want to highlight the importance of periodic monitoring of wheeze symptoms and simplify the identification of high-risk children for primary care providers and parents or caregivers,” said Dr. Subbarao, who is director of the CHILD study and professor of pediatrics at the University of Toronto.
The tool “does not identify the underlying biology, which could impact the efficacy of our current standard asthma treatment,” Dr. Subbarao emphasized. CHART has not been tested in low-prevalence settings or in countries in which the term “wheeze” is not commonly recognized, she added.
“CHART helps you focus your crystal ball a little bit, look into the future, and see what’s going to happen,” said Harold Farber, MD, a pediatric pulmonologist who was not involved in the study. “It’s useful even if it just confirms what I’m already doing clinically.”
Dr. Farber, who is professor of pediatrics at Baylor College of Medicine and the Texas Children’s Hospital, Houston, cautioned that the predictive value of CHART is based on the diagnosis of asthma, and that this can differ across health care communities. “Between the extremes and what’s considered borderline, there’s a lot of diagnostic variation in what we call asthma,” he explained in an interview. “The diagnosis is, to some extent, subjective.”
However, Dr. Farber agreed that two or more wheezing episodes in the past 12 months – enough to require treatment – puts a child at very high risk for future wheezing. “Kids with a bunch of wheezing problems at 3 years are likely to have wheezing problems at 5. We have to think about what we can do for a toddler today to keep him from wheezing later.”
CHART is simple to use, the investigators said. The information needed can be easily gathered through interviews and parent-reported questionnaires, then put into the electronic medical record to flag children at high risk for further investigation, and well as those at low or moderate risk for monitoring.
Parents and caregivers can also use CHART to document symptoms every 6 months in children older than 1 year of age, said Dr. Subbarao. This information can be brought to the attention of the doctor “to facilitate a deeper discussion,” she suggested.
This study was funded by the Canadian Institutes of Health Research, Allergy, Genes and Environment Network of Centers of Excellence; Don and Debbie Morrison; Women’s and Children Health Research Institute; and Canada Research Chairs. Dr Subbarao reported having no potential conflicts of interest. Coauthor Vanessa Breton, PhD, disclosed being employed by F. Hoffmann-La Roche Ltd., and coauthor Elinor Simons, MD, PhD, reported membership on the Sanofi-Genzyme Data Monitoring Board. No other conflicts of interest were reported by the study authors. Dr Farber disclosed having no potential conflicts of interest.
A symptom-based screening tool can identify 2-year-olds at increased risk of asthma, persistent symptoms of wheeze, and health care burden by the age of 5, according to researchers.
The validated CHILDhood Asthma Risk Tool (CHART) determines high, moderate, or low risk of asthma based on symptoms reported before the age of 3 years. It also recommends follow-up.
Potentially, CHART could be used “to identify children who need monitoring, timely symptom control, and introduction of preventive therapies,” said Padmaja Subbarao, MD, MSc, associate chief of clinical research at the Hospital for Sick Children, Toronto, and colleagues in JAMA Network Open.
“The implementation of CHART as a first-step screening tool in general practice could promote timely treatment control and, in turn, improve quality of life for patients and reduce the clinical and economic burden of asthma,” they wrote.
Dr. Subbarao and colleagues developed CHART using data from parent questionnaires and 3- and 5-year clinic visits in the CHILD study. Children were categorized as “high risk” when they experienced two or more episodes of wheeze annually at both 3 and 5 years of age, concurrent with ED visits, hospitalizations, asthma medication, or frequent dry cough. Children with only cough episodes or with cough episodes plus one episode of wheeze in the past 12 months were categorized as “low risk.”
“Our unique approach to classification of wheeze symptoms is important because it helps busy practitioners identify the smaller subset of children with more frequent or severe wheezing episodes who have a higher probability of continued symptoms and impaired lung function in adult life among most children with infrequent wheeze,” Dr. Sabbarao and coauthors said.
Their diagnostic study to evaluate CHART’s predictive capacity showed that the tool had the highest proportion of true-positive asthma at 5 years (sensitivity, 50.0%), compared with physicians’ diagnosis at 3 years (sensitivity, 43.5%), and positive standardized modified Asthma Predictive Index (mAPI) at 3 years (sensitivity, 24.4%).
CHART also outperformed physician assessments and mAPI for predicting persistent wheeze at 5 years and provided the highest predictive capacity for subsequent health care use at 5 years of age. The study showed that it identified 20% more children with emergency department visits or hospitalizations than the standardized mAPI (sensitivity 45.5% vs. 25.0%), and approximately 10% more at-risk children than physician diagnosis.
“These findings are especially important given that many hospitalizations are avoidable if appropriate treatment and management of asthma are implemented at primary care,” Dr. Subbarao and colleagues wrote.
CHART has been validated in two external cohorts: a general-population cohort of 2,185 children from the Raine Study in Australia at 5 years of age; and the other a high-risk cohort of 349 children from the Canadian Asthma Primary Prevention Study at 7 years of age.
“We want to highlight the importance of periodic monitoring of wheeze symptoms and simplify the identification of high-risk children for primary care providers and parents or caregivers,” said Dr. Subbarao, who is director of the CHILD study and professor of pediatrics at the University of Toronto.
The tool “does not identify the underlying biology, which could impact the efficacy of our current standard asthma treatment,” Dr. Subbarao emphasized. CHART has not been tested in low-prevalence settings or in countries in which the term “wheeze” is not commonly recognized, she added.
“CHART helps you focus your crystal ball a little bit, look into the future, and see what’s going to happen,” said Harold Farber, MD, a pediatric pulmonologist who was not involved in the study. “It’s useful even if it just confirms what I’m already doing clinically.”
Dr. Farber, who is professor of pediatrics at Baylor College of Medicine and the Texas Children’s Hospital, Houston, cautioned that the predictive value of CHART is based on the diagnosis of asthma, and that this can differ across health care communities. “Between the extremes and what’s considered borderline, there’s a lot of diagnostic variation in what we call asthma,” he explained in an interview. “The diagnosis is, to some extent, subjective.”
