User login
IHS Program Targets HIV/AIDs in Young Natives
More than half of the new HIV diagnoses among American Indians and Alaska Natives are estimated to be among those aged < 35 years, according to the CDC. To improve HIV prevention and care outcomes, an ongoing collaboration between IHS and the CDC is funding cooperative agreements with First Nations Community HealthSource, Albuquerque, and Inter Tribal Council of Arizona, Phoenix. The groups will receive up to $100,000 a year for up to 5 years for community health care services. “These awards increase access to culturally appropriate, high-quality HIV treatment for our American Indian and Alaska Native communities,” said Mary L. Smith, IHS principal deputy director.
First Nations, New Mexico’s urban Indian health center and a Federally Qualified Health Center, operates 2 clinic sites and 3 school-based health centers. The Inter Tribal Council of Arizona, representing 21 tribal governments, operates more than 30 projects and provides technical assistance and training to tribal governments in program planning and development, research and data collection, resource development, management and evaluation.
The awards support activities in 5 main areas:
- Increasing access to comprehensive pre-exposure prophylaxis;
- Identifying local-level priorities for HIV care needs and creating tools and resources;
- Making it easier for people living with HIV and AIDS to stay in treatment;
- Teaching people who inject drugs about reducing risks and extending access to services for medication-assisted therapies for people with opioid use disorder in accordance with federal, state, tribal, and local laws; and
- Increasing age-appropriate prevention education at the local levels.
“This multiyear collaboration supports a sustained, in-depth HIV prevention program that will benefit not only tribes, but also American Indians and Alaska Natives in urban locations,” said Eugene McCray, MD, director of CDC’s Division of HIV/AIDS Prevention. “We are bringing services right to the local level, reaching American Indian and Alaska Native communities.”
More than half of the new HIV diagnoses among American Indians and Alaska Natives are estimated to be among those aged < 35 years, according to the CDC. To improve HIV prevention and care outcomes, an ongoing collaboration between IHS and the CDC is funding cooperative agreements with First Nations Community HealthSource, Albuquerque, and Inter Tribal Council of Arizona, Phoenix. The groups will receive up to $100,000 a year for up to 5 years for community health care services. “These awards increase access to culturally appropriate, high-quality HIV treatment for our American Indian and Alaska Native communities,” said Mary L. Smith, IHS principal deputy director.
First Nations, New Mexico’s urban Indian health center and a Federally Qualified Health Center, operates 2 clinic sites and 3 school-based health centers. The Inter Tribal Council of Arizona, representing 21 tribal governments, operates more than 30 projects and provides technical assistance and training to tribal governments in program planning and development, research and data collection, resource development, management and evaluation.
The awards support activities in 5 main areas:
- Increasing access to comprehensive pre-exposure prophylaxis;
- Identifying local-level priorities for HIV care needs and creating tools and resources;
- Making it easier for people living with HIV and AIDS to stay in treatment;
- Teaching people who inject drugs about reducing risks and extending access to services for medication-assisted therapies for people with opioid use disorder in accordance with federal, state, tribal, and local laws; and
- Increasing age-appropriate prevention education at the local levels.
“This multiyear collaboration supports a sustained, in-depth HIV prevention program that will benefit not only tribes, but also American Indians and Alaska Natives in urban locations,” said Eugene McCray, MD, director of CDC’s Division of HIV/AIDS Prevention. “We are bringing services right to the local level, reaching American Indian and Alaska Native communities.”
More than half of the new HIV diagnoses among American Indians and Alaska Natives are estimated to be among those aged < 35 years, according to the CDC. To improve HIV prevention and care outcomes, an ongoing collaboration between IHS and the CDC is funding cooperative agreements with First Nations Community HealthSource, Albuquerque, and Inter Tribal Council of Arizona, Phoenix. The groups will receive up to $100,000 a year for up to 5 years for community health care services. “These awards increase access to culturally appropriate, high-quality HIV treatment for our American Indian and Alaska Native communities,” said Mary L. Smith, IHS principal deputy director.
First Nations, New Mexico’s urban Indian health center and a Federally Qualified Health Center, operates 2 clinic sites and 3 school-based health centers. The Inter Tribal Council of Arizona, representing 21 tribal governments, operates more than 30 projects and provides technical assistance and training to tribal governments in program planning and development, research and data collection, resource development, management and evaluation.
The awards support activities in 5 main areas:
- Increasing access to comprehensive pre-exposure prophylaxis;
- Identifying local-level priorities for HIV care needs and creating tools and resources;
- Making it easier for people living with HIV and AIDS to stay in treatment;
- Teaching people who inject drugs about reducing risks and extending access to services for medication-assisted therapies for people with opioid use disorder in accordance with federal, state, tribal, and local laws; and
- Increasing age-appropriate prevention education at the local levels.
“This multiyear collaboration supports a sustained, in-depth HIV prevention program that will benefit not only tribes, but also American Indians and Alaska Natives in urban locations,” said Eugene McCray, MD, director of CDC’s Division of HIV/AIDS Prevention. “We are bringing services right to the local level, reaching American Indian and Alaska Native communities.”
Aromatase Inhibitor as Adjuvant Therapy for Breast Cancer: Is Longer Treatment Better?
Study Overview
Objective. To assess the effect of extending adjuvant therapy with an aromatase inhibitor beyond 5 years in postmenopausal women with breast cancer.
Design. Phase 3, randomized, double-blind, placebo-controlled trial.
Setting and participants. This was a North American Breast Cancer Group trial, coordinated by the Canadian Cancer Trials Group. The trial was originally designed as an extension of the MA.17 trial evaluating the role for 5 years of letrozole versus placebo after 5 years of tamoxifen, with re-randomization of letrozole-assigned patients to an additional 5 years of letrozole versus placebo. The trial was then extended to include additional postmenopausal women with stage I-III breast cancer who had been treated with 4.5 to 6 years of adjuvant therapy with any aromatase inhibitor with or without prior tamoxifen.
Most patients had received adjuvant treatment with tamoxifen before the aromatase inhibitor. Patients were randomized within 2 years after completing treatment with the aromatase inhibitor to either letrozole 2.5 mg or placebo orally once a day, for another 5 years. The criteria for stratification included lymph node status, prior receipt of adjuvant chemotherapy, the interval between the last dose of aromatase inhibitor and randomization, and the duration of prior use of tamoxifen. Eligibility criteria included patients who were disease-free after 4.5 to 6 years of aromatase inhibitor, hormone-positive tumors (and unknown receptor status for participants in the MA.17 trial), ECOG performance status of 0 to 2, and life expectancy of 5 or more years.
Main outcome measures. The primary endpoint was disease-free survival, defined as the time from randomization to recurrence or the development of new primary breast cancer. Secondary endpoints included overall survival, incidence of contralateral breast cancer, quality of life using the Medical Outcomes Study 36-Item Short-Form Heath Survey (SF-36) and the Menopause-Specific Quality of Life (MENQOL) questionnaire, and long-term safety. The investigators calculated that 196 events were required for the study to have 80% power to detect a 33% lower hazard of recurrence with letrozole as compared with placebo. At the 6-year point, only 176 events had been observed, and the study design was amended to have a time-based analysis instead of event-based. On 13 Nov 2015 the final database had 165 events, with 80% power to detect a hazard ratio for disease-free survival of 0.655. The analysis of time-to-event outcomes was performed utilizing a log-rank test with adjustment for stratification factors. Fisher’s exact test was used to assess binary outcomes, and Wilcoxon test, to assess continuous outcomes. Comparisons between the letrozole and the placebo groups were made using a 2-sided test with an alpha level of 5%.
Main results. A total of 1918 patients were randomized to receive either letrozole (n = 959) or placebo (n = 959). The rate of adherence to the study regimen was approximately 62% for both arms. The median duration of prior treatment with tamoxifen was 5 years; 20.7% of patients did not receive tamoxifen. The median duration of prior treatment with aromatase inhibitor was 5 years, and the median time interval between the last dose of aromatase inhibitor and randomization was less than 6 months. The median duration of the study regimen (letrozole or placebo) was 5 years, and the median follow-up was 6.3 years. Approximately 90% of patients had stage T1 or T2 tumors at diagnosis, and 94% of nodal stage were N0 or N1. Estrogen receptor, progesterone receptor or both were known to be positive in 98.8% of patients.
Disease recurrence or contralateral breast cancer occurred in 67 patients (7%) in the letrozole group and 98 patients (10.2%) in the placebo group. The hazard ratio for recurrence or occurrence of contralateral breast cancer was 0.66 (95% confidence interval [CI], 0.48–0.91, P = 0.01). In the letrozole group, 55 patients had disease recurrence and 13 patients had contralateral breast cancer. Among the patients in the placebo group, 68 had recurrence of disease and 31 had contralateral breast cancer. Both disease recurrence and contralateral breast cancer occurred in one patient in each group. Distant disease recurrence was 5.5% in the placebo group and 4.4% in the letrozole group.
Five-year disease-free survival, the primary endpoint of this study, was 95% in the letrozole group (95% CI, 93–96) and 91% in the placebo group (95% CI, 89–93). The rate of 5-year disease free-survival was higher in the letrozole group in all subgroups. A total of 200 deaths were observed, 100 in each group. The rate of 5-year overall survival was not statistically different between the 2 groups (93% in the letrozole group and 94% in the placebo group, HR 0.97, P = 0.83). The annual incidence rate of contralateral breast cancer favored the letrozole group, with a rate of 0.21% in comparison with 0.49% in the placebo group (HR 0.42, P = 0.007).
Discontinuation of treatment occurred in 5.4% of patients in the letrozole group and 3.7% in the placebo group. The majority of toxic effects had a similar incidence in both groups, however bone-related side effects were more common in the letrozole group. Bone fractures occurred in 14% of patients in the letrozole group and 9% in the placebo group (P = 0.001). New-onset osteoporosis was also more common in the letrozole group (11% versus 6%, P < 0.001). Of note, 5 patients developed a hip fracture after discontinuation of letrozole. In regards to quality of life, patients receiving letrozole had a greater reduction in scores in the role-physical subscale of the SF-36 survey, indicating worse quality of life, but the difference was less than the minimum clinically important difference. There were no differences in the MENQOL questionnaire subscales.
Conclusion. Treatment with an aromatase inhibitor for additional 4.5 to 6 years was beneficial in preventing disease recurrence. There was no difference in overall survival.
Commentary
Adjuvant endocrine therapy reduces the risk of recurrence and increases survival in women with hormone receptor–positive breast cancer. The use of tamoxifen as adjuvant therapy for women with early stage breast cancer has been extensively studied. A metanalysis performed by the Early Breast Cancer Trialists’ Collaborative Group (EBCTG) demonstrated that tamoxifen reduces breast cancer mortality by a third when given as adjuvant therapy for women with hormone positive breast cancer [1].
Two important studies published in the last decade demonstrated that extending therapy with tamoxifen beyond 5 years reduces the chance of recurrence and improves survival. In the ATLAS (Adjuvant Tamoxifen: Longer Against Shorter) trial, women with early stage breast cancer who had completed 5 years of adjuvant tamoxifen were randomized to stop therapy or to continue tamoxifen for 5 additional years. Among patients with estrogen receptor (ER)–positive disease, the results demonstrated an absolute recurrence reduction of 3.7% and an absolute mortality reduction of 2.8% in 15 years after diagnosis [2].The aTTom trial randomized 6953 women with ER-positive breast cancer to discontinue tamoxifen after 5 years or to continue to complete 10 years of treatment and confirmed a benefit in recurrence rates and breast cancer mortality with 10 years of adjuvant tamoxifen [3].
Although tamoxifen is active in both pre- and postmenopausal patients, therapy with an aromatase inhibitor either as first-line or following treatment with tamoxifen has been demonstrated to be superior to tamoxifen alone in hormone receptor–positive postmenopausal women. In the ATAC (The Arimidex, Tamoxifen, Alone or in Combination) trial, postmenopausal patients were randomized to receive 5 years of either tamoxifen or anastrozole as adjuvant therapy. The anastrozole group had higher disease-free survival, time to recurrence and time to distant recurrence [4].In the Breast Intergroup (BIG) 1-98 trial, postmenopausal women were assigned to 4 different arms: 5 years of letrozole, 5 years of tamoxifen, letrozole for 2 years followed by tamoxifen for 3 years, or tamoxifen for 2 years followed by letrozole for 3 years. The 2 groups assigned to receive letrozole initially were compared to the 2 groups assigned to receive tamoxifen initially. Compared with tamoxifen, letrozole significantly decrease the risk of recurrence [5].The MA-17 trial demonstrated a disease-free survival advantage with 5 years of letrozole compared with placebo in women who had been treated with tamoxifen for 5 years [6]. Based on these data, current guidelines for adjuvant endocrine therapy for postmenopausal women recommend an aromatase inhibitor for 5 years as primary therapy or after 2 to 3 years of tamoxifen [7].
Results from studies with extended endocrine therapy, either 10 years of tamoxifen or 5 years of aromatase inhibitor after up to 5 years of tamoxifen, provide rationale to study the effect of therapy with aromatase inhibitor beyond 5 years. The current study by Goss et al (the MA 17.R trial) addresses the relevant question of whether extended adjuvant therapy with an aromatase inhibitor in post-menopausal women beyond 5 years provides additional benefit. The design of this study has several strengths including being randomized, phase 3, placebo-controlled and double-blind. Another strength was the large number of patients enrolled. The choice of disease-free survival as the primary endpoint is in accordance with the natural course of ER-positive breast cancer, which has a prolonged rate of recurrence. The study results showed that patients who received 10 years of letrozole had a 34% lower risk of recurrence, with an absolute improvement of 4% in disease-free survival. However, no overall survival benefit was demonstrated at a median follow-up of 6.3 years. This might be a result of the fact that the highest proportional benefit was reduction in incidence of contralateral breast cancer. It is also possible that an overall survival benefit would be observed with a longer follow-up.
As highlighted by the authors, the benefit of extended adjuvant therapy is higher in the first years. Given that the majority of patients enrolled in this study had received prior tamoxifen, it is possible that patients who receive only an aromatase inhibitor for 5 years without prior tamoxifen would benefit even more from extended aromatase inhibitor therapy. On the other hand, the 1.1% numerical advantage observed in reducing distant recurrence is quite modest, with the majority of the disease-free survival advantage seen with extended aromatase inhibition being due to a reduction in local recurrence and contralateral new concerns.
The quality of life assessment enhanced this trial, since adherence to adjuvant endocrine therapy remains a challenge. It should be noted, however, that patients willing to participate in a trial of extended therapy are likely to be those who have tolerated therapy reasonably well. The increase in body pain and differences in the role-emotional subscale in the letrozole reflect side effects of aromatase inhibitors that are seen in clinical practice. The higher rates of new-onset osteoporosis and bone fractures underscore the need to balance potential benefits and risks with extended aromatase inhibitor therapy.
Results from other trials evaluating extended adjuvant therapy will be helpful. The NSABP B-42 study randomized ER-positive postmenopausal patients to receive 5 years of letrozole or placebo after completing 5 years of hormonal therapy with an aromatase inhibitor for 5 years or ≤ 3 years of tamoxifen followed by an aromatase inhibitor. This study has completed enrollment and should provide additional insight regarding duration of therapy with aromatase inhibitors.
Applications for Clinical Practice
These trial results showed a benefit with extended aromatase inhibitor therapy; however, the magnitude of benefit was relatively small, particularly with respect to impacting distant recurrence risk. Given that extended therapy has potential side effects, it is appropriate to have a detailed discussion with patients regarding potential benefits and risks. A reasonable clinical strategy is to discuss extended therapy with patients who have a higher chance of relapse and those who are motivated to continue therapy to reduce new breast cancer events.
—Leticia Varella, MD, and Halle Moore, MD,
Cleveland Clinic Taussig Cancer Institute, Cleveland, OH
1. Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005;365:1687–717.
2. Davies C, Pan H, Godwin J, at al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet 2013;381:805–16.
3. Gray RG, Rea D, Handley K, et al. aTTom: Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years in 6,953 women with early breast cancer. J Clin Oncol 2013;31(suppl;abstr 5).
4. Cuzick J, Sestak I, Baum M, et al; ATAC/LATTE investigators. Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 10-year analysis of the ATAC trial. Lancet Oncol 2010;11:113541.
5. Breast International Group (BIG) 1-98 Collaborative Group, Thürlimann B, Keshaviah A, Coates AS, et al. A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl J Med 2005;353:2747–57.
6. Goss PE, Ingle JN, Martino S, et al. A randomized trial of letrozole in postmenopausal women after five years of tamoxifen therapy for early-stage breast cancer. N Engl J Med 2003;349:1793–802.
7. Burstein HJ, Prestrud AA, Seidenfeld J, et al; American Society of Clinical Oncology. American Society of Clinical Oncology clinical practice guideline: update on adjuvant endocrine therapy for women with hormone receptor-positive breast cancer. J Clin Oncol 2010;28:3784–96.
Study Overview
Objective. To assess the effect of extending adjuvant therapy with an aromatase inhibitor beyond 5 years in postmenopausal women with breast cancer.
Design. Phase 3, randomized, double-blind, placebo-controlled trial.
Setting and participants. This was a North American Breast Cancer Group trial, coordinated by the Canadian Cancer Trials Group. The trial was originally designed as an extension of the MA.17 trial evaluating the role for 5 years of letrozole versus placebo after 5 years of tamoxifen, with re-randomization of letrozole-assigned patients to an additional 5 years of letrozole versus placebo. The trial was then extended to include additional postmenopausal women with stage I-III breast cancer who had been treated with 4.5 to 6 years of adjuvant therapy with any aromatase inhibitor with or without prior tamoxifen.
Most patients had received adjuvant treatment with tamoxifen before the aromatase inhibitor. Patients were randomized within 2 years after completing treatment with the aromatase inhibitor to either letrozole 2.5 mg or placebo orally once a day, for another 5 years. The criteria for stratification included lymph node status, prior receipt of adjuvant chemotherapy, the interval between the last dose of aromatase inhibitor and randomization, and the duration of prior use of tamoxifen. Eligibility criteria included patients who were disease-free after 4.5 to 6 years of aromatase inhibitor, hormone-positive tumors (and unknown receptor status for participants in the MA.17 trial), ECOG performance status of 0 to 2, and life expectancy of 5 or more years.
Main outcome measures. The primary endpoint was disease-free survival, defined as the time from randomization to recurrence or the development of new primary breast cancer. Secondary endpoints included overall survival, incidence of contralateral breast cancer, quality of life using the Medical Outcomes Study 36-Item Short-Form Heath Survey (SF-36) and the Menopause-Specific Quality of Life (MENQOL) questionnaire, and long-term safety. The investigators calculated that 196 events were required for the study to have 80% power to detect a 33% lower hazard of recurrence with letrozole as compared with placebo. At the 6-year point, only 176 events had been observed, and the study design was amended to have a time-based analysis instead of event-based. On 13 Nov 2015 the final database had 165 events, with 80% power to detect a hazard ratio for disease-free survival of 0.655. The analysis of time-to-event outcomes was performed utilizing a log-rank test with adjustment for stratification factors. Fisher’s exact test was used to assess binary outcomes, and Wilcoxon test, to assess continuous outcomes. Comparisons between the letrozole and the placebo groups were made using a 2-sided test with an alpha level of 5%.
Main results. A total of 1918 patients were randomized to receive either letrozole (n = 959) or placebo (n = 959). The rate of adherence to the study regimen was approximately 62% for both arms. The median duration of prior treatment with tamoxifen was 5 years; 20.7% of patients did not receive tamoxifen. The median duration of prior treatment with aromatase inhibitor was 5 years, and the median time interval between the last dose of aromatase inhibitor and randomization was less than 6 months. The median duration of the study regimen (letrozole or placebo) was 5 years, and the median follow-up was 6.3 years. Approximately 90% of patients had stage T1 or T2 tumors at diagnosis, and 94% of nodal stage were N0 or N1. Estrogen receptor, progesterone receptor or both were known to be positive in 98.8% of patients.
Disease recurrence or contralateral breast cancer occurred in 67 patients (7%) in the letrozole group and 98 patients (10.2%) in the placebo group. The hazard ratio for recurrence or occurrence of contralateral breast cancer was 0.66 (95% confidence interval [CI], 0.48–0.91, P = 0.01). In the letrozole group, 55 patients had disease recurrence and 13 patients had contralateral breast cancer. Among the patients in the placebo group, 68 had recurrence of disease and 31 had contralateral breast cancer. Both disease recurrence and contralateral breast cancer occurred in one patient in each group. Distant disease recurrence was 5.5% in the placebo group and 4.4% in the letrozole group.
Five-year disease-free survival, the primary endpoint of this study, was 95% in the letrozole group (95% CI, 93–96) and 91% in the placebo group (95% CI, 89–93). The rate of 5-year disease free-survival was higher in the letrozole group in all subgroups. A total of 200 deaths were observed, 100 in each group. The rate of 5-year overall survival was not statistically different between the 2 groups (93% in the letrozole group and 94% in the placebo group, HR 0.97, P = 0.83). The annual incidence rate of contralateral breast cancer favored the letrozole group, with a rate of 0.21% in comparison with 0.49% in the placebo group (HR 0.42, P = 0.007).
Discontinuation of treatment occurred in 5.4% of patients in the letrozole group and 3.7% in the placebo group. The majority of toxic effects had a similar incidence in both groups, however bone-related side effects were more common in the letrozole group. Bone fractures occurred in 14% of patients in the letrozole group and 9% in the placebo group (P = 0.001). New-onset osteoporosis was also more common in the letrozole group (11% versus 6%, P < 0.001). Of note, 5 patients developed a hip fracture after discontinuation of letrozole. In regards to quality of life, patients receiving letrozole had a greater reduction in scores in the role-physical subscale of the SF-36 survey, indicating worse quality of life, but the difference was less than the minimum clinically important difference. There were no differences in the MENQOL questionnaire subscales.
Conclusion. Treatment with an aromatase inhibitor for additional 4.5 to 6 years was beneficial in preventing disease recurrence. There was no difference in overall survival.
Commentary
Adjuvant endocrine therapy reduces the risk of recurrence and increases survival in women with hormone receptor–positive breast cancer. The use of tamoxifen as adjuvant therapy for women with early stage breast cancer has been extensively studied. A metanalysis performed by the Early Breast Cancer Trialists’ Collaborative Group (EBCTG) demonstrated that tamoxifen reduces breast cancer mortality by a third when given as adjuvant therapy for women with hormone positive breast cancer [1].
Two important studies published in the last decade demonstrated that extending therapy with tamoxifen beyond 5 years reduces the chance of recurrence and improves survival. In the ATLAS (Adjuvant Tamoxifen: Longer Against Shorter) trial, women with early stage breast cancer who had completed 5 years of adjuvant tamoxifen were randomized to stop therapy or to continue tamoxifen for 5 additional years. Among patients with estrogen receptor (ER)–positive disease, the results demonstrated an absolute recurrence reduction of 3.7% and an absolute mortality reduction of 2.8% in 15 years after diagnosis [2].The aTTom trial randomized 6953 women with ER-positive breast cancer to discontinue tamoxifen after 5 years or to continue to complete 10 years of treatment and confirmed a benefit in recurrence rates and breast cancer mortality with 10 years of adjuvant tamoxifen [3].
Although tamoxifen is active in both pre- and postmenopausal patients, therapy with an aromatase inhibitor either as first-line or following treatment with tamoxifen has been demonstrated to be superior to tamoxifen alone in hormone receptor–positive postmenopausal women. In the ATAC (The Arimidex, Tamoxifen, Alone or in Combination) trial, postmenopausal patients were randomized to receive 5 years of either tamoxifen or anastrozole as adjuvant therapy. The anastrozole group had higher disease-free survival, time to recurrence and time to distant recurrence [4].In the Breast Intergroup (BIG) 1-98 trial, postmenopausal women were assigned to 4 different arms: 5 years of letrozole, 5 years of tamoxifen, letrozole for 2 years followed by tamoxifen for 3 years, or tamoxifen for 2 years followed by letrozole for 3 years. The 2 groups assigned to receive letrozole initially were compared to the 2 groups assigned to receive tamoxifen initially. Compared with tamoxifen, letrozole significantly decrease the risk of recurrence [5].The MA-17 trial demonstrated a disease-free survival advantage with 5 years of letrozole compared with placebo in women who had been treated with tamoxifen for 5 years [6]. Based on these data, current guidelines for adjuvant endocrine therapy for postmenopausal women recommend an aromatase inhibitor for 5 years as primary therapy or after 2 to 3 years of tamoxifen [7].
Results from studies with extended endocrine therapy, either 10 years of tamoxifen or 5 years of aromatase inhibitor after up to 5 years of tamoxifen, provide rationale to study the effect of therapy with aromatase inhibitor beyond 5 years. The current study by Goss et al (the MA 17.R trial) addresses the relevant question of whether extended adjuvant therapy with an aromatase inhibitor in post-menopausal women beyond 5 years provides additional benefit. The design of this study has several strengths including being randomized, phase 3, placebo-controlled and double-blind. Another strength was the large number of patients enrolled. The choice of disease-free survival as the primary endpoint is in accordance with the natural course of ER-positive breast cancer, which has a prolonged rate of recurrence. The study results showed that patients who received 10 years of letrozole had a 34% lower risk of recurrence, with an absolute improvement of 4% in disease-free survival. However, no overall survival benefit was demonstrated at a median follow-up of 6.3 years. This might be a result of the fact that the highest proportional benefit was reduction in incidence of contralateral breast cancer. It is also possible that an overall survival benefit would be observed with a longer follow-up.
As highlighted by the authors, the benefit of extended adjuvant therapy is higher in the first years. Given that the majority of patients enrolled in this study had received prior tamoxifen, it is possible that patients who receive only an aromatase inhibitor for 5 years without prior tamoxifen would benefit even more from extended aromatase inhibitor therapy. On the other hand, the 1.1% numerical advantage observed in reducing distant recurrence is quite modest, with the majority of the disease-free survival advantage seen with extended aromatase inhibition being due to a reduction in local recurrence and contralateral new concerns.
The quality of life assessment enhanced this trial, since adherence to adjuvant endocrine therapy remains a challenge. It should be noted, however, that patients willing to participate in a trial of extended therapy are likely to be those who have tolerated therapy reasonably well. The increase in body pain and differences in the role-emotional subscale in the letrozole reflect side effects of aromatase inhibitors that are seen in clinical practice. The higher rates of new-onset osteoporosis and bone fractures underscore the need to balance potential benefits and risks with extended aromatase inhibitor therapy.
Results from other trials evaluating extended adjuvant therapy will be helpful. The NSABP B-42 study randomized ER-positive postmenopausal patients to receive 5 years of letrozole or placebo after completing 5 years of hormonal therapy with an aromatase inhibitor for 5 years or ≤ 3 years of tamoxifen followed by an aromatase inhibitor. This study has completed enrollment and should provide additional insight regarding duration of therapy with aromatase inhibitors.
Applications for Clinical Practice
These trial results showed a benefit with extended aromatase inhibitor therapy; however, the magnitude of benefit was relatively small, particularly with respect to impacting distant recurrence risk. Given that extended therapy has potential side effects, it is appropriate to have a detailed discussion with patients regarding potential benefits and risks. A reasonable clinical strategy is to discuss extended therapy with patients who have a higher chance of relapse and those who are motivated to continue therapy to reduce new breast cancer events.
—Leticia Varella, MD, and Halle Moore, MD,
Cleveland Clinic Taussig Cancer Institute, Cleveland, OH
Study Overview
Objective. To assess the effect of extending adjuvant therapy with an aromatase inhibitor beyond 5 years in postmenopausal women with breast cancer.
Design. Phase 3, randomized, double-blind, placebo-controlled trial.
Setting and participants. This was a North American Breast Cancer Group trial, coordinated by the Canadian Cancer Trials Group. The trial was originally designed as an extension of the MA.17 trial evaluating the role for 5 years of letrozole versus placebo after 5 years of tamoxifen, with re-randomization of letrozole-assigned patients to an additional 5 years of letrozole versus placebo. The trial was then extended to include additional postmenopausal women with stage I-III breast cancer who had been treated with 4.5 to 6 years of adjuvant therapy with any aromatase inhibitor with or without prior tamoxifen.
Most patients had received adjuvant treatment with tamoxifen before the aromatase inhibitor. Patients were randomized within 2 years after completing treatment with the aromatase inhibitor to either letrozole 2.5 mg or placebo orally once a day, for another 5 years. The criteria for stratification included lymph node status, prior receipt of adjuvant chemotherapy, the interval between the last dose of aromatase inhibitor and randomization, and the duration of prior use of tamoxifen. Eligibility criteria included patients who were disease-free after 4.5 to 6 years of aromatase inhibitor, hormone-positive tumors (and unknown receptor status for participants in the MA.17 trial), ECOG performance status of 0 to 2, and life expectancy of 5 or more years.
Main outcome measures. The primary endpoint was disease-free survival, defined as the time from randomization to recurrence or the development of new primary breast cancer. Secondary endpoints included overall survival, incidence of contralateral breast cancer, quality of life using the Medical Outcomes Study 36-Item Short-Form Heath Survey (SF-36) and the Menopause-Specific Quality of Life (MENQOL) questionnaire, and long-term safety. The investigators calculated that 196 events were required for the study to have 80% power to detect a 33% lower hazard of recurrence with letrozole as compared with placebo. At the 6-year point, only 176 events had been observed, and the study design was amended to have a time-based analysis instead of event-based. On 13 Nov 2015 the final database had 165 events, with 80% power to detect a hazard ratio for disease-free survival of 0.655. The analysis of time-to-event outcomes was performed utilizing a log-rank test with adjustment for stratification factors. Fisher’s exact test was used to assess binary outcomes, and Wilcoxon test, to assess continuous outcomes. Comparisons between the letrozole and the placebo groups were made using a 2-sided test with an alpha level of 5%.
Main results. A total of 1918 patients were randomized to receive either letrozole (n = 959) or placebo (n = 959). The rate of adherence to the study regimen was approximately 62% for both arms. The median duration of prior treatment with tamoxifen was 5 years; 20.7% of patients did not receive tamoxifen. The median duration of prior treatment with aromatase inhibitor was 5 years, and the median time interval between the last dose of aromatase inhibitor and randomization was less than 6 months. The median duration of the study regimen (letrozole or placebo) was 5 years, and the median follow-up was 6.3 years. Approximately 90% of patients had stage T1 or T2 tumors at diagnosis, and 94% of nodal stage were N0 or N1. Estrogen receptor, progesterone receptor or both were known to be positive in 98.8% of patients.
Disease recurrence or contralateral breast cancer occurred in 67 patients (7%) in the letrozole group and 98 patients (10.2%) in the placebo group. The hazard ratio for recurrence or occurrence of contralateral breast cancer was 0.66 (95% confidence interval [CI], 0.48–0.91, P = 0.01). In the letrozole group, 55 patients had disease recurrence and 13 patients had contralateral breast cancer. Among the patients in the placebo group, 68 had recurrence of disease and 31 had contralateral breast cancer. Both disease recurrence and contralateral breast cancer occurred in one patient in each group. Distant disease recurrence was 5.5% in the placebo group and 4.4% in the letrozole group.
Five-year disease-free survival, the primary endpoint of this study, was 95% in the letrozole group (95% CI, 93–96) and 91% in the placebo group (95% CI, 89–93). The rate of 5-year disease free-survival was higher in the letrozole group in all subgroups. A total of 200 deaths were observed, 100 in each group. The rate of 5-year overall survival was not statistically different between the 2 groups (93% in the letrozole group and 94% in the placebo group, HR 0.97, P = 0.83). The annual incidence rate of contralateral breast cancer favored the letrozole group, with a rate of 0.21% in comparison with 0.49% in the placebo group (HR 0.42, P = 0.007).
Discontinuation of treatment occurred in 5.4% of patients in the letrozole group and 3.7% in the placebo group. The majority of toxic effects had a similar incidence in both groups, however bone-related side effects were more common in the letrozole group. Bone fractures occurred in 14% of patients in the letrozole group and 9% in the placebo group (P = 0.001). New-onset osteoporosis was also more common in the letrozole group (11% versus 6%, P < 0.001). Of note, 5 patients developed a hip fracture after discontinuation of letrozole. In regards to quality of life, patients receiving letrozole had a greater reduction in scores in the role-physical subscale of the SF-36 survey, indicating worse quality of life, but the difference was less than the minimum clinically important difference. There were no differences in the MENQOL questionnaire subscales.
Conclusion. Treatment with an aromatase inhibitor for additional 4.5 to 6 years was beneficial in preventing disease recurrence. There was no difference in overall survival.
Commentary
Adjuvant endocrine therapy reduces the risk of recurrence and increases survival in women with hormone receptor–positive breast cancer. The use of tamoxifen as adjuvant therapy for women with early stage breast cancer has been extensively studied. A metanalysis performed by the Early Breast Cancer Trialists’ Collaborative Group (EBCTG) demonstrated that tamoxifen reduces breast cancer mortality by a third when given as adjuvant therapy for women with hormone positive breast cancer [1].
Two important studies published in the last decade demonstrated that extending therapy with tamoxifen beyond 5 years reduces the chance of recurrence and improves survival. In the ATLAS (Adjuvant Tamoxifen: Longer Against Shorter) trial, women with early stage breast cancer who had completed 5 years of adjuvant tamoxifen were randomized to stop therapy or to continue tamoxifen for 5 additional years. Among patients with estrogen receptor (ER)–positive disease, the results demonstrated an absolute recurrence reduction of 3.7% and an absolute mortality reduction of 2.8% in 15 years after diagnosis [2].The aTTom trial randomized 6953 women with ER-positive breast cancer to discontinue tamoxifen after 5 years or to continue to complete 10 years of treatment and confirmed a benefit in recurrence rates and breast cancer mortality with 10 years of adjuvant tamoxifen [3].
Although tamoxifen is active in both pre- and postmenopausal patients, therapy with an aromatase inhibitor either as first-line or following treatment with tamoxifen has been demonstrated to be superior to tamoxifen alone in hormone receptor–positive postmenopausal women. In the ATAC (The Arimidex, Tamoxifen, Alone or in Combination) trial, postmenopausal patients were randomized to receive 5 years of either tamoxifen or anastrozole as adjuvant therapy. The anastrozole group had higher disease-free survival, time to recurrence and time to distant recurrence [4].In the Breast Intergroup (BIG) 1-98 trial, postmenopausal women were assigned to 4 different arms: 5 years of letrozole, 5 years of tamoxifen, letrozole for 2 years followed by tamoxifen for 3 years, or tamoxifen for 2 years followed by letrozole for 3 years. The 2 groups assigned to receive letrozole initially were compared to the 2 groups assigned to receive tamoxifen initially. Compared with tamoxifen, letrozole significantly decrease the risk of recurrence [5].The MA-17 trial demonstrated a disease-free survival advantage with 5 years of letrozole compared with placebo in women who had been treated with tamoxifen for 5 years [6]. Based on these data, current guidelines for adjuvant endocrine therapy for postmenopausal women recommend an aromatase inhibitor for 5 years as primary therapy or after 2 to 3 years of tamoxifen [7].
Results from studies with extended endocrine therapy, either 10 years of tamoxifen or 5 years of aromatase inhibitor after up to 5 years of tamoxifen, provide rationale to study the effect of therapy with aromatase inhibitor beyond 5 years. The current study by Goss et al (the MA 17.R trial) addresses the relevant question of whether extended adjuvant therapy with an aromatase inhibitor in post-menopausal women beyond 5 years provides additional benefit. The design of this study has several strengths including being randomized, phase 3, placebo-controlled and double-blind. Another strength was the large number of patients enrolled. The choice of disease-free survival as the primary endpoint is in accordance with the natural course of ER-positive breast cancer, which has a prolonged rate of recurrence. The study results showed that patients who received 10 years of letrozole had a 34% lower risk of recurrence, with an absolute improvement of 4% in disease-free survival. However, no overall survival benefit was demonstrated at a median follow-up of 6.3 years. This might be a result of the fact that the highest proportional benefit was reduction in incidence of contralateral breast cancer. It is also possible that an overall survival benefit would be observed with a longer follow-up.
As highlighted by the authors, the benefit of extended adjuvant therapy is higher in the first years. Given that the majority of patients enrolled in this study had received prior tamoxifen, it is possible that patients who receive only an aromatase inhibitor for 5 years without prior tamoxifen would benefit even more from extended aromatase inhibitor therapy. On the other hand, the 1.1% numerical advantage observed in reducing distant recurrence is quite modest, with the majority of the disease-free survival advantage seen with extended aromatase inhibition being due to a reduction in local recurrence and contralateral new concerns.
The quality of life assessment enhanced this trial, since adherence to adjuvant endocrine therapy remains a challenge. It should be noted, however, that patients willing to participate in a trial of extended therapy are likely to be those who have tolerated therapy reasonably well. The increase in body pain and differences in the role-emotional subscale in the letrozole reflect side effects of aromatase inhibitors that are seen in clinical practice. The higher rates of new-onset osteoporosis and bone fractures underscore the need to balance potential benefits and risks with extended aromatase inhibitor therapy.
Results from other trials evaluating extended adjuvant therapy will be helpful. The NSABP B-42 study randomized ER-positive postmenopausal patients to receive 5 years of letrozole or placebo after completing 5 years of hormonal therapy with an aromatase inhibitor for 5 years or ≤ 3 years of tamoxifen followed by an aromatase inhibitor. This study has completed enrollment and should provide additional insight regarding duration of therapy with aromatase inhibitors.
Applications for Clinical Practice
These trial results showed a benefit with extended aromatase inhibitor therapy; however, the magnitude of benefit was relatively small, particularly with respect to impacting distant recurrence risk. Given that extended therapy has potential side effects, it is appropriate to have a detailed discussion with patients regarding potential benefits and risks. A reasonable clinical strategy is to discuss extended therapy with patients who have a higher chance of relapse and those who are motivated to continue therapy to reduce new breast cancer events.
—Leticia Varella, MD, and Halle Moore, MD,
Cleveland Clinic Taussig Cancer Institute, Cleveland, OH
1. Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005;365:1687–717.
2. Davies C, Pan H, Godwin J, at al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet 2013;381:805–16.
3. Gray RG, Rea D, Handley K, et al. aTTom: Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years in 6,953 women with early breast cancer. J Clin Oncol 2013;31(suppl;abstr 5).
4. Cuzick J, Sestak I, Baum M, et al; ATAC/LATTE investigators. Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 10-year analysis of the ATAC trial. Lancet Oncol 2010;11:113541.
5. Breast International Group (BIG) 1-98 Collaborative Group, Thürlimann B, Keshaviah A, Coates AS, et al. A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl J Med 2005;353:2747–57.
6. Goss PE, Ingle JN, Martino S, et al. A randomized trial of letrozole in postmenopausal women after five years of tamoxifen therapy for early-stage breast cancer. N Engl J Med 2003;349:1793–802.
7. Burstein HJ, Prestrud AA, Seidenfeld J, et al; American Society of Clinical Oncology. American Society of Clinical Oncology clinical practice guideline: update on adjuvant endocrine therapy for women with hormone receptor-positive breast cancer. J Clin Oncol 2010;28:3784–96.
1. Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005;365:1687–717.
2. Davies C, Pan H, Godwin J, at al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet 2013;381:805–16.
3. Gray RG, Rea D, Handley K, et al. aTTom: Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years in 6,953 women with early breast cancer. J Clin Oncol 2013;31(suppl;abstr 5).
4. Cuzick J, Sestak I, Baum M, et al; ATAC/LATTE investigators. Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 10-year analysis of the ATAC trial. Lancet Oncol 2010;11:113541.
5. Breast International Group (BIG) 1-98 Collaborative Group, Thürlimann B, Keshaviah A, Coates AS, et al. A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl J Med 2005;353:2747–57.
6. Goss PE, Ingle JN, Martino S, et al. A randomized trial of letrozole in postmenopausal women after five years of tamoxifen therapy for early-stage breast cancer. N Engl J Med 2003;349:1793–802.
7. Burstein HJ, Prestrud AA, Seidenfeld J, et al; American Society of Clinical Oncology. American Society of Clinical Oncology clinical practice guideline: update on adjuvant endocrine therapy for women with hormone receptor-positive breast cancer. J Clin Oncol 2010;28:3784–96.
Intimate Partner and Sexual Violence Experienced by Women Serving in the Military
Study Overview
Objective. To understand how the experience of intimate partner violence and non-partner sexual assault (IPV/SA) in women in the military intersects with military service.
Design. Qualitative interviews conducted as part of a larger study focused on experiences of IPV/SA and health care needs and preferences among women veteran patients.
Setting and participants. Participants were 25 women veterans from all branches of the service, ages 22 to 58 years (mean 44.6), who were patients at the Veteran’s Medical Center in Philadelphia, PA. The sample was diverse: 56% self-identified as black or African American, 20% as white or Caucasian, 16% as Hispanic or Latina, and 8% as “other” or multiple race/ethnicity.
Interviews. Researchers conducted face-to-face interviews using a semi-structured interview guide to gather in-depth narratives related to the participants’ lives in the military and their experiences of IPV/SA. The Military Occupational Mental Health Model was used as a framework to understand the experience of IPV/SA within the cultural context of the military and how that context influences health and well-being. The model considers the unique context of the military, including the importance of the values of mission over individual well-being, hierarchy and subordination, leadership, and unit support, as well as what resources are made available.
Data analysis. The authors followed an inductive approach informed by grounded theory, with the goal of identifying themes and a unifying theory empirically grounded in the interview data. First, 2 members of the research team conducted independent, close readings of each transcript and applied open coding, then compared their coding to identify common patterns across transcripts. Through this process, they developed and refined a codebook to define a set of codes and guide application of codes to text. Research team members conducted line-by-line coding of each transcript, based on the codebook definitions. Then the authors read all coded text and met to discuss patterns within and between transcripts, leading to identification of 2 core categories pertaining to the relationship betweenIPV/SA and military service, as well as several subthemes within each core category.
Main results. The 2 core categories identified had both positive and negative influences. The first was the “experience of IPV/SA affects participation in military service, including entering and leaving military service,” and included the subthemes of coercion by the perpetrator to enter or leave military service, effects on service and work performance such as physical and mental health problems that interfered with their ability to do their job, and survival strategies that had negative repercussions on the woman’s career. The second was the “military context shapes responses to, and coping with, experiences of IPV/SA,” and included the subthemes of military sanction for IPV (but not sexual assault) if both partners were in the military, lack of accountability for and protection of service member perpetrators due to the value of unit support, military service as an opportunity to escape through relocation, even preferring a combat zone over home, and resistance to seeking help because of expectations of invulnerability related to the warrior identity.
Conclusion. The military context can provide personal and occupational resources for women who experience IPV/SA, but the institutional (ie, chain of command reporting) and cultural context can constrain women’s ability to access resources and support, negatively affecting outcomes.
Commentary
Intimate partner violence (IPV) is a widespread public health problem in the United States and women in the military are no exception. According to Black and Merrick [1], 36.3% of active duty women experienced sexual violence in their lifetime and 39.7% experienced IPV. Violence has significant health, economic, and social consequences for women in all settings, including serious short- and long-term physical and mental health problems, economic hardship, isolation, and decreased quality of life [2–5]. Women who experience IPV/SA in any setting face challenges in protecting themselves, overcoming violence, and seeking justice, however, the context in which the violence occurs can significantly influence the individual experiences of women. This study used a qualitative approach to understand how it is experienced by service women in the context of the military.
As the authors note, military culture can both facilitate and hamper women’s recovery from the physical, psychological, and economic sequelae of IPV/SA. The rigid hierarchal structure of the military and the expectation that one supports the unit and fellow soldiers above all else makes it very difficult for women to disclose IPV/SA and seek and receive protection and justice. On the other hand, military training and service provides women with the skills and means to be independent and to physically distance themselves from the perpetrator. However, the comment of one woman that facing bombs in Iraq was preferable to facing the violence at home should serve as a reminder of how devastating IPV/SA is and suggests that victims do not think there are effective institutional deterrents or protection available to them.
