User login
Recommendations for Cancer Moonshot overlook a few issues, YSC says
Overall, the response to Blue Ribbon Panel recommendations for guiding the Cancer Moonshot initiative were well received, though some patient advocates say a few key issues were overlooked.
In early September 2016, the Blue Ribbon Panel, a group of more than 150 scientists, clinicians, patient advocates, and industry representatives convened by the National Cancer Institutes’s National Cancer Advisory Board, published its Top 10 recommendations to guide future endeavors of the Cancer Moonshot Initiative.
The recommendations, which were informed by input from the research community and the public, emphasized “the importance of direct patient engagement in cancer research, a deeper understanding of why some therapies work and others do not, the dynamics of tumor evolution, and the need for mechanisms of data sharing, access, and analysis,” wrote Dinah S. Singer, PhD, and two other cochairs of the Blue Ribbon Panel in an article published in Science (2016 Sep 7. doi: 10.1126/science.aai7862).
“The recommendations that were announced today by the Cancer Moonshot Blue Ribbon Panel are vitally important to accomplishing the goal of the National Cancer Moonshot Initiative, which is to achieve a decade’s worth of advances in five years,” wrote American Association for Cancer Research President Nancy E. Davidson, MD, in a statement.
“The panel’s thoughtful work makes an important contribution to the Cancer Moonshot Initiative,” wrote American Society for Clinical Oncology President Daniel F. Hayes, MD, in a statement. In an interview, Dr. Hayes added that innovations in information technology and the focus on improving interoperability of electronic health records were two important strengths of the recommendations that will be “critically important to deliver high-quality, high-value oncology services to individuals with cancer.”
Michelle Esser, senior program manager at the Young Survival Coalition (YSC), agreed that the recommendations are good initial steps. However, she pointed out two issues that the recommendations overlooked. “First, is the lack of mention or understanding of the adolescent and young adult (AYA) oncology patient population,” Ms. Esser noted during an interview. “The report specifically called out pediatric cancer as an area of needed research, but AYAs, whose survival rates lag behind those of older and younger patients with a similar diagnosis, and for whom cancer is the leading cause of disease-related death, were not mentioned.”
Second, there was little mention of cancer metastasis, she said. “It is not an early-stage cancer diagnosis that kills, it is when cancer metastasizes and spreads that it becomes deadly. Out of the 10 recommendations only 1 mentions metastasis. If we want to make a difference in cancer outcomes, there needs to be focus on understanding why metastasis occurs, how to prevent it, and how to cure it.”
In order for these recommendations to really expedite the nation’s progress against cancer, “It is crucial that Congress provide the necessary funding to support the priority projects identified by the Blue Ribbon Panel and those we will hear about from the Task Force and Vice President’s Executive Reports later this year,” reported Dr. Hayes, a sentiment echoed by Dr. Davidson.
On Twitter @jessnicolecraig
Overall, the response to Blue Ribbon Panel recommendations for guiding the Cancer Moonshot initiative were well received, though some patient advocates say a few key issues were overlooked.
In early September 2016, the Blue Ribbon Panel, a group of more than 150 scientists, clinicians, patient advocates, and industry representatives convened by the National Cancer Institutes’s National Cancer Advisory Board, published its Top 10 recommendations to guide future endeavors of the Cancer Moonshot Initiative.
The recommendations, which were informed by input from the research community and the public, emphasized “the importance of direct patient engagement in cancer research, a deeper understanding of why some therapies work and others do not, the dynamics of tumor evolution, and the need for mechanisms of data sharing, access, and analysis,” wrote Dinah S. Singer, PhD, and two other cochairs of the Blue Ribbon Panel in an article published in Science (2016 Sep 7. doi: 10.1126/science.aai7862).
“The recommendations that were announced today by the Cancer Moonshot Blue Ribbon Panel are vitally important to accomplishing the goal of the National Cancer Moonshot Initiative, which is to achieve a decade’s worth of advances in five years,” wrote American Association for Cancer Research President Nancy E. Davidson, MD, in a statement.
“The panel’s thoughtful work makes an important contribution to the Cancer Moonshot Initiative,” wrote American Society for Clinical Oncology President Daniel F. Hayes, MD, in a statement. In an interview, Dr. Hayes added that innovations in information technology and the focus on improving interoperability of electronic health records were two important strengths of the recommendations that will be “critically important to deliver high-quality, high-value oncology services to individuals with cancer.”
Michelle Esser, senior program manager at the Young Survival Coalition (YSC), agreed that the recommendations are good initial steps. However, she pointed out two issues that the recommendations overlooked. “First, is the lack of mention or understanding of the adolescent and young adult (AYA) oncology patient population,” Ms. Esser noted during an interview. “The report specifically called out pediatric cancer as an area of needed research, but AYAs, whose survival rates lag behind those of older and younger patients with a similar diagnosis, and for whom cancer is the leading cause of disease-related death, were not mentioned.”
Second, there was little mention of cancer metastasis, she said. “It is not an early-stage cancer diagnosis that kills, it is when cancer metastasizes and spreads that it becomes deadly. Out of the 10 recommendations only 1 mentions metastasis. If we want to make a difference in cancer outcomes, there needs to be focus on understanding why metastasis occurs, how to prevent it, and how to cure it.”
In order for these recommendations to really expedite the nation’s progress against cancer, “It is crucial that Congress provide the necessary funding to support the priority projects identified by the Blue Ribbon Panel and those we will hear about from the Task Force and Vice President’s Executive Reports later this year,” reported Dr. Hayes, a sentiment echoed by Dr. Davidson.
On Twitter @jessnicolecraig
Overall, the response to Blue Ribbon Panel recommendations for guiding the Cancer Moonshot initiative were well received, though some patient advocates say a few key issues were overlooked.
In early September 2016, the Blue Ribbon Panel, a group of more than 150 scientists, clinicians, patient advocates, and industry representatives convened by the National Cancer Institutes’s National Cancer Advisory Board, published its Top 10 recommendations to guide future endeavors of the Cancer Moonshot Initiative.
The recommendations, which were informed by input from the research community and the public, emphasized “the importance of direct patient engagement in cancer research, a deeper understanding of why some therapies work and others do not, the dynamics of tumor evolution, and the need for mechanisms of data sharing, access, and analysis,” wrote Dinah S. Singer, PhD, and two other cochairs of the Blue Ribbon Panel in an article published in Science (2016 Sep 7. doi: 10.1126/science.aai7862).
“The recommendations that were announced today by the Cancer Moonshot Blue Ribbon Panel are vitally important to accomplishing the goal of the National Cancer Moonshot Initiative, which is to achieve a decade’s worth of advances in five years,” wrote American Association for Cancer Research President Nancy E. Davidson, MD, in a statement.
“The panel’s thoughtful work makes an important contribution to the Cancer Moonshot Initiative,” wrote American Society for Clinical Oncology President Daniel F. Hayes, MD, in a statement. In an interview, Dr. Hayes added that innovations in information technology and the focus on improving interoperability of electronic health records were two important strengths of the recommendations that will be “critically important to deliver high-quality, high-value oncology services to individuals with cancer.”
Michelle Esser, senior program manager at the Young Survival Coalition (YSC), agreed that the recommendations are good initial steps. However, she pointed out two issues that the recommendations overlooked. “First, is the lack of mention or understanding of the adolescent and young adult (AYA) oncology patient population,” Ms. Esser noted during an interview. “The report specifically called out pediatric cancer as an area of needed research, but AYAs, whose survival rates lag behind those of older and younger patients with a similar diagnosis, and for whom cancer is the leading cause of disease-related death, were not mentioned.”
Second, there was little mention of cancer metastasis, she said. “It is not an early-stage cancer diagnosis that kills, it is when cancer metastasizes and spreads that it becomes deadly. Out of the 10 recommendations only 1 mentions metastasis. If we want to make a difference in cancer outcomes, there needs to be focus on understanding why metastasis occurs, how to prevent it, and how to cure it.”
In order for these recommendations to really expedite the nation’s progress against cancer, “It is crucial that Congress provide the necessary funding to support the priority projects identified by the Blue Ribbon Panel and those we will hear about from the Task Force and Vice President’s Executive Reports later this year,” reported Dr. Hayes, a sentiment echoed by Dr. Davidson.
On Twitter @jessnicolecraig
CSF lactate concentration identifies postneurosurgical bacterial meningitis
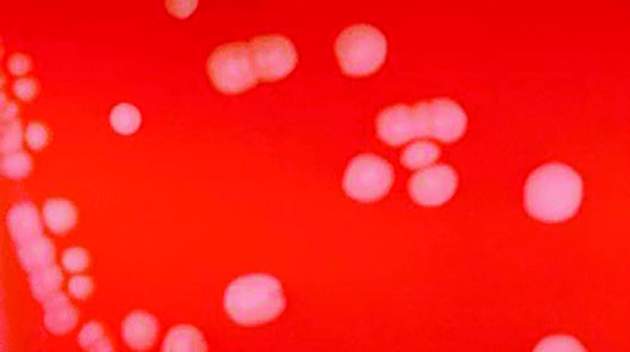
The concentration of lactate in the cerebrospinal fluid accurately identifies bacterial meningitis that develops after neurosurgery, distinguishing it from other conditions, according to a report published in BMC Infectious Diseases.
In patients who have undergone neurosurgery, failure to promptly identify and treat bacterial meningitis is associated with patient mortality as high as 50%, reported Xiong Xiao of the department of neurosurgery and the China National Clinical Research Center for Neurological Diseases at Beijing Tiantan Hospital and Capital Medical University, Beijing, and associates.
A recent small study suggested that cerebrospinal fluid (CSF) lactate was accurate at differentiating postoperative bacterial meningitis from aseptic meningitis. To examine this possibility in a larger patient population, Dr. Xiao and associates reviewed 1,672 articles in the medical literature. They found few high-quality studies of this topic, but were able to perform a meta-analysis and pool the data from five studies involving 404 postneurosurgical patients treated during a 15-year period.
CSF lactate concentration identified bacterial meningitis with a pooled sensitivity of 92% and a pooled specificity of 88%. “Moreover, this test is fast, simple, objective, and affordable, and can be widely applied in hospitals,” the investigators wrote (BMC Infect Dis. 2016;16:483. doi: 10.1186/s12879-016-1818-2).Larger prospective studies are needed to confirm this finding and to provide a more thorough understanding of the indicators of postneurosurgical meningitis, Dr. Xiao and associates added.
This study was supported by Beijing Tiantan Hospital Funds for Young Scholars, the Ministry of Science and Technology of China, and the Beijing Talents Fund. Dr. Xiao and associates reported having no relevant financial disclosures.
The concentration of lactate in the cerebrospinal fluid accurately identifies bacterial meningitis that develops after neurosurgery, distinguishing it from other conditions, according to a report published in BMC Infectious Diseases.
In patients who have undergone neurosurgery, failure to promptly identify and treat bacterial meningitis is associated with patient mortality as high as 50%, reported Xiong Xiao of the department of neurosurgery and the China National Clinical Research Center for Neurological Diseases at Beijing Tiantan Hospital and Capital Medical University, Beijing, and associates.
A recent small study suggested that cerebrospinal fluid (CSF) lactate was accurate at differentiating postoperative bacterial meningitis from aseptic meningitis. To examine this possibility in a larger patient population, Dr. Xiao and associates reviewed 1,672 articles in the medical literature. They found few high-quality studies of this topic, but were able to perform a meta-analysis and pool the data from five studies involving 404 postneurosurgical patients treated during a 15-year period.
