User login
Rigosertib falls short for high-risk myelodysplastic syndromes after failure on azacitidine or decitabine
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
A randomized phase III trial of rigosertib (NCT 02562443) is now underway in specific subgroups of high-risk patients, including patients with very high risk on the basis of the Revised International Prognostic Scoring System criteria, to determine whether the drug may benefit specific patient subgroups, according to Dr. Guillermo Garcia-Manero of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
The ONTIME study (NCT01241500) was an open-label, randomized controlled trial at 74 medical centers in the US and Europe. Patients with refractory anemia with excess blasts ([RAEB]-1, RAEB-2, RAEB-t, or chronic myelomonocytic leukemia) were enrolled based on local site assessment and treatment failure with a hypomethylating drug in the past 2 years.
Patients were randomly assigned on a 2:1 basis to receive rigosertib or best supportive care with or without low-dose cytarabine. Randomization was stratified by pretreatment bone marrow blast percentage. The 199 patients given rigosertib received 1,800 mg per 24 hours via a 72-hour continuous intravenous infusion administered every other week. Another 100 patients were assigned to best supportive care.
Median follow-up was 19.5 months. Median overall survival was 8.2 months (95% confidence interval, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group (hazard ratio, 0.87; 95% CI, 0.67-1.14; P = 0.33), the researchers reported (Lancet Oncol. 2016;17(4):496-508. doi: 10.1016/S1470-2045(16)00009-7).
The most common grade 3 or higher adverse events were anemia (18% of 184 patients in the rigosertib group and 8% of 91 patients in the best supportive care group), thrombocytopenia (19% vs 7%), neutropenia (17% vs. 8%), febrile neutropenia (12% vs 11%], and pneumonia (12% vs 11%). Adverse events led to death in 22% of 184 patients in the rigosertib group and 33% of 91 patients in the best supportive care group; three deaths were attributed to rigosertib treatment.
The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society.
On Twitter @maryjodales
THE LANCET ONCOLOGY
Key clinical point: Rigosertib failed to extend overall survival beyond that seen with best supportive care in a trial of patients who had myelodysplastic syndrome with excess blasts after failure of azacitidine or decitabine treatment.
Major finding: Median overall survival was 8.2 months (95% CI, 6.1-10.1) in the rigosertib group and 5.9 months (95% CI, 4.1-9.3) in the best supportive care group.
Data source: An open-label, randomized controlled trial involving 299 patients at 74 medical centers.
Disclosures: The study was funded by Onconova Therapeutics and the Leukemia and Lymphoma Society..
Study Finds: Blood Pressure Medication and Stain Cholesterol Fighter Decreases the Risk of Heart Attack and Stroke in Patients with Hypertension and Moderate Risk of Heart Disease
(Reuters) - Patients with hypertension and moderate risk of heart disease slashed their long-term risk of heart attack and stroke 40 percent by taking a blood pressure medication as well as a statin cholesterol fighter, according to a large global study that could change medical practice.
Results from the trial, called HOPE-3, could prod far more doctors to add a statin to antihypertensive therapy for such patients who have no prior history of heart attack or stroke, researchers said.
The data was presented on Saturday at the annual scientific session of the American College of Cardiology in Chicago.
To enroll in the trial, patients had to have at least one risk factor for heart disease such as obesity or smoking, in addition to being over 60 for women and over 55 for men.
"Intermediate-risk people with hypertension had a clear benefit when taking both a statin and an agent that lowers blood pressure," Dr. Salim Yusuf, a professor of cardiology at McMaster University in Ontario, Canada who headed the 12,000-patient global study, said in an interview.
Patients with systolic blood pressure of 140 and higher were deemed in the study to have high blood pressure. They experienced a 40 percent reduced risk of heart attack and stroke over a six-year period when taking AstraZeneca Plc's statin Crestor (rosuvastatin) as well as a combination tablet containing blood pressure treatment candesartan and the diuretic hydrochlorothiazide.
Patients with normal or low systolic pressure had the same approximate 25 percent reduction in cardiovascular events as seen among patients in one arm of the study who took only statins.
Yusuf said the trial underscores that if a patient at moderate heart risk has high blood pressure, defined as 140 or higher, "give them both a statin and a blood pressure medication as a matter of course." He said statins are not automatically given now to patients with hypertension that are at only moderate risk of heart attack or stroke.
Yusuf's trial included research centers in China, India, Latin America, Africa and Canada, but not the United States because of far greater research costs there. The trial was funded by the Canadian Institutes of Health Research and AstraZeneca.
A separate study published in November found that lowering blood pressure to below 120 dramatically reduced heart failure and risk of death in adults aged 50 and older. But the five-year U.S. government-sponsored study of more than 9,300 patients showed a higher rate of adverse side effects, including kidney damage, in the aggressively treated patients.
(Reuters) - Patients with hypertension and moderate risk of heart disease slashed their long-term risk of heart attack and stroke 40 percent by taking a blood pressure medication as well as a statin cholesterol fighter, according to a large global study that could change medical practice.
Results from the trial, called HOPE-3, could prod far more doctors to add a statin to antihypertensive therapy for such patients who have no prior history of heart attack or stroke, researchers said.
The data was presented on Saturday at the annual scientific session of the American College of Cardiology in Chicago.
To enroll in the trial, patients had to have at least one risk factor for heart disease such as obesity or smoking, in addition to being over 60 for women and over 55 for men.
"Intermediate-risk people with hypertension had a clear benefit when taking both a statin and an agent that lowers blood pressure," Dr. Salim Yusuf, a professor of cardiology at McMaster University in Ontario, Canada who headed the 12,000-patient global study, said in an interview.
Patients with systolic blood pressure of 140 and higher were deemed in the study to have high blood pressure. They experienced a 40 percent reduced risk of heart attack and stroke over a six-year period when taking AstraZeneca Plc's statin Crestor (rosuvastatin) as well as a combination tablet containing blood pressure treatment candesartan and the diuretic hydrochlorothiazide.
Patients with normal or low systolic pressure had the same approximate 25 percent reduction in cardiovascular events as seen among patients in one arm of the study who took only statins.
Yusuf said the trial underscores that if a patient at moderate heart risk has high blood pressure, defined as 140 or higher, "give them both a statin and a blood pressure medication as a matter of course." He said statins are not automatically given now to patients with hypertension that are at only moderate risk of heart attack or stroke.
Yusuf's trial included research centers in China, India, Latin America, Africa and Canada, but not the United States because of far greater research costs there. The trial was funded by the Canadian Institutes of Health Research and AstraZeneca.
A separate study published in November found that lowering blood pressure to below 120 dramatically reduced heart failure and risk of death in adults aged 50 and older. But the five-year U.S. government-sponsored study of more than 9,300 patients showed a higher rate of adverse side effects, including kidney damage, in the aggressively treated patients.
(Reuters) - Patients with hypertension and moderate risk of heart disease slashed their long-term risk of heart attack and stroke 40 percent by taking a blood pressure medication as well as a statin cholesterol fighter, according to a large global study that could change medical practice.
Results from the trial, called HOPE-3, could prod far more doctors to add a statin to antihypertensive therapy for such patients who have no prior history of heart attack or stroke, researchers said.
The data was presented on Saturday at the annual scientific session of the American College of Cardiology in Chicago.
To enroll in the trial, patients had to have at least one risk factor for heart disease such as obesity or smoking, in addition to being over 60 for women and over 55 for men.
"Intermediate-risk people with hypertension had a clear benefit when taking both a statin and an agent that lowers blood pressure," Dr. Salim Yusuf, a professor of cardiology at McMaster University in Ontario, Canada who headed the 12,000-patient global study, said in an interview.
Patients with systolic blood pressure of 140 and higher were deemed in the study to have high blood pressure. They experienced a 40 percent reduced risk of heart attack and stroke over a six-year period when taking AstraZeneca Plc's statin Crestor (rosuvastatin) as well as a combination tablet containing blood pressure treatment candesartan and the diuretic hydrochlorothiazide.
Patients with normal or low systolic pressure had the same approximate 25 percent reduction in cardiovascular events as seen among patients in one arm of the study who took only statins.
Yusuf said the trial underscores that if a patient at moderate heart risk has high blood pressure, defined as 140 or higher, "give them both a statin and a blood pressure medication as a matter of course." He said statins are not automatically given now to patients with hypertension that are at only moderate risk of heart attack or stroke.
