User login
New colorectal cancer data reveal troubling trends
Colorectal cancer (CRC) remains the second most common cause of cancer-related death in the United States. Although the past several decades have seen significantly greater emphasis on screening and disease prevention for CRC, it has also become increasingly apparent that the age profile and associated risks for this cancer are rapidly changing.
Evidence of this can be found in recently released CRC statistics from the American Cancer Society, which are updated every 3 years using population-based cancer registries.
The incidence in CRC has shown a progressive decline over the past 4 decades. However, whereas in the 2000s there was an average decline of approximately 3%-4% annually, it slowed to 1% per year between 2011 and 2019. This effect is in part because of the trends among younger individuals (< 55 years), in whom the incidence of CRC has increased by 9% over the past 25 years.
The incidence of regional-stage disease also increased by 2%-3% per year for those younger than 65 years, with an additional increase in the incidence of more advanced/distant disease by 0.5%-3% per year. The latter finding represents a reversal of earlier trends observed for staged disease in the decade from 1995 to 2005.
These recent statistics reveal other notable changes that occurred in parallel with the increased incidence of younger-onset CRC. There was a significant shift to left-sided tumors, with a 4% increase in rectal cancers in the decades spanning 1995–2019.
Although the overall mortality declined 2% from 2011 to 2020, the reverse was seen in patients younger than 50 years, in whom there was an increase by 0.5%-3% annually.
Available incidence and mortality data for the current year are understandably lacking, as there is a 2- to 4-year lag for data collection and assimilation, and there have also been methodological changes for tracking and projections. Nonetheless, 2023 projections estimate that there will be 153,020 new cases in the United States, with 19,550 (13%) to occur in those younger than 50 years and 33% in those aged 50-64 years. Overall, 43% of cases are projected to occur in those aged 45-49 years, which is noteworthy given that these ages are now included in the most current CRC screening recommendations.
Further underscoring the risks posed by earlier-onset trends is the projection of 52,550 CRC-related deaths in 2023, with 7% estimated to occur in those younger than 50 years.
What’s behind the trend toward younger onset?
The specific factors contributing to increasing rates of CRC in younger individuals are not well known, but there are several plausible explanations. Notable possible contributing factors reported in the literature include obesity, smoking, alcohol, diet, and microbial changes, among other demographic variables. Exposure to high-fructose corn syrup, sugar-sweetened beverages, and processed meats has also recently received attention as contributing dietary risk factors.
The shifting trends toward the onset of CRC among younger patients are now clearly established, with approximately 20% of new cases occurring in those in their early 50s or younger and a higher rate of left-sided tumor development. Unfortunately, these shifts are also associated with a more advanced stage of disease.
There are unique clinical challenges when it comes to identifying younger-onset CRC. A low level of suspicion among primary care providers that their younger patients may have CRC can result in delays in their receiving clinically appropriate diagnostic testing (particularly for overt or occult bleeding/iron deficiency). Younger patients may also be less likely to know about or adhere to new recommendations that they undergo screening.
The landscape for age-related CRC is changing. Although there are many obstacles for implementing new practices, these recent findings from the ACS also highlight a clear path for improvement.
David A. Johnson, MD, is professor of medicine and chief of gastroenterology at Eastern Virginia Medical School, Norfolk, and a past president of the American College of Gastroenterology.
A version of this article first appeared on Medscape.com.
Colorectal cancer (CRC) remains the second most common cause of cancer-related death in the United States. Although the past several decades have seen significantly greater emphasis on screening and disease prevention for CRC, it has also become increasingly apparent that the age profile and associated risks for this cancer are rapidly changing.
Evidence of this can be found in recently released CRC statistics from the American Cancer Society, which are updated every 3 years using population-based cancer registries.
The incidence in CRC has shown a progressive decline over the past 4 decades. However, whereas in the 2000s there was an average decline of approximately 3%-4% annually, it slowed to 1% per year between 2011 and 2019. This effect is in part because of the trends among younger individuals (< 55 years), in whom the incidence of CRC has increased by 9% over the past 25 years.
The incidence of regional-stage disease also increased by 2%-3% per year for those younger than 65 years, with an additional increase in the incidence of more advanced/distant disease by 0.5%-3% per year. The latter finding represents a reversal of earlier trends observed for staged disease in the decade from 1995 to 2005.
These recent statistics reveal other notable changes that occurred in parallel with the increased incidence of younger-onset CRC. There was a significant shift to left-sided tumors, with a 4% increase in rectal cancers in the decades spanning 1995–2019.
Although the overall mortality declined 2% from 2011 to 2020, the reverse was seen in patients younger than 50 years, in whom there was an increase by 0.5%-3% annually.
Available incidence and mortality data for the current year are understandably lacking, as there is a 2- to 4-year lag for data collection and assimilation, and there have also been methodological changes for tracking and projections. Nonetheless, 2023 projections estimate that there will be 153,020 new cases in the United States, with 19,550 (13%) to occur in those younger than 50 years and 33% in those aged 50-64 years. Overall, 43% of cases are projected to occur in those aged 45-49 years, which is noteworthy given that these ages are now included in the most current CRC screening recommendations.
Further underscoring the risks posed by earlier-onset trends is the projection of 52,550 CRC-related deaths in 2023, with 7% estimated to occur in those younger than 50 years.
What’s behind the trend toward younger onset?
The specific factors contributing to increasing rates of CRC in younger individuals are not well known, but there are several plausible explanations. Notable possible contributing factors reported in the literature include obesity, smoking, alcohol, diet, and microbial changes, among other demographic variables. Exposure to high-fructose corn syrup, sugar-sweetened beverages, and processed meats has also recently received attention as contributing dietary risk factors.
The shifting trends toward the onset of CRC among younger patients are now clearly established, with approximately 20% of new cases occurring in those in their early 50s or younger and a higher rate of left-sided tumor development. Unfortunately, these shifts are also associated with a more advanced stage of disease.
There are unique clinical challenges when it comes to identifying younger-onset CRC. A low level of suspicion among primary care providers that their younger patients may have CRC can result in delays in their receiving clinically appropriate diagnostic testing (particularly for overt or occult bleeding/iron deficiency). Younger patients may also be less likely to know about or adhere to new recommendations that they undergo screening.
The landscape for age-related CRC is changing. Although there are many obstacles for implementing new practices, these recent findings from the ACS also highlight a clear path for improvement.
David A. Johnson, MD, is professor of medicine and chief of gastroenterology at Eastern Virginia Medical School, Norfolk, and a past president of the American College of Gastroenterology.
A version of this article first appeared on Medscape.com.
Colorectal cancer (CRC) remains the second most common cause of cancer-related death in the United States. Although the past several decades have seen significantly greater emphasis on screening and disease prevention for CRC, it has also become increasingly apparent that the age profile and associated risks for this cancer are rapidly changing.
Evidence of this can be found in recently released CRC statistics from the American Cancer Society, which are updated every 3 years using population-based cancer registries.
The incidence in CRC has shown a progressive decline over the past 4 decades. However, whereas in the 2000s there was an average decline of approximately 3%-4% annually, it slowed to 1% per year between 2011 and 2019. This effect is in part because of the trends among younger individuals (< 55 years), in whom the incidence of CRC has increased by 9% over the past 25 years.
The incidence of regional-stage disease also increased by 2%-3% per year for those younger than 65 years, with an additional increase in the incidence of more advanced/distant disease by 0.5%-3% per year. The latter finding represents a reversal of earlier trends observed for staged disease in the decade from 1995 to 2005.
These recent statistics reveal other notable changes that occurred in parallel with the increased incidence of younger-onset CRC. There was a significant shift to left-sided tumors, with a 4% increase in rectal cancers in the decades spanning 1995–2019.
Although the overall mortality declined 2% from 2011 to 2020, the reverse was seen in patients younger than 50 years, in whom there was an increase by 0.5%-3% annually.
Available incidence and mortality data for the current year are understandably lacking, as there is a 2- to 4-year lag for data collection and assimilation, and there have also been methodological changes for tracking and projections. Nonetheless, 2023 projections estimate that there will be 153,020 new cases in the United States, with 19,550 (13%) to occur in those younger than 50 years and 33% in those aged 50-64 years. Overall, 43% of cases are projected to occur in those aged 45-49 years, which is noteworthy given that these ages are now included in the most current CRC screening recommendations.
Further underscoring the risks posed by earlier-onset trends is the projection of 52,550 CRC-related deaths in 2023, with 7% estimated to occur in those younger than 50 years.
What’s behind the trend toward younger onset?
The specific factors contributing to increasing rates of CRC in younger individuals are not well known, but there are several plausible explanations. Notable possible contributing factors reported in the literature include obesity, smoking, alcohol, diet, and microbial changes, among other demographic variables. Exposure to high-fructose corn syrup, sugar-sweetened beverages, and processed meats has also recently received attention as contributing dietary risk factors.
The shifting trends toward the onset of CRC among younger patients are now clearly established, with approximately 20% of new cases occurring in those in their early 50s or younger and a higher rate of left-sided tumor development. Unfortunately, these shifts are also associated with a more advanced stage of disease.
There are unique clinical challenges when it comes to identifying younger-onset CRC. A low level of suspicion among primary care providers that their younger patients may have CRC can result in delays in their receiving clinically appropriate diagnostic testing (particularly for overt or occult bleeding/iron deficiency). Younger patients may also be less likely to know about or adhere to new recommendations that they undergo screening.
The landscape for age-related CRC is changing. Although there are many obstacles for implementing new practices, these recent findings from the ACS also highlight a clear path for improvement.
David A. Johnson, MD, is professor of medicine and chief of gastroenterology at Eastern Virginia Medical School, Norfolk, and a past president of the American College of Gastroenterology.
A version of this article first appeared on Medscape.com.
Study: Prenatal supplements fail to meet nutrient needs
Although drugstore shelves might suggest otherwise,
In a new study published in the American Journal of Clinical Nutrition, investigators observed what many physicians have long suspected: Most prenatal vitamins and other supplements do not adequately make up the difference of what food-based intake of nutrients leave lacking. Despite patients believing they are getting everything they need with their product purchase, they fall short of guideline-recommended requirements.
“There is no magic pill,” said Katherine A. Sauder, PhD, an associate professor of pediatrics at the University of Colorado Anschutz Medical Campus, Aurora, and lead author of the study. “There is no easy answer here.”
The researchers analyzed 24-hour dietary intake data from 2,450 study participants across five states from 2007 to 2019. Dr. Sauder and colleagues focused on six of the more than 20 key nutrients recommended for pregnant people and determined the target dose for vitamin A, vitamin D, folate, calcium, iron, and omega-3 fatty acids.
The researchers tested more than 20,500 dietary supplements, of which 421 were prenatal products. Only 69 products – three prenatal – included all six nutrients. Just seven products – two prenatal – contained target doses for five nutrients. Only one product, which was not marketed as prenatal, contained target doses for all six nutrients but required seven tablets a serving and cost patients approximately $200 a month.
For many years, Dr. Sauder and her colleagues have struggled to identify the gold standard of vitamins for pregnant patients.
More than half of pregnant people in the United States are at risk of inadequate intake of vitamin D, folate, and iron from their diet alone, and one-third are at risk for insufficient intake of vitamin A and calcium.
Although more than 70% of pregnant women take dietary supplements, the products do not eliminate the risks for deficiencies.
The effects of inadequate nutrition during pregnancy may include neural tube defects, alterations in cardiovascular structure, and impaired neurocognitive development.
The researchers also looked at the challenges within the dietary supplement industry. The U.S. Food and Drug Administration regulates dietary supplements as foods rather than drugs and therefore does not require third-party verification that would ensure product ingredients match labels.
The researchers acknowledged the challenges in creating a one-size-fits-all nutritional supplement.
“The supplement industry is difficult, because you’re trying to create a product that works for a large, diverse group of people, but nutrition is very personal,” Dr. Sauder said.
Kendra Segura, MD, an ob.gyn. at the To Help Everyone Health and Wellness Center, Los Angeles, said she was unsurprised by the results.
“There’s no good prenatal vitamin out there,” Dr. Segura said. “There’s no ‘best.’ ”
Dr. Segura said she advises her patients to focus on increased nutritional intake with foods but added that that the lack of nutrients in diets and the need for supplements reflects the lack of availability of healthy food in some communities (known as “food deserts”), as well as poor dietary choices.
Diana Racusin, MD, an assistant professor of obstetrics, gynecology, and reproductive services at the University of Texas Health Science Center’s McGovern Medical School, Houston, also “wasn’t terribly surprised” by the findings. She stresses the importance of what patients eat more than the availability of supplements.
“What this is really showing us is we have work to do with our nutrition,” Dr. Racusin said.
Dr. Sauder’s biggest takeaway from her study is the need for more patient guidance for their nutrition beyond advising a supplement.
“We need better support for women to help them improve their diet during pregnancy so that they’re getting the nutrients they need from food,” she said, “and not having to rely on supplements as much.”
The study was supported by the Environmental Influences on Child Health Outcomes Program of the National Institutes of Health and by the nonprofit organization Autism Speaks. Dr. Sauder reports no relevant financial relationships. Two coauthors reported various conflicts of interest.
A version of this article first appeared on Medscape.com.
Although drugstore shelves might suggest otherwise,
In a new study published in the American Journal of Clinical Nutrition, investigators observed what many physicians have long suspected: Most prenatal vitamins and other supplements do not adequately make up the difference of what food-based intake of nutrients leave lacking. Despite patients believing they are getting everything they need with their product purchase, they fall short of guideline-recommended requirements.
“There is no magic pill,” said Katherine A. Sauder, PhD, an associate professor of pediatrics at the University of Colorado Anschutz Medical Campus, Aurora, and lead author of the study. “There is no easy answer here.”
The researchers analyzed 24-hour dietary intake data from 2,450 study participants across five states from 2007 to 2019. Dr. Sauder and colleagues focused on six of the more than 20 key nutrients recommended for pregnant people and determined the target dose for vitamin A, vitamin D, folate, calcium, iron, and omega-3 fatty acids.
The researchers tested more than 20,500 dietary supplements, of which 421 were prenatal products. Only 69 products – three prenatal – included all six nutrients. Just seven products – two prenatal – contained target doses for five nutrients. Only one product, which was not marketed as prenatal, contained target doses for all six nutrients but required seven tablets a serving and cost patients approximately $200 a month.
For many years, Dr. Sauder and her colleagues have struggled to identify the gold standard of vitamins for pregnant patients.
More than half of pregnant people in the United States are at risk of inadequate intake of vitamin D, folate, and iron from their diet alone, and one-third are at risk for insufficient intake of vitamin A and calcium.
Although more than 70% of pregnant women take dietary supplements, the products do not eliminate the risks for deficiencies.
The effects of inadequate nutrition during pregnancy may include neural tube defects, alterations in cardiovascular structure, and impaired neurocognitive development.
The researchers also looked at the challenges within the dietary supplement industry. The U.S. Food and Drug Administration regulates dietary supplements as foods rather than drugs and therefore does not require third-party verification that would ensure product ingredients match labels.
The researchers acknowledged the challenges in creating a one-size-fits-all nutritional supplement.
“The supplement industry is difficult, because you’re trying to create a product that works for a large, diverse group of people, but nutrition is very personal,” Dr. Sauder said.
Kendra Segura, MD, an ob.gyn. at the To Help Everyone Health and Wellness Center, Los Angeles, said she was unsurprised by the results.
“There’s no good prenatal vitamin out there,” Dr. Segura said. “There’s no ‘best.’ ”
Dr. Segura said she advises her patients to focus on increased nutritional intake with foods but added that that the lack of nutrients in diets and the need for supplements reflects the lack of availability of healthy food in some communities (known as “food deserts”), as well as poor dietary choices.
Diana Racusin, MD, an assistant professor of obstetrics, gynecology, and reproductive services at the University of Texas Health Science Center’s McGovern Medical School, Houston, also “wasn’t terribly surprised” by the findings. She stresses the importance of what patients eat more than the availability of supplements.
“What this is really showing us is we have work to do with our nutrition,” Dr. Racusin said.
Dr. Sauder’s biggest takeaway from her study is the need for more patient guidance for their nutrition beyond advising a supplement.
“We need better support for women to help them improve their diet during pregnancy so that they’re getting the nutrients they need from food,” she said, “and not having to rely on supplements as much.”
The study was supported by the Environmental Influences on Child Health Outcomes Program of the National Institutes of Health and by the nonprofit organization Autism Speaks. Dr. Sauder reports no relevant financial relationships. Two coauthors reported various conflicts of interest.
A version of this article first appeared on Medscape.com.
Although drugstore shelves might suggest otherwise,
In a new study published in the American Journal of Clinical Nutrition, investigators observed what many physicians have long suspected: Most prenatal vitamins and other supplements do not adequately make up the difference of what food-based intake of nutrients leave lacking. Despite patients believing they are getting everything they need with their product purchase, they fall short of guideline-recommended requirements.
“There is no magic pill,” said Katherine A. Sauder, PhD, an associate professor of pediatrics at the University of Colorado Anschutz Medical Campus, Aurora, and lead author of the study. “There is no easy answer here.”
The researchers analyzed 24-hour dietary intake data from 2,450 study participants across five states from 2007 to 2019. Dr. Sauder and colleagues focused on six of the more than 20 key nutrients recommended for pregnant people and determined the target dose for vitamin A, vitamin D, folate, calcium, iron, and omega-3 fatty acids.