However, Dr. Farber agreed that two or more wheezing episodes in the past 12 months – enough to require treatment – puts a child at very high risk for future wheezing. “Kids with a bunch of wheezing problems at 3 years are likely to have wheezing problems at 5. We have to think about what we can do for a toddler today to keep him from wheezing later.”
CHART is simple to use, the investigators said. The information needed can be easily gathered through interviews and parent-reported questionnaires, then put into the electronic medical record to flag children at high risk for further investigation, and well as those at low or moderate risk for monitoring.
Parents and caregivers can also use CHART to document symptoms every 6 months in children older than 1 year of age, said Dr. Subbarao. This information can be brought to the attention of the doctor “to facilitate a deeper discussion,” she suggested.
This study was funded by the Canadian Institutes of Health Research, Allergy, Genes and Environment Network of Centers of Excellence; Don and Debbie Morrison; Women’s and Children Health Research Institute; and Canada Research Chairs. Dr Subbarao reported having no potential conflicts of interest. Coauthor Vanessa Breton, PhD, disclosed being employed by F. Hoffmann-La Roche Ltd., and coauthor Elinor Simons, MD, PhD, reported membership on the Sanofi-Genzyme Data Monitoring Board. No other conflicts of interest were reported by the study authors. Dr Farber disclosed having no potential conflicts of interest.
A symptom-based screening tool can identify 2-year-olds at increased risk of asthma, persistent symptoms of wheeze, and health care burden by the age of 5, according to researchers.
The validated CHILDhood Asthma Risk Tool (CHART) determines high, moderate, or low risk of asthma based on symptoms reported before the age of 3 years. It also recommends follow-up.
Potentially, CHART could be used “to identify children who need monitoring, timely symptom control, and introduction of preventive therapies,” said Padmaja Subbarao, MD, MSc, associate chief of clinical research at the Hospital for Sick Children, Toronto, and colleagues in JAMA Network Open.
“The implementation of CHART as a first-step screening tool in general practice could promote timely treatment control and, in turn, improve quality of life for patients and reduce the clinical and economic burden of asthma,” they wrote.
Dr. Subbarao and colleagues developed CHART using data from parent questionnaires and 3- and 5-year clinic visits in the CHILD study. Children were categorized as “high risk” when they experienced two or more episodes of wheeze annually at both 3 and 5 years of age, concurrent with ED visits, hospitalizations, asthma medication, or frequent dry cough. Children with only cough episodes or with cough episodes plus one episode of wheeze in the past 12 months were categorized as “low risk.”
“Our unique approach to classification of wheeze symptoms is important because it helps busy practitioners identify the smaller subset of children with more frequent or severe wheezing episodes who have a higher probability of continued symptoms and impaired lung function in adult life among most children with infrequent wheeze,” Dr. Sabbarao and coauthors said.
Their diagnostic study to evaluate CHART’s predictive capacity showed that the tool had the highest proportion of true-positive asthma at 5 years (sensitivity, 50.0%), compared with physicians’ diagnosis at 3 years (sensitivity, 43.5%), and positive standardized modified Asthma Predictive Index (mAPI) at 3 years (sensitivity, 24.4%).
CHART also outperformed physician assessments and mAPI for predicting persistent wheeze at 5 years and provided the highest predictive capacity for subsequent health care use at 5 years of age. The study showed that it identified 20% more children with emergency department visits or hospitalizations than the standardized mAPI (sensitivity 45.5% vs. 25.0%), and approximately 10% more at-risk children than physician diagnosis.
“These findings are especially important given that many hospitalizations are avoidable if appropriate treatment and management of asthma are implemented at primary care,” Dr. Subbarao and colleagues wrote.
CHART has been validated in two external cohorts: a general-population cohort of 2,185 children from the Raine Study in Australia at 5 years of age; and the other a high-risk cohort of 349 children from the Canadian Asthma Primary Prevention Study at 7 years of age.
“We want to highlight the importance of periodic monitoring of wheeze symptoms and simplify the identification of high-risk children for primary care providers and parents or caregivers,” said Dr. Subbarao, who is director of the CHILD study and professor of pediatrics at the University of Toronto.
The tool “does not identify the underlying biology, which could impact the efficacy of our current standard asthma treatment,” Dr. Subbarao emphasized. CHART has not been tested in low-prevalence settings or in countries in which the term “wheeze” is not commonly recognized, she added.
“CHART helps you focus your crystal ball a little bit, look into the future, and see what’s going to happen,” said Harold Farber, MD, a pediatric pulmonologist who was not involved in the study. “It’s useful even if it just confirms what I’m already doing clinically.”
Dr. Farber, who is professor of pediatrics at Baylor College of Medicine and the Texas Children’s Hospital, Houston, cautioned that the predictive value of CHART is based on the diagnosis of asthma, and that this can differ across health care communities. “Between the extremes and what’s considered borderline, there’s a lot of diagnostic variation in what we call asthma,” he explained in an interview. “The diagnosis is, to some extent, subjective.”
However, Dr. Farber agreed that two or more wheezing episodes in the past 12 months – enough to require treatment – puts a child at very high risk for future wheezing. “Kids with a bunch of wheezing problems at 3 years are likely to have wheezing problems at 5. We have to think about what we can do for a toddler today to keep him from wheezing later.”
CHART is simple to use, the investigators said. The information needed can be easily gathered through interviews and parent-reported questionnaires, then put into the electronic medical record to flag children at high risk for further investigation, and well as those at low or moderate risk for monitoring.
Parents and caregivers can also use CHART to document symptoms every 6 months in children older than 1 year of age, said Dr. Subbarao. This information can be brought to the attention of the doctor “to facilitate a deeper discussion,” she suggested.
This study was funded by the Canadian Institutes of Health Research, Allergy, Genes and Environment Network of Centers of Excellence; Don and Debbie Morrison; Women’s and Children Health Research Institute; and Canada Research Chairs. Dr Subbarao reported having no potential conflicts of interest. Coauthor Vanessa Breton, PhD, disclosed being employed by F. Hoffmann-La Roche Ltd., and coauthor Elinor Simons, MD, PhD, reported membership on the Sanofi-Genzyme Data Monitoring Board. No other conflicts of interest were reported by the study authors. Dr Farber disclosed having no potential conflicts of interest.
