User login
Management of the Child With Cystic Fibrosis
All 50 states require newborn screening for cystic fibrosis, and pediatricians play an important role when a newborn is diagnosed. The positive screens from your state laboratory will include referral options for confirmatory testing and specialty care at an accredited Cystic Fibrosis Center or CF center affiliate in your area. Pediatricians remain the patient's “medical home,” help to coordinate this specialty care, and remain in close communication with the patient, families, and specialists at a CF center as these children grow.
Optimal outcomes come from assessment and treatment by a multidisciplinary team at an accredited CF center. Encourage your CF patient and families to be seen there regularly. You want those specialists on board to help you take optimal care of the child. Monitoring at least every 3 months is recommended and is called “expectant” or “proactive management” for an individual with CF. A more thorough assessment occurs at least annually.
Pediatricians are essential, in particular, when patients live far from a CF center. We have patients who live a 3-hour drive from our center at the University of Chicago. In some states, patients may live hundreds of miles from a center and can be seen for specialty care only once per year.
There are some specialist outreach efforts as well for children who live in extremely remote, rural areas: Clinicians in Seattle fly to Anchorage, Alaska, to monitor and treat children with CF.
If a sick child with CF comes as a new patient to your office and the records are not available, you should always feel free to call the closest CF center to speak to one of the specialists there and eventually refer them for care. Physicians at CF centers work in collaboration with primary care physicians who are the “go to” professionals, often treating other members of a CF child's family.
Consultation and referral are important. Pediatricians tend to be very, very busy and see 20-40 patients a day in their office for a wide range of indications, including earaches, stomach aches, and well-child exams. But if you are taking care of a sick child with CF who is just not getting better with antibiotic or other treatment, definitely communicate with a CF care provider.
Many pediatricians we know well in the Chicago area will call us up and say, “I have so-and-so in my office. They are coughing a little bit more. I know you sent a letter before saying I should try this particular antibiotic. Is there anything else I should do at this point?” They stay in close touch, and we always have a center physician or nurse available to speak with them.
Regular assessment by a pediatric pulmonologist is part of the CF center care. If a child has an increased cough and they have certain bacteria such as Pseudomonas, we aggressively treat them so they don't get worse. We monitor lung function and obtain frequent respiratory cultures.
In addition, up to 90% of these children and adolescents develop digestive problems and may benefit from consultation with a gastroenterologist. Some patients develop sinus-related problems and referral to an ENT may be warranted. Accredited centers are required to provide these specialists, as well as dieticians, social workers, and respiratory therapists, who are experienced and knowledgeable about CF and who are involved in providing a care plan for children with CF.
Pediatricians play an important role in the facilitation of regular testing of children and adolescents with cystic fibrosis. At a minimum of once a year, they require blood work and chest x-rays. Many patients do their annual visits in the summer because testing takes almost a whole day. The lab work and chest x-ray copy (on a CD) can then be brought to CF physicians on the day of that “annual” visit. Depending on the patient's insurance, it may be less expensive and more convenient for the family for the pediatrician to coordinate this annual testing at the local community hospital. Lung function testing typically needs to be done at the center.
We also now do an oral glucose tolerance test for CF-related diabetes in any patient older than 10 years. That often can be done locally as well. Patients with CF may develop a specific type of diabetes. Most patients with CF have pancreatic insufficiency, which results in problems with digestion and the need to take medication (pancreatic enzymes) with every meal. Over time, scarring of the pancreas results and insufficient insulin may be produced.
The Cystic Fibrosis Foundation, which approves and accredits CF centers, is a great source of information for patients and families. Advise parents to visit www.cff.org
All 50 states require newborn screening for cystic fibrosis, and pediatricians play an important role when a newborn is diagnosed. The positive screens from your state laboratory will include referral options for confirmatory testing and specialty care at an accredited Cystic Fibrosis Center or CF center affiliate in your area. Pediatricians remain the patient's “medical home,” help to coordinate this specialty care, and remain in close communication with the patient, families, and specialists at a CF center as these children grow.
Optimal outcomes come from assessment and treatment by a multidisciplinary team at an accredited CF center. Encourage your CF patient and families to be seen there regularly. You want those specialists on board to help you take optimal care of the child. Monitoring at least every 3 months is recommended and is called “expectant” or “proactive management” for an individual with CF. A more thorough assessment occurs at least annually.
Pediatricians are essential, in particular, when patients live far from a CF center. We have patients who live a 3-hour drive from our center at the University of Chicago. In some states, patients may live hundreds of miles from a center and can be seen for specialty care only once per year.
There are some specialist outreach efforts as well for children who live in extremely remote, rural areas: Clinicians in Seattle fly to Anchorage, Alaska, to monitor and treat children with CF.
If a sick child with CF comes as a new patient to your office and the records are not available, you should always feel free to call the closest CF center to speak to one of the specialists there and eventually refer them for care. Physicians at CF centers work in collaboration with primary care physicians who are the “go to” professionals, often treating other members of a CF child's family.
Consultation and referral are important. Pediatricians tend to be very, very busy and see 20-40 patients a day in their office for a wide range of indications, including earaches, stomach aches, and well-child exams. But if you are taking care of a sick child with CF who is just not getting better with antibiotic or other treatment, definitely communicate with a CF care provider.
Many pediatricians we know well in the Chicago area will call us up and say, “I have so-and-so in my office. They are coughing a little bit more. I know you sent a letter before saying I should try this particular antibiotic. Is there anything else I should do at this point?” They stay in close touch, and we always have a center physician or nurse available to speak with them.
Regular assessment by a pediatric pulmonologist is part of the CF center care. If a child has an increased cough and they have certain bacteria such as Pseudomonas, we aggressively treat them so they don't get worse. We monitor lung function and obtain frequent respiratory cultures.
In addition, up to 90% of these children and adolescents develop digestive problems and may benefit from consultation with a gastroenterologist. Some patients develop sinus-related problems and referral to an ENT may be warranted. Accredited centers are required to provide these specialists, as well as dieticians, social workers, and respiratory therapists, who are experienced and knowledgeable about CF and who are involved in providing a care plan for children with CF.
Pediatricians play an important role in the facilitation of regular testing of children and adolescents with cystic fibrosis. At a minimum of once a year, they require blood work and chest x-rays. Many patients do their annual visits in the summer because testing takes almost a whole day. The lab work and chest x-ray copy (on a CD) can then be brought to CF physicians on the day of that “annual” visit. Depending on the patient's insurance, it may be less expensive and more convenient for the family for the pediatrician to coordinate this annual testing at the local community hospital. Lung function testing typically needs to be done at the center.
We also now do an oral glucose tolerance test for CF-related diabetes in any patient older than 10 years. That often can be done locally as well. Patients with CF may develop a specific type of diabetes. Most patients with CF have pancreatic insufficiency, which results in problems with digestion and the need to take medication (pancreatic enzymes) with every meal. Over time, scarring of the pancreas results and insufficient insulin may be produced.
The Cystic Fibrosis Foundation, which approves and accredits CF centers, is a great source of information for patients and families. Advise parents to visit www.cff.org
All 50 states require newborn screening for cystic fibrosis, and pediatricians play an important role when a newborn is diagnosed. The positive screens from your state laboratory will include referral options for confirmatory testing and specialty care at an accredited Cystic Fibrosis Center or CF center affiliate in your area. Pediatricians remain the patient's “medical home,” help to coordinate this specialty care, and remain in close communication with the patient, families, and specialists at a CF center as these children grow.
Optimal outcomes come from assessment and treatment by a multidisciplinary team at an accredited CF center. Encourage your CF patient and families to be seen there regularly. You want those specialists on board to help you take optimal care of the child. Monitoring at least every 3 months is recommended and is called “expectant” or “proactive management” for an individual with CF. A more thorough assessment occurs at least annually.
Pediatricians are essential, in particular, when patients live far from a CF center. We have patients who live a 3-hour drive from our center at the University of Chicago. In some states, patients may live hundreds of miles from a center and can be seen for specialty care only once per year.
There are some specialist outreach efforts as well for children who live in extremely remote, rural areas: Clinicians in Seattle fly to Anchorage, Alaska, to monitor and treat children with CF.
If a sick child with CF comes as a new patient to your office and the records are not available, you should always feel free to call the closest CF center to speak to one of the specialists there and eventually refer them for care. Physicians at CF centers work in collaboration with primary care physicians who are the “go to” professionals, often treating other members of a CF child's family.
Consultation and referral are important. Pediatricians tend to be very, very busy and see 20-40 patients a day in their office for a wide range of indications, including earaches, stomach aches, and well-child exams. But if you are taking care of a sick child with CF who is just not getting better with antibiotic or other treatment, definitely communicate with a CF care provider.
Many pediatricians we know well in the Chicago area will call us up and say, “I have so-and-so in my office. They are coughing a little bit more. I know you sent a letter before saying I should try this particular antibiotic. Is there anything else I should do at this point?” They stay in close touch, and we always have a center physician or nurse available to speak with them.
Regular assessment by a pediatric pulmonologist is part of the CF center care. If a child has an increased cough and they have certain bacteria such as Pseudomonas, we aggressively treat them so they don't get worse. We monitor lung function and obtain frequent respiratory cultures.
In addition, up to 90% of these children and adolescents develop digestive problems and may benefit from consultation with a gastroenterologist. Some patients develop sinus-related problems and referral to an ENT may be warranted. Accredited centers are required to provide these specialists, as well as dieticians, social workers, and respiratory therapists, who are experienced and knowledgeable about CF and who are involved in providing a care plan for children with CF.
Pediatricians play an important role in the facilitation of regular testing of children and adolescents with cystic fibrosis. At a minimum of once a year, they require blood work and chest x-rays. Many patients do their annual visits in the summer because testing takes almost a whole day. The lab work and chest x-ray copy (on a CD) can then be brought to CF physicians on the day of that “annual” visit. Depending on the patient's insurance, it may be less expensive and more convenient for the family for the pediatrician to coordinate this annual testing at the local community hospital. Lung function testing typically needs to be done at the center.
We also now do an oral glucose tolerance test for CF-related diabetes in any patient older than 10 years. That often can be done locally as well. Patients with CF may develop a specific type of diabetes. Most patients with CF have pancreatic insufficiency, which results in problems with digestion and the need to take medication (pancreatic enzymes) with every meal. Over time, scarring of the pancreas results and insufficient insulin may be produced.
The Cystic Fibrosis Foundation, which approves and accredits CF centers, is a great source of information for patients and families. Advise parents to visit www.cff.org
Hospitalists Can Be Champions of Clinical Documentation
To improve your hospital’s reimbursements and key indicators, including observed and expected (O/E) mortality ratios, personalize your collaboration with clinical documentation specialists (CDSs). That’s what has worked at two medical centers where hospitalists teamed up with CDSs to improve their hospitals’ claims processes.
At Northwestern Memorial Hospital in Chicago, the hematology/oncology service was selected for a pilot program to focus on improving expected mortality rates. The specialists needed to ensure that coded data sent to state- and hospital-associated databases (as well as payor claims, such as those submitted to Medicare) accurately represented the severity of patients’ conditions upon admission. To do that, they needed buy-in from hospitalists to make their notes as complete as possible.
Hospitalists usually encounter CDSs anonymously, through an electronic query in the electronic health record (EHR). Kristine Green, RN, a CDS, quality leader, and interim manager at Northwestern’s clinical documentation program, approached hospitalist Charlotta Weaver, MD, medical director of the oncology HM service and a clinical instructor at Northwestern University’s Feinberg School of Medicine. Green suggested she shadow Dr. Weaver on rounds.
“We had implemented this technique in a couple of our other service lines, with good results,” Green says. She compared her notes on patient visits with Dr. Weaver’s notes and was able to catch conditions that were being undercoded. They generated a list, now posted in the work room, disseminated via email, and included in the orientation binder, of frequently missed coding diagnoses.
For example, Dr. Weaver explains, “instead of writing ‘AKI-obstructive,’ we now write ‘AKI due to ureteral obstruction from peritoneal carcinomatosis from metastatic gastric cancer.’ ”
Such specificity in physicians’ notes translates to a more accurate level of billing for the hospital and a more accurate reflection of patients’ acuity in comparative databases. With Dr. Weaver paving the way, Green has forged “a nice rapport” with the other hospitalists in the oncology medicine service.
Audiences for Your Notes
CDS and hospitalists might initially view notes differently. Most physicians train in programs where the “primary intent of a note” is to communicate to the rest of the medical team what’s happening with the patient, Dr. Weaver says.
