User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Boys may carry the weight, or overweight, of adults’ infertility
Overweight boy, infertile man?
When it comes to causes of infertility, history and science have generally focused on women. A lot of the research overlooks men, but some previous studies have suggested that male infertility contributes to about half of the cases of couple infertility. The reason for much of that male infertility, however, has been a mystery. Until now.
A group of Italian investigators looked at the declining trend in sperm counts over the past 40 years and the increase of childhood obesity. Is there a correlation? The researchers think so. Childhood obesity can be linked to multiple causes, but the researchers zeroed in on the effect that obesity has on metabolic rates and, therefore, testicular growth.
Collecting data on testicular volume, body mass index (BMI), and insulin resistance from 268 boys aged 2-18 years, the researchers discovered that those with normal weight and normal insulin levels had testicular volumes 1.5 times higher than their overweight counterparts and 1.5-2 times higher than those with hyperinsulinemia, building a case for obesity being a factor for infertility later in life.
Since low testicular volume is associated with lower sperm count and production as an adult, putting two and two together makes a compelling argument for childhood obesity being a major male infertility culprit. It also creates even more urgency for the health care industry and community decision makers to focus on childhood obesity.
It sure would be nice to be able to take one of the many risk factors for future human survival off the table. Maybe by taking something, like cake, off the table.
Fecal transplantation moves to the kitchen
Fecal microbiota transplantation is an effective way to treat Clostridioides difficile infection, but, in the end, it’s still a transplantation procedure involving a nasogastric or colorectal tube or rather large oral capsules with a demanding (30-40 capsules over 2 days) dosage. Please, Science, tell us there’s a better way.
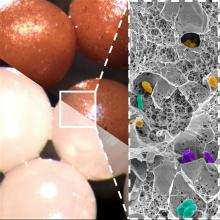
Science, in the form of investigators at the University of Geneva and Lausanne University Hospital in Switzerland, has spoken, and there may be a better way. Presenting fecal beads: All the bacterial goodness of donor stool without the tubal insertions or massive quantities of giant capsules.
We know you’re scoffing out there, but it’s true. All you need is a little alginate, which is a “biocompatible polysaccharide isolated from brown algae” of the Phaeophyceae family. The donor feces is microencapsulated by mixing it with the alginate, dropping that mixture into water containing calcium chloride, turning it into a gel, and then freeze-drying the gel into small (just 2 mm), solid beads.
Sounds plausible enough, but what do you do with them? “These brownish beads can be easily dispersed in a liquid or food that is pleasant to eat. They also have no taste,” senior author Eric Allémann, PhD, said in a statement released by the University of Geneva.
Pleasant to eat? No taste? So which is it? If you really want to know, watch fecal beads week on the new season of “The Great British Baking Show,” when Paul and Prue judge poop baked into crumpets, crepes, and crostatas. Yum.
We’re on the low-oxygen diet
Nine out of ten doctors agree: Oxygen is more important to your continued well-being than food. After all, a human can go weeks without food, but just minutes without oxygen. However, ten out of ten doctors agree that the United States has an obesity problem. They all also agree that previous research has shown soldiers who train at high altitudes lose more weight than those training at lower altitudes.
So, on the one hand, we have a country full of overweight people, and on the other, we have low oxygen levels causing weight loss. The solution, then, is obvious: Stop breathing.
More specifically (and somewhat less facetiously), researchers from Louisiana have launched the Low Oxygen and Weight Status trial and are currently recruiting individuals with BMIs of 30-40 to, uh, suffocate themselves. No, no, it’s okay, it’s just when they’re sleeping.
Fine, straight face. Participants in the LOWS trial will undergo an 8-week period when they will consume a controlled weight-loss diet and spend their nights in a hypoxic sealed tent, where they will sleep in an environment with an oxygen level equivalent to 8,500 feet above sea level (roughly equivalent to Aspen, Colo.). They will be compared with people on the same diet who sleep in a normal, sea-level oxygen environment.
The study’s goal is to determine whether or not spending time in a low-oxygen environment will suppress appetite, increase energy expenditure, and improve weight loss and insulin sensitivity. Excessive weight loss in high-altitude environments isn’t a good thing for soldiers – they kind of need their muscles and body weight to do the whole soldiering thing – but it could be great for people struggling to lose those last few pounds. And it also may prove LOTME’s previous thesis: Air is not good.
Overweight boy, infertile man?
When it comes to causes of infertility, history and science have generally focused on women. A lot of the research overlooks men, but some previous studies have suggested that male infertility contributes to about half of the cases of couple infertility. The reason for much of that male infertility, however, has been a mystery. Until now.
A group of Italian investigators looked at the declining trend in sperm counts over the past 40 years and the increase of childhood obesity. Is there a correlation? The researchers think so. Childhood obesity can be linked to multiple causes, but the researchers zeroed in on the effect that obesity has on metabolic rates and, therefore, testicular growth.
Collecting data on testicular volume, body mass index (BMI), and insulin resistance from 268 boys aged 2-18 years, the researchers discovered that those with normal weight and normal insulin levels had testicular volumes 1.5 times higher than their overweight counterparts and 1.5-2 times higher than those with hyperinsulinemia, building a case for obesity being a factor for infertility later in life.
Since low testicular volume is associated with lower sperm count and production as an adult, putting two and two together makes a compelling argument for childhood obesity being a major male infertility culprit. It also creates even more urgency for the health care industry and community decision makers to focus on childhood obesity.
It sure would be nice to be able to take one of the many risk factors for future human survival off the table. Maybe by taking something, like cake, off the table.
Fecal transplantation moves to the kitchen
Fecal microbiota transplantation is an effective way to treat Clostridioides difficile infection, but, in the end, it’s still a transplantation procedure involving a nasogastric or colorectal tube or rather large oral capsules with a demanding (30-40 capsules over 2 days) dosage. Please, Science, tell us there’s a better way.
Science, in the form of investigators at the University of Geneva and Lausanne University Hospital in Switzerland, has spoken, and there may be a better way. Presenting fecal beads: All the bacterial goodness of donor stool without the tubal insertions or massive quantities of giant capsules.
We know you’re scoffing out there, but it’s true. All you need is a little alginate, which is a “biocompatible polysaccharide isolated from brown algae” of the Phaeophyceae family. The donor feces is microencapsulated by mixing it with the alginate, dropping that mixture into water containing calcium chloride, turning it into a gel, and then freeze-drying the gel into small (just 2 mm), solid beads.
Sounds plausible enough, but what do you do with them? “These brownish beads can be easily dispersed in a liquid or food that is pleasant to eat. They also have no taste,” senior author Eric Allémann, PhD, said in a statement released by the University of Geneva.
Pleasant to eat? No taste? So which is it? If you really want to know, watch fecal beads week on the new season of “The Great British Baking Show,” when Paul and Prue judge poop baked into crumpets, crepes, and crostatas. Yum.
We’re on the low-oxygen diet
Nine out of ten doctors agree: Oxygen is more important to your continued well-being than food. After all, a human can go weeks without food, but just minutes without oxygen. However, ten out of ten doctors agree that the United States has an obesity problem. They all also agree that previous research has shown soldiers who train at high altitudes lose more weight than those training at lower altitudes.
So, on the one hand, we have a country full of overweight people, and on the other, we have low oxygen levels causing weight loss. The solution, then, is obvious: Stop breathing.
More specifically (and somewhat less facetiously), researchers from Louisiana have launched the Low Oxygen and Weight Status trial and are currently recruiting individuals with BMIs of 30-40 to, uh, suffocate themselves. No, no, it’s okay, it’s just when they’re sleeping.
Fine, straight face. Participants in the LOWS trial will undergo an 8-week period when they will consume a controlled weight-loss diet and spend their nights in a hypoxic sealed tent, where they will sleep in an environment with an oxygen level equivalent to 8,500 feet above sea level (roughly equivalent to Aspen, Colo.). They will be compared with people on the same diet who sleep in a normal, sea-level oxygen environment.
The study’s goal is to determine whether or not spending time in a low-oxygen environment will suppress appetite, increase energy expenditure, and improve weight loss and insulin sensitivity. Excessive weight loss in high-altitude environments isn’t a good thing for soldiers – they kind of need their muscles and body weight to do the whole soldiering thing – but it could be great for people struggling to lose those last few pounds. And it also may prove LOTME’s previous thesis: Air is not good.
Overweight boy, infertile man?
When it comes to causes of infertility, history and science have generally focused on women. A lot of the research overlooks men, but some previous studies have suggested that male infertility contributes to about half of the cases of couple infertility. The reason for much of that male infertility, however, has been a mystery. Until now.
A group of Italian investigators looked at the declining trend in sperm counts over the past 40 years and the increase of childhood obesity. Is there a correlation? The researchers think so. Childhood obesity can be linked to multiple causes, but the researchers zeroed in on the effect that obesity has on metabolic rates and, therefore, testicular growth.
Collecting data on testicular volume, body mass index (BMI), and insulin resistance from 268 boys aged 2-18 years, the researchers discovered that those with normal weight and normal insulin levels had testicular volumes 1.5 times higher than their overweight counterparts and 1.5-2 times higher than those with hyperinsulinemia, building a case for obesity being a factor for infertility later in life.
Since low testicular volume is associated with lower sperm count and production as an adult, putting two and two together makes a compelling argument for childhood obesity being a major male infertility culprit. It also creates even more urgency for the health care industry and community decision makers to focus on childhood obesity.
It sure would be nice to be able to take one of the many risk factors for future human survival off the table. Maybe by taking something, like cake, off the table.
Fecal transplantation moves to the kitchen
Fecal microbiota transplantation is an effective way to treat Clostridioides difficile infection, but, in the end, it’s still a transplantation procedure involving a nasogastric or colorectal tube or rather large oral capsules with a demanding (30-40 capsules over 2 days) dosage. Please, Science, tell us there’s a better way.
Science, in the form of investigators at the University of Geneva and Lausanne University Hospital in Switzerland, has spoken, and there may be a better way. Presenting fecal beads: All the bacterial goodness of donor stool without the tubal insertions or massive quantities of giant capsules.
We know you’re scoffing out there, but it’s true. All you need is a little alginate, which is a “biocompatible polysaccharide isolated from brown algae” of the Phaeophyceae family. The donor feces is microencapsulated by mixing it with the alginate, dropping that mixture into water containing calcium chloride, turning it into a gel, and then freeze-drying the gel into small (just 2 mm), solid beads.
Sounds plausible enough, but what do you do with them? “These brownish beads can be easily dispersed in a liquid or food that is pleasant to eat. They also have no taste,” senior author Eric Allémann, PhD, said in a statement released by the University of Geneva.
Pleasant to eat? No taste? So which is it? If you really want to know, watch fecal beads week on the new season of “The Great British Baking Show,” when Paul and Prue judge poop baked into crumpets, crepes, and crostatas. Yum.
We’re on the low-oxygen diet
Nine out of ten doctors agree: Oxygen is more important to your continued well-being than food. After all, a human can go weeks without food, but just minutes without oxygen. However, ten out of ten doctors agree that the United States has an obesity problem. They all also agree that previous research has shown soldiers who train at high altitudes lose more weight than those training at lower altitudes.
So, on the one hand, we have a country full of overweight people, and on the other, we have low oxygen levels causing weight loss. The solution, then, is obvious: Stop breathing.
More specifically (and somewhat less facetiously), researchers from Louisiana have launched the Low Oxygen and Weight Status trial and are currently recruiting individuals with BMIs of 30-40 to, uh, suffocate themselves. No, no, it’s okay, it’s just when they’re sleeping.
Fine, straight face. Participants in the LOWS trial will undergo an 8-week period when they will consume a controlled weight-loss diet and spend their nights in a hypoxic sealed tent, where they will sleep in an environment with an oxygen level equivalent to 8,500 feet above sea level (roughly equivalent to Aspen, Colo.). They will be compared with people on the same diet who sleep in a normal, sea-level oxygen environment.
The study’s goal is to determine whether or not spending time in a low-oxygen environment will suppress appetite, increase energy expenditure, and improve weight loss and insulin sensitivity. Excessive weight loss in high-altitude environments isn’t a good thing for soldiers – they kind of need their muscles and body weight to do the whole soldiering thing – but it could be great for people struggling to lose those last few pounds. And it also may prove LOTME’s previous thesis: Air is not good.
Part-time physician: Is it a viable career choice?
On average, physicians reported in the Medscape Physician Compensation Report 2023 that they worked 50 hours per week. Five specialties, including critical care, cardiology, and general surgery reported working 55 or more hours weekly.
In 2011, The New England Journal of Medicine reported that part-time physician careers were rising. At the time, part-time doctors made up 21% of the physician workforce, up from 13% in 2005.
In a more recent survey from the California Health Care Foundation, only 12% of California physicians said they devoted 20-29 hours a week to patient care.
Amy Knoup, a senior recruitment adviser with Provider Solutions & Development), has been helping doctors find jobs for over a decade, and she’s noticed a trend.
“Not only are more physicians seeking part-time roles than they were 10 years ago, but more large health care systems are also offering part time or per diem as well,” said Ms. Knoup.
Who’s working part time, and why?
Ten years ago, the fastest growing segment of part-timers were men nearing retirement and early- to mid-career women.
Pediatricians led the part-time pack in 2002, according to an American Academy of Pediatrics study. At the time, 15% of pediatricians reported their hours as part time. However, the numbers may have increased over the years. For example, a 2021 study by the department of pediatrics, Boston Medical Center, and Boston University found that almost 30% of graduating pediatricians sought part-time work at the end of their training.
At PS&D, Ms. Knoup said she has noticed a trend toward part-timers among primary care, behavioral health, and outpatient specialties such as endocrinology. “We’re also seeing it with the inpatient side in roles that are more shift based like hospitalists, radiologists, and critical care and ER doctors.”
Another trend Ms. Knoup has noticed is with early-career doctors. “They have a different mindset,” she said. “Younger generations are acutely aware of burnout. They may have experienced it in residency or during the pandemic. They’ve had a taste of that and don’t want to go down that road again, so they’re seeking part-time roles. It’s an intentional choice.”
Tracey O’Connell, MD, a radiologist, always knew that she wanted to work part time. “I had a baby as a resident, and I was pregnant with my second child as a fellow,” she said. “I was already feeling overwhelmed with medical training and having a family.”
Dr. O’Connell worked in private practice for 16 years on Mondays, Wednesdays, and Fridays, with no nights or weekends.
“I still found it completely overwhelming,” she said. “Even though I had more days not working than working, I felt like the demands of medical life had advanced faster than human beings could adapt, and I still feel that way.”
Today she runs a part-time teleradiology practice from home but spends more time on her second career as a life coach. “Most of my clients are physicians looking for more fulfillment and sustainable ways of practicing medicine while maintaining their own identity as human beings, not just the all-consuming identity of ‘doctor,’ ” she said.
On the other end of the career spectrum is Lois Goodman, MD, an ob.gyn. in her late 70s. After 42 years in a group practice, she started her solo practice at 72, seeing patients 3 days per week. “I’m just happy to be working. That’s a tremendous payoff for me. I need to keep working for my mental health.”
How does part-time work affect physician shortages and care delivery?
Reducing clinical effort is one of the strategies physicians use to scale down overload. Still, it’s not viable as a long-term solution, said Christine Sinsky, MD, AMA’s vice president of professional satisfaction and a nationally regarded researcher on physician burnout.
“If all the physicians in a community went from working 100% FTE clinical to 50% FTE clinical, then the people in that community would have half the access to care that they had,” said Dr. Sinsky. “There’s less capacity in the system to care for patients.”
Some could argue, then, that part-time physician work may contribute to physician shortage predictions. An Association of American Medical Colleges report estimates there will be a shortage of 37,800 to 124,000 physicians by 2034.
But physicians working part-time express a contrasting point of view. “I don’t believe that part-time workers are responsible for the health care shortage but rather, a great solution,” said Dr. O’Connell. “Because in order to continue working for a long time rather than quitting when the demands exceed human capacity, working part time is a great compromise to offer a life of more sustainable well-being and longevity as a physician, and still live a wholehearted life.”