FROM JAMA NETWORK OPEN
Opioids leading cause of poisoning deaths in young children
ANAHEIM, CALIF. – Opioids are the most common cause of fatal poisonings in young children, and their contribution to children’s deaths has been increasing, according to research presented at the American Academy of Pediatrics National Conference.
The study found that the proportion of deaths in U.S. children linked to opioids has doubled since the mid-2000s, tracking the course of the epidemic in adults in this country.
“What is striking about our study is how the opioid epidemic has not spared our nation’s infants or young children,” Christopher Gaw, MD, MA, a pediatric emergency medicine fellow physician at Children’s Hospital of Philadelphia, said in an interview. “There is important work being done to reduce unnecessary opioid prescribing, drug diversion, and treatment of substance use disorders. These efforts – though not directly related to children – also help protect them, since they can reduce the chance of exposure to opioids in the home.”
Dr. Gaw and his colleagues analyzed data in Child Death Reviews from 40 states that participate in the National Fatality Review Case Reporting System, focusing on children aged 5 years and younger who died from a poisoning between 2005 and 2018. During that time, 731 child poisoning deaths were reported to the system – of which nearly half (47%) involved opioids as the poisoning agent – up from 24% in 2005. More than 4 in 10 deaths (42%) involved children under age 1.
Most of the deaths (61%) occurred in the child’s home, and in even more cases (71%) the child was being supervised when the poisoning occurred, most often by a parent (58.5%). The others supervising children were usually a grandparent (11%) or another relative (5.5%). The child was in view of the supervising individual in 28.5% of the deaths. A child protective services case was opened in 13% of the cases.
“Supervising a child is hard. Kids are constantly exploring and moving,” Dr. Gaw said. “A child may find a dropped medication on the floor that a caregiver doesn’t see, or a child may get into a bag or a purse when a caregiver is looking the other way. Poisonings can happen in a split second.”
Expecting caregivers to be able to watch kids every moment and always be within arm’s reach to prevent an accident is unrealistic, Dr. Gaw said, so families should focus on preparedness.
“Young children can’t tell the difference between a deadly substance versus a substance that is harmless or would only cause some harm. The best way to protect children is to prevent the poisoning from happening in the first place,” Dr. Gaw said. ”
It is recommended that caregivers keep the Poison Control Center’s national 24/7 hotline in their phones: (800) 222-1222.
Two-thirds of the cases Dr. Gaw examined did not involve a call to a poison control center, but most did involve a call to 911.
“My guess is that caregivers likely called 911 instead of poison control because the child was likely critically ill or deceased when found,” Dr. Gaw said, noting that his group did not have access to descriptive information about 911 calls. “If a child is critically ill and a caregiver called poison control first, they would be referred to 911.”
If a child looks healthy but has just swallowed something dangerous or deadly, Dr. Gaw said poison control can guide the family to getting prompt medical attention that could be lifesaving.
“We don’t expect the public to know what substances are harmless, harmful, or deadly,” he said. “People should always call poison control if there is any concern, even if the child looks well.”
Some poison control centers are working to increase the ways people can reach them, including through texting, apps, or online chat, he added.
Gary A. Smith, MD, DrPH, president of the nonprofit Child Injury Prevention Alliance in Columbus, Ohio, and director of the Center for Injury Research and Policy at Nationwide Children’s Hospital, said the high level of supervision in these cases was not surprising.
”We have shown that most children are being directly supervised at the moment of injury for baby walker–related injuries, firework-related injuries, and other types of injuries that we have studied,” Dr. Smith said in an interview. “Injuries happen quickly and generally do not give a parent or caregiver time to react.”
“This dispels the myth that parental supervision is the key to injury prevention,” Dr. Smith said. “Although supervision helps, it is not adequate. These injuries occur to children of good and caring parents. The message for pediatricians is that we must create safe environments for children and design hazards out of existence to effectively prevent poisoning and other injuries.”
That preventive approach has been used for infectious disease and other public health problems, he added.
“Prescription opioids must be kept in their original containers with children-resistant closures and be stored up, away, and out of sight of children, preferably in a locked location,” Dr. Smith said. “If adults use illicit opioids or any other illicit substances – which are commonly laced with fentanyl – they should not use or store them in the home where children can access them.”
Over-the-counter pain, cold, and allergy medications were the second most common cause of death, occurring in 15% of cases.
“There has been a lot of work over the years among health care providers to counsel families on the proper dosing and use of medications such as Tylenol, Motrin, and Benadryl,” Dr. Gaw said. “There has also been a push to educate families that using antihistamines, such as Benadryl, to sedate their children can be dangerous and, depending on the dose, potentially deadly.”
Another 14% of cases were an unspecified illicit drug, and 10% were an unspecified over-the-counter or prescription medication. Carbon monoxide poisoning made up 6% of cases, and the remaining substances included amphetamines, antidepressants, cocaine, and alcohol.
Over half the deaths in 1-year-olds (61%) and children aged 2-5 (54%) were due to opioid poisoning, as were a third of deaths in infants (34%). Most of the poisonings involving amphetamines (81%), cocaine (84%), and alcohol (61.5%) occurred in infants under age 1.
Dr. Smith said that harm-reduction strategies, such as having naloxone on hand and using fentanyl test strips, can reduce the likelihood of death from illicit drugs.
Reducing stigma can save lives
“Referring parents to services for individuals who use drugs is key,” Dr. Smith said. “Treating this as a public health problem without stigmatizing the behavior is something that pediatricians and other health care professionals must remember.” As a resource for other pediatricians, Dr. Gaw noted that CHOP’s poison control center medical director Kevin Osterhoudt, MD produced a 25-minute podcast that covers common causes of poisonings, use of naloxone in children, and prevention tips.
“Naloxone is an effective antidote to opioid poisonings,” Dr. Gaw said. “We often think of using it in adults, but this is also a lifesaving medication for children poisoned by opioids. Educating people on recognizing the signs and symptoms of opioid poisoning and helping them feel empowered to use naloxone is something the public health world is working on.”
Dr. Gaw and Dr. Smith had no relevant disclosures. No external funding was noted for the study.
ANAHEIM, CALIF. – Opioids are the most common cause of fatal poisonings in young children, and their contribution to children’s deaths has been increasing, according to research presented at the American Academy of Pediatrics National Conference.