“When we train, we’re always thinking about communicating with each other,” says Theodore (Ted) Tsomides, MD, PhD, an attending physician on the hospital medicine service at WakeMed Hospital and assistant professor of medicine at the University of North Carolina’s School of Medicine in Raleigh. “But as we get into the system, we realize that there are a lot of eyes on those documents. And whether we think about it or not, those are all our different audiences.”
Once hospitalists develop confidence and comfort on the job, Dr. Tsomides says, they can move on to aligning themselves with the hospital’s interests. Dr. Weaver thinks hospitalists are uniquely positioned to help champion the CDI efforts. “We’re here to improve the mission of the hospital,” she says.
As physician liaison for quality programs, Dr. Tsomides began working on clinical documentation improvement. He became a resource for the department, and then worked to achieve a financial incentive plan for hospital physicians when their documentation improved. He’s also been pushing his institution to make the documentation process easier by using electronic queries, and by introducing residents to the “real world” of clinical documentation in their curriculum. (Click here to listen to more of Dr. Tsomides’ ideas to improve clinical documentation.)
He advises hospitalists meet their clinical documentation specialists face to face. “Once you know there are people who are doing their part, and have a relationship with them, you approach the whole problem differently,” Dr. Tsomides says, “as opposed to [viewing them] as anonymous reviewers breathing down your neck and giving you yet another thing to worry about.”
Gretchen Henkel is a freelance writer based in California.
To improve your hospital’s reimbursements and key indicators, including observed and expected (O/E) mortality ratios, personalize your collaboration with clinical documentation specialists (CDSs). That’s what has worked at two medical centers where hospitalists teamed up with CDSs to improve their hospitals’ claims processes.
At Northwestern Memorial Hospital in Chicago, the hematology/oncology service was selected for a pilot program to focus on improving expected mortality rates. The specialists needed to ensure that coded data sent to state- and hospital-associated databases (as well as payor claims, such as those submitted to Medicare) accurately represented the severity of patients’ conditions upon admission. To do that, they needed buy-in from hospitalists to make their notes as complete as possible.
Hospitalists usually encounter CDSs anonymously, through an electronic query in the electronic health record (EHR). Kristine Green, RN, a CDS, quality leader, and interim manager at Northwestern’s clinical documentation program, approached hospitalist Charlotta Weaver, MD, medical director of the oncology HM service and a clinical instructor at Northwestern University’s Feinberg School of Medicine. Green suggested she shadow Dr. Weaver on rounds.
“We had implemented this technique in a couple of our other service lines, with good results,” Green says. She compared her notes on patient visits with Dr. Weaver’s notes and was able to catch conditions that were being undercoded. They generated a list, now posted in the work room, disseminated via email, and included in the orientation binder, of frequently missed coding diagnoses.
For example, Dr. Weaver explains, “instead of writing ‘AKI-obstructive,’ we now write ‘AKI due to ureteral obstruction from peritoneal carcinomatosis from metastatic gastric cancer.’ ”
Such specificity in physicians’ notes translates to a more accurate level of billing for the hospital and a more accurate reflection of patients’ acuity in comparative databases. With Dr. Weaver paving the way, Green has forged “a nice rapport” with the other hospitalists in the oncology medicine service.
Audiences for Your Notes
CDS and hospitalists might initially view notes differently. Most physicians train in programs where the “primary intent of a note” is to communicate to the rest of the medical team what’s happening with the patient, Dr. Weaver says.
“When we train, we’re always thinking about communicating with each other,” says Theodore (Ted) Tsomides, MD, PhD, an attending physician on the hospital medicine service at WakeMed Hospital and assistant professor of medicine at the University of North Carolina’s School of Medicine in Raleigh. “But as we get into the system, we realize that there are a lot of eyes on those documents. And whether we think about it or not, those are all our different audiences.”
Once hospitalists develop confidence and comfort on the job, Dr. Tsomides says, they can move on to aligning themselves with the hospital’s interests. Dr. Weaver thinks hospitalists are uniquely positioned to help champion the CDI efforts. “We’re here to improve the mission of the hospital,” she says.
As physician liaison for quality programs, Dr. Tsomides began working on clinical documentation improvement. He became a resource for the department, and then worked to achieve a financial incentive plan for hospital physicians when their documentation improved. He’s also been pushing his institution to make the documentation process easier by using electronic queries, and by introducing residents to the “real world” of clinical documentation in their curriculum. (Click here to listen to more of Dr. Tsomides’ ideas to improve clinical documentation.)
He advises hospitalists meet their clinical documentation specialists face to face. “Once you know there are people who are doing their part, and have a relationship with them, you approach the whole problem differently,” Dr. Tsomides says, “as opposed to [viewing them] as anonymous reviewers breathing down your neck and giving you yet another thing to worry about.”
Gretchen Henkel is a freelance writer based in California.
To improve your hospital’s reimbursements and key indicators, including observed and expected (O/E) mortality ratios, personalize your collaboration with clinical documentation specialists (CDSs). That’s what has worked at two medical centers where hospitalists teamed up with CDSs to improve their hospitals’ claims processes.
At Northwestern Memorial Hospital in Chicago, the hematology/oncology service was selected for a pilot program to focus on improving expected mortality rates. The specialists needed to ensure that coded data sent to state- and hospital-associated databases (as well as payor claims, such as those submitted to Medicare) accurately represented the severity of patients’ conditions upon admission. To do that, they needed buy-in from hospitalists to make their notes as complete as possible.
Hospitalists usually encounter CDSs anonymously, through an electronic query in the electronic health record (EHR). Kristine Green, RN, a CDS, quality leader, and interim manager at Northwestern’s clinical documentation program, approached hospitalist Charlotta Weaver, MD, medical director of the oncology HM service and a clinical instructor at Northwestern University’s Feinberg School of Medicine. Green suggested she shadow Dr. Weaver on rounds.
“We had implemented this technique in a couple of our other service lines, with good results,” Green says. She compared her notes on patient visits with Dr. Weaver’s notes and was able to catch conditions that were being undercoded. They generated a list, now posted in the work room, disseminated via email, and included in the orientation binder, of frequently missed coding diagnoses.
For example, Dr. Weaver explains, “instead of writing ‘AKI-obstructive,’ we now write ‘AKI due to ureteral obstruction from peritoneal carcinomatosis from metastatic gastric cancer.’ ”
Such specificity in physicians’ notes translates to a more accurate level of billing for the hospital and a more accurate reflection of patients’ acuity in comparative databases. With Dr. Weaver paving the way, Green has forged “a nice rapport” with the other hospitalists in the oncology medicine service.
Audiences for Your Notes
CDS and hospitalists might initially view notes differently. Most physicians train in programs where the “primary intent of a note” is to communicate to the rest of the medical team what’s happening with the patient, Dr. Weaver says.
“When we train, we’re always thinking about communicating with each other,” says Theodore (Ted) Tsomides, MD, PhD, an attending physician on the hospital medicine service at WakeMed Hospital and assistant professor of medicine at the University of North Carolina’s School of Medicine in Raleigh. “But as we get into the system, we realize that there are a lot of eyes on those documents. And whether we think about it or not, those are all our different audiences.”
Once hospitalists develop confidence and comfort on the job, Dr. Tsomides says, they can move on to aligning themselves with the hospital’s interests. Dr. Weaver thinks hospitalists are uniquely positioned to help champion the CDI efforts. “We’re here to improve the mission of the hospital,” she says.
As physician liaison for quality programs, Dr. Tsomides began working on clinical documentation improvement. He became a resource for the department, and then worked to achieve a financial incentive plan for hospital physicians when their documentation improved. He’s also been pushing his institution to make the documentation process easier by using electronic queries, and by introducing residents to the “real world” of clinical documentation in their curriculum. (Click here to listen to more of Dr. Tsomides’ ideas to improve clinical documentation.)
He advises hospitalists meet their clinical documentation specialists face to face. “Once you know there are people who are doing their part, and have a relationship with them, you approach the whole problem differently,” Dr. Tsomides says, “as opposed to [viewing them] as anonymous reviewers breathing down your neck and giving you yet another thing to worry about.”
Gretchen Henkel is a freelance writer based in California.
CT Screening Cuts Lung Cancer Mortality; Raises Policy Questions
Final results from the National Lung Screening Trial show a significant reduction in lung cancer mortality with the use of annual low-dose CT screening, compared with standard chest x-rays among former heavy smokers at high risk for lung cancer.
Low-dose CT screening led to a relative reduction of 20% in the rate of death from lung cancer, according to findings released online by the New England Journal of Medicine on June 29 (doi: 10.1056/NEJMoa1102873).The number needed to screen with low-dose CT to prevent one death from lung cancer was 320.
Although preliminary study results were announced in November 2010, the article by the National Lung Screening Trial (NLST) research team marks the first time that the results appear in a peer-reviewed journal. Acknowledging that the earlier announcement has led to calls for lung cancer screening, the authors urge rigorous analysis of cost-effectiveness before public policy recommendations are made.
"The reduction in lung-cancer mortality must be weighed against the harms from positive screening results and overdiagnosis, as well as the costs," they wrote.
In the study, 53,454 men and women aged 55-74 years – who were current or former smokers with a smoking history of at least 30 pack-years – were recruited at 33 U.S. medical centers. A total of 26,722 participants were randomized to receive three annual screens with low-dose helical CT; 26,732 were randomized to three annual screens using chest x-ray. The two groups were virtually identical in demographics and smoking history.
In all three screening rounds, positive screening tests were substantially more common in the low-dose CT group than in the radiography group (27.3% vs. 9.2% in the first round; 27.9% vs. 6.2% in the second; and 16.8% vs. 5% in the third). All told, 39.1% of the CT group and 16% of the radiography group had at least one positive result.
The percentage of screening tests that identified a clinically significant abnormality -- other than an abnormality suspicious for lung cancer – also was more than three times as high in the low-dose CT group as in the radiography group (7.5% vs. 2.1%).
More than 90% of positive screenings in the first round of the study led to a diagnostic evaluation, though the follow-up rates were lower in the later rounds. Diagnostic evaluation most often consisted of additional imaging with invasive procedures being performed infrequently.
Across the three screenings, most of the positive results were false positives – 96.4% in the CT group and 94.5% in the radiography group. Of the total number of low-dose CT screening tests, 24.2% were classified as positive and 23.4% had false-positive results; of the total number of radiographic screening tests, 6.9% were classified as positive and 6.5% were false-positive results.
In all, 1,060 lung cancers were diagnosed in the low-dose CT group (645/100,000 person-years) vs. 941 in the radiography group (572/100,000 person-years). Of these cancers, 649 in the low-dose CT group were diagnosed after a positive screening test and 44 were diagnosed after a negative screening test. In the radiography group, 279 cancers were diagnosed after a positive screening test and 137 were diagnosed after a negative screening test.
In both groups, the remaining cases were among participants who missed screening or were diagnosed after their trial screening phase was over
Analysis of lung cancer-specific mortality showed that in the CT group 356 lung cancer deaths occurred after 144,103 person-years; in the radiography group 443 lung cancer deaths occurred after 143,368 person-years. This corresponded to 247 and 309 lung cancer deaths, respectively, per 100,000 person-years in the CT and radiography groups.
There were 1,877 and 2,000 deaths from all causes in the CT and radiography groups, respectively, "representing a significant reduction with low-dose CT screening of 6.7% ... in the rate of death from any cause," the investigators wrote. While lung cancer accounted for 24.1% of all the deaths in the trial, 60.3% of the excess deaths in the radiography group were due to lung cancer.
The authors concluded that "although some agencies and organizations are contemplating the establishment of lung-cancer screening recommendations on the basis of the findings of the NLST, the current NLST data alone are, in our opinion, insufficient to fully inform such important decisions."
They noted that "The observation that low-dose CT screening can reduce the rate of death from lung cancer has generated many questions." Among these they listed: Will populations with different risk profiles benefit from screening? Could less frequent screening programs be equally effective? Would the use of different criteria for a positive screening result translate to similar benefit? For how long should people be screened?
In an accompanying editorial, Dr. Harold C. Sox, professor of medicine at the Dartmouth Institute in Hanover, N. H., agreed with the investigators’ reservations. In particular, the cost effectiveness of low-dose CT screening for lung cancer must be analyzed, he said: "Policy makers should wait for cost-effectiveness analyses to determine the amount of overdiagnosis in the NLST, and, perhaps identification of biologic markers of cancers that do not progress."
