User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Early or delayed menopause and irregular periods tied to new-onset atrial fibrillation
Takeaway
- Early or delayed menopause and a history of irregular menstrual cycles were significantly associated with a greater risk of new-onset atrial fibrillation (AF) in women.
- Women with nulliparity and multiparity had a greater risk of new-onset AF compared with those with one to two live births.
Why this matters
- Findings highlight the significance of considering the reproductive history of women while developing tailored screening and prevention strategies for AF.
Study design
- A population-based cohort study of 235,191 women (age, 40-69 years) without AF and a history of hysterectomy and/or bilateral oophorectomy, identified from the UK Biobank (2006-2010).
- Funding: Gender and Prevention Grant from ZonMw and other.
Key results
- During a median follow-up of 11.6 years, 4,629 (2.0%) women were diagnosed with new-onset AF.
- A history of irregular menstrual cycle was associated with higher risk of new-onset AF (adjusted HR, 1.34; 95% confidence interval, 1.01-1.79; P = .04).
- Compared with women who experienced menarche at the age of 12 years, the risk of new-onset AF was significantly higher in those who experienced menarche:
- –Earlier between the ages of 7 and 11 years (aHR, 1.10; 95% CI, 1.00-1.21; P = .04) and
- –Later between the ages of 13 and 18 years (aHR, 1.08; 95% CI, 1.00-1.17; P = .05).
- The risk of new-onset AF was significantly higher in women who experienced menopause:
- –At the age of < 35 years (aHR, 2.25; 95% CI, 1.48-3.43; P < .001);
- –Between the ages of 35 and 44 years (aHR, 1.24; 95% CI, 1.10-1.39; P < .001); and
- –At the age of ≥ 60 years (aHR, 1.34; 95% CI, 1.10-1.78; P = .04).
- Women with no live births (aHR, 1.13; 95% CI, 1.04-1.24; P < .01), four to six live births (aHR, 1.12; 95% CI, 1.01-1.24; P = .04), and ≥ seven live births (aHR, 1.67; 95% CI, 1.03-2.70; P = .03) vs. those with one to two live births had a significantly higher risk of new-onset AF.
Limitations
- Observational design.
A version of this article first appeared on Medscape UK.
Reference
Lu Z, Aribas E, Geurts S, Roeters van Lennep JE, Ikram MA, Bos MM, de Groot NMS, Kavousi M. Association Between Sex-Specific Risk Factors and Risk of New-Onset Atrial Fibrillation Among Women. JAMA Netw Open. 2022;5(9):e2229716. doi: 10.1001/jamanetworkopen.2022.29716. PMID: 36048441.
Takeaway
- Early or delayed menopause and a history of irregular menstrual cycles were significantly associated with a greater risk of new-onset atrial fibrillation (AF) in women.
- Women with nulliparity and multiparity had a greater risk of new-onset AF compared with those with one to two live births.
Why this matters
- Findings highlight the significance of considering the reproductive history of women while developing tailored screening and prevention strategies for AF.
Study design
- A population-based cohort study of 235,191 women (age, 40-69 years) without AF and a history of hysterectomy and/or bilateral oophorectomy, identified from the UK Biobank (2006-2010).
- Funding: Gender and Prevention Grant from ZonMw and other.
Key results
- During a median follow-up of 11.6 years, 4,629 (2.0%) women were diagnosed with new-onset AF.
- A history of irregular menstrual cycle was associated with higher risk of new-onset AF (adjusted HR, 1.34; 95% confidence interval, 1.01-1.79; P = .04).
- Compared with women who experienced menarche at the age of 12 years, the risk of new-onset AF was significantly higher in those who experienced menarche:
- –Earlier between the ages of 7 and 11 years (aHR, 1.10; 95% CI, 1.00-1.21; P = .04) and
- –Later between the ages of 13 and 18 years (aHR, 1.08; 95% CI, 1.00-1.17; P = .05).
- The risk of new-onset AF was significantly higher in women who experienced menopause:
- –At the age of < 35 years (aHR, 2.25; 95% CI, 1.48-3.43; P < .001);
- –Between the ages of 35 and 44 years (aHR, 1.24; 95% CI, 1.10-1.39; P < .001); and
- –At the age of ≥ 60 years (aHR, 1.34; 95% CI, 1.10-1.78; P = .04).
- Women with no live births (aHR, 1.13; 95% CI, 1.04-1.24; P < .01), four to six live births (aHR, 1.12; 95% CI, 1.01-1.24; P = .04), and ≥ seven live births (aHR, 1.67; 95% CI, 1.03-2.70; P = .03) vs. those with one to two live births had a significantly higher risk of new-onset AF.
Limitations
- Observational design.
A version of this article first appeared on Medscape UK.
Reference
Lu Z, Aribas E, Geurts S, Roeters van Lennep JE, Ikram MA, Bos MM, de Groot NMS, Kavousi M. Association Between Sex-Specific Risk Factors and Risk of New-Onset Atrial Fibrillation Among Women. JAMA Netw Open. 2022;5(9):e2229716. doi: 10.1001/jamanetworkopen.2022.29716. PMID: 36048441.
Takeaway
- Early or delayed menopause and a history of irregular menstrual cycles were significantly associated with a greater risk of new-onset atrial fibrillation (AF) in women.
- Women with nulliparity and multiparity had a greater risk of new-onset AF compared with those with one to two live births.
Why this matters
- Findings highlight the significance of considering the reproductive history of women while developing tailored screening and prevention strategies for AF.
Study design
- A population-based cohort study of 235,191 women (age, 40-69 years) without AF and a history of hysterectomy and/or bilateral oophorectomy, identified from the UK Biobank (2006-2010).
- Funding: Gender and Prevention Grant from ZonMw and other.
Key results
- During a median follow-up of 11.6 years, 4,629 (2.0%) women were diagnosed with new-onset AF.
- A history of irregular menstrual cycle was associated with higher risk of new-onset AF (adjusted HR, 1.34; 95% confidence interval, 1.01-1.79; P = .04).
- Compared with women who experienced menarche at the age of 12 years, the risk of new-onset AF was significantly higher in those who experienced menarche:
- –Earlier between the ages of 7 and 11 years (aHR, 1.10; 95% CI, 1.00-1.21; P = .04) and
- –Later between the ages of 13 and 18 years (aHR, 1.08; 95% CI, 1.00-1.17; P = .05).
- The risk of new-onset AF was significantly higher in women who experienced menopause:
- –At the age of < 35 years (aHR, 2.25; 95% CI, 1.48-3.43; P < .001);
- –Between the ages of 35 and 44 years (aHR, 1.24; 95% CI, 1.10-1.39; P < .001); and
- –At the age of ≥ 60 years (aHR, 1.34; 95% CI, 1.10-1.78; P = .04).
- Women with no live births (aHR, 1.13; 95% CI, 1.04-1.24; P < .01), four to six live births (aHR, 1.12; 95% CI, 1.01-1.24; P = .04), and ≥ seven live births (aHR, 1.67; 95% CI, 1.03-2.70; P = .03) vs. those with one to two live births had a significantly higher risk of new-onset AF.
Limitations
- Observational design.
A version of this article first appeared on Medscape UK.
Reference
Lu Z, Aribas E, Geurts S, Roeters van Lennep JE, Ikram MA, Bos MM, de Groot NMS, Kavousi M. Association Between Sex-Specific Risk Factors and Risk of New-Onset Atrial Fibrillation Among Women. JAMA Netw Open. 2022;5(9):e2229716. doi: 10.1001/jamanetworkopen.2022.29716. PMID: 36048441.
FROM JAMA NETWORK OPEN
Nonsurgical treatments for patients with urinary incontinence
CASE Patient has urine leakage that worsens with exercise
At her annual preventative health visit, a 39-year-old woman reports that she has leakage of urine. She states that she drinks “a gallon of water daily” to help her lose the 20 lb she gained during the COVID-19 pandemic. She wants to resume Zumba fitness classes, but exercise makes her urine leakage worse. She started wearing protective pads because she finds herself often leaking urine on the way to the bathroom.
What nonsurgical treatment options are available for this patient?
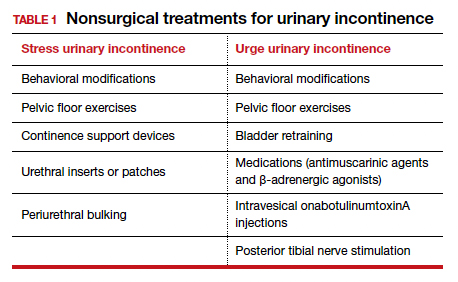
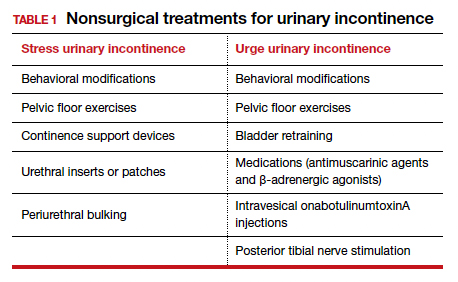
Nearly half of all women experience urinary incontinence (UI), the involuntary loss of urine, and the condition increases with age.1 This common condition negatively impacts physical and psychological health and has been associated with social isolation, sexual dysfunction, and reduced independence.2,3 Symptoms of UI are underreported, and therefore universal screening is recommended for women of all ages.4 The diversity of available treatments (TABLE 1) provides patients and clinicians an opportunity to develop a plan that aligns with their symptom severity, goals, preferences, and resources.
Types of UI
The most common types of UI are stress urinary incontinence (SUI) and urgency urinary incontinence (UUI). Mixed urinary incontinence (MUI) occurs when symptoms of both SUI and UUI are present. Although the mechanisms that lead to urine leakage vary by the type of incontinence, many primary interventions improve both types of leakage, so a clinical diagnosis is sufficient to initiate treatment.
Stress urinary incontinence results from an impaired or weakened sphincter, which leads to involuntary, yet predictable, urine loss during increased abdominal pressure, such as coughing, laughing, sneezing, lifting, or physical activity.5 In UUI, involuntary loss of urine often accompanies the sudden urge to void. UUI is associated with overactive bladder (OAB), defined as urinary urgency, with or without urinary incontinence, usually accompanied by urinary frequency and/or nocturia (urination that interrupts sleep).6
In OAB, the detrusor muscle contracts randomly, leading to a sudden urge to void. When bladder pressure exceeds urethral sphincter closure pressure, urine leakage occurs. Women describe the urgency episodes as unpredictable, the urine leakage as prolonged with large volumes, and often occurring as they seek the toilet. Risk factors include age, obesity, parity, history of vaginal delivery, family history, ethnicity/race, medical comorbidities, menopausal status, and tobacco use.5
Making a diagnosis
A basic office evaluation is the most key step for diagnostic accuracy that leads to treatment success. This includes a detailed history, assessment of symptom severity, physical exam, pelvic exam, urinalysis, postvoid residual (to rule out urinary retention), and a cough stress test (to demonstrate SUI). The goal is to assess symptom severity, determine the type of UI, and identify contributing and potentially reversible factors, such as a urinary tract infection, medications, pelvic organ prolapse, incomplete bladder emptying, or impaired neurologic status. In the absence of the latter, advanced diagnostic tests, such as urodynamics, contribute little toward discerning the type of incontinence or changing first-line treatment plans.7
During the COVID-19 pandemic, abbreviated, virtual assessments for urinary symptoms were associated with high degrees of satisfaction (91% for fulfillment of personal needs, 94% overall satisfaction).8 This highlights the value of validated symptom questionnaires that help establish a working diagnosis and treatment plan in the absence of a physical exam. Questionnaire-based diagnoses have acceptable accuracy for classifying UUI and SUI among women with uncomplicated medical and surgical histories and for initiating low-risk therapies for defined intervals.
The 3 incontinence questions (3IQ) screen is an example of a useful, quick diagnostic tool designed for the primary care setting (FIGURE 1).9 It has been used in pharmaceutical treatment trials for UUI, with low frequency of misdiagnosis (1%–4%), resulting in no harm by the drug treatment prescribed or by the delay in appropriate care.10 Due to the limitations of an abbreviated remote evaluation, however, clinicians should assess patient response to primary interventions in a timely window. Patients who fail to experience satisfactory symptom reduction within 6 to 12 weeks should complete their evaluation in person or through a referral to a urogynecology program.

Continue to: Primary therapies for UI...
Primary therapies for UI
Primary therapies for UUI and SUI target strength training of the pelvic floor muscles, moderation of fluid intake, and adjustment in voiding behaviors and medications. Any functional barriers to continence also should be identified and addressed. Simple interventions, including a daily bowel regimen to address constipation, a bedside commode, and scheduled voiding, may reduce incontinence episodes without incurring significant cost or risk. For women suspected of having MUI, the treatment plan should prioritize their most bothersome symptoms.
Lifestyle and behavioral modifications
Everyday habits, medical comorbidities, and medications may exacerbate the severity of both SUI and UUI. Behavioral therapy alone or in combination with other interventions effectively reduces both SUI and UUI symptoms and has been shown to improve the efficacy of continence surgery.11 Information gained from a 3-day bladder diary (FIGURE 2)12 can guide clinicians on personalized patient recommendations, such as reducing excessive consumption of fluids and bladder irritants, limiting late evening drinking in the setting of bothersome nocturia, and scheduling voids (every 2–3 hours) to preempt incontinence episodes.

Weight loss
Obesity is a strong, independent, modifiable risk factor for both SUI and UUI. Each 5 kg/m2 increase in body mass index (BMI) has been associated with a 20% to 70% increased risk of UI, while weight loss of 5% or greater in overweight or obese women can lead to at least a 50% decrease in UI frequency.13
Reducing fluid intake and bladder irritants
Overactive bladder symptoms often respond to moderation of excessive fluid intake and reduction of bladder irritants (caffeine, carbonated beverages, diet beverages, and alcohol). While there is no established definition of excess caffeine intake, one study categorized high caffeine intake as greater than 400 mg/day (approximately four 8-oz cups of coffee).14
Information provided in a bladder diary can guide individualized recommendations for reducing fluid intake, particularly when 24-hour urine production exceeds the normative range (> 50–60 oz or 1.5-1.8 L/day).15 Hydration needs vary by activity, environment, and food; some general guidelines suggest 48 to 64 oz/day.5,16
Continue to: Pelvic floor muscle training...
Pelvic floor muscle training
An effective treatment for both UUI and SUI symptoms, pelvic floor muscle training (PFMT) leads to high degrees of patient satisfaction and improvement in quality of life.17 The presumed mechanisms of action of PFMT include improved urethral closure pressure and inhibition of detrusor muscle contractions.
Common exercise protocols recommend 3 sets of 10 contractions, held for 6 to 10 seconds per day, in varying positions of sitting, standing, and lying. While many women may be familiar with Kegel exercises, poor technique with straining and recruitment of gluteal and abdominal muscles can undermine the effect of PFMT. Clinicians can confirm successful pelvic muscle contractions by placing a finger in the vagina to appreciate contraction around and elevation of the finger toward the pubic symphysis in the absence of pushing.
Referral to supervised physical therapy and use of such teaching aid tools as booklets, mobile applications, and biofeedback can improve exercise adherence and outcomes.18,19 Systematic reviews report initial cure or improvement of incontinence symptoms as high as 74%, although little information is available about the long-term duration of effect.17
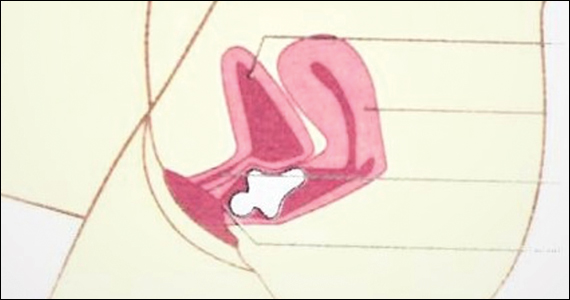
Vaginal pessaries
Vaginal continence support pessaries and devices work by stabilizing urethral mobility and compression of the bladder neck. Continence devices are particularly effective for situational SUI (such as during exercise).
The reusable medical grade silicone pessaries are available in numerous shapes and sizes and are fitted by a health care clinician (FIGURE 3). Uresta is a self-fitted intravaginal device that women can purchase online with a prescription. The Poise Impressa bladder support is a disposable intravaginal device marketed for incontinence and available over-the-counter, without a prescription (FIGURE 4). Anecdotally, many women find that menstrual tampons provide a similar effect, but outcome data are lacking.
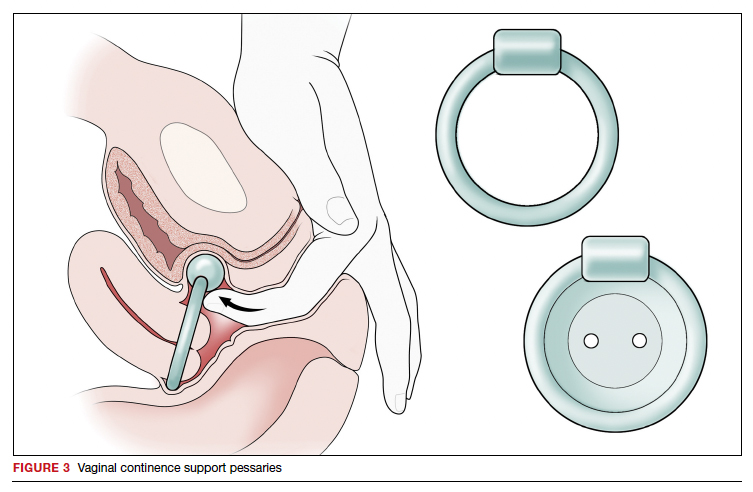
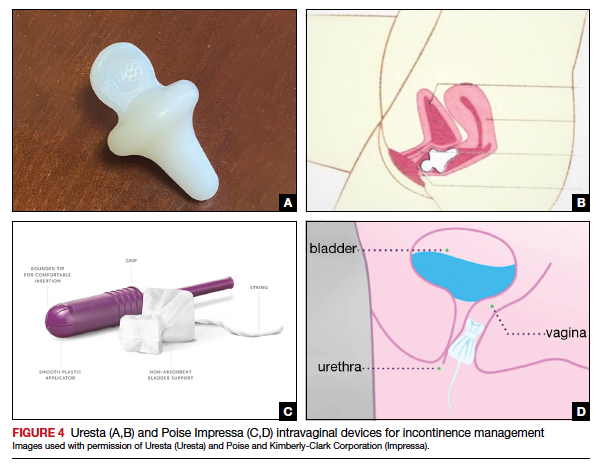
In a comparative effectiveness trial of a continence pessary and behavior therapy, behavioral therapy was more likely to result in no bothersome incontinence symptoms (49% vs 33%, P = .006) and greater treatment satisfaction at 3 months.20 However, these short-term group differences did not persist at 12 months, presumably due to waning adherence.
UUI-specific nonsurgical treatments
Drug therapy
All medications approved by the US Food and Drug Administration (FDA) for UI are for the indications of OAB or UUI. These second-line treatments are most effective as adjuncts to behavioral modifications and PFMT.
A multicenter randomized trial that evaluated the efficacy of drug therapy alone compared with drug therapy in combination with behavioral modification, PFMT, urge suppression strategies, timed voiding, and fluid management for UUI found that combined therapy was more successful in achieving greater than 70% reduction in incontinence episodes (58% for drug therapy vs 69% for combined therapy).21
Of the 8 medications currently marketed in the United States for OAB or UUI, 6 are anticholinergic agents that block muscarinic receptors in the smooth muscle of the bladder, leading to inhibition of detrusor contractions, and 2 are β-adrenergic receptor agonists that promote bladder storage capacity by relaxing the detrusor muscle (TABLE 2). Similar efficacies lead most clinicians to initiate drug therapy based on formulary coverage and tolerance for adverse effects. Patients can expect a 53% to 80% reduction in UUI episodes and a 12% to 32% reduction in urinary frequency.22
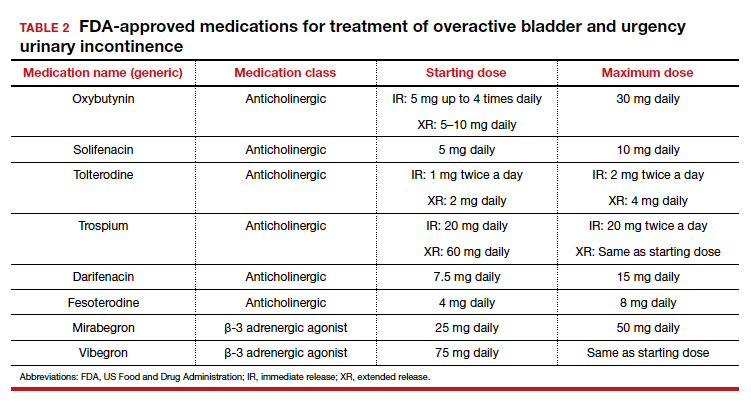
Extended-release formulations are associated with reduced anticholinergic side effects (dry mouth, constipation, somnolence, dry eyes), leading to improved adherence. Notably, the anticholinergic medications are contraindicated in patients with untreated narrow-angle glaucoma, gastric retention, and supraventricular tachycardia. Mirabegron should be used with caution in patients with poorly controlled hypertension. 5 Due to concerns regarding the association between cumulative anticholinergic burden and the development of dementia, clinicians may consider avoiding the anticholinergic medications in older and at-risk patients.23
Continue to: UUI office-based procedure treatments...
UUI office-based procedure treatments
If behavioral therapies and medications are ineffective, contraindicated, or not the patient’s preference, additional FDA-approved therapies for UUI are available, typically through referral to a urogynecologist, urologist, or continence center.
Posterior tibial nerve stimulation (PTNS) is a nondrug treatment that delivers electrical stimulation using an acupuncture needle for 12 weekly 30-minute sessions followed by monthly maintenance for responders. The time commitment for this treatment plan can be a barrier for some patients. However, patients who adhere to the recommended protocol can expect a 60% improvement in symptoms, with minimal adverse events. Treatment efficacy is comparable to that of anticholinergic medication.24
OnabotulinumtoxinA injections into the bladder muscle are performed cystoscopically under local anesthetic. The toxin blocks the presynaptic release of acetylcholine at the neuromuscular junction, resulting in temporary muscle paralysis. This treatment is associated with high satisfaction. Efficacy varies by study population and outcome measure.
In one US comparative effectiveness trial, 67% of study participants with UUI symptoms refractory to oral medication reported a greater than 50% reduction in OAB symptoms at 6 months, 20% reported complete resolution of UUI, and 72% requested a second injection within 24 months.25 The interval between the first and second injection was nearly 1 year (350 days).Risks include urinary tract infection (12% within 1 month of the procedure and 35% through 6 months); urinary retention requiring catheterization has decreased to 6% with recognition that most moderate retention is tolerated by patients.
Some insurers limit onabotulinumtoxinA treatment coverage to patients who have failed to achieve symptom control with first- and second-line treatments.
SUI-specific nonsurgical treatments
Cystoscopic injection of urethral bulking agents into the urethral submucosa is designed to improve urethral coaptation. It is a minor procedure that can be performed in an ambulatory setting under local anesthetic with or without sedation.
Various bulking agents have been approved for use in the United States, some of which have been withdrawn due to complications of migration, erosion, and pseudoabscess formation. Cure or improvement after bulking agent injection was found to be superior to a home pelvic floor exercise program but inferior to a midurethral sling procedure for cure (9% vs 89%).26
The durability of currently available urethral bulking agents beyond 1 year is unknown. Complications are typically minor and transient and include pain at the injection site, urinary retention, de novo urgency, and implant leakage. The advantages include no postprocedure activity restrictions.
CASE Symptom presentation guides treatment plan
Our patient described symptoms of stress-predominant MUI. She was counseled to moderate her fluid intake to 2 L per day and to strategically time voids (before exercise, and at least every 4 hours). The patient was fitted with an incontinence pessary, and she elected to pursue a course of supervised physical therapy for pelvic floor muscle strengthening. Her follow-up visit is scheduled in 3 months to determine if other interventions are warranted. ●
1. Lee UJ, Feinstein L, Ward JB, et al. Prevalence of urinary incontinence among a nationally representative sample of women, 2005–2016: findings from the Urologic Diseases in America Project. J Urol. 2021;205:1718-1724. doi:10.1097 /JU.0000000000001634
2. Sims J, Browning C, Lundgren-Lindquist B, et al. Urinary incontinence in a community sample of older adults: prevalence and impact on quality of life. Disabil Rehabil. 2011;33:1389-1398. doi:10.3109/09638288.2010.532284
3. Sarikaya S, Yildiz FG, Senocak C, et al. Urinary incontinence as a cause of depression and sexual dysfunction: questionnaire-based study. Rev Int Androl. 2020:18:50-54. doi:10.1016 /j.androl.2018.08.003
4. O’Reilly N, Nelson HD, Conry JM, et al; Women’s Preventive Services Initiative. Screening for urinary incontinence in women: a recommendation from the Women’s Preventive Services Initiative. Ann Intern Med. 2018;169(5):320-328. doi:10.7326/M18-0595
5. Barber MD, Walters MD, Karram MM, et al. Walters & Karram Urogynecology and Reconstructive Pelvic Surgery. 5th ed. Elsevier Saunders; 2021.
6. Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21: 5-26. doi:10.1007/s00192-009-0976-9
7. ACOG practice bulletin no. 155. Urinary incontinence in women. Obstet Gynecol. 2015;126:e66-e81. doi:10.1097 /AOG.0000000000001148
8. Sansone S, Lu J, Drangsholt S, et al. No pelvic exam, no problem: patient satisfaction following the integration of comprehensive urogynecology telemedicine. Int Urogynecol J. 2022;1:3. doi:10.1007/s00192-022-05104-w
9. Brown JS, Bradley CS, Subak LL, et al; Diagnostic Aspects of Incontinence Study (DAISy) Research Group. The sensitivity and specificity of a simple test to distinguish between urge and stress urinary incontinence. Ann Intern Med. 2006;144:715723. doi:10.7326/0003-4819-144-10-200605160-00005
10. Hess R, Huang AJ, Richter HE, et al. Long-term efficacy and safety of questionnaire-based initiation of urgency urinary incontinence treatment. Am J Obstet Gynecol. 2013;209:244. e1-9. doi:10.1016/j.ajog.2013.05.008
11. Sung VW, Borello-France D, Newman DK, et al; NICHD Pelvic Floor Disorders Network. Effect of behavioral and pelvic floor muscle therapy combined with surgery vs surgery alone on incontinence symptoms among women with mixed urinary incontinence. JAMA. 2019;322:1066-1076. doi:10.1001 /jama.2019.12467
12. American Urogynecologic Society. Voices for PFD: intake and voiding diary. Accessed August 11, 2022. https://www .voicesforpfd.org/assets/2/6/Voiding_Diary.pdf
13. Subak LL, Richter HE, Hunskaar S. Obesity and urinary incontinence: epidemiology and clinical research update. J Urol. 2009;182(6 suppl):S2-7. doi:10.1016/j.juro.2009.08.071
14. Arya LA, Myers DL, Jackson ND. Dietary caffeine intake and the risk for detrusor instability: a case-control study. Obstet Gynecol. 2000;96:85-89. doi:10.1016/s0029-7844(00)00808-5
15. Wyman JF, Zhou J, LaCoursiere DY, et al. Normative noninvasive bladder function measurements in healthy women: a systematic review and meta-analysis. Neurourol Urodyn. 2020;39:507-522. doi:10.1002/nau.24265
16. Hashim H, Al Mousa R. Management of fluid intake in patients with overactive bladder. Curr Urol Rep. 2009;10: 428-433. doi:10.1007/s11934-009-0068-x
17. Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2018;10:CD005654. doi:10.1002/14651858.CD005654.pub4
18. Araujo CC, de A Marques A, Juliato CRT. The adherence of home pelvic floor muscles training using a mobile device application for women with urinary incontinence: a randomized controlled trial. Female Pelvic Med Reconstr Surg. 2020;26:697-703. doi:10.1097/SPV.0000000000000670
19. Sjöström M, Umefjord G, Stenlund H, et al. Internet-based treatment of stress urinary incontinence: a randomized controlled study with focus on pelvic floor muscle training. BJU Int. 2013;112:362-372. doi:10.1111/j.1464 -410X.2012.11713.x
20. Richter HE, Burgio KL, Brubaker L, et al; Pelvic Floor Disorders Network. Continence pessary compared with behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Obstet Gynecol. 2010;115:609617. doi:10.1097/AOG.0b013e3181d055d4
21. Burgio KL, Kraus SR, Menefee S, et al. Behavioral therapy to enable women with urge incontinence to discontinue drug treatment: a randomized trial. Ann Intern Med. 2008;149(3): 161-169. doi:10.7326/0003-4819-149-3-200808050 -00005
22. Lukacz ES, Santiago-Lastra Y, Albo ME, et al. Urinary incontinence in women: a review. JAMA. 2017;318:1592-1604. doi:10.1001/jama.2017.12137
23. Welk B, Richardson K, Panicker JN. The cognitive effect of anticholinergics for patients with overactive bladder. Nat Rev Urol. 2021;18:686-700. doi:10.1038/s41585-021-00504-x
24. Burton C, Sajja A, Latthe PM. Effectiveness of percutaneous posterior tibial nerve stimulation for overactive bladder: a systematic review and meta-analysis. Neurourol Urodyn. 2012;31:1206-1216. doi:10.1002/nau.22251
25. Amundsen CL, Richter HE, Menefee SA, et al. OnabotulinumtoxinA vs sacral neuromodulation on refractory urgency urinary incontinence in women: A randomized clinical trial. JAMA. 2016;316:1366-1374. doi:10.1001/jama.2016.14617
26. Kirchin V, Page T, Keegan PE, et al. Urethral injection therapy for urinary incontinence in women. Cochrane Database Syst Rev. 2017;7:CD003881. doi:10.1002/14651858.CD003881.pub4
CASE Patient has urine leakage that worsens with exercise
At her annual preventative health visit, a 39-year-old woman reports that she has leakage of urine. She states that she drinks “a gallon of water daily” to help her lose the 20 lb she gained during the COVID-19 pandemic. She wants to resume Zumba fitness classes, but exercise makes her urine leakage worse. She started wearing protective pads because she finds herself often leaking urine on the way to the bathroom.
What nonsurgical treatment options are available for this patient?
Nearly half of all women experience urinary incontinence (UI), the involuntary loss of urine, and the condition increases with age.1 This common condition negatively impacts physical and psychological health and has been associated with social isolation, sexual dysfunction, and reduced independence.2,3 Symptoms of UI are underreported, and therefore universal screening is recommended for women of all ages.4 The diversity of available treatments (TABLE 1) provides patients and clinicians an opportunity to develop a plan that aligns with their symptom severity, goals, preferences, and resources.
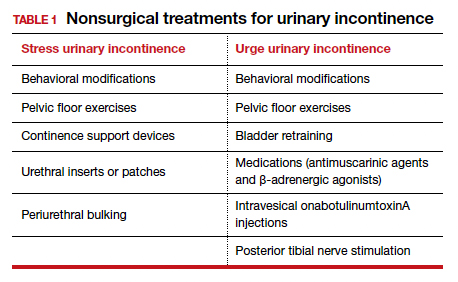
Types of UI
The most common types of UI are stress urinary incontinence (SUI) and urgency urinary incontinence (UUI). Mixed urinary incontinence (MUI) occurs when symptoms of both SUI and UUI are present. Although the mechanisms that lead to urine leakage vary by the type of incontinence, many primary interventions improve both types of leakage, so a clinical diagnosis is sufficient to initiate treatment.
Stress urinary incontinence results from an impaired or weakened sphincter, which leads to involuntary, yet predictable, urine loss during increased abdominal pressure, such as coughing, laughing, sneezing, lifting, or physical activity.5 In UUI, involuntary loss of urine often accompanies the sudden urge to void. UUI is associated with overactive bladder (OAB), defined as urinary urgency, with or without urinary incontinence, usually accompanied by urinary frequency and/or nocturia (urination that interrupts sleep).6
In OAB, the detrusor muscle contracts randomly, leading to a sudden urge to void. When bladder pressure exceeds urethral sphincter closure pressure, urine leakage occurs. Women describe the urgency episodes as unpredictable, the urine leakage as prolonged with large volumes, and often occurring as they seek the toilet. Risk factors include age, obesity, parity, history of vaginal delivery, family history, ethnicity/race, medical comorbidities, menopausal status, and tobacco use.5
Making a diagnosis
A basic office evaluation is the most key step for diagnostic accuracy that leads to treatment success. This includes a detailed history, assessment of symptom severity, physical exam, pelvic exam, urinalysis, postvoid residual (to rule out urinary retention), and a cough stress test (to demonstrate SUI). The goal is to assess symptom severity, determine the type of UI, and identify contributing and potentially reversible factors, such as a urinary tract infection, medications, pelvic organ prolapse, incomplete bladder emptying, or impaired neurologic status. In the absence of the latter, advanced diagnostic tests, such as urodynamics, contribute little toward discerning the type of incontinence or changing first-line treatment plans.7
During the COVID-19 pandemic, abbreviated, virtual assessments for urinary symptoms were associated with high degrees of satisfaction (91% for fulfillment of personal needs, 94% overall satisfaction).8 This highlights the value of validated symptom questionnaires that help establish a working diagnosis and treatment plan in the absence of a physical exam. Questionnaire-based diagnoses have acceptable accuracy for classifying UUI and SUI among women with uncomplicated medical and surgical histories and for initiating low-risk therapies for defined intervals.
The 3 incontinence questions (3IQ) screen is an example of a useful, quick diagnostic tool designed for the primary care setting (FIGURE 1).9 It has been used in pharmaceutical treatment trials for UUI, with low frequency of misdiagnosis (1%–4%), resulting in no harm by the drug treatment prescribed or by the delay in appropriate care.10 Due to the limitations of an abbreviated remote evaluation, however, clinicians should assess patient response to primary interventions in a timely window. Patients who fail to experience satisfactory symptom reduction within 6 to 12 weeks should complete their evaluation in person or through a referral to a urogynecology program.

Continue to: Primary therapies for UI...
Primary therapies for UI
Primary therapies for UUI and SUI target strength training of the pelvic floor muscles, moderation of fluid intake, and adjustment in voiding behaviors and medications. Any functional barriers to continence also should be identified and addressed. Simple interventions, including a daily bowel regimen to address constipation, a bedside commode, and scheduled voiding, may reduce incontinence episodes without incurring significant cost or risk. For women suspected of having MUI, the treatment plan should prioritize their most bothersome symptoms.
Lifestyle and behavioral modifications
Everyday habits, medical comorbidities, and medications may exacerbate the severity of both SUI and UUI. Behavioral therapy alone or in combination with other interventions effectively reduces both SUI and UUI symptoms and has been shown to improve the efficacy of continence surgery.11 Information gained from a 3-day bladder diary (FIGURE 2)12 can guide clinicians on personalized patient recommendations, such as reducing excessive consumption of fluids and bladder irritants, limiting late evening drinking in the setting of bothersome nocturia, and scheduling voids (every 2–3 hours) to preempt incontinence episodes.