The study found that the proportion of deaths in U.S. children linked to opioids has doubled since the mid-2000s, tracking the course of the epidemic in adults in this country.
“What is striking about our study is how the opioid epidemic has not spared our nation’s infants or young children,” Christopher Gaw, MD, MA, a pediatric emergency medicine fellow physician at Children’s Hospital of Philadelphia, said in an interview. “There is important work being done to reduce unnecessary opioid prescribing, drug diversion, and treatment of substance use disorders. These efforts – though not directly related to children – also help protect them, since they can reduce the chance of exposure to opioids in the home.”
Dr. Gaw and his colleagues analyzed data in Child Death Reviews from 40 states that participate in the National Fatality Review Case Reporting System, focusing on children aged 5 years and younger who died from a poisoning between 2005 and 2018. During that time, 731 child poisoning deaths were reported to the system – of which nearly half (47%) involved opioids as the poisoning agent – up from 24% in 2005. More than 4 in 10 deaths (42%) involved children under age 1.
Most of the deaths (61%) occurred in the child’s home, and in even more cases (71%) the child was being supervised when the poisoning occurred, most often by a parent (58.5%). The others supervising children were usually a grandparent (11%) or another relative (5.5%). The child was in view of the supervising individual in 28.5% of the deaths. A child protective services case was opened in 13% of the cases.
“Supervising a child is hard. Kids are constantly exploring and moving,” Dr. Gaw said. “A child may find a dropped medication on the floor that a caregiver doesn’t see, or a child may get into a bag or a purse when a caregiver is looking the other way. Poisonings can happen in a split second.”
Expecting caregivers to be able to watch kids every moment and always be within arm’s reach to prevent an accident is unrealistic, Dr. Gaw said, so families should focus on preparedness.
“Young children can’t tell the difference between a deadly substance versus a substance that is harmless or would only cause some harm. The best way to protect children is to prevent the poisoning from happening in the first place,” Dr. Gaw said. ”
It is recommended that caregivers keep the Poison Control Center’s national 24/7 hotline in their phones: (800) 222-1222.
Two-thirds of the cases Dr. Gaw examined did not involve a call to a poison control center, but most did involve a call to 911.
“My guess is that caregivers likely called 911 instead of poison control because the child was likely critically ill or deceased when found,” Dr. Gaw said, noting that his group did not have access to descriptive information about 911 calls. “If a child is critically ill and a caregiver called poison control first, they would be referred to 911.”
If a child looks healthy but has just swallowed something dangerous or deadly, Dr. Gaw said poison control can guide the family to getting prompt medical attention that could be lifesaving.
“We don’t expect the public to know what substances are harmless, harmful, or deadly,” he said. “People should always call poison control if there is any concern, even if the child looks well.”
Some poison control centers are working to increase the ways people can reach them, including through texting, apps, or online chat, he added.
Gary A. Smith, MD, DrPH, president of the nonprofit Child Injury Prevention Alliance in Columbus, Ohio, and director of the Center for Injury Research and Policy at Nationwide Children’s Hospital, said the high level of supervision in these cases was not surprising.
”We have shown that most children are being directly supervised at the moment of injury for baby walker–related injuries, firework-related injuries, and other types of injuries that we have studied,” Dr. Smith said in an interview. “Injuries happen quickly and generally do not give a parent or caregiver time to react.”
“This dispels the myth that parental supervision is the key to injury prevention,” Dr. Smith said. “Although supervision helps, it is not adequate. These injuries occur to children of good and caring parents. The message for pediatricians is that we must create safe environments for children and design hazards out of existence to effectively prevent poisoning and other injuries.”
That preventive approach has been used for infectious disease and other public health problems, he added.
“Prescription opioids must be kept in their original containers with children-resistant closures and be stored up, away, and out of sight of children, preferably in a locked location,” Dr. Smith said. “If adults use illicit opioids or any other illicit substances – which are commonly laced with fentanyl – they should not use or store them in the home where children can access them.”
Over-the-counter pain, cold, and allergy medications were the second most common cause of death, occurring in 15% of cases.
“There has been a lot of work over the years among health care providers to counsel families on the proper dosing and use of medications such as Tylenol, Motrin, and Benadryl,” Dr. Gaw said. “There has also been a push to educate families that using antihistamines, such as Benadryl, to sedate their children can be dangerous and, depending on the dose, potentially deadly.”
Another 14% of cases were an unspecified illicit drug, and 10% were an unspecified over-the-counter or prescription medication. Carbon monoxide poisoning made up 6% of cases, and the remaining substances included amphetamines, antidepressants, cocaine, and alcohol.
Over half the deaths in 1-year-olds (61%) and children aged 2-5 (54%) were due to opioid poisoning, as were a third of deaths in infants (34%). Most of the poisonings involving amphetamines (81%), cocaine (84%), and alcohol (61.5%) occurred in infants under age 1.
Dr. Smith said that harm-reduction strategies, such as having naloxone on hand and using fentanyl test strips, can reduce the likelihood of death from illicit drugs.
Reducing stigma can save lives
“Referring parents to services for individuals who use drugs is key,” Dr. Smith said. “Treating this as a public health problem without stigmatizing the behavior is something that pediatricians and other health care professionals must remember.” As a resource for other pediatricians, Dr. Gaw noted that CHOP’s poison control center medical director Kevin Osterhoudt, MD produced a 25-minute podcast that covers common causes of poisonings, use of naloxone in children, and prevention tips.
“Naloxone is an effective antidote to opioid poisonings,” Dr. Gaw said. “We often think of using it in adults, but this is also a lifesaving medication for children poisoned by opioids. Educating people on recognizing the signs and symptoms of opioid poisoning and helping them feel empowered to use naloxone is something the public health world is working on.”
Dr. Gaw and Dr. Smith had no relevant disclosures. No external funding was noted for the study.
ANAHEIM, CALIF. – Opioids are the most common cause of fatal poisonings in young children, and their contribution to children’s deaths has been increasing, according to research presented at the American Academy of Pediatrics National Conference.
The study found that the proportion of deaths in U.S. children linked to opioids has doubled since the mid-2000s, tracking the course of the epidemic in adults in this country.