In addition, "it may be possible to define subgroups of smokers who are at higher or lower risk for lung cancer and tailor the screening strategy accordingly," he said. "The findings of the NLST regarding lung-cancer mortality signal the beginning of the end of one era of research on lung-cancer screening and the start of another. The focus will shift to informing the difficult patient-centered and policy decisions that are yet to come."
Dr. Sox also noted that "overdiagnosis is a problem because predicting which early-stage cancers will not progress is in an early stage of development, so that everyone with screen-detected cancer receives treatment that some do not need," he wrote in an accompanying editorial (doi: 10.1056/NEJME1103776).
All but two of the NLST study authors reported that they have no relevant financial relationships. Jonathan D. Clap reported having financial interest in Human Genome Sciences. Constantine Gatsonis, Ph.D., is a consultant for Wilex AG, Mela Sciences, and Endocyte Inc., has received speaker fees from Bayer Health and payment for education development by the Radiologic Society of North America. He also has invested in the Vanguard Health Fund. Dr. Sox had no conflicts.
This is an exciting
study that does show an impact on mortality, which has not been a screening
result from previous studies. What it doesn’t tell us exactly is: What does
this mean from a policy standpoint?
We need to look at a lot
more to see what’s the best model with this kind of screening and when this is
screening appropriate. I think the authors of this study were right to say that
this is a very positive result and it’s helpful … but that the best way to
implement this in day-to-day practice still is not completely resolved. There’s
a lot more work to be done in that regard.
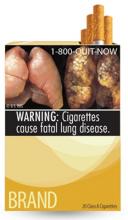
One message that is still
very clear is that if you don’t want to die from lung cancer, you need to stop
smoking or never start smoking. This still has to be foremost in our public
health preventative message.
The study results do help
by saying that screening can have a role in day-to-day practice. The fact that
these patients were treated in a community setting showed that … the process
for diagnosing lung cancer can be handled by community physicians. I’m a
pulmonary physician. So when I sit down with patients who have the risk of
smoking, and we talk about what is the role of getting a low-dose CT scan for
screening, I think I have a lot more information to help both me and the
patient to decide whether this is beneficial to them versus a risk.
In the past, with CT
screening there was certainly risk from the radiation and risks for having
unnecessary procedures done, but no real proven benefit that we were going to
impact mortality if we found an early cancer. The study results do add value on
a day-to-day basis.
We just don’t know whether
it’s something that should be applied to everybody. Another question is whether
there are there markers that might help in this group of individuals to
identify who is at high risk for fast-growing tumors or for slow-growing tumors
Are there biologic markers that we can find with a blood test that might add to
this information to help us sort out who would benefit from screening or not?
[Other questions to
answer] from these data or from other ongoing studies include: Are there
subgroups of this 55- to 74-year-old population that are at higher risk? Are
there individuals who with less frequent screening can do just as well? Are
there individuals for whom more screening is necessary? The population looked
at [in the study] was a narrow window of high-risk individuals … It represents
about 7 million people out of the 94 million current and former smokers that we
have in this country.
We may even be able to
look at genetic markers at some point in the near future to determine who is at
higher risk and that will help us better identify who needs to be screened. I
think biomarkers and genetic markers all could be added to the formula when
we’re trying to decide what the best risk population to be screened is.
Screening tools work best when the screening population is well defined.
So now we have evidence
that screening in general can have an impact on disease. Unfortunately, prior
to this, lung cancer was diagnosed too late to make a big impact for most
patients. In lung cancer, an earlier diagnosis hopefully impacts mortality.
Lung cancer could become a curable disease if it’s found early enough to be
completely resected.
Dr. Albert A. Rizzo is
chair-elect of the American Lung Association board and chief of Christiana
Care’s pulmonary and critical care medicine section in Newark, Del.
He has no conflicts of interest.
This is an exciting
study that does show an impact on mortality, which has not been a screening
result from previous studies. What it doesn’t tell us exactly is: What does
this mean from a policy standpoint?
We need to look at a lot
more to see what’s the best model with this kind of screening and when this is
screening appropriate. I think the authors of this study were right to say that
this is a very positive result and it’s helpful … but that the best way to
implement this in day-to-day practice still is not completely resolved. There’s
a lot more work to be done in that regard.
One message that is still
very clear is that if you don’t want to die from lung cancer, you need to stop
smoking or never start smoking. This still has to be foremost in our public
health preventative message.
The study results do help
by saying that screening can have a role in day-to-day practice. The fact that
these patients were treated in a community setting showed that … the process
for diagnosing lung cancer can be handled by community physicians. I’m a
pulmonary physician. So when I sit down with patients who have the risk of
smoking, and we talk about what is the role of getting a low-dose CT scan for
screening, I think I have a lot more information to help both me and the
patient to decide whether this is beneficial to them versus a risk.
In the past, with CT
screening there was certainly risk from the radiation and risks for having
unnecessary procedures done, but no real proven benefit that we were going to
impact mortality if we found an early cancer. The study results do add value on
a day-to-day basis.
We just don’t know whether
it’s something that should be applied to everybody. Another question is whether
there are there markers that might help in this group of individuals to
identify who is at high risk for fast-growing tumors or for slow-growing tumors
Are there biologic markers that we can find with a blood test that might add to
this information to help us sort out who would benefit from screening or not?
[Other questions to
answer] from these data or from other ongoing studies include: Are there
subgroups of this 55- to 74-year-old population that are at higher risk? Are
there individuals who with less frequent screening can do just as well? Are
there individuals for whom more screening is necessary? The population looked
at [in the study] was a narrow window of high-risk individuals … It represents
about 7 million people out of the 94 million current and former smokers that we
have in this country.
We may even be able to
look at genetic markers at some point in the near future to determine who is at
higher risk and that will help us better identify who needs to be screened. I
think biomarkers and genetic markers all could be added to the formula when
we’re trying to decide what the best risk population to be screened is.
Screening tools work best when the screening population is well defined.
So now we have evidence
that screening in general can have an impact on disease. Unfortunately, prior
to this, lung cancer was diagnosed too late to make a big impact for most
patients. In lung cancer, an earlier diagnosis hopefully impacts mortality.
Lung cancer could become a curable disease if it’s found early enough to be
completely resected.
Dr. Albert A. Rizzo is
chair-elect of the American Lung Association board and chief of Christiana
Care’s pulmonary and critical care medicine section in Newark, Del.
He has no conflicts of interest.
This is an exciting
study that does show an impact on mortality, which has not been a screening
result from previous studies. What it doesn’t tell us exactly is: What does
this mean from a policy standpoint?
We need to look at a lot
more to see what’s the best model with this kind of screening and when this is
screening appropriate. I think the authors of this study were right to say that
this is a very positive result and it’s helpful … but that the best way to
implement this in day-to-day practice still is not completely resolved. There’s
a lot more work to be done in that regard.
One message that is still
very clear is that if you don’t want to die from lung cancer, you need to stop
smoking or never start smoking. This still has to be foremost in our public
health preventative message.
The study results do help
by saying that screening can have a role in day-to-day practice. The fact that
these patients were treated in a community setting showed that … the process
for diagnosing lung cancer can be handled by community physicians. I’m a
pulmonary physician. So when I sit down with patients who have the risk of
smoking, and we talk about what is the role of getting a low-dose CT scan for
screening, I think I have a lot more information to help both me and the
patient to decide whether this is beneficial to them versus a risk.
In the past, with CT
screening there was certainly risk from the radiation and risks for having
unnecessary procedures done, but no real proven benefit that we were going to
impact mortality if we found an early cancer. The study results do add value on
a day-to-day basis.
We just don’t know whether
it’s something that should be applied to everybody. Another question is whether
there are there markers that might help in this group of individuals to
identify who is at high risk for fast-growing tumors or for slow-growing tumors
Are there biologic markers that we can find with a blood test that might add to
this information to help us sort out who would benefit from screening or not?
[Other questions to
answer] from these data or from other ongoing studies include: Are there
subgroups of this 55- to 74-year-old population that are at higher risk? Are
there individuals who with less frequent screening can do just as well? Are
there individuals for whom more screening is necessary? The population looked
at [in the study] was a narrow window of high-risk individuals … It represents
about 7 million people out of the 94 million current and former smokers that we
have in this country.
We may even be able to
look at genetic markers at some point in the near future to determine who is at
higher risk and that will help us better identify who needs to be screened. I
think biomarkers and genetic markers all could be added to the formula when
we’re trying to decide what the best risk population to be screened is.
Screening tools work best when the screening population is well defined.
So now we have evidence
that screening in general can have an impact on disease. Unfortunately, prior
to this, lung cancer was diagnosed too late to make a big impact for most
patients. In lung cancer, an earlier diagnosis hopefully impacts mortality.
Lung cancer could become a curable disease if it’s found early enough to be
completely resected.
Dr. Albert A. Rizzo is
chair-elect of the American Lung Association board and chief of Christiana
Care’s pulmonary and critical care medicine section in Newark, Del.
He has no conflicts of interest.
Final results from the National Lung Screening Trial show a significant reduction in lung cancer mortality with the use of annual low-dose CT screening, compared with standard chest x-rays among former heavy smokers at high risk for lung cancer.
Low-dose CT screening led to a relative reduction of 20% in the rate of death from lung cancer, according to findings released online by the New England Journal of Medicine on June 29 (doi: 10.1056/NEJMoa1102873).The number needed to screen with low-dose CT to prevent one death from lung cancer was 320.
Although preliminary study results were announced in November 2010, the article by the National Lung Screening Trial (NLST) research team marks the first time that the results appear in a peer-reviewed journal. Acknowledging that the earlier announcement has led to calls for lung cancer screening, the authors urge rigorous analysis of cost-effectiveness before public policy recommendations are made.
"The reduction in lung-cancer mortality must be weighed against the harms from positive screening results and overdiagnosis, as well as the costs," they wrote.
In the study, 53,454 men and women aged 55-74 years – who were current or former smokers with a smoking history of at least 30 pack-years – were recruited at 33 U.S. medical centers. A total of 26,722 participants were randomized to receive three annual screens with low-dose helical CT; 26,732 were randomized to three annual screens using chest x-ray. The two groups were virtually identical in demographics and smoking history.
In all three screening rounds, positive screening tests were substantially more common in the low-dose CT group than in the radiography group (27.3% vs. 9.2% in the first round; 27.9% vs. 6.2% in the second; and 16.8% vs. 5% in the third). All told, 39.1% of the CT group and 16% of the radiography group had at least one positive result.
The percentage of screening tests that identified a clinically significant abnormality -- other than an abnormality suspicious for lung cancer – also was more than three times as high in the low-dose CT group as in the radiography group (7.5% vs. 2.1%).
More than 90% of positive screenings in the first round of the study led to a diagnostic evaluation, though the follow-up rates were lower in the later rounds. Diagnostic evaluation most often consisted of additional imaging with invasive procedures being performed infrequently.
Across the three screenings, most of the positive results were false positives – 96.4% in the CT group and 94.5% in the radiography group. Of the total number of low-dose CT screening tests, 24.2% were classified as positive and 23.4% had false-positive results; of the total number of radiographic screening tests, 6.9% were classified as positive and 6.5% were false-positive results.
In all, 1,060 lung cancers were diagnosed in the low-dose CT group (645/100,000 person-years) vs. 941 in the radiography group (572/100,000 person-years). Of these cancers, 649 in the low-dose CT group were diagnosed after a positive screening test and 44 were diagnosed after a negative screening test. In the radiography group, 279 cancers were diagnosed after a positive screening test and 137 were diagnosed after a negative screening test.
In both groups, the remaining cases were among participants who missed screening or were diagnosed after their trial screening phase was over
Analysis of lung cancer-specific mortality showed that in the CT group 356 lung cancer deaths occurred after 144,103 person-years; in the radiography group 443 lung cancer deaths occurred after 143,368 person-years. This corresponded to 247 and 309 lung cancer deaths, respectively, per 100,000 person-years in the CT and radiography groups.
There were 1,877 and 2,000 deaths from all causes in the CT and radiography groups, respectively, "representing a significant reduction with low-dose CT screening of 6.7% ... in the rate of death from any cause," the investigators wrote. While lung cancer accounted for 24.1% of all the deaths in the trial, 60.3% of the excess deaths in the radiography group were due to lung cancer.
The authors concluded that "although some agencies and organizations are contemplating the establishment of lung-cancer screening recommendations on the basis of the findings of the NLST, the current NLST data alone are, in our opinion, insufficient to fully inform such important decisions."
