User login
ACIP weighs in on meningococcal B vaccines
The Advisory Committee on Immunization Practices (ACIP) voted at its June 2015 meeting to make a “B” recommendation for the use of meningococcal B vaccine for individuals 16 through 23 years of age. The Committee felt that the vaccine can be used if one desires it, but at this time it should not be included in the category of a routinely recommended vaccine.
Meningococcal meningitis caused by serogroup B is a serious disease, but it is rare. From 2009 to 2013, the annual number of meningococcal B cases in individuals ages 11 to 24 years ranged from 54 to 67, with 5 to 10 deaths and 5 to 13 serious sequelae.1 Since 2009, there have been outbreaks on 7 university campuses with cases-per-outbreak numbering 2 to 13.1 These well publicized outbreaks created much disruption and an impression of increased risk among college students. But the surveillance system of the Centers for Disease Control and Prevention (CDC) demonstrates that the rate of infection among college students is actually lower than it is among individuals the same age who are not in college (TABLE 1).1
The combined incidence of 0.14/100,000 means that to prevent one case, 714,000 individuals need to be vaccinated; 5 million need to be vaccinated to prevent one death.1 These numbers are subject to yearly variation and would be more favorable should the incidence of the disease increase. (For a look at the historical incidence of meningococcal meningitis from all serotypes, see the FIGURE.1) The question facing ACIP was whether the current very low levels of meningococcal B disease merit widespread, routinely-recommended use of the vaccine.
A look at the 2 meningococcal B vaccines
Two meningococcal B vaccines are now licensed for use in the United States. MenB-FHbp (Trumenba, Pfizer) was licensed in October 2014 as a 3-dose series given at 0, 2, and 6 months.2 MenB-4C (Bexsero, Novartis/GSK) was licensed in January 2015 and requires 2 doses at 0 and ≥1 month.3 Both vaccines induce a level of antibody production that is considered immunogenic in a high proportion of those vaccinated, but the level of immunity wanes after 6 to 24 months. The clinical significance of this drop in immunity is unknown and cannot be tested currently because of the rarity of the disease. Unfortunately, the rate of asymptomatic carriage of meningococcal B does not appear to be affected by vaccination.1
Both vaccines produce local and systemic reactions at rates higher than other recommended vaccines for this age group: pain at the injection site (83%-85%), headache (33%-35%), myalgia (30%-48%), fatigue (35%-40%), induration (28%), nausea (18%), chills (15%), and arthralgia (13%).2,3 There is some theoretical concern about the potential for autoimmune disease from the use of meningococcal B vaccines that will be studied as the vaccines are used more widely.1 In addition, the CDC estimates that serious anaphylactic reactions can occur after administration of any vaccine, estimated at about one per every million doses.1
Meningococcal serotype B bacteria consist of different strains. The 2 approved vaccines cover today’s most frequently found strains in the United States, but it’s uncertain if this will hold true in the future.
USPSTF: Screen obese/overweight adults for type 2 diabetes
The United States Preventive Services Task Force (USPSTF) recently updated its recommendation for screening for type 2 diabetes in adults. USPSTF recommends screening adults, ages 40 to 70 years, who are obese or overweight and referring those who have abnormal blood glucose to intensive behavioral counseling to promote a healthful diet and physical activity.
The Task Force gave this recommendation a grade of B, meaning that it is likely to result in a moderate level of benefit from a reduction in progression to diabetes. The Task Force also emphasized that lifestyle modifications have a greater risk-reducing effect than metformin and other medications.
The recommendation rationale points out that screening might also benefit those at high risk of diabetes based on family history or race/ethnicity and does not apply to those with signs and symptoms of diabetes; testing in this latter group is considered diagnostic testing, not screening.
Screening can be done by measuring glycated hemoglobin A1c or fasting glucose or with a glucose tolerance test. The recommendation includes tables that list the cutoffs for abnormal glucose levels for impaired fasting glucose, impaired glucose tolerance, and increased average glucose level. Obesity is defined as a body mass index ≥30 kg/m2 and overweight as >25 kg/m2.
This new recommendation expands the list of those at risk and those who should be screened compared to the previous recommendation, but the Task Force found no evidence to support universal screening in adults as advocated by other organizations.
Source: USPSTF. Final recommendation statement. Abnormal blood glucose and type 2 diabetes mellitus: screening. Available at: http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/screening-for-abnormal-blood-glucose-and-type-2-diabetes. Accessed November 13, 2015.
Recommendation considerations that came into play
A number of factors affected ACIP’s recommendation decision: the low incidence of the meningococcal B disease; the large number-needed-to-vaccinate to prevent a case and a death; uncertainties regarding the duration of protection; cost, lack of effect on carriage rates, and limited safety data with the potential for serious reactions to exceed the number of cases prevented; and the severity of the disease and the concern it elicits.
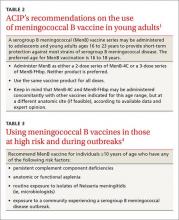
ACIP has multiple options when considering a vaccine: recommend it routinely for everyone or everyone in a defined group (A recommendation), recommend for individual decision making (B recommendation), recommend against use, and make no recommendation at all. Given that 2 meningococcal B vaccines are licensed in the United States and can be used by those who want them—and the Committee’s opinion that these vaccines should not (at this time) be included in the schedule of routinely-recommended vaccines—ACIP chose to make a B recommendation on their use (TABLE 2).1 Vaccines recommended by ACIP (both A and B recommendations) are mandated in the Affordable Care Act to be provided by commercial health insurance at no out-of-pocket expense to the patient.
A word about high-risk populations
At its February 2015 meeting, ACIP voted to recommend meningococcal B vaccine for use in high-risk populations and during outbreaks (TABLE 3).4 This recommendation—plus the most recent B recommendation for general use—comprise the totality of current recommendations for the prevention of meningococcal B disease in the United States.
1. MacNeil J. Considerations for the use of serogroup B meningococcal (MenB) vaccines in adolescents. Presented at: Advisory Committee on Immunization Practices; June 24, 2015; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2015-06/mening-03-macneil.pdf. Accessed October 14, 2015.
2. Trumenba [package insert]. Philadelphia, PA: Wyeth Pharmaceuticals Inc. (Pfizer); 2014. Available at: http://www.fda.gov/downloads/BiologicsBloodVaccines/Vaccines/ApprovedProducts/UCM421139.pdf. Accessed October 14, 2015.
3. Bexsero [package insert]. Cambridge, MA: Novartis Vaccines and Diagnostics Inc; 2015. Available at: http://www.fda.gov/downloads/BiologicsBloodVaccines/Vaccines/ApprovedProducts/UCM431447.pdf. Accessed October 14, 2015.
4. Folaranmi T, Rubin L, Martin SW, et al. Use of serogroup B meningococcal vaccines in persons aged ≥10 years at increased risk for serogroup B meningococcal disease: recommendations of the Advisory Committee on Immunization Practices, 2015. MMWR Morb Mortal Wkly Rep. 2015;64:608-612.
The Advisory Committee on Immunization Practices (ACIP) voted at its June 2015 meeting to make a “B” recommendation for the use of meningococcal B vaccine for individuals 16 through 23 years of age. The Committee felt that the vaccine can be used if one desires it, but at this time it should not be included in the category of a routinely recommended vaccine.
Meningococcal meningitis caused by serogroup B is a serious disease, but it is rare. From 2009 to 2013, the annual number of meningococcal B cases in individuals ages 11 to 24 years ranged from 54 to 67, with 5 to 10 deaths and 5 to 13 serious sequelae.1 Since 2009, there have been outbreaks on 7 university campuses with cases-per-outbreak numbering 2 to 13.1 These well publicized outbreaks created much disruption and an impression of increased risk among college students. But the surveillance system of the Centers for Disease Control and Prevention (CDC) demonstrates that the rate of infection among college students is actually lower than it is among individuals the same age who are not in college (TABLE 1).1
The combined incidence of 0.14/100,000 means that to prevent one case, 714,000 individuals need to be vaccinated; 5 million need to be vaccinated to prevent one death.1 These numbers are subject to yearly variation and would be more favorable should the incidence of the disease increase. (For a look at the historical incidence of meningococcal meningitis from all serotypes, see the FIGURE.1) The question facing ACIP was whether the current very low levels of meningococcal B disease merit widespread, routinely-recommended use of the vaccine.
A look at the 2 meningococcal B vaccines
Two meningococcal B vaccines are now licensed for use in the United States. MenB-FHbp (Trumenba, Pfizer) was licensed in October 2014 as a 3-dose series given at 0, 2, and 6 months.2 MenB-4C (Bexsero, Novartis/GSK) was licensed in January 2015 and requires 2 doses at 0 and ≥1 month.3 Both vaccines induce a level of antibody production that is considered immunogenic in a high proportion of those vaccinated, but the level of immunity wanes after 6 to 24 months. The clinical significance of this drop in immunity is unknown and cannot be tested currently because of the rarity of the disease. Unfortunately, the rate of asymptomatic carriage of meningococcal B does not appear to be affected by vaccination.1
Both vaccines produce local and systemic reactions at rates higher than other recommended vaccines for this age group: pain at the injection site (83%-85%), headache (33%-35%), myalgia (30%-48%), fatigue (35%-40%), induration (28%), nausea (18%), chills (15%), and arthralgia (13%).2,3 There is some theoretical concern about the potential for autoimmune disease from the use of meningococcal B vaccines that will be studied as the vaccines are used more widely.1 In addition, the CDC estimates that serious anaphylactic reactions can occur after administration of any vaccine, estimated at about one per every million doses.1
Meningococcal serotype B bacteria consist of different strains. The 2 approved vaccines cover today’s most frequently found strains in the United States, but it’s uncertain if this will hold true in the future.
USPSTF: Screen obese/overweight adults for type 2 diabetes
The United States Preventive Services Task Force (USPSTF) recently updated its recommendation for screening for type 2 diabetes in adults. USPSTF recommends screening adults, ages 40 to 70 years, who are obese or overweight and referring those who have abnormal blood glucose to intensive behavioral counseling to promote a healthful diet and physical activity.
The Task Force gave this recommendation a grade of B, meaning that it is likely to result in a moderate level of benefit from a reduction in progression to diabetes. The Task Force also emphasized that lifestyle modifications have a greater risk-reducing effect than metformin and other medications.
The recommendation rationale points out that screening might also benefit those at high risk of diabetes based on family history or race/ethnicity and does not apply to those with signs and symptoms of diabetes; testing in this latter group is considered diagnostic testing, not screening.
Screening can be done by measuring glycated hemoglobin A1c or fasting glucose or with a glucose tolerance test. The recommendation includes tables that list the cutoffs for abnormal glucose levels for impaired fasting glucose, impaired glucose tolerance, and increased average glucose level. Obesity is defined as a body mass index ≥30 kg/m2 and overweight as >25 kg/m2.
This new recommendation expands the list of those at risk and those who should be screened compared to the previous recommendation, but the Task Force found no evidence to support universal screening in adults as advocated by other organizations.
Source: USPSTF. Final recommendation statement. Abnormal blood glucose and type 2 diabetes mellitus: screening. Available at: http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/screening-for-abnormal-blood-glucose-and-type-2-diabetes. Accessed November 13, 2015.
Recommendation considerations that came into play
A number of factors affected ACIP’s recommendation decision: the low incidence of the meningococcal B disease; the large number-needed-to-vaccinate to prevent a case and a death; uncertainties regarding the duration of protection; cost, lack of effect on carriage rates, and limited safety data with the potential for serious reactions to exceed the number of cases prevented; and the severity of the disease and the concern it elicits.
ACIP has multiple options when considering a vaccine: recommend it routinely for everyone or everyone in a defined group (A recommendation), recommend for individual decision making (B recommendation), recommend against use, and make no recommendation at all. Given that 2 meningococcal B vaccines are licensed in the United States and can be used by those who want them—and the Committee’s opinion that these vaccines should not (at this time) be included in the schedule of routinely-recommended vaccines—ACIP chose to make a B recommendation on their use (TABLE 2).1 Vaccines recommended by ACIP (both A and B recommendations) are mandated in the Affordable Care Act to be provided by commercial health insurance at no out-of-pocket expense to the patient.
A word about high-risk populations
At its February 2015 meeting, ACIP voted to recommend meningococcal B vaccine for use in high-risk populations and during outbreaks (TABLE 3).4 This recommendation—plus the most recent B recommendation for general use—comprise the totality of current recommendations for the prevention of meningococcal B disease in the United States.
The Advisory Committee on Immunization Practices (ACIP) voted at its June 2015 meeting to make a “B” recommendation for the use of meningococcal B vaccine for individuals 16 through 23 years of age. The Committee felt that the vaccine can be used if one desires it, but at this time it should not be included in the category of a routinely recommended vaccine.
Meningococcal meningitis caused by serogroup B is a serious disease, but it is rare. From 2009 to 2013, the annual number of meningococcal B cases in individuals ages 11 to 24 years ranged from 54 to 67, with 5 to 10 deaths and 5 to 13 serious sequelae.1 Since 2009, there have been outbreaks on 7 university campuses with cases-per-outbreak numbering 2 to 13.1 These well publicized outbreaks created much disruption and an impression of increased risk among college students. But the surveillance system of the Centers for Disease Control and Prevention (CDC) demonstrates that the rate of infection among college students is actually lower than it is among individuals the same age who are not in college (TABLE 1).1
The combined incidence of 0.14/100,000 means that to prevent one case, 714,000 individuals need to be vaccinated; 5 million need to be vaccinated to prevent one death.1 These numbers are subject to yearly variation and would be more favorable should the incidence of the disease increase. (For a look at the historical incidence of meningococcal meningitis from all serotypes, see the FIGURE.1) The question facing ACIP was whether the current very low levels of meningococcal B disease merit widespread, routinely-recommended use of the vaccine.
A look at the 2 meningococcal B vaccines
Two meningococcal B vaccines are now licensed for use in the United States. MenB-FHbp (Trumenba, Pfizer) was licensed in October 2014 as a 3-dose series given at 0, 2, and 6 months.2 MenB-4C (Bexsero, Novartis/GSK) was licensed in January 2015 and requires 2 doses at 0 and ≥1 month.3 Both vaccines induce a level of antibody production that is considered immunogenic in a high proportion of those vaccinated, but the level of immunity wanes after 6 to 24 months. The clinical significance of this drop in immunity is unknown and cannot be tested currently because of the rarity of the disease. Unfortunately, the rate of asymptomatic carriage of meningococcal B does not appear to be affected by vaccination.1
Both vaccines produce local and systemic reactions at rates higher than other recommended vaccines for this age group: pain at the injection site (83%-85%), headache (33%-35%), myalgia (30%-48%), fatigue (35%-40%), induration (28%), nausea (18%), chills (15%), and arthralgia (13%).2,3 There is some theoretical concern about the potential for autoimmune disease from the use of meningococcal B vaccines that will be studied as the vaccines are used more widely.1 In addition, the CDC estimates that serious anaphylactic reactions can occur after administration of any vaccine, estimated at about one per every million doses.1
Meningococcal serotype B bacteria consist of different strains. The 2 approved vaccines cover today’s most frequently found strains in the United States, but it’s uncertain if this will hold true in the future.
USPSTF: Screen obese/overweight adults for type 2 diabetes
The United States Preventive Services Task Force (USPSTF) recently updated its recommendation for screening for type 2 diabetes in adults. USPSTF recommends screening adults, ages 40 to 70 years, who are obese or overweight and referring those who have abnormal blood glucose to intensive behavioral counseling to promote a healthful diet and physical activity.
The Task Force gave this recommendation a grade of B, meaning that it is likely to result in a moderate level of benefit from a reduction in progression to diabetes. The Task Force also emphasized that lifestyle modifications have a greater risk-reducing effect than metformin and other medications.
The recommendation rationale points out that screening might also benefit those at high risk of diabetes based on family history or race/ethnicity and does not apply to those with signs and symptoms of diabetes; testing in this latter group is considered diagnostic testing, not screening.
Screening can be done by measuring glycated hemoglobin A1c or fasting glucose or with a glucose tolerance test. The recommendation includes tables that list the cutoffs for abnormal glucose levels for impaired fasting glucose, impaired glucose tolerance, and increased average glucose level. Obesity is defined as a body mass index ≥30 kg/m2 and overweight as >25 kg/m2.
This new recommendation expands the list of those at risk and those who should be screened compared to the previous recommendation, but the Task Force found no evidence to support universal screening in adults as advocated by other organizations.
Source: USPSTF. Final recommendation statement. Abnormal blood glucose and type 2 diabetes mellitus: screening. Available at: http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/screening-for-abnormal-blood-glucose-and-type-2-diabetes. Accessed November 13, 2015.
Recommendation considerations that came into play
A number of factors affected ACIP’s recommendation decision: the low incidence of the meningococcal B disease; the large number-needed-to-vaccinate to prevent a case and a death; uncertainties regarding the duration of protection; cost, lack of effect on carriage rates, and limited safety data with the potential for serious reactions to exceed the number of cases prevented; and the severity of the disease and the concern it elicits.
ACIP has multiple options when considering a vaccine: recommend it routinely for everyone or everyone in a defined group (A recommendation), recommend for individual decision making (B recommendation), recommend against use, and make no recommendation at all. Given that 2 meningococcal B vaccines are licensed in the United States and can be used by those who want them—and the Committee’s opinion that these vaccines should not (at this time) be included in the schedule of routinely-recommended vaccines—ACIP chose to make a B recommendation on their use (TABLE 2).1 Vaccines recommended by ACIP (both A and B recommendations) are mandated in the Affordable Care Act to be provided by commercial health insurance at no out-of-pocket expense to the patient.
A word about high-risk populations
At its February 2015 meeting, ACIP voted to recommend meningococcal B vaccine for use in high-risk populations and during outbreaks (TABLE 3).4 This recommendation—plus the most recent B recommendation for general use—comprise the totality of current recommendations for the prevention of meningococcal B disease in the United States.
1. MacNeil J. Considerations for the use of serogroup B meningococcal (MenB) vaccines in adolescents. Presented at: Advisory Committee on Immunization Practices; June 24, 2015; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2015-06/mening-03-macneil.pdf. Accessed October 14, 2015.
2. Trumenba [package insert]. Philadelphia, PA: Wyeth Pharmaceuticals Inc. (Pfizer); 2014. Available at: http://www.fda.gov/downloads/BiologicsBloodVaccines/Vaccines/ApprovedProducts/UCM421139.pdf. Accessed October 14, 2015.
3. Bexsero [package insert]. Cambridge, MA: Novartis Vaccines and Diagnostics Inc; 2015. Available at: http://www.fda.gov/downloads/BiologicsBloodVaccines/Vaccines/ApprovedProducts/UCM431447.pdf. Accessed October 14, 2015.
4. Folaranmi T, Rubin L, Martin SW, et al. Use of serogroup B meningococcal vaccines in persons aged ≥10 years at increased risk for serogroup B meningococcal disease: recommendations of the Advisory Committee on Immunization Practices, 2015. MMWR Morb Mortal Wkly Rep. 2015;64:608-612.
1. MacNeil J. Considerations for the use of serogroup B meningococcal (MenB) vaccines in adolescents. Presented at: Advisory Committee on Immunization Practices; June 24, 2015; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2015-06/mening-03-macneil.pdf. Accessed October 14, 2015.
2. Trumenba [package insert]. Philadelphia, PA: Wyeth Pharmaceuticals Inc. (Pfizer); 2014. Available at: http://www.fda.gov/downloads/BiologicsBloodVaccines/Vaccines/ApprovedProducts/UCM421139.pdf. Accessed October 14, 2015.
3. Bexsero [package insert]. Cambridge, MA: Novartis Vaccines and Diagnostics Inc; 2015. Available at: http://www.fda.gov/downloads/BiologicsBloodVaccines/Vaccines/ApprovedProducts/UCM431447.pdf. Accessed October 14, 2015.
4. Folaranmi T, Rubin L, Martin SW, et al. Use of serogroup B meningococcal vaccines in persons aged ≥10 years at increased risk for serogroup B meningococcal disease: recommendations of the Advisory Committee on Immunization Practices, 2015. MMWR Morb Mortal Wkly Rep. 2015;64:608-612.
Being honest about diagnostic uncertainty
Like everyone else’s grandmother, mine gave me all kinds of advice while I was growing up. Some tips I still remember.
One came when I was home for Thanksgiving during my first year of medical school. She was frustrated over her recent visit to an internist. He kept ordering more tests but wouldn’t answer questions about what might be causing her symptoms.
She told me that, if I didn’t know what was going on, to just say so. As a patient, she felt that an honest answer was better than silence.
Today, as a doctor, I agree with her. So, while I may still be doing tests to crack the case, I have no problem, when asked what I think is going on, with saying “I don’t know.”
This approach isn’t perfect for everyone. Some docs (and patients) may see it as a sign of incompetence or weakness, thinking that admitting fallibility is a breach of the relationship or that with some tests the doctor becomes omniscient. Of course, that’s far from the truth.
In my experience, patients prefer the honesty of my saying “I don’t know.” I’m not saying I’ll never know, I’m just saying that, at present, I’m still looking for the answer.
Nobody likes being in the dark about their health, but at the same time they don’t want to feel their doctor is keeping a secret from them. By making it clear that I’m not, I’m hoping to keep a strong therapeutic relationship. I promise them that when I know, they’ll know, and that I’m honest when stumped. If I need to refer elsewhere for an answer, I have no problem doing that. Medicine, and neurology in particular, is a complex field. If every diagnosis were a slam-dunk, we wouldn’t need specialists and subspecialists (and even subsubspecialists).
Most people know and understand that, recognize the inherent uncertainty of this job, and know that I don’t know. I promise them that “I don’t know” doesn’t mean I’m done looking, it just means I’m going to keep trying. That’s the best anyone can do. Right, Granny?
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Like everyone else’s grandmother, mine gave me all kinds of advice while I was growing up. Some tips I still remember.
One came when I was home for Thanksgiving during my first year of medical school. She was frustrated over her recent visit to an internist. He kept ordering more tests but wouldn’t answer questions about what might be causing her symptoms.
She told me that, if I didn’t know what was going on, to just say so. As a patient, she felt that an honest answer was better than silence.
Today, as a doctor, I agree with her. So, while I may still be doing tests to crack the case, I have no problem, when asked what I think is going on, with saying “I don’t know.”
This approach isn’t perfect for everyone. Some docs (and patients) may see it as a sign of incompetence or weakness, thinking that admitting fallibility is a breach of the relationship or that with some tests the doctor becomes omniscient. Of course, that’s far from the truth.
In my experience, patients prefer the honesty of my saying “I don’t know.” I’m not saying I’ll never know, I’m just saying that, at present, I’m still looking for the answer.
Nobody likes being in the dark about their health, but at the same time they don’t want to feel their doctor is keeping a secret from them. By making it clear that I’m not, I’m hoping to keep a strong therapeutic relationship. I promise them that when I know, they’ll know, and that I’m honest when stumped. If I need to refer elsewhere for an answer, I have no problem doing that. Medicine, and neurology in particular, is a complex field. If every diagnosis were a slam-dunk, we wouldn’t need specialists and subspecialists (and even subsubspecialists).
Most people know and understand that, recognize the inherent uncertainty of this job, and know that I don’t know. I promise them that “I don’t know” doesn’t mean I’m done looking, it just means I’m going to keep trying. That’s the best anyone can do. Right, Granny?
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Like everyone else’s grandmother, mine gave me all kinds of advice while I was growing up. Some tips I still remember.
One came when I was home for Thanksgiving during my first year of medical school. She was frustrated over her recent visit to an internist. He kept ordering more tests but wouldn’t answer questions about what might be causing her symptoms.
She told me that, if I didn’t know what was going on, to just say so. As a patient, she felt that an honest answer was better than silence.
Today, as a doctor, I agree with her. So, while I may still be doing tests to crack the case, I have no problem, when asked what I think is going on, with saying “I don’t know.”
This approach isn’t perfect for everyone. Some docs (and patients) may see it as a sign of incompetence or weakness, thinking that admitting fallibility is a breach of the relationship or that with some tests the doctor becomes omniscient. Of course, that’s far from the truth.
In my experience, patients prefer the honesty of my saying “I don’t know.” I’m not saying I’ll never know, I’m just saying that, at present, I’m still looking for the answer.
Nobody likes being in the dark about their health, but at the same time they don’t want to feel their doctor is keeping a secret from them. By making it clear that I’m not, I’m hoping to keep a strong therapeutic relationship. I promise them that when I know, they’ll know, and that I’m honest when stumped. If I need to refer elsewhere for an answer, I have no problem doing that. Medicine, and neurology in particular, is a complex field. If every diagnosis were a slam-dunk, we wouldn’t need specialists and subspecialists (and even subsubspecialists).
Most people know and understand that, recognize the inherent uncertainty of this job, and know that I don’t know. I promise them that “I don’t know” doesn’t mean I’m done looking, it just means I’m going to keep trying. That’s the best anyone can do. Right, Granny?
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Cardiovascular Disease: From Milestones to Innovations
Supplement Editor:
Maan A. Fares, MD
Contents
Introduction: The transition from milestones to innovations
Maan a. Fares, MD
Transcatheter aortic valve replacement: History and current indications
Ahmad Zeeshan, MD; E. Murat Tuzcu, MD; Amar Krishnaswamy, MD; Samir Kapadia, MD; and Stephanie Mick, MD
Evolving strategies to prevent stroke and thromboembolism in nonvalvular atrial fibrillation
Ayman Hussein, MD; Walid Saliba, MD; and Oussama Wazni, MD
Stroke management and the impact of mobile stroke treatment units
Peter A. Rasmussen, MD
Biomarkers: Their potential in the diagnosis and treatment of heart failure
Barbara Heil, MD, and W.H. Wilson Tang, MD
Clinical challenges in diagnosing and managing adult hypertension
Joel Handler, MD
Supplement Editor:
Maan A. Fares, MD
Contents
Introduction: The transition from milestones to innovations
Maan a. Fares, MD
Transcatheter aortic valve replacement: History and current indications
Ahmad Zeeshan, MD; E. Murat Tuzcu, MD; Amar Krishnaswamy, MD; Samir Kapadia, MD; and Stephanie Mick, MD
Evolving strategies to prevent stroke and thromboembolism in nonvalvular atrial fibrillation
Ayman Hussein, MD; Walid Saliba, MD; and Oussama Wazni, MD
Stroke management and the impact of mobile stroke treatment units
Peter A. Rasmussen, MD
Biomarkers: Their potential in the diagnosis and treatment of heart failure
Barbara Heil, MD, and W.H. Wilson Tang, MD
Clinical challenges in diagnosing and managing adult hypertension
Joel Handler, MD
Supplement Editor:
Maan A. Fares, MD
Contents
Introduction: The transition from milestones to innovations
Maan a. Fares, MD
Transcatheter aortic valve replacement: History and current indications
Ahmad Zeeshan, MD; E. Murat Tuzcu, MD; Amar Krishnaswamy, MD; Samir Kapadia, MD; and Stephanie Mick, MD
Evolving strategies to prevent stroke and thromboembolism in nonvalvular atrial fibrillation
Ayman Hussein, MD; Walid Saliba, MD; and Oussama Wazni, MD
Stroke management and the impact of mobile stroke treatment units
Peter A. Rasmussen, MD
Biomarkers: Their potential in the diagnosis and treatment of heart failure
Barbara Heil, MD, and W.H. Wilson Tang, MD
Clinical challenges in diagnosing and managing adult hypertension
Joel Handler, MD
Introduction: The transition from milestones to innovations
Physicians who were educated and began practicing in the 20th century have witnessed some of the most significant innovations and discoveries in the history of healthcare. While major surgical and therapeutic milestones defined the previous century, our current century is defined by the high-speed pace of technological innovations that affect the practice of medicine. For example, the proliferation of hand-held communication devices now provides immediate access to a wealth of healthcare information. Ultimately, recollecting information will be less necessary and far less valuable than understanding the concepts behind it. The challenge for providers is to recognize how to incorporate these innovations into the traditional model of treating diseases with the goal of improving outcomes and containing costs.
With that objective in mind, the articles in this Cleveland Clinic Journal of Medicine supplement on cardiovascular disease aim to not only review traditional treatment models for cardiovascular disease but, more importantly, to address the broad implications of new innovations on day-to-day clinical practice.
Stephanie Mick, MD, and colleagues look at how the emergence of new devices and technologies has dramatically improved the treatment of severe aortic valve stenosis and expanded the patient population eligible for aortic valve replacement. The authors review the expanded array of surgical approaches to transcatheter aortic valve replacement and the development of new devices in light of their impact on reducing the risks and improving the outcomes associated with this therapy.
Oussama Wazni, MD, and colleagues present evidence underlying the evolving strategies to prevent serious complications of stroke and thromboembolism in patients with atrial fibrillation. Newer anticoagulants are changing the strategic picture. The article includes discussion of the safety and efficacy of the available anticoagulants, as well as nonpharmacologic approaches, and considers how the new data and medications affect traditional treatment models. The authors integrate the data into an evidence-based appraisal of how to best use these innovations to reduce stroke risk in this patient population.
Acute strokes have a significant impact on morbidity and mortality worldwide. Findings that stress the importance of reducing the “time to treatment”—the shorter the time, the better the outcomes—have pushed treatment approaches to center stage. A key factor is the time it takes for patients to arrive in the emergency department. One way to reduce this time is to take the treatment to the patient. Peter A. Rasmussen, MD, looks at how innovations in scanning technologies and wireless data transmissions have led to the development of spe- cially equipped mobile stroke units that can accurately differentiate the types of stroke and enable practitioners to more quickly begin appropriate thromboembolic therapy and reduce the time to therapy.
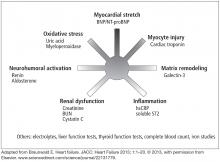
Barbara Heil, MD, and W. H. Wilson Tang, MD, review the use of cardiac biomarkers to diagnose and treat heart failure. Studies have shown the efficacy of using biomarkers to identify high-risk patients, but various factors limit their diagnostic accuracy and clinical adaptability. The authors summarize the data and explain how to incorporate biomarkers into clinical practice.
Hypertension control remains an elusive goal for practitioners. Joel Handler, MD, reviews how new evidence and innovations are revising the diagnostic guidelines and the recommended treatment strategies. He discusses innovations associated with out-of-office monitoring and new data from clinical trials that are changing the clinical practice model. He also addresses the controversy regarding systolic blood pressure goals in elderly patients and how these data have affected evidence-based guidelines.
We hope you find this supplement both informative and thought-provoking.
Physicians who were educated and began practicing in the 20th century have witnessed some of the most significant innovations and discoveries in the history of healthcare. While major surgical and therapeutic milestones defined the previous century, our current century is defined by the high-speed pace of technological innovations that affect the practice of medicine. For example, the proliferation of hand-held communication devices now provides immediate access to a wealth of healthcare information. Ultimately, recollecting information will be less necessary and far less valuable than understanding the concepts behind it. The challenge for providers is to recognize how to incorporate these innovations into the traditional model of treating diseases with the goal of improving outcomes and containing costs.
With that objective in mind, the articles in this Cleveland Clinic Journal of Medicine supplement on cardiovascular disease aim to not only review traditional treatment models for cardiovascular disease but, more importantly, to address the broad implications of new innovations on day-to-day clinical practice.
Stephanie Mick, MD, and colleagues look at how the emergence of new devices and technologies has dramatically improved the treatment of severe aortic valve stenosis and expanded the patient population eligible for aortic valve replacement. The authors review the expanded array of surgical approaches to transcatheter aortic valve replacement and the development of new devices in light of their impact on reducing the risks and improving the outcomes associated with this therapy.
Oussama Wazni, MD, and colleagues present evidence underlying the evolving strategies to prevent serious complications of stroke and thromboembolism in patients with atrial fibrillation. Newer anticoagulants are changing the strategic picture. The article includes discussion of the safety and efficacy of the available anticoagulants, as well as nonpharmacologic approaches, and considers how the new data and medications affect traditional treatment models. The authors integrate the data into an evidence-based appraisal of how to best use these innovations to reduce stroke risk in this patient population.
Acute strokes have a significant impact on morbidity and mortality worldwide. Findings that stress the importance of reducing the “time to treatment”—the shorter the time, the better the outcomes—have pushed treatment approaches to center stage. A key factor is the time it takes for patients to arrive in the emergency department. One way to reduce this time is to take the treatment to the patient. Peter A. Rasmussen, MD, looks at how innovations in scanning technologies and wireless data transmissions have led to the development of spe- cially equipped mobile stroke units that can accurately differentiate the types of stroke and enable practitioners to more quickly begin appropriate thromboembolic therapy and reduce the time to therapy.
Barbara Heil, MD, and W. H. Wilson Tang, MD, review the use of cardiac biomarkers to diagnose and treat heart failure. Studies have shown the efficacy of using biomarkers to identify high-risk patients, but various factors limit their diagnostic accuracy and clinical adaptability. The authors summarize the data and explain how to incorporate biomarkers into clinical practice.
Hypertension control remains an elusive goal for practitioners. Joel Handler, MD, reviews how new evidence and innovations are revising the diagnostic guidelines and the recommended treatment strategies. He discusses innovations associated with out-of-office monitoring and new data from clinical trials that are changing the clinical practice model. He also addresses the controversy regarding systolic blood pressure goals in elderly patients and how these data have affected evidence-based guidelines.
We hope you find this supplement both informative and thought-provoking.
Physicians who were educated and began practicing in the 20th century have witnessed some of the most significant innovations and discoveries in the history of healthcare. While major surgical and therapeutic milestones defined the previous century, our current century is defined by the high-speed pace of technological innovations that affect the practice of medicine. For example, the proliferation of hand-held communication devices now provides immediate access to a wealth of healthcare information. Ultimately, recollecting information will be less necessary and far less valuable than understanding the concepts behind it. The challenge for providers is to recognize how to incorporate these innovations into the traditional model of treating diseases with the goal of improving outcomes and containing costs.
With that objective in mind, the articles in this Cleveland Clinic Journal of Medicine supplement on cardiovascular disease aim to not only review traditional treatment models for cardiovascular disease but, more importantly, to address the broad implications of new innovations on day-to-day clinical practice.
Stephanie Mick, MD, and colleagues look at how the emergence of new devices and technologies has dramatically improved the treatment of severe aortic valve stenosis and expanded the patient population eligible for aortic valve replacement. The authors review the expanded array of surgical approaches to transcatheter aortic valve replacement and the development of new devices in light of their impact on reducing the risks and improving the outcomes associated with this therapy.
Oussama Wazni, MD, and colleagues present evidence underlying the evolving strategies to prevent serious complications of stroke and thromboembolism in patients with atrial fibrillation. Newer anticoagulants are changing the strategic picture. The article includes discussion of the safety and efficacy of the available anticoagulants, as well as nonpharmacologic approaches, and considers how the new data and medications affect traditional treatment models. The authors integrate the data into an evidence-based appraisal of how to best use these innovations to reduce stroke risk in this patient population.
Acute strokes have a significant impact on morbidity and mortality worldwide. Findings that stress the importance of reducing the “time to treatment”—the shorter the time, the better the outcomes—have pushed treatment approaches to center stage. A key factor is the time it takes for patients to arrive in the emergency department. One way to reduce this time is to take the treatment to the patient. Peter A. Rasmussen, MD, looks at how innovations in scanning technologies and wireless data transmissions have led to the development of spe- cially equipped mobile stroke units that can accurately differentiate the types of stroke and enable practitioners to more quickly begin appropriate thromboembolic therapy and reduce the time to therapy.
Barbara Heil, MD, and W. H. Wilson Tang, MD, review the use of cardiac biomarkers to diagnose and treat heart failure. Studies have shown the efficacy of using biomarkers to identify high-risk patients, but various factors limit their diagnostic accuracy and clinical adaptability. The authors summarize the data and explain how to incorporate biomarkers into clinical practice.
Hypertension control remains an elusive goal for practitioners. Joel Handler, MD, reviews how new evidence and innovations are revising the diagnostic guidelines and the recommended treatment strategies. He discusses innovations associated with out-of-office monitoring and new data from clinical trials that are changing the clinical practice model. He also addresses the controversy regarding systolic blood pressure goals in elderly patients and how these data have affected evidence-based guidelines.
We hope you find this supplement both informative and thought-provoking.
Transcatheter aortic valve replacement: History and current indications
Transcatheter aortic valve replacement (TAVR) has established itself as an effective way of treating high-risk patients with severe aortic valve stenosis. With new generations of existing valves and newer alternative devices, the procedure promises to become increasingly safer. The field is evolving rapidly and it will be important for interventional cardiologists and cardiac surgeons alike to stay abreast of developments. This article reviews the history of this promising procedure and examines its use in current practice.
HISTORICAL PERSPECTIVE
In 1980, Danish researcher H. R. Anderson reported developing and testing a balloon-expandable valve in animals.1 The technology was eventually acquired and further developed by Edwards Life Sciences (Irvine, California).
Alain Cribier started early work in humans in 2002 in France.2 He used a transfemoral arterial access to approach the aortic valve transseptally, but this procedure was associated with high rates of mortality and stroke.3 At the same time, in the United States, animal studies were being carried out by Lars G. Svensson, Todd Dewey, and Michael Mack to develop a transapical method of implantation,4,5 while John Webb and colleagues were also developing a transapical aortic valve implantation technique,6,7 and later went on to develop a retrograde transfemoral technique. This latter technique became feasible once Edwards developed a catheter that could be flexed to get around the aortic arch and across the aortic valve.
As the Edwards balloon-expandable valve (Sapien) was being developed, a nitinol-based self-expandable valve system was introduced by Medtronic: the CoreValve. Following feasibility studies,5,8 the safety and efficacy of these valves were established thorough the Placement of Aortic Transcatheter Valves (PARTNER) trial and the US Core Valve Pivotal Trial. These valves are currently approved by the US Food and Drug Administration (FDA) for patients for whom conventional surgery would pose an extreme or high risk.9–11
CLINICAL TRIALS OF TAVR
The two landmark prospective randomized trials of TAVR were the PARTNER trial and CoreValve Pivotal Trial.
The PARTNER trial consisted of two parts: PARTNER A, which compared the Sapien balloon-expandable transcatheter valve with surgical aortic valve replacement in patients at high surgical risk (Society of Thoracic Surgeons [STS] score > 10%), and PARTNER B, which compared TAVR with medical therapy in patients who could not undergo surgery (combined risk of serious morbidity or death of 50% or more, and two surgeons agreeing that the patient was inoperable).
Similarly, the CoreValve Pivotal Trial compared the self-expandable transcatheter valve with conventional medical and surgical treatment.
TAVR is comparable to surgery in outcomes, with caveats
In the PARTNER A trial, mortality rates were similar between patients who underwent Sapien TAVR and those who underwent surgical valve replacement at 30 days (3.4% and 6.5%, P = .07), 1 year (24.2% and 26.8%), and 2 years (33.9% and 35.0%). The patients in this group were randomized to either Sapien TAVR or surgery (Table 1).10,12
The combined rate of stroke and transient ischemic attack was higher in the patients assigned to TAVR at 30 days (5.5% with TAVR vs 2.4% with surgery, P = .04) and at 1 year (8.3% with TAVR vs 4.3% with surgery, P = .04). The difference was of small significance at 2 years (11.2% vs 6.5%, P = .05). At 30 days, the rate of major vascular complications was higher with TAVR (11.0% vs 3.2%), while surgery was associated with more frequent major bleeding episodes (19.5% vs 9.3%) and new-onset atrial fibrillation (16.0% vs 8.6%). The rate of new pacemaker requirement at 30 days was similar between the TAVR and surgical groups (3.8% vs 3.6%). Moderate or severe paravalvular aortic regurgitation was more common after TAVR at 30 days, 1 year, and 2 years. This aortic insufficiency was associated with increased late mortality.10,12
In the US CoreValve High Risk Study, no difference was found in the 30-day mortality rate in patients at high surgical risk randomized to CoreValve TAVR or surgery (3.3% and 4.5%) (Table 1). Surprisingly, the 1-year mortality rate was lower in the TAVR group than in the surgical group (14.1% vs 18.9%, respectively), a finding sustained at 2 years in data presented at the American College of Cardiology conference in March 2015.13–16
TAVR is superior to medical management, but the risk of stroke is higher
In the PARTNER B trial, inoperable patients were randomly assigned to undergo TAVR with a Sapien valve or medical management. TAVR resulted in lower mortality rates at 1 year (30.7% vs 50.7%) and 2 years (43.4% vs 68.0%) compared with medical management (Table 1).17 Of note, medical management included balloon valvuloplasty. The rate of the composite end point of death or repeat hospitalization was also lower with TAVR compared with medical therapy (44.1% vs 71.6%, respectively, at 1 year and 56.7% and 87.9%, respectively, at 2 years).17 The TAVR group had a higher stroke rate than the medical therapy group at 30 days (11.2% vs 5.5%, respectively) and at 2 years (13.8% vs 5.5%).17 Survival improved with TAVR in patients with an STS score of less than 15% but not in those with an STS score of 15% or higher.9
The very favorable results from the PARTNER trial rendered a randomized trial comparing self-expanding (CoreValve) TAVR and medical therapy unethical. Instead, a prospective single-arm study, the CoreValve Extreme Risk US Pivotal Trial, was used to compare the 12-month rate of death or major stroke with CoreValve TAVR vs a prespecified estimate of this rate with medical therapy.14 In about 500 patients who had a CoreValve attempt, the rate of all-cause mortality or major stroke at 1 year was significantly lower than the prespecified expected rate (26% vs 43%), reinforcing the results from the PARTNER Trial.14
Five-year outcomes
The 5-year PARTNER clinical and valve performance outcomes were published recently18 and continued to demonstrate equivalent outcomes for high-risk patients who underwent surgical aortic valve replacement or TAVR; there were no significant differences in all-cause mortality, cardiovascular mortality, stroke, or need for readmission to the hospital. The functional outcomes were similar as well, and no differences were demonstrated between surgical and TAVR valve performance.
Of note, moderate or severe aortic regurgitation occurred in 14% of patients in the TAVR group compared with 1% in the surgical aortic valve replacement group (P < .0001). This was associated with increased 5-year risk of death in the TAVR group (72.4% in those with moderate or severe aortic regurgitation vs 56.6% in those with mild aortic regurgitation or less; P = .003).
If the available randomized data are combined with observational reports, overall mortality and stroke rates are comparable between surgical aortic valve replacement and balloon-expandable or self-expandable TAVR in high-risk surgical candidates. Vascular complications, aortic regurgitation and permanent pacemaker insertion occur more frequently after TAVR, while major bleeding is more likely to occur after surgery.19 As newer generations of valves are developed, it is expected that aortic regurgitation and pacemaker rates will decrease over time. Indeed, trial data presented at the American College of Cardiology meeting in March 2015 for the third-generation Sapien valve (Sapien S3) showed only a 3.0% to 4.2% rate of significant paravalvular leak.