CSF lactate concentration identified bacterial meningitis with a pooled sensitivity of 92% and a pooled specificity of 88%. “Moreover, this test is fast, simple, objective, and affordable, and can be widely applied in hospitals,” the investigators wrote (BMC Infect Dis. 2016;16:483. doi: 10.1186/s12879-016-1818-2).Larger prospective studies are needed to confirm this finding and to provide a more thorough understanding of the indicators of postneurosurgical meningitis, Dr. Xiao and associates added.
This study was supported by Beijing Tiantan Hospital Funds for Young Scholars, the Ministry of Science and Technology of China, and the Beijing Talents Fund. Dr. Xiao and associates reported having no relevant financial disclosures.
The concentration of lactate in the cerebrospinal fluid accurately identifies bacterial meningitis that develops after neurosurgery, distinguishing it from other conditions, according to a report published in BMC Infectious Diseases.
In patients who have undergone neurosurgery, failure to promptly identify and treat bacterial meningitis is associated with patient mortality as high as 50%, reported Xiong Xiao of the department of neurosurgery and the China National Clinical Research Center for Neurological Diseases at Beijing Tiantan Hospital and Capital Medical University, Beijing, and associates.
A recent small study suggested that cerebrospinal fluid (CSF) lactate was accurate at differentiating postoperative bacterial meningitis from aseptic meningitis. To examine this possibility in a larger patient population, Dr. Xiao and associates reviewed 1,672 articles in the medical literature. They found few high-quality studies of this topic, but were able to perform a meta-analysis and pool the data from five studies involving 404 postneurosurgical patients treated during a 15-year period.
CSF lactate concentration identified bacterial meningitis with a pooled sensitivity of 92% and a pooled specificity of 88%. “Moreover, this test is fast, simple, objective, and affordable, and can be widely applied in hospitals,” the investigators wrote (BMC Infect Dis. 2016;16:483. doi: 10.1186/s12879-016-1818-2).Larger prospective studies are needed to confirm this finding and to provide a more thorough understanding of the indicators of postneurosurgical meningitis, Dr. Xiao and associates added.
This study was supported by Beijing Tiantan Hospital Funds for Young Scholars, the Ministry of Science and Technology of China, and the Beijing Talents Fund. Dr. Xiao and associates reported having no relevant financial disclosures.
FROM BMC INFECTIOUS DISEASES
Key clinical point: CSF lactate concentration accurately identifies bacterial meningitis that develops after neurosurgery.
Major finding: CSF lactate concentration identified bacterial meningitis with a pooled sensitivity of 92% and a pooled specificity of 88%.
Data source: A meta-analysis of five published studies involving 404 patients during a 15-year period.
Disclosures: This study was supported by Beijing Tiantan Hospital Funds for Young Scholars, the Ministry of Science and Technology of China, and the Beijing Talents Fund. Dr. Xiao and associates reported having no relevant financial disclosures.
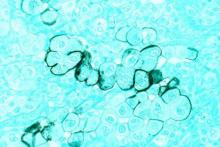
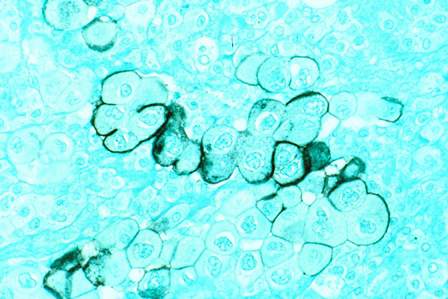
‘Meaningful’ antitumor activity with lenalidomide monotherapy in ATL
Lenalidomide monotherapy demonstrated “meaningful” antitumor activity in patients with relapsed or recurrent aggressive adult T-cell leukemia/lymphoma (ATL), according to new findings.
Among 26 patients enrolled in the study, 11 responses were observed, for an overall response rate of 42% (95% CI, 23%-63%). This included four complete responses and one unconfirmed complete response.
The tumor control rate was 73%, achieved in 19 patients, and the toxicity profile was manageable. Overall, these findings hint at the potential of lenalidomide to “become a treatment option in this patient population,” wrote Takashi Ishida, MD, of Nagoya City University Graduate School of Medical Sciences, Aichi, Japan, and his colleagues (J Clin Oncol. 2016 Sep 12. doi: 10.1200/JCO.2016.67.7732).
ATL is a difficult disease to treat, and it has a poor prognosis, as it is resistant to conventional chemotherapeutic agents and treatment options are currently limited. Lenalidomide, an oral immunomodulatory agent, has demonstrated both antiproliferative and antineoplastic activity in B-cell lymphomas in preclinical studies, and a previous phase I trial established a maximum tolerated dosage (25 mg/d) in a small cohort of Japanese patients with relapsed ATL or other peripheral T-cell lymphomas (PTCL).
Based on these preliminary results, Dr. Ishida and his coauthors designed the current multicenter phase II study, to evaluate the efficacy and safety of lenalidomide monotherapy in 26 patients with relapsed or recurrent ATL.
At a median follow-up of 3.9 months, responses were observed in 33% of patients (5 of 15) with acute disease, 57% (4 of 7) with lymphoma, and 50% (2 of 4) for unfavorable chronic ATL. Patient responses according to disease site were 31% for target (nodal and extranodal) lesions, 75% for cutaneous lesions, and 60% for peripheral blood.
The median time to relapse was 1.9 months (range, 1.8-3.7 months), while the median time to progression was 3.8 months (95% CI, 1.9 to not estimable [NE]). The median and mean duration of response for the entire cohort were NE (95% CI, 0.5 months to NE) and 5.2 months (range, 0 to 16.6 months), respectively.
Progression-free survival was 3.8 months (95% CI, 1.9 months to NE) and for overall survival, it was 20.3 months (95% CI, 9.1 months to NE).
Adverse events occurred in more than 20% of patients and the most common hematologic event was thrombocytopenia (77%). The most common nonhematologic event was increased C-reactive protein (42%), and hypoalbuminemia and hypoproteinemia were observed in about a third of patients, as were constipation, hyponatremia, and hypocalcemia (all 31%).
Dr. Ishida and several coauthors reported multiple relationships with industry, including Celgene K.K. (Tokyo), the study’s sponsor.
Lenalidomide monotherapy demonstrated “meaningful” antitumor activity in patients with relapsed or recurrent aggressive adult T-cell leukemia/lymphoma (ATL), according to new findings.
Among 26 patients enrolled in the study, 11 responses were observed, for an overall response rate of 42% (95% CI, 23%-63%). This included four complete responses and one unconfirmed complete response.
The tumor control rate was 73%, achieved in 19 patients, and the toxicity profile was manageable. Overall, these findings hint at the potential of lenalidomide to “become a treatment option in this patient population,” wrote Takashi Ishida, MD, of Nagoya City University Graduate School of Medical Sciences, Aichi, Japan, and his colleagues (J Clin Oncol. 2016 Sep 12. doi: 10.1200/JCO.2016.67.7732).
ATL is a difficult disease to treat, and it has a poor prognosis, as it is resistant to conventional chemotherapeutic agents and treatment options are currently limited. Lenalidomide, an oral immunomodulatory agent, has demonstrated both antiproliferative and antineoplastic activity in B-cell lymphomas in preclinical studies, and a previous phase I trial established a maximum tolerated dosage (25 mg/d) in a small cohort of Japanese patients with relapsed ATL or other peripheral T-cell lymphomas (PTCL).
Based on these preliminary results, Dr. Ishida and his coauthors designed the current multicenter phase II study, to evaluate the efficacy and safety of lenalidomide monotherapy in 26 patients with relapsed or recurrent ATL.
At a median follow-up of 3.9 months, responses were observed in 33% of patients (5 of 15) with acute disease, 57% (4 of 7) with lymphoma, and 50% (2 of 4) for unfavorable chronic ATL. Patient responses according to disease site were 31% for target (nodal and extranodal) lesions, 75% for cutaneous lesions, and 60% for peripheral blood.
The median time to relapse was 1.9 months (range, 1.8-3.7 months), while the median time to progression was 3.8 months (95% CI, 1.9 to not estimable [NE]). The median and mean duration of response for the entire cohort were NE (95% CI, 0.5 months to NE) and 5.2 months (range, 0 to 16.6 months), respectively.
Progression-free survival was 3.8 months (95% CI, 1.9 months to NE) and for overall survival, it was 20.3 months (95% CI, 9.1 months to NE).
Adverse events occurred in more than 20% of patients and the most common hematologic event was thrombocytopenia (77%). The most common nonhematologic event was increased C-reactive protein (42%), and hypoalbuminemia and hypoproteinemia were observed in about a third of patients, as were constipation, hyponatremia, and hypocalcemia (all 31%).
Dr. Ishida and several coauthors reported multiple relationships with industry, including Celgene K.K. (Tokyo), the study’s sponsor.
Lenalidomide monotherapy demonstrated “meaningful” antitumor activity in patients with relapsed or recurrent aggressive adult T-cell leukemia/lymphoma (ATL), according to new findings.
Among 26 patients enrolled in the study, 11 responses were observed, for an overall response rate of 42% (95% CI, 23%-63%). This included four complete responses and one unconfirmed complete response.
The tumor control rate was 73%, achieved in 19 patients, and the toxicity profile was manageable. Overall, these findings hint at the potential of lenalidomide to “become a treatment option in this patient population,” wrote Takashi Ishida, MD, of Nagoya City University Graduate School of Medical Sciences, Aichi, Japan, and his colleagues (J Clin Oncol. 2016 Sep 12. doi: 10.1200/JCO.2016.67.7732).
ATL is a difficult disease to treat, and it has a poor prognosis, as it is resistant to conventional chemotherapeutic agents and treatment options are currently limited. Lenalidomide, an oral immunomodulatory agent, has demonstrated both antiproliferative and antineoplastic activity in B-cell lymphomas in preclinical studies, and a previous phase I trial established a maximum tolerated dosage (25 mg/d) in a small cohort of Japanese patients with relapsed ATL or other peripheral T-cell lymphomas (PTCL).
Based on these preliminary results, Dr. Ishida and his coauthors designed the current multicenter phase II study, to evaluate the efficacy and safety of lenalidomide monotherapy in 26 patients with relapsed or recurrent ATL.
At a median follow-up of 3.9 months, responses were observed in 33% of patients (5 of 15) with acute disease, 57% (4 of 7) with lymphoma, and 50% (2 of 4) for unfavorable chronic ATL. Patient responses according to disease site were 31% for target (nodal and extranodal) lesions, 75% for cutaneous lesions, and 60% for peripheral blood.
The median time to relapse was 1.9 months (range, 1.8-3.7 months), while the median time to progression was 3.8 months (95% CI, 1.9 to not estimable [NE]). The median and mean duration of response for the entire cohort were NE (95% CI, 0.5 months to NE) and 5.2 months (range, 0 to 16.6 months), respectively.
Progression-free survival was 3.8 months (95% CI, 1.9 months to NE) and for overall survival, it was 20.3 months (95% CI, 9.1 months to NE).
Adverse events occurred in more than 20% of patients and the most common hematologic event was thrombocytopenia (77%). The most common nonhematologic event was increased C-reactive protein (42%), and hypoalbuminemia and hypoproteinemia were observed in about a third of patients, as were constipation, hyponatremia, and hypocalcemia (all 31%).
Dr. Ishida and several coauthors reported multiple relationships with industry, including Celgene K.K. (Tokyo), the study’s sponsor.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Lenalidomide demonstrated clinical activity with acceptable toxicity in recurrent or relapsed ATL.
Major finding: The overall response rate was 42%, and this included four complete responses and one unconfirmed complete response.