As the authors note, this was a small convenience sample of women at one VA medical center. This qualitative study provides a beginning understanding that should be expanded on with multisite quantitative research with large samples. Sexual assault in the military has been recognized as a significant problem, particularly for women but also for men. We need to continue to study this problem from many different perspectives to determine how to prevent violence and to ensure all victims get the resources and effective services they need.
Applications for Clinical Practice
This study has implications for all health care providers, as active duty and veteran service women seek care outside as well as within the VA. An important finding that has direct application to practice in all settings is the influence of the warrior identity. The warrior identity has been widely acknowledged as a barrier to seeking help for depression or PTSD in service men returning from combat but not as much in service women and not in the context of IPV/SA. It is important that providers consider warrior identity in assessing and treating women for IPV/SA. Not only can this affect disclosure and prevent a victim from seeking help, but the expectation that they should have been invulnerable and strong may increase feelings of self-blame and worsen psychological distress.
—Karen Roush, PhD, RN
1. Black MC, Merrick MT. Prevalence of intimate partner violence, sexual violence, and stalking among active duty women and wives of active duty men: Comparisons with women in the U.S. general population, 2010. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2013.
2. Bonomi AE, Anderson ML, Reid RJ, et al. Medical and psychosocial diagnoses in women with a history of intimate partner violence. Arch Intern Med 2009;169:1692–7.
3. Campbell J, Jones AS, Dienemann J, et al. Intimate partner violence and physical health consequences. Arch Intern Med 2002;162:1157–63.
4. Rees S, Silove D, Chey T, et al. Lifetime prevalence of gender-based violence in women and the relationship with mental disorders and psychosocial function. JAMA 2011;306:513–21.
5. Zlotnick C, Johnson DM, Kohn R. Intimate partner violence and long-term psychosocial functioning in a national sample of American women. J Interpers Violence 2006;21:
262–75.
Study Overview
Objective. To understand how the experience of intimate partner violence and non-partner sexual assault (IPV/SA) in women in the military intersects with military service.
Design. Qualitative interviews conducted as part of a larger study focused on experiences of IPV/SA and health care needs and preferences among women veteran patients.
Setting and participants. Participants were 25 women veterans from all branches of the service, ages 22 to 58 years (mean 44.6), who were patients at the Veteran’s Medical Center in Philadelphia, PA. The sample was diverse: 56% self-identified as black or African American, 20% as white or Caucasian, 16% as Hispanic or Latina, and 8% as “other” or multiple race/ethnicity.
Interviews. Researchers conducted face-to-face interviews using a semi-structured interview guide to gather in-depth narratives related to the participants’ lives in the military and their experiences of IPV/SA. The Military Occupational Mental Health Model was used as a framework to understand the experience of IPV/SA within the cultural context of the military and how that context influences health and well-being. The model considers the unique context of the military, including the importance of the values of mission over individual well-being, hierarchy and subordination, leadership, and unit support, as well as what resources are made available.
Data analysis. The authors followed an inductive approach informed by grounded theory, with the goal of identifying themes and a unifying theory empirically grounded in the interview data. First, 2 members of the research team conducted independent, close readings of each transcript and applied open coding, then compared their coding to identify common patterns across transcripts. Through this process, they developed and refined a codebook to define a set of codes and guide application of codes to text. Research team members conducted line-by-line coding of each transcript, based on the codebook definitions. Then the authors read all coded text and met to discuss patterns within and between transcripts, leading to identification of 2 core categories pertaining to the relationship betweenIPV/SA and military service, as well as several subthemes within each core category.
Main results. The 2 core categories identified had both positive and negative influences. The first was the “experience of IPV/SA affects participation in military service, including entering and leaving military service,” and included the subthemes of coercion by the perpetrator to enter or leave military service, effects on service and work performance such as physical and mental health problems that interfered with their ability to do their job, and survival strategies that had negative repercussions on the woman’s career. The second was the “military context shapes responses to, and coping with, experiences of IPV/SA,” and included the subthemes of military sanction for IPV (but not sexual assault) if both partners were in the military, lack of accountability for and protection of service member perpetrators due to the value of unit support, military service as an opportunity to escape through relocation, even preferring a combat zone over home, and resistance to seeking help because of expectations of invulnerability related to the warrior identity.
Conclusion. The military context can provide personal and occupational resources for women who experience IPV/SA, but the institutional (ie, chain of command reporting) and cultural context can constrain women’s ability to access resources and support, negatively affecting outcomes.
Commentary
Intimate partner violence (IPV) is a widespread public health problem in the United States and women in the military are no exception. According to Black and Merrick [1], 36.3% of active duty women experienced sexual violence in their lifetime and 39.7% experienced IPV. Violence has significant health, economic, and social consequences for women in all settings, including serious short- and long-term physical and mental health problems, economic hardship, isolation, and decreased quality of life [2–5]. Women who experience IPV/SA in any setting face challenges in protecting themselves, overcoming violence, and seeking justice, however, the context in which the violence occurs can significantly influence the individual experiences of women. This study used a qualitative approach to understand how it is experienced by service women in the context of the military.
As the authors note, military culture can both facilitate and hamper women’s recovery from the physical, psychological, and economic sequelae of IPV/SA. The rigid hierarchal structure of the military and the expectation that one supports the unit and fellow soldiers above all else makes it very difficult for women to disclose IPV/SA and seek and receive protection and justice. On the other hand, military training and service provides women with the skills and means to be independent and to physically distance themselves from the perpetrator. However, the comment of one woman that facing bombs in Iraq was preferable to facing the violence at home should serve as a reminder of how devastating IPV/SA is and suggests that victims do not think there are effective institutional deterrents or protection available to them.
As the authors note, this was a small convenience sample of women at one VA medical center. This qualitative study provides a beginning understanding that should be expanded on with multisite quantitative research with large samples. Sexual assault in the military has been recognized as a significant problem, particularly for women but also for men. We need to continue to study this problem from many different perspectives to determine how to prevent violence and to ensure all victims get the resources and effective services they need.
Applications for Clinical Practice
This study has implications for all health care providers, as active duty and veteran service women seek care outside as well as within the VA. An important finding that has direct application to practice in all settings is the influence of the warrior identity. The warrior identity has been widely acknowledged as a barrier to seeking help for depression or PTSD in service men returning from combat but not as much in service women and not in the context of IPV/SA. It is important that providers consider warrior identity in assessing and treating women for IPV/SA. Not only can this affect disclosure and prevent a victim from seeking help, but the expectation that they should have been invulnerable and strong may increase feelings of self-blame and worsen psychological distress.
—Karen Roush, PhD, RN
Study Overview
Objective. To understand how the experience of intimate partner violence and non-partner sexual assault (IPV/SA) in women in the military intersects with military service.
Design. Qualitative interviews conducted as part of a larger study focused on experiences of IPV/SA and health care needs and preferences among women veteran patients.
Setting and participants. Participants were 25 women veterans from all branches of the service, ages 22 to 58 years (mean 44.6), who were patients at the Veteran’s Medical Center in Philadelphia, PA. The sample was diverse: 56% self-identified as black or African American, 20% as white or Caucasian, 16% as Hispanic or Latina, and 8% as “other” or multiple race/ethnicity.
Interviews. Researchers conducted face-to-face interviews using a semi-structured interview guide to gather in-depth narratives related to the participants’ lives in the military and their experiences of IPV/SA. The Military Occupational Mental Health Model was used as a framework to understand the experience of IPV/SA within the cultural context of the military and how that context influences health and well-being. The model considers the unique context of the military, including the importance of the values of mission over individual well-being, hierarchy and subordination, leadership, and unit support, as well as what resources are made available.
Data analysis. The authors followed an inductive approach informed by grounded theory, with the goal of identifying themes and a unifying theory empirically grounded in the interview data. First, 2 members of the research team conducted independent, close readings of each transcript and applied open coding, then compared their coding to identify common patterns across transcripts. Through this process, they developed and refined a codebook to define a set of codes and guide application of codes to text. Research team members conducted line-by-line coding of each transcript, based on the codebook definitions. Then the authors read all coded text and met to discuss patterns within and between transcripts, leading to identification of 2 core categories pertaining to the relationship betweenIPV/SA and military service, as well as several subthemes within each core category.
Main results. The 2 core categories identified had both positive and negative influences. The first was the “experience of IPV/SA affects participation in military service, including entering and leaving military service,” and included the subthemes of coercion by the perpetrator to enter or leave military service, effects on service and work performance such as physical and mental health problems that interfered with their ability to do their job, and survival strategies that had negative repercussions on the woman’s career. The second was the “military context shapes responses to, and coping with, experiences of IPV/SA,” and included the subthemes of military sanction for IPV (but not sexual assault) if both partners were in the military, lack of accountability for and protection of service member perpetrators due to the value of unit support, military service as an opportunity to escape through relocation, even preferring a combat zone over home, and resistance to seeking help because of expectations of invulnerability related to the warrior identity.
Conclusion. The military context can provide personal and occupational resources for women who experience IPV/SA, but the institutional (ie, chain of command reporting) and cultural context can constrain women’s ability to access resources and support, negatively affecting outcomes.
Commentary
Intimate partner violence (IPV) is a widespread public health problem in the United States and women in the military are no exception. According to Black and Merrick [1], 36.3% of active duty women experienced sexual violence in their lifetime and 39.7% experienced IPV. Violence has significant health, economic, and social consequences for women in all settings, including serious short- and long-term physical and mental health problems, economic hardship, isolation, and decreased quality of life [2–5]. Women who experience IPV/SA in any setting face challenges in protecting themselves, overcoming violence, and seeking justice, however, the context in which the violence occurs can significantly influence the individual experiences of women. This study used a qualitative approach to understand how it is experienced by service women in the context of the military.
As the authors note, military culture can both facilitate and hamper women’s recovery from the physical, psychological, and economic sequelae of IPV/SA. The rigid hierarchal structure of the military and the expectation that one supports the unit and fellow soldiers above all else makes it very difficult for women to disclose IPV/SA and seek and receive protection and justice. On the other hand, military training and service provides women with the skills and means to be independent and to physically distance themselves from the perpetrator. However, the comment of one woman that facing bombs in Iraq was preferable to facing the violence at home should serve as a reminder of how devastating IPV/SA is and suggests that victims do not think there are effective institutional deterrents or protection available to them.
As the authors note, this was a small convenience sample of women at one VA medical center. This qualitative study provides a beginning understanding that should be expanded on with multisite quantitative research with large samples. Sexual assault in the military has been recognized as a significant problem, particularly for women but also for men. We need to continue to study this problem from many different perspectives to determine how to prevent violence and to ensure all victims get the resources and effective services they need.
Applications for Clinical Practice
This study has implications for all health care providers, as active duty and veteran service women seek care outside as well as within the VA. An important finding that has direct application to practice in all settings is the influence of the warrior identity. The warrior identity has been widely acknowledged as a barrier to seeking help for depression or PTSD in service men returning from combat but not as much in service women and not in the context of IPV/SA. It is important that providers consider warrior identity in assessing and treating women for IPV/SA. Not only can this affect disclosure and prevent a victim from seeking help, but the expectation that they should have been invulnerable and strong may increase feelings of self-blame and worsen psychological distress.
—Karen Roush, PhD, RN
1. Black MC, Merrick MT. Prevalence of intimate partner violence, sexual violence, and stalking among active duty women and wives of active duty men: Comparisons with women in the U.S. general population, 2010. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2013.
2. Bonomi AE, Anderson ML, Reid RJ, et al. Medical and psychosocial diagnoses in women with a history of intimate partner violence. Arch Intern Med 2009;169:1692–7.
3. Campbell J, Jones AS, Dienemann J, et al. Intimate partner violence and physical health consequences. Arch Intern Med 2002;162:1157–63.
4. Rees S, Silove D, Chey T, et al. Lifetime prevalence of gender-based violence in women and the relationship with mental disorders and psychosocial function. JAMA 2011;306:513–21.
5. Zlotnick C, Johnson DM, Kohn R. Intimate partner violence and long-term psychosocial functioning in a national sample of American women. J Interpers Violence 2006;21:
262–75.
1. Black MC, Merrick MT. Prevalence of intimate partner violence, sexual violence, and stalking among active duty women and wives of active duty men: Comparisons with women in the U.S. general population, 2010. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2013.
2. Bonomi AE, Anderson ML, Reid RJ, et al. Medical and psychosocial diagnoses in women with a history of intimate partner violence. Arch Intern Med 2009;169:1692–7.
3. Campbell J, Jones AS, Dienemann J, et al. Intimate partner violence and physical health consequences. Arch Intern Med 2002;162:1157–63.
4. Rees S, Silove D, Chey T, et al. Lifetime prevalence of gender-based violence in women and the relationship with mental disorders and psychosocial function. JAMA 2011;306:513–21.
5. Zlotnick C, Johnson DM, Kohn R. Intimate partner violence and long-term psychosocial functioning in a national sample of American women. J Interpers Violence 2006;21:
262–75.
A Mobile Health App for Weight Loss that Incorporates Social Networking
Study Overview
Objective. To test the efficacy of a weight loss app with incorporated social support and self-monitoring of diet, physical activity, and weight compared to a commercially available diet and PA tracking app.
Design. 2-group, randomized controlled trial.
Setting and participants. From October 2014 to January 2015, potential study participants were recruited via university/worksite listserv announcements, flyers, electronic newsletters, newspaper advertisements, social media posts, and a local research fair in 2 cities in South Carolina. Exclusion criteria included body mass index (BMI) outside the range of 25.0 to 49.9 kg/m2, unable to attend required measurement sessions, unable to access a computer or internet for completing assessments, having a psychiatric illness, receiving treatment for drug or alcohol dependency, having an eating disorder, participating in another weight loss program, reporting weight loss of 10+ pounds in the past 6 months, being pregnant or planning on becoming pregnant during study, or breastfeeding, or endorsing items on the Physical Activity Readiness Questionnaire (PAR-Q) regarding having a heart condition, feeling chest pain during physical activity, experiencing chest pain, becoming dizzy/ever losing balance or consciousness, and not having a physician give consent to participate despite reporting joint problems or taking blood pressure medication. Those who were eligible were invited to an orientation to the study, signed consent, and completed baseline assessments.
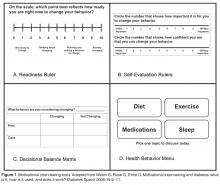
Intervention. Participants were randomized to either the experimental group (theory-based podcasts plus the Social POD app) or the comparison group (theory-based podcasts plus a standard app [“Fat Secret” app]). Both groups attended a training session on how to access the podcasts and download and use their app, and also had their baseline height and weight taken by study staff. Both groups received 2 podcasts per week, tracked their diet, weight, and physical activity, completed weekly surveys to report use of their assigned tracking app, and had their weight measures taken after 3 months. Objective measures of podcast usage and app usage were collected by study staff (experimental group only).
Both apps had diet and physical activity tracking features, but the Social POD app also included notifications to track diet and physical activity, messages sent from frequent app users to re-engage infrequent app users, a newsfeed to view other participants app tracking activity, stars awarded to frequent users of the app, points awarded for tracking, and prizes for earning points distributed at the final session by study staff. The Fat Secret app did not have any social support components but included a recipe database for looking up recipes by category.
Main outcome measures. The primary outcome was between-group differences in kilograms lost at 3 months. Secondary outcomes included group change in BMI after 3 months, as well as group differences in self-reported caloric intake, caloric expenditure, social support, self-efficacy, and outcome expectations scores, controlled for baseline measures.
Main results. Of the potential participants that inquired about the study (n = 189), those found to be eligible (n = 78) were invited to an orientation. Of those that attended the orientation (n = 62), 51 were randomized after completing baseline assessments (n = 25 to experimental group with Social POD app, n = 25 to comparison group with Fat Secret app), and 42 completed final weight measurements after 3 months. Participants were mostly white (57%) females (82%) with a mean BMI of 34.7 ± 6.0 kg/m2 and mean age of 46.2 ± 12.4 years. Baseline characteristics were similar between groups except that more comparison group participants reported previously downloading an app to track their diet than experimental participants. Participation attrition was 12% (n = 3 in each group).
Experimental group participants lost significantly more weight (–5.3 kg [95% CI, –7.5 to –3.0]) than the comparison group (–2.23 kg [95% CI, –3.6 to 1.0; P = 0.02). Experimental group participants also had a greater reduction in mean BMI (–1.9 kg/m2 [95% CI, –2.6 to –1.2]) vs. the comparison group (mean –0.9 kg/m2 [95% CI, –1.4 to – 0.05], P = 0.02). While there were significant differences in positive outcome expectations between groups (P = 0.04), other secondary outcomes were not significant.
Conclusions. An intervention with theory-based podcasts, social support, and incentivized self-monitoring resulted in significantly greater weight loss than a comparison intervention with theory-based podcasts and a commercially available standard self-monitoring app. This study highlights key features to add to mobile health interventions for adult weight loss.
Commentary
Obesity prevalence rates have increased over the past several decades across all genders, ages, ethnicities, income levels, and education levels [1], and recent data show that over one-third of adults in the US are obese and over two-thirds are overweight [2,3]. Behavior or lifestyle modification, which incorporates (often tailored) diet, physical activity, and behavior therapy, is highly recommended as the first strategy for losing initial weight and sustaining weight management efforts [4,5]. Mobile health (mHealth) technologies and other web-based and technology-assisted approaches (eg, mobile applications or “apps”) to facilitate behavior change for weight loss and management have aimed to address many of the limitations posed by traditional face-to-face weight loss approaches [6–8]. Prevailing theories of health behavior change imply key intervention design features that may increase their likelihood of promoting and sustaining desired behavior changes, particularly those that impact self-efficacy, self-regulation, and social facilitation [9,10].
Despite the plethora of weight loss mobile apps available to the public, it remains unclear if these are guided by evidence-based behavior change strategies typically used in traditional programs and approaches [11,12]. Further, very few of these apps have been rigorously evaluated with scientific testing to determine true effectiveness and safety [13,14]. This study adds to the literature by evaluating a mobile app for weight loss (Social POD) that was developed by researchers and utilizes theory-based components to target specific constructs that lead to health behavior change. Additionally, while self-monitoring is commonly incorporated into most available weight loss/management apps [11], the Social POD mobile app also incorporates social support and motivational strategies, which are less often included. The findings from this study add to the limited literature that mobile phone app-based interventions may be useful tools for weight loss [13].
The authors outlined several strengths and limitations. Briefly, this study was particularly strengthened by its randomized assignment to equivalent intervention groups, the use of a researcher-developed experimental group app that targets several key theory-based constructs for behavior change, measurement of objective use of the intervention group app, a racially diverse sample (over one-third of participants in both groups identified as black), measurement of secondary psycho-social behavioral outcomes, significant efforts to ensure survey completion and compliance with the intervention (increase retention), as well efforts to decrease participation burden by limiting required in-person sessions.
However, several important aspects of the study limit the internal validity and generalizability of its findings. The study had a small sample size and included a highly educated study population. If possible, future studies should consider including a large, diverse population to enhance generalizability. Also, this study was limited to those with an Android device, and significant demographic differences between Android and iPhone users have been reported [15]. The comparison group reported significantly more prior downloading of a diet-tracking app compared to the experimental group, which may have impacted use of the comparison app. The extrinsic reward system built into the experimental group intervention could have impacted adherence to experimental app, and is likely not feasible in real-world application of the experimental group app. Findings may have been subject to recall bias and measurement error due to self-reporting of outcomes measures. Importantly, this was a short-term weight loss study, and long-term weight loss/maintenance data is needed to support findings since in the usual course of weight-loss therapy the greatest weight loss occurs within 6 months of treatment, after which weight is often regained, sometimes near original level [16].
Applications for Clinical Practice
With the increasing popularity of technology-assisted and mHealth applications for weight loss and other health behaviors, it is important for practitioners to be familiar with proven, theory-based approaches and advise patients accordingly. This study demonstrated that social support components added to self-monitoring components in a weight loss app can lead to significant weight loss compared to self-monitoring alone. Thus, those that offer obesity counseling should be mindful that tracking and controlling dietary and physical activity behaviors alone may not prove to be successful. Opportunities for social facilitation to support weight loss efforts should be discussed with patients, including sources of social influence, support and collaboration between individuals, families, and health care professionals.
—Katrina F. Mateo, MPH
1. Mitchell NS, Catenacci VA, Wyatt HR, Hill JO. Obesity: overview of an epidemic. Psychiatr Clin North Am 2011;34:717–32.
2. Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA 2010;303:235–41.
3. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014;311:806–14.
4. Wadden TA, Butryn ML, Wilson C. Lifestyle modification for the management of obesity. Gastroenterology 2007;132:2226–38.
5. Butryn ML, Webb V, Wadden TA. Behavioral treatment of obesity. Psychiatr Clin North Am 2011;34:841–59.
6. Okorodudu DE, Bosworth HB, Corsino L. Innovative interventions to promote behavioral change in overweight or obese individuals: a review of the literature. Ann Med 2015;47:179–85.
7. Taylor RW, Roy M, Jospe MR, et al. Determining how best to support overweight adults to adhere to lifestyle change: protocol for the SWIFT study. BMC Public Health 2015;15:861.
8. Laing BY, Mangione CM, Tseng C-H, et al. Effectiveness of a smartphone application for weight loss compared with usual care in overweight primary care patients: a randomized, controlled trial. Ann Intern Med 2014;161(10 Suppl):
S5–S12.
9. Teixeira PJ, Carraça E V, Marques MM, et al. Successful behavior change in obesity interventions in adults: a systematic review of self-regulation mediators. BMC Med 2015;13:84.
10. Ryan P. Integrated theory of health behavior change: background and intervention development. Clin Nurse Spec 2009;23:161–70.
11. Rivera J, McPherson A, Hamilton J, et al. Mobile apps for weight management: a scoping review. JMIR mHealth uHealth 2016;4:e87.
12. Pellegrini CA, Pfammatter AF, Conroy DE, Spring B. Smartphone applications to support weight loss: current perspectives. Adv Health Care Technol 2015;1:13–22.
13. Flores Mateo G, Granado-Font E, Ferré-Grau C, Montaña-Carreras X. Mobile phone apps to promote weight loss and increase physical activity: a systematic review and meta-analysis. J Med Internet Res 2015;17:e253.
14. Stephens J, Allen J. Mobile phone interventions to increase physical activity and reduce weight: a systematic review. J Cardiovasc Nurs 28:320–9.
15. Smith A. Smartphone ownership 2013. Pew Research Center.
16. Jeffery RW, Drewnowski A, Epstein LH, et al. Long-term maintenance of weight loss: current status. Health Psychol 2000;19(1 Suppl):5–16.
Study Overview
Objective. To test the efficacy of a weight loss app with incorporated social support and self-monitoring of diet, physical activity, and weight compared to a commercially available diet and PA tracking app.
Design. 2-group, randomized controlled trial.
Setting and participants. From October 2014 to January 2015, potential study participants were recruited via university/worksite listserv announcements, flyers, electronic newsletters, newspaper advertisements, social media posts, and a local research fair in 2 cities in South Carolina. Exclusion criteria included body mass index (BMI) outside the range of 25.0 to 49.9 kg/m2, unable to attend required measurement sessions, unable to access a computer or internet for completing assessments, having a psychiatric illness, receiving treatment for drug or alcohol dependency, having an eating disorder, participating in another weight loss program, reporting weight loss of 10+ pounds in the past 6 months, being pregnant or planning on becoming pregnant during study, or breastfeeding, or endorsing items on the Physical Activity Readiness Questionnaire (PAR-Q) regarding having a heart condition, feeling chest pain during physical activity, experiencing chest pain, becoming dizzy/ever losing balance or consciousness, and not having a physician give consent to participate despite reporting joint problems or taking blood pressure medication. Those who were eligible were invited to an orientation to the study, signed consent, and completed baseline assessments.
Intervention. Participants were randomized to either the experimental group (theory-based podcasts plus the Social POD app) or the comparison group (theory-based podcasts plus a standard app [“Fat Secret” app]). Both groups attended a training session on how to access the podcasts and download and use their app, and also had their baseline height and weight taken by study staff. Both groups received 2 podcasts per week, tracked their diet, weight, and physical activity, completed weekly surveys to report use of their assigned tracking app, and had their weight measures taken after 3 months. Objective measures of podcast usage and app usage were collected by study staff (experimental group only).
Both apps had diet and physical activity tracking features, but the Social POD app also included notifications to track diet and physical activity, messages sent from frequent app users to re-engage infrequent app users, a newsfeed to view other participants app tracking activity, stars awarded to frequent users of the app, points awarded for tracking, and prizes for earning points distributed at the final session by study staff. The Fat Secret app did not have any social support components but included a recipe database for looking up recipes by category.
Main outcome measures. The primary outcome was between-group differences in kilograms lost at 3 months. Secondary outcomes included group change in BMI after 3 months, as well as group differences in self-reported caloric intake, caloric expenditure, social support, self-efficacy, and outcome expectations scores, controlled for baseline measures.
Main results. Of the potential participants that inquired about the study (n = 189), those found to be eligible (n = 78) were invited to an orientation. Of those that attended the orientation (n = 62), 51 were randomized after completing baseline assessments (n = 25 to experimental group with Social POD app, n = 25 to comparison group with Fat Secret app), and 42 completed final weight measurements after 3 months. Participants were mostly white (57%) females (82%) with a mean BMI of 34.7 ± 6.0 kg/m2 and mean age of 46.2 ± 12.4 years. Baseline characteristics were similar between groups except that more comparison group participants reported previously downloading an app to track their diet than experimental participants. Participation attrition was 12% (n = 3 in each group).
Experimental group participants lost significantly more weight (–5.3 kg [95% CI, –7.5 to –3.0]) than the comparison group (–2.23 kg [95% CI, –3.6 to 1.0; P = 0.02). Experimental group participants also had a greater reduction in mean BMI (–1.9 kg/m2 [95% CI, –2.6 to –1.2]) vs. the comparison group (mean –0.9 kg/m2 [95% CI, –1.4 to – 0.05], P = 0.02). While there were significant differences in positive outcome expectations between groups (P = 0.04), other secondary outcomes were not significant.
Conclusions. An intervention with theory-based podcasts, social support, and incentivized self-monitoring resulted in significantly greater weight loss than a comparison intervention with theory-based podcasts and a commercially available standard self-monitoring app. This study highlights key features to add to mobile health interventions for adult weight loss.
Commentary
Obesity prevalence rates have increased over the past several decades across all genders, ages, ethnicities, income levels, and education levels [1], and recent data show that over one-third of adults in the US are obese and over two-thirds are overweight [2,3]. Behavior or lifestyle modification, which incorporates (often tailored) diet, physical activity, and behavior therapy, is highly recommended as the first strategy for losing initial weight and sustaining weight management efforts [4,5]. Mobile health (mHealth) technologies and other web-based and technology-assisted approaches (eg, mobile applications or “apps”) to facilitate behavior change for weight loss and management have aimed to address many of the limitations posed by traditional face-to-face weight loss approaches [6–8]. Prevailing theories of health behavior change imply key intervention design features that may increase their likelihood of promoting and sustaining desired behavior changes, particularly those that impact self-efficacy, self-regulation, and social facilitation [9,10].
Despite the plethora of weight loss mobile apps available to the public, it remains unclear if these are guided by evidence-based behavior change strategies typically used in traditional programs and approaches [11,12]. Further, very few of these apps have been rigorously evaluated with scientific testing to determine true effectiveness and safety [13,14]. This study adds to the literature by evaluating a mobile app for weight loss (Social POD) that was developed by researchers and utilizes theory-based components to target specific constructs that lead to health behavior change. Additionally, while self-monitoring is commonly incorporated into most available weight loss/management apps [11], the Social POD mobile app also incorporates social support and motivational strategies, which are less often included. The findings from this study add to the limited literature that mobile phone app-based interventions may be useful tools for weight loss [13].
The authors outlined several strengths and limitations. Briefly, this study was particularly strengthened by its randomized assignment to equivalent intervention groups, the use of a researcher-developed experimental group app that targets several key theory-based constructs for behavior change, measurement of objective use of the intervention group app, a racially diverse sample (over one-third of participants in both groups identified as black), measurement of secondary psycho-social behavioral outcomes, significant efforts to ensure survey completion and compliance with the intervention (increase retention), as well efforts to decrease participation burden by limiting required in-person sessions.
However, several important aspects of the study limit the internal validity and generalizability of its findings. The study had a small sample size and included a highly educated study population. If possible, future studies should consider including a large, diverse population to enhance generalizability. Also, this study was limited to those with an Android device, and significant demographic differences between Android and iPhone users have been reported [15]. The comparison group reported significantly more prior downloading of a diet-tracking app compared to the experimental group, which may have impacted use of the comparison app. The extrinsic reward system built into the experimental group intervention could have impacted adherence to experimental app, and is likely not feasible in real-world application of the experimental group app. Findings may have been subject to recall bias and measurement error due to self-reporting of outcomes measures. Importantly, this was a short-term weight loss study, and long-term weight loss/maintenance data is needed to support findings since in the usual course of weight-loss therapy the greatest weight loss occurs within 6 months of treatment, after which weight is often regained, sometimes near original level [16].
Applications for Clinical Practice
With the increasing popularity of technology-assisted and mHealth applications for weight loss and other health behaviors, it is important for practitioners to be familiar with proven, theory-based approaches and advise patients accordingly. This study demonstrated that social support components added to self-monitoring components in a weight loss app can lead to significant weight loss compared to self-monitoring alone. Thus, those that offer obesity counseling should be mindful that tracking and controlling dietary and physical activity behaviors alone may not prove to be successful. Opportunities for social facilitation to support weight loss efforts should be discussed with patients, including sources of social influence, support and collaboration between individuals, families, and health care professionals.
—Katrina F. Mateo, MPH
Study Overview
Objective. To test the efficacy of a weight loss app with incorporated social support and self-monitoring of diet, physical activity, and weight compared to a commercially available diet and PA tracking app.
Design. 2-group, randomized controlled trial.
Setting and participants. From October 2014 to January 2015, potential study participants were recruited via university/worksite listserv announcements, flyers, electronic newsletters, newspaper advertisements, social media posts, and a local research fair in 2 cities in South Carolina. Exclusion criteria included body mass index (BMI) outside the range of 25.0 to 49.9 kg/m2, unable to attend required measurement sessions, unable to access a computer or internet for completing assessments, having a psychiatric illness, receiving treatment for drug or alcohol dependency, having an eating disorder, participating in another weight loss program, reporting weight loss of 10+ pounds in the past 6 months, being pregnant or planning on becoming pregnant during study, or breastfeeding, or endorsing items on the Physical Activity Readiness Questionnaire (PAR-Q) regarding having a heart condition, feeling chest pain during physical activity, experiencing chest pain, becoming dizzy/ever losing balance or consciousness, and not having a physician give consent to participate despite reporting joint problems or taking blood pressure medication. Those who were eligible were invited to an orientation to the study, signed consent, and completed baseline assessments.
Intervention. Participants were randomized to either the experimental group (theory-based podcasts plus the Social POD app) or the comparison group (theory-based podcasts plus a standard app [“Fat Secret” app]). Both groups attended a training session on how to access the podcasts and download and use their app, and also had their baseline height and weight taken by study staff. Both groups received 2 podcasts per week, tracked their diet, weight, and physical activity, completed weekly surveys to report use of their assigned tracking app, and had their weight measures taken after 3 months. Objective measures of podcast usage and app usage were collected by study staff (experimental group only).
Both apps had diet and physical activity tracking features, but the Social POD app also included notifications to track diet and physical activity, messages sent from frequent app users to re-engage infrequent app users, a newsfeed to view other participants app tracking activity, stars awarded to frequent users of the app, points awarded for tracking, and prizes for earning points distributed at the final session by study staff. The Fat Secret app did not have any social support components but included a recipe database for looking up recipes by category.
Main outcome measures. The primary outcome was between-group differences in kilograms lost at 3 months. Secondary outcomes included group change in BMI after 3 months, as well as group differences in self-reported caloric intake, caloric expenditure, social support, self-efficacy, and outcome expectations scores, controlled for baseline measures.
Main results. Of the potential participants that inquired about the study (n = 189), those found to be eligible (n = 78) were invited to an orientation. Of those that attended the orientation (n = 62), 51 were randomized after completing baseline assessments (n = 25 to experimental group with Social POD app, n = 25 to comparison group with Fat Secret app), and 42 completed final weight measurements after 3 months. Participants were mostly white (57%) females (82%) with a mean BMI of 34.7 ± 6.0 kg/m2 and mean age of 46.2 ± 12.4 years. Baseline characteristics were similar between groups except that more comparison group participants reported previously downloading an app to track their diet than experimental participants. Participation attrition was 12% (n = 3 in each group).
Experimental group participants lost significantly more weight (–5.3 kg [95% CI, –7.5 to –3.0]) than the comparison group (–2.23 kg [95% CI, –3.6 to 1.0; P = 0.02). Experimental group participants also had a greater reduction in mean BMI (–1.9 kg/m2 [95% CI, –2.6 to –1.2]) vs. the comparison group (mean –0.9 kg/m2 [95% CI, –1.4 to – 0.05], P = 0.02). While there were significant differences in positive outcome expectations between groups (P = 0.04), other secondary outcomes were not significant.
Conclusions. An intervention with theory-based podcasts, social support, and incentivized self-monitoring resulted in significantly greater weight loss than a comparison intervention with theory-based podcasts and a commercially available standard self-monitoring app. This study highlights key features to add to mobile health interventions for adult weight loss.
Commentary
Obesity prevalence rates have increased over the past several decades across all genders, ages, ethnicities, income levels, and education levels [1], and recent data show that over one-third of adults in the US are obese and over two-thirds are overweight [2,3]. Behavior or lifestyle modification, which incorporates (often tailored) diet, physical activity, and behavior therapy, is highly recommended as the first strategy for losing initial weight and sustaining weight management efforts [4,5]. Mobile health (mHealth) technologies and other web-based and technology-assisted approaches (eg, mobile applications or “apps”) to facilitate behavior change for weight loss and management have aimed to address many of the limitations posed by traditional face-to-face weight loss approaches [6–8]. Prevailing theories of health behavior change imply key intervention design features that may increase their likelihood of promoting and sustaining desired behavior changes, particularly those that impact self-efficacy, self-regulation, and social facilitation [9,10].
Despite the plethora of weight loss mobile apps available to the public, it remains unclear if these are guided by evidence-based behavior change strategies typically used in traditional programs and approaches [11,12]. Further, very few of these apps have been rigorously evaluated with scientific testing to determine true effectiveness and safety [13,14]. This study adds to the literature by evaluating a mobile app for weight loss (Social POD) that was developed by researchers and utilizes theory-based components to target specific constructs that lead to health behavior change. Additionally, while self-monitoring is commonly incorporated into most available weight loss/management apps [11], the Social POD mobile app also incorporates social support and motivational strategies, which are less often included. The findings from this study add to the limited literature that mobile phone app-based interventions may be useful tools for weight loss [13].
The authors outlined several strengths and limitations. Briefly, this study was particularly strengthened by its randomized assignment to equivalent intervention groups, the use of a researcher-developed experimental group app that targets several key theory-based constructs for behavior change, measurement of objective use of the intervention group app, a racially diverse sample (over one-third of participants in both groups identified as black), measurement of secondary psycho-social behavioral outcomes, significant efforts to ensure survey completion and compliance with the intervention (increase retention), as well efforts to decrease participation burden by limiting required in-person sessions.
However, several important aspects of the study limit the internal validity and generalizability of its findings. The study had a small sample size and included a highly educated study population. If possible, future studies should consider including a large, diverse population to enhance generalizability. Also, this study was limited to those with an Android device, and significant demographic differences between Android and iPhone users have been reported [15]. The comparison group reported significantly more prior downloading of a diet-tracking app compared to the experimental group, which may have impacted use of the comparison app. The extrinsic reward system built into the experimental group intervention could have impacted adherence to experimental app, and is likely not feasible in real-world application of the experimental group app. Findings may have been subject to recall bias and measurement error due to self-reporting of outcomes measures. Importantly, this was a short-term weight loss study, and long-term weight loss/maintenance data is needed to support findings since in the usual course of weight-loss therapy the greatest weight loss occurs within 6 months of treatment, after which weight is often regained, sometimes near original level [16].
Applications for Clinical Practice
With the increasing popularity of technology-assisted and mHealth applications for weight loss and other health behaviors, it is important for practitioners to be familiar with proven, theory-based approaches and advise patients accordingly. This study demonstrated that social support components added to self-monitoring components in a weight loss app can lead to significant weight loss compared to self-monitoring alone. Thus, those that offer obesity counseling should be mindful that tracking and controlling dietary and physical activity behaviors alone may not prove to be successful. Opportunities for social facilitation to support weight loss efforts should be discussed with patients, including sources of social influence, support and collaboration between individuals, families, and health care professionals.
—Katrina F. Mateo, MPH
1. Mitchell NS, Catenacci VA, Wyatt HR, Hill JO. Obesity: overview of an epidemic. Psychiatr Clin North Am 2011;34:717–32.
2. Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA 2010;303:235–41.
3. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014;311:806–14.
4. Wadden TA, Butryn ML, Wilson C. Lifestyle modification for the management of obesity. Gastroenterology 2007;132:2226–38.
5. Butryn ML, Webb V, Wadden TA. Behavioral treatment of obesity. Psychiatr Clin North Am 2011;34:841–59.
6. Okorodudu DE, Bosworth HB, Corsino L. Innovative interventions to promote behavioral change in overweight or obese individuals: a review of the literature. Ann Med 2015;47:179–85.
7. Taylor RW, Roy M, Jospe MR, et al. Determining how best to support overweight adults to adhere to lifestyle change: protocol for the SWIFT study. BMC Public Health 2015;15:861.
8. Laing BY, Mangione CM, Tseng C-H, et al. Effectiveness of a smartphone application for weight loss compared with usual care in overweight primary care patients: a randomized, controlled trial. Ann Intern Med 2014;161(10 Suppl):
S5–S12.
9. Teixeira PJ, Carraça E V, Marques MM, et al. Successful behavior change in obesity interventions in adults: a systematic review of self-regulation mediators. BMC Med 2015;13:84.
10. Ryan P. Integrated theory of health behavior change: background and intervention development. Clin Nurse Spec 2009;23:161–70.
11. Rivera J, McPherson A, Hamilton J, et al. Mobile apps for weight management: a scoping review. JMIR mHealth uHealth 2016;4:e87.
12. Pellegrini CA, Pfammatter AF, Conroy DE, Spring B. Smartphone applications to support weight loss: current perspectives. Adv Health Care Technol 2015;1:13–22.
13. Flores Mateo G, Granado-Font E, Ferré-Grau C, Montaña-Carreras X. Mobile phone apps to promote weight loss and increase physical activity: a systematic review and meta-analysis. J Med Internet Res 2015;17:e253.
14. Stephens J, Allen J. Mobile phone interventions to increase physical activity and reduce weight: a systematic review. J Cardiovasc Nurs 28:320–9.
15. Smith A. Smartphone ownership 2013. Pew Research Center.
16. Jeffery RW, Drewnowski A, Epstein LH, et al. Long-term maintenance of weight loss: current status. Health Psychol 2000;19(1 Suppl):5–16.
1. Mitchell NS, Catenacci VA, Wyatt HR, Hill JO. Obesity: overview of an epidemic. Psychiatr Clin North Am 2011;34:717–32.
2. Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA 2010;303:235–41.
3. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014;311:806–14.
4. Wadden TA, Butryn ML, Wilson C. Lifestyle modification for the management of obesity. Gastroenterology 2007;132:2226–38.
5. Butryn ML, Webb V, Wadden TA. Behavioral treatment of obesity. Psychiatr Clin North Am 2011;34:841–59.
6. Okorodudu DE, Bosworth HB, Corsino L. Innovative interventions to promote behavioral change in overweight or obese individuals: a review of the literature. Ann Med 2015;47:179–85.
7. Taylor RW, Roy M, Jospe MR, et al. Determining how best to support overweight adults to adhere to lifestyle change: protocol for the SWIFT study. BMC Public Health 2015;15:861.
8. Laing BY, Mangione CM, Tseng C-H, et al. Effectiveness of a smartphone application for weight loss compared with usual care in overweight primary care patients: a randomized, controlled trial. Ann Intern Med 2014;161(10 Suppl):
S5–S12.
9. Teixeira PJ, Carraça E V, Marques MM, et al. Successful behavior change in obesity interventions in adults: a systematic review of self-regulation mediators. BMC Med 2015;13:84.
10. Ryan P. Integrated theory of health behavior change: background and intervention development. Clin Nurse Spec 2009;23:161–70.
11. Rivera J, McPherson A, Hamilton J, et al. Mobile apps for weight management: a scoping review. JMIR mHealth uHealth 2016;4:e87.
12. Pellegrini CA, Pfammatter AF, Conroy DE, Spring B. Smartphone applications to support weight loss: current perspectives. Adv Health Care Technol 2015;1:13–22.
13. Flores Mateo G, Granado-Font E, Ferré-Grau C, Montaña-Carreras X. Mobile phone apps to promote weight loss and increase physical activity: a systematic review and meta-analysis. J Med Internet Res 2015;17:e253.
14. Stephens J, Allen J. Mobile phone interventions to increase physical activity and reduce weight: a systematic review. J Cardiovasc Nurs 28:320–9.
15. Smith A. Smartphone ownership 2013. Pew Research Center.
16. Jeffery RW, Drewnowski A, Epstein LH, et al. Long-term maintenance of weight loss: current status. Health Psychol 2000;19(1 Suppl):5–16.
Hypotension Prevalence Among Treated Hypertensive Patients
Study Overview
Objective. To determine the prevalence of hypotension using both clinic and ambulatory blood pressure monitoring (ABPM) in treated hypertensive patients and the factors associated with its presence.
Design. Registry-based study.
Setting and participants. Researchers studied patients in the Spanish Society of Hypertension ABPM Registry, which was established to evaluate the utility of the wider use of ABPM with the distribution of >1000 ambulatory BP monitors for routine use by primary care physicians and physicians from specialist units across Spain. The registry continues to expand since the first patient was recruited in June 2004. In June 2015, a total of 135,500 hypertensive patients were in the registry.
Measurements. Blood pressure readings in the clinic were taken according to current recommendations, with the patients in a seated position and their backs supported, after a 5-minute rest, using calibrated sphygmomanometers or validated automatic devices. The visit BP was the average of 2 separate readings. Validated devices (Spacelabs) were used for ABPM, which was performed during a working day with measurements taken every 30 minutes. Patients were told to keep their activity normal and to extend the arm without any movement during BP measurements. ABPM was considered successful in ≥ 80% systolic and diastolic BP valid readings. Patients were classified into 3 categories: hypotension, adequate BP control, or poor BP control for each type of blood pressure (office, daytime, nighttime, and 24-hour). The definitions for hypotension for each BP type were mainly based of the PROVE IT-TIMI study, ie, < 110 and/or 70 mm Hg for office, < 105 and/or 65 mm Hg for daytime ABPM, < 90 and or 50 mm Hg for nightime ABPM, and < 100 and/or 60 mm Hg for 24-hr ABPM.
Results. Of the 135,500 patients in the registry, only data from treated hypertensive patients were analyzed (n = 70,997). Mean age was 61.8 ± 12.8 years and 52.5% were men. The prevalence of hypotension was 8.2% with office BP, 12.2% with daytime ABPM, 3.9% with nightime ABPM, and 6.8% with 24-hour ABPM. Low diastolic BP values were responsible for the majority of hypotension. More than 68% of patients with hypotension detected with ABPM did not have hypotension according to office BP. Patients with hypotension were older, more likely to be female, and more likely to have high pulse pressue, lower heart rate, ischemic heart disease, and renal insufficiency. They were also more likely to be taking 3 or more drugs for hypertension.
