User login
Plan Good Discharges
It was probably just the ramblings of a mad woman. Only she wasn’t mad, so I searched for a hint of delirium. Nothing. She was mentally fit and lucid—perhaps too lucid. Could it be true … had I become my archenemy?
To decide, I put her utterance to the test through the Kubler-Ross obstacle course, hopping the denial hurdle, quick-footing through the anger tire course, wading through the bargaining pool, and finally swinging safely across the depression crevasse to acceptance.
She was my eighth patient that day, a 78-year-old woman admitted to the orthopedic service with a hip fracture. I was asked to do a preoperative risk assessment and comanage her diabetes and heart failure. During our introductions she asked what kind of doctor I was.
“A hospitalist,” I replied.
“Oh … that’s nice,” she answered, her furrowed eyebrow transforming her crow’s feet into a question mark.
“You know, a doctor who only cares for patients in the hospital,” I clarified. “I just take care of your acute problems.”
“You think a broken hip is cute?”
“No, no, not ‘cute.’ Acute. You know, I only deal with your urgent problems. When you leave here you will go back to see your primary care doctor, who will follow up your hip fracture and your more chronic issues.”
That’s when she dropped the bomb.
“Oh, I see; you’re sort of like a contractor for my body then—just helping when things get broke.”
I should explain my aversion to this comment. Reared by a 10-thumbed father, I’m genetically incapable of curing even the simplest household hiccup. This doesn’t mean I haven’t or won’t try. In fact, I’m willing to try anything. My wife, however, is too smart to allow that. She knows that home improvement project plus me equals larger home improvement project. Combine this mathematical axiom with our turn-of-the-(20th)-century home, and it’s easy to see why I find myself betrothed in nearly continuous engagement with contractors.
But this is a marriage on the rocks. As dependent as I am on home contractors, I generally dislike working with them. They’re all fine people I’m sure, and truth be told most of them are quite skilled at their work. The problem is that they go about their job as if they are allergic to customer service.
The only contractors who are not perpetually late are those who won’t give you a time to meet. “I’ll meet you in the morning,” they’ll say, only to define morning as any time after the sun comes up.
Then there’s the estimate, which appears to be an approximation calculated in a cavernous ballpark using an underestimater. It’s also not exactly clear how or what goes into the calculation of an estimate.
I recently got a written estimate that read as follows: “Fix sink, $400.” When I asked what the $400 would go toward, I got the ever-so-helpful reply: “Fixing the sink.” I responded, “No, I mean, how much are the parts and the labor and things like that?” He gruffly countered, “Four hundred dollars.” Uncovering how he came up with this estimate was about as easy as solving a Rubik’s cube. I gave up trying—and eventually paid $550.
Another time, a contractor agreed to fix a plumbing leak in our upstairs bathroom that had caused water damage to our first-floor ceiling. While tearing out the floor to reach the leak, he mistakenly ran a circular saw through a pipe, causing a considerably larger gusher that quickly destroyed said ceiling.
I understand these things happen. However, imagine my surprise when the eventual project cost was more than twice the estimated cost. He explained that repairing the new water damage was quite expensive and accounted for the variance with the estimate. We “discussed” this development, during which time I explained to him in no uncertain terms what the temperature in hell would be when I paid for his mistake.
So, it stung a bit to be called a “contractor.” But I could live with it. In fact, on the surface my patient’s analogy was quite good. Hospitalists do swoop in and fix patients’ problems only to then leave their lives, most often for good. It was only after a few days that her statement started to sour in my amygdala.
Habitual tardiness, sketchy response times, vague payment structures, lack of transparency in pricing, pricing errors into the cost of the job—I don’t think the analogy was intended to be so perceptive. I and the healthcare system within which I work really had adopted some of the less-desirable attributes of the contracting world.
I usually tell patients I’ll be back in an hour to give them their test results, knowing that I’m on “doctor time” and this could mean several hours or more. My tardiness usually results from being delayed while caring for another patient—but it’s all the same to the patient left waiting. Trying to build in cushion time for these unforeseen delays leaves a patient with a disagreeable contractor-like window of time to wait. For those who want to have their family at our daily rounds, an “I’ll come see you in the morning” is not just unhelpful—it disrespects the importance of their time.
Then there’s our payment system. It’s a mystery even to me: $12 aspirins, $100,000 cancer drugs, intentionally inflated professional fees and hospital bills that aren’t expected to be paid in full (unless the patient lacks an insurer to negotiate a lower price when they ironically are expected to foot the entire bill). All of which is made worse by the lack of transparency in our pricing. Patients (and most often I) simply are not privy to the costs of various tests and interventions. And, costs for the same procedure often differ among hospitals.
Few of us would contract for work without playing a role in choosing the supplies and knowing the rough cost of the materials. Yet that’s the situation our patients find themselves in daily.
Finally, expecting patients or their insurers to pay for my mistakes is not fair. I recognize there are adverse events that are unavoidable and should be reimbursed. However, many errors are as avoidable as being careful not to cut through a working pipe. Payment for these outcomes should be shouldered by the health system—not the patient.
I limped through the next few days re-examining my patient interactions. I licked my wounds, vowing to eschew those traits that so offend me as a consumer. I might not be able to repair a broken healthcare system, but I can refurbish the way I interact with my patients by being timely and responsive and not underestimating the effect of poor customer service. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado, Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
It was probably just the ramblings of a mad woman. Only she wasn’t mad, so I searched for a hint of delirium. Nothing. She was mentally fit and lucid—perhaps too lucid. Could it be true … had I become my archenemy?
To decide, I put her utterance to the test through the Kubler-Ross obstacle course, hopping the denial hurdle, quick-footing through the anger tire course, wading through the bargaining pool, and finally swinging safely across the depression crevasse to acceptance.
She was my eighth patient that day, a 78-year-old woman admitted to the orthopedic service with a hip fracture. I was asked to do a preoperative risk assessment and comanage her diabetes and heart failure. During our introductions she asked what kind of doctor I was.
“A hospitalist,” I replied.
“Oh … that’s nice,” she answered, her furrowed eyebrow transforming her crow’s feet into a question mark.
“You know, a doctor who only cares for patients in the hospital,” I clarified. “I just take care of your acute problems.”
“You think a broken hip is cute?”
“No, no, not ‘cute.’ Acute. You know, I only deal with your urgent problems. When you leave here you will go back to see your primary care doctor, who will follow up your hip fracture and your more chronic issues.”
That’s when she dropped the bomb.
“Oh, I see; you’re sort of like a contractor for my body then—just helping when things get broke.”
I should explain my aversion to this comment. Reared by a 10-thumbed father, I’m genetically incapable of curing even the simplest household hiccup. This doesn’t mean I haven’t or won’t try. In fact, I’m willing to try anything. My wife, however, is too smart to allow that. She knows that home improvement project plus me equals larger home improvement project. Combine this mathematical axiom with our turn-of-the-(20th)-century home, and it’s easy to see why I find myself betrothed in nearly continuous engagement with contractors.
But this is a marriage on the rocks. As dependent as I am on home contractors, I generally dislike working with them. They’re all fine people I’m sure, and truth be told most of them are quite skilled at their work. The problem is that they go about their job as if they are allergic to customer service.
The only contractors who are not perpetually late are those who won’t give you a time to meet. “I’ll meet you in the morning,” they’ll say, only to define morning as any time after the sun comes up.
Then there’s the estimate, which appears to be an approximation calculated in a cavernous ballpark using an underestimater. It’s also not exactly clear how or what goes into the calculation of an estimate.
I recently got a written estimate that read as follows: “Fix sink, $400.” When I asked what the $400 would go toward, I got the ever-so-helpful reply: “Fixing the sink.” I responded, “No, I mean, how much are the parts and the labor and things like that?” He gruffly countered, “Four hundred dollars.” Uncovering how he came up with this estimate was about as easy as solving a Rubik’s cube. I gave up trying—and eventually paid $550.
Another time, a contractor agreed to fix a plumbing leak in our upstairs bathroom that had caused water damage to our first-floor ceiling. While tearing out the floor to reach the leak, he mistakenly ran a circular saw through a pipe, causing a considerably larger gusher that quickly destroyed said ceiling.
I understand these things happen. However, imagine my surprise when the eventual project cost was more than twice the estimated cost. He explained that repairing the new water damage was quite expensive and accounted for the variance with the estimate. We “discussed” this development, during which time I explained to him in no uncertain terms what the temperature in hell would be when I paid for his mistake.
So, it stung a bit to be called a “contractor.” But I could live with it. In fact, on the surface my patient’s analogy was quite good. Hospitalists do swoop in and fix patients’ problems only to then leave their lives, most often for good. It was only after a few days that her statement started to sour in my amygdala.
Habitual tardiness, sketchy response times, vague payment structures, lack of transparency in pricing, pricing errors into the cost of the job—I don’t think the analogy was intended to be so perceptive. I and the healthcare system within which I work really had adopted some of the less-desirable attributes of the contracting world.
I usually tell patients I’ll be back in an hour to give them their test results, knowing that I’m on “doctor time” and this could mean several hours or more. My tardiness usually results from being delayed while caring for another patient—but it’s all the same to the patient left waiting. Trying to build in cushion time for these unforeseen delays leaves a patient with a disagreeable contractor-like window of time to wait. For those who want to have their family at our daily rounds, an “I’ll come see you in the morning” is not just unhelpful—it disrespects the importance of their time.
Then there’s our payment system. It’s a mystery even to me: $12 aspirins, $100,000 cancer drugs, intentionally inflated professional fees and hospital bills that aren’t expected to be paid in full (unless the patient lacks an insurer to negotiate a lower price when they ironically are expected to foot the entire bill). All of which is made worse by the lack of transparency in our pricing. Patients (and most often I) simply are not privy to the costs of various tests and interventions. And, costs for the same procedure often differ among hospitals.
Few of us would contract for work without playing a role in choosing the supplies and knowing the rough cost of the materials. Yet that’s the situation our patients find themselves in daily.
Finally, expecting patients or their insurers to pay for my mistakes is not fair. I recognize there are adverse events that are unavoidable and should be reimbursed. However, many errors are as avoidable as being careful not to cut through a working pipe. Payment for these outcomes should be shouldered by the health system—not the patient.
I limped through the next few days re-examining my patient interactions. I licked my wounds, vowing to eschew those traits that so offend me as a consumer. I might not be able to repair a broken healthcare system, but I can refurbish the way I interact with my patients by being timely and responsive and not underestimating the effect of poor customer service. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado, Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
It was probably just the ramblings of a mad woman. Only she wasn’t mad, so I searched for a hint of delirium. Nothing. She was mentally fit and lucid—perhaps too lucid. Could it be true … had I become my archenemy?
To decide, I put her utterance to the test through the Kubler-Ross obstacle course, hopping the denial hurdle, quick-footing through the anger tire course, wading through the bargaining pool, and finally swinging safely across the depression crevasse to acceptance.
She was my eighth patient that day, a 78-year-old woman admitted to the orthopedic service with a hip fracture. I was asked to do a preoperative risk assessment and comanage her diabetes and heart failure. During our introductions she asked what kind of doctor I was.
“A hospitalist,” I replied.
“Oh … that’s nice,” she answered, her furrowed eyebrow transforming her crow’s feet into a question mark.
“You know, a doctor who only cares for patients in the hospital,” I clarified. “I just take care of your acute problems.”
“You think a broken hip is cute?”
“No, no, not ‘cute.’ Acute. You know, I only deal with your urgent problems. When you leave here you will go back to see your primary care doctor, who will follow up your hip fracture and your more chronic issues.”
That’s when she dropped the bomb.
“Oh, I see; you’re sort of like a contractor for my body then—just helping when things get broke.”
I should explain my aversion to this comment. Reared by a 10-thumbed father, I’m genetically incapable of curing even the simplest household hiccup. This doesn’t mean I haven’t or won’t try. In fact, I’m willing to try anything. My wife, however, is too smart to allow that. She knows that home improvement project plus me equals larger home improvement project. Combine this mathematical axiom with our turn-of-the-(20th)-century home, and it’s easy to see why I find myself betrothed in nearly continuous engagement with contractors.
But this is a marriage on the rocks. As dependent as I am on home contractors, I generally dislike working with them. They’re all fine people I’m sure, and truth be told most of them are quite skilled at their work. The problem is that they go about their job as if they are allergic to customer service.
The only contractors who are not perpetually late are those who won’t give you a time to meet. “I’ll meet you in the morning,” they’ll say, only to define morning as any time after the sun comes up.
Then there’s the estimate, which appears to be an approximation calculated in a cavernous ballpark using an underestimater. It’s also not exactly clear how or what goes into the calculation of an estimate.
I recently got a written estimate that read as follows: “Fix sink, $400.” When I asked what the $400 would go toward, I got the ever-so-helpful reply: “Fixing the sink.” I responded, “No, I mean, how much are the parts and the labor and things like that?” He gruffly countered, “Four hundred dollars.” Uncovering how he came up with this estimate was about as easy as solving a Rubik’s cube. I gave up trying—and eventually paid $550.
Another time, a contractor agreed to fix a plumbing leak in our upstairs bathroom that had caused water damage to our first-floor ceiling. While tearing out the floor to reach the leak, he mistakenly ran a circular saw through a pipe, causing a considerably larger gusher that quickly destroyed said ceiling.
I understand these things happen. However, imagine my surprise when the eventual project cost was more than twice the estimated cost. He explained that repairing the new water damage was quite expensive and accounted for the variance with the estimate. We “discussed” this development, during which time I explained to him in no uncertain terms what the temperature in hell would be when I paid for his mistake.
So, it stung a bit to be called a “contractor.” But I could live with it. In fact, on the surface my patient’s analogy was quite good. Hospitalists do swoop in and fix patients’ problems only to then leave their lives, most often for good. It was only after a few days that her statement started to sour in my amygdala.
Habitual tardiness, sketchy response times, vague payment structures, lack of transparency in pricing, pricing errors into the cost of the job—I don’t think the analogy was intended to be so perceptive. I and the healthcare system within which I work really had adopted some of the less-desirable attributes of the contracting world.
I usually tell patients I’ll be back in an hour to give them their test results, knowing that I’m on “doctor time” and this could mean several hours or more. My tardiness usually results from being delayed while caring for another patient—but it’s all the same to the patient left waiting. Trying to build in cushion time for these unforeseen delays leaves a patient with a disagreeable contractor-like window of time to wait. For those who want to have their family at our daily rounds, an “I’ll come see you in the morning” is not just unhelpful—it disrespects the importance of their time.
Then there’s our payment system. It’s a mystery even to me: $12 aspirins, $100,000 cancer drugs, intentionally inflated professional fees and hospital bills that aren’t expected to be paid in full (unless the patient lacks an insurer to negotiate a lower price when they ironically are expected to foot the entire bill). All of which is made worse by the lack of transparency in our pricing. Patients (and most often I) simply are not privy to the costs of various tests and interventions. And, costs for the same procedure often differ among hospitals.
Few of us would contract for work without playing a role in choosing the supplies and knowing the rough cost of the materials. Yet that’s the situation our patients find themselves in daily.
Finally, expecting patients or their insurers to pay for my mistakes is not fair. I recognize there are adverse events that are unavoidable and should be reimbursed. However, many errors are as avoidable as being careful not to cut through a working pipe. Payment for these outcomes should be shouldered by the health system—not the patient.
I limped through the next few days re-examining my patient interactions. I licked my wounds, vowing to eschew those traits that so offend me as a consumer. I might not be able to repair a broken healthcare system, but I can refurbish the way I interact with my patients by being timely and responsive and not underestimating the effect of poor customer service. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado, Denver, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Coat Tales
Russ Cucina, MD, MS, a hospitalist at the University of California San Francisco (UCSF) Medical Center, and a colleague once spent a week wearing pedometers on the job to study how much ground they covered in the course of managing their patient caseloads in a huge hospital like UCSF. The result: an average of four miles walked per day.
“The usual productivity infrastructure for physicians in their offices is simply not as available to hospitalists, or isn’t under our control,” Dr. Cucina says. There may be networked computer terminals throughout the hospital, but how many there are, how accessible they are, and how much competition there is for them varies. Hospitalists may have their own offices, desks or shared office space, depending on institutional commitments, but these may be a trek from patient care areas.
As a result, they must bring essential tools of their trade on their persons. Some carry a briefcase or wear a fanny pack, but more often these essential tools are stuffed into every available pocket of their medical lab coats.
Dr. Cucina’s short list of essentials is typical of working hospitalists. It includes his “smart phone,” combining a personal digital assistant (PDA) and cell phone, pens, a reflex hammer, a tuning fork for testing neurologic sensitivities, a stethoscope, swabs for sterilizing the stethoscope, a stash of large hospital gloves (which can be a hard size to find), and a bulky and awkward—but secure—prescription pad in a cardstock wrapper.
He also totes a stack of 3-by-5-inch index cards held together with a steel ring—one card for each active patient, updated daily by hand with medication changes, lab results and other information provided by the residents. “I have tried higher-tech approaches,” he explains. “I am the hospital’s associate medical director for information technology, and I need to keep up to date and try new things, including the various applications for keeping patient lists on line. But nothing has yet beaten out hand-written index cards for efficiency and ease of use. The time it takes to input this information electronically just isn’t worth it.”
Hospitalists say additional medical tools, such as an otoscope or ophthalmoscope, could be helpful but may pile on too much bulk and weight. “I’m often challenged to find one on the floor when I really need it,” Dr. Cucina says. Portable scopes are also quite valuable and at some risk for disappearing from an unattended lab coat in the highly trafficked hospital setting.
PDA Is No Panacea
For many hospitalists, one key to efficient mobility on the job is the PDA or laptop computer, with basic references such as UpToDate, Epocrates, Tarascon Pocket Pharmacopoeia, or the Washington Manual of Medical Therapeutics, either loaded or accessed via the Internet. PDAs involve serious compromises balancing size and weight with ease of keyboard use, ease of reading the screen, and memory or processing speed. (See “Tackle Technology,” November 2007, p. 22 for a discussion of how hospitalists use portable computing devices on the job.)
“We’ve come a long way from tongue depressors and otoscopes,” says William Ford, MD, program medical director for Cogent Healthcare’s large and expanding hospitalist group based at Temple University, Collegeville, Pa. “Some of us at Temple, depending on the service, carry one or more cell phones and between one and three pagers, in a pocket or attached to a belt.” The doctors may have their own PDAs, but Cogent no longer supplies them, having converted to a Web-based tool that offers a variety of practice management resources accessed by laptop computers via the Internet.
Dr. Cucina believes the technology is evolving toward a tablet device that will integrate more of the resource databases hospitalists need in their daily practice with other essential functions, such as lab results, billing, and communications with primary physicians—all in a user-friendly scale and format. In the meantime, there’s still a lot that has to be stuffed into pockets.
Some hospitalists also prefer to hold favorite reference resources, such as the pocket-sized Sanford Guide to Antimicrobial Therapy in their hands. That also involves tradeoffs, notes Michelle Pezzani, MD, hospitalist at El Camino Hospital in Mountain View, Calif.
“I tried carrying a book bag over my shoulder, but I felt like a school kid,” Dr. Pezzani relates. “I also noticed that the more reference books I had stuffed into my pockets, the less confidence other people seemed to have in me as a physician.” Not to mention that her pockets ripped open from the weight. She even developed a sore neck from her ergonomically unbalanced, overstuffed lab coat.
“Although I love being a hospitalist, it’s getting to the point where I feel disorganized because I have no real home base,” Dr. Pezzani laments. She finds her hospitalist group’s shared office—a converted labor-and-delivery room with no windows and three desktop computers for nine doctors—less than ideal. She spends as little time as possible there.
“My life would be easier if I didn’t have to carry my office in my pockets—my ink-stained pockets,” she says. “I can’t carry my laptop around with me because of the neck pain, so I asked the hospital to give me a locker closer to the middle of the building. It has also become a kind of science for me to transfer a few personal essentials into a little satchel with a string that I wear around my neck,” since a purse is not feasible.
Love/Hate Situation
Dr. Cucina uses an online custom supplier of medical lab coats with extra, zippered pockets on the inside and outside. He’s careful not to let the lab coat of out his sight when he takes it off.
Randy Ferrance, MD, a hospitalist in internal medicine and pediatrics at Riverside Tappahannock Hospital in Tappahannock, Va., acknowledges his own love-hate relationship with the lab coat. In his pockets, he carries a stack of 3-by-5-inch index cards, an 8.5-by-11-inch hospital census sheet, folded over, a prescription pad, a highlighter pen and spare pens, the ubiquitous stethoscope, an EKG caliper, a reflex hammer with microfilament test for diabetes, and a pocket Sanford Guide.
“I’d love to ditch the lab coat,” Dr. Ferrance says. “I often take it off when I sit down and sometimes end up leaving it behind, such as in the medical dictation area. I never want to wear one when I’m talking to a child. But for a lot of families of patients who are critically ill, it is a symbol, almost like the armor of the knighthood of medicine. You have to read each family, but for some, you lose credibility when you take it off. They’re looking for everything that medicine can offer, and the lab coat gives them more confidence in you.”
