User login
TB with Pott's Disease and Psoas Abscess
A 22‐year‐old man was referred from an outside hospital with 2 weeks of generalized weakness and difficulty ambulating. He also reported a 6‐month history of abdominal pain, right‐sided lumbar back pain, malaise, night sweats, cough, and weight loss of 30 kg. The patient was born in Mexico but had lived in the US for 10 years, working as a construction worker in northern California. He had had no prior medical care. On examination, the patient had a temperature of 40C, a heart rate of 109, and a respiratory rate of 20. His oxygen saturation was 97% on room air, and lung fields were clear bilaterally. Strength was slightly decreased in the right leg, with tenderness in the posterolateral aspect of the right thigh and thoracic lumbar spine.
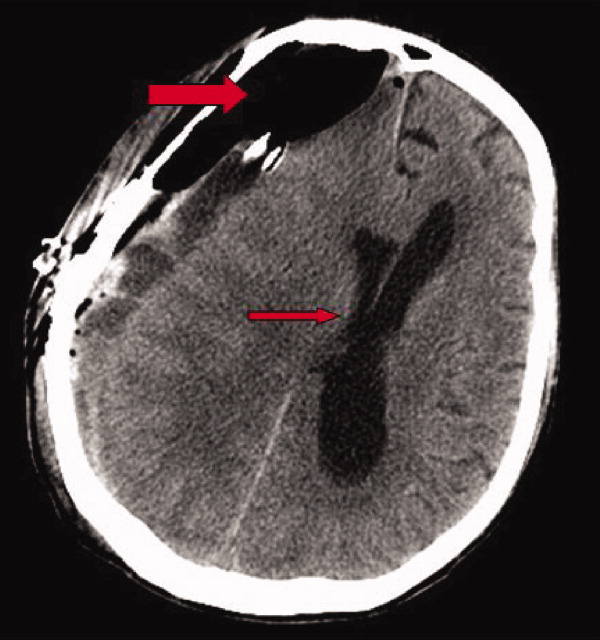
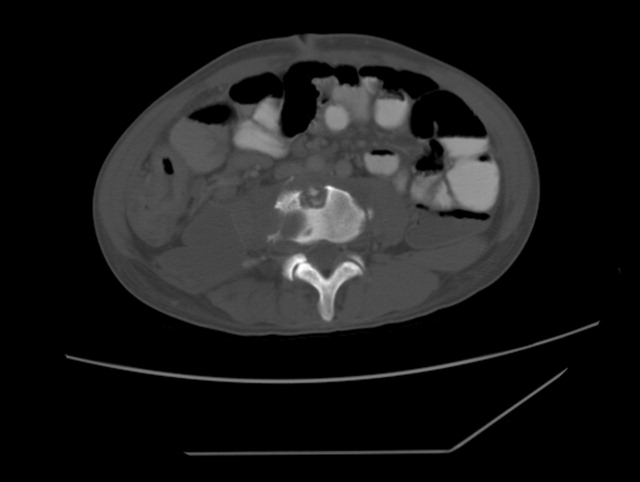
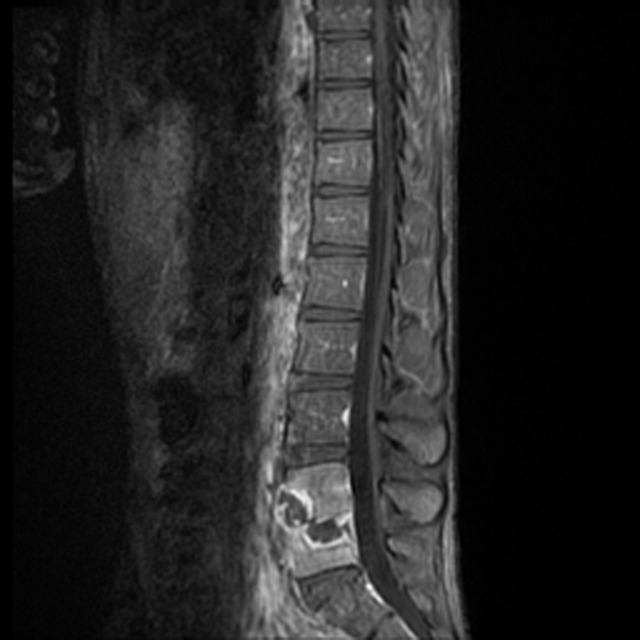
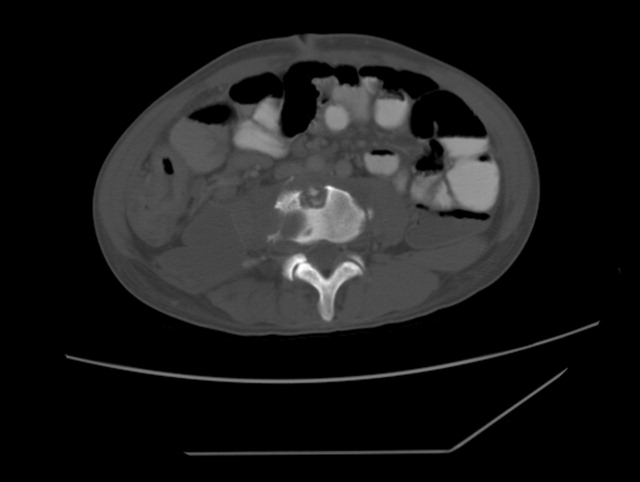
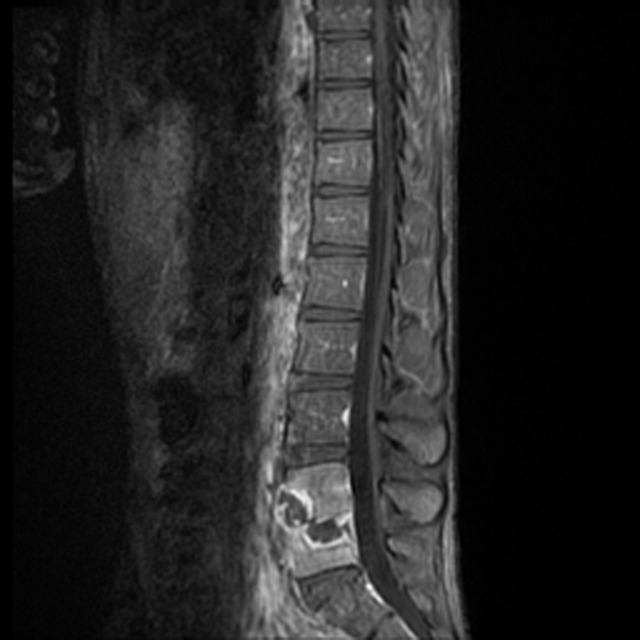
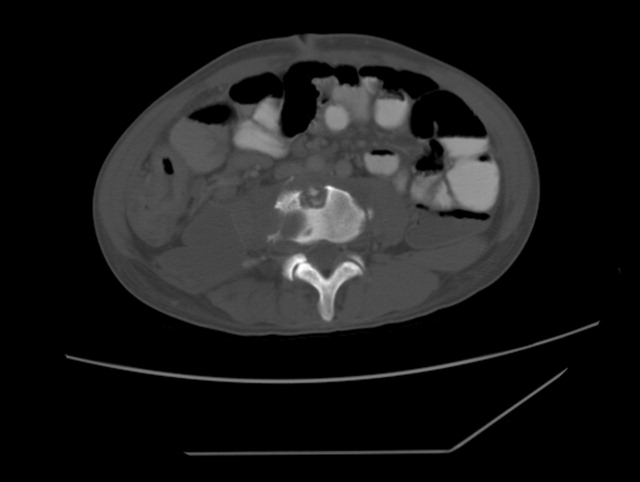
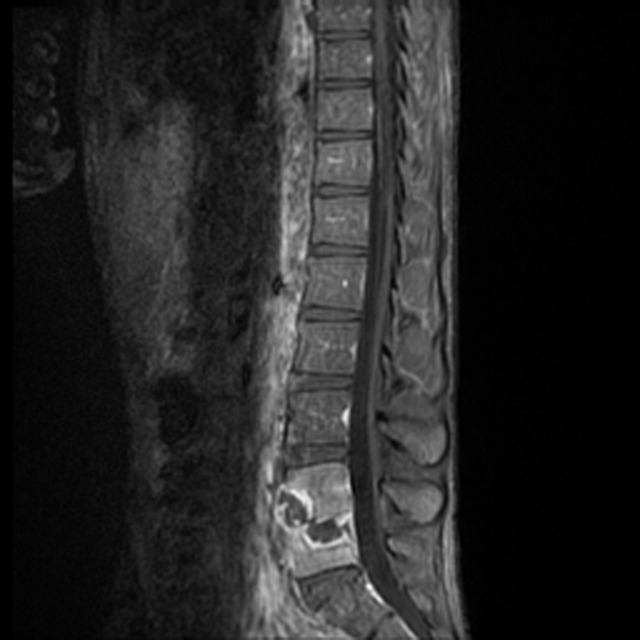
Radiograph of the chest showed bilateral upper lobe reticulonodular infiltrates, cavitation, and pleural thickening (Figure 1). Computed tomography (CT) showed innumerable pulmonary nodules throughout the mid and lower lungs, a loss of disc space between L4 and L5, and a large multiloculated abscess of the right iliacus and psoas muscles that extended into the right thigh (Figure 2). Longitudinal relaxation time (T1)‐weighted magnetic resonance imaging (MRI) of the lumbar spine revealed vertebral destruction of L4 and L5 (Figure 3).

The patient underwent vertebrectomy of L4 and L5, anterior/posterior fixation and fusion from L4 to S1, and drainage of a large right‐sided psoas abscess. Acid‐fast bacilli were seen in abscess fluid and vertebral bone. Subsequently, the intraoperative cultures and 6 sequential sputum cultures all grew Mycobacterium tuberculosis. The patient was begun on rifampin, isoniazid, pyrazinamide, and ethambutol with a good clinical response, and subsequently transferred back to his referring hospital for continued medical care and rehabilitation.
Extrapulmonary manifestations of tuberculosis should be suspected in patients from a tuberculosis‐endemic country of origin. Bone and joint tuberculosis account for up to 35% of cases of extrapulmonary tuberculosis. Spinal tuberculosis (Pott's disease) most commonly involves the anteroinferior aspect of vertebral bodies in the thoracic spine. Tuberculosis is a disease with diverse manifestations and can elude even the most astute physician if it is not considered as a diagnosis.
A 22‐year‐old man was referred from an outside hospital with 2 weeks of generalized weakness and difficulty ambulating. He also reported a 6‐month history of abdominal pain, right‐sided lumbar back pain, malaise, night sweats, cough, and weight loss of 30 kg. The patient was born in Mexico but had lived in the US for 10 years, working as a construction worker in northern California. He had had no prior medical care. On examination, the patient had a temperature of 40C, a heart rate of 109, and a respiratory rate of 20. His oxygen saturation was 97% on room air, and lung fields were clear bilaterally. Strength was slightly decreased in the right leg, with tenderness in the posterolateral aspect of the right thigh and thoracic lumbar spine.
Radiograph of the chest showed bilateral upper lobe reticulonodular infiltrates, cavitation, and pleural thickening (Figure 1). Computed tomography (CT) showed innumerable pulmonary nodules throughout the mid and lower lungs, a loss of disc space between L4 and L5, and a large multiloculated abscess of the right iliacus and psoas muscles that extended into the right thigh (Figure 2). Longitudinal relaxation time (T1)‐weighted magnetic resonance imaging (MRI) of the lumbar spine revealed vertebral destruction of L4 and L5 (Figure 3).

The patient underwent vertebrectomy of L4 and L5, anterior/posterior fixation and fusion from L4 to S1, and drainage of a large right‐sided psoas abscess. Acid‐fast bacilli were seen in abscess fluid and vertebral bone. Subsequently, the intraoperative cultures and 6 sequential sputum cultures all grew Mycobacterium tuberculosis. The patient was begun on rifampin, isoniazid, pyrazinamide, and ethambutol with a good clinical response, and subsequently transferred back to his referring hospital for continued medical care and rehabilitation.
Extrapulmonary manifestations of tuberculosis should be suspected in patients from a tuberculosis‐endemic country of origin. Bone and joint tuberculosis account for up to 35% of cases of extrapulmonary tuberculosis. Spinal tuberculosis (Pott's disease) most commonly involves the anteroinferior aspect of vertebral bodies in the thoracic spine. Tuberculosis is a disease with diverse manifestations and can elude even the most astute physician if it is not considered as a diagnosis.
A 22‐year‐old man was referred from an outside hospital with 2 weeks of generalized weakness and difficulty ambulating. He also reported a 6‐month history of abdominal pain, right‐sided lumbar back pain, malaise, night sweats, cough, and weight loss of 30 kg. The patient was born in Mexico but had lived in the US for 10 years, working as a construction worker in northern California. He had had no prior medical care. On examination, the patient had a temperature of 40C, a heart rate of 109, and a respiratory rate of 20. His oxygen saturation was 97% on room air, and lung fields were clear bilaterally. Strength was slightly decreased in the right leg, with tenderness in the posterolateral aspect of the right thigh and thoracic lumbar spine.
Radiograph of the chest showed bilateral upper lobe reticulonodular infiltrates, cavitation, and pleural thickening (Figure 1). Computed tomography (CT) showed innumerable pulmonary nodules throughout the mid and lower lungs, a loss of disc space between L4 and L5, and a large multiloculated abscess of the right iliacus and psoas muscles that extended into the right thigh (Figure 2). Longitudinal relaxation time (T1)‐weighted magnetic resonance imaging (MRI) of the lumbar spine revealed vertebral destruction of L4 and L5 (Figure 3).

The patient underwent vertebrectomy of L4 and L5, anterior/posterior fixation and fusion from L4 to S1, and drainage of a large right‐sided psoas abscess. Acid‐fast bacilli were seen in abscess fluid and vertebral bone. Subsequently, the intraoperative cultures and 6 sequential sputum cultures all grew Mycobacterium tuberculosis. The patient was begun on rifampin, isoniazid, pyrazinamide, and ethambutol with a good clinical response, and subsequently transferred back to his referring hospital for continued medical care and rehabilitation.
Extrapulmonary manifestations of tuberculosis should be suspected in patients from a tuberculosis‐endemic country of origin. Bone and joint tuberculosis account for up to 35% of cases of extrapulmonary tuberculosis. Spinal tuberculosis (Pott's disease) most commonly involves the anteroinferior aspect of vertebral bodies in the thoracic spine. Tuberculosis is a disease with diverse manifestations and can elude even the most astute physician if it is not considered as a diagnosis.
Evidence for Thromboembolism Prophylaxis
Deep venous thrombosis (DVT) and pulmonary embolism (PE), collectively referred to as venous thromboembolism (VTE), are common events in hospitalized patients and result in significant morbidity and mortality. Often silent and frequently unexpected, VTE is preventable. Accordingly, the American College of Chest Physicians recommends that pharmacologic prophylaxis be given to acutely ill medical patients admitted to the hospital with congestive heart failure or severe respiratory disease, or to patients who are confined to bed who have additional risk factors, such as cancer or previous VTE.1 Three recent meta‐analyses24 demonstrated significant reductions in VTE in general medicine patients with pharmacologic prophylaxis. Recently the National Quality Forum advocated that hospitals evaluate each patient upon admission and regularly thereafter, for the risk of developing DVT/VTE and utilize clinically appropriate methods to prevent DVT/VTE.5
Despite recommendations for prophylaxis, multiple studies demonstrate utilization in <50% of at‐risk general medical patients.68 Physicians' lack of awareness may partially explain this underutilization, but other likely factors include physicians' questions about the clinical importance of the outcome (eg, some studies have shown reductions primarily in asymptomatic distal DVT), doubt regarding the best form of prophylaxis (ie, unfractionated heparin [UFH] vs. low molecular weight heparin [LMWH]), uncertainty regarding optimal dosing regimens, and comparable uncertainty regarding which patients have sufficiently high risk for VTE to outweigh the risks of anticoagulation.
We undertook the current meta‐analysis to address questions about thromboembolism prevention in general medicine patients. Does pharmacologic prophylaxis prevent clinically relevant events? Is LMWH or UFH preferable in terms of either efficacy or safety?
MATERIALS AND METHODS
Search Strategy
We conducted an extensive search that included reviewing electronic databases (MEDLINE, EMBASE, and CINAHL) through June 2008, reviewing conference proceedings, and contacting drug manufacturers. The MEDLINE search combined the key words deep venous thrombosis, thromboembolism, AND pulmonary embolism with the terms primary prevention, prophylaxis, OR prevention. We limited the search results using the filter for randomized controlled trials in PubMed. Similar strategies (available on request) were used to search EMBASE, CINAHL, and the Cochrane Central Register of Controlled Trials. We also searched the Cochrane Database of Systematic Reviews to identify previous reviews on the same topic. We obtained translations of eligible, non‐English‐language articles.
The proceedings of annual meetings from the American Thoracic Society, the American Society of Hematology, and the Society for General Internal Medicine from 1994 to 2008 were hand‐searched for reports on DVT or PE prevention published in abstract form only. (Note: the American Society of Hematology was only available through 2007). We contacted the 3 main manufacturers of LMWHPfizer (dalteparin), Aventis (enoxaparin), Glaxo Smith Kline (nadoparin)and requested information on unpublished pharmaceutical sponsored trials. First authors from the trials included in this meta‐analysis were also contacted to determine if they knew of additional published or unpublished trials.
Inclusion and Exclusion Criteria
Studies were required to be prospective randomized controlled trials comparing UFH or LMWH to mechanical prophylaxis, placebo, or no intervention. We also included randomized head‐to‐head comparisons of UFH and LMWH. Eligible studies enrolled general medical patients. Trials including predominantly intensive care unit (ICU) patients; stroke, spinal cord, or acute myocardial infarction patients were excluded. We excluded trials focused on these populations because the risk for VTE may differ from that for general medical patients and because patients in these groups already commonly receive anticoagulants as a preventive measure or as active treatment (eg, for acute myocardial infarction [MI] care). Trials assessing thrombosis in patients with long‐term central venous access/catheters were also excluded. Articles focusing on long‐term rehabilitation patients were excluded.
Studies had to employ objective criteria for diagnosing VTE. For DVT these included duplex ultrasonography, venography, fibrinogen uptake scanning, impedance plethysmography, or autopsy as a primary or secondary outcome. Studies utilizing thermographic techniques were excluded.9 Eligible diagnostic modalities for PE consisted of pulmonary arteriogram, ventilation/perfusion scan, CT angiography, and autopsy.
After an initial review of article titles and abstracts, the full texts of all articles that potentially met our inclusion criteria were independently reviewed for eligibility by 2 authors (G.M.B., M.D.). In cases of disagreement, a third author (S.F.) independently reviewed the article and adjudicated decisions.
Quantitative Data Synthesis and Statistical Analysis
For all included articles, 2 reviewers independently abstracted data on key study features (including population size, trial design, modality of VTE diagnosis, and interventions delivered to treatment and control groups), results (including the rates of all DVT, proximal DVT, symptomatic DVT, PE, and death), as well as adverse events (such as bleeding and thrombocytopenia). We accepted the endpoint of DVT when assessed by duplex ultrasonography, venography, autopsy, or when diagnosed by fibrinogen uptake scanning or impedance plethysmography. For all endpoints we abstracted event rates as number of events based on intention to treat. Each study was assessed for quality using the Jadad scale.10 The Jadad scale is a validated tool for characterizing study quality that accounts for randomization, blinding, and description of withdrawals and dropouts in individual trials. The Jadad score ranges from 0 to 5 with higher numbers identifying trials of greater methodological rigor.
The trials were divided into 4 groups based on the prophylaxis agent used and the method of comparison (UFH vs. control, LMWH vs. control, LMWH vs. UFH, and LMWH/UFH combined vs. control). After combining trials for each group, we calculated a pooled relative risk (RR) and a 95% confidence interval (CI) based on both fixed and a random effects model using the DerSimonian and Laird method. Heterogeneity of the included studies was evaluated with a chi‐square statistic. The percentage of variation in the pooled RR attributable to heterogeneity was calculated and reported using the I‐squared statistic.11 Sensitivity analyses were performed and included repeating all analyses using high‐quality studies only (Jadad score 3 or higher). Publication bias was assessed using the methods developed by Egger et al.12 and Begg and Mazumdar.13 All analyses were performed using STATA SE version 9 (Stata Corp, College Station, TX).
RESULTS
Study Identification and Selection
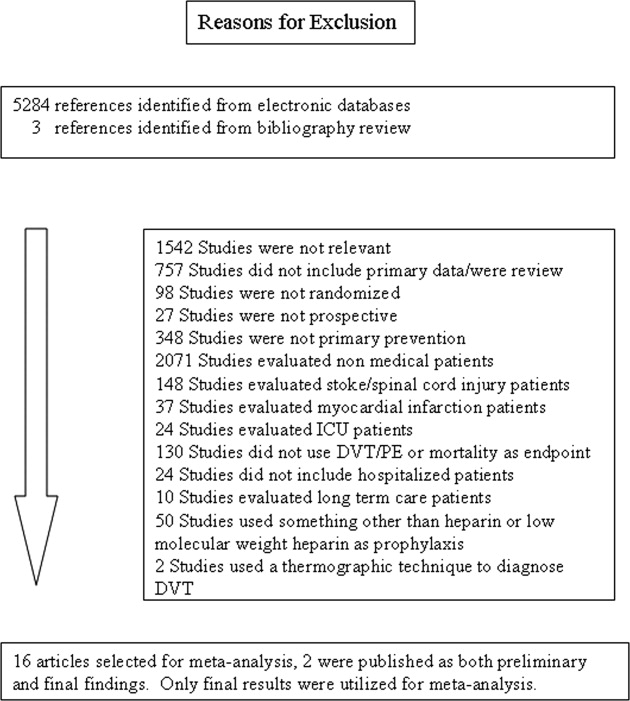
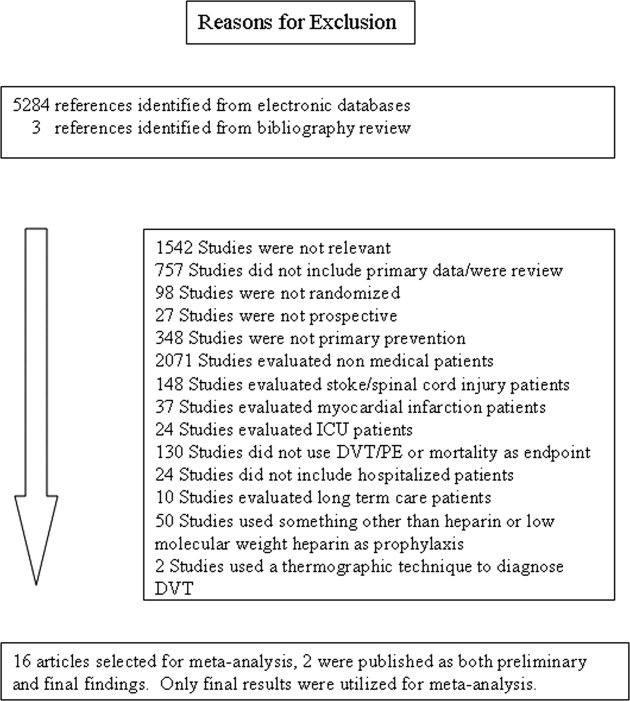
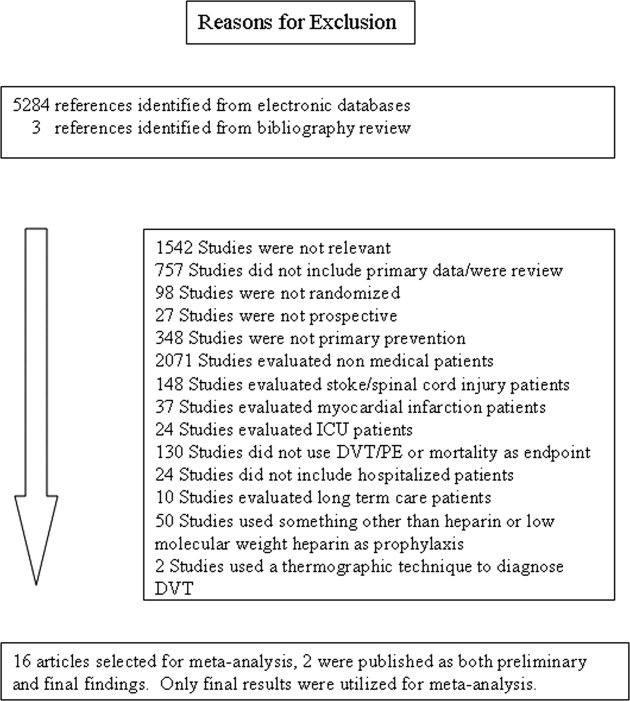
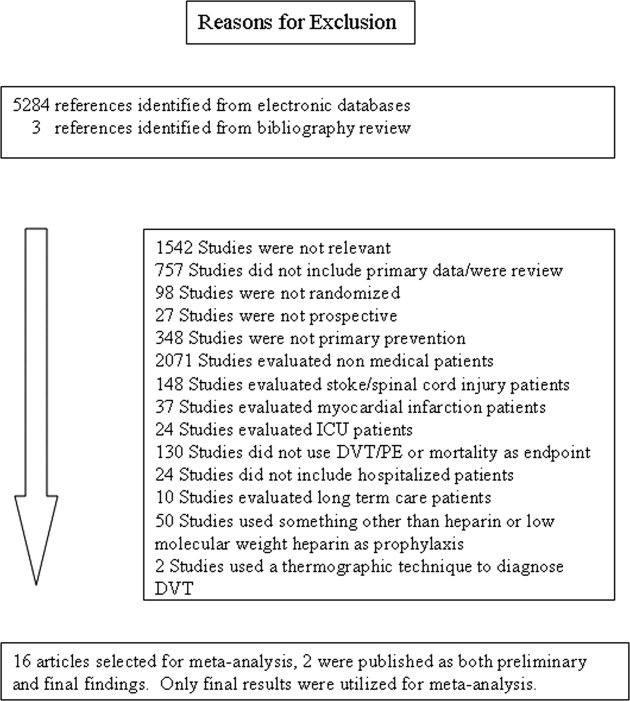
The computerized literature search resulted in 5284 articles. Three additional citations were found by review of bibliographies. No additional trials were identified from reviews of abstracts from national meetings. Representatives from the 3 pharmaceutical companies reported no knowledge of additional published or unpublished data. Of the 5287 studies identified by the search, 14 studies met all eligibility criteria (Figure 1).
Study Characteristics
The 14 trials eligible for inclusion in the analysis consisted of 8 comparisons of UFH or LMWH vs. control (Table 1) and 6 head‐to‐head comparisons of UFH and LMWH (Table 2). The 14 studies included 8 multicenter trials and enrolled a total of 24,515 patients: 20,594 in the 8 trials that compared UFH or LMWH with placebo and 3921 in the 6 trials that compared LMWH with UFH. Two trials exclusively enrolled patients with either congestive heart failure or severe respiratory disease,14, 15 while 12 trials enrolled mixed populations. In 8 trials a period of immobility was necessary for study entry,14, 1621 while in 2 trials immobility was not required.22, 23 In the 4 remaining trials immobility was not explicitly discussed.15, 2426 One‐half of the trials required a length of stay greater than 3 days.1719, 2225
| Study (Year)Reference | Patients (n) | Duration (days) | VTE Risk Factors | Drug Dose | Comparison | DVT Assessed | PE Assessed | Double Blind | Jadad Score |
|---|---|---|---|---|---|---|---|---|---|
| |||||||||
| Belch et al. (1981)15 | 100 | 8 | Age 40‐80 years; CHF; chest infection | UFH TID | None | FUS | VQ | No | 1 |
| Dahan et al. (1986)23 | 270 | 10* | Age >65 years | Enoxaparin 60 mg | Placebo | FUS | Autopsy | Yes | 3 |
| Halkin et al. (1982)20 | 1358 | Not reported | Age >40 years; immobile | UFH BID | None | No | No | No | 1 |
| Mahe et al. (2005)16 | 2474 | 13.08 | Age >40 years; immobile | Nadroparin 7500 IU | Placebo | Autopsy | Autopsy | Yes | 5 |
| Gardlund (1996)21 | 11693 | 8.2 | Age >55 years; immobile | UFH BID | None | Autopsy | Autopsy | No | 2 |
| Samama et al. (1999)24 | 738 | 7 | Age >40 years; length of stay 6 days; CHF; respiratory failure or 1 additional risk factor | Enoxaparin 40 mg | Placebo | Venography | Composite | Yes | 4 |
| Leizorovicz et al. (2004)25 | 3681 | 12.6 | Age >40 years; length of stay 4 days; CHF; respiratory failure or 1 additional risk factor | Dalteparin 5000 IU | Placebo | DUS | Composite | Yes | 4 |
| Lederle et al. (2006)22 | 280 | 13.4 | Age >60 years; length of stay 3 days | Enoxaparin 40 mg | Placebo | DUS | Composite | Yes | 5 |
| Study (Year)reference | Patients (n) | Duration (days) | VTE Risk Factors | Drug/Dose | Comparison | DVT Assessed | PE Assessed | Double Blind | Jadad Score |
|---|---|---|---|---|---|---|---|---|---|
| |||||||||
| Bergmann and Neuhart (1996)27 | 442 | 9.5 | Age >65 years; immobile | Enoxaparin 20 mg | UFH BID | FUS | Composite | Yes | 5 |
| Harenberg et al. (1990)19 | 166 | 10* | Age 40‐80 years; 1 week of bed rest | LMWH 1.500 aPTT units QD | UFH TID | IP | No | Yes | 3 |
| Kleber et al. (2003)14 | 665 | 9.8 | Age 18 years; severe CHF or respiratory disease; immobile | Enoxaparin 40 mg | UFH TID | Venography | Composite | No | 3 |
| Aquino et al. (1990)26 | 99 | Not reported | Age >70 years | Nadoparine 7500 IU | UFH BID | DUS | Composite | No | 1 |
| Harenberg et al. (1996)18 | 1590 | 10* | Age 50‐80 years; immobile + 1 additional risk factor | Nadoparine 36 mg | UFH TID | DUS | Composite | Yes | 4 |
| Lechler et al. (1996)17 | 959 | 7* | Age >18 years; immobile + 1 additional risk factor | Enoxaparin 40 mg | UFH TID | DUS | Composite | Yes | 3 |
While minimum age for study entry varied, the patient population predominantly ranged from 65 to 85 years of age. Many of the trials reported expected, not actual, treatment duration. The range of expected treatment was 7 to 21 days, with 10 days of treatment the most frequently mentioned. In the 8 trials1416, 21, 22, 24, 25, 27 that reported actual treatment duration, the range was 8 to 13.4 days. Most trials did not report number of VTE risk factors per patient, nor was there uniform acceptance of risk factors across trials.