The researchers tested more than 20,500 dietary supplements, of which 421 were prenatal products. Only 69 products – three prenatal – included all six nutrients. Just seven products – two prenatal – contained target doses for five nutrients. Only one product, which was not marketed as prenatal, contained target doses for all six nutrients but required seven tablets a serving and cost patients approximately $200 a month.
For many years, Dr. Sauder and her colleagues have struggled to identify the gold standard of vitamins for pregnant patients.
More than half of pregnant people in the United States are at risk of inadequate intake of vitamin D, folate, and iron from their diet alone, and one-third are at risk for insufficient intake of vitamin A and calcium.
Although more than 70% of pregnant women take dietary supplements, the products do not eliminate the risks for deficiencies.
The effects of inadequate nutrition during pregnancy may include neural tube defects, alterations in cardiovascular structure, and impaired neurocognitive development.
The researchers also looked at the challenges within the dietary supplement industry. The U.S. Food and Drug Administration regulates dietary supplements as foods rather than drugs and therefore does not require third-party verification that would ensure product ingredients match labels.
The researchers acknowledged the challenges in creating a one-size-fits-all nutritional supplement.
“The supplement industry is difficult, because you’re trying to create a product that works for a large, diverse group of people, but nutrition is very personal,” Dr. Sauder said.
Kendra Segura, MD, an ob.gyn. at the To Help Everyone Health and Wellness Center, Los Angeles, said she was unsurprised by the results.
“There’s no good prenatal vitamin out there,” Dr. Segura said. “There’s no ‘best.’ ”
Dr. Segura said she advises her patients to focus on increased nutritional intake with foods but added that that the lack of nutrients in diets and the need for supplements reflects the lack of availability of healthy food in some communities (known as “food deserts”), as well as poor dietary choices.
Diana Racusin, MD, an assistant professor of obstetrics, gynecology, and reproductive services at the University of Texas Health Science Center’s McGovern Medical School, Houston, also “wasn’t terribly surprised” by the findings. She stresses the importance of what patients eat more than the availability of supplements.
“What this is really showing us is we have work to do with our nutrition,” Dr. Racusin said.
Dr. Sauder’s biggest takeaway from her study is the need for more patient guidance for their nutrition beyond advising a supplement.
“We need better support for women to help them improve their diet during pregnancy so that they’re getting the nutrients they need from food,” she said, “and not having to rely on supplements as much.”
The study was supported by the Environmental Influences on Child Health Outcomes Program of the National Institutes of Health and by the nonprofit organization Autism Speaks. Dr. Sauder reports no relevant financial relationships. Two coauthors reported various conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF CLINICAL NUTRITION
Phototherapy a safe, effective, inexpensive new option for dementia?
It may be “one of the most promising interventions for improving core symptoms” of the disease.
A new meta-analysis shows that patients with dementia who received phototherapy experienced significant cognitive improvement, compared with those who received usual treatment. However, there were no differences between study groups in terms of improved depression, agitation, or sleep problems.
“Our meta-analysis indicates that phototherapy improved cognitive function in patients with dementia. ... This suggests that phototherapy may be one of the most promising non-pharmacological interventions for improving core symptoms of dementia,” wrote the investigators, led by Xinlian Lu, Peking University, Beijing.
The study was published online in Brain and Behavior.
A new treatment option?
“As drug treatment for dementia has limitations such as medical contraindications, limited efficacy, and adverse effects, nonpharmacological therapy has been increasingly regarded as a critical part of comprehensive dementia care,” the investigators noted.
Phototherapy, which utilizes full-spectrum bright light (usually > 600 lux) or wavelength-specific light (for example, blue-enriched or blue-green), is a “promising nonpharmacological therapy” that is noninvasive, inexpensive, and safe.
Most studies of phototherapy have focused on sleep. Findings have shown “high heterogeneity” among the interventions and the populations in the studies, and results have been “inconsistent.” In addition, the effect of phototherapy on cognitive function and behavioral and psychological symptoms of dementia (BPSD) “still need to be clarified.”
In the systematic review and meta-analysis, the investigators examined the effects of phototherapy on cognitive function, BPSD, and sleep in older adults with dementia.
They searched several databases for randomized controlled trials that investigated phototherapy interventions for elderly patients. The primary outcome was cognitive function, which was assessed via the Mini-Mental State Examination (MMSE).
Secondary outcomes included BPSD, including agitation, anxiety, irritability, depression, anxiety, and sleep disturbances, as assessed by the Cornell Scale for Depression in Dementia (CSDD), the Cohen-Mansfield Agitation Inventory (CMAI), the Neuropsychiatric Inventory (NPI), and measures of sleep, including total sleep time (TST), sleep efficiency (SE), and sleep disorders, as assessed by the Sleep Disorder Inventory (SDI).
To be included in the analysis, individual studies had to focus on elderly adults who had some form of dementia. In addition, a group receiving a phototherapy intervention had to be compared with a nonintervention group, and the study had to specify one of the above-defined outcomes.
The review included phototherapy interventions of all forms, frequencies, and durations, including use of bright light, LED light, and blue or blue-green light.
Regulating circadian rhythm
Twelve studies met the researchers’ criteria. They included a total of 766 patients with dementia – 426 in the intervention group and 340 in the control group. The mean ages ranged from 73.73 to 85.9 years, and there was a greater number of female than male participants.
Of the studies, seven employed routine daily light in the control group, while the others used either dim light (≤ 50 lux) or devices without light.
The researchers found “significant positive intervention effects” for global cognitive function. Improvements in postintervention MMSE scores differed significantly between the experimental groups and control groups (mean difference, 2.68; 95% confidence interval, 1.38-3.98; I2 = 0%).
No significant differences were found in the effects of intervention on depression symptoms, as evidenced in CSDD scores (MD, −0.70; 95% CI, −3.10 to 1.70; I2 = 81%).
Among patients with higher CMAI scores, which indicate more severe agitation behaviors, there was a “trend of decreasing CMAI scores” after phototherapy (MD, −3.12; 95% CI, −8.05 to 1.82; I2 = 0%). No significant difference in NPI scores was observed between the two groups.
Similarly, no significant difference was found between the two groups in TST, SE, or SDI scores.
Adverse effects were infrequent and were not severe. Two of the 426 patients in the intervention group experienced mild ocular irritation, and one experienced slight transient redness of the forehead.
Light “may compensate for the reduction in the visual sensory input of patients with dementia and stimulate specific neurons in the suprachiasmatic nucleus of the hypothalamus to regulate circadian rhythm,” the researchers suggested.
“As circadian rhythms are involved in optimal brain function, light supplementation may act on the synchronizing/phase-shifting effects of circadian rhythms to improve cognitive function,” they added.
They note that the light box is the “most commonly used device in phototherapy.” Light boxes provide full-spectrum bright light, usually greater than 2,500 lux. The duration is 30 minutes in the daytime, and treatment lasts 4-8 weeks.
The investigators cautioned that the light box should be placed 60 cm away from the patient or above the patient’s eye level. They said that a ceiling-mounted light is a “good choice” for providing whole-day phototherapy, since such lights do not interfere with the patient’s daily routine, reduce the demand on staff, and contribute to better adherence.
Phototherapy helmets and glasses are also available. These portable devices “allow for better control of light intensity and are ergonomic without interfering with patients’ normal activities.”
The researchers noted that “further well-designed studies are needed to explore the most effective clinical implementation conditions, including device type, duration, frequency, and time.”
Easy to use
Mariana Figueiro, PhD, professor and director of the Light and Health Research Center, department of population health medicine, Icahn School of Medicine at Mount Sinai, New York, said light is the “major stimulus for the circadian system, and a robust light-dark pattern daily (which can be given by light therapy during the day) improves sleep and behavior and reduces depression and agitation.”
Dr. Figueiro, who was not involved with the current study, noted that patients with dementia “have sleep issues, which can further affect their cognition; improvement in sleep leads to improvement in cognition,” and this may be an underlying mechanism associated with these results.
The clinical significance of the study “is that this is a nonpharmacological intervention and can be easily applied in the homes or controlled facilities, and it can be used with any other medication,” she pointed out.
“More importantly, sleep medications have negative side effects, so the use of nonpharmacological interventions improving sleep and cognition is great for clinical practice,” she added.
However, she took issue with the finding that phototherapy was not effective for depression and agitation, noting that there were “too few studies to say for sure that light therapy is ineffective at improving these outcomes.”
The research received no external funding. The authors and Dr. Figueiro disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It may be “one of the most promising interventions for improving core symptoms” of the disease.
A new meta-analysis shows that patients with dementia who received phototherapy experienced significant cognitive improvement, compared with those who received usual treatment. However, there were no differences between study groups in terms of improved depression, agitation, or sleep problems.
“Our meta-analysis indicates that phototherapy improved cognitive function in patients with dementia. ... This suggests that phototherapy may be one of the most promising non-pharmacological interventions for improving core symptoms of dementia,” wrote the investigators, led by Xinlian Lu, Peking University, Beijing.
The study was published online in Brain and Behavior.
A new treatment option?
“As drug treatment for dementia has limitations such as medical contraindications, limited efficacy, and adverse effects, nonpharmacological therapy has been increasingly regarded as a critical part of comprehensive dementia care,” the investigators noted.
Phototherapy, which utilizes full-spectrum bright light (usually > 600 lux) or wavelength-specific light (for example, blue-enriched or blue-green), is a “promising nonpharmacological therapy” that is noninvasive, inexpensive, and safe.
Most studies of phototherapy have focused on sleep. Findings have shown “high heterogeneity” among the interventions and the populations in the studies, and results have been “inconsistent.” In addition, the effect of phototherapy on cognitive function and behavioral and psychological symptoms of dementia (BPSD) “still need to be clarified.”
In the systematic review and meta-analysis, the investigators examined the effects of phototherapy on cognitive function, BPSD, and sleep in older adults with dementia.
They searched several databases for randomized controlled trials that investigated phototherapy interventions for elderly patients. The primary outcome was cognitive function, which was assessed via the Mini-Mental State Examination (MMSE).
Secondary outcomes included BPSD, including agitation, anxiety, irritability, depression, anxiety, and sleep disturbances, as assessed by the Cornell Scale for Depression in Dementia (CSDD), the Cohen-Mansfield Agitation Inventory (CMAI), the Neuropsychiatric Inventory (NPI), and measures of sleep, including total sleep time (TST), sleep efficiency (SE), and sleep disorders, as assessed by the Sleep Disorder Inventory (SDI).
To be included in the analysis, individual studies had to focus on elderly adults who had some form of dementia. In addition, a group receiving a phototherapy intervention had to be compared with a nonintervention group, and the study had to specify one of the above-defined outcomes.
The review included phototherapy interventions of all forms, frequencies, and durations, including use of bright light, LED light, and blue or blue-green light.
Regulating circadian rhythm
Twelve studies met the researchers’ criteria. They included a total of 766 patients with dementia – 426 in the intervention group and 340 in the control group. The mean ages ranged from 73.73 to 85.9 years, and there was a greater number of female than male participants.
Of the studies, seven employed routine daily light in the control group, while the others used either dim light (≤ 50 lux) or devices without light.
The researchers found “significant positive intervention effects” for global cognitive function. Improvements in postintervention MMSE scores differed significantly between the experimental groups and control groups (mean difference, 2.68; 95% confidence interval, 1.38-3.98; I2 = 0%).
No significant differences were found in the effects of intervention on depression symptoms, as evidenced in CSDD scores (MD, −0.70; 95% CI, −3.10 to 1.70; I2 = 81%).
Among patients with higher CMAI scores, which indicate more severe agitation behaviors, there was a “trend of decreasing CMAI scores” after phototherapy (MD, −3.12; 95% CI, −8.05 to 1.82; I2 = 0%). No significant difference in NPI scores was observed between the two groups.
Similarly, no significant difference was found between the two groups in TST, SE, or SDI scores.
Adverse effects were infrequent and were not severe. Two of the 426 patients in the intervention group experienced mild ocular irritation, and one experienced slight transient redness of the forehead.
Light “may compensate for the reduction in the visual sensory input of patients with dementia and stimulate specific neurons in the suprachiasmatic nucleus of the hypothalamus to regulate circadian rhythm,” the researchers suggested.
“As circadian rhythms are involved in optimal brain function, light supplementation may act on the synchronizing/phase-shifting effects of circadian rhythms to improve cognitive function,” they added.
They note that the light box is the “most commonly used device in phototherapy.” Light boxes provide full-spectrum bright light, usually greater than 2,500 lux. The duration is 30 minutes in the daytime, and treatment lasts 4-8 weeks.
The investigators cautioned that the light box should be placed 60 cm away from the patient or above the patient’s eye level. They said that a ceiling-mounted light is a “good choice” for providing whole-day phototherapy, since such lights do not interfere with the patient’s daily routine, reduce the demand on staff, and contribute to better adherence.
Phototherapy helmets and glasses are also available. These portable devices “allow for better control of light intensity and are ergonomic without interfering with patients’ normal activities.”
The researchers noted that “further well-designed studies are needed to explore the most effective clinical implementation conditions, including device type, duration, frequency, and time.”
Easy to use
Mariana Figueiro, PhD, professor and director of the Light and Health Research Center, department of population health medicine, Icahn School of Medicine at Mount Sinai, New York, said light is the “major stimulus for the circadian system, and a robust light-dark pattern daily (which can be given by light therapy during the day) improves sleep and behavior and reduces depression and agitation.”
Dr. Figueiro, who was not involved with the current study, noted that patients with dementia “have sleep issues, which can further affect their cognition; improvement in sleep leads to improvement in cognition,” and this may be an underlying mechanism associated with these results.
The clinical significance of the study “is that this is a nonpharmacological intervention and can be easily applied in the homes or controlled facilities, and it can be used with any other medication,” she pointed out.
“More importantly, sleep medications have negative side effects, so the use of nonpharmacological interventions improving sleep and cognition is great for clinical practice,” she added.
However, she took issue with the finding that phototherapy was not effective for depression and agitation, noting that there were “too few studies to say for sure that light therapy is ineffective at improving these outcomes.”
The research received no external funding. The authors and Dr. Figueiro disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It may be “one of the most promising interventions for improving core symptoms” of the disease.
A new meta-analysis shows that patients with dementia who received phototherapy experienced significant cognitive improvement, compared with those who received usual treatment. However, there were no differences between study groups in terms of improved depression, agitation, or sleep problems.
“Our meta-analysis indicates that phototherapy improved cognitive function in patients with dementia. ... This suggests that phototherapy may be one of the most promising non-pharmacological interventions for improving core symptoms of dementia,” wrote the investigators, led by Xinlian Lu, Peking University, Beijing.
The study was published online in Brain and Behavior.
A new treatment option?
“As drug treatment for dementia has limitations such as medical contraindications, limited efficacy, and adverse effects, nonpharmacological therapy has been increasingly regarded as a critical part of comprehensive dementia care,” the investigators noted.
Phototherapy, which utilizes full-spectrum bright light (usually > 600 lux) or wavelength-specific light (for example, blue-enriched or blue-green), is a “promising nonpharmacological therapy” that is noninvasive, inexpensive, and safe.
Most studies of phototherapy have focused on sleep. Findings have shown “high heterogeneity” among the interventions and the populations in the studies, and results have been “inconsistent.” In addition, the effect of phototherapy on cognitive function and behavioral and psychological symptoms of dementia (BPSD) “still need to be clarified.”
In the systematic review and meta-analysis, the investigators examined the effects of phototherapy on cognitive function, BPSD, and sleep in older adults with dementia.
They searched several databases for randomized controlled trials that investigated phototherapy interventions for elderly patients. The primary outcome was cognitive function, which was assessed via the Mini-Mental State Examination (MMSE).
Secondary outcomes included BPSD, including agitation, anxiety, irritability, depression, anxiety, and sleep disturbances, as assessed by the Cornell Scale for Depression in Dementia (CSDD), the Cohen-Mansfield Agitation Inventory (CMAI), the Neuropsychiatric Inventory (NPI), and measures of sleep, including total sleep time (TST), sleep efficiency (SE), and sleep disorders, as assessed by the Sleep Disorder Inventory (SDI).
To be included in the analysis, individual studies had to focus on elderly adults who had some form of dementia. In addition, a group receiving a phototherapy intervention had to be compared with a nonintervention group, and the study had to specify one of the above-defined outcomes.
The review included phototherapy interventions of all forms, frequencies, and durations, including use of bright light, LED light, and blue or blue-green light.
Regulating circadian rhythm
Twelve studies met the researchers’ criteria. They included a total of 766 patients with dementia – 426 in the intervention group and 340 in the control group. The mean ages ranged from 73.73 to 85.9 years, and there was a greater number of female than male participants.
Of the studies, seven employed routine daily light in the control group, while the others used either dim light (≤ 50 lux) or devices without light.
The researchers found “significant positive intervention effects” for global cognitive function. Improvements in postintervention MMSE scores differed significantly between the experimental groups and control groups (mean difference, 2.68; 95% confidence interval, 1.38-3.98; I2 = 0%).
No significant differences were found in the effects of intervention on depression symptoms, as evidenced in CSDD scores (MD, −0.70; 95% CI, −3.10 to 1.70; I2 = 81%).