Dr. Ferrance appreciates the smaller size of his 47-bed hospital, where he is never a long walk from anyplace. He frequently returns during the day to his office, which he doesn’t have to share with other doctors. He uses it for family conferences and to store larger manuals, his laptop, and diagnostic kits.
He also values his Treo Smart phone, which incorporates a variety of programs, including a drug reference, billing program, lab reports on active patients, pediatric growth chart program, pneumonia severity index calculator, a medical calculator, Geriatrics At Your Fingertips, the Harriet Lane Handbook: A Manual for Pediatric House Officers, the American Association of Pediatrics’ Redbook comprehensive online infectious disease resource, hospice eligibility criteria, a camera—“to take pictures of odd lesions”—and access to e-mail and sports scores.
Although a briefcase is one more thing to lug around and risk losing, Julia Wright, MD, director of hospital medicine at the University of Wisconsin Hospital in Madison, says she carries a bag that is a woman’s version of a briefcase, with her laptop and active administrative files required for her growing administrative duties as director of an academic hospitalist group.
“There are advantages to being mobile, but disadvantages as well,” Dr. Wright says. “You just can’t get everything done. I get between 50 and 60 phone pages a day, and a lot of curbside consults, as well.” The medical center is restructuring teaching services so a hospitalist’s assigned patients would be more often concentrated in one area, with less running from floor to floor, as well as exploring new office facilities for the hospitalist group.
Currently, 11 University of Wisconsin hospitalists share a room with five cubicles. “I’ve put my pictures up on the wall anyway, and I keep my files, stapler, and office supplies there. A couple of my partners keep their reference books there. What I like about sharing space like this is it can help with communication and collegiality within the group. We do a lot of patient hand-offs there. But as we grow and it becomes more crowded, we’re going to need some more dedicated space.” TH
Larry Beresford is a medical writer based in California.
Russ Cucina, MD, MS, a hospitalist at the University of California San Francisco (UCSF) Medical Center, and a colleague once spent a week wearing pedometers on the job to study how much ground they covered in the course of managing their patient caseloads in a huge hospital like UCSF. The result: an average of four miles walked per day.
“The usual productivity infrastructure for physicians in their offices is simply not as available to hospitalists, or isn’t under our control,” Dr. Cucina says. There may be networked computer terminals throughout the hospital, but how many there are, how accessible they are, and how much competition there is for them varies. Hospitalists may have their own offices, desks or shared office space, depending on institutional commitments, but these may be a trek from patient care areas.
As a result, they must bring essential tools of their trade on their persons. Some carry a briefcase or wear a fanny pack, but more often these essential tools are stuffed into every available pocket of their medical lab coats.
Dr. Cucina’s short list of essentials is typical of working hospitalists. It includes his “smart phone,” combining a personal digital assistant (PDA) and cell phone, pens, a reflex hammer, a tuning fork for testing neurologic sensitivities, a stethoscope, swabs for sterilizing the stethoscope, a stash of large hospital gloves (which can be a hard size to find), and a bulky and awkward—but secure—prescription pad in a cardstock wrapper.
He also totes a stack of 3-by-5-inch index cards held together with a steel ring—one card for each active patient, updated daily by hand with medication changes, lab results and other information provided by the residents. “I have tried higher-tech approaches,” he explains. “I am the hospital’s associate medical director for information technology, and I need to keep up to date and try new things, including the various applications for keeping patient lists on line. But nothing has yet beaten out hand-written index cards for efficiency and ease of use. The time it takes to input this information electronically just isn’t worth it.”
Hospitalists say additional medical tools, such as an otoscope or ophthalmoscope, could be helpful but may pile on too much bulk and weight. “I’m often challenged to find one on the floor when I really need it,” Dr. Cucina says. Portable scopes are also quite valuable and at some risk for disappearing from an unattended lab coat in the highly trafficked hospital setting.
PDA Is No Panacea
For many hospitalists, one key to efficient mobility on the job is the PDA or laptop computer, with basic references such as UpToDate, Epocrates, Tarascon Pocket Pharmacopoeia, or the Washington Manual of Medical Therapeutics, either loaded or accessed via the Internet. PDAs involve serious compromises balancing size and weight with ease of keyboard use, ease of reading the screen, and memory or processing speed. (See “Tackle Technology,” November 2007, p. 22 for a discussion of how hospitalists use portable computing devices on the job.)
“We’ve come a long way from tongue depressors and otoscopes,” says William Ford, MD, program medical director for Cogent Healthcare’s large and expanding hospitalist group based at Temple University, Collegeville, Pa. “Some of us at Temple, depending on the service, carry one or more cell phones and between one and three pagers, in a pocket or attached to a belt.” The doctors may have their own PDAs, but Cogent no longer supplies them, having converted to a Web-based tool that offers a variety of practice management resources accessed by laptop computers via the Internet.
Dr. Cucina believes the technology is evolving toward a tablet device that will integrate more of the resource databases hospitalists need in their daily practice with other essential functions, such as lab results, billing, and communications with primary physicians—all in a user-friendly scale and format. In the meantime, there’s still a lot that has to be stuffed into pockets.
Some hospitalists also prefer to hold favorite reference resources, such as the pocket-sized Sanford Guide to Antimicrobial Therapy in their hands. That also involves tradeoffs, notes Michelle Pezzani, MD, hospitalist at El Camino Hospital in Mountain View, Calif.
“I tried carrying a book bag over my shoulder, but I felt like a school kid,” Dr. Pezzani relates. “I also noticed that the more reference books I had stuffed into my pockets, the less confidence other people seemed to have in me as a physician.” Not to mention that her pockets ripped open from the weight. She even developed a sore neck from her ergonomically unbalanced, overstuffed lab coat.
“Although I love being a hospitalist, it’s getting to the point where I feel disorganized because I have no real home base,” Dr. Pezzani laments. She finds her hospitalist group’s shared office—a converted labor-and-delivery room with no windows and three desktop computers for nine doctors—less than ideal. She spends as little time as possible there.
“My life would be easier if I didn’t have to carry my office in my pockets—my ink-stained pockets,” she says. “I can’t carry my laptop around with me because of the neck pain, so I asked the hospital to give me a locker closer to the middle of the building. It has also become a kind of science for me to transfer a few personal essentials into a little satchel with a string that I wear around my neck,” since a purse is not feasible.
Love/Hate Situation
Dr. Cucina uses an online custom supplier of medical lab coats with extra, zippered pockets on the inside and outside. He’s careful not to let the lab coat of out his sight when he takes it off.
Randy Ferrance, MD, a hospitalist in internal medicine and pediatrics at Riverside Tappahannock Hospital in Tappahannock, Va., acknowledges his own love-hate relationship with the lab coat. In his pockets, he carries a stack of 3-by-5-inch index cards, an 8.5-by-11-inch hospital census sheet, folded over, a prescription pad, a highlighter pen and spare pens, the ubiquitous stethoscope, an EKG caliper, a reflex hammer with microfilament test for diabetes, and a pocket Sanford Guide.
“I’d love to ditch the lab coat,” Dr. Ferrance says. “I often take it off when I sit down and sometimes end up leaving it behind, such as in the medical dictation area. I never want to wear one when I’m talking to a child. But for a lot of families of patients who are critically ill, it is a symbol, almost like the armor of the knighthood of medicine. You have to read each family, but for some, you lose credibility when you take it off. They’re looking for everything that medicine can offer, and the lab coat gives them more confidence in you.”
Dr. Ferrance appreciates the smaller size of his 47-bed hospital, where he is never a long walk from anyplace. He frequently returns during the day to his office, which he doesn’t have to share with other doctors. He uses it for family conferences and to store larger manuals, his laptop, and diagnostic kits.
He also values his Treo Smart phone, which incorporates a variety of programs, including a drug reference, billing program, lab reports on active patients, pediatric growth chart program, pneumonia severity index calculator, a medical calculator, Geriatrics At Your Fingertips, the Harriet Lane Handbook: A Manual for Pediatric House Officers, the American Association of Pediatrics’ Redbook comprehensive online infectious disease resource, hospice eligibility criteria, a camera—“to take pictures of odd lesions”—and access to e-mail and sports scores.
Although a briefcase is one more thing to lug around and risk losing, Julia Wright, MD, director of hospital medicine at the University of Wisconsin Hospital in Madison, says she carries a bag that is a woman’s version of a briefcase, with her laptop and active administrative files required for her growing administrative duties as director of an academic hospitalist group.
“There are advantages to being mobile, but disadvantages as well,” Dr. Wright says. “You just can’t get everything done. I get between 50 and 60 phone pages a day, and a lot of curbside consults, as well.” The medical center is restructuring teaching services so a hospitalist’s assigned patients would be more often concentrated in one area, with less running from floor to floor, as well as exploring new office facilities for the hospitalist group.
Currently, 11 University of Wisconsin hospitalists share a room with five cubicles. “I’ve put my pictures up on the wall anyway, and I keep my files, stapler, and office supplies there. A couple of my partners keep their reference books there. What I like about sharing space like this is it can help with communication and collegiality within the group. We do a lot of patient hand-offs there. But as we grow and it becomes more crowded, we’re going to need some more dedicated space.” TH
Larry Beresford is a medical writer based in California.
Russ Cucina, MD, MS, a hospitalist at the University of California San Francisco (UCSF) Medical Center, and a colleague once spent a week wearing pedometers on the job to study how much ground they covered in the course of managing their patient caseloads in a huge hospital like UCSF. The result: an average of four miles walked per day.
“The usual productivity infrastructure for physicians in their offices is simply not as available to hospitalists, or isn’t under our control,” Dr. Cucina says. There may be networked computer terminals throughout the hospital, but how many there are, how accessible they are, and how much competition there is for them varies. Hospitalists may have their own offices, desks or shared office space, depending on institutional commitments, but these may be a trek from patient care areas.
As a result, they must bring essential tools of their trade on their persons. Some carry a briefcase or wear a fanny pack, but more often these essential tools are stuffed into every available pocket of their medical lab coats.
Dr. Cucina’s short list of essentials is typical of working hospitalists. It includes his “smart phone,” combining a personal digital assistant (PDA) and cell phone, pens, a reflex hammer, a tuning fork for testing neurologic sensitivities, a stethoscope, swabs for sterilizing the stethoscope, a stash of large hospital gloves (which can be a hard size to find), and a bulky and awkward—but secure—prescription pad in a cardstock wrapper.
He also totes a stack of 3-by-5-inch index cards held together with a steel ring—one card for each active patient, updated daily by hand with medication changes, lab results and other information provided by the residents. “I have tried higher-tech approaches,” he explains. “I am the hospital’s associate medical director for information technology, and I need to keep up to date and try new things, including the various applications for keeping patient lists on line. But nothing has yet beaten out hand-written index cards for efficiency and ease of use. The time it takes to input this information electronically just isn’t worth it.”
Hospitalists say additional medical tools, such as an otoscope or ophthalmoscope, could be helpful but may pile on too much bulk and weight. “I’m often challenged to find one on the floor when I really need it,” Dr. Cucina says. Portable scopes are also quite valuable and at some risk for disappearing from an unattended lab coat in the highly trafficked hospital setting.
PDA Is No Panacea
For many hospitalists, one key to efficient mobility on the job is the PDA or laptop computer, with basic references such as UpToDate, Epocrates, Tarascon Pocket Pharmacopoeia, or the Washington Manual of Medical Therapeutics, either loaded or accessed via the Internet. PDAs involve serious compromises balancing size and weight with ease of keyboard use, ease of reading the screen, and memory or processing speed. (See “Tackle Technology,” November 2007, p. 22 for a discussion of how hospitalists use portable computing devices on the job.)
“We’ve come a long way from tongue depressors and otoscopes,” says William Ford, MD, program medical director for Cogent Healthcare’s large and expanding hospitalist group based at Temple University, Collegeville, Pa. “Some of us at Temple, depending on the service, carry one or more cell phones and between one and three pagers, in a pocket or attached to a belt.” The doctors may have their own PDAs, but Cogent no longer supplies them, having converted to a Web-based tool that offers a variety of practice management resources accessed by laptop computers via the Internet.
Dr. Cucina believes the technology is evolving toward a tablet device that will integrate more of the resource databases hospitalists need in their daily practice with other essential functions, such as lab results, billing, and communications with primary physicians—all in a user-friendly scale and format. In the meantime, there’s still a lot that has to be stuffed into pockets.
Some hospitalists also prefer to hold favorite reference resources, such as the pocket-sized Sanford Guide to Antimicrobial Therapy in their hands. That also involves tradeoffs, notes Michelle Pezzani, MD, hospitalist at El Camino Hospital in Mountain View, Calif.
“I tried carrying a book bag over my shoulder, but I felt like a school kid,” Dr. Pezzani relates. “I also noticed that the more reference books I had stuffed into my pockets, the less confidence other people seemed to have in me as a physician.” Not to mention that her pockets ripped open from the weight. She even developed a sore neck from her ergonomically unbalanced, overstuffed lab coat.
“Although I love being a hospitalist, it’s getting to the point where I feel disorganized because I have no real home base,” Dr. Pezzani laments. She finds her hospitalist group’s shared office—a converted labor-and-delivery room with no windows and three desktop computers for nine doctors—less than ideal. She spends as little time as possible there.
“My life would be easier if I didn’t have to carry my office in my pockets—my ink-stained pockets,” she says. “I can’t carry my laptop around with me because of the neck pain, so I asked the hospital to give me a locker closer to the middle of the building. It has also become a kind of science for me to transfer a few personal essentials into a little satchel with a string that I wear around my neck,” since a purse is not feasible.
Love/Hate Situation
Dr. Cucina uses an online custom supplier of medical lab coats with extra, zippered pockets on the inside and outside. He’s careful not to let the lab coat of out his sight when he takes it off.
Randy Ferrance, MD, a hospitalist in internal medicine and pediatrics at Riverside Tappahannock Hospital in Tappahannock, Va., acknowledges his own love-hate relationship with the lab coat. In his pockets, he carries a stack of 3-by-5-inch index cards, an 8.5-by-11-inch hospital census sheet, folded over, a prescription pad, a highlighter pen and spare pens, the ubiquitous stethoscope, an EKG caliper, a reflex hammer with microfilament test for diabetes, and a pocket Sanford Guide.
“I’d love to ditch the lab coat,” Dr. Ferrance says. “I often take it off when I sit down and sometimes end up leaving it behind, such as in the medical dictation area. I never want to wear one when I’m talking to a child. But for a lot of families of patients who are critically ill, it is a symbol, almost like the armor of the knighthood of medicine. You have to read each family, but for some, you lose credibility when you take it off. They’re looking for everything that medicine can offer, and the lab coat gives them more confidence in you.”
Dr. Ferrance appreciates the smaller size of his 47-bed hospital, where he is never a long walk from anyplace. He frequently returns during the day to his office, which he doesn’t have to share with other doctors. He uses it for family conferences and to store larger manuals, his laptop, and diagnostic kits.
He also values his Treo Smart phone, which incorporates a variety of programs, including a drug reference, billing program, lab reports on active patients, pediatric growth chart program, pneumonia severity index calculator, a medical calculator, Geriatrics At Your Fingertips, the Harriet Lane Handbook: A Manual for Pediatric House Officers, the American Association of Pediatrics’ Redbook comprehensive online infectious disease resource, hospice eligibility criteria, a camera—“to take pictures of odd lesions”—and access to e-mail and sports scores.
Although a briefcase is one more thing to lug around and risk losing, Julia Wright, MD, director of hospital medicine at the University of Wisconsin Hospital in Madison, says she carries a bag that is a woman’s version of a briefcase, with her laptop and active administrative files required for her growing administrative duties as director of an academic hospitalist group.
“There are advantages to being mobile, but disadvantages as well,” Dr. Wright says. “You just can’t get everything done. I get between 50 and 60 phone pages a day, and a lot of curbside consults, as well.” The medical center is restructuring teaching services so a hospitalist’s assigned patients would be more often concentrated in one area, with less running from floor to floor, as well as exploring new office facilities for the hospitalist group.
Currently, 11 University of Wisconsin hospitalists share a room with five cubicles. “I’ve put my pictures up on the wall anyway, and I keep my files, stapler, and office supplies there. A couple of my partners keep their reference books there. What I like about sharing space like this is it can help with communication and collegiality within the group. We do a lot of patient hand-offs there. But as we grow and it becomes more crowded, we’re going to need some more dedicated space.” TH
Larry Beresford is a medical writer based in California.
The Patient Has Left the Building
The hospitalist service at the University of Wisconsin Hospital and Clinics in the Department of Medicine recently admitted a patient with altered sensorium, which the team determined most likely was narcotic-related. Going the extra distance, they did a spinal tap to rule out meningitis.
Within a day of changing the medication, the patient got better and was ready for discharge. However, says Julia S. Wright, MD, director of the Madison-based service, an important test remained from the spinal tap. “We thought that those results would not change the medical management of the case, but we knew if it were positive, it would be a big deal,” she recalls.
Not all medical-legal experts would agree the responsibility for patient care ends when patients leave the hospital. Often there are extenuating circumstances that may warrant the hospitalist’s continued communication and contact with patients and/or their providers and caregivers. Although there are no universally accepted standards of care that define these post-discharge issues, several hospitalists recently discussed their institutions’ and groups’ guiding principles for managing the nuances of post-discharge protocol.
Who’s Responsible?
Hospitalist Jeffrey Greenwald, MD, associate professor of medicine at Boston University School of Medicine, is a member of SHM’s Hospital Quality and Patient Safety Committee and also has been investigating pre- and post-discharge interventions through a grant-funded project from the Agency for Healthcare Research and Quality (AHRQ) called “Project RED” (the Re-Engineered Discharge, online at www.ahrq.gov/qual/pips).
One reason the post-discharge period is a “gray zone” of responsibility for care, he believes, is that the hospital system was designed to have a finite endpoint—the discharge. “This ‘out of sight, out of mind’ mentality has existed forever in the inpatient service, but it has become more highlighted in the post-hospitalist era,” he notes.
That mentality can sometimes take over in the hospitalists’ minds. “I think a lot of hospitalists are burying their heads [in the sand] about how these patients are being sent home and the chances for miscommunication and a ‘bounce-back,’ ” notes David Yu, MD, FACP, ABIM, medical director of hospitalist services, Decatur Memorial Hospital, Decatur, Ill., and clinical assistant professor of family and community medicine, Southern Illinois University School of Medicine. “This is going to be more of an issue as hospitalists become increasingly busy. The temptation is to squeeze time on discharges, because it takes an effort to reconcile medications and tie up loose ends at time of discharge. It is not acceptable to write, ‘resume current medications and follow up with PCP’ and think the job is done. It is magical thinking that discharge medications and follow-up instructions will be figured out somehow by the patient and discharging nurse.”
Cover the Gray Zone
Hospitalists describe differing approaches to ensuring patients get the care they need when they leave the hospital.
In the case of the UWHC patient who wanted to leave the hospital, the hospitalist team arranged to stay in touch with the patient. They watched for the test results during the next 24 hours. When the test came back positive, they called the patient back to the hospital, and began treatment.
“Although tracking test results may be out of the hospitalist’s purview, I think we have a strong obligation to make sure we look at some of that data,” Dr. Wright says. “I think there has to be some redundancy, otherwise, the patient probably would not have seen the primary care physician in time and would have become more ill.”
Attention to detail before discharge can avoid problems in the post-discharge period. Partnering with the pharmacy to achieve medication reconciliation has been shown to reduce risk of readmission, notes Tom Bookwalter, PharmD, associate professor of health sciences at the University of California San Francisco School of Medicine and formerly clinical pharmacist there. Using standardized templates and electronic medical records (EMR), hospitalists at many academic centers can furnish real-time discharge summaries to patients’ primary care physicians.
Dr. Yu is especially proud of the EMR system at his institution, by which discharge summaries are faxed to the primary care physician (PCP) in real time. “A patient can call their primary care physician right after discharge, and that physician will know exactly what happened during the hospital course, and what the medications and the discharge plan are,” he explains.
In addition, computerized entry and transmission eliminates the risk of error introduced when handwritten instructions are given to patients. “We believe that communication is the ‘mother’s milk’ of the hospitalist,” Dr. Yu says. Accordingly, his hospitalist service also makes a courtesy call to the PCP following transmission of the EMR for the patient.
Attorney Patrick T. O’Rourke of the Office of University Counsel at Colorado University in Denver and legal columnist for The Hospitalist, advises how to avoid inviting unintended legal consequences. “It’s important for hospitalists to understand that they are the conduit of information about what happened during the hospitalization,” he notes. “Failing to define everyone’s job in the discharge process can expose people to liability.”
In that vein, he urges hospitalists not to delegate the process of giving discharge instructions to the patient. Patients should hear directly from the hospitalist about their condition, the recommended course of action, and how to respond in case of emergency post-discharge. When returning the patient to their regular physician, the hospitalist should also touch base with the patient’s physician via e-mail or telephone to prevent gaps in communication.
Other Strategies
If budgets allow, some groups employ ancillary staff who call patients after discharge.