Pros and cons of being a part-time physician
Pros
Less burnout: The American Medical Association has tracked burnout rates for 22 years. By the end of 2021, nearly 63% of physicians reported burnout symptoms, compared with 38% the year before. Going part time appears to reduce burnout, suggests a study published in Mayo Clinic Proceedings.
Better work-life balance: Rachel Miller, MD, an ob.gyn., worked 60-70 hours weekly for 9 years. In 2022, she went to work as an OB hospitalist for a health care system that welcomes part-time clinicians. Since then, she has achieved a better work-life balance, putting in 26-28 hours a week. Dr. Miller now spends more time with her kids and in her additional role as an executive coach to leaders in the medical field.
More focus: “When I’m at work, I’m 100% mentally in and focused,” said Dr. Miller. “My interactions with patients are different because I’m not burned out. My demeanor and my willingness to connect are stronger.”
Better health: Mehmet Cilingiroglu, MD, with CardioSolution, traded full-time work for part time when health issues and a kidney transplant sidelined his 30-year career in 2018. “Despite my significant health issues, I’ve been able to continue working at a pace that suits me rather than having to retire,” he said. “Part-time physicians can still enjoy patient care, research, innovation, education, and training while balancing that with other areas of life.”
Errin Weisman, a DO who gave up full-time work in 2016, said cutting back makes her feel healthier, happier, and more energized. “Part-time work helps me to bring my A game each day I work and deliver the best care.” She’s also a life coach encouraging other physicians to find balance in their professional and personal lives.
Cons
Cut in pay: Obviously, the No. 1 con is you’ll make less working part time, so adjusting to a salary decrease can be a huge issue, especially if you don’t have other sources of income. Physicians paying off student loans, those caring for children or elderly parents, or those in their prime earning years needing to save for retirement may not be able to go part time.
Diminished career: The chance for promotions or being well known in your field can be diminished, as well as a loss of proficiency if you’re only performing surgery or procedures part time. In some specialties, working part time and not keeping up with (or being able to practice) newer technology developments can harm your career or reputation in the long run.
Missing out: While working part time has many benefits, physicians also experience a wide range of drawbacks. Dr. Goodman, for example, said she misses delivering babies and doing surgeries. Dr. Miller said she gave up some aspects of her specialty, like performing hysterectomies, participating in complex cases, and no longer having an office like she did as a full-time ob.gyn.
Loss of fellowship: Dr. O’Connell said she missed the camaraderie and sense of belonging when she scaled back her hours. “I felt like a fish out of water, that my values didn’t align with the group’s values,” she said. This led to self-doubt, frustrated colleagues, and a reduction in benefits.
Lost esteem: Dr. O’Connell also felt she was expected to work overtime without additional pay and was no longer eligible for bonuses. “I was treated as a team player when I was needed, but not when it came to perks and benefits and insider privilege,” she said. There may be a loss of esteem among colleagues and supervisors.
Overcoming stigma: Because part-time physician work is still not prevalent among colleagues, some may resist the idea, have less respect for it, perceive it as not being serious about your career as a physician, or associate it with being lazy or entitled.
Summing it up
Every physician must weigh the value and drawbacks of part-time work, but the more physicians who go this route, the more part-time medicine gains traction and the more physicians can learn about its values versus its drawbacks.
A version of this article first appeared on Medscape.com.
On average, physicians reported in the Medscape Physician Compensation Report 2023 that they worked 50 hours per week. Five specialties, including critical care, cardiology, and general surgery reported working 55 or more hours weekly.
In 2011, The New England Journal of Medicine reported that part-time physician careers were rising. At the time, part-time doctors made up 21% of the physician workforce, up from 13% in 2005.
In a more recent survey from the California Health Care Foundation, only 12% of California physicians said they devoted 20-29 hours a week to patient care.
Amy Knoup, a senior recruitment adviser with Provider Solutions & Development), has been helping doctors find jobs for over a decade, and she’s noticed a trend.
“Not only are more physicians seeking part-time roles than they were 10 years ago, but more large health care systems are also offering part time or per diem as well,” said Ms. Knoup.
Who’s working part time, and why?
Ten years ago, the fastest growing segment of part-timers were men nearing retirement and early- to mid-career women.
Pediatricians led the part-time pack in 2002, according to an American Academy of Pediatrics study. At the time, 15% of pediatricians reported their hours as part time. However, the numbers may have increased over the years. For example, a 2021 study by the department of pediatrics, Boston Medical Center, and Boston University found that almost 30% of graduating pediatricians sought part-time work at the end of their training.
At PS&D, Ms. Knoup said she has noticed a trend toward part-timers among primary care, behavioral health, and outpatient specialties such as endocrinology. “We’re also seeing it with the inpatient side in roles that are more shift based like hospitalists, radiologists, and critical care and ER doctors.”
Another trend Ms. Knoup has noticed is with early-career doctors. “They have a different mindset,” she said. “Younger generations are acutely aware of burnout. They may have experienced it in residency or during the pandemic. They’ve had a taste of that and don’t want to go down that road again, so they’re seeking part-time roles. It’s an intentional choice.”
Tracey O’Connell, MD, a radiologist, always knew that she wanted to work part time. “I had a baby as a resident, and I was pregnant with my second child as a fellow,” she said. “I was already feeling overwhelmed with medical training and having a family.”
Dr. O’Connell worked in private practice for 16 years on Mondays, Wednesdays, and Fridays, with no nights or weekends.
“I still found it completely overwhelming,” she said. “Even though I had more days not working than working, I felt like the demands of medical life had advanced faster than human beings could adapt, and I still feel that way.”
Today she runs a part-time teleradiology practice from home but spends more time on her second career as a life coach. “Most of my clients are physicians looking for more fulfillment and sustainable ways of practicing medicine while maintaining their own identity as human beings, not just the all-consuming identity of ‘doctor,’ ” she said.
On the other end of the career spectrum is Lois Goodman, MD, an ob.gyn. in her late 70s. After 42 years in a group practice, she started her solo practice at 72, seeing patients 3 days per week. “I’m just happy to be working. That’s a tremendous payoff for me. I need to keep working for my mental health.”
How does part-time work affect physician shortages and care delivery?
Reducing clinical effort is one of the strategies physicians use to scale down overload. Still, it’s not viable as a long-term solution, said Christine Sinsky, MD, AMA’s vice president of professional satisfaction and a nationally regarded researcher on physician burnout.
“If all the physicians in a community went from working 100% FTE clinical to 50% FTE clinical, then the people in that community would have half the access to care that they had,” said Dr. Sinsky. “There’s less capacity in the system to care for patients.”
Some could argue, then, that part-time physician work may contribute to physician shortage predictions. An Association of American Medical Colleges report estimates there will be a shortage of 37,800 to 124,000 physicians by 2034.
But physicians working part-time express a contrasting point of view. “I don’t believe that part-time workers are responsible for the health care shortage but rather, a great solution,” said Dr. O’Connell. “Because in order to continue working for a long time rather than quitting when the demands exceed human capacity, working part time is a great compromise to offer a life of more sustainable well-being and longevity as a physician, and still live a wholehearted life.”
Pros and cons of being a part-time physician
Pros
Less burnout: The American Medical Association has tracked burnout rates for 22 years. By the end of 2021, nearly 63% of physicians reported burnout symptoms, compared with 38% the year before. Going part time appears to reduce burnout, suggests a study published in Mayo Clinic Proceedings.
Better work-life balance: Rachel Miller, MD, an ob.gyn., worked 60-70 hours weekly for 9 years. In 2022, she went to work as an OB hospitalist for a health care system that welcomes part-time clinicians. Since then, she has achieved a better work-life balance, putting in 26-28 hours a week. Dr. Miller now spends more time with her kids and in her additional role as an executive coach to leaders in the medical field.
More focus: “When I’m at work, I’m 100% mentally in and focused,” said Dr. Miller. “My interactions with patients are different because I’m not burned out. My demeanor and my willingness to connect are stronger.”
Better health: Mehmet Cilingiroglu, MD, with CardioSolution, traded full-time work for part time when health issues and a kidney transplant sidelined his 30-year career in 2018. “Despite my significant health issues, I’ve been able to continue working at a pace that suits me rather than having to retire,” he said. “Part-time physicians can still enjoy patient care, research, innovation, education, and training while balancing that with other areas of life.”
Errin Weisman, a DO who gave up full-time work in 2016, said cutting back makes her feel healthier, happier, and more energized. “Part-time work helps me to bring my A game each day I work and deliver the best care.” She’s also a life coach encouraging other physicians to find balance in their professional and personal lives.
Cons
Cut in pay: Obviously, the No. 1 con is you’ll make less working part time, so adjusting to a salary decrease can be a huge issue, especially if you don’t have other sources of income. Physicians paying off student loans, those caring for children or elderly parents, or those in their prime earning years needing to save for retirement may not be able to go part time.
Diminished career: The chance for promotions or being well known in your field can be diminished, as well as a loss of proficiency if you’re only performing surgery or procedures part time. In some specialties, working part time and not keeping up with (or being able to practice) newer technology developments can harm your career or reputation in the long run.
Missing out: While working part time has many benefits, physicians also experience a wide range of drawbacks. Dr. Goodman, for example, said she misses delivering babies and doing surgeries. Dr. Miller said she gave up some aspects of her specialty, like performing hysterectomies, participating in complex cases, and no longer having an office like she did as a full-time ob.gyn.
Loss of fellowship: Dr. O’Connell said she missed the camaraderie and sense of belonging when she scaled back her hours. “I felt like a fish out of water, that my values didn’t align with the group’s values,” she said. This led to self-doubt, frustrated colleagues, and a reduction in benefits.
Lost esteem: Dr. O’Connell also felt she was expected to work overtime without additional pay and was no longer eligible for bonuses. “I was treated as a team player when I was needed, but not when it came to perks and benefits and insider privilege,” she said. There may be a loss of esteem among colleagues and supervisors.
Overcoming stigma: Because part-time physician work is still not prevalent among colleagues, some may resist the idea, have less respect for it, perceive it as not being serious about your career as a physician, or associate it with being lazy or entitled.
Summing it up
Every physician must weigh the value and drawbacks of part-time work, but the more physicians who go this route, the more part-time medicine gains traction and the more physicians can learn about its values versus its drawbacks.
A version of this article first appeared on Medscape.com.
On average, physicians reported in the Medscape Physician Compensation Report 2023 that they worked 50 hours per week. Five specialties, including critical care, cardiology, and general surgery reported working 55 or more hours weekly.
In 2011, The New England Journal of Medicine reported that part-time physician careers were rising. At the time, part-time doctors made up 21% of the physician workforce, up from 13% in 2005.
In a more recent survey from the California Health Care Foundation, only 12% of California physicians said they devoted 20-29 hours a week to patient care.
Amy Knoup, a senior recruitment adviser with Provider Solutions & Development), has been helping doctors find jobs for over a decade, and she’s noticed a trend.
“Not only are more physicians seeking part-time roles than they were 10 years ago, but more large health care systems are also offering part time or per diem as well,” said Ms. Knoup.
Who’s working part time, and why?
Ten years ago, the fastest growing segment of part-timers were men nearing retirement and early- to mid-career women.
Pediatricians led the part-time pack in 2002, according to an American Academy of Pediatrics study. At the time, 15% of pediatricians reported their hours as part time. However, the numbers may have increased over the years. For example, a 2021 study by the department of pediatrics, Boston Medical Center, and Boston University found that almost 30% of graduating pediatricians sought part-time work at the end of their training.
At PS&D, Ms. Knoup said she has noticed a trend toward part-timers among primary care, behavioral health, and outpatient specialties such as endocrinology. “We’re also seeing it with the inpatient side in roles that are more shift based like hospitalists, radiologists, and critical care and ER doctors.”
Another trend Ms. Knoup has noticed is with early-career doctors. “They have a different mindset,” she said. “Younger generations are acutely aware of burnout. They may have experienced it in residency or during the pandemic. They’ve had a taste of that and don’t want to go down that road again, so they’re seeking part-time roles. It’s an intentional choice.”
Tracey O’Connell, MD, a radiologist, always knew that she wanted to work part time. “I had a baby as a resident, and I was pregnant with my second child as a fellow,” she said. “I was already feeling overwhelmed with medical training and having a family.”
Dr. O’Connell worked in private practice for 16 years on Mondays, Wednesdays, and Fridays, with no nights or weekends.
“I still found it completely overwhelming,” she said. “Even though I had more days not working than working, I felt like the demands of medical life had advanced faster than human beings could adapt, and I still feel that way.”
Today she runs a part-time teleradiology practice from home but spends more time on her second career as a life coach. “Most of my clients are physicians looking for more fulfillment and sustainable ways of practicing medicine while maintaining their own identity as human beings, not just the all-consuming identity of ‘doctor,’ ” she said.
On the other end of the career spectrum is Lois Goodman, MD, an ob.gyn. in her late 70s. After 42 years in a group practice, she started her solo practice at 72, seeing patients 3 days per week. “I’m just happy to be working. That’s a tremendous payoff for me. I need to keep working for my mental health.”
How does part-time work affect physician shortages and care delivery?
Reducing clinical effort is one of the strategies physicians use to scale down overload. Still, it’s not viable as a long-term solution, said Christine Sinsky, MD, AMA’s vice president of professional satisfaction and a nationally regarded researcher on physician burnout.
“If all the physicians in a community went from working 100% FTE clinical to 50% FTE clinical, then the people in that community would have half the access to care that they had,” said Dr. Sinsky. “There’s less capacity in the system to care for patients.”
Some could argue, then, that part-time physician work may contribute to physician shortage predictions. An Association of American Medical Colleges report estimates there will be a shortage of 37,800 to 124,000 physicians by 2034.
But physicians working part-time express a contrasting point of view. “I don’t believe that part-time workers are responsible for the health care shortage but rather, a great solution,” said Dr. O’Connell. “Because in order to continue working for a long time rather than quitting when the demands exceed human capacity, working part time is a great compromise to offer a life of more sustainable well-being and longevity as a physician, and still live a wholehearted life.”
Pros and cons of being a part-time physician
Pros
Less burnout: The American Medical Association has tracked burnout rates for 22 years. By the end of 2021, nearly 63% of physicians reported burnout symptoms, compared with 38% the year before. Going part time appears to reduce burnout, suggests a study published in Mayo Clinic Proceedings.
Better work-life balance: Rachel Miller, MD, an ob.gyn., worked 60-70 hours weekly for 9 years. In 2022, she went to work as an OB hospitalist for a health care system that welcomes part-time clinicians. Since then, she has achieved a better work-life balance, putting in 26-28 hours a week. Dr. Miller now spends more time with her kids and in her additional role as an executive coach to leaders in the medical field.
More focus: “When I’m at work, I’m 100% mentally in and focused,” said Dr. Miller. “My interactions with patients are different because I’m not burned out. My demeanor and my willingness to connect are stronger.”
Better health: Mehmet Cilingiroglu, MD, with CardioSolution, traded full-time work for part time when health issues and a kidney transplant sidelined his 30-year career in 2018. “Despite my significant health issues, I’ve been able to continue working at a pace that suits me rather than having to retire,” he said. “Part-time physicians can still enjoy patient care, research, innovation, education, and training while balancing that with other areas of life.”
Errin Weisman, a DO who gave up full-time work in 2016, said cutting back makes her feel healthier, happier, and more energized. “Part-time work helps me to bring my A game each day I work and deliver the best care.” She’s also a life coach encouraging other physicians to find balance in their professional and personal lives.
Cons
Cut in pay: Obviously, the No. 1 con is you’ll make less working part time, so adjusting to a salary decrease can be a huge issue, especially if you don’t have other sources of income. Physicians paying off student loans, those caring for children or elderly parents, or those in their prime earning years needing to save for retirement may not be able to go part time.
Diminished career: The chance for promotions or being well known in your field can be diminished, as well as a loss of proficiency if you’re only performing surgery or procedures part time. In some specialties, working part time and not keeping up with (or being able to practice) newer technology developments can harm your career or reputation in the long run.
Missing out: While working part time has many benefits, physicians also experience a wide range of drawbacks. Dr. Goodman, for example, said she misses delivering babies and doing surgeries. Dr. Miller said she gave up some aspects of her specialty, like performing hysterectomies, participating in complex cases, and no longer having an office like she did as a full-time ob.gyn.