Data source: Multicenter phase II trial comprising 26 patients with relapsed or recurrent ATL.
Disclosures: Dr. Ishida and several coauthors reported multiple relationships with industry, including Celgene K.K. (Tokyo), the study’s sponsor.
Worry may attenuate link between psychiatric symptoms, poorer cognitive performance
SAN FRANCISCO – Unexpectedly, worry predicted better cognitive performance among older adults with mild symptoms of anxiety and depression, according to a cross-sectional, community-based study.
“This just flies in the face of everything that we know about worry in the adult literature,” said Sherry A. Beaudreau, PhD, of the department of psychiatry and behavioral sciences at Stanford (Calif.) University. The findings suggest that older worriers might score lower on some cognitive measures if their worry declines through treatment, she said at the 2016 congress of the International Psychogeriatric Association.
Old age often is marked by mild symptoms of anxiety and depression that do not meet criteria for a psychiatric diagnosis, but nonetheless predict poorer cognitive performance and mild dementia, Dr. Beaudreau said. Recent work has linked anxiety to decreased attentional control, and late life depression, to slow information processing, delayed verbal memory, and other cognitive deficits. Emerging evidence also suggests that worry leads to worse performance on tests of inhibitory ability and delayed memory, Dr. Beaudreau added.
To further test these relationships, she and her associates studied 119 older adults who were living in the San Francisco Bay area between 2010 and 2012. They averaged 74 years of age (range, 65-91 years), 92% were non-Hispanic white, and 56% were women.
Most of the cohort performed well on the Rey Auditory Verbal Learning test, which assesses word recall after a delay of 20-30 minutes, and also scored above average on condition 3 of the Delis-Kaplan Executive Function System, which is a color word assessment of inhibitory control, Dr. Beaudreau reported. Individuals also tended to score low on the Beck Anxiety Inventory and the Beck Depressive Inventory II, with average scores of 3.7 (range, 0-29) and 5.6 (0-41), respectively. The mean score on the Penn State Worry Questionnaire was 37.7, with a range of 16-76.
Regardless of whether their anxiety score was low or high, those who worried more had significantly better inhibitory control than those who worried less (P = .003), Dr. Beaudreau said. “So folks with high worry actually seemed to be doing better in terms of their inhibitory ability,” she added. “This is intriguing to me, because we assume that anxiety is affecting cognition, but worry seems to be doing something different.”
High worry also predicted significantly better inhibitory control among individuals with both low and high depression scores (P = .03), she reported. For the word recall test, worry did not seem to affect performance in the absence of depression, but high worry predicted significantly better word recall among individuals with high depression scores (P = .009).
“These results suggest that psychiatric symptoms of anxiety and depression are modulated by worry severity, and it’s interesting that this finding was so consistent throughout the analyses,” Dr. Beaudreau said. Future studies should examine these relationships in groups of older psychiatric patients stratified by symptom severity rather than diagnosis, she added.
The work was supported by the Alzheimer’s Association and the Stanford/VA Alzheimer’s Center. Dr. Beaudreau had no relevant financial disclosures.
SAN FRANCISCO – Unexpectedly, worry predicted better cognitive performance among older adults with mild symptoms of anxiety and depression, according to a cross-sectional, community-based study.
“This just flies in the face of everything that we know about worry in the adult literature,” said Sherry A. Beaudreau, PhD, of the department of psychiatry and behavioral sciences at Stanford (Calif.) University. The findings suggest that older worriers might score lower on some cognitive measures if their worry declines through treatment, she said at the 2016 congress of the International Psychogeriatric Association.
Old age often is marked by mild symptoms of anxiety and depression that do not meet criteria for a psychiatric diagnosis, but nonetheless predict poorer cognitive performance and mild dementia, Dr. Beaudreau said. Recent work has linked anxiety to decreased attentional control, and late life depression, to slow information processing, delayed verbal memory, and other cognitive deficits. Emerging evidence also suggests that worry leads to worse performance on tests of inhibitory ability and delayed memory, Dr. Beaudreau added.
To further test these relationships, she and her associates studied 119 older adults who were living in the San Francisco Bay area between 2010 and 2012. They averaged 74 years of age (range, 65-91 years), 92% were non-Hispanic white, and 56% were women.
Most of the cohort performed well on the Rey Auditory Verbal Learning test, which assesses word recall after a delay of 20-30 minutes, and also scored above average on condition 3 of the Delis-Kaplan Executive Function System, which is a color word assessment of inhibitory control, Dr. Beaudreau reported. Individuals also tended to score low on the Beck Anxiety Inventory and the Beck Depressive Inventory II, with average scores of 3.7 (range, 0-29) and 5.6 (0-41), respectively. The mean score on the Penn State Worry Questionnaire was 37.7, with a range of 16-76.
Regardless of whether their anxiety score was low or high, those who worried more had significantly better inhibitory control than those who worried less (P = .003), Dr. Beaudreau said. “So folks with high worry actually seemed to be doing better in terms of their inhibitory ability,” she added. “This is intriguing to me, because we assume that anxiety is affecting cognition, but worry seems to be doing something different.”
High worry also predicted significantly better inhibitory control among individuals with both low and high depression scores (P = .03), she reported. For the word recall test, worry did not seem to affect performance in the absence of depression, but high worry predicted significantly better word recall among individuals with high depression scores (P = .009).
“These results suggest that psychiatric symptoms of anxiety and depression are modulated by worry severity, and it’s interesting that this finding was so consistent throughout the analyses,” Dr. Beaudreau said. Future studies should examine these relationships in groups of older psychiatric patients stratified by symptom severity rather than diagnosis, she added.
The work was supported by the Alzheimer’s Association and the Stanford/VA Alzheimer’s Center. Dr. Beaudreau had no relevant financial disclosures.
SAN FRANCISCO – Unexpectedly, worry predicted better cognitive performance among older adults with mild symptoms of anxiety and depression, according to a cross-sectional, community-based study.
“This just flies in the face of everything that we know about worry in the adult literature,” said Sherry A. Beaudreau, PhD, of the department of psychiatry and behavioral sciences at Stanford (Calif.) University. The findings suggest that older worriers might score lower on some cognitive measures if their worry declines through treatment, she said at the 2016 congress of the International Psychogeriatric Association.
Old age often is marked by mild symptoms of anxiety and depression that do not meet criteria for a psychiatric diagnosis, but nonetheless predict poorer cognitive performance and mild dementia, Dr. Beaudreau said. Recent work has linked anxiety to decreased attentional control, and late life depression, to slow information processing, delayed verbal memory, and other cognitive deficits. Emerging evidence also suggests that worry leads to worse performance on tests of inhibitory ability and delayed memory, Dr. Beaudreau added.
To further test these relationships, she and her associates studied 119 older adults who were living in the San Francisco Bay area between 2010 and 2012. They averaged 74 years of age (range, 65-91 years), 92% were non-Hispanic white, and 56% were women.
Most of the cohort performed well on the Rey Auditory Verbal Learning test, which assesses word recall after a delay of 20-30 minutes, and also scored above average on condition 3 of the Delis-Kaplan Executive Function System, which is a color word assessment of inhibitory control, Dr. Beaudreau reported. Individuals also tended to score low on the Beck Anxiety Inventory and the Beck Depressive Inventory II, with average scores of 3.7 (range, 0-29) and 5.6 (0-41), respectively. The mean score on the Penn State Worry Questionnaire was 37.7, with a range of 16-76.
Regardless of whether their anxiety score was low or high, those who worried more had significantly better inhibitory control than those who worried less (P = .003), Dr. Beaudreau said. “So folks with high worry actually seemed to be doing better in terms of their inhibitory ability,” she added. “This is intriguing to me, because we assume that anxiety is affecting cognition, but worry seems to be doing something different.”
High worry also predicted significantly better inhibitory control among individuals with both low and high depression scores (P = .03), she reported. For the word recall test, worry did not seem to affect performance in the absence of depression, but high worry predicted significantly better word recall among individuals with high depression scores (P = .009).
“These results suggest that psychiatric symptoms of anxiety and depression are modulated by worry severity, and it’s interesting that this finding was so consistent throughout the analyses,” Dr. Beaudreau said. Future studies should examine these relationships in groups of older psychiatric patients stratified by symptom severity rather than diagnosis, she added.
The work was supported by the Alzheimer’s Association and the Stanford/VA Alzheimer’s Center. Dr. Beaudreau had no relevant financial disclosures.
AT IPA 2016
Key clinical point: In older adults, worry seems to attenuate the relationship between anxiety and depression and poorer cognitive performance.
Major finding: High worry predicted significantly better inhibitory control and delayed word recall, even in the presence of high anxiety and depression symptoms.
Data source: A cross-sectional study of 119 community-dwelling adults who averaged 74 years old.
Disclosures: The work was supported by the Alzheimer’s Association and the Stanford/VA Alzheimer’s Center. Dr. Beaudreau had no relevant financial disclosures.
Neoadjuvant therapy improves survival in pancreatic cancer
Pancreatic cancer patients who received neoadjuvant therapy (NAT) followed by resection had better outcomes than did those who underwent upfront resection, investigators report.
Among patients with clinical stage I or II resected pancreatic head adenocarcinoma, the median survival was higher among those who had received NAT, compared with those who had upfront resection (26 months vs. 21 months; P less than .01).
The survival benefit remained consistent for both clinical stage I (29 months vs. 23 months; P less than .01) and clinical stage II (24 months vs. 20 months; P less than .01).
“This study lends further support for the use of NAT as a favorable patient selection strategy in the management of resectable, early-stage pancreatic adenocarcinoma,” wrote Ali A. Mokdad, MD, of the University of Texas Southwestern Medical Center, Dallas, and his colleagues (J Clin Oncol. 2016 Sep 19. doi: 10.1200/JCO.2016.68.5081).
The researchers compared overall survival between patients who received NAT with subsequent resection with those who received upfront resection, and they also looked at the patient subset of those who received adjuvant therapy.
The cohort included 15,237 patients with clinical stage I or II resected pancreatic head adenocarcinoma who were identified from the National Cancer Database (2006-2012). The patients who received NAT followed by curative-intent resection were matched with patients whose tumors were resected upfront, and the researchers evaluated early postoperative and oncologic outcomes.
Overall survival at 1, 3, and 5 years was 83%, 35%, and 21% in the NAT arm, compared to 71%, 29%, and 18% among patients who underwent upfront surgery, respectively. In the NAT arm, overall mortality was reduced, with an estimated hazard ratio (HR) of 0.72 (95% CI, 0.68-0.76).
In comparison with the subset of patients who received adjuvant therapy, median survival was statistically significantly longer in the NAT group (26 months vs. 23 months; stratified log-rank P less than .01). Overall survival for the adjuvant therapy group at 1, 3, and 5 years was 78%, 31%, and 18%, respectively.
Upon multivariable analysis, the overall survival difference continued to favor the NAT group vs. the adjuvant therapy arm (adjusted HR, 0.83; 95% CI, 0.78-0.89).
Early postoperative morbidity and mortality did not differ between groups. Compared with patients who received NAT, the upfront surgery group had a higher pathologic T stage (pT3 and T4: 86% vs. 73%; P less than .01) and were more likely to have positive lymph nodes (73% vs. 48%; P less than .01) and positive resection margin (24% vs. 17%; P less than .01).
The data “will hopefully provide support and encouragement for participation in the currently open clinical trials evaluating the role of NAT for clinically staged patients with resectable pancreatic cancer,” the authors concluded.
No outside funding source was disclosed. Coauthor Sam C. Wang, MD, declared a relationship with patent/intellectual panel for a prognostic gene panel for gastric cancer. All other authors declared no disclosures.