Hospitalist David Grace, MD, area medical officer for the Schumacher Group, Hospital Medicine Division, in Lafayette, La., reports that having a practice coordinator who calls patients within 48 hours of discharge “adds one more layer of safety to the process.” “Yes” answers to some questions (e.g., “Have your symptoms worsened? Do you have any new symptoms?”) trigger follow-up calls to the on-call hospitalist to take appropriate steps. However, O’Rourke cautions that midlevel providers should possess adequate training to be able to act appropriately upon patients’ information.
Hospitalist Randy Ferrance, DC, MD, medical director at Riverside Tappahannock Hospice in Tappahannock, Va., agrees follow-up calls to patients are a good idea. “I think more aggressive follow up in the short term, and then turning the patient over, for continuity reasons, to their primary care physician as quickly as possible is very important.” His hospitalist group, comprising only four staff, struggles with having the time to devote to such activities. However, with an average inpatient age of 72, their patients often transition to home healthcare. His group enjoys an “excellent relationship” with all the area home health agencies. Those agencies are asked to call the hospitalist group during their first visit with the patient, in addition to sending their usual report to the primary care physician. “At that first home health visit, we consider ourselves still responsible for the patient,” he says.
Beyond Liability Protection
Adhering to the “higher standard” of patient safety can improve transitions of care even further, Dr. Greenwald believes. Such actions might include a mechanism for patients to reach a member of the hospitalist team (nurse, pharmacist or physician) if they have post-discharge concerns; empowering patients and family members to know what to do if an adverse event occurs; and enabling patients to have copies of their own medical information (discharge summary, lab tests, medication reconciliations).
“In addition, we need to involve the nonmedical caregivers who are going to help the patient recuperate,” he asserts. Physicians can educate patients and their caregivers about what happened while they were in the hospital, what treatments are planned, and what information is pending at discharge. While these efforts might require that hospitalists shift their thinking about doctor-patient roles, they can help to create a more comprehensive approach to patient care.
Inherent Dangers
Ironically, what hospitalists do best—promote effective inpatient management—can also lead to a disconnect when the patient leaves the hospital. “Part of what we do, as hospitalists, is to drive down the patient’s length of stay and get them home sooner,” Dr. Grace says. “While unquestionably beneficial for a variety of reasons, it increases the chance that a patient can leave before a result comes back.”
“This change from the continuity of healthcare [provided by a physician who also saw his or her hospitalized patients] to a division of labor does have some inherent fragmentation,” agrees Dr. Wright. “We need to still look at the patient as a whole and be in communication with [our primary care colleagues] and supporting each other on both ends so that the patient does get this more comprehensive care.” TH
Gretchen Henkel is a medical writer based in California.
The hospitalist service at the University of Wisconsin Hospital and Clinics in the Department of Medicine recently admitted a patient with altered sensorium, which the team determined most likely was narcotic-related. Going the extra distance, they did a spinal tap to rule out meningitis.
Within a day of changing the medication, the patient got better and was ready for discharge. However, says Julia S. Wright, MD, director of the Madison-based service, an important test remained from the spinal tap. “We thought that those results would not change the medical management of the case, but we knew if it were positive, it would be a big deal,” she recalls.
Not all medical-legal experts would agree the responsibility for patient care ends when patients leave the hospital. Often there are extenuating circumstances that may warrant the hospitalist’s continued communication and contact with patients and/or their providers and caregivers. Although there are no universally accepted standards of care that define these post-discharge issues, several hospitalists recently discussed their institutions’ and groups’ guiding principles for managing the nuances of post-discharge protocol.
Who’s Responsible?
Hospitalist Jeffrey Greenwald, MD, associate professor of medicine at Boston University School of Medicine, is a member of SHM’s Hospital Quality and Patient Safety Committee and also has been investigating pre- and post-discharge interventions through a grant-funded project from the Agency for Healthcare Research and Quality (AHRQ) called “Project RED” (the Re-Engineered Discharge, online at www.ahrq.gov/qual/pips).
One reason the post-discharge period is a “gray zone” of responsibility for care, he believes, is that the hospital system was designed to have a finite endpoint—the discharge. “This ‘out of sight, out of mind’ mentality has existed forever in the inpatient service, but it has become more highlighted in the post-hospitalist era,” he notes.
That mentality can sometimes take over in the hospitalists’ minds. “I think a lot of hospitalists are burying their heads [in the sand] about how these patients are being sent home and the chances for miscommunication and a ‘bounce-back,’ ” notes David Yu, MD, FACP, ABIM, medical director of hospitalist services, Decatur Memorial Hospital, Decatur, Ill., and clinical assistant professor of family and community medicine, Southern Illinois University School of Medicine. “This is going to be more of an issue as hospitalists become increasingly busy. The temptation is to squeeze time on discharges, because it takes an effort to reconcile medications and tie up loose ends at time of discharge. It is not acceptable to write, ‘resume current medications and follow up with PCP’ and think the job is done. It is magical thinking that discharge medications and follow-up instructions will be figured out somehow by the patient and discharging nurse.”
Cover the Gray Zone
Hospitalists describe differing approaches to ensuring patients get the care they need when they leave the hospital.
In the case of the UWHC patient who wanted to leave the hospital, the hospitalist team arranged to stay in touch with the patient. They watched for the test results during the next 24 hours. When the test came back positive, they called the patient back to the hospital, and began treatment.
“Although tracking test results may be out of the hospitalist’s purview, I think we have a strong obligation to make sure we look at some of that data,” Dr. Wright says. “I think there has to be some redundancy, otherwise, the patient probably would not have seen the primary care physician in time and would have become more ill.”
Attention to detail before discharge can avoid problems in the post-discharge period. Partnering with the pharmacy to achieve medication reconciliation has been shown to reduce risk of readmission, notes Tom Bookwalter, PharmD, associate professor of health sciences at the University of California San Francisco School of Medicine and formerly clinical pharmacist there. Using standardized templates and electronic medical records (EMR), hospitalists at many academic centers can furnish real-time discharge summaries to patients’ primary care physicians.
Dr. Yu is especially proud of the EMR system at his institution, by which discharge summaries are faxed to the primary care physician (PCP) in real time. “A patient can call their primary care physician right after discharge, and that physician will know exactly what happened during the hospital course, and what the medications and the discharge plan are,” he explains.
In addition, computerized entry and transmission eliminates the risk of error introduced when handwritten instructions are given to patients. “We believe that communication is the ‘mother’s milk’ of the hospitalist,” Dr. Yu says. Accordingly, his hospitalist service also makes a courtesy call to the PCP following transmission of the EMR for the patient.
Attorney Patrick T. O’Rourke of the Office of University Counsel at Colorado University in Denver and legal columnist for The Hospitalist, advises how to avoid inviting unintended legal consequences. “It’s important for hospitalists to understand that they are the conduit of information about what happened during the hospitalization,” he notes. “Failing to define everyone’s job in the discharge process can expose people to liability.”
In that vein, he urges hospitalists not to delegate the process of giving discharge instructions to the patient. Patients should hear directly from the hospitalist about their condition, the recommended course of action, and how to respond in case of emergency post-discharge. When returning the patient to their regular physician, the hospitalist should also touch base with the patient’s physician via e-mail or telephone to prevent gaps in communication.
Other Strategies
If budgets allow, some groups employ ancillary staff who call patients after discharge.
Hospitalist David Grace, MD, area medical officer for the Schumacher Group, Hospital Medicine Division, in Lafayette, La., reports that having a practice coordinator who calls patients within 48 hours of discharge “adds one more layer of safety to the process.” “Yes” answers to some questions (e.g., “Have your symptoms worsened? Do you have any new symptoms?”) trigger follow-up calls to the on-call hospitalist to take appropriate steps. However, O’Rourke cautions that midlevel providers should possess adequate training to be able to act appropriately upon patients’ information.
Hospitalist Randy Ferrance, DC, MD, medical director at Riverside Tappahannock Hospice in Tappahannock, Va., agrees follow-up calls to patients are a good idea. “I think more aggressive follow up in the short term, and then turning the patient over, for continuity reasons, to their primary care physician as quickly as possible is very important.” His hospitalist group, comprising only four staff, struggles with having the time to devote to such activities. However, with an average inpatient age of 72, their patients often transition to home healthcare. His group enjoys an “excellent relationship” with all the area home health agencies. Those agencies are asked to call the hospitalist group during their first visit with the patient, in addition to sending their usual report to the primary care physician. “At that first home health visit, we consider ourselves still responsible for the patient,” he says.
Beyond Liability Protection
Adhering to the “higher standard” of patient safety can improve transitions of care even further, Dr. Greenwald believes. Such actions might include a mechanism for patients to reach a member of the hospitalist team (nurse, pharmacist or physician) if they have post-discharge concerns; empowering patients and family members to know what to do if an adverse event occurs; and enabling patients to have copies of their own medical information (discharge summary, lab tests, medication reconciliations).
“In addition, we need to involve the nonmedical caregivers who are going to help the patient recuperate,” he asserts. Physicians can educate patients and their caregivers about what happened while they were in the hospital, what treatments are planned, and what information is pending at discharge. While these efforts might require that hospitalists shift their thinking about doctor-patient roles, they can help to create a more comprehensive approach to patient care.
Inherent Dangers
Ironically, what hospitalists do best—promote effective inpatient management—can also lead to a disconnect when the patient leaves the hospital. “Part of what we do, as hospitalists, is to drive down the patient’s length of stay and get them home sooner,” Dr. Grace says. “While unquestionably beneficial for a variety of reasons, it increases the chance that a patient can leave before a result comes back.”
“This change from the continuity of healthcare [provided by a physician who also saw his or her hospitalized patients] to a division of labor does have some inherent fragmentation,” agrees Dr. Wright. “We need to still look at the patient as a whole and be in communication with [our primary care colleagues] and supporting each other on both ends so that the patient does get this more comprehensive care.” TH
Gretchen Henkel is a medical writer based in California.
The hospitalist service at the University of Wisconsin Hospital and Clinics in the Department of Medicine recently admitted a patient with altered sensorium, which the team determined most likely was narcotic-related. Going the extra distance, they did a spinal tap to rule out meningitis.
Within a day of changing the medication, the patient got better and was ready for discharge. However, says Julia S. Wright, MD, director of the Madison-based service, an important test remained from the spinal tap. “We thought that those results would not change the medical management of the case, but we knew if it were positive, it would be a big deal,” she recalls.
Not all medical-legal experts would agree the responsibility for patient care ends when patients leave the hospital. Often there are extenuating circumstances that may warrant the hospitalist’s continued communication and contact with patients and/or their providers and caregivers. Although there are no universally accepted standards of care that define these post-discharge issues, several hospitalists recently discussed their institutions’ and groups’ guiding principles for managing the nuances of post-discharge protocol.
Who’s Responsible?
Hospitalist Jeffrey Greenwald, MD, associate professor of medicine at Boston University School of Medicine, is a member of SHM’s Hospital Quality and Patient Safety Committee and also has been investigating pre- and post-discharge interventions through a grant-funded project from the Agency for Healthcare Research and Quality (AHRQ) called “Project RED” (the Re-Engineered Discharge, online at www.ahrq.gov/qual/pips).
One reason the post-discharge period is a “gray zone” of responsibility for care, he believes, is that the hospital system was designed to have a finite endpoint—the discharge. “This ‘out of sight, out of mind’ mentality has existed forever in the inpatient service, but it has become more highlighted in the post-hospitalist era,” he notes.
That mentality can sometimes take over in the hospitalists’ minds. “I think a lot of hospitalists are burying their heads [in the sand] about how these patients are being sent home and the chances for miscommunication and a ‘bounce-back,’ ” notes David Yu, MD, FACP, ABIM, medical director of hospitalist services, Decatur Memorial Hospital, Decatur, Ill., and clinical assistant professor of family and community medicine, Southern Illinois University School of Medicine. “This is going to be more of an issue as hospitalists become increasingly busy. The temptation is to squeeze time on discharges, because it takes an effort to reconcile medications and tie up loose ends at time of discharge. It is not acceptable to write, ‘resume current medications and follow up with PCP’ and think the job is done. It is magical thinking that discharge medications and follow-up instructions will be figured out somehow by the patient and discharging nurse.”
Cover the Gray Zone
Hospitalists describe differing approaches to ensuring patients get the care they need when they leave the hospital.
In the case of the UWHC patient who wanted to leave the hospital, the hospitalist team arranged to stay in touch with the patient. They watched for the test results during the next 24 hours. When the test came back positive, they called the patient back to the hospital, and began treatment.
“Although tracking test results may be out of the hospitalist’s purview, I think we have a strong obligation to make sure we look at some of that data,” Dr. Wright says. “I think there has to be some redundancy, otherwise, the patient probably would not have seen the primary care physician in time and would have become more ill.”
Attention to detail before discharge can avoid problems in the post-discharge period. Partnering with the pharmacy to achieve medication reconciliation has been shown to reduce risk of readmission, notes Tom Bookwalter, PharmD, associate professor of health sciences at the University of California San Francisco School of Medicine and formerly clinical pharmacist there. Using standardized templates and electronic medical records (EMR), hospitalists at many academic centers can furnish real-time discharge summaries to patients’ primary care physicians.
Dr. Yu is especially proud of the EMR system at his institution, by which discharge summaries are faxed to the primary care physician (PCP) in real time. “A patient can call their primary care physician right after discharge, and that physician will know exactly what happened during the hospital course, and what the medications and the discharge plan are,” he explains.
In addition, computerized entry and transmission eliminates the risk of error introduced when handwritten instructions are given to patients. “We believe that communication is the ‘mother’s milk’ of the hospitalist,” Dr. Yu says. Accordingly, his hospitalist service also makes a courtesy call to the PCP following transmission of the EMR for the patient.
Attorney Patrick T. O’Rourke of the Office of University Counsel at Colorado University in Denver and legal columnist for The Hospitalist, advises how to avoid inviting unintended legal consequences. “It’s important for hospitalists to understand that they are the conduit of information about what happened during the hospitalization,” he notes. “Failing to define everyone’s job in the discharge process can expose people to liability.”
In that vein, he urges hospitalists not to delegate the process of giving discharge instructions to the patient. Patients should hear directly from the hospitalist about their condition, the recommended course of action, and how to respond in case of emergency post-discharge. When returning the patient to their regular physician, the hospitalist should also touch base with the patient’s physician via e-mail or telephone to prevent gaps in communication.
Other Strategies
If budgets allow, some groups employ ancillary staff who call patients after discharge.
Hospitalist David Grace, MD, area medical officer for the Schumacher Group, Hospital Medicine Division, in Lafayette, La., reports that having a practice coordinator who calls patients within 48 hours of discharge “adds one more layer of safety to the process.” “Yes” answers to some questions (e.g., “Have your symptoms worsened? Do you have any new symptoms?”) trigger follow-up calls to the on-call hospitalist to take appropriate steps. However, O’Rourke cautions that midlevel providers should possess adequate training to be able to act appropriately upon patients’ information.
Hospitalist Randy Ferrance, DC, MD, medical director at Riverside Tappahannock Hospice in Tappahannock, Va., agrees follow-up calls to patients are a good idea. “I think more aggressive follow up in the short term, and then turning the patient over, for continuity reasons, to their primary care physician as quickly as possible is very important.” His hospitalist group, comprising only four staff, struggles with having the time to devote to such activities. However, with an average inpatient age of 72, their patients often transition to home healthcare. His group enjoys an “excellent relationship” with all the area home health agencies. Those agencies are asked to call the hospitalist group during their first visit with the patient, in addition to sending their usual report to the primary care physician. “At that first home health visit, we consider ourselves still responsible for the patient,” he says.
Beyond Liability Protection
Adhering to the “higher standard” of patient safety can improve transitions of care even further, Dr. Greenwald believes. Such actions might include a mechanism for patients to reach a member of the hospitalist team (nurse, pharmacist or physician) if they have post-discharge concerns; empowering patients and family members to know what to do if an adverse event occurs; and enabling patients to have copies of their own medical information (discharge summary, lab tests, medication reconciliations).
“In addition, we need to involve the nonmedical caregivers who are going to help the patient recuperate,” he asserts. Physicians can educate patients and their caregivers about what happened while they were in the hospital, what treatments are planned, and what information is pending at discharge. While these efforts might require that hospitalists shift their thinking about doctor-patient roles, they can help to create a more comprehensive approach to patient care.
Inherent Dangers
Ironically, what hospitalists do best—promote effective inpatient management—can also lead to a disconnect when the patient leaves the hospital. “Part of what we do, as hospitalists, is to drive down the patient’s length of stay and get them home sooner,” Dr. Grace says. “While unquestionably beneficial for a variety of reasons, it increases the chance that a patient can leave before a result comes back.”
“This change from the continuity of healthcare [provided by a physician who also saw his or her hospitalized patients] to a division of labor does have some inherent fragmentation,” agrees Dr. Wright. “We need to still look at the patient as a whole and be in communication with [our primary care colleagues] and supporting each other on both ends so that the patient does get this more comprehensive care.” TH
Gretchen Henkel is a medical writer based in California.
Do post-discharge telephone calls to patients reduce the rate of complications?
Case
A 75-year-old male with history of diabetes and heart disease is discharged from the hospital after treatment for pneumonia. He has eight medications on his discharge list and is given two new prescriptions at discharge. He has a primary care provider but will not be able to see her until three weeks after discharge. Will a follow-up call decrease potential complications?
Overview
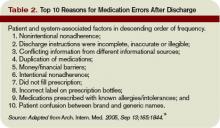
Medication errors are prevalent, especially during the transition period from discharge to follow-up with primary care physicians. There are more than 700,000 emergency department (ED) visits each year for adverse drug events with nearly 120,000 of these episodes resulting in hospitalization.1
The likelihood of an adverse drug event increases in patients using more than five medications and when there is a lack of understanding of how and why they are taking certain medications, scenarios common on hospital discharge.2 Studies evaluating effective means to reduce medication errors during transitions out of the hospital offer few solutions. One effective method, however, appears to be follow-up telephone calls.
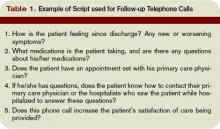
Telephone calls have been looked at in multiple studies and usually are performed in the studies by nurses, nurse practitioners, or pharmacists and occur within days of discharge from the hospital. These calls offer a mechanism to provide answers to questions about their medical condition or medications.
Review of the Data
There is a wide range of studies evaluating the benefit of a post-discharge telephone call. Unfortunately, most of the data are of low methodological quality with low patient numbers and high risk of bias.3
Much of the data are divided into subgroups of patients, including ED patients, cardiac patients, surgical patients, medicine patients, and other small groups. The end points also vary and examine areas such as patient satisfaction, reduction in medication errors, and effect on readmissions or repeat ED visits. The bulk of studies used a standardized script. These calls lasted only minutes, which could make it user-friendly, especially for a busy hospitalist’s schedule. Unfortunately, the effect of these interventions is mixed.
With ED patients, phone calls have been shown to be an effective means of communication between patients and physicians. In a study of 297 patients, the authors were only able to reach half the patients but still were able to identify medical problems needing referral or further intervention in 37% of the patients contacted.4 Another two studies revealed similar results with approximately 40% of the contacted patients requiring further clarification on their discharge instructions.5,6
Importantly, 95% of these patients felt the call was beneficial. Thus, more than one-third of patients discharged from an ED are likely to have problems and a follow-up telephone call offers an opportunity to intervene on these potential problems. Another ED study evaluated patients older than 75 and found a nurse liaison could effectively assess the complexity of a patient’s questions and appropriately advise them over the phone or triage them to the correct care provider for further care.7
Post-discharge follow-up telephone calls also can benefit patients discharged from the hospital. A recent paper reported that approximately 12% of patients develop new or worsening symptoms within a few days post-discharge and adverse drug events can occur in between 23% to 49% of people during this transition period.8-10
Another study evaluating resource use in heart failure patients found follow-up telephone calls significantly decreased the average number of hospital days over six months time and readmission rate at six months in the call group, as well as increased patient satisfaction.11
A randomized placebo-controlled trial evaluating follow-up calls from pharmacists to discharged medical patients found the call group patients were more satisfied with their post-discharge care. Additionally, there were less ED visits within 30 days of discharge in the call group compared to placebo or standard care.12
On the other hand, several studies have questioned the utility of follow-up telephone calls for improving transitions of care. A Stanford University group divided medical and surgical patients into three groups with one receiving routine follow-up calls, another requiring a patient-initiated call and a final group without any intervention and found there was no difference between these groups in regards to patient satisfaction or 30-day readmission rates.13
An outpatient trial completed at a South Dakota Veterans Affairs clinic also determined telephone calls had little effect on decreasing resources or hospital admissions.14
Although this study did not include inpatients, it demonstrates the fact that follow-up telephone calls may not be as helpful as shown in other trials and that more thorough and well-designed trials are needed to more definitively answer this question.
Back to the Case
The hospitalist makes a call to the patient to follow-up after he is discharged, and he says he is glad she called. He had questions about one of his medications that was discontinued while he was hospitalized and wants to know if he should restart it. He also says he is having low-grade fevers again and is not sure if he should come back in for evaluation.