“What is striking about our study is how the opioid epidemic has not spared our nation’s infants or young children,” Christopher Gaw, MD, MA, a pediatric emergency medicine fellow physician at Children’s Hospital of Philadelphia, said in an interview. “There is important work being done to reduce unnecessary opioid prescribing, drug diversion, and treatment of substance use disorders. These efforts – though not directly related to children – also help protect them, since they can reduce the chance of exposure to opioids in the home.”
Dr. Gaw and his colleagues analyzed data in Child Death Reviews from 40 states that participate in the National Fatality Review Case Reporting System, focusing on children aged 5 years and younger who died from a poisoning between 2005 and 2018. During that time, 731 child poisoning deaths were reported to the system – of which nearly half (47%) involved opioids as the poisoning agent – up from 24% in 2005. More than 4 in 10 deaths (42%) involved children under age 1.
Most of the deaths (61%) occurred in the child’s home, and in even more cases (71%) the child was being supervised when the poisoning occurred, most often by a parent (58.5%). The others supervising children were usually a grandparent (11%) or another relative (5.5%). The child was in view of the supervising individual in 28.5% of the deaths. A child protective services case was opened in 13% of the cases.
“Supervising a child is hard. Kids are constantly exploring and moving,” Dr. Gaw said. “A child may find a dropped medication on the floor that a caregiver doesn’t see, or a child may get into a bag or a purse when a caregiver is looking the other way. Poisonings can happen in a split second.”
Expecting caregivers to be able to watch kids every moment and always be within arm’s reach to prevent an accident is unrealistic, Dr. Gaw said, so families should focus on preparedness.
“Young children can’t tell the difference between a deadly substance versus a substance that is harmless or would only cause some harm. The best way to protect children is to prevent the poisoning from happening in the first place,” Dr. Gaw said. ”
It is recommended that caregivers keep the Poison Control Center’s national 24/7 hotline in their phones: (800) 222-1222.
Two-thirds of the cases Dr. Gaw examined did not involve a call to a poison control center, but most did involve a call to 911.
“My guess is that caregivers likely called 911 instead of poison control because the child was likely critically ill or deceased when found,” Dr. Gaw said, noting that his group did not have access to descriptive information about 911 calls. “If a child is critically ill and a caregiver called poison control first, they would be referred to 911.”
If a child looks healthy but has just swallowed something dangerous or deadly, Dr. Gaw said poison control can guide the family to getting prompt medical attention that could be lifesaving.
“We don’t expect the public to know what substances are harmless, harmful, or deadly,” he said. “People should always call poison control if there is any concern, even if the child looks well.”
Some poison control centers are working to increase the ways people can reach them, including through texting, apps, or online chat, he added.
Gary A. Smith, MD, DrPH, president of the nonprofit Child Injury Prevention Alliance in Columbus, Ohio, and director of the Center for Injury Research and Policy at Nationwide Children’s Hospital, said the high level of supervision in these cases was not surprising.
”We have shown that most children are being directly supervised at the moment of injury for baby walker–related injuries, firework-related injuries, and other types of injuries that we have studied,” Dr. Smith said in an interview. “Injuries happen quickly and generally do not give a parent or caregiver time to react.”
“This dispels the myth that parental supervision is the key to injury prevention,” Dr. Smith said. “Although supervision helps, it is not adequate. These injuries occur to children of good and caring parents. The message for pediatricians is that we must create safe environments for children and design hazards out of existence to effectively prevent poisoning and other injuries.”
That preventive approach has been used for infectious disease and other public health problems, he added.
“Prescription opioids must be kept in their original containers with children-resistant closures and be stored up, away, and out of sight of children, preferably in a locked location,” Dr. Smith said. “If adults use illicit opioids or any other illicit substances – which are commonly laced with fentanyl – they should not use or store them in the home where children can access them.”
Over-the-counter pain, cold, and allergy medications were the second most common cause of death, occurring in 15% of cases.
“There has been a lot of work over the years among health care providers to counsel families on the proper dosing and use of medications such as Tylenol, Motrin, and Benadryl,” Dr. Gaw said. “There has also been a push to educate families that using antihistamines, such as Benadryl, to sedate their children can be dangerous and, depending on the dose, potentially deadly.”
Another 14% of cases were an unspecified illicit drug, and 10% were an unspecified over-the-counter or prescription medication. Carbon monoxide poisoning made up 6% of cases, and the remaining substances included amphetamines, antidepressants, cocaine, and alcohol.
Over half the deaths in 1-year-olds (61%) and children aged 2-5 (54%) were due to opioid poisoning, as were a third of deaths in infants (34%). Most of the poisonings involving amphetamines (81%), cocaine (84%), and alcohol (61.5%) occurred in infants under age 1.
Dr. Smith said that harm-reduction strategies, such as having naloxone on hand and using fentanyl test strips, can reduce the likelihood of death from illicit drugs.
Reducing stigma can save lives
“Referring parents to services for individuals who use drugs is key,” Dr. Smith said. “Treating this as a public health problem without stigmatizing the behavior is something that pediatricians and other health care professionals must remember.” As a resource for other pediatricians, Dr. Gaw noted that CHOP’s poison control center medical director Kevin Osterhoudt, MD produced a 25-minute podcast that covers common causes of poisonings, use of naloxone in children, and prevention tips.
“Naloxone is an effective antidote to opioid poisonings,” Dr. Gaw said. “We often think of using it in adults, but this is also a lifesaving medication for children poisoned by opioids. Educating people on recognizing the signs and symptoms of opioid poisoning and helping them feel empowered to use naloxone is something the public health world is working on.”
Dr. Gaw and Dr. Smith had no relevant disclosures. No external funding was noted for the study.