Loss of fellowship: Dr. O’Connell said she missed the camaraderie and sense of belonging when she scaled back her hours. “I felt like a fish out of water, that my values didn’t align with the group’s values,” she said. This led to self-doubt, frustrated colleagues, and a reduction in benefits.
Lost esteem: Dr. O’Connell also felt she was expected to work overtime without additional pay and was no longer eligible for bonuses. “I was treated as a team player when I was needed, but not when it came to perks and benefits and insider privilege,” she said. There may be a loss of esteem among colleagues and supervisors.
Overcoming stigma: Because part-time physician work is still not prevalent among colleagues, some may resist the idea, have less respect for it, perceive it as not being serious about your career as a physician, or associate it with being lazy or entitled.
Summing it up
Every physician must weigh the value and drawbacks of part-time work, but the more physicians who go this route, the more part-time medicine gains traction and the more physicians can learn about its values versus its drawbacks.
A version of this article first appeared on Medscape.com.
New USPSTF draft suggests mammography start at 40, not 50
The major change: USPSTF proposed reducing the recommended start age for routine screening mammograms from age 50 to age 40. The latest recommendation, which carries a B grade, also calls for screening every other year and sets a cutoff age of 74.
The task force’s A and B ratings indicate strong confidence in the evidence for benefit, meaning that clinicians should encourage their patients to get these services as appropriate.
The influential federal advisory panel last updated these recommendations in 2016. At the time, USPSTF recommended routine screening mammograms starting at age 50, and gave a C grade to starting before that.
In the 2016 recommendations, “we felt a woman could start screening in her 40s depending on how she feels about the harms and benefits in an individualized personal decision,” USPSTF member John Wong, MD, chief of clinical decision making and a primary care physician at Tufts Medical Center in Boston, said in an interview. “In this draft recommendation, we now recommend that all women get screened starting at age 40.”
Two major factors prompted the change, explained Dr. Wong. One is that more women are being diagnosed with breast cancer in their 40s. The other is that a growing body of evidence showing that Black women get breast cancer younger, are more likely to die of breast cancer, and would benefit from earlier screening.
“It is now clear that screening every other year starting at age 40 has the potential to save about 20% more lives among all women and there is even greater potential benefit for Black women, who are much more likely to die from breast cancer,” Dr. Wong said.
The American Cancer Society (ACS) called the draft recommendations a “significant positive change,” while noting that the task force recommendations only apply to women at average risk for breast cancer.
The American College of Radiology (ACR) already recommends yearly mammograms for average risk women starting at age 40. Its latest guidelines on mammography call for women at higher-than-average risk for breast cancer to undergo a risk assessment by age 25 to determine if screening before age 40 is needed.
When asked about the differing views, Debra Monticciolo, MD, division chief for breast imaging at Massachusetts General Hospital, said annual screenings that follow ACR recommendations would save more lives than the every-other-year approach backed by the task force. Dr. Monticciolo also highlighted that the available scientific evidence supports earlier assessment as well as augmented and earlier-than-age-40 screening of many women – particularly Black women.
“These evidence-based updates should spur more-informed doctor–patient conversations and help providers save more lives,” Dr. Monticciolo said in a press release.
Insurance access
Typically, upgrading a USPSTF recommendation from C to B leads to better access and insurance coverage for patients. The Affordable Care Act (ACA) of 2010 requires insurers to cover the cost of services that get A and B recommendations from the USPSTF without charging copays – a mandate intended to promote greater use for highly regarded services.
But Congress created a special workaround that effectively makes the ACA mandate apply to the 2002 task force recommendations on mammography. In those recommendations, the task force gave a B grade to screening mammograms every 1 or 2 years starting at age 40 without an age limit.
Federal lawmakers have sought to provide copay-free access to mammograms for this entire population even when the USPSTF recommendations in 2009 and 2016 gave a C grade to routine screening for women under 50.
Still, “it is important to note that our recommendation is based solely on the science of what works to prevent breast cancer and it is not a recommendation for or against insurance coverage,” the task force acknowledged when unveiling the new draft update. “Coverage decisions involve considerations beyond the evidence about clinical benefit, and in the end, these decisions are the responsibility of payors, regulators, and legislators.”
Uncertainties persist
The new draft recommendations also highlight the persistent gaps in knowledge about the uses of mammography, despite years of widespread use of this screening tool.
The updated draft recommendations emphasize the lack of sufficient evidence to address major areas of concern related to screening and treating Black women, older women, women with dense breasts, and those with ductal carcinoma in situ (DCIS).
The task force called for more research addressing the underlying causes of elevated breast cancer mortality rates among Black women.
The USPSTF also issued an ‘I’ statement for providing women with dense breasts additional screening with breast ultrasound or MRI and for screening women older than 75 for breast cancer. Such statements indicate that the available evidence is lacking, poor quality, or conflicting, and thus the USPSTF can’t assess the benefits and harms or make a recommendation for or against providing the preventive service.
“Nearly half of all women have dense breasts, which increases their risk for breast cancer and means that mammograms may not work as well for them. We need to know more about whether and how additional screening might help women with dense breasts stay healthy,” the task force explained.
The task force also called for more research on approaches to reduce the risk for overdiagnosis and overtreatment for breast lesions, such as DCIS, which are identified through screening.
One analysis – the COMET study – is currently underway to assess whether women could be spared surgery for DCIS and opt for watchful waiting instead.
“If we can find that monitoring them carefully, either with or without some sort of endocrine therapy, is just as effective in keeping patients free of invasive cancer as surgery, then I think we could help to de-escalate treatment for this very low-risk group of patients,” Shelley Hwang, MD, MPH, principal investigator of the COMET study, told this news organization in December.
The task force will accept comments from the public on this draft update through June 5.
A version of this article first appeared on Medscape.com.
The major change: USPSTF proposed reducing the recommended start age for routine screening mammograms from age 50 to age 40. The latest recommendation, which carries a B grade, also calls for screening every other year and sets a cutoff age of 74.
The task force’s A and B ratings indicate strong confidence in the evidence for benefit, meaning that clinicians should encourage their patients to get these services as appropriate.
The influential federal advisory panel last updated these recommendations in 2016. At the time, USPSTF recommended routine screening mammograms starting at age 50, and gave a C grade to starting before that.
In the 2016 recommendations, “we felt a woman could start screening in her 40s depending on how she feels about the harms and benefits in an individualized personal decision,” USPSTF member John Wong, MD, chief of clinical decision making and a primary care physician at Tufts Medical Center in Boston, said in an interview. “In this draft recommendation, we now recommend that all women get screened starting at age 40.”
Two major factors prompted the change, explained Dr. Wong. One is that more women are being diagnosed with breast cancer in their 40s. The other is that a growing body of evidence showing that Black women get breast cancer younger, are more likely to die of breast cancer, and would benefit from earlier screening.
“It is now clear that screening every other year starting at age 40 has the potential to save about 20% more lives among all women and there is even greater potential benefit for Black women, who are much more likely to die from breast cancer,” Dr. Wong said.
The American Cancer Society (ACS) called the draft recommendations a “significant positive change,” while noting that the task force recommendations only apply to women at average risk for breast cancer.
The American College of Radiology (ACR) already recommends yearly mammograms for average risk women starting at age 40. Its latest guidelines on mammography call for women at higher-than-average risk for breast cancer to undergo a risk assessment by age 25 to determine if screening before age 40 is needed.
When asked about the differing views, Debra Monticciolo, MD, division chief for breast imaging at Massachusetts General Hospital, said annual screenings that follow ACR recommendations would save more lives than the every-other-year approach backed by the task force. Dr. Monticciolo also highlighted that the available scientific evidence supports earlier assessment as well as augmented and earlier-than-age-40 screening of many women – particularly Black women.
“These evidence-based updates should spur more-informed doctor–patient conversations and help providers save more lives,” Dr. Monticciolo said in a press release.
Insurance access
Typically, upgrading a USPSTF recommendation from C to B leads to better access and insurance coverage for patients. The Affordable Care Act (ACA) of 2010 requires insurers to cover the cost of services that get A and B recommendations from the USPSTF without charging copays – a mandate intended to promote greater use for highly regarded services.
But Congress created a special workaround that effectively makes the ACA mandate apply to the 2002 task force recommendations on mammography. In those recommendations, the task force gave a B grade to screening mammograms every 1 or 2 years starting at age 40 without an age limit.
Federal lawmakers have sought to provide copay-free access to mammograms for this entire population even when the USPSTF recommendations in 2009 and 2016 gave a C grade to routine screening for women under 50.
Still, “it is important to note that our recommendation is based solely on the science of what works to prevent breast cancer and it is not a recommendation for or against insurance coverage,” the task force acknowledged when unveiling the new draft update. “Coverage decisions involve considerations beyond the evidence about clinical benefit, and in the end, these decisions are the responsibility of payors, regulators, and legislators.”
Uncertainties persist
The new draft recommendations also highlight the persistent gaps in knowledge about the uses of mammography, despite years of widespread use of this screening tool.
The updated draft recommendations emphasize the lack of sufficient evidence to address major areas of concern related to screening and treating Black women, older women, women with dense breasts, and those with ductal carcinoma in situ (DCIS).
The task force called for more research addressing the underlying causes of elevated breast cancer mortality rates among Black women.
The USPSTF also issued an ‘I’ statement for providing women with dense breasts additional screening with breast ultrasound or MRI and for screening women older than 75 for breast cancer. Such statements indicate that the available evidence is lacking, poor quality, or conflicting, and thus the USPSTF can’t assess the benefits and harms or make a recommendation for or against providing the preventive service.
“Nearly half of all women have dense breasts, which increases their risk for breast cancer and means that mammograms may not work as well for them. We need to know more about whether and how additional screening might help women with dense breasts stay healthy,” the task force explained.
The task force also called for more research on approaches to reduce the risk for overdiagnosis and overtreatment for breast lesions, such as DCIS, which are identified through screening.
One analysis – the COMET study – is currently underway to assess whether women could be spared surgery for DCIS and opt for watchful waiting instead.
“If we can find that monitoring them carefully, either with or without some sort of endocrine therapy, is just as effective in keeping patients free of invasive cancer as surgery, then I think we could help to de-escalate treatment for this very low-risk group of patients,” Shelley Hwang, MD, MPH, principal investigator of the COMET study, told this news organization in December.
The task force will accept comments from the public on this draft update through June 5.
A version of this article first appeared on Medscape.com.
The major change: USPSTF proposed reducing the recommended start age for routine screening mammograms from age 50 to age 40. The latest recommendation, which carries a B grade, also calls for screening every other year and sets a cutoff age of 74.
The task force’s A and B ratings indicate strong confidence in the evidence for benefit, meaning that clinicians should encourage their patients to get these services as appropriate.
The influential federal advisory panel last updated these recommendations in 2016. At the time, USPSTF recommended routine screening mammograms starting at age 50, and gave a C grade to starting before that.
In the 2016 recommendations, “we felt a woman could start screening in her 40s depending on how she feels about the harms and benefits in an individualized personal decision,” USPSTF member John Wong, MD, chief of clinical decision making and a primary care physician at Tufts Medical Center in Boston, said in an interview. “In this draft recommendation, we now recommend that all women get screened starting at age 40.”
Two major factors prompted the change, explained Dr. Wong. One is that more women are being diagnosed with breast cancer in their 40s. The other is that a growing body of evidence showing that Black women get breast cancer younger, are more likely to die of breast cancer, and would benefit from earlier screening.
“It is now clear that screening every other year starting at age 40 has the potential to save about 20% more lives among all women and there is even greater potential benefit for Black women, who are much more likely to die from breast cancer,” Dr. Wong said.
The American Cancer Society (ACS) called the draft recommendations a “significant positive change,” while noting that the task force recommendations only apply to women at average risk for breast cancer.
The American College of Radiology (ACR) already recommends yearly mammograms for average risk women starting at age 40. Its latest guidelines on mammography call for women at higher-than-average risk for breast cancer to undergo a risk assessment by age 25 to determine if screening before age 40 is needed.
When asked about the differing views, Debra Monticciolo, MD, division chief for breast imaging at Massachusetts General Hospital, said annual screenings that follow ACR recommendations would save more lives than the every-other-year approach backed by the task force. Dr. Monticciolo also highlighted that the available scientific evidence supports earlier assessment as well as augmented and earlier-than-age-40 screening of many women – particularly Black women.
“These evidence-based updates should spur more-informed doctor–patient conversations and help providers save more lives,” Dr. Monticciolo said in a press release.
Insurance access
Typically, upgrading a USPSTF recommendation from C to B leads to better access and insurance coverage for patients. The Affordable Care Act (ACA) of 2010 requires insurers to cover the cost of services that get A and B recommendations from the USPSTF without charging copays – a mandate intended to promote greater use for highly regarded services.
But Congress created a special workaround that effectively makes the ACA mandate apply to the 2002 task force recommendations on mammography. In those recommendations, the task force gave a B grade to screening mammograms every 1 or 2 years starting at age 40 without an age limit.
Federal lawmakers have sought to provide copay-free access to mammograms for this entire population even when the USPSTF recommendations in 2009 and 2016 gave a C grade to routine screening for women under 50.
Still, “it is important to note that our recommendation is based solely on the science of what works to prevent breast cancer and it is not a recommendation for or against insurance coverage,” the task force acknowledged when unveiling the new draft update. “Coverage decisions involve considerations beyond the evidence about clinical benefit, and in the end, these decisions are the responsibility of payors, regulators, and legislators.”
Uncertainties persist
The new draft recommendations also highlight the persistent gaps in knowledge about the uses of mammography, despite years of widespread use of this screening tool.
The updated draft recommendations emphasize the lack of sufficient evidence to address major areas of concern related to screening and treating Black women, older women, women with dense breasts, and those with ductal carcinoma in situ (DCIS).
The task force called for more research addressing the underlying causes of elevated breast cancer mortality rates among Black women.
The USPSTF also issued an ‘I’ statement for providing women with dense breasts additional screening with breast ultrasound or MRI and for screening women older than 75 for breast cancer. Such statements indicate that the available evidence is lacking, poor quality, or conflicting, and thus the USPSTF can’t assess the benefits and harms or make a recommendation for or against providing the preventive service.
“Nearly half of all women have dense breasts, which increases their risk for breast cancer and means that mammograms may not work as well for them. We need to know more about whether and how additional screening might help women with dense breasts stay healthy,” the task force explained.
The task force also called for more research on approaches to reduce the risk for overdiagnosis and overtreatment for breast lesions, such as DCIS, which are identified through screening.
One analysis – the COMET study – is currently underway to assess whether women could be spared surgery for DCIS and opt for watchful waiting instead.
“If we can find that monitoring them carefully, either with or without some sort of endocrine therapy, is just as effective in keeping patients free of invasive cancer as surgery, then I think we could help to de-escalate treatment for this very low-risk group of patients,” Shelley Hwang, MD, MPH, principal investigator of the COMET study, told this news organization in December.
The task force will accept comments from the public on this draft update through June 5.
A version of this article first appeared on Medscape.com.
Familial cancer risk complex, not limited to same site
The researchers found, for instance, that children of breast cancer patients had a 27% higher risk of any discordant early-onset cancer, and patients’ siblings had a 7.6-fold higher risk of early pancreatic cancer. The analysis also indicated that children of patients’ siblings had a significantly increased risk of testicular and ovarian cancers.
“The findings suggest that the familial risk extends to discordant early-onset cancers, including ovarian, testicular, and pancreatic cancers, as well as beyond first-degree relatives,” the researchers, led by Janne M. Pitkäniemi, PhD, Finnish Cancer Registry, Institute for Statistical and Epidemiological Cancer Research, Helsinki, say. “Our findings are interesting but raise some questions about unknown [genetic] and environmental mechanisms that need to be further studied.”
Erin F. Cobain, MD, who was not involved in the research, said the findings are “not very surprising to me.”
Dr. Cobain said that at her institution, she has seen “many, many cases” of family members of early-onset breast cancer patients with discordant cancers “where we are unable to find a clear genetic cause.”
Not being able to find an identifiable cause for the clustering of early-onset cancers can be “very frustrating” for patients and their families, said Dr. Cobain, a medical oncologist at the University of Michigan Health, Ann Arbor.