The hospitalist is able to answer his questions about his medication list and instructs him to restart the metformin they had stopped while he was an inpatient. The hospitalist also is able to better explain what symptoms to be aware of and when the patient should come in for re-evaluation. The patient appreciates the five-minute call, and the hospitalist is glad she cleared up the patient’s confusion regarding his medications before a serious error or unnecessary readmission to the hospital occurred. TH
Dr. Moulds is a third-year internal medicine resident at the University of Colorado Denver. Dr. Epstein is director of medical affairs and clinical research at IPC-The Hospitalist Company.
References
- www.cdc.gov.
- Epstein K, Juarez E, Loya K, Gorman MJ, Singer A. Frequency of new or worsening symptoms in the post-hospitalization period. J Hosp Med. 2007 Mar;2(2):58-68.
- Mistiaen P, Poot E. Telephone follow-up, initiated by a hospital-based health professional, for post-discharge problems in patients discharged from hospital to home. Cochrane Database Syst Rev. 2006, Issue 4. Art. No.: CD004510. DOI:10.1002/14651858.CD004510.pub3.
- Shesser R, Smith M, Adams S, Walls R, Paxton M. The effectiveness of an organized follow-up system. Ann Emerg Med. 1986 Aug;15(8):911-915.
- Jones J, Clark W, Bradford J, Dougherty J. Efficacy of a telephone follow-up system in the emergency department. J Emerg Med. 1988 May-June;6(3):249-254.
- Jones JS, Young MS, LaFleur RA, Brown MD. Effectiveness of an organized follow-up system for elder patients released from the emergency department. Acad Emerg Med. 1997 Dec;4(12):1147-1152.
- Poncia HD, Ryan J, Carver M. Next day telephone follow up of the elderly: a needs assessment and critical incident monitoring tool for the accident and emergency department. J Accid Emerg Med. 2000 Sep;17(5):337-340.
- Kripalani S, Price M, Vigil V, Epstein K. Frequency and predictors of prescription-related issues after hospital discharge. J Hosp Med. 2008 Jan/Feb;3(1):12-19.
- Forster A, Murff H, Peterson J, Gandhi T, Bates D. Adverse drug events occurring following hospital discharge. J Gen Intern Med. 2005;20:317-323.
- Forster A, Murff H, Peterson J, Gandhi T, Bates D. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161-167.
- Riegel B, Carlson B, Kopp Z, LePetri B, Glaser D, Unger A. Effect of a standardized nurse case-management telephone intervention on resource use in patients with chronic heart failure. Arch Intern Med. 2002 Mar 25;162(6):705-712.
- Dudas V, Bookwalter T, Kerr KM, Pantilat SZ. The impact of follow-up telephone calls to patients after hospitalization. Am J Med. 2001 Dec 21;111(9B):26S-30S.
- Bostrom J, Caldwell J, McGuire K, Everson D. Telephone follow-up after discharge from the hospital: does it make a difference? Appl Nurs Res. 1996 May;9(2):47-52.
- Welch HG, Johnson DJ, Edson R. Telephone care as an adjunct to routine medical follow-up. A negative randomized trial. Eff Clin Pract. 2000 May-June;3(3):123-130.
- Coleman E, Smith J, Raha D, Min S. Posthospital medication discrepancies. Arch Intern Med. 2005;165:1842-1847.
Case
A 75-year-old male with history of diabetes and heart disease is discharged from the hospital after treatment for pneumonia. He has eight medications on his discharge list and is given two new prescriptions at discharge. He has a primary care provider but will not be able to see her until three weeks after discharge. Will a follow-up call decrease potential complications?
Overview
Medication errors are prevalent, especially during the transition period from discharge to follow-up with primary care physicians. There are more than 700,000 emergency department (ED) visits each year for adverse drug events with nearly 120,000 of these episodes resulting in hospitalization.1
The likelihood of an adverse drug event increases in patients using more than five medications and when there is a lack of understanding of how and why they are taking certain medications, scenarios common on hospital discharge.2 Studies evaluating effective means to reduce medication errors during transitions out of the hospital offer few solutions. One effective method, however, appears to be follow-up telephone calls.
Telephone calls have been looked at in multiple studies and usually are performed in the studies by nurses, nurse practitioners, or pharmacists and occur within days of discharge from the hospital. These calls offer a mechanism to provide answers to questions about their medical condition or medications.
Review of the Data
There is a wide range of studies evaluating the benefit of a post-discharge telephone call. Unfortunately, most of the data are of low methodological quality with low patient numbers and high risk of bias.3
Much of the data are divided into subgroups of patients, including ED patients, cardiac patients, surgical patients, medicine patients, and other small groups. The end points also vary and examine areas such as patient satisfaction, reduction in medication errors, and effect on readmissions or repeat ED visits. The bulk of studies used a standardized script. These calls lasted only minutes, which could make it user-friendly, especially for a busy hospitalist’s schedule. Unfortunately, the effect of these interventions is mixed.
With ED patients, phone calls have been shown to be an effective means of communication between patients and physicians. In a study of 297 patients, the authors were only able to reach half the patients but still were able to identify medical problems needing referral or further intervention in 37% of the patients contacted.4 Another two studies revealed similar results with approximately 40% of the contacted patients requiring further clarification on their discharge instructions.5,6
Importantly, 95% of these patients felt the call was beneficial. Thus, more than one-third of patients discharged from an ED are likely to have problems and a follow-up telephone call offers an opportunity to intervene on these potential problems. Another ED study evaluated patients older than 75 and found a nurse liaison could effectively assess the complexity of a patient’s questions and appropriately advise them over the phone or triage them to the correct care provider for further care.7
Post-discharge follow-up telephone calls also can benefit patients discharged from the hospital. A recent paper reported that approximately 12% of patients develop new or worsening symptoms within a few days post-discharge and adverse drug events can occur in between 23% to 49% of people during this transition period.8-10
Another study evaluating resource use in heart failure patients found follow-up telephone calls significantly decreased the average number of hospital days over six months time and readmission rate at six months in the call group, as well as increased patient satisfaction.11
A randomized placebo-controlled trial evaluating follow-up calls from pharmacists to discharged medical patients found the call group patients were more satisfied with their post-discharge care. Additionally, there were less ED visits within 30 days of discharge in the call group compared to placebo or standard care.12
On the other hand, several studies have questioned the utility of follow-up telephone calls for improving transitions of care. A Stanford University group divided medical and surgical patients into three groups with one receiving routine follow-up calls, another requiring a patient-initiated call and a final group without any intervention and found there was no difference between these groups in regards to patient satisfaction or 30-day readmission rates.13
An outpatient trial completed at a South Dakota Veterans Affairs clinic also determined telephone calls had little effect on decreasing resources or hospital admissions.14
Although this study did not include inpatients, it demonstrates the fact that follow-up telephone calls may not be as helpful as shown in other trials and that more thorough and well-designed trials are needed to more definitively answer this question.
Back to the Case
The hospitalist makes a call to the patient to follow-up after he is discharged, and he says he is glad she called. He had questions about one of his medications that was discontinued while he was hospitalized and wants to know if he should restart it. He also says he is having low-grade fevers again and is not sure if he should come back in for evaluation.
The hospitalist is able to answer his questions about his medication list and instructs him to restart the metformin they had stopped while he was an inpatient. The hospitalist also is able to better explain what symptoms to be aware of and when the patient should come in for re-evaluation. The patient appreciates the five-minute call, and the hospitalist is glad she cleared up the patient’s confusion regarding his medications before a serious error or unnecessary readmission to the hospital occurred. TH
Dr. Moulds is a third-year internal medicine resident at the University of Colorado Denver. Dr. Epstein is director of medical affairs and clinical research at IPC-The Hospitalist Company.
References
- www.cdc.gov.
- Epstein K, Juarez E, Loya K, Gorman MJ, Singer A. Frequency of new or worsening symptoms in the post-hospitalization period. J Hosp Med. 2007 Mar;2(2):58-68.
- Mistiaen P, Poot E. Telephone follow-up, initiated by a hospital-based health professional, for post-discharge problems in patients discharged from hospital to home. Cochrane Database Syst Rev. 2006, Issue 4. Art. No.: CD004510. DOI:10.1002/14651858.CD004510.pub3.
- Shesser R, Smith M, Adams S, Walls R, Paxton M. The effectiveness of an organized follow-up system. Ann Emerg Med. 1986 Aug;15(8):911-915.
- Jones J, Clark W, Bradford J, Dougherty J. Efficacy of a telephone follow-up system in the emergency department. J Emerg Med. 1988 May-June;6(3):249-254.
- Jones JS, Young MS, LaFleur RA, Brown MD. Effectiveness of an organized follow-up system for elder patients released from the emergency department. Acad Emerg Med. 1997 Dec;4(12):1147-1152.
- Poncia HD, Ryan J, Carver M. Next day telephone follow up of the elderly: a needs assessment and critical incident monitoring tool for the accident and emergency department. J Accid Emerg Med. 2000 Sep;17(5):337-340.
- Kripalani S, Price M, Vigil V, Epstein K. Frequency and predictors of prescription-related issues after hospital discharge. J Hosp Med. 2008 Jan/Feb;3(1):12-19.
- Forster A, Murff H, Peterson J, Gandhi T, Bates D. Adverse drug events occurring following hospital discharge. J Gen Intern Med. 2005;20:317-323.
- Forster A, Murff H, Peterson J, Gandhi T, Bates D. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161-167.
- Riegel B, Carlson B, Kopp Z, LePetri B, Glaser D, Unger A. Effect of a standardized nurse case-management telephone intervention on resource use in patients with chronic heart failure. Arch Intern Med. 2002 Mar 25;162(6):705-712.
- Dudas V, Bookwalter T, Kerr KM, Pantilat SZ. The impact of follow-up telephone calls to patients after hospitalization. Am J Med. 2001 Dec 21;111(9B):26S-30S.
- Bostrom J, Caldwell J, McGuire K, Everson D. Telephone follow-up after discharge from the hospital: does it make a difference? Appl Nurs Res. 1996 May;9(2):47-52.
- Welch HG, Johnson DJ, Edson R. Telephone care as an adjunct to routine medical follow-up. A negative randomized trial. Eff Clin Pract. 2000 May-June;3(3):123-130.
- Coleman E, Smith J, Raha D, Min S. Posthospital medication discrepancies. Arch Intern Med. 2005;165:1842-1847.
Case
A 75-year-old male with history of diabetes and heart disease is discharged from the hospital after treatment for pneumonia. He has eight medications on his discharge list and is given two new prescriptions at discharge. He has a primary care provider but will not be able to see her until three weeks after discharge. Will a follow-up call decrease potential complications?
Overview
Medication errors are prevalent, especially during the transition period from discharge to follow-up with primary care physicians. There are more than 700,000 emergency department (ED) visits each year for adverse drug events with nearly 120,000 of these episodes resulting in hospitalization.1
The likelihood of an adverse drug event increases in patients using more than five medications and when there is a lack of understanding of how and why they are taking certain medications, scenarios common on hospital discharge.2 Studies evaluating effective means to reduce medication errors during transitions out of the hospital offer few solutions. One effective method, however, appears to be follow-up telephone calls.
Telephone calls have been looked at in multiple studies and usually are performed in the studies by nurses, nurse practitioners, or pharmacists and occur within days of discharge from the hospital. These calls offer a mechanism to provide answers to questions about their medical condition or medications.
Review of the Data
There is a wide range of studies evaluating the benefit of a post-discharge telephone call. Unfortunately, most of the data are of low methodological quality with low patient numbers and high risk of bias.3
Much of the data are divided into subgroups of patients, including ED patients, cardiac patients, surgical patients, medicine patients, and other small groups. The end points also vary and examine areas such as patient satisfaction, reduction in medication errors, and effect on readmissions or repeat ED visits. The bulk of studies used a standardized script. These calls lasted only minutes, which could make it user-friendly, especially for a busy hospitalist’s schedule. Unfortunately, the effect of these interventions is mixed.
With ED patients, phone calls have been shown to be an effective means of communication between patients and physicians. In a study of 297 patients, the authors were only able to reach half the patients but still were able to identify medical problems needing referral or further intervention in 37% of the patients contacted.4 Another two studies revealed similar results with approximately 40% of the contacted patients requiring further clarification on their discharge instructions.5,6
Importantly, 95% of these patients felt the call was beneficial. Thus, more than one-third of patients discharged from an ED are likely to have problems and a follow-up telephone call offers an opportunity to intervene on these potential problems. Another ED study evaluated patients older than 75 and found a nurse liaison could effectively assess the complexity of a patient’s questions and appropriately advise them over the phone or triage them to the correct care provider for further care.7
Post-discharge follow-up telephone calls also can benefit patients discharged from the hospital. A recent paper reported that approximately 12% of patients develop new or worsening symptoms within a few days post-discharge and adverse drug events can occur in between 23% to 49% of people during this transition period.8-10
Another study evaluating resource use in heart failure patients found follow-up telephone calls significantly decreased the average number of hospital days over six months time and readmission rate at six months in the call group, as well as increased patient satisfaction.11
A randomized placebo-controlled trial evaluating follow-up calls from pharmacists to discharged medical patients found the call group patients were more satisfied with their post-discharge care. Additionally, there were less ED visits within 30 days of discharge in the call group compared to placebo or standard care.12
On the other hand, several studies have questioned the utility of follow-up telephone calls for improving transitions of care. A Stanford University group divided medical and surgical patients into three groups with one receiving routine follow-up calls, another requiring a patient-initiated call and a final group without any intervention and found there was no difference between these groups in regards to patient satisfaction or 30-day readmission rates.13
An outpatient trial completed at a South Dakota Veterans Affairs clinic also determined telephone calls had little effect on decreasing resources or hospital admissions.14
Although this study did not include inpatients, it demonstrates the fact that follow-up telephone calls may not be as helpful as shown in other trials and that more thorough and well-designed trials are needed to more definitively answer this question.
Back to the Case
The hospitalist makes a call to the patient to follow-up after he is discharged, and he says he is glad she called. He had questions about one of his medications that was discontinued while he was hospitalized and wants to know if he should restart it. He also says he is having low-grade fevers again and is not sure if he should come back in for evaluation.
The hospitalist is able to answer his questions about his medication list and instructs him to restart the metformin they had stopped while he was an inpatient. The hospitalist also is able to better explain what symptoms to be aware of and when the patient should come in for re-evaluation. The patient appreciates the five-minute call, and the hospitalist is glad she cleared up the patient’s confusion regarding his medications before a serious error or unnecessary readmission to the hospital occurred. TH
Dr. Moulds is a third-year internal medicine resident at the University of Colorado Denver. Dr. Epstein is director of medical affairs and clinical research at IPC-The Hospitalist Company.
References
- www.cdc.gov.
- Epstein K, Juarez E, Loya K, Gorman MJ, Singer A. Frequency of new or worsening symptoms in the post-hospitalization period. J Hosp Med. 2007 Mar;2(2):58-68.
- Mistiaen P, Poot E. Telephone follow-up, initiated by a hospital-based health professional, for post-discharge problems in patients discharged from hospital to home. Cochrane Database Syst Rev. 2006, Issue 4. Art. No.: CD004510. DOI:10.1002/14651858.CD004510.pub3.
- Shesser R, Smith M, Adams S, Walls R, Paxton M. The effectiveness of an organized follow-up system. Ann Emerg Med. 1986 Aug;15(8):911-915.
- Jones J, Clark W, Bradford J, Dougherty J. Efficacy of a telephone follow-up system in the emergency department. J Emerg Med. 1988 May-June;6(3):249-254.
- Jones JS, Young MS, LaFleur RA, Brown MD. Effectiveness of an organized follow-up system for elder patients released from the emergency department. Acad Emerg Med. 1997 Dec;4(12):1147-1152.
- Poncia HD, Ryan J, Carver M. Next day telephone follow up of the elderly: a needs assessment and critical incident monitoring tool for the accident and emergency department. J Accid Emerg Med. 2000 Sep;17(5):337-340.
- Kripalani S, Price M, Vigil V, Epstein K. Frequency and predictors of prescription-related issues after hospital discharge. J Hosp Med. 2008 Jan/Feb;3(1):12-19.
- Forster A, Murff H, Peterson J, Gandhi T, Bates D. Adverse drug events occurring following hospital discharge. J Gen Intern Med. 2005;20:317-323.
- Forster A, Murff H, Peterson J, Gandhi T, Bates D. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161-167.
- Riegel B, Carlson B, Kopp Z, LePetri B, Glaser D, Unger A. Effect of a standardized nurse case-management telephone intervention on resource use in patients with chronic heart failure. Arch Intern Med. 2002 Mar 25;162(6):705-712.
- Dudas V, Bookwalter T, Kerr KM, Pantilat SZ. The impact of follow-up telephone calls to patients after hospitalization. Am J Med. 2001 Dec 21;111(9B):26S-30S.
- Bostrom J, Caldwell J, McGuire K, Everson D. Telephone follow-up after discharge from the hospital: does it make a difference? Appl Nurs Res. 1996 May;9(2):47-52.
- Welch HG, Johnson DJ, Edson R. Telephone care as an adjunct to routine medical follow-up. A negative randomized trial. Eff Clin Pract. 2000 May-June;3(3):123-130.
- Coleman E, Smith J, Raha D, Min S. Posthospital medication discrepancies. Arch Intern Med. 2005;165:1842-1847.
Seek Work Wisely
Hospital medicine has come a long way since the term hospitalist was coined slightly more than a decade ago. SHM estimates the need for 30,000 practicing hospitalists within the next decade.
Filling an available hospitalist position is a two-way process that involves considerations and negotiations at various levels. When looking for the suitable hospitalist job, it is critical that you think both about what your potential employer needs and what you expect from the role you seek. The following insights provide a gauge of what an employer is looking for in a hospitalist applicant.
1) Clinical and procedural skills. Good clinical acumen is fundamental to being a successful hospitalist. As you complete residency training, your professional references are a reliable means for others to judge clinical skills. It’s important that your references comment on your clinical proficiency in their letters. Procedural skills always are welcome but by no means mandatory.
In larger facilities, where residents in training or specialists do many procedures, the program may not insist on procedural skills. On the other hand, some hospital medicine programs may require a proficiency in ICU procedures, which include intubations, central line placement, and A-line placements to mention a few. The SHM publication The Core Competencies in Hospital Medicine: A Framework for Curriculum Development is a great resource for understanding the knowledge and skills expected of a hospitalist physician.
2) Professionalism and teamwork. There are an extraordinary number of healthcare providers a hospitalist needs to work with. In addition to establishing a courteous rapport with patients and their families, good communication with primary care physicians, specialists, nursing staff, case managers, midlevel providers, and administrative and secretarial staff is essential. With this diversity of interactions, professionalism and teamwork are highly regarded and go a long way in establishing you as proficient hospitalist. An applicant’s professionalism is not only judged during the interview period but also confirmed by references. An unwavering positive attitude and commitment to a healthy work environment also are attributes that are recognized by a potential employer.
3) Quality improvement focus. Quality improvement activities and participation in such programs have rightly received unprecedented attention. SHM data indicate that 86% of hospitalist groups are active in quality improvement initiatives. Many hospital medicine programs participate in some form of Medicare pay-for-performance initiatives in order to ensure evidence-based patient care, better health outcomes, and reduce preventable complications.
A commitment to and active interest in quality improvement is highly desirable. Prior participation in and/or research for programs such as venous thromboembolism (VTE) prophylaxis, inpatient glycemic control, fall preventions, CHF optimization, medicine reconciliation pathways, and other evidence-based measures are a definite plus. In addition, specific training in areas such as perioperative care, improving safety of transitions of care, and stroke management are beneficial. Elaborating on any systems enhancement projects undertaken especially during hospital medicine clinical rotations/electives and/or fellowships will be invaluable.
4) Leadership skills. Nonclinical and administrative responsibilities are an important element of many hospitalist programs. Interest in various committees and an ability to assume leadership roles reflect favorably on your application. A good hospital medicine program will often encourage your interest in fostering the program and invite your involvement in initiatives to promote good patient care and facilitate fiscal strength.
An applicant should inquire about opportunities to participate in organizational committees and develop leadership skills, as this will be important for your professional growth. Take the time to point out any previous committee involvement in national healthcare organizations such as SHM.
5) Workflow efficiency. The ability to multitask and be organized are great skills to have as a hospitalist. Hospitalist work often involves managing several things during a short time span (i.e., rounding, admitting, teaching, holding family conferences, answering pages, and running codes). Successfully completing these responsibilities involves patience, structure, and resourcefulness during the course of any given day.
6) Teaching and research skills. In academic hospital medicine programs, good teaching and research skills can be very desirable. Chief residency or assistant chief residency experience is a good sign of teaching experience. Participation in research projects will boost your chances when looking for an academic hospitalist job. In non-academic practices, the employer may not focus much on these skills. Nevertheless, it is of significant value when the practice also hires midlevel practitioners like nurse practitioners or physician’s assistants or is thinking about how to evaluate the effects of a new program or intervention.
7) Local ties and durability. In view of the significant demand for hospitalists, recruiting can be challenging for any program. Another important aspect an employer looks at is whether you have any local ties or other compelling reasons to stay in the area for a long time. If you do have some geographic attachments or other reasons to be in the area for an extended duration, it will make the program more receptive toward you. Also, obtaining or applying for state licensure will save significant time and put you ahead of the curve.