Pancreatic cancer patients who received neoadjuvant therapy (NAT) followed by resection had better outcomes than did those who underwent upfront resection, investigators report.
Among patients with clinical stage I or II resected pancreatic head adenocarcinoma, the median survival was higher among those who had received NAT, compared with those who had upfront resection (26 months vs. 21 months; P less than .01).
The survival benefit remained consistent for both clinical stage I (29 months vs. 23 months; P less than .01) and clinical stage II (24 months vs. 20 months; P less than .01).
“This study lends further support for the use of NAT as a favorable patient selection strategy in the management of resectable, early-stage pancreatic adenocarcinoma,” wrote Ali A. Mokdad, MD, of the University of Texas Southwestern Medical Center, Dallas, and his colleagues (J Clin Oncol. 2016 Sep 19. doi: 10.1200/JCO.2016.68.5081).
The researchers compared overall survival between patients who received NAT with subsequent resection with those who received upfront resection, and they also looked at the patient subset of those who received adjuvant therapy.
The cohort included 15,237 patients with clinical stage I or II resected pancreatic head adenocarcinoma who were identified from the National Cancer Database (2006-2012). The patients who received NAT followed by curative-intent resection were matched with patients whose tumors were resected upfront, and the researchers evaluated early postoperative and oncologic outcomes.
Overall survival at 1, 3, and 5 years was 83%, 35%, and 21% in the NAT arm, compared to 71%, 29%, and 18% among patients who underwent upfront surgery, respectively. In the NAT arm, overall mortality was reduced, with an estimated hazard ratio (HR) of 0.72 (95% CI, 0.68-0.76).
In comparison with the subset of patients who received adjuvant therapy, median survival was statistically significantly longer in the NAT group (26 months vs. 23 months; stratified log-rank P less than .01). Overall survival for the adjuvant therapy group at 1, 3, and 5 years was 78%, 31%, and 18%, respectively.
Upon multivariable analysis, the overall survival difference continued to favor the NAT group vs. the adjuvant therapy arm (adjusted HR, 0.83; 95% CI, 0.78-0.89).
Early postoperative morbidity and mortality did not differ between groups. Compared with patients who received NAT, the upfront surgery group had a higher pathologic T stage (pT3 and T4: 86% vs. 73%; P less than .01) and were more likely to have positive lymph nodes (73% vs. 48%; P less than .01) and positive resection margin (24% vs. 17%; P less than .01).
The data “will hopefully provide support and encouragement for participation in the currently open clinical trials evaluating the role of NAT for clinically staged patients with resectable pancreatic cancer,” the authors concluded.
No outside funding source was disclosed. Coauthor Sam C. Wang, MD, declared a relationship with patent/intellectual panel for a prognostic gene panel for gastric cancer. All other authors declared no disclosures.
Pancreatic cancer patients who received neoadjuvant therapy (NAT) followed by resection had better outcomes than did those who underwent upfront resection, investigators report.
Among patients with clinical stage I or II resected pancreatic head adenocarcinoma, the median survival was higher among those who had received NAT, compared with those who had upfront resection (26 months vs. 21 months; P less than .01).
The survival benefit remained consistent for both clinical stage I (29 months vs. 23 months; P less than .01) and clinical stage II (24 months vs. 20 months; P less than .01).
“This study lends further support for the use of NAT as a favorable patient selection strategy in the management of resectable, early-stage pancreatic adenocarcinoma,” wrote Ali A. Mokdad, MD, of the University of Texas Southwestern Medical Center, Dallas, and his colleagues (J Clin Oncol. 2016 Sep 19. doi: 10.1200/JCO.2016.68.5081).
The researchers compared overall survival between patients who received NAT with subsequent resection with those who received upfront resection, and they also looked at the patient subset of those who received adjuvant therapy.
The cohort included 15,237 patients with clinical stage I or II resected pancreatic head adenocarcinoma who were identified from the National Cancer Database (2006-2012). The patients who received NAT followed by curative-intent resection were matched with patients whose tumors were resected upfront, and the researchers evaluated early postoperative and oncologic outcomes.
Overall survival at 1, 3, and 5 years was 83%, 35%, and 21% in the NAT arm, compared to 71%, 29%, and 18% among patients who underwent upfront surgery, respectively. In the NAT arm, overall mortality was reduced, with an estimated hazard ratio (HR) of 0.72 (95% CI, 0.68-0.76).
In comparison with the subset of patients who received adjuvant therapy, median survival was statistically significantly longer in the NAT group (26 months vs. 23 months; stratified log-rank P less than .01). Overall survival for the adjuvant therapy group at 1, 3, and 5 years was 78%, 31%, and 18%, respectively.
Upon multivariable analysis, the overall survival difference continued to favor the NAT group vs. the adjuvant therapy arm (adjusted HR, 0.83; 95% CI, 0.78-0.89).
Early postoperative morbidity and mortality did not differ between groups. Compared with patients who received NAT, the upfront surgery group had a higher pathologic T stage (pT3 and T4: 86% vs. 73%; P less than .01) and were more likely to have positive lymph nodes (73% vs. 48%; P less than .01) and positive resection margin (24% vs. 17%; P less than .01).
The data “will hopefully provide support and encouragement for participation in the currently open clinical trials evaluating the role of NAT for clinically staged patients with resectable pancreatic cancer,” the authors concluded.
No outside funding source was disclosed. Coauthor Sam C. Wang, MD, declared a relationship with patent/intellectual panel for a prognostic gene panel for gastric cancer. All other authors declared no disclosures.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Neoadjuvant therapy improves outcomes in pancreatic cancer.
Major finding: Neoadjuvant therapy was associated with improved survival compared with surgery alone, with a median survival of 26 months vs. 21 months.
Data source: Retrospective database study that included 15,237 patients with clinical stage I or II resected pancreatic head adenocarcinoma.
Disclosures: No outside funding source was disclosed. Coauthor Sam C. Wang, MD, declared a relationship with patent/intellectual panel for a prognostic gene panel for gastric cancer. All other authors declared no disclosures.
Try non-TNF biologics for RA if anti-TNF fails
Rheumatoid arthritis patients who were unsuccessfully treated with anti–tumor necrosis factor drugs fared significantly better when treated with a non-TNF biologic than with a second anti-TNF drug in a 52-week, randomized, clinical trial of 300 adults.
Overall, 69% of patients who received a non-TNF biologic achieved clinical response, defined as a good or moderate EULAR response at 24 weeks, compared with 52% of patients who received a second anti-TNF drug, wrote Jacques-Eric Gottenberg, MD, PhD, of Strasbourg (France) University Hospital and his colleagues.
Patients were randomized to a non-TNF biologic or a second anti-TNF drug, with the choice of biologic left to the clinician. Patients were assessed at 12, 24, and 52 weeks.
“In addition to the superiority of the non-TNF treatment for the primary outcome at week 24, the non-TNF treatment was associated with a better EULAR response than a second anti-TNF drug at weeks 12 and 52,” the researchers noted. Significantly more patients in the non-TNF group reported low disease activity at 6 months and 12 months, compared with the second anti-TNF group, they added.
A total of 18 patients in the non-TNF group and 13 patients in the second anti-TNF group experienced serious adverse events; the most common were serious infections (in 33% and 77% of the non-TNF and anti-TNF groups, respectively) and cardiovascular events (33% vs. 8%, respectively).
The study was supported by the French Ministry of Health and promoted by Strasbourg University Hospital. Dr. Gottenberg disclosed financial support from AbbVie, Pfizer, and Roche, and personal fees from Bristol-Myers Squibb, Merck Sharp & Dohme, UCB, GlaxoSmithKline, and Novartis.
The findings were published online Sept. 20 (JAMA 2016;316[11]:1172-80).
Rheumatoid arthritis patients who were unsuccessfully treated with anti–tumor necrosis factor drugs fared significantly better when treated with a non-TNF biologic than with a second anti-TNF drug in a 52-week, randomized, clinical trial of 300 adults.
Overall, 69% of patients who received a non-TNF biologic achieved clinical response, defined as a good or moderate EULAR response at 24 weeks, compared with 52% of patients who received a second anti-TNF drug, wrote Jacques-Eric Gottenberg, MD, PhD, of Strasbourg (France) University Hospital and his colleagues.
Patients were randomized to a non-TNF biologic or a second anti-TNF drug, with the choice of biologic left to the clinician. Patients were assessed at 12, 24, and 52 weeks.
“In addition to the superiority of the non-TNF treatment for the primary outcome at week 24, the non-TNF treatment was associated with a better EULAR response than a second anti-TNF drug at weeks 12 and 52,” the researchers noted. Significantly more patients in the non-TNF group reported low disease activity at 6 months and 12 months, compared with the second anti-TNF group, they added.
A total of 18 patients in the non-TNF group and 13 patients in the second anti-TNF group experienced serious adverse events; the most common were serious infections (in 33% and 77% of the non-TNF and anti-TNF groups, respectively) and cardiovascular events (33% vs. 8%, respectively).
The study was supported by the French Ministry of Health and promoted by Strasbourg University Hospital. Dr. Gottenberg disclosed financial support from AbbVie, Pfizer, and Roche, and personal fees from Bristol-Myers Squibb, Merck Sharp & Dohme, UCB, GlaxoSmithKline, and Novartis.
The findings were published online Sept. 20 (JAMA 2016;316[11]:1172-80).
Rheumatoid arthritis patients who were unsuccessfully treated with anti–tumor necrosis factor drugs fared significantly better when treated with a non-TNF biologic than with a second anti-TNF drug in a 52-week, randomized, clinical trial of 300 adults.
Overall, 69% of patients who received a non-TNF biologic achieved clinical response, defined as a good or moderate EULAR response at 24 weeks, compared with 52% of patients who received a second anti-TNF drug, wrote Jacques-Eric Gottenberg, MD, PhD, of Strasbourg (France) University Hospital and his colleagues.
Patients were randomized to a non-TNF biologic or a second anti-TNF drug, with the choice of biologic left to the clinician. Patients were assessed at 12, 24, and 52 weeks.
“In addition to the superiority of the non-TNF treatment for the primary outcome at week 24, the non-TNF treatment was associated with a better EULAR response than a second anti-TNF drug at weeks 12 and 52,” the researchers noted. Significantly more patients in the non-TNF group reported low disease activity at 6 months and 12 months, compared with the second anti-TNF group, they added.
A total of 18 patients in the non-TNF group and 13 patients in the second anti-TNF group experienced serious adverse events; the most common were serious infections (in 33% and 77% of the non-TNF and anti-TNF groups, respectively) and cardiovascular events (33% vs. 8%, respectively).
The study was supported by the French Ministry of Health and promoted by Strasbourg University Hospital. Dr. Gottenberg disclosed financial support from AbbVie, Pfizer, and Roche, and personal fees from Bristol-Myers Squibb, Merck Sharp & Dohme, UCB, GlaxoSmithKline, and Novartis.
The findings were published online Sept. 20 (JAMA 2016;316[11]:1172-80).
FROM JAMA
Buprenorphine restrictions don’t hinder addiction therapy
Restrictions on the number of buprenorphine prescriptions a physician can write in a given year do not hinder addiction treatment, as some had feared, according to a Research Letter published online Sept. 20 in JAMA.
Physicians who wish to treat opioid use disorders using buprenorphine are allowed to prescribe the drug to up to 30 patients during the first year they offer the treatment, and after that, they may request that the limit be increased to 100 patients. Some experts have expressed concern that this requirement may pose a barrier to buprenorphine therapy. To examine this possibility, researchers analyzed information in a database of prescriptions filled at retail pharmacies across the United States.