The study was published online in the International Journal of Cancer.
Family members of patients with early-onset breast cancer are at elevated risk for early-onset breast cancer. However, it is “unclear whether the familial risk is limited to early-onset cancer of the same site,” the authors explained.
To investigate, the researchers studied data from the Finnish Cancer Registry and the Finnish Population System, which included 54,753 relatives from 5,562 families of females diagnosed with early-onset breast cancer, defined as probands. A proband was the first member of the family diagnosed with female breast cancer at age 40 years or younger in Finland between January 1970 and December 31, 2012. Cancers were considered familial if they occurred in a family with a previously diagnosed proband and were deemed early onset if diagnosed before age 41.
The researchers found that only 5.5% of probands’ families had a family member with a discordant early-onset cancer. The most common diagnoses were testicular cancer (0.6% of families) and cancer of the thyroid gland (also 0.6%), followed by melanoma (0.5%).
Overall, the risk of any nonbreast early-onset cancer among first-degree relatives of probands was comparable with the risk in the general population (standardized incidence ratio, 0.99; 95% confidence interval, 0.84-1.16).
However, the risk was elevated for certain family members and certain cancers.
Specifically, the children of probands had an increased risk for any discordant cancer (SIR, 1.27; 95% CI, 1.05-1.55).
The siblings of probands had an elevated risk for early-onset pancreatic cancer (SIR, 7.61) but not overall for any discordant cancer (SIR, 0.93; 95% CI, 0.68-1.25).
And siblings’ children faced an elevated risk for testicular (SIR, 1.74) and ovarian (SIR, 2.69) cancer, though not of any discordant cancer (SIR, 1.16; 95% CI, 0.97-1.37).
The researchers also found that the fathers (SIR, 0.43), mothers (SIR, 0.48), and spouses (SIR, 0.58) of probands appeared to have a decreased risk of any discordant early-onset cancer.
A potential limitation to the study was that the authors could not identify individuals with hereditary cancer syndromes or concerning gene mutations, such as BRCA carriers, because “registry data do not include comprehensive information on the gene mutation carriage status.” But the authors note that the number of BRCA carriers is likely low because of the low number of ovarian cancers observed in first-degree relatives of probands.
Dr. Cobain noted as well that the current study is potentially limited by its “very homogeneous” cohort.
But, overall, the findings indicate that familial risk is often “a much more complicated problem, mathematically and statistically,” than were there a single genetic culprit, Dr. Cobain said. One possibility is that some shared environmental exposure may be increasing the cancer risk among members of the same family.
“Genetic diversity is so vast and understanding how the interplay of multiple genes can influence an individual’s cancer risk is so much more complicated than a single BRCA1 mutation that clearly influences your breast cancer risk,” she added. However, “we’re starting to get there.”
The study was funded by the Cancer Foundation Finland and Academy of Finland. The authors and Dr. Cobain had no relevant financial relationships to declare.
A version of this article originally appeared on Medscape.com.
The researchers found, for instance, that children of breast cancer patients had a 27% higher risk of any discordant early-onset cancer, and patients’ siblings had a 7.6-fold higher risk of early pancreatic cancer. The analysis also indicated that children of patients’ siblings had a significantly increased risk of testicular and ovarian cancers.
“The findings suggest that the familial risk extends to discordant early-onset cancers, including ovarian, testicular, and pancreatic cancers, as well as beyond first-degree relatives,” the researchers, led by Janne M. Pitkäniemi, PhD, Finnish Cancer Registry, Institute for Statistical and Epidemiological Cancer Research, Helsinki, say. “Our findings are interesting but raise some questions about unknown [genetic] and environmental mechanisms that need to be further studied.”
Erin F. Cobain, MD, who was not involved in the research, said the findings are “not very surprising to me.”
Dr. Cobain said that at her institution, she has seen “many, many cases” of family members of early-onset breast cancer patients with discordant cancers “where we are unable to find a clear genetic cause.”
Not being able to find an identifiable cause for the clustering of early-onset cancers can be “very frustrating” for patients and their families, said Dr. Cobain, a medical oncologist at the University of Michigan Health, Ann Arbor.
The study was published online in the International Journal of Cancer.
Family members of patients with early-onset breast cancer are at elevated risk for early-onset breast cancer. However, it is “unclear whether the familial risk is limited to early-onset cancer of the same site,” the authors explained.
To investigate, the researchers studied data from the Finnish Cancer Registry and the Finnish Population System, which included 54,753 relatives from 5,562 families of females diagnosed with early-onset breast cancer, defined as probands. A proband was the first member of the family diagnosed with female breast cancer at age 40 years or younger in Finland between January 1970 and December 31, 2012. Cancers were considered familial if they occurred in a family with a previously diagnosed proband and were deemed early onset if diagnosed before age 41.
The researchers found that only 5.5% of probands’ families had a family member with a discordant early-onset cancer. The most common diagnoses were testicular cancer (0.6% of families) and cancer of the thyroid gland (also 0.6%), followed by melanoma (0.5%).
Overall, the risk of any nonbreast early-onset cancer among first-degree relatives of probands was comparable with the risk in the general population (standardized incidence ratio, 0.99; 95% confidence interval, 0.84-1.16).
However, the risk was elevated for certain family members and certain cancers.
Specifically, the children of probands had an increased risk for any discordant cancer (SIR, 1.27; 95% CI, 1.05-1.55).
The siblings of probands had an elevated risk for early-onset pancreatic cancer (SIR, 7.61) but not overall for any discordant cancer (SIR, 0.93; 95% CI, 0.68-1.25).
And siblings’ children faced an elevated risk for testicular (SIR, 1.74) and ovarian (SIR, 2.69) cancer, though not of any discordant cancer (SIR, 1.16; 95% CI, 0.97-1.37).
The researchers also found that the fathers (SIR, 0.43), mothers (SIR, 0.48), and spouses (SIR, 0.58) of probands appeared to have a decreased risk of any discordant early-onset cancer.
A potential limitation to the study was that the authors could not identify individuals with hereditary cancer syndromes or concerning gene mutations, such as BRCA carriers, because “registry data do not include comprehensive information on the gene mutation carriage status.” But the authors note that the number of BRCA carriers is likely low because of the low number of ovarian cancers observed in first-degree relatives of probands.
Dr. Cobain noted as well that the current study is potentially limited by its “very homogeneous” cohort.
But, overall, the findings indicate that familial risk is often “a much more complicated problem, mathematically and statistically,” than were there a single genetic culprit, Dr. Cobain said. One possibility is that some shared environmental exposure may be increasing the cancer risk among members of the same family.
“Genetic diversity is so vast and understanding how the interplay of multiple genes can influence an individual’s cancer risk is so much more complicated than a single BRCA1 mutation that clearly influences your breast cancer risk,” she added. However, “we’re starting to get there.”
The study was funded by the Cancer Foundation Finland and Academy of Finland. The authors and Dr. Cobain had no relevant financial relationships to declare.
A version of this article originally appeared on Medscape.com.
The researchers found, for instance, that children of breast cancer patients had a 27% higher risk of any discordant early-onset cancer, and patients’ siblings had a 7.6-fold higher risk of early pancreatic cancer. The analysis also indicated that children of patients’ siblings had a significantly increased risk of testicular and ovarian cancers.
“The findings suggest that the familial risk extends to discordant early-onset cancers, including ovarian, testicular, and pancreatic cancers, as well as beyond first-degree relatives,” the researchers, led by Janne M. Pitkäniemi, PhD, Finnish Cancer Registry, Institute for Statistical and Epidemiological Cancer Research, Helsinki, say. “Our findings are interesting but raise some questions about unknown [genetic] and environmental mechanisms that need to be further studied.”
Erin F. Cobain, MD, who was not involved in the research, said the findings are “not very surprising to me.”
Dr. Cobain said that at her institution, she has seen “many, many cases” of family members of early-onset breast cancer patients with discordant cancers “where we are unable to find a clear genetic cause.”
Not being able to find an identifiable cause for the clustering of early-onset cancers can be “very frustrating” for patients and their families, said Dr. Cobain, a medical oncologist at the University of Michigan Health, Ann Arbor.
The study was published online in the International Journal of Cancer.
Family members of patients with early-onset breast cancer are at elevated risk for early-onset breast cancer. However, it is “unclear whether the familial risk is limited to early-onset cancer of the same site,” the authors explained.
To investigate, the researchers studied data from the Finnish Cancer Registry and the Finnish Population System, which included 54,753 relatives from 5,562 families of females diagnosed with early-onset breast cancer, defined as probands. A proband was the first member of the family diagnosed with female breast cancer at age 40 years or younger in Finland between January 1970 and December 31, 2012. Cancers were considered familial if they occurred in a family with a previously diagnosed proband and were deemed early onset if diagnosed before age 41.
The researchers found that only 5.5% of probands’ families had a family member with a discordant early-onset cancer. The most common diagnoses were testicular cancer (0.6% of families) and cancer of the thyroid gland (also 0.6%), followed by melanoma (0.5%).
Overall, the risk of any nonbreast early-onset cancer among first-degree relatives of probands was comparable with the risk in the general population (standardized incidence ratio, 0.99; 95% confidence interval, 0.84-1.16).
However, the risk was elevated for certain family members and certain cancers.
Specifically, the children of probands had an increased risk for any discordant cancer (SIR, 1.27; 95% CI, 1.05-1.55).
The siblings of probands had an elevated risk for early-onset pancreatic cancer (SIR, 7.61) but not overall for any discordant cancer (SIR, 0.93; 95% CI, 0.68-1.25).
And siblings’ children faced an elevated risk for testicular (SIR, 1.74) and ovarian (SIR, 2.69) cancer, though not of any discordant cancer (SIR, 1.16; 95% CI, 0.97-1.37).
The researchers also found that the fathers (SIR, 0.43), mothers (SIR, 0.48), and spouses (SIR, 0.58) of probands appeared to have a decreased risk of any discordant early-onset cancer.
A potential limitation to the study was that the authors could not identify individuals with hereditary cancer syndromes or concerning gene mutations, such as BRCA carriers, because “registry data do not include comprehensive information on the gene mutation carriage status.” But the authors note that the number of BRCA carriers is likely low because of the low number of ovarian cancers observed in first-degree relatives of probands.
Dr. Cobain noted as well that the current study is potentially limited by its “very homogeneous” cohort.
But, overall, the findings indicate that familial risk is often “a much more complicated problem, mathematically and statistically,” than were there a single genetic culprit, Dr. Cobain said. One possibility is that some shared environmental exposure may be increasing the cancer risk among members of the same family.
“Genetic diversity is so vast and understanding how the interplay of multiple genes can influence an individual’s cancer risk is so much more complicated than a single BRCA1 mutation that clearly influences your breast cancer risk,” she added. However, “we’re starting to get there.”
The study was funded by the Cancer Foundation Finland and Academy of Finland. The authors and Dr. Cobain had no relevant financial relationships to declare.
A version of this article originally appeared on Medscape.com.
FROM INTERNATIONAL JOURNAL OF CANCER
Pausing endocrine therapy to attempt pregnancy is safe
The results provide the “strongest evidence to date on the short-term safety of this choice,” Sharon Giordano, MD, MPH, with University of Texas M.D. Anderson Cancer Center, Houston, wrote in an editorial accompanying the study.
“Physicians should now incorporate these positive data into their shared decision-making process with patients,” Dr. Giordano said.
The POSITIVE trial findings were published online in The New England Journal of Medicine.
Before the analysis, the risks associated with taking a break from endocrine therapy among young women with hormone receptor (HR)–positive breast cancer remained unclear.
In the current trial, Ann Partridge, MD, MPH, and colleagues sought prospective data on the safety associated with taking a temporary break from therapy to attempt pregnancy.
The single-group trial enrolled more than 500 premenopausal women who had received 18-30 months of endocrine therapy for mostly stage I or II HR-positive breast cancer. After a 3-month washout, the women were given 2 years to conceive, deliver, and breastfeed, if desired, before resuming treatment. Breast cancer events – the primary outcome – were defined as local, regional, or distant recurrence of invasive breast cancer or new contralateral invasive breast cancer.
The results, initially reported at San Antonio Breast Cancer Symposium (SABCS) 2022, showed that a temporary interruption of therapy to attempt pregnancy did not appear to lead to worse breast cancer outcomes.
Among 497 women who were followed for pregnancy status, 368 (74%) had at least one pregnancy, and 317 (64%) had at least one live birth.
After a median follow-up of 3.4 years, 44 women had had a breast cancer event – a result that was close to, but did not exceed, the safety threshold of 46 breast cancer events.
The 3-year incidence of breast cancer events was 8.9% (95% confidence interval [CI], 6.3-11.6) in the treatment-interruption group compared with 9.2% (95% CI, 7.6-10.8) among historical controls, which included women who would have met the entry criteria for the trial.
“These results suggest that although endocrine therapy for a period of 5-10 years substantially improves disease outcomes in patients with hormone receptor–positive early breast cancer, a temporary interruption of therapy to attempt pregnancy does not appear to have an appreciable negative short-term effect,” wrote Dr. Partridge, vice chair of medical oncology at Dana-Farber Cancer Institute and professor of medicine at Harvard Medical School, Boston, and colleagues.
The authors cautioned, however, that the median follow-up was only 3.4 years and that 10-year follow-up data will be “critical” to confirm the safety of interruption of adjuvant endocrine therapy.
Dr. Giordano agreed, noting that “recurrences of breast cancer are reported to occur at a steady rate for up to 20 years after diagnosis among patients with hormone receptor–positive disease; the protocol-specified 10-year follow-up data will be essential to establish longer-term safety.”
The study was supported by the International Breast Cancer Study Group and by the Alliance for Clinical Trials in Oncology in North America in collaboration with the Breast International Group (BIG). Disclosures for authors and editorial writer are available at NEJM.org.
A version of this article first appeared on Medscape.com.
The results provide the “strongest evidence to date on the short-term safety of this choice,” Sharon Giordano, MD, MPH, with University of Texas M.D. Anderson Cancer Center, Houston, wrote in an editorial accompanying the study.
“Physicians should now incorporate these positive data into their shared decision-making process with patients,” Dr. Giordano said.
The POSITIVE trial findings were published online in The New England Journal of Medicine.
Before the analysis, the risks associated with taking a break from endocrine therapy among young women with hormone receptor (HR)–positive breast cancer remained unclear.
In the current trial, Ann Partridge, MD, MPH, and colleagues sought prospective data on the safety associated with taking a temporary break from therapy to attempt pregnancy.
The single-group trial enrolled more than 500 premenopausal women who had received 18-30 months of endocrine therapy for mostly stage I or II HR-positive breast cancer. After a 3-month washout, the women were given 2 years to conceive, deliver, and breastfeed, if desired, before resuming treatment. Breast cancer events – the primary outcome – were defined as local, regional, or distant recurrence of invasive breast cancer or new contralateral invasive breast cancer.
The results, initially reported at San Antonio Breast Cancer Symposium (SABCS) 2022, showed that a temporary interruption of therapy to attempt pregnancy did not appear to lead to worse breast cancer outcomes.
Among 497 women who were followed for pregnancy status, 368 (74%) had at least one pregnancy, and 317 (64%) had at least one live birth.
After a median follow-up of 3.4 years, 44 women had had a breast cancer event – a result that was close to, but did not exceed, the safety threshold of 46 breast cancer events.
The 3-year incidence of breast cancer events was 8.9% (95% confidence interval [CI], 6.3-11.6) in the treatment-interruption group compared with 9.2% (95% CI, 7.6-10.8) among historical controls, which included women who would have met the entry criteria for the trial.
“These results suggest that although endocrine therapy for a period of 5-10 years substantially improves disease outcomes in patients with hormone receptor–positive early breast cancer, a temporary interruption of therapy to attempt pregnancy does not appear to have an appreciable negative short-term effect,” wrote Dr. Partridge, vice chair of medical oncology at Dana-Farber Cancer Institute and professor of medicine at Harvard Medical School, Boston, and colleagues.
The authors cautioned, however, that the median follow-up was only 3.4 years and that 10-year follow-up data will be “critical” to confirm the safety of interruption of adjuvant endocrine therapy.