8) Board certification. Most programs require you to be board certified or eligible when hired. Many programs expect you to obtain board certification within one to two years of starting your job. The sooner this is accomplished the more beneficial for the applicant.
Other Considerations
The diversity of hospital medicine programs provides an array of opportunities to choose from. Broadly speaking, the practice type could be academic or community based. The choice would depend upon your interest and proficiency in teaching.
In terms of schedules offered, several models exist. Many hospitalist programs are increasingly becoming 24/7, and it may be expected that you work different shifts. Also look into the licensure requirements of the state where you want to practice and be prepared with the required documentation, as some states may take longer to issue the license.
Above all, always remember: As much as it is important for you to find a befitting job, it is similarly essential for hospital medicine programs to hire worthy and valuable physicians. TH
Dr. Asudani is assistant clinical professor of medicine and a hospitalist at Baystate Medical Center, Tufts School of Medicine. Dr. Gandla is program medical director, Cogent Healthcare, High Point Regional Health System.
Hospital medicine has come a long way since the term hospitalist was coined slightly more than a decade ago. SHM estimates the need for 30,000 practicing hospitalists within the next decade.
Filling an available hospitalist position is a two-way process that involves considerations and negotiations at various levels. When looking for the suitable hospitalist job, it is critical that you think both about what your potential employer needs and what you expect from the role you seek. The following insights provide a gauge of what an employer is looking for in a hospitalist applicant.
1) Clinical and procedural skills. Good clinical acumen is fundamental to being a successful hospitalist. As you complete residency training, your professional references are a reliable means for others to judge clinical skills. It’s important that your references comment on your clinical proficiency in their letters. Procedural skills always are welcome but by no means mandatory.
In larger facilities, where residents in training or specialists do many procedures, the program may not insist on procedural skills. On the other hand, some hospital medicine programs may require a proficiency in ICU procedures, which include intubations, central line placement, and A-line placements to mention a few. The SHM publication The Core Competencies in Hospital Medicine: A Framework for Curriculum Development is a great resource for understanding the knowledge and skills expected of a hospitalist physician.
2) Professionalism and teamwork. There are an extraordinary number of healthcare providers a hospitalist needs to work with. In addition to establishing a courteous rapport with patients and their families, good communication with primary care physicians, specialists, nursing staff, case managers, midlevel providers, and administrative and secretarial staff is essential. With this diversity of interactions, professionalism and teamwork are highly regarded and go a long way in establishing you as proficient hospitalist. An applicant’s professionalism is not only judged during the interview period but also confirmed by references. An unwavering positive attitude and commitment to a healthy work environment also are attributes that are recognized by a potential employer.
3) Quality improvement focus. Quality improvement activities and participation in such programs have rightly received unprecedented attention. SHM data indicate that 86% of hospitalist groups are active in quality improvement initiatives. Many hospital medicine programs participate in some form of Medicare pay-for-performance initiatives in order to ensure evidence-based patient care, better health outcomes, and reduce preventable complications.
A commitment to and active interest in quality improvement is highly desirable. Prior participation in and/or research for programs such as venous thromboembolism (VTE) prophylaxis, inpatient glycemic control, fall preventions, CHF optimization, medicine reconciliation pathways, and other evidence-based measures are a definite plus. In addition, specific training in areas such as perioperative care, improving safety of transitions of care, and stroke management are beneficial. Elaborating on any systems enhancement projects undertaken especially during hospital medicine clinical rotations/electives and/or fellowships will be invaluable.
4) Leadership skills. Nonclinical and administrative responsibilities are an important element of many hospitalist programs. Interest in various committees and an ability to assume leadership roles reflect favorably on your application. A good hospital medicine program will often encourage your interest in fostering the program and invite your involvement in initiatives to promote good patient care and facilitate fiscal strength.
An applicant should inquire about opportunities to participate in organizational committees and develop leadership skills, as this will be important for your professional growth. Take the time to point out any previous committee involvement in national healthcare organizations such as SHM.
5) Workflow efficiency. The ability to multitask and be organized are great skills to have as a hospitalist. Hospitalist work often involves managing several things during a short time span (i.e., rounding, admitting, teaching, holding family conferences, answering pages, and running codes). Successfully completing these responsibilities involves patience, structure, and resourcefulness during the course of any given day.
6) Teaching and research skills. In academic hospital medicine programs, good teaching and research skills can be very desirable. Chief residency or assistant chief residency experience is a good sign of teaching experience. Participation in research projects will boost your chances when looking for an academic hospitalist job. In non-academic practices, the employer may not focus much on these skills. Nevertheless, it is of significant value when the practice also hires midlevel practitioners like nurse practitioners or physician’s assistants or is thinking about how to evaluate the effects of a new program or intervention.
7) Local ties and durability. In view of the significant demand for hospitalists, recruiting can be challenging for any program. Another important aspect an employer looks at is whether you have any local ties or other compelling reasons to stay in the area for a long time. If you do have some geographic attachments or other reasons to be in the area for an extended duration, it will make the program more receptive toward you. Also, obtaining or applying for state licensure will save significant time and put you ahead of the curve.
8) Board certification. Most programs require you to be board certified or eligible when hired. Many programs expect you to obtain board certification within one to two years of starting your job. The sooner this is accomplished the more beneficial for the applicant.
Other Considerations
The diversity of hospital medicine programs provides an array of opportunities to choose from. Broadly speaking, the practice type could be academic or community based. The choice would depend upon your interest and proficiency in teaching.
In terms of schedules offered, several models exist. Many hospitalist programs are increasingly becoming 24/7, and it may be expected that you work different shifts. Also look into the licensure requirements of the state where you want to practice and be prepared with the required documentation, as some states may take longer to issue the license.
Above all, always remember: As much as it is important for you to find a befitting job, it is similarly essential for hospital medicine programs to hire worthy and valuable physicians. TH
Dr. Asudani is assistant clinical professor of medicine and a hospitalist at Baystate Medical Center, Tufts School of Medicine. Dr. Gandla is program medical director, Cogent Healthcare, High Point Regional Health System.
Hospital medicine has come a long way since the term hospitalist was coined slightly more than a decade ago. SHM estimates the need for 30,000 practicing hospitalists within the next decade.
Filling an available hospitalist position is a two-way process that involves considerations and negotiations at various levels. When looking for the suitable hospitalist job, it is critical that you think both about what your potential employer needs and what you expect from the role you seek. The following insights provide a gauge of what an employer is looking for in a hospitalist applicant.
1) Clinical and procedural skills. Good clinical acumen is fundamental to being a successful hospitalist. As you complete residency training, your professional references are a reliable means for others to judge clinical skills. It’s important that your references comment on your clinical proficiency in their letters. Procedural skills always are welcome but by no means mandatory.
In larger facilities, where residents in training or specialists do many procedures, the program may not insist on procedural skills. On the other hand, some hospital medicine programs may require a proficiency in ICU procedures, which include intubations, central line placement, and A-line placements to mention a few. The SHM publication The Core Competencies in Hospital Medicine: A Framework for Curriculum Development is a great resource for understanding the knowledge and skills expected of a hospitalist physician.
2) Professionalism and teamwork. There are an extraordinary number of healthcare providers a hospitalist needs to work with. In addition to establishing a courteous rapport with patients and their families, good communication with primary care physicians, specialists, nursing staff, case managers, midlevel providers, and administrative and secretarial staff is essential. With this diversity of interactions, professionalism and teamwork are highly regarded and go a long way in establishing you as proficient hospitalist. An applicant’s professionalism is not only judged during the interview period but also confirmed by references. An unwavering positive attitude and commitment to a healthy work environment also are attributes that are recognized by a potential employer.
3) Quality improvement focus. Quality improvement activities and participation in such programs have rightly received unprecedented attention. SHM data indicate that 86% of hospitalist groups are active in quality improvement initiatives. Many hospital medicine programs participate in some form of Medicare pay-for-performance initiatives in order to ensure evidence-based patient care, better health outcomes, and reduce preventable complications.
A commitment to and active interest in quality improvement is highly desirable. Prior participation in and/or research for programs such as venous thromboembolism (VTE) prophylaxis, inpatient glycemic control, fall preventions, CHF optimization, medicine reconciliation pathways, and other evidence-based measures are a definite plus. In addition, specific training in areas such as perioperative care, improving safety of transitions of care, and stroke management are beneficial. Elaborating on any systems enhancement projects undertaken especially during hospital medicine clinical rotations/electives and/or fellowships will be invaluable.
4) Leadership skills. Nonclinical and administrative responsibilities are an important element of many hospitalist programs. Interest in various committees and an ability to assume leadership roles reflect favorably on your application. A good hospital medicine program will often encourage your interest in fostering the program and invite your involvement in initiatives to promote good patient care and facilitate fiscal strength.
An applicant should inquire about opportunities to participate in organizational committees and develop leadership skills, as this will be important for your professional growth. Take the time to point out any previous committee involvement in national healthcare organizations such as SHM.
5) Workflow efficiency. The ability to multitask and be organized are great skills to have as a hospitalist. Hospitalist work often involves managing several things during a short time span (i.e., rounding, admitting, teaching, holding family conferences, answering pages, and running codes). Successfully completing these responsibilities involves patience, structure, and resourcefulness during the course of any given day.
6) Teaching and research skills. In academic hospital medicine programs, good teaching and research skills can be very desirable. Chief residency or assistant chief residency experience is a good sign of teaching experience. Participation in research projects will boost your chances when looking for an academic hospitalist job. In non-academic practices, the employer may not focus much on these skills. Nevertheless, it is of significant value when the practice also hires midlevel practitioners like nurse practitioners or physician’s assistants or is thinking about how to evaluate the effects of a new program or intervention.
7) Local ties and durability. In view of the significant demand for hospitalists, recruiting can be challenging for any program. Another important aspect an employer looks at is whether you have any local ties or other compelling reasons to stay in the area for a long time. If you do have some geographic attachments or other reasons to be in the area for an extended duration, it will make the program more receptive toward you. Also, obtaining or applying for state licensure will save significant time and put you ahead of the curve.
8) Board certification. Most programs require you to be board certified or eligible when hired. Many programs expect you to obtain board certification within one to two years of starting your job. The sooner this is accomplished the more beneficial for the applicant.
Other Considerations
The diversity of hospital medicine programs provides an array of opportunities to choose from. Broadly speaking, the practice type could be academic or community based. The choice would depend upon your interest and proficiency in teaching.
In terms of schedules offered, several models exist. Many hospitalist programs are increasingly becoming 24/7, and it may be expected that you work different shifts. Also look into the licensure requirements of the state where you want to practice and be prepared with the required documentation, as some states may take longer to issue the license.
Above all, always remember: As much as it is important for you to find a befitting job, it is similarly essential for hospital medicine programs to hire worthy and valuable physicians. TH
Dr. Asudani is assistant clinical professor of medicine and a hospitalist at Baystate Medical Center, Tufts School of Medicine. Dr. Gandla is program medical director, Cogent Healthcare, High Point Regional Health System.
Medical Board Maneuvers
There are a few pieces of mail that bring an instant feeling of dread—an audit letter from the IRS, a credit card bill after a Las Vegas vacation, and a letter from the medical board. We have no good solutions for the first two pieces of correspondence, but we have a few suggestions when communicating with the medical board.
1) Understand the medical board’s purpose. Every state regulates the practice of medicine for the same reason: Medicine requires highly specialized knowledge, and the average patient does not have the knowledge or experience to determine which physicians are qualified to practice.
Think of the harm that could result if incompetent physicians could practice medicine without oversight. Even worse, think of the harm that could result if non-physicians could provide medical services without proper education and training. That’s why, in every state, the legislatures have passed laws to regulate and control the practice of medicine so people can be properly protected against the unauthorized, unqualified, and improper practice of medicine. Almost everyone agrees regulation of this nature serves a legitimate public purpose.
Consequently, whenever a physician deals with a medical board, they are best served by remembering that the medical board exists to protect the public from the unauthorized, unqualified and improper practice of medicine. The physician’s ultimate goal is to reassure that medical board that their practice is authorized, well-grounded in medicine, and within the standards of professional care. Even if the patient has complained because of a questionable motive, such as attempting to gain an advantage in a billing dispute, a physician cannot use the patient’s motive as grounds for defending poor medical care. Medical boards often distrust physicians who try to shift the focus from the adequacy of their medical care to a patient’s shortcomings.
2) Do I need a lawyer? In most states, the medical board will ask a physician to respond to every patient complaint—even if the complaint is outlandish. Rather than judging the complaint when it arrives, the medical board is more interested in assessing the physician’s response to the complaint. An unhappy patient may lack the acumen to explain the course of treatment and the specifics of their condition, so the medical board relies upon the physician to describe their conduct and the course of care.
Unless the patient’s complaint is in the category of “the doctor placed transmitters in my brain and now the aliens won’t leave me alone,” we always recommend a physician review the complaint and the proposed response with an attorney. In every state, there are attorneys who specialize in representing physicians before medical boards.
Because they’ve dealt with the medical board in many cases throughout a number of years, these attorneys have a good idea of what the medical board expects to see in a response, and, more importantly, what the medical board does not want to see in a response. Investing in an attorney’s services at the outset is money well spent.
Far too often, we see physicians who tried to save a couple of hundred dollars by responding to the medical board, but their response was ineffective. The physician is then faced with spending several thousand dollars defending a disciplinary proceeding. Even worse, if the physician has made a sufficiently serious mistake in the initial response, the physician is going to be stuck with that mistake, severely limiting the attorney’s ability to defend the disciplinary proceeding. Some medical malpractice insurers reimburse physicians for attorney’s fees incurred in responding to a medical board complaint, so check your policy.
3) Candor is your friend. Undoubtedly, there are occasions when a patient complains about medical care without justification. Patients have unrealistic expectations and often fail to understand that each patient’s condition presents a unique challenge. Conversely, some complaints absolutely are legitimate. Every physician makes mistakes, and the medical board will react negatively to a physician who defends an unreasonable course of care. In fact, the medical board will view the physician’s defense of unreasonable care as evidence the mistake is not an aberration in the physician’s practice.
When confronted with one of those instances where the patient’s complaint is legitimate, we doubly recommend you confer with an attorney about your response. At a minimum, however, a physician must be able to explain:
- Why a mistake occurred;
- What steps the physician took to minimize the consequences of the mistake for the patient;
- Why the mistake represents an aberration, not a reason for continued concern; and
- What changes the physician has implemented to ensure the mistake will not reoccur.
In preparing a response to the medical board, we’ve recommended physicians take continuing education in the areas of the patients’ complaints. By taking this remedial measure voluntarily, a physician reduces the likelihood the medical board will impose it as a remedial sanction.
When we first began defending healthcare professionals before their licensing agencies, we thought we’d be spending lots of time dealing with complicated medical issues. We were wrong.
By an overwhelming proportion, the majority of disciplinary actions against physicians arise from three sources:
- Allegations of improper sexual conduct;
- Allegations of substance abuse; or
- Allegations of financial impropriety.
Physicians face the same problems that affect non-physicians—but a physician’s breach of the obligations owed to patients allows a medical board to take disciplinary action. The physician-patient relationship has an inherent disparity of power that makes patients vulnerable to a physician’s abuse of trust. For this reason, medical boards view allegations of this nature quite seriously.
The first question a physician has to ask when accused of these form of misconduct is, “Is it true?” If you are tempted, to answer, “no,” even if the real answer is “yes,” think twice. If you lie to the medical board about one of these issues, you almost certainly will lose your medical license. You will have demonstrated to the board that you not only lack judgment, but that you can’t be trusted. If it even crossed your mind to alter the medical or billing records, don’t. The medical board will probably obtain copies of those records from another source.
If the answer to the question, “Is it true?” is “yes,” the physician faces the prospect that the medical board will revoke or suspend their license. In these situations, we regularly recommend physicians embark on a course of action designed to save the medical license—even if the physician will be subject to arduous probationary terms.
We will recommend the physicians engage practice monitors, seek substance abuse counseling, and repay any wrongfully obtained money. In many states, there are specialized programs that provide mental health and addiction counseling for physicians, and these programs represent potential lifelines for physicians in crisis. Your goal is demonstrate to the medical board that you’ve seen the error of your ways and have committed to a program that will return you to good standing.
Responding to the medical board is a scary proposition. The majority of complaints are dismissed without any disciplinary action against a physician—but no physician should take a complaint lightly. Be thoughtful and candid in your response to maximize the likelihood that the medical board will dismiss the complaint. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, University of Colorado, Denver.
There are a few pieces of mail that bring an instant feeling of dread—an audit letter from the IRS, a credit card bill after a Las Vegas vacation, and a letter from the medical board. We have no good solutions for the first two pieces of correspondence, but we have a few suggestions when communicating with the medical board.
1) Understand the medical board’s purpose. Every state regulates the practice of medicine for the same reason: Medicine requires highly specialized knowledge, and the average patient does not have the knowledge or experience to determine which physicians are qualified to practice.
Think of the harm that could result if incompetent physicians could practice medicine without oversight. Even worse, think of the harm that could result if non-physicians could provide medical services without proper education and training. That’s why, in every state, the legislatures have passed laws to regulate and control the practice of medicine so people can be properly protected against the unauthorized, unqualified, and improper practice of medicine. Almost everyone agrees regulation of this nature serves a legitimate public purpose.
Consequently, whenever a physician deals with a medical board, they are best served by remembering that the medical board exists to protect the public from the unauthorized, unqualified and improper practice of medicine. The physician’s ultimate goal is to reassure that medical board that their practice is authorized, well-grounded in medicine, and within the standards of professional care. Even if the patient has complained because of a questionable motive, such as attempting to gain an advantage in a billing dispute, a physician cannot use the patient’s motive as grounds for defending poor medical care. Medical boards often distrust physicians who try to shift the focus from the adequacy of their medical care to a patient’s shortcomings.
2) Do I need a lawyer? In most states, the medical board will ask a physician to respond to every patient complaint—even if the complaint is outlandish. Rather than judging the complaint when it arrives, the medical board is more interested in assessing the physician’s response to the complaint. An unhappy patient may lack the acumen to explain the course of treatment and the specifics of their condition, so the medical board relies upon the physician to describe their conduct and the course of care.
Unless the patient’s complaint is in the category of “the doctor placed transmitters in my brain and now the aliens won’t leave me alone,” we always recommend a physician review the complaint and the proposed response with an attorney. In every state, there are attorneys who specialize in representing physicians before medical boards.
Because they’ve dealt with the medical board in many cases throughout a number of years, these attorneys have a good idea of what the medical board expects to see in a response, and, more importantly, what the medical board does not want to see in a response. Investing in an attorney’s services at the outset is money well spent.
Far too often, we see physicians who tried to save a couple of hundred dollars by responding to the medical board, but their response was ineffective. The physician is then faced with spending several thousand dollars defending a disciplinary proceeding. Even worse, if the physician has made a sufficiently serious mistake in the initial response, the physician is going to be stuck with that mistake, severely limiting the attorney’s ability to defend the disciplinary proceeding. Some medical malpractice insurers reimburse physicians for attorney’s fees incurred in responding to a medical board complaint, so check your policy.
3) Candor is your friend. Undoubtedly, there are occasions when a patient complains about medical care without justification. Patients have unrealistic expectations and often fail to understand that each patient’s condition presents a unique challenge. Conversely, some complaints absolutely are legitimate. Every physician makes mistakes, and the medical board will react negatively to a physician who defends an unreasonable course of care. In fact, the medical board will view the physician’s defense of unreasonable care as evidence the mistake is not an aberration in the physician’s practice.
When confronted with one of those instances where the patient’s complaint is legitimate, we doubly recommend you confer with an attorney about your response. At a minimum, however, a physician must be able to explain:
- Why a mistake occurred;
- What steps the physician took to minimize the consequences of the mistake for the patient;
- Why the mistake represents an aberration, not a reason for continued concern; and
- What changes the physician has implemented to ensure the mistake will not reoccur.
In preparing a response to the medical board, we’ve recommended physicians take continuing education in the areas of the patients’ complaints. By taking this remedial measure voluntarily, a physician reduces the likelihood the medical board will impose it as a remedial sanction.
When we first began defending healthcare professionals before their licensing agencies, we thought we’d be spending lots of time dealing with complicated medical issues. We were wrong.
By an overwhelming proportion, the majority of disciplinary actions against physicians arise from three sources:
- Allegations of improper sexual conduct;
- Allegations of substance abuse; or
- Allegations of financial impropriety.
Physicians face the same problems that affect non-physicians—but a physician’s breach of the obligations owed to patients allows a medical board to take disciplinary action. The physician-patient relationship has an inherent disparity of power that makes patients vulnerable to a physician’s abuse of trust. For this reason, medical boards view allegations of this nature quite seriously.
The first question a physician has to ask when accused of these form of misconduct is, “Is it true?” If you are tempted, to answer, “no,” even if the real answer is “yes,” think twice. If you lie to the medical board about one of these issues, you almost certainly will lose your medical license. You will have demonstrated to the board that you not only lack judgment, but that you can’t be trusted. If it even crossed your mind to alter the medical or billing records, don’t. The medical board will probably obtain copies of those records from another source.