They noted that "The observation that low-dose CT screening can reduce the rate of death from lung cancer has generated many questions." Among these they listed: Will populations with different risk profiles benefit from screening? Could less frequent screening programs be equally effective? Would the use of different criteria for a positive screening result translate to similar benefit? For how long should people be screened?
In an accompanying editorial, Dr. Harold C. Sox, professor of medicine at the Dartmouth Institute in Hanover, N. H., agreed with the investigators’ reservations. In particular, the cost effectiveness of low-dose CT screening for lung cancer must be analyzed, he said: "Policy makers should wait for cost-effectiveness analyses to determine the amount of overdiagnosis in the NLST, and, perhaps identification of biologic markers of cancers that do not progress."
In addition, "it may be possible to define subgroups of smokers who are at higher or lower risk for lung cancer and tailor the screening strategy accordingly," he said. "The findings of the NLST regarding lung-cancer mortality signal the beginning of the end of one era of research on lung-cancer screening and the start of another. The focus will shift to informing the difficult patient-centered and policy decisions that are yet to come."
Dr. Sox also noted that "overdiagnosis is a problem because predicting which early-stage cancers will not progress is in an early stage of development, so that everyone with screen-detected cancer receives treatment that some do not need," he wrote in an accompanying editorial (doi: 10.1056/NEJME1103776).
All but two of the NLST study authors reported that they have no relevant financial relationships. Jonathan D. Clap reported having financial interest in Human Genome Sciences. Constantine Gatsonis, Ph.D., is a consultant for Wilex AG, Mela Sciences, and Endocyte Inc., has received speaker fees from Bayer Health and payment for education development by the Radiologic Society of North America. He also has invested in the Vanguard Health Fund. Dr. Sox had no conflicts.
Final results from the National Lung Screening Trial show a significant reduction in lung cancer mortality with the use of annual low-dose CT screening, compared with standard chest x-rays among former heavy smokers at high risk for lung cancer.
Low-dose CT screening led to a relative reduction of 20% in the rate of death from lung cancer, according to findings released online by the New England Journal of Medicine on June 29 (doi: 10.1056/NEJMoa1102873).The number needed to screen with low-dose CT to prevent one death from lung cancer was 320.
Although preliminary study results were announced in November 2010, the article by the National Lung Screening Trial (NLST) research team marks the first time that the results appear in a peer-reviewed journal. Acknowledging that the earlier announcement has led to calls for lung cancer screening, the authors urge rigorous analysis of cost-effectiveness before public policy recommendations are made.
"The reduction in lung-cancer mortality must be weighed against the harms from positive screening results and overdiagnosis, as well as the costs," they wrote.
In the study, 53,454 men and women aged 55-74 years – who were current or former smokers with a smoking history of at least 30 pack-years – were recruited at 33 U.S. medical centers. A total of 26,722 participants were randomized to receive three annual screens with low-dose helical CT; 26,732 were randomized to three annual screens using chest x-ray. The two groups were virtually identical in demographics and smoking history.
In all three screening rounds, positive screening tests were substantially more common in the low-dose CT group than in the radiography group (27.3% vs. 9.2% in the first round; 27.9% vs. 6.2% in the second; and 16.8% vs. 5% in the third). All told, 39.1% of the CT group and 16% of the radiography group had at least one positive result.
The percentage of screening tests that identified a clinically significant abnormality -- other than an abnormality suspicious for lung cancer – also was more than three times as high in the low-dose CT group as in the radiography group (7.5% vs. 2.1%).
More than 90% of positive screenings in the first round of the study led to a diagnostic evaluation, though the follow-up rates were lower in the later rounds. Diagnostic evaluation most often consisted of additional imaging with invasive procedures being performed infrequently.
Across the three screenings, most of the positive results were false positives – 96.4% in the CT group and 94.5% in the radiography group. Of the total number of low-dose CT screening tests, 24.2% were classified as positive and 23.4% had false-positive results; of the total number of radiographic screening tests, 6.9% were classified as positive and 6.5% were false-positive results.
In all, 1,060 lung cancers were diagnosed in the low-dose CT group (645/100,000 person-years) vs. 941 in the radiography group (572/100,000 person-years). Of these cancers, 649 in the low-dose CT group were diagnosed after a positive screening test and 44 were diagnosed after a negative screening test. In the radiography group, 279 cancers were diagnosed after a positive screening test and 137 were diagnosed after a negative screening test.
In both groups, the remaining cases were among participants who missed screening or were diagnosed after their trial screening phase was over
Analysis of lung cancer-specific mortality showed that in the CT group 356 lung cancer deaths occurred after 144,103 person-years; in the radiography group 443 lung cancer deaths occurred after 143,368 person-years. This corresponded to 247 and 309 lung cancer deaths, respectively, per 100,000 person-years in the CT and radiography groups.
There were 1,877 and 2,000 deaths from all causes in the CT and radiography groups, respectively, "representing a significant reduction with low-dose CT screening of 6.7% ... in the rate of death from any cause," the investigators wrote. While lung cancer accounted for 24.1% of all the deaths in the trial, 60.3% of the excess deaths in the radiography group were due to lung cancer.
The authors concluded that "although some agencies and organizations are contemplating the establishment of lung-cancer screening recommendations on the basis of the findings of the NLST, the current NLST data alone are, in our opinion, insufficient to fully inform such important decisions."
They noted that "The observation that low-dose CT screening can reduce the rate of death from lung cancer has generated many questions." Among these they listed: Will populations with different risk profiles benefit from screening? Could less frequent screening programs be equally effective? Would the use of different criteria for a positive screening result translate to similar benefit? For how long should people be screened?
In an accompanying editorial, Dr. Harold C. Sox, professor of medicine at the Dartmouth Institute in Hanover, N. H., agreed with the investigators’ reservations. In particular, the cost effectiveness of low-dose CT screening for lung cancer must be analyzed, he said: "Policy makers should wait for cost-effectiveness analyses to determine the amount of overdiagnosis in the NLST, and, perhaps identification of biologic markers of cancers that do not progress."
In addition, "it may be possible to define subgroups of smokers who are at higher or lower risk for lung cancer and tailor the screening strategy accordingly," he said. "The findings of the NLST regarding lung-cancer mortality signal the beginning of the end of one era of research on lung-cancer screening and the start of another. The focus will shift to informing the difficult patient-centered and policy decisions that are yet to come."
Dr. Sox also noted that "overdiagnosis is a problem because predicting which early-stage cancers will not progress is in an early stage of development, so that everyone with screen-detected cancer receives treatment that some do not need," he wrote in an accompanying editorial (doi: 10.1056/NEJME1103776).
All but two of the NLST study authors reported that they have no relevant financial relationships. Jonathan D. Clap reported having financial interest in Human Genome Sciences. Constantine Gatsonis, Ph.D., is a consultant for Wilex AG, Mela Sciences, and Endocyte Inc., has received speaker fees from Bayer Health and payment for education development by the Radiologic Society of North America. He also has invested in the Vanguard Health Fund. Dr. Sox had no conflicts.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major Finding: Low-dose CT screening reduced the relative rate of death from lung cancer by 20%, compared with chest x-ray screening.
Data Source: A study of 53,454 Americans aged 55-74 years, who were current or former smokers with a smoking history of at least 30 pack-years.
Disclosures: All but two of the NLST study authors reported that they have no relevant financial relationships. Jonathan Clap reported having financial interest in Human Genome Sciences Inc. Constantine Gatsonis is a consultant for Wilex AG, Mela Sciences, and Endocyte Inc., has received speaker fees from Bayer Health, and payment for education development by the Radiologic Society of North America. He also has invested in the Vanguard Health Fund. Dr. Sox had no conflicts.
The Government, Undercover
A quickly-scuttled plan by the Department of Health and Human Services (HHS) to use "mystery shoppers" to test the availability of primary-care physicians (PCPs) would likely never be extended to HM—but the federal tack has certainly touched a nerve with some practitioners. (Ed note: updated June 29, 2011)
"Using surrogate patients or a sneaky way to get the data feels a bit less straightforward," says James Levy, PA-C, vice president of personnel for Traverse City-based Hospitalists of Northern Michigan. "If I were the government, I'm sure it would occur to me to do it that way. Nobody is going to be comfortable with surreptitious observations. That would seem to carry the message that the government doesn’t trust the providers it's reimbursing."
The government proposed using people pretending to be patients, both insured and uninsured, to gauge how long it takes to get PCP appointments. The action was proposed in the April 28 Federal Register. Comments were solicited, but negative feedback prompted HHS to drop the plan in a June 29 announcement.
Levy and David Friar, MD, CEO of Northern Hospitalists, say that the logistics of hospital admission make it near impossible for the government to have anybody pose as something they're not. Still, in an email, Dr. Friar adds that, aside from "philosophical indignation," he would likely not object should HHS try a similar tack with hospitalist groups.
"In essence, every patient that sees a hospitalist is a mystery patient," he writes. "We don't control who comes in, or what their diagnosis is or when they'll arrive. We have little control over any of those things. Since payors are collecting data on every aspect of hospitalists’ performance, and what they aren't, the hospitals we work for are, we have little left to hide."
A quickly-scuttled plan by the Department of Health and Human Services (HHS) to use "mystery shoppers" to test the availability of primary-care physicians (PCPs) would likely never be extended to HM—but the federal tack has certainly touched a nerve with some practitioners. (Ed note: updated June 29, 2011)
"Using surrogate patients or a sneaky way to get the data feels a bit less straightforward," says James Levy, PA-C, vice president of personnel for Traverse City-based Hospitalists of Northern Michigan. "If I were the government, I'm sure it would occur to me to do it that way. Nobody is going to be comfortable with surreptitious observations. That would seem to carry the message that the government doesn’t trust the providers it's reimbursing."
The government proposed using people pretending to be patients, both insured and uninsured, to gauge how long it takes to get PCP appointments. The action was proposed in the April 28 Federal Register. Comments were solicited, but negative feedback prompted HHS to drop the plan in a June 29 announcement.
Levy and David Friar, MD, CEO of Northern Hospitalists, say that the logistics of hospital admission make it near impossible for the government to have anybody pose as something they're not. Still, in an email, Dr. Friar adds that, aside from "philosophical indignation," he would likely not object should HHS try a similar tack with hospitalist groups.
"In essence, every patient that sees a hospitalist is a mystery patient," he writes. "We don't control who comes in, or what their diagnosis is or when they'll arrive. We have little control over any of those things. Since payors are collecting data on every aspect of hospitalists’ performance, and what they aren't, the hospitals we work for are, we have little left to hide."
A quickly-scuttled plan by the Department of Health and Human Services (HHS) to use "mystery shoppers" to test the availability of primary-care physicians (PCPs) would likely never be extended to HM—but the federal tack has certainly touched a nerve with some practitioners. (Ed note: updated June 29, 2011)
"Using surrogate patients or a sneaky way to get the data feels a bit less straightforward," says James Levy, PA-C, vice president of personnel for Traverse City-based Hospitalists of Northern Michigan. "If I were the government, I'm sure it would occur to me to do it that way. Nobody is going to be comfortable with surreptitious observations. That would seem to carry the message that the government doesn’t trust the providers it's reimbursing."
The government proposed using people pretending to be patients, both insured and uninsured, to gauge how long it takes to get PCP appointments. The action was proposed in the April 28 Federal Register. Comments were solicited, but negative feedback prompted HHS to drop the plan in a June 29 announcement.
Levy and David Friar, MD, CEO of Northern Hospitalists, say that the logistics of hospital admission make it near impossible for the government to have anybody pose as something they're not. Still, in an email, Dr. Friar adds that, aside from "philosophical indignation," he would likely not object should HHS try a similar tack with hospitalist groups.
"In essence, every patient that sees a hospitalist is a mystery patient," he writes. "We don't control who comes in, or what their diagnosis is or when they'll arrive. We have little control over any of those things. Since payors are collecting data on every aspect of hospitalists’ performance, and what they aren't, the hospitals we work for are, we have little left to hide."
Statewide Initiative To Tackle Hospital Readmissions, Infections
The Quality Institute of the Ohio Hospital Association (OHA) recently launched its fifth regional quality collaborative in the state, bringing together hospital administrators, physicians, and other clinicians to tackle statewide goals of reducing infections, readmissions, and adverse events while increasing patient satisfaction. A hospitalist involved in the initiative says it sets an example for other states to follow.