UFH or LMWH vs. Control
DVT
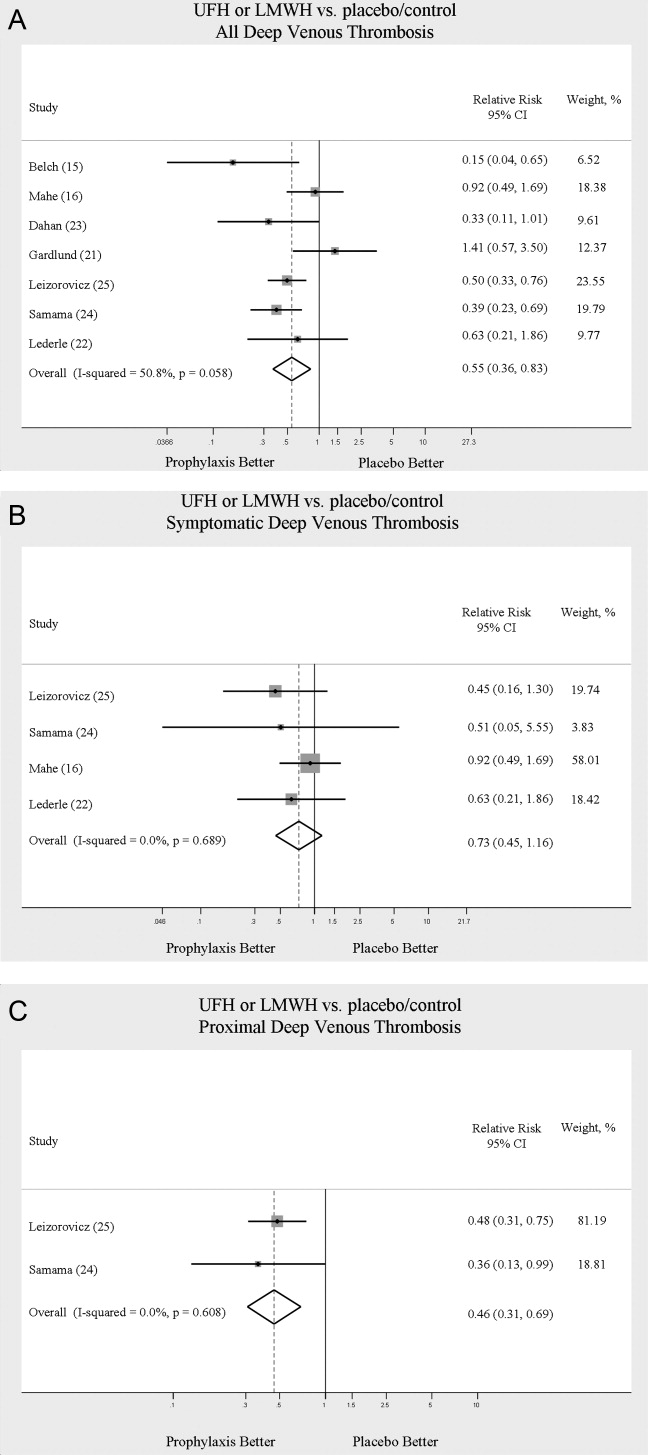
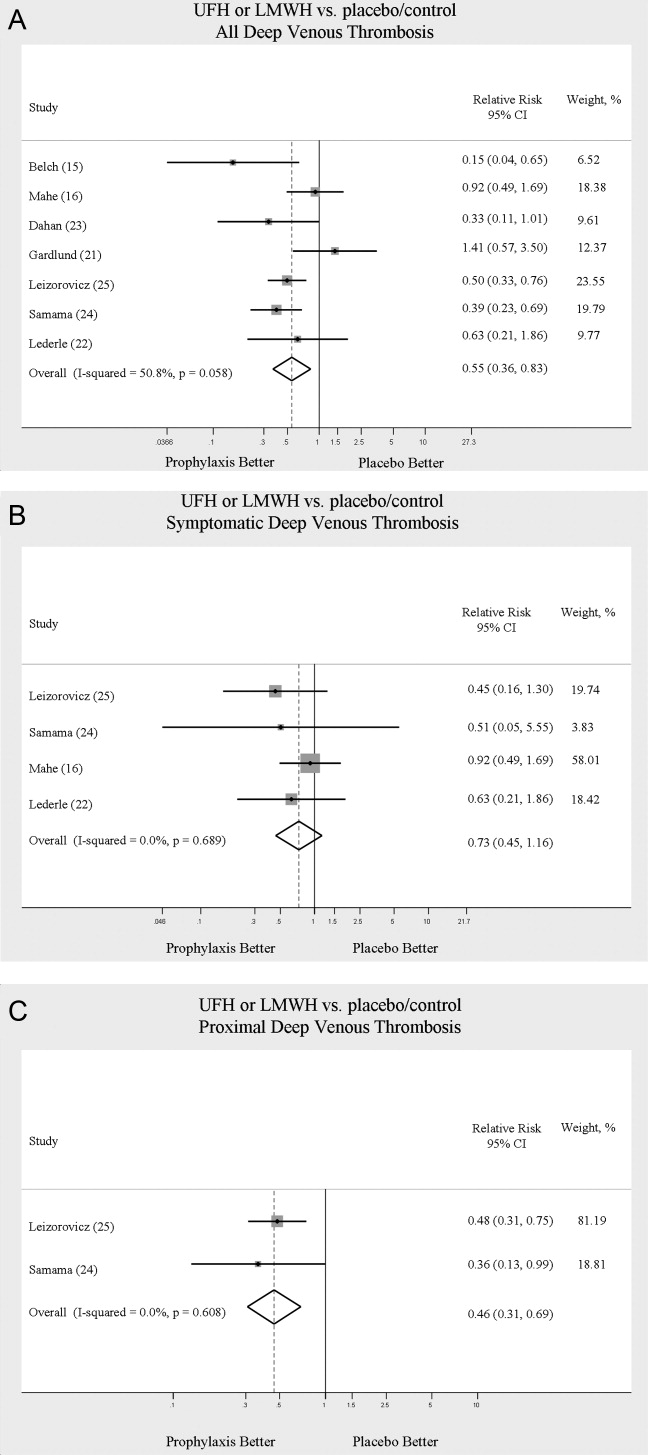
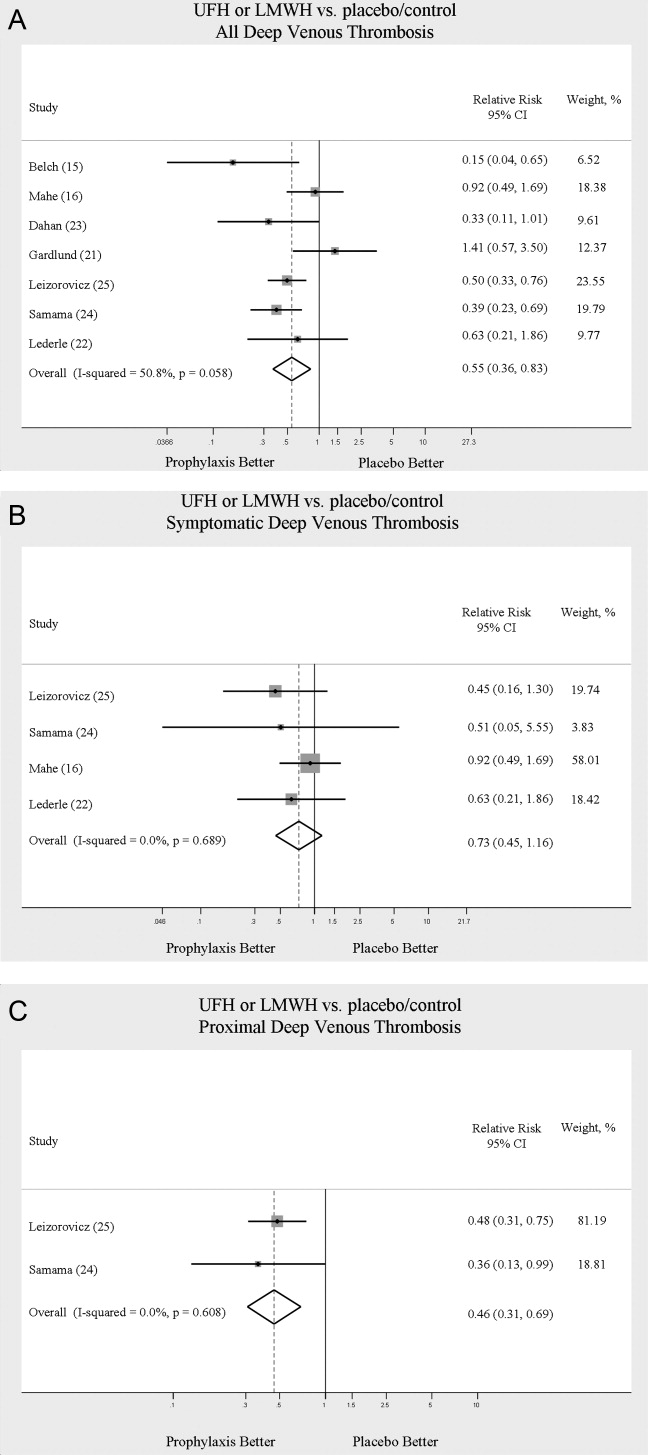
Across 7 trials comparing either UFH or LMWH to control, heparin products significantly decreased the risk of all DVT (RR = 0.55; 95% CI: 0.36‐0.83) (Figure 2A). When stratified by methodological quality, 5 trials16, 2225 with Jadad scores of 3 or higher showed an RR reduction of 0.53 (95% CI: 0.38‐0.72) in reducing all DVT. All of the higher‐quality trials compared LMWH to placebo. Across 4 trials that reported data for symptomatic DVT there was a nonsignificant reduction in RR compared with placebo (RR = 0.73; 95% CI: 0.45‐1.16) (Figure 2B). Only 2 trials24, 25 (both LMWH trials) reported results for proximal DVT and demonstrated significant benefit of prophylaxis with a pooled RR of 0.46 (95% CI: 0.31‐0.69) (Figure 2C).
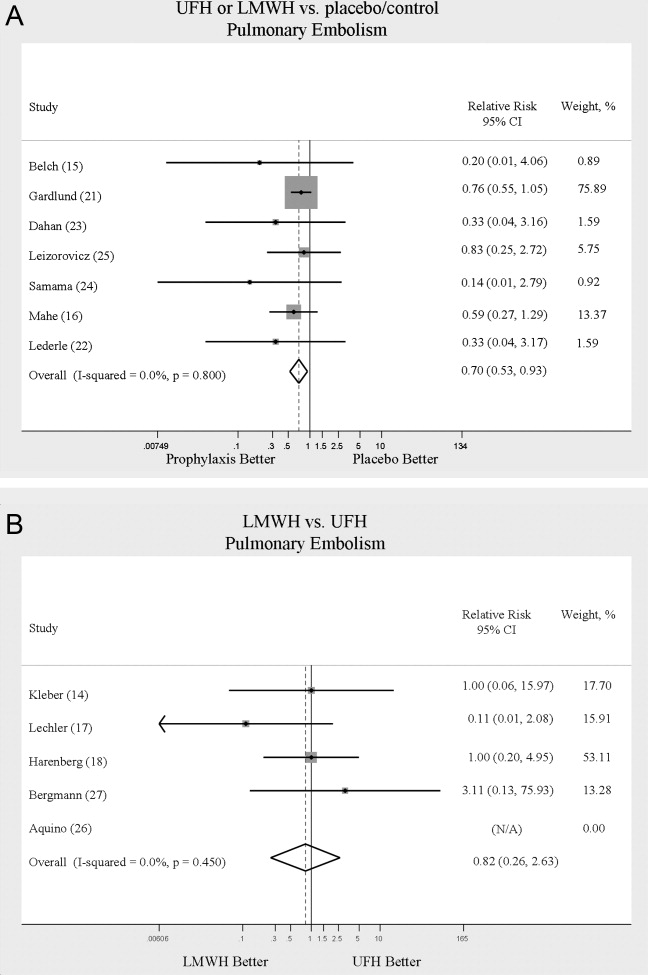
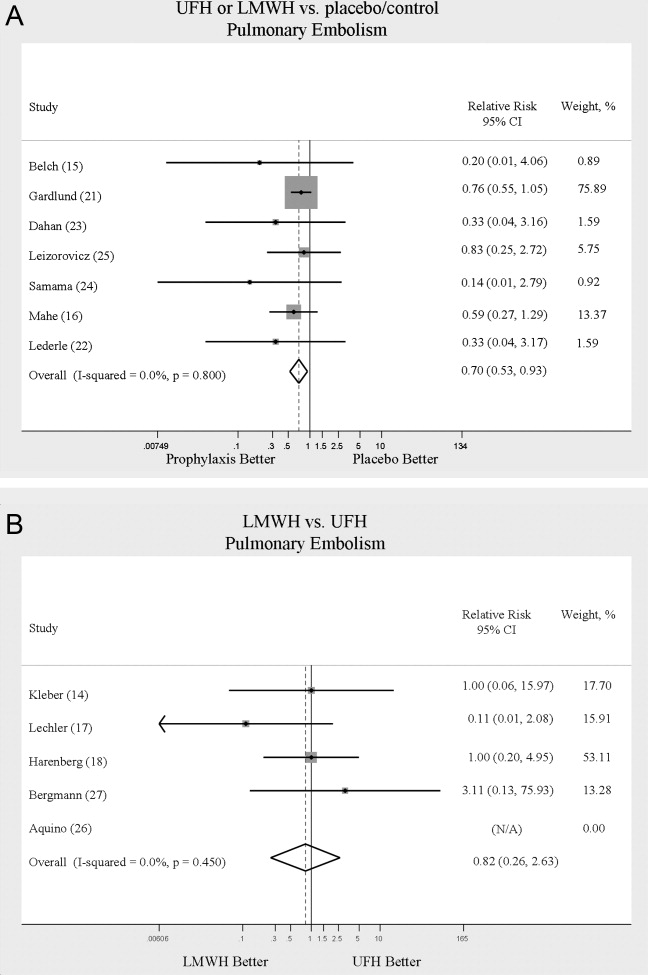
PE
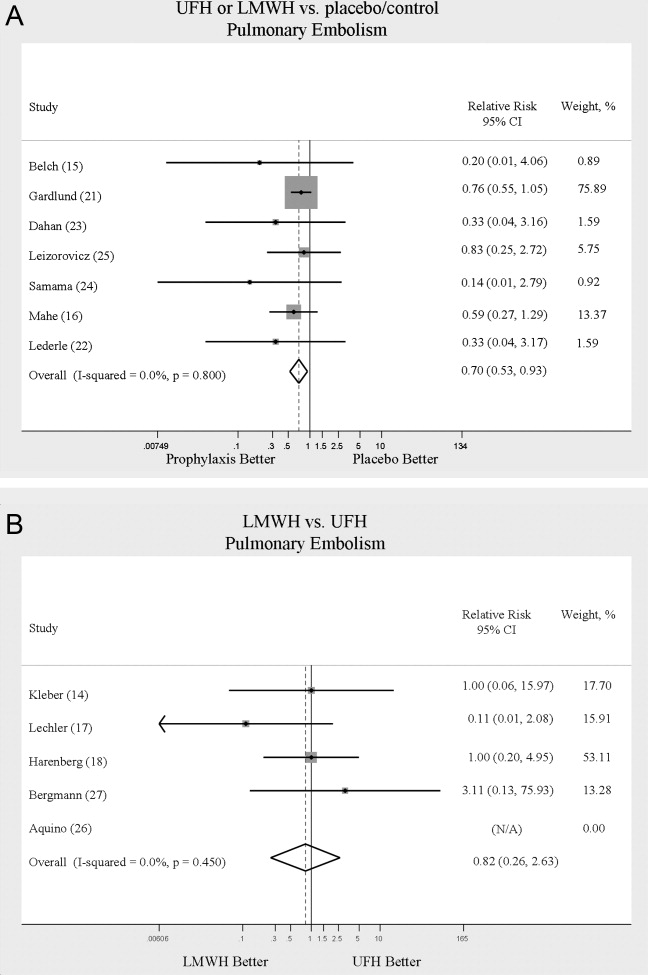
Across 7 trials comparing either UFH or LMWH to control, heparin products significantly decreased the risk of PE (RR = 0.70; 95% CI: 0.53‐0.93) (Figure 3A). The 5 trials16, 2225 with Jadad scores of 3 or greater showed a similar relative risk reduction, but the result was no longer statistically significant (RR = 0.56; 95% CI: 0.31‐1.02). Two of the trials16, 21 relied solely on the results of autopsy to diagnose PE, which may have given rise to chance differences in detection due to generally low autopsy rates. Eliminating these 2 studies from the analysis resulted in loss of statistical significance for the reduction in risk for PE (RR = 0.48; 95% CI: 0.20‐1.15).
Death
Seven trials16, 2025 comparing either UFH or LMWH to control examined the impact of pharmacologic prophylaxis on death and found no significant difference between treated and untreated patients across all trials (RR = 0.92; 95% CI: 0.82‐1.03) and those limited to studies with Jadad scores of 3 or higher (RR = 0.97; 95% CI: 0.80‐1.17).
LMWH vs. UFH
DVT
In 6 trials14, 1719, 26, 27 comparing LMWH to UFH given either twice a day (BID) or 3 times a day (TID), there was no statistically significant difference in all DVT (RR = 0.90; 95% CI: 0.57‐1.43). (For all analyses RRs <1 favor LMWH, while RRs >1 favor UFH.) A total of 2 trials14, 18 reported results separately for proximal DVT with no statistically significant difference noted between UFH and LMWH (RR = 1.60; 95% CI: 0.53‐4.88). One small trial26 reported findings comparing UFH to LMWH for prevention of symptomatic DVT with no difference noted.
PE
Pooled data from the 5 trials14, 17, 18, 26, 27 comparing UFH to LMWH in the prevention of PE showed no statistically significant difference in rates of pulmonary embolism (RR = 0.82; 95% CI: 0.26‐2.63) (Figure 3B). In sensitivity analysis this result was not impacted by Jadad score.
Death
When UFH was compared to LMWH no statistically significant difference in the rate of death was found (RR = 0.96; 95% CI: 0.50‐1.85). Here again, no difference was noted when limited to studies with Jadad scores of 3 or higher.
Complications
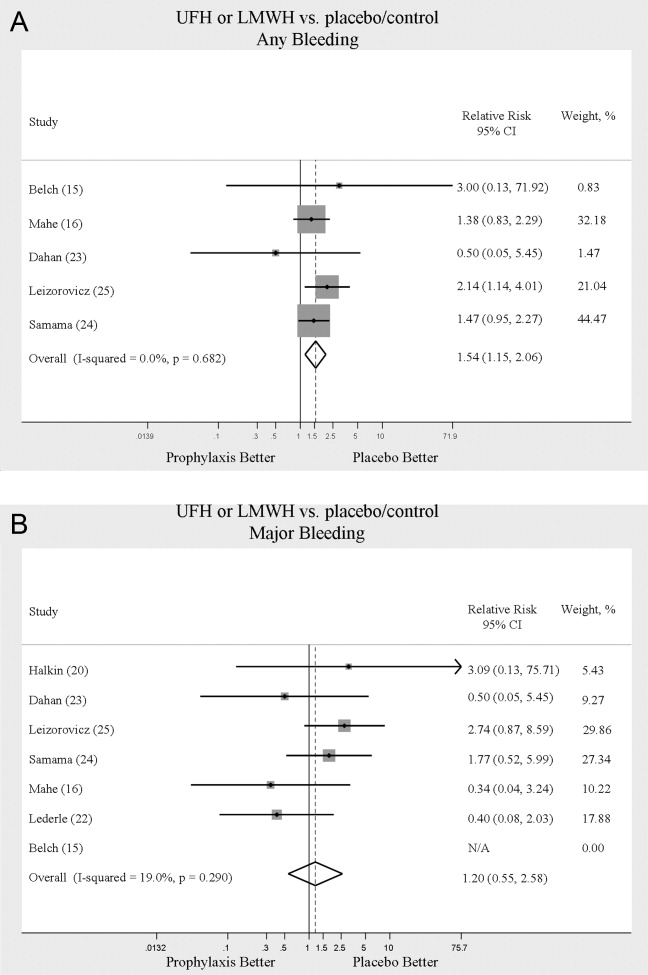
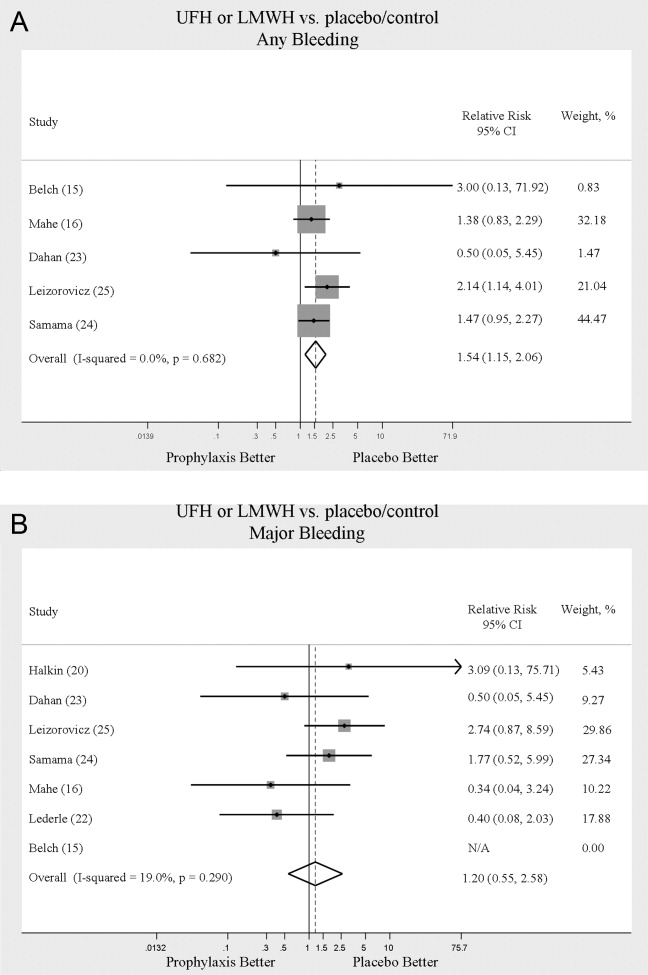
We evaluated adverse events of heparin products used for prophylaxis and whether there were differences between UFH and LMWH. Reporting of complications was not uniform from study to study, making pooling more difficult. However, we were able to abstract data on any bleeding, major bleeding, and thrombocytopenia from several studies. In 5 studies15, 16, 2325 of either UFH or LMWH vs. control, a significantly increased risk of any bleeding (RR = 1.54; 95% CI: 1.15‐2.06) (Figure 4A) was found. When only major bleeding was evaluated, no statistically significant difference was noted (RR = 1.20; 95% CI: 0.55‐2.58) (Figure 4B). In 4 trials16, 22, 24, 25 the occurrence of thrombocytopenia was not significantly different when comparing UFH or LMWH to control (RR = 0.92; 95% CI: 0.46‐1.86).
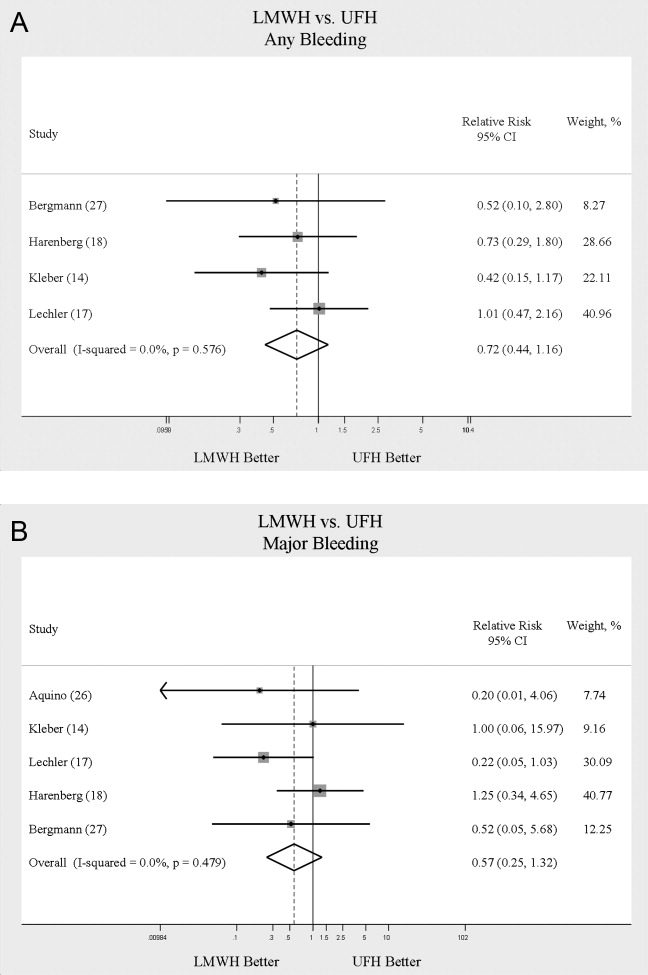
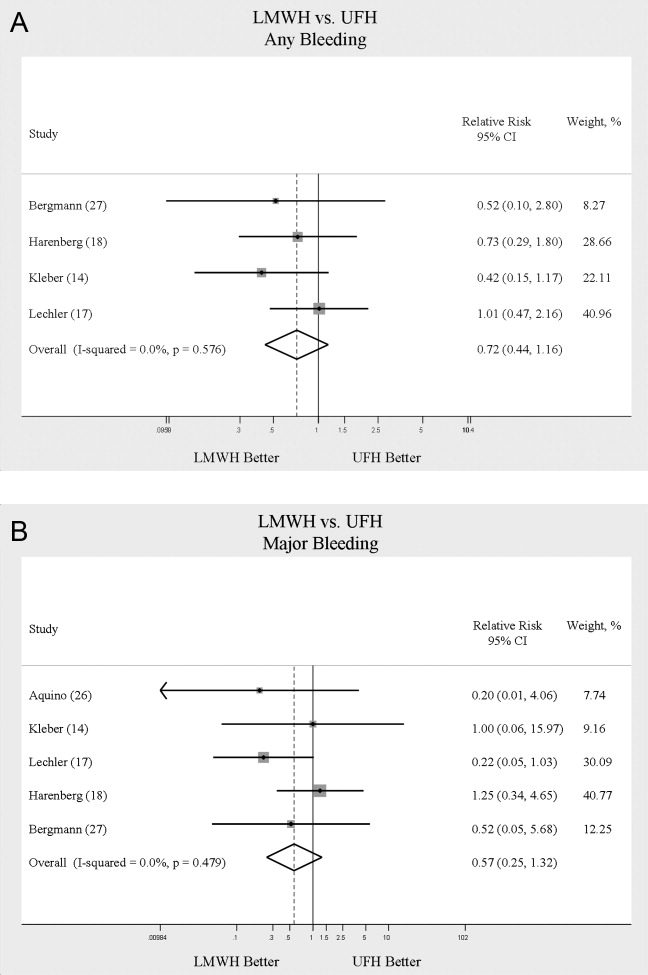
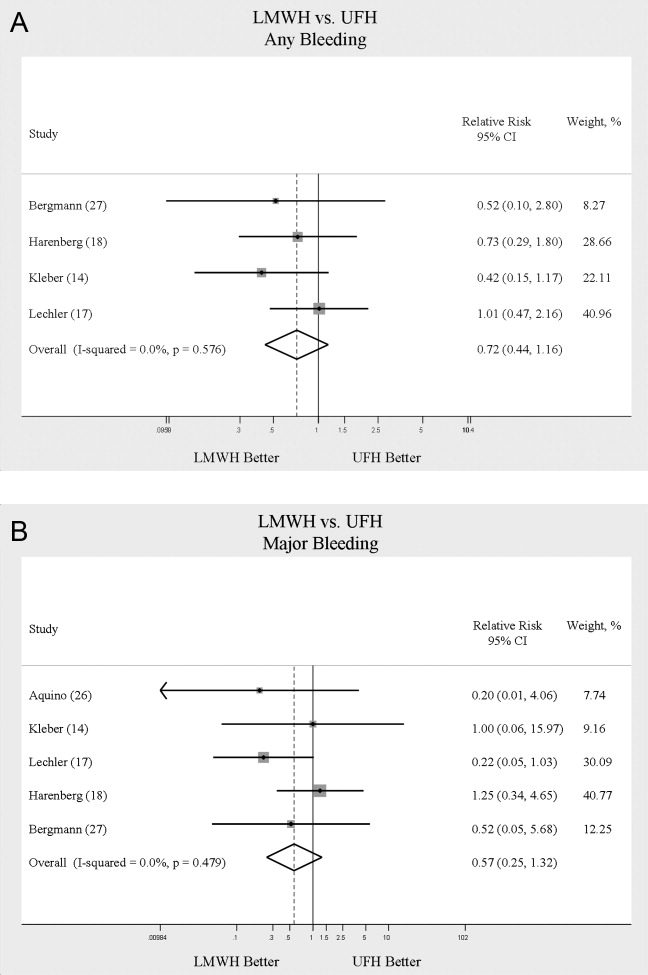
When LMWH was compared to UFH in 4 trials,14, 17, 18, 27 a nonsignificant trend toward a decrease in any bleeding was found in the LMWH group (RR = 0.72; 95% CI: 0.44‐1.16) (Figure 5A). A similar trend was seen favoring LMWH in rates of major bleeding (RR = 0.57; 95% CI: 0.25‐1.32) (Figure 5B). Neither trend was statistically significant. Three trials comparing LMWH to UFH reported on thrombocytopenia17, 18, 27 with no significant difference noted (RR = 0.52; 95% CI: 0.06‐4.18).
Heterogeneity and Publication Bias
No statistically significant heterogeneity was identified between trials for any outcomes. The highest I‐squared value was 54.5% (P = 0.14) for the endpoint of thrombocytopenia when UFH was compared to LMWH. In some cases, the nonsignificant results for tests of heterogeneity may have reflected small numbers of trials, but the values for I‐squared for all other endpoints were close to zero indicating that little nonrandom variation existed in the results across studies. All analyses were run using both random effects and fixed effects modeling. While we report results for random effects, no significant differences were observed using fixed effects.
We tested for publication bias using the methods developed by Egger et al.12 and Begg and Mazumdar.13 There was evidence of bias only for the outcome of PE when prophylaxis was compared to control, as the results for both tests were significant (Begg and Mazumdar:13 P = 0.035; Egger et al.:12 P = 0.010). For other outcomes tested, including all DVT (prophylaxis compared to control, and LMWH vs. UFH) as well as PE (LMWH vs. UFH), the P‐values were not significant.
DISCUSSION
When compared to control, LMWH or UFH decreased the risk of all DVT by 45% (RR = 0.55; 95% CI: 0.36‐0.83) and proximal DVT by 54% (RR = 0.46; 95% CI: 0.31‐0.69). PE was also decreased by 30% (RR = 0.70; 95% CI: 0.53‐0.93). Of note, when prophylaxis was compared with placebo all of the high‐quality studies showing a benefit were done using LMWH. The benefits of prophylaxis occurred at the cost of a 54% increased overall risk of bleeding (RR = 1.54; 95% CI 1.15‐2.06). However, the risk of major bleeding was not significantly increased. We did not find a mortality benefit to pharmacologic thromboembolism prophylaxis.
When comparing UFH to LMWH, we noted no difference in all DVT, symptomatic DVT, proximal DVT, PE, or death. While there was a trend toward less bleeding with LMWH, this was not statistically significant.
Taken in aggregate, our findings are in agreement with previous published meta‐analyses reporting net benefit for thromboembolism prophylaxis in medical patients.24, 22, 28, 29 Our meta‐analysis has several methodological strengths over the prior studies, including a comprehensive search of both the published and unpublished literature and assessment of the relationship between methodological quality of included trials and reported benefit. In contrast to previous reviews, our analysis highlights several limitations of the current evidence.
First, many of the studies are older, with predicted lengths of stay of greater than 1 week. The 8‐13‐day range of treatment duration we found in this study is longer than the average length of stay in today's hospitals. Second, there is variability in the diagnostic tests used to diagnose DVT, as well as variation in the definition of DVT among studies. Studies using fibrinogen uptake scanning reported rates of DVT as high as 26%15 while studies using venography reported DVT rates of almost 15% in the placebo arm.24 These rates are higher than most physicians' routine practice. One reason for this discrepancy is most studies did not distinguish below‐the‐knee DVT from more clinically relevant above‐the‐knee DVT. Systematic reviews of medical and surgical patients have found rates of proximal propagation from 0% to 29% in untreated patients.30, 31 Though controversial, below‐the‐knee DVT is believed less morbid than proximal DVT or symptomatic DVT. We addressed this by focusing specifically on clinically relevant endpoints of proximal and symptomatic DVT. When we restricted our analysis to proximal DVT we found a 54% RR reduction in 2 pooled trials of LMWH compared to placebo. In pooled analyses symptomatic DVT was not affected by prophylaxis. When compared head‐to‐head there were no differences between LMWH and UFH for proximal DVT or symptomatic DVT.
When considering PE, the utilization of autopsy as the sole diagnostic method in 2 large trials16, 21 is particularly problematic. In the trial by Garlund,21 the mortality rate was 5.4%, with an autopsy rate of 60.1%. Similarly, in the trial by Mahe et al.,16 the mortality rate was 10%, with an autopsy rate of 49%. Given the low absolute number of deaths and substantial proportion of decedents without autopsy, the potential for chance to produce an imbalance in detection of PE is high in these studies. When we excluded these 2 trials, we found that PE was no longer reduced to a statistically significant degree by prophylaxis. Loss of significance for PE in 2 sensitivity analyses (when excluding studies of lower quality, or using autopsy as a sole diagnostic study) is problematic and calls into question the true benefit of prophylaxis for prevention of PE.
Another limitation of the current literature centers on the variability of dosing used. We pooled trials of UFH whether given BID or TID. Given the small number of trials we did not do sensitivity analyses by dosage. A recent meta‐analysis3 found both doses are efficacious, while a recent review article32 suggested superiority of TID dosing. We believe the available literature does not clearly address this issue. Regarding comparisons of LMWH to UFH, dosing variability was also noted. The trial by Bergmann and Neuhart27 used enoxaparin 20 mg per day and found similar efficacy to UFH BID, while the Samama et al.24 trial found enoxaparin 20 mg per day no more efficacious than placebo. While the literature does not clearly define a best dose, we believe enoxaparin doses lower than 40 mg daily do not reflect the standard of care.
An additional limitation of the literature is publication bias. We assessed the possibility of publication bias by a variety of means. We did find statistical evidence of publication bias for the outcome of PE when prophylaxis was compared to control. Importantly, two meta‐analyses2, 4 on thromboembolism prophylaxis for general medicine patients suggested publication bias is present and our finding supports this conclusion. While no test for publication bias is foolproof, the best protection against publication bias, which we pursued in our study, consists of a thorough search for unpublished studies, including a search of conference proceedings, contact with experts in the field, and manufacturers of LMWH.
A final limitation of the current literature centers on risk assessment. All of the trials in this meta‐analysis included patients with an elevated level of risk. Unfortunately, risk was not clearly defined in many studies, and there was no minimum level of risk between trials. While immobility, age, and length of stay were reported for most studies, other risk factors such as personal history of thromboembolism and malignancy were not uniformly reported. Based on our analysis we are not confident our results can be extrapolated to all general medicine patients.
In conclusion, we found good evidence that pharmacologic prophylaxis significantly decreases the risk of all DVT and proximal DVT in at‐risk general medical patients. However, only LMWH was shown to prevent proximal DVT. We found inconclusive evidence that prophylaxis prevents PE. When compared directly we did not find clear superiority between UFH and LMWH, though several limitations of the current literature hamper decision‐making. Given the lower cost, it may seem justified to use UFH. However, there are other practical issues, such as the fact that LMWH is given once daily, and so potentially preferred by patients and more efficient for nurses. All of these results pertain to patients with elevated risk. While we did not find significant safety concerns with prophylaxis we do not know if these results can be extrapolated to lower‐risk patients. We believe that recommending widespread prophylaxis of all general medicine patients requires additional evidence about appropriate patient selection.
Acknowledgements
The authors thank Emmanuelle Williams, MD, for translating articles from French; Claudia Figueroa, MS, for translating articles from Spanish; Vikas Gulani, MD, for translating articles from German; and Rebecca Lee, MS, for translating articles from German, Dutch, and Italian. In addition, the authors thank Dr. Dilzer from Pfizer Global Pharmaceuticals, Kathleen E. Moigis from Aventis, and Carol McCullen from Glaxo Smith Kline for their search for unpublished pharmaceutical trials of low molecular weight heparins. Finally, the authors thank the Veterans Administration/University of Michigan Patient Safety Enhancement Program for research support.
- ,,, et al.Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy.Chest.2004;126(suppl):338S–400S.
- ,,,,.Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients: a meta‐analysis of randomized controlled trials.Arch Intern Med.2007;167(14):1476–1486.
- ,,,,.Twice vs three times daily heparin dosing for thromboembolism prophylaxis in the general medical population: a metaanalysis.Chest.2007;131(2):507–516.
- ,,,,.Meta‐analysis: anticoagulant prophylaxis to prevent symptomatic venous thromboembolism in hospitalized medical patients.Ann Intern Med.2007;146(4):278–288.
- National Quality Forum. National Consensus Standards for the Prevention and Care of Venous Thromboembolism (including Deep Vein Thrombosis and Pulmonary Embolism). Available at: http://www.qualityforum.org/projects/completed/vte/index.asp. Accessed May2009.
- ,.A prospective registry of 5,451 patients with ultrasound‐confirmed deep vein thrombosis.Am J Cardiol.2004;93(2):259–262.
- ,,, et al.Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross‐sectional study.Lancet.2008;371(9610):387–394.
- ,,,.Pharmacological thromboembolic prophylaxis in a medical ward: room for improvement.J Gen Intern Med.2002;17(10):788–791.
- ,,,.[Effectiveness of low molecular weight heparin (Fragmin) in the prevention of thromboembolism in internal medicine patients. A randomized double‐blind study].Med Klin (Munich).1988;83(7):241–245, 278.
- ,,, et al.Assessing the quality of reports of randomized clinical trials: is blinding necessary?Control Clin Trials.1996;17(1):1–12.
- ,.Quantifying heterogeneity in a meta‐analysis.Stat Med.2002;21(11):1539–1558.
- ,,,.Bias in meta‐analysis detected by a simple, graphical test.BMJ.1997;315(7109):629–634.
- ,.Operating characteristics of a rank correlation test for publication bias.Biometrics.1994;50(4):1088–1101.
- ,,,,,.Randomized comparison of enoxaparin with unfractionated heparin for the prevention of venous thromboembolism in medical patients with heart failure or severe respiratory disease.Am Heart J.2003;145(4):614–621.
- ,,,,.Prevention of deep vein thrombosis in medical patients by low‐dose heparin.Scott Med J.1981;26(2):115–117.
- ,,,,.Lack of effect of a low‐molecular‐weight heparin (nadroparin) on mortality in bedridden medical in‐patients: a prospective randomised double‐blind study.Eur J Clin Pharmacol.2005;61(5‐6):347–351.