Conclusion. The prevalence of hypotension is relatively high in treated hypertensive patients, and two-thirds are not identified with office BP measurement. Prevalence was higher in patients who were very elderly or with coronary or renal disease.
Commentary
Hypertension is a major public health concern worldwide [1]. In 2011–12 among US adults with hypertension, only 51.9% had their blood pressure controlled [2]. High blood pressure can effectively be reduced with antihypertensive treatment, and efforts are needed to improve clinical management of hypertension. However, excessive BP reduction may lead to patient harm.
In this study, researchers aimed to determine the prevalence of hypotension using both clinic and ABPM in hypertensive-treated patients and the factors associated with its presence, using descriptive statistics and multivariate analysis. The results highlight the need for health care providers to be aware of the individual response to antihypertensives in patients with high blood pressure and to individualize treatment to avoid complications of hypotension. A strength of this study was it large sample size.
Adherence to treatment recommendations was not a variable taken into consideration for this study and could be considered a confounder. Diet and behavioral interventions can have a significantly beneficial effect on hypertension and can reduce the need for drug therapy [3]. If patients were highly engaged and adopted lifestyle habits that can contribute to better blood pressure levels along with taking prescribed medications, this could have contributed to levels of hypotension.
Hypotension among hypertensive patients can be difficult to identify during clinical consultations due the “white coat effect.” This syndrome is characterized by a peak of high blood pressure caused by the stress of the individual in the presence of a healthcare provider or in a stressful medical environment [4]. This study showed that more than half of the patients in the sample with detected hypotension in the ABPM did not show hypotension during consultation at the medical office. This finding highlights the challenge in identifying hypotension and making adjustments to antihypertensive medication regimens as needed.
Women, patients with low body weight, and elderly patients were the groups more likely to develop hypo-tension. Thus, strategies specifically targeting these vulnerable groups are required. As suggested by the authors of this study, further longitudinal research is needed in order to identify gaps in the state of science in regards this topic and changes in the prevalence this population. The replication of this study in different populations is also encouraged.
Applications for Clinical Practice
The prevalence of hypotension is relatively high and may not be detected during office BP measurement. In patients with a higher risk of hypotension, such as the elderly those with cardiovascular disease, the use of ABPM should be considered.
—Paloma Cesar de Sales, BS, RN, MS
1. Kantachuvessiri A. Hypertension in public health. Southeast Asian J Trop Med Public Health 2002;33:425–31.
2. Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. NCHS Data Brief 2013;1–8.
3. Nicoll R, Henein MY. Hypertension and lifestyle modification: how useful are the guidelines? Br J Gen Pract 2010; 60:879–80.
4. Celis H, Fagard RH. White-coat hypertension: a clinical review. Eur J Intern Med 2004;15:348–57.
Study Overview
Objective. To determine the prevalence of hypotension using both clinic and ambulatory blood pressure monitoring (ABPM) in treated hypertensive patients and the factors associated with its presence.
Design. Registry-based study.
Setting and participants. Researchers studied patients in the Spanish Society of Hypertension ABPM Registry, which was established to evaluate the utility of the wider use of ABPM with the distribution of >1000 ambulatory BP monitors for routine use by primary care physicians and physicians from specialist units across Spain. The registry continues to expand since the first patient was recruited in June 2004. In June 2015, a total of 135,500 hypertensive patients were in the registry.
Measurements. Blood pressure readings in the clinic were taken according to current recommendations, with the patients in a seated position and their backs supported, after a 5-minute rest, using calibrated sphygmomanometers or validated automatic devices. The visit BP was the average of 2 separate readings. Validated devices (Spacelabs) were used for ABPM, which was performed during a working day with measurements taken every 30 minutes. Patients were told to keep their activity normal and to extend the arm without any movement during BP measurements. ABPM was considered successful in ≥ 80% systolic and diastolic BP valid readings. Patients were classified into 3 categories: hypotension, adequate BP control, or poor BP control for each type of blood pressure (office, daytime, nighttime, and 24-hour). The definitions for hypotension for each BP type were mainly based of the PROVE IT-TIMI study, ie, < 110 and/or 70 mm Hg for office, < 105 and/or 65 mm Hg for daytime ABPM, < 90 and or 50 mm Hg for nightime ABPM, and < 100 and/or 60 mm Hg for 24-hr ABPM.
Results. Of the 135,500 patients in the registry, only data from treated hypertensive patients were analyzed (n = 70,997). Mean age was 61.8 ± 12.8 years and 52.5% were men. The prevalence of hypotension was 8.2% with office BP, 12.2% with daytime ABPM, 3.9% with nightime ABPM, and 6.8% with 24-hour ABPM. Low diastolic BP values were responsible for the majority of hypotension. More than 68% of patients with hypotension detected with ABPM did not have hypotension according to office BP. Patients with hypotension were older, more likely to be female, and more likely to have high pulse pressue, lower heart rate, ischemic heart disease, and renal insufficiency. They were also more likely to be taking 3 or more drugs for hypertension.
Conclusion. The prevalence of hypotension is relatively high in treated hypertensive patients, and two-thirds are not identified with office BP measurement. Prevalence was higher in patients who were very elderly or with coronary or renal disease.
Commentary
Hypertension is a major public health concern worldwide [1]. In 2011–12 among US adults with hypertension, only 51.9% had their blood pressure controlled [2]. High blood pressure can effectively be reduced with antihypertensive treatment, and efforts are needed to improve clinical management of hypertension. However, excessive BP reduction may lead to patient harm.
In this study, researchers aimed to determine the prevalence of hypotension using both clinic and ABPM in hypertensive-treated patients and the factors associated with its presence, using descriptive statistics and multivariate analysis. The results highlight the need for health care providers to be aware of the individual response to antihypertensives in patients with high blood pressure and to individualize treatment to avoid complications of hypotension. A strength of this study was it large sample size.
Adherence to treatment recommendations was not a variable taken into consideration for this study and could be considered a confounder. Diet and behavioral interventions can have a significantly beneficial effect on hypertension and can reduce the need for drug therapy [3]. If patients were highly engaged and adopted lifestyle habits that can contribute to better blood pressure levels along with taking prescribed medications, this could have contributed to levels of hypotension.
Hypotension among hypertensive patients can be difficult to identify during clinical consultations due the “white coat effect.” This syndrome is characterized by a peak of high blood pressure caused by the stress of the individual in the presence of a healthcare provider or in a stressful medical environment [4]. This study showed that more than half of the patients in the sample with detected hypotension in the ABPM did not show hypotension during consultation at the medical office. This finding highlights the challenge in identifying hypotension and making adjustments to antihypertensive medication regimens as needed.
Women, patients with low body weight, and elderly patients were the groups more likely to develop hypo-tension. Thus, strategies specifically targeting these vulnerable groups are required. As suggested by the authors of this study, further longitudinal research is needed in order to identify gaps in the state of science in regards this topic and changes in the prevalence this population. The replication of this study in different populations is also encouraged.
Applications for Clinical Practice
The prevalence of hypotension is relatively high and may not be detected during office BP measurement. In patients with a higher risk of hypotension, such as the elderly those with cardiovascular disease, the use of ABPM should be considered.
—Paloma Cesar de Sales, BS, RN, MS
Study Overview
Objective. To determine the prevalence of hypotension using both clinic and ambulatory blood pressure monitoring (ABPM) in treated hypertensive patients and the factors associated with its presence.
Design. Registry-based study.
Setting and participants. Researchers studied patients in the Spanish Society of Hypertension ABPM Registry, which was established to evaluate the utility of the wider use of ABPM with the distribution of >1000 ambulatory BP monitors for routine use by primary care physicians and physicians from specialist units across Spain. The registry continues to expand since the first patient was recruited in June 2004. In June 2015, a total of 135,500 hypertensive patients were in the registry.
Measurements. Blood pressure readings in the clinic were taken according to current recommendations, with the patients in a seated position and their backs supported, after a 5-minute rest, using calibrated sphygmomanometers or validated automatic devices. The visit BP was the average of 2 separate readings. Validated devices (Spacelabs) were used for ABPM, which was performed during a working day with measurements taken every 30 minutes. Patients were told to keep their activity normal and to extend the arm without any movement during BP measurements. ABPM was considered successful in ≥ 80% systolic and diastolic BP valid readings. Patients were classified into 3 categories: hypotension, adequate BP control, or poor BP control for each type of blood pressure (office, daytime, nighttime, and 24-hour). The definitions for hypotension for each BP type were mainly based of the PROVE IT-TIMI study, ie, < 110 and/or 70 mm Hg for office, < 105 and/or 65 mm Hg for daytime ABPM, < 90 and or 50 mm Hg for nightime ABPM, and < 100 and/or 60 mm Hg for 24-hr ABPM.
Results. Of the 135,500 patients in the registry, only data from treated hypertensive patients were analyzed (n = 70,997). Mean age was 61.8 ± 12.8 years and 52.5% were men. The prevalence of hypotension was 8.2% with office BP, 12.2% with daytime ABPM, 3.9% with nightime ABPM, and 6.8% with 24-hour ABPM. Low diastolic BP values were responsible for the majority of hypotension. More than 68% of patients with hypotension detected with ABPM did not have hypotension according to office BP. Patients with hypotension were older, more likely to be female, and more likely to have high pulse pressue, lower heart rate, ischemic heart disease, and renal insufficiency. They were also more likely to be taking 3 or more drugs for hypertension.
Conclusion. The prevalence of hypotension is relatively high in treated hypertensive patients, and two-thirds are not identified with office BP measurement. Prevalence was higher in patients who were very elderly or with coronary or renal disease.
Commentary
Hypertension is a major public health concern worldwide [1]. In 2011–12 among US adults with hypertension, only 51.9% had their blood pressure controlled [2]. High blood pressure can effectively be reduced with antihypertensive treatment, and efforts are needed to improve clinical management of hypertension. However, excessive BP reduction may lead to patient harm.
In this study, researchers aimed to determine the prevalence of hypotension using both clinic and ABPM in hypertensive-treated patients and the factors associated with its presence, using descriptive statistics and multivariate analysis. The results highlight the need for health care providers to be aware of the individual response to antihypertensives in patients with high blood pressure and to individualize treatment to avoid complications of hypotension. A strength of this study was it large sample size.
Adherence to treatment recommendations was not a variable taken into consideration for this study and could be considered a confounder. Diet and behavioral interventions can have a significantly beneficial effect on hypertension and can reduce the need for drug therapy [3]. If patients were highly engaged and adopted lifestyle habits that can contribute to better blood pressure levels along with taking prescribed medications, this could have contributed to levels of hypotension.
Hypotension among hypertensive patients can be difficult to identify during clinical consultations due the “white coat effect.” This syndrome is characterized by a peak of high blood pressure caused by the stress of the individual in the presence of a healthcare provider or in a stressful medical environment [4]. This study showed that more than half of the patients in the sample with detected hypotension in the ABPM did not show hypotension during consultation at the medical office. This finding highlights the challenge in identifying hypotension and making adjustments to antihypertensive medication regimens as needed.
Women, patients with low body weight, and elderly patients were the groups more likely to develop hypo-tension. Thus, strategies specifically targeting these vulnerable groups are required. As suggested by the authors of this study, further longitudinal research is needed in order to identify gaps in the state of science in regards this topic and changes in the prevalence this population. The replication of this study in different populations is also encouraged.
Applications for Clinical Practice
The prevalence of hypotension is relatively high and may not be detected during office BP measurement. In patients with a higher risk of hypotension, such as the elderly those with cardiovascular disease, the use of ABPM should be considered.
—Paloma Cesar de Sales, BS, RN, MS
1. Kantachuvessiri A. Hypertension in public health. Southeast Asian J Trop Med Public Health 2002;33:425–31.
2. Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. NCHS Data Brief 2013;1–8.
3. Nicoll R, Henein MY. Hypertension and lifestyle modification: how useful are the guidelines? Br J Gen Pract 2010; 60:879–80.
4. Celis H, Fagard RH. White-coat hypertension: a clinical review. Eur J Intern Med 2004;15:348–57.
1. Kantachuvessiri A. Hypertension in public health. Southeast Asian J Trop Med Public Health 2002;33:425–31.
2. Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. NCHS Data Brief 2013;1–8.
3. Nicoll R, Henein MY. Hypertension and lifestyle modification: how useful are the guidelines? Br J Gen Pract 2010; 60:879–80.
4. Celis H, Fagard RH. White-coat hypertension: a clinical review. Eur J Intern Med 2004;15:348–57.
A Computer-Assisted Process to Reduce Discharge of Emergency Department Patients with Abnormal Vital Signs
From Case Western Reserve University, MetroHealth Medical Center, Cleveland, OH.
Abstract
- Objective: To describe a computer-assisted process for reducing the number of patients discharged from the emergency department with abnormal vital signs.
- Methods: We devised a best practice alert in the Epic electronic medical record that triggers when the clinician attempts to print an after visit summary (discharge paperwork) at the time of discharge from the emergency department.
- Results: We saw no change in the percentage of patients discharged with elevated blood pressures, consistent with national recommendations. Removing that category of patients, we saw a decrease in the percentage of patients discharged with abnormal vital signs, primarily driven by a decrease in the percentage of patients discharged with tachycardia.
- Conclusion: A computer-assisted process can reduce the percentage of patients discharged with abnormal vital signs. Since based on national recommendations ED physicians do not address most elevated blood pressures in the ED, hypertension should not trigger an alert.
Abnormal vital signs in the emergency department (ED) have been associated with adverse outcomes [1,2]. While most patients discharged from the ED do well, some studies have found that the death rate within days to weeks post–ED discharge may be as high as 200 per 100,000 visits, although other studies have found a much lower rate [1]. A study by Sklar et al, although not specifically focused on vital signs at discharge, found that unexpected death within 7 days of ED discharge occurred at a rate of 30 per 100,000 patients. Abnormal vital signs, most commonly tachycardia, were present in 83% of cases [2].
In busy EDs, the combination of patient volume, frequent interruptions, and the intensity of tasks can result in deficiencies in vital sign monitoring [3–5] as well as abnormal vital signs not being recognized by the clinician at the time of patient discharge [6]. The importance of addressing this quality problem has been recognized. Prior efforts to address the problem have included nurses using manual methods to alert the physician to the presence of abnormal vital signs at the time of discharge [7]. Recommendations have been made to use electronic medical record (EMR) functions for prospectively addressing the problem of ED discharge with abnormal vital signs [8]. The utility of the EMR to identify potentially septic patients earlier and reduce mortality from sepsis via an algorithm that incorporated vital signs and other clinical crieria has been demonstrated [9,10]. In addition, automated vital signs advisories have been associated with increased survival on general hospital wards [11].
An adverse event that occurred at our institution prompted us to review this issue for our ED. We designed an EMR-assisted intervention to reduce the rate of patients discharged from the ED with abnormal vital signs.
Methods
Setting
Our ED is a busy, urban, Level 1 trauma center within a teaching facility. It sees over 100,000 patients per year and is segmented into resuscitation, high acuity, moderate acuity, and fast tract areas, in addition to the observation unit. Our organization uses the Epic (Madison, Wisconsin) electronic health record, which we have been using for over a decade.
Discharge Instructions—Old Process
In our ED, providers, attending physicians, residents and advance practice nurses enter and print their own discharge instructions, which are given to nursing staff to review with patients. Prior to the project, nurses were expected to notify a physician if they thought a vital sign was abnormal. Each nurse made independent decisions on what constituted a vital sign abnormality based on the patient’s condition and could communicate that to the provider at their discretion prior to discharge. This process created inconsistencies in care.
Development of Alert
We created an alert that appears within the provider workflow at the time the provider attempts to print discharge instructions. Based on literature review and operational leadership consensus, we set the parameters for abnormal vital signs (Table 1). We chose parameters to identify abnormalities important to
The alert displays when a user attempts to print discharge instructions on a patient whose last recorded vital signs are not all normal. The display informs that there are abnormal vital signs (Figure). Upon display of the alert, the user can click on the message, which would take them to the vital sign entry activity in the EMR, or they can proceed with printing by clicking the print button (not visible in the Figure). The alert is not a forcing function; the user can proceed with printing the discharge instructions without addressing the abnormality that triggered the alert.
Pre-Post Evaluation
We would have liked to have determined how often the abnormal vital signs alert triggered, how it was responded to, and whether the patient was subsequently discharged with normal vital signs; however, our system does not record these events. Instead, we used the system to compare the percentage of adult patients who were discharged with abnormal vital signs for 2 time periods: the period prior to our December 2014 implementation (1 Oct to 1 Dec 2014) and the post implementation period (15 Dec 2014 to 15 Feb 2015). Our presumption was that the use of the alert system would reduce the percentage of patients discharged with abnormal vital signs, including an abnormal pulse oximetry.
To conduct our analysis, we identified adult patients seen during the 2 time periods. We eliminated those patients who died, left without being seen, eloped, were admitted or were transferred to other institutions. This resulted in 3664 patients, with 2179 in the pre-implementation group and 1485 in the post-implementation group. The higher volume in the pre group reflects the early occurrence of influenza season in our area during the study period, along with our generally busier time in late fall compared to winter.
The analysis was performed as a likelihood ratio chi-square analysis using SAS (Cary, NC) software.
Results
The analysis demonstrated that physicians were, by and large, following recommendations consistent with policies of the American College of Emergency Physicians regarding the management of elevated blood pressures, which do not mandate that patients with asymptomatic elevations of blood pressure receive medical intervention in the ED [12]. In our analysis, the percentage of patients discharged with elevated blood pressures actually increased from 7.5% to 9.9% following the intervention. Importantly, however, the percentage of patients discharged with low blood pressures decreased from 6.9% to 5.0% (P < 0.01).Tthe percent of patients discharged with an elevated heart rate, decreased from 58% in the pre alert group to 42% in the post alert group (P < 0.02).
Discussion
In our study, we used features of the EMR prospectively to affect discharge and then used the database functions of the EMR to assess the effectiveness of those efforts. Previous studies that have looked at the incidence of abnormal vital signs at discharge have been manual, retrospective reviews of records. We are not aware of any studies reporting the results of introducing an EMR alert to prospectively identify patients with abnormal vital signs prior to discharge
While we found that this intervention was successful in reducing clinically relevant abnormal vital signs at discharge, we have realized that the elevated blood pressure alert was unnecessary and we have eliminated it from the programming. We will revisit our strategy to determine if further reducing the high blood pressure alerts can lead to greater improvements in reducing the percentage of patients discharged with abnormal vital signs.
Future plans include a review of the re-visit or hospitalization rate for patients discharged with abnormal vital signs. A companion study evaluating a similar approach to the care of children is under consideration. We are also considering including a field in the EMR for the clinician to document why they discharged a patient with abnormal vital signs.
Corresponding author: Jonathan E. Siff, MD 2500 MetroHealth Drive BG3-65 Cleveland, Ohio 44109 [email protected].
Financial disclosures: None.
1. Gunnarsdottir OS, Rafnsson V. Death within 8 days after discharge to home from the emergency department. Eur J of Public Health 2008;18:522–6.
2. Sklar DP, Crandall CS, Loeliger E, et al. Unanticipated death after discharge home from the emergency department. Ann Emerg Med 2007;49:735–45.
3. Johnson KD, Winkelman C, Burant CJ, et al. The factors that affect the frequency of vital sign monitoring in the emergency department. J Emerg Nurs 2014;40:27–35.
4. Gravel J, Opatrny L, Gouin S. High rate of missing vital signs data at triage in a paediatric emergency department. Paediatr Child Health 2006;11:211–5.
5. Depinet HE, Iyer SB, Hornung R, et al. The effect of emergency department crowding on reassessment of children with critically abnormal vital signs. Acad Emerg Med 2014;21:1116–20.
6. Hafner JW, Parrish SE, Hubler JR, et al. Repeat assessment of abnormal vital signs and patient re-examination in us emergency department patients. Ann Emerg Med 2006;48(4 Suppl):S66.
7. Domagala SE. Discharge vital signs: an enhancement to ED quality and patient outcomes. J Emerg Nursing 2009;35:138–40.
8. Welch S. Red flags: abnormal vital signs at discharge.Emerg Med News 2011:33;7–8.
9. Nguyen SQ, Mwakalindile E, Booth JS, et al. Automated electronic medical record sepsis detection in the emergency department. PeerJ 2014;2:e343.
10. Narayanan N, Gross AK, Pintens M, et al. Effect of an electronic medical record alert for severe sepsis among ED patients. Am J Emerg Med 2016;34:185–8.
11. Bellomo R, Ackerman M, Bailey M, et al. A controlled trial of electronic automated advisory vital signs monitoring in general hospital wards. Crit Care Med 2012;40:2349–61.
12. Wolf SJ, Lo B, Smith MD, et al. Clinical policy: critical issues in the evaluation and management of adult patients in the emergency department with asymptomatic elevated blood pressure. Ann Emerg Med 2013:62;59–68.
From Case Western Reserve University, MetroHealth Medical Center, Cleveland, OH.
Abstract
- Objective: To describe a computer-assisted process for reducing the number of patients discharged from the emergency department with abnormal vital signs.
- Methods: We devised a best practice alert in the Epic electronic medical record that triggers when the clinician attempts to print an after visit summary (discharge paperwork) at the time of discharge from the emergency department.
- Results: We saw no change in the percentage of patients discharged with elevated blood pressures, consistent with national recommendations. Removing that category of patients, we saw a decrease in the percentage of patients discharged with abnormal vital signs, primarily driven by a decrease in the percentage of patients discharged with tachycardia.
- Conclusion: A computer-assisted process can reduce the percentage of patients discharged with abnormal vital signs. Since based on national recommendations ED physicians do not address most elevated blood pressures in the ED, hypertension should not trigger an alert.
Abnormal vital signs in the emergency department (ED) have been associated with adverse outcomes [1,2]. While most patients discharged from the ED do well, some studies have found that the death rate within days to weeks post–ED discharge may be as high as 200 per 100,000 visits, although other studies have found a much lower rate [1]. A study by Sklar et al, although not specifically focused on vital signs at discharge, found that unexpected death within 7 days of ED discharge occurred at a rate of 30 per 100,000 patients. Abnormal vital signs, most commonly tachycardia, were present in 83% of cases [2].
In busy EDs, the combination of patient volume, frequent interruptions, and the intensity of tasks can result in deficiencies in vital sign monitoring [3–5] as well as abnormal vital signs not being recognized by the clinician at the time of patient discharge [6]. The importance of addressing this quality problem has been recognized. Prior efforts to address the problem have included nurses using manual methods to alert the physician to the presence of abnormal vital signs at the time of discharge [7]. Recommendations have been made to use electronic medical record (EMR) functions for prospectively addressing the problem of ED discharge with abnormal vital signs [8]. The utility of the EMR to identify potentially septic patients earlier and reduce mortality from sepsis via an algorithm that incorporated vital signs and other clinical crieria has been demonstrated [9,10]. In addition, automated vital signs advisories have been associated with increased survival on general hospital wards [11].
An adverse event that occurred at our institution prompted us to review this issue for our ED. We designed an EMR-assisted intervention to reduce the rate of patients discharged from the ED with abnormal vital signs.
Methods
Setting
Our ED is a busy, urban, Level 1 trauma center within a teaching facility. It sees over 100,000 patients per year and is segmented into resuscitation, high acuity, moderate acuity, and fast tract areas, in addition to the observation unit. Our organization uses the Epic (Madison, Wisconsin) electronic health record, which we have been using for over a decade.
Discharge Instructions—Old Process
In our ED, providers, attending physicians, residents and advance practice nurses enter and print their own discharge instructions, which are given to nursing staff to review with patients. Prior to the project, nurses were expected to notify a physician if they thought a vital sign was abnormal. Each nurse made independent decisions on what constituted a vital sign abnormality based on the patient’s condition and could communicate that to the provider at their discretion prior to discharge. This process created inconsistencies in care.
Development of Alert
We created an alert that appears within the provider workflow at the time the provider attempts to print discharge instructions. Based on literature review and operational leadership consensus, we set the parameters for abnormal vital signs (Table 1). We chose parameters to identify abnormalities important to
The alert displays when a user attempts to print discharge instructions on a patient whose last recorded vital signs are not all normal. The display informs that there are abnormal vital signs (Figure). Upon display of the alert, the user can click on the message, which would take them to the vital sign entry activity in the EMR, or they can proceed with printing by clicking the print button (not visible in the Figure). The alert is not a forcing function; the user can proceed with printing the discharge instructions without addressing the abnormality that triggered the alert.
Pre-Post Evaluation
We would have liked to have determined how often the abnormal vital signs alert triggered, how it was responded to, and whether the patient was subsequently discharged with normal vital signs; however, our system does not record these events. Instead, we used the system to compare the percentage of adult patients who were discharged with abnormal vital signs for 2 time periods: the period prior to our December 2014 implementation (1 Oct to 1 Dec 2014) and the post implementation period (15 Dec 2014 to 15 Feb 2015). Our presumption was that the use of the alert system would reduce the percentage of patients discharged with abnormal vital signs, including an abnormal pulse oximetry.
To conduct our analysis, we identified adult patients seen during the 2 time periods. We eliminated those patients who died, left without being seen, eloped, were admitted or were transferred to other institutions. This resulted in 3664 patients, with 2179 in the pre-implementation group and 1485 in the post-implementation group. The higher volume in the pre group reflects the early occurrence of influenza season in our area during the study period, along with our generally busier time in late fall compared to winter.
The analysis was performed as a likelihood ratio chi-square analysis using SAS (Cary, NC) software.
Results
The analysis demonstrated that physicians were, by and large, following recommendations consistent with policies of the American College of Emergency Physicians regarding the management of elevated blood pressures, which do not mandate that patients with asymptomatic elevations of blood pressure receive medical intervention in the ED [12]. In our analysis, the percentage of patients discharged with elevated blood pressures actually increased from 7.5% to 9.9% following the intervention. Importantly, however, the percentage of patients discharged with low blood pressures decreased from 6.9% to 5.0% (P < 0.01).Tthe percent of patients discharged with an elevated heart rate, decreased from 58% in the pre alert group to 42% in the post alert group (P < 0.02).
Discussion
In our study, we used features of the EMR prospectively to affect discharge and then used the database functions of the EMR to assess the effectiveness of those efforts. Previous studies that have looked at the incidence of abnormal vital signs at discharge have been manual, retrospective reviews of records. We are not aware of any studies reporting the results of introducing an EMR alert to prospectively identify patients with abnormal vital signs prior to discharge
While we found that this intervention was successful in reducing clinically relevant abnormal vital signs at discharge, we have realized that the elevated blood pressure alert was unnecessary and we have eliminated it from the programming. We will revisit our strategy to determine if further reducing the high blood pressure alerts can lead to greater improvements in reducing the percentage of patients discharged with abnormal vital signs.
Future plans include a review of the re-visit or hospitalization rate for patients discharged with abnormal vital signs. A companion study evaluating a similar approach to the care of children is under consideration. We are also considering including a field in the EMR for the clinician to document why they discharged a patient with abnormal vital signs.
Corresponding author: Jonathan E. Siff, MD 2500 MetroHealth Drive BG3-65 Cleveland, Ohio 44109 [email protected].
Financial disclosures: None.
From Case Western Reserve University, MetroHealth Medical Center, Cleveland, OH.
Abstract
- Objective: To describe a computer-assisted process for reducing the number of patients discharged from the emergency department with abnormal vital signs.
- Methods: We devised a best practice alert in the Epic electronic medical record that triggers when the clinician attempts to print an after visit summary (discharge paperwork) at the time of discharge from the emergency department.
- Results: We saw no change in the percentage of patients discharged with elevated blood pressures, consistent with national recommendations. Removing that category of patients, we saw a decrease in the percentage of patients discharged with abnormal vital signs, primarily driven by a decrease in the percentage of patients discharged with tachycardia.
- Conclusion: A computer-assisted process can reduce the percentage of patients discharged with abnormal vital signs. Since based on national recommendations ED physicians do not address most elevated blood pressures in the ED, hypertension should not trigger an alert.
Abnormal vital signs in the emergency department (ED) have been associated with adverse outcomes [1,2]. While most patients discharged from the ED do well, some studies have found that the death rate within days to weeks post–ED discharge may be as high as 200 per 100,000 visits, although other studies have found a much lower rate [1]. A study by Sklar et al, although not specifically focused on vital signs at discharge, found that unexpected death within 7 days of ED discharge occurred at a rate of 30 per 100,000 patients. Abnormal vital signs, most commonly tachycardia, were present in 83% of cases [2].
In busy EDs, the combination of patient volume, frequent interruptions, and the intensity of tasks can result in deficiencies in vital sign monitoring [3–5] as well as abnormal vital signs not being recognized by the clinician at the time of patient discharge [6]. The importance of addressing this quality problem has been recognized. Prior efforts to address the problem have included nurses using manual methods to alert the physician to the presence of abnormal vital signs at the time of discharge [7]. Recommendations have been made to use electronic medical record (EMR) functions for prospectively addressing the problem of ED discharge with abnormal vital signs [8]. The utility of the EMR to identify potentially septic patients earlier and reduce mortality from sepsis via an algorithm that incorporated vital signs and other clinical crieria has been demonstrated [9,10]. In addition, automated vital signs advisories have been associated with increased survival on general hospital wards [11].
An adverse event that occurred at our institution prompted us to review this issue for our ED. We designed an EMR-assisted intervention to reduce the rate of patients discharged from the ED with abnormal vital signs.
Methods
Setting
Our ED is a busy, urban, Level 1 trauma center within a teaching facility. It sees over 100,000 patients per year and is segmented into resuscitation, high acuity, moderate acuity, and fast tract areas, in addition to the observation unit. Our organization uses the Epic (Madison, Wisconsin) electronic health record, which we have been using for over a decade.
Discharge Instructions—Old Process
In our ED, providers, attending physicians, residents and advance practice nurses enter and print their own discharge instructions, which are given to nursing staff to review with patients. Prior to the project, nurses were expected to notify a physician if they thought a vital sign was abnormal. Each nurse made independent decisions on what constituted a vital sign abnormality based on the patient’s condition and could communicate that to the provider at their discretion prior to discharge. This process created inconsistencies in care.
Development of Alert
We created an alert that appears within the provider workflow at the time the provider attempts to print discharge instructions. Based on literature review and operational leadership consensus, we set the parameters for abnormal vital signs (Table 1). We chose parameters to identify abnormalities important to
The alert displays when a user attempts to print discharge instructions on a patient whose last recorded vital signs are not all normal. The display informs that there are abnormal vital signs (Figure). Upon display of the alert, the user can click on the message, which would take them to the vital sign entry activity in the EMR, or they can proceed with printing by clicking the print button (not visible in the Figure). The alert is not a forcing function; the user can proceed with printing the discharge instructions without addressing the abnormality that triggered the alert.
Pre-Post Evaluation
We would have liked to have determined how often the abnormal vital signs alert triggered, how it was responded to, and whether the patient was subsequently discharged with normal vital signs; however, our system does not record these events. Instead, we used the system to compare the percentage of adult patients who were discharged with abnormal vital signs for 2 time periods: the period prior to our December 2014 implementation (1 Oct to 1 Dec 2014) and the post implementation period (15 Dec 2014 to 15 Feb 2015). Our presumption was that the use of the alert system would reduce the percentage of patients discharged with abnormal vital signs, including an abnormal pulse oximetry.
To conduct our analysis, we identified adult patients seen during the 2 time periods. We eliminated those patients who died, left without being seen, eloped, were admitted or were transferred to other institutions. This resulted in 3664 patients, with 2179 in the pre-implementation group and 1485 in the post-implementation group. The higher volume in the pre group reflects the early occurrence of influenza season in our area during the study period, along with our generally busier time in late fall compared to winter.
The analysis was performed as a likelihood ratio chi-square analysis using SAS (Cary, NC) software.
Results
The analysis demonstrated that physicians were, by and large, following recommendations consistent with policies of the American College of Emergency Physicians regarding the management of elevated blood pressures, which do not mandate that patients with asymptomatic elevations of blood pressure receive medical intervention in the ED [12]. In our analysis, the percentage of patients discharged with elevated blood pressures actually increased from 7.5% to 9.9% following the intervention. Importantly, however, the percentage of patients discharged with low blood pressures decreased from 6.9% to 5.0% (P < 0.01).Tthe percent of patients discharged with an elevated heart rate, decreased from 58% in the pre alert group to 42% in the post alert group (P < 0.02).
Discussion
In our study, we used features of the EMR prospectively to affect discharge and then used the database functions of the EMR to assess the effectiveness of those efforts. Previous studies that have looked at the incidence of abnormal vital signs at discharge have been manual, retrospective reviews of records. We are not aware of any studies reporting the results of introducing an EMR alert to prospectively identify patients with abnormal vital signs prior to discharge
While we found that this intervention was successful in reducing clinically relevant abnormal vital signs at discharge, we have realized that the elevated blood pressure alert was unnecessary and we have eliminated it from the programming. We will revisit our strategy to determine if further reducing the high blood pressure alerts can lead to greater improvements in reducing the percentage of patients discharged with abnormal vital signs.
Future plans include a review of the re-visit or hospitalization rate for patients discharged with abnormal vital signs. A companion study evaluating a similar approach to the care of children is under consideration. We are also considering including a field in the EMR for the clinician to document why they discharged a patient with abnormal vital signs.
Corresponding author: Jonathan E. Siff, MD 2500 MetroHealth Drive BG3-65 Cleveland, Ohio 44109 [email protected].
Financial disclosures: None.
1. Gunnarsdottir OS, Rafnsson V. Death within 8 days after discharge to home from the emergency department. Eur J of Public Health 2008;18:522–6.
2. Sklar DP, Crandall CS, Loeliger E, et al. Unanticipated death after discharge home from the emergency department. Ann Emerg Med 2007;49:735–45.
3. Johnson KD, Winkelman C, Burant CJ, et al. The factors that affect the frequency of vital sign monitoring in the emergency department. J Emerg Nurs 2014;40:27–35.
4. Gravel J, Opatrny L, Gouin S. High rate of missing vital signs data at triage in a paediatric emergency department. Paediatr Child Health 2006;11:211–5.
5. Depinet HE, Iyer SB, Hornung R, et al. The effect of emergency department crowding on reassessment of children with critically abnormal vital signs. Acad Emerg Med 2014;21:1116–20.
6. Hafner JW, Parrish SE, Hubler JR, et al. Repeat assessment of abnormal vital signs and patient re-examination in us emergency department patients. Ann Emerg Med 2006;48(4 Suppl):S66.
7. Domagala SE. Discharge vital signs: an enhancement to ED quality and patient outcomes. J Emerg Nursing 2009;35:138–40.
8. Welch S. Red flags: abnormal vital signs at discharge.Emerg Med News 2011:33;7–8.
9. Nguyen SQ, Mwakalindile E, Booth JS, et al. Automated electronic medical record sepsis detection in the emergency department. PeerJ 2014;2:e343.
10. Narayanan N, Gross AK, Pintens M, et al. Effect of an electronic medical record alert for severe sepsis among ED patients. Am J Emerg Med 2016;34:185–8.
11. Bellomo R, Ackerman M, Bailey M, et al. A controlled trial of electronic automated advisory vital signs monitoring in general hospital wards. Crit Care Med 2012;40:2349–61.
12. Wolf SJ, Lo B, Smith MD, et al. Clinical policy: critical issues in the evaluation and management of adult patients in the emergency department with asymptomatic elevated blood pressure. Ann Emerg Med 2013:62;59–68.
1. Gunnarsdottir OS, Rafnsson V. Death within 8 days after discharge to home from the emergency department. Eur J of Public Health 2008;18:522–6.
2. Sklar DP, Crandall CS, Loeliger E, et al. Unanticipated death after discharge home from the emergency department. Ann Emerg Med 2007;49:735–45.
3. Johnson KD, Winkelman C, Burant CJ, et al. The factors that affect the frequency of vital sign monitoring in the emergency department. J Emerg Nurs 2014;40:27–35.
4. Gravel J, Opatrny L, Gouin S. High rate of missing vital signs data at triage in a paediatric emergency department. Paediatr Child Health 2006;11:211–5.
5. Depinet HE, Iyer SB, Hornung R, et al. The effect of emergency department crowding on reassessment of children with critically abnormal vital signs. Acad Emerg Med 2014;21:1116–20.
6. Hafner JW, Parrish SE, Hubler JR, et al. Repeat assessment of abnormal vital signs and patient re-examination in us emergency department patients. Ann Emerg Med 2006;48(4 Suppl):S66.
7. Domagala SE. Discharge vital signs: an enhancement to ED quality and patient outcomes. J Emerg Nursing 2009;35:138–40.
8. Welch S. Red flags: abnormal vital signs at discharge.Emerg Med News 2011:33;7–8.
9. Nguyen SQ, Mwakalindile E, Booth JS, et al. Automated electronic medical record sepsis detection in the emergency department. PeerJ 2014;2:e343.
10. Narayanan N, Gross AK, Pintens M, et al. Effect of an electronic medical record alert for severe sepsis among ED patients. Am J Emerg Med 2016;34:185–8.
11. Bellomo R, Ackerman M, Bailey M, et al. A controlled trial of electronic automated advisory vital signs monitoring in general hospital wards. Crit Care Med 2012;40:2349–61.
12. Wolf SJ, Lo B, Smith MD, et al. Clinical policy: critical issues in the evaluation and management of adult patients in the emergency department with asymptomatic elevated blood pressure. Ann Emerg Med 2013:62;59–68.
Nonsurgical biomarkers show potential in chronic endometriosis
SALT LAKE CITY – and might soon spare patients from years of misdiagnosis and the costs and burden of diagnostic surgery, according to experts at the annual meeting of the American Society for Reproductive Medicine.
Most notably, expression levels of three microRNAs, 125-b-5p, 451a, and 3613-5p, correctly distinguished patients with chronic endometriosis from healthy controls, said Hugh S. Taylor, MD, of Yale University in New Haven, Conn.
Chronic endometriosis affects about 10% of women and up to half of those with infertility, Dr. Taylor noted. The disease costs the United States at least $22 billion annually and is the second most-common reason for hysterectomy (Reprod Sci. 2009 Apr;16[4]:335-46). Its complexity means that patients face many barriers to diagnosis, particularly young women, who are often told they have “routine” menstrual pain, Dr. Taylor said.
Patients may go up to 12 years and see five or more physicians before they are diagnosed. Clinicians tend to rely on surgical diagnosis, but “there is a reluctance to perform surgery unless there is severe disease,” he added. “The lack of nonsurgical biomarkers contributes significantly to delays in diagnosis and timely intervention.”
These concerns prompted Dr. Taylor and his associates to study microRNAs – the short, noncoding, functional RNAs that promote messenger RNA breakdown or repress its translation. MicroRNA expression varies by tissue type and disease status, and occurs in a variety of body fluids, giving them real potential as nonsurgical biomarkers, Dr. Taylor said. To examine their role in endometriosis, he and his associates performed microarray profiling and confirmatory quantitative real-time polymerase chain reaction testing of serum samples from 24 women with chronic endometriosis and 24 healthy women who served as controls (Fertil Steril. 2016 Aug;106[2]:402-9).
MicroRNA 125b-5p was upregulated the most in endometriosis patients and distinguished patients from controls with a “giant” area under the receiver operating characteristic curve value of 0.974, Dr. Taylor said. Remarkably, this value rose to 1 – meaning that sensitivity and specificity both were 100% – when the researchers added another upregulated microRNA (451a) and a downregulated microRNA (3613-5p) to the model. More work is underway to understand how a test for these microRNAs would perform in larger populations, Dr. Taylor said.
MicroRNAs also are likely to play functional roles in chronic endometriosis and may mediate treatment response, he noted. For example, the microRNA 125b-5p, which is upregulated in endometriosis, increases the expression of inflammatory cytokines and tumor necrosis factor alpha in macrophages, and the aromatase inhibitor letrozole, which reduces pelvic pain in the disease, increases the expression of let-7 microRNAs, with corresponding decreases in the migration of endometrial cells (Fertil Steril. 2016 Sep 1;106[3]:673-80). “Maybe these microRNAs are changing metabolism. Maybe they are changing immune cell activity,” Dr. Taylor said. “I think they are doing a lot more than sitting around waiting for us to discover them.”
None of the 24 patients with endometriosis in his study had taken oral contraceptives in the 3 months prior to serum sampling, Dr. Taylor noted. “We need to look at oral contraception as a potential confounder,” he acknowledged. “If something is independent of the menstrual cycle phase, that is much better than a marker that is dependent on cycle phase.”
Menstrual cycle phase and oral contraceptives are just two of many potential confounders of biomarkers in chronic endometriosis, according to Linda Giudice, MD, PhD, of the University of California, San Francisco. Disease severity, as well as the type, number, and location of lesions and the presence or absence of coexisting inflammatory disorders all can potentially affect the sensitivity and specificity of a marker, she said. Consequently, “there is no single biomarker for chronic endometriosis,” but there are several candidates besides microRNAs, she added. For example, studies show that menstrual blood is readily distinguishable from peripheral blood, and closely resembles the immune environment of the uterus. Another study found that urinary peptides distinguished patients with moderate to severe endometriosis from healthy controls, and mild disease from severe disease, with sensitivities and specificities ranging from 72% to 88% (Fertil Steril. 2011 Mar 15;95[4]:1261-6).
Other potential sources of diagnostic tests include the endometrial proteome, transcriptome, and methylome, as well as endometrial stem cells, Dr. Giudice said. But for now, surgical diagnosis remains the gold standard, and the World Endometriosis Research Foundation is working to homogenize recording of surgical phenotypic information and laparoscopic specimens to improve data quality, she added.
Dr. Taylor did not report funding sources. He disclosed financial ties to Pfizer, OvaScience AbbVie, Bayer, and Euroscreen. Dr. Giudice acknowledged support from the National Institutes of Health and the UCSF NIH Human Endometrial Tissue and DNA Bank. She disclosed ties to Merck, Pfizer, NextGen Jane, AbbVie, and Juniper Pharmaceuticals.
SALT LAKE CITY – and might soon spare patients from years of misdiagnosis and the costs and burden of diagnostic surgery, according to experts at the annual meeting of the American Society for Reproductive Medicine.
Most notably, expression levels of three microRNAs, 125-b-5p, 451a, and 3613-5p, correctly distinguished patients with chronic endometriosis from healthy controls, said Hugh S. Taylor, MD, of Yale University in New Haven, Conn.
Chronic endometriosis affects about 10% of women and up to half of those with infertility, Dr. Taylor noted. The disease costs the United States at least $22 billion annually and is the second most-common reason for hysterectomy (Reprod Sci. 2009 Apr;16[4]:335-46). Its complexity means that patients face many barriers to diagnosis, particularly young women, who are often told they have “routine” menstrual pain, Dr. Taylor said.
Patients may go up to 12 years and see five or more physicians before they are diagnosed. Clinicians tend to rely on surgical diagnosis, but “there is a reluctance to perform surgery unless there is severe disease,” he added. “The lack of nonsurgical biomarkers contributes significantly to delays in diagnosis and timely intervention.”
These concerns prompted Dr. Taylor and his associates to study microRNAs – the short, noncoding, functional RNAs that promote messenger RNA breakdown or repress its translation. MicroRNA expression varies by tissue type and disease status, and occurs in a variety of body fluids, giving them real potential as nonsurgical biomarkers, Dr. Taylor said. To examine their role in endometriosis, he and his associates performed microarray profiling and confirmatory quantitative real-time polymerase chain reaction testing of serum samples from 24 women with chronic endometriosis and 24 healthy women who served as controls (Fertil Steril. 2016 Aug;106[2]:402-9).