If the answer to the question, “Is it true?” is “yes,” the physician faces the prospect that the medical board will revoke or suspend their license. In these situations, we regularly recommend physicians embark on a course of action designed to save the medical license—even if the physician will be subject to arduous probationary terms.
We will recommend the physicians engage practice monitors, seek substance abuse counseling, and repay any wrongfully obtained money. In many states, there are specialized programs that provide mental health and addiction counseling for physicians, and these programs represent potential lifelines for physicians in crisis. Your goal is demonstrate to the medical board that you’ve seen the error of your ways and have committed to a program that will return you to good standing.
Responding to the medical board is a scary proposition. The majority of complaints are dismissed without any disciplinary action against a physician—but no physician should take a complaint lightly. Be thoughtful and candid in your response to maximize the likelihood that the medical board will dismiss the complaint. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, University of Colorado, Denver.
There are a few pieces of mail that bring an instant feeling of dread—an audit letter from the IRS, a credit card bill after a Las Vegas vacation, and a letter from the medical board. We have no good solutions for the first two pieces of correspondence, but we have a few suggestions when communicating with the medical board.
1) Understand the medical board’s purpose. Every state regulates the practice of medicine for the same reason: Medicine requires highly specialized knowledge, and the average patient does not have the knowledge or experience to determine which physicians are qualified to practice.
Think of the harm that could result if incompetent physicians could practice medicine without oversight. Even worse, think of the harm that could result if non-physicians could provide medical services without proper education and training. That’s why, in every state, the legislatures have passed laws to regulate and control the practice of medicine so people can be properly protected against the unauthorized, unqualified, and improper practice of medicine. Almost everyone agrees regulation of this nature serves a legitimate public purpose.
Consequently, whenever a physician deals with a medical board, they are best served by remembering that the medical board exists to protect the public from the unauthorized, unqualified and improper practice of medicine. The physician’s ultimate goal is to reassure that medical board that their practice is authorized, well-grounded in medicine, and within the standards of professional care. Even if the patient has complained because of a questionable motive, such as attempting to gain an advantage in a billing dispute, a physician cannot use the patient’s motive as grounds for defending poor medical care. Medical boards often distrust physicians who try to shift the focus from the adequacy of their medical care to a patient’s shortcomings.
2) Do I need a lawyer? In most states, the medical board will ask a physician to respond to every patient complaint—even if the complaint is outlandish. Rather than judging the complaint when it arrives, the medical board is more interested in assessing the physician’s response to the complaint. An unhappy patient may lack the acumen to explain the course of treatment and the specifics of their condition, so the medical board relies upon the physician to describe their conduct and the course of care.
Unless the patient’s complaint is in the category of “the doctor placed transmitters in my brain and now the aliens won’t leave me alone,” we always recommend a physician review the complaint and the proposed response with an attorney. In every state, there are attorneys who specialize in representing physicians before medical boards.
Because they’ve dealt with the medical board in many cases throughout a number of years, these attorneys have a good idea of what the medical board expects to see in a response, and, more importantly, what the medical board does not want to see in a response. Investing in an attorney’s services at the outset is money well spent.
Far too often, we see physicians who tried to save a couple of hundred dollars by responding to the medical board, but their response was ineffective. The physician is then faced with spending several thousand dollars defending a disciplinary proceeding. Even worse, if the physician has made a sufficiently serious mistake in the initial response, the physician is going to be stuck with that mistake, severely limiting the attorney’s ability to defend the disciplinary proceeding. Some medical malpractice insurers reimburse physicians for attorney’s fees incurred in responding to a medical board complaint, so check your policy.
3) Candor is your friend. Undoubtedly, there are occasions when a patient complains about medical care without justification. Patients have unrealistic expectations and often fail to understand that each patient’s condition presents a unique challenge. Conversely, some complaints absolutely are legitimate. Every physician makes mistakes, and the medical board will react negatively to a physician who defends an unreasonable course of care. In fact, the medical board will view the physician’s defense of unreasonable care as evidence the mistake is not an aberration in the physician’s practice.
When confronted with one of those instances where the patient’s complaint is legitimate, we doubly recommend you confer with an attorney about your response. At a minimum, however, a physician must be able to explain:
- Why a mistake occurred;
- What steps the physician took to minimize the consequences of the mistake for the patient;
- Why the mistake represents an aberration, not a reason for continued concern; and
- What changes the physician has implemented to ensure the mistake will not reoccur.
In preparing a response to the medical board, we’ve recommended physicians take continuing education in the areas of the patients’ complaints. By taking this remedial measure voluntarily, a physician reduces the likelihood the medical board will impose it as a remedial sanction.
When we first began defending healthcare professionals before their licensing agencies, we thought we’d be spending lots of time dealing with complicated medical issues. We were wrong.
By an overwhelming proportion, the majority of disciplinary actions against physicians arise from three sources:
- Allegations of improper sexual conduct;
- Allegations of substance abuse; or
- Allegations of financial impropriety.
Physicians face the same problems that affect non-physicians—but a physician’s breach of the obligations owed to patients allows a medical board to take disciplinary action. The physician-patient relationship has an inherent disparity of power that makes patients vulnerable to a physician’s abuse of trust. For this reason, medical boards view allegations of this nature quite seriously.
The first question a physician has to ask when accused of these form of misconduct is, “Is it true?” If you are tempted, to answer, “no,” even if the real answer is “yes,” think twice. If you lie to the medical board about one of these issues, you almost certainly will lose your medical license. You will have demonstrated to the board that you not only lack judgment, but that you can’t be trusted. If it even crossed your mind to alter the medical or billing records, don’t. The medical board will probably obtain copies of those records from another source.
If the answer to the question, “Is it true?” is “yes,” the physician faces the prospect that the medical board will revoke or suspend their license. In these situations, we regularly recommend physicians embark on a course of action designed to save the medical license—even if the physician will be subject to arduous probationary terms.
We will recommend the physicians engage practice monitors, seek substance abuse counseling, and repay any wrongfully obtained money. In many states, there are specialized programs that provide mental health and addiction counseling for physicians, and these programs represent potential lifelines for physicians in crisis. Your goal is demonstrate to the medical board that you’ve seen the error of your ways and have committed to a program that will return you to good standing.
Responding to the medical board is a scary proposition. The majority of complaints are dismissed without any disciplinary action against a physician—but no physician should take a complaint lightly. Be thoughtful and candid in your response to maximize the likelihood that the medical board will dismiss the complaint. TH
Patrick O’Rourke works in the Office of University Counsel, Department of Litigation, University of Colorado, Denver.
Sort Out Surgical Cases
Hospitalists often are involved in the care of a surgical patient. Reimbursement for surgical procedures includes payment for pre-, intra-, and post-operative care.
Knowing the billing and coding responsibilities apart from those of the surgeon is imperative for the hospitalist’s accurate charge capture. There are several critical misconceptions in this regard:
- Hospitalists cannot bill for services when involved in a surgical case;
- Surgeons are not responsible for inpatient care if the patient is stable and does not require additional inpatient post-op visits; and
- Modifiers are not required for hospitalist claims unless the hospitalist reports under the same tax identification number as the surgeon.
Determine Global Period
Procedures are categorized as major or minor surgery. A global period is assigned to each procedure code, designating post-operative periods of zero, 10, or 90 days. Physician services during this global period are considered part of the packaged payment and not separately reimbursed.
The global period for any given CPT code can be identified in the Medicare Physician Fee Schedule and accessed at www.cms.hhs.gov/PfsLookup. In addition to zero, 10, and 90 days, services can be noted with:
- XXX, indicating the global period concept does not apply; or
- ZZZ, indicating an “add-on” procedure that must always be reported with the relevant primary procedure code; “add-on” procedures assume the global period of the primary procedure.
Major surgery routinely is allotted 90-day global periods. Therefore, the surgeon is responsible for the patient and must provide all related care one day prior to the surgery forward thru 90 postoperative days at no additional charge. Minor surgery, including endoscopy, has zero or 10-day postoperative periods, bundling all services on the surgical day only, or the surgical day and the subsequent 10 days, respectively (see Table 1, p. above).
The Surgeon Defined
Any qualified physician able to perform “surgical” services within his scope of practice is considered a “surgeon” for billing purposes. For example, a pulmonologist, or primary care physician, must meet the surgical billing and documentation requirements when performing bronchoscopies or uncomplicated incision-and-drainage services, respectively.
Surgical services easily are identified as any code included in range 20000-69999. This code series includes major, minor, and endoscopic procedures. The “surgeon” and all physicians in the same group practice (i.e., reporting services under the same tax identification number) with the same specialty designation must adhere to the global period billing rules.
Alternately, physicians with different specialty designations in the same group practice (e.g., multispecialty group that reports services under the same tax identification number) or different group practices can perform and separately report medically necessary services during the surgeon’s global period, as long as a formal (mutually agreed upon) transfer of care did not occur. Information on physician specialty designations is available at www.highmarkmedicareservices.com/partb/refman/appendix-d.html.
Package Components
The following services are included in the surgeon’s packaged payment:
- Preoperative visits after the decision for surgery is made beginning one day prior to surgery;
- All additional post-operative medical or surgical services provided by the surgeon related to complications, but not require additional trips to the operating room;
- Post-operative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes; local incisional care; removal of cutaneous sutures and staples; line removals; changes and removal of tracheostomy tubes; and discharge services; and
- Post-operative pain management provided by the surgeon.
Services not included are:
- The initial consultation or evaluation of the problem by the surgeon to determine the need for surgery. Append modifier 57 to this visit if provided the day before or day of major surgery to alert the payer that the service resulted in the decision for surgery. Append modifier 25 to this visit if provided the day of minor surgery;
- Services of other physicians except where the other physicians are providing coverage for the surgeon or agree on a transfer of care. This agreement may be in the form of a letter or an annotation in the discharge summary, hospital record, or ASC record;
- Post-operative visits by the surgeon unrelated to the diagnosis for which the surgical procedure is performed, unless the visits occur due to complications of the surgery. These services only are payable after the patient has been discharged from the hospitalization in which the surgery occurred. Append modifier 24 to these unrelated post-op visits;
- Diagnostic tests and procedures, including diagnostic radiological procedures;
- Clearly distinct surgical procedures during the post-operative period that do not result in repeat operations or treatment for complications;
- Treatment for post-operative complications that require a return trip to the operating room, catheterization lab, or endoscopy suite;
- Immunosuppressive therapy for organ transplants; and
- Critical care services (CPT codes 99291 and 99292) unrelated to the surgery in which a seriously injured or burned patient is critically ill and requires constant attendance of the surgeon. Append modifier 24 to these unrelated critical care services (see Table 2, above).
Payer Variations
While Medicare does not require modifier usage by hospitalists providing medically necessary services on surgical cases, some private payers do. Their electronic claim systems may not differentiate services by non-surgical specialists, requiring all physicians to append the appropriate modifier depending on the reason and timing of the service (see “Key Modifiers” below). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
Hospitalists often are involved in the care of a surgical patient. Reimbursement for surgical procedures includes payment for pre-, intra-, and post-operative care.
Knowing the billing and coding responsibilities apart from those of the surgeon is imperative for the hospitalist’s accurate charge capture. There are several critical misconceptions in this regard:
- Hospitalists cannot bill for services when involved in a surgical case;
- Surgeons are not responsible for inpatient care if the patient is stable and does not require additional inpatient post-op visits; and
- Modifiers are not required for hospitalist claims unless the hospitalist reports under the same tax identification number as the surgeon.
Determine Global Period
Procedures are categorized as major or minor surgery. A global period is assigned to each procedure code, designating post-operative periods of zero, 10, or 90 days. Physician services during this global period are considered part of the packaged payment and not separately reimbursed.
The global period for any given CPT code can be identified in the Medicare Physician Fee Schedule and accessed at www.cms.hhs.gov/PfsLookup. In addition to zero, 10, and 90 days, services can be noted with:
- XXX, indicating the global period concept does not apply; or
- ZZZ, indicating an “add-on” procedure that must always be reported with the relevant primary procedure code; “add-on” procedures assume the global period of the primary procedure.
Major surgery routinely is allotted 90-day global periods. Therefore, the surgeon is responsible for the patient and must provide all related care one day prior to the surgery forward thru 90 postoperative days at no additional charge. Minor surgery, including endoscopy, has zero or 10-day postoperative periods, bundling all services on the surgical day only, or the surgical day and the subsequent 10 days, respectively (see Table 1, p. above).
The Surgeon Defined
Any qualified physician able to perform “surgical” services within his scope of practice is considered a “surgeon” for billing purposes. For example, a pulmonologist, or primary care physician, must meet the surgical billing and documentation requirements when performing bronchoscopies or uncomplicated incision-and-drainage services, respectively.
Surgical services easily are identified as any code included in range 20000-69999. This code series includes major, minor, and endoscopic procedures. The “surgeon” and all physicians in the same group practice (i.e., reporting services under the same tax identification number) with the same specialty designation must adhere to the global period billing rules.
Alternately, physicians with different specialty designations in the same group practice (e.g., multispecialty group that reports services under the same tax identification number) or different group practices can perform and separately report medically necessary services during the surgeon’s global period, as long as a formal (mutually agreed upon) transfer of care did not occur. Information on physician specialty designations is available at www.highmarkmedicareservices.com/partb/refman/appendix-d.html.
Package Components
The following services are included in the surgeon’s packaged payment:
- Preoperative visits after the decision for surgery is made beginning one day prior to surgery;
- All additional post-operative medical or surgical services provided by the surgeon related to complications, but not require additional trips to the operating room;
- Post-operative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes; local incisional care; removal of cutaneous sutures and staples; line removals; changes and removal of tracheostomy tubes; and discharge services; and
- Post-operative pain management provided by the surgeon.
Services not included are:
- The initial consultation or evaluation of the problem by the surgeon to determine the need for surgery. Append modifier 57 to this visit if provided the day before or day of major surgery to alert the payer that the service resulted in the decision for surgery. Append modifier 25 to this visit if provided the day of minor surgery;
- Services of other physicians except where the other physicians are providing coverage for the surgeon or agree on a transfer of care. This agreement may be in the form of a letter or an annotation in the discharge summary, hospital record, or ASC record;
- Post-operative visits by the surgeon unrelated to the diagnosis for which the surgical procedure is performed, unless the visits occur due to complications of the surgery. These services only are payable after the patient has been discharged from the hospitalization in which the surgery occurred. Append modifier 24 to these unrelated post-op visits;
- Diagnostic tests and procedures, including diagnostic radiological procedures;
- Clearly distinct surgical procedures during the post-operative period that do not result in repeat operations or treatment for complications;
- Treatment for post-operative complications that require a return trip to the operating room, catheterization lab, or endoscopy suite;
- Immunosuppressive therapy for organ transplants; and
- Critical care services (CPT codes 99291 and 99292) unrelated to the surgery in which a seriously injured or burned patient is critically ill and requires constant attendance of the surgeon. Append modifier 24 to these unrelated critical care services (see Table 2, above).
Payer Variations
While Medicare does not require modifier usage by hospitalists providing medically necessary services on surgical cases, some private payers do. Their electronic claim systems may not differentiate services by non-surgical specialists, requiring all physicians to append the appropriate modifier depending on the reason and timing of the service (see “Key Modifiers” below). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
Hospitalists often are involved in the care of a surgical patient. Reimbursement for surgical procedures includes payment for pre-, intra-, and post-operative care.
Knowing the billing and coding responsibilities apart from those of the surgeon is imperative for the hospitalist’s accurate charge capture. There are several critical misconceptions in this regard:
- Hospitalists cannot bill for services when involved in a surgical case;
- Surgeons are not responsible for inpatient care if the patient is stable and does not require additional inpatient post-op visits; and
- Modifiers are not required for hospitalist claims unless the hospitalist reports under the same tax identification number as the surgeon.
Determine Global Period
Procedures are categorized as major or minor surgery. A global period is assigned to each procedure code, designating post-operative periods of zero, 10, or 90 days. Physician services during this global period are considered part of the packaged payment and not separately reimbursed.
The global period for any given CPT code can be identified in the Medicare Physician Fee Schedule and accessed at www.cms.hhs.gov/PfsLookup. In addition to zero, 10, and 90 days, services can be noted with:
- XXX, indicating the global period concept does not apply; or
- ZZZ, indicating an “add-on” procedure that must always be reported with the relevant primary procedure code; “add-on” procedures assume the global period of the primary procedure.
Major surgery routinely is allotted 90-day global periods. Therefore, the surgeon is responsible for the patient and must provide all related care one day prior to the surgery forward thru 90 postoperative days at no additional charge. Minor surgery, including endoscopy, has zero or 10-day postoperative periods, bundling all services on the surgical day only, or the surgical day and the subsequent 10 days, respectively (see Table 1, p. above).
The Surgeon Defined
Any qualified physician able to perform “surgical” services within his scope of practice is considered a “surgeon” for billing purposes. For example, a pulmonologist, or primary care physician, must meet the surgical billing and documentation requirements when performing bronchoscopies or uncomplicated incision-and-drainage services, respectively.
Surgical services easily are identified as any code included in range 20000-69999. This code series includes major, minor, and endoscopic procedures. The “surgeon” and all physicians in the same group practice (i.e., reporting services under the same tax identification number) with the same specialty designation must adhere to the global period billing rules.
Alternately, physicians with different specialty designations in the same group practice (e.g., multispecialty group that reports services under the same tax identification number) or different group practices can perform and separately report medically necessary services during the surgeon’s global period, as long as a formal (mutually agreed upon) transfer of care did not occur. Information on physician specialty designations is available at www.highmarkmedicareservices.com/partb/refman/appendix-d.html.
Package Components
The following services are included in the surgeon’s packaged payment:
- Preoperative visits after the decision for surgery is made beginning one day prior to surgery;
- All additional post-operative medical or surgical services provided by the surgeon related to complications, but not require additional trips to the operating room;
- Post-operative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes; local incisional care; removal of cutaneous sutures and staples; line removals; changes and removal of tracheostomy tubes; and discharge services; and
- Post-operative pain management provided by the surgeon.
Services not included are:
- The initial consultation or evaluation of the problem by the surgeon to determine the need for surgery. Append modifier 57 to this visit if provided the day before or day of major surgery to alert the payer that the service resulted in the decision for surgery. Append modifier 25 to this visit if provided the day of minor surgery;
- Services of other physicians except where the other physicians are providing coverage for the surgeon or agree on a transfer of care. This agreement may be in the form of a letter or an annotation in the discharge summary, hospital record, or ASC record;
- Post-operative visits by the surgeon unrelated to the diagnosis for which the surgical procedure is performed, unless the visits occur due to complications of the surgery. These services only are payable after the patient has been discharged from the hospitalization in which the surgery occurred. Append modifier 24 to these unrelated post-op visits;
- Diagnostic tests and procedures, including diagnostic radiological procedures;
- Clearly distinct surgical procedures during the post-operative period that do not result in repeat operations or treatment for complications;
- Treatment for post-operative complications that require a return trip to the operating room, catheterization lab, or endoscopy suite;
- Immunosuppressive therapy for organ transplants; and
- Critical care services (CPT codes 99291 and 99292) unrelated to the surgery in which a seriously injured or burned patient is critically ill and requires constant attendance of the surgeon. Append modifier 24 to these unrelated critical care services (see Table 2, above).
Payer Variations
While Medicare does not require modifier usage by hospitalists providing medically necessary services on surgical cases, some private payers do. Their electronic claim systems may not differentiate services by non-surgical specialists, requiring all physicians to append the appropriate modifier depending on the reason and timing of the service (see “Key Modifiers” below). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
Presidential Opportunity
Next year, a new president will take the White House and likely will be the one to lead the United States toward much-needed healthcare reform. What does the near future hold? What should hospitalists know about each candidate’s healthcare policies and proposals? Here, a hospitalist and a government advocate for hospitalists each weigh in.
Are the Times a-Changin’?
Laura Allendorf, SHM’s senior adviser for advocacy and government affairs, keeps a close eye on healthcare legislation, values, and trends in Washington, D.C. She predicts that regardless of which candidate takes office in 2009, change is coming fast.
“Healthcare will definitely be a top priority for the new administration … regardless of who wins the White House,” she says. “There’s been an unprecedented level of discussion already. Congressional committees have already held hearings to prepare for changes next year. They’re laying the groundwork now.”
However, not everyone agrees that we’ll see healthcare reform so soon: Bradley Flansbaum, DO, MPH, chief of hospitalist section at Lenox Hill Hospital in New York City, believes other major issues, such as the slow economy and the war in Iraq, may take precedence.
—Laura Allendorf, SHM senior adviser for advocacy and government affairs
“There are a lot of things on the agenda in Congress right now,” he points out. “I’m not sure how fast [healthcare reform] will really happen.” He says regardless of which man (Barack Obama or John McCain) wins, “he will have two or three top priorities as soon as he takes office—if healthcare reform is one of those priorities, some changes will happen.”