Yusuf's trial included research centers in China, India, Latin America, Africa and Canada, but not the United States because of far greater research costs there. The trial was funded by the Canadian Institutes of Health Research and AstraZeneca.
A separate study published in November found that lowering blood pressure to below 120 dramatically reduced heart failure and risk of death in adults aged 50 and older. But the five-year U.S. government-sponsored study of more than 9,300 patients showed a higher rate of adverse side effects, including kidney damage, in the aggressively treated patients.
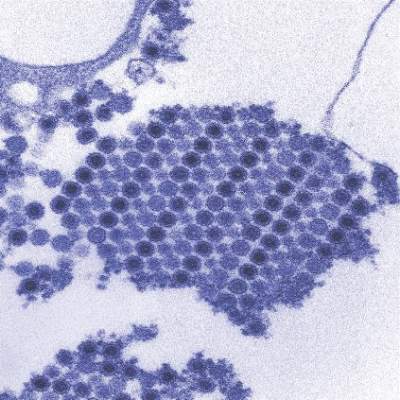
TCD screening underused in sickle cell patients

with sickle cell anemia
Photo courtesy of St. Jude
Results of a large, retrospective study suggest the use of transcranial Doppler (TCD) screening is on the rise in US children and adolescents with sickle cell anemia.
However, the rate of TCD screening in these patients falls well below national recommendations.
In addition, TCD screening rates vary greatly by state, and the use of screening tends to decrease as patients grow older.
Sarah L. Reeves, PhD, of University of Michigan, Ann Arbor, and her colleagues reported these findings in JAMA Pediatrics.
The researchers noted that guidelines from the National Heart, Lung, and Blood Institute recommend that patients with sickle cell anemia receive annual TCD screenings from age 2 to 16 to identify those patients at the highest risk of stroke.
Dr Reeves and her colleagues wanted to determine if this recommendation is being followed. So they analyzed Medicaid claims data from 2005 through 2010 for Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas.
The data included 4775 patients, ages 2 to 16, with sickle cell anemia. For these patients, TCD screening rates increased from 22% in 2005 to 44% in 2010 (P<0.001).
The researchers found that TCD screening rates varied significantly by state (P=0.004), and Texas had the lowest screening rate at any time point (7% in 2005).
The team also analyzed a subset of 2388 patients who were enrolled for 2 or more consecutive years to examine potential predictors of TCD screening.
This analysis revealed that, with each year of increasing age, a patient’s odds of receiving TCD screening decreased (odds ratio=0.97, P=0.002).
On the other hand, an increasing number of well-child visits was associated with higher odds of receiving TCD screening (odds ratio=1.10, P=0.007).
And the odds of receiving TCD screening were higher for patients who previously underwent TCD screening (odds ratio=2.44, P<0.001).
The researchers said these results suggest that, despite national recommendations, TCD screening rates remain low in young patients with sickle cell anemia in the US. ![]()

with sickle cell anemia
Photo courtesy of St. Jude
Results of a large, retrospective study suggest the use of transcranial Doppler (TCD) screening is on the rise in US children and adolescents with sickle cell anemia.
However, the rate of TCD screening in these patients falls well below national recommendations.
In addition, TCD screening rates vary greatly by state, and the use of screening tends to decrease as patients grow older.
Sarah L. Reeves, PhD, of University of Michigan, Ann Arbor, and her colleagues reported these findings in JAMA Pediatrics.
The researchers noted that guidelines from the National Heart, Lung, and Blood Institute recommend that patients with sickle cell anemia receive annual TCD screenings from age 2 to 16 to identify those patients at the highest risk of stroke.
Dr Reeves and her colleagues wanted to determine if this recommendation is being followed. So they analyzed Medicaid claims data from 2005 through 2010 for Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas.
The data included 4775 patients, ages 2 to 16, with sickle cell anemia. For these patients, TCD screening rates increased from 22% in 2005 to 44% in 2010 (P<0.001).
The researchers found that TCD screening rates varied significantly by state (P=0.004), and Texas had the lowest screening rate at any time point (7% in 2005).
The team also analyzed a subset of 2388 patients who were enrolled for 2 or more consecutive years to examine potential predictors of TCD screening.
This analysis revealed that, with each year of increasing age, a patient’s odds of receiving TCD screening decreased (odds ratio=0.97, P=0.002).
On the other hand, an increasing number of well-child visits was associated with higher odds of receiving TCD screening (odds ratio=1.10, P=0.007).
And the odds of receiving TCD screening were higher for patients who previously underwent TCD screening (odds ratio=2.44, P<0.001).
The researchers said these results suggest that, despite national recommendations, TCD screening rates remain low in young patients with sickle cell anemia in the US. ![]()

with sickle cell anemia
Photo courtesy of St. Jude
Results of a large, retrospective study suggest the use of transcranial Doppler (TCD) screening is on the rise in US children and adolescents with sickle cell anemia.
However, the rate of TCD screening in these patients falls well below national recommendations.
In addition, TCD screening rates vary greatly by state, and the use of screening tends to decrease as patients grow older.
Sarah L. Reeves, PhD, of University of Michigan, Ann Arbor, and her colleagues reported these findings in JAMA Pediatrics.
The researchers noted that guidelines from the National Heart, Lung, and Blood Institute recommend that patients with sickle cell anemia receive annual TCD screenings from age 2 to 16 to identify those patients at the highest risk of stroke.
Dr Reeves and her colleagues wanted to determine if this recommendation is being followed. So they analyzed Medicaid claims data from 2005 through 2010 for Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas.
The data included 4775 patients, ages 2 to 16, with sickle cell anemia. For these patients, TCD screening rates increased from 22% in 2005 to 44% in 2010 (P<0.001).
The researchers found that TCD screening rates varied significantly by state (P=0.004), and Texas had the lowest screening rate at any time point (7% in 2005).
The team also analyzed a subset of 2388 patients who were enrolled for 2 or more consecutive years to examine potential predictors of TCD screening.
This analysis revealed that, with each year of increasing age, a patient’s odds of receiving TCD screening decreased (odds ratio=0.97, P=0.002).
On the other hand, an increasing number of well-child visits was associated with higher odds of receiving TCD screening (odds ratio=1.10, P=0.007).
And the odds of receiving TCD screening were higher for patients who previously underwent TCD screening (odds ratio=2.44, P<0.001).
The researchers said these results suggest that, despite national recommendations, TCD screening rates remain low in young patients with sickle cell anemia in the US. ![]()
Company recalls hemostasis valves

Photo courtesy of
Vascular Solutions, Inc.
Vascular Solutions, Inc. has issued a US-wide recall of Guardian II hemostasis valves used in catheterization procedures.
Specific lots of the products have been recalled because they pose an increased risk of air leakage that may lead to an air embolism, which could result in serious injury or death.
This recall only affects the Guardian II hemostasis valves and does not include the Guardian II NC hemostasis valves.
No injuries have been reported in association with this issue to date.
Healthcare facilities that have the affected Guardian II hemostasis valves should remove the products from their inventory and return them to Vascular Solutions.
The recalled products were manufactured from March 2015 to February 2016 and distributed from April 2015 to February 2016.
The recalled products are specific lots of Model Numbers 8210 and 8211. A listing of the recalled lots is available from Vascular Solutions and has been provided to each facility that purchased the affected products.
A total of 26,550 devices have been manufactured, with 5283 distributed in the US. The condition that led to the recall may affect approximately 2.4% of recalled devices.
Vascular Solutions voluntarily initiated the recall on March 3, 2016, through an Urgent Medical Device Recall notification distributed to purchasers of the affected products. The notification identified the specific lots subject to the recall and included instructions on how to return the affected products.
The US Food and Drug Administration (FDA) classified this as a Class I recall. The FDA defines Class I recalls as “a situation in which there is a reasonable probability that the use of, or exposure to, a violative product will cause serious adverse health consequences or death.”
Consumers with questions may contact the company by phone at 1-888-240-6001, Monday through Friday, between the hours of 8:00 am and 5:00 pm Central Time or by email at [email protected].
Adverse reactions or quality problems associated with the use of this product may be reported to the FDA’s MedWatch Adverse Event Reporting Program. ![]()

Photo courtesy of
Vascular Solutions, Inc.