"Hospitalists are on the front lines of quality," says Craig Cairns, MD, MPH, a hospitalist and vice president of medical affairs at Licking Memorial Health Systems in Newark, Ohio. "But it helps to get a statewide or regional group together to share problems and potential solutions."
Licking Memorial, for example, participates in OHA's statewide quality initiatives, including one on physician handwashing and STAAR (State Action on Avoidable Rehospitalizations), a multistate care-transitions initiative developed by the Institute for Healthcare Improvement.
Licking has set a goal of reducing its readmission rate to 10.5%, Dr. Cairns says. "Trying to get the patient back to the primary medical home as quickly as possible can be difficult," he adds. "We work with support people at medical offices to try to ensure a spot for our patients going home."
Because one of the risk factors for preventable rehospitalizations is heart failure, Licking also recently instituted a heart-failure clinic, staffed by two hospital cardiologists.
The first of the regional collaborations started in the Dayton area in 1998, according to David Engler, PhD, vice president of OHA's Quality Institute. The collaborative has posted a 36% reduction in heart-attack mortality over the past three years, the equivalent of 52 lives saved.
"We were brought in to help them on a specific issue: a higher-than-expected acute myocardial infarction mortality rate," Dr. Engler says. "We held collaborative meetings, developed risk management models, and began to track data across sites." Peer-review protocols developed by OHA make it possible to share quality data among the participating hospitals, with participants agreeing not to use these for marketing or competitive advantage.
A total of 133 hospitals participate in one of OHA's regional or statewide quality collaborations.
The Quality Institute of the Ohio Hospital Association (OHA) recently launched its fifth regional quality collaborative in the state, bringing together hospital administrators, physicians, and other clinicians to tackle statewide goals of reducing infections, readmissions, and adverse events while increasing patient satisfaction. A hospitalist involved in the initiative says it sets an example for other states to follow.
"Hospitalists are on the front lines of quality," says Craig Cairns, MD, MPH, a hospitalist and vice president of medical affairs at Licking Memorial Health Systems in Newark, Ohio. "But it helps to get a statewide or regional group together to share problems and potential solutions."
Licking Memorial, for example, participates in OHA's statewide quality initiatives, including one on physician handwashing and STAAR (State Action on Avoidable Rehospitalizations), a multistate care-transitions initiative developed by the Institute for Healthcare Improvement.
Licking has set a goal of reducing its readmission rate to 10.5%, Dr. Cairns says. "Trying to get the patient back to the primary medical home as quickly as possible can be difficult," he adds. "We work with support people at medical offices to try to ensure a spot for our patients going home."
Because one of the risk factors for preventable rehospitalizations is heart failure, Licking also recently instituted a heart-failure clinic, staffed by two hospital cardiologists.
The first of the regional collaborations started in the Dayton area in 1998, according to David Engler, PhD, vice president of OHA's Quality Institute. The collaborative has posted a 36% reduction in heart-attack mortality over the past three years, the equivalent of 52 lives saved.
"We were brought in to help them on a specific issue: a higher-than-expected acute myocardial infarction mortality rate," Dr. Engler says. "We held collaborative meetings, developed risk management models, and began to track data across sites." Peer-review protocols developed by OHA make it possible to share quality data among the participating hospitals, with participants agreeing not to use these for marketing or competitive advantage.
A total of 133 hospitals participate in one of OHA's regional or statewide quality collaborations.
The Quality Institute of the Ohio Hospital Association (OHA) recently launched its fifth regional quality collaborative in the state, bringing together hospital administrators, physicians, and other clinicians to tackle statewide goals of reducing infections, readmissions, and adverse events while increasing patient satisfaction. A hospitalist involved in the initiative says it sets an example for other states to follow.
"Hospitalists are on the front lines of quality," says Craig Cairns, MD, MPH, a hospitalist and vice president of medical affairs at Licking Memorial Health Systems in Newark, Ohio. "But it helps to get a statewide or regional group together to share problems and potential solutions."
Licking Memorial, for example, participates in OHA's statewide quality initiatives, including one on physician handwashing and STAAR (State Action on Avoidable Rehospitalizations), a multistate care-transitions initiative developed by the Institute for Healthcare Improvement.
Licking has set a goal of reducing its readmission rate to 10.5%, Dr. Cairns says. "Trying to get the patient back to the primary medical home as quickly as possible can be difficult," he adds. "We work with support people at medical offices to try to ensure a spot for our patients going home."
Because one of the risk factors for preventable rehospitalizations is heart failure, Licking also recently instituted a heart-failure clinic, staffed by two hospital cardiologists.
The first of the regional collaborations started in the Dayton area in 1998, according to David Engler, PhD, vice president of OHA's Quality Institute. The collaborative has posted a 36% reduction in heart-attack mortality over the past three years, the equivalent of 52 lives saved.
"We were brought in to help them on a specific issue: a higher-than-expected acute myocardial infarction mortality rate," Dr. Engler says. "We held collaborative meetings, developed risk management models, and began to track data across sites." Peer-review protocols developed by OHA make it possible to share quality data among the participating hospitals, with participants agreeing not to use these for marketing or competitive advantage.
A total of 133 hospitals participate in one of OHA's regional or statewide quality collaborations.
Impact of Fellowship Programs on Residents' Case Logs Examined
BOCA RATON, FLA. – Coexisting subspecialty fellowship programs have at most only minimal adverse impact on general surgery residency training operative volumes, according to a national study sponsored by the American Board of Surgery.
The analysis also demonstrated that fellowship-bound general surgery residents tend to select additional cases in their chosen future subspecialty, thereby in effect creating a self-directed early tracking program, Dr. John B. Hanks said at the annual meeting of the American Surgical Association.
The American Board of Surgery (ABS) conducted the study in response to concerns that because 80% of general surgery residents pursue fellowship training, an insufficient number of cases could be available for resident training. But the national data indicate that this is not a problem, according to Dr. Hanks, professor and chief of general surgery at the University of Virginia, Charlottesville.
The study entailed detailed analysis of the operative logs of 976 applicants to the 2009 ABS qualifying exam. The applicants came from 246 general surgery residency programs. In all, 97 of these residency programs coexisted with a vascular surgery fellowship program, 35 with a colorectal surgery fellowship program, 80 with a minimally invasive surgery training program, and 12 with an endocrine surgery fellowship program. The investigators scrutinized case volumes for predefined key operations in the areas of vascular, colorectal, endocrine, and minimally invasive surgery (MIS).
Residents bound for fellowships in vascular, colorectal, and endocrine surgery performed significantly more total cases in each of those areas than did general surgery residents who were not bound for fellowships. For example, operative logs for the 90 vascular surgery fellowship–bound residents showed a mean experience of 165 vascular cases, compared with 123 cases for the other general surgery residents. And residents headed for colorectal surgery fellowships had a mean of 204 colorectal surgery cases, compared with 163 for all other general surgery residents.
In contrast, residents who were headed for an MIS fellowship and those who were not averaged a similar number of minimally invasive operations.
With regard to the effect of coexisting fellowship programs on general surgery residents’ operative experience in those specific areas, there was a negative impact only for MIS. Residents in general surgery training programs with a coexisting MIS fellowship averaged about 10% fewer MIS cases than did residents in institutions without a fellowship.
"That difference reaches statistical significance, although the practical significance of this effect may be open for debate," Dr. Hanks observed.
The situation was different for residents at institutions with coexisting colorectal or vascular surgery fellowships; those fellowships had no impact on general surgery residents’ case volumes in those specialty-specific areas. And the presence of a coexisting endocrine surgery fellowship was actually associated with a significant increase in endocrine surgery case volumes for all residents, he continued.
Discussant Dr. Layton F. Rikkers cautioned that the ABS study describes national trends using broad strokes, and the data don’t necessarily apply to any individual residency program.
"As an example, the only fellowship we developed at the University of Wisconsin, Madison, during the time I was chairman there was a vascular surgery fellowship," said Dr. Rikkers, professor of surgery at the university and past president of the ABS. "The year prior to developing the fellowship, our residents were in the 93rd percentile nationally with respect to vascular surgery cases done. Over the many years since that fellowship was established, our residents are in the 10th to 20th percentile for vascular surgery cases."
Dr. Hanks declared having no financial conflict of interest.
The significance of this is hard to determine, precisely because of the reason stated by Dr. Rikkers – impact on individual programs cannot be assessed, and likely varies greatly from program to program. For example, in some instances the additional specialty cases may be uncovered by residents, and in that situation no impact would be seen. In others, the cases might be directly "poached" from the general surgery residencies. A final scenario might be one in which an initial downturn is seen in general surgery cases, which is overcome over a period of years as the presence of a fellowship often drives up case volumes at an institution.
Another confounding issue generated by the lack of individual institutional information is that the case volumes in certain specialties may be higher in institutions that attract more residents to a specific field – prominence of a specialty in a given institution may impact resident choice of specialty. Indeed, rather than residents choosing to do more cases in their chosen field, they may in fact have chosen their field based on greater exposure to the specialty. This cannot be parsed out from the data at hand.
No mention is made of the involvement of the residents in the pre-operative and post-operative care of the patients when participation is outside of usual service assignments. If this is not robust, benefits to patients and trainees may be lessened.
Dr. Cynthia K. Shortell is a professor of surgery and chief of vascular surgery and program director, vascular residency at Duke University Medical Center, Durham, N.C., and an associate medical editor for Vascular Specialist.
The significance of this is hard to determine, precisely because of the reason stated by Dr. Rikkers – impact on individual programs cannot be assessed, and likely varies greatly from program to program. For example, in some instances the additional specialty cases may be uncovered by residents, and in that situation no impact would be seen. In others, the cases might be directly "poached" from the general surgery residencies. A final scenario might be one in which an initial downturn is seen in general surgery cases, which is overcome over a period of years as the presence of a fellowship often drives up case volumes at an institution.
Another confounding issue generated by the lack of individual institutional information is that the case volumes in certain specialties may be higher in institutions that attract more residents to a specific field – prominence of a specialty in a given institution may impact resident choice of specialty. Indeed, rather than residents choosing to do more cases in their chosen field, they may in fact have chosen their field based on greater exposure to the specialty. This cannot be parsed out from the data at hand.
No mention is made of the involvement of the residents in the pre-operative and post-operative care of the patients when participation is outside of usual service assignments. If this is not robust, benefits to patients and trainees may be lessened.
Dr. Cynthia K. Shortell is a professor of surgery and chief of vascular surgery and program director, vascular residency at Duke University Medical Center, Durham, N.C., and an associate medical editor for Vascular Specialist.
The significance of this is hard to determine, precisely because of the reason stated by Dr. Rikkers – impact on individual programs cannot be assessed, and likely varies greatly from program to program. For example, in some instances the additional specialty cases may be uncovered by residents, and in that situation no impact would be seen. In others, the cases might be directly "poached" from the general surgery residencies. A final scenario might be one in which an initial downturn is seen in general surgery cases, which is overcome over a period of years as the presence of a fellowship often drives up case volumes at an institution.
Another confounding issue generated by the lack of individual institutional information is that the case volumes in certain specialties may be higher in institutions that attract more residents to a specific field – prominence of a specialty in a given institution may impact resident choice of specialty. Indeed, rather than residents choosing to do more cases in their chosen field, they may in fact have chosen their field based on greater exposure to the specialty. This cannot be parsed out from the data at hand.
No mention is made of the involvement of the residents in the pre-operative and post-operative care of the patients when participation is outside of usual service assignments. If this is not robust, benefits to patients and trainees may be lessened.
Dr. Cynthia K. Shortell is a professor of surgery and chief of vascular surgery and program director, vascular residency at Duke University Medical Center, Durham, N.C., and an associate medical editor for Vascular Specialist.
BOCA RATON, FLA. – Coexisting subspecialty fellowship programs have at most only minimal adverse impact on general surgery residency training operative volumes, according to a national study sponsored by the American Board of Surgery.
The analysis also demonstrated that fellowship-bound general surgery residents tend to select additional cases in their chosen future subspecialty, thereby in effect creating a self-directed early tracking program, Dr. John B. Hanks said at the annual meeting of the American Surgical Association.
The American Board of Surgery (ABS) conducted the study in response to concerns that because 80% of general surgery residents pursue fellowship training, an insufficient number of cases could be available for resident training. But the national data indicate that this is not a problem, according to Dr. Hanks, professor and chief of general surgery at the University of Virginia, Charlottesville.