Dr. Giordano agreed, noting that “recurrences of breast cancer are reported to occur at a steady rate for up to 20 years after diagnosis among patients with hormone receptor–positive disease; the protocol-specified 10-year follow-up data will be essential to establish longer-term safety.”
The study was supported by the International Breast Cancer Study Group and by the Alliance for Clinical Trials in Oncology in North America in collaboration with the Breast International Group (BIG). Disclosures for authors and editorial writer are available at NEJM.org.
A version of this article first appeared on Medscape.com.
The results provide the “strongest evidence to date on the short-term safety of this choice,” Sharon Giordano, MD, MPH, with University of Texas M.D. Anderson Cancer Center, Houston, wrote in an editorial accompanying the study.
“Physicians should now incorporate these positive data into their shared decision-making process with patients,” Dr. Giordano said.
The POSITIVE trial findings were published online in The New England Journal of Medicine.
Before the analysis, the risks associated with taking a break from endocrine therapy among young women with hormone receptor (HR)–positive breast cancer remained unclear.
In the current trial, Ann Partridge, MD, MPH, and colleagues sought prospective data on the safety associated with taking a temporary break from therapy to attempt pregnancy.
The single-group trial enrolled more than 500 premenopausal women who had received 18-30 months of endocrine therapy for mostly stage I or II HR-positive breast cancer. After a 3-month washout, the women were given 2 years to conceive, deliver, and breastfeed, if desired, before resuming treatment. Breast cancer events – the primary outcome – were defined as local, regional, or distant recurrence of invasive breast cancer or new contralateral invasive breast cancer.
The results, initially reported at San Antonio Breast Cancer Symposium (SABCS) 2022, showed that a temporary interruption of therapy to attempt pregnancy did not appear to lead to worse breast cancer outcomes.
Among 497 women who were followed for pregnancy status, 368 (74%) had at least one pregnancy, and 317 (64%) had at least one live birth.
After a median follow-up of 3.4 years, 44 women had had a breast cancer event – a result that was close to, but did not exceed, the safety threshold of 46 breast cancer events.
The 3-year incidence of breast cancer events was 8.9% (95% confidence interval [CI], 6.3-11.6) in the treatment-interruption group compared with 9.2% (95% CI, 7.6-10.8) among historical controls, which included women who would have met the entry criteria for the trial.
“These results suggest that although endocrine therapy for a period of 5-10 years substantially improves disease outcomes in patients with hormone receptor–positive early breast cancer, a temporary interruption of therapy to attempt pregnancy does not appear to have an appreciable negative short-term effect,” wrote Dr. Partridge, vice chair of medical oncology at Dana-Farber Cancer Institute and professor of medicine at Harvard Medical School, Boston, and colleagues.
The authors cautioned, however, that the median follow-up was only 3.4 years and that 10-year follow-up data will be “critical” to confirm the safety of interruption of adjuvant endocrine therapy.
Dr. Giordano agreed, noting that “recurrences of breast cancer are reported to occur at a steady rate for up to 20 years after diagnosis among patients with hormone receptor–positive disease; the protocol-specified 10-year follow-up data will be essential to establish longer-term safety.”
The study was supported by the International Breast Cancer Study Group and by the Alliance for Clinical Trials in Oncology in North America in collaboration with the Breast International Group (BIG). Disclosures for authors and editorial writer are available at NEJM.org.
A version of this article first appeared on Medscape.com.
FROM NEJM
Clinic responsible for misdiagnosing newborn’s meningitis, must pay millions
according to a report in the Star Tribune, among other news outlets.
The story of the jury verdict begins in 2013, when the boy, Johnny Galligan, was just 8 days old.
Alarmed by the newborn’s crying, lack of appetite, and fever, his parents, Alina and Steve Galligan, brought him to Essentia-Health-Ashland Clinic, located in Memorial Medical Center, Ashland, Wisc. There, the baby was seen by Andrew D. Snider, MD, a family physician. Dr. Snider noted the baby’s extreme fussiness and irritability and was concerned that he was being overfed. Without ordering additional tests, the family physician sent the baby home but arranged for the Galligans to be visited by a county nurse the following day.
Her visit raised concerns, as court documents make clear. She contacted Dr. Snider’s office and explained that the baby needed to be seen immediately. After writing a script for reflux and constipation, Dr. Snider arranged for the baby to be taken to his office later that day.
Events proceeded rapidly from this point.
Following an x-ray, Johnny appeared lethargic and in respiratory distress. He was then taken down the hall to Memorial’s emergency department, where doctors suspected a critical bowel obstruction. Arrangements were made for him to be transported by helicopter to Essentia Health, Duluth, Minn. There, doctors saw that Johnny was acidotic and in respiratory failure. Once again, he was rerouted, this time to Children’s Hospital, Minneapolis, where physicians finally arrived at a definitive diagnosis: meningitis.
In 2020, the Galligans filed a medical malpractice claim against several parties, including Dr. Snider, Duluth Clinic (doing business as Essentia Health and Essentia Health–Ashland Clinic), and Memorial Hospital. In their suit, Johnny’s parents alleged that the collective failure to diagnose their son’s severe infection led directly to his permanent brain damage.
But a Bayfield County, Wisconsin, jury didn’t quite see things that way. After deliberating, it dismissed the claim against Dr. Snider and the other named defendants and found the staff of Duluth Clinic to be solely responsible for injuries to Johnny Galligan.
Duluth must pay $19 million to the Galligan family, of which the largest amount ($7,500,00) is to be directed to Johnny’s “future medical expenses and care needs.”
These expenses and costs are likely to be significant. Currently, at 10 years of age, Johnny can’t walk and is confined to a wheelchair. He has serious neurologic problems and is almost completely deaf and blind.
“He’s doing fairly well, which I attribute to his family providing care for him,” says the attorney who represented the Galligans. “They care for him 24/7. They take him swimming and on four-wheeler rides. He’s not bedridden. He has the best possible quality of life he could have, in my opinion.”
In a statement following the verdict, Essentia Health said that, while it felt “compassion for the family,” it stood by the care it had provided in 2013: “We are exploring our options regarding next steps and remain committed to delivering high-quality care to the patients and communities we are privileged to serve.”
ED physician found not liable for embolism, jury finds
A Missouri doctor accused of incorrectly treating a woman’s embolism has been found not liable for her death, reports a story in Missouri Lawyers Media.
The woman went to her local hospital’s ED complaining of pain and swelling in her leg. At the ED, an emergency physician examined her and discovered an extensive, visible thrombosis. No other symptoms were noted.
In the past, such a finding would have prompted immediate hospital admission. But the standard of care has evolved. Now, many doctors first prescribe enoxaparin sodium (Lovenox), an anticoagulant used to treat deep-vein thrombosis. This was the option chosen by the Missouri emergency physician to treat his patient. After administering a first dose of the drug, he wrote a script for additional doses; consulted with his patient’s primary care physician; and arranged for the patient to be seen by him, the ED physician, the following day.
At the drugstore, though, the woman became ill, and an emergency medical services crew was alerted. Despite its quick response, the woman died en route to the hospital. No autopsy was later performed, and it was generally presumed that she had died of a pulmonary embolism.
Following the woman’s death, her family sued the emergency physician, alleging that his failure to admit the woman to the hospital most likely delayed treatment that could have saved her life.
The defense pushed back, arguing that the ED physician had followed the standard of care. “Even if she [had] come into the ER with full-blown [pulmonary embolism],” says the attorney representing the emergency physician, “the first thing you do is give Lovenox. It is just one of those rare circumstances where you can do everything right, but the patient can still die.”
The trial jury agreed. After deliberating for more than an hour, it found that the emergency physician was not responsible for the patient’s death.
At press time, there was no word on whether the plaintiffs planned to appeal.
A version of this article first appeared on Medscape.com.
according to a report in the Star Tribune, among other news outlets.
The story of the jury verdict begins in 2013, when the boy, Johnny Galligan, was just 8 days old.
Alarmed by the newborn’s crying, lack of appetite, and fever, his parents, Alina and Steve Galligan, brought him to Essentia-Health-Ashland Clinic, located in Memorial Medical Center, Ashland, Wisc. There, the baby was seen by Andrew D. Snider, MD, a family physician. Dr. Snider noted the baby’s extreme fussiness and irritability and was concerned that he was being overfed. Without ordering additional tests, the family physician sent the baby home but arranged for the Galligans to be visited by a county nurse the following day.
Her visit raised concerns, as court documents make clear. She contacted Dr. Snider’s office and explained that the baby needed to be seen immediately. After writing a script for reflux and constipation, Dr. Snider arranged for the baby to be taken to his office later that day.
Events proceeded rapidly from this point.
Following an x-ray, Johnny appeared lethargic and in respiratory distress. He was then taken down the hall to Memorial’s emergency department, where doctors suspected a critical bowel obstruction. Arrangements were made for him to be transported by helicopter to Essentia Health, Duluth, Minn. There, doctors saw that Johnny was acidotic and in respiratory failure. Once again, he was rerouted, this time to Children’s Hospital, Minneapolis, where physicians finally arrived at a definitive diagnosis: meningitis.
In 2020, the Galligans filed a medical malpractice claim against several parties, including Dr. Snider, Duluth Clinic (doing business as Essentia Health and Essentia Health–Ashland Clinic), and Memorial Hospital. In their suit, Johnny’s parents alleged that the collective failure to diagnose their son’s severe infection led directly to his permanent brain damage.
But a Bayfield County, Wisconsin, jury didn’t quite see things that way. After deliberating, it dismissed the claim against Dr. Snider and the other named defendants and found the staff of Duluth Clinic to be solely responsible for injuries to Johnny Galligan.
Duluth must pay $19 million to the Galligan family, of which the largest amount ($7,500,00) is to be directed to Johnny’s “future medical expenses and care needs.”
These expenses and costs are likely to be significant. Currently, at 10 years of age, Johnny can’t walk and is confined to a wheelchair. He has serious neurologic problems and is almost completely deaf and blind.
“He’s doing fairly well, which I attribute to his family providing care for him,” says the attorney who represented the Galligans. “They care for him 24/7. They take him swimming and on four-wheeler rides. He’s not bedridden. He has the best possible quality of life he could have, in my opinion.”
In a statement following the verdict, Essentia Health said that, while it felt “compassion for the family,” it stood by the care it had provided in 2013: “We are exploring our options regarding next steps and remain committed to delivering high-quality care to the patients and communities we are privileged to serve.”
ED physician found not liable for embolism, jury finds
A Missouri doctor accused of incorrectly treating a woman’s embolism has been found not liable for her death, reports a story in Missouri Lawyers Media.
The woman went to her local hospital’s ED complaining of pain and swelling in her leg. At the ED, an emergency physician examined her and discovered an extensive, visible thrombosis. No other symptoms were noted.
In the past, such a finding would have prompted immediate hospital admission. But the standard of care has evolved. Now, many doctors first prescribe enoxaparin sodium (Lovenox), an anticoagulant used to treat deep-vein thrombosis. This was the option chosen by the Missouri emergency physician to treat his patient. After administering a first dose of the drug, he wrote a script for additional doses; consulted with his patient’s primary care physician; and arranged for the patient to be seen by him, the ED physician, the following day.
At the drugstore, though, the woman became ill, and an emergency medical services crew was alerted. Despite its quick response, the woman died en route to the hospital. No autopsy was later performed, and it was generally presumed that she had died of a pulmonary embolism.
Following the woman’s death, her family sued the emergency physician, alleging that his failure to admit the woman to the hospital most likely delayed treatment that could have saved her life.
The defense pushed back, arguing that the ED physician had followed the standard of care. “Even if she [had] come into the ER with full-blown [pulmonary embolism],” says the attorney representing the emergency physician, “the first thing you do is give Lovenox. It is just one of those rare circumstances where you can do everything right, but the patient can still die.”
The trial jury agreed. After deliberating for more than an hour, it found that the emergency physician was not responsible for the patient’s death.
At press time, there was no word on whether the plaintiffs planned to appeal.
A version of this article first appeared on Medscape.com.
according to a report in the Star Tribune, among other news outlets.
The story of the jury verdict begins in 2013, when the boy, Johnny Galligan, was just 8 days old.
Alarmed by the newborn’s crying, lack of appetite, and fever, his parents, Alina and Steve Galligan, brought him to Essentia-Health-Ashland Clinic, located in Memorial Medical Center, Ashland, Wisc. There, the baby was seen by Andrew D. Snider, MD, a family physician. Dr. Snider noted the baby’s extreme fussiness and irritability and was concerned that he was being overfed. Without ordering additional tests, the family physician sent the baby home but arranged for the Galligans to be visited by a county nurse the following day.
Her visit raised concerns, as court documents make clear. She contacted Dr. Snider’s office and explained that the baby needed to be seen immediately. After writing a script for reflux and constipation, Dr. Snider arranged for the baby to be taken to his office later that day.
Events proceeded rapidly from this point.
Following an x-ray, Johnny appeared lethargic and in respiratory distress. He was then taken down the hall to Memorial’s emergency department, where doctors suspected a critical bowel obstruction. Arrangements were made for him to be transported by helicopter to Essentia Health, Duluth, Minn. There, doctors saw that Johnny was acidotic and in respiratory failure. Once again, he was rerouted, this time to Children’s Hospital, Minneapolis, where physicians finally arrived at a definitive diagnosis: meningitis.
In 2020, the Galligans filed a medical malpractice claim against several parties, including Dr. Snider, Duluth Clinic (doing business as Essentia Health and Essentia Health–Ashland Clinic), and Memorial Hospital. In their suit, Johnny’s parents alleged that the collective failure to diagnose their son’s severe infection led directly to his permanent brain damage.
But a Bayfield County, Wisconsin, jury didn’t quite see things that way. After deliberating, it dismissed the claim against Dr. Snider and the other named defendants and found the staff of Duluth Clinic to be solely responsible for injuries to Johnny Galligan.
Duluth must pay $19 million to the Galligan family, of which the largest amount ($7,500,00) is to be directed to Johnny’s “future medical expenses and care needs.”
These expenses and costs are likely to be significant. Currently, at 10 years of age, Johnny can’t walk and is confined to a wheelchair. He has serious neurologic problems and is almost completely deaf and blind.
“He’s doing fairly well, which I attribute to his family providing care for him,” says the attorney who represented the Galligans. “They care for him 24/7. They take him swimming and on four-wheeler rides. He’s not bedridden. He has the best possible quality of life he could have, in my opinion.”
In a statement following the verdict, Essentia Health said that, while it felt “compassion for the family,” it stood by the care it had provided in 2013: “We are exploring our options regarding next steps and remain committed to delivering high-quality care to the patients and communities we are privileged to serve.”
ED physician found not liable for embolism, jury finds
A Missouri doctor accused of incorrectly treating a woman’s embolism has been found not liable for her death, reports a story in Missouri Lawyers Media.
The woman went to her local hospital’s ED complaining of pain and swelling in her leg. At the ED, an emergency physician examined her and discovered an extensive, visible thrombosis. No other symptoms were noted.
In the past, such a finding would have prompted immediate hospital admission. But the standard of care has evolved. Now, many doctors first prescribe enoxaparin sodium (Lovenox), an anticoagulant used to treat deep-vein thrombosis. This was the option chosen by the Missouri emergency physician to treat his patient. After administering a first dose of the drug, he wrote a script for additional doses; consulted with his patient’s primary care physician; and arranged for the patient to be seen by him, the ED physician, the following day.
At the drugstore, though, the woman became ill, and an emergency medical services crew was alerted. Despite its quick response, the woman died en route to the hospital. No autopsy was later performed, and it was generally presumed that she had died of a pulmonary embolism.
Following the woman’s death, her family sued the emergency physician, alleging that his failure to admit the woman to the hospital most likely delayed treatment that could have saved her life.
The defense pushed back, arguing that the ED physician had followed the standard of care. “Even if she [had] come into the ER with full-blown [pulmonary embolism],” says the attorney representing the emergency physician, “the first thing you do is give Lovenox. It is just one of those rare circumstances where you can do everything right, but the patient can still die.”
The trial jury agreed. After deliberating for more than an hour, it found that the emergency physician was not responsible for the patient’s death.