However, the business of Washington still can get in the way of a new administration. Dr. Flansbaum points to a House bill (HR 6331) that requests a delay in implementation of the Medicare competitive bidding program for durable medical equipment. “Lobbyists have sway over what legislators do in Washington, D.C.,” he notes. “Just because Obama or McCain come into office doesn’t mean those lobbyists will go away.”
Despite the forces against change, each candidate is touting major changes to healthcare access.
McCain and Tax Credits
Republican candidate McCain has released a healthcare plan based on instituting a federal tax credit to be used by individuals to purchase their own health insurance—regardless of whether they are covered (or can be covered) through an employer or through the non-group market.
His plan would replace a tax break for those who receive health insurance from their employers with a refundable tax credit of as much as $2,500 per individual and $5,000 per family, to be used for buying private coverage of their choice.
McCain’s plan proposes compensating physicians and hospitals based on performance, including tying Medicaid and Medicare reimbursements to results. His plan also includes ideas for containing healthcare spending by better treating chronic diseases, such as diabetes and heart disease.
“I believe that the best way to help small businesses and employers afford health care is not to increase government control of health care but to bring the rising cost of care under control and give people the option of having personal, portable health insurance,” McCain has said. He added that his proposal would allow individuals to retain their health insurance “even when they move or change jobs.”
Obama’s Funding Plan
Meanwhile, Democratic candidate Obama approaches the issue with a different solution. He proposes universal coverage through the following:
- The proposal would mandate all children have healthcare coverage, and would expand eligibility for Medicaid and SCHIP (State Children’s Health Insurance Program);
- A new public insurance program that would bridge the gap of the uninsured, covering Americans who don’t quality for Medicaid or SCHIP and have no access to coverage through their employer. The coverage would be similar to that offered to members of Congress; and
- A National Health Insurance Exchange to aid individuals and businesses that want to purchase private health insurance directly. Obama’s plan would require all employers to contribute toward health coverage for their employees or toward the cost of the public plan—all, that is, except small businesses who meet certain exemptions.
Congress Is the Decider
“McCain’s plan is, far and away, the more daring, and will present a greater shock to the system,” Dr. Flansbaum maintains. “It would probably lead to gridlock in Congress, because it would need bipartisan agreement to pass and I don’t think the Democrats would agree to it.” If, on the other hand, Obama wins the election, he would almost certainly have a sympathetic Democratic Congress to work with. “He’d have a greater chance of leading change along his lines,” predicts Dr. Flansbaum. “In this case, we might see a Massachusetts-esque plan.”
In either case, the candidate’s proposal may not become reality. “Folks have to remember, it’s Congress that has to come up with the plan” for reform, Allendorf cautions.
A strong president may carry some weight in this regard. “Like all presidents able to effect change, once [the 2009 electee] has the bully pulpit and can sway opinion, Congress should fall into line,” says Dr. Flansbaum. “There will be pressure to change things.”
That change, whatever shape it takes, is almost certain to include some belt-tightening for hospitals, he says. “You have to look at the facts: One-third of healthcare dollars are spent in hospitals … and the numbers given for waste in care in the system are upwards of 30%. You have to assume that hospitals are the logical place to cut.” Regardless of the election outcome, he cautions: “Hospitals will probably have to make painful cuts and changes. It’s going to happen at some point, though I’m not sure that Congress has the political will to push through any changes soon.”
Luckily, hospitalists are accustomed to continuous change and shifting policies, roles, and responsibilities. Their skills at adapting to changing conditions should serve them well in the post-election months. TH
Jane Jerrard is a medical writer based in Chicago.
Next year, a new president will take the White House and likely will be the one to lead the United States toward much-needed healthcare reform. What does the near future hold? What should hospitalists know about each candidate’s healthcare policies and proposals? Here, a hospitalist and a government advocate for hospitalists each weigh in.
Are the Times a-Changin’?
Laura Allendorf, SHM’s senior adviser for advocacy and government affairs, keeps a close eye on healthcare legislation, values, and trends in Washington, D.C. She predicts that regardless of which candidate takes office in 2009, change is coming fast.
“Healthcare will definitely be a top priority for the new administration … regardless of who wins the White House,” she says. “There’s been an unprecedented level of discussion already. Congressional committees have already held hearings to prepare for changes next year. They’re laying the groundwork now.”
However, not everyone agrees that we’ll see healthcare reform so soon: Bradley Flansbaum, DO, MPH, chief of hospitalist section at Lenox Hill Hospital in New York City, believes other major issues, such as the slow economy and the war in Iraq, may take precedence.
—Laura Allendorf, SHM senior adviser for advocacy and government affairs
“There are a lot of things on the agenda in Congress right now,” he points out. “I’m not sure how fast [healthcare reform] will really happen.” He says regardless of which man (Barack Obama or John McCain) wins, “he will have two or three top priorities as soon as he takes office—if healthcare reform is one of those priorities, some changes will happen.”
However, the business of Washington still can get in the way of a new administration. Dr. Flansbaum points to a House bill (HR 6331) that requests a delay in implementation of the Medicare competitive bidding program for durable medical equipment. “Lobbyists have sway over what legislators do in Washington, D.C.,” he notes. “Just because Obama or McCain come into office doesn’t mean those lobbyists will go away.”
Despite the forces against change, each candidate is touting major changes to healthcare access.
McCain and Tax Credits
Republican candidate McCain has released a healthcare plan based on instituting a federal tax credit to be used by individuals to purchase their own health insurance—regardless of whether they are covered (or can be covered) through an employer or through the non-group market.
His plan would replace a tax break for those who receive health insurance from their employers with a refundable tax credit of as much as $2,500 per individual and $5,000 per family, to be used for buying private coverage of their choice.
McCain’s plan proposes compensating physicians and hospitals based on performance, including tying Medicaid and Medicare reimbursements to results. His plan also includes ideas for containing healthcare spending by better treating chronic diseases, such as diabetes and heart disease.
“I believe that the best way to help small businesses and employers afford health care is not to increase government control of health care but to bring the rising cost of care under control and give people the option of having personal, portable health insurance,” McCain has said. He added that his proposal would allow individuals to retain their health insurance “even when they move or change jobs.”
Obama’s Funding Plan
Meanwhile, Democratic candidate Obama approaches the issue with a different solution. He proposes universal coverage through the following:
- The proposal would mandate all children have healthcare coverage, and would expand eligibility for Medicaid and SCHIP (State Children’s Health Insurance Program);
- A new public insurance program that would bridge the gap of the uninsured, covering Americans who don’t quality for Medicaid or SCHIP and have no access to coverage through their employer. The coverage would be similar to that offered to members of Congress; and
- A National Health Insurance Exchange to aid individuals and businesses that want to purchase private health insurance directly. Obama’s plan would require all employers to contribute toward health coverage for their employees or toward the cost of the public plan—all, that is, except small businesses who meet certain exemptions.
Congress Is the Decider
“McCain’s plan is, far and away, the more daring, and will present a greater shock to the system,” Dr. Flansbaum maintains. “It would probably lead to gridlock in Congress, because it would need bipartisan agreement to pass and I don’t think the Democrats would agree to it.” If, on the other hand, Obama wins the election, he would almost certainly have a sympathetic Democratic Congress to work with. “He’d have a greater chance of leading change along his lines,” predicts Dr. Flansbaum. “In this case, we might see a Massachusetts-esque plan.”
In either case, the candidate’s proposal may not become reality. “Folks have to remember, it’s Congress that has to come up with the plan” for reform, Allendorf cautions.
A strong president may carry some weight in this regard. “Like all presidents able to effect change, once [the 2009 electee] has the bully pulpit and can sway opinion, Congress should fall into line,” says Dr. Flansbaum. “There will be pressure to change things.”
That change, whatever shape it takes, is almost certain to include some belt-tightening for hospitals, he says. “You have to look at the facts: One-third of healthcare dollars are spent in hospitals … and the numbers given for waste in care in the system are upwards of 30%. You have to assume that hospitals are the logical place to cut.” Regardless of the election outcome, he cautions: “Hospitals will probably have to make painful cuts and changes. It’s going to happen at some point, though I’m not sure that Congress has the political will to push through any changes soon.”
Luckily, hospitalists are accustomed to continuous change and shifting policies, roles, and responsibilities. Their skills at adapting to changing conditions should serve them well in the post-election months. TH
Jane Jerrard is a medical writer based in Chicago.
Next year, a new president will take the White House and likely will be the one to lead the United States toward much-needed healthcare reform. What does the near future hold? What should hospitalists know about each candidate’s healthcare policies and proposals? Here, a hospitalist and a government advocate for hospitalists each weigh in.
Are the Times a-Changin’?
Laura Allendorf, SHM’s senior adviser for advocacy and government affairs, keeps a close eye on healthcare legislation, values, and trends in Washington, D.C. She predicts that regardless of which candidate takes office in 2009, change is coming fast.
“Healthcare will definitely be a top priority for the new administration … regardless of who wins the White House,” she says. “There’s been an unprecedented level of discussion already. Congressional committees have already held hearings to prepare for changes next year. They’re laying the groundwork now.”
However, not everyone agrees that we’ll see healthcare reform so soon: Bradley Flansbaum, DO, MPH, chief of hospitalist section at Lenox Hill Hospital in New York City, believes other major issues, such as the slow economy and the war in Iraq, may take precedence.
—Laura Allendorf, SHM senior adviser for advocacy and government affairs
“There are a lot of things on the agenda in Congress right now,” he points out. “I’m not sure how fast [healthcare reform] will really happen.” He says regardless of which man (Barack Obama or John McCain) wins, “he will have two or three top priorities as soon as he takes office—if healthcare reform is one of those priorities, some changes will happen.”
However, the business of Washington still can get in the way of a new administration. Dr. Flansbaum points to a House bill (HR 6331) that requests a delay in implementation of the Medicare competitive bidding program for durable medical equipment. “Lobbyists have sway over what legislators do in Washington, D.C.,” he notes. “Just because Obama or McCain come into office doesn’t mean those lobbyists will go away.”
Despite the forces against change, each candidate is touting major changes to healthcare access.
McCain and Tax Credits
Republican candidate McCain has released a healthcare plan based on instituting a federal tax credit to be used by individuals to purchase their own health insurance—regardless of whether they are covered (or can be covered) through an employer or through the non-group market.
His plan would replace a tax break for those who receive health insurance from their employers with a refundable tax credit of as much as $2,500 per individual and $5,000 per family, to be used for buying private coverage of their choice.
McCain’s plan proposes compensating physicians and hospitals based on performance, including tying Medicaid and Medicare reimbursements to results. His plan also includes ideas for containing healthcare spending by better treating chronic diseases, such as diabetes and heart disease.
“I believe that the best way to help small businesses and employers afford health care is not to increase government control of health care but to bring the rising cost of care under control and give people the option of having personal, portable health insurance,” McCain has said. He added that his proposal would allow individuals to retain their health insurance “even when they move or change jobs.”
Obama’s Funding Plan
Meanwhile, Democratic candidate Obama approaches the issue with a different solution. He proposes universal coverage through the following:
- The proposal would mandate all children have healthcare coverage, and would expand eligibility for Medicaid and SCHIP (State Children’s Health Insurance Program);
- A new public insurance program that would bridge the gap of the uninsured, covering Americans who don’t quality for Medicaid or SCHIP and have no access to coverage through their employer. The coverage would be similar to that offered to members of Congress; and
- A National Health Insurance Exchange to aid individuals and businesses that want to purchase private health insurance directly. Obama’s plan would require all employers to contribute toward health coverage for their employees or toward the cost of the public plan—all, that is, except small businesses who meet certain exemptions.
Congress Is the Decider
“McCain’s plan is, far and away, the more daring, and will present a greater shock to the system,” Dr. Flansbaum maintains. “It would probably lead to gridlock in Congress, because it would need bipartisan agreement to pass and I don’t think the Democrats would agree to it.” If, on the other hand, Obama wins the election, he would almost certainly have a sympathetic Democratic Congress to work with. “He’d have a greater chance of leading change along his lines,” predicts Dr. Flansbaum. “In this case, we might see a Massachusetts-esque plan.”
In either case, the candidate’s proposal may not become reality. “Folks have to remember, it’s Congress that has to come up with the plan” for reform, Allendorf cautions.
A strong president may carry some weight in this regard. “Like all presidents able to effect change, once [the 2009 electee] has the bully pulpit and can sway opinion, Congress should fall into line,” says Dr. Flansbaum. “There will be pressure to change things.”
That change, whatever shape it takes, is almost certain to include some belt-tightening for hospitals, he says. “You have to look at the facts: One-third of healthcare dollars are spent in hospitals … and the numbers given for waste in care in the system are upwards of 30%. You have to assume that hospitals are the logical place to cut.” Regardless of the election outcome, he cautions: “Hospitals will probably have to make painful cuts and changes. It’s going to happen at some point, though I’m not sure that Congress has the political will to push through any changes soon.”
Luckily, hospitalists are accustomed to continuous change and shifting policies, roles, and responsibilities. Their skills at adapting to changing conditions should serve them well in the post-election months. TH
Jane Jerrard is a medical writer based in Chicago.
Beat the Boss Blues
A sour relationship with your immediate superior can ruin an otherwise fulfilling job. When you report to someone you continually disagree with or simply don’t understand, just showing up for work can become a misery. If you’re in a situation like this, don’t despair; there is a possible solution.
Power Struggle
Whether the conflict you feel with your boss is over care decisions, personal style, or scope of work, it really boils down to who gets control over your time and your patients.
“For physicians especially, autonomy is very important,” says Tosha B. Wetterneck, MD, associate professor of medicine at University of Wisconsin Hospital/Clinics in Madison. “Physicians are people who work hard, are very smart, and like to control what they do. There is obviously a lot of complexity and variation to the job, which adds to the workload. Plus, decision-making processes need to be happening all the time. This creates stress—and the way to control that stress is to have control over what they do.”
—Russell L. Holman, MD, chief operating officer, Cogent Healthcare, and immediate past president of SHM
A hospitalist who continually butts heads with a superior over issues—or one who subjugates his or her opinion and decisions to the boss’s—is not likely to be satisfied with their job.
“Certainly, an individual’s autonomy is influenced by what they want to have control over and they’re allowed to have control over,” says Dr. Wetterneck. “If there’s a discrepancy between the two, that’s definitely going to have a negative effect on that hospitalist. If there’s a mismatch between what they want control over and what their boss wants, that’s going to be a problem.”
Manage Up
Russell L. Holman, MD, chief operating officer for Brentwood, Tenn.-based Cogent Healthcare and immediate past president of SHM, has worked his way through problems like this—both as the reportee and the boss. He worked out some particularly valuable lessons in a past job where, as medical director, he had trouble connecting with his boss.
“There seemed to be a tremendous communication gap, and there was a mismatch between what I felt was important and what my superior felt was important,” he recalls. “It seemed really hard to get on the same page.”
So he set out to solve the problem: “What I learned was that it’s not sufficient in a leadership role to just focus on who is reporting to you and manage in that direction,” says Dr. Holman. “No one ever tells you this, but you need to spend time managing up.”
Managing up primarily means initiating conversations to get information you need to better work with your boss.
“You need a clear understanding about the priorities and hot buttons of the person you’re reporting to, what they’re personally invested in, how they’re being managed, and what their incentives are,” advises Dr. Holman. “In my situation, I felt that I needed to understand my superior’s background—his career progression, areas of interest, things he felt were important in the organization.”
How do you uncover these facts? It’s simple: Request a one-on-one meeting with your superior and have a direct conversation where you ask those questions.
Next, continues Dr. Holman: “Have what I would call a translational conversation … ‘How do your priorities translate to me and my daily work?’ Again, ask this directly.”
But be warned. “This can be a very productive conversation, but it’s not an easy one to have,” he says. “The reason it’s hard is because whether you’re a frontline hospitalist or a group leader of some kind, you’re a highly educated, highly paid professional. Why would you want to redirect yourself to someone else’s priorities?”
That is the crux of the problem in working for a boss you don’t agree with—you need to relinquish some control to make the situation work.
“This may be difficult for some people but by giving up a little bit, you’ll get a much more productive relationship,” says Dr. Holman. “It also helps you understand how your daily work fits into the broader organizational vision, and you build political capital. You’ll build trust, respect, and equity. If there’s a project you want to engage in and you want support for it, you can trade on that equity.”
Learn their Style
Even as you’re practicing the art of managing up, you may face barriers in dealing with the boss. Consider whether it is a matter of understanding their personal and professional style.
“Maybe you’re just having trouble connecting,” Dr. Holman suggests. “Learn their style, how they communicate. Invest a little time to get a better understanding of their personality style. One way is to ask about their preferences—do they prefer e-mail, phone, or in-person conversations?—and to observe.”
You may discover that the boss is brusque with everyone, not just you, or that they don’t reply to your e-mails because they never check their in-box. The better you understand them, the less stress you’ll suffer from interactions.
The Last Resort
If you’re not getting along with your boss, or don’t like the answers you’re getting, should you consider going over their head to the next level up?
“The temptation may be to use workarounds or back channels—what I call leapfrogging—until you get the answer you want,” Dr. Holman says. “But there’s a lot of damage you can do in leapfrogging. I typically do not recommend that someone going over or around their supervisor unless the circumstances are egregious.”
Ultimately, if you’re still at odds with your boss and the conflict makes you unhappy with your job, you may need to consider finding a better environment.
“If your superior’s personal priorities are in conflict with yours, you owe it to both the boss and yourself to try to converse and reconcile those priorities,” says Dr. Holman. “You should still use the steps, but you may end up leaving anyway. [Managing up] doesn’t guarantee success, but it stacks the deck in your favor.”
He recalls an example where he was the superior to a dissatisfied hospitalist: “There was a hospitalist working for me who had a priority of working in an environment where he could use subjective judgment to make patient decisions. My priority was to standardize care as much as possible. The individual viewed [guidelines, checklists] as an encroachment on his autonomy. This came down to a very fundamental issue. I knew he’d be unhappy in this environment, and we agreed that he would be better off working for another group.”
Perhaps the best advice for coping with a difficult hospitalist-boss relationship is to avoid it in the first place. By recognizing what’s most important to you—what areas you need autonomy in—you can ask questions and perhaps negotiate during the interview or promotion stages. Dr. Wetterneck suggests that hospitalists take the control/autonomy survey included in the SHM white paper “A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction,” which she co-wrote. (The white paper is available under “Publications” on www.hospitalmedicine.org). TH
Jane Jerrard also writes “Public Policy” for The Hospitalist.
A sour relationship with your immediate superior can ruin an otherwise fulfilling job. When you report to someone you continually disagree with or simply don’t understand, just showing up for work can become a misery. If you’re in a situation like this, don’t despair; there is a possible solution.
Power Struggle
Whether the conflict you feel with your boss is over care decisions, personal style, or scope of work, it really boils down to who gets control over your time and your patients.
“For physicians especially, autonomy is very important,” says Tosha B. Wetterneck, MD, associate professor of medicine at University of Wisconsin Hospital/Clinics in Madison. “Physicians are people who work hard, are very smart, and like to control what they do. There is obviously a lot of complexity and variation to the job, which adds to the workload. Plus, decision-making processes need to be happening all the time. This creates stress—and the way to control that stress is to have control over what they do.”
—Russell L. Holman, MD, chief operating officer, Cogent Healthcare, and immediate past president of SHM
A hospitalist who continually butts heads with a superior over issues—or one who subjugates his or her opinion and decisions to the boss’s—is not likely to be satisfied with their job.
“Certainly, an individual’s autonomy is influenced by what they want to have control over and they’re allowed to have control over,” says Dr. Wetterneck. “If there’s a discrepancy between the two, that’s definitely going to have a negative effect on that hospitalist. If there’s a mismatch between what they want control over and what their boss wants, that’s going to be a problem.”
Manage Up
Russell L. Holman, MD, chief operating officer for Brentwood, Tenn.-based Cogent Healthcare and immediate past president of SHM, has worked his way through problems like this—both as the reportee and the boss. He worked out some particularly valuable lessons in a past job where, as medical director, he had trouble connecting with his boss.
“There seemed to be a tremendous communication gap, and there was a mismatch between what I felt was important and what my superior felt was important,” he recalls. “It seemed really hard to get on the same page.”
So he set out to solve the problem: “What I learned was that it’s not sufficient in a leadership role to just focus on who is reporting to you and manage in that direction,” says Dr. Holman. “No one ever tells you this, but you need to spend time managing up.”
Managing up primarily means initiating conversations to get information you need to better work with your boss.
“You need a clear understanding about the priorities and hot buttons of the person you’re reporting to, what they’re personally invested in, how they’re being managed, and what their incentives are,” advises Dr. Holman. “In my situation, I felt that I needed to understand my superior’s background—his career progression, areas of interest, things he felt were important in the organization.”
How do you uncover these facts? It’s simple: Request a one-on-one meeting with your superior and have a direct conversation where you ask those questions.
Next, continues Dr. Holman: “Have what I would call a translational conversation … ‘How do your priorities translate to me and my daily work?’ Again, ask this directly.”
But be warned. “This can be a very productive conversation, but it’s not an easy one to have,” he says. “The reason it’s hard is because whether you’re a frontline hospitalist or a group leader of some kind, you’re a highly educated, highly paid professional. Why would you want to redirect yourself to someone else’s priorities?”