The investigators focused on buprenorphine prescriptions filled during a 3-year period in seven states with the highest rates of addiction therapy: California, Florida, Massachusetts, Michigan, New York, Pennsylvania, and Texas. They identified 3,234 physician prescribers and 245,016 patients receiving a new buprenorphine prescription during the study period, said Bradley D. Stein, MD, PhD, of the RAND Corporation, Pittsburgh, and his associates.
A substantial proportion of the physician prescribers – 20% – treated only 1-3 patients, and an additional 49% treated fewer than the 30-patient limit. Only 9% of physician prescribers treated more than 75 patients. So the restrictions on the number of concurrent prescriptions do not appear to pose a barrier to buprenorphine therapy, Dr. Stein and his associates said (JAMA. 2016 Sep 20;316[11]:1211-2).
An unexpected finding was that the median duration of buprenorphine therapy was only 53 days, even though clinical recommendations specify that up to 12 months of treatment is beneficial, and longer duration of therapy is associated with better outcomes.
These findings indicate that strategies for improving access to addiction therapy may not need to target prescription limits, the investigators said.
Dr. Stein and his associates said their research was supported by the National Institute on Drug Abuse. He reported having served on the advisory board of Otsuka Pharmaceuticals, and the other investigators reported receiving royalties from Cambridge University Press and UpToDate.
Restrictions on the number of buprenorphine prescriptions a physician can write in a given year do not hinder addiction treatment, as some had feared, according to a Research Letter published online Sept. 20 in JAMA.
Physicians who wish to treat opioid use disorders using buprenorphine are allowed to prescribe the drug to up to 30 patients during the first year they offer the treatment, and after that, they may request that the limit be increased to 100 patients. Some experts have expressed concern that this requirement may pose a barrier to buprenorphine therapy. To examine this possibility, researchers analyzed information in a database of prescriptions filled at retail pharmacies across the United States.
The investigators focused on buprenorphine prescriptions filled during a 3-year period in seven states with the highest rates of addiction therapy: California, Florida, Massachusetts, Michigan, New York, Pennsylvania, and Texas. They identified 3,234 physician prescribers and 245,016 patients receiving a new buprenorphine prescription during the study period, said Bradley D. Stein, MD, PhD, of the RAND Corporation, Pittsburgh, and his associates.
A substantial proportion of the physician prescribers – 20% – treated only 1-3 patients, and an additional 49% treated fewer than the 30-patient limit. Only 9% of physician prescribers treated more than 75 patients. So the restrictions on the number of concurrent prescriptions do not appear to pose a barrier to buprenorphine therapy, Dr. Stein and his associates said (JAMA. 2016 Sep 20;316[11]:1211-2).
An unexpected finding was that the median duration of buprenorphine therapy was only 53 days, even though clinical recommendations specify that up to 12 months of treatment is beneficial, and longer duration of therapy is associated with better outcomes.
These findings indicate that strategies for improving access to addiction therapy may not need to target prescription limits, the investigators said.
Dr. Stein and his associates said their research was supported by the National Institute on Drug Abuse. He reported having served on the advisory board of Otsuka Pharmaceuticals, and the other investigators reported receiving royalties from Cambridge University Press and UpToDate.
Restrictions on the number of buprenorphine prescriptions a physician can write in a given year do not hinder addiction treatment, as some had feared, according to a Research Letter published online Sept. 20 in JAMA.
Physicians who wish to treat opioid use disorders using buprenorphine are allowed to prescribe the drug to up to 30 patients during the first year they offer the treatment, and after that, they may request that the limit be increased to 100 patients. Some experts have expressed concern that this requirement may pose a barrier to buprenorphine therapy. To examine this possibility, researchers analyzed information in a database of prescriptions filled at retail pharmacies across the United States.
The investigators focused on buprenorphine prescriptions filled during a 3-year period in seven states with the highest rates of addiction therapy: California, Florida, Massachusetts, Michigan, New York, Pennsylvania, and Texas. They identified 3,234 physician prescribers and 245,016 patients receiving a new buprenorphine prescription during the study period, said Bradley D. Stein, MD, PhD, of the RAND Corporation, Pittsburgh, and his associates.
A substantial proportion of the physician prescribers – 20% – treated only 1-3 patients, and an additional 49% treated fewer than the 30-patient limit. Only 9% of physician prescribers treated more than 75 patients. So the restrictions on the number of concurrent prescriptions do not appear to pose a barrier to buprenorphine therapy, Dr. Stein and his associates said (JAMA. 2016 Sep 20;316[11]:1211-2).
An unexpected finding was that the median duration of buprenorphine therapy was only 53 days, even though clinical recommendations specify that up to 12 months of treatment is beneficial, and longer duration of therapy is associated with better outcomes.
These findings indicate that strategies for improving access to addiction therapy may not need to target prescription limits, the investigators said.
Dr. Stein and his associates said their research was supported by the National Institute on Drug Abuse. He reported having served on the advisory board of Otsuka Pharmaceuticals, and the other investigators reported receiving royalties from Cambridge University Press and UpToDate.
FROM JAMA
Key clinical point: Restrictions on the number of buprenorphine prescriptions a physician can write in a given year do not hinder addiction treatment.
Major finding: Most (69%) of physician prescribers treated fewer than the 30-patient limit for buprenorphine prescriptions in a given year
Data source: An analysis of pharmacy data regarding 3,234 buprenorphine prescribers in seven states during a 3-year period.
Disclosures: This work was supported by the National Institute on Drug Abuse. Dr. Stein reported having served on an advisory board of Otsuka Pharmaceuticals; the other investigators reported receiving royalties from Cambridge University Press and UpToDate.
Analyses strengthen FLAME’s findings
LONDON – In chronic obstructive pulmonary disease (COPD), the advantage of a long-acting beta agonist (LABA) plus a long-acting muscarinic antagonist (LAMA) over a LABA plus an inhaled corticosteroid (ICS) was observed in every subgroup in the FLAME trial evaluated, according to post hoc analyses presented at the annual congress of the European Respiratory Society.
“We thought that we might not see the difference in the COPD patients with more severe disease, but the advantage was consistent even among those who entered the trial on triple therapy,” reported Jadwiga A. Wedzicha, MD, professor of respiratory medicine at the National Heart and Lung Institute, Imperial College, London.
FLAME, the recently published study that compared LABA/LAMA to LABA/ICS, was planned as a noninferiority study with the underlying hypothesis that LABA/LAMA would perform as well as LABA/ICS for the primary outcome of annual rate of COPD exacerbations (N Engl J Med. 2016;374:2222-34). Instead, the 11% lower rate of exacerbations for LABA/LAMA proved statistically significant (P = .003).
Six post hoc FLAME analyses were presented at the 2016 ERS Congress to further explore this result. All supported the main result. In addition to evaluating those who entered the trial on a LABA/LAMA/ICS triple-therapy combination, the analyses covered a broad array of subgroups defined by age, smoking history, and COPD severity as defined by Global Initiative for Chronic Obstructive Lung Disease (GOLD) classifications.
In FLAME, 3,362 COPD patients who had at least one exacerbation in the preceding year were randomized to the LABA indacaterol (110 mcg) plus the LAMA glycopyrronium (50 mcg) once daily or the combination of the LABA salmeterol (50 mcg) and the ICS fluticasone (500 mcg) twice daily. In addition to the relative advantage on the primary outcome of any exacerbation, the LABA/LAMA combination also significantly reduced the rate of moderate to severe exacerbations (P less than .001), and it extended the times to the first moderate to severe exacerbation (P less than .001) and the first severe exacerbation (P = .046), according to the published data.
In the post hoc analyses, the advantage of LABA/LAMA relative to LAMA/ICS was remarkably consistent. For example, in stratifications made for age (less than 55 years, 55 to less than 65 years, 65-75 years, and greater than or equal to 75 years) at least a numerical advantage of LABA/LAMA was seen in all age groups for prevention of any exacerbation, and the difference reached statistical significance for those in the age group 55 to greater than 65 years. For prevention of moderate to severe exacerbations, the treatments were found to be equivalent for individuals younger than 55 years, but LABA/LAMA was statistically superior for the other three age categories.
For ex-smokers, unlike current smokers, the numerical advantage of LABA/LAMA over LABA/ICS for reduction in the rate ratio of all exacerbations did not reach statistical significance, but the LABA/LAMA combination did provide a statistically significant advantage for both ex-smokers and current smokers for moderate to severe exacerbations.
For patients with two or more exacerbations in the year prior to enrollment in FLAME, the relative degree of protection was of magnitude similar to that of patients with only one exacerbation even though the relative advantage in those with multiple prior exacerbations did not reach statistical significance. However, the lack of significance was likely due to the relatively small number of patients in this subpopulation, according to Dr. Wedzicha.
Similarly, the LABA/LAMA combination was at least numerically superior to LABA/ICS for all exacerbations and for moderate to severe exacerbations across GOLD classifications with one exception. When compared for relative protection against moderate to severe exacerbations, there was a slight and nonsignificant disadvantage for LABA/LAMA, but, again, Dr. Wedzicha reported, “the number of patients in this subgroup was quite small.”
In another FLAME post hoc analysis, the odds ratio (OR) for exacerbations among the 1,893 patients (56.3%) who were on ICS at study entry was found to be almost identical to the OR among those who were not. Specifically, the ORs for all exacerbations and moderate to severe exacerbations were 0.88 (P = .008) and 0.86 (P = .018), respectively, for those previously treated with ICS and 0.88 (P = .021) and 0.78 (P = .002), respectively, for those who had not been treated with ICS.
The LABA/LAMA combination was also superior to LABA/ICS for improvements in quality of life, which was measured via the St. George’s Respiratory Questionnaire. With an improvement of at least four units on the St. George’s Respiratory Questionnaire defined as clinically meaningful, 49.5% of LABA/LAMA patients versus 43.8% of LABA/ICS patients (P less than .024) benefited on this measure.
Overall, the results from the FLAME post hoc analyses have demonstrated “remarkable consistency,” Dr. Wedzicha reported. Taken together, she said the data “imply that LABA/LAMA is the first choice of treatment for COPD patients at risk of exacerbation.”
LONDON – In chronic obstructive pulmonary disease (COPD), the advantage of a long-acting beta agonist (LABA) plus a long-acting muscarinic antagonist (LAMA) over a LABA plus an inhaled corticosteroid (ICS) was observed in every subgroup in the FLAME trial evaluated, according to post hoc analyses presented at the annual congress of the European Respiratory Society.
“We thought that we might not see the difference in the COPD patients with more severe disease, but the advantage was consistent even among those who entered the trial on triple therapy,” reported Jadwiga A. Wedzicha, MD, professor of respiratory medicine at the National Heart and Lung Institute, Imperial College, London.
FLAME, the recently published study that compared LABA/LAMA to LABA/ICS, was planned as a noninferiority study with the underlying hypothesis that LABA/LAMA would perform as well as LABA/ICS for the primary outcome of annual rate of COPD exacerbations (N Engl J Med. 2016;374:2222-34). Instead, the 11% lower rate of exacerbations for LABA/LAMA proved statistically significant (P = .003).
Six post hoc FLAME analyses were presented at the 2016 ERS Congress to further explore this result. All supported the main result. In addition to evaluating those who entered the trial on a LABA/LAMA/ICS triple-therapy combination, the analyses covered a broad array of subgroups defined by age, smoking history, and COPD severity as defined by Global Initiative for Chronic Obstructive Lung Disease (GOLD) classifications.