Weight loss
Obesity is a strong, independent, modifiable risk factor for both SUI and UUI. Each 5 kg/m2 increase in body mass index (BMI) has been associated with a 20% to 70% increased risk of UI, while weight loss of 5% or greater in overweight or obese women can lead to at least a 50% decrease in UI frequency.13
Reducing fluid intake and bladder irritants
Overactive bladder symptoms often respond to moderation of excessive fluid intake and reduction of bladder irritants (caffeine, carbonated beverages, diet beverages, and alcohol). While there is no established definition of excess caffeine intake, one study categorized high caffeine intake as greater than 400 mg/day (approximately four 8-oz cups of coffee).14
Information provided in a bladder diary can guide individualized recommendations for reducing fluid intake, particularly when 24-hour urine production exceeds the normative range (> 50–60 oz or 1.5-1.8 L/day).15 Hydration needs vary by activity, environment, and food; some general guidelines suggest 48 to 64 oz/day.5,16
Continue to: Pelvic floor muscle training...
Pelvic floor muscle training
An effective treatment for both UUI and SUI symptoms, pelvic floor muscle training (PFMT) leads to high degrees of patient satisfaction and improvement in quality of life.17 The presumed mechanisms of action of PFMT include improved urethral closure pressure and inhibition of detrusor muscle contractions.
Common exercise protocols recommend 3 sets of 10 contractions, held for 6 to 10 seconds per day, in varying positions of sitting, standing, and lying. While many women may be familiar with Kegel exercises, poor technique with straining and recruitment of gluteal and abdominal muscles can undermine the effect of PFMT. Clinicians can confirm successful pelvic muscle contractions by placing a finger in the vagina to appreciate contraction around and elevation of the finger toward the pubic symphysis in the absence of pushing.
Referral to supervised physical therapy and use of such teaching aid tools as booklets, mobile applications, and biofeedback can improve exercise adherence and outcomes.18,19 Systematic reviews report initial cure or improvement of incontinence symptoms as high as 74%, although little information is available about the long-term duration of effect.17
Vaginal pessaries
Vaginal continence support pessaries and devices work by stabilizing urethral mobility and compression of the bladder neck. Continence devices are particularly effective for situational SUI (such as during exercise).
The reusable medical grade silicone pessaries are available in numerous shapes and sizes and are fitted by a health care clinician (FIGURE 3). Uresta is a self-fitted intravaginal device that women can purchase online with a prescription. The Poise Impressa bladder support is a disposable intravaginal device marketed for incontinence and available over-the-counter, without a prescription (FIGURE 4). Anecdotally, many women find that menstrual tampons provide a similar effect, but outcome data are lacking.
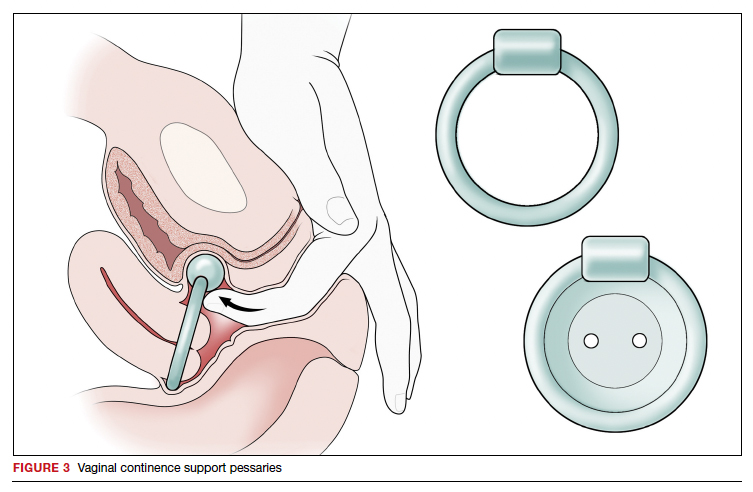
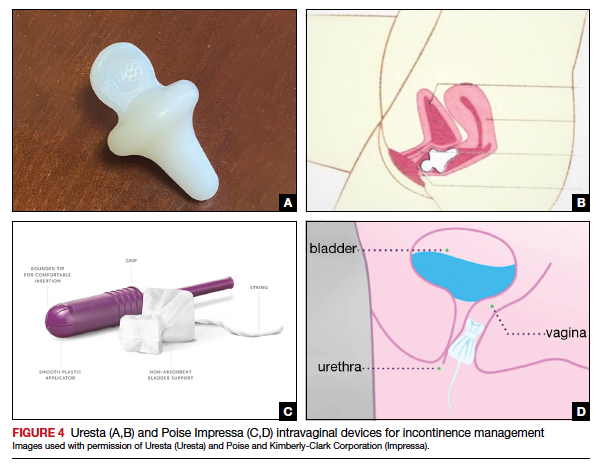
In a comparative effectiveness trial of a continence pessary and behavior therapy, behavioral therapy was more likely to result in no bothersome incontinence symptoms (49% vs 33%, P = .006) and greater treatment satisfaction at 3 months.20 However, these short-term group differences did not persist at 12 months, presumably due to waning adherence.
UUI-specific nonsurgical treatments
Drug therapy
All medications approved by the US Food and Drug Administration (FDA) for UI are for the indications of OAB or UUI. These second-line treatments are most effective as adjuncts to behavioral modifications and PFMT.
A multicenter randomized trial that evaluated the efficacy of drug therapy alone compared with drug therapy in combination with behavioral modification, PFMT, urge suppression strategies, timed voiding, and fluid management for UUI found that combined therapy was more successful in achieving greater than 70% reduction in incontinence episodes (58% for drug therapy vs 69% for combined therapy).21
Of the 8 medications currently marketed in the United States for OAB or UUI, 6 are anticholinergic agents that block muscarinic receptors in the smooth muscle of the bladder, leading to inhibition of detrusor contractions, and 2 are β-adrenergic receptor agonists that promote bladder storage capacity by relaxing the detrusor muscle (TABLE 2). Similar efficacies lead most clinicians to initiate drug therapy based on formulary coverage and tolerance for adverse effects. Patients can expect a 53% to 80% reduction in UUI episodes and a 12% to 32% reduction in urinary frequency.22
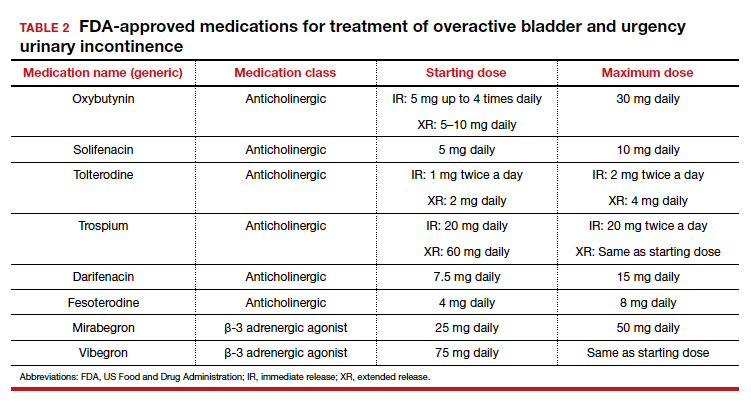
Extended-release formulations are associated with reduced anticholinergic side effects (dry mouth, constipation, somnolence, dry eyes), leading to improved adherence. Notably, the anticholinergic medications are contraindicated in patients with untreated narrow-angle glaucoma, gastric retention, and supraventricular tachycardia. Mirabegron should be used with caution in patients with poorly controlled hypertension. 5 Due to concerns regarding the association between cumulative anticholinergic burden and the development of dementia, clinicians may consider avoiding the anticholinergic medications in older and at-risk patients.23
Continue to: UUI office-based procedure treatments...
UUI office-based procedure treatments
If behavioral therapies and medications are ineffective, contraindicated, or not the patient’s preference, additional FDA-approved therapies for UUI are available, typically through referral to a urogynecologist, urologist, or continence center.
Posterior tibial nerve stimulation (PTNS) is a nondrug treatment that delivers electrical stimulation using an acupuncture needle for 12 weekly 30-minute sessions followed by monthly maintenance for responders. The time commitment for this treatment plan can be a barrier for some patients. However, patients who adhere to the recommended protocol can expect a 60% improvement in symptoms, with minimal adverse events. Treatment efficacy is comparable to that of anticholinergic medication.24
OnabotulinumtoxinA injections into the bladder muscle are performed cystoscopically under local anesthetic. The toxin blocks the presynaptic release of acetylcholine at the neuromuscular junction, resulting in temporary muscle paralysis. This treatment is associated with high satisfaction. Efficacy varies by study population and outcome measure.
In one US comparative effectiveness trial, 67% of study participants with UUI symptoms refractory to oral medication reported a greater than 50% reduction in OAB symptoms at 6 months, 20% reported complete resolution of UUI, and 72% requested a second injection within 24 months.25 The interval between the first and second injection was nearly 1 year (350 days).Risks include urinary tract infection (12% within 1 month of the procedure and 35% through 6 months); urinary retention requiring catheterization has decreased to 6% with recognition that most moderate retention is tolerated by patients.
Some insurers limit onabotulinumtoxinA treatment coverage to patients who have failed to achieve symptom control with first- and second-line treatments.
SUI-specific nonsurgical treatments
Cystoscopic injection of urethral bulking agents into the urethral submucosa is designed to improve urethral coaptation. It is a minor procedure that can be performed in an ambulatory setting under local anesthetic with or without sedation.
Various bulking agents have been approved for use in the United States, some of which have been withdrawn due to complications of migration, erosion, and pseudoabscess formation. Cure or improvement after bulking agent injection was found to be superior to a home pelvic floor exercise program but inferior to a midurethral sling procedure for cure (9% vs 89%).26
The durability of currently available urethral bulking agents beyond 1 year is unknown. Complications are typically minor and transient and include pain at the injection site, urinary retention, de novo urgency, and implant leakage. The advantages include no postprocedure activity restrictions.
CASE Symptom presentation guides treatment plan
Our patient described symptoms of stress-predominant MUI. She was counseled to moderate her fluid intake to 2 L per day and to strategically time voids (before exercise, and at least every 4 hours). The patient was fitted with an incontinence pessary, and she elected to pursue a course of supervised physical therapy for pelvic floor muscle strengthening. Her follow-up visit is scheduled in 3 months to determine if other interventions are warranted. ●
CASE Patient has urine leakage that worsens with exercise
At her annual preventative health visit, a 39-year-old woman reports that she has leakage of urine. She states that she drinks “a gallon of water daily” to help her lose the 20 lb she gained during the COVID-19 pandemic. She wants to resume Zumba fitness classes, but exercise makes her urine leakage worse. She started wearing protective pads because she finds herself often leaking urine on the way to the bathroom.
What nonsurgical treatment options are available for this patient?
Nearly half of all women experience urinary incontinence (UI), the involuntary loss of urine, and the condition increases with age.1 This common condition negatively impacts physical and psychological health and has been associated with social isolation, sexual dysfunction, and reduced independence.2,3 Symptoms of UI are underreported, and therefore universal screening is recommended for women of all ages.4 The diversity of available treatments (TABLE 1) provides patients and clinicians an opportunity to develop a plan that aligns with their symptom severity, goals, preferences, and resources.
Types of UI
The most common types of UI are stress urinary incontinence (SUI) and urgency urinary incontinence (UUI). Mixed urinary incontinence (MUI) occurs when symptoms of both SUI and UUI are present. Although the mechanisms that lead to urine leakage vary by the type of incontinence, many primary interventions improve both types of leakage, so a clinical diagnosis is sufficient to initiate treatment.
Stress urinary incontinence results from an impaired or weakened sphincter, which leads to involuntary, yet predictable, urine loss during increased abdominal pressure, such as coughing, laughing, sneezing, lifting, or physical activity.5 In UUI, involuntary loss of urine often accompanies the sudden urge to void. UUI is associated with overactive bladder (OAB), defined as urinary urgency, with or without urinary incontinence, usually accompanied by urinary frequency and/or nocturia (urination that interrupts sleep).6
In OAB, the detrusor muscle contracts randomly, leading to a sudden urge to void. When bladder pressure exceeds urethral sphincter closure pressure, urine leakage occurs. Women describe the urgency episodes as unpredictable, the urine leakage as prolonged with large volumes, and often occurring as they seek the toilet. Risk factors include age, obesity, parity, history of vaginal delivery, family history, ethnicity/race, medical comorbidities, menopausal status, and tobacco use.5
Making a diagnosis
A basic office evaluation is the most key step for diagnostic accuracy that leads to treatment success. This includes a detailed history, assessment of symptom severity, physical exam, pelvic exam, urinalysis, postvoid residual (to rule out urinary retention), and a cough stress test (to demonstrate SUI). The goal is to assess symptom severity, determine the type of UI, and identify contributing and potentially reversible factors, such as a urinary tract infection, medications, pelvic organ prolapse, incomplete bladder emptying, or impaired neurologic status. In the absence of the latter, advanced diagnostic tests, such as urodynamics, contribute little toward discerning the type of incontinence or changing first-line treatment plans.7
During the COVID-19 pandemic, abbreviated, virtual assessments for urinary symptoms were associated with high degrees of satisfaction (91% for fulfillment of personal needs, 94% overall satisfaction).8 This highlights the value of validated symptom questionnaires that help establish a working diagnosis and treatment plan in the absence of a physical exam. Questionnaire-based diagnoses have acceptable accuracy for classifying UUI and SUI among women with uncomplicated medical and surgical histories and for initiating low-risk therapies for defined intervals.
The 3 incontinence questions (3IQ) screen is an example of a useful, quick diagnostic tool designed for the primary care setting (FIGURE 1).9 It has been used in pharmaceutical treatment trials for UUI, with low frequency of misdiagnosis (1%–4%), resulting in no harm by the drug treatment prescribed or by the delay in appropriate care.10 Due to the limitations of an abbreviated remote evaluation, however, clinicians should assess patient response to primary interventions in a timely window. Patients who fail to experience satisfactory symptom reduction within 6 to 12 weeks should complete their evaluation in person or through a referral to a urogynecology program.

Continue to: Primary therapies for UI...
Primary therapies for UI
Primary therapies for UUI and SUI target strength training of the pelvic floor muscles, moderation of fluid intake, and adjustment in voiding behaviors and medications. Any functional barriers to continence also should be identified and addressed. Simple interventions, including a daily bowel regimen to address constipation, a bedside commode, and scheduled voiding, may reduce incontinence episodes without incurring significant cost or risk. For women suspected of having MUI, the treatment plan should prioritize their most bothersome symptoms.
Lifestyle and behavioral modifications
Everyday habits, medical comorbidities, and medications may exacerbate the severity of both SUI and UUI. Behavioral therapy alone or in combination with other interventions effectively reduces both SUI and UUI symptoms and has been shown to improve the efficacy of continence surgery.11 Information gained from a 3-day bladder diary (FIGURE 2)12 can guide clinicians on personalized patient recommendations, such as reducing excessive consumption of fluids and bladder irritants, limiting late evening drinking in the setting of bothersome nocturia, and scheduling voids (every 2–3 hours) to preempt incontinence episodes.

Weight loss
Obesity is a strong, independent, modifiable risk factor for both SUI and UUI. Each 5 kg/m2 increase in body mass index (BMI) has been associated with a 20% to 70% increased risk of UI, while weight loss of 5% or greater in overweight or obese women can lead to at least a 50% decrease in UI frequency.13
Reducing fluid intake and bladder irritants
Overactive bladder symptoms often respond to moderation of excessive fluid intake and reduction of bladder irritants (caffeine, carbonated beverages, diet beverages, and alcohol). While there is no established definition of excess caffeine intake, one study categorized high caffeine intake as greater than 400 mg/day (approximately four 8-oz cups of coffee).14
Information provided in a bladder diary can guide individualized recommendations for reducing fluid intake, particularly when 24-hour urine production exceeds the normative range (> 50–60 oz or 1.5-1.8 L/day).15 Hydration needs vary by activity, environment, and food; some general guidelines suggest 48 to 64 oz/day.5,16
Continue to: Pelvic floor muscle training...
Pelvic floor muscle training
An effective treatment for both UUI and SUI symptoms, pelvic floor muscle training (PFMT) leads to high degrees of patient satisfaction and improvement in quality of life.17 The presumed mechanisms of action of PFMT include improved urethral closure pressure and inhibition of detrusor muscle contractions.
Common exercise protocols recommend 3 sets of 10 contractions, held for 6 to 10 seconds per day, in varying positions of sitting, standing, and lying. While many women may be familiar with Kegel exercises, poor technique with straining and recruitment of gluteal and abdominal muscles can undermine the effect of PFMT. Clinicians can confirm successful pelvic muscle contractions by placing a finger in the vagina to appreciate contraction around and elevation of the finger toward the pubic symphysis in the absence of pushing.
Referral to supervised physical therapy and use of such teaching aid tools as booklets, mobile applications, and biofeedback can improve exercise adherence and outcomes.18,19 Systematic reviews report initial cure or improvement of incontinence symptoms as high as 74%, although little information is available about the long-term duration of effect.17
Vaginal pessaries
Vaginal continence support pessaries and devices work by stabilizing urethral mobility and compression of the bladder neck. Continence devices are particularly effective for situational SUI (such as during exercise).
The reusable medical grade silicone pessaries are available in numerous shapes and sizes and are fitted by a health care clinician (FIGURE 3). Uresta is a self-fitted intravaginal device that women can purchase online with a prescription. The Poise Impressa bladder support is a disposable intravaginal device marketed for incontinence and available over-the-counter, without a prescription (FIGURE 4). Anecdotally, many women find that menstrual tampons provide a similar effect, but outcome data are lacking.
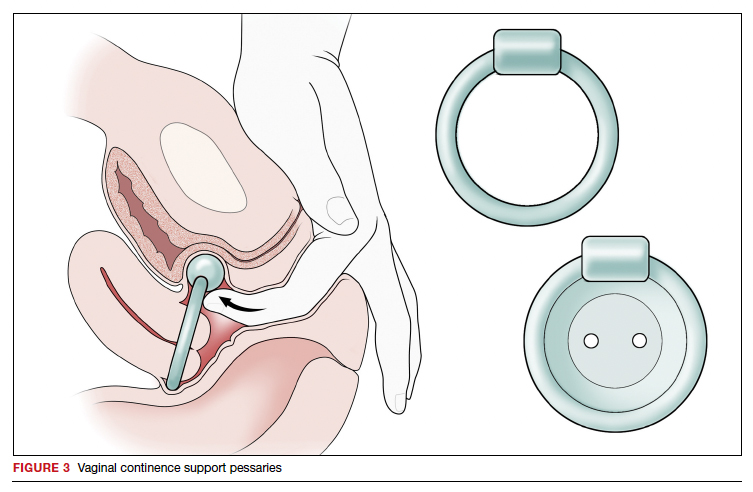
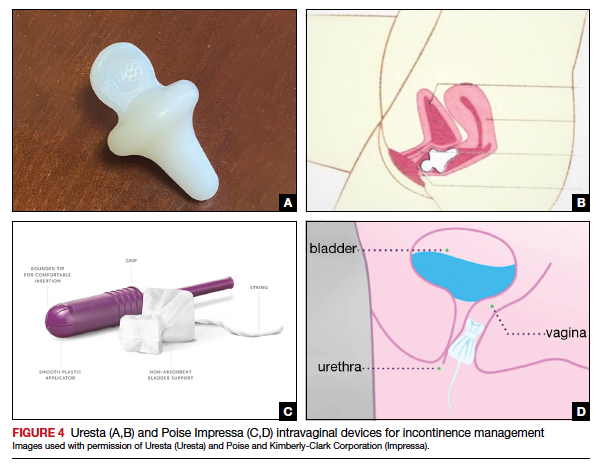
In a comparative effectiveness trial of a continence pessary and behavior therapy, behavioral therapy was more likely to result in no bothersome incontinence symptoms (49% vs 33%, P = .006) and greater treatment satisfaction at 3 months.20 However, these short-term group differences did not persist at 12 months, presumably due to waning adherence.
UUI-specific nonsurgical treatments
Drug therapy
All medications approved by the US Food and Drug Administration (FDA) for UI are for the indications of OAB or UUI. These second-line treatments are most effective as adjuncts to behavioral modifications and PFMT.
A multicenter randomized trial that evaluated the efficacy of drug therapy alone compared with drug therapy in combination with behavioral modification, PFMT, urge suppression strategies, timed voiding, and fluid management for UUI found that combined therapy was more successful in achieving greater than 70% reduction in incontinence episodes (58% for drug therapy vs 69% for combined therapy).21
Of the 8 medications currently marketed in the United States for OAB or UUI, 6 are anticholinergic agents that block muscarinic receptors in the smooth muscle of the bladder, leading to inhibition of detrusor contractions, and 2 are β-adrenergic receptor agonists that promote bladder storage capacity by relaxing the detrusor muscle (TABLE 2). Similar efficacies lead most clinicians to initiate drug therapy based on formulary coverage and tolerance for adverse effects. Patients can expect a 53% to 80% reduction in UUI episodes and a 12% to 32% reduction in urinary frequency.22
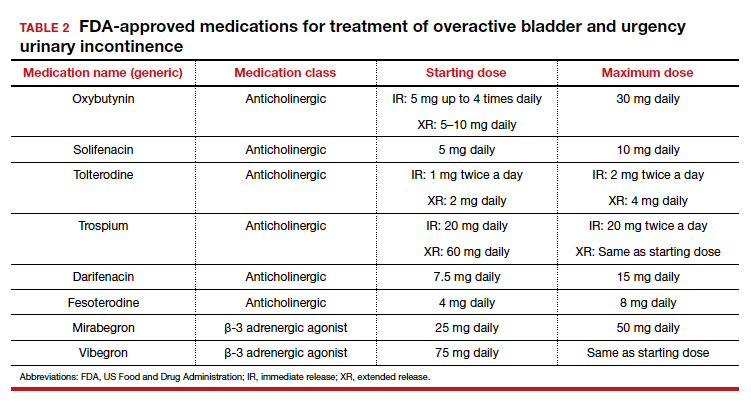
Extended-release formulations are associated with reduced anticholinergic side effects (dry mouth, constipation, somnolence, dry eyes), leading to improved adherence. Notably, the anticholinergic medications are contraindicated in patients with untreated narrow-angle glaucoma, gastric retention, and supraventricular tachycardia. Mirabegron should be used with caution in patients with poorly controlled hypertension. 5 Due to concerns regarding the association between cumulative anticholinergic burden and the development of dementia, clinicians may consider avoiding the anticholinergic medications in older and at-risk patients.23
Continue to: UUI office-based procedure treatments...
UUI office-based procedure treatments
If behavioral therapies and medications are ineffective, contraindicated, or not the patient’s preference, additional FDA-approved therapies for UUI are available, typically through referral to a urogynecologist, urologist, or continence center.
Posterior tibial nerve stimulation (PTNS) is a nondrug treatment that delivers electrical stimulation using an acupuncture needle for 12 weekly 30-minute sessions followed by monthly maintenance for responders. The time commitment for this treatment plan can be a barrier for some patients. However, patients who adhere to the recommended protocol can expect a 60% improvement in symptoms, with minimal adverse events. Treatment efficacy is comparable to that of anticholinergic medication.24
OnabotulinumtoxinA injections into the bladder muscle are performed cystoscopically under local anesthetic. The toxin blocks the presynaptic release of acetylcholine at the neuromuscular junction, resulting in temporary muscle paralysis. This treatment is associated with high satisfaction. Efficacy varies by study population and outcome measure.
In one US comparative effectiveness trial, 67% of study participants with UUI symptoms refractory to oral medication reported a greater than 50% reduction in OAB symptoms at 6 months, 20% reported complete resolution of UUI, and 72% requested a second injection within 24 months.25 The interval between the first and second injection was nearly 1 year (350 days).Risks include urinary tract infection (12% within 1 month of the procedure and 35% through 6 months); urinary retention requiring catheterization has decreased to 6% with recognition that most moderate retention is tolerated by patients.
Some insurers limit onabotulinumtoxinA treatment coverage to patients who have failed to achieve symptom control with first- and second-line treatments.
SUI-specific nonsurgical treatments
Cystoscopic injection of urethral bulking agents into the urethral submucosa is designed to improve urethral coaptation. It is a minor procedure that can be performed in an ambulatory setting under local anesthetic with or without sedation.
Various bulking agents have been approved for use in the United States, some of which have been withdrawn due to complications of migration, erosion, and pseudoabscess formation. Cure or improvement after bulking agent injection was found to be superior to a home pelvic floor exercise program but inferior to a midurethral sling procedure for cure (9% vs 89%).26
The durability of currently available urethral bulking agents beyond 1 year is unknown. Complications are typically minor and transient and include pain at the injection site, urinary retention, de novo urgency, and implant leakage. The advantages include no postprocedure activity restrictions.
CASE Symptom presentation guides treatment plan
Our patient described symptoms of stress-predominant MUI. She was counseled to moderate her fluid intake to 2 L per day and to strategically time voids (before exercise, and at least every 4 hours). The patient was fitted with an incontinence pessary, and she elected to pursue a course of supervised physical therapy for pelvic floor muscle strengthening. Her follow-up visit is scheduled in 3 months to determine if other interventions are warranted. ●
1. Lee UJ, Feinstein L, Ward JB, et al. Prevalence of urinary incontinence among a nationally representative sample of women, 2005–2016: findings from the Urologic Diseases in America Project. J Urol. 2021;205:1718-1724. doi:10.1097 /JU.0000000000001634
2. Sims J, Browning C, Lundgren-Lindquist B, et al. Urinary incontinence in a community sample of older adults: prevalence and impact on quality of life. Disabil Rehabil. 2011;33:1389-1398. doi:10.3109/09638288.2010.532284
3. Sarikaya S, Yildiz FG, Senocak C, et al. Urinary incontinence as a cause of depression and sexual dysfunction: questionnaire-based study. Rev Int Androl. 2020:18:50-54. doi:10.1016 /j.androl.2018.08.003
4. O’Reilly N, Nelson HD, Conry JM, et al; Women’s Preventive Services Initiative. Screening for urinary incontinence in women: a recommendation from the Women’s Preventive Services Initiative. Ann Intern Med. 2018;169(5):320-328. doi:10.7326/M18-0595
5. Barber MD, Walters MD, Karram MM, et al. Walters & Karram Urogynecology and Reconstructive Pelvic Surgery. 5th ed. Elsevier Saunders; 2021.
6. Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21: 5-26. doi:10.1007/s00192-009-0976-9
7. ACOG practice bulletin no. 155. Urinary incontinence in women. Obstet Gynecol. 2015;126:e66-e81. doi:10.1097 /AOG.0000000000001148
8. Sansone S, Lu J, Drangsholt S, et al. No pelvic exam, no problem: patient satisfaction following the integration of comprehensive urogynecology telemedicine. Int Urogynecol J. 2022;1:3. doi:10.1007/s00192-022-05104-w
9. Brown JS, Bradley CS, Subak LL, et al; Diagnostic Aspects of Incontinence Study (DAISy) Research Group. The sensitivity and specificity of a simple test to distinguish between urge and stress urinary incontinence. Ann Intern Med. 2006;144:715723. doi:10.7326/0003-4819-144-10-200605160-00005
10. Hess R, Huang AJ, Richter HE, et al. Long-term efficacy and safety of questionnaire-based initiation of urgency urinary incontinence treatment. Am J Obstet Gynecol. 2013;209:244. e1-9. doi:10.1016/j.ajog.2013.05.008
11. Sung VW, Borello-France D, Newman DK, et al; NICHD Pelvic Floor Disorders Network. Effect of behavioral and pelvic floor muscle therapy combined with surgery vs surgery alone on incontinence symptoms among women with mixed urinary incontinence. JAMA. 2019;322:1066-1076. doi:10.1001 /jama.2019.12467
12. American Urogynecologic Society. Voices for PFD: intake and voiding diary. Accessed August 11, 2022. https://www .voicesforpfd.org/assets/2/6/Voiding_Diary.pdf
13. Subak LL, Richter HE, Hunskaar S. Obesity and urinary incontinence: epidemiology and clinical research update. J Urol. 2009;182(6 suppl):S2-7. doi:10.1016/j.juro.2009.08.071
14. Arya LA, Myers DL, Jackson ND. Dietary caffeine intake and the risk for detrusor instability: a case-control study. Obstet Gynecol. 2000;96:85-89. doi:10.1016/s0029-7844(00)00808-5
15. Wyman JF, Zhou J, LaCoursiere DY, et al. Normative noninvasive bladder function measurements in healthy women: a systematic review and meta-analysis. Neurourol Urodyn. 2020;39:507-522. doi:10.1002/nau.24265
16. Hashim H, Al Mousa R. Management of fluid intake in patients with overactive bladder. Curr Urol Rep. 2009;10: 428-433. doi:10.1007/s11934-009-0068-x
17. Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2018;10:CD005654. doi:10.1002/14651858.CD005654.pub4
18. Araujo CC, de A Marques A, Juliato CRT. The adherence of home pelvic floor muscles training using a mobile device application for women with urinary incontinence: a randomized controlled trial. Female Pelvic Med Reconstr Surg. 2020;26:697-703. doi:10.1097/SPV.0000000000000670
19. Sjöström M, Umefjord G, Stenlund H, et al. Internet-based treatment of stress urinary incontinence: a randomized controlled study with focus on pelvic floor muscle training. BJU Int. 2013;112:362-372. doi:10.1111/j.1464 -410X.2012.11713.x
20. Richter HE, Burgio KL, Brubaker L, et al; Pelvic Floor Disorders Network. Continence pessary compared with behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Obstet Gynecol. 2010;115:609617. doi:10.1097/AOG.0b013e3181d055d4
21. Burgio KL, Kraus SR, Menefee S, et al. Behavioral therapy to enable women with urge incontinence to discontinue drug treatment: a randomized trial. Ann Intern Med. 2008;149(3): 161-169. doi:10.7326/0003-4819-149-3-200808050 -00005
22. Lukacz ES, Santiago-Lastra Y, Albo ME, et al. Urinary incontinence in women: a review. JAMA. 2017;318:1592-1604. doi:10.1001/jama.2017.12137
23. Welk B, Richardson K, Panicker JN. The cognitive effect of anticholinergics for patients with overactive bladder. Nat Rev Urol. 2021;18:686-700. doi:10.1038/s41585-021-00504-x
24. Burton C, Sajja A, Latthe PM. Effectiveness of percutaneous posterior tibial nerve stimulation for overactive bladder: a systematic review and meta-analysis. Neurourol Urodyn. 2012;31:1206-1216. doi:10.1002/nau.22251
25. Amundsen CL, Richter HE, Menefee SA, et al. OnabotulinumtoxinA vs sacral neuromodulation on refractory urgency urinary incontinence in women: A randomized clinical trial. JAMA. 2016;316:1366-1374. doi:10.1001/jama.2016.14617
26. Kirchin V, Page T, Keegan PE, et al. Urethral injection therapy for urinary incontinence in women. Cochrane Database Syst Rev. 2017;7:CD003881. doi:10.1002/14651858.CD003881.pub4
1. Lee UJ, Feinstein L, Ward JB, et al. Prevalence of urinary incontinence among a nationally representative sample of women, 2005–2016: findings from the Urologic Diseases in America Project. J Urol. 2021;205:1718-1724. doi:10.1097 /JU.0000000000001634
2. Sims J, Browning C, Lundgren-Lindquist B, et al. Urinary incontinence in a community sample of older adults: prevalence and impact on quality of life. Disabil Rehabil. 2011;33:1389-1398. doi:10.3109/09638288.2010.532284
3. Sarikaya S, Yildiz FG, Senocak C, et al. Urinary incontinence as a cause of depression and sexual dysfunction: questionnaire-based study. Rev Int Androl. 2020:18:50-54. doi:10.1016 /j.androl.2018.08.003
4. O’Reilly N, Nelson HD, Conry JM, et al; Women’s Preventive Services Initiative. Screening for urinary incontinence in women: a recommendation from the Women’s Preventive Services Initiative. Ann Intern Med. 2018;169(5):320-328. doi:10.7326/M18-0595
5. Barber MD, Walters MD, Karram MM, et al. Walters & Karram Urogynecology and Reconstructive Pelvic Surgery. 5th ed. Elsevier Saunders; 2021.
6. Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21: 5-26. doi:10.1007/s00192-009-0976-9
7. ACOG practice bulletin no. 155. Urinary incontinence in women. Obstet Gynecol. 2015;126:e66-e81. doi:10.1097 /AOG.0000000000001148
8. Sansone S, Lu J, Drangsholt S, et al. No pelvic exam, no problem: patient satisfaction following the integration of comprehensive urogynecology telemedicine. Int Urogynecol J. 2022;1:3. doi:10.1007/s00192-022-05104-w
9. Brown JS, Bradley CS, Subak LL, et al; Diagnostic Aspects of Incontinence Study (DAISy) Research Group. The sensitivity and specificity of a simple test to distinguish between urge and stress urinary incontinence. Ann Intern Med. 2006;144:715723. doi:10.7326/0003-4819-144-10-200605160-00005
10. Hess R, Huang AJ, Richter HE, et al. Long-term efficacy and safety of questionnaire-based initiation of urgency urinary incontinence treatment. Am J Obstet Gynecol. 2013;209:244. e1-9. doi:10.1016/j.ajog.2013.05.008
11. Sung VW, Borello-France D, Newman DK, et al; NICHD Pelvic Floor Disorders Network. Effect of behavioral and pelvic floor muscle therapy combined with surgery vs surgery alone on incontinence symptoms among women with mixed urinary incontinence. JAMA. 2019;322:1066-1076. doi:10.1001 /jama.2019.12467
12. American Urogynecologic Society. Voices for PFD: intake and voiding diary. Accessed August 11, 2022. https://www .voicesforpfd.org/assets/2/6/Voiding_Diary.pdf
13. Subak LL, Richter HE, Hunskaar S. Obesity and urinary incontinence: epidemiology and clinical research update. J Urol. 2009;182(6 suppl):S2-7. doi:10.1016/j.juro.2009.08.071
14. Arya LA, Myers DL, Jackson ND. Dietary caffeine intake and the risk for detrusor instability: a case-control study. Obstet Gynecol. 2000;96:85-89. doi:10.1016/s0029-7844(00)00808-5
15. Wyman JF, Zhou J, LaCoursiere DY, et al. Normative noninvasive bladder function measurements in healthy women: a systematic review and meta-analysis. Neurourol Urodyn. 2020;39:507-522. doi:10.1002/nau.24265
16. Hashim H, Al Mousa R. Management of fluid intake in patients with overactive bladder. Curr Urol Rep. 2009;10: 428-433. doi:10.1007/s11934-009-0068-x
17. Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2018;10:CD005654. doi:10.1002/14651858.CD005654.pub4
18. Araujo CC, de A Marques A, Juliato CRT. The adherence of home pelvic floor muscles training using a mobile device application for women with urinary incontinence: a randomized controlled trial. Female Pelvic Med Reconstr Surg. 2020;26:697-703. doi:10.1097/SPV.0000000000000670
19. Sjöström M, Umefjord G, Stenlund H, et al. Internet-based treatment of stress urinary incontinence: a randomized controlled study with focus on pelvic floor muscle training. BJU Int. 2013;112:362-372. doi:10.1111/j.1464 -410X.2012.11713.x
20. Richter HE, Burgio KL, Brubaker L, et al; Pelvic Floor Disorders Network. Continence pessary compared with behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Obstet Gynecol. 2010;115:609617. doi:10.1097/AOG.0b013e3181d055d4
21. Burgio KL, Kraus SR, Menefee S, et al. Behavioral therapy to enable women with urge incontinence to discontinue drug treatment: a randomized trial. Ann Intern Med. 2008;149(3): 161-169. doi:10.7326/0003-4819-149-3-200808050 -00005
22. Lukacz ES, Santiago-Lastra Y, Albo ME, et al. Urinary incontinence in women: a review. JAMA. 2017;318:1592-1604. doi:10.1001/jama.2017.12137
23. Welk B, Richardson K, Panicker JN. The cognitive effect of anticholinergics for patients with overactive bladder. Nat Rev Urol. 2021;18:686-700. doi:10.1038/s41585-021-00504-x
24. Burton C, Sajja A, Latthe PM. Effectiveness of percutaneous posterior tibial nerve stimulation for overactive bladder: a systematic review and meta-analysis. Neurourol Urodyn. 2012;31:1206-1216. doi:10.1002/nau.22251
25. Amundsen CL, Richter HE, Menefee SA, et al. OnabotulinumtoxinA vs sacral neuromodulation on refractory urgency urinary incontinence in women: A randomized clinical trial. JAMA. 2016;316:1366-1374. doi:10.1001/jama.2016.14617
26. Kirchin V, Page T, Keegan PE, et al. Urethral injection therapy for urinary incontinence in women. Cochrane Database Syst Rev. 2017;7:CD003881. doi:10.1002/14651858.CD003881.pub4
2022 Update on abnormal uterine bleeding
In this Update, we focus on therapies for abnormal uterine bleeding (AUB) that include a new formulation of a progesterone-only pill (POP), drospirenone 4 mg in a 24/4 regimen (24 days of drospirenone/4 days of inert tablets), which recently showed benefit over the use of desogestrel in a European randomized clinical trial (RCT). Two other commonly used treatments for AUB— the levonorgestrel-releasing intrauterine system (LNG IUS) and endometrial ablation—were studied in terms of cost-effectiveness as well as whether they should be used in combination for added efficacy. In addition, although at times either COVID-19 disease or the COVID-19 vaccine has been blamed for societal and medical problems, one study showed that it is unlikely that significant changes in the menstrual cycle are a result of the COVID-19 vaccine.
COVID-19 vaccination had minimal effects on menstrual cycle length
Edelman A, Boniface ER, Benhar W, et al. Association between menstrual cycle length and coronavirus disease 2019 (COVID-19) vaccination: a US cohort. Obstet Gynecol. 2022;139:481-489.
Does receiving the COVID-19 vaccination result in abnormal menstrual cycles? Patients often ask this question, and it has been a topic of social media discussion (including NPR) and concerns about the possibility of vaccine hesitancy,1,2 as the menstrual cycle is often considered a sign of health and fertility.
To better understand this possible association, Edelman and colleagues conducted a study that prospectively tracked menstrual cycle data using the digital app Natural Cycles in US residents aged 18 to 45 years for 3 consecutive cycles in both a vaccinated and an unvaccinated cohort.3 Almost 4,000 individuals were studied; 2,403 were vaccinated and 1,556 were unvaccinated. The study vaccine types included the BioNTech (Pfizer), Moderna, Johnson & Johnson/Janssen, and unspecified vaccines.
The primary outcome was the within-individual change in cycle length in days, comparing a 3-cycle postvaccine average to a 3-cycle prevaccination average in the 2 groups. (For the unvaccinated group, cycles 1, 2, and 3 were considered the equivalent of prevaccination cycles; cycle 4 was designated as the artificial first vaccine dose-cycle and cycle 5 as the artificial second-dose cycle.)
Increase in cycle length clinically negligible
The investigators found that the vaccinated cohort had less than a 1-day unadjusted increase in the length of their menstrual cycle, which was essentially a 0.71-day increase (98.75% confidence interval [CI], 0.47–0.94). Although this is considered statistically significant, it is likely clinically insignificant in that the overlaid histograms comparing the distribution of change showed a cycle length distribution in vaccinated individuals that is essentially equivalent to that in unvaccinated individuals. After adjusting for confounders, the difference in cycle length was reduced to a 0.64 day (98.75% CI, 0.27–1.01).
An interesting finding was that a subset of individuals who received both vaccine doses in a single cycle had, on average, an adjusted 2-day increase in their menstrual cycle compared with unvaccinated individuals. To explain this slightly longer cycle length, the authors postulated that mRNA vaccines create an immune response, or stressor, which could temporarily affect the hypothalamic-pituitary-ovarian axis if timed correctly. It is certainly possible for an individual to receive 2 doses in a single cycle, which could have both been administered in the early follicular phase. Such cycle length variability can be caused by events, including stressors, that affect the recruitment and maturation of the dominant follicle.
Counseling takeaway
This study provides reassurance to most individuals who receive a COVID-19 vaccine that it likely will not affect their menstrual cycle in a clinically significant manner.
This robust study by Edelman and colleagues on COVID-19 vaccination effects on menstrual cycle length had more than 99% power to detect an unadjusted 1-day difference in cycle length. However, given that most of the study participants were White and had access to the Natural Cycles app, the results may not be generalizable to all individuals who receive the vaccine.
Continue to: Drospirenone improved bleeding profiles, lowered discontinuation rates compared with desogestrel...
Drospirenone improved bleeding profiles, lowered discontinuation rates compared with desogestrel
Regidor PA, Colli E, Palacios S. Overall and bleeding-related discontinuation rates of a new oral contraceptive containing 4 mg drospirenone only in a 24/4 regimen and comparison to 0.075 mg desogestrel. Gynecol Endocrinol. 2021;37:1121-1127.
A new POP, marketed under the name Slynd, recently came to market. It contains the progestin drospirenone (DRSP) 4 mg in a 24/4 regimen. This formulation has the advantage of being an antiandrogenic progestin, with a long enough half-life to allow for managing a missed pill in the same fashion as combined oral contraceptives (COCs).
Investigators in Europe conducted a double-blind, randomized trial to assess discontinuation rates due to adverse events (mainly bleeding disorders) in participants taking DRSP 4 mg in a 24/4 regimen compared with those taking the POP desogestrel (DSG) 0.075 mg, which is commonly used in Europe.4 Regidor and colleagues compared 858 women with 6,691 DRSP treatment cycles with 332 women with 2,487 DSG treatment cycles.
Top reasons for stopping a POP
The discontinuation rate for abnormal bleeding was 3.7% in the DRSP group versus 7.3% in the DSG group (55.7% lower). The most common reasons for stopping either POP formulation were vaginal bleeding and acne. Both of these adverse events were less common in the DRSP group. Pill discontinuation due to vaginal bleeding was 2.6% in the DRSP group versus 5.4% in the DSG group, while discontinuation due to acne occurred in 1% in the DRSP group versus 2.7% in the DSG group.
New oral contraception option
This study shows improved acceptability and bleeding profiles in women using this new DRSP contraception pill regimen.
Adherence to a contraceptive method is influenced by patient satisfaction, and this is particularly important in patients who cannot take COCs. It also should be noted that the discontinuation rate for DRSP as a POP used in this 24/4 regimen was similar to discontinuation rates for COCs containing 20 µg and 30 µg of ethinyl estradiol. Cost, however, may be an issue with DRSP, depending on a patient’s insurance coverage.
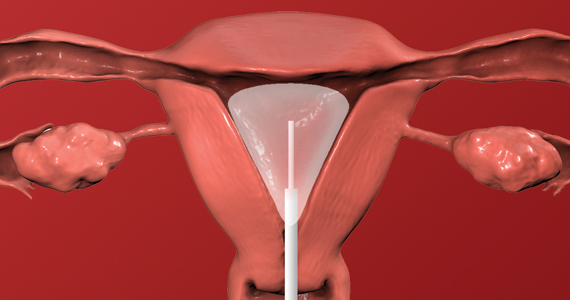
Continue to: Placing an LNG IUS after endometrial ablation for heavy menstrual bleeding reduced risk of hysterectomy...
Placing an LNG IUS after endometrial ablation for heavy menstrual bleeding reduced risk of hysterectomy
Oderkerk TJ, van de Kar MMA, van der Zanden CHM, et al. The combined use of endometrial ablation or resection and levonorgestrel-releasing intrauterine system in women with heavy menstrual bleeding: a systematic review. Acta Obstet Gynecol Scand. 2021;100:1779-1787.
Over the years, a smattering of articles have suggested that a reduction in uterine bleeding was associated with placement of an LNG IUS at the conclusion of endometrial ablation. We now have a systematic review of this surgical modification.
Oderkerk and colleagues sifted through 747 articles to find 7 publications that could provide meaningful data on the impact of combined use of endometrial ablation and LNG IUS insertion for women with heavy menstrual bleeding.5 These included 4 retrospective cohort studies with control groups, 2 retrospective studies without control groups, and 1 case series. The primary outcome was the hysterectomy rate after therapy.
Promising results for combined therapy
Although no statistically significant intergroup differences were seen in the combined treatment group versus the endometrial ablation alone group for the first 6 months of treatment, significant differences existed at the 12- and 24-month mark. Hysterectomy rates after combined treatment varied from 0% to 11% versus 9.4% to 24% after endometrial ablation alone. Complication rates for combined treatment did not appear higher than those for endometrial ablation alone.
The authors postulated that the failure of endometrial ablation is generally caused by either remaining or regenerating endometrial tissue and that the addition of an LNG IUS allows for suppression of endometrial tissue. Also encouraging was that, in general, the removal of the LNG IUS was relatively simple. A single difficult removal was described due to uterine synechiae, but hysteroscopic resection was not necessary. The authors acknowledged that the data from these 7 retrospective studies are limited and that high-quality research from prospective studies is needed.
Bottom line
The data available from this systematic review suggest that placement of an LNG IUS at the completion of an endometrial ablation may result in lower hysterectomy rates, without apparent risk, and without significantly difficult LNG IUS removal when needed.
The data provided by Oderkerk and colleagues’ systematic review are promising and, although not studied in the reviewed publications, the potential may exist to reduce the risk of endometrial hyperplasia and endometrial cancer by adding an LNG IUS.
Continue to: LNG IUS is less expensive, and less effective, than endometrial ablation for heavy menstrual bleeding, cost analysis shows...
LNG IUS is less expensive, and less effective, than endometrial ablation for heavy menstrual bleeding, cost analysis shows
van den Brink MJ, Beelen P, Herman MC, et al. The levonorgestrel intrauterine system versus endometrial ablation for heavy menstrual bleeding: a cost-effectiveness analysis. BJOG. 2021;128:2003-2011.
To assess the cost-effectiveness of the LNG IUS versus endometrial ablation in the treatment of heavy menstrual bleeding, van den Brink and colleagues conducted a randomized, noninferiority trial.6
Part of the rationale for this study was to better understand the cost differences between the LNG IUS and second-generation endometrial ablation. Some data have suggested that the LNG IUS is cost-effective when compared with first-generation endometrial ablation; however, definitive evidence about its cost compared with second-generation endometrial ablation is lacking, as these procedures should be less expensive than first-generation endometrial ablation since they frequently are performed in the office rather than in an operating room.
Cost-effectiveness and noninferiority assessed
A total of 270 women were randomly assigned to 1 of 2 treatment strategies. Eventually, 132 women were treated first with the 52-mg LNG IUS, and 138 were treated first with endometrial ablation by radiofrequency ablation. Menstrual blood loss after 24 months was the primary outcome.
At 24 months, the mean pictorial blood loss assessment chart (PBAC) scores were 64.8 in the LNG IUS group compared with 14.2 in the endometrial ablation group. Given that the noninferiority margin was defined as 25 points, noninferiority could not be demonstrated. However, when looking at PBAC scores less than 75 points, the LNG IUS group met this secondary end point in 87% of women versus 94% in the endometrial ablation group. When satisfaction was assessed, 74% of women in the LNG IUS group were satisfied compared with 84% in the endometrial ablation group.
Overall, the total costs per patient were €2,285 in the LNG IUS strategy and €3,465 in the endometrial ablation strategy (costs convert to $2,285 and $3,465 as of this writing).
Key takeaway
Treatment of heavy menstrual bleeding starting with the LNG IUS is cheaper, but it is slightly less effective than endometrial ablation. ●
It is interesting that there are minimal differences between satisfaction rates and PBAC scores less than 75, yet the mean PBAC scores were significantly more favorable for endometrial ablation. This study’s results support the use of a sequential therapy of a less invasive therapy, such as the LNG IUS, prior to performing endometrial ablation.
- Blumfiel G. Why reports of menstrual changes after COVID vaccine are tough to study. NPR. August 9, 2021. Accessed August 30, 2022. https://www.npr.org/sections/health-shots/2021/08/09/1024190379/covid-vaccine-period-menstrual-cycle-research
- Lee KMN, Junkins EJ, Fatima UA, et al. Characterizing menstrual bleeding changes occurring after SARSCoV-2 vaccinations. MedRxiv. February 11, 2022. doi:10.1101/2021.10.11.21264863
- Edelman A, Boniface ER, Benhar W, et al. Association between menstrual cycle length and coronavirus disease 2019 (COVID-19) vaccination: a US cohort. Obstet Gynecol. 2022;139:481-489.
- Regidor PA, Colli E, Palacios S. Overall and bleeding-related discontinuation rates of a new oral contraceptive containing 4 mg drospirenone only in a 24/4 regimen and comparison to 0.075 mg desogestrel. Gynecol Endocrinol. 2021;37:1121-1127.
- Oderkerk TJ, van de Kar MMA, van der Zanden CHM, et al. T he combined use of endometrial ablation or resection and levonorgestrel-releasing intrauterine system in women with heavy menstrual bleeding: a systematic review. Acta Obstet Gynecol Scand. 2021;100:1779-1787.
- van den Brink MJ, Beelen P, Herman MC, et al. The levonorgestrel intrauterine system versus endometrial ablation for heavy menstrual bleeding: a cost-effectiveness analysis. BJOG. 2021;128:2003-2011.
In this Update, we focus on therapies for abnormal uterine bleeding (AUB) that include a new formulation of a progesterone-only pill (POP), drospirenone 4 mg in a 24/4 regimen (24 days of drospirenone/4 days of inert tablets), which recently showed benefit over the use of desogestrel in a European randomized clinical trial (RCT). Two other commonly used treatments for AUB— the levonorgestrel-releasing intrauterine system (LNG IUS) and endometrial ablation—were studied in terms of cost-effectiveness as well as whether they should be used in combination for added efficacy. In addition, although at times either COVID-19 disease or the COVID-19 vaccine has been blamed for societal and medical problems, one study showed that it is unlikely that significant changes in the menstrual cycle are a result of the COVID-19 vaccine.
COVID-19 vaccination had minimal effects on menstrual cycle length
Edelman A, Boniface ER, Benhar W, et al. Association between menstrual cycle length and coronavirus disease 2019 (COVID-19) vaccination: a US cohort. Obstet Gynecol. 2022;139:481-489.
Does receiving the COVID-19 vaccination result in abnormal menstrual cycles? Patients often ask this question, and it has been a topic of social media discussion (including NPR) and concerns about the possibility of vaccine hesitancy,1,2 as the menstrual cycle is often considered a sign of health and fertility.
To better understand this possible association, Edelman and colleagues conducted a study that prospectively tracked menstrual cycle data using the digital app Natural Cycles in US residents aged 18 to 45 years for 3 consecutive cycles in both a vaccinated and an unvaccinated cohort.3 Almost 4,000 individuals were studied; 2,403 were vaccinated and 1,556 were unvaccinated. The study vaccine types included the BioNTech (Pfizer), Moderna, Johnson & Johnson/Janssen, and unspecified vaccines.
The primary outcome was the within-individual change in cycle length in days, comparing a 3-cycle postvaccine average to a 3-cycle prevaccination average in the 2 groups. (For the unvaccinated group, cycles 1, 2, and 3 were considered the equivalent of prevaccination cycles; cycle 4 was designated as the artificial first vaccine dose-cycle and cycle 5 as the artificial second-dose cycle.)
Increase in cycle length clinically negligible
The investigators found that the vaccinated cohort had less than a 1-day unadjusted increase in the length of their menstrual cycle, which was essentially a 0.71-day increase (98.75% confidence interval [CI], 0.47–0.94). Although this is considered statistically significant, it is likely clinically insignificant in that the overlaid histograms comparing the distribution of change showed a cycle length distribution in vaccinated individuals that is essentially equivalent to that in unvaccinated individuals. After adjusting for confounders, the difference in cycle length was reduced to a 0.64 day (98.75% CI, 0.27–1.01).
An interesting finding was that a subset of individuals who received both vaccine doses in a single cycle had, on average, an adjusted 2-day increase in their menstrual cycle compared with unvaccinated individuals. To explain this slightly longer cycle length, the authors postulated that mRNA vaccines create an immune response, or stressor, which could temporarily affect the hypothalamic-pituitary-ovarian axis if timed correctly. It is certainly possible for an individual to receive 2 doses in a single cycle, which could have both been administered in the early follicular phase. Such cycle length variability can be caused by events, including stressors, that affect the recruitment and maturation of the dominant follicle.
Counseling takeaway
This study provides reassurance to most individuals who receive a COVID-19 vaccine that it likely will not affect their menstrual cycle in a clinically significant manner.
This robust study by Edelman and colleagues on COVID-19 vaccination effects on menstrual cycle length had more than 99% power to detect an unadjusted 1-day difference in cycle length. However, given that most of the study participants were White and had access to the Natural Cycles app, the results may not be generalizable to all individuals who receive the vaccine.
Continue to: Drospirenone improved bleeding profiles, lowered discontinuation rates compared with desogestrel...
Drospirenone improved bleeding profiles, lowered discontinuation rates compared with desogestrel
Regidor PA, Colli E, Palacios S. Overall and bleeding-related discontinuation rates of a new oral contraceptive containing 4 mg drospirenone only in a 24/4 regimen and comparison to 0.075 mg desogestrel. Gynecol Endocrinol. 2021;37:1121-1127.
A new POP, marketed under the name Slynd, recently came to market. It contains the progestin drospirenone (DRSP) 4 mg in a 24/4 regimen. This formulation has the advantage of being an antiandrogenic progestin, with a long enough half-life to allow for managing a missed pill in the same fashion as combined oral contraceptives (COCs).
Investigators in Europe conducted a double-blind, randomized trial to assess discontinuation rates due to adverse events (mainly bleeding disorders) in participants taking DRSP 4 mg in a 24/4 regimen compared with those taking the POP desogestrel (DSG) 0.075 mg, which is commonly used in Europe.4 Regidor and colleagues compared 858 women with 6,691 DRSP treatment cycles with 332 women with 2,487 DSG treatment cycles.
Top reasons for stopping a POP
The discontinuation rate for abnormal bleeding was 3.7% in the DRSP group versus 7.3% in the DSG group (55.7% lower). The most common reasons for stopping either POP formulation were vaginal bleeding and acne. Both of these adverse events were less common in the DRSP group. Pill discontinuation due to vaginal bleeding was 2.6% in the DRSP group versus 5.4% in the DSG group, while discontinuation due to acne occurred in 1% in the DRSP group versus 2.7% in the DSG group.
New oral contraception option
This study shows improved acceptability and bleeding profiles in women using this new DRSP contraception pill regimen.
Adherence to a contraceptive method is influenced by patient satisfaction, and this is particularly important in patients who cannot take COCs. It also should be noted that the discontinuation rate for DRSP as a POP used in this 24/4 regimen was similar to discontinuation rates for COCs containing 20 µg and 30 µg of ethinyl estradiol. Cost, however, may be an issue with DRSP, depending on a patient’s insurance coverage.
Continue to: Placing an LNG IUS after endometrial ablation for heavy menstrual bleeding reduced risk of hysterectomy...
Placing an LNG IUS after endometrial ablation for heavy menstrual bleeding reduced risk of hysterectomy
Oderkerk TJ, van de Kar MMA, van der Zanden CHM, et al. The combined use of endometrial ablation or resection and levonorgestrel-releasing intrauterine system in women with heavy menstrual bleeding: a systematic review. Acta Obstet Gynecol Scand. 2021;100:1779-1787.
Over the years, a smattering of articles have suggested that a reduction in uterine bleeding was associated with placement of an LNG IUS at the conclusion of endometrial ablation. We now have a systematic review of this surgical modification.
Oderkerk and colleagues sifted through 747 articles to find 7 publications that could provide meaningful data on the impact of combined use of endometrial ablation and LNG IUS insertion for women with heavy menstrual bleeding.5 These included 4 retrospective cohort studies with control groups, 2 retrospective studies without control groups, and 1 case series. The primary outcome was the hysterectomy rate after therapy.
Promising results for combined therapy
Although no statistically significant intergroup differences were seen in the combined treatment group versus the endometrial ablation alone group for the first 6 months of treatment, significant differences existed at the 12- and 24-month mark. Hysterectomy rates after combined treatment varied from 0% to 11% versus 9.4% to 24% after endometrial ablation alone. Complication rates for combined treatment did not appear higher than those for endometrial ablation alone.
The authors postulated that the failure of endometrial ablation is generally caused by either remaining or regenerating endometrial tissue and that the addition of an LNG IUS allows for suppression of endometrial tissue. Also encouraging was that, in general, the removal of the LNG IUS was relatively simple. A single difficult removal was described due to uterine synechiae, but hysteroscopic resection was not necessary. The authors acknowledged that the data from these 7 retrospective studies are limited and that high-quality research from prospective studies is needed.
Bottom line
The data available from this systematic review suggest that placement of an LNG IUS at the completion of an endometrial ablation may result in lower hysterectomy rates, without apparent risk, and without significantly difficult LNG IUS removal when needed.
The data provided by Oderkerk and colleagues’ systematic review are promising and, although not studied in the reviewed publications, the potential may exist to reduce the risk of endometrial hyperplasia and endometrial cancer by adding an LNG IUS.
Continue to: LNG IUS is less expensive, and less effective, than endometrial ablation for heavy menstrual bleeding, cost analysis shows...
LNG IUS is less expensive, and less effective, than endometrial ablation for heavy menstrual bleeding, cost analysis shows
van den Brink MJ, Beelen P, Herman MC, et al. The levonorgestrel intrauterine system versus endometrial ablation for heavy menstrual bleeding: a cost-effectiveness analysis. BJOG. 2021;128:2003-2011.
To assess the cost-effectiveness of the LNG IUS versus endometrial ablation in the treatment of heavy menstrual bleeding, van den Brink and colleagues conducted a randomized, noninferiority trial.6
Part of the rationale for this study was to better understand the cost differences between the LNG IUS and second-generation endometrial ablation. Some data have suggested that the LNG IUS is cost-effective when compared with first-generation endometrial ablation; however, definitive evidence about its cost compared with second-generation endometrial ablation is lacking, as these procedures should be less expensive than first-generation endometrial ablation since they frequently are performed in the office rather than in an operating room.
Cost-effectiveness and noninferiority assessed
A total of 270 women were randomly assigned to 1 of 2 treatment strategies. Eventually, 132 women were treated first with the 52-mg LNG IUS, and 138 were treated first with endometrial ablation by radiofrequency ablation. Menstrual blood loss after 24 months was the primary outcome.
At 24 months, the mean pictorial blood loss assessment chart (PBAC) scores were 64.8 in the LNG IUS group compared with 14.2 in the endometrial ablation group. Given that the noninferiority margin was defined as 25 points, noninferiority could not be demonstrated. However, when looking at PBAC scores less than 75 points, the LNG IUS group met this secondary end point in 87% of women versus 94% in the endometrial ablation group. When satisfaction was assessed, 74% of women in the LNG IUS group were satisfied compared with 84% in the endometrial ablation group.
Overall, the total costs per patient were €2,285 in the LNG IUS strategy and €3,465 in the endometrial ablation strategy (costs convert to $2,285 and $3,465 as of this writing).
Key takeaway
Treatment of heavy menstrual bleeding starting with the LNG IUS is cheaper, but it is slightly less effective than endometrial ablation. ●
It is interesting that there are minimal differences between satisfaction rates and PBAC scores less than 75, yet the mean PBAC scores were significantly more favorable for endometrial ablation. This study’s results support the use of a sequential therapy of a less invasive therapy, such as the LNG IUS, prior to performing endometrial ablation.
In this Update, we focus on therapies for abnormal uterine bleeding (AUB) that include a new formulation of a progesterone-only pill (POP), drospirenone 4 mg in a 24/4 regimen (24 days of drospirenone/4 days of inert tablets), which recently showed benefit over the use of desogestrel in a European randomized clinical trial (RCT). Two other commonly used treatments for AUB— the levonorgestrel-releasing intrauterine system (LNG IUS) and endometrial ablation—were studied in terms of cost-effectiveness as well as whether they should be used in combination for added efficacy. In addition, although at times either COVID-19 disease or the COVID-19 vaccine has been blamed for societal and medical problems, one study showed that it is unlikely that significant changes in the menstrual cycle are a result of the COVID-19 vaccine.
COVID-19 vaccination had minimal effects on menstrual cycle length
Edelman A, Boniface ER, Benhar W, et al. Association between menstrual cycle length and coronavirus disease 2019 (COVID-19) vaccination: a US cohort. Obstet Gynecol. 2022;139:481-489.
Does receiving the COVID-19 vaccination result in abnormal menstrual cycles? Patients often ask this question, and it has been a topic of social media discussion (including NPR) and concerns about the possibility of vaccine hesitancy,1,2 as the menstrual cycle is often considered a sign of health and fertility.
To better understand this possible association, Edelman and colleagues conducted a study that prospectively tracked menstrual cycle data using the digital app Natural Cycles in US residents aged 18 to 45 years for 3 consecutive cycles in both a vaccinated and an unvaccinated cohort.3 Almost 4,000 individuals were studied; 2,403 were vaccinated and 1,556 were unvaccinated. The study vaccine types included the BioNTech (Pfizer), Moderna, Johnson & Johnson/Janssen, and unspecified vaccines.
The primary outcome was the within-individual change in cycle length in days, comparing a 3-cycle postvaccine average to a 3-cycle prevaccination average in the 2 groups. (For the unvaccinated group, cycles 1, 2, and 3 were considered the equivalent of prevaccination cycles; cycle 4 was designated as the artificial first vaccine dose-cycle and cycle 5 as the artificial second-dose cycle.)
Increase in cycle length clinically negligible
The investigators found that the vaccinated cohort had less than a 1-day unadjusted increase in the length of their menstrual cycle, which was essentially a 0.71-day increase (98.75% confidence interval [CI], 0.47–0.94). Although this is considered statistically significant, it is likely clinically insignificant in that the overlaid histograms comparing the distribution of change showed a cycle length distribution in vaccinated individuals that is essentially equivalent to that in unvaccinated individuals. After adjusting for confounders, the difference in cycle length was reduced to a 0.64 day (98.75% CI, 0.27–1.01).
An interesting finding was that a subset of individuals who received both vaccine doses in a single cycle had, on average, an adjusted 2-day increase in their menstrual cycle compared with unvaccinated individuals. To explain this slightly longer cycle length, the authors postulated that mRNA vaccines create an immune response, or stressor, which could temporarily affect the hypothalamic-pituitary-ovarian axis if timed correctly. It is certainly possible for an individual to receive 2 doses in a single cycle, which could have both been administered in the early follicular phase. Such cycle length variability can be caused by events, including stressors, that affect the recruitment and maturation of the dominant follicle.
Counseling takeaway
This study provides reassurance to most individuals who receive a COVID-19 vaccine that it likely will not affect their menstrual cycle in a clinically significant manner.
This robust study by Edelman and colleagues on COVID-19 vaccination effects on menstrual cycle length had more than 99% power to detect an unadjusted 1-day difference in cycle length. However, given that most of the study participants were White and had access to the Natural Cycles app, the results may not be generalizable to all individuals who receive the vaccine.
Continue to: Drospirenone improved bleeding profiles, lowered discontinuation rates compared with desogestrel...
Drospirenone improved bleeding profiles, lowered discontinuation rates compared with desogestrel
Regidor PA, Colli E, Palacios S. Overall and bleeding-related discontinuation rates of a new oral contraceptive containing 4 mg drospirenone only in a 24/4 regimen and comparison to 0.075 mg desogestrel. Gynecol Endocrinol. 2021;37:1121-1127.
A new POP, marketed under the name Slynd, recently came to market. It contains the progestin drospirenone (DRSP) 4 mg in a 24/4 regimen. This formulation has the advantage of being an antiandrogenic progestin, with a long enough half-life to allow for managing a missed pill in the same fashion as combined oral contraceptives (COCs).
Investigators in Europe conducted a double-blind, randomized trial to assess discontinuation rates due to adverse events (mainly bleeding disorders) in participants taking DRSP 4 mg in a 24/4 regimen compared with those taking the POP desogestrel (DSG) 0.075 mg, which is commonly used in Europe.4 Regidor and colleagues compared 858 women with 6,691 DRSP treatment cycles with 332 women with 2,487 DSG treatment cycles.
Top reasons for stopping a POP
The discontinuation rate for abnormal bleeding was 3.7% in the DRSP group versus 7.3% in the DSG group (55.7% lower). The most common reasons for stopping either POP formulation were vaginal bleeding and acne. Both of these adverse events were less common in the DRSP group. Pill discontinuation due to vaginal bleeding was 2.6% in the DRSP group versus 5.4% in the DSG group, while discontinuation due to acne occurred in 1% in the DRSP group versus 2.7% in the DSG group.
New oral contraception option
This study shows improved acceptability and bleeding profiles in women using this new DRSP contraception pill regimen.
Adherence to a contraceptive method is influenced by patient satisfaction, and this is particularly important in patients who cannot take COCs. It also should be noted that the discontinuation rate for DRSP as a POP used in this 24/4 regimen was similar to discontinuation rates for COCs containing 20 µg and 30 µg of ethinyl estradiol. Cost, however, may be an issue with DRSP, depending on a patient’s insurance coverage.
Continue to: Placing an LNG IUS after endometrial ablation for heavy menstrual bleeding reduced risk of hysterectomy...
Placing an LNG IUS after endometrial ablation for heavy menstrual bleeding reduced risk of hysterectomy
Oderkerk TJ, van de Kar MMA, van der Zanden CHM, et al. The combined use of endometrial ablation or resection and levonorgestrel-releasing intrauterine system in women with heavy menstrual bleeding: a systematic review. Acta Obstet Gynecol Scand. 2021;100:1779-1787.
Over the years, a smattering of articles have suggested that a reduction in uterine bleeding was associated with placement of an LNG IUS at the conclusion of endometrial ablation. We now have a systematic review of this surgical modification.
Oderkerk and colleagues sifted through 747 articles to find 7 publications that could provide meaningful data on the impact of combined use of endometrial ablation and LNG IUS insertion for women with heavy menstrual bleeding.5 These included 4 retrospective cohort studies with control groups, 2 retrospective studies without control groups, and 1 case series. The primary outcome was the hysterectomy rate after therapy.
Promising results for combined therapy
Although no statistically significant intergroup differences were seen in the combined treatment group versus the endometrial ablation alone group for the first 6 months of treatment, significant differences existed at the 12- and 24-month mark. Hysterectomy rates after combined treatment varied from 0% to 11% versus 9.4% to 24% after endometrial ablation alone. Complication rates for combined treatment did not appear higher than those for endometrial ablation alone.
The authors postulated that the failure of endometrial ablation is generally caused by either remaining or regenerating endometrial tissue and that the addition of an LNG IUS allows for suppression of endometrial tissue. Also encouraging was that, in general, the removal of the LNG IUS was relatively simple. A single difficult removal was described due to uterine synechiae, but hysteroscopic resection was not necessary. The authors acknowledged that the data from these 7 retrospective studies are limited and that high-quality research from prospective studies is needed.
Bottom line
The data available from this systematic review suggest that placement of an LNG IUS at the completion of an endometrial ablation may result in lower hysterectomy rates, without apparent risk, and without significantly difficult LNG IUS removal when needed.
The data provided by Oderkerk and colleagues’ systematic review are promising and, although not studied in the reviewed publications, the potential may exist to reduce the risk of endometrial hyperplasia and endometrial cancer by adding an LNG IUS.
Continue to: LNG IUS is less expensive, and less effective, than endometrial ablation for heavy menstrual bleeding, cost analysis shows...
LNG IUS is less expensive, and less effective, than endometrial ablation for heavy menstrual bleeding, cost analysis shows
van den Brink MJ, Beelen P, Herman MC, et al. The levonorgestrel intrauterine system versus endometrial ablation for heavy menstrual bleeding: a cost-effectiveness analysis. BJOG. 2021;128:2003-2011.
To assess the cost-effectiveness of the LNG IUS versus endometrial ablation in the treatment of heavy menstrual bleeding, van den Brink and colleagues conducted a randomized, noninferiority trial.6
Part of the rationale for this study was to better understand the cost differences between the LNG IUS and second-generation endometrial ablation. Some data have suggested that the LNG IUS is cost-effective when compared with first-generation endometrial ablation; however, definitive evidence about its cost compared with second-generation endometrial ablation is lacking, as these procedures should be less expensive than first-generation endometrial ablation since they frequently are performed in the office rather than in an operating room.
Cost-effectiveness and noninferiority assessed
A total of 270 women were randomly assigned to 1 of 2 treatment strategies. Eventually, 132 women were treated first with the 52-mg LNG IUS, and 138 were treated first with endometrial ablation by radiofrequency ablation. Menstrual blood loss after 24 months was the primary outcome.
At 24 months, the mean pictorial blood loss assessment chart (PBAC) scores were 64.8 in the LNG IUS group compared with 14.2 in the endometrial ablation group. Given that the noninferiority margin was defined as 25 points, noninferiority could not be demonstrated. However, when looking at PBAC scores less than 75 points, the LNG IUS group met this secondary end point in 87% of women versus 94% in the endometrial ablation group. When satisfaction was assessed, 74% of women in the LNG IUS group were satisfied compared with 84% in the endometrial ablation group.
Overall, the total costs per patient were €2,285 in the LNG IUS strategy and €3,465 in the endometrial ablation strategy (costs convert to $2,285 and $3,465 as of this writing).