AT AAP 2022
Children and COVID: Downward trend reverses with small increase in new cases
A small increase in new cases brought COVID-19’s latest losing streak to an end at 4 weeks, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
The 40,656 new cases reported bring the U.S. cumulative count of child COVID-19 cases to over 14.8 million since the pandemic began, which represents 18.4% of all cases, the AAP and CHA said in their weekly report based on state-level data.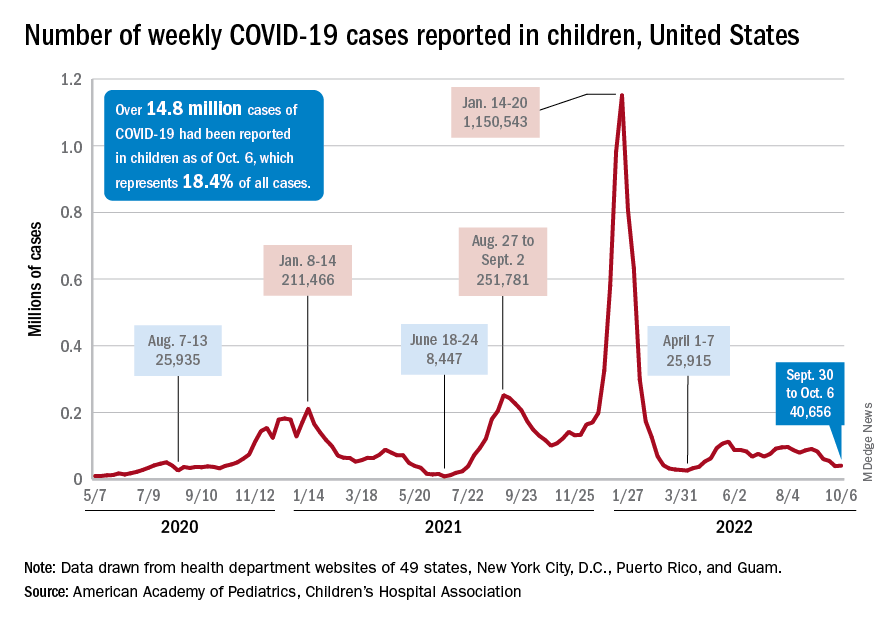
The increase in new cases was not reflected in emergency department visits or hospital admissions, which both continued sustained declines that started in August. In the week from Sept. 27 to Oct. 4, the 7-day averages for ED visits with diagnosed COVID were down by 21.5% (age 0-11), 27.3% (12-15), and 18.2% (16-17), the Centers for Disease Control and Prevention said, while the most recent 7-day average for new admissions – 127 per day for Oct. 2-8 – among children aged 0-17 years with confirmed COVID was down from 161 per day the previous week, a drop of over 21%.
The state-level data that are currently available (several states are no longer reporting) show Alaska (25.5%) and Vermont (25.4%) have the highest proportions of cumulative cases in children, and Florida (12.3%) and Utah (13.5%) have the lowest. Rhode Island has the highest rate of COVID-19 per 100,000 children at 40,427, while Missouri has the lowest at 14,252. The national average is 19,687 per 100,000, the AAP and CHA reported.
Taking a look at vaccination
Vaccinations were up slightly in children aged 12-17 years, as 20,000 initial doses were given during the week of Sept. 29 to Oct. 5, compared with 17,000 and 18,000 the previous 2 weeks. Initial vaccinations in younger children, however, continued declines dating back to August, the AAP said in its weekly vaccination trends report.
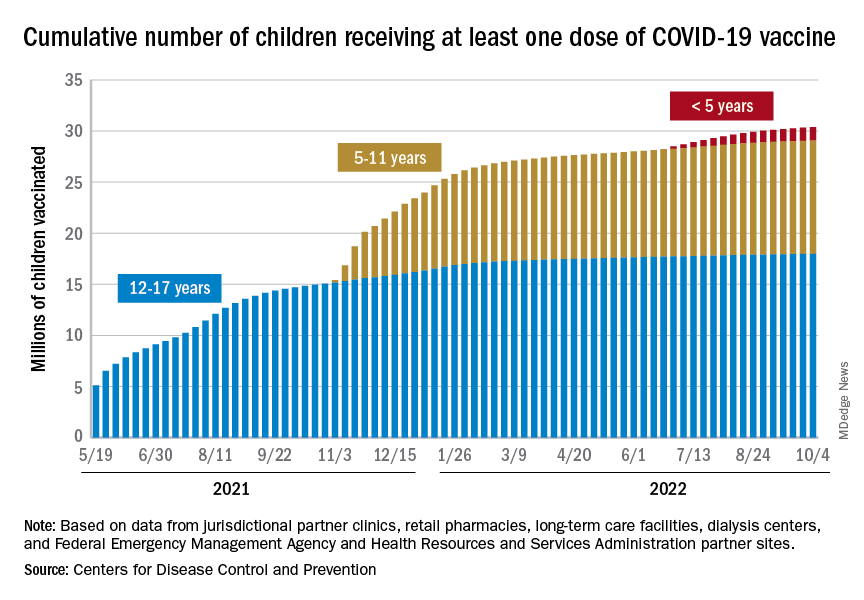
The District of Columbia and Massachusetts have the most highly vaccinated groups of 12- to 17-year-olds, as 100% and 95%, respectively, have received initial doses, while Wyoming (39%) and Idaho (42%) have the lowest. D.C. (73%) and Vermont (68%) have the highest proportions of vaccinated 5- to 11-year-olds, and Alabama (17%) and Mississippi (18%) have the lowest. For children under age 5 years, those in D.C. (33%) and Vermont (26%) are the most likely to have received an initial COVID vaccination, while Alabama, Louisiana, and Mississippi share national-low rates of 2%, the AAP said its report, which is based on CDC data.
When all states and territories are combined, 71% of children aged 12-17 have received at least one dose of vaccine, as have 38.6% of all children 5-11 years old and 6.7% of those under age 5. Almost 61% of the nation’s 16- to 17-year-olds have been fully vaccinated, along with 31.5% of those aged 5-11 and 2.4% of children younger than 5 years, the CDC said on its COVID Data Tracker.
About 42 million children – 58% of the population under the age of 18 years – have not received any vaccine yet, the AAP noted. Meanwhile, CDC data indicate that 36 children died of COVID in the last week, with pediatric deaths now totaling 1,781 over the course of the pandemic.