Vascular Solutions, Inc. has issued a US-wide recall of Guardian II hemostasis valves used in catheterization procedures.
Specific lots of the products have been recalled because they pose an increased risk of air leakage that may lead to an air embolism, which could result in serious injury or death.
This recall only affects the Guardian II hemostasis valves and does not include the Guardian II NC hemostasis valves.
No injuries have been reported in association with this issue to date.
Healthcare facilities that have the affected Guardian II hemostasis valves should remove the products from their inventory and return them to Vascular Solutions.
The recalled products were manufactured from March 2015 to February 2016 and distributed from April 2015 to February 2016.
The recalled products are specific lots of Model Numbers 8210 and 8211. A listing of the recalled lots is available from Vascular Solutions and has been provided to each facility that purchased the affected products.
A total of 26,550 devices have been manufactured, with 5283 distributed in the US. The condition that led to the recall may affect approximately 2.4% of recalled devices.
Vascular Solutions voluntarily initiated the recall on March 3, 2016, through an Urgent Medical Device Recall notification distributed to purchasers of the affected products. The notification identified the specific lots subject to the recall and included instructions on how to return the affected products.
The US Food and Drug Administration (FDA) classified this as a Class I recall. The FDA defines Class I recalls as “a situation in which there is a reasonable probability that the use of, or exposure to, a violative product will cause serious adverse health consequences or death.”
Consumers with questions may contact the company by phone at 1-888-240-6001, Monday through Friday, between the hours of 8:00 am and 5:00 pm Central Time or by email at [email protected].
Adverse reactions or quality problems associated with the use of this product may be reported to the FDA’s MedWatch Adverse Event Reporting Program. ![]()

Photo courtesy of
Vascular Solutions, Inc.
Vascular Solutions, Inc. has issued a US-wide recall of Guardian II hemostasis valves used in catheterization procedures.
Specific lots of the products have been recalled because they pose an increased risk of air leakage that may lead to an air embolism, which could result in serious injury or death.
This recall only affects the Guardian II hemostasis valves and does not include the Guardian II NC hemostasis valves.
No injuries have been reported in association with this issue to date.
Healthcare facilities that have the affected Guardian II hemostasis valves should remove the products from their inventory and return them to Vascular Solutions.
The recalled products were manufactured from March 2015 to February 2016 and distributed from April 2015 to February 2016.
The recalled products are specific lots of Model Numbers 8210 and 8211. A listing of the recalled lots is available from Vascular Solutions and has been provided to each facility that purchased the affected products.
A total of 26,550 devices have been manufactured, with 5283 distributed in the US. The condition that led to the recall may affect approximately 2.4% of recalled devices.
Vascular Solutions voluntarily initiated the recall on March 3, 2016, through an Urgent Medical Device Recall notification distributed to purchasers of the affected products. The notification identified the specific lots subject to the recall and included instructions on how to return the affected products.
The US Food and Drug Administration (FDA) classified this as a Class I recall. The FDA defines Class I recalls as “a situation in which there is a reasonable probability that the use of, or exposure to, a violative product will cause serious adverse health consequences or death.”
Consumers with questions may contact the company by phone at 1-888-240-6001, Monday through Friday, between the hours of 8:00 am and 5:00 pm Central Time or by email at [email protected].
Adverse reactions or quality problems associated with the use of this product may be reported to the FDA’s MedWatch Adverse Event Reporting Program. ![]()
Survey says docs don’t know FDA requirements

A survey of nearly 700 US physicians revealed that many do not know the basic requirements for a drug to receive approval from the US Food and
Drug Administration (FDA).
The results also suggested that most physicians don’t understand the FDA’s “breakthrough therapy” designation.
Since 2012, the FDA has been able to designate a drug as a breakthrough therapy if preliminary clinical evidence suggests it provides an advantage
over existing options.
Aaron S. Kesselheim, MD, of Brigham and Women’s Hospital in Boston, Massachusetts, and his colleagues wanted to determine how much physicians understood about this designation and if they had a basic understanding of the FDA’s requirements for drug approval.
So the researchers surveyed internists and specialists from the American Board of Internal Medicine’s diplomate list and reported the results of this survey in JAMA.
Of the 1148 physicians contacted, 692 (60%) responded. Participants were asked 3 questions about FDA approval and 5 about breakthrough therapies.
FDA approval
Seventy-three percent of respondents incorrectly believed that, for a drug to gain FDA approval, it must be as effective as drugs that are already approved.
However, 85% of respondents answered correctly that FDA-approved drugs typically have a favorable benefit/harm ratio.
Seventy percent of respondents incorrectly believed that FDA approval requires a drug to have both a statistically significant and a clinically important effect.
Only 6% of respondents knew the correct answer—that neither is required.
Breakthrough designation
Twenty percent of respondents said they were “familiar” (17%) or “very familiar” (3%) with breakthrough therapy designation, while 37% said they were “a little familiar,” and 42% said they were “not familiar at all.”
Fifty-eight percent of respondents said they were “fairly certain” that an FDA-approved breakthrough drug represents a major advance over currently approved treatments for its indication. Thirty-one percent said they were “fairly uncertain,” 5% said they were “very uncertain,” and 6% said they were “very certain.”
Fifty-two percent of respondents incorrectly believed that strong evidence (ie, randomized trials) is needed to earn the breakthrough designation.
However, 45% correctly answered that only preliminary evidence (eg, uncontrolled studies or studies testing surrogate outcomes) is needed. Four percent said very preliminary evidence (eg, in vitro laboratory or animal studies) is needed.
Seventy-seven percent of respondents incorrectly believed that, when the FDA grants breakthrough designation, there is high-quality evidence that the drug is more effective than currently approved treatments.
But 74% of respondents answered correctly that breakthrough designation does not mean there is high-quality evidence that the drug is safer than currently approved treatments.
Dr Kesselheim and his colleagues said the misconceptions identified in this survey may lead physicians to overprescribe newly approved drugs—particularly breakthrough therapies—and inadequately communicate how well these drugs work to patients. ![]()

A survey of nearly 700 US physicians revealed that many do not know the basic requirements for a drug to receive approval from the US Food and
Drug Administration (FDA).
The results also suggested that most physicians don’t understand the FDA’s “breakthrough therapy” designation.
Since 2012, the FDA has been able to designate a drug as a breakthrough therapy if preliminary clinical evidence suggests it provides an advantage
over existing options.
Aaron S. Kesselheim, MD, of Brigham and Women’s Hospital in Boston, Massachusetts, and his colleagues wanted to determine how much physicians understood about this designation and if they had a basic understanding of the FDA’s requirements for drug approval.
So the researchers surveyed internists and specialists from the American Board of Internal Medicine’s diplomate list and reported the results of this survey in JAMA.
Of the 1148 physicians contacted, 692 (60%) responded. Participants were asked 3 questions about FDA approval and 5 about breakthrough therapies.
FDA approval
Seventy-three percent of respondents incorrectly believed that, for a drug to gain FDA approval, it must be as effective as drugs that are already approved.
However, 85% of respondents answered correctly that FDA-approved drugs typically have a favorable benefit/harm ratio.
Seventy percent of respondents incorrectly believed that FDA approval requires a drug to have both a statistically significant and a clinically important effect.
Only 6% of respondents knew the correct answer—that neither is required.
Breakthrough designation
Twenty percent of respondents said they were “familiar” (17%) or “very familiar” (3%) with breakthrough therapy designation, while 37% said they were “a little familiar,” and 42% said they were “not familiar at all.”
Fifty-eight percent of respondents said they were “fairly certain” that an FDA-approved breakthrough drug represents a major advance over currently approved treatments for its indication. Thirty-one percent said they were “fairly uncertain,” 5% said they were “very uncertain,” and 6% said they were “very certain.”
Fifty-two percent of respondents incorrectly believed that strong evidence (ie, randomized trials) is needed to earn the breakthrough designation.
However, 45% correctly answered that only preliminary evidence (eg, uncontrolled studies or studies testing surrogate outcomes) is needed. Four percent said very preliminary evidence (eg, in vitro laboratory or animal studies) is needed.
Seventy-seven percent of respondents incorrectly believed that, when the FDA grants breakthrough designation, there is high-quality evidence that the drug is more effective than currently approved treatments.