MicroRNA 125b-5p was upregulated the most in endometriosis patients and distinguished patients from controls with a “giant” area under the receiver operating characteristic curve value of 0.974, Dr. Taylor said. Remarkably, this value rose to 1 – meaning that sensitivity and specificity both were 100% – when the researchers added another upregulated microRNA (451a) and a downregulated microRNA (3613-5p) to the model. More work is underway to understand how a test for these microRNAs would perform in larger populations, Dr. Taylor said.
MicroRNAs also are likely to play functional roles in chronic endometriosis and may mediate treatment response, he noted. For example, the microRNA 125b-5p, which is upregulated in endometriosis, increases the expression of inflammatory cytokines and tumor necrosis factor alpha in macrophages, and the aromatase inhibitor letrozole, which reduces pelvic pain in the disease, increases the expression of let-7 microRNAs, with corresponding decreases in the migration of endometrial cells (Fertil Steril. 2016 Sep 1;106[3]:673-80). “Maybe these microRNAs are changing metabolism. Maybe they are changing immune cell activity,” Dr. Taylor said. “I think they are doing a lot more than sitting around waiting for us to discover them.”
None of the 24 patients with endometriosis in his study had taken oral contraceptives in the 3 months prior to serum sampling, Dr. Taylor noted. “We need to look at oral contraception as a potential confounder,” he acknowledged. “If something is independent of the menstrual cycle phase, that is much better than a marker that is dependent on cycle phase.”
Menstrual cycle phase and oral contraceptives are just two of many potential confounders of biomarkers in chronic endometriosis, according to Linda Giudice, MD, PhD, of the University of California, San Francisco. Disease severity, as well as the type, number, and location of lesions and the presence or absence of coexisting inflammatory disorders all can potentially affect the sensitivity and specificity of a marker, she said. Consequently, “there is no single biomarker for chronic endometriosis,” but there are several candidates besides microRNAs, she added. For example, studies show that menstrual blood is readily distinguishable from peripheral blood, and closely resembles the immune environment of the uterus. Another study found that urinary peptides distinguished patients with moderate to severe endometriosis from healthy controls, and mild disease from severe disease, with sensitivities and specificities ranging from 72% to 88% (Fertil Steril. 2011 Mar 15;95[4]:1261-6).
Other potential sources of diagnostic tests include the endometrial proteome, transcriptome, and methylome, as well as endometrial stem cells, Dr. Giudice said. But for now, surgical diagnosis remains the gold standard, and the World Endometriosis Research Foundation is working to homogenize recording of surgical phenotypic information and laparoscopic specimens to improve data quality, she added.
Dr. Taylor did not report funding sources. He disclosed financial ties to Pfizer, OvaScience AbbVie, Bayer, and Euroscreen. Dr. Giudice acknowledged support from the National Institutes of Health and the UCSF NIH Human Endometrial Tissue and DNA Bank. She disclosed ties to Merck, Pfizer, NextGen Jane, AbbVie, and Juniper Pharmaceuticals.
SALT LAKE CITY – and might soon spare patients from years of misdiagnosis and the costs and burden of diagnostic surgery, according to experts at the annual meeting of the American Society for Reproductive Medicine.
Most notably, expression levels of three microRNAs, 125-b-5p, 451a, and 3613-5p, correctly distinguished patients with chronic endometriosis from healthy controls, said Hugh S. Taylor, MD, of Yale University in New Haven, Conn.
Chronic endometriosis affects about 10% of women and up to half of those with infertility, Dr. Taylor noted. The disease costs the United States at least $22 billion annually and is the second most-common reason for hysterectomy (Reprod Sci. 2009 Apr;16[4]:335-46). Its complexity means that patients face many barriers to diagnosis, particularly young women, who are often told they have “routine” menstrual pain, Dr. Taylor said.
Patients may go up to 12 years and see five or more physicians before they are diagnosed. Clinicians tend to rely on surgical diagnosis, but “there is a reluctance to perform surgery unless there is severe disease,” he added. “The lack of nonsurgical biomarkers contributes significantly to delays in diagnosis and timely intervention.”
These concerns prompted Dr. Taylor and his associates to study microRNAs – the short, noncoding, functional RNAs that promote messenger RNA breakdown or repress its translation. MicroRNA expression varies by tissue type and disease status, and occurs in a variety of body fluids, giving them real potential as nonsurgical biomarkers, Dr. Taylor said. To examine their role in endometriosis, he and his associates performed microarray profiling and confirmatory quantitative real-time polymerase chain reaction testing of serum samples from 24 women with chronic endometriosis and 24 healthy women who served as controls (Fertil Steril. 2016 Aug;106[2]:402-9).
MicroRNA 125b-5p was upregulated the most in endometriosis patients and distinguished patients from controls with a “giant” area under the receiver operating characteristic curve value of 0.974, Dr. Taylor said. Remarkably, this value rose to 1 – meaning that sensitivity and specificity both were 100% – when the researchers added another upregulated microRNA (451a) and a downregulated microRNA (3613-5p) to the model. More work is underway to understand how a test for these microRNAs would perform in larger populations, Dr. Taylor said.
MicroRNAs also are likely to play functional roles in chronic endometriosis and may mediate treatment response, he noted. For example, the microRNA 125b-5p, which is upregulated in endometriosis, increases the expression of inflammatory cytokines and tumor necrosis factor alpha in macrophages, and the aromatase inhibitor letrozole, which reduces pelvic pain in the disease, increases the expression of let-7 microRNAs, with corresponding decreases in the migration of endometrial cells (Fertil Steril. 2016 Sep 1;106[3]:673-80). “Maybe these microRNAs are changing metabolism. Maybe they are changing immune cell activity,” Dr. Taylor said. “I think they are doing a lot more than sitting around waiting for us to discover them.”
None of the 24 patients with endometriosis in his study had taken oral contraceptives in the 3 months prior to serum sampling, Dr. Taylor noted. “We need to look at oral contraception as a potential confounder,” he acknowledged. “If something is independent of the menstrual cycle phase, that is much better than a marker that is dependent on cycle phase.”
Menstrual cycle phase and oral contraceptives are just two of many potential confounders of biomarkers in chronic endometriosis, according to Linda Giudice, MD, PhD, of the University of California, San Francisco. Disease severity, as well as the type, number, and location of lesions and the presence or absence of coexisting inflammatory disorders all can potentially affect the sensitivity and specificity of a marker, she said. Consequently, “there is no single biomarker for chronic endometriosis,” but there are several candidates besides microRNAs, she added. For example, studies show that menstrual blood is readily distinguishable from peripheral blood, and closely resembles the immune environment of the uterus. Another study found that urinary peptides distinguished patients with moderate to severe endometriosis from healthy controls, and mild disease from severe disease, with sensitivities and specificities ranging from 72% to 88% (Fertil Steril. 2011 Mar 15;95[4]:1261-6).
Other potential sources of diagnostic tests include the endometrial proteome, transcriptome, and methylome, as well as endometrial stem cells, Dr. Giudice said. But for now, surgical diagnosis remains the gold standard, and the World Endometriosis Research Foundation is working to homogenize recording of surgical phenotypic information and laparoscopic specimens to improve data quality, she added.
Dr. Taylor did not report funding sources. He disclosed financial ties to Pfizer, OvaScience AbbVie, Bayer, and Euroscreen. Dr. Giudice acknowledged support from the National Institutes of Health and the UCSF NIH Human Endometrial Tissue and DNA Bank. She disclosed ties to Merck, Pfizer, NextGen Jane, AbbVie, and Juniper Pharmaceuticals.
EXPERT ANALYSIS FROM 2016 ASRM
Patient-Physician Communication and Diabetes Self-Care
Abstract
- Objective: To summarize the current literature, research findings, and interventions for self-care communication in the physician-patient relationship.
- Methods: Literature review.
- Results: Diabetes management requires patients to follow complex self-care recommendations for nutrition, physical activity, blood glucose monitoring, and medication. Adherence to these recommendations improves glycemic control and mitigates the risk of diabetes complications; however, many patients struggle to follow these behaviors in everyday life. In the physician-patient relationship, self-care communication is largely influenced by interpersonal trust. Physicians need to incorporate interpersonal and relational skills to establish a trusting relationship. Physician-level barriers to self-care communication include lack of time, lack of collaboration and teamwork among health care providers, lack of patients’ access to resources, and lack of psychosocial support for diabetes patients. Among patients, psychosocial barriers and health literacy may affect willingness to discuss self-care. Motivational interviewing techniques may be helpful for improving communication around patient self-management and promotion of healthy behaviors.
- Conclusion: Physicians can assist patients with their diabetes self-care by discussing self-care challenges during medical visits.
Diabetes is one of the most significant and growing chronic health problems in the world, affecting approximately 415 million people [1]. Diabetes is marked by the body’s inability to make insulin as well as the body’s inability to effectively use the insulin it produces [2]. Diagnosis of diabetes has increased sharply in recent decades and is expected to increase even more, with the largest increases in middle- and low-income countries [3]. Diabetes is a leading cause of blindness, kidney failure, myocardial infarction, stroke, and amputation [3], and in 2015 it accounted for 5 million deaths worldwide [1]. Further, diabetes’s costs to society represent 12% ($673 billion) of global health expenditures [1]. By 2040, models predict that 642 million people will be diagnosed with diabetes and costs will continue to grow as the population ages [1]. Thus, prevention of diabetes is the ultimate goal; however, more effective management for individuals already diagnosed with diabetes is critical to reduce the risk of complications and the economic burden of the disease.
Diabetes management requires patients to perform complex self-care regimens, including weight reduction, frequent blood glucose monitoring, taking oral and/or insulin medications, engaging in physical activity, adhering to diabetes nutrition guidelines, and attending clinic appointments [4–9]. These self-care behaviors are critically linked to improved glycemic control, however, integrating them into one’s daily life can be challenging [10–12]. Recent National Health and Nutrition Examination Survey (NHANES) data show that approximately half of adults with diabetes are not meeting recommended goals for diabetes care [13]. Physicians can assist patients with their diabetes self-care by scheduling frequent follow-up visits and discussing self-care challenges with their patients [14].
In this review, we discuss the current literature on physician-patient communication and diabetes self-care. First, we discuss the qualities of an effective physician-patient relationship followed by the importance of self-care communication in diabetes care. Next, we discuss barriers and facilitators to self-care communication. Finally, we review interventions for improving physician-patient communication in diabetes self-care.
Qualities of an Effective Physician-Patient Relationship
Successful diabetes care requires teamwork between physicians and patients [15]. Two components of successful teamwork are physician-patient communication and shared decision-making, both of which have been shown to improve patient satisfaction, adherence to treatment plans and health outcomes [16–23]. In shared decision-making, the physician and patient share medical information [24–26]. Specifically, the physician presents different treatment options to the patient and describes the risks and benefits of each option. Then the patient expresses his or her preferences for treatment to ensure that the care provided aligns with the patient’s values and needs [27]. Thus, shared decision-making in the treatment relationship is predicated on effective communication between the physician and patient [19].
Effective physician-patient communication is supported by continuous care [19,28], a secure attachment style [29, 30], shared goals [19], a mutual understanding of respective roles and tasks [15,31–33], and a bond characterized by liking, confidence, and trust [19,28,31]. Trust is paramount in physician-patient communication. Interpersonal trust and social trust are the 2 predominant types [34]. Interpersonal trust refers to the relationship the patient has with the physician, specifically the confidence the patient has in the physician as well as the responsibility, competence, compassion, and regard the physician has for the patient’s welfare [34–36]. For patients and physicians, interpersonal trust is developed over time with repeated interactions [34–36]. On the other hand, social trust refers to the beliefs of honesty, integrity, and reliability in others [36]. Social trust is influenced by social constructs, including the media and institutions of higher education [36].
In the physician-patient relationship, self-care communication is largely influenced by interpersonal trust. A patient’s trust can be acquired through multiple medical appointments with the physician. Further, how the patient is treated during these appointments as well as how much time and attention the physician invests in the patient’s care influences the level of interpersonal trust. A high level of trust in the relationship can lead to in improvements in adherence to self-care, continuity of care, physician-patient communication, and overall quality of the physician-patient relationship [37–39].
In the diabetes physician-patient relationship, minimal research has explored how trust in one’s physician impacts self-care communication. In a study by Beverly and colleagues, diabetes patients emphasized the importance of a trusting physician-patient relationship for diabetes care [27]. Another study by Ritholz and colleagues found that physicians and patients both stress the importance of developing trust to facilitate self-care communication [40]. Specifically, trust as well as acceptance from the physician contributes to open and honest self-care communication in the physician-patient diabetes relationship[40]. Additional research is needed to determine whether a high level of physician-patient trust is associated with increased self-care behaviors and improved diabetes outcomes over time.
Importance of Diabetes Self-Care Communication
Diabetes self-care communication in the physician-patient relationship increases patient satisfaction, improves adherence to treatment regimens, and leads to better clinical outcomes [22,41–43]. For physicians, effective self-care communication requires the performance of specific communication tasks and behaviors, including collecting a medical history, explaining a diagnosis and prognosis, and providing clear and concise therapeutic instructions [44]. In addition, physicians must incorporate interpersonal and relational skills to establish a trusting relationship [44,45]. Both physicians and patients agree that a trusting treatment relationship is a requirement for open and honest self-care communication [45]. For patients, effective communication necessitates the disclosure of self-care successes and failures [46]. Diabetes patients face challenging self-care regimens, and these challenges can interfere with glycemic control and increase the risk for diabetes complications [47,48]. For this reason, patients must feel comfortable discussing their self-are challenges so that their physician can individualize treatment prescriptions and recommendations, thereby increasing the likelihood of treatment success.
Barriers to Self-Care Communication
Physician-patient self-care communication is essential to improving patient adherence [29,49] yet numerous barriers exist that undermine effective physician-patient self-care communication. From the physician perspective, the most commonly cited barrier to self-care communication is time [50]. A recent study of family medicine practices found that the time physicians spent discussing self-care with their patients varied from 1 to 17 minutes, suggesting that time is a major barrier to self-care communication [51]. Other barriers include lack of collaboration and teamwork among health care providers, lack of patients’ access to resources, and lack of psychosocial support for patients with diabetes [50]. Relatedly, Beverly and colleagues [52] found that physicians often feel inadequately trained to address diabetes patients’ psychosocial issues and this perceived lack of expertise may contribute to physicians feeling overwhelmed and frustrated within the physician-patient relationship, which may hinder open self-care communication.
For patients, barriers tend to differ from those perceived by physicians. A qualitative study using semi-structured interviews with patients and clinicians, and direct observation of clinical encounters at an inner-city family practice training site, revealed different perceptions of the term “control” between physicians and patients. In practice, physicians used the term “control” to focus on the management of blood glucose levels rather than trying to understand the patients’ understanding of diabetes and subsequent treatment goals. Differing viewpoints contributed to frustration and hindered effective communication [53]. In another qualitative study with physicians and patients, both noted that patients were reluctant to discuss self-care for fear being judged or shamed about food intake and weight [45]. This finding was supported in a quantitative follow-up study assessing patient reluctance to discuss self-care. Thirty percent of surveyed patients reported reluctance to discussing self-care with their physicians for fear of being judged, not wanting to disappoint their doctors, guilt, and shame [14]. Interestingly, patients reporting elevated depressive symptoms were more likely to be reluctant to discuss their self-care [14]. Cognitive behavioral changes (eg, cognitive distortions, avoidance behavior, attention deficits) associated with major depression and depressive symptoms may impair patients’ ability to recall self-care information. Also, patients reporting more depressive symptoms may be more socially withdrawn during a medical appointment, and thus less willing to communicate with their physician about self-care.
Other studies found that psychosocial factors such as diabetes distress [54,55] and pessimistic attitudes [56–59], cultural differences [60–66], lack of family and social support [60,67–70], lack of readiness to change behavior [71], introversion and social isolation [72,73], hypo-glycemia fear [74,75] and ineffectual coping styles [76,77] interfere with self-care and glycemic control. Further, low health literacy is associated with difficulty adhering to self-care, particular medication regimens, and negative health outcomes [78].
In summary psychosocial barriers and health literacy may affect a patients’ willingness to discuss self-care during a medical visit. Therefore, routine assessment of psychosocial factors and health literacy may be necessary to address a patient’s barriers to self-care as well as to promote open and honest self-care communication. Interventions and evidenced-based approaches that address psychosocial factors, health literacy, and physician-patient self-care communication are needed.
Facilitators to Self-Care Communication
Despite numerous barriers to self-care communication, several factors promote self-care communication in the physician-patient relationship. For example, direct and non-accusatory communication from physicians as well as providing patients with hope for living with diabetes both support physician-patient self-care communication [45]. A recent systematic review by Sohal and colleagues [79] found that trust in physicians, the use of culturally appropriate exercise and dietary advice, and increasing family involvement improved physician-patient communication and diabetes self-care [79]. Lastly, a study by Schillinger and colleagues [80] found that physician assessment of patient recall and comprehension of new concepts during medical visits improved diabetes outcomes [80].
Patient-Physician Self-Care Communication Interventions
One of the more successful interventions for improving diabetes self-care and patient-physician communication is motivational interviewing (MI). MI is a non-judgmental communication style designed to explore a patient’s intrinsic motivation to change health behaviors [81]. Inherent to MI is the belief that motivation for change is malleable and that it can be transformed in the context of the patient-physician relationship [81]. MI is a patient-centered method designed to empower a patient’s ability and responsibility to make health-related decisions, with the physician supporting the patient’s autonomy in the process [82]. Recent meta-analyses and systematic reviews [83–87] showed that MI interventions improve self-care behaviors and glycemic control in the short-term; long-term effects of MI on self-care and glycemia remain inconclusive. More high-quality research is needed to evaluate the MI training content of these interventions in order to determine its long-term effectiveness and replicate outcomes in various healthcare settings [87].
Other studies not included in the meta-analyses and reviews found MI interventions improved self-care behaviors [88–90], glycemic control [90,91], and quality of life [91]. A qualitative study exploring diabetes patients’ experiences with MI and self-care behaviors revealed that patients’ appreciate when providers initiate discussions that result in new ways of thinking about self-care and promote a sense of well-being in patients [92]. New research utilizing patient navigators to connect diabetes patients’ to their primary care providers showed MI techniques improved patient self-efficacy and glycemic control [93]. Another study, an internet-based incentives study, found that the application of a brief MI interviewing session improved blood glucose monitoring in adolescents with type 1 diabetes [94]. Thus, creative strategies that employ MI techniques in collaboration with other members of the health care team (ie, patient navigation [93], telehealth [89], health coaching [95], internet-based tools [94]) hold promise for improving self-care and patient-physician communication. Increased collaboration with members of the health care team (eg, certified diabetes educators, nurses, dietitians, pharmacists, exercise physiologists), community health workers [96,97] and peer mentors [98,99] may help reinforce messages, promote shared decision-making, improve diabetes outcomes, increase patient satisfaction, and reduce medical costs [100].
Few other interventions have directly addressed physician-patient diabetes self-care communication. One older study examined the effectiveness of an intervention designed to increase of diabetes patients’ involvement in medical decision-making [16]. Patients randomized to the intervention arm participated in a 20-minute session prior to meeting with their physician, in which researchers reviewed their medical chart and used systematic prompts to encourage patients to negotiate medical decisions with their physician. Patients in the control arm received standard educational materials in a session of equal length. Patients in the intervention arm improved glycemia and elicited twice the amount of medical information from their physician compared to controls [16]. These findings suggest that brief interventions prior to medical appointments can improve patient communication, self-care behavior, and in turn, diabetes outcomes [16].
A recent study evaluated the effectiveness of a training program in communication skills for pediatric diabetes care providers in the UK [101, 102]. In this cluster randomized controlled trial, pediatric providers allocated to the Talking Diabetes intervention participated in web-based material and face-to-face seminars designed to prepare providers for constructive self-care conversations with patients as well as skills for promoting behavior change. The psychoeducational training emphasized shared decision-making and utilized motivational interviewing techniques [101]. Twenty-six centers and 693 young people with type 1 diabetes participated in the study [102]. At 12-month follow-up, the Talking Diabetes intervention did not demonstrate improvements in glycemic control. Further, the intervention had a negative effect on patients’ quality of life but a short-term improvement in coping [102]. Interestingly, parents of patients in the intervention arm reported greater continuity of care, which suggests that parents benefited more from the intervention than their children. Future communication interventions targeting the pediatric population should provide ongoing support to children of physicians exposed to interventions such as Talking Diabetes [102].
Currently, 3 ongoing studies aim to improve self-care and clinical outcomes via physician-patient communication interventions. A study by Ricci-Cabello and colleagues [103] aims to improve diabetes self-care by enhancing patient-physician communication in an underserved community of adults with uncontrolled type 2 diabetes. In this 3-arm randomized controlled trial, patients allocated to groups A and B received communication skills training and graphic feedback about glycosylated hemoglobin A1c levels; patients in group C received usual care. Patients in group B also received telephone reinforcement [103]. The second study, by Billimek and colleagues, aims to improve physician-patient communication about medication regimens via diabetes coaching [104]. In this intervention, 190 Mexican-American adult patients with type 2 diabetes were randomly assigned to complete a Coached Care visit with trained community health workers or a Coached Care visit plus the EMPATHy software toolkit, a computer-based activity with strategies and resources to overcome self-care barriers. The primary endpoints are (1) the development of care plan that addresses everyday barriers to medication adherence and (2) completion of a concrete behavioral goal [104]. Finally, the third study, by Grant and colleagues, aims to improve physician-patient communication via a pre-visit prioritization of diabetes concerns. In this controlled, cluster-randomized, multisite trial, primary care physicians were randomized to the Pre-Visit Prioritization for Complex Patients with Diabetes or the control group [105]. The Pre-Visit Prioritization IT-tool is designed to help patients identify one or two concerns prior to a medical visit and then send these priorities to the primary care physician via an electronic health record. The overall goal of the intervention is to improve communication of self-care concerns during a medical visit [105]. Findings from these 3 interventions are forthcoming; findings may provide evidence for validated interventions that improve physician-patient self-care communication in diabetes.
Techniques to Improve Self-Care Communication
Incorporating communication skills in continuing medical education and diabetes education may improve self-care communication in the physician-patient relationship. Educational programs that teach physicians how to provide consistent messages, repeat information, reinforce and offer feedback regarding specific self-care behaviors, and problem-solve self-care challenges may improve patients’ willingness to discuss self-care [14,106]. Most patients will remember only a small portion of the information given to them during medical visit. Studies that compare how much information patients retain versus how much information physicians provide show that patients forget 31% to 71% of information [107]. Therefore, physicians need techniques that promote open self-care communication during a visit. The following techniques can help physicians improve self-care communication [108]:
- Discuss the most important self-care information first; patients tend to remember the information that is presented first.
- Use the phrase “This is very important…” when discussing key points because patients will remember things that are perceived as important.
- Deliver simple, clear, and concrete instructions; patients are more likely to forget complex or confusing instructions. For example, “Check your blood glucose every morning within five minutes of waking up and before you eat breakfast” is more specific and easier to follow than “Check your blood glucose”.
- Ask open-ended questions to allow patients to verbalize feelings or concerns about their diabetes self-care.
- Employ MI techniques to help patients who are struggling to initiate and adhere to self-care behaviors. MI tools, such as the Readiness Ruler, Self-Evaluation Rulers, Decisional Balance Matrix, and Health Behavior Menu (Figure), may help patients and physicians discuss self-care behaviors during a medical visit [109].
– Express empathy by reflective listening and asking patients for permission before offering information or advice about diabetes self-care.
– Roll with resistance by engaging the patient in the process of problem solving rather than opposing a patient’s resistance to change behaviors.
– Develop discrepancy by helping the patient recognize that there is an inconsistency between his/her behavior and personal goals.
– Support self-efficacy by empowering the patient to believe that he/she can change behaviors.
6. Demonstrate active listening skills by reflecting and summarizing the patient’s statements. Reflecting and summarizing show the patient that the physician has been listening to concerns and understands what the patient is saying. This is also an opportunity to correct any miscommunications from the visit.
7. Write down instructions or provide handouts to the patient to help reinforce learning and information retention.
8. Ask patients to write a list of questions a few days prior to the medical appointment and bring it with them. Patients are more likely to remember information about issues they have previously considered that directly relate to them.
9. Consider collaborating with community health workers, patient navigators, peer mentors, and other members of the healthcare team to improve communication, diabetes outcomes, and patient satisfaction.
Summary
Physician-patient self-care communication is essential to achieving optimal diabetes outcomes [15,22,33,110] Patients’ ability to inform physicians about their self-care challenges [14], and physicians’ ability to respond to patients’ self-care reports directly and in non-accusatory language, are vital factors in effective diabetes care [45]. Interventions and education that promote open and honest conversations are particularly important given patients’ well-documented struggles achieving self-care and glycemic goals [111] and physicians’ feelings of inadequacy, frustration, and fatigue when they are not making an impact on patients’ outcomes [48,112]. More research is needed to determine the best strategies to improve self-care communication in the physician-patient relationship.
Corresponding author: Elizabeth A. Beverly, PhD, Department of Family Medicine, Ohio University Heritage College of Osteopathic Medicine, Athens, OH 45701, [email protected].
Financial disclosures: None.
Author contributions: drafting of article, EAB, MFW, ABC, KEP, NNI; critical revision of the article, EAB, MFW, ABC, KEP, NNI.
1. Anderson E, Kian EM. Examining media contestation of masculinity and head trauma in the National Football League. J Men Masculinities 2011;1–22.
2. CDC. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011.
3. Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986.
4. Jacobson AM, Adler AG, Derby L, et al. Clinic attendance and glycemic control. Study of contrasting groups of patients with IDDM. Diabetes Care 1991;14:599–601.
5. Dyer PH, Lloyd CE, Lancashire RJ, et al. Factors associated with clinic non-attendance in adults with type 1 diabetes mellitus. Diab Med 1998;15:339–43.
6. Conn VS, Hafdahl AR, Mehr DR, et al. Metabolic effects of interventions to increase exercise in adults with type 2 diabetes. Diabetologia 2007;50:913–21.
7. Maiorana A, O’Driscoll G, Goodman C, et al. Combined aerobic and resistance exercise improves glycemic control and fitness in type 2 diabetes. Diab Res Clin Pract 2002;56:115–23.
8. Pi-Sunyer FX, Maggio CA, McCarron DA, et al. Multicenter randomized trial of a comprehensive prepared meal program in type 2 diabetes. Diabetes Care 1999;22:191–7.
9. Delahanty LM, Halford BN. The role of diet behaviors in achieving improved glycemic control in intensively treated patients in the Diabetes Control and Complications Trial. Diabetes Care 1993;16:1453–8.
10. Gafarian CT, Heiby EM, Blair P, Singer F. The Diabetes Time Management Questionnaire. Diabetes Educ 1999;25:585–92.
11. Wdowik MJ, Kendall PA, Harris MA. College students with diabetes: using focus groups and interviews to determine psychosocial issues and barriers to control. Diabetes Educ 1997;23:558–62.
12. Rubin RR, Peyrot M. Psychological issues and treatment for people with diabetes. J Clin Psychol 2001;57:457–78.
13. Ali MK, Bullard KM, Gregg EW. Achievement of goals in U.S. Diabetes Care, 1999-2010. N Engl J Med 2013;369:287–8.
14. Beverly EA, Ganda OP, Ritholz MD, et al. Look who’s (not) talking: diabetic patients’ willingness to discuss self-care with physicians. Diabetes Care 2012;35:1466–72.
15. Heisler M, Vijan S, Anderson RM, et al. When do patients and their physicians agree on diabetes treatment goals and strategies, and what difference does it make? J Gen Intern Med 2003;18:893–902.
16. Greenfield S, Kaplan SH, Ware JE Jr, et al. Patients’ participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med 1988;3:448–57.
17. Greenfield S, Kaplan S, Ware JE Jr. Expanding patient involvement in care. Effects on patient outcomes. Ann Intern Med 1985;102:520–8.
18. Anderson RM, Funnell MM, Butler PM, et al. Patient empowerment. Results of a randomized controlled trial. Diabetes Care 1995;18:943–9.
19. Von Korff M, Gruman J, Schaefer J, et al. Collaborative management of chronic illness. Ann Intern Med 1997;127:1097–102.
20. Campbell SM, Hann M, Hacker J, et al. Identifying predictors of high quality care in English general practice: observational study. BMJ 2001;323:784–7.
21. Bower P, Campbell S, Bojke C, Sibbald B. Team structure, team climate and the quality of care in primary care: an observational study. Qual Saf Health Care 2003;12:273–9.
22. Piette JD, Schillinger D, Potter MB, Heisler M. Dimensions of patient-provider communication and diabetes self-care in an ethnically diverse population. J Gen Intern Med 2003;18:624-33.
23. Kerr EA, Smith DM, Kaplan SH, Hayward RA. The association between three different measures of health status and satisfaction among patients with diabetes. Med Care Res Rev 2003;60:158-77.
24. Oshima Lee E, Emanuel EJ. Shared decision making to improve care and reduce costs. N Engl J Med 2013;368:6-8.
25. Barry MJ, Edgman-Levitan S. Shared decision making--pinnacle of patient-centered care. N Engl J Med 2012;366:780–1.
26. Truog RD. Patients and doctors--evolution of a relationship. N Engl J Med 2012;366:581–5.
27. Beverly EA, Wray LA, LaCoe CL, Gabbay R. Listening to older adults’ values and preferences for type 2 diabetes care: a qualitative study. Diabetes Spectrum 2014;27:44–9.
28. Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy 1979;26:252–60.
29. Ciechanowski PS, Katon WJ, Russo JE, Walker EA. The patient-provider relationship: attachment theory and adherence to treatment in diabetes. Am J Psychiatry 2001;158:29–35.
30. Ciechanowski P, Russo J, Katon W, et al. Influence of patient attachment style on self-care and outcomes in diabetes. Psychosom Med 2004;66:720–8.
31. Jahng KH, Martin LR, Golin CE, DiMatteo MR. Preferences for medical collaboration: patient-physician congruence and patient outcomes. Patient Educ Couns 2005;57:308–14.
32. Street RL Jr, Krupat E, Bell RA, et al. Beliefs about control in the physician-patient relationship: effect on communication in medical encounters. J Gen Intern Med 2003;18:609–16.
33. Heisler M, Bouknight RR, Hayward RA, et al. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med 2002;17:243–52.
34. Mechanic D. Changing medical organization and the erosion of trust. Milbank Q 1996;74:171–89.
35. Mechanic D, Schlesinger M. The impact of managed care on patients’ trust in medical care and their physicians. JAMA 1996;275:1693–7.
36. Pearson SD, Raeke LH. Patients’ trust in physicians: many theories, few measures, and little data. J Gen Intern Med 2000;15:509–13.
37. Jones DE, Carson KA, Bleich SN, Cooper LA. Patient trust in physicians and adoption of lifestyle behaviors to control high blood pressure. Patient Educ Couns 2012;89:57–62.
38. Mostashari F, Riley E, Selwyn PA, Altice FL. Acceptance and adherence with antiretroviral therapy among HIV-infected women in a correctional facility. J Acquired Immun Def Syndr Hum Retrovir 1998;18:341–8.
39. Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA 1999;282:583–9.
40. Ritholz MD, Beverly EA, Brooks KM, et al. Barriers and facilitators to self-care communication during medical appointments in the United States for adults with type 2 diabetes. Chronic Illn 2014;10:303–13.
41. Aikens JE, Bingham R, Piette JD. Patient-provider communication and self-care behavior among type 2 diabetes patients. Diabetes Educ 2005;31:681–90.
42. Bundesmann R, Kaplowitz SA. Provider communication and patient participation in diabetes self-care. Patient Educ Couns 2011;85:143–7.
43. Heisler M, Cole I, Weir D, et al. Does physician communication influence older patients’ diabetes self-management and glycemic control? Results from the Health and Retirement Study (HRS). J Gerontol A Biol Sci Med Sci 2007;62:1435–42.
44. Duffy FD, Gordon GH, Whelan G, et al. Assessing competence in communication and interpersonal skills: the Kalamazoo II report. Acad Med 2004;79:495–507.
45. Ritholz MD, Beverly EA, Brooks KM, et al. Barriers and facilitators to self-care communication during medical appointments in the United States for adults with type 2 diabetes. Chronic Illn 2014;10:303–13.
46. Ciechanowski P, Katon WJ. The interpersonal experience of health care through the eyes of patients with diabetes. Soc Sci Med 2006;63:3067–79.
47. Diabetes Control and Complications Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med 1993;329:977–86.
48. Peyrot M, Rubin RR, Lauritzen T, et al. Psychosocial problems and barriers to improved diabetes management: results of the Cross-National Diabetes Attitudes, Wishes and Needs (DAWN) Study. Diab Med 2005;22:1379–85.
49. DiMatteo MR, Linn LS, Chang BL, Cope DW. Affect and neutrality in physician behavior: a study of patients’ values and satisfaction. J Behav Med 1985;8:397–409.
50. Stuckey HL, Vallis M, Kovacs Burns K, et al. “I do my best to listen to patients”: qualitative insights into DAWN2 (Diabetes Psychosocial Care From the Perspective of Health Care Professionals in the Second Diabetes Attitudes, Wishes and Needs Study). Clin Ther 2015;37:1986–98.
51. Kruse RL, Olsberg JE, Oliver DP, et al. Patient-provider communication about diabetes self-care activities. Fam Med 2013;45:319–22.
52. Beverly EA, Hultgren BA, Brooks KM, et al. Understanding physicians’ challenges when treating type 2 diabetic patients’ social and emotional difficulties: a qualitative study. Diabetes Care 2011;34:1086–8.
53. Freeman J, Loewe R. Barriers to communication about diabetes mellitus. Patients’ and physicians’ different view of the disease. J Fam Pract 2000;49:507–12.
54. Gonzalez JS, Delahanty LM, Safren SA, et al. Differentiating symptoms of depression from diabetes-specific distress: relationships with self-care in type 2 diabetes. Diabetologia 2008;51:1822–5.
55. Fisher L, Hessler DM, Polonsky WH, Mullan J. When is diabetes distress clinically meaningful?: establishing cut points for the Diabetes Distress Scale. Diabetes Care 2012;35:259–64.
56. Polonsky WH, Anderson BJ, Lohrer PA, et al. Assessment of diabetes-related distress. Diabetes Care 1995;18:754–60.
57. Welch G, Weinger K, Anderson B, Polonsky WH. Responsiveness of the Problem Areas In Diabetes (PAID) questionnaire. Diabetic Med 2003;20:69–72.
58. Weinger K, Kinsley BT, Bajaj M, et al. Diabetes-related emotional distress: A barrier to improving glycemic control during intensive diabetes treatment. Abstract. Diabetes 1997;46:Supp1:268A.
59. Weinger K, Jacobson AM. Psychosocial and quality of life correlates of glycemic control during intensive treatment of type 1 diabetes. Patient Educ Couns 2001;42:123–31.
60. Fisher L, Chesla CA, Skaff MM, et al. The family and disease management in Hispanic and European-American patients with type 2 diabetes. Diabetes Care 2000;23:267–72.
61. Wen LK, Parchman ML, Shepherd MD. Family support and diet barriers among older Hispanic adults with type 2 diabetes. Fam Med 2004;36:423–30.
62. Chesla CA, Fisher L, Mullan JT, et al. Family and disease management in African-American patients with type 2 diabetes. Diabetes Care 2004;27:2850–5.
63. Brown SA, Harrist RB, Villagomez ET, et al. Gender and treatment differences in knowledge, health beliefs, and metabolic control in Mexican Americans with type 2 diabetes. Diabetes Educ 2000;26:425–38.
64. Fisher L, Chesla CA, Chun KM, et al. Patient-appraised couple emotion management and disease management among Chinese American patients with type 2 diabetes. J Fam Psychol 2004;18:302–10.
65. Akimoto M, Fukunishi I, Kanno K, et al. Psychosocial predictors of relapse among diabetes patients: a 2-year follow-up after inpatient diabetes education. Psychosomatics 2004;45:343–9.
66. Samuel-Hodge CD, Headen SW, Skelly AH, et al. Influences on day-to-day self-management of type 2 diabetes among African-American women: spirituality, the multi-caregiver role, and other social context factors. Diabetes Care 2000;23:928–33.
67. Wing RR, Marcus MD, Epstein LH, Jawad A. A “family-based” approach to the treatment of obese type II diabetic patients. J Consult Clin Psychol 1991;59:156–62.
68. Trief PM, Ploutz-Snyder R, Britton KD, Weinstock RS. The relationship between marital quality and adherence to the diabetes care regimen. Ann Behav Med 2004;27:148–54.
69. Gleeson-Kreig J, Bernal H, Woolley S. The role of social support in the self-management of diabetes mellitus among a Hispanic population. Pub Health Nurs 2002;19:215–22.
70. Wen LK, Shepherd MD, Parchman ML. Family support, diet, and exercise among older Mexican Americans with type 2 diabetes. Diabetes Educ 2004;30:980–93.
71. Ruggiero L. Helping people with diabetes change behavior: from theory to practice. Diab Spectrum 2000;13:125–32.
72. Orr DP, Golden MP, Myers G, Marrero DG. Characteristics of adolescents with poorly controlled diabetes referred to a tertiary care center. Diabetes Care 1983;6:170–5.
73. Lane JD, Stabler B, Ross SL, et al. Psychological predictors of glucose control in patients with IDDM. Diabetes Care 1988;11:798–800.
74. Irvine AA, Cox D, Gonder-Frederick L. Fear of hypoglycemia: relationship to physical and psychological symptoms in patients with insulin-dependent diabetes mellitus. Health Psychology 1992;11:135–8.
75. Irvine A, Cox D, Gonder-Frederick L. The fear of hypoglycemia scale. In: Bradley C, editor. Handbook of psychology and diabetes. Harwood Academic; 1994.
76. Peyrot MF, McMurry JF Jr. Stress buffering and glycemic control. The role of coping styles. Diabetes Care 1992;15:842–6.
77. Peyrot M, McMurry JF Jr, Kruger DF. A biopsychosocial model of glycemic control in diabetes: stress, coping and regimen adherence. J Health Soc Behav 1999;40:141–58.
78. Berkman ND, Sheridan SL, Donahue KE, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155:97–107.
79. Sohal S, Sohal P, King-Shier KM, Khan NA. Barriers and facilitators for type-2 diabetes management in South Asians: a systematic review. PloS One 2015:1–15.
80. Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med 2003;163:83–90.
81. Miller WR, Rollnick S. Motivational interviewing: preparing people for change. New York: Guilford Press; 2002.
82. Powell PW, Corathers SD, Raymond J, Streisand R. New approaches to providing individualized diabetes care in the 21st century. Curr Diabetes Rev 2015;11:222–30.
83. Jones AJ, Gladstone BP, Lubeck M, et al. Motivational interventions in the management of HbA1c levels: A systematic review and meta-analysis. Prim Care Diabetes 2014;8:91–100.
84. Song D, Xu TZ, Sun QH. Effect of motivational interviewing on self-management in patients with type 2 diabetes mellitus: a meta-analysis. Intl J Nurs Sci 2014;1:291–7.
85. Clifford Mulimba A, Byron-Daniel J. Motivational interviewing-based interventions and diabetes mellitus. Br J Nurs 2014;23:8–14.
86. Noordman J, van der Weijden T, van Dulmen S. Communication-related behavior change techniques used in face-to-face lifestyle interventions in primary care: a systematic review of the literature. Patient Educ Couns 2012;89:227–44.
87. Soderlund LL, Madson MB, Rubak S, Nilsen P. A systematic review of motivational interviewing training for general health care practitioners. Patient Educ Couns 2011;84:16–26.
88. Kang SH, Kim BG, Lee GM. Justification of continuous packed-bed reactor for retroviral vector production from amphotropic PsiCRIP murine producer cell. Cytotechnology 2000;34(1–2):151–8.
89. Holmen H, Torbjornsen A, Wahl AK, et al. A mobile health intervention for self-management and lifestyle change for persons with type 2 diabetes, part 2: one-year results from the Norwegian randomized controlled trial RENEWING HEALTH. JMIR mHealth uHealth 2014;2(4):e57.
90. Chlebowy DO, El-Mallakh P, Myers J, et al. Motivational interviewing to improve diabetes outcomes in African Americans adults with diabetes. West J Nurs Res 2015;37:566–80.
91. Kang HY, Gu MO. [Development and effects of a motivational interviewing self-management program for elderly patients with diabetes mellitus]. J Kor Acad Nurs 2015;45:533–43.
92. Brobeck E, Odencrants S, Bergh H, Hildingh C. Patients’ experiences of lifestyle discussions based on motivational interviewing: a qualitative study. BMC Nursing 2014;13:13.
93. Loskutova NY, Tsai AG, Fisher EB, et al. Patient navigators connecting patients to community resources to improve diabetes outcomes. J Am Board Fam Med 2016;29:78–89.
94. Raiff BR, Barry VB, Ridenour TA, Jitnarin N. Internet-based incentives increase blood glucose testing with a non-adherent, diverse sample of teens with type 1 diabetes mellitus: a randomized controlled Trial. Trans Behav Med 2016;6:179–88.
95. Sahlen KG, Johansson H, Nystrom L, Lindholm L. Health coaching to promote healthier lifestyle among older people at moderate risk for cardiovascular diseases, diabetes and depression: a study protocol for a randomized controlled trial in Sweden. BMC Public Health 2013;13:199.
96. Kane EP, Collinsworth AW, Schmidt KL, et al. Improving diabetes care and outcomes with community health workers. Fam Pract 2016;33:523–8.
97. Wagner JA, Bermudez-Millan A, Damio G, et al. A randomized, controlled trial of a stress management intervention for Latinos with type 2 diabetes delivered by community health workers: Outcomes for psychological wellbeing, glycemic control, and cortisol. Diabetes Res Clin Pract 2016;120:162–70.
98. Rogers EA, Hessler DM, Bodenheimer TS, et al. Diabetes peer coaching: do “better patients” make better coaches? Diabetes Educ 2014;40:107–15.
99. Long JA, Jahnle EC, Richardson DM, et al. Peer mentoring and financial incentives to improve glucose control in African American veterans: a randomized trial. Ann Intern Med 2012;156:416–24.
100. Mundt MP, Agneessens F, Tuan WJ, et al. Primary care team communication networks, team climate, quality of care, and medical costs for patients with diabetes: A cross-sectional study. Int J Nurs Stud 2016;58:1–11.
101. Fisher L, Mullan JT, Arean P, et al. Diabetes distress but not clinical depression or depressive symptoms is associated with glycemic control in both cross-sectional and longitudinal analyses. Diabetes Care 2010;33:23–8.
102. Fisher L, Glasgow RE, Strycker LA. The relationship between diabetes distress and clinical depression with glycemic control among patients with type 2 diabetes. Diabetes Care 2010;33:1034–6.
103. Ricci-Cabello I, Olry de Labry-Lima A, Bolivar-Munoz J, et al. Effectiveness of two interventions based on improving patient-practitioner communication on diabetes self-management in patients with low educational level: study protocol of a clustered randomized trial in primary care. BMC Health Serv Res 2013;13:433.
104. Billimek J, Guzman H, Angulo MA. Effectiveness and feasibility of a software tool to help patients communicate with doctors about problems they face with their medication regimen (EMPATHy): study protocol for a randomized controlled trial. Trials 2015;16:145.
105. Grant RW, Uratsu CS, Estacio KR, et al. Pre-Visit Prioritization for complex patients with diabetes: Randomized trial design and implementation within an integrated health care system. Contemp Clin Trials 2016;47:196–201.
106. Ritholz MD, Beverly EA, Abrahamson MJ, et al. Physicians’ perceptions of the type 2 diabetes multidisciplinary treatment team: a qualitative study. Diabetes Educ 2011.