Contemporary valve comparison data
The valve used in the original PARTNER data was the first-generation Sapien valve. Since then, the second generation of this valve, the Sapien XT, has been introduced and is the model currently used in the United States (with the third-generation valve mentioned above, the Sapien S3, still available only through clinical trials). Thus, the two contemporary valves available for commercial use in the United States are the Edwards Sapien XT and Medtronic CoreValve. There are limited data comparing these valves head-to-head, but one recent trial attempted to do just that.
The Comparison of Transcatheter Heart Valves in High Risk Patients with Severe Aortic Stenosis: Medtronic CoreValve vs Edwards Sapien XT (CHOICE) trial compared the Edwards Sapien XT and CoreValve devices. Two hundred and forty-one patients were randomized. The primary end point of this trial was “device success” (a composite end point of four components: successful vascular access and deployment of the device with retrieval of the delivery system, correct position of the device, intended performance of the valve without moderate or severe insufficiency, and only one valve implanted in the correct anatomical location).
In this trial, the balloon-expandable Sapien XT valve showed a significantly higher device success rate than the self-expanding CoreValve, due to a significantly lower rate of aortic regurgitation (4.1% vs 18.3%, P < .001) and the less frequent need for implantation of more than one valve (0.8% vs 5.8%, P = .03). Placement of a permanent pacemaker was considerably less frequent in the balloon-expandable valve group (17.3% vs 37.6%, P = .001).20
PREOPERATIVE CONSIDERATIONS AND EVALUATION CRITERIA
Currently, TAVR is indicated for patients with symptomatic severe native aortic valve stenosis who are deemed at high risk or inoperable by a heart team including interventional cardiologists and cardiac surgeons. The CoreValve was also recently approved for valve-in-valve insertion in high-risk or inoperable patients with a prosthetic aortic valve in place.
The STS risk score is a reasonable preliminary risk assessment tool and is applicable to most patients being evaluated for aortic valve replacement. The STS risk score represents the percentage risk of unfavorable outcomes based on certain clinical variables. A calculator is available at riskcalc.sts.org. Patients considered at high risk are those with an STS operative risk score of 8% or higher or a postoperative 30-day risk of death of 15% or higher.
It is important to remember, though, that the STS score does not account for certain severe surgical risk factors. These include the presence of a "porcelain aorta" (heavy circumferential calcification of the ascending aorta precluding cross-clamping), history of mediastinal radiation, “hostile chest” (kyphoscoliosis, other deformities, previous coronary artery bypass grafting with adhesion of internal mammary artery to the back of sternum), severely compromised respiratory function (forced expiratory volume in 1 second < 1 L or < 40% predicted, diffusing capacity for carbon monoxide < 30%), severe pulmonary hypertension, severe liver disease (Model for End-stage Liver Disease score 8–20), severe dementia, severe cerebrovascular disease, and frailty.
With regard to this last risk factor, frailty is not simply old age but rather a measurable characteristic akin to weakness or disability. Several tests exist to measure frailty, including the “eyeball test” (the physician’s subjective assessment), Mini-Mental State Examination, gait speed/15-foot walk test, hand grip strength, serum albumin, and assessment of activities of daily living. Formal frailty testing is recommended during the course of a TAVR workup.
Risk assessment and patient suitability for TAVR is ultimately determined by the combined judgment of the heart valve team using both the STS score and consideration of these other factors.
Implantation approaches
Today, TAVR could be performed by several approaches: transfemoral arterial, transapical, transaortic via partial sternotomy or right anterior thoracotomy,21,22 transcarotid,23–25 and transaxillary or subclavian.26,27 Less commonly, transfemoral-venous routes have been performed utilizing either transseptal28 or caval-aortic puncture.29
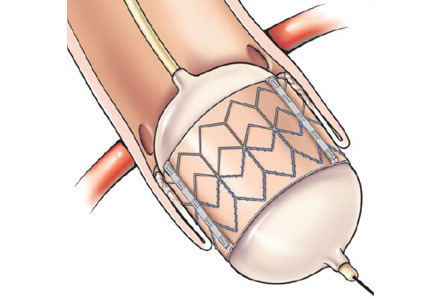
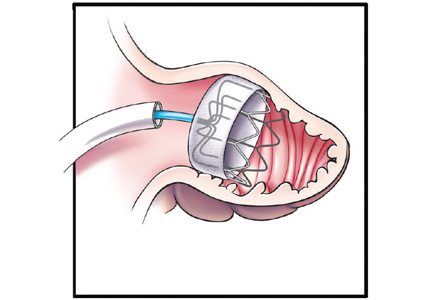
The transfemoral approach is used most commonly by most institutions, including Cleveland Clinic. It allows for a completely percutaneous insertion and, in select cases, without endotracheal intubation and general anesthesia (Figure 1).
In patients with difficult femoral access due to severe calcification, extreme tortuosity, or small diameter, alternative access routes become a consideration. In this situation, at our institution, we favor the transaortic approach in patients who have not undergone cardiac surgery in the past, while the transapical approach is used in patients who had previous cardiac surgery. With the transapical approach, we have found the outcomes similar to those of transfemoral TAVR after propensity matching.30,31 Although there is a learning curve,32 transapical TAVR can be performed with very limited mortality and morbidity. In a recent series at Cleveland Clinic, the mortality rate with the transapical approach was 1.2%, renal failure occurred in 4.7%, and a pacemaker was placed in 5.9% of patients; there were no strokes.33 This approach can be utilized for simultaneous additional procedures like transcatheter mitral valve reimplantation and percutaneous coronary interventions.34–36
- Andersen HR, Knudsen LL, Hasenkam JM. Transluminal implantation of artificial heart valves. Description of a new expandable aortic valve and initial results with implantation by catheter technique in closed chest pigs. Eur Heart J 1992; 13:704– 708.
- Cribier A, Eltchaninoff H, Bash A, et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case descrip- tion. Circulation 2002; 106:3006–3008.
- Cribier A, Eltchaninoff H, Tron C, et al. Early experience with percutaneous transcatheter implantation of heart valve prosthesis for the treatment of end-stage inoperable patients with calcific aortic stenosis. J Am Coll Cardiol 2004; 43:698– 703.
- Dewey TM, Walther T, Doss M, et al. Transapical aortic valve implantation: an animal feasibility study. Ann Thorac Surg 2006; 82:110–116.
- Svensson LG, Dewey T, Kapadia S, et al. United States feasibility study of trans- catheter insertion of a stented aortic valve by the left ventricular apex. Ann Thorac Surg 2008; 86:46–54.
- Lichtenstein SV, Cheung A, Ye J, et al. Transapical transcatheter aortic valve im- plantation in humans: initial clinical experience. Circulation 2006; 114:591–596.
- Webb JG, Pasupati S, Hyumphries K, et al. Percutaneous transarterial aortic valve replacement in selected high-risk patients with aortic stenosis. Circulation 2007; 116:755–763.
- Leon MB, Kodali S, Williams M, et al. Transcatheter aortic valve replacement in patients with critical aortic stenosis: rationale, device descriptions, early clinical experiences, and perspectives. Semin Thorac Cardiovasc Surg 2006; 18:165–174.
- Leon MB, Smith CR, Mack M, et al; PARTNER Trial Investigators. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo sur- gery. N Engl J Med 2010; 363:1597–1607.
- Smith CR, Leon MB, Mack MJ, et al; PARTNER Trial Investigators. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 2011; 364:2187–2198.
- Adams DH, Popma JJ, Reardon MJ, et al; U.S. CoreValve Clinical Investigators. Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med 2014; 370:1790–1798.
- Kodali SK, Williams MR, Smith CR, et al; PARTNER Trial Investigators. Two- year outcomes after transcatheter or surgical aortic-valve replacement. N Engl J Med 2012; 366:1686–1695.
- Reardon M, et al. A randomized comparison of self-expanding
- Popma JJ, Adams DH, Reardon MJ, et al; CoreValve United States Clinical In- vestigators. Transcatheter aortic valve replacement using a self-expanding biopros- thesis in patients with severe aortic stenosis at extreme risk for surgery. J Am Coll Cardiol 2014; 63:1972–1981.
- Adams DH, Popma JJ, Reardon MJ. Transcatheter aortic-valve replacement with a self-expanding prosthesis (letter). N Engl J Med 2014; 371:967–968.
- Kaul S. Transcatheter aortic-valve replacement with a self-expanding prosthesis (letter). N Engl J Med 2014; 371:967.
- Makkar RR, Fontana GP, Jilaihawi H, et al. Transcathether aortic-valve re- placement for inoperable severe aortic stenosis. N Engl J Med 2012; 366: 1696–704.
- Mack MJ, Leon MB, Smith CR, et al; PARTNER 1 trial investigators. 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve re- placement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet 2015; 385:2477–2484.
- Cao C, Ang SC, Indraratna P, et al. Systematic review and meta-analysis of trans- catheter aortic valve implantation versus surgical aortic valve replacement for severe aortic stenosis. Ann Cardiothorac Surg 2013; 2:10–23.
- Abdel-Wahab M, Mehilli J, Frerker C, et al; CHOICE investigators. Comparison of balloon-expandable vs self-expandable valves in patients undergoing transcath- eter aortic valve replacement: the CHOICE randomized clinical trial. JAMA 2014; 311:1503–1514.
- Okuyama K, Jilaihawi H, Mirocha J, et al. Alternative access for balloon-ex- pandable transcatheter aortic valve replacement: comparison of the transaortic approach using right anterior thoracotomy to partial J-sternotomy. J Thorac Car- diovasc Surg 2014; 149:789–797.
- Lardizabal JA, O’Neill BP, Desai HV, et al. The transaortic approach for transcath- eter aortic valve replacement: initial clinical experience in the United States. J Am Coll Cardiol 2013; 61:2341–2345.
- Thourani VH, Gunter RL, Neravetla S, et al. Use of transaortic, transapical, and transcarotid transcatheter aortic valve replacement in inoperable patients. Ann Thorac Surg 2013; 96:1349–1357.
- Azmoun A, Amabile N, Ramadan R, et al. Transcatheter aortic valve implantation through carotid artery access under local anaesthesia. Eur J Cardiothorac Surg 2014; 46: 693–698.
- Rajagopal R, More RS, Roberts DH. Transcatheter aortic valve implantation through a transcarotid approach under local anesthesia. Catheter Cardiovasc In- terv 2014; 84:903–907.
- Fraccaro C, Napodano M, Tarantini G, et al. Expanding the eligibility for trans- catheter aortic valve implantation the trans-subclavian retrograde approach using: the III generation CoreValve revalving system. JACC Cardiovasc Interv 2009; 2:828–333.
- Petronio AS, De Carlo M, Bedogni F, et al. Safety and efficacy of the subclavian approach for transcatheter aortic valve implantation with the CoreValve revalving system. Circ Cardiovasc Interv 2010; 3:359–366.
- Cohen MG, Singh V, Martinez CA, et al. Transseptal antegrade transcatheter aor- tic valve replacement for patients with no other access approach—a contemporary experience. Catheter Cardiovasc Interv 2013; 82:987–993.
- Greenbaum AB, O’Neill WW, Paone G, et al. Caval-aortic access to allow trans- catheter aortic valve replacement in otherwise ineligible patients: initial human experience. J Am Coll Cardiol 2014; 63:2795–2804.
- D’Onofrio A, Salizzoni S, Agrifoglio M, et al. Medium term outcomes of trans- apical aortic valve implantation: results from the Italian Registry of Trans-Apical Aortic Valve Implantation. Ann Thorac Surg 2013; 96:830–835.
- Johansson M, Nozohoor S, Kimblad PO, Harnek J, Olivecrona GK, Sjögren J. Transapical versus transfemoral aortic valve implantation: a comparison of survival and safety. Ann Thorac Surg 2011; 91:57–63.
- Kempfert J, Rastan A, Holzhey D, et al. Transapical aortic valve implantation: analysis of risk factors and learning experience in 299 patients. Circulation 2011; 124(suppl):S124–S129.
- Aguirre J, Waskowski R, Poddar K, et al. Transcatheter aortic valve replacement: experience with the transapical approach, alternate access sites, and concomitant cardiac repairs. J Thorac Cardiovasc Surg 2014; 148:1417–1422.
- Al Kindi AH, Salhab KF, Roselli EE, Kapadia S, Tuzcu EM, Svensson LG. Alternative access options for transcatheter aortic valve replacement in patients with no conventional access and chest pathology. J Thorac Cardiovasc Surg 2014; 147:644–651.
- Salhab KF, Al Kindi AH, Lane JH, et al. Concomitant percutaneous coronary intervention and transcatheter aortic valve replacement: safe and feasible replace- ment alternative approaches in high-risk patients with severe aortic stenosis and coronary artery disease. J Card Surg 2013; 28:481–483.
- Al Kindi AH, Salhab KF, Kapadia S, et al. Simultaneous transapical transcatheter aortic and mitral valve replacement in a high-risk patient with a previous mitral bioprosthesis. J Thorac Cardiovasc Surg 2012; 144:e90–e91.
Transcatheter aortic valve replacement (TAVR) has established itself as an effective way of treating high-risk patients with severe aortic valve stenosis. With new generations of existing valves and newer alternative devices, the procedure promises to become increasingly safer. The field is evolving rapidly and it will be important for interventional cardiologists and cardiac surgeons alike to stay abreast of developments. This article reviews the history of this promising procedure and examines its use in current practice.
HISTORICAL PERSPECTIVE
In 1980, Danish researcher H. R. Anderson reported developing and testing a balloon-expandable valve in animals.1 The technology was eventually acquired and further developed by Edwards Life Sciences (Irvine, California).
Alain Cribier started early work in humans in 2002 in France.2 He used a transfemoral arterial access to approach the aortic valve transseptally, but this procedure was associated with high rates of mortality and stroke.3 At the same time, in the United States, animal studies were being carried out by Lars G. Svensson, Todd Dewey, and Michael Mack to develop a transapical method of implantation,4,5 while John Webb and colleagues were also developing a transapical aortic valve implantation technique,6,7 and later went on to develop a retrograde transfemoral technique. This latter technique became feasible once Edwards developed a catheter that could be flexed to get around the aortic arch and across the aortic valve.
As the Edwards balloon-expandable valve (Sapien) was being developed, a nitinol-based self-expandable valve system was introduced by Medtronic: the CoreValve. Following feasibility studies,5,8 the safety and efficacy of these valves were established thorough the Placement of Aortic Transcatheter Valves (PARTNER) trial and the US Core Valve Pivotal Trial. These valves are currently approved by the US Food and Drug Administration (FDA) for patients for whom conventional surgery would pose an extreme or high risk.9–11
CLINICAL TRIALS OF TAVR
The two landmark prospective randomized trials of TAVR were the PARTNER trial and CoreValve Pivotal Trial.
The PARTNER trial consisted of two parts: PARTNER A, which compared the Sapien balloon-expandable transcatheter valve with surgical aortic valve replacement in patients at high surgical risk (Society of Thoracic Surgeons [STS] score > 10%), and PARTNER B, which compared TAVR with medical therapy in patients who could not undergo surgery (combined risk of serious morbidity or death of 50% or more, and two surgeons agreeing that the patient was inoperable).
Similarly, the CoreValve Pivotal Trial compared the self-expandable transcatheter valve with conventional medical and surgical treatment.
TAVR is comparable to surgery in outcomes, with caveats
In the PARTNER A trial, mortality rates were similar between patients who underwent Sapien TAVR and those who underwent surgical valve replacement at 30 days (3.4% and 6.5%, P = .07), 1 year (24.2% and 26.8%), and 2 years (33.9% and 35.0%). The patients in this group were randomized to either Sapien TAVR or surgery (Table 1).10,12
The combined rate of stroke and transient ischemic attack was higher in the patients assigned to TAVR at 30 days (5.5% with TAVR vs 2.4% with surgery, P = .04) and at 1 year (8.3% with TAVR vs 4.3% with surgery, P = .04). The difference was of small significance at 2 years (11.2% vs 6.5%, P = .05). At 30 days, the rate of major vascular complications was higher with TAVR (11.0% vs 3.2%), while surgery was associated with more frequent major bleeding episodes (19.5% vs 9.3%) and new-onset atrial fibrillation (16.0% vs 8.6%). The rate of new pacemaker requirement at 30 days was similar between the TAVR and surgical groups (3.8% vs 3.6%). Moderate or severe paravalvular aortic regurgitation was more common after TAVR at 30 days, 1 year, and 2 years. This aortic insufficiency was associated with increased late mortality.10,12
In the US CoreValve High Risk Study, no difference was found in the 30-day mortality rate in patients at high surgical risk randomized to CoreValve TAVR or surgery (3.3% and 4.5%) (Table 1). Surprisingly, the 1-year mortality rate was lower in the TAVR group than in the surgical group (14.1% vs 18.9%, respectively), a finding sustained at 2 years in data presented at the American College of Cardiology conference in March 2015.13–16
TAVR is superior to medical management, but the risk of stroke is higher
In the PARTNER B trial, inoperable patients were randomly assigned to undergo TAVR with a Sapien valve or medical management. TAVR resulted in lower mortality rates at 1 year (30.7% vs 50.7%) and 2 years (43.4% vs 68.0%) compared with medical management (Table 1).17 Of note, medical management included balloon valvuloplasty. The rate of the composite end point of death or repeat hospitalization was also lower with TAVR compared with medical therapy (44.1% vs 71.6%, respectively, at 1 year and 56.7% and 87.9%, respectively, at 2 years).17 The TAVR group had a higher stroke rate than the medical therapy group at 30 days (11.2% vs 5.5%, respectively) and at 2 years (13.8% vs 5.5%).17 Survival improved with TAVR in patients with an STS score of less than 15% but not in those with an STS score of 15% or higher.9
The very favorable results from the PARTNER trial rendered a randomized trial comparing self-expanding (CoreValve) TAVR and medical therapy unethical. Instead, a prospective single-arm study, the CoreValve Extreme Risk US Pivotal Trial, was used to compare the 12-month rate of death or major stroke with CoreValve TAVR vs a prespecified estimate of this rate with medical therapy.14 In about 500 patients who had a CoreValve attempt, the rate of all-cause mortality or major stroke at 1 year was significantly lower than the prespecified expected rate (26% vs 43%), reinforcing the results from the PARTNER Trial.14
Five-year outcomes
The 5-year PARTNER clinical and valve performance outcomes were published recently18 and continued to demonstrate equivalent outcomes for high-risk patients who underwent surgical aortic valve replacement or TAVR; there were no significant differences in all-cause mortality, cardiovascular mortality, stroke, or need for readmission to the hospital. The functional outcomes were similar as well, and no differences were demonstrated between surgical and TAVR valve performance.
Of note, moderate or severe aortic regurgitation occurred in 14% of patients in the TAVR group compared with 1% in the surgical aortic valve replacement group (P < .0001). This was associated with increased 5-year risk of death in the TAVR group (72.4% in those with moderate or severe aortic regurgitation vs 56.6% in those with mild aortic regurgitation or less; P = .003).
If the available randomized data are combined with observational reports, overall mortality and stroke rates are comparable between surgical aortic valve replacement and balloon-expandable or self-expandable TAVR in high-risk surgical candidates. Vascular complications, aortic regurgitation and permanent pacemaker insertion occur more frequently after TAVR, while major bleeding is more likely to occur after surgery.19 As newer generations of valves are developed, it is expected that aortic regurgitation and pacemaker rates will decrease over time. Indeed, trial data presented at the American College of Cardiology meeting in March 2015 for the third-generation Sapien valve (Sapien S3) showed only a 3.0% to 4.2% rate of significant paravalvular leak.
Contemporary valve comparison data
The valve used in the original PARTNER data was the first-generation Sapien valve. Since then, the second generation of this valve, the Sapien XT, has been introduced and is the model currently used in the United States (with the third-generation valve mentioned above, the Sapien S3, still available only through clinical trials). Thus, the two contemporary valves available for commercial use in the United States are the Edwards Sapien XT and Medtronic CoreValve. There are limited data comparing these valves head-to-head, but one recent trial attempted to do just that.
The Comparison of Transcatheter Heart Valves in High Risk Patients with Severe Aortic Stenosis: Medtronic CoreValve vs Edwards Sapien XT (CHOICE) trial compared the Edwards Sapien XT and CoreValve devices. Two hundred and forty-one patients were randomized. The primary end point of this trial was “device success” (a composite end point of four components: successful vascular access and deployment of the device with retrieval of the delivery system, correct position of the device, intended performance of the valve without moderate or severe insufficiency, and only one valve implanted in the correct anatomical location).
In this trial, the balloon-expandable Sapien XT valve showed a significantly higher device success rate than the self-expanding CoreValve, due to a significantly lower rate of aortic regurgitation (4.1% vs 18.3%, P < .001) and the less frequent need for implantation of more than one valve (0.8% vs 5.8%, P = .03). Placement of a permanent pacemaker was considerably less frequent in the balloon-expandable valve group (17.3% vs 37.6%, P = .001).20
PREOPERATIVE CONSIDERATIONS AND EVALUATION CRITERIA
Currently, TAVR is indicated for patients with symptomatic severe native aortic valve stenosis who are deemed at high risk or inoperable by a heart team including interventional cardiologists and cardiac surgeons. The CoreValve was also recently approved for valve-in-valve insertion in high-risk or inoperable patients with a prosthetic aortic valve in place.
The STS risk score is a reasonable preliminary risk assessment tool and is applicable to most patients being evaluated for aortic valve replacement. The STS risk score represents the percentage risk of unfavorable outcomes based on certain clinical variables. A calculator is available at riskcalc.sts.org. Patients considered at high risk are those with an STS operative risk score of 8% or higher or a postoperative 30-day risk of death of 15% or higher.
It is important to remember, though, that the STS score does not account for certain severe surgical risk factors. These include the presence of a "porcelain aorta" (heavy circumferential calcification of the ascending aorta precluding cross-clamping), history of mediastinal radiation, “hostile chest” (kyphoscoliosis, other deformities, previous coronary artery bypass grafting with adhesion of internal mammary artery to the back of sternum), severely compromised respiratory function (forced expiratory volume in 1 second < 1 L or < 40% predicted, diffusing capacity for carbon monoxide < 30%), severe pulmonary hypertension, severe liver disease (Model for End-stage Liver Disease score 8–20), severe dementia, severe cerebrovascular disease, and frailty.
With regard to this last risk factor, frailty is not simply old age but rather a measurable characteristic akin to weakness or disability. Several tests exist to measure frailty, including the “eyeball test” (the physician’s subjective assessment), Mini-Mental State Examination, gait speed/15-foot walk test, hand grip strength, serum albumin, and assessment of activities of daily living. Formal frailty testing is recommended during the course of a TAVR workup.
Risk assessment and patient suitability for TAVR is ultimately determined by the combined judgment of the heart valve team using both the STS score and consideration of these other factors.
Implantation approaches
Today, TAVR could be performed by several approaches: transfemoral arterial, transapical, transaortic via partial sternotomy or right anterior thoracotomy,21,22 transcarotid,23–25 and transaxillary or subclavian.26,27 Less commonly, transfemoral-venous routes have been performed utilizing either transseptal28 or caval-aortic puncture.29
The transfemoral approach is used most commonly by most institutions, including Cleveland Clinic. It allows for a completely percutaneous insertion and, in select cases, without endotracheal intubation and general anesthesia (Figure 1).
In patients with difficult femoral access due to severe calcification, extreme tortuosity, or small diameter, alternative access routes become a consideration. In this situation, at our institution, we favor the transaortic approach in patients who have not undergone cardiac surgery in the past, while the transapical approach is used in patients who had previous cardiac surgery. With the transapical approach, we have found the outcomes similar to those of transfemoral TAVR after propensity matching.30,31 Although there is a learning curve,32 transapical TAVR can be performed with very limited mortality and morbidity. In a recent series at Cleveland Clinic, the mortality rate with the transapical approach was 1.2%, renal failure occurred in 4.7%, and a pacemaker was placed in 5.9% of patients; there were no strokes.33 This approach can be utilized for simultaneous additional procedures like transcatheter mitral valve reimplantation and percutaneous coronary interventions.34–36
Transcatheter aortic valve replacement (TAVR) has established itself as an effective way of treating high-risk patients with severe aortic valve stenosis. With new generations of existing valves and newer alternative devices, the procedure promises to become increasingly safer. The field is evolving rapidly and it will be important for interventional cardiologists and cardiac surgeons alike to stay abreast of developments. This article reviews the history of this promising procedure and examines its use in current practice.
HISTORICAL PERSPECTIVE
In 1980, Danish researcher H. R. Anderson reported developing and testing a balloon-expandable valve in animals.1 The technology was eventually acquired and further developed by Edwards Life Sciences (Irvine, California).
Alain Cribier started early work in humans in 2002 in France.2 He used a transfemoral arterial access to approach the aortic valve transseptally, but this procedure was associated with high rates of mortality and stroke.3 At the same time, in the United States, animal studies were being carried out by Lars G. Svensson, Todd Dewey, and Michael Mack to develop a transapical method of implantation,4,5 while John Webb and colleagues were also developing a transapical aortic valve implantation technique,6,7 and later went on to develop a retrograde transfemoral technique. This latter technique became feasible once Edwards developed a catheter that could be flexed to get around the aortic arch and across the aortic valve.
As the Edwards balloon-expandable valve (Sapien) was being developed, a nitinol-based self-expandable valve system was introduced by Medtronic: the CoreValve. Following feasibility studies,5,8 the safety and efficacy of these valves were established thorough the Placement of Aortic Transcatheter Valves (PARTNER) trial and the US Core Valve Pivotal Trial. These valves are currently approved by the US Food and Drug Administration (FDA) for patients for whom conventional surgery would pose an extreme or high risk.9–11
CLINICAL TRIALS OF TAVR
The two landmark prospective randomized trials of TAVR were the PARTNER trial and CoreValve Pivotal Trial.
The PARTNER trial consisted of two parts: PARTNER A, which compared the Sapien balloon-expandable transcatheter valve with surgical aortic valve replacement in patients at high surgical risk (Society of Thoracic Surgeons [STS] score > 10%), and PARTNER B, which compared TAVR with medical therapy in patients who could not undergo surgery (combined risk of serious morbidity or death of 50% or more, and two surgeons agreeing that the patient was inoperable).
Similarly, the CoreValve Pivotal Trial compared the self-expandable transcatheter valve with conventional medical and surgical treatment.
TAVR is comparable to surgery in outcomes, with caveats
In the PARTNER A trial, mortality rates were similar between patients who underwent Sapien TAVR and those who underwent surgical valve replacement at 30 days (3.4% and 6.5%, P = .07), 1 year (24.2% and 26.8%), and 2 years (33.9% and 35.0%). The patients in this group were randomized to either Sapien TAVR or surgery (Table 1).10,12
The combined rate of stroke and transient ischemic attack was higher in the patients assigned to TAVR at 30 days (5.5% with TAVR vs 2.4% with surgery, P = .04) and at 1 year (8.3% with TAVR vs 4.3% with surgery, P = .04). The difference was of small significance at 2 years (11.2% vs 6.5%, P = .05). At 30 days, the rate of major vascular complications was higher with TAVR (11.0% vs 3.2%), while surgery was associated with more frequent major bleeding episodes (19.5% vs 9.3%) and new-onset atrial fibrillation (16.0% vs 8.6%). The rate of new pacemaker requirement at 30 days was similar between the TAVR and surgical groups (3.8% vs 3.6%). Moderate or severe paravalvular aortic regurgitation was more common after TAVR at 30 days, 1 year, and 2 years. This aortic insufficiency was associated with increased late mortality.10,12
In the US CoreValve High Risk Study, no difference was found in the 30-day mortality rate in patients at high surgical risk randomized to CoreValve TAVR or surgery (3.3% and 4.5%) (Table 1). Surprisingly, the 1-year mortality rate was lower in the TAVR group than in the surgical group (14.1% vs 18.9%, respectively), a finding sustained at 2 years in data presented at the American College of Cardiology conference in March 2015.13–16
TAVR is superior to medical management, but the risk of stroke is higher
In the PARTNER B trial, inoperable patients were randomly assigned to undergo TAVR with a Sapien valve or medical management. TAVR resulted in lower mortality rates at 1 year (30.7% vs 50.7%) and 2 years (43.4% vs 68.0%) compared with medical management (Table 1).17 Of note, medical management included balloon valvuloplasty. The rate of the composite end point of death or repeat hospitalization was also lower with TAVR compared with medical therapy (44.1% vs 71.6%, respectively, at 1 year and 56.7% and 87.9%, respectively, at 2 years).17 The TAVR group had a higher stroke rate than the medical therapy group at 30 days (11.2% vs 5.5%, respectively) and at 2 years (13.8% vs 5.5%).17 Survival improved with TAVR in patients with an STS score of less than 15% but not in those with an STS score of 15% or higher.9
The very favorable results from the PARTNER trial rendered a randomized trial comparing self-expanding (CoreValve) TAVR and medical therapy unethical. Instead, a prospective single-arm study, the CoreValve Extreme Risk US Pivotal Trial, was used to compare the 12-month rate of death or major stroke with CoreValve TAVR vs a prespecified estimate of this rate with medical therapy.14 In about 500 patients who had a CoreValve attempt, the rate of all-cause mortality or major stroke at 1 year was significantly lower than the prespecified expected rate (26% vs 43%), reinforcing the results from the PARTNER Trial.14
Five-year outcomes
The 5-year PARTNER clinical and valve performance outcomes were published recently18 and continued to demonstrate equivalent outcomes for high-risk patients who underwent surgical aortic valve replacement or TAVR; there were no significant differences in all-cause mortality, cardiovascular mortality, stroke, or need for readmission to the hospital. The functional outcomes were similar as well, and no differences were demonstrated between surgical and TAVR valve performance.
Of note, moderate or severe aortic regurgitation occurred in 14% of patients in the TAVR group compared with 1% in the surgical aortic valve replacement group (P < .0001). This was associated with increased 5-year risk of death in the TAVR group (72.4% in those with moderate or severe aortic regurgitation vs 56.6% in those with mild aortic regurgitation or less; P = .003).
If the available randomized data are combined with observational reports, overall mortality and stroke rates are comparable between surgical aortic valve replacement and balloon-expandable or self-expandable TAVR in high-risk surgical candidates. Vascular complications, aortic regurgitation and permanent pacemaker insertion occur more frequently after TAVR, while major bleeding is more likely to occur after surgery.19 As newer generations of valves are developed, it is expected that aortic regurgitation and pacemaker rates will decrease over time. Indeed, trial data presented at the American College of Cardiology meeting in March 2015 for the third-generation Sapien valve (Sapien S3) showed only a 3.0% to 4.2% rate of significant paravalvular leak.
Contemporary valve comparison data
The valve used in the original PARTNER data was the first-generation Sapien valve. Since then, the second generation of this valve, the Sapien XT, has been introduced and is the model currently used in the United States (with the third-generation valve mentioned above, the Sapien S3, still available only through clinical trials). Thus, the two contemporary valves available for commercial use in the United States are the Edwards Sapien XT and Medtronic CoreValve. There are limited data comparing these valves head-to-head, but one recent trial attempted to do just that.
The Comparison of Transcatheter Heart Valves in High Risk Patients with Severe Aortic Stenosis: Medtronic CoreValve vs Edwards Sapien XT (CHOICE) trial compared the Edwards Sapien XT and CoreValve devices. Two hundred and forty-one patients were randomized. The primary end point of this trial was “device success” (a composite end point of four components: successful vascular access and deployment of the device with retrieval of the delivery system, correct position of the device, intended performance of the valve without moderate or severe insufficiency, and only one valve implanted in the correct anatomical location).
In this trial, the balloon-expandable Sapien XT valve showed a significantly higher device success rate than the self-expanding CoreValve, due to a significantly lower rate of aortic regurgitation (4.1% vs 18.3%, P < .001) and the less frequent need for implantation of more than one valve (0.8% vs 5.8%, P = .03). Placement of a permanent pacemaker was considerably less frequent in the balloon-expandable valve group (17.3% vs 37.6%, P = .001).20
PREOPERATIVE CONSIDERATIONS AND EVALUATION CRITERIA
Currently, TAVR is indicated for patients with symptomatic severe native aortic valve stenosis who are deemed at high risk or inoperable by a heart team including interventional cardiologists and cardiac surgeons. The CoreValve was also recently approved for valve-in-valve insertion in high-risk or inoperable patients with a prosthetic aortic valve in place.
The STS risk score is a reasonable preliminary risk assessment tool and is applicable to most patients being evaluated for aortic valve replacement. The STS risk score represents the percentage risk of unfavorable outcomes based on certain clinical variables. A calculator is available at riskcalc.sts.org. Patients considered at high risk are those with an STS operative risk score of 8% or higher or a postoperative 30-day risk of death of 15% or higher.
It is important to remember, though, that the STS score does not account for certain severe surgical risk factors. These include the presence of a "porcelain aorta" (heavy circumferential calcification of the ascending aorta precluding cross-clamping), history of mediastinal radiation, “hostile chest” (kyphoscoliosis, other deformities, previous coronary artery bypass grafting with adhesion of internal mammary artery to the back of sternum), severely compromised respiratory function (forced expiratory volume in 1 second < 1 L or < 40% predicted, diffusing capacity for carbon monoxide < 30%), severe pulmonary hypertension, severe liver disease (Model for End-stage Liver Disease score 8–20), severe dementia, severe cerebrovascular disease, and frailty.
With regard to this last risk factor, frailty is not simply old age but rather a measurable characteristic akin to weakness or disability. Several tests exist to measure frailty, including the “eyeball test” (the physician’s subjective assessment), Mini-Mental State Examination, gait speed/15-foot walk test, hand grip strength, serum albumin, and assessment of activities of daily living. Formal frailty testing is recommended during the course of a TAVR workup.
Risk assessment and patient suitability for TAVR is ultimately determined by the combined judgment of the heart valve team using both the STS score and consideration of these other factors.
Implantation approaches
Today, TAVR could be performed by several approaches: transfemoral arterial, transapical, transaortic via partial sternotomy or right anterior thoracotomy,21,22 transcarotid,23–25 and transaxillary or subclavian.26,27 Less commonly, transfemoral-venous routes have been performed utilizing either transseptal28 or caval-aortic puncture.29
The transfemoral approach is used most commonly by most institutions, including Cleveland Clinic. It allows for a completely percutaneous insertion and, in select cases, without endotracheal intubation and general anesthesia (Figure 1).
In patients with difficult femoral access due to severe calcification, extreme tortuosity, or small diameter, alternative access routes become a consideration. In this situation, at our institution, we favor the transaortic approach in patients who have not undergone cardiac surgery in the past, while the transapical approach is used in patients who had previous cardiac surgery. With the transapical approach, we have found the outcomes similar to those of transfemoral TAVR after propensity matching.30,31 Although there is a learning curve,32 transapical TAVR can be performed with very limited mortality and morbidity. In a recent series at Cleveland Clinic, the mortality rate with the transapical approach was 1.2%, renal failure occurred in 4.7%, and a pacemaker was placed in 5.9% of patients; there were no strokes.33 This approach can be utilized for simultaneous additional procedures like transcatheter mitral valve reimplantation and percutaneous coronary interventions.34–36
- Andersen HR, Knudsen LL, Hasenkam JM. Transluminal implantation of artificial heart valves. Description of a new expandable aortic valve and initial results with implantation by catheter technique in closed chest pigs. Eur Heart J 1992; 13:704– 708.
- Cribier A, Eltchaninoff H, Bash A, et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case descrip- tion. Circulation 2002; 106:3006–3008.
- Cribier A, Eltchaninoff H, Tron C, et al. Early experience with percutaneous transcatheter implantation of heart valve prosthesis for the treatment of end-stage inoperable patients with calcific aortic stenosis. J Am Coll Cardiol 2004; 43:698– 703.
- Dewey TM, Walther T, Doss M, et al. Transapical aortic valve implantation: an animal feasibility study. Ann Thorac Surg 2006; 82:110–116.
- Svensson LG, Dewey T, Kapadia S, et al. United States feasibility study of trans- catheter insertion of a stented aortic valve by the left ventricular apex. Ann Thorac Surg 2008; 86:46–54.
- Lichtenstein SV, Cheung A, Ye J, et al. Transapical transcatheter aortic valve im- plantation in humans: initial clinical experience. Circulation 2006; 114:591–596.
- Webb JG, Pasupati S, Hyumphries K, et al. Percutaneous transarterial aortic valve replacement in selected high-risk patients with aortic stenosis. Circulation 2007; 116:755–763.
- Leon MB, Kodali S, Williams M, et al. Transcatheter aortic valve replacement in patients with critical aortic stenosis: rationale, device descriptions, early clinical experiences, and perspectives. Semin Thorac Cardiovasc Surg 2006; 18:165–174.
- Leon MB, Smith CR, Mack M, et al; PARTNER Trial Investigators. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo sur- gery. N Engl J Med 2010; 363:1597–1607.
- Smith CR, Leon MB, Mack MJ, et al; PARTNER Trial Investigators. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 2011; 364:2187–2198.
- Adams DH, Popma JJ, Reardon MJ, et al; U.S. CoreValve Clinical Investigators. Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med 2014; 370:1790–1798.
- Kodali SK, Williams MR, Smith CR, et al; PARTNER Trial Investigators. Two- year outcomes after transcatheter or surgical aortic-valve replacement. N Engl J Med 2012; 366:1686–1695.
- Reardon M, et al. A randomized comparison of self-expanding
- Popma JJ, Adams DH, Reardon MJ, et al; CoreValve United States Clinical In- vestigators. Transcatheter aortic valve replacement using a self-expanding biopros- thesis in patients with severe aortic stenosis at extreme risk for surgery. J Am Coll Cardiol 2014; 63:1972–1981.
- Adams DH, Popma JJ, Reardon MJ. Transcatheter aortic-valve replacement with a self-expanding prosthesis (letter). N Engl J Med 2014; 371:967–968.
- Kaul S. Transcatheter aortic-valve replacement with a self-expanding prosthesis (letter). N Engl J Med 2014; 371:967.
- Makkar RR, Fontana GP, Jilaihawi H, et al. Transcathether aortic-valve re- placement for inoperable severe aortic stenosis. N Engl J Med 2012; 366: 1696–704.
- Mack MJ, Leon MB, Smith CR, et al; PARTNER 1 trial investigators. 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve re- placement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet 2015; 385:2477–2484.
- Cao C, Ang SC, Indraratna P, et al. Systematic review and meta-analysis of trans- catheter aortic valve implantation versus surgical aortic valve replacement for severe aortic stenosis. Ann Cardiothorac Surg 2013; 2:10–23.
- Abdel-Wahab M, Mehilli J, Frerker C, et al; CHOICE investigators. Comparison of balloon-expandable vs self-expandable valves in patients undergoing transcath- eter aortic valve replacement: the CHOICE randomized clinical trial. JAMA 2014; 311:1503–1514.
- Okuyama K, Jilaihawi H, Mirocha J, et al. Alternative access for balloon-ex- pandable transcatheter aortic valve replacement: comparison of the transaortic approach using right anterior thoracotomy to partial J-sternotomy. J Thorac Car- diovasc Surg 2014; 149:789–797.
- Lardizabal JA, O’Neill BP, Desai HV, et al. The transaortic approach for transcath- eter aortic valve replacement: initial clinical experience in the United States. J Am Coll Cardiol 2013; 61:2341–2345.
- Thourani VH, Gunter RL, Neravetla S, et al. Use of transaortic, transapical, and transcarotid transcatheter aortic valve replacement in inoperable patients. Ann Thorac Surg 2013; 96:1349–1357.
- Azmoun A, Amabile N, Ramadan R, et al. Transcatheter aortic valve implantation through carotid artery access under local anaesthesia. Eur J Cardiothorac Surg 2014; 46: 693–698.
- Rajagopal R, More RS, Roberts DH. Transcatheter aortic valve implantation through a transcarotid approach under local anesthesia. Catheter Cardiovasc In- terv 2014; 84:903–907.
- Fraccaro C, Napodano M, Tarantini G, et al. Expanding the eligibility for trans- catheter aortic valve implantation the trans-subclavian retrograde approach using: the III generation CoreValve revalving system. JACC Cardiovasc Interv 2009; 2:828–333.
- Petronio AS, De Carlo M, Bedogni F, et al. Safety and efficacy of the subclavian approach for transcatheter aortic valve implantation with the CoreValve revalving system. Circ Cardiovasc Interv 2010; 3:359–366.
- Cohen MG, Singh V, Martinez CA, et al. Transseptal antegrade transcatheter aor- tic valve replacement for patients with no other access approach—a contemporary experience. Catheter Cardiovasc Interv 2013; 82:987–993.
- Greenbaum AB, O’Neill WW, Paone G, et al. Caval-aortic access to allow trans- catheter aortic valve replacement in otherwise ineligible patients: initial human experience. J Am Coll Cardiol 2014; 63:2795–2804.
- D’Onofrio A, Salizzoni S, Agrifoglio M, et al. Medium term outcomes of trans- apical aortic valve implantation: results from the Italian Registry of Trans-Apical Aortic Valve Implantation. Ann Thorac Surg 2013; 96:830–835.
- Johansson M, Nozohoor S, Kimblad PO, Harnek J, Olivecrona GK, Sjögren J. Transapical versus transfemoral aortic valve implantation: a comparison of survival and safety. Ann Thorac Surg 2011; 91:57–63.
- Kempfert J, Rastan A, Holzhey D, et al. Transapical aortic valve implantation: analysis of risk factors and learning experience in 299 patients. Circulation 2011; 124(suppl):S124–S129.
- Aguirre J, Waskowski R, Poddar K, et al. Transcatheter aortic valve replacement: experience with the transapical approach, alternate access sites, and concomitant cardiac repairs. J Thorac Cardiovasc Surg 2014; 148:1417–1422.
- Al Kindi AH, Salhab KF, Roselli EE, Kapadia S, Tuzcu EM, Svensson LG. Alternative access options for transcatheter aortic valve replacement in patients with no conventional access and chest pathology. J Thorac Cardiovasc Surg 2014; 147:644–651.
- Salhab KF, Al Kindi AH, Lane JH, et al. Concomitant percutaneous coronary intervention and transcatheter aortic valve replacement: safe and feasible replace- ment alternative approaches in high-risk patients with severe aortic stenosis and coronary artery disease. J Card Surg 2013; 28:481–483.
- Al Kindi AH, Salhab KF, Kapadia S, et al. Simultaneous transapical transcatheter aortic and mitral valve replacement in a high-risk patient with a previous mitral bioprosthesis. J Thorac Cardiovasc Surg 2012; 144:e90–e91.
- Andersen HR, Knudsen LL, Hasenkam JM. Transluminal implantation of artificial heart valves. Description of a new expandable aortic valve and initial results with implantation by catheter technique in closed chest pigs. Eur Heart J 1992; 13:704– 708.
- Cribier A, Eltchaninoff H, Bash A, et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case descrip- tion. Circulation 2002; 106:3006–3008.
- Cribier A, Eltchaninoff H, Tron C, et al. Early experience with percutaneous transcatheter implantation of heart valve prosthesis for the treatment of end-stage inoperable patients with calcific aortic stenosis. J Am Coll Cardiol 2004; 43:698– 703.
- Dewey TM, Walther T, Doss M, et al. Transapical aortic valve implantation: an animal feasibility study. Ann Thorac Surg 2006; 82:110–116.