But 74% of respondents answered correctly that breakthrough designation does not mean there is high-quality evidence that the drug is safer than currently approved treatments.
Dr Kesselheim and his colleagues said the misconceptions identified in this survey may lead physicians to overprescribe newly approved drugs—particularly breakthrough therapies—and inadequately communicate how well these drugs work to patients. ![]()

A survey of nearly 700 US physicians revealed that many do not know the basic requirements for a drug to receive approval from the US Food and
Drug Administration (FDA).
The results also suggested that most physicians don’t understand the FDA’s “breakthrough therapy” designation.
Since 2012, the FDA has been able to designate a drug as a breakthrough therapy if preliminary clinical evidence suggests it provides an advantage
over existing options.
Aaron S. Kesselheim, MD, of Brigham and Women’s Hospital in Boston, Massachusetts, and his colleagues wanted to determine how much physicians understood about this designation and if they had a basic understanding of the FDA’s requirements for drug approval.
So the researchers surveyed internists and specialists from the American Board of Internal Medicine’s diplomate list and reported the results of this survey in JAMA.
Of the 1148 physicians contacted, 692 (60%) responded. Participants were asked 3 questions about FDA approval and 5 about breakthrough therapies.
FDA approval
Seventy-three percent of respondents incorrectly believed that, for a drug to gain FDA approval, it must be as effective as drugs that are already approved.
However, 85% of respondents answered correctly that FDA-approved drugs typically have a favorable benefit/harm ratio.
Seventy percent of respondents incorrectly believed that FDA approval requires a drug to have both a statistically significant and a clinically important effect.
Only 6% of respondents knew the correct answer—that neither is required.
Breakthrough designation
Twenty percent of respondents said they were “familiar” (17%) or “very familiar” (3%) with breakthrough therapy designation, while 37% said they were “a little familiar,” and 42% said they were “not familiar at all.”
Fifty-eight percent of respondents said they were “fairly certain” that an FDA-approved breakthrough drug represents a major advance over currently approved treatments for its indication. Thirty-one percent said they were “fairly uncertain,” 5% said they were “very uncertain,” and 6% said they were “very certain.”
Fifty-two percent of respondents incorrectly believed that strong evidence (ie, randomized trials) is needed to earn the breakthrough designation.
However, 45% correctly answered that only preliminary evidence (eg, uncontrolled studies or studies testing surrogate outcomes) is needed. Four percent said very preliminary evidence (eg, in vitro laboratory or animal studies) is needed.
Seventy-seven percent of respondents incorrectly believed that, when the FDA grants breakthrough designation, there is high-quality evidence that the drug is more effective than currently approved treatments.
But 74% of respondents answered correctly that breakthrough designation does not mean there is high-quality evidence that the drug is safer than currently approved treatments.
Dr Kesselheim and his colleagues said the misconceptions identified in this survey may lead physicians to overprescribe newly approved drugs—particularly breakthrough therapies—and inadequately communicate how well these drugs work to patients. ![]()
Manufacturing methods can damage red cells

Photo by Elise Amendola
Certain methods of manufacturing red cell concentrates (RCCs) may be less damaging than others, according to research published in Vox Sanguinis.
The study showed that damage-associated molecular patterns (DAMPs) in stored blood differ according to the process and materials used to collect or prepare RCCs for transfusion.
Researchers believe this discovery could help reduce adverse reactions in transfusion recipients and potentially impact how blood is collected around the world.
To conduct this study, the researchers compared RCCs collected at blood donation centers in the US and Canada. The team examined the influence of manufacturing methods on the levels of mitochondrial (mt) DNA and extracellular vesicle (EV) DAMPs in RCCs.
“Working with the American team at Blood Systems Research Institute was key to this research because of the wide variations in blood manufacturing processes present in the US,” said Jason Acker, PhD, of Canadian Blood Services’ Centre for Innovation in Edmonton, Alberta.
“In countries like Canada, where there is a national blood service, manufacturing methods are largely standardized, so it is difficult to compare various methods. But blood collection in the US is characterized by dozens of independent blood centers that use a variety of available manufacturing processes. The Americans provided the variations we needed to measure red cell damage and to ascertain whether it can be attributed to different manufacturing methods.”
Manufacturing methods
The researchers evaluated 87 RCCs prepared using 9 different methods, outlined in the following table.
| Name | Processing method | Collection/
manufacturing method |
Anticoagulant/
additive solution (AS) |
Leuko-reduction (LR) method | LR temperature and timing |
| FenBC (n=6) | Semi-automated whole blood (WB) processing
following overnight (O/N) hold at 18–24 °C: Buffy coat (BC) method |
Collection set: Fenwal CGR6494B, Quad OptiPure RC 9SBT WB 500 ml Component processing: Compomat G4 | Citrate phosphate dextrose (CPD)/saline adenine glucose mannitol (SAGM) | Filtration of RCC | 20–24°C within 24 h of the stop bleed time |
| MacoBC
(n=6) |
Semi-automated WB processing
following O/N hold at 18–24°C: BC method |
Collection set: Macopharma LQT 7291
LX Leucoflex LCR-Diamond Quadruple Bottom and Top System, WB 500 ml Component processing: Compomat G4 |
CPD/SAGM | Filtration of RCC | 20–24°C within 24 h of the stop bleed time |
| FenWBF
(n=6) |
Semi-automated WB processing:
WB filtration method |
Collection set: Fenwal CGR8441B, Quad
PackPure WB 500 ml Component processing: Compomat G4 |
CPD/SAGM | Filtration of WB | 1–6°C within 72 h of the stop bleed time |
| MacoWBF
(n=6) |
Semi-automated WB processing:
WB filtration method |
Collection set: Macopharma Leucoflex MTL1 Quadruple Top and Top System, WB 500 ml
Component processing: Compomat G4 |
CPD/SAGM | Filtration of WB | 1–6°C within 72 h of the stop bleed time |
| FenMAN
(n=12) |
Manual WB processing | Fenwal 4R1582 Double Blood-Pack Unit
500 ml, with Flex-Excel Red Cell Filter |
CPD/AS-1 | Filtration of RCC | Room temperature (RT) within 8 h of stop bleed time |
| FenMAN-non-LR
(n=12) |
Manual WB processing | Fenwal 4R1587P Triple Blood-Pack Unit 500 ml | CPD/AS-1 | Not applicable | Not applicable |
| Alyx (n=15) | Apheresis | Fenwal Software: 3.0; 4R5720 Alyx 2RBC-LR Kit | Acid citrate dextrose A (ACD-A)/AS-1 | Filtration of RCC | RT post-
collection |
| MCS+ (n=12) | Apheresis | Haemonetics; Software Rev H or L; 0832F-00, 2RBC filtered | CP2D/AS-3 | Filtration of RCC | RT if <8 h/
cold if >8 h post- collection |
| Trima (n=12) | Apheresis | Terumo BCT; Software 6.0.6; Trima Accel 80500 kit | ACD-A/AS-3 | Filtration of RCC | RT if <8 h/ cold if >8 h post-
collection |
Results
For all RCCs, the researchers assessed the levels of mtDNA and the number and cell of origin of EVs on storage days 5 and 42.
They observed a 100-fold difference in mtDNA levels between the different methods.
The highest mtDNA levels were in the non-leukoreduced RCCs, followed by the MCS+ and Trima apheresis RCCs. The mean levels were 5.3 x 105 copies/µL, 1.3 x 105 copies/µL, and 1.2 x 105 copies/µL, respectively.
The lowest mtDNA levels were seen with the semi-automated methods. The mean levels ranged from 3.8 x 103 copies/µL to 5.9 x 103 copies/µL.
The researchers also saw a 10-fold difference in EV levels between the different methods.
The team detected red blood cell-derived CD235a+ EVs in fresh RCCs, which increased in most RCCs over the storage period (but not for FenBC and MCS+).
Platelet-derived CD41a+ EVs were highest in non-leukoreduced and Trima RCCs and did not change significantly during storage.
White blood cell-derived CD11b+ and CD66b+ EVs were low in most RCCs (though not in Trima and FenMAN-non-LR RCCs), and their levels did not significantly change during storage.
White blood cell-derived CD14+ EVs were negligible in fresh RCCs but increased in several RCCs during storage (FenMAN, Alyx, MCS+, and Trima).