107. Ley P. Satisfaction, compliance and communication. Br J Clin Psychol 1982;21:241–54.
108. Weinger K, Smaldone A, Beverly EA. Psychosocial and educational implications of diabetic foot complications. In: Veves A, Giurini JM, LoGerfo FW, editors. The diabetic foot: medical and surgical management. Boston: Springer; 2012:503–18.
109. Welch G, Rose G, Ernst D. Motivational interviewing and diabetes: what is it, how is it used, and does it work? Diabetes Spectr 2006;19:5–11.
110. Kaplan SH, Greenfield S, Ware JE Jr. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care 1989;27(3 Suppl):S110–27.
111. Nelson KM, Reiber G, Boyko EJ. Diet and exercise among adults with type 2 diabetes: findings from the third national health and nutrition examination survey (NHANES III). Diabetes Care 2002;25:1722–8.
112. Wens J, Vermeire E, Royen PV, et al. GPs’ perspectives of type 2 diabetes patients’ adherence to treatment: A qualitative analysis of barriers and solutions. BMC Fam Pract 2005;6:20.
Abstract
- Objective: To summarize the current literature, research findings, and interventions for self-care communication in the physician-patient relationship.
- Methods: Literature review.
- Results: Diabetes management requires patients to follow complex self-care recommendations for nutrition, physical activity, blood glucose monitoring, and medication. Adherence to these recommendations improves glycemic control and mitigates the risk of diabetes complications; however, many patients struggle to follow these behaviors in everyday life. In the physician-patient relationship, self-care communication is largely influenced by interpersonal trust. Physicians need to incorporate interpersonal and relational skills to establish a trusting relationship. Physician-level barriers to self-care communication include lack of time, lack of collaboration and teamwork among health care providers, lack of patients’ access to resources, and lack of psychosocial support for diabetes patients. Among patients, psychosocial barriers and health literacy may affect willingness to discuss self-care. Motivational interviewing techniques may be helpful for improving communication around patient self-management and promotion of healthy behaviors.
- Conclusion: Physicians can assist patients with their diabetes self-care by discussing self-care challenges during medical visits.
Diabetes is one of the most significant and growing chronic health problems in the world, affecting approximately 415 million people [1]. Diabetes is marked by the body’s inability to make insulin as well as the body’s inability to effectively use the insulin it produces [2]. Diagnosis of diabetes has increased sharply in recent decades and is expected to increase even more, with the largest increases in middle- and low-income countries [3]. Diabetes is a leading cause of blindness, kidney failure, myocardial infarction, stroke, and amputation [3], and in 2015 it accounted for 5 million deaths worldwide [1]. Further, diabetes’s costs to society represent 12% ($673 billion) of global health expenditures [1]. By 2040, models predict that 642 million people will be diagnosed with diabetes and costs will continue to grow as the population ages [1]. Thus, prevention of diabetes is the ultimate goal; however, more effective management for individuals already diagnosed with diabetes is critical to reduce the risk of complications and the economic burden of the disease.
Diabetes management requires patients to perform complex self-care regimens, including weight reduction, frequent blood glucose monitoring, taking oral and/or insulin medications, engaging in physical activity, adhering to diabetes nutrition guidelines, and attending clinic appointments [4–9]. These self-care behaviors are critically linked to improved glycemic control, however, integrating them into one’s daily life can be challenging [10–12]. Recent National Health and Nutrition Examination Survey (NHANES) data show that approximately half of adults with diabetes are not meeting recommended goals for diabetes care [13]. Physicians can assist patients with their diabetes self-care by scheduling frequent follow-up visits and discussing self-care challenges with their patients [14].
In this review, we discuss the current literature on physician-patient communication and diabetes self-care. First, we discuss the qualities of an effective physician-patient relationship followed by the importance of self-care communication in diabetes care. Next, we discuss barriers and facilitators to self-care communication. Finally, we review interventions for improving physician-patient communication in diabetes self-care.
Qualities of an Effective Physician-Patient Relationship
Successful diabetes care requires teamwork between physicians and patients [15]. Two components of successful teamwork are physician-patient communication and shared decision-making, both of which have been shown to improve patient satisfaction, adherence to treatment plans and health outcomes [16–23]. In shared decision-making, the physician and patient share medical information [24–26]. Specifically, the physician presents different treatment options to the patient and describes the risks and benefits of each option. Then the patient expresses his or her preferences for treatment to ensure that the care provided aligns with the patient’s values and needs [27]. Thus, shared decision-making in the treatment relationship is predicated on effective communication between the physician and patient [19].
Effective physician-patient communication is supported by continuous care [19,28], a secure attachment style [29, 30], shared goals [19], a mutual understanding of respective roles and tasks [15,31–33], and a bond characterized by liking, confidence, and trust [19,28,31]. Trust is paramount in physician-patient communication. Interpersonal trust and social trust are the 2 predominant types [34]. Interpersonal trust refers to the relationship the patient has with the physician, specifically the confidence the patient has in the physician as well as the responsibility, competence, compassion, and regard the physician has for the patient’s welfare [34–36]. For patients and physicians, interpersonal trust is developed over time with repeated interactions [34–36]. On the other hand, social trust refers to the beliefs of honesty, integrity, and reliability in others [36]. Social trust is influenced by social constructs, including the media and institutions of higher education [36].
In the physician-patient relationship, self-care communication is largely influenced by interpersonal trust. A patient’s trust can be acquired through multiple medical appointments with the physician. Further, how the patient is treated during these appointments as well as how much time and attention the physician invests in the patient’s care influences the level of interpersonal trust. A high level of trust in the relationship can lead to in improvements in adherence to self-care, continuity of care, physician-patient communication, and overall quality of the physician-patient relationship [37–39].
In the diabetes physician-patient relationship, minimal research has explored how trust in one’s physician impacts self-care communication. In a study by Beverly and colleagues, diabetes patients emphasized the importance of a trusting physician-patient relationship for diabetes care [27]. Another study by Ritholz and colleagues found that physicians and patients both stress the importance of developing trust to facilitate self-care communication [40]. Specifically, trust as well as acceptance from the physician contributes to open and honest self-care communication in the physician-patient diabetes relationship[40]. Additional research is needed to determine whether a high level of physician-patient trust is associated with increased self-care behaviors and improved diabetes outcomes over time.
Importance of Diabetes Self-Care Communication
Diabetes self-care communication in the physician-patient relationship increases patient satisfaction, improves adherence to treatment regimens, and leads to better clinical outcomes [22,41–43]. For physicians, effective self-care communication requires the performance of specific communication tasks and behaviors, including collecting a medical history, explaining a diagnosis and prognosis, and providing clear and concise therapeutic instructions [44]. In addition, physicians must incorporate interpersonal and relational skills to establish a trusting relationship [44,45]. Both physicians and patients agree that a trusting treatment relationship is a requirement for open and honest self-care communication [45]. For patients, effective communication necessitates the disclosure of self-care successes and failures [46]. Diabetes patients face challenging self-care regimens, and these challenges can interfere with glycemic control and increase the risk for diabetes complications [47,48]. For this reason, patients must feel comfortable discussing their self-are challenges so that their physician can individualize treatment prescriptions and recommendations, thereby increasing the likelihood of treatment success.
Barriers to Self-Care Communication
Physician-patient self-care communication is essential to improving patient adherence [29,49] yet numerous barriers exist that undermine effective physician-patient self-care communication. From the physician perspective, the most commonly cited barrier to self-care communication is time [50]. A recent study of family medicine practices found that the time physicians spent discussing self-care with their patients varied from 1 to 17 minutes, suggesting that time is a major barrier to self-care communication [51]. Other barriers include lack of collaboration and teamwork among health care providers, lack of patients’ access to resources, and lack of psychosocial support for patients with diabetes [50]. Relatedly, Beverly and colleagues [52] found that physicians often feel inadequately trained to address diabetes patients’ psychosocial issues and this perceived lack of expertise may contribute to physicians feeling overwhelmed and frustrated within the physician-patient relationship, which may hinder open self-care communication.
For patients, barriers tend to differ from those perceived by physicians. A qualitative study using semi-structured interviews with patients and clinicians, and direct observation of clinical encounters at an inner-city family practice training site, revealed different perceptions of the term “control” between physicians and patients. In practice, physicians used the term “control” to focus on the management of blood glucose levels rather than trying to understand the patients’ understanding of diabetes and subsequent treatment goals. Differing viewpoints contributed to frustration and hindered effective communication [53]. In another qualitative study with physicians and patients, both noted that patients were reluctant to discuss self-care for fear being judged or shamed about food intake and weight [45]. This finding was supported in a quantitative follow-up study assessing patient reluctance to discuss self-care. Thirty percent of surveyed patients reported reluctance to discussing self-care with their physicians for fear of being judged, not wanting to disappoint their doctors, guilt, and shame [14]. Interestingly, patients reporting elevated depressive symptoms were more likely to be reluctant to discuss their self-care [14]. Cognitive behavioral changes (eg, cognitive distortions, avoidance behavior, attention deficits) associated with major depression and depressive symptoms may impair patients’ ability to recall self-care information. Also, patients reporting more depressive symptoms may be more socially withdrawn during a medical appointment, and thus less willing to communicate with their physician about self-care.
Other studies found that psychosocial factors such as diabetes distress [54,55] and pessimistic attitudes [56–59], cultural differences [60–66], lack of family and social support [60,67–70], lack of readiness to change behavior [71], introversion and social isolation [72,73], hypo-glycemia fear [74,75] and ineffectual coping styles [76,77] interfere with self-care and glycemic control. Further, low health literacy is associated with difficulty adhering to self-care, particular medication regimens, and negative health outcomes [78].
In summary psychosocial barriers and health literacy may affect a patients’ willingness to discuss self-care during a medical visit. Therefore, routine assessment of psychosocial factors and health literacy may be necessary to address a patient’s barriers to self-care as well as to promote open and honest self-care communication. Interventions and evidenced-based approaches that address psychosocial factors, health literacy, and physician-patient self-care communication are needed.
Facilitators to Self-Care Communication
Despite numerous barriers to self-care communication, several factors promote self-care communication in the physician-patient relationship. For example, direct and non-accusatory communication from physicians as well as providing patients with hope for living with diabetes both support physician-patient self-care communication [45]. A recent systematic review by Sohal and colleagues [79] found that trust in physicians, the use of culturally appropriate exercise and dietary advice, and increasing family involvement improved physician-patient communication and diabetes self-care [79]. Lastly, a study by Schillinger and colleagues [80] found that physician assessment of patient recall and comprehension of new concepts during medical visits improved diabetes outcomes [80].
Patient-Physician Self-Care Communication Interventions
One of the more successful interventions for improving diabetes self-care and patient-physician communication is motivational interviewing (MI). MI is a non-judgmental communication style designed to explore a patient’s intrinsic motivation to change health behaviors [81]. Inherent to MI is the belief that motivation for change is malleable and that it can be transformed in the context of the patient-physician relationship [81]. MI is a patient-centered method designed to empower a patient’s ability and responsibility to make health-related decisions, with the physician supporting the patient’s autonomy in the process [82]. Recent meta-analyses and systematic reviews [83–87] showed that MI interventions improve self-care behaviors and glycemic control in the short-term; long-term effects of MI on self-care and glycemia remain inconclusive. More high-quality research is needed to evaluate the MI training content of these interventions in order to determine its long-term effectiveness and replicate outcomes in various healthcare settings [87].
Other studies not included in the meta-analyses and reviews found MI interventions improved self-care behaviors [88–90], glycemic control [90,91], and quality of life [91]. A qualitative study exploring diabetes patients’ experiences with MI and self-care behaviors revealed that patients’ appreciate when providers initiate discussions that result in new ways of thinking about self-care and promote a sense of well-being in patients [92]. New research utilizing patient navigators to connect diabetes patients’ to their primary care providers showed MI techniques improved patient self-efficacy and glycemic control [93]. Another study, an internet-based incentives study, found that the application of a brief MI interviewing session improved blood glucose monitoring in adolescents with type 1 diabetes [94]. Thus, creative strategies that employ MI techniques in collaboration with other members of the health care team (ie, patient navigation [93], telehealth [89], health coaching [95], internet-based tools [94]) hold promise for improving self-care and patient-physician communication. Increased collaboration with members of the health care team (eg, certified diabetes educators, nurses, dietitians, pharmacists, exercise physiologists), community health workers [96,97] and peer mentors [98,99] may help reinforce messages, promote shared decision-making, improve diabetes outcomes, increase patient satisfaction, and reduce medical costs [100].
Few other interventions have directly addressed physician-patient diabetes self-care communication. One older study examined the effectiveness of an intervention designed to increase of diabetes patients’ involvement in medical decision-making [16]. Patients randomized to the intervention arm participated in a 20-minute session prior to meeting with their physician, in which researchers reviewed their medical chart and used systematic prompts to encourage patients to negotiate medical decisions with their physician. Patients in the control arm received standard educational materials in a session of equal length. Patients in the intervention arm improved glycemia and elicited twice the amount of medical information from their physician compared to controls [16]. These findings suggest that brief interventions prior to medical appointments can improve patient communication, self-care behavior, and in turn, diabetes outcomes [16].
A recent study evaluated the effectiveness of a training program in communication skills for pediatric diabetes care providers in the UK [101, 102]. In this cluster randomized controlled trial, pediatric providers allocated to the Talking Diabetes intervention participated in web-based material and face-to-face seminars designed to prepare providers for constructive self-care conversations with patients as well as skills for promoting behavior change. The psychoeducational training emphasized shared decision-making and utilized motivational interviewing techniques [101]. Twenty-six centers and 693 young people with type 1 diabetes participated in the study [102]. At 12-month follow-up, the Talking Diabetes intervention did not demonstrate improvements in glycemic control. Further, the intervention had a negative effect on patients’ quality of life but a short-term improvement in coping [102]. Interestingly, parents of patients in the intervention arm reported greater continuity of care, which suggests that parents benefited more from the intervention than their children. Future communication interventions targeting the pediatric population should provide ongoing support to children of physicians exposed to interventions such as Talking Diabetes [102].
Currently, 3 ongoing studies aim to improve self-care and clinical outcomes via physician-patient communication interventions. A study by Ricci-Cabello and colleagues [103] aims to improve diabetes self-care by enhancing patient-physician communication in an underserved community of adults with uncontrolled type 2 diabetes. In this 3-arm randomized controlled trial, patients allocated to groups A and B received communication skills training and graphic feedback about glycosylated hemoglobin A1c levels; patients in group C received usual care. Patients in group B also received telephone reinforcement [103]. The second study, by Billimek and colleagues, aims to improve physician-patient communication about medication regimens via diabetes coaching [104]. In this intervention, 190 Mexican-American adult patients with type 2 diabetes were randomly assigned to complete a Coached Care visit with trained community health workers or a Coached Care visit plus the EMPATHy software toolkit, a computer-based activity with strategies and resources to overcome self-care barriers. The primary endpoints are (1) the development of care plan that addresses everyday barriers to medication adherence and (2) completion of a concrete behavioral goal [104]. Finally, the third study, by Grant and colleagues, aims to improve physician-patient communication via a pre-visit prioritization of diabetes concerns. In this controlled, cluster-randomized, multisite trial, primary care physicians were randomized to the Pre-Visit Prioritization for Complex Patients with Diabetes or the control group [105]. The Pre-Visit Prioritization IT-tool is designed to help patients identify one or two concerns prior to a medical visit and then send these priorities to the primary care physician via an electronic health record. The overall goal of the intervention is to improve communication of self-care concerns during a medical visit [105]. Findings from these 3 interventions are forthcoming; findings may provide evidence for validated interventions that improve physician-patient self-care communication in diabetes.
Techniques to Improve Self-Care Communication
Incorporating communication skills in continuing medical education and diabetes education may improve self-care communication in the physician-patient relationship. Educational programs that teach physicians how to provide consistent messages, repeat information, reinforce and offer feedback regarding specific self-care behaviors, and problem-solve self-care challenges may improve patients’ willingness to discuss self-care [14,106]. Most patients will remember only a small portion of the information given to them during medical visit. Studies that compare how much information patients retain versus how much information physicians provide show that patients forget 31% to 71% of information [107]. Therefore, physicians need techniques that promote open self-care communication during a visit. The following techniques can help physicians improve self-care communication [108]:
- Discuss the most important self-care information first; patients tend to remember the information that is presented first.
- Use the phrase “This is very important…” when discussing key points because patients will remember things that are perceived as important.
- Deliver simple, clear, and concrete instructions; patients are more likely to forget complex or confusing instructions. For example, “Check your blood glucose every morning within five minutes of waking up and before you eat breakfast” is more specific and easier to follow than “Check your blood glucose”.
- Ask open-ended questions to allow patients to verbalize feelings or concerns about their diabetes self-care.
- Employ MI techniques to help patients who are struggling to initiate and adhere to self-care behaviors. MI tools, such as the Readiness Ruler, Self-Evaluation Rulers, Decisional Balance Matrix, and Health Behavior Menu (Figure), may help patients and physicians discuss self-care behaviors during a medical visit [109].
– Express empathy by reflective listening and asking patients for permission before offering information or advice about diabetes self-care.
– Roll with resistance by engaging the patient in the process of problem solving rather than opposing a patient’s resistance to change behaviors.
– Develop discrepancy by helping the patient recognize that there is an inconsistency between his/her behavior and personal goals.
– Support self-efficacy by empowering the patient to believe that he/she can change behaviors.
6. Demonstrate active listening skills by reflecting and summarizing the patient’s statements. Reflecting and summarizing show the patient that the physician has been listening to concerns and understands what the patient is saying. This is also an opportunity to correct any miscommunications from the visit.
7. Write down instructions or provide handouts to the patient to help reinforce learning and information retention.
8. Ask patients to write a list of questions a few days prior to the medical appointment and bring it with them. Patients are more likely to remember information about issues they have previously considered that directly relate to them.
9. Consider collaborating with community health workers, patient navigators, peer mentors, and other members of the healthcare team to improve communication, diabetes outcomes, and patient satisfaction.
Summary
Physician-patient self-care communication is essential to achieving optimal diabetes outcomes [15,22,33,110] Patients’ ability to inform physicians about their self-care challenges [14], and physicians’ ability to respond to patients’ self-care reports directly and in non-accusatory language, are vital factors in effective diabetes care [45]. Interventions and education that promote open and honest conversations are particularly important given patients’ well-documented struggles achieving self-care and glycemic goals [111] and physicians’ feelings of inadequacy, frustration, and fatigue when they are not making an impact on patients’ outcomes [48,112]. More research is needed to determine the best strategies to improve self-care communication in the physician-patient relationship.
Corresponding author: Elizabeth A. Beverly, PhD, Department of Family Medicine, Ohio University Heritage College of Osteopathic Medicine, Athens, OH 45701, [email protected].
Financial disclosures: None.
Author contributions: drafting of article, EAB, MFW, ABC, KEP, NNI; critical revision of the article, EAB, MFW, ABC, KEP, NNI.
Abstract
- Objective: To summarize the current literature, research findings, and interventions for self-care communication in the physician-patient relationship.
- Methods: Literature review.
- Results: Diabetes management requires patients to follow complex self-care recommendations for nutrition, physical activity, blood glucose monitoring, and medication. Adherence to these recommendations improves glycemic control and mitigates the risk of diabetes complications; however, many patients struggle to follow these behaviors in everyday life. In the physician-patient relationship, self-care communication is largely influenced by interpersonal trust. Physicians need to incorporate interpersonal and relational skills to establish a trusting relationship. Physician-level barriers to self-care communication include lack of time, lack of collaboration and teamwork among health care providers, lack of patients’ access to resources, and lack of psychosocial support for diabetes patients. Among patients, psychosocial barriers and health literacy may affect willingness to discuss self-care. Motivational interviewing techniques may be helpful for improving communication around patient self-management and promotion of healthy behaviors.
- Conclusion: Physicians can assist patients with their diabetes self-care by discussing self-care challenges during medical visits.
Diabetes is one of the most significant and growing chronic health problems in the world, affecting approximately 415 million people [1]. Diabetes is marked by the body’s inability to make insulin as well as the body’s inability to effectively use the insulin it produces [2]. Diagnosis of diabetes has increased sharply in recent decades and is expected to increase even more, with the largest increases in middle- and low-income countries [3]. Diabetes is a leading cause of blindness, kidney failure, myocardial infarction, stroke, and amputation [3], and in 2015 it accounted for 5 million deaths worldwide [1]. Further, diabetes’s costs to society represent 12% ($673 billion) of global health expenditures [1]. By 2040, models predict that 642 million people will be diagnosed with diabetes and costs will continue to grow as the population ages [1]. Thus, prevention of diabetes is the ultimate goal; however, more effective management for individuals already diagnosed with diabetes is critical to reduce the risk of complications and the economic burden of the disease.
Diabetes management requires patients to perform complex self-care regimens, including weight reduction, frequent blood glucose monitoring, taking oral and/or insulin medications, engaging in physical activity, adhering to diabetes nutrition guidelines, and attending clinic appointments [4–9]. These self-care behaviors are critically linked to improved glycemic control, however, integrating them into one’s daily life can be challenging [10–12]. Recent National Health and Nutrition Examination Survey (NHANES) data show that approximately half of adults with diabetes are not meeting recommended goals for diabetes care [13]. Physicians can assist patients with their diabetes self-care by scheduling frequent follow-up visits and discussing self-care challenges with their patients [14].
In this review, we discuss the current literature on physician-patient communication and diabetes self-care. First, we discuss the qualities of an effective physician-patient relationship followed by the importance of self-care communication in diabetes care. Next, we discuss barriers and facilitators to self-care communication. Finally, we review interventions for improving physician-patient communication in diabetes self-care.
Qualities of an Effective Physician-Patient Relationship
Successful diabetes care requires teamwork between physicians and patients [15]. Two components of successful teamwork are physician-patient communication and shared decision-making, both of which have been shown to improve patient satisfaction, adherence to treatment plans and health outcomes [16–23]. In shared decision-making, the physician and patient share medical information [24–26]. Specifically, the physician presents different treatment options to the patient and describes the risks and benefits of each option. Then the patient expresses his or her preferences for treatment to ensure that the care provided aligns with the patient’s values and needs [27]. Thus, shared decision-making in the treatment relationship is predicated on effective communication between the physician and patient [19].
Effective physician-patient communication is supported by continuous care [19,28], a secure attachment style [29, 30], shared goals [19], a mutual understanding of respective roles and tasks [15,31–33], and a bond characterized by liking, confidence, and trust [19,28,31]. Trust is paramount in physician-patient communication. Interpersonal trust and social trust are the 2 predominant types [34]. Interpersonal trust refers to the relationship the patient has with the physician, specifically the confidence the patient has in the physician as well as the responsibility, competence, compassion, and regard the physician has for the patient’s welfare [34–36]. For patients and physicians, interpersonal trust is developed over time with repeated interactions [34–36]. On the other hand, social trust refers to the beliefs of honesty, integrity, and reliability in others [36]. Social trust is influenced by social constructs, including the media and institutions of higher education [36].
In the physician-patient relationship, self-care communication is largely influenced by interpersonal trust. A patient’s trust can be acquired through multiple medical appointments with the physician. Further, how the patient is treated during these appointments as well as how much time and attention the physician invests in the patient’s care influences the level of interpersonal trust. A high level of trust in the relationship can lead to in improvements in adherence to self-care, continuity of care, physician-patient communication, and overall quality of the physician-patient relationship [37–39].
In the diabetes physician-patient relationship, minimal research has explored how trust in one’s physician impacts self-care communication. In a study by Beverly and colleagues, diabetes patients emphasized the importance of a trusting physician-patient relationship for diabetes care [27]. Another study by Ritholz and colleagues found that physicians and patients both stress the importance of developing trust to facilitate self-care communication [40]. Specifically, trust as well as acceptance from the physician contributes to open and honest self-care communication in the physician-patient diabetes relationship[40]. Additional research is needed to determine whether a high level of physician-patient trust is associated with increased self-care behaviors and improved diabetes outcomes over time.
Importance of Diabetes Self-Care Communication
Diabetes self-care communication in the physician-patient relationship increases patient satisfaction, improves adherence to treatment regimens, and leads to better clinical outcomes [22,41–43]. For physicians, effective self-care communication requires the performance of specific communication tasks and behaviors, including collecting a medical history, explaining a diagnosis and prognosis, and providing clear and concise therapeutic instructions [44]. In addition, physicians must incorporate interpersonal and relational skills to establish a trusting relationship [44,45]. Both physicians and patients agree that a trusting treatment relationship is a requirement for open and honest self-care communication [45]. For patients, effective communication necessitates the disclosure of self-care successes and failures [46]. Diabetes patients face challenging self-care regimens, and these challenges can interfere with glycemic control and increase the risk for diabetes complications [47,48]. For this reason, patients must feel comfortable discussing their self-are challenges so that their physician can individualize treatment prescriptions and recommendations, thereby increasing the likelihood of treatment success.
Barriers to Self-Care Communication
Physician-patient self-care communication is essential to improving patient adherence [29,49] yet numerous barriers exist that undermine effective physician-patient self-care communication. From the physician perspective, the most commonly cited barrier to self-care communication is time [50]. A recent study of family medicine practices found that the time physicians spent discussing self-care with their patients varied from 1 to 17 minutes, suggesting that time is a major barrier to self-care communication [51]. Other barriers include lack of collaboration and teamwork among health care providers, lack of patients’ access to resources, and lack of psychosocial support for patients with diabetes [50]. Relatedly, Beverly and colleagues [52] found that physicians often feel inadequately trained to address diabetes patients’ psychosocial issues and this perceived lack of expertise may contribute to physicians feeling overwhelmed and frustrated within the physician-patient relationship, which may hinder open self-care communication.
For patients, barriers tend to differ from those perceived by physicians. A qualitative study using semi-structured interviews with patients and clinicians, and direct observation of clinical encounters at an inner-city family practice training site, revealed different perceptions of the term “control” between physicians and patients. In practice, physicians used the term “control” to focus on the management of blood glucose levels rather than trying to understand the patients’ understanding of diabetes and subsequent treatment goals. Differing viewpoints contributed to frustration and hindered effective communication [53]. In another qualitative study with physicians and patients, both noted that patients were reluctant to discuss self-care for fear being judged or shamed about food intake and weight [45]. This finding was supported in a quantitative follow-up study assessing patient reluctance to discuss self-care. Thirty percent of surveyed patients reported reluctance to discussing self-care with their physicians for fear of being judged, not wanting to disappoint their doctors, guilt, and shame [14]. Interestingly, patients reporting elevated depressive symptoms were more likely to be reluctant to discuss their self-care [14]. Cognitive behavioral changes (eg, cognitive distortions, avoidance behavior, attention deficits) associated with major depression and depressive symptoms may impair patients’ ability to recall self-care information. Also, patients reporting more depressive symptoms may be more socially withdrawn during a medical appointment, and thus less willing to communicate with their physician about self-care.
Other studies found that psychosocial factors such as diabetes distress [54,55] and pessimistic attitudes [56–59], cultural differences [60–66], lack of family and social support [60,67–70], lack of readiness to change behavior [71], introversion and social isolation [72,73], hypo-glycemia fear [74,75] and ineffectual coping styles [76,77] interfere with self-care and glycemic control. Further, low health literacy is associated with difficulty adhering to self-care, particular medication regimens, and negative health outcomes [78].
In summary psychosocial barriers and health literacy may affect a patients’ willingness to discuss self-care during a medical visit. Therefore, routine assessment of psychosocial factors and health literacy may be necessary to address a patient’s barriers to self-care as well as to promote open and honest self-care communication. Interventions and evidenced-based approaches that address psychosocial factors, health literacy, and physician-patient self-care communication are needed.
Facilitators to Self-Care Communication
Despite numerous barriers to self-care communication, several factors promote self-care communication in the physician-patient relationship. For example, direct and non-accusatory communication from physicians as well as providing patients with hope for living with diabetes both support physician-patient self-care communication [45]. A recent systematic review by Sohal and colleagues [79] found that trust in physicians, the use of culturally appropriate exercise and dietary advice, and increasing family involvement improved physician-patient communication and diabetes self-care [79]. Lastly, a study by Schillinger and colleagues [80] found that physician assessment of patient recall and comprehension of new concepts during medical visits improved diabetes outcomes [80].
Patient-Physician Self-Care Communication Interventions
One of the more successful interventions for improving diabetes self-care and patient-physician communication is motivational interviewing (MI). MI is a non-judgmental communication style designed to explore a patient’s intrinsic motivation to change health behaviors [81]. Inherent to MI is the belief that motivation for change is malleable and that it can be transformed in the context of the patient-physician relationship [81]. MI is a patient-centered method designed to empower a patient’s ability and responsibility to make health-related decisions, with the physician supporting the patient’s autonomy in the process [82]. Recent meta-analyses and systematic reviews [83–87] showed that MI interventions improve self-care behaviors and glycemic control in the short-term; long-term effects of MI on self-care and glycemia remain inconclusive. More high-quality research is needed to evaluate the MI training content of these interventions in order to determine its long-term effectiveness and replicate outcomes in various healthcare settings [87].
Other studies not included in the meta-analyses and reviews found MI interventions improved self-care behaviors [88–90], glycemic control [90,91], and quality of life [91]. A qualitative study exploring diabetes patients’ experiences with MI and self-care behaviors revealed that patients’ appreciate when providers initiate discussions that result in new ways of thinking about self-care and promote a sense of well-being in patients [92]. New research utilizing patient navigators to connect diabetes patients’ to their primary care providers showed MI techniques improved patient self-efficacy and glycemic control [93]. Another study, an internet-based incentives study, found that the application of a brief MI interviewing session improved blood glucose monitoring in adolescents with type 1 diabetes [94]. Thus, creative strategies that employ MI techniques in collaboration with other members of the health care team (ie, patient navigation [93], telehealth [89], health coaching [95], internet-based tools [94]) hold promise for improving self-care and patient-physician communication. Increased collaboration with members of the health care team (eg, certified diabetes educators, nurses, dietitians, pharmacists, exercise physiologists), community health workers [96,97] and peer mentors [98,99] may help reinforce messages, promote shared decision-making, improve diabetes outcomes, increase patient satisfaction, and reduce medical costs [100].
Few other interventions have directly addressed physician-patient diabetes self-care communication. One older study examined the effectiveness of an intervention designed to increase of diabetes patients’ involvement in medical decision-making [16]. Patients randomized to the intervention arm participated in a 20-minute session prior to meeting with their physician, in which researchers reviewed their medical chart and used systematic prompts to encourage patients to negotiate medical decisions with their physician. Patients in the control arm received standard educational materials in a session of equal length. Patients in the intervention arm improved glycemia and elicited twice the amount of medical information from their physician compared to controls [16]. These findings suggest that brief interventions prior to medical appointments can improve patient communication, self-care behavior, and in turn, diabetes outcomes [16].
A recent study evaluated the effectiveness of a training program in communication skills for pediatric diabetes care providers in the UK [101, 102]. In this cluster randomized controlled trial, pediatric providers allocated to the Talking Diabetes intervention participated in web-based material and face-to-face seminars designed to prepare providers for constructive self-care conversations with patients as well as skills for promoting behavior change. The psychoeducational training emphasized shared decision-making and utilized motivational interviewing techniques [101]. Twenty-six centers and 693 young people with type 1 diabetes participated in the study [102]. At 12-month follow-up, the Talking Diabetes intervention did not demonstrate improvements in glycemic control. Further, the intervention had a negative effect on patients’ quality of life but a short-term improvement in coping [102]. Interestingly, parents of patients in the intervention arm reported greater continuity of care, which suggests that parents benefited more from the intervention than their children. Future communication interventions targeting the pediatric population should provide ongoing support to children of physicians exposed to interventions such as Talking Diabetes [102].
Currently, 3 ongoing studies aim to improve self-care and clinical outcomes via physician-patient communication interventions. A study by Ricci-Cabello and colleagues [103] aims to improve diabetes self-care by enhancing patient-physician communication in an underserved community of adults with uncontrolled type 2 diabetes. In this 3-arm randomized controlled trial, patients allocated to groups A and B received communication skills training and graphic feedback about glycosylated hemoglobin A1c levels; patients in group C received usual care. Patients in group B also received telephone reinforcement [103]. The second study, by Billimek and colleagues, aims to improve physician-patient communication about medication regimens via diabetes coaching [104]. In this intervention, 190 Mexican-American adult patients with type 2 diabetes were randomly assigned to complete a Coached Care visit with trained community health workers or a Coached Care visit plus the EMPATHy software toolkit, a computer-based activity with strategies and resources to overcome self-care barriers. The primary endpoints are (1) the development of care plan that addresses everyday barriers to medication adherence and (2) completion of a concrete behavioral goal [104]. Finally, the third study, by Grant and colleagues, aims to improve physician-patient communication via a pre-visit prioritization of diabetes concerns. In this controlled, cluster-randomized, multisite trial, primary care physicians were randomized to the Pre-Visit Prioritization for Complex Patients with Diabetes or the control group [105]. The Pre-Visit Prioritization IT-tool is designed to help patients identify one or two concerns prior to a medical visit and then send these priorities to the primary care physician via an electronic health record. The overall goal of the intervention is to improve communication of self-care concerns during a medical visit [105]. Findings from these 3 interventions are forthcoming; findings may provide evidence for validated interventions that improve physician-patient self-care communication in diabetes.
Techniques to Improve Self-Care Communication
Incorporating communication skills in continuing medical education and diabetes education may improve self-care communication in the physician-patient relationship. Educational programs that teach physicians how to provide consistent messages, repeat information, reinforce and offer feedback regarding specific self-care behaviors, and problem-solve self-care challenges may improve patients’ willingness to discuss self-care [14,106]. Most patients will remember only a small portion of the information given to them during medical visit. Studies that compare how much information patients retain versus how much information physicians provide show that patients forget 31% to 71% of information [107]. Therefore, physicians need techniques that promote open self-care communication during a visit. The following techniques can help physicians improve self-care communication [108]:
- Discuss the most important self-care information first; patients tend to remember the information that is presented first.
- Use the phrase “This is very important…” when discussing key points because patients will remember things that are perceived as important.
- Deliver simple, clear, and concrete instructions; patients are more likely to forget complex or confusing instructions. For example, “Check your blood glucose every morning within five minutes of waking up and before you eat breakfast” is more specific and easier to follow than “Check your blood glucose”.
- Ask open-ended questions to allow patients to verbalize feelings or concerns about their diabetes self-care.
- Employ MI techniques to help patients who are struggling to initiate and adhere to self-care behaviors. MI tools, such as the Readiness Ruler, Self-Evaluation Rulers, Decisional Balance Matrix, and Health Behavior Menu (Figure), may help patients and physicians discuss self-care behaviors during a medical visit [109].
– Express empathy by reflective listening and asking patients for permission before offering information or advice about diabetes self-care.
– Roll with resistance by engaging the patient in the process of problem solving rather than opposing a patient’s resistance to change behaviors.
– Develop discrepancy by helping the patient recognize that there is an inconsistency between his/her behavior and personal goals.
– Support self-efficacy by empowering the patient to believe that he/she can change behaviors.
6. Demonstrate active listening skills by reflecting and summarizing the patient’s statements. Reflecting and summarizing show the patient that the physician has been listening to concerns and understands what the patient is saying. This is also an opportunity to correct any miscommunications from the visit.
7. Write down instructions or provide handouts to the patient to help reinforce learning and information retention.
8. Ask patients to write a list of questions a few days prior to the medical appointment and bring it with them. Patients are more likely to remember information about issues they have previously considered that directly relate to them.
9. Consider collaborating with community health workers, patient navigators, peer mentors, and other members of the healthcare team to improve communication, diabetes outcomes, and patient satisfaction.
Summary
Physician-patient self-care communication is essential to achieving optimal diabetes outcomes [15,22,33,110] Patients’ ability to inform physicians about their self-care challenges [14], and physicians’ ability to respond to patients’ self-care reports directly and in non-accusatory language, are vital factors in effective diabetes care [45]. Interventions and education that promote open and honest conversations are particularly important given patients’ well-documented struggles achieving self-care and glycemic goals [111] and physicians’ feelings of inadequacy, frustration, and fatigue when they are not making an impact on patients’ outcomes [48,112]. More research is needed to determine the best strategies to improve self-care communication in the physician-patient relationship.
Corresponding author: Elizabeth A. Beverly, PhD, Department of Family Medicine, Ohio University Heritage College of Osteopathic Medicine, Athens, OH 45701, [email protected].
Financial disclosures: None.
Author contributions: drafting of article, EAB, MFW, ABC, KEP, NNI; critical revision of the article, EAB, MFW, ABC, KEP, NNI.
1. Anderson E, Kian EM. Examining media contestation of masculinity and head trauma in the National Football League. J Men Masculinities 2011;1–22.
2. CDC. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011.
3. Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986.
4. Jacobson AM, Adler AG, Derby L, et al. Clinic attendance and glycemic control. Study of contrasting groups of patients with IDDM. Diabetes Care 1991;14:599–601.
5. Dyer PH, Lloyd CE, Lancashire RJ, et al. Factors associated with clinic non-attendance in adults with type 1 diabetes mellitus. Diab Med 1998;15:339–43.
6. Conn VS, Hafdahl AR, Mehr DR, et al. Metabolic effects of interventions to increase exercise in adults with type 2 diabetes. Diabetologia 2007;50:913–21.
7. Maiorana A, O’Driscoll G, Goodman C, et al. Combined aerobic and resistance exercise improves glycemic control and fitness in type 2 diabetes. Diab Res Clin Pract 2002;56:115–23.
8. Pi-Sunyer FX, Maggio CA, McCarron DA, et al. Multicenter randomized trial of a comprehensive prepared meal program in type 2 diabetes. Diabetes Care 1999;22:191–7.
9. Delahanty LM, Halford BN. The role of diet behaviors in achieving improved glycemic control in intensively treated patients in the Diabetes Control and Complications Trial. Diabetes Care 1993;16:1453–8.
10. Gafarian CT, Heiby EM, Blair P, Singer F. The Diabetes Time Management Questionnaire. Diabetes Educ 1999;25:585–92.
11. Wdowik MJ, Kendall PA, Harris MA. College students with diabetes: using focus groups and interviews to determine psychosocial issues and barriers to control. Diabetes Educ 1997;23:558–62.
12. Rubin RR, Peyrot M. Psychological issues and treatment for people with diabetes. J Clin Psychol 2001;57:457–78.
13. Ali MK, Bullard KM, Gregg EW. Achievement of goals in U.S. Diabetes Care, 1999-2010. N Engl J Med 2013;369:287–8.
14. Beverly EA, Ganda OP, Ritholz MD, et al. Look who’s (not) talking: diabetic patients’ willingness to discuss self-care with physicians. Diabetes Care 2012;35:1466–72.
15. Heisler M, Vijan S, Anderson RM, et al. When do patients and their physicians agree on diabetes treatment goals and strategies, and what difference does it make? J Gen Intern Med 2003;18:893–902.
16. Greenfield S, Kaplan SH, Ware JE Jr, et al. Patients’ participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med 1988;3:448–57.
17. Greenfield S, Kaplan S, Ware JE Jr. Expanding patient involvement in care. Effects on patient outcomes. Ann Intern Med 1985;102:520–8.
18. Anderson RM, Funnell MM, Butler PM, et al. Patient empowerment. Results of a randomized controlled trial. Diabetes Care 1995;18:943–9.
19. Von Korff M, Gruman J, Schaefer J, et al. Collaborative management of chronic illness. Ann Intern Med 1997;127:1097–102.
20. Campbell SM, Hann M, Hacker J, et al. Identifying predictors of high quality care in English general practice: observational study. BMJ 2001;323:784–7.
21. Bower P, Campbell S, Bojke C, Sibbald B. Team structure, team climate and the quality of care in primary care: an observational study. Qual Saf Health Care 2003;12:273–9.
22. Piette JD, Schillinger D, Potter MB, Heisler M. Dimensions of patient-provider communication and diabetes self-care in an ethnically diverse population. J Gen Intern Med 2003;18:624-33.
23. Kerr EA, Smith DM, Kaplan SH, Hayward RA. The association between three different measures of health status and satisfaction among patients with diabetes. Med Care Res Rev 2003;60:158-77.
24. Oshima Lee E, Emanuel EJ. Shared decision making to improve care and reduce costs. N Engl J Med 2013;368:6-8.
25. Barry MJ, Edgman-Levitan S. Shared decision making--pinnacle of patient-centered care. N Engl J Med 2012;366:780–1.
26. Truog RD. Patients and doctors--evolution of a relationship. N Engl J Med 2012;366:581–5.
27. Beverly EA, Wray LA, LaCoe CL, Gabbay R. Listening to older adults’ values and preferences for type 2 diabetes care: a qualitative study. Diabetes Spectrum 2014;27:44–9.
28. Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy 1979;26:252–60.
29. Ciechanowski PS, Katon WJ, Russo JE, Walker EA. The patient-provider relationship: attachment theory and adherence to treatment in diabetes. Am J Psychiatry 2001;158:29–35.
30. Ciechanowski P, Russo J, Katon W, et al. Influence of patient attachment style on self-care and outcomes in diabetes. Psychosom Med 2004;66:720–8.
31. Jahng KH, Martin LR, Golin CE, DiMatteo MR. Preferences for medical collaboration: patient-physician congruence and patient outcomes. Patient Educ Couns 2005;57:308–14.
32. Street RL Jr, Krupat E, Bell RA, et al. Beliefs about control in the physician-patient relationship: effect on communication in medical encounters. J Gen Intern Med 2003;18:609–16.
33. Heisler M, Bouknight RR, Hayward RA, et al. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med 2002;17:243–52.
34. Mechanic D. Changing medical organization and the erosion of trust. Milbank Q 1996;74:171–89.
35. Mechanic D, Schlesinger M. The impact of managed care on patients’ trust in medical care and their physicians. JAMA 1996;275:1693–7.
36. Pearson SD, Raeke LH. Patients’ trust in physicians: many theories, few measures, and little data. J Gen Intern Med 2000;15:509–13.
37. Jones DE, Carson KA, Bleich SN, Cooper LA. Patient trust in physicians and adoption of lifestyle behaviors to control high blood pressure. Patient Educ Couns 2012;89:57–62.
38. Mostashari F, Riley E, Selwyn PA, Altice FL. Acceptance and adherence with antiretroviral therapy among HIV-infected women in a correctional facility. J Acquired Immun Def Syndr Hum Retrovir 1998;18:341–8.
39. Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA 1999;282:583–9.
40. Ritholz MD, Beverly EA, Brooks KM, et al. Barriers and facilitators to self-care communication during medical appointments in the United States for adults with type 2 diabetes. Chronic Illn 2014;10:303–13.
41. Aikens JE, Bingham R, Piette JD. Patient-provider communication and self-care behavior among type 2 diabetes patients. Diabetes Educ 2005;31:681–90.
42. Bundesmann R, Kaplowitz SA. Provider communication and patient participation in diabetes self-care. Patient Educ Couns 2011;85:143–7.
43. Heisler M, Cole I, Weir D, et al. Does physician communication influence older patients’ diabetes self-management and glycemic control? Results from the Health and Retirement Study (HRS). J Gerontol A Biol Sci Med Sci 2007;62:1435–42.
44. Duffy FD, Gordon GH, Whelan G, et al. Assessing competence in communication and interpersonal skills: the Kalamazoo II report. Acad Med 2004;79:495–507.
45. Ritholz MD, Beverly EA, Brooks KM, et al. Barriers and facilitators to self-care communication during medical appointments in the United States for adults with type 2 diabetes. Chronic Illn 2014;10:303–13.
46. Ciechanowski P, Katon WJ. The interpersonal experience of health care through the eyes of patients with diabetes. Soc Sci Med 2006;63:3067–79.