- ,,.The venous thrombotic risk in non‐surgical patients: epidemiological data and efficacy/safety profile of a low‐molecular‐weight heparin (enoxaparin). The Prime Study Group.Haemostasis.1996;26(suppl 2):49–56.
- ,,.Subcutaneous low‐molecular‐weight heparin versus standard heparin and the prevention of thromboembolism in medical inpatients. The Heparin Study in Internal Medicine Group.Haemostasis.1996;26(3):127–139.
- ,,, et al.Randomized controlled study of heparin and low molecular weight heparin for prevention of deep‐vein thrombosis in medical patients.Thromb Res.1990;59(3):639–650.
- ,,,.Reduction of mortality in general medical in‐patients by low‐dose heparin prophylaxis.Ann Intern Med.1982;96(5):561–565.
- .Randomised, controlled trial of low‐dose heparin for prevention of fatal pulmonary embolism in patients with infectious diseases. The Heparin Prophylaxis Study Group.Lancet.1996;347(9012):1357–1361.
- ,,, et al.The prophylaxis of medical patients for thromboembolism pilot study.Am J Med.2006;119(1):54–59.
- ,,, et al.Prevention of deep vein thrombosis in elderly medical in‐patients by a low molecular weight heparin: a randomized double‐blind trial.Haemostasis.1986;16(2):159–164.
- ,,, et al.A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. Prophylaxis in Medical Patients with Enoxaparin Study Group.N Engl J Med.1999;341(11):793–800.
- ,,,,,.Randomized, placebo‐controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients.Circulation.2004;110(7):874–879.
- ,,.Prevention of thromboembolic accidents in elderly subjects with Fraxiparine. In: Bounameaux H, Samama MM, Ten Cate JW, eds.Fraxiaparine. 2nd International Symposium. Recent pharmacological and clinical data.New York:Schattauer;1990:51‐54.
- ,.A multicenter randomized double‐blind study of enoxaparin compared with unfractionated heparin in the prevention of venous thromboembolic disease in elderly in‐patients bedridden for an acute medical illness. The Enoxaparin in Medicine Study Group.Thromb Haemost.1996;76(4):529–534.
- ,,, et al.Prevention of venous thromboembolism in internal medicine with unfractionated or low‐molecular‐weight heparins: a meta‐analysis of randomised clinical trials.Thromb Haemost.2000;83(1):14–19.
- ,,,,.Meta‐analysis of venous thromboembolism prophylaxis in medically Ill patients.Clin Ther.2007;29(11):2395–2405.
- ,,,,,.Clinical relevance of distal deep vein thrombosis. Review of literature data.Thromb Haemost.2006;95(1):56–64.
- .Natural history of venous thromboembolism.Circulation.2003;107(suppl 1):I22–I30.
- .Clinical practice. Prophylaxis for thromboembolism in hospitalized medical patients.N Engl J Med.2007;356(14):1438–1444.
Deep venous thrombosis (DVT) and pulmonary embolism (PE), collectively referred to as venous thromboembolism (VTE), are common events in hospitalized patients and result in significant morbidity and mortality. Often silent and frequently unexpected, VTE is preventable. Accordingly, the American College of Chest Physicians recommends that pharmacologic prophylaxis be given to acutely ill medical patients admitted to the hospital with congestive heart failure or severe respiratory disease, or to patients who are confined to bed who have additional risk factors, such as cancer or previous VTE.1 Three recent meta‐analyses24 demonstrated significant reductions in VTE in general medicine patients with pharmacologic prophylaxis. Recently the National Quality Forum advocated that hospitals evaluate each patient upon admission and regularly thereafter, for the risk of developing DVT/VTE and utilize clinically appropriate methods to prevent DVT/VTE.5
Despite recommendations for prophylaxis, multiple studies demonstrate utilization in <50% of at‐risk general medical patients.68 Physicians' lack of awareness may partially explain this underutilization, but other likely factors include physicians' questions about the clinical importance of the outcome (eg, some studies have shown reductions primarily in asymptomatic distal DVT), doubt regarding the best form of prophylaxis (ie, unfractionated heparin [UFH] vs. low molecular weight heparin [LMWH]), uncertainty regarding optimal dosing regimens, and comparable uncertainty regarding which patients have sufficiently high risk for VTE to outweigh the risks of anticoagulation.
We undertook the current meta‐analysis to address questions about thromboembolism prevention in general medicine patients. Does pharmacologic prophylaxis prevent clinically relevant events? Is LMWH or UFH preferable in terms of either efficacy or safety?
MATERIALS AND METHODS
Search Strategy
We conducted an extensive search that included reviewing electronic databases (MEDLINE, EMBASE, and CINAHL) through June 2008, reviewing conference proceedings, and contacting drug manufacturers. The MEDLINE search combined the key words deep venous thrombosis, thromboembolism, AND pulmonary embolism with the terms primary prevention, prophylaxis, OR prevention. We limited the search results using the filter for randomized controlled trials in PubMed. Similar strategies (available on request) were used to search EMBASE, CINAHL, and the Cochrane Central Register of Controlled Trials. We also searched the Cochrane Database of Systematic Reviews to identify previous reviews on the same topic. We obtained translations of eligible, non‐English‐language articles.
The proceedings of annual meetings from the American Thoracic Society, the American Society of Hematology, and the Society for General Internal Medicine from 1994 to 2008 were hand‐searched for reports on DVT or PE prevention published in abstract form only. (Note: the American Society of Hematology was only available through 2007). We contacted the 3 main manufacturers of LMWHPfizer (dalteparin), Aventis (enoxaparin), Glaxo Smith Kline (nadoparin)and requested information on unpublished pharmaceutical sponsored trials. First authors from the trials included in this meta‐analysis were also contacted to determine if they knew of additional published or unpublished trials.
Inclusion and Exclusion Criteria
Studies were required to be prospective randomized controlled trials comparing UFH or LMWH to mechanical prophylaxis, placebo, or no intervention. We also included randomized head‐to‐head comparisons of UFH and LMWH. Eligible studies enrolled general medical patients. Trials including predominantly intensive care unit (ICU) patients; stroke, spinal cord, or acute myocardial infarction patients were excluded. We excluded trials focused on these populations because the risk for VTE may differ from that for general medical patients and because patients in these groups already commonly receive anticoagulants as a preventive measure or as active treatment (eg, for acute myocardial infarction [MI] care). Trials assessing thrombosis in patients with long‐term central venous access/catheters were also excluded. Articles focusing on long‐term rehabilitation patients were excluded.
Studies had to employ objective criteria for diagnosing VTE. For DVT these included duplex ultrasonography, venography, fibrinogen uptake scanning, impedance plethysmography, or autopsy as a primary or secondary outcome. Studies utilizing thermographic techniques were excluded.9 Eligible diagnostic modalities for PE consisted of pulmonary arteriogram, ventilation/perfusion scan, CT angiography, and autopsy.
After an initial review of article titles and abstracts, the full texts of all articles that potentially met our inclusion criteria were independently reviewed for eligibility by 2 authors (G.M.B., M.D.). In cases of disagreement, a third author (S.F.) independently reviewed the article and adjudicated decisions.
Quantitative Data Synthesis and Statistical Analysis
For all included articles, 2 reviewers independently abstracted data on key study features (including population size, trial design, modality of VTE diagnosis, and interventions delivered to treatment and control groups), results (including the rates of all DVT, proximal DVT, symptomatic DVT, PE, and death), as well as adverse events (such as bleeding and thrombocytopenia). We accepted the endpoint of DVT when assessed by duplex ultrasonography, venography, autopsy, or when diagnosed by fibrinogen uptake scanning or impedance plethysmography. For all endpoints we abstracted event rates as number of events based on intention to treat. Each study was assessed for quality using the Jadad scale.10 The Jadad scale is a validated tool for characterizing study quality that accounts for randomization, blinding, and description of withdrawals and dropouts in individual trials. The Jadad score ranges from 0 to 5 with higher numbers identifying trials of greater methodological rigor.
The trials were divided into 4 groups based on the prophylaxis agent used and the method of comparison (UFH vs. control, LMWH vs. control, LMWH vs. UFH, and LMWH/UFH combined vs. control). After combining trials for each group, we calculated a pooled relative risk (RR) and a 95% confidence interval (CI) based on both fixed and a random effects model using the DerSimonian and Laird method. Heterogeneity of the included studies was evaluated with a chi‐square statistic. The percentage of variation in the pooled RR attributable to heterogeneity was calculated and reported using the I‐squared statistic.11 Sensitivity analyses were performed and included repeating all analyses using high‐quality studies only (Jadad score 3 or higher). Publication bias was assessed using the methods developed by Egger et al.12 and Begg and Mazumdar.13 All analyses were performed using STATA SE version 9 (Stata Corp, College Station, TX).
RESULTS
Study Identification and Selection
The computerized literature search resulted in 5284 articles. Three additional citations were found by review of bibliographies. No additional trials were identified from reviews of abstracts from national meetings. Representatives from the 3 pharmaceutical companies reported no knowledge of additional published or unpublished data. Of the 5287 studies identified by the search, 14 studies met all eligibility criteria (Figure 1).
Study Characteristics
The 14 trials eligible for inclusion in the analysis consisted of 8 comparisons of UFH or LMWH vs. control (Table 1) and 6 head‐to‐head comparisons of UFH and LMWH (Table 2). The 14 studies included 8 multicenter trials and enrolled a total of 24,515 patients: 20,594 in the 8 trials that compared UFH or LMWH with placebo and 3921 in the 6 trials that compared LMWH with UFH. Two trials exclusively enrolled patients with either congestive heart failure or severe respiratory disease,14, 15 while 12 trials enrolled mixed populations. In 8 trials a period of immobility was necessary for study entry,14, 1621 while in 2 trials immobility was not required.22, 23 In the 4 remaining trials immobility was not explicitly discussed.15, 2426 One‐half of the trials required a length of stay greater than 3 days.1719, 2225
| Study (Year)Reference | Patients (n) | Duration (days) | VTE Risk Factors | Drug Dose | Comparison | DVT Assessed | PE Assessed | Double Blind | Jadad Score |
|---|---|---|---|---|---|---|---|---|---|
| |||||||||
| Belch et al. (1981)15 | 100 | 8 | Age 40‐80 years; CHF; chest infection | UFH TID | None | FUS | VQ | No | 1 |
| Dahan et al. (1986)23 | 270 | 10* | Age >65 years | Enoxaparin 60 mg | Placebo | FUS | Autopsy | Yes | 3 |
| Halkin et al. (1982)20 | 1358 | Not reported | Age >40 years; immobile | UFH BID | None | No | No | No | 1 |
| Mahe et al. (2005)16 | 2474 | 13.08 | Age >40 years; immobile | Nadroparin 7500 IU | Placebo | Autopsy | Autopsy | Yes | 5 |
| Gardlund (1996)21 | 11693 | 8.2 | Age >55 years; immobile | UFH BID | None | Autopsy | Autopsy | No | 2 |
| Samama et al. (1999)24 | 738 | 7 | Age >40 years; length of stay 6 days; CHF; respiratory failure or 1 additional risk factor | Enoxaparin 40 mg | Placebo | Venography | Composite | Yes | 4 |
| Leizorovicz et al. (2004)25 | 3681 | 12.6 | Age >40 years; length of stay 4 days; CHF; respiratory failure or 1 additional risk factor | Dalteparin 5000 IU | Placebo | DUS | Composite | Yes | 4 |
| Lederle et al. (2006)22 | 280 | 13.4 | Age >60 years; length of stay 3 days | Enoxaparin 40 mg | Placebo | DUS | Composite | Yes | 5 |
| Study (Year)reference | Patients (n) | Duration (days) | VTE Risk Factors | Drug/Dose | Comparison | DVT Assessed | PE Assessed | Double Blind | Jadad Score |
|---|---|---|---|---|---|---|---|---|---|
| |||||||||
| Bergmann and Neuhart (1996)27 | 442 | 9.5 | Age >65 years; immobile | Enoxaparin 20 mg | UFH BID | FUS | Composite | Yes | 5 |
| Harenberg et al. (1990)19 | 166 | 10* | Age 40‐80 years; 1 week of bed rest | LMWH 1.500 aPTT units QD | UFH TID | IP | No | Yes | 3 |
| Kleber et al. (2003)14 | 665 | 9.8 | Age 18 years; severe CHF or respiratory disease; immobile | Enoxaparin 40 mg | UFH TID | Venography | Composite | No | 3 |
| Aquino et al. (1990)26 | 99 | Not reported | Age >70 years | Nadoparine 7500 IU | UFH BID | DUS | Composite | No | 1 |
| Harenberg et al. (1996)18 | 1590 | 10* | Age 50‐80 years; immobile + 1 additional risk factor | Nadoparine 36 mg | UFH TID | DUS | Composite | Yes | 4 |
| Lechler et al. (1996)17 | 959 | 7* | Age >18 years; immobile + 1 additional risk factor | Enoxaparin 40 mg | UFH TID | DUS | Composite | Yes | 3 |
While minimum age for study entry varied, the patient population predominantly ranged from 65 to 85 years of age. Many of the trials reported expected, not actual, treatment duration. The range of expected treatment was 7 to 21 days, with 10 days of treatment the most frequently mentioned. In the 8 trials1416, 21, 22, 24, 25, 27 that reported actual treatment duration, the range was 8 to 13.4 days. Most trials did not report number of VTE risk factors per patient, nor was there uniform acceptance of risk factors across trials.
UFH or LMWH vs. Control
DVT
Across 7 trials comparing either UFH or LMWH to control, heparin products significantly decreased the risk of all DVT (RR = 0.55; 95% CI: 0.36‐0.83) (Figure 2A). When stratified by methodological quality, 5 trials16, 2225 with Jadad scores of 3 or higher showed an RR reduction of 0.53 (95% CI: 0.38‐0.72) in reducing all DVT. All of the higher‐quality trials compared LMWH to placebo. Across 4 trials that reported data for symptomatic DVT there was a nonsignificant reduction in RR compared with placebo (RR = 0.73; 95% CI: 0.45‐1.16) (Figure 2B). Only 2 trials24, 25 (both LMWH trials) reported results for proximal DVT and demonstrated significant benefit of prophylaxis with a pooled RR of 0.46 (95% CI: 0.31‐0.69) (Figure 2C).
PE
Across 7 trials comparing either UFH or LMWH to control, heparin products significantly decreased the risk of PE (RR = 0.70; 95% CI: 0.53‐0.93) (Figure 3A). The 5 trials16, 2225 with Jadad scores of 3 or greater showed a similar relative risk reduction, but the result was no longer statistically significant (RR = 0.56; 95% CI: 0.31‐1.02). Two of the trials16, 21 relied solely on the results of autopsy to diagnose PE, which may have given rise to chance differences in detection due to generally low autopsy rates. Eliminating these 2 studies from the analysis resulted in loss of statistical significance for the reduction in risk for PE (RR = 0.48; 95% CI: 0.20‐1.15).
Death
Seven trials16, 2025 comparing either UFH or LMWH to control examined the impact of pharmacologic prophylaxis on death and found no significant difference between treated and untreated patients across all trials (RR = 0.92; 95% CI: 0.82‐1.03) and those limited to studies with Jadad scores of 3 or higher (RR = 0.97; 95% CI: 0.80‐1.17).
LMWH vs. UFH
DVT
In 6 trials14, 1719, 26, 27 comparing LMWH to UFH given either twice a day (BID) or 3 times a day (TID), there was no statistically significant difference in all DVT (RR = 0.90; 95% CI: 0.57‐1.43). (For all analyses RRs <1 favor LMWH, while RRs >1 favor UFH.) A total of 2 trials14, 18 reported results separately for proximal DVT with no statistically significant difference noted between UFH and LMWH (RR = 1.60; 95% CI: 0.53‐4.88). One small trial26 reported findings comparing UFH to LMWH for prevention of symptomatic DVT with no difference noted.
PE
Pooled data from the 5 trials14, 17, 18, 26, 27 comparing UFH to LMWH in the prevention of PE showed no statistically significant difference in rates of pulmonary embolism (RR = 0.82; 95% CI: 0.26‐2.63) (Figure 3B). In sensitivity analysis this result was not impacted by Jadad score.
Death
When UFH was compared to LMWH no statistically significant difference in the rate of death was found (RR = 0.96; 95% CI: 0.50‐1.85). Here again, no difference was noted when limited to studies with Jadad scores of 3 or higher.
Complications
We evaluated adverse events of heparin products used for prophylaxis and whether there were differences between UFH and LMWH. Reporting of complications was not uniform from study to study, making pooling more difficult. However, we were able to abstract data on any bleeding, major bleeding, and thrombocytopenia from several studies. In 5 studies15, 16, 2325 of either UFH or LMWH vs. control, a significantly increased risk of any bleeding (RR = 1.54; 95% CI: 1.15‐2.06) (Figure 4A) was found. When only major bleeding was evaluated, no statistically significant difference was noted (RR = 1.20; 95% CI: 0.55‐2.58) (Figure 4B). In 4 trials16, 22, 24, 25 the occurrence of thrombocytopenia was not significantly different when comparing UFH or LMWH to control (RR = 0.92; 95% CI: 0.46‐1.86).
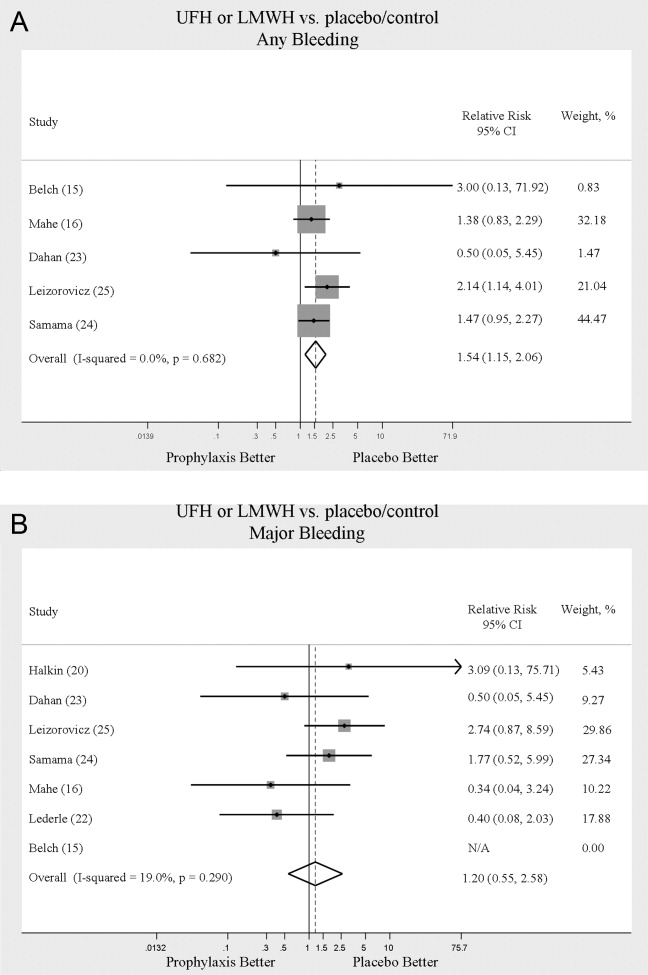
When LMWH was compared to UFH in 4 trials,14, 17, 18, 27 a nonsignificant trend toward a decrease in any bleeding was found in the LMWH group (RR = 0.72; 95% CI: 0.44‐1.16) (Figure 5A). A similar trend was seen favoring LMWH in rates of major bleeding (RR = 0.57; 95% CI: 0.25‐1.32) (Figure 5B). Neither trend was statistically significant. Three trials comparing LMWH to UFH reported on thrombocytopenia17, 18, 27 with no significant difference noted (RR = 0.52; 95% CI: 0.06‐4.18).
Heterogeneity and Publication Bias
No statistically significant heterogeneity was identified between trials for any outcomes. The highest I‐squared value was 54.5% (P = 0.14) for the endpoint of thrombocytopenia when UFH was compared to LMWH. In some cases, the nonsignificant results for tests of heterogeneity may have reflected small numbers of trials, but the values for I‐squared for all other endpoints were close to zero indicating that little nonrandom variation existed in the results across studies. All analyses were run using both random effects and fixed effects modeling. While we report results for random effects, no significant differences were observed using fixed effects.
We tested for publication bias using the methods developed by Egger et al.12 and Begg and Mazumdar.13 There was evidence of bias only for the outcome of PE when prophylaxis was compared to control, as the results for both tests were significant (Begg and Mazumdar:13 P = 0.035; Egger et al.:12 P = 0.010). For other outcomes tested, including all DVT (prophylaxis compared to control, and LMWH vs. UFH) as well as PE (LMWH vs. UFH), the P‐values were not significant.
DISCUSSION
When compared to control, LMWH or UFH decreased the risk of all DVT by 45% (RR = 0.55; 95% CI: 0.36‐0.83) and proximal DVT by 54% (RR = 0.46; 95% CI: 0.31‐0.69). PE was also decreased by 30% (RR = 0.70; 95% CI: 0.53‐0.93). Of note, when prophylaxis was compared with placebo all of the high‐quality studies showing a benefit were done using LMWH. The benefits of prophylaxis occurred at the cost of a 54% increased overall risk of bleeding (RR = 1.54; 95% CI 1.15‐2.06). However, the risk of major bleeding was not significantly increased. We did not find a mortality benefit to pharmacologic thromboembolism prophylaxis.
When comparing UFH to LMWH, we noted no difference in all DVT, symptomatic DVT, proximal DVT, PE, or death. While there was a trend toward less bleeding with LMWH, this was not statistically significant.
Taken in aggregate, our findings are in agreement with previous published meta‐analyses reporting net benefit for thromboembolism prophylaxis in medical patients.24, 22, 28, 29 Our meta‐analysis has several methodological strengths over the prior studies, including a comprehensive search of both the published and unpublished literature and assessment of the relationship between methodological quality of included trials and reported benefit. In contrast to previous reviews, our analysis highlights several limitations of the current evidence.
First, many of the studies are older, with predicted lengths of stay of greater than 1 week. The 8‐13‐day range of treatment duration we found in this study is longer than the average length of stay in today's hospitals. Second, there is variability in the diagnostic tests used to diagnose DVT, as well as variation in the definition of DVT among studies. Studies using fibrinogen uptake scanning reported rates of DVT as high as 26%15 while studies using venography reported DVT rates of almost 15% in the placebo arm.24 These rates are higher than most physicians' routine practice. One reason for this discrepancy is most studies did not distinguish below‐the‐knee DVT from more clinically relevant above‐the‐knee DVT. Systematic reviews of medical and surgical patients have found rates of proximal propagation from 0% to 29% in untreated patients.30, 31 Though controversial, below‐the‐knee DVT is believed less morbid than proximal DVT or symptomatic DVT. We addressed this by focusing specifically on clinically relevant endpoints of proximal and symptomatic DVT. When we restricted our analysis to proximal DVT we found a 54% RR reduction in 2 pooled trials of LMWH compared to placebo. In pooled analyses symptomatic DVT was not affected by prophylaxis. When compared head‐to‐head there were no differences between LMWH and UFH for proximal DVT or symptomatic DVT.
When considering PE, the utilization of autopsy as the sole diagnostic method in 2 large trials16, 21 is particularly problematic. In the trial by Garlund,21 the mortality rate was 5.4%, with an autopsy rate of 60.1%. Similarly, in the trial by Mahe et al.,16 the mortality rate was 10%, with an autopsy rate of 49%. Given the low absolute number of deaths and substantial proportion of decedents without autopsy, the potential for chance to produce an imbalance in detection of PE is high in these studies. When we excluded these 2 trials, we found that PE was no longer reduced to a statistically significant degree by prophylaxis. Loss of significance for PE in 2 sensitivity analyses (when excluding studies of lower quality, or using autopsy as a sole diagnostic study) is problematic and calls into question the true benefit of prophylaxis for prevention of PE.
Another limitation of the current literature centers on the variability of dosing used. We pooled trials of UFH whether given BID or TID. Given the small number of trials we did not do sensitivity analyses by dosage. A recent meta‐analysis3 found both doses are efficacious, while a recent review article32 suggested superiority of TID dosing. We believe the available literature does not clearly address this issue. Regarding comparisons of LMWH to UFH, dosing variability was also noted. The trial by Bergmann and Neuhart27 used enoxaparin 20 mg per day and found similar efficacy to UFH BID, while the Samama et al.24 trial found enoxaparin 20 mg per day no more efficacious than placebo. While the literature does not clearly define a best dose, we believe enoxaparin doses lower than 40 mg daily do not reflect the standard of care.
An additional limitation of the literature is publication bias. We assessed the possibility of publication bias by a variety of means. We did find statistical evidence of publication bias for the outcome of PE when prophylaxis was compared to control. Importantly, two meta‐analyses2, 4 on thromboembolism prophylaxis for general medicine patients suggested publication bias is present and our finding supports this conclusion. While no test for publication bias is foolproof, the best protection against publication bias, which we pursued in our study, consists of a thorough search for unpublished studies, including a search of conference proceedings, contact with experts in the field, and manufacturers of LMWH.
A final limitation of the current literature centers on risk assessment. All of the trials in this meta‐analysis included patients with an elevated level of risk. Unfortunately, risk was not clearly defined in many studies, and there was no minimum level of risk between trials. While immobility, age, and length of stay were reported for most studies, other risk factors such as personal history of thromboembolism and malignancy were not uniformly reported. Based on our analysis we are not confident our results can be extrapolated to all general medicine patients.
In conclusion, we found good evidence that pharmacologic prophylaxis significantly decreases the risk of all DVT and proximal DVT in at‐risk general medical patients. However, only LMWH was shown to prevent proximal DVT. We found inconclusive evidence that prophylaxis prevents PE. When compared directly we did not find clear superiority between UFH and LMWH, though several limitations of the current literature hamper decision‐making. Given the lower cost, it may seem justified to use UFH. However, there are other practical issues, such as the fact that LMWH is given once daily, and so potentially preferred by patients and more efficient for nurses. All of these results pertain to patients with elevated risk. While we did not find significant safety concerns with prophylaxis we do not know if these results can be extrapolated to lower‐risk patients. We believe that recommending widespread prophylaxis of all general medicine patients requires additional evidence about appropriate patient selection.
Acknowledgements
The authors thank Emmanuelle Williams, MD, for translating articles from French; Claudia Figueroa, MS, for translating articles from Spanish; Vikas Gulani, MD, for translating articles from German; and Rebecca Lee, MS, for translating articles from German, Dutch, and Italian. In addition, the authors thank Dr. Dilzer from Pfizer Global Pharmaceuticals, Kathleen E. Moigis from Aventis, and Carol McCullen from Glaxo Smith Kline for their search for unpublished pharmaceutical trials of low molecular weight heparins. Finally, the authors thank the Veterans Administration/University of Michigan Patient Safety Enhancement Program for research support.
Deep venous thrombosis (DVT) and pulmonary embolism (PE), collectively referred to as venous thromboembolism (VTE), are common events in hospitalized patients and result in significant morbidity and mortality. Often silent and frequently unexpected, VTE is preventable. Accordingly, the American College of Chest Physicians recommends that pharmacologic prophylaxis be given to acutely ill medical patients admitted to the hospital with congestive heart failure or severe respiratory disease, or to patients who are confined to bed who have additional risk factors, such as cancer or previous VTE.1 Three recent meta‐analyses24 demonstrated significant reductions in VTE in general medicine patients with pharmacologic prophylaxis. Recently the National Quality Forum advocated that hospitals evaluate each patient upon admission and regularly thereafter, for the risk of developing DVT/VTE and utilize clinically appropriate methods to prevent DVT/VTE.5
Despite recommendations for prophylaxis, multiple studies demonstrate utilization in <50% of at‐risk general medical patients.68 Physicians' lack of awareness may partially explain this underutilization, but other likely factors include physicians' questions about the clinical importance of the outcome (eg, some studies have shown reductions primarily in asymptomatic distal DVT), doubt regarding the best form of prophylaxis (ie, unfractionated heparin [UFH] vs. low molecular weight heparin [LMWH]), uncertainty regarding optimal dosing regimens, and comparable uncertainty regarding which patients have sufficiently high risk for VTE to outweigh the risks of anticoagulation.
We undertook the current meta‐analysis to address questions about thromboembolism prevention in general medicine patients. Does pharmacologic prophylaxis prevent clinically relevant events? Is LMWH or UFH preferable in terms of either efficacy or safety?
MATERIALS AND METHODS
Search Strategy
We conducted an extensive search that included reviewing electronic databases (MEDLINE, EMBASE, and CINAHL) through June 2008, reviewing conference proceedings, and contacting drug manufacturers. The MEDLINE search combined the key words deep venous thrombosis, thromboembolism, AND pulmonary embolism with the terms primary prevention, prophylaxis, OR prevention. We limited the search results using the filter for randomized controlled trials in PubMed. Similar strategies (available on request) were used to search EMBASE, CINAHL, and the Cochrane Central Register of Controlled Trials. We also searched the Cochrane Database of Systematic Reviews to identify previous reviews on the same topic. We obtained translations of eligible, non‐English‐language articles.
The proceedings of annual meetings from the American Thoracic Society, the American Society of Hematology, and the Society for General Internal Medicine from 1994 to 2008 were hand‐searched for reports on DVT or PE prevention published in abstract form only. (Note: the American Society of Hematology was only available through 2007). We contacted the 3 main manufacturers of LMWHPfizer (dalteparin), Aventis (enoxaparin), Glaxo Smith Kline (nadoparin)and requested information on unpublished pharmaceutical sponsored trials. First authors from the trials included in this meta‐analysis were also contacted to determine if they knew of additional published or unpublished trials.
Inclusion and Exclusion Criteria
Studies were required to be prospective randomized controlled trials comparing UFH or LMWH to mechanical prophylaxis, placebo, or no intervention. We also included randomized head‐to‐head comparisons of UFH and LMWH. Eligible studies enrolled general medical patients. Trials including predominantly intensive care unit (ICU) patients; stroke, spinal cord, or acute myocardial infarction patients were excluded. We excluded trials focused on these populations because the risk for VTE may differ from that for general medical patients and because patients in these groups already commonly receive anticoagulants as a preventive measure or as active treatment (eg, for acute myocardial infarction [MI] care). Trials assessing thrombosis in patients with long‐term central venous access/catheters were also excluded. Articles focusing on long‐term rehabilitation patients were excluded.
Studies had to employ objective criteria for diagnosing VTE. For DVT these included duplex ultrasonography, venography, fibrinogen uptake scanning, impedance plethysmography, or autopsy as a primary or secondary outcome. Studies utilizing thermographic techniques were excluded.9 Eligible diagnostic modalities for PE consisted of pulmonary arteriogram, ventilation/perfusion scan, CT angiography, and autopsy.
After an initial review of article titles and abstracts, the full texts of all articles that potentially met our inclusion criteria were independently reviewed for eligibility by 2 authors (G.M.B., M.D.). In cases of disagreement, a third author (S.F.) independently reviewed the article and adjudicated decisions.
Quantitative Data Synthesis and Statistical Analysis
For all included articles, 2 reviewers independently abstracted data on key study features (including population size, trial design, modality of VTE diagnosis, and interventions delivered to treatment and control groups), results (including the rates of all DVT, proximal DVT, symptomatic DVT, PE, and death), as well as adverse events (such as bleeding and thrombocytopenia). We accepted the endpoint of DVT when assessed by duplex ultrasonography, venography, autopsy, or when diagnosed by fibrinogen uptake scanning or impedance plethysmography. For all endpoints we abstracted event rates as number of events based on intention to treat. Each study was assessed for quality using the Jadad scale.10 The Jadad scale is a validated tool for characterizing study quality that accounts for randomization, blinding, and description of withdrawals and dropouts in individual trials. The Jadad score ranges from 0 to 5 with higher numbers identifying trials of greater methodological rigor.
The trials were divided into 4 groups based on the prophylaxis agent used and the method of comparison (UFH vs. control, LMWH vs. control, LMWH vs. UFH, and LMWH/UFH combined vs. control). After combining trials for each group, we calculated a pooled relative risk (RR) and a 95% confidence interval (CI) based on both fixed and a random effects model using the DerSimonian and Laird method. Heterogeneity of the included studies was evaluated with a chi‐square statistic. The percentage of variation in the pooled RR attributable to heterogeneity was calculated and reported using the I‐squared statistic.11 Sensitivity analyses were performed and included repeating all analyses using high‐quality studies only (Jadad score 3 or higher). Publication bias was assessed using the methods developed by Egger et al.12 and Begg and Mazumdar.13 All analyses were performed using STATA SE version 9 (Stata Corp, College Station, TX).
RESULTS
Study Identification and Selection
The computerized literature search resulted in 5284 articles. Three additional citations were found by review of bibliographies. No additional trials were identified from reviews of abstracts from national meetings. Representatives from the 3 pharmaceutical companies reported no knowledge of additional published or unpublished data. Of the 5287 studies identified by the search, 14 studies met all eligibility criteria (Figure 1).