Among patients with higher CMAI scores, which indicate more severe agitation behaviors, there was a “trend of decreasing CMAI scores” after phototherapy (MD, −3.12; 95% CI, −8.05 to 1.82; I2 = 0%). No significant difference in NPI scores was observed between the two groups.
Similarly, no significant difference was found between the two groups in TST, SE, or SDI scores.
Adverse effects were infrequent and were not severe. Two of the 426 patients in the intervention group experienced mild ocular irritation, and one experienced slight transient redness of the forehead.
Light “may compensate for the reduction in the visual sensory input of patients with dementia and stimulate specific neurons in the suprachiasmatic nucleus of the hypothalamus to regulate circadian rhythm,” the researchers suggested.
“As circadian rhythms are involved in optimal brain function, light supplementation may act on the synchronizing/phase-shifting effects of circadian rhythms to improve cognitive function,” they added.
They note that the light box is the “most commonly used device in phototherapy.” Light boxes provide full-spectrum bright light, usually greater than 2,500 lux. The duration is 30 minutes in the daytime, and treatment lasts 4-8 weeks.
The investigators cautioned that the light box should be placed 60 cm away from the patient or above the patient’s eye level. They said that a ceiling-mounted light is a “good choice” for providing whole-day phototherapy, since such lights do not interfere with the patient’s daily routine, reduce the demand on staff, and contribute to better adherence.
Phototherapy helmets and glasses are also available. These portable devices “allow for better control of light intensity and are ergonomic without interfering with patients’ normal activities.”
The researchers noted that “further well-designed studies are needed to explore the most effective clinical implementation conditions, including device type, duration, frequency, and time.”
Easy to use
Mariana Figueiro, PhD, professor and director of the Light and Health Research Center, department of population health medicine, Icahn School of Medicine at Mount Sinai, New York, said light is the “major stimulus for the circadian system, and a robust light-dark pattern daily (which can be given by light therapy during the day) improves sleep and behavior and reduces depression and agitation.”
Dr. Figueiro, who was not involved with the current study, noted that patients with dementia “have sleep issues, which can further affect their cognition; improvement in sleep leads to improvement in cognition,” and this may be an underlying mechanism associated with these results.
The clinical significance of the study “is that this is a nonpharmacological intervention and can be easily applied in the homes or controlled facilities, and it can be used with any other medication,” she pointed out.
“More importantly, sleep medications have negative side effects, so the use of nonpharmacological interventions improving sleep and cognition is great for clinical practice,” she added.
However, she took issue with the finding that phototherapy was not effective for depression and agitation, noting that there were “too few studies to say for sure that light therapy is ineffective at improving these outcomes.”
The research received no external funding. The authors and Dr. Figueiro disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM BRAIN AND BEHAVIOR
Disordered sleep tied to a marked increase in stroke risk
Results of a large international study show stroke risk was more than three times higher in those who slept too little, more than twice as high in those who sleep too much, and two to three times higher in those with symptoms of severe obstructive sleep apnea.
The study also showed that the greater the number of sleep disorder symptoms, the greater the stroke risk. The 11% of study participants with five or more symptoms of disordered sleep had a fivefold increased risk for stroke.
Although the study data do not show a causal link between disordered sleep and stroke, the association between the two was strong.
“Given the association, sleep disturbance may represent a marker of somebody at increased risk of stroke, and further interventional studies are required to see if management can reduce this risk,” lead investigator Christine McCarthy, MD, PhD, a geriatric and stroke medicine physician and researcher with the University of Galway (Ireland), told this news organization. “In the interim, however, management of sleep disturbance may have a positive impact on a patient’s quality of life.”
The findings were published online in the journal Neurology.
More symptoms, more risk
Previous research shows severe OSA doubles the risk of stroke and increases the chance of recurrent stroke. A 2019 study showed that people with insomnia had a small increased risk of stroke.
“Both snoring and extremes of sleep duration have been previously associated with an increased risk of stroke in observational research, but less is known about other symptoms of sleep impairment, with less consistent findings,” Dr. McCarthy said.
Prior studies have also generally come from a single geographic region, which Dr. McCarthy noted could limit their generalizability.
For this effort, investigators used data from 4,496 participants in INTERSTROKE, an international case-control study of risk factors for a first acute stroke. About half of the participants had a history of stroke.
Using information collected from a survey of sleep habits, researchers found an elevated stroke risk in those who received less than 5 hours of sleep per night (odds ratio, 3.15; 95% confidence interval, 2.09-4.76) or more than 9 hours of sleep per night (OR, 2.67; 95% CI, 1.89-3.78), compared with those who slept 7 hours a night.
Participants who took unplanned naps or naps lasting an hour or more (OR, 2.46; 95% CI, 1.69-3.57) and participants who reported poor quality sleep (OR,1.52; 95% CI, 1.32-1.75) were also at an increased risk for stroke.
Symptoms of OSA were also strongly associated with increased stroke risk, including snoring (OR, 1.91; 95% CI, 1.62-2.24), snorting (OR, 2.64; 95% CI, 2.17-3.20), and breathing cessation (OR, 2.87; 95% CI, 2.28-2.60).
Stroke risk increased as the number of sleep disturbance symptoms rose, with the greatest risk in the 11% of participants who had five or more symptoms (OR, 5.38; 95% CI, 4.03-7.18).
“This study finds an association between a broad range of sleep impairment symptoms and stroke, and a graded association with increasing symptoms, in an international setting,” Dr. McCarthy said.
Researchers aren’t sure what’s driving the higher stroke risk among people with sleep disturbances. Although the study did control for potential confounders, it wasn’t designed to get at what’s driving the association.
“Sleep disturbance may also have a bi-directional relationship with many stroke risk factors; for example, sleep disturbance may be a symptom of disease and exacerbate disease,” Dr. McCarthy said. “Future interventional studies are required to determine the true direction of the relationship.”
A marker of stroke risk
Daniel Lackland, DrPH, professor of neurology at the Medical University of South Carolina, Charleston, said the findings provide additional evidence of the link between sleep and stroke risk.
“The results confirm sleep disorders as a potential marker and part of the risk profile,” he said.
Collecting information about sleep using a validated assessment tool is an important piece of clinical care, Dr. Lackland said, especially among patients with other stroke risk factors.
One limitation of the study was that data on sleep was collected only at one point, and participants were not followed over time to see if changes in sleep affected stroke risk.
“This is an important point and should be a focus for future studies, as it is critical in the design of interventions,” Dr. Lackland said.
The INTERSTROKE study is funded by the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, Canadian Stroke Network, Swedish Research Council, Swedish Heart and Lung Foundation, The Health & Medical Care Committee of the Regional Executive Board, Region Västra Götaland, Astra Zeneca, Boehringer Ingelheim (Canada), Pfizer (Canada), MERCK, Sharp and Dohme, Swedish Heart and Lung Foundation, U.K. Chest, and U.K. Heart and Stroke. Dr. McCarthy and Lackland report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results of a large international study show stroke risk was more than three times higher in those who slept too little, more than twice as high in those who sleep too much, and two to three times higher in those with symptoms of severe obstructive sleep apnea.
The study also showed that the greater the number of sleep disorder symptoms, the greater the stroke risk. The 11% of study participants with five or more symptoms of disordered sleep had a fivefold increased risk for stroke.
Although the study data do not show a causal link between disordered sleep and stroke, the association between the two was strong.
“Given the association, sleep disturbance may represent a marker of somebody at increased risk of stroke, and further interventional studies are required to see if management can reduce this risk,” lead investigator Christine McCarthy, MD, PhD, a geriatric and stroke medicine physician and researcher with the University of Galway (Ireland), told this news organization. “In the interim, however, management of sleep disturbance may have a positive impact on a patient’s quality of life.”
The findings were published online in the journal Neurology.
More symptoms, more risk
Previous research shows severe OSA doubles the risk of stroke and increases the chance of recurrent stroke. A 2019 study showed that people with insomnia had a small increased risk of stroke.
“Both snoring and extremes of sleep duration have been previously associated with an increased risk of stroke in observational research, but less is known about other symptoms of sleep impairment, with less consistent findings,” Dr. McCarthy said.
Prior studies have also generally come from a single geographic region, which Dr. McCarthy noted could limit their generalizability.
For this effort, investigators used data from 4,496 participants in INTERSTROKE, an international case-control study of risk factors for a first acute stroke. About half of the participants had a history of stroke.
Using information collected from a survey of sleep habits, researchers found an elevated stroke risk in those who received less than 5 hours of sleep per night (odds ratio, 3.15; 95% confidence interval, 2.09-4.76) or more than 9 hours of sleep per night (OR, 2.67; 95% CI, 1.89-3.78), compared with those who slept 7 hours a night.
Participants who took unplanned naps or naps lasting an hour or more (OR, 2.46; 95% CI, 1.69-3.57) and participants who reported poor quality sleep (OR,1.52; 95% CI, 1.32-1.75) were also at an increased risk for stroke.
Symptoms of OSA were also strongly associated with increased stroke risk, including snoring (OR, 1.91; 95% CI, 1.62-2.24), snorting (OR, 2.64; 95% CI, 2.17-3.20), and breathing cessation (OR, 2.87; 95% CI, 2.28-2.60).
Stroke risk increased as the number of sleep disturbance symptoms rose, with the greatest risk in the 11% of participants who had five or more symptoms (OR, 5.38; 95% CI, 4.03-7.18).
“This study finds an association between a broad range of sleep impairment symptoms and stroke, and a graded association with increasing symptoms, in an international setting,” Dr. McCarthy said.
Researchers aren’t sure what’s driving the higher stroke risk among people with sleep disturbances. Although the study did control for potential confounders, it wasn’t designed to get at what’s driving the association.
“Sleep disturbance may also have a bi-directional relationship with many stroke risk factors; for example, sleep disturbance may be a symptom of disease and exacerbate disease,” Dr. McCarthy said. “Future interventional studies are required to determine the true direction of the relationship.”
A marker of stroke risk
Daniel Lackland, DrPH, professor of neurology at the Medical University of South Carolina, Charleston, said the findings provide additional evidence of the link between sleep and stroke risk.
“The results confirm sleep disorders as a potential marker and part of the risk profile,” he said.
Collecting information about sleep using a validated assessment tool is an important piece of clinical care, Dr. Lackland said, especially among patients with other stroke risk factors.
One limitation of the study was that data on sleep was collected only at one point, and participants were not followed over time to see if changes in sleep affected stroke risk.
“This is an important point and should be a focus for future studies, as it is critical in the design of interventions,” Dr. Lackland said.
The INTERSTROKE study is funded by the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, Canadian Stroke Network, Swedish Research Council, Swedish Heart and Lung Foundation, The Health & Medical Care Committee of the Regional Executive Board, Region Västra Götaland, Astra Zeneca, Boehringer Ingelheim (Canada), Pfizer (Canada), MERCK, Sharp and Dohme, Swedish Heart and Lung Foundation, U.K. Chest, and U.K. Heart and Stroke. Dr. McCarthy and Lackland report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results of a large international study show stroke risk was more than three times higher in those who slept too little, more than twice as high in those who sleep too much, and two to three times higher in those with symptoms of severe obstructive sleep apnea.
The study also showed that the greater the number of sleep disorder symptoms, the greater the stroke risk. The 11% of study participants with five or more symptoms of disordered sleep had a fivefold increased risk for stroke.
Although the study data do not show a causal link between disordered sleep and stroke, the association between the two was strong.
“Given the association, sleep disturbance may represent a marker of somebody at increased risk of stroke, and further interventional studies are required to see if management can reduce this risk,” lead investigator Christine McCarthy, MD, PhD, a geriatric and stroke medicine physician and researcher with the University of Galway (Ireland), told this news organization. “In the interim, however, management of sleep disturbance may have a positive impact on a patient’s quality of life.”
The findings were published online in the journal Neurology.
More symptoms, more risk
Previous research shows severe OSA doubles the risk of stroke and increases the chance of recurrent stroke. A 2019 study showed that people with insomnia had a small increased risk of stroke.
“Both snoring and extremes of sleep duration have been previously associated with an increased risk of stroke in observational research, but less is known about other symptoms of sleep impairment, with less consistent findings,” Dr. McCarthy said.
Prior studies have also generally come from a single geographic region, which Dr. McCarthy noted could limit their generalizability.
For this effort, investigators used data from 4,496 participants in INTERSTROKE, an international case-control study of risk factors for a first acute stroke. About half of the participants had a history of stroke.
Using information collected from a survey of sleep habits, researchers found an elevated stroke risk in those who received less than 5 hours of sleep per night (odds ratio, 3.15; 95% confidence interval, 2.09-4.76) or more than 9 hours of sleep per night (OR, 2.67; 95% CI, 1.89-3.78), compared with those who slept 7 hours a night.
Participants who took unplanned naps or naps lasting an hour or more (OR, 2.46; 95% CI, 1.69-3.57) and participants who reported poor quality sleep (OR,1.52; 95% CI, 1.32-1.75) were also at an increased risk for stroke.
Symptoms of OSA were also strongly associated with increased stroke risk, including snoring (OR, 1.91; 95% CI, 1.62-2.24), snorting (OR, 2.64; 95% CI, 2.17-3.20), and breathing cessation (OR, 2.87; 95% CI, 2.28-2.60).
Stroke risk increased as the number of sleep disturbance symptoms rose, with the greatest risk in the 11% of participants who had five or more symptoms (OR, 5.38; 95% CI, 4.03-7.18).
“This study finds an association between a broad range of sleep impairment symptoms and stroke, and a graded association with increasing symptoms, in an international setting,” Dr. McCarthy said.
Researchers aren’t sure what’s driving the higher stroke risk among people with sleep disturbances. Although the study did control for potential confounders, it wasn’t designed to get at what’s driving the association.
“Sleep disturbance may also have a bi-directional relationship with many stroke risk factors; for example, sleep disturbance may be a symptom of disease and exacerbate disease,” Dr. McCarthy said. “Future interventional studies are required to determine the true direction of the relationship.”
A marker of stroke risk
Daniel Lackland, DrPH, professor of neurology at the Medical University of South Carolina, Charleston, said the findings provide additional evidence of the link between sleep and stroke risk.
“The results confirm sleep disorders as a potential marker and part of the risk profile,” he said.
Collecting information about sleep using a validated assessment tool is an important piece of clinical care, Dr. Lackland said, especially among patients with other stroke risk factors.
One limitation of the study was that data on sleep was collected only at one point, and participants were not followed over time to see if changes in sleep affected stroke risk.
“This is an important point and should be a focus for future studies, as it is critical in the design of interventions,” Dr. Lackland said.
The INTERSTROKE study is funded by the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, Canadian Stroke Network, Swedish Research Council, Swedish Heart and Lung Foundation, The Health & Medical Care Committee of the Regional Executive Board, Region Västra Götaland, Astra Zeneca, Boehringer Ingelheim (Canada), Pfizer (Canada), MERCK, Sharp and Dohme, Swedish Heart and Lung Foundation, U.K. Chest, and U.K. Heart and Stroke. Dr. McCarthy and Lackland report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
Addressing the new mortality: Counseling on lethal means
Although I have worked with depressed patients for many years, I have come to realize that
Firearms are now the leading cause of death for U.S. children and youth aged 1-24 years, an increase of 29.5% from 2019 to 2020. Among all youth firearm deaths, homicides (58%), suicides (37%), unintentional shootings (2%), and legal intervention (1%) were causes. These horrific numbers do not even include almost 400,000 child ED visits from 2010 to 2019 for nonfatal firearm injuries that were unintentional (39.4%), assault-related (37.7%), or self-harm (1.7%).
Accidental injury from firearms is greater when the weapon is a handgun or pistol as these are small enough to be fired by a 2-year-old, more likely to be stored loaded with ammunition as “self-protection,” and less likely to be in a gun storage case.
While an overall decline in gun ownership has occurred in homes with children ages 1-5, the proportion of weapons that are handguns has actually increased, posing higher danger to the family itself. We can’t assume hiding a weapon is ever enough as children often know the location of guns and their keys or lock codes.
Many Americans fear for their safety, have doubts about policing as protective, and strongly assert the need to protect themselves. While asking about guns in the home is universally recommended, these beliefs need to be taken into account in the discussion. It is also important to speak with the firearm owner, most often the father. We might ask, “Do you feel that you need a firearm in your home to feel safe?” as a way to nonjudgmentally acknowledge their beliefs. Because women are more likely to be killed by their spouses than by all other types of assailants combined, we can ask, “What dangers worry you the most?” and “Do you feel safe in your current and any past relationships?” If their answer is worrisome, the discussion must first turn to dealing with the family situation. If the perceived threat is outside the family, we can inform families that having a gun in evidence in the home greatly increases the risk of being hurt by an assailant as well as risk for child injury and death. We might ask, “Can you think of any other ways to protect your home (for example, alarm system, outdoor lighting, dog, or pepper spray)?”
If parents insist on keeping a gun, we can strongly and directly recommend that all firearms be stored locked, unloaded, and with ammunition locked and stored separately. We can provide information on such locking and storage options. Programs in which information on devices to disable the gun were provided – such as cables to pass through the chamber or trigger locks – have shown big increases in safe gun storage. It may be worth saying/posting information on the Child Access Prevention (CAP) laws, enacted by many states, making adults owning firearms that are not stored safely unloaded legally responsible for any resulting injuries or deaths. Such laws have reduced injuries of both children and adults by 30%-40%, unintentional gun deaths by 23%, and gun suicides by 11% (for 14- to 17-year-olds).