At press time, there was no word on whether the plaintiffs planned to appeal.
A version of this article first appeared on Medscape.com.
Mammography after breast cancer: No benefit for older patients?
BOSTON – Older women who have had breast cancer frequently undergo annual surveillance mammography, even if there is only a small risk of their developing a second cancer or if they have other mortality risks associated with age and comorbidities.
In a study that included almost 45,000 women who were aged 67 years or older when they were diagnosed with breast cancer, investigators found that patients commonly underwent annual mammographies.
“Even 10 years after their initial diagnosis ... about 40% of them were still getting surveillance mammography well into their 80s and 90s,” noted lead investigator Elizabeth Berger, MD, assistant professor of breast surgical oncology, Yale University, New Haven, Conn.
“Ongoing surveillance mammography in these patients may lead to overdiagnosis and overtreatment of cancers that potentially would not harm patients if left untreated,” Dr. Berger said.
“A positive or false positive finding may unnecessarily erode patient quality of life and incur costs to the patient and health care system without benefit,” she said. She added: “If an elderly woman is in poor health and has significant competing mortality risks compared to breast cancer, annual mammography may not be necessary.”
The research was presented at the annual meeting of the American Society of Breast Surgeons (ASBrS). The study was highlighted in a preview press briefing.
Speaking at the press briefing, Dr. Berger said that the “risks and benefits of surveillance mammography, including its downstream effects, should be considered by both patients and their doctors together to create a shared decision plan.” She acknowledged that the idea of skipping mammograms may be a sensitive one for patients.
She also shared what she described as “exciting news”: “We have just recently received funding from our geriatric group here at Yale to start to evaluate the potential benefits and harms of these surveillance mammographies.”
The aim is to evaluate false positive rates and the potential for overdiagnosis and overtreatment, “so stay tuned,” she added.
Approached for comment, Mediget Teshome, MD, MPH, said it was “not surprising to see the high rates of surveillance mammography, especially in the short term after treatment.”
She said in an interview that the results suggest that it “may be being overused,” given the low rates of second primary breast cancer and the “competing health concerns” of these women.
Overuse can, on the other hand, “definitely be a complex issue,” said Dr. Teshome, associate professor, department of breast surgical oncology, University of Texas MD Anderson Cancer Center, Houston.
“The goal of mammography screening is to identify breast cancer at an early stage,” she explained. She noted that because of the “competing mortality risk from other challenging and life-threatening health problems,” early-stage breast cancer “may not contribute significantly” to the overall mortality risk.
“In general, in this patient population, consideration should be given to stratifying based on an individual patient’s risk of breast cancer recurrence or new breast cancer, estimated life expectancy, as well as shared decision-making with the patient based on their goals of care.”
Study details
To examine the use of surveillance mammography and the risk of subsequent cancers among older women, Dr. Berger and her team used data from the Surveillance, Epidemiology, and End Results (SEER) registry to identify women aged 67 years or older who were diagnosed with a first nonmetastatic beast cancer between 2003 and 2007.
The patients were followed beginning 1 year after diagnosis until the occurrence of a second primary breast cancer, death, or the end of follow-up in 2017.
Data on 44,475 women were analyzed. Of those patients, 30% were older than 80 years. The majority (74%) of breast cancers were of stage I or II, and 72% were hormone receptor–positive (HR+).
Comorbid conditions were common; 55% of women had at least one, and 16% had three or more.
Life expectancy, determined on the basis of age, sex, and comorbidities, was estimated at less than 5 years for 26% of women. For 36% of patients, life expectancy was 6-10 years, and for 38%, it was longer than 10 years.
The cumulative incidence of developing a second primary breast cancer varied by life expectancy and the tumor’s molecular subtype.
The incidence was 3.7% among women with a life expectancy of less than 5 years, 4.9% among those expected to live 6-10 years, and 7.6% among those predicted to live more than 10 years.
Among women with a life expectancy of less than 5 years, the cumulative incidence of a second primary tumor was 4.0% among those with triple-negative breast cancer, vs. 3.0% among those with HR+ breast cancer.
Among patients whose life expectancy was more than 10 years, the cumulative incidence of a second primary tumor was 9.2% among women with triple-negative disease, vs. 7.0% among those with HR+ cancers.
The team found that it was common for women across all the groups to undergo mammography.
Among women with a life expectancy of 6-10 years, 82% underwent at least one mammogram, and 65% underwent five mammograms. Even among women with a life expectancy of less than 1 year, 51% underwent at least one mammogram within 12 months of death.
Among women with a life expectancy of less than 5 years, 68% of women had received a mammogram 1 year after treatment; 53% underwent three mammograms within 3 years after treatment.
No funding for the study was declared. The investigators have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BOSTON – Older women who have had breast cancer frequently undergo annual surveillance mammography, even if there is only a small risk of their developing a second cancer or if they have other mortality risks associated with age and comorbidities.
In a study that included almost 45,000 women who were aged 67 years or older when they were diagnosed with breast cancer, investigators found that patients commonly underwent annual mammographies.
“Even 10 years after their initial diagnosis ... about 40% of them were still getting surveillance mammography well into their 80s and 90s,” noted lead investigator Elizabeth Berger, MD, assistant professor of breast surgical oncology, Yale University, New Haven, Conn.
“Ongoing surveillance mammography in these patients may lead to overdiagnosis and overtreatment of cancers that potentially would not harm patients if left untreated,” Dr. Berger said.
“A positive or false positive finding may unnecessarily erode patient quality of life and incur costs to the patient and health care system without benefit,” she said. She added: “If an elderly woman is in poor health and has significant competing mortality risks compared to breast cancer, annual mammography may not be necessary.”
The research was presented at the annual meeting of the American Society of Breast Surgeons (ASBrS). The study was highlighted in a preview press briefing.
Speaking at the press briefing, Dr. Berger said that the “risks and benefits of surveillance mammography, including its downstream effects, should be considered by both patients and their doctors together to create a shared decision plan.” She acknowledged that the idea of skipping mammograms may be a sensitive one for patients.
She also shared what she described as “exciting news”: “We have just recently received funding from our geriatric group here at Yale to start to evaluate the potential benefits and harms of these surveillance mammographies.”
The aim is to evaluate false positive rates and the potential for overdiagnosis and overtreatment, “so stay tuned,” she added.
Approached for comment, Mediget Teshome, MD, MPH, said it was “not surprising to see the high rates of surveillance mammography, especially in the short term after treatment.”
She said in an interview that the results suggest that it “may be being overused,” given the low rates of second primary breast cancer and the “competing health concerns” of these women.
Overuse can, on the other hand, “definitely be a complex issue,” said Dr. Teshome, associate professor, department of breast surgical oncology, University of Texas MD Anderson Cancer Center, Houston.
“The goal of mammography screening is to identify breast cancer at an early stage,” she explained. She noted that because of the “competing mortality risk from other challenging and life-threatening health problems,” early-stage breast cancer “may not contribute significantly” to the overall mortality risk.
“In general, in this patient population, consideration should be given to stratifying based on an individual patient’s risk of breast cancer recurrence or new breast cancer, estimated life expectancy, as well as shared decision-making with the patient based on their goals of care.”
Study details
To examine the use of surveillance mammography and the risk of subsequent cancers among older women, Dr. Berger and her team used data from the Surveillance, Epidemiology, and End Results (SEER) registry to identify women aged 67 years or older who were diagnosed with a first nonmetastatic beast cancer between 2003 and 2007.
The patients were followed beginning 1 year after diagnosis until the occurrence of a second primary breast cancer, death, or the end of follow-up in 2017.
Data on 44,475 women were analyzed. Of those patients, 30% were older than 80 years. The majority (74%) of breast cancers were of stage I or II, and 72% were hormone receptor–positive (HR+).
Comorbid conditions were common; 55% of women had at least one, and 16% had three or more.
Life expectancy, determined on the basis of age, sex, and comorbidities, was estimated at less than 5 years for 26% of women. For 36% of patients, life expectancy was 6-10 years, and for 38%, it was longer than 10 years.
The cumulative incidence of developing a second primary breast cancer varied by life expectancy and the tumor’s molecular subtype.
The incidence was 3.7% among women with a life expectancy of less than 5 years, 4.9% among those expected to live 6-10 years, and 7.6% among those predicted to live more than 10 years.
Among women with a life expectancy of less than 5 years, the cumulative incidence of a second primary tumor was 4.0% among those with triple-negative breast cancer, vs. 3.0% among those with HR+ breast cancer.
Among patients whose life expectancy was more than 10 years, the cumulative incidence of a second primary tumor was 9.2% among women with triple-negative disease, vs. 7.0% among those with HR+ cancers.
The team found that it was common for women across all the groups to undergo mammography.
Among women with a life expectancy of 6-10 years, 82% underwent at least one mammogram, and 65% underwent five mammograms. Even among women with a life expectancy of less than 1 year, 51% underwent at least one mammogram within 12 months of death.
Among women with a life expectancy of less than 5 years, 68% of women had received a mammogram 1 year after treatment; 53% underwent three mammograms within 3 years after treatment.
No funding for the study was declared. The investigators have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
BOSTON – Older women who have had breast cancer frequently undergo annual surveillance mammography, even if there is only a small risk of their developing a second cancer or if they have other mortality risks associated with age and comorbidities.
In a study that included almost 45,000 women who were aged 67 years or older when they were diagnosed with breast cancer, investigators found that patients commonly underwent annual mammographies.
“Even 10 years after their initial diagnosis ... about 40% of them were still getting surveillance mammography well into their 80s and 90s,” noted lead investigator Elizabeth Berger, MD, assistant professor of breast surgical oncology, Yale University, New Haven, Conn.
“Ongoing surveillance mammography in these patients may lead to overdiagnosis and overtreatment of cancers that potentially would not harm patients if left untreated,” Dr. Berger said.
“A positive or false positive finding may unnecessarily erode patient quality of life and incur costs to the patient and health care system without benefit,” she said. She added: “If an elderly woman is in poor health and has significant competing mortality risks compared to breast cancer, annual mammography may not be necessary.”
The research was presented at the annual meeting of the American Society of Breast Surgeons (ASBrS). The study was highlighted in a preview press briefing.
Speaking at the press briefing, Dr. Berger said that the “risks and benefits of surveillance mammography, including its downstream effects, should be considered by both patients and their doctors together to create a shared decision plan.” She acknowledged that the idea of skipping mammograms may be a sensitive one for patients.
She also shared what she described as “exciting news”: “We have just recently received funding from our geriatric group here at Yale to start to evaluate the potential benefits and harms of these surveillance mammographies.”
The aim is to evaluate false positive rates and the potential for overdiagnosis and overtreatment, “so stay tuned,” she added.
Approached for comment, Mediget Teshome, MD, MPH, said it was “not surprising to see the high rates of surveillance mammography, especially in the short term after treatment.”
She said in an interview that the results suggest that it “may be being overused,” given the low rates of second primary breast cancer and the “competing health concerns” of these women.
Overuse can, on the other hand, “definitely be a complex issue,” said Dr. Teshome, associate professor, department of breast surgical oncology, University of Texas MD Anderson Cancer Center, Houston.
“The goal of mammography screening is to identify breast cancer at an early stage,” she explained. She noted that because of the “competing mortality risk from other challenging and life-threatening health problems,” early-stage breast cancer “may not contribute significantly” to the overall mortality risk.
“In general, in this patient population, consideration should be given to stratifying based on an individual patient’s risk of breast cancer recurrence or new breast cancer, estimated life expectancy, as well as shared decision-making with the patient based on their goals of care.”
Study details
To examine the use of surveillance mammography and the risk of subsequent cancers among older women, Dr. Berger and her team used data from the Surveillance, Epidemiology, and End Results (SEER) registry to identify women aged 67 years or older who were diagnosed with a first nonmetastatic beast cancer between 2003 and 2007.
The patients were followed beginning 1 year after diagnosis until the occurrence of a second primary breast cancer, death, or the end of follow-up in 2017.
Data on 44,475 women were analyzed. Of those patients, 30% were older than 80 years. The majority (74%) of breast cancers were of stage I or II, and 72% were hormone receptor–positive (HR+).
Comorbid conditions were common; 55% of women had at least one, and 16% had three or more.
Life expectancy, determined on the basis of age, sex, and comorbidities, was estimated at less than 5 years for 26% of women. For 36% of patients, life expectancy was 6-10 years, and for 38%, it was longer than 10 years.
The cumulative incidence of developing a second primary breast cancer varied by life expectancy and the tumor’s molecular subtype.
The incidence was 3.7% among women with a life expectancy of less than 5 years, 4.9% among those expected to live 6-10 years, and 7.6% among those predicted to live more than 10 years.
Among women with a life expectancy of less than 5 years, the cumulative incidence of a second primary tumor was 4.0% among those with triple-negative breast cancer, vs. 3.0% among those with HR+ breast cancer.
Among patients whose life expectancy was more than 10 years, the cumulative incidence of a second primary tumor was 9.2% among women with triple-negative disease, vs. 7.0% among those with HR+ cancers.
The team found that it was common for women across all the groups to undergo mammography.
Among women with a life expectancy of 6-10 years, 82% underwent at least one mammogram, and 65% underwent five mammograms. Even among women with a life expectancy of less than 1 year, 51% underwent at least one mammogram within 12 months of death.
Among women with a life expectancy of less than 5 years, 68% of women had received a mammogram 1 year after treatment; 53% underwent three mammograms within 3 years after treatment.
No funding for the study was declared. The investigators have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ASBRS 2023
SCC from breast implants: Negligible risk, study finds
Findings from a large cohort study suggest the incidence of SCC is negligible. The analysis found one case of SCC among nearly 57,000 women who had undergone breast implant reconstruction over 421,227 person-years of follow-up.
The authors also confirmed the known risk of breast implant–associated anaplastic large-cell lymphoma (ALCL), identifying five cases in the population, which was considered a “significantly elevated” risk.
Although patients with breast cancer who are eligible for mastectomy should be counseled on the risks for cancer after implant reconstruction, patients “should not be dissuaded from pursuing implant-based reconstruction because of the risk of SCC,” lead author Connor J. Kinslow, MD, of Columbia University, New York, and colleagues concluded.
SCC cases associated with breast implants are distinct from breast implant–associated ALCL, the authors noted, explaining that this lymphoma “is the subject of a boxed warning on all saline- and silicone gel–filled breast implants since 2020.”
The results were published in a research letter in JAMA Surgery.
Last September, a safety communication from the FDA highlighted reports of SCC and other lymphomas associated with breast implants. The FDA said it was aware of fewer than 20 cases of SCC.
Following the safety communication, Dr. Kinslow and colleagues assessed SCC risk among 56,785 women who underwent cancer-directed mastectomy with implant reconstruction for breast tumors.
Women in the cohort were diagnosed between 2000 and 2018 and included in the Surveillance, Epidemiology, and End Results (SEER) 17 database. Patients had a median age of 51 years; most (84%) where White, 8.1% were Black, 7.4% were Asian or Pacific Islander, 0.4% were American Indian/Alaska Native, and race was unknown in 0.4%.
Across 421,227 person-years of follow-up, the team identified one case of SCC, corresponding to an incidence rate of 2.37 per million person-years vs. an expected incidence of 1.02 per million person-years in the general population. Although the 2.33 standardized incidence ratio (SIR) “appeared elevated vs. the general population,” it was “not significant given the low incidence” (95% confidence interval, 0.06-13.0).
The team also identified five cases of breast implant–associated ALCL. That corresponded to an incidence rate of 11.9 per million person-years compared with an expected incidence of 0.29 per million person-years – for a significantly elevated SIR of 40.9. The authors also noted more than 1,000 reported cases of breast implant–associated ALCL previous as well as a robust association with implants.
Regarding SCC, “whether the observed elevated risk is associated with the implants is difficult to interpret because it is based on only one case and wide [confidence intervals],” the authors said. But, overall, “we found that the incidence rate of SCC was extraordinarily low and of minimal public health concern.”
A version of this article first appeared on Medscape.com.
Findings from a large cohort study suggest the incidence of SCC is negligible. The analysis found one case of SCC among nearly 57,000 women who had undergone breast implant reconstruction over 421,227 person-years of follow-up.