- Svensson LG, Dewey T, Kapadia S, et al. United States feasibility study of trans- catheter insertion of a stented aortic valve by the left ventricular apex. Ann Thorac Surg 2008; 86:46–54.
- Lichtenstein SV, Cheung A, Ye J, et al. Transapical transcatheter aortic valve im- plantation in humans: initial clinical experience. Circulation 2006; 114:591–596.
- Webb JG, Pasupati S, Hyumphries K, et al. Percutaneous transarterial aortic valve replacement in selected high-risk patients with aortic stenosis. Circulation 2007; 116:755–763.
- Leon MB, Kodali S, Williams M, et al. Transcatheter aortic valve replacement in patients with critical aortic stenosis: rationale, device descriptions, early clinical experiences, and perspectives. Semin Thorac Cardiovasc Surg 2006; 18:165–174.
- Leon MB, Smith CR, Mack M, et al; PARTNER Trial Investigators. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo sur- gery. N Engl J Med 2010; 363:1597–1607.
- Smith CR, Leon MB, Mack MJ, et al; PARTNER Trial Investigators. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 2011; 364:2187–2198.
- Adams DH, Popma JJ, Reardon MJ, et al; U.S. CoreValve Clinical Investigators. Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med 2014; 370:1790–1798.
- Kodali SK, Williams MR, Smith CR, et al; PARTNER Trial Investigators. Two- year outcomes after transcatheter or surgical aortic-valve replacement. N Engl J Med 2012; 366:1686–1695.
- Reardon M, et al. A randomized comparison of self-expanding
- Popma JJ, Adams DH, Reardon MJ, et al; CoreValve United States Clinical In- vestigators. Transcatheter aortic valve replacement using a self-expanding biopros- thesis in patients with severe aortic stenosis at extreme risk for surgery. J Am Coll Cardiol 2014; 63:1972–1981.
- Adams DH, Popma JJ, Reardon MJ. Transcatheter aortic-valve replacement with a self-expanding prosthesis (letter). N Engl J Med 2014; 371:967–968.
- Kaul S. Transcatheter aortic-valve replacement with a self-expanding prosthesis (letter). N Engl J Med 2014; 371:967.
- Makkar RR, Fontana GP, Jilaihawi H, et al. Transcathether aortic-valve re- placement for inoperable severe aortic stenosis. N Engl J Med 2012; 366: 1696–704.
- Mack MJ, Leon MB, Smith CR, et al; PARTNER 1 trial investigators. 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve re- placement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet 2015; 385:2477–2484.
- Cao C, Ang SC, Indraratna P, et al. Systematic review and meta-analysis of trans- catheter aortic valve implantation versus surgical aortic valve replacement for severe aortic stenosis. Ann Cardiothorac Surg 2013; 2:10–23.
- Abdel-Wahab M, Mehilli J, Frerker C, et al; CHOICE investigators. Comparison of balloon-expandable vs self-expandable valves in patients undergoing transcath- eter aortic valve replacement: the CHOICE randomized clinical trial. JAMA 2014; 311:1503–1514.
- Okuyama K, Jilaihawi H, Mirocha J, et al. Alternative access for balloon-ex- pandable transcatheter aortic valve replacement: comparison of the transaortic approach using right anterior thoracotomy to partial J-sternotomy. J Thorac Car- diovasc Surg 2014; 149:789–797.
- Lardizabal JA, O’Neill BP, Desai HV, et al. The transaortic approach for transcath- eter aortic valve replacement: initial clinical experience in the United States. J Am Coll Cardiol 2013; 61:2341–2345.
- Thourani VH, Gunter RL, Neravetla S, et al. Use of transaortic, transapical, and transcarotid transcatheter aortic valve replacement in inoperable patients. Ann Thorac Surg 2013; 96:1349–1357.
- Azmoun A, Amabile N, Ramadan R, et al. Transcatheter aortic valve implantation through carotid artery access under local anaesthesia. Eur J Cardiothorac Surg 2014; 46: 693–698.
- Rajagopal R, More RS, Roberts DH. Transcatheter aortic valve implantation through a transcarotid approach under local anesthesia. Catheter Cardiovasc In- terv 2014; 84:903–907.
- Fraccaro C, Napodano M, Tarantini G, et al. Expanding the eligibility for trans- catheter aortic valve implantation the trans-subclavian retrograde approach using: the III generation CoreValve revalving system. JACC Cardiovasc Interv 2009; 2:828–333.
- Petronio AS, De Carlo M, Bedogni F, et al. Safety and efficacy of the subclavian approach for transcatheter aortic valve implantation with the CoreValve revalving system. Circ Cardiovasc Interv 2010; 3:359–366.
- Cohen MG, Singh V, Martinez CA, et al. Transseptal antegrade transcatheter aor- tic valve replacement for patients with no other access approach—a contemporary experience. Catheter Cardiovasc Interv 2013; 82:987–993.
- Greenbaum AB, O’Neill WW, Paone G, et al. Caval-aortic access to allow trans- catheter aortic valve replacement in otherwise ineligible patients: initial human experience. J Am Coll Cardiol 2014; 63:2795–2804.
- D’Onofrio A, Salizzoni S, Agrifoglio M, et al. Medium term outcomes of trans- apical aortic valve implantation: results from the Italian Registry of Trans-Apical Aortic Valve Implantation. Ann Thorac Surg 2013; 96:830–835.
- Johansson M, Nozohoor S, Kimblad PO, Harnek J, Olivecrona GK, Sjögren J. Transapical versus transfemoral aortic valve implantation: a comparison of survival and safety. Ann Thorac Surg 2011; 91:57–63.
- Kempfert J, Rastan A, Holzhey D, et al. Transapical aortic valve implantation: analysis of risk factors and learning experience in 299 patients. Circulation 2011; 124(suppl):S124–S129.
- Aguirre J, Waskowski R, Poddar K, et al. Transcatheter aortic valve replacement: experience with the transapical approach, alternate access sites, and concomitant cardiac repairs. J Thorac Cardiovasc Surg 2014; 148:1417–1422.
- Al Kindi AH, Salhab KF, Roselli EE, Kapadia S, Tuzcu EM, Svensson LG. Alternative access options for transcatheter aortic valve replacement in patients with no conventional access and chest pathology. J Thorac Cardiovasc Surg 2014; 147:644–651.
- Salhab KF, Al Kindi AH, Lane JH, et al. Concomitant percutaneous coronary intervention and transcatheter aortic valve replacement: safe and feasible replace- ment alternative approaches in high-risk patients with severe aortic stenosis and coronary artery disease. J Card Surg 2013; 28:481–483.
- Al Kindi AH, Salhab KF, Kapadia S, et al. Simultaneous transapical transcatheter aortic and mitral valve replacement in a high-risk patient with a previous mitral bioprosthesis. J Thorac Cardiovasc Surg 2012; 144:e90–e91.
KEY POINTS
- In randomized trials, transcatheter aortic valve replacement (TAVR) has produced results that are comparable to surgical aortic valve replacement in high-risk patients. TAVR is superior to medical management in patients who cannot undergo surgery, although it is associated with higher rates of stroke.
- Risk assessment and suitability for TAVR is determined by a heart team composed of interventional cardiologists and cardiac surgeons. Society of Thoracic Surgeons Score and a number of other criteria mentioned below are considered during this process.
- The transfemoral arterial approach is the most common approach used by most institutions, but other approaches such as transaortic, transapical, transaxillary, and transcarotid are utilized if suitable in patients who have difficult femoral access.
Evolving strategies to prevent stroke and thromboembolism in nonvalvular atrial fibrillation
Atrial fibrillation (AF), the most common cardiac arrhythmia, has become a major public health problem. In the United States, the prevalence of AF was estimated at 2.7 to 6.1 million in 2010, and it is expected to rise to between 5.6 and 12 million by 2050.1 The arrhythmia is associated with impaired quality of life and increased morbidity and mortality.1,2 Stroke remains the most devastating consequence of AF.
The clinical management of patients with AF typically targets two main goals: prevention of stroke or thromboembolism and control of symptoms. This article addresses the evolving pharmacologic and nonpharmacologic strategies in stroke prevention in nonvalvular AF; reviews clinical trials evaluating medical and procedural strategies, including the novel oral anticoagulants and left atrial appendage (LAA) exclusion devices; and assesses the impact of these novel strategies on clinical practice.
RISK OF STROKE AND THROMBOEMBOLISM IN NONVALVULAR AF
Stroke occurrence from AF is primarily caused by thrombi formation in the left atrium, most commonly in the LAA. It is important to recognize that the cardiovascular risk factors for AF are also risk factors for atheroembolism; therefore, specific risk factor management is as important as anticoagulation when addressing stroke risk.
The incidence of all-cause stroke in patients with AF is 5%, and it is believed that AF causes approximately 15% of all strokes in the United States.1 This risk appears to be more significant in older patients who are more vulnerable to ischemic strokes. Estimates are that AF independently increases the risk of stroke by fivefold throughout all ages, with a steep increase in percentage of strokes attributed to AF from 1.5% at ages 50 to 59 to 23.5% at ages 80 to 89.1 Importantly, the clinical course of ischemic stroke associated with AF is often more severe than for strokes of other causes,3 further emphasizing the need for stroke prevention.
Assessment of stroke risk/thromboembolism
Multiple risk estimation scores have been developed based on epidemiologic data. Until recently, the CHADS2 score4 was the most commonly used, but it has been superseded by the CHA2DS2-VASc score.5 The point system for this scoring system is shown in Table 1. In contrast with CHADS2, this updated system assigns 2 points for age over 75 years and accounts for stroke risk in the relatively younger group of patients (age 65–75) and in females, neither of whom were included in CHADS2. The CHA2DS2-VASc score ranges between 0 and 9 with a respective estimated stroke risk of 0 to 15.2% per year. Note that for females who are younger than 65 years, no points are given for sex. The major advantage of the CHA2DS2-VASc score over the CHADS2 score is that it is more accurate for lower-risk categories. It has been adopted in most of the recent guidelines that address stroke risk in AF.
In clinical practice, practitioners use these scores to define three primary stroke risk categories: low, intermediate, or high. In our practice, we use a 2% per year cut-off to identify high-risk patients in whom the risk of stroke significantly outweighs the risk of bleeding on anticoagulants. In general, patients with a CHA2DS2-VASc score equal to or greater than 2 have a greater than 2% stroke risk per year and are most likely to benefit from antithrombotic therapies.
In male patients with a CHA2DS2-VASc score of 0 and in most patients with a score of 1, the stroke risk is less than 1% per year. These patients are not likely to derive benefit from anticoagulant therapy. They are usually approached on a case-by-case basis with careful assessment of bleeding risk and discussion of risks and benefits of anticoagulant strategies.
Assessment of bleeding risk
Any general approach to thromboembolism risk assessment in patients with AF should include an analysis that weighs the benefits of anticoagulant therapies against the risks of bleeding. Although no precise tools exist to predict bleeding risk, the HAS-BLED score is increasingly used.6 This score assigns 1 point to each of the following:
- systolic blood pressure greater than 160 mm Hg
- abnormal renal function
- abnormal liver function
- age older than 65
- prior cerebrovascular event
- prior bleeding
- history of labile international normalized ratios (INR)
- alcohol intake (> 8 U/week)
- drug use, especially antiplatelet agents or nonsteroidal anti-inflammatory drugs (NSAIDs).
In general, a HAS-BLED score of 3 or greater indicates increased 1-year risk of intracranial bleed, bleeding requiring hospitalization, drop in hemoglobin of at least 2 g/dL, or need for transfusion.
One problem with the bleeding risk scores is that they were derived from studies that included bleeding events of differing severity. Most bleeding events do not lead to death or severe disability with the exception of intracranial bleeding, which is, therefore, the primary concern when assessing bleeding risk.
The estimated bleeding risk with anticoagulant therapy ranges from 0.2% to 0.4% per year but could be much higher in patients with prior severe bleeding, intracranial hemorrhage, thrombocytopenia, coagulopathies, recent surgery, or ongoing bleeding, aortic dissection, malignant hypertension, and in those receiving a combination of anticoagulant and antiplatelet agents.
MEDICAL THERAPIES TO PREVENT STROKE AND THROMBOEMBOLISM IN AF
In general, anticoagulation reduces the risk of ischemic stroke and thromboembolic events by approximately two-thirds, regardless of baseline risk. Anticoagulant options have increased substantially in the past few years with the introduction of novel oral anticoagulants, including the direct thrombin-inhibitor dabigatran and the factor Xa inhibitors rivaroxaban, apixaban, and edoxaban.
Warfarin
Warfarin has been used for decades for stroke prevention. It remains the only acceptable anticoagulant in patients with valvular AF. Multiple randomized clinical trials have assessed the efficacy of warfarin for stroke prevention in patients with nonvalvular AF.7 These trials demonstrated that warfarin significantly reduces stroke risk, stroke severity, and 30-day mortality compared with no anticoagulant therapy.7,8
Although warfarin is one of the most efficacious drugs to prevent stroke in AF, it has several key limitations. The most important is the need for dose adjustment to keep the INR in a narrow window (2.0 to 3.0) in which net clinical benefit is achieved without increased bleeding risk. The need for continuous monitoring is an inconvenience to patients and often leads to drug discontinuation and nonadherence. A meta-analysis found that patients are only in the therapeutic INR about half of the time.9 Importantly, the time spent in therapeutic INR range cor- relates significantly with the reduction in stroke risk.10 Furthermore, patients who spend less than 40% of the time in the therapeutic INR range are at a higher stroke risk than those not taking warfarin.10
Another limitation with the medication is the dietary restriction on intake of vitamin K-rich green vegetables, which are emphasized as healthy food choices especially in patients with heart disease. Higher warfarin doses are required in patients who consume greens and salads. It is important that patients be consistent in their intake of vitamin K-rich foods to avoid labile INRs, a difficult task for most patients.
Finally, there are several drugs that might interact with warfarin and potentially interfere with its safety or efficacy. These drugs include amiodarone, statins including simvastatin and rosuvastatin (not atorvastatin or pravastatin), fibrates (fenofibrate, gemfibrozil), antibiotics (sulfamethoxazole/trimethoprim, metronidazole), and azole antifungals (fluconazole, miconazole, voriconazole). The use of drugs that induce the cytochrome P450 enzyme CYP2C9, such as rifampin, decrease warfarin effectiveness by reducing INR values. Other non-CYP2C9-dependent drug interactions exist as well.
Aspirin monotherapy or in combination with other agents
Aspirin monotherapy or aspirin plus clopidogrel both increase the risk of bleeding without appreciable benefit, and, as such, their use for stroke prevention in patients with AF is not well supported. The combination of aspirin plus low-dose warfarin was assessed in the SPAF-III trial11 that randomized AF patients at stroke risk to either aspirin plus low-dose warfarin or to dose-adjusted warfarin to target a therapeutic INR. In this trial, patients on aspirin plus low-dose warfarin had significantly higher morbidity and mortality than patients who took adjusted-dose warfarin alone. Thus, the combination of low-dose warfarin plus aspirin should not be used for stroke prevention in AF.
In contrast, the combination of aspirin plus full anticoagulation with warfarin has not been well studied. Limited post-hoc data from the SPORTIF trials suggest, however, that this combination does not reduce the risk of stroke or thromboembolism more than warfarin alone.12
Novel oral anticoagulants
Dabigatran. The value of dabigatran for prevention of stroke or thromboembolism in AF was tested in the RE-LY trial (Randomized Evaluation of Long-Term Anticoagulation Therapy).13 In this trial, 18,113 patients with AF at high risk for stroke were randomized to dabigatran (110 mg or 150 mg twice daily) or adjusted-dose warfarin (INR target 2.0–3.0). By intention-to-treat analysis, dabigatran 150 mg was superior to warfarin for stroke prevention. Importantly, the risk of intracranial or life-threatening bleeding was significantly lower for both dabigatran doses compared with warfarin. Of note, gastrointestinal bleeding was more common with dabigatran 150 mg than warfarin; rates were similar for dabigatran 110 mg versus warfarin.
Rivaroxaban. This factor-Xa inhibitor was assessed in ROCKET-AF (Rivaroxaban Once-daily oral direct factor Xa inhibition Compared with vitamin K antagonism for prevention of stroke and Embolism Trial in Atrial Fibrillation).14 In this trial, 14,264 patients with AF and at risk for stroke were randomized to rivaroxaban (20 mg once daily) or warfarin (INR target 2.5). In the warfarin arm, INR was in the therapeutic range only 55% of the time. Results showed rivaroxaban was noninferior, but not superior, to warfarin for the prevention of stroke or systemic thromboembolism, the primary end points. From a safety standpoint, the overall bleeding rates were similar in the treatment arms with less life-threatening (fatal or intracranial) hemorrhage events with rivaroxaban.
Apixaban. This factor-Xa inhibitor was tested for stroke prevention in AF in two separate clinical trials.15,16 In the AVERROES trial (Apixaban Versus Acetylsalicylic Acid to Prevent Strokes),15 5,599 patients with AF deemed “unsuitable” for warfarin were randomized to apixaban (5 mg twice daily) or aspirin (81–324 mg daily). The trial was terminated early due to superiority of apixaban in achieving the primary end point: occurrence of stroke or systemic embolism. Importantly, the risk of major bleeding appeared to be similar with apixaban versus aspirin.
The ARISTOTLE (Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation) trial16 randomized 18,201 patients with AF and at least one additional risk factor for stroke to either apixaban 5 mg or warfarin (target INR 2.0–3.0). In this trial, apixaban was superior to warfarin for the prevention of stroke or systemic embolism, the primary efficacy end point. There also appeared to be a mortality benefit with apixaban versus warfarin. Importantly, the risk of major and intracranial bleeding, the primary safety outcomes, occurred at lower rates in the apixaban group.
All three of these oral anticoagulants require dose adjustment in patients with renal insufficiency and are contraindicated in patients with end-stage renal failure. They are not indicated in patients with valvular heart disease or a mechanical heart valves.
NONPHARMACOLOGIC INTERVENTIONS
Most atrial thrombi in patients with nonvalvular AF form in the LAA. Nonpharmacologic interventions have been developed to block the LAA to reduce the risk of stroke. These are especially valuable options for patients who are not candidates for chronic anticoagulation. In patients undergoing mitral valve surgery,17 ligation to close the LAA has become a standard practice at experienced centers. The introduction of less invasive catheter-based interventions to occlude the LAA has provided additional options.
Watchman device
The Watchman implant, a closure device that blocks the LAA, was recently approved by the US Food and Drug Administration (FDA) for stroke prevention in patients with nonvalvular AF who are at increased risk for stroke based on a CHA2DS2-VASc score of 2 or greater; candidates also must have an appropriate rationale for nonpharmacologic therapy. The expandable-cage device is surgically delivered into the LAA (Figure 1), which subsequently endothelializes and isolates the LAA. (Video 1 shows the delivery sheath positioned at the os of the appendage with a confirmatory contrast appendogram. Video 2 shows the delivery of the device into the appendage.) Therapeutic warfarin is required for a minimum of 45 days after implant followed by aspirin and clopidogrel for 6 months and then aspirin alone.
This device was initially tested in the PROTECT AF (Watchman Left Atrial Appendage System for Embolic PROTECTion in Patients with Atrial Fibrillation) trial, a noninferiority trial that randomized patients to either device implant or warfarin.18 Device implant was successful in 91% of patients in whom it was attempted. Overall, the study showed noninferiority of the device to warfarin in terms of the primary efficacy standpoint, which included stroke, systemic embolism, and cardiovascular death; however, this came at the expense of higher incidence of procedure-related complications, which seemed to be dependent on a learning curve with the device.
In the PREVAIL (Evaluation of the Watchman LAA Closure Device in Patients with Atrial Fibrillation Versus Long-Term Warfarin Therapy) trial,19 although noninferiority was not achieved, the event rates were low and the safety of the procedure was much improved. This was also demonstrated in registry data, which showed improved safety with device implantation with increased operator experience.
Of note, both of these trials included only patients who were eligible for warfarin. Another nonrandomized study20 assessed the use of this device in patients with a contraindication to long-term anticoagulation. Results showed a very low incidence of stroke, which was lower than CHADS2-matched controls taking either aspirin or clopidogrel. The FDA has approved this device for stroke prevention in AF.
Lariat system
The Lariat system is another percutaneous system for occlusion of the LAA. This device, which requires both atrial transseptal and epicardial access, ligates the appendage from the pericardial space. While some small studies have shown it safe and efficacious in patients with AF who cannot take anticoagulation,21 other reports have not been as encouraging.22 The device has been approved by the FDA for “soft tissue approximation”; it is not approved for stroke prevention.
SUMMARY
The most common serious complications of AF are stroke and thromboembolism. Medical and interventional therapies have been developed to prevent these complications. In patients with an estimated thromboembolic risk of greater than 1% to 2% per year, anticoagulation is warranted to reduce that risk. Warfarin remains one of the most studied and useful medications for this purpose, but its use is limited by the need for frequent monitoring, multiple drug interactions, dietary restrictions, and, most importantly, by the difficulty of consistently maintaining therapeutic INRs.
The recently introduced novel oral anticoagulants have been found to be at least noninferior to warfarin and for some agents to be superior to warfarin for the prevention of stroke and thromboembolism. Their main advantage is that they do not require monitoring and have fewer drug interactions and dietary restrictions. Most important, there appear to be fewer major and life-threatening bleeding events than with warfarin. However, use of these novel agents could be limited by patients’ renal function, which needs to be assessed when these agents are being considered. Another limitation with these agents (versus warfarin) is that patients are not therapeutically anticoagulated when they miss a dose, whereas missing a single dose of warfarin may not have the same effect.
In our practice, we have transitioned to use of these novel oral anticoagulants whenever possible using an approach that assesses the individual patient’s risks for both stroke and thromboembolism as well as the risk for bleeding. In patients who are at increased risk of bleeding but at risk of stroke in AF, percutaneous occlusion of the LAA using the Watchman device is offered. This device has been shown to be noninferior to warfarin for stroke prevention and may provide a survival benefit due to the reduction of life-threatening bleeding, which is an inherent risk with anticoagulants. One caveat is that there is a residual risk of stroke after undergoing LAA occlusion because the same risk factors for stroke in AF contribute to stroke from atherothrombosis and atheroembolism; also, thrombi can form in the body of the left atrium.
Clinical decision-making is often challenging in patients with AF who are at risk of stroke and bleeding. In fact, these risk factors often overlap. In our practice, we have established a multidisciplinary clinic for stroke prevention in AF that involves cardiologists, cardiac electrophysiologists, neurologists, gastroenterologists, and vascular medicine specialists. This model allows a multidisciplinary assessment of patients’ individual risks and ultimately facilitates clinical decision-making in terms of strategies to prevent stroke and thromboembolism in AF.
- Roger VL, Go AS, Lloyd-Jones DM, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation 2012; 125:e2–e220.
- January CT, Wann LS, Alpert JS, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2014; 64(21):e1–76.
- Dulli DA, Stanko H, Levine RL. Atrial fibrillation is associated with severe acute ischemic stroke. Neuroepidemiology 2003; 22:118–123.
- Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the national registry of atrial fibrillation. JAMA 2001; 285:2864–2870.
- Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 2010; 137:263-272.
- Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest 2010; 138:1093–1100.
- Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med 2007; 146:857–867.
- Johnsen SP, Svendsen ML, Hansen ML, Brandes A, Mehnert F, Husted SE. Preadmission oral anticoagulant treatment and clinical outcome among patients hospitalized with acute stroke and atrial fibrillation: a nationwide study. Stroke 2014; 45:168-175.
- Baker WL, Cios DA, Sander SD, Coleman CI. Meta-analysis to assess the quality of warfarin control in atrial fibrillation patients in the united states. J Manage Care Pharm 2009; 15:244-252.
- Morgan CL, McEwan P, Tukiendorf A, Robinson PA, Clemens A, Plumb JM. Warfarin treatment in patients with atrial fibrillation: observing outcomes associated with varying levels of INR control. Thromb Res 2009; 124:37–41.
- Adjusted-dose warfarin versus low-intensity, fixed-dose warfarin plus aspirin for high-risk patients with atrial fibrillation: Stroke prevention in atrial fibrillation III randomised clinical trial. Lancet 1996; 348(9028):633–638.
- Flaker GC, Gruber M, Connolly SJ, et al. Risks and benefits of combining aspirin with anticoagulant therapy in patients with atrial fibrillation: an exploratory analysis of stroke prevention using an oral thrombin inhibitor in atrial fibrillation (SPORTIF) trials. Am Heart J 2006; 152:967–973.
- Connolly SJ, Ezekowitz MD, Yusuf S, et al, and the RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009; 361:1139–1151.
- Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 2011; 365:883–891.
- Connolly SJ, Eikelboom J, Joyner C, et al. Apixaban in patients with atrial fibrillation. N Engl J Med 2011; 364:806–817.
- Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 2011; 365:981–992.
- Garcia-Fernandez MA, Perez-David E, Quiles J, et al. Role of left atrial appendage obliteration in stroke reduction in patients with mitral valve prosthesis: a transesophageal echocardiographic study. J Am Coll Cardiol 2003; 42:1253–1258.
- Holmes DR, Reddy VY, Turi ZG, et al. Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: a randomised non-inferiority trial. Lancet 2009; 374(9689):534–542.
- Holmes DR Jr, Kar S, Price MJ, et al. Prospective randomized evaluation of the Watchman left atrial appendage closure device in patients with atrial fibrillation versus long-term warfarin therapy: The PREVAIL trial. J Am Coll Cardiol 2014; 64:1–12.
- Reddy VY, Mobius-Winkler S, Miller MA, et al. Left atrial appendage closure with the Watchman device in patients with a contraindication for oral anticoagulation: the ASAP study (ASA plavix feasibility study with watchman left atrial appendage closure technology). J Am Coll Cardiol 2013; 61:2551–2556.
- Bartus K, Han FT, Bednarek J, et al. Percutaneous left atrial appendage suture ligation using the LARIAT device in patients with atrial fibrillation: initial clinical experience. J Am Coll Cardiol 2013; 62:108–118.
- Chatterjee S, Herrmann HC, Wilensky RL, et al. Safety and procedural success of left atrial appendage exclusion with the Lariat device: a systematic review of published reports and analytic review of the FDA MAUDE database. JAMA Intern Med 2015; 175(7):1104–9.
Atrial fibrillation (AF), the most common cardiac arrhythmia, has become a major public health problem. In the United States, the prevalence of AF was estimated at 2.7 to 6.1 million in 2010, and it is expected to rise to between 5.6 and 12 million by 2050.1 The arrhythmia is associated with impaired quality of life and increased morbidity and mortality.1,2 Stroke remains the most devastating consequence of AF.
The clinical management of patients with AF typically targets two main goals: prevention of stroke or thromboembolism and control of symptoms. This article addresses the evolving pharmacologic and nonpharmacologic strategies in stroke prevention in nonvalvular AF; reviews clinical trials evaluating medical and procedural strategies, including the novel oral anticoagulants and left atrial appendage (LAA) exclusion devices; and assesses the impact of these novel strategies on clinical practice.
RISK OF STROKE AND THROMBOEMBOLISM IN NONVALVULAR AF
Stroke occurrence from AF is primarily caused by thrombi formation in the left atrium, most commonly in the LAA. It is important to recognize that the cardiovascular risk factors for AF are also risk factors for atheroembolism; therefore, specific risk factor management is as important as anticoagulation when addressing stroke risk.
The incidence of all-cause stroke in patients with AF is 5%, and it is believed that AF causes approximately 15% of all strokes in the United States.1 This risk appears to be more significant in older patients who are more vulnerable to ischemic strokes. Estimates are that AF independently increases the risk of stroke by fivefold throughout all ages, with a steep increase in percentage of strokes attributed to AF from 1.5% at ages 50 to 59 to 23.5% at ages 80 to 89.1 Importantly, the clinical course of ischemic stroke associated with AF is often more severe than for strokes of other causes,3 further emphasizing the need for stroke prevention.
Assessment of stroke risk/thromboembolism
Multiple risk estimation scores have been developed based on epidemiologic data. Until recently, the CHADS2 score4 was the most commonly used, but it has been superseded by the CHA2DS2-VASc score.5 The point system for this scoring system is shown in Table 1. In contrast with CHADS2, this updated system assigns 2 points for age over 75 years and accounts for stroke risk in the relatively younger group of patients (age 65–75) and in females, neither of whom were included in CHADS2. The CHA2DS2-VASc score ranges between 0 and 9 with a respective estimated stroke risk of 0 to 15.2% per year. Note that for females who are younger than 65 years, no points are given for sex. The major advantage of the CHA2DS2-VASc score over the CHADS2 score is that it is more accurate for lower-risk categories. It has been adopted in most of the recent guidelines that address stroke risk in AF.
In clinical practice, practitioners use these scores to define three primary stroke risk categories: low, intermediate, or high. In our practice, we use a 2% per year cut-off to identify high-risk patients in whom the risk of stroke significantly outweighs the risk of bleeding on anticoagulants. In general, patients with a CHA2DS2-VASc score equal to or greater than 2 have a greater than 2% stroke risk per year and are most likely to benefit from antithrombotic therapies.
In male patients with a CHA2DS2-VASc score of 0 and in most patients with a score of 1, the stroke risk is less than 1% per year. These patients are not likely to derive benefit from anticoagulant therapy. They are usually approached on a case-by-case basis with careful assessment of bleeding risk and discussion of risks and benefits of anticoagulant strategies.
Assessment of bleeding risk
Any general approach to thromboembolism risk assessment in patients with AF should include an analysis that weighs the benefits of anticoagulant therapies against the risks of bleeding. Although no precise tools exist to predict bleeding risk, the HAS-BLED score is increasingly used.6 This score assigns 1 point to each of the following:
- systolic blood pressure greater than 160 mm Hg
- abnormal renal function
- abnormal liver function
- age older than 65
- prior cerebrovascular event
- prior bleeding
- history of labile international normalized ratios (INR)
- alcohol intake (> 8 U/week)
- drug use, especially antiplatelet agents or nonsteroidal anti-inflammatory drugs (NSAIDs).
In general, a HAS-BLED score of 3 or greater indicates increased 1-year risk of intracranial bleed, bleeding requiring hospitalization, drop in hemoglobin of at least 2 g/dL, or need for transfusion.
One problem with the bleeding risk scores is that they were derived from studies that included bleeding events of differing severity. Most bleeding events do not lead to death or severe disability with the exception of intracranial bleeding, which is, therefore, the primary concern when assessing bleeding risk.
The estimated bleeding risk with anticoagulant therapy ranges from 0.2% to 0.4% per year but could be much higher in patients with prior severe bleeding, intracranial hemorrhage, thrombocytopenia, coagulopathies, recent surgery, or ongoing bleeding, aortic dissection, malignant hypertension, and in those receiving a combination of anticoagulant and antiplatelet agents.
MEDICAL THERAPIES TO PREVENT STROKE AND THROMBOEMBOLISM IN AF
In general, anticoagulation reduces the risk of ischemic stroke and thromboembolic events by approximately two-thirds, regardless of baseline risk. Anticoagulant options have increased substantially in the past few years with the introduction of novel oral anticoagulants, including the direct thrombin-inhibitor dabigatran and the factor Xa inhibitors rivaroxaban, apixaban, and edoxaban.
Warfarin
Warfarin has been used for decades for stroke prevention. It remains the only acceptable anticoagulant in patients with valvular AF. Multiple randomized clinical trials have assessed the efficacy of warfarin for stroke prevention in patients with nonvalvular AF.7 These trials demonstrated that warfarin significantly reduces stroke risk, stroke severity, and 30-day mortality compared with no anticoagulant therapy.7,8
Although warfarin is one of the most efficacious drugs to prevent stroke in AF, it has several key limitations. The most important is the need for dose adjustment to keep the INR in a narrow window (2.0 to 3.0) in which net clinical benefit is achieved without increased bleeding risk. The need for continuous monitoring is an inconvenience to patients and often leads to drug discontinuation and nonadherence. A meta-analysis found that patients are only in the therapeutic INR about half of the time.9 Importantly, the time spent in therapeutic INR range cor- relates significantly with the reduction in stroke risk.10 Furthermore, patients who spend less than 40% of the time in the therapeutic INR range are at a higher stroke risk than those not taking warfarin.10
Another limitation with the medication is the dietary restriction on intake of vitamin K-rich green vegetables, which are emphasized as healthy food choices especially in patients with heart disease. Higher warfarin doses are required in patients who consume greens and salads. It is important that patients be consistent in their intake of vitamin K-rich foods to avoid labile INRs, a difficult task for most patients.
Finally, there are several drugs that might interact with warfarin and potentially interfere with its safety or efficacy. These drugs include amiodarone, statins including simvastatin and rosuvastatin (not atorvastatin or pravastatin), fibrates (fenofibrate, gemfibrozil), antibiotics (sulfamethoxazole/trimethoprim, metronidazole), and azole antifungals (fluconazole, miconazole, voriconazole). The use of drugs that induce the cytochrome P450 enzyme CYP2C9, such as rifampin, decrease warfarin effectiveness by reducing INR values. Other non-CYP2C9-dependent drug interactions exist as well.
Aspirin monotherapy or in combination with other agents
Aspirin monotherapy or aspirin plus clopidogrel both increase the risk of bleeding without appreciable benefit, and, as such, their use for stroke prevention in patients with AF is not well supported. The combination of aspirin plus low-dose warfarin was assessed in the SPAF-III trial11 that randomized AF patients at stroke risk to either aspirin plus low-dose warfarin or to dose-adjusted warfarin to target a therapeutic INR. In this trial, patients on aspirin plus low-dose warfarin had significantly higher morbidity and mortality than patients who took adjusted-dose warfarin alone. Thus, the combination of low-dose warfarin plus aspirin should not be used for stroke prevention in AF.
In contrast, the combination of aspirin plus full anticoagulation with warfarin has not been well studied. Limited post-hoc data from the SPORTIF trials suggest, however, that this combination does not reduce the risk of stroke or thromboembolism more than warfarin alone.12
Novel oral anticoagulants
Dabigatran. The value of dabigatran for prevention of stroke or thromboembolism in AF was tested in the RE-LY trial (Randomized Evaluation of Long-Term Anticoagulation Therapy).13 In this trial, 18,113 patients with AF at high risk for stroke were randomized to dabigatran (110 mg or 150 mg twice daily) or adjusted-dose warfarin (INR target 2.0–3.0). By intention-to-treat analysis, dabigatran 150 mg was superior to warfarin for stroke prevention. Importantly, the risk of intracranial or life-threatening bleeding was significantly lower for both dabigatran doses compared with warfarin. Of note, gastrointestinal bleeding was more common with dabigatran 150 mg than warfarin; rates were similar for dabigatran 110 mg versus warfarin.
Rivaroxaban. This factor-Xa inhibitor was assessed in ROCKET-AF (Rivaroxaban Once-daily oral direct factor Xa inhibition Compared with vitamin K antagonism for prevention of stroke and Embolism Trial in Atrial Fibrillation).14 In this trial, 14,264 patients with AF and at risk for stroke were randomized to rivaroxaban (20 mg once daily) or warfarin (INR target 2.5). In the warfarin arm, INR was in the therapeutic range only 55% of the time. Results showed rivaroxaban was noninferior, but not superior, to warfarin for the prevention of stroke or systemic thromboembolism, the primary end points. From a safety standpoint, the overall bleeding rates were similar in the treatment arms with less life-threatening (fatal or intracranial) hemorrhage events with rivaroxaban.
Apixaban. This factor-Xa inhibitor was tested for stroke prevention in AF in two separate clinical trials.15,16 In the AVERROES trial (Apixaban Versus Acetylsalicylic Acid to Prevent Strokes),15 5,599 patients with AF deemed “unsuitable” for warfarin were randomized to apixaban (5 mg twice daily) or aspirin (81–324 mg daily). The trial was terminated early due to superiority of apixaban in achieving the primary end point: occurrence of stroke or systemic embolism. Importantly, the risk of major bleeding appeared to be similar with apixaban versus aspirin.
The ARISTOTLE (Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation) trial16 randomized 18,201 patients with AF and at least one additional risk factor for stroke to either apixaban 5 mg or warfarin (target INR 2.0–3.0). In this trial, apixaban was superior to warfarin for the prevention of stroke or systemic embolism, the primary efficacy end point. There also appeared to be a mortality benefit with apixaban versus warfarin. Importantly, the risk of major and intracranial bleeding, the primary safety outcomes, occurred at lower rates in the apixaban group.
All three of these oral anticoagulants require dose adjustment in patients with renal insufficiency and are contraindicated in patients with end-stage renal failure. They are not indicated in patients with valvular heart disease or a mechanical heart valves.
NONPHARMACOLOGIC INTERVENTIONS
Most atrial thrombi in patients with nonvalvular AF form in the LAA. Nonpharmacologic interventions have been developed to block the LAA to reduce the risk of stroke. These are especially valuable options for patients who are not candidates for chronic anticoagulation. In patients undergoing mitral valve surgery,17 ligation to close the LAA has become a standard practice at experienced centers. The introduction of less invasive catheter-based interventions to occlude the LAA has provided additional options.
Watchman device
The Watchman implant, a closure device that blocks the LAA, was recently approved by the US Food and Drug Administration (FDA) for stroke prevention in patients with nonvalvular AF who are at increased risk for stroke based on a CHA2DS2-VASc score of 2 or greater; candidates also must have an appropriate rationale for nonpharmacologic therapy. The expandable-cage device is surgically delivered into the LAA (Figure 1), which subsequently endothelializes and isolates the LAA. (Video 1 shows the delivery sheath positioned at the os of the appendage with a confirmatory contrast appendogram. Video 2 shows the delivery of the device into the appendage.) Therapeutic warfarin is required for a minimum of 45 days after implant followed by aspirin and clopidogrel for 6 months and then aspirin alone.
This device was initially tested in the PROTECT AF (Watchman Left Atrial Appendage System for Embolic PROTECTion in Patients with Atrial Fibrillation) trial, a noninferiority trial that randomized patients to either device implant or warfarin.18 Device implant was successful in 91% of patients in whom it was attempted. Overall, the study showed noninferiority of the device to warfarin in terms of the primary efficacy standpoint, which included stroke, systemic embolism, and cardiovascular death; however, this came at the expense of higher incidence of procedure-related complications, which seemed to be dependent on a learning curve with the device.
In the PREVAIL (Evaluation of the Watchman LAA Closure Device in Patients with Atrial Fibrillation Versus Long-Term Warfarin Therapy) trial,19 although noninferiority was not achieved, the event rates were low and the safety of the procedure was much improved. This was also demonstrated in registry data, which showed improved safety with device implantation with increased operator experience.
Of note, both of these trials included only patients who were eligible for warfarin. Another nonrandomized study20 assessed the use of this device in patients with a contraindication to long-term anticoagulation. Results showed a very low incidence of stroke, which was lower than CHADS2-matched controls taking either aspirin or clopidogrel. The FDA has approved this device for stroke prevention in AF.
Lariat system
The Lariat system is another percutaneous system for occlusion of the LAA. This device, which requires both atrial transseptal and epicardial access, ligates the appendage from the pericardial space. While some small studies have shown it safe and efficacious in patients with AF who cannot take anticoagulation,21 other reports have not been as encouraging.22 The device has been approved by the FDA for “soft tissue approximation”; it is not approved for stroke prevention.
SUMMARY
The most common serious complications of AF are stroke and thromboembolism. Medical and interventional therapies have been developed to prevent these complications. In patients with an estimated thromboembolic risk of greater than 1% to 2% per year, anticoagulation is warranted to reduce that risk. Warfarin remains one of the most studied and useful medications for this purpose, but its use is limited by the need for frequent monitoring, multiple drug interactions, dietary restrictions, and, most importantly, by the difficulty of consistently maintaining therapeutic INRs.
The recently introduced novel oral anticoagulants have been found to be at least noninferior to warfarin and for some agents to be superior to warfarin for the prevention of stroke and thromboembolism. Their main advantage is that they do not require monitoring and have fewer drug interactions and dietary restrictions. Most important, there appear to be fewer major and life-threatening bleeding events than with warfarin. However, use of these novel agents could be limited by patients’ renal function, which needs to be assessed when these agents are being considered. Another limitation with these agents (versus warfarin) is that patients are not therapeutically anticoagulated when they miss a dose, whereas missing a single dose of warfarin may not have the same effect.
In our practice, we have transitioned to use of these novel oral anticoagulants whenever possible using an approach that assesses the individual patient’s risks for both stroke and thromboembolism as well as the risk for bleeding. In patients who are at increased risk of bleeding but at risk of stroke in AF, percutaneous occlusion of the LAA using the Watchman device is offered. This device has been shown to be noninferior to warfarin for stroke prevention and may provide a survival benefit due to the reduction of life-threatening bleeding, which is an inherent risk with anticoagulants. One caveat is that there is a residual risk of stroke after undergoing LAA occlusion because the same risk factors for stroke in AF contribute to stroke from atherothrombosis and atheroembolism; also, thrombi can form in the body of the left atrium.
Clinical decision-making is often challenging in patients with AF who are at risk of stroke and bleeding. In fact, these risk factors often overlap. In our practice, we have established a multidisciplinary clinic for stroke prevention in AF that involves cardiologists, cardiac electrophysiologists, neurologists, gastroenterologists, and vascular medicine specialists. This model allows a multidisciplinary assessment of patients’ individual risks and ultimately facilitates clinical decision-making in terms of strategies to prevent stroke and thromboembolism in AF.
Atrial fibrillation (AF), the most common cardiac arrhythmia, has become a major public health problem. In the United States, the prevalence of AF was estimated at 2.7 to 6.1 million in 2010, and it is expected to rise to between 5.6 and 12 million by 2050.1 The arrhythmia is associated with impaired quality of life and increased morbidity and mortality.1,2 Stroke remains the most devastating consequence of AF.
The clinical management of patients with AF typically targets two main goals: prevention of stroke or thromboembolism and control of symptoms. This article addresses the evolving pharmacologic and nonpharmacologic strategies in stroke prevention in nonvalvular AF; reviews clinical trials evaluating medical and procedural strategies, including the novel oral anticoagulants and left atrial appendage (LAA) exclusion devices; and assesses the impact of these novel strategies on clinical practice.
RISK OF STROKE AND THROMBOEMBOLISM IN NONVALVULAR AF
Stroke occurrence from AF is primarily caused by thrombi formation in the left atrium, most commonly in the LAA. It is important to recognize that the cardiovascular risk factors for AF are also risk factors for atheroembolism; therefore, specific risk factor management is as important as anticoagulation when addressing stroke risk.
The incidence of all-cause stroke in patients with AF is 5%, and it is believed that AF causes approximately 15% of all strokes in the United States.1 This risk appears to be more significant in older patients who are more vulnerable to ischemic strokes. Estimates are that AF independently increases the risk of stroke by fivefold throughout all ages, with a steep increase in percentage of strokes attributed to AF from 1.5% at ages 50 to 59 to 23.5% at ages 80 to 89.1 Importantly, the clinical course of ischemic stroke associated with AF is often more severe than for strokes of other causes,3 further emphasizing the need for stroke prevention.