That is the crux of the problem in working for a boss you don’t agree with—you need to relinquish some control to make the situation work.
“This may be difficult for some people but by giving up a little bit, you’ll get a much more productive relationship,” says Dr. Holman. “It also helps you understand how your daily work fits into the broader organizational vision, and you build political capital. You’ll build trust, respect, and equity. If there’s a project you want to engage in and you want support for it, you can trade on that equity.”
Learn their Style
Even as you’re practicing the art of managing up, you may face barriers in dealing with the boss. Consider whether it is a matter of understanding their personal and professional style.
“Maybe you’re just having trouble connecting,” Dr. Holman suggests. “Learn their style, how they communicate. Invest a little time to get a better understanding of their personality style. One way is to ask about their preferences—do they prefer e-mail, phone, or in-person conversations?—and to observe.”
You may discover that the boss is brusque with everyone, not just you, or that they don’t reply to your e-mails because they never check their in-box. The better you understand them, the less stress you’ll suffer from interactions.
The Last Resort
If you’re not getting along with your boss, or don’t like the answers you’re getting, should you consider going over their head to the next level up?
“The temptation may be to use workarounds or back channels—what I call leapfrogging—until you get the answer you want,” Dr. Holman says. “But there’s a lot of damage you can do in leapfrogging. I typically do not recommend that someone going over or around their supervisor unless the circumstances are egregious.”
Ultimately, if you’re still at odds with your boss and the conflict makes you unhappy with your job, you may need to consider finding a better environment.
“If your superior’s personal priorities are in conflict with yours, you owe it to both the boss and yourself to try to converse and reconcile those priorities,” says Dr. Holman. “You should still use the steps, but you may end up leaving anyway. [Managing up] doesn’t guarantee success, but it stacks the deck in your favor.”
He recalls an example where he was the superior to a dissatisfied hospitalist: “There was a hospitalist working for me who had a priority of working in an environment where he could use subjective judgment to make patient decisions. My priority was to standardize care as much as possible. The individual viewed [guidelines, checklists] as an encroachment on his autonomy. This came down to a very fundamental issue. I knew he’d be unhappy in this environment, and we agreed that he would be better off working for another group.”
Perhaps the best advice for coping with a difficult hospitalist-boss relationship is to avoid it in the first place. By recognizing what’s most important to you—what areas you need autonomy in—you can ask questions and perhaps negotiate during the interview or promotion stages. Dr. Wetterneck suggests that hospitalists take the control/autonomy survey included in the SHM white paper “A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction,” which she co-wrote. (The white paper is available under “Publications” on www.hospitalmedicine.org). TH
Jane Jerrard also writes “Public Policy” for The Hospitalist.
A sour relationship with your immediate superior can ruin an otherwise fulfilling job. When you report to someone you continually disagree with or simply don’t understand, just showing up for work can become a misery. If you’re in a situation like this, don’t despair; there is a possible solution.
Power Struggle
Whether the conflict you feel with your boss is over care decisions, personal style, or scope of work, it really boils down to who gets control over your time and your patients.
“For physicians especially, autonomy is very important,” says Tosha B. Wetterneck, MD, associate professor of medicine at University of Wisconsin Hospital/Clinics in Madison. “Physicians are people who work hard, are very smart, and like to control what they do. There is obviously a lot of complexity and variation to the job, which adds to the workload. Plus, decision-making processes need to be happening all the time. This creates stress—and the way to control that stress is to have control over what they do.”
—Russell L. Holman, MD, chief operating officer, Cogent Healthcare, and immediate past president of SHM
A hospitalist who continually butts heads with a superior over issues—or one who subjugates his or her opinion and decisions to the boss’s—is not likely to be satisfied with their job.
“Certainly, an individual’s autonomy is influenced by what they want to have control over and they’re allowed to have control over,” says Dr. Wetterneck. “If there’s a discrepancy between the two, that’s definitely going to have a negative effect on that hospitalist. If there’s a mismatch between what they want control over and what their boss wants, that’s going to be a problem.”
Manage Up
Russell L. Holman, MD, chief operating officer for Brentwood, Tenn.-based Cogent Healthcare and immediate past president of SHM, has worked his way through problems like this—both as the reportee and the boss. He worked out some particularly valuable lessons in a past job where, as medical director, he had trouble connecting with his boss.
“There seemed to be a tremendous communication gap, and there was a mismatch between what I felt was important and what my superior felt was important,” he recalls. “It seemed really hard to get on the same page.”
So he set out to solve the problem: “What I learned was that it’s not sufficient in a leadership role to just focus on who is reporting to you and manage in that direction,” says Dr. Holman. “No one ever tells you this, but you need to spend time managing up.”
Managing up primarily means initiating conversations to get information you need to better work with your boss.
“You need a clear understanding about the priorities and hot buttons of the person you’re reporting to, what they’re personally invested in, how they’re being managed, and what their incentives are,” advises Dr. Holman. “In my situation, I felt that I needed to understand my superior’s background—his career progression, areas of interest, things he felt were important in the organization.”
How do you uncover these facts? It’s simple: Request a one-on-one meeting with your superior and have a direct conversation where you ask those questions.
Next, continues Dr. Holman: “Have what I would call a translational conversation … ‘How do your priorities translate to me and my daily work?’ Again, ask this directly.”
But be warned. “This can be a very productive conversation, but it’s not an easy one to have,” he says. “The reason it’s hard is because whether you’re a frontline hospitalist or a group leader of some kind, you’re a highly educated, highly paid professional. Why would you want to redirect yourself to someone else’s priorities?”
That is the crux of the problem in working for a boss you don’t agree with—you need to relinquish some control to make the situation work.
“This may be difficult for some people but by giving up a little bit, you’ll get a much more productive relationship,” says Dr. Holman. “It also helps you understand how your daily work fits into the broader organizational vision, and you build political capital. You’ll build trust, respect, and equity. If there’s a project you want to engage in and you want support for it, you can trade on that equity.”
Learn their Style
Even as you’re practicing the art of managing up, you may face barriers in dealing with the boss. Consider whether it is a matter of understanding their personal and professional style.
“Maybe you’re just having trouble connecting,” Dr. Holman suggests. “Learn their style, how they communicate. Invest a little time to get a better understanding of their personality style. One way is to ask about their preferences—do they prefer e-mail, phone, or in-person conversations?—and to observe.”
You may discover that the boss is brusque with everyone, not just you, or that they don’t reply to your e-mails because they never check their in-box. The better you understand them, the less stress you’ll suffer from interactions.
The Last Resort
If you’re not getting along with your boss, or don’t like the answers you’re getting, should you consider going over their head to the next level up?
“The temptation may be to use workarounds or back channels—what I call leapfrogging—until you get the answer you want,” Dr. Holman says. “But there’s a lot of damage you can do in leapfrogging. I typically do not recommend that someone going over or around their supervisor unless the circumstances are egregious.”
Ultimately, if you’re still at odds with your boss and the conflict makes you unhappy with your job, you may need to consider finding a better environment.
“If your superior’s personal priorities are in conflict with yours, you owe it to both the boss and yourself to try to converse and reconcile those priorities,” says Dr. Holman. “You should still use the steps, but you may end up leaving anyway. [Managing up] doesn’t guarantee success, but it stacks the deck in your favor.”
He recalls an example where he was the superior to a dissatisfied hospitalist: “There was a hospitalist working for me who had a priority of working in an environment where he could use subjective judgment to make patient decisions. My priority was to standardize care as much as possible. The individual viewed [guidelines, checklists] as an encroachment on his autonomy. This came down to a very fundamental issue. I knew he’d be unhappy in this environment, and we agreed that he would be better off working for another group.”
Perhaps the best advice for coping with a difficult hospitalist-boss relationship is to avoid it in the first place. By recognizing what’s most important to you—what areas you need autonomy in—you can ask questions and perhaps negotiate during the interview or promotion stages. Dr. Wetterneck suggests that hospitalists take the control/autonomy survey included in the SHM white paper “A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction,” which she co-wrote. (The white paper is available under “Publications” on www.hospitalmedicine.org). TH
Jane Jerrard also writes “Public Policy” for The Hospitalist.
Use Outside Help
Addressing the clinical and political issues raised by the use of non-housestaff services is one of the biggest challenges facing hospitalists at academic medical centers, according to a paper in this month’s issue of the Journal of Hospital Medicine.
Lead author Niraj Sehgal, MD, assistant clinical professor of medicine at the University of California, San Francisco (UCSF), and colleagues studied the non-housestaff services at five academic medical centers around the United States to identify what it takes to make the best use of non-housestaff services.
Reliance on these services will grow largely because of restrictions established in 2003 by the Accreditation Council of Graduate Medical Education (ACGME), which limit residents to an 80-hour workweek.
What’s more, it is possible that the ACGME may cut hours even more, given that many other countries have lower restrictions.
In other words, “most academic medical centers now realize residents no longer will be providing as much patient care as they used to,” Dr. Sehgal says.
For example, at UCSF, residents’ hours have been reduced by one-third since the restrictions were established. One way to handle the situation was to reduce the number of patient-hours per resident.
However, at the same time that ruling went into effect, UCSF also increased the number of beds in its hospital. In an effort to determine who is best suited to care for these patients, UCSF and other academic centers turned to non-housestaff services to pick up the slack. “Every residency program has struggled with different models,” he explains.
In their paper, Dr. Sehgal and his colleagues identify nine questions to consider in developing non-housestaff medicine services. The questions reflect key challenges facing medical centers that are building these services, such as:
- System equities: Avoid creating a two-tiered system in which non-housestaff hospitalists who mostly provide clinical care are viewed as second-class citizens compared with academic hospitalists, who also teach and conduct research. This also raises the question of how to define an academic hospitalist;
- Define the patient mix: Should non-housestaff physicians handle less acute patients, specific patient populations, or all patients above the limit for residents?;
- Recruitment and retention: Academic centers may have to offer non-housestaff hospitalists incentives, such as teaching or research opportunities, or financial rewards such as student loan forgiveness, to attract talented clinicians; and
- Compensation and incentives: This should reflect all aspects of the physician’s job, including quality improvement efforts, research activities, and excellence in teaching, as well as clinical productivity.
“How these questions are answered is often driven by local factors, such as the vision of local leadership and the availability of important resources,” Dr. Sehgal and his coauthors write. “Nevertheless, it is important for hospitals to share their experiences since best practices remain unclear.”
To explore how different centers and services address these issues, they compared the non-housestaff medicine services at Brigham and Women’s Hospital in Boston, Emory University in Atlanta, the University of Michigan in Ann Arbor, Northwestern University Medical Center in Chicago, and UCSF. The information was obtained from representatives at each center and was current as of July 2007.
The services ranged in age from two to five years old and covered 168 to 212 clinical days per year, or 15 to 20 shifts per month. Depending on the number of hospitalists in the service, they saw anywhere from 12 to 95 patients per day.
Further, they all provided coverage for 50% of weekends. For night coverage, one service used dedicated nocturnists, two relied exclusively on moonlighters, and the remainder split coverage between the two.
All the services were located within the university hospital, except for the one at UCSF, which was at an outlying affiliated hospital.
Compensation for non-housestaff hospitalists matched that of staff physicians at two hospitals; the other three hospitals offered non-housestaff physicians some type of financial incentive, either in the form of higher salary, student loan forgiveness, or a combination of the two.
This is an interesting era for hospitalists, who are striving to carve an academic niche for themselves while still performing their clinical duties, Dr. Sehgal notes.
Among the ways they can achieve that is by becoming more involved in other areas of medical center operations, such as information technology, quality and system improvements, and committee work.
Handled properly, these opportunities to collaborate can increase hospitalist prestige and visibility, as they become more involved in hospital leadership and research and share management responsibilities with their medical and surgical colleagues.
Smoothly integrating non-housestaff services into day-to-day function is another opportunity for hospitalists to demonstrate their leadership skills, because the use of these services will increase, Dr. Sehgal adds. This makes it necessary to keep studying the outside services and identifying the ways in which they differ from their housestaff counterparts in order to maximize their contributions.
This study shows that creating non-housestaff services involves the consideration of several important elements, including the patients to be seen by those services, and staffing issues, such as whether the service should be composed exclusively of hospitalists, or if other specialties also should be included.
Hospitalists will have to monitor quality control issues and staff retention, and make sure a two-tiered system does not develop between housestaff and non-housestaff physicians. “So far, there has been very little written about this,” Dr. Sehgal concludes. TH
Norra MacReady is a medical writer based in California.
Addressing the clinical and political issues raised by the use of non-housestaff services is one of the biggest challenges facing hospitalists at academic medical centers, according to a paper in this month’s issue of the Journal of Hospital Medicine.
Lead author Niraj Sehgal, MD, assistant clinical professor of medicine at the University of California, San Francisco (UCSF), and colleagues studied the non-housestaff services at five academic medical centers around the United States to identify what it takes to make the best use of non-housestaff services.
Reliance on these services will grow largely because of restrictions established in 2003 by the Accreditation Council of Graduate Medical Education (ACGME), which limit residents to an 80-hour workweek.
What’s more, it is possible that the ACGME may cut hours even more, given that many other countries have lower restrictions.
In other words, “most academic medical centers now realize residents no longer will be providing as much patient care as they used to,” Dr. Sehgal says.
For example, at UCSF, residents’ hours have been reduced by one-third since the restrictions were established. One way to handle the situation was to reduce the number of patient-hours per resident.
However, at the same time that ruling went into effect, UCSF also increased the number of beds in its hospital. In an effort to determine who is best suited to care for these patients, UCSF and other academic centers turned to non-housestaff services to pick up the slack. “Every residency program has struggled with different models,” he explains.
In their paper, Dr. Sehgal and his colleagues identify nine questions to consider in developing non-housestaff medicine services. The questions reflect key challenges facing medical centers that are building these services, such as:
- System equities: Avoid creating a two-tiered system in which non-housestaff hospitalists who mostly provide clinical care are viewed as second-class citizens compared with academic hospitalists, who also teach and conduct research. This also raises the question of how to define an academic hospitalist;
- Define the patient mix: Should non-housestaff physicians handle less acute patients, specific patient populations, or all patients above the limit for residents?;
- Recruitment and retention: Academic centers may have to offer non-housestaff hospitalists incentives, such as teaching or research opportunities, or financial rewards such as student loan forgiveness, to attract talented clinicians; and
- Compensation and incentives: This should reflect all aspects of the physician’s job, including quality improvement efforts, research activities, and excellence in teaching, as well as clinical productivity.
“How these questions are answered is often driven by local factors, such as the vision of local leadership and the availability of important resources,” Dr. Sehgal and his coauthors write. “Nevertheless, it is important for hospitals to share their experiences since best practices remain unclear.”
To explore how different centers and services address these issues, they compared the non-housestaff medicine services at Brigham and Women’s Hospital in Boston, Emory University in Atlanta, the University of Michigan in Ann Arbor, Northwestern University Medical Center in Chicago, and UCSF. The information was obtained from representatives at each center and was current as of July 2007.
The services ranged in age from two to five years old and covered 168 to 212 clinical days per year, or 15 to 20 shifts per month. Depending on the number of hospitalists in the service, they saw anywhere from 12 to 95 patients per day.
Further, they all provided coverage for 50% of weekends. For night coverage, one service used dedicated nocturnists, two relied exclusively on moonlighters, and the remainder split coverage between the two.
All the services were located within the university hospital, except for the one at UCSF, which was at an outlying affiliated hospital.
Compensation for non-housestaff hospitalists matched that of staff physicians at two hospitals; the other three hospitals offered non-housestaff physicians some type of financial incentive, either in the form of higher salary, student loan forgiveness, or a combination of the two.
This is an interesting era for hospitalists, who are striving to carve an academic niche for themselves while still performing their clinical duties, Dr. Sehgal notes.
Among the ways they can achieve that is by becoming more involved in other areas of medical center operations, such as information technology, quality and system improvements, and committee work.
Handled properly, these opportunities to collaborate can increase hospitalist prestige and visibility, as they become more involved in hospital leadership and research and share management responsibilities with their medical and surgical colleagues.
Smoothly integrating non-housestaff services into day-to-day function is another opportunity for hospitalists to demonstrate their leadership skills, because the use of these services will increase, Dr. Sehgal adds. This makes it necessary to keep studying the outside services and identifying the ways in which they differ from their housestaff counterparts in order to maximize their contributions.
This study shows that creating non-housestaff services involves the consideration of several important elements, including the patients to be seen by those services, and staffing issues, such as whether the service should be composed exclusively of hospitalists, or if other specialties also should be included.
Hospitalists will have to monitor quality control issues and staff retention, and make sure a two-tiered system does not develop between housestaff and non-housestaff physicians. “So far, there has been very little written about this,” Dr. Sehgal concludes. TH
Norra MacReady is a medical writer based in California.
Addressing the clinical and political issues raised by the use of non-housestaff services is one of the biggest challenges facing hospitalists at academic medical centers, according to a paper in this month’s issue of the Journal of Hospital Medicine.
Lead author Niraj Sehgal, MD, assistant clinical professor of medicine at the University of California, San Francisco (UCSF), and colleagues studied the non-housestaff services at five academic medical centers around the United States to identify what it takes to make the best use of non-housestaff services.
Reliance on these services will grow largely because of restrictions established in 2003 by the Accreditation Council of Graduate Medical Education (ACGME), which limit residents to an 80-hour workweek.
What’s more, it is possible that the ACGME may cut hours even more, given that many other countries have lower restrictions.
In other words, “most academic medical centers now realize residents no longer will be providing as much patient care as they used to,” Dr. Sehgal says.
For example, at UCSF, residents’ hours have been reduced by one-third since the restrictions were established. One way to handle the situation was to reduce the number of patient-hours per resident.
However, at the same time that ruling went into effect, UCSF also increased the number of beds in its hospital. In an effort to determine who is best suited to care for these patients, UCSF and other academic centers turned to non-housestaff services to pick up the slack. “Every residency program has struggled with different models,” he explains.
In their paper, Dr. Sehgal and his colleagues identify nine questions to consider in developing non-housestaff medicine services. The questions reflect key challenges facing medical centers that are building these services, such as:
- System equities: Avoid creating a two-tiered system in which non-housestaff hospitalists who mostly provide clinical care are viewed as second-class citizens compared with academic hospitalists, who also teach and conduct research. This also raises the question of how to define an academic hospitalist;
- Define the patient mix: Should non-housestaff physicians handle less acute patients, specific patient populations, or all patients above the limit for residents?;
- Recruitment and retention: Academic centers may have to offer non-housestaff hospitalists incentives, such as teaching or research opportunities, or financial rewards such as student loan forgiveness, to attract talented clinicians; and
- Compensation and incentives: This should reflect all aspects of the physician’s job, including quality improvement efforts, research activities, and excellence in teaching, as well as clinical productivity.
“How these questions are answered is often driven by local factors, such as the vision of local leadership and the availability of important resources,” Dr. Sehgal and his coauthors write. “Nevertheless, it is important for hospitals to share their experiences since best practices remain unclear.”
To explore how different centers and services address these issues, they compared the non-housestaff medicine services at Brigham and Women’s Hospital in Boston, Emory University in Atlanta, the University of Michigan in Ann Arbor, Northwestern University Medical Center in Chicago, and UCSF. The information was obtained from representatives at each center and was current as of July 2007.
The services ranged in age from two to five years old and covered 168 to 212 clinical days per year, or 15 to 20 shifts per month. Depending on the number of hospitalists in the service, they saw anywhere from 12 to 95 patients per day.
Further, they all provided coverage for 50% of weekends. For night coverage, one service used dedicated nocturnists, two relied exclusively on moonlighters, and the remainder split coverage between the two.
All the services were located within the university hospital, except for the one at UCSF, which was at an outlying affiliated hospital.
Compensation for non-housestaff hospitalists matched that of staff physicians at two hospitals; the other three hospitals offered non-housestaff physicians some type of financial incentive, either in the form of higher salary, student loan forgiveness, or a combination of the two.
This is an interesting era for hospitalists, who are striving to carve an academic niche for themselves while still performing their clinical duties, Dr. Sehgal notes.
Among the ways they can achieve that is by becoming more involved in other areas of medical center operations, such as information technology, quality and system improvements, and committee work.
Handled properly, these opportunities to collaborate can increase hospitalist prestige and visibility, as they become more involved in hospital leadership and research and share management responsibilities with their medical and surgical colleagues.
Smoothly integrating non-housestaff services into day-to-day function is another opportunity for hospitalists to demonstrate their leadership skills, because the use of these services will increase, Dr. Sehgal adds. This makes it necessary to keep studying the outside services and identifying the ways in which they differ from their housestaff counterparts in order to maximize their contributions.
This study shows that creating non-housestaff services involves the consideration of several important elements, including the patients to be seen by those services, and staffing issues, such as whether the service should be composed exclusively of hospitalists, or if other specialties also should be included.
Hospitalists will have to monitor quality control issues and staff retention, and make sure a two-tiered system does not develop between housestaff and non-housestaff physicians. “So far, there has been very little written about this,” Dr. Sehgal concludes. TH
Norra MacReady is a medical writer based in California.