If the reason for owning a gun is for hunting, the owner is more likely to have had firearm safety training and use a long gun. Long guns are more difficult for a child. Discussing safe hunting gun storage is still worth recommending, as is removing any handguns they may own as these are most dangerous.
Removing or securing firearms is important for everyone’s safety but it is an essential and perhaps more difficult topic of discussion when a child is at risk for suicide or harming others. We need to consider some crucial facts about completed suicide, now the leading cause of death in children and adolescents and largely from guns. Most suicide attempts occur within 10 minutes of having a wave of suicidal thoughts. These waves of thoughts may be acted upon immediately when lethal means are available, with guns by far the most likely to result in death. It is therefore critical to assess access and counsel about lethal means in every family with a child reporting thoughts of killing themselves or others, or a history of violence or substance use. Even without imminent risk of self-harm, we can start a discussion about securing lethal means by saying, “It’s like wearing a seatbelt; you don’t expect a car crash, but if one happens, wearing a safety belt can greatly reduce injury. Guns are the most frequent cause of dying, so let’s make a plan to reduce access to those.”
Creating a written plan to deal with waves of suicidal thoughts is the basis of a Safety Plan. We can accurately remind families and youth that “When someone is struggling like this, sometimes suicidal feelings can show up and get worse fast. There are steps I routinely recommend to make things safer at home.”
It is important to assess the presence of guns in the primary home and other places the child spends time even if we have asked in the past, as things change. If firearms are present, even if locked up appropriately, when a child is having suicidal thoughts we can say, “What some gun owners in your situation do is store weapons elsewhere temporarily with someone they trust, at a self-storage unit, gun or pawn shop, or police department. I’d like to talk over storage options like that with you.” If the child themself owns the firearm, they need to agree with a removal or lock up plan for giving up their access.
If the gun owner is unwilling to remove firearms, even temporarily, we can ask them to lock them up separately from ammunition, a move that alone reduces danger a lot, and ensure the child has no access to the keys or combination. Better yet, we can ask, “Would you be willing to ask someone who doesn’t live in your home to hold the keys or to change the combination temporarily or at least store the ammunition?” They could also remove from the home a critical component of the gun so that it can’t fire, such as the slide or firing pin. If even those steps are not accepted, we can ask, “What other options would you be willing to consider to increase your child’s safety, at least until s/he is doing better?”
Whatever plan we negotiate with the family, as for any health behavior change strategy, it is more likely to be implemented if we summarize the specifics, write them down, and set a time-frame for carrying it out. We might say, “Let’s review who’s doing what and when: Dad will take the guns to his uncle’s house tomorrow and meanwhile, he will put them in the gun safe.” A follow-up call or contact soon, a key part of management of suicidal ideation, also signals how strongly we care about these safety measures and has been shown to increase implementation. We might call to say, “I wanted to check in and see how [you/your child] is doing and also ask how the plan is going that we talked about for gun storage.”
Discussions about firearms can spark strong emotions, especially if the family suspects political motivations. The Florida law prohibiting health care providers from discussing guns with patients was overturned but the thinking remains and may give us pause before having these important conversations. First of all, we need to stay calm and be prepared with key facts. The “sandwich” method is a useful approach to reduce resistance: start with something you can agree on (such as “What we hear on the news can make us all scared about safety”); then add the facts we want to convey (such as “You are actually less likely to get hurt in a break-in if you do not have a gun”); then conclude with a positive (such as “I can see that you are giving a lot of thought to how to keep your family safe”). Families generally trust our intentions and knowledge and appreciate rather than resent safety counseling when it is given in a nonjudgmental manner. Because we are protectors of child health, firearm safety must be an essential part of our anticipatory guidance.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
*Wording suggestions adapted from https://www.hsph.harvard.edu/means-matter/recommendations/clinicians.
Although I have worked with depressed patients for many years, I have come to realize that
Firearms are now the leading cause of death for U.S. children and youth aged 1-24 years, an increase of 29.5% from 2019 to 2020. Among all youth firearm deaths, homicides (58%), suicides (37%), unintentional shootings (2%), and legal intervention (1%) were causes. These horrific numbers do not even include almost 400,000 child ED visits from 2010 to 2019 for nonfatal firearm injuries that were unintentional (39.4%), assault-related (37.7%), or self-harm (1.7%).
Accidental injury from firearms is greater when the weapon is a handgun or pistol as these are small enough to be fired by a 2-year-old, more likely to be stored loaded with ammunition as “self-protection,” and less likely to be in a gun storage case.
While an overall decline in gun ownership has occurred in homes with children ages 1-5, the proportion of weapons that are handguns has actually increased, posing higher danger to the family itself. We can’t assume hiding a weapon is ever enough as children often know the location of guns and their keys or lock codes.
Many Americans fear for their safety, have doubts about policing as protective, and strongly assert the need to protect themselves. While asking about guns in the home is universally recommended, these beliefs need to be taken into account in the discussion. It is also important to speak with the firearm owner, most often the father. We might ask, “Do you feel that you need a firearm in your home to feel safe?” as a way to nonjudgmentally acknowledge their beliefs. Because women are more likely to be killed by their spouses than by all other types of assailants combined, we can ask, “What dangers worry you the most?” and “Do you feel safe in your current and any past relationships?” If their answer is worrisome, the discussion must first turn to dealing with the family situation. If the perceived threat is outside the family, we can inform families that having a gun in evidence in the home greatly increases the risk of being hurt by an assailant as well as risk for child injury and death. We might ask, “Can you think of any other ways to protect your home (for example, alarm system, outdoor lighting, dog, or pepper spray)?”
If parents insist on keeping a gun, we can strongly and directly recommend that all firearms be stored locked, unloaded, and with ammunition locked and stored separately. We can provide information on such locking and storage options. Programs in which information on devices to disable the gun were provided – such as cables to pass through the chamber or trigger locks – have shown big increases in safe gun storage. It may be worth saying/posting information on the Child Access Prevention (CAP) laws, enacted by many states, making adults owning firearms that are not stored safely unloaded legally responsible for any resulting injuries or deaths. Such laws have reduced injuries of both children and adults by 30%-40%, unintentional gun deaths by 23%, and gun suicides by 11% (for 14- to 17-year-olds).
If the reason for owning a gun is for hunting, the owner is more likely to have had firearm safety training and use a long gun. Long guns are more difficult for a child. Discussing safe hunting gun storage is still worth recommending, as is removing any handguns they may own as these are most dangerous.
Removing or securing firearms is important for everyone’s safety but it is an essential and perhaps more difficult topic of discussion when a child is at risk for suicide or harming others. We need to consider some crucial facts about completed suicide, now the leading cause of death in children and adolescents and largely from guns. Most suicide attempts occur within 10 minutes of having a wave of suicidal thoughts. These waves of thoughts may be acted upon immediately when lethal means are available, with guns by far the most likely to result in death. It is therefore critical to assess access and counsel about lethal means in every family with a child reporting thoughts of killing themselves or others, or a history of violence or substance use. Even without imminent risk of self-harm, we can start a discussion about securing lethal means by saying, “It’s like wearing a seatbelt; you don’t expect a car crash, but if one happens, wearing a safety belt can greatly reduce injury. Guns are the most frequent cause of dying, so let’s make a plan to reduce access to those.”
Creating a written plan to deal with waves of suicidal thoughts is the basis of a Safety Plan. We can accurately remind families and youth that “When someone is struggling like this, sometimes suicidal feelings can show up and get worse fast. There are steps I routinely recommend to make things safer at home.”
It is important to assess the presence of guns in the primary home and other places the child spends time even if we have asked in the past, as things change. If firearms are present, even if locked up appropriately, when a child is having suicidal thoughts we can say, “What some gun owners in your situation do is store weapons elsewhere temporarily with someone they trust, at a self-storage unit, gun or pawn shop, or police department. I’d like to talk over storage options like that with you.” If the child themself owns the firearm, they need to agree with a removal or lock up plan for giving up their access.
If the gun owner is unwilling to remove firearms, even temporarily, we can ask them to lock them up separately from ammunition, a move that alone reduces danger a lot, and ensure the child has no access to the keys or combination. Better yet, we can ask, “Would you be willing to ask someone who doesn’t live in your home to hold the keys or to change the combination temporarily or at least store the ammunition?” They could also remove from the home a critical component of the gun so that it can’t fire, such as the slide or firing pin. If even those steps are not accepted, we can ask, “What other options would you be willing to consider to increase your child’s safety, at least until s/he is doing better?”
Whatever plan we negotiate with the family, as for any health behavior change strategy, it is more likely to be implemented if we summarize the specifics, write them down, and set a time-frame for carrying it out. We might say, “Let’s review who’s doing what and when: Dad will take the guns to his uncle’s house tomorrow and meanwhile, he will put them in the gun safe.” A follow-up call or contact soon, a key part of management of suicidal ideation, also signals how strongly we care about these safety measures and has been shown to increase implementation. We might call to say, “I wanted to check in and see how [you/your child] is doing and also ask how the plan is going that we talked about for gun storage.”
Discussions about firearms can spark strong emotions, especially if the family suspects political motivations. The Florida law prohibiting health care providers from discussing guns with patients was overturned but the thinking remains and may give us pause before having these important conversations. First of all, we need to stay calm and be prepared with key facts. The “sandwich” method is a useful approach to reduce resistance: start with something you can agree on (such as “What we hear on the news can make us all scared about safety”); then add the facts we want to convey (such as “You are actually less likely to get hurt in a break-in if you do not have a gun”); then conclude with a positive (such as “I can see that you are giving a lot of thought to how to keep your family safe”). Families generally trust our intentions and knowledge and appreciate rather than resent safety counseling when it is given in a nonjudgmental manner. Because we are protectors of child health, firearm safety must be an essential part of our anticipatory guidance.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
*Wording suggestions adapted from https://www.hsph.harvard.edu/means-matter/recommendations/clinicians.
Although I have worked with depressed patients for many years, I have come to realize that
Firearms are now the leading cause of death for U.S. children and youth aged 1-24 years, an increase of 29.5% from 2019 to 2020. Among all youth firearm deaths, homicides (58%), suicides (37%), unintentional shootings (2%), and legal intervention (1%) were causes. These horrific numbers do not even include almost 400,000 child ED visits from 2010 to 2019 for nonfatal firearm injuries that were unintentional (39.4%), assault-related (37.7%), or self-harm (1.7%).
Accidental injury from firearms is greater when the weapon is a handgun or pistol as these are small enough to be fired by a 2-year-old, more likely to be stored loaded with ammunition as “self-protection,” and less likely to be in a gun storage case.
While an overall decline in gun ownership has occurred in homes with children ages 1-5, the proportion of weapons that are handguns has actually increased, posing higher danger to the family itself. We can’t assume hiding a weapon is ever enough as children often know the location of guns and their keys or lock codes.
Many Americans fear for their safety, have doubts about policing as protective, and strongly assert the need to protect themselves. While asking about guns in the home is universally recommended, these beliefs need to be taken into account in the discussion. It is also important to speak with the firearm owner, most often the father. We might ask, “Do you feel that you need a firearm in your home to feel safe?” as a way to nonjudgmentally acknowledge their beliefs. Because women are more likely to be killed by their spouses than by all other types of assailants combined, we can ask, “What dangers worry you the most?” and “Do you feel safe in your current and any past relationships?” If their answer is worrisome, the discussion must first turn to dealing with the family situation. If the perceived threat is outside the family, we can inform families that having a gun in evidence in the home greatly increases the risk of being hurt by an assailant as well as risk for child injury and death. We might ask, “Can you think of any other ways to protect your home (for example, alarm system, outdoor lighting, dog, or pepper spray)?”
If parents insist on keeping a gun, we can strongly and directly recommend that all firearms be stored locked, unloaded, and with ammunition locked and stored separately. We can provide information on such locking and storage options. Programs in which information on devices to disable the gun were provided – such as cables to pass through the chamber or trigger locks – have shown big increases in safe gun storage. It may be worth saying/posting information on the Child Access Prevention (CAP) laws, enacted by many states, making adults owning firearms that are not stored safely unloaded legally responsible for any resulting injuries or deaths. Such laws have reduced injuries of both children and adults by 30%-40%, unintentional gun deaths by 23%, and gun suicides by 11% (for 14- to 17-year-olds).
If the reason for owning a gun is for hunting, the owner is more likely to have had firearm safety training and use a long gun. Long guns are more difficult for a child. Discussing safe hunting gun storage is still worth recommending, as is removing any handguns they may own as these are most dangerous.
Removing or securing firearms is important for everyone’s safety but it is an essential and perhaps more difficult topic of discussion when a child is at risk for suicide or harming others. We need to consider some crucial facts about completed suicide, now the leading cause of death in children and adolescents and largely from guns. Most suicide attempts occur within 10 minutes of having a wave of suicidal thoughts. These waves of thoughts may be acted upon immediately when lethal means are available, with guns by far the most likely to result in death. It is therefore critical to assess access and counsel about lethal means in every family with a child reporting thoughts of killing themselves or others, or a history of violence or substance use. Even without imminent risk of self-harm, we can start a discussion about securing lethal means by saying, “It’s like wearing a seatbelt; you don’t expect a car crash, but if one happens, wearing a safety belt can greatly reduce injury. Guns are the most frequent cause of dying, so let’s make a plan to reduce access to those.”
Creating a written plan to deal with waves of suicidal thoughts is the basis of a Safety Plan. We can accurately remind families and youth that “When someone is struggling like this, sometimes suicidal feelings can show up and get worse fast. There are steps I routinely recommend to make things safer at home.”
It is important to assess the presence of guns in the primary home and other places the child spends time even if we have asked in the past, as things change. If firearms are present, even if locked up appropriately, when a child is having suicidal thoughts we can say, “What some gun owners in your situation do is store weapons elsewhere temporarily with someone they trust, at a self-storage unit, gun or pawn shop, or police department. I’d like to talk over storage options like that with you.” If the child themself owns the firearm, they need to agree with a removal or lock up plan for giving up their access.
If the gun owner is unwilling to remove firearms, even temporarily, we can ask them to lock them up separately from ammunition, a move that alone reduces danger a lot, and ensure the child has no access to the keys or combination. Better yet, we can ask, “Would you be willing to ask someone who doesn’t live in your home to hold the keys or to change the combination temporarily or at least store the ammunition?” They could also remove from the home a critical component of the gun so that it can’t fire, such as the slide or firing pin. If even those steps are not accepted, we can ask, “What other options would you be willing to consider to increase your child’s safety, at least until s/he is doing better?”
Whatever plan we negotiate with the family, as for any health behavior change strategy, it is more likely to be implemented if we summarize the specifics, write them down, and set a time-frame for carrying it out. We might say, “Let’s review who’s doing what and when: Dad will take the guns to his uncle’s house tomorrow and meanwhile, he will put them in the gun safe.” A follow-up call or contact soon, a key part of management of suicidal ideation, also signals how strongly we care about these safety measures and has been shown to increase implementation. We might call to say, “I wanted to check in and see how [you/your child] is doing and also ask how the plan is going that we talked about for gun storage.”
Discussions about firearms can spark strong emotions, especially if the family suspects political motivations. The Florida law prohibiting health care providers from discussing guns with patients was overturned but the thinking remains and may give us pause before having these important conversations. First of all, we need to stay calm and be prepared with key facts. The “sandwich” method is a useful approach to reduce resistance: start with something you can agree on (such as “What we hear on the news can make us all scared about safety”); then add the facts we want to convey (such as “You are actually less likely to get hurt in a break-in if you do not have a gun”); then conclude with a positive (such as “I can see that you are giving a lot of thought to how to keep your family safe”). Families generally trust our intentions and knowledge and appreciate rather than resent safety counseling when it is given in a nonjudgmental manner. Because we are protectors of child health, firearm safety must be an essential part of our anticipatory guidance.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
*Wording suggestions adapted from https://www.hsph.harvard.edu/means-matter/recommendations/clinicians.
Mississippi–Ohio River valley linked to higher risk of Parkinson’s disease
according to findings from a study that was released ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology.
The association was attributed to concentrations of particulate matter (PM) 2.5 in the Mississippi–Ohio River valley, which was on average higher than in other areas, but that didn’t entirely explain the increase in Parkinson’s disease in that region, Brittany Krzyzanowski, PhD, a postdoctoral research fellow in the neuroepidemiology research program of the department of neurology at Barrow Neurological Institute, Dignity Health St. Joseph’s Hospital and Medical Center, Phoenix, said in an interview.
“This study revealed Parkinson’s disease hot spots in the Mississippi–Ohio River valley, a region that has some of the highest levels of air pollution in the nation,” she said, “but we also still find a relationship between air pollution and Parkinson’s risk in the regions in the western half of the United States where Parkinson’s disease and air pollution levels are relatively low.”
Dr. Krzyzanowski and colleagues evaluated 22,546,965 Medicare beneficiaries in 2009, using a multimethod approach that included geospatial analytical techniques to categorize their exposure to PM2.5 based on age, sex, race, smoking status, and health care usage. The researchers also performed individual-level case-control analysis to assess PM2.5 results at the county level. The Medicare beneficiaries were grouped according to average exposure, with the lowest group having an average annual exposure of 5 mcg/m3 and the group with the highest exposure having an average annual exposure of 19 mcg/m3.