47. Diabetes Control and Complications Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med 1993;329:977–86.
48. Peyrot M, Rubin RR, Lauritzen T, et al. Psychosocial problems and barriers to improved diabetes management: results of the Cross-National Diabetes Attitudes, Wishes and Needs (DAWN) Study. Diab Med 2005;22:1379–85.
49. DiMatteo MR, Linn LS, Chang BL, Cope DW. Affect and neutrality in physician behavior: a study of patients’ values and satisfaction. J Behav Med 1985;8:397–409.
50. Stuckey HL, Vallis M, Kovacs Burns K, et al. “I do my best to listen to patients”: qualitative insights into DAWN2 (Diabetes Psychosocial Care From the Perspective of Health Care Professionals in the Second Diabetes Attitudes, Wishes and Needs Study). Clin Ther 2015;37:1986–98.
51. Kruse RL, Olsberg JE, Oliver DP, et al. Patient-provider communication about diabetes self-care activities. Fam Med 2013;45:319–22.
52. Beverly EA, Hultgren BA, Brooks KM, et al. Understanding physicians’ challenges when treating type 2 diabetic patients’ social and emotional difficulties: a qualitative study. Diabetes Care 2011;34:1086–8.
53. Freeman J, Loewe R. Barriers to communication about diabetes mellitus. Patients’ and physicians’ different view of the disease. J Fam Pract 2000;49:507–12.
54. Gonzalez JS, Delahanty LM, Safren SA, et al. Differentiating symptoms of depression from diabetes-specific distress: relationships with self-care in type 2 diabetes. Diabetologia 2008;51:1822–5.
55. Fisher L, Hessler DM, Polonsky WH, Mullan J. When is diabetes distress clinically meaningful?: establishing cut points for the Diabetes Distress Scale. Diabetes Care 2012;35:259–64.
56. Polonsky WH, Anderson BJ, Lohrer PA, et al. Assessment of diabetes-related distress. Diabetes Care 1995;18:754–60.
57. Welch G, Weinger K, Anderson B, Polonsky WH. Responsiveness of the Problem Areas In Diabetes (PAID) questionnaire. Diabetic Med 2003;20:69–72.
58. Weinger K, Kinsley BT, Bajaj M, et al. Diabetes-related emotional distress: A barrier to improving glycemic control during intensive diabetes treatment. Abstract. Diabetes 1997;46:Supp1:268A.
59. Weinger K, Jacobson AM. Psychosocial and quality of life correlates of glycemic control during intensive treatment of type 1 diabetes. Patient Educ Couns 2001;42:123–31.
60. Fisher L, Chesla CA, Skaff MM, et al. The family and disease management in Hispanic and European-American patients with type 2 diabetes. Diabetes Care 2000;23:267–72.
61. Wen LK, Parchman ML, Shepherd MD. Family support and diet barriers among older Hispanic adults with type 2 diabetes. Fam Med 2004;36:423–30.
62. Chesla CA, Fisher L, Mullan JT, et al. Family and disease management in African-American patients with type 2 diabetes. Diabetes Care 2004;27:2850–5.
63. Brown SA, Harrist RB, Villagomez ET, et al. Gender and treatment differences in knowledge, health beliefs, and metabolic control in Mexican Americans with type 2 diabetes. Diabetes Educ 2000;26:425–38.
64. Fisher L, Chesla CA, Chun KM, et al. Patient-appraised couple emotion management and disease management among Chinese American patients with type 2 diabetes. J Fam Psychol 2004;18:302–10.
65. Akimoto M, Fukunishi I, Kanno K, et al. Psychosocial predictors of relapse among diabetes patients: a 2-year follow-up after inpatient diabetes education. Psychosomatics 2004;45:343–9.
66. Samuel-Hodge CD, Headen SW, Skelly AH, et al. Influences on day-to-day self-management of type 2 diabetes among African-American women: spirituality, the multi-caregiver role, and other social context factors. Diabetes Care 2000;23:928–33.
67. Wing RR, Marcus MD, Epstein LH, Jawad A. A “family-based” approach to the treatment of obese type II diabetic patients. J Consult Clin Psychol 1991;59:156–62.
68. Trief PM, Ploutz-Snyder R, Britton KD, Weinstock RS. The relationship between marital quality and adherence to the diabetes care regimen. Ann Behav Med 2004;27:148–54.
69. Gleeson-Kreig J, Bernal H, Woolley S. The role of social support in the self-management of diabetes mellitus among a Hispanic population. Pub Health Nurs 2002;19:215–22.
70. Wen LK, Shepherd MD, Parchman ML. Family support, diet, and exercise among older Mexican Americans with type 2 diabetes. Diabetes Educ 2004;30:980–93.
71. Ruggiero L. Helping people with diabetes change behavior: from theory to practice. Diab Spectrum 2000;13:125–32.
72. Orr DP, Golden MP, Myers G, Marrero DG. Characteristics of adolescents with poorly controlled diabetes referred to a tertiary care center. Diabetes Care 1983;6:170–5.
73. Lane JD, Stabler B, Ross SL, et al. Psychological predictors of glucose control in patients with IDDM. Diabetes Care 1988;11:798–800.
74. Irvine AA, Cox D, Gonder-Frederick L. Fear of hypoglycemia: relationship to physical and psychological symptoms in patients with insulin-dependent diabetes mellitus. Health Psychology 1992;11:135–8.
75. Irvine A, Cox D, Gonder-Frederick L. The fear of hypoglycemia scale. In: Bradley C, editor. Handbook of psychology and diabetes. Harwood Academic; 1994.
76. Peyrot MF, McMurry JF Jr. Stress buffering and glycemic control. The role of coping styles. Diabetes Care 1992;15:842–6.
77. Peyrot M, McMurry JF Jr, Kruger DF. A biopsychosocial model of glycemic control in diabetes: stress, coping and regimen adherence. J Health Soc Behav 1999;40:141–58.
78. Berkman ND, Sheridan SL, Donahue KE, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155:97–107.
79. Sohal S, Sohal P, King-Shier KM, Khan NA. Barriers and facilitators for type-2 diabetes management in South Asians: a systematic review. PloS One 2015:1–15.
80. Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med 2003;163:83–90.
81. Miller WR, Rollnick S. Motivational interviewing: preparing people for change. New York: Guilford Press; 2002.
82. Powell PW, Corathers SD, Raymond J, Streisand R. New approaches to providing individualized diabetes care in the 21st century. Curr Diabetes Rev 2015;11:222–30.
83. Jones AJ, Gladstone BP, Lubeck M, et al. Motivational interventions in the management of HbA1c levels: A systematic review and meta-analysis. Prim Care Diabetes 2014;8:91–100.
84. Song D, Xu TZ, Sun QH. Effect of motivational interviewing on self-management in patients with type 2 diabetes mellitus: a meta-analysis. Intl J Nurs Sci 2014;1:291–7.
85. Clifford Mulimba A, Byron-Daniel J. Motivational interviewing-based interventions and diabetes mellitus. Br J Nurs 2014;23:8–14.
86. Noordman J, van der Weijden T, van Dulmen S. Communication-related behavior change techniques used in face-to-face lifestyle interventions in primary care: a systematic review of the literature. Patient Educ Couns 2012;89:227–44.
87. Soderlund LL, Madson MB, Rubak S, Nilsen P. A systematic review of motivational interviewing training for general health care practitioners. Patient Educ Couns 2011;84:16–26.
88. Kang SH, Kim BG, Lee GM. Justification of continuous packed-bed reactor for retroviral vector production from amphotropic PsiCRIP murine producer cell. Cytotechnology 2000;34(1–2):151–8.
89. Holmen H, Torbjornsen A, Wahl AK, et al. A mobile health intervention for self-management and lifestyle change for persons with type 2 diabetes, part 2: one-year results from the Norwegian randomized controlled trial RENEWING HEALTH. JMIR mHealth uHealth 2014;2(4):e57.
90. Chlebowy DO, El-Mallakh P, Myers J, et al. Motivational interviewing to improve diabetes outcomes in African Americans adults with diabetes. West J Nurs Res 2015;37:566–80.
91. Kang HY, Gu MO. [Development and effects of a motivational interviewing self-management program for elderly patients with diabetes mellitus]. J Kor Acad Nurs 2015;45:533–43.
92. Brobeck E, Odencrants S, Bergh H, Hildingh C. Patients’ experiences of lifestyle discussions based on motivational interviewing: a qualitative study. BMC Nursing 2014;13:13.
93. Loskutova NY, Tsai AG, Fisher EB, et al. Patient navigators connecting patients to community resources to improve diabetes outcomes. J Am Board Fam Med 2016;29:78–89.
94. Raiff BR, Barry VB, Ridenour TA, Jitnarin N. Internet-based incentives increase blood glucose testing with a non-adherent, diverse sample of teens with type 1 diabetes mellitus: a randomized controlled Trial. Trans Behav Med 2016;6:179–88.
95. Sahlen KG, Johansson H, Nystrom L, Lindholm L. Health coaching to promote healthier lifestyle among older people at moderate risk for cardiovascular diseases, diabetes and depression: a study protocol for a randomized controlled trial in Sweden. BMC Public Health 2013;13:199.
96. Kane EP, Collinsworth AW, Schmidt KL, et al. Improving diabetes care and outcomes with community health workers. Fam Pract 2016;33:523–8.
97. Wagner JA, Bermudez-Millan A, Damio G, et al. A randomized, controlled trial of a stress management intervention for Latinos with type 2 diabetes delivered by community health workers: Outcomes for psychological wellbeing, glycemic control, and cortisol. Diabetes Res Clin Pract 2016;120:162–70.
98. Rogers EA, Hessler DM, Bodenheimer TS, et al. Diabetes peer coaching: do “better patients” make better coaches? Diabetes Educ 2014;40:107–15.
99. Long JA, Jahnle EC, Richardson DM, et al. Peer mentoring and financial incentives to improve glucose control in African American veterans: a randomized trial. Ann Intern Med 2012;156:416–24.
100. Mundt MP, Agneessens F, Tuan WJ, et al. Primary care team communication networks, team climate, quality of care, and medical costs for patients with diabetes: A cross-sectional study. Int J Nurs Stud 2016;58:1–11.
101. Fisher L, Mullan JT, Arean P, et al. Diabetes distress but not clinical depression or depressive symptoms is associated with glycemic control in both cross-sectional and longitudinal analyses. Diabetes Care 2010;33:23–8.
102. Fisher L, Glasgow RE, Strycker LA. The relationship between diabetes distress and clinical depression with glycemic control among patients with type 2 diabetes. Diabetes Care 2010;33:1034–6.
103. Ricci-Cabello I, Olry de Labry-Lima A, Bolivar-Munoz J, et al. Effectiveness of two interventions based on improving patient-practitioner communication on diabetes self-management in patients with low educational level: study protocol of a clustered randomized trial in primary care. BMC Health Serv Res 2013;13:433.
104. Billimek J, Guzman H, Angulo MA. Effectiveness and feasibility of a software tool to help patients communicate with doctors about problems they face with their medication regimen (EMPATHy): study protocol for a randomized controlled trial. Trials 2015;16:145.
105. Grant RW, Uratsu CS, Estacio KR, et al. Pre-Visit Prioritization for complex patients with diabetes: Randomized trial design and implementation within an integrated health care system. Contemp Clin Trials 2016;47:196–201.
106. Ritholz MD, Beverly EA, Abrahamson MJ, et al. Physicians’ perceptions of the type 2 diabetes multidisciplinary treatment team: a qualitative study. Diabetes Educ 2011.
107. Ley P. Satisfaction, compliance and communication. Br J Clin Psychol 1982;21:241–54.
108. Weinger K, Smaldone A, Beverly EA. Psychosocial and educational implications of diabetic foot complications. In: Veves A, Giurini JM, LoGerfo FW, editors. The diabetic foot: medical and surgical management. Boston: Springer; 2012:503–18.
109. Welch G, Rose G, Ernst D. Motivational interviewing and diabetes: what is it, how is it used, and does it work? Diabetes Spectr 2006;19:5–11.
110. Kaplan SH, Greenfield S, Ware JE Jr. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care 1989;27(3 Suppl):S110–27.
111. Nelson KM, Reiber G, Boyko EJ. Diet and exercise among adults with type 2 diabetes: findings from the third national health and nutrition examination survey (NHANES III). Diabetes Care 2002;25:1722–8.
112. Wens J, Vermeire E, Royen PV, et al. GPs’ perspectives of type 2 diabetes patients’ adherence to treatment: A qualitative analysis of barriers and solutions. BMC Fam Pract 2005;6:20.
1. Anderson E, Kian EM. Examining media contestation of masculinity and head trauma in the National Football League. J Men Masculinities 2011;1–22.
2. CDC. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011.
3. Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986.
4. Jacobson AM, Adler AG, Derby L, et al. Clinic attendance and glycemic control. Study of contrasting groups of patients with IDDM. Diabetes Care 1991;14:599–601.
5. Dyer PH, Lloyd CE, Lancashire RJ, et al. Factors associated with clinic non-attendance in adults with type 1 diabetes mellitus. Diab Med 1998;15:339–43.
6. Conn VS, Hafdahl AR, Mehr DR, et al. Metabolic effects of interventions to increase exercise in adults with type 2 diabetes. Diabetologia 2007;50:913–21.
7. Maiorana A, O’Driscoll G, Goodman C, et al. Combined aerobic and resistance exercise improves glycemic control and fitness in type 2 diabetes. Diab Res Clin Pract 2002;56:115–23.
8. Pi-Sunyer FX, Maggio CA, McCarron DA, et al. Multicenter randomized trial of a comprehensive prepared meal program in type 2 diabetes. Diabetes Care 1999;22:191–7.
9. Delahanty LM, Halford BN. The role of diet behaviors in achieving improved glycemic control in intensively treated patients in the Diabetes Control and Complications Trial. Diabetes Care 1993;16:1453–8.
10. Gafarian CT, Heiby EM, Blair P, Singer F. The Diabetes Time Management Questionnaire. Diabetes Educ 1999;25:585–92.
11. Wdowik MJ, Kendall PA, Harris MA. College students with diabetes: using focus groups and interviews to determine psychosocial issues and barriers to control. Diabetes Educ 1997;23:558–62.
12. Rubin RR, Peyrot M. Psychological issues and treatment for people with diabetes. J Clin Psychol 2001;57:457–78.
13. Ali MK, Bullard KM, Gregg EW. Achievement of goals in U.S. Diabetes Care, 1999-2010. N Engl J Med 2013;369:287–8.
14. Beverly EA, Ganda OP, Ritholz MD, et al. Look who’s (not) talking: diabetic patients’ willingness to discuss self-care with physicians. Diabetes Care 2012;35:1466–72.
15. Heisler M, Vijan S, Anderson RM, et al. When do patients and their physicians agree on diabetes treatment goals and strategies, and what difference does it make? J Gen Intern Med 2003;18:893–902.
16. Greenfield S, Kaplan SH, Ware JE Jr, et al. Patients’ participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med 1988;3:448–57.
17. Greenfield S, Kaplan S, Ware JE Jr. Expanding patient involvement in care. Effects on patient outcomes. Ann Intern Med 1985;102:520–8.
18. Anderson RM, Funnell MM, Butler PM, et al. Patient empowerment. Results of a randomized controlled trial. Diabetes Care 1995;18:943–9.
19. Von Korff M, Gruman J, Schaefer J, et al. Collaborative management of chronic illness. Ann Intern Med 1997;127:1097–102.
20. Campbell SM, Hann M, Hacker J, et al. Identifying predictors of high quality care in English general practice: observational study. BMJ 2001;323:784–7.
21. Bower P, Campbell S, Bojke C, Sibbald B. Team structure, team climate and the quality of care in primary care: an observational study. Qual Saf Health Care 2003;12:273–9.
22. Piette JD, Schillinger D, Potter MB, Heisler M. Dimensions of patient-provider communication and diabetes self-care in an ethnically diverse population. J Gen Intern Med 2003;18:624-33.
23. Kerr EA, Smith DM, Kaplan SH, Hayward RA. The association between three different measures of health status and satisfaction among patients with diabetes. Med Care Res Rev 2003;60:158-77.
24. Oshima Lee E, Emanuel EJ. Shared decision making to improve care and reduce costs. N Engl J Med 2013;368:6-8.
25. Barry MJ, Edgman-Levitan S. Shared decision making--pinnacle of patient-centered care. N Engl J Med 2012;366:780–1.
26. Truog RD. Patients and doctors--evolution of a relationship. N Engl J Med 2012;366:581–5.
27. Beverly EA, Wray LA, LaCoe CL, Gabbay R. Listening to older adults’ values and preferences for type 2 diabetes care: a qualitative study. Diabetes Spectrum 2014;27:44–9.
28. Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy 1979;26:252–60.
29. Ciechanowski PS, Katon WJ, Russo JE, Walker EA. The patient-provider relationship: attachment theory and adherence to treatment in diabetes. Am J Psychiatry 2001;158:29–35.
30. Ciechanowski P, Russo J, Katon W, et al. Influence of patient attachment style on self-care and outcomes in diabetes. Psychosom Med 2004;66:720–8.
31. Jahng KH, Martin LR, Golin CE, DiMatteo MR. Preferences for medical collaboration: patient-physician congruence and patient outcomes. Patient Educ Couns 2005;57:308–14.
32. Street RL Jr, Krupat E, Bell RA, et al. Beliefs about control in the physician-patient relationship: effect on communication in medical encounters. J Gen Intern Med 2003;18:609–16.
33. Heisler M, Bouknight RR, Hayward RA, et al. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med 2002;17:243–52.
34. Mechanic D. Changing medical organization and the erosion of trust. Milbank Q 1996;74:171–89.
35. Mechanic D, Schlesinger M. The impact of managed care on patients’ trust in medical care and their physicians. JAMA 1996;275:1693–7.
36. Pearson SD, Raeke LH. Patients’ trust in physicians: many theories, few measures, and little data. J Gen Intern Med 2000;15:509–13.
37. Jones DE, Carson KA, Bleich SN, Cooper LA. Patient trust in physicians and adoption of lifestyle behaviors to control high blood pressure. Patient Educ Couns 2012;89:57–62.
38. Mostashari F, Riley E, Selwyn PA, Altice FL. Acceptance and adherence with antiretroviral therapy among HIV-infected women in a correctional facility. J Acquired Immun Def Syndr Hum Retrovir 1998;18:341–8.
39. Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA 1999;282:583–9.
40. Ritholz MD, Beverly EA, Brooks KM, et al. Barriers and facilitators to self-care communication during medical appointments in the United States for adults with type 2 diabetes. Chronic Illn 2014;10:303–13.
41. Aikens JE, Bingham R, Piette JD. Patient-provider communication and self-care behavior among type 2 diabetes patients. Diabetes Educ 2005;31:681–90.
42. Bundesmann R, Kaplowitz SA. Provider communication and patient participation in diabetes self-care. Patient Educ Couns 2011;85:143–7.
43. Heisler M, Cole I, Weir D, et al. Does physician communication influence older patients’ diabetes self-management and glycemic control? Results from the Health and Retirement Study (HRS). J Gerontol A Biol Sci Med Sci 2007;62:1435–42.
44. Duffy FD, Gordon GH, Whelan G, et al. Assessing competence in communication and interpersonal skills: the Kalamazoo II report. Acad Med 2004;79:495–507.
45. Ritholz MD, Beverly EA, Brooks KM, et al. Barriers and facilitators to self-care communication during medical appointments in the United States for adults with type 2 diabetes. Chronic Illn 2014;10:303–13.
46. Ciechanowski P, Katon WJ. The interpersonal experience of health care through the eyes of patients with diabetes. Soc Sci Med 2006;63:3067–79.
47. Diabetes Control and Complications Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med 1993;329:977–86.
48. Peyrot M, Rubin RR, Lauritzen T, et al. Psychosocial problems and barriers to improved diabetes management: results of the Cross-National Diabetes Attitudes, Wishes and Needs (DAWN) Study. Diab Med 2005;22:1379–85.
49. DiMatteo MR, Linn LS, Chang BL, Cope DW. Affect and neutrality in physician behavior: a study of patients’ values and satisfaction. J Behav Med 1985;8:397–409.
50. Stuckey HL, Vallis M, Kovacs Burns K, et al. “I do my best to listen to patients”: qualitative insights into DAWN2 (Diabetes Psychosocial Care From the Perspective of Health Care Professionals in the Second Diabetes Attitudes, Wishes and Needs Study). Clin Ther 2015;37:1986–98.
51. Kruse RL, Olsberg JE, Oliver DP, et al. Patient-provider communication about diabetes self-care activities. Fam Med 2013;45:319–22.
52. Beverly EA, Hultgren BA, Brooks KM, et al. Understanding physicians’ challenges when treating type 2 diabetic patients’ social and emotional difficulties: a qualitative study. Diabetes Care 2011;34:1086–8.
53. Freeman J, Loewe R. Barriers to communication about diabetes mellitus. Patients’ and physicians’ different view of the disease. J Fam Pract 2000;49:507–12.
54. Gonzalez JS, Delahanty LM, Safren SA, et al. Differentiating symptoms of depression from diabetes-specific distress: relationships with self-care in type 2 diabetes. Diabetologia 2008;51:1822–5.
55. Fisher L, Hessler DM, Polonsky WH, Mullan J. When is diabetes distress clinically meaningful?: establishing cut points for the Diabetes Distress Scale. Diabetes Care 2012;35:259–64.
56. Polonsky WH, Anderson BJ, Lohrer PA, et al. Assessment of diabetes-related distress. Diabetes Care 1995;18:754–60.
57. Welch G, Weinger K, Anderson B, Polonsky WH. Responsiveness of the Problem Areas In Diabetes (PAID) questionnaire. Diabetic Med 2003;20:69–72.
58. Weinger K, Kinsley BT, Bajaj M, et al. Diabetes-related emotional distress: A barrier to improving glycemic control during intensive diabetes treatment. Abstract. Diabetes 1997;46:Supp1:268A.
59. Weinger K, Jacobson AM. Psychosocial and quality of life correlates of glycemic control during intensive treatment of type 1 diabetes. Patient Educ Couns 2001;42:123–31.
60. Fisher L, Chesla CA, Skaff MM, et al. The family and disease management in Hispanic and European-American patients with type 2 diabetes. Diabetes Care 2000;23:267–72.
61. Wen LK, Parchman ML, Shepherd MD. Family support and diet barriers among older Hispanic adults with type 2 diabetes. Fam Med 2004;36:423–30.
62. Chesla CA, Fisher L, Mullan JT, et al. Family and disease management in African-American patients with type 2 diabetes. Diabetes Care 2004;27:2850–5.
63. Brown SA, Harrist RB, Villagomez ET, et al. Gender and treatment differences in knowledge, health beliefs, and metabolic control in Mexican Americans with type 2 diabetes. Diabetes Educ 2000;26:425–38.
64. Fisher L, Chesla CA, Chun KM, et al. Patient-appraised couple emotion management and disease management among Chinese American patients with type 2 diabetes. J Fam Psychol 2004;18:302–10.
65. Akimoto M, Fukunishi I, Kanno K, et al. Psychosocial predictors of relapse among diabetes patients: a 2-year follow-up after inpatient diabetes education. Psychosomatics 2004;45:343–9.
66. Samuel-Hodge CD, Headen SW, Skelly AH, et al. Influences on day-to-day self-management of type 2 diabetes among African-American women: spirituality, the multi-caregiver role, and other social context factors. Diabetes Care 2000;23:928–33.
67. Wing RR, Marcus MD, Epstein LH, Jawad A. A “family-based” approach to the treatment of obese type II diabetic patients. J Consult Clin Psychol 1991;59:156–62.
68. Trief PM, Ploutz-Snyder R, Britton KD, Weinstock RS. The relationship between marital quality and adherence to the diabetes care regimen. Ann Behav Med 2004;27:148–54.
69. Gleeson-Kreig J, Bernal H, Woolley S. The role of social support in the self-management of diabetes mellitus among a Hispanic population. Pub Health Nurs 2002;19:215–22.
70. Wen LK, Shepherd MD, Parchman ML. Family support, diet, and exercise among older Mexican Americans with type 2 diabetes. Diabetes Educ 2004;30:980–93.
71. Ruggiero L. Helping people with diabetes change behavior: from theory to practice. Diab Spectrum 2000;13:125–32.
72. Orr DP, Golden MP, Myers G, Marrero DG. Characteristics of adolescents with poorly controlled diabetes referred to a tertiary care center. Diabetes Care 1983;6:170–5.
73. Lane JD, Stabler B, Ross SL, et al. Psychological predictors of glucose control in patients with IDDM. Diabetes Care 1988;11:798–800.
74. Irvine AA, Cox D, Gonder-Frederick L. Fear of hypoglycemia: relationship to physical and psychological symptoms in patients with insulin-dependent diabetes mellitus. Health Psychology 1992;11:135–8.
75. Irvine A, Cox D, Gonder-Frederick L. The fear of hypoglycemia scale. In: Bradley C, editor. Handbook of psychology and diabetes. Harwood Academic; 1994.
76. Peyrot MF, McMurry JF Jr. Stress buffering and glycemic control. The role of coping styles. Diabetes Care 1992;15:842–6.
77. Peyrot M, McMurry JF Jr, Kruger DF. A biopsychosocial model of glycemic control in diabetes: stress, coping and regimen adherence. J Health Soc Behav 1999;40:141–58.
78. Berkman ND, Sheridan SL, Donahue KE, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155:97–107.
79. Sohal S, Sohal P, King-Shier KM, Khan NA. Barriers and facilitators for type-2 diabetes management in South Asians: a systematic review. PloS One 2015:1–15.
80. Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med 2003;163:83–90.
81. Miller WR, Rollnick S. Motivational interviewing: preparing people for change. New York: Guilford Press; 2002.
82. Powell PW, Corathers SD, Raymond J, Streisand R. New approaches to providing individualized diabetes care in the 21st century. Curr Diabetes Rev 2015;11:222–30.
83. Jones AJ, Gladstone BP, Lubeck M, et al. Motivational interventions in the management of HbA1c levels: A systematic review and meta-analysis. Prim Care Diabetes 2014;8:91–100.
84. Song D, Xu TZ, Sun QH. Effect of motivational interviewing on self-management in patients with type 2 diabetes mellitus: a meta-analysis. Intl J Nurs Sci 2014;1:291–7.
85. Clifford Mulimba A, Byron-Daniel J. Motivational interviewing-based interventions and diabetes mellitus. Br J Nurs 2014;23:8–14.
86. Noordman J, van der Weijden T, van Dulmen S. Communication-related behavior change techniques used in face-to-face lifestyle interventions in primary care: a systematic review of the literature. Patient Educ Couns 2012;89:227–44.
87. Soderlund LL, Madson MB, Rubak S, Nilsen P. A systematic review of motivational interviewing training for general health care practitioners. Patient Educ Couns 2011;84:16–26.
88. Kang SH, Kim BG, Lee GM. Justification of continuous packed-bed reactor for retroviral vector production from amphotropic PsiCRIP murine producer cell. Cytotechnology 2000;34(1–2):151–8.
89. Holmen H, Torbjornsen A, Wahl AK, et al. A mobile health intervention for self-management and lifestyle change for persons with type 2 diabetes, part 2: one-year results from the Norwegian randomized controlled trial RENEWING HEALTH. JMIR mHealth uHealth 2014;2(4):e57.
90. Chlebowy DO, El-Mallakh P, Myers J, et al. Motivational interviewing to improve diabetes outcomes in African Americans adults with diabetes. West J Nurs Res 2015;37:566–80.
91. Kang HY, Gu MO. [Development and effects of a motivational interviewing self-management program for elderly patients with diabetes mellitus]. J Kor Acad Nurs 2015;45:533–43.
92. Brobeck E, Odencrants S, Bergh H, Hildingh C. Patients’ experiences of lifestyle discussions based on motivational interviewing: a qualitative study. BMC Nursing 2014;13:13.
93. Loskutova NY, Tsai AG, Fisher EB, et al. Patient navigators connecting patients to community resources to improve diabetes outcomes. J Am Board Fam Med 2016;29:78–89.
94. Raiff BR, Barry VB, Ridenour TA, Jitnarin N. Internet-based incentives increase blood glucose testing with a non-adherent, diverse sample of teens with type 1 diabetes mellitus: a randomized controlled Trial. Trans Behav Med 2016;6:179–88.
95. Sahlen KG, Johansson H, Nystrom L, Lindholm L. Health coaching to promote healthier lifestyle among older people at moderate risk for cardiovascular diseases, diabetes and depression: a study protocol for a randomized controlled trial in Sweden. BMC Public Health 2013;13:199.
96. Kane EP, Collinsworth AW, Schmidt KL, et al. Improving diabetes care and outcomes with community health workers. Fam Pract 2016;33:523–8.
97. Wagner JA, Bermudez-Millan A, Damio G, et al. A randomized, controlled trial of a stress management intervention for Latinos with type 2 diabetes delivered by community health workers: Outcomes for psychological wellbeing, glycemic control, and cortisol. Diabetes Res Clin Pract 2016;120:162–70.
98. Rogers EA, Hessler DM, Bodenheimer TS, et al. Diabetes peer coaching: do “better patients” make better coaches? Diabetes Educ 2014;40:107–15.
99. Long JA, Jahnle EC, Richardson DM, et al. Peer mentoring and financial incentives to improve glucose control in African American veterans: a randomized trial. Ann Intern Med 2012;156:416–24.
100. Mundt MP, Agneessens F, Tuan WJ, et al. Primary care team communication networks, team climate, quality of care, and medical costs for patients with diabetes: A cross-sectional study. Int J Nurs Stud 2016;58:1–11.
101. Fisher L, Mullan JT, Arean P, et al. Diabetes distress but not clinical depression or depressive symptoms is associated with glycemic control in both cross-sectional and longitudinal analyses. Diabetes Care 2010;33:23–8.
102. Fisher L, Glasgow RE, Strycker LA. The relationship between diabetes distress and clinical depression with glycemic control among patients with type 2 diabetes. Diabetes Care 2010;33:1034–6.
103. Ricci-Cabello I, Olry de Labry-Lima A, Bolivar-Munoz J, et al. Effectiveness of two interventions based on improving patient-practitioner communication on diabetes self-management in patients with low educational level: study protocol of a clustered randomized trial in primary care. BMC Health Serv Res 2013;13:433.
104. Billimek J, Guzman H, Angulo MA. Effectiveness and feasibility of a software tool to help patients communicate with doctors about problems they face with their medication regimen (EMPATHy): study protocol for a randomized controlled trial. Trials 2015;16:145.
105. Grant RW, Uratsu CS, Estacio KR, et al. Pre-Visit Prioritization for complex patients with diabetes: Randomized trial design and implementation within an integrated health care system. Contemp Clin Trials 2016;47:196–201.
106. Ritholz MD, Beverly EA, Abrahamson MJ, et al. Physicians’ perceptions of the type 2 diabetes multidisciplinary treatment team: a qualitative study. Diabetes Educ 2011.
107. Ley P. Satisfaction, compliance and communication. Br J Clin Psychol 1982;21:241–54.
108. Weinger K, Smaldone A, Beverly EA. Psychosocial and educational implications of diabetic foot complications. In: Veves A, Giurini JM, LoGerfo FW, editors. The diabetic foot: medical and surgical management. Boston: Springer; 2012:503–18.
109. Welch G, Rose G, Ernst D. Motivational interviewing and diabetes: what is it, how is it used, and does it work? Diabetes Spectr 2006;19:5–11.
110. Kaplan SH, Greenfield S, Ware JE Jr. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care 1989;27(3 Suppl):S110–27.
111. Nelson KM, Reiber G, Boyko EJ. Diet and exercise among adults with type 2 diabetes: findings from the third national health and nutrition examination survey (NHANES III). Diabetes Care 2002;25:1722–8.
112. Wens J, Vermeire E, Royen PV, et al. GPs’ perspectives of type 2 diabetes patients’ adherence to treatment: A qualitative analysis of barriers and solutions. BMC Fam Pract 2005;6:20.
How to reduce early readmissions after bariatric surgery
NEW ORLEANS – A couple of home nursing visits early after bariatric surgery halved emergency department visits and hospital readmissions within the first 30 days in a case-control study, Linden A. Karas, MD, reported at Obesity Week 2016.
“Home nursing visits during the month following surgery, between doctor’s office visits, are a simple and inexpensive intervention that drastically decreases hospital revisits,” she declared at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
These early revisits to the hospital following bariatric surgery are not only common, they carry a substantial cost. An ED visit for hydration runs about $3,000 and a 2-day inpatient admission about $18,000. In contrast, the price tag for two home nursing visits in this study was $300, noted Dr. Karas, a surgeon at Mercy Catholic Medical Center in Philadelphia.
The triad of dehydration, nausea, and vomiting in addition to abdominal pain account for up to 40% of early readmissions following bariatric surgery. Because most hospital revisits for these reasons entail very little intervention other than IV fluids, Dr. Karas and her coinvestigators decided to investigate whether preemptive structured home visits by nurses prepared to administer IV fluids on the spot would cut down on hospital revisits. They found that indeed this strategy was successful.
Mercy Catholic Medical Center serves a largely low-income Medicare/Medicaid population. Part of the local culture is for many patients to obtain their primary care in the ED, so bariatric surgery patients are generally not reluctant to show up there if they don’t feel well in the first few weeks post surgery. That’s why in the year prior to the study the 30-day readmission rate was 23.6%, she explained.
The study included 193 consecutive prospectively followed adult participants in the home nursing program who underwent Roux-en-Y gastric bypass, laparoscopic adjustable banding, or revision surgery in 2014 and a control group of 267 matched bariatric surgery patients who underwent the same procedures in 2013, before introduction of the home nursing visits.
The first home visit occurred roughly 3 days after hospital discharge. The second one bridged the period between the first scheduled postoperative office visit at 2 weeks and the next office visit at 4 weeks. At discharge, patients were given a checklist concerning the signs and symptoms of dehydration, dietary recommendations, and lifestyle choices. Patients were encouraged to use the checklist to self-evaluate for dehydration and hand it over to the visiting nurses. The same checklist was provided to the home nurses. If the nurses found that patients met three or more criteria on the dehydration checklist, which included dry mucus membranes, heart rate greater than 90 beats/minute, headache, going more than 8 hours without urination, weakness, abdominal pain, and roughly a dozen other well-known criteria, they were instructed to initiate home hydration therapy with a banana bag and 2 L of normal saline.
If 1-2 days of home hydration failed to resolve the symptoms, the home care nurse was supposed to refer the patient to the ED. If the patient improved in response to home hydration therapy, the home nurse informed the surgeon’s office, which then set up a follow-up office visit to take place within the next 24 hours. Also, if the patient’s responses on the nutrition and behavioral health questionnaire raised any red flags regarding inadequate food and fluid intake, nonadherence to the recommended daily minimum of 30 minutes of physical activity, or depressive symptoms, the nurse was supposed to notify the surgeon to schedule a behavioral or nutrition appointment at the patient’s next scheduled visit.
The 30-day rate of all-cause hospital revisits in the home nursing care group was 11.9%, compared with 23.6% in controls. The rate of hospital revisits specifically for dehydration was 6.2% in the home visit group vs. 8.6% in controls, a 28% relative risk reduction in the home treatment group, which didn’t achieve statistical significance. However, in hindsight, it was evident that some of the visiting nurses didn’t fully understand the treatment protocol; they sent patients straight to the ED without first providing home hydration therapy. The visiting nurses were subcontracted out and weren’t part of the hospital’s bariatric surgery program.
Among those patients who did receive the therapy, however, it prevented readmission in 77% of cases. The 23% of patients who didn’t improve were referred to the hospital for further workup and treatment.
Patients with early hospital readmission had an average of 4.38 comorbid conditions, significantly more than the average 3.46 comorbidities in patients who weren’t readmitted. Several specific comorbid conditions were independently associated with significantly increased risk of hospital readmission: asthma, chronic obstructive pulmonary disease, anxiety, heart failure, and gastroesophageal reflux disease.
“Patients with those comorbidities are the ones to watch aggressively in the postop period,” according to Dr. Karas.
Insurers have paid for the home nursing visits without hesitation.
Her presentation met with an enthusiastic audience reception.
“I think it’s important that you’ve shown a return on investment for this initiative,” one surgeon commented.
Session cochair John J. Kelly, MD, chief of general and minimally invasive surgery at the University of Massachusetts in Worcester, declared, “I think this is a very-important paper. We’re obviously all faced with this dilemma in terms of readmission rates. If you can prevent them, it’s to be commended.”
Dr. Karas reported having no financial conflicts of interest regarding her study.
NEW ORLEANS – A couple of home nursing visits early after bariatric surgery halved emergency department visits and hospital readmissions within the first 30 days in a case-control study, Linden A. Karas, MD, reported at Obesity Week 2016.
“Home nursing visits during the month following surgery, between doctor’s office visits, are a simple and inexpensive intervention that drastically decreases hospital revisits,” she declared at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
These early revisits to the hospital following bariatric surgery are not only common, they carry a substantial cost. An ED visit for hydration runs about $3,000 and a 2-day inpatient admission about $18,000. In contrast, the price tag for two home nursing visits in this study was $300, noted Dr. Karas, a surgeon at Mercy Catholic Medical Center in Philadelphia.
The triad of dehydration, nausea, and vomiting in addition to abdominal pain account for up to 40% of early readmissions following bariatric surgery. Because most hospital revisits for these reasons entail very little intervention other than IV fluids, Dr. Karas and her coinvestigators decided to investigate whether preemptive structured home visits by nurses prepared to administer IV fluids on the spot would cut down on hospital revisits. They found that indeed this strategy was successful.
Mercy Catholic Medical Center serves a largely low-income Medicare/Medicaid population. Part of the local culture is for many patients to obtain their primary care in the ED, so bariatric surgery patients are generally not reluctant to show up there if they don’t feel well in the first few weeks post surgery. That’s why in the year prior to the study the 30-day readmission rate was 23.6%, she explained.
The study included 193 consecutive prospectively followed adult participants in the home nursing program who underwent Roux-en-Y gastric bypass, laparoscopic adjustable banding, or revision surgery in 2014 and a control group of 267 matched bariatric surgery patients who underwent the same procedures in 2013, before introduction of the home nursing visits.
The first home visit occurred roughly 3 days after hospital discharge. The second one bridged the period between the first scheduled postoperative office visit at 2 weeks and the next office visit at 4 weeks. At discharge, patients were given a checklist concerning the signs and symptoms of dehydration, dietary recommendations, and lifestyle choices. Patients were encouraged to use the checklist to self-evaluate for dehydration and hand it over to the visiting nurses. The same checklist was provided to the home nurses. If the nurses found that patients met three or more criteria on the dehydration checklist, which included dry mucus membranes, heart rate greater than 90 beats/minute, headache, going more than 8 hours without urination, weakness, abdominal pain, and roughly a dozen other well-known criteria, they were instructed to initiate home hydration therapy with a banana bag and 2 L of normal saline.
If 1-2 days of home hydration failed to resolve the symptoms, the home care nurse was supposed to refer the patient to the ED. If the patient improved in response to home hydration therapy, the home nurse informed the surgeon’s office, which then set up a follow-up office visit to take place within the next 24 hours. Also, if the patient’s responses on the nutrition and behavioral health questionnaire raised any red flags regarding inadequate food and fluid intake, nonadherence to the recommended daily minimum of 30 minutes of physical activity, or depressive symptoms, the nurse was supposed to notify the surgeon to schedule a behavioral or nutrition appointment at the patient’s next scheduled visit.
The 30-day rate of all-cause hospital revisits in the home nursing care group was 11.9%, compared with 23.6% in controls. The rate of hospital revisits specifically for dehydration was 6.2% in the home visit group vs. 8.6% in controls, a 28% relative risk reduction in the home treatment group, which didn’t achieve statistical significance. However, in hindsight, it was evident that some of the visiting nurses didn’t fully understand the treatment protocol; they sent patients straight to the ED without first providing home hydration therapy. The visiting nurses were subcontracted out and weren’t part of the hospital’s bariatric surgery program.
Among those patients who did receive the therapy, however, it prevented readmission in 77% of cases. The 23% of patients who didn’t improve were referred to the hospital for further workup and treatment.
Patients with early hospital readmission had an average of 4.38 comorbid conditions, significantly more than the average 3.46 comorbidities in patients who weren’t readmitted. Several specific comorbid conditions were independently associated with significantly increased risk of hospital readmission: asthma, chronic obstructive pulmonary disease, anxiety, heart failure, and gastroesophageal reflux disease.
“Patients with those comorbidities are the ones to watch aggressively in the postop period,” according to Dr. Karas.
Insurers have paid for the home nursing visits without hesitation.
Her presentation met with an enthusiastic audience reception.
“I think it’s important that you’ve shown a return on investment for this initiative,” one surgeon commented.
Session cochair John J. Kelly, MD, chief of general and minimally invasive surgery at the University of Massachusetts in Worcester, declared, “I think this is a very-important paper. We’re obviously all faced with this dilemma in terms of readmission rates. If you can prevent them, it’s to be commended.”
Dr. Karas reported having no financial conflicts of interest regarding her study.
NEW ORLEANS – A couple of home nursing visits early after bariatric surgery halved emergency department visits and hospital readmissions within the first 30 days in a case-control study, Linden A. Karas, MD, reported at Obesity Week 2016.
“Home nursing visits during the month following surgery, between doctor’s office visits, are a simple and inexpensive intervention that drastically decreases hospital revisits,” she declared at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
These early revisits to the hospital following bariatric surgery are not only common, they carry a substantial cost. An ED visit for hydration runs about $3,000 and a 2-day inpatient admission about $18,000. In contrast, the price tag for two home nursing visits in this study was $300, noted Dr. Karas, a surgeon at Mercy Catholic Medical Center in Philadelphia.
The triad of dehydration, nausea, and vomiting in addition to abdominal pain account for up to 40% of early readmissions following bariatric surgery. Because most hospital revisits for these reasons entail very little intervention other than IV fluids, Dr. Karas and her coinvestigators decided to investigate whether preemptive structured home visits by nurses prepared to administer IV fluids on the spot would cut down on hospital revisits. They found that indeed this strategy was successful.
Mercy Catholic Medical Center serves a largely low-income Medicare/Medicaid population. Part of the local culture is for many patients to obtain their primary care in the ED, so bariatric surgery patients are generally not reluctant to show up there if they don’t feel well in the first few weeks post surgery. That’s why in the year prior to the study the 30-day readmission rate was 23.6%, she explained.
The study included 193 consecutive prospectively followed adult participants in the home nursing program who underwent Roux-en-Y gastric bypass, laparoscopic adjustable banding, or revision surgery in 2014 and a control group of 267 matched bariatric surgery patients who underwent the same procedures in 2013, before introduction of the home nursing visits.
The first home visit occurred roughly 3 days after hospital discharge. The second one bridged the period between the first scheduled postoperative office visit at 2 weeks and the next office visit at 4 weeks. At discharge, patients were given a checklist concerning the signs and symptoms of dehydration, dietary recommendations, and lifestyle choices. Patients were encouraged to use the checklist to self-evaluate for dehydration and hand it over to the visiting nurses. The same checklist was provided to the home nurses. If the nurses found that patients met three or more criteria on the dehydration checklist, which included dry mucus membranes, heart rate greater than 90 beats/minute, headache, going more than 8 hours without urination, weakness, abdominal pain, and roughly a dozen other well-known criteria, they were instructed to initiate home hydration therapy with a banana bag and 2 L of normal saline.
If 1-2 days of home hydration failed to resolve the symptoms, the home care nurse was supposed to refer the patient to the ED. If the patient improved in response to home hydration therapy, the home nurse informed the surgeon’s office, which then set up a follow-up office visit to take place within the next 24 hours. Also, if the patient’s responses on the nutrition and behavioral health questionnaire raised any red flags regarding inadequate food and fluid intake, nonadherence to the recommended daily minimum of 30 minutes of physical activity, or depressive symptoms, the nurse was supposed to notify the surgeon to schedule a behavioral or nutrition appointment at the patient’s next scheduled visit.