Study Characteristics
The 14 trials eligible for inclusion in the analysis consisted of 8 comparisons of UFH or LMWH vs. control (Table 1) and 6 head‐to‐head comparisons of UFH and LMWH (Table 2). The 14 studies included 8 multicenter trials and enrolled a total of 24,515 patients: 20,594 in the 8 trials that compared UFH or LMWH with placebo and 3921 in the 6 trials that compared LMWH with UFH. Two trials exclusively enrolled patients with either congestive heart failure or severe respiratory disease,14, 15 while 12 trials enrolled mixed populations. In 8 trials a period of immobility was necessary for study entry,14, 1621 while in 2 trials immobility was not required.22, 23 In the 4 remaining trials immobility was not explicitly discussed.15, 2426 One‐half of the trials required a length of stay greater than 3 days.1719, 2225
| Study (Year)Reference | Patients (n) | Duration (days) | VTE Risk Factors | Drug Dose | Comparison | DVT Assessed | PE Assessed | Double Blind | Jadad Score |
|---|---|---|---|---|---|---|---|---|---|
| |||||||||
| Belch et al. (1981)15 | 100 | 8 | Age 40‐80 years; CHF; chest infection | UFH TID | None | FUS | VQ | No | 1 |
| Dahan et al. (1986)23 | 270 | 10* | Age >65 years | Enoxaparin 60 mg | Placebo | FUS | Autopsy | Yes | 3 |
| Halkin et al. (1982)20 | 1358 | Not reported | Age >40 years; immobile | UFH BID | None | No | No | No | 1 |
| Mahe et al. (2005)16 | 2474 | 13.08 | Age >40 years; immobile | Nadroparin 7500 IU | Placebo | Autopsy | Autopsy | Yes | 5 |
| Gardlund (1996)21 | 11693 | 8.2 | Age >55 years; immobile | UFH BID | None | Autopsy | Autopsy | No | 2 |
| Samama et al. (1999)24 | 738 | 7 | Age >40 years; length of stay 6 days; CHF; respiratory failure or 1 additional risk factor | Enoxaparin 40 mg | Placebo | Venography | Composite | Yes | 4 |
| Leizorovicz et al. (2004)25 | 3681 | 12.6 | Age >40 years; length of stay 4 days; CHF; respiratory failure or 1 additional risk factor | Dalteparin 5000 IU | Placebo | DUS | Composite | Yes | 4 |
| Lederle et al. (2006)22 | 280 | 13.4 | Age >60 years; length of stay 3 days | Enoxaparin 40 mg | Placebo | DUS | Composite | Yes | 5 |
| Study (Year)reference | Patients (n) | Duration (days) | VTE Risk Factors | Drug/Dose | Comparison | DVT Assessed | PE Assessed | Double Blind | Jadad Score |
|---|---|---|---|---|---|---|---|---|---|
| |||||||||
| Bergmann and Neuhart (1996)27 | 442 | 9.5 | Age >65 years; immobile | Enoxaparin 20 mg | UFH BID | FUS | Composite | Yes | 5 |
| Harenberg et al. (1990)19 | 166 | 10* | Age 40‐80 years; 1 week of bed rest | LMWH 1.500 aPTT units QD | UFH TID | IP | No | Yes | 3 |
| Kleber et al. (2003)14 | 665 | 9.8 | Age 18 years; severe CHF or respiratory disease; immobile | Enoxaparin 40 mg | UFH TID | Venography | Composite | No | 3 |
| Aquino et al. (1990)26 | 99 | Not reported | Age >70 years | Nadoparine 7500 IU | UFH BID | DUS | Composite | No | 1 |
| Harenberg et al. (1996)18 | 1590 | 10* | Age 50‐80 years; immobile + 1 additional risk factor | Nadoparine 36 mg | UFH TID | DUS | Composite | Yes | 4 |
| Lechler et al. (1996)17 | 959 | 7* | Age >18 years; immobile + 1 additional risk factor | Enoxaparin 40 mg | UFH TID | DUS | Composite | Yes | 3 |
While minimum age for study entry varied, the patient population predominantly ranged from 65 to 85 years of age. Many of the trials reported expected, not actual, treatment duration. The range of expected treatment was 7 to 21 days, with 10 days of treatment the most frequently mentioned. In the 8 trials1416, 21, 22, 24, 25, 27 that reported actual treatment duration, the range was 8 to 13.4 days. Most trials did not report number of VTE risk factors per patient, nor was there uniform acceptance of risk factors across trials.
UFH or LMWH vs. Control
DVT
Across 7 trials comparing either UFH or LMWH to control, heparin products significantly decreased the risk of all DVT (RR = 0.55; 95% CI: 0.36‐0.83) (Figure 2A). When stratified by methodological quality, 5 trials16, 2225 with Jadad scores of 3 or higher showed an RR reduction of 0.53 (95% CI: 0.38‐0.72) in reducing all DVT. All of the higher‐quality trials compared LMWH to placebo. Across 4 trials that reported data for symptomatic DVT there was a nonsignificant reduction in RR compared with placebo (RR = 0.73; 95% CI: 0.45‐1.16) (Figure 2B). Only 2 trials24, 25 (both LMWH trials) reported results for proximal DVT and demonstrated significant benefit of prophylaxis with a pooled RR of 0.46 (95% CI: 0.31‐0.69) (Figure 2C).
PE
Across 7 trials comparing either UFH or LMWH to control, heparin products significantly decreased the risk of PE (RR = 0.70; 95% CI: 0.53‐0.93) (Figure 3A). The 5 trials16, 2225 with Jadad scores of 3 or greater showed a similar relative risk reduction, but the result was no longer statistically significant (RR = 0.56; 95% CI: 0.31‐1.02). Two of the trials16, 21 relied solely on the results of autopsy to diagnose PE, which may have given rise to chance differences in detection due to generally low autopsy rates. Eliminating these 2 studies from the analysis resulted in loss of statistical significance for the reduction in risk for PE (RR = 0.48; 95% CI: 0.20‐1.15).
Death
Seven trials16, 2025 comparing either UFH or LMWH to control examined the impact of pharmacologic prophylaxis on death and found no significant difference between treated and untreated patients across all trials (RR = 0.92; 95% CI: 0.82‐1.03) and those limited to studies with Jadad scores of 3 or higher (RR = 0.97; 95% CI: 0.80‐1.17).
LMWH vs. UFH
DVT
In 6 trials14, 1719, 26, 27 comparing LMWH to UFH given either twice a day (BID) or 3 times a day (TID), there was no statistically significant difference in all DVT (RR = 0.90; 95% CI: 0.57‐1.43). (For all analyses RRs <1 favor LMWH, while RRs >1 favor UFH.) A total of 2 trials14, 18 reported results separately for proximal DVT with no statistically significant difference noted between UFH and LMWH (RR = 1.60; 95% CI: 0.53‐4.88). One small trial26 reported findings comparing UFH to LMWH for prevention of symptomatic DVT with no difference noted.
PE
Pooled data from the 5 trials14, 17, 18, 26, 27 comparing UFH to LMWH in the prevention of PE showed no statistically significant difference in rates of pulmonary embolism (RR = 0.82; 95% CI: 0.26‐2.63) (Figure 3B). In sensitivity analysis this result was not impacted by Jadad score.
Death
When UFH was compared to LMWH no statistically significant difference in the rate of death was found (RR = 0.96; 95% CI: 0.50‐1.85). Here again, no difference was noted when limited to studies with Jadad scores of 3 or higher.
Complications
We evaluated adverse events of heparin products used for prophylaxis and whether there were differences between UFH and LMWH. Reporting of complications was not uniform from study to study, making pooling more difficult. However, we were able to abstract data on any bleeding, major bleeding, and thrombocytopenia from several studies. In 5 studies15, 16, 2325 of either UFH or LMWH vs. control, a significantly increased risk of any bleeding (RR = 1.54; 95% CI: 1.15‐2.06) (Figure 4A) was found. When only major bleeding was evaluated, no statistically significant difference was noted (RR = 1.20; 95% CI: 0.55‐2.58) (Figure 4B). In 4 trials16, 22, 24, 25 the occurrence of thrombocytopenia was not significantly different when comparing UFH or LMWH to control (RR = 0.92; 95% CI: 0.46‐1.86).
When LMWH was compared to UFH in 4 trials,14, 17, 18, 27 a nonsignificant trend toward a decrease in any bleeding was found in the LMWH group (RR = 0.72; 95% CI: 0.44‐1.16) (Figure 5A). A similar trend was seen favoring LMWH in rates of major bleeding (RR = 0.57; 95% CI: 0.25‐1.32) (Figure 5B). Neither trend was statistically significant. Three trials comparing LMWH to UFH reported on thrombocytopenia17, 18, 27 with no significant difference noted (RR = 0.52; 95% CI: 0.06‐4.18).
Heterogeneity and Publication Bias
No statistically significant heterogeneity was identified between trials for any outcomes. The highest I‐squared value was 54.5% (P = 0.14) for the endpoint of thrombocytopenia when UFH was compared to LMWH. In some cases, the nonsignificant results for tests of heterogeneity may have reflected small numbers of trials, but the values for I‐squared for all other endpoints were close to zero indicating that little nonrandom variation existed in the results across studies. All analyses were run using both random effects and fixed effects modeling. While we report results for random effects, no significant differences were observed using fixed effects.
We tested for publication bias using the methods developed by Egger et al.12 and Begg and Mazumdar.13 There was evidence of bias only for the outcome of PE when prophylaxis was compared to control, as the results for both tests were significant (Begg and Mazumdar:13 P = 0.035; Egger et al.:12 P = 0.010). For other outcomes tested, including all DVT (prophylaxis compared to control, and LMWH vs. UFH) as well as PE (LMWH vs. UFH), the P‐values were not significant.
DISCUSSION
When compared to control, LMWH or UFH decreased the risk of all DVT by 45% (RR = 0.55; 95% CI: 0.36‐0.83) and proximal DVT by 54% (RR = 0.46; 95% CI: 0.31‐0.69). PE was also decreased by 30% (RR = 0.70; 95% CI: 0.53‐0.93). Of note, when prophylaxis was compared with placebo all of the high‐quality studies showing a benefit were done using LMWH. The benefits of prophylaxis occurred at the cost of a 54% increased overall risk of bleeding (RR = 1.54; 95% CI 1.15‐2.06). However, the risk of major bleeding was not significantly increased. We did not find a mortality benefit to pharmacologic thromboembolism prophylaxis.
When comparing UFH to LMWH, we noted no difference in all DVT, symptomatic DVT, proximal DVT, PE, or death. While there was a trend toward less bleeding with LMWH, this was not statistically significant.
Taken in aggregate, our findings are in agreement with previous published meta‐analyses reporting net benefit for thromboembolism prophylaxis in medical patients.24, 22, 28, 29 Our meta‐analysis has several methodological strengths over the prior studies, including a comprehensive search of both the published and unpublished literature and assessment of the relationship between methodological quality of included trials and reported benefit. In contrast to previous reviews, our analysis highlights several limitations of the current evidence.
First, many of the studies are older, with predicted lengths of stay of greater than 1 week. The 8‐13‐day range of treatment duration we found in this study is longer than the average length of stay in today's hospitals. Second, there is variability in the diagnostic tests used to diagnose DVT, as well as variation in the definition of DVT among studies. Studies using fibrinogen uptake scanning reported rates of DVT as high as 26%15 while studies using venography reported DVT rates of almost 15% in the placebo arm.24 These rates are higher than most physicians' routine practice. One reason for this discrepancy is most studies did not distinguish below‐the‐knee DVT from more clinically relevant above‐the‐knee DVT. Systematic reviews of medical and surgical patients have found rates of proximal propagation from 0% to 29% in untreated patients.30, 31 Though controversial, below‐the‐knee DVT is believed less morbid than proximal DVT or symptomatic DVT. We addressed this by focusing specifically on clinically relevant endpoints of proximal and symptomatic DVT. When we restricted our analysis to proximal DVT we found a 54% RR reduction in 2 pooled trials of LMWH compared to placebo. In pooled analyses symptomatic DVT was not affected by prophylaxis. When compared head‐to‐head there were no differences between LMWH and UFH for proximal DVT or symptomatic DVT.
When considering PE, the utilization of autopsy as the sole diagnostic method in 2 large trials16, 21 is particularly problematic. In the trial by Garlund,21 the mortality rate was 5.4%, with an autopsy rate of 60.1%. Similarly, in the trial by Mahe et al.,16 the mortality rate was 10%, with an autopsy rate of 49%. Given the low absolute number of deaths and substantial proportion of decedents without autopsy, the potential for chance to produce an imbalance in detection of PE is high in these studies. When we excluded these 2 trials, we found that PE was no longer reduced to a statistically significant degree by prophylaxis. Loss of significance for PE in 2 sensitivity analyses (when excluding studies of lower quality, or using autopsy as a sole diagnostic study) is problematic and calls into question the true benefit of prophylaxis for prevention of PE.
Another limitation of the current literature centers on the variability of dosing used. We pooled trials of UFH whether given BID or TID. Given the small number of trials we did not do sensitivity analyses by dosage. A recent meta‐analysis3 found both doses are efficacious, while a recent review article32 suggested superiority of TID dosing. We believe the available literature does not clearly address this issue. Regarding comparisons of LMWH to UFH, dosing variability was also noted. The trial by Bergmann and Neuhart27 used enoxaparin 20 mg per day and found similar efficacy to UFH BID, while the Samama et al.24 trial found enoxaparin 20 mg per day no more efficacious than placebo. While the literature does not clearly define a best dose, we believe enoxaparin doses lower than 40 mg daily do not reflect the standard of care.
An additional limitation of the literature is publication bias. We assessed the possibility of publication bias by a variety of means. We did find statistical evidence of publication bias for the outcome of PE when prophylaxis was compared to control. Importantly, two meta‐analyses2, 4 on thromboembolism prophylaxis for general medicine patients suggested publication bias is present and our finding supports this conclusion. While no test for publication bias is foolproof, the best protection against publication bias, which we pursued in our study, consists of a thorough search for unpublished studies, including a search of conference proceedings, contact with experts in the field, and manufacturers of LMWH.
A final limitation of the current literature centers on risk assessment. All of the trials in this meta‐analysis included patients with an elevated level of risk. Unfortunately, risk was not clearly defined in many studies, and there was no minimum level of risk between trials. While immobility, age, and length of stay were reported for most studies, other risk factors such as personal history of thromboembolism and malignancy were not uniformly reported. Based on our analysis we are not confident our results can be extrapolated to all general medicine patients.
In conclusion, we found good evidence that pharmacologic prophylaxis significantly decreases the risk of all DVT and proximal DVT in at‐risk general medical patients. However, only LMWH was shown to prevent proximal DVT. We found inconclusive evidence that prophylaxis prevents PE. When compared directly we did not find clear superiority between UFH and LMWH, though several limitations of the current literature hamper decision‐making. Given the lower cost, it may seem justified to use UFH. However, there are other practical issues, such as the fact that LMWH is given once daily, and so potentially preferred by patients and more efficient for nurses. All of these results pertain to patients with elevated risk. While we did not find significant safety concerns with prophylaxis we do not know if these results can be extrapolated to lower‐risk patients. We believe that recommending widespread prophylaxis of all general medicine patients requires additional evidence about appropriate patient selection.
Acknowledgements
The authors thank Emmanuelle Williams, MD, for translating articles from French; Claudia Figueroa, MS, for translating articles from Spanish; Vikas Gulani, MD, for translating articles from German; and Rebecca Lee, MS, for translating articles from German, Dutch, and Italian. In addition, the authors thank Dr. Dilzer from Pfizer Global Pharmaceuticals, Kathleen E. Moigis from Aventis, and Carol McCullen from Glaxo Smith Kline for their search for unpublished pharmaceutical trials of low molecular weight heparins. Finally, the authors thank the Veterans Administration/University of Michigan Patient Safety Enhancement Program for research support.
- ,,, et al.Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy.Chest.2004;126(suppl):338S–400S.
- ,,,,.Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients: a meta‐analysis of randomized controlled trials.Arch Intern Med.2007;167(14):1476–1486.
- ,,,,.Twice vs three times daily heparin dosing for thromboembolism prophylaxis in the general medical population: a metaanalysis.Chest.2007;131(2):507–516.
- ,,,,.Meta‐analysis: anticoagulant prophylaxis to prevent symptomatic venous thromboembolism in hospitalized medical patients.Ann Intern Med.2007;146(4):278–288.
- National Quality Forum. National Consensus Standards for the Prevention and Care of Venous Thromboembolism (including Deep Vein Thrombosis and Pulmonary Embolism). Available at: http://www.qualityforum.org/projects/completed/vte/index.asp. Accessed May2009.
- ,.A prospective registry of 5,451 patients with ultrasound‐confirmed deep vein thrombosis.Am J Cardiol.2004;93(2):259–262.
- ,,, et al.Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross‐sectional study.Lancet.2008;371(9610):387–394.
- ,,,.Pharmacological thromboembolic prophylaxis in a medical ward: room for improvement.J Gen Intern Med.2002;17(10):788–791.
- ,,,.[Effectiveness of low molecular weight heparin (Fragmin) in the prevention of thromboembolism in internal medicine patients. A randomized double‐blind study].Med Klin (Munich).1988;83(7):241–245, 278.
- ,,, et al.Assessing the quality of reports of randomized clinical trials: is blinding necessary?Control Clin Trials.1996;17(1):1–12.
- ,.Quantifying heterogeneity in a meta‐analysis.Stat Med.2002;21(11):1539–1558.
- ,,,.Bias in meta‐analysis detected by a simple, graphical test.BMJ.1997;315(7109):629–634.
- ,.Operating characteristics of a rank correlation test for publication bias.Biometrics.1994;50(4):1088–1101.
- ,,,,,.Randomized comparison of enoxaparin with unfractionated heparin for the prevention of venous thromboembolism in medical patients with heart failure or severe respiratory disease.Am Heart J.2003;145(4):614–621.
- ,,,,.Prevention of deep vein thrombosis in medical patients by low‐dose heparin.Scott Med J.1981;26(2):115–117.
- ,,,,.Lack of effect of a low‐molecular‐weight heparin (nadroparin) on mortality in bedridden medical in‐patients: a prospective randomised double‐blind study.Eur J Clin Pharmacol.2005;61(5‐6):347–351.
- ,,.The venous thrombotic risk in non‐surgical patients: epidemiological data and efficacy/safety profile of a low‐molecular‐weight heparin (enoxaparin). The Prime Study Group.Haemostasis.1996;26(suppl 2):49–56.
- ,,.Subcutaneous low‐molecular‐weight heparin versus standard heparin and the prevention of thromboembolism in medical inpatients. The Heparin Study in Internal Medicine Group.Haemostasis.1996;26(3):127–139.
- ,,, et al.Randomized controlled study of heparin and low molecular weight heparin for prevention of deep‐vein thrombosis in medical patients.Thromb Res.1990;59(3):639–650.
- ,,,.Reduction of mortality in general medical in‐patients by low‐dose heparin prophylaxis.Ann Intern Med.1982;96(5):561–565.
- .Randomised, controlled trial of low‐dose heparin for prevention of fatal pulmonary embolism in patients with infectious diseases. The Heparin Prophylaxis Study Group.Lancet.1996;347(9012):1357–1361.
- ,,, et al.The prophylaxis of medical patients for thromboembolism pilot study.Am J Med.2006;119(1):54–59.
- ,,, et al.Prevention of deep vein thrombosis in elderly medical in‐patients by a low molecular weight heparin: a randomized double‐blind trial.Haemostasis.1986;16(2):159–164.
- ,,, et al.A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. Prophylaxis in Medical Patients with Enoxaparin Study Group.N Engl J Med.1999;341(11):793–800.
- ,,,,,.Randomized, placebo‐controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients.Circulation.2004;110(7):874–879.
- ,,.Prevention of thromboembolic accidents in elderly subjects with Fraxiparine. In: Bounameaux H, Samama MM, Ten Cate JW, eds.Fraxiaparine. 2nd International Symposium. Recent pharmacological and clinical data.New York:Schattauer;1990:51‐54.
- ,.A multicenter randomized double‐blind study of enoxaparin compared with unfractionated heparin in the prevention of venous thromboembolic disease in elderly in‐patients bedridden for an acute medical illness. The Enoxaparin in Medicine Study Group.Thromb Haemost.1996;76(4):529–534.
- ,,, et al.Prevention of venous thromboembolism in internal medicine with unfractionated or low‐molecular‐weight heparins: a meta‐analysis of randomised clinical trials.Thromb Haemost.2000;83(1):14–19.
- ,,,,.Meta‐analysis of venous thromboembolism prophylaxis in medically Ill patients.Clin Ther.2007;29(11):2395–2405.
- ,,,,,.Clinical relevance of distal deep vein thrombosis. Review of literature data.Thromb Haemost.2006;95(1):56–64.
- .Natural history of venous thromboembolism.Circulation.2003;107(suppl 1):I22–I30.
- .Clinical practice. Prophylaxis for thromboembolism in hospitalized medical patients.N Engl J Med.2007;356(14):1438–1444.
- ,,, et al.Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy.Chest.2004;126(suppl):338S–400S.
- ,,,,.Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients: a meta‐analysis of randomized controlled trials.Arch Intern Med.2007;167(14):1476–1486.
- ,,,,.Twice vs three times daily heparin dosing for thromboembolism prophylaxis in the general medical population: a metaanalysis.Chest.2007;131(2):507–516.
- ,,,,.Meta‐analysis: anticoagulant prophylaxis to prevent symptomatic venous thromboembolism in hospitalized medical patients.Ann Intern Med.2007;146(4):278–288.
- National Quality Forum. National Consensus Standards for the Prevention and Care of Venous Thromboembolism (including Deep Vein Thrombosis and Pulmonary Embolism). Available at: http://www.qualityforum.org/projects/completed/vte/index.asp. Accessed May2009.
- ,.A prospective registry of 5,451 patients with ultrasound‐confirmed deep vein thrombosis.Am J Cardiol.2004;93(2):259–262.
- ,,, et al.Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross‐sectional study.Lancet.2008;371(9610):387–394.
- ,,,.Pharmacological thromboembolic prophylaxis in a medical ward: room for improvement.J Gen Intern Med.2002;17(10):788–791.
- ,,,.[Effectiveness of low molecular weight heparin (Fragmin) in the prevention of thromboembolism in internal medicine patients. A randomized double‐blind study].Med Klin (Munich).1988;83(7):241–245, 278.
- ,,, et al.Assessing the quality of reports of randomized clinical trials: is blinding necessary?Control Clin Trials.1996;17(1):1–12.
- ,.Quantifying heterogeneity in a meta‐analysis.Stat Med.2002;21(11):1539–1558.
- ,,,.Bias in meta‐analysis detected by a simple, graphical test.BMJ.1997;315(7109):629–634.
- ,.Operating characteristics of a rank correlation test for publication bias.Biometrics.1994;50(4):1088–1101.
- ,,,,,.Randomized comparison of enoxaparin with unfractionated heparin for the prevention of venous thromboembolism in medical patients with heart failure or severe respiratory disease.Am Heart J.2003;145(4):614–621.
- ,,,,.Prevention of deep vein thrombosis in medical patients by low‐dose heparin.Scott Med J.1981;26(2):115–117.
- ,,,,.Lack of effect of a low‐molecular‐weight heparin (nadroparin) on mortality in bedridden medical in‐patients: a prospective randomised double‐blind study.Eur J Clin Pharmacol.2005;61(5‐6):347–351.
- ,,.The venous thrombotic risk in non‐surgical patients: epidemiological data and efficacy/safety profile of a low‐molecular‐weight heparin (enoxaparin). The Prime Study Group.Haemostasis.1996;26(suppl 2):49–56.
- ,,.Subcutaneous low‐molecular‐weight heparin versus standard heparin and the prevention of thromboembolism in medical inpatients. The Heparin Study in Internal Medicine Group.Haemostasis.1996;26(3):127–139.
- ,,, et al.Randomized controlled study of heparin and low molecular weight heparin for prevention of deep‐vein thrombosis in medical patients.Thromb Res.1990;59(3):639–650.
- ,,,.Reduction of mortality in general medical in‐patients by low‐dose heparin prophylaxis.Ann Intern Med.1982;96(5):561–565.
- .Randomised, controlled trial of low‐dose heparin for prevention of fatal pulmonary embolism in patients with infectious diseases. The Heparin Prophylaxis Study Group.Lancet.1996;347(9012):1357–1361.
- ,,, et al.The prophylaxis of medical patients for thromboembolism pilot study.Am J Med.2006;119(1):54–59.
- ,,, et al.Prevention of deep vein thrombosis in elderly medical in‐patients by a low molecular weight heparin: a randomized double‐blind trial.Haemostasis.1986;16(2):159–164.
- ,,, et al.A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. Prophylaxis in Medical Patients with Enoxaparin Study Group.N Engl J Med.1999;341(11):793–800.
- ,,,,,.Randomized, placebo‐controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients.Circulation.2004;110(7):874–879.
- ,,.Prevention of thromboembolic accidents in elderly subjects with Fraxiparine. In: Bounameaux H, Samama MM, Ten Cate JW, eds.Fraxiaparine. 2nd International Symposium. Recent pharmacological and clinical data.New York:Schattauer;1990:51‐54.
- ,.A multicenter randomized double‐blind study of enoxaparin compared with unfractionated heparin in the prevention of venous thromboembolic disease in elderly in‐patients bedridden for an acute medical illness. The Enoxaparin in Medicine Study Group.Thromb Haemost.1996;76(4):529–534.
- ,,, et al.Prevention of venous thromboembolism in internal medicine with unfractionated or low‐molecular‐weight heparins: a meta‐analysis of randomised clinical trials.Thromb Haemost.2000;83(1):14–19.
- ,,,,.Meta‐analysis of venous thromboembolism prophylaxis in medically Ill patients.Clin Ther.2007;29(11):2395–2405.
- ,,,,,.Clinical relevance of distal deep vein thrombosis. Review of literature data.Thromb Haemost.2006;95(1):56–64.
- .Natural history of venous thromboembolism.Circulation.2003;107(suppl 1):I22–I30.
- .Clinical practice. Prophylaxis for thromboembolism in hospitalized medical patients.N Engl J Med.2007;356(14):1438–1444.
Copyright © 2009 Society of Hospital Medicine
Tension Pneumocephalus as Complication of Hematoma Evacuation
A 78‐year‐old man was transferred from an outside hospital where he presented with declining mental status and a history of falls. A computed tomography (CT) scan of the brain revealed a chronic subdural hematoma with superimposed acute hemorrhage. The subdural hematoma was attributed to a fall at home approximately 5 weeks prior to admission. He was taken to the operating room for urgent craniotomy and hemorrhage evacuation and postoperatively comanaged by neurosurgery, hospitalists, and medicine residents. He tolerated the procedure and was noted to have marked improvement in mental status after the procedure. He was monitored overnight in our intensive care unit without intracranial pressure monitoring.
Early on postoperative day 1, he was awake, alert, following commands, and felt to be stable enough to be transferred to our transitional intensive care unit. However, later in the day he became progressively more confused. A follow‐up CT scan of the brain was ordered (Fig. 1) by the medicine team which revealed a large collection of air (wide arrow) and marked midline shift (thin arrow) consistent with tension pneumocephaly and subfalcine herniation (Fig. 2; arrow). Examination revealed that he was grossly obtunded with marked anisocoria, decerebrate posturing, and rigid tone. Neurosurgery was immediately contacted and recommended accessing 2 indwelling catheters left in the cerebrum as part of the normal postoperative course. Approximately 100 mL of serosanguinous fluid and air was aspirated with immediate improvement in his mental status and exam findings. Over the next few days, he remained clinically stable, and repeat CT scan showed slow resolution of the pneumocephalus and a decrease of his mass effect and midline shift. He was ultimately transferred to our skilled nursing facility for physical therapy and has done relatively well.
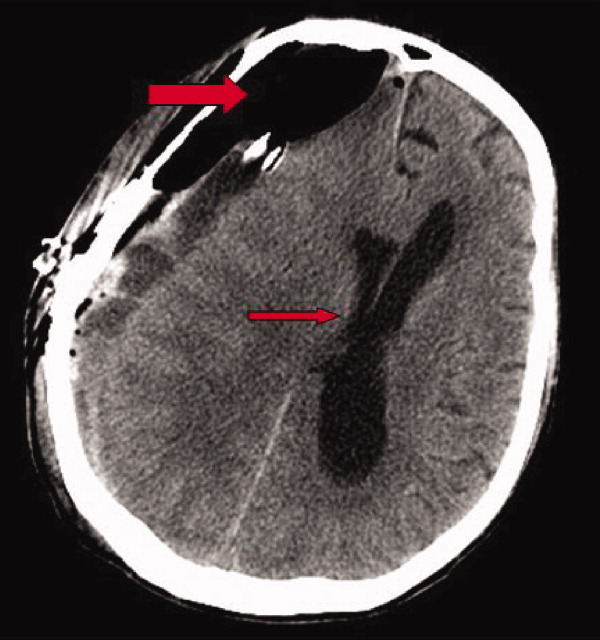

Pneumocephalus is a relatively common finding in many neurosurgical, intracranial procedures. However, tension pneumocephalus is a rare, life‐threatening form of pneumocephalus in which intracranial air causes mass effect and midline shift. In a review of 295 cases of pneumocephalus, 75% were caused by surgery, mostly intracranial and transsphenoidal, and head trauma. About 9% of cases resulted from infection with gas‐forming bacteria and rare causes include invasion of a nasopharyngeal carcinoma, frequent Valsalva maneuver, and air travel.1 Tension pneumocephalus occurs most commonly after the neurosurgical evacuation of a subdural hematoma. The prevalence of tension pneumocephalus following the evacuation of chronic subdural hematomas has been reported from 2.5% to 16%.2
There are 2 proposed mechanisms for the development of pneumocephalus; 1 proposes that air passes through a dural tear by a ball valve effect in which air can be forced into the intracranial cavity by a rapid increase in intrasinus pressure that occurs during sneezing, coughing, or straining. The air is then trapped intracranially. The second theory proposes that cerebrospinal fluid leakage permits air to enter the intracranial cavity because negative pressure is created as cerebrospinal fluid leaves the space.3 The conversion to tension physiology in either of these theories is less well understood.
- ,,,,.Pneumocephalus secondary to septic thrombosis of the superior sagittal sinus: report of a case.J Formos Med Assoc.2001;100(2):142‐144.
- ,,, et al.Subdural tension pneumocephalus following surgery for chronic subdural hematoma.J Neurosurg.1988;68:58‐61.
- ,,,.Nontraumatic tension pneumocephalus—a differential diagnosis of headache in the ED.Am J Emerg Med.2005, Vol.23, pp235‐236.
A 78‐year‐old man was transferred from an outside hospital where he presented with declining mental status and a history of falls. A computed tomography (CT) scan of the brain revealed a chronic subdural hematoma with superimposed acute hemorrhage. The subdural hematoma was attributed to a fall at home approximately 5 weeks prior to admission. He was taken to the operating room for urgent craniotomy and hemorrhage evacuation and postoperatively comanaged by neurosurgery, hospitalists, and medicine residents. He tolerated the procedure and was noted to have marked improvement in mental status after the procedure. He was monitored overnight in our intensive care unit without intracranial pressure monitoring.
Early on postoperative day 1, he was awake, alert, following commands, and felt to be stable enough to be transferred to our transitional intensive care unit. However, later in the day he became progressively more confused. A follow‐up CT scan of the brain was ordered (Fig. 1) by the medicine team which revealed a large collection of air (wide arrow) and marked midline shift (thin arrow) consistent with tension pneumocephaly and subfalcine herniation (Fig. 2; arrow). Examination revealed that he was grossly obtunded with marked anisocoria, decerebrate posturing, and rigid tone. Neurosurgery was immediately contacted and recommended accessing 2 indwelling catheters left in the cerebrum as part of the normal postoperative course. Approximately 100 mL of serosanguinous fluid and air was aspirated with immediate improvement in his mental status and exam findings. Over the next few days, he remained clinically stable, and repeat CT scan showed slow resolution of the pneumocephalus and a decrease of his mass effect and midline shift. He was ultimately transferred to our skilled nursing facility for physical therapy and has done relatively well.
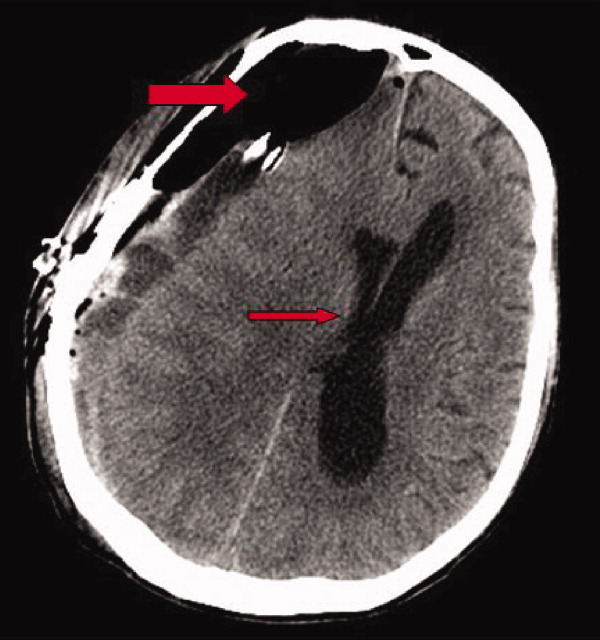

Pneumocephalus is a relatively common finding in many neurosurgical, intracranial procedures. However, tension pneumocephalus is a rare, life‐threatening form of pneumocephalus in which intracranial air causes mass effect and midline shift. In a review of 295 cases of pneumocephalus, 75% were caused by surgery, mostly intracranial and transsphenoidal, and head trauma. About 9% of cases resulted from infection with gas‐forming bacteria and rare causes include invasion of a nasopharyngeal carcinoma, frequent Valsalva maneuver, and air travel.1 Tension pneumocephalus occurs most commonly after the neurosurgical evacuation of a subdural hematoma. The prevalence of tension pneumocephalus following the evacuation of chronic subdural hematomas has been reported from 2.5% to 16%.2
There are 2 proposed mechanisms for the development of pneumocephalus; 1 proposes that air passes through a dural tear by a ball valve effect in which air can be forced into the intracranial cavity by a rapid increase in intrasinus pressure that occurs during sneezing, coughing, or straining. The air is then trapped intracranially. The second theory proposes that cerebrospinal fluid leakage permits air to enter the intracranial cavity because negative pressure is created as cerebrospinal fluid leaves the space.3 The conversion to tension physiology in either of these theories is less well understood.
A 78‐year‐old man was transferred from an outside hospital where he presented with declining mental status and a history of falls. A computed tomography (CT) scan of the brain revealed a chronic subdural hematoma with superimposed acute hemorrhage. The subdural hematoma was attributed to a fall at home approximately 5 weeks prior to admission. He was taken to the operating room for urgent craniotomy and hemorrhage evacuation and postoperatively comanaged by neurosurgery, hospitalists, and medicine residents. He tolerated the procedure and was noted to have marked improvement in mental status after the procedure. He was monitored overnight in our intensive care unit without intracranial pressure monitoring.
Early on postoperative day 1, he was awake, alert, following commands, and felt to be stable enough to be transferred to our transitional intensive care unit. However, later in the day he became progressively more confused. A follow‐up CT scan of the brain was ordered (Fig. 1) by the medicine team which revealed a large collection of air (wide arrow) and marked midline shift (thin arrow) consistent with tension pneumocephaly and subfalcine herniation (Fig. 2; arrow). Examination revealed that he was grossly obtunded with marked anisocoria, decerebrate posturing, and rigid tone. Neurosurgery was immediately contacted and recommended accessing 2 indwelling catheters left in the cerebrum as part of the normal postoperative course. Approximately 100 mL of serosanguinous fluid and air was aspirated with immediate improvement in his mental status and exam findings. Over the next few days, he remained clinically stable, and repeat CT scan showed slow resolution of the pneumocephalus and a decrease of his mass effect and midline shift. He was ultimately transferred to our skilled nursing facility for physical therapy and has done relatively well.