In total, researchers identified 83,674 Medicare beneficiaries with incident Parkinson’s disease, with 434 new cases per 100,000 people in the highest exposure group, compared with 359 new cases per 100,000 people in the lowest-exposure group. The relative risk for Parkinson’s disease increased in the highest quartile of PM2.5 by 25%, compared with the lowest quartile after adjusting for factors such as age, smoking status, and health care usage (95% confidence interval, 20%–29%).
The results showed the nationwide average annual PM2.5 was associated with incident Parkinson’s disease, and the Rocky Mountain region carried a strong association between PM2.5 and Parkson’s disease with a 16% increase in risk per level of exposure to PM2.5. While the Mississippi-Ohio River valley was also associated with Parkinson’s disease, there was a weaker association between PM2.5 and Parkinson’s disease, which the researchers attributed to a “ceiling effect” of PM2.5 between approximately 12-19 mcg/m3.
Dr. Krzyzanowski said that use of a large-population-based dataset and high-resolution location data were major strengths of the study. “Having this level of information leaves less room for uncertainty in our measures and analyses,” she said. “Our study also leveraged innovative geographic information systems which allowed us to refine local patterns of disease by using population behavior and demographic information (such as smoking and age) to ensure that we could provide the most accurate map representation available to date.”
A focus on air pollution
Existing research in examining the etiology of Parkinson’s mainly focused on exposure to pesticides,* Dr. Krzyzanowski explained, and “consists of studies using relatively small populations and low-resolution air pollution data.” Genetics is another possible cause, she noted, but only explains some Parkinson’s disease cases.
“Our work suggests that we should also be looking at air pollution as a contributor in the development of Parkinson’s disease,” she said.
Ray Dorsey, MD, professor of neurology at the University of Rochester (N.Y.), who was not involved with the study, said that evidence is mounting that “air pollution may be an important causal factor in Parkinson’s and especially Alzheimer’s disease.”
“This study by a well-regarded group of researchers adds epidemiological evidence for that association,” he said. Another strength is that the study was conducted in the United States, as many epidemiological studies evaluating air pollution and Parkinson’s disease have been performed outside the country because of “a dearth of reliable data sources.”
“This study, along with others, suggest that some of the important environmental toxicants tied to brain disease may be inhaled,” Dr. Dorsey said. “The nose may be the front door to the brain.”
Dr. Krzyzanowski said the next step in their research is further examination of different types of air pollution. “Air pollution contains a variety of toxic components which vary from region to region. Understanding the different components in air pollution and how they interact with climate, temperature, and topography could help explain the regional differences we observed.”
One potential limitation in the study is a lag between air pollution exposure and development of Parkinson’s disease, Dr. Dorsey noted.
“Here, it looks like (but I am not certain) that the investigators looked at current air pollution levels and new cases of Parkinson’s. Ideally, for incident cases of Parkinson’s disease, we would want to know historical data on exposure to air pollution,” he said.
Future studies should include prospective evaluation of adults as well as babies and children who have been exposed to both high and low levels of air pollution. That kind of study “would be incredibly valuable for determining the role of an important environmental toxicant in many brain diseases, including stroke, Alzheimer’s, and Parkinson’s,” he said.
Dr. Krzyzanowski and Dr. Dorsey reported no relevant financial disclosures. This study was supported by grants from the Department of Defense, the National Institute of Environmental Health Sciences, and The Michael J. Fox Foundation for Parkinson’s Research.
*Correction, 4/14/23: An earlier version of this article mischaracterized the disease that was the subject of this research.
according to findings from a study that was released ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology.
The association was attributed to concentrations of particulate matter (PM) 2.5 in the Mississippi–Ohio River valley, which was on average higher than in other areas, but that didn’t entirely explain the increase in Parkinson’s disease in that region, Brittany Krzyzanowski, PhD, a postdoctoral research fellow in the neuroepidemiology research program of the department of neurology at Barrow Neurological Institute, Dignity Health St. Joseph’s Hospital and Medical Center, Phoenix, said in an interview.
“This study revealed Parkinson’s disease hot spots in the Mississippi–Ohio River valley, a region that has some of the highest levels of air pollution in the nation,” she said, “but we also still find a relationship between air pollution and Parkinson’s risk in the regions in the western half of the United States where Parkinson’s disease and air pollution levels are relatively low.”
Dr. Krzyzanowski and colleagues evaluated 22,546,965 Medicare beneficiaries in 2009, using a multimethod approach that included geospatial analytical techniques to categorize their exposure to PM2.5 based on age, sex, race, smoking status, and health care usage. The researchers also performed individual-level case-control analysis to assess PM2.5 results at the county level. The Medicare beneficiaries were grouped according to average exposure, with the lowest group having an average annual exposure of 5 mcg/m3 and the group with the highest exposure having an average annual exposure of 19 mcg/m3.
In total, researchers identified 83,674 Medicare beneficiaries with incident Parkinson’s disease, with 434 new cases per 100,000 people in the highest exposure group, compared with 359 new cases per 100,000 people in the lowest-exposure group. The relative risk for Parkinson’s disease increased in the highest quartile of PM2.5 by 25%, compared with the lowest quartile after adjusting for factors such as age, smoking status, and health care usage (95% confidence interval, 20%–29%).
The results showed the nationwide average annual PM2.5 was associated with incident Parkinson’s disease, and the Rocky Mountain region carried a strong association between PM2.5 and Parkson’s disease with a 16% increase in risk per level of exposure to PM2.5. While the Mississippi-Ohio River valley was also associated with Parkinson’s disease, there was a weaker association between PM2.5 and Parkinson’s disease, which the researchers attributed to a “ceiling effect” of PM2.5 between approximately 12-19 mcg/m3.
Dr. Krzyzanowski said that use of a large-population-based dataset and high-resolution location data were major strengths of the study. “Having this level of information leaves less room for uncertainty in our measures and analyses,” she said. “Our study also leveraged innovative geographic information systems which allowed us to refine local patterns of disease by using population behavior and demographic information (such as smoking and age) to ensure that we could provide the most accurate map representation available to date.”
A focus on air pollution
Existing research in examining the etiology of Parkinson’s mainly focused on exposure to pesticides,* Dr. Krzyzanowski explained, and “consists of studies using relatively small populations and low-resolution air pollution data.” Genetics is another possible cause, she noted, but only explains some Parkinson’s disease cases.
“Our work suggests that we should also be looking at air pollution as a contributor in the development of Parkinson’s disease,” she said.
Ray Dorsey, MD, professor of neurology at the University of Rochester (N.Y.), who was not involved with the study, said that evidence is mounting that “air pollution may be an important causal factor in Parkinson’s and especially Alzheimer’s disease.”
“This study by a well-regarded group of researchers adds epidemiological evidence for that association,” he said. Another strength is that the study was conducted in the United States, as many epidemiological studies evaluating air pollution and Parkinson’s disease have been performed outside the country because of “a dearth of reliable data sources.”
“This study, along with others, suggest that some of the important environmental toxicants tied to brain disease may be inhaled,” Dr. Dorsey said. “The nose may be the front door to the brain.”
Dr. Krzyzanowski said the next step in their research is further examination of different types of air pollution. “Air pollution contains a variety of toxic components which vary from region to region. Understanding the different components in air pollution and how they interact with climate, temperature, and topography could help explain the regional differences we observed.”
One potential limitation in the study is a lag between air pollution exposure and development of Parkinson’s disease, Dr. Dorsey noted.
“Here, it looks like (but I am not certain) that the investigators looked at current air pollution levels and new cases of Parkinson’s. Ideally, for incident cases of Parkinson’s disease, we would want to know historical data on exposure to air pollution,” he said.
Future studies should include prospective evaluation of adults as well as babies and children who have been exposed to both high and low levels of air pollution. That kind of study “would be incredibly valuable for determining the role of an important environmental toxicant in many brain diseases, including stroke, Alzheimer’s, and Parkinson’s,” he said.
Dr. Krzyzanowski and Dr. Dorsey reported no relevant financial disclosures. This study was supported by grants from the Department of Defense, the National Institute of Environmental Health Sciences, and The Michael J. Fox Foundation for Parkinson’s Research.
*Correction, 4/14/23: An earlier version of this article mischaracterized the disease that was the subject of this research.
according to findings from a study that was released ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology.
The association was attributed to concentrations of particulate matter (PM) 2.5 in the Mississippi–Ohio River valley, which was on average higher than in other areas, but that didn’t entirely explain the increase in Parkinson’s disease in that region, Brittany Krzyzanowski, PhD, a postdoctoral research fellow in the neuroepidemiology research program of the department of neurology at Barrow Neurological Institute, Dignity Health St. Joseph’s Hospital and Medical Center, Phoenix, said in an interview.
“This study revealed Parkinson’s disease hot spots in the Mississippi–Ohio River valley, a region that has some of the highest levels of air pollution in the nation,” she said, “but we also still find a relationship between air pollution and Parkinson’s risk in the regions in the western half of the United States where Parkinson’s disease and air pollution levels are relatively low.”
Dr. Krzyzanowski and colleagues evaluated 22,546,965 Medicare beneficiaries in 2009, using a multimethod approach that included geospatial analytical techniques to categorize their exposure to PM2.5 based on age, sex, race, smoking status, and health care usage. The researchers also performed individual-level case-control analysis to assess PM2.5 results at the county level. The Medicare beneficiaries were grouped according to average exposure, with the lowest group having an average annual exposure of 5 mcg/m3 and the group with the highest exposure having an average annual exposure of 19 mcg/m3.
In total, researchers identified 83,674 Medicare beneficiaries with incident Parkinson’s disease, with 434 new cases per 100,000 people in the highest exposure group, compared with 359 new cases per 100,000 people in the lowest-exposure group. The relative risk for Parkinson’s disease increased in the highest quartile of PM2.5 by 25%, compared with the lowest quartile after adjusting for factors such as age, smoking status, and health care usage (95% confidence interval, 20%–29%).
The results showed the nationwide average annual PM2.5 was associated with incident Parkinson’s disease, and the Rocky Mountain region carried a strong association between PM2.5 and Parkson’s disease with a 16% increase in risk per level of exposure to PM2.5. While the Mississippi-Ohio River valley was also associated with Parkinson’s disease, there was a weaker association between PM2.5 and Parkinson’s disease, which the researchers attributed to a “ceiling effect” of PM2.5 between approximately 12-19 mcg/m3.
Dr. Krzyzanowski said that use of a large-population-based dataset and high-resolution location data were major strengths of the study. “Having this level of information leaves less room for uncertainty in our measures and analyses,” she said. “Our study also leveraged innovative geographic information systems which allowed us to refine local patterns of disease by using population behavior and demographic information (such as smoking and age) to ensure that we could provide the most accurate map representation available to date.”
A focus on air pollution
Existing research in examining the etiology of Parkinson’s mainly focused on exposure to pesticides,* Dr. Krzyzanowski explained, and “consists of studies using relatively small populations and low-resolution air pollution data.” Genetics is another possible cause, she noted, but only explains some Parkinson’s disease cases.
“Our work suggests that we should also be looking at air pollution as a contributor in the development of Parkinson’s disease,” she said.
Ray Dorsey, MD, professor of neurology at the University of Rochester (N.Y.), who was not involved with the study, said that evidence is mounting that “air pollution may be an important causal factor in Parkinson’s and especially Alzheimer’s disease.”
“This study by a well-regarded group of researchers adds epidemiological evidence for that association,” he said. Another strength is that the study was conducted in the United States, as many epidemiological studies evaluating air pollution and Parkinson’s disease have been performed outside the country because of “a dearth of reliable data sources.”
“This study, along with others, suggest that some of the important environmental toxicants tied to brain disease may be inhaled,” Dr. Dorsey said. “The nose may be the front door to the brain.”
Dr. Krzyzanowski said the next step in their research is further examination of different types of air pollution. “Air pollution contains a variety of toxic components which vary from region to region. Understanding the different components in air pollution and how they interact with climate, temperature, and topography could help explain the regional differences we observed.”
One potential limitation in the study is a lag between air pollution exposure and development of Parkinson’s disease, Dr. Dorsey noted.
“Here, it looks like (but I am not certain) that the investigators looked at current air pollution levels and new cases of Parkinson’s. Ideally, for incident cases of Parkinson’s disease, we would want to know historical data on exposure to air pollution,” he said.
Future studies should include prospective evaluation of adults as well as babies and children who have been exposed to both high and low levels of air pollution. That kind of study “would be incredibly valuable for determining the role of an important environmental toxicant in many brain diseases, including stroke, Alzheimer’s, and Parkinson’s,” he said.
Dr. Krzyzanowski and Dr. Dorsey reported no relevant financial disclosures. This study was supported by grants from the Department of Defense, the National Institute of Environmental Health Sciences, and The Michael J. Fox Foundation for Parkinson’s Research.
*Correction, 4/14/23: An earlier version of this article mischaracterized the disease that was the subject of this research.
FROM AAN 2023
Seven ‘simple’ cardiovascular health measures linked to reduced dementia risk in women
according to results of a study that was released early, ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology.
Epidemiologist Pamela M. Rist, ScD, assistant professor of medicine at Harvard Medical School and associate epidemiologist at Brigham and Women’s Hospital, both in Boston, and colleagues, used data from 13,720 women whose mean age was 54 when they enrolled in the Harvard-based Women’s Health Study between 1992 and 1995. Subjects in that study were followed up in 2004.
Putting ‘Life’s Simple 7’ to the test
Dr. Rist and colleagues used the Harvard data to discern how well closely women conformed, during the initial study period and at 10-year follow up, to what the American Heart Association describes as “Life’s Simple 7,” a list of behavioral and biometric measures that indicate and predict cardiovascular health. The measures include four modifiable behaviors – not smoking, healthy weight, a healthy diet, and being physically active – along with three biometric measures of blood pressure, cholesterol, and blood sugar (AHA has since added a sleep component).
Researchers assigned women one point for each desirable habit or measure on the list, with subjects’ average Simple 7 score at baseline 4.3, and 4.2 at 10 years’ follow-up.
The investigators then looked at Medicare data for the study subjects from 2011 to 2018 – approximately 20 years after their enrollment in the Women’s Health Study – seeking dementia diagnoses. Some 13% of the study cohort (n = 1,771) had gone on to develop dementia.
Each point on the Simple 7 score at baseline corresponded with a 6% reduction in later dementia risk, Dr. Rist and her colleagues found after adjusting for variables including age and education (odds ratio per one unit change in score, 0.94; 95% CI, 0.90-0.98). This effect was similar for Simple 7 scores measured at 10 years of follow-up (OR, 0.95; 95% CI, 0.91-1.00).
“It can be empowering for people to know that by taking steps such as exercising for a half an hour a day or keeping their blood pressure under control, they can reduce their risk of dementia,” Dr. Rist said in a statement on the findings.
‘A simple take-home message’
Reached for comment, Andrew E. Budson, MD, chief of cognitive-behavioral neurology at the VA Boston Healthcare System, praised Dr. Rist and colleagues’ study as one that “builds on existing knowledge to provide a simple take-home message that empowers women to take control of their dementia risk.”
Each of the seven known risk factors – being active, eating better, maintaining a healthy weight, not smoking, maintaining a healthy blood pressure, controlling cholesterol, and having low blood sugar – “was associated with a 6% reduced risk of dementia,” Dr. Budson continued. “So, women who work to address all seven risk factors can reduce their risk of developing dementia by 42%: a huge amount. Moreover, although this study only looked at women, I am confident that if men follow this same advice they will also be able to reduce their risk of dementia, although we don’t know if the size of the effect will be the same.”
Dr. Rist and colleagues’ study was supported by the National Institutes of Health. None of the study authors reported conflicts of interest. Dr. Budson has reported receiving past compensation as a speaker for Eli Lilly.
according to results of a study that was released early, ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology.
Epidemiologist Pamela M. Rist, ScD, assistant professor of medicine at Harvard Medical School and associate epidemiologist at Brigham and Women’s Hospital, both in Boston, and colleagues, used data from 13,720 women whose mean age was 54 when they enrolled in the Harvard-based Women’s Health Study between 1992 and 1995. Subjects in that study were followed up in 2004.
Putting ‘Life’s Simple 7’ to the test
Dr. Rist and colleagues used the Harvard data to discern how well closely women conformed, during the initial study period and at 10-year follow up, to what the American Heart Association describes as “Life’s Simple 7,” a list of behavioral and biometric measures that indicate and predict cardiovascular health. The measures include four modifiable behaviors – not smoking, healthy weight, a healthy diet, and being physically active – along with three biometric measures of blood pressure, cholesterol, and blood sugar (AHA has since added a sleep component).
Researchers assigned women one point for each desirable habit or measure on the list, with subjects’ average Simple 7 score at baseline 4.3, and 4.2 at 10 years’ follow-up.
The investigators then looked at Medicare data for the study subjects from 2011 to 2018 – approximately 20 years after their enrollment in the Women’s Health Study – seeking dementia diagnoses. Some 13% of the study cohort (n = 1,771) had gone on to develop dementia.
Each point on the Simple 7 score at baseline corresponded with a 6% reduction in later dementia risk, Dr. Rist and her colleagues found after adjusting for variables including age and education (odds ratio per one unit change in score, 0.94; 95% CI, 0.90-0.98). This effect was similar for Simple 7 scores measured at 10 years of follow-up (OR, 0.95; 95% CI, 0.91-1.00).