The 30-day rate of all-cause hospital revisits in the home nursing care group was 11.9%, compared with 23.6% in controls. The rate of hospital revisits specifically for dehydration was 6.2% in the home visit group vs. 8.6% in controls, a 28% relative risk reduction in the home treatment group, which didn’t achieve statistical significance. However, in hindsight, it was evident that some of the visiting nurses didn’t fully understand the treatment protocol; they sent patients straight to the ED without first providing home hydration therapy. The visiting nurses were subcontracted out and weren’t part of the hospital’s bariatric surgery program.
Among those patients who did receive the therapy, however, it prevented readmission in 77% of cases. The 23% of patients who didn’t improve were referred to the hospital for further workup and treatment.
Patients with early hospital readmission had an average of 4.38 comorbid conditions, significantly more than the average 3.46 comorbidities in patients who weren’t readmitted. Several specific comorbid conditions were independently associated with significantly increased risk of hospital readmission: asthma, chronic obstructive pulmonary disease, anxiety, heart failure, and gastroesophageal reflux disease.
“Patients with those comorbidities are the ones to watch aggressively in the postop period,” according to Dr. Karas.
Insurers have paid for the home nursing visits without hesitation.
Her presentation met with an enthusiastic audience reception.
“I think it’s important that you’ve shown a return on investment for this initiative,” one surgeon commented.
Session cochair John J. Kelly, MD, chief of general and minimally invasive surgery at the University of Massachusetts in Worcester, declared, “I think this is a very-important paper. We’re obviously all faced with this dilemma in terms of readmission rates. If you can prevent them, it’s to be commended.”
Dr. Karas reported having no financial conflicts of interest regarding her study.
AT OBESITY WEEK 2016
Key clinical point:
Major finding: The combined rate of ED visits and hospital readmissions within 30 days post–bariatric surgery was 11.9% in a group of patients who received two home nursing visits that included home hydration therapy as indicated, compared with 23.6% in bariatric surgery patients who weren’t involved in the home visit program.
Data source: This study compared 30-day hospital readmission rates in 193 consecutive prospectively followed bariatric surgery patients who received two structured home nursing visits in the first 4 postoperative weeks to readmissions in 267 matched controls whose surgery occurred prior to implementation of the home nursing program.
Disclosures: The presenter reported having no financial conflicts of interest regarding the study.
The Role of Self-Compassion in Chronic Illness Care
From the Department of Psychology, University of Sheffield, Sheffield, UK.
Abstract
- Objective: To present current research and theory on the potential of self-compassion for improving health-related outcomes in chronic illness, and make recommendations for the application of self-compassion interventions in clinical care to improve well-being and facilitate self-management of health in patients with chronic illness.
- Methods: Narrative review of the literature.
- Results: Current theory indicates that the self-kindness, common humanity, and mindfulness components of self-compassion can foster adaptive responses to the perceived setbacks and shortcomings that people experience in the context of living with a chronic illness. Research on self-compassion in relation to health has been examined primarily within non-medical populations. Cross-sectional and experimental studies have demonstrated clear links between self-compassion and lower levels of both perceived stress and physiological indictors of stress. A growing evidence base also indicates that self-compassion is associated with more frequent practice of health-promoting behaviors in healthy populations. Research on self-compassion with chronic illness populations is limited but has demonstrated cross-sectional links to adaptive coping, lower stress and distress, and the practice of important health behaviors. There are several interventions for increasing self-compassion in clinical settings, with limited data suggesting beneficial effects for clinical populations.
- Conclusion: Self-compassion holds promise as an important quality to cultivate to enhance health-related outcomes in those with chronic health conditions. Further systematic and rigorous research evaluating the effectiveness of self-compassion interventions in chronic illness populations is warranted to fully understand the role of this quality for chronic illness care.
Living with a chronic illness presents a number of challenges that can take a toll on both physical and psychological well-being. Pain, fatigue, and decreased daily functioning are symptoms common to many chronic illnesses that can negatively impact psychological well-being by creating uncertainty about attaining personal goals [1], and contributing to doubts and concerns about being able to fulfil one’s personal and work-related responsibilities [2]. The stress associated with negotiating the challenges of chronic illness can further complicate adjustment by exacerbating existing symptoms via stress-mediated and inflammation regulation pathways [3–5] and compromising the practice of important disease management and health maintenance behaviors [6,7]. These experiences can in turn fuel self-blame and other negative self-evaluations about not being able to meet personal and others’ expectations about managing one’s illness and create a downward spiral of poor adjustment and well-being [8,9].
A growing evidence base suggests that self-compassion is an important quality to help manage the stress and behavior-related issues that can compromise chronic illness care. Defined by Neff [10] as taking a kind, accepting, and non-judgmental stance towards oneself in times of failure or difficulty, self-compassion is associated with several indicators of adjustment in non-medical populations including resilience [11,12] and adaptive coping [13]. In support of the notion that self-compassion can play a role in promoting health behaviors, a recent meta-analysis found that self-compassion is linked to better practice of a range of health-promoting behaviors due in part to its links to adaptive emotions [14]. Research on the role of self-compassion for health-related outcomes with chronic illness populations is limited but nonetheless promising [15–17] , and suggests that self-compassion may be a worthwhile quality to cultivate to improve well-being and facilitate disease self-management.
In this article we present current research and theory on the potential of self-compassion as a clinical concept for improving health-related outcomes in chronic illness. After presenting a brief overview of the theoretical underpinnings of self-compassion and its measurement, we present the current state of research on the role of self-compassion in reducing stress and facilitating health behaviors in general medical populations. We then outline the emerging evidence illustrating a potential role for extending this research to chronic illness populations and make recommendations for the application of self-compassion interventions in clinical care, as a means to improving well-being and facilitating self-management of health for this group.
Self-Compassion: A Healthier Way of Responding to Challenges
Research into the correlates and effects of self-compassion has been primarily guided by the model of self-compassion proposed by Kristen Neff [10]. This view of self-compassion is derived from Buddhist psychology and reconceptualised in a secular manner to refer to the compassion expressed towards the self when experiencing suffering, whether it be due to circumstances beyond one’s control or within one’s control [18]. The 3 key components of self-compassion are proposed to work synergistically to promote kind rather than critical responses to failures and difficult circumstances. Self-kindness (versus self-judgment) involves taking a kind, caring and non-evaluative stance towards perceived inadequacies, shortcomings, and mistakes, and may be particularly valuable for countering the negative self-evaluations that can accompany not being able to meet one’s expectations due to the restrictions of living with a chronic condition [9]. Common humanity (versus isolation) refers to the sense of connection to others that arises from acknowledging the common human experience of imperfection and making mistakes, and being more aware that others may face similar challenging circumstances [18]. Framing hardship from this perspective can help people let go of the “why me?” view of their illness which can compromise adjustment [19], and instead foster a greater connection with others who live with similar conditions. Mindfulness (versus over identification) is the final component of self-compassion as conceptualised by Neff [10], and refers to taking a balanced and non-judgmental view of emotional experiences, grounding them in the present moment and neither ignoring nor becoming overly embroiled in the negative feelings that accompany painful experiences. Neff [10,18] proposes that mindfulness helps counteract the over-identification with one’s suffering that can reduce objectivity and taking a larger perspective on the situation. This mindful stance may be particularly beneficial for dealing with the ongoing pain and suffering of living with a chronic health condition, and encourage healthier ways of viewing the limitations associated with chronic illness. Correlational evidence from a study of healthy students further suggests that certain individual components of self-compassion may be particularly beneficial in the context of health, as the self-kindness and common humanity components were each found to be linked to better physical health and managing life stressors [20].
Although there are other conceptualizations of self-compassion [21], this 3-faceted model is the most widely used in research, in part because of the availability of a measure, the Self-compassion Scale [22], which explicitly assesses each of the facets of self-compassion. The 26-item scale is designed to assess positive and negative dimensions of each facet of self-compassion, but the total score is used more often than the separate subscales [23]. The measure assesses dispositional or trait self-compassion, with an underlying assumption that some individuals can be more or less self-compassionate in the way they regularly respond to challenges or failures. Importantly, self-compassion can also be prompted or fostered as a way of responding to failures and challenges, presenting the possibility that self-compassion can be increased among those who may benefit the most from responding with greater self-kindness and less self-judgement [24–26].
Whether conceived of as a momentary state or as an enduring quality, self-compassion has demonstrated consistent links with an array of indicators of psychological well-being. For example, one meta-analysis found that self-compassion is robustly and negatively linked with psychopathology (average r = –0.54), including depression and anxiety [27], 2 mental health issues that are prevalent in chronic illness populations [28,29]. Several studies have also noted associations of self-compassion with emotional resilience [18,30], and better coping and lower stress [12,13].
Self-Compassion Is Associated with Lower Perceived Stress
Relevant for our focus on chronic illness care, there is some evidence that self-compassion can be effective for improving well-being, and reducing stress in particular, in people with chronic illness. Across two illness samples, cancer and mixed chronic illnesses, those who scored low on a measure of self-compassion had higher levels of depression and stress compared to a healthy control sample [15], suggesting self-compassion may be protective against poor adjustment. Similar results have been found for breast cancer patients, with self-compassion explaining lower distress related to body image [16], and HIV patients, with self-compassion linked to lower stress, anxiety, and shame [31].
The protective role of self-compassion for stress appears to be explained primarily by the set of coping strategies that self-compassionate people use to deal with challenging circumstances. In their review, Allen and Leary [13] noted that self-compassionate people use coping styles that are adaptive and problem-focused (e.g., planning, social-support-seeking, and positive reframing), and tend to not use maladaptive coping styles (e.g., cognitively or behaviorally disengaging from the stressor and other escape-avoidance coping). Consistent with appraisal-based models of coping [32], adaptive coping strategies focus on removing the stressful event, garnering resources to better deal with the stressor, or recasting the stressor as less threatening, and therefore are instrumental in reducing the levels of stress that might normally be perceived in the absence of such coping approaches. Having access to a repertoire of adaptive coping strategies is particularly important in the context of chronic illness which can present a variety of daily challenges related to pain, functional and psychosocial limitations that require a flexible approach to changing demands.
Self-compassion with its links to adaptive coping may be particularly relevant for coping with such demands. One study put this assertion to the test by examining the role of coping strategies in explaining the link between self-compassion and stress in two chronic illness samples, inflammatory bowel disease (IBD) and arthritis [17]. In both samples, higher trait self-compassion was associated with a set of adaptive coping strategies which in turn explained greater coping efficacy and lower perceived stress, with the overall model explaining 43% of the variance in stress after controlling for health status and disease duration. Key adaptive coping strategies included greater use of active coping (a problem-focused coping strategy aimed at removing or reducing the stressor), positive reframing, and acceptance. The self-compassion–stress link was also explained in part by less use of maladaptive strategies, including denial, behavioral disengagement, and self-blame coping [17]. The latter coping strategy in particular is linked to poor adjustment in chronic illness as it reflects efforts to take control over uncontrollable symptoms by viewing illness-related changes, such as flare-ups, as a personal failure to manage one’s illness [9,33]. Together these findings, which were remarkably consistent across 2 distinct chronic illness groups, provide solid evidence to suggest that self-compassion provides individuals living with a chronic illness with a coping advantage that fosters adjustment through engaging in appropriate cognitive and behavioral coping strategies to minimize perceived stress.
Self-Compassion Can Reduce Physiological Stress
A caveat regarding the research to date on self-compassion and stress in chronic illness is that all studies are cross-sectional, which limits any conclusions about the direction of causality. Ignoring the fact that self-compassion in each of these studies was assessed as a relatively stable trait-like quality, one could argue that individuals who are less stressed have a greater opportunity to express kindness to themselves as they are not pre-occupied with illness-related demands and challenges. However, emerging research on self-compassion and the physiological correlates of stress provide a compelling case for the directionality assumed in the cross-sectional research. In one study, healthy young adults were subjected to a standard stress-inducing laboratory task (involving mental mathematics and public speaking), with plasma concentrations of the pro-inflammatory cytokine, interleukin-6 (IL-6), assessed before and after the task on 2 days [34]. Those with higher trait self-compassion responded to the stress task with significantly lower IL-6 levels even after controlling for other potential confounds such as demographics, self-esteem, depressive symptoms, and distress. Self-compassion was also linked to lower baseline levels of IL-6 on both days. These findings suggest that self-compassion may be both an enduring and response-specific protective factor against stress-induced inflammation.
There is also evidence supporting the efficacy of self-compassion interventions for reducing stress. In a study of healthy young women, those who underwent a brief training in self-compassion were found to have lower sympathetic nervous system reactivity (salivary alpha-amylase), and more adaptive parasympathetic nervous system reactivity (heart rate variability) in response to a stress-inducing lab task, compared to placebo control and no-training control groups [35]. That this study was conducted with women only is notable, as research indicates that women tend to have lower levels of self-compassion compared to men [18]. Together with the study on trait self-compassion and biomarkers of stress-induced inflammation, this research provides supportive evidence for the role of self-compassion in reducing the harmful physiological effects of stress. Self-compassion may therefore be particularly beneficial for both psychological and physical well-being in chronic illness given the known and negative impact of stress on symptoms for a number of chronic illnesses such as diabetes [36], cardiovascular disease [32], arthritis [4], and IBD [38].
Self-Compassion and the Regulation of Health Behaviors
Another key role for self-compassion in chronic illness care is through the facilitation of health-promoting behaviors. Health maintenance and disease management behaviors, such as getting diagnostic tests, taking medication, and weight management, are central for managing symptoms and minimizing the risk of disease progression or complications. For example, staying physically fit, maintaining a healthy diet, managing stress, and getting adequate sleep are critical for weight management and the behavioral control of symptoms for a number of chronic diseases [39,40]. Nonetheless, weight management behaviors often require initiating significant lifestyle changes which need to be maintained in order to be effective. Such behaviors can be particularly challenging for individuals with chronic illness symptoms such as pain and fatigue, which can present significant barriers [41] and trigger self-critical coping about not being able to adequately self-care or manage one’s disease [8,9]. Rather than being motivating, theory and evidence indicate that negative evaluations tend to increase stress and promote procrastination of important health behaviors [7,42].
In addition to theory noting why self-compassion may facilitate the regulation of important health behaviors [43,44], there is now a burgeoning body of research supporting the beneficial role of self-compassion in health behaviors [12,43,45]. Each of the 3 components of self-compassion (self-kindness, common humanity, and mindfulness) are posited to facilitate adaptive self-regulatory responses to the inevitable and momentary failures that occur when people try to enact their health goals. For example, not following through with dietary recommendations and giving into temptation can result in feelings of shame, negative self-evaluations, and reactive eating [46], which in turn can result in discontinuation of one’s diet. These minor failures would be viewed less negatively by people who are self-compassionate, because they realise that others have made similar mistakes (common humanity) and, therefore, do not become excessively self-critical (self-kindness) or immersed in feelings of guilt, shame or frustration (mindfulness), negative emotions which are known to interfere with self-regulation [43,47]. Indeed, self-compassion is associated with having fewer negative reactions in response to imagining a scenario in which a diet goal is transgressed [48].
There is also evidence that collectively, these components of self-compassion facilitate experiencing a healthy balance of positive and negative emotions in the context of health behavior change. Self-compassion appears to temper the negative responses to minor setbacks and failures that occur whilst trying to reach health goals, and foster the positive emotions required to maintain motivation during the pursuit of health goals. The most compelling support for this proposition comes from a meta-analysis of 15 samples (n = 3252) in which self-compassion was consistently and positively (average r = 0.25) associated with the practice of a range of health-promoting behaviors relevant for chronic illness care, including healthy eating, regular exercise, healthy sleep behaviors, and stress management [12]. The explanatory roles of positive and negative affect were also tested, with the results indicating that higher levels of positive affect and lower levels of negative affect were significant mediators of the link between self-compassion and health behaviors.
With respect to mood regulation, it is important to note that self-compassion is not simply an optimistic bias that predisposes individuals towards responding only in a positive way to perceived failures or setbacks. Rather, self-compassion fosters taking a balanced perspective on one’s failures, recognizing both the positive and negative aspects, and harnessing the negative mood that arises from a state of discrepancy to motivate self-improvement. For example, in experimental studies, both enduring and momentary self-compassionate states are associated with increased self-improvement motivation and behavior after experiencing failure and regret [49,50], in part because self-compassion fosters personal acceptance [50]. This adaptive responding can translate into better adherence and health behaviors in chronic health conditions after lapses in self-care which might otherwise foster self-criticism and poor disease management. Preliminary evidence from the author’s lab supports this proposition, as self-compassion was positively associated with both treatment adherence and the practice of wellness behaviors, due in part to lower levels of perceived stress, in samples of cancer patients and survivors [51], and people with chronic fatigue syndrome [52].
Clinical Applications of Self-Compassion for Chronic Illness Care
Given the growing evidence linking self-compassion to well-being and health behaviors, the next logical step is to consider ways of cultivating self-compassion for those individuals experiencing chronic health conditions.
Training in mindfulness might be one way to foster self-compassion within a health care setting. Mindfulness-Based Cognitive Behavior Therapy (MBCT [53]), and Mindfulness-Based Stress Reduction (MBSR [54]), are both programs that use mindfulness skills to notice distressing thoughts and feelings, hold these experiences in awareness, and cultivate acceptance and self-compassion [53]. MBSR, usually delivered as an 8-week group-based program, has been found to have significant effects on depression, anxiety and psychological distress in people with chronic somatic diseases [55]. However, fostering self-compassion forms only part of MBCT and MBSR. Indeed there are very few therapeutic interventions that specifically and primarily target self-compassion; however, where they are used they show promise.
Compassionate Mind Training (CMT [24]), Compassion-Focused Therapy (CFT [21]), and the Mindful Self-Compassion program [26] are examples of such targeted interventions. These therapeutic models, again usually delivered in group settings, aim to foster a kinder and more accepting attitude towards oneself through the use of formal meditations (such as living kindness meditation; LKM), home practice and informal practices for daily life (such as self-compassionate letter writing), and have been demonstrated to be effective with, for example, community participants [26], people who hear malevolent voices [56], and those with chronic mood difficulties [24].
Additionally, there are a number of brief self-compassion practices that have been evaluated as an intervention in their own right and demonstrate positive effects. LKM aiming to develop a state of unconditional kindness towards both oneself and others and compassion meditation (CM [57]), are the most commonly described. CM involves techniques to cultivate compassion, or deep, genuine sympathy for those stricken by misfortune, including oneself, “together with an earnest wish to ease this suffering” [58]. The effects of these kindness-based meditations on health and well-being have been summarized in a recent review [59] which illustrates that, whilst limited data exists currently, promising effects have been shown for a number of different groups. Positive effects have for example been demonstrated for patients with chronic back pain [60] and for people with experiences traditionally conceptualized as psychosis [61], suggesting these practice may also be beneficial for other chronic health conditions.
Alongside the potential benefits, how interventions cultivating self-compassion can be delivered in clinical practice is worthy of consideration. Previous applications have included group work (including MBCT, MBSR), one-to-one therapy (such as CFT) and self-directed practice via bibliotherapy or online materials. The different options available here suggest this kind of intervention is highly accessible, potentially inexpensive and could be used as a complimentary approach alongside other more traditional medical disease management treatments or as a stand-alone psychotherapeutic intervention when required.
In order to best support the successful introduction and evaluation of such interventions, consideration of compassionate practice by staff within health-care settings is also needed. Cultivating a culture of compassion through compassionate leadership [62] is required. We know services with higher levels of caring practice have higher quality care, greater well-being for staff and in turn more compassionate care for patients [63] than those services that are struggling. It is hoped that taking a broad systemic compassionate approach (via training, ongoing supervision and ethos cultivation) would ensure that the language used, information communicated, and disease management approaches are planned and delivered in a way that fosters patients’ sense of self-efficacy and kindness towards themselves, with all the benefits outlined above.
Conclusion
Theory and research indicate that self-compassion fosters adaptive responses to perceived failures and setbacks, and is therefore associated with well-being, reduced stress and more frequent health behaviors. The emerging evidence base on the benefits of self-compassion for coping with the challenges of chronic health conditions is promising, and suggests that the benefits of self-compassion noted in non-medical populations may extend to chronic illness care. Interventions cultivating self-compassion may be especially beneficial for those with chronic health conditions through the mechanisms identified earlier; reducing stress (and thereby impacting on an individual’s relationship with their physical health); improving self-management skills with condition related behaviors and health-promoting behaviors; altering one’s relationship with illness-related shame and self-blame; and in boosting resilience. Systematic and rigorous evaluation of such interventions with people with chronic health conditions is now needed, evaluating impacts on well-being, health behaviors, and disease management and outcomes.
Corresponding author: Fuschia M. Sirois, Dept. of Psychology, University of Sheffield, 1 Vicar Lane, Sheffeld, S1 1HD, [email protected].
Fianacial disclosures: None.
1. Hamilton N, Karoly P, Kitzman H. Self-regulation and chronic pain:The role of emotion. Cogn Ther Res 2007;28:559–576.
2. Luyten P, Kempke S, Van Wambeke P, et al. Self-critical perfectionism, stress generation, and stress sensitivity in patients with chronic fatigue syndrome: relationship with severity of depression. Psychiatry 2011;74:21–30.
3. Cohen S, Janicki-Deverts D, Doyle WJ, et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proceedings of the National Academy of Sciences 2012.
4. Evers AWM, Verhoeven EWM, van Middendorp H, et al. Does stress affect the joints? Daily stressors, stress vulnerability, immune and HPA axis activity, and short-term disease and symptom fluctuations in rheumatoid arthritis. Ann Rheum Dis 2014;73:1683–8.
5. Maunder RG, Levenstein S. The role of stress in the development and clinical course of inflammatory bowel disease: epidemiological evidence. Curr Molecular Med 2008;8:247–52.
6. Rod NH, Grønbæk M, Schnohr P, et al. Perceived stress as a risk factor for changes in health behavior and cardiac risk profile: a longitudinal study. J Intern Med 2009;266:467–75.
7. Sirois FM. Is procrastination a vulnerability factor for hypertension and cardiovascular disease? Testing an extension of the procrastination-health model. J Behav Med 2015;38:578–89.
8. Moskovitz DN, Maunder RG, Cohen Z, et al. Coping behavior and social support contribute independently to quality of life after surgery for inflammatory bowel disease. Dis Colon Rectum 2000;43:517–21.
9. Voth J, Sirois FM. The role of self-blame and responsibility in adjustment to inflammatory bowel disease. Rehab Psych 2009;54:99–108.
10. Neff KD. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self Ident 2003;2:85–101.
11. Neff KD, Kirkpatrick KL, Rude SS. Self-compassion and adaptive psychological functioning. J Res Personality 2007;41:139–54.
12. Sirois FM. Procrastination and stress: Exploring the role of self-compassion. Self Ident 2014;13:128–45.
13. Allen AB, Leary MR. Self-compassion, stress, and coping. Soc Person Psych Comp 2010;4:107–18.
14. Sirois FM, Kitner R, Hirsch JK. Self-compassion, affect, and health behaviors. Health Psychol 2014.
15. Pinto-Gouveia J, Duarte C, Matos M, Fráguas S. The protective role of self-compassion in relation to psychopathology symptoms and quality of life in chronic illness and in cancer patients. Clin Psychol Psychother 2014;21:311–23.
16. Przezdziecki A, Sherman KA, Baillie A, et al. My changed body: breast cancer, body image, distress and self-compassion. Psychooncology 2013;22:1872–9.
17. Sirois FM, Molnar DS, Hirsch JK. Self-compassion, stress, and coping in the context of chronic illness. Self Identity 2015:1–14.
18. Neff KD. Self-compassion, self-esteem, and well-being. Social Personality Psych Compass 2011;5:1–12.
19. Davis DG, Morgan MS. Finding meaning, perceiving growth, and acceptance of tinnitus. Rehabil Psych 2008;53:128–38.
20. Hall CW, Row KA, Wuensch KL, Godley KR. The role of self-compassion in physical and psychological well-being. J Psychology 2013;147:311–23.
21. Gilbert P. Introducing compassion-focused therapy. Advance Psych Treat 2009;15:199–208.
22. Neff KD. Development and validation of a scale to measure self-compassion. Self Identity 2003;2:223–50.
23. Neff KD. The self-compassion scale is a valid and theoretically coherent measure of self-compassion. Mindfulness 2016;7:264–74.
24. Gilbert P, Procter S. Compassionate mind training for people with high shame and self-criticism: overview and pilot study of a group therapy approach. Clin Psychol Psychother 2006;13:353–79.
25. Leary MR, Tate EB, Adams CE, et al. Self-compassion and reactions to unpleasant self-relevant events: the implications of treating oneself kindly. J Personality Social Psychol 2007;92:887–904.
26. Neff KD, Germer CK. A pilot study and randomized controlled trial of the mindful self-compassion program. J Clin Psychol 2013;69:28–44.
27. MacBeth A, Gumley A. Exploring compassion: A meta-analysis of the association between self-compassion and psychopathology. Clin Psych Rev 2012;32:545–52.
28. Murphy LB, Sacks JJ, Brady TJ, et al. Anxiety and depression among US adults with arthritis: Prevalence and correlates. Arthritis Care Res 2012:64:968–76.
29. Walker JR, Ediger JP, Graff LA, et al. The Manitoba IBD Cohort Study: a population-based study of the prevalence of lifetime and 12-month anxiety and mood disorders. Am J Gastroenterol 2008;103:1989–97.
30. Neff KD, McGehee P. Self-compassion and psychological resilience among adolescents and young adults. Self Ident 2009;9:225–40.
31. Brion J, Leary M, Drabkin A. Self-compassion and reactions to serious illness: The case of HIV. J Health Psychol 2014;19:218–29.
32. Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984.
33. Thompson SC, Cheek PR, Graham MA. The other side of perceived control: disadvantages and negative effects. In: Spacapan S, Oskamp S, editors. The social psychology of health. Newbury Park: Sage; 1988:69–93.
34. Breines JG, Thoma MV, Gianferante D, et al. Self-compassion as a predictor of interleukin-6 response to acute psychosocial stress. Brain, Behavior, and Immunity 2014;37:109–14.
36. Lloyd C, Smith J, Weinger K. Stress and diabetes: a review of the links. Diabetes Spectrum 2005;18:121–7.
35. Arch JJ, Brown KW, Dean DJ, et al. Self-compassion training modulates alpha-amylase, heart rate variability, and subjective responses to social evaluative threat in women. Psychoneuroendocrinology 2013;42:49–58.
37. Dimsdale JE. Psychological stress and cardiovascular disease. J Am Coll Cardiol 2008;51:1237–46.
38. Maunder RG. Evidence that stress contributes to inflammatory bowel disease: evaluation, synthesis, and future directions. Inflam Bowel Dis 2005;11:600–8.
39. Daskalopoulou SS, Khan NA, Quinn RR, et al. The 2012 Canadian Hypertension Education program recommendations for the management of hypertension: blood pressure measurement, diagnosis, assessment of risk, and therapy. Can J Cardiol 2012;28:270–87.
40. Gulliksson M, Burell G, Vessby B, et al. Randomized controlled trial of cognitive behavioral therapy vs standard treatment to prevent recurrent cardiovascular events in patients with coronary heart disease: Secondary prevention in uppsala primary health care project (suprim). Arch Intern Med 2011;171:134–40.
41. Jerant AF, Friederichs-Fitzwater MMV, Moore M. Patients’ perceived barriers to active self-management of chronic conditions. Patient Ed Couns 2005;57:300–7.
42. Sirois FM. Procrastination, stress, and chronic health conditions: a temporal perspective. In: Sirois FM, Pychyl T, editors. Procrastination, health, and well-being. Elsevier; 2016.
43. Sirois FM. A self-regulation resource model of self-compassion and health behavior intentions in emerging adults. Prev Med Rep 2015;2:218–22.
44. Terry ML, Leary MR. Self-compassion, self-regulation, and health. Self Identity 2011;10:352–62.
45. Dunne S, Sheffield D, Chilcot J. Brief report: Self-compassion, physical health and the mediating role of health-promoting behaviors. J Health Psychol 2016.
46. Polivy J, Herman CP, Deo R. Getting a bigger slice of the pie. Effects on eating and emotion in restrained and unrestrained eaters. Appetite 2010;55:426–30.
47. Wagner DD, Heatherton TF. Self-regulation and its failure: The seven deadly threats to self-regulation. In: Mikulincer M, Shaver PR, Borgida E, Bargh JA, editors. APA handbook of personality and social psychology, Volume 1: Attitudes and social cognition. Washington: American Psychological Association. Forthcoming.
48. Adams CE, Leary MR. Promoting self-compassionate attitudes toward eating among restrictive and guilty eaters. J Soc Clin Psychol 2007;26:1120–44.
49. Breines JG, Chen S. Self-compassion increases self-improvement motivation. Pers Social Psych Bull 2012;38:1133–43.
50. Zhang JW, Chen S. Self-compassion promotes personal improvement from regret experiences via acceptance. Pers Social Psych Bull 2016;42:244–58.
51. Sirois FM, Hirsch JK. Self-compassion is associated with health behaviors in cancer patients and survivors. Forthcoming.
52. Sirois FM. Self-compassion, adheremce, and health behaviors in chronic fatigue syndrome: The role of stress. Forthcoming.
53. Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. New York: Guilford Press; 2002.
54. Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Dell; 1990.
55. Bohlmeijer E, Prenger R, Taal E, Cuijpers P. The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: A meta-analysis. J Psychosom Res 2010;68:539–44.
56. Mayhew SL, Gilbert P. Compassionate mind training with people who hear malevolent voices: a case series report. Clin Psychol Psychother 2008;15:113–38.
57. Hofmann SG, Grossman P, Hinton DE. Loving-kindness and compassion meditation: potential for psychological interventions. Clin Psychol Rev 2011;31:1126–32.
58. Hopkins J. Cultivating compassion. New York: Broadway Books; 2001.
59. Galante J, Galante I, Bekkers M-J Gallacher. Effect of kindness-based meditation on health and well-being: a systematic review and meta-analysis. J Consult Clin Psychol 2014;82:1101–14.
60. Carson JW, Keefe FJ, Lynch TR, et al. Loving-kindness meditation for chronic low back pain: results from a pilot trial. J Holist Nurs 2005;23:287–304.
61. Johnson DP, Penn DL, Fredrickson BL, et al. A pilot study of loving-kindness meditation for the negative symptoms of schizophrenia. Schizophr Res 2011;129:137–40.
62. West M, Steward K, Eckert R, Pasmore B. Developing collective leadership for health care. London: The King’s Fund; 2014.
63. Dixon-Woods M, Baker R, Charles K, et al. Culture and behavior in the English National Health Service: overview of lessons from a large multimethod study. BMJ Qual Saf 2014;23:106–15.
From the Department of Psychology, University of Sheffield, Sheffield, UK.
Abstract
- Objective: To present current research and theory on the potential of self-compassion for improving health-related outcomes in chronic illness, and make recommendations for the application of self-compassion interventions in clinical care to improve well-being and facilitate self-management of health in patients with chronic illness.
- Methods: Narrative review of the literature.
- Results: Current theory indicates that the self-kindness, common humanity, and mindfulness components of self-compassion can foster adaptive responses to the perceived setbacks and shortcomings that people experience in the context of living with a chronic illness. Research on self-compassion in relation to health has been examined primarily within non-medical populations. Cross-sectional and experimental studies have demonstrated clear links between self-compassion and lower levels of both perceived stress and physiological indictors of stress. A growing evidence base also indicates that self-compassion is associated with more frequent practice of health-promoting behaviors in healthy populations. Research on self-compassion with chronic illness populations is limited but has demonstrated cross-sectional links to adaptive coping, lower stress and distress, and the practice of important health behaviors. There are several interventions for increasing self-compassion in clinical settings, with limited data suggesting beneficial effects for clinical populations.
- Conclusion: Self-compassion holds promise as an important quality to cultivate to enhance health-related outcomes in those with chronic health conditions. Further systematic and rigorous research evaluating the effectiveness of self-compassion interventions in chronic illness populations is warranted to fully understand the role of this quality for chronic illness care.
Living with a chronic illness presents a number of challenges that can take a toll on both physical and psychological well-being. Pain, fatigue, and decreased daily functioning are symptoms common to many chronic illnesses that can negatively impact psychological well-being by creating uncertainty about attaining personal goals [1], and contributing to doubts and concerns about being able to fulfil one’s personal and work-related responsibilities [2]. The stress associated with negotiating the challenges of chronic illness can further complicate adjustment by exacerbating existing symptoms via stress-mediated and inflammation regulation pathways [3–5] and compromising the practice of important disease management and health maintenance behaviors [6,7]. These experiences can in turn fuel self-blame and other negative self-evaluations about not being able to meet personal and others’ expectations about managing one’s illness and create a downward spiral of poor adjustment and well-being [8,9].
A growing evidence base suggests that self-compassion is an important quality to help manage the stress and behavior-related issues that can compromise chronic illness care. Defined by Neff [10] as taking a kind, accepting, and non-judgmental stance towards oneself in times of failure or difficulty, self-compassion is associated with several indicators of adjustment in non-medical populations including resilience [11,12] and adaptive coping [13]. In support of the notion that self-compassion can play a role in promoting health behaviors, a recent meta-analysis found that self-compassion is linked to better practice of a range of health-promoting behaviors due in part to its links to adaptive emotions [14]. Research on the role of self-compassion for health-related outcomes with chronic illness populations is limited but nonetheless promising [15–17] , and suggests that self-compassion may be a worthwhile quality to cultivate to improve well-being and facilitate disease self-management.
In this article we present current research and theory on the potential of self-compassion as a clinical concept for improving health-related outcomes in chronic illness. After presenting a brief overview of the theoretical underpinnings of self-compassion and its measurement, we present the current state of research on the role of self-compassion in reducing stress and facilitating health behaviors in general medical populations. We then outline the emerging evidence illustrating a potential role for extending this research to chronic illness populations and make recommendations for the application of self-compassion interventions in clinical care, as a means to improving well-being and facilitating self-management of health for this group.
Self-Compassion: A Healthier Way of Responding to Challenges
Research into the correlates and effects of self-compassion has been primarily guided by the model of self-compassion proposed by Kristen Neff [10]. This view of self-compassion is derived from Buddhist psychology and reconceptualised in a secular manner to refer to the compassion expressed towards the self when experiencing suffering, whether it be due to circumstances beyond one’s control or within one’s control [18]. The 3 key components of self-compassion are proposed to work synergistically to promote kind rather than critical responses to failures and difficult circumstances. Self-kindness (versus self-judgment) involves taking a kind, caring and non-evaluative stance towards perceived inadequacies, shortcomings, and mistakes, and may be particularly valuable for countering the negative self-evaluations that can accompany not being able to meet one’s expectations due to the restrictions of living with a chronic condition [9]. Common humanity (versus isolation) refers to the sense of connection to others that arises from acknowledging the common human experience of imperfection and making mistakes, and being more aware that others may face similar challenging circumstances [18]. Framing hardship from this perspective can help people let go of the “why me?” view of their illness which can compromise adjustment [19], and instead foster a greater connection with others who live with similar conditions. Mindfulness (versus over identification) is the final component of self-compassion as conceptualised by Neff [10], and refers to taking a balanced and non-judgmental view of emotional experiences, grounding them in the present moment and neither ignoring nor becoming overly embroiled in the negative feelings that accompany painful experiences. Neff [10,18] proposes that mindfulness helps counteract the over-identification with one’s suffering that can reduce objectivity and taking a larger perspective on the situation. This mindful stance may be particularly beneficial for dealing with the ongoing pain and suffering of living with a chronic health condition, and encourage healthier ways of viewing the limitations associated with chronic illness. Correlational evidence from a study of healthy students further suggests that certain individual components of self-compassion may be particularly beneficial in the context of health, as the self-kindness and common humanity components were each found to be linked to better physical health and managing life stressors [20].
Although there are other conceptualizations of self-compassion [21], this 3-faceted model is the most widely used in research, in part because of the availability of a measure, the Self-compassion Scale [22], which explicitly assesses each of the facets of self-compassion. The 26-item scale is designed to assess positive and negative dimensions of each facet of self-compassion, but the total score is used more often than the separate subscales [23]. The measure assesses dispositional or trait self-compassion, with an underlying assumption that some individuals can be more or less self-compassionate in the way they regularly respond to challenges or failures. Importantly, self-compassion can also be prompted or fostered as a way of responding to failures and challenges, presenting the possibility that self-compassion can be increased among those who may benefit the most from responding with greater self-kindness and less self-judgement [24–26].
Whether conceived of as a momentary state or as an enduring quality, self-compassion has demonstrated consistent links with an array of indicators of psychological well-being. For example, one meta-analysis found that self-compassion is robustly and negatively linked with psychopathology (average r = –0.54), including depression and anxiety [27], 2 mental health issues that are prevalent in chronic illness populations [28,29]. Several studies have also noted associations of self-compassion with emotional resilience [18,30], and better coping and lower stress [12,13].
Self-Compassion Is Associated with Lower Perceived Stress
Relevant for our focus on chronic illness care, there is some evidence that self-compassion can be effective for improving well-being, and reducing stress in particular, in people with chronic illness. Across two illness samples, cancer and mixed chronic illnesses, those who scored low on a measure of self-compassion had higher levels of depression and stress compared to a healthy control sample [15], suggesting self-compassion may be protective against poor adjustment. Similar results have been found for breast cancer patients, with self-compassion explaining lower distress related to body image [16], and HIV patients, with self-compassion linked to lower stress, anxiety, and shame [31].
The protective role of self-compassion for stress appears to be explained primarily by the set of coping strategies that self-compassionate people use to deal with challenging circumstances. In their review, Allen and Leary [13] noted that self-compassionate people use coping styles that are adaptive and problem-focused (e.g., planning, social-support-seeking, and positive reframing), and tend to not use maladaptive coping styles (e.g., cognitively or behaviorally disengaging from the stressor and other escape-avoidance coping). Consistent with appraisal-based models of coping [32], adaptive coping strategies focus on removing the stressful event, garnering resources to better deal with the stressor, or recasting the stressor as less threatening, and therefore are instrumental in reducing the levels of stress that might normally be perceived in the absence of such coping approaches. Having access to a repertoire of adaptive coping strategies is particularly important in the context of chronic illness which can present a variety of daily challenges related to pain, functional and psychosocial limitations that require a flexible approach to changing demands.
Self-compassion with its links to adaptive coping may be particularly relevant for coping with such demands. One study put this assertion to the test by examining the role of coping strategies in explaining the link between self-compassion and stress in two chronic illness samples, inflammatory bowel disease (IBD) and arthritis [17]. In both samples, higher trait self-compassion was associated with a set of adaptive coping strategies which in turn explained greater coping efficacy and lower perceived stress, with the overall model explaining 43% of the variance in stress after controlling for health status and disease duration. Key adaptive coping strategies included greater use of active coping (a problem-focused coping strategy aimed at removing or reducing the stressor), positive reframing, and acceptance. The self-compassion–stress link was also explained in part by less use of maladaptive strategies, including denial, behavioral disengagement, and self-blame coping [17]. The latter coping strategy in particular is linked to poor adjustment in chronic illness as it reflects efforts to take control over uncontrollable symptoms by viewing illness-related changes, such as flare-ups, as a personal failure to manage one’s illness [9,33]. Together these findings, which were remarkably consistent across 2 distinct chronic illness groups, provide solid evidence to suggest that self-compassion provides individuals living with a chronic illness with a coping advantage that fosters adjustment through engaging in appropriate cognitive and behavioral coping strategies to minimize perceived stress.
Self-Compassion Can Reduce Physiological Stress
A caveat regarding the research to date on self-compassion and stress in chronic illness is that all studies are cross-sectional, which limits any conclusions about the direction of causality. Ignoring the fact that self-compassion in each of these studies was assessed as a relatively stable trait-like quality, one could argue that individuals who are less stressed have a greater opportunity to express kindness to themselves as they are not pre-occupied with illness-related demands and challenges. However, emerging research on self-compassion and the physiological correlates of stress provide a compelling case for the directionality assumed in the cross-sectional research. In one study, healthy young adults were subjected to a standard stress-inducing laboratory task (involving mental mathematics and public speaking), with plasma concentrations of the pro-inflammatory cytokine, interleukin-6 (IL-6), assessed before and after the task on 2 days [34]. Those with higher trait self-compassion responded to the stress task with significantly lower IL-6 levels even after controlling for other potential confounds such as demographics, self-esteem, depressive symptoms, and distress. Self-compassion was also linked to lower baseline levels of IL-6 on both days. These findings suggest that self-compassion may be both an enduring and response-specific protective factor against stress-induced inflammation.
There is also evidence supporting the efficacy of self-compassion interventions for reducing stress. In a study of healthy young women, those who underwent a brief training in self-compassion were found to have lower sympathetic nervous system reactivity (salivary alpha-amylase), and more adaptive parasympathetic nervous system reactivity (heart rate variability) in response to a stress-inducing lab task, compared to placebo control and no-training control groups [35]. That this study was conducted with women only is notable, as research indicates that women tend to have lower levels of self-compassion compared to men [18]. Together with the study on trait self-compassion and biomarkers of stress-induced inflammation, this research provides supportive evidence for the role of self-compassion in reducing the harmful physiological effects of stress. Self-compassion may therefore be particularly beneficial for both psychological and physical well-being in chronic illness given the known and negative impact of stress on symptoms for a number of chronic illnesses such as diabetes [36], cardiovascular disease [32], arthritis [4], and IBD [38].
Self-Compassion and the Regulation of Health Behaviors
Another key role for self-compassion in chronic illness care is through the facilitation of health-promoting behaviors. Health maintenance and disease management behaviors, such as getting diagnostic tests, taking medication, and weight management, are central for managing symptoms and minimizing the risk of disease progression or complications. For example, staying physically fit, maintaining a healthy diet, managing stress, and getting adequate sleep are critical for weight management and the behavioral control of symptoms for a number of chronic diseases [39,40]. Nonetheless, weight management behaviors often require initiating significant lifestyle changes which need to be maintained in order to be effective. Such behaviors can be particularly challenging for individuals with chronic illness symptoms such as pain and fatigue, which can present significant barriers [41] and trigger self-critical coping about not being able to adequately self-care or manage one’s disease [8,9]. Rather than being motivating, theory and evidence indicate that negative evaluations tend to increase stress and promote procrastination of important health behaviors [7,42].
In addition to theory noting why self-compassion may facilitate the regulation of important health behaviors [43,44], there is now a burgeoning body of research supporting the beneficial role of self-compassion in health behaviors [12,43,45]. Each of the 3 components of self-compassion (self-kindness, common humanity, and mindfulness) are posited to facilitate adaptive self-regulatory responses to the inevitable and momentary failures that occur when people try to enact their health goals. For example, not following through with dietary recommendations and giving into temptation can result in feelings of shame, negative self-evaluations, and reactive eating [46], which in turn can result in discontinuation of one’s diet. These minor failures would be viewed less negatively by people who are self-compassionate, because they realise that others have made similar mistakes (common humanity) and, therefore, do not become excessively self-critical (self-kindness) or immersed in feelings of guilt, shame or frustration (mindfulness), negative emotions which are known to interfere with self-regulation [43,47]. Indeed, self-compassion is associated with having fewer negative reactions in response to imagining a scenario in which a diet goal is transgressed [48].