The study entailed detailed analysis of the operative logs of 976 applicants to the 2009 ABS qualifying exam. The applicants came from 246 general surgery residency programs. In all, 97 of these residency programs coexisted with a vascular surgery fellowship program, 35 with a colorectal surgery fellowship program, 80 with a minimally invasive surgery training program, and 12 with an endocrine surgery fellowship program. The investigators scrutinized case volumes for predefined key operations in the areas of vascular, colorectal, endocrine, and minimally invasive surgery (MIS).
Residents bound for fellowships in vascular, colorectal, and endocrine surgery performed significantly more total cases in each of those areas than did general surgery residents who were not bound for fellowships. For example, operative logs for the 90 vascular surgery fellowship–bound residents showed a mean experience of 165 vascular cases, compared with 123 cases for the other general surgery residents. And residents headed for colorectal surgery fellowships had a mean of 204 colorectal surgery cases, compared with 163 for all other general surgery residents.
In contrast, residents who were headed for an MIS fellowship and those who were not averaged a similar number of minimally invasive operations.
With regard to the effect of coexisting fellowship programs on general surgery residents’ operative experience in those specific areas, there was a negative impact only for MIS. Residents in general surgery training programs with a coexisting MIS fellowship averaged about 10% fewer MIS cases than did residents in institutions without a fellowship.
"That difference reaches statistical significance, although the practical significance of this effect may be open for debate," Dr. Hanks observed.
The situation was different for residents at institutions with coexisting colorectal or vascular surgery fellowships; those fellowships had no impact on general surgery residents’ case volumes in those specialty-specific areas. And the presence of a coexisting endocrine surgery fellowship was actually associated with a significant increase in endocrine surgery case volumes for all residents, he continued.
Discussant Dr. Layton F. Rikkers cautioned that the ABS study describes national trends using broad strokes, and the data don’t necessarily apply to any individual residency program.
"As an example, the only fellowship we developed at the University of Wisconsin, Madison, during the time I was chairman there was a vascular surgery fellowship," said Dr. Rikkers, professor of surgery at the university and past president of the ABS. "The year prior to developing the fellowship, our residents were in the 93rd percentile nationally with respect to vascular surgery cases done. Over the many years since that fellowship was established, our residents are in the 10th to 20th percentile for vascular surgery cases."
Dr. Hanks declared having no financial conflict of interest.
BOCA RATON, FLA. – Coexisting subspecialty fellowship programs have at most only minimal adverse impact on general surgery residency training operative volumes, according to a national study sponsored by the American Board of Surgery.
The analysis also demonstrated that fellowship-bound general surgery residents tend to select additional cases in their chosen future subspecialty, thereby in effect creating a self-directed early tracking program, Dr. John B. Hanks said at the annual meeting of the American Surgical Association.
The American Board of Surgery (ABS) conducted the study in response to concerns that because 80% of general surgery residents pursue fellowship training, an insufficient number of cases could be available for resident training. But the national data indicate that this is not a problem, according to Dr. Hanks, professor and chief of general surgery at the University of Virginia, Charlottesville.
The study entailed detailed analysis of the operative logs of 976 applicants to the 2009 ABS qualifying exam. The applicants came from 246 general surgery residency programs. In all, 97 of these residency programs coexisted with a vascular surgery fellowship program, 35 with a colorectal surgery fellowship program, 80 with a minimally invasive surgery training program, and 12 with an endocrine surgery fellowship program. The investigators scrutinized case volumes for predefined key operations in the areas of vascular, colorectal, endocrine, and minimally invasive surgery (MIS).
Residents bound for fellowships in vascular, colorectal, and endocrine surgery performed significantly more total cases in each of those areas than did general surgery residents who were not bound for fellowships. For example, operative logs for the 90 vascular surgery fellowship–bound residents showed a mean experience of 165 vascular cases, compared with 123 cases for the other general surgery residents. And residents headed for colorectal surgery fellowships had a mean of 204 colorectal surgery cases, compared with 163 for all other general surgery residents.
In contrast, residents who were headed for an MIS fellowship and those who were not averaged a similar number of minimally invasive operations.
With regard to the effect of coexisting fellowship programs on general surgery residents’ operative experience in those specific areas, there was a negative impact only for MIS. Residents in general surgery training programs with a coexisting MIS fellowship averaged about 10% fewer MIS cases than did residents in institutions without a fellowship.
"That difference reaches statistical significance, although the practical significance of this effect may be open for debate," Dr. Hanks observed.
The situation was different for residents at institutions with coexisting colorectal or vascular surgery fellowships; those fellowships had no impact on general surgery residents’ case volumes in those specialty-specific areas. And the presence of a coexisting endocrine surgery fellowship was actually associated with a significant increase in endocrine surgery case volumes for all residents, he continued.
Discussant Dr. Layton F. Rikkers cautioned that the ABS study describes national trends using broad strokes, and the data don’t necessarily apply to any individual residency program.
"As an example, the only fellowship we developed at the University of Wisconsin, Madison, during the time I was chairman there was a vascular surgery fellowship," said Dr. Rikkers, professor of surgery at the university and past president of the ABS. "The year prior to developing the fellowship, our residents were in the 93rd percentile nationally with respect to vascular surgery cases done. Over the many years since that fellowship was established, our residents are in the 10th to 20th percentile for vascular surgery cases."
Dr. Hanks declared having no financial conflict of interest.
New Options to Treat Hepatitis C
Enter text here
Enter text here
Enter text here
New Options to Treat Hepatitis C
Two new drug therapies to treat chronic hepatitis C (HCV) are the first new options for hospitalists in 20 years. But freedom of choice doesn't come cheap.
Telaprevir, from Vertex Pharmaceuticals, will cost $49,200 for a 12-week regimen, while boceprevir, from Merck & Co., will cost from $26,400 to $48,000 for regimens of 24 and 48 weeks, respectively, Reuters reports. Telaprevir will go by the brand name Incivek, while boceprevir is known as Victrelis.
"The price is expensive," but financial support for some patients is expected early on, says Satya Chelamkuri, MD, a hospitalist with Cogent Healthcare at Allegiance Health in Jackson, Mich. "When the generic comes out, it will be a great help to patients with hepatitis C. Cost is a worry, but with help from pharmaceutical companies, the majority of the patients who need it will hopefully get the treatment."
Still, Dr. Chelamkuri expects the drugs to appear relatively quickly on hospital formularies, in large part because of the efficacy they showed in trials. The standard treatment for years, a cocktail of peginterferon-alpha and ribavirin, has a roughly 50% response rate. Both of the new treatments, which have been formally approved by the FDA in the past six weeks, boost the cure rates to a range of 66% to 80% by working in tandem with the current therapy.
"A less than 50% [response rate] for the previous regime and around 70% for the new regime. That’s a considerable difference," Dr. Chelamkuri says.
Two new drug therapies to treat chronic hepatitis C (HCV) are the first new options for hospitalists in 20 years. But freedom of choice doesn't come cheap.
Telaprevir, from Vertex Pharmaceuticals, will cost $49,200 for a 12-week regimen, while boceprevir, from Merck & Co., will cost from $26,400 to $48,000 for regimens of 24 and 48 weeks, respectively, Reuters reports. Telaprevir will go by the brand name Incivek, while boceprevir is known as Victrelis.
"The price is expensive," but financial support for some patients is expected early on, says Satya Chelamkuri, MD, a hospitalist with Cogent Healthcare at Allegiance Health in Jackson, Mich. "When the generic comes out, it will be a great help to patients with hepatitis C. Cost is a worry, but with help from pharmaceutical companies, the majority of the patients who need it will hopefully get the treatment."
Still, Dr. Chelamkuri expects the drugs to appear relatively quickly on hospital formularies, in large part because of the efficacy they showed in trials. The standard treatment for years, a cocktail of peginterferon-alpha and ribavirin, has a roughly 50% response rate. Both of the new treatments, which have been formally approved by the FDA in the past six weeks, boost the cure rates to a range of 66% to 80% by working in tandem with the current therapy.
"A less than 50% [response rate] for the previous regime and around 70% for the new regime. That’s a considerable difference," Dr. Chelamkuri says.
Two new drug therapies to treat chronic hepatitis C (HCV) are the first new options for hospitalists in 20 years. But freedom of choice doesn't come cheap.
Telaprevir, from Vertex Pharmaceuticals, will cost $49,200 for a 12-week regimen, while boceprevir, from Merck & Co., will cost from $26,400 to $48,000 for regimens of 24 and 48 weeks, respectively, Reuters reports. Telaprevir will go by the brand name Incivek, while boceprevir is known as Victrelis.
"The price is expensive," but financial support for some patients is expected early on, says Satya Chelamkuri, MD, a hospitalist with Cogent Healthcare at Allegiance Health in Jackson, Mich. "When the generic comes out, it will be a great help to patients with hepatitis C. Cost is a worry, but with help from pharmaceutical companies, the majority of the patients who need it will hopefully get the treatment."
Still, Dr. Chelamkuri expects the drugs to appear relatively quickly on hospital formularies, in large part because of the efficacy they showed in trials. The standard treatment for years, a cocktail of peginterferon-alpha and ribavirin, has a roughly 50% response rate. Both of the new treatments, which have been formally approved by the FDA in the past six weeks, boost the cure rates to a range of 66% to 80% by working in tandem with the current therapy.
"A less than 50% [response rate] for the previous regime and around 70% for the new regime. That’s a considerable difference," Dr. Chelamkuri says.
In the Literature: Research You Need to Know
Clinical question: Does the mortality rate differ between patients treated perioperatively with atenolol versus metoprolol?
Background: Perioperative beta-blockers have been shown to reduce mortality in patients with significant cardiac risk factors. Different beta-blockers have been used in the studies demonstrating benefit, and it is uncertain which beta-blocker is the preferred agent. The purpose of this study was to compare the perioperative benefits of metoprolol versus atenolol.
Study design: Retrospective cohort study.
Setting: San Francisco Veterans Affairs Medical Center.
Synopsis: Computerized records of patients who underwent surgery from 1996 to 2008 were extracted into a database, and patients who received inpatient beta-blockers after surgery were included. Of these patients, 3,787 received beta-blockade exclusively with either atenolol (n=1,011) or metoprolol (n=2,776) during hospitalization. Perioperative risk reduction was better with atenolol versus metoprolol. Mortality rates were 1% versus 3% at 30 days (P=0.0008), and 7% versus 13% at one year (P=<0.0001) with atenolol and metoprolol, respectively. Similar results were found in the analysis of 1,871 patients who were on their respective beta-blocker as an outpatient before surgery.
Because the metoprolol group had higher prevalence of risk factors, such as coronary artery disease, peripheral vascular disease, and congestive heart failure, a propensity-matched analysis was performed to remove differences in risk factors between the groups. After propensity matching, the metoprolol group still had statistically significant higher mortality at 30 days and one year, even though causality cannot be established in this retrospective study.
Bottom line: Atenolol was associated with fewer cases of perioperative mortality compared with metoprolol in patients with cardiac risk factors or established cardiovascular disease.
Citation: Wallace AW, Au S, Cason BA. Perioperative ß-blockade: atenolol is associated with reduced mortality when compared to metoprolol. Anesthesiology. 2011;114:824-836.
For more physician reviews of HM-related research, visit our website.
Clinical question: Does the mortality rate differ between patients treated perioperatively with atenolol versus metoprolol?
Background: Perioperative beta-blockers have been shown to reduce mortality in patients with significant cardiac risk factors. Different beta-blockers have been used in the studies demonstrating benefit, and it is uncertain which beta-blocker is the preferred agent. The purpose of this study was to compare the perioperative benefits of metoprolol versus atenolol.
Study design: Retrospective cohort study.
Setting: San Francisco Veterans Affairs Medical Center.
Synopsis: Computerized records of patients who underwent surgery from 1996 to 2008 were extracted into a database, and patients who received inpatient beta-blockers after surgery were included. Of these patients, 3,787 received beta-blockade exclusively with either atenolol (n=1,011) or metoprolol (n=2,776) during hospitalization. Perioperative risk reduction was better with atenolol versus metoprolol. Mortality rates were 1% versus 3% at 30 days (P=0.0008), and 7% versus 13% at one year (P=<0.0001) with atenolol and metoprolol, respectively. Similar results were found in the analysis of 1,871 patients who were on their respective beta-blocker as an outpatient before surgery.