Assessment of stroke risk/thromboembolism
Multiple risk estimation scores have been developed based on epidemiologic data. Until recently, the CHADS2 score4 was the most commonly used, but it has been superseded by the CHA2DS2-VASc score.5 The point system for this scoring system is shown in Table 1. In contrast with CHADS2, this updated system assigns 2 points for age over 75 years and accounts for stroke risk in the relatively younger group of patients (age 65–75) and in females, neither of whom were included in CHADS2. The CHA2DS2-VASc score ranges between 0 and 9 with a respective estimated stroke risk of 0 to 15.2% per year. Note that for females who are younger than 65 years, no points are given for sex. The major advantage of the CHA2DS2-VASc score over the CHADS2 score is that it is more accurate for lower-risk categories. It has been adopted in most of the recent guidelines that address stroke risk in AF.
In clinical practice, practitioners use these scores to define three primary stroke risk categories: low, intermediate, or high. In our practice, we use a 2% per year cut-off to identify high-risk patients in whom the risk of stroke significantly outweighs the risk of bleeding on anticoagulants. In general, patients with a CHA2DS2-VASc score equal to or greater than 2 have a greater than 2% stroke risk per year and are most likely to benefit from antithrombotic therapies.
In male patients with a CHA2DS2-VASc score of 0 and in most patients with a score of 1, the stroke risk is less than 1% per year. These patients are not likely to derive benefit from anticoagulant therapy. They are usually approached on a case-by-case basis with careful assessment of bleeding risk and discussion of risks and benefits of anticoagulant strategies.
Assessment of bleeding risk
Any general approach to thromboembolism risk assessment in patients with AF should include an analysis that weighs the benefits of anticoagulant therapies against the risks of bleeding. Although no precise tools exist to predict bleeding risk, the HAS-BLED score is increasingly used.6 This score assigns 1 point to each of the following:
- systolic blood pressure greater than 160 mm Hg
- abnormal renal function
- abnormal liver function
- age older than 65
- prior cerebrovascular event
- prior bleeding
- history of labile international normalized ratios (INR)
- alcohol intake (> 8 U/week)
- drug use, especially antiplatelet agents or nonsteroidal anti-inflammatory drugs (NSAIDs).
In general, a HAS-BLED score of 3 or greater indicates increased 1-year risk of intracranial bleed, bleeding requiring hospitalization, drop in hemoglobin of at least 2 g/dL, or need for transfusion.
One problem with the bleeding risk scores is that they were derived from studies that included bleeding events of differing severity. Most bleeding events do not lead to death or severe disability with the exception of intracranial bleeding, which is, therefore, the primary concern when assessing bleeding risk.
The estimated bleeding risk with anticoagulant therapy ranges from 0.2% to 0.4% per year but could be much higher in patients with prior severe bleeding, intracranial hemorrhage, thrombocytopenia, coagulopathies, recent surgery, or ongoing bleeding, aortic dissection, malignant hypertension, and in those receiving a combination of anticoagulant and antiplatelet agents.
MEDICAL THERAPIES TO PREVENT STROKE AND THROMBOEMBOLISM IN AF
In general, anticoagulation reduces the risk of ischemic stroke and thromboembolic events by approximately two-thirds, regardless of baseline risk. Anticoagulant options have increased substantially in the past few years with the introduction of novel oral anticoagulants, including the direct thrombin-inhibitor dabigatran and the factor Xa inhibitors rivaroxaban, apixaban, and edoxaban.
Warfarin
Warfarin has been used for decades for stroke prevention. It remains the only acceptable anticoagulant in patients with valvular AF. Multiple randomized clinical trials have assessed the efficacy of warfarin for stroke prevention in patients with nonvalvular AF.7 These trials demonstrated that warfarin significantly reduces stroke risk, stroke severity, and 30-day mortality compared with no anticoagulant therapy.7,8
Although warfarin is one of the most efficacious drugs to prevent stroke in AF, it has several key limitations. The most important is the need for dose adjustment to keep the INR in a narrow window (2.0 to 3.0) in which net clinical benefit is achieved without increased bleeding risk. The need for continuous monitoring is an inconvenience to patients and often leads to drug discontinuation and nonadherence. A meta-analysis found that patients are only in the therapeutic INR about half of the time.9 Importantly, the time spent in therapeutic INR range cor- relates significantly with the reduction in stroke risk.10 Furthermore, patients who spend less than 40% of the time in the therapeutic INR range are at a higher stroke risk than those not taking warfarin.10
Another limitation with the medication is the dietary restriction on intake of vitamin K-rich green vegetables, which are emphasized as healthy food choices especially in patients with heart disease. Higher warfarin doses are required in patients who consume greens and salads. It is important that patients be consistent in their intake of vitamin K-rich foods to avoid labile INRs, a difficult task for most patients.
Finally, there are several drugs that might interact with warfarin and potentially interfere with its safety or efficacy. These drugs include amiodarone, statins including simvastatin and rosuvastatin (not atorvastatin or pravastatin), fibrates (fenofibrate, gemfibrozil), antibiotics (sulfamethoxazole/trimethoprim, metronidazole), and azole antifungals (fluconazole, miconazole, voriconazole). The use of drugs that induce the cytochrome P450 enzyme CYP2C9, such as rifampin, decrease warfarin effectiveness by reducing INR values. Other non-CYP2C9-dependent drug interactions exist as well.
Aspirin monotherapy or in combination with other agents
Aspirin monotherapy or aspirin plus clopidogrel both increase the risk of bleeding without appreciable benefit, and, as such, their use for stroke prevention in patients with AF is not well supported. The combination of aspirin plus low-dose warfarin was assessed in the SPAF-III trial11 that randomized AF patients at stroke risk to either aspirin plus low-dose warfarin or to dose-adjusted warfarin to target a therapeutic INR. In this trial, patients on aspirin plus low-dose warfarin had significantly higher morbidity and mortality than patients who took adjusted-dose warfarin alone. Thus, the combination of low-dose warfarin plus aspirin should not be used for stroke prevention in AF.
In contrast, the combination of aspirin plus full anticoagulation with warfarin has not been well studied. Limited post-hoc data from the SPORTIF trials suggest, however, that this combination does not reduce the risk of stroke or thromboembolism more than warfarin alone.12
Novel oral anticoagulants
Dabigatran. The value of dabigatran for prevention of stroke or thromboembolism in AF was tested in the RE-LY trial (Randomized Evaluation of Long-Term Anticoagulation Therapy).13 In this trial, 18,113 patients with AF at high risk for stroke were randomized to dabigatran (110 mg or 150 mg twice daily) or adjusted-dose warfarin (INR target 2.0–3.0). By intention-to-treat analysis, dabigatran 150 mg was superior to warfarin for stroke prevention. Importantly, the risk of intracranial or life-threatening bleeding was significantly lower for both dabigatran doses compared with warfarin. Of note, gastrointestinal bleeding was more common with dabigatran 150 mg than warfarin; rates were similar for dabigatran 110 mg versus warfarin.
Rivaroxaban. This factor-Xa inhibitor was assessed in ROCKET-AF (Rivaroxaban Once-daily oral direct factor Xa inhibition Compared with vitamin K antagonism for prevention of stroke and Embolism Trial in Atrial Fibrillation).14 In this trial, 14,264 patients with AF and at risk for stroke were randomized to rivaroxaban (20 mg once daily) or warfarin (INR target 2.5). In the warfarin arm, INR was in the therapeutic range only 55% of the time. Results showed rivaroxaban was noninferior, but not superior, to warfarin for the prevention of stroke or systemic thromboembolism, the primary end points. From a safety standpoint, the overall bleeding rates were similar in the treatment arms with less life-threatening (fatal or intracranial) hemorrhage events with rivaroxaban.
Apixaban. This factor-Xa inhibitor was tested for stroke prevention in AF in two separate clinical trials.15,16 In the AVERROES trial (Apixaban Versus Acetylsalicylic Acid to Prevent Strokes),15 5,599 patients with AF deemed “unsuitable” for warfarin were randomized to apixaban (5 mg twice daily) or aspirin (81–324 mg daily). The trial was terminated early due to superiority of apixaban in achieving the primary end point: occurrence of stroke or systemic embolism. Importantly, the risk of major bleeding appeared to be similar with apixaban versus aspirin.
The ARISTOTLE (Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation) trial16 randomized 18,201 patients with AF and at least one additional risk factor for stroke to either apixaban 5 mg or warfarin (target INR 2.0–3.0). In this trial, apixaban was superior to warfarin for the prevention of stroke or systemic embolism, the primary efficacy end point. There also appeared to be a mortality benefit with apixaban versus warfarin. Importantly, the risk of major and intracranial bleeding, the primary safety outcomes, occurred at lower rates in the apixaban group.
All three of these oral anticoagulants require dose adjustment in patients with renal insufficiency and are contraindicated in patients with end-stage renal failure. They are not indicated in patients with valvular heart disease or a mechanical heart valves.
NONPHARMACOLOGIC INTERVENTIONS
Most atrial thrombi in patients with nonvalvular AF form in the LAA. Nonpharmacologic interventions have been developed to block the LAA to reduce the risk of stroke. These are especially valuable options for patients who are not candidates for chronic anticoagulation. In patients undergoing mitral valve surgery,17 ligation to close the LAA has become a standard practice at experienced centers. The introduction of less invasive catheter-based interventions to occlude the LAA has provided additional options.
Watchman device
The Watchman implant, a closure device that blocks the LAA, was recently approved by the US Food and Drug Administration (FDA) for stroke prevention in patients with nonvalvular AF who are at increased risk for stroke based on a CHA2DS2-VASc score of 2 or greater; candidates also must have an appropriate rationale for nonpharmacologic therapy. The expandable-cage device is surgically delivered into the LAA (Figure 1), which subsequently endothelializes and isolates the LAA. (Video 1 shows the delivery sheath positioned at the os of the appendage with a confirmatory contrast appendogram. Video 2 shows the delivery of the device into the appendage.) Therapeutic warfarin is required for a minimum of 45 days after implant followed by aspirin and clopidogrel for 6 months and then aspirin alone.
This device was initially tested in the PROTECT AF (Watchman Left Atrial Appendage System for Embolic PROTECTion in Patients with Atrial Fibrillation) trial, a noninferiority trial that randomized patients to either device implant or warfarin.18 Device implant was successful in 91% of patients in whom it was attempted. Overall, the study showed noninferiority of the device to warfarin in terms of the primary efficacy standpoint, which included stroke, systemic embolism, and cardiovascular death; however, this came at the expense of higher incidence of procedure-related complications, which seemed to be dependent on a learning curve with the device.
In the PREVAIL (Evaluation of the Watchman LAA Closure Device in Patients with Atrial Fibrillation Versus Long-Term Warfarin Therapy) trial,19 although noninferiority was not achieved, the event rates were low and the safety of the procedure was much improved. This was also demonstrated in registry data, which showed improved safety with device implantation with increased operator experience.
Of note, both of these trials included only patients who were eligible for warfarin. Another nonrandomized study20 assessed the use of this device in patients with a contraindication to long-term anticoagulation. Results showed a very low incidence of stroke, which was lower than CHADS2-matched controls taking either aspirin or clopidogrel. The FDA has approved this device for stroke prevention in AF.
Lariat system
The Lariat system is another percutaneous system for occlusion of the LAA. This device, which requires both atrial transseptal and epicardial access, ligates the appendage from the pericardial space. While some small studies have shown it safe and efficacious in patients with AF who cannot take anticoagulation,21 other reports have not been as encouraging.22 The device has been approved by the FDA for “soft tissue approximation”; it is not approved for stroke prevention.
SUMMARY
The most common serious complications of AF are stroke and thromboembolism. Medical and interventional therapies have been developed to prevent these complications. In patients with an estimated thromboembolic risk of greater than 1% to 2% per year, anticoagulation is warranted to reduce that risk. Warfarin remains one of the most studied and useful medications for this purpose, but its use is limited by the need for frequent monitoring, multiple drug interactions, dietary restrictions, and, most importantly, by the difficulty of consistently maintaining therapeutic INRs.
The recently introduced novel oral anticoagulants have been found to be at least noninferior to warfarin and for some agents to be superior to warfarin for the prevention of stroke and thromboembolism. Their main advantage is that they do not require monitoring and have fewer drug interactions and dietary restrictions. Most important, there appear to be fewer major and life-threatening bleeding events than with warfarin. However, use of these novel agents could be limited by patients’ renal function, which needs to be assessed when these agents are being considered. Another limitation with these agents (versus warfarin) is that patients are not therapeutically anticoagulated when they miss a dose, whereas missing a single dose of warfarin may not have the same effect.
In our practice, we have transitioned to use of these novel oral anticoagulants whenever possible using an approach that assesses the individual patient’s risks for both stroke and thromboembolism as well as the risk for bleeding. In patients who are at increased risk of bleeding but at risk of stroke in AF, percutaneous occlusion of the LAA using the Watchman device is offered. This device has been shown to be noninferior to warfarin for stroke prevention and may provide a survival benefit due to the reduction of life-threatening bleeding, which is an inherent risk with anticoagulants. One caveat is that there is a residual risk of stroke after undergoing LAA occlusion because the same risk factors for stroke in AF contribute to stroke from atherothrombosis and atheroembolism; also, thrombi can form in the body of the left atrium.
Clinical decision-making is often challenging in patients with AF who are at risk of stroke and bleeding. In fact, these risk factors often overlap. In our practice, we have established a multidisciplinary clinic for stroke prevention in AF that involves cardiologists, cardiac electrophysiologists, neurologists, gastroenterologists, and vascular medicine specialists. This model allows a multidisciplinary assessment of patients’ individual risks and ultimately facilitates clinical decision-making in terms of strategies to prevent stroke and thromboembolism in AF.
- Roger VL, Go AS, Lloyd-Jones DM, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation 2012; 125:e2–e220.
- January CT, Wann LS, Alpert JS, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2014; 64(21):e1–76.
- Dulli DA, Stanko H, Levine RL. Atrial fibrillation is associated with severe acute ischemic stroke. Neuroepidemiology 2003; 22:118–123.
- Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the national registry of atrial fibrillation. JAMA 2001; 285:2864–2870.
- Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 2010; 137:263-272.
- Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest 2010; 138:1093–1100.
- Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med 2007; 146:857–867.
- Johnsen SP, Svendsen ML, Hansen ML, Brandes A, Mehnert F, Husted SE. Preadmission oral anticoagulant treatment and clinical outcome among patients hospitalized with acute stroke and atrial fibrillation: a nationwide study. Stroke 2014; 45:168-175.
- Baker WL, Cios DA, Sander SD, Coleman CI. Meta-analysis to assess the quality of warfarin control in atrial fibrillation patients in the united states. J Manage Care Pharm 2009; 15:244-252.
- Morgan CL, McEwan P, Tukiendorf A, Robinson PA, Clemens A, Plumb JM. Warfarin treatment in patients with atrial fibrillation: observing outcomes associated with varying levels of INR control. Thromb Res 2009; 124:37–41.
- Adjusted-dose warfarin versus low-intensity, fixed-dose warfarin plus aspirin for high-risk patients with atrial fibrillation: Stroke prevention in atrial fibrillation III randomised clinical trial. Lancet 1996; 348(9028):633–638.
- Flaker GC, Gruber M, Connolly SJ, et al. Risks and benefits of combining aspirin with anticoagulant therapy in patients with atrial fibrillation: an exploratory analysis of stroke prevention using an oral thrombin inhibitor in atrial fibrillation (SPORTIF) trials. Am Heart J 2006; 152:967–973.
- Connolly SJ, Ezekowitz MD, Yusuf S, et al, and the RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009; 361:1139–1151.
- Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 2011; 365:883–891.
- Connolly SJ, Eikelboom J, Joyner C, et al. Apixaban in patients with atrial fibrillation. N Engl J Med 2011; 364:806–817.
- Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 2011; 365:981–992.
- Garcia-Fernandez MA, Perez-David E, Quiles J, et al. Role of left atrial appendage obliteration in stroke reduction in patients with mitral valve prosthesis: a transesophageal echocardiographic study. J Am Coll Cardiol 2003; 42:1253–1258.
- Holmes DR, Reddy VY, Turi ZG, et al. Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: a randomised non-inferiority trial. Lancet 2009; 374(9689):534–542.
- Holmes DR Jr, Kar S, Price MJ, et al. Prospective randomized evaluation of the Watchman left atrial appendage closure device in patients with atrial fibrillation versus long-term warfarin therapy: The PREVAIL trial. J Am Coll Cardiol 2014; 64:1–12.
- Reddy VY, Mobius-Winkler S, Miller MA, et al. Left atrial appendage closure with the Watchman device in patients with a contraindication for oral anticoagulation: the ASAP study (ASA plavix feasibility study with watchman left atrial appendage closure technology). J Am Coll Cardiol 2013; 61:2551–2556.
- Bartus K, Han FT, Bednarek J, et al. Percutaneous left atrial appendage suture ligation using the LARIAT device in patients with atrial fibrillation: initial clinical experience. J Am Coll Cardiol 2013; 62:108–118.
- Chatterjee S, Herrmann HC, Wilensky RL, et al. Safety and procedural success of left atrial appendage exclusion with the Lariat device: a systematic review of published reports and analytic review of the FDA MAUDE database. JAMA Intern Med 2015; 175(7):1104–9.
- Roger VL, Go AS, Lloyd-Jones DM, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation 2012; 125:e2–e220.
- January CT, Wann LS, Alpert JS, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2014; 64(21):e1–76.
- Dulli DA, Stanko H, Levine RL. Atrial fibrillation is associated with severe acute ischemic stroke. Neuroepidemiology 2003; 22:118–123.
- Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the national registry of atrial fibrillation. JAMA 2001; 285:2864–2870.
- Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 2010; 137:263-272.
- Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest 2010; 138:1093–1100.
- Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med 2007; 146:857–867.
- Johnsen SP, Svendsen ML, Hansen ML, Brandes A, Mehnert F, Husted SE. Preadmission oral anticoagulant treatment and clinical outcome among patients hospitalized with acute stroke and atrial fibrillation: a nationwide study. Stroke 2014; 45:168-175.
- Baker WL, Cios DA, Sander SD, Coleman CI. Meta-analysis to assess the quality of warfarin control in atrial fibrillation patients in the united states. J Manage Care Pharm 2009; 15:244-252.
- Morgan CL, McEwan P, Tukiendorf A, Robinson PA, Clemens A, Plumb JM. Warfarin treatment in patients with atrial fibrillation: observing outcomes associated with varying levels of INR control. Thromb Res 2009; 124:37–41.
- Adjusted-dose warfarin versus low-intensity, fixed-dose warfarin plus aspirin for high-risk patients with atrial fibrillation: Stroke prevention in atrial fibrillation III randomised clinical trial. Lancet 1996; 348(9028):633–638.
- Flaker GC, Gruber M, Connolly SJ, et al. Risks and benefits of combining aspirin with anticoagulant therapy in patients with atrial fibrillation: an exploratory analysis of stroke prevention using an oral thrombin inhibitor in atrial fibrillation (SPORTIF) trials. Am Heart J 2006; 152:967–973.
- Connolly SJ, Ezekowitz MD, Yusuf S, et al, and the RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009; 361:1139–1151.
- Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 2011; 365:883–891.
- Connolly SJ, Eikelboom J, Joyner C, et al. Apixaban in patients with atrial fibrillation. N Engl J Med 2011; 364:806–817.
- Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 2011; 365:981–992.
- Garcia-Fernandez MA, Perez-David E, Quiles J, et al. Role of left atrial appendage obliteration in stroke reduction in patients with mitral valve prosthesis: a transesophageal echocardiographic study. J Am Coll Cardiol 2003; 42:1253–1258.
- Holmes DR, Reddy VY, Turi ZG, et al. Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: a randomised non-inferiority trial. Lancet 2009; 374(9689):534–542.
- Holmes DR Jr, Kar S, Price MJ, et al. Prospective randomized evaluation of the Watchman left atrial appendage closure device in patients with atrial fibrillation versus long-term warfarin therapy: The PREVAIL trial. J Am Coll Cardiol 2014; 64:1–12.
- Reddy VY, Mobius-Winkler S, Miller MA, et al. Left atrial appendage closure with the Watchman device in patients with a contraindication for oral anticoagulation: the ASAP study (ASA plavix feasibility study with watchman left atrial appendage closure technology). J Am Coll Cardiol 2013; 61:2551–2556.
- Bartus K, Han FT, Bednarek J, et al. Percutaneous left atrial appendage suture ligation using the LARIAT device in patients with atrial fibrillation: initial clinical experience. J Am Coll Cardiol 2013; 62:108–118.
- Chatterjee S, Herrmann HC, Wilensky RL, et al. Safety and procedural success of left atrial appendage exclusion with the Lariat device: a systematic review of published reports and analytic review of the FDA MAUDE database. JAMA Intern Med 2015; 175(7):1104–9.
KEY POINTS
- Specific risk factor management is as important as anticoagulation when addressing stroke risk.
- The CHADS2 score has been superseded by the CHA2DS2-VASc score, which is more accurate for lower-risk categories.
- Anticoagulant options have increased substantially in the past few years with the introduction of novel oral anticoagulants, including the direct thrombin-inhibitor dabigatran and the factor Xa inhibitors rivaroxaban, apixaban, and edoxaban.
- Most atrial thrombi in patients with nonvalvular atrial fibrillation form in the left atrial appendage (LAA); nonpharmacologic interventions have been developed to block the LAA and reduce the risk of stroke.
Stroke management and the impact of mobile stroke treatment units
Stroke is the fifth leading cause of death in the United States. Approximately 795,000 strokes occur every year and about 130,000 patients die.1 The impact of stroke-related medical costs and disability is significant, making it a key target for treatment and prevention strategies.
Stroke is defined as an acute loss of neurologic function caused by damaged brain tissue. There are two primary types: ischemic and hemorrhagic. Ischemic strokes are by far the most common, accounting for 87% of all strokes.2 An ischemic stroke is caused by an arterial occlusion that restricts cerebral blood flow; a hemorrhagic stroke is caused by a rupture or leak in the cerebrovasculature. Treatment of an ischemic stroke focuses on thrombolysis and revascularization strategies to restore blood flow, whereas with hemorrhagic stroke, treatment focuses on controlling intracerebral bleeding, elevated intracranial pressure, and secondary brain injury. This article addresses a key factor in improved stroke outcomes—time to treatment—and the impact that a mobile stroke treatment unit (MSTU) can have on this factor.
DECLINING MORBIDITY AND MORTALITY RATES
Although the morbidity and mortality associated with stroke are high, the rates have been declining. From 2001 o 2011, the stroke mortality rate declined by 35%.2 The American Heart Association attributes the reduction to improvements in both prevention and treatment.
A significant portion of the decline has come from population-wide stroke prevention efforts. These include community efforts to control the major cardiovascular risk factors for stroke, including hypertension and hypercholesterolemia. Treating hypertension can reduce the incidence of stroke by up to 40%.3 In addition, community education efforts aimed at improving awareness of stroke symptoms and early detection have contributed to the declining rates, although, by some estimates, only about one-third of the population knows the major signs and symptoms of stroke.
Improved stroke treatments have also contributed to better outcomes, primarily through the more widespread use of thrombolytics. When first approved by the US Food and Drug Administration (FDA), thrombolytics were primarily the purview of cardiologists. However, as outcomes data accumulated, neurologists recognized the utility of thrombolytics in treating ischemic cerebrovascular disease and began investigating their use in clinical trials. Positive outcomes from those trials led to their FDA approval for stroke treatment and universal recognition as the primary therapy for acute stroke. More recent efforts have concentrated on early treatment by bringing the therapy to the patient as opposed to the traditional treatment algorithm of providing care in the emergency department. If therapy is instituted quickly enough, ischemic stroke symptoms can be reversed.
TIME TO TREATMENT
Therapeutic use of tissue plasminogen activators (tPA) has had a major impact on morbidity and mortality in patients with acute ischemic strokes. The efficacy of tPA as thrombolytic therapy in this patient population is well documented.4
Also well documented is the significant impact of time-to-tPA treatment on outcomes. If therapy is started within 3 to 4.5 hours of ischemic stroke onset, patients have improved functional outcomes 3 to 6 months after the incident (Figure 1). Between 31% and 50% of patients treated with tPA within 3 hours experienced improved recovery at 3 months compared with 20% to 38% of patients treated with placebo.5–9 Faster onset to treatment, measured in 15-minute increments, has been shown to significantly reduce in-hospital mortality, reduce intracranial hemorrhage, increase ability to walk at discharge, and increase number discharged to home.6 Even a 1-minute delay in time-to-tPA treatment has a substantial impact on rates of morbidity and mortality (Table 1).10 National and international guidelines recommend starting intravenous tPA within 1 hour of patient arrival in the emergency department and not longer than 4.5 hours since symptom onset, although some evidence indicates a 3-hour window.5,11,12
Although the evidence supports the benefit of rapid therapy for acute ischemic stroke, the national percentage of patients who actually receive tPA within the therapeutic window is small, by some estimates as low as 3% to 5%.13 For optimal stroke care, the rate should be 30% to 50%.
IMPROVING TREATMENT TIMES
Studies have found that the major reason patients do not receive tPA is that they do not reach the hospital quickly enough to be assessed and treated within the treatment window.14,15 In essence, neurologists have the technology to treat most patients, but are waiting for the patients to arrive. Many factors contribute to this delayed arrival time. On the patient level, the primary factors are related to failure to recognize stroke symptoms as well as failure to understand their seriousness.
From the healthcare provider’s perspective, a major barrier to reducing the time-to-treatment window is the need to accurately assess patients with acute ischemic stroke who are eligible for thrombolytic therapy. This is difficult to achieve in clinical practice because it requires neurologic imaging primarily with computed tomography (CT) or magnetic resonance imaging (MRI) and laboratory analyses so that hemorrhagic stroke and other contraindications to thrombolysis can be excluded. Traditionally, this type of analytic equipment had been available only in emergency departments, requiring patients to be brought to those facilities.
Recent innovation in this area led to the development of specialized ambulances equipped with a CT scanner, point-of-care laboratory equipment, and telemedicine connection along with the appropriate treatment options/medications and trained healthcare personnel to provide prehospital stroke treatment. These specially equipped ambulances are known as MSTUs or stroke emergency mobile (STEMO) units. Their development has dramatically altered the strategy from one of taking the patient to the treatment to taking the treatment to the patient.
MOBILE STROKE TREATMENT UNITS
Two technological innovations have been fundamental to the creation and success of MSTU: portable CT scanners and high-speed wireless data transmission.
CT scanners. A key element was the development of a portable diagnostic-quality head and neck CT scanner that can be fit inside a typical-sized ambulance. This 8-slice CT scanner is capable of creating the same scan types and quality found in radiology department CT scanners, including axial imaging, helical angiography, and perfusion imaging. The resolution and slice thickness (1.25 mm) of the images are of suitable quality to enable neurologists and neuroradiologists to exclude hemorrhage in acute stroke, to assess the degree of brain injury, and to identify the vascular lesion responsible for the ischemic deficit. These technologies also enable diagnostic differentiation between brain tissue that is irreversibly infarcted from that which is potentially salvageable, thereby allowing more accurate patient assessment. The imaging data currently obtainable by CT scanners fitted on ambulances is only likely to improve with future technological advances.
Wireless data transmission. Cellular wireless providers have developed the technology and equipment to provide high-speed wireless broadband capable of transmitting high-quality CT and MRI images. It also enables encrypted feed of video telemedicine, data transmission, and download of patient data. This allows the MSTU to electronically sit inside the firewalls of healthcare facilities, providing access to the patients’ electronic health records and to on-site stroke experts.
The successes have been impressive. Studies have found that the deployment of an MSTU significantly reduces the median time from 9-1-1 alarm to intravenous thrombolysis without increasing adverse events.16–19 These data are primarily from the PHANTOM-S study, a pilot program conducted in Germany.18,19 Results showed a significant reduction in alarm-to-treatment times, from 76 minutes in the hospital control group to 52 minutes in the MSTU group (Table 2).17,19 Further, among patients who suffered an ischemic stroke, the proportion who received tPA within 1 hour of symptom onset was sixfold higher after MSTU deployment (Table 3).18 In a separate European study, prehospital stroke assessment using an MSTU significantly reduced the median time from alarm-to-therapy decision: 35 minutes versus 76 in the hospital group.16
The prehospital cerebrovascular diagnostic workup provided by an MSTU also can improve the emergency management of other stroke types. By providing more diagnostic data and higher quality imaging, the units improve the accuracy of the diagnosis. In turn, this enables emergency personnel to provide accurate therapy and to transfer patients to hospitals with the appropriate level of stroke care, decreasing the need for additional intrahospital transfers.20
Overall, it has been shown that an MSTU equipped with the necessary imaging and laboratory testing equipment can provide appropriate, accurate, and safe ambulance-based prehospital tPA administration, reduce the time to tPA administration, and increase the number of patients who receive tPA administration. All of these factors combine to improve outcomes in patients with acute ischemic stroke.
CLEVELAND CLINIC EXPERIENCE
Cleveland Clinic has a tradition of providing high-quality and innovative stroke care. Recognizing the importance of an appropriately equipped MSTU in reducing the time to stroke treatment, especially tPA administration, Cleveland Clinic instituted a plan to develop an MSTU for the care of patients in the Cleveland area. The development required several planning, funding, and development phases.
Planning. Establishing relations with both city planners and area hospitals was central to planning the MSTU startup. An agreement with the city of Cleveland included creating an emergency medical system (EMS) triage algorithm for the 9-1-1 dispatch center. When a call is received, the dispatcher uses a stroke checklist to perform an initial screening. If a stroke is suspected, the MSTU is dispatched along with a Cleveland EMS or other first-responder unit.
As part of the agreement, Cleveland officials required that the MSTU treat all patients, regardless of their ability to pay. This requirement has been beneficial to the MSTU mission as it allows for treating more patients with tPA as quickly as possible without concern for health insurance, which maximizes the potential for neurologic recovery.
Staffing and procedures. The MSTU staff is composed of a paramedic, a critical care nurse, a CT technologist, and an emergency medicine technician/EMS driver. They perform CT scans and point-of-care laboratory tests on patients who have stroke symptoms. The CT scans and laboratory results are wirelessly transmitted to Cleveland Clinic. A neurologist assesses the data, consults with the MSTU staff on history and neurologic examination, and diagnoses the patient remotely. Patients are then transported to the closest hospital with the resources to meet their clinical needs. If thrombolytic therapy is indicated, intravenous tPA is initiated immediately at the scene. If the patient has sustained a hemorrhagic stroke, reversal of anticoagulation therapy is initiated, if indicated.
Outcomes. The success rates also have been impressive, with dramatic reductions in time to treatment. On average, patients received tPA 40 minutes faster in the MSTU model than in the standard model of ambulance transport and in-hospital evaluation and treatment: 64 minutes versus 104 minutes. Further, more patients in the MSTU group received tPA: 26% versus 14%. Results also showed a 21-minute reduction in time-to-CT completion, an important aspect of providing more timely care.21–23 This CT scanner is also capable of CT angiography. This enables large-vessel occlusion strokes to be identified in the field. When these types of strokes are identified in the field, the patients are transported directly to a stroke center capable of endovascular therapy, even bypassing some primary stroke centers.
Using the MSTU to bring diagnostic and stroke care to the patient has shown that the time between the onset of stroke-like symptoms and the delivery of treatment can be reduced. Thus, an MSTU has the potential to minimize the mortality and long-term morbidity associated with strokes.
- Centers for Disease Control and Prevention (CDC). Prevalence of stroke— United States, 2006–2010. MMWR Morb Mortal Wkly Rep 2012; 61:379–382.
- Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation 2015; 131:e29–e322.
- Howard G, Banach M, Cushman M, et al. Is blood pressure control for stroke prevention the correct goal? The lost opportunity of preventing hypertension. Stroke 2015; 46:1595–1600.
- Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med 1995; 333:1581–1587.
- Lees KR, Bluhmki E, von Kummer R, et al; ECASS, ATLANTIS, NINDS, and EPITHET rt-PA Study Group. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet 2010; 375:1695–1703.
- Saver JL, Fonarow GC, Smith EE, et al. Time to treatment with intravenous tissue plasminogen activator and outcome from acute ischemic stroke. JAMA 2013; 309:2480–2488.
- Hacke W, Donnan G, Fieschi C, et al; ATLANTIS Trials Investigators; ECASS Trials Investigators; NINDS rt-PA Study Group Investigators. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet 2004; 363:768–774.
- Wardlaw JM, Murray V, Berge E, et al. Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis. Lancet 2012; 379:2364–2372.
- Prabhakaran S, Ruff I, Bernstein RA. Acute stroke intervention: a systematic review. JAMA 2015; 313:1451–1462.
- Saver JL. Time is brain—quantified. Stroke 2006; 37:263–266.
- Jauch EC, Saver JL, Adams HP Jr, et al; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Peripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013; 44:870–947.
- Hacke W, Kaste M, Bluhmki E, et al; ECASS Investigators. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008; 359:1317– 1329.
- Adeoye O, Hornung R, Khatri P, Kleindorfer D. Recombinant tissue-type plasminogen activator use for ischemic stroke in the United States: a doubling of treatment rates over the course of 5 years. Stroke 2011; 42:1952–1955.
- Barber PA, Zhang J, Demchuk AM, Hill MD, Buchan AM. Why are stroke patients excluded from TPA therapy? An analysis of patient eligibility. Neurology 2001; 56:1015–1020.
- Lichtman JH, Watanabe E, Allen NB, Jones SB, Dostal J, Goldstein LB. Hospital arrival time and intravenous t-PA use in US Academic Medical Centers, 2001– 2004. Stroke 2009; 40:3845–3850.
- Walter S, Kostopoulos P, Haass A, et al. Diagnosis and treatment of patients with stroke in a mobile stroke unit versus in hospital: a randomised controlled trial. Lancet Neurol 2012; 11:397–404.
- Ebinger M, Winter B, Wendt M, et al; STEMO Consortium. Effect of the use of ambulance-based thrombolysis on time to thrombolysis in acute ischemic stroke: a randomized clinical trial. JAMA 2014; 311:1622–1631.
- Ebinger M, Kunz A, Wendt M, et al. Effects of golden hour thrombolysis: a prehospital acute neurological treatment and optimization of medical care in stroke (PHANTOM-S) substudy. JAMA Neurol 2015; 72:25–30.
- Weber JE, Ebinger M, Rozansk M, et al; STEMO-Consortium. Prehospital thrombolysis in acute stroke: results of the PHANTOM-S pilot study. Neurology 2013; 80:163–168.
- Wendt M, Ebinger M, Kunz A, et al; STEMO Consortium. Improved prehospital triage of patients with stroke in a specialized stroke ambulance: results of the prehospital acute neurological therapy and optimization of medical care in stroke study. Stroke 2015; 46: 740–745.
- Cho S, Cerejo R, Taqui A, et al. Feasibility of telemedicine on a mobile stroke treatment unit. Stroke 2015; 46:ATP200.
- Sheikhi L, Itrat A, Cerejo R, et al. Does portable CT imaging in a mobile stroke treatment unit (MSTU) provide adequate quality for early critical decision making? Stroke 2015; 46:AWP31.
- Taqui A, Cerejo R, Itrat A, et al. Reduction in time to imaging and intravenous thrombolysis by in-field evaluation and treatment in a mobile stroke treatment unit. Stroke 2015; 46:A54.
Stroke is the fifth leading cause of death in the United States. Approximately 795,000 strokes occur every year and about 130,000 patients die.1 The impact of stroke-related medical costs and disability is significant, making it a key target for treatment and prevention strategies.
Stroke is defined as an acute loss of neurologic function caused by damaged brain tissue. There are two primary types: ischemic and hemorrhagic. Ischemic strokes are by far the most common, accounting for 87% of all strokes.2 An ischemic stroke is caused by an arterial occlusion that restricts cerebral blood flow; a hemorrhagic stroke is caused by a rupture or leak in the cerebrovasculature. Treatment of an ischemic stroke focuses on thrombolysis and revascularization strategies to restore blood flow, whereas with hemorrhagic stroke, treatment focuses on controlling intracerebral bleeding, elevated intracranial pressure, and secondary brain injury. This article addresses a key factor in improved stroke outcomes—time to treatment—and the impact that a mobile stroke treatment unit (MSTU) can have on this factor.
DECLINING MORBIDITY AND MORTALITY RATES
Although the morbidity and mortality associated with stroke are high, the rates have been declining. From 2001 o 2011, the stroke mortality rate declined by 35%.2 The American Heart Association attributes the reduction to improvements in both prevention and treatment.
A significant portion of the decline has come from population-wide stroke prevention efforts. These include community efforts to control the major cardiovascular risk factors for stroke, including hypertension and hypercholesterolemia. Treating hypertension can reduce the incidence of stroke by up to 40%.3 In addition, community education efforts aimed at improving awareness of stroke symptoms and early detection have contributed to the declining rates, although, by some estimates, only about one-third of the population knows the major signs and symptoms of stroke.
Improved stroke treatments have also contributed to better outcomes, primarily through the more widespread use of thrombolytics. When first approved by the US Food and Drug Administration (FDA), thrombolytics were primarily the purview of cardiologists. However, as outcomes data accumulated, neurologists recognized the utility of thrombolytics in treating ischemic cerebrovascular disease and began investigating their use in clinical trials. Positive outcomes from those trials led to their FDA approval for stroke treatment and universal recognition as the primary therapy for acute stroke. More recent efforts have concentrated on early treatment by bringing the therapy to the patient as opposed to the traditional treatment algorithm of providing care in the emergency department. If therapy is instituted quickly enough, ischemic stroke symptoms can be reversed.
TIME TO TREATMENT
Therapeutic use of tissue plasminogen activators (tPA) has had a major impact on morbidity and mortality in patients with acute ischemic strokes. The efficacy of tPA as thrombolytic therapy in this patient population is well documented.4
Also well documented is the significant impact of time-to-tPA treatment on outcomes. If therapy is started within 3 to 4.5 hours of ischemic stroke onset, patients have improved functional outcomes 3 to 6 months after the incident (Figure 1). Between 31% and 50% of patients treated with tPA within 3 hours experienced improved recovery at 3 months compared with 20% to 38% of patients treated with placebo.5–9 Faster onset to treatment, measured in 15-minute increments, has been shown to significantly reduce in-hospital mortality, reduce intracranial hemorrhage, increase ability to walk at discharge, and increase number discharged to home.6 Even a 1-minute delay in time-to-tPA treatment has a substantial impact on rates of morbidity and mortality (Table 1).10 National and international guidelines recommend starting intravenous tPA within 1 hour of patient arrival in the emergency department and not longer than 4.5 hours since symptom onset, although some evidence indicates a 3-hour window.5,11,12
Although the evidence supports the benefit of rapid therapy for acute ischemic stroke, the national percentage of patients who actually receive tPA within the therapeutic window is small, by some estimates as low as 3% to 5%.13 For optimal stroke care, the rate should be 30% to 50%.
IMPROVING TREATMENT TIMES
Studies have found that the major reason patients do not receive tPA is that they do not reach the hospital quickly enough to be assessed and treated within the treatment window.14,15 In essence, neurologists have the technology to treat most patients, but are waiting for the patients to arrive. Many factors contribute to this delayed arrival time. On the patient level, the primary factors are related to failure to recognize stroke symptoms as well as failure to understand their seriousness.
From the healthcare provider’s perspective, a major barrier to reducing the time-to-treatment window is the need to accurately assess patients with acute ischemic stroke who are eligible for thrombolytic therapy. This is difficult to achieve in clinical practice because it requires neurologic imaging primarily with computed tomography (CT) or magnetic resonance imaging (MRI) and laboratory analyses so that hemorrhagic stroke and other contraindications to thrombolysis can be excluded. Traditionally, this type of analytic equipment had been available only in emergency departments, requiring patients to be brought to those facilities.
Recent innovation in this area led to the development of specialized ambulances equipped with a CT scanner, point-of-care laboratory equipment, and telemedicine connection along with the appropriate treatment options/medications and trained healthcare personnel to provide prehospital stroke treatment. These specially equipped ambulances are known as MSTUs or stroke emergency mobile (STEMO) units. Their development has dramatically altered the strategy from one of taking the patient to the treatment to taking the treatment to the patient.
MOBILE STROKE TREATMENT UNITS
Two technological innovations have been fundamental to the creation and success of MSTU: portable CT scanners and high-speed wireless data transmission.
CT scanners. A key element was the development of a portable diagnostic-quality head and neck CT scanner that can be fit inside a typical-sized ambulance. This 8-slice CT scanner is capable of creating the same scan types and quality found in radiology department CT scanners, including axial imaging, helical angiography, and perfusion imaging. The resolution and slice thickness (1.25 mm) of the images are of suitable quality to enable neurologists and neuroradiologists to exclude hemorrhage in acute stroke, to assess the degree of brain injury, and to identify the vascular lesion responsible for the ischemic deficit. These technologies also enable diagnostic differentiation between brain tissue that is irreversibly infarcted from that which is potentially salvageable, thereby allowing more accurate patient assessment. The imaging data currently obtainable by CT scanners fitted on ambulances is only likely to improve with future technological advances.
Wireless data transmission. Cellular wireless providers have developed the technology and equipment to provide high-speed wireless broadband capable of transmitting high-quality CT and MRI images. It also enables encrypted feed of video telemedicine, data transmission, and download of patient data. This allows the MSTU to electronically sit inside the firewalls of healthcare facilities, providing access to the patients’ electronic health records and to on-site stroke experts.
The successes have been impressive. Studies have found that the deployment of an MSTU significantly reduces the median time from 9-1-1 alarm to intravenous thrombolysis without increasing adverse events.16–19 These data are primarily from the PHANTOM-S study, a pilot program conducted in Germany.18,19 Results showed a significant reduction in alarm-to-treatment times, from 76 minutes in the hospital control group to 52 minutes in the MSTU group (Table 2).17,19 Further, among patients who suffered an ischemic stroke, the proportion who received tPA within 1 hour of symptom onset was sixfold higher after MSTU deployment (Table 3).18 In a separate European study, prehospital stroke assessment using an MSTU significantly reduced the median time from alarm-to-therapy decision: 35 minutes versus 76 in the hospital group.16
The prehospital cerebrovascular diagnostic workup provided by an MSTU also can improve the emergency management of other stroke types. By providing more diagnostic data and higher quality imaging, the units improve the accuracy of the diagnosis. In turn, this enables emergency personnel to provide accurate therapy and to transfer patients to hospitals with the appropriate level of stroke care, decreasing the need for additional intrahospital transfers.20
Overall, it has been shown that an MSTU equipped with the necessary imaging and laboratory testing equipment can provide appropriate, accurate, and safe ambulance-based prehospital tPA administration, reduce the time to tPA administration, and increase the number of patients who receive tPA administration. All of these factors combine to improve outcomes in patients with acute ischemic stroke.