“It can be empowering for people to know that by taking steps such as exercising for a half an hour a day or keeping their blood pressure under control, they can reduce their risk of dementia,” Dr. Rist said in a statement on the findings.
‘A simple take-home message’
Reached for comment, Andrew E. Budson, MD, chief of cognitive-behavioral neurology at the VA Boston Healthcare System, praised Dr. Rist and colleagues’ study as one that “builds on existing knowledge to provide a simple take-home message that empowers women to take control of their dementia risk.”
Each of the seven known risk factors – being active, eating better, maintaining a healthy weight, not smoking, maintaining a healthy blood pressure, controlling cholesterol, and having low blood sugar – “was associated with a 6% reduced risk of dementia,” Dr. Budson continued. “So, women who work to address all seven risk factors can reduce their risk of developing dementia by 42%: a huge amount. Moreover, although this study only looked at women, I am confident that if men follow this same advice they will also be able to reduce their risk of dementia, although we don’t know if the size of the effect will be the same.”
Dr. Rist and colleagues’ study was supported by the National Institutes of Health. None of the study authors reported conflicts of interest. Dr. Budson has reported receiving past compensation as a speaker for Eli Lilly.
according to results of a study that was released early, ahead of its scheduled presentation at the annual meeting of the American Academy of Neurology.
Epidemiologist Pamela M. Rist, ScD, assistant professor of medicine at Harvard Medical School and associate epidemiologist at Brigham and Women’s Hospital, both in Boston, and colleagues, used data from 13,720 women whose mean age was 54 when they enrolled in the Harvard-based Women’s Health Study between 1992 and 1995. Subjects in that study were followed up in 2004.
Putting ‘Life’s Simple 7’ to the test
Dr. Rist and colleagues used the Harvard data to discern how well closely women conformed, during the initial study period and at 10-year follow up, to what the American Heart Association describes as “Life’s Simple 7,” a list of behavioral and biometric measures that indicate and predict cardiovascular health. The measures include four modifiable behaviors – not smoking, healthy weight, a healthy diet, and being physically active – along with three biometric measures of blood pressure, cholesterol, and blood sugar (AHA has since added a sleep component).
Researchers assigned women one point for each desirable habit or measure on the list, with subjects’ average Simple 7 score at baseline 4.3, and 4.2 at 10 years’ follow-up.
The investigators then looked at Medicare data for the study subjects from 2011 to 2018 – approximately 20 years after their enrollment in the Women’s Health Study – seeking dementia diagnoses. Some 13% of the study cohort (n = 1,771) had gone on to develop dementia.
Each point on the Simple 7 score at baseline corresponded with a 6% reduction in later dementia risk, Dr. Rist and her colleagues found after adjusting for variables including age and education (odds ratio per one unit change in score, 0.94; 95% CI, 0.90-0.98). This effect was similar for Simple 7 scores measured at 10 years of follow-up (OR, 0.95; 95% CI, 0.91-1.00).
“It can be empowering for people to know that by taking steps such as exercising for a half an hour a day or keeping their blood pressure under control, they can reduce their risk of dementia,” Dr. Rist said in a statement on the findings.
‘A simple take-home message’
Reached for comment, Andrew E. Budson, MD, chief of cognitive-behavioral neurology at the VA Boston Healthcare System, praised Dr. Rist and colleagues’ study as one that “builds on existing knowledge to provide a simple take-home message that empowers women to take control of their dementia risk.”
Each of the seven known risk factors – being active, eating better, maintaining a healthy weight, not smoking, maintaining a healthy blood pressure, controlling cholesterol, and having low blood sugar – “was associated with a 6% reduced risk of dementia,” Dr. Budson continued. “So, women who work to address all seven risk factors can reduce their risk of developing dementia by 42%: a huge amount. Moreover, although this study only looked at women, I am confident that if men follow this same advice they will also be able to reduce their risk of dementia, although we don’t know if the size of the effect will be the same.”
Dr. Rist and colleagues’ study was supported by the National Institutes of Health. None of the study authors reported conflicts of interest. Dr. Budson has reported receiving past compensation as a speaker for Eli Lilly.
FROM AAN 2023
Helping a patient buck the odds
I’m not going to get rich off Mike.
Of course, I’m not going to get rich off anyone, nor do I want to. I’m not here to rip anyone off.
Mike goes back with me, roughly 23 years.
He was born with cerebral palsy and refractory seizures. His birth mother gave him up quickly, and he was adopted by a couple who knew what they were getting into (to me that constitutes sainthood).
Over the years Mike has done his best to buck the odds. He’s tried to stay employed, in spite of his physical limitations, working variously as a janitor, grocery courtesy clerk, and store greeter. He tells me that he can still work and wants to, even with having to rely on public transportation.
By the time he came to me he’d been through several neurologists and even more failed epilepsy drugs. His brain MRI and EEGs showed multifocal seizures from numerous inoperable cortical heterotopias.
I dabbled with a few newer drugs at the time for him, without success. Finally, I reached for the neurological equivalent of unstable dynamite – Felbatol (felbamate).
As it often does, it worked. One of my attendings in training (you, Bob) told me it was the home-run drug. When nothing else worked, it might – but you had to handle it carefully.
Fortunately, after 23 years, that hasn’t happened. Mike’s labs have looked good. His seizures have dropped from several a week to a few per year.
Ten years ago Mike had to change insurance to one I don’t take, and had me forward his records to another neurologist. That office told him they don’t handle Felbatol. As did another. And another.
Mike, understandably, doesn’t want to change meds. This is the only drug that’s given him a decent quality of life, and let him have a job. That’s pretty important to him.
So, I see him for free now, once or twice a year. Sometimes he offers me a token payment of $5-$10, but I turn it down. He needs it more than I do, for bus fair to my office if nothing else.
I’m sure some would be critical of me, saying that I should be more open to new drugs and treatments. I am, believe me. But Mike can’t afford many of them, or the loss of work they’d entail if his seizures worsen. He doesn’t want to take that chance, and I don’t blame him.
Of course, none of us can see everyone for free. In fact, he’s the only one I do. I’m not greedy, but I also have to pay my rent, staff, and mortgage.
But taking money from Mike, who’s come up on the short end of the stick in so many ways, doesn’t seem right. I can’t do it, and really don’t want to.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I’m not going to get rich off Mike.
Of course, I’m not going to get rich off anyone, nor do I want to. I’m not here to rip anyone off.
Mike goes back with me, roughly 23 years.
He was born with cerebral palsy and refractory seizures. His birth mother gave him up quickly, and he was adopted by a couple who knew what they were getting into (to me that constitutes sainthood).
Over the years Mike has done his best to buck the odds. He’s tried to stay employed, in spite of his physical limitations, working variously as a janitor, grocery courtesy clerk, and store greeter. He tells me that he can still work and wants to, even with having to rely on public transportation.
By the time he came to me he’d been through several neurologists and even more failed epilepsy drugs. His brain MRI and EEGs showed multifocal seizures from numerous inoperable cortical heterotopias.
I dabbled with a few newer drugs at the time for him, without success. Finally, I reached for the neurological equivalent of unstable dynamite – Felbatol (felbamate).
As it often does, it worked. One of my attendings in training (you, Bob) told me it was the home-run drug. When nothing else worked, it might – but you had to handle it carefully.
Fortunately, after 23 years, that hasn’t happened. Mike’s labs have looked good. His seizures have dropped from several a week to a few per year.
Ten years ago Mike had to change insurance to one I don’t take, and had me forward his records to another neurologist. That office told him they don’t handle Felbatol. As did another. And another.
Mike, understandably, doesn’t want to change meds. This is the only drug that’s given him a decent quality of life, and let him have a job. That’s pretty important to him.
So, I see him for free now, once or twice a year. Sometimes he offers me a token payment of $5-$10, but I turn it down. He needs it more than I do, for bus fair to my office if nothing else.
I’m sure some would be critical of me, saying that I should be more open to new drugs and treatments. I am, believe me. But Mike can’t afford many of them, or the loss of work they’d entail if his seizures worsen. He doesn’t want to take that chance, and I don’t blame him.
Of course, none of us can see everyone for free. In fact, he’s the only one I do. I’m not greedy, but I also have to pay my rent, staff, and mortgage.
But taking money from Mike, who’s come up on the short end of the stick in so many ways, doesn’t seem right. I can’t do it, and really don’t want to.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I’m not going to get rich off Mike.
Of course, I’m not going to get rich off anyone, nor do I want to. I’m not here to rip anyone off.
Mike goes back with me, roughly 23 years.
He was born with cerebral palsy and refractory seizures. His birth mother gave him up quickly, and he was adopted by a couple who knew what they were getting into (to me that constitutes sainthood).
Over the years Mike has done his best to buck the odds. He’s tried to stay employed, in spite of his physical limitations, working variously as a janitor, grocery courtesy clerk, and store greeter. He tells me that he can still work and wants to, even with having to rely on public transportation.
By the time he came to me he’d been through several neurologists and even more failed epilepsy drugs. His brain MRI and EEGs showed multifocal seizures from numerous inoperable cortical heterotopias.
I dabbled with a few newer drugs at the time for him, without success. Finally, I reached for the neurological equivalent of unstable dynamite – Felbatol (felbamate).
As it often does, it worked. One of my attendings in training (you, Bob) told me it was the home-run drug. When nothing else worked, it might – but you had to handle it carefully.
Fortunately, after 23 years, that hasn’t happened. Mike’s labs have looked good. His seizures have dropped from several a week to a few per year.
Ten years ago Mike had to change insurance to one I don’t take, and had me forward his records to another neurologist. That office told him they don’t handle Felbatol. As did another. And another.
Mike, understandably, doesn’t want to change meds. This is the only drug that’s given him a decent quality of life, and let him have a job. That’s pretty important to him.
So, I see him for free now, once or twice a year. Sometimes he offers me a token payment of $5-$10, but I turn it down. He needs it more than I do, for bus fair to my office if nothing else.
I’m sure some would be critical of me, saying that I should be more open to new drugs and treatments. I am, believe me. But Mike can’t afford many of them, or the loss of work they’d entail if his seizures worsen. He doesn’t want to take that chance, and I don’t blame him.
Of course, none of us can see everyone for free. In fact, he’s the only one I do. I’m not greedy, but I also have to pay my rent, staff, and mortgage.
But taking money from Mike, who’s come up on the short end of the stick in so many ways, doesn’t seem right. I can’t do it, and really don’t want to.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Time to rebuild
A few months ago, after several months of considerable foot dragging, I wrote that I have accepted the American Academy of Pediatrics’ proclamation that we should begin to treat obesity as a disease.
While it may feel like we are just throwing in the towel, it sounds better if we admit that we may have reached the threshold beyond which total focus on prevention is not going to work.
I continue to be troubled by the lingering fear that, in declaring that obesity is a disease, we will suspend our current efforts at preventing the condition. Granted, most of these efforts at prevention have been woefully ineffective. However, I still believe that, much like ADHD, the rise in obesity in this country is a reflection of some serious flaws in our society. On the other hand, as an inveterate optimist I have not given up on the belief that we will find some yet-to-be-discovered changes in our societal fabric that will eventually turn the ship around.
With this somewhat contradictory combination of resignation and optimism in mind, I continue to seek out studies that hold some promise for prevention while we begin tinkering with the let’s-treat-it-like-a-disease approach.
I recently discovered a story about one such study from the Center for Economic and Social Research at the University of Southern California. Using data collected about adolescent dependents of military personnel, the researchers found that “exposure to a more advantageous built environment for more than 2 years was associated with lower probabilities of obesity.” Because more than half of these teenagers were living in housing that had been assigned by the military, the researchers could more easily control for a variety of factors some related to self-selection.
Interestingly, the data did not support associations between the adolescents’ diet, physical activity, or socioeconomic environments. The investigators noted that “more advantageous built environments were associated with lower consumption of unhealthy foods.” However, the study lacked the granularity to determine what segments of the built environment were most associated with the effect they were observing.
Like me, you may not be familiar with the term “built environment.” Turns out it is just exactly what we might expect – anything about the environment that is the result of human action – buildings, roadways, dams, neighborhoods – and what they do and don’t contain. For example, is the adolescent living in an environment that encourages walking or one that is overly motor vehicle–centric? Does his or her neighborhood have easily reachable grocery stores that offer a range of healthy foods or does the teenager live in a nutritional desert populated only by convenience stores? Is there ample space for outdoor physical activity?
The authors’ observation that the adolescents who benefited from living in advantageous environments had a lower consumption of unhealthy foods might suggest that access to a healthy diet might be a significant factor. For me, the take-home message is that in our search for preventive strategies we have barely scratched the surface. The observation that the associations these researchers were making was over a relatively short time span of 2 years should give us hope that if we think more broadly and creatively we may be to find solutions on a grand scale.
Over the last century we have built an environment that is clearly obesogenic. This paper offers a starting point from which we can learn which components of that environment are the most potent contributors to the obesity epidemic. Once we have that information the question remains: Can we find the political will to tear down and rebuilt?
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
A few months ago, after several months of considerable foot dragging, I wrote that I have accepted the American Academy of Pediatrics’ proclamation that we should begin to treat obesity as a disease.
While it may feel like we are just throwing in the towel, it sounds better if we admit that we may have reached the threshold beyond which total focus on prevention is not going to work.
I continue to be troubled by the lingering fear that, in declaring that obesity is a disease, we will suspend our current efforts at preventing the condition. Granted, most of these efforts at prevention have been woefully ineffective. However, I still believe that, much like ADHD, the rise in obesity in this country is a reflection of some serious flaws in our society. On the other hand, as an inveterate optimist I have not given up on the belief that we will find some yet-to-be-discovered changes in our societal fabric that will eventually turn the ship around.
With this somewhat contradictory combination of resignation and optimism in mind, I continue to seek out studies that hold some promise for prevention while we begin tinkering with the let’s-treat-it-like-a-disease approach.
I recently discovered a story about one such study from the Center for Economic and Social Research at the University of Southern California. Using data collected about adolescent dependents of military personnel, the researchers found that “exposure to a more advantageous built environment for more than 2 years was associated with lower probabilities of obesity.” Because more than half of these teenagers were living in housing that had been assigned by the military, the researchers could more easily control for a variety of factors some related to self-selection.
Interestingly, the data did not support associations between the adolescents’ diet, physical activity, or socioeconomic environments. The investigators noted that “more advantageous built environments were associated with lower consumption of unhealthy foods.” However, the study lacked the granularity to determine what segments of the built environment were most associated with the effect they were observing.
Like me, you may not be familiar with the term “built environment.” Turns out it is just exactly what we might expect – anything about the environment that is the result of human action – buildings, roadways, dams, neighborhoods – and what they do and don’t contain. For example, is the adolescent living in an environment that encourages walking or one that is overly motor vehicle–centric? Does his or her neighborhood have easily reachable grocery stores that offer a range of healthy foods or does the teenager live in a nutritional desert populated only by convenience stores? Is there ample space for outdoor physical activity?
The authors’ observation that the adolescents who benefited from living in advantageous environments had a lower consumption of unhealthy foods might suggest that access to a healthy diet might be a significant factor. For me, the take-home message is that in our search for preventive strategies we have barely scratched the surface. The observation that the associations these researchers were making was over a relatively short time span of 2 years should give us hope that if we think more broadly and creatively we may be to find solutions on a grand scale.
Over the last century we have built an environment that is clearly obesogenic. This paper offers a starting point from which we can learn which components of that environment are the most potent contributors to the obesity epidemic. Once we have that information the question remains: Can we find the political will to tear down and rebuilt?
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
A few months ago, after several months of considerable foot dragging, I wrote that I have accepted the American Academy of Pediatrics’ proclamation that we should begin to treat obesity as a disease.
While it may feel like we are just throwing in the towel, it sounds better if we admit that we may have reached the threshold beyond which total focus on prevention is not going to work.
I continue to be troubled by the lingering fear that, in declaring that obesity is a disease, we will suspend our current efforts at preventing the condition. Granted, most of these efforts at prevention have been woefully ineffective. However, I still believe that, much like ADHD, the rise in obesity in this country is a reflection of some serious flaws in our society. On the other hand, as an inveterate optimist I have not given up on the belief that we will find some yet-to-be-discovered changes in our societal fabric that will eventually turn the ship around.
With this somewhat contradictory combination of resignation and optimism in mind, I continue to seek out studies that hold some promise for prevention while we begin tinkering with the let’s-treat-it-like-a-disease approach.
I recently discovered a story about one such study from the Center for Economic and Social Research at the University of Southern California. Using data collected about adolescent dependents of military personnel, the researchers found that “exposure to a more advantageous built environment for more than 2 years was associated with lower probabilities of obesity.” Because more than half of these teenagers were living in housing that had been assigned by the military, the researchers could more easily control for a variety of factors some related to self-selection.
Interestingly, the data did not support associations between the adolescents’ diet, physical activity, or socioeconomic environments. The investigators noted that “more advantageous built environments were associated with lower consumption of unhealthy foods.” However, the study lacked the granularity to determine what segments of the built environment were most associated with the effect they were observing.