The authors also confirmed the known risk of breast implant–associated anaplastic large-cell lymphoma (ALCL), identifying five cases in the population, which was considered a “significantly elevated” risk.
Although patients with breast cancer who are eligible for mastectomy should be counseled on the risks for cancer after implant reconstruction, patients “should not be dissuaded from pursuing implant-based reconstruction because of the risk of SCC,” lead author Connor J. Kinslow, MD, of Columbia University, New York, and colleagues concluded.
SCC cases associated with breast implants are distinct from breast implant–associated ALCL, the authors noted, explaining that this lymphoma “is the subject of a boxed warning on all saline- and silicone gel–filled breast implants since 2020.”
The results were published in a research letter in JAMA Surgery.
Last September, a safety communication from the FDA highlighted reports of SCC and other lymphomas associated with breast implants. The FDA said it was aware of fewer than 20 cases of SCC.
Following the safety communication, Dr. Kinslow and colleagues assessed SCC risk among 56,785 women who underwent cancer-directed mastectomy with implant reconstruction for breast tumors.
Women in the cohort were diagnosed between 2000 and 2018 and included in the Surveillance, Epidemiology, and End Results (SEER) 17 database. Patients had a median age of 51 years; most (84%) where White, 8.1% were Black, 7.4% were Asian or Pacific Islander, 0.4% were American Indian/Alaska Native, and race was unknown in 0.4%.
Across 421,227 person-years of follow-up, the team identified one case of SCC, corresponding to an incidence rate of 2.37 per million person-years vs. an expected incidence of 1.02 per million person-years in the general population. Although the 2.33 standardized incidence ratio (SIR) “appeared elevated vs. the general population,” it was “not significant given the low incidence” (95% confidence interval, 0.06-13.0).
The team also identified five cases of breast implant–associated ALCL. That corresponded to an incidence rate of 11.9 per million person-years compared with an expected incidence of 0.29 per million person-years – for a significantly elevated SIR of 40.9. The authors also noted more than 1,000 reported cases of breast implant–associated ALCL previous as well as a robust association with implants.
Regarding SCC, “whether the observed elevated risk is associated with the implants is difficult to interpret because it is based on only one case and wide [confidence intervals],” the authors said. But, overall, “we found that the incidence rate of SCC was extraordinarily low and of minimal public health concern.”
A version of this article first appeared on Medscape.com.
Findings from a large cohort study suggest the incidence of SCC is negligible. The analysis found one case of SCC among nearly 57,000 women who had undergone breast implant reconstruction over 421,227 person-years of follow-up.
The authors also confirmed the known risk of breast implant–associated anaplastic large-cell lymphoma (ALCL), identifying five cases in the population, which was considered a “significantly elevated” risk.
Although patients with breast cancer who are eligible for mastectomy should be counseled on the risks for cancer after implant reconstruction, patients “should not be dissuaded from pursuing implant-based reconstruction because of the risk of SCC,” lead author Connor J. Kinslow, MD, of Columbia University, New York, and colleagues concluded.
SCC cases associated with breast implants are distinct from breast implant–associated ALCL, the authors noted, explaining that this lymphoma “is the subject of a boxed warning on all saline- and silicone gel–filled breast implants since 2020.”
The results were published in a research letter in JAMA Surgery.
Last September, a safety communication from the FDA highlighted reports of SCC and other lymphomas associated with breast implants. The FDA said it was aware of fewer than 20 cases of SCC.
Following the safety communication, Dr. Kinslow and colleagues assessed SCC risk among 56,785 women who underwent cancer-directed mastectomy with implant reconstruction for breast tumors.
Women in the cohort were diagnosed between 2000 and 2018 and included in the Surveillance, Epidemiology, and End Results (SEER) 17 database. Patients had a median age of 51 years; most (84%) where White, 8.1% were Black, 7.4% were Asian or Pacific Islander, 0.4% were American Indian/Alaska Native, and race was unknown in 0.4%.
Across 421,227 person-years of follow-up, the team identified one case of SCC, corresponding to an incidence rate of 2.37 per million person-years vs. an expected incidence of 1.02 per million person-years in the general population. Although the 2.33 standardized incidence ratio (SIR) “appeared elevated vs. the general population,” it was “not significant given the low incidence” (95% confidence interval, 0.06-13.0).
The team also identified five cases of breast implant–associated ALCL. That corresponded to an incidence rate of 11.9 per million person-years compared with an expected incidence of 0.29 per million person-years – for a significantly elevated SIR of 40.9. The authors also noted more than 1,000 reported cases of breast implant–associated ALCL previous as well as a robust association with implants.
Regarding SCC, “whether the observed elevated risk is associated with the implants is difficult to interpret because it is based on only one case and wide [confidence intervals],” the authors said. But, overall, “we found that the incidence rate of SCC was extraordinarily low and of minimal public health concern.”
A version of this article first appeared on Medscape.com.
FROM JAMA SURGERY
Study shows higher obesity-related cancer mortality in areas with more fast food
based on data from a new cross-sectional study of more than 3,000 communities.
Although increased healthy eating has been associated with reduced risk of obesity and with reduced cancer incidence and mortality, access to healthier eating remains a challenge in communities with less access to grocery stores and healthy food options (food deserts) and/or easy access to convenience stores and fast food (food swamps), Malcolm Seth Bevel, PhD, of the Medical College of Georgia, Augusta, and colleagues, wrote in their paper, published in JAMA Oncology.
In addition, data on the association between food deserts and swamps and obesity-related cancer mortality are limited, they said.
“We felt that the study was important given the fact that obesity is an epidemic in the United States, and multiple factors contribute to obesity, especially adverse food environments,” Dr. Bevel said in an interview. “Also, I lived in these areas my whole life, and saw how it affected underserved populations. There was a story that needed to be told, so we’re telling it,” he said in an interview.
In a study, the researchers analyzed food access and cancer mortality data from 3,038 counties across the United States. The food access data came from the U.S. Department of Agriculture Food Environment Atlas (FEA) for the years 2012, 2014, 2015, 2017, and 2020. Data on obesity-related cancer mortality came from the Centers for Disease Control and Prevention for the years from 2010 to 2020.
Food desert scores were calculated through data from the FEA, and food swamp scores were based on the ratio of fast-food restaurants and convenience stores to grocery stores and farmers markets in a modification of the Retail Food Environment Index score.
The researchers used an age-adjusted, multiple regression model to determine the association between food desert and food swamp scores and obesity-related cancer mortality rates. Higher food swamp and food desert scores (defined as 20.0 to 58.0 or higher) were used to classify counties as having fewer healthy food resources. The primary outcome was obesity-related cancer mortality, defined as high or low (71.8 or higher per 100,000 individuals and less than 71.8 per 100,000 individuals, respectively).
Overall, high rates of obesity-related cancer mortality were 77% more likely in the counties that met the criteria for high food swamp scores (adjusted odds ratio 1.77). In addition, researchers found a positive dose-response relationship among three levels of both food desert scores and food swamp scores and obesity-related cancer mortality.
A total of 758 counties had obesity-related cancer mortality rates in the highest quartile. Compared to counties with low rates of obesity-related cancer mortality, counties with high rates of obesity-related cancer mortality also had a higher percentage of non-Hispanic Black residents (3.26% vs. 1.77%), higher percentage of adults older than 65 years (15.71% vs. 15.40%), higher rates of adult obesity (33.0% vs. 32.10%), and higher rates of adult diabetes (12.50% vs. 10.70%).
Possible explanations for the results include the lack of interest in grocery stores in neighborhoods with a population with a lower socioeconomic status, which can create a food desert, the researchers wrote in their discussion. “Coupled with the increasing growth rate of fast-food restaurants in recent years and the intentional advertisement of unhealthy foods in urban neighborhoods with [people of lower income], the food desert may transform into a food swamp,” they said.
The findings were limited by several factors including the study design, which did not allow for showing a causal association of food deserts and food swamps with obesity-related cancer mortality, the researchers noted. Other limitations included the use of groups rather than individuals, the potential misclassification of food stores, and the use of county-level data on race, ethnicity, and income, they wrote.
The results indicate that “food swamps appear to be a growing epidemic across the U.S., likely because of systemic issues, and should draw concern and conversation from local and state officials,” the researchers concluded.
Community-level investments can benefit individual health
Dr. Bevel said he was not surprised by the findings, as he has seen firsthand the lack of healthy food options and growth of unhealthy food options, especially for certain populations in certain communities. “Typically, these are people who have lower socioeconomic status, primarily non-Hispanic Black or African American or Hispanic American,” he said “I have watched people have to choose between getting fruits/vegetables versus their medications or running to fast food places to feed their families. What is truly surprising is that we’re not talking about people’s lived environment enough for my taste,” he said.
“I hope that our data and results can inform local and state policymakers to truly invest in all communities, such as funding for community gardens, and realize that adverse food environments, including the barriers in navigating these environments, have significant consequences on real people,” said Dr. Bevel. “Also, I hope that the results can help clinicians realize that a patient’s lived environment can truly affect their obesity and/or obesity-related cancer status; being cognizant of that is the first step in holistic, comprehensive care,” he said.
“One role that oncologists might be able to play in improving patients’ access to healthier food is to create and/or implement healthy lifestyle programs with gardening components to combat the poorest food environments that their patients likely reside in,” said Dr. Bevel. Clinicians also could consider the innovative approach of “food prescriptions” to help reduce the effects of deprived, built environments, he noted.
Looking ahead, next steps for research include determining the severity of association between food swamps and obesity-related cancer by varying factors such as cancer type, and examining any potential racial disparities between people living in these environments and obesity-related cancer, Dr. Bevel added.
Data provide foundation for multilevel interventions
The current study findings “raise a clarion call to elevate the discussion on food availability and access to ensure an equitable emphasis on both the importance of lifestyle factors and the upstream structural, economic, and environmental contexts that shape these behaviors at the individual level,” Karriem S. Watson, DHSc, MS, MPH, of the National Institutes of Health, Bethesda, Md., and Angela Odoms-Young, PhD, of Cornell University, Ithaca, N.Y., wrote in an accompanying editorial.
The findings provide a foundation for studies of obesity-related cancer outcomes that take the community environment into consideration, they added.
The causes of both obesity and cancer are complex, and the study findings suggest that the links between unhealthy food environments and obesity-related cancer may go beyond dietary consumption alone and extend to social and psychological factors, the editorialists noted.
“Whether dealing with the lack of access to healthy foods or an overabundance of unhealthy food, there is a critical need to develop additional research that explores the associations between obesity-related cancer mortality and food inequities,” they concluded.
The study received no outside funding. The researchers and the editorialists had no financial conflicts to disclose.
based on data from a new cross-sectional study of more than 3,000 communities.
Although increased healthy eating has been associated with reduced risk of obesity and with reduced cancer incidence and mortality, access to healthier eating remains a challenge in communities with less access to grocery stores and healthy food options (food deserts) and/or easy access to convenience stores and fast food (food swamps), Malcolm Seth Bevel, PhD, of the Medical College of Georgia, Augusta, and colleagues, wrote in their paper, published in JAMA Oncology.
In addition, data on the association between food deserts and swamps and obesity-related cancer mortality are limited, they said.
“We felt that the study was important given the fact that obesity is an epidemic in the United States, and multiple factors contribute to obesity, especially adverse food environments,” Dr. Bevel said in an interview. “Also, I lived in these areas my whole life, and saw how it affected underserved populations. There was a story that needed to be told, so we’re telling it,” he said in an interview.
In a study, the researchers analyzed food access and cancer mortality data from 3,038 counties across the United States. The food access data came from the U.S. Department of Agriculture Food Environment Atlas (FEA) for the years 2012, 2014, 2015, 2017, and 2020. Data on obesity-related cancer mortality came from the Centers for Disease Control and Prevention for the years from 2010 to 2020.
Food desert scores were calculated through data from the FEA, and food swamp scores were based on the ratio of fast-food restaurants and convenience stores to grocery stores and farmers markets in a modification of the Retail Food Environment Index score.
The researchers used an age-adjusted, multiple regression model to determine the association between food desert and food swamp scores and obesity-related cancer mortality rates. Higher food swamp and food desert scores (defined as 20.0 to 58.0 or higher) were used to classify counties as having fewer healthy food resources. The primary outcome was obesity-related cancer mortality, defined as high or low (71.8 or higher per 100,000 individuals and less than 71.8 per 100,000 individuals, respectively).
Overall, high rates of obesity-related cancer mortality were 77% more likely in the counties that met the criteria for high food swamp scores (adjusted odds ratio 1.77). In addition, researchers found a positive dose-response relationship among three levels of both food desert scores and food swamp scores and obesity-related cancer mortality.
A total of 758 counties had obesity-related cancer mortality rates in the highest quartile. Compared to counties with low rates of obesity-related cancer mortality, counties with high rates of obesity-related cancer mortality also had a higher percentage of non-Hispanic Black residents (3.26% vs. 1.77%), higher percentage of adults older than 65 years (15.71% vs. 15.40%), higher rates of adult obesity (33.0% vs. 32.10%), and higher rates of adult diabetes (12.50% vs. 10.70%).
Possible explanations for the results include the lack of interest in grocery stores in neighborhoods with a population with a lower socioeconomic status, which can create a food desert, the researchers wrote in their discussion. “Coupled with the increasing growth rate of fast-food restaurants in recent years and the intentional advertisement of unhealthy foods in urban neighborhoods with [people of lower income], the food desert may transform into a food swamp,” they said.
The findings were limited by several factors including the study design, which did not allow for showing a causal association of food deserts and food swamps with obesity-related cancer mortality, the researchers noted. Other limitations included the use of groups rather than individuals, the potential misclassification of food stores, and the use of county-level data on race, ethnicity, and income, they wrote.
The results indicate that “food swamps appear to be a growing epidemic across the U.S., likely because of systemic issues, and should draw concern and conversation from local and state officials,” the researchers concluded.
Community-level investments can benefit individual health
Dr. Bevel said he was not surprised by the findings, as he has seen firsthand the lack of healthy food options and growth of unhealthy food options, especially for certain populations in certain communities. “Typically, these are people who have lower socioeconomic status, primarily non-Hispanic Black or African American or Hispanic American,” he said “I have watched people have to choose between getting fruits/vegetables versus their medications or running to fast food places to feed their families. What is truly surprising is that we’re not talking about people’s lived environment enough for my taste,” he said.
“I hope that our data and results can inform local and state policymakers to truly invest in all communities, such as funding for community gardens, and realize that adverse food environments, including the barriers in navigating these environments, have significant consequences on real people,” said Dr. Bevel. “Also, I hope that the results can help clinicians realize that a patient’s lived environment can truly affect their obesity and/or obesity-related cancer status; being cognizant of that is the first step in holistic, comprehensive care,” he said.
“One role that oncologists might be able to play in improving patients’ access to healthier food is to create and/or implement healthy lifestyle programs with gardening components to combat the poorest food environments that their patients likely reside in,” said Dr. Bevel. Clinicians also could consider the innovative approach of “food prescriptions” to help reduce the effects of deprived, built environments, he noted.
Looking ahead, next steps for research include determining the severity of association between food swamps and obesity-related cancer by varying factors such as cancer type, and examining any potential racial disparities between people living in these environments and obesity-related cancer, Dr. Bevel added.
Data provide foundation for multilevel interventions
The current study findings “raise a clarion call to elevate the discussion on food availability and access to ensure an equitable emphasis on both the importance of lifestyle factors and the upstream structural, economic, and environmental contexts that shape these behaviors at the individual level,” Karriem S. Watson, DHSc, MS, MPH, of the National Institutes of Health, Bethesda, Md., and Angela Odoms-Young, PhD, of Cornell University, Ithaca, N.Y., wrote in an accompanying editorial.
The findings provide a foundation for studies of obesity-related cancer outcomes that take the community environment into consideration, they added.
The causes of both obesity and cancer are complex, and the study findings suggest that the links between unhealthy food environments and obesity-related cancer may go beyond dietary consumption alone and extend to social and psychological factors, the editorialists noted.
“Whether dealing with the lack of access to healthy foods or an overabundance of unhealthy food, there is a critical need to develop additional research that explores the associations between obesity-related cancer mortality and food inequities,” they concluded.