CLEVELAND CLINIC EXPERIENCE
Cleveland Clinic has a tradition of providing high-quality and innovative stroke care. Recognizing the importance of an appropriately equipped MSTU in reducing the time to stroke treatment, especially tPA administration, Cleveland Clinic instituted a plan to develop an MSTU for the care of patients in the Cleveland area. The development required several planning, funding, and development phases.
Planning. Establishing relations with both city planners and area hospitals was central to planning the MSTU startup. An agreement with the city of Cleveland included creating an emergency medical system (EMS) triage algorithm for the 9-1-1 dispatch center. When a call is received, the dispatcher uses a stroke checklist to perform an initial screening. If a stroke is suspected, the MSTU is dispatched along with a Cleveland EMS or other first-responder unit.
As part of the agreement, Cleveland officials required that the MSTU treat all patients, regardless of their ability to pay. This requirement has been beneficial to the MSTU mission as it allows for treating more patients with tPA as quickly as possible without concern for health insurance, which maximizes the potential for neurologic recovery.
Staffing and procedures. The MSTU staff is composed of a paramedic, a critical care nurse, a CT technologist, and an emergency medicine technician/EMS driver. They perform CT scans and point-of-care laboratory tests on patients who have stroke symptoms. The CT scans and laboratory results are wirelessly transmitted to Cleveland Clinic. A neurologist assesses the data, consults with the MSTU staff on history and neurologic examination, and diagnoses the patient remotely. Patients are then transported to the closest hospital with the resources to meet their clinical needs. If thrombolytic therapy is indicated, intravenous tPA is initiated immediately at the scene. If the patient has sustained a hemorrhagic stroke, reversal of anticoagulation therapy is initiated, if indicated.
Outcomes. The success rates also have been impressive, with dramatic reductions in time to treatment. On average, patients received tPA 40 minutes faster in the MSTU model than in the standard model of ambulance transport and in-hospital evaluation and treatment: 64 minutes versus 104 minutes. Further, more patients in the MSTU group received tPA: 26% versus 14%. Results also showed a 21-minute reduction in time-to-CT completion, an important aspect of providing more timely care.21–23 This CT scanner is also capable of CT angiography. This enables large-vessel occlusion strokes to be identified in the field. When these types of strokes are identified in the field, the patients are transported directly to a stroke center capable of endovascular therapy, even bypassing some primary stroke centers.
Using the MSTU to bring diagnostic and stroke care to the patient has shown that the time between the onset of stroke-like symptoms and the delivery of treatment can be reduced. Thus, an MSTU has the potential to minimize the mortality and long-term morbidity associated with strokes.
Stroke is the fifth leading cause of death in the United States. Approximately 795,000 strokes occur every year and about 130,000 patients die.1 The impact of stroke-related medical costs and disability is significant, making it a key target for treatment and prevention strategies.
Stroke is defined as an acute loss of neurologic function caused by damaged brain tissue. There are two primary types: ischemic and hemorrhagic. Ischemic strokes are by far the most common, accounting for 87% of all strokes.2 An ischemic stroke is caused by an arterial occlusion that restricts cerebral blood flow; a hemorrhagic stroke is caused by a rupture or leak in the cerebrovasculature. Treatment of an ischemic stroke focuses on thrombolysis and revascularization strategies to restore blood flow, whereas with hemorrhagic stroke, treatment focuses on controlling intracerebral bleeding, elevated intracranial pressure, and secondary brain injury. This article addresses a key factor in improved stroke outcomes—time to treatment—and the impact that a mobile stroke treatment unit (MSTU) can have on this factor.
DECLINING MORBIDITY AND MORTALITY RATES
Although the morbidity and mortality associated with stroke are high, the rates have been declining. From 2001 o 2011, the stroke mortality rate declined by 35%.2 The American Heart Association attributes the reduction to improvements in both prevention and treatment.
A significant portion of the decline has come from population-wide stroke prevention efforts. These include community efforts to control the major cardiovascular risk factors for stroke, including hypertension and hypercholesterolemia. Treating hypertension can reduce the incidence of stroke by up to 40%.3 In addition, community education efforts aimed at improving awareness of stroke symptoms and early detection have contributed to the declining rates, although, by some estimates, only about one-third of the population knows the major signs and symptoms of stroke.
Improved stroke treatments have also contributed to better outcomes, primarily through the more widespread use of thrombolytics. When first approved by the US Food and Drug Administration (FDA), thrombolytics were primarily the purview of cardiologists. However, as outcomes data accumulated, neurologists recognized the utility of thrombolytics in treating ischemic cerebrovascular disease and began investigating their use in clinical trials. Positive outcomes from those trials led to their FDA approval for stroke treatment and universal recognition as the primary therapy for acute stroke. More recent efforts have concentrated on early treatment by bringing the therapy to the patient as opposed to the traditional treatment algorithm of providing care in the emergency department. If therapy is instituted quickly enough, ischemic stroke symptoms can be reversed.
TIME TO TREATMENT
Therapeutic use of tissue plasminogen activators (tPA) has had a major impact on morbidity and mortality in patients with acute ischemic strokes. The efficacy of tPA as thrombolytic therapy in this patient population is well documented.4
Also well documented is the significant impact of time-to-tPA treatment on outcomes. If therapy is started within 3 to 4.5 hours of ischemic stroke onset, patients have improved functional outcomes 3 to 6 months after the incident (Figure 1). Between 31% and 50% of patients treated with tPA within 3 hours experienced improved recovery at 3 months compared with 20% to 38% of patients treated with placebo.5–9 Faster onset to treatment, measured in 15-minute increments, has been shown to significantly reduce in-hospital mortality, reduce intracranial hemorrhage, increase ability to walk at discharge, and increase number discharged to home.6 Even a 1-minute delay in time-to-tPA treatment has a substantial impact on rates of morbidity and mortality (Table 1).10 National and international guidelines recommend starting intravenous tPA within 1 hour of patient arrival in the emergency department and not longer than 4.5 hours since symptom onset, although some evidence indicates a 3-hour window.5,11,12
Although the evidence supports the benefit of rapid therapy for acute ischemic stroke, the national percentage of patients who actually receive tPA within the therapeutic window is small, by some estimates as low as 3% to 5%.13 For optimal stroke care, the rate should be 30% to 50%.
IMPROVING TREATMENT TIMES
Studies have found that the major reason patients do not receive tPA is that they do not reach the hospital quickly enough to be assessed and treated within the treatment window.14,15 In essence, neurologists have the technology to treat most patients, but are waiting for the patients to arrive. Many factors contribute to this delayed arrival time. On the patient level, the primary factors are related to failure to recognize stroke symptoms as well as failure to understand their seriousness.
From the healthcare provider’s perspective, a major barrier to reducing the time-to-treatment window is the need to accurately assess patients with acute ischemic stroke who are eligible for thrombolytic therapy. This is difficult to achieve in clinical practice because it requires neurologic imaging primarily with computed tomography (CT) or magnetic resonance imaging (MRI) and laboratory analyses so that hemorrhagic stroke and other contraindications to thrombolysis can be excluded. Traditionally, this type of analytic equipment had been available only in emergency departments, requiring patients to be brought to those facilities.
Recent innovation in this area led to the development of specialized ambulances equipped with a CT scanner, point-of-care laboratory equipment, and telemedicine connection along with the appropriate treatment options/medications and trained healthcare personnel to provide prehospital stroke treatment. These specially equipped ambulances are known as MSTUs or stroke emergency mobile (STEMO) units. Their development has dramatically altered the strategy from one of taking the patient to the treatment to taking the treatment to the patient.
MOBILE STROKE TREATMENT UNITS
Two technological innovations have been fundamental to the creation and success of MSTU: portable CT scanners and high-speed wireless data transmission.
CT scanners. A key element was the development of a portable diagnostic-quality head and neck CT scanner that can be fit inside a typical-sized ambulance. This 8-slice CT scanner is capable of creating the same scan types and quality found in radiology department CT scanners, including axial imaging, helical angiography, and perfusion imaging. The resolution and slice thickness (1.25 mm) of the images are of suitable quality to enable neurologists and neuroradiologists to exclude hemorrhage in acute stroke, to assess the degree of brain injury, and to identify the vascular lesion responsible for the ischemic deficit. These technologies also enable diagnostic differentiation between brain tissue that is irreversibly infarcted from that which is potentially salvageable, thereby allowing more accurate patient assessment. The imaging data currently obtainable by CT scanners fitted on ambulances is only likely to improve with future technological advances.
Wireless data transmission. Cellular wireless providers have developed the technology and equipment to provide high-speed wireless broadband capable of transmitting high-quality CT and MRI images. It also enables encrypted feed of video telemedicine, data transmission, and download of patient data. This allows the MSTU to electronically sit inside the firewalls of healthcare facilities, providing access to the patients’ electronic health records and to on-site stroke experts.
The successes have been impressive. Studies have found that the deployment of an MSTU significantly reduces the median time from 9-1-1 alarm to intravenous thrombolysis without increasing adverse events.16–19 These data are primarily from the PHANTOM-S study, a pilot program conducted in Germany.18,19 Results showed a significant reduction in alarm-to-treatment times, from 76 minutes in the hospital control group to 52 minutes in the MSTU group (Table 2).17,19 Further, among patients who suffered an ischemic stroke, the proportion who received tPA within 1 hour of symptom onset was sixfold higher after MSTU deployment (Table 3).18 In a separate European study, prehospital stroke assessment using an MSTU significantly reduced the median time from alarm-to-therapy decision: 35 minutes versus 76 in the hospital group.16
The prehospital cerebrovascular diagnostic workup provided by an MSTU also can improve the emergency management of other stroke types. By providing more diagnostic data and higher quality imaging, the units improve the accuracy of the diagnosis. In turn, this enables emergency personnel to provide accurate therapy and to transfer patients to hospitals with the appropriate level of stroke care, decreasing the need for additional intrahospital transfers.20
Overall, it has been shown that an MSTU equipped with the necessary imaging and laboratory testing equipment can provide appropriate, accurate, and safe ambulance-based prehospital tPA administration, reduce the time to tPA administration, and increase the number of patients who receive tPA administration. All of these factors combine to improve outcomes in patients with acute ischemic stroke.
CLEVELAND CLINIC EXPERIENCE
Cleveland Clinic has a tradition of providing high-quality and innovative stroke care. Recognizing the importance of an appropriately equipped MSTU in reducing the time to stroke treatment, especially tPA administration, Cleveland Clinic instituted a plan to develop an MSTU for the care of patients in the Cleveland area. The development required several planning, funding, and development phases.
Planning. Establishing relations with both city planners and area hospitals was central to planning the MSTU startup. An agreement with the city of Cleveland included creating an emergency medical system (EMS) triage algorithm for the 9-1-1 dispatch center. When a call is received, the dispatcher uses a stroke checklist to perform an initial screening. If a stroke is suspected, the MSTU is dispatched along with a Cleveland EMS or other first-responder unit.
As part of the agreement, Cleveland officials required that the MSTU treat all patients, regardless of their ability to pay. This requirement has been beneficial to the MSTU mission as it allows for treating more patients with tPA as quickly as possible without concern for health insurance, which maximizes the potential for neurologic recovery.
Staffing and procedures. The MSTU staff is composed of a paramedic, a critical care nurse, a CT technologist, and an emergency medicine technician/EMS driver. They perform CT scans and point-of-care laboratory tests on patients who have stroke symptoms. The CT scans and laboratory results are wirelessly transmitted to Cleveland Clinic. A neurologist assesses the data, consults with the MSTU staff on history and neurologic examination, and diagnoses the patient remotely. Patients are then transported to the closest hospital with the resources to meet their clinical needs. If thrombolytic therapy is indicated, intravenous tPA is initiated immediately at the scene. If the patient has sustained a hemorrhagic stroke, reversal of anticoagulation therapy is initiated, if indicated.
Outcomes. The success rates also have been impressive, with dramatic reductions in time to treatment. On average, patients received tPA 40 minutes faster in the MSTU model than in the standard model of ambulance transport and in-hospital evaluation and treatment: 64 minutes versus 104 minutes. Further, more patients in the MSTU group received tPA: 26% versus 14%. Results also showed a 21-minute reduction in time-to-CT completion, an important aspect of providing more timely care.21–23 This CT scanner is also capable of CT angiography. This enables large-vessel occlusion strokes to be identified in the field. When these types of strokes are identified in the field, the patients are transported directly to a stroke center capable of endovascular therapy, even bypassing some primary stroke centers.
Using the MSTU to bring diagnostic and stroke care to the patient has shown that the time between the onset of stroke-like symptoms and the delivery of treatment can be reduced. Thus, an MSTU has the potential to minimize the mortality and long-term morbidity associated with strokes.
- Centers for Disease Control and Prevention (CDC). Prevalence of stroke— United States, 2006–2010. MMWR Morb Mortal Wkly Rep 2012; 61:379–382.
- Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation 2015; 131:e29–e322.
- Howard G, Banach M, Cushman M, et al. Is blood pressure control for stroke prevention the correct goal? The lost opportunity of preventing hypertension. Stroke 2015; 46:1595–1600.
- Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med 1995; 333:1581–1587.
- Lees KR, Bluhmki E, von Kummer R, et al; ECASS, ATLANTIS, NINDS, and EPITHET rt-PA Study Group. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet 2010; 375:1695–1703.
- Saver JL, Fonarow GC, Smith EE, et al. Time to treatment with intravenous tissue plasminogen activator and outcome from acute ischemic stroke. JAMA 2013; 309:2480–2488.
- Hacke W, Donnan G, Fieschi C, et al; ATLANTIS Trials Investigators; ECASS Trials Investigators; NINDS rt-PA Study Group Investigators. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet 2004; 363:768–774.
- Wardlaw JM, Murray V, Berge E, et al. Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis. Lancet 2012; 379:2364–2372.
- Prabhakaran S, Ruff I, Bernstein RA. Acute stroke intervention: a systematic review. JAMA 2015; 313:1451–1462.
- Saver JL. Time is brain—quantified. Stroke 2006; 37:263–266.
- Jauch EC, Saver JL, Adams HP Jr, et al; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Peripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013; 44:870–947.
- Hacke W, Kaste M, Bluhmki E, et al; ECASS Investigators. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008; 359:1317– 1329.
- Adeoye O, Hornung R, Khatri P, Kleindorfer D. Recombinant tissue-type plasminogen activator use for ischemic stroke in the United States: a doubling of treatment rates over the course of 5 years. Stroke 2011; 42:1952–1955.
- Barber PA, Zhang J, Demchuk AM, Hill MD, Buchan AM. Why are stroke patients excluded from TPA therapy? An analysis of patient eligibility. Neurology 2001; 56:1015–1020.
- Lichtman JH, Watanabe E, Allen NB, Jones SB, Dostal J, Goldstein LB. Hospital arrival time and intravenous t-PA use in US Academic Medical Centers, 2001– 2004. Stroke 2009; 40:3845–3850.
- Walter S, Kostopoulos P, Haass A, et al. Diagnosis and treatment of patients with stroke in a mobile stroke unit versus in hospital: a randomised controlled trial. Lancet Neurol 2012; 11:397–404.
- Ebinger M, Winter B, Wendt M, et al; STEMO Consortium. Effect of the use of ambulance-based thrombolysis on time to thrombolysis in acute ischemic stroke: a randomized clinical trial. JAMA 2014; 311:1622–1631.
- Ebinger M, Kunz A, Wendt M, et al. Effects of golden hour thrombolysis: a prehospital acute neurological treatment and optimization of medical care in stroke (PHANTOM-S) substudy. JAMA Neurol 2015; 72:25–30.
- Weber JE, Ebinger M, Rozansk M, et al; STEMO-Consortium. Prehospital thrombolysis in acute stroke: results of the PHANTOM-S pilot study. Neurology 2013; 80:163–168.
- Wendt M, Ebinger M, Kunz A, et al; STEMO Consortium. Improved prehospital triage of patients with stroke in a specialized stroke ambulance: results of the prehospital acute neurological therapy and optimization of medical care in stroke study. Stroke 2015; 46: 740–745.
- Cho S, Cerejo R, Taqui A, et al. Feasibility of telemedicine on a mobile stroke treatment unit. Stroke 2015; 46:ATP200.
- Sheikhi L, Itrat A, Cerejo R, et al. Does portable CT imaging in a mobile stroke treatment unit (MSTU) provide adequate quality for early critical decision making? Stroke 2015; 46:AWP31.
- Taqui A, Cerejo R, Itrat A, et al. Reduction in time to imaging and intravenous thrombolysis by in-field evaluation and treatment in a mobile stroke treatment unit. Stroke 2015; 46:A54.
- Centers for Disease Control and Prevention (CDC). Prevalence of stroke— United States, 2006–2010. MMWR Morb Mortal Wkly Rep 2012; 61:379–382.
- Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation 2015; 131:e29–e322.
- Howard G, Banach M, Cushman M, et al. Is blood pressure control for stroke prevention the correct goal? The lost opportunity of preventing hypertension. Stroke 2015; 46:1595–1600.
- Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med 1995; 333:1581–1587.
- Lees KR, Bluhmki E, von Kummer R, et al; ECASS, ATLANTIS, NINDS, and EPITHET rt-PA Study Group. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet 2010; 375:1695–1703.
- Saver JL, Fonarow GC, Smith EE, et al. Time to treatment with intravenous tissue plasminogen activator and outcome from acute ischemic stroke. JAMA 2013; 309:2480–2488.
- Hacke W, Donnan G, Fieschi C, et al; ATLANTIS Trials Investigators; ECASS Trials Investigators; NINDS rt-PA Study Group Investigators. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet 2004; 363:768–774.
- Wardlaw JM, Murray V, Berge E, et al. Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis. Lancet 2012; 379:2364–2372.
- Prabhakaran S, Ruff I, Bernstein RA. Acute stroke intervention: a systematic review. JAMA 2015; 313:1451–1462.
- Saver JL. Time is brain—quantified. Stroke 2006; 37:263–266.
- Jauch EC, Saver JL, Adams HP Jr, et al; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Peripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013; 44:870–947.
- Hacke W, Kaste M, Bluhmki E, et al; ECASS Investigators. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008; 359:1317– 1329.
- Adeoye O, Hornung R, Khatri P, Kleindorfer D. Recombinant tissue-type plasminogen activator use for ischemic stroke in the United States: a doubling of treatment rates over the course of 5 years. Stroke 2011; 42:1952–1955.
- Barber PA, Zhang J, Demchuk AM, Hill MD, Buchan AM. Why are stroke patients excluded from TPA therapy? An analysis of patient eligibility. Neurology 2001; 56:1015–1020.
- Lichtman JH, Watanabe E, Allen NB, Jones SB, Dostal J, Goldstein LB. Hospital arrival time and intravenous t-PA use in US Academic Medical Centers, 2001– 2004. Stroke 2009; 40:3845–3850.
- Walter S, Kostopoulos P, Haass A, et al. Diagnosis and treatment of patients with stroke in a mobile stroke unit versus in hospital: a randomised controlled trial. Lancet Neurol 2012; 11:397–404.
- Ebinger M, Winter B, Wendt M, et al; STEMO Consortium. Effect of the use of ambulance-based thrombolysis on time to thrombolysis in acute ischemic stroke: a randomized clinical trial. JAMA 2014; 311:1622–1631.
- Ebinger M, Kunz A, Wendt M, et al. Effects of golden hour thrombolysis: a prehospital acute neurological treatment and optimization of medical care in stroke (PHANTOM-S) substudy. JAMA Neurol 2015; 72:25–30.
- Weber JE, Ebinger M, Rozansk M, et al; STEMO-Consortium. Prehospital thrombolysis in acute stroke: results of the PHANTOM-S pilot study. Neurology 2013; 80:163–168.
- Wendt M, Ebinger M, Kunz A, et al; STEMO Consortium. Improved prehospital triage of patients with stroke in a specialized stroke ambulance: results of the prehospital acute neurological therapy and optimization of medical care in stroke study. Stroke 2015; 46: 740–745.
- Cho S, Cerejo R, Taqui A, et al. Feasibility of telemedicine on a mobile stroke treatment unit. Stroke 2015; 46:ATP200.
- Sheikhi L, Itrat A, Cerejo R, et al. Does portable CT imaging in a mobile stroke treatment unit (MSTU) provide adequate quality for early critical decision making? Stroke 2015; 46:AWP31.
- Taqui A, Cerejo R, Itrat A, et al. Reduction in time to imaging and intravenous thrombolysis by in-field evaluation and treatment in a mobile stroke treatment unit. Stroke 2015; 46:A54.
KEY POINTS
- Therapeutic use of tissue plasminogen activators (tPA) has had a major impact on morbidity and mortality rates in patients with acute ischemic strokes.
- Even a 1-minute delay in time-to-tPA treatment affects morbidity and mortality rates.
- The major reason patients do not receive tPA is that they do not reach the hospital quickly enough to be assessed and treated within the treatment window.
- Portable computed tomography and high-speed wireless data transmission are fundamental to the success of mobile stroke treatment units.
Biomarkers: Their potential in the diagnosis and treatment of heart failure
The growth in recognition and clinical adoption of blood and urine biomarkers over the last 20 years has been a major advance in the diagnosis and prognosis of heart failure (HF). While there have been numerous research studies and prospective clinical trials on this topic, healthcare providers often face limited availability of biomarker testing and a relative paucity of data to guide individual patient management. This is especially true since many guideline-directed medical therapies have long-established clinical indications and target populations, predating the clinical availability of biomarkers testing. This article addresses the salient insights gained from broad clinical use of biomarkers, as well as from clinical studies that helped define their appropriate use and lay the foundations of the major changes presented in the recently published clinical guidelines for the management of HF.
WHAT MAKES A BIOMARKER CLINICALLY USEFUL?
To appreciate the appropriate use of any clinical tool, clinicians need to first understand its indications and limitations and how they are defined. There are four major criteria regarding the clinical utility of a biomarker.
First, we have to establish what we are measuring, particularly with accurate and reproducible methods, with rapid turnaround, and at a reasonable cost. Second, we have to determine why we need the biomarker: ie, we need to determine if its measurement provides valuable new information to the clinician, if there is a strong and consistent association between the marker and the disease or outcome, and if this has been validated in a way that is generalizable. Third, we have to determine when measuring the biomarker would help clinical management, whether it is superior to existing tests, and whether there is evidence that it improves outcomes. Last, and perhaps most commonly overlooked, is practicality: ie, how can measuring the biomarkers be incorporated into the clinical workflow?
Not all biomarkers need to fulfill all these criteria in order to be useful, and the usefulness of a biomarker may differ from one patient population to another, from one clinician to another, or from one clinical scenario to another.1 Many clinical biomarkers are applied based on their ability to indicate a specific diagnosis or treatment (eg, glycated hemoglobin), and some have been used to determine the limits of therapy (eg, creatinine or liver function tests to detect end-organ damage). Nevertheless, the overarching goal is to establish the clinical role of a biomarker to provide the opportunity to gain additional insight into a disease state beyond that provided by a standard clinical assessment, and to determine if using the biomarker favorably alters the clinical course.
WHICH BIOMARKERS DO WE ALREADY ROUTINELY MEASURE?
Traditionally, the management of HF requires meticulous monitoring for adverse effects of drug therapy (eg, electrolyte and renal abnormalities with diuretics or drugs targeting the renin-angiotensin-aldosterone system). Although no specific clinical studies have been conducted to support their routine use, electrolytes (sodium, potassium, chloride, bicarbonate) and renal function measurements (blood urea nitrogen [BUN], creatinine) are often repeated periodically in the longitudinal care of patients with HF.2 Diagnostic tests for hemochromatosis, human immunodeficiency virus, rheumatologic disease, amyloidosis, and pheochromocytoma are reasonable in patients presenting with HF in whom there is a clinical suspicion of these diseases.2
For risk stratification, biomarkers that reflect renal insufficiency (particularly sodium, BUN, creatinine, and the estimated glomerular filtration rate [eGFR]) are powerful prognosticators.3 Newer renal markers of glomerular function (such as cystatin C)4,5 or of acute kidney injury (such as neutrophil gelatinase-associated lipocalin)6,7 have been proposed, although their clinical utility beyond prognostication remains to be determined. In fact, head- to-head comparisons have revealed that BUN appeared to be superior to most other renal biomarkers in stratifying short-term and long-term risk.8
Liver function, blood cell count, and thyroid function profiles are checked on some occasions to determine underlying end-organ dysfunction.2 Interestingly, several common laboratory values have consistently been associated with more advanced disease states or with a higher risk of future adverse events. These include serum uric acid (likely reflecting oxidative stress and nucleotide catabolism),9 anemia or red cell distribution width (likely reflecting iron deficiency or hematopoietic insufficiency),10 lymphocytopenia (likely reflecting immune dysfunction), and total bilirubin (likely reflection of hepatobiliary congestion).11
Some biomarkers have been incorporated into risk-stratification in patients with HF.2 However, drugs targeting these biomarkers have yet to be shown to improve clinical outcomes in prospective clinical trials. Several recent examples in chronic systolic HF include allopurinol for elevated uric acid levels12 and darbepoetin alfa for anemia (low hemoglobin).13 Thus, improving the biomarker level with specific treatment may not translate to improved clinical outcomes.
GUIDELINE RECOMMENDATIONS FOR CARDIAC BIOMARKERS IN HEART FAILURE
Clinical guidelines from several countries on the management of HF have expanded the role of biomarker testing in patients with HF.2,14–16 Table 1 shows the recommendations for biomarker testing in HF from the most recent joint guidelines of the American College of Cardiology and the American Heart Association. These recommendations will form the basis of the following discussion of clinically available biomarkers of HF that reflect distinct pathophysiologic processes and that have been cleared by the US Food and Drug Administration (Figure 1).
Biomarkers of myocardial stress: Natriuretic peptides
Natriuretic peptides are primary counterregulatory hormones produced in response to myocardial stress. Natriuretic peptide receptors stimulated by B-type (also “brain”) natriuretic peptide (BNP) lead to an increase in natriuresis, vasodilation, and opposing effects of other overactive neurohormonal systems. The contemporary understanding of how natriuretic peptides are being produced and metabolized is beyond the scope of this review, but generally it is now recognized that natriuretic peptide levels vary widely among patients with the same degree of symptoms or echocardiographic features.17
Of the several types of natriuretic peptide detectable by immunoassay, the two main types available for clinical use in the United States are BNP and amino acid N-terminal pro-BNP (NT-proBNP). Although there is no direct conversion available (NT-proBNP levels are five to eight times higher than BNP levels), their levels are often concordant and both are influenced by factors such as age, body mass index, and renal function. Specifically, natriuretic peptide levels in morbidly obese patients range 30% to 40% lower than levels in patients who are not morbidly obese.18
Studies over the past 10 years of natriuretic peptides in the diagnosis of HF have shown that levels are invariably elevated in underlying HF, while stable (and especially low) levels often track with clinical stability. In the latest clinical guidelines, natriuretic peptide testing has gained the highest level of recommendation for clinical use for any biomarker in HF, especially in the setting of clinical uncertainty (class 1 recommendation, level of evidence A).2,16 Two common clinical scenarios are represented in this indication. When patients present with signs and symptoms suspicious of HF (shortness of breath, fluid retention, peripheral edema, evidence of central congestion), natriuretic peptide testing provides confirmation of an underlying cardiac cause of these symptoms when elevated. Conversely, when there are alternative explanations or if the presentation is subtle and there is some degree of uncertainty, testing natriuretic peptide levels helps establish the diagnosis of HF when levels are higher than the cut-off values, and levels below the cut-off have a high negative predictive value (Table 2).19,20
Meanwhile, for patients with established HF, a deviation from “stable” natriuretic peptide levels (particularly an increase of more than 30%) may represent evolving destabilization that may warrant an intensification of therapy, whereas an unchanged or reduced level may be taken as objective evidence of clinical stability or favorable response to medical therapy. Table 3 outlines the latest Canadian guidelines that offer a practical approach as ongoing studies attempt to clarify the benefits of these strategies.15
The consistent association between elevated natriuretic peptide levels and worse prognosis21 has led to the promise that intensification of medical therapy in those with elevated natriuretic peptide levels can lead to better outcomes. Nevertheless, the rise in natriuretic peptide levels requires interpretation in the clinical context, as not all factors affecting the levels can be relieved by intensifying medical therapy (eg, age, renal insufficiency).
Several prospective, randomized controlled trials have tested this hypothesis, with favorable yet mixed results. Most studies have utilized a BNP measurement less than 100 pg/mL or an NT-proBNP measurement less than 1,000 pg/mL as a therapeutic target. In a recent prospective study that utilized the NT-proBNP threshold, only about half of patients were able to reach the target of less than 1,000 pg/mL.22 Often overlooked is the fact that in the same study, the inability to reach less than 5,000 pg/mL within 3 months after discharge clearly identified advanced, “nonresponsive” HF refractory to medical therapy and with a poor prognosis.23 This is an important point when assessing the clinical utility of biomarkers, as incremental prognostic values may not guarantee the feasibility or ultimate benefit of intensifying drug therapy according to specific biomarker targets. Until we have more insight into whether a care pathway guided by NT-proBNP measurements can lead to a consistent reduction in rates of hospitalization and mortality in HF, it is reasonable to target those with elevated natriuretic peptide levels by reevaluating their treatment regimen to achieve optimal dosing of guideline-directed medical therapy (Class 2a recommendation, level of evidence B).2 Also, the usefulness of BNP and NT-proBNP in guiding therapy for acutely decompensated HF is not well established (Class 2b recommendation, level of evidence C).2
Biomarkers of myocardial injury: Cardiac troponin
Whereas detecting circulating cardiac troponin is helpful in the diagnosis of acute coronary syndrome, the role of cardiac troponin levels in HF is primarily for risk stratification (Class 1 recommendation, level of evidence A in both acute and chronic HF).2 In patients hospitalized with acute decompensated HF, those with elevated troponin I or troponin T at the time of admission had lower systolic blood pressures, lower ejection fractions, and higher rate of in-hospital mortality.24,25 In chronic HF, elevations in both standard and high-sensitivity cardiac troponin levels were associated with increases in all-cause mortality,26 and rise in serial measurements appeared to correlate with an increased risk of future cardiovascular events.27 And with regard to cardiotoxicity, an increase in cardiac troponin over time (either after chemotherapy or with amyloidosis) is indicative of progressive cardiac dysfunction.28,29
Nevertheless, how to adjust medical therapy according to a rise in cardiac troponin levels remains unclear, as levels of cardiac troponin beyond the setting of acute coronary syndrome have appeared not to fluctuate significantly over time and do not seem to be related to underlying coronary events. Newer-generation cardiac troponin assays have yet to provide incremental value compared with standard clinical troponin assays despite their higher sensitivities.26
One common and underappreciated clinical application that combines both diagnostic and prognostic properties of both natriuretic peptide and cardiac troponin testing is the concept of HF staging. This is particularly relevant when there is a progressive change in clinical status (eg, need for hospitalization, change in signs or symptoms) or when a new therapy is started that may promote adverse effects. For example, a patient with pre-existing HF hospitalized with atypical symptoms and deemed not to have HF could be found to have subclinical myocardial necrosis as detected by low concentration of cardiac troponin or higher-than-baseline natriuretic peptide levels in the absence of hypervolemia. Careful assessment of the potential triggers of fluctuations from previous stable levels of cardiac biomarkers is also warranted (eg, atrial fibrillation, dietary indiscretion, infection, and ischemia). Indeed, these may represent objective rather than subjective changes in clinical manifestation of HF, which may warrant a reassessment of disease severity (eg, objective testing for functional capacity or hemodynamics, or even referral for consideration of advanced HF therapeutic options).
Biomarkers of inflammation and fibrosis: Soluble ST2 and galectin-3
Inflammation has long been associated with HF, and clinically available markers of inflammation such as high-sensitivity C-reactive protein (CRP)30,31 and myeloperoxidase32 have consistently tracked with prognosis. The search for a stable biomarker of inflammation has been challenging because inflammation is a dynamic process and because of the lack of treatment options for heightened inflammation.
A promising new protein biomarker, ST2 (suppression of tumorigenicity-2), has been identified in a soluble form (sST2) that binds to interleukin 33 (IL-33) to antagonize the maladaptive response of the myocardium to overload states.33 The levels of sST2 inversely correlate with the ejection fraction and have a positive association with increasing New York Heart Association class, worsening symptoms, and indicators of HF severity, such as norepinephrine levels, diastolic filling pressures, CRP, and natriuretic peptide levels.34 Unlike natriuretic peptides, levels of sST2 are not significantly affected by age, sex, body mass index, and valve disease,34 although recent observations have challenged its cardiac associations.35 In patients with chronic HF, elevated levels of sST2 (especially >35 ng/mL) have been associated with poorer clinical outcomes36 and increased risk of sudden cardiac death in HF.37 In addition, persistently elevated sST2 levels consistently confer poor long-term prognosis. Several studies have also demonstrated the prognostic value of elevated sST2 in predicting long-term risk of death in acute HF, either at baseline38,39 or on serial testing.40
Another new biomarker, galectin-3, has been implicated in fibrosis and in structural and pathophysiologic changes seen in HF.41 Studies have shown that higher levels of galectin-3 in patients with acute HF and chronic HF were associated with more severe cardiac fibrosis and with an increase in left ventricular remodeling.42–44 Serial measurements also confer prognostic information.45 However, many of these studies did not fully account for renal dysfunction as a major confounder, and the relationship between circulating galectin-3 and estimated GFR is strong.46,47 Meanwhile, head-to-head comparisons among galectin-3 and other clinically available biomarkers also revealed that the prognostic value of galectin-3 can be attenuated in the presence of sST2 and NT-proBNP.48,49 Furthermore, careful evaluation of diastolic parameters only showed a modest relationship with galectin-3 levels, especially in those with HF with preserved ejection fraction.50,51
In animal infarction models, disruption of the galectin-3 and IL-33/ST2 pathway with pharmacologic therapy such as mineralocorticoid receptor antagonists may attenuate cardiac remodeling.52,53 It is conceivable that these biomarkers may have mechanistic links with therapeutic benefits. However, the practical uses of galectin-3 and sST2 are still debated (Class 2b recommendation by the latest guidelines2) despite strong statistical associations between biomarker levels and adverse outcomes. The majority of biomarker substudies from clinical trials have suggested that improvements following drug or device therapy were largely confined to patients with lower rather than higher biomarker levels.54,55 Furthermore, validation studies have challenged the incremental prognostic value of these markers when natriuretic peptide levels are available.54,56–58 Thus, more clinical experience and research are warranted, and current clinical applications may be restricted to patient subsets.
BIOMARKERS IN EARLY STAGES OF HEART FAILURE
The potential benefit of biomarker testing may reside in the earlier end of the HF spectrum, especially in patients at risk of but not yet diagnosed with HF (so-called stage A). In the HealthABC study, the future risk of HF in elderly patients can be predicted with a combination of clinical risk factors (age, sex, left ventricular hypertrophy, systolic blood pressure, heart rate, smoking), as well as biochemical risk factors such as albumin, creatinine, and glucose.59 Patients with elevated natriuretic peptide levels are more likely to have underlying cardiac abnormalities and to have poorer long-term outcomes.60 In a recent prospective, randomized controlled trial, participants with a BNP-guided transition to HF therapies (when BNP >50 pg/mL) had a lower incidence of HF than participants without knowledge of BNP levels.61 Elevated levels of clinically available biomarkers of inflammation, such as myeloperoxidase,29,62 ceruloplasmin,63 and CRP,64 have also been associated with an increased risk of future HF. These findings support the notion that biomarkers, especially when combined with clinical risk factors, can serve as indicators of HF vulnerability. If independently confirmed, this will be an important therapeutic approach to the prevention of HF.
PRACTICAL CONSIDERATIONS
An important perspective often overlooked concerns the variability of a biomarker level as it is utilized in clinical practice (Table 4). In general, point-of-care assays are often more variable than the same tests done in clinical laboratories. Sample collection, handling, and processing also introduce a degree of variability. The biologic variability of specific measurements can significantly affect the precision of the measurement. In the case of HF, the biologic variability (as measured in stable patients over time) of natriuretic peptides and galectin-3 are significantly higher than those observed in cardiac troponins or sST2 (> 130% vs approximately 30%).65 Nevertheless because of their relative cardiac specificity, natriuretic peptides have maintained their clinical utility.
- Morrow DA, de Lemos JA. Benchmarks for the assessment of novel cardiovascular biomarkers. Circulation 2007; 115:949–952.
- Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 2013; 128:e240–327.
- Halkar M, Tang WH. Incorporating common biomarkers into the clinical management of heart failure. Curr Heart Fail Rep 2013; 10:450–457.
- Dupont M, Wu Y, Hazen SL, Tang WH. Cystatin C identifies patients with stable chronic heart failure at increased risk for adverse cardiovascular events. Circ Heart Fail 2012; 5:602–609.
- Tang WH, Van Lente F, Shrestha K, et al. Impact of myocardial function on cystatin C measurements in chronic systolic heart failure. J Card Fail 2008; 14:394– 399.
- Dupont M, Shrestha K, Singh D, et al. Lack of significant renal tubular injury despite acute kidney injury in acute decompensated heart failure. Eur J Heart Fail 2012; 14:597–604.
- Verbrugge FH, Dupont M, Shao Z, et al. Novel urinary biomarkers in detecting acute kidney injury, persistent renal impairment, and all-cause mortality following decongestive therapy in acute decompensated heart failure. J Card Fail 2013; 19:621–628.
- Tang WH, Dupont M, Hernandez AF, et al. Comparative assessment of short-term adverse events in acute heart failure with cystatin C and other estimates of renal function: results from the ASCEND-HF trial. JACC Heart Fail 2015; 3:40–49.
- Vaduganathan M, Greene SJ, Ambrosy AP, et al. Relation of serum uric acid levels and outcomes among patients hospitalized for worsening heart failure with reduced ejection fraction (from the efficacy of vasopressin antagonism in heart failure outcome study with tolvaptan trial). Am J Cardiol 2014; 114:1713–1721.
- Felker GM, Allen LA, Pocock SJ, et al. Red cell distribution width as a novel prognostic marker in heart failure: data from the CHARM Program and the Duke Databank. J Am Coll Cardiol 2007; 50:40–47.
- Wu AH, Levy WC, Welch KB, et al. Association between bilirubin and mode of death in severe systolic heart failure. Am J Cardiol 2013; 111:1192–1197.
- Givertz MM, Anstrom KJ, Redfield MM, et al. Effects of xanthine oxidase inhibition in hyperuricemic heart failure patients: the Xanthine Oxidase Inhibition for Hyperuricemic Heart Failure Patients (EXACT-HF) study. Circulation 2015; 131:1763–1771.
- Swedberg K, Young JB, Anand IS, et al. Treatment of anemia with darbepoetin alfa in systolic heart failure. N Engl J Med 2013; 368:1210–1219.
- McMurray JJ, Adamopoulos S, Anker SD, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 2012; 33:1787–1847.
- Moe GW, Ezekowitz JA, O’Meara E, et al. The 2014 Canadian Cardiovascular Society Heart Failure Management Guidelines Focus Update: anemia, biomarkers, and recent therapeutic trial implications. Can J Cardiol 2015; 31:3–16.
- Tang WH, Francis GS, Morrow DA, et al. National Academy of Clinical Biochemistry Laboratory Medicine practice guidelines: clinical utilization of cardiac biomarker testing in heart failure. Circulation 2007; 116:e99–109.
- Maisel AS, Daniels LB. Breathing not properly 10 years later: what we have learned and what we still need to learn. J Am Coll Cardiol 2012; 60:277–282.
- Mehra MR, Uber PA, Park MH, et al. Obesity and suppressed B-type natriuretic peptide levels in heart failure. J Am Coll Cardiol 2004; 43:1590–1595.
- Januzzi JL, Jr, Camargo CA, Anwaruddin S, et al. The N-terminal Pro-BNP Investigation of Dyspnea in the Emergency Department (PRIDE) study. Am J Cardiol 2005; 95:948–954.
- Maisel AS, Krishnaswamy P, Nowak RM, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 2002; 347:161–167.
- Fonarow GC, Peacock WF, Phillips CO, Givertz MM, Lopatin M. Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. J Am Coll Cardiol 2007; 49:1943–1950.
- Januzzi JL, Jr, Rehman SU, Mohammed AA, et al. Use of amino-terminal pro-B- type natriuretic peptide to guide outpatient therapy of patients with chronic left ventricular systolic dysfunction. J Am Coll Cardiol 2011; 58:1881–1889.
- Gaggin HK, Truong QA, Rehman SU, et al. Characterization and prediction of natriuretic peptide ‘nonresponse’ during heart failure management: results from the ProBNP Outpatient Tailored Chronic Heart Failure (PROTECT) and the NT-proBNP-Assisted Treatment to Lessen Serial Cardiac Readmissions and Death (BATTLESCARRED) study. Congest Heart Fail 2013; 19:135–142.
- Peacock WF 4th, De Marco T, Fonarow GC, et al. Cardiac troponin and outcome in acute heart failure. N Engl J Med 2008; 358:2117–2126.
- Felker GM, Hasselblad V, Tang WH, et al. Troponin I in acute decompen- sated heart failure: insights from the ASCEND-HF study. Eur J Heart Fail 2012; 14:1257–1264.
- Grodin JL, Neale S, Wu Y, Hazen SL, Tang WH. Prognostic comparison of different sensitivity cardiac troponin assays in stable heart failure. Am J Med 2015; 128:276–282.
- Masson S, Anand I, Favero C, et al. Serial measurement of cardiac troponin T using a highly sensitive assay in patients with chronic heart failure: data from 2 large randomized clinical trials. Circulation 2012; 125:280–288.
- Cardinale D, Sandri MT, Colombo A, et al. Prognostic value of troponin I in cardiac risk stratification of cancer patients undergoing high-dose chemotherapy. Circulation 2004; 109:2749–2754.
- Ky B, Putt M, Sawaya H, et al. Early increases in multiple biomarkers predict subsequent cardiotoxicity in breast cancer patients treated with doxorubicin, taxanes, and trastuzumab. J Am Coll Cardiol 2014; 63:809–816.
- Kalogeropoulos AP, Tang WH, Hsu A, et al. High-sensitivity C-reactive protein in acute heart failure: insights from the ASCEND-HF trial. J Card Fail 2014; 20:319–326.
- Tang WH, Shrestha K, Van Lente F, et al. Usefulness of C-reactive protein and left ventricular diastolic performance for prognosis in patients with left ventricular systolic heart failure. Am J Cardiol 2008; 101:370–373.
- Tang WH, Wu Y, Nicholls SJ, Hazen SL. Plasma myeloperoxidase predicts incident cardiovascular risks in stable patients undergoing medical management for coronary artery disease. Clin Chem 2011; 57:33–39.
- Sanada S, Hakuno D, Higgins LJ, Schreiter ER, McKenzie AN, Lee RT. IL-33 and ST2 comprise a critical biomechanically induced and cardioprotective signaling system. J Clin Invest 2007; 117:1538–1549.
- Rehman SU, Mueller T, Januzzi JL, Jr. Characteristics of the novel interleukin family biomarker ST2 in patients with acute heart failure. J Am Coll Cardiol 2008; 52:1458–1465.