Next steps
“There must be more testing of the apheresis collections equipment, blood bags, leukoreduction filters, and other variations in manufacturing methods to determine what single element or combination of elements in the various red blood cell manufacturing processes result in high levels of DAMPs and why,” said Michael Busch, MD, PhD, of Blood Systems Research Institute in San Francisco, California.
“We also need to understand how mitochondrial DAMPs are involved in adverse reactions to red blood cell transfusions,” added Sonia Bakkour, PhD, also from Blood Systems Research Institute.
“Some recently published studies on platelet components link high levels of mitochondrial DAMPs to adverse transfusion reactions. We need to see if DAMPs have similar adverse effects on recipients of red blood cell transfusions.”
“We think that our research could lead to finding the best way to manufacture red blood cells,” Dr Acker noted.
“It’s clear now that manufacturing methods matter. We . . . are keen to explore what’s in the blood bag or in the filters or in the tubing, for example, that can be minimized or eliminated, improving the outcome in patients who receive blood transfusions.” ![]()

Photo by Elise Amendola
Certain methods of manufacturing red cell concentrates (RCCs) may be less damaging than others, according to research published in Vox Sanguinis.
The study showed that damage-associated molecular patterns (DAMPs) in stored blood differ according to the process and materials used to collect or prepare RCCs for transfusion.
Researchers believe this discovery could help reduce adverse reactions in transfusion recipients and potentially impact how blood is collected around the world.
To conduct this study, the researchers compared RCCs collected at blood donation centers in the US and Canada. The team examined the influence of manufacturing methods on the levels of mitochondrial (mt) DNA and extracellular vesicle (EV) DAMPs in RCCs.
“Working with the American team at Blood Systems Research Institute was key to this research because of the wide variations in blood manufacturing processes present in the US,” said Jason Acker, PhD, of Canadian Blood Services’ Centre for Innovation in Edmonton, Alberta.
“In countries like Canada, where there is a national blood service, manufacturing methods are largely standardized, so it is difficult to compare various methods. But blood collection in the US is characterized by dozens of independent blood centers that use a variety of available manufacturing processes. The Americans provided the variations we needed to measure red cell damage and to ascertain whether it can be attributed to different manufacturing methods.”
Manufacturing methods
The researchers evaluated 87 RCCs prepared using 9 different methods, outlined in the following table.
| Name | Processing method | Collection/
manufacturing method |
Anticoagulant/
additive solution (AS) |
Leuko-reduction (LR) method | LR temperature and timing |
| FenBC (n=6) | Semi-automated whole blood (WB) processing
following overnight (O/N) hold at 18–24 °C: Buffy coat (BC) method |
Collection set: Fenwal CGR6494B, Quad OptiPure RC 9SBT WB 500 ml Component processing: Compomat G4 | Citrate phosphate dextrose (CPD)/saline adenine glucose mannitol (SAGM) | Filtration of RCC | 20–24°C within 24 h of the stop bleed time |
| MacoBC
(n=6) |
Semi-automated WB processing
following O/N hold at 18–24°C: BC method |
Collection set: Macopharma LQT 7291
LX Leucoflex LCR-Diamond Quadruple Bottom and Top System, WB 500 ml Component processing: Compomat G4 |
CPD/SAGM | Filtration of RCC | 20–24°C within 24 h of the stop bleed time |
| FenWBF
(n=6) |
Semi-automated WB processing:
WB filtration method |
Collection set: Fenwal CGR8441B, Quad
PackPure WB 500 ml Component processing: Compomat G4 |
CPD/SAGM | Filtration of WB | 1–6°C within 72 h of the stop bleed time |
| MacoWBF
(n=6) |
Semi-automated WB processing:
WB filtration method |
Collection set: Macopharma Leucoflex MTL1 Quadruple Top and Top System, WB 500 ml
Component processing: Compomat G4 |
CPD/SAGM | Filtration of WB | 1–6°C within 72 h of the stop bleed time |
| FenMAN
(n=12) |
Manual WB processing | Fenwal 4R1582 Double Blood-Pack Unit
500 ml, with Flex-Excel Red Cell Filter |
CPD/AS-1 | Filtration of RCC | Room temperature (RT) within 8 h of stop bleed time |
| FenMAN-non-LR
(n=12) |
Manual WB processing | Fenwal 4R1587P Triple Blood-Pack Unit 500 ml | CPD/AS-1 | Not applicable | Not applicable |
| Alyx (n=15) | Apheresis | Fenwal Software: 3.0; 4R5720 Alyx 2RBC-LR Kit | Acid citrate dextrose A (ACD-A)/AS-1 | Filtration of RCC | RT post-
collection |
| MCS+ (n=12) | Apheresis | Haemonetics; Software Rev H or L; 0832F-00, 2RBC filtered | CP2D/AS-3 | Filtration of RCC | RT if <8 h/
cold if >8 h post- collection |
| Trima (n=12) | Apheresis | Terumo BCT; Software 6.0.6; Trima Accel 80500 kit | ACD-A/AS-3 | Filtration of RCC | RT if <8 h/ cold if >8 h post-
collection |
Results
For all RCCs, the researchers assessed the levels of mtDNA and the number and cell of origin of EVs on storage days 5 and 42.
They observed a 100-fold difference in mtDNA levels between the different methods.
The highest mtDNA levels were in the non-leukoreduced RCCs, followed by the MCS+ and Trima apheresis RCCs. The mean levels were 5.3 x 105 copies/µL, 1.3 x 105 copies/µL, and 1.2 x 105 copies/µL, respectively.
The lowest mtDNA levels were seen with the semi-automated methods. The mean levels ranged from 3.8 x 103 copies/µL to 5.9 x 103 copies/µL.
The researchers also saw a 10-fold difference in EV levels between the different methods.
The team detected red blood cell-derived CD235a+ EVs in fresh RCCs, which increased in most RCCs over the storage period (but not for FenBC and MCS+).
Platelet-derived CD41a+ EVs were highest in non-leukoreduced and Trima RCCs and did not change significantly during storage.
White blood cell-derived CD11b+ and CD66b+ EVs were low in most RCCs (though not in Trima and FenMAN-non-LR RCCs), and their levels did not significantly change during storage.
White blood cell-derived CD14+ EVs were negligible in fresh RCCs but increased in several RCCs during storage (FenMAN, Alyx, MCS+, and Trima).
Next steps
“There must be more testing of the apheresis collections equipment, blood bags, leukoreduction filters, and other variations in manufacturing methods to determine what single element or combination of elements in the various red blood cell manufacturing processes result in high levels of DAMPs and why,” said Michael Busch, MD, PhD, of Blood Systems Research Institute in San Francisco, California.
“We also need to understand how mitochondrial DAMPs are involved in adverse reactions to red blood cell transfusions,” added Sonia Bakkour, PhD, also from Blood Systems Research Institute.
“Some recently published studies on platelet components link high levels of mitochondrial DAMPs to adverse transfusion reactions. We need to see if DAMPs have similar adverse effects on recipients of red blood cell transfusions.”
“We think that our research could lead to finding the best way to manufacture red blood cells,” Dr Acker noted.
“It’s clear now that manufacturing methods matter. We . . . are keen to explore what’s in the blood bag or in the filters or in the tubing, for example, that can be minimized or eliminated, improving the outcome in patients who receive blood transfusions.” ![]()

Photo by Elise Amendola
Certain methods of manufacturing red cell concentrates (RCCs) may be less damaging than others, according to research published in Vox Sanguinis.
The study showed that damage-associated molecular patterns (DAMPs) in stored blood differ according to the process and materials used to collect or prepare RCCs for transfusion.
Researchers believe this discovery could help reduce adverse reactions in transfusion recipients and potentially impact how blood is collected around the world.
To conduct this study, the researchers compared RCCs collected at blood donation centers in the US and Canada. The team examined the influence of manufacturing methods on the levels of mitochondrial (mt) DNA and extracellular vesicle (EV) DAMPs in RCCs.
“Working with the American team at Blood Systems Research Institute was key to this research because of the wide variations in blood manufacturing processes present in the US,” said Jason Acker, PhD, of Canadian Blood Services’ Centre for Innovation in Edmonton, Alberta.