In FLAME, 3,362 COPD patients who had at least one exacerbation in the preceding year were randomized to the LABA indacaterol (110 mcg) plus the LAMA glycopyrronium (50 mcg) once daily or the combination of the LABA salmeterol (50 mcg) and the ICS fluticasone (500 mcg) twice daily. In addition to the relative advantage on the primary outcome of any exacerbation, the LABA/LAMA combination also significantly reduced the rate of moderate to severe exacerbations (P less than .001), and it extended the times to the first moderate to severe exacerbation (P less than .001) and the first severe exacerbation (P = .046), according to the published data.
In the post hoc analyses, the advantage of LABA/LAMA relative to LAMA/ICS was remarkably consistent. For example, in stratifications made for age (less than 55 years, 55 to less than 65 years, 65-75 years, and greater than or equal to 75 years) at least a numerical advantage of LABA/LAMA was seen in all age groups for prevention of any exacerbation, and the difference reached statistical significance for those in the age group 55 to greater than 65 years. For prevention of moderate to severe exacerbations, the treatments were found to be equivalent for individuals younger than 55 years, but LABA/LAMA was statistically superior for the other three age categories.
For ex-smokers, unlike current smokers, the numerical advantage of LABA/LAMA over LABA/ICS for reduction in the rate ratio of all exacerbations did not reach statistical significance, but the LABA/LAMA combination did provide a statistically significant advantage for both ex-smokers and current smokers for moderate to severe exacerbations.
For patients with two or more exacerbations in the year prior to enrollment in FLAME, the relative degree of protection was of magnitude similar to that of patients with only one exacerbation even though the relative advantage in those with multiple prior exacerbations did not reach statistical significance. However, the lack of significance was likely due to the relatively small number of patients in this subpopulation, according to Dr. Wedzicha.
Similarly, the LABA/LAMA combination was at least numerically superior to LABA/ICS for all exacerbations and for moderate to severe exacerbations across GOLD classifications with one exception. When compared for relative protection against moderate to severe exacerbations, there was a slight and nonsignificant disadvantage for LABA/LAMA, but, again, Dr. Wedzicha reported, “the number of patients in this subgroup was quite small.”
In another FLAME post hoc analysis, the odds ratio (OR) for exacerbations among the 1,893 patients (56.3%) who were on ICS at study entry was found to be almost identical to the OR among those who were not. Specifically, the ORs for all exacerbations and moderate to severe exacerbations were 0.88 (P = .008) and 0.86 (P = .018), respectively, for those previously treated with ICS and 0.88 (P = .021) and 0.78 (P = .002), respectively, for those who had not been treated with ICS.
The LABA/LAMA combination was also superior to LABA/ICS for improvements in quality of life, which was measured via the St. George’s Respiratory Questionnaire. With an improvement of at least four units on the St. George’s Respiratory Questionnaire defined as clinically meaningful, 49.5% of LABA/LAMA patients versus 43.8% of LABA/ICS patients (P less than .024) benefited on this measure.
Overall, the results from the FLAME post hoc analyses have demonstrated “remarkable consistency,” Dr. Wedzicha reported. Taken together, she said the data “imply that LABA/LAMA is the first choice of treatment for COPD patients at risk of exacerbation.”
LONDON – In chronic obstructive pulmonary disease (COPD), the advantage of a long-acting beta agonist (LABA) plus a long-acting muscarinic antagonist (LAMA) over a LABA plus an inhaled corticosteroid (ICS) was observed in every subgroup in the FLAME trial evaluated, according to post hoc analyses presented at the annual congress of the European Respiratory Society.
“We thought that we might not see the difference in the COPD patients with more severe disease, but the advantage was consistent even among those who entered the trial on triple therapy,” reported Jadwiga A. Wedzicha, MD, professor of respiratory medicine at the National Heart and Lung Institute, Imperial College, London.
FLAME, the recently published study that compared LABA/LAMA to LABA/ICS, was planned as a noninferiority study with the underlying hypothesis that LABA/LAMA would perform as well as LABA/ICS for the primary outcome of annual rate of COPD exacerbations (N Engl J Med. 2016;374:2222-34). Instead, the 11% lower rate of exacerbations for LABA/LAMA proved statistically significant (P = .003).
Six post hoc FLAME analyses were presented at the 2016 ERS Congress to further explore this result. All supported the main result. In addition to evaluating those who entered the trial on a LABA/LAMA/ICS triple-therapy combination, the analyses covered a broad array of subgroups defined by age, smoking history, and COPD severity as defined by Global Initiative for Chronic Obstructive Lung Disease (GOLD) classifications.
In FLAME, 3,362 COPD patients who had at least one exacerbation in the preceding year were randomized to the LABA indacaterol (110 mcg) plus the LAMA glycopyrronium (50 mcg) once daily or the combination of the LABA salmeterol (50 mcg) and the ICS fluticasone (500 mcg) twice daily. In addition to the relative advantage on the primary outcome of any exacerbation, the LABA/LAMA combination also significantly reduced the rate of moderate to severe exacerbations (P less than .001), and it extended the times to the first moderate to severe exacerbation (P less than .001) and the first severe exacerbation (P = .046), according to the published data.
In the post hoc analyses, the advantage of LABA/LAMA relative to LAMA/ICS was remarkably consistent. For example, in stratifications made for age (less than 55 years, 55 to less than 65 years, 65-75 years, and greater than or equal to 75 years) at least a numerical advantage of LABA/LAMA was seen in all age groups for prevention of any exacerbation, and the difference reached statistical significance for those in the age group 55 to greater than 65 years. For prevention of moderate to severe exacerbations, the treatments were found to be equivalent for individuals younger than 55 years, but LABA/LAMA was statistically superior for the other three age categories.
For ex-smokers, unlike current smokers, the numerical advantage of LABA/LAMA over LABA/ICS for reduction in the rate ratio of all exacerbations did not reach statistical significance, but the LABA/LAMA combination did provide a statistically significant advantage for both ex-smokers and current smokers for moderate to severe exacerbations.
For patients with two or more exacerbations in the year prior to enrollment in FLAME, the relative degree of protection was of magnitude similar to that of patients with only one exacerbation even though the relative advantage in those with multiple prior exacerbations did not reach statistical significance. However, the lack of significance was likely due to the relatively small number of patients in this subpopulation, according to Dr. Wedzicha.
Similarly, the LABA/LAMA combination was at least numerically superior to LABA/ICS for all exacerbations and for moderate to severe exacerbations across GOLD classifications with one exception. When compared for relative protection against moderate to severe exacerbations, there was a slight and nonsignificant disadvantage for LABA/LAMA, but, again, Dr. Wedzicha reported, “the number of patients in this subgroup was quite small.”
In another FLAME post hoc analysis, the odds ratio (OR) for exacerbations among the 1,893 patients (56.3%) who were on ICS at study entry was found to be almost identical to the OR among those who were not. Specifically, the ORs for all exacerbations and moderate to severe exacerbations were 0.88 (P = .008) and 0.86 (P = .018), respectively, for those previously treated with ICS and 0.88 (P = .021) and 0.78 (P = .002), respectively, for those who had not been treated with ICS.
The LABA/LAMA combination was also superior to LABA/ICS for improvements in quality of life, which was measured via the St. George’s Respiratory Questionnaire. With an improvement of at least four units on the St. George’s Respiratory Questionnaire defined as clinically meaningful, 49.5% of LABA/LAMA patients versus 43.8% of LABA/ICS patients (P less than .024) benefited on this measure.
Overall, the results from the FLAME post hoc analyses have demonstrated “remarkable consistency,” Dr. Wedzicha reported. Taken together, she said the data “imply that LABA/LAMA is the first choice of treatment for COPD patients at risk of exacerbation.”
At THE ERS CONGRESS 2016
Key clinical point: The advantage of a LABA/LAMA combination over LABA/ICS in COPD patients persists regardless of patient subgroup.
Major finding: In a series of post hoc analyses from the FLAME trial, the advantage of LABA/LAMA was observed in every subgroup evaluated.
Data source: Post hoc analyses of phase III trial.
Disclosures: Dr Wedzicha reported financial relationships with Bayer, Chiesi, Boehringer Ingelheim, GlaxoSmithKline, Johnson & Johnson, Novartis, Pfizer, Takeda, and Vifor Pharma
EPO improves cognitive impairment in depression
VIENNA – Recombinant human erythropoietin appears to be a cognitive enhancer in patients with unipolar or bipolar depression accompanied by cognitive impairment, Kamilla W. Miskowiak, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
She presented a pooled analysis of her two pilot randomized, placebo-controlled clinical trials totaling 79 patients with treatment-resistant unipolar or partly remitted bipolar depression associated with baseline cognitive impairment. She found that 8 weeks of once-weekly intravenous infusions of high-dose human recombinant erythropoetin (Epogen), also known as epoetin alfa (EPO), resulted in clinically meaningful improvement in cognition 1 week post treatment, as measured on neuropsychological tests assessing the speed of complex cognitive processing, verbal memory, attention span, concentration, working memory, and strategic planning ability. Saline infusions had no effect.
Moreover, follow-up testing conducted 6 weeks after the final treatment session showed continued full maintenance of the initial cognitive gains, which averaged an 11% improvement over baseline. The full duration of effect will be determined in the next round of studies, which will feature 12 weeks of EPO and 6 months of off-treatment follow-up, added Dr. Miskowiak, a senior research psychologist at the University of Copenhagen.
In an interview, she emphasized that the mechanism of benefit doesn’t appear to be related to EPO’s signature ability to boost red blood cell (RBC) production and raise hemoglobin levels. After all, she noted, RBCs were back to normal within 2 weeks after treatment ended, yet the objective cognitive improvements continued. Instead, the mechanism involves EPO’s capacity to enhance brain neuroplasticity, an effect that was demonstrated first in animal studies and subsequently in Dr. Miskowiak’s clinical trials.
“We did MRI functional and structural brain scans at baseline and after completion of treatment, and we saw that EPO increased left hippocampal volume. In fact, it was the structural change in hippocampal volume in response to EPO that was the single strongest predictor of cognitive improvement in multivariate analyses adjusted for age, illness chronicity, depressive symptom severity, gender, and other factors,” according to Dr. Miskowiak.
Physicians who use EPO to treat anemia might blanch at the doses of EPO administered to improve cognitive impairments in patients with affective disorders. Instead of giving 50-100 U/kg of body weight several times per week, as is common in treating anemia, the patients in her studies typically received 40,000 U/wk.
“We used much, much higher doses than are given to affect the bone marrow in patients with anemia, because only about 1% of the IV dose passes across the blood/brain barrier,” she explained.
Because EPO, even in conventional doses, is associated with an increased risk of blood clots, patients were ineligible for the cognition-improvement trials if they had a history of venous thromboembolism, coronary disease, or cancer. Moreover, their RBC and platelet activity levels were monitored on a weekly basis. No untoward effects were seen, Dr. Miskowiak continued.
“Patients really liked coming in for this therapy. Many of them were quite chronic, with years of illness, yet adherence was excellent,” she said.
Early in the developmental pipeline are an intranasal variant of EPO and a carbamylated EPO designed to cross the blood/brain barrier efficiently in order to achieve direct brain neuroplasticity-stimulating effects with minimal impact on RBC production.
Dr. Miskowiak stressed that EPO as a treatment for cognitive dysfunction associated with affective disorders is not ready for prime time use in clinical practice. The next round of randomized, placebo-controlled clinical trials, due to start early in 2017, will attempt to replicate her pilot study findings while pinning down the optimal dosing regimen. The new trials will feature longer off-treatment follow-up as well as quality-of-life measures and an economic analysis that includes assessment of the ability to return to work.