Like me, you may not be familiar with the term “built environment.” Turns out it is just exactly what we might expect – anything about the environment that is the result of human action – buildings, roadways, dams, neighborhoods – and what they do and don’t contain. For example, is the adolescent living in an environment that encourages walking or one that is overly motor vehicle–centric? Does his or her neighborhood have easily reachable grocery stores that offer a range of healthy foods or does the teenager live in a nutritional desert populated only by convenience stores? Is there ample space for outdoor physical activity?
The authors’ observation that the adolescents who benefited from living in advantageous environments had a lower consumption of unhealthy foods might suggest that access to a healthy diet might be a significant factor. For me, the take-home message is that in our search for preventive strategies we have barely scratched the surface. The observation that the associations these researchers were making was over a relatively short time span of 2 years should give us hope that if we think more broadly and creatively we may be to find solutions on a grand scale.
Over the last century we have built an environment that is clearly obesogenic. This paper offers a starting point from which we can learn which components of that environment are the most potent contributors to the obesity epidemic. Once we have that information the question remains: Can we find the political will to tear down and rebuilt?
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Family violence after COVID: Understanding coercive relationships
Despite the ability of some couples to pull together and manage through the COVID-19 pandemic, other couples and families failed to thrive. Increasing divorce rates have been noted nationwide with many disagreements being specifically about COVID.1
A review of over 1 million tweets, between April 12 and July 16, 2020, found an increase in calls to hotlines and increased reports of a variety of types of family violence. There were also more inquiries about social services for family violence, an increased presence from social movements, and more domestic violence-related news.2
The literature addressing family violence uses a variety of terms, so here are some definitions.
Domestic violence is defined as a pattern of behaviors used to gain or maintain power and control. Broadly speaking, domestic violence includes elder abuse, sibling abuse, child abuse, intimate partner abuse, parent abuse, and can also include people who don’t necessarily live together but who have an intimate relationship. Domestic violence centers use the Power and Control Wheel (see graphic) developed by the Domestic Abuse Intervention Project in Duluth, Minn., to describe how domestic violence occurs.
Intimate partner violence is more specific, referring to violence that happens between people in an ongoing or former intimate or romantic relationship, and is a subcategory of domestic violence.
Coercive control is the use of power for control and compliance. It is a dynamic and systematic process described in the top left corner of the Power and Control Wheel. Overt control occurs with the implication that “if you don’t follow the rules, I’ll kill you.” More subtle control is when obedience is forced through monopolizing resources, dictating preferred choices, microregulating a partner’s behavior, and deprivation of supports needed to exercise independent judgment.
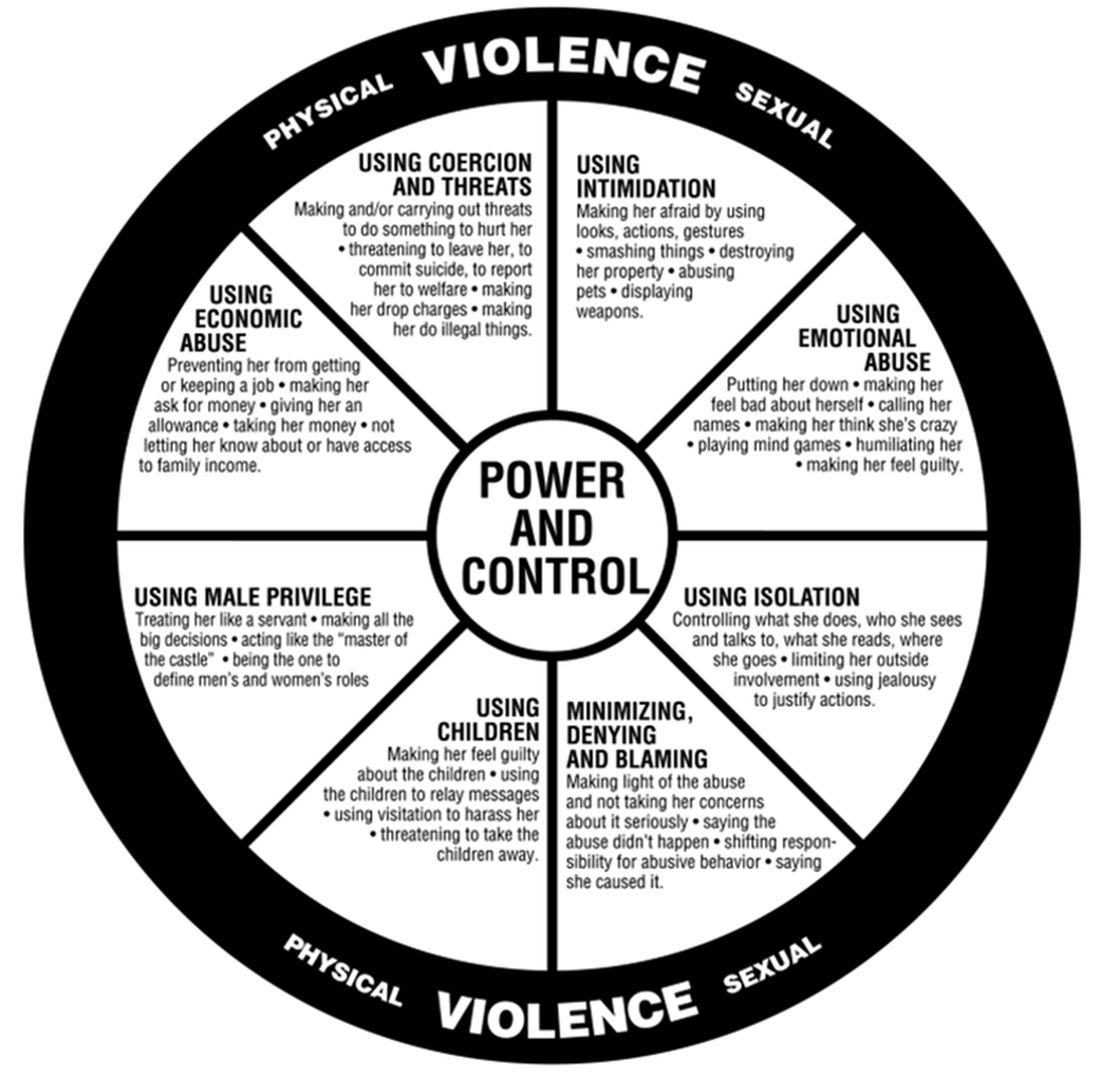
All interpersonal relationships have elements of persuasion and influence; however, the goal of coercive relationships is to maintain power and control. It is a dynamic of the relationship. Coercive control emphasizes the systematic, organized, multifaceted, and patterned nature of this interpersonal dynamic and can be considered to originate in the patriarchal dynamic where men control women.
Most professionals who work in this interdisciplinary area now refer to domestic violence as coercive control. Victimizers target women whom they sense they can control to get their own needs met. They are disinclined to invest in relationships with women who stress their own points of view, who do not readily accept blame when there is a disagreement, and who offer nurturing only when it is reciprocated.
In my office, if I think there are elements of coercion in a relationship, I bring out the Power and Control Wheel and the patient and I go over it. Good education is our responsibility. However, we all have met women who decide to stay in unhealthy relationships.
Assessing people who stay in coercive relationships
Fear
The most important first step is to assess safety. Are they afraid of increased violence if they challenge their partner? Restraining orders or other legal deterrents may not offer solace, as many women are clear that their spouse will come after them, if not tomorrow, then next week, or even next month. They are sure that they will not be safe.
In these cases, I go over safety steps with them so that if they decide to go, they will be prepared. I bring out the “safety box,” which includes the following action steps:
- Memorize important phone numbers of people to call in an emergency.
- If your children are old enough, teach them important phone numbers, including when to dial 911.
- If you can, open your own bank account.
- Stay in touch with friends. Get to know your neighbors. Don’t cut yourself off from people, even if you feel like you want to be alone.
- Rehearse your escape plan until you know it by heart.
- Leave a set of car keys, extra money, a change of clothes and copies of important documents with a trusted friend or relative: your own and your children’s birth certificates, children’s school and medical records, bank books, welfare identification, passport/green card, immigration papers, social security card, lease agreements or mortgage payment books, insurance papers, important addresses, and telephone numbers.
- Keep information about domestic violence in a safe place, where your abuser won’t find it, but where you can get it when you need to review it.
Some women may acknowledge that the risk of physical violence is not the determining factor in their decision to stay and have difficulty explaining why they choose to stay. I suggest that we then consider the following frames that have their origin in the study of the impact of trauma.
Shame
From this lens, abusive events are humiliating experiences, now represented as shame experiences. Humiliation and shame hide hostile feelings that the patient is not able to acknowledge.
“In shame, the self is the failure and others may reject or be critical of this exposed, flawed self.”3 Women will therefore remain attached to an abuser to avoid the exposure of their defective self.
Action steps: Empathic engagement and acknowledgment of shame and humiliation are key. For someone to overcome shame, they must face their sense of their defective self and have strategies to manage these feelings. The development of such strategies is the next step.
Trauma repetition and trauma bonding
Women subjected to domestic violence often respond with incapacitating traumatic syndromes. The concept of “trauma repetition” is suggested as a cause of vulnerability to repeated abuse, and “trauma bonding” is the term for the intense and tenacious bond that can form between abusers and victims.4
Trauma bonding implies that a sense of safety and closeness and secure attachment can only be reached through highly abusive engagement; anything else is experienced as “superficial, cold, or irrelevant.”5 Trauma bonding may have its origins in emotional neglect, according to self reports of 116 women.6Action steps: The literature on trauma is growing and many patients will benefit from good curated sources. Having a good list of books and website on hand is important. Discussion and exploration of the impact of trauma will be needed, and can be provided by someone who is available on a consistent and frequent basis. This work may be time consuming and difficult.
Some asides
1. Some psychiatrists proffer the explanation that these women who stay must be masochistic. The misogynistic concept of masochism still haunts the halls of psychiatry. It is usually offered as a way to dismiss these women’s concerns.
2. One of the obstacles to recognizing chronic mistreatment in relationships is that most abusive men simply “do not seem like abusers.” They have many good qualities, including times of kindness, warmth, and humor, especially in the initial period of a relationship. An abuser’s friends may think the world of him. He may have a successful work life and have no problems with drugs or alcohol. He may simply not fit anyone’s image of a cruel or intimidating person. So, when a woman feels her relationship spinning out of control, it may not occur to her that her partner is an abuser. Even if she does consider her partner to be overly controlling, others may question her perception.
3. Neutrality in family courts is systemic sexism/misogyny. When it comes to domestic violence, family courts tend to split the difference. Stephanie Brandt, MD, notes that The assumption that it is violence alone that matters has formed the basis of much clinical and legal confusion.7 As an analyst, she has gone against the grain of a favored neutrality and become active in the courts, noting the secondary victimization that occurs when a woman enters the legal system.
In summary, psychiatrists must reclaim our expertise in systemic dynamics and point out the role of systemic misogyny. Justices and other court officials need to be educated. Ideally, justice should be based on the equality of men and women in a society free of systemic misogyny. Unfortunately our society has not yet reached this position. In the meanwhile, we must think systemically about interpersonal dynamics. This is our lane. This should not be controversial.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at [email protected]. Dr. Heru would like to thank Dr. Stephanie Brandt for discussing this topic with her and supporting this work.
References
1. Ellyatt H. Arguing with your partner over Covid? You’re not alone, with the pandemic straining many relationships. 2022 Jan 21. https://www.cnbc.com/2022/01/21/covid-has-put-pressures-and-strains-on-relationships.html
2. Xue J et al. J Med Internet Res. 2020 Nov 6;22(11):e24361. doi: 10.2196/24361.
3. Dorahy MJ. J Trauma Dissociation. 2017 May-Jun;18(3):383-96. doi: 10.1080/15299732.2017.1295422.
4. Dutton DG and Painter SL. Victimology. 1981 Jan;6(1):139-55.
5. Sachs A. J Trauma Dissociation. 2017 May-Jun;18(3):319-39. doi: 10.1080/15299732.2017.1295400.
6. Krüger C and Fletcher L. J Trauma Dissociation. 2017 May-Jun;18(3):356-72. doi: 10.1080/15299732.2017.1295420.
7. Brandt S and Rudden M. Int J Appl Psychoanal Studies. 2020 Sept;17(3):215-31. doi: 10.1002/aps.1671.
Despite the ability of some couples to pull together and manage through the COVID-19 pandemic, other couples and families failed to thrive. Increasing divorce rates have been noted nationwide with many disagreements being specifically about COVID.1
A review of over 1 million tweets, between April 12 and July 16, 2020, found an increase in calls to hotlines and increased reports of a variety of types of family violence. There were also more inquiries about social services for family violence, an increased presence from social movements, and more domestic violence-related news.2
The literature addressing family violence uses a variety of terms, so here are some definitions.
Domestic violence is defined as a pattern of behaviors used to gain or maintain power and control. Broadly speaking, domestic violence includes elder abuse, sibling abuse, child abuse, intimate partner abuse, parent abuse, and can also include people who don’t necessarily live together but who have an intimate relationship. Domestic violence centers use the Power and Control Wheel (see graphic) developed by the Domestic Abuse Intervention Project in Duluth, Minn., to describe how domestic violence occurs.
Intimate partner violence is more specific, referring to violence that happens between people in an ongoing or former intimate or romantic relationship, and is a subcategory of domestic violence.
Coercive control is the use of power for control and compliance. It is a dynamic and systematic process described in the top left corner of the Power and Control Wheel. Overt control occurs with the implication that “if you don’t follow the rules, I’ll kill you.” More subtle control is when obedience is forced through monopolizing resources, dictating preferred choices, microregulating a partner’s behavior, and deprivation of supports needed to exercise independent judgment.
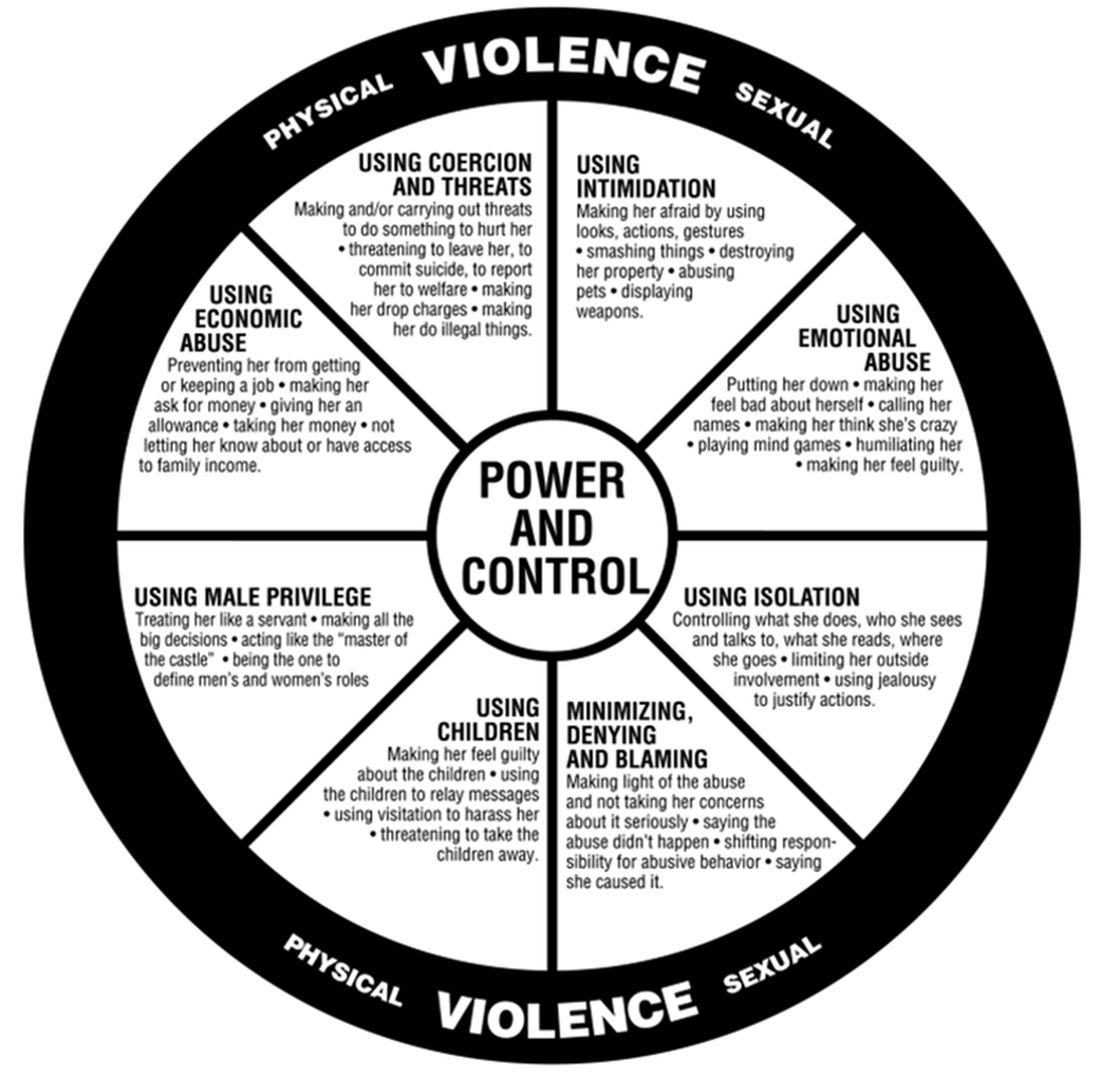
All interpersonal relationships have elements of persuasion and influence; however, the goal of coercive relationships is to maintain power and control. It is a dynamic of the relationship. Coercive control emphasizes the systematic, organized, multifaceted, and patterned nature of this interpersonal dynamic and can be considered to originate in the patriarchal dynamic where men control women.