There is also evidence that collectively, these components of self-compassion facilitate experiencing a healthy balance of positive and negative emotions in the context of health behavior change. Self-compassion appears to temper the negative responses to minor setbacks and failures that occur whilst trying to reach health goals, and foster the positive emotions required to maintain motivation during the pursuit of health goals. The most compelling support for this proposition comes from a meta-analysis of 15 samples (n = 3252) in which self-compassion was consistently and positively (average r = 0.25) associated with the practice of a range of health-promoting behaviors relevant for chronic illness care, including healthy eating, regular exercise, healthy sleep behaviors, and stress management [12]. The explanatory roles of positive and negative affect were also tested, with the results indicating that higher levels of positive affect and lower levels of negative affect were significant mediators of the link between self-compassion and health behaviors.
With respect to mood regulation, it is important to note that self-compassion is not simply an optimistic bias that predisposes individuals towards responding only in a positive way to perceived failures or setbacks. Rather, self-compassion fosters taking a balanced perspective on one’s failures, recognizing both the positive and negative aspects, and harnessing the negative mood that arises from a state of discrepancy to motivate self-improvement. For example, in experimental studies, both enduring and momentary self-compassionate states are associated with increased self-improvement motivation and behavior after experiencing failure and regret [49,50], in part because self-compassion fosters personal acceptance [50]. This adaptive responding can translate into better adherence and health behaviors in chronic health conditions after lapses in self-care which might otherwise foster self-criticism and poor disease management. Preliminary evidence from the author’s lab supports this proposition, as self-compassion was positively associated with both treatment adherence and the practice of wellness behaviors, due in part to lower levels of perceived stress, in samples of cancer patients and survivors [51], and people with chronic fatigue syndrome [52].
Clinical Applications of Self-Compassion for Chronic Illness Care
Given the growing evidence linking self-compassion to well-being and health behaviors, the next logical step is to consider ways of cultivating self-compassion for those individuals experiencing chronic health conditions.
Training in mindfulness might be one way to foster self-compassion within a health care setting. Mindfulness-Based Cognitive Behavior Therapy (MBCT [53]), and Mindfulness-Based Stress Reduction (MBSR [54]), are both programs that use mindfulness skills to notice distressing thoughts and feelings, hold these experiences in awareness, and cultivate acceptance and self-compassion [53]. MBSR, usually delivered as an 8-week group-based program, has been found to have significant effects on depression, anxiety and psychological distress in people with chronic somatic diseases [55]. However, fostering self-compassion forms only part of MBCT and MBSR. Indeed there are very few therapeutic interventions that specifically and primarily target self-compassion; however, where they are used they show promise.
Compassionate Mind Training (CMT [24]), Compassion-Focused Therapy (CFT [21]), and the Mindful Self-Compassion program [26] are examples of such targeted interventions. These therapeutic models, again usually delivered in group settings, aim to foster a kinder and more accepting attitude towards oneself through the use of formal meditations (such as living kindness meditation; LKM), home practice and informal practices for daily life (such as self-compassionate letter writing), and have been demonstrated to be effective with, for example, community participants [26], people who hear malevolent voices [56], and those with chronic mood difficulties [24].
Additionally, there are a number of brief self-compassion practices that have been evaluated as an intervention in their own right and demonstrate positive effects. LKM aiming to develop a state of unconditional kindness towards both oneself and others and compassion meditation (CM [57]), are the most commonly described. CM involves techniques to cultivate compassion, or deep, genuine sympathy for those stricken by misfortune, including oneself, “together with an earnest wish to ease this suffering” [58]. The effects of these kindness-based meditations on health and well-being have been summarized in a recent review [59] which illustrates that, whilst limited data exists currently, promising effects have been shown for a number of different groups. Positive effects have for example been demonstrated for patients with chronic back pain [60] and for people with experiences traditionally conceptualized as psychosis [61], suggesting these practice may also be beneficial for other chronic health conditions.
Alongside the potential benefits, how interventions cultivating self-compassion can be delivered in clinical practice is worthy of consideration. Previous applications have included group work (including MBCT, MBSR), one-to-one therapy (such as CFT) and self-directed practice via bibliotherapy or online materials. The different options available here suggest this kind of intervention is highly accessible, potentially inexpensive and could be used as a complimentary approach alongside other more traditional medical disease management treatments or as a stand-alone psychotherapeutic intervention when required.
In order to best support the successful introduction and evaluation of such interventions, consideration of compassionate practice by staff within health-care settings is also needed. Cultivating a culture of compassion through compassionate leadership [62] is required. We know services with higher levels of caring practice have higher quality care, greater well-being for staff and in turn more compassionate care for patients [63] than those services that are struggling. It is hoped that taking a broad systemic compassionate approach (via training, ongoing supervision and ethos cultivation) would ensure that the language used, information communicated, and disease management approaches are planned and delivered in a way that fosters patients’ sense of self-efficacy and kindness towards themselves, with all the benefits outlined above.
Conclusion
Theory and research indicate that self-compassion fosters adaptive responses to perceived failures and setbacks, and is therefore associated with well-being, reduced stress and more frequent health behaviors. The emerging evidence base on the benefits of self-compassion for coping with the challenges of chronic health conditions is promising, and suggests that the benefits of self-compassion noted in non-medical populations may extend to chronic illness care. Interventions cultivating self-compassion may be especially beneficial for those with chronic health conditions through the mechanisms identified earlier; reducing stress (and thereby impacting on an individual’s relationship with their physical health); improving self-management skills with condition related behaviors and health-promoting behaviors; altering one’s relationship with illness-related shame and self-blame; and in boosting resilience. Systematic and rigorous evaluation of such interventions with people with chronic health conditions is now needed, evaluating impacts on well-being, health behaviors, and disease management and outcomes.
Corresponding author: Fuschia M. Sirois, Dept. of Psychology, University of Sheffield, 1 Vicar Lane, Sheffeld, S1 1HD, [email protected].
Fianacial disclosures: None.
From the Department of Psychology, University of Sheffield, Sheffield, UK.
Abstract
- Objective: To present current research and theory on the potential of self-compassion for improving health-related outcomes in chronic illness, and make recommendations for the application of self-compassion interventions in clinical care to improve well-being and facilitate self-management of health in patients with chronic illness.
- Methods: Narrative review of the literature.
- Results: Current theory indicates that the self-kindness, common humanity, and mindfulness components of self-compassion can foster adaptive responses to the perceived setbacks and shortcomings that people experience in the context of living with a chronic illness. Research on self-compassion in relation to health has been examined primarily within non-medical populations. Cross-sectional and experimental studies have demonstrated clear links between self-compassion and lower levels of both perceived stress and physiological indictors of stress. A growing evidence base also indicates that self-compassion is associated with more frequent practice of health-promoting behaviors in healthy populations. Research on self-compassion with chronic illness populations is limited but has demonstrated cross-sectional links to adaptive coping, lower stress and distress, and the practice of important health behaviors. There are several interventions for increasing self-compassion in clinical settings, with limited data suggesting beneficial effects for clinical populations.
- Conclusion: Self-compassion holds promise as an important quality to cultivate to enhance health-related outcomes in those with chronic health conditions. Further systematic and rigorous research evaluating the effectiveness of self-compassion interventions in chronic illness populations is warranted to fully understand the role of this quality for chronic illness care.
Living with a chronic illness presents a number of challenges that can take a toll on both physical and psychological well-being. Pain, fatigue, and decreased daily functioning are symptoms common to many chronic illnesses that can negatively impact psychological well-being by creating uncertainty about attaining personal goals [1], and contributing to doubts and concerns about being able to fulfil one’s personal and work-related responsibilities [2]. The stress associated with negotiating the challenges of chronic illness can further complicate adjustment by exacerbating existing symptoms via stress-mediated and inflammation regulation pathways [3–5] and compromising the practice of important disease management and health maintenance behaviors [6,7]. These experiences can in turn fuel self-blame and other negative self-evaluations about not being able to meet personal and others’ expectations about managing one’s illness and create a downward spiral of poor adjustment and well-being [8,9].
A growing evidence base suggests that self-compassion is an important quality to help manage the stress and behavior-related issues that can compromise chronic illness care. Defined by Neff [10] as taking a kind, accepting, and non-judgmental stance towards oneself in times of failure or difficulty, self-compassion is associated with several indicators of adjustment in non-medical populations including resilience [11,12] and adaptive coping [13]. In support of the notion that self-compassion can play a role in promoting health behaviors, a recent meta-analysis found that self-compassion is linked to better practice of a range of health-promoting behaviors due in part to its links to adaptive emotions [14]. Research on the role of self-compassion for health-related outcomes with chronic illness populations is limited but nonetheless promising [15–17] , and suggests that self-compassion may be a worthwhile quality to cultivate to improve well-being and facilitate disease self-management.
In this article we present current research and theory on the potential of self-compassion as a clinical concept for improving health-related outcomes in chronic illness. After presenting a brief overview of the theoretical underpinnings of self-compassion and its measurement, we present the current state of research on the role of self-compassion in reducing stress and facilitating health behaviors in general medical populations. We then outline the emerging evidence illustrating a potential role for extending this research to chronic illness populations and make recommendations for the application of self-compassion interventions in clinical care, as a means to improving well-being and facilitating self-management of health for this group.
Self-Compassion: A Healthier Way of Responding to Challenges
Research into the correlates and effects of self-compassion has been primarily guided by the model of self-compassion proposed by Kristen Neff [10]. This view of self-compassion is derived from Buddhist psychology and reconceptualised in a secular manner to refer to the compassion expressed towards the self when experiencing suffering, whether it be due to circumstances beyond one’s control or within one’s control [18]. The 3 key components of self-compassion are proposed to work synergistically to promote kind rather than critical responses to failures and difficult circumstances. Self-kindness (versus self-judgment) involves taking a kind, caring and non-evaluative stance towards perceived inadequacies, shortcomings, and mistakes, and may be particularly valuable for countering the negative self-evaluations that can accompany not being able to meet one’s expectations due to the restrictions of living with a chronic condition [9]. Common humanity (versus isolation) refers to the sense of connection to others that arises from acknowledging the common human experience of imperfection and making mistakes, and being more aware that others may face similar challenging circumstances [18]. Framing hardship from this perspective can help people let go of the “why me?” view of their illness which can compromise adjustment [19], and instead foster a greater connection with others who live with similar conditions. Mindfulness (versus over identification) is the final component of self-compassion as conceptualised by Neff [10], and refers to taking a balanced and non-judgmental view of emotional experiences, grounding them in the present moment and neither ignoring nor becoming overly embroiled in the negative feelings that accompany painful experiences. Neff [10,18] proposes that mindfulness helps counteract the over-identification with one’s suffering that can reduce objectivity and taking a larger perspective on the situation. This mindful stance may be particularly beneficial for dealing with the ongoing pain and suffering of living with a chronic health condition, and encourage healthier ways of viewing the limitations associated with chronic illness. Correlational evidence from a study of healthy students further suggests that certain individual components of self-compassion may be particularly beneficial in the context of health, as the self-kindness and common humanity components were each found to be linked to better physical health and managing life stressors [20].
Although there are other conceptualizations of self-compassion [21], this 3-faceted model is the most widely used in research, in part because of the availability of a measure, the Self-compassion Scale [22], which explicitly assesses each of the facets of self-compassion. The 26-item scale is designed to assess positive and negative dimensions of each facet of self-compassion, but the total score is used more often than the separate subscales [23]. The measure assesses dispositional or trait self-compassion, with an underlying assumption that some individuals can be more or less self-compassionate in the way they regularly respond to challenges or failures. Importantly, self-compassion can also be prompted or fostered as a way of responding to failures and challenges, presenting the possibility that self-compassion can be increased among those who may benefit the most from responding with greater self-kindness and less self-judgement [24–26].
Whether conceived of as a momentary state or as an enduring quality, self-compassion has demonstrated consistent links with an array of indicators of psychological well-being. For example, one meta-analysis found that self-compassion is robustly and negatively linked with psychopathology (average r = –0.54), including depression and anxiety [27], 2 mental health issues that are prevalent in chronic illness populations [28,29]. Several studies have also noted associations of self-compassion with emotional resilience [18,30], and better coping and lower stress [12,13].
Self-Compassion Is Associated with Lower Perceived Stress
Relevant for our focus on chronic illness care, there is some evidence that self-compassion can be effective for improving well-being, and reducing stress in particular, in people with chronic illness. Across two illness samples, cancer and mixed chronic illnesses, those who scored low on a measure of self-compassion had higher levels of depression and stress compared to a healthy control sample [15], suggesting self-compassion may be protective against poor adjustment. Similar results have been found for breast cancer patients, with self-compassion explaining lower distress related to body image [16], and HIV patients, with self-compassion linked to lower stress, anxiety, and shame [31].
The protective role of self-compassion for stress appears to be explained primarily by the set of coping strategies that self-compassionate people use to deal with challenging circumstances. In their review, Allen and Leary [13] noted that self-compassionate people use coping styles that are adaptive and problem-focused (e.g., planning, social-support-seeking, and positive reframing), and tend to not use maladaptive coping styles (e.g., cognitively or behaviorally disengaging from the stressor and other escape-avoidance coping). Consistent with appraisal-based models of coping [32], adaptive coping strategies focus on removing the stressful event, garnering resources to better deal with the stressor, or recasting the stressor as less threatening, and therefore are instrumental in reducing the levels of stress that might normally be perceived in the absence of such coping approaches. Having access to a repertoire of adaptive coping strategies is particularly important in the context of chronic illness which can present a variety of daily challenges related to pain, functional and psychosocial limitations that require a flexible approach to changing demands.
Self-compassion with its links to adaptive coping may be particularly relevant for coping with such demands. One study put this assertion to the test by examining the role of coping strategies in explaining the link between self-compassion and stress in two chronic illness samples, inflammatory bowel disease (IBD) and arthritis [17]. In both samples, higher trait self-compassion was associated with a set of adaptive coping strategies which in turn explained greater coping efficacy and lower perceived stress, with the overall model explaining 43% of the variance in stress after controlling for health status and disease duration. Key adaptive coping strategies included greater use of active coping (a problem-focused coping strategy aimed at removing or reducing the stressor), positive reframing, and acceptance. The self-compassion–stress link was also explained in part by less use of maladaptive strategies, including denial, behavioral disengagement, and self-blame coping [17]. The latter coping strategy in particular is linked to poor adjustment in chronic illness as it reflects efforts to take control over uncontrollable symptoms by viewing illness-related changes, such as flare-ups, as a personal failure to manage one’s illness [9,33]. Together these findings, which were remarkably consistent across 2 distinct chronic illness groups, provide solid evidence to suggest that self-compassion provides individuals living with a chronic illness with a coping advantage that fosters adjustment through engaging in appropriate cognitive and behavioral coping strategies to minimize perceived stress.
Self-Compassion Can Reduce Physiological Stress
A caveat regarding the research to date on self-compassion and stress in chronic illness is that all studies are cross-sectional, which limits any conclusions about the direction of causality. Ignoring the fact that self-compassion in each of these studies was assessed as a relatively stable trait-like quality, one could argue that individuals who are less stressed have a greater opportunity to express kindness to themselves as they are not pre-occupied with illness-related demands and challenges. However, emerging research on self-compassion and the physiological correlates of stress provide a compelling case for the directionality assumed in the cross-sectional research. In one study, healthy young adults were subjected to a standard stress-inducing laboratory task (involving mental mathematics and public speaking), with plasma concentrations of the pro-inflammatory cytokine, interleukin-6 (IL-6), assessed before and after the task on 2 days [34]. Those with higher trait self-compassion responded to the stress task with significantly lower IL-6 levels even after controlling for other potential confounds such as demographics, self-esteem, depressive symptoms, and distress. Self-compassion was also linked to lower baseline levels of IL-6 on both days. These findings suggest that self-compassion may be both an enduring and response-specific protective factor against stress-induced inflammation.
There is also evidence supporting the efficacy of self-compassion interventions for reducing stress. In a study of healthy young women, those who underwent a brief training in self-compassion were found to have lower sympathetic nervous system reactivity (salivary alpha-amylase), and more adaptive parasympathetic nervous system reactivity (heart rate variability) in response to a stress-inducing lab task, compared to placebo control and no-training control groups [35]. That this study was conducted with women only is notable, as research indicates that women tend to have lower levels of self-compassion compared to men [18]. Together with the study on trait self-compassion and biomarkers of stress-induced inflammation, this research provides supportive evidence for the role of self-compassion in reducing the harmful physiological effects of stress. Self-compassion may therefore be particularly beneficial for both psychological and physical well-being in chronic illness given the known and negative impact of stress on symptoms for a number of chronic illnesses such as diabetes [36], cardiovascular disease [32], arthritis [4], and IBD [38].
Self-Compassion and the Regulation of Health Behaviors
Another key role for self-compassion in chronic illness care is through the facilitation of health-promoting behaviors. Health maintenance and disease management behaviors, such as getting diagnostic tests, taking medication, and weight management, are central for managing symptoms and minimizing the risk of disease progression or complications. For example, staying physically fit, maintaining a healthy diet, managing stress, and getting adequate sleep are critical for weight management and the behavioral control of symptoms for a number of chronic diseases [39,40]. Nonetheless, weight management behaviors often require initiating significant lifestyle changes which need to be maintained in order to be effective. Such behaviors can be particularly challenging for individuals with chronic illness symptoms such as pain and fatigue, which can present significant barriers [41] and trigger self-critical coping about not being able to adequately self-care or manage one’s disease [8,9]. Rather than being motivating, theory and evidence indicate that negative evaluations tend to increase stress and promote procrastination of important health behaviors [7,42].
In addition to theory noting why self-compassion may facilitate the regulation of important health behaviors [43,44], there is now a burgeoning body of research supporting the beneficial role of self-compassion in health behaviors [12,43,45]. Each of the 3 components of self-compassion (self-kindness, common humanity, and mindfulness) are posited to facilitate adaptive self-regulatory responses to the inevitable and momentary failures that occur when people try to enact their health goals. For example, not following through with dietary recommendations and giving into temptation can result in feelings of shame, negative self-evaluations, and reactive eating [46], which in turn can result in discontinuation of one’s diet. These minor failures would be viewed less negatively by people who are self-compassionate, because they realise that others have made similar mistakes (common humanity) and, therefore, do not become excessively self-critical (self-kindness) or immersed in feelings of guilt, shame or frustration (mindfulness), negative emotions which are known to interfere with self-regulation [43,47]. Indeed, self-compassion is associated with having fewer negative reactions in response to imagining a scenario in which a diet goal is transgressed [48].
There is also evidence that collectively, these components of self-compassion facilitate experiencing a healthy balance of positive and negative emotions in the context of health behavior change. Self-compassion appears to temper the negative responses to minor setbacks and failures that occur whilst trying to reach health goals, and foster the positive emotions required to maintain motivation during the pursuit of health goals. The most compelling support for this proposition comes from a meta-analysis of 15 samples (n = 3252) in which self-compassion was consistently and positively (average r = 0.25) associated with the practice of a range of health-promoting behaviors relevant for chronic illness care, including healthy eating, regular exercise, healthy sleep behaviors, and stress management [12]. The explanatory roles of positive and negative affect were also tested, with the results indicating that higher levels of positive affect and lower levels of negative affect were significant mediators of the link between self-compassion and health behaviors.
With respect to mood regulation, it is important to note that self-compassion is not simply an optimistic bias that predisposes individuals towards responding only in a positive way to perceived failures or setbacks. Rather, self-compassion fosters taking a balanced perspective on one’s failures, recognizing both the positive and negative aspects, and harnessing the negative mood that arises from a state of discrepancy to motivate self-improvement. For example, in experimental studies, both enduring and momentary self-compassionate states are associated with increased self-improvement motivation and behavior after experiencing failure and regret [49,50], in part because self-compassion fosters personal acceptance [50]. This adaptive responding can translate into better adherence and health behaviors in chronic health conditions after lapses in self-care which might otherwise foster self-criticism and poor disease management. Preliminary evidence from the author’s lab supports this proposition, as self-compassion was positively associated with both treatment adherence and the practice of wellness behaviors, due in part to lower levels of perceived stress, in samples of cancer patients and survivors [51], and people with chronic fatigue syndrome [52].
Clinical Applications of Self-Compassion for Chronic Illness Care
Given the growing evidence linking self-compassion to well-being and health behaviors, the next logical step is to consider ways of cultivating self-compassion for those individuals experiencing chronic health conditions.
Training in mindfulness might be one way to foster self-compassion within a health care setting. Mindfulness-Based Cognitive Behavior Therapy (MBCT [53]), and Mindfulness-Based Stress Reduction (MBSR [54]), are both programs that use mindfulness skills to notice distressing thoughts and feelings, hold these experiences in awareness, and cultivate acceptance and self-compassion [53]. MBSR, usually delivered as an 8-week group-based program, has been found to have significant effects on depression, anxiety and psychological distress in people with chronic somatic diseases [55]. However, fostering self-compassion forms only part of MBCT and MBSR. Indeed there are very few therapeutic interventions that specifically and primarily target self-compassion; however, where they are used they show promise.
Compassionate Mind Training (CMT [24]), Compassion-Focused Therapy (CFT [21]), and the Mindful Self-Compassion program [26] are examples of such targeted interventions. These therapeutic models, again usually delivered in group settings, aim to foster a kinder and more accepting attitude towards oneself through the use of formal meditations (such as living kindness meditation; LKM), home practice and informal practices for daily life (such as self-compassionate letter writing), and have been demonstrated to be effective with, for example, community participants [26], people who hear malevolent voices [56], and those with chronic mood difficulties [24].
Additionally, there are a number of brief self-compassion practices that have been evaluated as an intervention in their own right and demonstrate positive effects. LKM aiming to develop a state of unconditional kindness towards both oneself and others and compassion meditation (CM [57]), are the most commonly described. CM involves techniques to cultivate compassion, or deep, genuine sympathy for those stricken by misfortune, including oneself, “together with an earnest wish to ease this suffering” [58]. The effects of these kindness-based meditations on health and well-being have been summarized in a recent review [59] which illustrates that, whilst limited data exists currently, promising effects have been shown for a number of different groups. Positive effects have for example been demonstrated for patients with chronic back pain [60] and for people with experiences traditionally conceptualized as psychosis [61], suggesting these practice may also be beneficial for other chronic health conditions.
Alongside the potential benefits, how interventions cultivating self-compassion can be delivered in clinical practice is worthy of consideration. Previous applications have included group work (including MBCT, MBSR), one-to-one therapy (such as CFT) and self-directed practice via bibliotherapy or online materials. The different options available here suggest this kind of intervention is highly accessible, potentially inexpensive and could be used as a complimentary approach alongside other more traditional medical disease management treatments or as a stand-alone psychotherapeutic intervention when required.
In order to best support the successful introduction and evaluation of such interventions, consideration of compassionate practice by staff within health-care settings is also needed. Cultivating a culture of compassion through compassionate leadership [62] is required. We know services with higher levels of caring practice have higher quality care, greater well-being for staff and in turn more compassionate care for patients [63] than those services that are struggling. It is hoped that taking a broad systemic compassionate approach (via training, ongoing supervision and ethos cultivation) would ensure that the language used, information communicated, and disease management approaches are planned and delivered in a way that fosters patients’ sense of self-efficacy and kindness towards themselves, with all the benefits outlined above.
Conclusion
Theory and research indicate that self-compassion fosters adaptive responses to perceived failures and setbacks, and is therefore associated with well-being, reduced stress and more frequent health behaviors. The emerging evidence base on the benefits of self-compassion for coping with the challenges of chronic health conditions is promising, and suggests that the benefits of self-compassion noted in non-medical populations may extend to chronic illness care. Interventions cultivating self-compassion may be especially beneficial for those with chronic health conditions through the mechanisms identified earlier; reducing stress (and thereby impacting on an individual’s relationship with their physical health); improving self-management skills with condition related behaviors and health-promoting behaviors; altering one’s relationship with illness-related shame and self-blame; and in boosting resilience. Systematic and rigorous evaluation of such interventions with people with chronic health conditions is now needed, evaluating impacts on well-being, health behaviors, and disease management and outcomes.
Corresponding author: Fuschia M. Sirois, Dept. of Psychology, University of Sheffield, 1 Vicar Lane, Sheffeld, S1 1HD, [email protected].
Fianacial disclosures: None.
1. Hamilton N, Karoly P, Kitzman H. Self-regulation and chronic pain:The role of emotion. Cogn Ther Res 2007;28:559–576.
2. Luyten P, Kempke S, Van Wambeke P, et al. Self-critical perfectionism, stress generation, and stress sensitivity in patients with chronic fatigue syndrome: relationship with severity of depression. Psychiatry 2011;74:21–30.
3. Cohen S, Janicki-Deverts D, Doyle WJ, et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proceedings of the National Academy of Sciences 2012.
4. Evers AWM, Verhoeven EWM, van Middendorp H, et al. Does stress affect the joints? Daily stressors, stress vulnerability, immune and HPA axis activity, and short-term disease and symptom fluctuations in rheumatoid arthritis. Ann Rheum Dis 2014;73:1683–8.
5. Maunder RG, Levenstein S. The role of stress in the development and clinical course of inflammatory bowel disease: epidemiological evidence. Curr Molecular Med 2008;8:247–52.
6. Rod NH, Grønbæk M, Schnohr P, et al. Perceived stress as a risk factor for changes in health behavior and cardiac risk profile: a longitudinal study. J Intern Med 2009;266:467–75.
7. Sirois FM. Is procrastination a vulnerability factor for hypertension and cardiovascular disease? Testing an extension of the procrastination-health model. J Behav Med 2015;38:578–89.
8. Moskovitz DN, Maunder RG, Cohen Z, et al. Coping behavior and social support contribute independently to quality of life after surgery for inflammatory bowel disease. Dis Colon Rectum 2000;43:517–21.
9. Voth J, Sirois FM. The role of self-blame and responsibility in adjustment to inflammatory bowel disease. Rehab Psych 2009;54:99–108.
10. Neff KD. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self Ident 2003;2:85–101.
11. Neff KD, Kirkpatrick KL, Rude SS. Self-compassion and adaptive psychological functioning. J Res Personality 2007;41:139–54.
12. Sirois FM. Procrastination and stress: Exploring the role of self-compassion. Self Ident 2014;13:128–45.
13. Allen AB, Leary MR. Self-compassion, stress, and coping. Soc Person Psych Comp 2010;4:107–18.
14. Sirois FM, Kitner R, Hirsch JK. Self-compassion, affect, and health behaviors. Health Psychol 2014.
15. Pinto-Gouveia J, Duarte C, Matos M, Fráguas S. The protective role of self-compassion in relation to psychopathology symptoms and quality of life in chronic illness and in cancer patients. Clin Psychol Psychother 2014;21:311–23.
16. Przezdziecki A, Sherman KA, Baillie A, et al. My changed body: breast cancer, body image, distress and self-compassion. Psychooncology 2013;22:1872–9.
17. Sirois FM, Molnar DS, Hirsch JK. Self-compassion, stress, and coping in the context of chronic illness. Self Identity 2015:1–14.
18. Neff KD. Self-compassion, self-esteem, and well-being. Social Personality Psych Compass 2011;5:1–12.
19. Davis DG, Morgan MS. Finding meaning, perceiving growth, and acceptance of tinnitus. Rehabil Psych 2008;53:128–38.
20. Hall CW, Row KA, Wuensch KL, Godley KR. The role of self-compassion in physical and psychological well-being. J Psychology 2013;147:311–23.
21. Gilbert P. Introducing compassion-focused therapy. Advance Psych Treat 2009;15:199–208.
22. Neff KD. Development and validation of a scale to measure self-compassion. Self Identity 2003;2:223–50.
23. Neff KD. The self-compassion scale is a valid and theoretically coherent measure of self-compassion. Mindfulness 2016;7:264–74.
24. Gilbert P, Procter S. Compassionate mind training for people with high shame and self-criticism: overview and pilot study of a group therapy approach. Clin Psychol Psychother 2006;13:353–79.
25. Leary MR, Tate EB, Adams CE, et al. Self-compassion and reactions to unpleasant self-relevant events: the implications of treating oneself kindly. J Personality Social Psychol 2007;92:887–904.
26. Neff KD, Germer CK. A pilot study and randomized controlled trial of the mindful self-compassion program. J Clin Psychol 2013;69:28–44.
27. MacBeth A, Gumley A. Exploring compassion: A meta-analysis of the association between self-compassion and psychopathology. Clin Psych Rev 2012;32:545–52.
28. Murphy LB, Sacks JJ, Brady TJ, et al. Anxiety and depression among US adults with arthritis: Prevalence and correlates. Arthritis Care Res 2012:64:968–76.
29. Walker JR, Ediger JP, Graff LA, et al. The Manitoba IBD Cohort Study: a population-based study of the prevalence of lifetime and 12-month anxiety and mood disorders. Am J Gastroenterol 2008;103:1989–97.
30. Neff KD, McGehee P. Self-compassion and psychological resilience among adolescents and young adults. Self Ident 2009;9:225–40.
31. Brion J, Leary M, Drabkin A. Self-compassion and reactions to serious illness: The case of HIV. J Health Psychol 2014;19:218–29.
32. Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984.
33. Thompson SC, Cheek PR, Graham MA. The other side of perceived control: disadvantages and negative effects. In: Spacapan S, Oskamp S, editors. The social psychology of health. Newbury Park: Sage; 1988:69–93.
34. Breines JG, Thoma MV, Gianferante D, et al. Self-compassion as a predictor of interleukin-6 response to acute psychosocial stress. Brain, Behavior, and Immunity 2014;37:109–14.
36. Lloyd C, Smith J, Weinger K. Stress and diabetes: a review of the links. Diabetes Spectrum 2005;18:121–7.
35. Arch JJ, Brown KW, Dean DJ, et al. Self-compassion training modulates alpha-amylase, heart rate variability, and subjective responses to social evaluative threat in women. Psychoneuroendocrinology 2013;42:49–58.
37. Dimsdale JE. Psychological stress and cardiovascular disease. J Am Coll Cardiol 2008;51:1237–46.
38. Maunder RG. Evidence that stress contributes to inflammatory bowel disease: evaluation, synthesis, and future directions. Inflam Bowel Dis 2005;11:600–8.
39. Daskalopoulou SS, Khan NA, Quinn RR, et al. The 2012 Canadian Hypertension Education program recommendations for the management of hypertension: blood pressure measurement, diagnosis, assessment of risk, and therapy. Can J Cardiol 2012;28:270–87.
40. Gulliksson M, Burell G, Vessby B, et al. Randomized controlled trial of cognitive behavioral therapy vs standard treatment to prevent recurrent cardiovascular events in patients with coronary heart disease: Secondary prevention in uppsala primary health care project (suprim). Arch Intern Med 2011;171:134–40.
41. Jerant AF, Friederichs-Fitzwater MMV, Moore M. Patients’ perceived barriers to active self-management of chronic conditions. Patient Ed Couns 2005;57:300–7.
42. Sirois FM. Procrastination, stress, and chronic health conditions: a temporal perspective. In: Sirois FM, Pychyl T, editors. Procrastination, health, and well-being. Elsevier; 2016.
43. Sirois FM. A self-regulation resource model of self-compassion and health behavior intentions in emerging adults. Prev Med Rep 2015;2:218–22.
44. Terry ML, Leary MR. Self-compassion, self-regulation, and health. Self Identity 2011;10:352–62.
45. Dunne S, Sheffield D, Chilcot J. Brief report: Self-compassion, physical health and the mediating role of health-promoting behaviors. J Health Psychol 2016.
46. Polivy J, Herman CP, Deo R. Getting a bigger slice of the pie. Effects on eating and emotion in restrained and unrestrained eaters. Appetite 2010;55:426–30.
47. Wagner DD, Heatherton TF. Self-regulation and its failure: The seven deadly threats to self-regulation. In: Mikulincer M, Shaver PR, Borgida E, Bargh JA, editors. APA handbook of personality and social psychology, Volume 1: Attitudes and social cognition. Washington: American Psychological Association. Forthcoming.
48. Adams CE, Leary MR. Promoting self-compassionate attitudes toward eating among restrictive and guilty eaters. J Soc Clin Psychol 2007;26:1120–44.
49. Breines JG, Chen S. Self-compassion increases self-improvement motivation. Pers Social Psych Bull 2012;38:1133–43.
50. Zhang JW, Chen S. Self-compassion promotes personal improvement from regret experiences via acceptance. Pers Social Psych Bull 2016;42:244–58.
51. Sirois FM, Hirsch JK. Self-compassion is associated with health behaviors in cancer patients and survivors. Forthcoming.
52. Sirois FM. Self-compassion, adheremce, and health behaviors in chronic fatigue syndrome: The role of stress. Forthcoming.
53. Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. New York: Guilford Press; 2002.
54. Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Dell; 1990.
55. Bohlmeijer E, Prenger R, Taal E, Cuijpers P. The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: A meta-analysis. J Psychosom Res 2010;68:539–44.
56. Mayhew SL, Gilbert P. Compassionate mind training with people who hear malevolent voices: a case series report. Clin Psychol Psychother 2008;15:113–38.
57. Hofmann SG, Grossman P, Hinton DE. Loving-kindness and compassion meditation: potential for psychological interventions. Clin Psychol Rev 2011;31:1126–32.
58. Hopkins J. Cultivating compassion. New York: Broadway Books; 2001.
59. Galante J, Galante I, Bekkers M-J Gallacher. Effect of kindness-based meditation on health and well-being: a systematic review and meta-analysis. J Consult Clin Psychol 2014;82:1101–14.
60. Carson JW, Keefe FJ, Lynch TR, et al. Loving-kindness meditation for chronic low back pain: results from a pilot trial. J Holist Nurs 2005;23:287–304.
61. Johnson DP, Penn DL, Fredrickson BL, et al. A pilot study of loving-kindness meditation for the negative symptoms of schizophrenia. Schizophr Res 2011;129:137–40.
62. West M, Steward K, Eckert R, Pasmore B. Developing collective leadership for health care. London: The King’s Fund; 2014.
63. Dixon-Woods M, Baker R, Charles K, et al. Culture and behavior in the English National Health Service: overview of lessons from a large multimethod study. BMJ Qual Saf 2014;23:106–15.
1. Hamilton N, Karoly P, Kitzman H. Self-regulation and chronic pain:The role of emotion. Cogn Ther Res 2007;28:559–576.
2. Luyten P, Kempke S, Van Wambeke P, et al. Self-critical perfectionism, stress generation, and stress sensitivity in patients with chronic fatigue syndrome: relationship with severity of depression. Psychiatry 2011;74:21–30.
3. Cohen S, Janicki-Deverts D, Doyle WJ, et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proceedings of the National Academy of Sciences 2012.
4. Evers AWM, Verhoeven EWM, van Middendorp H, et al. Does stress affect the joints? Daily stressors, stress vulnerability, immune and HPA axis activity, and short-term disease and symptom fluctuations in rheumatoid arthritis. Ann Rheum Dis 2014;73:1683–8.
5. Maunder RG, Levenstein S. The role of stress in the development and clinical course of inflammatory bowel disease: epidemiological evidence. Curr Molecular Med 2008;8:247–52.
6. Rod NH, Grønbæk M, Schnohr P, et al. Perceived stress as a risk factor for changes in health behavior and cardiac risk profile: a longitudinal study. J Intern Med 2009;266:467–75.
7. Sirois FM. Is procrastination a vulnerability factor for hypertension and cardiovascular disease? Testing an extension of the procrastination-health model. J Behav Med 2015;38:578–89.
8. Moskovitz DN, Maunder RG, Cohen Z, et al. Coping behavior and social support contribute independently to quality of life after surgery for inflammatory bowel disease. Dis Colon Rectum 2000;43:517–21.
9. Voth J, Sirois FM. The role of self-blame and responsibility in adjustment to inflammatory bowel disease. Rehab Psych 2009;54:99–108.
10. Neff KD. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self Ident 2003;2:85–101.
11. Neff KD, Kirkpatrick KL, Rude SS. Self-compassion and adaptive psychological functioning. J Res Personality 2007;41:139–54.
12. Sirois FM. Procrastination and stress: Exploring the role of self-compassion. Self Ident 2014;13:128–45.
13. Allen AB, Leary MR. Self-compassion, stress, and coping. Soc Person Psych Comp 2010;4:107–18.
14. Sirois FM, Kitner R, Hirsch JK. Self-compassion, affect, and health behaviors. Health Psychol 2014.
15. Pinto-Gouveia J, Duarte C, Matos M, Fráguas S. The protective role of self-compassion in relation to psychopathology symptoms and quality of life in chronic illness and in cancer patients. Clin Psychol Psychother 2014;21:311–23.
16. Przezdziecki A, Sherman KA, Baillie A, et al. My changed body: breast cancer, body image, distress and self-compassion. Psychooncology 2013;22:1872–9.
17. Sirois FM, Molnar DS, Hirsch JK. Self-compassion, stress, and coping in the context of chronic illness. Self Identity 2015:1–14.
18. Neff KD. Self-compassion, self-esteem, and well-being. Social Personality Psych Compass 2011;5:1–12.
19. Davis DG, Morgan MS. Finding meaning, perceiving growth, and acceptance of tinnitus. Rehabil Psych 2008;53:128–38.
20. Hall CW, Row KA, Wuensch KL, Godley KR. The role of self-compassion in physical and psychological well-being. J Psychology 2013;147:311–23.
21. Gilbert P. Introducing compassion-focused therapy. Advance Psych Treat 2009;15:199–208.
22. Neff KD. Development and validation of a scale to measure self-compassion. Self Identity 2003;2:223–50.
23. Neff KD. The self-compassion scale is a valid and theoretically coherent measure of self-compassion. Mindfulness 2016;7:264–74.
24. Gilbert P, Procter S. Compassionate mind training for people with high shame and self-criticism: overview and pilot study of a group therapy approach. Clin Psychol Psychother 2006;13:353–79.
25. Leary MR, Tate EB, Adams CE, et al. Self-compassion and reactions to unpleasant self-relevant events: the implications of treating oneself kindly. J Personality Social Psychol 2007;92:887–904.
26. Neff KD, Germer CK. A pilot study and randomized controlled trial of the mindful self-compassion program. J Clin Psychol 2013;69:28–44.
27. MacBeth A, Gumley A. Exploring compassion: A meta-analysis of the association between self-compassion and psychopathology. Clin Psych Rev 2012;32:545–52.
28. Murphy LB, Sacks JJ, Brady TJ, et al. Anxiety and depression among US adults with arthritis: Prevalence and correlates. Arthritis Care Res 2012:64:968–76.
29. Walker JR, Ediger JP, Graff LA, et al. The Manitoba IBD Cohort Study: a population-based study of the prevalence of lifetime and 12-month anxiety and mood disorders. Am J Gastroenterol 2008;103:1989–97.
30. Neff KD, McGehee P. Self-compassion and psychological resilience among adolescents and young adults. Self Ident 2009;9:225–40.
31. Brion J, Leary M, Drabkin A. Self-compassion and reactions to serious illness: The case of HIV. J Health Psychol 2014;19:218–29.
32. Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984.
33. Thompson SC, Cheek PR, Graham MA. The other side of perceived control: disadvantages and negative effects. In: Spacapan S, Oskamp S, editors. The social psychology of health. Newbury Park: Sage; 1988:69–93.
34. Breines JG, Thoma MV, Gianferante D, et al. Self-compassion as a predictor of interleukin-6 response to acute psychosocial stress. Brain, Behavior, and Immunity 2014;37:109–14.
36. Lloyd C, Smith J, Weinger K. Stress and diabetes: a review of the links. Diabetes Spectrum 2005;18:121–7.
35. Arch JJ, Brown KW, Dean DJ, et al. Self-compassion training modulates alpha-amylase, heart rate variability, and subjective responses to social evaluative threat in women. Psychoneuroendocrinology 2013;42:49–58.
37. Dimsdale JE. Psychological stress and cardiovascular disease. J Am Coll Cardiol 2008;51:1237–46.
38. Maunder RG. Evidence that stress contributes to inflammatory bowel disease: evaluation, synthesis, and future directions. Inflam Bowel Dis 2005;11:600–8.
39. Daskalopoulou SS, Khan NA, Quinn RR, et al. The 2012 Canadian Hypertension Education program recommendations for the management of hypertension: blood pressure measurement, diagnosis, assessment of risk, and therapy. Can J Cardiol 2012;28:270–87.
40. Gulliksson M, Burell G, Vessby B, et al. Randomized controlled trial of cognitive behavioral therapy vs standard treatment to prevent recurrent cardiovascular events in patients with coronary heart disease: Secondary prevention in uppsala primary health care project (suprim). Arch Intern Med 2011;171:134–40.
41. Jerant AF, Friederichs-Fitzwater MMV, Moore M. Patients’ perceived barriers to active self-management of chronic conditions. Patient Ed Couns 2005;57:300–7.
42. Sirois FM. Procrastination, stress, and chronic health conditions: a temporal perspective. In: Sirois FM, Pychyl T, editors. Procrastination, health, and well-being. Elsevier; 2016.
43. Sirois FM. A self-regulation resource model of self-compassion and health behavior intentions in emerging adults. Prev Med Rep 2015;2:218–22.
44. Terry ML, Leary MR. Self-compassion, self-regulation, and health. Self Identity 2011;10:352–62.
45. Dunne S, Sheffield D, Chilcot J. Brief report: Self-compassion, physical health and the mediating role of health-promoting behaviors. J Health Psychol 2016.
46. Polivy J, Herman CP, Deo R. Getting a bigger slice of the pie. Effects on eating and emotion in restrained and unrestrained eaters. Appetite 2010;55:426–30.
47. Wagner DD, Heatherton TF. Self-regulation and its failure: The seven deadly threats to self-regulation. In: Mikulincer M, Shaver PR, Borgida E, Bargh JA, editors. APA handbook of personality and social psychology, Volume 1: Attitudes and social cognition. Washington: American Psychological Association. Forthcoming.
48. Adams CE, Leary MR. Promoting self-compassionate attitudes toward eating among restrictive and guilty eaters. J Soc Clin Psychol 2007;26:1120–44.
49. Breines JG, Chen S. Self-compassion increases self-improvement motivation. Pers Social Psych Bull 2012;38:1133–43.
50. Zhang JW, Chen S. Self-compassion promotes personal improvement from regret experiences via acceptance. Pers Social Psych Bull 2016;42:244–58.
51. Sirois FM, Hirsch JK. Self-compassion is associated with health behaviors in cancer patients and survivors. Forthcoming.
52. Sirois FM. Self-compassion, adheremce, and health behaviors in chronic fatigue syndrome: The role of stress. Forthcoming.
53. Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. New York: Guilford Press; 2002.
54. Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Dell; 1990.
55. Bohlmeijer E, Prenger R, Taal E, Cuijpers P. The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: A meta-analysis. J Psychosom Res 2010;68:539–44.
56. Mayhew SL, Gilbert P. Compassionate mind training with people who hear malevolent voices: a case series report. Clin Psychol Psychother 2008;15:113–38.
57. Hofmann SG, Grossman P, Hinton DE. Loving-kindness and compassion meditation: potential for psychological interventions. Clin Psychol Rev 2011;31:1126–32.
58. Hopkins J. Cultivating compassion. New York: Broadway Books; 2001.
59. Galante J, Galante I, Bekkers M-J Gallacher. Effect of kindness-based meditation on health and well-being: a systematic review and meta-analysis. J Consult Clin Psychol 2014;82:1101–14.
60. Carson JW, Keefe FJ, Lynch TR, et al. Loving-kindness meditation for chronic low back pain: results from a pilot trial. J Holist Nurs 2005;23:287–304.
61. Johnson DP, Penn DL, Fredrickson BL, et al. A pilot study of loving-kindness meditation for the negative symptoms of schizophrenia. Schizophr Res 2011;129:137–40.
62. West M, Steward K, Eckert R, Pasmore B. Developing collective leadership for health care. London: The King’s Fund; 2014.
63. Dixon-Woods M, Baker R, Charles K, et al. Culture and behavior in the English National Health Service: overview of lessons from a large multimethod study. BMJ Qual Saf 2014;23:106–15.