“This therapy may be attractive from an economic perspective,” according to the psychologist. “I don’t see this as first-line therapy in clinical practice, though,” she added. “It will be reserved for the more severely cognitively impaired patients.”
Eduard Vieta, MD, professor and chair of the department of psychiatry and psychology at the University of Barcelona, commented that cognitive impairment is now recognized as a core aspect of affective disorders. There is a huge unmet need for treatments that address this disease aspect. The drugs now available for treatment of bipolar disorder and unipolar depression don’t improve the associated cognitive impairments. Indeed, up to 40% of patients in remission from major depressive disorder and 70% in remission from bipolar disorder continue to experience neurocognitive symptoms.
Dr. Miskowiak’s work was funded by the Danish Ministry of Science, Innovation, and Higher Education. She reported having no relevant financial conflicts of interest.
VIENNA – Recombinant human erythropoietin appears to be a cognitive enhancer in patients with unipolar or bipolar depression accompanied by cognitive impairment, Kamilla W. Miskowiak, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
She presented a pooled analysis of her two pilot randomized, placebo-controlled clinical trials totaling 79 patients with treatment-resistant unipolar or partly remitted bipolar depression associated with baseline cognitive impairment. She found that 8 weeks of once-weekly intravenous infusions of high-dose human recombinant erythropoetin (Epogen), also known as epoetin alfa (EPO), resulted in clinically meaningful improvement in cognition 1 week post treatment, as measured on neuropsychological tests assessing the speed of complex cognitive processing, verbal memory, attention span, concentration, working memory, and strategic planning ability. Saline infusions had no effect.
Moreover, follow-up testing conducted 6 weeks after the final treatment session showed continued full maintenance of the initial cognitive gains, which averaged an 11% improvement over baseline. The full duration of effect will be determined in the next round of studies, which will feature 12 weeks of EPO and 6 months of off-treatment follow-up, added Dr. Miskowiak, a senior research psychologist at the University of Copenhagen.
In an interview, she emphasized that the mechanism of benefit doesn’t appear to be related to EPO’s signature ability to boost red blood cell (RBC) production and raise hemoglobin levels. After all, she noted, RBCs were back to normal within 2 weeks after treatment ended, yet the objective cognitive improvements continued. Instead, the mechanism involves EPO’s capacity to enhance brain neuroplasticity, an effect that was demonstrated first in animal studies and subsequently in Dr. Miskowiak’s clinical trials.
“We did MRI functional and structural brain scans at baseline and after completion of treatment, and we saw that EPO increased left hippocampal volume. In fact, it was the structural change in hippocampal volume in response to EPO that was the single strongest predictor of cognitive improvement in multivariate analyses adjusted for age, illness chronicity, depressive symptom severity, gender, and other factors,” according to Dr. Miskowiak.
Physicians who use EPO to treat anemia might blanch at the doses of EPO administered to improve cognitive impairments in patients with affective disorders. Instead of giving 50-100 U/kg of body weight several times per week, as is common in treating anemia, the patients in her studies typically received 40,000 U/wk.
“We used much, much higher doses than are given to affect the bone marrow in patients with anemia, because only about 1% of the IV dose passes across the blood/brain barrier,” she explained.
Because EPO, even in conventional doses, is associated with an increased risk of blood clots, patients were ineligible for the cognition-improvement trials if they had a history of venous thromboembolism, coronary disease, or cancer. Moreover, their RBC and platelet activity levels were monitored on a weekly basis. No untoward effects were seen, Dr. Miskowiak continued.
“Patients really liked coming in for this therapy. Many of them were quite chronic, with years of illness, yet adherence was excellent,” she said.
Early in the developmental pipeline are an intranasal variant of EPO and a carbamylated EPO designed to cross the blood/brain barrier efficiently in order to achieve direct brain neuroplasticity-stimulating effects with minimal impact on RBC production.
Dr. Miskowiak stressed that EPO as a treatment for cognitive dysfunction associated with affective disorders is not ready for prime time use in clinical practice. The next round of randomized, placebo-controlled clinical trials, due to start early in 2017, will attempt to replicate her pilot study findings while pinning down the optimal dosing regimen. The new trials will feature longer off-treatment follow-up as well as quality-of-life measures and an economic analysis that includes assessment of the ability to return to work.
“This therapy may be attractive from an economic perspective,” according to the psychologist. “I don’t see this as first-line therapy in clinical practice, though,” she added. “It will be reserved for the more severely cognitively impaired patients.”
Eduard Vieta, MD, professor and chair of the department of psychiatry and psychology at the University of Barcelona, commented that cognitive impairment is now recognized as a core aspect of affective disorders. There is a huge unmet need for treatments that address this disease aspect. The drugs now available for treatment of bipolar disorder and unipolar depression don’t improve the associated cognitive impairments. Indeed, up to 40% of patients in remission from major depressive disorder and 70% in remission from bipolar disorder continue to experience neurocognitive symptoms.
Dr. Miskowiak’s work was funded by the Danish Ministry of Science, Innovation, and Higher Education. She reported having no relevant financial conflicts of interest.
VIENNA – Recombinant human erythropoietin appears to be a cognitive enhancer in patients with unipolar or bipolar depression accompanied by cognitive impairment, Kamilla W. Miskowiak, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
She presented a pooled analysis of her two pilot randomized, placebo-controlled clinical trials totaling 79 patients with treatment-resistant unipolar or partly remitted bipolar depression associated with baseline cognitive impairment. She found that 8 weeks of once-weekly intravenous infusions of high-dose human recombinant erythropoetin (Epogen), also known as epoetin alfa (EPO), resulted in clinically meaningful improvement in cognition 1 week post treatment, as measured on neuropsychological tests assessing the speed of complex cognitive processing, verbal memory, attention span, concentration, working memory, and strategic planning ability. Saline infusions had no effect.
Moreover, follow-up testing conducted 6 weeks after the final treatment session showed continued full maintenance of the initial cognitive gains, which averaged an 11% improvement over baseline. The full duration of effect will be determined in the next round of studies, which will feature 12 weeks of EPO and 6 months of off-treatment follow-up, added Dr. Miskowiak, a senior research psychologist at the University of Copenhagen.
In an interview, she emphasized that the mechanism of benefit doesn’t appear to be related to EPO’s signature ability to boost red blood cell (RBC) production and raise hemoglobin levels. After all, she noted, RBCs were back to normal within 2 weeks after treatment ended, yet the objective cognitive improvements continued. Instead, the mechanism involves EPO’s capacity to enhance brain neuroplasticity, an effect that was demonstrated first in animal studies and subsequently in Dr. Miskowiak’s clinical trials.
“We did MRI functional and structural brain scans at baseline and after completion of treatment, and we saw that EPO increased left hippocampal volume. In fact, it was the structural change in hippocampal volume in response to EPO that was the single strongest predictor of cognitive improvement in multivariate analyses adjusted for age, illness chronicity, depressive symptom severity, gender, and other factors,” according to Dr. Miskowiak.
Physicians who use EPO to treat anemia might blanch at the doses of EPO administered to improve cognitive impairments in patients with affective disorders. Instead of giving 50-100 U/kg of body weight several times per week, as is common in treating anemia, the patients in her studies typically received 40,000 U/wk.
“We used much, much higher doses than are given to affect the bone marrow in patients with anemia, because only about 1% of the IV dose passes across the blood/brain barrier,” she explained.
Because EPO, even in conventional doses, is associated with an increased risk of blood clots, patients were ineligible for the cognition-improvement trials if they had a history of venous thromboembolism, coronary disease, or cancer. Moreover, their RBC and platelet activity levels were monitored on a weekly basis. No untoward effects were seen, Dr. Miskowiak continued.
“Patients really liked coming in for this therapy. Many of them were quite chronic, with years of illness, yet adherence was excellent,” she said.
Early in the developmental pipeline are an intranasal variant of EPO and a carbamylated EPO designed to cross the blood/brain barrier efficiently in order to achieve direct brain neuroplasticity-stimulating effects with minimal impact on RBC production.
Dr. Miskowiak stressed that EPO as a treatment for cognitive dysfunction associated with affective disorders is not ready for prime time use in clinical practice. The next round of randomized, placebo-controlled clinical trials, due to start early in 2017, will attempt to replicate her pilot study findings while pinning down the optimal dosing regimen. The new trials will feature longer off-treatment follow-up as well as quality-of-life measures and an economic analysis that includes assessment of the ability to return to work.
“This therapy may be attractive from an economic perspective,” according to the psychologist. “I don’t see this as first-line therapy in clinical practice, though,” she added. “It will be reserved for the more severely cognitively impaired patients.”
Eduard Vieta, MD, professor and chair of the department of psychiatry and psychology at the University of Barcelona, commented that cognitive impairment is now recognized as a core aspect of affective disorders. There is a huge unmet need for treatments that address this disease aspect. The drugs now available for treatment of bipolar disorder and unipolar depression don’t improve the associated cognitive impairments. Indeed, up to 40% of patients in remission from major depressive disorder and 70% in remission from bipolar disorder continue to experience neurocognitive symptoms.
Dr. Miskowiak’s work was funded by the Danish Ministry of Science, Innovation, and Higher Education. She reported having no relevant financial conflicts of interest.
AT THE ECNP CONGRESS
Key clinical point: Recombinant human erythropoietin enhances brain neuroplasticity and achieves measurable improvements in cognitive impairment associated with unipolar or bipolar depression.
Major finding: Patients with cognitive impairment related to unipolar or bipolar depression responded to a series of infusions of recombinant human erythropoietin with a significant improvement in neuropsychological test scores that was maintained unabated 6 weeks after their final infusion.
Data source: A retrospective analysis of pooled data from two randomized, placebo-controlled trials totaling 79 patients with unipolar or bipolar depression.
Disclosures: This work was funded by the Danish Ministry of Science, Innovation, and Higher Education. The presenter reported having no relevant financial conflicts of interest.
Siponimod curbs disability in secondary progressive multiple sclerosis
LONDON – Siponimod delayed disability progression in patients with secondary progressive multiple sclerosis, according to top-line findings from the phase III EXPAND study.
Siponimod reduced the primary endpoint of the time to 3-month confirmed disease progression (CDP) assessed via the Expanded Disability Status Scale (EDSS) by 21%, compared with placebo (P = .013).
“It is reassuring that this primary outcome is supported by an important secondary outcome of the time to CDP at 6 months,” presenting author Ludwig Kappos, MD, of University Hospital Basel (Switzerland), said at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
He reported that a 26% reduction in the 6-month CDP was also observed comparing the active and placebo treatments (P = .006) in the multicenter, randomized, double-blind trial that involved 1,646 patients “with the whole spectrum” of secondary progressive multiple sclerosis (SPMS).
The findings build on those of the phase II BOLD study in patients with relapsing-remitting MS (RRMS) (Lancet Neurol. 2013;12[8]:756-67) and showed a reduction in relapse rates and a reduction in the number of brain lesions seen on MRI scans for siponimod, compared with placebo.
Recently reported data from the 24-month extension of the BOLD phase II trial (JAMA Neurol. 2016;73[9]:1089-98) also showed that disease activity was low in patients treated with siponimod, and that there were no new safety signals. Dose reduction during initiation mitigated cardiac adverse effects, an approach that was also used successfully in the phase III study.