Key takeaway
Treatment of heavy menstrual bleeding starting with the LNG IUS is cheaper, but it is slightly less effective than endometrial ablation. ●
It is interesting that there are minimal differences between satisfaction rates and PBAC scores less than 75, yet the mean PBAC scores were significantly more favorable for endometrial ablation. This study’s results support the use of a sequential therapy of a less invasive therapy, such as the LNG IUS, prior to performing endometrial ablation.
- Blumfiel G. Why reports of menstrual changes after COVID vaccine are tough to study. NPR. August 9, 2021. Accessed August 30, 2022. https://www.npr.org/sections/health-shots/2021/08/09/1024190379/covid-vaccine-period-menstrual-cycle-research
- Lee KMN, Junkins EJ, Fatima UA, et al. Characterizing menstrual bleeding changes occurring after SARSCoV-2 vaccinations. MedRxiv. February 11, 2022. doi:10.1101/2021.10.11.21264863
- Edelman A, Boniface ER, Benhar W, et al. Association between menstrual cycle length and coronavirus disease 2019 (COVID-19) vaccination: a US cohort. Obstet Gynecol. 2022;139:481-489.
- Regidor PA, Colli E, Palacios S. Overall and bleeding-related discontinuation rates of a new oral contraceptive containing 4 mg drospirenone only in a 24/4 regimen and comparison to 0.075 mg desogestrel. Gynecol Endocrinol. 2021;37:1121-1127.
- Oderkerk TJ, van de Kar MMA, van der Zanden CHM, et al. T he combined use of endometrial ablation or resection and levonorgestrel-releasing intrauterine system in women with heavy menstrual bleeding: a systematic review. Acta Obstet Gynecol Scand. 2021;100:1779-1787.
- van den Brink MJ, Beelen P, Herman MC, et al. The levonorgestrel intrauterine system versus endometrial ablation for heavy menstrual bleeding: a cost-effectiveness analysis. BJOG. 2021;128:2003-2011.
- Blumfiel G. Why reports of menstrual changes after COVID vaccine are tough to study. NPR. August 9, 2021. Accessed August 30, 2022. https://www.npr.org/sections/health-shots/2021/08/09/1024190379/covid-vaccine-period-menstrual-cycle-research
- Lee KMN, Junkins EJ, Fatima UA, et al. Characterizing menstrual bleeding changes occurring after SARSCoV-2 vaccinations. MedRxiv. February 11, 2022. doi:10.1101/2021.10.11.21264863
- Edelman A, Boniface ER, Benhar W, et al. Association between menstrual cycle length and coronavirus disease 2019 (COVID-19) vaccination: a US cohort. Obstet Gynecol. 2022;139:481-489.
- Regidor PA, Colli E, Palacios S. Overall and bleeding-related discontinuation rates of a new oral contraceptive containing 4 mg drospirenone only in a 24/4 regimen and comparison to 0.075 mg desogestrel. Gynecol Endocrinol. 2021;37:1121-1127.
- Oderkerk TJ, van de Kar MMA, van der Zanden CHM, et al. T he combined use of endometrial ablation or resection and levonorgestrel-releasing intrauterine system in women with heavy menstrual bleeding: a systematic review. Acta Obstet Gynecol Scand. 2021;100:1779-1787.
- van den Brink MJ, Beelen P, Herman MC, et al. The levonorgestrel intrauterine system versus endometrial ablation for heavy menstrual bleeding: a cost-effectiveness analysis. BJOG. 2021;128:2003-2011.
The SCOTUS 2021–2022 Term: Decisions and analysis
The 2021–2022 US Supreme Court Term was a blockbuster medical Term. The bookends of the Term were COVID-19 vaccinations and abortion rights. Between the bookends were Medicare reimbursement, criminal liability for prescribing controlled substances, gun control, and carbon dioxide emissions. In this article, we focus on the significant medical issues, briefly note other important decisions, and consider the implications of this Term.
Abortion decisions
Dobbs v Jackson Women’s Health Organization1 was the most controversial decision and, for ObGyns, perhaps the most important decision in decades. The basic holding of the case can be stated simply: Roe v Wade2 and Planned Parenthood of Southeastern Pennsylvania v Casey3 (which essentially created a constitutional right to abortion) are overruled. The law related to abortion is for the states and Congress to determine, not federal courts. (For a review of earlier reproductive freedom cases in the Court, see our previous article, “The Supreme Court and reproductive rights.”4)
Dobbs arose from a Mississippi statute that made it illegal to perform abortions after 15 weeks of gestation, well before viability. Six members of the Court held that the Mississippi law was constitutional and 3 would have struck down the state law. There were 5 opinions, covering a total of 213 pages in the U.S. Reports. The Court fell into 4 camps, ranging from the most to the least protective of abortion rights, as follows:
- Three justices (Breyer, Kagan, and Sotomayor) voted to strike down the Mississippi statute and uphold Roe and Casey and wrote a joint dissent. They believe the Constitution makes abortion an issue “off limits to majority rule.” They also warned that other areas of “substantive due process” (discussed below), including contraception and same-sex marriage, might be under threat.
- The Chief Justice voted to uphold the statute but wanted an incremental approach; that is, not to overturn Roe and Casey entirely in this case because the Dobbs case required the Court only to determine the more limited question of whether the 15-week limit on abortion was constitutional. He found that the viability standard did not make sense, but he suggested that the Court “leave for another day” whether to overturn Roe.
- Five justices joined the opinion to uphold the statute and overturn Roe. Justice Alito wrote the decision joined by Justices Thomas, Kavanaugh, Gorsuch, and Barrett. They found that a right to abortion was not “deeply rooted in our Nation’s history,” as evidenced by the fact that when the 14th Amendment was adopted, abortion was a criminal offense in most states and not a protected right in any state. In 2 lengthy appendices, the Court reviewed the criminalization of abortion in the states in 1868 and in the territories that later became states. Even when Roe was decided in 1973, abortion was not “deeply rooted” because it was not generally legal in the states. Justice Kavanaugh joined this opinion and wrote separately to emphasize that the majority opinion does not outlaw abortion, but rather leaves the issue to “the people and their representatives.” He also emphasized that the case did not overturn all of the substantive due process cases.
- Justice Thomas would have gone further and abandoned “substantive due process” completely.
The constitutional issue
The majority said that the issue before the Court was not whether the law should permit or prohibit abortions—that is a question for the political branches. Rather, the question was only whether the Constitution precludes the political branches from allowing abortions. There is no mention of abortion in the Constitution and no specific reference to a right to privacy that includes medical decisions. A central constitutional question has been to identify where exactly in the Constitution the right to privacy resides. The Court has generally used “substantive due process” to locate privacy rights. The 14th Amendment provides, in part, that no state may “deprive any person of life, liberty, or property, without due process of law.” “Process” generally refers to procedural protections, but the Court sometimes has used it to encompass substantive rights (for example, privacy)—hence, “substantive due process.”
Over the decades, the legitimacy of substantive due process has remained controversial. Justice Thomas called it an “oxymoron” to turn “process” into substantive rights. And its use has a somewhat checkered history. For nearly 50 years (1890–1937), it was used to preclude states from protecting employees (for example, hour and wage laws violated “the right to contract”) and was discredited. More recently the Court has used substantive due process to protect contraception access, abortion, and same-sex marriages.
A critical question is knowing what rights substantive due process protects. The Court sometimes has said that it protects rights “deeply rooted in the Nation’s history and traditions” and “implicit in the concept of ordered liberty,”5 although in other cases suggested a more ambiguous definition.6 The next constitutional question is how to state or define the right to be protected. For example, is it the right to intimately personal decisions, bodily integrity, reproductive choice, abortion, or late-term abortion? Some of those may be deeply rooted in history and traditions (intimate decisions), and others not so much (late-term abortion). Finally, a question is whether a substantive right is defined at the time the 14th Amendment was adopted (1868) or now—is it a “living Constitution” that, without much guidance, means whatever 5 justices believe at the moment, or is it a Constitution grounded in the distant past?
The future of substantive due process is uncertain following Dobbs. Although the majority said it was not disclaiming substantive due process, the dissent said it doubted that claim because other rights are “part of the same constitutional fabric” (substantive due process). The Court might, in future cases, find some other constitutional provision in which to ground rights. The source of those rights might be the 9th Amendment (in addition to the Constitution’s enumerated rights, there are “others retained by the people”) or another provision of the 14th (“No State shall make or enforce any law which shall abridge the privileges or immunities of citizens of the United States…”). Each of these possibilities has its problems, many of which are similar to substantive due process, but they avoid the “oxymoron” issue.
Among the other important cases this Term, the Court made these determinations:
- Held that the 2nd Amendment, as applied to the states through the 14th Amendment, includes a general right to carry a gun for self-defense outside the home.1 It struck down a New York law that required people to show a special need to have and carry a gun.
- Determined that the US Environmental Protection Agency exceeded the authority Congress had granted it with a “Clean Power Plan” that was intended to reduce carbon dioxide emissions.2 It is up to Congress, not the agency, to expand agency authority.
- Gave trial courts discretion in determining whether (and under what conditions) children in international custody disputes must be returned to their home countries where there is a serious risk of harm to them.3
- Held that there is an implied right of action to sue medical providers for disability discrimination, but under the Rehabilitation Act and the Affordable Care Act the damages do not include emotional harm.4
- Decided several “free exercise of religion” cases, and in each found the state had violated religious rights, holding that: A state improperly prevented religious schools from being eligible for a state tuition grant system,5 a coach was wrongfully fired for kneeling in prayer following football games,6 Boston denied free speech in allowing other organizations to fly their flags but denying a Christian flag to be displayed,7 and a state must permit prisoners to have a spiritual advisor to be present and pray and touch them during their execution.8
- Held that the administration’s rescission of the “stay in Mexico” immigration policy was permitted by existing statutes.9
References
1. New York State Rifle & Pistol Association, Inc. v Bruen, 20-843, decided June 23, 2022. https://www.supremecourt.gov/opinions/21pdf/20-843_7j80.pdf
2. West Virginia v Environmental Protection Agency, 20-1530, decided June 30, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1530_new_l537.pdf
3. Golan v Saada, 20-1034, decided June 15, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1034_b8dg.pdf
4. Cummings v Premier Rehab Keller, 20-219, decided April 28, 2022. https://www.supremecourt.gov/opinions/21pdf/20-219_1b82.pdf
5. Carson v Makin, 20-1088, decided June 21, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1088_dbfi.pdf
6. Kennedy v Bremerton School District., 21-418, decided June 27, 2022. https://www.supremecourt.gov/opinions/21pdf/21-418_new_onkq.pdf
7. Shurtleff v Boston, 20-1800, decided May 2, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1800_7lho.pdf
8. Ramirez v Collier, 21-5592, decided March 24, 2022. https://www.supremecourt.gov/opinions/21pdf/21-5592_feah.pdf
9. Biden v Texas, 21-9 54, decided June 30, 2022. https://www.supremecourt.gov/opinions/21pdf/21-954_7l48.pdf
Continue to: ObGyn briefs in the case...
ObGyn briefs in the case
The medical profession filed several amicus curiae briefs in the Dobbs case. (These are “friends of the court” briefs filed by nonparties to the litigation. The purpose is to give a court a perspective on the case not presented by the parties.) The American College of Obstetricians and Gynecologists (ACOG) took the lead in filing an amicus brief.7 Nearly 2 dozen other medical organizations joined the brief, including the American Academy of Pediatrics, American College of Osteopathic Obstetricians and Gynecologists, American Gynecological and Obstetrical Society, American Society for Reproductive Medicine, Council of University Chairs of Obstetrics and Gynecology, North American Society for Pediatric and Adolescent Gynecology, Society for Academic Specialists in General Obstetrics and Gynecology, Society of Gynecologic Oncology, and Society of OB/GYN Hospitalists.
The brief argued that abortion is a safe procedure, an abortion ban would harm the health of pregnant patients, and it would undermine the physician-patient relationship and interfere with patient autonomy. It also discussed the issue of fetal pain,8 telling the Court that “Every major medical organization that has examined the issue of fetal pain and peer-reviewed studies on the matter have consistently concluded that pre-viability abortion does not result in fetal pain perception.”9 The brief was cited in the dissent for the fact that “About 18 percent of pregnancies in this country end in abortion, and about one-quarter of American women will have an abortion before the age of 45.”10
The Court received a different view from an amicus brief filed by the American Association of Pro-Life Obstetricians and Gynecologists.11 It told the Court that abortion, especially later-term, poses health risks: the abortion process itself may injure the woman, abortion puts women at risk for future preterm births, later-term abortion raises a woman’s risk of developing breast cancer, and abortions (especially those later in the pregnancy) are linked to a greater risk of psychological harm.12 The brief also noted that 93% of obstetrician-gynecologists do not perform abortions, and “abortion has been deemed contrary to sound medicine for thousands of years” (citing the Hippocratic oath).13 The brief was not cited by the Court.
Many other medical and pro-life medical groups presented amicus briefs. A list of and links to all the briefs is available on the SCOTUSblog website at https://www.scotusblog.com/case-files/cases/dobbs-v-jackson-womens-health-organization/.
Ramifications
The Court decision does not make abortion illegal but allows states (and possibly Congress) to decide whether, when, and how abortions may be performed. Some states may ban most abortions (making it illegal to have or to perform abortions). Thirteen states had “trigger laws” to go into effect limiting abortion if the Court permitted such limitations. Most of those states were almost immediately entangled in lawsuits challenging the state laws. Some states, for example, have privacy provisions in their state constitution that state courts could interpret as allowing abortion, thereby voiding the state statutes prohibiting abortion.
At least a few states have abortion laws still on the books that were passed decades ago (perhaps before Roe) and were never repealed. Those laws may once again be valid, although state courts might hold that those statutes were repealed by Roe and must be passed again to be valid. Some experts anticipate that 28 states will eventually have significant limitations on abortion.
The Guttmacher Institute maintains a frequently updated table on the abortion laws in each state.14 According to one estimate, 29 states are hostile to abortion rights (or lean that way), with about 40 million women aged 13 to 44 (58% of the United States) living in states with some hostility to abortion.15 Congress may pass some national abortion laws, but that seems unlikely and there may be some limits on its ability to control private medical practice within states.
An additional legal issue will arise from medication-induced abortions, generally through the use of mifepristone and misoprostol. They now account for the majority of abortions. These medications might be used for abortion, up to about 9 weeks of pregnancy, in states prohibiting abortion. The drugs once were available only with an in-person visit, but now the US Food and Drug Administration (FDA) permits mail-order delivery. The potential exists, therefore, to circumvent states’ prohibition on abortion through mail-order postal shipments. The FDA controls the licensing of pharmaceuticals in interstate commerce, but not the practice of medicine within a state. Therefore the ability of individuals (within a state) to possess or use drugs is unclear.
The abortion wars of the last 50 years gave rise to state laws related to abortion, including consent by minors, information to parents, special informed consent, and facilities requirements. If these laws were once struck down because they were inconsistent with Roe, but were never formally repealed, they may now become legal requirements.
In the foreseeable future, abortion laws generally will not be determined by federal courts but by state law, generally legislatures. In legislative hearings, town hall meetings, and conversations with lawmakers, ObGyns should engage the topic of abortion with scientific expertise, reason, openness, and humility. It will be impossible for the profession to speak with a single voice, as the briefs filed this Term demonstrate. Where there are honest differences in science, the reasons for the different interpretations should be explainable to lay decision makers. The profession, who are not being pseudo-lobbyists, can contribute a great deal to the rational consideration of this emotional topic.
On January 27, 2022, Justice Stephen Breyer informed President Biden of his intention to retire from the Court at the end of the Term. At age 84, he was the oldest member of the Court, but he continued to be among the most active of the justices and seemed to relish the work of the Court. He had been under pressure from liberal groups to retire earlier so a successor could be confirmed by a Democratic Senate. In many ways he was the Renaissance man of the Court: he spoke fluent French, wrote books, and famously sprinkled his questions with complex and funny hypotheticals.
Justice Breyer was a law professor before becoming a judge and enjoyed presentations to many groups, from children to law professors. He loved the Court and defended it—most recently against partisan attacks from both the right and the left. In the decisions of the Court, he was one of the more liberal justices. He had, for example, indicated that the death penalty is unconstitutional.
In his January retirement letter, he said that he would step down at the end of the Term if his replacement had been appointed and confirmed. She had. The new justice had clerked for Justice Breyer in 1999–2000.
Ketanji Brown Jackson was nominated by President Biden on February 28, confirmed by the Senate on April 7 by a 53–47 margin, and sworn in on June 30, 2022. Justice Jackson had previously been a federal district court judge and on the Court of Appeals for the D.C. Circuit. She attended Harvard-Radcliffe College and received her law degree from Harvard Law School. She worked as a criminal defense attorney and was active in the US Sentencing Commission.
Continue to: What is a practitioner to do?...
What is a practitioner to do?
For many practitioners, the Dobbs decision will have little effect because their state laws are consistent with Roe, and the legislature is not going to change the law. They may, of course, see an influx of patients from other states (that restrict abortion) seeking treatment. At the other extreme, in some states, most abortions will become prohibited. State courts may ease the restrictions. In many states, there will be an ongoing battle over when abortion is legal and when it is not, resulting in shifting laws and regulations. Keeping up with the shifts that affect practice will be a challenge.
All states are likely to permit abortions “to save the life of the mother,” and many will have a version of “to preserve the health of the mother.” Other exceptions may be for pregnancy resulting from rape or incest or in the case of serious fetal abnormality. ObGyns, of course, will be called on to certify that one of these exceptions exists. Determining that pregnancy resulted from rape or incest, of course, can be challenging. Before Roe, there was a cottage industry opining that pregnancy seriously affected the health of the mother, which often involved physical manifestations of mental health. ObGyns in some states may be asked once again to make such determinations.
Laws not directly related to abortions will, in some states, be changed as a way of discouraging abortion. For example, child abuse reporting laws may be modified to require reporting of any known or suspected abortion or attempted abortion, and medical licensing standards may make it a violation to participate in or facilitate abortion in any way.
Particularly in states where the rules keep shifting, practitioners must keep up with the current law. Professional organizations can help with that, but there is no substitute for practitioners having an ongoing professional relationship with an attorney who has expertise in health law.
Other abortion decisions this Term
In other abortion decisions this Term, the Court refused to suspend a Texas law that prohibited abortions after a fetal heartbeat could be detected.16 The law has remarkable enforcement mechanisms that preclude state officers from enforcing it; instead, it creates what amounts to a private attorney general (PAG) provision that allows private citizens to file suit against anyone performing or assisting in performing abortions. This PAG made pre-enforcement challenges to the law difficult.17
In a Kentucky case, the Court allowed the Kentucky attorney general to intervene in a case that challenged a Kentucky law that prohibits physicians from using dilation and evacuation procedures to end second-trimester pregnancies.18
Criminal convictions for physicians’ overprescription of controlled substances
Perhaps the least sympathetic of the physicians involved with the Court this Term were the 2 in Ruan v U.S.19 Their trials indicate that Dr. Ruan’s clinic issued more than 300,000 controlled substance prescriptions over 4 years and was one of the most frequent prescribers of fentanyl. Dr. Kahn prescribed controlled substances without an examination, falsified notes, and sold controlled substances for cash and guns.20
Both physicians were convicted of “knowingly or intentionally” dispensing a controlled substance without authorization.21 They were authorized to prescribe drugs, but only “for a legitimate medical purpose.”22 Appeals to their respective Circuit courts confirmed their convictions. The Supreme Court, however, held that to convict them, the government must prove that they knowingly or intentionally acted in an unauthorized manner. That proof can be by circumstantial evidence, but it must be beyond a reasonable doubt.
Health care reimbursement
Hospitals won one and lost one Medicare-Medicaid reimbursement case that involved payments for low-income patients.
In the loss, the Court held that the US Department of Health and Human Services (HHS) properly calculated the disproportionate share adjustments (DSH), or Medicare fraction,23 that provides a supplemental payment for hospitals with a large proportion of low-income patients. The lower DSH payments calculated by HHS were upheld, thereby reducing the number of hospitals receiving DSH payments and decreasing the amounts others will receive.
The win involved payments for prescription drugs that hospitals provide to outpatients in safety-net hospitals.24 HHS determined that it was overpaying hospitals for drugs and cut the reimbursement rate. The Court held that before HHS can change the drug rate, it must conduct a survey of hospitals regarding actual costs. It had not done that, so the rate reduction was not permitted by the law.
An accidental disincentive to (some) malpractice suits
Medicaid requires states to obtain part of a tort recovery that recipients obtain if Medicaid is covering medical expenses related to their injuries. In implementing that law, a state may provide a disincentive for injured beneficiaries to file malpractice cases. At issue was a Florida law that provided the Medicaid state would take 37.5% of the beneficiary’s total tort recovery (being one-half of the recovery after deducting 25% for attorney’s fees and costs). In a 7-2 decision, the Court upheld the Florida law.25
The disincentive to filing a lawsuit is that the state is taking 37.5%, plus contingency fee attorneys will typically take 33.3% (and there will be some fees). This is especially true when there is a state cap on noneconomic damages. In the case the Court decided, the plaintiff received a settlement of $850,000. If we assume a typical contingency fee, less the state’s Medicaid claim of $300,000, the plaintiff possibly received $266,667. That is not trivial, but it is only 31% of the settlement.
The Medicaid expectation of reimbursement and the Florida approach, however, impose heavy burdens on severely injured beneficiaries. The plaintiff had catastrophic injuries and was in a vegetative state. There are some things Medicaid does not pay for, as well as nonmedical expenses. The amount left for such expenses is likely well below what the family will need.
Continue to: COVID-19 vaccinations...
COVID-19 vaccinations
Had it not been for the abortion decisions, 2021–2022 might have been “the COVID Term.” Two of the most anticipated decisions involved mandatory vaccinations (or masking/testing instead). The question in each of these cases was whether Congress had authorized 2 federal agencies to issue the emergency regulations requiring vaccination. Emergency regulations are held to higher standards because they bypass the usual protections of the Administrative Procedure Act.
One case involved a regulation issued by the Occupational Safety and Health Administration (OSHA) that employers (with more than 100 employees) must require their employees to be vaccinated. In a 6-3 decision, the Court held that OSHA did not have the authority to enforce this as an emergency regulation. The other case was a regulation issued by HHS that health care institutions receiving Medicare and Medicaid funding must require all staff to be vaccinated.26 In a 5-4 decision, the Court upheld this emergency regulation because of the very broad authority Congress had given HHS to ensure the safety of patients and the quality of Medicare- and Medicaid-funded programs.27
In another case, in the shadow docket (orders and opinions in cases without full arguments), the Court struck down the Centers for Disease Control and Prevention’s eviction moratorium.28 The Court said the government claimed “a breathtaking amount of authority” that Congress did not intend. In other shadow docket cases, the Court refused to hold unconstitutional state laws that require COVID-19 vaccination but did not have religious exemptions.29
Analysis of this Term
It was an extraordinary Term. The Court decided 66 cases (excluding most cases in the shadow docket), a low number historically. Not only were there many seminal cases but also the Court appears to be shifting toward a new direction. That direction may be oriented more toward the original understanding of the words of the Constitution and statutes and less toward policy; Congress rather than administrative agencies; racial nondiscrimination rather than preferences; and the free exercise rather than the establishment of religion. Whether there is such a shift or not, of course, only time will tell.
Chief Justice Roberts and Justice Kavanaugh were in the majority most often (95% of the cases), followed by Justices Barrett (90%), Alito (85%), Thomas (80%), and Gorsuch (75%). Justices Kagan (69%) and Breyer (68%) were not far behind. Justice Sotomayor was in the majority 58%. The Court was unanimous 29% of the time, well below the decade average (43%), and 6-3 accounted for 30% of the decisions.
A major, potentially scarring, event this Term was the leak of an early draft of the majority opinion in Dobbs. Although leaks have occurred before, the early leak of an opinion was unprecedented. It will almost inevitably change the openness and candor within the Court and the justices’ clerks. Although not unprecedented, the attempt on the life of Justice Kavanaugh and the organized efforts to harass some justices in their homes are likely to have lasting impact. Almost certainly it means that justices and their families will have constant security and their movements and connection with the general public will become less frequent, which is sad for the justices and our democracy.
Looking toward the next Term
When the Court next convenes, Justice Ketanji Brown Jackson will take her seat on the left end of the Court (the traditional seat for a new justice, not a commentary on judicial philosophy). The Court has already taken many cases, including issues about university affirmative action programs, web designers and same-sex couples, redistricting and voting rights, DNA testing in criminal cases, and overtime pay for someone making over $200,000 per year. It begins Monday, October 3, and promises to be another interesting Term. ●
- Dobbs v Jackson Women’s Health Organization, 19-1392, decided June 24, 2022. https://www.supremecourt.gov /opinions/21pdf/19-1392_6j37.pdf
- Roe v Wade, 410 U.S. 113, 163 (1973).
- Planned Parenthood of Southeastern Pennsylvania v Casey, 505 U.S. 833 (1992).
- Smith SR, Sanfilippo JR. The Supreme Court and reproductive rights. OBG Manag. 2022;34(1):36-41, 46. https://cdn.mdedge. com/files/s3fs-public/issues/articles/obgm0340136_smith.pdf
- Washington v Glucksberg, 521 U.S. 702 (1997).
- Obergefell v Hodges, 576 U.S. 644, 654-70 (2015).
- Brief of amici curiae of American College of Obstetricians and Gynecologists, American Medical Association, et al, in Dobbs v Jackson Women’s Health Organization, in Support of Respondents (Sep. 2021). https://www.supremecourt .gov/DocketPDF/19/19-1392/193074/20210920174518042 _19-1392%20bsacACOGetal.pdf
- Id. at 8, 13-15.
- Id. at 14.
- Justices Breyer, Kagan, and Sotomayor, dissenting, at 48, note 22.
- Brief for American Association of Pro-Life Obstetricians And Gynecologists as Amicus Curiae, in Dobbs v Jackson Women’s Health Organization, in Support of Petitioners (July 2021). https://www.supremecourt.gov /DocketPDF/19/19-1392/185350/20210729163532595_No. %2019-1392%20-%20American%20Association%20of%20 Pro-Life%20Obstetricians%20and%20Gynecologists%20-%20 Amicus%20Brief%20in%20Support%20of%20Petitioner%20-%20 7-29-21.pdf
- Id. at 3-4, 7-29.
- Id. at 30.
- Guttmacher Institute. An overview of abortion laws. July 11, 2022. https://www.guttmacher.org/state-policy/explore/overview -abortion-laws
- Guttmacher Institute. State abortion policy landscape: from hostile to supportive. Dec. 2020. https://www .guttmacher.org/article/2019/08/state-abortion-policy -landscape-hostile-supportive
- Whole Woman’s Health v Jackson, 21-463, decided Dec. 10, 2021. https://www.supremecourt.gov/opinions/21pdf/21-463_ new_8o6b.pdf
- United States v Texas, 21-588, decided Dec. 10, 2021. (Per curiam, Sotomayor dissenting). https://www.supremecourt.gov /opinions/21pdf/21-588_c07d.pdf
- Cameron v EMW Women’s Surgical Center, 20-601, decided Mar. 3, 2022. https://www.supremecourt.gov/opinions/21pdf/20-601 _new_g20h.pdf
- Xiulu Ruan v United States, 20-1410, decided June 27, 2022. https:// www.supremecourt.gov/opinions/21pdf/20-1410_1an2.pdf
- Adam Liptak. Supreme Court sides with doctors accused of running pill mills. The New York Times. June 27, 2022. https://www .nytimes.com/2022/06/27/us/politics/supreme-court-controlled -substance-act.html
- 84 Stat. 1260, 21 U.S.C. §841(a).
- 21 CFR §1306.04(a) (2021).
- Becerra v Empire Health Foundation, For Valley Hospital Medical Center, 20-1312, decided June 24, 2022. https://www.supremecourt .gov/opinions/21pdf/20-1312_j42l.pdf
- American Hospital Association v Becerra, 20-1114, decided June 15, 2022. https://www.supremecourt.gov/opinions/21pdf/20 -1114_09m1.pdf
- Gallardo v Marstiller, 20-1263, decided June 6, 2022. https:// www.supremecourt.gov/opinions/21pdf/20-1263_new_hfci.pdf
- National Federation of Independent Business v Department of Labor, Occupational Safety and Health Administration, 21A244, decided Jan. 13, 2022. https://www.supremecourt.gov /opinions/21pdf/21a244_hgci.pdf
- Biden v Missouri, 21A240, decided Jan. 13, 2022. https://www .supremecourt.gov/opinions/21pdf/21a240_d18e.pdf
- Alabama Association of Realtors v Department of Health and Human Services, 21A23, decided Aug. 26, 2021. https://www .supremecourt.gov/opinions/20pdf/21a23_ap6c.pdf
- Does v Mills, 21A90, decided Oct. 29, 2021. https://www .supremecourt.gov/opinions/21pdf/21a90_6j37.pdf
The 2021–2022 US Supreme Court Term was a blockbuster medical Term. The bookends of the Term were COVID-19 vaccinations and abortion rights. Between the bookends were Medicare reimbursement, criminal liability for prescribing controlled substances, gun control, and carbon dioxide emissions. In this article, we focus on the significant medical issues, briefly note other important decisions, and consider the implications of this Term.
Abortion decisions
Dobbs v Jackson Women’s Health Organization1 was the most controversial decision and, for ObGyns, perhaps the most important decision in decades. The basic holding of the case can be stated simply: Roe v Wade2 and Planned Parenthood of Southeastern Pennsylvania v Casey3 (which essentially created a constitutional right to abortion) are overruled. The law related to abortion is for the states and Congress to determine, not federal courts. (For a review of earlier reproductive freedom cases in the Court, see our previous article, “The Supreme Court and reproductive rights.”4)
Dobbs arose from a Mississippi statute that made it illegal to perform abortions after 15 weeks of gestation, well before viability. Six members of the Court held that the Mississippi law was constitutional and 3 would have struck down the state law. There were 5 opinions, covering a total of 213 pages in the U.S. Reports. The Court fell into 4 camps, ranging from the most to the least protective of abortion rights, as follows:
- Three justices (Breyer, Kagan, and Sotomayor) voted to strike down the Mississippi statute and uphold Roe and Casey and wrote a joint dissent. They believe the Constitution makes abortion an issue “off limits to majority rule.” They also warned that other areas of “substantive due process” (discussed below), including contraception and same-sex marriage, might be under threat.
- The Chief Justice voted to uphold the statute but wanted an incremental approach; that is, not to overturn Roe and Casey entirely in this case because the Dobbs case required the Court only to determine the more limited question of whether the 15-week limit on abortion was constitutional. He found that the viability standard did not make sense, but he suggested that the Court “leave for another day” whether to overturn Roe.
- Five justices joined the opinion to uphold the statute and overturn Roe. Justice Alito wrote the decision joined by Justices Thomas, Kavanaugh, Gorsuch, and Barrett. They found that a right to abortion was not “deeply rooted in our Nation’s history,” as evidenced by the fact that when the 14th Amendment was adopted, abortion was a criminal offense in most states and not a protected right in any state. In 2 lengthy appendices, the Court reviewed the criminalization of abortion in the states in 1868 and in the territories that later became states. Even when Roe was decided in 1973, abortion was not “deeply rooted” because it was not generally legal in the states. Justice Kavanaugh joined this opinion and wrote separately to emphasize that the majority opinion does not outlaw abortion, but rather leaves the issue to “the people and their representatives.” He also emphasized that the case did not overturn all of the substantive due process cases.
- Justice Thomas would have gone further and abandoned “substantive due process” completely.
The constitutional issue
The majority said that the issue before the Court was not whether the law should permit or prohibit abortions—that is a question for the political branches. Rather, the question was only whether the Constitution precludes the political branches from allowing abortions. There is no mention of abortion in the Constitution and no specific reference to a right to privacy that includes medical decisions. A central constitutional question has been to identify where exactly in the Constitution the right to privacy resides. The Court has generally used “substantive due process” to locate privacy rights. The 14th Amendment provides, in part, that no state may “deprive any person of life, liberty, or property, without due process of law.” “Process” generally refers to procedural protections, but the Court sometimes has used it to encompass substantive rights (for example, privacy)—hence, “substantive due process.”
Over the decades, the legitimacy of substantive due process has remained controversial. Justice Thomas called it an “oxymoron” to turn “process” into substantive rights. And its use has a somewhat checkered history. For nearly 50 years (1890–1937), it was used to preclude states from protecting employees (for example, hour and wage laws violated “the right to contract”) and was discredited. More recently the Court has used substantive due process to protect contraception access, abortion, and same-sex marriages.
A critical question is knowing what rights substantive due process protects. The Court sometimes has said that it protects rights “deeply rooted in the Nation’s history and traditions” and “implicit in the concept of ordered liberty,”5 although in other cases suggested a more ambiguous definition.6 The next constitutional question is how to state or define the right to be protected. For example, is it the right to intimately personal decisions, bodily integrity, reproductive choice, abortion, or late-term abortion? Some of those may be deeply rooted in history and traditions (intimate decisions), and others not so much (late-term abortion). Finally, a question is whether a substantive right is defined at the time the 14th Amendment was adopted (1868) or now—is it a “living Constitution” that, without much guidance, means whatever 5 justices believe at the moment, or is it a Constitution grounded in the distant past?
The future of substantive due process is uncertain following Dobbs. Although the majority said it was not disclaiming substantive due process, the dissent said it doubted that claim because other rights are “part of the same constitutional fabric” (substantive due process). The Court might, in future cases, find some other constitutional provision in which to ground rights. The source of those rights might be the 9th Amendment (in addition to the Constitution’s enumerated rights, there are “others retained by the people”) or another provision of the 14th (“No State shall make or enforce any law which shall abridge the privileges or immunities of citizens of the United States…”). Each of these possibilities has its problems, many of which are similar to substantive due process, but they avoid the “oxymoron” issue.
Among the other important cases this Term, the Court made these determinations:
- Held that the 2nd Amendment, as applied to the states through the 14th Amendment, includes a general right to carry a gun for self-defense outside the home.1 It struck down a New York law that required people to show a special need to have and carry a gun.
- Determined that the US Environmental Protection Agency exceeded the authority Congress had granted it with a “Clean Power Plan” that was intended to reduce carbon dioxide emissions.2 It is up to Congress, not the agency, to expand agency authority.