Because the metoprolol group had higher prevalence of risk factors, such as coronary artery disease, peripheral vascular disease, and congestive heart failure, a propensity-matched analysis was performed to remove differences in risk factors between the groups. After propensity matching, the metoprolol group still had statistically significant higher mortality at 30 days and one year, even though causality cannot be established in this retrospective study.
Bottom line: Atenolol was associated with fewer cases of perioperative mortality compared with metoprolol in patients with cardiac risk factors or established cardiovascular disease.
Citation: Wallace AW, Au S, Cason BA. Perioperative ß-blockade: atenolol is associated with reduced mortality when compared to metoprolol. Anesthesiology. 2011;114:824-836.
For more physician reviews of HM-related research, visit our website.
Clinical question: Does the mortality rate differ between patients treated perioperatively with atenolol versus metoprolol?
Background: Perioperative beta-blockers have been shown to reduce mortality in patients with significant cardiac risk factors. Different beta-blockers have been used in the studies demonstrating benefit, and it is uncertain which beta-blocker is the preferred agent. The purpose of this study was to compare the perioperative benefits of metoprolol versus atenolol.
Study design: Retrospective cohort study.
Setting: San Francisco Veterans Affairs Medical Center.
Synopsis: Computerized records of patients who underwent surgery from 1996 to 2008 were extracted into a database, and patients who received inpatient beta-blockers after surgery were included. Of these patients, 3,787 received beta-blockade exclusively with either atenolol (n=1,011) or metoprolol (n=2,776) during hospitalization. Perioperative risk reduction was better with atenolol versus metoprolol. Mortality rates were 1% versus 3% at 30 days (P=0.0008), and 7% versus 13% at one year (P=<0.0001) with atenolol and metoprolol, respectively. Similar results were found in the analysis of 1,871 patients who were on their respective beta-blocker as an outpatient before surgery.
Because the metoprolol group had higher prevalence of risk factors, such as coronary artery disease, peripheral vascular disease, and congestive heart failure, a propensity-matched analysis was performed to remove differences in risk factors between the groups. After propensity matching, the metoprolol group still had statistically significant higher mortality at 30 days and one year, even though causality cannot be established in this retrospective study.
Bottom line: Atenolol was associated with fewer cases of perioperative mortality compared with metoprolol in patients with cardiac risk factors or established cardiovascular disease.
Citation: Wallace AW, Au S, Cason BA. Perioperative ß-blockade: atenolol is associated with reduced mortality when compared to metoprolol. Anesthesiology. 2011;114:824-836.
For more physician reviews of HM-related research, visit our website.
FDA Unveils Graphic Cigarette Packaging Intended to Deter Smoking
The Food and Drug Administration unveiled on June 21 the final nine warning images that will appear on every package of cigarettes by 2012 – graphic photos and drawings intended to educate and even deter consumers from buying cigarettes.
The images, set to debut in stores this September, are required by the 2009 Tobacco Control Act, according to FDA spokesman Jeffrey Ventura, who added that these are the first changes to cigarette pack warnings in 25 years. By Oct. 22, 2012, cigarette manufacturers will no longer be able to distribute cigarettes for sale in the United States unless they display these warnings.
The law required the warnings to cover the top half of the front and back of cigarette packs and 20% of cigarette advertisements, and they must contain color graphics depicting the negative health consequences of smoking.
"This is something Congress wanted to happen and mandated that the FDA carry out," Mr. Ventura said in an interview. Based on a study of 18,000 smokers conducted for the FDA by RTI International, federal officials said they firmly believe that visually communicating smoking’s harm will deter cigarette consumption over the long run.
The images include photos of tobacco-diseased lungs beside healthy lungs, a corpse in casket, a man exhaling smoke though a tracheostomy, and lip cancer. There are also several cartoons and photos of mothers blowing smoke into infants’ faces. One positive image shows a burly man exposing a T-shirt saying, "I Quit."
Blunt statements accompany each image, intended to drive home the messages that cigarette smoke not only directly harms the smoker, but the smokers’ children and people in close proximity.
"The introduction of these warnings is expected to have a significant public health impact by decreasing the number of smokers, resulting in lives saved, increased life expectancy, and improved health status," FDA officials said in a press statement.
Mr. Ventura said the images were selected after the consumer study involving smokers aged 15-50 years. After viewing each of the images, subjects rated their emotional and cognitive responses, their ability to recall the images, and their opinions on whether the pictures could alter their beliefs about the danger of smoking and the desire to buy tobacco products and quitting tobacco.
Young people responded most strongly to a cartoon image depicting tobacco addiction – a cigarette being injected into an arm vein as well as a puppet controlled by strings.
Adults, on the other hand, responded most strongly to photos showing the direct effects of cancer on their bodies – the man with the tracheostomy and a woman smoking in the pouring rain, trying to shield her cigarette with a folded newspaper. Adults also reacted more strongly than did young people to images depicting harm to young children.
The study did conclude, however, that none of the images were significantly related to an increased likelihood of quitting smoking within the next 30 days, or the likelihood of smoking a year after viewing the images. Thus, the report noted, the campaign is more likely to exert a long-term behavioral impact than any immediate effects.
"Eliciting strong emotional and cognitive reactions to the graphic cigarette warning label enhances recall and processing of the health warning, which helps ensure that the warning is better processed, understood, and remembered," the study said. "As attitudes and beliefs change, they eventually lead to changes in intentions to quit or start smoking and then later to lower smoking initiation and successful cessation. The time scale on which this behavior change process occurs is largely unknown in the context of the impact of exposure to graphic warning labels on smoking behaviors, but the effects on behavior change are unlikely to be immediate or short-term.
Nevertheless, groups promoting antitobacco messages – including the American Heart Association – strongly believe that the warnings will enhance consumer education and change behavior.
"Undoubtedly, the new graphic health warnings will heighten awareness about the dangers of smoking and, more importantly, encourage smokers to quit and discourage smoking initiation," an AHA press statement read. "We’re confident that the new labels will move us closer to our goal of making the nation 100% smoke free."
Tobacco-Free Kids, a group dedicated to educating children and teens about the dangers of smoking, also issued a statement of support, but with a moderated view on the campaign’s possible impact. The group also called on political leaders to financially commit to "waging war" against tobacco.
"The warnings and other FDA regulations are powerful tools, but they are a complement – not a replacement – to other federal and state strategies to reduce tobacco use," Matthew L. Meyers, the group’s president, said in the statement. "To win the fight against tobacco, elected leaders must also fund and implement public education campaigns, expand health care coverage for therapies to help smokers quit, increase tobacco taxes, and enact strong smoke-free laws in every state."
I give the FDA a
“B” on this action, but I don’t think it’s enough. Congress could have decided on
much stronger pictures. It could have made them larger, not just 20% of the
pack and located on the back . In other countries that use such warnings, the
pictures cover almost 80% of the packaging.
Plainly put, the United States is a Third
World country when it comes to warning about cigarettes. Similar
pictorial warnings have been used in Canada
for almost a decade; Australia,
almost all of the European Union countries, and even Uruguay have similar warnings.
Having said that, we do know
that pictures speak louder than words and may help motivate smokers to quit.
But here is the hard reality: Even though nearly everyone wants to quit smoking
and many are trying to do so every day, the ability to sustain that motivation
is not always present.
Two factors are highly
predictive of a successful quit: the clinical predictor of personal biology and
the financial predictor of cigarette engineering.
Biologically, some people
are more prone to developing addictions than others. If you have a patient who
reaches for a cigarette before their feet even hit the floor in the morning,
that patient is going to need more medical assistance to be successful.
The second factor is
cigarette engineering. Cigarettes are designed to get people hooked and keep
them hooked. This is what makes quitting so hard despite strong personal motivation.
If we look back in
history, around 1900 there were only a few hundred cases of lung cancer
diagnosed in the U.S.
each year. This year it will be around 160,000. What has happened since then?
People were indeed smoking
then – pipes, cigars, and roll-your-own cigarettes. But this was not a daily-use
situation, mostly because the pH of the smoke made it very hard to inhale.
Right around 1920, commercially available cigarette brands reformulated their
tobacco to make the smoke milder. This allowed people to smoke more, loading
their brains up with lots more nicotine, lots faster.
Around 1950, manufacturers
began adding chemicals to moderate the pH, facilitating deep inhalation. the
lungs. These ingredients – diammonium phosphate, urea, and hydrochloride among
them – are still on the packs’ ingredient list, although manufacturers call
them “flavorings.”
Filters were the next step
in developing an addictive product. Manufacturers presented filters as making
cigarettes safer. Their real purpose was both to break down the tar into
smaller particles and to force people to suck on the cigarette harder to get
the smoke. Filters actually make things worse by forcing rapid inhalation and
rapid absorption – delivering the nicotine to the brain within seconds.
These things were done
secretly and purposefully to promote tobacco addiction and maintain profits. Tobacco
companies deliberately suppressed this information until 2006, when a
racketeering lawsuit forced the disclosure of dozens of documents showing the
intention behind these decisions. U.S District Court Judge Gladys Kessler determined
that tobacco companies conspired to lie about the dangers of smoking and, in
her 1,600-page ruling, called the conspiracy “decades long.”
“In short, the defendants
have marketed and sold their lethal product with zeal, with deception, with a
single-minded focus on their financial success, and without regard for the
human tragedy or social costs that success exacted,” according to her ruling.
Despite lawsuits, public
information campaigns, and the current warnings on cigarette packs, Americans
continue to smoke and I continue to see the effects.
About a third of the
patients I see at the Roswell Park Cancer Institute have smoking-related
cancers. Imagine a vaccine that would prevent a third of cancers. The inventor would
be a Nobel Laureate, globally praised.
We already have this – but
it’s not a vaccine. It’s much simpler.
Just stop smoking.
K. Michael Cummings,
Ph.D, is the director of the New York State Smokers’ Quitline and a senior research
scientist at the Roswell Park cancer Institute, Buffalo.
The images, set to debut in stores this September, are required by the 2009 Tobacco Control Act, according to FDA spokesman Jeffrey Ventura, who added that these are the first changes to cigarette pack warnings
I give the FDA a
“B” on this action, but I don’t think it’s enough. Congress could have decided on
much stronger pictures. It could have made them larger, not just 20% of the
pack and located on the back . In other countries that use such warnings, the
pictures cover almost 80% of the packaging.
Plainly put, the United States is a Third
World country when it comes to warning about cigarettes. Similar
pictorial warnings have been used in Canada
for almost a decade; Australia,
almost all of the European Union countries, and even Uruguay have similar warnings.
Having said that, we do know
that pictures speak louder than words and may help motivate smokers to quit.
But here is the hard reality: Even though nearly everyone wants to quit smoking
and many are trying to do so every day, the ability to sustain that motivation
is not always present.
Two factors are highly
predictive of a successful quit: the clinical predictor of personal biology and
the financial predictor of cigarette engineering.
Biologically, some people
are more prone to developing addictions than others. If you have a patient who
reaches for a cigarette before their feet even hit the floor in the morning,
that patient is going to need more medical assistance to be successful.
The second factor is
cigarette engineering. Cigarettes are designed to get people hooked and keep
them hooked. This is what makes quitting so hard despite strong personal motivation.
If we look back in
history, around 1900 there were only a few hundred cases of lung cancer
diagnosed in the U.S.
each year. This year it will be around 160,000. What has happened since then?
People were indeed smoking
then – pipes, cigars, and roll-your-own cigarettes. But this was not a daily-use
situation, mostly because the pH of the smoke made it very hard to inhale.
Right around 1920, commercially available cigarette brands reformulated their
tobacco to make the smoke milder. This allowed people to smoke more, loading
their brains up with lots more nicotine, lots faster.
Around 1950, manufacturers
began adding chemicals to moderate the pH, facilitating deep inhalation. the
lungs. These ingredients – diammonium phosphate, urea, and hydrochloride among
them – are still on the packs’ ingredient list, although manufacturers call
them “flavorings.”
Filters were the next step
in developing an addictive product. Manufacturers presented filters as making
cigarettes safer. Their real purpose was both to break down the tar into
smaller particles and to force people to suck on the cigarette harder to get
the smoke. Filters actually make things worse by forcing rapid inhalation and
rapid absorption – delivering the nicotine to the brain within seconds.
These things were done
secretly and purposefully to promote tobacco addiction and maintain profits. Tobacco
companies deliberately suppressed this information until 2006, when a
racketeering lawsuit forced the disclosure of dozens of documents showing the
intention behind these decisions. U.S District Court Judge Gladys Kessler determined
that tobacco companies conspired to lie about the dangers of smoking and, in
her 1,600-page ruling, called the conspiracy “decades long.”