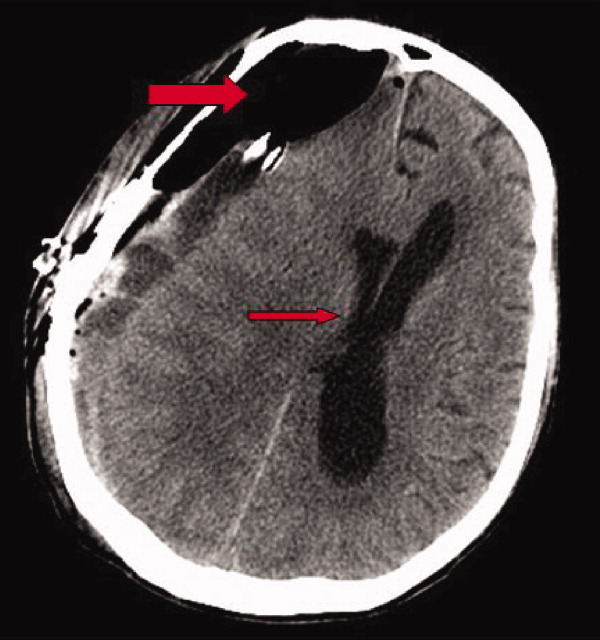

Pneumocephalus is a relatively common finding in many neurosurgical, intracranial procedures. However, tension pneumocephalus is a rare, life‐threatening form of pneumocephalus in which intracranial air causes mass effect and midline shift. In a review of 295 cases of pneumocephalus, 75% were caused by surgery, mostly intracranial and transsphenoidal, and head trauma. About 9% of cases resulted from infection with gas‐forming bacteria and rare causes include invasion of a nasopharyngeal carcinoma, frequent Valsalva maneuver, and air travel.1 Tension pneumocephalus occurs most commonly after the neurosurgical evacuation of a subdural hematoma. The prevalence of tension pneumocephalus following the evacuation of chronic subdural hematomas has been reported from 2.5% to 16%.2
There are 2 proposed mechanisms for the development of pneumocephalus; 1 proposes that air passes through a dural tear by a ball valve effect in which air can be forced into the intracranial cavity by a rapid increase in intrasinus pressure that occurs during sneezing, coughing, or straining. The air is then trapped intracranially. The second theory proposes that cerebrospinal fluid leakage permits air to enter the intracranial cavity because negative pressure is created as cerebrospinal fluid leaves the space.3 The conversion to tension physiology in either of these theories is less well understood.
- ,,,,.Pneumocephalus secondary to septic thrombosis of the superior sagittal sinus: report of a case.J Formos Med Assoc.2001;100(2):142‐144.
- ,,, et al.Subdural tension pneumocephalus following surgery for chronic subdural hematoma.J Neurosurg.1988;68:58‐61.
- ,,,.Nontraumatic tension pneumocephalus—a differential diagnosis of headache in the ED.Am J Emerg Med.2005, Vol.23, pp235‐236.
- ,,,,.Pneumocephalus secondary to septic thrombosis of the superior sagittal sinus: report of a case.J Formos Med Assoc.2001;100(2):142‐144.
- ,,, et al.Subdural tension pneumocephalus following surgery for chronic subdural hematoma.J Neurosurg.1988;68:58‐61.
- ,,,.Nontraumatic tension pneumocephalus—a differential diagnosis of headache in the ED.Am J Emerg Med.2005, Vol.23, pp235‐236.
Quantification of Bedside Teaching
Bedside teaching, defined as teaching in the presence of a patient, has been an integral, respected part of medical education throughout the history of modern medicine. There is widespread concern among medical educators that bedside teaching is declining, and in particular, physical examination teaching.1‐5 Learning at the bedside accounted for 75% of clinical teaching in the 1960s and only 16% by 1978.2 Current estimates range from 8% to 19%.1
The bedside is the ideal venue for demonstrating, observing, and evaluating medical interviewing skills, physical examination techniques, and interpersonal and communication skills. Role modeling is the primary method by which clinical teachers demonstrate and teach professionalism and humanistic behavior.6 The bedside is also a place to develop clinical reasoning skills, stimulate problem‐based learning,7 and demonstrate teamwork.4 Thus, the decline in bedside teaching is of major concern for more than just the dying of a time‐honored tradition, but for the threat to the development of skills and attitudes essential for the practice of medicine.
With the rapid growth in the number of hospitalists and their presence at most major U.S. teaching hospitals, internal medicine residents and medical students in their medicine clerkships receive much of their inpatient training from attending physicians who are hospitalists.8 Little is known about the teaching practices of hospitalist attending physicians. We investigated the fraction of time hospitalist attending physicians spend at the bedside during attending teaching rounds and the frequency of the demonstration of physical examination skills at 1 academic teaching hospital.
Patients and Methods
The Brigham & Women's Hospitalist Service, a 28‐member academic hospitalist group who serve as both the teaching attendings and patient care attendings on 4 general medicine teams, was studied in a prospective, observational fashion. Internal medicine residents at Brigham & Women's Hospital rotating on the hospitalist service were identified by examining the schedule of inpatient rotations during the 2007‐2008 academic year and were asked to participate in the study via an e‐mail invitation. The Institutional Review Board of Brigham & Women's Hospital approved the study.
Teams were made up of 1 senior resident and 2 interns. Call frequency was every fourth day. Over a period of 23 sequential weekdays, medical residents and interns from each of the 4 hospitalist teams observed and reported the behavior of their attendings on rounds. Their reports captured the fraction of time spent at the bedside during rounds and the frequency of physical examination teaching. Residents and interns were asked to respond to 3 questions in a daily e‐mail. Respondents reported (1) total time spent with their hospitalist attending during attending rounds, (2) time spent inside patient rooms during attending rounds, and (3) whether or not a physical examination finding or skill was demonstrated by their hospitalist attending. When more than 1 team member responded, time reported among team members was averaged and if there was a discrepancy between whether or not a physical examination finding or skill was demonstrated, it was defaulted to the positive response. Hospitalist attendings remained unaware of the daily observations.
Hospitalist attendings were independently invited to complete a baseline needs assessment survey on bedside teaching. Surveys addressed attitudes toward bedside teaching, confidence in ability to lead bedside teaching rounds and teach the physical examination, and adequacy of their own training in these skills. Respondents were asked to comment on obstacles to bedside teaching. Residents were surveyed at the completion of a rotation with a hospitalist attending regarding the value of the time spent at the bedside and their self‐perceived improvement in physical examination skills and bedside teaching skills. The survey solicited the residents' opinion of the most valuable aspect of bedside teaching. The survey questions used a 4‐point Likert scale with response options ranging from 1 = strongly disagree to 4 = strongly agree.
The fraction of time spent at the bedside during attending hospitalist rounds was calculated from the average time spent in patient rooms and the average time of attending rounds. The frequency of physical examination teaching was expressed as a percent of all teaching encounters. Interrater reliability was calculated using the intraclass correlation coefficient with the Spearman‐Brown adjustment. Differences between groups were calculated using the Fisher's exact test for counts and the Wilcoxon rank‐sum test for continuous data. Significance was accepted for P < 0.05.
Results
Thirty‐five residents provided observations on 61 of 92 potentially observed attending rounds (66% response rate) over 23 weekdays, including observations of the rounding behavior of 12 different hospitalists. The interrater reliability was 0.91. The average patient census on each team during this time period was 12 (range 6‐19).
Residents reported that their attendings went to the bedside at least once during 37 of these 61 rounds (61%), and provided physical examination teaching during 23 of these 61 (38%) encounters. Hospitalists spent an average of 101 minutes on rounds and an average of 17 minutes (17%) of their time inside patient rooms.
Rounds that included time spent at the bedside were significantly longer on average than rounds that did not include time spent at the bedside (122 vs. 69 minutes, P < 0.001). During rounds that included bedside teaching, teams spent an average of 29 minutes (24% of the total time) in patient rooms, and rounds were significantly more likely to include teaching on physical diagnosis (23/37 rounds vs. 0/24 rounds, P < 0.001). Physical examination teaching did not significantly prolong those rounds that included bedside teaching (124 vs. 119 minutes, P = 0.56), but did significantly increase the amount of time spent at the bedside (32 vs. 22 minutes, P = 0.046).
Eighteen hospitalists (64% response) with a mean of 5.9 years of experience as attending physicians completed a needs‐assessment survey (Table 1). Fourteen of the 18 hospitalists (78%) reported that they prioritize bedside teaching and 16 (89%) requested more emphasis on bedside teaching in the residency curriculum. Twelve hospitalists (67%) indicated that they were confident in their ability to lead bedside teaching rounds; 9 (50%) were confident in their ability to teach physical examination. Eleven (61%) of the respondents felt poorly prepared to do bedside teaching after completing their residency, and 12 (67%) felt that they had received inadequate training in how to teach the physical examination. Of the obstacles to bedside teaching, time and inadequate training and skills were the most frequently noted, present in 11 and 6 of the reports, respectively. Lack of confidence and lack of role models were also cited in 4 and 2 of the reports, respectively.
| Strongly Disagree (%) | Disagree (%) | Agree (%) | Strongly Agree (%) | |
|---|---|---|---|---|
| ||||
| I make bedside teaching a priority | 0 | 22 | 56 | 22 |
| More emphasis on bedside teaching in the residency curriculum is needed | 0 | 11 | 39 | 50 |
| I feel confident in my ability to lead bedside teaching rounds | 11 | 22 | 50 | 17 |
| I was well‐prepared to do bedside teaching after residency training | 22 | 39 | 28 | 11 |
| I feel confident in my ability to teach the physical exam | 11 | 39 | 33 | 17 |
| I have received adequate training in how to teach the physical exam | 17 | 50 | 22 | 11 |
Seventeen medical residents (49% response) completed a survey regarding their general medical service rotation with a hospitalist upon its completion (Table 2). Sixteen of the respondents (94%) agreed that time spent at the bedside during hospitalist attending teaching rounds that specific rotation was valuable, and 15 (82%) of the residents sought more emphasis on bedside teaching in the residency curriculum. Four of the respondents (24%) reported that their physical examination skills improved over the rotation, 5 (29%) felt better prepared to teach the physical examination, and 9 (53%) felt better prepared to lead bedside teaching rounds. Only 3 (18%) of the respondents reported that they had received helpful feedback on their physical examination skills from their attending. Responding residents noted physical examination teaching, communication and interpersonal skills, focus on patient‐centered care, and integrating the clinical examination with diagnostic and management decisions as the most valuable aspects of bedside teaching.
| Strongly Disagree (%) | Disagree (%) | Agree (%) | Strongly Agree (%) | |
|---|---|---|---|---|
| ||||
| Time spent at the bedside during teaching rounds was valuable | 0 | 6 | 65 | 29 |
| More emphasis on bedside teaching in the residency curriculum is needed | 0 | 18 | 53 | 29 |
| I feel better prepared to lead bedside teaching rounds | 6 | 41 | 53 | 0 |
| My physical exam skills improved over the rotation | 6 | 71 | 24 | 0 |
| I feel better prepared to teach the physical exam | 6 | 65 | 29 | 0 |
| I received helpful feedback on my physical exam skills | 18 | 65 | 18 | 0 |
Discussion
Bedside teaching is highly valued by clinicians and trainees, though there is little evidence supporting its efficacy. Patients also enjoy and are accepting of bedside presentations7, 9, 10 if certain rules are adhered to (eg, avoid medical jargon) and benefit by having a better understanding of their illness.9 This study supports previous views of medical residents, students,1, 5, 7 and faculty11 of the value and need for greater emphasis on bedside teaching in medical education.
This study of rounding behavior found that hospitalists in this academic center go to the bedside most days, but 39% of attending teaching rounds did not include a bedside encounter. Physical examination teaching is infrequent. Though time spent at the bedside was only a small fraction of total teaching time (17%) in this practice, this fraction is at the high end of previous reports. Teaching rounds that did not include bedside teaching most likely occurred in the confines of a conference room.
Many factors appear to contribute to the paucity of time spent at the bedside: time constraints, shorter hospital stays, greater work demands,11 residency duty‐hour regulations,12 declining bedside teaching skills, unrealistic expectations of the encounter, and erosion of the teaching ethic.3 A decline in clinical examination skills among trainees and attending physicians leads to a growing reliance on data and technology, thereby perpetuating the cycle of declining bedside skills.4
The hospitalists in this study identify time as the most dominant obstacle to bedside teaching. On days when hospitalist attending physicians went to the bedside, rounds were on average 53 minutes longer than on those days when they did not go to the bedside. This time increase varied little whether or not physical examination teaching occurred. The difference in rounding time may be partially explained by the admitting cycle and patient census. Teaching attendings are likely to go to the bedside to see new patients on postcall days when the patient census is also the highest.
Many members of this hospitalist group indicated that they felt inadequately prepared to lead bedside teaching rounds. Of those who responded to the survey, 67% did not feel that they received adequate training in how to teach the physical examination. Consequently, only one‐half of responding hospitalists expressed confidence in their ability to teach the physical examination. Not surprisingly, physical examination skills were a component of a minority of teaching sessions and only one‐quarter of the medical residents perceived that their physical examination skills improved during the rotation with a hospitalist attending. The paucity of feedback to the house‐staff likely contributed to this stagnancy. Residents who become hospitalists ill‐prepared to lead bedside teaching and teach the physical examination will perpetuate the decline in bedside teaching.
Though a substantial portion of the hospitalists in this study lacked confidence, an overwhelming majority of medical residents found their time spent at the bedside with a hospitalist to be valuable. More than one‐half of residents reported that they were better prepared to lead bedside teaching after the rotation. Residents recognize that bedside teaching can include communication and clinical reasoning skills. Hospitalists should be made aware that a broad range of skills and content can be taught at the bedside.
Hospitalists have an increasing influence on the education of medical residents and students and are appropriate targets for faculty development programs aimed at improving bedside teaching. As a newer, growing specialty, hospitalists tend to be younger physicians, and are therefore more reliant on the education attained during residency to support their bedside activities. Many residencies have developed resident as educator programs in an attempt to create a future generation of attendings better able to teach.13
Several limitations should be acknowledged when interpreting the results of this study. The study was limited to a hospitalist group at a single academic medical center and relied on resident recall. Though the response rate to the daily e‐mails was relatively low, the interrater reliability was high, and a broad range of residents and attendings were represented. Residents with greater patient censuses may have been too busy to respond, but it is unclear in which direction this would bias the results.
Conclusions
This study provides additional evidence that bedside and physical examination teaching are in decline. Time is an increasingly precious commodity for hospitalists; though many commentators echo the sentiments of the respondents in this study that more time at the bedside is needed, the amount of time that should be optimally spent at the bedside remains unclear. Research to improve the quality of bedside learning and its influence on patient care outcomes is needed.
- ,,,.Improving bedside teaching: findings from a focus group study of learners.Acad Med.2008;83(3):257–264.
- .On bedside teaching.Ann Intern Med.1997;126(3):217–220.
- ,,,.Whither bedside teaching? A focus‐group study of clinical teachers.Acad Med.2003;78(4):384–390.
- .Bedside rounds revisited.N Engl J Med.1997;336(16):1174–1175.
- ,,,.Effect of a physical examination teaching program on the behavior of medical residents.J Gen Intern Med.2005;20(8):710–714.
- ,,,,.Role modeling humanistic behavior: learning bedside manner from the experts.Acad Med.2006;81(7):661–667.
- ,,.Student and patient perspectives on bedside teaching.Med Educ.1997;31(5):341–346.
- .Hospitalists in the United States—mission accomplished or work in progress?N Engl J Med.2004;350(19):1935–1936.
- ,,,,.The effect of bedside case presentations on patients' perceptions of their medical care.N Engl J Med.1997;336(16):1150–1155.
- ,,,.A randomized, controlled trial of bedside versus conference‐room case presentation in a pediatric intensive care unit.Pediatrics.2007;120(2):275–280.
- ,,.Impediments to bed‐side teaching.Med Educ.1998;32(2):159–162.
- ,,, et al.Internal medicine and general surgery residents' attitudes about the ACGME duty hours regulations: a multicenter study.Acad Med.2006;81(12):1052–1058.
- ,,.Resident as teacher: educating the educators.Mt Sinai J Med.2006;73(8):1165–1169.
Bedside teaching, defined as teaching in the presence of a patient, has been an integral, respected part of medical education throughout the history of modern medicine. There is widespread concern among medical educators that bedside teaching is declining, and in particular, physical examination teaching.1‐5 Learning at the bedside accounted for 75% of clinical teaching in the 1960s and only 16% by 1978.2 Current estimates range from 8% to 19%.1
The bedside is the ideal venue for demonstrating, observing, and evaluating medical interviewing skills, physical examination techniques, and interpersonal and communication skills. Role modeling is the primary method by which clinical teachers demonstrate and teach professionalism and humanistic behavior.6 The bedside is also a place to develop clinical reasoning skills, stimulate problem‐based learning,7 and demonstrate teamwork.4 Thus, the decline in bedside teaching is of major concern for more than just the dying of a time‐honored tradition, but for the threat to the development of skills and attitudes essential for the practice of medicine.
With the rapid growth in the number of hospitalists and their presence at most major U.S. teaching hospitals, internal medicine residents and medical students in their medicine clerkships receive much of their inpatient training from attending physicians who are hospitalists.8 Little is known about the teaching practices of hospitalist attending physicians. We investigated the fraction of time hospitalist attending physicians spend at the bedside during attending teaching rounds and the frequency of the demonstration of physical examination skills at 1 academic teaching hospital.
Patients and Methods
The Brigham & Women's Hospitalist Service, a 28‐member academic hospitalist group who serve as both the teaching attendings and patient care attendings on 4 general medicine teams, was studied in a prospective, observational fashion. Internal medicine residents at Brigham & Women's Hospital rotating on the hospitalist service were identified by examining the schedule of inpatient rotations during the 2007‐2008 academic year and were asked to participate in the study via an e‐mail invitation. The Institutional Review Board of Brigham & Women's Hospital approved the study.
Teams were made up of 1 senior resident and 2 interns. Call frequency was every fourth day. Over a period of 23 sequential weekdays, medical residents and interns from each of the 4 hospitalist teams observed and reported the behavior of their attendings on rounds. Their reports captured the fraction of time spent at the bedside during rounds and the frequency of physical examination teaching. Residents and interns were asked to respond to 3 questions in a daily e‐mail. Respondents reported (1) total time spent with their hospitalist attending during attending rounds, (2) time spent inside patient rooms during attending rounds, and (3) whether or not a physical examination finding or skill was demonstrated by their hospitalist attending. When more than 1 team member responded, time reported among team members was averaged and if there was a discrepancy between whether or not a physical examination finding or skill was demonstrated, it was defaulted to the positive response. Hospitalist attendings remained unaware of the daily observations.
Hospitalist attendings were independently invited to complete a baseline needs assessment survey on bedside teaching. Surveys addressed attitudes toward bedside teaching, confidence in ability to lead bedside teaching rounds and teach the physical examination, and adequacy of their own training in these skills. Respondents were asked to comment on obstacles to bedside teaching. Residents were surveyed at the completion of a rotation with a hospitalist attending regarding the value of the time spent at the bedside and their self‐perceived improvement in physical examination skills and bedside teaching skills. The survey solicited the residents' opinion of the most valuable aspect of bedside teaching. The survey questions used a 4‐point Likert scale with response options ranging from 1 = strongly disagree to 4 = strongly agree.
The fraction of time spent at the bedside during attending hospitalist rounds was calculated from the average time spent in patient rooms and the average time of attending rounds. The frequency of physical examination teaching was expressed as a percent of all teaching encounters. Interrater reliability was calculated using the intraclass correlation coefficient with the Spearman‐Brown adjustment. Differences between groups were calculated using the Fisher's exact test for counts and the Wilcoxon rank‐sum test for continuous data. Significance was accepted for P < 0.05.
Results
Thirty‐five residents provided observations on 61 of 92 potentially observed attending rounds (66% response rate) over 23 weekdays, including observations of the rounding behavior of 12 different hospitalists. The interrater reliability was 0.91. The average patient census on each team during this time period was 12 (range 6‐19).
Residents reported that their attendings went to the bedside at least once during 37 of these 61 rounds (61%), and provided physical examination teaching during 23 of these 61 (38%) encounters. Hospitalists spent an average of 101 minutes on rounds and an average of 17 minutes (17%) of their time inside patient rooms.
Rounds that included time spent at the bedside were significantly longer on average than rounds that did not include time spent at the bedside (122 vs. 69 minutes, P < 0.001). During rounds that included bedside teaching, teams spent an average of 29 minutes (24% of the total time) in patient rooms, and rounds were significantly more likely to include teaching on physical diagnosis (23/37 rounds vs. 0/24 rounds, P < 0.001). Physical examination teaching did not significantly prolong those rounds that included bedside teaching (124 vs. 119 minutes, P = 0.56), but did significantly increase the amount of time spent at the bedside (32 vs. 22 minutes, P = 0.046).
Eighteen hospitalists (64% response) with a mean of 5.9 years of experience as attending physicians completed a needs‐assessment survey (Table 1). Fourteen of the 18 hospitalists (78%) reported that they prioritize bedside teaching and 16 (89%) requested more emphasis on bedside teaching in the residency curriculum. Twelve hospitalists (67%) indicated that they were confident in their ability to lead bedside teaching rounds; 9 (50%) were confident in their ability to teach physical examination. Eleven (61%) of the respondents felt poorly prepared to do bedside teaching after completing their residency, and 12 (67%) felt that they had received inadequate training in how to teach the physical examination. Of the obstacles to bedside teaching, time and inadequate training and skills were the most frequently noted, present in 11 and 6 of the reports, respectively. Lack of confidence and lack of role models were also cited in 4 and 2 of the reports, respectively.
| Strongly Disagree (%) | Disagree (%) | Agree (%) | Strongly Agree (%) | |
|---|---|---|---|---|
| ||||
| I make bedside teaching a priority | 0 | 22 | 56 | 22 |
| More emphasis on bedside teaching in the residency curriculum is needed | 0 | 11 | 39 | 50 |
| I feel confident in my ability to lead bedside teaching rounds | 11 | 22 | 50 | 17 |
| I was well‐prepared to do bedside teaching after residency training | 22 | 39 | 28 | 11 |
| I feel confident in my ability to teach the physical exam | 11 | 39 | 33 | 17 |
| I have received adequate training in how to teach the physical exam | 17 | 50 | 22 | 11 |
Seventeen medical residents (49% response) completed a survey regarding their general medical service rotation with a hospitalist upon its completion (Table 2). Sixteen of the respondents (94%) agreed that time spent at the bedside during hospitalist attending teaching rounds that specific rotation was valuable, and 15 (82%) of the residents sought more emphasis on bedside teaching in the residency curriculum. Four of the respondents (24%) reported that their physical examination skills improved over the rotation, 5 (29%) felt better prepared to teach the physical examination, and 9 (53%) felt better prepared to lead bedside teaching rounds. Only 3 (18%) of the respondents reported that they had received helpful feedback on their physical examination skills from their attending. Responding residents noted physical examination teaching, communication and interpersonal skills, focus on patient‐centered care, and integrating the clinical examination with diagnostic and management decisions as the most valuable aspects of bedside teaching.
| Strongly Disagree (%) | Disagree (%) | Agree (%) | Strongly Agree (%) | |
|---|---|---|---|---|
| ||||
| Time spent at the bedside during teaching rounds was valuable | 0 | 6 | 65 | 29 |
| More emphasis on bedside teaching in the residency curriculum is needed | 0 | 18 | 53 | 29 |
| I feel better prepared to lead bedside teaching rounds | 6 | 41 | 53 | 0 |
| My physical exam skills improved over the rotation | 6 | 71 | 24 | 0 |
| I feel better prepared to teach the physical exam | 6 | 65 | 29 | 0 |
| I received helpful feedback on my physical exam skills | 18 | 65 | 18 | 0 |
Discussion
Bedside teaching is highly valued by clinicians and trainees, though there is little evidence supporting its efficacy. Patients also enjoy and are accepting of bedside presentations7, 9, 10 if certain rules are adhered to (eg, avoid medical jargon) and benefit by having a better understanding of their illness.9 This study supports previous views of medical residents, students,1, 5, 7 and faculty11 of the value and need for greater emphasis on bedside teaching in medical education.
This study of rounding behavior found that hospitalists in this academic center go to the bedside most days, but 39% of attending teaching rounds did not include a bedside encounter. Physical examination teaching is infrequent. Though time spent at the bedside was only a small fraction of total teaching time (17%) in this practice, this fraction is at the high end of previous reports. Teaching rounds that did not include bedside teaching most likely occurred in the confines of a conference room.
Many factors appear to contribute to the paucity of time spent at the bedside: time constraints, shorter hospital stays, greater work demands,11 residency duty‐hour regulations,12 declining bedside teaching skills, unrealistic expectations of the encounter, and erosion of the teaching ethic.3 A decline in clinical examination skills among trainees and attending physicians leads to a growing reliance on data and technology, thereby perpetuating the cycle of declining bedside skills.4
The hospitalists in this study identify time as the most dominant obstacle to bedside teaching. On days when hospitalist attending physicians went to the bedside, rounds were on average 53 minutes longer than on those days when they did not go to the bedside. This time increase varied little whether or not physical examination teaching occurred. The difference in rounding time may be partially explained by the admitting cycle and patient census. Teaching attendings are likely to go to the bedside to see new patients on postcall days when the patient census is also the highest.
Many members of this hospitalist group indicated that they felt inadequately prepared to lead bedside teaching rounds. Of those who responded to the survey, 67% did not feel that they received adequate training in how to teach the physical examination. Consequently, only one‐half of responding hospitalists expressed confidence in their ability to teach the physical examination. Not surprisingly, physical examination skills were a component of a minority of teaching sessions and only one‐quarter of the medical residents perceived that their physical examination skills improved during the rotation with a hospitalist attending. The paucity of feedback to the house‐staff likely contributed to this stagnancy. Residents who become hospitalists ill‐prepared to lead bedside teaching and teach the physical examination will perpetuate the decline in bedside teaching.
Though a substantial portion of the hospitalists in this study lacked confidence, an overwhelming majority of medical residents found their time spent at the bedside with a hospitalist to be valuable. More than one‐half of residents reported that they were better prepared to lead bedside teaching after the rotation. Residents recognize that bedside teaching can include communication and clinical reasoning skills. Hospitalists should be made aware that a broad range of skills and content can be taught at the bedside.
Hospitalists have an increasing influence on the education of medical residents and students and are appropriate targets for faculty development programs aimed at improving bedside teaching. As a newer, growing specialty, hospitalists tend to be younger physicians, and are therefore more reliant on the education attained during residency to support their bedside activities. Many residencies have developed resident as educator programs in an attempt to create a future generation of attendings better able to teach.13
Several limitations should be acknowledged when interpreting the results of this study. The study was limited to a hospitalist group at a single academic medical center and relied on resident recall. Though the response rate to the daily e‐mails was relatively low, the interrater reliability was high, and a broad range of residents and attendings were represented. Residents with greater patient censuses may have been too busy to respond, but it is unclear in which direction this would bias the results.
Conclusions
This study provides additional evidence that bedside and physical examination teaching are in decline. Time is an increasingly precious commodity for hospitalists; though many commentators echo the sentiments of the respondents in this study that more time at the bedside is needed, the amount of time that should be optimally spent at the bedside remains unclear. Research to improve the quality of bedside learning and its influence on patient care outcomes is needed.
Bedside teaching, defined as teaching in the presence of a patient, has been an integral, respected part of medical education throughout the history of modern medicine. There is widespread concern among medical educators that bedside teaching is declining, and in particular, physical examination teaching.1‐5 Learning at the bedside accounted for 75% of clinical teaching in the 1960s and only 16% by 1978.2 Current estimates range from 8% to 19%.1
The bedside is the ideal venue for demonstrating, observing, and evaluating medical interviewing skills, physical examination techniques, and interpersonal and communication skills. Role modeling is the primary method by which clinical teachers demonstrate and teach professionalism and humanistic behavior.6 The bedside is also a place to develop clinical reasoning skills, stimulate problem‐based learning,7 and demonstrate teamwork.4 Thus, the decline in bedside teaching is of major concern for more than just the dying of a time‐honored tradition, but for the threat to the development of skills and attitudes essential for the practice of medicine.
With the rapid growth in the number of hospitalists and their presence at most major U.S. teaching hospitals, internal medicine residents and medical students in their medicine clerkships receive much of their inpatient training from attending physicians who are hospitalists.8 Little is known about the teaching practices of hospitalist attending physicians. We investigated the fraction of time hospitalist attending physicians spend at the bedside during attending teaching rounds and the frequency of the demonstration of physical examination skills at 1 academic teaching hospital.
Patients and Methods
The Brigham & Women's Hospitalist Service, a 28‐member academic hospitalist group who serve as both the teaching attendings and patient care attendings on 4 general medicine teams, was studied in a prospective, observational fashion. Internal medicine residents at Brigham & Women's Hospital rotating on the hospitalist service were identified by examining the schedule of inpatient rotations during the 2007‐2008 academic year and were asked to participate in the study via an e‐mail invitation. The Institutional Review Board of Brigham & Women's Hospital approved the study.
Teams were made up of 1 senior resident and 2 interns. Call frequency was every fourth day. Over a period of 23 sequential weekdays, medical residents and interns from each of the 4 hospitalist teams observed and reported the behavior of their attendings on rounds. Their reports captured the fraction of time spent at the bedside during rounds and the frequency of physical examination teaching. Residents and interns were asked to respond to 3 questions in a daily e‐mail. Respondents reported (1) total time spent with their hospitalist attending during attending rounds, (2) time spent inside patient rooms during attending rounds, and (3) whether or not a physical examination finding or skill was demonstrated by their hospitalist attending. When more than 1 team member responded, time reported among team members was averaged and if there was a discrepancy between whether or not a physical examination finding or skill was demonstrated, it was defaulted to the positive response. Hospitalist attendings remained unaware of the daily observations.
Hospitalist attendings were independently invited to complete a baseline needs assessment survey on bedside teaching. Surveys addressed attitudes toward bedside teaching, confidence in ability to lead bedside teaching rounds and teach the physical examination, and adequacy of their own training in these skills. Respondents were asked to comment on obstacles to bedside teaching. Residents were surveyed at the completion of a rotation with a hospitalist attending regarding the value of the time spent at the bedside and their self‐perceived improvement in physical examination skills and bedside teaching skills. The survey solicited the residents' opinion of the most valuable aspect of bedside teaching. The survey questions used a 4‐point Likert scale with response options ranging from 1 = strongly disagree to 4 = strongly agree.
The fraction of time spent at the bedside during attending hospitalist rounds was calculated from the average time spent in patient rooms and the average time of attending rounds. The frequency of physical examination teaching was expressed as a percent of all teaching encounters. Interrater reliability was calculated using the intraclass correlation coefficient with the Spearman‐Brown adjustment. Differences between groups were calculated using the Fisher's exact test for counts and the Wilcoxon rank‐sum test for continuous data. Significance was accepted for P < 0.05.
Results
Thirty‐five residents provided observations on 61 of 92 potentially observed attending rounds (66% response rate) over 23 weekdays, including observations of the rounding behavior of 12 different hospitalists. The interrater reliability was 0.91. The average patient census on each team during this time period was 12 (range 6‐19).
Residents reported that their attendings went to the bedside at least once during 37 of these 61 rounds (61%), and provided physical examination teaching during 23 of these 61 (38%) encounters. Hospitalists spent an average of 101 minutes on rounds and an average of 17 minutes (17%) of their time inside patient rooms.
Rounds that included time spent at the bedside were significantly longer on average than rounds that did not include time spent at the bedside (122 vs. 69 minutes, P < 0.001). During rounds that included bedside teaching, teams spent an average of 29 minutes (24% of the total time) in patient rooms, and rounds were significantly more likely to include teaching on physical diagnosis (23/37 rounds vs. 0/24 rounds, P < 0.001). Physical examination teaching did not significantly prolong those rounds that included bedside teaching (124 vs. 119 minutes, P = 0.56), but did significantly increase the amount of time spent at the bedside (32 vs. 22 minutes, P = 0.046).
Eighteen hospitalists (64% response) with a mean of 5.9 years of experience as attending physicians completed a needs‐assessment survey (Table 1). Fourteen of the 18 hospitalists (78%) reported that they prioritize bedside teaching and 16 (89%) requested more emphasis on bedside teaching in the residency curriculum. Twelve hospitalists (67%) indicated that they were confident in their ability to lead bedside teaching rounds; 9 (50%) were confident in their ability to teach physical examination. Eleven (61%) of the respondents felt poorly prepared to do bedside teaching after completing their residency, and 12 (67%) felt that they had received inadequate training in how to teach the physical examination. Of the obstacles to bedside teaching, time and inadequate training and skills were the most frequently noted, present in 11 and 6 of the reports, respectively. Lack of confidence and lack of role models were also cited in 4 and 2 of the reports, respectively.
| Strongly Disagree (%) | Disagree (%) | Agree (%) | Strongly Agree (%) | |
|---|---|---|---|---|
| ||||
| I make bedside teaching a priority | 0 | 22 | 56 | 22 |
| More emphasis on bedside teaching in the residency curriculum is needed | 0 | 11 | 39 | 50 |
| I feel confident in my ability to lead bedside teaching rounds | 11 | 22 | 50 | 17 |
| I was well‐prepared to do bedside teaching after residency training | 22 | 39 | 28 | 11 |
| I feel confident in my ability to teach the physical exam | 11 | 39 | 33 | 17 |
| I have received adequate training in how to teach the physical exam | 17 | 50 | 22 | 11 |
Seventeen medical residents (49% response) completed a survey regarding their general medical service rotation with a hospitalist upon its completion (Table 2). Sixteen of the respondents (94%) agreed that time spent at the bedside during hospitalist attending teaching rounds that specific rotation was valuable, and 15 (82%) of the residents sought more emphasis on bedside teaching in the residency curriculum. Four of the respondents (24%) reported that their physical examination skills improved over the rotation, 5 (29%) felt better prepared to teach the physical examination, and 9 (53%) felt better prepared to lead bedside teaching rounds. Only 3 (18%) of the respondents reported that they had received helpful feedback on their physical examination skills from their attending. Responding residents noted physical examination teaching, communication and interpersonal skills, focus on patient‐centered care, and integrating the clinical examination with diagnostic and management decisions as the most valuable aspects of bedside teaching.
| Strongly Disagree (%) | Disagree (%) | Agree (%) | Strongly Agree (%) | |
|---|---|---|---|---|
| ||||
| Time spent at the bedside during teaching rounds was valuable | 0 | 6 | 65 | 29 |
| More emphasis on bedside teaching in the residency curriculum is needed | 0 | 18 | 53 | 29 |
| I feel better prepared to lead bedside teaching rounds | 6 | 41 | 53 | 0 |
| My physical exam skills improved over the rotation | 6 | 71 | 24 | 0 |
| I feel better prepared to teach the physical exam | 6 | 65 | 29 | 0 |
| I received helpful feedback on my physical exam skills | 18 | 65 | 18 | 0 |
Discussion
Bedside teaching is highly valued by clinicians and trainees, though there is little evidence supporting its efficacy. Patients also enjoy and are accepting of bedside presentations7, 9, 10 if certain rules are adhered to (eg, avoid medical jargon) and benefit by having a better understanding of their illness.9 This study supports previous views of medical residents, students,1, 5, 7 and faculty11 of the value and need for greater emphasis on bedside teaching in medical education.
This study of rounding behavior found that hospitalists in this academic center go to the bedside most days, but 39% of attending teaching rounds did not include a bedside encounter. Physical examination teaching is infrequent. Though time spent at the bedside was only a small fraction of total teaching time (17%) in this practice, this fraction is at the high end of previous reports. Teaching rounds that did not include bedside teaching most likely occurred in the confines of a conference room.