- Gave trial courts discretion in determining whether (and under what conditions) children in international custody disputes must be returned to their home countries where there is a serious risk of harm to them.3
- Held that there is an implied right of action to sue medical providers for disability discrimination, but under the Rehabilitation Act and the Affordable Care Act the damages do not include emotional harm.4
- Decided several “free exercise of religion” cases, and in each found the state had violated religious rights, holding that: A state improperly prevented religious schools from being eligible for a state tuition grant system,5 a coach was wrongfully fired for kneeling in prayer following football games,6 Boston denied free speech in allowing other organizations to fly their flags but denying a Christian flag to be displayed,7 and a state must permit prisoners to have a spiritual advisor to be present and pray and touch them during their execution.8
- Held that the administration’s rescission of the “stay in Mexico” immigration policy was permitted by existing statutes.9
References
1. New York State Rifle & Pistol Association, Inc. v Bruen, 20-843, decided June 23, 2022. https://www.supremecourt.gov/opinions/21pdf/20-843_7j80.pdf
2. West Virginia v Environmental Protection Agency, 20-1530, decided June 30, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1530_new_l537.pdf
3. Golan v Saada, 20-1034, decided June 15, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1034_b8dg.pdf
4. Cummings v Premier Rehab Keller, 20-219, decided April 28, 2022. https://www.supremecourt.gov/opinions/21pdf/20-219_1b82.pdf
5. Carson v Makin, 20-1088, decided June 21, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1088_dbfi.pdf
6. Kennedy v Bremerton School District., 21-418, decided June 27, 2022. https://www.supremecourt.gov/opinions/21pdf/21-418_new_onkq.pdf
7. Shurtleff v Boston, 20-1800, decided May 2, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1800_7lho.pdf
8. Ramirez v Collier, 21-5592, decided March 24, 2022. https://www.supremecourt.gov/opinions/21pdf/21-5592_feah.pdf
9. Biden v Texas, 21-9 54, decided June 30, 2022. https://www.supremecourt.gov/opinions/21pdf/21-954_7l48.pdf
Continue to: ObGyn briefs in the case...
ObGyn briefs in the case
The medical profession filed several amicus curiae briefs in the Dobbs case. (These are “friends of the court” briefs filed by nonparties to the litigation. The purpose is to give a court a perspective on the case not presented by the parties.) The American College of Obstetricians and Gynecologists (ACOG) took the lead in filing an amicus brief.7 Nearly 2 dozen other medical organizations joined the brief, including the American Academy of Pediatrics, American College of Osteopathic Obstetricians and Gynecologists, American Gynecological and Obstetrical Society, American Society for Reproductive Medicine, Council of University Chairs of Obstetrics and Gynecology, North American Society for Pediatric and Adolescent Gynecology, Society for Academic Specialists in General Obstetrics and Gynecology, Society of Gynecologic Oncology, and Society of OB/GYN Hospitalists.
The brief argued that abortion is a safe procedure, an abortion ban would harm the health of pregnant patients, and it would undermine the physician-patient relationship and interfere with patient autonomy. It also discussed the issue of fetal pain,8 telling the Court that “Every major medical organization that has examined the issue of fetal pain and peer-reviewed studies on the matter have consistently concluded that pre-viability abortion does not result in fetal pain perception.”9 The brief was cited in the dissent for the fact that “About 18 percent of pregnancies in this country end in abortion, and about one-quarter of American women will have an abortion before the age of 45.”10
The Court received a different view from an amicus brief filed by the American Association of Pro-Life Obstetricians and Gynecologists.11 It told the Court that abortion, especially later-term, poses health risks: the abortion process itself may injure the woman, abortion puts women at risk for future preterm births, later-term abortion raises a woman’s risk of developing breast cancer, and abortions (especially those later in the pregnancy) are linked to a greater risk of psychological harm.12 The brief also noted that 93% of obstetrician-gynecologists do not perform abortions, and “abortion has been deemed contrary to sound medicine for thousands of years” (citing the Hippocratic oath).13 The brief was not cited by the Court.
Many other medical and pro-life medical groups presented amicus briefs. A list of and links to all the briefs is available on the SCOTUSblog website at https://www.scotusblog.com/case-files/cases/dobbs-v-jackson-womens-health-organization/.
Ramifications
The Court decision does not make abortion illegal but allows states (and possibly Congress) to decide whether, when, and how abortions may be performed. Some states may ban most abortions (making it illegal to have or to perform abortions). Thirteen states had “trigger laws” to go into effect limiting abortion if the Court permitted such limitations. Most of those states were almost immediately entangled in lawsuits challenging the state laws. Some states, for example, have privacy provisions in their state constitution that state courts could interpret as allowing abortion, thereby voiding the state statutes prohibiting abortion.
At least a few states have abortion laws still on the books that were passed decades ago (perhaps before Roe) and were never repealed. Those laws may once again be valid, although state courts might hold that those statutes were repealed by Roe and must be passed again to be valid. Some experts anticipate that 28 states will eventually have significant limitations on abortion.
The Guttmacher Institute maintains a frequently updated table on the abortion laws in each state.14 According to one estimate, 29 states are hostile to abortion rights (or lean that way), with about 40 million women aged 13 to 44 (58% of the United States) living in states with some hostility to abortion.15 Congress may pass some national abortion laws, but that seems unlikely and there may be some limits on its ability to control private medical practice within states.
An additional legal issue will arise from medication-induced abortions, generally through the use of mifepristone and misoprostol. They now account for the majority of abortions. These medications might be used for abortion, up to about 9 weeks of pregnancy, in states prohibiting abortion. The drugs once were available only with an in-person visit, but now the US Food and Drug Administration (FDA) permits mail-order delivery. The potential exists, therefore, to circumvent states’ prohibition on abortion through mail-order postal shipments. The FDA controls the licensing of pharmaceuticals in interstate commerce, but not the practice of medicine within a state. Therefore the ability of individuals (within a state) to possess or use drugs is unclear.
The abortion wars of the last 50 years gave rise to state laws related to abortion, including consent by minors, information to parents, special informed consent, and facilities requirements. If these laws were once struck down because they were inconsistent with Roe, but were never formally repealed, they may now become legal requirements.
In the foreseeable future, abortion laws generally will not be determined by federal courts but by state law, generally legislatures. In legislative hearings, town hall meetings, and conversations with lawmakers, ObGyns should engage the topic of abortion with scientific expertise, reason, openness, and humility. It will be impossible for the profession to speak with a single voice, as the briefs filed this Term demonstrate. Where there are honest differences in science, the reasons for the different interpretations should be explainable to lay decision makers. The profession, who are not being pseudo-lobbyists, can contribute a great deal to the rational consideration of this emotional topic.
On January 27, 2022, Justice Stephen Breyer informed President Biden of his intention to retire from the Court at the end of the Term. At age 84, he was the oldest member of the Court, but he continued to be among the most active of the justices and seemed to relish the work of the Court. He had been under pressure from liberal groups to retire earlier so a successor could be confirmed by a Democratic Senate. In many ways he was the Renaissance man of the Court: he spoke fluent French, wrote books, and famously sprinkled his questions with complex and funny hypotheticals.
Justice Breyer was a law professor before becoming a judge and enjoyed presentations to many groups, from children to law professors. He loved the Court and defended it—most recently against partisan attacks from both the right and the left. In the decisions of the Court, he was one of the more liberal justices. He had, for example, indicated that the death penalty is unconstitutional.
In his January retirement letter, he said that he would step down at the end of the Term if his replacement had been appointed and confirmed. She had. The new justice had clerked for Justice Breyer in 1999–2000.
Ketanji Brown Jackson was nominated by President Biden on February 28, confirmed by the Senate on April 7 by a 53–47 margin, and sworn in on June 30, 2022. Justice Jackson had previously been a federal district court judge and on the Court of Appeals for the D.C. Circuit. She attended Harvard-Radcliffe College and received her law degree from Harvard Law School. She worked as a criminal defense attorney and was active in the US Sentencing Commission.
Continue to: What is a practitioner to do?...
What is a practitioner to do?
For many practitioners, the Dobbs decision will have little effect because their state laws are consistent with Roe, and the legislature is not going to change the law. They may, of course, see an influx of patients from other states (that restrict abortion) seeking treatment. At the other extreme, in some states, most abortions will become prohibited. State courts may ease the restrictions. In many states, there will be an ongoing battle over when abortion is legal and when it is not, resulting in shifting laws and regulations. Keeping up with the shifts that affect practice will be a challenge.
All states are likely to permit abortions “to save the life of the mother,” and many will have a version of “to preserve the health of the mother.” Other exceptions may be for pregnancy resulting from rape or incest or in the case of serious fetal abnormality. ObGyns, of course, will be called on to certify that one of these exceptions exists. Determining that pregnancy resulted from rape or incest, of course, can be challenging. Before Roe, there was a cottage industry opining that pregnancy seriously affected the health of the mother, which often involved physical manifestations of mental health. ObGyns in some states may be asked once again to make such determinations.
Laws not directly related to abortions will, in some states, be changed as a way of discouraging abortion. For example, child abuse reporting laws may be modified to require reporting of any known or suspected abortion or attempted abortion, and medical licensing standards may make it a violation to participate in or facilitate abortion in any way.
Particularly in states where the rules keep shifting, practitioners must keep up with the current law. Professional organizations can help with that, but there is no substitute for practitioners having an ongoing professional relationship with an attorney who has expertise in health law.
Other abortion decisions this Term
In other abortion decisions this Term, the Court refused to suspend a Texas law that prohibited abortions after a fetal heartbeat could be detected.16 The law has remarkable enforcement mechanisms that preclude state officers from enforcing it; instead, it creates what amounts to a private attorney general (PAG) provision that allows private citizens to file suit against anyone performing or assisting in performing abortions. This PAG made pre-enforcement challenges to the law difficult.17
In a Kentucky case, the Court allowed the Kentucky attorney general to intervene in a case that challenged a Kentucky law that prohibits physicians from using dilation and evacuation procedures to end second-trimester pregnancies.18
Criminal convictions for physicians’ overprescription of controlled substances
Perhaps the least sympathetic of the physicians involved with the Court this Term were the 2 in Ruan v U.S.19 Their trials indicate that Dr. Ruan’s clinic issued more than 300,000 controlled substance prescriptions over 4 years and was one of the most frequent prescribers of fentanyl. Dr. Kahn prescribed controlled substances without an examination, falsified notes, and sold controlled substances for cash and guns.20
Both physicians were convicted of “knowingly or intentionally” dispensing a controlled substance without authorization.21 They were authorized to prescribe drugs, but only “for a legitimate medical purpose.”22 Appeals to their respective Circuit courts confirmed their convictions. The Supreme Court, however, held that to convict them, the government must prove that they knowingly or intentionally acted in an unauthorized manner. That proof can be by circumstantial evidence, but it must be beyond a reasonable doubt.
Health care reimbursement
Hospitals won one and lost one Medicare-Medicaid reimbursement case that involved payments for low-income patients.
In the loss, the Court held that the US Department of Health and Human Services (HHS) properly calculated the disproportionate share adjustments (DSH), or Medicare fraction,23 that provides a supplemental payment for hospitals with a large proportion of low-income patients. The lower DSH payments calculated by HHS were upheld, thereby reducing the number of hospitals receiving DSH payments and decreasing the amounts others will receive.
The win involved payments for prescription drugs that hospitals provide to outpatients in safety-net hospitals.24 HHS determined that it was overpaying hospitals for drugs and cut the reimbursement rate. The Court held that before HHS can change the drug rate, it must conduct a survey of hospitals regarding actual costs. It had not done that, so the rate reduction was not permitted by the law.
An accidental disincentive to (some) malpractice suits
Medicaid requires states to obtain part of a tort recovery that recipients obtain if Medicaid is covering medical expenses related to their injuries. In implementing that law, a state may provide a disincentive for injured beneficiaries to file malpractice cases. At issue was a Florida law that provided the Medicaid state would take 37.5% of the beneficiary’s total tort recovery (being one-half of the recovery after deducting 25% for attorney’s fees and costs). In a 7-2 decision, the Court upheld the Florida law.25
The disincentive to filing a lawsuit is that the state is taking 37.5%, plus contingency fee attorneys will typically take 33.3% (and there will be some fees). This is especially true when there is a state cap on noneconomic damages. In the case the Court decided, the plaintiff received a settlement of $850,000. If we assume a typical contingency fee, less the state’s Medicaid claim of $300,000, the plaintiff possibly received $266,667. That is not trivial, but it is only 31% of the settlement.
The Medicaid expectation of reimbursement and the Florida approach, however, impose heavy burdens on severely injured beneficiaries. The plaintiff had catastrophic injuries and was in a vegetative state. There are some things Medicaid does not pay for, as well as nonmedical expenses. The amount left for such expenses is likely well below what the family will need.
Continue to: COVID-19 vaccinations...
COVID-19 vaccinations
Had it not been for the abortion decisions, 2021–2022 might have been “the COVID Term.” Two of the most anticipated decisions involved mandatory vaccinations (or masking/testing instead). The question in each of these cases was whether Congress had authorized 2 federal agencies to issue the emergency regulations requiring vaccination. Emergency regulations are held to higher standards because they bypass the usual protections of the Administrative Procedure Act.
One case involved a regulation issued by the Occupational Safety and Health Administration (OSHA) that employers (with more than 100 employees) must require their employees to be vaccinated. In a 6-3 decision, the Court held that OSHA did not have the authority to enforce this as an emergency regulation. The other case was a regulation issued by HHS that health care institutions receiving Medicare and Medicaid funding must require all staff to be vaccinated.26 In a 5-4 decision, the Court upheld this emergency regulation because of the very broad authority Congress had given HHS to ensure the safety of patients and the quality of Medicare- and Medicaid-funded programs.27
In another case, in the shadow docket (orders and opinions in cases without full arguments), the Court struck down the Centers for Disease Control and Prevention’s eviction moratorium.28 The Court said the government claimed “a breathtaking amount of authority” that Congress did not intend. In other shadow docket cases, the Court refused to hold unconstitutional state laws that require COVID-19 vaccination but did not have religious exemptions.29
Analysis of this Term
It was an extraordinary Term. The Court decided 66 cases (excluding most cases in the shadow docket), a low number historically. Not only were there many seminal cases but also the Court appears to be shifting toward a new direction. That direction may be oriented more toward the original understanding of the words of the Constitution and statutes and less toward policy; Congress rather than administrative agencies; racial nondiscrimination rather than preferences; and the free exercise rather than the establishment of religion. Whether there is such a shift or not, of course, only time will tell.
Chief Justice Roberts and Justice Kavanaugh were in the majority most often (95% of the cases), followed by Justices Barrett (90%), Alito (85%), Thomas (80%), and Gorsuch (75%). Justices Kagan (69%) and Breyer (68%) were not far behind. Justice Sotomayor was in the majority 58%. The Court was unanimous 29% of the time, well below the decade average (43%), and 6-3 accounted for 30% of the decisions.
A major, potentially scarring, event this Term was the leak of an early draft of the majority opinion in Dobbs. Although leaks have occurred before, the early leak of an opinion was unprecedented. It will almost inevitably change the openness and candor within the Court and the justices’ clerks. Although not unprecedented, the attempt on the life of Justice Kavanaugh and the organized efforts to harass some justices in their homes are likely to have lasting impact. Almost certainly it means that justices and their families will have constant security and their movements and connection with the general public will become less frequent, which is sad for the justices and our democracy.
Looking toward the next Term
When the Court next convenes, Justice Ketanji Brown Jackson will take her seat on the left end of the Court (the traditional seat for a new justice, not a commentary on judicial philosophy). The Court has already taken many cases, including issues about university affirmative action programs, web designers and same-sex couples, redistricting and voting rights, DNA testing in criminal cases, and overtime pay for someone making over $200,000 per year. It begins Monday, October 3, and promises to be another interesting Term. ●
The 2021–2022 US Supreme Court Term was a blockbuster medical Term. The bookends of the Term were COVID-19 vaccinations and abortion rights. Between the bookends were Medicare reimbursement, criminal liability for prescribing controlled substances, gun control, and carbon dioxide emissions. In this article, we focus on the significant medical issues, briefly note other important decisions, and consider the implications of this Term.
Abortion decisions
Dobbs v Jackson Women’s Health Organization1 was the most controversial decision and, for ObGyns, perhaps the most important decision in decades. The basic holding of the case can be stated simply: Roe v Wade2 and Planned Parenthood of Southeastern Pennsylvania v Casey3 (which essentially created a constitutional right to abortion) are overruled. The law related to abortion is for the states and Congress to determine, not federal courts. (For a review of earlier reproductive freedom cases in the Court, see our previous article, “The Supreme Court and reproductive rights.”4)
Dobbs arose from a Mississippi statute that made it illegal to perform abortions after 15 weeks of gestation, well before viability. Six members of the Court held that the Mississippi law was constitutional and 3 would have struck down the state law. There were 5 opinions, covering a total of 213 pages in the U.S. Reports. The Court fell into 4 camps, ranging from the most to the least protective of abortion rights, as follows:
- Three justices (Breyer, Kagan, and Sotomayor) voted to strike down the Mississippi statute and uphold Roe and Casey and wrote a joint dissent. They believe the Constitution makes abortion an issue “off limits to majority rule.” They also warned that other areas of “substantive due process” (discussed below), including contraception and same-sex marriage, might be under threat.
- The Chief Justice voted to uphold the statute but wanted an incremental approach; that is, not to overturn Roe and Casey entirely in this case because the Dobbs case required the Court only to determine the more limited question of whether the 15-week limit on abortion was constitutional. He found that the viability standard did not make sense, but he suggested that the Court “leave for another day” whether to overturn Roe.
- Five justices joined the opinion to uphold the statute and overturn Roe. Justice Alito wrote the decision joined by Justices Thomas, Kavanaugh, Gorsuch, and Barrett. They found that a right to abortion was not “deeply rooted in our Nation’s history,” as evidenced by the fact that when the 14th Amendment was adopted, abortion was a criminal offense in most states and not a protected right in any state. In 2 lengthy appendices, the Court reviewed the criminalization of abortion in the states in 1868 and in the territories that later became states. Even when Roe was decided in 1973, abortion was not “deeply rooted” because it was not generally legal in the states. Justice Kavanaugh joined this opinion and wrote separately to emphasize that the majority opinion does not outlaw abortion, but rather leaves the issue to “the people and their representatives.” He also emphasized that the case did not overturn all of the substantive due process cases.
- Justice Thomas would have gone further and abandoned “substantive due process” completely.
The constitutional issue
The majority said that the issue before the Court was not whether the law should permit or prohibit abortions—that is a question for the political branches. Rather, the question was only whether the Constitution precludes the political branches from allowing abortions. There is no mention of abortion in the Constitution and no specific reference to a right to privacy that includes medical decisions. A central constitutional question has been to identify where exactly in the Constitution the right to privacy resides. The Court has generally used “substantive due process” to locate privacy rights. The 14th Amendment provides, in part, that no state may “deprive any person of life, liberty, or property, without due process of law.” “Process” generally refers to procedural protections, but the Court sometimes has used it to encompass substantive rights (for example, privacy)—hence, “substantive due process.”
Over the decades, the legitimacy of substantive due process has remained controversial. Justice Thomas called it an “oxymoron” to turn “process” into substantive rights. And its use has a somewhat checkered history. For nearly 50 years (1890–1937), it was used to preclude states from protecting employees (for example, hour and wage laws violated “the right to contract”) and was discredited. More recently the Court has used substantive due process to protect contraception access, abortion, and same-sex marriages.
A critical question is knowing what rights substantive due process protects. The Court sometimes has said that it protects rights “deeply rooted in the Nation’s history and traditions” and “implicit in the concept of ordered liberty,”5 although in other cases suggested a more ambiguous definition.6 The next constitutional question is how to state or define the right to be protected. For example, is it the right to intimately personal decisions, bodily integrity, reproductive choice, abortion, or late-term abortion? Some of those may be deeply rooted in history and traditions (intimate decisions), and others not so much (late-term abortion). Finally, a question is whether a substantive right is defined at the time the 14th Amendment was adopted (1868) or now—is it a “living Constitution” that, without much guidance, means whatever 5 justices believe at the moment, or is it a Constitution grounded in the distant past?
The future of substantive due process is uncertain following Dobbs. Although the majority said it was not disclaiming substantive due process, the dissent said it doubted that claim because other rights are “part of the same constitutional fabric” (substantive due process). The Court might, in future cases, find some other constitutional provision in which to ground rights. The source of those rights might be the 9th Amendment (in addition to the Constitution’s enumerated rights, there are “others retained by the people”) or another provision of the 14th (“No State shall make or enforce any law which shall abridge the privileges or immunities of citizens of the United States…”). Each of these possibilities has its problems, many of which are similar to substantive due process, but they avoid the “oxymoron” issue.
Among the other important cases this Term, the Court made these determinations:
- Held that the 2nd Amendment, as applied to the states through the 14th Amendment, includes a general right to carry a gun for self-defense outside the home.1 It struck down a New York law that required people to show a special need to have and carry a gun.
- Determined that the US Environmental Protection Agency exceeded the authority Congress had granted it with a “Clean Power Plan” that was intended to reduce carbon dioxide emissions.2 It is up to Congress, not the agency, to expand agency authority.
- Gave trial courts discretion in determining whether (and under what conditions) children in international custody disputes must be returned to their home countries where there is a serious risk of harm to them.3
- Held that there is an implied right of action to sue medical providers for disability discrimination, but under the Rehabilitation Act and the Affordable Care Act the damages do not include emotional harm.4
- Decided several “free exercise of religion” cases, and in each found the state had violated religious rights, holding that: A state improperly prevented religious schools from being eligible for a state tuition grant system,5 a coach was wrongfully fired for kneeling in prayer following football games,6 Boston denied free speech in allowing other organizations to fly their flags but denying a Christian flag to be displayed,7 and a state must permit prisoners to have a spiritual advisor to be present and pray and touch them during their execution.8
- Held that the administration’s rescission of the “stay in Mexico” immigration policy was permitted by existing statutes.9
References
1. New York State Rifle & Pistol Association, Inc. v Bruen, 20-843, decided June 23, 2022. https://www.supremecourt.gov/opinions/21pdf/20-843_7j80.pdf
2. West Virginia v Environmental Protection Agency, 20-1530, decided June 30, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1530_new_l537.pdf
3. Golan v Saada, 20-1034, decided June 15, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1034_b8dg.pdf
4. Cummings v Premier Rehab Keller, 20-219, decided April 28, 2022. https://www.supremecourt.gov/opinions/21pdf/20-219_1b82.pdf
5. Carson v Makin, 20-1088, decided June 21, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1088_dbfi.pdf
6. Kennedy v Bremerton School District., 21-418, decided June 27, 2022. https://www.supremecourt.gov/opinions/21pdf/21-418_new_onkq.pdf
7. Shurtleff v Boston, 20-1800, decided May 2, 2022. https://www.supremecourt.gov/opinions/21pdf/20-1800_7lho.pdf
8. Ramirez v Collier, 21-5592, decided March 24, 2022. https://www.supremecourt.gov/opinions/21pdf/21-5592_feah.pdf
9. Biden v Texas, 21-9 54, decided June 30, 2022. https://www.supremecourt.gov/opinions/21pdf/21-954_7l48.pdf
Continue to: ObGyn briefs in the case...
ObGyn briefs in the case
The medical profession filed several amicus curiae briefs in the Dobbs case. (These are “friends of the court” briefs filed by nonparties to the litigation. The purpose is to give a court a perspective on the case not presented by the parties.) The American College of Obstetricians and Gynecologists (ACOG) took the lead in filing an amicus brief.7 Nearly 2 dozen other medical organizations joined the brief, including the American Academy of Pediatrics, American College of Osteopathic Obstetricians and Gynecologists, American Gynecological and Obstetrical Society, American Society for Reproductive Medicine, Council of University Chairs of Obstetrics and Gynecology, North American Society for Pediatric and Adolescent Gynecology, Society for Academic Specialists in General Obstetrics and Gynecology, Society of Gynecologic Oncology, and Society of OB/GYN Hospitalists.
The brief argued that abortion is a safe procedure, an abortion ban would harm the health of pregnant patients, and it would undermine the physician-patient relationship and interfere with patient autonomy. It also discussed the issue of fetal pain,8 telling the Court that “Every major medical organization that has examined the issue of fetal pain and peer-reviewed studies on the matter have consistently concluded that pre-viability abortion does not result in fetal pain perception.”9 The brief was cited in the dissent for the fact that “About 18 percent of pregnancies in this country end in abortion, and about one-quarter of American women will have an abortion before the age of 45.”10
The Court received a different view from an amicus brief filed by the American Association of Pro-Life Obstetricians and Gynecologists.11 It told the Court that abortion, especially later-term, poses health risks: the abortion process itself may injure the woman, abortion puts women at risk for future preterm births, later-term abortion raises a woman’s risk of developing breast cancer, and abortions (especially those later in the pregnancy) are linked to a greater risk of psychological harm.12 The brief also noted that 93% of obstetrician-gynecologists do not perform abortions, and “abortion has been deemed contrary to sound medicine for thousands of years” (citing the Hippocratic oath).13 The brief was not cited by the Court.
Many other medical and pro-life medical groups presented amicus briefs. A list of and links to all the briefs is available on the SCOTUSblog website at https://www.scotusblog.com/case-files/cases/dobbs-v-jackson-womens-health-organization/.
Ramifications
The Court decision does not make abortion illegal but allows states (and possibly Congress) to decide whether, when, and how abortions may be performed. Some states may ban most abortions (making it illegal to have or to perform abortions). Thirteen states had “trigger laws” to go into effect limiting abortion if the Court permitted such limitations. Most of those states were almost immediately entangled in lawsuits challenging the state laws. Some states, for example, have privacy provisions in their state constitution that state courts could interpret as allowing abortion, thereby voiding the state statutes prohibiting abortion.
At least a few states have abortion laws still on the books that were passed decades ago (perhaps before Roe) and were never repealed. Those laws may once again be valid, although state courts might hold that those statutes were repealed by Roe and must be passed again to be valid. Some experts anticipate that 28 states will eventually have significant limitations on abortion.
The Guttmacher Institute maintains a frequently updated table on the abortion laws in each state.14 According to one estimate, 29 states are hostile to abortion rights (or lean that way), with about 40 million women aged 13 to 44 (58% of the United States) living in states with some hostility to abortion.15 Congress may pass some national abortion laws, but that seems unlikely and there may be some limits on its ability to control private medical practice within states.
An additional legal issue will arise from medication-induced abortions, generally through the use of mifepristone and misoprostol. They now account for the majority of abortions. These medications might be used for abortion, up to about 9 weeks of pregnancy, in states prohibiting abortion. The drugs once were available only with an in-person visit, but now the US Food and Drug Administration (FDA) permits mail-order delivery. The potential exists, therefore, to circumvent states’ prohibition on abortion through mail-order postal shipments. The FDA controls the licensing of pharmaceuticals in interstate commerce, but not the practice of medicine within a state. Therefore the ability of individuals (within a state) to possess or use drugs is unclear.
The abortion wars of the last 50 years gave rise to state laws related to abortion, including consent by minors, information to parents, special informed consent, and facilities requirements. If these laws were once struck down because they were inconsistent with Roe, but were never formally repealed, they may now become legal requirements.
In the foreseeable future, abortion laws generally will not be determined by federal courts but by state law, generally legislatures. In legislative hearings, town hall meetings, and conversations with lawmakers, ObGyns should engage the topic of abortion with scientific expertise, reason, openness, and humility. It will be impossible for the profession to speak with a single voice, as the briefs filed this Term demonstrate. Where there are honest differences in science, the reasons for the different interpretations should be explainable to lay decision makers. The profession, who are not being pseudo-lobbyists, can contribute a great deal to the rational consideration of this emotional topic.
On January 27, 2022, Justice Stephen Breyer informed President Biden of his intention to retire from the Court at the end of the Term. At age 84, he was the oldest member of the Court, but he continued to be among the most active of the justices and seemed to relish the work of the Court. He had been under pressure from liberal groups to retire earlier so a successor could be confirmed by a Democratic Senate. In many ways he was the Renaissance man of the Court: he spoke fluent French, wrote books, and famously sprinkled his questions with complex and funny hypotheticals.
Justice Breyer was a law professor before becoming a judge and enjoyed presentations to many groups, from children to law professors. He loved the Court and defended it—most recently against partisan attacks from both the right and the left. In the decisions of the Court, he was one of the more liberal justices. He had, for example, indicated that the death penalty is unconstitutional.
In his January retirement letter, he said that he would step down at the end of the Term if his replacement had been appointed and confirmed. She had. The new justice had clerked for Justice Breyer in 1999–2000.
Ketanji Brown Jackson was nominated by President Biden on February 28, confirmed by the Senate on April 7 by a 53–47 margin, and sworn in on June 30, 2022. Justice Jackson had previously been a federal district court judge and on the Court of Appeals for the D.C. Circuit. She attended Harvard-Radcliffe College and received her law degree from Harvard Law School. She worked as a criminal defense attorney and was active in the US Sentencing Commission.
Continue to: What is a practitioner to do?...
What is a practitioner to do?
For many practitioners, the Dobbs decision will have little effect because their state laws are consistent with Roe, and the legislature is not going to change the law. They may, of course, see an influx of patients from other states (that restrict abortion) seeking treatment. At the other extreme, in some states, most abortions will become prohibited. State courts may ease the restrictions. In many states, there will be an ongoing battle over when abortion is legal and when it is not, resulting in shifting laws and regulations. Keeping up with the shifts that affect practice will be a challenge.
All states are likely to permit abortions “to save the life of the mother,” and many will have a version of “to preserve the health of the mother.” Other exceptions may be for pregnancy resulting from rape or incest or in the case of serious fetal abnormality. ObGyns, of course, will be called on to certify that one of these exceptions exists. Determining that pregnancy resulted from rape or incest, of course, can be challenging. Before Roe, there was a cottage industry opining that pregnancy seriously affected the health of the mother, which often involved physical manifestations of mental health. ObGyns in some states may be asked once again to make such determinations.
Laws not directly related to abortions will, in some states, be changed as a way of discouraging abortion. For example, child abuse reporting laws may be modified to require reporting of any known or suspected abortion or attempted abortion, and medical licensing standards may make it a violation to participate in or facilitate abortion in any way.
Particularly in states where the rules keep shifting, practitioners must keep up with the current law. Professional organizations can help with that, but there is no substitute for practitioners having an ongoing professional relationship with an attorney who has expertise in health law.
Other abortion decisions this Term
In other abortion decisions this Term, the Court refused to suspend a Texas law that prohibited abortions after a fetal heartbeat could be detected.16 The law has remarkable enforcement mechanisms that preclude state officers from enforcing it; instead, it creates what amounts to a private attorney general (PAG) provision that allows private citizens to file suit against anyone performing or assisting in performing abortions. This PAG made pre-enforcement challenges to the law difficult.17
In a Kentucky case, the Court allowed the Kentucky attorney general to intervene in a case that challenged a Kentucky law that prohibits physicians from using dilation and evacuation procedures to end second-trimester pregnancies.18
Criminal convictions for physicians’ overprescription of controlled substances
Perhaps the least sympathetic of the physicians involved with the Court this Term were the 2 in Ruan v U.S.19 Their trials indicate that Dr. Ruan’s clinic issued more than 300,000 controlled substance prescriptions over 4 years and was one of the most frequent prescribers of fentanyl. Dr. Kahn prescribed controlled substances without an examination, falsified notes, and sold controlled substances for cash and guns.20
Both physicians were convicted of “knowingly or intentionally” dispensing a controlled substance without authorization.21 They were authorized to prescribe drugs, but only “for a legitimate medical purpose.”22 Appeals to their respective Circuit courts confirmed their convictions. The Supreme Court, however, held that to convict them, the government must prove that they knowingly or intentionally acted in an unauthorized manner. That proof can be by circumstantial evidence, but it must be beyond a reasonable doubt.
Health care reimbursement
Hospitals won one and lost one Medicare-Medicaid reimbursement case that involved payments for low-income patients.
In the loss, the Court held that the US Department of Health and Human Services (HHS) properly calculated the disproportionate share adjustments (DSH), or Medicare fraction,23 that provides a supplemental payment for hospitals with a large proportion of low-income patients. The lower DSH payments calculated by HHS were upheld, thereby reducing the number of hospitals receiving DSH payments and decreasing the amounts others will receive.
The win involved payments for prescription drugs that hospitals provide to outpatients in safety-net hospitals.24 HHS determined that it was overpaying hospitals for drugs and cut the reimbursement rate. The Court held that before HHS can change the drug rate, it must conduct a survey of hospitals regarding actual costs. It had not done that, so the rate reduction was not permitted by the law.
An accidental disincentive to (some) malpractice suits
Medicaid requires states to obtain part of a tort recovery that recipients obtain if Medicaid is covering medical expenses related to their injuries. In implementing that law, a state may provide a disincentive for injured beneficiaries to file malpractice cases. At issue was a Florida law that provided the Medicaid state would take 37.5% of the beneficiary’s total tort recovery (being one-half of the recovery after deducting 25% for attorney’s fees and costs). In a 7-2 decision, the Court upheld the Florida law.25
The disincentive to filing a lawsuit is that the state is taking 37.5%, plus contingency fee attorneys will typically take 33.3% (and there will be some fees). This is especially true when there is a state cap on noneconomic damages. In the case the Court decided, the plaintiff received a settlement of $850,000. If we assume a typical contingency fee, less the state’s Medicaid claim of $300,000, the plaintiff possibly received $266,667. That is not trivial, but it is only 31% of the settlement.
The Medicaid expectation of reimbursement and the Florida approach, however, impose heavy burdens on severely injured beneficiaries. The plaintiff had catastrophic injuries and was in a vegetative state. There are some things Medicaid does not pay for, as well as nonmedical expenses. The amount left for such expenses is likely well below what the family will need.
Continue to: COVID-19 vaccinations...
COVID-19 vaccinations
Had it not been for the abortion decisions, 2021–2022 might have been “the COVID Term.” Two of the most anticipated decisions involved mandatory vaccinations (or masking/testing instead). The question in each of these cases was whether Congress had authorized 2 federal agencies to issue the emergency regulations requiring vaccination. Emergency regulations are held to higher standards because they bypass the usual protections of the Administrative Procedure Act.
One case involved a regulation issued by the Occupational Safety and Health Administration (OSHA) that employers (with more than 100 employees) must require their employees to be vaccinated. In a 6-3 decision, the Court held that OSHA did not have the authority to enforce this as an emergency regulation. The other case was a regulation issued by HHS that health care institutions receiving Medicare and Medicaid funding must require all staff to be vaccinated.26 In a 5-4 decision, the Court upheld this emergency regulation because of the very broad authority Congress had given HHS to ensure the safety of patients and the quality of Medicare- and Medicaid-funded programs.27
In another case, in the shadow docket (orders and opinions in cases without full arguments), the Court struck down the Centers for Disease Control and Prevention’s eviction moratorium.28 The Court said the government claimed “a breathtaking amount of authority” that Congress did not intend. In other shadow docket cases, the Court refused to hold unconstitutional state laws that require COVID-19 vaccination but did not have religious exemptions.29
Analysis of this Term
It was an extraordinary Term. The Court decided 66 cases (excluding most cases in the shadow docket), a low number historically. Not only were there many seminal cases but also the Court appears to be shifting toward a new direction. That direction may be oriented more toward the original understanding of the words of the Constitution and statutes and less toward policy; Congress rather than administrative agencies; racial nondiscrimination rather than preferences; and the free exercise rather than the establishment of religion. Whether there is such a shift or not, of course, only time will tell.