- Kaye DM, Mariani JA, van Empel V, Maeder MT. Determinants and implications of elevated soluble ST2 levels in heart failure. Int J Cardiol 2014; 176:1242–1243.
- Ky B, French B, McCloskey K, et al. High-sensitivity ST2 for prediction of adverse outcomes in chronic heart failure. Circ Heart Fail 2011; 4:180–187.
- Ahmad T, Fiuzat M, Neely B, et al. Biomarkers of myocardial stress and fibrosis as predictors of mode of death in patients with chronic heart failure. JACC Heart Fail 2014; 2:260–268.
- Pascual-Figal DA, Manzano-Fernandez S, Boronat M, et al. Soluble ST2, high-sensitivity troponin T- and N-terminal pro-B-type natriuretic peptide: complementary role for risk stratification in acutely decompensated heart failure. Eur J Heart Fail 2011; 13:718–725.
- Januzzi JL, Jr, Peacock WF, Maisel AS, et al. Measurement of the interleukin family member ST2 in patients with acute dyspnea: results from the PRIDE (Pro-Brain Natriuretic Peptide Investigation of Dyspnea in the Emergency Department) study. J Am Coll Cardiol 2007; 50:607-613.
- Boisot S, Beede J, Isakson S, et al. Serial sampling of ST2 predicts 90-day mortality following destabilized heart failure. J Card Fail 2008; 14:732–738.
- Sharma UC, Pokharel S, van Brakel TJ, et al. Galectin-3 marks activated macrophages in failure-prone hypertrophied hearts and contributes to cardiac dysfunction. Circulation 2004; 110:3121–3128.
- van Kimmenade RR, Januzzi JL, Jr., Ellinor PT, et al. Utility of amino-terminal pro-brain natriuretic peptide, galectin-3, and apelin for the evaluation of patients with acute heart failure. J Am Coll Cardiol 2006; 48:1217–1224.
- Lok DJ, Van Der Meer P, de la Porte PW, et al. Prognostic value of galectin-3, a novel marker of fibrosis, in patients with chronic heart failure: data from the DEAL-HF study. Clin Res Cardiol 2010; 99:323–328.
- Shah RV, Chen-Tournoux AA, Picard MH, van Kimmenade RR, Januzzi JL. Ga- lectin-3, cardiac structure and function, and long-term mortality in patients with acutely decompensated heart failure. Eur J Heart Fail 2010; 12:826–832.
- van der Velde AR, Gullestad L, Ueland T, et al. Prognostic value of changes in galectin-3 levels over time in patients with heart failure: data from CORONA and COACH. Circ Heart Fail 2013; 6:219–226.
- Tang WH, Shrestha K, Shao Z, et al. Usefulness of plasma galectin-3 levels in systolic heart failure to predict renal insufficiency and survival. Am J Cardiol 2011; 108:385–390.
- Gopal DM, Kommineni M, Ayalon N, et al. Relationship of plasma galectin-3 to renal function in patients with heart failure: effects of clinical status, pathophysiology of heart failure, and presence or absence of heart failure. J Am Heart Assoc 2012; 1:e000760.
- Bayes-Genis A, de Antonio M, Vila J, et al. Head-to-head comparison of 2 myocardial fibrosis biomarkers for long-term heart failure risk stratification: ST2 versus galectin-3. J Am Coll Cardiol 2014; 63:158–166.
- Felker GM, Fiuzat M, Shaw LK, et al. Galectin-3 in ambulatory patients with heart failure: results from the HF-ACTION study. Circ Heart Fail 2012; 5:72–78.
- Edelmann F, Holzendorf V, Wachter R, et al. Galectin-3 in patients with heart failure with preserved ejection fraction: results from the Aldo-DHF trial. Eur J Heart Fail 2015; 17:214–223.
- AbouEzzeddine OF, Haines P, Stevens S, et al. Galectin-3 in heart failure with preserved ejection fraction. A RELAX trial substudy (Phosphodiesterase-5 Inhibition to Improve Clinical Status and Exercise Capacity in Diastolic Heart Failure). JACC Heart failure 2015; 3:245–252.
- Lax A, Sanchez-Mas J, Asensio-Lopez MC, et al. Mineralocorticoid receptor antagonists modulate galectin-3 and interleukin-33/ST2 signaling in left ventricular systolic dysfunction after acute myocardial infarction. JACC Heart failure 2015; 3:50–58.
- Calvier L, Martinez-Martinez E, Miana M, et al. The impact of galectin-3 inhibition on aldosterone-induced cardiac and renal injuries. JACC Heart failure 2015; 3:59–67.
- Anand IS, Rector TS, Kuskowski M, Adourian A, Muntendam P, Cohn JN. Baseline and serial measurements of galectin-3 in patients with heart failure: relationship to prognosis and effect of treatment with valsartan in the Val-HeFT. Eur J Heart Fail 2013; 15:511–518.
- Gullestad L, Ueland T, Kjekshus J, et al. Galectin-3 predicts response to statin therapy in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CO- RONA). Eur Heart J 2012; 33:2290–2296.
- Felker GM, Fiuzat M, Thompson V, et al. Soluble ST2 in ambulatory patients with heart failure: association with functional capacity and long-term outcomes. Circ Heart Fail 2013; 6:1172–1179.
- Anand IS, Rector TS, Kuskowski M, Snider J, Cohn JN. Prognostic value of soluble ST2 in the Valsartan Heart Failure Trial. Circ Heart Fail 2014; 7:418–426.
- Gullestad L, Ueland T, Kjekshus J, et al. The predictive value of galectin-3 for mortality and cardiovascular events in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CORONA). Am Heart J 2012; 164:878–883.
- Butler J, Kalogeropoulos A, Georgiopoulou V, et al. Incident heart failure prediction in the elderly: the health ABC heart failure score. Circ Heart Fail 2008; 1:125–133.
- McKie PM, Rodeheffer RJ, Cataliotti A, et al. Amino-terminal pro-B-type natriuretic peptide and B-type natriuretic peptide: biomarkers for mortality in a large community-based cohort free of heart failure. Hypertension 2006; 47:874–880.
- Ledwidge M, Gallagher J, Conlon C, et al. Natriuretic peptide-based screening and collaborative care for heart failure: the STOP-HF randomized trial. JAMA 2013; 310:66–74.
- Tang WH, Katz R, Brennan ML, et al. Usefulness of myeloperoxidase levels in healthy elderly subjects to predict risk of developing heart failure. Am J Cardiol 2009; 103:1269–1274.
- Dadu RT, Dodge R, Nambi V, et al. Ceruloplasmin and heart failure in the Atherosclerosis Risk in Communities study. Circ Heart Fail 2013; 6:936–943.
- Kalogeropoulos A, Georgiopoulou V, Psaty BM, et al. Inflammatory markers and incident heart failure risk in older adults: the Health ABC (Health, Aging, and Body Composition) study. J Am Coll Cardiol 2010; 55:2129–2137.
- Wu AH, Wians F, Jaffe A. Biological variation of galectin-3 and soluble ST2 for chronic heart failure: implication on interpretation of test results. Am Heart J 2013; 165:995–999.
The growth in recognition and clinical adoption of blood and urine biomarkers over the last 20 years has been a major advance in the diagnosis and prognosis of heart failure (HF). While there have been numerous research studies and prospective clinical trials on this topic, healthcare providers often face limited availability of biomarker testing and a relative paucity of data to guide individual patient management. This is especially true since many guideline-directed medical therapies have long-established clinical indications and target populations, predating the clinical availability of biomarkers testing. This article addresses the salient insights gained from broad clinical use of biomarkers, as well as from clinical studies that helped define their appropriate use and lay the foundations of the major changes presented in the recently published clinical guidelines for the management of HF.
WHAT MAKES A BIOMARKER CLINICALLY USEFUL?
To appreciate the appropriate use of any clinical tool, clinicians need to first understand its indications and limitations and how they are defined. There are four major criteria regarding the clinical utility of a biomarker.
First, we have to establish what we are measuring, particularly with accurate and reproducible methods, with rapid turnaround, and at a reasonable cost. Second, we have to determine why we need the biomarker: ie, we need to determine if its measurement provides valuable new information to the clinician, if there is a strong and consistent association between the marker and the disease or outcome, and if this has been validated in a way that is generalizable. Third, we have to determine when measuring the biomarker would help clinical management, whether it is superior to existing tests, and whether there is evidence that it improves outcomes. Last, and perhaps most commonly overlooked, is practicality: ie, how can measuring the biomarkers be incorporated into the clinical workflow?
Not all biomarkers need to fulfill all these criteria in order to be useful, and the usefulness of a biomarker may differ from one patient population to another, from one clinician to another, or from one clinical scenario to another.1 Many clinical biomarkers are applied based on their ability to indicate a specific diagnosis or treatment (eg, glycated hemoglobin), and some have been used to determine the limits of therapy (eg, creatinine or liver function tests to detect end-organ damage). Nevertheless, the overarching goal is to establish the clinical role of a biomarker to provide the opportunity to gain additional insight into a disease state beyond that provided by a standard clinical assessment, and to determine if using the biomarker favorably alters the clinical course.
WHICH BIOMARKERS DO WE ALREADY ROUTINELY MEASURE?
Traditionally, the management of HF requires meticulous monitoring for adverse effects of drug therapy (eg, electrolyte and renal abnormalities with diuretics or drugs targeting the renin-angiotensin-aldosterone system). Although no specific clinical studies have been conducted to support their routine use, electrolytes (sodium, potassium, chloride, bicarbonate) and renal function measurements (blood urea nitrogen [BUN], creatinine) are often repeated periodically in the longitudinal care of patients with HF.2 Diagnostic tests for hemochromatosis, human immunodeficiency virus, rheumatologic disease, amyloidosis, and pheochromocytoma are reasonable in patients presenting with HF in whom there is a clinical suspicion of these diseases.2
For risk stratification, biomarkers that reflect renal insufficiency (particularly sodium, BUN, creatinine, and the estimated glomerular filtration rate [eGFR]) are powerful prognosticators.3 Newer renal markers of glomerular function (such as cystatin C)4,5 or of acute kidney injury (such as neutrophil gelatinase-associated lipocalin)6,7 have been proposed, although their clinical utility beyond prognostication remains to be determined. In fact, head- to-head comparisons have revealed that BUN appeared to be superior to most other renal biomarkers in stratifying short-term and long-term risk.8
Liver function, blood cell count, and thyroid function profiles are checked on some occasions to determine underlying end-organ dysfunction.2 Interestingly, several common laboratory values have consistently been associated with more advanced disease states or with a higher risk of future adverse events. These include serum uric acid (likely reflecting oxidative stress and nucleotide catabolism),9 anemia or red cell distribution width (likely reflecting iron deficiency or hematopoietic insufficiency),10 lymphocytopenia (likely reflecting immune dysfunction), and total bilirubin (likely reflection of hepatobiliary congestion).11
Some biomarkers have been incorporated into risk-stratification in patients with HF.2 However, drugs targeting these biomarkers have yet to be shown to improve clinical outcomes in prospective clinical trials. Several recent examples in chronic systolic HF include allopurinol for elevated uric acid levels12 and darbepoetin alfa for anemia (low hemoglobin).13 Thus, improving the biomarker level with specific treatment may not translate to improved clinical outcomes.
GUIDELINE RECOMMENDATIONS FOR CARDIAC BIOMARKERS IN HEART FAILURE
Clinical guidelines from several countries on the management of HF have expanded the role of biomarker testing in patients with HF.2,14–16 Table 1 shows the recommendations for biomarker testing in HF from the most recent joint guidelines of the American College of Cardiology and the American Heart Association. These recommendations will form the basis of the following discussion of clinically available biomarkers of HF that reflect distinct pathophysiologic processes and that have been cleared by the US Food and Drug Administration (Figure 1).
Biomarkers of myocardial stress: Natriuretic peptides
Natriuretic peptides are primary counterregulatory hormones produced in response to myocardial stress. Natriuretic peptide receptors stimulated by B-type (also “brain”) natriuretic peptide (BNP) lead to an increase in natriuresis, vasodilation, and opposing effects of other overactive neurohormonal systems. The contemporary understanding of how natriuretic peptides are being produced and metabolized is beyond the scope of this review, but generally it is now recognized that natriuretic peptide levels vary widely among patients with the same degree of symptoms or echocardiographic features.17
Of the several types of natriuretic peptide detectable by immunoassay, the two main types available for clinical use in the United States are BNP and amino acid N-terminal pro-BNP (NT-proBNP). Although there is no direct conversion available (NT-proBNP levels are five to eight times higher than BNP levels), their levels are often concordant and both are influenced by factors such as age, body mass index, and renal function. Specifically, natriuretic peptide levels in morbidly obese patients range 30% to 40% lower than levels in patients who are not morbidly obese.18
Studies over the past 10 years of natriuretic peptides in the diagnosis of HF have shown that levels are invariably elevated in underlying HF, while stable (and especially low) levels often track with clinical stability. In the latest clinical guidelines, natriuretic peptide testing has gained the highest level of recommendation for clinical use for any biomarker in HF, especially in the setting of clinical uncertainty (class 1 recommendation, level of evidence A).2,16 Two common clinical scenarios are represented in this indication. When patients present with signs and symptoms suspicious of HF (shortness of breath, fluid retention, peripheral edema, evidence of central congestion), natriuretic peptide testing provides confirmation of an underlying cardiac cause of these symptoms when elevated. Conversely, when there are alternative explanations or if the presentation is subtle and there is some degree of uncertainty, testing natriuretic peptide levels helps establish the diagnosis of HF when levels are higher than the cut-off values, and levels below the cut-off have a high negative predictive value (Table 2).19,20
Meanwhile, for patients with established HF, a deviation from “stable” natriuretic peptide levels (particularly an increase of more than 30%) may represent evolving destabilization that may warrant an intensification of therapy, whereas an unchanged or reduced level may be taken as objective evidence of clinical stability or favorable response to medical therapy. Table 3 outlines the latest Canadian guidelines that offer a practical approach as ongoing studies attempt to clarify the benefits of these strategies.15
The consistent association between elevated natriuretic peptide levels and worse prognosis21 has led to the promise that intensification of medical therapy in those with elevated natriuretic peptide levels can lead to better outcomes. Nevertheless, the rise in natriuretic peptide levels requires interpretation in the clinical context, as not all factors affecting the levels can be relieved by intensifying medical therapy (eg, age, renal insufficiency).
Several prospective, randomized controlled trials have tested this hypothesis, with favorable yet mixed results. Most studies have utilized a BNP measurement less than 100 pg/mL or an NT-proBNP measurement less than 1,000 pg/mL as a therapeutic target. In a recent prospective study that utilized the NT-proBNP threshold, only about half of patients were able to reach the target of less than 1,000 pg/mL.22 Often overlooked is the fact that in the same study, the inability to reach less than 5,000 pg/mL within 3 months after discharge clearly identified advanced, “nonresponsive” HF refractory to medical therapy and with a poor prognosis.23 This is an important point when assessing the clinical utility of biomarkers, as incremental prognostic values may not guarantee the feasibility or ultimate benefit of intensifying drug therapy according to specific biomarker targets. Until we have more insight into whether a care pathway guided by NT-proBNP measurements can lead to a consistent reduction in rates of hospitalization and mortality in HF, it is reasonable to target those with elevated natriuretic peptide levels by reevaluating their treatment regimen to achieve optimal dosing of guideline-directed medical therapy (Class 2a recommendation, level of evidence B).2 Also, the usefulness of BNP and NT-proBNP in guiding therapy for acutely decompensated HF is not well established (Class 2b recommendation, level of evidence C).2
Biomarkers of myocardial injury: Cardiac troponin
Whereas detecting circulating cardiac troponin is helpful in the diagnosis of acute coronary syndrome, the role of cardiac troponin levels in HF is primarily for risk stratification (Class 1 recommendation, level of evidence A in both acute and chronic HF).2 In patients hospitalized with acute decompensated HF, those with elevated troponin I or troponin T at the time of admission had lower systolic blood pressures, lower ejection fractions, and higher rate of in-hospital mortality.24,25 In chronic HF, elevations in both standard and high-sensitivity cardiac troponin levels were associated with increases in all-cause mortality,26 and rise in serial measurements appeared to correlate with an increased risk of future cardiovascular events.27 And with regard to cardiotoxicity, an increase in cardiac troponin over time (either after chemotherapy or with amyloidosis) is indicative of progressive cardiac dysfunction.28,29
Nevertheless, how to adjust medical therapy according to a rise in cardiac troponin levels remains unclear, as levels of cardiac troponin beyond the setting of acute coronary syndrome have appeared not to fluctuate significantly over time and do not seem to be related to underlying coronary events. Newer-generation cardiac troponin assays have yet to provide incremental value compared with standard clinical troponin assays despite their higher sensitivities.26
One common and underappreciated clinical application that combines both diagnostic and prognostic properties of both natriuretic peptide and cardiac troponin testing is the concept of HF staging. This is particularly relevant when there is a progressive change in clinical status (eg, need for hospitalization, change in signs or symptoms) or when a new therapy is started that may promote adverse effects. For example, a patient with pre-existing HF hospitalized with atypical symptoms and deemed not to have HF could be found to have subclinical myocardial necrosis as detected by low concentration of cardiac troponin or higher-than-baseline natriuretic peptide levels in the absence of hypervolemia. Careful assessment of the potential triggers of fluctuations from previous stable levels of cardiac biomarkers is also warranted (eg, atrial fibrillation, dietary indiscretion, infection, and ischemia). Indeed, these may represent objective rather than subjective changes in clinical manifestation of HF, which may warrant a reassessment of disease severity (eg, objective testing for functional capacity or hemodynamics, or even referral for consideration of advanced HF therapeutic options).
Biomarkers of inflammation and fibrosis: Soluble ST2 and galectin-3
Inflammation has long been associated with HF, and clinically available markers of inflammation such as high-sensitivity C-reactive protein (CRP)30,31 and myeloperoxidase32 have consistently tracked with prognosis. The search for a stable biomarker of inflammation has been challenging because inflammation is a dynamic process and because of the lack of treatment options for heightened inflammation.
A promising new protein biomarker, ST2 (suppression of tumorigenicity-2), has been identified in a soluble form (sST2) that binds to interleukin 33 (IL-33) to antagonize the maladaptive response of the myocardium to overload states.33 The levels of sST2 inversely correlate with the ejection fraction and have a positive association with increasing New York Heart Association class, worsening symptoms, and indicators of HF severity, such as norepinephrine levels, diastolic filling pressures, CRP, and natriuretic peptide levels.34 Unlike natriuretic peptides, levels of sST2 are not significantly affected by age, sex, body mass index, and valve disease,34 although recent observations have challenged its cardiac associations.35 In patients with chronic HF, elevated levels of sST2 (especially >35 ng/mL) have been associated with poorer clinical outcomes36 and increased risk of sudden cardiac death in HF.37 In addition, persistently elevated sST2 levels consistently confer poor long-term prognosis. Several studies have also demonstrated the prognostic value of elevated sST2 in predicting long-term risk of death in acute HF, either at baseline38,39 or on serial testing.40
Another new biomarker, galectin-3, has been implicated in fibrosis and in structural and pathophysiologic changes seen in HF.41 Studies have shown that higher levels of galectin-3 in patients with acute HF and chronic HF were associated with more severe cardiac fibrosis and with an increase in left ventricular remodeling.42–44 Serial measurements also confer prognostic information.45 However, many of these studies did not fully account for renal dysfunction as a major confounder, and the relationship between circulating galectin-3 and estimated GFR is strong.46,47 Meanwhile, head-to-head comparisons among galectin-3 and other clinically available biomarkers also revealed that the prognostic value of galectin-3 can be attenuated in the presence of sST2 and NT-proBNP.48,49 Furthermore, careful evaluation of diastolic parameters only showed a modest relationship with galectin-3 levels, especially in those with HF with preserved ejection fraction.50,51
In animal infarction models, disruption of the galectin-3 and IL-33/ST2 pathway with pharmacologic therapy such as mineralocorticoid receptor antagonists may attenuate cardiac remodeling.52,53 It is conceivable that these biomarkers may have mechanistic links with therapeutic benefits. However, the practical uses of galectin-3 and sST2 are still debated (Class 2b recommendation by the latest guidelines2) despite strong statistical associations between biomarker levels and adverse outcomes. The majority of biomarker substudies from clinical trials have suggested that improvements following drug or device therapy were largely confined to patients with lower rather than higher biomarker levels.54,55 Furthermore, validation studies have challenged the incremental prognostic value of these markers when natriuretic peptide levels are available.54,56–58 Thus, more clinical experience and research are warranted, and current clinical applications may be restricted to patient subsets.
BIOMARKERS IN EARLY STAGES OF HEART FAILURE
The potential benefit of biomarker testing may reside in the earlier end of the HF spectrum, especially in patients at risk of but not yet diagnosed with HF (so-called stage A). In the HealthABC study, the future risk of HF in elderly patients can be predicted with a combination of clinical risk factors (age, sex, left ventricular hypertrophy, systolic blood pressure, heart rate, smoking), as well as biochemical risk factors such as albumin, creatinine, and glucose.59 Patients with elevated natriuretic peptide levels are more likely to have underlying cardiac abnormalities and to have poorer long-term outcomes.60 In a recent prospective, randomized controlled trial, participants with a BNP-guided transition to HF therapies (when BNP >50 pg/mL) had a lower incidence of HF than participants without knowledge of BNP levels.61 Elevated levels of clinically available biomarkers of inflammation, such as myeloperoxidase,29,62 ceruloplasmin,63 and CRP,64 have also been associated with an increased risk of future HF. These findings support the notion that biomarkers, especially when combined with clinical risk factors, can serve as indicators of HF vulnerability. If independently confirmed, this will be an important therapeutic approach to the prevention of HF.
PRACTICAL CONSIDERATIONS
An important perspective often overlooked concerns the variability of a biomarker level as it is utilized in clinical practice (Table 4). In general, point-of-care assays are often more variable than the same tests done in clinical laboratories. Sample collection, handling, and processing also introduce a degree of variability. The biologic variability of specific measurements can significantly affect the precision of the measurement. In the case of HF, the biologic variability (as measured in stable patients over time) of natriuretic peptides and galectin-3 are significantly higher than those observed in cardiac troponins or sST2 (> 130% vs approximately 30%).65 Nevertheless because of their relative cardiac specificity, natriuretic peptides have maintained their clinical utility.
The growth in recognition and clinical adoption of blood and urine biomarkers over the last 20 years has been a major advance in the diagnosis and prognosis of heart failure (HF). While there have been numerous research studies and prospective clinical trials on this topic, healthcare providers often face limited availability of biomarker testing and a relative paucity of data to guide individual patient management. This is especially true since many guideline-directed medical therapies have long-established clinical indications and target populations, predating the clinical availability of biomarkers testing. This article addresses the salient insights gained from broad clinical use of biomarkers, as well as from clinical studies that helped define their appropriate use and lay the foundations of the major changes presented in the recently published clinical guidelines for the management of HF.
WHAT MAKES A BIOMARKER CLINICALLY USEFUL?
To appreciate the appropriate use of any clinical tool, clinicians need to first understand its indications and limitations and how they are defined. There are four major criteria regarding the clinical utility of a biomarker.
First, we have to establish what we are measuring, particularly with accurate and reproducible methods, with rapid turnaround, and at a reasonable cost. Second, we have to determine why we need the biomarker: ie, we need to determine if its measurement provides valuable new information to the clinician, if there is a strong and consistent association between the marker and the disease or outcome, and if this has been validated in a way that is generalizable. Third, we have to determine when measuring the biomarker would help clinical management, whether it is superior to existing tests, and whether there is evidence that it improves outcomes. Last, and perhaps most commonly overlooked, is practicality: ie, how can measuring the biomarkers be incorporated into the clinical workflow?
Not all biomarkers need to fulfill all these criteria in order to be useful, and the usefulness of a biomarker may differ from one patient population to another, from one clinician to another, or from one clinical scenario to another.1 Many clinical biomarkers are applied based on their ability to indicate a specific diagnosis or treatment (eg, glycated hemoglobin), and some have been used to determine the limits of therapy (eg, creatinine or liver function tests to detect end-organ damage). Nevertheless, the overarching goal is to establish the clinical role of a biomarker to provide the opportunity to gain additional insight into a disease state beyond that provided by a standard clinical assessment, and to determine if using the biomarker favorably alters the clinical course.
WHICH BIOMARKERS DO WE ALREADY ROUTINELY MEASURE?
Traditionally, the management of HF requires meticulous monitoring for adverse effects of drug therapy (eg, electrolyte and renal abnormalities with diuretics or drugs targeting the renin-angiotensin-aldosterone system). Although no specific clinical studies have been conducted to support their routine use, electrolytes (sodium, potassium, chloride, bicarbonate) and renal function measurements (blood urea nitrogen [BUN], creatinine) are often repeated periodically in the longitudinal care of patients with HF.2 Diagnostic tests for hemochromatosis, human immunodeficiency virus, rheumatologic disease, amyloidosis, and pheochromocytoma are reasonable in patients presenting with HF in whom there is a clinical suspicion of these diseases.2
For risk stratification, biomarkers that reflect renal insufficiency (particularly sodium, BUN, creatinine, and the estimated glomerular filtration rate [eGFR]) are powerful prognosticators.3 Newer renal markers of glomerular function (such as cystatin C)4,5 or of acute kidney injury (such as neutrophil gelatinase-associated lipocalin)6,7 have been proposed, although their clinical utility beyond prognostication remains to be determined. In fact, head- to-head comparisons have revealed that BUN appeared to be superior to most other renal biomarkers in stratifying short-term and long-term risk.8
Liver function, blood cell count, and thyroid function profiles are checked on some occasions to determine underlying end-organ dysfunction.2 Interestingly, several common laboratory values have consistently been associated with more advanced disease states or with a higher risk of future adverse events. These include serum uric acid (likely reflecting oxidative stress and nucleotide catabolism),9 anemia or red cell distribution width (likely reflecting iron deficiency or hematopoietic insufficiency),10 lymphocytopenia (likely reflecting immune dysfunction), and total bilirubin (likely reflection of hepatobiliary congestion).11
Some biomarkers have been incorporated into risk-stratification in patients with HF.2 However, drugs targeting these biomarkers have yet to be shown to improve clinical outcomes in prospective clinical trials. Several recent examples in chronic systolic HF include allopurinol for elevated uric acid levels12 and darbepoetin alfa for anemia (low hemoglobin).13 Thus, improving the biomarker level with specific treatment may not translate to improved clinical outcomes.
GUIDELINE RECOMMENDATIONS FOR CARDIAC BIOMARKERS IN HEART FAILURE
Clinical guidelines from several countries on the management of HF have expanded the role of biomarker testing in patients with HF.2,14–16 Table 1 shows the recommendations for biomarker testing in HF from the most recent joint guidelines of the American College of Cardiology and the American Heart Association. These recommendations will form the basis of the following discussion of clinically available biomarkers of HF that reflect distinct pathophysiologic processes and that have been cleared by the US Food and Drug Administration (Figure 1).
Biomarkers of myocardial stress: Natriuretic peptides
Natriuretic peptides are primary counterregulatory hormones produced in response to myocardial stress. Natriuretic peptide receptors stimulated by B-type (also “brain”) natriuretic peptide (BNP) lead to an increase in natriuresis, vasodilation, and opposing effects of other overactive neurohormonal systems. The contemporary understanding of how natriuretic peptides are being produced and metabolized is beyond the scope of this review, but generally it is now recognized that natriuretic peptide levels vary widely among patients with the same degree of symptoms or echocardiographic features.17
Of the several types of natriuretic peptide detectable by immunoassay, the two main types available for clinical use in the United States are BNP and amino acid N-terminal pro-BNP (NT-proBNP). Although there is no direct conversion available (NT-proBNP levels are five to eight times higher than BNP levels), their levels are often concordant and both are influenced by factors such as age, body mass index, and renal function. Specifically, natriuretic peptide levels in morbidly obese patients range 30% to 40% lower than levels in patients who are not morbidly obese.18
Studies over the past 10 years of natriuretic peptides in the diagnosis of HF have shown that levels are invariably elevated in underlying HF, while stable (and especially low) levels often track with clinical stability. In the latest clinical guidelines, natriuretic peptide testing has gained the highest level of recommendation for clinical use for any biomarker in HF, especially in the setting of clinical uncertainty (class 1 recommendation, level of evidence A).2,16 Two common clinical scenarios are represented in this indication. When patients present with signs and symptoms suspicious of HF (shortness of breath, fluid retention, peripheral edema, evidence of central congestion), natriuretic peptide testing provides confirmation of an underlying cardiac cause of these symptoms when elevated. Conversely, when there are alternative explanations or if the presentation is subtle and there is some degree of uncertainty, testing natriuretic peptide levels helps establish the diagnosis of HF when levels are higher than the cut-off values, and levels below the cut-off have a high negative predictive value (Table 2).19,20
Meanwhile, for patients with established HF, a deviation from “stable” natriuretic peptide levels (particularly an increase of more than 30%) may represent evolving destabilization that may warrant an intensification of therapy, whereas an unchanged or reduced level may be taken as objective evidence of clinical stability or favorable response to medical therapy. Table 3 outlines the latest Canadian guidelines that offer a practical approach as ongoing studies attempt to clarify the benefits of these strategies.15
The consistent association between elevated natriuretic peptide levels and worse prognosis21 has led to the promise that intensification of medical therapy in those with elevated natriuretic peptide levels can lead to better outcomes. Nevertheless, the rise in natriuretic peptide levels requires interpretation in the clinical context, as not all factors affecting the levels can be relieved by intensifying medical therapy (eg, age, renal insufficiency).
Several prospective, randomized controlled trials have tested this hypothesis, with favorable yet mixed results. Most studies have utilized a BNP measurement less than 100 pg/mL or an NT-proBNP measurement less than 1,000 pg/mL as a therapeutic target. In a recent prospective study that utilized the NT-proBNP threshold, only about half of patients were able to reach the target of less than 1,000 pg/mL.22 Often overlooked is the fact that in the same study, the inability to reach less than 5,000 pg/mL within 3 months after discharge clearly identified advanced, “nonresponsive” HF refractory to medical therapy and with a poor prognosis.23 This is an important point when assessing the clinical utility of biomarkers, as incremental prognostic values may not guarantee the feasibility or ultimate benefit of intensifying drug therapy according to specific biomarker targets. Until we have more insight into whether a care pathway guided by NT-proBNP measurements can lead to a consistent reduction in rates of hospitalization and mortality in HF, it is reasonable to target those with elevated natriuretic peptide levels by reevaluating their treatment regimen to achieve optimal dosing of guideline-directed medical therapy (Class 2a recommendation, level of evidence B).2 Also, the usefulness of BNP and NT-proBNP in guiding therapy for acutely decompensated HF is not well established (Class 2b recommendation, level of evidence C).2
Biomarkers of myocardial injury: Cardiac troponin
Whereas detecting circulating cardiac troponin is helpful in the diagnosis of acute coronary syndrome, the role of cardiac troponin levels in HF is primarily for risk stratification (Class 1 recommendation, level of evidence A in both acute and chronic HF).2 In patients hospitalized with acute decompensated HF, those with elevated troponin I or troponin T at the time of admission had lower systolic blood pressures, lower ejection fractions, and higher rate of in-hospital mortality.24,25 In chronic HF, elevations in both standard and high-sensitivity cardiac troponin levels were associated with increases in all-cause mortality,26 and rise in serial measurements appeared to correlate with an increased risk of future cardiovascular events.27 And with regard to cardiotoxicity, an increase in cardiac troponin over time (either after chemotherapy or with amyloidosis) is indicative of progressive cardiac dysfunction.28,29
Nevertheless, how to adjust medical therapy according to a rise in cardiac troponin levels remains unclear, as levels of cardiac troponin beyond the setting of acute coronary syndrome have appeared not to fluctuate significantly over time and do not seem to be related to underlying coronary events. Newer-generation cardiac troponin assays have yet to provide incremental value compared with standard clinical troponin assays despite their higher sensitivities.26
One common and underappreciated clinical application that combines both diagnostic and prognostic properties of both natriuretic peptide and cardiac troponin testing is the concept of HF staging. This is particularly relevant when there is a progressive change in clinical status (eg, need for hospitalization, change in signs or symptoms) or when a new therapy is started that may promote adverse effects. For example, a patient with pre-existing HF hospitalized with atypical symptoms and deemed not to have HF could be found to have subclinical myocardial necrosis as detected by low concentration of cardiac troponin or higher-than-baseline natriuretic peptide levels in the absence of hypervolemia. Careful assessment of the potential triggers of fluctuations from previous stable levels of cardiac biomarkers is also warranted (eg, atrial fibrillation, dietary indiscretion, infection, and ischemia). Indeed, these may represent objective rather than subjective changes in clinical manifestation of HF, which may warrant a reassessment of disease severity (eg, objective testing for functional capacity or hemodynamics, or even referral for consideration of advanced HF therapeutic options).
Biomarkers of inflammation and fibrosis: Soluble ST2 and galectin-3
Inflammation has long been associated with HF, and clinically available markers of inflammation such as high-sensitivity C-reactive protein (CRP)30,31 and myeloperoxidase32 have consistently tracked with prognosis. The search for a stable biomarker of inflammation has been challenging because inflammation is a dynamic process and because of the lack of treatment options for heightened inflammation.
A promising new protein biomarker, ST2 (suppression of tumorigenicity-2), has been identified in a soluble form (sST2) that binds to interleukin 33 (IL-33) to antagonize the maladaptive response of the myocardium to overload states.33 The levels of sST2 inversely correlate with the ejection fraction and have a positive association with increasing New York Heart Association class, worsening symptoms, and indicators of HF severity, such as norepinephrine levels, diastolic filling pressures, CRP, and natriuretic peptide levels.34 Unlike natriuretic peptides, levels of sST2 are not significantly affected by age, sex, body mass index, and valve disease,34 although recent observations have challenged its cardiac associations.35 In patients with chronic HF, elevated levels of sST2 (especially >35 ng/mL) have been associated with poorer clinical outcomes36 and increased risk of sudden cardiac death in HF.37 In addition, persistently elevated sST2 levels consistently confer poor long-term prognosis. Several studies have also demonstrated the prognostic value of elevated sST2 in predicting long-term risk of death in acute HF, either at baseline38,39 or on serial testing.40
Another new biomarker, galectin-3, has been implicated in fibrosis and in structural and pathophysiologic changes seen in HF.41 Studies have shown that higher levels of galectin-3 in patients with acute HF and chronic HF were associated with more severe cardiac fibrosis and with an increase in left ventricular remodeling.42–44 Serial measurements also confer prognostic information.45 However, many of these studies did not fully account for renal dysfunction as a major confounder, and the relationship between circulating galectin-3 and estimated GFR is strong.46,47 Meanwhile, head-to-head comparisons among galectin-3 and other clinically available biomarkers also revealed that the prognostic value of galectin-3 can be attenuated in the presence of sST2 and NT-proBNP.48,49 Furthermore, careful evaluation of diastolic parameters only showed a modest relationship with galectin-3 levels, especially in those with HF with preserved ejection fraction.50,51
In animal infarction models, disruption of the galectin-3 and IL-33/ST2 pathway with pharmacologic therapy such as mineralocorticoid receptor antagonists may attenuate cardiac remodeling.52,53 It is conceivable that these biomarkers may have mechanistic links with therapeutic benefits. However, the practical uses of galectin-3 and sST2 are still debated (Class 2b recommendation by the latest guidelines2) despite strong statistical associations between biomarker levels and adverse outcomes. The majority of biomarker substudies from clinical trials have suggested that improvements following drug or device therapy were largely confined to patients with lower rather than higher biomarker levels.54,55 Furthermore, validation studies have challenged the incremental prognostic value of these markers when natriuretic peptide levels are available.54,56–58 Thus, more clinical experience and research are warranted, and current clinical applications may be restricted to patient subsets.
BIOMARKERS IN EARLY STAGES OF HEART FAILURE
The potential benefit of biomarker testing may reside in the earlier end of the HF spectrum, especially in patients at risk of but not yet diagnosed with HF (so-called stage A). In the HealthABC study, the future risk of HF in elderly patients can be predicted with a combination of clinical risk factors (age, sex, left ventricular hypertrophy, systolic blood pressure, heart rate, smoking), as well as biochemical risk factors such as albumin, creatinine, and glucose.59 Patients with elevated natriuretic peptide levels are more likely to have underlying cardiac abnormalities and to have poorer long-term outcomes.60 In a recent prospective, randomized controlled trial, participants with a BNP-guided transition to HF therapies (when BNP >50 pg/mL) had a lower incidence of HF than participants without knowledge of BNP levels.61 Elevated levels of clinically available biomarkers of inflammation, such as myeloperoxidase,29,62 ceruloplasmin,63 and CRP,64 have also been associated with an increased risk of future HF. These findings support the notion that biomarkers, especially when combined with clinical risk factors, can serve as indicators of HF vulnerability. If independently confirmed, this will be an important therapeutic approach to the prevention of HF.
PRACTICAL CONSIDERATIONS
An important perspective often overlooked concerns the variability of a biomarker level as it is utilized in clinical practice (Table 4). In general, point-of-care assays are often more variable than the same tests done in clinical laboratories. Sample collection, handling, and processing also introduce a degree of variability. The biologic variability of specific measurements can significantly affect the precision of the measurement. In the case of HF, the biologic variability (as measured in stable patients over time) of natriuretic peptides and galectin-3 are significantly higher than those observed in cardiac troponins or sST2 (> 130% vs approximately 30%).65 Nevertheless because of their relative cardiac specificity, natriuretic peptides have maintained their clinical utility.
- Morrow DA, de Lemos JA. Benchmarks for the assessment of novel cardiovascular biomarkers. Circulation 2007; 115:949–952.
- Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 2013; 128:e240–327.
- Halkar M, Tang WH. Incorporating common biomarkers into the clinical management of heart failure. Curr Heart Fail Rep 2013; 10:450–457.
- Dupont M, Wu Y, Hazen SL, Tang WH. Cystatin C identifies patients with stable chronic heart failure at increased risk for adverse cardiovascular events. Circ Heart Fail 2012; 5:602–609.
- Tang WH, Van Lente F, Shrestha K, et al. Impact of myocardial function on cystatin C measurements in chronic systolic heart failure. J Card Fail 2008; 14:394– 399.
- Dupont M, Shrestha K, Singh D, et al. Lack of significant renal tubular injury despite acute kidney injury in acute decompensated heart failure. Eur J Heart Fail 2012; 14:597–604.
- Verbrugge FH, Dupont M, Shao Z, et al. Novel urinary biomarkers in detecting acute kidney injury, persistent renal impairment, and all-cause mortality following decongestive therapy in acute decompensated heart failure. J Card Fail 2013; 19:621–628.
- Tang WH, Dupont M, Hernandez AF, et al. Comparative assessment of short-term adverse events in acute heart failure with cystatin C and other estimates of renal function: results from the ASCEND-HF trial. JACC Heart Fail 2015; 3:40–49.
- Vaduganathan M, Greene SJ, Ambrosy AP, et al. Relation of serum uric acid levels and outcomes among patients hospitalized for worsening heart failure with reduced ejection fraction (from the efficacy of vasopressin antagonism in heart failure outcome study with tolvaptan trial). Am J Cardiol 2014; 114:1713–1721.
- Felker GM, Allen LA, Pocock SJ, et al. Red cell distribution width as a novel prognostic marker in heart failure: data from the CHARM Program and the Duke Databank. J Am Coll Cardiol 2007; 50:40–47.
- Wu AH, Levy WC, Welch KB, et al. Association between bilirubin and mode of death in severe systolic heart failure. Am J Cardiol 2013; 111:1192–1197.
- Givertz MM, Anstrom KJ, Redfield MM, et al. Effects of xanthine oxidase inhibition in hyperuricemic heart failure patients: the Xanthine Oxidase Inhibition for Hyperuricemic Heart Failure Patients (EXACT-HF) study. Circulation 2015; 131:1763–1771.
- Swedberg K, Young JB, Anand IS, et al. Treatment of anemia with darbepoetin alfa in systolic heart failure. N Engl J Med 2013; 368:1210–1219.
- McMurray JJ, Adamopoulos S, Anker SD, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 2012; 33:1787–1847.
- Moe GW, Ezekowitz JA, O’Meara E, et al. The 2014 Canadian Cardiovascular Society Heart Failure Management Guidelines Focus Update: anemia, biomarkers, and recent therapeutic trial implications. Can J Cardiol 2015; 31:3–16.
- Tang WH, Francis GS, Morrow DA, et al. National Academy of Clinical Biochemistry Laboratory Medicine practice guidelines: clinical utilization of cardiac biomarker testing in heart failure. Circulation 2007; 116:e99–109.
- Maisel AS, Daniels LB. Breathing not properly 10 years later: what we have learned and what we still need to learn. J Am Coll Cardiol 2012; 60:277–282.
- Mehra MR, Uber PA, Park MH, et al. Obesity and suppressed B-type natriuretic peptide levels in heart failure. J Am Coll Cardiol 2004; 43:1590–1595.
- Januzzi JL, Jr, Camargo CA, Anwaruddin S, et al. The N-terminal Pro-BNP Investigation of Dyspnea in the Emergency Department (PRIDE) study. Am J Cardiol 2005; 95:948–954.
- Maisel AS, Krishnaswamy P, Nowak RM, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 2002; 347:161–167.
- Fonarow GC, Peacock WF, Phillips CO, Givertz MM, Lopatin M. Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. J Am Coll Cardiol 2007; 49:1943–1950.
- Januzzi JL, Jr, Rehman SU, Mohammed AA, et al. Use of amino-terminal pro-B- type natriuretic peptide to guide outpatient therapy of patients with chronic left ventricular systolic dysfunction. J Am Coll Cardiol 2011; 58:1881–1889.
- Gaggin HK, Truong QA, Rehman SU, et al. Characterization and prediction of natriuretic peptide ‘nonresponse’ during heart failure management: results from the ProBNP Outpatient Tailored Chronic Heart Failure (PROTECT) and the NT-proBNP-Assisted Treatment to Lessen Serial Cardiac Readmissions and Death (BATTLESCARRED) study. Congest Heart Fail 2013; 19:135–142.
- Peacock WF 4th, De Marco T, Fonarow GC, et al. Cardiac troponin and outcome in acute heart failure. N Engl J Med 2008; 358:2117–2126.
- Felker GM, Hasselblad V, Tang WH, et al. Troponin I in acute decompen- sated heart failure: insights from the ASCEND-HF study. Eur J Heart Fail 2012; 14:1257–1264.
- Grodin JL, Neale S, Wu Y, Hazen SL, Tang WH. Prognostic comparison of different sensitivity cardiac troponin assays in stable heart failure. Am J Med 2015; 128:276–282.
- Masson S, Anand I, Favero C, et al. Serial measurement of cardiac troponin T using a highly sensitive assay in patients with chronic heart failure: data from 2 large randomized clinical trials. Circulation 2012; 125:280–288.
- Cardinale D, Sandri MT, Colombo A, et al. Prognostic value of troponin I in cardiac risk stratification of cancer patients undergoing high-dose chemotherapy. Circulation 2004; 109:2749–2754.