“In short, the defendants
have marketed and sold their lethal product with zeal, with deception, with a
single-minded focus on their financial success, and without regard for the
human tragedy or social costs that success exacted,” according to her ruling.
Despite lawsuits, public
information campaigns, and the current warnings on cigarette packs, Americans
continue to smoke and I continue to see the effects.
About a third of the
patients I see at the Roswell Park Cancer Institute have smoking-related
cancers. Imagine a vaccine that would prevent a third of cancers. The inventor would
be a Nobel Laureate, globally praised.
We already have this – but
it’s not a vaccine. It’s much simpler.
Just stop smoking.
K. Michael Cummings,
Ph.D, is the director of the New York State Smokers’ Quitline and a senior research
scientist at the Roswell Park cancer Institute, Buffalo.
I give the FDA a
“B” on this action, but I don’t think it’s enough. Congress could have decided on
much stronger pictures. It could have made them larger, not just 20% of the
pack and located on the back . In other countries that use such warnings, the
pictures cover almost 80% of the packaging.
Plainly put, the United States is a Third
World country when it comes to warning about cigarettes. Similar
pictorial warnings have been used in Canada
for almost a decade; Australia,
almost all of the European Union countries, and even Uruguay have similar warnings.
Having said that, we do know
that pictures speak louder than words and may help motivate smokers to quit.
But here is the hard reality: Even though nearly everyone wants to quit smoking
and many are trying to do so every day, the ability to sustain that motivation
is not always present.
Two factors are highly
predictive of a successful quit: the clinical predictor of personal biology and
the financial predictor of cigarette engineering.
Biologically, some people
are more prone to developing addictions than others. If you have a patient who
reaches for a cigarette before their feet even hit the floor in the morning,
that patient is going to need more medical assistance to be successful.
The second factor is
cigarette engineering. Cigarettes are designed to get people hooked and keep
them hooked. This is what makes quitting so hard despite strong personal motivation.
If we look back in
history, around 1900 there were only a few hundred cases of lung cancer
diagnosed in the U.S.
each year. This year it will be around 160,000. What has happened since then?
People were indeed smoking
then – pipes, cigars, and roll-your-own cigarettes. But this was not a daily-use
situation, mostly because the pH of the smoke made it very hard to inhale.
Right around 1920, commercially available cigarette brands reformulated their
tobacco to make the smoke milder. This allowed people to smoke more, loading
their brains up with lots more nicotine, lots faster.
Around 1950, manufacturers
began adding chemicals to moderate the pH, facilitating deep inhalation. the
lungs. These ingredients – diammonium phosphate, urea, and hydrochloride among
them – are still on the packs’ ingredient list, although manufacturers call
them “flavorings.”
Filters were the next step
in developing an addictive product. Manufacturers presented filters as making
cigarettes safer. Their real purpose was both to break down the tar into
smaller particles and to force people to suck on the cigarette harder to get
the smoke. Filters actually make things worse by forcing rapid inhalation and
rapid absorption – delivering the nicotine to the brain within seconds.
These things were done
secretly and purposefully to promote tobacco addiction and maintain profits. Tobacco
companies deliberately suppressed this information until 2006, when a
racketeering lawsuit forced the disclosure of dozens of documents showing the
intention behind these decisions. U.S District Court Judge Gladys Kessler determined
that tobacco companies conspired to lie about the dangers of smoking and, in
her 1,600-page ruling, called the conspiracy “decades long.”
“In short, the defendants
have marketed and sold their lethal product with zeal, with deception, with a
single-minded focus on their financial success, and without regard for the
human tragedy or social costs that success exacted,” according to her ruling.
Despite lawsuits, public
information campaigns, and the current warnings on cigarette packs, Americans
continue to smoke and I continue to see the effects.
About a third of the
patients I see at the Roswell Park Cancer Institute have smoking-related
cancers. Imagine a vaccine that would prevent a third of cancers. The inventor would
be a Nobel Laureate, globally praised.
We already have this – but
it’s not a vaccine. It’s much simpler.
Just stop smoking.
K. Michael Cummings,
Ph.D, is the director of the New York State Smokers’ Quitline and a senior research
scientist at the Roswell Park cancer Institute, Buffalo.
The Food and Drug Administration unveiled on June 21 the final nine warning images that will appear on every package of cigarettes by 2012 – graphic photos and drawings intended to educate and even deter consumers from buying cigarettes.
The images, set to debut in stores this September, are required by the 2009 Tobacco Control Act, according to FDA spokesman Jeffrey Ventura, who added that these are the first changes to cigarette pack warnings in 25 years. By Oct. 22, 2012, cigarette manufacturers will no longer be able to distribute cigarettes for sale in the United States unless they display these warnings.
The law required the warnings to cover the top half of the front and back of cigarette packs and 20% of cigarette advertisements, and they must contain color graphics depicting the negative health consequences of smoking.
"This is something Congress wanted to happen and mandated that the FDA carry out," Mr. Ventura said in an interview. Based on a study of 18,000 smokers conducted for the FDA by RTI International, federal officials said they firmly believe that visually communicating smoking’s harm will deter cigarette consumption over the long run.
The images include photos of tobacco-diseased lungs beside healthy lungs, a corpse in casket, a man exhaling smoke though a tracheostomy, and lip cancer. There are also several cartoons and photos of mothers blowing smoke into infants’ faces. One positive image shows a burly man exposing a T-shirt saying, "I Quit."
Blunt statements accompany each image, intended to drive home the messages that cigarette smoke not only directly harms the smoker, but the smokers’ children and people in close proximity.
"The introduction of these warnings is expected to have a significant public health impact by decreasing the number of smokers, resulting in lives saved, increased life expectancy, and improved health status," FDA officials said in a press statement.
Mr. Ventura said the images were selected after the consumer study involving smokers aged 15-50 years. After viewing each of the images, subjects rated their emotional and cognitive responses, their ability to recall the images, and their opinions on whether the pictures could alter their beliefs about the danger of smoking and the desire to buy tobacco products and quitting tobacco.
Young people responded most strongly to a cartoon image depicting tobacco addiction – a cigarette being injected into an arm vein as well as a puppet controlled by strings.
Adults, on the other hand, responded most strongly to photos showing the direct effects of cancer on their bodies – the man with the tracheostomy and a woman smoking in the pouring rain, trying to shield her cigarette with a folded newspaper. Adults also reacted more strongly than did young people to images depicting harm to young children.
The study did conclude, however, that none of the images were significantly related to an increased likelihood of quitting smoking within the next 30 days, or the likelihood of smoking a year after viewing the images. Thus, the report noted, the campaign is more likely to exert a long-term behavioral impact than any immediate effects.
"Eliciting strong emotional and cognitive reactions to the graphic cigarette warning label enhances recall and processing of the health warning, which helps ensure that the warning is better processed, understood, and remembered," the study said. "As attitudes and beliefs change, they eventually lead to changes in intentions to quit or start smoking and then later to lower smoking initiation and successful cessation. The time scale on which this behavior change process occurs is largely unknown in the context of the impact of exposure to graphic warning labels on smoking behaviors, but the effects on behavior change are unlikely to be immediate or short-term.
Nevertheless, groups promoting antitobacco messages – including the American Heart Association – strongly believe that the warnings will enhance consumer education and change behavior.
"Undoubtedly, the new graphic health warnings will heighten awareness about the dangers of smoking and, more importantly, encourage smokers to quit and discourage smoking initiation," an AHA press statement read. "We’re confident that the new labels will move us closer to our goal of making the nation 100% smoke free."
Tobacco-Free Kids, a group dedicated to educating children and teens about the dangers of smoking, also issued a statement of support, but with a moderated view on the campaign’s possible impact. The group also called on political leaders to financially commit to "waging war" against tobacco.
"The warnings and other FDA regulations are powerful tools, but they are a complement – not a replacement – to other federal and state strategies to reduce tobacco use," Matthew L. Meyers, the group’s president, said in the statement. "To win the fight against tobacco, elected leaders must also fund and implement public education campaigns, expand health care coverage for therapies to help smokers quit, increase tobacco taxes, and enact strong smoke-free laws in every state."
The Food and Drug Administration unveiled on June 21 the final nine warning images that will appear on every package of cigarettes by 2012 – graphic photos and drawings intended to educate and even deter consumers from buying cigarettes.
The images, set to debut in stores this September, are required by the 2009 Tobacco Control Act, according to FDA spokesman Jeffrey Ventura, who added that these are the first changes to cigarette pack warnings in 25 years. By Oct. 22, 2012, cigarette manufacturers will no longer be able to distribute cigarettes for sale in the United States unless they display these warnings.
The law required the warnings to cover the top half of the front and back of cigarette packs and 20% of cigarette advertisements, and they must contain color graphics depicting the negative health consequences of smoking.
"This is something Congress wanted to happen and mandated that the FDA carry out," Mr. Ventura said in an interview. Based on a study of 18,000 smokers conducted for the FDA by RTI International, federal officials said they firmly believe that visually communicating smoking’s harm will deter cigarette consumption over the long run.
The images include photos of tobacco-diseased lungs beside healthy lungs, a corpse in casket, a man exhaling smoke though a tracheostomy, and lip cancer. There are also several cartoons and photos of mothers blowing smoke into infants’ faces. One positive image shows a burly man exposing a T-shirt saying, "I Quit."
Blunt statements accompany each image, intended to drive home the messages that cigarette smoke not only directly harms the smoker, but the smokers’ children and people in close proximity.
"The introduction of these warnings is expected to have a significant public health impact by decreasing the number of smokers, resulting in lives saved, increased life expectancy, and improved health status," FDA officials said in a press statement.
Mr. Ventura said the images were selected after the consumer study involving smokers aged 15-50 years. After viewing each of the images, subjects rated their emotional and cognitive responses, their ability to recall the images, and their opinions on whether the pictures could alter their beliefs about the danger of smoking and the desire to buy tobacco products and quitting tobacco.
Young people responded most strongly to a cartoon image depicting tobacco addiction – a cigarette being injected into an arm vein as well as a puppet controlled by strings.
Adults, on the other hand, responded most strongly to photos showing the direct effects of cancer on their bodies – the man with the tracheostomy and a woman smoking in the pouring rain, trying to shield her cigarette with a folded newspaper. Adults also reacted more strongly than did young people to images depicting harm to young children.
The study did conclude, however, that none of the images were significantly related to an increased likelihood of quitting smoking within the next 30 days, or the likelihood of smoking a year after viewing the images. Thus, the report noted, the campaign is more likely to exert a long-term behavioral impact than any immediate effects.
"Eliciting strong emotional and cognitive reactions to the graphic cigarette warning label enhances recall and processing of the health warning, which helps ensure that the warning is better processed, understood, and remembered," the study said. "As attitudes and beliefs change, they eventually lead to changes in intentions to quit or start smoking and then later to lower smoking initiation and successful cessation. The time scale on which this behavior change process occurs is largely unknown in the context of the impact of exposure to graphic warning labels on smoking behaviors, but the effects on behavior change are unlikely to be immediate or short-term.
Nevertheless, groups promoting antitobacco messages – including the American Heart Association – strongly believe that the warnings will enhance consumer education and change behavior.
"Undoubtedly, the new graphic health warnings will heighten awareness about the dangers of smoking and, more importantly, encourage smokers to quit and discourage smoking initiation," an AHA press statement read. "We’re confident that the new labels will move us closer to our goal of making the nation 100% smoke free."
Tobacco-Free Kids, a group dedicated to educating children and teens about the dangers of smoking, also issued a statement of support, but with a moderated view on the campaign’s possible impact. The group also called on political leaders to financially commit to "waging war" against tobacco.
"The warnings and other FDA regulations are powerful tools, but they are a complement – not a replacement – to other federal and state strategies to reduce tobacco use," Matthew L. Meyers, the group’s president, said in the statement. "To win the fight against tobacco, elected leaders must also fund and implement public education campaigns, expand health care coverage for therapies to help smokers quit, increase tobacco taxes, and enact strong smoke-free laws in every state."
The images, set to debut in stores this September, are required by the 2009 Tobacco Control Act, according to FDA spokesman Jeffrey Ventura, who added that these are the first changes to cigarette pack warnings
The images, set to debut in stores this September, are required by the 2009 Tobacco Control Act, according to FDA spokesman Jeffrey Ventura, who added that these are the first changes to cigarette pack warnings