“In countries like Canada, where there is a national blood service, manufacturing methods are largely standardized, so it is difficult to compare various methods. But blood collection in the US is characterized by dozens of independent blood centers that use a variety of available manufacturing processes. The Americans provided the variations we needed to measure red cell damage and to ascertain whether it can be attributed to different manufacturing methods.”
Manufacturing methods
The researchers evaluated 87 RCCs prepared using 9 different methods, outlined in the following table.
| Name | Processing method | Collection/
manufacturing method |
Anticoagulant/
additive solution (AS) |
Leuko-reduction (LR) method | LR temperature and timing |
| FenBC (n=6) | Semi-automated whole blood (WB) processing
following overnight (O/N) hold at 18–24 °C: Buffy coat (BC) method |
Collection set: Fenwal CGR6494B, Quad OptiPure RC 9SBT WB 500 ml Component processing: Compomat G4 | Citrate phosphate dextrose (CPD)/saline adenine glucose mannitol (SAGM) | Filtration of RCC | 20–24°C within 24 h of the stop bleed time |
| MacoBC
(n=6) |
Semi-automated WB processing
following O/N hold at 18–24°C: BC method |
Collection set: Macopharma LQT 7291
LX Leucoflex LCR-Diamond Quadruple Bottom and Top System, WB 500 ml Component processing: Compomat G4 |
CPD/SAGM | Filtration of RCC | 20–24°C within 24 h of the stop bleed time |
| FenWBF
(n=6) |
Semi-automated WB processing:
WB filtration method |
Collection set: Fenwal CGR8441B, Quad
PackPure WB 500 ml Component processing: Compomat G4 |
CPD/SAGM | Filtration of WB | 1–6°C within 72 h of the stop bleed time |
| MacoWBF
(n=6) |
Semi-automated WB processing:
WB filtration method |
Collection set: Macopharma Leucoflex MTL1 Quadruple Top and Top System, WB 500 ml
Component processing: Compomat G4 |
CPD/SAGM | Filtration of WB | 1–6°C within 72 h of the stop bleed time |
| FenMAN
(n=12) |
Manual WB processing | Fenwal 4R1582 Double Blood-Pack Unit
500 ml, with Flex-Excel Red Cell Filter |
CPD/AS-1 | Filtration of RCC | Room temperature (RT) within 8 h of stop bleed time |
| FenMAN-non-LR
(n=12) |
Manual WB processing | Fenwal 4R1587P Triple Blood-Pack Unit 500 ml | CPD/AS-1 | Not applicable | Not applicable |
| Alyx (n=15) | Apheresis | Fenwal Software: 3.0; 4R5720 Alyx 2RBC-LR Kit | Acid citrate dextrose A (ACD-A)/AS-1 | Filtration of RCC | RT post-
collection |
| MCS+ (n=12) | Apheresis | Haemonetics; Software Rev H or L; 0832F-00, 2RBC filtered | CP2D/AS-3 | Filtration of RCC | RT if <8 h/
cold if >8 h post- collection |
| Trima (n=12) | Apheresis | Terumo BCT; Software 6.0.6; Trima Accel 80500 kit | ACD-A/AS-3 | Filtration of RCC | RT if <8 h/ cold if >8 h post-
collection |
Results
For all RCCs, the researchers assessed the levels of mtDNA and the number and cell of origin of EVs on storage days 5 and 42.
They observed a 100-fold difference in mtDNA levels between the different methods.
The highest mtDNA levels were in the non-leukoreduced RCCs, followed by the MCS+ and Trima apheresis RCCs. The mean levels were 5.3 x 105 copies/µL, 1.3 x 105 copies/µL, and 1.2 x 105 copies/µL, respectively.
The lowest mtDNA levels were seen with the semi-automated methods. The mean levels ranged from 3.8 x 103 copies/µL to 5.9 x 103 copies/µL.
The researchers also saw a 10-fold difference in EV levels between the different methods.
The team detected red blood cell-derived CD235a+ EVs in fresh RCCs, which increased in most RCCs over the storage period (but not for FenBC and MCS+).
Platelet-derived CD41a+ EVs were highest in non-leukoreduced and Trima RCCs and did not change significantly during storage.
White blood cell-derived CD11b+ and CD66b+ EVs were low in most RCCs (though not in Trima and FenMAN-non-LR RCCs), and their levels did not significantly change during storage.
White blood cell-derived CD14+ EVs were negligible in fresh RCCs but increased in several RCCs during storage (FenMAN, Alyx, MCS+, and Trima).
Next steps
“There must be more testing of the apheresis collections equipment, blood bags, leukoreduction filters, and other variations in manufacturing methods to determine what single element or combination of elements in the various red blood cell manufacturing processes result in high levels of DAMPs and why,” said Michael Busch, MD, PhD, of Blood Systems Research Institute in San Francisco, California.
“We also need to understand how mitochondrial DAMPs are involved in adverse reactions to red blood cell transfusions,” added Sonia Bakkour, PhD, also from Blood Systems Research Institute.
“Some recently published studies on platelet components link high levels of mitochondrial DAMPs to adverse transfusion reactions. We need to see if DAMPs have similar adverse effects on recipients of red blood cell transfusions.”
“We think that our research could lead to finding the best way to manufacture red blood cells,” Dr Acker noted.
“It’s clear now that manufacturing methods matter. We . . . are keen to explore what’s in the blood bag or in the filters or in the tubing, for example, that can be minimized or eliminated, improving the outcome in patients who receive blood transfusions.” ![]()
Suicidal ideation: Team-based care requires knowledge, resources
Continuity of care for the 18-year-old male who told Dr. Lillian M. Beard about his depression requires collaboration with colleagues, but coordinating that care takes resources. Who is in charge of ensuring care?
“This is where teams come in,” says Dr. April Barbour, associate professor of medicine and chief of general internal medicine George Washington University, Washington. “Because it doesn’t necessarily need to be the psychiatrist. A discharge coordinator could serve that role and send that information back.”
“I agree. And then we come back to the next thing: Who’s going to pay for the team? Who’s going to manage the team? Also, the other thing – with any team, someone’s got to be the quarterback – someone has to make sure or verify that it happened,” says Dr. Lorenzo Norris, cohost of Mental Health Consult, and assistant professor of psychiatry and behavioral sciences at George Washington University.
“When you are treating mental illness, you need a team-based approach so that you can look at everything that is going on. If you are strictly algorithmic based, there are going to be fatal errors,” Dr. Norris says. “It doesn’t reduce down to that level.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Continuity of care for the 18-year-old male who told Dr. Lillian M. Beard about his depression requires collaboration with colleagues, but coordinating that care takes resources. Who is in charge of ensuring care?
“This is where teams come in,” says Dr. April Barbour, associate professor of medicine and chief of general internal medicine George Washington University, Washington. “Because it doesn’t necessarily need to be the psychiatrist. A discharge coordinator could serve that role and send that information back.”
“I agree. And then we come back to the next thing: Who’s going to pay for the team? Who’s going to manage the team? Also, the other thing – with any team, someone’s got to be the quarterback – someone has to make sure or verify that it happened,” says Dr. Lorenzo Norris, cohost of Mental Health Consult, and assistant professor of psychiatry and behavioral sciences at George Washington University.
“When you are treating mental illness, you need a team-based approach so that you can look at everything that is going on. If you are strictly algorithmic based, there are going to be fatal errors,” Dr. Norris says. “It doesn’t reduce down to that level.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Continuity of care for the 18-year-old male who told Dr. Lillian M. Beard about his depression requires collaboration with colleagues, but coordinating that care takes resources. Who is in charge of ensuring care?
“This is where teams come in,” says Dr. April Barbour, associate professor of medicine and chief of general internal medicine George Washington University, Washington. “Because it doesn’t necessarily need to be the psychiatrist. A discharge coordinator could serve that role and send that information back.”
“I agree. And then we come back to the next thing: Who’s going to pay for the team? Who’s going to manage the team? Also, the other thing – with any team, someone’s got to be the quarterback – someone has to make sure or verify that it happened,” says Dr. Lorenzo Norris, cohost of Mental Health Consult, and assistant professor of psychiatry and behavioral sciences at George Washington University.