- Ky B, Putt M, Sawaya H, et al. Early increases in multiple biomarkers predict subsequent cardiotoxicity in breast cancer patients treated with doxorubicin, taxanes, and trastuzumab. J Am Coll Cardiol 2014; 63:809–816.
- Kalogeropoulos AP, Tang WH, Hsu A, et al. High-sensitivity C-reactive protein in acute heart failure: insights from the ASCEND-HF trial. J Card Fail 2014; 20:319–326.
- Tang WH, Shrestha K, Van Lente F, et al. Usefulness of C-reactive protein and left ventricular diastolic performance for prognosis in patients with left ventricular systolic heart failure. Am J Cardiol 2008; 101:370–373.
- Tang WH, Wu Y, Nicholls SJ, Hazen SL. Plasma myeloperoxidase predicts incident cardiovascular risks in stable patients undergoing medical management for coronary artery disease. Clin Chem 2011; 57:33–39.
- Sanada S, Hakuno D, Higgins LJ, Schreiter ER, McKenzie AN, Lee RT. IL-33 and ST2 comprise a critical biomechanically induced and cardioprotective signaling system. J Clin Invest 2007; 117:1538–1549.
- Rehman SU, Mueller T, Januzzi JL, Jr. Characteristics of the novel interleukin family biomarker ST2 in patients with acute heart failure. J Am Coll Cardiol 2008; 52:1458–1465.
- Kaye DM, Mariani JA, van Empel V, Maeder MT. Determinants and implications of elevated soluble ST2 levels in heart failure. Int J Cardiol 2014; 176:1242–1243.
- Ky B, French B, McCloskey K, et al. High-sensitivity ST2 for prediction of adverse outcomes in chronic heart failure. Circ Heart Fail 2011; 4:180–187.
- Ahmad T, Fiuzat M, Neely B, et al. Biomarkers of myocardial stress and fibrosis as predictors of mode of death in patients with chronic heart failure. JACC Heart Fail 2014; 2:260–268.
- Pascual-Figal DA, Manzano-Fernandez S, Boronat M, et al. Soluble ST2, high-sensitivity troponin T- and N-terminal pro-B-type natriuretic peptide: complementary role for risk stratification in acutely decompensated heart failure. Eur J Heart Fail 2011; 13:718–725.
- Januzzi JL, Jr, Peacock WF, Maisel AS, et al. Measurement of the interleukin family member ST2 in patients with acute dyspnea: results from the PRIDE (Pro-Brain Natriuretic Peptide Investigation of Dyspnea in the Emergency Department) study. J Am Coll Cardiol 2007; 50:607-613.
- Boisot S, Beede J, Isakson S, et al. Serial sampling of ST2 predicts 90-day mortality following destabilized heart failure. J Card Fail 2008; 14:732–738.
- Sharma UC, Pokharel S, van Brakel TJ, et al. Galectin-3 marks activated macrophages in failure-prone hypertrophied hearts and contributes to cardiac dysfunction. Circulation 2004; 110:3121–3128.
- van Kimmenade RR, Januzzi JL, Jr., Ellinor PT, et al. Utility of amino-terminal pro-brain natriuretic peptide, galectin-3, and apelin for the evaluation of patients with acute heart failure. J Am Coll Cardiol 2006; 48:1217–1224.
- Lok DJ, Van Der Meer P, de la Porte PW, et al. Prognostic value of galectin-3, a novel marker of fibrosis, in patients with chronic heart failure: data from the DEAL-HF study. Clin Res Cardiol 2010; 99:323–328.
- Shah RV, Chen-Tournoux AA, Picard MH, van Kimmenade RR, Januzzi JL. Ga- lectin-3, cardiac structure and function, and long-term mortality in patients with acutely decompensated heart failure. Eur J Heart Fail 2010; 12:826–832.
- van der Velde AR, Gullestad L, Ueland T, et al. Prognostic value of changes in galectin-3 levels over time in patients with heart failure: data from CORONA and COACH. Circ Heart Fail 2013; 6:219–226.
- Tang WH, Shrestha K, Shao Z, et al. Usefulness of plasma galectin-3 levels in systolic heart failure to predict renal insufficiency and survival. Am J Cardiol 2011; 108:385–390.
- Gopal DM, Kommineni M, Ayalon N, et al. Relationship of plasma galectin-3 to renal function in patients with heart failure: effects of clinical status, pathophysiology of heart failure, and presence or absence of heart failure. J Am Heart Assoc 2012; 1:e000760.
- Bayes-Genis A, de Antonio M, Vila J, et al. Head-to-head comparison of 2 myocardial fibrosis biomarkers for long-term heart failure risk stratification: ST2 versus galectin-3. J Am Coll Cardiol 2014; 63:158–166.
- Felker GM, Fiuzat M, Shaw LK, et al. Galectin-3 in ambulatory patients with heart failure: results from the HF-ACTION study. Circ Heart Fail 2012; 5:72–78.
- Edelmann F, Holzendorf V, Wachter R, et al. Galectin-3 in patients with heart failure with preserved ejection fraction: results from the Aldo-DHF trial. Eur J Heart Fail 2015; 17:214–223.
- AbouEzzeddine OF, Haines P, Stevens S, et al. Galectin-3 in heart failure with preserved ejection fraction. A RELAX trial substudy (Phosphodiesterase-5 Inhibition to Improve Clinical Status and Exercise Capacity in Diastolic Heart Failure). JACC Heart failure 2015; 3:245–252.
- Lax A, Sanchez-Mas J, Asensio-Lopez MC, et al. Mineralocorticoid receptor antagonists modulate galectin-3 and interleukin-33/ST2 signaling in left ventricular systolic dysfunction after acute myocardial infarction. JACC Heart failure 2015; 3:50–58.
- Calvier L, Martinez-Martinez E, Miana M, et al. The impact of galectin-3 inhibition on aldosterone-induced cardiac and renal injuries. JACC Heart failure 2015; 3:59–67.
- Anand IS, Rector TS, Kuskowski M, Adourian A, Muntendam P, Cohn JN. Baseline and serial measurements of galectin-3 in patients with heart failure: relationship to prognosis and effect of treatment with valsartan in the Val-HeFT. Eur J Heart Fail 2013; 15:511–518.
- Gullestad L, Ueland T, Kjekshus J, et al. Galectin-3 predicts response to statin therapy in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CO- RONA). Eur Heart J 2012; 33:2290–2296.
- Felker GM, Fiuzat M, Thompson V, et al. Soluble ST2 in ambulatory patients with heart failure: association with functional capacity and long-term outcomes. Circ Heart Fail 2013; 6:1172–1179.
- Anand IS, Rector TS, Kuskowski M, Snider J, Cohn JN. Prognostic value of soluble ST2 in the Valsartan Heart Failure Trial. Circ Heart Fail 2014; 7:418–426.
- Gullestad L, Ueland T, Kjekshus J, et al. The predictive value of galectin-3 for mortality and cardiovascular events in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CORONA). Am Heart J 2012; 164:878–883.
- Butler J, Kalogeropoulos A, Georgiopoulou V, et al. Incident heart failure prediction in the elderly: the health ABC heart failure score. Circ Heart Fail 2008; 1:125–133.
- McKie PM, Rodeheffer RJ, Cataliotti A, et al. Amino-terminal pro-B-type natriuretic peptide and B-type natriuretic peptide: biomarkers for mortality in a large community-based cohort free of heart failure. Hypertension 2006; 47:874–880.
- Ledwidge M, Gallagher J, Conlon C, et al. Natriuretic peptide-based screening and collaborative care for heart failure: the STOP-HF randomized trial. JAMA 2013; 310:66–74.
- Tang WH, Katz R, Brennan ML, et al. Usefulness of myeloperoxidase levels in healthy elderly subjects to predict risk of developing heart failure. Am J Cardiol 2009; 103:1269–1274.
- Dadu RT, Dodge R, Nambi V, et al. Ceruloplasmin and heart failure in the Atherosclerosis Risk in Communities study. Circ Heart Fail 2013; 6:936–943.
- Kalogeropoulos A, Georgiopoulou V, Psaty BM, et al. Inflammatory markers and incident heart failure risk in older adults: the Health ABC (Health, Aging, and Body Composition) study. J Am Coll Cardiol 2010; 55:2129–2137.
- Wu AH, Wians F, Jaffe A. Biological variation of galectin-3 and soluble ST2 for chronic heart failure: implication on interpretation of test results. Am Heart J 2013; 165:995–999.
- Morrow DA, de Lemos JA. Benchmarks for the assessment of novel cardiovascular biomarkers. Circulation 2007; 115:949–952.
- Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 2013; 128:e240–327.
- Halkar M, Tang WH. Incorporating common biomarkers into the clinical management of heart failure. Curr Heart Fail Rep 2013; 10:450–457.
- Dupont M, Wu Y, Hazen SL, Tang WH. Cystatin C identifies patients with stable chronic heart failure at increased risk for adverse cardiovascular events. Circ Heart Fail 2012; 5:602–609.
- Tang WH, Van Lente F, Shrestha K, et al. Impact of myocardial function on cystatin C measurements in chronic systolic heart failure. J Card Fail 2008; 14:394– 399.
- Dupont M, Shrestha K, Singh D, et al. Lack of significant renal tubular injury despite acute kidney injury in acute decompensated heart failure. Eur J Heart Fail 2012; 14:597–604.
- Verbrugge FH, Dupont M, Shao Z, et al. Novel urinary biomarkers in detecting acute kidney injury, persistent renal impairment, and all-cause mortality following decongestive therapy in acute decompensated heart failure. J Card Fail 2013; 19:621–628.
- Tang WH, Dupont M, Hernandez AF, et al. Comparative assessment of short-term adverse events in acute heart failure with cystatin C and other estimates of renal function: results from the ASCEND-HF trial. JACC Heart Fail 2015; 3:40–49.
- Vaduganathan M, Greene SJ, Ambrosy AP, et al. Relation of serum uric acid levels and outcomes among patients hospitalized for worsening heart failure with reduced ejection fraction (from the efficacy of vasopressin antagonism in heart failure outcome study with tolvaptan trial). Am J Cardiol 2014; 114:1713–1721.
- Felker GM, Allen LA, Pocock SJ, et al. Red cell distribution width as a novel prognostic marker in heart failure: data from the CHARM Program and the Duke Databank. J Am Coll Cardiol 2007; 50:40–47.
- Wu AH, Levy WC, Welch KB, et al. Association between bilirubin and mode of death in severe systolic heart failure. Am J Cardiol 2013; 111:1192–1197.
- Givertz MM, Anstrom KJ, Redfield MM, et al. Effects of xanthine oxidase inhibition in hyperuricemic heart failure patients: the Xanthine Oxidase Inhibition for Hyperuricemic Heart Failure Patients (EXACT-HF) study. Circulation 2015; 131:1763–1771.
- Swedberg K, Young JB, Anand IS, et al. Treatment of anemia with darbepoetin alfa in systolic heart failure. N Engl J Med 2013; 368:1210–1219.
- McMurray JJ, Adamopoulos S, Anker SD, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 2012; 33:1787–1847.
- Moe GW, Ezekowitz JA, O’Meara E, et al. The 2014 Canadian Cardiovascular Society Heart Failure Management Guidelines Focus Update: anemia, biomarkers, and recent therapeutic trial implications. Can J Cardiol 2015; 31:3–16.
- Tang WH, Francis GS, Morrow DA, et al. National Academy of Clinical Biochemistry Laboratory Medicine practice guidelines: clinical utilization of cardiac biomarker testing in heart failure. Circulation 2007; 116:e99–109.
- Maisel AS, Daniels LB. Breathing not properly 10 years later: what we have learned and what we still need to learn. J Am Coll Cardiol 2012; 60:277–282.
- Mehra MR, Uber PA, Park MH, et al. Obesity and suppressed B-type natriuretic peptide levels in heart failure. J Am Coll Cardiol 2004; 43:1590–1595.
- Januzzi JL, Jr, Camargo CA, Anwaruddin S, et al. The N-terminal Pro-BNP Investigation of Dyspnea in the Emergency Department (PRIDE) study. Am J Cardiol 2005; 95:948–954.
- Maisel AS, Krishnaswamy P, Nowak RM, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 2002; 347:161–167.
- Fonarow GC, Peacock WF, Phillips CO, Givertz MM, Lopatin M. Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. J Am Coll Cardiol 2007; 49:1943–1950.
- Januzzi JL, Jr, Rehman SU, Mohammed AA, et al. Use of amino-terminal pro-B- type natriuretic peptide to guide outpatient therapy of patients with chronic left ventricular systolic dysfunction. J Am Coll Cardiol 2011; 58:1881–1889.
- Gaggin HK, Truong QA, Rehman SU, et al. Characterization and prediction of natriuretic peptide ‘nonresponse’ during heart failure management: results from the ProBNP Outpatient Tailored Chronic Heart Failure (PROTECT) and the NT-proBNP-Assisted Treatment to Lessen Serial Cardiac Readmissions and Death (BATTLESCARRED) study. Congest Heart Fail 2013; 19:135–142.
- Peacock WF 4th, De Marco T, Fonarow GC, et al. Cardiac troponin and outcome in acute heart failure. N Engl J Med 2008; 358:2117–2126.
- Felker GM, Hasselblad V, Tang WH, et al. Troponin I in acute decompen- sated heart failure: insights from the ASCEND-HF study. Eur J Heart Fail 2012; 14:1257–1264.
- Grodin JL, Neale S, Wu Y, Hazen SL, Tang WH. Prognostic comparison of different sensitivity cardiac troponin assays in stable heart failure. Am J Med 2015; 128:276–282.
- Masson S, Anand I, Favero C, et al. Serial measurement of cardiac troponin T using a highly sensitive assay in patients with chronic heart failure: data from 2 large randomized clinical trials. Circulation 2012; 125:280–288.
- Cardinale D, Sandri MT, Colombo A, et al. Prognostic value of troponin I in cardiac risk stratification of cancer patients undergoing high-dose chemotherapy. Circulation 2004; 109:2749–2754.
- Ky B, Putt M, Sawaya H, et al. Early increases in multiple biomarkers predict subsequent cardiotoxicity in breast cancer patients treated with doxorubicin, taxanes, and trastuzumab. J Am Coll Cardiol 2014; 63:809–816.
- Kalogeropoulos AP, Tang WH, Hsu A, et al. High-sensitivity C-reactive protein in acute heart failure: insights from the ASCEND-HF trial. J Card Fail 2014; 20:319–326.
- Tang WH, Shrestha K, Van Lente F, et al. Usefulness of C-reactive protein and left ventricular diastolic performance for prognosis in patients with left ventricular systolic heart failure. Am J Cardiol 2008; 101:370–373.
- Tang WH, Wu Y, Nicholls SJ, Hazen SL. Plasma myeloperoxidase predicts incident cardiovascular risks in stable patients undergoing medical management for coronary artery disease. Clin Chem 2011; 57:33–39.
- Sanada S, Hakuno D, Higgins LJ, Schreiter ER, McKenzie AN, Lee RT. IL-33 and ST2 comprise a critical biomechanically induced and cardioprotective signaling system. J Clin Invest 2007; 117:1538–1549.
- Rehman SU, Mueller T, Januzzi JL, Jr. Characteristics of the novel interleukin family biomarker ST2 in patients with acute heart failure. J Am Coll Cardiol 2008; 52:1458–1465.
- Kaye DM, Mariani JA, van Empel V, Maeder MT. Determinants and implications of elevated soluble ST2 levels in heart failure. Int J Cardiol 2014; 176:1242–1243.
- Ky B, French B, McCloskey K, et al. High-sensitivity ST2 for prediction of adverse outcomes in chronic heart failure. Circ Heart Fail 2011; 4:180–187.
- Ahmad T, Fiuzat M, Neely B, et al. Biomarkers of myocardial stress and fibrosis as predictors of mode of death in patients with chronic heart failure. JACC Heart Fail 2014; 2:260–268.
- Pascual-Figal DA, Manzano-Fernandez S, Boronat M, et al. Soluble ST2, high-sensitivity troponin T- and N-terminal pro-B-type natriuretic peptide: complementary role for risk stratification in acutely decompensated heart failure. Eur J Heart Fail 2011; 13:718–725.
- Januzzi JL, Jr, Peacock WF, Maisel AS, et al. Measurement of the interleukin family member ST2 in patients with acute dyspnea: results from the PRIDE (Pro-Brain Natriuretic Peptide Investigation of Dyspnea in the Emergency Department) study. J Am Coll Cardiol 2007; 50:607-613.
- Boisot S, Beede J, Isakson S, et al. Serial sampling of ST2 predicts 90-day mortality following destabilized heart failure. J Card Fail 2008; 14:732–738.
- Sharma UC, Pokharel S, van Brakel TJ, et al. Galectin-3 marks activated macrophages in failure-prone hypertrophied hearts and contributes to cardiac dysfunction. Circulation 2004; 110:3121–3128.
- van Kimmenade RR, Januzzi JL, Jr., Ellinor PT, et al. Utility of amino-terminal pro-brain natriuretic peptide, galectin-3, and apelin for the evaluation of patients with acute heart failure. J Am Coll Cardiol 2006; 48:1217–1224.
- Lok DJ, Van Der Meer P, de la Porte PW, et al. Prognostic value of galectin-3, a novel marker of fibrosis, in patients with chronic heart failure: data from the DEAL-HF study. Clin Res Cardiol 2010; 99:323–328.
- Shah RV, Chen-Tournoux AA, Picard MH, van Kimmenade RR, Januzzi JL. Ga- lectin-3, cardiac structure and function, and long-term mortality in patients with acutely decompensated heart failure. Eur J Heart Fail 2010; 12:826–832.
- van der Velde AR, Gullestad L, Ueland T, et al. Prognostic value of changes in galectin-3 levels over time in patients with heart failure: data from CORONA and COACH. Circ Heart Fail 2013; 6:219–226.
- Tang WH, Shrestha K, Shao Z, et al. Usefulness of plasma galectin-3 levels in systolic heart failure to predict renal insufficiency and survival. Am J Cardiol 2011; 108:385–390.
- Gopal DM, Kommineni M, Ayalon N, et al. Relationship of plasma galectin-3 to renal function in patients with heart failure: effects of clinical status, pathophysiology of heart failure, and presence or absence of heart failure. J Am Heart Assoc 2012; 1:e000760.
- Bayes-Genis A, de Antonio M, Vila J, et al. Head-to-head comparison of 2 myocardial fibrosis biomarkers for long-term heart failure risk stratification: ST2 versus galectin-3. J Am Coll Cardiol 2014; 63:158–166.
- Felker GM, Fiuzat M, Shaw LK, et al. Galectin-3 in ambulatory patients with heart failure: results from the HF-ACTION study. Circ Heart Fail 2012; 5:72–78.
- Edelmann F, Holzendorf V, Wachter R, et al. Galectin-3 in patients with heart failure with preserved ejection fraction: results from the Aldo-DHF trial. Eur J Heart Fail 2015; 17:214–223.
- AbouEzzeddine OF, Haines P, Stevens S, et al. Galectin-3 in heart failure with preserved ejection fraction. A RELAX trial substudy (Phosphodiesterase-5 Inhibition to Improve Clinical Status and Exercise Capacity in Diastolic Heart Failure). JACC Heart failure 2015; 3:245–252.
- Lax A, Sanchez-Mas J, Asensio-Lopez MC, et al. Mineralocorticoid receptor antagonists modulate galectin-3 and interleukin-33/ST2 signaling in left ventricular systolic dysfunction after acute myocardial infarction. JACC Heart failure 2015; 3:50–58.
- Calvier L, Martinez-Martinez E, Miana M, et al. The impact of galectin-3 inhibition on aldosterone-induced cardiac and renal injuries. JACC Heart failure 2015; 3:59–67.
- Anand IS, Rector TS, Kuskowski M, Adourian A, Muntendam P, Cohn JN. Baseline and serial measurements of galectin-3 in patients with heart failure: relationship to prognosis and effect of treatment with valsartan in the Val-HeFT. Eur J Heart Fail 2013; 15:511–518.
- Gullestad L, Ueland T, Kjekshus J, et al. Galectin-3 predicts response to statin therapy in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CO- RONA). Eur Heart J 2012; 33:2290–2296.
- Felker GM, Fiuzat M, Thompson V, et al. Soluble ST2 in ambulatory patients with heart failure: association with functional capacity and long-term outcomes. Circ Heart Fail 2013; 6:1172–1179.
- Anand IS, Rector TS, Kuskowski M, Snider J, Cohn JN. Prognostic value of soluble ST2 in the Valsartan Heart Failure Trial. Circ Heart Fail 2014; 7:418–426.
- Gullestad L, Ueland T, Kjekshus J, et al. The predictive value of galectin-3 for mortality and cardiovascular events in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CORONA). Am Heart J 2012; 164:878–883.
- Butler J, Kalogeropoulos A, Georgiopoulou V, et al. Incident heart failure prediction in the elderly: the health ABC heart failure score. Circ Heart Fail 2008; 1:125–133.
- McKie PM, Rodeheffer RJ, Cataliotti A, et al. Amino-terminal pro-B-type natriuretic peptide and B-type natriuretic peptide: biomarkers for mortality in a large community-based cohort free of heart failure. Hypertension 2006; 47:874–880.
- Ledwidge M, Gallagher J, Conlon C, et al. Natriuretic peptide-based screening and collaborative care for heart failure: the STOP-HF randomized trial. JAMA 2013; 310:66–74.
- Tang WH, Katz R, Brennan ML, et al. Usefulness of myeloperoxidase levels in healthy elderly subjects to predict risk of developing heart failure. Am J Cardiol 2009; 103:1269–1274.
- Dadu RT, Dodge R, Nambi V, et al. Ceruloplasmin and heart failure in the Atherosclerosis Risk in Communities study. Circ Heart Fail 2013; 6:936–943.
- Kalogeropoulos A, Georgiopoulou V, Psaty BM, et al. Inflammatory markers and incident heart failure risk in older adults: the Health ABC (Health, Aging, and Body Composition) study. J Am Coll Cardiol 2010; 55:2129–2137.
- Wu AH, Wians F, Jaffe A. Biological variation of galectin-3 and soluble ST2 for chronic heart failure: implication on interpretation of test results. Am Heart J 2013; 165:995–999.
KEY POINTS
- The usefulness of a biomarker may differ from one patient population to another, from one clinician to another, or from one clinical scenario to another.
- For risk stratification in heart failure (HF), biomarkers that reflect renal insufficiency are especially powerful prognosticators.
- In the latest clinical guidelines, natriuretic peptide testing has gained the highest level of recommendation for clinical use for any biomarker in HF.
- In general, point-of-care assays are often more variable than the same tests done in clinical laboratories; sample collection, handling, and processing also introduce variability.
Clinical challenges in diagnosing and managing adult hypertension
Hypertension is a primary care specialty. Most of the 70,000,000 adult Americans with hypertension are cared for by primary care providers. Medications are readily available that achieve high control rates when used in combination. Primary care providers are uniquely positioned to lead team-oriented approaches to improve medication adherence and provide equitable care that addresses racial disparity in hypertension control.
This review focuses on some of the challenges that primary care providers face, including diagnosis of hypertension, medication options, controversy regarding the goal systolic blood pressure in the elderly, and population care strategies in our fractured healthcare system.
USING OUT-OF-OFFICE AND AUTOMATED MEASUREMENTS FOR DIAGNOSIS
A systematic review performed for the US Preventive Services Task Force concluded that the evidence supports ambulatory monitoring to confirm blood pressure in the office in all but the most severe cases of office-based blood pressure elevation in order to avoid misdiagnosis and overtreatment.1 Elevated ambulatory pressure is the best predictor of cardiovascular events in prospective cohort studies.1 A new hypertension diagnostic algorithm for Canada2 is similar to an earlier American Heart Association algorithm3 in recommending diagnostic confirmation by out-of-office measures including home blood pressure, ambulatory pressure, or automated office blood pressures. With automated blood pressure measurement, the clinician or medical assistant initiates preprogrammed oscillometric devices to take sequential blood pressure measurements after the assistant leaves the examining room. Thresholds for the diagnosis of hypertension are1,2:
- Office measurements: ≥ 140/90 mm Hg
- Automated office measurements (mean): ≥ 135/ 85 mm Hg
- Home blood pressure measurements: ≥ 135/85 mm Hg
- Ambulatory monitoring (mean of daytime readings): ≥ 135/85 mm Hg
- Ambulatory monitoring (mean 24-hour reading): ≥ 130/80 mm Hg.
However, evidence supporting the use of ambulatory monitoring, home measurements, and automated office measurements has significant limitations. There is no evidence from prospective randomized controlled trials that withholding treatment on the basis of these measurements when office blood pressures are elevated leads to cardiovascular outcomes equivalent to normotensive outcomes. Also, the Centers for Medicare and Medicaid Services do not reimburse for ambulatory blood pressure monitoring, which would lead to inconsistent implementation and more disparity in healthcare. Moreover, when ambulatory monitoring is used to diagnose hypertension, how to determine response to treatment has not been defined.
Table 1 summarizes recommendations for the use of out-of-office measurements to diagnose hypertension.1–4 System-wide efforts can reduce the need for out-of-office confirmation; these include improving competence in measuring office blood pressure through peer validator spot-checking in the normal workflow, performance feedback reporting of repeat measurements when the first is elevated, and extensive use of walk-in measurements to reduce the white-coat effect.5,6 Two well-performed office measurements performed on each of two or three visits over at least a month will continue to be the diagnostic standard for most patients. Small errors in technique introduce inaccuracies in blood pressure readings, which, if falsely high, can lead to unnecessary treatment or, conversely, if falsely low can lead to inadequate treatment. Table 2 lists several common measurement errors that need to be consistently avoided.7–9
ANTIHYPERTENSIVE DRUG TREATMENT STRATEGIES
The Eighth Joint National Committee (JNC 8)10 issued a strictly evidence-based guideline based on adequate randomized controlled trials comparing representative drugs of different antihypertensive classes with respect to hard cardiovascular outcomes to arrive at well-supported recommendations (Table 3). The three groups of agents with the greatest evidence to support their use are:
- Thiazide-type diuretics
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers
- Calcium channel blockers.
Beta-blockers did not make the first tier because the beta-blocker atenolol was found to be inferior to the angiotensin receptor blocker losartan in terms of the rate of the primary end point (death, myocardial infarction, or stroke) in the Losartan Intervention For Endpoint Reduction in Hypertension (LIFE) trial,11 and we lack hard end point evidence to support other beta-blockers. However, patients with coronary artery disease or heart failure have a compelling drug-specific indication for a beta-blocker outside of blood pressure reduction.
There is an important race-based difference in the initial antihypertensive drug treatment options based on the findings of the prespecified subgroup of more than 10,000 black patients in the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT).12 The thiazide-type diuretic chlorthalidone was more effective than the ACE inhibitor lisinopril in improving the rates of adverse cardiovascular and cerebrovascular outcomes, including stroke and heart failure, and the calcium channel blocker amlodipine was more effective than lisinopril in improving the rate of stroke. There have been no randomized controlled trials or prespecified subgroups in randomized controlled trials evaluating angiotensin receptor blockers in black patients. Therefore, thiazide-type diuretics and calcium channel blockers are the preferred initial options for reducing cardiovascular outcomes in the general black population. ACE inhibitors and angiotensin receptor blockers are preferred across all races for patients with chronic kidney disease to improve renal outcomes.10 However, a strategy using initial combination therapy with an ACE inhibitor or an angioten sin receptor blocker together with a thiazide diuretic or calcium channel blocker does satisfy the evidence, improving both cardiovascular and renal outcomes in black patients with and without chronic kidney disease.
JNC 8 recommended thiazide-type diuretics as a class rather than specifically recommending chlorthalidone because confirmatory trials used thiazide-type diuretics other than chlorthalidone, such as hydrochlorothiazide. For example, whereas the ALLHAT trial found that chlorthalidone 12.5 or 25 mg was superior to the calcium channel blocker amlodipine in terms of reducing the incidence of heart failure, the International Nifedipine Study: Intervention as a Goal in Hypertension Treatment (INSIGHT) similarly found that hydrochlorothiazide titrated up to 50 mg was superior to the calcium channel blocker nifedipine in reducing the incidence of heart failure.13
Dose as well as drug is important. Inadequately dosed hydrochlorothiazide (12.5–25 mg/day) in the Second Australian National Blood Pressure (ANBP2) and the Avoiding Cardiovascular Events through Combination Therapy in Patients with Systolic Hypertension (ACCOMPLISH) trials14,15 did not fare as well as comparator agents. The hydrochlorothiazide dosage in these trials was decided on the basis of usual prescribing practices rather than strict examination of prior comparators. Common rationales for prescribing lower doses of diuretics are fear of renal fail- ure in the elderly or drug-induced incident diabetes. However, analyses of ALLHAT patients did not reveal increased renal failure or worsened outcomes due to drug-related diabetes.16,17 A supplement to the JNC 8 report, available online, provides a rationale for the target hydrochlorothiazide dose of 50 mg.18
ACE inhibitors and angiotensin receptor blockers should not be prescribed together to control hypertension in the general population, due to increased risk of acute renal failure.19 However, a nonprogressive decrease in creatinine clearance of up to 30% at the beginning of ACE inhibitor or angiotensin receptor blocker therapy in patients who have chronic kidney disease can be viewed as a good sign, indicating that intraglomerular pressure has been reduced and the kidneys are better protected against structural damage.20
Intensifying therapy
While the first-tier antihypertensive drug classes have been identified by randomized controlled trials, most patients require drug intensification. In the absence of randomized controlled trials examining second-step options, the JNC 8 recommended adding a drug from another of the first-tier treatment classes, based on expert opinion. The preferred medication intensification strategies are:
- Maximizing the first medication before adding a second, as was done in the randomized controlled trials
- Adding a second medication before reaching the maximum dose of the first, recognizing dose plateau relationships
- Starting with two medication classes separately or as a fixed-dose combination, a strategy that enhances hypertension control in large populations.
At the conclusion of the process, three drug classes are maximized as needed to achieve the goal blood pressure (Table 3).
CONTROVERSY REGARDING GOAL SYSTOLIC PRESSURE IN THE ELDERLY
JNC 8 set a systolic blood pressure target of less than 150 mm Hg in patients 60 years and older without diabetes or chronic kidney disease. This target was based on results of the Systolic Hypertension in the Elderly Program (SHEP)21 and the Systolic Hypertension in Europe (Syst-Eur) trial.22 In SHEP,21 the goal systolic pressure was individually tailored on the basis of the systolic pressure at study entry, and mean of the trial participants’ goal systolic pressure was less than 148 mm Hg, compared with less than 150 mm Hg in Syst-Eur.22 Participants in these two trials were representative of a broad spectrum of cardiovascular risk. In SHEP, 14% of the patients were black, compared with 12.6% in the US population, and both studies included patients with a history of myocardial infarction and stroke. In SHEP, 61% of the patients had a baseline electrocardiographic abnormality, and 30% of patients in Syst-Eur had a prior “cardiovascular complication.” In these randomized controlled trials, stroke, the primary end point, was reduced by 32% and 31% respectively, and major cardiovascular events were reduced by 32% and 31%, respectively.21,22
The JNC 8 panel followed a process mandated by the National Heart, Lung, and Blood Institute (NHLBI) that excluded “as-treated” or “achieved” blood pressure trials such as the Felodipine Event Reduction study (FEVER)23 because of bias due to selection of patients of inherently low cardiovascular risk who were associated with lower achieved systolic pressures. Cochrane methodologists independently arrived at the same conclusion.24 In fact, in the landmark African American Study of Kidney Disease and Hypertension (AASK), a post hoc analysis according to the blood pressure achieved indicated improved renal outcomes associated with lower achieved blood pressures—the opposite conclusion of the intention-to-treat blood pressure analysis.25 Alternative viewpoints and guidelines recommending the older goal of less than 140/90 mm Hg for elderly patients rely on observational and post hoc data, which were excluded by the National Heart, Lung, and Blood Institute process.26
As this article is prepared for publication, a press release from the NHLBI announced that the Safety and Monitoring Committee of the Systolic Blood Pressure Intervention trial (SPRINT) stopped the study early because of fewer cardiovascular complications and lower mortality in the more intensely treated group.27 SPRINT randomized more than 9,300 patients age 50 years and older with at least one additional cardiovascular disease risk factor to an intensive treatment arm targeting goal systolic pressure less than 120 mm Hg vs a standard treatment arm targeting goal systolic pressure less than 140 mm Hg. Approximately 25% of patients were age 75 years and older. Preliminary data indicate reduction of the primary composite outcome of fatal and nonfatal cardiovascular disease events by 30% and a 25% reduction in overall mortality that was homogeneous across major prespecified subgroups including those above and below age 75 years. The intensive treatment protocol was based upon combination therapy with a thiazide-type diuretic and/or an ACE inhibitor or angiotensin receptor blocker (but not both) and/or a calcium channel blocker.28
Hypertension treatment guidelines need to be based upon the results of high value randomized clinical trials and the federally funded NHLBI sponsored SHEP, ALLHAT, Action to Control Cardiovascular Risk in Diabetes (ACCORD),29 and SPRINT trials are noteworthy. Because the results of SPRINT are preliminary, updated recommendations need to await a peer reviewed publication. Important questions include the magnitude of the absolute risk reductions in SPRINT, and the apparent disparity between the ACCORD and SPRINT outcomes. ACCORD was similar in design to SPRINT, examining the same primary composite outcome and comparing goal systolic pressure less than 120 mm Hg to goal systolic pressure less than 140 mm Hg in patients with diabetes defined as glycated hemoglobin at least 7.5%. The principle finding was that there was no difference in benefit, but there was a significant increase in adverse events driven by hypotension.29
Additionally, rather than dialing in blood pressures for patients, the effect of antihypertensive treatment of large populations is to move mean population pressure and the bell shaped curve of blood pressure distribution. For example, in the southern California Kaiser Permanente hypertension population age 60 years and over, a hypertension control rate of almost 90% achieving goal blood pressure less than 140/90 mm Hg has moved the mean systolic pressure to 127 mm Hg. Almost 10% of treated patients have a last systolic pressure less than 110 mm Hg, and safety net features have been introduced to downtitrate medications for these individuals. Achieving 90% control with goal systolic pressure less than 120 mm Hg would be proportionally forecasted to move the population mean systolic pressure to 107 mm Hg, with systolic pressures in the 80s and 90s for sizable numbers of patients. Potential SPRINT implementation would require strong anticipatory safety net features. How many antihypertensive medications should be used to drive systolic pressure less than 120 mm Hg in more resistant patients? Certainly SPRINT raises important strategic population care issues.
POPULATION CARE STRATEGIES IN A FRACTURED HEALTHCARE DELIVERY SYSTEM
High rates of hypertension control have been achieved in large, very well-integrated healthcare systems even before widespread adoption of the electronic health record,5,30,31 and the essential implementation principles can be adapted to large and small health plans (Table 4).
A hypertension registry is necessary to generate regular performance feedback reports, and performance feedback provides factual information to drive improvement via competition and sharing of best practices. Those experienced in registry building can share their experience.5,31 Creating a hypertension registry may be as simple as identifying all patients who have an International Classification of Diseases 9 (ICD 9) code of 401.9 (essential hypertension) twice within a rolling 12-month period.
Antihypertensive drug treatment protocols should be simple, inclusive, and evidence-based. Although there are thousands of individual drug permutations of the JNC 8 treatment algorithm, ease of implementation should always be the tie-breaker. Most often, a treatment algorithm based on single-pill combination therapy will fulfill those requirements.
For example, one could start with one-half of a combination pill containing lisinopril 20 mg and hydrochlorothiazide 25 mg and then, at intervals of 2 to 4 weeks, titrate this dosage up to a full pill and then to two pills (ie, lisinopril 40 mg plus hydrochlorothiazide 50 mg) before adding amlodipine in sequentially higher doses to achieve goal blood pressure. This algorithm is inclusive for black patients, patients with stage 1, 2, or 3 chronic kidney disease, and patients with diabetes. There is good physiologic support for combination drugs, and goal blood pressure is achieved more rapidly than with sequential monotherapy.32,33 The ACCOMPLISH trial, which showed an ACE inhibitor-calcium channel blocker combination to be superior to an ACE inhibitor plus a thiazide diuretic, was not considered definitive in either the JNC 8 or European guideline reports.5,34 Implementation success supports protocol-driven algorithmic care,35 which can be practiced by physician providers, nurse practitioners, and clinical pharmacists within their scope of practice.
Given the large number of hypertensive patients, the multiple medication titration encounters necessary to attain high control rates, and the limited numbers of providers who can prescribe medication, medical and clinical assistants play a key role. The protocol-driven no-copayment walk-in or scheduled blood pressure check is an essential component of hypertension care.5,31
These principles focus on simplicity and inclusiveness and can drive high hypertension control rates nationally across a wide spectrum of healthcare plan capabilities. Health plans practicing equitable care, assigning priority and additional resources to black patients with hypertension, can close the racial performance gap.36
- Piper MA, Evans CV, Burda BU, Margolis KL, O’Connor E, Whitlock EP. Diagnostic and predictive accuracy of blood pressure screening methods with consideragnostic and predictive accuracy of blood pressure screening methods with consideration of rescreening intervals: an updated systematic review for the U.S. Preventive Services Task Force. Ann Intern Med 2015; 162:192–204.
- Cloutier L, Daskalopoulu SS, Padwal RS, et al. A new algorithm for the diagnosis of hypertension in Canada. Can J Cardiol 2015; 31:620–630.
- Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D. Call to action on use and reimbursement for home blood pressure monitoring: executive summary. A joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. J Am Soc Hypertens 2008; 2:192–202.
- Chobanian AV, Bakris GL, Black HR, et al; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42:1206–1252.
- Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved blood pressure control associated with a large-scale hypertension program. JAMA 2013; 310: 699–705.
- Ringerman E, Flint LJ, Hughes DE. An innovative education program. The peer competency validator model. J Nurses in Staff Development 2006; 22:114–121.
- Reeves RA. Does this patient have hypertension? How to measure blood pressure. JAMA 1995; 273:1211–1218.
- Le Pailleur C, Helft G, Landais P, et al. The effects of talking, reading, and silence on the “white coat” phenomenon in hypertensive patients. Am J Hypertens 1998; 11:203–207.
- Kaplan NM. Chapter 2. Measurement of blood pressure. In: Kaplan NM, Victor RG, eds. Kaplan’s Clinical Hypertension, 11th ed. Philadelphia, PA: Wolters Kluwer, 2015:1–39.
- James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014; 311:507–520.
- Dahlöf B, Devereux RB, Kjeldsen SE, et al; LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention for Endpoint reduction in hypertension study (LIFE): a randomized trial against atenolol. Lancet 2002; 359:995–1003.
- Wright JT Jr, Dunn JK, Cutler JA, et al; ALLHAT Collaborative Research Group. Outcomes in hypertensive black and nonblack patients treated with chlorthalidone, amlodipine, and lisinopril. JAMA 2005; 293:1595–1608.
- Brown MJ, Palmer CR, Castaigne A, et al. Morbidity and mortality in patients randomized to double-blind treatment with a long-acting calcium-channel blocker or diuretic in the International Nifedipine GITS study: Intervention as a goal in Hypertension Treatment (INSIGHT). Lancet 2000; 356:366–372.
- Wing LM, Reid CM, Ryan P, et al; Second Australian National Blood Pressure Study Group. A comparison of outcomes with angiotensin-converting-enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med 2003; 348:583–592.
- Jamerson K, Weber MA, Bakris GL, et al; ACCOMPLISH Trial Investigators. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med 2008; 359:2417–2428.
- Rahman M, Pressel S, Davis BR, et al. Renal outcomes in high-risk hypertensive patients treated with an angiotensin-converting enzyme inhibitor or a calcium channel blocker vs a diuretic: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med 2005; 165:936–946.
- Barzilay JI, Davis BR, Cutler JA, et al; ALLHAT Collaborative Research Group. Fasting glucose levels and incident diabetes mellitus in older nondiabetic adults randomized to receive 3 different classes of antihypertensive treatment: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med 2006; 166:2191–2201.
- James PA, Oparil S, Carter BL, et al. Supplement to 2014 evidence-based guideline for the management of high blood pressure in adults: report by the panel appointed to the Eighth Joint National Committee (JNC 8). Available at http://jama. jamanetwork.com/article.aspx?articleid=1791497. Accessed August 3, 2015.
- ONTARGET Investigators; Yusuf S, Teo KK, Pogue J, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med 2008; 358: 1547–1559.
- Palmer BF. Renal dysfunction complicating the treatment of hypertension. N Engl J Med 2002; 347:1256–1261.
- SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA 1991; 265:3255–3264.
- Staessen JA, Fagard R, Thijs L, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet 1997; 350:757–764.
- Liu L, Zhang Y, Liu G, Zhang X, Zanchetti A; FEVER Study Group. The Felodipine Event Reduction (FEVER) study: a randomized long-term placebo-controlled trial in Chinese hypertensive patients. J Hypertens 2005; 23:2157–2172.
- Arguedas JA, Perez MI, Wright JM. Treatment blood pressure targets for hypertension. Cochrane Database of Syst Rev 2009 Jul 8; (3):CD004349.
- Davis EM, Appel LJ, Wang X, et al; African American Study of Kidney Disease and Hypertension Research Collaborative Group. Limitations of analyses based on achieved blood pressure: lessons from the African American Study of Kidney Disease and Hypertension Trial. Hypertension 2011; 57:1061–1068.
- Handler J. 2014 Hypertension guideline: recommendation for a change in systolic blood pressure. Perm J 2015; 19:64–72.
- National Heart Lung and Blood Institute. Landmark NIH study shows intensive blood pressure management may save lives. Available at: http://www.nhlbi.nih.gov/ news/press-releases/2015/landmark-nih-study-shows-intensive-blood-pressure-management-may-save-lives. Published September 11, 2015. Accessed September 16, 2015.
- Ambrosius WT, Sink KM, Foy CG, et al; SPRINT Study Research Group. The design and rationale of a multicenter clinical trial comparing two strategies for control of systolic blood pressure: the Systolic Blood Pressure Intervention Trial (SPRINT) Clin Trials 2014; 11:1–15.
- The ACCORD Study Group, Cushman WC, Evans GW, Byington RP, et al. Effects of intensive blood pressure control in type 2 diabetes mellitus. N Engl J Med 2010; 362:1575–1585.
- Shaw KM, Handler J, Wall HK, Kanter MH. Improving blood pressure control in a large multiethnic California population through changes in health care delivery, 2004–2012. Prev Chronic Dis 2014; 11:E191.
- Sim JJ, Handler J, Jacobsen SJ, Kanter MH. Systematic implementation strategies to improve hypertension: the Kaiser Permanente Southern California experience. Can J Cardiol 2014; 30:544–552.
- Gradman AH, Basile JN, Carter BL, Bakris GL; American Society of Hypertension Writing Group. Combination therapy in hypertension. J Am Soc Hypertens 2010; 4:42–50.