Siponimod is a once-daily oral treatment being developed by Novartis for the treatment of MS. Like fingolimod (Gilenya), which is licensed for the treatment of RRMS, siponimod is a selective sphingosine 1-phosphate receptor (S1P) modulator. Unlike fingolimod, which targets S1P subtypes 1, 3, 4, and 5, siponimod only targets the S1P 1 and 5 subtypes.
Fingolimod is also known to cause temporary changes in heart rate, heartbeat, and blood pressure, which necessitates early electrocardiographic monitoring during the first 6 hours when the drug is first given. At the present time, it doesn’t seem that siponimod will have unwanted cardiac effects, but longer-term follow-up data are needed.
“Adverse events were as you would expect with an S1P receptor modulator,” Dr. Kappos said, noting that there was nothing new. Overall, any adverse event occurred in 88% of actively-treated and 81% of placebo-treated patients. The rate of serious adverse events was similar in the siponimod (3.8%) and placebo (3.7%) arms, and a similar percentage of patients were reported to have infections (48% and 49%, respectively).
Analysis of all the various secondary endpoints is still ongoing; Dr. Kappos noted that the primary endpoint data had just recently become available. Some initial findings, however, show benefit for siponimod over placebo.
The change in T2 lesion volume from baseline to both 12 and 24 months was significantly less with siponimod than with placebo, at a 79.1% lower average change (P less than .0001).
The annualized relapse rate was reduced by 55% with the active treatment versus placebo, and there was less percent change in brain volume with active therapy versus placebo from baseline to 12 and 24 months’ follow-up (23.4% lower average change, P = .0002).
The time to 3-month confirmed worsening by 20% or more from baseline in the timed 25-foot walk test was reduced by 6.2%. Although not significant, the trend was “in the right direction,” Dr. Kappos said.
The mean age of recruited patients was 48 years, with an average duration of MS of 16-17 years, and just under 4 years since their conversion to SPMS. Baseline EDSS was a mean of 5.4, around 35%-37% had one or more relapses in the 2 years before screening, and 20% had gadolinium-enhancing lesions at baseline.
A variety of predefined subgroup analyses showed a benefit for siponimod over placebo. These included analyses looking at the effect by the number of gadolinium-enhancing lesions at baseline, previous disease-modifying treatment, whether patients’ MS was rapidly progressing, whether patients’ disease was moderate or severe, the baseline EDSS, and the duration of MS since the first recognition of symptoms.
“What is the optimal patient population?” an audience member asked Dr. Kappos during the Q&A period following his presentation at the ECTRIMS meeting. He responded: “I think younger patients with the more active disease will certainly be the best candidates.” But, he added, it was reassuring to note that the drug seems to work equally well in all patient subtypes.
Novartis funded the study. Dr. Kappos disclosed that his institution has received financial support for research purposes from multiple MS drug manufacturers – including Novartis – and charitable organizations.
LONDON – Siponimod delayed disability progression in patients with secondary progressive multiple sclerosis, according to top-line findings from the phase III EXPAND study.
Siponimod reduced the primary endpoint of the time to 3-month confirmed disease progression (CDP) assessed via the Expanded Disability Status Scale (EDSS) by 21%, compared with placebo (P = .013).
“It is reassuring that this primary outcome is supported by an important secondary outcome of the time to CDP at 6 months,” presenting author Ludwig Kappos, MD, of University Hospital Basel (Switzerland), said at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
He reported that a 26% reduction in the 6-month CDP was also observed comparing the active and placebo treatments (P = .006) in the multicenter, randomized, double-blind trial that involved 1,646 patients “with the whole spectrum” of secondary progressive multiple sclerosis (SPMS).
The findings build on those of the phase II BOLD study in patients with relapsing-remitting MS (RRMS) (Lancet Neurol. 2013;12[8]:756-67) and showed a reduction in relapse rates and a reduction in the number of brain lesions seen on MRI scans for siponimod, compared with placebo.
Recently reported data from the 24-month extension of the BOLD phase II trial (JAMA Neurol. 2016;73[9]:1089-98) also showed that disease activity was low in patients treated with siponimod, and that there were no new safety signals. Dose reduction during initiation mitigated cardiac adverse effects, an approach that was also used successfully in the phase III study.
Siponimod is a once-daily oral treatment being developed by Novartis for the treatment of MS. Like fingolimod (Gilenya), which is licensed for the treatment of RRMS, siponimod is a selective sphingosine 1-phosphate receptor (S1P) modulator. Unlike fingolimod, which targets S1P subtypes 1, 3, 4, and 5, siponimod only targets the S1P 1 and 5 subtypes.
Fingolimod is also known to cause temporary changes in heart rate, heartbeat, and blood pressure, which necessitates early electrocardiographic monitoring during the first 6 hours when the drug is first given. At the present time, it doesn’t seem that siponimod will have unwanted cardiac effects, but longer-term follow-up data are needed.
“Adverse events were as you would expect with an S1P receptor modulator,” Dr. Kappos said, noting that there was nothing new. Overall, any adverse event occurred in 88% of actively-treated and 81% of placebo-treated patients. The rate of serious adverse events was similar in the siponimod (3.8%) and placebo (3.7%) arms, and a similar percentage of patients were reported to have infections (48% and 49%, respectively).
Analysis of all the various secondary endpoints is still ongoing; Dr. Kappos noted that the primary endpoint data had just recently become available. Some initial findings, however, show benefit for siponimod over placebo.
The change in T2 lesion volume from baseline to both 12 and 24 months was significantly less with siponimod than with placebo, at a 79.1% lower average change (P less than .0001).
The annualized relapse rate was reduced by 55% with the active treatment versus placebo, and there was less percent change in brain volume with active therapy versus placebo from baseline to 12 and 24 months’ follow-up (23.4% lower average change, P = .0002).
The time to 3-month confirmed worsening by 20% or more from baseline in the timed 25-foot walk test was reduced by 6.2%. Although not significant, the trend was “in the right direction,” Dr. Kappos said.
The mean age of recruited patients was 48 years, with an average duration of MS of 16-17 years, and just under 4 years since their conversion to SPMS. Baseline EDSS was a mean of 5.4, around 35%-37% had one or more relapses in the 2 years before screening, and 20% had gadolinium-enhancing lesions at baseline.
A variety of predefined subgroup analyses showed a benefit for siponimod over placebo. These included analyses looking at the effect by the number of gadolinium-enhancing lesions at baseline, previous disease-modifying treatment, whether patients’ MS was rapidly progressing, whether patients’ disease was moderate or severe, the baseline EDSS, and the duration of MS since the first recognition of symptoms.
“What is the optimal patient population?” an audience member asked Dr. Kappos during the Q&A period following his presentation at the ECTRIMS meeting. He responded: “I think younger patients with the more active disease will certainly be the best candidates.” But, he added, it was reassuring to note that the drug seems to work equally well in all patient subtypes.
Novartis funded the study. Dr. Kappos disclosed that his institution has received financial support for research purposes from multiple MS drug manufacturers – including Novartis – and charitable organizations.
LONDON – Siponimod delayed disability progression in patients with secondary progressive multiple sclerosis, according to top-line findings from the phase III EXPAND study.
Siponimod reduced the primary endpoint of the time to 3-month confirmed disease progression (CDP) assessed via the Expanded Disability Status Scale (EDSS) by 21%, compared with placebo (P = .013).
“It is reassuring that this primary outcome is supported by an important secondary outcome of the time to CDP at 6 months,” presenting author Ludwig Kappos, MD, of University Hospital Basel (Switzerland), said at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
He reported that a 26% reduction in the 6-month CDP was also observed comparing the active and placebo treatments (P = .006) in the multicenter, randomized, double-blind trial that involved 1,646 patients “with the whole spectrum” of secondary progressive multiple sclerosis (SPMS).
The findings build on those of the phase II BOLD study in patients with relapsing-remitting MS (RRMS) (Lancet Neurol. 2013;12[8]:756-67) and showed a reduction in relapse rates and a reduction in the number of brain lesions seen on MRI scans for siponimod, compared with placebo.
Recently reported data from the 24-month extension of the BOLD phase II trial (JAMA Neurol. 2016;73[9]:1089-98) also showed that disease activity was low in patients treated with siponimod, and that there were no new safety signals. Dose reduction during initiation mitigated cardiac adverse effects, an approach that was also used successfully in the phase III study.
Siponimod is a once-daily oral treatment being developed by Novartis for the treatment of MS. Like fingolimod (Gilenya), which is licensed for the treatment of RRMS, siponimod is a selective sphingosine 1-phosphate receptor (S1P) modulator. Unlike fingolimod, which targets S1P subtypes 1, 3, 4, and 5, siponimod only targets the S1P 1 and 5 subtypes.
Fingolimod is also known to cause temporary changes in heart rate, heartbeat, and blood pressure, which necessitates early electrocardiographic monitoring during the first 6 hours when the drug is first given. At the present time, it doesn’t seem that siponimod will have unwanted cardiac effects, but longer-term follow-up data are needed.
“Adverse events were as you would expect with an S1P receptor modulator,” Dr. Kappos said, noting that there was nothing new. Overall, any adverse event occurred in 88% of actively-treated and 81% of placebo-treated patients. The rate of serious adverse events was similar in the siponimod (3.8%) and placebo (3.7%) arms, and a similar percentage of patients were reported to have infections (48% and 49%, respectively).
Analysis of all the various secondary endpoints is still ongoing; Dr. Kappos noted that the primary endpoint data had just recently become available. Some initial findings, however, show benefit for siponimod over placebo.
The change in T2 lesion volume from baseline to both 12 and 24 months was significantly less with siponimod than with placebo, at a 79.1% lower average change (P less than .0001).
The annualized relapse rate was reduced by 55% with the active treatment versus placebo, and there was less percent change in brain volume with active therapy versus placebo from baseline to 12 and 24 months’ follow-up (23.4% lower average change, P = .0002).
The time to 3-month confirmed worsening by 20% or more from baseline in the timed 25-foot walk test was reduced by 6.2%. Although not significant, the trend was “in the right direction,” Dr. Kappos said.
The mean age of recruited patients was 48 years, with an average duration of MS of 16-17 years, and just under 4 years since their conversion to SPMS. Baseline EDSS was a mean of 5.4, around 35%-37% had one or more relapses in the 2 years before screening, and 20% had gadolinium-enhancing lesions at baseline.
A variety of predefined subgroup analyses showed a benefit for siponimod over placebo. These included analyses looking at the effect by the number of gadolinium-enhancing lesions at baseline, previous disease-modifying treatment, whether patients’ MS was rapidly progressing, whether patients’ disease was moderate or severe, the baseline EDSS, and the duration of MS since the first recognition of symptoms.
“What is the optimal patient population?” an audience member asked Dr. Kappos during the Q&A period following his presentation at the ECTRIMS meeting. He responded: “I think younger patients with the more active disease will certainly be the best candidates.” But, he added, it was reassuring to note that the drug seems to work equally well in all patient subtypes.
Novartis funded the study. Dr. Kappos disclosed that his institution has received financial support for research purposes from multiple MS drug manufacturers – including Novartis – and charitable organizations.
AT ECTRIMS 2016
Key clinical point: Siponimod is an investigational treatment that could help patients with secondary progressive multiple sclerosis.
Major finding: Siponimod reduced the 3-month confirmed disability progression by 21%, compared with placebo (hazard ratio, 0.79; P = .013).
Data source: Phase III, multicenter, randomized, double-blind, placebo-controlled trial of siponimod versus placebo in the treatment of 1,646 patients with SPMS.
Disclosures: Novartis funded the study. Dr. Kappos disclosed that his institution has received financial support for research purposes from many MS drug manufacturers – including Novartis – and charitable organizations.