Chief Justice Roberts and Justice Kavanaugh were in the majority most often (95% of the cases), followed by Justices Barrett (90%), Alito (85%), Thomas (80%), and Gorsuch (75%). Justices Kagan (69%) and Breyer (68%) were not far behind. Justice Sotomayor was in the majority 58%. The Court was unanimous 29% of the time, well below the decade average (43%), and 6-3 accounted for 30% of the decisions.
A major, potentially scarring, event this Term was the leak of an early draft of the majority opinion in Dobbs. Although leaks have occurred before, the early leak of an opinion was unprecedented. It will almost inevitably change the openness and candor within the Court and the justices’ clerks. Although not unprecedented, the attempt on the life of Justice Kavanaugh and the organized efforts to harass some justices in their homes are likely to have lasting impact. Almost certainly it means that justices and their families will have constant security and their movements and connection with the general public will become less frequent, which is sad for the justices and our democracy.
Looking toward the next Term
When the Court next convenes, Justice Ketanji Brown Jackson will take her seat on the left end of the Court (the traditional seat for a new justice, not a commentary on judicial philosophy). The Court has already taken many cases, including issues about university affirmative action programs, web designers and same-sex couples, redistricting and voting rights, DNA testing in criminal cases, and overtime pay for someone making over $200,000 per year. It begins Monday, October 3, and promises to be another interesting Term. ●
- Dobbs v Jackson Women’s Health Organization, 19-1392, decided June 24, 2022. https://www.supremecourt.gov /opinions/21pdf/19-1392_6j37.pdf
- Roe v Wade, 410 U.S. 113, 163 (1973).
- Planned Parenthood of Southeastern Pennsylvania v Casey, 505 U.S. 833 (1992).
- Smith SR, Sanfilippo JR. The Supreme Court and reproductive rights. OBG Manag. 2022;34(1):36-41, 46. https://cdn.mdedge. com/files/s3fs-public/issues/articles/obgm0340136_smith.pdf
- Washington v Glucksberg, 521 U.S. 702 (1997).
- Obergefell v Hodges, 576 U.S. 644, 654-70 (2015).
- Brief of amici curiae of American College of Obstetricians and Gynecologists, American Medical Association, et al, in Dobbs v Jackson Women’s Health Organization, in Support of Respondents (Sep. 2021). https://www.supremecourt .gov/DocketPDF/19/19-1392/193074/20210920174518042 _19-1392%20bsacACOGetal.pdf
- Id. at 8, 13-15.
- Id. at 14.
- Justices Breyer, Kagan, and Sotomayor, dissenting, at 48, note 22.
- Brief for American Association of Pro-Life Obstetricians And Gynecologists as Amicus Curiae, in Dobbs v Jackson Women’s Health Organization, in Support of Petitioners (July 2021). https://www.supremecourt.gov /DocketPDF/19/19-1392/185350/20210729163532595_No. %2019-1392%20-%20American%20Association%20of%20 Pro-Life%20Obstetricians%20and%20Gynecologists%20-%20 Amicus%20Brief%20in%20Support%20of%20Petitioner%20-%20 7-29-21.pdf
- Id. at 3-4, 7-29.
- Id. at 30.
- Guttmacher Institute. An overview of abortion laws. July 11, 2022. https://www.guttmacher.org/state-policy/explore/overview -abortion-laws
- Guttmacher Institute. State abortion policy landscape: from hostile to supportive. Dec. 2020. https://www .guttmacher.org/article/2019/08/state-abortion-policy -landscape-hostile-supportive
- Whole Woman’s Health v Jackson, 21-463, decided Dec. 10, 2021. https://www.supremecourt.gov/opinions/21pdf/21-463_ new_8o6b.pdf
- United States v Texas, 21-588, decided Dec. 10, 2021. (Per curiam, Sotomayor dissenting). https://www.supremecourt.gov /opinions/21pdf/21-588_c07d.pdf
- Cameron v EMW Women’s Surgical Center, 20-601, decided Mar. 3, 2022. https://www.supremecourt.gov/opinions/21pdf/20-601 _new_g20h.pdf
- Xiulu Ruan v United States, 20-1410, decided June 27, 2022. https:// www.supremecourt.gov/opinions/21pdf/20-1410_1an2.pdf
- Adam Liptak. Supreme Court sides with doctors accused of running pill mills. The New York Times. June 27, 2022. https://www .nytimes.com/2022/06/27/us/politics/supreme-court-controlled -substance-act.html
- 84 Stat. 1260, 21 U.S.C. §841(a).
- 21 CFR §1306.04(a) (2021).
- Becerra v Empire Health Foundation, For Valley Hospital Medical Center, 20-1312, decided June 24, 2022. https://www.supremecourt .gov/opinions/21pdf/20-1312_j42l.pdf
- American Hospital Association v Becerra, 20-1114, decided June 15, 2022. https://www.supremecourt.gov/opinions/21pdf/20 -1114_09m1.pdf
- Gallardo v Marstiller, 20-1263, decided June 6, 2022. https:// www.supremecourt.gov/opinions/21pdf/20-1263_new_hfci.pdf
- National Federation of Independent Business v Department of Labor, Occupational Safety and Health Administration, 21A244, decided Jan. 13, 2022. https://www.supremecourt.gov /opinions/21pdf/21a244_hgci.pdf
- Biden v Missouri, 21A240, decided Jan. 13, 2022. https://www .supremecourt.gov/opinions/21pdf/21a240_d18e.pdf
- Alabama Association of Realtors v Department of Health and Human Services, 21A23, decided Aug. 26, 2021. https://www .supremecourt.gov/opinions/20pdf/21a23_ap6c.pdf
- Does v Mills, 21A90, decided Oct. 29, 2021. https://www .supremecourt.gov/opinions/21pdf/21a90_6j37.pdf
- Dobbs v Jackson Women’s Health Organization, 19-1392, decided June 24, 2022. https://www.supremecourt.gov /opinions/21pdf/19-1392_6j37.pdf
- Roe v Wade, 410 U.S. 113, 163 (1973).
- Planned Parenthood of Southeastern Pennsylvania v Casey, 505 U.S. 833 (1992).
- Smith SR, Sanfilippo JR. The Supreme Court and reproductive rights. OBG Manag. 2022;34(1):36-41, 46. https://cdn.mdedge. com/files/s3fs-public/issues/articles/obgm0340136_smith.pdf
- Washington v Glucksberg, 521 U.S. 702 (1997).
- Obergefell v Hodges, 576 U.S. 644, 654-70 (2015).
- Brief of amici curiae of American College of Obstetricians and Gynecologists, American Medical Association, et al, in Dobbs v Jackson Women’s Health Organization, in Support of Respondents (Sep. 2021). https://www.supremecourt .gov/DocketPDF/19/19-1392/193074/20210920174518042 _19-1392%20bsacACOGetal.pdf
- Id. at 8, 13-15.
- Id. at 14.
- Justices Breyer, Kagan, and Sotomayor, dissenting, at 48, note 22.
- Brief for American Association of Pro-Life Obstetricians And Gynecologists as Amicus Curiae, in Dobbs v Jackson Women’s Health Organization, in Support of Petitioners (July 2021). https://www.supremecourt.gov /DocketPDF/19/19-1392/185350/20210729163532595_No. %2019-1392%20-%20American%20Association%20of%20 Pro-Life%20Obstetricians%20and%20Gynecologists%20-%20 Amicus%20Brief%20in%20Support%20of%20Petitioner%20-%20 7-29-21.pdf
- Id. at 3-4, 7-29.
- Id. at 30.
- Guttmacher Institute. An overview of abortion laws. July 11, 2022. https://www.guttmacher.org/state-policy/explore/overview -abortion-laws
- Guttmacher Institute. State abortion policy landscape: from hostile to supportive. Dec. 2020. https://www .guttmacher.org/article/2019/08/state-abortion-policy -landscape-hostile-supportive
- Whole Woman’s Health v Jackson, 21-463, decided Dec. 10, 2021. https://www.supremecourt.gov/opinions/21pdf/21-463_ new_8o6b.pdf
- United States v Texas, 21-588, decided Dec. 10, 2021. (Per curiam, Sotomayor dissenting). https://www.supremecourt.gov /opinions/21pdf/21-588_c07d.pdf
- Cameron v EMW Women’s Surgical Center, 20-601, decided Mar. 3, 2022. https://www.supremecourt.gov/opinions/21pdf/20-601 _new_g20h.pdf
- Xiulu Ruan v United States, 20-1410, decided June 27, 2022. https:// www.supremecourt.gov/opinions/21pdf/20-1410_1an2.pdf
- Adam Liptak. Supreme Court sides with doctors accused of running pill mills. The New York Times. June 27, 2022. https://www .nytimes.com/2022/06/27/us/politics/supreme-court-controlled -substance-act.html
- 84 Stat. 1260, 21 U.S.C. §841(a).
- 21 CFR §1306.04(a) (2021).
- Becerra v Empire Health Foundation, For Valley Hospital Medical Center, 20-1312, decided June 24, 2022. https://www.supremecourt .gov/opinions/21pdf/20-1312_j42l.pdf
- American Hospital Association v Becerra, 20-1114, decided June 15, 2022. https://www.supremecourt.gov/opinions/21pdf/20 -1114_09m1.pdf
- Gallardo v Marstiller, 20-1263, decided June 6, 2022. https:// www.supremecourt.gov/opinions/21pdf/20-1263_new_hfci.pdf
- National Federation of Independent Business v Department of Labor, Occupational Safety and Health Administration, 21A244, decided Jan. 13, 2022. https://www.supremecourt.gov /opinions/21pdf/21a244_hgci.pdf
- Biden v Missouri, 21A240, decided Jan. 13, 2022. https://www .supremecourt.gov/opinions/21pdf/21a240_d18e.pdf
- Alabama Association of Realtors v Department of Health and Human Services, 21A23, decided Aug. 26, 2021. https://www .supremecourt.gov/opinions/20pdf/21a23_ap6c.pdf
- Does v Mills, 21A90, decided Oct. 29, 2021. https://www .supremecourt.gov/opinions/21pdf/21a90_6j37.pdf
Eighty percent of U.S. maternal deaths are preventable: Study
More than 80% of U.S. maternal deaths across a 2-year period were due to preventable causes, according to a new CDC report.
Black mothers made up about a third of deaths, and more than 90% of deaths among Indigenous mothers were preventable.
“It’s significant. It’s staggering. It’s heartbreaking,” Allison Bryant, MD, a high-risk pregnancy specialist and senior medical director for health equity at Massachusetts General Hospital, told USA Today.
“It just means that we have so much work to do,” she said.
In the report, CDC researchers looked at pregnancy-related deaths between 2017 to 2019 based on numbers from maternal mortality review committees, which are multidisciplinary groups in 36 states that investigate the circumstances around maternal deaths.
Of the 1,018 deaths during the 2-year period, 839 occurred up to a year after delivery. About 22% of deaths happened during pregnancy, and 25% happened on the day of delivery or within a week after delivery. But 53% occurred more than 7 days after delivery.
Mental health conditions, such as overdoses and deaths by suicide, were the top underlying cause, followed by hemorrhage, or extreme bleeding. About a quarter of deaths were due to mental health conditions, followed by 14% due to hemorrhage and 13% due to heart problems. The rest were related to infection, embolism, cardiomyopathy, and high blood pressure-related disorders.
The analysis included a section on maternal deaths for American Indian and Alaska Native mothers, who are more than twice as likely as White mothers to die but are often undercounted in health data due to misclassification. More than 90% of their deaths were preventable between 2017 to 2019, with most due to mental health conditions and hemorrhage.
“It’s incredibly distressful,” Brian Thompson, MD, of the Oneida Nation and assistant professor of obstetrics and gynecology at Upstate Medical University, New York, told USA Today.
Dr. Thompson is working with the National Indian Health Board to create the first national tribal review committee for maternal deaths.
“It really needs to be looked at and examined why that is the case if essentially all of them are preventable,” he said.
Black mothers were also three times as likely as White mothers to die and more likely to die from heart problems. Hispanic mothers, who made up 14% of deaths, were more likely to die from mental health conditions.
Some of the deaths, such as hemorrhage, should be highly preventable. Existing toolkits for clinicians provide evidence-based guidelines to prevent and treat excessive bleeding.
“No pregnant person should be passing away from a hemorrhage,” Andrea Jackson, MD, division chief of obstetrics and gynecology at the University of California, San Francisco, told USA Today.
“We have the tools in the United States, and we know how to deal with it,” she said. “That was really disheartening to see.”
What’s more, the new CDC report highlights the need for more mental health resources during pregnancy and the postpartum period – up to a year or more after delivery – including improvements in access to care, diagnosis, and treatment.
“These are things that need to happen systemically,” LeThenia Baker, MD, an obstetrician and gynecologist at Wellstar Health, Georgia, told USA Today.
“It can’t just be a few practices here or there who are adopting best practices,” she said. “It has to be a systemic change.”
A version of this article first appeared on WebMD.com.
More than 80% of U.S. maternal deaths across a 2-year period were due to preventable causes, according to a new CDC report.
Black mothers made up about a third of deaths, and more than 90% of deaths among Indigenous mothers were preventable.
“It’s significant. It’s staggering. It’s heartbreaking,” Allison Bryant, MD, a high-risk pregnancy specialist and senior medical director for health equity at Massachusetts General Hospital, told USA Today.
“It just means that we have so much work to do,” she said.
In the report, CDC researchers looked at pregnancy-related deaths between 2017 to 2019 based on numbers from maternal mortality review committees, which are multidisciplinary groups in 36 states that investigate the circumstances around maternal deaths.
Of the 1,018 deaths during the 2-year period, 839 occurred up to a year after delivery. About 22% of deaths happened during pregnancy, and 25% happened on the day of delivery or within a week after delivery. But 53% occurred more than 7 days after delivery.
Mental health conditions, such as overdoses and deaths by suicide, were the top underlying cause, followed by hemorrhage, or extreme bleeding. About a quarter of deaths were due to mental health conditions, followed by 14% due to hemorrhage and 13% due to heart problems. The rest were related to infection, embolism, cardiomyopathy, and high blood pressure-related disorders.
The analysis included a section on maternal deaths for American Indian and Alaska Native mothers, who are more than twice as likely as White mothers to die but are often undercounted in health data due to misclassification. More than 90% of their deaths were preventable between 2017 to 2019, with most due to mental health conditions and hemorrhage.
“It’s incredibly distressful,” Brian Thompson, MD, of the Oneida Nation and assistant professor of obstetrics and gynecology at Upstate Medical University, New York, told USA Today.
Dr. Thompson is working with the National Indian Health Board to create the first national tribal review committee for maternal deaths.
“It really needs to be looked at and examined why that is the case if essentially all of them are preventable,” he said.
Black mothers were also three times as likely as White mothers to die and more likely to die from heart problems. Hispanic mothers, who made up 14% of deaths, were more likely to die from mental health conditions.
Some of the deaths, such as hemorrhage, should be highly preventable. Existing toolkits for clinicians provide evidence-based guidelines to prevent and treat excessive bleeding.
“No pregnant person should be passing away from a hemorrhage,” Andrea Jackson, MD, division chief of obstetrics and gynecology at the University of California, San Francisco, told USA Today.
“We have the tools in the United States, and we know how to deal with it,” she said. “That was really disheartening to see.”
What’s more, the new CDC report highlights the need for more mental health resources during pregnancy and the postpartum period – up to a year or more after delivery – including improvements in access to care, diagnosis, and treatment.
“These are things that need to happen systemically,” LeThenia Baker, MD, an obstetrician and gynecologist at Wellstar Health, Georgia, told USA Today.
“It can’t just be a few practices here or there who are adopting best practices,” she said. “It has to be a systemic change.”
A version of this article first appeared on WebMD.com.
More than 80% of U.S. maternal deaths across a 2-year period were due to preventable causes, according to a new CDC report.
Black mothers made up about a third of deaths, and more than 90% of deaths among Indigenous mothers were preventable.
“It’s significant. It’s staggering. It’s heartbreaking,” Allison Bryant, MD, a high-risk pregnancy specialist and senior medical director for health equity at Massachusetts General Hospital, told USA Today.
“It just means that we have so much work to do,” she said.
In the report, CDC researchers looked at pregnancy-related deaths between 2017 to 2019 based on numbers from maternal mortality review committees, which are multidisciplinary groups in 36 states that investigate the circumstances around maternal deaths.
Of the 1,018 deaths during the 2-year period, 839 occurred up to a year after delivery. About 22% of deaths happened during pregnancy, and 25% happened on the day of delivery or within a week after delivery. But 53% occurred more than 7 days after delivery.
Mental health conditions, such as overdoses and deaths by suicide, were the top underlying cause, followed by hemorrhage, or extreme bleeding. About a quarter of deaths were due to mental health conditions, followed by 14% due to hemorrhage and 13% due to heart problems. The rest were related to infection, embolism, cardiomyopathy, and high blood pressure-related disorders.
The analysis included a section on maternal deaths for American Indian and Alaska Native mothers, who are more than twice as likely as White mothers to die but are often undercounted in health data due to misclassification. More than 90% of their deaths were preventable between 2017 to 2019, with most due to mental health conditions and hemorrhage.
“It’s incredibly distressful,” Brian Thompson, MD, of the Oneida Nation and assistant professor of obstetrics and gynecology at Upstate Medical University, New York, told USA Today.
Dr. Thompson is working with the National Indian Health Board to create the first national tribal review committee for maternal deaths.
“It really needs to be looked at and examined why that is the case if essentially all of them are preventable,” he said.
Black mothers were also three times as likely as White mothers to die and more likely to die from heart problems. Hispanic mothers, who made up 14% of deaths, were more likely to die from mental health conditions.
Some of the deaths, such as hemorrhage, should be highly preventable. Existing toolkits for clinicians provide evidence-based guidelines to prevent and treat excessive bleeding.
“No pregnant person should be passing away from a hemorrhage,” Andrea Jackson, MD, division chief of obstetrics and gynecology at the University of California, San Francisco, told USA Today.
“We have the tools in the United States, and we know how to deal with it,” she said. “That was really disheartening to see.”
What’s more, the new CDC report highlights the need for more mental health resources during pregnancy and the postpartum period – up to a year or more after delivery – including improvements in access to care, diagnosis, and treatment.
“These are things that need to happen systemically,” LeThenia Baker, MD, an obstetrician and gynecologist at Wellstar Health, Georgia, told USA Today.
“It can’t just be a few practices here or there who are adopting best practices,” she said. “It has to be a systemic change.”
A version of this article first appeared on WebMD.com.
Dignity
Queen Elizabeth is everywhere. She was even on the last slide of a presentation on COVID, monkeypox, and influenza vaccines given by our physician in charge of quality. This was odd. The presenter wasn’t English. The Queen had nothing to do with vaccines. Nor apparently would she have said even if she did have an opinion about them. But there we were, an audience of physicians and staff pausing for a moment of remembrance of her.
I’m not a Monarchist – except perhaps for the Kennedys. I grew up in New England. I don’t have an opinion on whether or not the British Crown should endure. But I do marvel at the astounding effect Queen Elizabeth’s passing had on so many around the world. Her personal qualities, particularly her steadiness and humane sympathy, might explain why so many are sad hearing the news. But also I think there was something in her role that we all wished for: Not the owning of palaces and sceptres, but rather, the respect that was given to her.
She was a stateswoman of “unmatched dignity,” the White House wrote. That was true, but it seems being the Queen might have been the last job on earth where such dignity is still possible. Certainly in politics, education, and even health care, there doesn’t seem to be much left lately.
The same day of that presentation I walked into the room of a patient 22 minutes late, she held her arm forth tapping her watch to indicate the time and my tardiness. Unnecessary, if not impertinent. Covering for one of my female physician colleagues, I read an email from a patient which began, “Dear Julie, With all due respect …” Another patient submitted a photo for us to review that was clearly taken from her car while waiting at a stop light. Hardly the consideration a clinical encounter should be given.
Much has been lost for patients. too. There are patients trying to make appointments lately who are told: “There are none. Call back later.” . There is no dignified way to remove exam paper stuck to your backside before introducing yourself to the doctor. Maybe that last slide of Her Majesty was in fact for us to have a moment of silence for what we’ve all lost.
Walter Bagehot (pronounce it “Baj-et” if you tell this story to your Harlan wine friends) was a political writer and editor of The Economist in the 1860s. He famously said that the secret to the English government was having two kinds of institutions, the dignified and the efficient. The efficient, Parliament, was responsible for all the work. The dignified, the Crown, gives significance and holds everyone’s respect. If medicine ever once was both dignified and efficient, we aren’t lately. We push to reduce backlogs, offer same-time virtual care, work to reduce costs. We’ve driven medicine to the efficient and left little of the dignity it seems.
The Queen will be remembered for her lifelong dedication to the laborious service of others. Even though each of us in medicine pledges the same, we also mourn this week the loss of dignity that once came with it.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Queen Elizabeth is everywhere. She was even on the last slide of a presentation on COVID, monkeypox, and influenza vaccines given by our physician in charge of quality. This was odd. The presenter wasn’t English. The Queen had nothing to do with vaccines. Nor apparently would she have said even if she did have an opinion about them. But there we were, an audience of physicians and staff pausing for a moment of remembrance of her.
I’m not a Monarchist – except perhaps for the Kennedys. I grew up in New England. I don’t have an opinion on whether or not the British Crown should endure. But I do marvel at the astounding effect Queen Elizabeth’s passing had on so many around the world. Her personal qualities, particularly her steadiness and humane sympathy, might explain why so many are sad hearing the news. But also I think there was something in her role that we all wished for: Not the owning of palaces and sceptres, but rather, the respect that was given to her.
She was a stateswoman of “unmatched dignity,” the White House wrote. That was true, but it seems being the Queen might have been the last job on earth where such dignity is still possible. Certainly in politics, education, and even health care, there doesn’t seem to be much left lately.
The same day of that presentation I walked into the room of a patient 22 minutes late, she held her arm forth tapping her watch to indicate the time and my tardiness. Unnecessary, if not impertinent. Covering for one of my female physician colleagues, I read an email from a patient which began, “Dear Julie, With all due respect …” Another patient submitted a photo for us to review that was clearly taken from her car while waiting at a stop light. Hardly the consideration a clinical encounter should be given.
Much has been lost for patients. too. There are patients trying to make appointments lately who are told: “There are none. Call back later.” . There is no dignified way to remove exam paper stuck to your backside before introducing yourself to the doctor. Maybe that last slide of Her Majesty was in fact for us to have a moment of silence for what we’ve all lost.
Walter Bagehot (pronounce it “Baj-et” if you tell this story to your Harlan wine friends) was a political writer and editor of The Economist in the 1860s. He famously said that the secret to the English government was having two kinds of institutions, the dignified and the efficient. The efficient, Parliament, was responsible for all the work. The dignified, the Crown, gives significance and holds everyone’s respect. If medicine ever once was both dignified and efficient, we aren’t lately. We push to reduce backlogs, offer same-time virtual care, work to reduce costs. We’ve driven medicine to the efficient and left little of the dignity it seems.
The Queen will be remembered for her lifelong dedication to the laborious service of others. Even though each of us in medicine pledges the same, we also mourn this week the loss of dignity that once came with it.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Queen Elizabeth is everywhere. She was even on the last slide of a presentation on COVID, monkeypox, and influenza vaccines given by our physician in charge of quality. This was odd. The presenter wasn’t English. The Queen had nothing to do with vaccines. Nor apparently would she have said even if she did have an opinion about them. But there we were, an audience of physicians and staff pausing for a moment of remembrance of her.
I’m not a Monarchist – except perhaps for the Kennedys. I grew up in New England. I don’t have an opinion on whether or not the British Crown should endure. But I do marvel at the astounding effect Queen Elizabeth’s passing had on so many around the world. Her personal qualities, particularly her steadiness and humane sympathy, might explain why so many are sad hearing the news. But also I think there was something in her role that we all wished for: Not the owning of palaces and sceptres, but rather, the respect that was given to her.
She was a stateswoman of “unmatched dignity,” the White House wrote. That was true, but it seems being the Queen might have been the last job on earth where such dignity is still possible. Certainly in politics, education, and even health care, there doesn’t seem to be much left lately.
The same day of that presentation I walked into the room of a patient 22 minutes late, she held her arm forth tapping her watch to indicate the time and my tardiness. Unnecessary, if not impertinent. Covering for one of my female physician colleagues, I read an email from a patient which began, “Dear Julie, With all due respect …” Another patient submitted a photo for us to review that was clearly taken from her car while waiting at a stop light. Hardly the consideration a clinical encounter should be given.
Much has been lost for patients. too. There are patients trying to make appointments lately who are told: “There are none. Call back later.” . There is no dignified way to remove exam paper stuck to your backside before introducing yourself to the doctor. Maybe that last slide of Her Majesty was in fact for us to have a moment of silence for what we’ve all lost.
Walter Bagehot (pronounce it “Baj-et” if you tell this story to your Harlan wine friends) was a political writer and editor of The Economist in the 1860s. He famously said that the secret to the English government was having two kinds of institutions, the dignified and the efficient. The efficient, Parliament, was responsible for all the work. The dignified, the Crown, gives significance and holds everyone’s respect. If medicine ever once was both dignified and efficient, we aren’t lately. We push to reduce backlogs, offer same-time virtual care, work to reduce costs. We’ve driven medicine to the efficient and left little of the dignity it seems.
The Queen will be remembered for her lifelong dedication to the laborious service of others. Even though each of us in medicine pledges the same, we also mourn this week the loss of dignity that once came with it.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
ObGyn: A leader in academic medicine, with progress still to be made in diversity
The nation’s population is quickly diversifying, making racial/ethnic disparities in health care outcomes even more apparent. Minority and non-English-speaking populations have grown and may become a majority in the next generation.1 A proposed strategy to reduce disparities in health care is to recruit more practitioners who better reflect the patient populations.2 Improved access to care with racial concordance between physicians and patients has been reported.3
Being increasingly aware of access-to-care data, more patients are advocating and asking for physicians of color to be their providers.4 Despite progress (ie, more women entering the medical profession), the proportion of physicians who are underrepresented in medicine (URiM—eg, Black, Hispanic, and Native American) still lags US population demographics.3
Why diversity in medicine matters
In addition to improving access to care, diversity in medicine offers other benefits. Working within diverse learning environments has demonstrated educational advantages.5,6 Medical students and residents from diverse backgrounds are less likely to report depression symptoms, regardless of their race. Diversity may accelerate advancements in health care as well, since it is well-established that diverse teams outperform nondiverse teams when it comes to innovation and productivity.7 Finally, as a profession committed to equity, advocacy, and justice, physicians are positioned to lead the way toward racial equity.
Overall, racial and gender diversity in all clinical specialties is improving, but not at the same pace. While the diversity of US medical students and residents by sex and race/ethnicity is greater than among faculty, change in racial diversity has been slow for all 3 groups.8 During the past 40 years the number of full-time faculty has increased 6-fold for females and more than tripled for males.8 However, this rise has not favored URiM faculty, because their proportion is still underrepresented relative to their group in the general population. Clinical departments that are making the most progress in recruiting URiM residents and faculty are often primary or preventive care specialties rather than surgical or service or hospital-based specialties.8,9 ObGyn has consistently had a proportion of URiM residents (18%) that is highest in the surgical specialties and comparable to family medicine and pediatrics.10
When examining physician workforce diversity, it is important to “drill down” to individual specialties to obtain a clearer understanding of trends. The continued need for increased resident and faculty diversity prompted us to examine ObGyn departments. The most recent nationwide data were gathered about full-time faculty from the 2021 AAMC Faculty Roster, residents from the 2021 Accreditation Counsel for Graduate Medical Education (ACGME) Data Resource Book, medical student matriculants from 2021 AAMC, and US adult women (defined arbitrarily as 15 years or older) from the 2019 American Community Survey.11-13
Increase in female faculty and residents
The expanding numbers of faculty and residents over a 40-year period (from 1973 to 2012) led to more women and underrepresented minorities in ObGyn than in other major clinical departments.14,15 Women now constitute two-thirds of all ObGyn faculty and are more likely to be junior rather than senior faculty.9 When looking at junior faculty, a higher proportion of junior faculty who are URiM are female. While more junior faculty and residents are female, male faculty are also racially and ethnically diverse.9
- ObGyn is a leader in racial/ethnic diversity in academic medicine.
- The rapid rise of faculty numbers in the past has not favored underrepresented faculty.
- The rise in ObGyn faculty and residents, who were predominantly female, has contributed to greater racial/ethnic diversity.
- Improved patient outcomes with racial concordance between physicians and patients have been reported.
- More patients are advocating and asking for physicians of color to be their clinicians.
- Racial/ethnic diversity of junior faculty and residents is similar to medical students.
- The most underrepresented group is Hispanic, due in part to its rapid growth in the US population.
Continue to: Growth of URiM physicians in ObGyn...
Growth of URiM physicians in ObGyn
The distribution of racial/ethnic groups in 2021 were compared between senior and junior ObGyn faculty and residents with the US adult female population.9 As shown in the FIGURE, the proportion of ObGyn faculty who are White approximates the White US adult female population. The most rapidly growing racial/ethnic group in the US population is Hispanic. Although Hispanic is the best represented ethnicity among junior faculty, the proportions of Hispanics among faculty and residents lag well behind the US population. The proportion of ObGyn faculty who are Black has consistently been less than in the US adult female population. ObGyns who are Asian constitute higher proportions of faculty and residents than in the US adult female population. This finding about Asians is consistent across all clinical specialties.7
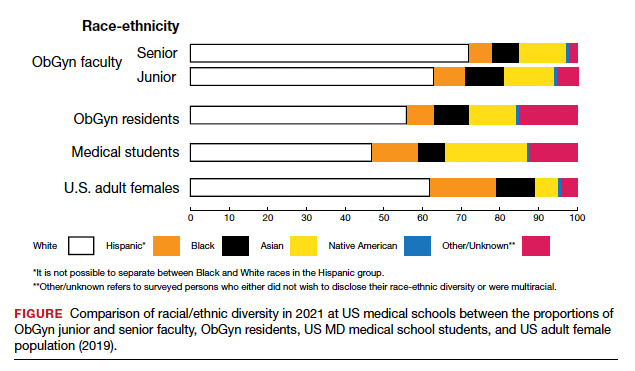
Recruiting URiM students into ObGyn is important. Racial and ethnic representation in surgical and nonsurgical residency programs has not substantially improved in the past decade and continues to lag the changing demographics of the US population.10 More students than residents and faculty are Hispanic, which represents a much-needed opportunity for recruitment. By contrast, junior ObGyn faculty are more likely to be Black than residents and students. Native Americans constitute less than 1% of all faculty, residents, students, and US adult females.9 Lastly, race/ethnicity being self-reported as “other” or “unknown” is most common among students and residents, which perhaps represents greater diversity.
Looking back
Increasing diversity in medicine and in ObGyn has not happened by accident. Transformational change requires rectifying any factors that detrimentally affect the racial/ethnic diversity of our medical students, residents, and faculty. For example, biases inherent in key residency application metrics are being recognized, and use of holistic review is increasing. Change is also accelerated by an explicit and public commitment from national organizations. In 2009, the Liaison Committee of Medical Education (LCME) mandated that medical schools engage in practices that focus on recruitment and retention of a diverse workforce. Increases in Black and Hispanic medical students were noted after implementation of this new mandate.16 The ACGME followed suit with similar guidelines in 2019.10
Diversity is one of the foundational strengths of the ObGyn specialty. Important aspects of the specialty are built upon the contributions of women of color, some voluntary and some not. One example is the knowledge of gynecology that was gained through the involuntary and nonanesthetized surgeries performed on
Moving forward
Advancing diversity in ObGyn offers advantages: better representation of patient populations, improving public health by better access to care, enhancing learning in medical education, building more comprehensive research agendas, and driving institutional excellence. While progress has been made, significant work is still to be done. We must continue to critically examine the role of biases and structural racism that are embedded in evaluating medical students, screening of residency applicants, and selecting and retaining faculty. In future work, we should explore the hypothesis that continued change in racial/ethnic diversity of faculty will only occur once more URiM students, especially the growing number of Hispanics, are admitted into medical schools and recruited for residency positions. We should also examine whether further diversity improves patient outcomes.
It is encouraging to realize that ObGyn departments are leaders in racial/ethnic diversity at US medical schools. It is also critical that the specialty commits to the progress that still needs to be made, including increasing diversity among faculty and institutional leadership. To maintain diversity that mirrors the US adult female population, the specialty of ObGyn will require active surveillance and continued recruitment of Black and, especially Hispanic, faculty and residents.19 The national strategies aimed at building medical student and residency diversity are beginning to yield results. For those gains to help faculty diversity, institutional and departmental leaders will need to implement best practices for recruiting, retaining, and advancing URiM faculty.19 Those practices would include making workforce diversity an explicit priority, building diverse applicant pools, and establishing infrastructure and mentorship to advance URiM faculty to senior leadership positions.20
In conclusion
Building a physician workforce that is more representative of the US population should aid in addressing inequalities in health and health care. Significant strides have been made in racial/ethnic diversity in ObGyn. This has resulted in a specialty that is among the most diverse in academic medicine. At the same time, there is more work to be done. For example, the specialty is far from reaching racial equity for Hispanic physicians. Also, continued efforts are necessary to advance URiM faculty to leadership positions. The legacy of racial/ethnic diversity in ObGyn did not happen by accident and will not be maintained without intention. ●
- Hummes KR, Jones NA, Ramierez RR. United States Census: overview of race and Hispanic origin: 2010. http//www. census.gov/prod/cen2010/briefs/c2010br-02.pdf. Accessed May 22, 2022.
- Xierali IM, Castillo-Page L, Zhang K, et al. AM last page: the urgency of physician workforce diversity. Acad Med. 2014;89:1192.
- Association of American Medical College. Diversity in the physician workforce. Facts & figures 2014. http://www .aamcdiversityfactsandfigures.org. Accessed April 9, 2022.
- Marrast LM, Zallman L, Woolhandler S, et al. Minority physicians’ role in the care of underserved patients: Diversifying the physician workforce may be key in addressing health disparities. JAMA Int Med. 2014;174:289-291.
- Amalba A, Abantanga FA, Scherpbier AJ, et al. Community-based education: The influence of role modeling on career choice and practice location. Med Teac. 2017;39:174-180.
- Umbach PD. The contribution of faculty of color to undergraduate education. Res High Educ. 2006;47:317-345.
- Gonzalo JD, Chuang CH, Glod SA, et al. General internists as change agents: opportunities and barriers to leadership in health systems and medical education transformation. J Gen Intern Med. 2020;35:1865-1869.
- Xierali IM, Fair MA, Nivet MA. Faculty diversity in U.S. medical schools: Progress and gaps coexist. AAMC Analysis in Brief. 2016;16. https://www.aamc.org/system/files/reports/1/decem ber2016facultydiversityinu.s.medicalschoolsprogressandga ps.pdf. Accessed May 4, 2022.