A small increase in new cases brought COVID-19’s latest losing streak to an end at 4 weeks, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
The 40,656 new cases reported bring the U.S. cumulative count of child COVID-19 cases to over 14.8 million since the pandemic began, which represents 18.4% of all cases, the AAP and CHA said in their weekly report based on state-level data.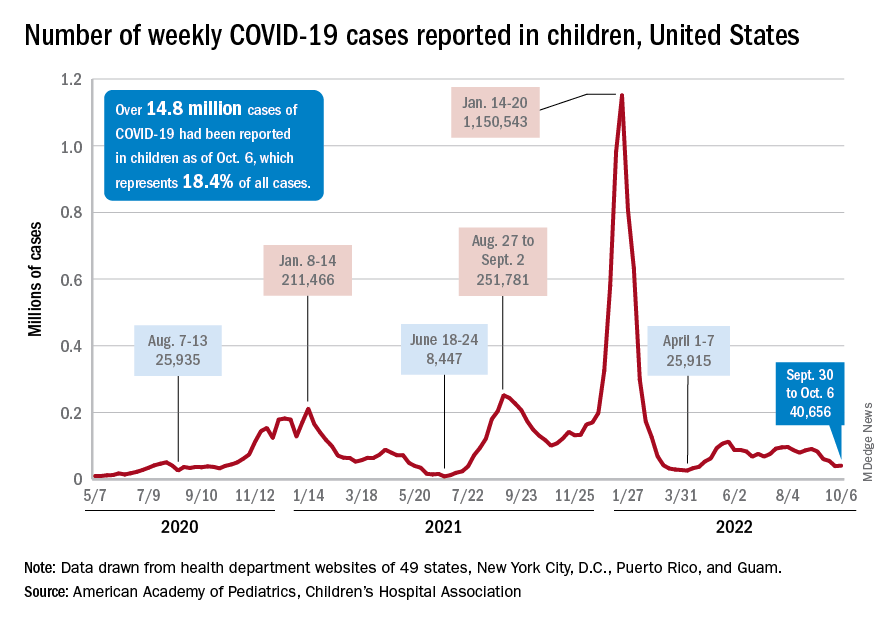
The increase in new cases was not reflected in emergency department visits or hospital admissions, which both continued sustained declines that started in August. In the week from Sept. 27 to Oct. 4, the 7-day averages for ED visits with diagnosed COVID were down by 21.5% (age 0-11), 27.3% (12-15), and 18.2% (16-17), the Centers for Disease Control and Prevention said, while the most recent 7-day average for new admissions – 127 per day for Oct. 2-8 – among children aged 0-17 years with confirmed COVID was down from 161 per day the previous week, a drop of over 21%.
The state-level data that are currently available (several states are no longer reporting) show Alaska (25.5%) and Vermont (25.4%) have the highest proportions of cumulative cases in children, and Florida (12.3%) and Utah (13.5%) have the lowest. Rhode Island has the highest rate of COVID-19 per 100,000 children at 40,427, while Missouri has the lowest at 14,252. The national average is 19,687 per 100,000, the AAP and CHA reported.
Taking a look at vaccination
Vaccinations were up slightly in children aged 12-17 years, as 20,000 initial doses were given during the week of Sept. 29 to Oct. 5, compared with 17,000 and 18,000 the previous 2 weeks. Initial vaccinations in younger children, however, continued declines dating back to August, the AAP said in its weekly vaccination trends report.
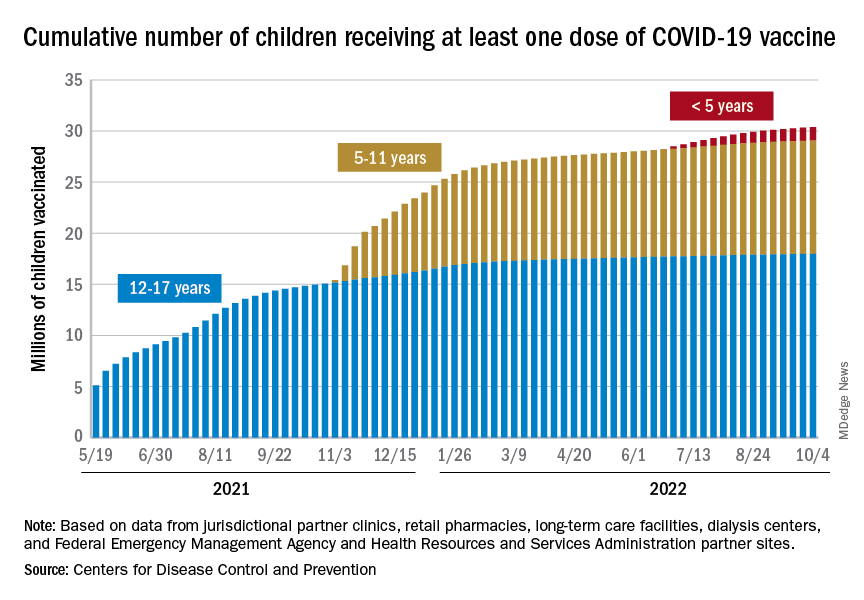
The District of Columbia and Massachusetts have the most highly vaccinated groups of 12- to 17-year-olds, as 100% and 95%, respectively, have received initial doses, while Wyoming (39%) and Idaho (42%) have the lowest. D.C. (73%) and Vermont (68%) have the highest proportions of vaccinated 5- to 11-year-olds, and Alabama (17%) and Mississippi (18%) have the lowest. For children under age 5 years, those in D.C. (33%) and Vermont (26%) are the most likely to have received an initial COVID vaccination, while Alabama, Louisiana, and Mississippi share national-low rates of 2%, the AAP said its report, which is based on CDC data.
When all states and territories are combined, 71% of children aged 12-17 have received at least one dose of vaccine, as have 38.6% of all children 5-11 years old and 6.7% of those under age 5. Almost 61% of the nation’s 16- to 17-year-olds have been fully vaccinated, along with 31.5% of those aged 5-11 and 2.4% of children younger than 5 years, the CDC said on its COVID Data Tracker.
About 42 million children – 58% of the population under the age of 18 years – have not received any vaccine yet, the AAP noted. Meanwhile, CDC data indicate that 36 children died of COVID in the last week, with pediatric deaths now totaling 1,781 over the course of the pandemic.