“When you are treating mental illness, you need a team-based approach so that you can look at everything that is going on. If you are strictly algorithmic based, there are going to be fatal errors,” Dr. Norris says. “It doesn’t reduce down to that level.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Suicidal ideation: An 18-year-old male presents in crisis
When a patient presents with depression, how is it possible to determine whether serious mental illnesses such as first-episode psychosis are unfolding? In this video, Dr. Lillian M. Beard, who practices pediatrics in Silver Spring, Md., discusses the case of an 18-year-old male with thoughts of suicide whose situation was exacerbated by poor continuity of care.
“From the crisis center, [the patient] was admitted to a hospital, but there wasn’t a follow-up,” Dr. Beard says.
This discussion between Dr. Beard; Dr. Lorenzo Norris, cohost of Mental Health Consult and medical director of psychiatric and behavioral services at George Washington University Hospital, Washington; and Dr. David Pickar, adjunct professor of psychiatry at Johns Hopkins University, Baltimore, explores how these kinds of circumstances might affect the patient’s case, as well as other clinical considerations that should help guide referral.
When a patient presents with depression, how is it possible to determine whether serious mental illnesses such as first-episode psychosis are unfolding? In this video, Dr. Lillian M. Beard, who practices pediatrics in Silver Spring, Md., discusses the case of an 18-year-old male with thoughts of suicide whose situation was exacerbated by poor continuity of care.
“From the crisis center, [the patient] was admitted to a hospital, but there wasn’t a follow-up,” Dr. Beard says.
This discussion between Dr. Beard; Dr. Lorenzo Norris, cohost of Mental Health Consult and medical director of psychiatric and behavioral services at George Washington University Hospital, Washington; and Dr. David Pickar, adjunct professor of psychiatry at Johns Hopkins University, Baltimore, explores how these kinds of circumstances might affect the patient’s case, as well as other clinical considerations that should help guide referral.
When a patient presents with depression, how is it possible to determine whether serious mental illnesses such as first-episode psychosis are unfolding? In this video, Dr. Lillian M. Beard, who practices pediatrics in Silver Spring, Md., discusses the case of an 18-year-old male with thoughts of suicide whose situation was exacerbated by poor continuity of care.
“From the crisis center, [the patient] was admitted to a hospital, but there wasn’t a follow-up,” Dr. Beard says.
This discussion between Dr. Beard; Dr. Lorenzo Norris, cohost of Mental Health Consult and medical director of psychiatric and behavioral services at George Washington University Hospital, Washington; and Dr. David Pickar, adjunct professor of psychiatry at Johns Hopkins University, Baltimore, explores how these kinds of circumstances might affect the patient’s case, as well as other clinical considerations that should help guide referral.
VIDEO: Proposed revision of medullary thyroid cancer staging improves risk-stratification analysis
BOSTON – An analysis of data from medullary thyroid cancer patients that partitioned the patients into groups with similar overall survival has spurred a rethink of the current American Joint Committee on Cancer (AJCC) staging system.
The results from researchers at Duke University, Durham, N.C., presented at the annual meeting of the Endocrine Society by Dr. Mohamed Abdelgadir Adam, are timely, as the AJCC has embarked on a reconsideration of the staging of cancers, including medullary thyroid cancer (MTC), as part revisions for the eighth edition of the staging system.
“The existing AJCC staging system for MTC appears to be less than optimal in discriminating the risk of mortality among disease stage groups,” said Dr. Adam, who discussed the findings in a video interview.
MTC, a neuroendocrine tumor that affects C cells of the thyroid, comprises 3%-5% of all cases of thyroid cancer and it can be a more aggressive disease than differentiated thyroid cancer. Yet the current AJCC MTC staging system has been extrapolated from differentiated thyroid cancer data.
“We sought to evaluate how well the current AJCC seventh edition stage groupings predict survival for patients with MTC, to suggest a possible staging revision to sharpen estimates of prognosis,” said Dr. Adam.
The researchers utilized the National Cancer Data Base, representing over 70% of incident cancer cases in the United States.
MTC patients who underwent thyroid surgery from 1998 to 2012 were identified. Patients with missing values for pathologic T, N, or M were excluded. The primary outcome in the 3,315 patients was survival.
The researchers used a form of decision-tree analysis called recursive partitioning. In general, recursive partitioning is able to classify a population by splitting subjects into subgroups, each of which is homogeneous based on the particular outcome. In this study, the subgroup allocations were based on T, N, and M stages, with the outcome being overall survival. Kaplan-Meier and adjusted survival analyses enabled survival differences among the four subgroups (groups I, II, III and IV) to be explored.
The four groups were distinct in terms of survival time and allowed more accurate risk stratification. In particular, groups I and II were markedly better distinguished from one another than is the case with the current staging system. Survival differences across the stages were more distinct with the newly created T, N, and M groupings, compared with the current AJCC staging system.
After adjustment, survival differences across TNM groups were more distinct with the newly created TNM groupings (compared to subgroup I, hazard ratio of 3.06 for subgroup II; HR, 6.79 for III; and HR, 17.03 for IV), compared with the current AJCC staging (compared to stage I, HR, 1.45 for stage II; HR, 2.17 for III; and HR, 5.33 for IV).
“The AJCC is reevaluating all staging schemas, including MTC. The current AJCC staging system could be improved with the newly identified TNM groupings suggested here for more accurate patient risk stratification and possibly treatment selection,” said Dr. Adam.
Dr. Adam had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – An analysis of data from medullary thyroid cancer patients that partitioned the patients into groups with similar overall survival has spurred a rethink of the current American Joint Committee on Cancer (AJCC) staging system.
The results from researchers at Duke University, Durham, N.C., presented at the annual meeting of the Endocrine Society by Dr. Mohamed Abdelgadir Adam, are timely, as the AJCC has embarked on a reconsideration of the staging of cancers, including medullary thyroid cancer (MTC), as part revisions for the eighth edition of the staging system.
“The existing AJCC staging system for MTC appears to be less than optimal in discriminating the risk of mortality among disease stage groups,” said Dr. Adam, who discussed the findings in a video interview.
MTC, a neuroendocrine tumor that affects C cells of the thyroid, comprises 3%-5% of all cases of thyroid cancer and it can be a more aggressive disease than differentiated thyroid cancer. Yet the current AJCC MTC staging system has been extrapolated from differentiated thyroid cancer data.
“We sought to evaluate how well the current AJCC seventh edition stage groupings predict survival for patients with MTC, to suggest a possible staging revision to sharpen estimates of prognosis,” said Dr. Adam.
The researchers utilized the National Cancer Data Base, representing over 70% of incident cancer cases in the United States.
MTC patients who underwent thyroid surgery from 1998 to 2012 were identified. Patients with missing values for pathologic T, N, or M were excluded. The primary outcome in the 3,315 patients was survival.
The researchers used a form of decision-tree analysis called recursive partitioning. In general, recursive partitioning is able to classify a population by splitting subjects into subgroups, each of which is homogeneous based on the particular outcome. In this study, the subgroup allocations were based on T, N, and M stages, with the outcome being overall survival. Kaplan-Meier and adjusted survival analyses enabled survival differences among the four subgroups (groups I, II, III and IV) to be explored.
The four groups were distinct in terms of survival time and allowed more accurate risk stratification. In particular, groups I and II were markedly better distinguished from one another than is the case with the current staging system. Survival differences across the stages were more distinct with the newly created T, N, and M groupings, compared with the current AJCC staging system.
After adjustment, survival differences across TNM groups were more distinct with the newly created TNM groupings (compared to subgroup I, hazard ratio of 3.06 for subgroup II; HR, 6.79 for III; and HR, 17.03 for IV), compared with the current AJCC staging (compared to stage I, HR, 1.45 for stage II; HR, 2.17 for III; and HR, 5.33 for IV).
“The AJCC is reevaluating all staging schemas, including MTC. The current AJCC staging system could be improved with the newly identified TNM groupings suggested here for more accurate patient risk stratification and possibly treatment selection,” said Dr. Adam.
Dr. Adam had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – An analysis of data from medullary thyroid cancer patients that partitioned the patients into groups with similar overall survival has spurred a rethink of the current American Joint Committee on Cancer (AJCC) staging system.
The results from researchers at Duke University, Durham, N.C., presented at the annual meeting of the Endocrine Society by Dr. Mohamed Abdelgadir Adam, are timely, as the AJCC has embarked on a reconsideration of the staging of cancers, including medullary thyroid cancer (MTC), as part revisions for the eighth edition of the staging system.