- Feldman RD, Zou GY, Vandervoort MK, Wong CJ, Nelson SAE, Feagan BG. A simplified approach to the treatment of uncomplicated hypertension: a cluster randomized, controlled trial. Hypertension 2009; 53:646–653.
- Mancia G, Fagard R, Narkiewicz K, et al; Task Force Members. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013; 31:1281–1357.
- Frieden TR, King SM, Wright JS. Protocol-based treatment of hypertension: a critical step on the pathway to progress. JAMA 2014; 311:21–22.
- Ayanian JZ, Landon BE, Newhouse JP, Zaslavsky AM. Racial and ethnic disparities among enrollees in Medicare advantage plans. N Engl J Med 2014; 371: 2288–2297.
Hypertension is a primary care specialty. Most of the 70,000,000 adult Americans with hypertension are cared for by primary care providers. Medications are readily available that achieve high control rates when used in combination. Primary care providers are uniquely positioned to lead team-oriented approaches to improve medication adherence and provide equitable care that addresses racial disparity in hypertension control.
This review focuses on some of the challenges that primary care providers face, including diagnosis of hypertension, medication options, controversy regarding the goal systolic blood pressure in the elderly, and population care strategies in our fractured healthcare system.
USING OUT-OF-OFFICE AND AUTOMATED MEASUREMENTS FOR DIAGNOSIS
A systematic review performed for the US Preventive Services Task Force concluded that the evidence supports ambulatory monitoring to confirm blood pressure in the office in all but the most severe cases of office-based blood pressure elevation in order to avoid misdiagnosis and overtreatment.1 Elevated ambulatory pressure is the best predictor of cardiovascular events in prospective cohort studies.1 A new hypertension diagnostic algorithm for Canada2 is similar to an earlier American Heart Association algorithm3 in recommending diagnostic confirmation by out-of-office measures including home blood pressure, ambulatory pressure, or automated office blood pressures. With automated blood pressure measurement, the clinician or medical assistant initiates preprogrammed oscillometric devices to take sequential blood pressure measurements after the assistant leaves the examining room. Thresholds for the diagnosis of hypertension are1,2:
- Office measurements: ≥ 140/90 mm Hg
- Automated office measurements (mean): ≥ 135/ 85 mm Hg
- Home blood pressure measurements: ≥ 135/85 mm Hg
- Ambulatory monitoring (mean of daytime readings): ≥ 135/85 mm Hg
- Ambulatory monitoring (mean 24-hour reading): ≥ 130/80 mm Hg.
However, evidence supporting the use of ambulatory monitoring, home measurements, and automated office measurements has significant limitations. There is no evidence from prospective randomized controlled trials that withholding treatment on the basis of these measurements when office blood pressures are elevated leads to cardiovascular outcomes equivalent to normotensive outcomes. Also, the Centers for Medicare and Medicaid Services do not reimburse for ambulatory blood pressure monitoring, which would lead to inconsistent implementation and more disparity in healthcare. Moreover, when ambulatory monitoring is used to diagnose hypertension, how to determine response to treatment has not been defined.
Table 1 summarizes recommendations for the use of out-of-office measurements to diagnose hypertension.1–4 System-wide efforts can reduce the need for out-of-office confirmation; these include improving competence in measuring office blood pressure through peer validator spot-checking in the normal workflow, performance feedback reporting of repeat measurements when the first is elevated, and extensive use of walk-in measurements to reduce the white-coat effect.5,6 Two well-performed office measurements performed on each of two or three visits over at least a month will continue to be the diagnostic standard for most patients. Small errors in technique introduce inaccuracies in blood pressure readings, which, if falsely high, can lead to unnecessary treatment or, conversely, if falsely low can lead to inadequate treatment. Table 2 lists several common measurement errors that need to be consistently avoided.7–9
ANTIHYPERTENSIVE DRUG TREATMENT STRATEGIES
The Eighth Joint National Committee (JNC 8)10 issued a strictly evidence-based guideline based on adequate randomized controlled trials comparing representative drugs of different antihypertensive classes with respect to hard cardiovascular outcomes to arrive at well-supported recommendations (Table 3). The three groups of agents with the greatest evidence to support their use are:
- Thiazide-type diuretics
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers
- Calcium channel blockers.
Beta-blockers did not make the first tier because the beta-blocker atenolol was found to be inferior to the angiotensin receptor blocker losartan in terms of the rate of the primary end point (death, myocardial infarction, or stroke) in the Losartan Intervention For Endpoint Reduction in Hypertension (LIFE) trial,11 and we lack hard end point evidence to support other beta-blockers. However, patients with coronary artery disease or heart failure have a compelling drug-specific indication for a beta-blocker outside of blood pressure reduction.
There is an important race-based difference in the initial antihypertensive drug treatment options based on the findings of the prespecified subgroup of more than 10,000 black patients in the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT).12 The thiazide-type diuretic chlorthalidone was more effective than the ACE inhibitor lisinopril in improving the rates of adverse cardiovascular and cerebrovascular outcomes, including stroke and heart failure, and the calcium channel blocker amlodipine was more effective than lisinopril in improving the rate of stroke. There have been no randomized controlled trials or prespecified subgroups in randomized controlled trials evaluating angiotensin receptor blockers in black patients. Therefore, thiazide-type diuretics and calcium channel blockers are the preferred initial options for reducing cardiovascular outcomes in the general black population. ACE inhibitors and angiotensin receptor blockers are preferred across all races for patients with chronic kidney disease to improve renal outcomes.10 However, a strategy using initial combination therapy with an ACE inhibitor or an angioten sin receptor blocker together with a thiazide diuretic or calcium channel blocker does satisfy the evidence, improving both cardiovascular and renal outcomes in black patients with and without chronic kidney disease.
JNC 8 recommended thiazide-type diuretics as a class rather than specifically recommending chlorthalidone because confirmatory trials used thiazide-type diuretics other than chlorthalidone, such as hydrochlorothiazide. For example, whereas the ALLHAT trial found that chlorthalidone 12.5 or 25 mg was superior to the calcium channel blocker amlodipine in terms of reducing the incidence of heart failure, the International Nifedipine Study: Intervention as a Goal in Hypertension Treatment (INSIGHT) similarly found that hydrochlorothiazide titrated up to 50 mg was superior to the calcium channel blocker nifedipine in reducing the incidence of heart failure.13
Dose as well as drug is important. Inadequately dosed hydrochlorothiazide (12.5–25 mg/day) in the Second Australian National Blood Pressure (ANBP2) and the Avoiding Cardiovascular Events through Combination Therapy in Patients with Systolic Hypertension (ACCOMPLISH) trials14,15 did not fare as well as comparator agents. The hydrochlorothiazide dosage in these trials was decided on the basis of usual prescribing practices rather than strict examination of prior comparators. Common rationales for prescribing lower doses of diuretics are fear of renal fail- ure in the elderly or drug-induced incident diabetes. However, analyses of ALLHAT patients did not reveal increased renal failure or worsened outcomes due to drug-related diabetes.16,17 A supplement to the JNC 8 report, available online, provides a rationale for the target hydrochlorothiazide dose of 50 mg.18
ACE inhibitors and angiotensin receptor blockers should not be prescribed together to control hypertension in the general population, due to increased risk of acute renal failure.19 However, a nonprogressive decrease in creatinine clearance of up to 30% at the beginning of ACE inhibitor or angiotensin receptor blocker therapy in patients who have chronic kidney disease can be viewed as a good sign, indicating that intraglomerular pressure has been reduced and the kidneys are better protected against structural damage.20
Intensifying therapy
While the first-tier antihypertensive drug classes have been identified by randomized controlled trials, most patients require drug intensification. In the absence of randomized controlled trials examining second-step options, the JNC 8 recommended adding a drug from another of the first-tier treatment classes, based on expert opinion. The preferred medication intensification strategies are:
- Maximizing the first medication before adding a second, as was done in the randomized controlled trials
- Adding a second medication before reaching the maximum dose of the first, recognizing dose plateau relationships
- Starting with two medication classes separately or as a fixed-dose combination, a strategy that enhances hypertension control in large populations.
At the conclusion of the process, three drug classes are maximized as needed to achieve the goal blood pressure (Table 3).
CONTROVERSY REGARDING GOAL SYSTOLIC PRESSURE IN THE ELDERLY
JNC 8 set a systolic blood pressure target of less than 150 mm Hg in patients 60 years and older without diabetes or chronic kidney disease. This target was based on results of the Systolic Hypertension in the Elderly Program (SHEP)21 and the Systolic Hypertension in Europe (Syst-Eur) trial.22 In SHEP,21 the goal systolic pressure was individually tailored on the basis of the systolic pressure at study entry, and mean of the trial participants’ goal systolic pressure was less than 148 mm Hg, compared with less than 150 mm Hg in Syst-Eur.22 Participants in these two trials were representative of a broad spectrum of cardiovascular risk. In SHEP, 14% of the patients were black, compared with 12.6% in the US population, and both studies included patients with a history of myocardial infarction and stroke. In SHEP, 61% of the patients had a baseline electrocardiographic abnormality, and 30% of patients in Syst-Eur had a prior “cardiovascular complication.” In these randomized controlled trials, stroke, the primary end point, was reduced by 32% and 31% respectively, and major cardiovascular events were reduced by 32% and 31%, respectively.21,22
The JNC 8 panel followed a process mandated by the National Heart, Lung, and Blood Institute (NHLBI) that excluded “as-treated” or “achieved” blood pressure trials such as the Felodipine Event Reduction study (FEVER)23 because of bias due to selection of patients of inherently low cardiovascular risk who were associated with lower achieved systolic pressures. Cochrane methodologists independently arrived at the same conclusion.24 In fact, in the landmark African American Study of Kidney Disease and Hypertension (AASK), a post hoc analysis according to the blood pressure achieved indicated improved renal outcomes associated with lower achieved blood pressures—the opposite conclusion of the intention-to-treat blood pressure analysis.25 Alternative viewpoints and guidelines recommending the older goal of less than 140/90 mm Hg for elderly patients rely on observational and post hoc data, which were excluded by the National Heart, Lung, and Blood Institute process.26
As this article is prepared for publication, a press release from the NHLBI announced that the Safety and Monitoring Committee of the Systolic Blood Pressure Intervention trial (SPRINT) stopped the study early because of fewer cardiovascular complications and lower mortality in the more intensely treated group.27 SPRINT randomized more than 9,300 patients age 50 years and older with at least one additional cardiovascular disease risk factor to an intensive treatment arm targeting goal systolic pressure less than 120 mm Hg vs a standard treatment arm targeting goal systolic pressure less than 140 mm Hg. Approximately 25% of patients were age 75 years and older. Preliminary data indicate reduction of the primary composite outcome of fatal and nonfatal cardiovascular disease events by 30% and a 25% reduction in overall mortality that was homogeneous across major prespecified subgroups including those above and below age 75 years. The intensive treatment protocol was based upon combination therapy with a thiazide-type diuretic and/or an ACE inhibitor or angiotensin receptor blocker (but not both) and/or a calcium channel blocker.28
Hypertension treatment guidelines need to be based upon the results of high value randomized clinical trials and the federally funded NHLBI sponsored SHEP, ALLHAT, Action to Control Cardiovascular Risk in Diabetes (ACCORD),29 and SPRINT trials are noteworthy. Because the results of SPRINT are preliminary, updated recommendations need to await a peer reviewed publication. Important questions include the magnitude of the absolute risk reductions in SPRINT, and the apparent disparity between the ACCORD and SPRINT outcomes. ACCORD was similar in design to SPRINT, examining the same primary composite outcome and comparing goal systolic pressure less than 120 mm Hg to goal systolic pressure less than 140 mm Hg in patients with diabetes defined as glycated hemoglobin at least 7.5%. The principle finding was that there was no difference in benefit, but there was a significant increase in adverse events driven by hypotension.29
Additionally, rather than dialing in blood pressures for patients, the effect of antihypertensive treatment of large populations is to move mean population pressure and the bell shaped curve of blood pressure distribution. For example, in the southern California Kaiser Permanente hypertension population age 60 years and over, a hypertension control rate of almost 90% achieving goal blood pressure less than 140/90 mm Hg has moved the mean systolic pressure to 127 mm Hg. Almost 10% of treated patients have a last systolic pressure less than 110 mm Hg, and safety net features have been introduced to downtitrate medications for these individuals. Achieving 90% control with goal systolic pressure less than 120 mm Hg would be proportionally forecasted to move the population mean systolic pressure to 107 mm Hg, with systolic pressures in the 80s and 90s for sizable numbers of patients. Potential SPRINT implementation would require strong anticipatory safety net features. How many antihypertensive medications should be used to drive systolic pressure less than 120 mm Hg in more resistant patients? Certainly SPRINT raises important strategic population care issues.
POPULATION CARE STRATEGIES IN A FRACTURED HEALTHCARE DELIVERY SYSTEM
High rates of hypertension control have been achieved in large, very well-integrated healthcare systems even before widespread adoption of the electronic health record,5,30,31 and the essential implementation principles can be adapted to large and small health plans (Table 4).
A hypertension registry is necessary to generate regular performance feedback reports, and performance feedback provides factual information to drive improvement via competition and sharing of best practices. Those experienced in registry building can share their experience.5,31 Creating a hypertension registry may be as simple as identifying all patients who have an International Classification of Diseases 9 (ICD 9) code of 401.9 (essential hypertension) twice within a rolling 12-month period.
Antihypertensive drug treatment protocols should be simple, inclusive, and evidence-based. Although there are thousands of individual drug permutations of the JNC 8 treatment algorithm, ease of implementation should always be the tie-breaker. Most often, a treatment algorithm based on single-pill combination therapy will fulfill those requirements.
For example, one could start with one-half of a combination pill containing lisinopril 20 mg and hydrochlorothiazide 25 mg and then, at intervals of 2 to 4 weeks, titrate this dosage up to a full pill and then to two pills (ie, lisinopril 40 mg plus hydrochlorothiazide 50 mg) before adding amlodipine in sequentially higher doses to achieve goal blood pressure. This algorithm is inclusive for black patients, patients with stage 1, 2, or 3 chronic kidney disease, and patients with diabetes. There is good physiologic support for combination drugs, and goal blood pressure is achieved more rapidly than with sequential monotherapy.32,33 The ACCOMPLISH trial, which showed an ACE inhibitor-calcium channel blocker combination to be superior to an ACE inhibitor plus a thiazide diuretic, was not considered definitive in either the JNC 8 or European guideline reports.5,34 Implementation success supports protocol-driven algorithmic care,35 which can be practiced by physician providers, nurse practitioners, and clinical pharmacists within their scope of practice.
Given the large number of hypertensive patients, the multiple medication titration encounters necessary to attain high control rates, and the limited numbers of providers who can prescribe medication, medical and clinical assistants play a key role. The protocol-driven no-copayment walk-in or scheduled blood pressure check is an essential component of hypertension care.5,31
These principles focus on simplicity and inclusiveness and can drive high hypertension control rates nationally across a wide spectrum of healthcare plan capabilities. Health plans practicing equitable care, assigning priority and additional resources to black patients with hypertension, can close the racial performance gap.36
Hypertension is a primary care specialty. Most of the 70,000,000 adult Americans with hypertension are cared for by primary care providers. Medications are readily available that achieve high control rates when used in combination. Primary care providers are uniquely positioned to lead team-oriented approaches to improve medication adherence and provide equitable care that addresses racial disparity in hypertension control.
This review focuses on some of the challenges that primary care providers face, including diagnosis of hypertension, medication options, controversy regarding the goal systolic blood pressure in the elderly, and population care strategies in our fractured healthcare system.
USING OUT-OF-OFFICE AND AUTOMATED MEASUREMENTS FOR DIAGNOSIS
A systematic review performed for the US Preventive Services Task Force concluded that the evidence supports ambulatory monitoring to confirm blood pressure in the office in all but the most severe cases of office-based blood pressure elevation in order to avoid misdiagnosis and overtreatment.1 Elevated ambulatory pressure is the best predictor of cardiovascular events in prospective cohort studies.1 A new hypertension diagnostic algorithm for Canada2 is similar to an earlier American Heart Association algorithm3 in recommending diagnostic confirmation by out-of-office measures including home blood pressure, ambulatory pressure, or automated office blood pressures. With automated blood pressure measurement, the clinician or medical assistant initiates preprogrammed oscillometric devices to take sequential blood pressure measurements after the assistant leaves the examining room. Thresholds for the diagnosis of hypertension are1,2:
- Office measurements: ≥ 140/90 mm Hg
- Automated office measurements (mean): ≥ 135/ 85 mm Hg
- Home blood pressure measurements: ≥ 135/85 mm Hg
- Ambulatory monitoring (mean of daytime readings): ≥ 135/85 mm Hg
- Ambulatory monitoring (mean 24-hour reading): ≥ 130/80 mm Hg.
However, evidence supporting the use of ambulatory monitoring, home measurements, and automated office measurements has significant limitations. There is no evidence from prospective randomized controlled trials that withholding treatment on the basis of these measurements when office blood pressures are elevated leads to cardiovascular outcomes equivalent to normotensive outcomes. Also, the Centers for Medicare and Medicaid Services do not reimburse for ambulatory blood pressure monitoring, which would lead to inconsistent implementation and more disparity in healthcare. Moreover, when ambulatory monitoring is used to diagnose hypertension, how to determine response to treatment has not been defined.
Table 1 summarizes recommendations for the use of out-of-office measurements to diagnose hypertension.1–4 System-wide efforts can reduce the need for out-of-office confirmation; these include improving competence in measuring office blood pressure through peer validator spot-checking in the normal workflow, performance feedback reporting of repeat measurements when the first is elevated, and extensive use of walk-in measurements to reduce the white-coat effect.5,6 Two well-performed office measurements performed on each of two or three visits over at least a month will continue to be the diagnostic standard for most patients. Small errors in technique introduce inaccuracies in blood pressure readings, which, if falsely high, can lead to unnecessary treatment or, conversely, if falsely low can lead to inadequate treatment. Table 2 lists several common measurement errors that need to be consistently avoided.7–9
ANTIHYPERTENSIVE DRUG TREATMENT STRATEGIES
The Eighth Joint National Committee (JNC 8)10 issued a strictly evidence-based guideline based on adequate randomized controlled trials comparing representative drugs of different antihypertensive classes with respect to hard cardiovascular outcomes to arrive at well-supported recommendations (Table 3). The three groups of agents with the greatest evidence to support their use are:
- Thiazide-type diuretics
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers
- Calcium channel blockers.
Beta-blockers did not make the first tier because the beta-blocker atenolol was found to be inferior to the angiotensin receptor blocker losartan in terms of the rate of the primary end point (death, myocardial infarction, or stroke) in the Losartan Intervention For Endpoint Reduction in Hypertension (LIFE) trial,11 and we lack hard end point evidence to support other beta-blockers. However, patients with coronary artery disease or heart failure have a compelling drug-specific indication for a beta-blocker outside of blood pressure reduction.
There is an important race-based difference in the initial antihypertensive drug treatment options based on the findings of the prespecified subgroup of more than 10,000 black patients in the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT).12 The thiazide-type diuretic chlorthalidone was more effective than the ACE inhibitor lisinopril in improving the rates of adverse cardiovascular and cerebrovascular outcomes, including stroke and heart failure, and the calcium channel blocker amlodipine was more effective than lisinopril in improving the rate of stroke. There have been no randomized controlled trials or prespecified subgroups in randomized controlled trials evaluating angiotensin receptor blockers in black patients. Therefore, thiazide-type diuretics and calcium channel blockers are the preferred initial options for reducing cardiovascular outcomes in the general black population. ACE inhibitors and angiotensin receptor blockers are preferred across all races for patients with chronic kidney disease to improve renal outcomes.10 However, a strategy using initial combination therapy with an ACE inhibitor or an angioten sin receptor blocker together with a thiazide diuretic or calcium channel blocker does satisfy the evidence, improving both cardiovascular and renal outcomes in black patients with and without chronic kidney disease.
JNC 8 recommended thiazide-type diuretics as a class rather than specifically recommending chlorthalidone because confirmatory trials used thiazide-type diuretics other than chlorthalidone, such as hydrochlorothiazide. For example, whereas the ALLHAT trial found that chlorthalidone 12.5 or 25 mg was superior to the calcium channel blocker amlodipine in terms of reducing the incidence of heart failure, the International Nifedipine Study: Intervention as a Goal in Hypertension Treatment (INSIGHT) similarly found that hydrochlorothiazide titrated up to 50 mg was superior to the calcium channel blocker nifedipine in reducing the incidence of heart failure.13
Dose as well as drug is important. Inadequately dosed hydrochlorothiazide (12.5–25 mg/day) in the Second Australian National Blood Pressure (ANBP2) and the Avoiding Cardiovascular Events through Combination Therapy in Patients with Systolic Hypertension (ACCOMPLISH) trials14,15 did not fare as well as comparator agents. The hydrochlorothiazide dosage in these trials was decided on the basis of usual prescribing practices rather than strict examination of prior comparators. Common rationales for prescribing lower doses of diuretics are fear of renal fail- ure in the elderly or drug-induced incident diabetes. However, analyses of ALLHAT patients did not reveal increased renal failure or worsened outcomes due to drug-related diabetes.16,17 A supplement to the JNC 8 report, available online, provides a rationale for the target hydrochlorothiazide dose of 50 mg.18
ACE inhibitors and angiotensin receptor blockers should not be prescribed together to control hypertension in the general population, due to increased risk of acute renal failure.19 However, a nonprogressive decrease in creatinine clearance of up to 30% at the beginning of ACE inhibitor or angiotensin receptor blocker therapy in patients who have chronic kidney disease can be viewed as a good sign, indicating that intraglomerular pressure has been reduced and the kidneys are better protected against structural damage.20
Intensifying therapy
While the first-tier antihypertensive drug classes have been identified by randomized controlled trials, most patients require drug intensification. In the absence of randomized controlled trials examining second-step options, the JNC 8 recommended adding a drug from another of the first-tier treatment classes, based on expert opinion. The preferred medication intensification strategies are:
- Maximizing the first medication before adding a second, as was done in the randomized controlled trials
- Adding a second medication before reaching the maximum dose of the first, recognizing dose plateau relationships
- Starting with two medication classes separately or as a fixed-dose combination, a strategy that enhances hypertension control in large populations.
At the conclusion of the process, three drug classes are maximized as needed to achieve the goal blood pressure (Table 3).
CONTROVERSY REGARDING GOAL SYSTOLIC PRESSURE IN THE ELDERLY
JNC 8 set a systolic blood pressure target of less than 150 mm Hg in patients 60 years and older without diabetes or chronic kidney disease. This target was based on results of the Systolic Hypertension in the Elderly Program (SHEP)21 and the Systolic Hypertension in Europe (Syst-Eur) trial.22 In SHEP,21 the goal systolic pressure was individually tailored on the basis of the systolic pressure at study entry, and mean of the trial participants’ goal systolic pressure was less than 148 mm Hg, compared with less than 150 mm Hg in Syst-Eur.22 Participants in these two trials were representative of a broad spectrum of cardiovascular risk. In SHEP, 14% of the patients were black, compared with 12.6% in the US population, and both studies included patients with a history of myocardial infarction and stroke. In SHEP, 61% of the patients had a baseline electrocardiographic abnormality, and 30% of patients in Syst-Eur had a prior “cardiovascular complication.” In these randomized controlled trials, stroke, the primary end point, was reduced by 32% and 31% respectively, and major cardiovascular events were reduced by 32% and 31%, respectively.21,22
The JNC 8 panel followed a process mandated by the National Heart, Lung, and Blood Institute (NHLBI) that excluded “as-treated” or “achieved” blood pressure trials such as the Felodipine Event Reduction study (FEVER)23 because of bias due to selection of patients of inherently low cardiovascular risk who were associated with lower achieved systolic pressures. Cochrane methodologists independently arrived at the same conclusion.24 In fact, in the landmark African American Study of Kidney Disease and Hypertension (AASK), a post hoc analysis according to the blood pressure achieved indicated improved renal outcomes associated with lower achieved blood pressures—the opposite conclusion of the intention-to-treat blood pressure analysis.25 Alternative viewpoints and guidelines recommending the older goal of less than 140/90 mm Hg for elderly patients rely on observational and post hoc data, which were excluded by the National Heart, Lung, and Blood Institute process.26
As this article is prepared for publication, a press release from the NHLBI announced that the Safety and Monitoring Committee of the Systolic Blood Pressure Intervention trial (SPRINT) stopped the study early because of fewer cardiovascular complications and lower mortality in the more intensely treated group.27 SPRINT randomized more than 9,300 patients age 50 years and older with at least one additional cardiovascular disease risk factor to an intensive treatment arm targeting goal systolic pressure less than 120 mm Hg vs a standard treatment arm targeting goal systolic pressure less than 140 mm Hg. Approximately 25% of patients were age 75 years and older. Preliminary data indicate reduction of the primary composite outcome of fatal and nonfatal cardiovascular disease events by 30% and a 25% reduction in overall mortality that was homogeneous across major prespecified subgroups including those above and below age 75 years. The intensive treatment protocol was based upon combination therapy with a thiazide-type diuretic and/or an ACE inhibitor or angiotensin receptor blocker (but not both) and/or a calcium channel blocker.28
Hypertension treatment guidelines need to be based upon the results of high value randomized clinical trials and the federally funded NHLBI sponsored SHEP, ALLHAT, Action to Control Cardiovascular Risk in Diabetes (ACCORD),29 and SPRINT trials are noteworthy. Because the results of SPRINT are preliminary, updated recommendations need to await a peer reviewed publication. Important questions include the magnitude of the absolute risk reductions in SPRINT, and the apparent disparity between the ACCORD and SPRINT outcomes. ACCORD was similar in design to SPRINT, examining the same primary composite outcome and comparing goal systolic pressure less than 120 mm Hg to goal systolic pressure less than 140 mm Hg in patients with diabetes defined as glycated hemoglobin at least 7.5%. The principle finding was that there was no difference in benefit, but there was a significant increase in adverse events driven by hypotension.29
Additionally, rather than dialing in blood pressures for patients, the effect of antihypertensive treatment of large populations is to move mean population pressure and the bell shaped curve of blood pressure distribution. For example, in the southern California Kaiser Permanente hypertension population age 60 years and over, a hypertension control rate of almost 90% achieving goal blood pressure less than 140/90 mm Hg has moved the mean systolic pressure to 127 mm Hg. Almost 10% of treated patients have a last systolic pressure less than 110 mm Hg, and safety net features have been introduced to downtitrate medications for these individuals. Achieving 90% control with goal systolic pressure less than 120 mm Hg would be proportionally forecasted to move the population mean systolic pressure to 107 mm Hg, with systolic pressures in the 80s and 90s for sizable numbers of patients. Potential SPRINT implementation would require strong anticipatory safety net features. How many antihypertensive medications should be used to drive systolic pressure less than 120 mm Hg in more resistant patients? Certainly SPRINT raises important strategic population care issues.
POPULATION CARE STRATEGIES IN A FRACTURED HEALTHCARE DELIVERY SYSTEM
High rates of hypertension control have been achieved in large, very well-integrated healthcare systems even before widespread adoption of the electronic health record,5,30,31 and the essential implementation principles can be adapted to large and small health plans (Table 4).
A hypertension registry is necessary to generate regular performance feedback reports, and performance feedback provides factual information to drive improvement via competition and sharing of best practices. Those experienced in registry building can share their experience.5,31 Creating a hypertension registry may be as simple as identifying all patients who have an International Classification of Diseases 9 (ICD 9) code of 401.9 (essential hypertension) twice within a rolling 12-month period.
Antihypertensive drug treatment protocols should be simple, inclusive, and evidence-based. Although there are thousands of individual drug permutations of the JNC 8 treatment algorithm, ease of implementation should always be the tie-breaker. Most often, a treatment algorithm based on single-pill combination therapy will fulfill those requirements.
For example, one could start with one-half of a combination pill containing lisinopril 20 mg and hydrochlorothiazide 25 mg and then, at intervals of 2 to 4 weeks, titrate this dosage up to a full pill and then to two pills (ie, lisinopril 40 mg plus hydrochlorothiazide 50 mg) before adding amlodipine in sequentially higher doses to achieve goal blood pressure. This algorithm is inclusive for black patients, patients with stage 1, 2, or 3 chronic kidney disease, and patients with diabetes. There is good physiologic support for combination drugs, and goal blood pressure is achieved more rapidly than with sequential monotherapy.32,33 The ACCOMPLISH trial, which showed an ACE inhibitor-calcium channel blocker combination to be superior to an ACE inhibitor plus a thiazide diuretic, was not considered definitive in either the JNC 8 or European guideline reports.5,34 Implementation success supports protocol-driven algorithmic care,35 which can be practiced by physician providers, nurse practitioners, and clinical pharmacists within their scope of practice.
Given the large number of hypertensive patients, the multiple medication titration encounters necessary to attain high control rates, and the limited numbers of providers who can prescribe medication, medical and clinical assistants play a key role. The protocol-driven no-copayment walk-in or scheduled blood pressure check is an essential component of hypertension care.5,31
These principles focus on simplicity and inclusiveness and can drive high hypertension control rates nationally across a wide spectrum of healthcare plan capabilities. Health plans practicing equitable care, assigning priority and additional resources to black patients with hypertension, can close the racial performance gap.36
- Piper MA, Evans CV, Burda BU, Margolis KL, O’Connor E, Whitlock EP. Diagnostic and predictive accuracy of blood pressure screening methods with consideragnostic and predictive accuracy of blood pressure screening methods with consideration of rescreening intervals: an updated systematic review for the U.S. Preventive Services Task Force. Ann Intern Med 2015; 162:192–204.
- Cloutier L, Daskalopoulu SS, Padwal RS, et al. A new algorithm for the diagnosis of hypertension in Canada. Can J Cardiol 2015; 31:620–630.
- Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D. Call to action on use and reimbursement for home blood pressure monitoring: executive summary. A joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. J Am Soc Hypertens 2008; 2:192–202.
- Chobanian AV, Bakris GL, Black HR, et al; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42:1206–1252.
- Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved blood pressure control associated with a large-scale hypertension program. JAMA 2013; 310: 699–705.
- Ringerman E, Flint LJ, Hughes DE. An innovative education program. The peer competency validator model. J Nurses in Staff Development 2006; 22:114–121.
- Reeves RA. Does this patient have hypertension? How to measure blood pressure. JAMA 1995; 273:1211–1218.
- Le Pailleur C, Helft G, Landais P, et al. The effects of talking, reading, and silence on the “white coat” phenomenon in hypertensive patients. Am J Hypertens 1998; 11:203–207.
- Kaplan NM. Chapter 2. Measurement of blood pressure. In: Kaplan NM, Victor RG, eds. Kaplan’s Clinical Hypertension, 11th ed. Philadelphia, PA: Wolters Kluwer, 2015:1–39.
- James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014; 311:507–520.
- Dahlöf B, Devereux RB, Kjeldsen SE, et al; LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention for Endpoint reduction in hypertension study (LIFE): a randomized trial against atenolol. Lancet 2002; 359:995–1003.
- Wright JT Jr, Dunn JK, Cutler JA, et al; ALLHAT Collaborative Research Group. Outcomes in hypertensive black and nonblack patients treated with chlorthalidone, amlodipine, and lisinopril. JAMA 2005; 293:1595–1608.
- Brown MJ, Palmer CR, Castaigne A, et al. Morbidity and mortality in patients randomized to double-blind treatment with a long-acting calcium-channel blocker or diuretic in the International Nifedipine GITS study: Intervention as a goal in Hypertension Treatment (INSIGHT). Lancet 2000; 356:366–372.
- Wing LM, Reid CM, Ryan P, et al; Second Australian National Blood Pressure Study Group. A comparison of outcomes with angiotensin-converting-enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med 2003; 348:583–592.
- Jamerson K, Weber MA, Bakris GL, et al; ACCOMPLISH Trial Investigators. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med 2008; 359:2417–2428.
- Rahman M, Pressel S, Davis BR, et al. Renal outcomes in high-risk hypertensive patients treated with an angiotensin-converting enzyme inhibitor or a calcium channel blocker vs a diuretic: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med 2005; 165:936–946.
- Barzilay JI, Davis BR, Cutler JA, et al; ALLHAT Collaborative Research Group. Fasting glucose levels and incident diabetes mellitus in older nondiabetic adults randomized to receive 3 different classes of antihypertensive treatment: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med 2006; 166:2191–2201.
- James PA, Oparil S, Carter BL, et al. Supplement to 2014 evidence-based guideline for the management of high blood pressure in adults: report by the panel appointed to the Eighth Joint National Committee (JNC 8). Available at http://jama. jamanetwork.com/article.aspx?articleid=1791497. Accessed August 3, 2015.
- ONTARGET Investigators; Yusuf S, Teo KK, Pogue J, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med 2008; 358: 1547–1559.
- Palmer BF. Renal dysfunction complicating the treatment of hypertension. N Engl J Med 2002; 347:1256–1261.
- SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA 1991; 265:3255–3264.
- Staessen JA, Fagard R, Thijs L, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet 1997; 350:757–764.
- Liu L, Zhang Y, Liu G, Zhang X, Zanchetti A; FEVER Study Group. The Felodipine Event Reduction (FEVER) study: a randomized long-term placebo-controlled trial in Chinese hypertensive patients. J Hypertens 2005; 23:2157–2172.
- Arguedas JA, Perez MI, Wright JM. Treatment blood pressure targets for hypertension. Cochrane Database of Syst Rev 2009 Jul 8; (3):CD004349.
- Davis EM, Appel LJ, Wang X, et al; African American Study of Kidney Disease and Hypertension Research Collaborative Group. Limitations of analyses based on achieved blood pressure: lessons from the African American Study of Kidney Disease and Hypertension Trial. Hypertension 2011; 57:1061–1068.
- Handler J. 2014 Hypertension guideline: recommendation for a change in systolic blood pressure. Perm J 2015; 19:64–72.
- National Heart Lung and Blood Institute. Landmark NIH study shows intensive blood pressure management may save lives. Available at: http://www.nhlbi.nih.gov/ news/press-releases/2015/landmark-nih-study-shows-intensive-blood-pressure-management-may-save-lives. Published September 11, 2015. Accessed September 16, 2015.
- Ambrosius WT, Sink KM, Foy CG, et al; SPRINT Study Research Group. The design and rationale of a multicenter clinical trial comparing two strategies for control of systolic blood pressure: the Systolic Blood Pressure Intervention Trial (SPRINT) Clin Trials 2014; 11:1–15.
- The ACCORD Study Group, Cushman WC, Evans GW, Byington RP, et al. Effects of intensive blood pressure control in type 2 diabetes mellitus. N Engl J Med 2010; 362:1575–1585.
- Shaw KM, Handler J, Wall HK, Kanter MH. Improving blood pressure control in a large multiethnic California population through changes in health care delivery, 2004–2012. Prev Chronic Dis 2014; 11:E191.
- Sim JJ, Handler J, Jacobsen SJ, Kanter MH. Systematic implementation strategies to improve hypertension: the Kaiser Permanente Southern California experience. Can J Cardiol 2014; 30:544–552.
- Gradman AH, Basile JN, Carter BL, Bakris GL; American Society of Hypertension Writing Group. Combination therapy in hypertension. J Am Soc Hypertens 2010; 4:42–50.
- Feldman RD, Zou GY, Vandervoort MK, Wong CJ, Nelson SAE, Feagan BG. A simplified approach to the treatment of uncomplicated hypertension: a cluster randomized, controlled trial. Hypertension 2009; 53:646–653.
- Mancia G, Fagard R, Narkiewicz K, et al; Task Force Members. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013; 31:1281–1357.
- Frieden TR, King SM, Wright JS. Protocol-based treatment of hypertension: a critical step on the pathway to progress. JAMA 2014; 311:21–22.
- Ayanian JZ, Landon BE, Newhouse JP, Zaslavsky AM. Racial and ethnic disparities among enrollees in Medicare advantage plans. N Engl J Med 2014; 371: 2288–2297.
- Piper MA, Evans CV, Burda BU, Margolis KL, O’Connor E, Whitlock EP. Diagnostic and predictive accuracy of blood pressure screening methods with consideragnostic and predictive accuracy of blood pressure screening methods with consideration of rescreening intervals: an updated systematic review for the U.S. Preventive Services Task Force. Ann Intern Med 2015; 162:192–204.
- Cloutier L, Daskalopoulu SS, Padwal RS, et al. A new algorithm for the diagnosis of hypertension in Canada. Can J Cardiol 2015; 31:620–630.
- Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D. Call to action on use and reimbursement for home blood pressure monitoring: executive summary. A joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. J Am Soc Hypertens 2008; 2:192–202.
- Chobanian AV, Bakris GL, Black HR, et al; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42:1206–1252.
- Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved blood pressure control associated with a large-scale hypertension program. JAMA 2013; 310: 699–705.
- Ringerman E, Flint LJ, Hughes DE. An innovative education program. The peer competency validator model. J Nurses in Staff Development 2006; 22:114–121.
- Reeves RA. Does this patient have hypertension? How to measure blood pressure. JAMA 1995; 273:1211–1218.
- Le Pailleur C, Helft G, Landais P, et al. The effects of talking, reading, and silence on the “white coat” phenomenon in hypertensive patients. Am J Hypertens 1998; 11:203–207.
- Kaplan NM. Chapter 2. Measurement of blood pressure. In: Kaplan NM, Victor RG, eds. Kaplan’s Clinical Hypertension, 11th ed. Philadelphia, PA: Wolters Kluwer, 2015:1–39.
- James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014; 311:507–520.
- Dahlöf B, Devereux RB, Kjeldsen SE, et al; LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention for Endpoint reduction in hypertension study (LIFE): a randomized trial against atenolol. Lancet 2002; 359:995–1003.
- Wright JT Jr, Dunn JK, Cutler JA, et al; ALLHAT Collaborative Research Group. Outcomes in hypertensive black and nonblack patients treated with chlorthalidone, amlodipine, and lisinopril. JAMA 2005; 293:1595–1608.
- Brown MJ, Palmer CR, Castaigne A, et al. Morbidity and mortality in patients randomized to double-blind treatment with a long-acting calcium-channel blocker or diuretic in the International Nifedipine GITS study: Intervention as a goal in Hypertension Treatment (INSIGHT). Lancet 2000; 356:366–372.
- Wing LM, Reid CM, Ryan P, et al; Second Australian National Blood Pressure Study Group. A comparison of outcomes with angiotensin-converting-enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med 2003; 348:583–592.
- Jamerson K, Weber MA, Bakris GL, et al; ACCOMPLISH Trial Investigators. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med 2008; 359:2417–2428.
- Rahman M, Pressel S, Davis BR, et al. Renal outcomes in high-risk hypertensive patients treated with an angiotensin-converting enzyme inhibitor or a calcium channel blocker vs a diuretic: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med 2005; 165:936–946.
- Barzilay JI, Davis BR, Cutler JA, et al; ALLHAT Collaborative Research Group. Fasting glucose levels and incident diabetes mellitus in older nondiabetic adults randomized to receive 3 different classes of antihypertensive treatment: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med 2006; 166:2191–2201.
- James PA, Oparil S, Carter BL, et al. Supplement to 2014 evidence-based guideline for the management of high blood pressure in adults: report by the panel appointed to the Eighth Joint National Committee (JNC 8). Available at http://jama. jamanetwork.com/article.aspx?articleid=1791497. Accessed August 3, 2015.
- ONTARGET Investigators; Yusuf S, Teo KK, Pogue J, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med 2008; 358: 1547–1559.
- Palmer BF. Renal dysfunction complicating the treatment of hypertension. N Engl J Med 2002; 347:1256–1261.
- SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA 1991; 265:3255–3264.
- Staessen JA, Fagard R, Thijs L, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet 1997; 350:757–764.
- Liu L, Zhang Y, Liu G, Zhang X, Zanchetti A; FEVER Study Group. The Felodipine Event Reduction (FEVER) study: a randomized long-term placebo-controlled trial in Chinese hypertensive patients. J Hypertens 2005; 23:2157–2172.
- Arguedas JA, Perez MI, Wright JM. Treatment blood pressure targets for hypertension. Cochrane Database of Syst Rev 2009 Jul 8; (3):CD004349.
- Davis EM, Appel LJ, Wang X, et al; African American Study of Kidney Disease and Hypertension Research Collaborative Group. Limitations of analyses based on achieved blood pressure: lessons from the African American Study of Kidney Disease and Hypertension Trial. Hypertension 2011; 57:1061–1068.
- Handler J. 2014 Hypertension guideline: recommendation for a change in systolic blood pressure. Perm J 2015; 19:64–72.
- National Heart Lung and Blood Institute. Landmark NIH study shows intensive blood pressure management may save lives. Available at: http://www.nhlbi.nih.gov/ news/press-releases/2015/landmark-nih-study-shows-intensive-blood-pressure-management-may-save-lives. Published September 11, 2015. Accessed September 16, 2015.
- Ambrosius WT, Sink KM, Foy CG, et al; SPRINT Study Research Group. The design and rationale of a multicenter clinical trial comparing two strategies for control of systolic blood pressure: the Systolic Blood Pressure Intervention Trial (SPRINT) Clin Trials 2014; 11:1–15.
- The ACCORD Study Group, Cushman WC, Evans GW, Byington RP, et al. Effects of intensive blood pressure control in type 2 diabetes mellitus. N Engl J Med 2010; 362:1575–1585.
- Shaw KM, Handler J, Wall HK, Kanter MH. Improving blood pressure control in a large multiethnic California population through changes in health care delivery, 2004–2012. Prev Chronic Dis 2014; 11:E191.
- Sim JJ, Handler J, Jacobsen SJ, Kanter MH. Systematic implementation strategies to improve hypertension: the Kaiser Permanente Southern California experience. Can J Cardiol 2014; 30:544–552.
- Gradman AH, Basile JN, Carter BL, Bakris GL; American Society of Hypertension Writing Group. Combination therapy in hypertension. J Am Soc Hypertens 2010; 4:42–50.
- Feldman RD, Zou GY, Vandervoort MK, Wong CJ, Nelson SAE, Feagan BG. A simplified approach to the treatment of uncomplicated hypertension: a cluster randomized, controlled trial. Hypertension 2009; 53:646–653.
- Mancia G, Fagard R, Narkiewicz K, et al; Task Force Members. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013; 31:1281–1357.
- Frieden TR, King SM, Wright JS. Protocol-based treatment of hypertension: a critical step on the pathway to progress. JAMA 2014; 311:21–22.
- Ayanian JZ, Landon BE, Newhouse JP, Zaslavsky AM. Racial and ethnic disparities among enrollees in Medicare advantage plans. N Engl J Med 2014; 371: 2288–2297.
KEY POINTS
- Diagnosing hypertension continues to require a sufficient number of well-performed office blood pressure measurements for most patients.
- First-tier drug choices are angiotensin-converting enzyme inhibitors and angiotensin receptor blockers (but not both together), calcium channel blockers, and thiazide-type diuretics. Add-ons to achieve blood pressure targets should come from first-tier classes not used initially.
- Simple implementation principles can achieve high control rates across a fractured healthcare delivery landscape. Equitable care can reduce racial disparities in hypertension control.