- Rayburn WF, Xierali IM, McDade WA. Racial-ethnic diversity of obstetrics and gynecology faculty at medical schools in the United States. Am J Obstet Gynecol. 2022;S00029378(22)00106-5. doi: 10.1016/j.ajog.2022.02.007.
- Hucko L, Al-khersan H, Lopez Dominguez J, et al. Racial and ethnic diversity of U.S. residency programs, 2011-2019. N Engl J Med. 2022;386:22-23.
- Accreditation Council for Graduate Medical Education. Data Resource Book Academic Year 2020-2021. https://www.acgme.org/globalassets/pfassets /publicationsbooks/2020-2021_acgme_databook _document.pdf. Accessed October 24, 2021
- United States Census Bureau. The 2019 American Community Survey 5-Year Public Use Microdata Sample (PUMS) Files.
- Accreditation Council for Graduate Medical Education. Data Resource Book Academic Year 2020-2021. https://www.acgme .org/globalassets/pfassets/publicationsbooks/2020-2021 _acgme_databook_document.pdf. Accessed October 24, 2021.
- Rayburn WF, Liu CQ, Elwell EC, et al. Diversity of physician faculty in obstetrics and gynecology. J Reprod Med. 2016;61:22-26.
- Xierali IM, Nivet MA, Rayburn WF. Full-time faculty in clinical and basic science departments by sex and underrepresented in medicine status: A 40-year review. Acad Med. 2021;96: 568-575.
- Boatright DH, Samuels EA, Cramer LJ, et al. Association between the Liaison Committee on Medical Education’s Diversity Standards and Changes in percentage of medical student sex, race, and ethnicity. JAMA. 2018;320:2267-2269.
- United States National Library of Medicine. Changing the face of medicine.
- https://cfmedicine.nlm.nih.gov/physicians/biography_82. html. Accessed May 5, 2022.
- Christmas M. #SayHerName: Should obstetrics and gynecology reckon with the legacy of JM Sims? Reprod Sci. 2021;28:3282-3284.
- Morgan HK, Winkel AF, Bands E, et al. Promoting diversity, equity, and inclusion in the selection of obstetrician-gynecologists. Obstet Gynecol. 2021;138:272-277.
- Peek ME, Kim KE, Johnson JK, et al. “URM candidates are encouraged to apply”: a national study to identify effective strategies to enhance racial and ethnic faculty diversity in academic departments of medicine. Acad Med. 2013;88:405-412.
The nation’s population is quickly diversifying, making racial/ethnic disparities in health care outcomes even more apparent. Minority and non-English-speaking populations have grown and may become a majority in the next generation.1 A proposed strategy to reduce disparities in health care is to recruit more practitioners who better reflect the patient populations.2 Improved access to care with racial concordance between physicians and patients has been reported.3
Being increasingly aware of access-to-care data, more patients are advocating and asking for physicians of color to be their providers.4 Despite progress (ie, more women entering the medical profession), the proportion of physicians who are underrepresented in medicine (URiM—eg, Black, Hispanic, and Native American) still lags US population demographics.3
Why diversity in medicine matters
In addition to improving access to care, diversity in medicine offers other benefits. Working within diverse learning environments has demonstrated educational advantages.5,6 Medical students and residents from diverse backgrounds are less likely to report depression symptoms, regardless of their race. Diversity may accelerate advancements in health care as well, since it is well-established that diverse teams outperform nondiverse teams when it comes to innovation and productivity.7 Finally, as a profession committed to equity, advocacy, and justice, physicians are positioned to lead the way toward racial equity.
Overall, racial and gender diversity in all clinical specialties is improving, but not at the same pace. While the diversity of US medical students and residents by sex and race/ethnicity is greater than among faculty, change in racial diversity has been slow for all 3 groups.8 During the past 40 years the number of full-time faculty has increased 6-fold for females and more than tripled for males.8 However, this rise has not favored URiM faculty, because their proportion is still underrepresented relative to their group in the general population. Clinical departments that are making the most progress in recruiting URiM residents and faculty are often primary or preventive care specialties rather than surgical or service or hospital-based specialties.8,9 ObGyn has consistently had a proportion of URiM residents (18%) that is highest in the surgical specialties and comparable to family medicine and pediatrics.10
When examining physician workforce diversity, it is important to “drill down” to individual specialties to obtain a clearer understanding of trends. The continued need for increased resident and faculty diversity prompted us to examine ObGyn departments. The most recent nationwide data were gathered about full-time faculty from the 2021 AAMC Faculty Roster, residents from the 2021 Accreditation Counsel for Graduate Medical Education (ACGME) Data Resource Book, medical student matriculants from 2021 AAMC, and US adult women (defined arbitrarily as 15 years or older) from the 2019 American Community Survey.11-13
Increase in female faculty and residents
The expanding numbers of faculty and residents over a 40-year period (from 1973 to 2012) led to more women and underrepresented minorities in ObGyn than in other major clinical departments.14,15 Women now constitute two-thirds of all ObGyn faculty and are more likely to be junior rather than senior faculty.9 When looking at junior faculty, a higher proportion of junior faculty who are URiM are female. While more junior faculty and residents are female, male faculty are also racially and ethnically diverse.9
- ObGyn is a leader in racial/ethnic diversity in academic medicine.
- The rapid rise of faculty numbers in the past has not favored underrepresented faculty.
- The rise in ObGyn faculty and residents, who were predominantly female, has contributed to greater racial/ethnic diversity.
- Improved patient outcomes with racial concordance between physicians and patients have been reported.
- More patients are advocating and asking for physicians of color to be their clinicians.
- Racial/ethnic diversity of junior faculty and residents is similar to medical students.
- The most underrepresented group is Hispanic, due in part to its rapid growth in the US population.
Continue to: Growth of URiM physicians in ObGyn...
Growth of URiM physicians in ObGyn
The distribution of racial/ethnic groups in 2021 were compared between senior and junior ObGyn faculty and residents with the US adult female population.9 As shown in the FIGURE, the proportion of ObGyn faculty who are White approximates the White US adult female population. The most rapidly growing racial/ethnic group in the US population is Hispanic. Although Hispanic is the best represented ethnicity among junior faculty, the proportions of Hispanics among faculty and residents lag well behind the US population. The proportion of ObGyn faculty who are Black has consistently been less than in the US adult female population. ObGyns who are Asian constitute higher proportions of faculty and residents than in the US adult female population. This finding about Asians is consistent across all clinical specialties.7
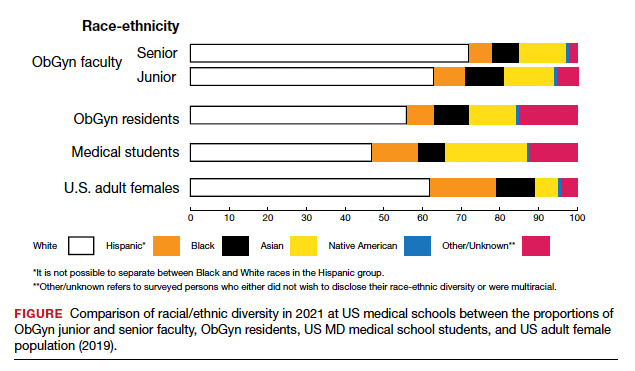
Recruiting URiM students into ObGyn is important. Racial and ethnic representation in surgical and nonsurgical residency programs has not substantially improved in the past decade and continues to lag the changing demographics of the US population.10 More students than residents and faculty are Hispanic, which represents a much-needed opportunity for recruitment. By contrast, junior ObGyn faculty are more likely to be Black than residents and students. Native Americans constitute less than 1% of all faculty, residents, students, and US adult females.9 Lastly, race/ethnicity being self-reported as “other” or “unknown” is most common among students and residents, which perhaps represents greater diversity.
Looking back
Increasing diversity in medicine and in ObGyn has not happened by accident. Transformational change requires rectifying any factors that detrimentally affect the racial/ethnic diversity of our medical students, residents, and faculty. For example, biases inherent in key residency application metrics are being recognized, and use of holistic review is increasing. Change is also accelerated by an explicit and public commitment from national organizations. In 2009, the Liaison Committee of Medical Education (LCME) mandated that medical schools engage in practices that focus on recruitment and retention of a diverse workforce. Increases in Black and Hispanic medical students were noted after implementation of this new mandate.16 The ACGME followed suit with similar guidelines in 2019.10
Diversity is one of the foundational strengths of the ObGyn specialty. Important aspects of the specialty are built upon the contributions of women of color, some voluntary and some not. One example is the knowledge of gynecology that was gained through the involuntary and nonanesthetized surgeries performed on
Moving forward
Advancing diversity in ObGyn offers advantages: better representation of patient populations, improving public health by better access to care, enhancing learning in medical education, building more comprehensive research agendas, and driving institutional excellence. While progress has been made, significant work is still to be done. We must continue to critically examine the role of biases and structural racism that are embedded in evaluating medical students, screening of residency applicants, and selecting and retaining faculty. In future work, we should explore the hypothesis that continued change in racial/ethnic diversity of faculty will only occur once more URiM students, especially the growing number of Hispanics, are admitted into medical schools and recruited for residency positions. We should also examine whether further diversity improves patient outcomes.
It is encouraging to realize that ObGyn departments are leaders in racial/ethnic diversity at US medical schools. It is also critical that the specialty commits to the progress that still needs to be made, including increasing diversity among faculty and institutional leadership. To maintain diversity that mirrors the US adult female population, the specialty of ObGyn will require active surveillance and continued recruitment of Black and, especially Hispanic, faculty and residents.19 The national strategies aimed at building medical student and residency diversity are beginning to yield results. For those gains to help faculty diversity, institutional and departmental leaders will need to implement best practices for recruiting, retaining, and advancing URiM faculty.19 Those practices would include making workforce diversity an explicit priority, building diverse applicant pools, and establishing infrastructure and mentorship to advance URiM faculty to senior leadership positions.20
In conclusion
Building a physician workforce that is more representative of the US population should aid in addressing inequalities in health and health care. Significant strides have been made in racial/ethnic diversity in ObGyn. This has resulted in a specialty that is among the most diverse in academic medicine. At the same time, there is more work to be done. For example, the specialty is far from reaching racial equity for Hispanic physicians. Also, continued efforts are necessary to advance URiM faculty to leadership positions. The legacy of racial/ethnic diversity in ObGyn did not happen by accident and will not be maintained without intention. ●
The nation’s population is quickly diversifying, making racial/ethnic disparities in health care outcomes even more apparent. Minority and non-English-speaking populations have grown and may become a majority in the next generation.1 A proposed strategy to reduce disparities in health care is to recruit more practitioners who better reflect the patient populations.2 Improved access to care with racial concordance between physicians and patients has been reported.3
Being increasingly aware of access-to-care data, more patients are advocating and asking for physicians of color to be their providers.4 Despite progress (ie, more women entering the medical profession), the proportion of physicians who are underrepresented in medicine (URiM—eg, Black, Hispanic, and Native American) still lags US population demographics.3
Why diversity in medicine matters
In addition to improving access to care, diversity in medicine offers other benefits. Working within diverse learning environments has demonstrated educational advantages.5,6 Medical students and residents from diverse backgrounds are less likely to report depression symptoms, regardless of their race. Diversity may accelerate advancements in health care as well, since it is well-established that diverse teams outperform nondiverse teams when it comes to innovation and productivity.7 Finally, as a profession committed to equity, advocacy, and justice, physicians are positioned to lead the way toward racial equity.
Overall, racial and gender diversity in all clinical specialties is improving, but not at the same pace. While the diversity of US medical students and residents by sex and race/ethnicity is greater than among faculty, change in racial diversity has been slow for all 3 groups.8 During the past 40 years the number of full-time faculty has increased 6-fold for females and more than tripled for males.8 However, this rise has not favored URiM faculty, because their proportion is still underrepresented relative to their group in the general population. Clinical departments that are making the most progress in recruiting URiM residents and faculty are often primary or preventive care specialties rather than surgical or service or hospital-based specialties.8,9 ObGyn has consistently had a proportion of URiM residents (18%) that is highest in the surgical specialties and comparable to family medicine and pediatrics.10
When examining physician workforce diversity, it is important to “drill down” to individual specialties to obtain a clearer understanding of trends. The continued need for increased resident and faculty diversity prompted us to examine ObGyn departments. The most recent nationwide data were gathered about full-time faculty from the 2021 AAMC Faculty Roster, residents from the 2021 Accreditation Counsel for Graduate Medical Education (ACGME) Data Resource Book, medical student matriculants from 2021 AAMC, and US adult women (defined arbitrarily as 15 years or older) from the 2019 American Community Survey.11-13
Increase in female faculty and residents
The expanding numbers of faculty and residents over a 40-year period (from 1973 to 2012) led to more women and underrepresented minorities in ObGyn than in other major clinical departments.14,15 Women now constitute two-thirds of all ObGyn faculty and are more likely to be junior rather than senior faculty.9 When looking at junior faculty, a higher proportion of junior faculty who are URiM are female. While more junior faculty and residents are female, male faculty are also racially and ethnically diverse.9
- ObGyn is a leader in racial/ethnic diversity in academic medicine.
- The rapid rise of faculty numbers in the past has not favored underrepresented faculty.
- The rise in ObGyn faculty and residents, who were predominantly female, has contributed to greater racial/ethnic diversity.
- Improved patient outcomes with racial concordance between physicians and patients have been reported.
- More patients are advocating and asking for physicians of color to be their clinicians.
- Racial/ethnic diversity of junior faculty and residents is similar to medical students.
- The most underrepresented group is Hispanic, due in part to its rapid growth in the US population.
Continue to: Growth of URiM physicians in ObGyn...
Growth of URiM physicians in ObGyn
The distribution of racial/ethnic groups in 2021 were compared between senior and junior ObGyn faculty and residents with the US adult female population.9 As shown in the FIGURE, the proportion of ObGyn faculty who are White approximates the White US adult female population. The most rapidly growing racial/ethnic group in the US population is Hispanic. Although Hispanic is the best represented ethnicity among junior faculty, the proportions of Hispanics among faculty and residents lag well behind the US population. The proportion of ObGyn faculty who are Black has consistently been less than in the US adult female population. ObGyns who are Asian constitute higher proportions of faculty and residents than in the US adult female population. This finding about Asians is consistent across all clinical specialties.7
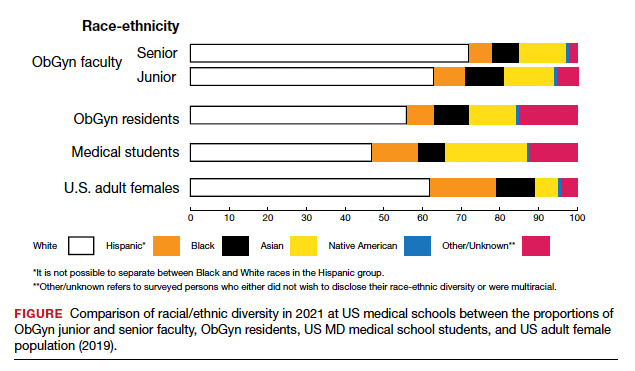
Recruiting URiM students into ObGyn is important. Racial and ethnic representation in surgical and nonsurgical residency programs has not substantially improved in the past decade and continues to lag the changing demographics of the US population.10 More students than residents and faculty are Hispanic, which represents a much-needed opportunity for recruitment. By contrast, junior ObGyn faculty are more likely to be Black than residents and students. Native Americans constitute less than 1% of all faculty, residents, students, and US adult females.9 Lastly, race/ethnicity being self-reported as “other” or “unknown” is most common among students and residents, which perhaps represents greater diversity.
Looking back
Increasing diversity in medicine and in ObGyn has not happened by accident. Transformational change requires rectifying any factors that detrimentally affect the racial/ethnic diversity of our medical students, residents, and faculty. For example, biases inherent in key residency application metrics are being recognized, and use of holistic review is increasing. Change is also accelerated by an explicit and public commitment from national organizations. In 2009, the Liaison Committee of Medical Education (LCME) mandated that medical schools engage in practices that focus on recruitment and retention of a diverse workforce. Increases in Black and Hispanic medical students were noted after implementation of this new mandate.16 The ACGME followed suit with similar guidelines in 2019.10
Diversity is one of the foundational strengths of the ObGyn specialty. Important aspects of the specialty are built upon the contributions of women of color, some voluntary and some not. One example is the knowledge of gynecology that was gained through the involuntary and nonanesthetized surgeries performed on
Moving forward
Advancing diversity in ObGyn offers advantages: better representation of patient populations, improving public health by better access to care, enhancing learning in medical education, building more comprehensive research agendas, and driving institutional excellence. While progress has been made, significant work is still to be done. We must continue to critically examine the role of biases and structural racism that are embedded in evaluating medical students, screening of residency applicants, and selecting and retaining faculty. In future work, we should explore the hypothesis that continued change in racial/ethnic diversity of faculty will only occur once more URiM students, especially the growing number of Hispanics, are admitted into medical schools and recruited for residency positions. We should also examine whether further diversity improves patient outcomes.
It is encouraging to realize that ObGyn departments are leaders in racial/ethnic diversity at US medical schools. It is also critical that the specialty commits to the progress that still needs to be made, including increasing diversity among faculty and institutional leadership. To maintain diversity that mirrors the US adult female population, the specialty of ObGyn will require active surveillance and continued recruitment of Black and, especially Hispanic, faculty and residents.19 The national strategies aimed at building medical student and residency diversity are beginning to yield results. For those gains to help faculty diversity, institutional and departmental leaders will need to implement best practices for recruiting, retaining, and advancing URiM faculty.19 Those practices would include making workforce diversity an explicit priority, building diverse applicant pools, and establishing infrastructure and mentorship to advance URiM faculty to senior leadership positions.20
In conclusion
Building a physician workforce that is more representative of the US population should aid in addressing inequalities in health and health care. Significant strides have been made in racial/ethnic diversity in ObGyn. This has resulted in a specialty that is among the most diverse in academic medicine. At the same time, there is more work to be done. For example, the specialty is far from reaching racial equity for Hispanic physicians. Also, continued efforts are necessary to advance URiM faculty to leadership positions. The legacy of racial/ethnic diversity in ObGyn did not happen by accident and will not be maintained without intention. ●
- Hummes KR, Jones NA, Ramierez RR. United States Census: overview of race and Hispanic origin: 2010. http//www. census.gov/prod/cen2010/briefs/c2010br-02.pdf. Accessed May 22, 2022.
- Xierali IM, Castillo-Page L, Zhang K, et al. AM last page: the urgency of physician workforce diversity. Acad Med. 2014;89:1192.
- Association of American Medical College. Diversity in the physician workforce. Facts & figures 2014. http://www .aamcdiversityfactsandfigures.org. Accessed April 9, 2022.
- Marrast LM, Zallman L, Woolhandler S, et al. Minority physicians’ role in the care of underserved patients: Diversifying the physician workforce may be key in addressing health disparities. JAMA Int Med. 2014;174:289-291.
- Amalba A, Abantanga FA, Scherpbier AJ, et al. Community-based education: The influence of role modeling on career choice and practice location. Med Teac. 2017;39:174-180.
- Umbach PD. The contribution of faculty of color to undergraduate education. Res High Educ. 2006;47:317-345.
- Gonzalo JD, Chuang CH, Glod SA, et al. General internists as change agents: opportunities and barriers to leadership in health systems and medical education transformation. J Gen Intern Med. 2020;35:1865-1869.
- Xierali IM, Fair MA, Nivet MA. Faculty diversity in U.S. medical schools: Progress and gaps coexist. AAMC Analysis in Brief. 2016;16. https://www.aamc.org/system/files/reports/1/decem ber2016facultydiversityinu.s.medicalschoolsprogressandga ps.pdf. Accessed May 4, 2022.
- Rayburn WF, Xierali IM, McDade WA. Racial-ethnic diversity of obstetrics and gynecology faculty at medical schools in the United States. Am J Obstet Gynecol. 2022;S00029378(22)00106-5. doi: 10.1016/j.ajog.2022.02.007.
- Hucko L, Al-khersan H, Lopez Dominguez J, et al. Racial and ethnic diversity of U.S. residency programs, 2011-2019. N Engl J Med. 2022;386:22-23.
- Accreditation Council for Graduate Medical Education. Data Resource Book Academic Year 2020-2021. https://www.acgme.org/globalassets/pfassets /publicationsbooks/2020-2021_acgme_databook _document.pdf. Accessed October 24, 2021
- United States Census Bureau. The 2019 American Community Survey 5-Year Public Use Microdata Sample (PUMS) Files.
- Accreditation Council for Graduate Medical Education. Data Resource Book Academic Year 2020-2021. https://www.acgme .org/globalassets/pfassets/publicationsbooks/2020-2021 _acgme_databook_document.pdf. Accessed October 24, 2021.
- Rayburn WF, Liu CQ, Elwell EC, et al. Diversity of physician faculty in obstetrics and gynecology. J Reprod Med. 2016;61:22-26.
- Xierali IM, Nivet MA, Rayburn WF. Full-time faculty in clinical and basic science departments by sex and underrepresented in medicine status: A 40-year review. Acad Med. 2021;96: 568-575.
- Boatright DH, Samuels EA, Cramer LJ, et al. Association between the Liaison Committee on Medical Education’s Diversity Standards and Changes in percentage of medical student sex, race, and ethnicity. JAMA. 2018;320:2267-2269.
- United States National Library of Medicine. Changing the face of medicine.
- https://cfmedicine.nlm.nih.gov/physicians/biography_82. html. Accessed May 5, 2022.
- Christmas M. #SayHerName: Should obstetrics and gynecology reckon with the legacy of JM Sims? Reprod Sci. 2021;28:3282-3284.
- Morgan HK, Winkel AF, Bands E, et al. Promoting diversity, equity, and inclusion in the selection of obstetrician-gynecologists. Obstet Gynecol. 2021;138:272-277.
- Peek ME, Kim KE, Johnson JK, et al. “URM candidates are encouraged to apply”: a national study to identify effective strategies to enhance racial and ethnic faculty diversity in academic departments of medicine. Acad Med. 2013;88:405-412.
- Hummes KR, Jones NA, Ramierez RR. United States Census: overview of race and Hispanic origin: 2010. http//www. census.gov/prod/cen2010/briefs/c2010br-02.pdf. Accessed May 22, 2022.
- Xierali IM, Castillo-Page L, Zhang K, et al. AM last page: the urgency of physician workforce diversity. Acad Med. 2014;89:1192.
- Association of American Medical College. Diversity in the physician workforce. Facts & figures 2014. http://www .aamcdiversityfactsandfigures.org. Accessed April 9, 2022.
- Marrast LM, Zallman L, Woolhandler S, et al. Minority physicians’ role in the care of underserved patients: Diversifying the physician workforce may be key in addressing health disparities. JAMA Int Med. 2014;174:289-291.
- Amalba A, Abantanga FA, Scherpbier AJ, et al. Community-based education: The influence of role modeling on career choice and practice location. Med Teac. 2017;39:174-180.
- Umbach PD. The contribution of faculty of color to undergraduate education. Res High Educ. 2006;47:317-345.
- Gonzalo JD, Chuang CH, Glod SA, et al. General internists as change agents: opportunities and barriers to leadership in health systems and medical education transformation. J Gen Intern Med. 2020;35:1865-1869.
- Xierali IM, Fair MA, Nivet MA. Faculty diversity in U.S. medical schools: Progress and gaps coexist. AAMC Analysis in Brief. 2016;16. https://www.aamc.org/system/files/reports/1/decem ber2016facultydiversityinu.s.medicalschoolsprogressandga ps.pdf. Accessed May 4, 2022.
- Rayburn WF, Xierali IM, McDade WA. Racial-ethnic diversity of obstetrics and gynecology faculty at medical schools in the United States. Am J Obstet Gynecol. 2022;S00029378(22)00106-5. doi: 10.1016/j.ajog.2022.02.007.
- Hucko L, Al-khersan H, Lopez Dominguez J, et al. Racial and ethnic diversity of U.S. residency programs, 2011-2019. N Engl J Med. 2022;386:22-23.
- Accreditation Council for Graduate Medical Education. Data Resource Book Academic Year 2020-2021. https://www.acgme.org/globalassets/pfassets /publicationsbooks/2020-2021_acgme_databook _document.pdf. Accessed October 24, 2021
- United States Census Bureau. The 2019 American Community Survey 5-Year Public Use Microdata Sample (PUMS) Files.
- Accreditation Council for Graduate Medical Education. Data Resource Book Academic Year 2020-2021. https://www.acgme .org/globalassets/pfassets/publicationsbooks/2020-2021 _acgme_databook_document.pdf. Accessed October 24, 2021.
- Rayburn WF, Liu CQ, Elwell EC, et al. Diversity of physician faculty in obstetrics and gynecology. J Reprod Med. 2016;61:22-26.
- Xierali IM, Nivet MA, Rayburn WF. Full-time faculty in clinical and basic science departments by sex and underrepresented in medicine status: A 40-year review. Acad Med. 2021;96: 568-575.
- Boatright DH, Samuels EA, Cramer LJ, et al. Association between the Liaison Committee on Medical Education’s Diversity Standards and Changes in percentage of medical student sex, race, and ethnicity. JAMA. 2018;320:2267-2269.
- United States National Library of Medicine. Changing the face of medicine.
- https://cfmedicine.nlm.nih.gov/physicians/biography_82. html. Accessed May 5, 2022.
- Christmas M. #SayHerName: Should obstetrics and gynecology reckon with the legacy of JM Sims? Reprod Sci. 2021;28:3282-3284.
- Morgan HK, Winkel AF, Bands E, et al. Promoting diversity, equity, and inclusion in the selection of obstetrician-gynecologists. Obstet Gynecol. 2021;138:272-277.
- Peek ME, Kim KE, Johnson JK, et al. “URM candidates are encouraged to apply”: a national study to identify effective strategies to enhance racial and ethnic faculty diversity in academic departments of medicine. Acad Med. 2013;88:405-412.
House passes prior authorization bill, Senate path unclear
The path through the U.S. Senate is not yet certain for a bill intended to speed the prior authorization process of insurer-run Medicare Advantage plans, despite the measure having breezed through the House.
House leaders opted to move the Improving Seniors’ Timely Access to Care Act of 2021 (HR 3173) without requiring a roll-call vote. The measure was passed on Sept. 14 by a voice vote, an approach used in general with only uncontroversial measures that have broad support. The bill has 191 Democratic and 135 Republican sponsors, representing about three-quarters of the members of the House.
“There is no reason that patients should be waiting for medically appropriate care, especially when we know that this can lead to worse outcomes,” Rep. Earl Blumenauer (D-Ore.) said in a Sept. 14 speech on the House floor. “The fundamental promise of Medicare Advantage is undermined when people are delaying care, getting sicker, and ultimately costing Medicare more money.”
Rep. Greg Murphy, MD (R-N.C.), spoke on the House floor that day as well, bringing up cases he has seen in his own urology practice in which prior authorization delays disrupted medical care. One patient wound up in the hospital with abscess after an insurer denied an antibiotic prescription, Rep. Murphy said.
But the Senate appears unlikely at this time to move the prior authorization bill as a standalone measure. Instead, the bill may become part of a larger legislative package focused on health care that the Senate Finance Committee intends to prepare later this year.
The House-passed bill would require insurer-run Medicare plans to respond to expedited requests for prior authorization of services within 24 hours and to other requests within 7 days. This bill also would establish an electronic program for prior authorizations and mandate increased transparency as to how insurers use this tool.
CBO: Cost of change would be billions
In seeking to mandate changes in prior authorization, lawmakers likely will need to contend with the issue of a $16 billion cumulative cost estimate for the bill from the Congressional Budget Office. Members of Congress often seek to offset new spending by pairing bills that add to expected costs for the federal government with ones expected to produce savings.
Unlike Rep. Blumenauer, Rep. Murphy, and other backers of the prior authorization streamlining bill, CBO staff estimates that making the mandated changes would raise federal spending, inasmuch as there would be “a greater use of services.”
On Sept. 14, CBO issued a one-page report on the costs of the bill. The CBO report concerns only the bill in question, as is common practice with the office’s estimates.
Prior authorization changes would begin in fiscal 2025 and would add $899 million in spending, or outlays, that year, CBO said. The annual costs from the streamlined prior authorization practices through fiscal 2026 to 2032 range from $1.6 billion to $2.7 billion.
Looking at the CBO estimate against a backdrop of total Medicare Advantage costs, though, may provide important context.
The increases in spending estimated by CBO may suggest that there would be little change in federal spending as a result of streamlining prior authorization practices. These estimates of increased annual spending of $1.6 billion–$2.7 billion are only a small fraction of the current annual cost of insurer-run Medicare, and they represent an even smaller share of the projected expense.
The federal government last year spent about $350 billion on insurer-run plans, excluding Part D drug plan payments, according to the Medicare Advisory Payment Commission (MedPAC).
As of 2021, about 27 million people were enrolled in these plans, accounting for about 46% of the total Medicare population. Enrollment has doubled since 2010, MedPAC said, and it is expected to continue to grow. By 2027, insurer-run Medicare could cover 50% of the program’s population, a figure that may reach 53% by 2031.
Federal payments to these plans will accelerate in the years ahead as insurers attract more people eligible for Medicare as customers. Payments to these private health plans could rise from an expected $418 billion this year to $940.6 billion by 2031, according to the most recent Medicare trustees report.
Good intentions, poor implementation?
Insurer-run Medicare has long enjoyed deep bipartisan support in Congress. That’s due in part to its potential for reducing spending on what are considered low-value treatments, or ones considered unlikely to provide a significant medical benefit, but Rep. Blumenauer is among the members of Congress who see insurer-run Medicare as a path for preserving the giant federal health program. Traditional Medicare has far fewer restrictions on services, which sometimes opens a path for tests and treatments that offer less value for patients.
“I believe that the way traditional fee-for-service Medicare operates is not sustainable and that Medicare Advantage is one of the tools we can use to demonstrate how we can incentivize value,” Rep. Blumenauer said on the House floor. “But this is only possible when the program operates as intended. I have been deeply concerned about the reports of delays in care” caused by the clunky prior authorization processes.
He highlighted a recent report from the internal watchdog group for the Department of Health & Human Services that raises concerns about denials of appropriate care. About 18% of a set of payment denials examined by the Office of Inspector General of HHS in April actually met Medicare coverage rules and plan billing rules.
“For patients and their families, being told that you need to wait longer for care that your doctor tells you that you need is incredibly frustrating and frightening,” Rep. Blumenauer said. “There’s no comfort to be found in the fact that your insurance company needs time to decide if your doctor is right.”
Trends in prior authorization
The CBO report does not provide detail on what kind of medical spending would increase under a streamlined prior authorization process in insurer-run Medicare plans.
From trends reported in prior authorization, though, two factors could be at play in what appear to be relatively small estimated increases in Medicare spending from streamlined prior authorization.
One is the work already underway to create less burdensome electronic systems for these requests, such as the Fast Prior Authorization Technology Highway initiative run by the trade association America’s Health Insurance Plans.
The other factor could be the number of cases in which prior authorization merely causes delays in treatments and tests and thus simply postpones spending while adding to clinicians’ administrative work.
An analysis of prior authorization requests for dermatologic practices affiliated with the University of Utah may represent an extreme example. In a report published in JAMA Dermatology in 2020, researchers described what happened with requests made during 1 month, September 2016.
The approval rate for procedures was 99.6% – 100% (95 of 95) for Mohs surgery, and 96% (130 of 131, with 4 additional cases pending) for excisions. These findings supported calls for simplifying prior authorization procedures, “perhaps first by eliminating unnecessary PAs [prior authorizations] and appeals,” Aaron M. Secrest, MD, PhD, of the University of Utah, Salt Lake City, and coauthors wrote in the article.
Still, there is some evidence that insurer-run Medicare policies reduce the use of low-value care.
In a study published in JAMA Health Forum, Emily Boudreau, PhD, of insurer Humana Inc, and coauthors from Tufts University, Boston, and the University of Pennsylvania, Philadelphia investigated whether insurer-run Medicare could do a better job in reducing the amount of low-value care delivered than the traditional program. They analyzed a set of claims data from 2017 to 2019 for people enrolled in insurer-run and traditional Medicare.
They reported a rate of 23.07 low-value services provided per 100 people in insurer-run Medicare, compared with 25.39 for those in traditional Medicare. Some of the biggest differences reported in the article were in cancer screenings for older people.
As an example, the U.S. Preventive Services Task Force recommends that women older than 65 years not be screened for cervical cancer if they have undergone adequate screening in the past and are not at high risk for cervical cancer. There was an annual count of 1.76 screenings for cervical cancer per 100 women older than 65 in the insurer-run Medicare group versus 3.18 for those in traditional Medicare.
The Better Medicare Alliance issued a statement in favor of the House passage of the Improving Seniors’ Timely Access to Care Act.
In it, the group said the measure would “modernize prior authorization while protecting its essential function in facilitating safe, high-value, evidence-based care.” The alliance promotes use of insurer-run Medicare. The board of the Better Medicare Alliance includes executives who serve with firms that run Advantage plans as well as medical organizations and universities.
“With studies showing that up to one-quarter of all health care expenditures are wasted on services with no benefit to the patient, we need a robust, next-generation prior authorization program to deter low-value, and even harmful, care while protecting access to needed treatment and effective therapies,” said A. Mark Fendrick, MD, director of the University of Michigan’s Center for Value-Based Insurance Design in Ann Arbor, in a statement issued by the Better Medicare Alliance. He is a member of the group’s council of scholars.
On the House floor on September 14, Rep. Ami Bera, MD (D-Calif.), said he has heard from former colleagues and his medical school classmates that they now spend as much as 40% of their time on administrative work. These distractions from patient care are helping drive physicians away from the practice of medicine.
Still, the internist defended the basic premise of prior authorization while strongly appealing for better systems of handling it.
“Yes, there is a role for prior authorization in limited cases. There is also a role to go back and retrospectively look at how care is being delivered,” Rep. Bera said. “But what is happening today is a travesty. It wasn’t the intention of prior authorization. It is a prior authorization process gone awry.”
A version of this article first appeared on Medscape.com.
The path through the U.S. Senate is not yet certain for a bill intended to speed the prior authorization process of insurer-run Medicare Advantage plans, despite the measure having breezed through the House.
House leaders opted to move the Improving Seniors’ Timely Access to Care Act of 2021 (HR 3173) without requiring a roll-call vote. The measure was passed on Sept. 14 by a voice vote, an approach used in general with only uncontroversial measures that have broad support. The bill has 191 Democratic and 135 Republican sponsors, representing about three-quarters of the members of the House.
“There is no reason that patients should be waiting for medically appropriate care, especially when we know that this can lead to worse outcomes,” Rep. Earl Blumenauer (D-Ore.) said in a Sept. 14 speech on the House floor. “The fundamental promise of Medicare Advantage is undermined when people are delaying care, getting sicker, and ultimately costing Medicare more money.”