“The existing AJCC staging system for MTC appears to be less than optimal in discriminating the risk of mortality among disease stage groups,” said Dr. Adam, who discussed the findings in a video interview.
MTC, a neuroendocrine tumor that affects C cells of the thyroid, comprises 3%-5% of all cases of thyroid cancer and it can be a more aggressive disease than differentiated thyroid cancer. Yet the current AJCC MTC staging system has been extrapolated from differentiated thyroid cancer data.
“We sought to evaluate how well the current AJCC seventh edition stage groupings predict survival for patients with MTC, to suggest a possible staging revision to sharpen estimates of prognosis,” said Dr. Adam.
The researchers utilized the National Cancer Data Base, representing over 70% of incident cancer cases in the United States.
MTC patients who underwent thyroid surgery from 1998 to 2012 were identified. Patients with missing values for pathologic T, N, or M were excluded. The primary outcome in the 3,315 patients was survival.
The researchers used a form of decision-tree analysis called recursive partitioning. In general, recursive partitioning is able to classify a population by splitting subjects into subgroups, each of which is homogeneous based on the particular outcome. In this study, the subgroup allocations were based on T, N, and M stages, with the outcome being overall survival. Kaplan-Meier and adjusted survival analyses enabled survival differences among the four subgroups (groups I, II, III and IV) to be explored.
The four groups were distinct in terms of survival time and allowed more accurate risk stratification. In particular, groups I and II were markedly better distinguished from one another than is the case with the current staging system. Survival differences across the stages were more distinct with the newly created T, N, and M groupings, compared with the current AJCC staging system.
After adjustment, survival differences across TNM groups were more distinct with the newly created TNM groupings (compared to subgroup I, hazard ratio of 3.06 for subgroup II; HR, 6.79 for III; and HR, 17.03 for IV), compared with the current AJCC staging (compared to stage I, HR, 1.45 for stage II; HR, 2.17 for III; and HR, 5.33 for IV).
“The AJCC is reevaluating all staging schemas, including MTC. The current AJCC staging system could be improved with the newly identified TNM groupings suggested here for more accurate patient risk stratification and possibly treatment selection,” said Dr. Adam.
Dr. Adam had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Key clinical point: A proposed revision of the AJCC thyroid cancer staging system improves risk stratification analysis.
Major finding: In the proposed staging system, compared to subgroup I, hazard ratio for survival was 3.06 for subgroup II; HR, 6.79 for III; and HR, 17.03 for IV, compared with the current AJCC staging of HR, 1.45 for stage II; HR, 2.17 for III; and HR, 5.33 for IV.
Data source: Data from 3,315 patients with medullary thyroid cancer was drawn from the National Cancer Database.
Disclosures: Dr. Adam had no disclosures.
Severe sepsis and septic shock syndrome linked to chikungunya
Severe sepsis and septic shock syndrome may be rare complications of chikungunya virus infection, according to a recent study in Guadeloupe.
Dr. Bruno Hoen, of the department of infectious diseases, dermatology, and internal medicine at the University Medical Center of Guadeloupe, and his associates studied 110 nonpregnant adults hospitalized at the University Hospital of Pointe-à-Pitre, Guadeloupe, with chikungunya (CHIKV) after a November 2013 outbreak in Guadeloupe. Of all patients who had a positive CHIKV reverse transcription–polymerase chain reaction (RT-PCR) test result, 34 had a common form, 34 had an atypical form, and 42 had a severe form. Among the 42 patients with severe forms, 25 patients had illness consistent with the case definition for severe sepsis and had no other identified cause for this syndrome, and 12 died.
The 25 patients identified as having severe sepsis had significantly higher occurrences of cardiac, respiratory, and renal manifestations upon admission to hospital. They also had significantly higher leukocyte counts and levels of serum lactate dehydrogenase, aspartate aminotransferase, and creatinine – all clinical and laboratory indicators of sepsis – than patients without severe sepsis or septic shock. In addition, the mortality rate for the patients with severe sepsis was significantly higher than that in patients without severe sepsis or septic shock (48% vs. 3%; P less than .001).
As none of the 25 patients with severe sepsis or septic shock in the early stages of CHIKV had another organism that could be identified as a potential cause of sepsis, the researchers concluded that this finding strongly suggests that CHIKV can, in rare cases, cause severe sepsis and septic shock syndromes, an observation that had not been reported until very recently.
Dr. Hoen and his colleagues said additional studies are needed to identify any background characteristics that might be associated with the onset of severe sepsis or septic shock. The authors reported no conflicts of interest.
Read the full study in Emerging Infectious Diseases (2016 May. doi: 10.3201/eid2205.151449).
Severe sepsis and septic shock syndrome may be rare complications of chikungunya virus infection, according to a recent study in Guadeloupe.
Dr. Bruno Hoen, of the department of infectious diseases, dermatology, and internal medicine at the University Medical Center of Guadeloupe, and his associates studied 110 nonpregnant adults hospitalized at the University Hospital of Pointe-à-Pitre, Guadeloupe, with chikungunya (CHIKV) after a November 2013 outbreak in Guadeloupe. Of all patients who had a positive CHIKV reverse transcription–polymerase chain reaction (RT-PCR) test result, 34 had a common form, 34 had an atypical form, and 42 had a severe form. Among the 42 patients with severe forms, 25 patients had illness consistent with the case definition for severe sepsis and had no other identified cause for this syndrome, and 12 died.
The 25 patients identified as having severe sepsis had significantly higher occurrences of cardiac, respiratory, and renal manifestations upon admission to hospital. They also had significantly higher leukocyte counts and levels of serum lactate dehydrogenase, aspartate aminotransferase, and creatinine – all clinical and laboratory indicators of sepsis – than patients without severe sepsis or septic shock. In addition, the mortality rate for the patients with severe sepsis was significantly higher than that in patients without severe sepsis or septic shock (48% vs. 3%; P less than .001).
As none of the 25 patients with severe sepsis or septic shock in the early stages of CHIKV had another organism that could be identified as a potential cause of sepsis, the researchers concluded that this finding strongly suggests that CHIKV can, in rare cases, cause severe sepsis and septic shock syndromes, an observation that had not been reported until very recently.
Dr. Hoen and his colleagues said additional studies are needed to identify any background characteristics that might be associated with the onset of severe sepsis or septic shock. The authors reported no conflicts of interest.
Read the full study in Emerging Infectious Diseases (2016 May. doi: 10.3201/eid2205.151449).
Severe sepsis and septic shock syndrome may be rare complications of chikungunya virus infection, according to a recent study in Guadeloupe.
Dr. Bruno Hoen, of the department of infectious diseases, dermatology, and internal medicine at the University Medical Center of Guadeloupe, and his associates studied 110 nonpregnant adults hospitalized at the University Hospital of Pointe-à-Pitre, Guadeloupe, with chikungunya (CHIKV) after a November 2013 outbreak in Guadeloupe. Of all patients who had a positive CHIKV reverse transcription–polymerase chain reaction (RT-PCR) test result, 34 had a common form, 34 had an atypical form, and 42 had a severe form. Among the 42 patients with severe forms, 25 patients had illness consistent with the case definition for severe sepsis and had no other identified cause for this syndrome, and 12 died.
The 25 patients identified as having severe sepsis had significantly higher occurrences of cardiac, respiratory, and renal manifestations upon admission to hospital. They also had significantly higher leukocyte counts and levels of serum lactate dehydrogenase, aspartate aminotransferase, and creatinine – all clinical and laboratory indicators of sepsis – than patients without severe sepsis or septic shock. In addition, the mortality rate for the patients with severe sepsis was significantly higher than that in patients without severe sepsis or septic shock (48% vs. 3%; P less than .001).
As none of the 25 patients with severe sepsis or septic shock in the early stages of CHIKV had another organism that could be identified as a potential cause of sepsis, the researchers concluded that this finding strongly suggests that CHIKV can, in rare cases, cause severe sepsis and septic shock syndromes, an observation that had not been reported until very recently.
Dr. Hoen and his colleagues said additional studies are needed to identify any background characteristics that might be associated with the onset of severe sepsis or septic shock. The authors reported no conflicts of interest.
Read the full study in Emerging Infectious Diseases (2016 May. doi: 10.3201/eid2205.151449).
FROM EMERGING INFECTIOUS DISEASES