Many factors appear to contribute to the paucity of time spent at the bedside: time constraints, shorter hospital stays, greater work demands,11 residency duty‐hour regulations,12 declining bedside teaching skills, unrealistic expectations of the encounter, and erosion of the teaching ethic.3 A decline in clinical examination skills among trainees and attending physicians leads to a growing reliance on data and technology, thereby perpetuating the cycle of declining bedside skills.4
The hospitalists in this study identify time as the most dominant obstacle to bedside teaching. On days when hospitalist attending physicians went to the bedside, rounds were on average 53 minutes longer than on those days when they did not go to the bedside. This time increase varied little whether or not physical examination teaching occurred. The difference in rounding time may be partially explained by the admitting cycle and patient census. Teaching attendings are likely to go to the bedside to see new patients on postcall days when the patient census is also the highest.
Many members of this hospitalist group indicated that they felt inadequately prepared to lead bedside teaching rounds. Of those who responded to the survey, 67% did not feel that they received adequate training in how to teach the physical examination. Consequently, only one‐half of responding hospitalists expressed confidence in their ability to teach the physical examination. Not surprisingly, physical examination skills were a component of a minority of teaching sessions and only one‐quarter of the medical residents perceived that their physical examination skills improved during the rotation with a hospitalist attending. The paucity of feedback to the house‐staff likely contributed to this stagnancy. Residents who become hospitalists ill‐prepared to lead bedside teaching and teach the physical examination will perpetuate the decline in bedside teaching.
Though a substantial portion of the hospitalists in this study lacked confidence, an overwhelming majority of medical residents found their time spent at the bedside with a hospitalist to be valuable. More than one‐half of residents reported that they were better prepared to lead bedside teaching after the rotation. Residents recognize that bedside teaching can include communication and clinical reasoning skills. Hospitalists should be made aware that a broad range of skills and content can be taught at the bedside.
Hospitalists have an increasing influence on the education of medical residents and students and are appropriate targets for faculty development programs aimed at improving bedside teaching. As a newer, growing specialty, hospitalists tend to be younger physicians, and are therefore more reliant on the education attained during residency to support their bedside activities. Many residencies have developed resident as educator programs in an attempt to create a future generation of attendings better able to teach.13
Several limitations should be acknowledged when interpreting the results of this study. The study was limited to a hospitalist group at a single academic medical center and relied on resident recall. Though the response rate to the daily e‐mails was relatively low, the interrater reliability was high, and a broad range of residents and attendings were represented. Residents with greater patient censuses may have been too busy to respond, but it is unclear in which direction this would bias the results.
Conclusions
This study provides additional evidence that bedside and physical examination teaching are in decline. Time is an increasingly precious commodity for hospitalists; though many commentators echo the sentiments of the respondents in this study that more time at the bedside is needed, the amount of time that should be optimally spent at the bedside remains unclear. Research to improve the quality of bedside learning and its influence on patient care outcomes is needed.
- ,,,.Improving bedside teaching: findings from a focus group study of learners.Acad Med.2008;83(3):257–264.
- .On bedside teaching.Ann Intern Med.1997;126(3):217–220.
- ,,,.Whither bedside teaching? A focus‐group study of clinical teachers.Acad Med.2003;78(4):384–390.
- .Bedside rounds revisited.N Engl J Med.1997;336(16):1174–1175.
- ,,,.Effect of a physical examination teaching program on the behavior of medical residents.J Gen Intern Med.2005;20(8):710–714.
- ,,,,.Role modeling humanistic behavior: learning bedside manner from the experts.Acad Med.2006;81(7):661–667.
- ,,.Student and patient perspectives on bedside teaching.Med Educ.1997;31(5):341–346.
- .Hospitalists in the United States—mission accomplished or work in progress?N Engl J Med.2004;350(19):1935–1936.
- ,,,,.The effect of bedside case presentations on patients' perceptions of their medical care.N Engl J Med.1997;336(16):1150–1155.
- ,,,.A randomized, controlled trial of bedside versus conference‐room case presentation in a pediatric intensive care unit.Pediatrics.2007;120(2):275–280.
- ,,.Impediments to bed‐side teaching.Med Educ.1998;32(2):159–162.
- ,,, et al.Internal medicine and general surgery residents' attitudes about the ACGME duty hours regulations: a multicenter study.Acad Med.2006;81(12):1052–1058.
- ,,.Resident as teacher: educating the educators.Mt Sinai J Med.2006;73(8):1165–1169.
- ,,,.Improving bedside teaching: findings from a focus group study of learners.Acad Med.2008;83(3):257–264.
- .On bedside teaching.Ann Intern Med.1997;126(3):217–220.
- ,,,.Whither bedside teaching? A focus‐group study of clinical teachers.Acad Med.2003;78(4):384–390.
- .Bedside rounds revisited.N Engl J Med.1997;336(16):1174–1175.
- ,,,.Effect of a physical examination teaching program on the behavior of medical residents.J Gen Intern Med.2005;20(8):710–714.
- ,,,,.Role modeling humanistic behavior: learning bedside manner from the experts.Acad Med.2006;81(7):661–667.
- ,,.Student and patient perspectives on bedside teaching.Med Educ.1997;31(5):341–346.
- .Hospitalists in the United States—mission accomplished or work in progress?N Engl J Med.2004;350(19):1935–1936.
- ,,,,.The effect of bedside case presentations on patients' perceptions of their medical care.N Engl J Med.1997;336(16):1150–1155.
- ,,,.A randomized, controlled trial of bedside versus conference‐room case presentation in a pediatric intensive care unit.Pediatrics.2007;120(2):275–280.
- ,,.Impediments to bed‐side teaching.Med Educ.1998;32(2):159–162.
- ,,, et al.Internal medicine and general surgery residents' attitudes about the ACGME duty hours regulations: a multicenter study.Acad Med.2006;81(12):1052–1058.
- ,,.Resident as teacher: educating the educators.Mt Sinai J Med.2006;73(8):1165–1169.
Copyright © 2009 Society of Hospital Medicine
A numbered day in the life
It seemed like years had passed since he was told he had cancer. While he basked in the cool white ambiance of the examination room, Jim mentally traced his many steps up and down the nearby hospital hallways. From this room to that, he had shuffled through most of the rooms on this hospital ward. Jim had read every outdated Time and National Geographic magazine, and all of the kids' books. From sitting in waiting rooms, he had even developed a deep appreciation for Thomas the Tank Engine. As he sat there, he realized that he had only spent 8 days in this hospital ward. But in here, 8 days might as well be 11 years. Time doesn't so much pass in hospital wards as it stands perfectly still on your chest. The total isolation for those who must stay is startling. Jim had begun judging time by the movements of those lucky enough to go home. Instead of Mondays, Tuesdays, and Wednesdays, he was also measuring time by food. Days of the week had become known as Styrofoam meatloaf, highly suspect lasagna, and inedible beef Wellington; all had become units of time measurement.
When he was told about his cancerthe doctor told him it was a type of hematological neo‐something‐or‐otherJim felt strangely aroused by the news. He felt energy racing through his body as he geared for battle. His immediate response was to think about how he would volunteer for the harshest, meanest, nastiest treatment he could get the doctor to agree with. Poke him full of holes, pour poison straight in his veins, run him on treadmills while doing all of thatit didn't matter. There was nothing he would not do to beat this thing. The doctor had finished telling Jim about all those options at the very minute Jim was ready to hear them. Whatever, whatever, Doc, let's get going with this, was his response.
Then, he had gradually noticed that the pace of medicine was something a little less urgent than he had thought. On TV the doctors run everywhere, but here they walked with a brisk but awkward gait, as if afraid of falling on the floor by going too fast. While waiting for his appointments, Jim noticed that everything was about waitingwaiting for everything. Nothing happens in the hospital. There are people walking everywhere with some projected sense of purpose but it all seems so meaningless when there's a hundred people in hospital uniforms walking past a whole room of patients.
Finally, the door to the examination room burst open and in walked Dr. Day. Standing slightly less than 6 feet tall, Docas Jim called himwas one of those well‐preserved 50‐year‐olds who could be found wind‐surfing his way back to his convertible sports car during his off‐hours. Jim imagined that Doc had been the star student, the handsome rover, the jock. Age had started to claw at his youthful looks, but vanity had led the charge against age for Doc. His behavior and choices worked against his clock, and he was not going quietly into that dark night. Doc's athletic stride made it seem like his feet never touched the floor, and he wafted deep into the room before the doors had even fully opened. Doc never looked forward, but always studied the charts in front of him. He was intense; it was as if he had to truly concentrate sometimes to keep pace with his own mind. Doc was talking, but it was unclear to whom. Finally, he looked up with an expectant pause, and Jim, battered with indifference, nodded in affirmationto what, he didn't care. Doc then gave Jim the thumbs‐up, turned on his heel and headed toward the door; he spun around on the spot and looked back, Yeah, you'll need to change into a robe with nothing on underneath it. He gestured to the one wall where a shelf held neatly folded paper‐thin gowns. Jim put one on and could barely believe how sheer it was. It had the density of a paper napkin, he thought. Then again, this was hardly a cause for modesty. The cancer, he had learned, was actually lymphoma, and it had settled in his groin. At first, Jim was ashamed to have doctors and nurses poke and prod his nether regions, but after a while he became quite causal about it with the usual array of doctors and nurses who populated his monotonous life in this shiny new white palace. After the requisite 15 minutes of unexplained absence, Dr. Day returned through the doors. There was something different about him now, and in a world so dominated by sameness, predictability, and routine, change was a dark storm cloud and sudden wind in Jim's mind.
Lie down on that table please, Doc said in his usual my hand may be making a tactile map of your groin, but my mind is in Bermuda manner. As Jim hopped up on the table and shifted his diseased area closer to the end, the Doc seemed to brighten up, Stay right there, he said as he moved quickly from the room once again. Jim pondered the instruction. As opposed to going where? Jim groaned. He would go somewhere, but his treatment, eventually, would happen here. If he left, he didn't know if would ever come back.
In through the door, one more time, came Dr. Day, but this time he seemed to be leading some kind of tour. Trailing behind him in different states of interest and alertness was a team of young people, all in the little training smocks they give them that look just like the big‐boy coat that Dr. Day wore. Their smocks were more wrinkled and more ivory colored, but they still looked official. Dr. Day hardly looked toward the patient as he smoothly rolled into the side of the table nearest Jim's now‐exposed groin.
Jim looked up between his upstretched knees to see them, all of them, standing around trying to decide if they should be looking at the Doc or looking at the affected area. Jim was embarrassed. Jim was mad. Jim was embarrassed again. He tried to make eye contact with every single visitor in the room, and all he could see were eyes looking straight down under the flap of his hospital gown. Doc had broken into his whole song and dance when he stopped short and looked to Jim, almost apologetically, You're alright with this, right? These are first‐year residents and I wanted them to see this kind of tumor up close. Doc hardly took a full breath and he had turned and was back into his blather about mito, crypto, this, that, and some other bullshit. Jim felt like if he rested his head back maybe no one would ever know that he was the real fleshy cadaver that they stared at that day. He might never see any of these students again, and even if he did, none of them could bring themselves to look him anywhere near the eye anyway. Not much danger that any of them could pick him out of a police lineup, even if he did it without any pants on.
It's important to palpate the region, each of you need to feel what this is like, starting with you. Jim heard this particular instruction and snapped his head up to see exactly where the students were now headed to see and feel the thing they just had to touch. Imagine his dismay when he saw that all of them were still there, still transfixed on whatever they had found to look at studiously during this whole period of time. Doc had motioned to the smallest, frailest, most out‐of‐her‐element young woman he had ever seen. She visibly swallowed hard at the news that she would be first. Her eyes, previously fixed without distraction on some point on Jim's leg, now began to frantically search the eyes of others, possibly looking for some permission to run away. Her eyes met Jim's quite by accident, and she shared with him a look of total and complete shame. He took out his annoyance on her by fixing her with a murderous stare, while he watched as her hand inched ever closer to his leg. In a continuous, but painfully slow motion, she reached under the robe and Jim felt the slightest touch of what he assumed was her finger come to rest on the lowest part of his abdomen. She held her finger there, motionless, and then drew it away quickly while nodding to the Doc. No, no, no, you have to really feel it! Doc chided. He reached down and poked the area firmly, but with a certainty and comfort that comes only from unspoken familiarity. Doc then grabbed the poor girl's hand and guided it and proceeded, with his hand holding her wrist, to make the poking motion with her hand. She was clearly horrified and would have rather been poking through the exposed abdomen of a cadaver at that point. Jim's mood became even more annoyed at her response. It was okay to be embarrassed, but she was now acting like his groin was Elephant‐Man‐esque in its hideousness. He wondered if Doc would set up a barker stand and call to the passers‐by to see the bulbous freak, 50 cents for a viewing! Don't forget about our snack tents! Nobody should go home without candy, everybody loves candy!
After the young resident had endured all that the Doc thought she should, he motioned to the next one and repeated the same process; one after another, after another. The students instinctively formed a line that snaked around the table and spilled out through the room. Jim became callous at this point and began chatting up the students while they stood, quietly waiting their turn for the guided poking, to make them feel even more uncomfortable and intimidated. Jim spied one extremely uncomfortable‐looking male student. You know, if you like this, it doesn't make you gay, Jim shared in an almost caring tone. As the target of his comments shuffled forward, eyes never leaving the floor, Jim targeted another victim with his comments, and then another, and then another. Jim became a sniper of sarcasm, picking off helpless young residents as they stood helplessly in his aim. Doc finally reacted to Jim and shot him a scolding look. Doc leaned into Jim's ear, Fun is fun, but let's just take it easy now, ok? Jim grunted in disagreement, but complied. There was no anger left to vent, and really no need to vent it. Residents weren't the problem, but it was easy to treat them that way. Besides, Jim figured there was many more days for him to make it up to them by being a nicer patient. Today was today, but there were probably 20 more tomorrows for him here.
Finally, the last student had his moment. Jim noticed that the region was now sore from the guiding probing, and Doc had his back to him while addressing the students about what they had seen there today. Jim hopped off the table and proceeded to change back into his clothes while Doc carried on talking. Then, Doc was gone; he sped from the room with his entourage in close pursuit. Jim finished dressing and shuffled down the hallway to his room. Jim sighed under the weight of monotony. Every day was the same, and only the torturous delight he enjoyed at the expense of those residents made the day unique. It was, for the most part, emotion that broke the routine. Emotion was the only thing that Jim controlled at this point, and occasionally, selfishly, he would let it loose on the unsuspecting, simply to bookmark his day. Cancer was not killing Jim, but boredom quite possibly could. As Jim passed the drink machine around the corner from his ward, he saw nurse Janet coming in to work with her neon pink lunch kit slung over her shoulder. She smiled at Jim and asked him how he was feeling. Jim smiled, told her all was getting better, and then made his way back to his room. Janet's arrival meant it was almost supper time, and today was lasagna.
It seemed like years had passed since he was told he had cancer. While he basked in the cool white ambiance of the examination room, Jim mentally traced his many steps up and down the nearby hospital hallways. From this room to that, he had shuffled through most of the rooms on this hospital ward. Jim had read every outdated Time and National Geographic magazine, and all of the kids' books. From sitting in waiting rooms, he had even developed a deep appreciation for Thomas the Tank Engine. As he sat there, he realized that he had only spent 8 days in this hospital ward. But in here, 8 days might as well be 11 years. Time doesn't so much pass in hospital wards as it stands perfectly still on your chest. The total isolation for those who must stay is startling. Jim had begun judging time by the movements of those lucky enough to go home. Instead of Mondays, Tuesdays, and Wednesdays, he was also measuring time by food. Days of the week had become known as Styrofoam meatloaf, highly suspect lasagna, and inedible beef Wellington; all had become units of time measurement.
When he was told about his cancerthe doctor told him it was a type of hematological neo‐something‐or‐otherJim felt strangely aroused by the news. He felt energy racing through his body as he geared for battle. His immediate response was to think about how he would volunteer for the harshest, meanest, nastiest treatment he could get the doctor to agree with. Poke him full of holes, pour poison straight in his veins, run him on treadmills while doing all of thatit didn't matter. There was nothing he would not do to beat this thing. The doctor had finished telling Jim about all those options at the very minute Jim was ready to hear them. Whatever, whatever, Doc, let's get going with this, was his response.
Then, he had gradually noticed that the pace of medicine was something a little less urgent than he had thought. On TV the doctors run everywhere, but here they walked with a brisk but awkward gait, as if afraid of falling on the floor by going too fast. While waiting for his appointments, Jim noticed that everything was about waitingwaiting for everything. Nothing happens in the hospital. There are people walking everywhere with some projected sense of purpose but it all seems so meaningless when there's a hundred people in hospital uniforms walking past a whole room of patients.
Finally, the door to the examination room burst open and in walked Dr. Day. Standing slightly less than 6 feet tall, Docas Jim called himwas one of those well‐preserved 50‐year‐olds who could be found wind‐surfing his way back to his convertible sports car during his off‐hours. Jim imagined that Doc had been the star student, the handsome rover, the jock. Age had started to claw at his youthful looks, but vanity had led the charge against age for Doc. His behavior and choices worked against his clock, and he was not going quietly into that dark night. Doc's athletic stride made it seem like his feet never touched the floor, and he wafted deep into the room before the doors had even fully opened. Doc never looked forward, but always studied the charts in front of him. He was intense; it was as if he had to truly concentrate sometimes to keep pace with his own mind. Doc was talking, but it was unclear to whom. Finally, he looked up with an expectant pause, and Jim, battered with indifference, nodded in affirmationto what, he didn't care. Doc then gave Jim the thumbs‐up, turned on his heel and headed toward the door; he spun around on the spot and looked back, Yeah, you'll need to change into a robe with nothing on underneath it. He gestured to the one wall where a shelf held neatly folded paper‐thin gowns. Jim put one on and could barely believe how sheer it was. It had the density of a paper napkin, he thought. Then again, this was hardly a cause for modesty. The cancer, he had learned, was actually lymphoma, and it had settled in his groin. At first, Jim was ashamed to have doctors and nurses poke and prod his nether regions, but after a while he became quite causal about it with the usual array of doctors and nurses who populated his monotonous life in this shiny new white palace. After the requisite 15 minutes of unexplained absence, Dr. Day returned through the doors. There was something different about him now, and in a world so dominated by sameness, predictability, and routine, change was a dark storm cloud and sudden wind in Jim's mind.
Lie down on that table please, Doc said in his usual my hand may be making a tactile map of your groin, but my mind is in Bermuda manner. As Jim hopped up on the table and shifted his diseased area closer to the end, the Doc seemed to brighten up, Stay right there, he said as he moved quickly from the room once again. Jim pondered the instruction. As opposed to going where? Jim groaned. He would go somewhere, but his treatment, eventually, would happen here. If he left, he didn't know if would ever come back.
In through the door, one more time, came Dr. Day, but this time he seemed to be leading some kind of tour. Trailing behind him in different states of interest and alertness was a team of young people, all in the little training smocks they give them that look just like the big‐boy coat that Dr. Day wore. Their smocks were more wrinkled and more ivory colored, but they still looked official. Dr. Day hardly looked toward the patient as he smoothly rolled into the side of the table nearest Jim's now‐exposed groin.
Jim looked up between his upstretched knees to see them, all of them, standing around trying to decide if they should be looking at the Doc or looking at the affected area. Jim was embarrassed. Jim was mad. Jim was embarrassed again. He tried to make eye contact with every single visitor in the room, and all he could see were eyes looking straight down under the flap of his hospital gown. Doc had broken into his whole song and dance when he stopped short and looked to Jim, almost apologetically, You're alright with this, right? These are first‐year residents and I wanted them to see this kind of tumor up close. Doc hardly took a full breath and he had turned and was back into his blather about mito, crypto, this, that, and some other bullshit. Jim felt like if he rested his head back maybe no one would ever know that he was the real fleshy cadaver that they stared at that day. He might never see any of these students again, and even if he did, none of them could bring themselves to look him anywhere near the eye anyway. Not much danger that any of them could pick him out of a police lineup, even if he did it without any pants on.
It's important to palpate the region, each of you need to feel what this is like, starting with you. Jim heard this particular instruction and snapped his head up to see exactly where the students were now headed to see and feel the thing they just had to touch. Imagine his dismay when he saw that all of them were still there, still transfixed on whatever they had found to look at studiously during this whole period of time. Doc had motioned to the smallest, frailest, most out‐of‐her‐element young woman he had ever seen. She visibly swallowed hard at the news that she would be first. Her eyes, previously fixed without distraction on some point on Jim's leg, now began to frantically search the eyes of others, possibly looking for some permission to run away. Her eyes met Jim's quite by accident, and she shared with him a look of total and complete shame. He took out his annoyance on her by fixing her with a murderous stare, while he watched as her hand inched ever closer to his leg. In a continuous, but painfully slow motion, she reached under the robe and Jim felt the slightest touch of what he assumed was her finger come to rest on the lowest part of his abdomen. She held her finger there, motionless, and then drew it away quickly while nodding to the Doc. No, no, no, you have to really feel it! Doc chided. He reached down and poked the area firmly, but with a certainty and comfort that comes only from unspoken familiarity. Doc then grabbed the poor girl's hand and guided it and proceeded, with his hand holding her wrist, to make the poking motion with her hand. She was clearly horrified and would have rather been poking through the exposed abdomen of a cadaver at that point. Jim's mood became even more annoyed at her response. It was okay to be embarrassed, but she was now acting like his groin was Elephant‐Man‐esque in its hideousness. He wondered if Doc would set up a barker stand and call to the passers‐by to see the bulbous freak, 50 cents for a viewing! Don't forget about our snack tents! Nobody should go home without candy, everybody loves candy!
After the young resident had endured all that the Doc thought she should, he motioned to the next one and repeated the same process; one after another, after another. The students instinctively formed a line that snaked around the table and spilled out through the room. Jim became callous at this point and began chatting up the students while they stood, quietly waiting their turn for the guided poking, to make them feel even more uncomfortable and intimidated. Jim spied one extremely uncomfortable‐looking male student. You know, if you like this, it doesn't make you gay, Jim shared in an almost caring tone. As the target of his comments shuffled forward, eyes never leaving the floor, Jim targeted another victim with his comments, and then another, and then another. Jim became a sniper of sarcasm, picking off helpless young residents as they stood helplessly in his aim. Doc finally reacted to Jim and shot him a scolding look. Doc leaned into Jim's ear, Fun is fun, but let's just take it easy now, ok? Jim grunted in disagreement, but complied. There was no anger left to vent, and really no need to vent it. Residents weren't the problem, but it was easy to treat them that way. Besides, Jim figured there was many more days for him to make it up to them by being a nicer patient. Today was today, but there were probably 20 more tomorrows for him here.
Finally, the last student had his moment. Jim noticed that the region was now sore from the guiding probing, and Doc had his back to him while addressing the students about what they had seen there today. Jim hopped off the table and proceeded to change back into his clothes while Doc carried on talking. Then, Doc was gone; he sped from the room with his entourage in close pursuit. Jim finished dressing and shuffled down the hallway to his room. Jim sighed under the weight of monotony. Every day was the same, and only the torturous delight he enjoyed at the expense of those residents made the day unique. It was, for the most part, emotion that broke the routine. Emotion was the only thing that Jim controlled at this point, and occasionally, selfishly, he would let it loose on the unsuspecting, simply to bookmark his day. Cancer was not killing Jim, but boredom quite possibly could. As Jim passed the drink machine around the corner from his ward, he saw nurse Janet coming in to work with her neon pink lunch kit slung over her shoulder. She smiled at Jim and asked him how he was feeling. Jim smiled, told her all was getting better, and then made his way back to his room. Janet's arrival meant it was almost supper time, and today was lasagna.
It seemed like years had passed since he was told he had cancer. While he basked in the cool white ambiance of the examination room, Jim mentally traced his many steps up and down the nearby hospital hallways. From this room to that, he had shuffled through most of the rooms on this hospital ward. Jim had read every outdated Time and National Geographic magazine, and all of the kids' books. From sitting in waiting rooms, he had even developed a deep appreciation for Thomas the Tank Engine. As he sat there, he realized that he had only spent 8 days in this hospital ward. But in here, 8 days might as well be 11 years. Time doesn't so much pass in hospital wards as it stands perfectly still on your chest. The total isolation for those who must stay is startling. Jim had begun judging time by the movements of those lucky enough to go home. Instead of Mondays, Tuesdays, and Wednesdays, he was also measuring time by food. Days of the week had become known as Styrofoam meatloaf, highly suspect lasagna, and inedible beef Wellington; all had become units of time measurement.
When he was told about his cancerthe doctor told him it was a type of hematological neo‐something‐or‐otherJim felt strangely aroused by the news. He felt energy racing through his body as he geared for battle. His immediate response was to think about how he would volunteer for the harshest, meanest, nastiest treatment he could get the doctor to agree with. Poke him full of holes, pour poison straight in his veins, run him on treadmills while doing all of thatit didn't matter. There was nothing he would not do to beat this thing. The doctor had finished telling Jim about all those options at the very minute Jim was ready to hear them. Whatever, whatever, Doc, let's get going with this, was his response.
Then, he had gradually noticed that the pace of medicine was something a little less urgent than he had thought. On TV the doctors run everywhere, but here they walked with a brisk but awkward gait, as if afraid of falling on the floor by going too fast. While waiting for his appointments, Jim noticed that everything was about waitingwaiting for everything. Nothing happens in the hospital. There are people walking everywhere with some projected sense of purpose but it all seems so meaningless when there's a hundred people in hospital uniforms walking past a whole room of patients.
Finally, the door to the examination room burst open and in walked Dr. Day. Standing slightly less than 6 feet tall, Docas Jim called himwas one of those well‐preserved 50‐year‐olds who could be found wind‐surfing his way back to his convertible sports car during his off‐hours. Jim imagined that Doc had been the star student, the handsome rover, the jock. Age had started to claw at his youthful looks, but vanity had led the charge against age for Doc. His behavior and choices worked against his clock, and he was not going quietly into that dark night. Doc's athletic stride made it seem like his feet never touched the floor, and he wafted deep into the room before the doors had even fully opened. Doc never looked forward, but always studied the charts in front of him. He was intense; it was as if he had to truly concentrate sometimes to keep pace with his own mind. Doc was talking, but it was unclear to whom. Finally, he looked up with an expectant pause, and Jim, battered with indifference, nodded in affirmationto what, he didn't care. Doc then gave Jim the thumbs‐up, turned on his heel and headed toward the door; he spun around on the spot and looked back, Yeah, you'll need to change into a robe with nothing on underneath it. He gestured to the one wall where a shelf held neatly folded paper‐thin gowns. Jim put one on and could barely believe how sheer it was. It had the density of a paper napkin, he thought. Then again, this was hardly a cause for modesty. The cancer, he had learned, was actually lymphoma, and it had settled in his groin. At first, Jim was ashamed to have doctors and nurses poke and prod his nether regions, but after a while he became quite causal about it with the usual array of doctors and nurses who populated his monotonous life in this shiny new white palace. After the requisite 15 minutes of unexplained absence, Dr. Day returned through the doors. There was something different about him now, and in a world so dominated by sameness, predictability, and routine, change was a dark storm cloud and sudden wind in Jim's mind.
Lie down on that table please, Doc said in his usual my hand may be making a tactile map of your groin, but my mind is in Bermuda manner. As Jim hopped up on the table and shifted his diseased area closer to the end, the Doc seemed to brighten up, Stay right there, he said as he moved quickly from the room once again. Jim pondered the instruction. As opposed to going where? Jim groaned. He would go somewhere, but his treatment, eventually, would happen here. If he left, he didn't know if would ever come back.
In through the door, one more time, came Dr. Day, but this time he seemed to be leading some kind of tour. Trailing behind him in different states of interest and alertness was a team of young people, all in the little training smocks they give them that look just like the big‐boy coat that Dr. Day wore. Their smocks were more wrinkled and more ivory colored, but they still looked official. Dr. Day hardly looked toward the patient as he smoothly rolled into the side of the table nearest Jim's now‐exposed groin.
Jim looked up between his upstretched knees to see them, all of them, standing around trying to decide if they should be looking at the Doc or looking at the affected area. Jim was embarrassed. Jim was mad. Jim was embarrassed again. He tried to make eye contact with every single visitor in the room, and all he could see were eyes looking straight down under the flap of his hospital gown. Doc had broken into his whole song and dance when he stopped short and looked to Jim, almost apologetically, You're alright with this, right? These are first‐year residents and I wanted them to see this kind of tumor up close. Doc hardly took a full breath and he had turned and was back into his blather about mito, crypto, this, that, and some other bullshit. Jim felt like if he rested his head back maybe no one would ever know that he was the real fleshy cadaver that they stared at that day. He might never see any of these students again, and even if he did, none of them could bring themselves to look him anywhere near the eye anyway. Not much danger that any of them could pick him out of a police lineup, even if he did it without any pants on.
It's important to palpate the region, each of you need to feel what this is like, starting with you. Jim heard this particular instruction and snapped his head up to see exactly where the students were now headed to see and feel the thing they just had to touch. Imagine his dismay when he saw that all of them were still there, still transfixed on whatever they had found to look at studiously during this whole period of time. Doc had motioned to the smallest, frailest, most out‐of‐her‐element young woman he had ever seen. She visibly swallowed hard at the news that she would be first. Her eyes, previously fixed without distraction on some point on Jim's leg, now began to frantically search the eyes of others, possibly looking for some permission to run away. Her eyes met Jim's quite by accident, and she shared with him a look of total and complete shame. He took out his annoyance on her by fixing her with a murderous stare, while he watched as her hand inched ever closer to his leg. In a continuous, but painfully slow motion, she reached under the robe and Jim felt the slightest touch of what he assumed was her finger come to rest on the lowest part of his abdomen. She held her finger there, motionless, and then drew it away quickly while nodding to the Doc. No, no, no, you have to really feel it! Doc chided. He reached down and poked the area firmly, but with a certainty and comfort that comes only from unspoken familiarity. Doc then grabbed the poor girl's hand and guided it and proceeded, with his hand holding her wrist, to make the poking motion with her hand. She was clearly horrified and would have rather been poking through the exposed abdomen of a cadaver at that point. Jim's mood became even more annoyed at her response. It was okay to be embarrassed, but she was now acting like his groin was Elephant‐Man‐esque in its hideousness. He wondered if Doc would set up a barker stand and call to the passers‐by to see the bulbous freak, 50 cents for a viewing! Don't forget about our snack tents! Nobody should go home without candy, everybody loves candy!
After the young resident had endured all that the Doc thought she should, he motioned to the next one and repeated the same process; one after another, after another. The students instinctively formed a line that snaked around the table and spilled out through the room. Jim became callous at this point and began chatting up the students while they stood, quietly waiting their turn for the guided poking, to make them feel even more uncomfortable and intimidated. Jim spied one extremely uncomfortable‐looking male student. You know, if you like this, it doesn't make you gay, Jim shared in an almost caring tone. As the target of his comments shuffled forward, eyes never leaving the floor, Jim targeted another victim with his comments, and then another, and then another. Jim became a sniper of sarcasm, picking off helpless young residents as they stood helplessly in his aim. Doc finally reacted to Jim and shot him a scolding look. Doc leaned into Jim's ear, Fun is fun, but let's just take it easy now, ok? Jim grunted in disagreement, but complied. There was no anger left to vent, and really no need to vent it. Residents weren't the problem, but it was easy to treat them that way. Besides, Jim figured there was many more days for him to make it up to them by being a nicer patient. Today was today, but there were probably 20 more tomorrows for him here.
Finally, the last student had his moment. Jim noticed that the region was now sore from the guiding probing, and Doc had his back to him while addressing the students about what they had seen there today. Jim hopped off the table and proceeded to change back into his clothes while Doc carried on talking. Then, Doc was gone; he sped from the room with his entourage in close pursuit. Jim finished dressing and shuffled down the hallway to his room. Jim sighed under the weight of monotony. Every day was the same, and only the torturous delight he enjoyed at the expense of those residents made the day unique. It was, for the most part, emotion that broke the routine. Emotion was the only thing that Jim controlled at this point, and occasionally, selfishly, he would let it loose on the unsuspecting, simply to bookmark his day. Cancer was not killing Jim, but boredom quite possibly could. As Jim passed the drink machine around the corner from his ward, he saw nurse Janet coming in to work with her neon pink lunch kit slung over her shoulder. She smiled at Jim and asked him how he was feeling. Jim smiled, told her all was getting better, and then made his way back to his room. Janet's arrival meant it was almost supper time, and today was lasagna.
PRESsed for time
A 36‐year‐old woman was admitted after new‐onset Hseizures. She had been diagnosed with breast cancer 5 years prior to admission. At that time, she underwent left radical mastectomy and lymph node dissection. Lymph nodes were positive for metastatic disease with negative HER‐2‐Neu and positive estrogen and progesterone receptors. She was treated with docetaxel and tamoxifen but subsequently developed metastatic left hip lesions and was treated with letrozole and anastrozole. Three years later, scans revealed further metastatic disease to the liver, lung, and vertebral column. She was subsequently treated with capecitabine, until further disease progression led to the use of carboplatin and paclitaxel. Seven months prior to admission, her cancer was progressing and she was switched to doxorubicin, gemcitabine, and bevacizumab. Six weeks prior to admission, both positron emission tomography (PET) and computed tomography (CT) scan of her whole body and magnetic resonance imaging (MRI) of the brain illustrated significant improvement. Her last dose of bevacizumab was given 3 weeks prior to her admission.
Two weeks prior to admission, patient reported new‐onset daily headache. These were often localized in the occipital region. She reported some associated nausea and occasional emesis. Subsequently, she developed photophobia and phonophobia. On seeking outpatient treatment for her headache, it was noted that her systolic blood pressure had increased from a baseline of 100 mm Hg to 170 mm Hg. On the day prior to admission, she reported severe headache and several episodes of emesis and later that evening had a witnessed tonic‐clonic seizure.
The patient presented to an outside hospital and had an unremarkable noncontrast CT scan of her brain. An examination of her cerebrospinal fluid revealed negative gram stain, and a normal white blood cell count and protein level. She was treated with lorazepam, phenytoin, and decadron. On becoming more alert, she insisted on going home, where she later developed recurrent headache and presented to our emergency room.
On admission to our service, she was noted to be confused and irritable, and unable to provide any history. Her exam revealed a blood pressure of 143/102 mmHg. No localizing neurologic signs were noted and her laboratory values were normal. After sedation, MRI of the brain was obtained (Figure 1). This revealed diffuse and patchy gyriform hyperintensity of the white matter, most consistent with posterior reversible encephalopathy syndrome (PRES).