The study received no outside funding. The researchers and the editorialists had no financial conflicts to disclose.
based on data from a new cross-sectional study of more than 3,000 communities.
Although increased healthy eating has been associated with reduced risk of obesity and with reduced cancer incidence and mortality, access to healthier eating remains a challenge in communities with less access to grocery stores and healthy food options (food deserts) and/or easy access to convenience stores and fast food (food swamps), Malcolm Seth Bevel, PhD, of the Medical College of Georgia, Augusta, and colleagues, wrote in their paper, published in JAMA Oncology.
In addition, data on the association between food deserts and swamps and obesity-related cancer mortality are limited, they said.
“We felt that the study was important given the fact that obesity is an epidemic in the United States, and multiple factors contribute to obesity, especially adverse food environments,” Dr. Bevel said in an interview. “Also, I lived in these areas my whole life, and saw how it affected underserved populations. There was a story that needed to be told, so we’re telling it,” he said in an interview.
In a study, the researchers analyzed food access and cancer mortality data from 3,038 counties across the United States. The food access data came from the U.S. Department of Agriculture Food Environment Atlas (FEA) for the years 2012, 2014, 2015, 2017, and 2020. Data on obesity-related cancer mortality came from the Centers for Disease Control and Prevention for the years from 2010 to 2020.
Food desert scores were calculated through data from the FEA, and food swamp scores were based on the ratio of fast-food restaurants and convenience stores to grocery stores and farmers markets in a modification of the Retail Food Environment Index score.
The researchers used an age-adjusted, multiple regression model to determine the association between food desert and food swamp scores and obesity-related cancer mortality rates. Higher food swamp and food desert scores (defined as 20.0 to 58.0 or higher) were used to classify counties as having fewer healthy food resources. The primary outcome was obesity-related cancer mortality, defined as high or low (71.8 or higher per 100,000 individuals and less than 71.8 per 100,000 individuals, respectively).
Overall, high rates of obesity-related cancer mortality were 77% more likely in the counties that met the criteria for high food swamp scores (adjusted odds ratio 1.77). In addition, researchers found a positive dose-response relationship among three levels of both food desert scores and food swamp scores and obesity-related cancer mortality.
A total of 758 counties had obesity-related cancer mortality rates in the highest quartile. Compared to counties with low rates of obesity-related cancer mortality, counties with high rates of obesity-related cancer mortality also had a higher percentage of non-Hispanic Black residents (3.26% vs. 1.77%), higher percentage of adults older than 65 years (15.71% vs. 15.40%), higher rates of adult obesity (33.0% vs. 32.10%), and higher rates of adult diabetes (12.50% vs. 10.70%).
Possible explanations for the results include the lack of interest in grocery stores in neighborhoods with a population with a lower socioeconomic status, which can create a food desert, the researchers wrote in their discussion. “Coupled with the increasing growth rate of fast-food restaurants in recent years and the intentional advertisement of unhealthy foods in urban neighborhoods with [people of lower income], the food desert may transform into a food swamp,” they said.
The findings were limited by several factors including the study design, which did not allow for showing a causal association of food deserts and food swamps with obesity-related cancer mortality, the researchers noted. Other limitations included the use of groups rather than individuals, the potential misclassification of food stores, and the use of county-level data on race, ethnicity, and income, they wrote.
The results indicate that “food swamps appear to be a growing epidemic across the U.S., likely because of systemic issues, and should draw concern and conversation from local and state officials,” the researchers concluded.
Community-level investments can benefit individual health
Dr. Bevel said he was not surprised by the findings, as he has seen firsthand the lack of healthy food options and growth of unhealthy food options, especially for certain populations in certain communities. “Typically, these are people who have lower socioeconomic status, primarily non-Hispanic Black or African American or Hispanic American,” he said “I have watched people have to choose between getting fruits/vegetables versus their medications or running to fast food places to feed their families. What is truly surprising is that we’re not talking about people’s lived environment enough for my taste,” he said.
“I hope that our data and results can inform local and state policymakers to truly invest in all communities, such as funding for community gardens, and realize that adverse food environments, including the barriers in navigating these environments, have significant consequences on real people,” said Dr. Bevel. “Also, I hope that the results can help clinicians realize that a patient’s lived environment can truly affect their obesity and/or obesity-related cancer status; being cognizant of that is the first step in holistic, comprehensive care,” he said.
“One role that oncologists might be able to play in improving patients’ access to healthier food is to create and/or implement healthy lifestyle programs with gardening components to combat the poorest food environments that their patients likely reside in,” said Dr. Bevel. Clinicians also could consider the innovative approach of “food prescriptions” to help reduce the effects of deprived, built environments, he noted.
Looking ahead, next steps for research include determining the severity of association between food swamps and obesity-related cancer by varying factors such as cancer type, and examining any potential racial disparities between people living in these environments and obesity-related cancer, Dr. Bevel added.
Data provide foundation for multilevel interventions
The current study findings “raise a clarion call to elevate the discussion on food availability and access to ensure an equitable emphasis on both the importance of lifestyle factors and the upstream structural, economic, and environmental contexts that shape these behaviors at the individual level,” Karriem S. Watson, DHSc, MS, MPH, of the National Institutes of Health, Bethesda, Md., and Angela Odoms-Young, PhD, of Cornell University, Ithaca, N.Y., wrote in an accompanying editorial.
The findings provide a foundation for studies of obesity-related cancer outcomes that take the community environment into consideration, they added.
The causes of both obesity and cancer are complex, and the study findings suggest that the links between unhealthy food environments and obesity-related cancer may go beyond dietary consumption alone and extend to social and psychological factors, the editorialists noted.
“Whether dealing with the lack of access to healthy foods or an overabundance of unhealthy food, there is a critical need to develop additional research that explores the associations between obesity-related cancer mortality and food inequities,” they concluded.
The study received no outside funding. The researchers and the editorialists had no financial conflicts to disclose.
FROM JAMA ONCOLOGY
Adherence to cancer prevention guidance linked with reduced breast cancer recurrence, death risk
Following such recommendations surrounding smoking, physical activity (PA), eating fruits and vegetables and reducing or eliminating sugar-sweetened beverages seemed to be the most beneficial, wrote the authors of the paper published online in JAMA Network Open.
Rikki A. Cannioto, PhD, EdD, with the department of cancer prevention & control, Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., led the prospective cohort study of 1,340 patients.
The American Institute for Cancer Research and American Cancer Society regularly recommend and publish lifestyle modifications for cancer prevention. To conduct this study Dr. Cannioto and colleagues developed an aggregate lifestyle scoring index to investigate whether those recommendations have an effect on high-risk breast cancer survival.
Highest adherence vs. lowest cut death risk by more than half
The researchers found patients with highest vs. lowest lifestyle index scores saw a 37% reduction in cancer recurrence (hazard ratio, 0.63; 95% confidence interval, 0.48-0.82) and a 58% reduction in mortality (HR, 0.42; 95% CI, 0.30-0.59).
“As a person who has based her career on the belief that our modifiable lifestyle behaviors are associated with cancer survival, I was actually surprised about how strong these associations were, especially for breast cancer recurrence,” Dr. Cannioto said in an interview,
The author also expressed surprise about the associations that were seen “in patients diagnosed with triple-negative breast cancer and HER2-positive breast cancer, which are the two subtypes traditionally more aggressive and more difficult to treat.”
Most patients in the study were diagnosed with hormone receptor–positive breast cancer (873 [65.3%]); completed some education beyond high school (954 [71.2%]); were postmenopausal (696 [52.5%]); and self-identified as non-Hispanic White (1,118 [83.7%]).
Patients were drawn from the Diet, Exercise, Lifestyles, and Cancer Prognosis (DELCaP) study, a prospective, observational cohort study ancillary to a multicenter phase 3 trial led by the Southwest Oncology Group (SWOG). The DELCaP study was designed to examine lifestyles before diagnosis, during treatment, and at 1 and 2 years after treatment.
Never smoking, physical activity had strongest links
Never smoking and meeting or exceeding PA guidelines had the strongest and most consistent associations with outcomes; each factor was linked with a 44%-45% reduced risk of mortality and a 35% reduced risk of recurrence.
Strongest adherence to the alcohol and body mass index (BMI) recommendations were not significantly associated with improved outcomes.
Partial and full adherence to red and processed meat recommendations were associated with significant reductions in mortality, but not recurrence.
The authors note that, while medications are the foundation for breast cancer treatment, lifestyle interventions could be a safe and inexpensive additional strategy for delaying and preventing recurrence and death.
“Such developments could be especially impactful for patients diagnosed with more aggressive tumors that do not respond well to current therapies,” they write.
Dr. Cannioto says the guidelines around physical activity advise 150 minutes or more of moderate to vigorous intensity a week. But she noted that this research shows that any physical activity can lead to longer survival.
“The greatest benefits from physical activity occur from moving from a sedentary lifestyle to beginning to be active,” she said.
Dr. Cannioto acknowledged the homogeneity of the study population as a limitation and recommended the associations next be tested in a more racially and ethnically diverse population of breast cancer patients.
This work was supported by the National Cancer Institute, the Breast Cancer Research Foundation, and Amgen.
The authors report receiving grants from the Southwest Oncology Group and the National Cancer Institute during the conduct of the study and receiving personal fees, grants, or serving on the boards or independent monitoring committees of many pharmaceutical companies. A full list of disclosures is available with the paper.
Following such recommendations surrounding smoking, physical activity (PA), eating fruits and vegetables and reducing or eliminating sugar-sweetened beverages seemed to be the most beneficial, wrote the authors of the paper published online in JAMA Network Open.
Rikki A. Cannioto, PhD, EdD, with the department of cancer prevention & control, Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., led the prospective cohort study of 1,340 patients.
The American Institute for Cancer Research and American Cancer Society regularly recommend and publish lifestyle modifications for cancer prevention. To conduct this study Dr. Cannioto and colleagues developed an aggregate lifestyle scoring index to investigate whether those recommendations have an effect on high-risk breast cancer survival.
Highest adherence vs. lowest cut death risk by more than half
The researchers found patients with highest vs. lowest lifestyle index scores saw a 37% reduction in cancer recurrence (hazard ratio, 0.63; 95% confidence interval, 0.48-0.82) and a 58% reduction in mortality (HR, 0.42; 95% CI, 0.30-0.59).
“As a person who has based her career on the belief that our modifiable lifestyle behaviors are associated with cancer survival, I was actually surprised about how strong these associations were, especially for breast cancer recurrence,” Dr. Cannioto said in an interview,
The author also expressed surprise about the associations that were seen “in patients diagnosed with triple-negative breast cancer and HER2-positive breast cancer, which are the two subtypes traditionally more aggressive and more difficult to treat.”
Most patients in the study were diagnosed with hormone receptor–positive breast cancer (873 [65.3%]); completed some education beyond high school (954 [71.2%]); were postmenopausal (696 [52.5%]); and self-identified as non-Hispanic White (1,118 [83.7%]).
Patients were drawn from the Diet, Exercise, Lifestyles, and Cancer Prognosis (DELCaP) study, a prospective, observational cohort study ancillary to a multicenter phase 3 trial led by the Southwest Oncology Group (SWOG). The DELCaP study was designed to examine lifestyles before diagnosis, during treatment, and at 1 and 2 years after treatment.
Never smoking, physical activity had strongest links
Never smoking and meeting or exceeding PA guidelines had the strongest and most consistent associations with outcomes; each factor was linked with a 44%-45% reduced risk of mortality and a 35% reduced risk of recurrence.
Strongest adherence to the alcohol and body mass index (BMI) recommendations were not significantly associated with improved outcomes.
Partial and full adherence to red and processed meat recommendations were associated with significant reductions in mortality, but not recurrence.
The authors note that, while medications are the foundation for breast cancer treatment, lifestyle interventions could be a safe and inexpensive additional strategy for delaying and preventing recurrence and death.
“Such developments could be especially impactful for patients diagnosed with more aggressive tumors that do not respond well to current therapies,” they write.
Dr. Cannioto says the guidelines around physical activity advise 150 minutes or more of moderate to vigorous intensity a week. But she noted that this research shows that any physical activity can lead to longer survival.
“The greatest benefits from physical activity occur from moving from a sedentary lifestyle to beginning to be active,” she said.
Dr. Cannioto acknowledged the homogeneity of the study population as a limitation and recommended the associations next be tested in a more racially and ethnically diverse population of breast cancer patients.
This work was supported by the National Cancer Institute, the Breast Cancer Research Foundation, and Amgen.
The authors report receiving grants from the Southwest Oncology Group and the National Cancer Institute during the conduct of the study and receiving personal fees, grants, or serving on the boards or independent monitoring committees of many pharmaceutical companies. A full list of disclosures is available with the paper.
Following such recommendations surrounding smoking, physical activity (PA), eating fruits and vegetables and reducing or eliminating sugar-sweetened beverages seemed to be the most beneficial, wrote the authors of the paper published online in JAMA Network Open.
Rikki A. Cannioto, PhD, EdD, with the department of cancer prevention & control, Roswell Park Comprehensive Cancer Center in Buffalo, N.Y., led the prospective cohort study of 1,340 patients.
The American Institute for Cancer Research and American Cancer Society regularly recommend and publish lifestyle modifications for cancer prevention. To conduct this study Dr. Cannioto and colleagues developed an aggregate lifestyle scoring index to investigate whether those recommendations have an effect on high-risk breast cancer survival.
Highest adherence vs. lowest cut death risk by more than half
The researchers found patients with highest vs. lowest lifestyle index scores saw a 37% reduction in cancer recurrence (hazard ratio, 0.63; 95% confidence interval, 0.48-0.82) and a 58% reduction in mortality (HR, 0.42; 95% CI, 0.30-0.59).
“As a person who has based her career on the belief that our modifiable lifestyle behaviors are associated with cancer survival, I was actually surprised about how strong these associations were, especially for breast cancer recurrence,” Dr. Cannioto said in an interview,
The author also expressed surprise about the associations that were seen “in patients diagnosed with triple-negative breast cancer and HER2-positive breast cancer, which are the two subtypes traditionally more aggressive and more difficult to treat.”
Most patients in the study were diagnosed with hormone receptor–positive breast cancer (873 [65.3%]); completed some education beyond high school (954 [71.2%]); were postmenopausal (696 [52.5%]); and self-identified as non-Hispanic White (1,118 [83.7%]).
Patients were drawn from the Diet, Exercise, Lifestyles, and Cancer Prognosis (DELCaP) study, a prospective, observational cohort study ancillary to a multicenter phase 3 trial led by the Southwest Oncology Group (SWOG). The DELCaP study was designed to examine lifestyles before diagnosis, during treatment, and at 1 and 2 years after treatment.
Never smoking, physical activity had strongest links
Never smoking and meeting or exceeding PA guidelines had the strongest and most consistent associations with outcomes; each factor was linked with a 44%-45% reduced risk of mortality and a 35% reduced risk of recurrence.
Strongest adherence to the alcohol and body mass index (BMI) recommendations were not significantly associated with improved outcomes.
Partial and full adherence to red and processed meat recommendations were associated with significant reductions in mortality, but not recurrence.
The authors note that, while medications are the foundation for breast cancer treatment, lifestyle interventions could be a safe and inexpensive additional strategy for delaying and preventing recurrence and death.
“Such developments could be especially impactful for patients diagnosed with more aggressive tumors that do not respond well to current therapies,” they write.
Dr. Cannioto says the guidelines around physical activity advise 150 minutes or more of moderate to vigorous intensity a week. But she noted that this research shows that any physical activity can lead to longer survival.
“The greatest benefits from physical activity occur from moving from a sedentary lifestyle to beginning to be active,” she said.
Dr. Cannioto acknowledged the homogeneity of the study population as a limitation and recommended the associations next be tested in a more racially and ethnically diverse population of breast cancer patients.
This work was supported by the National Cancer Institute, the Breast Cancer Research Foundation, and Amgen.
The authors report receiving grants from the Southwest Oncology Group and the National Cancer Institute during the conduct of the study and receiving personal fees, grants, or serving on the boards or independent monitoring committees of many pharmaceutical companies. A full list of disclosures is available with the paper.
FROM JAMA NETWORK OPEN