Rep. Greg Murphy, MD (R-N.C.), spoke on the House floor that day as well, bringing up cases he has seen in his own urology practice in which prior authorization delays disrupted medical care. One patient wound up in the hospital with abscess after an insurer denied an antibiotic prescription, Rep. Murphy said.
But the Senate appears unlikely at this time to move the prior authorization bill as a standalone measure. Instead, the bill may become part of a larger legislative package focused on health care that the Senate Finance Committee intends to prepare later this year.
The House-passed bill would require insurer-run Medicare plans to respond to expedited requests for prior authorization of services within 24 hours and to other requests within 7 days. This bill also would establish an electronic program for prior authorizations and mandate increased transparency as to how insurers use this tool.
CBO: Cost of change would be billions
In seeking to mandate changes in prior authorization, lawmakers likely will need to contend with the issue of a $16 billion cumulative cost estimate for the bill from the Congressional Budget Office. Members of Congress often seek to offset new spending by pairing bills that add to expected costs for the federal government with ones expected to produce savings.
Unlike Rep. Blumenauer, Rep. Murphy, and other backers of the prior authorization streamlining bill, CBO staff estimates that making the mandated changes would raise federal spending, inasmuch as there would be “a greater use of services.”
On Sept. 14, CBO issued a one-page report on the costs of the bill. The CBO report concerns only the bill in question, as is common practice with the office’s estimates.
Prior authorization changes would begin in fiscal 2025 and would add $899 million in spending, or outlays, that year, CBO said. The annual costs from the streamlined prior authorization practices through fiscal 2026 to 2032 range from $1.6 billion to $2.7 billion.
Looking at the CBO estimate against a backdrop of total Medicare Advantage costs, though, may provide important context.
The increases in spending estimated by CBO may suggest that there would be little change in federal spending as a result of streamlining prior authorization practices. These estimates of increased annual spending of $1.6 billion–$2.7 billion are only a small fraction of the current annual cost of insurer-run Medicare, and they represent an even smaller share of the projected expense.
The federal government last year spent about $350 billion on insurer-run plans, excluding Part D drug plan payments, according to the Medicare Advisory Payment Commission (MedPAC).
As of 2021, about 27 million people were enrolled in these plans, accounting for about 46% of the total Medicare population. Enrollment has doubled since 2010, MedPAC said, and it is expected to continue to grow. By 2027, insurer-run Medicare could cover 50% of the program’s population, a figure that may reach 53% by 2031.
Federal payments to these plans will accelerate in the years ahead as insurers attract more people eligible for Medicare as customers. Payments to these private health plans could rise from an expected $418 billion this year to $940.6 billion by 2031, according to the most recent Medicare trustees report.
Good intentions, poor implementation?
Insurer-run Medicare has long enjoyed deep bipartisan support in Congress. That’s due in part to its potential for reducing spending on what are considered low-value treatments, or ones considered unlikely to provide a significant medical benefit, but Rep. Blumenauer is among the members of Congress who see insurer-run Medicare as a path for preserving the giant federal health program. Traditional Medicare has far fewer restrictions on services, which sometimes opens a path for tests and treatments that offer less value for patients.
“I believe that the way traditional fee-for-service Medicare operates is not sustainable and that Medicare Advantage is one of the tools we can use to demonstrate how we can incentivize value,” Rep. Blumenauer said on the House floor. “But this is only possible when the program operates as intended. I have been deeply concerned about the reports of delays in care” caused by the clunky prior authorization processes.
He highlighted a recent report from the internal watchdog group for the Department of Health & Human Services that raises concerns about denials of appropriate care. About 18% of a set of payment denials examined by the Office of Inspector General of HHS in April actually met Medicare coverage rules and plan billing rules.
“For patients and their families, being told that you need to wait longer for care that your doctor tells you that you need is incredibly frustrating and frightening,” Rep. Blumenauer said. “There’s no comfort to be found in the fact that your insurance company needs time to decide if your doctor is right.”
Trends in prior authorization
The CBO report does not provide detail on what kind of medical spending would increase under a streamlined prior authorization process in insurer-run Medicare plans.
From trends reported in prior authorization, though, two factors could be at play in what appear to be relatively small estimated increases in Medicare spending from streamlined prior authorization.
One is the work already underway to create less burdensome electronic systems for these requests, such as the Fast Prior Authorization Technology Highway initiative run by the trade association America’s Health Insurance Plans.
The other factor could be the number of cases in which prior authorization merely causes delays in treatments and tests and thus simply postpones spending while adding to clinicians’ administrative work.
An analysis of prior authorization requests for dermatologic practices affiliated with the University of Utah may represent an extreme example. In a report published in JAMA Dermatology in 2020, researchers described what happened with requests made during 1 month, September 2016.
The approval rate for procedures was 99.6% – 100% (95 of 95) for Mohs surgery, and 96% (130 of 131, with 4 additional cases pending) for excisions. These findings supported calls for simplifying prior authorization procedures, “perhaps first by eliminating unnecessary PAs [prior authorizations] and appeals,” Aaron M. Secrest, MD, PhD, of the University of Utah, Salt Lake City, and coauthors wrote in the article.
Still, there is some evidence that insurer-run Medicare policies reduce the use of low-value care.
In a study published in JAMA Health Forum, Emily Boudreau, PhD, of insurer Humana Inc, and coauthors from Tufts University, Boston, and the University of Pennsylvania, Philadelphia investigated whether insurer-run Medicare could do a better job in reducing the amount of low-value care delivered than the traditional program. They analyzed a set of claims data from 2017 to 2019 for people enrolled in insurer-run and traditional Medicare.
They reported a rate of 23.07 low-value services provided per 100 people in insurer-run Medicare, compared with 25.39 for those in traditional Medicare. Some of the biggest differences reported in the article were in cancer screenings for older people.
As an example, the U.S. Preventive Services Task Force recommends that women older than 65 years not be screened for cervical cancer if they have undergone adequate screening in the past and are not at high risk for cervical cancer. There was an annual count of 1.76 screenings for cervical cancer per 100 women older than 65 in the insurer-run Medicare group versus 3.18 for those in traditional Medicare.
The Better Medicare Alliance issued a statement in favor of the House passage of the Improving Seniors’ Timely Access to Care Act.
In it, the group said the measure would “modernize prior authorization while protecting its essential function in facilitating safe, high-value, evidence-based care.” The alliance promotes use of insurer-run Medicare. The board of the Better Medicare Alliance includes executives who serve with firms that run Advantage plans as well as medical organizations and universities.
“With studies showing that up to one-quarter of all health care expenditures are wasted on services with no benefit to the patient, we need a robust, next-generation prior authorization program to deter low-value, and even harmful, care while protecting access to needed treatment and effective therapies,” said A. Mark Fendrick, MD, director of the University of Michigan’s Center for Value-Based Insurance Design in Ann Arbor, in a statement issued by the Better Medicare Alliance. He is a member of the group’s council of scholars.
On the House floor on September 14, Rep. Ami Bera, MD (D-Calif.), said he has heard from former colleagues and his medical school classmates that they now spend as much as 40% of their time on administrative work. These distractions from patient care are helping drive physicians away from the practice of medicine.
Still, the internist defended the basic premise of prior authorization while strongly appealing for better systems of handling it.
“Yes, there is a role for prior authorization in limited cases. There is also a role to go back and retrospectively look at how care is being delivered,” Rep. Bera said. “But what is happening today is a travesty. It wasn’t the intention of prior authorization. It is a prior authorization process gone awry.”
A version of this article first appeared on Medscape.com.
The path through the U.S. Senate is not yet certain for a bill intended to speed the prior authorization process of insurer-run Medicare Advantage plans, despite the measure having breezed through the House.
House leaders opted to move the Improving Seniors’ Timely Access to Care Act of 2021 (HR 3173) without requiring a roll-call vote. The measure was passed on Sept. 14 by a voice vote, an approach used in general with only uncontroversial measures that have broad support. The bill has 191 Democratic and 135 Republican sponsors, representing about three-quarters of the members of the House.
“There is no reason that patients should be waiting for medically appropriate care, especially when we know that this can lead to worse outcomes,” Rep. Earl Blumenauer (D-Ore.) said in a Sept. 14 speech on the House floor. “The fundamental promise of Medicare Advantage is undermined when people are delaying care, getting sicker, and ultimately costing Medicare more money.”
Rep. Greg Murphy, MD (R-N.C.), spoke on the House floor that day as well, bringing up cases he has seen in his own urology practice in which prior authorization delays disrupted medical care. One patient wound up in the hospital with abscess after an insurer denied an antibiotic prescription, Rep. Murphy said.
But the Senate appears unlikely at this time to move the prior authorization bill as a standalone measure. Instead, the bill may become part of a larger legislative package focused on health care that the Senate Finance Committee intends to prepare later this year.
The House-passed bill would require insurer-run Medicare plans to respond to expedited requests for prior authorization of services within 24 hours and to other requests within 7 days. This bill also would establish an electronic program for prior authorizations and mandate increased transparency as to how insurers use this tool.
CBO: Cost of change would be billions
In seeking to mandate changes in prior authorization, lawmakers likely will need to contend with the issue of a $16 billion cumulative cost estimate for the bill from the Congressional Budget Office. Members of Congress often seek to offset new spending by pairing bills that add to expected costs for the federal government with ones expected to produce savings.
Unlike Rep. Blumenauer, Rep. Murphy, and other backers of the prior authorization streamlining bill, CBO staff estimates that making the mandated changes would raise federal spending, inasmuch as there would be “a greater use of services.”
On Sept. 14, CBO issued a one-page report on the costs of the bill. The CBO report concerns only the bill in question, as is common practice with the office’s estimates.
Prior authorization changes would begin in fiscal 2025 and would add $899 million in spending, or outlays, that year, CBO said. The annual costs from the streamlined prior authorization practices through fiscal 2026 to 2032 range from $1.6 billion to $2.7 billion.
Looking at the CBO estimate against a backdrop of total Medicare Advantage costs, though, may provide important context.
The increases in spending estimated by CBO may suggest that there would be little change in federal spending as a result of streamlining prior authorization practices. These estimates of increased annual spending of $1.6 billion–$2.7 billion are only a small fraction of the current annual cost of insurer-run Medicare, and they represent an even smaller share of the projected expense.
The federal government last year spent about $350 billion on insurer-run plans, excluding Part D drug plan payments, according to the Medicare Advisory Payment Commission (MedPAC).
As of 2021, about 27 million people were enrolled in these plans, accounting for about 46% of the total Medicare population. Enrollment has doubled since 2010, MedPAC said, and it is expected to continue to grow. By 2027, insurer-run Medicare could cover 50% of the program’s population, a figure that may reach 53% by 2031.
Federal payments to these plans will accelerate in the years ahead as insurers attract more people eligible for Medicare as customers. Payments to these private health plans could rise from an expected $418 billion this year to $940.6 billion by 2031, according to the most recent Medicare trustees report.
Good intentions, poor implementation?
Insurer-run Medicare has long enjoyed deep bipartisan support in Congress. That’s due in part to its potential for reducing spending on what are considered low-value treatments, or ones considered unlikely to provide a significant medical benefit, but Rep. Blumenauer is among the members of Congress who see insurer-run Medicare as a path for preserving the giant federal health program. Traditional Medicare has far fewer restrictions on services, which sometimes opens a path for tests and treatments that offer less value for patients.
“I believe that the way traditional fee-for-service Medicare operates is not sustainable and that Medicare Advantage is one of the tools we can use to demonstrate how we can incentivize value,” Rep. Blumenauer said on the House floor. “But this is only possible when the program operates as intended. I have been deeply concerned about the reports of delays in care” caused by the clunky prior authorization processes.
He highlighted a recent report from the internal watchdog group for the Department of Health & Human Services that raises concerns about denials of appropriate care. About 18% of a set of payment denials examined by the Office of Inspector General of HHS in April actually met Medicare coverage rules and plan billing rules.
“For patients and their families, being told that you need to wait longer for care that your doctor tells you that you need is incredibly frustrating and frightening,” Rep. Blumenauer said. “There’s no comfort to be found in the fact that your insurance company needs time to decide if your doctor is right.”
Trends in prior authorization
The CBO report does not provide detail on what kind of medical spending would increase under a streamlined prior authorization process in insurer-run Medicare plans.
From trends reported in prior authorization, though, two factors could be at play in what appear to be relatively small estimated increases in Medicare spending from streamlined prior authorization.
One is the work already underway to create less burdensome electronic systems for these requests, such as the Fast Prior Authorization Technology Highway initiative run by the trade association America’s Health Insurance Plans.
The other factor could be the number of cases in which prior authorization merely causes delays in treatments and tests and thus simply postpones spending while adding to clinicians’ administrative work.
An analysis of prior authorization requests for dermatologic practices affiliated with the University of Utah may represent an extreme example. In a report published in JAMA Dermatology in 2020, researchers described what happened with requests made during 1 month, September 2016.
The approval rate for procedures was 99.6% – 100% (95 of 95) for Mohs surgery, and 96% (130 of 131, with 4 additional cases pending) for excisions. These findings supported calls for simplifying prior authorization procedures, “perhaps first by eliminating unnecessary PAs [prior authorizations] and appeals,” Aaron M. Secrest, MD, PhD, of the University of Utah, Salt Lake City, and coauthors wrote in the article.
Still, there is some evidence that insurer-run Medicare policies reduce the use of low-value care.
In a study published in JAMA Health Forum, Emily Boudreau, PhD, of insurer Humana Inc, and coauthors from Tufts University, Boston, and the University of Pennsylvania, Philadelphia investigated whether insurer-run Medicare could do a better job in reducing the amount of low-value care delivered than the traditional program. They analyzed a set of claims data from 2017 to 2019 for people enrolled in insurer-run and traditional Medicare.
They reported a rate of 23.07 low-value services provided per 100 people in insurer-run Medicare, compared with 25.39 for those in traditional Medicare. Some of the biggest differences reported in the article were in cancer screenings for older people.
As an example, the U.S. Preventive Services Task Force recommends that women older than 65 years not be screened for cervical cancer if they have undergone adequate screening in the past and are not at high risk for cervical cancer. There was an annual count of 1.76 screenings for cervical cancer per 100 women older than 65 in the insurer-run Medicare group versus 3.18 for those in traditional Medicare.
The Better Medicare Alliance issued a statement in favor of the House passage of the Improving Seniors’ Timely Access to Care Act.
In it, the group said the measure would “modernize prior authorization while protecting its essential function in facilitating safe, high-value, evidence-based care.” The alliance promotes use of insurer-run Medicare. The board of the Better Medicare Alliance includes executives who serve with firms that run Advantage plans as well as medical organizations and universities.
“With studies showing that up to one-quarter of all health care expenditures are wasted on services with no benefit to the patient, we need a robust, next-generation prior authorization program to deter low-value, and even harmful, care while protecting access to needed treatment and effective therapies,” said A. Mark Fendrick, MD, director of the University of Michigan’s Center for Value-Based Insurance Design in Ann Arbor, in a statement issued by the Better Medicare Alliance. He is a member of the group’s council of scholars.
On the House floor on September 14, Rep. Ami Bera, MD (D-Calif.), said he has heard from former colleagues and his medical school classmates that they now spend as much as 40% of their time on administrative work. These distractions from patient care are helping drive physicians away from the practice of medicine.
Still, the internist defended the basic premise of prior authorization while strongly appealing for better systems of handling it.
“Yes, there is a role for prior authorization in limited cases. There is also a role to go back and retrospectively look at how care is being delivered,” Rep. Bera said. “But what is happening today is a travesty. It wasn’t the intention of prior authorization. It is a prior authorization process gone awry.”
A version of this article first appeared on Medscape.com.
Experts sound alarm on ruling threatening preventive cancer care
In a statement, the groups highlighted that the decision “would result in a return to financial and other barriers proven to discourage Americans from obtaining lifesaving, preventive care.”
The ruling, issued earlier in September by a federal district judge in Texas, essentially says that the U.S. Preventive Services Task Force has no authority to determine which preventive care services must be fully covered by insurance companies – an ability granted by the Affordable Care Act (ACA).
Judge Reed O’Connor ruled that the method of appointing officers to the USPSTF is unconstitutional, which means the task force’s recommendations for no-cost preventive health care may no longer be guaranteed under the ACA for millions of insured Americans.
The judgment, however, is not yet final, and individuals still have access to these preventive services. The judge must first make the scope of the ruling clear, and the decision will likely be appealed. In addition, the decision does not affect the authority of two other entities that make recommendations about vaccinations and preventive care for infants, children, and adolescents.
But experts are concerned that the ruling will force some individuals to pay out of pocket for preventive cancer screenings and other care that would otherwise have been fully covered by insurance.
After the ruling, a group of 26 patient groups, including the American Cancer Society Cancer Action Network and the Leukemia and Lymphoma Society, took a stand.
In a statement, the groups highlighted that “access to preventive health care can prevent both disease and early death.” Under the ACA, more than 150 million Americans have benefited from expanded access to these services, and research reveals that high-quality coverage – which includes preventive services – improves health, reduces health disparities, and lowers health care costs. “This ruling directly threatens these benefits,” they explained.
Lisa Lacasse, MBA, president of ACS CAN, agreed that the ruling “threatens to erode more than a decade of progress reducing cancer deaths and suffering.”
In a statement, the ACS CAN urged the government to “swiftly appeal” the decision.
“We cannot risk returning to a system wherein every individual has to interpret their complex insurance plans to determine if a recommended mammogram will be covered or to determine how much their colonoscopy may cost,” Ms. Lacasse told this news organization.
For now, Ms. Lacasse urged patients and providers to remember that no changes to coverage requirements will occur while litigation continues.
“All preventive services required under the Affordable Care Act remain in place with no cost sharing for enrollees,” she said. “ACS CAN will continue to support and advocate for coverage of preventive services at no cost sharing.”
A version of this article first appeared on Medscape.com.
In a statement, the groups highlighted that the decision “would result in a return to financial and other barriers proven to discourage Americans from obtaining lifesaving, preventive care.”
The ruling, issued earlier in September by a federal district judge in Texas, essentially says that the U.S. Preventive Services Task Force has no authority to determine which preventive care services must be fully covered by insurance companies – an ability granted by the Affordable Care Act (ACA).
Judge Reed O’Connor ruled that the method of appointing officers to the USPSTF is unconstitutional, which means the task force’s recommendations for no-cost preventive health care may no longer be guaranteed under the ACA for millions of insured Americans.
The judgment, however, is not yet final, and individuals still have access to these preventive services. The judge must first make the scope of the ruling clear, and the decision will likely be appealed. In addition, the decision does not affect the authority of two other entities that make recommendations about vaccinations and preventive care for infants, children, and adolescents.
But experts are concerned that the ruling will force some individuals to pay out of pocket for preventive cancer screenings and other care that would otherwise have been fully covered by insurance.
After the ruling, a group of 26 patient groups, including the American Cancer Society Cancer Action Network and the Leukemia and Lymphoma Society, took a stand.
In a statement, the groups highlighted that “access to preventive health care can prevent both disease and early death.” Under the ACA, more than 150 million Americans have benefited from expanded access to these services, and research reveals that high-quality coverage – which includes preventive services – improves health, reduces health disparities, and lowers health care costs. “This ruling directly threatens these benefits,” they explained.
Lisa Lacasse, MBA, president of ACS CAN, agreed that the ruling “threatens to erode more than a decade of progress reducing cancer deaths and suffering.”
In a statement, the ACS CAN urged the government to “swiftly appeal” the decision.
“We cannot risk returning to a system wherein every individual has to interpret their complex insurance plans to determine if a recommended mammogram will be covered or to determine how much their colonoscopy may cost,” Ms. Lacasse told this news organization.
For now, Ms. Lacasse urged patients and providers to remember that no changes to coverage requirements will occur while litigation continues.
“All preventive services required under the Affordable Care Act remain in place with no cost sharing for enrollees,” she said. “ACS CAN will continue to support and advocate for coverage of preventive services at no cost sharing.”
A version of this article first appeared on Medscape.com.
In a statement, the groups highlighted that the decision “would result in a return to financial and other barriers proven to discourage Americans from obtaining lifesaving, preventive care.”
The ruling, issued earlier in September by a federal district judge in Texas, essentially says that the U.S. Preventive Services Task Force has no authority to determine which preventive care services must be fully covered by insurance companies – an ability granted by the Affordable Care Act (ACA).
Judge Reed O’Connor ruled that the method of appointing officers to the USPSTF is unconstitutional, which means the task force’s recommendations for no-cost preventive health care may no longer be guaranteed under the ACA for millions of insured Americans.
The judgment, however, is not yet final, and individuals still have access to these preventive services. The judge must first make the scope of the ruling clear, and the decision will likely be appealed. In addition, the decision does not affect the authority of two other entities that make recommendations about vaccinations and preventive care for infants, children, and adolescents.
But experts are concerned that the ruling will force some individuals to pay out of pocket for preventive cancer screenings and other care that would otherwise have been fully covered by insurance.
After the ruling, a group of 26 patient groups, including the American Cancer Society Cancer Action Network and the Leukemia and Lymphoma Society, took a stand.
In a statement, the groups highlighted that “access to preventive health care can prevent both disease and early death.” Under the ACA, more than 150 million Americans have benefited from expanded access to these services, and research reveals that high-quality coverage – which includes preventive services – improves health, reduces health disparities, and lowers health care costs. “This ruling directly threatens these benefits,” they explained.
Lisa Lacasse, MBA, president of ACS CAN, agreed that the ruling “threatens to erode more than a decade of progress reducing cancer deaths and suffering.”
In a statement, the ACS CAN urged the government to “swiftly appeal” the decision.
“We cannot risk returning to a system wherein every individual has to interpret their complex insurance plans to determine if a recommended mammogram will be covered or to determine how much their colonoscopy may cost,” Ms. Lacasse told this news organization.
For now, Ms. Lacasse urged patients and providers to remember that no changes to coverage requirements will occur while litigation continues.
“All preventive services required under the Affordable Care Act remain in place with no cost sharing for enrollees,” she said. “ACS CAN will continue to support and advocate for coverage of preventive services at no cost sharing.”
A version of this article first appeared on Medscape.com.
New science reveals the best way to take a pill
I want to tell you a story about forgetfulness and haste, and how the combination of the two can lead to frightening consequences. A few years ago, I was lying in bed about to turn out the light when I realized I’d forgotten to take “my pill.”
Like some 161 million other American adults, I was then a consumer of a prescription medication. Being conscientious, I got up, retrieved said pill, and tossed it back. Being lazy, I didn’t bother to grab a glass of water to help the thing go down. Instead, I promptly returned to bed, threw a pillow over my head, and prepared for sleep.
Within seconds, I began to feel a burning sensation in my chest. After about a minute, that burn became a crippling pain. Not wanting to alarm my wife, I went into the living room, where I spent the next 30 minutes doubled over in agony. Was I having a heart attack? I phoned my sister, a hospitalist in Texas. She advised me to take myself to the ED to get checked out.
If only I’d known then about “Duke.” He could have told me how critical body posture is when people swallow pills.
Who’s Duke?
Duke is a computer representation of a 34-year-old, anatomically normal human male created by computer scientists at the IT’IS Foundation, a nonprofit group based in Switzerland that works on a variety of projects in health care technology. Using Duke, Rajat Mittal, PhD, a professor of medicine at the Johns Hopkins University, Baltimore, created a computer model called “StomachSim” to explore the process of digestion.
Their research, published in the journal Physics of Fluids, turned up several surprising findings about the dynamics of swallowing pills – the most common way medication is used worldwide.
Dr. Mittal said he chose to study the stomach because the functions of most other organ systems, from the heart to the brain, have already attracted plenty of attention from scientists.
“As I was looking to initiate research in some new directions, the implications of stomach biomechanics on important conditions such as diabetes, obesity, and gastroparesis became apparent to me,” he said. “It was clear that bioengineering research in this arena lags other more ‘sexy’ areas such as cardiovascular flows by at least 20 years, and there seemed to be a great opportunity to do impactful work.”
Your posture may help a pill work better
Several well-known things affect a pill’s ability to disperse its contents into the gut and be used by the body, such as the stomach’s contents (a heavy breakfast, a mix of liquids like juice, milk, and coffee) and the motion of the organ’s walls. But Dr. Mittal’s group learned that Duke’s posture also played a major role.
The researchers ran Duke through computer simulations in varying postures: upright, leaning right, leaning left, and leaning back, while keeping all the other parts of their analyses (like the things mentioned above) the same.
They found that posture determined as much as 83% of how quickly a pill disperses into the intestines. The most efficient position was leaning right. The least was leaning left, which prevented the pill from reaching the antrum, or bottom section of the stomach, and thus kept all but traces of the dissolved drug from entering the duodenum, where the stomach joins the small intestine. (Interestingly, Jews who observe Passover are advised to recline to the left during the meal as a symbol of freedom and leisure.)
That makes sense if you think about the stomach’s shape, which looks kind of like a bean, curving from the left to the right side of the body. Because of gravity, your position will change where the pill lands.
a condition in which the stomach loses the ability to empty properly.
How this could help people
Among the groups most likely to benefit from such studies, Dr. Mittal said, are the elderly – who both take a lot of pills and are more prone to trouble swallowing because of age-related changes in their esophagus – and the bedridden, who can’t easily shift their posture. The findings may also lead to improvements in the ability to treat people with gastroparesis, a particular problem for people with diabetes.
Future studies with Duke and similar simulations will look at how the GI system digests proteins, carbohydrates, and fatty meals, Dr. Mittal said.
In the meantime, Dr. Mittal offered the following advice: “Standing or sitting upright after taking a pill is fine. If you have to take a pill lying down, stay on your back or on your right side. Avoid lying on your left side after taking a pill.”
As for what happened to me, any gastroenterologist reading this has figured out that my condition was not heart-related. Instead, I likely was having a bout of pill esophagitis, irritation that can result from medications that aggravate the mucosa of the food tube. Although painful, esophagitis isn’t life-threatening. After about an hour, the pain began to subside, and by the next morning I was fine, with only a faint ache in my chest to remind me of my earlier torment. (Researchers noted an increase in the condition early in the COVID-19 pandemic, linked to the antibiotic doxycycline.)
And, in the interest of accuracy, my pill problem began above the stomach. Nothing in the Hopkins research suggests that the alignment of the esophagus plays a role in how drugs disperse in the gut – unless, of course, it prevents those pills from reaching the stomach in the first place.
A version of this article first appeared on WebMD.com.
I want to tell you a story about forgetfulness and haste, and how the combination of the two can lead to frightening consequences. A few years ago, I was lying in bed about to turn out the light when I realized I’d forgotten to take “my pill.”
Like some 161 million other American adults, I was then a consumer of a prescription medication. Being conscientious, I got up, retrieved said pill, and tossed it back. Being lazy, I didn’t bother to grab a glass of water to help the thing go down. Instead, I promptly returned to bed, threw a pillow over my head, and prepared for sleep.
Within seconds, I began to feel a burning sensation in my chest. After about a minute, that burn became a crippling pain. Not wanting to alarm my wife, I went into the living room, where I spent the next 30 minutes doubled over in agony. Was I having a heart attack? I phoned my sister, a hospitalist in Texas. She advised me to take myself to the ED to get checked out.
If only I’d known then about “Duke.” He could have told me how critical body posture is when people swallow pills.
Who’s Duke?
Duke is a computer representation of a 34-year-old, anatomically normal human male created by computer scientists at the IT’IS Foundation, a nonprofit group based in Switzerland that works on a variety of projects in health care technology. Using Duke, Rajat Mittal, PhD, a professor of medicine at the Johns Hopkins University, Baltimore, created a computer model called “StomachSim” to explore the process of digestion.
Their research, published in the journal Physics of Fluids, turned up several surprising findings about the dynamics of swallowing pills – the most common way medication is used worldwide.
Dr. Mittal said he chose to study the stomach because the functions of most other organ systems, from the heart to the brain, have already attracted plenty of attention from scientists.
“As I was looking to initiate research in some new directions, the implications of stomach biomechanics on important conditions such as diabetes, obesity, and gastroparesis became apparent to me,” he said. “It was clear that bioengineering research in this arena lags other more ‘sexy’ areas such as cardiovascular flows by at least 20 years, and there seemed to be a great opportunity to do impactful work.”
Your posture may help a pill work better
Several well-known things affect a pill’s ability to disperse its contents into the gut and be used by the body, such as the stomach’s contents (a heavy breakfast, a mix of liquids like juice, milk, and coffee) and the motion of the organ’s walls. But Dr. Mittal’s group learned that Duke’s posture also played a major role.
The researchers ran Duke through computer simulations in varying postures: upright, leaning right, leaning left, and leaning back, while keeping all the other parts of their analyses (like the things mentioned above) the same.
They found that posture determined as much as 83% of how quickly a pill disperses into the intestines. The most efficient position was leaning right. The least was leaning left, which prevented the pill from reaching the antrum, or bottom section of the stomach, and thus kept all but traces of the dissolved drug from entering the duodenum, where the stomach joins the small intestine. (Interestingly, Jews who observe Passover are advised to recline to the left during the meal as a symbol of freedom and leisure.)
That makes sense if you think about the stomach’s shape, which looks kind of like a bean, curving from the left to the right side of the body. Because of gravity, your position will change where the pill lands.
a condition in which the stomach loses the ability to empty properly.
How this could help people
Among the groups most likely to benefit from such studies, Dr. Mittal said, are the elderly – who both take a lot of pills and are more prone to trouble swallowing because of age-related changes in their esophagus – and the bedridden, who can’t easily shift their posture. The findings may also lead to improvements in the ability to treat people with gastroparesis, a particular problem for people with diabetes.
Future studies with Duke and similar simulations will look at how the GI system digests proteins, carbohydrates, and fatty meals, Dr. Mittal said.
In the meantime, Dr. Mittal offered the following advice: “Standing or sitting upright after taking a pill is fine. If you have to take a pill lying down, stay on your back or on your right side. Avoid lying on your left side after taking a pill.”
As for what happened to me, any gastroenterologist reading this has figured out that my condition was not heart-related. Instead, I likely was having a bout of pill esophagitis, irritation that can result from medications that aggravate the mucosa of the food tube. Although painful, esophagitis isn’t life-threatening. After about an hour, the pain began to subside, and by the next morning I was fine, with only a faint ache in my chest to remind me of my earlier torment. (Researchers noted an increase in the condition early in the COVID-19 pandemic, linked to the antibiotic doxycycline.)
And, in the interest of accuracy, my pill problem began above the stomach. Nothing in the Hopkins research suggests that the alignment of the esophagus plays a role in how drugs disperse in the gut – unless, of course, it prevents those pills from reaching the stomach in the first place.
A version of this article first appeared on WebMD.com.
I want to tell you a story about forgetfulness and haste, and how the combination of the two can lead to frightening consequences. A few years ago, I was lying in bed about to turn out the light when I realized I’d forgotten to take “my pill.”
Like some 161 million other American adults, I was then a consumer of a prescription medication. Being conscientious, I got up, retrieved said pill, and tossed it back. Being lazy, I didn’t bother to grab a glass of water to help the thing go down. Instead, I promptly returned to bed, threw a pillow over my head, and prepared for sleep.
Within seconds, I began to feel a burning sensation in my chest. After about a minute, that burn became a crippling pain. Not wanting to alarm my wife, I went into the living room, where I spent the next 30 minutes doubled over in agony. Was I having a heart attack? I phoned my sister, a hospitalist in Texas. She advised me to take myself to the ED to get checked out.
If only I’d known then about “Duke.” He could have told me how critical body posture is when people swallow pills.
Who’s Duke?
Duke is a computer representation of a 34-year-old, anatomically normal human male created by computer scientists at the IT’IS Foundation, a nonprofit group based in Switzerland that works on a variety of projects in health care technology. Using Duke, Rajat Mittal, PhD, a professor of medicine at the Johns Hopkins University, Baltimore, created a computer model called “StomachSim” to explore the process of digestion.
Their research, published in the journal Physics of Fluids, turned up several surprising findings about the dynamics of swallowing pills – the most common way medication is used worldwide.
Dr. Mittal said he chose to study the stomach because the functions of most other organ systems, from the heart to the brain, have already attracted plenty of attention from scientists.
“As I was looking to initiate research in some new directions, the implications of stomach biomechanics on important conditions such as diabetes, obesity, and gastroparesis became apparent to me,” he said. “It was clear that bioengineering research in this arena lags other more ‘sexy’ areas such as cardiovascular flows by at least 20 years, and there seemed to be a great opportunity to do impactful work.”
Your posture may help a pill work better
Several well-known things affect a pill’s ability to disperse its contents into the gut and be used by the body, such as the stomach’s contents (a heavy breakfast, a mix of liquids like juice, milk, and coffee) and the motion of the organ’s walls. But Dr. Mittal’s group learned that Duke’s posture also played a major role.
The researchers ran Duke through computer simulations in varying postures: upright, leaning right, leaning left, and leaning back, while keeping all the other parts of their analyses (like the things mentioned above) the same.
They found that posture determined as much as 83% of how quickly a pill disperses into the intestines. The most efficient position was leaning right. The least was leaning left, which prevented the pill from reaching the antrum, or bottom section of the stomach, and thus kept all but traces of the dissolved drug from entering the duodenum, where the stomach joins the small intestine. (Interestingly, Jews who observe Passover are advised to recline to the left during the meal as a symbol of freedom and leisure.)
That makes sense if you think about the stomach’s shape, which looks kind of like a bean, curving from the left to the right side of the body. Because of gravity, your position will change where the pill lands.
a condition in which the stomach loses the ability to empty properly.
How this could help people
Among the groups most likely to benefit from such studies, Dr. Mittal said, are the elderly – who both take a lot of pills and are more prone to trouble swallowing because of age-related changes in their esophagus – and the bedridden, who can’t easily shift their posture. The findings may also lead to improvements in the ability to treat people with gastroparesis, a particular problem for people with diabetes.
Future studies with Duke and similar simulations will look at how the GI system digests proteins, carbohydrates, and fatty meals, Dr. Mittal said.
In the meantime, Dr. Mittal offered the following advice: “Standing or sitting upright after taking a pill is fine. If you have to take a pill lying down, stay on your back or on your right side. Avoid lying on your left side after taking a pill.”
As for what happened to me, any gastroenterologist reading this has figured out that my condition was not heart-related. Instead, I likely was having a bout of pill esophagitis, irritation that can result from medications that aggravate the mucosa of the food tube. Although painful, esophagitis isn’t life-threatening. After about an hour, the pain began to subside, and by the next morning I was fine, with only a faint ache in my chest to remind me of my earlier torment. (Researchers noted an increase in the condition early in the COVID-19 pandemic, linked to the antibiotic doxycycline.)
And, in the interest of accuracy, my pill problem began above the stomach. Nothing in the Hopkins research suggests that the alignment of the esophagus plays a role in how drugs disperse in the gut – unless, of course, it prevents those pills from reaching the stomach in the first place.
A version of this article first appeared on WebMD.com.