A small increase in new cases brought COVID-19’s latest losing streak to an end at 4 weeks, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
The 40,656 new cases reported bring the U.S. cumulative count of child COVID-19 cases to over 14.8 million since the pandemic began, which represents 18.4% of all cases, the AAP and CHA said in their weekly report based on state-level data.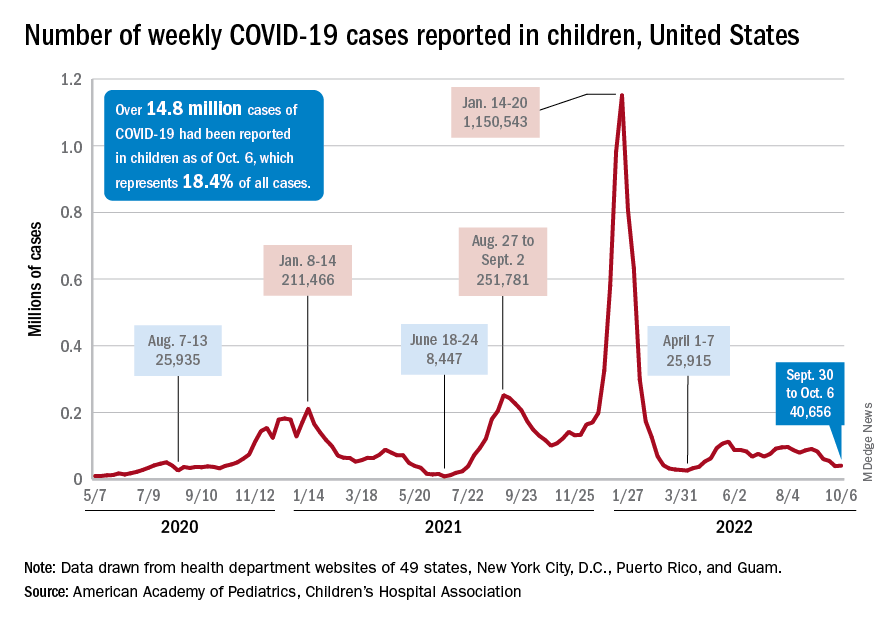
The increase in new cases was not reflected in emergency department visits or hospital admissions, which both continued sustained declines that started in August. In the week from Sept. 27 to Oct. 4, the 7-day averages for ED visits with diagnosed COVID were down by 21.5% (age 0-11), 27.3% (12-15), and 18.2% (16-17), the Centers for Disease Control and Prevention said, while the most recent 7-day average for new admissions – 127 per day for Oct. 2-8 – among children aged 0-17 years with confirmed COVID was down from 161 per day the previous week, a drop of over 21%.
The state-level data that are currently available (several states are no longer reporting) show Alaska (25.5%) and Vermont (25.4%) have the highest proportions of cumulative cases in children, and Florida (12.3%) and Utah (13.5%) have the lowest. Rhode Island has the highest rate of COVID-19 per 100,000 children at 40,427, while Missouri has the lowest at 14,252. The national average is 19,687 per 100,000, the AAP and CHA reported.
Taking a look at vaccination
Vaccinations were up slightly in children aged 12-17 years, as 20,000 initial doses were given during the week of Sept. 29 to Oct. 5, compared with 17,000 and 18,000 the previous 2 weeks. Initial vaccinations in younger children, however, continued declines dating back to August, the AAP said in its weekly vaccination trends report.
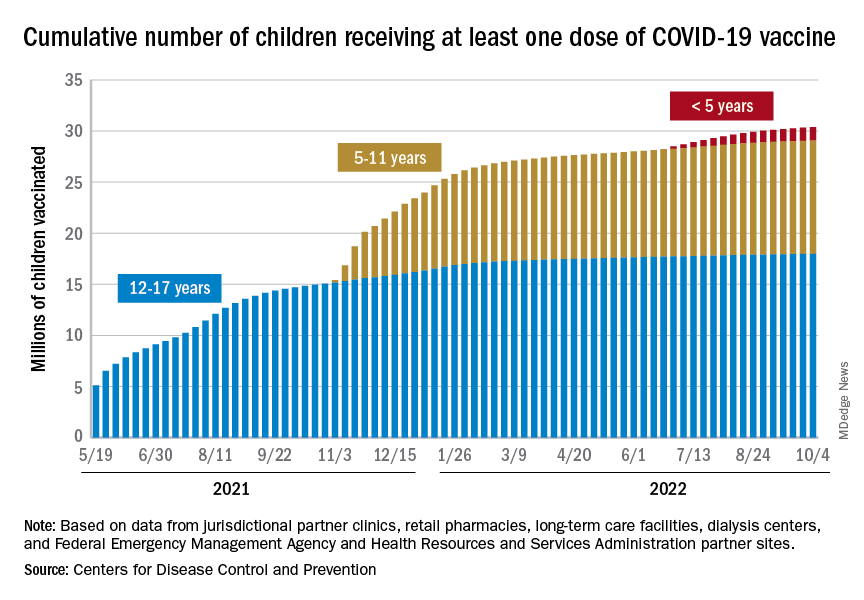
The District of Columbia and Massachusetts have the most highly vaccinated groups of 12- to 17-year-olds, as 100% and 95%, respectively, have received initial doses, while Wyoming (39%) and Idaho (42%) have the lowest. D.C. (73%) and Vermont (68%) have the highest proportions of vaccinated 5- to 11-year-olds, and Alabama (17%) and Mississippi (18%) have the lowest. For children under age 5 years, those in D.C. (33%) and Vermont (26%) are the most likely to have received an initial COVID vaccination, while Alabama, Louisiana, and Mississippi share national-low rates of 2%, the AAP said its report, which is based on CDC data.
When all states and territories are combined, 71% of children aged 12-17 have received at least one dose of vaccine, as have 38.6% of all children 5-11 years old and 6.7% of those under age 5. Almost 61% of the nation’s 16- to 17-year-olds have been fully vaccinated, along with 31.5% of those aged 5-11 and 2.4% of children younger than 5 years, the CDC said on its COVID Data Tracker.
About 42 million children – 58% of the population under the age of 18 years – have not received any vaccine yet, the AAP noted. Meanwhile, CDC data indicate that 36 children died of COVID in the last week, with pediatric deaths now totaling 1,781 over the course of the pandemic.