Most professionals who work in this interdisciplinary area now refer to domestic violence as coercive control. Victimizers target women whom they sense they can control to get their own needs met. They are disinclined to invest in relationships with women who stress their own points of view, who do not readily accept blame when there is a disagreement, and who offer nurturing only when it is reciprocated.
In my office, if I think there are elements of coercion in a relationship, I bring out the Power and Control Wheel and the patient and I go over it. Good education is our responsibility. However, we all have met women who decide to stay in unhealthy relationships.
Assessing people who stay in coercive relationships
Fear
The most important first step is to assess safety. Are they afraid of increased violence if they challenge their partner? Restraining orders or other legal deterrents may not offer solace, as many women are clear that their spouse will come after them, if not tomorrow, then next week, or even next month. They are sure that they will not be safe.
In these cases, I go over safety steps with them so that if they decide to go, they will be prepared. I bring out the “safety box,” which includes the following action steps:
- Memorize important phone numbers of people to call in an emergency.
- If your children are old enough, teach them important phone numbers, including when to dial 911.
- If you can, open your own bank account.
- Stay in touch with friends. Get to know your neighbors. Don’t cut yourself off from people, even if you feel like you want to be alone.
- Rehearse your escape plan until you know it by heart.
- Leave a set of car keys, extra money, a change of clothes and copies of important documents with a trusted friend or relative: your own and your children’s birth certificates, children’s school and medical records, bank books, welfare identification, passport/green card, immigration papers, social security card, lease agreements or mortgage payment books, insurance papers, important addresses, and telephone numbers.
- Keep information about domestic violence in a safe place, where your abuser won’t find it, but where you can get it when you need to review it.
Some women may acknowledge that the risk of physical violence is not the determining factor in their decision to stay and have difficulty explaining why they choose to stay. I suggest that we then consider the following frames that have their origin in the study of the impact of trauma.
Shame
From this lens, abusive events are humiliating experiences, now represented as shame experiences. Humiliation and shame hide hostile feelings that the patient is not able to acknowledge.
“In shame, the self is the failure and others may reject or be critical of this exposed, flawed self.”3 Women will therefore remain attached to an abuser to avoid the exposure of their defective self.
Action steps: Empathic engagement and acknowledgment of shame and humiliation are key. For someone to overcome shame, they must face their sense of their defective self and have strategies to manage these feelings. The development of such strategies is the next step.
Trauma repetition and trauma bonding
Women subjected to domestic violence often respond with incapacitating traumatic syndromes. The concept of “trauma repetition” is suggested as a cause of vulnerability to repeated abuse, and “trauma bonding” is the term for the intense and tenacious bond that can form between abusers and victims.4
Trauma bonding implies that a sense of safety and closeness and secure attachment can only be reached through highly abusive engagement; anything else is experienced as “superficial, cold, or irrelevant.”5 Trauma bonding may have its origins in emotional neglect, according to self reports of 116 women.6Action steps: The literature on trauma is growing and many patients will benefit from good curated sources. Having a good list of books and website on hand is important. Discussion and exploration of the impact of trauma will be needed, and can be provided by someone who is available on a consistent and frequent basis. This work may be time consuming and difficult.
Some asides
1. Some psychiatrists proffer the explanation that these women who stay must be masochistic. The misogynistic concept of masochism still haunts the halls of psychiatry. It is usually offered as a way to dismiss these women’s concerns.
2. One of the obstacles to recognizing chronic mistreatment in relationships is that most abusive men simply “do not seem like abusers.” They have many good qualities, including times of kindness, warmth, and humor, especially in the initial period of a relationship. An abuser’s friends may think the world of him. He may have a successful work life and have no problems with drugs or alcohol. He may simply not fit anyone’s image of a cruel or intimidating person. So, when a woman feels her relationship spinning out of control, it may not occur to her that her partner is an abuser. Even if she does consider her partner to be overly controlling, others may question her perception.
3. Neutrality in family courts is systemic sexism/misogyny. When it comes to domestic violence, family courts tend to split the difference. Stephanie Brandt, MD, notes that The assumption that it is violence alone that matters has formed the basis of much clinical and legal confusion.7 As an analyst, she has gone against the grain of a favored neutrality and become active in the courts, noting the secondary victimization that occurs when a woman enters the legal system.
In summary, psychiatrists must reclaim our expertise in systemic dynamics and point out the role of systemic misogyny. Justices and other court officials need to be educated. Ideally, justice should be based on the equality of men and women in a society free of systemic misogyny. Unfortunately our society has not yet reached this position. In the meanwhile, we must think systemically about interpersonal dynamics. This is our lane. This should not be controversial.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at [email protected]. Dr. Heru would like to thank Dr. Stephanie Brandt for discussing this topic with her and supporting this work.
References
1. Ellyatt H. Arguing with your partner over Covid? You’re not alone, with the pandemic straining many relationships. 2022 Jan 21. https://www.cnbc.com/2022/01/21/covid-has-put-pressures-and-strains-on-relationships.html
2. Xue J et al. J Med Internet Res. 2020 Nov 6;22(11):e24361. doi: 10.2196/24361.
3. Dorahy MJ. J Trauma Dissociation. 2017 May-Jun;18(3):383-96. doi: 10.1080/15299732.2017.1295422.
4. Dutton DG and Painter SL. Victimology. 1981 Jan;6(1):139-55.
5. Sachs A. J Trauma Dissociation. 2017 May-Jun;18(3):319-39. doi: 10.1080/15299732.2017.1295400.
6. Krüger C and Fletcher L. J Trauma Dissociation. 2017 May-Jun;18(3):356-72. doi: 10.1080/15299732.2017.1295420.
7. Brandt S and Rudden M. Int J Appl Psychoanal Studies. 2020 Sept;17(3):215-31. doi: 10.1002/aps.1671.
Despite the ability of some couples to pull together and manage through the COVID-19 pandemic, other couples and families failed to thrive. Increasing divorce rates have been noted nationwide with many disagreements being specifically about COVID.1
A review of over 1 million tweets, between April 12 and July 16, 2020, found an increase in calls to hotlines and increased reports of a variety of types of family violence. There were also more inquiries about social services for family violence, an increased presence from social movements, and more domestic violence-related news.2
The literature addressing family violence uses a variety of terms, so here are some definitions.
Domestic violence is defined as a pattern of behaviors used to gain or maintain power and control. Broadly speaking, domestic violence includes elder abuse, sibling abuse, child abuse, intimate partner abuse, parent abuse, and can also include people who don’t necessarily live together but who have an intimate relationship. Domestic violence centers use the Power and Control Wheel (see graphic) developed by the Domestic Abuse Intervention Project in Duluth, Minn., to describe how domestic violence occurs.
Intimate partner violence is more specific, referring to violence that happens between people in an ongoing or former intimate or romantic relationship, and is a subcategory of domestic violence.
Coercive control is the use of power for control and compliance. It is a dynamic and systematic process described in the top left corner of the Power and Control Wheel. Overt control occurs with the implication that “if you don’t follow the rules, I’ll kill you.” More subtle control is when obedience is forced through monopolizing resources, dictating preferred choices, microregulating a partner’s behavior, and deprivation of supports needed to exercise independent judgment.
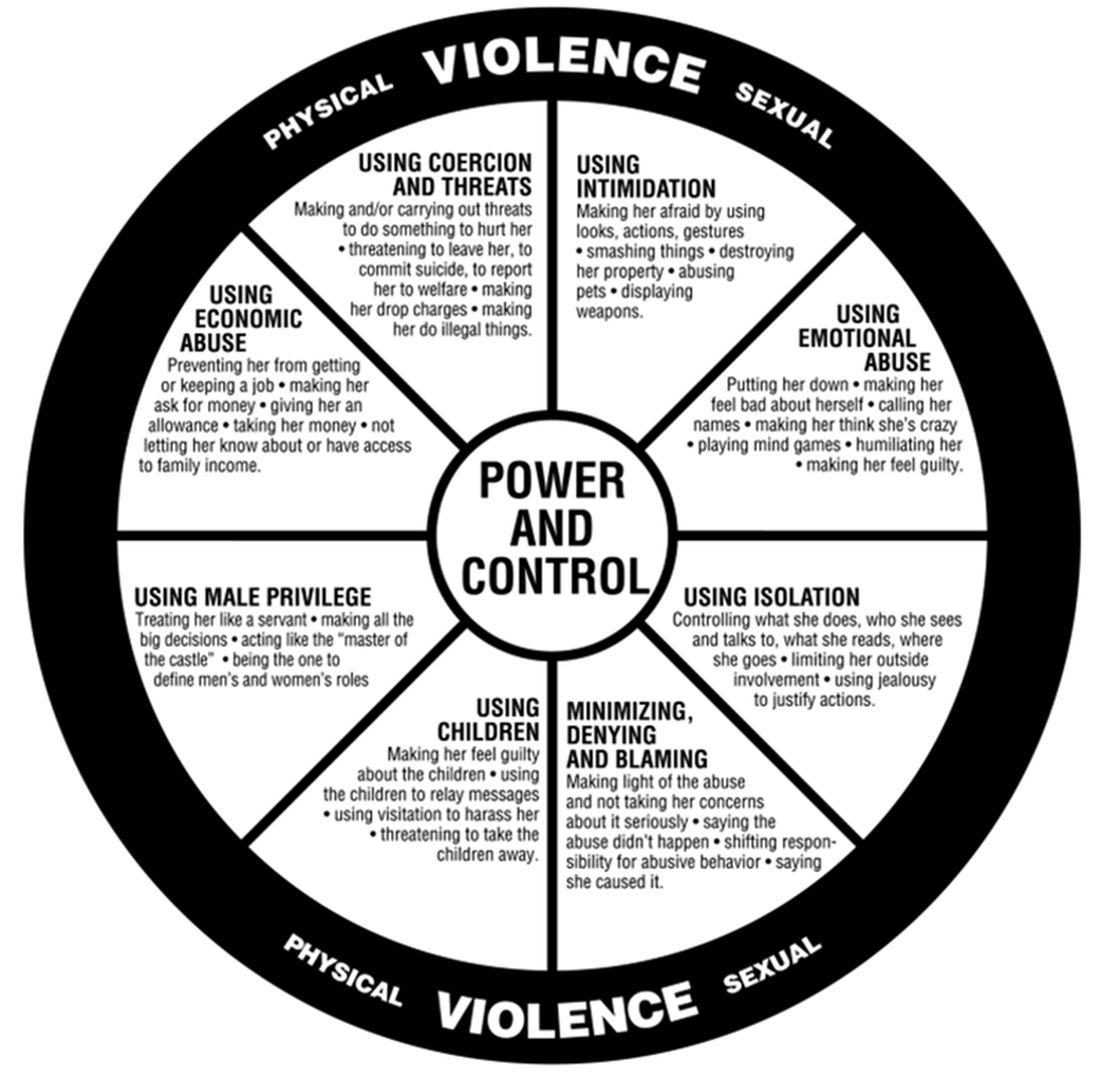
All interpersonal relationships have elements of persuasion and influence; however, the goal of coercive relationships is to maintain power and control. It is a dynamic of the relationship. Coercive control emphasizes the systematic, organized, multifaceted, and patterned nature of this interpersonal dynamic and can be considered to originate in the patriarchal dynamic where men control women.
Most professionals who work in this interdisciplinary area now refer to domestic violence as coercive control. Victimizers target women whom they sense they can control to get their own needs met. They are disinclined to invest in relationships with women who stress their own points of view, who do not readily accept blame when there is a disagreement, and who offer nurturing only when it is reciprocated.
In my office, if I think there are elements of coercion in a relationship, I bring out the Power and Control Wheel and the patient and I go over it. Good education is our responsibility. However, we all have met women who decide to stay in unhealthy relationships.
Assessing people who stay in coercive relationships
Fear
The most important first step is to assess safety. Are they afraid of increased violence if they challenge their partner? Restraining orders or other legal deterrents may not offer solace, as many women are clear that their spouse will come after them, if not tomorrow, then next week, or even next month. They are sure that they will not be safe.
In these cases, I go over safety steps with them so that if they decide to go, they will be prepared. I bring out the “safety box,” which includes the following action steps:
- Memorize important phone numbers of people to call in an emergency.
- If your children are old enough, teach them important phone numbers, including when to dial 911.
- If you can, open your own bank account.
- Stay in touch with friends. Get to know your neighbors. Don’t cut yourself off from people, even if you feel like you want to be alone.
- Rehearse your escape plan until you know it by heart.
- Leave a set of car keys, extra money, a change of clothes and copies of important documents with a trusted friend or relative: your own and your children’s birth certificates, children’s school and medical records, bank books, welfare identification, passport/green card, immigration papers, social security card, lease agreements or mortgage payment books, insurance papers, important addresses, and telephone numbers.
- Keep information about domestic violence in a safe place, where your abuser won’t find it, but where you can get it when you need to review it.
Some women may acknowledge that the risk of physical violence is not the determining factor in their decision to stay and have difficulty explaining why they choose to stay. I suggest that we then consider the following frames that have their origin in the study of the impact of trauma.
Shame
From this lens, abusive events are humiliating experiences, now represented as shame experiences. Humiliation and shame hide hostile feelings that the patient is not able to acknowledge.
“In shame, the self is the failure and others may reject or be critical of this exposed, flawed self.”3 Women will therefore remain attached to an abuser to avoid the exposure of their defective self.
Action steps: Empathic engagement and acknowledgment of shame and humiliation are key. For someone to overcome shame, they must face their sense of their defective self and have strategies to manage these feelings. The development of such strategies is the next step.
Trauma repetition and trauma bonding
Women subjected to domestic violence often respond with incapacitating traumatic syndromes. The concept of “trauma repetition” is suggested as a cause of vulnerability to repeated abuse, and “trauma bonding” is the term for the intense and tenacious bond that can form between abusers and victims.4
Trauma bonding implies that a sense of safety and closeness and secure attachment can only be reached through highly abusive engagement; anything else is experienced as “superficial, cold, or irrelevant.”5 Trauma bonding may have its origins in emotional neglect, according to self reports of 116 women.6Action steps: The literature on trauma is growing and many patients will benefit from good curated sources. Having a good list of books and website on hand is important. Discussion and exploration of the impact of trauma will be needed, and can be provided by someone who is available on a consistent and frequent basis. This work may be time consuming and difficult.
Some asides
1. Some psychiatrists proffer the explanation that these women who stay must be masochistic. The misogynistic concept of masochism still haunts the halls of psychiatry. It is usually offered as a way to dismiss these women’s concerns.
2. One of the obstacles to recognizing chronic mistreatment in relationships is that most abusive men simply “do not seem like abusers.” They have many good qualities, including times of kindness, warmth, and humor, especially in the initial period of a relationship. An abuser’s friends may think the world of him. He may have a successful work life and have no problems with drugs or alcohol. He may simply not fit anyone’s image of a cruel or intimidating person. So, when a woman feels her relationship spinning out of control, it may not occur to her that her partner is an abuser. Even if she does consider her partner to be overly controlling, others may question her perception.
3. Neutrality in family courts is systemic sexism/misogyny. When it comes to domestic violence, family courts tend to split the difference. Stephanie Brandt, MD, notes that The assumption that it is violence alone that matters has formed the basis of much clinical and legal confusion.7 As an analyst, she has gone against the grain of a favored neutrality and become active in the courts, noting the secondary victimization that occurs when a woman enters the legal system.
In summary, psychiatrists must reclaim our expertise in systemic dynamics and point out the role of systemic misogyny. Justices and other court officials need to be educated. Ideally, justice should be based on the equality of men and women in a society free of systemic misogyny. Unfortunately our society has not yet reached this position. In the meanwhile, we must think systemically about interpersonal dynamics. This is our lane. This should not be controversial.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at [email protected]. Dr. Heru would like to thank Dr. Stephanie Brandt for discussing this topic with her and supporting this work.
References
1. Ellyatt H. Arguing with your partner over Covid? You’re not alone, with the pandemic straining many relationships. 2022 Jan 21. https://www.cnbc.com/2022/01/21/covid-has-put-pressures-and-strains-on-relationships.html
2. Xue J et al. J Med Internet Res. 2020 Nov 6;22(11):e24361. doi: 10.2196/24361.
3. Dorahy MJ. J Trauma Dissociation. 2017 May-Jun;18(3):383-96. doi: 10.1080/15299732.2017.1295422.
4. Dutton DG and Painter SL. Victimology. 1981 Jan;6(1):139-55.
5. Sachs A. J Trauma Dissociation. 2017 May-Jun;18(3):319-39. doi: 10.1080/15299732.2017.1295400.
6. Krüger C and Fletcher L. J Trauma Dissociation. 2017 May-Jun;18(3):356-72. doi: 10.1080/15299732.2017.1295420.
7. Brandt S and Rudden M. Int J Appl Psychoanal Studies. 2020 Sept;17(3):215-31. doi: 10.1002/aps.1671.

