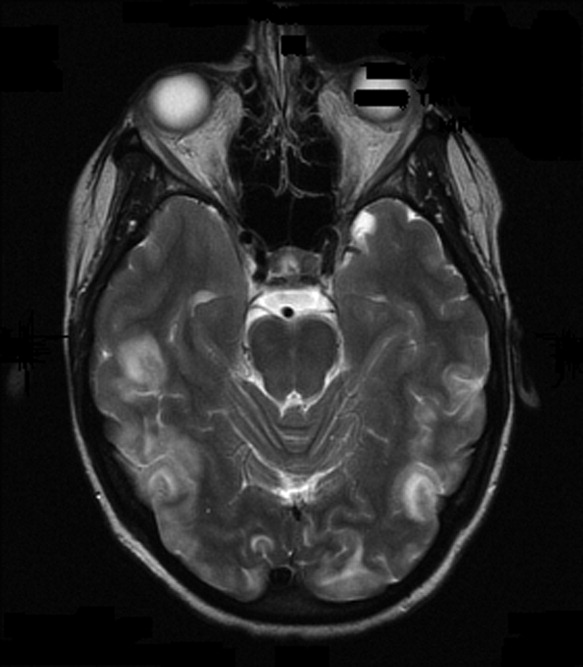
Upon reflection, the patient had new onset hypertension that coincided with the initiation and dosing of bevacizumab. Bevacizumab, an antineoplastic agent, is a recombinant humanized monoclonal antibody that binds to and neutralizes vascular endothelial growth factor, thereby preventing angiogenesis.1 It is known to cause grade 3 hypertension in a minority of patients. Therefore, it was postulated that the patient's persistent blood pressure elevation resulted in vasogenic brain edema, precipitating her seizure. Subsequent to the diagnosis, her blood pressure was aggressively controlled with oral enalapril, metoprolol, triamterene/hydrochlorothiazide, and hydralazine. By hospital day 7, her headache had subsided and her altered mental status had resolved. She had no further episodes of seizures and bevacizumab was discontinued.
PRES has a distinct constellation of clinical symptoms and radiologic findings. The name PRES is a misnomer, as this syndrome is not always reversible, nor is it restricted to the white matter or to the posterior areas of the brain.2 It is hypothesized that a sudden rise in blood pressure leads to elevations in intracranial pressure, which exceeds the brain's autoregulatory mechanisms. This subsequently leads to transudation of fluid into the brain parenchyma. Interestingly, it appears that it is not the absolute level of systolic blood pressure that is critical in the development of PRES, but the rate of change in blood pressure. Hence, patients with chronic hypertension have developed adaptive vascular changes that protect them from this type of parenchymal damage.
PRES has gained increasing recognition due to the use of immunosuppressive and chemotherapeutic medications in organ transplant and oncology patients. Drugs such as cyclosporine, tacrolimus, fludarabine, vincristine, cisplatin, cytarabine, interferon‐alpha, interleukin, antiretroviral therapy, erythropoietin, granulocyte stimulating factor, and intravenous immunoglobulin have all been implicated.3 In addition to increasing blood pressure, these agents likely cause direct toxic injury to the brain, disrupting the blood‐brain barrier and resulting in subsequent edema. Other conditions associated with PRES include renal disease, vasculitis, endocrine disorders, porphyria, cocaine or amphetamine abuse, and stimulant abuse.
Clinically, PRES can present as headache, altered mental status, confusion, drowsiness progressing to stupor, emesis, abnormal visual perceptions, visual neglect, cortical blindness, difficulty with memory and concentration, brisk deep tendon reflexes, weakness, ataxia, and seizure activity. PRES has a characteristic appearance on neuroimaging that differentiates it from other forms of hypertensive encephalopathy. Edema of the white or gray matter in the posterior cerebral hemispheres, particularly the bilateral parietooccipital regions, is seen. PRES can also diffusely involve the brain stem, cerebellum, basal ganglia, and the frontal lobes. Abnormalities on neuroimaging are often symmetric but clinical manifestations can be asymmetric. MRI and CT scans can both be utilized for characterization of PRES.4
There are currently no published guidelines for the management of PRES. Expert opinion suggests removing the underlying cause and aggressively treating the hypertension.5 Furthermore, initiation and duration of antiepileptics remains controversial. After aggressive blood pressure control, resolution of findings on neuroimaging studies are expected anywhere from 8 days to 17 months.
Timely recognition of PRES is critical for prevention of further neurologic compromise. Immediate discontinuation of offending agents, as well as aggressive treatment of blood pressure, is the cornerstone treatment for PRES. In the future, a better understanding of the pathophysiology of PRES can lead to improved diagnostic and management options.
- ,,.Reversible posterior leukoencephalopathy syndrome and bevacizumab.N Engl J Med.2006;354(9):980–982.
- ,,, et al.A reversible posterior leukoencephalopathy syndrome.N Engl J Med.1996;334(8):494–500.
- ,,,,,.Reversible posterior leukoencephalopathy syndrome complicating cytotoxic chemotherapy for hematologic malignancies.Am J Hematol.2004;77(1):72–76.
- ,,, et al.Posterior leukoencephalopathy without severe hypertension: utility of diffusion‐weighted MRI.Neurology.1998;51(5):1369–1376.
- .Posterior leukoencephalopathy syndrome.Postgrad Med J.2001;77(903):24–28.
A 36‐year‐old woman was admitted after new‐onset Hseizures. She had been diagnosed with breast cancer 5 years prior to admission. At that time, she underwent left radical mastectomy and lymph node dissection. Lymph nodes were positive for metastatic disease with negative HER‐2‐Neu and positive estrogen and progesterone receptors. She was treated with docetaxel and tamoxifen but subsequently developed metastatic left hip lesions and was treated with letrozole and anastrozole. Three years later, scans revealed further metastatic disease to the liver, lung, and vertebral column. She was subsequently treated with capecitabine, until further disease progression led to the use of carboplatin and paclitaxel. Seven months prior to admission, her cancer was progressing and she was switched to doxorubicin, gemcitabine, and bevacizumab. Six weeks prior to admission, both positron emission tomography (PET) and computed tomography (CT) scan of her whole body and magnetic resonance imaging (MRI) of the brain illustrated significant improvement. Her last dose of bevacizumab was given 3 weeks prior to her admission.
Two weeks prior to admission, patient reported new‐onset daily headache. These were often localized in the occipital region. She reported some associated nausea and occasional emesis. Subsequently, she developed photophobia and phonophobia. On seeking outpatient treatment for her headache, it was noted that her systolic blood pressure had increased from a baseline of 100 mm Hg to 170 mm Hg. On the day prior to admission, she reported severe headache and several episodes of emesis and later that evening had a witnessed tonic‐clonic seizure.
The patient presented to an outside hospital and had an unremarkable noncontrast CT scan of her brain. An examination of her cerebrospinal fluid revealed negative gram stain, and a normal white blood cell count and protein level. She was treated with lorazepam, phenytoin, and decadron. On becoming more alert, she insisted on going home, where she later developed recurrent headache and presented to our emergency room.
On admission to our service, she was noted to be confused and irritable, and unable to provide any history. Her exam revealed a blood pressure of 143/102 mmHg. No localizing neurologic signs were noted and her laboratory values were normal. After sedation, MRI of the brain was obtained (Figure 1). This revealed diffuse and patchy gyriform hyperintensity of the white matter, most consistent with posterior reversible encephalopathy syndrome (PRES).
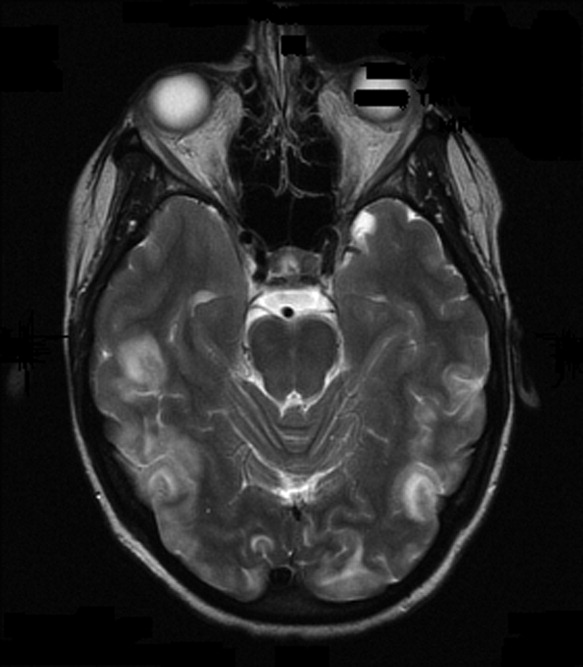
Upon reflection, the patient had new onset hypertension that coincided with the initiation and dosing of bevacizumab. Bevacizumab, an antineoplastic agent, is a recombinant humanized monoclonal antibody that binds to and neutralizes vascular endothelial growth factor, thereby preventing angiogenesis.1 It is known to cause grade 3 hypertension in a minority of patients. Therefore, it was postulated that the patient's persistent blood pressure elevation resulted in vasogenic brain edema, precipitating her seizure. Subsequent to the diagnosis, her blood pressure was aggressively controlled with oral enalapril, metoprolol, triamterene/hydrochlorothiazide, and hydralazine. By hospital day 7, her headache had subsided and her altered mental status had resolved. She had no further episodes of seizures and bevacizumab was discontinued.
PRES has a distinct constellation of clinical symptoms and radiologic findings. The name PRES is a misnomer, as this syndrome is not always reversible, nor is it restricted to the white matter or to the posterior areas of the brain.2 It is hypothesized that a sudden rise in blood pressure leads to elevations in intracranial pressure, which exceeds the brain's autoregulatory mechanisms. This subsequently leads to transudation of fluid into the brain parenchyma. Interestingly, it appears that it is not the absolute level of systolic blood pressure that is critical in the development of PRES, but the rate of change in blood pressure. Hence, patients with chronic hypertension have developed adaptive vascular changes that protect them from this type of parenchymal damage.
PRES has gained increasing recognition due to the use of immunosuppressive and chemotherapeutic medications in organ transplant and oncology patients. Drugs such as cyclosporine, tacrolimus, fludarabine, vincristine, cisplatin, cytarabine, interferon‐alpha, interleukin, antiretroviral therapy, erythropoietin, granulocyte stimulating factor, and intravenous immunoglobulin have all been implicated.3 In addition to increasing blood pressure, these agents likely cause direct toxic injury to the brain, disrupting the blood‐brain barrier and resulting in subsequent edema. Other conditions associated with PRES include renal disease, vasculitis, endocrine disorders, porphyria, cocaine or amphetamine abuse, and stimulant abuse.
Clinically, PRES can present as headache, altered mental status, confusion, drowsiness progressing to stupor, emesis, abnormal visual perceptions, visual neglect, cortical blindness, difficulty with memory and concentration, brisk deep tendon reflexes, weakness, ataxia, and seizure activity. PRES has a characteristic appearance on neuroimaging that differentiates it from other forms of hypertensive encephalopathy. Edema of the white or gray matter in the posterior cerebral hemispheres, particularly the bilateral parietooccipital regions, is seen. PRES can also diffusely involve the brain stem, cerebellum, basal ganglia, and the frontal lobes. Abnormalities on neuroimaging are often symmetric but clinical manifestations can be asymmetric. MRI and CT scans can both be utilized for characterization of PRES.4
There are currently no published guidelines for the management of PRES. Expert opinion suggests removing the underlying cause and aggressively treating the hypertension.5 Furthermore, initiation and duration of antiepileptics remains controversial. After aggressive blood pressure control, resolution of findings on neuroimaging studies are expected anywhere from 8 days to 17 months.
Timely recognition of PRES is critical for prevention of further neurologic compromise. Immediate discontinuation of offending agents, as well as aggressive treatment of blood pressure, is the cornerstone treatment for PRES. In the future, a better understanding of the pathophysiology of PRES can lead to improved diagnostic and management options.
A 36‐year‐old woman was admitted after new‐onset Hseizures. She had been diagnosed with breast cancer 5 years prior to admission. At that time, she underwent left radical mastectomy and lymph node dissection. Lymph nodes were positive for metastatic disease with negative HER‐2‐Neu and positive estrogen and progesterone receptors. She was treated with docetaxel and tamoxifen but subsequently developed metastatic left hip lesions and was treated with letrozole and anastrozole. Three years later, scans revealed further metastatic disease to the liver, lung, and vertebral column. She was subsequently treated with capecitabine, until further disease progression led to the use of carboplatin and paclitaxel. Seven months prior to admission, her cancer was progressing and she was switched to doxorubicin, gemcitabine, and bevacizumab. Six weeks prior to admission, both positron emission tomography (PET) and computed tomography (CT) scan of her whole body and magnetic resonance imaging (MRI) of the brain illustrated significant improvement. Her last dose of bevacizumab was given 3 weeks prior to her admission.
Two weeks prior to admission, patient reported new‐onset daily headache. These were often localized in the occipital region. She reported some associated nausea and occasional emesis. Subsequently, she developed photophobia and phonophobia. On seeking outpatient treatment for her headache, it was noted that her systolic blood pressure had increased from a baseline of 100 mm Hg to 170 mm Hg. On the day prior to admission, she reported severe headache and several episodes of emesis and later that evening had a witnessed tonic‐clonic seizure.
The patient presented to an outside hospital and had an unremarkable noncontrast CT scan of her brain. An examination of her cerebrospinal fluid revealed negative gram stain, and a normal white blood cell count and protein level. She was treated with lorazepam, phenytoin, and decadron. On becoming more alert, she insisted on going home, where she later developed recurrent headache and presented to our emergency room.
On admission to our service, she was noted to be confused and irritable, and unable to provide any history. Her exam revealed a blood pressure of 143/102 mmHg. No localizing neurologic signs were noted and her laboratory values were normal. After sedation, MRI of the brain was obtained (Figure 1). This revealed diffuse and patchy gyriform hyperintensity of the white matter, most consistent with posterior reversible encephalopathy syndrome (PRES).
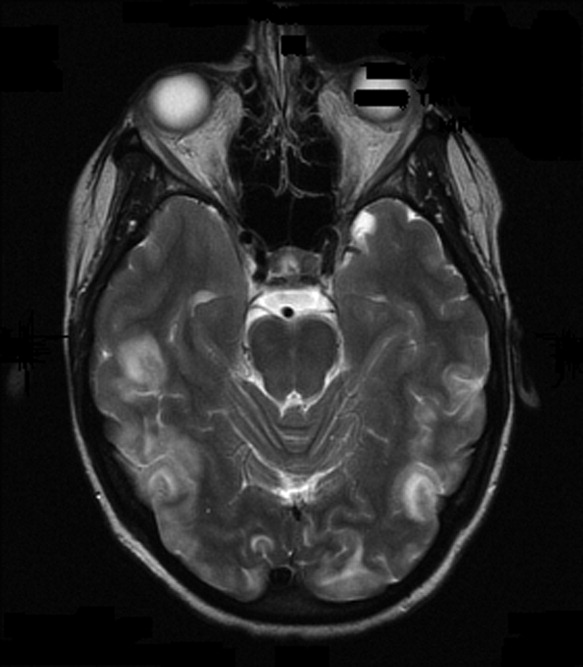
Upon reflection, the patient had new onset hypertension that coincided with the initiation and dosing of bevacizumab. Bevacizumab, an antineoplastic agent, is a recombinant humanized monoclonal antibody that binds to and neutralizes vascular endothelial growth factor, thereby preventing angiogenesis.1 It is known to cause grade 3 hypertension in a minority of patients. Therefore, it was postulated that the patient's persistent blood pressure elevation resulted in vasogenic brain edema, precipitating her seizure. Subsequent to the diagnosis, her blood pressure was aggressively controlled with oral enalapril, metoprolol, triamterene/hydrochlorothiazide, and hydralazine. By hospital day 7, her headache had subsided and her altered mental status had resolved. She had no further episodes of seizures and bevacizumab was discontinued.
PRES has a distinct constellation of clinical symptoms and radiologic findings. The name PRES is a misnomer, as this syndrome is not always reversible, nor is it restricted to the white matter or to the posterior areas of the brain.2 It is hypothesized that a sudden rise in blood pressure leads to elevations in intracranial pressure, which exceeds the brain's autoregulatory mechanisms. This subsequently leads to transudation of fluid into the brain parenchyma. Interestingly, it appears that it is not the absolute level of systolic blood pressure that is critical in the development of PRES, but the rate of change in blood pressure. Hence, patients with chronic hypertension have developed adaptive vascular changes that protect them from this type of parenchymal damage.
PRES has gained increasing recognition due to the use of immunosuppressive and chemotherapeutic medications in organ transplant and oncology patients. Drugs such as cyclosporine, tacrolimus, fludarabine, vincristine, cisplatin, cytarabine, interferon‐alpha, interleukin, antiretroviral therapy, erythropoietin, granulocyte stimulating factor, and intravenous immunoglobulin have all been implicated.3 In addition to increasing blood pressure, these agents likely cause direct toxic injury to the brain, disrupting the blood‐brain barrier and resulting in subsequent edema. Other conditions associated with PRES include renal disease, vasculitis, endocrine disorders, porphyria, cocaine or amphetamine abuse, and stimulant abuse.
Clinically, PRES can present as headache, altered mental status, confusion, drowsiness progressing to stupor, emesis, abnormal visual perceptions, visual neglect, cortical blindness, difficulty with memory and concentration, brisk deep tendon reflexes, weakness, ataxia, and seizure activity. PRES has a characteristic appearance on neuroimaging that differentiates it from other forms of hypertensive encephalopathy. Edema of the white or gray matter in the posterior cerebral hemispheres, particularly the bilateral parietooccipital regions, is seen. PRES can also diffusely involve the brain stem, cerebellum, basal ganglia, and the frontal lobes. Abnormalities on neuroimaging are often symmetric but clinical manifestations can be asymmetric. MRI and CT scans can both be utilized for characterization of PRES.4
There are currently no published guidelines for the management of PRES. Expert opinion suggests removing the underlying cause and aggressively treating the hypertension.5 Furthermore, initiation and duration of antiepileptics remains controversial. After aggressive blood pressure control, resolution of findings on neuroimaging studies are expected anywhere from 8 days to 17 months.
Timely recognition of PRES is critical for prevention of further neurologic compromise. Immediate discontinuation of offending agents, as well as aggressive treatment of blood pressure, is the cornerstone treatment for PRES. In the future, a better understanding of the pathophysiology of PRES can lead to improved diagnostic and management options.
- ,,.Reversible posterior leukoencephalopathy syndrome and bevacizumab.N Engl J Med.2006;354(9):980–982.
- ,,, et al.A reversible posterior leukoencephalopathy syndrome.N Engl J Med.1996;334(8):494–500.
- ,,,,,.Reversible posterior leukoencephalopathy syndrome complicating cytotoxic chemotherapy for hematologic malignancies.Am J Hematol.2004;77(1):72–76.
- ,,, et al.Posterior leukoencephalopathy without severe hypertension: utility of diffusion‐weighted MRI.Neurology.1998;51(5):1369–1376.
- .Posterior leukoencephalopathy syndrome.Postgrad Med J.2001;77(903):24–28.
- ,,.Reversible posterior leukoencephalopathy syndrome and bevacizumab.N Engl J Med.2006;354(9):980–982.
- ,,, et al.A reversible posterior leukoencephalopathy syndrome.N Engl J Med.1996;334(8):494–500.
- ,,,,,.Reversible posterior leukoencephalopathy syndrome complicating cytotoxic chemotherapy for hematologic malignancies.Am J Hematol.2004;77(1):72–76.
- ,,, et al.Posterior leukoencephalopathy without severe hypertension: utility of diffusion‐weighted MRI.Neurology.1998;51(5):1369–1376.
- .Posterior leukoencephalopathy syndrome.Postgrad Med J.2001;77(903):24–28.
Pemetrexed
Dr. Chandra P. Belani reports that maintenance therapy with pemetrexed significantly improves overall survival in advanced non-small cell lung cancer. Damian McNamara of the Global Medical News Network (GMNN) reports from the annual meeting of the American Society of Clinical Oncology in Orlando.
Dr. Chandra P. Belani reports that maintenance therapy with pemetrexed significantly improves overall survival in advanced non-small cell lung cancer. Damian McNamara of the Global Medical News Network (GMNN) reports from the annual meeting of the American Society of Clinical Oncology in Orlando.
Dr. Chandra P. Belani reports that maintenance therapy with pemetrexed significantly improves overall survival in advanced non-small cell lung cancer. Damian McNamara of the Global Medical News Network (GMNN) reports from the annual meeting of the American Society of Clinical Oncology in Orlando.
Elderly Patients & Pneumonia, Metoprolol after Vascular Surgery, and More
Elderly Pneumonia Patients after Antibiotic Switch
Nathan RV, Rhew DC, Bratzler DW, et al. In-hospital observation after antibiotic switch in pneumonia: a national evaluation. Am J Med. 2006 Jun;119(6):512.e1-7.
Community-acquired pneumonia (CAP) continues to be a common reason for hospital admission—especially among the elderly. As with many infectious diseases, the duration and route of antibiotic therapy is often based on expert recommendations rather than prospective randomized trials. The Patient Outcome Research Team (PORT) trials address the decision to admit a patient, but not other aspects of care. For hospitalists, the decision of when to discharge any patient with reasonable safety is often fraught with uncertainty. This study addresses the necessity of observing a patient for one day following the switch from IV to oral therapy. Two previous smaller retrospective studies have suggested this was unnecessary.
The current study is also retrospective but involves a large database derived from the U.S. Medicare National Pneumonia Project database. Ultimately 5,248 patients over 65 (mean age=80) were selected for analysis; 2,536 were not observed; and 2,712 were observed for one day.) Patients were excluded if their length of stay was greater than seven days or less than two days, suggesting complicated cases in the former instance and mild illness in the latter (i.e., perhaps not even requiring admission). Immunosupressed patients were also excluded. There was no significant difference in the observed 30-day mortality (5.1% in the “not observed” versus 4.4% in the “observed” cohort, respectively).
The obvious limitation of this study is that it was retrospective/observational and thus potentially subject to the bias inherent in this study design. It is possible that the sicker patients were logically watched longer. Propensity analysis was not a component of this study. The authors do present reasons why certain structural weaknesses would have favored the “observed “group.
Certainly there may be other reasons to observe a patient after the switch to oral therapy. A patient with associated gastrointestinal disturbance or a questionable history of GI or other intolerance to a class of antibiotics is an obvious example. Nevertheless, this study should convey a certain confidence to hospitalists when they assess the suitability for discharge for the type of patient covered in this analysis. Interestingly the recently published guidelines for treatment of community acquired pneumonia are concordant with this study.1
Reference
- Mandell L, Wundrelink A, Bartlett J. Guideline for the treatment of community acquired pneumonia. Clin Infect Dis. 2007;44: S27-72.
The Revised Geneva Score for PE
Le Gal G, Righini M, Roy PM, et al. Prediction of pulmonary embolism in the emergency department. Ann Intern Med. 2006 Feb 7:144(3):165-171. Comment in: ACP J Club. 2006 Jul-Aug;145(1):25 & Ann Intern Med. 2006 Feb 7;144(3):210-212.
Pulmonary embolism is a diagnosis frequently considered by the hospitalist—both as an explanation for the admitting clinical picture, as well as a complication arising during the course of a hospitalization for another condition.
My institutions’ ability to identify patients with this potentially lethal condition has greatly improved with the advent of multidetector CT angiography and various diagnostic schemata that include d-dimer testing and estimations of pre-test probability. It is a classic consideration whenever there is a onset of pleurisy, dyspnea, or aggravation thereof. Nevertheless multiple other situations arise in the hospital setting, such as unexplained tachycardia, hemoptysis, or vaguely possible but not clear-cut pleuritic chest pain, in which one feels obligated to at least consider the diagnosis. Further, to have to incorporate d-dimer testing into the diagnostic strategy is problematic as up to 80% of hospitalized patients are likely to be positive. Hospitalists need a reasonable strategy to avoid going down that proverbial pathway in certain low risk situations.
The Geneva scoring system and the Wells system are two methodologies that have been used in lieu of or as an adjunct to “clinical judgment.” The former requires arterial blood gases and the latter has as criteria “other diagnosis more likely than pulmonary embolus” that can be problematic and difficult to standardize.
This article presents a revised Geneva scoring system based solely on elements of the history and physical examination. The elements were derived retrospectively from a prior different study on diagnostic strategies for pulmonary thromboembolism (PTE). A different prospective study on PTE was utilized for the validation arm of this study. By logistical regression analysis the following eight elements were incorporated into the revised Geneva score: Age greater than 65 (1 point), previous deep venous thrombosis or pulmonary embolism (3 points), surgery or fracture within one month (2 points), active malignant condition (2 points), unilateral lower limb pain (3 points), hemoptysis (2 points), heart rate 75 to 94 beats/min (3 points) or heart rate 95 beats /minute or more (5 points), and pain on lower limb palpation and unilateral edema (4 points). The prevalence for pulmonary embolism was as follows: low probability or 8% (0 to 3 points), intermediate probability or 28% (4 to 10 points), and high probability or 74% (equal or greater than 11 points).
Significance for hospitalists: This scoring system is not validated a management system per se. However in the imperfect world of clinical reasoning it can help reinforce a thoughtful decision not to embark on the diagnostic path for pulmonary embolism, with its own inherent risks.
Metoprolol after Vascular Surgery
Yang H, Raymer K, Butler R, et al. The effects of perioperative beta-blockade: results of metoprolol after vascular surgery (MaVS) study, a randomized controlled trial. Am Heart J. 2006 Nov;152(5):983-990. Comment in Am Heart J. 2006 Nov;152(5):815-818. McCullough PA. Failure of beta-blockers in the reduction of perioperative events: where did we go wrong? Am Heart J. 2006 Nov;152(5):815-818. Comment in: Am Heart J. 2006 Nov;152(5):983-990.
Hospitalists are frequently consulted regarding perioperative risk assessment and reduction for patients undergoing non-cardiac surgery. Over the last decade and supported by a few studies, the perioperative use of beta-blocker therapy has resolved the uncertainty frequently encountered. The McFalls study in 2004 showed no benefit to routine coronary revascularization for patients undergoing vascular surgery deemed at risk for myocardial ischemia.1 This provided further confidence for those of us supplying these preoperative assessments. However, the Lindenauer study in 2005 (a retrospective cohort analysis) was the first indication that perioperative beta blockade could be harmful.2 Lower-risk patients based on the revised cardiovascular index (RCRI) score actually did worse when treated. Still the ACC guidelines published in 2006 suggested perioperative beta blockers be considered for lower risk patients undergoing vascular surgery.3
This study is a randomized placebo-controlled trial of perioperative beta-blocker therapy in 500 treatment-naïve patients undergoing vascular surgery. Metoprolol was started two hours before surgery and continued for one week. Cardiovascular endpoints included cardiac death, arrhythmia requiring treatment, acute myocardial infarction or acute coronary syndrome, and congestive heart failure. No benefit was found for treatment with metoprolol regardless of the number of Revised Cardiac Risk Index (RCRI) factors present. No excess adverse outcomes were noted for therapy although intraoperative bradycardia and hypotension were significantly increased in the active treatment group.
In the accompanying editorial McCullough discusses possible reasons and implications of these findings. In fact, two other trials have reported similar findings. In contrast to the older trials suggesting a benefit to perioperative beta blockade these newer trials are larger and have a stronger design. He also notes that the patients in the more recent trials are more likely to have prior revascularization and hence are less prone to demand-type events, reflective of the type of insult beta blockade would most likely be helpful in preventing. These events may be more closely allied with plaque destabilization of subcritical lesions, with factors such as perioperative hypercoagulability and perhaps inflammation being more important. In this regard it is notable that recent trials on the perioperative use of statins have demonstrated favorable results, with these agents presumably acting to promote plaque stability, the so-called “pleiotropic” function of statins.
Significance for hospitalists: It is reasonable to be more circumspect in the recommendation of perioperative beta blockade. This practice is not likely the magic bullet, which is a common misconcpetion. An indicative situation is an 80-year-old patient undergoing total hip replacement. He has diabetes, COPD, and hypertension, a pulse of 65, a blood pressure of 110/50. There may also be concerns about bradycardia, hypotension, and bronchospasm. Given this analysis a clinician can be confident in withholding perioperative treatment.
The use of beta-blocker therapy in a patient with a single RCRI factor, which is not coronary artery disease, does not seem justified. On the other hand the use of perioperative statins should be more actively entertained. Emerging recommendations from various specialty organizations and other relevant professional entities should be anticipated and sought.
Bibliography
- McFalls EO, Ward HB, Moritz TE, et al. Coronary-artery revascularization before elective major vascular surgery. N Eng J Med. 2004Dec 30;351(27):2795-2804.
- Lindenauer PK, Pekow P, Wang K, et al. Perioperative beta-blocker therapy and mortality after major noncardiac surgery. N Eng J Med. 2005 Jul 28;353(4):349-361.
- Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2006 guideline update on perioperative cardiovascular evaluation for noncardiac surgery. J Am Coll Cardiol. 2006;47: 2343-2355
The New C. Diff Epidemic
Bartlett JG. Narrative review: the new epidemic of Clostridium difficile-associated enteric disease. Ann Intern Med. 2006 Nov 21;145(10):758-764.
C. difficile infection is emerging as one of the most important illnesses for hospitalists to be facile with. It not only occurs frequently, but is also often severe or life threatening, and most importantly iatrogenic and preventable. This review by Bartlett, who elucidated the cause of this disease in 1978, reviews important up-to-date information on C. difficile, focusing on the recent emergence of a more virulent form of the disease.
Infectious diarrhea that develops in the hospital is almost always due to C. difficile. The tissue culture cytotoxic assay (first described in 1978) remains the most sensitive and specific diagnostic tool. The toxin immunoassay used most routinely is only 75% sensitive.
An epidemic of unusually severe C. difficile was first described in Quebec in 2001. Important features include a higher tendency for toxic megacolon and a need for colectomy, protein-losing enteropathy, leukemoid reactions, refractoriness to treatment, a high rate of relapse and an astonishing 16.5% attributable mortality. Fluoroquinolones are the leading associated antibiotic causal factor, although extended spectrum cephalosporins remain important as well in this regard. The new strain is characterized by high levels of toxin production due to the deletion of a toxin production regulatory gene. The strain is also fluoroquinolone resistant, explaining the role of that antibiotic in its genesis.
Treatment of C. difficile colitis (especially the emergent strain) remains problematic. In particular the role of metronidazole versus vancomycin as initial therapy is often contentious. Bartlett cites some evidence suggesting vancomycin may be more effective and is especially recommended for severe disease, characteristics of which are often manifested by this new strain.
This review cites important considerations that hospitalist ought to vigilant and proactive in. Given the high risk of fluoroquinolone treatment we must be sure that these drugs are used appropriately. Nonchalantly stacking on levofloxacin therapy for the COPD flair without evidence for pneumonia should be discouraged. When possible antibiotics with a lower risk for C. difficile (sulfonamides, macrolides, tetracyclines) should be used for any infection. When disease is suspected, a negative toxin immunoassay should not discourage empiric treatment especially in a very ill patient. Isolation and barrier precautions are important in preventing the spread of this potentially lethal infection. C. difficile spores are not killed by alcohol-based detergents, and either soap and water or gloves are necessary to care for these patients. When your hospital experiences a clustering of severe C. difficile infection, alert appropriate infection control personnel. Administrative control of antibiotic use may be indicated.
Baclofen Versus Diazepam to Treat Alcohol Withdrawal
Addolorato G, Leggio L, Abenavoli L, et al. Baclofen in the treatment of alcohol withdrawal syndrome: a comparative study vs diazepam. Am J Med. 2006 Mar;119 (3):276.e13-18.
Alcohol withdrawal syndrome (AWS) is a frequent problem encountered in hospitalized patients; its management is considered one of SHM’s core competencies for hospitalists. Benzodiazepines are the gold standard of therapy for this problem given their established record for safety and efficacy; however, their use can be problematic in certain instances.
This study involved 37 outpatients, as inpatients may often be sicker and at higher risk of severe withdrawal.
There is a definite risk of oversedation—especially in patients with COPD or chronic liver disease. Some patients require inordinately high doses of benzodiazepines, thus setting the stage for a prolonged hospitalization. Occasional paradoxical or disinhibition reactions to benzodiazepines can also be problematic. Addiction and or diversion are also a concern in patients prone to substance abuse. An otherwise stable patient, ready for discharge, may still be on a relatively high dose of lorazepam, but it is generally not prudent to send the patient out with a supply of medication to finish the course given concerns over resumption of drinking while on the sedative. Conversely, the solution can be cold comfort for the attending physician if the patient resumes drinking, thus eliminating the need for additional medication.
Baclofen, a stereoselective gamma-aminobutyric acid agonist, has a long history of safety in the treatment of spasticity. As such it can counter balance the activation of the glutamate excitatory pathway that characterizes AWS. It has been proposed as an alternative treatment for AWS that would not share the above concerns cited for benzodiazepines.
This study is a randomized controlled trial of baclofen versus valium in the treatment for AWS. Thirty-seven subjects with a history of heavy alcohol use were randomized to either baclofen 30 mg per day or valium 0.5 to 0.75 mg/kg. All were outpatients treated for 10 days. Clinical Institute Withdrawal Assessment-Alcohol (CIWA) scores were assessed daily. Both regimens continuously decreased the baseline elevation of CIWA scores daily over the course of the study, without a significant difference in treatment efficacy. No adverse events or side effects were reported in either group.
Other than baseline CIWA and daily alcohol consumption, it is not clear that the two groups were at equal risk for severe withdrawal reactions. Relevant baseline characteristics such as history of seizures or delirium tremens, factors that raise this risk were not noted.
Significance for hospitalists: With a long history of safety and efficacy, benzodiazepines remain the drugs of choice for hospitalists treating patients with AWS. In certain instances it may be desirable to limit or even avoid their use. How effective and safe baclofen would be in filling this role remains to be fully established. In particular the relative risk for sedation and respiratory depression has not been defined. Nevertheless at least in my institutions, as guided by expert consultation, its use has been carefully considered and proven helpful in some of the situations noted above. TH
Elderly Pneumonia Patients after Antibiotic Switch
Nathan RV, Rhew DC, Bratzler DW, et al. In-hospital observation after antibiotic switch in pneumonia: a national evaluation. Am J Med. 2006 Jun;119(6):512.e1-7.
Community-acquired pneumonia (CAP) continues to be a common reason for hospital admission—especially among the elderly. As with many infectious diseases, the duration and route of antibiotic therapy is often based on expert recommendations rather than prospective randomized trials. The Patient Outcome Research Team (PORT) trials address the decision to admit a patient, but not other aspects of care. For hospitalists, the decision of when to discharge any patient with reasonable safety is often fraught with uncertainty. This study addresses the necessity of observing a patient for one day following the switch from IV to oral therapy. Two previous smaller retrospective studies have suggested this was unnecessary.
The current study is also retrospective but involves a large database derived from the U.S. Medicare National Pneumonia Project database. Ultimately 5,248 patients over 65 (mean age=80) were selected for analysis; 2,536 were not observed; and 2,712 were observed for one day.) Patients were excluded if their length of stay was greater than seven days or less than two days, suggesting complicated cases in the former instance and mild illness in the latter (i.e., perhaps not even requiring admission). Immunosupressed patients were also excluded. There was no significant difference in the observed 30-day mortality (5.1% in the “not observed” versus 4.4% in the “observed” cohort, respectively).
The obvious limitation of this study is that it was retrospective/observational and thus potentially subject to the bias inherent in this study design. It is possible that the sicker patients were logically watched longer. Propensity analysis was not a component of this study. The authors do present reasons why certain structural weaknesses would have favored the “observed “group.
Certainly there may be other reasons to observe a patient after the switch to oral therapy. A patient with associated gastrointestinal disturbance or a questionable history of GI or other intolerance to a class of antibiotics is an obvious example. Nevertheless, this study should convey a certain confidence to hospitalists when they assess the suitability for discharge for the type of patient covered in this analysis. Interestingly the recently published guidelines for treatment of community acquired pneumonia are concordant with this study.1
Reference
- Mandell L, Wundrelink A, Bartlett J. Guideline for the treatment of community acquired pneumonia. Clin Infect Dis. 2007;44: S27-72.
The Revised Geneva Score for PE
Le Gal G, Righini M, Roy PM, et al. Prediction of pulmonary embolism in the emergency department. Ann Intern Med. 2006 Feb 7:144(3):165-171. Comment in: ACP J Club. 2006 Jul-Aug;145(1):25 & Ann Intern Med. 2006 Feb 7;144(3):210-212.
Pulmonary embolism is a diagnosis frequently considered by the hospitalist—both as an explanation for the admitting clinical picture, as well as a complication arising during the course of a hospitalization for another condition.
My institutions’ ability to identify patients with this potentially lethal condition has greatly improved with the advent of multidetector CT angiography and various diagnostic schemata that include d-dimer testing and estimations of pre-test probability. It is a classic consideration whenever there is a onset of pleurisy, dyspnea, or aggravation thereof. Nevertheless multiple other situations arise in the hospital setting, such as unexplained tachycardia, hemoptysis, or vaguely possible but not clear-cut pleuritic chest pain, in which one feels obligated to at least consider the diagnosis. Further, to have to incorporate d-dimer testing into the diagnostic strategy is problematic as up to 80% of hospitalized patients are likely to be positive. Hospitalists need a reasonable strategy to avoid going down that proverbial pathway in certain low risk situations.
The Geneva scoring system and the Wells system are two methodologies that have been used in lieu of or as an adjunct to “clinical judgment.” The former requires arterial blood gases and the latter has as criteria “other diagnosis more likely than pulmonary embolus” that can be problematic and difficult to standardize.
This article presents a revised Geneva scoring system based solely on elements of the history and physical examination. The elements were derived retrospectively from a prior different study on diagnostic strategies for pulmonary thromboembolism (PTE). A different prospective study on PTE was utilized for the validation arm of this study. By logistical regression analysis the following eight elements were incorporated into the revised Geneva score: Age greater than 65 (1 point), previous deep venous thrombosis or pulmonary embolism (3 points), surgery or fracture within one month (2 points), active malignant condition (2 points), unilateral lower limb pain (3 points), hemoptysis (2 points), heart rate 75 to 94 beats/min (3 points) or heart rate 95 beats /minute or more (5 points), and pain on lower limb palpation and unilateral edema (4 points). The prevalence for pulmonary embolism was as follows: low probability or 8% (0 to 3 points), intermediate probability or 28% (4 to 10 points), and high probability or 74% (equal or greater than 11 points).
Significance for hospitalists: This scoring system is not validated a management system per se. However in the imperfect world of clinical reasoning it can help reinforce a thoughtful decision not to embark on the diagnostic path for pulmonary embolism, with its own inherent risks.
Metoprolol after Vascular Surgery
Yang H, Raymer K, Butler R, et al. The effects of perioperative beta-blockade: results of metoprolol after vascular surgery (MaVS) study, a randomized controlled trial. Am Heart J. 2006 Nov;152(5):983-990. Comment in Am Heart J. 2006 Nov;152(5):815-818. McCullough PA. Failure of beta-blockers in the reduction of perioperative events: where did we go wrong? Am Heart J. 2006 Nov;152(5):815-818. Comment in: Am Heart J. 2006 Nov;152(5):983-990.
Hospitalists are frequently consulted regarding perioperative risk assessment and reduction for patients undergoing non-cardiac surgery. Over the last decade and supported by a few studies, the perioperative use of beta-blocker therapy has resolved the uncertainty frequently encountered. The McFalls study in 2004 showed no benefit to routine coronary revascularization for patients undergoing vascular surgery deemed at risk for myocardial ischemia.1 This provided further confidence for those of us supplying these preoperative assessments. However, the Lindenauer study in 2005 (a retrospective cohort analysis) was the first indication that perioperative beta blockade could be harmful.2 Lower-risk patients based on the revised cardiovascular index (RCRI) score actually did worse when treated. Still the ACC guidelines published in 2006 suggested perioperative beta blockers be considered for lower risk patients undergoing vascular surgery.3
This study is a randomized placebo-controlled trial of perioperative beta-blocker therapy in 500 treatment-naïve patients undergoing vascular surgery. Metoprolol was started two hours before surgery and continued for one week. Cardiovascular endpoints included cardiac death, arrhythmia requiring treatment, acute myocardial infarction or acute coronary syndrome, and congestive heart failure. No benefit was found for treatment with metoprolol regardless of the number of Revised Cardiac Risk Index (RCRI) factors present. No excess adverse outcomes were noted for therapy although intraoperative bradycardia and hypotension were significantly increased in the active treatment group.
In the accompanying editorial McCullough discusses possible reasons and implications of these findings. In fact, two other trials have reported similar findings. In contrast to the older trials suggesting a benefit to perioperative beta blockade these newer trials are larger and have a stronger design. He also notes that the patients in the more recent trials are more likely to have prior revascularization and hence are less prone to demand-type events, reflective of the type of insult beta blockade would most likely be helpful in preventing. These events may be more closely allied with plaque destabilization of subcritical lesions, with factors such as perioperative hypercoagulability and perhaps inflammation being more important. In this regard it is notable that recent trials on the perioperative use of statins have demonstrated favorable results, with these agents presumably acting to promote plaque stability, the so-called “pleiotropic” function of statins.
Significance for hospitalists: It is reasonable to be more circumspect in the recommendation of perioperative beta blockade. This practice is not likely the magic bullet, which is a common misconcpetion. An indicative situation is an 80-year-old patient undergoing total hip replacement. He has diabetes, COPD, and hypertension, a pulse of 65, a blood pressure of 110/50. There may also be concerns about bradycardia, hypotension, and bronchospasm. Given this analysis a clinician can be confident in withholding perioperative treatment.
The use of beta-blocker therapy in a patient with a single RCRI factor, which is not coronary artery disease, does not seem justified. On the other hand the use of perioperative statins should be more actively entertained. Emerging recommendations from various specialty organizations and other relevant professional entities should be anticipated and sought.
Bibliography
- McFalls EO, Ward HB, Moritz TE, et al. Coronary-artery revascularization before elective major vascular surgery. N Eng J Med. 2004Dec 30;351(27):2795-2804.
- Lindenauer PK, Pekow P, Wang K, et al. Perioperative beta-blocker therapy and mortality after major noncardiac surgery. N Eng J Med. 2005 Jul 28;353(4):349-361.
- Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2006 guideline update on perioperative cardiovascular evaluation for noncardiac surgery. J Am Coll Cardiol. 2006;47: 2343-2355
The New C. Diff Epidemic
Bartlett JG. Narrative review: the new epidemic of Clostridium difficile-associated enteric disease. Ann Intern Med. 2006 Nov 21;145(10):758-764.
C. difficile infection is emerging as one of the most important illnesses for hospitalists to be facile with. It not only occurs frequently, but is also often severe or life threatening, and most importantly iatrogenic and preventable. This review by Bartlett, who elucidated the cause of this disease in 1978, reviews important up-to-date information on C. difficile, focusing on the recent emergence of a more virulent form of the disease.
Infectious diarrhea that develops in the hospital is almost always due to C. difficile. The tissue culture cytotoxic assay (first described in 1978) remains the most sensitive and specific diagnostic tool. The toxin immunoassay used most routinely is only 75% sensitive.
An epidemic of unusually severe C. difficile was first described in Quebec in 2001. Important features include a higher tendency for toxic megacolon and a need for colectomy, protein-losing enteropathy, leukemoid reactions, refractoriness to treatment, a high rate of relapse and an astonishing 16.5% attributable mortality. Fluoroquinolones are the leading associated antibiotic causal factor, although extended spectrum cephalosporins remain important as well in this regard. The new strain is characterized by high levels of toxin production due to the deletion of a toxin production regulatory gene. The strain is also fluoroquinolone resistant, explaining the role of that antibiotic in its genesis.
Treatment of C. difficile colitis (especially the emergent strain) remains problematic. In particular the role of metronidazole versus vancomycin as initial therapy is often contentious. Bartlett cites some evidence suggesting vancomycin may be more effective and is especially recommended for severe disease, characteristics of which are often manifested by this new strain.
This review cites important considerations that hospitalist ought to vigilant and proactive in. Given the high risk of fluoroquinolone treatment we must be sure that these drugs are used appropriately. Nonchalantly stacking on levofloxacin therapy for the COPD flair without evidence for pneumonia should be discouraged. When possible antibiotics with a lower risk for C. difficile (sulfonamides, macrolides, tetracyclines) should be used for any infection. When disease is suspected, a negative toxin immunoassay should not discourage empiric treatment especially in a very ill patient. Isolation and barrier precautions are important in preventing the spread of this potentially lethal infection. C. difficile spores are not killed by alcohol-based detergents, and either soap and water or gloves are necessary to care for these patients. When your hospital experiences a clustering of severe C. difficile infection, alert appropriate infection control personnel. Administrative control of antibiotic use may be indicated.
Baclofen Versus Diazepam to Treat Alcohol Withdrawal
Addolorato G, Leggio L, Abenavoli L, et al. Baclofen in the treatment of alcohol withdrawal syndrome: a comparative study vs diazepam. Am J Med. 2006 Mar;119 (3):276.e13-18.
Alcohol withdrawal syndrome (AWS) is a frequent problem encountered in hospitalized patients; its management is considered one of SHM’s core competencies for hospitalists. Benzodiazepines are the gold standard of therapy for this problem given their established record for safety and efficacy; however, their use can be problematic in certain instances.
This study involved 37 outpatients, as inpatients may often be sicker and at higher risk of severe withdrawal.
There is a definite risk of oversedation—especially in patients with COPD or chronic liver disease. Some patients require inordinately high doses of benzodiazepines, thus setting the stage for a prolonged hospitalization. Occasional paradoxical or disinhibition reactions to benzodiazepines can also be problematic. Addiction and or diversion are also a concern in patients prone to substance abuse. An otherwise stable patient, ready for discharge, may still be on a relatively high dose of lorazepam, but it is generally not prudent to send the patient out with a supply of medication to finish the course given concerns over resumption of drinking while on the sedative. Conversely, the solution can be cold comfort for the attending physician if the patient resumes drinking, thus eliminating the need for additional medication.
Baclofen, a stereoselective gamma-aminobutyric acid agonist, has a long history of safety in the treatment of spasticity. As such it can counter balance the activation of the glutamate excitatory pathway that characterizes AWS. It has been proposed as an alternative treatment for AWS that would not share the above concerns cited for benzodiazepines.
This study is a randomized controlled trial of baclofen versus valium in the treatment for AWS. Thirty-seven subjects with a history of heavy alcohol use were randomized to either baclofen 30 mg per day or valium 0.5 to 0.75 mg/kg. All were outpatients treated for 10 days. Clinical Institute Withdrawal Assessment-Alcohol (CIWA) scores were assessed daily. Both regimens continuously decreased the baseline elevation of CIWA scores daily over the course of the study, without a significant difference in treatment efficacy. No adverse events or side effects were reported in either group.
Other than baseline CIWA and daily alcohol consumption, it is not clear that the two groups were at equal risk for severe withdrawal reactions. Relevant baseline characteristics such as history of seizures or delirium tremens, factors that raise this risk were not noted.
Significance for hospitalists: With a long history of safety and efficacy, benzodiazepines remain the drugs of choice for hospitalists treating patients with AWS. In certain instances it may be desirable to limit or even avoid their use. How effective and safe baclofen would be in filling this role remains to be fully established. In particular the relative risk for sedation and respiratory depression has not been defined. Nevertheless at least in my institutions, as guided by expert consultation, its use has been carefully considered and proven helpful in some of the situations noted above. TH
Elderly Pneumonia Patients after Antibiotic Switch
Nathan RV, Rhew DC, Bratzler DW, et al. In-hospital observation after antibiotic switch in pneumonia: a national evaluation. Am J Med. 2006 Jun;119(6):512.e1-7.
Community-acquired pneumonia (CAP) continues to be a common reason for hospital admission—especially among the elderly. As with many infectious diseases, the duration and route of antibiotic therapy is often based on expert recommendations rather than prospective randomized trials. The Patient Outcome Research Team (PORT) trials address the decision to admit a patient, but not other aspects of care. For hospitalists, the decision of when to discharge any patient with reasonable safety is often fraught with uncertainty. This study addresses the necessity of observing a patient for one day following the switch from IV to oral therapy. Two previous smaller retrospective studies have suggested this was unnecessary.
The current study is also retrospective but involves a large database derived from the U.S. Medicare National Pneumonia Project database. Ultimately 5,248 patients over 65 (mean age=80) were selected for analysis; 2,536 were not observed; and 2,712 were observed for one day.) Patients were excluded if their length of stay was greater than seven days or less than two days, suggesting complicated cases in the former instance and mild illness in the latter (i.e., perhaps not even requiring admission). Immunosupressed patients were also excluded. There was no significant difference in the observed 30-day mortality (5.1% in the “not observed” versus 4.4% in the “observed” cohort, respectively).
The obvious limitation of this study is that it was retrospective/observational and thus potentially subject to the bias inherent in this study design. It is possible that the sicker patients were logically watched longer. Propensity analysis was not a component of this study. The authors do present reasons why certain structural weaknesses would have favored the “observed “group.
Certainly there may be other reasons to observe a patient after the switch to oral therapy. A patient with associated gastrointestinal disturbance or a questionable history of GI or other intolerance to a class of antibiotics is an obvious example. Nevertheless, this study should convey a certain confidence to hospitalists when they assess the suitability for discharge for the type of patient covered in this analysis. Interestingly the recently published guidelines for treatment of community acquired pneumonia are concordant with this study.1
Reference
- Mandell L, Wundrelink A, Bartlett J. Guideline for the treatment of community acquired pneumonia. Clin Infect Dis. 2007;44: S27-72.
The Revised Geneva Score for PE
Le Gal G, Righini M, Roy PM, et al. Prediction of pulmonary embolism in the emergency department. Ann Intern Med. 2006 Feb 7:144(3):165-171. Comment in: ACP J Club. 2006 Jul-Aug;145(1):25 & Ann Intern Med. 2006 Feb 7;144(3):210-212.
Pulmonary embolism is a diagnosis frequently considered by the hospitalist—both as an explanation for the admitting clinical picture, as well as a complication arising during the course of a hospitalization for another condition.
My institutions’ ability to identify patients with this potentially lethal condition has greatly improved with the advent of multidetector CT angiography and various diagnostic schemata that include d-dimer testing and estimations of pre-test probability. It is a classic consideration whenever there is a onset of pleurisy, dyspnea, or aggravation thereof. Nevertheless multiple other situations arise in the hospital setting, such as unexplained tachycardia, hemoptysis, or vaguely possible but not clear-cut pleuritic chest pain, in which one feels obligated to at least consider the diagnosis. Further, to have to incorporate d-dimer testing into the diagnostic strategy is problematic as up to 80% of hospitalized patients are likely to be positive. Hospitalists need a reasonable strategy to avoid going down that proverbial pathway in certain low risk situations.
The Geneva scoring system and the Wells system are two methodologies that have been used in lieu of or as an adjunct to “clinical judgment.” The former requires arterial blood gases and the latter has as criteria “other diagnosis more likely than pulmonary embolus” that can be problematic and difficult to standardize.
This article presents a revised Geneva scoring system based solely on elements of the history and physical examination. The elements were derived retrospectively from a prior different study on diagnostic strategies for pulmonary thromboembolism (PTE). A different prospective study on PTE was utilized for the validation arm of this study. By logistical regression analysis the following eight elements were incorporated into the revised Geneva score: Age greater than 65 (1 point), previous deep venous thrombosis or pulmonary embolism (3 points), surgery or fracture within one month (2 points), active malignant condition (2 points), unilateral lower limb pain (3 points), hemoptysis (2 points), heart rate 75 to 94 beats/min (3 points) or heart rate 95 beats /minute or more (5 points), and pain on lower limb palpation and unilateral edema (4 points). The prevalence for pulmonary embolism was as follows: low probability or 8% (0 to 3 points), intermediate probability or 28% (4 to 10 points), and high probability or 74% (equal or greater than 11 points).
Significance for hospitalists: This scoring system is not validated a management system per se. However in the imperfect world of clinical reasoning it can help reinforce a thoughtful decision not to embark on the diagnostic path for pulmonary embolism, with its own inherent risks.
Metoprolol after Vascular Surgery
Yang H, Raymer K, Butler R, et al. The effects of perioperative beta-blockade: results of metoprolol after vascular surgery (MaVS) study, a randomized controlled trial. Am Heart J. 2006 Nov;152(5):983-990. Comment in Am Heart J. 2006 Nov;152(5):815-818. McCullough PA. Failure of beta-blockers in the reduction of perioperative events: where did we go wrong? Am Heart J. 2006 Nov;152(5):815-818. Comment in: Am Heart J. 2006 Nov;152(5):983-990.
Hospitalists are frequently consulted regarding perioperative risk assessment and reduction for patients undergoing non-cardiac surgery. Over the last decade and supported by a few studies, the perioperative use of beta-blocker therapy has resolved the uncertainty frequently encountered. The McFalls study in 2004 showed no benefit to routine coronary revascularization for patients undergoing vascular surgery deemed at risk for myocardial ischemia.1 This provided further confidence for those of us supplying these preoperative assessments. However, the Lindenauer study in 2005 (a retrospective cohort analysis) was the first indication that perioperative beta blockade could be harmful.2 Lower-risk patients based on the revised cardiovascular index (RCRI) score actually did worse when treated. Still the ACC guidelines published in 2006 suggested perioperative beta blockers be considered for lower risk patients undergoing vascular surgery.3
This study is a randomized placebo-controlled trial of perioperative beta-blocker therapy in 500 treatment-naïve patients undergoing vascular surgery. Metoprolol was started two hours before surgery and continued for one week. Cardiovascular endpoints included cardiac death, arrhythmia requiring treatment, acute myocardial infarction or acute coronary syndrome, and congestive heart failure. No benefit was found for treatment with metoprolol regardless of the number of Revised Cardiac Risk Index (RCRI) factors present. No excess adverse outcomes were noted for therapy although intraoperative bradycardia and hypotension were significantly increased in the active treatment group.
In the accompanying editorial McCullough discusses possible reasons and implications of these findings. In fact, two other trials have reported similar findings. In contrast to the older trials suggesting a benefit to perioperative beta blockade these newer trials are larger and have a stronger design. He also notes that the patients in the more recent trials are more likely to have prior revascularization and hence are less prone to demand-type events, reflective of the type of insult beta blockade would most likely be helpful in preventing. These events may be more closely allied with plaque destabilization of subcritical lesions, with factors such as perioperative hypercoagulability and perhaps inflammation being more important. In this regard it is notable that recent trials on the perioperative use of statins have demonstrated favorable results, with these agents presumably acting to promote plaque stability, the so-called “pleiotropic” function of statins.
Significance for hospitalists: It is reasonable to be more circumspect in the recommendation of perioperative beta blockade. This practice is not likely the magic bullet, which is a common misconcpetion. An indicative situation is an 80-year-old patient undergoing total hip replacement. He has diabetes, COPD, and hypertension, a pulse of 65, a blood pressure of 110/50. There may also be concerns about bradycardia, hypotension, and bronchospasm. Given this analysis a clinician can be confident in withholding perioperative treatment.
The use of beta-blocker therapy in a patient with a single RCRI factor, which is not coronary artery disease, does not seem justified. On the other hand the use of perioperative statins should be more actively entertained. Emerging recommendations from various specialty organizations and other relevant professional entities should be anticipated and sought.
Bibliography
- McFalls EO, Ward HB, Moritz TE, et al. Coronary-artery revascularization before elective major vascular surgery. N Eng J Med. 2004Dec 30;351(27):2795-2804.
- Lindenauer PK, Pekow P, Wang K, et al. Perioperative beta-blocker therapy and mortality after major noncardiac surgery. N Eng J Med. 2005 Jul 28;353(4):349-361.
- Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2006 guideline update on perioperative cardiovascular evaluation for noncardiac surgery. J Am Coll Cardiol. 2006;47: 2343-2355
The New C. Diff Epidemic
Bartlett JG. Narrative review: the new epidemic of Clostridium difficile-associated enteric disease. Ann Intern Med. 2006 Nov 21;145(10):758-764.
C. difficile infection is emerging as one of the most important illnesses for hospitalists to be facile with. It not only occurs frequently, but is also often severe or life threatening, and most importantly iatrogenic and preventable. This review by Bartlett, who elucidated the cause of this disease in 1978, reviews important up-to-date information on C. difficile, focusing on the recent emergence of a more virulent form of the disease.
Infectious diarrhea that develops in the hospital is almost always due to C. difficile. The tissue culture cytotoxic assay (first described in 1978) remains the most sensitive and specific diagnostic tool. The toxin immunoassay used most routinely is only 75% sensitive.
An epidemic of unusually severe C. difficile was first described in Quebec in 2001. Important features include a higher tendency for toxic megacolon and a need for colectomy, protein-losing enteropathy, leukemoid reactions, refractoriness to treatment, a high rate of relapse and an astonishing 16.5% attributable mortality. Fluoroquinolones are the leading associated antibiotic causal factor, although extended spectrum cephalosporins remain important as well in this regard. The new strain is characterized by high levels of toxin production due to the deletion of a toxin production regulatory gene. The strain is also fluoroquinolone resistant, explaining the role of that antibiotic in its genesis.
Treatment of C. difficile colitis (especially the emergent strain) remains problematic. In particular the role of metronidazole versus vancomycin as initial therapy is often contentious. Bartlett cites some evidence suggesting vancomycin may be more effective and is especially recommended for severe disease, characteristics of which are often manifested by this new strain.
This review cites important considerations that hospitalist ought to vigilant and proactive in. Given the high risk of fluoroquinolone treatment we must be sure that these drugs are used appropriately. Nonchalantly stacking on levofloxacin therapy for the COPD flair without evidence for pneumonia should be discouraged. When possible antibiotics with a lower risk for C. difficile (sulfonamides, macrolides, tetracyclines) should be used for any infection. When disease is suspected, a negative toxin immunoassay should not discourage empiric treatment especially in a very ill patient. Isolation and barrier precautions are important in preventing the spread of this potentially lethal infection. C. difficile spores are not killed by alcohol-based detergents, and either soap and water or gloves are necessary to care for these patients. When your hospital experiences a clustering of severe C. difficile infection, alert appropriate infection control personnel. Administrative control of antibiotic use may be indicated.
Baclofen Versus Diazepam to Treat Alcohol Withdrawal
Addolorato G, Leggio L, Abenavoli L, et al. Baclofen in the treatment of alcohol withdrawal syndrome: a comparative study vs diazepam. Am J Med. 2006 Mar;119 (3):276.e13-18.
Alcohol withdrawal syndrome (AWS) is a frequent problem encountered in hospitalized patients; its management is considered one of SHM’s core competencies for hospitalists. Benzodiazepines are the gold standard of therapy for this problem given their established record for safety and efficacy; however, their use can be problematic in certain instances.
This study involved 37 outpatients, as inpatients may often be sicker and at higher risk of severe withdrawal.
There is a definite risk of oversedation—especially in patients with COPD or chronic liver disease. Some patients require inordinately high doses of benzodiazepines, thus setting the stage for a prolonged hospitalization. Occasional paradoxical or disinhibition reactions to benzodiazepines can also be problematic. Addiction and or diversion are also a concern in patients prone to substance abuse. An otherwise stable patient, ready for discharge, may still be on a relatively high dose of lorazepam, but it is generally not prudent to send the patient out with a supply of medication to finish the course given concerns over resumption of drinking while on the sedative. Conversely, the solution can be cold comfort for the attending physician if the patient resumes drinking, thus eliminating the need for additional medication.
Baclofen, a stereoselective gamma-aminobutyric acid agonist, has a long history of safety in the treatment of spasticity. As such it can counter balance the activation of the glutamate excitatory pathway that characterizes AWS. It has been proposed as an alternative treatment for AWS that would not share the above concerns cited for benzodiazepines.
This study is a randomized controlled trial of baclofen versus valium in the treatment for AWS. Thirty-seven subjects with a history of heavy alcohol use were randomized to either baclofen 30 mg per day or valium 0.5 to 0.75 mg/kg. All were outpatients treated for 10 days. Clinical Institute Withdrawal Assessment-Alcohol (CIWA) scores were assessed daily. Both regimens continuously decreased the baseline elevation of CIWA scores daily over the course of the study, without a significant difference in treatment efficacy. No adverse events or side effects were reported in either group.
Other than baseline CIWA and daily alcohol consumption, it is not clear that the two groups were at equal risk for severe withdrawal reactions. Relevant baseline characteristics such as history of seizures or delirium tremens, factors that raise this risk were not noted.
Significance for hospitalists: With a long history of safety and efficacy, benzodiazepines remain the drugs of choice for hospitalists treating patients with AWS. In certain instances it may be desirable to limit or even avoid their use. How effective and safe baclofen would be in filling this role remains to be fully established. In particular the relative risk for sedation and respiratory depression has not been defined. Nevertheless at least in my institutions, as guided by expert consultation, its use has been carefully considered and proven helpful in some of the situations noted above. TH
New Path to Primary Care?
A new bill that could steer more medical school students toward primary care is winding its way through Congress and will receive a careful look from SHM.
The Preserving Patient Access to Primary Care Act of 2009 (HR 2350) would provide financial assistance to medical students choosing a primary-care career, proposes changes to Medicare reimbursement, and suggests the development of measures to support and expand the patient-centered medical home (PCMH) model of care.
The bill, sponsored by U.S. Rep. Allyson Schwartz, D-Pa., has been endorsed by the American College of Physicians (ACP). In a press release, the ACP referred to the proposal as "the best medicine for curing the growing crisis in primary care."
SHM's Public Policy Committee will discuss HR 2350 during its June meeting. "SHM has been supportive of improving and expanding primary care because a strong primary-care base creates opportunities for a partnership with hospitalists," says Larry Wellikson, MD, FHM, CEO of SHM. "The committee also will look at HR 2350 from the hospitalist perspective and how it fits in with many of the other proposals that are part of healthcare reform."
A new bill that could steer more medical school students toward primary care is winding its way through Congress and will receive a careful look from SHM.
The Preserving Patient Access to Primary Care Act of 2009 (HR 2350) would provide financial assistance to medical students choosing a primary-care career, proposes changes to Medicare reimbursement, and suggests the development of measures to support and expand the patient-centered medical home (PCMH) model of care.
The bill, sponsored by U.S. Rep. Allyson Schwartz, D-Pa., has been endorsed by the American College of Physicians (ACP). In a press release, the ACP referred to the proposal as "the best medicine for curing the growing crisis in primary care."
SHM's Public Policy Committee will discuss HR 2350 during its June meeting. "SHM has been supportive of improving and expanding primary care because a strong primary-care base creates opportunities for a partnership with hospitalists," says Larry Wellikson, MD, FHM, CEO of SHM. "The committee also will look at HR 2350 from the hospitalist perspective and how it fits in with many of the other proposals that are part of healthcare reform."
A new bill that could steer more medical school students toward primary care is winding its way through Congress and will receive a careful look from SHM.
The Preserving Patient Access to Primary Care Act of 2009 (HR 2350) would provide financial assistance to medical students choosing a primary-care career, proposes changes to Medicare reimbursement, and suggests the development of measures to support and expand the patient-centered medical home (PCMH) model of care.
The bill, sponsored by U.S. Rep. Allyson Schwartz, D-Pa., has been endorsed by the American College of Physicians (ACP). In a press release, the ACP referred to the proposal as "the best medicine for curing the growing crisis in primary care."
SHM's Public Policy Committee will discuss HR 2350 during its June meeting. "SHM has been supportive of improving and expanding primary care because a strong primary-care base creates opportunities for a partnership with hospitalists," says Larry Wellikson, MD, FHM, CEO of SHM. "The committee also will look at HR 2350 from the hospitalist perspective and how it fits in with many of the other proposals that are part of healthcare reform."
In the Literature: The Latest Research You Need to Know
Clinical question: Are elevated fasting blood glucose levels independently associated with poor outcomes in all types of acute coronary syndromes (ACS)?
Background: Elevated admission blood glucose levels have been associated with poor outcomes in ACS patients; however, the role of fasting blood glucose levels in these settings, especially non-ST elevation myocardial infarction (NSTEMI), is unclear. It also is uncertain if one is a better predictor of outcomes than the other.
Study design: Prospective cohort of 57,406 patients in the Global Registry of Acute Coronary Events (GRACE).
Setting: 106 hospitals located in 14 countries in North and South America, Europe, Australia, and New Zealand.
Synopsis: 22,001 admission and 13,526 fasting blood glucose levels were extracted from GRACE and categorized into groups ranging from <100 mg/dL to =300 mg/dL. Multivariate logistic regression analysis of the association between these and the primary outcomes of in-hospital and six-month post-discharge all-cause mortality was carried out.
Fasting glucose levels higher than 100 mg/dL were associated with a linear increase in inpatient mortality (irrespective of diagnosis of diabetes) with an eightfold increase at levels =300mg/dL (17.22% vs. 1.71%). Increased six-month mortality, especially in patients with NSTEMI and STEMI, was also noted. However, this was a nonlinear relationship due to a lower mortality at 200-299 mg/dL, possibly reflecting the higher number of diabetics undergoing treatment in this group.
Admission glucose levels showed a linear increase in inpatient mortality at levels higher than 126 mg/dL. In contrast to fasting levels, admission levels were not associated with poor long-term outcome.
Study limitations included the use of registry data from a subgroup analysis and the possibility that fasting glucose levels in severely ill patients might not be representative of actual metabolic state.
Bottom line: Elevated fasting blood glucose in patients with acute coronary syndromes may portend a worse outcome and may be a better predictor than admission glucose levels.
Citation: Sinnaeve PR, Steg PG, Fox KA, et al. Association of elevated fasting glucose with increased short-term and 6-month mortality in ST-segment elevation and non-ST-segment elevation acute coronary syndromes: the Global Registry of Acute Coronary Events. Arch Intern Med. 2009;169(4):401-409.
— Reviewed for "TH eWire" by Mital Patel, MD, Alraies Chadi, MD, Saurabh Kandpal, MD, Iqbal Masood, MD, Anuradha Ramaswamy, MD, Department of Hospital Medicine, Cleveland Clinic
Clinical question: Are elevated fasting blood glucose levels independently associated with poor outcomes in all types of acute coronary syndromes (ACS)?
Background: Elevated admission blood glucose levels have been associated with poor outcomes in ACS patients; however, the role of fasting blood glucose levels in these settings, especially non-ST elevation myocardial infarction (NSTEMI), is unclear. It also is uncertain if one is a better predictor of outcomes than the other.
Study design: Prospective cohort of 57,406 patients in the Global Registry of Acute Coronary Events (GRACE).
Setting: 106 hospitals located in 14 countries in North and South America, Europe, Australia, and New Zealand.
Synopsis: 22,001 admission and 13,526 fasting blood glucose levels were extracted from GRACE and categorized into groups ranging from <100 mg/dL to =300 mg/dL. Multivariate logistic regression analysis of the association between these and the primary outcomes of in-hospital and six-month post-discharge all-cause mortality was carried out.
Fasting glucose levels higher than 100 mg/dL were associated with a linear increase in inpatient mortality (irrespective of diagnosis of diabetes) with an eightfold increase at levels =300mg/dL (17.22% vs. 1.71%). Increased six-month mortality, especially in patients with NSTEMI and STEMI, was also noted. However, this was a nonlinear relationship due to a lower mortality at 200-299 mg/dL, possibly reflecting the higher number of diabetics undergoing treatment in this group.
Admission glucose levels showed a linear increase in inpatient mortality at levels higher than 126 mg/dL. In contrast to fasting levels, admission levels were not associated with poor long-term outcome.
Study limitations included the use of registry data from a subgroup analysis and the possibility that fasting glucose levels in severely ill patients might not be representative of actual metabolic state.
Bottom line: Elevated fasting blood glucose in patients with acute coronary syndromes may portend a worse outcome and may be a better predictor than admission glucose levels.
Citation: Sinnaeve PR, Steg PG, Fox KA, et al. Association of elevated fasting glucose with increased short-term and 6-month mortality in ST-segment elevation and non-ST-segment elevation acute coronary syndromes: the Global Registry of Acute Coronary Events. Arch Intern Med. 2009;169(4):401-409.
— Reviewed for "TH eWire" by Mital Patel, MD, Alraies Chadi, MD, Saurabh Kandpal, MD, Iqbal Masood, MD, Anuradha Ramaswamy, MD, Department of Hospital Medicine, Cleveland Clinic
Clinical question: Are elevated fasting blood glucose levels independently associated with poor outcomes in all types of acute coronary syndromes (ACS)?
Background: Elevated admission blood glucose levels have been associated with poor outcomes in ACS patients; however, the role of fasting blood glucose levels in these settings, especially non-ST elevation myocardial infarction (NSTEMI), is unclear. It also is uncertain if one is a better predictor of outcomes than the other.
Study design: Prospective cohort of 57,406 patients in the Global Registry of Acute Coronary Events (GRACE).
Setting: 106 hospitals located in 14 countries in North and South America, Europe, Australia, and New Zealand.
Synopsis: 22,001 admission and 13,526 fasting blood glucose levels were extracted from GRACE and categorized into groups ranging from <100 mg/dL to =300 mg/dL. Multivariate logistic regression analysis of the association between these and the primary outcomes of in-hospital and six-month post-discharge all-cause mortality was carried out.
Fasting glucose levels higher than 100 mg/dL were associated with a linear increase in inpatient mortality (irrespective of diagnosis of diabetes) with an eightfold increase at levels =300mg/dL (17.22% vs. 1.71%). Increased six-month mortality, especially in patients with NSTEMI and STEMI, was also noted. However, this was a nonlinear relationship due to a lower mortality at 200-299 mg/dL, possibly reflecting the higher number of diabetics undergoing treatment in this group.
Admission glucose levels showed a linear increase in inpatient mortality at levels higher than 126 mg/dL. In contrast to fasting levels, admission levels were not associated with poor long-term outcome.
Study limitations included the use of registry data from a subgroup analysis and the possibility that fasting glucose levels in severely ill patients might not be representative of actual metabolic state.
Bottom line: Elevated fasting blood glucose in patients with acute coronary syndromes may portend a worse outcome and may be a better predictor than admission glucose levels.
Citation: Sinnaeve PR, Steg PG, Fox KA, et al. Association of elevated fasting glucose with increased short-term and 6-month mortality in ST-segment elevation and non-ST-segment elevation acute coronary syndromes: the Global Registry of Acute Coronary Events. Arch Intern Med. 2009;169(4):401-409.
— Reviewed for "TH eWire" by Mital Patel, MD, Alraies Chadi, MD, Saurabh Kandpal, MD, Iqbal Masood, MD, Anuradha Ramaswamy, MD, Department of Hospital Medicine, Cleveland Clinic